Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0608-10147. The contractual start date was in February 2010. The final report began editorial review in August 2015 and was accepted for publication in June 2016. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Sue Ziebland declares that she is deputy chairperson of the National Institute for Health Research (NIHR) Doctoral Research Fellowship Panel, is a Policy Research Panel Committee Member and is a NIHR Senior Investigator. Louise Locock declares current membership of the Health Services and Delivery Research Commissioning Board. John Powell declares current membership of the Health Technology Assessment and Efficacy and Mechanism Evaluation Editorial Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Ziebland et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Overview of the programme
Health-care decisions are made at every stage of an illness from the point at which we first experience a symptom and try to identify what it might mean. The dilemmas that people face include a lot of ‘whether, how and for how long’ questions about self-management, seeking professional help, using treatments and minimising the disruptive effects of illness on daily life, work, and relationships. The programme of work reported in this monograph grew from the awareness that the public and patients need reliable health information to support these decisions and the recognition that the relatively new ability to find other patients’ experiences online could be transforming the health information landscape and the information that patients seek, find and use.
When the programme began in 2010, it was already becoming routine for people in the UK to seek health information online. There was also an evident growth in online ‘patient experience’ (PEx) in many formats, including social networking, reputation systems (an approach borrowed from e-commerce and now widespread in health), peer-to-peer forums, chat rooms, blogs and personal experience sections on health and voluntary sector websites. However, there were also many concerns being voiced about whether or not the internet was too overwhelming and confusing (especially for people with low heath literacy), whether patients would misinform or alarm themselves, and how all of this might affect their choices and communication with NHS staff, in particular during the brief consultation in primary care.
We therefore proposed a 5-year programme to examine the phenomenon of the online experiences of patients, to understand its potential for both benefit and harm and identify whether, when and how the NHS might recommend incorporating people’s health and care experiences (hereafter referred to as PEx) into online health information.
When we began this work, the role of online PEx was a new field with no agreed theoretical and methodological basis: almost all of the research had been exploratory or descriptive. It has long been recognised that people seek knowledge about their health from others who have been through the same experiences. 1,2 What was unknown was how the online environment might be transforming this behaviour, perhaps opening up opportunities for support, information and new forms of connection. Our own work had indicated that exposure to online PEx had the potential to both improve health and do harm. 3 We were aware that PEx might be of greater or lesser value depending on how it is presented, the type of condition involved, the stage in the patient journey and individual preference.
Aim
The aim of the programme was to find out whether, when and how the NHS should incorporate PEx into online health information.
To achieve the aim of the programme, we needed to understand the mechanisms through which PEx may influence health, develop the tools to measure the effects, explore how PEx is used and test prototype websites in exemplar patient groups: (1) people who wanted to stop smoking, (2) people with asthma and (3) carers of people with multiple sclerosis (MS). The programme was delivered through three work packages (WPs) which used mixed methods comprising a conceptual literature review, a qualitative secondary analysis, the development and testing of a new questionnaire, an online ethnography, observational and experimental studies in an internet café environment and, last, some exploratory feasibility trials.
Our WPs were designed and implemented by a multidisciplinary team led by a medical sociologist and including health psychologists, a public health doctor, academic general practitioners (GPs), experts in questionnaire design, statistics and website design, and clinical trialists, with coinvestigators from health policy and a service user perspective.
We summarise below the full programme and the relevance of each of the WPs.
Note: we acknowledge that there are many different ways of referring to people who are interviewed about their health, who contribute to or seek health-related information, or who publish their own material about their health experiences online. These terms include ‘patients’, ‘the public’, ‘people’, ‘consumers’ and ‘health service users’. For the sake of brevity and to conform with other NHS and National Institute for Health Research (NIHR) documents, we use PEx or ‘patient experience’ to encompass the various roles of the public and patients in this field.
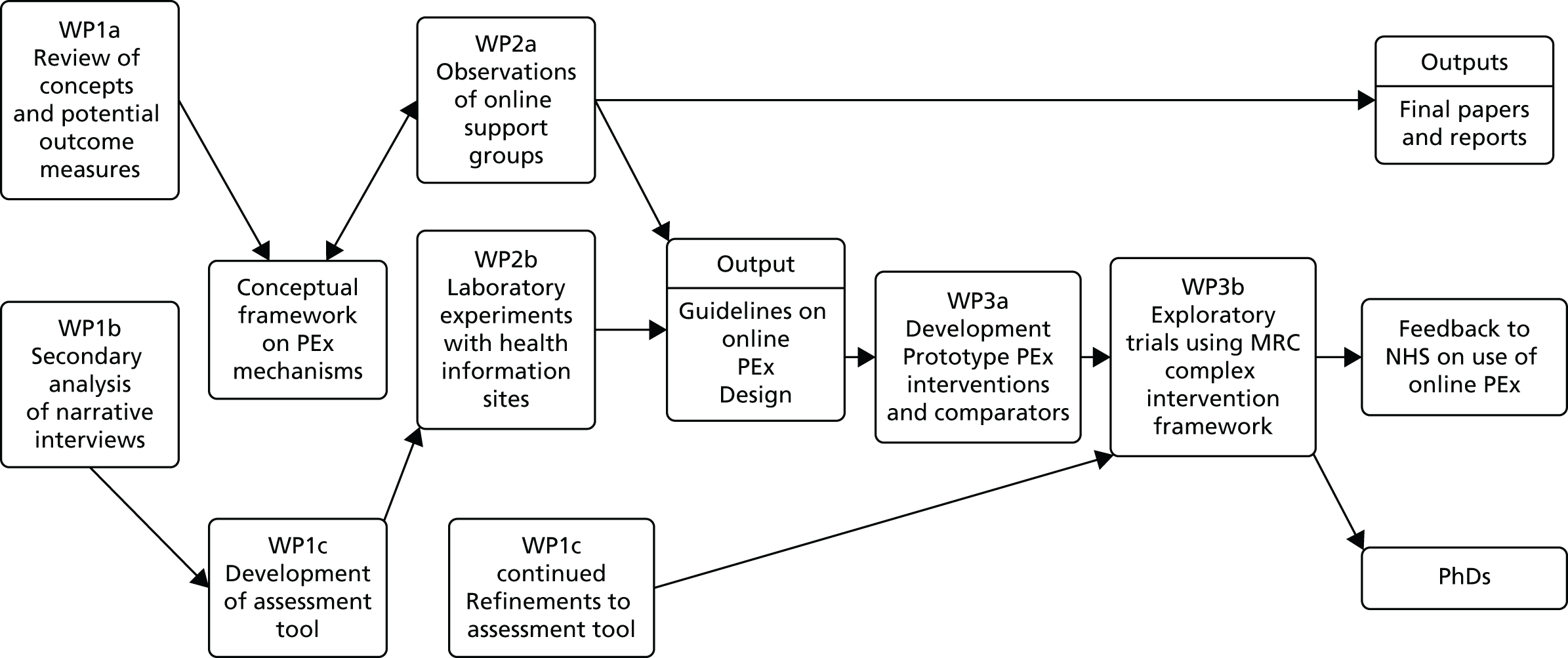
Figure 1 shows the connections between the elements of the programme and the main outputs.
FIGURE 1.
Overview of the programme.
Work package 1
Conceptual and literature review
We used reviews and secondary analysis to clarify the theoretical mechanisms and the domains of health that we expected to be affected by exposure to online PEx. An approach drawing on ‘realist’ literature review methods was conducted to identify theories, mechanisms of action and the potential impact of PEx and to establish the conceptual and theoretical framework for the whole programme. The review identified seven domains through which access to other people’s experiences of a health condition could affect health; these comprised finding information, feeling supported, maintaining relationships, using health services, changing behaviours, learning to tell the story and visualising illness.
Secondary analysis of narrative interviews
Interviews from a unique Oxford archive of interviews, held by the Health Experiences Research Group (HERG), were used for a qualitative secondary analysis. At the time of the study, the archive included over 60 health conditions, which were sampled to (1) gather evidence through thematic analysis about how and why information based on real experience is sought and used, and (2) select quotations from interview transcripts which illustrate participants’ views on their use of the internet for health information, to inform the item pool for a questionnaire tool.
Development and piloting of the e-Health Impact Questionnaire
Trials to evaluate the impact of online PEx need to identify the most appropriate outcomes to be measured. The range of outcomes is potentially large and may be addressed, in part, by existing measures. However, as research on online patient experiential information was in its infancy at the time this WP commenced, there was no valid and reliable assessment tool to capture the health effects of using websites which contain PEx. We therefore developed the e-Health Impact Questionnaire (eHIQ) to assess health-related websites which contain either experiential or factual information. The tool was developed and tested for use across a range of health groups (e.g. people with long-term conditions, carers and those viewing websites aimed at changing health behaviour) and can also be used for websites that include different styles of online information (e.g. factual or experiential information and discussion forums). This WP was written up by LK as her doctorate (awarded in 2014, supervised by CJ and SZ).
Work package 2
Online ethnographic observations
In this WP, we explored internet behaviour using in-depth observational research methods to establish how different types and formats of online PEx are used and how online PEx material might be optimised. We studied how and why people share experiences of health and illness on the internet in the context of MS. Through a content analysis of online settings, ethnographic observation of online activity and telephone interviews, we studied how people living with MS and those who care for them seek out others’ experiences, how they share their own experiences, and how this affects their understanding of MS, their relationship with health-care practitioners, their health-care decision-making and their general well-being.
Observations and experimental studies
Acknowledging the diverse quality of online PEx, we conducted three studies using observational and internet laboratory café methods to discover how patients find and use PEx to inform health and lifestyle choices. The first study was expanded from that stipulated in the proposal and included, in addition to the asthma and MS carers elements, two further elements with people who wished to stop smoking. The second study, which focused on people with asthma and MS carers, involved the collection of eye-tracking data, to identify where people spend time, what holds their attention and how they organise their searches, and a comprehensive interview. From these studies, we developed a model of patients’ peer-to-peer engagement online, which was used to develop the prototype PEx websites that were used in the feasibility trials in the final WP.
The third study involved a sample of smokers. We sought to examine the effect of (1) message type (i.e. PEx vs. information only), (2) the palatability of material in terms of pre-existing beliefs (attitude towards quitting by using or not using aids and support) and (3) perceived similarity (based on gender) between the reader and the author of the PEx on a participant’s readiness to accept the message. The study adopted a longitudinal approach to examine the potential impact of these variables on behavioural intentions and actions 2 weeks and 3 months after exposure.
Work package 3
Development and testing of patient experience web interventions for exploratory trials
We developed six prototype multimedia websites featuring either PEx information (intervention) or non-PEx factual information (comparator) for each of three exemplar health issues (adults with asthma, carers of people with MS and people considering giving up smoking cigarettes). We used established qualitative research methods, led by experienced qualitative social scientists based in the Oxford team, to collect unstructured, narrative interviews about the experiences, information and support needs of people in each of the three exemplar groups. The design and presentation of PEx information on the websites were developed in accord with the guidelines developed in WP2. The comparator websites were based on non-PEx material from NHS Choices and were presented in a similar design to that of the intervention sites.
Exploratory trials
As originally proposed, we conducted a phase II pilot randomised single-blind trial, in which eligible participants were randomly allocated to a condition-specific PEx-based health information website or to a comparator website which contained no PEx information, stratified by one of three health conditions. The original application described three separate pilot randomised trials, one for each health condition. For operational efficiency, the three trials were run under the governance of a single trial protocol and analysed by condition (smoking cessation, asthma or caring for someone with MS). As this was an exploratory study, our main aim was to establish the feasibility of undertaking this research and to identify any emergent evidence of efficacy or harm. We measured recruitment and retention rates, usage of the intervention and comparator, and any adverse events. We measured the impact of all six websites on health status, and we assessed attitudes towards the websites using the new instrument, the eHIQ. We also included some condition-specific measures as secondary outcomes (such as self-efficacy measures). We also undertook qualitative interviews with 30 purposively selected trial participants to explore why and how they took part and used the websites (or did not).
Chapter 2 Work package 1a: how might sharing experiences on the internet affect people’s health? A conceptual overview
Abstract
Introduction: the role of information based on online PEx is a new field with no agreed theoretical and methodological basis. As a first step to improving the scientific base and policy guidance, we aimed to provide an overview, or conceptual map, of the potential health effects of online PEx in health and health care.
Methods: we drew on realist review methods in three stages: (1) a wide-ranging review of literature in social and health sciences distilled in a matrix that covered potential positive and negative impacts (we continued reading until we reached data saturation); (2) further refinement of the results with reference to a public panel; and (3) even further refinement after testing with expert colleagues.
Findings: seven domains characterise how online PEx could affect health, each with the potential for positive and negative impacts. The domains are finding information, feeling supported, maintaining relationships with others, affecting behaviour, experiencing health services, learning to tell the story and visualising disease.
Conclusions: the value of first-person accounts, the appeal and memorability of stories, and the need to make contact with peers all suggest that reading and hearing others’ accounts of their own experiences of health and illnesss will remain a key feature of e-health.
Introduction
As we have seen, the role of information based on online PEx is a new field with no agreed theoretical and methodological basis. As a first step to improving the scientific base and policy guidance on the provision of information based on people’s experiences, we drew on a wide literature in the social and health sciences to provide an overview, or conceptual map, of the potential health effects of online PEx in health and health care. The below contains extracts from and represents an abridged version of material first published in the Milbank Quarterly © (2012) The Milbank Memorial Fund. 4
We identified seven domains of the online PEx terrain. In this section of the report, we describe the methods we used to develop this conceptual map before going on to describe the seven domains of the terrain in turn.
Methods
We conducted the overview in three stages: a literature review, a public panel, and a final review and revision after we presented our initial findings at a specialists’ workshop.
Literature review
Our approach was informed by realist review, a method for synthesising research evidence regarding complex interventions. 5,6 It is based on the idea that research should pass on collective wisdom about the successes and failures of previous initiatives in particular policy domains ‘before the leap into policy and practice’. 5 Its main purpose is to identify explanations through which complex social programmes might operate so that policy-makers can learn how to introduce or adapt programmes based on a good understanding of why and how they might work.
This approach was suited to our task because the science of the role of information based on online PEx is epistemologically complex and methodologically diverse. 6 However, in our case, there was no set of theories or even defined social or health programmes to identify and evaluate: the field is too new. We therefore adapted the approach to allow us to identify and describe the domains of the territory rather than to develop programme theories of how it may work. Our approach was iterative and collaborative; SZ and SW worked intensively face to face, through e-mails and by telephone over 6 months in 2010. Box 1 summarises the review’s five overlapping steps.
-
Settled the review question: ‘what is written in peer-reviewed journals and scholarly books about the health effects of access to and use of online patients’ experiences?’.
-
Refined the purpose of our review: to provide ‘a conceptual map’ of what is known about the health effects of access to and use of online PEx about health and illness.
-
Articulated the key ideas to be explored in a multidisciplinary project meeting in which we developed our initial matrix.
-
Exploratory background reading gave ‘a feel’ for the literature based on our own and colleagues’ bibliographic databases (concurrent with steps 1a and 1b).
-
Pragmatic and wide-ranging search (with assistance from a librarian at the Oxford Knowledge Centre) sought to identify any studies that had tested the effects of exposure to online PEx or that described theories or ideas about the potential effects of exposure to online PEx.
-
Both authors scanned all resulting titles and abstracts and, after discussion, chose potentially promising papers that could inform our thinking.
-
Sought more papers and books by ‘snowballing’ from reference lists as promising ideas emerged.
-
Our final search for additional studies came when we had nearly completed our review or when we came across them in the course of our professional lives, for example through discussions and seminars.
-
At least one of us read full papers. Although we used no formal quality appraisal tools, we considered papers in relation to their:
-
relevance – does the research address the topic and enable us to add to, adapt, or amend the initial matrix developed in step 1c?
-
rigour – does the research support the conclusions drawn from it by the researchers or the reviewers?
-
-
Both of us identified papers containing important ideas, explained them, and discussed their relevance during a period of intensive working together.
-
We added categories and specific instances to the initial matrix, which became our main data extraction framework.
-
We developed our initial ‘map’ or overview in a tabular form, identifying potential effects of access to and use of personal experiences of health and illness on the internet, the potential negatives and the potential mechanisms through which it might work.
-
A constant comparison between our reading and the working table identified the point at which no new ideas were emerging and we were confident that we had achieved data saturation.
-
We drew up a glossary of terms defining, recording and explaining key concepts; our understanding of them; and their application in this overview.
-
We presented and discussed the table and glossary at a full team meeting and made some modifications and clarifications regarding how the table should be presented.
-
We discussed the table in a workshop with 30 members of a health service public panel, who suggested the emphasis and importance of topics.
-
A final search and discussions at a conference identified the importance of visual as well as written and read presentations of experiences.
-
We identified and described seven domains.
Public panel of health website users
To check our interpretation of the literature, we convened a public panel which consisted of 30 participants primarily recruited through an invitation from Oxfordshire Primary Care Trust sent to a list of people who had previously agreed to help with research (see Chapter 11). We selected the respondents to ensure that they were representative of a cross-section of the community (gender, age, occupation and ethnic group) and included those who had used the internet for heath information in a variety of ways (websites, forums, blogs) and for a variety of health conditions (either for themselves or on behalf of family and friends).
We first showed examples of health information with and without the inclusion of ‘personal experiences of health and illness’. The panel was divided into four groups, each with a rapporteur, and asked to think about how people might be positively and negatively affected by experiential information. The rapporteurs delivered the feedback to the whole group. In a final plenary session, we summarised the results of the conceptual review and discussed how they compared with the results of the group discussions. A final questionnaire asked participants what, in their view, were the most important ways in which experiences might affect people, both positively and negatively, from the perspective of someone with a condition and that of a caregiver of someone with a condition. A report was circulated and feedback was sought.
Final review and revision
During our final search for relevant papers we presented our findings at a specialists’ workshop at the 25th British Computing Society conference on Human–Computer Interaction, July 2011, Northumbria University, Newcastle upon Tyne, as part of the workshop ‘Online patient experience (PEx) and its role in e-health’, organised by the authors. During discussion, we identified the importance of the visual presentations of online PEx. We had not identified this topic in our reading but on realising its importance we included it in our matrix. Finally, we agreed on the seven ‘domains’ of our conceptual map of the potential health effects of online PEx.
Results
The potential health effects of seeing and sharing experiences online: seven domains
Our approach allowed us to identify seven domains which broadly map the role of online PEx:
-
finding information
-
feeling supported
-
maintaining relationships with others
-
experiencing health services
-
learning to tell the story
-
visualising disease
-
affecting behaviour.
For each of these we considered the potential for both positive and negative effects.
Finding information
Other people’s experiences of illness can provide information that is valued in its own right. They can make information more relevant,7,8 provide contextual information about causes and consequences, and help people to understand what may happen. 9,10 Hearing about how others have coped may change one’s orientation to the illness11 and offer a framework for managing the uncertainties. Simple, practical tips on how to manage problems encountered in everyday life, coping strategies that others use, and advice based on what has worked for others are highly valued for their pragmatism12,13 and because they are easy to understand. 14
In making decisions, people draw on many sources of information. They discuss using their own and others’ experiences as well as more traditional ‘factual’ information for decisions,15 and they often say that they prefer not to base their health decisions solely on other people’s experiences. 16 However, hearing about other people’s decisions can help them to recognise that a decision must be made, understand what the range of options might be and clarify the alternatives (e.g. in relation to treatment, lifestyle and attitude). 16,17
Learning through other people’s accounts of their experiences can be memorable because the accounts are vivid,18,19 but if the experiences presented are not typical,16 are inaccurate and biased, or if the sites are sponsored by vested interests or open to commercial exploitation,16 the information may be distorted, which could lead to worse decisions if people are not aware of this. 1,20 Our public panel emphasised that the internet’s unregulated nature means that all sources of information might be seen as having equivalent status, regardless of their trustworthiness. The panel also raised the issue of information overload. Descriptions of negative or dramatic outcomes might mean that more numerous but unremarkable experiences remain unwritten or unnoticed. The difficulty of providing ‘balanced’ information has been previously addressed21 but no clear solutions are yet available.
Feeling supported
Having an illness, facing a health issue or being a family caregiver can challenge one’s personal identity, and some people may feel embarrassed or even stigmatised by their condition. Knowing that others are tackling similar problems and learning how they deal with difficult issues can reduce these feelings of isolation, bringing a sense of belonging to a group and reassurance that one’s experiences and reactions are ‘normal’22 so that one feels more supported.
People who have joined an online peer-to-peer group may also benefit from feeling that they are connected by helping and supporting others. 23,24 Online contacts can provide a safe environment for ‘emotional labour’. 25,26 Hearing about others’ experiences can induce feelings of compassion, so that one becomes less self-absorbed and gains a better perspective. 27 In their study of participation in online support groups, van Uden-Kraan et al. 13 describe ‘emotional empowerment’ as the process through which information is exchanged, emotional support is encountered, and recognition is gained through sharing experiences. Cohen28 calls this ‘emotional support’ and suggests that it can make people simply feel better. Our public panel considered this process important, saying that it meant that you knew you ‘were not alone’ because hearing about other people’s experiences gave you a sense of ‘being supported’. For people who have rare conditions, who are undergoing unusual treatments or who are geographically isolated, the internet may be their only source of this type of support and, therefore, be especially important. 29,30
In contrast, depending on their content, others’ experiences may arouse feelings of anxiety and lead to unrealistic expectations, false hopes or even despair, fear, guilt, anger and inadequacy if others seem to be managing better. Patients’ feelings of despair at their own condition may become worse if they find out that peers have fared badly;31 internet-based support groups are sometimes dominated by a single viewpoint. How one responds to other people’s experiences depends greatly on one’s mood at the time of the encounter, and, if that goes badly, it can reinforce one’s vulnerability or feelings of inferiority. The public panel were particularly concerned that people with mental illness might be adversely affected by negative postings, especially from those they described as the ‘trolls and fruitcakes’.
Maintaining relationships with others
The internet raises the possibility of having a distinct set of ‘online’ and ‘offline’ relationships that can be helpful when it is hard to maintain both an illness identity and an everyday identity. Online and offline relationships need not, of course, be mutually exclusive; many people keep in touch with friends via the internet and people who meet on the internet can become real-life friends. 32 There are, however, big differences in the way that people communicate and establish relationships online and offline. In an online forum, the usual requirement for conversational give-and-take need not apply: although a person may choose to write in extensive detail about their experiences, their audience can quickly browse through the account, break off at any point, or go back and review a section in more detail. Needless to say, such actions might be difficult to achieve in real-world interactions without causing offence.
Learning about how others cope may help patients become socialised into a new role in relationships (e.g. as a patient or as the spouse or parent of a patient). Finding that other people are facing similar problems may help one to feel more ‘normal’ and confident in managing one’s health condition in other contexts, including family, work, relationships and travel. Thus, online support may even help to sustain ‘real-world’ relationships by providing another sounding board and emotional outlet for health concerns, thereby ‘saving’ real-world relationships from that role.
Paradoxically, isolation in the real world could increase if people feel that only those who have been through exactly the same thing can understand them. For example, Hinton et al. ,31 writing about the use of online infertility support groups, drew attention to the possibility that web support could increase real-world isolation by reinforcing the notion that only those who have dealt with infertility themselves could possibly understand what it is like. A related idea, drawing on the work of Nicholas Negroponte,33 is that by enabling people to refine and personalise all of the information they receive (characterised as ‘The Daily Me’), they will rarely be exposed to any ideas that challenge their own. In this way the internet could reinforce entrenched interests and misunderstandings. Our public panel endorsed the idea that over-reliance on ‘virtual support’ can lead to ‘wasted time’ browsing and posting on the web, which could be to the detriment of face-to-face social contact in their own locality.
Experiencing health services
Finding out about other people’s experiences of care can affect the use of health services. In health systems that encourage patients to make choices about health-care providers, feedback and commentary about others’ experiences of providers can often be found either on ‘reputation’ sites (designed to present public ratings) or on patients’ chat rooms, forums or social networking sites. Accessing this information can contribute to decisions about which clinic to attend, which professionals to consult or which treatment to request or avoid17,34 and may even help to raise and address safety issues for patients. 35
Health consultations may be more efficient and patient centered if patients pick up useful ideas about the questions to ask, the best terms to use, and the symptoms or side effects to mention to their doctor. 36 Learning through other people’s experiences of symptoms and consultations may reassure the ‘worried well’ that they do not have the health problem they feared, thereby preventing unnecessary consultations. Our public panel expressed concern about ‘hypochondria heaven’, in which the unnecessary use of health services might be encouraged by seeing other people’s experiences online. People often look online to ‘follow up’ on the advice given by health professionals or to seek validation for their own interpretations or feelings. 37–39 Responses may spur them to seek a second opinion or further clarification from their health-care team. 40
At a macro level, by finding out how stigmatized conditions affect others or through restricted access to care and support, people can become more aware of inequalities and injustices which might foster changes in social attitudes or a more equitable provision of care. 41 It may also stimulate advocacy and campaigns. In some cases, shared experiences have been used to challenge not only the provision of services but the very parameters of what counts as an illness, particularly for contested illnesses such as fibromyalgia and contested treatments such as vascular surgery for MS. 42 Patients who compare what ‘counts’ as an illness or a recognised treatment in different health systems find ample examples of inconsistency, which are used to fuel campaigns for either better evidence or more treatment options.
Although there are clearly several potential benefits for the way in which people use health services and influence the development of care services,43 clinical relationships may be strained if unrealistic expectations are raised or if alarming stories from other patients damage people’s confidence in professionals and adherence to treatment. Those who take the time to provide feedback on services may feel frustrated if this does not lead to improvements. Finding out about other people’s experiences of poor care could increase anxiety in situations in which they have little choice or control.
Learning to tell the story
From childhood onward, stories provide a powerful, palatable and memorable way of learning about the world. 44 An engaging narrative can immerse the audience in the account and thereby transfer information in a particularly effective manner. 45,46 When a story is well told and encountered at an opportune moment, it can reassure and ground the reader or listener. It can also help her make sense of her own situation by suggesting a practical and emotional frame for her response. 12–14 We can see stories as a conduit for memorable and meaningful information and support.
Another relatively neglected aspect of stories, which we believe is important and distinct, concerns the very language, including the terms of reference and the figures of speech, that is used to construct an account. Hearing how others describe what has happened to them (as well as what has happened) adds to the richness of the vocabulary and can help to construct our own account. Although it is well understood that we learn through stories, the effect of hearing about other people’s experiences on our ability to relate our own narrative is less well understood. The consequences of gaining an enriched and more powerful vocabulary, being able to tell their story well, may help people to develop an appropriate professional interest by giving a concise and relevant account in a clinical setting, help them explain salient points to professionals11 and elicit understanding, support and affirmation from friends, family and wider audiences via the media and web blogs. We therefore see ‘learning to tell the story’ as distinct from other aspects of the exchange of information and support because it focuses on the ‘how’ rather than the ‘what’ of the accounts that we are able to relate.
Frank47 and Pennebaker and Seagal48 suggested that even the very process of constructing a coherent story may help the healing process. Narrative construction (and reconstruction) may also help people make sense of what has happened to them and thus support emotional recovery. 49 The internet allows those who want to share their stories with others to do so by adding a posting on a forum or chat room or perhaps setting up a site or blog of their own. Such sharing can feel empowering, especially if it attracts many followers or elicits approving commentary. 24
The question of verification cannot be ignored: how can we know whether or not accounts of people’s health experiences are true? ‘Telling’ or ‘spinning’ stories is sometimes used as a synonym for telling lies, but Bury50 recommends that we view people’s accounts of their illness as ‘factions’, a meld of facts and fiction that weave interpretation and presentation into the account of what actually happened. As Entwistle et al. 16 observed, people rarely present themselves as naive users of any information, yet we know relatively little about the effects (which could include incoherence and confusion) of exposure to numerous, and sometimes conflicting, accounts of health experiences on the web. Schwartz51 proposes that, far from helping, a plethora of options may prevent one from being able to make (and live with) a choice. Those who post their own stories online may be harmed if their account is misappropriated, criticised, ridiculed or even just corrected for facts. A mental health service user on our panel pointed out that a person posting a story when he or she is in the ‘wrong’ frame of mind may later regret their action. Internet posts can expose people to ‘flaming’ criticism from others. Yet if no-one comments on a heartfelt posting, the writer may feel even more isolated and ignored precisely because the potential audience was so vast. It may also be intimidating for some people to encounter a highly articulate account of an experience similar to their own.
Visualising disease
Many health-related websites include images; even some that were originally intended to be based on text now link to video clips on sites such as YouTube (YouTube LLC, San Bruno, CA, USA). The incorporation of photographs and videos on health websites has been treated mainly as a design issue rather than considered in terms of the potential consequences for the way in which people deal with their health problems. Williams and Cameron52 argued that images – in a variety of forms – are increasingly used in health-care communication and can be powerful ways of communicating important messages. The internet is inherently visual and the ability to post and access images of people dealing with health issues may be another important, albeit rarely explored, feature of health experiences and the internet.
How do people use images of PEx online? Dermatological conditions are undeniably visual; photographs can help people to compare and evaluate the effects of different treatments ‘with their own eyes’. Hardey (University of York, 2011, personal communication) reviewed video postings of eczema on YouTube and found more than 1000 clips, some of which had more than 2 million viewers. Some types of behaviour change are documented online through repeated images. Weight loss blogs, for example, often include a visual chronicle (a series of before, during and after photographs) of a person’s changing body shape. Sometimes these blogs feature a weekly picture of feet standing on a set of bathroom scales, adding ‘objective’ evidence to the bloggers’ claims about their progress. 53 There also is evidence that adding imagery to text-based website information about the risk of cardiovascular disease can work better than text alone in increasing the perception of risk and motivating protective behaviour. 54
Among the thousands of YouTube films of people with different health conditions, some capture a single moment, some record progress by following treatment and some are undoubtedly positioned to promote a particular treatment (although the presentation may or may not make this explicit). Like stories, imagery can be powerful and memorable; like stories, this has both positive and negative consequences. Illness can dramatically change a person’s appearance. People with serious progressive conditions, such as motor neurone disease (MND) (also known as amyotrophic lateral sclerosis), may choose to avoid looking at images of other people whose appearance may grimly foreshadow their own future. 55
Affecting behaviour
Advertising has long recognised the persuasive power of testimonials in changing behaviour. The field of health education and health promotion was quick to see the potential of the internet to deliver efficient, tailored advice56 to help people lose weight, do more exercise, give up smoking, tackle depression, control diabetes or high blood pressure and practise safe sex. 57 Some behaviour change sites have evident commercial backing, and others are funded through government or health insurance and promoted in self-management programmes. Testimonials and stories may be used to advertise a particular product, but they also may be intended as illustrations or for general encouragement and inspiration.
In her study of weight loss bloggers, Oostveen53 suggests that, through public blogging, people may feel accountable to an audience, and that by being aware that their progress is being watched, they may feel motivated to adhere to their programme. Reflecting on what they have posted may make people feel proud and in control, or embarrassed and regretful. For some health behaviours, such as cigarette smoking, people acknowledge that health professionals now are unlikely ever to have been smokers themselves, so advice from those who have ‘been there’ may have greater weight (through empathy and resonance) with those trying to make changes. Hearing about how others deal with a problem or a concern can also build confidence and self-efficacy. 58
Narratives or stories hold people’s attention by melding imagery and feeling. De Wit et al. 45 studied the effect of statistical and narrative evidence on the perceived threat of hepatitis B infection among men who have sex with men. They found that the intention to be vaccinated was higher among those who were presented with a personal narrative, and they believe that this is because narratives are less susceptible to the defensive processing through which people distance themselves from health education messages. In their study in South Wales, Davison et al. 59 noted that people use a ‘lay epidemiology’ (e.g. the popular image of an elderly relative who lived into his nineties despite smoking and drinking) to resist acknowledging that health education messages apply to them. This tendency to distance oneself from an unwelcome message (e.g. about susceptibility to a smoking-related disease or a sexually transmitted infection) may be strongly challenged by a resonant account from someone else who had held the same belief that they would not be affected yet was shown to be mistaken in their optimism.
In some circumstances, hearing about other people’s experiences may reinforce unhealthy behaviours. Some sites contain messages that contradict or challenge medical advice and suggest or reinforce unhealthy behaviours. Several studies have examined the content of online pro-anorexia support groups;60 people with diabetes can learn from forums about non-prescribed ways to use (misuse) their insulin for weight loss. Some online forums promote unsafe sexual practices and even provide advice on how to most effectively contract human immunodeficiency virus (HIV). At the extreme end of harm, those who are inclined toward suicide can even find forums that offer advice (and possibly encouragement) about how to end their life.
Conclusions
The profusion of patients’ experiences online has dramatically influenced the health information field. Health choices cannot be made without information,61 and the importance of internet health information is not disputed. Yet our conceptual review demonstrates that the full gamut of effects (for both the ‘poster’ and the ‘consumer’) of websites that cite patients’ experiences go far beyond the provision of ‘information’or ‘support’, at least as they are conventionally conceived. Our conceptual review shows that we are unlikely to identify the effects of exposure to online PEx simply by measuring outcomes such as knowledge acquisition, coping or decisional quality alone.
We were careful to consider the potential for harm as well as benefit, trying to avoid the temptation to be either pessimists and optimists. 62 Online PEx may help people make better health-care choices and alert them to health issues, improve their health literacy and understanding of susceptibility to illness, compare their situation with that of others, improve their own illness narration, access more appropriate services and develop better relationships. Yet we cannot assume that the effects of exposure to online PEx are always benign. They may raise anxiety. They may be disadvantageous if they feature only a small number of unrepresentative patients’ stories. A single story with strong emotional content can distort decisions. 1,20 Overengagement with online communities can be detrimental to life ‘offline’. The powerful and memorable delivery of a personal experience could be used for a deliberately misleading or exploitative message. The benefits and disadvantages are unlikely to be evenly distributed across socioeconomic, age and gender groups, yet little is known about these patterns, and, as the digital ground shifts again, new applications may encourage new types of use and users.
Guided by realist review methods,6 we considered the processes through which PEx may operate. The literature suggests that the processes may differ depending on, for example, whether people are reading about others’ experiences or writing about their own. Those who help to create health content may be participating in a different way from those who consume rather than post their own contributions, yet the widespread use of social media and blogs is already blurring these boundaries. Some of the outcomes or consequences (e.g. the ability to make sense of what has happened and construct a coherent account) may be similar, whether one has learned from other people’s stories or from constructing a coherent account of one’s own.
The extent to which patients and members of the public have turned to other people’s experiences on the internet has provoked both surprise and, in some quarters, concern, although with the rise of social media and access from multiple platforms it is becoming the norm across health systems. Our review sheds some light on the features that make first-hand accounts compelling and the processes through which they operate. The value of first-person accounts, the appeal and memorability of stories, and the need to make contact with peers all strongly suggest that reading and hearing others’ accounts of personal experiences of health and illness will remain a key feature of e-health.
Chapter 3 Work package 1b: how, why and with what effect do people seek out and share health information online? Secondary analysis of the Oxford Health Experiences Group archive
Abstract
Introduction: the HERG archive contained almost 3000 interviews on over 60 health conditions. We conducted a secondary analysis on a subset of interviews to gain insight into how, why and with what effect people seek out and share health information online.
Methods: information relating to internet use and/or PEx was extracted from 276 interviews. First, 95 interviews were analysed in depth with a focus on seeking and sharing PEx. Second, statements relating to the use of health-related websites were extracted, recast as questionnaire items and reviewed by an expert panel for the eHIQ.
Findings: perceptions and experiences of online PEx differ between individuals and across conditions. Factors influencing people’s desire for and response to PEx include personal characteristics and preferences; condition and stage of illness; health-care environment; source and type of PEx; and the format and medium through which PEx is communicated. Eighty-two items relevant to the impact of health-related websites were identified for use in the eHIQ.
Conclusions: online PEx is widely available, diverse and hard to control. Reasons for, practices of and the health effects of seeking and sharing PEx are complex and relationally contingent. A secondary analysis of the HERG archive enabled us to explore key aspects of this complexity across multiple conditions and develop new questionnaire items suitable for use across health conditions.
Introduction
At the time of this study, the Oxford HERG archive contained almost 3000 qualitative interviews covering more than 60 different conditions. It is ethically approved for secondary analysis and is an invaluable resource for health-related research. As interviewees are routinely asked about their experiences of seeking and receiving information, internet use, professional and peer support, it was thought that the archive would contain a great deal of information of relevance to the iPEx (Internet Patient Experiences) programme grant. To benefit from these data, a secondary analysis, or more accurately, a series of iterative secondary analyses, was conducted on the material. 63 The aims of this process were (1) to inform the design and implementation of subsequent WPs (especially WP1c and WP2b; see Chapters 4 and 6); (2) to contribute to extant knowledge on how, why and in what ways seeking and sharing PEx online affects people’s health and well-being; and (3) to identify the main reasons that people use online health information in order to construct a set of items for an assessment tool that measures the impact of using health-related websites to be used later in the programme (WP1c; see Chapter 4).
The analysis was conducted in two stages (Figure 2). In stage 1, two researchers (FM and LK) conducted a high-level thematic analysis on a subset of 276 strategically selected interviews. The aim of this preliminary stage was to familiarise ourselves with the data, develop appropriate sampling approaches and forms of analysis for subsequent work, generate a high-level list of themes relating to people’s perceptions and experiences of online PEx and select key topics and questions for further analysis. To ensure that a range of experiences, practices and perceptions of online health information was included, we aimed for breadth rather than depth of coverage.
FIGURE 2.
Work package 1b: high-level overview of the secondary analysis process.
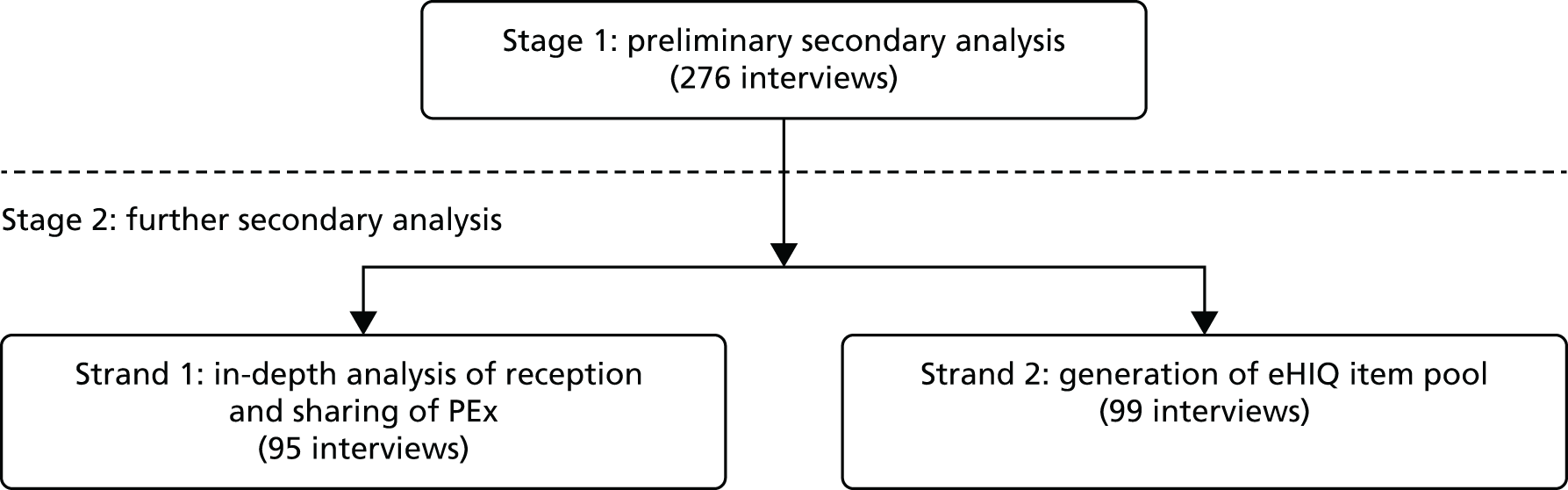
In stage 2, two distinct strands of work were conducted. In the first strand, FM, JP and LL investigated two areas of interest that emerged during the first stage of analysis, and were new contributions to research in this area. The first, focused on issues around the reception of PEx, was an exploration into how processes of identification and visualisation mediated the ways in which people with serious neurological conditions (MND and Parkinson’s disease) communicated and responded to PEx. 55,64 The second, focused on issues around the sharing of PEx, explored the ‘value’ that people who actively shared their experiences attributed to doing so. 65 In the second strand, drawing on the theoretical framework outlined in the previous chapter (WP1a), LK conducted further analysis to generate an item pool for the development of the eHIQ. This secondary analysis enabled the incorporation of internet users’ actual words as a basis for questionnaire items and helped enhance content validity of the assessment tool.
In this chapter, we provide a high-level overview of the methods used for the secondary analyses and present overarching findings. Much of the research discussed here has been published elsewhere. 55,64–66 To avoid duplication, we do not go into the details of published work, but rather (1) provide a high-level overview of the findings from stage 1 of the secondary analyses that have not been published elsewhere and (2) summarise and contextualise key findings from both strands of stage 2 (which have been published) in relation to this wider secondary analysis. 55,64–66
Methods
Secondary analysis, broadly defined as the use of an existing data set to answer questions not posed in the original research,67 has long been conducted on quantitative data. In qualitative research, where the need for contextual sensitivity and specificity is seen as paramount, secondary analysis is less well established. More recently, as evidenced by the creation of the Economic and Social Research Council Qualitative Archival Research Data Centre (QUALIDATA) in the mid-1990s and its incorporation into the UK Data Service, there has been an increased interest in the value of conducting secondary analyses on qualitative data. In spite of this acceptance and, indeed, in some cases, active encouragement (e.g. from funding bodies) of the secondary analysis of qualitative data, persistent concerns remain. According to Heaton,63 these can be broken down into three main areas: (1) the ‘fit’ between the data and the questions posed in the secondary analysis; (2) the position of the researcher and their relationship with the data; and (3) verification of the data and findings generated from it. All three of these concerns were taken into consideration and addressed during the course of our secondary analysis.
The interviews collected by the HERG are in-depth narrative ones, conducted with a view to soliciting as wide a range of experiences of illness as possible, which makes them particularly suitable for secondary analysis. 68 In the first half of the interview, participants are invited to tell their story for as long as they want with as little interruption as possible. In the second half, a semistructured interviewing approach is adopted to enquire after topics of interest that have not already been raised and to explore key topics in more depth, including questions on information seeking, internet use and peer support. The interviews are collected using maximum variation sampling, with variation across demographic variables and type of experience. 69 Ethics approval for secondary data sharing and analysis was received from the Eastern Multi-Centre Research Ethics Committee (reference 03/05/016) and the interviews have been successfully used for secondary analysis in extant studies on health-related use of the internet. 10,15 Further information about the methods used to collect and conduct the interviews is available elsewhere. 70,71
Stage 1: preliminary analysis
Given the range of conditions contained in the archive, it was not possible to undertake an exhaustive analysis of all available interviews. Key findings of HERG interview collections are published as online resources (www.healthtalk.org). These website sections were explored to gain an insight into the topics that the primary researchers had identified in each interview collection and to help select which interviews to use in the secondary analysis. We decided, in the first instance, to focus our analysis on those deemed to have closest relevance to the three exemplar conditions being investigated by the iPEx programme (smoking cessation, asthma and carers of people with MS). To maximise the chances of finding information about internet technologies, only interviews published from 2005 onwards were included. Based on this, seven complete collections and a further nine ‘pilot’ interviews with people affected by MS were included in the first round of analysis (Table 1). These were selected through discussions with key members of the project team, including those who were very familiar with the content of the HERG archive.
| Title of collection | Date | Number of interviews |
|---|---|---|
| Carers of people with dementia | 2005 | 31 |
| MS | N/A | 9 |
| MND | 2008 | 47 |
| Parkinson’s disease | 2008 | 40 |
| Young people with type 1 diabetes | 2006 | 39 |
| Young people with epilepsy | 2008 | 41 |
| Young people with depression and low mood | 2009 | 39 |
| Young people with long-term health conditions | 2007 | 30 |
| Total | 276 |
With the exception of the MS-related interviews, thematic summaries and interview extracts are available online for all of these conditions (see www.healthtalk.org). The summaries contain sections of direct relevance to the secondary analysis (e.g. ‘information and support’, ‘support and support groups’). The interviews were read (by FM or LK and in many cases by both) and all information relating to internet use and/or sharing or seeking experiences (online and off) was extracted. Scoping summary reports were compiled to identify the extent to which the collections had content relating to using the internet for health. A list of key emergent themes and associated statements (examples of the exact wording and language used by interviewees) was created for each condition. This list was subjected to an additional round of constant comparison coding, and key cross-cutting themes and areas for further investigation were summarised. This summary was not intended to be an exhaustive assessment of all the interviews. Instead, alongside the conceptual review (WP1a; see Chapter 2), it was used to highlight areas of interest for more in-depth secondary analysis and to index interviews and excerpts for the development of the assessment tool (WP1c; see Chapter 4).
The sample design and suitability of the data was further informed by consulting the original researchers of the selected interview collections. The researchers (most of whom are still employed in the HERG) provided input and advice based on their experiences of the collections they had created and their expertise in terms of online PEx more generally, which was incorporated into the analysis. Following discussions about the suitability of an interview collection for the research purpose, the original researchers provided coding reports [generated at the time of their own research using either the NUD*IST or NVivo (both QSR International, Warrington, UK) qualitative analysis software] that they believed would be particularly relevant to the topic. Coding reports took the form of electronic reports of sections of interview transcripts which related to a specific topic and were subsequently reviewed to inform the sample selection. Examples of coding reports were entitled ‘Web forums’, ‘Information’, ‘Support groups’ and ‘Information carer’.
The steps outlined above aided familiarisation with the data sets and helped us to assess the suitability of particular interview collections for further analysis. Sampling and selection of interview transcripts were not finalised at the outset, but, as is usual in qualitative analysis, remained continuous throughout the process.
Stage 2: further secondary analysis
Strand 1: secondary analysis to explore the sharing and receiving of patient experience in more depth
Numerous topics of interest emerged from the first round of analysis, and it was not possible to explore all of them in depth. We decided to focus on areas that have been underexplored in the extant literature and had wider implications for our understanding of online PEx. Based on this and in discussion with the project team, two areas were chosen for further analysis. The first was an exploration into the ways in which people articulated and responded to different types of PEx in relation to neurological conditions. Here, we performed a secondary analysis on 87 interviews conducted between 2006 and 2008 in the UK with people (patients and carers) affected by MND (46 interviews) and Parkinson’s disease (41 interviews). The second was an examination of people’s self-reported reasons why they shared their experiences through the internet and other mediums. We were interested not in psychological motivations, but in using these data to develop a nuanced understanding of the value(s) associated with sharing PEx. Here, we selected and analysed a strategic sample of 37 interviews conducted with people affected by 15 different conditions who had reflected on why they chose to share their experiences (Table 2).
| Condition | Number of interviews |
|---|---|
| Alzheimer’s disease | 1 |
| Autism spectrum disorders | 2 |
| Cervical abnormalities | 6 |
| Colorectal cancer | 2 |
| HIV | 2 |
| Leukaemia | 1 |
| Ethnic minority experiences of mental health | 2 |
| Organ donation | 1 |
| Osteoporosis | 5 |
| Pancreatic cancer | 1 |
| Experiences of psychosis | 2 |
| Rheumatoid arthritis | 2 |
| Testicular cancer | 1 |
| Parkinson’s disease | 7 |
| MND | 2 |
| Total | 37 |
In both cases, a supra-analysis (analysis of existing data from a new theoretical perspective)63 was conducted using a modified grounded theory approach. 72 All of the interviews were read in their entirety, online summaries were, once again, consulted and discussions were held with primary researchers. One of the authors (LL) was the original researcher for the MND module and hence was able to contribute to the analysis with contextual knowledge. Constant comparison coding was used, with discussions held among FM, LL and JP at regular intervals to validate and further conceptualise key themes. Throughout the course of the analysis, we presented the work in progress at programme grant meetings and conferences, receiving useful feedback that assisted with the development of key ideas. For more detail on the methods used please refer to Mazanderani et al. ,55 Locock et al. 64 and Mazanderani et al. 65
Strand 2: secondary analysis for the development of the e-Health Impact Questionnaire
Following the preliminary analysis in stage 1, interview collections were reviewed which were likely to be rich in data regarding the use of online health information. Of the 203 interviews reviewed, relevant extracts from 99 transcripts were identified and analysed using a modified version of the framework method73 (Table 3). Framework analysis allows a researcher to look at the data and conduct analysis in a systematic and comprehensive manner. 74 The framework method involves five stages: (1) familiarisation with the data gathered; (2) identification of a thematic framework which allows emerging issues, concepts and themes to be listed; (3) indexing the transcripts according to the thematic framework; (4) charting the data through extracting and synthesising it in a manner which allows within-case and between-case comparison; and (5) mapping and interpretation of the data. 75,76 Many of the themes that were expected to be raised during analysis had been identified in the WP1a review of the literature (see Chapter 2). This stage of the secondary analysis sought to gain a deeper understanding of existing (‘anticipated’) themes found in the literature while being mindful of any new (‘emergent’) ones that arose.
| Condition group | Male | Female | Total |
|---|---|---|---|
| Long term condition (younger people) | 3 | 12 | 15 |
| Diabetes (younger people) | 5 | 14 | 19 |
| Depression (younger people) | 3 | 6 | 9 |
| Parkinson’s disease (carers) | 2 | 4 | 6 |
| Motor neuron disease (carers) | 3 | 6 | 9 |
| Dementia (carers) | 5 | 8 | 13 |
| Antenatal screening | 1 | 4 | 5 |
| Fetal abnormality | 5 | 8 | 13 |
| Menopause | 0 | 6 | 6 |
| Mental health: BME (carers) | 1 | 3 | 4 |
| Total | 28 | 71 | 99 |
Two further sources of data were used to corroborate the themes identified for inclusion in the item pool: (1) focus group transcripts (n = 16) from research carried out on trust and online health information at Northumbria University76 and (2) comment forms (n = 29) completed by members of the programme’s public panel (WP1a; see Chapter 2) consisting of lay persons using local primary health-care services. Using more than one data source served as a method of ‘data triangulation’, enhancing rigour in the research. 77
This process contributed to the development of an item pool relating to the impact of using health-related websites which would be subsequently entered into psychometric testing (see Chapter 4). The assessment tool needed to be suitable for use in the WP3b Phase II pilot randomised controlled trial (RCT). Therefore, for each theme identified, candidate items were developed and checked for applicability to people viewing a website containing scientific information only and a website containing scientific information plus experiential health information. Emphasis was also placed on checking the suitability of the items among the WP3 exemplar condition groups (i.e. smoking cessation, asthma and carers of people with MS). Candidate items were circulated among colleagues in the project team for review and the feedback received was incorporated into the development of the final questionnaire.
Results and discussion
Key findings from the preliminary secondary analysis (stage 1)
The conceptual review presented in Chapter 2 drew attention to how practices of seeking and sharing PEx can have numerous and often profound (both positive and negative) consequences for people affected by different conditions. 4 Our secondary analysis of patient interviews reinforced and supported the findings of the review.
The first five domains of how online PEx could affect health (‘information’, ‘feeling supported’, ‘relationships with others’, ‘experiencing health services’ and ‘affecting behaviour’) identified in the review were evident across all the modules analysed. The sixth (‘learning to tell your story’) emerged in interviews with people who had actively shared their experiences online or in other forums. As many more people seek out others’ experiences rather than share their own, this domain was less prevalent than the first five. Interestingly, the seventh domain (‘visualising disease’), although not common across the corpus of interviews, was evident in certain conditions with visible and highly variable symptoms (namely MND and Parkinson’s disease). Given their importance in both our secondary analysis and the extant literature, the first five domains were used as a key structuring device for the development of the assessment tool for measuring the impact of health-related websites. 66 Owing to the lack of research on the sixth and seventh domains, they were selected for further secondary analysis. 55,64,65
In our secondary analysis we found both variations and similarities between how people affected by different conditions used the internet and responded to PEx. This is significant, as a great deal of current research on health-related use of the internet is condition specific and hence unlikely to pick up on wider cross-condition trends and differences. Although it is not possible to provide an exhaustive list of all the factors that influence how people respond to online PEx, we list some particularly notable ones that emerged from our high-level analysis.
The first is the condition in question and, linked to this, the age of the people affected by it. This was especially striking in relation to carers of people with dementia, where, despite the fact that interviewees spoke about benefiting from sharing PEx in face-to-face environments, there was very little evidence of them using online PEx. This may be because interviewees tended to be older and used the internet less, but it may also be related to the nature of the condition and the types of PEx available about dementia. In contrast, young people are particularly active online, seeking and sharing PEx across a variety of technologies and platforms [e.g. patient forums, Facebook (Facebook Inc., Menlo Park, CA, USA), YouTube]. However, in the case of young people with serious chronic conditions, such as cystic fibrosis, interviewees spoke of being upset by and in some cases actively avoiding ‘negative’ or distressing information, including PEx.
It has long been recognised that PEx can be a highly ambivalent source of information with the potential to bring about feelings of both hope and fear, provide support and increase isolation, and be perceived as ‘true’ knowledge or discarded as irrelevant. 31,78 In our secondary analysis we found that this was most definitely the case, with interviewees speaking of having had both ‘positive’ (e.g. feeling ‘supported’, ‘empowered’, ‘inspired’) and ‘negative’ (e.g. feeling ‘depressed’, ‘upset’, ‘devastated’) responses to online PEx. In relation to the former, interviewees said that PEx was an extremely valuable source of information that was simply not available elsewhere. Key areas of information provided by PEx discussed across interviews were practical hints and tips about actually living with a condition, information about diagnosis, prognosis, treatment, side effects, family and personal relations, finances, jokes and humour. Furthermore, PEx affected the health and well-being of interviewees not only by virtue of its informational content (important as this was), but from the sense of support and mutual understanding that was gained from speaking to, sharing with and identifying with other people affected by the same condition. In terms of ‘negative’ responses to PEx, the two most common concerns were fears about the danger of misinformation and the emotional difficulties of dealing with PEx. Interestingly, we found that people with serious chronic or terminal conditions tended to respond especially strongly to PEx, seeing it as an extremely valuable source of information and support, but at the same time often finding others’ experiences very distressing.
It is important to note that what were perceived as ‘negative’ versus ‘positive’ experiences of PEx were not static but, as with other forms of health information, changed over time, sometimes radically. For many people diagnosis was a crucial time for seeking out PEx, while others preferred to wait and seek out PEx once they had adjusted to their new diagnosis. The fact that for many people the internet is available at any time and can be customised to filter and select different PEx was seen as an important feature of the technology. Indeed, interviewees were selective about the source of the PEx they found online (who and where was it coming from), as well as the format and medium through which it was communicated (e.g. text written on a patient forum or a video on YouTube). Thus, the value and, crucially, evaluation of PEx as either ‘good’ or ‘bad’ was highly relational and contingent not only across interviews, but over time, and in relation to different modes of communication. For example, in the case of MND and Parkinson’s disease, a number of interviewees expressed a strong preference for PEx communicated in writing rather than face to face to avoid seeing physical symptoms of the disease that they found upsetting.
Moreover, when interviewees spoke of how online PEx had affected their health and well-being they situated it in relation to their wider health-care environment and informational landscape (both online and offline). In some rare cases health-care practitioners had encouraged patients to look up PEx, occasionally suggesting websites and other sources; in others (again often in relation to more severe conditions), the use of the internet was actively discouraged by medical practitioners. Either way, across all of the collections we analysed, interviewees interpreted and used PEx in conjunction with information they received from numerous different sources, including the information they received from their health-care practitioner(s), NHS services, charitable organisations, the media, family and friends.
Key findings from the further secondary analysis (stage 2, strand 1)
Identification, mediation and visualisation in online patient experience
In our secondary analysis of the HERG interviews, interviewees regularly stated that PEx was a valuable source of ‘experiential knowledge’: ‘truth based on personal experience with a phenomenon’. 79 However, not all PEx was considered equally useful or relevant. Interviewees often spoke about how they were particularly interested in and affected by PEx from people they could relate to. Although the importance of relationships has been discussed in the sociological literature on ‘experiential knowledge’,18,80,81 little explicit attention has been given to examining the different forms of relationality at play in whether or not PEx is deemed as a valid source of ‘knowledge’. We explored this question in more depth through a secondary analysis on the MND and Parkinson’s disease collections. The main findings have been published55 and are summarised here.
A key factor that influenced whether or not interviewees considered someone else’s experience to be relevant to them was based on the recipient’s identification with the person sharing their experience. In the case of health-related PEx, this sense of identification was premised, in the first instance, on a shared diagnosis. Interviewees regularly said that only someone else living with the same condition as them could understand what they were going through and, therefore, be able to provide them with appropriate advice and support. However, a shared medical condition was not the only factor that affected whose experiences were considered relevant and useful. Interviewees sought out and responded most strongly to PEx provided by people they felt were ‘the same’ or similar to them. The key factors that informed whether or not someone was deemed similar, and hence that their experience was relevant, can be broadly classified as medical (e.g. stage and severity of illness, medication and symptoms) or personal and/or social (e.g. age, gender, lifestyle, family situation, education or job).
However, although the subtle processes of identification play key roles in underpinning how people respond to PEx, identifying with a ‘disease’ and with people living with it can be a source of emotional distress that is particularly acute in people with serious, stigmatised and/or degenerative conditions. 31 This results in a tension. To learn from PEx and consider it relevant to his or her own situation, the recipient of the PEx needs to identify with the person sharing it. At the same time, to minimise the negative associations and emotional distress that results from this identification, the recipient seeks out ways to distance him- or herself from the sharer. A key way people manage this tension is through emphasising both the similarities and the differences between their experiences and those of others: what, drawing on Ricoeur’s work on metaphor,82 we have conceptualised as ‘being differently the same’. 55
The tension between making someone else’s experience relevant and, at the same time, avoiding becoming upset by the more ‘negative’ or distressing aspects of the experience was also managed through mediating the way in which that experience was communicated. This is expressed in the excerpt below from an interview with a woman with MND:
You like the support you have helping one another but you’re scared that, I think, well I’m personally scared that if I met up with someone face-to-face and we started meeting up that if they needed to become reliant on me or to talk to me about their problems with MND that I wouldn’t be strong enough for that. I mean it might not be the case that they would do that but you don’t know. So I think too. I like having the e-mail contact but I don’t think I would want personal contact with someone else with MND because I think it gets too involved then.
MND collection, interview 10
It was precisely in contexts like the one described above, seeing other people with the same condition as them experiencing poor health or visible disability, that interviewees said the internet could be very helpful. Indeed, the ability to control seeing people and being seen was a key reason interviewees gave for using internet technologies for seeking out PEx and meeting people, rather than going to face-to-face support groups. This is illustrated in a quotation below, which was taken from an interview with a woman living with Parkinson’s disease:
[. . .] whilst I’m happy to go onto the web forum and communicate with people who’ve, with, who have had Parkinson’s for twenty years. I’m anxious about meeting people in the flesh, I don’t want to, I don’t want to see my future.
Parkinson’s disease collection, interview 17
When people speak about their experiences of illness, they often use extremely vivid imagery and metaphors that can have a powerful impact on others. 64 The articulation of PEx through written and verbal language, especially in the form of narratives and stories,14,47,50,83 has received a considerable amount of academic attention. In contrast, the visual dimensions of PEx through images and video has been relatively under-researched. We explored this topic further in WP2a, as discussed in Chapter 5. 84
Exploring the multiple ‘values’ of patient experience in contemporary health care
Patient experience has become an increasingly central part of contemporary health care. Patients’ experiential accounts are used for many different purposes, ranging from artistic expression through to fundraising for biomedical research and lobbying for changes to health-care policy. Yet relatively little is known about why people choose to share their personal experiences of illness.
Everyone who took part in the HERG interviews knew that text, audio and/or video clips of their interviews would be made available on a publicly accessible website with the specific aim of making their experience available to others. In addition, some interviewees had already shared their experiences in other mediums (e.g. blogs, support groups, face to face, books, documentaries, etc.). This meant that the archive contained a considerable number of data on this rarely discussed topic. In the first round of secondary analysis, we noted a number of cases in which interviewees reflected on why they had chosen to share their experiences and what they thought the effects of this had been on themselves and on others. To explore this topic, we selected additional interviews where this had been elaborated on in more depth and subjected them to a further round of analysis (for more detail on our sampling approach see the full account of this research, published elsewhere65). A significant portion of what we found related to the emotional and therapeutic benefits of peer support. As this has already been discussed in depth elsewhere,25,84 we chose to focus on other aspects of why interviewees share their experiences, especially in more public forums.
In summary, interviewees said that they shared their experiences because they believed that living with a condition on a daily basis meant that they had unique insights, which could be of value to others. They explicitly distinguished the type of knowledge and ways of knowing that came about as a result of embodied experiences of illness from both fictional accounts of illness and medical knowledge. This is illustrated in the quotation below taken from an interview with a man with colorectal cancer:
They’ve [hospital staff and stoma care nurses] got a bit of learning from books but it ain’t nothing like living with it. It really is quite a different thing and all their ideas really as I say are book learning which I don’t know who writes the books but they haven’t had one [colostomy] either if you know what I mean. And when you live with one you learn that it can be quite capricious at times and it can do all sorts of things, odd things that you can’t expect or you don’t expect and really and truthfully the best thing is to find somebody who’s got one.
Colorectal cancer collection, interview 4
Moreover, interviewees said that they had decided to share their experiences because they believed that doing so could help others in some way. In a number of cases people said this was because they had been similarly helped by others who had done so. Thus, sharing PEx was seen as a means of contributing to the community affected by a particular condition. The value attributed to PEx was, therefore, both epistemic (in that it was seen as a form of knowledge and way of knowing) and ethical (in that it was intended to help others). In a few, rarer, cases interviewees spoke of generating tangible economic value from sharing their experiences, for example through fundraising activities, advertising on websites or selling books. Rather than being an end in itself, this economic value was articulated by interviewees as part of a broader ethical project of sharing knowledge and helping others. The coconstitution of these three forms of value, the epistemic, ethical and economic – what we have conceptualised as ‘biographical value’65 – in the sharing of PEx is succinctly illustrated by the quotation below taken from an interview with a man with osteoporosis:
I go out and I meet people and then win them over and tell them my story and go away feeling happy. And, and that’s how I’d describe my NOS [National Osteoporosis Society] work. And in the meantime it raises money and it raises awareness. So . . . it’s a win–win. So that’s the therapy, that’s my therapy if you like.
Osteoporosis collection, interview 28
There was a general belief among interviewees who actively shared their experiences that doing so was a ‘good’ thing for the reasons articulated above. At the same time, PEx produced about or by well-known figures were viewed as particularly powerful in terms of raising public awareness of a condition, fundraising and research. This was reinforced by findings from stage 1 of the secondary analysis, in which famous people with different conditions (e.g. Michael J Fox in relation to Parkinson’s disease, Stephen Hawking in relation to MND, Jade Goody in relation to cervical cancer) were frequently mentioned. This raises questions about the differential effects that the public articulation, be it in books, websites or any other media, of people’s experiences can have not only on the health and well-being of particular individuals, but on public perceptions of different conditions and the field of medicine more generally (see Mazanderani et al. 65 for more details).
Findings from further secondary analysis for the development of the e-Health Impact Questionnaire (stage 2, strand 2)
As discussed above, it was clear from the analysis that preferences for various types of online health information varied between participants. This was viewed as an individual’s ‘baseline’ acceptance or openness towards using the web for health information which could potentially have an influence on using a specific website. Therefore, a pool of items assessing general attitudes towards online health information was constructed (eHIQ part 1).
To inform the second pool of items relevant to using a specific health-related website (eHIQ part 2), themes derived from the secondary data analysis were mapped onto five of the seven domains identified in the review of literature in WP1a (see Chapter 2). These themes are outlined briefly here, but are discussed further in Kelly et al. 66 The first theme, ‘information’, incorporated learning about a health condition, becoming informed of what to expect and recognising decisions that may need to be made in the future. Health-related websites were also a valuable resource for finding practical tips and advice to help manage health.
The second theme, ‘feeling supported’, related to finding support through others going through similar health experiences. In some cases, accessing a particular health-related website was the first time participants learnt that other people had similar health concerns. Increased hope and confidence was also found through gaining and lending support.
The third theme, ‘relationships with others’, referred to a person feeling less isolated and that others understood what they were experiencing (e.g. in an online community). Using websites also had the potential to ease offline relationships, as these provided an area in which they could discuss their health concerns with people going through similar experiences and learn to articulate what they were feeling.
The fourth theme, ‘experiencing health services’, concerned the use of websites when deciding whether or not medical advice should be sought. The use of the internet could help participants to navigate the health system and helped to prepare people for upcoming decisions. Participants could corroborate advice, find out more information and reflect on decisions made after accessing health services.
The final theme, ‘affecting behaviour’, incorporated the motivational effect some website content may have on the individual. For example, learning of the consequences of ignoring best practice when managing a long-term condition encouraged people to improve their own health-care regime.
The Northumbrian focus group transcripts and the public panel comment forms were subsequently reviewed to ensure that each theme identified had been fully explored and that no additional themes were evident. No new overarching themes were evident; however, the confirmatory sources did provide greater insight into some themes identified. For example, the focus group transcripts provided further insight to the fourth theme, ‘experiencing health services’, as participants discussed the dangers of using misleading information found online instead of consulting a health professional. These concerns were also highlighted in the public panel group.
Overall, the five themes were consistent with the domains identified in the WP1a literature review, providing a strong basis for the conceptual underpinning of the eHIQ part 2 item pool. Although the two remaining themes (‘learning to tell your story’ and ‘visualising disease’) were less pervasive across the transcripts analysed, issues relevant to each domain were dispersed throughout the five confirmed themes. For example, ‘learning to tell your story’ was incorporated into ‘relationships with others’ when a participant discussed being able to communicate more succinctly with their partner after using an online forum. ‘Visualising disease’ was incorporated throughout the five themes identified when participants described images reinforcing people’s stories or messages. It was therefore felt that the issues addressed in domains 6 and 7 were adequately represented in the item pool.
In total, 376 participant statements were extracted from the transcripts to represent all the themes present. LK identified 149 generic statements that could be answered by people across health conditions. Statements were recast as questionnaire items and reduced to 67 items in an iterative process involving LK, SZ and CJ. LK, CJ and SZ added a further 15 items to ensure that all themes were adequately represented. On review, the expert group recommended changes to two items to make them acceptable to people with a low level of health literacy. All members agreed that the items reflected the impact of using health-related websites. Eighty-two items were, therefore, entered into patient interviews and psychometric testing (see Chapter 4 for a full description of the development of the eHIQ).
Conclusions
We analysed over 276 interviews about people’s experiences of 24 different health issues. This large and diverse sample included experiences of a wide range of conditions, across different time periods and locations in the UK. Moreover, our sample included people of different ages, gender, race and ethnicity. In the time available it would not have been possible to access this diversity or richness of experience without using the HERG archive. Being able to meet with and, in some cases, work closely with the original researchers was of great value, as it helped us to select particularly salient interviews and contextualise our findings. 68 We were also fortunate in that the topics we were interested in (internet use and/or sharing PEx) were explicitly asked about in the interviews. However, there were some limitations. First, as the internet changes so rapidly it can be hard to get a sense of people’s experiences of the latest platforms and technologies. Second, there was sometimes insufficient depth on specific issues. To mitigate these limitations, additional focused interviews were carried out during the process of developing the eHIQ (see Chapters 4 and 5 for more details).
A huge quantity and variety of PEx is shared through internet technologies and, as society becomes ever more connected, and more and more people share their experiences of health and illness online, this will only grow. What counts as PEx is highly diverse in terms of the topics discussed as well as the formats and mediums through which it is communicated. Studies on how health is affected by online PEx tend to focus on the informational content of PEx. Our analysis and the conceptual review, outlined in Chapter 2, show that, although PEx can indeed be a source of information, in order to understand how seeking and sharing PEx affects people’s health and well-being it is essential to study the practices, technologies, forms of identification and relationships that shape how people engage with PEx. PEx must, moreover, be situated in relation to the wider health-care environment and people’s lives.
Our secondary analysis drew attention to a number of contextual factors that affect how and why people respond to and share PEx. These included personal characteristics and preferences; condition and stage of illness; health-care environment; source and type of PEx; and the format and medium through which it is communicated. To ensure that this variety and contextual sensitivity was reflected in the item pool which would inform the assessment tool relevant to the impact of health-related websites (see Chapter 4), the secondary analysis was used alongside the conceptual review. The item pool was, therefore, based on five core domains that were prevalent in the secondary analysis and conceptual review of relevance to both PEx and other forms of health information: ‘information’, ‘feeling supported’, ‘relationships with others’, ‘experiencing health services’ and ‘affecting behaviour’. Eighty-two items were tested for acceptability among experts and were considered suitable to enter cognitive testing with users and subsequent psychometric testing.
Patient experience is a very important source of information and support for many people, but not all PEx is considered equally important or relevant. Beyond a shared diagnosis, one of the main ways people decide if PEx is relevant to them is based on whether or not they identify with the person sharing his or her experience. However, identifying with a ‘disease identity’, and being exposed to others’ at times very distressing experiences, can be a cause of emotional upset. To manage this, people use internet technologies to control their levels and extent of communication with others, thereby enabling them to benefit from PEx without being overwhelmed by it. A key factor in this is whether PEx is communicated in writing, images or video, when and at what times. Based on our secondary analysis, the ways in which experiences of illness and disease are articulated and visualised online has been highlighted as an area for further research in WP2a (see Chapter 5).
People share their experiences because they believe that PEx is a valuable form of knowledge and, moreover, that sharing their experiences can help others and, in some cases, influence wider public perception, fundraising, research and policy related to particular health conditions and topics. For the most part PEx is not considered a replacement for biomedical or clinical knowledge, but is seen as complementary to it. The relationship between PEx and other forms of knowledge in medicine is a topic that is developed further in Chapter 5.
Chapter 4 Work package 1c: refining and validation of the e-Health Impact Questionnaire
Abstract
Introduction: this chapter outlines the development of an assessment tool to capture the impact of using health-related websites. In earlier chapters we described using a literature review (see Chapter 2) and a secondary analysis of narrative interviews (see Chapter 3) to inform questionnaire items relating to issues that matter to people using health-related websites. In this chapter we explain how we refined and reduced the 82-item pool and assessed appropriateness across a range of health conditions.
Methods: the initial set of items was refined following cognitive interviews with 21 people who had experience of a range of health conditions. Item reduction steps were then conducted using a data set during a pilot survey (n = 167). We then conducted tests of validity and reliability on a further data set (n = 170) to determine the psychometric properties of the questionnaire.
Findings: following cognitive interviews, 62 items were entered into psychometric testing. Two independent questionnaire parts were identified: part 1 consisted of items relating to general views of using the internet in relation to health and part 2 consisted of items relating to the consequences of using a health-related website. Subscales were found to have high construct validity, internal consistency and test–retest reliability.
Conclusions: analyses confirmed good psychometric properties in the new eHIQ part 1 (11 items) and part 2 (26 items). The questionnaire was found to be suitable for use in assessing the health-related effects of using websites containing different types of material (scientific facts and figures, blogs, experiences, images) across a range of health conditions.
Introduction
This WP aimed to develop a valid and reliable instrument to capture the impact of using health-related websites. The instrument, the eHIQ, was designed for use in the WP3b feasibility trial to compare prototype health-related websites. To be suitable for use in the trial, the questionnaire needed to be appropriate for assessing different types of material (e.g. scientific facts and figures, and patients’ accounts of their experiences in blogs and forums) and appropriate across a range of health groups (e.g. people with chronic conditions, carers of people with a health condition and people viewing websites designed to influence health behaviour).
Candidate items for the questionnaire were informed by the literature review reported in Chapter 2 and the qualitative secondary analysis of narrative interviews with patients and carers with experience of a wide range of health conditions (reported in Chapter 3). Draft questionnaire items were subsequently reviewed by an expert panel to assess whether or not they adequately represented the potential effects of using health-related websites. In this chapter we describe how we tested the items with members of the public, reduced the number of items and then assessed the psychometric properties of the questionnaire.
Methods
Following the expert review described in Chapter 3, questionnaire items were divided into two pools: (1) items relating to general views of using the internet in relation to health (which became the eHIQ part 1); and (2) items relating to a specific health-related website (which became the eHIQ part 2).
Analyses of the item pools were carried out over four stages. In stage 1, items were discussed in cognitive face-to-face interview with people who had experience of various health conditions, either as patients or as family carers. The aim of this stage was to check that the items and questionnaire structure were understandable, clear, acceptable and applicable to a range of different health groups. In the second stage, a pilot version of the questionnaire was administered online to a large sample across a range of health groups. The aim of this stage was to reduce the number of items by identifying any poorly performing items and examining the internal structure of the questionnaire. The third stage involved administering the reduced questionnaire to a further sample of participants. By analysing these data we were able to finalise the subscales of the questionnaire and evaluate their validity and reliability. Further analysis of the data was carried out in stage 4 to assess the appropriateness of creating a summary score for each questionnaire part (eHIQ parts 1 and 2).
Participants
Participants were aged ≥ 18 years with access to the internet and living in the UK. To ensure that items were appropriate for inclusion in a generic questionnaire, we included participants with different types of experience (e.g. family carers, people with chronic conditions and people interested in changing a health behaviour).
Recruitment
Stage 1: cognitive interviews
Potential participants were recruited through a list of people who had responded to the original invitation from the Oxfordshire Primary Care Trust to attend a panel for the conceptual review (see Chapter 2) and who had indicated that they would be interested in taking part in our research. The available demographic information for list members was used to ensure that people with a range of conditions and ages were contacted. Potential participants were asked to contact LK to arrange a suitable time to be interviewed. The interviews took place in the Department of Public Health (as it was then named), University of Oxford, or in the participant’s own home if preferred.
Stage 2: pilot questionnaire
We invited people to complete the pilot questionnaire through a variety of methods, including health blogs, online discussion forums, social networking sites [Facebook and Twitter (Twitter, Inc., San Francisco, CA, USA)], news pages on health websites, research volunteer pages, local news advertisements and a research volunteer e-mail list. Potential participants were asked to click on an electronic link which led them to the questionnaire.
Stage 3: validation questionnaire
We used a variety of methods to recruit participants for the validation questionnaire. We used some direct recruitment (stage 3a) by sending postal research invitations [through the Oxfordshire Primary Care Trust (n = 520) and the Birmingham branch of the MS Society (n = 235)]. We also used open recruitment (stage 3b), including advertisements on health-related websites and social networking sites but not those that had been used in the previous stage. Data were also obtained from a separate website evaluation study carried out in the HERG which incorporated the candidate eHIQ items. This evaluation study ran in parallel with stage 3 recruitment.
Ethics
Recruitment methods for stages 1, 2 and 3b were approved by the University of Oxford’s Medical Sciences Division Research Ethics Committee (reference numbers MSD/IDREC/C1/2011/98, MSD/IDREC/C1/2011/77 and MSD/IDREC/C1/2013/063). Stage 3a was approved by the NHS Research Ethics Committee (reference number 12/SW/0209).
Instrument development and testing
In each stage, participants were asked to spend 10–15 minutes browsing a pre-selected health website; these included government websites (e.g. NHS Choices), charity websites (e.g. HealthTalk) and commercial websites (e.g. BootsWebMD). The websites were chosen to test the items with information based on facts, figures and personal experiences and other features such as discussion boards, video clips and ratings.
Stage 1: cognitive interviews with patients
Cognitive interviewing, a qualitative method used to find out how respondents understood and answered structured questions and the response categories, was used to improve the validity and acceptability of items. 85,86 The ‘verbal probing’ method gave the 21 respondents an opportunity to provide uninterrupted answers to the items, followed by a focused interview85,87 in which the participant’s understanding of an item and their interpretation of the instructions and response options were checked. 75
Items were checked for consistency of interpretation between participants and across health groups. Recurring problems with specific items or wording were highlighted. The analysis was carried out throughout the interview process so that revisions to the wording of items could be tested. We continued until we judged that all problems with questionnaire completion had been identified, revised and retested.
Stage 2: pilot questionnaire
Analyses of the eHIQ parts 1 and 2 were carried out separately in IBM SPSS Statistics, version 20 (2011, IBM Corporation, Armonk, NY, USA). The items were subjected to preliminary data checks to confirm their suitability for inclusion in further analysis. A priori decision rules for item removal included items with high floor and ceiling effects (> 40% of respondents selecting one of the extreme response options) and items that had large numbers of missing data (> 10% non-response). Items demonstrating poor correlations (< 0.2) with a large number of other items were considered for removal and analysis was carried out to identify items with low item-to-total correlations (< 0.3) and items that decreased the internal consistency (Cronbach’s alpha value). Items were iteratively removed when displaying a high number of poor correlations with other items or if they reduced the Cronbach’s alpha value.
An exploratory factor analysis (EFA) was carried out to identify subscales within the item pools and to exclude items that did not group in conceptually sound subscales. We carried out standard preliminary tests to confirm the suitability of using factor analysis on each data set [Bartlett’s test of sphericity (p < 0.05)88 and the Kaiser–Meyer–Olkin statistic89]. Factors with eigenvalues of > 1 were extracted, and an oblique, direct oblimin rotation of the factors was sought so that axes were not restricted to right angles. This permitted correlation between the factors where appropriate. 90,91 The output, in the form of the structure and pattern matrices, was used to interpret the factors (or subscales) within the questionnaire, with the structure matrix offering primary guidance for interpretation. 92 Items that had been removed were examined to ensure that no further scales were present.
At this point, a ‘translatability assessment’ was carried out in collaboration with experts in the field. Translatability assessments consider whether or not items can be meaningfully translated into another language while remaining conceptually equivalent to the source language and culturally and linguistically appropriate to the target country. 93 Assessing the translatability of a questionnaire during its development should help to reduce problems in future translations. A concept elaboration document was initially produced which aimed to clarify any ambiguities or nuances within the questionnaire. With the help of the concept elaboration document, the questionnaire was then reviewed by the following selected language (and country) combinations: Arabic (Tunisia), French (France), German (Germany), Japanese (Japan), Simplified Chinese (China) and Spanish (USA). We noted that the translation exercise also helped us to refine the English-language version.
Stage 3: validation questionnaire
Convergent validity assesses whether or not theoretically similar scales are statistically related to the newly developed questionnaire. To assess convergent validity, participants in stage 3 were asked to complete two reference questionnaires in addition to the reduced eHIQ. These questionnaires were hypothesised to have moderate correlations with the eHIQ items.
The first questionnaire which was predicted to have a moderate correlation to eHIQ part 1 scores was a single item from the Health Information National Trends Survey (‘in general, how much would you trust information about health or medical topics on the internet?’). 94 The second questionnaire was predicted to have moderate correlations with all subscales of the eHIQ part 2 and consisted of one subscale, ‘access to quality information’, from the Web Trust Questionnaire. 95 Two of the eight items in the ‘access to quality information’ subscale overlapped with two items already included in the eHIQ part 2 questionnaire. The relationship of the eHIQ subscales with an adjusted 6-item subscale was, therefore, undertaken without the overlapping items.
We used Pearson’s correlation coefficients (r) to compare the identified subscales with their respective reference measure. 90,96 Internal consistency was tested for each unidimensional subscale using the Cronbach’s alpha statistic (> 0.7). Participants were also asked to complete the eHIQ items on two occasions with a 2-week interval to examine test–retest reliability. The test–retest procedure was used to establish whether or not responses were reliable over time. The level of agreement between scores from the two occasions was assessed using the intraclass correlation coefficient (ICC), where coefficients > 0.70 were considered satisfactory. 97
Stage 4: summary scores
We explored whether or not it would be appropriate to create summary scores for each questionnaire part. The factor correlation matrices from stage 3 were used to examine whether or not the identified factors loaded on a single overall ‘higher order’ factor for each questionnaire part. The use of the factor correlation matrices was preferred over the use of first-order factor raw scores, as variance which did not contribute to the first-order factors may still have been useful in explaining the variance within a second-order factor. 98 The summary scores were calculated through summing the subscale scores and dividing by the number of subscales to get a 0–100 metric.
Results
An overview of recruitment at each stage of the study is shown in Figure 3 and participant characteristics are given in Table 4. The results are reported below by study stage.
FIGURE 3.
Work package 1c: stages overview.
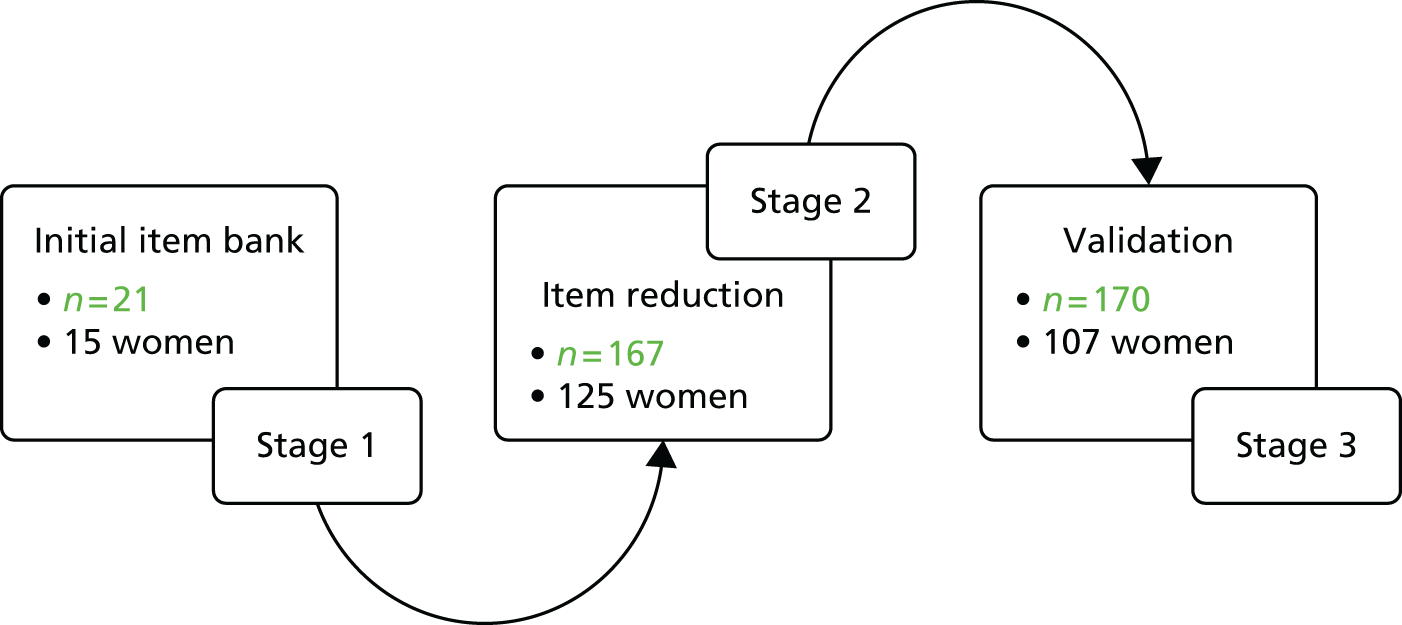
| Characteristic | n (%) |
|---|---|
| Stage 1 (n = 21) | |
| Sex | |
| Male | 6 (28.6) |
| Female | 15 (71.4) |
| Age, mean years (SD) | 45 (16.2) |
| Stage 2 (n = 167) | |
| Sex | |
| Male | 41 (24.7) |
| Female | 125 (75.3) |
| Missing | 1 (–) |
| Age, mean years (SD) | 38.80 (14.04) |
| Condition | |
| Alcohol reduction | 25 |
| Asthma | 92 |
| MND (carer) | 11 |
| MS (carer) | 22 |
| Smoking cessation | 17 |
| Stage 3 (n = 170) | |
| Sex | |
| Male | 59 (35.5) |
| Female | 107 (64.5) |
| Missing | 4 (–) |
| Age, mean years (SD) | 50.4 (13.0)a |
| Condition | |
| Asthma | 17 |
| Cancer | 27 |
| Generic (carer) | 2 |
| Healthy eating | 49 |
| Menopause | 7 |
| MND | 32 |
| MS | 26 |
| MS (carer) | 4 |
| Smoking cessation | 6 |
Stage 1: cognitive interviews
Participants (n = 21) were six men and 15 women with a mean age of 45 years [standard deviation (SD) 16.2 years]. Five were carers and 16 had one of a number of chronic health conditions. Three rounds of cognitive interviewing were carried out to ensure that (1) the instructions were easy to understand and the rubric clearly indicated how participants were supposed to answer items, (2) participants considered items relevant to the topic and acceptable to answer, (3) the response options were appropriate to the item stem and adequately covered the potential range of agreement, and (4) the electronic format was appropriate for use among participants with varying levels of confidence in using computers. Twenty-nine items were deleted and nine items were added, leaving 62 items to enter the next stage.
Two independent item pools were identified to enter psychometric testing. The first item pool contained 23 items on general attitudes towards health websites, while the second item pool contained 39 items asking about attitudes towards a specific health website. All items were given a 5-point response scale (strongly disagree to strongly agree).
Stage 2: pilot questionnaire
The two-part questionnaire was completed by 167 participants. The mean age of the sample was 38.8 years (SD 14.04 years); 125 participants were female and 41 were male (the sex of one participant was unknown) (see Table 4). Checks for floor and ceiling effects confirmed that no item had > 40% of respondents selecting one of the extreme response options and that no item had a large number of missing data (> 10% non-response). Therefore, no items were removed owing to floor or ceiling effects or missing responses.
Seven items (eHIQ part 1) and five items (eHIQ part 2) were iteratively removed owing to poor correlations (< 0.2) with a large number of items in the same item pool and decreasing the overall Cronbach’s alpha value. An EFA was carried out on the remaining eHIQ part 1 items. Five factors with eigenvalues of > 1 were initially extracted. These factors explained 63.85% of the variance. The first two factors were believed to constitute conceptually meaningful factors. These two factors explained 61.06% of the total variance.
In a further separate analysis, the eight items which had been removed following the EFA were examined to investigate the presence of any further conceptually relevant scales. This analysis resulted in a scale of six items which had Cronbach’s alpha value of 0.64. Therefore, 14 items in total for eHIQ part 1 entered stage 3.
An EFA was carried out on the remaining eHIQ part 2 items, resulting in six factors explaining 66.26% of the variance. All factors had a Cronbach’s alpha value of ≥ 0.76. The 34 items asking about using a specific health-related website were, therefore, identified as suitable to enter the next stage of development.
The translatability assessment suggested several minor changes to the instructions and item wording. Changes were suggested to improve consistency with wording, to ensure that all wording was culturally and linguistically relevant to the selected countries and to avoid ambiguities which could jeopardise future translations. Seven minor modifications were made to improve grammar and consistency with wording. Two items were amended to improve their cultural or linguistic suitability and six items were amended to avoid ambiguous wording. Three further items were identified as potentially problematic for translation. These items were:
-
I feel I have a sense of solidarity with other people using the website.
-
I can identify with other people using the website.
-
I feel I have a lot in common with other people using the website.
Although the above items had similar, yet subtly different meanings in the English language, translators were concerned that some languages may not have the capacity to express those differences (e.g. because of fewer adjectives or forms of expression in the target language). Following discussions, we decided to retain the items to capture the intended concept in English.
Stage 3: validation questionnaire
The reduced questionnaire was completed by 170 participants (see Table 4). Stage 3a recruited 47 participants, stage 3b recruited 96 participants and the separate website evaluation study recruited 27 participants. Of the 170 respondents, 59 were men and 107 were women (four unknown). Of those who consented to take part in either stage 3a or 3b, 71.1% (n = 143) completed the full questionnaire.
The items for each questionnaire part were entered into an EFA to examine the questionnaire structure and find the optimal factor solutions. An EFA for items in the eHIQ part 1 confirmed four factors. An item which did not load with other similar items and had poor distributions across response options (i.e. no participant selected the ‘strongly disagree’ response category) was removed. A further EFA suggested three factors; however, two items which formed the third factor were removed due to poor internal consistency (α = 0.59). The two remaining subscales explained 56.58% of the variance with the structure and pattern matrices (Table 5) demonstrating high loadings on their respective factors. The two remaining subscales were entitled ‘attitudes towards online health information’ and ‘attitudes towards sharing health experiences online’. Both subscales demonstrated good internal consistency (≥ 0.77) and were conceptually relevant to overall attitudes towards online health information (Table 6).
| Item | Structure | Pattern | ||
|---|---|---|---|---|
| 1 | 2 | 1 | 2 | |
| 2 | 0.32 | 0.61 | –0.002 | 0.61 |
| 5 | 0.39 | 0.65 | 0.063 | 0.62 |
| 6 | 0.39 | 0.79 | –0.03 | 0.81 |
| 7 | 0.41 | 0.80 | –0.013 | 0.81 |
| 8 | 0.37 | 0.71 | 0.000 | 0.71 |
| 9 | 0.84 | 0.31 | 0.93 | –0.18 |
| 10 | 0.84 | 0.48 | 0.81 | 0.06 |
| 11 | 0.67 | 0.38 | 0.65 | 0.04 |
| 12 | 0.62 | 0.59 | 0.43 | 0.36 |
| 13 | 0.84 | 0.45 | 0.83 | 0.02 |
| 14 | 0.77 | 0.49 | 0.71 | 0.11 |
| Scale and items | Item to total correlation | Cronbach’s alpha |
|---|---|---|
| 1.1 Attitudes towards online health information | 0.77 | |
| 2. The internet is a reliable resource to help me understand what a doctor tells me | 0.39 | |
| 7. I would use the internet if I needed help to make a decision about my health (for example, whether I should see a doctor, take medication or seek other types of treatment) | 0.64 | |
| 6. The internet can be useful to help people decide if their symptoms are important enough to go to see a doctor | 0.60 | |
| 8. I would use the internet to check that the doctor is giving me appropriate advice | 0.58 | |
| 5. The internet can help the public to know what it is like to live with a health problem | 0.52 | |
| 1.2 Attitudes towards sharing health experiences online | 0.89 | |
| 13. The internet is a good way of finding other people who are facing health-related decisions I may also face | 0.72 | |
| 9. The internet is a good way of finding other people who are experiencing similar health problems | 0.68 | |
| 10. It can be helpful to see other people’s health-related experiences on the internet | 0.72 | |
| 14. Looking at health websites reassures me that I am not alone with my health concerns | 0.67 | |
| 11. The internet is useful if you don’t want to tell people around you (for example, your family or people at work) how you feel | 0.56 | |
| 12. It can be reassuring to know that I can access health-related websites at any time of the day or night | 0.56 |
An EFA for items in the eHIQ part 2 identified six subscales explaining 66.34% of the variance. One of the six factors consisted of two items which exhibited poor internal consistency (Cronbach’s alpha = 0.50). Inspection of the structure and pattern matrices indicated that one of the two items loaded on another, conceptually relevant, factor, while the remaining item did not. The item which did not load on any other factor was, therefore, removed and all remaining items were entered into a further EFA producing five factors. Reflections on the fourth and fifth factors concluded with a consensus between the team (LK, CJ and SZ) that, grouped together, items did not constitute theoretically sound factors and explained very little variance. The seven items in factors four and five were, therefore, removed and a final EFA confirmed the three remaining factors explaining 61.68% of the variance. The structure and pattern matrices (Table 7) were used to interpret the final factor structure and confirmed high loadings of each item on their respective factor. The three subscales were entitled: ‘Confidence and identification’, ‘Information and presentation’ and ‘Understanding and motivation’. All scales had good internal reliability (≥ 0.80) and are listed in Table 8.
| Item | Structure | Pattern | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | |
| 1 | 0.36 | 0.36 | –0.80 | –0.08 | –0.01 | –0.84 |
| 2 | 0.20 | 0.42 | –0.68 | –0.23 | 0.15 | –0.72 |
| 3 | 0.26 | 0.74 | –0.36 | 0.02 | 0.74 | 0.01 |
| 4 | 0.40 | 0.52 | –0.79 | –0.03 | 0.19 | –0.71 |
| 6 | 0.48 | 0.72 | –0.52 | 0.21 | 0.59 | –0.13 |
| 7 | 0.36 | 0.81 | –0.53 | 0.02 | 0.72 | –0.18 |
| 9 | 0.53 | 0.23 | –0.73 | 0.23 | –0.18 | –0.69 |
| 10 | 0.52 | 0.44 | –0.69 | 0.21 | 0.12 | –0.52 |
| 11 | 0.23 | 0.78 | –0.35 | –0.03 | 0.79 | 0.01 |
| 13 | 0.62 | 0.34 | –0.57 | 0.44 | 0.04 | –0.33 |
| 15 | 0.70 | 0.37 | –0.49 | 0.59 | 0.11 | –0.13 |
| 17 | 0.45 | 0.74 | –0.60 | 0.11 | 0.57 | –0.27 |
| 18 | 0.52 | 0.53 | –0.66 | 0.22 | 0.25 | –0.43 |
| 19 | 0.87 | 0.30 | –0.42 | 0.89 | 0.03 | 0.06 |
| 21 | 0.84 | 0.31 | –0.36 | 0.88 | 0.08 | 0.14 |
| 22 | 0.63 | 0.58 | –0.68 | 0.35 | 0.30 | –0.36 |
| 24 | 0.72 | 0.64 | –0.66 | 0.47 | 0.37 | –0.24 |
| 25 | 0.73 | 0.57 | –0.65 | 0.50 | 0.27 | –0.26 |
| 26 | 0.81 | 0.24 | –0.37 | 0.85 | –0.01 | 0.08 |
| 27 | 0.77 | 0.26 | –0.60 | 0.64 | –0.10 | –0.31 |
| 28 | 0.69 | 0.44 | –0.74 | 0.41 | 0.06 | –0.49 |
| 29 | 0.56 | 0.41 | –0.76 | 0.22 | 0.04 | –0.63 |
| 30 | 0.73 | 0.35 | –0.67 | 0.52 | –0.02 | –0.41 |
| 31 | 0.56 | 0.70 | –0.51 | 0.34 | 0.56 | –0.07 |
| 32 | 0.04 | 0.67 | –0.18 | –0.17 | 0.77 | 0.09 |
| 34 | 0.40 | 0.81 | –0.43 | 0.15 | 0.77 | 0.02 |
| Items | Item to total correlation | Cronbach’s alpha |
|---|---|---|
| 2.1 Confidence and identification | 0.92 | |
| 19. I feel I have a sense of solidarity with other people using the website | 0.79 | |
| 21. I can identify with other people using the website | 0.72 | |
| 26. I feel I have a lot in common with other people using the website | 0.70 | |
| 27. The website gives me the confidence to explain my health concerns to others | 0.72 | |
| 30. The website makes me more confident to discuss my health with the people around me (for example, my family or people at work) | 0.73 | |
| 25. The website gives me confidence that I am able to manage my health | 0.75 | |
| 24. I value the advice given on the website | 0.74 | |
| 15. The people who have contributed to the website understand what is important to me | 0.65 | |
| 13. The website prepares me for what might happen to my health | 0.61 | |
| 2.2 Information and presentation | 0.89 | |
| 7. The language on the website made it easy to understand | 0.75 | |
| 11. I can easily understand the information on the website | 0.66 | |
| 34. The website is easy to use | 0.74 | |
| 3. The information on the website left me feeling confused | 0.65 | |
| 6. The website provides a wide range of information | 0.68 | |
| 17. I trust the information on the website | 0.69 | |
| 32. I found the images on the website distressing | 0.51 | |
| 31. Photographs and other images were used appropriately on the website | 0.67 | |
| 2.3 Understanding and motivation | 0.90 | |
| 4. The website includes useful tips on how to make life better | 0.71 | |
| 1. The website encourages me to take actions that could be beneficial to my health | 0.67 | |
| 2. The website has a positive outlook | 0.55 | |
| 9. I feel more inclined to look after myself after visiting the website | 0.65 | |
| 29. The website encourages me to play a more active role in my health care | 0.70 | |
| 28. The website helps me to have a better understanding of my personal health | 0.74 | |
| 22. On the whole, I find the website reassuring | 0.69 | |
| 10. I have learnt something new from the website | 0.64 | |
| 18. I would consult the website if I had to make a decision about my health | 0.64 |
Scale distributions and validation
Each scale was transformed to a 0–100 metric, where 0 = low perceived value of the internet (or a specific website) for health and 100 = high perceived benefit of using the internet (or website) in relation to health. Descriptive statistics for the final eHIQ subscales are shown in Table 9. The eHIQ subscale scores followed a relatively normal distribution across the study sample. Scores were examined for floor and ceiling effects. High frequencies at the limits of the scales can suggest a lack of sensitivity at the extreme points. No scales exhibited floor or ceiling effects.
| Subscale | n | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|---|
| 1.1 Attitudes towards online health information | 169 | 0.0 | 100.0 | 63.31 | 16.90 |
| 1.2 Attitudes towards sharing health experiences online | 169 | 0.00 | 100 | 70.69 | 16.30 |
| 2.1 Confidence and identification | 165 | 0.0 | 100.0 | 58.17 | 17.54 |
| 2.2 Information and presentation | 167 | 0.0 | 100.0 | 73.18 | 13.93 |
| 2.3 Understanding and motivation | 167 | 8.33 | 97.22 | 61.23 | 16.07 |
The relationships between the subscales and a range of variables were examined. No significant differences were found for either sex (t-tests) or age (Pearson’s correlations) among all subscale scores on the eHIQ. A significant difference [analysis of variance (ANOVA)] was observed between subscale 1.2 (‘attitudes towards sharing health experiences online’) [F(2,166) = 4.60, p = 0.011] scales and mode of recruitment. Post hoc comparisons using Tukey’s indicated that there were significant differences between those in stage 3a (mean = 65.51, SD = 14.89) and the website evaluation study (mean = 76.85, SD = 15.17). This difference may have been due to the sample size; however, it is conceivable that those in the website evaluation study were more open to sharing experiential information as they had agreed to help evaluate a website built around experiences of cancer.
Relationships (Pearson’s correlation coefficients) between eHIQ scores and the selected reference measures were examined to assess convergent validity. Correlations between the eHIQ part 1 subscales and the Health Information National Trends Survey single item were weak to moderate (r = 0.35 to 0.52; p < 0.01). Correlations between the eHIQ part 2 subscales and the adjusted Web Trust Questionnaire subscale were good (r = 0.75 to 0.76; p < 0.01). The results confirmed expectations that the scales are significantly related but sufficiently divergent.
Participants were invited to complete the eHIQ on two separate occasions with a 2-week interval. Of the 170 sample, 143 were asked to complete a second questionnaire (those in the independent HERG website evaluation study which ran in parallel to this stage were not asked to complete a second questionnaire). Of the 143 people asked, 90 (62.94%) people responded. A computer error meant that 22 MND responses were not valid and seven respondents did not fully complete the eHIQ part 2. The levels of agreement (ICC = 0.76 to 0.91) indicated good test–retest reliability for all subscales.
Stage 4: summary score
The factor correlation matrix for eHIQ part 1 was entered into a factor analysis. One factor with an eigenvalue of > 1 was extracted, explaining 76.2% of the variance. No rotation was needed, as all subscales loaded sufficiently on the factor extracted (Table 10, eHIQ part 1). The higher order factor, referred to here as ‘attitudes towards the use of the internet in relation to health’ was assessed for internal consistency achieving a Cronbach’s alpha of 0.78 (n = 169). This supported summing all eHIQ part 1 subscales to create a total index score. After the summed score for the higher-order factor had been standardised to 0–100 metric, the mean summary score was 67.0 [SD 15.04, 95% confidence interval (CI) 64.72 to 69.28; n = 169].
| First-order factor | Factor loading on higher-order factor |
|---|---|
| eHIQ part 1 | |
| Scale 1.2 | 0.873 |
| Scale 1.1 | 0.873 |
| eHIQ part 2 | |
| Scale 2.3 | –0.854 |
| Scale 2.1 | 0.779 |
| Scale 2.2 | 0.747 |
The factor correlation matrix for eHIQ part 2 was subsequently entered into a factor analysis. One factor with an eigenvalue of > 1 was extracted, explaining 63.1% of the variance. No rotation was needed, as all subscales loaded sufficiently on the factor extracted (see Table 10, eHIQ part 2). The higher-order factor, referred to as ‘overall impact of using a specific health-related website’, was assessed for internal consistency, achieving a Cronbach’s alpha of 0.87 (n = 163). The mean summary score was 64.22 (SD 14.20, 95% CI 62.02 to 66.41; n = 163).
Discussion
This chapter outlines the stages taken to develop an instrument which is suitable for use in the WP3b trial comparing websites based on different types of health information. We followed best practice guidelines in health-related questionnaire development100,101 and tested the applicability of the questionnaire items across a range of health groups and different types of health-related websites. The items and questionnaire design were tested for suitability among (1) people with chronic conditions, (2) people hoping to modify their health behaviour and (3) carers of people with a health condition. The questionnaire was also tested on websites containing standard ‘scientific’ health information, experiential health information, and forums and blogs.
Items were identified through secondary analysis and expert review and were pre-tested among patients and carers. Cognitive interviews established that the instructions, items, response options and electronic format of the instrument were acceptable to patients and carers. Two independent item pools were confirmed as suitable for psychometric testing. The first item pool (eHIQ part 1) contained 23 items concerning general attitudes towards health-related websites, while the second item pool (eHIQ part 2) contained 39 items about attitudes towards a specific health-related website. The online questionnaire was administered in a pilot survey and items were removed using a series of a priori item reduction decisions and EFA.
The reduced 48-item questionnaire was subsequently administered in stage 3 to explore the validity and reliability of the new measure. The analyses resulted in the removal of three items from the eHIQ part 1 and confirmed the presence of two subscales: 1.1 ‘attitudes towards online health information‘ and 1.2 ‘attitudes towards sharing health experiences online’. The two subscales in the eHIQ part 1 explained 56.6% of the variance and higher-order factor analysis in stage 4 confirmed the appropriateness of creating a summary index score for ‘overall attitides towards using the internet for health information’.
In relation to the eHIQ part 2, eight items were removed and three subscales were retained: 2.1 ‘confidence and identification’, 2.2 ‘information and presentation’ and 2.3 ‘understanding and motivation’. The three subscales in the eHIQ part 2 explained 61.9% of the variance. The subscales identified were considered conceptually relevant to the impact of using health-related websites. The first eHIQ part 2 subscale, ‘confidence and identification’, measures the extent to which an individual identifies with others using a specific website and whether or not they feel that visiting the website has affected their confidence in discussing and managing their health. The second subscale, ‘information and presentation’, measures ease of use, ease of understanding, the perceived trustworthiness of information and the appropriateness of images. The final eHIQ part 2 subscale, ‘understanding and motivation’, measures the extent to which the respondent felt reassured, better understood their condition and felt motivated to manage their health after viewing a specific website.
Statistical analyses confirmed the hypotheses that the eHIQ subscales were moderately related to the chosen reference measures. Correlations between the eHIQ part 1 and the Health Information National Trends Survey trust item were weak to moderate, while correlations between the eHIQ part 2 and the adjusted ‘access to quality information’ scale were moderate to good. This demonstrated that the eHIQ subscales were sufficiently related to each respective reference measure to demonstrate convergent validity, yet sufficiently dissimilar to validate the independent construct. 102 The scaling properties of the eHIQ subscales were also satisfactory, showing little or no floor and ceiling effects. All subscales had some evidence of negative skew, indicating that the distribution was concentrated on the positive end of the scale (i.e. positive view of the websites). This was expected, as participants were asked to view established websites run by government organisations (e.g. NHS Choices) or major charities (e.g. the MS Society). Despite the concentration of scores at the positive end of the construct, the distributions were relatively normal.
All subscales showed good internal consistency, achieving a Cronbach’s alpha of ≥ 0.77. This gave a good indication that all items within each subscale were measuring the same latent variable. Good test–retest reliability was found among those who completed the eHIQ again after a 2-week interval (n = 83, ICC = 0.76 to 0.91). This indicated that, providing there had been no change in the construct being measured, the items in each eHIQ subscale are answered consistently over time. 103,104 Overall, the eHIQ subscales are highly relevant to attitudes towards using the internet for health information (eHIQ part 1) and using a specific health-related website (eHIQ part 2).
Conclusions
We developed an instrument (the eHIQ) to capture the impact of different types of health-related website. The questionnaire consists of two independently administered and scored parts. The eHIQ part 1 consists of 11 items asking about a person’s general attitudes towards health-related websites. The eHIQ part 2 consists of 26 items asking about a person’s views of a specific health-related website.
The development of a questionnaire which can be used to compare responses to different types of websites was important both in general and in particular to be used in a subsequent intervention study within this same programme of work (see Chapter 8). A focused internet-specific instrument may pick up important yet subtle aspects associated with using information from the web.
Chapter 5 Work package 2a: practices and platforms for sharing experiences of multiple sclerosis patient experience online – interviews, participant observation and content analysis
Abstract
Introduction: this chapter explores the construction and exchange of MS-related PEx on the internet across different websites, platforms and services, with a focus on online support groups and YouTube.
Methods: between June 2011 and July 2012, we studied online MS-related PEx through non-participant observation, content analysis of forums, blogs, websites and YouTube videos, and 24 interviews [people affected by MS (n = 17) and professionals working in relation to online PEx (n = 7)].
Findings: the MS-related PEx shared online is extremely diverse. Three categories of PEx were particularly prominent: advice and information on ‘living with’ MS, PEx focused on medical research and treatment, and PEx as creative and emotional expression. What and how PEx is shared online is shaped by various factors, including the design, management and dynamics of the platforms on which it is shared. People affected by MS not only seek out and share individual PEx, but experiment with, link up and aggregate their experiences, creating databases of experience that can be turned into, at times highly contested, forms of ‘experiential evidence’.
Conclusions: online PEx is an integral part of the MS health information landscape. Developing and maintaining productive spaces for sharing PEx requires work and expertise (emotional and technical). People affected by MS share PEx as a means of actively engaging with and sometimes challenging mainstream medicine. This has consequences for biomedical research, health-care policy and practice. More research is needed on how health-care professionals, patient organisations, charities and patients produce and respond to online PEx in different conditions.
Introduction
The aim of WP2a was to explore how PEx is constructed and exchanged in online support groups, and the ways people respond to and interpret PEx-related information in these settings. Given the time scale of WP2a, it was not possible to conduct in-depth ethnographically informed research on all three exemplar conditions. Through discussions with the project team, it was decided that WP2a would focus on the use of online support groups by people, both patients and carers, affected by MS. This decision was informed by a number of factors. As MS is the most common neurological condition to affect young adults,105 there is a large amount of related PEx information available online (e.g. patient blogs, MS-based Facebook pages, patient forums, YouTube videos). In addition, MS is a long-term condition with highly variable symptoms and severity, and there is a range of treatment options, some of which conform to mainstream ‘Western’ medicine and some of which do not. People’s experiences (and discussions) of MS are, therefore, extremely diverse. 106–108 Although considerable social science research has been conducted on the experiences of people affected by MS, the majority of this pre-dates the rise of the internet as a health information resource. Consequently, there is a relative paucity of research on internet use in relation to MS. 109,110 A focus on MS, therefore, enabled us to combine the specificity required for qualitative research with a wide-ranging analytical scope that touched on numerous issues of relevance to the exchange of PEx.
At the start of WP2a we were already sensitive to a number of themes and possible areas for further exploration. However, the findings from WP1a and 1b informed our thinking but did not predetermine the focus of WP2a. Instead, informed by grounded theory,111 we approached the field in as open a manner as possible, using an ethnographically informed mixed-methods approach that included extended periods of observation of online MS related patient forums, blogs and websites; interviews with people affected by MS [carers (n = 5) and patients (n = 12)]; interviews with people working in relation to the production, editing and moderation of online MS research, support, community and information services (n = 7); and a content analysis of YouTube videos.
This chapter contains a high-level overview of this research with a focus on three core elements. First, drawing on both online and interview material, we provide a high-level summary of MS-related PEx online. Second, we discuss the (often overlooked) importance of platform-specific factors, such as forum design and management, in the construction and exchange of PEx in different online spaces. Third, we present findings from the research we conducted on the use of YouTube in relation to a chronic cerebrospinal venous insufficiency (CCSVI), a controversial causal theory and associated treatment for MS proposed by Italian physician Paolo Zamboni in 2009. 112 This was a much debated topic when we were conducting our fieldwork. In the conclusion, we bring these three areas together, focusing specifically on the relevance of this research for the NHS and health-care practitioners.
Methods
Researching patient forums and other online PEx raises a number of ethical questions. We followed the ethical guidelines of the British Sociological Association and the Association of Internet Researchers. To minimise any inadvertent breaches of privacy, we limited the scope of our analysis to publicly available content. Ethics approval was received from Warwick Medical School’s Biomedical Research Ethics Committee. For a more detailed discussion of methodological and ethical questions in relation to analysing PEx online, see Mazanderani and Powell. 113
The research was conducted in a series of iterative stages. We started by using the publicly available issuecrawler software (www.issuecrawler.net, Govcom.org Foundation, Amsterdam, the Netherlands) to map out the network of MS-related websites available online and to identify websites, personal blogs and patient forums for further analysis. 114 We found that, in the UK, the NHS website (www.nhs.uk) is a key source of information to which many other websites link. Large charities such as the MS Society and Citizens Advice are prominent, but smaller charities, such as the MS Trust and the MS Resource Centre, also have a strong online presence. Following this initial mapping of the MS-related web content, we developed a three-tiered research strategy. First, we observed a range of different MS-related websites, blogs and forums, recording key topics and themes that emerged within and across these sites. Second, we performed a content analysis on YouTube videos about CCSVI. 84 Third, we used telephone interviews to further develop the themes emerging from our online observations. These methods were supplemented by an advisory workshop with people affected by MS that took place in November 2011 at the University of Oxford (see Chapter 10).
Observation and analysis of patient forums and online information sharing
Between June 2011 and July 2012, one researcher (FM) spent extended periods of time (approximately 1–3 hours per day, 3–4 days per week) reading MS-related websites, following news items and analysing forums. She familiarised herself with different platforms and key debates, analysing current as well as historic data within and across different websites. Although this involved moving between websites and sources of information, three forums were chosen as key ‘sites’ to focus on: the MS Society forum (www.mssociety.org.uk/forum); Shift.MS (http://shift.ms); and ThisIsMS (referred to as TIMS by its members) (www.thisisms.com).
The forums were analysed in terms of topics and themes (what people were talking about); the ways in which PEx were articulated and responded to (discourse and imagery, the types of language used, colours, avatars and emoticons), and patterns of communication (e.g. what types of topics received most responses, how many people engaged in different types of conversations, and when, if ever, did moderators intervene). Notes were taken and, where relevant, discussions were copied and stored as text files for further analysis. Rather than limiting our analysis to the patient forums (as is often the case in the analysis of online health forums), links and references to other sources of information, such as biomedical publications or newspaper articles, YouTube videos or blogs, were followed up. In this way the content of the forums was contextualised in relation to broader information practices and topics being debated in the field of MS research and care at the time.
Analysis of YouTube videos
While conducting our research we became aware of the large number of MS-related videos online, many of which contain PEx. As there is relatively little research on YouTube as a source of PEx, and the visual dimensions of PEx were highlighted in both the literature review (see Chapter 2) and the secondary analysis (see Chapter 3), we decided to pursue further research on YouTube.
In January 2012, we searched for the term ‘CCSVI’ using the YouTube search facility. Four thousand videos were returned, and we selected the top 100 most viewed videos for a quantitative and qualitative analysis. A sample of the 15 most viewed videos were analysed by FM, Braden O’Neill and JP. Each researcher developed their own coding scheme and after discussion a final coding scheme was agreed. Next, FM and Braden O’Neill separately coded the full sample of 100 videos. Thirty videos were excluded because either they were not about CCSVI107 or they were not in English (videos with English subtitles were kept). 115 This left 70 videos, with number of views per video ranging from 7103 to 79,956.
The title, channel, number of views, date uploaded and country of origin were recorded for each of the videos. We also categorised videos into two broad groups: ‘patient’ and ‘non-patient’. Videos that focused on the experiences or thoughts of a particular person with MS were categorised as ‘patient’ videos; videos that discussed CCSVI in ways that did not draw on the experiences of individual patients were categorised as ‘non-patient’ videos. Where possible, the gender, type of MS and current medical treatment were additionally recorded for each ‘patient’ video. All videos were then coded in terms of the type of information they provided and whether they portrayed CCSVI positively, negatively, neutrally or ambiguously. Coding was consistent across both coders, with a basic percentage agreement intercoder reliability of 90%. 116 Any discrepancies were resolved through discussion.
In addition, we performed a qualitative thematic analysis on the full sample of ‘patient’ videos (n = 46). Some ‘patient’ videos belonged to a ‘channel’ that contained more videos uploaded by the same YouTube user, often posted over a period of time as a video diary. When this was the case, we analysed the entire channel to contextualise specific videos. We focused on what patients said and how they said it. For each video we noted key emergent themes, transcribed portions of the video and read the comments posted by people who had watched the videos. For further details on the methods used and results please refer to the article published on this work. 84
Interviews
The analysis of online material provides only a partial view of the dynamics of sharing PEx online. It cannot provide insight into people’s motivations for, or perceptions of, sharing their experiences. Moreover, only observing what is available online misses out on the experiences of ‘lurkers’: those who read PEx, but do not post. 117 We used telephone interviews as a method for exploring aspects of PEx that could not be studied through the analysis of online data. The telephone interviews captured the views of two groups of informants: first, people affected by MS (people with MS, and carers) and, second, people who worked on the production or ‘back-end’ of patient forums and online services (e.g. forum moderators, web managers, researchers and designers).
To recruit people affected by MS, the study was advertised on the MS Society, MS Trust and MS Resource Centre research pages, the MS pages of NHS Choices, Shift.MS and a MS National Therapy Centre blog. Regional MS Society groups were e-mailed and asked to circulate information about the study to their user groups. We recruited 17 people affected by MS (five carers and 12 patients) to the study (Table 11). The interviewees included people who had been diagnosed relatively recently and those who had had MS for many years. Some interviewees used the internet and shared PEx prolifically, while others were more circumspect in their use. Three interviewees had undergone venoplasty in response to a diagnosis with CCSVI and one was the mother of a young woman who had had this treatment. In all four of these cases, the interviewees had shared some of their experiences online.
| Description of interviewee | Gender | ||
|---|---|---|---|
| Men | Women | Total | |
| People living with MS | 3 | 9 | 12 |
| Family members and friends of people living with MS | 1 | 4 | 5 |
| People involved in the provision and management of online services | 4 | 3 | 7 |
| Total | 24 | ||
To recruit people who worked on the production and management of patient forums and online services, we made direct contact with representatives from major websites and organisations involved in MS-related PEx. In all cases our informants agreed to take part in an interview (seven interviewees representing five organisations in total; see Table 11).
Both sets of interviews were semistructured and used a common interview protocol that was based on themes that emerged from the earlier analysis of the online material. Each interview lasted for approximately 1 hour. Informed consent was taken and interviews were audio recorded and transcribed verbatim. Constant comparison thematic coding was performed by FM on the interviews with the assistance of the qualitative analysis software tool NVivo. The findings were analysed in conjunction with the online material and observations and discussed at regular intervals with JP and other members of the project team.
Results
Multiple sclerosis-related patient experience on the internet
The MS-related PEx circulating online is extremely large and diverse, ranging from YouTube video diaries and brief postings on Facebook pages through to detailed biographical information provided on blogs. Accounts of PEx are not limited to patient forums, blogs and social networking sites, but permeate the internet, appearing regularly on the websites of pharmaceutical companies, health service providers (including the NHS), charities and patient organisations (e.g. in the UK the MS Society, MS Trust, MS Resource Centre and Shift.MS). Despite this, only a relatively small number of people actually share PEx on the internet as producers of content. The majority are consumers (sometimes referred to as ‘lurkers’): people who draw on other people’s experiences, but do not share their own. As our study focused on online PEx, the majority of our participants had shared their experiences online at some stage, but a few said that they preferred not to do so. The most frequently cited reasons for this were concerns about privacy; fears of being subjected to negative or aggressive responses; the desire to maintain an emotional distance from the condition; and, for carers, concerns about breaking trust or breaching the privacy of their family member. Nonetheless, even participants who preferred not to share their experiences online or expressed concern about the reliability of PEx at times searched for other people’s experiences.
Three inter-related categories and associated practices of PEx emerged as particularly prominent in our analysis of both online and interview material. The first, to adopt Corbin and Strauss’ terminology,118 was PEx dealing with the everyday ‘work’ of living with MS. This includes seeking and sharing experiences about practical concerns and the challenges of living with MS that fall beyond the remit of medicine and health care as strictly defined (e.g. employment, financial concerns, home adaptations, mobility and transport). This type of PEx was frequently mentioned in interviews as a relatively uncontroversial source of very useful information that supplemented biomedical knowledge and expertise.
The second category was PEx directly linked to health-care practices and/or biomedical treatment and research. This takes many forms. It includes the sharing of PEx-based personal experiences and decision-making in relation to treatment and care (e.g. when someone was experiencing particularly troubling symptoms or side effects), discussions about interactions with health-care services and practitioners, and debates on biomedical research. As MS is a degenerative condition for which there are a number of different treatment options, but no cure, it is unsurprising that treatments and research are frequently discussed online. At times, these discussions include an activist component, with people advocating for different theories and treatments, including those that are controversial (such as goat serum, stem cell therapy or long-term antibiotic therapy).
Traditionally, a distinction has been made in social studies of medicine between ‘subjective’ experiences of illness and ‘objective’ biomedical knowledge about disease. 119 However, at least in Western Europe and North America, the majority of people experience illness in relation to some aspect of orthodox biomedicine (even if that relationship is an antithetical one). This is reflected in MS-related PEx on the internet where what might be more narrowly conceived of as ‘medical’ information is combined and supplemented with ‘experiential’ information, and vice versa, and personal accounts often include discussions on biomedical disease models, research and treatments. Despite this blurring, in both interviews and online comments, distinctions were frequently made between ‘facts’ and ‘opinions’, with people frequently caveating what they said with statements such as ‘This is just my subjective opinion’; ‘I know this is not scientific, but . . .’; and ‘I’m not a medical practitioner, so please check this with your doctor.’
Yet there was a strong sense (espoused online and in interviews) that individual, personal experiences of living with MS were a valuable source of knowledge and constituted a distinct way of knowing and source of knowledge that needed to be taken into consideration. In most cases this ‘experiential’79 or ‘patient knowledge’120 was seen as (by interviewees and in online comments) as complementary to rather than as a challenge to medical knowledge and traditional medical expertise. However, some patients did draw on their experiences to question or even directly challenge biomedical theories, treatments and practitioners (discussed in more depth in YouTube and the sharing of patient experience in relation to chronic cerebrospinal venous insufficiency).
The third category and associated practices of PEx shared online (very much inter-related and inseparable from both of the above) centred on self-expression, community building and mutual support. The focus here was less on imparting specific information (although this was included) than on emotional and creative expression. This included, for example, initial forums posts in which people introduced themselves to the community, and creative writing based on experiences of MS. These types of interaction differed between platforms and spaces, and in many cases were linked to forum cultures that encouraged particular types of engagement.
We have separated these three categories for analytical purposes only. In practice one online post will often combine elements of all three. Indeed, we contend that it is precisely through the interweaving of lived experience, biomedical knowledge, creative expression and emotional support in how it is constructed that makes PEx so valuable, and distinguishes it from other sources of health-related information and support. However, although the blurring of categories is a key characteristic of PEx, we found that these three categories and their various combinations were not equally distributed online. For example, with regard to the three forums we analysed, one slanted toward non-mainstream MS research and treatments, whereas another was geared towards providing a platform for sharing everyday experiences of living with MS and peer support, and the third specifically encouraged creative engagement (e.g. through shorts films and video clips). This highlights the role that the design and management of online spaces for sharing PEx play in how and what PEx is shared on the internet, a topic that has been relatively understudied in e-health research and which we discuss in more depth below in the specific context of MS.
Constructing patient experience: the role of the design and management of online spaces
In the early days of the internet, the most common sites for sharing PEx were blogs and text-based health forums. In a relatively short space of time, social media platforms such as Facebook and YouTube have emerged, and e-health and tele-health services have grown and diversified. Consequently, how and what PEx is shared online has changed radically. ‘Traditional’ text-based health forums still exist and continue to flourish, but they operate as part of a complex ‘polymedia’ landscape in which different mediums and platforms are situated in relation to each other. 121 Users can choose between platforms and technologies, while service providers learn from and adapt in relation to each other. In our interviews, participants (especially those who used the internet regularly in relation to MS) often expressed a strong preference for a specific site or service that they had become familiar with and found helpful to them. It would, however, be inaccurate to characterise this as a free or ‘open’ market where people can simply choose the service they prefer.
It is well recognised that search engines [predominantly GoogleTM (Mountain View, CA, USA)] and large health-care incumbents (the NHS, pharmaceutical companies, established patient organisations) play a significant role in how and what health information people access online. 122 However, considerably less is known about how the design and management of online forums shape online experiential information sharing. Our data suggest that various, often subtle and pervasive, factors shape these different services, and that this affects who ends up using these services, what PEx they share online, how they share it and the consequences this use has for them. This was recognised and clearly articulated by interviewees working on sites and services for sharing PEx online, for example in the quotation below:
[T]he context in which you encourage people to submit data has a massive impact on the culture that’s developed there as well as the type of people who are attracted to your system. So if you want Daily Strength and you make a system where people can give each other hugs and smiley faces, you attract people who want hugs and smiley faces and put butterflies in their email. If you make a system that tries to mimic clinical trials and does scientific studies you’re going to attract highly educated, quantified-self type people who want to manage their illness better.
Interviewee 7, research director of health information organisation
Although the people we interviewed who worked on websites and forums were aware of and very sensitive to the fact that the technical, aesthetic and management decisions they made had an effect on their users and could even alienate some people, as one interviewee pointed out ‘nobody can be everything to everyone’, and, often, difficult decisions had to be made. In some cases the individual, group or organisation providing the platform, forum or online service (such as an organisational Facebook page) was able to make design and management decisions that reflected and supported their aims, ambitions and relative positioning in the field. Their ability to do so was, however, constrained by numerous factors; four key ones which emerged from our interviews were the nature and aims of the individual or organisation providing the service (e.g. funding, capacity, time); the condition in question and the service provider’s position in the wider field of information and support providers (e.g. competition, target users); technical dynamics, challenges and opportunities, often ones beyond their control (e.g. changes to underlying infrastructure and platforms such as Google and Facebook); and user dynamics, initiative and resistance.
Moreover, the rise of Facebook and YouTube as popular sites for sharing PEx has resulted in a decline in the number of people using more ‘traditional’ patient forums. However, Facebook and YouTube have not simply replaced these forums; instead, they are used for other purposes, and in some cases are directly linked to patient forums. For example, in the case of one charity that has both a Facebook page and a forum, Facebook was used for shorter messages, campaigns and less private information, while forums were perceived as more anonymous and intimate spaces:
I think that the overwhelming difference is that the forums allow people to be much more anonymous and we even go so far as not only can you create an online identity which conceals who you are, but you can actually ask a question completely anonymously on top of that as well. The older generation particularly don’t trust Facebook as a way of putting personal issues out there and even, to a certain extent, the kind of traffic we get on Facebook is quite different really.
Interviewee 1, social media officer, MS charity
However, platforms such as Facebook are not neutral or stable. They have their own commitments and politics,123 and regularly update their services in ways that can have unexpected effects on user interaction. For example, a change made by Facebook to their settings, something beyond the control of the MS charity using it, had a dramatic effect on the usage patterns of the page:
[I]t [the group] hasn’t actually been this active until the last year or so because Facebook have changed the settings or something. Once they changed their group settings so the groups were automated in their updates so suddenly people would see that something had happened on the group. People started looking much more at them and they became much more involved. So I would say up to about 2010 we didn’t have an awful lot of activity going on on there. There was, you know, now and again, but now it is . . . back then we might have had to send one question a week to information where now we have to send say five a day, so it is quite different.
Interviewee 6, web editor, MS charity
As these sites are often important sources of information and support for people affected by MS, changes, intentional or unintentional, can have dramatic effects, in some cases leaving users feeling powerless and bereft. This was brought forcibly to our attention in August 2011 when one of the forums we were observing underwent an extensive upgrade. The forum had been in operation for approximately 10 years and had a very dedicated group of users. When its layout, colour and functionality changed, many users responded very critically. The distress and upheaval brought about by the changes were evident in the large number of posts in which members expressed their unhappiness, in some cases stating that they would no longer use the forum. Some of the criticism was attributed to problems with functionality (e.g. users struggling to move their profiles over, customise their avatars and usernames, send private messages), but many focused on aesthetics, such as the change in the colours – from pastel to brighter shades – and the overall ‘feel’ of the forum. Numerous members stated that the forum no longer felt ‘like home’ and complained that it was now ‘stark and clinical’ as opposed to warm and friendly: for example, ‘I just feel emptiness now when I go in this site. I hardly come here now . . .’; ‘It’s cold in here. The sense of community and support has gone.’ The people working on the ‘back-end’ of this forum were obviously very aware of these responses, and were surprised by them.
This case illustrates how what might seem as ‘trivial’ aesthetic decisions, such as colour or where branding is placed, can influence what PEx is shared and how people respond to it. This was reiterated by research participants who worked on websites and forums, who spoke of how important aesthetics, including, colour, wording, visuals, branding, links and so on, were in not only attracting and retaining users, but in the creation of appropriate online spaces for sharing PEx that not only provided information, but a sense of care and support. Previous work has indicated that visual design elements unrelated to the actual health information content can influence trust and credibility;124 in a review of design features used in effective e-health interventions aesthetics, was raised as salient feature. 121 Similarly, in our research, what can be broadly classified as aesthetic factors played a key role in how people affected by MS perceived and used online spaces for sharing PEx. What counts as a ‘good’ design is not, however, easy to pin down. Some interviewees spoke of being instantly ‘attracted’ to a specific site or service, while others felt that the same service was unappealing or off-putting.
Familiarity with a given service also played an important role in how users perceived and used it. Different forum cultures and networks of exchange develop over time among specific groups of people in ways that can differ considerably from the original intentions of the service or platform provider. In all three of the forums we studied a core group of users played a significant role in shaping the overall tone and type of PEx shared on the forum. Sometimes they were volunteers and moderators with an official, if usually unpaid, role, but in the many cases they were simply prolific users.
These ‘super users’ spent considerable amounts of time online: welcoming people, responding to their queries, creating a friendly environment, and sometimes policing the forums. It is well recognised that health forums have specific cultures and that users play a crucial role in developing this. 125,126 However, the forms of emotional labour – broadly defined as labour involved in dealing with other people’s emotions and regulating your own – involved in the creation and maintenance of supportive and effective platforms for sharing PEx are rarely discussed in the e-health literature. 127 The importance of this form of ‘work’ was especially evident when there were breakdowns in relations, for example when a user or group of users ‘flamed’ – engaging in hostile and disruptive behaviour – a particular service or an individual. When this happened it not only disrupted the service (sometimes for a considerable time), but also prevented people from using it, or indeed any online platform for sharing experiences, in the future. Forums have different procedures for handling disruptive users and behaviours, from extremely light-touch moderation through to actively removing posts and banning some users. In the majority of cases when conflicts or disagreements arose on the forums we observed that they were resolved relatively swiftly with minimal intervention. However, during the period we were conducting our research the topic of CCSVI was a particular source of conflict and disagreement, and we observed many heated exchanges on it. It was also a topic in relation to which a great deal of PEx had been and was being shared. We, therefore, chose to focus on it as a specific area of interest.
YouTube and the sharing of patient experience in relation to chronic cerebrospinal venous insufficiency
In 2009 Zamboni proposed that abnormal venous drainage, what he called CCSVI, was a possible cause for MS. Furthermore, he suggested that venoplasty of the azygous and jugular veins – dubbed the ‘liberation procedure’ by its supporters – might improve symptoms and slow disease progression. 128 Although Zamboni’s research ran counter to much orthodox biomedical thinking about MS, between 2009 and 2012 it received a great deal of media and popular attention, with thousands of people across the world undergoing venoplasty in private clinics and/or as part of research studies. 29,129
Many people affected by MS shared their thoughts about CCSVI and venoplasty on blogs, forums, Facebook and YouTube, with some using their experiences to lobby for further research and treatment. 84,115,129,130 In particular, YouTube emerged as an important medium for sharing CCSVI-related PEx. To study this further we analysed the top 100 most viewed YouTube videos relating to CCSVI. The results of this analysis are published in detail elsewhere;84 therefore, we provide just a brief summary of the key findings here.
Although many neurologists and the representatives of international MS Societies expressed skepticism about Zamboni’s research, the YouTube videos we analysed adopted an overwhelmingly positive attitude towards it (67/70; 96%). Many of the videos were uploaded by patients (46/70; 66%). Videos in which people posted vivid pre- and post-treatment comparisons were particularly popular. Here, video posters did not simply share their experiences verbally, but tried to quantify and communicate the changes they experienced through performing various tests, such as walking up stairs, balancing on one leg or bending. Many of these tests drew on clinical and diagnostic practices as well as medical explanations and terminology, with patients frequently discussing MS treatments, medical professionals and the role of pharmaceutical companies. These videos, some of which form part of extensive video diaries that document people’s experiences over years, were often highly personal: videoed in people’s homes, showing their families, and embedding PEx not only in the clinical aspects of MS, but in everyday living with the condition.
Three key themes emerged from our analysis of these videos: (1) the visual medium enabled vivid depictions of pre- and post-treatment comparisons, often drawing on medical explanations, terminology and tests adapted from clinical practice; (2) patients not only displayed their own medical knowledge, but discussed current MS treatments, medical professionals and ‘big pharma’; and (3) videos were situated in relation to specific people’s experiences, conferring a sense of authenticity and personal immediacy. Thus, patients drew on medical knowledge to explain and reinforce their message, but, at the same time, their status as patients rather than practitioners conferred their thoughts, experiences, and, in some cases, advice, with a particular type of authority. The evidence generated through the YouTube videos we analysed was, therefore, predicated both on the language and practices of contemporary biomedicine and personal experiences of living with MS. This was most notably actualised in personal experience diaries, through which trust and legitimacy can be particularly developed, enhancing the strength of the ‘evidence’ portrayed.
Our aim in the study was not to comment on the scientific validity of or treatment efficacy for CCSVI. Nonetheless, an obvious question prompted by our findings is why were the YouTube videos (at least at the time of our study) so positive? There are of course numerous possible answers to this. Many of the most-viewed videos were uploaded by early adopters and strong advocates of CCSVI before later, more critical studies were published. 115 Thus, simply by virtue of being online for longer these videos had higher view counts and emerged more prominently in our sample. There is, moreover, a more general bias towards reporting positive experiences with medical treatments online. 131 Additionally, a few interviewees (including some who were supportive of CCSVI and Zamboni’s work) noted that those who might have been more critical of CCSVI often chose to stay silent because they were afraid of being criticised by their fellow patients or did not want to dampen other people’s hopes. This was reinforced by CCSVI advocates who worked actively to provide positive information about CCSVI on different online spaces, including forums and Facebook pages:
We got to the point on Facebook where there were people initiating conversations about it [CCSVI] and then somebody was replying to it and somebody would reply to that reply and all members of the ‘pro’, if you like, camp, and basically it was a very sort of stage managed dialogue and it got a lot of people’s backs up because they kind of felt like they were being patronised by a special interest group.
Interviewee 1, social media manager, MS charity
This resulted in a disconnect between the very positive information about CCSVI being posted online and the far less positive response of mainstream neurologists, policy-makers and funding bodies. Consequently, many people affected by MS who were interested in CCSVI or personally had a positive experience with venoplasty became disillusioned with the critical mainstream biomedical response to it. At the same time, other patients and practitioners expressed frustration that an unproven theory received so much attention and funding, a situation they saw as a hijacking of the MS research agenda by a partisan group, with detrimental effects on patients’ well-being. 132
Although CCSVI is a specific and controversial case, the way that CCSVI activists used internet technologies to generate new forms of knowledge is not an isolated event, but indicative of a wider phenomenon in which online ‘communities of practice’ can generate new forms of knowledge, becoming, albeit non-traditional, ‘epistemic communities’. 133 For example, in addition to the use of YouTube described above, users on the TIMS forum (which was and continues to be a hub for discussions on CCSVI) created a thread to collect experiences in a more systematic manner than is typical on patient forums (this is discussed in depth in a book on CCSVI written by one of the community members);130 and a group based in the Netherlands developed a tracking website (www.ccsvi-tracking.com) to aggregate and visualise outcomes post venoplasty. This results in the collection and interlinking of PEx that might not be ‘evidence-based’ as typically understood in medicine, but for many people serves as a form of ‘experiential evidence’, which they turn to in order to help them make decisions and, to a lesser extent, advocate for policy changes and particular research agendas.
Conclusions
Patient experience is now fully established as a key part of the internet health information landscape. Even in the context of one condition, MS, there are numerous websites and sources of PEx online. What counts as PEx is, moreover, extremely diverse in terms of content, format and associated practices. It can, simultaneously, be a form of knowledge, a source of information, a set of practices, support and a means of creative expression. In this chapter, we highlighted key categories and associated practices of PEx linked to ‘everyday’ life with MS; health care and biomedicine; and emotional support and creative expression. However, rather than belonging to only one category, what makes PEx such an importance resource for people affected by serious health conditions is how it operates across these categories, combining everyday experience with knowledge of health care and medicine, and emotional support.
Although individual preferences and practices clearly play a key role in what and how PEx is shared, here we focused on the less discussed topic of how the infrastructure, technologies, design and management of online platforms and forums shape the construction and exchange of PEx online. We found that a relatively small group of influential people play a crucial role in shaping online spaces for sharing PEx in MS, and highlighted the importance of the work, both technical and emotional, that goes into their creation. As the internet is becoming increasingly integrated into health care and more services move online, more research is needed on how often subtle design and management decisions shape these online spaces and the nature of the services and care provided through them.
One of the key concerns expressed about the sharing of PEx online is that it can spread misinformation that is detrimental to people’s health and well-being. Health-care practitioners cannot, however, stop people from sharing their experiences or seeking out others’ experiences on the internet, even if these experiences contravene the advice of medical practitioners. Regardless of how CCSVI is perceived – either as a revolutionary theory about neurodegenerative diseases or as dangerous pseudo-science – it is an excellent illustration of the relevance of social media and PEx for the health and well-being of individual patients as well as the field of medicine more generally. In many cases, interested patients will seek out information about new and controversial treatments regardless of what they are told in clinical consultations. Thus, instead of dismissing information they do not consider ‘evidence-based’, health-care practitioners need to enhance their understanding of the forms of evidence considered significant to patients, even if they themselves would not consider it valid. By gaining a better understanding of the experiences and priorities of different patients presented in social media, health-care practitioners may be better able to focus on issues of importance to patients and avoid the polarisation that has taken place in the case of CCSVI. It is essential for practitioners to be aware of what is circulated online and, although they do not need to endorse it, dismissing it can have serious consequences for their relationship with the patient (in fact, many interviewees said that they wished their doctor and/or nurse had provided them with more links to online information). This emerged clearly from the research on CCSVI, but was also reiterated in interviews. Participants strongly expressed the need for appropriate ‘frameworks’ or systems that enable people to share their experiences in ‘helpful’ ways. One of the key ways interviewees felt this could be done was through access to a wide range of different experiences that would reflect the different perspectives and experiences of people with this variable condition.
Chapter 6 Work package 2b: understanding the important factors for user engagement with online personal experiences
Abstract
Introduction: both the source and the nature of e-health content have changed rapidly over the past few years, such that other people themselves now provide a significant source of health material online. This chapter explores the important factors for user engagement with online PEx.
Methods: in the first half of the chapter we describe a series of qualitative user studies in which we capture information from three groups of people (n = 36: people with asthma, carers for people with MS and smokers wishing to quit) about the various new types of peer-led information, support and advice online and the processes by which these individuals might select from the vast range of online stories available. In the second half of the chapter, we employ an experimental methodology with smokers wishing to quit (n = 113) to identify those source and message elements of personal stories that are most able to influence health intentions and behaviour.
Findings: the analysis of the qualitative user studies has led to a new research framework that captures not only the different kinds of personal experience available online, but also the decision process by which people chose one source of information over another. The experimental study found some limited effects regarding preference matching and personal experience-based health messages.
Conclusions: the qualitative and quantitative investigations have allowed us to tease out issues of individual preference and trust and have given us a better grasp of the way in which different design elements may influence user engagement and ultimately affect health outcomes.
Background
There is increasing evidence that the sharing of PEx forms an important part of health-related internet use. 4,134 Data from the 2013 Pew Internet Survey, which asked adults about their online health experience over the past year, showed that one in four adults (24%) had turned to others with the same health condition online, one in four internet users (26%) had recently read or watched someone else’s health experience and 16% of internet users had gone online to find others who might share the same health concerns. Furthermore, of the 8% of internet users who had posted a health-related question online, 40% said that they had shared stories about their own experiences. 135
The online sharing of experience is particularly prevalent in people who have health conditions that are serious, sensitive in nature or involve making a decision. Examples explored in the research literature include HIV/AIDS (acquired immunodeficiency syndrome),134 antenatal diagnostic testing,15 and infertility. 31 Carers also use the internet to find and proffer information, share experiences and opinions, and provide encouragement and support across a range of groups, including those with cancer136,137 and Alzheimer’s disease138 and parents caring for children with special health-care needs. 139 The internet is also becoming a popular mechanism for supporting behavioural and lifestyle changes, for example weight loss and smoking cessation, through the use of tailored interventions, reminders and online support groups. 140,141
Why have personal experiences become so prevalent online? The most obvious answer is that they fulfil some critical role and recent studies have highlighted different elements of this role. For example, people welcome opportunities for social comparison in helping them understand how well they are coping with a particular illness. 78 They can also draw on others’ accounts of their experiences of disease in order to become more optimistic about their own condition142 or to adjust to the reality of the disease in order to prepare them for what is to come. In either case, others’ experiences can seem to leave them feeling less isolated in their ‘patient journey’. 4 PEx can also be used to inform health decisions. 15,16
The story is not unequivocally positive, as the ability to harvest health experiences with no online ‘quality control’ can cause problems. Individuals may struggle with experiences that contain very strong emotional content, or be left feeling that their condition will isolate them from other healthy individuals when accounts suggest that only those who have personally dealt with the condition could know what it feels like. 31 The findings from some studies suggest that online groups can even exacerbate a process in which an illness comes to define the individual. 55,78
Furthermore, when an individual uses online experiences to aid decision-making, he or she is engaged in a sampling or selection process, given the diverse experiences available online. This, in turn, raises the important question of what drives the sampling process. From a theoretical standpoint we already know something about how people come to select one health website over another: it is a staged process that involves both a heuristic decision that is influenced by web design factors, and an analytic decision that involves a careful exploration of the content of the online material. 8,143,144 This mirrors a number of two-stage process models in the persuasion literature (e.g. Chaiken145) in which people use cognitively intense analytical processing when the task is an important or particularly engaging one, but use affect or other simple heuristics to guide their decisions when they lack the motivation or capacity to think properly about the issues involved.
We also know that the presence of personal stories or of personalised content will influence this decision; people are drawn to material offered by and written for ‘people like me’,8,45,146,147 with some suggestion that PEx may be more effective in reducing defensive responding to threatening health messages. However, although we know that the inclusion of personally authored material can affect patient decision-making, this has typically been demonstrated in experimental settings and we do not yet know how individuals sift through these personalised stories in order to determine the sample of experiences that they will use to influence subsequent decisions. Understanding the processes that drive engagement with online PEx is important, given their likely impact on patient decision-making and subsequent health outcomes. 148
A recent review of the potential health-related effects of access to online personal experiences4 (see Chapter 2) has placed health-based personal accounts centre stage, and means that we are now in a position to examine online personal experiences from users’ perspective in more detail, with a view to understanding the process by which people come to engage, or not, with a particular individual experience. Although we already have models detailing how users engage with and trust online health information over time,8,95 we as yet have no similar framework for understanding engagement with online personal experiences. Currently, understanding of how those motivated to find information and advice (relating to their own or a close other’s health condition) navigate through the vast array of personal experiences online is still not well developed. We can assume from the literature that factors such as credibility or trustworthiness and relevance will play a role in the use of PEx149 but it remains unclear as to the relative importance of these and other factors and the way in which they interact with different stages of the engagement process. What kinds of sites do people visit, which sites do they choose to explore further, and with what purpose in mind? These are important questions for health information providers, web designers and the voluntary sector.
A framework for user engagement with online patient experience
Our introduction has documented the growth in shared personal experience online and the associated rise in peer-to-peer health care. Increasingly, we recognise that people turn to their peers for information, advice and support, but it is not clear how they make the decision to accept or reject the peer advice they find online. What are the factors that underpin user engagement in this arena? In a series of qualitative studies, we set out to explore individuals’ preferences for particular forms of PEx and to gain a sense of how people from different health groups may seek peer support.
Qualitative studies
Consistent with the focus of the wider iPEx programme, our participants were drawn from three different health populations: smokers wanting to quit, people with asthma and carers of people with MS. Participants were recruited using a number of sources, including newsletters and flyers and through various health support groups, and were compensated £20 for their participation. In total, we recruited 36 participants (20 male) aged between 20 and 65 years, with a mean age of 38.7 years. All were experienced internet users (9.92 average number of years using the internet). Sixteen of the participants took part in the follow-up interviews.
Breaking these down into health groups, we recruited:
-
10 smokers (nine male and one female) aged between 20 and 47 years, with a mean age of 29.5 years, who had been smoking an average of 12 years
-
15 people with mild to severe asthma (seven male and eight female) aged between 22 and 60 years, with a mean age of 34.07 years and an average length of asthma diagnosis of 20.58 years
-
11 MS carers (four male and seven female) aged between 39 and 65 years, with a mean age of 53 years, comprising 10 spouses and one mother of someone with MS. They had been carers for an average of 13.61 years.
The participants visited a laboratory styled as an internet café at Northumbria University. They were asked to search a subset of the health materials available on the internet for approximately 1 hour, seeking information and advice on issues relevant to their personal circumstances (smoking, asthma or MS caring). They were then asked to take part in a group discussion led by a facilitator and to complete log books detailing their impressions of the sites they visited. These sites were also automatically logged by the computer. Each participant was given access to seven predetermined sites during the search phase. Every site contained user-relevant material, but only four of the seven sites contained personal experiences. This selection was informed by content analyses of available e-health material reported in an earlier study. 150 Sites were chosen to be representative of those generally available to users, with the proviso that those requiring registration before access were excluded.
Following the initial search, when first impressions were recorded, participants were asked to choose two sites to explore in more detail. They then shared their experiences in group discussions that addressed the following main areas: (1) site selection and rejection; (2) site likes and dislikes; (3) aspects of personal experience; and (4) trusted elements. Participants were then directed to personal experiences sections on two further sites and took part in a final discussion around the content of these last two sites which addressed: (1) recall of experiential material; (2) level of interest and usefulness of personal experiences; (3) variety and type of experiences (i.e. individual accounts such as blogs or testimonials vs. interactive forum-style content containing multiple experiences); and (4) trust and behaviour.
Two weeks later, participants were contacted for a 1-hour semistructured telephone interview. The discussion covered the following main areas: (1) information searching behaviours since phase 1; (2) recall of the websites and their content; (3) information sharing activities; and (4) decision-making and current behavioural intentions.
We also conducted a follow-up qualitative study with two of our groups (people with asthma and MS carers). For this second study, we recruited 14 additional participants to the asthma group (five male and nine female) aged between 19 and 64 years, with a mean age of 28.21 years, and we recruited nine additional MS carers (three male and six female) with an age range of 40–73 years and a mean age of 58.9 years. These additional participants followed the same protocol as in the first study, but all were then asked to take part in a more extensive, structured interview that also involved the use of the repertory grid technique151 as a means of eliciting uniquely personal constructs about the ways in which they viewed the sites they found. This work has been published. 152
All focus group discussions and interviews were audio recorded and transcribed for analysis. The transcripts were read and reread separately by two of the research team and then were subject to thematic methods153 to identify both anticipated themes, for example design and reputation factors, and emergent issues such as comparison processes. The themes were then subject to discussion with the rest of the team to ensure validity in the interpretation and representation of data. For ethical reasons all participants were given a participant number and all quotations used in the results have been stripped of any information that could potentially identify the participant.
Resulting framework
The analysis revealed a three-phase process by which users engage with online personal experiences. Phase 1 is a ‘gating’ process, whereby people determine the suitability of the material they encounter; phase 2 comprises an ‘engagement loop’, whereby people look for support or advice from others with similar or relevant experience; and phase 3 is an ‘evaluation and outcomes’ process, whereby individuals make a judgement about the costs and benefits of engaging with the site in the longer term and in some cases experience outcomes related to that engagement. This three-phase process is captured in the framework (Figure 4), with the three phases described in more detail below.
FIGURE 4.
Schematic representation of the online health user experience (PEx) engagement framework. The stages are shown on the left-hand side of the framework (i.e. gating, engagement loop, and then evaluation and outcomes) and the dominating factors influencing engagement at each respective stage are shown on the right-hand side. Each box displays the questions and factors that users address during each stage of the engagement process. Reproduced with permission from Sillence E, Hardy C, Harris P, Briggs P. Modelling Patient Engagement in Peer-to-Peer Healthcare. 23rd International World Wide Web Conference, Korea, April 2014. 154

Phase 1: gating
Participants reported making a swift initial judgment about whether they should engage further with the site or move swiftly on to an alternative. We know from other studies that this ‘gating’ decision relies heavily on the look and feel of the site, as users are known to make snap decisions on the basis of site design elements. 8,155 We found similar evidence that the first impression was influenced by the design elements of a site, but also that people looked for assurance that the site was hosted by a credible and impartial agency with a known reputation.
It was very easy to access what you wanted [. . .] it was easy to navigate round the website whereas some of the other ones you got lost and it threw you into perhaps something else you didn’t want to get into or wasn’t really appropriate.
MS, participant 9
So yeah, I probably like the NHS and the Asthma UK site. They were both obviously well established and really really well liked from it seemed so I’d say that they’re easy to trust . . . And the British Lung Foundation as well ‘cos they’re a charity.
Asthma, participant 5
Phase 2: engagement loop
Having made their initial selections, participants began to examine the content of the websites and the personal experiences in more detail. For participants in all three health groups, engaging with the experiences involved an iterative process during which they discovered who was making the contribution, assessed what was being said, and then compared the online stories with their own experiences – in part to see how credible the material was – while also assessing the extent to which these experiences were shared directly between participants (in which case they could add their own) or were scripted as part of a more controlled environment. These four processes – who, what, compare and share – were critical to meaningful engagement with personal experiences and are discussed in more detail below with evidence from participant transcripts.
Who?
Personal experiences reveal something about the person posting the experience, and our participants were keen to understand who that person was. They were quick to reject experiences that came from an individual who seemed different from them, either because that person came from a different age group, region or demographic, or because their health profile or severity of condition was a poor match. Sometimes these judgements were made on the basis of quite superficial information (such as the photograph of the story-teller), whereas on other occasions the judgements reflected a more nuanced interpretation of the underlying ‘voice’ in the story. Differences in age and severity of condition were the main reasons for rejecting an account of an experience altogether:
The first one, the three stories, they were older people. I think they were a little bit extreme. I don’t think they’re typical of an everyday asthma sufferer . . . So I don’t see the relevance of those particular ones. I think it would probably be more useful to have younger people’s experiences, what triggers them more, how people have reacted if they needed help that kind of thing.
Asthma, participant 15 (aged 46 years). Reproduced with permission from Sillence E, Hardy C, Briggs P, Harris PR. How do people with asthma use Internet sites containing patient experiences? Patient Educ Couns 2013;93:439–43156
So I don’t know if it’s helpful because I can’t really relate to it. I couldn’t really relate to those people. I can’t say how. Definitely not Maria from Michigan [laughs].
Smoking, participant 7
What?
Participants appeared have very different needs when searching the online PEx. Some were seeking out basic information, while others looked for advice on how to proceed, make changes or decisions, and some simply acknowledged the social and emotional support on offer. Participants rejected information offered by their peers if it did not resonate with their own understanding of a condition, or if the mixture of information, advice and support on offer was unbalanced or a poor match with their needs. However, even those who felt that they were quite knowledgeable about their condition were generally interested in the different kinds of individual journey that others had experienced:
I feel quite confident in what I actually know about it in terms of just the base level of information but I found I learned a lot more from actually listening to, and reading about the other peoples’ experiences, and how they handle different situations in comparison to how I do and also just the different range of treatments.
Asthma, participant 6
Compare
Some participants saw clear and direct comparisons between their situation and the online experiences:
The first one about 47-aged smoking for 30 years. But she got this, she got stroke, and I was thinking, when I read it I thought, well it’s me. I couldn’t sleep because my chest is hurting, it could be me! That kind of that experience and you can share it, and when I read that experience I thought yes, 30 years of smoking, she is younger than me, one year younger than me, and she got stroke, it could be me.
Smoking, participant 9
Other people, who differed in the extent to which they were coping with their varying circumstances, said that they found it difficult to read stories that might be overly optimistic or pessimistic and that challenged their own worldview. The MS carers were particularly vulnerable here, as they found that reading about other people’s experiences could highlight imagined futures that they simply did not want to consider.
Share
For some participants, the presence of a forum or some means whereby people could share information directly was important, as it provided the opportunity to interact directly with others who shared similar health conditions and histories. The presence of a forum could also lend the site greater credibility, as the stories were more variable and less like artificial or scripted individual testimonials:
The forums are better than the real life stories because we can interact with other people and share their experiences with us and we can gain some knowledge.
Asthma, participant 6
However, some participants, while recognising the potential benefits of sharing, simply felt that it was not something they were likely to engage in:
Forums are . . . definitely people would find it useful, but personally I wouldn’t because I won’t tend to go on post about my stuff, I’m not a sharing kind of person in that way.
Smoking, participant 10
Phase 3: evaluation and outcomes
Participants expected – and in some cases had already experienced – a range of outcomes resulting from their interactions with online experiences. The advantages and disadvantages described by our participants mapped well onto the domains described in the recent literature. For example, Ziebland and Wyke4 have argued that access to patients’ stories is associated with seven domains of engagement: (1) finding information; (2) feeling supported; (3) maintaining relationships with others; (4) experiencing health services; (5) learning to tell the story; (6) visualising disease; and (7) affecting behaviour. We found evidence to support each of these here (Table 12). The personal experiences provided participants with the opportunity to learn more about their condition, to acquire knowledge about the practicalities of managing their condition, dealing with the NHS and other services, to understand more about what they might expect, to motivate themselves through positive stories or to remind themselves about the seriousness of their condition or outlook, and to develop supportive relationships with others.
| Domain | Description | Example |
|---|---|---|
| Finding information | The majority of smokers felt that they were familiar with the facts about smoking and health and so did not rate the information content particularly highly. However, several appreciated the sharing of practical tips and new ideas to help them quit. For people with asthma, the issues were often about acquiring hints and tips on management | It just helps you, if someone telling you about the mistakes they have made and help you avoid it. That’s the ideal for what forum is for really. That’s why people are using because they are so usefulSmoking, participant 2I have learned something from looking at those sites that I didn’t knowAsthma, participant 5 |
| Feeling supported | Smokers in particular also recognised the supportive or motivational function of personal experiences For some smokers, simply knowing that other people (like them) fail but persist until they succeed was felt to be valuable For those MS carers with a recently diagnosed partner, son or daughter, the experiences satisfied a strong desire for basic information about the condition and allowed them to test out possible symptoms with other MS experiences in a more meaningful manner Even those people who managed their asthma well recognised the possibility that online support could be important to others Some MS carers also recognised that their future selves may benefit from online support |
I don’t feel alone on the forum because there are different people who try to quit smoking. And it’s kind of encouragingSmoking, participant 3There’s a certain personality to it [the inclusion of PEx] one you sort of connect to even at a very superficial level of reading. It still gives you kind of sort of hope and motivation that if other people can do it so can ISmoking, participant 10[The forums] are useful for both carers and sufferers . . . if they get something that they haven’t experienced before they can find out whether it’s a symptom or not a symptom of the conditionMS, participant 1Yeah I think it’s good, good support, especially for people that sort of whose asthma’s quite bad and can’t get out as much as they’d like to and interact with people. It’s good for communicating and letting off steamAsthma, participant 6You know, it’s not changed everything about the way we live. But as things progress then yeah I might well find myself doing that kind of thing [using forums]MS, participant 2 |
| Maintaining relationships with others | For most of our participants, the significant longer-term potential of the internet was in developing new supportive relationships | It felt like people knew each other and they were saying so and so are you OK, I hear you’ve been in hospital and you can see that there would be that real peer support network, which for me, I suppose is the benefit of doing this kind of thing online. That could never happen just normally without the internetAsthma, participant 7 |
| Experiencing health services | For people with asthma the online experiences sometimes provided pointers as to how other people had interacted with their doctors and this in turn led to our participants drawing up plans for their own use of health services | It gave me a few places to look at myself when I get back home and some things my doctor or nurse next time might be able to review what’s happening, maybe sort of help meAsthma, participant 6 |
| Learning to tell the story | For some people with asthma the online personal experiences allowed them to make sense of aspects of their treatment that they had not previously considered. They were able to talk more knowledgably with others about their condition. Others described how they had begun to discuss their asthma with family and friends | Several participants had discussed the online personal experiences with their close friends and family. These discussions had helped the participants to construct a narrative around asthma that highlighted the seriousness of the condition, as well as allowing them to pass on practical guidance as to what to do in the case of emergency |
| Visualising disease | For people with asthma the issues were often about visualising the potential seriousness of their condition For those people or for carers with less recent MS diagnoses, the perceived benefit of reading such experiences was less clear. Other people’s experiences were sometimes regarded as too gloomy and few carers wished to be reminded of what was coming |
It was interesting to read the discussions and some of the stories of people who’ve been in hospital for a lengthy amount of time and how they deal with things and really how bad it can getAsthma, participant 5I got so far and then I started to feel really sickly because it was talking about the future and I really don’t want to think about things in that way. I tried, I thought I’ll have a go, but I just couldn’t, I didn’t enjoy it, it’s not what I want to doMS, participant 7 |
| Affecting behaviour | There were some signs across the groups that the experiences had initiated behaviour change | At the 2-week follow-up, one of the MS carers, triggered by the experiences online, had begun applying for power of attorney (the authority to represent or act on another’s behalf in legal matters), and another had started asking for more help and support from other family members and requested a social worker |
Using the framework to improve the design of online patient experience
Overall, the engagement framework supports findings from earlier research, reflecting the importance of good design, visual appeal, credibility, reputation and trust in phase 1144,155 and the recognition of a range of outcomes from engagement with people’s stories in phase 3. 4 We have made the greatest contribution in developing the engagement loop in phase 2, where we have clarified the kinds of questions different people may ask of the PEx they encounter. This can be a useful framework, then, for comparing the needs of different health groups against the seven domains identified in WP1,4 as we imagine, for example, that some groups may be more concerned with seeking information, whereas others may seek greater levels of support or an improvement in their use of health services. Some of these needs are illustrated by the three cases studies below, which present a narrative account of the ways in which health users engaged with online PEx.
Case study 1: re-engaging with your asthma
Asthma patients were initially drawn to websites showing good design quality. In line with previous studies,8,155 we noted that participants preferred sites that were easy to navigate and looked professional. Participants were then subsequently drawn to those sites containing PEx, but only if the contributions seemed to come from individuals judged to be similar to themselves (e.g. in terms of age and length of time since diagnosis) and could offer ‘relevant’ stories. Before the study, participants were unsure what else they could or should know about asthma but, as they started to engage with the online personal experiences, many chose to explore certain stories in more detail by comparing their own experiences with those of others online. This comparison process allowed for recognition of their experiential asthma knowledge,157 with participants able to reflect on the ways in which they had experienced and handled certain situations with regard to their asthma. Despite many participants reporting a high level of asthma knowledge before the study, many were still able to acquire hints and tips from others regarding the management of their condition. For others it was a case of confirming or even fine-tuning their existing knowledge. However, one consequence of this comparison process was that participants sometimes dismissed potentially useful hints and tips for managing their asthma on the grounds that the online experience was written by someone different from them. Most participants thought that the online contributions came from people who were worse off or had more severe asthma than they did. This process of downward social comparison has been noted in other health settings in which people under threat evaluate themselves favourably in comparison with others. 158 A consequence of this process is that, for some, the personal experiences served as a reminder of the potentially serious nature of the condition and triggered some re-engagement with the self-management programme through the asthma nurse.
Case study 2: multiple sclerosis carers and coping in the here and now
Shared PEx online can be used to support both the problem-focused and the emotion-focused coping strategies of the MS carers. Problem-based coping was seen as the norm when caring for people in the early stages of MS, as carers needed to understand both the symptoms and behaviours they might expect of someone with MS, and may also need practical support to establish daily care routines or understand entitlements. This is consistent with other findings showing that coping strategies for MS carers are often focused on the current situation, the ‘here and now’ of coping. Carers felt that problem-coping strategies would give way to emotion-focused strategies as they became reconciled to the progression of the disease in the person with MS, accepting that knowing more about MS would not change anything. Consistent with this shift to emotional-coping, carers valued personal stories that fuelled empathy and a greater understanding of what the person with MS was experiencing. Participants recognised that, ultimately, individuals would have different needs and that each would come to employ their own distinctive coping strategies, better served by separate online resources. A sense that carers should be able to pick and choose from the stories available was strong here. Carers recognised that although they were not always likely to be receptive to some of the more difficult messages from other carers, they valued the fact that the PEx offered both practical and emotional support.
Case study 3: smokers and their mistrust of the commercial testimonial
The smokers’ engagement with PEx was characterised by strong preferences for certain kinds of experiential material. The interactive forums were seen as valuable in terms of providing support and motivation for those wishing to quit. Smokers identified with those authors who seemed well matched in terms of gender, age and location. Smokers noted unusual tips and hints for giving up smoking but, overall, preferred realistic yet positive support messages. Such messages acknowledged the difficulties associated with quitting but often included an inspirational message and a positive, successful outcome. The testimonials were viewed with more suspicion. For smokers, at least, there was a sense that this form of PEx might not always be genuine and in large part this reflected the strong commercial overtones associated with PEx around this topic area. Many of the websites featured commercial advertising and products associated with quitting. Celebrity and non-celebrity endorsements or testimonials were seen as difficult to trust and the smokers thought it highly unlikely that they would return to this kind of website. Overall, there was less evidence of longer-term engagement with the PEx for the smokers. The participants commented on the difficulty of navigating to useful sections of the forums or finding relevant experiences in the dense message threads.
Implications of the framework for further studies
Our framework highlights both the source and the message of PEx (the ‘who’ and ‘what’ of PEx) as critical factors in user engagement. We believe that people are quick to make judgements about the person offering information and advice, judgements that reflect the extent to which they are seen to be ‘like me’ but also judgements that take into account their motivation in shared storytelling that in turn raise issues around trust. Individuals are also concerned about the extent to which the content of a health message fits with their own experience and pre-existing beliefs and reflects their particular journey. For example, the MS carers we observed in the framework studies above tended to exhibit information-based coping strategies if they were caring for someone in the early stages of MS, but more emotion-based strategies when caring for someone in the later stages of MS, and their responses to available PEx varied accordingly. 159 In the two studies that follow, we explore these source and message issues in more detail by exploring smoking cessation.
Do smokers trust the source of the patient experience message?
People who listen and respond to others’ stories must consider whether or not the account is trustworthy. Trust is a key construct here, as online PEx is often unregulated. Our own large-scale surveys of trust in online health information have revealed a paradox, in that people like PEx and are drawn to sites containing PEx, but are then less likely to trust the information and advice they find there. 160 A subsequent analysis suggested that this paradox may be related to the extent to which the contributor is seen as impartial. Not all PEx is benign. Much of it is explicitly intended to persuade, and the prevalence of advertising as a funding model for online support communities and health information sites only complicates this issue further.
We know, from a range of previous studies,8,144 that the presence of advertising on a site can give a negative first impression that can lead to disengagement or to mistrust of the messages on that site. In a recent study, for example,124 the presence of advertising on a website showing the link between drinking alcohol and breast cancer had no immediate effect on alcohol drinkers’ overall attitude to the site, but did subsequently affect health behaviours: those who drank heavily reported no reduction in drinking after viewing a ‘commercial’ site but a significant reduction in drinking following exposure to a non-commercial site that presented them with the same health message with the advertising removed. To better understand these issues, we explored one health domain (smoking cessation) in greater depth, inviting participants to search for relevant material and then discuss their ability to trust the different contributors they found online.
Method
We used a similar paradigm to that reported earlier in this chapter (A framework for user engagement with online patient experience, Qualitative studies), asking 15 smokers to search for health-related smoking material online and then discuss their findings. Participants were recruited using a number of sources including council newsletters, leaflets and flyers. The smokers (seven male and eight female, with a mean age of 23 years) were all experienced internet users. They had been smoking on average for 7 years and smoked an average of 11 cigarettes per day.
Each participant was allocated to one of four focus groups and asked to attend a 2-hour session held in an internet café-styled laboratory in Newcastle upon Tyne, UK. During the first hour of the session, participants were invited to search the internet freely, looking for information and advice on smoking and health. We logged the sites they visited, but also asked them to record their perceptions of each site in a log book and to use this information during a subsequent group discussion with a facilitator. These group discussions covered four main themes: (1) selection and rejection factors, (2) liked and disliked websites, (3) PEx/account features and (4) trust and behaviour. Thematic analysis and coding practice followed that of the earlier qualitative studies. Coders were primed to highlight comments in relation to trust or mistrust and like or dislike of sites, and were also interested in the presence or absence of a ‘commercial voice’.
Results and discussion
Participants visited 8.5 websites on average. The most commonly viewed sites (in order of number of participants who visited the site) were the UK NHS Smokefree website (www.nhs.uk/smokefree), Netdoctor (www.netdoctor.co.uk), Wikipedia [www.en.wikipedia.org/wiki/Smoking_cessation (accessed 1 July 2011)] and the British Broadcasting Corporation’s smoking website [www.bbc.co.uk/health/physical_health/conditions/smoking_health_effects.shtml (accessed 1 July 2011)]. The consistency in sites viewed suggested that participants may have employed similar strategies and/or been influenced by similar factors when deciding which sites to examine. From the discussions, data logs and log books, all participants attempted to locate relevant websites using Google, although some participants also employed a more targeted search via the NHS.
As anticipated from our earlier work, we found that people said that they very much liked having access to other people’s experiences online and found the material engaging.
Well the patient UK one did have experiences of people who’ve smoked and who’ve quit and health issues that they’ve had whilst smoking and once giving up and things like that and that was quite good I think – reading about other people’s experiences.
Focus group 1, participant 3
We also found support for the claims that such experiences can help make the health issues seem more real and engaging as people felt that they could relate more to other people who are in similar situations.
[It’s more helpful] If they’re more realistic if they’re not just literally a doctor’s sat and written it like ‘Mrs C has done this’. If it’s an actual person saying ‘look it’s really hard. I’ve shouted a lot. I’ve done this, I’ve done that,’ then you can relate to them.
Focus group 1, participant 2
However, the presence of advertising was almost universally raised as something that was disliked about some of the sites.
There’s lots of adverts as well which annoyed me. It’s like they get some form of gain out of telling people to quit. There’s adverts and even some adverts weren’t even related to smoking.
Focus group 1, participant 2
As predicted, we found considerable evidence that users were suspicious about site content and that advertising had an important role to play in this. Sites that appeared to be selling a product or that were otherwise viewed as commercial created very negative first impressions in the sample, and participants often felt that information contained on such a site would not be impartial or trustworthy.
More tellingly, participants became particularly suspicious if it seemed that the PEx had been used cynically to advertise a particular product or manipulate beliefs.
There is one particular one that got like a few . . . a review of stories of how people are doing with the product, but I think those websites try to sell their products rather than they are really trying to be help.
Focus group 3, participant 10
Participants also seemed very aware of the potential for PEx to be manipulated and were concerned about the extent to which the experiences might be honest, questioning if they might have been scripted rather than represent an actual experience:
That kind of story from an actual person or something would have way more impact than some typed words on the internet that could have been put there by anyone. You don’t know who typed the website.
Focus group 1, participant 7
These discussion points are revealing as they show that people are drawn to PEx material, but can also mistrust PEx when it appears to be used for commercial gain. Indeed, users may come to question the genuineness of PEx that sits in an overly commercial context (at least in a context such as the UK, where health care is provided free at the point of delivery). In our subsequent study with smokers, we explore the extent to which matching the source and recipient characteristics of PEx can influence smokers’ perceptions of the acceptability of the advice presented to them and also directly influence health outcomes in terms of reducing the number of cigarettes smoked.
Source and message elements of patient experience that can impact on smoking cessation
Campaigns to promote healthier lifestyles face many obstacles including message resistance: a refusal to see that the message is relevant by those individuals for whom it is most relevant. 161,162 For example, overweight individuals might ignore or denigrate a campaign designed to promote dietary improvement, or smokers, targeted by a quit campaign, may be less likely to accept its key messages. Intriguingly, there is evidence that presenting information as PEx may reduce such resistance and facilitate message uptake. 45,147 If so, this would clearly be a major practical advantage of presenting information using PEx but, as yet, relatively few studies have addressed this. In this final study, we tested whether or not PEx would reduce the tendency of a targeted audience (smokers) to resist a quit message and thereby promote greater message acceptance.
We asked smokers to view pro-quitting information online, with the material presented to them either as PEx (the PEx condition) or as a simple information factsheet. All of the information was based on current evidence and suggested that attempting to quit smoking using support and aids is more likely to be successful than attempting to quit unsupported. 163 We wanted to know if information presented as PEx would be more likely to reduce message resistance and promote message acceptance.
From our earlier studies and framework (see Figure 4) we knew that participants exhibit ‘homophily’, that is, they seem drawn to experiences from similar others. We assessed this in two ways. First, we manipulated the perceived gender of the PEx ‘voice’, with the prediction that people would be more accepting of PEx from same-sex others. Consequently, we randomly allocated half of those in the PEx condition to read PEx ostensibly written by a woman, and half to read PEx ostensibly written by a man. Second, we assessed the effects of the palatability of the material in terms of participants’ pre-existing beliefs (attitudes towards quitting by using or not using aids and support). To do this, we established participants’ preferences for mode of quitting (supported vs. unsupported) and their previous quit experiences and practices, and we used this information to classify them as having received information that either matched their preferences (the information advocated quitting by using aids and support) or did not match their preferences. The study thus contained an experimental manipulation involving gender matching (random allocation to no PEx, male PEx or female PEx conditions) and a separate, measurement component, involving preference matching (the classification post hoc of participants as having read preference-consistent or preference-inconsistent information, irrespective of the gender of the ostensible PEx author). The data involving these two separate elements were analysed separately.
We were primarily interested in the results of these variables on message acceptance, which we assessed with a wide range of indicators that included participant mood, message believability and responses to the website, as measured by the eHIQ (described in Chapter 4). We also measured message knowledge and intentions to change at time 1 (i.e. immediately following exposure to the website) and reported quit attempts and nicotine dependency in two follow-up phases, conducted 14 days and 3 months later.
Method
We recruited smokers to an online study using poster advertising, e-mail and word of mouth. A total of 113 participants (mean age 24.7 years, n = 63, 55.7% female) completed all three phases of the study. Most (n = 74; 65.5%) were students.
Measures
In a participant’s first visit to the website, we measured basic demographics, as well as smoking behaviour, internet use, preferences for and experiences of quitting (supported vs. unsupported), nicotine dependency and motivation to quit. 164 The primary outcome measures addressed message acceptance as indicated by measures of mood,165 message believability, message derogation and personal relevance, and evaluation of the website, assessed using the 26 items from the eHIQ part 2. 66 We also employed a range of secondary outcome measures that included message knowledge, nicotine dependency, intentions to cut down and intentions to quit. After 14 days and again after 3 months, participants received an e-mail inviting them to log on to the website and complete a brief follow-up that included the measures of reported quit attempts and nicotine dependency.
Materials
The health message was presented as a single web page and contained evidence about quitting smoking taken from an authoritative source. 163 Two different but similarly sized versions of the web page were created, both containing exactly the same design features and layout but varying in terms of the way in which the information was presented. In the factsheet condition, the quitting smoking facts were presented as a bullet point list of statements. In the PEx conditions, the same facts were presented as a personal story of quitting.
Procedure
Testing was done online. Participants logged in using a unique identification code and were randomly assigned to one of the experimental conditions. They worked their way through the pre-manipulation questions before being shown the condition-relevant webpage. They then completed the outcome measures. After completing the session, participants were asked to provide an e-mail address so that follow-up surveys could be sent to them automatically at 14 days and 3 months after the initial session. The initial session lasted approximately 20 minutes and each follow-up lasted approximately 5 minutes. Those who completed all three parts were compensated £20 for their time. Ethics approval was granted for the study by Northumbria University’s Psychology Department Ethics Committee.
Results
For the gender-match analyses, participants were matched on the basis of the correspondence between their gender and that of the ostensible author of the PEx. For the preference-match analyses, participants were matched on the basis of the correspondence between the information and their preferences for quitting supported (match) or unsupported (no match). Alpha was set at p ≤ 0.05 for all analyses.
Baseline measures
The sample comprised regular internet users who smoked, on average, eight cigarettes per day. Men (mean 9.58, SD 7.59) reported smoking significantly more than women (mean 7.00, SD 6.27, ηp2 = 0.59). The men (mean 1.92, SD 1.71) also had significantly higher nicotine dependency scores than the women (mean 1.21, SD 1.56, ηp2 = 0.48). Motivation to quit was high; participants reported moderate to high urges to smoke and 75 people said that they had made a quit attempt in the previous 2 weeks.
Time 1 results
The time 1 gender-match effects were analysed using one-way between-subjects ANOVA with three levels (no PEx, gender-matched PEx or gender-unmatched PEx) followed by Helmert contrasts. Contrast 1 tests the question ‘Does PEx make a difference?’. Contrast 2 tests the question ‘Are there differences between the types of PEx?’. Analyses were conducted separately within gender. Men who viewed PEx found it more believable than no PEx information (mean 5.4 vs. 4.4, ηp2 = 0.14) and were also in a better mood after viewing (mean 5.4 vs. 3.9, ηp2 = 0.25). It made little difference whether the PEx was gender matched or unmatched. No other time 1 effects were significant.
The time 1 preference-match effects were analysed using a two (information type: information only, PEx) × two (preference match: preference consistent, preference inconsistent) between-subjects ANOVA. Missing data on dependent variables resulted in the following cell sizes for most analyses: information only, n = 21 (preference consistent), n = 16 (preference inconsistent); PEx, n = 50 (preference consistent), n = 20 (preference inconsistent).
There were significant main effects of preference match on several of the dependent measures: when the message was preference-consistent, participants spent more time viewing the material (consistent mean 95.2 seconds, inconsistent mean 67.8 seconds, ηp2 = 0.06), were more motivated to quit smoking (consistent mean 4.7, inconsistent mean 4.0, ηp2 = 0.04), reported thinking more deeply about the information (consistent mean 3.7, inconsistent mean 2.7, ηp2 = 0.08), reported being more worried by it (consistent mean 4.2, inconsistent mean 3.4, ηp2 = 0.04), and worrying more about the health risks of their smoking (consistent mean 4.0, inconsistent mean 2.9, ηp2 = 0.09). In terms of responses to the site, they had higher scores on eHIQ confidence (consistent mean 30.4, inconsistent mean 26.7, ηp2 = 0.06) and eHIQ understanding (consistent mean 31.3, inconsistent mean 27.6, ηp2 = 0.06), but not on eHIQ information (consistent mean 26.9, inconsistent mean 25.9, ηp2 = 0.01).
There was only one significant main effect of information type: the PEx promoted more positive mood (mean 4.6) than did the information only (mean 4.2, ηp2 = 0.04). The key preference match × information type interaction was significant for only one dependent measure (ηp2 = 0.05): preference consistency affected intentions to cut down in the information-only condition (consistent mean 5.5, inconsistent mean 4.2) but not in the PEx condition (consistent mean 5.0, inconsistent mean 5.2).
Follow-ups
There were no effects of preference match at follow-up and so the subsequent analyses deal with only the gender-match effects. The follow-up measures taken at time 2 (14 days) and time 3 (3 months) were therefore analysed using two-way ANOVA for mixed designs with gender-match condition (no PEx, gender-matched PEx, gender-unmatched PEx) as the between-subjects independent variable and time as a three-level (times 1, 2 and 3) repeated measures independent variable.
Men reported a significant increase in quit attempts over time (ηp2 = 0.08). Both men (ηp2 = 0.20) and women (ηp2 = 0.17) showed a significant decrease in nicotine dependency over time. For both sexes there were also significant effects of condition on nicotine dependency; however, the pattern varied. Men had significantly higher nicotine dependency in the matched PEx than the unmatched PEx condition (95% CI 0.29 to 2.27; p = 0.013), but women had significantly higher dependency in the no PEx than PEx condition (95% CI 0.15 to 1.42; p = 0.017). However, these findings may reflect the lingering impact of differences observed at baseline. There were no other significant findings.
Discussion
We explored the effect of PEx in conjunction with an exploration of the effect of matching PEx to the gender of the participant. We found little effect of gender matching and only observed a PEx effect in the men. Men found PEx preferable in terms of both mood and message believability, but it mattered little whether the experience seemed to come from a man or woman. PEx did not affect message knowledge or website evaluation as measured by the eHIQ in either sex.
Over time, other effects emerged. Men showed increases in quit attempts and decreases in nicotine dependency over the 3-month period. Women also showed decreases in nicotine dependency over this period. There were also some significant effects of condition on nicotine dependency. However, these effects may reflect the lingering impact of gender differences in dependency at baseline.
We also found some initial effects (at baseline) of matching for preference in terms of the way people might choose to give up smoking (supported or unsupported). Health information expressed in a way that is preference consistent led to higher levels of engagement with online content, which supports the general health literature on the role of homophily as a component of effective health behaviour change.
Conclusion
In this chapter we have proposed a framework that captures the ways in which people engage with the experiences of others online. This framework was drawn from qualitative studies with three groups (people with asthma, MS carers and smokers wishing to quit). The framework is useful in that it helps us to understand the decision process by which users chose one source of information over another and gives us a structured means to interpret the different components of the users ‘voice’. In subsequent studies, we have explored some of the elements of this framework further with one of our participant groups: smokers seeking advice about quitting. We have seen that some of the commercial elements of website design can be counterproductive; smokers were suspicious of websites that contained advertising and other more commercial elements and were drawn, instead, to those sites that appeared to offer impartial information and advice. We have also seen that many people like to be given information in the form of PEx. Our MS carers, for example, were able to turn to PEx for both practical and emotional support in ways that echoed the seven domains of PEx engagement proposed by Ziebland and Wyke4 and presented in Chapter 2. However, we must exercise a note of caution about the health outcomes associated with PEx. We found only a limited advantage (and primarily for men) in presenting material as PEx in our final study, where men viewing PEx reported being in a better mood and finding the material more believable, and we found no real advantage in gender matching stories to individuals. These are early days for such explorations and there are a number of PEx variables that may be more critical in supporting health and well-being. We have found our engagement framework to be a useful tool in helping to identify some of the design questions we should be asking, but there is some way to go in terms of collecting a solid evidence base for the usefulness of PEx as a persuasive tool.
Chapter 7 Work package 3a: development and user testing of prototype websites based on (1) patients’ experiences and (2) ‘facts and figures’
Abstract
Introduction: the sharing of online PEx could bring health and social benefits in a number of ways. One of our interests was to explore whether or not the value of these experiences could be harnessed as an intervention and ultimately compared with ‘facts and figures’ sites as part of a feasibility trial.
Methods: narrative interviews were conducted to explore the experiences and information and support needs of people in each of the three exemplar groups (smokers, people with asthma and family or friend carers of people with MS). Using guidelines on how best to present experiential information online, three prototype multimedia web resources were developed.
Findings: three prototype multimedia experience-based web resources were developed, together with three comparator websites which presented health information in a ‘facts and figures’ format without experiential information from patients, although they did include video clips from health professionals. All sites used the same ‘look and feel’. We recruited 47 members of the public to pilot the entire participant journey, from the initial invitation to the completion of the follow-up measures.
Conclusions: the sites were successfully developed in line with the guidelines and provided new, password-protected access for the WP3 trial.
Introduction
As we have discussed, the sharing of online PEx could bring health and social benefits in a number of ways. One of our interests was in exploring whether or not the value of these experiences could be harnessed as an intervention. In the next two chapters we describe the design of a novel PEx-based internet intervention, and the subsequent randomised controlled exploratory trial undertaken to assess feasibility and measure the impact of the intervention on a range of outcome measures. As with the rest of the programme of work, we examined three exemplar groups: people with asthma, people wishing to quit smoking and people caring for someone with MS.
In this chapter we describe the conduct of three qualitative interview studies of our three exemplar conditions and describe how guidelines on how best to present health information online (see Chapter 6) were used to design three multimedia online resources based on contextualised information derived from PEx. We also describe the development of three comparator websites which contain facts and figures without experiential information from patients.
Interview methods
The exemplar health conditions were chosen to allow an exploration of different aspects of the effects of exposure to online health experiences: behaviour change, management of a chronic condition and preparedness for a caring role.
Three separate qualitative interview studies were conducted by experienced qualitative social scientists working within the Oxford HERG. Each study aimed to collect 30–50 narrative interviews with respondents from the target groups. These groups were (1) smokers or ex-smokers, describing their experiences of quitting or attempting to quit; (2) people with asthma describing in particular how they live with and manage their illness; and (3) family and friend carers of people with MS, talking about their caregiving role. Each study sought to explore the experiences, and information and support needs, of these populations. Each project was informed by a literature and field review and by the appointment of a specialist advisory panel comprising researchers, clinicians, lay persons, representatives from the voluntary sector and other stakeholders. The panel advised on all aspects of the studies, including the scope, selection of participants, sampling and content of the interviews, the analysis and the preparation of thematic summaries for the websites.
In each of these studies, interviews started with an appropriate variation on an open-ended question intended to invite a narrative response from the participant. This was followed by a guided series of questions and prompts about any issues of interest that may not have been fully discussed in the narrative. These typically included questions about signs and symptoms, treatment decisions, emotions, information and support needs, self-management, and communication with health professionals. All participants were asked if they had messages for others starting out on the same journey and if there was anything they would like health professionals to learn from their experiences.
As diverse a sample as possible was generated through national, purposive sampling so as to gather experiences which might be considered ‘typical’ as well as experiences which were more unusual. 166 Participants in each of the three conditions had had a wide variety of different experiences and were from a broad range of sociodemographic backgrounds. Participants were recruited through primary care staff, hospital consultants and specialist nurses, advisory panel members, local and national support groups, advertising online and in local newspapers and snowballing through participants’ and personal contacts. Using established qualitative research methods, analysis and data collection proceeded simultaneously and continued until ‘data saturation’ was reached to ensure that the widest practical range of experiences had been included.
The interviews, which usually took place in people’s homes or other place of their choosing, were digitally audio or video recorded (depending on the participant’s preference), transcribed, checked by the interview participant and copyrighted to the University of Oxford. The methods were approved by the Berkshire Research Ethics Committee, reference 12/SC/0495.
Specialist software (NVivo) was used to support the analysis which explored different aspects of people’s accounts and to group similar themes across all of the interviews. The method of constant comparison was used to ensure that all perspectives on the issues that are important to participants were included, not just the anticipated themes that health professionals and researchers consider important. 70 For each of the three studies, topic summaries were produced, written in lay language, accompanied by video, audio or text-only extracts from the interviews (in total approximately 250 clips per study), chosen to illustrate each topic. The titles of these topics summaries are shown in Table 13.
| Asthma intervention site | Giving up smoking intervention site | MS carers intervention site |
|---|---|---|
| What is asthma? Early signs and symptoms Childhood onset Adult onset Triggers What asthma feels like Changing symptoms over time Being diagnosed with asthma Medications treatment: inhalers Medication and treatment: other treatments Alternative and complementary therapies Managing asthma: reviews and action plans Managing asthma: adjusting medication and other self-care strategies Asthma attack and emergencies Dealing with health professionals Remembering to take medication Finding information about asthma Emotions and coping Asthma and the workplace Finances and benefits Exercise, diet, weight and other lifestyle issues Support and support groups Relationships, family and friends Advice to others Messages to health professionals |
Parents, friends and first cigarettes Smoking: memories and experiences Nicotine, dependence and cravings Cannabis, alcohol and coffee The image of smoking and smoking in secret First thinking about quitting Life events and their effect on people’s motivation to stop smoking Appearance and physical health Smoking-related diseases The role of others in the decision to quit Changing culture, public health campaigns and the smoking ban Money and smoking Help from pharmacists, GPs and nicotine replacement therapies Complementary approaches to quitting Going it alone Giving up with others and online support ‘Cutting down’, unsuccessful attempts and trying again Being a non-smoker Effects of not smoking Messages to others Unsolicited advice from health professionals, family and friends Reflecting on relapses |
What is MS? First symptoms Getting a diagnosis Reactions to diagnosis Deciding whether to tell others Looking for information Decisions about treatment Work Financial impact Family life Being a ‘carer’ Maintaining a social life Normality and optimism Love and relationships Changing symptoms over time Adaptations, aids and equipment Dealing with emotions Getting help with care needs Feelings of loss, grief and bereavement Support from family, friends and neighbours Contacts with health, social services and voluntary organisations Advocacy and activism Thoughts about the future Talking about end of life Messages to health and social care services Messages to carers, relatives and friends |
For rigour, the thematic analyses were checked by another experienced qualitative researcher from the Oxford HERG team and the summaries were checked by this person and by at least one medically qualified member of the advisory panel. Brief biographies of the study participants were included to add context to the individual clips from each interview.
We also video recorded health professionals (a professor of behavioural medicine and a GP on the smoking site; a respiratory nurse, a professor of environmental and respiratory medicine and a GP for the asthma site; and a MS nurse consultant, a MS specialist nurse and a GP for the MS carers site) talking about aspects of each health area, including an explanation of the condition or health topic, and treatments. These professional accounts were used to create multimedia ‘health professionals corners’ which included text and video excerpts from the interviews. They were included on both the intervention and comparator sites.
Design of intervention websites
Three separate websites were designed using guidelines which were developed in WP2b (see Chapter 6). As far as possible, all guideline points were incorporated into the prototype sites. Examples of how this was applied are shown in tabular form in Table 14. For example, one important point arising from the guidelines was to provide a means to help people locate the experience material most relevant to them. To address this we allowed people to search for ‘experiences by group’. These groups varied by health ‘condition’ and included, for example, age at diagnosis (asthma), time since giving up (smoking) and relationship to person with MS (MS carers). As the material was based on sampling to data saturation on themes, participants should have found a perspective akin to their own in most of the lay summaries, although this might not be reported by a person of the same age, family situation or social class as them.
| Design element | Adherence to design element |
|---|---|
| Gating | Logos used: Oxford University and the Thames Valley Primary Care Research Partnership NHS logo |
| Two ways of accessing the same information are provided: topic headings are presented down the side and across the top of the page. User can return to the home page from any point, can access material via topic or through ‘experiences by group’ (groupings as appropriate) | |
| The videos of health professionals are separate and clearly labelled | |
| No advertising | |
| Engagement: who | Experiences are grouped (e.g. for smoking cessation, by gender, age of participant at interview, relapses, time since giving up, time since diagnosis). The participants’ location was not included to protect anonymity, although it was clear that all were based in England or Wales. Brief individual biographies were included |
| Wide sample of experiences which are grouped into analytic themes. This should provide resonant PEx | |
| Engagement: what | The strapline provides an overview of each interview clip – biography gives more detail |
| Video and transcript are provided. Video clips have a time bar at the bottom; the total length of the clip is indicated | |
| The collections aimed to include the widest practicable range of experiences, which are then organised into topic summaries to reflect different perspectives on each issue. Analysis was checked by a second researcher to ensure balance and final material reviewed by an advisory panel to make sure that material presented was not misleading | |
| A maximum variation sample of interviewees was sought | |
| The research team strove for an appropriate balance when writing the topic summaries | |
| Engagement: compare | All of the experiences are grouped according to topic – to present full range of perspectives – and also by subsection of participants (e.g. age group, caring status and time since quitting smoking) |
| Points are broken down into lay summaries. Internal links at the bottom of the summaries guide reader to related issues and there is the easy option of getting back to the home page with one click | |
| Engagement: share | Ratings box included. However, ratings not displayed to avoid changing the site for subsequent participants |
| Comments box included so that people can interact with the site. However, comments not displayed to avoid changing the site for subsequent participants |
There were a few exceptions to the adherence with the guidelines as we decided to exclude features that would be incompatible with the subsequent intervention study (randomised trial). For example, the facility to leave public comments and to rate web pages are standard features of modern websites, but it was decided that these may present problems for the randomised trial design, as the presence of comments could alter the intervention for other users. To address this issue, the websites were designed to allow comments to be posted and pages rated but these were not visible to other trial participants. In other words users could submit comments and feedback to the ‘site owners’, but these would not be published. We did not include external links to other sites as we did not want to encourage trial participants to use other resources instead of their allocated website. Screenshots of the final websites are shown in Figures 5–7.
FIGURE 5.
Work package 3a: the home pages of the intervention sites.
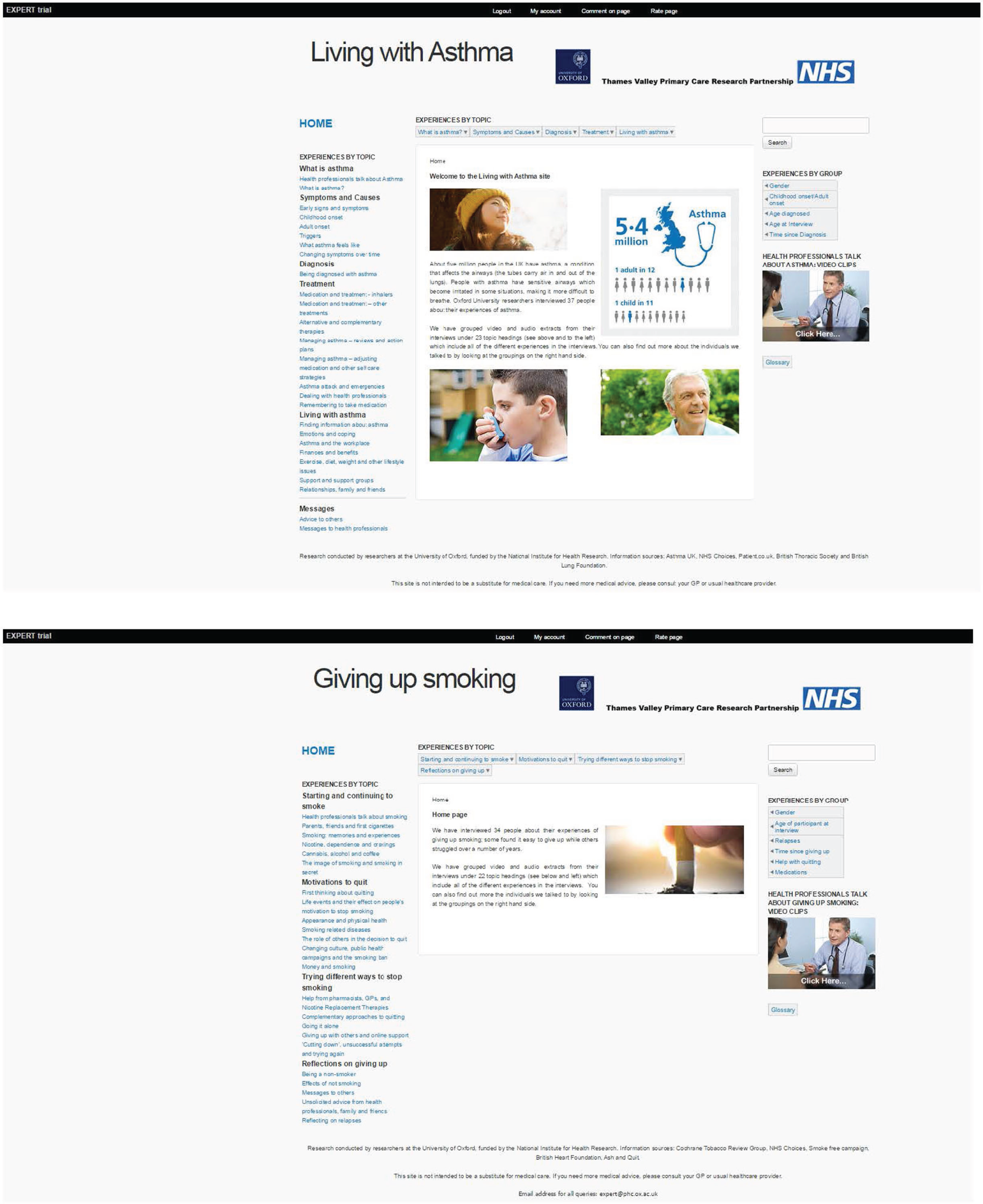
FIGURE 6.
Work package 3a: example of an illustrated lay summary from the asthma intervention.
FIGURE 7.
Work package 3a: presentation of a video clip and transcript from the asthma intervention.
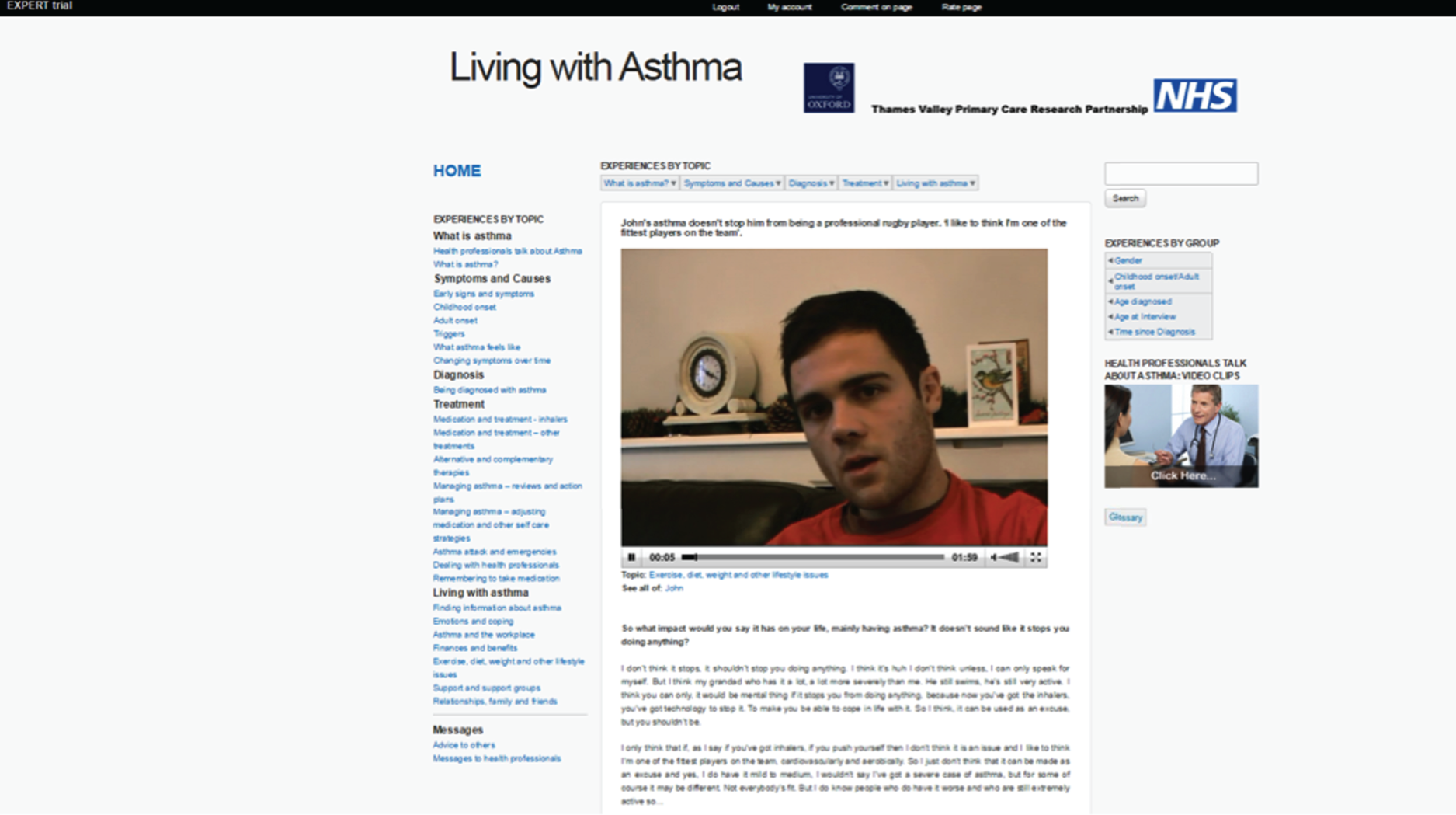
Design of comparator websites
For the randomised trial, we also required three comparator websites, one for each of the three conditions, containing ‘facts and figures’ about each condition, but no PEx. We decided that, as far as possible, these websites should have exactly the same ‘look and feel’ and navigation characteristics as the intervention websites, so that the only difference was in their content. To test the value of the PEx-based sites against the ‘gold standard’, these multimedia websites were populated with information from NHS Choices, the NHS health information website. Where necessary, minor changes were required, for example to remove experiential information that had been included in NHS Choices or to add in sections that were present on the intervention sites but not on NHS Choices. In this case, material was identified from other reputable sources (the MS Society, Asthma UK and NHS Smokefree). The material was then presented in a similar way to that of the intervention websites, with similar numbers of topic headings, pictures and other features. Screenshots of the final websites are shown in Figure 8.
FIGURE 8.
Work package 3a: the home pages of the comparator sites.
The list of topic areas included on each of the three comparator websites is given in Table 15.
| Asthma comparator site | Giving up smoking comparator site | MS carers comparator site |
|---|---|---|
|
|
|
Participant activity tracking and data portal development
In addition to the six information websites, we developed a ‘portal’ website through which the randomised trial could be administered. This contained all sensitive trial data (including all personal information and the questionnaire responses pre and post website exposure). It was linked to the content server hosting the information websites by means of a ‘wrapper’. The participant-facing interface comprised:
-
a welcome page where the participant entered their assigned participant code
-
a home page with an introduction explaining the trial
-
a participant-facing system for capturing baseline questionnaire data
-
a system for the user to fill in the post-exposure questionnaire data
-
a password recovery system
-
a forgotten login details link.
The interface for the research team comprised:
-
A participant registration system which, in conjunction with the randomisation system, put the participant into the correct branch of the trial.
-
A participant randomisation system.
-
A registration handover system to hand over user baseline and registration sessions to the content server.
-
A system for sending a welcome e-mail to a participant on completion of registration. Participants were e-mailed the URL to the login page of the information sites, their username and their password.
-
A system to pull usage tracking data from the content server on a daily basis via public–private key pair encryption, as an automated scheduled task. This was fed into a system to hold a decrypted copy of user tracking data linked to correct users.
-
A facility to send participant reminders to view the intervention sites at defined time periods.
-
A trial completion system that performed the following tasks 2 weeks after participant registration:
-
The portal e-mailed the participant to explain that the trial was over and that they no longer had access to the information sites, and directed them to return to the portal to fill in the post-exposure questionnaires.
-
The portal interacted with the content sites to block the users from being able to log in to the system.
-
If questionnaires were not returned within 24 hours then e-mail reminders were sent at defined time intervals.
-
Once post-exposure questionnaires were completed, the portal interacted with the content sites to reinstate the user login and e-mailed the participant to advise that they were able to view their allocated website again if they wished. After this point the participants’ usage of the website was no longer tracked.
-
-
An online issue tracker.
Assessment of use of the websites
Participants’ usage of their allocated website was tracked and logged by means of a ‘wrapper’ which facilitated communication between the content server (which hosted the six information websites) and the data ‘portal’. User activity was tracked by both page views (number and type) and interaction with web pages (e.g. if a participant viewed videos or listened to audio clips). We also tracked if participants used the search facility and what search words they used. The recorded data were linked to baseline and follow-up questionnaire data by a unique participant identification number.
Tracking data was collected in the following ways by individual user:
-
total visits to site (including times and date stamps)
-
total time spent on site
-
total number of page views
-
breakdown of session times (start and finish)
-
breakdown of page type visited and time spent on each
-
breakdown of clips viewed and length of time they were viewed for, split by the three formats: video, audio and text only
-
JavaScript (www.javascript.com) enabled/disabled in participants’ browser.
User testing
Before commencement of the randomised trial, we recruited 47 members of the public to pilot the entire participant journey, from the initial invitation to the completion of the follow-up measures. A primary goal of this pilot testing was to determine the functionality of the information websites and data portal and the credibility of the comparator sites. Twenty participants were recruited from the programme public panel and 27 participants were recruited externally. As part of the full pilot, participants were invited to undertake an informal heuristic evaluation of the websites, with particular focus on the design and appeal of the websites, the tone of the material, ease of navigation, perceived trustworthiness and participants’ overall level of engagement.
Participants were registered on the trial’s online data portal and their usage of the websites was tracked. They also provided additional information regarding platform and browser use, which was useful to the team when troubleshooting some access problems that turned out to be related to the user’s browser. A total of 41 participants completed the evaluation (i.e. submitted follow-up measures) and 31 provided feedback by e-mail and/or telephone interview. Feedback on individual website pages was also provided using the comments and ratings options on the websites themselves.
All feedback was examined and discussed by the research team. On the whole, feedback from participants across all sites was positive, for example:
It was a logically laid out website which made it easy to use. The use of colour and graphics was good, it made it easier and more enjoyable to use and helped to bring the information alive.
Smoking comparator site, user tester 5
I liked watching the videos though and feeling like they were real people’s experiences was good. I did find the website trustworthy and the design was professional.
Smoking intervention site, user tester 2
Seemed liked a good website, trustworthy and professional. It contained a lot of information which was very clearly laid out and easy to access.
Asthma comparator site, user tester 3
Other feedback was very useful in suggesting minor modifications which were incorporated into the design. For example, a ‘no smoking’ sign on the home page of the giving up smoking websites was seen as punitive by smokers and was replaced. The image chosen for the ‘health professionals’ section on the websites was also altered in response to consistently negative feedback.
Some people were unhappy with the aesthetics of the websites. This illustrated the challenge in designing online information sites to appeal to all. Example comments were:
Seems authoritative and boring, not particularly engaging on the homepage, but once you delve further in the testimonies are very good.
Smoking intervention site, user tester 3
Design of website is offering lot of text, can improve with more visual links (perhaps colour coding topics/groups) which will invite for easy navigation though steps.
Smoking intervention site, user tester 4
Looks a bit academic and pages are a bit ‘too busy’.
Asthma comparator site, user tester 5
Participants’ comments both agreed with and sometimes challenged the guidelines used to develop the prototype websites, with the duplicate menu being the most controversial:
The NHS logo really helped, as did the Oxford Uni one.
MS carer intervention site, user tester 5
Anything with an Oxford badge appears trustworthy.
Smoking comparator site, user tester 3
Irritated by having menu on the left and across the top.
Asthma intervention site, user tester 3
I do not think it is necessary to have ‘Information by topic’ at the top when it is on the side.
Asthma comparator site, user tester 6
Importantly, participant feedback and the tracked user data on the online portal also revealed that the material had not been optimised for viewing across multiple platforms with multiple browsers, especially using iOS devices [such as iPhone (Apple Inc., Cupertino, CA, USA)]. In addition, some participants were unable to stream videos while others were able to watch the videos but this was not registered as ‘usage’ by the online portal. This had direct implications for the quality and quantity of the usage data we would be able to collect during the main trial. As a result the software expert producing the online portal further optimised the site for multiple platforms, and tested and retested the tracking capability across platforms and devices. In addition, full trial participants were subsequently advised of the optimal platform and browser combinations in the study information sheet.
Conclusions
We successfully developed three multimedia prototype websites based entirely on experiential data from a maximum variation sample of narrative interviews on three health topics. The summaries which formed the basis of the sites were grounded in what was important to the study participants as detailed in their personal accounts. Three multimedia comparator websites, with the same look and feel as the intervention websites, were also constructed based on ‘facts and figures’ style information from a ‘gold-standard’ source, the NHS Choices website. The intervention websites were developed to adhere to guidelines on how best to present online PEx based on work conducted earlier in this programme. We also developed a data portal website which collected two distinct sets of data: clinical data (participants’ screening and demographic data and all baseline and outcome questionnaire data) and the user activity tracking data. User testing led to minor amendments of the information websites and the data collection portal prior to their use in the randomised trial, which is described in the next chapter.
Chapter 8 Work package 3b: the EXPERT study – randomised trial of patient experience-based websites
Abstract
Introduction: the aim was to assess the feasibility and measure the impact of a PEx-based website using a randomised trial. We did this for three conditions: smoking cessation, asthma and caring for someone with MS.
Methods: in this phase II pilot randomised single-blind trial, eligible participants were allocated randomly to a PEx website or a non-PEx comparator website, stratified by health topic. Participants completed baseline measures, were given access to their allocated website for 2 weeks, and completed follow-up measures. Website usage was tracked. Semistructured interviews were conducted with purposively selected participants and analysed using an interpretative thematic analysis.
Findings: in the three conditions (smoking cessation, asthma and caring for someone with MS) we randomised 87, 148 and 42 participants, respectively. At 2-week follow-up, retention rates were 75%, 82% and 86%, respectively. The median numbers of logins to the websites were 2, 2 and 4; the median numbers of page views were 10, 15 and 27.5; and the median total duration on site was 9 minutes, 17 minutes and 31.5 minutes, respectively. We found no evidence of differences on self-report measures which included condition-specific outcomes, health status and attitudes of users towards health websites. There were no adverse events.
Conclusions: the trials demonstrated ‘technical feasibility’ and had good internal validity, although usage of allocated websites was low. Carers were difficult to recruit. Future, more pragmatic work needs to consider how to evaluate PEx tools in the context of ‘real-world’ internet use and information-seeking behaviour.
Introduction
In this chapter we describe the design, conduct and findings of a phase II pilot randomised single-blind trial, in which eligible participants were randomly allocated to a condition-specific PEx-based health information website or to a comparator website which contained facts and figures information, stratified by one of three health conditions. The original application described three separate pilot randomised trials, one for each health condition. For operational efficiency, the three trials were run under the governance of a single trial protocol and analysed by condition. In this programme of work we followed the Medical Research Council (MRC) guidance for complex interventions. 167 The conceptual and literature review work described in Chapter 2 established what was already known on this topic and identified the theoretical ways in which the online sharing of personal experiences of health and illness may yield benefits. This theoretical understanding was developed by the work described in Chapter 3, where we further explored the ways in which experiences are reported as helpful, using data from interviews with patients. Chapter 6 explained how we established the factors which maximise engagement with online information and which we then used to inform the optimum design of our intervention (as described in Chapter 7). The next step for us in developing and evaluating this complex intervention was to undertake this exploratory study, with our main aim being to establish the feasibility of undertaking this research and to identify any emergent evidence of efficacy or harm. This work will inform further, more pragmatic effectiveness research. As discussed previously, the three exemplar conditions were chosen to assess the impact of experiential information on (1) confidence to self-manage a chronic disease (asthma); (2) motivation to change an unhealthy behaviour (smoking); and (3) preparedness to undertake a caring role (carers of people with MS): our initial theoretical work suggested that these are three of the several ways in which experiential information may be beneficial. We also measured the impact of all six websites on health status, and we assessed attitudes towards the websites using the new instrument, the eHIQ (see Chapter 4). Our objectives are as follows.
Primary objective
-
To evaluate the feasibility issues in an online randomised study providing health information websites containing PEx information compared with matched health information websites that do not contain experiential information.
Secondary objectives
-
To assess the efficacy of two types of online health information (PEx accounts compared with matched health information websites that do not contain experiential information) on a range of self-reported outcomes.
-
To explore whether or not the interventions have differential effects on pre-specified subgroups of participants.
-
To measure the impact of the intervention and comparator websites using the eHIQ.
Methods
Design
A phase II pilot randomised single-blind trial, in which eligible participants were randomly allocate to a PEx website or a comparator ‘facts and figures’ website stratified by health topic.
Interventions
As described in the previous chapter, for each condition (asthma, smoking cessation, MS carer) two websites were developed: one containing PEx information and the other containing information solely based on facts and figures with no experience-based content. Each were password protected, multimedia internet sites based on guidelines which were developed by the team working on WP2b. The comparator sites shared the design and multimedia features (such as video) of the intervention sites but the content excluded any accounts of personal experience. They used source material from the national health information portal NHS Choices with all experiential information removed.
Participants
Trial participants had asthma, were smokers with a willingness to quit or were carers of a person with MS. To be eligible for the asthma condition, participants were required to have clinically diagnosed asthma as coded in their primary care electronic record, and have been prescribed inhaled corticosteroids for at least 3 months in the previous year. To be eligible for the smoking cessation condition, participants were required to be current smokers, who had been smokers for at least 1 year, and who indicated some willingness to quit, including those referred to smoking cessation services. To be eligible as carers of people with MS, participants were required to identify themselves as an unpaid caregiver (i.e. not a professional carer) for another person who had a diagnosis of MS. Participants who matched more than one condition could be included only once, and only one participant per household could be included.
We included participants who were male or female, over the age of 18 years, resident in the UK, with access to the internet and able to use websites. We excluded people who could not understand English (owing to the nature of the intervention), who were terminally ill or who had a significant disease or disorder that may have put that person at risk because of participation in the research, or may have influenced the result of the research, or which affected that person’s ability to participate.
Recruitment
The recruitment of participants eligible for the asthma and smoking cessation conditions was predominantly through primary care practices in two regions of England, facilitated by the local primary care research networks. GPs who agreed to take part were asked to identify eligible individuals from their practices and to send them full information on the research study. In addition, for the smoking cessation recruitment, posters advertising the study were placed in public places, such as GP waiting rooms and libraries, and online adverts were placed on Facebook. The recruitment invitations and posters gave contact details for the study team so that potential participants could make initial contact to indicate their willingness to take part.
The recruitment of participants eligible as carers of people with MS took a different approach. Being a carer for someone with MS is not routinely recorded in primary care records. We took a broad and iterative approach to the recruitment of carers, helped by our patient and public advisory panel. Recruitment was not easy, and over time we used many routes. We placed posters and leaflets in GP practices, neurology clinics, MS therapy centres, local enablement and well-being services, and local leisure centres. We enlisted the support of several third-sector organisations that distributed recruitment adverts on their websites and social media feeds, including the MS Society, Shift.MS, Carers UK and the Carers Trust. We met with the local carers group, advertised in their newsletter and staffed a stand at a local carers’ conference. We placed paid-for adverts in Enable magazine, in local newspapers, in the London Metro paper and on Facebook. We had our own study recruitment webpage and promoted this through various channels, including the Oxford Daily Info website and tweets sent to key organisations and public figures. We were supported by members of the programme public panel and the MS patient and carer panel who helped us to identify recruitment avenues as well as potential participants. Further participants were recruited through word of mouth and personal contact.
Study procedures
For each condition, potential participants who indicated a willingness to take part completed screening questionnaires to assess their eligibility against our inclusion/exclusion criteria (see above). All eligible participants were sent a patient information sheet and consent form by post to be signed and returned to the research office in a reply-paid envelope. Once consent had been received participants’ details were entered into a secure trial management portal and they were sent a unique ‘welcome code’ with a link to the trial registration webpage. If after 1 week the participant had not used their welcome code, a reminder was sent by automatic e-mail inviting them to visit the trial registration page. If the participant no longer wished to take part, they could simply ignore this reminder. If the participant did wish to take part they could use the link in the e-mail to access the trial registration page where they were asked to complete baseline questionnaires on the online portal. Once these measures had been completed they were invited to create a unique user identification and password and then they were randomised to have access to either the intervention or the comparator website, for a period of 2 weeks. Randomisation used a computer-generated random number sequence in a 1 : 1 ratio. The sequence was generated by a trial statistician independent of the study. Participants did not know whether they were receiving the comparator or the intervention website, only that we were evaluating two approaches to giving health information. Nevertheless, the nature of the intervention meant that they could not be blind to whether they were looking at personal experiences or facts and figures information. The study investigators undertaking the analyses were blind to allocation, which was an automated process. Participants were able to log on and access the website interventions as much or as little as they wanted. At the end of the 2-week period, participants were invited by e-mail to complete final follow-up measures, using the same portal. Up to two e-mails and one telephone call were used to remind those who did not initially respond. Participants’ usage of their allocated website was also tracked.
Measures
The outcome measures for each condition are shown in Table 16. As a feasibility trial, our primary measures concerned the number of participants consented and recruited, the usage of the websites (in terms of numbers of logins, page views and time on site) and the numbers with completed outcome measures or lost to follow-up. For secondary outcomes, we used condition-specific self-report measures as well as the widely used and well-validated Short Form questionnaire-36 items (SF-36) health status measure (including both physical and mental dimensions and all subscales), and the eHIQ, a new self-completion measure designed earlier in this programme of work to measure the effects of accessing online health information. The eHIQ part 1 contains 11 items covering general attitudes towards using the internet to access health information. The eHIQ part 2, which contains 26 items, is administered at follow-up, as it captures the attitudes of the respondents towards the website they have recently viewed. Both parts of the questionnaire use five-point response categories, from ‘strongly agree’ to ‘strongly disagree’, for all items. 66,99 The eHIQ part 2 scores are combined to make three subscales: confidence and identification (reflecting confidence to discuss health with others and a person’s ability to identify with the website); information and presentation (reflecting trust and suitability of website content); and understanding and motivation (reflecting understanding and learning about relevant information and motivation to take action (see Chapter 4). Each subscale is scored between 0 and 100, with higher scores indicating a more positive rating.
| Outcome measure | Asthma | Smoking | MS carers |
|---|---|---|---|
| Feasibility measures | |||
| Numbers of participants recruited | ✓ | ✓ | ✓ |
| Numbers of participants retained | ✓ | ✓ | ✓ |
| Completeness of outcome measures | ✓ | ✓ | ✓ |
| Intervention usage | ✓ | ✓ | ✓ |
| Secondary outcomes | |||
| eHIQ | ✓ | ✓ | ✓ |
| SF-36 health status | ✓ | ✓ | ✓ |
| PIH questionnaire | ✓ | ||
| CDSES | ✓ | ||
| Single-item asthma control question | ✓ | ||
| MTSS | ✓ | ||
| Abstinence rates | ✓ | ||
| Number of quit attempts | ✓ | ||
| SASEQ | ✓ | ||
| PFCS | ✓ | ||
The choice of condition-specific outcome measures was informed by our theoretical understanding of what the benefit of shared personal experiences might be. So, for the asthma condition, we were specifically interested in whether or not other people’s experiences could have effects on aspects of self-management including self-efficacy and asthma control. For asthma we therefore used the Chronic Disease Self-Efficacy Scale (CDSES), which is a six-item questionnaire assessing confidence in self-managing a chronic condition. 168 (The score is the mean of the six items. If more than two items were missing, the scale was not scored.) We also used the 12-item Partners in Health (PIH) scale, which assesses knowledge and behaviour in relation to self-management for a chronic condition. 169 The 12 items cover four domains of competency in relation to self-management (knowledge, coping, management of condition and adherence to treatment), and the total sum score is used (the higher score indicating greater competency). We also used a single-item asthma control question taken from the 5-item Asthma Control Test (which was used as a baseline descriptive measure), whereby participants rated their asthma control on a five-point scale from ‘not controlled’ to ‘completely controlled’. 170
For smoking cessation, we were interested in whether or not other people’s experiences could be harnessed to achieve health behaviour change, namely to quit smoking or to change the motivation to quit. We therefore used the following self-report measures: abstinence rates (single self-report question), quit attempts (single self-report question), the single-item Motivation To Stop Scale (MTSS) to measure whether motivation had changed, on a 7-point scale (where a rating of 1 reflected the absence of any belief, desire or intention to stop smoking, and a rating of 7 reflected a strong desire and short-term intention to stop),164 and the Smoking Abstinence Self-Efficacy Questionnaire (SASEQ), a six-item questionnaire on which smokers are required to indicate, using a five-point Likert scale, how confident they are in abstaining from smoking in six example situations. 171
For carers of someone with MS, we wanted to assess whether or not other people’s experiences of caring could help carers feel more confident and supported in their own caring roles. Most of the validated instruments in this area are specific to dementia care and this restricted our choice of questionnaires. We did not find any instruments specific to the caring role in MS. We used the 8-item Preparedness For Caregiving Scale (PFCS), which assesses how well prepared participants think they are. 172 Each question is scored 0–4, with 4 representing ‘very well prepared’, and the higher the score the more prepared the caregiver feels for caregiving. The score for the PFCS is calculated as the mean of the eight items.
Sample size and statistical analyses
We planned to recruit a total of 300 participants, 100 for each of the three conditions. The focus of the study was to assess feasibility, which could usually be addressed using a smaller sample but we anticipated that this sample size would provide enough power to estimate acceptability judged by engagement with the PEx components of the site with a precision of ± 14% in each condition/arm (50 participants) and 8% for the whole trial/per arm (150 participants). This was based on a worst-case scenario of acceptability being 50%. We assumed the acceptability rate to be in the region of 80%. We also wanted sufficient participants to be able to adequately assess issues of recruitment and retention, as attrition rates are often high in fully internet-based trials.
Feasibility outcome measures were summarised using descriptive statistics such as rates reported as percentages. We undertook descriptive statistics to characterise participants at baseline; constructed a Consolidated Standards of Reporting Trials (CONSORT) diagram to show the flow of participants through the trial, including the proportion who completed each stage to trial entry; and measured usage of the interventions in terms of total visits to site, total time on site and total number of website pages visited. Formal hypothesis testing of the self-report outcome measures was not performed, as this was a feasibility trial and was not intended (or powered) to assess evidence of significant treatment effect. However, the estimated difference in outcome measures of efficacy and corresponding 95% CIs were calculated using analysis of covariance (ANCOVA) adjusting for baseline values. In terms of effect sizes, based on a balanced randomisation of intervention–comparator groups in a ratio of 1 : 1 (i.e. 50 intervention and 50 comparator for each condition), the trial would detect potential large effects of the intervention for each condition; for dichotomous outcomes these were equivalent to relative risks of ≥ 2.1 for a baseline rate of ≤ 30% given an alpha of 0.05 and 90% power, and for continuous outcomes these detectable differences would be of the order of 0.4 SD based on the same power and significance.
Qualitative study
Following completion of final follow-up measures, a subset of study participants was purposively selected and invited to be interviewed by one of three qualitative researchers from the HERG at the University of Oxford. The participants were selected for maximum variation of their demographic characteristics and use of the intervention (determined by usage data), to give us a diverse sample. Information sheets and consent forms were sent out by e-mail following an expression of interest by participants (who were asked to indicate their willingness to take part when filling in their online measures). The consent forms were completed in person. The interviews focused on reasons for participating in the trial, engagement with the online resources, and attitudes towards online interventions and generic health resources and support. Participants from both intervention and comparator arms in each of the three conditions were included to explore differences which may have been attributable to the allocated website. The interviews used two semistructured interview guides: one for participants allocated to the intervention websites and one for those allocated to the comparator websites. These were based on reviews of existing literature and earlier, exploratory work. The guides differed to ensure that the participant remained blind to trial allocation and purpose. For example, those participants in the intervention arm of the trial were asked specifically about how they chose which PEx clips to view. The guides covered the following topics: motivation for participation, acceptability of trial procedure, experience of taking part in the online intervention and trial, use of the internet for health-related purposes and attitudes towards different types of health information. We used a set of laminated ‘home pages’ from six different types of websites to facilitate this discussion. Open-ended questions and prompts were used to further explore participants’ experiences of taking part in this online study and their attitudes towards the website content. The researchers did not ‘unblind’ the participants by telling them more about the study until the end of the interview.
The interviews were transcribed and analysed by thematic analysis using the method of constant comparison. A specialist software package (NVivo 10) was used to organise the data. Recurrent themes and subthemes were identified, as they emerged from the data, by the three interviewers, who initially coded their own interviews. This was followed by extensive discussion and comparison of the emergent themes between the researchers.
Changes from the original proposal
The original protocol stated that follow-up measurements would be collected at 1 month and 3 months, and that participants would be randomised in a 2 : 1 active–comparator ratio. After discussion with our trial statistician and the rest of the trial team, we reduced the follow-up to one measurement immediately post exposure to the website, and changed the randomisation ratio to 1 : 1. The change to a shorter follow-up (immediately post exposure to the website intervention) was for a number of reasons: that this would maximise blinding and minimise contamination; that our primary aim was to establish feasibility; that our main measures related to the immediate effect of the website exposure; and that we wanted to minimise attrition. This decision was discussed and agreed with the funder.
Ethics and governance
Ethics approval for this study was provided by the NHS Health Research Authority Research Ethics Committee, reference 13/NW/0162. The trials were overseen by a Trial Steering Committee chaired by Professor Elizabeth Murray of University College London. The trial registration number is ISRCTN29549695 and it was registered on 17 May 2013.
Results
The results for each of the three conditions in the trial are presented separately. There were no adverse events for any participant.
Smoking cessation
Recruitment through primary care was relatively slow, and we engaged more primary care practices (23 in total) than anticipated. The first participant was recruited in June 2013, and the last participant completed follow-up in August 2014. The trial ended as we had recruited > 80% of target sample size and the funding was ending. A total of 129 invitations were sent in response to expressions of interest in the study, and 89 individuals (69%) completed registration (i.e. they consented and completed baseline questionnaires). Two participants withdrew before randomisation, leaving 87 randomised participants (recruitment rate of 87/89 = 98%). Of these, 44 (51%) were allocated to the PEx website. Of the randomised participants, 22 out of 87 (25%) were lost to follow-up (please see the CONSORT flow diagram in Figure 9).
FIGURE 9.
Work package 3b: CONSORT flow diagram – smoking cessation.
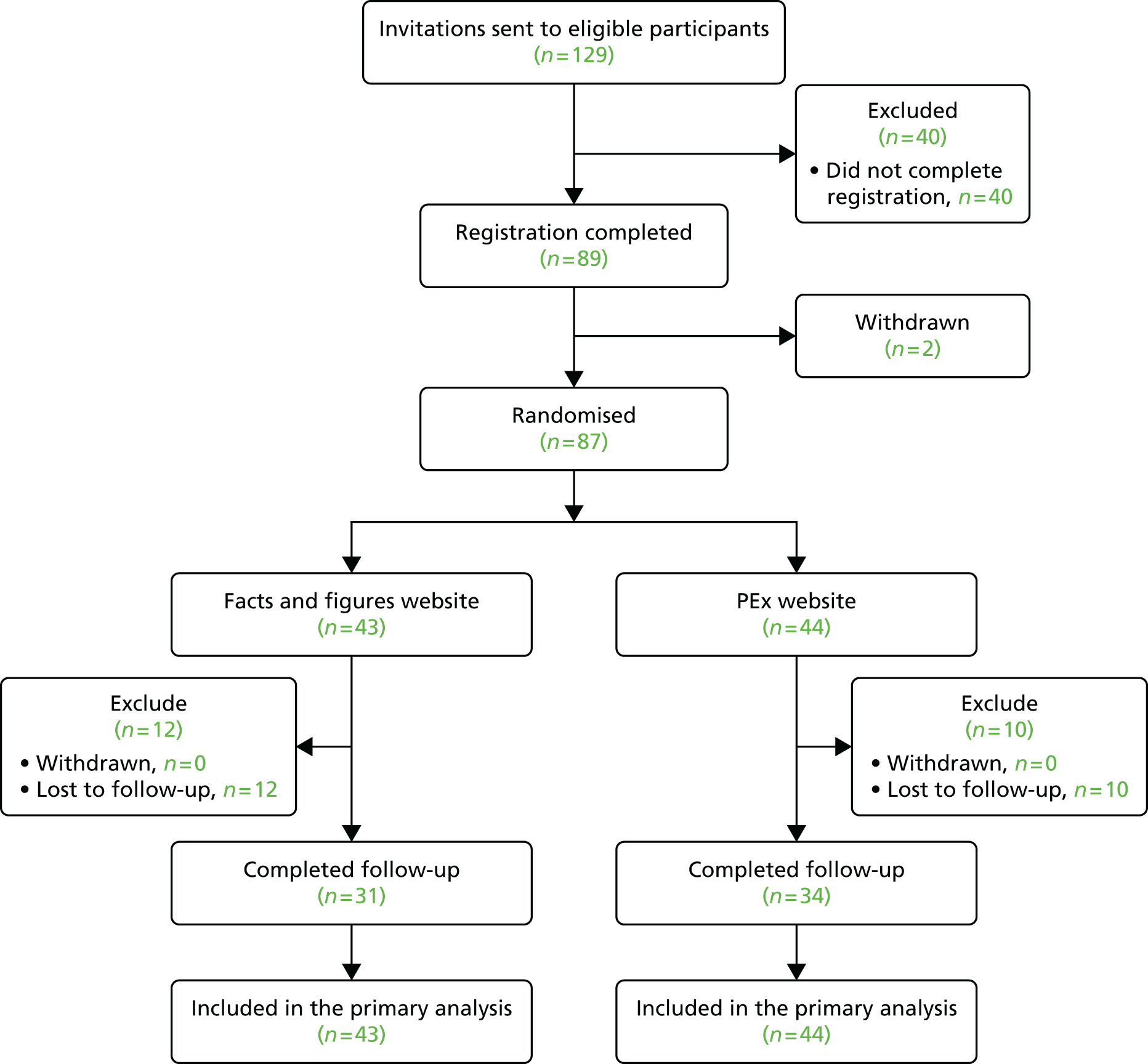
The baseline demographic, internet use and smoking characteristics of randomised participants are presented in Table 17. These were balanced between groups. Most were regular users of the internet with good to excellent self-reported internet abilities. Of the 87 participants, 45 (52%) were women. The majority of participants reported smoking < 20 cigarettes per day, with most smoking between 11 and 20 cigarettes per day (53% of the sample). Most had intentions to quit smoking, with only three participants reporting either not wanting to quit (3%) or knowing that they should quit but not ‘really’ wanting to (18%, n = 16). Twenty-seven participants reported having made an attempt to quit during the 2 weeks before they started the study (31%).
| Baseline variable | Comparator (N = 43), n (%) | Intervention (N = 44), n (%) |
|---|---|---|
| Age | ||
| Mean (SD); minimum–maximum | 53.6 (15.1); 17–80 | 55.1 (12.9); 24–92 |
| Gender | ||
| Female | 23 (53.5) | 22 (50.0) |
| Male | 20 (46.5) | 22 (50.0) |
| Self-rated ability to use the internet | ||
| Excellent | 9 (20.9) | 10 (22.7) |
| Good | 15 (34.9) | 21 (47.7) |
| Fair | 16 (37.2) | 11 (25.0) |
| Poor | 3 (7.0) | 2 (4.5) |
| Bad | 0 (0) | 0 (0) |
| Internet use | ||
| At least once per day | 26 (60.5) | 28 (63.6) |
| Several times per week | 17 (39.5) | 10 (22.7) |
| Once per week | 0 (0) | 3 (6.8) |
| Less than once per week | 0 (0) | 3 (6.8) |
| Ethnicity | ||
| White: English/Welsh/Scottish/Northern Irish/British | 39 (90.7) | 41 (93.2) |
| White: any other white background | 2 (4.7) | 2 (4.5) |
| Mixed | 1 (2.3) | 0 (0) |
| Asian: Pakistani | 0 (0) | 1 (2.3) |
| Black: Caribbean | 1 (2.3) | 0 (0) |
| Number of cigarettes smoked per day | ||
| ≤ 10 | 12 (27.9) | 15 (34.1) |
| 11–20 | 25 (58.1) | 21 (47.7) |
| 21–30 | 4 (9.3) | 7 (15.9) |
| ≥ 31 | 2 (4.7) | 0 (0) |
| Did not answer | 0 (0) | 1 (2.3) |
| Time from waking up to smoking first cigarette | ||
| After 60 minutes | 8 (18.6) | 13 (29.5) |
| 31–60 minutes | 9 (20.9) | 11 (25.0) |
| 6–30 minutes | 17 (39.5) | 15 (34.1) |
| Within 5 minutes | 8 (18.6) | 4 (9.1) |
| Did not answer | 1 (2.3) | 1 (2.3) |
| Serious attempt to stop smoking in past 2 weeks? | ||
| No | 32 (74.4) | 27 (61.4) |
| Yes | 11 (25.6) | 16 (36.4) |
| Did not answer | 0 (0) | 1 (2.3) |
| Which of the following describes you? | ||
| I don’t want to stop smoking | 1 (2.3) | 2 (4.5) |
| I think I should stop smoking but don’t really want to | 9 (20.9) | 7 (15.9) |
| I want to stop smoking but haven’t thought about when | 5 (11.6) | 2 (4.5) |
| I REALLY want to stop smoking but I don’t know when I will | 15 (34.9) | 16 (36.4) |
| I want to stop smoking and hope to soon | 6 (14.0) | 6 (13.6) |
| I REALLY want to stop smoking and intend to in the next 3 months | 2 (4.7) | 4 (9.1) |
| I REALLY want to stop smoking and intend to in the next month | 3 (7.0) | 5 (11.4) |
| Don’t know | 2 (4.6) | 2 (4.6) |
The usage of the websites is shown in Table 18. This shows that the median number of logins during the 2-week period for both smoking cessation sites was 2, with a median number of page views of 11.5 for the intervention site and 7 for the comparator site. The median duration of use was 15 minutes for the intervention site and 5 minutes for the comparator site. One user never logged in to their allocated site, and two other users logged in but did not record a page view or spend any time on the site. Table 18 also presents the results of post hoc significance tests for differences in usage between groups. This was a post hoc analysis suggested by the chairperson of our Trial Steering Committee. The differences between groups for number of logins and number of page views were not statistically significant. The total duration on site was significantly longer (p = 0.013) for the PEx website.
| Usage measure | All participants (n = 87) | Comparator (n = 43) | PEx (n = 44) |
|---|---|---|---|
| Total number of logins to website | |||
| n | 86 | 42 | 44 |
| Median (minimum–maximum) | 2 (1–20) | 2 (1–8) | 2 (1–20) |
| IQR | 1–3 | 1–3 | 1.5–3 |
| p-value | 0.419a | ||
| Total number of pages visited | |||
| n | 84 | 42 | 42 |
| Median (minimum–maximum) | 10 (1–237) | 7 (1–225) | 11.5 (1–237) |
| IQR | 4–24.5 | 3–20 | 5–30 |
| Adjusted difference in medians (95% CI) | 3 (–9.142 to 15.142)b | ||
| p-value | 0.624 | ||
| Total duration on site (minutes)c | |||
| n | 86 | 42 | 44 |
| Median (minimum–maximum) | 9 (0.5–213) | 5 (0.5–69) | 15 (0.5–213) |
| IQR | 1–26 | 1–16 | 3–35 |
| Adjusted difference in medians (95% CI) | 12 (2.608 to 21.392)b | ||
| p-value | 0.013 | ||
Figures 10 and 11 are dot plots of the total number of logins and total number of pages, respectively, visited by the randomised group. The solid blue line indicates the median, and the lower and upper quartiles are shown by the dotted lines.
FIGURE 10.
Work package 3b: dot plot graphs of total number of logins by the randomised group for smoking cessation. IQR, interquartile range.
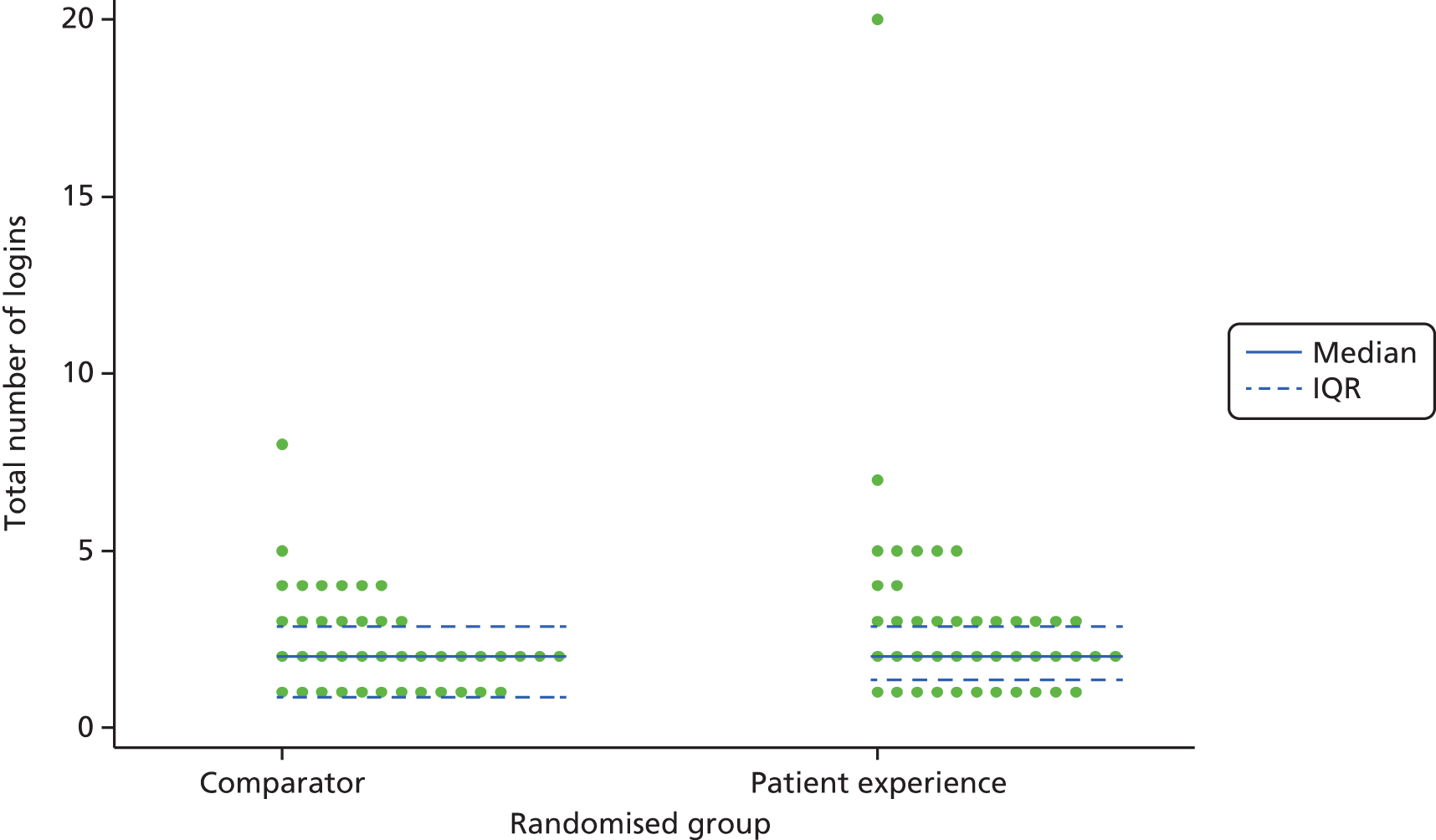
FIGURE 11.
Work package 3b: dot plot graph of total number of pages visited by the randomised group for smoking cessation. IQR, interquartile range.
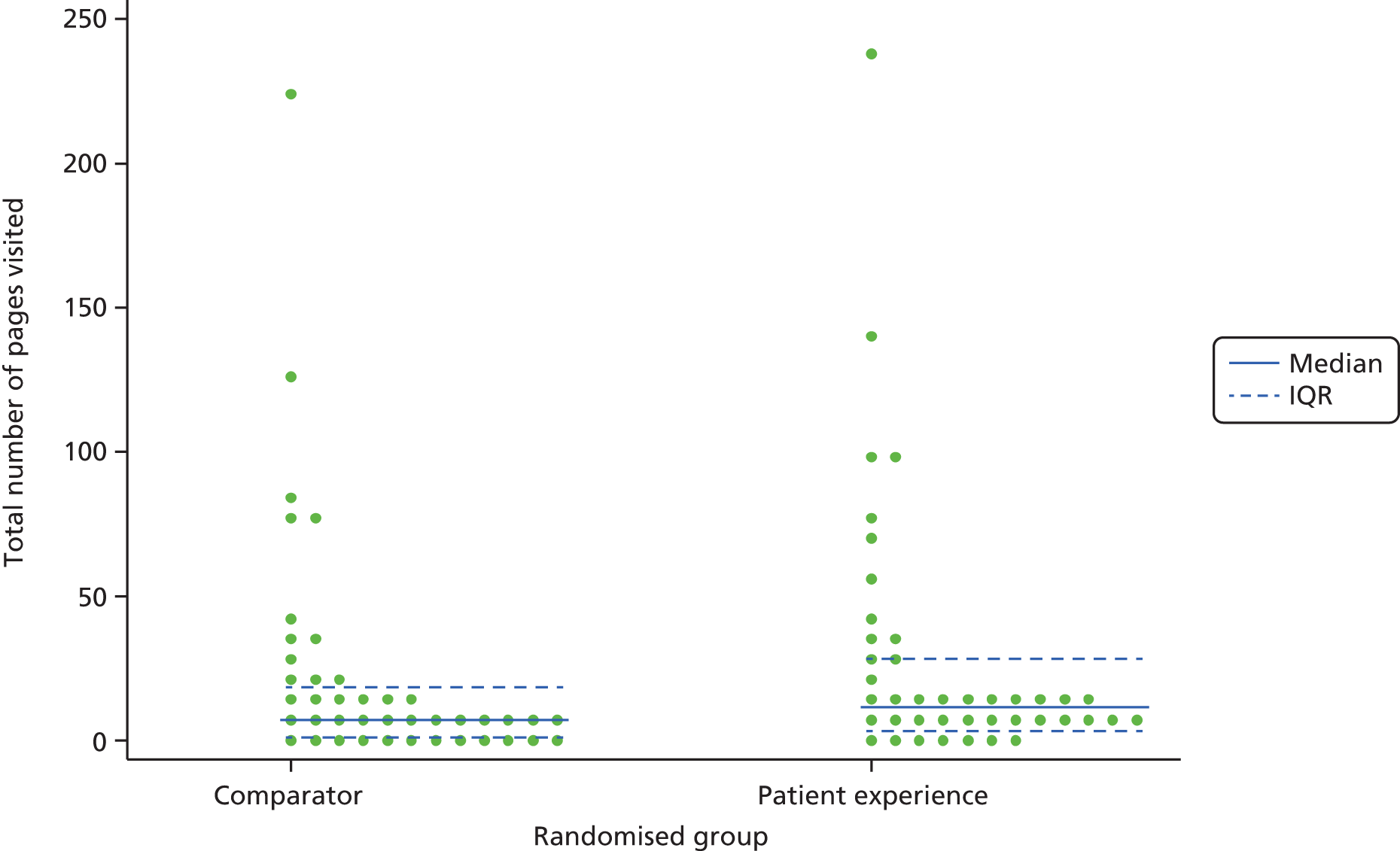
Figure 12 shows dot plots of the total duration on the website in minutes by randomised group. The solid blue line indicates the median, and the lower and upper quartiles are shown by the dotted lines.
FIGURE 12.
Work package 3b: dot plot graphs of total duration (minutes) on website by the randomised group for smoking cessation. IQR, interquartile range.
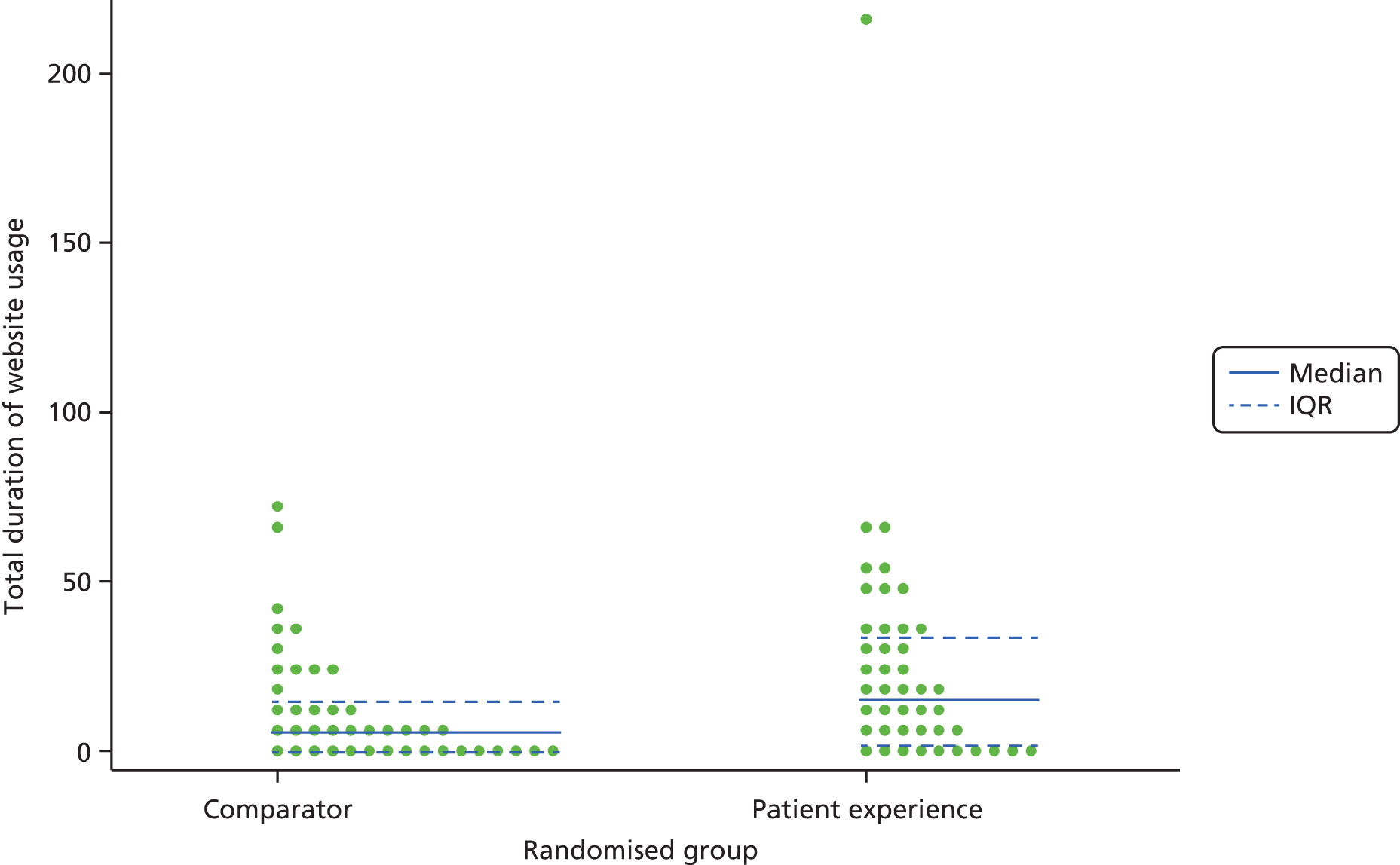
The mean SASEQ scores were similar between the randomised groups. The baseline mean score (SD) for the intervention group was 1.94 (1.02) and for the comparator group was 1.84 (0.89); at 2-week follow-up these scores were 1.89 (0.99) and 1.71 (0.95), respectively. Both groups had low mean SASEQ scores, indicating low self-confidence in abstaining from smoking in a variety of situations. An ANCOVA found an adjusted mean difference for the change in SASEQ scores between the two randomised groups of 0.155 (95% CI –0.262 to 0.573), adjusted for baseline SASEQ scores.
The findings from the other exploratory comparisons of the smoking-specific outcome measures are shown in Table 19. This table shows that the baseline and follow-up scores and the change scores for the MTSS, abstinence rates and quit attempts were similar between groups for baseline and follow-up measures and for change scores.
| Measure | All participants (N = 87), n (%) | Comparator (N = 43), n (%) | Intervention (N = 44), n (%) |
|---|---|---|---|
| MTSS | |||
| Change in MTSS from baseline | |||
| Decreased motivation | 14 (16) | 6 (14) | 8 (18) |
| Improved motivation | 19 (22) | 9 (20) | 10 (23) |
| No change | 28 (32) | 14 (33) | 14 (32) |
| Unknown | 26 (30) | 14 (33) | 12 (27) |
| Abstinence at follow-up | |||
| Cigarettes or other tobacco used in the last 7 days at 2 weeks | |||
| Yes | 57 (65) | 28 (65) | 29 (66) |
| No | 8 (9) | 3 (7) | 5 (11) |
| Unknown | 22 (25) | 12 (28) | 10 (23) |
| Quit attempts | |||
| Quit attempts in the last 2 weeks at baseline | |||
| Yes | 27 (31) | 11 (26) | 16 (36) |
| No | 59 (68) | 32 (74) | 27 (62) |
| Unknown | 1 (1) | 0 (0) | 1 (2) |
| Quit attempts in the last 2 weeks at 2 weeks | |||
| Yes | 25 (29) | 11 (26) | 14 (32) |
| No | 39 (45) | 20 (46) | 19 (43) |
| Unknown | 23 (26) | 12 (28) | 11 (25) |
The results for the SF-36 were also similar between groups and are shown in Table 20. Participants in both arms showed non-significant improvement in health state from baseline in the mental component and a very small, non-significant worsening in the physical component. There was no visible pattern between the two groups. The adjusted mean differences between the two groups (ANCOVA, n = 64 participants with full data) for the absolute change in physical component summary (PCS) score of the SF-36 was 1.393 (95% CI –0.702 to 3.489) and for the absolute change in mental component summary (MCS) score of the SF-36 was 0.785 (95% CI –3.09 to 4.648).
| Measure | Comparator (N = 43) | Intervention (N = 44) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | Minimum to maximum | n | Mean (SD) | Minimum to maximum | |
| Baseline PCS | 43 | 44.08 (11.02) | 19.63 to 64.91 | 44 | 48.59 (8.41) | 24.91 to 61.07 |
| 2-week PCS | 31 | 43.21 (11.10) | 19.85 to 61.88 | 33 | 48.43 (8.76) | 21.29 to 63.73 |
| Change in PCS from baseline | 31 | –0.92 (4.12) | –11.74 to 5.92 | 33 | –0.14 (4.49) | –7.77 to 14.20 |
| Baseline MCS | 43 | 43.00 (13.57) | 10.56 to 65.69 | 44 | 46.68 (11.19) | 17.94 to 67.15 |
| 2-week MCS | 31 | 43.42 (15.18) | 10.45 to 69.15 | 33 | 47.99 (10.25) | 25.38 to 62.54 |
| Change in MCS from baseline | 31 | 2.20 (8.79) | –19.14 to 26.82 | 33 | 1.89 (7.44) | –10.78 to 21.02 |
Asthma
Recruitment was rapid through nine primary care practices. The first participant was recruited in June 2013, and the last participant completed follow-up in November 2013. The trial ended as we had recruited in excess of the target sample size. Two hundred invitations were sent in response to expressions of interest in the study, and 150 individuals (75%) completed registration (i.e. they consented and completed baseline questionnaires). Two participants withdrew before randomisation, leaving 148 randomised participants (a recruitment rate of 148/150 = 99%). Seventy-three of these (49%) were allocated to the PEx website. Of the randomised participants, 27 (18%) were lost to follow-up (please see the CONSORT flow diagram in Figure 13).
FIGURE 13.
Work package 3b: CONSORT flow diagram – asthma.
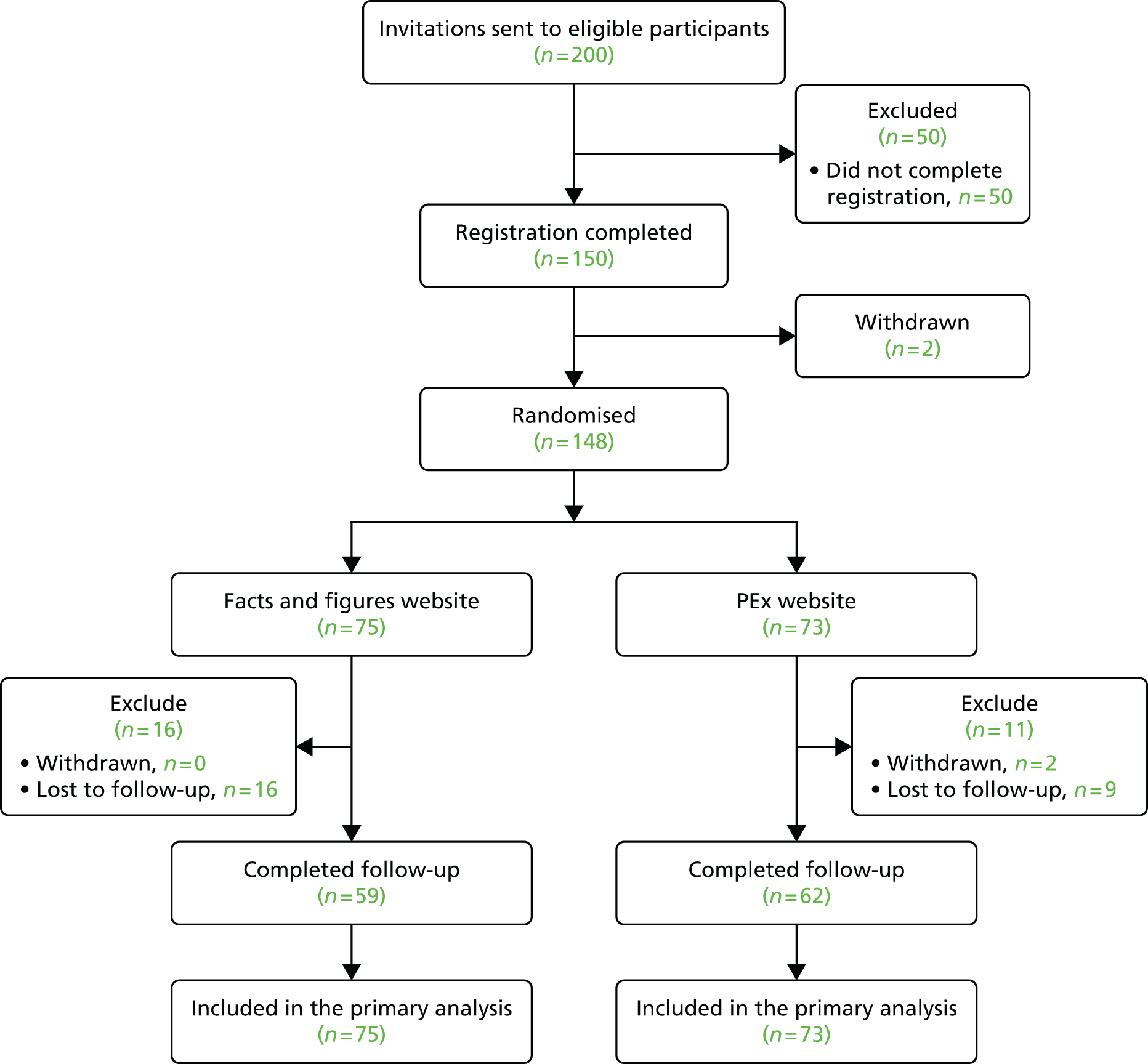
The baseline demographic and internet use characteristics of randomised participants are presented in Table 21 and were balanced between groups. Most were regular users of the internet with good to excellent self-reported internet abilities. Of the 148 participants, 87 (58.8%) were women.
| Baseline variable | Comparator (N = 75), n (%) | Intervention (N = 73), n (%) |
|---|---|---|
| Age | ||
| Mean (SD); minimum–maximum | 55.7(13.9); 19–84 | 58.2 (11.7); 27–77 |
| Gender | ||
| Female | 41 (54.7) | 46 (63.0) |
| Male | 34 (45.3) | 27 (37.0) |
| Self-rated ability to use the internet | ||
| Excellent | 26 (34.7) | 18 (24.7) |
| Good | 35 (46.7) | 34 (46.6) |
| Fair | 12 (16.0) | 17 (23.3) |
| Poor | 2 (2.7) | 3 (4.1) |
| Bad | 0 (0) | 1 (1.4) |
| Internet use | ||
| At least once per day | 49 (65.3) | 37 (50.7) |
| Several times per week | 19 (25.3) | 21 (28.8) |
| Once per week | 6 (8.0) | 6 (8.2) |
| Less than once per week | 1 (1.3) | 9 (12.3) |
| Ethnicity | ||
| White: English/Welsh/Scottish/Northern Irish/British | 66 (88.0) | 66 (90.4) |
| White: any other white background | 4 (5.3) | 1 (1.4) |
| Mixed | 0 (0) | 1 (1.4) |
| Asian: Indian | 1 (1.3) | 2 (2.7) |
| Black: Caribbean | 0 (0) | 1 (1.4) |
| Black: African | 1 (1.3) | 0 (0) |
| Not reported | 3 (4.0) | 2 (2.7) |
In general, the participants’ asthma symptoms were well controlled and did not interfere with daily living to a great extent (Table 22).
| Item | All participants (N = 148), n (%) | Comparator (N = 75), n (%) | PEx (N = 73), n (%) |
|---|---|---|---|
| How often did your asthma keep you from getting as much done at work, school or home? | |||
| All of the time | 1 (0.7) | 1 (1.3) | 0 (0) |
| Most of the time | 5 (3.4) | 3 (4.0) | 2 (2.7) |
| Some of the time | 11 (7.4) | 3 (4.0) | 8 (11.0) |
| A little of the time | 33 (22.3) | 16 (21.3) | 17 (23.3) |
| None of the time | 98 (66.2) | 52 (69.3) | 46 (63.0) |
| How often have you had shortness of breath? | |||
| More than once per day | 11 (7.4) | 6 (8.0) | 5 (6.8) |
| Once per day | 6 (4.1) | 1 (1.3) | 5 (6.8) |
| Three to six times per week | 12 (8.1) | 7 (9.3) | 5 (6.8) |
| Once or twice per week | 63 (42.6) | 36 (48.0) | 27 (37.0) |
| Not at all | 56 (37.8) | 25 (33.3) | 31 (42.5) |
| How often did your asthma symptoms (wheezing, coughing, chest tightness, shortness of breath) wake you up at night or earlier than usual in the morning? | |||
| Four or more times per day | 9 (6.1) | 4 (5.3) | 5 (6.8) |
| Two to three nights per week | 8 (5.4) | 5 (6.7) | 3 (4.1) |
| Once per week | 4 (2.7) | 2 (2.7) | 2 (2.7) |
| Once or twice per week | 37 (25.0) | 17 (22.7) | 20 (27.4) |
| Not at all | 90 (60.8) | 47 (62.7) | 43 (58.9) |
| How often have you used your reliever inhaler (usually blue)? | |||
| Three or more times per day | 12 (8.1) | 5 (6.7) | 7 (9.6) |
| Once or twice per day | 26 (17.6) | 13 (17.3) | 13 (17.8) |
| Two or three times per week | 21 (14.2) | 11 (14.7) | 10 (13.7) |
| Once per week or less | 42 (28.4) | 27 (36.0) | 15 (20.5) |
| Not at all | 47 (31.8) | 19 (25.3) | 28 (38.4) |
| How would you rate your asthma control? | |||
| Not controlled | 2 (1.4) | 1 (1.3) | 1 (1.4) |
| Poorly controlled | 2 (1.4) | 1 (1.3) | 1 (1.4) |
| Somewhat controlled | 22 (14.9) | 9 (12.0) | 13 (17.8) |
| Well controlled | 72 (48.6) | 41 (54.7) | 31 (42.5) |
| Completely controlled | 50 (33.8) | 23 (30.7) | 27 (37.0) |
The usage of the websites is shown in Table 23. This shows that the median number of logins in the 2-week period for both sites was 2, with a median number of page views of 14 for the intervention site and 15 for the comparator site. The median duration of use of the intervention site was 15 minutes and for the comparator site was 19 minutes. Three users never logged in to their allocated site. Table 23 also presents the results of post hoc significance tests for differences in usage between groups. This was a post hoc analysis suggested by the chairperson of our Trial Steering Committee. The differences between groups for number of logins and number of page views and total duration on the sites were not statistically significant.
| Usage measure | All participants (n = 148)a | Comparator (n = 75) | PEx (n = 73)a |
|---|---|---|---|
| Total number of logins to website | |||
| Median (minimum–maximum); IQR | 2 (1–48); 2–3 | 2 (1–32); 2–3 | 2 (1–48); 2–4 |
| p-value | 0.716b | ||
| Total number of pages visited | |||
| Median (minimum–maximum); IQR | 15 (1–65); 5–27 | 15 (1–65); 5–27 | 14 (1–62); 5–27 |
| Adjusted difference in medians (95% CI) | –1 (–7.830 to 5.830)c | ||
| p-value | 0.773 | ||
| Total duration on site (minutes)d | |||
| Median (minimum–maximum); IQR | 17 (0.5–471); 5–42 | 19 (0.5–471); 5–41 | 15 (0.5–119); 4–43 |
| Adjusted difference in medians (95% CI) | –3 (–14.946 to 8.946)c | ||
| p-value | 0.620 | ||
Figures 14 and 15 show dot plots of the total number of logins by randomised group with and without the extreme observations, respectively. The solid blue line indicates the median, and the lower and upper quartiles are shown by the dotted lines.
FIGURE 14.
Work package 3b: dot plot graphs of total number of logins by the randomised group for asthma (with extreme values). IQR, interquartile range.
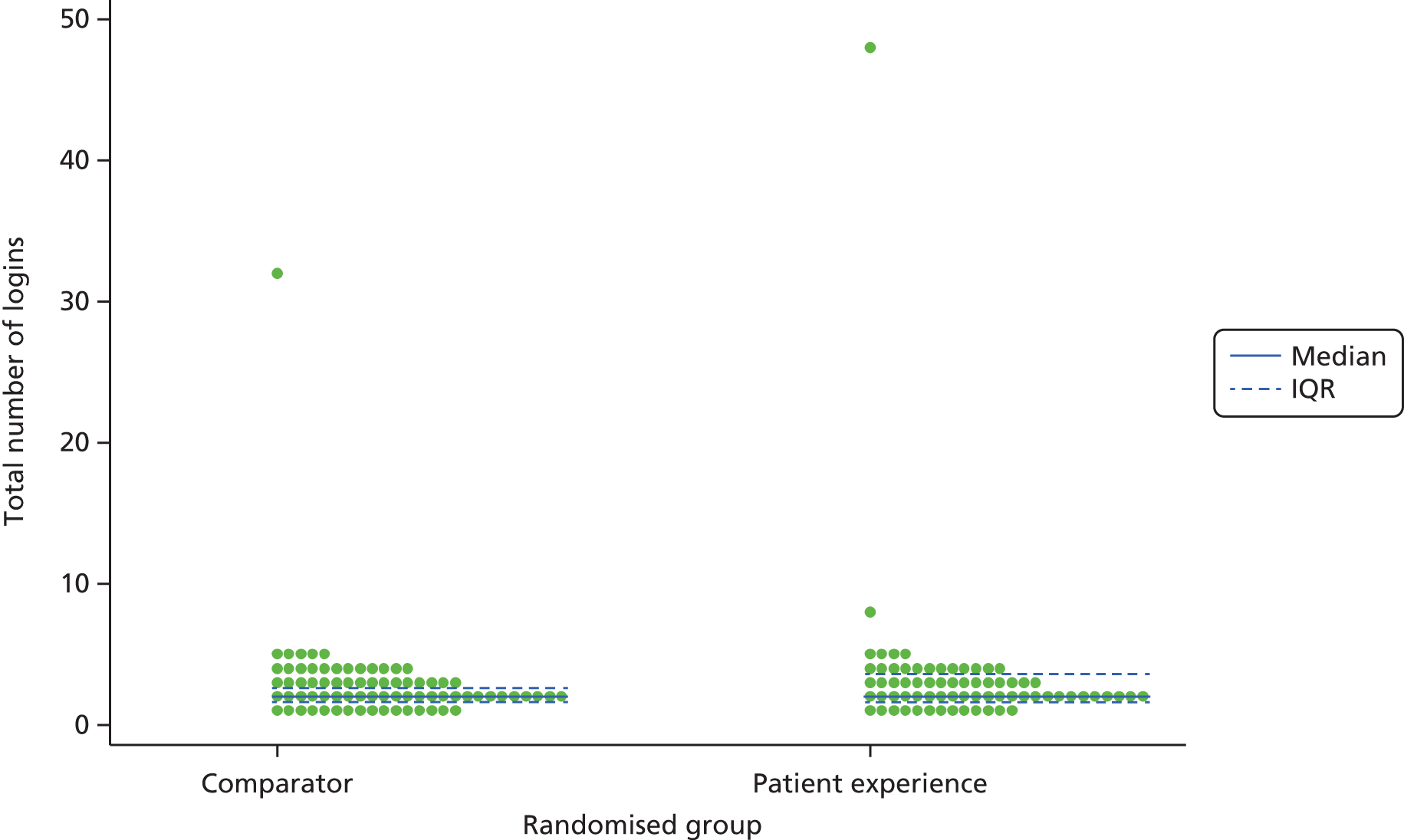
FIGURE 15.
Work package 3b: dot plot graphs of total number of logins by the randomised group for asthma (without the extreme values). IQR, interquartile range.
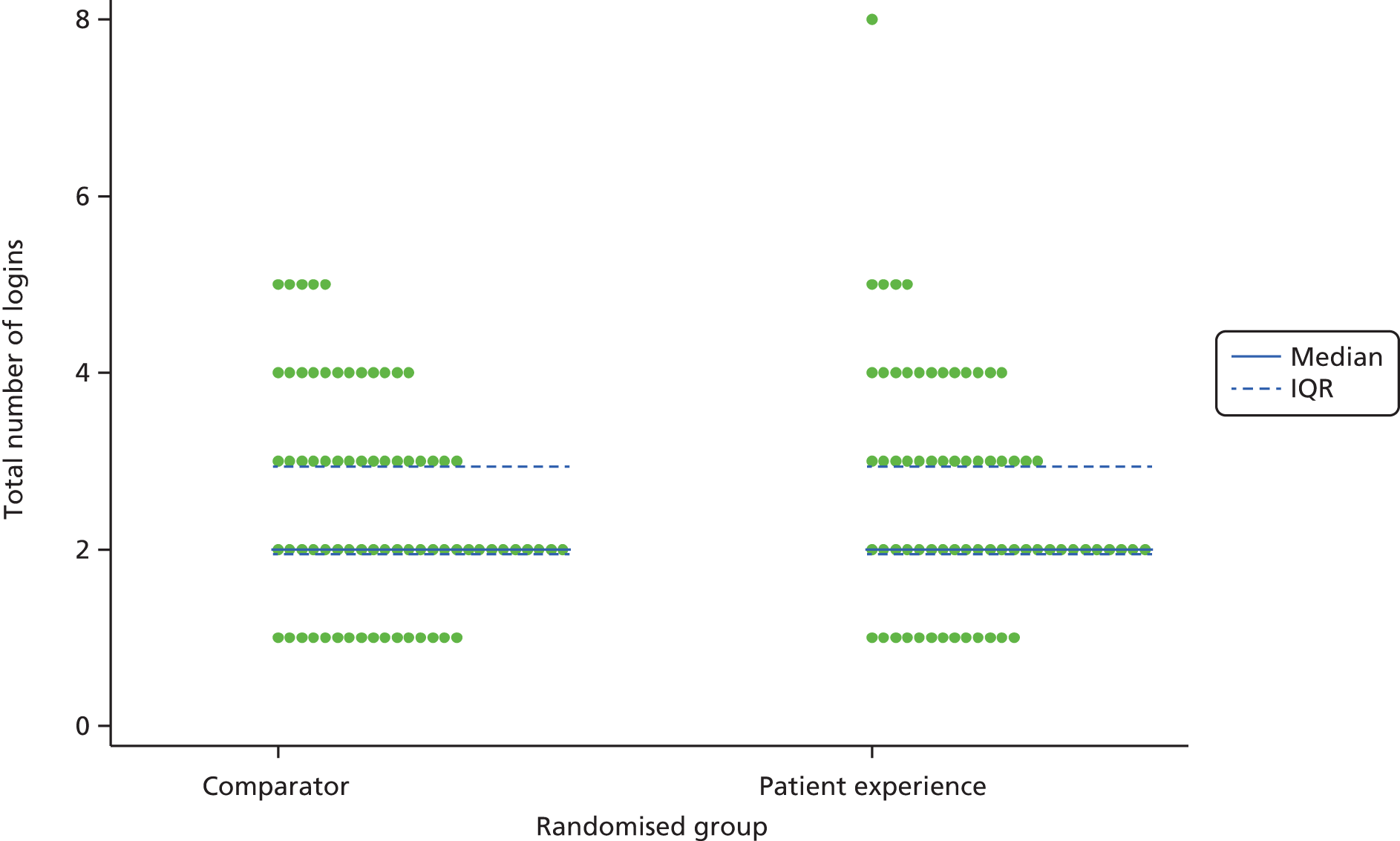
Figure 16 shows dot plots of the total number of pages visited by randomised group. The solid blue line indicates the median, and the lower and upper quartiles are shown by the dotted lines.
FIGURE 16.
Dot plot graph of total number of pages visited by the randomised group for asthma. IQR, interquartile range.
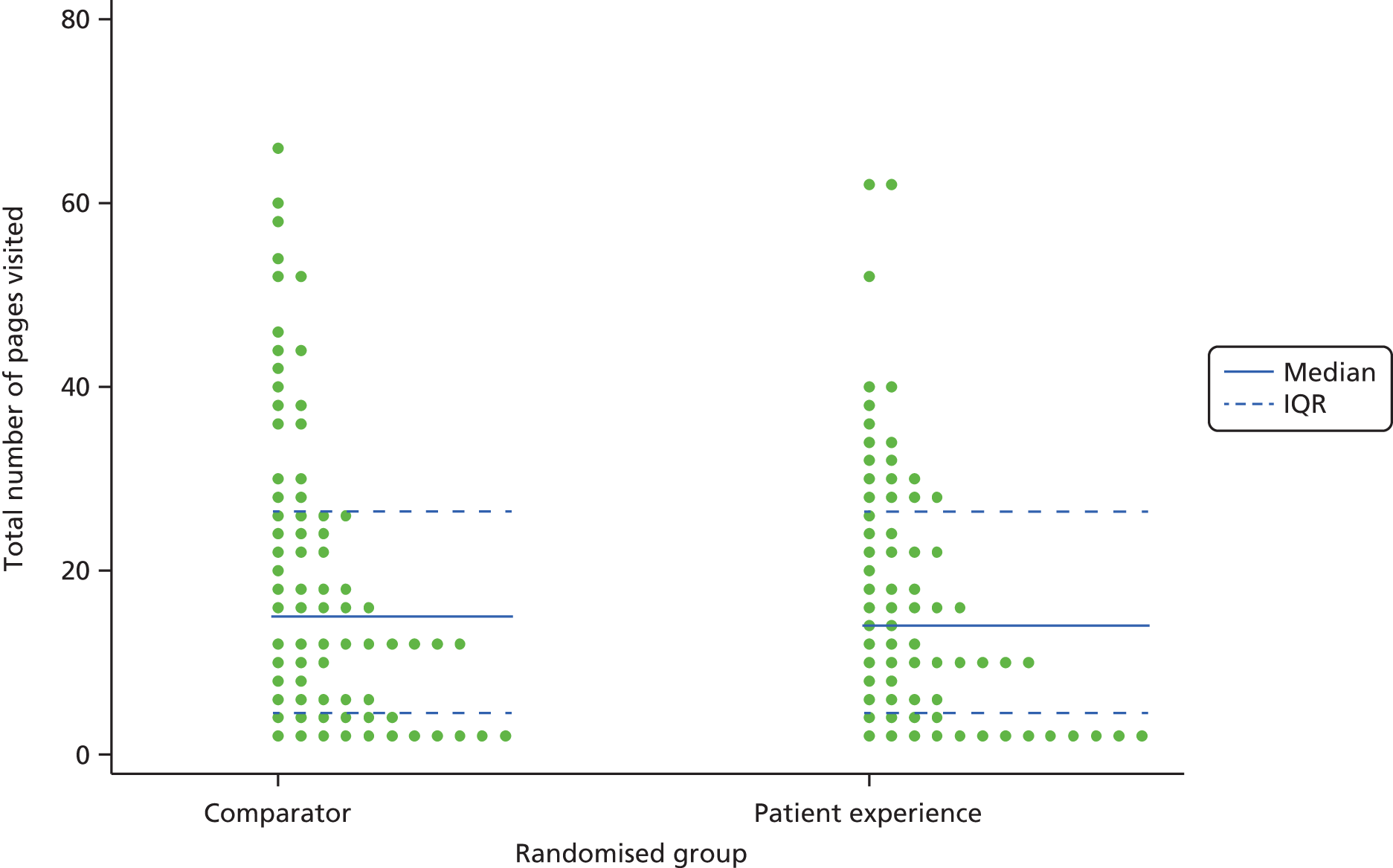
Figures 17 and 18 show dot plots of the total duration (minutes) on website by randomised group with and without the extreme observations, respectively. The solid blue line indicates the median, and the lower and upper quartiles are shown by the dotted lines.
FIGURE 17.
Work package 3b: dot plot graphs of total duration (minutes) on website by the randomised group for asthma (with extreme values). IQR, interquartile range.
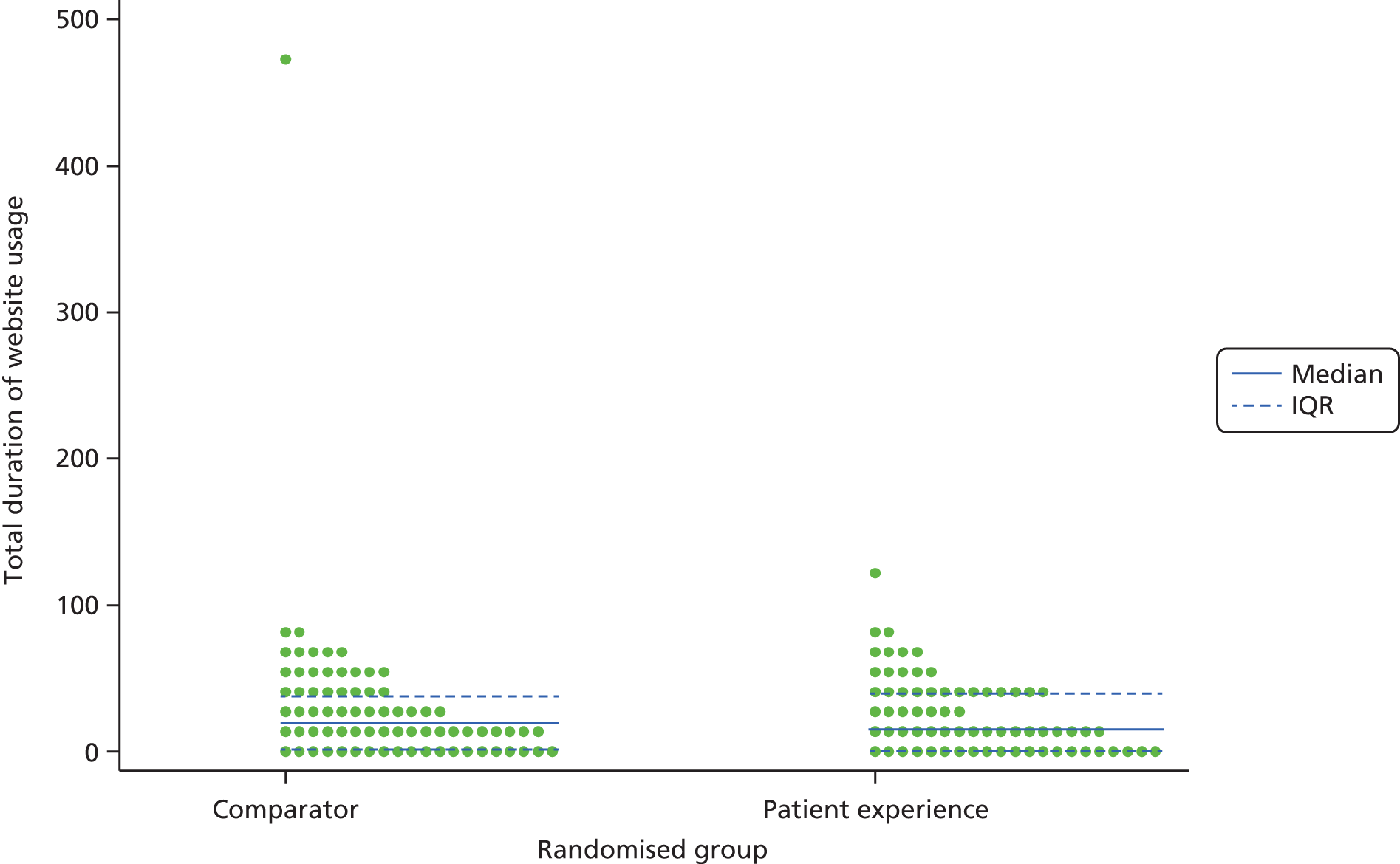
FIGURE 18.
Work package 3b: dot plot graphs of total duration (minutes) on website by the randomised group for asthma (without extreme values). IQR, interquartile range.
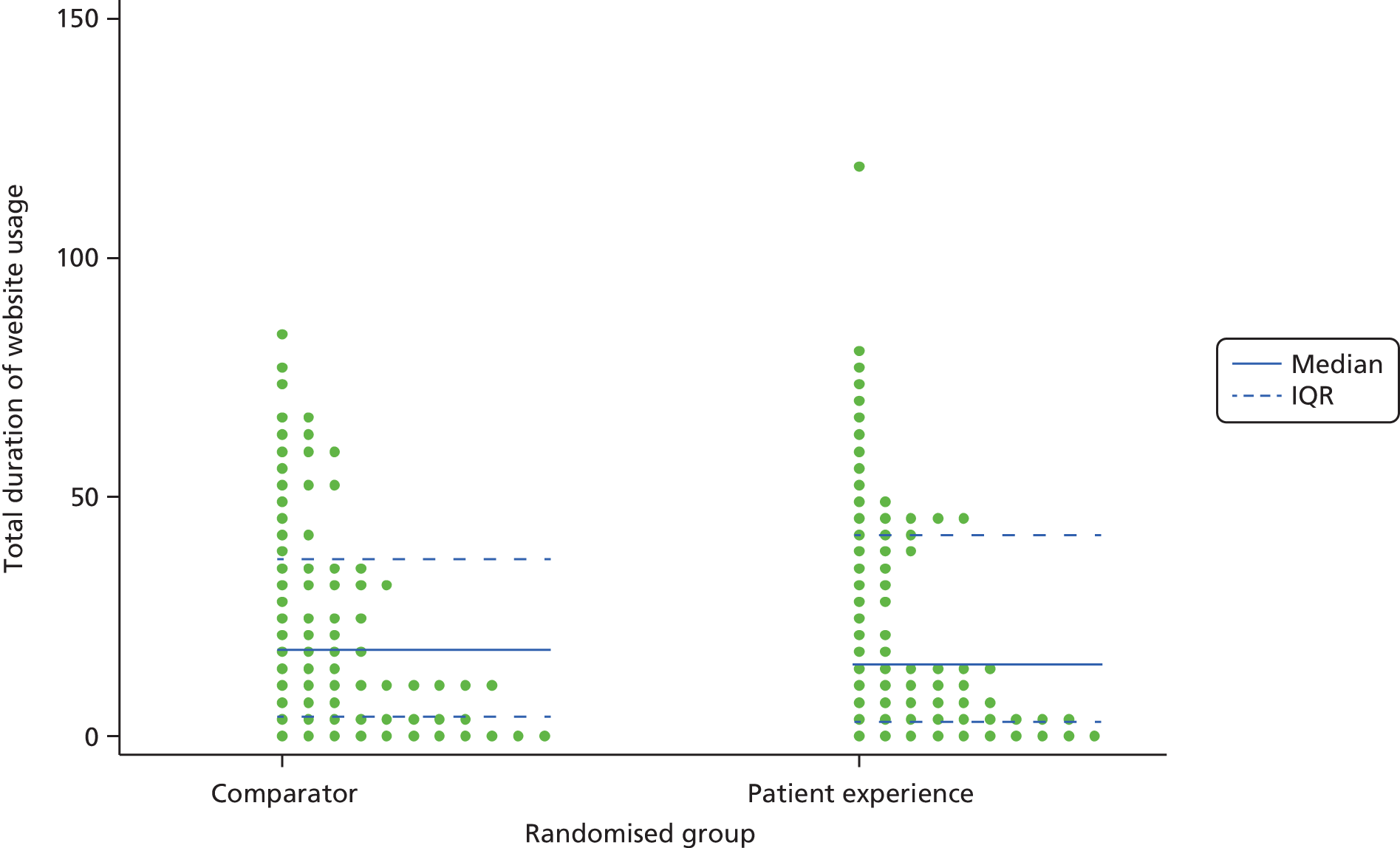
Table 24 shows summary statistics for baseline, 2-week follow-up and mean PIH scores. The mean (SD) change from baseline in the PEx (intervention) group was an increase of 0.068 (0.61), compared with an increase of 0.073 (0.64) in the comparator group. Treatment effect (mean differences with CI) was estimated using ANCOVA adjusting for baseline mean PIH scores, and showed that there were no significant differences between groups.
| Measure | Comparator (N = 75) | PEx (N = 73) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | Minimum to maximum | n | Mean (SD) | Minimum to maximum | |
| Mean baseline PIH scores | 71 | 6.816 (0.864) | 4.250 to 8.0 | 72 | 6.690 (0.888) | 4.083 to 8.0 |
| Mean 2-week PIH scores | 55 | 6.974 (0.995) | 3.750 to 8.0 | 61 | 6.847 (0.863) | 4.333 to 8.0 |
| Change from baseline | 54 | 0.073 (0.639) | –1.583 to 1.5 | 61 | 0.068 (0.606) | –1.833 to 1.25 |
| ANCOVA | ||||||
| PEx | 115 | aAdjusted mean difference –0.0186 | 95% CI –0.2475 to 0.2103 | |||
For the CDSES, two participants completed five of the six items at baseline (the mean of the five items was calculated) and four participants completed five items at follow-up (the mean of the five items was calculated). Higher scores indicate higher self-efficacy. The mean change from baseline to 2-week follow-up in the comparator group was an increase of 0.093, compared with a decrease of –0.068 in the PEx group. Treatment effect (mean differences with CI) was estimated using ANCOVA adjusting for baseline mean CDSES scores, which showed no significant difference between groups (Table 25).
| Measure | Comparator (N = 75) | PEx (N = 73) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | Minimum to maximum | n | Mean (SD) | Minimum to maximum | |
| Baseline CDSES scoresa | 74 | 8.207 (1.530) | 2.33 to 10.0 | 73 | 8.231 (1.611) | 1.83 to 10.0 |
| 2-week CDSES scoresb | 59 | 8.401 (1.501) | 4.00 to 10.0 | 62 | 8.238 (1.389) | 4.40 to 10.0 |
| Change in mean CDSES scores | 58 | 0.093 (0.951) | –3.00 to 2.33 | 62 | –0.068 (0.910) | –1.33 to 3.67 |
| ANCOVA | ||||||
| PEx | 120 | Adjusted mean differencec –0.1574 | 95% CI –0.4661 to 0.1512 | |||
The results for self-rated asthma control at the follow-up measurement are shown in Table 26.
| Self-rated asthma control during the past 2 weeks | All participants (N = 148), n (%) | Comparator (N = 75), n (%) | PEx (N = 73), n (%) |
|---|---|---|---|
| Not reporteda | 27 (18.2) | 16 (21.3) | 11 (15.1) |
| Poorly controlled | 2 (1.4) | 1 (1.3) | 1 (1.4) |
| Somewhat controlled | 11 (7.4) | 8 (10.7) | 3 (4.1) |
| Well controlled | 61 (41.2) | 26 (34.7) | 35 (47.9) |
| Completely controlled | 47 (31.8) | 24 (32.0) | 23 (31.5) |
The results for the SF-36 were also similar between groups and are shown in Table 27. Participants in both arms showed a small, non-significant improvement in health state from baseline in both the mental and physical components. The adjusted mean differences between the two groups (ANCOVA, n = 119 participants with full data) for the absolute change in PCS score of the SF-36 was 0.196 (95% CI –1.454 to 1.846) and for the absolute change in MCS score of the SF-36 was 0.843 (95% CI –1.066 to 2.750).
| Measure | Comparator (N = 75) | Intervention (N = 73) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | Minimum to maximum | n | Mean (SD) | Minimum to maximum | |
| Baseline PCS | 74 | 48.30 (10.34) | 18.38 to 60.88 | 72 | 48.40 (8.88) | 25.77 to 61.76 |
| 2-week PCS | 59 | 49.48 (9.12) | 20.02 to 60.43 | 61 | 49.56 (9.33) | 18.00 to 64.45 |
| Change in PCS from baseline | 58 | 0.67 (4.76) | –11.68 to 15.10 | 61 | 0.91 (4.80) | –11.11 to 17.15 |
| Baseline MCS | 74 | 49.62 (11.09) | 10.43 to 62.13 | 72 | 49.74 (9.16) | 24.01 to 63.05 |
| 2-week MCS | 59 | 50.59 (10.82) | 15.53 to 62.5 | 61 | 51.74 (8.01) | 28.67 to 63.16 |
| Change in MCS from baseline | 58 | 0.48 (5.63) | –17.56 to 18.08 | 61 | 1.25 (5.43) | –10.10 to 25.62 |
Multiple sclerosis carers
The recruitment of carers of people with MS proved challenging and was reviewed by the project team and the Trial Steering Committee on several occasions. As detailed in Methods, multiple routes to recruitment were used. Recruitment was slow, with usually between one and four carers recruited per month over the course of the study. Targeted advertising proved relatively unsuccessful and snowballing through personal contacts was more helpful. The first participant was recruited in June 2013 and the last participant completed follow-up in August 2014. The trial ended as the funding was ending and we had exhausted approaches to recruitment. Eventually, 47 invitations were sent in response to expressions of interest in the study, and 42 individuals (89%) completed registration (i.e. they consented and completed baseline questionnaires). No participants withdrew before randomisation and there were, therefore, 42 randomised participants (a recruitment rate of 100%). Twenty-two of these (52%) were allocated to the PEx website. Of the randomised participants, 6 out of 42 (14%) were lost to follow-up (please see the CONSORT flow diagram in Figure 19).
FIGURE 19.
Work package 3b: CONSORT flow diagram – carers of people with MS.
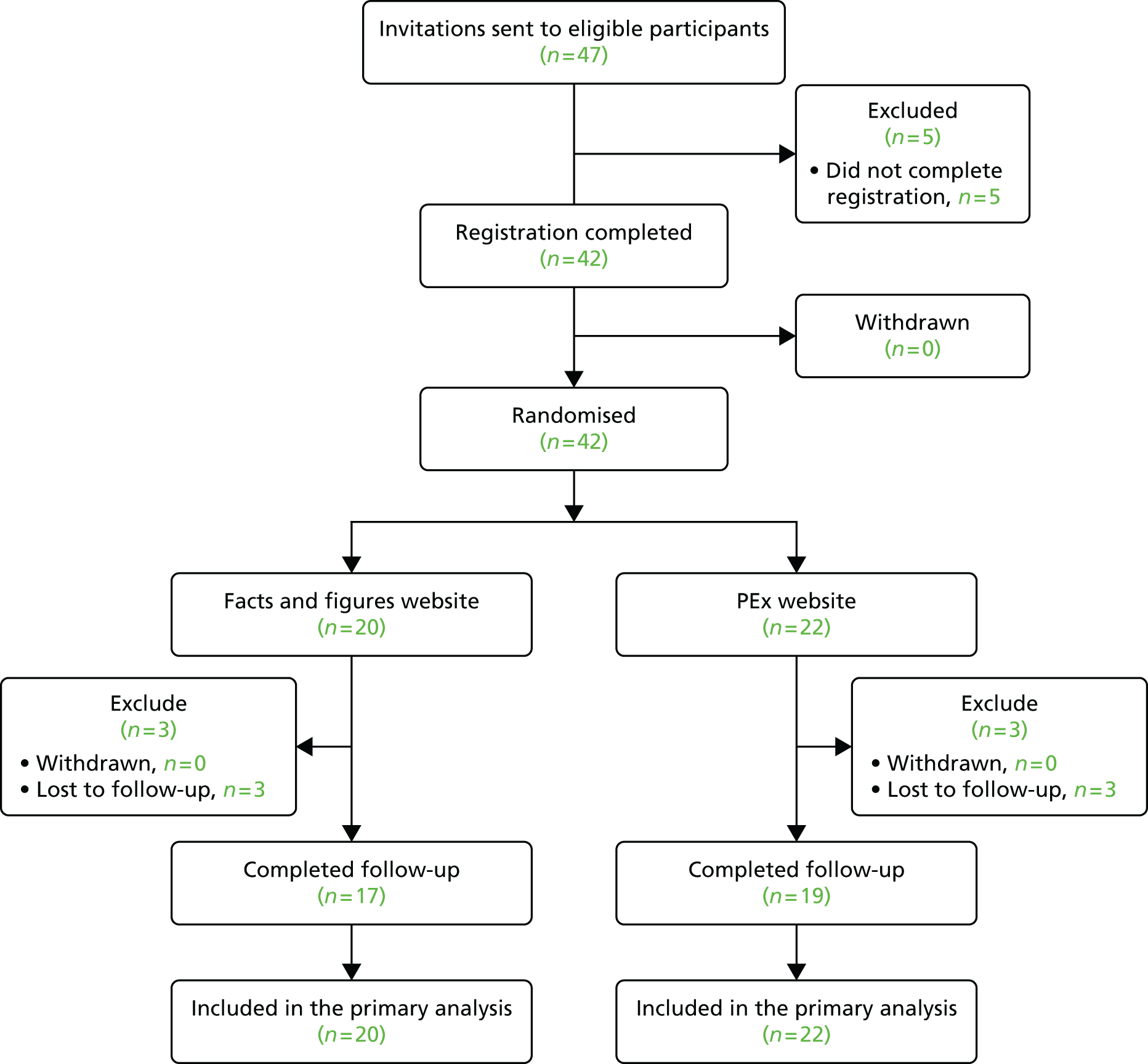
The baseline demographic and internet use characteristics of randomised participants are presented in Table 28 and were balanced between groups. Most were regular users of the internet with good to excellent self-reported internet abilities. Of the 42 participants, 18 (42.3%) were women.
| Baseline variable | Comparator (N = 20), n (%) | Intervention (N = 22), n (%) |
|---|---|---|
| Age | ||
| Mean (SD); minimum–maximum | 61.5 (11.6); 28.0–78.8 | 60.3 (13.2); 21.0–77.0 |
| Gender | ||
| Female | 8 (40.0) | 10 (45.5) |
| Male | 12 (60.0) | 12 (54.5) |
| Self-rated ability to use the internet | ||
| Excellent | 8 (40.0) | 8 (36.4) |
| Good | 8 (40.0) | 9 (40.9) |
| Fair | 4 (20.0) | 3 (13.6) |
| Poor | 0 (0) | 2 (9.1) |
| Bad | 0 (0) | 0 (0) |
| Internet use | ||
| At least once per day | 16 (80.0) | 19 (86.4) |
| Several times per week | 4 (20.0) | 2 (9.1) |
| Once per week | 0 (0) | 0 (0) |
| Less than once per week | 0 (0) | 1 (4.5) |
| Ethnicity | ||
| White: English/Welsh/Scottish/Northern Irish/British | 19 (95.0) | 22 (100.0) |
| White: any other white background | 1 (5.0) | 0 (0) |
The usage of the websites is shown in Table 29. This shows that the median number of logins in the 2-week period for both sites was 4, with a median number of page views of 27.5 for both the intervention and comparator sites. The median duration of use was 31 minutes for the intervention site and 31.5 minutes for the comparator site. Table 29 also presents the results of post-hoc significance tests for differences in usage between groups. This was a post hoc analysis suggested by the chairperson of our Trial Steering Committee. The differences between groups for number of logins and number of page views and total duration on site were not statistically significant.
| Usage measure | All participants (N = 42) | Comparator (N = 20) | PEx (N = 22) |
|---|---|---|---|
| Total number of logins to website | |||
| n | 42 | 20 | 22 |
| Median (minimum–maximum); IQR | 4 (1–12); 2–5 | 4 (1–9); 2–5 | 4.5 (1–12); 2–5 |
| p-value | 0.692a | ||
| Total number of pages visited | |||
| n | 42 | 20 | 22 |
| Median (minimum–maximum); IQR | 27.5 (1–438); 13–61 | 27.5 (1–291); 12–46 | 27.5 (1–438); 14–67 |
| Adjusted difference in medians (95% CI) | 19 (–11.40 to 49.40) | ||
| p-value | 0.214b | ||
| Total duration on site (minutes)c | |||
| Median (minimum–maximum); IQR | 31.5 (0.5–143); 10–61 | 31.5 (1–143); 13–50 | 31 (0.5–139); 8–84 |
| Adjusted difference in medians (95% CI) | 1 (–34.34 to 36.34) | ||
| p-value | 0.955b | ||
Figure 20 shows a dot plot of the total number of logins by the randomised group. The solid blue line indicates the median, and the lower and upper quartiles are shown by the dotted lines.
FIGURE 20.
Work package 3b: dot plot graphs of total number of logins by randomised group for carers of people with MS. IQR, interquartile range.
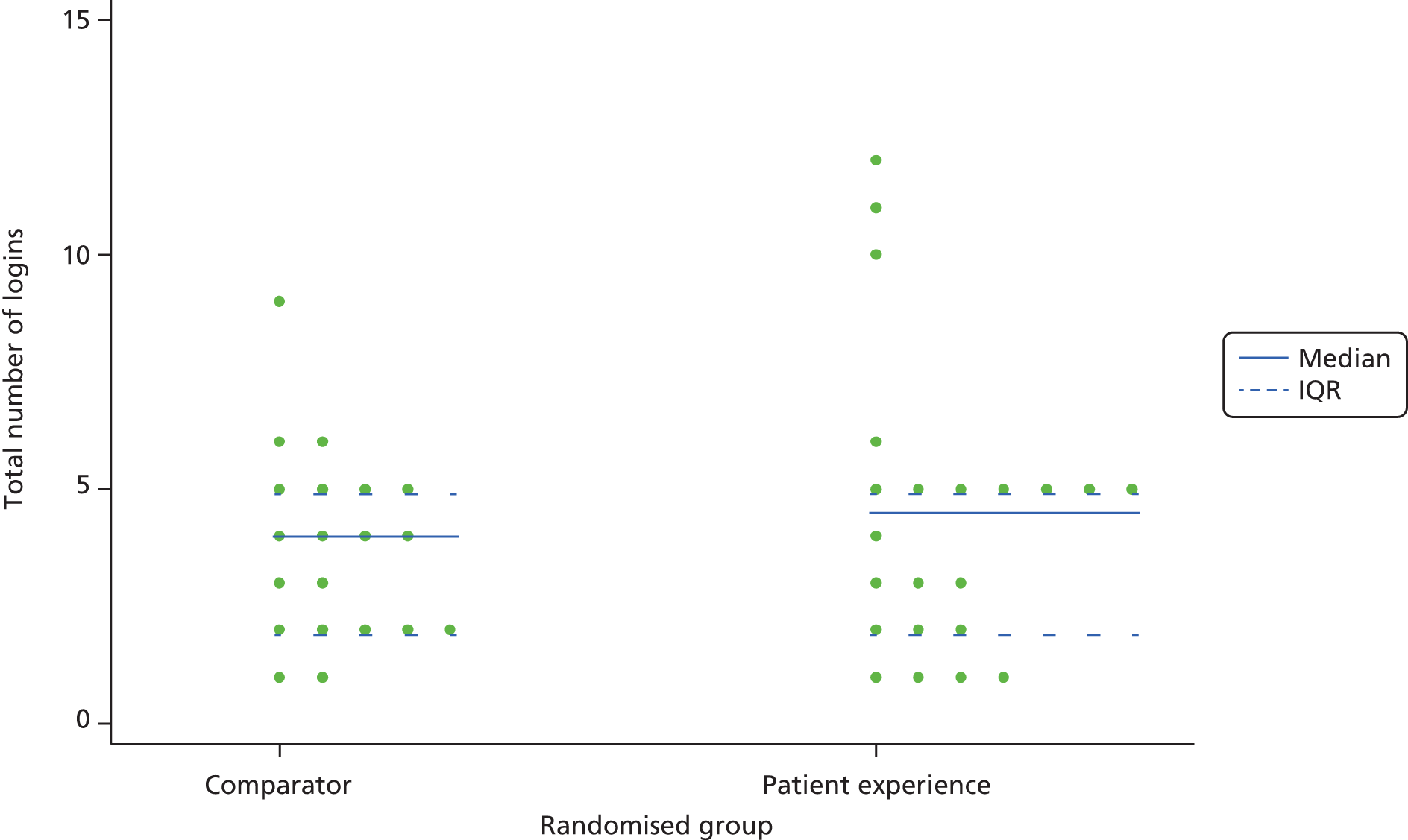
Figure 21 shows dot plots of the total number of pages visited by the randomised group. The solid blue line indicates the median, and the lower and upper quartiles are shown by the dotted lines.
FIGURE 21.
Work package 3b: dot plot graph of total number of pages visited by randomised group for carers of people with MS. IQR, interquartile range.
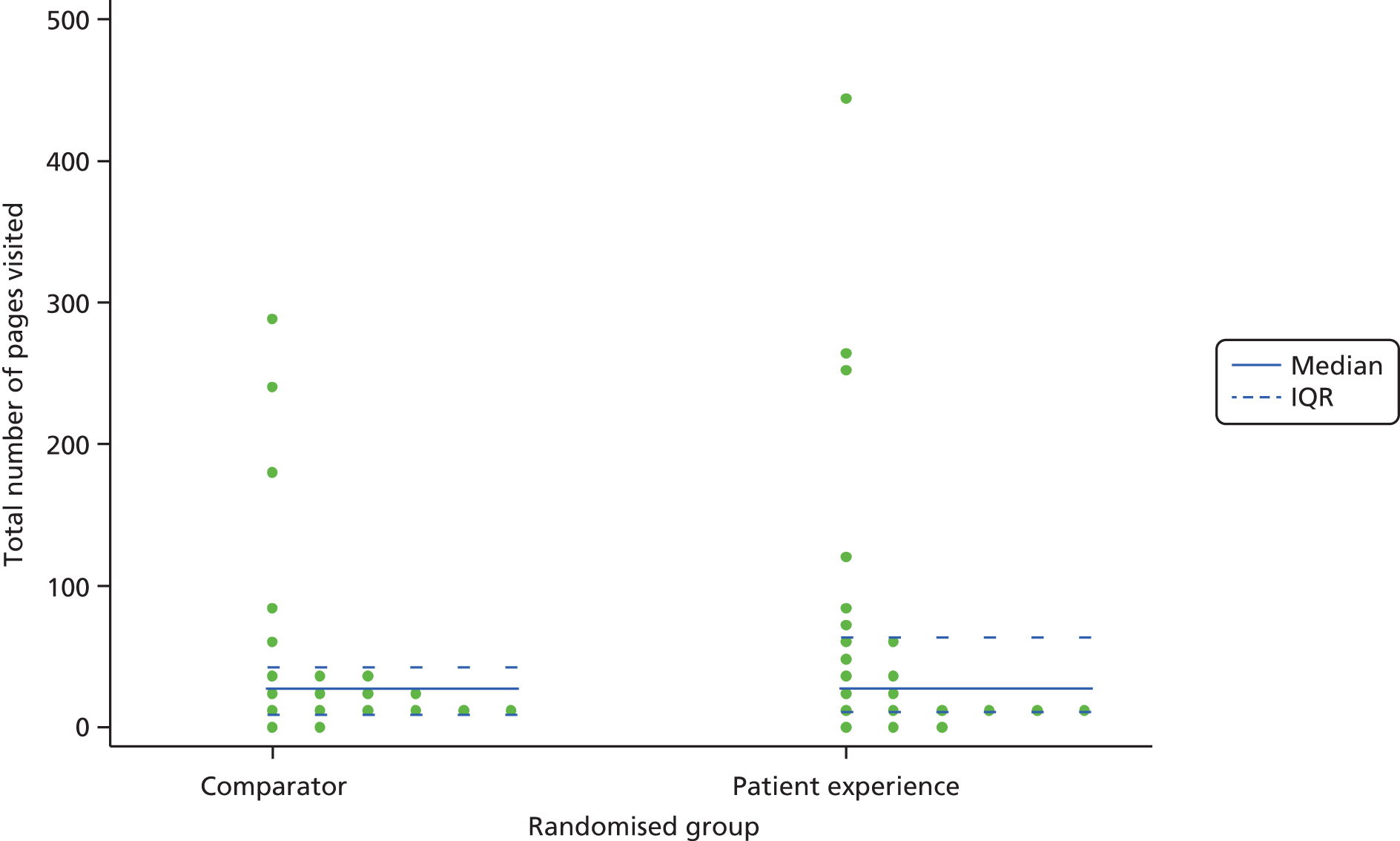
Figure 22 shows a dot plot of the total duration (minutes) on website by the randomised group. The solid blue line indicates the median, and the lower and upper quartiles are shown by the dotted lines.
FIGURE 22.
Work package 3b: dot plot graphs of total duration (minutes) on website by randomised group for carers of people with MS. IQR, interquartile range.
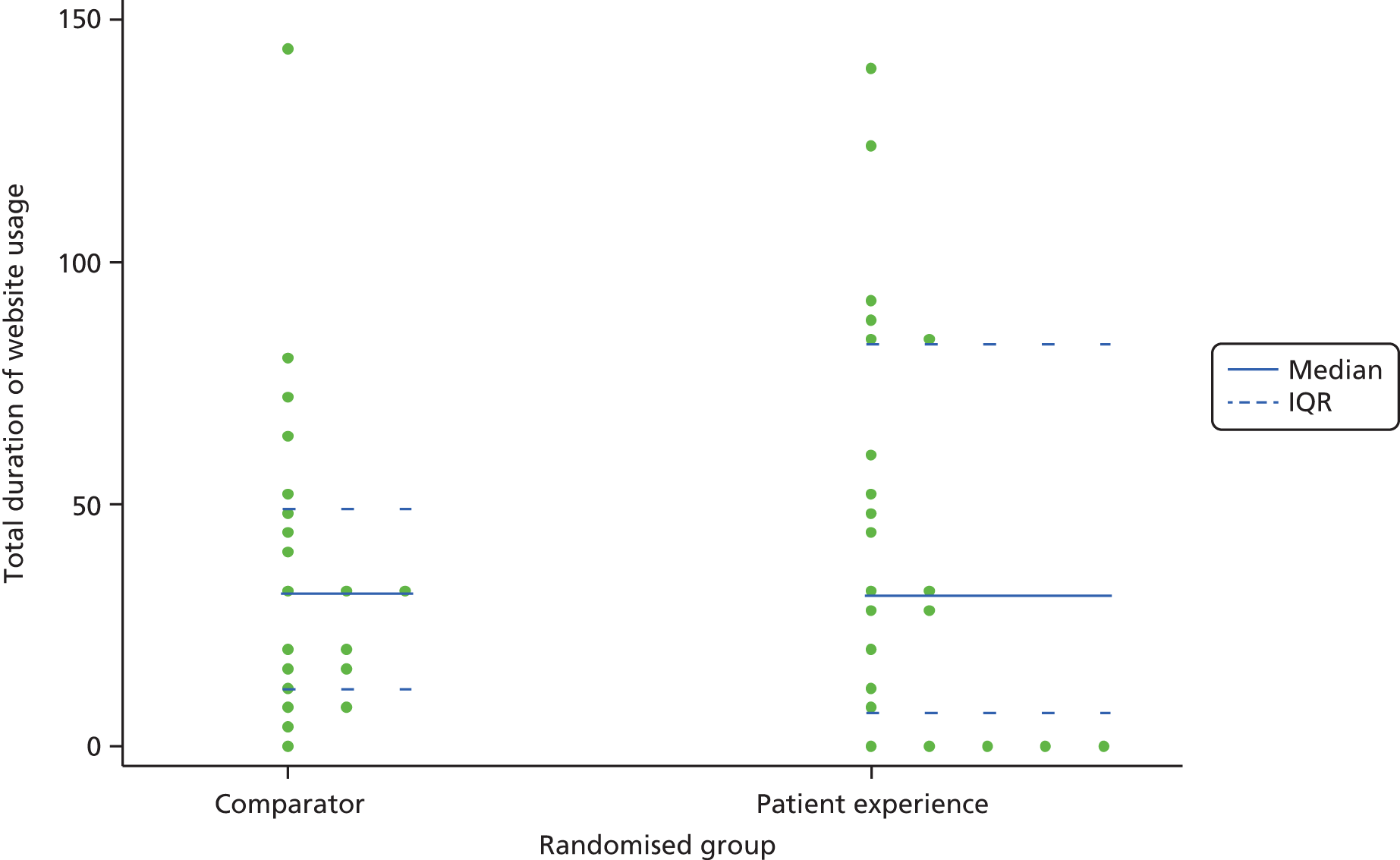
The mean PFCS scores were similar between the randomised groups. The summary of PFCS scores are shown in Table 30. The change in PFCS score from baseline was very similar in both groups (intervention –0.16, comparator –0.15), with both groups showing a small decrease in PFCS score at the 2-week follow-up.
| Measure | Comparator (N = 20) | PEx (N = 22) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | Minimum to maximum | n | Mean(SD) | Minimum to maximum | |
| Baseline PFCS | 20 | 2.42 (1.03) | 0.63 to 4.00 | 22 | 2.28 (0.75) | 0.88 to 3.88 |
| 2-week PFCS | 17 | 2.19 (1.01) | 0.50 to 4.00 | 19 | 1.97 (0.77) | 0.13 to 3.25 |
| Change in PFCS score from baseline | 17 | –0.15 (0.78) | –2.38 to 0.88 | 19 | –0.16 (0.59) | –1.38 to 0.75 |
The results for the SF-36 were also similar between groups and are shown in Table 31. Participants in both arms showed non-significant worsening in health state from baseline in the physical component scores. The adjusted mean differences between the two groups (ANCOVA, n = 36 participants with full data) for the absolute change in PCS score of the SF-36 was 0.365 (95% CI –2.756 to 3.486) and for the absolute change in MCS score of the SF-36 was 2.655 (95% CI –1.788 to 7.099).
| Measure | Comparator (N = 20) | Intervention (N = 22) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | Minimum to maximum | n | Mean (SD) | Minimum to maximum | |
| Baseline PCS | 20 | 51.01 (11.70) | 18.23 to 63.01 | 22 | 50.00 (9.08) | 31.51 to 67.26 |
| 2-week PCS | 17 | 50.72 (10.63) | 18.79 to 63.26 | 19 | 48.80 (7.47) | 30.21 to 61.27 |
| Change in PCS from baseline | 17 | –1.73 (2.84) | –6.33 to 5.12 | 19 | –0.72 (6.33) | –15.32 to 15.19 |
| Baseline MCS | 20 | 48.64 (8.75) | 28.26 to 58.55 | 22 | 45.68 (14.55) | 15.08 to 64.06 |
| 2-week MCS | 17 | 46.22 (9.02) | 26.86 to 57.55 | 19 | 44.19 (14.70) | 17.59 to 60.57 |
| Change in MCS from baseline | 17 | –3.11 (5.80) | –18.06 to 6.03 | 19 | 0.21 (7.00) | –15.89 to 14.21 |
e-Health Impact Questionnaire findings
The eHIQ part 2 is administered at follow-up only, as it captures the attitudes of the respondents towards the website they have recently viewed. Tables 32 and 33 show the eHIQ part 2 results comparing the responses from participants who viewed the PEx website with those of participants who viewed the comparator websites, for all three conditions combined. Table 32 shows that there were only small, non-significant differences between the PEx and the non-PEx groups, both overall and on the three subscales (confidence and identification; information and presentation; and understanding and motivation).
| Measure | Comparator | PEx |
|---|---|---|
| eHIQ-part 2 overall scores | ||
| n | 103 | 110 |
| Mean (SD) | 67.15 (11.99) | 65.07 (10.12) |
| Minimum–maximum | 23.38–98.03 | 36.11–96.99 |
| Subscales | ||
| Confidence and identification | ||
| n | 105 | 112 |
| Mean (SD) | 60.08 (15.22) | 58.85 (12.62) |
| Minimum–maximum | 2.78–97.22 | 16.67–97.22 |
| Information and presentation | ||
| n | 106 | 114 |
| Mean (SD) | 75.32 (10.84) | 73.25 (10.73) |
| Minimum–maximum | 43.75–100 | 46.88–100 |
| Understanding and motivation | ||
| n | 106 | 112 |
| Mean (SD) | 64.62 (15.30) | 68.87 (12.85) |
| Minimum–maximum | 11.11–100 | 19.44–100 |
| Measure | n | Unadjusted mean difference | 95% CI |
|---|---|---|---|
| Overall score | 213 | –2.085 | –5.076 to 0.906 |
| Subscales | |||
| Confidence and identification | 217 | –1.225 | –4.957 to 2.506 |
| Information and presentation | 220 | –2.079 | –4.946 to 0.789 |
| Understanding and motivation | 218 | –1.751 | –5.516 to 2.014 |
Qualitative interviews
The qualitative interviews are discussed in detail in Chapter 9. Here we present only brief findings in relation to the trial design and process. The demographic characteristics of the interview participants are discussed in Chapter 9. In brief, the 30 interview participants were slightly older, and more likely to be retired, than those in the feasibility trials. The interviews demonstrated that the interventions and the online trial process were acceptable and usable. We did not identify major barriers to participation in the trial nor to use of the interventions: the interviews confirmed the pilot study findings that the technical aspects of the online trial had worked well, that the reminders were considered appropriate and that the questionnaires were not too burdensome.
People were motivated to take part in the trial for a fairly narrow range of reasons, including because the condition was relevant to them, the study sounded interesting, they were asked by their general practice and they liked to help with research.
There were few problems reported with accessing the websites (underlining the value of the pilot work and troubleshooting), although a couple of the participants had had difficulty on at least one occasion with opening the video clips. During the pilot study this had been associated with particular browsers. In the interviews people sometimes appeared unsure which ‘browser’ they had been using. The amount of time needed to complete the questionnaires at baseline and follow-up and the frequency of reminders were generally acceptable. Several of the participants said that they would have preferred longer access to the website as the limited period of 2 weeks meant that they had not had time to visit it as much as they would have liked. One man commented that, despite the e-mail reminders, he had been taken aback to discover that he no longer had access.
Participants were generally positive towards the website content, navigation and layout (comparator and intervention). Participants confirmed that certain aspects of the guidelines which had been used to develop the sites, such as the importance of reputable branding and the lack of commercial advertising, supported their impression of the trustworthiness of the website.
The interviews also shed light on the nature of usage and engagement with the websites, and how this differed from a pragmatic ‘real-world’ use of online resources. Some participants (including those allocated to the intervention and to the comparator) reported methodically working through their allocated websites in the order that the material appeared, as they felt that this was the task required of them, rather than selecting the information that interested them. Similarly, some reported logging on to the site only in response to automated reminder e-mails.
Discussion
The primary objective of this trial was to assess the feasibility and measure the impact of a PEx-based website in comparison with a ‘facts and figures’ website using a randomised trial. Our findings show that it was possible to recruit people with asthma and people who smoke to the studies. People with asthma were, in particular, relatively easily recruited through primary care. In contrast, carers of people with MS were very hard to recruit, despite our trying multiple routes and making serial amendments to our approved strategies with the ethics committee. This may indicate that carers, by the nature of their role, have other priorities or are simply too busy to take part in research studies. It may also reflect the fact that many people with MS do not have someone who has this role, or, if they do, that person may not define themselves as a ‘carer’ or may resist this terminology. 173 The qualitative interviews suggest that the eligibility criteria were not always applied correctly: some smokers had already given up, while others had no desire to quit. Similarly, participants in the asthma trial did not take part with a motive to improve self-management. There are clearly lessons here for recruitment and eligibility assessment in subsequent work.
As might be expected, recruited participants had a relatively high self-rated ability to use the internet. The interventions were delivered successfully and there were no adverse events. Retention rates were moderate (75% for smoking cessation, 82% for asthma and 86% for carers), considering the short period of follow-up. We sent up to two reminder e-mails and one telephone contact to participants to complete their self-report follow-up measures. Other work has shown the high levels of attrition in online trials of fully automated internet interventions, and the value of more intensive contact in reducing this. 174 The absence of face-to-face contact (between participants and researchers) in a study such as this is one attraction of internet trials, as it lowers the cost and allows the trial to be more geographically dispersed. However, there is a trade-off between this lack of personal contact and rates of loss to follow-up.
Our comparisons between randomised groups showed no differences on the self-report measures, which included condition-specific outcomes, health status and a questionnaire specifically designed to capture the attitudes of users towards a health website. In this study, the comparator group received access to factual information from the leading health information site in the UK (NHS Choices), so it would be surprising if our novel interventions containing personal accounts were to show major comparative benefits, and, in any case, as ours was a feasibility study we did not have the statistical power to examine these differences. The findings from our secondary outcome measures may be useful to derive effect sizes to inform power calculations for future studies which are designed to look for these differences. It is encouraging that the experience-based intervention groups showed no harms compared with the fact-based website comparators. Our choice of a best-practice comparator was appropriate to determine whether or not the novel interventions may be ‘harmful’, but future work should consider evaluating experience-based information as additional rather than as alternative, especially given the comments in the qualitative interviews about the place of experience-based information as a complement rather than a contrast to more factual information.
With the caveats of the difficulty in recruiting carers of people with MS, and the eligibility issues, we believe that the trial demonstrated adequate ‘technical feasibility’ and had good internal validity. However, we believe that there are significant questions to address regarding external validity and generalisability to ‘real-world’ internet use and information-seeking behaviour. On average, actual use of the websites (both intervention and comparator) was infrequent. The median numbers of logins in the smoking cessation, asthma and carers trials were (respectively) 2, 2 and 4; the median numbers of page views were 10, 15 and 27.5; and the median total duration on site was 9 minutes, 17 minutes and 31.5 minutes. This suggests that the MS carers sites were used more frequently than the asthma site, which in turn was used more frequently than the smoking sites. It is important to note that there was wide variation between the minimum and maximum users. This low actual use of an internet intervention is common in many e-health trials, and the plausibility of this level of exposure having an effect should be considered, as well as some determination of what level of engagement with the intervention would be sufficient. The low usage of both intervention and comparator also suggests that participants were ‘assessing’ the websites (as instructed), rather than using them in a more natural way. The qualitative interview findings also raised questions over the nature of engagement and whether the participants were using the sites to help themselves or because they were undertaking a task to help researchers.
In designing further work and addressing engagement and use, it will be important to address the issue of what constitutes ‘exposure’ and ‘dose’ in relation to online information, and whether or not these are appropriate conceptualisations for information behaviour. We used a period of 2 weeks during which we invited participants to access their allocated website. In practice, people do not use a single source of information for a short defined period of time (unless, as with a patient decision aid, it is designed to influence a single decision at one point in an illness trajectory which may more easily fit a trial design). In packaging up experience-based interventions designed to influence outcomes such as self-efficacy or health behaviour change, rather than a single decision, we used a randomised trial design, in line with conventional approaches to generating evidence for an intervention. In a real-world setting, experiential information is rarely isolated from other resources, and internet users do not all use websites in the same way or ‘consume’ them in a 2-week period. Internet users search and browse, and do not generally visit sites ‘on prescription’. They can also produce and share experiences as well as consume them, thus contributing to the experiences made available to others, and websites which gather people’s experiences tend to evolve over time. Any future larger efficacy study of these or similar web-based resources needs to address these issues and understand how to embed such interventions in people’s everyday lives. This could draw on the MRC’s new guidance on developing and evaluating complex interventions, including the recent additional guidance on process evaluation. 167,175
Such future work should incorporate an understanding of real-world online information behaviour, including the use of social media. Future work could assess the potential value in being able to tell your story, in addition to hearing about others’, as well as the opportunity for an experience-based intervention to be changed by its users. There is also a need to establish the place of other people’s accounts: should they be ‘stand-alone’, or incorporated into other internet-based interventions, or used as an adjunct alongside them? It will also be important to identify which user groups, and at what points within a trajectory of illness (or health behaviour), this type of intervention may be most useful for, as our qualitative interviews demonstrated that people, not surprisingly, have their own personal preferences for types of information, at different times. Future work should consider how information, including experiential information, can best be tailored for an individual. Finally, future health economic work could examine the cost benefit of PEx-based web resources, especially given the absence of harm demonstrated in this study, and the low marginal cost of a highly scalable public website intervention.
This study adds to a nascent literature looking at the value of digital interventions which attempt to harness narrative information from peers to influence health attitudes and behaviour. 176,177 Emerging work by others is testing the value that narrative accounts could have in modifying attitudes to breast screening among African American women,178,179 in helping people with hypertension achieve control of their blood pressure180 and in achieving lifestyle change for people with coronary heart disease and low-back pain. 181
Conclusion
The internet is playing a significant role in health and health care and offers one opportunity for innovative, low-cost, highly scalable approaches to health challenges. The online sharing of personal experiences of health and illness is a relatively new phenomenon and we have tested the feasibility of assessing its impact in a randomised trial. Our original intention for this programme of work was to identify whether or not, when and how to incorporate PEx into online health information. We showed that PEx-based interventions could be developed and used and that a trial was technically feasible, with some recruitment issues. We showed no harm from the interventions. In common with many internet interventions, actual use of the websites was relatively low and there was attrition from the trials. In beginning to address the ‘whether or not, when and how’ questions (also addressed by our other workstreams, from different perspectives), one contribution of this feasibility trial was to establish the limitations of a RCT approach. In the next chapter we discuss how personal preference for style of information is an important factor that does not fit easily with a standard RCT design, and future work also needs to understand how to maximise engagement with information-based websites and how to assess the value of such interventions in more pragmatic, everyday use, rather than (as with a drug intervention) an isolated ‘dose of information’ with a 2-week exposure.
Chapter 9 Qualitative interviews with a subset of the feasibility trial participants
Abstract
Introduction: qualitative interviews were conducted to explore the process of taking part in the trial, to gain an understanding of participants’ perspectives on their allocated website and to encourage reflections on the pros and cons of different types of online health information.
Methods: thirty of the trial participants took part in an interview within a few weeks of completing their follow up measures. The interviews were conducted in people’s homes, or at their workplace if they preferred, and were audio recorded and transcribed for thematic analysis.
Findings: the interviews included perspectives on the process of the trial, which was acceptable and not burdensome to the participants (data are discussed in Chapter 8), and a discussion of a variety of different types of websites, prompted by laminated cards. The results were analysed in relation to the seven domains identified in the conceptual review. The relevance of the seven domains were supported by the interviews and there was evidence (as anticipated) that different domains were applicable to different conditions; for example, the negative impact of visualisation was raised only in MS and smoking, not in asthma. Facts and figures were seen as important, particularly soon after diagnosis (asthma and MS).
Conclusions: the interviews underlined the highly individual manner in which patients assemble their own online information landscape, the requirements of which change at different stages. Personal experiences are valued and approached, with some caution, as a supplement, but not a substitute, for facts and figures from a trustworthy source.
Background and methods
Trial participants were asked to indicate if they would be willing to take part in a face-to-face interview in the weeks after they completed their follow-up measures. We selected participants purposively to cover the three different groups (asthma, MS carers and smoking cessation) and to include those from the intervention and comparator arms of the trial. We interviewed men and women and also aimed for a range of different types of engagement with the websites (some who had visited the site often and some who had only looked at it a couple of times). More details about the qualitative interview sample can be seen in Table 34.
| Characteristic | Smoking cessation | Asthma | MS carers |
|---|---|---|---|
| Mean participant age | 62 years (range 47–72 years) | 54 years (range 21–72 years) | 61 years (range 23–79 years) |
| Allocated to intervention (n) | 7 (3 male, 4 female) | 3 (2 male, 1 female) | 6 (2 male, 4 female) |
| Allocated to comparator (n) | 5 (4 male, 1 female) | 4 (1 male, 3 female) | 5 (4 male, 1 female) |
The interviews were conducted by SZ (12 interviews), coinvestigator LL (nine interviews) and research assistant NN (nine interviews). A researcher arranged to visit people’s homes to conduct the interview at a time that suited the respondent. Interviews lasted between 45 and 90 minutes and were digital audio recorded for transcription and analysis. The interview schedule was developed with assistance from the wider programme team and covered:
-
Taking part in the trial: motivation to participate, views of the trial procedures, the questionnaire measures and reminders. These data are discussed in Chapter 8.
-
Specific questions (different for each arm of the study) about the website: what they looked at, how they decided what to look at, thoughts about the straplines, visual design and different ways of presenting material. To prompt discussion and help remind people about the site layout, we took laminated cards showing different pages. These questions drew on the engagement framework aspects of gating, engagement and outcomes (see Chapter 6). These data are discussed in Chapter 8.
-
Content comparisons: participants were asked to discuss the pros and cons of six different types of health website. Participants were shown laminated cards with (1) a health blog, (2) a patients’ forum, (3) a national charity home page with facts and figures, (4) a national charity page with a personal experience, (5) a hospital trust ‘rating’ page and (6) the Patients’ Opinion home page. Participants were also asked which of these they might use or contribute to and discuss the reasons for their answers. This content comparison helped us to explore the seven domains from the conceptual review, which is the focus of this chapter.
-
Finally, participants were asked about their views of ‘sharing experiences’ online and whether or not (and why) this was something they could imagine doing themselves. They were asked if there were any other issues they wanted to raise in relation to the study and if they would like to be sent results of the study in due course (all said that they would).
Approach to analysis
The three researchers who had conducted the interviews and coinvestigator SW read the same few interviews and agreed a coding frame based on the elements of the engagement framework (gating, engagement and outcomes) and the seven domains from the conceptual review (finding information, feeling supported, maintaining relationships with others, affecting behaviour, experiencing health services, learning to tell the story and visualising disease). We also coded ‘trust’ and the emerging issue of ‘timing/need’, which reflected an important set of comments around the point(s) in any given health trajectory at which experiential information might be regarded as more relevant or helpful. Each of the researchers coded her own interviews using the coding frame and NVivo. We used constant comparison to develop our coding, and considered the reasons for any differences between the three conditions in preparing the thematic analysis for this chapter.
The qualitative analysis presented in this chapter is based on all of the interviews because people in both arms of the study were asked to discuss and compare the six different types of websites. People in the comparator arm as well as the intervention arm had some very interesting things to say about the pros and cons of PEx and facts and figures, sometimes prompted by the laminated cards that we used in the interviews and sometimes due to their reflections on the value, and limitations, of the website they had access to in the study. Quotations from the interviews are presented along with brief sociodemographic information about the participant and whether they had been in the comparator or intervention arm.
Findings
Findings about the trial process (sections 1 and 2 of the interview, described above) contributed to the interpretation of the feasibility trial results and are discussed in Chapter 8. In this chapter we discuss the findings from the interviews (mainly, but not exclusively, drawn from section 3 of the interview) in relation to the seven domains from the conceptual review. Finally, we discuss comparisons between different types of sites and the importance of timing of access.
Finding information
The research interviewers were careful not to assume that people were approaching the websites primarily as a source of ‘health information’ (we were, after all, aware that there were at least six other domains that might be relevant). All of the participants made it clear that the need for ‘information’ was what often motivated them to look at health websites, and that they would all want to be able to find reliable factual information about their condition or health issue (see also Timing and need). There were people in both the comparator and intervention groups who said this kind of factual information was either the only or the main type of information they wanted. For example, one person in the asthma comparator arm volunteered the following comment in relation to not wanting to look at videos, before any interview prompts had been raised about the sharing of personal experiences:
I prefer reading information and I would view a site like this, not for chatty, touchy-feely stuff, but for information because I’m not particularly interested in other people’s experiences of asthma, because I’ve had it so long that I feel that, you know, they’re not going to be particularly interesting or helpful.
Asthma comparator, 58-year-old woman
This is also an indication of the importance of timing and need, to which we return below.
An asthma intervention participant commented on the relative priority they would attach to experiential information:
Well I would think that the most important part of it is the symptoms and the available choices and medication.
So the medical kind of factual?
Yeah. The other thing about people’s experiences and what have you, although interesting, are not as important. I mean what everybody wants is to alleviate their symptoms and if the money’s there to break it up a bit with some personal experiences so much the better because it does make it easier to read if you get my meaning?
Asthma intervention, 66-year-old man
As anticipated, for the MS carers learning through other people’s experiences included getting practical advice about equipment and adaptations to the home. The value of hearing from other people who have ‘been there’ was frequently raised among those who had access to the intervention site.
So, and what was useful was, it’s all very well going to a site that tells you what’s available but it doesn’t tell you how people have coped with it, and that’s why the carers’ thing is so much more valuable. You know the physio will tell me but, it’s not quite the same as somebody who’s been in that situation and said, ‘This has worked for us,’ and you think, ‘Ah yeah, that might work for me’.
MS intervention, 59-year-old woman
Hearing other people’s experiences also helped some MS carers to make sense of what they had been told by various health professionals.
Because it highlighted . . . you go to, you go to see various people, you know take my partner and you go to see a consultant and people say different things and that was really useful because then you could see exactly what it was that they were, you know, meaning – for example benign MS.
MS intervention, 50-year-old woman
One person with asthma thought that people’s ‘detailed descriptions’ on the website were useful for those who had not talked about their illness to others.
To hear other people’s detailed descriptions of what they went through if you can put it that way, you know, because I’ve never talked to anybody about it. You know I know quite a few people who have asthma in various degrees but it’s not that we sort of talk about it, but it was interesting to hear other people’s views.
Asthma intervention, 78-year-old man
Concerns about the potential for harm included that information drawn from other people’s experiences could be either irrelevant or misleading. People with asthma and those caring for someone with MS pointed out that these conditions affect people very differently and therefore other people’s advice may not be relevant. One MS carer said that when it comes to adaptations to the home, even information from health professionals can be misleading ‘particularly in terms of finances and things’ as they might not understand that people struggling with limited funds may be encouraged to make expensive mistakes if they do not know what is going to work.
People who had many years’ experience of living with asthma or caring for someone with MS thought that it was unlikely that they would find anything new on a website; however, some who had looked at the PEx material in detail had been pleased and surprised to discover something new.
It was really interesting to see how other carers were coping with the idea of getting people in and things like that and how much problems there can be.
. . . We’ve had that a while so it’s not a major problem but you have to then buy new beds and things. And also you need two people. Well, really he prefers, and I do, that we can cope on our own as best we can. So there was a gentleman who mentioned the ceiling hoists which a friend of mine with MS also has, and that confirmed that that’s the only way to go you know.
So that was a really useful piece of information otherwise we’d have perhaps got hoists in and . . . I’ve been and tried them; I had a nice afternoon trying them out but, I did realise that they have limited potential.
MS intervention, 59-year-old woman
The ‘smoking cessation’ group felt, somewhat wearily, that they already knew everything there was to know about why it would be beneficial to give up. Some were evidently resistant to any more ‘information’ about the harms of smoking being thrust at them.
Feeling supported
Much of the literature about the role of health websites has focused on the potential for ‘peer-to-peer support’, which is arguably one of the most transformational aspects of the internet, especially for people who might be socially or geographically isolated, or who find it difficult to talk to others about their emotional responses. In our data this was particularly evident in the MS carers interviews; the following extract is from a woman who felt that she had benefited from access to the trial PEx website.
As someone who’s on my own, basically because relatives are far away, it’s quite useful; reassuring; encapsulates the most helpful comments of other carers; helps me realise aspects of [my husband’s] symptoms and behaviour which are to be expected, because it’s very difficult for him to know if it’s the MS if he has a tummy problem, or if it’s something else and then it’s easier for both of us to accept quite regularly. Reinforces the path we’re on – like I mentioned with carers – and you can see any alternatives might have bigger problems than they’d solve. And it helped about equipment; it helped more about emotions and every carer seemed to be unique and was finding the best way through which helped me think about the best way through.
MS intervention, 59-year-old woman
One of the participants with asthma commented that, among the benefits of seeing what other people have written about and dealt with, it is:
. . . also helpful to know (a) that you’re not alone and (b) how other people cope in those circumstances.
Asthma comparator, 45-year-old woman
The MS carer interviews included several examples of when hearing from another carer had helped (or could help) people to feel less alone and better able to cope. The MS carer quoted above had attended a face-to-face support group but felt that the PEx site was ‘a more useful thing’ for her:
I’ve been to carers’ meetings and they’re very helpful about what might be out there but it doesn’t get you into the emotion of being a carer in the same way. And I found out things, I can’t specify, but information about [husband’s] emotions which helps me to deal with them, and they don’t crop up at, you know other venues. So, it’s really useful when people talk about how they’re . . . I don’t know what you call them . . . the person you’re caring for feels and how their emotions are affected and it helps you to deal with it as well.
MS intervention, 59-year-old woman
Hearing about what other people are going through can sometimes help people to feel that they are comparatively well off. A woman in her sixties who was in her first few weeks of giving up smoking had not seen the PEx website, but volunteered early in the interview that she would have liked to see some other people’s experiences of trying to give up. She wanted to see not only the positive accounts but also what it was like for those who were struggling to give up, partly for ‘downward comparisons’, but also because she would ‘mistrust’ a site that was only positive. A person with asthma commented on the value of these ‘downward comparisons’ with people on the PEx website:
You also are thankful that you’re not as bad as some people you know because for some people it is really debilitating [. . .] I mean it doesn’t stop me doing what I want to do.
Asthma intervention, 78-year-old man
Carers of people with MS were aware that looking at other people’s experiences could be either uplifting or depressing. Online peer-to-peer contact could be a ‘mixed blessing’ or a ‘double-edged sword’, and it would not always be easy to predict how someone might respond to hearing someone else’s account:
It’s a balance the stories isn’t it . . . I mean the personal dimension where people have struggled and have, you know, made some progress or have come through well is very positive and inspiring but then equally without being, you know, depressing is also useful to know about the sort of difficulties where people have where, you know, the challenges that emerge as people become doubly incontinent and what you have to do about caring for that and all the rest of it because it’s something’s real and you don’t want people feeling, ‘Oh god I . . .’ you know either the person who’s suffering or the person . . . sounds awful when the person’s dealing with this, or the carer, ‘Oh god I’m inadequate, I can’t cope with this’.
MS comparator, 65-year-old man
Apologetic that he might be sounding unsympathetic, one person with asthma pointed out that people can tend to ‘witter on’ in forums and on blogs. Of course, a benefit of an online group is that one can remove oneself without causing the offence that might ensue in a face-to-face meeting. 4 Others wondered why it seemed to be that some people wanted to live their lives, and rehearse their health problems, in public and online. Those in the smoking cessation group differed from the asthma and MS carer participants in that several said that they really did not like the idea of being advised what to do – and they were doubtful that other people would want to hear about their experiences either:
. . . because, to me, it’s self-evident – if you want to give up smoking, you give up smoking.
Smoking intervention, 59-year-old man
Another smoker said that they would not want to ‘shove my opinions down other people’s throats’.
I don’t know . . . if I had breast cancer I wouldn’t want to read people’s last diaries maybe necessarily while I was undergoing my chemotherapy.
Yeah.
But if we’re talking about something like this I think it’s really helpful to have people who’ve had bad experiences or who have failed at various things because then it makes you just feel a lot better about, you know, the fact that you’re not coping well or you know you’ve given up smoking seven times in the last eight months you know and each time you’ve lapsed and you think, ‘Oh I’m hopeless,’ and you think, ‘Well so and so that happened to them and they persisted or they tried this other thing and it really worked,’ so I think that’s really good. I would always . . . I would mistrust a site I think that only had positive things.
Smoking intervention, 78-year-old woman
This perspective was echoed by some of the people with asthma or MS carers who, although a little concerned about unmoderated content on online forums, reasoned that it also would not be helpful to exclude negative stories:
Well there is a danger there isn’t there that if you’re feeling vulnerable and in need of support anyway and you don’t have any other support network and you know if there are forums they’re usually . . . I wouldn’t say uncensored but they do tell [. . .] they shouldn’t exclude people who tell a negative story otherwise there’s not much point in having a forum, it just becomes a controlled network, so there is that danger. Now as an individual you might come away from there feeling, ‘Well at least I’m not as bad as that,’ which isn’t necessarily a good idea but it might give some people some support to say look there’s people who are worse off, you could do better or you might identify them as a bit, you know, you’re being just as good, as bad as they are. So I don’t know about that one, could be a double edged sword. Overall I’d think it would come down as perhaps helping people who are seeking support overall.
Asthma intervention, 60-year-old man
The same participant drew attention to the value of the curated collection of clips on the intervention PEx site, which avoided being repetitive or presenting only one perspective.
Those were interesting as well and I thought that would also give support to people who perhaps are a little bit anxious particularly if they’ve been recently diagnosed or it’s grown over, you know, in recent times, so yeah, so that’s where I first went yeah.
OK. And did you look at any of the clips, the video clips?
Yes yes. I suppose also those are well put together. I think the . . . sometimes if they’re too repetitive or the people aren’t explaining themselves very well that might put you off, but if they’re put together in a supportive way I think they would provide people with encouragement yeah [. . .] I thought overall they were well put together; people . . . it’s always a danger if you’re using non-professionals I suppose or people . . . they just look at it from their own angle but then I suppose that’s the point and as long as they put it over clearly then yeah I think they were . . . they added to the website yeah.
Asthma intervention, 60-year-old man
The PEx site was designed to cover many different perspectives on each topic so that people using the site could find material that resonated with their own views and experiences. This had not been successful for one of the MS carers, who felt that her perspective was not included because she cared for a partner with MS but they did not live together:
In some ways it was quite disappointing to use partly because the examples . . . I think I was looking for something that wasn’t there, possibly because our situation is so different from most people in that situation. Because we don’t live in the same place; because we’re not man and wife; so I’m much more like a friend and I appreciate that this is designed for friends as well. But obviously a lot of the things that were said were, where somebody was in a very intimate relationship 24/7. So there were times when I thought, ‘Ah now that might give me a clue,’ and it didn’t quite hit the spot.
MS intervention, 59-year-old woman
Maintaining relationships with others
Carers of people with MS talked about the unmet need for support for people who are caring for a spouse with MS. One participant (in the non-PEx arm) explained how much he had gained from meeting someone else who was caring for a wife with MS. He reflected that he had not found anything similar on a website, although the need, evidenced by the high divorce rate (especially in cases when the woman has MS), seemed clear to him:
And we’d talked about things and we had exactly the same experiences of, when you go through that diagnosis it’s a big shock and then you worry a lot for a long time, and then things become normal. But, you redefine yourself as the partner of someone who has MS, and I found myself telling people that all the time. If they asked who I was, it was almost the first thing that came out all the time. And, it’s like you’ve . . . someone’s flicked a switch and you’re not who you were before and your partner isn’t who they were before. And, it’s really, really weird. I had never spoken to anyone else before who’d had that. And, it was just really incredibly helpful.
Yeah.
And that’s not . . . I haven’t found that on any website anywhere or anything like that. All you do see is that, you know statistics like; I think this is roughly right but, men who are partners, 75% of men who are partners of women with MS, divorce them. And, it’s about 25% of women whose male partners got MS, divorce them. And there’s a very big difference there but, I think there’s probably . . . and there is probably a need for some sort of support there that isn’t, that just isn’t there at the moment. Because, I think, MS is like one of those things . . . you know people try and hide Alzheimer’s because we’ve been through this with parents and god knows what, and partners of people with Alzheimer’s try and cover it up and everything. MS is one of those completely hidden things . . .
MS comparator, 59-year-old man
Sometimes the online environment can offer welcome anonymity. One of the smoking participants commented that it might be easier to share personal issues with strangers rather than with friends, family or health professionals:
. . . with a professional it’s a bit more like more like going to confession, do you know what I mean? There’s a sort of barrier . . . sometimes it’s easier to share personal things with someone you don’t know.
Smoking intervention, 78-year-old woman
One of the asthma participants recognised the potential value of the online forum because of his daughter’s experience of online communities for people with fibromyalgia:
What she does find is that it’s easier to cope with now there is a fair bit of it on the web and things like Facebook where they discuss how their days have been and that sort of thing and she’s not alone . . . this is . . . she’s found very much a great help, you know, that there’s people she can talk to over the web whereas she doesn’t physically know anybody in her local friendly circle that’s got it but there are people out there that she can contact and talk to and sort of say, ‘Oh I’ve had a rotten day,’ or, ‘I’ve felt better today,’ or whatever you know.
Asthma intervention, 78-year-old man
Affecting behaviour
Stories can inspire people to cope with their health problems. One man who had been diagnosed with asthma as a child was inspired and reassured to discover that a famous cricketer also had asthma:
I do remember there was an interview with I can’t remember who it was – it was a famous cricketer – who had asthma or who has asthma, and I do remember thinking, ‘Gosh well you know if this person can be a, you know, a test cricketer and he’s got asthma, you know, that’s a good thing I can run,’ because as a child, although Ventolin had been invented my GP had obviously never heard of it so I didn’t have any treatment; you know the only treatment for an asthma attack was to lie down and gasp on the floor and, you know, try and get fresh air. And so I was always scared of running and that sort of thing and so then in the second phase when I was older and then got the drugs I suppose at that point seeing success stories and thinking, ‘I can run if these other people can do things’.
Asthma comparator, 58-year-old woman
Interestingly, this was the same person quoted above in Finding Information who said, ‘I’m not particularly interested in other people’s experiences of asthma, because I’ve had it so long that I feel that, you know, they’re not going to be particularly interesting or helpful.’ Again, this illustrates how shared experience at the right time – success stories ‘at that point’, as she puts it – may be valuable.
One participant (in the non-PEx arm of the smoking study) felt that other people’s experiences of quitting (or trying to quit), if they were ‘smokers like me’, might be a ‘worthwhile addition’ to a website for smokers trying to give up:
But a worthwhile addition to it would be, people who have been smokers like me, for 47-odd years, and you know what’s your experience been actually finally quitting?
Right.
And how have you stuck with it? How have you done it? And there are lots of little things that help; there’s one thing in my view except my own inner decision.
Yes.
My decision.
So what other, you know what other types of experiences would you like to see? People who’ve . . . just people who have been successful or people who’ve tried and . . .?
People who’ve been . . . people who tried and failed even and are willing to try again.
Yeah.
And even people who say, you know, ‘Look this is the hardest thing you’ll probably ever do in your life’. It is very hard.
Smoking comparator, 59-year-old woman
Experiencing health services
There were a few accounts from people who had been encouraged to seek health care, although not necessarily because of the 2-week exposure to the trial websites. An asthma study participant said that taking part had reminded them that they were overdue to see their asthma nurse, which was probably simply a beneficial side effect of taking part in the research rather than a consequence of exposure to the intervention.
It has been suggested that health websites (in general) might support self-care by increasing people’s confidence in their ability to look after themselves. One of the participants from the asthma study described being reassured by the PEx website that their current approach to their health care was satisfactory, and a MS carer said that they felt a ‘bit more confident to go to the GP’ to ask for help:
Perhaps if anything it reassured me that I was doing just about most of what I could do to control the asthma and keep it in check, and it perhaps confirmed that there was nothing contradictory to what I’d been told or any course of action that, you know, any medication that I’m taking at the moment. There was nothing contradicting what I’d been told – different terminology but mounting to the same thing so I suppose if anything I came away feeling that this is . . . I had more confidence, it was reinforcing. If there was something glaringly different to what I’d been following then I might have gone back to my doctors and said, ‘Oi’. [laughs]
Yeah OK. Has anything that you looked at prompted you to go and talk to anyone else; go back to your GP; talk to support groups?
I think it’s made me a little bit more confident to go to the GP with problems.
[. . .] Yeah and I suppose websites could go either way couldn’t they, you know that online stuff might put you into downward spiral or, it might prompt you to think, ‘Actually there’s other people out there who’ve gone and got help, maybe I should do that’.
MS intervention, 59-year-old woman
It has made me think more and more that that’s what I should be doing. [Interviewer: Hm mm.] And it’s my mind-set and also habit as well and I think these e-cigarettes is to look . . . well say a lot of friends are doing those now and that seems . . . they seem quite happy with that. [Interviewer: Yeah.] And I think that might be sort of one of the aids to . . . and also I need to go and see the doctor and say, ‘Right, can I have some patches as well,’ and work out the best way for me to stop smoking.
Smoking comparator, 47-year-old man
Learning to tell the story
Our conceptual review indicated that one of the consequences of accessing online PEx might be that people would learn new ways to talk about their health, which might help them to describe their condition more accurately (or more persuasively). Any such change would probably be gradual, diffuse and difficult to assign to any one influence. However, one man who was caring for his partner with MS explained how hearing men talk about their emotions might help others to express themselves. This is, of course, related to ‘support’ but provides a particular stimulus to action:
I think there’s a gender issue here too because women have traditionally, for historical reasons, had a greater caring role and they still do because we still have a patriarchal society [. . .] but many women find it more easy to talk about their emotions and their feelings and to exchange. Men tend to not do that so easily and tend to internalise and block down, and I think the opportunity for, you know, a male person, for everyone, but maybe to actually see other male carers talking [. . .], ‘Oh so you know, actually I’m not alone; actually those are issues and actually I have these feelings of, you know anger and upset and whatever and it’s actually OK to feel those things because that’s an understandable human reaction, but then I’ve got to sort of deal with those and channel onto . . .,’ you know so all of that’s . . . and I guess this must be true . . . lots of support and therapy across all sorts of issues and conditions, not just MS but yes, I’ll take the view that the ability to share that is quite important.
MS comparator, 65-year-old man
Another man caring for his wife with MS expressed a similar idea about how hearing about other people’s problems might encourage a person to ‘talk to someone else about how they feel’:
I think, actually getting things off your chest or talking about things is always helpful. And, if it’s something that you find difficult to talk about with other people then it’s probably even more helpful to you to get it off your chest. And, if someone experiences someone else doing that it can possibly help them. Either just to read about it or, hear about it or, to encourage them to go and talk to somebody about how they’re feeling I think. For their own sort of mental health really.
MS comparator, 59-year-old man
In contrast, several of the participants in the asthma and smoking cessation groups were sceptical about the value of telling other people about health problems. Some expressed amazement that anyone would want to write, or read, a health blog. A person with asthma commented:
People are all different. It might be a generational thing as well in that it was the way I was brought up – basically, you know, you sort yourself out, you don’t go lumbering other people with your problems; or nod and say yes but by and large they’re not interested, they have their problems and so why should they want to hear yours?
[laughs]
I don’t know yeah.
If you thought they were going to help someone.
I mean the worst person to meet in an office environment is when you ask them how are you and you get the whole nine yards and you think oh . . . that’s unkind to some extent but because there are people who definitely need help and support and you would do – give them support – but I mean as a general rule, you know I’ve done it myself – you know you’re feeling like death but yeah you’re fine.
Asthma intervention, 60-year-old man
Visualising disease
The conceptual review drew attention to the inherently visual nature of health websites. Many sites include pictures of people with a health condition, and other illustrations. These images, intentionally or otherwise, position the condition in particular ways.
In the interviews we asked people if there were any images they would prefer not to see on a health website. Responses were clearly divided by condition. While a few of the people with asthma discussed design issues and talked in general about the benefits of breaking up text with images, they did raise concerns about negative or distressing images. In comparison, MS carers were aware that images of people with advanced disability might be distressing, particularly for the person with MS, although one remarked that ‘with MS there aren’t so many gory pictures because it’s not that sort of disease’:
They don’t want it in their face; they’ve got it, they want access to things to help them but they don’t want to really be reminded of it in a sad sort of way and that’s . . . websites can do that too seeing people severely disabled in a wheelchair, for my husband for example, probably wouldn’t do him any favours and it doesn’t actually interest me that much other than from the practical point of view that that particular piece of kit being suitable for my husband, then I would want to see it.
MS comparator, 64-year-old woman
The smoking cessation group expressed some quite strong feelings about the images that have been used in anti-smoking campaigns, which some suggested could be counterproductive:
That I do not want to see? Pictures of diseased lungs. [Interviewer: Hm mm.] I know that and I don’t want to see it because it makes me instantly want to go and smoke a packet of cigarettes. [Interviewer: Hm mm.] Because it makes me so nervous.
Are there any things that you’d really rather not see on a site that’s supposed to be helping and supporting people to give up smoking?
Well yes. I mean we’ve all seen the photographs, the medical photographs of lungs of someone with cancer. [Interviewer: Yeah.] And I don’t think we need to see them any more. [Interviewer: No.] You know I mean that kind of shock tactic it didn’t make me want to stop. [Interviewer: No.]
I just didn’t bother to look at the picture; I would open the packet in such a way that I didn’t look at the picture. And so I think most people see through that.
Yeah. You know you can’t . . . ultimately there is only one way and that is really through understanding and loving support.
Smoking intervention, 59-year-old woman
In contrast, the next quotation was from the one participant who suggested that images should be more graphic to shock people – on the grounds that everyone now knows that smoking is ‘not a good thing’ and people may need an extra push to stop:
I think people use the pictures which have a more hard-hitting effect.
OK so by graphic you mean sort of like . . .?
Images of lungs and that sort of thing yeah.
Lungs yeah. OK yeah.
And also the effect it has on others. I think that’s more of a positive for people to say, ‘Right . . .’ because I do think it’s . . . it’s not so much educational because I think most people have got a general, you know, they know it’s not a good thing. But I think if you can actually show it through and through and show that, you know, from start to finish, this is what will happen, not could happen, will happen.
Smoking comparator, 47-year-old man
One participant in her mid-sixties, who had just given up smoking, also commented on the image of a professor and expert on smoking cessation research, who was filmed for the website, talking in his office. She reacted to the way that he was positioned ‘against his files and his study papers and all the rest of it; his research documentation’. As someone who admitted that she had rather enjoyed her self-image as a bit of a rebel, she was not persuaded by the image of ‘authority figures’ telling her what to do:
But the photograph is totally, it’s just totally inappropriate you know [. . .] You see it interests me why I’m an addictive personality but the photo . . . he’s a great guy, no problem with that, but why put that, why? What is the reason for showing the professor’s photograph against his files and his study papers and all the rest of it; his research documentation – why, why do that? What purpose does it serve me who’s trying to stop smoking?
Authority? [laughs]
It’s an authority figure. Well you know [makes a ‘V sign’ with fingers and laughs], they’re closed, they’re closed. I used to put a cigarette between those [laughs].
Smoking comparator, 66-year-old woman
Facts, figures, experiences and blogs
People were asked to compare and comment on the different types of health websites, using a series of laminated cards with screengrabs from different types of sites accompanied by an explanation from their interviewer. Among all three groups and both arms of the feasibility trial, there was general agreement that everyone needs the facts and figures from reliable, non-commercial sources such as the NHS, well-known universities and voluntary organisations. People were very alert to the dangers of advertising and commercial influence on the site content:
I quite like the idea of factual information; again it’s just telling it straight and being able to work your way through something logically and forming your own thought process over it and that way you’ve got something to take away and discuss with your health professional or friends and family, whatever, to try and ascertain the meaning. I suppose that’s the way I tend to work so I’d say that was quite useful.
Asthma comparator, 45-year-old woman
When it came to patients’ experiences, there was considerably more variation in response. As we have indicated previously, some of the people we interviewed were at a loss to understand why anyone would ever want to talk about, or hear, anyone’s experiences of their health issues. People who had experience of caring for someone with MS had often realised the value of hearing about other people’s experiences, but they and the people with asthma emphasised that the conditions affect people very differently, making it hard to learn from a single blog, or an individual posting on a forum. There were also concerns about unmoderated content which might attract highly damaging comment and activity from ‘trolls’ on forums.
Those who had visited the PEx repeatedly commented on the benefit of being able to see many different people’s experiences gathered together under topics so that they did not become too repetitive (see Feeling supported).
It was also clear from the interviews that although there are some functions that can be very well performed by a website, the material is seen as a supplement, not an alternative, to care from a professional. Similarly, those who valued the PEx material also wanted to see facts and figures:
And that’s where a website is very handy because you can back-up what you’ve been listening to and also give you that little bit . . . well no GP’s going to know exactly how much you can take in or how much you want to as some people don’t want to know do they?
Mm yes or don’t want to know right now but they might want to know later.
No they might want to know later yes quite. If you’d just had a really serious diagnosis you might not want to know immediately anything more but you might . . .
MS intervention, 59-year-old woman
I think things like this, well the factual ones should encourage people to use the services less but when they do go it’s for more important issue which can’t be resolved you know outside the health service.
OK and is that something that would make you think, ‘Ooh quite like to know more about that, I might ask the GP,’ or . . . or look it up further on Google or something or other?
I would probably try and read more about it I suppose yeah. I suppose if I wanted more information after I’d tried to do that then I’d probably would talk to the GP or the nurse who deals with it.
Asthma comparator, 57-year-old man
Yeah. I’d want the facts first, only then would I perhaps want to look at individual stories and that’s only if I could search them to follow somebody who’d perhaps got as near enough the same condition as myself and I’d then follow them through but if I had a condition that was concerning me I’d want facts and information about it and then I’d go to my doctor and take a conventional approach to it.
Asthma intervention, 60-year-old man
Timing and need
Timing and need was a strongly emergent theme from the interviews. We have already touched on this in the example of the 58-year-old woman in the asthma comparator group who said that she was now ‘not particularly interested in other people’s experiences of asthma, because I’ve had it so long that I feel that, you know, they’re not going to be particularly interesting or helpful’. The same participant also told us that at one stage in her illness she had found the example of a famous cricketer with asthma helpful in encouraging her to think she could still go running.
Many of the people recruited for the asthma feasibility trial had had the condition for some time; they generally felt well informed and their condition was well controlled. It is not surprising, therefore, that they often felt that they had little to gain from either the facts and figures or the personal experiences sites. However, they could see that they or others might have benefited from information at a different point in their illness, such as when they were newly diagnosed or experiencing changing symptoms. The same woman in the asthma comparator group as mentioned above explained further:
But of course somebody who’s newly diagnosed . . . or particularly if they had a child who was newly diagnosed, would be looking for totally different things . . . and probably with the other conditions you’ve been looking at as well, somebody who is newly diagnosed is going to be in a sort of, you know, shock/horror ‘What do I actually do? What does it mean? Am I the only one?’ sort of thing. It’s almost a completely different thing . . . I suppose it almost feels like making a bit too much of a fuss about it – talking to other people about it. But then you see my asthma’s pretty well controlled most of the time . . . I mean going back to a parent of a child who’d been newly diagnosed, that’s such a completely different sort of experience. I think if you’re afraid of the condition then I think having discussions with other people is going to be perhaps more effective. So I think again it comes back to this difference between, you know, if you’ve had asthma for, you know, over half a century as I have, versus if it’s all completely new and you don’t know anything about it – you’re going to want completely different sorts of support and information.
Asthma comparator, 58-year-old woman
This example is typical of how people talked about personal variation in the time at which they might need different sorts of information.
One woman in the intervention arm, who was caring for her husband with MS, explained that the trial had come at a particularly helpful point for some pieces of information and emotional support, as she had been experiencing some depression because of her sense of isolation and sadness at her husband’s disease progression. The following extracts show how she selected material for her own current needs. In addition, searching the site online was, for her, a more efficient way of gleaning others’ experiences than a support group would have been:
I find it difficult to find the time to talk to people a lot and go to MS meetings and things like that, and very often you’re talking about people’s relatives and things, whereas I find that the website condensed the sort of information that I needed. So I did find out things which could have taken quite a long time to find out otherwise . . . I had to by-pass a lot of things because my husband is now chair bound. So, I didn’t need to look at anything about mobility cars, scooters, you know anything like that because we’ve already been through that. So, it was particularly things for the future. He’s not too worried but I like to be prepared.
OK so quite selective, quite targeted?
Very targeted, yes, probably missed half of it because it’s no longer appropriate, which doesn’t mean it wasn’t of real value to people who are in a different position . . .
What kinds of things were useful?
Well I did look at some of the things that we’re sort of currently in, like [paid] carers and things, and it was really interesting to see how other carers were coping with the idea of getting people in and things like that, and how much problems there can be . . . I was particularly interested in hoists because he doesn’t need one yet, but we need to know what sort of hoists might be available [. . .] I think initially when you’re diagnosed you want to look at a whole lot of information. [partner] and I were very different; he didn’t want to know, he just wanted to get on. I wanted to be prepared . . . so I wanted to get hold of literature and find out as much as I could. So it’s very useful in those early stages I think . . . And what was useful was, it’s all very well going to a site that tells you what’s available but it doesn’t tell you how people have coped with it, and that’s why the carers’ thing is so much more valuable. You know, the physio will tell me but, it’s not quite the same as somebody who’s been in that situation and said, ‘This has worked for us,’ and you think, ‘Ah yeah, that might work for me’.
MS intervention, 59-year-old woman
At the same time, she was selective about experiences that she knew she did not want to see, perhaps because they were upsetting:
When people were in a similar situation to myself then I would, you know watch the whole clip. And I think I tried to look at every clip where it might be relevant. As opposed to clips where people were in the very early stages and talking about holidays – dream on [laughs] – you know, they were irrelevant and probably painful.
Conclusions
The above extracts touch on many of the seven domains. What the domains can tell us is what the benefits (and possible adverse consequences) from shared experience can be. The theme of ‘timing and need’ helps to explain why and when these benefits and harms may be realised. This discussion further underlines the importance of the person’s point along a trajectory, as well as their specific needs at that point and their personal information preferences for facts, figures and experience. We discuss the implications of these findings further in Chapter 10.
Chapter 10 Discussion
During the 5 years since we started the programme, we have seen considerable changes in how people access the internet, for example the rapid growth in mobile access through tablets and smartphones and the rise of Twitter and other social media. Although this period has also seen substantial changes in health and care policy and responsibilities, the Department of Health remains committed to giving reliable and timely health information to the public and patients. The primacy of the internet as a conduit for essential information is rarely disputed; the UK government has committed that everyone who has the capacity to be online will be by 2020. In 2015, those without internet access tended to be older and more disadvantaged with greater health and social care needs; for example, the Office for National Statistics reported in May 2015 that 27% of adults with disabilities had never used the internet, compared with 11% of non-disabled adults. Recognising the risk that the shift to online information and service provision in the NHS might exacerbate current inequalities in access to health information, NHS England is working to widen digital participation through a programme with the Tinder Foundation (www.tinderfoundation.org).
When we began this programme there was no agreed conceptual and theoretical basis for research on the effects of accessing other patients’ experiences online. We started the programme with a conceptual literature review (based on a realist approach), conducted by the principal investigator and coinvestigator Professor Sally Wyke, to identify the mechanisms through which PEx might influence health. The review included numerous different types of studies, as well as editorials and opinion pieces, to understand what might be the positive and negative consequences of looking at other patients’ experiences online. We concluded that there were seven ways that health might be affected: through finding information, feeling supported, maintaining relationships, experiencing health services, learning to tell the story, visualising disease and affecting behaviour. Our review successfully established the theoretical underpinnings for the study and guided all subsequent WPs. Published in Milbank Quarterly in 2012,4 the review has been widely cited in the field (38 citations by July 2015 and an Altmetric score of 54, putting the paper in the top 5% of all publications).
We established that there was no validated outcome measure that could be used to compare the effects of a ‘facts and figures’ with the effects of a PEx website, and we therefore set about developing and validating a new measure, the eHIQ, for this purpose. The item pool for the questionnaire was based on a secondary analysis of qualitative interviews in the HERG archive from a range of conditions, and included young, middle-aged and older people’s experiences of chronic conditions, cancers, learning disability, neurodegenerative conditions and mental illness. This proved a highly efficient method of identifying an item pool.
We conducted online ethnographic studies to observe what happened in online support groups and interviewed people who participated and managed the sites. The ethnographic study focused on online MS support groups and examined how people affected by MS (patients, family members and friends) responded to and interpreted PEx in these settings. Methods included online observations and content analysis of forums and YouTube videos, particularly in relation to controversial theories and treatments. This work was important in helping us understand what people actually do in online environments, which is sometimes in contrast to what they report they do.
We conducted detailed internet café-style laboratory observations to help us to understand the various ways in which PEx is used in online support groups and how patients use and respond to a variety of different types of health information websites that present PEx as single stories, testimonials or ‘maximum variation’ samples. These studies fed into the development of new ‘engagement guidelines’ for incorporating PEx in websites.
We conducted three national qualitative interview studies of the experiences of people with asthma, carers of people with MS and smokers’ experiences of trying to give up. Interviews were collected by experienced qualitative social scientists based in the principal investigator’s team in Oxford. The interview collections were analysed and edited so that written, audio and video extracts from the interviews could be published on three new prototype PEx websites, based on the engagement guidelines. This material has now been published on three website sections on www.healthtalk.org, where it is available to the public as part of a voluntary sector website covering over 90 different health conditions. A matched set of three very similar websites was developed to be used in the feasibility trials; the comparator websites featured information from NHS Choices without PEx.
The prototype websites and methods for an online trial were piloted. We then conducted a feasibility trial to see if we could use RCT methods to understand and compare the effects of PEx using prototype websites on the three exemplar conditions. Finally, we interviewed a subset of 30 of the people who had participated in the three arms of the feasibility trial.
We demonstrated that it is feasible and acceptable to compare a PEx website with a ‘facts and figures’ website in a randomised trial. However, our findings suggest that, although this may be feasible, the requirements of our phase II trial design may mean that the websites are used in a way that is divorced from how people use the internet and other sources of information in real life. Although methods to evaluate complex interventions can help to address this issue, we believe that challenges remain for researchers in conceptualising online sources of information and support as interventions with doses and exposures.
The qualitative interviews with trial participants underlined that everyone wants and needs facts and figures and that online experiential information is not seen as an alternative to facts, or to care from a health professional, but is used in addition to other sources of information, support and expression. Future work needs to ensure that personal stories are not isolated from the rest of the information landscape, in addition to allowing for the iterative nature of information behaviour.
We have had strong patient and public involvement (PPI) support throughout the programme, led by coinvestigator Margaret Booth. The project was both consultative and collaborative in user involvement. We consulted users in preparing the proposal; Margaret Booth attended regular meetings throughout the programme and ensured that we gave appropriate consideration to when and how to involve members of the public in advising our design and reflecting on our findings. We have also benefited from a good link to English health policy through coinvestigator Bob Gann, who has kept us informed about policy developments and helped to organise presentations of our findings to NHS England colleagues.
In summary, we achieved all that we set out to do and were also able to include some associated studies (e.g. we were pleased to attract an additional doctoral student to the programme to explore the feasibility data on health literacy; a doctorate was awarded to Braden O’Neill in 2014).
Limitations
This programme used a mixed-methods and interdisciplinary approach. We made some pragmatic adaptations to established methods, for example in our wide-ranging conceptual review which deviated somewhat from a conventional realist review.
The conceptual review provided a framework for the whole programme but we did not draw on a single overarching theoretically informed approach. Instead, we used relevant theory and methods from the WP leads, who represented a range of disciplines.
The leads for the different WPs drew on their own disciplinary backgrounds in medical sociology, public health, health psychology, health policy, primary care trials and sociology of technology and science. We believed that the overall aim of the programme was best served through a series of connected, and regularly communicated, WPs which drew on relevant theory and method from the disciplinary lead of the package. This seemed preferable, and more mutually respectful, than an approach which attempted to drive an entire programme of work from one of the contributing disciplines. We were able to do this because the topic was of central scholarly interest to all of the authors and we were genuinely committed to learning through an interdisciplinary approach which has enriched our knowledge of the field. Hence the programme was multiply theoretically informed but not driven by a single theoretical perspective.
Patient experience in policy
During the last 5 years there has been a noticeable shift in the perceived value of PEx in health policy. The Mid Staffordshire NHS Foundation Trust Public Inquiry and the Francis Report drew attention to the importance of listening to patients’ experiences and the accounts of their family carers. Analyses of online feedback and ‘hard’ statistics on hospital trust infection rates suggest that patients and their visitors may become aware of problems before they are evident to managers. PEx is now viewed as an essential indicator, indeed the ‘final arbiter’, of heath care, and all attenders at NHS facilities are encouraged to complete a brief questionnaire (the Friends and Family Test). It is an indication of the importance of PEx in health policy that there is now a NHS England Director for Patients’ Experience.
Accompanying this focus on collecting PEx, there is increasing emphasis on the need to use what we find to improve services; indeed, some of us have argued that it is unethical to do otherwise. 182 Whereas policy-makers seem keen that hospital staff should learn from PEx, there is evidence of reluctance, or uncertainty, from health and care professionals. In January 2015 the National Quality Board published Improving Experiences of Care: Our Shared Understanding and Ambition, which suggests that there is a problem in how staff view and value PEx:
If we are to make sure experience is thought of in the same way as other aspects of high-quality care and that people’s experiences continually improve, there will need to be a fundamental shift in how people’s experiences are viewed and valued.
National Quality Board. 183 Contains public sector information licensed under the Open Government Licence v3.0
Traditionally, health information has been based on facts and figures, not experiences. There are now many popular websites containing PEx; for example, healthtalk.org alone received 2 million unique visits in the first quarter of 2015. Against the backdrop of increased policy interest in learning from PEx to guide clinical practice and priorities, our programme has shed some light on the role that online PEx has for people coping with a long-term health condition, caring for someone with MS or contemplating giving up smoking.
The findings from our observations, internet café studies, exploratory trials and qualitative work all suggest that, at least in the context of a health issue that affects them or a close friend or family member, people are cautious and reflective consumers of PEx information. This contrasts with earlier concerns in the literature that people might be swayed towards inappropriate choices through the power of the patient ‘testimonial’. 1,20 Indeed, in the internet café observations and the qualitative studies with trial participants, people consistently reported, not surprisingly, being more cautious about PEx than about ‘facts and figures’. There was consensus among the qualitative study participants that everyone wants and needs facts and figures from a reliable source. When narratives from other patients were valued, it was as a supplement, not a replacement, for facts and figures from trusted non-commercial sources and advice and hands-on care from health-care professionals. In practice, some people, at some stages of any particular illness trajectory, will prefer to see only facts and figures, while others will want to access other people’s experiences as an additional source of information, fulfilling a rather different purpose. Admittedly the distinctions are not always clear-cut, as narratives may incorporate facts (e.g. some narrators mention evidence about the effects of a treatment). Indeed, we contend that it is precisely the interweaving of lived experience, biomedical knowledge, creative expression and emotional support that makes PEx so valuable, and distinguishes it from other sources of health-related information and support.
It would be considered very poor practice to develop a health information leaflet without checking its readability level and thinking carefully about how facts and figures (e.g. risk information) are conveyed. The internet, however, is different: material can be presented in numerous different ways and competent users can choose their own ‘playlist’, selecting the images, videos, text, graphs and interactions that they want. They can, in effect, fashion their own information landscape.
What we have observed repeatedly in this programme, using different methods and approaches, is that people personalise the range of resources they may use according to the timing, stage of illness and their own preferences. There may be times when people prefer to avoid certain facts or particular images, which is why clear design and signposting are needed. A person may choose to use the web, share experiences or look at survival data at one stage of their illness and choose not to at another.
We could see a parallel with the growth of personalised medicine and the choice of the right ‘drug’, before we consider how much and how often it should be given. In the world of personalised medicine, drug treatments will increasingly be customised for individuals based on their personal genetic and disease profile. Similarly, our findings on personal preference, timing and need suggest that we need a more tailored offering, whereby people can select information styles that suit them at a particular moment, rather than a standard intervention package. The evidence for segmenting and customising in personalised medicine relies on new forms of ‘big data’, from large cohort studies, biobanks, genome sequencing and record linkage. In the provision of online information, big data studies – tracking real-life use of high volume sites and surveying users – may help us to understand better how and why some people benefit from some information sources and not from others, and who these people are likely to be.
There may be some broad observable patterns in what people ‘on average’ want at different times, but one of the transformational changes that the internet has brought is that it is no longer relevant to think of designing a resource that everyone will access in the same manner. The challenge now is to find ways to conduct robust research in an environment characterised by this highly individual, personalised use.
Recommendations for research
The NIHR and academic community may benefit from research in the following areas (in order of priority).
-
Future intervention research evaluating online health interventions should reflect the way that people use the internet in everyday life. This is challenging within the specification of a randomised trial, which is generally designed for repeatable, consistent, controllable exposure. In practice, people search, browse, digest and comment on multiple information sources to varying degrees, within a landscape of other sources of help and advice, and with varying personal preferences for types of information. Although it is possible to package up an online health information intervention in the same way as a ‘dose’ of a medication, and to administer an exposure by allocating or denying access to the intervention, researchers need to consider critically if this reflects real information-seeking behaviour. Further theoretical and methodological work is, therefore, needed to consider the issues of ‘exposure’ and ‘dose’ in the context of online health information interventions. This present programme of work makes a significant contribution to this area, and the 2008 MRC guidance on developing and evaluating complex interventions167,175 and the recent additional MRC guidance on process evaluation167,175 can help to systematically examine these issues in future work.
-
Future intervention research evaluating online health interventions should examine and explain issues of engagement and use, and seek to identify how to increase engagement. In common with many online trials, we showed that actual usage of the website intervention was low (in terms of numbers of logins, page views and duration on site) for both the intervention and comparator sites. Further research is required to understand the nature of engagement with online interventions and the determinants of this. The reliability of tracking data should also be assessed.
-
Future research should harness qualitative methods, including online ethnography and offline interview research, to further explore how and why people use online sources of experience-based health information, and what effect this may or may not have on subsequent behaviour and health and social outcomes in different conditions. In particular, studies might consider who chooses to share experiences online, who is influenced by these and to what extent online sources of PEx (both solicited and unsolicited) are representative of patients’ experiences more generally, and, indeed, what representative means in this context. Areas of particular interest are online patient activism, especially around contested illnesses and treatments, and online comments on health services (including reviews and ratings).
-
Future studies evaluating health information websites should make use of the eHIQ, which we have demonstrated to be an acceptable, valid and reliable measure for examining individual attitudes towards websites presenting different types of information.
-
In designing online interventions which harness PEx, researchers should note the guidelines on intervention design. We demonstrated that these guidelines can be successfully applied in building three intervention and three comparator websites.
-
The seven domains (identified through our review) have been demonstrated to be a valid conceptual basis for research on how online PEx affects health and should inform research in digital health.
Chapter 11 Patient and public involvement
It was planned from the start that there would be an important public role in the research programme. Margaret Booth, who had extensive experience in serving as a lay member and patient representative on health-related bodies, led this and attended all of the programme steering group meetings.
It was agreed at the first programme steering group meeting in February 2010 that ‘patients and the public’ for this work should be anyone who used the internet for health information. It would be too restrictive to confine user involvement to those who used the internet to access PEx. Different public panels would be convened to inform different WPs as appropriate.
The initial public panel was recruited through an invitation sent via the Oxfordshire Primary Care Trust to lay people who had previously expressed interest in helping with research of this nature. From 89 respondents, panellists were selected to maximise representation from a cross-section of the community (gender, age, occupation and ethnic group). The panel included those who had used the internet for health information in a variety of ways (websites, forums, blogs) and for a variety of health conditions (either for themselves or on behalf of family and friends). People who were or had been health professionals were excluded. It was apparent that non-manual workers were over-represented in the group and so additional user advisors were invited through personal contacts and snowballing to generate a final panel of 30 individuals.
This panel was maintained throughout the programme. Its members were invited to participate in subsequent WPs as appropriate. They were sent updates and briefing reports to maintain their interest and engagement during periods when there was no need for active involvement. A separate panel was selected to inform the MS work of WP2a. Additional arrangements for public participation were used for WP3a to correspond to an existing framework.
An initial meeting of the core panel was held in Oxford in November 2010 to introduce the research and to discuss the preliminary results from WP1a, the literature review. To facilitate attendance, the meeting took place in the early evening. Travel expenses were reimbursed and an honorarium and refreshments were offered. A brief presentation by the researchers was followed by discussion in groups facilitated by members of the research team, who took notes on the discussion. There was then a final overall feedback and discussion session. Participants were also able to add comments in writing. A note summarising the conclusions was then sent to the participants. A similar approach was adopted for the two subsequent public panel sessions (on WP2a and overall dissemination of the results).
Details of the involvement of users in the various WPs and their contribution are set out below.
Work package 1a: the literature review
The public panel was asked to comment on the initial findings of the WP1a conceptual literature review and, in particular, the advantages and disadvantages of accessing PEx via the internet from the perspectives of patients and family carers. The panel proved to have a clear appreciation of the pros and cons of online PEx and provided many comments which largely reflected the findings of the conceptual review. However, we became aware that the distinction between different types of online information was not always straightforward to describe or discern in the discussions. This alerted us to the need to provide clear examples of the different types of website (e.g. in the WP3 qualitative interviews). It was also evident that not all of the panel had used online PEx. It was not always possible to distinguish comments which related to PEx from those relating to other types of health information on the internet. In general the public panel members tended to concentrate on practical benefits (e.g. the value of the internet for providing information about a health condition vs. potential drawbacks such as information overload and the difficulty of identifying inaccurate information). However, some members raised the possible positive and negative emotional impacts of internet PEx (memorably described by one participant as the dangers of ‘fruitcakes and trolls’). A panel member drew attention to the potential negative consequences for people with mental illness who might subsequently regret having shared their experience or participated in forums. This was a new perspective, one not raised in any of the literature we had read, and was included in the publication based on this WP. 4 A report was circulated to the group and feedback was sought. This WP was drawn on during all subsequent WPs.
Work package 2a: the construction and exchange of multiple sclerosis-related patient experience on the internet
A specialised public panel was convened. This comprised MS patients and their carers (10 attended on the day and a further two expressed interest and contributed to later activities). Panellists responded to an invitation sent through local branches of the MS Society. In November 2011, a meeting was held at which participants were split into two discussion groups, one for patients and another for carers. In practice, the carers were not substantial users of the internet for health information of any kind. Some mentioned that they already used face-to-face support groups (they had, after all, been recruited through a local MS Society group) and so did not report having much need to seek out or share experiences online. The MS patients, in contrast, were regular users of the internet both for information about MS and for looking at others’ experiences and sharing their own (one had a blog). In some cases this was a supplement to face-to-face groups. Patients and carers valued sharing personal experiences, whatever the medium, as a source of practical information and personal support. Both groups voiced major concerns about the quality of information on the internet and the potential for damage through hearing about other people’s experiences (e.g. if the observer was shocked to hear what might be in store for them). Depression is a symptom of MS and can affect both the way in which experiences are reported and the way in which they are received. The patients were well informed about the controversies regarding alternative treatments for MS and some had participated in internet exchanges about these. However, others expressed concerns that these controversies had led to some MS forums having an aggressive culture and that they preferred to use general social networking sites such as Facebook to access other people with MS. Other valuable points made by patients were that use of the internet is likely to vary over the course of the condition, with heavier use likely around the time of initial diagnosis. At times, severe MS symptoms could prevent use of the internet; MS symptoms are very variable and sites for other conditions with similar symptoms could be valuable to MS patients. A message felt to be important by users was that that generalisations should be avoided; it is necessary to contextualise internet use and the sharing of experiences.
Work package 3a: the development of prototype online interventions based on patient experience
Website interventions were developed based on qualitative analyses of interviews about a wide range of people’s experiences of quitting smoking, having asthma or caring for friends and family with MS. In accordance with the HERG’s normal practice, advisory panels were set up for each of these studies. These comprised representatives from national and local volunteer groups and service users, in addition to the usual professional stakeholders. They met at an early stage in the work to inform the sampling strategy and content of the interviews, and again mid-project. The panels also critically reviewed the thematic summaries that formed the basis of each website.
Work package 3b: the EXPERT feasibility trial
In preparation for the trial, members of the WP1a and WP2a public panels, together with new recruits chosen to represent younger age groups and men, were invited to help pilot the methods and advise on various aspects of the online trial. In total, 47 people participated. They were asked to log in to the trial portal, complete the baseline measures, view one of the (allocated) six information websites and complete the follow-up measures. Users were asked to provide feedback on their journey through the process and on the acceptability of the measures. Feedback was received from 41 users by e-mail and was followed up with a telephone call. The researchers were particularly interested to learn if the length of the questionnaires and the time it took to complete them all (both at baseline and at follow-up) were reasonable. The research group was also interested in the users’ general impression of their allocated website (design and attractiveness, whether or not it appeared trustworthy, if the tone was appropriate, if it was easy to navigate) and users were asked to suggest improvements. Where possible, users were given an arm of the trial that was relevant to them, but the main purpose was to get their views on the process and general impressions, and so no particular knowledge of the health conditions was needed.
This exercise identified technical problems, a few of which were significant and were resolved. Most participants navigated the process without substantial problems, although some felt that it was too lengthy. There were both positive and negative comments about all the websites. Suggested improvements to the websites were discussed and implemented when feasible; for example, both smoking cessation sites originally had the ‘no smoking’ sign on their home pages, but this sign was described as too negative by users who were smokers and it was replaced with another image.
During the recruitment phase for the WP3b trial, it proved difficult to locate and recruit the planned number of MS carers. An attempt was made to arrange a meeting with members of the MS carers’ panel, carers from the core panel and people from relevant voluntary organisations to discuss ways to boost recruitment. This proved to be impractical (it was difficult to find any date and time that was suitable for more than a few people) and instead members of the MS carers’ panel were asked by e-mail if they could suggest improvements to the recruitment advertisement and alternative ways to find and recruit carers. Responses were obtained by telephone and e-mail. As a result, changes were made to recruitment documents and other recruitment routes pursued, but, despite all efforts, we agreed to close recruitment for the trial with 42 participants.
The lay coinvestigator was also a member of the Trial Steering Committee.
Dissemination of results
A final public panel meeting was held in Oxford on 8 May 2014 to discuss the best way of disseminating the results of the research project. The members of both the original panel and the MS panel were invited; nine of the former and two of the latter attended. In addition, there were seven representatives of voluntary organisations in relevant fields, where possible from the communications departments. Following an introduction from the research team, the participants were divided into two groups for a discussion. The representatives of organisations formed one group and public panel members formed a second group. The meeting concentrated on the results from the conceptual review, health literacy and the web design guideline work and the proposed dissemination strategy.
There were good discussions in both groups but few additional ideas about dissemination routes for the study findings. Both groups expressed the view that the term ‘people’ should be used in referring to PEx and not ‘patient’. They said that people do not generally think of themselves as patients and are interested in the impact of health conditions on all aspects of their lives, not just on their interactions with health services. It was felt that websites featuring PEx could be particularly suited to young people and ethnic minority groups, who are hard to reach with health messages. Ways to disseminate the PEx sites to these groups include doing so via schools or ‘champions’.
The groups discussed the role of recommendations from professionals; few of the public panel had been directed to internet sites by health professionals, and some members said that they were reluctant to discuss their use of the internet for health information with professionals, especially doctors. This was partly because of shortage of time during consultations, but some thought that health professionals were uncomfortable if patients were well informed about their condition and questioned the professionals’ views. This suggests that health professionals may need to find ways to assure patients that their use of the internet to self-manage their conditions is welcome and appropriate, and that the doctor is happy to recommend reliable websites.
A member of the original public panel attended and actively participated in the June 2014 meeting on dissemination held by the research team with representatives of the Department of Health and NHS England.
Discussion
In a 5-year programme there are challenges in finding the best and most convenient method of involving users in the research. A number of issues with public participation in the research were identified and discussed at an early stage of the work. These were as follows.
-
There might be difficulty in selecting an appropriate group of users whose knowledge and experience were such that they would find participation in a public panel interesting and worthwhile and also provide a helpful input to the work.
-
When the research involved individuals, these would generally be as members of the public rather than as patients and the research would relate to their experiences in using the internet for health information rather than to experiences of obtaining treatment or health care. We anticipated that care would have to be taken to avoid the public panel merely going over the same ground as study participants but less rigorously.
-
The research teams responsible for the different WPs were in different parts of the country and the overall programme covered separate WPs spanning several years. This raised issues of whether there should be a single public panel or several, and where meetings should be held.
In practice, there was no difficulty in obtaining a good number of volunteers for the original public panel, although older age groups and professional workers were over-represented. Small numbers of additional members were invited to join the panels to balance this. The panel members proved to be knowledgeable about health information on the internet and issues arising from its use. They were interested in the work and had lively discussions, providing useful material for the researchers. The only problem was that it was sometimes difficult for those leading the sessions to keep the discussion focused on the topic of online PEx rather than health information on the internet more generally. Sometimes it was not clear whether a comment or concern was intended to apply to all types of online health information, or to PEx only.
We decided that we would not try to find some way of involving users in every WP. Participation would be concentrated in those packages where there was a clear role for the users, distinct from the input of study participants.
The largest group of research staff was based in Oxford and this, together with the nature of the research in different locations, made it sensible to base all of the user involvement in Oxford, with appropriate panels for different WPs. The research project and user involvement continued for some 5 years. It was difficult to maintain contact with all of the original public panel throughout this period, in spite of the effort put into doing so. A little under half of the original panel remained actively involved throughout the period of the research, though most of the MS panel did so.
Discussions in small groups sparked ideas and brought a range of views to the fore, which was useful to the research team. We endeavoured to ensure that meetings were interesting and enjoyable for participants. However, it could be difficult to arrange meetings at a time convenient for all members of the panels. The larger meetings required the involvement of a considerable number of the research team as it was desirable to have separate members of the team facilitating and recording all the discussions. Other approaches, such as contacting individual members of the panels by e-mail and/or telephone, had both advantages and disadvantages. The nature of the research meant that all members of the public panels were experienced users of the internet and happy to communicate and comment by e-mail. It was essential for them to comment on the trial process for WP3b after following it through on the internet. When it was possible to discuss views over the telephone, these could be explored fully, and people who were not confident about speaking in a group may have been more forthcoming in one-to-one conversations. However, conducting and recording telephone calls was time-consuming. Comments made only in e-mails tended to be briefer and lacked the opportunity for development and discussion that was afforded by the face-to-face group meetings.
Lessons learned
Organising PPI uses time and resources. It is important to use the public only in ways which give the participants a genuinely useful and worthwhile role in the research and justify both their input and that of the research team.
Members of the public are likely to have a wide range of views largely reflecting their personal experience. Those volunteering to be members of PPI groups may hold particularly strong views which may not lead to clear consensus.
It might have resulted in better and more focussed discussions, especially on dissemination, if material on the topics to be discussed had been sent to participants in advance. However, to do so would have required an even greater time commitment from the participants, as well as the preparation of new material by the research team.
It was a challenge to maintain the involvement of the same members of the original public panel throughout the long period of the research. We tried to mitigate this with e-mail updates. We also needed to supplement the original panel of PPI volunteers with under-represented sociodemographic groups at later stages of the programme.
It can be difficult to arrange face-to-face meetings of a PPI group, especially if the health conditions of members restrict their mobility or a relatively uncommon condition means that they are drawn from a wide geographical area. In this programme there were particular challenges in convening the MS and MS carers group, but the point is generalisable to other health conditions.
Acknowledgements
The authors would like to thank the following:
The participants of all the separate studies that made up this programme, without whom we would not have had the privilege of conducting this work. These include the participants who gave their time for the numerous studies that were the subject of the WP1b secondary analyses; those who helped develop and pilot the eHIQ, whether through cognitive interview or testing of the questionnaire; those who were the subject of the exploration of the exchange of PEx in online communities in WP2a; those in the studies that led to the development of the guidelines on how to best present experiential information online and the subsequent follow-up study; those in the three narrative interview studies on giving up smoking, living with asthma and caring for someone with MS; and, finally, the EXPERT trial participants, particularly those who also gave a follow-up interview.
Patient and public representatives. The first group contributed to the conceptual mapping (WP1a) at the beginning of the programme and to the piloting of the EXPERT trial. The second, a MS patient and carer group, contributed to the exploration of the exchange of PEx in online communities study (WP2a). Both groups convened later in the programme to advise on dissemination.
David Mant (retired head of the Department of Primary Health Care, University of Oxford) for providing advice on the programme design.
Ruth Sanders, who prepared the WP3a narrative interviews on giving up smoking, living with asthma and caring for someone with MS for delivery to the DIPEx charity and developed the comparator websites used in the EXPERT trial. She also updated and reworked the three intervention websites prior to them being published on healthtalk.org.
Susan Kirkpatrick, Nic Hughes and Laura Griffith, the three senior qualitative researchers who collected the narrative interviews for the development of the EXPERT intervention websites. Thanks are also due to the enthusiastic members of the three qualitative study advisory panels.
Graham Shaw and Luís Carrasqueiro (both former Chief Executives of the DIPEx charity), Adam Barnett (the DIPEx Head of Technical Development and Operations), and Jo Kidd (communications officer) who developed the intervention and comparator websites used in the EXPERT trial and who worked with Codeface (Brighton, UK; www.codeface.com) on the technical aspects of the trial. DIPEx also published the qualitative studies from WP3a on the healthtalk.org website, have developed the project website ipexonline.org and managed a very positively received end-of-project dissemination event.
Richard McGregor from Codeface, an information technology consultant who developed the web portal used in the EXPERT trial and who worked closely with the DIPEx charity to construct the ‘wrapper’ that facilitated communication between the content server and the data portal.
Phoenix Mo and Claire Hardy, postdoctoral researchers who worked sequentially at Northumbria University on the WP2b guidelines for the presentation of experiential information online.
Braden O’Neill, a Rhodes scholar and doctoral student, supervised by SZ, who worked closely with FM on WP2a and also on health literacy, particularly in relation to the EXPERT asthma data set.
Sena Jawad (Clinical Trials Statistician) and Milensu Shanyinde (Clinical Trials Statistician), under the supervision of Ly-Mee Yu (Lead Trial Statistician and Deputy Director Academic of the Oxford Primary Care Clinical Trials Unit), undertook the statistical analyses for the EXPERT trial which are presented in Chapter 8. Ly-Mee Yu and Milensu Shanyinde developed the statistical analysis plan for the three conditions in the trial. Milensu Shanyinde analysed the asthma data. Sena Jawad analysed the smoking cessation and carers of people with MS data. They conducted all of the statistical analyses which are presented, and constructed the tables and plots which are included in this chapter. Nicola Williams (Senior Trial Statistician) also helped in the validation of the analyses. Their statistical expertise and analysis work was vital to the conduct of the EXPERT trial.
Maria Breen (Clinical Trials Unit Manager), David Judge (Clinical Trials Programmer), Brendon Bradley (Clinical Data Manager) and Mina Davoudianfar, Faye Alexander and Ally Bradley (Clinical Trial Managers) all contributed to the EXPERT trial as members of the Oxford Primary Care Clinical Trials Unit. We thank them for all their advice and practical input during the development of the EXPERT trial protocol and during all phases of the trial itself.
The Trial Steering Committee chairperson, Professor Elizabeth Murray (University College London), and external committee member Professor Peter Davidson (University of Southampton) for their highly valued insights and enthusiasm for the EXPERT trial.
The health professionals (Helen Salisbury, Paul Aveyard, Jo Riley, Audrey Owen, Jon Ayres and Richard Warner) who agreed to be interviewed for the health professionals’ corner, used in the three arms of the EXPERT trial.
Sophie Pask for providing general research assistant support and Anasztazia Gubijev for providing practical support during the production of this report.
Nicola Small and Clare Wickings from the Nuffield Department of Primary Care Health Sciences for departmental financial and administrative support, and also Caroline Jordan, Vanessa Eade and Kristy Ravenhall, who provided support to the researchers in the HERG, University of Oxford.
Sula Wiltshire (Coinvestigator, Oxfordshire Clinical Commissioning Group) contributed to the overall study design to ensure relevance for local NHS strategy. She also provided access to the register, held by the then Oxfordshire Primary Care Trust, of patients interested in participating in research, from which the majority of the core public panel was drawn. She remains supportive of the research and would like PEx to be used more widely in the NHS.
We are grateful for funding from the National Institute for Health Research Programme Grants for Applied Research funding scheme (RP-PG-0608–10147). The views expressed in this publication are those of the authors, representing iPEx, and not necessarily those of the NHS, the NIHR or the Department of Health.
Contributions of authors
Sue Ziebland (Principal Investigator, Director of the HERG and Professor of Medical Sociology, University of Oxford) led the overall design of the study, led WP1a, the conceptual review, and coauthored the WP1a chapter, cosupervised the doctoral student who conducted WP1c on development of the eHIQ, led WP3a, the qualitative studies leading to the development of the trial websites, sat on the WP3b EXPERT Trial Steering Committee and led the trial qualitative interviews, chaired the broader programme steering group and led the writing of the final report.
John Powell (Coinvestigator, Senior Clinical Researcher and Associate Professor, University of Oxford) contributed to the overall study design, led WP1b on the secondary analysis of narrative interviews, WP2a on the exploration of the exchange of PEx in online communities and WP3b, the EXPERT randomised trial. He coauthored the chapters describing WP1b, WP2a and WP3a and was the lead author on WP3b. He sat on both the EXPERT Trial Steering Committee and the broader programme steering group, contributed to the final report and gave final approval of the manuscript.
Pamela Briggs (Coinvestigator, Professor of Applied Psychology, Northumbria University) contributed to the overall study design, led WP2b on the development of the guidelines on how best to present experiential information online and coauthored the WP2b chapter. She sat on the programme steering group, contributed to the final report and gave final approval of the manuscript.
Crispin Jenkinson (Coinvestigator, Professor of Health Services Research, University of Oxford) contributed to the overall study design, led WP1c on the development of the eHIQ and coauthored the WP1c chapter. He sat on the programme steering group, contributed to the final report and gave final approval of the manuscript.
Sally Wyke (Coinvestigator, Deputy Director, Institute of Health and Wellbeing, University of Glasgow) contributed to the overall study design, worked closely with Sue Ziebland on the conceptual review (WP1a) and provided expert guidance throughout, especially on the development of the WP1c assessment tool. She coauthored the WP1a chapter, sat on the programme steering group, contributed to the final report and gave final approval of the manuscript.
Elizabeth Sillence (Coinvestigator, Senior Lecturer in Psychology, Northumbria University) contributed to the overall study design, contributed to WP2b on the development of the guidelines on how best to present experiential information online and coauthored the WP2b chapter. She sat on the programme steering group, contributed to the final report and gave final approval of the manuscript.
Peter Harris (Coinvestigator, Professor of Psychology, University of Sussex) contributed to the overall study design, contributed to WP2b on the development of the guidelines on how best to present experiential information online and coauthored the WP2b chapter. He was also a member of the EXPERT Trial Steering Committee and sat on the programme steering group. He contributed to the final report and gave final approval of the manuscript.
Rafael Perera (Coinvestigator, Professor of Medical Statistics, University of Oxford) contributed to the overall study design, was heavily involved in the development of the protocol and the statistical analysis plan for the EXPERT trial (WP3b), sat on the programme steering group, contributed to the final report and gave final approval of the manuscript.
Fadhila Mazanderani (Chancellors’ Fellow, University of Edinburgh) contributed to the design of and was the main researcher on WP1b (secondary analyses of narrative interviews) and WP2a (exploration of the exchange of PEx in online communities). She also worked closely with Braden O’Neill, who conducted the health literacy work with the asthma data from the EXPERT trial. She sat on the programme steering group, coauthored the WP1b and WP2a chapters, contributed to the final report and gave final approval of the manuscript.
Angela Martin (Programme Co-ordinator, University of Oxford) managed and contributed to all WPs bar WP2b, coauthored the chapter describing WP3a, sat on the steering group, contributed to the final report and gave final approval of the manuscript.
Louise Locock (Director of Applied Research, HERG, University of Oxford) contributed to the overall study design and to the conduct of WP1b and WP2a. She contributed to the qualitative study on experiences of asthma (WP3a), and conducted a large proportion of the qualitative interviews with trial participants (WP3b). She coauthored the chapter describing WP3b and the discussion. She sat on the programme steering group, contributed to the final report and gave final approval of the manuscript.
Laura Kelly (Researcher, University of Oxford) contributed to the design of and was the main researcher on WP1c, development of the eHIQ. She sat on the programme steering group, coauthored the chapter describing WP1c, contributed to the final report and gave final approval of the manuscript.
Margaret Booth (Coinvestigator and Lay Representative) contributed to the design of the PPI activities that informed WP1a (the conceptual review), WP2a (the exploration of the exchange of PEx in online communities) and the piloting of the participant journey through the EXPERT trial. She was a member of the EXPERT Trial Steering Committee, sat on the programme steering group, wrote the PPI chapter of the final report and gave final approval of the manuscript.
Bob Gann (Coinvestigator, Programme Director Widening Digital Participation, NHS England) contributed to the overall study design and was involved throughout by providing insight into the relevance of the programme for NHS information policy. He sat on the programme steering group, contributed to the final report and gave final approval of the manuscript.
Nicola Newhouse (Researcher, University of Oxford) contributed to the design and development of the EXPERT trial websites (WP3a), was the main researcher responsible for the EXPERT piloting work and was part of the EXPERT trial team (WP3b). She sat on the programme steering group, contributed to the report chapters describing WP3a and WP3b and gave final approval of the manuscript.
Andrew Farmer (Coinvestigator, Professor of General Practice, University of Oxford) contributed to the overall study design, was involved in the initial development of the protocol for the EXPERT trial (WP3b), sat on the programme steering group, contributed to the final report, in particular the chapter describing WP3b, and gave final approval of the manuscript.
Publications
Locock L, Mazanderani F, Powell J. Metaphoric language and the articulation of emotions by people affected by motor neurone disease. Chronic Illn 2012;8:201–13.
Mazanderani F, Locock L, Powell J. Being differently the same: an exploration of the mediation of identity tensions in the sharing of illness experiences. Soc Sci Med 2012;74:546–53.
O’Neill B, Mazanderani F, Powell J. ‘People power’ or ‘pester power’? YouTube, multiple sclerosis, and the liberation procedure. Lancet 2012;380:S20.
Ziebland S, Wyke S. Health and illness in a connected world: how might sharing experiences on the internet affect people’s health? Milbank Q 2012;90:219–49.
Hughes N, Locock L, Ziebland S. Personal identity and the role of ‘carer’ among relatives and friends of people with multiple sclerosis. Soc Sci Med 2013;96:78–85.
Kelly L, Jenkinson C, Ziebland S. Measuring the effects of online health information for patients: item generation for an e-health impact questionnaire. Patient Educ Couns 2013;93:433–8.
Mazanderani F, Locock L, Powell J. Biographical value: towards a conceptualisaton of the commodification of illness narratives in contemporary healthcare. Sociol Health Ill 2013;35:891–905.
Mazanderani F, O’Neill B, Powell J. ‘People power’ or ‘pester power’? YouTube as a forum for the generation of evidence and patient advocacy. Patient Educ Couns 2013;93:420–5.
Mazanderani F, Powell J. Using the Internet as a Source of Information about Patients’ Experiences. In Ziebland S, Coulter A, Calabrese JD, Locock L, editors. Understanding and Using Health Experiences: Improving Patient Care. Oxford: Oxford University Press; 2013. pp. 94–103.
Sillence E, Hardy C, Briggs P, Harris PR. How do people with asthma use Internet sites containing patient experiences? Patient Educ Couns 2013;93:439–43.
Sillence E, Hardy C, Briggs P, Harris PR. Online health information and patient adherence. J Patient Compliance 2013;2:24–6.
O’Neill B, Gonçalves D, Ricci-Cabello I, Ziebland S, Valderas J. An overview of self-administered health literacy instruments. PLOS ONE 2014;9:e109110.
Kelly L, Ziebland S, Jenkinson C. Measuring the effects of online health information: scale validation for the e-Health Impact Questionnaire. Patient Educ Couns 2015;98:1418–24.
Sillence E, Briggs P. A Timeline to Approach the Study of Trust and Engagement in Online Health and Wellness. In Sundar SS, editor. The Handbook of Psychology and Communication Technology. West Sussex: Wiley-Blackwell; 2015. pp. 469–87.
Sillence E, Hardy C, Briggs P, Harris PR. How do carers of people with multiple sclerosis engage with websites containing the personal experiences of other carers and patients? [Published online ahead of print 11 October 2015.] Health Inform J 2015.
Newhouse N, Martin A, Jawad S, Yu L-M, Davoudianfar M, Locock L, et al. Randomised feasibility study of a novel experience-based Internet intervention to support self-management in chronic asthma. BMJ Open 2016; in press.
Powell J, Newhouse N, Martin A, Jawad S, Yu L-M, Davoudianfar M, Locock L, Ziebland S. A novel experience-based internet intervention for smoking cessation: feasibility randomised controlled trial. BMC Public Health 2016; in press.
Conference presentations
Work package 1a and overview
Ziebland S, Wyke S. Health and Illness in a Wired World: How Might Access to Patients Experiences on the Internet Affect People’s Health? Oral presentation given at the 25th British Computing Society conference on Human-Computer Interaction as part of an iPEx organised workshop, ‘Online patient experience (PEx) and its role in e-health’, Northumbria University, Newcastle upon Tyne, UK, July 2011.
Wyke S, Ziebland S. Health in (Y)our Hands. Oral presentation, Radboud University, Nijmegen, the Netherlands, October 2012.
Wyke S, Ziebland S. Health and Illness in a Connected World: How Might Patients’ Experiences on the Internet Affect People’s Health? Oral presentation, University of British Colombia, Vancouver, BC, Canada, November 2011.
Ziebland S. Health and Illness in a Connected World. Keynote. Qualitative Inquiry Conference, Ben Gurion University, Negev, Israel, February 2012.
Ziebland S. Health and Illness in a Connected World. Invited seminar, DIPEx International and Social Change, University of Monash, Melbourne, VIC, Australia, February 2012.
Ziebland S. The Rise of ‘Patients’ Experiences’: Evidence, Distraction or Final Arbiter. Cochrane Lecture, London School of Hygiene and Tropical Medicine, Society for Social Medicine, 2012.
Ziebland S, Wyke S. Health and Illness in a Connected World: How Might Sharing Experiences on the Internet Affect People’s Health? Abstract and oral presentation, Science and Technology Studies Unit Conference, University of York, York, UK, July 2012.
Ziebland S, Wyke S. Health and Illness in a Connected World: How Might Sharing Experiences on the Internet Affect People’s Health? Oral presentation, British Sociological Association Medical Sociology Annual Conference, University of Leicester, Leicester, UK, September 2012.
Ziebland S, Powell J, Wyke S, Locock L, Farmer A, Perera R, et al. Examining the Role of Patients’ Experiences as a Resource for Choice and Decision-Making in Health Care: An NIHR Programme for Applied Research. South West Society for Academic Primary Care, January 2013.
Work package 1b
Mazanderani F, Powell J, Locock L. Being Differently the Same in the Sharing of Experiences in Healthcare. Oral presentation given at the 25th British Computing Society conference on Human-Computer Interaction as part of an iPEx organised workshop, ‘Online patient experience (PEx) and its role in ehealth’, Northumbria University, Newcastle upon Tyne, UK, July 2011.
Mazanderani F, Powell J, Locock L. Biographical Value: Exploring the Economics, Epistemics and Ethics of Patients’ Experiential Narratives. Oral presentation given at the British Sociological Association, Medical Sociology Annual Conference, University of Chester, Chester, UK, September 2011.
Work package 1c
Hardy C, Hinton L. Mazanderani F, Kelly L. Communicating with Other Patients Online: Exploring the Effects of Sharing Health Experiences on the Internet. Oral presentation given at the European Association of Communication in Healthcare Annual Conference, as part of an iPEx organised symposium, ‘Communicating with other patients online: exploring the effects of sharing health experiences on the internet,’ University of St Andrews, St Andrews, UK, September 2012.
Kelly L, Jenkinson C, Ziebland S. Measuring the Effects of Exposure to Health Websites. Oral presentation given at the European Association of Communication in Healthcare Annual Conference as part of an iPEx organised symposium, ‘Communicating with other patients online: exploring the effects of sharing health experiences on the internet,’ University of St Andrews, St Andrews, UK, September 2012.
Kelly L, Ziebland S, Jenkinson C. Developing and Pre-Testing an Item Pool Relating to the Effects of Exposure to Health Websites. Abstract and poster presentation at International Society for Quality of Life Research, Budapest, Hungary, October 2012.
Kelly L, Simpson H, Verjee-Lorenz A, Clayson D, Churchman D, Jenkinson C, Ziebland S. Translatability Assessment of the e-Health Impact Questionnaire (eHIQ). Poster presentation at the 18th International Society of Pharmacoeconomics and Outcomes Research, New Orleans, LA, May 2013.
Kelly L, Simpson H, Two R, Ziebland S, Jenkinson C. Measuring the Effects of Using Health-Related Websites: Translatability Assessment of Questionnaire Items in the E-Health Impact Questionnaire (eHIQ). Poster presentation at Med 2.0, London, UK, September 2013.
Kelly L, Jenkinson C, Ziebland S. Developing a Tool to Measure the Effects of using Health-Related Websites (the e-Health Impact Questionnaire). Oral presentation, International Society for Quality of Life Research, Miami, FL, October 2013.
Kelly L, Ziebland S, Jenkinson C. The e-Health Impact Questionnaire: Developing a Tool to Measure the Effects of using Health-Related Websites. Value Health 2013;16:A605. Poster presented at International Society of Pharmacoeconomics and Outcomes Research 16th Annual European Congress, Dublin, Ireland, November 2013.
Work package 2a
Mazanderani F, Powell J. Bodies of Knowledge: Reconfiguring Multiple Sclerosis as a Vascular Disease. Making (In)Appropriate Bodies Conference, hosted by the Science Studies Department, University of Vienna, Vienna, Austria, December 2011.
Mazanderani F, Powell J. Anecdote and Evidence: Social Media and the Enactment of ‘Proof’ in a Controversial Theory about Multiple Sclerosis. Oral presentation, The Co-Production of Knowledge: Social Media, STS and . . ., hosted by the University of York, York, UK, July 2012.
Mazanderani F, Powell J. Platforms, Patients and the Production of Experience. Oral presentation given at the European Association of Communication in Healthcare Annual Conference as part of an iPEx organised symposium, ‘Communicating with other patients online: exploring the effects of sharing health experiences on the internet’, University of St Andrews, St Andrews, UK, September 2012.
Mazanderani F, Powell J. An Aesthetics of Care? Attraction, Attachment and Alignment in Online Multiple Sclerosis Communities. Abstract and oral presentation, Society for Social Studies of Science and European Association for the Study of Science and Technology Joint Conference, Copenhagen, Denmark, October 2012.
O’Neill BG, Mazanderani F, Powell J. ‘People Power’ or ‘Pester Power’? YouTube as a Forum for the Generation of Evidence and Patient Advocacy. Oral presentation, Royal Society of Medicine, London, UK, November 2012.
Mazanderani F. Illness Narratives, Experiential Knowledge and Contemporary Regimes of ‘Living With’ Disease. Oral presentation, Medical Sociology Annual Conference, University of York, York, UK, September 2013.
Mazanderani F, O’Neill B, Powell, J. YouTube and Patient Activism: Online Video and the Generation of ‘Experiential’ Evidence. Oral presentation, Med 2.0, London, UK, September 2013.
Mazanderani F and Powell J. When Bodies Fall Apart. Internet Use, Patient Activism and the Mediation of Medical Knowledge. Oral presentation, Medical Sociology Annual Conference, University of York, York, UK, September 2013.
O’Neill B, Ziebland S, Powell J. Health Literacy and the Internet: EXperiences Evaluated in a Randomised Trial (EXPERT). Oral presentation, Connected Life, Oxford, UK, 2014.
Work package 2b
Mo P, Sillence E, Briggs P, Harris P. What Kind of Information on Smoking Cessation is Available Online? A Content Analysis of Common Websites. Oral presentation, 25th British Computing Society conference on Human–Computer Interaction as part of an iPEx organised workshop ‘Online patient experience (PEx) and its role in ehealth’, Northumbria University, Newcastle upon Tyne, UK, July 2011.
Hardy C, Sillence E, Briggs P, Harris PR. A Toolkit Approach for eHealth research: Using Focus Groups, Interviews, Data Logging, and Eye Tracking to Examine Individuals across a Range of Health Conditions. Oral presentation, European Association of Communication in Healthcare Annual Conference as part of an iPEx organised symposium ‘Communicating with other patients online: exploring the effects of sharing health experiences on the internet’, University of St Andrews, St Andrews, UK, September 2012.
Hardy C, Sillence E, Briggs P, Harris P. Engaging With Online Patient Experiences: Exploring Differences Between Health Groups. Abstract and oral presentation, Global Health Conference, Venice, Austria, October 2012.
Briggs P, Hardy C, Sillence E, Harris P. An Engagement Framework for Understanding the Communication Needs of Different Health Groups. Poster and extended abstract, CHI Conference on Human Factors in Computing Systems, Paris, France, 27 April–2 May 2013.
Sillence E, Hardy C, Briggs P. Why Don’t We Trust Health Websites that Help Us Help Each Other? ACM Web Science 2013, Paris, May 2013.
Hardy C, Sillence E, Briggs P, Harris P. Online Peer-to-Peer Healthcare: Exploring Push-Pull Factors of Engagement. Oral presentation, Med 2.0, London, UK, September 2013.
Briggs P, Hardy C, Harris PR, Sillence E. Patient-led Perspectives on eHealth: How Might Hyperpersonal Data inform Design? Proceedings of HCIK, ACM Press, Korea, 2014.
Sillence E, Hardy C, Harris P, Briggs P. Modelling Patient Engagement in Peer-to-Peer Healthcare. 23rd International World Wide Web Conference, Korea, April 2014.
Sillence E, Harris P, Briggs P. Assessing Patient Experience and Patient Preference when Designing Web Support for Smoking Cessation. Extended abstract and oral presentation, Association for Computing Machinery conference on Digital Health, Florence, Italy, May 2015.
Work package 3a
Hughes N. Personal Identity and Caring: Stories Told by Relatives and Friends of People with Multiple Sclerosis. Oral presentation, Contemporary Narratives of Care, Birkbeck, London, October 2013.
Kirkpatrick S, Locock L, Salisbury H, Ziebland S. ‘I’d Always Seen Myself as Invincible but Suddenly I’d Got this Condition that Wasn’t Going to Go Away’: The Emotional Impact of a Diagnosis of Asthma in Adulthood. British Sociological Association Medical Sociology Annual Conference, Aston University, Birmingham, UK, September 2014.
Hughes N. Personal identity and role of ‘carer’ among relatives and friends of people with MS. Oral presentation, 6th National Conference for Psychologists Working in MS, Genoa, Italy, October 2014.
Work package 3b
Newhouse N, Ziebland S, Locock L, Perera R, Farmer A, Powell J. Sharing Experiences Online: Design of a Randomised Trial to Determine the Feasibility and Efficacy of Three Novel Internet-Based Interventions Based on Patient Experience. Oral presentation, Med 2.0, London, UK, September 2013.
Newhouse N. The EXPERT study: Patient Experience as Information Resource: What Does the Right ‘Dose’ Look Like? Oral presentation, UK Society for Behavioural Medicine, Oxford, UK, December 2013.
Powell J, Ziebland S, Newhouse N. The EXPERT Study: Randomised Controlled Trial of an Internet-Based Intervention Harnessing Patient Experiences to Support Self-Management of Asthma. Oral presentation, Med 2.0, Malaga, Spain, October 2014.
Newhouse N. The EXPERT Study. Patient Experience as Information Resource: What Does the Right ‘Dose’ Look Like? Oral presentation, Centre for Behaviour Change Conference, London, UK, February 2015.
Powell P, Newhouse N, Martin A, Jawad S, Yu L-M, Davoudianfar M, et al. Randomised Feasibility Study of a Novel Experience-based Internet Intervention for Smoking Cessation. Poster presentation, Association for Computing Machinery Conference on Digital Health, Florence, Italy, May 2015.
Powell P, Newhouse N, Martin A, Jawad S, Yu L-M, Davoudianfar M, et al. The EXPERT Study: Feasibility Randomised Controlled Trial of an Internet-Based Intervention using Patient Experience to Support Self-Management of Asthma. Oral presentation, Society for Academic Primary Care Conference, Oxford, UK, July 2015.
Overarching programme
Ziebland S. Health and Illness in a Connected World: Understanding the Role and Value of ‘Patients’ Experiences’ Online. British Sociological Association Medical Sociology South Coast Conference, Brighton, UK, July 2015.
Other outputs
Series of presentations for undergraduate students from Radboud University, Nijmegen, the Netherlands, October 2013:
-
O’Neill B. ‘People Power’ or ‘Pester Power’? YouTube as a Forum for the Generation of Evidence and Patient Advocacy.
-
Newhouse N. EXPERT Trial.
-
O’Neill B. Technology of Stories: Health Literacy and EXPERT.
A secondary analysis of the asthma qualitative interviews in WP3a contributed to the evidence considered by the National Institute for Health and Care Excellence Quality Standard on asthma.
A new website on experiences of asthma: www.healthtalk.org/asthma.
A new website on experiences of giving up smoking: www.healthtalk.org/giving-up-smoking.
A new resource for the family and friends of people with MS: www.healthtalk.org/ms-friends-family.
Examining the Role of Patients’ Experiences as a Resource for Choice and Decision-Making in Health Care. iPEx programme dissemination event for senior policy-makers, London, June 2014.
Examining the Role of Patients’ Experiences as a Resource for Choice and Decision-Making in Health Care. iPEx programme final dissemination event, London, June 2015.
Data sharing statement
Data can be obtained on application to the corresponding author, Professor Sue Ziebland: e-mail sue.ziebland@phc.ox.ac.uk.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- Leydon GM, Boulton M, Moynihan C, Jones A, Mossman J, Boudioni M, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ 2000;320:909-13. http://dx.doi.org/10.1136/bmj.320.7239.909.
- Glenton C. Developing patient-centred information for back pain sufferers. Health Expect 2002;5:319-29. http://dx.doi.org/10.1046/j.1369-6513.2002.00196.x.
- Sillence E, Mo PK. Communicating health decisions: an analysis of messages posted to online prostate cancer forums. Health Expect 2014;17:244-53. http://dx.doi.org/10.1111/j.1369-7625.2011.00745.x.
- Ziebland S, Wyke S. Health and illness in a connected world: how might sharing experiences on the internet affect people’s health?. Milbank Q 2012;90:219-49. http://dx.doi.org/10.1111/j.1468-0009.2012.00662.x.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: Sage; 2006.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. http://dx.doi.org/10.1258/1355819054308530.
- Broemer P. Ease of imagination moderates reactions to differently framed health messages. Eur J Soc Psychol 2004;34:103-19. http://dx.doi.org/10.1002/ejsp.185.
- Sillence E, Briggs P, Harris PR, Fishwick L. How do patients evaluate and make use of online health information?. Soc Sci Med 2007;64:1853-62. http://dx.doi.org/10.1016/j.socscimed.2007.01.012.
- Rothman AJ, Kiviniemi MT. Treating people with information: an analysis and review of approaches to communicating health risk information. J Natl Cancer Inst Monographs 1999;25:44-51. http://dx.doi.org/10.1093/oxfordjournals.jncimonographs.a024207.
- Lowe P, Powell J, Griffiths F, Thorogood M, Locock L. Making it all normal: the role of the internet in problematic pregnancy. Qual Health Res 2009;19:1476-84. http://dx.doi.org/10.1177/1049732309348368.
- Caiata Zufferey M, Schulz PJ. Self-management of chronic low back pain: an exploration of the impact of a patient-centered website. Patient Educ Couns 2009;77:27-32. http://dx.doi.org/10.1016/j.pec.2009.01.016.
- Sandaunet AG. A space for suffering? Communicating breast cancer in an online self-help context. Qual Health Res 2008;18:1631-41. http://dx.doi.org/10.1177/1049732308327076.
- van Uden-Kraan CF, Drossaert CH, Taal E, Shaw BR, Seydel ER, van de Laar MA. Empowering processes and outcomes of participation in online support groups for patients with breast cancer, arthritis, or fibromyalgia. Qual Health Res 2008;18:405-17. http://dx.doi.org/10.1177/1049732307313429.
- Steffen V. Life stories and shared experience. Soc Sci Med 1997;45:99-111. http://dx.doi.org/10.1016/S0277-9536(96)00319-X.
- France EF, Wyke S, Ziebland S, Entwistle VA, Hunt K. How personal experiences feature in women’s accounts of use of information for decisions about antenatal diagnostic testing for foetal abnormality. Soc Sci Med 2011;72:755-62. http://dx.doi.org/10.1016/j.socscimed.2010.11.031.
- Entwistle VA, France EF, Wyke S, Jepson R, Hunt K, Ziebland S, et al. How information about other people’s personal experiences can help with healthcare decision-making: a qualitative study. Patient Educ Couns 2011;85:e291-8. http://dx.doi.org/10.1016/j.pec.2011.05.014.
- Bruce B, Lorig K, Laurent D, Ritter P. The impact of a moderated e-mail discussion group on use of complementary and alternative therapies in subjects with recurrent back pain. Patient Educ Couns 2005;58:305-11. http://dx.doi.org/10.1016/j.pec.2004.08.012.
- Etchegary H, Potter B, Howley H, Cappelli M, Coyle D, Graham I, et al. The influence of experiential knowledge on prenatal screening and testing decisions. Genet Test 2008;12:115-24. http://dx.doi.org/10.1089/gte.2007.0057.
- Taylor SE, Thompson SC. Stalking the elusive ‘vividness’ effect. Psychol Rev 1982;89:155-81. http://dx.doi.org/10.1037/0033-295X.89.2.155.
- Winterbottom A, Bekker HL, Conner M, Mooney A. Does narrative information bias individual’s decision making? A systematic review. Soc Sci Med 2008;67:2079-88. http://dx.doi.org/10.1016/j.socscimed.2008.09.037.
- Entwistle V. Considering ‘balance’ in information. Health Expect 2007;10:307-8. http://dx.doi.org/10.1111/j.1369-7625.2007.00469.x.
- Harvey KJ, Brown B, Crawford P, Macfarlane A, McPherson A. ‘Am I normal?’ Teenagers, sexual health and the internet. Soc Sci Med 2007;65:771-81. http://dx.doi.org/10.1016/j.socscimed.2007.04.005.
- Adair CE, Marcoux G, Williams A, Reimer M. The Internet as a source of data to support the development of a quality-of-life measure for eating disorders. Qual Health Res 2006;16:538-46. http://dx.doi.org/10.1177/1049732305285850.
- Gillett J. Media activism and Internet use by people with HIV/AIDS. Sociol Health Illn 2003;25:608-24. http://dx.doi.org/10.1111/1467-9566.00361.
- Bar-Lev S. ‘We are here to give you emotional support’: performing emotions in an online HIV/AIDS support group. Qual Health Res 2008;18:509-21. http://dx.doi.org/10.1177/1049732307311680.
- Drentea P, Moren-Cross JL. Social capital and social support on the web: the case of an internet mother site. Sociol Health Illn 2005;27:920-43. http://dx.doi.org/10.1111/j.1467-9566.2005.00464.x.
- Radley A. The aesthetics of illness: narrative, horror and the sublime. Sociol Health Ill 1999;21:778-96. http://dx.doi.org/10.1111/1467-9566.00183.
- Cohen S. Social relationships and health. Am Psychol 2004;59:676-84. http://dx.doi.org/10.1037/0003-066X.59.8.676.
- Armstrong N, Powell J. Patient perspectives on health advice posted on Internet discussion boards: a qualitative study. Health Expect 2009;12:313-20. http://dx.doi.org/10.1111/j.1369-7625.2009.00543.x.
- Coulson NS, Buchanan H, Aubeeluck A. Social support in cyberspace: a content analysis of communication within a Huntington’s disease online support group. Patient Educ Couns 2007;68:173-8. http://dx.doi.org/10.1016/j.pec.2007.06.002.
- Hinton L, Kurinczuk JJ, Ziebland S. Infertility; isolation and the Internet: a qualitative interview study. Patient Educ Couns 2010;81:436-41. http://dx.doi.org/10.1016/j.pec.2010.09.023.
- Chapple A, Ziebland S. How the Internet is changing the experience of bereavement by suicide: a qualitative study in the UK. Health 2011;15:173-87. http://dx.doi.org/10.1177/1363459309360792.
- Negroponte N. Being Digital. New York, NY: Vintage Books; 1995.
- Sharf BF. Communicating breast cancer on-line: support and empowerment on the Internet. Women Health 1997;26:65-84. http://dx.doi.org/10.1300/J013v26n01_05.
- Ricketts M, Shanteau J, McSpadden B, Fernandez-Medina KM. Using stories to battle unintentional injuries: narratives in safety and health communication. Soc Sci Med 2010;70:1441-9. http://dx.doi.org/10.1016/j.socscimed.2009.12.036.
- Caiata-Zufferey M, Abraham A, Sommerhalder K, Schulz PJ. Online health information seeking in the context of the medical consultation in Switzerland. Qual Health Res 2010;20:1050-61. http://dx.doi.org/10.1177/1049732310368404.
- Fredriksen EH, Moland KM, Sundby J. ‘Listen to your body’. A qualitative text analysis of Internet discussions related to pregnancy health and pelvic girdle pain in pregnancy. Patient Educ Couns 2008;73:294-9. http://dx.doi.org/10.1016/j.pec.2008.02.002.
- Ziebland S. The importance of being expert: the quest for cancer information on the internet. Soc Sci Med 2004;59:1783-93. http://dx.doi.org/10.1016/j.socscimed.2004.02.019.
- Ziebland S, Chapple A, Dumelow C, Evans J, Prinjha S, Rozmovits L. How the Internet affects patients’ experience of cancer: a qualitative study. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.328.7439.564.
- Pitts V. Illness and Internet empowerment: writing and reading breast cancer in cyberspace. Health 2004;8:33-59. http://dx.doi.org/10.1177/1363459304038794.
- Dumit J. Illnesses you have to fight to get: facts as forces in uncertain, emergent illnesses. Soc Sci Med 2006;62:577-90. http://dx.doi.org/10.1016/j.socscimed.2005.06.018.
- Qiu J. Venous abnormalities and multiple sclerosis: another breakthrough claim?. Lancet Neurol 2010;9:464-5. http://dx.doi.org/10.1016/S1474-4422(10)70098-3.
- Wicks P, Massagli M, Frost J, Brownstein C, Okun S, Vaughan T, et al. Sharing health data for better outcomes on PatientsLikeMe. J Med Internet Res 2010;12. http://dx.doi.org/10.2196/jmir.1549.
- Bettelheim B. The Uses of Enchantment: The Meaning and Importance of Fairy Tales. New York, NY: Knopf; 1976.
- de Wit JB, Das E, Vet R. What works best: objective statistics or a personal testimonial? An assessment of the persuasive effects of different types of message evidence on risk perception. Health Psychol 2008;27:110-15. http://dx.doi.org/10.1037/0278-6133.27.1.110.
- Green MC, Brock TC. The role of transportation in the persuasiveness of public narratives. J Pers Soc Psychol 2000;79:701-21. http://dx.doi.org/10.1037/0022-3514.79.5.701.
- Frank AW. The Wounded Storyteller: Body, Illness, and Ethics. Chicago, IL: University of Chicago Press; 1995.
- Pennebaker JW, Seagal JD. Forming a story: the health benefits of narrative. J Clin Psychol 1999;55:1243-54. http://dx.doi.org/10.1002/(SICI)1097-4679(199910)55:10<1243::AID-JCLP6>3.0.CO;2-N.
- Carlick A, Biley FC. Thoughts on the therapeutic use of narrative in the promotion of coping in cancer care. Eur J Cancer Care 2004;13:308-17. http://dx.doi.org/10.1111/j.1365-2354.2004.00466.x.
- Bury M. Illness narratives: fact or fiction?. Sociol Health Ill 2001;23:263-85. http://dx.doi.org/10.1111/1467-9566.00252.
- Schwartz B. The Paradox of Choice: Why More Is Less. New York, NY: Ecco; 2004.
- Williams B, Cameron L. Images in health care: potential and problems. J Health Serv Res Policy 2009;14:251-4. http://dx.doi.org/10.1258/jhsrp.2009.008168.
- Oostveen A. The Internet As an Empowering Technology for Stigmatized Groups: A Case Study of Weight Loss Bloggers n.d.
- Lee TJ, Cameron LD, Wünsche B, Stevens C. A randomized trial of computer-based communications using imagery and text information to alter representations of heart disease risk and motivate protective behaviour. Br J Health Psychol 2011;16:72-91. http://dx.doi.org/10.1348/135910710X511709.
- Mazanderani F, Locock L, Powell J. Being differently the same: the mediation of identity tensions in the sharing of illness experiences. Soc Sci Med 2012;74:546-53. http://dx.doi.org/10.1016/j.socscimed.2011.10.036.
- Cline RJ, Haynes KM. Consumer health information seeking on the Internet: the state of the art. Health Educ Res 2001;16:671-92. http://dx.doi.org/10.1093/her/16.6.671.
- Rothman AJ, Kelly KM, Weinstein ND, O’Leary A. Increasing the salience of risky sexual behavior: promoting interest in HIV-antibody testing among heterosexually active young adults. J Appl Soc Psychol 1999;29:531-51. http://dx.doi.org/10.1111/j.1559-1816.1999.tb01400.x.
- Buchanan H, Coulson NS. Accessing dental anxiety online support groups: an exploratory qualitative study of motives and experiences. Patient Educ Couns 2007;66:263-9. http://dx.doi.org/10.1016/j.pec.2006.12.011.
- Davison C, Smith GD, Frankel S. Lay epidemiology and the prevention paradox – the implications of coronary candidacy for health-education. Sociol Health Ill 1991;13:1-19. http://dx.doi.org/10.1111/1467-9566.ep11340301.
- Gavin J, Rodham K, Poyer H. The presentation of ‘pro-anorexia’ in online group interactions. Qual Health Res 2008;18:325-33. http://dx.doi.org/10.1177/1049732307311640.
- Ubel PA, Jepson C, Baron J. The inclusion of patient testimonials in decision aids: effects on treatment choices. Med Decis Making 2001;21:60-8. http://dx.doi.org/10.1177/0272989X0102100108.
- Blumenthal D. Doctors in a wired world: can professionalism survive connectivity?. Milbank Q 2002;80:525-46. http://dx.doi.org/10.1111/1468-0009.00021.
- Heaton J. Reworking Qualitative Data. London: Sage; 2004.
- Locock L, Mazanderani F, Powell J. Metaphoric language and the articulation of emotions by people affected by motor neurone disease. Chronic Illn 2012;8:201-13. http://dx.doi.org/10.1177/1742395312443390.
- Mazanderani F, Locock L, Powell J. Biographical value: towards a conceptualisation of the commodification of illness narratives in contemporary healthcare. Sociol Health Illn 2013;35:891-905. http://dx.doi.org/10.1111/1467-9566.12001.
- Kelly L, Jenkinson C, Ziebland S. Measuring the effects of online health information for patients: item generation for an e-health impact questionnaire. Patient Educ Couns 2013;93:433-8. http://dx.doi.org/10.1016/j.pec.2013.03.012.
- Hinds PS, Vogel RJ, ClarkeSteffen L. The possibilities and pitfalls of doing a secondary analysis of a qualitative data set. Qual Health Res 1997;7:408-24. http://dx.doi.org/10.1177/104973239700700306.
- Ziebland S, Hunt K. Using secondary analysis of qualitative data of patient experiences of health care to inform health services research and policy. J Health Serv Res Policy 2014;19:177-82. http://dx.doi.org/10.1177/1355819614524187.
- Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries?. J Adv Nurs 1997;26:623-30. http://dx.doi.org/10.1046/j.1365-2648.1997.t01-25-00999.x.
- Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ 2006;40:405-14. http://dx.doi.org/10.1111/j.1365-2929.2006.02467.x.
- Herxheimer A, McPherson A, Miller R, Shepperd S, Yaphe J, Ziebland S. Database of patients’ experiences (DIPEx): a multi-media approach to sharing experiences and information. Lancet 2000;355:1540-3. http://dx.doi.org/10.1016/S0140-6736(00)02174-7.
- Charmaz K. ‘Discovering’ chronic illness: using grounded theory. Soc Sci Med 1990;30:1161-72. http://dx.doi.org/10.1016/0277-9536(90)90256-R.
- NatCen Social Research . NATCEN Social Research n.d. www.natcen.ac.uk/ (accessed 2 June 2016).
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. Abingdon: Routledge; 1994.
- McColl E, Fayers R, Hays R. Assessing Quality of Life in Clinical Trials. Oxford: Oxford University Press; 2005.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Robson C. Real World Research: A Resource for Social Scientists and Practitioner-Researchers. Oxford: Blackwell Publishers; 2002.
- Locock L, Brown JB. ‘All in the same boat’? Patient and carer attitudes to peer support and social comparison in Motor Neurone Disease (MND). Soc Sci Med 2010;71:1498-505. http://dx.doi.org/10.1016/j.socscimed.2010.06.043.
- Borkman T. Experiential knowledge: a new concept for the analysis of self-help groups. Soc Sci Rev 1976;50:445-56. http://dx.doi.org/10.1086/643401.
- Abel K, Browner C, Lock MM, Kaufert PA. Pragmatic Women and Body Politics. Cambridge: Cambridge University Press; 1998.
- Boardman FK. Knowledge is power? The role of experiential knowledge in genetically ‘risky’ reproductive decisions. Sociol Health Illn 2014;36:137-50. http://dx.doi.org/10.1111/1467-9566.12048.
- Ricoeur P. The Rule of Metaphor: The Creation of Meaning in Language. London: Routledge; 2003.
- Charon R. Narrative Medicine: Honoring the Stories of Illness. New York, NY: Oxford University Press; 2008.
- Mazanderani F, O’Neill B, Powell J. ‘People power’ or ‘pester power’? YouTube as a forum for the generation of evidence and patient advocacy. Patient Educ Couns 2013;93:420-5. http://dx.doi.org/10.1016/j.pec.2013.06.006.
- Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. London: Sage Publications; 2005.
- Willis GB. Cognitive Interviewing: A ‘How To’ Guide n.d.
- Wilson M. Constructing Measures: An Item Response Modeling Approach. Mahwah, NJ: Lawrence Erlbaum Associates; 2005.
- Bartlett MS. A note on multiplying factors for various chi-squared approximations. J R Stat Soc Series B Stat Methodol 1954;16:296-8.
- Kaiser HF, Rice J. Little Jiffy, Mark IV. Educ Psychol Meas 1974;34:111-17. http://dx.doi.org/10.1177/001316447403400115.
- Norman G, Streiner D. Biostatistics: The Bare Essentials. London: B.C. Decker; 2000.
- Matsunaga M. How to factor-analyze your data right: do’s, don’ts, and how-to’s. Int J Psychol Res 2010;3:97-110.
- Pett MA, Lackey NR, Sullivan JJ. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research. Thousand Oaks, CA: Sage Publications; 2003.
- Conway K, Patrick DL, Gauchon T. Enhancing cross-cultural appropriateness for newly developed patient-reported outcome (PRO) instruments: the use of translatability assessment. PRO Newsletter 2010;44:9-11.
- Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun 2004;9:443-60. http://dx.doi.org/10.1080/10810730490504233.
- Harris PR, Sillence E, Briggs P. Perceived threat and corroboration: key factors that improve a predictive model of trust in internet-based health information and advice. J Med Internet Res 2011;13. http://dx.doi.org/10.2196/jmir.1821.
- Williams G, Detels R, Beaglehole R, Lansang MA, Gulliford M. Oxford Textbook of Public Health 1. New York, NY: Oxford University Press; 2009.
- Nunnally J, Bernstein IH. Psychometric Theory. New York, NY: McGraw-Hill; 1994.
- Gorsuch RL. Factor Analysis. Hillsdale, NJ: L Erlbaum Associates; 1983.
- Kelly L, Ziebland S, Jenkinson C. Measuring the effects of online health information: scale validation for the e-Health Impact Questionnaire. Patient Educ Couns 2015;98:1418-24. http://dx.doi.org/10.1016/j.pec.2015.06.008.
- European Medicine Agency . Reflection Paper on the Regulatory Guidance for the Use of Health-Related Quality Of Life (HRQL) Measures in the Evaluation of Medicinal Products n.d. www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/general/general_content_001238.jsp&mid=WC0b01ac0580032ec4 (accessed 23 August 2016).
- US Department of Health and Human Services Food and Drug Administration . Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims 2009. www.fda.gov/downloads/Drugs/. /Guidances/UCM193282.pdf (accessed 23 August 2016).
- Hinkin TR. A brief tutorial on the development of measures for use in survey questionnaires. Organ Res Methods 1998;1:104-21. http://dx.doi.org/10.1177/109442819800100106.
- Jenkinson C, McGee H, Jenkinson C. Assessment and Evaluation of Health and Medical Care: A Methods Text. Philadelphia, PA: Open University Press; 1997.
- Hays RD, Revicki D, Fayers P, Hays R. Reliability and Validity (Including Responsiveness). New York, NY: Oxford University Press; 2005.
- Murray TJ. Diagnosis and treatment of multiple sclerosis. BMJ 2006;332:525-7. http://dx.doi.org/10.1136/bmj.332.7540.525.
- Robinson I. Multiple Sclerosis (Experience of Illness). London: Routledge; 1988.
- Lexell EM, Lund ML, Iwarsson S. Constantly changing lives: experiences of people with multiple sclerosis. Am J Occup Ther 2009;63:772-81. http://dx.doi.org/10.5014/ajot.63.6.772.
- Dyck I. Hidden geographies: the changing lifeworlds of women with multiple sclerosis. Soc Sci Med 1995;40:307-20. http://dx.doi.org/10.1016/0277-9536(94)E0091-6.
- Hay MC, Strathmann C, Lieber E, Wick K, Giesser B. Why patients go online: multiple sclerosis, the internet, and physician-patient communication. Neurologist 2008;14:374-81. http://dx.doi.org/10.1097/NRL.0b013e31817709bb.
- Fernandez-Luque L, Elahi N, Grajales FJ. An analysis of personal medical information disclosed in YouTube videos created by patients with multiple sclerosis. Stud Health Technol Inform 2009;150:292-6.
- Charmaz K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. London: Sage; 2006.
- Zamboni P, Menegatti E, Weinstock-Guttman B, Schirda C, Cox JL, Malagoni AM, et al. The severity of chronic cerebrospinal venous insufficiency in patients with multiple sclerosis is related to altered cerebrospinal fluid dynamics. Funct Neurol 2009;24:133-8.
- Mazanderani F, Powell J, Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and Using Health Experiences: Improving Patient Care. Oxford: Oxford University Press; 2013.
- Orgad S. How Can Researchers Make Sense of the Issues Involved in Collecting and Interpreting Online and Offline Data?. Thousand Oaks, CA: Sage; 2009.
- Gafson AR, Giovannoni G. CCSVI-A. A call to clinicans and scientists to vocalise in an Internet age. Mult Scler Relat Disord 2014;3:143-6. http://dx.doi.org/10.1016/j.msard.2013.10.005.
- Lombard M, Snyder-Duch J, Bracken CC. Content analysis in mass communication: assessment and reporting of intercoder reliability. Hum Commun Res 2002;28:587-604. http://dx.doi.org/10.1111/j.1468-2958.2002.tb00826.x.
- Nonnecke B, Preece J, Lueg C, Fisher D. From Usenet to CoWebs: Interacting with Social Information Spaces. London: Springer-Verlag; 2003.
- Corbin JM, Strauss A. Unending Work and Care: Managing Chronic Illness at Home. San Francisco, CA: Jossey-Bass Publishers; 1988.
- Timmermans S, Haas S. Towards a sociology of disease. Sociol Health Illn 2008;30:659-76. http://dx.doi.org/10.1111/j.1467-9566.2008.01097.x.
- Pols J. Knowing patients: turning patient knowledge into science. Sci Technol Hum Val 2014;39:73-97. http://dx.doi.org/10.1177/0162243913504306.
- Morrison LG, Yardley L, Powell J, Michie S. What design features are used in effective e-health interventions? A review using techniques from Critical Interpretive Synthesis. Telemed J E Health 2012;18:137-44. http://dx.doi.org/10.1089/tmj.2011.0062.
- Seale C. New directions for critical internet health studies: representing cancer experience on the web. Sociol Health Illn 2005;27:515-40. http://dx.doi.org/10.1111/j.1467-9566.2005.00454.x.
- Gillespie T. The politics of ‘platforms’. New Media Soc 2010;12:347-64. http://dx.doi.org/10.1177/1461444809342738.
- Harris PR, Sillence E, Briggs P. The effect of credibility-related design cues on responses to a web-based message about the breast cancer risks from alcohol: randomized controlled trial. J Med Internet Res 2009;11. http://dx.doi.org/10.2196/jmir.1097.
- Orgad S. The cultural dimensions of online communication: a study of breast cancer patients’ internet spaces. New Media Soc 2006;8:877-99. http://dx.doi.org/10.1177/1461444806069643.
- Armstrong N, Koteyko N, Powell J. ‘Oh dear, should I really be saying that on here?’: issues of identity and authority in an online diabetes community. Health 2012;16:347-65. http://dx.doi.org/10.1177/1363459311425514.
- James N. Emotional labor – skill and work in the social regulation of feelings. Sociol Rev 1989;37:15-42. http://dx.doi.org/10.1111/j.1467-954X.1989.tb00019.x.
- Zamboni P, Galeotti R, Menegatti E, Malagoni AM, Tacconi G, Dall’Ara S, et al. Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis. J Neurol Neurosurg Psychiatr 2009;80:392-9. http://dx.doi.org/10.1136/jnnp.2008.157164.
- Chafe R, Born KB, Slutsky AS, Laupacis A. The rise of people power. Nature 2011;472:410-11. http://dx.doi.org/10.1038/472410a.
- Rhodes MA. CCSVI as the Cause Of Multiple Sclerosis: The Science Behind the Controversial Theory. Jefferson, NC: McFarland & Co.; 2011.
- de Barra M, Eriksson K, Strimling P. How feedback biases give ineffective medical treatments a good reputation. J Med Internet Res 2014;16. http://dx.doi.org/10.2196/jmir.3214.
- Reekers JA. CCSVI and MS: a never-ending story. Eur J Vasc Endovasc Surg 2012;43:127-8. http://dx.doi.org/10.1016/j.ejvs.2011.09.019.
- Akrich M. From communities of practice to epistemic communities: health mobilizations on the internet. Sociol Res Online 2010;15. http://dx.doi.org/10.5153/sro.2152.
- Mo PK, Coulson NS. Exploring the communication of social support within virtual communities: a content analysis of messages posted to an online HIV/AIDS support group. Cyberpsychol Behav 2008;11:371-4. http://dx.doi.org/10.1089/cpb.2007.0118.
- Fox S, Duggan M. Peer-to-Peer Health Care 2013. www.pewinternet.org/2013/01/15/peer-to-peer-health-care/ (accessed 2 June 2016).
- Coleman J, Olsen SJ, Sauter PK, Baker D, Hodgin MB, Stanfield C, et al. The effect of a frequently asked questions module on a pancreatic cancer web site patient/family chat room. Cancer Nurs 2005;28:460-8. http://dx.doi.org/10.1097/00002820-200511000-00009.
- James N, Daniels H, Rahman R, McConkey C, Derry J, Young A. A study of information seeking by cancer patients and their carers. Clin Oncol 2007;19:356-62. http://dx.doi.org/10.1016/j.clon.2007.02.005.
- White MH, Dorman SM. Online support for caregivers. Analysis of an internet Alzheimer mailgroup. Comput Nurs 2000;18:168-76.
- Baum LS. Internet parent support groups for primary caregivers of a child with special health care needs. Pediatr Nurs 2004;30:381-8.
- Brindal E, Freyne J, Saunders I, Berkovsky S, Smith G, Noakes M. Features predicting weight loss in overweight or obese participants in a web-based intervention: randomized trial. J Med Internet Res 2012;14:114-29. http://dx.doi.org/10.2196/jmir.2156.
- van Mierlo T, Voci S, Lee S, Fournier R, Selby P. Superusers in social networks for smoking cessation: analysis of demographic characteristics and posting behavior from the Canadian Cancer Society’s Smokers’ Helpline Online and StopSmokingCenter.net. J Med Internet Res 2012;14:45-59. http://dx.doi.org/10.2196/jmir.1854.
- Powell J, Clarke A. Information in mental health: qualitative study of mental health service users. Health Expect 2006;9:359-65. http://dx.doi.org/10.1111/j.1369-7625.2006.00403.x.
- Sillence E, Briggs P, Peter H, Fishwick L. A framework for understanding trust factors in web-based health advice. Int J Hum-Comput St 2006;64:697-713. http://dx.doi.org/10.1016/j.ijhcs.2006.02.007.
- Sillence E, Briggs P, Fishwick L, Harris PR. Trust and Mistrust of Online Health Sites n.d. http://dx.doi.org/10.1145/985692.985776.
- Chaiken S. Heuristic versus systematic information-processing and the use of source versus message cues in persuasion. J Pers Soc Psychol 1980;39:752-66. http://dx.doi.org/10.1037/0022-3514.39.5.752.
- Wang Z, Walther JB, Pingree S, Hawkins RP. Health information, credibility, homophily, and influence via the Internet: web sites versus discussion groups. Health Commun 2008;23:358-68. http://dx.doi.org/10.1080/10410230802229738.
- Winterbottom AE, Bekker HL, Conner M, Mooney AF. Patient stories about their dialysis experience biases others’ choices regardless of doctor’s advice: an experimental study. Nephrol Dial Transplant 2012;27:325-31. http://dx.doi.org/10.1093/ndt/gfr266.
- O’Grady LA, Witteman H, Wathen CN. The experiential health information processing model: supporting collaborative web-based patient education. BMC Med Inform Decis Mak 2008;8. http://dx.doi.org/10.1186/1472-6947-8-58.
- Metzger MJ, Flanagin AJ. Using Web 2.0 technologies to enhance evidence-based medical information. J Health Commun 2011;16:45-58. http://dx.doi.org/10.1080/10810730.2011.589881.
- Mo PKH, Sillence E, Briggs P, Harris PR. Patient Experience Information Online: A Content Analysis of Smoking Related Websites n.d.
- Kelly GA. The Psychology of Personal Constructs. New York, NY: Norton; 1955.
- Briggs P, Hardy C, Harris PR, Sillence E. Proceedings of HCI Korea. Seoul: Hanbit Media, Inc.; 2014.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Sillence E, Hardy C, Harris P, Briggs P. Modelling Patient Engagement in Peer-to-Peer Healthcare n.d.
- Fogg BJ, Marshall J, Laraki O, Osipovish A, Varma C, Fang N, et al. What Makes Web Sites Credible? A Report on a Large Quantitative Study n.d.
- Sillence E, Hardy C, Briggs P, Harris PR. How do people with asthma use Internet sites containing patient experiences?. Patient Educ Couns 2013;93:439-43. http://dx.doi.org/10.1016/j.pec.2013.01.009.
- Ring N, Jepson R, Hoskins G, Wilson C, Pinnock H, Sheikh A, et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Couns 2011;85:e131-43. http://dx.doi.org/10.1016/j.pec.2011.01.025.
- Taylor SE, Lobel M. Social comparison activity under threat: downward evaluation and upward contacts. Psychol Rev 1989;96:569-75. http://dx.doi.org/10.1037/0033-295X.96.4.569.
- Sillence E, Hardy C, Briggs P, Harris PR. How do carers of people with multiple sclerosis engage with websites containing the personal experiences of other carers and patients? [published online ahead of print October 11 2015]. Health Informatics J 2015. http://dx.doi.org/10.1177/1460458215607938.
- Sillence E, Hardy C, Briggs P. Why Don’t We Trust Health Websites That Help Us Help Each Other? An Analysis of Online Peer-to-Peer Healthcare n.d.
- Liberman A, Chaiken S. Defensive processing of personally relevant health messages. Pers Soc Psychol B 1992;18:669-79. http://dx.doi.org/10.1177/0146167292186002.
- Van’t Riet J, Ruiter RAC. Defensive reactions to health-promoting information: an overview and implications for future research. Health Psychol Rev 2013;7:S104-36. http://dx.doi.org/10.1080/17437199.2011.606782.
- West R. Finding better ways of motivating and assisting smokers to stop: research at the CRUK Health Behaviour Research Centre. Eur Health Psychol 2008;10:54-8.
- Kotz D, Brown J, West R. Predictive validity of the Motivation To Stop Scale (MTSS): a single-item measure of motivation to stop smoking. Drug Alcohol Depend 2013;128:15-9. http://dx.doi.org/10.1016/j.drugalcdep.2012.07.012.
- Aarts H, Dijksterhuis A. The silence of the library: environment, situational norm, and social behavior. J Pers Soc Psychol 2003;84:18-2. http://dx.doi.org/10.1037/0022-3514.84.1.18.
- Morse JM, Morse JM. Qualitative Nursing Research: A Contemporary Dialogue. Newbury Park, CA: Sage; 1991.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract 2001;4:256-62.
- Petkov J, Harvey P, Battersby M. The internal consistency and construct validity of the partners in health scale: validation of a patient rated chronic condition self-management measure. Qual Life Res 2010;19:1079-85. http://dx.doi.org/10.1007/s11136-010-9661-1.
- Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004;113:59-65. http://dx.doi.org/10.1016/j.jaci.2003.09.008.
- Spek V, Lemmens F, Chatrou M, van Kempen S, Pouwer F, Pop V. Development of a smoking abstinence self-efficacy questionnaire. Int J Behav Med 2013;20:444-9. http://dx.doi.org/10.1007/s12529-012-9229-2.
- Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Res Nurs Health 1990;13:375-84. http://dx.doi.org/10.1002/nur.4770130605.
- Hughes N, Locock L, Ziebland S. Personal identity and the role of ‘carer’ among relatives and friends of people with multiple sclerosis. Soc Sci Med 2013;96:78-85. http://dx.doi.org/10.1016/j.socscimed.2013.07.023.
- Wangberg SC, Bergmo TS, Johnsen JA. Adherence in Internet-based interventions. Patient Prefer Adherence 2008;2:57-65.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h1258.
- Hinyard LJ, Kreuter MW. Using narrative communication as a tool for health behavior change: a conceptual, theoretical, and empirical overview. Health Educ Behav 2007;34:777-92. http://dx.doi.org/10.1177/1090198106291963.
- Petraglia J. Narrative intervention in behavior and public health. J Health Commun 2007;12:493-505. http://dx.doi.org/10.1080/10810730701441371.
- Pérez M, Sefko JA, Ksiazek D, Golla B, Casey C, Margenthaler JA, et al. A novel intervention using interactive technology and personal narratives to reduce cancer disparities: African American breast cancer survivor stories. J Cancer Surviv 2014;8:21-30. http://dx.doi.org/10.1007/s11764-013-0308-4.
- Kreuter MW, Holmes K, Alcaraz K, Kalesan B, Rath S, Richert M, et al. Comparing narrative and informational videos to increase mammography in low-income African American women. Patient Educ Couns 2010;81:S6-14. http://dx.doi.org/10.1016/j.pec.2010.09.008.
- Ashton CM, Houston TK, Williams JH, Larkin D, Trobaugh J, Crenshaw K, et al. A stories-based interactive DVD intended to help people with hypertension achieve blood pressure control through improved communication with their doctors. Patient Educ Couns 2010;79:245-50. http://dx.doi.org/10.1016/j.pec.2009.09.021.
- Schweier R, Romppel M, Richter C, Hoberg E, Hahmann H, Scherwinski I, et al. A web-based peer-modeling intervention aimed at lifestyle changes in patients with coronary heart disease and chronic back pain: sequential controlled trial. J Med Internet Res 2014;16. http://dx.doi.org/10.2196/jmir.3434.
- Coulter A, Locock L, Ziebland S, Calabrese J. Collecting data on patient experience is not enough: they must be used to improve care. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g2225.
- National Quality Board . Improving Experiences of Care: Our Shared Understanding and Ambition 2015.
- Patient Opinion . Desmond Course for Diabetes n.d. www.patientopinion.org.uk/opinions/103675.
- Diabetes UK . Diabetes Support Forum n.d. www.diabetes.org.uk/How_we_help/Community/Diabetes-Support-Forum/.
- NHS Choices . Churchill Hospital n.d. www.nhs.uk/Services/hospitals/Overview/DefaultView.aspx?id=1675.
- Diabetes UK . My New Year’s Resolution Has Become Part of Who I Am n.d. www.nhs.uk/Services/hospitals/Overview/DefaultView.aspx?id=1675.
- Diabetes UK . Diabetes Symptoms n.d. www.diabetes.org.uk/Guide-to-diabetes/What-is-diabetes/Diabetes-Symptoms/.
Appendix 1 EXPERT trial protocol
Reproduced with permission from the University of Oxford.
Appendix 2 Topic guides for the EXPERT qualitative interviews
EXPERT qualitative interviews with trial participants: patient experience version
DO NOT UNBLIND.
Preamble
You have been taking part in a trial of different types of health website. We’d like to hear your views about taking part in the study, and understand more about how people may use such sites and why.
Reassure that this is not a test.
-
Could you start by telling me why you agreed to take part?
-
What were you expecting would be involved?
-
Did it meet your expectations?
-
What browser did you use?
Part A: ‘process questions’
General usage
Turning now to how you used the site:
-
How often do you think you visited the site?
-
How much time did you spend on it?
-
How did you decide what to look at?
Feelings about it
-
What do you think about the design of the site?
-
Tell me what you thought about it . . . (Pick up burden, pleasure, etc.)
-
What did you get from it? Did you find it useful? Interesting?
-
Likes or dislikes?
-
Was there anything you did not know before?
-
Did you come across anything that worried you?
-
Anything you think was missing from the site?
-
Has looking at the site made you feel differently about giving up smoking/having asthma/looking after a relative with MS? In what way?
Specific questions about the design of the patient experience site
-
Was it user friendly?
-
Were all the links working?
-
Did you notice that you could comment?
-
IF YES: what did you feel about the opportunity to comment – did you? If not, any reason why not? Would you like to see other people’s comments too on a site like this one? (May need to explain that we did not show any comments so we made sure everyone in the trial saw the same thing.)
-
Explore specific comments.
-
Also, whether participants are reluctant to be the first to leave a comment; is a comment needed first. [Also analyse qualitative comments.] Consequences of comments on others’ experiences.
Clip use and selection
-
Did you look at any of the interview clips (video, audio, written)?
-
Did you have a preference for video or written text (i.e. did they listen to the clip or read the transcript)?
-
How did you choose which clips to look at?
-
How much do you want to know about the people whose clips you looked at (did you want to know anything that wasn’t available on the site?)
-
Was there enough information in strapline (show examples)? Would shorter/longer straplines have been more inviting?
Trustworthiness
-
Anything misleading? Why?
-
What it was about it that led to you feeling that way (e.g. how it was presented, or who was providing it)?
Further action/health service use
-
Did it encourage you to talk to other people about what you found? Or go to the doctor’s?
Using other sites
-
If you hadn’t been looking at this site would you have been looking elsewhere? (This is to learn about the landscape of use.)
-
Did looking at it encourage you to look at other materials (on other websites, books, etc.)?
-
Do you use other health websites occasionally or regularly? Which? Why?
NOTE: encourage comparisons with other named sites – we will avoid surfing during the interview but are very happy to look at sites afterwards if people want to show them to us.
-
One of our aims in running this study is to see how practical it is to run a trial comparing different health websites. This means we’ve been testing a lot of things for the first time, such as the questionnaire measures, the log-in process, setting up the websites . . .
-
Can you tell us what the process of taking part was like and whether there are any practical or technical aspects you think we could improve in future?
Part B: principles of PEx and other content – a key area
We’d like to talk a bit now about the different types of health-related content that people may visit online.
Broadly, we might distinguish between web site content that is:
-
content provided by professionals or medical charities – facts and figures about conditions
-
collections of people’s experiences of particular health issues or conditions
-
individual people’s blogs about their health
-
patients’ forums/chat rooms
-
feedback and reputation sites about people’s experience of particular services.
Show laminated cards
-
What do you think of all these different types of site?
-
Do you use any similar sites yourself?
-
Would you be interested in doing so?
-
Which sort/why?
Encourage people to speak freely and mention any other sites they are familiar with
-
We wonder why it is people in general may use various websites like these – what do you think?
-
We are interested in what it may do for them, what might be positive?
-
And what about the downsides?
-
How do you think looking at any of these different kinds of content may affect how much people use health services? (More? Less?)
-
What difference does it make seeing pictures on websites, those people upload themselves, anything you’d prefer not to see? (Visualisation domain.)
-
Where people are looking at other people’s health experiences do you think they look for positive experiences of ‘success stories’, for example stories showing how other people have coped?
-
Or is it also useful to see accounts from people who are finding it all too much?
PART C: sharing your own experiences
We are interested to know what you think about sharing your own experiences with other people (apart from health professionals).
-
Have you ever told people who you do not know, or do not know well, about your experiences of asthma/being a carer/trying to give up smoking? This might be in a face to face support group, an interview, an article, in an online forum or blog, or in a book.
-
Do you feel you ever would?
-
Are there some types of experiences you think people might be more or less likely to tell others about (expand if possible).
-
Do you feel any more likely to tell YOUR story since seeing these other people’s experiences – if so, why do you think this might be? If not, why not – has it put you off in any way? Do you feel that your experiences are already covered and there is no need to add?
-
Other reasons – would be good to explore this quite thoroughly since not much known about why people do and don’t.
Final questions
‘Trade off‘ questions.
-
If voluntary organisations and the NHS are going to fund websites what type of content do you think it is most important for them to provide (could ask respondents to rank the laminated cards and tell us why)?
-
Would you like a summary of the findings in due course?
EXPERT qualitative interviews with trial participants: non-patient experience version
DO NOT UNBLIND.
Preamble
You have been taking part in a trial of different types of health website. We’d like to hear your views about taking part in the study, and understand more about how people may use such sites and why.
Reassure that this is not a test.
-
Could you start by telling me why you agreed to take part?
-
What were you expecting would be involved?
-
Did it meet your expectations?
-
What browser did you use?
Part A: ‘process questions’
General usage
Turning now to how you used the site:
-
How often do you think you visited the site?
-
How much time did you spend on it?
-
How did you decide what to look at?
Feelings about it
-
What do you think about the design of the site?
-
Tell me what you thought about it . . . (Pick up burden, pleasure, etc.)
-
What did you get from it? Did you find it useful? Interesting?
-
Likes or dislikes?
-
Was there anything you did not know before?
-
Did you come across anything that worried you?
-
Anything you think was missing from the site?
-
Has looking at the site made you feel differently about giving up smoking/having asthma/looking after a relative with MS? In what way?
Specific questions about the design of the non-patient experience site
-
Was it user friendly?
-
Were all the links working?
-
Did you notice that you could comment?
-
IF YES: what did you feel about the opportunity to comment – did you? If not, any reason why not? Would you like to see other people’s comments too on a site like this one? (May need to explain that we did not show any comments so we made sure everyone in the trial saw the same thing.)
-
Explore specific comments.
-
Also, whether participants are reluctant to be the first to leave a comment; is a comment needed first. [Also analyse qualitative comments.] Consequences of comments on others’ experiences.
Clip use and selection
-
Did you look at any of the HP interview clips?
-
Did you have a preference for video or written text (i.e. did they listen to the clip or read the transcript)?
-
How did you choose which clips to look at?
-
Did you want to know anything that wasn’t available on the site?
-
Was there enough information in the strapline (show examples). Would shorter/longer straplines have been more inviting?
Trustworthiness
-
Anything misleading? Why?
-
What was it about it that led to you feeling that way? (e.g. how it was presented, or who was providing it. NB – all health professionals).
Further action/health service use
-
Did it encourage you to talk to other people about what you found? Or go to the doctor’s?
Using other sites
-
If you hadn’t been looking at this site would you have been looking elsewhere? (This is to learn about the landscape of use.)
-
Did looking at it encourage you to look at other materials (on other websites, books, etc.)?
-
Do you use other health websites occasionally or regularly? Which? Why?
NOTE: encourage comparisons with other named sites – we will avoid surfing during the interview but are very happy to look at sites afterwards if people want to show them to us.
-
One of our aims in running this study is to see how practical it is to run a trial comparing different health websites. This means we’ve been testing a lot of things for the first time, such as the questionnaire measures, the log-in process, setting up the websites.
-
Can you tell us what the process of taking part was like and whether there are any practical or technical aspects you think we could improve in future?
Part B: principles of patient experience and other content – a key area
We’d like to talk a bit now about the different types of health-related content that people may visit online.
Broadly, we might distinguish between website content that is:
-
content provided by professionals or medical charities – facts and figures about conditions
-
collections of people’s experiences of particular health issues or conditions
-
individual people’s blogs about their health
-
patients’ forums/chat rooms
-
feedback and reputation sites about people’s experience of particular services.
Show laminated cards
-
What do you think of all these different types of site?
-
Do you use any similar sites yourself?
-
Would you be interested in doing so?
-
Which sort/why?
Encourage people to speak freely and mention any other sites they are familiar with
-
We wonder why it is people in general may use various websites like these – what do you think?
-
We are interested in what it may do for them, what might be positive?
-
And what about the downsides?
-
How do you think looking at any of these different kinds of content may affect how much people use health services? (More? Less?)
-
What difference does it make seeing pictures on websites, those people upload themselves, anything you’d prefer not to see? (Visualisation domain.)
-
Where people are looking at other people’s health experiences do you think they look for positive experiences of ‘success stories’, for example stories showing how other people have coped?
-
Or is it also useful to see accounts from people who are finding it all too much?
PART C: sharing your own experiences
-
We are interested to know what you think about sharing your own experiences with other people (apart from health professionals).
-
Have you ever told people who you do not know, or do not know well, about your experiences of asthma/being a carer/trying to give up smoking? This might be in a face to face support group, an interview, an article, in an online forum or blog, or in a book. Do you feel you ever would?
-
Are there some types of experiences you think people might be more or less likely to tell others about (expand if possible).
-
Are you likely to tell YOUR story on a website? If not, why not?
-
Other reasons – would be good to explore this quite thoroughly since not much known about why people do and don’t.
Final questions
‘Trade-off‘ questions:
-
If voluntary organisations and the NHS are going to fund websites what type of content do you think it is most important for them to provide (could ask respondents to rank the laminated cards and tell us why)?
-
Would you like a summary of the findings in due course?
Appendix 3 Screenshots shown to the work package 3b trial interviewees to illustrate types of health websites available online
Reproduced from Patient Opinion184 under the terms of the Creative Commons Attribution Licence (CC BY-NC-SA 4.0).
Reproduced with permission from the author of the blog post.
Reproduced with permission from Diabetes Support. 185
Reproduced with permission from NHS Choices. 186
Reproduced with permission from Diabetes UK. 187
Reproduced with permission from Diabetes UK. 188
Appendix 4 Series of eight briefing sheets produced for dissemination activities
List of abbreviations
- ANCOVA
- analysis of covariance
- ANOVA
- analysis of variance
- CCSVI
- chronic cerebrospinal venous insufficiency
- CDSES
- Chronic Disease Self-Efficacy Scale
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- EFA
- exploratory factor analysis
- eHIQ
- e-Health Impact Questionnaire
- GP
- general practitioner
- HERG
- Health Experiences Research Group
- HIV
- human immunodeficiency virus
- ICC
- intraclass correlation coefficient
- iPEx
- Internet Patient Experiences
- MCS
- mental component summary
- MND
- motor neurone disease
- MRC
- Medical Research Council
- MS
- multiple sclerosis
- MTSS
- Motivation To Stop Scale
- PCS
- physical component summary
- PEx
- patient experience
- PFCS
- Preparedness For Caregiving Scale
- PIH
- Partners in Health
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- SASEQ
- Smoking Abstinence Self-Efficacy Questionnaire
- SD
- standard deviation
- SF-36
- Short Form questionnaire-36 items
- WP
- work package