Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0606-1006. The contractual start date was in August 2007. The final report began editorial review in November 2014 and was accepted for publication in March 2016. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Burns et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Part 1 Introduction to the programme
Chapter 1 Overview
The Oxford Mental Health Coercion Programme focused on two key areas: formal and informal coercion. Formal coercion, hereafter referred to as compulsion, is authorised in mental health legislation. Within community mental health care, this takes the form of outpatient compulsion: community treatment orders (CTOs) in England and Wales. Informal coercion comprises a range of treatment pressures that mental health professionals may use with patients, including but not limited to leverage, defined as the use of an explicit and specific treatment lever.
The Oxford Mental Health Coercion Programme, which took place from 2007 to 2014, comprised three studies: the Oxford Community Treatment Order Evaluation Trial (OCTET) and the OCTET Follow-up Study, evaluating and exploring compulsion in the form of CTOs, and the Use of Leverage Tools to Improve Adherence in community Mental Health care (ULTIMA) Study, evaluating and exploring informal coercion, including leverage.
The OCTET Study was built around the OCTET Trial, a randomised controlled trial (RCT) of the effectiveness of CTOs, but also encompassed a number of substudies, including an economic evaluation; a qualitative study of patients’, family carers’ and professionals’ perspectives; a substudy developing and testing a measure of capabilities; an ethical analysis of the implications of CTOs; and an analysis of the lawfulness of an RCT of CTOs leading to the development of the OCTET Trial design. The OCTET Follow-up Study determined long-term outcomes of CTO use, focused on disengagement and continuity of care, through a follow-up study of the cohort from the OCTET Trial at 36 months after randomisation. The ULTIMA Study assessed patients’ experiences and perceptions of informal coercion in community mental health care in a cross-sectional quantitative study, and investigated patients’ and mental health professionals’ views in a qualitative study.
Although the literature uses a range of terminology (see Part 2, Chapter 5 and Part 4, Chapter 17), we use the terms described above throughout this report. Thus we use the term compulsion to indicate formal or statutory coercion through mental health legislation; our focus is on compulsion within community mental health care, but other types of compulsion are discussed when this is relevant to understand CTO legislation or the procedures of our trial. We use informal coercion to cover the range of treatment pressures mental health professionals may exert over patients, and reserve leverage for those in which a particular explicit treatment lever is utilised. We use the term perceived coercion to indicate patients’ assessments of coercion in their care (Figure 1). For clarity, the term discharge is used to indicate discharge from inpatient care rather than from an involuntary to a voluntary legal status; for the latter, we use discharge from section (referring to a section of the mental health legislation).
FIGURE 1.
Coercion in community mental health care.

Each study reported here – the OCTET Study, the OCTET Follow-up Study and the ULTIMA Study – appears in a separate section of the report (see Parts 2–4, respectively). Each has its own introduction, including the background to the study, and its own discussion section. Individual chapters within these three parts then report the main study and the related substudies, such as the OCTET Trial within the OCTET Study.
The OCTET Study, and in particular the OCTET Trial, was a tremendous undertaking in its scope and complexity, as well as in its international importance. We describe the development of the OCTET Trial design, including extensive consultation with stakeholders and legal experts, in an introductory section to the OCTET Study (see Part 2, Chapter 6, Introduction), along with the complicated logistics involved in the trial’s execution.
The OCTET Trial had a tremendous impact when its findings were first published, and international interest in it has been extensive. We have given 109 presentations on the whole programme to date, of which 67 were on the findings of the OCTET Trial, across 22 countries. The OCTET Trial also generated considerable controversy. We describe these aspects in the final section of the report (see Part 5) and here we also detail the dissemination of the studies in the Oxford Mental Health Coercion Programme (henceforth referred to as the OCTET Coercion Programme). We also describe the range of additional research generated through the programme’s capacity building. This is also where we discuss the findings of the entire programme and give recommendations for future research.
In the remainder of Part 1, we describe the rationale for the OCTET Coercion Programme, its objectives and how the three studies met these objectives, and its overall governance structures.
Chapter 2 Rationale
We designed the OCTET Coercion Programme to fill significant gaps in the evidence base concerning compulsion and informal coercion by conducting a series of high-quality linked studies. Our aim was to improve understanding of the care of severely unwell patients experiencing multiple admissions, particularly patients with psychosis, and to guide the targeting of the new powers conferred by CTO legislation. We also designed the programme to form the basis of effective evidence-based practice guidance for both this group and a wider group of patients whose treatment is not subject to compulsion but who, nevertheless, experience high degrees of dependency on mental health services. It was designed to address public, professional and policy concerns,1,2 with the aim of facilitating a more balanced, less stigmatising, public engagement with the issues.
The management of people with severe mental illness in the community (and, in particular, failures to achieve it) has been the yardstick used by the public to judge mental health services. There is a pressing need to understand better and improve how professionals succeed in maintaining contact and support treatment adherence with these patients.
The introduction of compulsory treatment in the community has been intensely controversial, and has remained so, sustained by the absence of convincing scientific evidence for its effects (despite its widespread adoption internationally) (see Part 2, Chapter 5). Providing such evidence is particularly necessary because of the complex ethical balance of personal autonomy against the need for care and public safety, and because there are strongly held conflicting opinions. There is also a pressing need to determine whether or not a reduction in personal autonomy resulting from being on a CTO is sufficiently justified by concomitant clinical improvements.
As we describe below (see Part 2, Chapter 5), there is a substantial gap in the evidence base for supervised community treatment. 3,4 There is thus a compelling need to provide the most robust evidence possible, for both clinical and ethical reasons. To conduct such research in the form of an RCT, the accepted gold standard for evidence of the effectiveness of interventions, is hugely important both for patients and for the clinicians who have responsibility for making decisions about their care. Without such a study, a clear estimate of the effects of CTOs cannot be acquired, and understanding of their target patient group and implementation would accrue only slowly and unsystematically.
We therefore designed the most extensive of the studies in this programme, the OCTET Trial, to provide robust evidence of the effectiveness for patients with psychosis of CTOs, which had just been introduced in England and Wales at the time of the study’s inception, and to give a clear and early indication of the specific clinical groups that might or might not benefit from them. The trial included a rigorous economic analysis in order to inform policy and resource planning. It was anticipated that the OCTET Study might identify a trade-off between improved outcomes and the duration of compulsion. We investigated this by developing and testing a new instrument to measure capabilities.
In the OCTET Follow-up Study, the longer-term implications of CTO use for these patients were investigated through a follow-up of the original OCTET Trial cohort focusing on disengagement, hospitalisation, discontinuity and the use of involuntary treatment at 36 months after randomisation. Until now, no empirical study has been published about persisting effects of CTOs. Serious concerns about CTO use motivated this study, particularly that the compulsion involved might be excessively prolonged5,6 and might lead to disengagement from services. We thus designed the study to determine whether or not CTOs might drive patients away from services.
Establishing the extent and form of informal coercion, including leverage, and its variation across different clinical groups is an essential precursor to an informed debate on its place in modern community mental health care. Such a debate would also inform the inclusion of discussions of what informal coercion is and how patients experience it in mental health training. The ULTIMA Study represents the largest systematic study of patient-reported informal coercion and leverage in European mental health services to date. We designed this study to identify the frequency and pattern of leverage and replicate the methods of a key study from the USA,7 thus providing both the first English data and an international comparison. The ULTIMA Study also expanded on the previous research by examining patterns of leverage and informal coercion more widely across different patient populations, and investigating the association of leverage with important clinical characteristics.
Both the OCTET Study and the ULTIMA Study included qualitative substudies conducted with patients and mental health professionals and, in the OCTET Study, family carers, in order to access insights beyond those which would be achievable by quantitative and experimental means. 8 Qualitative methods are recognised as an excellent way of exploring areas for which there is a paucity of data. They are flexible and adaptable and can allow for changes or refinement of instruments during the course of the research. They commonly encourage discussion of issues deemed important by research participants. We designed the qualitative substudies in OCTET and ULTIMA to access perspectives on CTO use and informal coercion, respectively, which might be key to understanding their mechanisms of action and guiding policy decisions. 9,10 They included close attention to patients’ and professionals’ understanding of the use of compulsion and informal coercion within therapeutic relationships. Given the central role of therapeutic relationships in current mental health policy,11 investigating the conceptualisations of these relationships by those involved in them has the potential to shed light on how such policy is implemented in practice.
The programme also included an extensive exploration of the ethical issues surrounding the use of community coercion. The two qualitative substudies provided an opportunity to identify dilemmas and ethical aspects of compulsion and informal coercion. The ethical substudies were designed to break new ground in informing development of training in good practice, relate findings to the wider context and promote a more nuanced public discourse.
Chapter 3 Aims, objectives and programme design
The overall aim of the OCTET Coercion Programme was to obtain a detailed understanding of the compulsion and informal coercion experienced by patients with mental health problems, including testing the effectiveness of CTOs following their introduction into English and Welsh mental health legislation in 2008.
This aim was to be achieved by six overarching objectives [as expressed in the original National Institute of Health Research (NIHR) grant application]. We follow each objective listed here by a brief description of how it was met by different studies or substudies within the OCTET Coercion Programme (Table 1).
| Objective | Study/substudy | Part/chapter |
|---|---|---|
| 1. Informal coercion | ULTIMA | Part 4 |
| ULTIMA Quantitative Study | Chapter 18 | |
| 2. Obstacles, ethical, legal, clinical and practical | OCTET | Part 2 |
| Legal Analysis | Chapter 11 | |
| 3. CTO trial | OCTET | Part 2 |
| OCTET Trial | Chapter 6 | |
| 4. Experiences of patients, carers and staff, including ethical dilemmas | ULTIMA | Part 4 |
| ULTIMA Qualitative Study | Chapter 19 | |
| ULTIMA Ethical Analysis | Chapter 20 | |
| OCTET | Part 2 | |
| OCTET Qualitative Study | Chapter 8 | |
| OCTET Ethical Analysis | Chapter 9 | |
| 5. Economic evaluation | OCTET | Part 2 |
| Economic Evaluation | Chapter 7 | |
| Capabilities Project | Chapter 10 | |
| 6. Disengagement and readmission at 36 months | OCTET Follow-up | Part 3 |
Objective 1
To investigate levels of informal coercion (‘leverage’) in differing UK clinical populations and investigate their sociodemographic and clinical correlates.
We addressed this objective by conducting the ULTIMA Quantitative Study of informal coercion (see Part 4, Chapter 19). We interviewed four distinct samples [psychosis patients in Assertive Outreach Teams (AOTs), psychosis and non-psychosis patients in Community Mental Health Teams (CMHTs) and substance misuse patients] about their lifetime experiences of four forms of leverage (housing, finance, avoidance of criminal sanction and child access). We also explored associations between these leverages and patient and treatment characteristics and perceived coercion.
Objective 2
To explore and address the ethical, legal, clinical and practical obstacles to designing and conducting the most powerful study possible for testing the efficacy of community treatment orders, which will maximise the power of the conclusions for policy and practice.
We addressed this objective in a preliminary substudy within the OCTET Study conducted as a means of designing the most appropriate and most powerful RCT possible. The aim was to establish the feasibility of, and obtain agreement about and support for, the strongest test of the intervention, in order to produce a detailed study brief. We held a series of meetings with clinicians and legal, policy and ethical groups in order to carry out a detailed investigation of ethical, legal and practical issues of methodologies to test the impact of CTOs (see Part 2, Chapter 5). The need for a detailed legal analysis emerged through this process and we report this in detail in a separate chapter (see Part 2, Chapter 11).
Objective 3
To conduct the most rigorous trial possible of community treatment orders, with prolonged, high-quality care incorporating a broad range of outcomes, and identify patient and service predictors of response.
Following the successful completion of the analysis of obstacles meeting objective 2, we met objective 3 by conducting the OCTET Trial (see Part 2, Chapter 6). The objective was to compare CTO use with voluntary outpatient care, although legal advice required that patients be randomised to leave hospital either on a CTO or via Section 17 Leave. Independent researchers conducted interviews with patients at baseline and at 6 and 12 months, and examined case notes. The primary outcome was rate of readmission. Other outcomes included Mental Health Act (MHA)12 use and patterns of care and social and quality of life outcomes. We also explored patient and treatment characteristics that were associated with outcomes.
Objective 4
To conduct a detailed qualitative assessment of the experiences (including ethical dilemmas) of patients, staff and carers in both studies.
We met this objective by conducting two qualitative substudies: the ULTIMA Qualitative Study (see Part 4, Chapter 19) and the OCTET Qualitative Study (see Part 2, Chapter 8), each of which conducted a qualitative exploration of the experiences and perceptions of patients in the study and other key groups. We sampled from each study in order to conduct a series of semistructured, in-depth interviews with a subsample. For mental health professionals in the ULTIMA Study, we used focus group methods. We did not seek the experiences of family carers in the ULTIMA Qualitative Study, for reasons given below (see Part 4, Chapter 19), but we included their experiences of informal coercion as well as CTOs in the OCTET Qualitative Study. In both substudies, we analysed the qualitative data in two ways: first, to explore experiences and perceptions of CTOs (OCTET) and informal coercion (ULTIMA), and, second, to address ethical questions raised by the use of CTOs (OCTET) and informal coercion (ULTIMA). We report the Ethical Analyses arising from this secondary aim of the two substudies separately (see Part 2, Chapter 9 and Part 4, Chapter 20, respectively).
Objective 5
To conduct a cost-effectiveness analysis of community treatment orders and model the costs of their national introduction.
We met this objective by conducting an economic evaluation as part of the OCTET Trial (see Part 2, Chapter 7). This comprised a detailed cost analysis of health, social care and other broader societal costs, and an incremental cost-effectiveness analysis. We also developed a capabilities and well-being index13 from the capabilities framework. 14 We report the development of this index separately (see Part 2, Chapter 10).
We later added an additional objective, to be met by a further study, as agreed by the funder.
Objective 6
To compare disengagement and clinical outcomes between those randomised to community treatment order and those randomised to non-community treatment order treatment at 36 months after randomisation.
We met this objective by conducting the OCTET Follow-up Study (see Part 3). It aimed to establish whether or not CTO use had a significant effect on rates and duration of readmission, engagement with services and service use at 36 months after randomisation. This was based on medical records and a follow-up to patients to measure longer-term outcomes.
The original proposal also included a further objective: ‘to develop a training package for best clinical and ethical practice in CTOs and use of leverage’. We subsequently omitted this, by agreement with the funder, as Department of Health training programmes in CTO use had already been initiated by this time. The OCTET team held an annual conference involving clinicians involved in the trial and other interested clinicians, attended by up to 90 people each time (see Appendix 4). The contribution towards training was also indirectly met by the considerable amount of discussion and debate generated by the study, along with dissemination conferences, associated studies and replication studies (see Part 5, Chapter 22).
Chapter 4 Ethical approval, registrations, user involvement and data
The Oxfordshire Research Ethics Committee A gave ethical approval for the ULTIMA Study (22/02/2006, reference no. 05/Q1604/180).
The Staffordshire NHS Research Ethics Committee gave ethical approval for the OCTET Study (30/10/2008, reference no. 08/H1204/131). An amendment to the ethical approval (20/07/2011) covered the additional work required for the OCTET Follow-up Study, which was funded by a supplementary grant held from 2012 to 2014.
The OCTET Trial is registered with the International Standard Randomised Controlled Trial Number Register (reference: ISRCTN73110773). All three studies were part of the UK Clinical Research Network Study Portfolio.
We performed all three studies in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. 15 Some changes to the original research protocols were agreed with the funder and the relevant ethics committees during the course of the research, as we describe below (see Part 2, Chapter 6, Methods and Part 4, Chapter 19, Methods).
We held a number of meetings with service user and carer representatives during the course of the programme to discuss the procedures for the studies. (We give details about governance for the OCTET Study in more detail below; see Part 2, Chapter 5, Governance.) The service user and carer representatives on the OCTET Steering Group formed part of the OCTET Follow-up Study’s governance structure. We designed the OCTET Follow-up Study partly to meet concerns raised by service users and service user representatives in the consultation phase of the OCTET Trial.
Part 2 The OCTET Study
Abstract
Background
Community treatment orders were introduced in England and Wales in 2008, despite equivocal evidence of effectiveness.
Design
The study comprised an RCT (OCTET Trial) comparing treatment on CTO to voluntary treatment via Section 17 Leave, over 12 months; an Economic Evaluation; a Qualitative Study and an Ethical Analysis. A new measure of capabilities was developed.
Methods
Trial participants were patients with psychosis diagnoses currently admitted involuntarily and considered for ongoing community treatment under supervision. The trial primary outcome was psychiatric readmission. Secondary and tertiary outcomes included hospitalisation and a range of clinical and social measures. A subsample of patients, carers and mental health professionals was interviewed in depth.
Results
A total of 336 patients were randomised. CTO use did not reduce rates of readmissions to hospital {[59/166 (36%)] of patients in the CTO group vs. 60/167 (36%) of patients in the non-CTO group; adjusted relative risk 1.0 (95% CI 0.75 to 1.33)} or any other secondary or tertiary outcome. There were no differences for any subgroups. It did not reduce hospitalisation costs and there was no evidence that it might be cost-effective. The results from in-depth interviews about CTO experiences with 26 patients, 24 family carers and 25 psychiatrists showed divergent views and that CTOs’ (perceived) focus on medication adherence may influence how they are experienced. No general ethical justification was found for the use of a CTO regime.
Conclusions
Community treatment orders do not confer early patient benefits despite substantial curtailment of individual freedoms.
Chapter 5 Introduction to the OCTET Study
Overview
The OCTET Study was built around the OCTET Trial. It comprised the following:
-
OCTET Trial An RCT evaluating the effectiveness of CTO use.
-
OCTET Economic Evaluation A detailed cost analysis of health, social care and other broader societal costs and an incremental cost-effectiveness analysis.
-
OCTET Qualitative Study An in-depth investigation of patient, carer and professional views and experiences of CTOs, utilising interviews with a subgroup from the OCTET Trial cohort and recruited groups of carers and mental health professionals.
-
OCTET Ethical Analysis A detailed empirical ethical analysis drawing on the OCTET Trial and qualitative data from the Qualitative Study.
-
OCTET Capabilities Project A study of the operationalisation of the capability model for outcome measurement in mental health studies, tested in the OCTET cohort.
-
OCTET Legal Analysis An investigation of the legal implications of designing an RCT of CTO use which preceded and informed the design of the trial.
The rigorous RCT design of the OCTET Trial (see Chapter 6) was designed to test the use of CTOs in the target group considered by most clinicians to be likely to benefit from the new regime. It included an economic evaluation (see Chapter 7), which also applied the newly developed multidimensional capabilities instrument and the resulting capability index, developed and tested in the trial cohort (see Chapter 10).
The OCTET Qualitative Study (see Chapter 8) was designed to complement and extend the trial results. Rather than testing a predetermined hypothesis, the objective here was to explore personal experiences of and perspectives on CTOs that might turn out to be the key to understanding their mechanism of action. This was particularly important given that CTOs were new at the time of the study’s inception, and it was impossible to anticipate all of the potential relevant outcomes in the trial. It was also important to explore the reasoning of psychiatrists, patients and family carers about their perceptions of the advantages and disadvantages of CTOs.
The OCTET Qualitative Study also provided an opportunity to identify the dilemmas and ethical aspects of using compulsion in community mental health care. We conducted a detailed ethical analysis in the context of the relevant empirical data and the ethics literature: the OCTET Ethical Analysis (see Chapter 9). A thorough exploration of ethical, legal, clinical and practical obstacles to developing the OCTET Trial preceded the finalisation of the OCTET protocol. The consultation exercise undertaken to this end is summarised below (see Chapter 6, Introduction), whereas the OCTET Legal Analysis is given in full in Chapter 11.
Background
This section draws substantially on papers by members of the OCTET Coercion Programme Group (Burns et al. ,16 with permission from Elsevier; Molodynski et al. ,17 with permission from Oxford Journals; and Rugkåsa et al. ,18 with permission from Springer Publishing Company).
Mental health care in the community
Mental health care is an international priority. 19 In the UK, expenditure on mental health care accounts for between 3% and 4% of gross domestic product. 20 Mental ill health is the leading cause of invalidity benefit in the UK21 and mental disorders are set to become the major causes of disability worldwide. 22
Psychiatry is the only area of medicine in which adult, competent patients can be treated against their will. This is governed by specific mental health legislation (in the UK, the MHA). Compulsory treatment is integral to mental health care and was originally restricted to inpatient settings. 23 Over the last 50 years or so, however, a policy focus on deinstitutionalisation has gradually moved psychiatric services from hospital settings into the community. The psychiatric inpatient population has fallen drastically in developed countries since its peak in the mid-1950s. 24 In England and Wales, for example, although there were 154,000 psychiatric beds in 1954, this had been reduced to 33,000 by 2005,25 despite the overall increase in the population. This has placed new demands on practices, policies and legislation for managing individuals with mental illness and their associated complex vulnerabilities.
Community psychiatry creates difficulties for professionals in terms of how to encourage and monitor patients to ensure both their safety and well-being and that of others. Community services may subject patients to intense levels of supervision, restrictions on their behaviour and elements of compulsion. 26 In fact, it is now commonly accepted that coercive treatment is provided outside hospitals. 27 This has been reflected in several amendments and challenges to mental health legislation over the last 30 years, as new models for more assertive treatment in the community have emerged, often monitoring patients closely while seeking to assist them to achieve stability, insight and independence. 28–30
Various provisions to maintain contact with outpatients are used where required, at differing levels of intensity and regularity as appropriate. Mental health services are increasingly delivered via case management approaches by multidisciplinary teams consisting of psychiatrists, nurses, psychologists, social workers, support workers and occasionally other professionals such as occupational therapists. 28,31,32 Such case management may be provided by the CMHT, a multidisciplinary team with diagnostically mixed caseloads (usually 1 : 25) and some provision of outreach. An alternative model, the AOT, was introduced in England from 1999,20 modelled closely on Assertive Community Treatment (ACT) teams as developed in the USA. 33 AOT teams target hard-to-engage patients with psychosis and provide much more intensive multidisciplinary outreach with small caseloads (1 : 12). These services operate within policy frameworks such as the Care Programme Approach20 and, less often, within legal frameworks provided by mental health legislation. The terms and implications of these provisions tend to vary by jurisdiction. 34,35 In England, specialist mental health services are provided by area-based UK NHS mental health trusts, each divided into catchment areas where, at the start of the OCTET Trial, community teams provided both community and inpatient care. As we discuss below (see Chapter 6, Introduction), during the recruitment phase of the trial, many trusts separated their inpatient from their community services, and CTOs were then increasingly initiated by specialist inpatient psychiatrists. 36
Community care37 has been a success for the majority of patients who have been discharged from long-term inpatient care to more dignified and rewarding lives in the community. It increasingly provides for severely disabled patients requiring complex and expensive care. 38 Despite these efforts, a substantial minority of patients are subject to repeated compulsory admissions (‘the revolving-door syndrome’39). The absolute rate of these involuntary admissions has increased following deinstitutionalisation. 40
At the same time as community mental health services have evolved, public confidence in community care has, in many countries, been profoundly undermined by a series of high-profile violent offences: usually by individuals with psychosis who, although known to mental health services, were not effectively engaged in treatment. 41 This has given rise to significant public concern about the ability of services to manage severely ill patients in the community, possibly contributing to recent trends of increasing compulsion and institutional care, with its attendant high costs. Policy-makers and clinicians have long been concerned to address such concerns about the safe management of severely ill patients. 42 In the UK, however, a number of alterations to the MHA such as Supervision Registers43 and Supervised Discharge44 are widely regarded as having achieved only limited results. The introduction of CTOs in 2008,45 described in Community treatment orders: the legislation, was designed to ensure that this group of very ill patients could be more successfully monitored and treated.
Detailed accounts of the literature on CTOs also appear in papers by members of the OCTET Coercion Programme Group. 17,18
Compulsion in community mental health care
In attempting to increase patients’ adherence to treatment and thereby improve their outcomes, mental health professionals use a range of formal and informal techniques. (We discuss informal techniques, or informal coercion, in Part 4, Chapter 17.) At the formal end of the spectrum, legislation for compulsory outpatient psychiatric treatment (compulsion) has been introduced in around 75 jurisdictions worldwide, across the USA, Australasia, some Canadian provinces, the UK and several other European countries. 4
Community treatment orders were designed with the aim of helping so-called revolving-door patients: those who have a long history of psychotic illness and experience multiple hospital admissions. They were principally aimed at preventing this revolving-door scenario by helping patients experience a period of stability after leaving hospital.
Community treatment orders were introduced in England and Wales in November 2008. 45 CTOs require patients to accept treatment and clinical monitoring, and allow rapid recall to hospital when necessary, as is described more fully in Community treatment orders: the legislation. This provision had been sought for at least 15 years by some professionals,46 but it was heavily debated and resisted during the build-up to its introduction by a coalition of 32 professional and patient organisations. 47
Mental health legislation in England and Wales
Patients in England and Wales who meet the legal criteria can be treated in hospital against their will under Section 3 of the MHA. While on Section 3, they can be given leave of absence for some hours or days, or even – exceptionally – weeks, for instance to spend time with family or engage in other social activities. This is called Section 17 Leave. Its purpose is to assess recovery before granting voluntary status. Section 17 Leave is a well-established rehabilitation practice used for brief periods to assess the stability of a patient’s recovery after or during a period of involuntary hospital treatment. Under Section 17 Leave, the treatment order (Section 3) remains active and the patient can be immediately readmitted without additional legal process. Section 17 Leave is extensively used but, as it is a continuation of Section 3, no routine national data on its use are collated. Its frequency and duration are therefore unknown, but both are believed to be highly variable, with some clinicians using it for extended periods and others hardly at all. The use of this extended leave of absence from involuntary hospital admission under Section 3 of the MHA has been shaped by several legal challenges. 25 It is generally agreed, however, that such leave has a place in mental health services. Indeed, the Code of Practice that accompanies the 1983 MHA48 states that such leave may constitute an important part of a patient’s treatment plan.
Prior to the introduction of CTOs, a series of attempts was made to introduce outpatient compulsion. Guardianship (Section 7) had been available since 1983 and remains unchanged today. It can require a patient to attend medical appointments and can direct where he or she should reside. 49 It has never really been used for patients other than those with learning disability and dementia. Since 1983, Section 117 has required that aftercare be provided for those treated under section (e.g. Section 3) following their discharge from hospital. To meet the needs of those who rejected their right to this aftercare provision, aftercare under supervision (known as Supervised Discharge or Section 25) was introduced in 1996. 25 This required the patient to attend for treatment, live where directed and make themselves available for assessments. It was widely perceived to be ineffective because it could not insist on medication adherence and it was removed from the legislation in 2008.
Community treatment orders: the legislation
The introduction of CTOs in England and Wales in 2008, as part of the amended MHA 2007,45 marked the next step in this evolution of forms of compulsory treatment in the community. This regime authorises compulsory treatment for patients in the community following a period of involuntary hospital treatment. Enforcement is provided via the power of recall, which permits patients to be returned to hospital for treatment or assessment without conducting a formal MHA assessment. The intention is to prevent relapse or harm (to self or others), help maintain a period of stability and provide a least restrictive alternative to hospital (i.e. one in which the intervention given restricts the patient’s freedom the least). 48
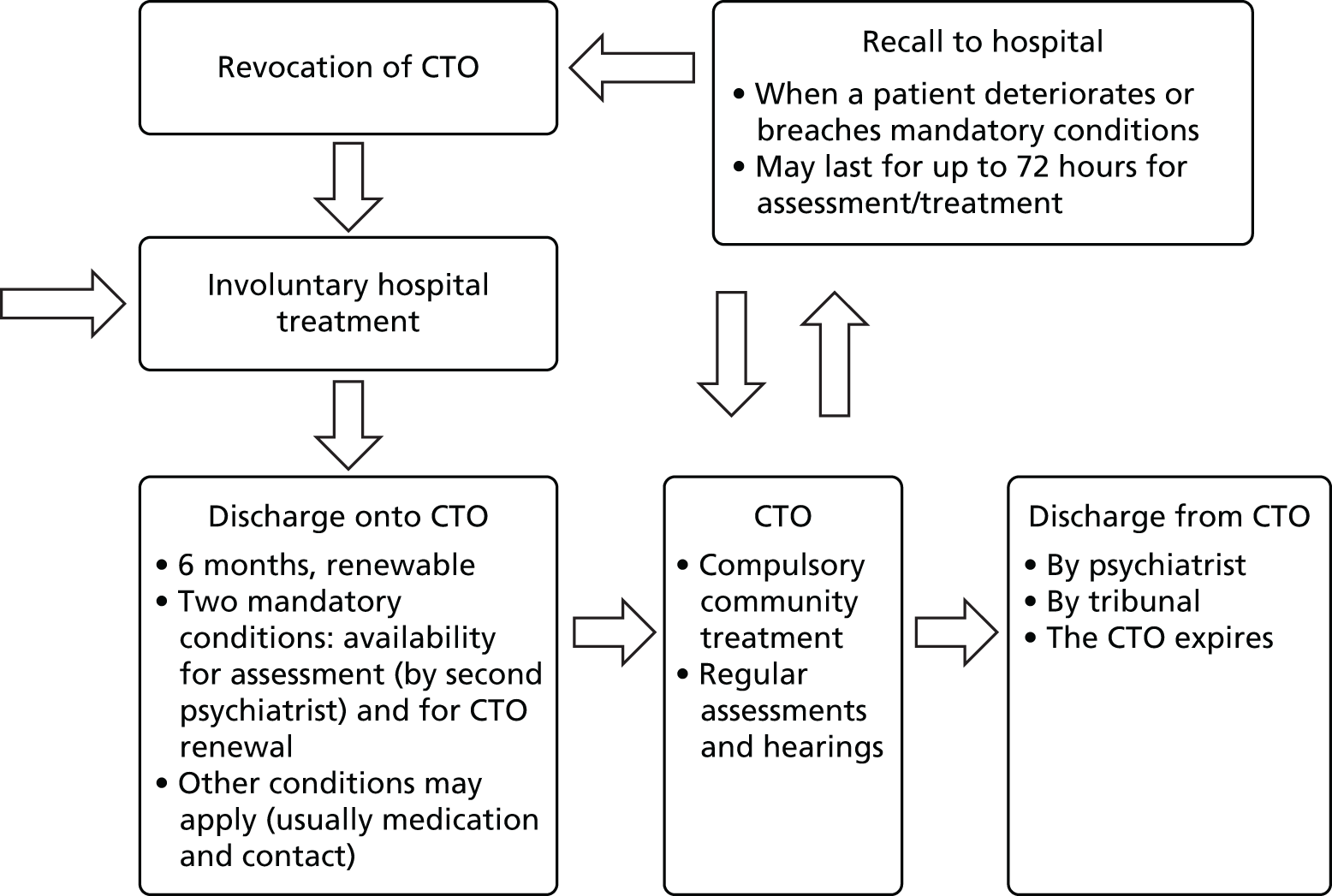
A CTO can be imposed when the responsible clinician (RC) (usually a consultant psychiatrist) and an approved mental health professional (AMHP) (usually a social worker) deem that a patient needs supervision after a period of involuntary hospital treatment and that, without it, he or she is highly likely to relapse and be readmitted involuntarily. The AMHP is required to consult with the patient and with family carers. The formal process is intentionally time-consuming to ensure that the CTO is not used for clinical convenience. Several days, sometimes more, elapse between the clinical decision and CTO activation. Alternatively, RCs may choose to use Section 17 Leave (described above). Unlike with Section 25, CTOs can insist on medication. Medication cannot be given by force in the community, however, regardless of whether or not a CTO or Section 17 Leave is used. Forceful administration is permitted only if the patient has been recalled to a ‘safe place’. Patients can be discharged directly from Section 3 without the need for either Section 17 Leave or a CTO, and most are. (Such patients would not be eligible for recruitment to this trial.)
The CTO requires the patient to comply with treatment and he or she can be recalled to hospital without delay if necessary. The regime in England and Wales specifies two mandatory conditions that apply to all CTOs. 48 First, a second opinion appointed doctor (SOAD) must assess patients who refuse medication or who lack capacity, to confirm that the treatment specified is appropriate. 50 Second, all patients must make themselves available for assessment for renewal of the CTO. The RC and AMHP who initiate the CTO may also specify discretionary conditions based on their knowledge of an individual patient. The most frequently stipulated conditions are to take prescribed treatment and remain in contact with the mental health team. 51–53 The power of recall can be used when the patient:
-
requires treatment in hospital and in the absence of recall there would be a risk of harm to self or others, or
-
does not comply with one of the mandatory conditions.
Recall can be used for the purpose of giving treatment or for assessment for up to 72 hours, after which the patient returns to the community under the CTO or the CTO is revoked and the patient remains in hospital for involuntary treatment under Section 3 of the MHA. The MHA Code of Practice states that patients and their families should be consulted about the CTO, its conditions and the need to recall, not least because family carers are likely to hold information of importance. 48
A CTO is imposed for up to 6 months in the first instance and is then renewable for a further 6 months and subsequently for 1-year terms; frequent clinical monitoring was anticipated in the Code. 48 It can be discharged at any time by the RC or by a Mental Health Review Tribunal (MHRT) if the patient’s mental state or circumstances change. During the period covered by the CTO, the hospital treatment order (Section 3) remains in place but is inactive; it is reactivated if the CTO is revoked after a recall to hospital (Box 1 and Figure 2).
FIGURE 2.
The CTO process.
Community treatment orders were introduced via a 2007 amendment to the MHA for England and Wales, with effect from 3 November 2008. They are referred to in the Act under the heading of supervised community treatment.
To be placed on a CTO, a patient must fulfil all the following criteria:
-
suffering from a mental disorder of a nature or degree which makes it appropriate for them to receive medical treatment
-
it is necessary for that person’s health or safety or for the protection of others that the person should receive treatment
-
treatment can continue in the community without the person being detained in hospital
-
it is necessary that it be possible to recall that person swiftly to hospital if needed
-
appropriate medical treatment is available.
The order is made by a responsible clinician (usually a psychiatrist) and an approved mental health professional (usually a social worker). The order lasts for 6 months initially, can be renewed for another 6 months and thereafter for 12-month periods. The responsible clinician can end the order when clinically indicated, and it may also be ended by the managers of the treating hospital or the MHRT.
The order includes two mandatory conditions. Patients on CTOs must make themselves available:
-
to be assessed by a second psychiatrist to complete the mandatory peer review process concerning treatment without consent, when required
-
for assessment concerning renewal of the CTO.
The RC and AMHP may also specify discretionary conditions that are needed to ensure the patient receives medical treatment, or to prevent risks of harm to the patient or others, based on their knowledge of an individual patient. These may subsequently be varied by the RC.
Patients on CTOs may be recalled to hospital for up to 72 hours when they:
-
breach the mandatory conditions, or
-
require further treatment in hospital and there would be a risk of harm to self or others if they were not recalled.
Recall can be used for assessment or to provide treatment without consent. When 72 hours have elapsed, the patient returns to the community under the CTO, remains in hospital for involuntary treatment under Section 3 of the MHA or is discharged from involuntary care under the MHA.
Section 17 Leave remains an available option under the new law, but since the amendment to the MHA, clinicians must consider using a CTO instead if they are granting leave for more than seven consecutive days, as is stated in the Code. This change, along with the removal of supervised discharge, signalled that the government saw CTOs as the primary means of providing involuntary supervision in the community.
Controversy surrounding community treatment orders in England and Wales
The introduction of supervised community treatment was highly controversial and was preceded by a heated debate lasting for at least 15 years. In other countries there had been similar levels of debate and controversy,54 but when the orders were made available, they were incorporated into practice swiftly. Initial proposals in England and Wales were met with broad opposition from service users, psychiatrists and mental health charities. The amended proposals, once enshrined in law, continued to provoke vigorous debate and to divide the psychiatric profession. Some viewed CTOs as ethically unacceptable because of the infringement of rights and freedoms. 55 Others believed they were potentially beneficial to patients and their families4,56 or argued that they constituted only a minor amendment to current law or practice. 25
The arguments emphasising individual human rights and people’s rights to make lawful decisions about their own lives were particularly forceful. This position provided powerful arguments against coercive treatment6 but was vulnerable to the criticism that such a purely rights-based approach could leave revolving-door patients in unacceptable circumstances, preventing them from improving their lives. Not to pursue compulsory interventions could be seen as conflicting with mental health practitioners’ primary obligation to help. 6
Much of the debate centred on issues of an individual’s capacity to make decisions about his or her treatment. Such competence might, of course, be compromised or even absent in those with severe mental illness. Others might have to make decisions on their behalf. This would require good knowledge about the person’s values and opinions based on when he or she had full capacity. It is commonly viewed as appropriate that when the patient’s views are not available, ‘best-interest’ standards should be applied. 6
It has been argued that although politicians sought to introduce CTOs in order to address the public’s fear of crimes committed by people with mental health problems, the protection of society is an insufficient reason to justify detention. 57 This is particularly the case given the difficulty in predicting serious violence by those with mental health problems. 58 The ‘principle of reciprocity’ requires that restrictions of civil liberties must be matched by the provision of adequate and high-quality services. 27,57 This was one of the underpinning principles of the amended MHA in Scotland, which introduced compulsory powers in the community in 2005. 59 Some have suggested that the use of compulsion may be enabling and consistent with the recovery model if adequately resourced and accompanied by clear goals for treatment and progress. 3
The change in the law in England and Wales was thus highly controversial. A fierce debate continued about how it impacts on patients’ lives and mental health services. It was argued, for instance, that even if compulsion in the community may be necessary in itself, CTOs in the form introduced in the 2007 MHA may not be in patients’ best interests. In particular, the following issues were identified that needed to be resolved:
-
whether or not capacity should have been a fundamental principle of the new MHA
-
whether or not having CTOs would increase the overall level of coercion
-
whether or not CTOs would contribute to better outcomes
-
which patient groups might benefit from CTOs and in what ways
-
whether or not it might be relatively easy to be placed on a CTO but harder to get off one (a lobster pot effect), leading to an inexorable rise in numbers over time
-
whether or not potential benefits would justify the restrictions in civil liberties. 17
Evidence base for community treatment orders
Although early opposition to CTOs focused on civil liberties6 or lack of improvement on the existing leave regime,25 more recent opposition has emphasised the absence of experimental evidence. 3,60
Around 40 published non-randomised studies have investigated CTO effectiveness by measuring outcomes, particularly in Australia, New Zealand, the USA and Canada,3,4,61,62 but prior to the OCTET Trial there had been only two published RCTs. 63,64 Most of the studies have methodological limitations. 65 It is therefore problematic to generalise from these findings. Generalisability is also problematic because of significant differences between the contexts into which CTOs have been introduced, such as the mental health systems and legal procedures. Neither of the two RCTs demonstrated a difference in the primary outcome measure of readmission rates, as detailed below.
The most common research designs used in studies of CTOs conducted prior to the OCTET Trial (which have been reviewed in detail by Dawson,4 Churchill et al. 3 and by the OCTET Coercion Programme Group18,66,67) have been controlled before-and-after (CBA) studies and uncontrolled before-and-after (UBA) studies, in which patient outcomes are compared before and after the intervention. Some epidemiological studies have also been conducted in which CTO and non-CTO populations have been observed but not matched. Studies using routine administrative data in this way have the advantage of including data on all CTO patients in whole areas or jurisdictions, avoiding selection bias following from excluding, for instance, violent or non-consenting patients.
Observational studies
Numerous studies describe local CTO patient cohort characteristics or stakeholder views. Overall, these studies suggest that clinicians prefer to work in systems where CTOs are available,68 views among psychiatrists may become more positive over time,69 and many believe CTOs to have positive clinical outcomes. 70,71 Many of these studies report perceptions of reduced readmission rates or that positive change occurs after many months on a CTO. Study designs preclude conclusions being drawn, and observed effects could be influenced by regression to the mean and rater bias.
A review by Dawson4 points out that after an initial ‘bedding in’ period, the use of CTOs often increases, particularly when there is a reduction in hospital beds and build-up of community teams. Some studies report therapeutic benefits for patients, such as greater compliance with outpatient treatment (particularly medication) and reduced rates of hospital admission. Some studies show better relationships between patients and their families, enhanced social contact, reduced levels of violence or self-harm and earlier identification of relapse. Dawson’s review4 also identifies some potentially negative effects of CTOs, such as a strong focus on medication (particularly depot medication) as opposed to other treatments, and that they are often used for the maximum time allowed and possibly overused.
The literature on personal experience of CTOs is very limited and derived from surveys and qualitative studies. It suggests that patients hold ambivalent, and sometimes contradictory, views about CTOs; for instance that they appreciate the sense of security and attribute health improvements to CTO use, but do not appreciate the restriction of their choices, particularly about residence, travel and medication. 72,73 Similarly, patients may appreciate a sense of safety,74 but dislike the sense of external control,75,76 and they may feel coerced but believe the CTOs provide a necessary structure in their lives. 77 Family carers generally find them helpful,77 albeit with similar misgivings,75 and regard them as providing relief and a supportive structure for the patient’s care. 78 They tend to consider the community services offered to be inadequate. 77,79 When professionals have been studied, they generally report finding CTOs useful,77 particularly for engaging the patient in a therapeutic relationship and increasing adherence to medication,78 although some also report disliking the sense of external control. 75 The main expressed concern of all three stakeholder groups is usually to avoid hospital admissions. 80
Controlled before-and-after studies
A handful of studies from the 1980s and early 1990s, mainly from the USA with UBA designs, led to initial optimism about positive effects of CTOs on hospital outcomes. 3 Since then, however, studies from a number of jurisdictions have reported discrepant findings. 3,81 Eight out of 12 studies published since 2006 and measuring readmission18 reported reductions under CTOs, but several of these were uncontrolled studies. Some reported reductions for subgroups of CTO patients. Four studies reported increased readmissions. The picture is equally complex for duration of admissions and community service use, with some studies reporting no difference and some reporting benefits for subgroups. There is considerable variability in outcome measurement and it is not always clear whether reported measures are considered part of the CTO intervention or as an outcome of it. 81
A number of studies analyse outcomes at different time periods under the CTO, frequently the first 6 months and then periods beyond that. These studies commonly report benefits from the second 6-month period on the CTO onwards. This might be a result of long-term benefits from CTOs,64 but an alternative interpretation would be that those on the CTO over a longer period were kept on it because things were going well clinically and the CTO was presumed to be responsible. 82 The latter interpretation would be supported by the evidence that psychiatrists are reluctant to change treatment in long-term conditions when the patient is stable. 83,84
These studies do not always include all available CTO patients, which affects generalisability. Many analyse CTOs in conjunction with other interventions, such as ACT. Many utilise routine administrative registers providing data on large numbers of patients over time. The two most frequently used registers are the Victoria register in Australia and the New York State register in the USA. There is a trend for the Victoria register studies to report increases in admission, whereas those using the New York State register report reductions. 67 This may be due to prioritisation of CTO patients for enhanced community services in the USA, whereas such services form part of standard care in the Australian context. Improved patient outcomes may thus be an effect of the services rather than compulsion.
Studies with non-randomised designs may be confounded by methodological limitations. Their results are vulnerable to changes being made over time. 67 CBA studies may be confounded by problems in adequate matching of patient characteristics, particularly lack of insight or adherence. UBA studies eliminate the problem of matching using patients as their own controls, but may be confounded by regression to the mean, that is, patients may improve as part of the natural fluctuation of their illness after they are placed on the CTO, which is often initiated at a time of maximal instability in their condition.
Overall, the evidence from these studies shows no strong or consistent effect for CTOs in any direction. These conflicting findings are complicated by the variation in study designs including the lack of standardised outcome measures.
Randomised controlled trials
By randomising the treatment condition, RCTs reduce the risk of sample and observer bias and the effects of regression to the mean.
The New York RCT63 recruited patients referred to the outpatient commitment programme at an acute hospital in New York City. It randomised 142 patients to either treatment under court-ordered CTO or voluntary status. It was not possible to randomise patients with a history of violence. No difference was found in the primary outcome of readmission or any of the other outcomes measured at 11-month follow-up. Both groups received case management and close follow-up during the trial (which was not standard care) and both had significantly fewer admissions in the trial period than in the preceding 12 months. The trial took place within a pilot CTO project and no police pick-up procedures were in place in case of non-adherence, so there was no systematic enforcement of the CTOs. The trial also experienced considerable problems, including lack of adherence to the protocol and an apparent confusion among staff and patients that some in the control arm were in fact on CTOs. A smaller than expected sample size and high attrition rates (45% at 11 months) could mean that the trial lacked statistical power to detect differences. 63 The New York data are therefore usually treated with caution.
The North Carolina trial64 was more rigorously conducted and has been highly influential. It recruited 264 patients from one state hospital and three public inpatient services, and randomised them between court-ordered CTO and voluntary status. All received case management, which went beyond standard care. The control group was ‘immunised’ from being on a CTO for 1 year. Attrition was low (18%) and equally distributed between the two groups. The primary outcome of readmission to hospital showed no difference between the two groups at 12 months. 64 No difference was found in treatment adherence, quality of life, service intensity, arrests, homelessness, quality of life or perceived coercion. A significant difference was detected in victimisation (being a victim of crime) with those in the CTO group less likely to report this. Outcomes for both groups improved during follow-up.
A secondary analysis showed significant reductions in readmissions for patients who were on a CTO for > 6 months while also receiving frequent service contacts (three or more per month). This analysis has been criticised for potentially introducing a selection bias if only patients who were considered to do well on the CTO were kept on the order long term. Several other outcomes (adherence, violence, arrest, quality of life) also reached statistical significance when dividing up patients according to duration of the CTO or including the non-randomised violent patient group, but this does not represent RCT-level evidence. 3,81
Systematic reviews and meta-analyses
A Cochrane review of these two RCTs61 found no advantage to CTO for readmission, service use, social functioning, mental state, homelessness, satisfaction with services or perceived coercion. There was some evidence that CTOs reduced the risk of victimisation. The authors suggested that the generalisability of the USA trials may be limited by the exclusion of violent patients and the court-initiated nature of the CTOs. 81 They subsequently reviewed non-randomised studies to identify those that measured relevant outcomes and were of sufficient quality to be pooled with the RCT data. Three further studies were included, bringing the number of patients to 1108, including those with a history of violence and those on clinician-initiated CTOs. No outcome reached statistical significance, including admissions, duration of admissions, total days in hospital and treatment adherence. 81
Churchill et al. 3 conducted a systematic review including 72 papers published up until 2006. Most reported descriptive or observational studies. They found the quality of the evidence base to be poor, with studies showing discrepant results, and concluded that there was no robust evidence of positive or negative outcomes of CTOs. They also found that various stakeholder groups hold very different views about CTOs. Avoiding involuntary hospitalisation was, however, the shared top priority for patients, family members, clinicians and members of the general public alike.
Churchill et al. 3 found, however, that when CTOs are implemented, they are used for the same patient group, usually men around 40 years of age, in the middle phase of their illness, with a diagnosis of schizophrenia, several prior hospital admissions and a history of non-compliance with outpatient care: features characterising the revolving-door stereotype. Many had problems with substance misuse and had experienced imprisonment or forensic care. Most were single and living in rented accommodation alone or, less often, with their family.
As the Cochrane review61 concluded, there is clearly an urgent need for high-quality RCTs in this field, particularly to establish whether or not it is the intensity of treatment or the compulsion in itself that is responsible for any outcomes achieved by CTOs. This is consistent with Churchill et al. ’s3 conclusion that:
Research in this area has been beset by conceptual, practical and methodological problems, and the general quality of the empirical evidence is poor . . . [T]here is currently no robust evidence about either the positive or negative effects of CTOs on key outcomes, including hospital readmission, length of hospital stay, improved medication compliance, or patients’ quality of life. 3
How to measure relevant outcomes
There have been different opinions on what constitutes the best measure to assess the outcome of CTOs. This relates to whether the chief purpose of CTOs is considered to be prevention of relapse or the provision of a least restrictive alternative. Readmission to hospital has been the most widely used outcome measure of success in preventing relapse in patients with psychosis. The term relapse has different meanings in the literature and no unambiguous measure of it has emerged. Readmission is the measure that has been the most consistently used, not only as the primary outcome of the two RCTs, but also in most of the non-randomised studies. It has also been widely used as the primary outcome measure in most antipsychotic maintenance trials. 85 Measures obtained directly from patients have been vulnerable to attrition and difficult to standardise. Despite criticism of it as being a crude proxy for relapse, readmission is a measure for which data are obtainable. A binary measure of readmission, excluding brief recall or breach admissions, where they are permitted, may be least sensitive to particularities of service organisation and other contextual issues. (This was the primary outcome measure we used in our trial; see Chapter 6, Methods.) When recall admissions are not routinely distinguished, it may be difficult to ascertain the effect of CTOs. Similarly, frequent contact with the community team may indicate that the CTO is working, whereas contact with a crisis team may suggest relapse, and these situations must be carefully distinguished. 67
Some have argued that the duration of admission should be the preferred measure because shorter admissions may reduce the overall restrictiveness of CTOs. Duration of admission does measure relapse, but it also measures the clinical response to that relapse. Although duration of admission conveys important information, it does not measure the effectiveness of CTOs in their purpose of stabilising patients in the community and reducing or preventing relapse. It may therefore be more suitable as a secondary measure (as we used it in our trial; see Chapter 6, Methods). It is of obvious importance in cost-effectiveness studies.
The outcomes most frequently measured in the existing literature include readmission rates, time to readmission, duration of admissions and use of community services. The ways in which these outcomes have been measured has varied. Duration of admission, for example, has been measured by the number of days from admission to release from hospital for each episode,86 and as the patient’s mean number of days in hospital during months in which a hospitalisation occurred, compared across 6-month periods. 87 Other outcomes, such as medication possession, adherence, victimisation, arrest, mortality and quality of life, have been measured in some studies. 3,81 This means that the total number of outcome measures applied has been rather large for a relatively small body of research.
The clinical ambition of a CTO is to foster longer-term changes in patient well-being and insight as a result of a protracted period of treatment. Churchill et al. 3 argue that ‘if CTOs are intended to improve outcomes for patients, then . . . patient relevant outcomes should be prioritised in future research.’ Their review reveals the paucity of data on such patient-level outcomes as symptoms, social functioning, quality of life and satisfaction. Churchill et al. 3 also argue for the inclusion of measures of perceived coercion, found to be associated with CTO use in the literature, which they argue may be mediated by factors such as treatment adherence and therapeutic relationship. In fact, measuring perceptions of the therapeutic relationship and the patient’s experience of the service may be particularly important given the indications in the literature that the use of CTOs may threaten the patient–professional relationship, although Churchill et al. 3 note that ‘the impact and duration of such problems have not yet been properly investigated’.
The literature on CTOs suggests that any effect of CTOs on admission to hospital may be achieved by improving treatment compliance. Although, as noted above, there is no robust evidence to support either contention, it is clearly important to understand the factors that might affect treatment compliance or engagement. Churchill et al. 3 note the emphasis in the literature on insight, or awareness of the need for treatment, along with other factors such as previous experience of the mental health system (including coercion) or poor access to services.
In designing the most robust possible study of CTOs, there is thus a clear need to include data on patient-level outcomes such as these. As well as the hospitalisation outcomes described above, the OCTET Trial used well-established measures of clinical and social outcomes, attitudes to medication and experiences of services and of coercion, including measures of insight and therapeutic relationship (see Chapter 6, Methods). We also identified a need to develop a measure capable of capturing quality of life for people with severe mental illness, in particular one that would capture their capabilities (things that they are free to do or be). We therefore developed and tested such a measure as part of the OCTET Study (see Chapter 10) and it was utilised as part of the Economic Evaluation (see Chapter 7).
Ethical implications of community treatment orders
Ethicists studying CTOs have largely been critical of what has been taken to be a new paternalistic approach to the delivery of community-based mental health services. Instigating involuntary outpatient treatment into patients’ care regimens outside of hospital has been argued to constitute an unjustified restriction of patients’ personal freedoms and autonomy, undermining the principles of respect for liberty and self-determination. 6,88,89 These ethical arguments have moved beyond the use of catch-all normative concepts such as coercion, and have been accompanied by a more general recognition of, and concern about, the use of a range of pressures to influence patients’ adherence to treatment within community mental health settings, as investigated in the ULTIMA Study.
In response to these principle-led attacks on the justification of CTOs, other commentators have offered spirited defences of the new legal powers by highlighting the difficult realities of the lives of those patients who have severe illnesses that undermine treatment adherence and frequently require readmission to hospital. Established to support these so-called revolving-door patients in ways that could secure the longer-term positive outcomes associated with continued treatment and prompt intervention in the face of crisis, CTOs have been claimed to be liberty enhancing and potentially beneficial to those in receipt of them. 90,91
Although the ethical discussion has begun to take seriously the realities of the treatment settings within which CTOs are used, the academic psychiatric literature continues to scrutinise whether or not the ethical considerations identified can be balanced in such a way as to defend the use of CTO regimes in different jurisdictions. Moreover, little is known about how these considerations translate into practice, given the complex and varied mental health and social support needs of the patients who will be subject to these powers. The empirical studies that have explored the experiences of mental health professionals and patients have highlighted positive and negative views about the use of CTOs in practice,73,77,92 but the authors of these studies have not sought to explicate their findings in ways that directly address the ethical questions that concern the use of this new legal power. These complex ethical considerations provided the starting point for the ethical analyses conducted in the OCTET Coercion Programme.
Governance
We established a clear governance framework for the OCTET Study, which covered all its substudies as well as the OCTET Trial.
Host/sponsor
The study protocol was reviewed and approved by the research and development (R&D) office of the then Oxfordshire and Buckinghamshire NHS Mental Health Foundation Trust (from March 2011, Oxford Health NHS Foundation Trust). The trust accepted its role as study sponsor and issued the necessary indemnity documentation.
Ethical approval
Details of ethical approval are given above (see Part I, Chapter 4). During the course of the study, seven amendments to the original protocol were sought and approved (see Appendix 1). All were communicated to all participating trusts.
Steering group and data monitoring committee
The OCTET Study Steering Group consisted of an independent clinician, a service user, a service user organisation representative, a carer representative and a mental health lawyer. Its function was to advise on the implementation process and on how to translate our findings into policy and practice.
The OCTET Trial also had a data monitoring committee (DMC) as part of its governance structure, as is a prerequisite for all high-quality RCTs. The purpose of a DMC is to judge at agreed intervals whether or not it is ethical and desirable to continue with the trial, by examining reports of interim data. The DMC is asked to assess on the basis of these reports whether or not the trial should be stopped because:
-
there are unanticipated adverse outcomes clustered in one arm, or
-
the result is already clear (i.e. there is a statistically clear advantage to one arm because of a very large effect size).
It was anticipated in the OCTET Trial protocol that the first report could be delivered for the committee’s consideration 12 months after the study’s inception. Recruitment was delayed, however, by delays in obtaining R&D approval and negotiating researcher access in the participating NHS Trusts, so at 12 months we had follow-up data for only about 30 patients. This was deemed insufficient to give any meaningful indication as to the trial’s progress. With the agreement of the DMC, we therefore decided to postpone the first report to 18 months and the second to 24 months after the study’s inception. The statistical data were prepared by a statistician who was independent from all data collection. Although the OCTET research team assisted in her work, in particular by preparing the background information, they were kept blind from all calculations of outcome data. The committee reviewed the project at the agreed time points and saw no reason to stop the trial.
The composition of the OCTET Steering Group and DMC is given in Appendix 5.
Chapter 6 OCTET Trial
Introduction
The need for a randomised controlled trial of community treatment orders
As the Introduction to this study made clear, CTOs were highly controversial when they were introduced and have remained so (see Chapter 5). The key issues of contention in the period before their implementation included:
-
ethics – whether or not CTOs ought to be enacted
-
legality – whether or not CTOs would comply with constitutional and/or human rights
-
empirical issues – whether or not established CTO schemes had the intended beneficial outcomes.
The only methodology which could convincingly address concerns about the effectiveness of CTOs was an RCT. We therefore designed the OCTET Trial to:
-
provide rigorous evidence to inform the debate about CTOs
-
demonstrate whether or not adding CTOs to community care reduced readmission rates and affected a range of other outcomes
-
identify patient characteristics and care patterns associated with positive and negative outcomes
-
inform an economic evaluation.
This chapter draws substantially on papers by members of the OCTET Coercion Programme Group: the trial protocol summarised in The Lancet (Burns et al. ,93 with permission from Elsevier); its primary and secondary outcome findings as published in The Lancet (Burns et al. ,16 with permission from Elsevier) and the tertiary outcome and subgroup findings (Rugkåsa et al. ,94 with permission from John Wiley & Sons).
Development of the Trial design: consultation exercise
The aim of the OCTET Trial was to compare CTO use to voluntary outpatient treatment. A number of ethical, legal and practical issues rendered this a complex undertaking.
In view of concerns being raised about the ethical, legal and practical issues of methodologies to test the impact of CTOs, we conducted a consultation exercise with clinicians and legal, policy and ethical groups in the spring and summer of 2008, before finalising the protocol for the OCTET Trial. As is reported below, the exploratory work on the legal constraints involved led to our seeking a detailed legal opinion; we report this separately (see Chapter 11).
This detailed consultation exercise involved numerous opportunistic discussions and a series of more structured meetings to explore the ethical, legal, clinical and practical aspects to the proposed study methodology and to obtain agreement about, and support for, the strongest test of the intervention, in order to produce a detailed study protocol. The consultation exercise involved > 50 people from the full range of stakeholders from the following groups:
-
patients and carer organisations and mental health voluntary organisations
-
MHA practitioners
-
mental health lawyers
-
academic legal experts
-
the MHRT
-
approved social workers
-
clinicians in inpatient and outpatient services
-
ethicists.
There were some differences between the different groups of stakeholders, in particular between those working with patients in a clinical capacity and those who practised mental health law as solicitors or as representatives of the MHRT. Here we summarise the views expressed by each group, in turn. The summaries represent the breadth of views in each group and the main points, from across the groups, which were of relevance to the trial’s feasibility and design. It should be noted that this consultation was conducted after the legislation had been passed by Parliament in 2007 but prior to the actual introduction of CTOs on 3 November 2008, so none of the consultees had any practical experience of the new regime.
Clinicians and approved social workers
The long and heated debate preceding the introduction of CTOs nationally was reflected in the views raised during our consultations. Some were concerned that CTOs constituted ‘incarceration in the community’ and that CTOs might lead to a lowering of the threshold for compulsion so that a larger proportion of people at relatively low risk might be subject to compulsion. Others commented that, in practice, the new provision did not represent much change and that ‘we are doing it anyway with Section 17 as a long leash: at least a CTO is honest’.
Clinicians noted that attitudes to CTO use had changed since the new legislation had been passed by Parliament. Much of the opposition had dissolved and CTOs were rapidly becoming accepted as part of the provision that was soon to be implemented. This was expressed in concerns or even fear associated with not complying with the new legislation: ‘As a clinician, I will opt for a CTO because of the new law [when it takes effect]. We would be frightened what will happen if we do not.’ They were also concerned about public harm and liabilities in the event that tribunals would discharge patients in the non-CTO group who subsequently committed crimes. As such, CTOs were considered the more restrictive option, with more control remaining with the clinician.
At the time of the consultation, few mental health professionals had received training on the amended MHA and how it would impact on services. There was considerable uncertainty about how CTOs would work in practice and whether or how Section 17 Leave would change. Prolonging Section 17 Leave was seen as being likely to be challenged by tribunals, as the new Code of Practice indicated that this would not constitute ‘good practice’. Psychiatrists were concerned that mental health lawyers might be eager to test the amended MHA, and worries were expressed about how to explain to tribunals why an RC had repeated Section 17 Leave instead of placing the person on a CTO. Several psychiatrists stated ‘I don’t want to be involved in the first judicial review’.
Mental health lawyers
Lawyers representing patients in tribunals emphasised the right of patients to make decisions about their treatment, including taking part in trials; they suggested that legal representatives would be obliged to take a client’s participation in any study into account when representing them at a hearing. They strongly emphasised that patients must be fully informed about the trial and that the different mechanisms for treatment following from randomisation should be made clear to patients prior to enrolment in the study.
The legal representatives we spoke to expressed surprise at the degree of fear of the MHRT among clinicians. Their view was that a tribunal only recommends treatment and that it is a matter for clinicians to ‘stick to their guns’ regarding what they consider an appropriate course of action.
Academic legal experts
Unlike many clinicians, who believed that the clinical effectiveness of CTOs needed to be tested, some of the academic legal experts we consulted saw the overall research question as being of limited interest to the law, since the amended MHA had already been passed by Parliament and CTOs were soon to become part of the MHA.
Some legal experts expressed uncertainty whether or not the new Act presented the option of using Section 17 Leave as the control arm of the trial, given the directions in the Code of Practice; they anticipated that MHRT hearings would insist on the Code being followed. They thus saw the MHRT, despite its inability to go beyond recommending treatment, as potentially exerting influence over the trial.
The legal experts also identified a worry about a shifting threshold for detention, and they described the new Act as ‘vague’ on this point. Some believed that the introduction of CTOs might lead to an increasingly ‘defensive practice’ in which clinicians might leave it to tribunals to discharge patients from CTOs. Moreover, would some such ‘defensive’ clinicians, if a patient were randomly allocated to be managed without CTO, end up using Section 17 Leave for longer periods than they would have done otherwise and thus threatening the naturalistic design of the trial? Some experts were also sceptical as to whether or not clinicians would be willing to put patients forward given that the randomisation would lead to some patients who were deemed appropriate for CTOs not being put on to CTOs.
The legal experts raised two related issues regarding clinical equipoise. First, would there be genuine equipoise when the clinical judgement was that CTO would be appropriate? Second, would clinicians who were willing to put patients on to a CTO be in equipoise? In other words, once a clinician deemed that a CTO was appropriate for a particular patient, would they then deem CTOs to have benefits and by definition not be in equipoise?
Mental Health Review Tribunal
Those representing the MHRT expressed a different view of the Code of Practice compared with some academic lawyers. Although, from the point of view of Government, there would be little point in issuing a new Act with provision for CTOs without a steer as to their use, they argued that case law illustrates that the Code does not constitute a statute; making decisions contrary to the Code might therefore be in adherence with the MHA. 95 Moreover, they pointed out that the Code is directed towards clinicians rather than tribunals.
Regarding the appropriate treatment arms for a study, the MHRT stakeholders raised the issue of what would constitute the least restrictive option. Established case law and European law require a tribunal to apply the least restrictive option. As a matter of law, the MHRT stakeholders considered that if a patient were subject to Section 17 Leave, this would mean that Section 3 was still active and the patient was still detained, whereas a CTO would represent a form of discharge from Section 3 (unless the patient was recalled), so that the patient would not be considered to be detained despite the restrictions to their personal freedom. Contrary to the impression of most clinicians, they thus saw CTOs as the least restrictive option, based on Article 5 of the European Convention on Human Rights (albeit not yet tested in a court of law). 96 Following from this, they considered that it would be difficult for a tribunal to believe simultaneously both that Section 17 Leave was appropriate and that a CTO was appropriate for a particular patient. They expressed a degree of surprise at what they saw as ‘liberal’ views and uses of Section 17 Leave among clinicians, as, from their point of view, it constituted part of Section 3.
This position on the relative restrictedness of CTO and Section 17 Leave was seen as relevant to the equipoise of any clinician participating in a trial. The MHRT stakeholders explained that when a tribunal looked at a patient’s circumstances (e.g. treatment, potential risks) and decided whether or not, on balance, continued detention or a CTO was justified, only clinical arguments would be considered. If the clinician were in genuine equipoise, it was suggested, they might be unable to provide such an argument. They advised us to seek separate legal advice to address this issue.
From the viewpoint of the MHRT stakeholders, it was mental health lawyers who might provide a challenge to the trial: they might be eager to test the new provision via judicial review should they believe that a tribunal had been influenced in any way by any factors other than Statute. They also noted, however, that a robust clinical argument would in most cases suffice for the use of either option; while the tribunal might recommend a CTO, clinicians did not have to follow their recommendation. They commented that perhaps some clinicians ‘fear the tribunals too much’.
Service user representatives
There was less enthusiasm for taking part in the consultations among service user representatives and mental health organisations than among the other groups of stakeholders and thus fewer people took part or expressed their views. Overall, there was strong support for testing the effectiveness of CTOs, but they expressed concern over the lawfulness of randomisation and whether or not clinicians would find it ethical to randomise. They also reiterated the importance of fully informing patients about what taking part would entail and of their right to withdraw, and recommended using a wide range of outcome measures.
Key issues raised in the consultation exercise
The consultation exercise thus elicited a range of views as to the various legal, clinical and practical aspects of the proposed protocol. In particular, although many clinicians considered CTO to represent a more coercive alternative than Section 17 Leave, many lawyers considered it to be less restrictive. Three issues emerged overall:
-
what would constitute appropriate treatment arms of the study
-
issues of equipoise
-
whether randomisation between different legal statuses would be lawful.
These are summarised here along with the conclusions we reached about our trial design based on the consultation.
Treatment arms It was clear that to randomise between a CTO and voluntary status, as the two US RCTs had been able to do, would be unacceptable to clinicians and ethicists, and might be considered unlawful should it be tried in the courts. The consultation exercise confirmed that patients in the control arm of our trial should instead leave hospital via Section 17 Leave. Many consultees were concerned about the lawfulness of prolonged use of Section 17 Leave or how it would impact on the research. To preclude the threat of prolonged use of Section 17 Leave during the trial, which would serve as a de facto CTO and contaminate the results, we decided that we would recruit only from clinicians who used Section 17 Leave as intended by the Code of Practice that accompanies the amended MHA. This states that if extending Section 17 Leave beyond seven consecutive days, the RC should consider a CTO instead. This gives a clear indication that Section 17 Leave should be treated as a short-term measure, whereas prolonged community compulsion should be managed by a CTO.
As the legal analysis indicated, for the trial to be lawful, patients needed to be randomised to two equally restrictive positions. Therefore, this confirmed that it would not be lawful to randomise a patient either to be put on a CTO or to be discharged to voluntary status. The solution, which our experts deemed to be both ethically and legally valid, was to randomise the patients to leave hospital either on a CTO or via Section 17 Leave. Those in the control arm (henceforth referred to as the ‘non-CTO arm’) would then proceed to voluntary care.
Equipoise The issue of equipoise is central to all RCTs, as no clinician should put forward a patient to a trial if he or she considers treatment in one arm to be inferior to that in the other. Given the fact that there was no robust evidence for CTO effectiveness at the time and that English psychiatrists did not have any clinical experience on which to base an opinion, by definition a state of equipoise existed. We decided to recruit only from psychiatrists who accepted this. This was in order to address the concern that a psychiatrist might be willing to refer one patient but not another (cherry-picking the RCT patients). Given the state of the evidence, if one were in equipoise in one case, one must be in equipoise on all cases. We did accept, however, that there might be exceptional circumstances (such as insistence from family) when an eligible patient was not put forward. Moreover, there were psychiatrists who, perhaps as a result of the heated debate preceding the introduction of CTOs, were convinced that CTOs would be the best option, and there were also psychiatrists who were equally convinced that CTOs were not effective or should not be used for ethical reasons. It was considered unlikely that either of these groups of psychiatrists would participate in the trial. This is a limitation that applies to most RCTs. (For further details about the state of equipoise, see Chapter 11.)
Lawfulness of randomisation The legal experts involved in our consultation exercise identified a need for further work on understanding the legal issues arising from our proposed trial design and this issue was also raised by the Research Ethics Committee. Following their initial review, and the stakeholder consultation, we therefore commissioned a formal legal opinion from John Dawson, Professor of Law, and Marion Rickman, mental health lawyer (and subsequently tribunal judge). This concluded that our protocol was lawful. To arrive at this decision, they examined three features of the law in detail to answer the questions:
-
Do the legal criteria for the two chosen treatment arms overlap? Is there therefore a group of patients who may simultaneously meet the legal criteria for both treatments?
-
Are both the treatment arms equally restrictive in terms of the patient’s liberty?
-
Is there a situation in which RCs can be genuinely uncertain as to which of the two treatments is the more appropriate option for an individual patient?
They concluded, respectively, that:
-
there would be a number of patients fulfilling the criteria for detention under both regimes
-
it was difficult to ascertain which of the two treatment arms would constitute a more or less restrictive option
-
genuine equipoise existed, making it both ethical and lawful for RCs to allow a specific group of patients to be randomised between a CTO and Section 17 Leave.
Thus, within particular constraints, their legal opinion was that an RCT of CTOs would be feasible. (The legal analysis is reported in detail in Chapter 11.)
The legal analysis also concluded that the period soon after the change in the MHA would provide a window of opportunity to study the outcomes for patients of the varying clinical practices that were likely to emerge from the position of equipoise in which clinicians would find themselves at that point, because of genuine uncertainty about both treatment efficacy and the proper application of the law. The legal analysis also advised on the correct procedure for randomisation and advised that clinical decision-making should not be influenced by the patient’s participation in the trial or randomised allocation (see Overview of the OCTET Trial).
The exploration of legal, ethical and feasibility issues during the consultation period shaped the final research protocol. In addition to clarifying the randomisation process, it also helped shape the design of eligibility criteria, outcome measurement and strategies for recruitment and data collection, all of which we describe next.
Overview of the OCTET Trial
Design
The OCTET Trial was a single-outcome, parallel-arm, non-blinded randomised trial. Its primary objective was ‘to conduct the most rigorous trial possible of CTOs with prolonged, high-quality care incorporating a broad range of outcomes, and identify patient and service predictors of response’. Our aim was to compare CTO use to voluntary outpatient treatment. This aim was modified on the basis of the legal analysis, as explained above. Our trial therefore randomised the patients to leave hospital either on a CTO or via Section 17 Leave. There was an understanding that for patients in the non-CTO arm, Section 17 Leave was to be used according to the MHA Code of Practice48 and be restricted to a short period of days, or at most weeks, before discharge to voluntary care took place. The trial thus randomly assigned patients to receive one of two forms of mandatory outpatient care at the point of discharge from inpatient care: the two main options for clinicians regarding patients who needed ongoing supervision in the community from November 2008 onwards. Patients were assessed at baseline, and at 6 and 12 months, and the primary outcome measure was readmission to hospital, as detailed below and represented in the OCTET flow chart (Figure 3).
FIGURE 3.
The OCTET Trial procedure.
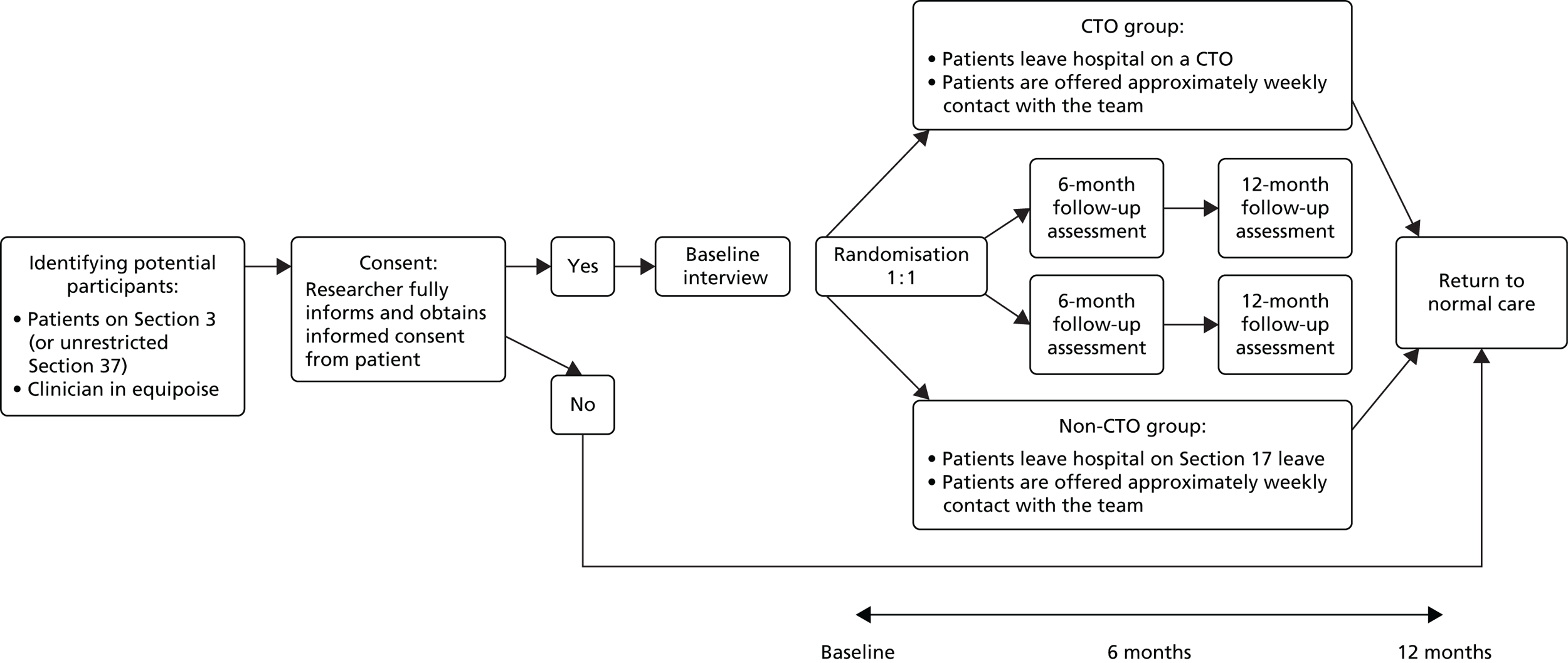
Taking into account the findings from the North Carolina RCT,64 which suggested a correlation between outcomes and the combination of duration of CTO and intensity of services, we designed the OCTET Trial so that patients in both arms would receive approximately weekly contact with services. This was in line with common practice for this group of patients in English services.
Eligibility
Patients were deemed eligible for the study when the RC and AMHP agreed that they needed ongoing supervision in the community, but (after having considered the relevant legal standards, including the guidelines in the Code of Practice) when clinicians recognised the uncertainty as to which option was more appropriate (CTO or non-CTO). Potential referring clinicians who held strong views in favour of certain patients being likely to be more or less well on a CTO were actively discouraged from referring any patients to the trial, so that the referring clinicians would be those, reflecting the evidence base, with a neutral view (accepting the state of equipoise), thus avoiding cherry-picking. Clinicians who used Section 17 Leave as a de facto CTO were excluded from recruiting to the trial.
During the preparations for the amendment of the MHA, discussions around CTOs focused almost exclusively on the situation of so-called revolving-door patients, that is, patients experiencing frequent relapse and readmission to hospital. Both expert views and the evidence from other jurisdictions suggested that CTOs were likely to be mostly used for patients with psychosis in adult mental health services. The amendment did, however, pave the way for the use of CTOs for a much wider group of patients, including those with learning disabilities and in forensic detention. Given the potentially different clinical uses of CTOs for different patient groups, we decided to design the trial to focus on a relatively homogeneous group of patients. We therefore decided to exclude those on restricted forensic sections and those without a primary diagnosis of psychosis, as well as those in adolescent or older adult services. Including the other groups would require a significantly larger sample size, which could prove unachievable given restrictions of time and resources. The group included matched those studied in the majority of CTO studies internationally, to facilitate comparisons.
Clinical decision-making
Once we had recruited a patient and conducted the baseline interview, legal advice indicated that the correct procedure was for the independent statistician to advise the RC on the random allocation, who would then allocate the patient to either the CTO group or the non-CTO group. In practice, RCs referring to the trial undertook to allocate the patient according to the statistician’s advice; this is no different from the usual randomisation procedure in any RCT. This procedure is referred to simply as ‘randomisation’ below.
After patients had been recruited and randomised, it was stipulated that when RCs made decisions about them, they should strictly adhere to the statutory process and criteria in every case, as the law required, and should fully consider every option open to them within the legal regime and the relevant factors listed in the statute or the Code of Practice. We thus did not exercise control over clinical decisions subsequent to randomisation. Patients in both groups retained all their usual legal rights, including their right of access to the MHRT, which might discharge them from compulsory treatment. No attempt was made to influence how clinicians subsequently managed these patients, including whether the clinicians decided to renew a patient’s treatment on Section 17 Leave or renew their CTO. When a patient was discharged from involuntary treatment by the RC or the MHRT, or transferred from Section 17 Leave to a CTO, for instance, as required by law, this would simply be counted as one outcome of the process for that patient.
Patients in the CTO arm of the study might therefore, during the follow-up period, be recalled to hospital, have their CTO revoked or be discharged from it. Patients in the non-CTO arm might be discharged to voluntary status after the initial period of leave, or might have it renewed, or they might, in exceptional cases, be put on a CTO. (Details of which of these scenarios we handled as protocol violations are given below, under Methods, while actual protocol violations appear under Results.) Given the Code of Practice, there was a reasonable expectation that the majority of patients randomised to the non-CTO arm of the trial might proceed fairly swiftly to voluntary status. We collected data on changes to legal status systematically as part of the trial.
Recruitment of trusts, teams and patients
Procedures and NHS permissions
Permission to carry out the trial needed to be obtained for each trust, and each research assistant needed to obtain personal permission to access professionals, patients and medical records in each trust. We sought permission to conduct the trial locally from R&D offices in around 60 NHS trusts that provided mental health services in England. All trusts within a reasonable travelling distance were approached.
Having secured R&D approval, we carefully mapped that trust’s services before embarking on extensive information sharing and a series of meetings with the mental health teams to secure their collaboration.
We then identified potentially eligible patients from a network of CMHTs and AOTs agreeing to participate in the trial. In NHS trusts with a split between inpatient and outpatient services, patients were recruited via the inpatient service. This happened, however, in agreement with the outpatient service to which the patient would be transferred when leaving hospital. All community teams had to be able to provide approximately weekly contact with the patient.
Following identification of an eligible patient, a member of the care team then approached the patient and secured agreement that one of the study researchers could make contact. This researcher then assessed and recorded the patient’s capacity to participate in research and sought written informed consent for inclusion in the study. Once the consent form had been signed and the baseline assessment completed, the patient was randomised.
For the follow-up interviews, the researcher contacted the mental health team to confirm that the patient was still in their care or, if not, where they were then based; and whether they believed that it was appropriate to contact the patient.
Obtaining access in NHS trusts
Obtaining permission in the NHS trusts we approached proved much more time-consuming than expected. The time required to deal with our applications varied considerably. Although one trust was able to process the necessary paperwork in a matter of days, for others it took nearly a year; in some cases, it took longer and we were eventually obliged to give up. The extent of documentation required varied and, although this was usually easily dealt with, it caused some delays, in particular in the cases when a trust required specific contracts drawn up between themselves and the host trust. One trust refused collaboration because the service leads did not give their support to the study. Two others refused as a result of their own internal peer reviews of the protocol: one review concluded that there was no immediate benefit to that trust; the other deemed the protocol unethical. It took us between 2 days and, in one case, 11 months, to gain R&D permissions in the 44 trusts. Of these 44 trusts, 32 trusts – predominantly in the Midlands and southern England – recruited to the trial (see Results, below).
Each of our research assistants (14 in all, over the 28 months of recruitment and data collection) was required to obtain individual permissions in each of the collaborating trusts in which they were working. We found that a wide range of procedures for obtaining such letters of access was required. Despite NHS guidelines, a number of trusts required new Criminal Records Bureau (CRB) checks to be conducted, which caused several months delay in each case. In total, 607 letters of access, 56 honorary contracts, 17 research passports and seven clinical licences were processed and issued to our researchers: on average, 21 contracts per trust. In addition to this, 51 CRB checks were also performed (on top of those issued on behalf of the employing trust).
Getting mental health teams and their patients on board
We initially focused on recruiting from AOTs, so began by mapping the location and contact details of these teams in the participating trusts. It proved more difficult than we had expected to find out the number and location of AOTs, as it was hard to find people within each trust with an overview of how services were organised and divided both geographically and functionally. This process resulted in a largely complete map of AOTs across our chosen trust areas, of which there were approximately 200.
We had initially envisaged that the vast majority of the patients placed on CTOs in England would come from AOTs, as both AOTs and CTOs were designed to be employed for revolving-door patients. We quickly realised, however, that a considerable proportion of patients from regular adult CMHTs were also being placed on CTOs, and we therefore made the decision to recruit from these CMHTs as well as AOTs. This was a huge undertaking. Not only were there on average three times the number of CMHTs as AOTs in each trust, but also the functional split between inpatient and outpatient care meant that all of the inpatient services into which CMHTs fed had to be contacted separately. This meant that we had a total of approximately 1000 potential teams, including CMHTs and AOTs, as well as approximately 500 inpatient units.
We contacted by e-mail and telephone the team leaders, the consultant psychiatrist for each team and the medical directors for each trust. It was at this point that it became apparent to us that services were increasingly being split into those providing care for inpatients and those providing care for outpatients. This situation differed from the pre-existing arrangement in which a consultant psychiatrist was attached to a particular geographical area, within which he or she had responsibility for the care of patients regardless of whether they were currently in hospital or in the community. This increased the number of consultant psychiatrists we were to contact considerably.
Once contact had been established with the mental health teams and information about the OCTET Trial had been sent to them, we used a combination of large meetings, forums, academic meetings and individual team meetings to inform teams and doctors about the study and agree a plan for the recruitment of their patients to the study by their own referral. We also met with ward managers and inpatient consultants to secure their agreement for us to monitor the inpatient wards for eligible patients. We then e-mailed or telephoned the clinicians responsible for potentially eligible candidates to seek their permission to meet the patient and proceed with the consent process. Our recruitment therefore proceeded along two routes: both through the direct referral of patients by the consultant and team and through the identification of eligible patients from wards.
In getting teams on board, holding large meetings in which many teams and doctors were present was most successful. In these meetings, the issues surrounding the OCTET Trial were thoroughly discussed. In each case, we then held a series of smaller meetings with individual interested teams and consultants, to discuss practicalities and specifically to ascertain whether or not there were any suitable patients known to the team. This ensured that research assistants mainly travelled to individual teams that had already expressed interest in the study and that were aware of the broad outline of the study. Even so, many teams were unable to find eligible candidates once they heard the inclusion criteria in more detail, even when they were happy to do so in principle. In these cases, the inpatient ward monitoring process was designed to ensure that should any eligible candidates exist in the future, they would be identified.
Ultimately, recruitment was most successful with teams and doctors who had met a member of the team in person and had the opportunity to discuss any issues and concerns in detail. Owing to the number of teams involved, this initial setting-up phase of the study was both resource heavy and time-consuming. Once the teams and doctors were familiar with the study team, however, they were often happy to receive further e-mails prompting them to refer or asking permission to see a patient identified on the ward. This system made recruitment reliable and efficient, despite requiring a considerable input of effort initially. Because of the complexity of the study, the recruitment of patients by a less personal process, for example solely by e-mail, often resulted either in a refusal to recruit, or in confusions and misunderstandings about the study process, and ultimately wasted time. As teams were located in such disparate locations as Cornwall, Lincolnshire, Greater Manchester and Birmingham, one of the biggest challenges in the OCTET Trial was to use this personal and hands-on approach with a team of six researchers, all of whom were based in Oxford.
Potential obstacles to referral were many and varied. First, some team members or consultants were not in equipoise, so were opposed in principle to allocating their patients randomly to one of two different legal statuses. Both the multidisciplinary nature of mental health teams and the functional inpatient–outpatient split increased the number of professionals involved in, and responsible for, the care of individual patients, which ultimately increased the likelihood of at least one of those professionals objecting to the patient’s involvement in the trial. This proved to be the biggest problem: when the parties in disagreement were the inpatient and outpatient clinicians for one patient, one of whom would implement the CTO, or not, depending on the outcome of randomisation, and the other of whom would manage the patient in the community. If these parties could not agree on the acceptability of randomisation then recruitment could not go ahead. Once a patient had been identified as eligible and permission had been gained from both the inpatient and outpatient consultants, and the relevant team members where necessary, we would be able to approach the patient.
This final stage of recruitment also posed several problems. First, access to wards in trusts that were remote from our own proved at times unreasonably difficult, given that we had official researcher access to all relevant sites. Second, a lack of communication between doctors and ward staff, or within the ward, resulted in a few cases in patients being sent on leave or discharged before we could see them. This was despite the rapidity with which the research team responded to patient referrals, often seeing patients no more than a few hours after they had been referred. A third issue was premature referral, which resulted in some patients being too unwell at the time we saw them to give informed consent. This did not often prevent the patient being recruited, as the researchers would return to the ward when they were well enough, but it did waste time and resources. Last, patients themselves sometimes refused to take part or were judged by the research team to lack the capacity to consent. We stayed in contact with the recruiting teams regularly via e-mails or phone calls, and we produced a monthly newsletter in which we provided information about the progress of the trial and relevant information about CTOs. We stayed in touch with patients via postcards at Christmas and made contact again some weeks before each 6-monthly interview.
In these extensive recruitment activities, we got considerable support from the Mental Health Research Network, the clinical support officers of which often provided considerable practical assistance in local NHS trusts, such as making contact with hospital wards and local clinicians, and in some cases helping with obtaining R&D access and accessing medical records.
In total, the study team assessed 442 patients, of whom 336 were randomised, as we detail in Results.
Methods
Sample
Recruitment took place from 10 November 2008 to 22 February 2011.
Eligible patients were those:
-
aged 18–65 years (in line with local administrative procedures for adult mental health services)
-
diagnosed with psychosis
-
currently admitted under Section 3 or Section 37 (without restrictions) of the MHA
-
not currently subject to any other legal restrictions
-
judged by their clinicians (RC and AMHP) to need ongoing community treatment under supervision
-
able to consent to take part in research and give written and informed consent
-
not participating in the study already (i.e. patients with multiple admissions throughout the recruitment period should participate in the study only once).
We did not exclude patients with insufficient English language to complete the interview. As the research instruments were not validated in different languages, these patients could not be interviewed, but we collected data from their medical records and invited them to take part in the Qualitative Study in their own language.
Patients were not eligible if they were:
-
unable to give informed consent (e.g. advanced dementia or mental disorder too severe)
-
subject to incompatible legal restrictions on treatment
-
considered to be clear candidates for immediate discharge to voluntary treatment
-
already on Section 17 Leave for > 30 days.
We invited mental health professionals to complete questionnaires about their therapeutic relationships with the patient and the patient’s quality of life if they were:
-
currently the care co-ordinators of the recruited patient and employed by the NHS at baseline and/or 12 months
-
providing care for the recruited patient (for at least the past 3 months).
We originally intended to recruit family carers of the sampled patients to undertake a questionnaire survey at the 6-month follow-up point. We later decided to omit this, however (see Changes to protocol from original proposal).
Objectives and hypotheses
The primary objective of the OCTET Trial was to test the hypothesis that patients with psychosis and a history of compulsory admissions in the CTO arm of the trial would experience a reduction in readmissions to hospital compared with those not placed on a CTO. The secondary and tertiary objectives were to investigate whether or not such patients would experience a greater delay to readmission, shorter admissions or improvements in a range of clinical and social outcomes.
The exploratory objectives of the trial were to identify the baseline characteristics of patients associated with differential treatment effects; to examine the factors (other than treatment group) associated with readmission; and to explore the effect on readmission of process variables such as rate of contact.
Cost-effectiveness was also evaluated and this is reported separately (see Chapter 7).
Sample size and power calculation
The North Carolina trial64 demonstrated a difference of 16% in the proportions readmitted to a psychiatric hospital within 12 months (32% in the group under outpatient commitment vs. 48% in the control arm). We calculated that to detect a similar difference with a significance level of 5% and power of 80%, assuming that rates of readmission would be comparable in our control group, would require a sample size of 288 patients. We predicted that attrition would be negligible, as primary outcome data would be available from medical records. With this number of patients, we calculated that we would also be able to detect either of the following differences as statistically significant at the 5% level with 80% power:
-
a 14-day difference in the mean number of days spent in hospital over 12 months (e.g. a reduction of 28 days to 14 days)
-
a difference of 0.43 in the mean number of readmissions over 12 months.
Data collection
We collected data from medical notes and structured patient interviews with independent, trained researchers at baseline and at 6 and 12 months. Detailed assessments included demographics, clinical history, prior MHA use and criminal justice history. We assessed current status using well-validated and widely used structured questionnaires, as detailed in Instruments. The researcher read out the questions and recorded the patient’s replies. The full assessment battery took between 45 and 90 minutes to complete. We pursued notes from other teams or hospitals or from MHA offices when applicable. In all cases, we collected all primary outcome data from Trust information systems. We collected data on diagnosis and current medication from case notes. We also confirmed data on sociodemographics and psychiatric history, collected in the Socio-demographic Schedule (see Instruments), from case notes.
We collected 6-month data for use in the analyses along with the 12-month data, but did not intend to report them independently. We used the three data points in order to have sufficient power for the modelling of the within-patient variability in the multilevel analysis. Collecting 6-month data also ensured that the research team was able to keep in contact with the patients and as a safety net in case there proved to be significant difficulties in follow-up at 12 months.
Outcomes
We chose outcome measures for the trial based on the evidence in the literature about the most appropriate hospitalisation outcomes to capture the outcome and process of CTOs, as well as relevant clinical and social functioning outcomes (see Chapter 5, Background). We chose the rate of readmission as our primary outcome because CTOs had been legislated explicitly for this outcome. It was the primary outcome in most major studies,3,4,61 including the only two published randomised trials. 63,64 It is also accepted as the best measure for relapse prevention85 and therefore a proxy for community stability.
The primary outcome measure was therefore psychiatric readmission in the 12-month follow-up period, as a binary outcome. We defined a readmission as the period between the patient’s admission date and the date on which the patient left hospital, which should include at least one overnight stay. Readmissions could be either voluntary or involuntary. We did not classify recall to hospital of a patient on a CTO as a readmission, as it was understood as being part of the CTO process rather than an outcome. If a recall ended in the CTO being revoked, we counted this as a readmission, calculated from the first day of the recall. The follow-up point was defined as 365 days after randomisation (referred to below as ‘follow-up’).
Secondary outcomes related to readmission followed the same readmission definition and constraints. We mainly obtained these from medical records. They represented patterns of readmission, as follows:
-
number of nights in psychiatric hospital from randomisation (index) to follow-up
-
days in community until first readmission
-
number of readmissions from first discharge to follow-up, per patient
-
days under legal compulsion (measured by time being subject to the MHA 2007 under Sections 2, 3, 4, 37, 48, 49, 135, 136 or on a CTO) from randomisation (index) to follow-up
-
number of patients with multiple readmissions.
Tertiary outcomes were mainly self-reported patient outcomes. These were:
-
clinical and social outcomes
-
medication
-
experiences of and satisfaction with services
-
experiences of leverage and perceived coercion
-
employment.
Safety outcomes were covered by self-reported items in the clinical research forms. Additional safety outcomes included death and cause of death.
Instruments
We utilised the following instruments with patients to measure the outcomes detailed above. Unless otherwise specified, they were patient rated at baseline and at 6- and 12-month follow-up, and relate to the 6-month period prior to interview.
Demographics and psychiatric history
-
The OCTET Socio-demographic Schedule This collected data on three areas:
-
‘Self and Home’ (basic information including age, sex, ethnicity and educational achievement, employment, family, including marital status; living situation).
-
‘Clinical History’ (diagnosis, psychiatric history, current psychiatric medication), which was corroborated from medical records.
-
‘Legal History’ (criminal convictions, imprisonments).
-
Clinical and social outcomes
-
Symptom severity The Brief Psychiatric Rating Scale (BPRS),97 a researcher-rated instrument, was used to assess symptom severity on a scale from ‘1’ (not present) to ‘7’ (extremely severe) over the last 2 weeks. The total score (range 24–168) is a sum of ratings across 24 symptom domains.
-
Insight The Insight and Treatment Attitudes Questionnaire (ITAQ)98 is an 11-item questionnaire assessing patient awareness of illness and need for treatment on a three-point Likert scale (no = 0, possibly = 1, yes = 2). Total scores range from ‘0’ (no insight) to ‘22’ (full insight). Its two subscales are the Awareness of Illness Scale and the Attitude to Treatment Scales (range 0–10 and 0–12, respectively).
-
Substance misuse The CAGE99,100 is a screening questionnaire for alcohol and drug misuse. Four items are rated for each area, covering the last 30 days, with yes/no responses. Two or more positive responses indicate a drink/drug problem. Its four questions focus on ‘Cutting down’, ‘Annoyance by criticism’, ‘Guilty feeling’ and ‘Eye-openers’, providing the acronym for the scale.
-
Social functioning The Global Assessment of Functioning (GAF),101 a researcher-rated, single-item scale, was used to assess impairment in functioning over the previous 2 weeks. Scores range from ‘1’ (severe, life-threatening impairment) to ‘100’ (superior functioning). The rating is based on the information collected during the course of the interview.
-
Overall social outcomes The Objective Social Outcomes Index (SIX)102 summarises objective indicators of social outcomes (employment, housing, living status and social contacts) in one overall score (range 0–6), with higher scores indicating better social outcome.
-
Health-related quality of life The EuroQol-5 Dimensions (EQ-5D),103 a non-disease-specific five-item scale, is commonly applied in health economics research and was used to ascertain the patient’s self-description and valuation of their health status. Data from this measure are reported under OCTET Economic Evaluation (see Chapter 7).
Medication
-
Type of medication We collected data on prescribed psychotropic medication from medical records.
-
Attitudes and adherence to medication The Drug Attitude Inventory, 10-item version (DAI-10)104,105 assesses experiences of, and attitudes towards, medication. Patients rate 10 statements as true or false (variously scored as ‘–1’ or ‘1’). The total score ranges from ‘–10’ (negative subjective response/adherence) to ‘10’ (positive subjective response/adherence).
Experiences of services
-
Therapeutic relationships The Scale To Assess Therapeutic Relationship–Patient Version (STAR-P)106 assesses community patients’ relationships with their care co-ordinators. Patients rate, on a five-point Likert scale (0–4), the frequency with which communication, consultation and trust is present in interactions across 12 items, which constitute three subscales: Positive Collaboration (range 0–24), Positive Clinician Input (range 0–12) and Non-Supportive Clinician Input (range 0–12). The total STAR-P score ranges from ‘0’ to ‘48’. Higher scores indicate better relationships on all scales (with Non-Supportive Clinician Input being reverse scored).
-
Satisfaction with services The Client Satisfaction Questionnaire (CSQ-8)107 assesses satisfaction with health services on eight items using a four-point Likert scale (1–4). It yields a total score ranging from ‘8’ (low satisfaction) to ‘32’ (high satisfaction).
-
Preference for joint decision-making and information-seeking The Autonomy Preference Index (API),108 adjusted to the mental health setting,109 is a 23-item questionnaire on preferred autonomy (14 items were utilised for the purposes of our analysis). Its two subscales are the Decision Making Preference Scale, which measures patients’ desire for their own rather than their psychiatrists’ involvement in clinical decision-making, and the Information Seeking Preference Scale, which measures patients’ desire to be informed about their illness and treatment. Both use five-point Likert scales (strongly agree = 1, strongly disagree = 5). Adjusted scores for each subscale range from ‘0’ to ‘100’, where ‘0’ is a lack of desire to be involved/informed, ‘100’ the strongest possible desire and ‘50’ indicates a neutral stance.
Experience of leverage and informal coercion
-
Experience of coercion The MacArthur Leverage Interview7 ascertains patients’ experience of leverage. Leverage was defined as making support to obtain housing, money and child custody conditional on treatment adherence or reducing or dropping criminal charges if patients adhered. It is a semistructured interview designed to ascertain experience of leverage during the 6 months prior to interview and across the patient’s lifetime. Here we report experience over only the previous 6 months. We adapted it for use in the English setting for the ULTIMA Study, including adding a section asking about child access. Questions test for both access to, and potential withdrawal of, benefits. Any positive response within a specific coercion area counts as ‘reported’ (Box 2).
-
Perceived coercion The MacArthur Admission Experience Survey (AES),111 adapted for outpatient use,112 contains 14 statements rated on a five-point Likert scale (1 = strongly agree, 5 = strongly disagree). There are three subscales:113 the Perceived Coercion Scale assesses perception of influence and control in treatment decisions (range 5–25, with a high score indicating a high level of perceived coercion); the Negative Pressures Scale assesses experienced threats and force (range 6–30, with a high score indicating higher negative pressure after reverse scoring); and the Procedural Justice Scale assesses experience of having a say in one’s care (range 3–15, with a high score indicating feeling less involved in one’s care). No total score for the AES was utilised.
-
Fairness and effectiveness of pressure The Index of Fairness assesses patient agreement with statements on the fairness of any treatment pressure they have experienced in the last 6 months, and the Index of Effectiveness assesses their views of how effective this pressure has been in making them stay in treatment and gain control. 114,115 It is rated on a five-point Likert scale (1 = strongly agree, 5 = strongly disagree) with a total score for each scale (range 4–20), with higher scores indicating that the pressure is viewed as more fair/effective.
Have you ever lived somewhere where you were required to stay in mental health or substance use treatment (or required to continue taking your medication) to keep living there (including family home)?
Have you ever been told that obtaining new accommodation is dependent on you taking treatment?
FinanceHas a financial manager/guardian ever made giving you your money or giving you spending money depend on whether you did what he or she wanted in terms of getting mental health, alcohol or drug treatment (or taking medication?)
Whether or not you have a financial manager/guardian, has anyone who handles your money for you or helps you manage your money ever made giving you the money or giving you spending money depend on whether you did what he or she wanted in terms of getting mental health, alcohol or drug treatment (or taking medication?)
Criminal justiceHas anyone in the legal system ever told you or your lawyer that the charges will be dropped or reduced if you get treatment in the community for your mental health, alcohol or drug problems?
Has a mental health professional, or anyone in the legal system (a judge, a magistrate or your lawyer), or their report, suggested that you take treatment for a mental health problem as a condition of not going to prison?
Child custodyHave you ever been told that your children might be taken into care if you did not participate in mental health, alcohol or drug treatment (or taking your medication)?
Have you ever been told that your access to see your children would be reduced if you did not participate in mental health, alcohol or drug treatment (or taking your medication)?
Service usage
-
A modified version of the Client Service Receipt Inventory (CSRI),116 which measures the number and duration of contacts the patient has had with a range of health and social care professionals during the 6 months prior to interview and the location of these meetings (24 items). (Some data from this measure are reported below but it was most extensively used for the OCTET Economic Evaluation reported in Chapter 7.)
(The full Schedule of Procedures and the instruments listed here are available from the authors on request.)
Outcome data from medical records
We collected outcome data on readmissions and MHA use from patients’ medical records. This included questions on legal status (whether under section or not), CTO recalls and conditions (both over 12 months), tribunals and managers’ hearings. We also pursued notes from other hospitals and from the criminal justice system where applicable.
Blinding
It would, of course, be impossible to blind clinicians or patients in a trial for which knowledge of the intervention is part of the intervention itself. Moreover, it would be unlawful not to inform each party of legal status. It was not possible to blind researchers to randomisation. Research assistants were blind to randomised status during the baseline assessment.
Randomisation and masking
Randomisation was a stratified block design with a 1 : 1 allocation ratio. Eligible patients had an equal probability of assignment to each arm of the trial. Patients were randomised individually to either the CTO or the non-CTO arm by an independent statistician using stratified block randomisation for gender (male/female), schizophrenic status (yes/no) and duration of illness (< 2 years, ≥ 2 years). We developed the randomisation code using a computer random number generator to select random permuted blocks. The block lengths were two, four and six, varied randomly.
A researcher independent to the trial team enclosed assignments in sequentially numbered, opaque, sealed envelopes and stored them. The details of the sequence remained unknown to all members of the trial team until recruitment, data collection and analyses had been completed. The sealed envelope was labelled with the stratum number, gender, schizophrenic status, duration of illness and an envelope number. A matching label inside, also numbered, specified the intervention arm. Randomisation took place after consent had been obtained and the baseline interview had been performed. The envelope was opened on the day of the interview by the independent researcher after recording the patient’s trial identification number on the envelope. She then communicated the randomised allocation to the recruiting researcher by telephone. As randomisation involved allocation to different legal statuses, it was both impossible and unlawful to mask research assistants, treating clinicians or patients.
Protocol violations
Protocol violations were predefined as arising when patients were:
-
withdrawn
-
ineligible
-
discharged to the wrong treatment arm
-
never discharged from hospital.
Patients who were protocol violators of any of these predefined types were included in our intention-to-treat analysis. We counted those patients who never left hospital during the follow-up period as having had one readmission of 365 days.
Statistical methods
All analyses were performed using Stata/SE version 12 (StataCorp LP, College Station, TX, USA).
The trial team wrote and signed off a detailed statistical analytical plan before any data were analysed (see Appendix 2). All analyses were done according to the analysis plan. Blinding of the statistical analysis, methods for dealing with outliers, missing data, computation and methods are detailed there.
Intention-to-treat population
Analysis was carried out on an intention-to-treat basis (n = 336), except for the tertiary analyses for which the sample was 333. The intention-to-treat population included all randomised patients; we thus analysed data from dropouts or protocol violators according to their randomised group.
Baseline characteristics, interview refusers and loss to follow-up
We assessed the baseline comparability of the two randomised groups by tabulating patient characteristics and treatment experiences; we did not perform any statistical tests on baseline data. We compared the baseline characteristics of any patients who refused to participate in follow-up interviews (or who had inadequate English language for this) to those of patients completing the follow-up interviews.
Primary analysis
The primary analysis was a test of the difference in the proportion of patients readmitted to a psychiatric hospital during the 12-month follow-up period between the CTO arm and the non-CTO arm. We analysed the primary outcome using a log-binomial regression model adjusted for the stratification factors (sex, schizophrenic status and duration of illness). Results are presented as the relative risk of readmission for the CTO group compared with the non-CTO group, with appropriate 95% confidence intervals (CIs) and two-sided p-values.
Secondary analyses
We conducted secondary analyses using the intention-to-treat population. There were no missing data for secondary outcomes. We analysed secondary outcomes in the same way as primary outcomes, using multiple regression models with adjustment for stratification factors. The type of regression model depended on the data distribution. All model assumptions were assessed.
Number of readmissions and number of nights in psychiatric hospitalisation are count outcomes, and we analysed these using adjusted zero-inflated Poisson and negative-binomial regression models, respectively. Results are presented as adjusted incidence–density ratios (IDRs) with 95% CIs, and interpreted in the same way as relative risks.
The number of nights from first discharge to first readmission and the time spent under compulsion are time-to-event outcomes. We therefore performed these analyses using adjusted proportional hazards regression, and present the results as hazard ratios (HRs) with 95% CIs. Kaplan–Meier plots are also presented and the median time to readmission is calculated with 95% CIs. We used the log-rank test to compare the median time under compulsion between the two arms, whereas we used the Wilcoxon rank-sum test for comparison of time to first readmission, as this variable violated the log-rank test assumptions.
Tertiary analyses
We conducted tertiary analyses using the population of 333 patients (omitting the three exclusions). Thus we included all available data from all of the patients, and imputed missing values intrinsically within the model rather than requiring multiple imputations.
Sensitivity analyses
We conducted a repeated measures sensitivity analysis for end points measured at multiple time points using multivariable mixed-effects regression models. We used the Stata command xtmixed for continuous end points, xtlogit for binary end points and xtmelogit for multiple category end points. We included all available data from all patients, with missing values intrinsically imputed within the model rather than requiring multiple imputations. We entered treatment, stratification factors and time point (time since randomisation) into the model as fixed effects, and the model contained a patient-specific random intercept. We treated an interaction between time point and treatment group as a fixed effect to allow estimation of treatment effect at each time point. We also used likelihood ratio tests to assess whether or not time should be included in the model as a random effect. We also explored different covariance structures.
As a sensitivity analysis, we imputed missing data in self-reported outcomes using multiple imputations117 in the mi routine in Stata. Subsequently, we used regression modelling to estimate the association between change from baseline to 12 months and study arm, adjusting for baseline end point and randomisation factors. We chose the regression models according to the distribution of the end points (logistic models for CAGE, leverage and employment; linear models for CSQ-8, STAR-P, BPRS, GAF, ITAQ, DAI-10, API, SIX, AES subscales, Index of Fairness and Index of Effectiveness).
We performed safety analyses according to the statistical analysis plan (see Appendix 2).
Subgroup analysis
Subgroup analyses are designed to explore whether or not any treatment effect tested in an RCT varies across subgroups defined by baseline patient characteristics. 118
We defined binary subgroups a priori, as identified in the literature to be related to outcomes. We performed subgroup analysis for the primary outcome, all of the secondary outcomes apart from time under compulsion and for the main clinical outcomes, BPRS and GAF. Potential errors (i.e. increased type 1 error and decreased type 2 error) introduced by a subgroup analysis were controlled by selecting the subgroups and stabilising the hypothesis to test (i.e. equal direction of effect as for the overall sample) prior to accessing the data and thus performing the analysis. With 13 subgroups there is a 12% chance of at least one subgroup resulting significant at the 5% level. All conclusions were written paying due consideration to this fact.
We evaluated 13 groups in this analysis, the first three of which were used as stratification factors during randomisation:
-
diagnosis: schizophrenia spectrum versus other psychoses
-
duration of illness: < 2 years versus ≥ 2 years
-
gender: male versus female
-
age: ≤ 40 years versus > 40 years
-
ethnicity: white, black, Asian, mixed race and ‘other’
-
immigration history: UK versus other
-
marital status: married/co-habiting versus single/separated/divorced
-
living status: living alone (including homelessness) versus living with others
-
accommodation status: independent versus supported/homeless
-
years of education: ≤ 12 years versus > 12 years (as 12 years of education is compulsory in England)
-
tertiary education: ‘yes’ versus ‘no’
-
BPRS: ≤ 33 versus > 33
-
GAF: ≤ 49 versus > 49.
We performed the subgroup analysis by fitting the same models as for primary and secondary outcome measures plus an additional interaction effect for interactions between study arm and the relevant subgroup variable. The p-value of interest is that for the interaction test.
Data management
The researchers recorded data in the clinical research forms by hand and two different researchers double-entered them into IBM SPSS version 20 (IBM Corporation, Armonk, NY, USA). Double-entered data were compared against each other, and discrepancies were discussed and corrected by the research assistants under supervision. The statistician responsible for the analysis conducted additional data quality evaluations. These included range checks and logical and consistency checks that might not be picked up by checks at the individual patient level by the research staff who collected and entered the data. In the case of variables that were a function of other variables (e.g. length of a particular readmission), these were checked by automatic calculation of the variable’s values, except for total scoring of the individual instruments, which was performed automatically using a validated code. We froze the final cleaned data before analysis commenced.
Changes to protocol from original proposal
Family carers questionnaire
According to the original protocol, we were to ask the patients to identify family carers and ask their consent to contact the carer. These carers were then to be sent a carer questionnaire by post, enclosing a letter with full information about the study. We initially undertook this part of the trial but it had a poor response rate. In July 2010, of the 135 patients who had reached the 6-month follow-up point, 38 had agreed to a carer being contacted and only two of those carers had returned a questionnaire. It was anticipated that many of the patients who were eligible for the trial had limited contact with their family, so this result was not surprising. With a response rate of 3%, we decided not to pursue this part of the study, as the results would not be representative or robust. Some of the items covered in the questionnaire, such as carer strain and perceptions of patient well-being, were included in the topic guide for the qualitative interviews with family carers.
Clinical staff questionnaire
According to the original protocol, care co-ordinators were to be asked to complete two validated instruments covering demographics, the therapeutic relationship with the patient, and their assessment of the patients’ health-related quality of life, at both baseline and 12 months. The questionnaires were handed to the relevant staff, or were posted to them, or both. A poor response rate at baseline, however, was compounded by multiple changes of staff, which made identifying the appropriate staff group at follow-up almost impossible. The information sought was designed to be analysed in conjunction with patients’ views of their own health, quality of life and therapeutic relationships, and was thus time sensitive and dependent on a response from a particular individual. Given the difficulties in obtaining this, we therefore decided not to pursue this part of the study.
Statistical analysis
We conducted an additional sensitivity analysis for the primary outcome. This analysis excluded all protocol violators. It was not a prespecified analysis but was conducted to address concerns raised about the number of protocol violators, particularly those who had been discharged to the wrong arm of the trial.
The analyses undertaken were all in line with the spirit of the analyses detailed in the original proposal, but we made some changes to the original proposal when writing the statistical analysis plan: these were changes to the types of statistical models or tests performed to allow for more sophisticated adjusted regression models to be used as the primary comparisons, with the simpler unadjusted tests used for secondary sensitivity analyses. Adjusted regression models have more statistical power (i.e. are more precise) than unadjusted tests such as t-tests, and thus make better use of the data collected.
The original protocol makes reference to minimisation factors. No minimisation procedure was carried out during treatment assignment. Instead, a stratified block design was used. Tertiary outcomes were specified. In particular, we decided to treat satisfaction with service as a tertiary outcome instead of a secondary one. We did not analyse the effect of the discipline of the clinical supervisor in readmissions, as originally planned, as information on this outcome was not available.
We added type of medication as a tertiary outcome, as we considered this to be clinically relevant, given a reported association between CTOs and the use of depot injections. 4 We included this before any of the data analyses were conducted. Patient-rated adherence to medication could not be adequately measured at baseline (patients were recruited while detained in hospital for treatment) and data collected on this during follow-up were of insufficient quality to be included as an outcome. We therefore used the DAI-10, which correlates with clinician-rated adherence,104 as the reported measure for adherence. Missing data made it impossible to analyse different types of leverage separately or divide leverage experience into types of pressure. We originally planned to analyse tertiary outcomes by type of service (e.g. ACT, early intervention, crisis teams), but ongoing service reconfigurations rendered this analysis redundant.
Results
Recruitment
We recruited patients from 32 trusts to the trial, predominantly in the Midlands and southern England (Figures 4 and 5).
FIGURE 4.
Recruiting counties.

FIGURE 5.
Recruitment rates in participating NHS mental health trusts in England.
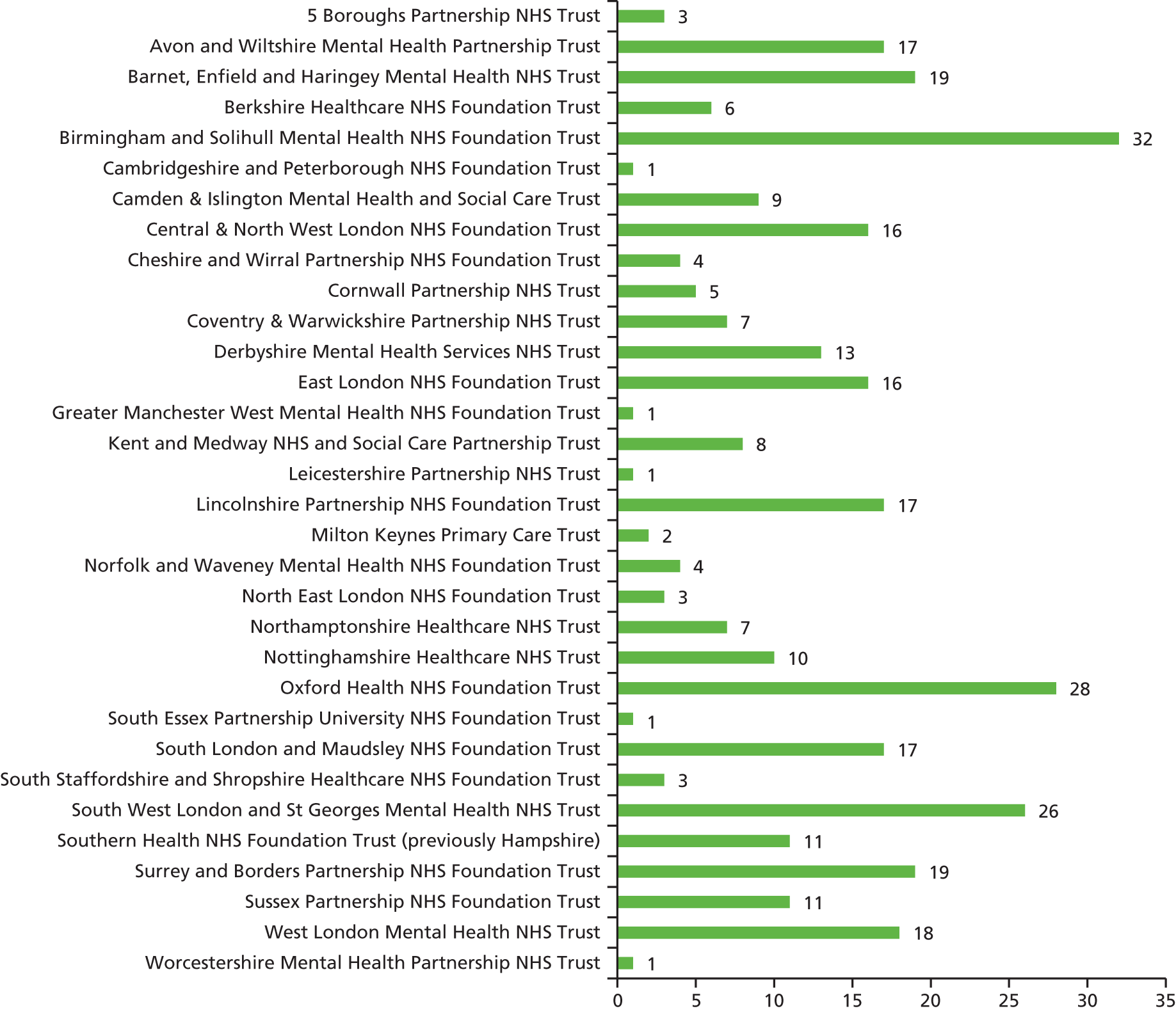
The study team assessed 442 patients in total, of whom we recruited 336. The 106 patients who were not recruited after being approached either refused (n = 91), were found not to be eligible (n = 6) or lacked capacity (n = 9) (Figure 6). The Ethics Committee did not grant us permission to collect any data on those who refused to enter the study or were considered for referral to the study by their clinicians but then not referred.
FIGURE 6.
Trial profile. a, Including three patients deceased during follow-up period; b, including two patients deceased during follow-up period. Reproduced from Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet 2013;381:1627–33,16 with permission from Elsevier.
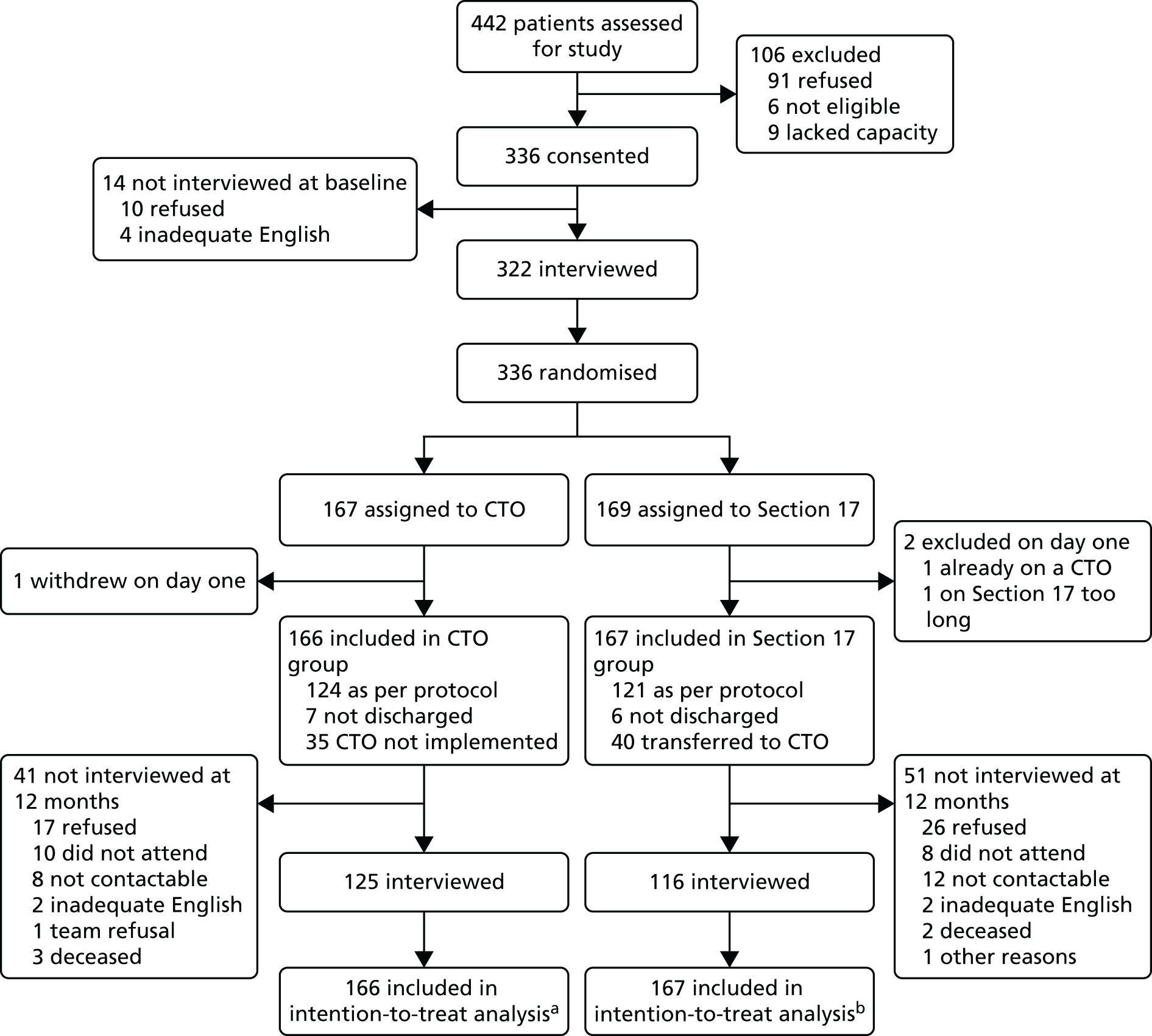
Participant flow
Participant flow is presented in our CONSORT (Consolidated Standards of Reporting Trials) diagram (see Figure 6). The 336 recruited patients were randomly assigned to either the CTO arm (167 patients) or the non-CTO (169 patients) arm of the trial. One patient withdrew and two patients were identified as ineligible directly after randomisation.
Primary and secondary outcome data
We based all of our analyses (apart from the tertiary analyses) on all 336 patients, as we conducted them on an intention-to-treat basis. We had data on the primary and secondary measures for all 333 patients at baseline and 12 months. We included the three patients who either withdrew or were ineligible, with their data missing for all variables, apart from data on the inclusion criteria and the randomisation factors.
Interview data
Of the 336 patients in the trial, 14 were not interviewed at baseline (10 because they wanted to take part but did not want to be interviewed and four because of inadequate English). The remaining 322 patients completed baseline interviews. We compared the baseline characteristics of the 14 patients not interviewed to those of the interviewed patients; there were no obvious differences that might have skewed the subsequent analyses.
At 12 months, we interviewed 241 patients [72%: 125 (75%) of the CTO group and 116 (69%) of the non-CTO group], of whom 189 (56%) completed all three interviews [98 (59%) of the CTO group and 91 (54%) of the non-CTO group]. Those not interviewed at 12 months either refused or did not attend [61 (18%) overall: 27 (16%) of the CTO and 34 (20%) of the non-CTO group], were non-contactable (20 (6%) overall: 8 (5%) of the CTO and 12 (7%) of the non-CTO group), had inadequate English language [4 (1%) overall: 2 (1%) of each group], were deceased [5 (1%) overall: 3 (2%) of the CTO and 2 (1%) of the non-CTO group] or were not interviewed because the clinical team advised against it (one patient in the CTO group) or for other reasons (one patient in the non-CTO group).
Sample: baseline data
Baseline sociodemographic data and data on psychiatric and legal history are shown in Table 2. Of the 336 patients included in the final data analyses, 225 (67%) were males. The vast majority (n = 316, 98%) were not employed. The majority of the patients (n = 206, 61%) were white, with 78 (23%) being black. The majority (n = 259, 77%) had been born in the UK. They had received 12 years of education on average. The majority (n = 241, 72%) were living in independent accommodation and were living alone or homeless (n = 239, 75%). Only a minority (n = 112, 37%) had an identified carer. They had been ill for 12 years on average, with only 14 patients (4%) having been ill for < 2 years. They had experienced an average of four involuntary psychiatric hospital admissions in the past and reported that they had spent a total of 15 months in psychiatric hospital in their lifetime. A substantial minority (n = 133, 40%) had criminal convictions and just over one-quarter (n = 86, 26%) had previously been in prison (see Table 2).
| Patient characteristics | Sample size | CTO (N = 167) | Non-CTO (N = 169) | Total (N = 336) |
|---|---|---|---|---|
| n (%)/mean {SD}/median [IQR] | n (%)/mean{SD}/median [IQR] | n (%)/mean {SD}/median [IQR] | ||
| Age (years) | 336 | 39.8 {11.2} | 39.5 {11.7} | 39.7 {11.4} |
| Male | 336 | 111 (66) | 114 (67) | 225 (67) |
| General education (years) | 332 | 11.8 {1.7} | 12.0 {2.1} | 11.9 {1.9} |
| Ethnicity | 336 | |||
| White | – | 102 (61) | 104 (62) | 206 (61) |
| Black | – | 38 (23) | 40 (24) | 78 (23) |
| Asian | – | 15 (9) | 14 (8) | 29 (9) |
| Mixed and other | – | 12 (7) | 11 (7) | 23 (7) |
| Born in UK | 335 | 135 (81) | 124 (74) | 259 (77) |
| Married or cohabiting | 334 | 11 (7) | 18 (11) | 29 (9) |
| Identified carer | 306 | 62 (41) | 50 (32) | 112 (37) |
| Independent accommodation | 334 | 118 (71) | 123 (73) | 241 (72) |
| Living alonea | 318 | 123 (79) | 116 (72) | 239 (75) |
| Employment | 321 | |||
| None | – | 156 (99) | 160 (98) | 316 (98) |
| Voluntary/protected/sheltered | – | 2 (1) | 1 (1) | 3 (1) |
| Regular employment | – | 0 (0) | 2 (1) | 2 (1) |
| Duration of illness (years) | 327 | 12 [6–20] | 12.5 [5–21] | 12.0 [6–21] |
| < 2 years’ illness duration | 336 | 7 (4) | 7 (4) | 14 (4) |
| Number of hospital admissions | 314 | 6.0 [3–8] | 5.0 [3–9] | 5.0 [3–9] |
| Duration of past psychiatric hospital admissions (months) | 278 | 14.0 [6–28] | 15.0 [7–30] | 15.0 [7–30] |
| Number of involuntary hospital admissions | 303 | 4.0 [2–7] | 3.0 [2–8] | 4.0 [2–7] |
| Any criminal convictions | 305 | 65 (43) | 68 (44) | 133 (44) |
| Any imprisonment | 312 | 41 (27) | 45 (28) | 86 (28) |
Table 3 shows baseline values of clinical characteristics, experiences of services variables and experiences of leverage and perceived coercion. The majority (n = 286, 85%) had a primary clinical diagnosis of schizophrenia. The sample was only mildly to moderately symptomatic (BPRS, median: 38), as would be expected for patients being discharged to the community following successful inpatient treatment. They were a significantly impaired group, however, in terms of their functioning (GAF, mean: 39). Five patients (2%) screened as positive for alcohol or drugs. The sample reported a fairly low level of overall social outcome (SIX, mean: 2.5). They had fairly high levels of insight (ITAQ, median: 13.5), including more positive attitudes to treatment but less awareness of illness (medians: 9 and 6, respectively). The majority (n = 265, 79%) were on oral medication, a small minority were prescribed clozapine (Clozaril, Novartis, Basel, Switzerland) (n = 43, 13%) and a substantial proportion (n = 188, 56%) were on depot medication. They reported somewhat negative attitudes and adherence to medication (DAI-10, median: –2), which was mainly first generation antipsychotic medication.
| Patient characteristics | CTO (N = 167) | Non-CTO (N = 169) | Total (N = 336) | |||
|---|---|---|---|---|---|---|
| Sample size | n (%)/mean {SD}/median [IQR] | Sample size | n (%)/mean {SD}/median [IQR] | Sample size | n (%)/mean {SD}/median [IQR] | |
| Schizophrenia | 167 | 141 (84) | 169 | 145 (86) | 336 | 286 (85) |
| BPRS | 153 | 38.0 [30–48] | 161 | 38.0 [32–49] | 314 | 38.0 [31–49] |
| GAF | 153 | 38.3 {9.4} | 158 | 39.3 {10.2} | 311 | 38.8 {9.8} |
| CAGE: positive for alcohol | 153 | 12 (7) | 153 | 4 (2) | 306 | 16 (5) |
| CAGE: positive for drug | 158 | 14 (8) | 158 | 14 (8) | 316 | 28 (8) |
| CAGE: positive for drug and alcohol | 156 | 4 (2) | 157 | 1 (1) | 313 | 5 (2) |
| SIX | 155 | 2.5 {1.1} | 160 | 2.5 {1.1} | 315 | 2.5 {1.1} |
| ITAQ | ||||||
| Total score | 129 | 14.0 [9–18] | 131 | 14.0 [6–19] | 260 | 14.0 [7–18] |
| Awareness of Illness | 132 | 6.0 [3–8] | 136 | 6.0 [3–8] | 268 | 6.0 [3–8] |
| Attitude to Treatment | 130 | 9.0 [5–11] | 136 | 8.0 [3–11] | 266 | 8.5 [4–11] |
| Prescribed oral medication | 166 | 137 (83) | 167 | 128 (77) | 333 | 265 (79) |
| Prescribed clozapine | 166 | 26 (16) | 167 | 17 (10) | 333 | 43 (13) |
| Prescribed depot medication | 166 | 85 (51) | 167 | 103 (62) | 333 | 188 (56) |
| DAI-10 | 117 | –2.0 [–6 to 4] | 108 | –2.0 [–6 to 4] | 225 | –2.0 [–6 to 4] |
| STAR-P | ||||||
| Total score | 100 | 31.2 {8.9} | 101 | 29.4 {10.4} | 201 | 30.3 {9.7} |
| Positive collaboration | 111 | 15.9 {5.4} | 110 | 14.5 {6.2} | 221 | 15.2 {5.8} |
| Positive Clinician Input | 107 | 7.1 {2.6} | 103 | 6.9 {3.0} | 210 | 7.0 {2.8} |
| Non-Supportive Clinician Input | 109 | 7.9 {2.7} | 110 | 7.9 {2.6} | 219 | 7.9 {2.7} |
| API Decision Making | 135 | 54.8 (16.3) | 142 | 58.4 {19.0} | 277 | 56.6 {17.7} |
| API Information Seeking | 130 | 76.4 (11.2) | 129 | 76.6 {14.6} | 259 | 76.5 {12.9} |
| CSQ-8 | 125 | 21.7 (5.9) | 137 | 20.8 {6.6} | 262 | 21.3 {6.2} |
| Any leverage | 151 | 30 (20) | 151 | 40 (27) | 302 | 70 (23) |
| AES Perceived Coercion | 109 | 14.7 (3.8) | 112 | 15 {4.3} | 221 | 14.8 {4.1} |
| AES Negative Pressures | 114 | 14.4 (4.8) | 116 | 14.6 {4.7} | 230 | 14.5 {4.8} |
| AES Procedural Justice | 112 | 8.3 (2.3) | 109 | 8.5 {2.6} | 221 | 8.4 {2.5} |
| Index of Fairness | 120 | 13.2 (3.2) | 119 | 12.3 {3.6} | 239 | 12.8 {3.4} |
| Index of Effectiveness | 120 | 13.0 (3.4) | 121 | 11.6 {3.7} | 241 | 12.3 {3.6} |
Patients reported their therapeutic relationships to be fairly positive (STAR-P, mean: 30.3), with similar levels across the three subscales. They reported fairly neutral attitudes to being involved in clinical decision-making (API, mean: 56.6) but a greater desire to be informed about their illness and treatment (API, mean: 76.5). They were fairly satisfied with services (CSQ-8, mean: 21.3).
Seventy (23%) of the patients reported having had experience of leverage in the previous 6 months. They rated their care as fairly coercive (Perceived Coercion Scale, mean: 14.8) and reported that they had experienced a fairly high number of negative pressures (Negative Pressures Scale, mean: 14.5). They reported not having much of a say in their own care (Procedural Justice Scale, mean: 8.4). They regarded the treatment pressure they had experienced as only moderately fair (Index of Fairness, mean: 12.8) and effective (Index of Effectiveness, mean: 12.3) (see Table 3).
Baseline characteristics did not differ between those who were interviewed at 12 months and those who were not (Table 4).
| Patient characteristics | Interviewed at 12 months (N = 241) | Not interviewed at 12 months (N = 95) | ||||
|---|---|---|---|---|---|---|
| Sample size | n (%)/mean {SD}/median [IQR] | Sample size | n (%)/mean {SD}/median [IQR] | |||
| CTO (N = 125) | Non-CTO (N = 116) | CTO (N = 42) | Non-CTO (N = 53) | |||
| Age (years) | 241 | 38.9 {10.6} | 40.1 {11.8} | 95 | 42.5 {12.5} | 38.3 {11.3} |
| Male | 241 | 84 (67) | 78 (67) | 95 | 27 (4) | 36 (68) |
| General education, years | 241 | 11.0 [11–13] | 11.0 [11–13] | 93 | 12 [11–13] | 12 [11–13] |
| Ethnicity | 241 | 95 | ||||
| White | – | 77 (62) | 76 (66) | – | 25 (60) | 28 (53) |
| Black | – | 24 (19) | 25 (22) | – | 14 (33) | 15 (28) |
| Asian | – | 12 (10) | 5 (4) | – | 3 (7) | 9 (17) |
| Mixed and other | – | 12 (10) | 10 (9) | – | 0 (0) | 1 (2) |
| Born in UK | 240 | 105 (84) | 87 (76) | 95 | 30 (71) | 37 (70) |
| Married or cohabiting | 240 | 9 (7) | 12 (10) | 94 | 2 (5) | 6 (11) |
| Identified carer | 229 | 51 (43) | 32 (29) | 77 | 11 (33) | 18 (41) |
| Independent accommodation | 241 | 90 (72) | 84 (72) | 93 | 28 (68) | 39 (75) |
| Living alone or homeless | 234 | 92 (77) | 86 (75) | 84 | 31 (84) | 30 (64) |
| Schizophrenia | 241 | 106 (85) | 97 (84) | 95 | 35 (83) | 48 (91) |
| BPRS | 232 | 38.0 [28.4–49] | 38.0 [31–47] | 82 | 39 [33–48] | 38 [34–54.8] |
| GAF | 229 | 38.0 [32–45] | 40.0 [32–47] | 82 | 40 [31–46] | 39 [32–45] |
| Duration of illness (years) | 236 | 10.5 [6–20] | 13.0 [5–21] | 91 | 15 [8–25] | 12 [5.5–21.5] |
| < 2 years’ illness duration | 241 | 5 (4) | 6 (5) | 95 | 2 (5) | 1 (2) |
| Number of hospital admissions | 225 | 6.0 [3–8] | 5.0 [3–8] | 89 | 6 [3–8] | 6 [2–12] |
| Duration of past psychiatric hospital admissions (months) | 203 | 14.0 [6–29] | 15.0 [7–30] | 75 | 14.5 [6–26] | 15 [6–33] |
| Number of involuntary hospital admissions | 215 | 4.0 [2–7] | 3.0 [2–7] | 88 | 5 [2–8] | 5 [2–9] |
| Any criminal conviction | 228 | 49 (42) | 51 (46) | 77 | 16 (47) | 17 (40) |
| Any imprisonment | 233 | 32 (27) | 31 (27) | 79 | 9 (26) | 14 (32) |
Protocol violations
It was impossible to control for protocol violations, as clinical decision-making needed to be unconstrained by the study design for the trial to be lawful (see Introduction/Overview of the OCTET Trial). The treatment of 35 patients in the CTO arm and 40 in the non-CTO arm (22.5% of the whole sample) did not follow the randomised status: these 35 patients from the CTO arm of the trial were never put on a CTO, whereas the 40 patients from the non-CTO arm were put on a CTO directly after leaving hospital. Seven further patients from the CTO arm of the trial and six from the non-CTO arm were never discharged from hospital, making a total of 42 protocol violations in the CTO group and 46 in the non-CTO group: 88 in total. Combined with the three patients who were withdrawn or ineligible, this made a total of 91 protocol violations (Table 5).
| Protocol violation | CTO group (n = 167) | Non-CTO group (n = 169) | Total (n = 336) |
|---|---|---|---|
| Never put on CTO (CTO group only) | 35 | – | 35 |
| Put on CTO when left hospital (non-CTO group only) | – | 40 | 40 |
| Never discharged from hospital | 7 | 6 | 13 |
| Total | 42 | 46 | 88 |
Primary outcome
There was no difference in the primary outcome of psychiatric readmission in the 12-month follow-up period between the two groups, with 59 and 60 patients readmitted in the CTO and non-CTO groups, respectively (see Table 6).
Secondary and major clinical outcomes
There were no differences in any of the secondary hospitalisation outcomes between the two groups or in the major clinical outcomes of symptoms and functioning. At 12 months, neither the total duration of all psychiatric hospitalisations, nor the number of readmissions per patient, the number of patients experiencing multiple readmissions and the number of days spent in the community until the first readmission differed between the two groups (Table 6). (Time to first readmission is also presented in Figure 7.) The pattern of duration of individual readmissions was similar for each group (Figure 8). Neither severity of symptoms nor social functioning differed between the groups at 12 months (see Table 6).
| Outcome | CTO (N = 167) | Non-CTO (N = 169) | Treatment effect (N = 336) | ||||
|---|---|---|---|---|---|---|---|
| Sample size | n (%)/mean {SD} | Median [IQR] | Sample size | n (%)/mean {SD} | Median [IQR] | ||
| Primary outcome | |||||||
| Psychiatric hospital readmission | 166 | 59 (36) | – | 167 | 60 (36) | – | 1.00 (0.75 to 1.33)a |
| Secondary outcomes | |||||||
| Total duration of all psychiatric hospitalisations (nights) | 166 | 82.2 {102.0} | 41.5 [8–109] | 167 | 90.9 {104.5} | 48.0 [10–133] | 0.90 (0.65 to 1.26)b |
| Number of readmissions | 59 | 1.2 {0.6} | 1.0 [1–1] | 60 | 1.4 {0.8} | 1.0 [1–2] | 0.82 (0.58 to 1.16)b |
| Multiple readmissions | 166 | 10.0 (6) | – | 167 | 18.0 (10.8) | – | – |
| Days in community until first readmission | 166 | 246.0 {122.4} | 295.0 [140–357] | 167 | 241.0 {126.5} | 292.0 [126–354] | p = 0.755c |
| BPRS | 122 | 38.2 {11.5} | 35.0 [29–44] | 112 | 38.3 {12.4} | 34.0 [30–43.5] | −1.09 (−3.25 to 1.07)d |
| GAF | 123 | 39.0 {12.0} | 36.0 [31–45] | 114 | 39.7 {13.1} | 35.5 [30–45] | −0.86 (−2.93 to 1.20)d |
FIGURE 7.
Time to first readmission. Reproduced from Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet 2013;381:1627–33,16 with permission from Elsevier.
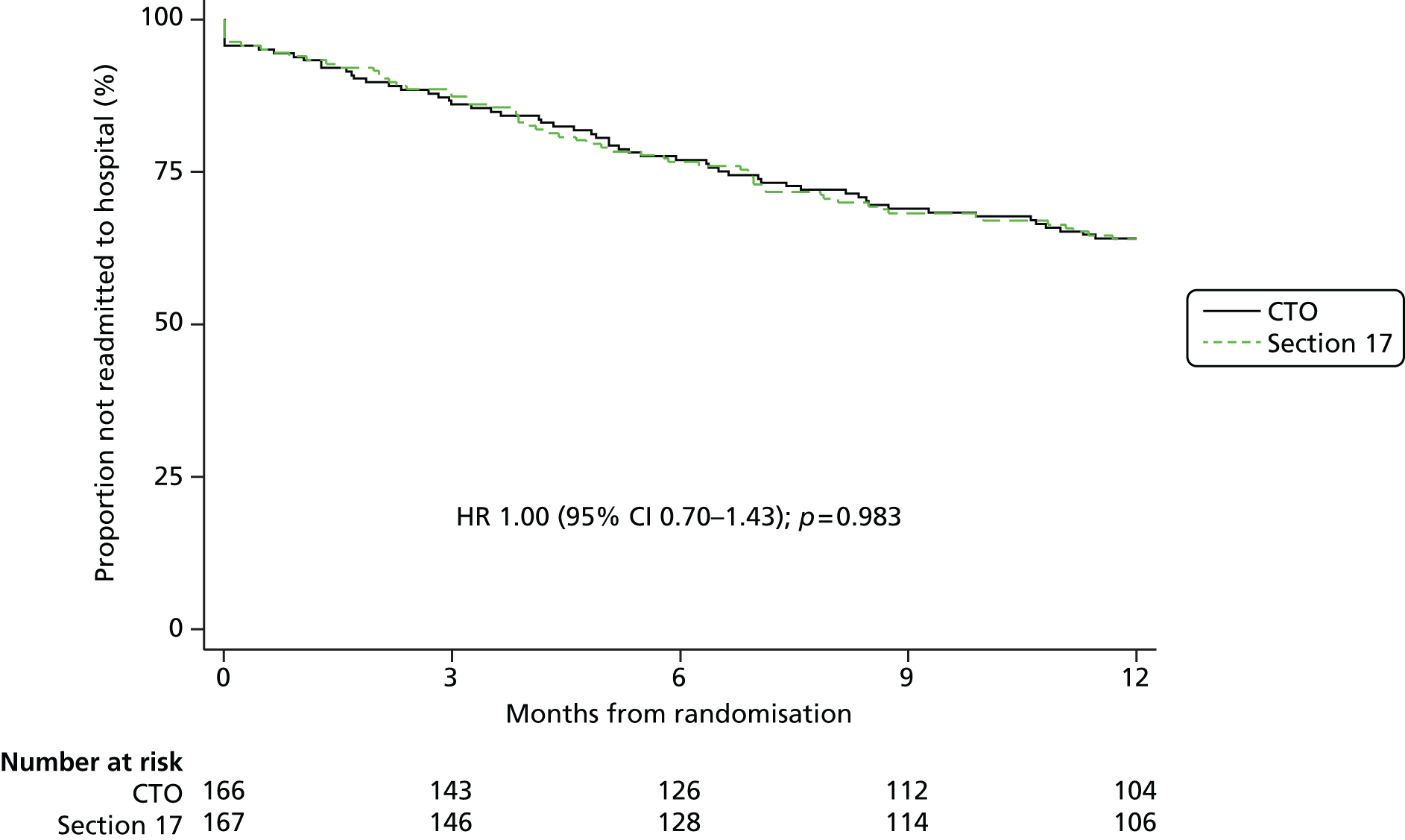
FIGURE 8.
Duration of admissions in months. Reproduced from Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet 2013;381:1627–33,16 with permission from Elsevier.
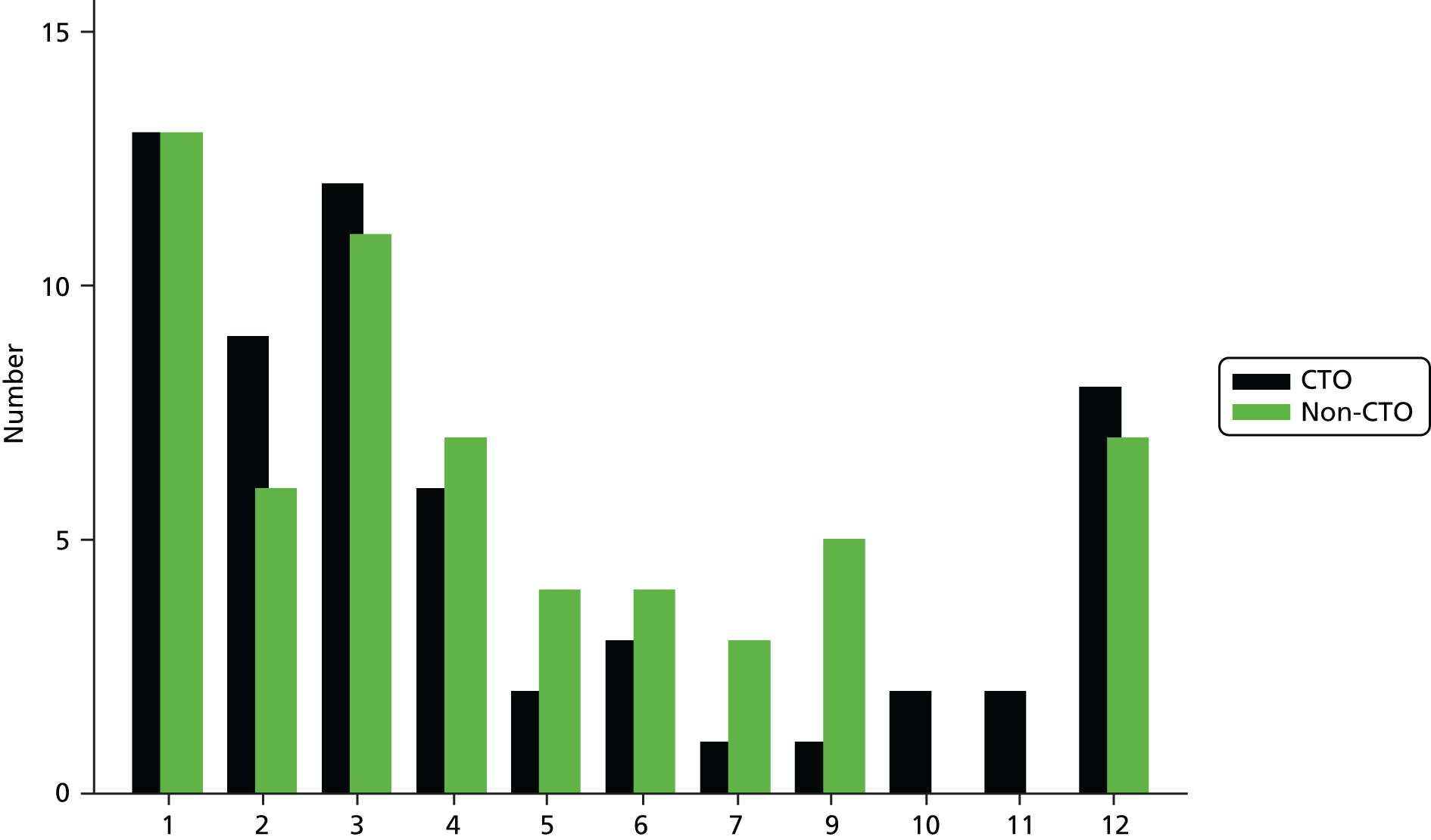
We conducted a per-protocol sensitivity analysis for the primary and secondary outcomes, removing the 91 protocol violations (i.e. excluding those patients who were discharged to the wrong arm of the trial or were not discharged, and the three ineligible or withdrawn patients, for whom we had no data on the primary outcome). This analysis was based on 245 cases with no protocol violations. It did not alter the findings (Table 7).
| Patient characteristics | Sample size (N = 245) | CTO (N = 124) | Non-CTO (N = 127) |
|---|---|---|---|
| n (%)/mean {SD}/median [IQR] | n (%)/mean {SD}/median [IQR] | ||
| Age (years) | 245 | 39.9 {11.6} | 39.7 {12.2} |
| Male | 245 | 84 (68) | 81 (67) |
| General education (years) | 242 | 11.5 [11–13] | 11 [11–13] |
| Ethnicity | 245 | ||
| White | – | 73 (59) | 76 (63) |
| Black | – | 29 (23) | 27 (22) |
| Asian | – | 12 (10) | 9 (7) |
| Mixed and other | – | 10 (8) | 9 (7) |
| Born in UK | 244 | 98 (79) | 85 (71) |
| Married or cohabiting | 243 | 8 (7) | 13 (11) |
| Identified carer | 221 | 50 (45) | 36 (32) |
| Independent accommodation | 244 | 90 (73) | 90 (74) |
| Living alone or homeless | 229 | 92 (81) | 84 (73) |
| Schizophrenia | 245 | 102 (82) | 103 (85) |
| BPRS | 226 | 37.3 [29–47] | 37 [31–48] |
| GAF | 225 | 40 [33–45] | 40 [32–45] |
| Duration of illness (years) | 238 | 11 [6–20] | 11 [5–21] |
| < 2 years’ illness duration | 245 | 4 (3) | 5 (4) |
| Number of psychiatric hospital admissions | 230 | 6 [3–8] | 4 [3–9] |
| Duration of past psychiatric hospital admissions (months) | 201 | 14 [6–25] | 12 [6–24] |
| Previous involuntary hospitalisations | 219 | 4 [2–7] | 3 [2–8] |
| Any criminal convictions | 225 | 47 (42) | 42 (39) |
| Any imprisonment | 221 | 29 (26) | 26 (23) |
Table 8 shows details of the treatment process (days in the community under the randomised legal compulsion, days under any legal compulsion during the follow-up period, and the number of contacts with the service per month). The number of days spent in the community after hospital discharge under the randomised compulsory outpatient supervision (i.e. randomised compulsion) was substantially longer in the CTO group (median: 183 days compared with 8 days for the non-CTO group) and this was highly statistically significant. The time to first voluntary status was also substantially longer for the CTO group (Figure 9). Overall, the total number of days under any compulsion during the 12-month follow-up period was significantly greater in the CTO group (median: 255 days) than in the non-CTO group (102 days), which was again highly statistically significant (p < 0.0001). This total number of days included compulsion under the randomised regime (either CTO or non-CTO), any time on CTOs for crossover patients in the non-CTO group and any time as a compulsory inpatient or on a subsequent CTO. The self-reported number of contacts with the service per month during the time outside hospital did not differ between the two groups (with a median of two contacts reported in each group) (see Table 8).
| Process characteristic | CTO (N = 167) | Non-CTO (N = 169) | Treatment effect (N = 336) | ||
|---|---|---|---|---|---|
| Mean {SD} | Median [IQR] | Mean {SD} | Median [IQR] | ||
| Days in community under randomised legal compulsion | 170.1 {134.4} | 183 [0–299] | 45.5 {80.7} | 8 [0–37] | p < 0.0001a |
| Days under any legal compulsion during follow-up | 241.4 {121.1} | 255 [148–365] | 134.6 {114.1} | 102 [31–212] | p < 0.0001a |
| Number of contacts with service per month | 3.0 {3.1} | 2.1 [0.8–4.4] | 3.9 {5.9} | 2.2 [0.8–4.7] | 0.77 (0.47 to 1.26)b |
FIGURE 9.
Time to first voluntary status. Reproduced from Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet 2013;381:1627–33,16 with permission from Elsevier.
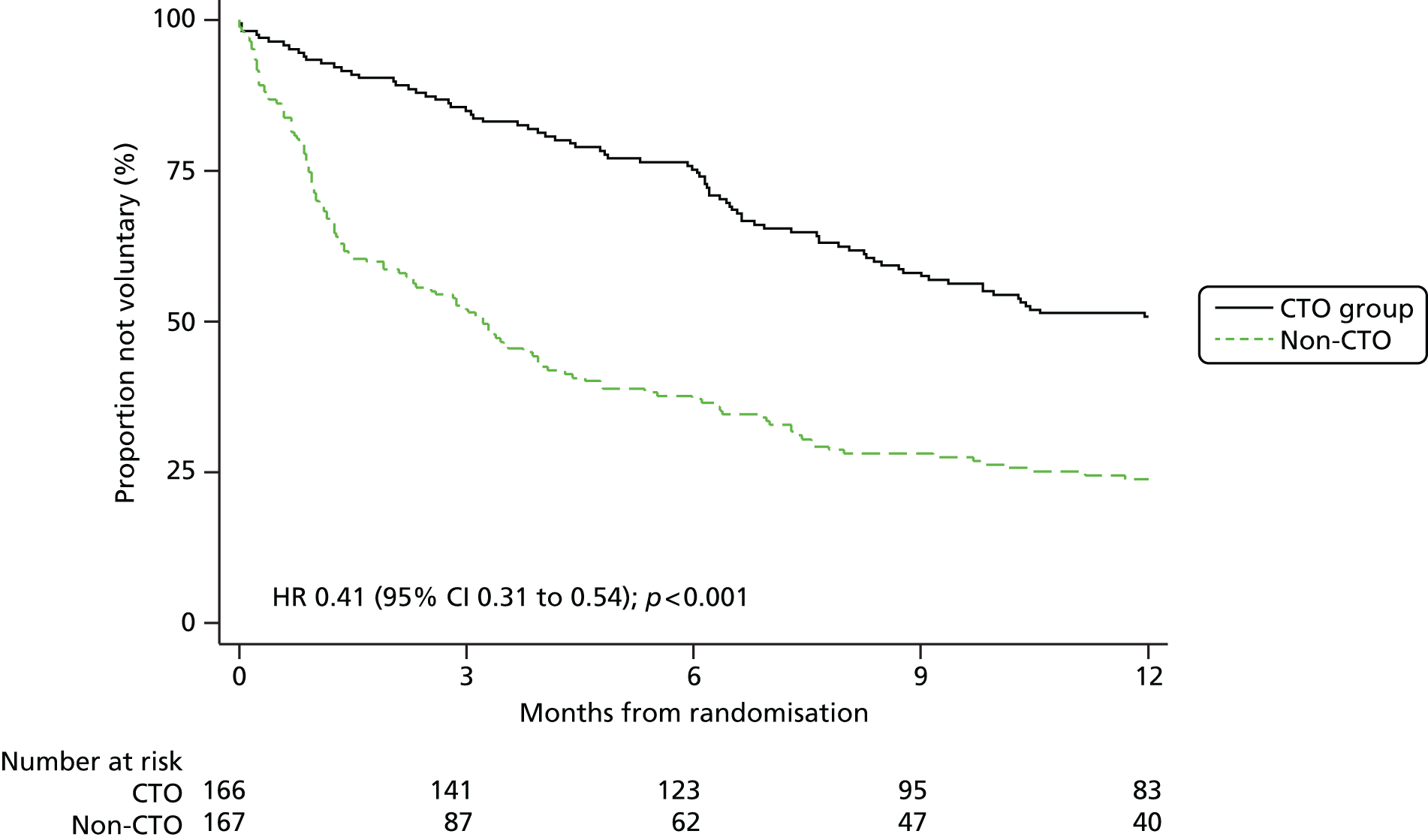
Table 9 shows the number of nights spent in psychiatric hospital during the 12-month follow-up period for the whole sample and for those patients who were readmitted. For the whole sample, the number of nights in hospital from randomisation (index) to 12 months did not differ significantly between the two groups [incident rate for CTO group 0.9 times the incident rate for the non-CTO group (95% CI 0.65 to 1.26; p = 0.550; not tabulated]. When patients who were never discharged were excluded from this analysis, the difference remained non-significant. The time from randomisation to discharge from hospital was similar between groups [median 8 days in the CTO group vs. 16 days in the non-CTO group, HR 1.08 (95% CI 0.86 to 1.34); not tabulated; Figure 10]. For those 119 patients who were readmitted only, the number of nights in hospital from randomisation to 12 months did not differ between the CTO and non-CTO groups and nor did the number of nights from randomisation to first discharge from hospital or the number of nights from the first readmission to the end of the follow-up period (whether or not excluding those who were never discharged) (see Table 9).
| Hospitalisation characteristic | CTO | Non-CTO | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean {SD} | Median [IQR] | n | Mean {SD} | Median [IQR] | n | Mean {SD} | Median [IQR] | |
| Whole sample | N = 167 | N = 169 | N = 336 | ||||||
| Index to 365 daysa | 166 | 82.2 {102.0} | 41.5 [8–109] | 167 | 90.9 {104.5} | 48.0 [10–133] | 333 | 86.6 {103.2} | 45.0 [8–127] |
| Index to first discharge | 166 | 37.3 {61.6} | 8.0 [0–47] | 167 | 44.2 {66.6} | 16.0 [0–67] | 333 | 40.8 {64.1} | 14.0 [0–51] |
| Index to 365 daysb | 159 | 69.8 {84.6} | 37.0 [7–99] | 161 | 80.7 {91.7} | 42.0 [9–124] | 320 | 75.3 {88.3} | 40.5 [7–107.5] |
| Readmitted patients | N = 59 | N = 60 | N = 119 | ||||||
| Index to 365 days | 59 | 145.7 {121.0} | 99.0 [56–264] | 60 | 160.5 {113.3} | 135.0 [75.5–238.5] | 119 | 153.2 {116.9} | 109.0 [61–239] |
| Index to first discharge | 59 | 19.2 {41.2} | 0.0 [0–24] | 60 | 30.6 {44.3} | 14.5 [0–39] | 119 | 24.9 {43} | 6.0 [0–35] |
| First readmission to 365 days | 59 | 126.5 {122.4} | 78 [32–170] | 60 | 129.9 {111.2} | 94.5 [44–186.5] | 119 | 128.2 {116.4} | 90 [35–175] |
| First readmission to 365 daysb | 52 | 94.4 {90.4} | 68.5 [29.5–102] | 54 | 103.8 {82.6} | 86.0 [35–148] | 106 | 99.2 {86.2} | 71.5 [31–139] |
FIGURE 10.
Time to first discharge (n = 333). Reproduced from Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet 2013;381:1627–33,16 with permission from Elsevier.
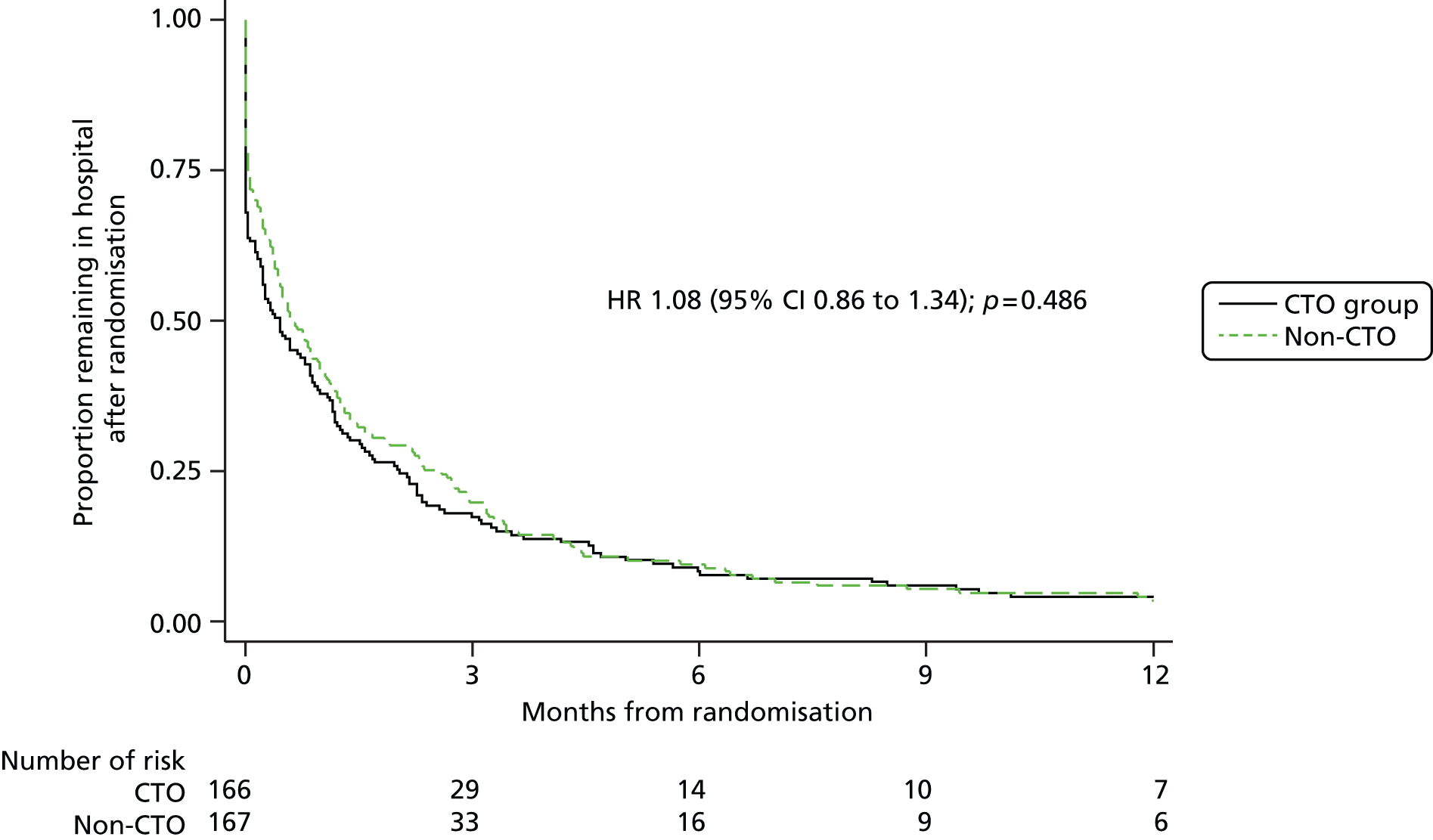
Tertiary outcomes
Table 10 presents the clinical and social factors for the whole sample at baseline and 12 months, along with the estimated average change over time. Table 11 presents the same clinical and social factors at 12 months for the CTO and non-CTO groups, along with the test statistics for the difference in change over time between the two groups.
| Factor | Baseline (N = 166) | 12 months (N = 167) | Change over time, total sample | p-valuea | ||
|---|---|---|---|---|---|---|
| Sample size | n (%)/mean {SD}/median [IQR] | Sample size | n (%)/mean {SD}/median [IQR] | |||
| BPRS | 254 | 37.0 [30–46] | 207 | 33.0 [29–42] | 1.21 | – |
| GAF | 309 | 39.0 [32–45] | 237 | 36.0 [31–45] | 0.38 | – |
| CAGE: alcohol | 306 | 16 (5) | 230 | 19 (6) | OR 5.01 | 0.050 |
| CAGE: drug | 316 | 28 (8) | 232 | 24 (7) | OR 1.06 | – |
| CAGE: drug and alcohol | 313 | 5 (2) | 233 | 5 (2) | OR 36.20 | – |
| SIX | 315 | 2.5 {1.1} | 236 | 2.6 {1.2} | 0.15 | – |
| Employment | 321 | – | 238 | – | 2.74 | < 0.010 |
| None | – | 316 (98) | – | 222 (93) | – | – |
| Voluntary/protected/sheltered | – | 3 (1) | – | 9 (4) | – | – |
| Regular employment | – | 2 (1) | – | 7 (3) | – | – |
| ITAQ | ||||||
| Total score | 260 | 14.0 [7.5–18] | 196 | 13.5 [7–19.5] | 0.41 | – |
| Awareness of Illness | 268 | 6.0 [3–8] | 200 | 6.0 [3–8.5] | 0.10 | – |
| Attitude to Treatment | 266 | 8.5 [4–11] | 200 | 9.0 [4–11] | 0.21 | – |
| Prescribed oral medication | 333 | 265 (80) | 333 | 266 (80) | OR 1.00 | – |
| Prescribed clozapine | 333 | 43 (13) | 333 | 30 (9) | OR 0.13 | < 0.050 |
| Prescribed depot medication | 333 | 188 (56) | 333 | 139 (42) | OR 0.04 | < 0.001 |
| DAI-10 | 255 | –2.0 [–6 to 4] | 172 | 2.0 [–2 to 6] | 1.74 | < 0.010 |
| STAR-P | ||||||
| Total score | 201 | 30.3 {9.7} | 178 | 32.5 {9.3} | 2.97 | < 0.010 |
| Positive Collaboration | 221 | 15.2 {5.8} | 186 | 16.2 {5.4} | 1.81 | < 0.010 |
| Positive Clinician Input | 210 | 7.0 {2.8} | 189 | 7.5 {2.8} | 0.61 | – |
| Non-Supportive Clinician Input | 219 | 7.9 {2.7} | 187 | 8.8 {2.5} | 0.66 | < 0.050 |
| API Decision Making | 277 | 56.6 {17.8} | 207 | 52.9 {16.9} | –4.83 | < 0.010 |
| API Information Seeking | 259 | 76.5 {13.0} | 201 | 74.3 {13.5} | –3.94 | < 0.050 |
| CSQ-8 | 262 | 21.3 {6.3} | 203 | 21.8 {6.0} | 0.95 | – |
| Any leverage in the past 6 months | 302 | 70 (23) | 229 | 50 (22) | 0.70 | – |
| AES Perceived Coercion | 221 | 14.8 {4.1} | 182 | 14.0 {4.2} | –0.34 | – |
| AES Negative Pressures | 230 | 21.4 {4.8} | 184 | 22.1 {4.3} | 0.41 | – |
| AES Procedural Justice | 221 | 8.4 {2.5} | 183 | 8.0 {2.5} | –0.07 | – |
| Index of Fairness | 239 | 12.8 {3.4} | 179 | 13.6 {3.1} | 1.31 | 0.001 |
| Index of Effectiveness | 241 | 12.3 {3.6} | 180 | 13.8 {3.2} | 2.10 | < 0.001 |
| Factor | Baseline (N = 333) | 12 months (N = 333) | Change over time, CTO vs. non-CTO | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CTO (n = 166) | Non-CTO (n = 167) | CTO (n = 166) | Non-CTO (n = 167) | ||||||
| Sample size | n (%)/mean {SD}/median [IQR] | Sample size | n (%)/mean {SD}/median [IQR] | Sample size | n (%)/mean {SD}/median [IQR] | Sample size | n (%)/mean {SD}/median [IQR] | ||
| BPRS | 126 | 36.0 [29–47] | 128 | 37.0 [31–45.5] | 101 | 34.0 [28–41] | 105 | 33.0 [29–43] | –1.20 |
| GAF | 153 | 38.0 [32–45] | 156 | 40.0 [32–46] | 123 | 36.0 [31–45] | 114 | 35.5 [30–45] | 0.26 |
| CAGE: alcohol | 153 | 12 (7) | 153 | 4 (2) | 120 | 9 (5) | 110 | 10 (6) | OR 0.20 |
| CAGE: drug | 158 | 14 (8) | 158 | 14 (8) | 119 | 14 (8) | 113 | 10 (6) | OR 1.40 |
| CAGE: drug and alcohol | 156 | 4 (2) | 157 | 1 (1) | 120 | 1 (1) | 113 | 4 (2) | OR 0.01 |
| SIX | 155 | 2.5 {1.1} | 160 | 2.5 {1.1} | 123 | 2.6 {1.0} | 113 | 2.7 {1.3} | –0.05 |
| Employment | 158 | – | 163 | – | 124 | – | 114 | – | –0.53 |
| None | – | 156 (99) | – | 160 (98) | – | 117 (94) | – | 105 (92) | – |
| Voluntary/protected/sheltered | – | 2 (1) | – | 1 (1) | – | 6 (5) | – | 3 (3) | – |
| Regular employment | – | 0 (0) | – | 2 (1) | – | 1 (1) | – | 6 (5) | – |
| ITAQ | |||||||||
| Total score | 129 | 14.0 [9–18] | 131 | 14.0 [6–19] | 100 | 16.0 [6.5–19] | 96 | 13.0 [7–20] | –0.37 |
| Awareness of Illness | 132 | 6.0 [3–8] | 136 | 6.0 [3–8] | 100 | 5.5 [3–8] | 100 | 6.0 [2.5–9] | 0.17 |
| Attitude to Treatment | 130 | 9.0 [5–11] | 136 | 8.0 [3–11] | 102 | 9.0 [4–11] | 98 | 8.5 [4–12] | –0.44 |
| Prescribed oral medication | 166 | 137 (83) | 167 | 128 (77) | 166 | 138 (83) | 167 | 128 (77) | OR 1.14 |
| Prescribed clozapine | 166 | 26 (16) | 167 | 17 (10) | 166 | 21 (13) | 167 | 9 (5) | OR 3.33 |
| Prescribed depot medication | 166 | 85 (51) | 167 | 103 (62) | 166 | 65 (39) | 166 | 74 (45) | OR 6.08a |
| DAI-10 | 117 | –2.0 [–6 to 4] | 108 | –2.0 [–6 to 4] | 89 | 2.0 [–2 to 6] | 83 | 0.0 [–2 to 4] | 0.15 |
| STAR-P | |||||||||
| Total score | 100 | 31.2 {8.9} | 101 | 29.4 {10.4} | 90 | 32.5 {10.2} | 88 | 32.4 {8.3} | –0.92 |
| Positive Collaboration | 111 | 15.9 {5.4} | 110 | 14.5 {6.2} | 95 | 16.1 {5.9} | 91 | 16.3 {4.7} | –1.15 |
| Positive Clinician Input | 107 | 7.1 {2.6} | 103 | 6.9 {3} | 95 | 7.5 {2.9} | 94 | 7.6 {2.6} | –0.10 |
| Non-Supportive Clinician Input | 109 | 7.9 {2.7} | 110 | 7.9 {2.7} | 92 | 8.9 {2.6} | 95 | 8.6 {2.5} | 0.43 |
| API Decision Making | 135 | 54.8 {16.3} | 142 | 58.4 {19} | 106 | 52.4 {16.8} | 101 | 53.4 {17.1} | 1.99 |
| API Information Seeking | 130 | 76.4 {11.2} | 129 | 76.6 {14.6} | 104 | 75.6 {13.5} | 97 | 72.8 {13.4} | 3.05 |
| CSQ-8 | 125 | 21.7 {5.9} | 137 | 20.8 {6.6} | 106 | 21.9 {6.2} | 97 | 21.7 {5.9} | –0.61 |
| Any leverage | 151 | 30 (20) | 151 | 40 (26) | 119 | 28 (24) | 110 | 22 (20) | 1.87 |
| AES Perceived Coercion | 109 | 14.7 {3.8} | 112 | 15.0 {4.3} | 97 | 13.8 {4.3} | 85 | 14.3 {4} | –0.45 |
| AES Negative Pressures | 113 | 14.4 {4.8} | 116 | 14.6 {4.7} | 97 | 13.6 {4.6} | 87 | 14.2 {3.9} | 0.51 |
| AES Procedural Justice | 112 | 8.3 {2.3} | 109 | 8.5 {2.6} | 97 | 7.7 {2.4} | 86 | 8.3 {2.5} | –0.51 |
| Index of Fairness | 120 | 13.2 {3.2} | 119 | 12.3 {3.6} | 95 | 13.6 {3.2} | 84 | 13.7 {3.0} | –0.94 |
| Index of Effectiveness | 120 | 13.0 {3.4} | 121 | 11.6 {3.7} | 95 | 13.8 {3.4} | 85 | 13.8 {2.9} | –1.22a |
There were some statistically significant changes over the 12 months in the total sample of 333 (see Table 10). Patients reported higher effectiveness of treatment pressure (Index of Effectiveness, average change 2.10 points, 95% CI 1.32 to 2.89 points; p < 0.001) and more positive views of the fairness of the pressure applied (Index of Fairness, average change 1.31 points, 95% CI 0.54 to 2.08 points; p = 0.001). They also reported more positive relationships with clinicians at 12 months compared with baseline (STAR-P, average change 2.97 points, 95% CI 0.97 to 4.97 points; p = 0.004). This included more positive collaboration (average change: 1.81 points, 95% CI 0.71 to 2.93 points; p = 0.001) and less non-supportive clinician input (average change: 0.66 points, 95% CI 0.06 to 1.25 points; p = 0.031). Although the sample expressed a desire for gaining control in decision-making and to be given information about their illness, the scores were lower at 12 months than at baseline (Decision Making Preference, average change –4.83 points, 95% CI –8.24 to –1.41 points; p = 0.006 – Information Seeking Preference, average change –3.94 points, 95% CI –6.98 to –0.90; p = 0.011). There was an increase over time in patients scoring positively for potential problem drinking [odds ratio (OR) 5.01, 95% CI 1.31 to 19.19; p = 0.019]. Attitudes to medication were more positive across the sample (DAI-10, average change 1.74 points, 95% CI 0.57 to 2.91 points; p = 0.004) and more patients were in employment at 12 months (2.74 points, 95% CI 0.99 to 4.48 points; p = 0.002). Significantly fewer patients were prescribed clozapine (OR 0.13, 95% CI 0.03 to 0.63; p = 0.011) and depot medication (OR 0.09, 95% CI 0.03 to 0.24; p < 0.001) at 12 months compared with baseline.
There were no significant differences between the two arms in the change from baseline to 12 months in any of the reported outcomes except for the Index of Effectiveness (see Table 11). Those in the CTO group showed a smaller increase over time than those in the non-CTO group in their agreement that the treatment pressure they had experienced had been helpful. The difference was small (–1.22 points, 95% CI –2.32 to –0.14; p = 0.028).
The sensitivity analysis using multiple imputation did not alter the outcome results.
Subgroup analyses
The observed values for the primary outcome (psychiatric hospital readmission) and main secondary outcomes (nights in hospital and days to first readmission) in the subgroup analysis are shown in Table 12, and for the main clinical outcomes (BPRS and GAF) in Table 13. Adjusted values for the statistically significant interactions (adjusted for the randomisation factors) are presented in the text.
| Subgroup | Hospital readmission: n (%) | Nights in hospital: median [IQR] | Days to first readmission: median [IQR] | |||
|---|---|---|---|---|---|---|
| CTO (N = 59)a | Non-CTO (N = 60a) | CTO (N = 166) | Non-CTO (N = 167) | CTO (N = 59a) | Non-CTO (N = 60a) | |
| Age (years) | ||||||
| > 40 | 25 (42) | 27 (45) | 59.0 [8–109] | 63.5 [12–137] | 287.0 [128–357] | 282.0 [152–350] |
| ≤ 40 | 34 (58) | 33 (55) | 36.0 [5–112] | 37.0 [5–131] | 305.0 [150–356] | 298.0 [115–360] |
| Gender | ||||||
| Male | 44 (75) | 41 (68) | 35.0 [5–103] | 45.0 [9–117] | 304.0 [127–359] | 292.0 [115–356] |
| Female | 15 (25) | 19 (32) | 56.0 [18–127] | 57.5 [11–155] | 287.0 [193–344] | 280.0 [152–353] |
| Ethnicity | ||||||
| Other | 47 (80) | 47 (78) | 43.5 [9–107] | 57.5 [9.5–140] | 298.0 [128–355] | 289.0 [108–354.8] |
| Black | 12 (20) | 13 (22) | 39.0 [1–112] | 42.0 [11–117] | 288.0 [209–358] | 297.0 [161.3–354] |
| Country of birth | ||||||
| Other | 8 (14) | 14 (23) | 26.0 [0–105.5] | 46.0 [14.5–101.5] | 298.0 [187–365] | 306.0 [135–351] |
| Britain | 51 (86) | 46 (77) | 46.5 [9–109] | 84.0 [9–137] | 294.0 [139–354] | 282.0 [115–356] |
| Marital status | ||||||
| Married/co-habiting | 2 (3) | 8 (13) | 36.0 [18–143] | 72.0 [10–106] | 329.0 [214–347] | 286.0 [129–342] |
| Single/separated/divorced | 56 (97) | 52 (87) | 41.5 [7–109] | 44.5 [10–132.5] | 294.0 [139–357] | 293.0 [123–355] |
| Living status | ||||||
| Living with others | 11 (20) | 15 (26) | 39.0 [6–93] | 32.5 [5–105] | 319.0 [231–359] | 322.0 [212–360] |
| Living alone/homeless/sheltered | 44 (80) | 43 (74) | 42.0 [9–120] | 53.5 [11–137] | 287.0 [127–353] | 275.0 [115–353] |
| Diagnosis | ||||||
| Other diagnosis | 10 (17) | 9 (15) | 43.0 [7–109] | 83.0 [13–119] | 270.0 [176–355] | 268.0 [132.5–352] |
| Schizophrenia | 49 (83) | 51 (85) | 41.5 [8–109.5] | 42.0 [7–137] | 296.0 [140–357] | 292.0 [126–358] |
| Duration of illness (years)b | ||||||
| < 2 | 1 (2) | 2 (3) | 1.0 [0–96] | 27.0 [2–202] | 364.0 [231–365] | 338.0 [108–363] |
| ≥ 2 | 58 (98) | 58 (97) | 42.0 [8–112] | 49.5 [10.5–132.5] | 294.0 [139–355] | 288.0 [128–353.8] |
| General education (years) | ||||||
| ≤ 12 | 38 (66) | 35 (58) | 36.0 [7–120] | 45.0 [7–132] | 294.0 [127–357] | 295.0 [132–358] |
| > 12 | 20 (34) | 25 (42) | 46.0 [11–98] | 50.0 [12–132] | 299.0 [207–351] | 238.0 [115–348] |
| Tertiary education | ||||||
| No | 44 (76) | 44 (73) | 46.0 [7–120] | 67.0 [12–154] | 296.0 [127–357] | 281.0 [115–353] |
| Yes | 14 (24) | 16 (27) | 39.0 [18–83] | 40.0 [4–91] | 287.0 [182–343] | 322.0 [208–361] |
| BPRS score, baseline | ||||||
| ≤ 33 | 17 (31) | 11 (20) | 28 [1–93] | 27 [1–81] | 337.0 [231–364] | 336.0 [248–364] |
| > 33 | 37 (69) | 45 (80) | 50 [11.5–131] | 70.5 [12–176.5] | 255.0 [122–346] | 260.0 [105–351] |
| GAF score, baseline | ||||||
| ≤ 49 | 46 (88) | 49 (91) | 44 [7–109] | 49.5 [11–132] | 291.0 [140–357] | 283.0 [141–353] |
| > 49 | 6 (12) | 5 (9) | 38 [0–107] | 20.5 [2–82] | 327.0 [253–365] | 345.0 [180–363] |
| Subgroup | GAF score: mean {SD} | BPRS: mean {SD} | ||
|---|---|---|---|---|
| CTO (N = 166) | Non-CTO (N = 167) | CTO (N = 166) | Non-CTO (N = 167) | |
| Age (years) | ||||
| > 40 | 38.9 {12.6} | 38.4 {12.5} | 36.2a {9.8} | 39.6a {13.5} |
| ≤ 40 | 39.0 {11.7} | 40.9 {13.7} | 39.5a {12.3} | 37.1a {11.3} |
| Gender | ||||
| Male | 39.0 {11.8} | 40.0 {13.1} | 38.3 {12.6} | 36.9 {10.9} |
| Female | 39.0 {12.6} | 39.1 {13.3} | 38.0 {8.7} | 41.3 {15.0} |
| Ethnicity | ||||
| Other | 38.5 {12.5} | 38.1 {12.3} | 39.2 {12.1} | 39.8 {12.8} |
| Black | 41.0 {9.6} | 45.7 {14.6} | 34.2 {6.9} | 32.7 {9.3} |
| Country of birth | ||||
| Other | 40.4 {11.7} | 41.3 {14} | 35.6 {9.5} | 35.5 {10.2} |
| Britain | 38.7 {12.1} | 39.3 {12.9} | 38.7 {11.8} | 39.3 {13.1} |
| Marital status | ||||
| Married/co-habiting | 50.1 {16.6} | 40.3 {14.2} | 32.2 {8.4} | 39.4 {13.4} |
| Single | 38.2 {11.3} | 39.7 {13.1} | 38.6 {11.5} | 38.3 {12.4} |
| Living status | ||||
| Living with others | 42.3 {14.8} | 41.5 {15.8} | 37.3 {10.9} | 37.7 {12.0} |
| Living alone | 38.5 {11.3} | 39.2 {12.1} | 38.2 {11.6} | 38.6 {12.7} |
| Diagnosis | ||||
| Other diagnosis | 44.2 {13.9} | 37.5 {12.2} | 34.9 {8.1} | 39.8 {11.9} |
| Schizophrenia | 38.0 {11.4} | 40.1 {13.3} | 38.8 {11.9} | 38.0 {12.6} |
| Duration of illness (years) | ||||
| < 2 | 45.6 {12} | 40.0 {8.9} | 29.9 {5.1} | 33.5 {7.3} |
| ≥ 2 | 38.7 {12} | 39.7 {13.3} | 38.6 {11.5} | 38.6 {12.6} |
| General education (years) | ||||
| ≤ 12 | 37.6 {10.6} | 37.2 {10.9} | 39.7 {12.6} | 38.9 {12.4} |
| > 12 | 41.6 {14.1} | 43.9 {15.3} | 35.4 {8.2} | 37.5 {12.7} |
| Tertiary education | ||||
| No | 37.7 {10.8} | 38.2 {11.6} | 39.6a {12} | 39.4a {12.9} |
| Yes | 43 {14.5} | 43.9 {16} | 34.0a {8.3} | 35.7a {11.1} |
| BPRS score, baseline | ||||
| ≤ 33 | 43.9 {12.2} | 46.1 {13.9} | 33.2 {9.3} | 33.1 {8.7} |
| > 33 | 35.9 {11.3} | 36.5 {11.5} | 41.9 {11.8} | 41.4 {13.6} |
| GAF score, baseline | ||||
| ≤ 49 | 37.5 {11.7} | 38.4 {12.2} | 39.8 {12} | 39.2 {12.7} |
| > 49 | 48.1 {11.1} | 49.9 {14} | 30.0 {3.9} | 33.0 {11.3} |
There were no statistically significant interactions between any of the subgroups and the primary outcome measure of readmission or for time to first readmission, duration of readmissions or social functioning.
Severity of symptoms (BPRS) demonstrated crossover interactions with age in the two arms (interaction coefficient –4.49; p = 0.043). In the CTO group, those aged < 40 years had more severe symptoms than those aged > 40 years [39.54 (95% CI 37.55 to 41.52) vs. 37.96 (95% CI 35.58 to 40.34)]. Among the non-CTO group, those aged < 40 years had less severe symptoms than the older group [38.64 (95% CI 36.53 to 40.75) vs. 41.56 (95% CI 39.35 to 43.78)].
There were also crossover interactions between symptoms and subgroups with and without some tertiary education (interaction coefficient = –5.62; p = 0.024). In the CTO group, those without tertiary education had more severe symptoms than those with tertiary education [40.05 (95% CI 38.35 to 41.76) vs. 34.92 (95% CI 31.78 to 38.07)]. Among the non-CTO group, those without tertiary education had less severe symptoms than those with tertiary education [39.93 (95% CI 38.13 to 41.73) vs. 40.42 (95% CI 37.62 to 43.22)].
The proportion of patients on depot medication at baseline was not statistically different between the two groups [85/166 (51%) in the CTO arm vs. 103/167 (62%) in the non-CTO arm; p = 0.054). The statistically significant reduction in the number of patients prescribed depot medication over time was unexpected. Our exploratory analyses showed that the reduction was significant in both groups (OR 0.04, 95% CI 0.01 to 0.11; p < 0.001) and that it was significantly larger in the CTO group than among the non-CTO group (OR 6.08, 95% CI 1.48 to 24.97; p = 0.012). There was no statistically significant difference in the primary outcome measure of readmission between those on depot and those not. There was also no interaction effect of the CTO and non-CTO groups with being prescribed depot (interaction coefficient 0.85; p = 0.586).
Deaths
Five patients died during follow-up: two deaths by suicide and one by accidental death from a drug overdose were recorded in the CTO group, and one death by suicide and one death from natural causes were recorded in the non-CTO group. The DMC did not regard these deaths as necessitating the ending of the trial.
Conclusions
-
CTO use did not reduce the rate of readmission to hospital.
-
The length of the initial compulsory outpatient treatment was hugely greater for the CTO group than the non-CTO group (median 183 days vs. 8 days).
-
CTO use had no impact on:
-
time to readmission
-
number and duration of hospital admissions
-
any measured clinical and social outcomes.
-
-
There were no differences between CTO and non-CTO outcomes for any of the prespecified subgroups.
Chapter 7 OCTET Economic Evaluation
Introduction
Although we hypothesised that CTO use might lead to improved health outcomes in terms of reduced hospital admissions and hence to significant cost savings for the health and social care system, we also recognised that the additional coercion posed on patients might have a significant negative impact on their quality of life and freedom of choice (i.e. their capabilities). To assess the trade-off between these potentially conflicting impacts of CTOs, we carried out a prospective within-trial economic evaluation.
Economic evaluations compare the costs and the benefits of relevant alternative health care options to assess their incremental cost-effectiveness. The current economic evaluation included:
-
a detailed cost analysis of health, social care and other broader societal costs
-
an incremental cost-effectiveness analysis comparing the CTO and non-CTO groups from the OCTET Trial over the 12-month trial period.
Methods
Study population
Of the 336 randomised patients in the OCTET Trial, three were excluded and five died during the follow-up period (see Chapter 6, Results). In order to reduce the potential bias in the cost-effectiveness results due to the imbalanced timing of deaths, we removed these eight patients from the Economic Evaluation, which was therefore based on 328 patients. Table 14 shows the sociodemographic and clinical characteristics of these 328 patients (CTO 163; non-CTO 165).
| Variables | CTO (N = 163) | Non-CTO (N = 165) | ||
|---|---|---|---|---|
| Sample size | n (%)/mean {SD} | Sample size | n (%)/mean {SD} | |
| Age (years) | 163 | 39.9 {11.28} | 165 | 39.3 {11.60} |
| Male | 163 | 109 (67) | 165 | 112 (68) |
| Marital status | 162 | – | 164 | – |
| Single (never married) | – | 122 (75) | – | 122 (74) |
| Married/co-habiting | – | 11 (7) | – | 17 (10) |
| Separated/divorced | – | 29 (18) | – | 25 (15) |
| Have children | 162 | 72 (44) | 164 | 59 (36) |
| General education (years) | 161 | 11.7 {1.75} | 163 | 12.0 {2.11} |
| Accommodation | 162 | – | 164 | – |
| Independent | – | 116 (71) | – | 119 (72) |
| Supported | – | 29 (18) | – | 27 (16) |
| Homeless | – | 17 (10) | – | 18 (11) |
| Employment | 162 | – | 165 | – |
| Regular paid | – | 0 (0) | – | 2 (1) |
| Voluntary/protected/sheltered | – | 1 (1) | – | 1 (1) |
| Jobseeker’s Allowance | – | 9 (6) | – | 5 (3) |
| Sickness benefit | – | 141 (87) | – | 146 (88) |
| Unemployed | – | 8 (5) | – | 5 (3) |
| Other (student/pensioner) | – | 3 (2) | – | 6 (4) |
| Religious denomination | 146 | – | 153 | – |
| Christian | – | 64 (39) | – | 71 (43) |
| Jewish | – | 3 (2) | – | 2 (1) |
| Muslim | – | 9 (6) | – | 9 (5) |
| Other | – | 27 (17) | – | 15 (9) |
| None | – | 43 (26) | – | 56 (34) |
| Duration of illness (years) | 158 | 14.6 {10.40} | 162 | 14.0 {10.29} |
| Diagnosis | 163 | – | 165 | – |
| Schizophrenia, schizotypal and delusional disorders | – | 138 (85) | – | 141 (85) |
| Other psychosis (including bipolar disorder) | – | 25 (15) | – | 24 (15) |
| BMI (kg/m2) | 124 | – | 132 | – |
| Underweight (BMI < 18.5) | – | 6 (4) | – | 1 (1) |
| Normal (18.5 ≤ BMI < 25) | – | 48 (29) | – | 46 (28) |
| Overweight (25 ≤ BMI < 30) | – | 47 (29) | – | 42 (25) |
| Obese (30 ≤ BMI) | – | 23 (14) | – | 43 (26) |
| Ethnicity | 163 | – | 165 | – |
| White | – | 100 (61) | – | 102 (62) |
| Black | – | 36 (22) | – | 38 (23) |
| Asian | – | 15 (9) | – | 14 (8) |
| Mixed | – | 12 (7) | – | 11 (7) |
Data collection
We collected all outcome and resource-use data through face-to-face interviews with the trial patients at baseline and at 6 and 12 months. We based the cost analysis on an amended version of the CSRI instrument,116 a widely used and well-validated instrument for collection of resource-use data in mental health. Collected data included all hospital and community health and social services, psychotropic medication, productivity losses and informal care. Information on manager hearings and tribunals were extracted from the trial clinical research forms.
Outcomes
The primary economic analysis was a cost–utility analysis, for which the quality-adjusted life-year (QALY) calculated using the EuroQol-5 Dimensions, three-level version (EQ-5D-3L) was adopted as the effectiveness measure. 119 The EQ-5D-3L is a standardised, non-disease-specific instrument used for describing and valuing health-related quality of life. 120 It is widely used in health economics and it is the preferred measure by the National Institute for Health and Care Excellence (NICE). 121 We valued EQ-5D-3L responses using the UK ‘tariff’ of utility values for discrete health states, and expressed changes in terms of QALYs gained over 12 months in comparison to the relevant baseline values. 122 Quality of life was assumed to change linearly between health states. We also compared the changes between baseline and 12 months on the EQ-5D visual analogue scale (EQ-5D VAS), in which patients rate their overall health status on a visual analogue scale (range 0–100). We carried out a secondary economic analysis using the newly developed multidimensional capabilities instrument, the Oxford Capabilities Questionnaire – Mental Health (OxCAP-MH) (Table 15) and the resulting 16-question capability index (CAPINDEX16) as outcome measures. The development of this measure is described later in the report (see Chapter 10).
| Number | Question | Response | |||||
|---|---|---|---|---|---|---|---|
| 1 | Does your health in any way limit your daily activities, compared to most people of your age? [Please tick one] 1. Domain: DAILY ACTIVITIES |
□ Yes □ No |
|||||
| 2 | Are you able to meet socially with friends or relatives? [Please tick one] 2. Domain: SOCIAL NETWORKS |
□ Yes □ No |
|||||
| 3 | In the past 4 weeks, how often have you lost sleep over worry? [Please tick one] 3. Domain: LOSING SLEEP |
□ Always □ Most of the time □ Some of the time □ Hardly ever □ Never |
|||||
| 4 | In the past 4 weeks, how often have you been able to enjoy your recreational activities? [Please tick one] 4. Domain: ENJOY RECREATION |
□ Always □ Most of the time □ Some of the time □ Hardly ever □ Never |
|||||
| 5 | Do you own your home (outright/or on a mortgage)? [Please tick one] 5. Domain: PROPERTY OWNERSHIP |
□ Yes □ No |
|||||
| 6 | How suitable or unsuitable is your accommodation for your current needs? [Please tick one] 6. Domain: SUITABLE ACCOMODATION |
□ Very suitable □ Fairly suitable □ Neither suitable nor unsuitable □ Fairly unsuitable □ Very unsuitable |
|||||
| 7 | Please indicate how safe you feel walking alone in the area near your home: [Please tick one] 7. Domain: NEIGHBOURHOOD SAFETY |
□ Very safe □ Fairly safe □ Neither safe nor unsafe □ Fairly unsafe □ Very unsafe |
|||||
| 8 | Please indicate how likely you believe it to be that you will be assaulted in the future (including sexual and domestic assault): [Please tick one] 8. Domain: POTENTIAL FOR ASSAULT |
□ Very likely □ Fairly likely □ Neither likely nor unlikely □ Fairly unlikely □ Very unlikely |
|||||
| 9A | How likely do you think it is that you will experience discrimination? [Please tick one] 9. Domain: DISCRIMINATION |
□ Very likely □ Fairly likely □ Neither likely nor unlikely □ Fairly unlikely □ Very unlikely |
|||||
| 9B | On what grounds do you think it is likely that you will be discriminated against? (Please complete only if your answer to question 8A is ‘Very likely’ or ‘Fairly likely’) [Please tick up to three] 9. Domain: DISCRIMINATION |
□ Race/ethnicity □ Gender □ Religion □ Sexual orientation □ Age □ Health or disability (including mental health) |
|||||
| 10 | Please indicate how strongly you agree or disagree with the following statements: [Please tick one box for each statement] |
||||||
| Strongly Agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | |||
| 10A | I am able to influence decisions affecting my local area 10. Domain: INFLUENCE LOCAL DECISIONS |
||||||
| 10B | I am free to express my views, including political and religious views 11. Domain: FREEDOM OF EXPERESSION |
||||||
| 10C | I am able to appreciate and value plants, animals and the world of nature 12. Domain: APPRECIATE NATURE |
||||||
| 10D | I respect, value and appreciate people around me 13. Domain: RESPECT AND APPRECIATION |
||||||
| 10E | I find it easy to enjoy the love, care and support of my family and friends 14. Domain: LOVE AND SUPPORT |
||||||
| 10F | I am free to decide for myself how to live my life 15. Domain: PLANINNG ONE’S LIFE |
||||||
| 10G | I am free to use my imagination and to express myself creatively (e.g. through art, literature, music, etc.) 16. Domain: IMAGINATION AND CREATIVITY |
||||||
| 10H | I have access to interesting forms of activity (or employment) 17. Domain: ACCESS |
||||||
| 11 | The next question asks you to think about your life expectancy: The average life expectancy in the UK is 77 years for men and 81 years for women. Some people think they are going to live longer than the average person whilst other people believe they are going to live shorter than the average person |
||||||
| 11A | Given your family history, dietary habits, lifestyle and health status, do you expect to live . . .? [Please tick one] 18. Domain: LIFE EXPECTANCY |
□ Longer than average □ Same as average □ Shorter than average |
|||||
| 11B | Until what age do you believe you are going to live? (Please complete only if your answer to question 10A is ‘Longer than average’ or ‘Shorter than average’.) 18. Domain: LIFE EXPECTANCY |
□□□ years | |||||
Costs
We applied national-level unit costs to each resource-use item to calculate the total cost of resources used by each patient (Tables 16–18). All unit costs were for the financial year 2012–13 and were expressed in British Pounds (£). We calculated medication costs using daily dose data and multiplying this with the average unit price for each compound based on the British National Formulary. 123 We estimated lost productivity costs using the human capital approach. We multiplied days off work by the average daily UK national salary for patients who were employed or self-employed. 124,125 We estimated informal care costs by multiplying the average UK hourly salary for 2012–13 by the number of hours family and friends spent on helping patients because of their illness.
| Resource use | Unit costs (£) | Unit | Source of estimate |
|---|---|---|---|
| Psychiatric medication | |||
| Oral medication | Various | Per daily dose (mg) | BNF123 |
| Depot medication | Various | Per administered depot (ml/mg) | BNF123 |
| Mental health community/outpatient | |||
| Community mental health nurse – telephone contact | 6.7 | Per contact | Curtis126 |
| Community mental health nurse – face-to-face contact in NHS setting | 16.8 | Per visit | Curtis126 |
| Community mental health nurse – face-to-face contact in community | 35.6 | Per visit | Curtis126 |
| Psychiatrist – telephone contact | 24.4 | Per contact | NHS Reference Costs 2012–13,127 Curtis126 |
| Psychiatrist – face-to-face contact in NHS setting | 40.0 | Per visit | NHS Reference Costs 2012–13,127 Curtis126 |
| Psychiatrist – face-to-face contact in community | 102.2 | Per visit | NHS Reference Costs 2012–13,127 Curtis126 |
| Psychologist – telephone contact | 16.1 | Per contact | Curtis126 |
| Psychologist – face-to-face contact in NHS setting | 136.0 | Per visit | Curtis126 |
| Psychologist – face-to-face contact in community | 173.5 | Per visit | Curtis126 |
| Drug/alcohol service worker – face-to-face contact in NHS setting | 48.0 | Per visit | Curtis126 |
| Drug/alcohol service worker – face-to-face contact in community | 122.7 | Per visit | Curtis126 |
| Other secondary care worker (e.g. occupational therapist) – face-to-face contact in NHS setting | 51.9a | Per visit | Curtis128 |
| Other secondary care worker (e.g. occupational therapist) – face-to-face contact in community | 66.1a | Per visit | Curtis128 |
| Day centre (groups/programmes, non-health-care staff) | 37.0 | Per session | Curtis126 |
| Day hospital (group therapies etc., health-care staff, regular) | 100.0 | Per day | Curtis126 |
| Drop-in centre (including street agencies) (informal) | 37.0 | Per session | Curtis126 |
| Self-help group/support group | 59.0 | Per session | Curtis126 |
| Attendance in other facility (social club, dinner club) | 6.9a | Per visit | Community Accountancy Self Help129 |
| Mental health inpatient | |||
| Psychiatric hospital inpatient general ward | 345.9 | Per day | Curtis 2012126 |
| Psychiatric hospital inpatient PICU | 669.3 | Per day | Curtis 2012126 |
| Resource use | Unit costs (£) | Unit | Source of estimate |
|---|---|---|---|
| Non-mental health outpatient | |||
| Alternative therapies (NHS) – face-to-face contact in NHS setting | 43.8 | Per visit | NHS Choices, www.nhs.uk/conditions/acupuncture/Pages/Introduction.aspx (accessed 1 July 2014) |
| Alternative therapies (NHS) – face-to-face contact in community | 43.8 | Per visit | NHS Choices, www.nhs.uk/conditions/acupuncture/Pages/Introduction.aspx (accessed 1 July 2014) |
| Alternative therapies (private) – face-to-face contact in private health care facility | 67.0 | Per visit | Private Healthcare Tariff130 |
| Alternative therapies (private) – face-to-face contacts in community | 67.0 | Per visit | Private Healthcare Tariff130 |
| Day patient hospital attendance/accident and emergency attendance | 117.0 | Per attendance | NHS Reference Costs 2012–13 127 |
| Other medical/surgical outpatient visits | 3.0–204.0 | Per visit | NHS Reference Costs 2012–13 127 |
| Non-mental health inpatient | |||
| Other medical/surgical inpatient department | 61.0–1964.0 | Per day | Scottish National Tariff 2012–13,131 NHS Reference Costs 2012–13127 |
| Resource use | Unit costs (£) | Unit | Source of estimate |
|---|---|---|---|
| Primary care | |||
| GP – telephone contact | 22.0 | Per contact | Curtis126 |
| GP – face-to-face contact in NHS setting | 38.0 | Per visit | Curtis126 |
| GP – face-to-face contact in community | 92.0 | Per visit | Curtis126 |
| Practice nurse – telephone contact | 4.5 | Per contact | Curtis126 |
| Practice nurse – face-to-face contact in NHS setting | 11.6 | Per visit | Curtis126 |
| Practice nurse – face-to-face contact in community | 23.9 | Per visit | Curtis126 |
| Other primary care worker (e.g. dietitian or nutritionist) – phone contact | 3.6 | Per contact | Curtis126 |
| Other primary care worker (e.g. dietitian or nutritionist) – face-to-face contact in NHS setting | 30.0 | Per visit | Curtis126 |
| Other primary care worker (e.g. dietitian or nutritionist) – face-to-face contact in community | 38.3 | Per visit | Curtis126 |
| Social care | |||
| Community support worker – face-to-face contact in NHS setting | 8.1 | Per visit | Curtis126 |
| Community support worker – face-to-face contact in community | 10.3 | Per visit | Curtis126 |
| Social worker – telephone contact | 18.5 | Per contact | Curtis126 |
| Social worker – face-to-face contact in NHS setting | 52.0 | Per visit | Curtis126 |
| Social worker – face-to-face contact in community | 66.3 | Per visit | Curtis126 |
| Home help/home care worker – phone contact | 5.7 | Per contact | Curtis126 |
| Home help/home care worker – face-to-face contact in NHS setting | 25.5 | Per visit | Curtis126 |
| Home help/home care worker – face-to-face contact in community | 25.5 | Per visit | Curtis126 |
| Housing worker – phone contact | 2.6 | Per contact | Assuming national average salary, ONS132 |
| Housing worker – face-to-face contact in NHS setting | 5.2 | Per visit | Assuming national average salary, ONS132 |
| Housing worker – face-to-face contact in community | 6.6 | Per visit | Assuming national average salary, ONS132 |
| Voluntary/charity worker (e.g. advocacy) – phone contact | 2.6 | Per contact | Assuming national average salary, ONS132 |
| Voluntary/charity worker (e.g. advocacy) – face-to-face contact in NHS setting | 5.2 | Per visit | Assuming national average salary, ONS132 |
| Voluntary/charity worker (e.g. advocacy) – face-to-face contact in community | 6.6 | Per visit | Assuming national average salary, ONS132 |
| Indirect costs | |||
| Lost productivity (sick leave) | 116.8 | Per day | Assuming national average salary, ONS132 |
| Informal care | 15.6 | Per hour | Assuming national average salary, ONS132 |
Analyses
Although we primarily assessed cost-effectiveness from the health and social care perspective preferred by NICE,121 we thus also conducted separate analyses including indirect costs such as lost productivity and informal care. We assessed independently the impact of CTOs on the number of manager hearings and tribunals. We also investigated the impact of missing data in contrast with the complete cases data set in our sensitivity analysis. For this, we assumed missing data to be missing at random, and estimated values using multiple imputation with randomisation group, age, gender, main clinical diagnosis, illness duration and length of inpatient stay as covariates. 133 The number of imputations sets was kept at 30 for costs and EQ-5D, and 50 for the OxCAP-MH index (CAPINDEX16), driven by the percentage of cases that were incomplete. 134 Further sensitivity analyses addressed the potential impact of the assumed pattern of transition between health states on the outcome results.
Results are reported as means with standard deviations (SDs) or as mean differences with 95% CIs. We compared differences in mean costs and effects in a regression framework, with a p-value of < 5% considered as statistically significant. We used non-parametric bootstrapping135 from the cost and effectiveness data to generate a joint distribution of the mean incremental costs and effects for the options under comparison and to calculate the 95% CIs of the incremental cost-effectiveness ratio (ICER). We represented uncertainty around the main cost-effectiveness estimates by cost-effectiveness acceptability curves (CEACs) using the net benefit approach. 136,137 CEACs show the probability that each option is cost-effective to a range of maximum values (ceiling ratio) that a decision-maker might be willing to pay for an additional unit of improvement in outcomes. We carried out all analyses according to the intention-to-treat principle, using Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA) and Stata 13 software.
Results
Outcomes
Table 19 shows the mean value of the different outcome measures (EQ-5D-3L, EQ-5D VAS and OxCAP-MH index) at baseline and at 6 and 12 months. There was no significant difference in the change in QALYs gained during the 12 months in comparison with baseline between the CTO and non-CTO groups (Table 20). Neither could we find an indication of benefit for CTO in comparison with non-CTO in terms of patients’ capabilities either in the complete case analysis (n = 67, mean OxCAP-MH index difference: 0.818, 95% CI –2.04 to 3.68; p = 0.58) or in the full imputed data set (n = 328, mean OxCAP-MH index difference: 0.527, 95% CI –0.62 to 1.68; p = 0.37).
| Measures | Baseline | 6 months | 12 months | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CTO (N = 163) | Non-CTO (N = 165) | CTO (N = 163) | Non-CTO (N = 165) | CTO (N = 163) | Non-CTO (N = 165) | |||||||
| Sample size | Mean {SD} | Sample size | Mean {SD} | Sample size | Mean {SD} | Sample size | Mean {SD} | Sample size | Mean {SD} | Sample size | Mean {SD} | |
| Complete case analysis | ||||||||||||
| EQ-5D-3L utility | 133 | 0.7 {0.27} | 139 | 0.7 {0.29} | 93 | 0.8 {0.28} | 90 | 0.7 {0.28} | 113 | 0.7 {0.34} | 109 | 0.7 {0.28} |
| EQ-5D VAS | 133 | 66.5 {23.05} | 138 | 65.3 {24.60} | 90 | 73.1 {17.66} | 87 | 68.8 {21.72} | 111 | 68.9 {21.74} | 105 | 71.0 {21.60} |
| OxCAP-MH index | 83 | 59.3 {10.03} | 87 | 57.4 {8.63} | 72 | 61.5 {8.22} | 64 | 59.0 {8.52} | 81 | 61.0 {8.38} | 85 | 59.7 {7.50} |
| Imputed full data set | ||||||||||||
| EQ-5D-3L utility | 163 | 0.7 {0.26} | 165 | 0.7 {0.27} | 163 | 0.8 {0.23} | 165 | 0.7 {0.22} | 163 | 0.7 {0.30} | 165 | 0.7 {0.25} |
| EQ-5D VAS | 163 | 65.7 {21.37} | 165 | 64.9 {22.73} | 163 | 72.8 {13.92} | 165 | 69.6 {16.31} | 163 | 68.2 {18.80} | 165 | 71.6 {18.29} |
| OxCAP-MH index | 163 | 59.0 {7.46} | 165 | 57.6 {6.51} | 163 | 61.4 {6.02} | 165 | 59.1 {5.80} | 163 | 60.9 {6.52} | 165 | 59.4 {6.37} |
| QALYs gained | CTO | Non-CTO | CTO vs. Non-CTO | ||||
|---|---|---|---|---|---|---|---|
| Sample size | Mean {SD} | Sample size | Mean {SD} | Mean difference | 95% CI | p-value | |
| Complete case analysis | |||||||
| QALYs gained | 69 | 0.03 {0.19} | 74 | 0.03 {0.23} | 0.003 | –0.07 to 0.07 | 0.94 |
| Imputed full data set | |||||||
| QALYs gained | 163 | 0.02 {0.19} | 165 | 0.02 {0.20} | 0.006 | –0.04 to 0.05 | 0.79 |
Costs
The mean costs per patient over the 12-month follow-up are listed according to the different resource-use categories and analysis scenarios in Table 21. Further discussion of the main cost results are based on the full imputed data set. The mean total health and social care costs were £35,959 per patient (SD £44,886) in the CTO group and £36,003 per patient (SD £41,406) in the non-CTO group. The costs of mental health hospitalisation accounted for > 85% of the annual health and social care costs. There was no indication of a significant difference between the groups in any of the investigated health and social care cost categories, either in the complete case or in the full imputed data set analyses.
| Costs | CTO (N = 163) | Non-CTO (N = 165) | CTO vs. non-CTO | |||
|---|---|---|---|---|---|---|
| n | Mean {SD} | n | Mean {SD} | Mean difference | 95% CI | |
| Complete case analysis | ||||||
| Total medication costs | 163 | 1266.0 {2123.03} | 165 | 1432.5 {1487.47} | –166.5 | –458.74 to 125.68 |
| Oral medication | 163 | 920.9 {44,862.35} | 165 | 895.6 {997.22} | 25.4 | –197.98 to 248.67 |
| Depot medication | 163 | 345.1 {348.30} | 165 | 536.9 {1281.88} | –191.9 | –421.08 to 37.34 |
| Total other health and social care costs | 95 | 35,984.9 {400.79} | 90 | 30,343.8 {34,974.91} | 5641.1 | –6665.50 to 17,947.63 |
| Mental health community/outpatient | 99 | 2172.8 {259.17} | 92 | 2054.1 {2565.27} | 118.7 | –551.86 to 789.29 |
| Mental health inpatient | 163 | 30,655.1 {1951.87} | 165 | 30,393.4 {41,341.95} | 261.7 | –9077.69 to 9601.07 |
| Non-mental health outpatient | 104 | 98.0 {49,540.10} | 100 | 133.0 {286.59} | –34.9 | –122.32 to 52.45 |
| Non-mental health inpatient | 106 | 75.9 {1064.80} | 101 | 405.1 {1827.76} | –329.2 | –693.68 to 35.38 |
| Primary care | 105 | 145.2 {778.43} | 99 | 238.8 {478.03} | –93.6 | –200.02 to 12.81 |
| Social care | 101 | 1216.5 {1198.90} | 98 | 1335.1 {2343.42} | –118.7 | –718.79 to 481.48 |
| Total health and social care costs | 95 | 37,197.9 {49,438.91} | 90 | 31,809.9 {35,064.79} | 5388.1 | –6912.97 to 17,689.07 |
| Indirect costs | 81 | 5307.6 {16,774.04} | 72 | 1355.0 {3647.60} | 3952.6a | 203.77 to 7701.47 |
| Lost productivity (sick leave) | 97 | 0.00 {0.00} | 85 | 55.00 {506.64} | –55.0 | –162.66 to 52.75 |
| Informal care | 83 | 5243.2 {16,574.11} | 76 | 1283.7 {3562.04} | 3959.5a | 304.97 to 7613.92 |
| Total societal costs | 59 | 37,756.4 {44,469.28} | 57 | 30,689.5 {33,045.08} | 7066.9 | –7157.99 to 21,291.81 |
| Imputed full data set | ||||||
| Total medication costs | 163 | 1266.0 {1198.90} | 165 | 1432.5 {1487.47} | –166.5 | –458.74 to 125.68 |
| Oral medication | 163 | 920.9 {1064.80} | 165 | 895.6 {997.22} | 25.4 | –197.98 to 248.67 |
| Depot medication | 163 | 345.1 {778.43} | 165 | 536.9 {1281.88} | –191.9 | –421.08 to 37.34 |
| Total other health and social care costs | 163 | 34,693.1 {44,928.06} | 165 | 34,570.7 {41,382.25} | 122.4 | –9228.61 to 9473.33 |
| Mental health community/outpatient | 163 | 2417.1 {2019.22} | 165 | 2280.8 {2424.34} | 136.3 | –346.30 to 618.94 |
| Mental health inpatient | 163 | 30,655.1 {44,862.35} | 165 | 30,393.4 {41,341.95} | 261.7 | –9077.69 to 9601.07 |
| Non-mental health outpatient | 163 | 92.6 {281.59} | 165 | 125.8 {238.42} | –33.2 | –89.71 to 23.29 |
| Non-mental health inpatient | 163 | 78.6 {332.40} | 165 | 312.4 {1439.77} | –233.7 | –459.27 to –8.21 |
| Primary care | 163 | 150.0 {221.39} | 165 | 207.8 {377.03} | –57.8 | –124.63 to 9.01 |
| Social care | 163 | 1299.7 {1707.99} | 165 | 1250.5 {1885.22} | 49.1 | –340.10 to 438.34 |
| Total health and social care costs | 163 | 35,959.0 {44,886.29} | 165 | 36,003.2 {41,406.39} | –44.2 | –9392.90 to 9304.56 |
| Indirect costs | 163 | 6138.4 {13,752.46} | 165 | 2992.6 {8407.44} | 3145.8a | 675.40 to 5616.22 |
| Lost productivity (sick leave) | 163 | 0.0 {0.00} | 165 | 28.3 {363.64} | –28.3 | –83.79 to 27.18 |
| Informal care | 163 | 6138.4 {13,752.46} | 165 | 2964.3 {8404.91} | 3174.1a | 703.91 to 5644.33 |
| Total societal costs | 163 | 42,097.4 {45,977.40} | 165 | 38,995.8 {41,475.12} | 3101.6 | –6378.23 to 12,581.51 |
Only one patient in the CTO group and five patients in the non-CTO group had any period of employment or self-employment during the 12-month follow-up period, and from these only one reported lost productivity due to sick leave. Patients in the CTO group had significantly higher mean informal care costs than patients in the non-CTO group: £6138 versus £2993, respectively (see Table 21). The mean number of manager hearings and tribunals per patient was also significantly higher in the CTO group, as would be expected (Table 22).
| Hearings/tribunals | CTO | Non-CTO | CTO vs. Non-CTO | ||||
|---|---|---|---|---|---|---|---|
| Sample size | Mean {SD} | Sample size | Mean {SD} | Mean difference | 95% CI | p-value | |
| Complete case analysis | |||||||
| Number of tribunals (MHRT) | 163 | 0.6 {0.72} | 164 | 0.3 {0.54} | 0.3 | 0.12 to 0.40 | < 0.050 |
| Number of manager hearings | 163 | 0.4 {0.55} | 164 | 0.2 {0.53} | 0.1 | 0.01 to 0.25 | < 0.050 |
| Imputed full data set | |||||||
| Number of tribunals (MHRT) | 163 | 0.6 {0.72} | 164 | 0.3 {0.54} | 0.3 | 0.12 to 0.40 | < 0.050 |
| Number of manager hearings | 163 | 0.4 {0.55} | 164 | 0.2 {0.53} | 0.1 | 0.01 to 0.25 | < 0.050 |
Cost-effectiveness
In the complete case analysis, the non-significant differences in mean costs (health and social care perspective £5388, societal perspective £7067) and mean effects (0.003 QALY gained) between the CTO and the non-CTO groups resulted in ICERs of £1,893,388/QALY gained from the health and social care perspective and £2,483,349/QALY gained from the societal perspective. After conducting multiple imputation of missing data, we found non-significant mean cost differences of –£44 from the health and social care perspective and £3102 from the societal perspective between the CTO and non-CTO groups. The mean effects difference (0.006 QALY gained) was also non-significant resulting in ICER point estimates of –£7651/QALY gained (health and social care perspective) and £537,292/QALY gained (societal perspective), respectively.
Figure 11 illustrates the uncertainty around the ICER point estimates using scatterplots of the bootstrapped cost and effectiveness pairs for CTO compared with non-CTO for the different analysis scenarios. The points in the scatterplot fall in all four quadrants of the cost-effectiveness plane, suggesting that there is no unequivocal conclusion to be drawn regarding the cost-effectiveness of CTO in terms of QALYs gained. Figure 12 shows the relevant statistical uncertainty in the form of CEACs. These clearly illustrate that, independently of the analysis scenario, the probability of CTO being cost-effective remains at ≤ 50% or below at the currently considered maximum UK cost-effectiveness threshold value of £30,000/QALY. 121
FIGURE 11.
Bootstrapped mean differences in costs and effects of CTO vs. non-CTO. (a) Health and social care costs, complete case analysis (n = 121); (b) health and social care costs, imputed full data set (n = 328); (c) societal costs and effects, complete case analysis (n = 102); and (d) societal costs and effects, imputed full data set (n = 328).
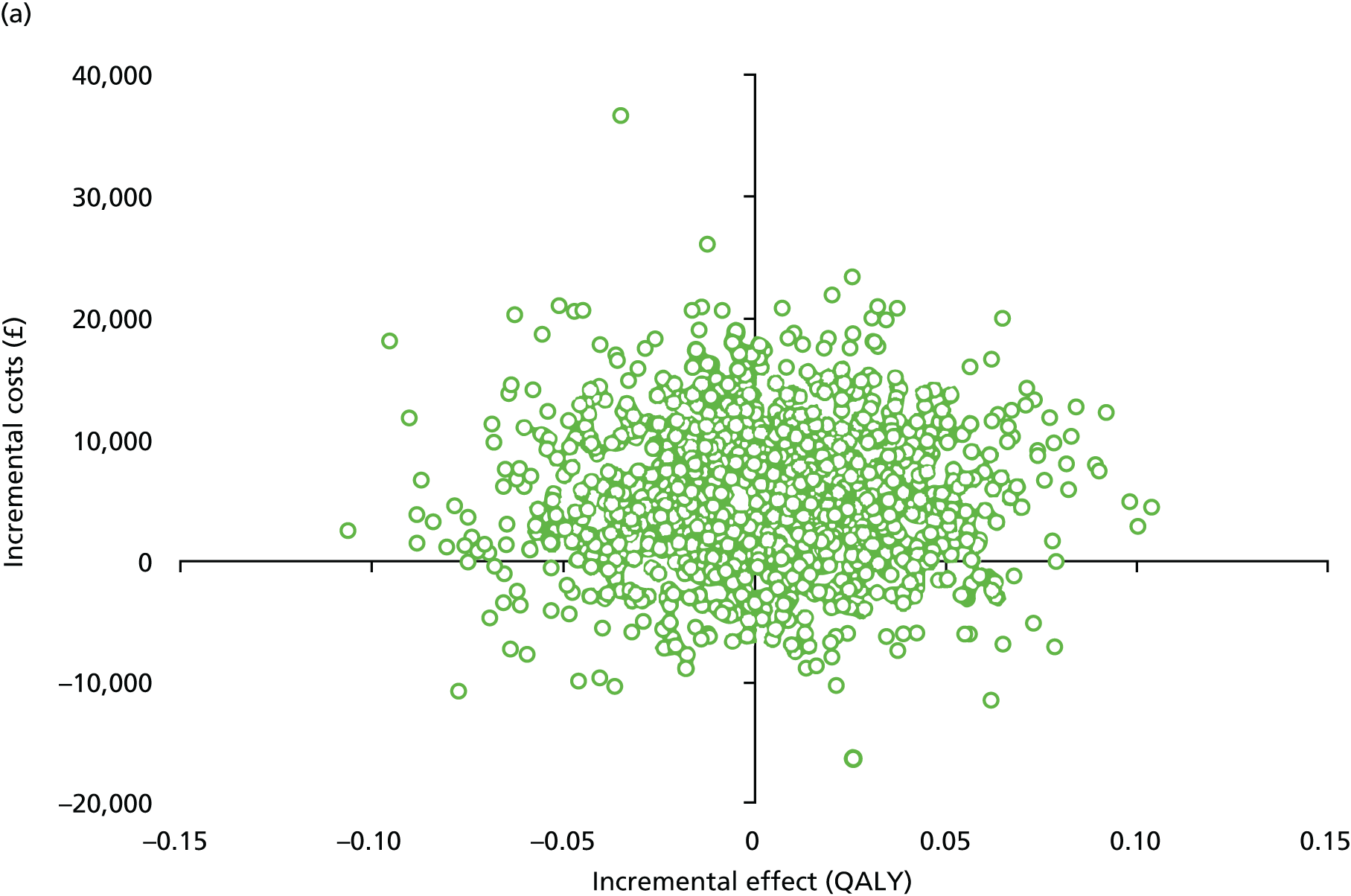
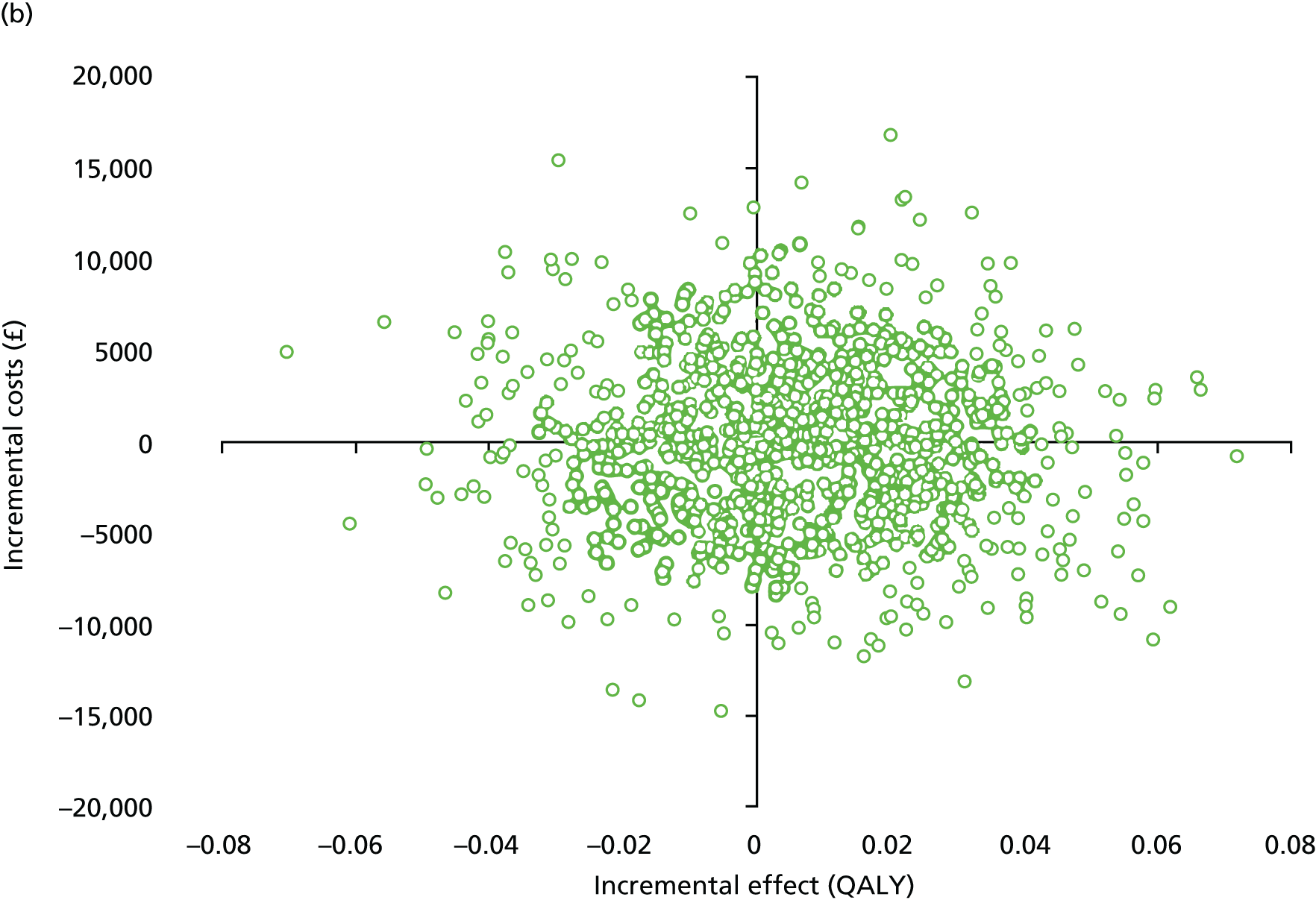

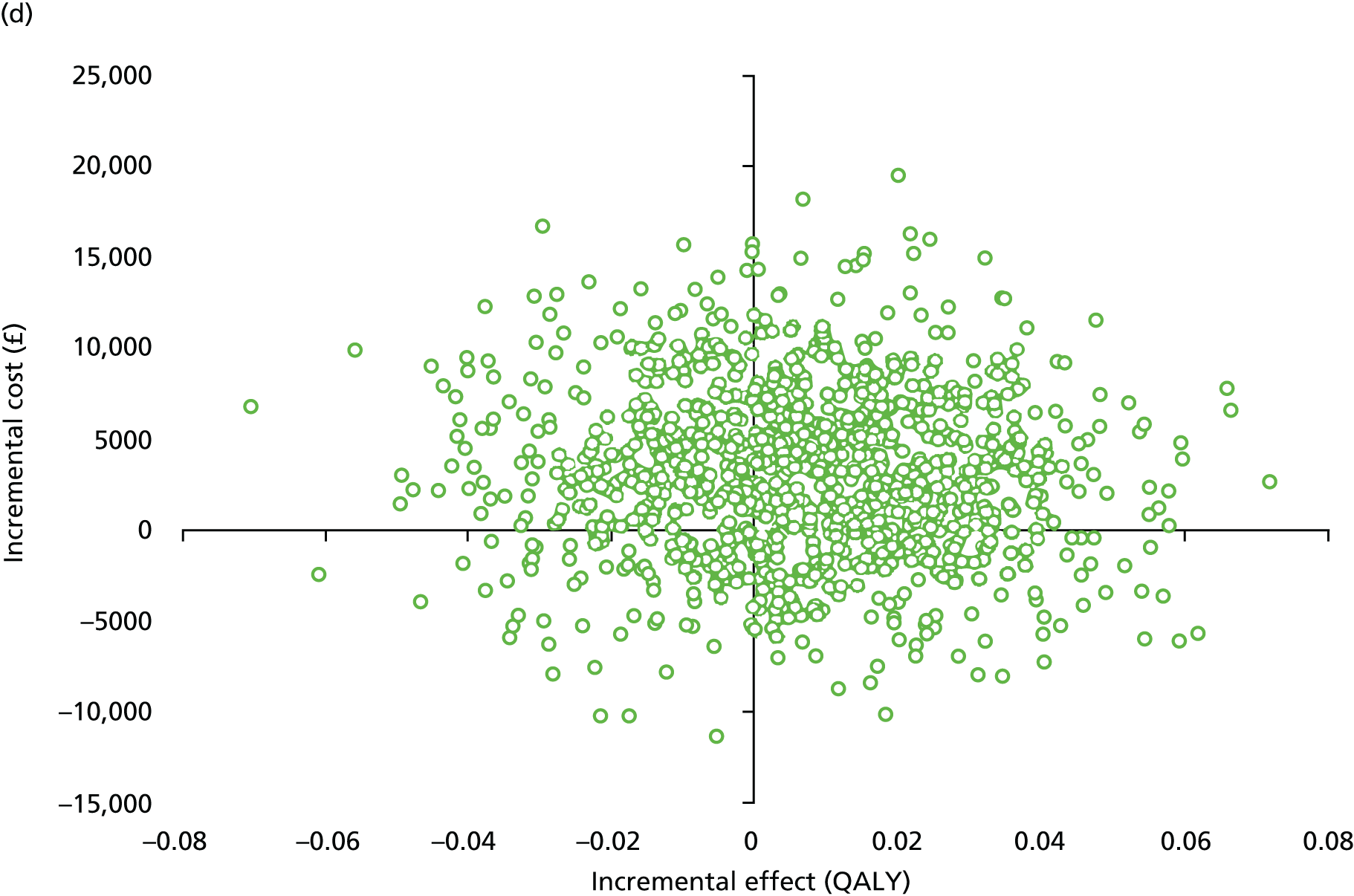
FIGURE 12.
Cost-effectiveness acceptability curves. (a) Health and social care costs, complete case analysis (n = 121); (b) health and social care costs, imputed full data set (n = 328); (c) societal costs, complete case analysis (n = 102); and (d) societal costs, imputed full data set (n = 328).
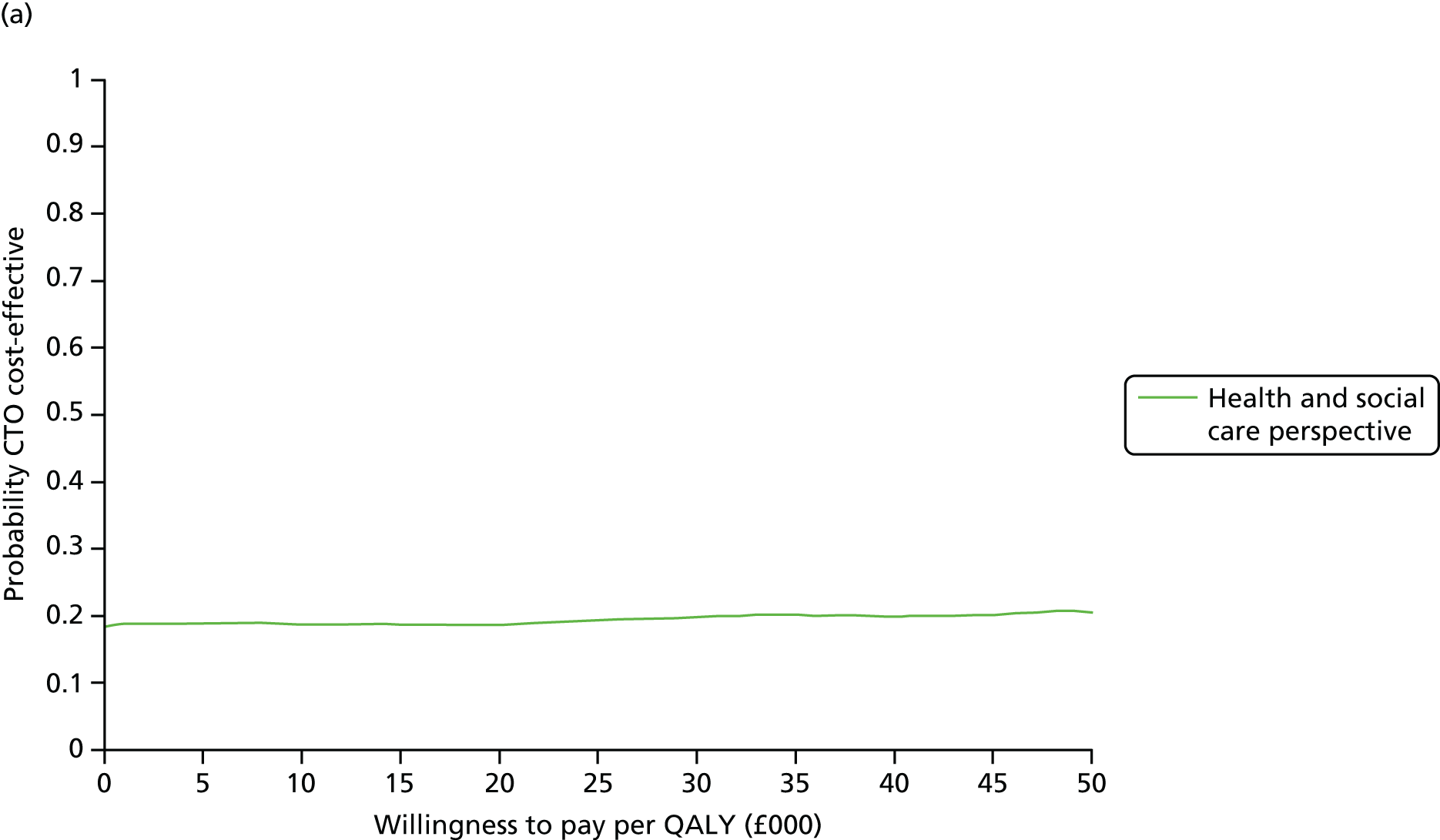
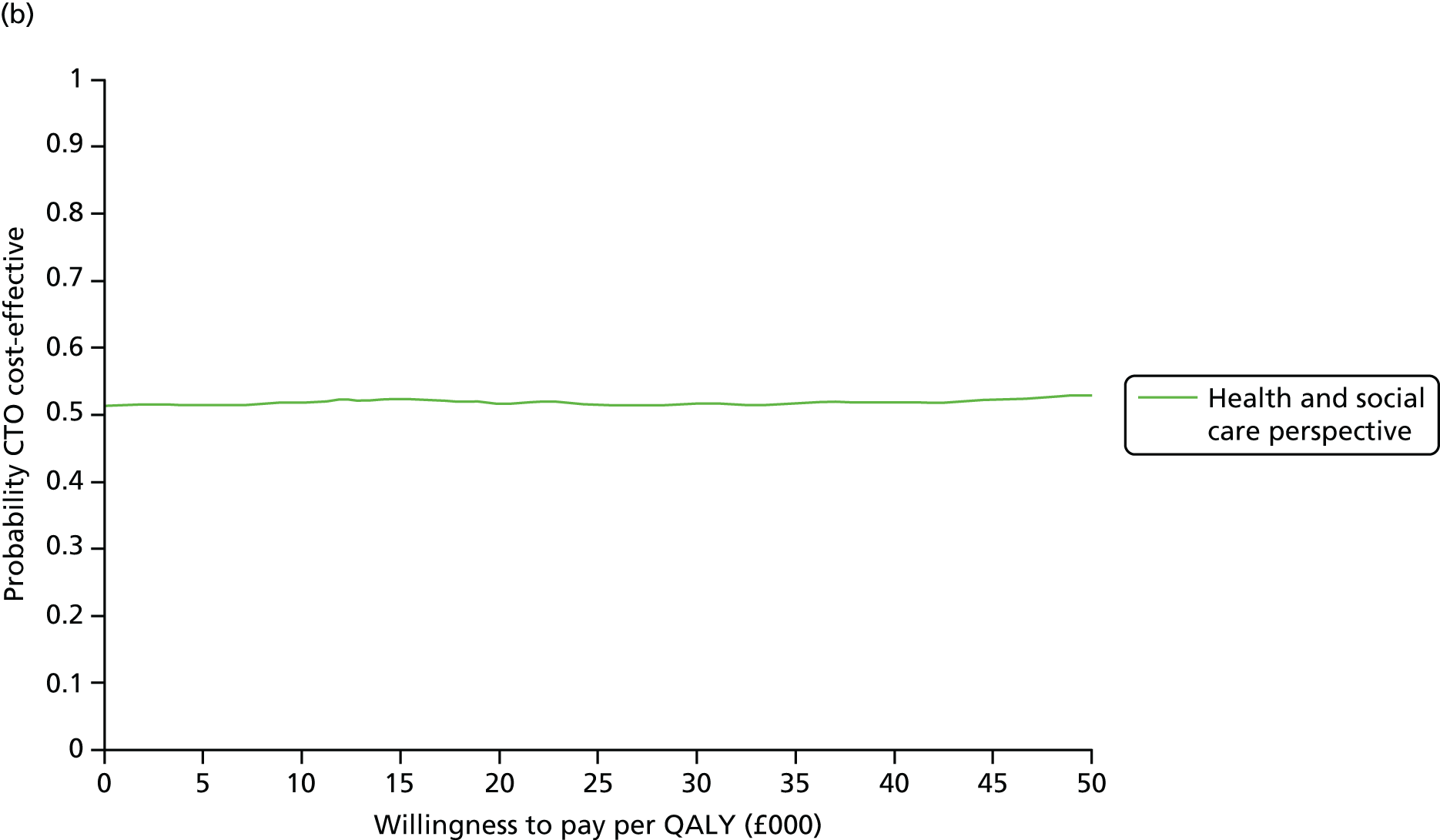
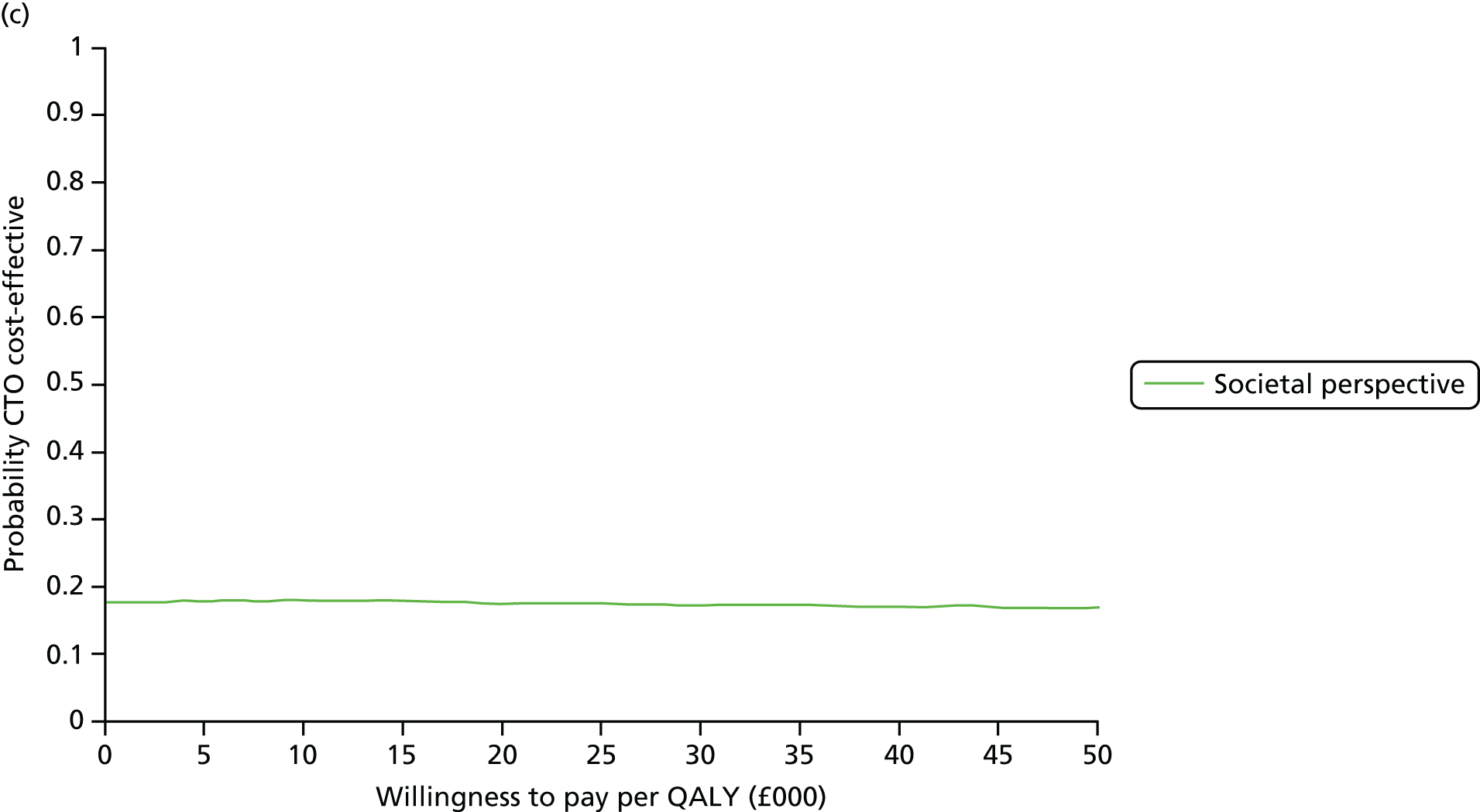
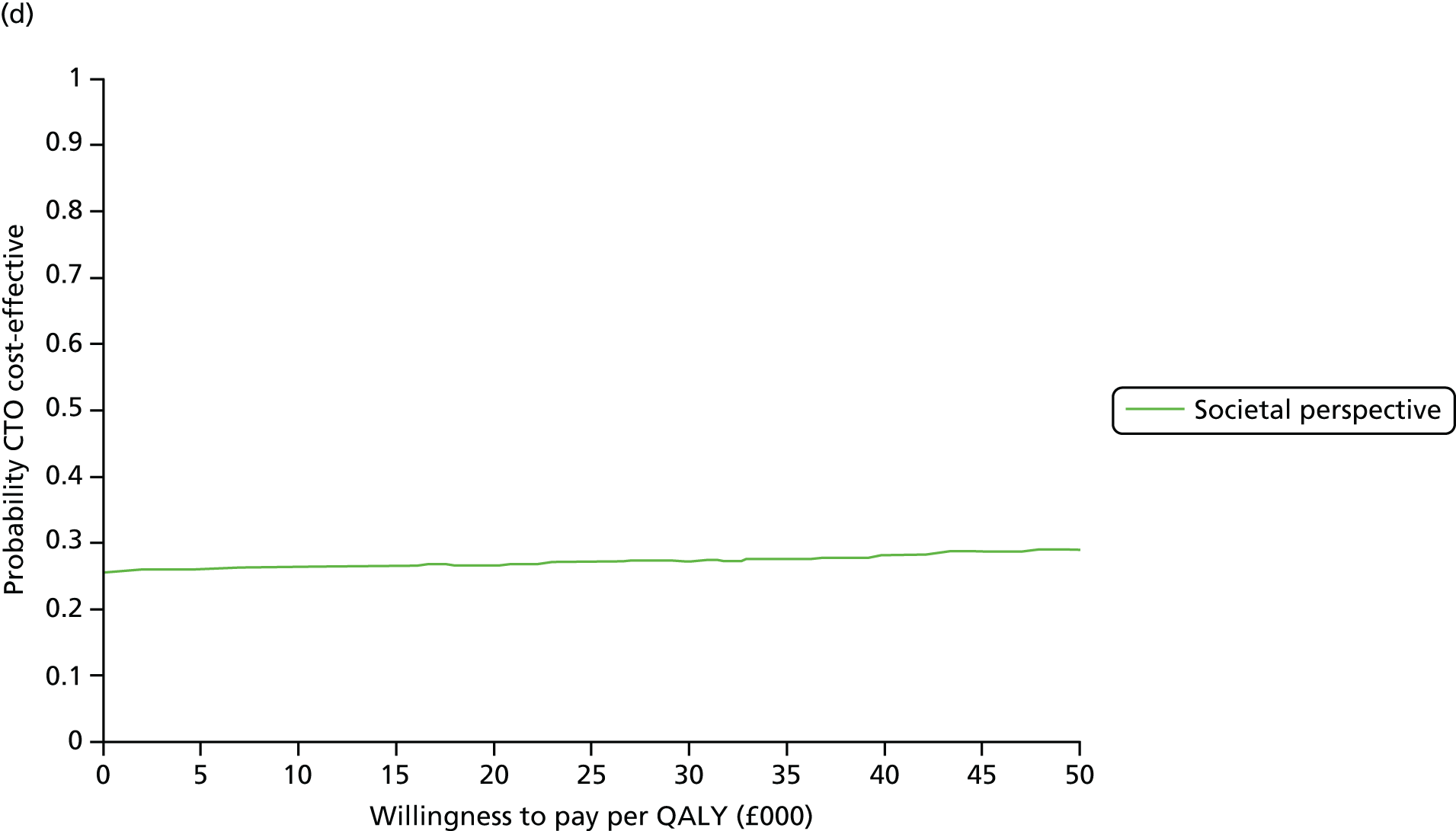
The assumed pattern of transition between health states had no impact on the final results and conclusions. The mean QALY difference was –0.008 (95% CI –0.10 to 0.08; p = 0.87) between CTO and non-CTO when transition was assumed at the beginning of the time period, and 0.017 (95% CI –0.03 to 0.07; p = 0.49) when transition was assumed at the end of the time period.
Conclusions
-
The results did not support the hypothesis that CTOs would result in reduced hospitalisation costs.
-
There was no evidence of any health or social care cost savings in the CTO group.
-
CTOs significantly increased informal care costs and the costs of legal procedures.
-
CTO use had no significant impact on patients’ health-related quality of life or capabilities.
-
CTOs are unlikely to be cost-effective from a health and social care or a broader societal perspective.
Chapter 8 OCTET Qualitative Study
Introduction
We designed the OCTET Qualitative Study in order to study the social mechanisms of compulsion in community mental health care, and to explore in depth participants’ perceptions of compulsion under CTOs. The objective was ‘to conduct a detailed qualitative assessment of the experiences of patients, staff and carers with Community Treatment Orders’. Current literature on personal experiences of CTOs is very limited and suggests that patients hold ambivalent, and sometimes contradictory, views about CTOs; family carers generally find them helpful, though limited; and most psychiatrists find them useful. 68,73,75–78 Given that CTOs were introduced so recently in England and Wales, no study of personal experiences of the English CTO regime exists. The OCTET Qualitative Study therefore aimed to contribute to a fuller picture of how the law is implemented and how CTOs operate in practice by examining psychiatrists’, patients’ and family carers’ experiences.
This chapter draws substantially on a paper published by members of the members of the OCTET Coercion Programme Group: Canvin et al. ,138 with permission from Springer Publishing Company.
Methods
Design
Individual in-depth interviews provide rich data on personal experience and are particularly appropriate for studying sensitive research topics. We conducted interviews with patients (AS), family carers (JR) and psychiatrists (KC), respectively. We initially invited participants to tell their story freely and then used a semistructured topic guide to ensure that the same topics were covered in each interview (allowing for within- and between-case comparisons). The topic guide was developed in co-operation with service user and carer representatives. (It is available from the authors by request.) The interviewers were Anna Sulman (AS, social science graduate, white British female, early thirties), Jorun Rugkåsa (JR, PhD in sociology, white Norwegian, early forties) and Krysia Canvin (KR, PhD in Law, white British, late thirties).
The interviews with each subsample used a specifically designed topic guide containing open-ended questions in order to spark discussion of specific topics, followed by open, participant-driven elaboration. We developed the topic guide from emerging findings in the OCTET Trial and from the literature, and piloted it to ensure its acceptability to participants. Topics included experiences of and views about:
-
mental health services (views on compulsion and, in particular, its use in mental health care)
-
CTOs and Section 17 Leave and how they work
-
other types of coercion and how they work.
Interviewers prompted participants about CTO conditions and recall. We probed for nuance, including changes over time and circumstances, and differences between CTOs and other inpatient and outpatient interventions. We also asked family carers questions regarding their views and experience of informal coercion in general and of leverage in particular. We asked psychiatrists about the ethical challenges of working with CTOs and Section 17 Leave. We offered patients and family carers £25 as a compensation for their time. After the interview, we gave participants the opportunity to review their transcript before providing consent for the use of direct quotations. We audio-taped all interviews and transcribed them ad verbatim. A researcher checked the transcripts for accuracy and returned them to the participant if the participant had indicated that they wished to review it. If a participant did not want a particular section quoted, this was marked in the transcript. Atlas.ti qualitative analysis software version 6.2. (Scientific Software Development, Berlin) aided the storage, management and retrieval of data.
Sampling and data collection
Sampling was purposive and aimed to achieve maximum variation139 of characteristics that were expected to influence views, experiences and use of CTOs. The sampling pool for patient interviews comprised the 237 patients (119 CTO, 118 non-CTO) from the OCTET Trial sample who had agreed to be approached about the Qualitative Study (93 declined, 3 were deceased). As we were primarily interested in personal experiences of being under a CTO, we aimed to sample 75% of interviewees from the CTO arm. We recruited psychiatrists from the pool of those with whom we had discussed recruitment to the trial. This included psychiatrists from both inpatient and outpatient settings and psychiatrists who did and did not recruit to the trial. We recruited family carers via carer organisations, research collaborators and via snowballing.
Analysis
We utilised a modified version of Grounded Theory,140 an inductive methodology concerned with producing theoretical and conceptual insights grounded in empirical data. Following initial line-by-line ‘open’ coding of the transcripts,141 we identified patterns and deviant cases using the constant comparative method. 142 Coding and initial analyses were undertaken while the relevant researcher was blind to the OCTET Trial results.
When conducting qualitative analysis, as we elaborate in more detail in relation to the ULTIMA Qualitative Study (see Part 4, Chapter 19), researchers usually decide a posteriori which analytical strands to pursue and in what order. Given the aim of the overall programme, we decided first to pursue analysis of participants’ experience of the mechanisms by which CTOs were designed to work (conditions and recall) and their impression of how they worked.
The four themes discussed below originated from different aspects of the Grounded Theory analytical approach used. Taking a deductive approach, we specifically asked about and coded for participants’ experiences and views of CTO recall and conditions. An inductive analytical approach led to the emergence of the notion of legal clout. We also sought data on participants’ considerations about the effectiveness of CTOs, as this was part of the overall agenda for the OCTET Study. Rather than using a preconceived definition of effectiveness, here we used participants’ descriptions compared against their perceptions of the purpose of CTOs, combining the deductive and inductive approaches. We conducted focused coding141 in order to identify and analyse all mentions of these themes. All members of the qualitative research team provided input into the analysis through regular discussion of the findings and their interpretation.
We also examined the interview transcripts closely to identify ethical issues arising (as reported separately; see Chapter 9).
Results
Sample
Of the 45 patients with whom we made contact, three in the CTO arm of the RCT and one in the non-CTO arm declined to participate. Two CTO patients and two non-CTO patients cancelled their interviews. None of the 25 psychiatrists approached declined to participate. A total of 26 family carers volunteered and were interviewed. Participants were geographically spread across England and attached to a range of mental health teams, including Early Intervention Services (EIS), CMHTs, AOTs and forensic teams, and together they had experience of the various aspects of CTOs. Interviews lasted on average 65 minutes (range 25–135 minutes). The sample is described in Table 23.
| Characteristic | Psychiatrists (N = 25) | Patients (N = 37) | Carers, N = 26a (patients cared for, N = 23)b | |
|---|---|---|---|---|
| With CTO experience (n = 26) | Without CTO experience (n = 11) | |||
| Male | 19 | 18 | 6 | 7 |
| Ethnicity | ||||
| White | 18 | 14 | 11 | 23c |
| Black | 1 | 7 | 0 | 0 |
| Others | 7 | 5 | 0 | 3 |
| Diagnosis | ||||
| Schizophrenia | – | 18 | 7 | (21) |
| Bipolar disorder | – | 7 | 0 | (3) |
| Other psychosis | – | 1 | 4 | (2c) |
| Depot medication | – | 14 | NK | (11) |
| History of violence | – | NK | NK | (12) |
| Team | ||||
| CMHT | 6 | 11 | 6 | – |
| AOT | 6 | 9 | 2 | – |
| EIS | 2 | 1 | 1 | – |
| Forensic | 1 | 0 | 0 | – |
| Unknown | 0 | 5 | 2 | – |
| Setting/role | ||||
| Inpatient | 7 | – | – | – |
| Community | 14 | – | – | – |
| Inpatient/community | 4 | – | – | – |
| SOAD | 1 | – | – | – |
| Recruited for OCTET | 19 | – | – | – |
| Relationship to patient | ||||
| Parent | – | – | – | 22 |
| Spouse | – | – | – | 3c |
| Sibling | – | – | – | 1 |
| CTOs used | ||||
| 0 | 2 | – | – | – |
| 1–10 | 11 | – | – | – |
| 11–20 | 4 | – | – | – |
| ≥ 20 | 8 | – | – | – |
| CTO status | ||||
| Ongoing CTO | – | 13 | – | (14) |
| Revoked | – | 4 | – | (2) |
| Ended (reason unknown) | 8 | – | (0) | |
| Discharged | – | 0 | – | (3) |
| Unknown | – | 0 | – | (5c) |
| Duration of CTO (months) | ||||
| < 6 | – | 15 | – | (1) |
| 6–12 | – | 8 | – | (9) |
| ≥ 12 | – | 2 | – | (8) |
| Unknown | – | 0 | – | (5c) |
| Experience of recall | – | 7 | – | (8) |
The topic of the analysis reported here was the experience of CTOs, so this did not include patients in the non-CTO arm. Two family carers were also excluded as the person they cared for had not been on a CTO. We therefore report from interviews with samples of the 26 patients with CTO experience, 24 family carers and 25 psychiatrists.
Quotations from the transcripts are included to illustrate and validate our interpretations. 143 Words and short phrases appearing in the text in quotation marks are examples of the language used by participants. Words appearing in italics indicate descriptive analytical labels reflecting themes. Quotations are attributed to patients identified by a unique patient identification (ID) number, team and CTO status (e.g. ‘CTO ongoing’); family carers identified by a unique carer ID number and relationship to the patient; and professionals identified by profession, unique ID number and type of service. When this is a dialogue with the interviewer, speakers are identified in full, where first mentioned, and by P (patient), C (carer) or I (interviewer) subsequently.
Views and experiences of community treatment order conditions
As described above (see Part 2, Chapter 5), the CTO regime in England and Wales specifies two mandatory conditions that apply to all CTOs:48 first, patients who refuse medication or who lack capacity must be assessed by a second opinion appointed doctor (SOAD) to confirm that the treatment specified is appropriate; and second, all patients must make themselves available for assessment for renewal of the CTO. The RC and AMHP who initiate the CTO may also specify discretionary conditions based on their knowledge of an individual patient. We asked psychiatrists, patients and family carers about their experience of CTO conditions.
Psychiatrists’ perspectives
Psychiatrists’ accounts of inserting discretionary conditions were strikingly pragmatic. Overall, they proposed that conditions could be as useful as only their content and design allowed. Most designed conditions primarily with effectiveness in mind. Many described inserting only ‘minimal’ conditions, the ‘usual’ ones being adherence to medication and contact with the mental health team. The criteria that psychiatrists repeatedly mentioned as guiding their design of conditions were achievability and enforceability: conditions that were neither achievable nor enforceable were reportedly avoided. Similarly, it was considered important to make the wording as ‘broad’ as possible to accommodate probable changes in personnel or treatment and permit control over detail by the CMHT. None of the psychiatrists interviewed described inserting conditions related to work or social activities: such conditions were dismissed as ‘unworkable and pointless’ (consultant psychiatrist 2, inpatient/community).
There was variation in psychiatrists’ attitudes towards and use of other conditions, such as those stipulating, for example, abstinence/moderation of substance or alcohol use, participation in psychological therapies or, as the two following excerpts demonstrate, residence in a specified place:
We might specify a residence if that’s a particularly important element that needs to be in place. It may be supported accommodation. A lot of our people have been through a variety of housing set-ups, have failed to maintain tenancies and a lot of them tend to drift around a bit and it can be sometimes difficult to sort of keep tabs.
Consultant psychiatrist 4, AOT
There’s often some confusion about whether you can [stipulate a specific residence]; and I’ve seen people who’ve had it on them [. . .]. I don’t think, as far as I’m aware, that it’s the right use of [CTO].
Consultant psychiatrist 13, inpatient
This variation and other deviations from the criteria described arose out of the need, albeit infrequent, to insert a condition that catered for the specific needs of an individual patient. They took into account, for example, factors such as patient safety, the practicality of monitoring patients’ whereabouts and the likelihood of substance misuse-related deterioration (despite treatment adherence).
Patients’ perspectives
From the patient perspective, the CTO and its conditions were synonymous. Most patients described ‘having to’ do various things as part of their CTO, including ‘having to’ take medication:
They just want me to take the medication but I think the mental health services rely too much on medication and not enough on other means of solving people’s problems.
Patient 1, CMHT, ongoing CTO
Despite this, some expressed confusion about whether or not their CTO included conditions and few spontaneously referred to conditions per se. None of the patients interviewed distinguished between mandatory and discretionary conditions.
Patients’ reported responses to their conditions ranged from matter-of-fact acceptance to outright rejection; some patients questioned their necessity (and the need for compulsion): ‘I’m not criminal; I don’t know why I have to report everything I do’ (patient 2, CMHT, CTO finished). ‘Medication ties’, travel restrictions and accommodation conditions were viewed by patients as restricting their freedom; a few expressed feelings of being ‘trapped’ or ‘imprisoned’. One or two welcomed the CTO as a ‘safeguard’ and compared it to being sectioned in hospital:
On the surface [the CTO] does seem freer [. . .]. It was better than being on section [involuntarily detained in hospital] because you would end up in hospital being away from everybody.
Patient 37, AOT, CTO finished
Family carers’ perspectives
Family carers portrayed conditions as a helpful mechanism because the CTO carried legal authority that carers did not, or could not, apply themselves, at least not without risk of damaging their relationship with the person for whom they cared. Taking medication and keeping in contact with services were the most frequently mentioned conditions. Understanding of CTO conditions varied, however. Many, but not all, had seen formal documentation, or had been otherwise informed of what conditions applied. Others struggled to distinguish the conditions of the CTO from what mental health teams encouraged patients to do (e.g. give notice of travel) or confused them with other obligations, for example parole conditions or curfew rules imposed by supported housing. Some reported that the mental health teams also appeared uncertain about how CTO conditions could be used. Some said, for example, that they had been told that depot medication was a necessary CTO condition (although there were cases when this was challenged and amended). One carer reported being told that abstinence from alcohol could not constitute a CTO condition. Others pointed out that the mental health team restricted the use of conditions:
Can you remember what conditions were put on the CTO? What kind of things he had to do?
I think it was just medication. Because the other things like his drinking or his cannabis smoking, that was very much left to him, he had to approach the services for support.
Some expressed disappointment about this and mentioned further conditions that they would have liked further to have been included, such as social engagement:
If the team were active and found something for this intelligent man to do [. . .] then I would see a way of recovery in terms of being included in things and going out and getting fresh air.
Would he do it do you think if [the team] came knocking on the door?
If he had to.
OK, so it would have to be made conditional?
Absolutely. If it meant that rather than hospital he would [do it].
Views and experiences of recall to hospital under the community treatment order
Under a CTO, a patient may be recalled to hospital when the patient (1) requires treatment in hospital and in the absence of recall there would be a risk of harm to self or others, or (2) does not comply with one of the mandatory conditions. As described above, the Code of Practice states that patients and their families should be consulted about the CTO, its conditions and the need to recall. 48 We asked psychiatrists, patients and family carers about their experience of recall.
Psychiatrists’ perspectives
The majority of psychiatrists perceived the power of recall to be the mechanism that gave the CTO its ‘teeth’, at least theoretically. From psychiatrists’ perspectives, adherence was driven by patients’ belief that non-adherence would (automatically) lead to hospitalisation via recall.
Interpretations of the law and the Code of Practice relating to the use of recall varied. Some psychiatrists expressed continuing uncertainty about the lawfulness of using recall to give depot injections to patients for refusing medication or for non-compliance with discretionary conditions. Most – but not all – interpreted the Code as requiring evidence of deterioration in the patient’s mental health for recall. For some, this requirement set the threshold for recall disappointingly high and limited the utility of CTOs in practice. Regardless of their interpretation, however, some psychiatrists’ accounts of how they explained the CTO to patients suggested that they did not share their concerns about the limitations with patients:
The patient is not always entirely clear what happens and I don’t always clarify exactly what happens either.
Consultant psychiatrist 24, Forensic inpatient/community
Although some psychiatrists reported reminding non-compliant patients about the potential for recall as a way of enforcing medication adherence, some expressed concern about doing so: ‘Is it blackmailing when you say ‘recall or injection’?’ (consultant psychiatrist 11, CMHT).
Although the overall view of recall was positive, many psychiatrists described the recall procedure as ‘a hassle’, complex or too time-consuming. Various limitations were mentioned: the 72-hour assessment period was thought to be inadequate; insufficient availability of inpatient beds was said to limit use of recall; and lack of clarity about out-of-hours or out-of-area procedures had reportedly caused logistical difficulties in several cases. A few psychiatrists thought that the recall procedure permitted quicker hospital admission but others indicated that, given its limitations, the CTO added little and expressed a preference for conducting MHA assessment:
Sometimes the whole thing gets so cumbersome that you will feel, ‘Golly, let’s forget about this and go back to normal service with the Mental Health Act’.
Consultant psychiatrist 4, AOT
Patients’ perspectives
Patients were acutely aware of what they viewed as the ‘threat’ of recall ‘hanging over’ them. Only two patients used the term ‘recall’ unprompted, and some could not remember whether or not they had ever been recalled. In contrast with psychiatrists, patients generally perceived that recall had a relatively low threshold and could be used for non-compliance with conditions, one-off refusal of medication, general non-co-operation or simply ‘on a whim’ (patient 17, CMHT, CTO finished). A few patients with experience of recall said the power could be used if they exhibited signs of illness:
All I know is that if I don’t take my depot and they think – and my CPN [community psychiatric nurse] or my doctor thinks I’m not very well then they can put me back into hospital without me having a say in it really.
Patient 35, EIS, ongoing CTO
Although most expressed the view that: ‘I would rather take my medication’ than go to hospital, the potential for recall to hospital was only one reason that patients gave for medication adherence. One or two said ‘nothing would happen’ if they did not adhere.
Patients recognised that recall was a ‘new’ power:
Well basically when I was on my section they would give me the Clopixol injection and then when I come off my section I would say I didn’t want to have the injection any more and I’d stop the injection. [. . .]
[. . .] You refused to take it?
Yeah I refused to take it.
[. . .] What did they use to do or say to try and encourage you?
There was nothing they could do.
Nevertheless, patients expressed the sentiment that there was little difference between recall and being involuntarily detained: both led to involuntary hospitalisation. Some expressed a preference for the recall procedure because of, for example, being recalled by letter rather than ‘everybody coming round’, being taken to hospital by car rather than ambulance, and being admitted more quickly.
Family carers’ perspectives
Family carers also described the power of recall as giving ‘teeth’ to CTOs and the ‘threat’ or ‘fear’ of readmission as instrumental in increasing medication adherence. Knowing that their relative could be returned to hospital without fully relapsing relieved some carers’ anxiety about patient well-being and, for a few, their own safety. One carer said that the power of recall meant she was ‘not the nervous wreck I was’ (carer 2, parent). Some noted that as the recall function had not yet been tested in their case, it was unclear if it represented an improvement. Most of those who did have experience of recall said that, helpfully, it had happened without delay [e.g. via general practitioner (GP) referral or MHA assessment]:
He wouldn’t take his medication when he relapsed and that was the reason they could take him back into hospital. So we would have perhaps a fortnight of it instead of four months. [. . .] It makes such a difference. It saves us all so much distress.
Carer 2, parent
One carer, however, said that she had successfully intervened to prevent what she considered premature recalls of her daughter on several occasions. Another, after alerting the mental health team to her son’s deterioration, had the recall stopped when she realised that no beds were available locally. Not all carers reported this level of influence, however.
The criteria for recall were unclear to many: some thought it followed automatically if a condition, particularly pertaining to medication, was breached. Others believed signs of deterioration were required.
It wasn’t clearly spelled out to him. I couldn’t get a clear grip on that if you don’t do A then B will happen; what B was. [. . .]. All of that was very unclear.
Carer 26, parent
Influence of legal clout
All three groups referred to respect for the legal powers of the CTO and those administering them and how this influenced patients’ behaviour: we refer to this as legal clout.
Psychiatrists’ perspectives
For psychiatrists, the main purpose of the CTO was legally to oblige patients to engage with services and be compliant with prescribed medication:
I think a bit of the law actually helps because they worry, ‘Oo, better keep going with it. This is the law. The doctor says it’s the law so I’ll stick with it’.
Consultant psychiatrist 2, inpatient/community
The legal clout dimension of the CTO was perceived to be pivotal for some patients: ‘Certain people, just because they’re on a [CTO], toe the line’ (consultant psychiatrist, 12, EIS).
Patients’ perspectives
Patients’ perceived the CTO as a legal tool for enforcing their adherence to treatment:
They use the law to keep somebody to do things against their will like to give them medication.
Patient 1, CMHT, ongoing CTO
Most seemed to understand that adherence to the CTO and its conditions was a ‘legal requirement’. These patients viewed the CTO as tantamount to being ‘forced’ to take medication and feeling forced was one of the main reasons given by patients for adhering to medication: ‘If it was free choice I would say, “No, I do not want it”’ (patient 6, ongoing CTO). All patients, however, appeared to understand that medication could not be administered by force in the community setting: ‘They can’t treat you at home, but they can inject me without sectioning’ (patient 31, AOT, ongoing CTO).
Family carers’ perspectives
Like patients, family carers also largely saw the main rationale of the CTO as obliging patients to take medication:
He’s been on a regular depot medication and he knows that if he attempted to refuse it, which he’s done many times in the past, he could be taken back into hospital without further ado.
Carer 24, parent
Family carers considered their relative’s respect for the law and/or the power of recall to be the key mechanism for achieving adherence: ‘He’s getting the consequences. This really is up to him’ (carer 2, parent). As such, legal clout could be more effective than familial pressure.
Impressions of community treatment orders’ effectiveness
All three groups expressed the idea that the desired effects of CTO would be adherence and avoiding hospitalisation. The extent to which they thought this was achieved in practice varied within and between the groups.
Psychiatrists’ impressions
Most psychiatrists interviewed reported examples of when they thought that the CTO had been effective in terms of adherence to medication and readmissions, and when it had not. One AOT psychiatrist with 15–20 patients on CTOs commented that in his experience:
One third or so have a major beneficial response. There’s another third who it makes some difference [to] but it’s not the entire answer (and it’s never going to be) and the other third it doesn’t make a shadow of difference.
Consultant psychiatrist 4, AOT
Some said, however, that it was ‘too early’ to tell and some were awaiting the OCTET Trial results. Others said that the numbers seen in their own practice were too small to be able to judge: ‘You’ve got to look at hundreds of cases before you are actually able to draw a conclusion’ (consultant psychiatrist 7, inpatient/community). There was also reluctance to attribute changes in patients’ outcomes to the CTO alone: ‘It is really difficult to disentangle how much of this is due to the CTO’ (consultant psychiatrist 9, AOT).
None of the psychiatrists interviewed said that CTO patients received anything different or extra compared with non-CTO patients. Nevertheless, some referred to potential benefits afforded by the CTO, such as structure and a period of stability. Also, some described pairing the CTO with depot medication with a view to facilitating enforcement:
Unless [the patient’s] family take a keen interest in monitoring the medication there usually are issues with non-compliance; with the depot we know when they have missed and we can sort of enforce that.
Consultant psychiatrist 17, AOT
Patients’ impressions
Some patients described feeling well and enjoying greater stability since being on a CTO, but not many thought that they spent less time in hospital or had fewer admissions: ‘I’m the sort of person who is in and out of hospital like a yo-yo with CTOs or without them’ (patient 17, CMHT, CTO revoked). A few patients attributed their improved treatment adherence to the CTO: ‘I would have just carried on the way I was before really which, no not as good. I prefer this’ (patient 21, ongoing CTO).
One reason identified by patients for their improved adherence to medication was the use of depot medication:
Before I used to miss my medication and with the depot, they know I’m taking the depot. [. . .]
What’s made you take it?
Because before, there wasn’t any CTO I think they got a new CTO on their scheme you know. And from then you have to take the depot if you don’t you will be staying in the hospital for a bit of time. [. . .] They’ve got more power than me. Yes that’s why.
Another reason was being generally monitored and/or observed taking oral medication by professionals or family carers: ‘They see the tabs in my hands and [watch] me put them in my mouth’ (patient 17, CMHT, CTO ended). This kind of close monitoring of medication was experienced by some as unnecessarily intrusive and disempowering, and as getting in the way of living a ‘normal life’, including a social life and ability to work. Other factors affecting adherence were also described, including change of mental health team, retention of social security benefits (one patient believed receipt of benefits was dependent upon treatment adherence) and doing it for their family.
Family carers’ impressions
Most carers reported unprecedented or improved adherence (during and beyond the CTO period) and several said that their relative had not been back to hospital (either voluntarily or via recall) under the CTO. Some described improvements in social functioning, including two patients in part-time employment and two who had formed romantic relationships. Although some attributed these outcomes to the CTOs working as intended, others suggested that there could be factors in addition to CTOs causing this. Moreover, they posed the question of whether or not, with the right resources and attitude, intensive community services could achieve similar results without the need for a legal, coercive regime that patients often opposed.
Lack of support beyond medication was a grave concern shared by all family carers:
He’s simply being held by a drug really. A drug he needs, but that isn’t all that he needs [. . .] I’d like to see compliance strengthened by [a] really good CMHT. Some people say well he has more freedom on a CTO because he takes the medication. But I don’t see that. I see that he doesn’t have more freedom because it doesn’t address the other issues.
Carer 13, parent
Some said that the focus on medication meant that CTOs addressed only positive symptoms such as hearing voices or hallucinations, and not negative symptoms such as blunted affect, lack of motivation or desire to engage socially. Addressing positive symptoms alone was considered insufficient for recovery or for ‘having a life’ (carer 24, parent). One woman said her son was simply ‘contained at home’ rather than hospital and his social functioning had not improved, ‘not an iota’ (carer 13, parent). A couple compared hospital favourably to CTOs because patients there could at least engage in activities and with other people.
Many of the family carers saw their involvement as potentially contributing to the effectiveness of CTOs. Good communication with mental health teams, including obtaining the right information at the right time, was a precursor to achieving this. Some family carers monitored compliance with conditions and were in continuous communication about this with clinicians. Others said they were ignored or excluded from decision-making, whereas others again welcomed the opportunity to take a step back: ‘It’s nice being just mum’, because ‘the onus now is on the services’ (carer 17, parent). In this way, the CTO relieved pressure on some carers.
Conclusions
-
The implementation of CTOs may be influenced by:
-
interactions between patients, psychiatrists and family carers
-
their interpretation of the legislation
-
how they act on these interpretations.
-
-
Despite participants’ keen awareness of legal clout, there was considerable uncertainty about whether or not patient deterioration was required prior to recall.
-
The (perceived) focus of the CTO on medication adherence may have consequences for:
-
how CTOs are viewed and subsequently experienced
-
broader goals in patient care and patient and carer involvement.
-
Chapter 9 OCTET Ethical Analysis
Introduction
The OCTET Ethical Analysis substudy sought to identify and analyse ethical issues surrounding CTOs as identified and experienced by patients, family carers and mental health professionals. It drew on a specific analysis of the data from the OCTET Qualitative Study (see Chapter 8). Its objective was ‘to conduct a detailed qualitative assessment of the . . . ethical dilemmas . . . of patients, staff and carers’ in the OCTET Study. The aim was to identify the real-world experiences and attitudes of patients, professionals and family carers in order to determine how key ethical considerations should underpin practical judgements about any ethical justification for the use of CTOs. The analysis presented here focuses on potential benefits of CTOs to patients and does not include potential benefits to family carers, services or society at large.
Methods
In the interviews for the Qualitative Study, we invited participants to describe their experiences of the CTO. The interviewer probed participants’ views about the positive and negative aspects of the CTO, and encouraged reflection upon differences between the new and previous regimes, as well as inpatient and outpatient care. We gave particular attention to potential ethical considerations.
For the Ethical Analysis, we undertook a focused thematic reanalysis of the qualitative data. The reanalysis of the data involved recoding the relevant sections of the interviews in order explicitly to highlight ethical dimensions in the data. The analysis of ethical themes was conducted by categorising the data according to the three ethical values of patient benefit, autonomy and liberty, which had been identified in the literature as the considerations relevant to making ethical judgements about the use of CTOs.
Drawing directly on the literature, we interpreted the theme of benefit as an outcome-orientated consideration that revealed how, and in what ways, a patient was judged to be better or worse off through the use of a CTO. We interpreted the theme of autonomy in terms of the relationship between the patient’s ability to pursue a life of value to him or her, and his or her experience of being subject to a CTO. We interpreted the theme of liberty by considering the extent to which patients’ freedoms of action were restricted by the use of CTOs. In contrast with the themes of benefit and autonomy – which necessarily include reference to accounts of the individual patient’s well-being and personal values and therefore have a subjective component – freedom was taken to be an objectively determined characteristic of the care regime provided under a CTO. Therefore, in those instances for which a subjective account of patients’ experiences of being more or less free under a CTO were given, these accounts were classed under the theme of benefit (if they were explicated in terms of a positive or negative outcome) or the theme of autonomy (if they were explicated in terms of the patient’s ability or inability to make decisions in line with his or her values). Most of the emphasis of the analysis therefore focuses on considerations relating to benefit and autonomy, but it is important to recognise that all three themes were identified frequently within this process of data reanalysis.
Results
We report on in-depth interviews conducted with 25 consultant psychiatrists, 26 patients and 24 family carers (including three couples): the majority of the sample interviewed in the OCTET Qualitative Study, excluding those who had no experience of CTOs (see Chapter 8).
The analysis of the data revealed the complex ways in which the ethical considerations of benefit, autonomy and liberty are perceived to play out in the context of individual patient care. The theme of benefit in particular requires careful interpretation. The OCTET Trial made clear that no wider clinical or social benefits accrued to patients on CTOs, including any improvements to quality of life or the perceived coerciveness of services, compared with those in the non-CTO group. Moreover, no subgroup of patients benefited more than others. In terms of the medical and personal outcome measures adopted in these studies, therefore, there looks to be no benefit for patients from the use of CTOs. The qualitative data on benefit described below thus represent participants’ perceptions of benefit.
For all three ethical considerations, there was evidence both in support of, and against, the use of CTOs. We consider this evidence in turn.
Patient benefit
A number of participants talked about the benefits that they perceived to accrue from a patient being placed on a CTO.
Some family carers stressed the speed of response that could be instigated under a CTO as supporting positive outcomes for the patient, even if that patient was recalled to hospital:
Chiefly it’s the speed with which he’s dealt with which prevents all this deterioration and building up of bills and filth and ends up in criminal behaviour. I mean that is all saved ‘cos they take him in as soon as he stops co-operating.
Carer 2, parent
This was a view endorsed by some psychiatrists who saw benefits accruing to a patient when recall took place, minimising the decline in a patient’s distress and reducing the time required in hospital:
Their difficulty with this man is what to do when he becomes unwell because he just starts moving so fast that organising a Mental Health Act assessment, the logistics of getting two doctors and an AMHP and him and the police all in one place is so difficult that there’s a delay of some days before, between the time they decide he has to come back and where they actually can go through the mechanics of getting him in . . . And during that delay there is a lot of risk to himself, he deteriorates and that probably costs him some weeks in hospital later on and [the AMHP] said actually if we could just recall him then it would be much better.
Consultant psychiatrist 8, inpatient
Some patients also perceived that they were able to get appropriate treatment more quickly under a CTO than was possible as a voluntary outpatient, and regarded this as a positive outcome:
That is another important point, when I get ill and I’m under the [CTO], I get admitted to hospital quicker than when I’m alone like now, so I save time and I catch up with my illness straightaway and quickly. With myself, not under the [CTO], I will have to see a doctor then the doctor will see another doctor and then they will decide to get me into the hospital and then they will send the police. That procedure, nobody likes that procedure.
Patient 3, CMHT, CTO ended
These patients emphasised the possibility that CTOs could provide a ‘window of opportunity’ to maintain their stability in the longer term by allowing them to establish a new collaborative relationship with the community team. Two psychiatrists suggested that CTOs could improve patients’ engagement with services because of the requirement for the patient to agree to the original care plan set in place to govern the use of the CTO. When the CTO was perceived to make longer-term stability possible, the legal regime of care management under a CTO was seen as crucial for patients:
The thing is when I was unwell I’d function and I’d do the groceries and make the dinner and stuff but I’d be drinking and making up all this stuff in my head and I’m not doing that now. I’m well and I’m stable but I think CTO just because it is threat, threat is the wrong word but it’s the safeguard, it’s the safeguard that if I was to think of going on a bender I just wouldn’t because I wouldn’t want to jeopardise all this work that I’ve put into being well again.
Patient 10, CMHT, CTO ongoing
Although this patient identified that the safeguards associated with her CTO had led to increased stability, other psychiatrists, patients and family carers expressed concerns that patients were no better off under a CTO. Some highlighted a difficulty in accessing treatment as a particular concern:
The point is a CTO, the most important thing is that they can access treatment, and I don’t think – well [patient’s name] definitely couldn’t access the treatment. The following weekend which was the . . . cos there’s no out of hours service. After 5 o’clock that’s it. And the home treatment team you almost have to book them.
Carer 9, parent
A second concern expressed was that the process of placing a patient on a CTO could ossify care planning, preventing an individual’s broader needs being met and undermining a dynamic process of reviewing changes in the services required:
My disappointment with the community treatment order is that . . . it keeps [patient’s name] quiet. It keeps him very under the weather. I feel in a way that it – if only the community treatment order was not just a medical model . . . if there was a social side going along with it then it would be useful, but I think it just simply holds a situation. OK [patient’s name] doesn’t become psychotic because of the medication and I know he’d get taken in very quickly if he did stop medicating but it doesn’t do anything for recovery or a plan forward. I think it simply contains him, here.
Carer 13, parent
Patient autonomy
Although previous ethical analyses have emphasised that imposing a CTO on a patient who has the capacity to refuse treatment fails to respect patients’ autonomy, the restriction of choice in the act of being placed on a CTO was specifically mentioned as a concern by only about half of the patients whom we interviewed. Otherwise, the patients focused their attention on the positive and negative impacts of CTOs on their self-identity and their ability to modify their life plans in order to act in line with their own values.
One view expressed was that the clarity of knowing how a service would respond if patients were to act in certain ways was important for these patients, and that this opportunity was not available to them when on short-term leave from hospital:
I suppose potentially I think CTOs could be seen as being the better of the two from the patient’s perspective because at least the conditions are clear and sort of it’s not, whereas in Section 17 Leave it can you know, it can just be used completely in a coercive way because you’re not really sort of setting out what you want, you’re saying, you’re still under the section.
Consultant psychiatrist 14, CMHT
This insight was seen as important to patients as well, not just because of the benefit that accrued from understanding where they stood, but in that it provided a route back to a normal life:
I feel very, very well, very confident to take steps back to a normal life. I go and see my kids every time – I am separated from the mother who lives in the same house as them, but I visit them like anytime, it’s open. I am searching for a job at the moment, I claimed – what is it called – I applied for chances with volunteer organisations, I filled the forms and gave it to them, just to fill my time and to give me the idea of the work environment and having people around you and stuff and getting used to normal people and things.
Patient 3, CMHT, CTO ended
Again, this suggests that instigating a new legal regime provided a ‘window of opportunity’ for the patient to evaluate what was of importance to them, and to take active steps to achieve these goals. Interestingly, one patient accounted for this transition in terms of how a legal regime – in which he was expected to fulfil certain tasks directly associated with his illness – freed him from the constraints that he had placed on himself:
I’m not under pressure. I’m an entirely free agent. I’ve got a little area on top of my writing bureau; I’ve got all my things set out and I know what time, exactly what time I take [medication] and the quantity, how many and yeah I’ve got a little – it’s like a little altar it is to my medication and these little pots.
Patient 32, forensic, CTO ongoing
For other patients, however, CTOs were viewed as infantilising, placing them under a regime of supervision that held them back from pursuing options in their lives, rather than enabling them to pursue valuable activities. The following patient illustrated this by commenting on his experiences having been discharged from a CTO:
I feel that I’m a free man again you know. I don’t need to tell, to let them know of everything I want to do. I’ve got a bit of privacy. I’m a grown man and I should be able to look after myself.
Patient 2, CMHT, CTO ended
From the perspective of many family carers, a CTO was viewed as containment: a way of managing the patient in the community that was not associated with the requisite supports that the patient needed to become independent and to act autonomously in their lives:
It would be a lot better if the team were active and found something for this intelligent man to do. You know he just sits doing crosswords from the newspaper and that’s about it now. You know, he’s becoming more and more isolated and more and more withdrawn. I think the CTOs just contain him.
Carer 13, parent
The lack of support that accompanied a CTO was also mentioned by one patient, who equated the imposition of this legal power with the limited opportunities he felt he had to embark on a range of activities:
You know it’s imprisoning them, it’s imprisoning them in a system that can only just maintain some sort of degree of normality you know. They think they can preserve some degree of normality whereas people can if given the opportunity of being allowed off of a CTO for 6 months . . .
Patient 17, CMHT, CTO ended
There was qualified support for CTOs in view of the obligation to promote a patient’s autonomy, even if it is correct to observe that the original decision to place a competent patient on a CTO fails to respect that patient’s autonomy. It is again important, however, to note that the majority of the accounts of patients’ abilities to act autonomously within the community setting hinged on whether or not appropriate personal and social support was provided within the mental health service, rather than being determined by the use of the legal power itself. It is only for those small numbers of patients who viewed the legal regime of the CTO as liberating them from the difficulties of managing their illness to focus on other life goals that mandated community treatment looked to be justified from the standpoint of autonomy.
Patient liberty
Given that clinicians are able to determine the specific content of the discretionary conditions of the order, it is unsurprising that the impact that CTOs can have on patients’ liberty was identified as an ethical concern. It is also clear, however, that CTOs are less liberty restricting than the use of compulsory powers of detention and treatment within inpatient settings. This position was endorsed widely by psychiatrists, patients and family carers, who all recognised that patients’ freedoms were better protected by CTOs when contrasted with inpatient care.
The interview data yielded several insights into how patients experienced freedom under a CTO compared with their experiences of outpatient care more generally. Perhaps surprisingly, the CTO regime was seen by a number of patients as being no more restrictive than being a voluntary outpatient. This observation was explained in terms of the ways in which patients and carers saw community services supporting those with severe and enduring mental disorders. Three patients expressed concerns that, as people eligible to receive mental health services, their freedoms were constantly at risk on the grounds that they were caught up in a system that demanded compliance from them. Although, in legal terms, patients enjoyed greater freedoms when not subject to such powers, the same patients identified that they could not easily differentiate between the restrictions imposed by the CTO and their experiences of being treated as voluntary outpatients. This is illustrated by the following patient’s account of rehospitalisation:
I mean I just want to be free from the mental health services and get on with my life. Go to college and I’m able to do that but I feel like I’m not being allowed to because all it takes is for you to go unwell once like with drugs and be taken to hospital and then they’re all talking about, oh he’s got schizophrenia again . . .
Patient 1, CMHT, CTO ongoing
Importantly, however, the implications of such experiences for ethical considerations of liberty need to be reviewed carefully. Although this patient might feel that her liberty is being restricted when receiving community mental health care, it is incorrect that her liberty is restricted – as a matter of fact – when she is not subject to legal powers in the community (although, of course, how she exercises her freedom might lead to the imposition of legal powers in the future). The concerns she raises are better viewed in terms of the other ethical considerations identified above, such as personal autonomy. Here, her autonomy might fail to be respected within a service that does not support the person to pursue her own life choices adequately, quite independently of whether or not that patient is being treated under a CTO.
Conclusions
-
There is no general ethical justification for the introduction or use of a CTO regime.
-
In some limited situations, the promotion of patient autonomy could provide sufficient reason for using a CTO, but this should not be done when the patient’s autonomy could be promoted by another means.
Chapter 10 OCTET Capabilities Project
Introduction
The objective of this substudy was to develop and test a multidimensional instrument – the OxCAP-MH – that could be used to measure the capabilities of people with mental health problems. Here, we describe the theoretical background to the capability approach, report the methods used in the development and early application of the OxCAP-MH, and then present the baseline findings on social functioning, health-related quality of life and capabilities among patients in the OCTET Trial. The substudy reported here was part of a wider programme of work on operationalising the capability approach for outcome measurement in mental health research. This chapter substantially reproduces a paper published by members of the OCTET Coercion Programme Group: Simon et al. ,144 with permission from Elsevier. Further details of the development of the measure are also given in a further paper by members of the group. 145
The capability approach
In evaluating the quality of life of those with severe mental illness, concerns have been raised about the extent to which existing measures sufficiently capture key domains. In particular, existing measures fail to capture capabilities (things that people are free to do or be) which is one of the central concepts of Amartya Sen’s capability approach. 14 Beyond the intrinsic value of freedom of choice, other central concepts of the capability approach include multidimensionality, equity and the objective valuation of welfare for use in interpersonal comparisons and social policies. The OCTET Study represented an invaluable opportunity to apply the capability approach as a means of measuring the broader well-being and freedom of severely ill mental health patients.
Many people with severe mental illness experience significant social challenges. This may be due to stigma or discrimination, or to limitations on their freedom of choice and their opportunities to enjoy social relationships. These factors may all impact on their social participation, roles and opportunities for self-support. Current mental health services seek to address such issues by targeting both health and social impairments. 146,147
The latest guidance by NICE advocates the adoption of a joint health and social care perspective when measuring costs in evaluations,148 and highlights the importance of distributive considerations when developing recommendations. As the preferred outcome measure for decision-making, NICE supports the use of QALYs. A QALY is a unit that combines both quantity (length) of life and health-related quality of life into a single measure of health gain. NICE also supports the use of the EQ-5D103 – a generic, multi-attribute health status classification scale commonly used for QALY calculations – to develop utility weights. 120,148 Health-related quality of life is anchored on a utility scale rated on a 0–1 scale, with ‘0’ being the value of ‘dead’ and ‘1’ being the value of ‘perfect health’. 119 In their current form, QALYs have limited ability to capture non-health effects and may be insensitive to the impact of social care interventions, thus underestimating the full welfare impact of mental health interventions. 149 Some concerns have also emerged about the fitness of the EQ-5D when administered to patients with psychosis diagnoses or severe non-psychosis disorders. 150
The capability approach was introduced by Amartya Sen in the early 1980s as an alternative to standard utilitarian welfare economics. 151 Sen argues that outcomes (functional utilities) should not be the sole object of welfare assessments and that capabilities (things that people are free to do or be) should also be included in the overall assessment of a person’s well-being. The capabilities framework has already been very influential in development economics and led to the introduction of the Human Development Index by the United Nations Development Programme in 1990. The Human Development Index measures levels of national development using a composite statistic comprising national income, education and life expectancy. 152 The framework has, more recently, become influential through the Beyond Gross Domestic Product work of the Organisation for Economic Cooperation and Development, the European Union and the Sarkozy report. 153 The inclusion of life expectancy in all these indexes and dashboards highlights the central position of health in a person’s well-being. Moreover, health is causally related to other capabilities, influencing the broader opportunities someone has in life while also being directly influenced by other factors such as nutrition, environmental elements, education and income.
There is now quite a significant literature on capabilities and health, covering issues such as health outcome measurement, ethics, autonomy, life chances and inequalities. 154–159 Furthermore, more and more health economists and social scientists agree that the capabilities framework has the potential to offer a richer theoretical evaluative space than the traditional QALY approach and may have particular strengths when assessing complex interventions in social care and public health. 149,160 Although substantial progress has been made since the mid-2000s, major themes and points of discussion include:
-
determining a comprehensive or appropriate general set of capabilities
-
differentiating between evidence of functioning and that of capabilities
-
measuring objective versus perceived capabilities
-
objectively valuing capability sets for interpersonal and cross-contextual comparisons
-
providing useful information on both efficiency and equity for policy-making.
Despite the contribution of Sen’s original critique of utilitarian welfarism (the underlying theory of cost–benefit analyses) to the current interest in extra-welfarist health economics (the underlying theory of cost–utility analyses and QALYs), significant disparities exist between the theoretical foundations of the capability approach and the QALY approach. 161–163 Although QALYs allow for the use of societal-level preference measurement and consequently for the interpersonal comparison of well-being, currently they focus on maximising health outcomes measured at the level of functioning and expressed as utilities in a single composite index value. 164 When designing or evaluating policy, a major distinction may also be made between observable health achievements and the capability to achieve good health. 165 Moreover, it is important to recognise that within a QALY maximisation framework, people with chronic disabilities (mental, physical or social) may be disadvantaged to the extent that their capacity to return to full health is limited. The framework therefore prioritises resources for those who can produce more health. The so-called capability QALY framework introduced by Cookson154 – one of the first attempts to link the capability and QALY approaches directly – retains these limitations.
In this substudy, we built on the work of Anand et al. ,166 which sought to identify direct measures of capabilities from large population survey data and produce new measures that demonstrate how additional data on capabilities can be developed. This work produced the Oxford Capabilities (OCAP) instrument for measuring capabilities and provided an operationalisation of Nussbaum’s list of 10 central human capabilities: ‘life’, ‘bodily health’, ‘bodily integrity’, ‘senses, imagination and thought’, ‘emotions’, ‘practical reason’, ‘affiliation’, ‘other species’, ‘play’ and ‘control over one’s environment’. 167 Although Nussbaum’s list and the criteria for inclusion have been debated, its contents overlap with many other such lists (see, for example, the review by Alkire168) and have been taken to be a relatively comprehensive generic list of the most important human capabilities. To date, this programme of research has concluded that commonly collected survey data do provide information about capabilities; it is feasible to collect direct evidence on a wide range of capabilities; and many different types of capabilities are related to experienced subjective well-being. 166
Initial development of the OxCAP-MH and the CAPINDEX16
In the absence of an established capabilities instrument to be used in clinical study settings, or of any previous applications of the capabilities framework in mental health outcome research, we sought to develop an instrument that would:
-
be suitable for the identification of the most important capabilities dimensions in this context
-
be sensitive to different levels of coercion or compulsion and to changes in health status over time
-
potentially provide a richer evaluative space for economic evaluations than the currently used measures of well-being or functioning (e.g. EQ-5D and GAF, both also collected in the trial).
We could identify only one relevant earlier attempt to develop such a measure (although not in a mental health context) by Lorgelly et al. ,169 who reduced and refined the original OCAP measure by Anand et al. 166 into an 18-item capability index (OCAP-18), and validated it for the assessment of public health interventions in Glasgow using qualitative and quantitative methods. The Glasgow study was driven by the identified challenges health economists have been facing in producing public health guidance, namely benefit measurement, public choice compared with individual choice, equity against efficiency, an analytical perspective, extrapolation of results to the appropriate time horizon, the quality of evidence and the cost-effectiveness threshold. 160 Many of these showed major synergies with the issues health economists working in the mental health field have to handle.
Our approach to instrument development began by assessing whether or not the items in the OCAP-18 could be adapted, with specific attention being paid to applicability and validity in the mental health context, as well as feasibility, because of the underlying cognitive task. The initial component included expert focus group discussions involving psychiatrists, psychologists, social scientists and health economists. The resulting preliminary version of the OxCAP-MH questionnaire was piloted with 20 OCTET Trial patients to assess content validity and feasibility. We identified four questions that needed modification, either because they were not relevant for this population group (discrimination at work, meeting socially with work colleagues), resulted in distress in the interview situation (life expectancy) or because they were not easily interpretable in their original form (love and support). We also identified one additional capability dimension (access to activities/employment) that was deemed important for people with mental health problems, but was not part of the OCAP-18. The resultant OxCAP-MH instrument has 18 domains (see Table 15). Table 24 shows the relationships of the individual items in the OxCAP-MH instrument to Nussbaum’s list of 10 central human capabilities dimensions (shown in the left-hand column) and the relevant OCAP-18 items. (For the evolution of the exact wording of the questions from the original OCAP survey to the OxCAP-MH, see Appendix 3.)
| Central human capabilities | OCAP-18 | OxCAP-MH |
|---|---|---|
| Life | Life expectancy | Life expectancy |
| Bodily health | Daily activities | Daily activities |
| Suitable accommodation | Suitable accommodation | |
| Bodily integrity | Neighbourhood safety | Neighbourhood safety |
| Potential for assault | Potential for assault | |
| Senses, imagination and thought | Freedom of expression | Freedom of expression |
| Imagination and creativity | Imagination and creativity | |
| Emotions | Love and support | Love and support |
| Losing sleep | Losing sleep | |
| Practical reason | Planning one’s life | Planning one’s life |
| Affiliation | Respect and appreciation | Respect and appreciation |
| Social networks | Social networks | |
| Discrimination | Discrimination | |
| Species | Appreciate nature | Appreciate nature |
| Play | Enjoy recreation | Enjoy recreation |
| Control over one’s environment | Influence local decisions | Influence local decisions |
| Property ownership | Property ownership | |
| Employment discrimination | Access |
After introducing response cards and reordering the questions, the initial problems with feasibility of completion and patient apprehensiveness disappeared, and interviewers were able to complete the full set of capability questions in, on average, less than 10 minutes in the pilot interviews. In the finalised OCTET schedules, some of the OxCAP-MH items appeared later in the overall interview schedule than others because it was important to keep up the flow of questioning over the whole hour-long interview.
From the OxCAP-MH items, we also developed a single index of capabilities, 16-question Capability Index (CAPINDEX16). For reasons given below [see Results, Capability index (CAPINDEX16), below], this used 16 of the 18 capability questions. This was scored by assigning equal weights to each potential level of answers on a 1–5 scale, where ‘1’ means very severe limitation and ‘5’ means no limitation in the given capability domain. Answers to the ‘Meet socially’ and ‘Daily activities’ domains originally measured as a yes/no dichotomous rating were transformed to fit this 1–5 scale by scoring a ‘yes’ on the ‘Meet socially’ domain as ‘5’ (and ‘no’ as ‘1’) and a ‘yes’ in the ‘Daily activities’ domain as ‘1’ (and ‘no’ as ‘5’). The resulting capability index (CAPINDEX16) therefore had a minimum value of 16 (very severe limitation) and a maximum value of 80 (very high level of capability) for living respondents, although it could be set to ‘0’ following death.
Testing the OxCAP-MH with the OCTET Trial Cohort
Methods
The OxCAP-MH was utilised in interviews with the cohort of patients in the OCTET Trial at each time point, in order to test its feasibility and validity for this patient group. The final list of functioning/well-being-related outcome measures used in the OCTET Trial included the GAF scale101 and the EQ-5D-3L120 as well as the OxCAP-MH. This enabled us to test the construct validity of the OxCAP-MH. The reliability of the CAPINDEX16 was tested using Cronbach’s alpha. Factor analysis was performed in order to confirm the scoring of the CAPINDEX16 (details from the authors on request). The effects of age, gender, illness duration and primary clinical diagnosis, and the association between the EQ-5D-3L, the GAF and the OxCAP-MH items, were investigated using multiple regression analyses. Statistical significance was investigated at a two-sided p < 0.05 level. All data analyses were carried out using Stata 11.
Results
Cohort characteristics
Baseline characteristics for the whole OCTET Trial cohort are given in Chapter 6. Complete OxCAP-MH data were available for 172 patients. Response rates ranged from 299 (90%) for the ‘Social networks’ question to 225 (68%) for the ‘Life expectancy’ question. Response rates were primarily influenced by the order of the questions within the broader assessment interview rather than the question itself. The later the question appeared in the clinical research form, the lower was the response rate.
Patients reported their health-related quality of life using the EQ-5D visual analogue score (EQ-5D VAS), as 65.70 (SD 23.75, n = 275). Health-related quality of life was further assessed on the EQ-5D-3L utility scale using UK tariff values. 170 The utility scores ranged between –0.239 and 1.0, with a mean score of 0.725 (SD 0.28, n = 277). Correlations between the EQ-5D VAS scores and utility values were high (correlation 0.50). As Table 25 shows, the EQ-5D-3L also proved to be a feasible and sensitive measure of health limitations for this patient group, with age- and gender-stratified mean utility values being substantially lower than the UK population norms170 for all categories. Female patients and those with longer illness duration reported significantly lower health-related quality of life scores, expressed either on the EQ-5D VAS or as EQ-5D-3L utility values (all p < 0.01). Variations in health-related quality of life did not show significant associations with the primary clinical diagnostic category or age (Table 26).
| Age (years) | Males | Females | ||
|---|---|---|---|---|
| OCTET, mean (sample size) | UK norms (mean) | OCTET, mean (sample size) | UK norms (mean) | |
| < 25 | 0.84 (25) | 0.94 | 0.71 (3) | 0.94 |
| > 25 to < 35 | 0.78 (63) | 0.93 | 0.71 (16) | 0.93 |
| > 35 to < 45 | 0.72 (58) | 0.91 | 0.75 (29) | 0.91 |
| > 45 to < 55 | 0.78 (25) | 0.84 | 0.51 (24) | 0.85 |
| > 55 to < 65 | 0.73 (21) | 0.78 | 0.56 (10) | 0.84 |
| > 65 to < 75 | 0.055 (1) | 0.78 | 0.35 (2) | 0.78 |
| > 75 | NA (0) | 0.75 | NA (0) | 0.71 |
| Scales | Sample size | Constant | Age (years) | Female gender | Other psychosis diagnosis (including bipolar disorder) | Illness duration (years) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| b | p-value | b | p-value | b | p-value | b | p-value | b | p-value | ||
| GAF | 304 | 40.822 | 0.000 | –0.039 | 0.579 | 0.625 | 0.604 | 2.143 | 0.171 | –0.084 | 0.264 |
| EQ-5D VAS | 271 | 72.938 | 0.000 | 0.072 | 0.679 | –8.950 | 0.004 | 4.829 | 0.234 | –0.584 | 0.002 |
| EQ-5D utility | 274 | 0.852 | 0.000 | –0.000 | 0.898 | –0.101 | 0.007 | 0.007 | 0.885 | –0.006 | 0.007 |
| CAPINDEX16 | 172 | 59.876 | 0.000 | 0.048 | 0.604 | –3.317 | 0.040 | 5.161 | 0.026 | –0.217 | 0.033 |
Based on the 309 (93%) interviewer-completed measurements of functioning, just over half of the cohort (158, 51%) was assigned a functioning score of less than 40 (GAF: mean 38.69, SD 9.67), showing at least major impairments in reality-testing or communication (e.g. ‘speech is at times illogical, obscure or irrelevant’) and in several areas of functioning (e.g. work/school, family relations, judgement, thinking, mood, hygiene). 101 Variations in the functioning score did not show any significant associations with age, gender, the primary clinical diagnostic category or illness duration (see Table 26).
OxCAP-MH capability domains
Figures 13 and 14 show the distribution of capability levels across the 18 capability domains of the OxCAP-MH, with lower-level responses indicating more limitations in the given capability dimension. The vast majority (246, 88%) answered ‘No’ to the ‘Property ownership’ domain. A smaller majority (145, 56%) reported some level of limitations in carrying out their ‘Daily activities’ because of health problems. Over 30% of the sample also reported very severe or severe limitations (level 1 or 2 answers on a 1–5 scale) in their capabilities to ‘Influence local decisions’ (109, 48%), to ‘Enjoy recreation’ (83, 32%) or in ‘Planning one’s life’ (71, 31%). One-third (80, 33%) reported having a very high or high likelihood of experiencing ‘Discrimination’ and just over one-third (83, 37%) reported a subjective ‘Life expectancy’ that was lower than that of the general population.
FIGURE 13.
Capability domain scores (two- and three-level answers). Reproduced from Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187–96,144 with permission from Elsevier. LE, life expectancy.
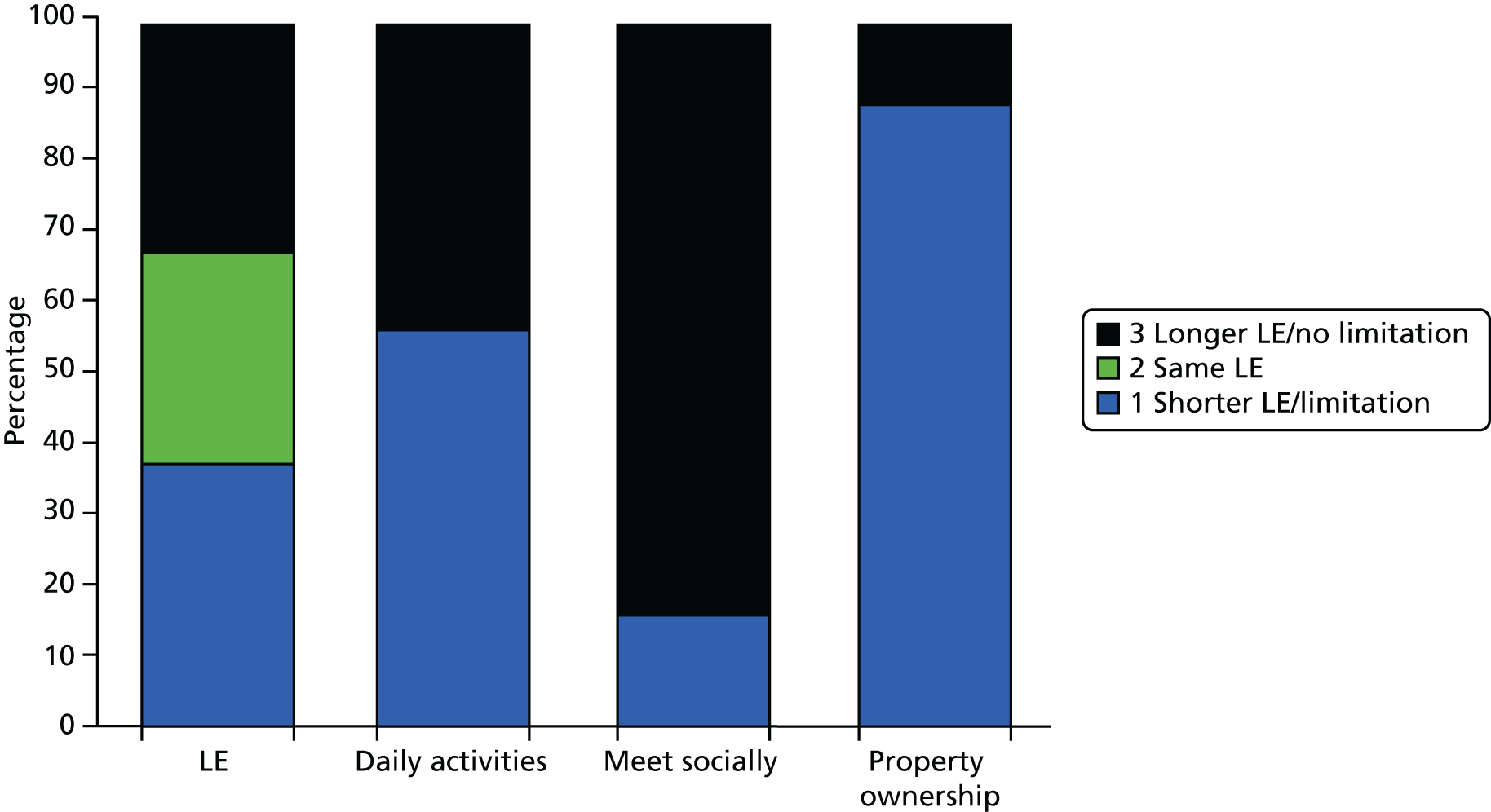
FIGURE 14.
Capability domain scores (five-level answers). Reproduced from Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187–96,144 with permission from Elsevier.
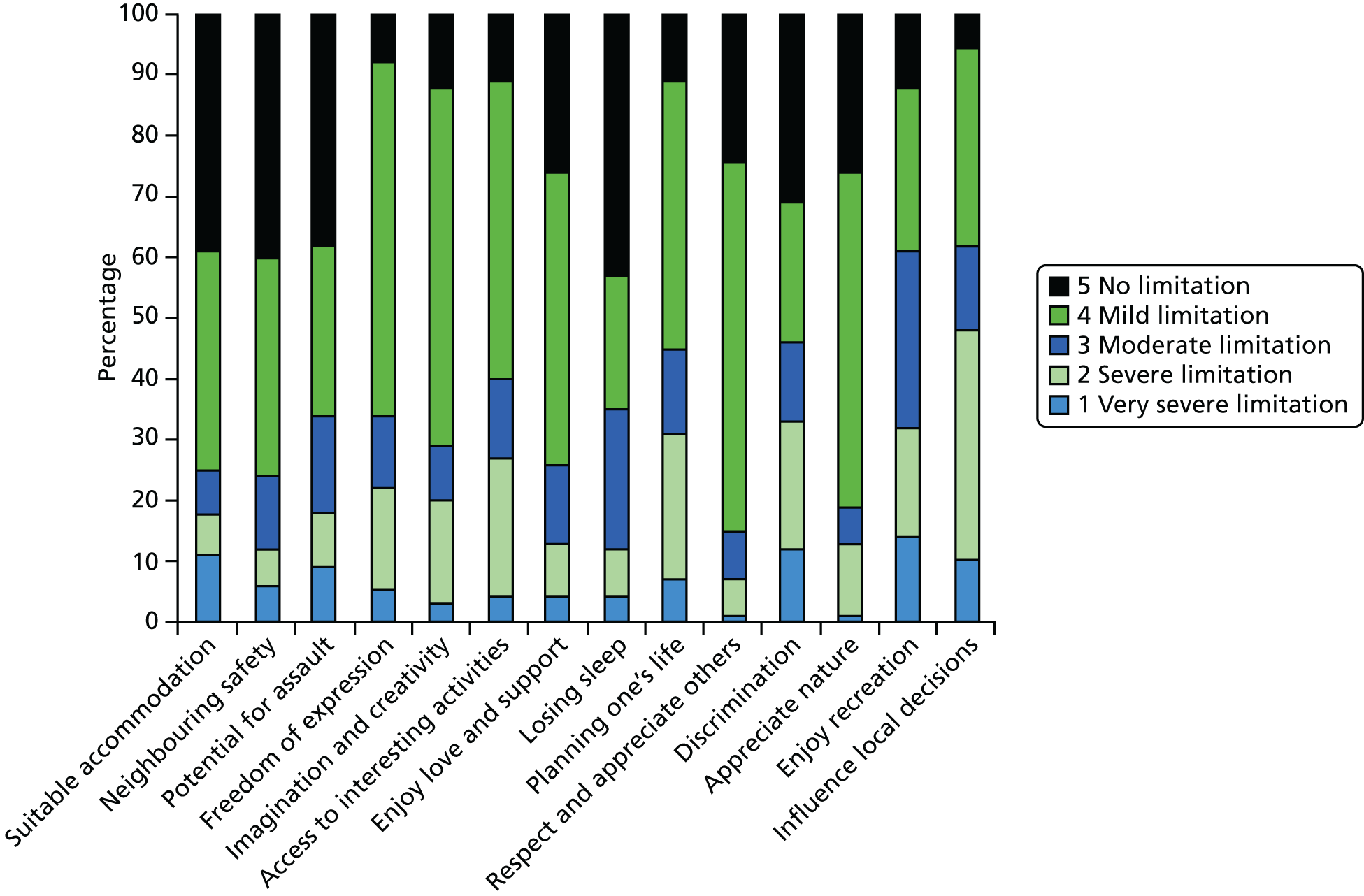
Female patients scored lower than male patients, on average, on most capability domains except for ‘Property ownership’, ‘Access to interesting forms of activities’, ‘Influence local decisions’ and enjoying the ‘Love and support’ of family and friends (Figure 15). The limiting effects of female gender proved statistically significant for the ‘Suitable accommodation’, ‘Neighbourhood safety’ and ‘Life expectancy’ domains, and resulted in greater ‘Potential for assault’ (Table 27).
FIGURE 15.
Mean capability levels by gender: 1, very severe limitations, 5 = no limitation. Reproduced from Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187–96,144 with permission from Elsevier.
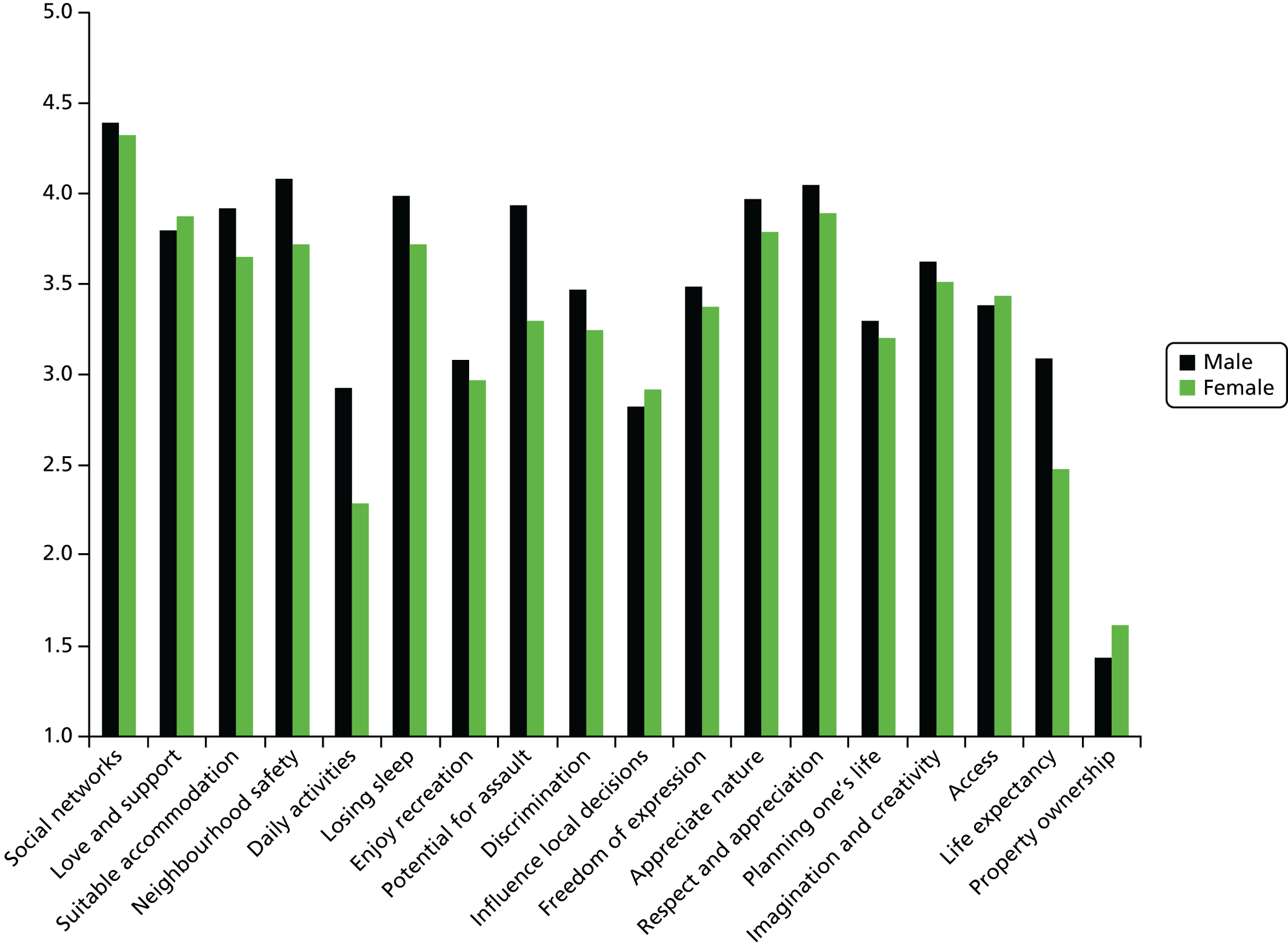
| Capability domainsa | Sample size | Age (years) | Female gender | Other psychosis diagnoses (including bipolar disorder | Illness duration (years) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | p-value | Coefficient | p-value | Coefficient | p-value | Coefficient | p-value | ||
| Life expectancy | 221 | 0.030 | 0.063 | –0.814 | 0.006 | 0.172 | 0.654 | –0.037 | 0.035 |
| Daily activities | 254 | –0.000 | 0.993 | –0.514 | 0.093 | 0.291 | 0.463 | –0.053 | 0.006 |
| Suitable accommodation | 263 | 0.028 | 0.061 | –0.503 | 0.050 | –0.048 | 0.887 | –0.012 | 0.442 |
| Neighbourhood safety | 264 | 0.041 | 0.008 | –0.689 | 0.007 | –0.276 | 0.414 | –0.038 | 0.020 |
| Potential for assault | 238 | 0.044 | 0.006 | –0.950 | 0.001 | 0.495 | 0.174 | –0.056 | 0.001 |
| Freedom of expression | 226 | 0.006 | 0.757 | –0.138 | 0.640 | 0.937 | 0.021 | –0.029 | 0.128 |
| Imagination and creativity | 225 | 0.014 | 0.448 | –0.114 | 0.703 | 1.236 | 0.002 | –0.037 | 0.062 |
| Access | 223 | –0.010 | 0.547 | 0.135 | 0.642 | 1.251 | 0.002 | –0.004 | 0.843 |
| Love and support | 283 | 0.009 | 0.534 | –0.018 | 0.942 | 0.748 | 0.028 | –0.004 | 0.792 |
| Losing sleep | 252 | –0.017 | 0.267 | –0.266 | 0.313 | –0.333 | 0.311 | 0.001 | 0.949 |
| Planning one’s life | 224 | 0.009 | 0.595 | –0.145 | 0.605 | 0.381 | 0.295 | –0.022 | 0.222 |
| Respect and appreciation | 223 | 0.016 | 0.370 | –0.314 | 0.310 | 0.546 | 0.166 | –0.026 | 0.187 |
| Social networks | 294 | –0.024 | 0.255 | 0.051 | 0.886 | 0.182 | 0.696 | –0.021 | 0.330 |
| Discrimination | 243 | 0.026 | 0.094 | –0.315 | 0.238 | –0.046 | 0.895 | –0.031 | 0.071 |
| Appreciate nature | 224 | 0.005 | 0.801 | –0.195 | 0.511 | 0.929 | 0.016 | –0.023 | 0.232 |
| Enjoy recreation | 252 | –0.002 | 0.910 | –0.128 | 0.621 | 0.433 | 0.188 | 0.010 | 0.506 |
| Influence local decisions | 224 | –0.040 | 0.021 | 0.279 | 0.327 | 0.096 | 0.791 | 0.025 | 0.182 |
| Property ownership | 276 | 0.069 | 0.002 | 0.132 | 0.735 | –0.127 | 0.805 | –0.025 | 0.247 |
Patients with a primary clinical diagnosis of schizophrenia reported lower mean scores than those with other psychosis diagnoses (including bipolar disorder) for 11 of the OxCAP-MH domains. They reported the same mean score for the ‘Suitable accommodation’ domain and somewhat higher mean scores for the remaining six capability domains: ‘Social networks’, ‘Influence local decisions’, ‘Daily activities’, ‘Discrimination’, ‘Losing sleep’ and ‘Neighbourhood safety’ (Figure 16). The greater limiting effects of schizophrenia reached statistical significance for ‘Love and support’ of family and friends, ‘Freedom of expression’, ‘Appreciate nature’, ‘Imagination and creativity’ and ‘Access’ to interesting activities (see Table 27).
FIGURE 16.
Mean capability levels by primary diagnosis: 1, very severe limitations, 5 = no limitation. Reproduced from Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187–96,144 with permission from Elsevier.

Higher age had a significant negative effect on the capability to ‘Influence local decisions’, but significant positive effects on ‘Neighbourhood safety’ and ‘Property ownership’, and it was protective against ‘Potential for assault’ (see Table 27). Patients with longer illness duration had significantly more limitations in ‘Neighbourhood safety’, ‘Daily activities’ and ‘Life expectancy’ and had significantly greater ‘Potential for assault’ (see Table 27).
Being less limited in ‘Daily activities’ because of health (β = 0.051; p < 0.01) and not ‘Losing sleep’ over worry (β = 0.058; p < 0.01) were the only individual capability domains that were found to be significantly related to better health-related quality of life measured by the EQ-5D-3L utility scores. Being less limited in ‘Daily activities’ because of health also had a significant positive effect on the EQ-5D VAS (β = 4.793; p < 0.01) and GAF scores (β = 1.274; p < 0.01), similar to ‘Suitable accommodation’ (β = 3.053; p = 0.031) and the ability to enjoy the ‘Love and support’ of family and friends (β = 2.681; p < 0.01), respectively. No other associations between individual capability domains and the EQ-5D VAS and the GAF scores were significant and they are therefore not shown.
Capability index (CAPINDEX16)
The ‘Property ownership’ question had low variability and was eventually deemed irrelevant in the context of mental health. This question and the question on ‘Life expectancy’ were excluded from the overall capability index, which was therefore based on 16 rather than 18 domains. Factor analysis confirmed these decisions. Just over half of the patients (172, 52%) answered all of the other 16 capabilities questions used in the final calculation for the CAPINDEX16. Their characteristics did not differ significantly from those of the full cohort, with a mean age of 38.94 (SD 11.51) years and the majority being male (72%) and having a primary diagnosis of schizophrenia, schizotypal disorders or delusional disorders (89%). A Cronbach’s alpha of 0.79 indicated that the capability index had good internal reliability. The CAPINDEX16 scores ranged from 26 to 75, with a mean of 58.40 (SD 9.32) (Figure 17).
FIGURE 17.
Distribution of the capability index (CAPINDEX16). Reproduced from Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187–96,144 with permission from Elsevier.
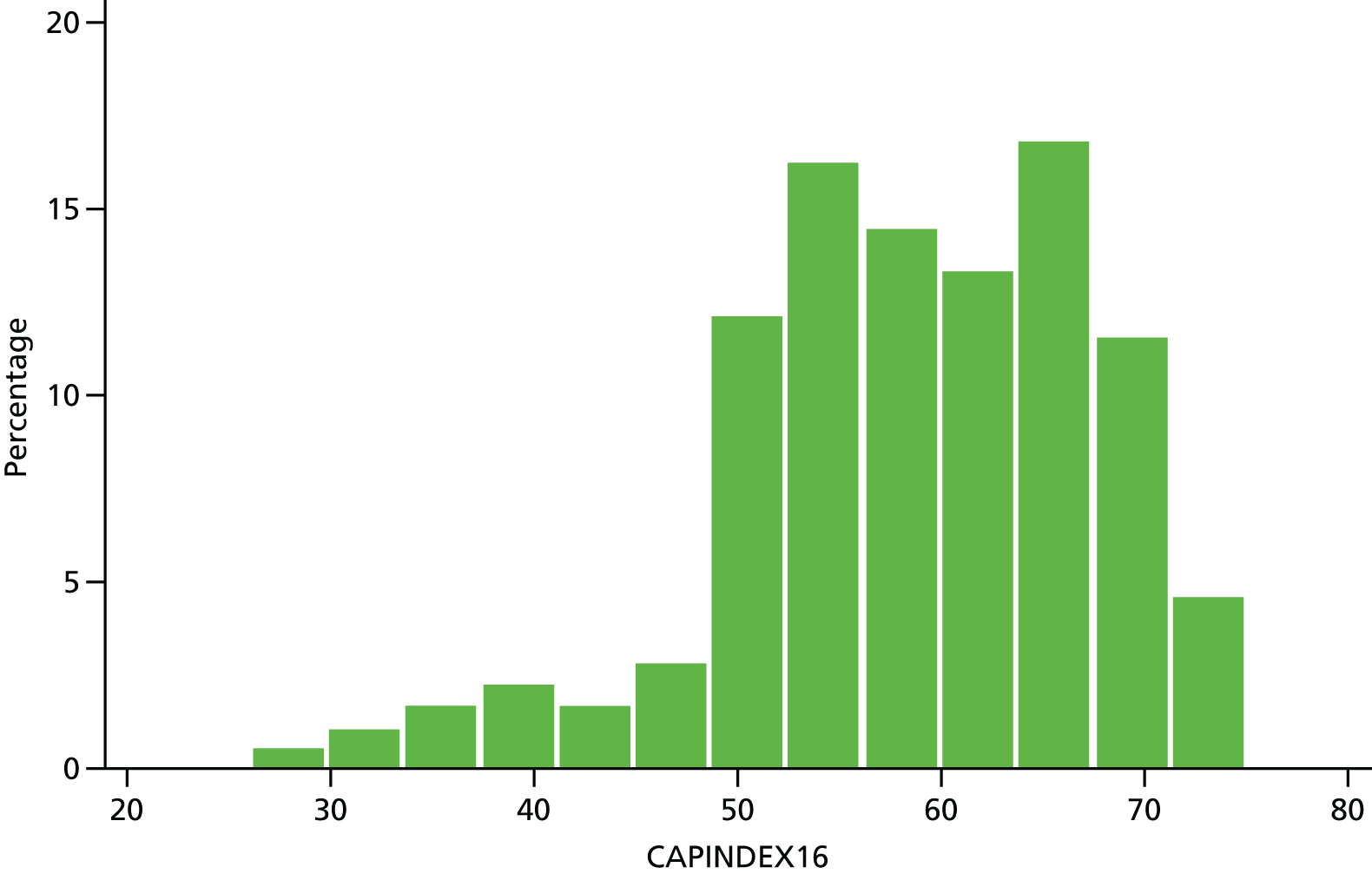
Female patients and those with a primary clinical diagnosis of schizophrenia or longer illness duration reported significantly lower CAPINDEX16 scores (all p < 0.05) (see Table 26). On average, patients with a diagnosis of schizophrenia had five points lower and female patients had three points lower CAPINDEX16 scores (see Table 26). The correlations between the CAPINDEX16 and the EQ-5D VAS scores, the EQ-5D-3L utility values and the GAF scores were 0.51, 0.42 and 0.25, respectively (Figure 18).
FIGURE 18.
Correlation between the capability index (CAPINDEX16) and other measures of well-being. Reproduced from Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187–96,144 with permission from Elsevier.
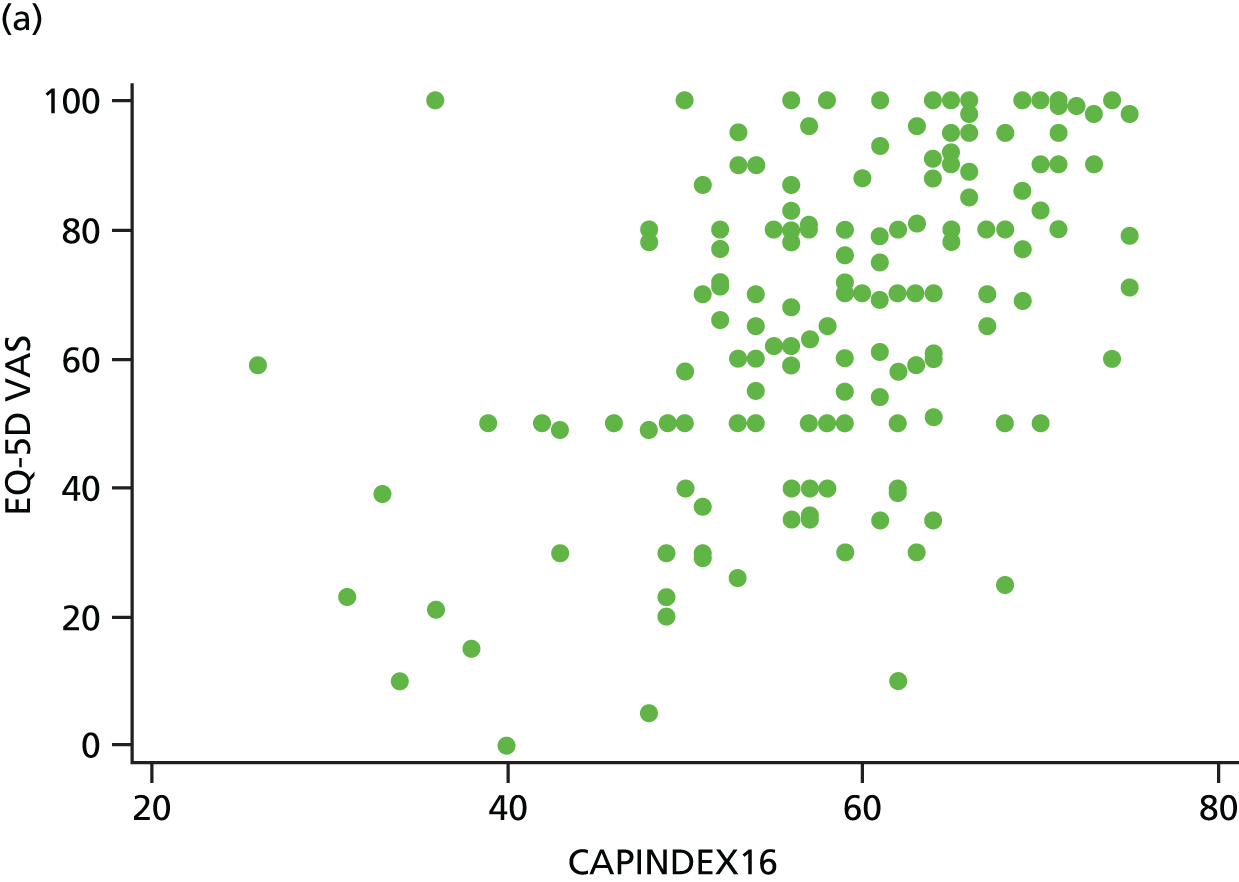
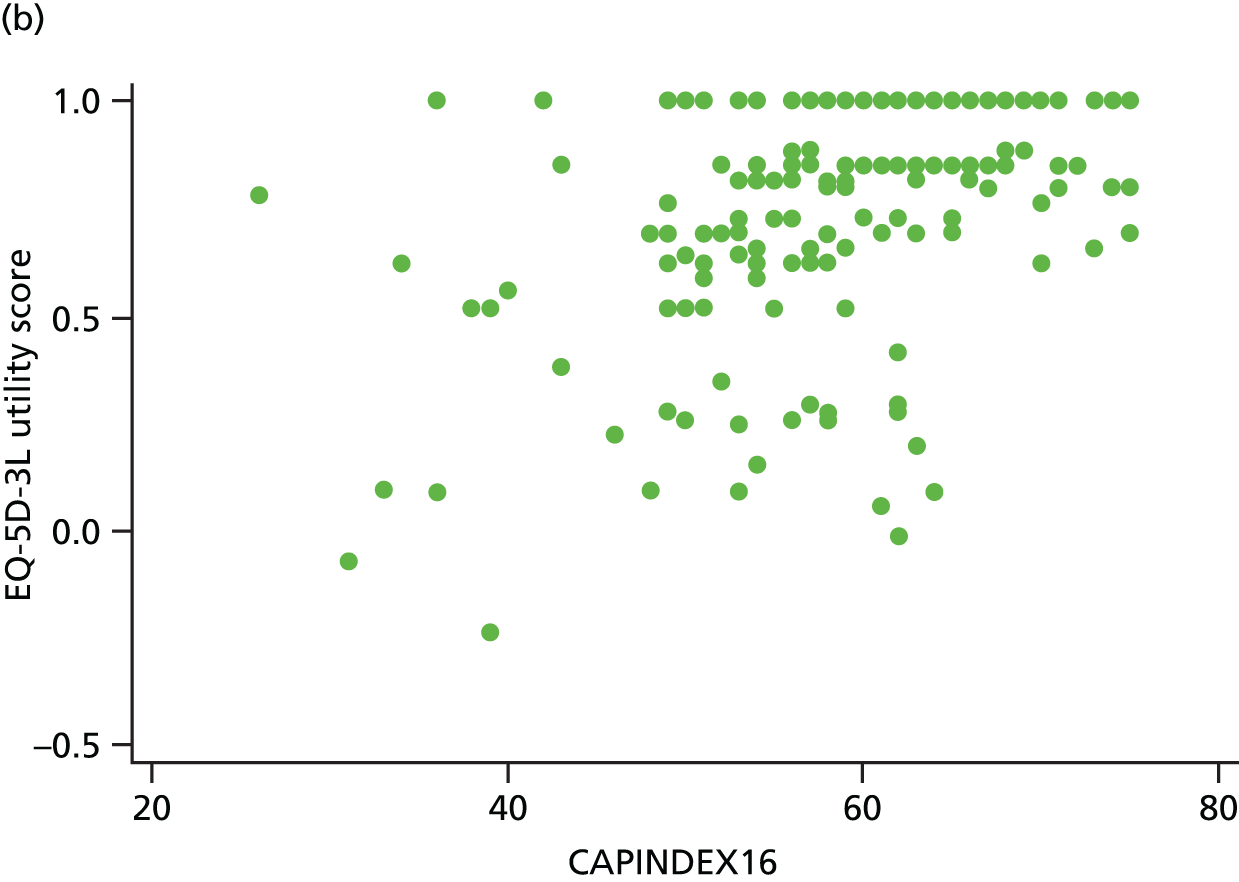

Feasibility
In general, the achieved completion rates for the OxCAP-MH questions reached the required standards of > 70% for patient-reported outcome measures. 171 Neither the response rates nor the interviewers’ final observations suggested feasibility issues despite the relatively large number and somewhat abstract nature of the OxCAP-MH questions. Focused debriefing sessions with the interviewers showed that, overall, patients gave positive feedback and felt that the questions allowed them to express their views and experience on topics that they considered to be important but which were often left out of clinical or research interviews.
Specific concerns, however, remained about both the quantity and quality of the responses to the ‘Life expectancy’ question. Despite the amended two-stage format to address initial feasibility and acceptability concerns from the pilot phase, only 68% of the cohort completed the question. Furthermore, 63% of the responders predicted their life expectancy being the same or longer than that of the general population. The low completion rate together with the overall responses clearly indicated a general lack of insight into or denial of objective life expectancy. The ‘Property ownership’ question was also deemed irrelevant and non-informative in the mental health context, as opposed to the ‘Suitable accommodation’ question. These two questions were thus cut from the OxCAP-MH and also excluded from the CAPINDEX16 (as mentioned above).
Validity
The baseline results from the OCTET Trial showed significant correlations between patients’ investigated OxCAP-MH scores and their social functioning as measured by the GAF scale, and an even stronger correlation with their health-related quality of life as measured by the EQ-5D. This confirmed the connection originally hypothesised between capabilities, social functioning and health-related quality of life, thus supporting the instrument’s construct validity. The capability domains most affected by patients’ characteristics were ‘Daily activities’, ‘Influencing local decisions’, ‘Enjoying recreation’, ‘Planning one’s life’ and ‘Discrimination’. Age had a mixed effect, whereas female patients and those with a primary clinical diagnosis of schizophrenia or a longer duration of illness reported significantly lower capability scores. Some capability domains were more affected by these effects than others. The results also suggest that the current multi-domain capability approach is not prone to the commonly observed end-of-scale bias of the EQ-5D and allows for a more sensitive measurement of well-being than either the EQ-5D or the GAF (see Figure 18).
Although the EQ-5D was prone to end-of-scale bias (see Figure 18), the 83% completion rate of the EQ-5D questionnaire, and the EQ-5D-3L utility results being significantly and substantially lower than the UK population norms for all age- and gender-stratified categories, support the feasibility and sensitivity of the EQ-5D-3L as a measure of health limitations for patients with psychosis. 170 The significant association between the EQ-5D-3L utility values and the individual OxCAP-MH domains of ‘Daily activities’ limitations due to health and ‘Losing sleep’ over worry are not surprising if we consider the affinities between these domains and the usual activities and anxiety/depression domains of the EQ-5D-3L.
The GAF scale is an interviewer-rated measure, which explains its higher completion rate in comparison with either the EQ-5D or the OxCAP-MH. For the same reason, the GAF scores are expected to be less sensitive to individual patient factors, potentially explaining the lack of correlations with age, gender, illness duration or primary clinical diagnosis. Although the GAF scale is held to be a sensitive measure of changes in the social functioning of a given individual, its usefulness in evaluating differences and inequities across individuals is therefore likely to be limited. In the current study, both the EQ-5D and the OxCAP-MH proved superior in this aspect.
Conclusions
-
We developed and tested a new measure, the OxCAP-MH, to be able to assess the comprehensive capability profile of mental health patients.
-
This provides a complementary outcome measure of well-being in addition to health-related quality of life and social functioning.
Chapter 11 OCTET Legal Analysis
Introduction
The substudy reported here was part of the preparatory work conducted prior to the OCTET Trial (see Chapter 6, Introduction). It constitutes an investigation into the question of whether or not an RCT could be designed that would permit researchers to collect – lawfully – the treatment outcomes required to evaluate rigorously involuntary outpatient care. All references to the provisions of legislation are to the MHA 1983 unless otherwise indicated.
Ideally, the best approach might be to conduct an RCT in which the outcome of treatment on a CTO would be directly compared with that of voluntary outpatient care. The consent of several hundred patients, who had recently been placed under involuntary outpatient care, might be obtained for inclusion in the trial. Half would remain under the statutory scheme, whereas the other half would be discharged immediately to voluntary outpatient treatment, with the choice between the two randomly made.
Such a randomised trial would permit the element of compulsion to be isolated as the central point of difference in the treatment of the two groups and independently assessed. The random allocation of patients would reduce the potential for bias. The results of treatment could then be readily compared. From a methodological perspective, therefore, this would be the strongest test of compulsory outpatient treatment.
The random discharge of half of the patients from supervised treatment, however, would appear to be unlawful172 if they were discharged directly from the compulsory treatment regime, for which they had been considered suitable by their RC. Their discharge, in such circumstances – for the purposes of the research – would not be governed by the criteria governing the release from compulsory treatment set by the MHA. It would therefore appear to involve an unlawful exercise of the statutory discharge power.
This chapter draws substantially on a paper published by members of the OCTET Coercion Programme Group: Dawson et al. ,173 with permission from Oxford Journals.
Our proposed research design
We believed that a rigorous – and lawful – alternative method could be found to evaluate involuntary outpatient care; this is represented by the OCTET Trial.
The method did not set up a direct comparison between compulsory and voluntary outpatient care, nor did it lead to the random discharge of compulsory patients from the MHA. Instead, it compared the treatment outcomes for patients randomised to the two parallel compulsory outpatient treatment schemes now authorised by the reformed legislation for England and Wales (i.e. Section 17 Leave and CTOs). Our study aimed to compare the outcomes for patients who, at the point of randomisation, were due to leave hospital under one or other of these two similar forms of compulsory outpatient care.
The patients were all considered proper candidates for supervised outpatient treatment, but all were recruited by RCs who recognised that the evidence left them genuinely uncertain about which legal mechanism to employ. After randomisation, these patients were treated under the authority of the Act in the usual way. The usual powers and procedures applicable to the treatment mechanism to which they had been assigned continued to apply, without interference from researchers. They could thus be discharged from the Act by their RC or by the Tribunal as the law allowed, be returned to hospital from Section 17 Leave or the CTO, or be switched from Section 17 Leave to a CTO, and so on, in the usual way.
We believed that this would produce data that would permit us to evaluate the efficacy of compulsory outpatient care because it might transpire that the patients in the two arms of the trial were, on average, treated under these two very similar schemes for different lengths of time. If different outcomes were found, we might then reasonably infer that those differences had been caused by the duration of their compulsion. The average length of time for which a person’s involuntary outpatient treatment was likely to continue under the Section 17 Leave or the CTO regime could not be known when our study commenced, on the day of the introduction of the new CTO regime. Nor is any maximum period for the use of Section 17 Leave or a CTO currently specified by law, because both can be renewed repeatedly as long as the ruling legal criteria continue to apply. Patients could therefore be treated under either regime for lengthy periods of time although the Code of Practice insisted that when use of Section 17 Leave was protracted beyond 1 week, the alternative of a CTO should always be considered.
Lawfulness of this research method
The focus of this chapter is therefore on the lawfulness of our research design. Our analysis focuses mainly on the decisions made by the RCs who exercise key functions under the Act concerning patients in our trial. The RCs must decide whether or not to place sectioned patients under compulsory outpatient care in the first place; allocate them to Section 17 Leave or a CTO; keep them in that position for a certain length of time; recall them to hospital from community care; and so on. In making those decisions, RCs exercise specific statutory powers. Simultaneously, they are pursuing therapeutic aims, such as maintaining the stability of the patient’s condition, and ensuring continuity of care. In addition to this, in setting up this study, we were asking the RCs to collaborate with us on a trial that would compare the treatment outcomes of the two regimes. Would they act lawfully in doing so?
Responsible clinicians are not the only decision-makers to exercise relevant powers over compulsory outpatients. The Mental Health Tribunal can also order a patient’s release from compulsion, for instance. RCs undoubtedly exercise considerable powers, however, particularly the power to direct compulsory outpatient treatment in the first place and to direct the form that treatment will take. The exercise of RCs’ statutory powers during the research process was thus our primary concern. In particular, we had to consider whether or not following our research protocol could cause RCs to commit any legal error in the exercise of their statutory powers that might expose them to judicial review, and might lead a court to declare the research process unlawful or to halt its progress. To avoid that possibility, nothing in our methods should prevent the RCs applying the correct legal criteria to decisions about compulsory patients, or prevent them following the correct procedures, or induce them to make what could be viewed, in law, as an unreasonable or irrational decision. In short, the RCs should avoid all the usual grounds for judicial review when following the research protocol. Moreover, the RCs must act lawfully when exercising any residual element of statutory discretion concerning patients in our trial. They exercise considerable discretion because the Act often authorises – but does not require – certain decisions to be made. An RC ‘may’ place a sectioned patient on Section 17 Leave or a CTO, ‘may’ impose certain conditions on outpatients’ treatment and ‘may’ recall them to hospital in certain circumstances. Permissive language is used in the empowering provisions conferring significant discretion. But the exercise of these powers has important implications for patients’ rights. The manner in which this discretion is exercised is thus governed by important legal principles, drawn from administrative and human rights law. RCs must exercise their discretion for proper purposes. They must take into account all relevant considerations. They should avoid predetermination or bias. Their decisions should not have a disproportionate or overly restrictive impact on the rights of patients involved in the research, nor should they expose patients in the trial, or any other person, to heightened risks of harm. We therefore needed to consider whether following our research protocol could cause RCs to breach any principle of that kind.
Two legal issues needed special scrutiny to determine whether it was lawful to allocate patients at random to Section 17 Leave or a CTO. First, we had to consider whether or not some overlap exists between the legal criteria that apply to these two different forms of outpatient care to determine whether or not some patients are simultaneously eligible for treatment under both regimes. If so, it may be possible to allocate them to either regime for the purposes of the research. Second, we had to consider whether or not placing a person under one or other regime would constitute a less restrictive form of intervention in that person’s life. This is important because if clinicians were left in a state of initial uncertainty as to the correct regime to use then they should use the less restrictive option, if one could properly be described in those terms. Only if neither the Section 17 Leave nor the CTO regime could be correctly described as less restrictive than the other – because they scored equally on that parameter – could RCs lawfully allocate eligible patients at random to one or other regime when in doubt. Those two legal issues – the degree of overlap between the legal criteria governing the use of CTOs and Section 17 Leave, and whether or not one regime is less restrictive than the other – were therefore central to our analysis.
Criteria governing use of Section 17 Leave and community treatment orders
Both the Section 17 Leave and the CTO regimes provide a cluster of powers designed to permit continuing contact to be maintained between compulsory outpatients and the members of a CMHT. Further provisions govern the likely duration, and extension, of a patient’s treatment under the scheme and stipulate the associated procedural requirements or entitlements, including the right of a patient to apply to the Tribunal for discharge from the scheme.
The rules concerning Section 17 Leave require there to be a continuing need for the person’s detention under the MHA. This requires the patient’s treatment to include a continuing, periodic element of hospital-based treatment, although this need not amount to inpatient care, overnight admission or physical detention of the patient in a hospital. Occasional attendance at a hospital-based service is enough to justify extended use of Section 17 Leave, along with the need for clinicians to retain the power to recall the patient swiftly to such a service for treatment, if required. It is sufficient that the patient attends ward rounds for discussion of progress and medication, or has regular sessions at the hospital with a psychologist. There is no requirement for the treatment to include the overnight admission or detention at the hospital.
Very similar standards govern the use of CTOs:
-
The patient is suffering from mental disorder of a nature or degree which makes it appropriate for him to receive medical treatment.
-
It is necessary for his or her health or safety or for the protection of other persons that he or she should receive such treatment.
-
Subject to his or her being liable to be recalled . . . such treatment can be provided without him or her continuing to be detained in hospital.
-
It is necessary that the responsible clinician should be able to exercise the power . . . to recall the patient to hospital.
-
Appropriate medical treatment is available for him or her. [Section 17 A(5)]
The one significant departure from the Section 17 Leave criteria is that when using a CTO there is no need for any current aspect of the treatment programme to take place in a hospital setting. Nevertheless, the clinicians must still be convinced that a patient on a CTO should remain liable to immediate recall to hospital, should that be required. The prospect that the patient will again require compulsory hospital care remains an important part of the equation.
Further factors are then listed in the Act and the Code of Practice that clinicians should take into account when deciding to use the Leave regime or a CTO. These factors strongly overlap in their content and virtually nothing is listed as a relevant factor for use of Section 17 Leave that would not be relevant to a CTO. The legal provisions do not, therefore, establish mutually exclusive zones for the operation of the two regimes.
There are legal provisions that directly address the choice between the two schemes. Section 17 Leave, it is said, is primarily intended to allow a patient ‘to be temporarily absent from hospital where further inpatient treatment as a detained patient is still thought to be necessary’, whereas CTOs are ‘principally aimed at preventing the “revolving-door” scenario and the prevention of harm which could arise from relapse . . . even if there is no reason to think that the patient will need further treatment as a detained inpatient for the time being’. Factors pointing to use of a CTO, for instance, are said to include ‘confidence that the patient is ready for discharge from hospital on an indefinite basis’; ‘good reasons to expect that the patient will not need to be detained for the treatment they need to be given’; the patient ‘appears prepared to consent or comply with the treatment they need’; and that the ‘risks of arrangements in the community breaking down, or of the patient needing to be recalled to hospital for treatment, is sufficiently serious’.
Ultimately, these provisions give little strong guidance, however, as to when a CTO must be used in preference to long-term Section 17 Leave and no final guillotine is imposed by law on use of Section 17 Leave. That RCs should ‘first consider’ using a CTO before putting a patient on longer-term Section 17 Leave ‘does not mean’ that they cannot use the latter. The Code states that Section 17 Leave ‘may also be useful in the longer-term where the clinical team wish to see how the patient manages outside hospital before making the decision to discharge’.
Uncertainty concerning the choice between regimes
Very similar legal criteria therefore govern the use of the two regimes and there is a strong degree of overlap in the factors to which clinicians are directed and very few mandatory indicators. Some continuing element of hospital-based treatment is required to extend a patient’s Section 17 Leave, but that element of treatment could also be suitable for a patient on a CTO, particularly visits to an outpatient clinic. That requirement therefore does not draw a sharp line between the proper uses of the two schemes. As a consequence, it was highly likely that varying practices would emerge as to the choice between CTOs and Section 17 Leave between different clinicians, hospitals and regions, just as Pinfold et al. 174 found great variation in the implementation of the prior supervised discharge scheme. These variations may simply reflect legitimate professional differences over the proper application of the law.
In these circumstances, some patients could lawfully be allocated to either Section 17 Leave or a CTO. Either decision would be a legitimate exercise of the discretion left in clinicians’ hands by the uncertainties surrounding use of the two schemes. Our research protocol therefore stated that patients might be included in our trial only when their RCs considered that they were proper candidates for involuntary outpatient care and acknowledged uncertainty as to whether to use Section 17 Leave or a CTO. In addition, the protocol stated that patients should not be included in the study if they were viewed as clear candidates for either Section 17 Leave or a CTO, or considered suitable, when leaving hospital, for immediate discharge to voluntary care. To reach those conclusions, the RCs would have to consider the relevant legal criteria, in the Act and the Code of Practice, and still recognise ambivalence between the two options. In that limited situation, it would be lawful, in our view, for RCs to allocate patients at random to one or other regime.
Least restrictive alternative
Responsible clinicians, when in doubt, should always allocate patients to the least restrictive regime. It is precisely when the other legal criteria fail to resolve the choice that this principle has most bite. Compulsory outpatient treatment can have a significant impact on patients’ human rights, such as the right to privacy and respect for family life, protected by the European Convention on Human Rights. 96 Such powers must be exercised in a ‘proportionate’ manner, and compliance with that ‘proportionality’ principle requires that the least restrictive (or least drastic) form of intervention that is viable should be employed. 175
This argument would apply in the current context, however, only if either the Section 17 Leave or the CTO regime could properly be described as less restrictive of patients’ rights. Determining that matter required a full inquiry into the means used to implement both regimes.
Restrictiveness of the two regimes
The general structure of the two regimes is very similar. The same kinds of conditions can be imposed on compulsory outpatients’ community tenure, similar powers may be exercised by clinicians over outpatients and in neither case is the patient’s consent required to their initial placement under the scheme. Both patients on Section 17 Leave and those on CTOs may be swiftly returned to compulsory hospital care; both have a regular right of access to independent review of their compulsory status before the Tribunal, both must be discharged by their RC or the Tribunal if they cease to meet the relevant criteria, and both are entitled to a second opinion from an approved doctor. In both cases, their involuntary outpatient treatment may be extended repeatedly, if the proper process is followed.
Nevertheless, there are significant differences between the two regimes. The provisions governing Section 17 Leave are more open-textured, so may confer more discretion on clinicians. They also place the authority for decisions more squarely on the shoulders of the RC, instead of requiring prior agreement to be reached between the RC and an AMHP, as is required for many decisions about patients on CTOs. There are differences in the timing of patients’ entitlements to have their position reviewed by the Tribunal and to have their treatment approved by an SOAD. The scope of the treatment powers in the community differs in the two cases, particularly regarding patients who retain their capacity to consent. Moreover, somewhat different legal consequences flow from any recall to hospital of patients treated under the different regimes.
Conditions of outpatient treatment
With regard to the conditions that may be imposed on a patient’s outpatient treatment, and the consequences that may flow from breach of those conditions, the CTO provisions appear somewhat more restrictive than the Section 17 Leave scheme because of the mandatory character of some conditions that must be imposed on treatment under a CTO, and the immediate power conferred to recall patients to hospital for breach of those mandatory conditions. Regarding Section 17 Leave, the Act establishes only very broad parameters concerning the conditions that may be imposed on outpatient care.
Recall may proceed only ‘when it appears to the responsible clinician that it is necessary to do so in the interests of the patient’s health or safety or for the protection of other persons’12 and should proceed only on the basis of an up-to-date medical opinion to meet the procedural requirements of detention for mental health purposes specified by the European Court of Human Rights.
Under the CTO regime, on the other hand, the Act requires certain mandatory conditions to be imposed on outpatient care. Patients on CTOs must make themselves available for medical examination at two key points in the process: when the order’s extension for another term is contemplated and when approval of treatment by the SOAD must occur. Breach of mandatory conditions authorises the patient’s immediate recall to hospital. Optional conditions may be imposed on a CTO that are ‘necessary or appropriate’ to ensure that the patient receives treatment. Agreement on those optional conditions must be reached in advance, however, between the RC and an AMHP: a somewhat more rigorous process than that which is required to set the conditions of Section 17 Leave. The patient cannot be recalled to hospital solely for breach of these optional conditions, but only when ‘(a) the patient requires medical treatment in hospital for his mental condition; and (b) there would be a risk of harm to the health or safety of the patient or to other persons if the patient were not recalled’. 12 Even when the patient is refusing treatment, those standards must be met for recall to occur.
Comparison of the two regimes on these parameters therefore yields very mixed results. A less rigorous process must be followed to set the conditions for Section 17 Leave, but no mandatory conditions are imposed, or is any automatic power conferred to recall patients to hospital simply for breaching the conditions of their Section 17 Leave. Regarding CTOs, on the other hand, a more rigorous process must be followed to set the conditions, but some mandatory conditions are imposed and their breach automatically authorises the use of the recall power. We might therefore say that a CTO is less restrictive of patients’ rights in certain respects (because a more rigorous process must be followed to set the conditions for outpatient care), but more restrictive in other respects (in imposing mandatory conditions linked to an immediate recall power).
Powers to treat without consent
The CTO and Section 17 Leave regimes confer slightly different powers to treat patients under them. The CTO regime distinguishes between the position of patients who have, and patients who lack, the capacity to consent to their community treatment and confers different powers to treat in each case. The Section 17 Leave regime makes no such distinction. It appears to confer a single set of powers to treat outpatients, regardless of their capacity.
Patients on Section 17 Leave remain ‘liable to be detained’. They are thus subject to compulsory treatment. This appears to authorise the administration of medication to patients on Section 17 Leave without their consent, regardless of their capacity, as long as the approval of an SOAD is obtained. The Act, however, confers no express power to administer medication through the use of physical force or restraint in a community setting to a patient on Section 17 Leave and it is doubtful whether or not that would be a safe health practice. Medication may therefore be lawfully administered to patients on Section 17 Leave who are not consenting and not resisting, provided that no significant physical force is used. When physical force is to be used, however, the patient should be recalled to hospital for treatment to proceed (except perhaps in an emergency). The Code of Practice therefore specifies that where treatment without consent of a patient on Section 17 Leave is contemplated, ‘consideration should be given to whether it would be more appropriate to recall the patient to hospital’. 12 Recall permits more extensive assessment of the patient’s condition before and after treatment, although it may also impose additional restrictions on liberty.
Treatment in the community of patients on CTOs distinguishes between patients with and without capacity. 176 Patients on CTOs who retain their capacity cannot be treated in the community without their consent, even in an emergency. To be treated without consent, they must be recalled to hospital premises. Community patients who lack capacity, on the other hand, can generally be treated without consent, even over their objection, provided that no ‘force’ is used.
A clear mechanism is therefore available for treating CTO patients without their consent, regardless of their capacity. Nevertheless, the treatment provisions governing patients on CTOs are more respectful of patients’ wishes than those governing patients who are ‘liable to be detained’.
It is a fair conclusion, therefore, that the CTO regime is somewhat less restrictive of a patient’s right to refuse treatment than Section 17 Leave, because a CTO does not confer any power to treat outpatients involuntarily who retain the capacity to consent. There is little difference between the two regimes, however, regarding the powers to treat patients who lack the capacity to consent (which may be a substantial proportion), and, ultimately, all patients on CTOs and Section 17 Leave can be treated without consent, regardless of their capacity, following their recall to hospital. The threat of involuntary treatment in hospital following recall therefore remains in all cases, and this may be the most important mechanism for the enforcement of compulsory outpatient care. The overall equation is thus still somewhat equivocal and, if the CTO regime is less restrictive of the right to refuse treatment than Section 17 Leave, that may balance out only its more restrictive aspects concerning the conditions that may be imposed on compulsory outpatient care and the consequences of their breach.
There is not space here to compare every feature of the two regimes, but the comparisons conducted above should be sufficient to support our claim that there is no obvious way to conclude which regime is the least restrictive overall. It is not safe to conclude that one is clearly more restrictive than the other, for two reasons: first, because the two regimes are very similar in many respects; and, second, because, when there are significant differences between them, these point, on some occasions, to Section 17 Leave being less restrictive and sometimes to the CTO regime.
Conclusions concerning the least restrictive regime
The conclusion we reach from such comparisons is that some indicators point to CTOs being more restrictive, whereas others point to Section 17 Leave. The two regimes simply have different kinds of impacts on different kinds of rights. Much will depend on the sequence of events in individual cases, and on how particular clinicians exercise their statutory powers. The indicators are too conflicting to reach any general conclusion about the least restrictive regime. Thus, the final legal principle we identified – that clinicians should always, when in doubt, allocate patients to the least restrictive option – cannot resolve our current dilemma because we cannot identify with confidence the least restrictive regime. Thus when clinicians encounter patients who meet the criteria for both Section 17 Leave and a CTO simultaneously, they could be lawfully allocated to either regime; they retain this important element of discretion. We incorporated that discretion into the methods for our research, taking the view that when patients met the legal criteria for both regimes, clinicians might allocate them at random between the two. In doing so, they would act lawfully, and would permit us to research the efficacy of compulsory outpatient care.
Conclusions
-
Patients can simultaneously meet the legal requirements for discharge to both a CTO and Section 17 Leave.
-
Neither CTO nor Section 17 Leave can be clearly demonstrated to be the least restrictive option.
-
The OCTET Trial was designed lawfully to compare the treatment outcomes of CTOs against treatment initially on Section 17 Leave.
-
The OCTET Trial tested the changes made to the law of compulsory outpatient treatment by the MHA 2007.
Chapter 12 OCTET Study discussion and conclusions
The key findings of the OCTET Study are shown in Box 3, below.
-
CTO use did not reduce the rate of readmission to hospital.
-
The length of the initial compulsory outpatient treatment was hugely greater for the CTO group than the non-CTO group (median 183 days vs. 8 days).
-
CTO use had no impact on time to readmission, number and duration of hospital admissions or the range of clinical and social outcomes.
-
There were no differences for any of the prespecified subgroups.
-
The results did not support the hypothesis that CTOs would result in reduced hospitalisation costs.
-
There was no evidence of any health or social care cost savings in the CTO group.
-
CTOs significantly increased informal care costs and the costs of legal procedures.
-
CTO use had no significant impact on patients’ health-related quality of life or capabilities.
-
CTOs are unlikely to be cost-effective from a health and social care or a broader societal perspective.
-
The implementation of CTOs may be influenced by interactions between patients, psychiatrists and family carers; their interpretation of the legislation; and how they act on these interpretations.
-
Despite participants’ keen awareness of legal clout, there was considerable uncertainty about whether or not patient deterioration was required prior to recall.
-
The (perceived) focus of the CTO on medication adherence may have consequences for how CTOs are viewed and subsequently experienced; broader goals in patient care, and patient and carer involvement.
-
There is no general ethical justification for the introduction or use of a CTO regime.
-
In some limited situations, the promotion of patient autonomy could provide sufficient reason for using a CTO, but this should not be done when the patient’s autonomy could be promoted by another means.
-
We developed and tested a new measure, the OxCAP-MH, to be able to assess the comprehensive capability profile of mental health patients.
-
This provides a complementary outcome measure of well-being in addition to health-related quality of life and social functioning.
-
Patients can simultaneously meet the legal requirements for discharge to both a CTO and Section 17 Leave.
-
Neither CTO nor Section 17 Leave can be clearly demonstrated to be the least restrictive option.
-
The OCTET Trial was designed lawfully to compare the treatment outcomes of CTOs against treatment initially on Section 17 Leave.
-
The OCTET Trial tested the changes made to the law of compulsory outpatient treatment by the MHA 2007.
This discussion chapter draws substantially on papers published by members of the OCTET Coercion Programme Group: Burns et al. ,16 with permission from Elsevier; Dawson et al. ,173 with permission from Oxford Journals; and Simon et al. ,144 with permission from Elsevier.
The OCTET Trial clearly demonstrated that CTOs do not reduce readmissions to hospital, confirming the findings of both the earlier RCTs,63,64 as well as the conclusions of two reviews conducted before the inception of our study3,4 and a more recent one. 67 As such, it is clear that CTOs have not achieved their stated aim of reducing revolving-door admissions to hospital. This was the case despite the fact that patients on a CTO spent far longer under the randomised regime than the non-CTO group (median 183 days vs. 8 days) and that they spent more than twice as long under compulsion in total as the non-CTO group (255 days vs. 102 days). As well as not affecting the rate of readmission, CTO use did not decrease the time to readmission, and there were no significant differences in the number or duration of hospital admissions.
There was also no demonstrable impact on clinical or social outcomes, quality of life or capabilities, and no differential effects of being in different subgroups. Neither the CTO nor the non-CTO group improved clinically over time. The only statistically significant result was a smaller increase among the CTO group than among the non-CTO group in their assessment of the effectiveness of treatment pressures. This difference was small (1.2 points on a scale from 4 to 20) and unlikely to be clinically meaningful. There was also no impact on health-care costs, including hospitalisation costs. In fact, CTOs significantly increased informal care and legal procedures costs. Our Ethical Analysis concluded that there is no general ethical justification for their use.
The OCTET Qualitative Study established that patients, psychiatrists and family carers alike see the main purpose of CTOs as being to ensure treatment adherence. As in international studies, most of the psychiatrists and family carers interviewed (although not all) expressed support for having a CTO regime. Patients held more ambivalent views and identified more disadvantages than the other groups. CTOs were seen as a potential safety net by all three groups, but there were divergent experiences of whether this was how they worked in practice. Many of the psychiatrists were careful not to give additional services to patients on a CTO in order to prevent the orders from becoming a ticket to better care. Family carers, however, were critical of services that contained patients on CTOs but did not provide services that enabled them to live more fulfilling lives. There were mixed opinions within and across the three groups whether or not adherence had improved under a CTO and whether or not it was the CTO that led to such improvement when found.
Community treatment orders and their impact
Our results add to the accumulating body of research into CTO effectiveness: while findings from non-randomised studies form an inconsistent pattern,67 randomised studies consistently fail to find support for patient benefit. 18,66
Not only did our results fail to support our hypothesis, but the total number of days in psychiatric hospital was very similar for both groups in our trial, as was the time from randomisation to readmission. Several patients remained in hospital for most of the trial period, including 13 who were never discharged because of deterioration in their clinical state, who had no opportunity to be supervised in the community.
Our trial sample was very similar to those in other RCTs. 18 The median length of illness was 12 years, during which time they had been hospitalised on average six times. One-third of the sample had been imprisoned and 43% had criminal convictions. The sample also closely matched descriptions in the literature of CTO populations internationally. 3
The OCTET Trial findings confirm those of the two previous RCTs63,64 that CTOs have no impact on hospital outcomes. In fact, the OCTET Trial found that patients on CTOs remained under compulsion for significantly longer periods than those in the non-CTO group without any demonstrable benefit. This raises the ethical question of whether or not such an imposition on personal liberty can be justified in the absence of any clinical benefit. Clinicians, after all, have a duty to provide treatment in the least restrictive environment.
The OCTET Trial was one of several studies, including the other two RCTs, which provided patients with case management and close clinical monitoring. In the US trials, this was added to standard care in both arms, leading to reported improvements, whereas in our trial such services were part of standard care already and neither group improved. This would seem to reinforce the conclusion that it is enhanced services that this group of patients requires rather than coercion. 65
Randomised controlled trials provide the most rigorous test of treatment effects, reducing the possible effects of researcher bias and regression to the mean, and identifying hypothesis and outcomes in advance. Conducting RCTs of CTOs is challenging, as our extensive investigation of methodological, ethical and legal issues demonstrated. Our trial design was not without imperfections and limitations (discussed below). This was also true of the previous trials. The New York RCT had considerable problems, including a smaller sample size than expected, high attrition and low adherence to the protocol. The North Carolina trial had a refusal rate of 12% and high attrition (18.2%). By comparison, only 1 of our 336 patients withdrew and we had primary outcome data for all. Our trial provided robust evidence that confirmed the main findings of the two other RCTs in this field.
Aspects of each RCT and differences between them could affect their comparability and generalisability. The US studies examined court-ordered CTOs, and randomised between CTO and voluntary status. Our trial examined clinician-ordered CTOs, and randomised between discharge via CTO and discharge via Section 17 Leave. The US studies actively excluded a proportion of patients with a history of violence. The OCTET and New York trials experienced more protocol violations than expected. Nevertheless, the clear differences between the length of compulsion imposed on patients and the comparability of the treatment in the two arms of the trials indicate that their common findings are comparable and noteworthy.
Trial design and its implications
The difficulties we faced in designing the OCTET Trial arose to a great degree from the need to maintain a lawful research method, that is, a method that avoided the random discharge of compulsory patients from the statutory scheme and ensured that patients were dealt with according to law. This requirement meant that we could not use the optimum research method: direct randomisation to either compulsory or voluntary outpatient care. Instead, after the lengthy study of the legal and ethical implications, we had to adopt a secondary strategy. This involved the patient being randomised to leave hospital either on a CTO or via Section 17 Leave, with an understanding that the latter was to be used according to the Code of Practice and be restricted to a short period of days, or at most weeks, before discharge to voluntary care. Protracted use of Section 17 Leave has been reined in by the courts176 and clinicians are required to consider using a CTO when extending Section 17 Leave beyond 1 week. 48 Section 17 Leave is commonly used as part of the discharge process, including when patients are discharged to a CTO. In our trial, clinicians discharged patients on Section 17 Leave to voluntary status after a median of 8 days, showing that their use of the Section 17 Leave regime was, on average, what we had anticipated it to be.
In effect, the OCTET Trial design allowed us to test a new form of treatment against the prior standard form of care, instead of against placebo. In the past, the standard approach to the treatment of those patients who are likely to be included in our trial was not their direct discharge to voluntary outpatient care, but discharge to voluntary care through Section 17 Leave. Our trial aimed to test the effectiveness of that older standard approach against the use of CTOs. If it was necessary to enact a new CTO regime, as the government claimed during the law reform process, then this new regime should have produced measurable differences in treatment outcomes.
The period immediately after the change of legislation provided a window of opportunity for this study, as the position of equipoise in which the clinicians then found themselves meant that varying clinical practices were likely to emerge. Therefore, this created the conditions for us to conduct an RCT that would be both lawful and ethical. This had the potential limitation that there might be a slow acquisition of confidence and skills in use of the CTO regime, thereby reducing trial generalisability. This does not appear to have been the case.
Centrally collected data on CTO usage show that clinicians were quick to use the new regime. Since 2008, CTOs have been used extensively (18,942 have been made so far) and there has been a 10 per cent increase year on year. The latest figures show that in 2012–13, in excess of 4600 orders were made, and 5218 individuals were subject to a CTO. That the total number of people on CTOs has consistently been higher than the number of CTOs made each year shows that some patients stay on CTOs for protracted periods. In 2012–13, 2272 recalls were made and on 1509 occasions a CTO was revoked. There were 2162 discharges. 177 The median duration of the initial CTOs in our trial was 6 months, indicating that about half were being renewed, which matches the national trends. Combined with clinical contacts averaging over two per month, this suggests that CTOs in the trial were being implemented in line with the legislators’ expectations of the regime being used for long-term community supervision with close monitoring.
Central figures correspond with local studies and audits in terms of the characteristics of patients being subjected to CTOs. Of those on CTO, 65% are male. 177 The majority (around 80%) of those on CTOs have a diagnosis of schizophrenia or schizoaffective disorder and almost half lack insight into their disorder. Around two-thirds are on depot antipsychotic medication. 178 This pattern is also reflected in small-scale studies, which report that patients on CTOs also have long histories of mental illness and of previous admissions. 52,53,179,180 Less than five per cent of CTOs were for people under forensic sections. 177 The OCTET Trial cohort is therefore in line with national and international CTO usage.
Clinical and social factors and subgroup analyses
Although there was no change in patients’ perceived coercion at the end of the trial, the sample as a whole was more positive about the effectiveness and fairness of the treatment pressure they had experienced. They were also more positive about their interaction with clinicians and expressed slightly reduced desires for involvement and information. As patients were hospitalised at baseline but most were in the community at 12 months, this could reflect a preference for community services. This would be consistent with what is reported elsewhere. 80 The increase in the number of patients screening positive for problem drinking and the small increase in the number in employment may reflect their restrictive environment at baseline. None of these changes was influenced by the presence or absence of a CTO.
The interactions between symptoms and age and between symptoms and tertiary education detected in the subgroup analysis were also small and unlikely to be of clinical significance. The lack of consistency both in the direction of the observed interactions and across outcomes for these subgroups suggest that they are chance findings. 118,181
There was no difference in readmission rate between those on depot medication and those not. The use of depot medication decreased over time in the entire sample, but significantly more in the CTO arm than the non-CTO arm. This overall reduction in depot use might explain some of the more positive attitudes to antipsychotic medication in the total sample at 12 months. Although the proportion of patients treated by depot (51% of the CTO group, 62% of the non-CTO group) was slightly lower than that reported in many other studies (60–90%4), it matches early reports for those on CTOs in England as a whole (65%178) and in London (54%182 and 61%183). Reduction in depot use over time for those on CTOs has also been reported in other contexts,184 although others suggest the opposite effect182 and that depot use may prolong the CTO. 183
We thus failed to find any benefits of being on a CTO for the identified subgroups or for any of the clinical and social outcomes. This is consistent with previous RCTs that did not find improvement for any of the outcomes of their randomised samples (with the exception of self-reported victimisation). 3 A range of improved outcomes has been reported in selected non-random subsets3 but no conclusions about effectiveness can be drawn from these studies. 3,185
Economic implications of community treatment orders
The Economic Evaluation was a prospectively designed, comprehensive analysis of the cost and outcome consequences of CTOs over a 12-month follow-up period, both from a health and social care perspective and from a broader societal perspective. The analysis was based on patient-level resource use and outcome data collected directly from patients and expanded with information from medical notes where needed. The analysis used data from the whole cohort apart from the three excluded patients and the five patients who died during the follow-up period (n = 328).
Despite the above, we encountered the problem of missing data on self-reported contacts with services and quality of life. To assess the potential impact of missing data on the cost-effectiveness results, we used multiple imputation of the missing information and conducted alternative analyses both on the complete cases and the full imputed data set. We assessed the quality of life/well-being consequences of CTOs across multiple outcome measures including the EQ-5D-3L, the EQ-5D-VAS and the OxCAP-MH capability index. We also looked at the potential impact of the assumed pattern of transition between health states on the outcome results in further sensitivity analyses. We applied non-parametric bootstrapping to assess the overall uncertainty in our cost-effectiveness results.
The analysis provided robust evidence against the hypothesis that CTOs may lead to reduced health and social services costs as a consequence of reduced hospitalisation, or that they may result in superior quality of life/well-being outcomes for patients. Neither could we find a significant opposite effect of CTOs on quality of life or well-being. Although substantial uncertainty remains about the exact incremental cost-effectiveness of CTOs, neither of the alternative analyses altered the final results and conclusions that CTOs are unlikely to be cost-effective. It is important that decision-makers consider our additional important findings on the increased informal care and legal procedure costs of CTOs.
Patients’, carers’ and professionals’ views of community treatment orders
The OCTET Qualitative Study contributes to an understanding of how the two mechanisms by which the England and Wales CTO regime was designed to work – conditions and power of recall – operate in practice. We examined psychiatrists’, patients’ and family carers’ experiences of these two inbuilt mechanisms, along with their impressions of CTOs’ effectiveness. A third dimension, legal clout, emerged during analysis. Three main issues arose.
First, all three groups perceived the chief purpose of CTOs to be the enforcement of medication and that legal clout was central to the achievement of medication adherence. Nevertheless, all three groups described CTOs as being helpful (i.e. leading to medication adherence and/or reduced admissions) for only some, and identified a variety of shortcomings in how the orders were used in practice. Family carers viewed the perceived focus on medication – to the exclusion of additional support or service provision – as a major flaw that impeded full recovery. By contrast, psychiatrists often emphasised that CTO patients were not treated preferentially, responding to concerns voiced prior to the introduction of CTOs about creating perverse incentives for their use. 186 All three groups also acknowledged that other, non-CTO-related factors might have contributed to any observed improvements in patients’ adherence.
Second, the way in which the CTO’s mechanisms worked in practice could be influenced by participants’ understanding of those mechanisms and by structural factors. Participants’ understanding of how the inbuilt mechanisms of the CTO (should) work varied considerably. It was clear that patients, carers and psychiatrists alike were unclear about the enforceability of discretionary conditions and the criteria for recall. This lack of clarity, which in part may have arisen as a result of the way in which the statute was written, was compounded by the way information was communicated between, and subsequently interpreted by, patients, psychiatrists and family carers. We found that some psychiatrists maintained patients’ uncertainty about recall for the purposes of enhancing adherence. Although some psychiatrists expressed disappointment about what they perceived as a too-high threshold for the use of recall, patients perceived the threshold for hospitalisation to be lower than when they were not on a CTO. The CTO mechanisms discussed here could therefore rely not only on how they were interpreted and applied by psychiatrists, but also on how patients responded to them and how carers were involved. Although recall was intended as a simplified means of responding to relapse or risk,48 we found mixed evidence from all three groups as to whether or not this was the case in practice. One reason for this was the lack of clarity about the requirement in the law regarding the role of conditions and the need to wait for patients’ deterioration. Structural factors, such as inpatient bed shortages and out-of-hours procedures, could also influence the use of recall.
Third, we identified a wide range of experiences and views within each group, indicating that there is no such thing as the definitive patient, psychiatrist or family carer experience of CTOs. Although some patients were motivated to comply with the conditions by the ‘threat’ of recall, others said that they did not feel compelled to comply and viewed the possibility of hospitalisation under the CTO as no different from their experiences before being on a CTO. We identified commonalities in psychiatrists’ overall pragmatism in their design and use of conditions and belief in the power of recall, but we also discovered more unusual practices and variation in views about the appropriateness of, for example, specifying and enforcing discretionary conditions. Family carers mostly welcomed the conditions and power of recall, but did not arrive at univocal conclusions about the usefulness of CTOs. The involvement of family carers in decision-making related to the CTO also varied widely.
Broadly speaking, our findings are not dissimilar to those of the small number of existing studies (mainly from the North America and Australasia) on experiences of CTOs. 73,75–78 The three sets of interviews yielded a large amount of rich data. Further analytical strands will be pursued after the completion of the programme grant period.
Ethical implications of community treatment orders
Our Ethical Analysis shows how ethical considerations concerning the use of legal powers in community mental health care map on to the different ways in which CTOs are used and experienced in practice. A complex and nuanced account emerged of how the ethical principles of respecting patients’ autonomy, respecting patients’ liberty and acting beneficently should be interpreted in order to make judgements about the ethical justification of CTOs.
Previous ethical analyses have pitched this ethical debate largely as a conflict between patient benefits, on the one hand, and liberty and autonomy, on the other, with the implication that this is a debate to be settled one way or the other. These analyses have not been sensitive to the ways in which CTOs are being used and experienced in practice. The varied range of experiences documented here, by contrast, suggests that ethical duties can pull in different directions, depending on the individual patient’s circumstances. The ethical picture is not as clear, nor as binary, as other commentators have suggested. Exploring these ethical considerations in light of a detailed qualitative account of stakeholders’ experiences of CTOs in England reveals a more complex ethical picture than has been presented previously.
The overall picture in participants’ personal accounts of outcomes resulting from the use of CTOs was mixed, with a range of positive and negative outcomes described. It predominantly related to claims about how well the mental health service was functioning when CTOs were being used, rather than simply describing the use of CTOs themselves (with the exception that some participants regarded the CTO as a new opportunity for stability for some patients). Little evidence came to light to suggest that the other benefits about personal and social support identified by patients could not have accrued independently of the CTO, if the service were appropriately responsive to patients’ own accounts of their needs. For instance, despite the speed of readmission being emphasised as a positive feature of patient care under (some) CTO orders, it should be recognised that it is not rapid readmission itself that constitutes a benefit to patients but rather the positive health, social and/or personal outcomes that can accrue for a patient in these circumstances. The evidence from the OCTET Trial reveals that such outcomes do not result from the use of a CTO. Moreover, it is unclear from these interviews whether it was the instigation of a CTO regime that led to the increased speed of readmission in some cases, or other factors relating to, for example, the efficiency and working patterns of the mental health professionals involved.
Although the legal powers are different, several North American studies similarly emphasise the importance of the legal regime of care management under a CTO. 65 Evidence reported from research conducted in response to the introduction of CTOs in New York State suggests that the experiences expressed by our participants are not uncommon. In that study, the data indicated that the intensive support required to meet the broad personal and social needs of some patients subject to CTOs did not materialise. 63 This evidence connects to the concerns raised by patient advocacy groups in the legal reform process in England and Wales. These groups expressed the concern that the CTO regime could legitimate the withdrawal of support to these patients on the grounds that their interests were safeguarded by narrow medical treatment-oriented care.
In considering the question of patients’ liberty, participants’ views and experiences must be read alongside the findings of the OCTET Trial. The OCTET Trial found important differences between the degree of freedom enjoyed by patients under CTOs compared with the non-CTO group. The CTO group were subject to this legal power for the subsequent 182 days (median) against 8 days for those in the non-CTO group. Similarly, across the entire 12-month follow-up period, those in the CTO group were subject to legal powers of compulsion for a total of 255 days against 102 days for the non-CTO group. Given that the CTO regime allows a range of conditions to be placed on what patients are able and not able to do, these figures clearly suggest that those placed upon CTOs have their liberties restricted, in more substantive ways and for longer periods of time, than other patients who receive mental health care in the community.
Two clear conclusions may thus be drawn from our Ethical Analysis, as the following sections explain.
No general ethical justification for community treatment orders
No general ethical justification for the legal framework of the CTO can be provided from our analysis. The reason for drawing this conclusion emerges from even a cursory review of how the relevant ethical considerations identified should be interpreted in practice.
Community treatment orders are not the least restrictive alternative when it comes to providing care within community mental health services, although they were widely interpreted when introduced as being less restrictive than the use of legal powers of detention in hospital. The conditions that clinicians can place on patients’ care regimes means that these clinicians must have good ethical reasons for using CTOs over less restrictive ways of supporting patients in the community. If such reasons are not available, CTOs cannot be justified.
Although our analysis indicates that some patients, carers and psychiatrists talked about different ways in which patients can benefit from the use of CTOs, it must be recognised that there is no RCT-level evidence that such perceived benefits actually result in improved outcomes for patients. It is therefore not possible to argue that CTOs can be justified from these accounts of perceived benefits – medical, social or personal – that are seen to accrue for some patients for whom CTOs are used. In other situations, clear accounts of difficulties or specific harms that patients faced under the CTO regime were described.
When considering whether or not the CTO regime functions to respect patients’ autonomy, there is a stronger ethical case to be made that CTOs can, for some patients at least, promote self-determination. A number of respondents clearly viewed the imposition of a community-based legal power as aiding patients in managing their illnesses in ways that enabled them to take control of their lives and to engage in new activities. Equally, for other patients the evidence suggested that they were constrained in their ability to exercise their autonomy in similar circumstances.
Promoting patients’ autonomy: a limited justification for the use of community treatment orders?
We therefore found that in some limited situations, the promotion of patient autonomy could provide sufficient reason for using a CTO when the patient’s circumstances suggest to the clinical team that this legal power is required to enable the patient to pursue life choices and activities in line with his or her values. This would not apply if the patient’s autonomy could be promoted by another means, for example by making additional multidisciplinary personal and social support available to him or her.
How the ethical argument regarding autonomy is developed here depends on resolving a practical and conceptual tension between respecting a patient’s autonomy and promoting that patient’s autonomy. Although this tension has been examined to some degree within psychiatric ethics187 and applied to discussions about mental health practice in view of interventions such as advance mental health directives (also known as ‘Ulysses Contracts’ or ‘Joint Crisis Plans’188–191), it is not an issue that has been discussed in previous ethical analysis of CTOs.
Participants prioritised the promotion of autonomy over mere respect for autonomy when thinking about the ethical legitimacy of CTOs, and usually contrasted the use of CTOs with being an inpatient. This position is understandable; given the long-term nature of community-based mental health services, it should be seen as entirely appropriate to foster a person’s self-development and support his or her life projects into the future, rather than treating that person’s values and abilities as static. By way of caution, however, it should be noted that the recent evidence from an RCT of advance directives for mental health suggests that the promotion of patient autonomy through the use of such interventions may not lead to clinical benefits. 188 This implies that it is also important to look very closely at whether or not autonomous choice would indeed be fostered through the use of CTOs in any given clinical situation.
There are two additional difficulties in drawing on an ethical requirement to promote a patient’s autonomy to provide an ethical justification for the use of CTOs. The first difficulty is an epistemological one. Although it may be correct that, in some cases, patients’ abilities to pursue choices and activities better, in line with their own values, will be enhanced by invoking a CTO, it will be difficult – if not impossible – for CMHTs to know whether or not patient autonomy will be promoted in any given case. Even if there are a small number of situations in which CTOs ought to be used to support the delivery of empowering and person-centred care, it is far from clear whether or not mental health professionals will be able to identify, in advance, when such situations have arisen.
The second difficulty in mounting an autonomy-based defence of CTOs is that our analysis has revealed that it is not possible to differentiate features associated with the use of a CTO from features of the broader care environment in which this power is invoked. As such, making an ethical judgement about the use of CTOs cannot be separated from the broader ethical requirement that professionals have to tailor the delivery of care and support services in ways that promote patients’ autonomy. The majority of concerns highlighted in the interviews concerned perceived failings in how interventions provided to patients were used to support their care and treatment, rather than constituting evidence that CTOs by themselves were harmful or disrespectful of patients’ autonomy. Equally, the benefits that participants felt emerged through the use of CTOs were commonly presented as being contingent on the availability and appropriateness of other interventions designed to provide personal and social support to patients in receipt of care in the community: features that are independent of these legal powers in a number of jurisdictions.
If patients’ autonomy can be promoted through the more optimal provision of multidisciplinary forms of personal and social support within community services, rather than through the use of CTOs, this is to be preferred, as these multidisciplinary interventions do not impose comparable restrictions on patients’ freedoms. There is clearly much more to say about the practical and ethical aspects of delivering good care to patients with complex needs within community mental health services, and we return to this in the ULTIMA Ethical Analysis (see Part 4, Chapter 20). Notwithstanding this observation, however, this Ethical Analysis does suggest that it is indeed possible that, in some situations, a CTO might be judged by the clinical team to be a valuable or indeed necessary component of a package of community-based care that promotes the autonomy of a patient. When such situations can be identified with some degree of certainty, it would be ethically defensible to use a CTO if available. This observation does not, however, legitimate the use of CTOs in general, nor does it provide a strong rationale for the introduction of these powers in jurisdictions for which they are currently unavailable.
Measuring capabilities: the development of the OxCAP-MH
As well as using previously established measures of clinical and social outcomes in the OCTET Trial, we also developed and tested a new measure of capabilities, the OxCAP-MH, which may in future be used to complement existing measures of health-related quality of life and social functioning. This work underlines the direct measurability of human capabilities for people with severe mental illness, and the practical potential for applying the capability approach to problems of health outcome measurement.
In developing the OxCAP-MH, we adopted an approach that draws heavily on the theoretical insights of Nussbaum167 and combined them with empirical focus group work used to develop the OCAP-18 questionnaire, which had previously been validated for the evaluation of public health interventions. Specifically, we focused on the contextual aspects of mental health research, particularly feasibility and content validity. Currently, although there may not be an agreement on any single unique account or list of capabilities, similar kinds of domains are beginning to emerge about the measurement of progress.
The single capability index derived from OxCAP-MH, the CAPINDEX16, is not in its current form intended to be used as a sole outcome measure for economic evaluations. We are aware of two projects that have tried to develop such composite, societal preference-based outcome measures using different capability instruments with the ultimate goal of a richer evaluative space. Netten et al. 192 have recently developed the Adult Social Care Outcomes Toolkit, a preference-weighted measure of social care-specific quality of life to be used in the evaluation of social care services. Using time-trade-off and best-worst scaling methods, a formula was developed to be able to generate a social care QALY comparable to a health QALY on a zero-to-one scale (where ‘0’ is equivalent to ‘being dead’ and ‘1’ is equivalent to ‘being in the ideal state’192). At the same time, Grewal et al. 193 have been developing a group of instruments also conceptually linked to Sen’s capability approach for assessing the impact of health and social care interventions for older adults, adults and carers [ICEpop CAPability measure for Older people (ICECAP-O), ICEpop CAPability measure for Adults (ICECAP-A), Carer Experience Scale, respectively] in an economic evaluation framework. To enable the application of capability well-being for economic evaluations, sets of preference-based index values are currently being estimated for these instruments (again on a ‘0–1’ capability scale using best–worst scaling methods). 159,194
Collapsing multidimensional capabilities information into single index scores in this way, using preference-based valuation techniques, is, however, conceptually in tension with the original capability approach. It is likely to be context-restricted and reduce the additional opportunities the capabilities framework can offer for policy-making (e.g. prioritisation of intervention areas, distributional information).
All approaches to self-reported outcome measurement in mental health are prone to similar difficulties. This substudy was not designed to investigate such issues surrounding adaptation. The use of numerous and explicit domains in OxCAP-MH, however, rather than the relatively catch-all term ‘daily activities’, may mitigate any impact of adaptation on self-reported results. If so, this would argue strongly for our capability approach. This idea remains to be tested, however, together with the potential impact of altered perception due to delusion or changed mood, such as mania or depression.
Limitations
OCTET Trial and Economic Evaluation
One in five of the patients approached refused to participate, which may have skewed our sample. The sample was, however, similar to those in the other two RCTs of CTOs.
Patients who lacked the capacity to consent to take part in research were excluded from our trial. These patients were excluded because of the ethical difficulties involved in engaging people in research who are incapable of understanding the implications of taking part on their treatment. This was a small group (nine patients), as only patients who were ready for discharge to the community were eligible to take part, and patients in that position should not be acutely unwell.
The number of protocol violations was noteworthy (42 violations in the CTO group and 46 in the non-CTO group, as well as the three patients who were ineligible or withdrew), although this is far from unique in pragmatic effectiveness trials. 195 Three factors contributed to this result. First, the legal position underpinning the lawfulness of the trial (see Chapter 11) required each subsequent clinical decision to be entirely unconstrained by the patient’s randomised status. Consequently, clinicians could not be encouraged to persist with the randomised assignment. Second, recruitment of patients took place at the point that the clinical team decided to initiate supervised outpatient care. Finalisation of a CTO requires detailed consultation both within the team and with the patient and their family, which can take from a few days to several weeks. During this time both the patient’s clinical condition and the commitment of the team to the trial can vary.
Third, adherence to randomisation was compromised by reorganisation in almost all of the collaborating mental health services, particularly by the separation of inpatient and outpatient consultant responsibility. As a result, many patients passed to being treated by psychiatrists who were unfamiliar with the trial and who might have had different opinions about management. Although these protocol violations are illustrative of key factors affecting the operation of CTOs, they did not alter the findings of our well-powered trial and this was confirmed by our sensitivity analysis.
The OCTET Trial was originally designed to capture the experience of family carers as well as patients, but this aspect of the trial had to be abandoned because of the low response rate. To some extent this was not unexpected as the patient group in question often have limited contact with their family. Carer views were, however, included in the OCTET Qualitative Study.
The Economic Evaluation encountered the common problem of missing data, as some relevant information could not be obtained from either the patient interviews or medical records. We addressed this according to current best practice using multiple imputation of the missing data and a sensitivity analysis carried out on the complete data set. Although the results of the sensitivity analysis did not alter the main findings, the potential impact of missing data on the results cannot be fully estimated.
OCTET Qualitative Study
Although we report the views of patients, carers and psychiatrists in the Qualitative Study, we could not sample patient–carer–psychiatrist triads or did we sample other professions involved in the administration of CTOs, such as AMHPs. The aim of this substudy, however, was not to examine dynamics and outcomes in case studies, but to identify experiences of the mechanisms at work in the operation of CTOs. The majority of family carers whom we interviewed were parents, and the experiences and views reported by this group might have differed if the sample had included, for example, more siblings or spouses. It is a strength of the OCTET Qualitative Study that our maximum variation sampling strategy captured a range of views and experiences within, and across, the three samples, minimising the likelihood that the findings were associated with a particular team, setting or NHS trust.
OCTET Ethical Analysis
We did not examine some potential benefits of CTOs, such as any impact on families. Some family carers felt that this was an important issue. The potential benefit for society at large was also not something our study assessed and this was one of the issues featuring in the debate preceding the introduction of CTOs.
OCTET Capabilities Project
In developing the capability approach for this patient group, our method did not capture effects on informal carers’ capabilities or those of the wider community who were likely to be affected by the inevitable externalities of mental disorders treated in the community. This is not uncommon in this area and currently it is not clear how these aspects could be aligned. So far the closest attempt to capture similar externalities is the development of the Carer Experience Scale. 196 Neither is it yet clear how people’s ‘agency goals’,197 another fundamental concept of the capability approach, might or should be incorporated in any of the existing capability measurement frameworks as applied to health status assessment.
Conclusions and implications
The OCTET Trial is the third, and largest, randomised trial of CTOs, and, similar to its predecessors, did not find any evidence that CTOs achieve their intended purpose of reducing readmission in so-called revolving-door patients with a diagnosis of psychosis. No benefit was found for any of the clinical or social outcomes measured or for any of the prespecified subgroups. Despite some positive experiences being reported, the qualitative study found no univocal views within or across the groups interviewed as to the effect of the intervention. The evidence is now strong that the use of CTOs does not confer early patient benefits despite substantial curtailment of individual freedoms. In view of the now consistent experimental evidence against any clear benefit, we believe any proposal to either introduce CTOs to new jurisdictions or extend their use would require a commitment to test their effects at least as rigorously as we have done.
Part 3 OCTET Follow-up Study
Abstract
Background
Serious concerns have been raised that CTOs might lead to disengagement.
Objectives
Our objectives were to investigate the association between compulsion and disengagement; the effect of the trial randomisation arm on disengagement and readmission; the association between CTO use and readmission to hospital for patients who experienced time on a CTO; and the differential impact of baseline characteristics on the effect of duration of compulsion on discontinuity of care.
Methods
The OCTET Follow-up Study followed up the OCTET Trial cohort (n = 333) at 36 months after randomisation, collecting data from medical records. The primary outcome was the level of disengagement during the 36-month follow-up period. Secondary and tertiary outcomes comprised a range of hospitalisation outcomes.
Results
Rates of consistent clinical follow-up were much greater than expected (94% at 36 months). Just over half of the sample (n = 187, 57%) had no discontinuity in their care. There was no significant difference between the CTO and non-CTO groups in the number of discontinuities (IDR 1.12, 95% CI 0.78 to 1.59; p = 0.537). Longer duration of compulsion was associated with longer time to disengagement (HR 0.946, 95% CI 0.90 to 0.99; p = 0.023) and fewer periods of discontinuity (IDR 0.96, 95% CI 0.95 to 0.98; p < 0.001). There was no difference in any readmission outcomes over the 36 months. We did not identify a linear relationship between readmission outcomes and duration of CTO. We identified no effect of baseline characteristics on the association between compulsion and disengagement.
Conclusions
There was no evidence that increased coercion led to disengagement from services. There was no convincing evidence for improved hospitalisation outcomes from CTOs at 36 months.
Chapter 13 Introduction to the OCTET Follow-up Study
The OCTET Follow-up Study took place from 1 August 2012 to 30 October 2014. Following on from the OCTET Trial, it aimed to investigate the association between compulsion and disengagement in the OCTET Trial cohort in the 36-month period following randomisation, as well as investigating any effect of the randomisation.
This was a revision of the original objective of the OCTET Follow-up Study, which was ‘to compare disengagement and clinical outcomes between those randomised to CTO and those randomised to non-CTO treatment at 36 months after randomisation’. We modified this in view of the findings of the OCTET Trial. Given that the OCTET Trial showed no difference between the two arms, our revised primary objective for the OCTET Follow-up Study was thus to examine compulsion and disengagement across the whole sample, with the effect of randomisation being explored as a secondary objective.
We designed the OCTET Follow-up Study to address serious concerns that CTOs might represent an increase in coercion that might lead to disengagement from services. No studies had previously addressed this question, although there are some anecdotal reports. 68,69 The purpose of CTOs, as discussed above (see Part 2, Chapter 5), is to ensure a period of improved mental health that optimally leads to subsequent voluntary engagement and treatment concordance. The possibility that their use might instead lead to great disengagement from services merits serious attention.
The OCTET Follow-up Study thus added a fourth time point, at 36 months after randomisation, in order to collect data over 24 additional months from the end of the initial 12-month follow-up period. The aims were to establish whether or not engagement with services and service use demonstrated any association with duration of compulsion; whether or not, in the long term, there was a difference in engagement with services and service use between patients in the two arms of the trial; and whether or not there was a difference in rates and duration of readmission between patients who spent any time on a CTO. We also sought to determine whether or not being in the CTO arm of the trial made any difference.
This chapter draws substantially on a paper published by members of the members of the OCTET Coercion Programme Group: Burns et al. ,198 with permission from Elsevier.
Chapter 14 OCTET Follow-up Study: methods
Sample
Participants in the OCTET Follow-up Study were the 336 patients who were participating in the OCTET Trial. We applied no further inclusion or exclusion criteria.
Objectives
Our objectives were to investigate:
-
the association between compulsion and levels of disengagement
-
the effect of randomisation arm (CTO or non-CTO) on levels of disengagement and readmission rates
-
the association between CTO use and readmission to hospital for patients who experienced time on a CTO
-
the differential impact of baseline characteristics on the effect of duration of compulsion on discontinuity of care.
The first objective was to test the hypothesis that a longer time under compulsion would increase disengagement from mental health services or discontinuity of contact. These were defined as:
-
disengagement: no service contact for at least 90 days immediately preceding final follow-up
-
discontinuity: any 60-day period (or more) of no service contact.
The second objective was to test the hypothesis that at 36-month follow-up, patients in the CTO arm of the trial, compared with those in the non-CTO arm, would:
-
be more likely to experience disengagement
-
experience more discontinuities
-
have a reduction in readmissions to hospital.
The third objective was to test the association between CTO use and (only for patients who experienced time on a CTO, regardless of the arm to which they were randomised):
-
hospitalisation rate
-
time to readmission
-
duration of admissions.
We also aimed to use subgroup analysis to test the hypothesis that the levels of disengagement (time to disengagement and discontinuity of treatment over time) would differ according to factors measured at baseline, and to test for a centre effect by comparing London patients to those in the other sites.
Data collection
We collected all data from medical records at 36 months after randomisation. This continued until 22 February 2014.
Outcomes
Disengagement outcomes
Two variables were used to measure the level of disengagement during the 36-month follow-up period from the first discharge (the date when the patient left the hospital) to the end of the study:
-
Time to disengagement Disengagement was defined as no service contact for 90 days (or longer) and no return to contact. Time to disengagement was therefore calculated as the number of days from the point of first discharge from hospital to the last clinical contact, if that last contact occurred at least 90 days (3 months) before the end of the study follow-up period. This was a continuous variable, expected to be skewed. Data were censored for patients who died, emigrated or were discharged or imprisoned, and the 90-day period no contact requirement was calculated to that date rather than 1095 days.
-
Discontinuity of treatment over time This was defined as the number of time periods of 60 days or more in community care without a contact with services. This was a continuous variable expected to be skewed.
The explanatory variable duration of compulsion was defined as follows:
-
Duration of compulsion This was defined for duration of total compulsion and for duration of community compulsion. Total compulsion was defined as the number of days under any legal compulsion (e.g. Sections 2, 3, 4, 136 or 37, CTO, and 40/48 of the MHA) during the 36-month follow-up period, including time under the initial Section 3 between randomisation and discharge to randomised status. This variable included inpatient and outpatient compulsion times.
-
Community compulsion This was defined as the number of days in the community on a CTO and excluded inpatient compulsion. Time under voluntary status was not included in this variable.
Readmission outcomes
We used the following readmission outcome variables:
-
Readmission to psychiatric hospital This was defined as a binary outcome (patient readmitted to hospital (voluntary and involuntary) during the 36-month follow-up period versus patient never readmitted).
-
Duration of admission Number of nights of psychiatric hospitalisation from first discharge from hospital to 1095 days. This included voluntary and involuntary hospitalisations; nights on recall were not included unless the recall ended in revocation.
-
Time to first readmission Number of nights from first discharge to first readmission. For patients (in both arms) who remained in hospital for the duration of the study, the time to first readmission was counted as zero. Nights on recall did not count as a readmission unless the recall ended in revocation.
-
Number of readmissions from first discharge to 1095 days This included voluntary and involuntary hospitalisations but not any recall that did not end in revocation of the CTO.
Community treatment order compulsion outcomes
The following CTO compulsion outcomes were used for patients who experienced a CTO at any point during the study (non-randomised group):
-
Duration of readmission Defined as above in Readmission outcomes.
-
Readmission rate Defined as the proportion of patients readmitted to hospital (subject to the constraints mentioned under Readmission outcomes);
-
Time to readmission Defined as the number of nights from the point of first discharge from hospital to the first readmission.
Data management
The study researchers entered most of the data directly into an Access® 2010 database (Microsoft Corporation). They subsequently cleaned these data using an Excel 2010 database. They recorded data for the first 66 patients in clinical research forms. For these 66 patient interviews, different researchers double-entered the data, compared them against each other, and discussed and corrected discrepancies under supervision. The statistician responsible for the analysis performed additional data quality evaluations. These included range checks and logical and consistency checks that might not be picked up by checks at the individual patient level by research staff. In the case of variables that were a function of other variables (e.g. length of a particular hospitalisation), these were checked by automatic calculation of its values. We froze the final cleaned data before starting the analysis.
Statistical methods
As with the OCTET Trial, the research team wrote and signed off a detailed statistical analytical plan before analysing any data (see Appendix 2). All analyses were done according to the statistical analysis plan, except for the analysis of non-randomised CTO group.
Disengagement
‘Time to disengagement’ is a time-to-event outcome. We therefore performed the analysis using a proportional hazards model adjusting for duration of compulsion and the stratification factors [gender (male/female), schizophrenia (yes/no) and duration of illness (< 2 years, > 2 years)]. We present the results as HRs with 95% CIs.
‘Discontinuity of treatment over time’ is a count outcome. We therefore analysed it using a negative-binomial regression model and adjusting for duration of compulsion and stratification factors. We present the results as IDRs, which are interpreted in the same way as relative risks.
We conducted this analysis for the whole sample (not splitting by trial arm).
Readmission
We conducted the analysis for the readmission outcomes using the intention-to-treat population. We analysed the readmission outcomes in the same way as the disengagement outcomes, using multiple regression models with adjustment for the stratification factors. The type of regression model depended on the data distribution. We assessed all model assumptions.
We compared the trial groups for time to disengagement with the non-parametric Wilcoxon rank-sum test because of the violation of the proportional hazards assumption of the proportional hazards model.
Similarly, the model used in the analysis for discontinuity of treatment was adjusted for trial arm, reporting its coefficient (and 95% CI and two-sided p-value) interpreted as an IDR.
We analysed psychiatric hospital readmission in the 36-month follow-up period, as a binary outcome, using log-binomial regression that was adjusted for the trial arm indicator and the stratification factors. We present the results as the relative risk of readmission in the CTO group compared with the non-CTO group, with appropriate 95% CIs and two-sided p-values.
The number of readmissions and duration of readmission are count outcomes. We analysed these using negative-binomial regression models and adjusting for trial arm indicator and the stratification factors. We present the results as IDRs.
The time to first readmission from first discharge to 1095 days is a time-to-event outcome. We therefore performed this analysis using a proportional hazards model, adjusting for the trial arm indicator and the stratification factors. We present the results as HRs with 95% CIs and also present Kaplan–Meier plots. We calculated the median readmission time with 95% CIs.
Community treatment order compulsion
Analyses of association of duration of CTO and readmission outcomes were conducted only on patients who had at least one CTO event so the sample size was restricted to 198 people. Owing to model assumptions violations, the explanatory variable CTO compulsion was split into quartiles.
We analysed the association between CTO compulsion groups and readmission rate using Poisson regression with robust error variances,199 as the log-binomial model was not possible because of model instability. The results are presented as relative risks with 95% CIs.
We performed the analysis for the time to readmission using the non-parametric Kruskal–Wallis test. The proportional hazards model was not used because of the violation of the proportional hazards assumption.
We analysed the duration of readmissions using a negative binomial regression model adjusting for the categorical CTO compulsion and stratification factors. We present the results as IDRs with 95% CIs.
Sensitivity analyses
We conducted a sensitivity analysis for the variables measuring the disengagement outcome, which consisted of repeating the above analyses without adjusting for the stratification factors.
Subgroup analyses
To identify patients’ baseline characteristics associated with a differential effect of duration of compulsion on discontinuity of care, we fitted the same model as for the disengagement outcome, with the inclusion of an additional interaction effect for the interaction between the duration of compulsion and the relevant subgroup variable. The p-value for the interaction test was the p-value of interest, as this was the test of the stated hypothesis. The significance of the compulsion variable was not considered of interest here.
We evaluated the following groups, defined a priori, the first three of which were stratification factors:
-
gender: male versus female
-
diagnosis: schizophrenia versus other
-
duration of illness: < 2 years versus ≥ 2 years
-
age: ≤ 40 years versus > 40 years
-
ethnicity: white versus others
-
born in UK: born in UK versus born in another country
-
marital status: (single + separated/divorced) versus married/cohabiting
-
accommodation: independent versus (supported + homeless)
-
living status: living alone versus living with others
-
educational level: ≤ 12 years versus > 12 years; tertiary education (yes/no)
-
BPRS: ≤ 33 versus > 33
-
GAF: ≤ 49 versus > 49.
A centre effect was evaluated through a similar subgroup analysis for both the disengagement and readmission outcomes. The subgroups were defined by the variable:
-
centre: London versus other sites.
Changes to protocol from original proposal
With the exception of the change in the primary objective, detailed above, the analyses we conducted were all in line with the spirit of the analyses detailed in the original proposal. As with the OCTET Trial, we made some changes to the original proposal when writing the statistical analysis plan. In particular, we used more sophisticated adjusted regression models as the primary comparisons, using the simpler unadjusted tests for secondary sensitivity analyses. We performed the adjustment for the variables used in the stratified block design method of randomisation. We did not conduct any minimisation process.
We performed all analyses over the 36-month follow-up period from randomisation (i.e. from randomisation to 1095 days) and not over the 24 months after the OCTET Trial ended, as the original proposal indicated.
Chapter 15 OCTET Follow-up Study: results
Participant flow
Of the original 336 OCTET Trial patients, three were excluded, as one withdrew and two were found to be ineligible (see Part 2, Chapter 6). Of the remaining 333 patients, one withdrew consent to continuing engagement in the Follow-up Study; data could therefore not be collected for this patient and was treated as missing data. For two further patients, data on contacts with services were missing for the entire study period as a result of their paper medical records being destroyed in a fire or lost. We therefore present data throughout the OCTET Follow-up Study for the sample of 330 patients.
A total of 20 patients died during the 36-month follow-up period. Five of these died during the 12 months of the OCTET Trial. In total, six of the deaths were suicides (four of the CTO group and two of the non-CTO group), one (in the CTO group) was an accidental death by drug overdose group and 13 patients died of natural causes (eight of the CTO and five of the non-CTO group).
There were 16 patients who were in general hospital care (three patients: one patient of the CTO group and two patients of the non-CTO group) or in prison (one patient from each group) for substantial periods leading up to the end of the study, or who moved abroad (three patients of the non-CTO group) or were discharged from secondary psychiatric services (eight patients: four patients from each group). Analysis was censored for these 16 patients.
Interventions received during the 36-month follow-up period
Table 28 presents the descriptive data for hospital care for the 36-month follow-up period. By 36 months, 213 patients (65%) had been readmitted [100 (61%) of the CTO and 113 (68%) of the non-CTO group]. The 213 who had been readmitted spent a median of 132 nights in hospital (117.5 for the CTO and 139.5 for the non-CTO group). Of these 213 patients with readmissions, 126 (59%) had experienced more than one readmission (60 of the CTO group and 66 of the non-CTO group). None of these differences was statistically significant.
| Hospitalisation | Total sample size | CTO (N = 165) | Non-CTO (N = 165) | Total sample (N = 330) | |||
|---|---|---|---|---|---|---|---|
| n (%)/mean {SD} | Median [IQR] | n (%)/mean {SD} | Median [IQR] | n (%)/mean {SD} | Median [IQR] | ||
| Psychiatric hospital readmission | |||||||
| Readmitted | 330 | 100 (61) | – | 113 (68) | – | 213 (65) | – |
| Not readmitted | 330 | 65 (39) | – | 52 (32) | – | 119 (36) | – |
| Duration of readmission (nights) | 212a | 237.1 {269.09} | 117.5 [63–303] | 252.1 {282.48} | 139.5 [63–309.5] | 245.0 {275.69} | 132.0 [63–307] |
| Number of readmissions | 213 | 2.4 {1.91} | 2.0 [1–3] | 2.2 {1.43} | 2.0 [1–3] | 2.2 {1.68} | 2.0 [1–3] |
| Number with multiple readmissionsb | 213 | 60 (60) | 66 (58) | 126 (59) | – | ||
| Average duration of readmission (days)a,c,d | 212 | 100.5 | 116.2 | 108.4 | |||
Table 29 presents details of patients’ community care and legal status. Not all of the data were obtainable and the listed sample sizes reflect this. Patients spent a median of 983.5 days out of the possible 1095 days in the community (992 for the CTO group and 976 for the non-CTO group). Overall, 198 patients (60%) were subject to a CTO at some point [127 (77%) of the CTO and 71 (43%) of the non-CTO group]. These 198 patients spent a median of 346 days on the CTO (364 days for the CTO group and 308 days for the non-CTO group). This included all CTO episodes during the 36-month follow-up period. When inpatient care was included, the time under total compulsion was a median of 399.5 days (513 days for the CTO group and 309 days for the non-CTO group). The CTO group had a higher number of MHA tribunals (179 vs. 129), managers’ hearings (170 vs. 110) and recalls from CTOs (87 vs. 49) than the non-CTO group. Most recalls (92, 68%) resulted in revocation of the CTO, with the rate marginally higher in the CTO group [62 (71%) vs. 30 (61%)]. Only two patients were discharged directly from recall to voluntary status.
| Outcomes | Sample size | CTO | Non-CTO | Total sample | |||
|---|---|---|---|---|---|---|---|
| N = 165 | N = 165 | N = 330 | |||||
| n (%)/mean {SD} | Median [IQR] | n (%)/mean {SD} | Median [IQR] | n (%)/mean {SD} | Median [IQR] | ||
| Number of days in community | 330 | 902.9 {249.20} | 992.0 [859–1065] | 870.2 {273.40} | 976.0 [791–1062] | 886.5 {261.78} | 983.5 [824–1063] |
| Patients subject to CTO | 330 | 127 (77) | – | 71 (43) | – | 198 (60) | – |
| Number of days on CTOa | 198 | 487.7 {347.23} | 364.0 [181–828] | 393.0 {287.42} | 308.0 [173–661] | 453.7 {329.45} | 346.0 [180–724] |
| Number of days under any compulsionb | 330 | 570.1 {387.98} | 513.0 [230–1081] | 408.6 {364.39} | 309.0 [98–697] | 489.4 {384.40} | 399.5 [161–839] |
| Number of successful contacts per month | 322c | 3.6 {3.01} | 2.5 [1.7–4.4] | 4.1 {3.64} | 2.9 [1.7–4.98] | 3.8 {3.34} | 2.8 [1.7–4.9] |
| Number of failed contacts per month | 278d | 0.5 {0.52} | 0.3 [0.1–0.7] | 0.5 {0.64} | 0.3 [0.1–0.7] | 0.5 {0.59} | 0.3 [0.1–0.7] |
| Total number of tribunals | 330 | 179 | – | 129 | – | 308 | – |
| Total number of managers’ hearings | 330 | 170 | – | 110 | – | 280 | – |
| Total number of recalls | 198 | 87 | – | 49 | – | 136 | – |
| Recalls’ outcomes | 136 | ||||||
| Remains on CTO | – | 23 (27) | – | 19 (39) | – | 42 (31) | – |
| Revoked | – | 62 (71) | – | 30 (61) | – | 92 (68) | – |
| Discharge form CTO | – | 2 (2) | – | 0 (0) | – | 2 (1) | – |
The care teams engaged in the original OCTET Trial were encouraged to aim for similar rates of community contacts during the 12 months of the trial follow-up, irrespective of the arm of the trial to which the patient was allocated. They achieved this with medians of 2.1 contacts per month for the CTO group and 2.2 contacts per month for the non-CTO group. Over the 36-month follow-up period, the rate of contacts per month was slightly higher than over the first 12 months, but there was no difference between the two groups (2.5 for the CTO and 2.9 for the non-CTO group). The rate of failed contacts recorded in the medical notes was 0.3 for the CTO group and 0.3 for the non-CTO group.
Table 30 details the professionals seen by the patients over the 36 months. (Some of the individual professionals may have been counted more than once if they had more than one patient in the study.) There were no obvious differences between the CTO and non-CTO groups. Over the 36-month follow-up period, patients were under the supervision of a mean of 2.2 care co-ordinators (2.3 for the CTO and 2.4 for the non-CTO group) and a mean of 3.6 consultant psychiatrists (3.6 for the CTO and 3.7 for the non-CTO group). The overwhelming majority of care co-ordinators [509 (68%)] were community psychiatric nurses [239 (66%) for the CTO group and 270 (70%) for the non-CTO group]. Of the 1169 consultants seen, only 182 (16%) were ‘integrated’ consultants responsible for inpatient and outpatient care [83 (14%) for the CTO group and 99 (17%) for the non-CTO group], whereas 492 (42%) were consultants [238 (41%) for the CTO and 254 (43%) for the non-CTO group] and 484 (41%) community consultants [253 (44%) for the CTO and 231 (39%) for the non-CTO group].
| Professionals | Sample size | CTO (N = 165) | Non-CTO (N = 165) | Total sample (N = 330) | |||
|---|---|---|---|---|---|---|---|
| n (%)/mean {SD} | Median [IQR] | n (%)/mean {SD} | Median [IQR] | n (%)/mean {SD} | Median [IQR] | ||
| Number of care co-ordinators, per patient | 328 | 2.2 {1.19} | 2.0 [1–3] | 2.4 {1.31} | 2.0 [1–3] | 2.3 {1.25} | 2.0 [1–3] |
| Number of consultant psychiatrists, per patient | 328 | 3.6 {2.66} | 3.0 [2–4] | 3.7 {2.83} | 3.0 [1–5] | 3.7 {2.74} | 3.0 [2–5] |
| Care co-ordinators’ profession | 749 | 361a | 388a | 749a | |||
| Social worker | – | 97 (27) | – | 95 (24) | – | 192 (26) | – |
| Community psychiatric nurse | – | 239 (66) | – | 270 (70) | – | 509 (68) | – |
| Occupational therapist | – | 13 (4) | – | 13 (3) | – | 26 (3) | – |
| Other mental health worker | – | 4 (1) | – | 5 (1) | – | 9 (1) | – |
| Psychiatrist | – | 5 (1) | – | 2 (1) | – | 7 (1) | – |
| Clinical psychiatrist | – | 3 (1) | – | 3 (1) | – | 6 (1) | – |
| Type of consultant | 1169 | 578b | 591b | 1169b | |||
| Integrated care | – | 83 (14) | – | 99 (17) | – | 182 (16) | – |
| Inpatient care | – | 238 (41) | – | 254 (43) | – | 492 (42) | – |
| Community/AOT | – | 253 (44) | – | 231 (39) | – | 484 (41) | – |
| Crises team/other | – | 4 (1) | – | 7 (1) | – | 11 (1) | – |
Disengagement outcomes
As Table 31 shows, of the 329 patients for whom data were available up to the 36-month follow-up point or up to the time of their death or the date of their leaving the UK permanently, only 19 (6%) were no longer in regular contact with services and had not been for at least 90 days (i.e. had disengaged). These patients had their final contact with services at least 3 months before the end of the study. A significant association was found between time to disengagement and duration of compulsion (HR 0.946, 95% CI 0.90 to 0.99; p = 0.023) with longer duration of compulsion being associated with a longer time before the patient disengaged, although this finding was based on a small number of disengaged patients (see Table 31). Table 32 reports disengagement (along with readmission) outcomes in the randomised groups. Out of the 19 patients that disengaged 12 were at the CTO group and seven in the non CTO-group and no significant difference was detected between the CTO and non-CTO groups (Wilcoxon rank-sum p-value = 0.274.)
| Outcomes | N = 330 | Treatment effecta (95% CI) | ||
|---|---|---|---|---|
| Sample size | n/mean {SD} | %/median [IQR] | ||
| Experienced discontinuity (≥ 60 days) | 327 | 140 | 43 | – |
| Number of patients with periods of discontinuity | ||||
| No discontinuity of care | 327 | 187 | 57 | |
| 1 period of discontinuity | – | 66 | 20 | – |
| 2 periods of discontinuity | – | 27 | 8 | – |
| 3 periods of discontinuity | – | 19 | 6 | – |
| 4 periods of discontinuity | – | 19 | 6 | – |
| ≥ 5 periods of discontinuity | – | 9 | 3 | – |
| Number of periods of discontinuity | 327 | 0.9 {1.42} | 0 [0–1] | IDR 0.973 (0.96 to 0.99) |
| Experienced disengagement [≥ 90 days (no return)] | 329b | 19 | 6 | – |
| Time to disengagement, monthsc | 329 | – | – | HR 0.946 (0.90 to 0.99) |
| Outcomes | CTO (N = 165) | Non-CTO (N = 165) | Treatment effect (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Sample size | n (%)/mean {SD} | Median [IQR]/median (95% CI) | Sample size | n (%)/mean {SD} | Median [IQR]/median (95% CI) | ||
| Psychiatric hospital readmission | 165 | 100 (61) | – | 165 | 113 (68) | – | RR 0.88 (0.75 to 1.03) |
| Duration of readmissions (nights) | 100 | 237.1 {269.09} | 117.5 [63–303] | 112a | 252.1 {282.48} | 139.5 [63–309.5] | IDR 0.84 (0.51 to 1.38) |
| Number of readmissions | 100 | 2.4 {1.91} | 2.0 [1–3] | 113 | 2.2 {1.43} | 2.0 [1–3] | IDR 0.97 (0.76 to 1.24) |
| Days in community until first readmission | 165 | 571.5 {410.80} | 601.0b (387 to 777) | 165 | 511.4 {401.66} | 420.0b (352 to 548) | HR 0.81 (0.62 to 1.06) |
| Number of periods of discontinuity | 162 | 1.0 {1.48} | 0.0 [0–2] | 165 | 0.85 {1.36} | 0.0 [0–1] | IDR 1.12 (0.78 to 1.59) |
| Time to disengagement, months | 164 | 32.5 {6.26} | 35.2 [31.9–36.0] | 165 | 32.3 {6.76} | 35.0 [32.8–35.9] | p = 0.274c |
Just over half of the sample (n = 187, 57%) had no discontinuity in their care (defined as any period of ≥ 60 days without any contact). One-fifth of the sample (n = 66, 20%) had only one such discontinuity and the remaining 74 patients (23%) had several discontinuities, with nine patients (3%) having more than four each. There were no significant differences between the CTO and non-CTO groups (IDR 1.12, 95% CI 0.78 to 1.59; p = 0.537) (see Table 32). A significant association was found between the number of periods of discontinuity in treatment and duration of compulsion (IDR 0.97, 95% CI 0.96 to 0.99; p < 0.001) (see Table 31), with those under longer compulsion experiencing fewer periods of discontinuity.
Readmission outcomes
Table 32 also reports the readmission outcomes, comparing the CTO and the non-CTO groups. The number of patients with readmissions and the time to readmission are both presented for the full sample. The duration of inpatient care and the number of admissions are presented for only those who were readmitted. None of the effect sizes reached statistical significance.
The survival curve for time to readmission is shown in Figure 19. The time to readmission does not show a significant difference over the 36-month follow-up period (HR 0.81; p = 0.118). Unlike in the OCTET Trial, time to readmission here was calculated from the time of first discharge rather than from randomisation. This shifts the duration of this variable for the non-CTO group, who were discharged on average 8 days later after randomisation than the CTO group (see Table 9) and explains why the curve looks somewhat different from that presented in relation to the OCTET Trial (see Figure 7). There is a striking divergence between the two curves at between 12 and 18 months. During the 12 months of the OCTET Trial, the admissions are effectively identical, but between 12 and 18 months there is an unexplained but noticeable increased rate of readmission in the non-CTO group. Between 18 and 36 months, the rates of admission are almost parallel.
FIGURE 19.
Time to first readmission during 36-month follow-up. This figure is reproduced from Burns T, Yeeles K, Koshiaris C, Vazquez-Montes M, Molodynski A, Puntis S, et al. Effect of increased compulsion on readmission to hospital or disengagement from community services for patients with psychosis: follow-up of a cohort from the OCTET Trial. Lancet Psychiatry 2005;2:881–90,198 with permission from Elsevier.

Compulsory treatment order compulsion outcomes
There was an association between the duration of overall compulsion and hospitalisation, which was not surprising as most of the hospitalisations were compulsory. We therefore completed analyses for duration of community compulsion (i.e. duration of being on a CTO) rather than compulsion overall. This analysis was limited to patients who had experienced at least one period of being on a CTO. We tested the association between our readmission outcomes (readmission rate, duration of psychiatric hospital readmission and time in the community between randomisation and first readmission) with the total duration of community compulsion (being on a CTO) in the 36-month follow-up period (as opposed to the randomised groups from the original OCTET Trial). The association between duration of all periods of CTO for the 198 patients with CTO experience and readmission rates was not significant. Duration of CTO was significantly associated with the duration of readmissions (p = 0.019) and the time to first readmission (p = 0.007); neither of these relationships were linear, however. For readmission rates, duration of readmission and time to first readmission, patients spending 6–12 months on a CTO did better than patients with either shorter or longer CTOs. We identified non-linear relationships between duration of CTO and relative risks of readmission, mean days in the community until first readmission and mean numbers of inpatient days.
Subgroup analyses
Table 33 presents the effects of predetermined subgroups on the outcomes of discontinuity and disengagement. A significant interaction was found between disengagement and age, but it should be interpreted with caution in view of the multiple comparisons.
| Subgroup | Discontinuity of treatment | Disengagement | ||||
|---|---|---|---|---|---|---|
| HRa | p-value | 95% CI | HRa | p-value | 95% CI | |
| Age > 40 years | 1.02 | 0.102 | 0.99 to 1.06 | 1.18 | 0.042 | 1.01 to 1.38 |
| Female (vs. male) | 1.01 | 0.583 | 0.98 to 1.04 | 1.09 | 0.126 | 0.97 to 1.24 |
| Black (vs. other ethnicities) | 1.01 | 0.708 | 0.97 to 1.04 | 1.03 | 0.562 | 0.93 to 1.14 |
| Born in other countries (vs. UK) | 1.01 | 0.764 | 0.97 to 1.04 | 1.03 | 0.636 | 0.92 to 1.14 |
| Married (vs. single) | 0.98 | 0.490 | 0.92 to 1.04 | 0.91 | 0.446 | 0.73 to 1.15 |
| Living with others (vs. alone) | 0.97 | 0.106 | 0.93 to 1.01 | 0.93 | 0.332 | 0.80 to 1.08 |
| General education > 12 years | 1.01 | 0.766 | 0.97 to 1.04 | 1.04 | 0.425 | 0.94 to 1.16 |
| Have tertiary education | 1.00 | 0.989 | 0.97 to 1.03 | 0.94 | 0.372 | 0.83 to 1.07 |
| BPRS > 33 | 1.02 | 0.202 | 0.99 to 1.05 | 0.90 | 0.291 | 0.75 to 1.09 |
| GAF > 49 | 1.01 | 0.893 | 0.96 to 1.05 | 0.96 | 0.703 | 0.77 to 1.20 |
| Duration of illness > 2 years | 1.01 | 0.837 | 0.93 to 1.11 | 0.98 | 0.908 | 0.82 to 1.19 |
| Diagnosis schizophrenia (vs. other diagnoses) | 0.98 | 0.382 | 0.95 to 1.02 | 1.01 | 0.882 | 0.90 to 1.13 |
| London (vs. other locations) | 0.99 | 0.723 | 0.97 to 1.03 | 0.95 | 0.510 | 0.80 to 1.12 |
Chapter 16 OCTET Follow-up Study: discussion and conclusions
The OCTET Follow-up Study was designed to answer two questions. First, was there evidence that increased use of compulsion resulted in disengagement of patients from services? Second, was there any long-term impact of being in the original CTO arm of the study on hospitalisation and care outcomes? Neither of these was found to be the case.
All of the hospitalisation outcome measures were favourable towards the CTO group but none of these differences was statistically significant. Given that all three published RCTs used a follow-up period of either 11 or 12 months and failed to demonstrate any difference, this would suggest that any further RCT should aim at an extended follow-up period of 2 or 3 years. The practical difficulties of conducting such a trial are considerable, but it seems the more logical test than a further RCT with a restricted follow-up.
What our study did show, however, is that CTO compulsion was extensive in both groups, with a median of 308 days of community compulsion for the non-CTO group and 364 days for the CTO group over the 3 years. Once CTOs are imposed they tend to be protracted. The median of 183 days in the original OCTET Trial was clearly a consequence of the trial cut-off at 12 months and we believe our current figures are still an underestimate because of censoring at 36 months. Certainly when reliable long-term data are available, it is clear that many patients, once established on CTOs, may continue on them for very long periods, sometimes for several years. 4
Recall was not common in our sample. Only 136 recalls were invoked in 198 patients. Of these, over two-thirds resulted in the patient being detained for treatment in hospital. This sparing use may reflect the opinions expressed by clinicians in the OCTET Qualitative Study (see Part 2, Chapter 8) that recalls were difficult to arrange and of limited practicality or use. Only two patients were discharged directly from a recall to voluntary status in the 36 months.
We were unable to distinguish confidently between managers’ hearings and MHA tribunals for CTOs and those for inpatient detention. That the lawfulness and appropriateness of detention were tested 558 times during the follow-up period does suggest that procedures were being followed and that effective scrutiny was provided. Similarly, the continued rate of contact over the 36 months (a slightly increased median of 2.8 per month compared with 2.1 CTO and 2.2 non-CTO during the first 12 months) is evidence that this patient group was receiving a substantial level of care. The rates of failed contacts emphasises just how seriously the clinical teams took their responsibilities to this very vulnerable group. That the rate of contact with the CTO group was so similar to the rate of contact with the non-CTO group would argue against the view that CTOs may work by ensuring that patients feel obliged to keep appointments through a respect for legal powers which in the USA is referred to as the ‘black robe effect’200 (i.e. respect for legal powers).
The OCTET Follow-up Study was conducted at a time of considerable reorganisation in mental health services. Many AOTs were being disbanded, crisis teams being reconfigured, and inpatient and outpatient consultant responsibilities being separated. Knock-on effects of these changes also included the redrawing of catchment area boundaries for teams. This is manifest in the number of consultant psychiatrists who were responsible for patients. The average patient changed consultant at least once a year. This was a consequence of the introduction of so-called ‘functional services’. In these services, inpatient and outpatient consultant responsibility is split, and this contrasts with the model of the traditional ‘integrated’ consultant who is responsible for patients both on the ward and in the community. This is a remarkable and disturbing change in provision for a group who are selected for their enhanced need for persistent supervision. Had our study been conducted a decade earlier, we would have anticipated that the majority of our patients would have had the same consultant for the whole period. This is a disruption in continuity of care that might undermine any potential benefits of CTOs or other community-based services and deserves more attention than it is currently receiving. 36
The figures for care co-ordinators were marginally more reassuring, with an average of just over two during the 36 months. There can, of course, be clinical reasons for changing care co-ordinators, such as from a CPN to a social worker, but these are probably rare. Most of the changes must reflect staff turnover and team changes. 201
Despite this turbulence, we found that only 19 patients (6%) were completely disengaged after 3 years. This shows a surprisingly high level of continuity of care, which contrasts with the discontinuities of professional staff. It testifies to the persistence of these teams and their active outreach. Further evidence of this persistence is provided by the fact that only 74 patients (23%) had experienced more than one discontinuity of contact over the 3 years. We also found no evidence that subgroups of patients generally considered to be more distrustful of care (such as younger patients or ethnic minority patients) experienced more disengagement or disruption of care with increasing compulsion.
There was no difference between the randomised groups in disengagement. The significant association observed between time to disengagement and duration of compulsion in the whole sample could therefore not be attributed to CTO use. In view of the low numbers who disengaged (n = 19, 6%) this needs to be interpreted cautiously.
This high level of clinical follow-up may explain why CTOs have not achieved the outcomes expected of them. Much of the motivation for the introduction of CTOs was based on the assumption that these patients were dropping out of care and consequently not being supported and encouraged to take their medicines to prevent relapse. This does not appear to be the case. English mental health teams appear to be remarkably focused and successful in providing relatively intensive and persisting contact with this patient group. This may hold for most patients with psychosis: in a parallel study of contingency management for patients treated with depot antipsychotics, the inclusion criteria had to be radically loosened because of the difficulty of finding sufficient non-adherent patients. 202
We have presented our data on the association between duration of community compulsion and hospitalisation in some detail. We cannot draw any conclusions about causality from this, however. Greater community compulsion was significantly associated with the duration of psychiatric rehospitalisation and time to first readmission in this non-randomised sample. The results in this sample should be interpreted with caution, however, because of the fact that patients could be placed on a CTO during follow-up only if they had been readmitted involuntary; there is therefore an inherent bias in the nature of these data. Similarly, the time available for inpatient days was inevitably reduced for patients with longer recorded community compulsion, thereby driving an association. Given that all three of the published RCTs find that CTOs do not reduce hospitalisation or improve other, wider, outcomes, these data do not undermine the conclusion that excessive compulsion is being used to no obvious benefit.
The OCTET Follow-up Study has demonstrated that the standard of outpatient care of patients with severe psychoses is higher than perhaps anticipated. English mental health teams are successful in persistent long-term clinical follow-up of this difficult group of patients, despite repeated service reorganisations. There is no support from our findings for the concern, expressed by many patient groups during consultations prior to the introduction of CTOs (see Part 2, Chapter 5), that they might lead to a disengagement from services perceived to be more concerned with social control than treatment.
There was an unexplained divergence in readmission rates between the CTO and non-CTO groups in the 6 months directly following the end of the OCTET Trial (between 12 and 18 months after randomisation). This may simply have been a random variation, as there was no significant overall difference in any of the hospitalisation outcomes over the full 36 months. We speculated that it might reflect teams reducing their input to patients in the non-CTO group once the requirements of the original trial had been removed. To explore this, we compared the rates of contact between the CTO and non-CTO groups for the period between the 12th and 18th months but could not find any support for this explanation. Overall, however, there was a non-significant trend favouring the CTO group in all the readmission outcomes, in contrast with the original OCTET Trial. This would lend further support to our contention that any future RCT should include an extended outcome period of at least 2 years, although we recognise the practical difficulties of accomplishing this.
Limitations
The OCTET Follow-up Study was not an RCT, as the disengagement outcome was not based on the treatment arm from the original trial and patients were not held in their original treatment arm. The evidence it provides is thus not as robust as the findings of the OCTET Trial.
We did not repeat the patient-rated clinical outcome measures used in the OCTET Trial, and so were unable to capture the range of clinical and social functioning and perceived coercion outcomes as the OCTET Trial.
We deviated from our original analytic plan (see Chapter 13), in view of the findings of the OCTET Trial and the strong association between duration of overall compulsion and hospitalisation.
That the subsample analysis used reduced samples and tested against CTO compulsion in quartiles may have led to a lack of statistical power.
Conclusions
-
There was no evidence that increased coercion led to disengagement from services.
-
Recent service reorganisations have introduced lower levels of continuity of care that deserve urgent attention.
-
Levels of successful clinical follow-up in this patient group were excellent, with only 6% of the sample no longer in regular contact with services at 36 months, with or without CTO; this may help explain why CTOs have failed to demonstrate any effect on outcomes.
-
There remains no convincing or significant evidence for improved hospitalisation outcomes from CTOs at 36 months.
-
The pattern of hospitalisation outcomes suggested (but did not prove) some possible advantage to CTOs, which should be tested in an RCT with a follow-up period of at least 2 years.
Part 4 The ULTIMA Study
Abstract
Background
There is a pressing need to understand the extent and nature of informal coercion.
Design
The study comprised a quantitative cross-sectional study of leverage in England, comparison with a previous US study7 and an exploration of perceived coercion; a qualitative study of patient and professional perceptions of informal coercion; and an ethical analysis.
Participants
Participants in the Quantitative Study comprised patients from AOTs, CMHTs (with and without psychosis diagnoses) and substance misuse services. Subsamples of patients and a sample of mental health professionals participated in the Qualitative Study.
Results
The Quantitative Study sample comprised 417 patients. One-third (35%) of the sample reported lifetime experiences of leverage, lower than in the USA (51%), although patterns of experienced leverage were similar. Rates of most leverages in the substance misuse sample (63% reporting any leverage) were higher than those in the USA and our other subgroups. Reporting leverage made little difference to patients’ perceived coercion. The Qualitative Study sample comprised 39 patients and 48 professionals. Patients’ experiences of pressure were wide-ranging and pervasive, perceived to come from family, friends and themselves, as well as professionals. Professionals were committed to patient-centred approaches, but felt obliged to assert authority when patients deteriorated. On the basis of our Ethical Analysis, we propose a five-step framework for determining the ethical status of offers by mental health professionals and give detailed guidance for professionals about how to exercise leverage.
Conclusion
Informal coercion is widespread and takes a range of different forms.
Chapter 17 Introduction to the ULTIMA Study
Overview
The Use of Leverage Tools to Improve Adherence in community Mental health care (ULTIMA) Study took place from January 2008 to June 2010. It was designed to investigate informal coercion by studying rates of leverage experience among patients who were using mental health and substance misuse services and by exploring, in depth, their perceptions about the nature and operation of informal coercion and those of professionals working with them.
In this study, the term informal coercion is used as an overarching term for all non-statutory coercion (see Part 1, Chapter 1). Within this overarching term, the narrower term leverage is used to denote the particular set of practices whereby an explicit and specific treatment lever is used to increase the patient’s adherence to treatment, whereas treatment pressure is used as a wider term for the range of pressures that may be exerted as part of informal coercion. Perceived coercion was also investigated and this term is used to indicate patients’ perceptions of the coerciveness of their care in general (and, in some cases, the coerciveness of specific treatment pressures).
The ULTIMA Study comprised:
-
The ULTIMA Quantitative Study A cross-sectional study of levels and patterns of leverage in four distinct clinical populations, with their sociodemographic and clinical correlates; a comparison of levels of these leverages to rates reported in the USA;7 and a quantitative exploration of patients’ perceived coercion.
-
The ULTIMA Qualitative Study An in-depth investigation of patient and mental health professional views and experiences of informal coercion in which we interviewed a subsample of patients in depth and accessed professionals’ views via focus groups.
-
The ULTIMA Ethical Analysis A detailed conceptual and empirical ethical analysis (using data from the Qualitative Study), leading to ethical guidance for professionals in the use of leverage.
The epidemiological approach used in the ULTIMA Quantitative Study (see Chapter 18) drew on international precedent, utilising similar methodology to the only previous study of leverage. 7 This enabled us to provide a comparison between the first English data and data from the USA. It expanded on that previous study by investigating the association of leverage use with important sociodemographic and clinical data, including criminal and psychiatric history as well as insight, experiences of services and perceived coercion. It also added more structured sampling than the US study7 by examining patterns of leverage experience across four distinct patient populations (patients in AOTs, patients with psychosis diagnoses in CMHTs, patients with non-psychosis diagnoses in CMHTs and substance misusers). It is the first study to have done so.
The ULTIMA Qualitative Study of patients’ and mental health professionals’ attitudes towards informal coercion (see Chapter 19) was the first in the area, enabling the identification of mechanisms of operation and a significant expansion of the concepts of informal coercion and leverage. This also offered an unprecedented opportunity to conduct a detailed ethical analysis of the qualitative data in the context of the relevant ethical literature, reported in the Ethical Analysis (see Chapter 20).
Background
Informal coercion in community mental health services
The shift towards providing mental health services in community rather than hospital settings presents an array of challenges. Mental health professionals working in community settings face a particular difficulty when patients for whom they hold responsibility do not wish to receive their services. The overarching therapeutic aim of these professionals is to prevent relapse and readmission to hospital by ensuring that treatment is adhered to, often by addressing their patients’ wider needs. Increasingly, services focus on assisting recovery, which refers to a patient’s ability to identify their needs, manage their symptoms and live fulfilling lives with a mental illness. 203 To achieve these aims, professionals become involved in a wide range of patients’ daily activities and interact with family members and those services with a remit for such matters as housing and social security benefits. 30,204
This approach to service delivery means that professionals are often involved across different spheres of patients’ personal lives, taking on roles which are both empowering and controlling, and which exert different types and degrees of pressure. 29,205 These roles and the numerous informal practices associated with them fall outside legal and policy provision or guidance. They include the identified practices used by ACT teams,206–209 such as ‘aggressive’ outreach or ‘intensive’ follow-up to patients, but they are also likely to include a wider range of techniques and pressures. This array of treatment pressures has been described as spanning:
a continuum of restrictiveness that includes verbal encouragement or admonition, contingent support or contracting, involvement of others, informal coercion, or formal coercion. 208
The terminology used in the literature regarding these informal practices is unclear. The terms leverage and informal coercion, for example, are often used interchangeably, whereas the term mandated community treatment is also used to indicate a potential form of leverage. 210 This is problematic, because although to ‘coerce’ or ‘mandate’ implies a lack of choice, leverage may not always amount to coercion. 34,204 Researchers also use the terms ‘treatment pressure’204 and ‘therapeutic limit setting’208 to refer to informal coercion. The lack of conceptual clarity has led some to suggest that additional conceptual work relating to coercion and related practices is required. 204
In making sense of the types of pressure and the different terms used, Szmukler et al. 204,211,212 have proposed a hierarchy that ranges from persuasion at the least coercive end of the spectrum, through interpersonal leverage, inducement and threat, to the use of formal compulsion through mental health legislation. They differentiate between these different kinds of pressure on the basis of morally salient distinctions between them, which can be identified using conceptual and ethical analysis. Figure 20 (reproduced from a publication by the OCTET Coercion Group17) which was developed from the work of Szmukler and Appelbaum,185,204 represents this five-level hierarchy.
FIGURE 20.
Hierarchy of treatment pressures. Reproduced from Molodynski A, Rugkåsa J, Burns T. Coercion and compulsion in community mental health care. Br Med Bull 2010;95:105–19,17 with permission from Oxford Journals.
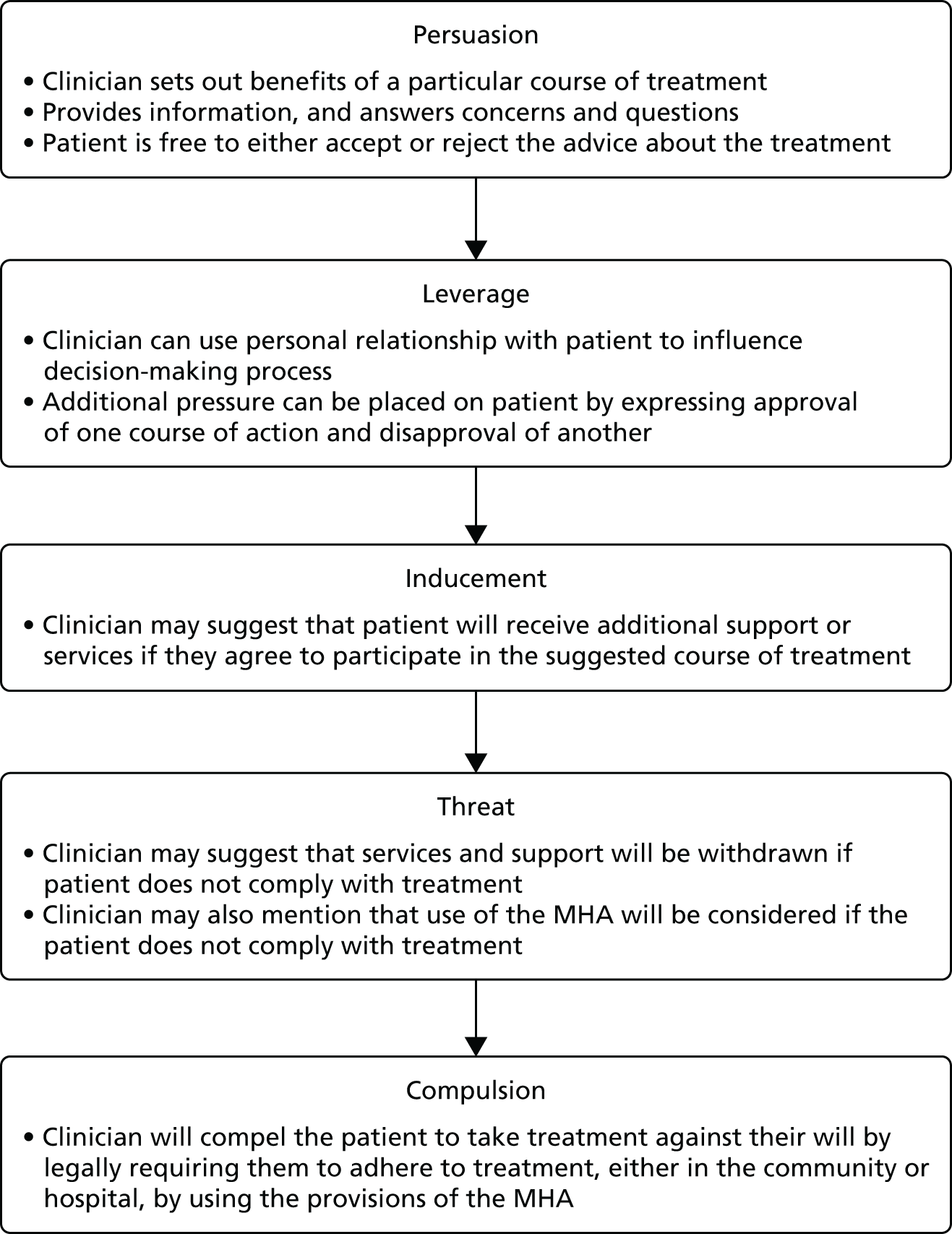
The literature to date has used the term leverage, as we do in this report, to refer to an informal practice whereby professionals attempt to influence patients’ treatment adherence using a lever. The study by Monahan et al. 7 measured four types of leverage, thus defined: leverage related to housing; leverage related to finance; leverage related to the avoidance of criminal sanction; and leverage relating to outpatient commitment. 7,213–217
Perceived coercion
Coercion can be perceived both as what is done to someone and what is experienced by someone: ‘it is thus both an objective set of actions and a subjectively experienced result of particular actions’. 218 In addition to formal and informal coercion, the notion of perceived coercion is also often applied in the literature. Perceived coercion represents that which is experienced by the patient to be coercive and that affects their treatment decisions.
Perceived coercion, particularly in relation to the range of influencing behaviours comprising informal coercion and leverage, has received little attention until recently, although a small but growing literature has started to investigate this. Patients may perceive the ways in which professionals seek to influence their behaviour as both helpful or caring and also pressurising or coercive. 208 Indeed, many so-called voluntary patients have been found to perceive their involvement with mental health care as coerced. 219 Investigation of this area has been hampered by the fact that the majority of empirical studies measuring patient experiences uses concepts of pressure constructed from a professional perspective rather than a patient perspective.
Leverage levels and patterns
The US study7 of public mental health service patients found that half of the sample reported experiencing one or more of the four leverages described above. Despite the fact that it was thought anecdotally to be widely used, there were no English data on the extent, distribution or impact of leverage prior to the ULTIMA Study.
There are marked differences between the US and European social welfare systems in terms of whether basic needs are seen as rights or privileges. This might give rise to substantial differences in the rate of experiences of leverage in England and the USA. The US mental health-care system has a relatively fragmented community provision, limited availability of adequate benefits214 and some availability of ‘mental health courts’. 220 Bonnie and Monahan34 also draw attention to the relevance of the legal jurisdiction within which techniques such as leverage are applied, examining differences across states in the USA. The difference in rates of the use of leverage they report, coupled with variations between social welfare and legal cultures within the USA and between the USA and Europe, raises questions as to the international comparability of leverage practices described in the literature. Leverage may, specifically, be less common in a European setting, in which the provision of, for example, accommodation and welfare payments, is a basic universal entitlement and should not be made conditional on treatment adherence.
Mental health professionals and informal coercion
Although only limited attention has been given to patient perspectives on informal coercion, still less has been given to community mental health professionals’ perspectives on how they exert influence over patients. 206 In addition to ascertaining which influencing behaviours are used, and to what extent, there is a significant gap in the literature regarding how these behaviours or strategies are conceptualised by those applying them. 208 A few studies, largely from the USA, identify and measure the use of different influencing behaviours. These are summarised in Box 4.
-
Creating partnerships through listening to patients’ views, including their resistance, and communicating that one sees patients’ viewpoint. 223–225
-
Showing ‘human’ and not exclusively ‘professional’ responses, developing ‘therapeutic friendliness’. 221,223,226–228
-
Developing skills to overcome hostility and conflict. 223
-
Reminding or persuading, including appealing to obligations to reciprocate. 225,228–231
-
Educating patients through motivational interviewing and psychosocial interventions, CBT or behavioural interventions. 225,231–233
-
Giving verbal reminders about potential consequences of non-adherence, drug use or self-neglect, or confronting patients with these consequences. 11,112,207,225
-
Negotiating deals, including presenting choices (e.g. about use of medication). 223,230,234
-
Using reinforcement strategies, such as praise or taking patients out for coffee. 225
-
Using incentives, such as food, shelter or money. 207,225,235,236
-
Structuring adherence through routines, for example by bundling medication delivery with disbursement of money. 207,225
-
Intensive monitoring of medication or observed consumption. 11,207,237
-
Involving family, friends or family doctors in the monitoring of medication. 207,223
-
Holding back support or refraining from activities (such as caring for pets or homes). 225
-
Making unwanted contacts or increasing attention from care co-ordinator. 112,207
-
Making access to housing, children or social security benefits contingent on treatment adherence. 7,110,214,238–241
-
Initiating actions to bring about consequences, such as invoking the threat of or threaten with (re-)hospitalisation or the involvement of legal authorities. 207,225
-
Holding back, delaying or playing down information (e.g. about side effects of medication) or telling something that is untrue. 223,229
-
Making treatment a condition for parole or in lieu of incarceration. 216
This box has been reproduced from Rugkåsa J, Canvin K, Sinclair J, Sulman A, Burns T. Trust, deals and authority: community mental health professionals’ experiences of influencing reluctant patients. Community Ment Health J 2014;50:866–95,244 with permission from Springer Publishing Company.
The issue of mental health professionals’ relationships with patients has been a central feature of current discourse on mental health services in the UK147,221,245–247 and elsewhere. 30,248 In this discourse, the ideal relationship is presented as supporting recovery and moving beyond a more narrow focus on treatment to foster ‘patient-centred care’. 146,203 The (albeit limited) literature on health professionals’ descriptions of their relationships vis-à-vis patients suggests that professionals also view these relationships as central mechanisms for the delivery of care, and that they perceive their approaches to be patient centred. 223 Indeed, in the literature, mental health professionals (particularly nurses) describe building trusting relationships as a core aspect of their practice,223,224,226 and argue that coercive measures often result from a failure to achieve this. 223,227
The development of trusting relationships, however, can be impeded by difficulties in balancing trust-building with insistence on change,11,208,230 and with moving in and out of the authoritative part of the professional role. 223 In fact, the context within which these relationships occur, for which one party ultimately holds authority to compel the other, makes them unlike many other social relationships and, arguably, ones in which reciprocal exchange cannot be balanced249 because the relationships are played out in what has been described as a ‘coercion context’. 250 Whether or not such a coercion context may impact on the operation of leverage and informal coercion has received little attention, particularly as it may be seen from patients’ and professionals’ perspectives.
Informal coercion and ethical practice
Empirical studies show that threats and offers are used to increase treatment adherence (see Box 4), particularly among patients with severe mental illness who have experienced repeated hospitalisations and intensive outpatient service use and who display severe, disabling and longer-lasting psychopathology. 7,206,207,217 Distinguishing between threats and offers, however, may be complex in practice.
Contemporary accounts of the distinction between threats and offers centre around Wertheimer’s claims that, first, a threat or offer will be credible if the patient perceives the practitioner as having the power to act on the proposal; and, second, a threat should be understood in terms of a proposal which, if not accepted, leads to a person ‘being made worse off’ compared with a relevant pre-proposal baseline. 251 By contrast, not accepting an offer would leave the person no worse off compared with that baseline. According to such an account, threats reduce the range of options available compared with the pre-proposal baseline, whereas offers expand that range.
The picture becomes more complex, however, when one tries to define this pre-proposal baseline. Two broad approaches have been taken. One understands the baseline in empirical terms; the other understands it in normative terms. The empirical approach – at least in its ‘statistical’ form251,252 – asks what, as a matter of fact, the baseline was. A normative approach asks what it should have been. 251,253 The dominant approach in the literature has been to substantiate the normative account of the pre-proposal baseline within an ethical theory based upon individuals’ rights. 251,254 A threat, according to this account, is one in which X proposes to violate Y’s rights and the wrong of such a threat involves making adherence contingent upon a course of action that violates the person’s rights. Bonnie and Monahan34 endorse this position in the context of community mental health care. They argue that examining how the law interprets the scope of an individual’s rights sets the pre-proposal baseline and determines whether, for example, making a proposal that involves withholding disability benefits or restricting access to housing if it is not accepted, is, or is not, a threat. (The validity of this claim is discussed elsewhere. 255)
Given that patients’ subjective well-being may be reduced in circumstances in which they feel coerced or threatened,210,227,256,257 it is crucial to understand the impact of such threats and offers on them, as well as the pressures facing mental health professionals as they attempt to engage with patients in ways that are both effective and ethical.
Chapter 18 ULTIMA Quantitative Study
Introduction
The ULTIMA Quantitative Study was designed to examine levels and patterns of informal coercion in England, with a primary focus on leverage. It was designed to replicate the methodology of the US study of leverage by Monahan et al. 7 Of the four types of leverage reported in the US study,7 the ULTIMA Study focused on three (excluding community compulsion, as CTOs had not yet been introduced in England at the inception of this study) and added a fourth type of leverage relating to patients’ access to their children.
We collected data on these four predefined types of leverage in this study, and also sought to explore a range of ways in which patients might experience either their care in general, treatment pressures or the specific forms of leverage they reported as more or less coercive or more or less fair (perceived coercion). We also explored how this related to their preferences for being involved in decisions about their treatment and having information about it shared with them. When patients reported their experience of leverage (of the four types) in this study, this reflected their subjective perception, and this study did not seek to validate this against other evidence of what had taken place. Nevertheless, for the sake of clarity, we distinguish between reported leverage and perceived coercion, using the latter as a broad term for the variety of ways in which we explicitly asked the patient to judge how coercive they experienced their care to be or how fair or effective they perceived any treatment pressure to be (Table 34). (As Table 34 shows, we also used perceived coercion more explicitly to refer to a specific three-part measure of patients’ perceived coercion.) (An in-depth investigation of both leverage and wider treatment pressures is provided in the ULTIMA Qualitative Study – see Chapter 19.)
| Term | Measuresa |
|---|---|
| Leverage | |
| Four types of leverage Financial Housing Child access Criminal justice |
|
| Perceived coercion | |
| Perceived coercion | Perceived coercion |
| Influence and control in treatment decisions | |
| Negative pressures | |
| Experience of threats and force | |
| Procedural justice | |
| Having a say in one’s care | |
| Fairness and effectiveness of pressure | Index of fairness |
| How fair any treatment pressure was | |
| Index of effectiveness | |
| How effective any treatment pressure was | |
| Categorisation of leverage | Types of pressure |
| Perceived type of pressure ranging from persuasion to compulsion for each reported leverage | |
This chapter draws substantially on a paper published by members of the OCTET Coercion Programme Group: Burns et al. ,110 with permission from the Royal College of Psychiatrists.
Methods
The study’s overarching objective was ‘to investigate levels of informal coercion (‘leverage’) in differing English clinical populations and to investigate their sociodemographic and clinical correlates’. Its more specific objectives were to:
-
assess the prevalence and pattern of leverage among four patient groups in England:
-
AOT patients (majority with psychoses diagnoses)
-
CMHT patients with diagnosis of psychosis
-
CMHT patients with non-psychosis diagnoses; patients with a substance misuse diagnosis (currently treated with substitution medication: methadone or buprenorphine (Subutex, Reckitt Benckiser, Seoul, South Korea)
-
-
compare the prevalence and patterns of leverage found in England to those reported in the USA.
Design
This cross-sectional study was designed to determine the extent and pattern of leverage reported. We therefore compared the four patient groups to each other and also to the sample from the US study,7 with respect to their sociodemographic and clinical characteristics and their leverage experience. We then explored associations between patient characteristics and the leverage rates in analyses modelled on those conducted in the US study. 7 We also investigated patients’ experiences of services along with their perceived coercion.
Sample
We sampled patients from four differing clinical populations in three settings (AOT, CMHT and substance misuse services) from the then Oxfordshire and Buckinghamshire NHS Mental Health Foundation Trust (from March 2011, Oxford Health NHS Foundation Trust), which serves a mixed urban and rural population of one million. This sampling was designed to cover the range of patients likely to be subject to leverage, allowing the results to be generalisable nationally and to be comparable to the replicated US study. 7
We aimed to recruit 100 patients from each group. The substance misuse group either attended dispersed local clinics run by the mental health services or attended their general practice.
Inclusion criteria for all four groups were having been in the team’s care continuously for at least 6 months and having had at least one contact with services during that period. There were no exclusion criteria apart from severe dementia (i.e. precluding the ability to give informed consent) and having insufficient English for the interview, as the instruments were validated for use only in English language.
Recruitment procedures varied between the different teams. We approached all patients on the caseloads of the four AOTs in the trust. We recruited CMHT patients from the caseloads of eight teams out of the 23 teams in the trust (drawn from both counties served by the trust and from both urban and rural settings) in randomly selected blocks of 25 with either psychosis or non-psychosis diagnoses. Selection of the CMHT groups used independent random number lists for patients with psychosis and non-psychosis diagnoses, restricted to patients who had received care by the team for over 6 months. We over-sampled in all four groups, as we could not always reliably identify the duration of contact (required to confirm eligibility) from the case notes. Comprehensive caseload lists were not available in the substance misuse services and many of their patients were ‘shared care’ patients, with local GPs prescribing and following up. We obtained a consecutive convenience sample from the four methadone clinics in the Oxfordshire County and the Oxford City shared-care methadone services. Box 5 shows the different teams from which we recruited.
Abingdon.
Didcot.
North East Buckinghamshire (Aylesbury).
Oxford City.
Oxford City East.
Oxford City Central South.
Oxford City Central West.
Oxford City Central North.
Four assertive outreach teamsOxford City.
North Buckinghamshire (Aylesbury).
South Buckinghamshire (Aylesbury).
Oxfordshire County.
Four methadone clinicsOxford.
Didcot.
Abingdon.
Witney.
Three general practice surgeriesOxford Shared Care.
Interviews and researcher training
We conducted the interviews between January 2008 and April 2009.
The ethical approval for the study required that the clinician approach each potential participant before any researcher did; only those agreeing were then contacted by the researcher. This independent researcher fully explained the study, and obtained written, informed consent to conduct an interview and examine the case notes. The interview lasted an average of 50 minutes and we offered patients £10 in compensation for their time.
A senior researcher and a psychiatrist provided training in the clinical rating scales for the research assistants who conducted the patient interviews. During the training period for each trainee researcher, two research assistants (one experienced and the trainee) jointly rated 10 interviewed patients. After each interview, they discussed and compared their ratings for training purposes.
We tested inter-rater reliability twice among the three research assistants who used the researcher-rated scales (BPRS and GAF; see Instruments). Inter-rater reliability at the two time points for the GAF was confirmed as fair [intraclass correlation coefficient (ICC) = 0.489)] and moderate (ICC = 0.689), and for the BPRS was moderate (ICC = 0.789) and substantial (ICC = 0.923) (see below). We conducted refresher sessions with the research assistants and the senior researcher every 6 months to guard against rater drift.
Instruments
We used the following well-established, validated questionnaires and rating instruments in the interviews. The research assistants read out the questions for all of the instruments, as this was more motivating for the patients, and recorded them in the clinical research forms. All scales are patient rated and relate to the 6 months prior to interview unless otherwise stated. We confirmed all data on clinical history in the case notes. (All cross-references to the OCTET Trial Instruments are to Part 2, Chapter 6, Methods.)
Demographics and psychiatric history
-
The ULTIMA Socio-demographic Schedule: this was the same as the OCTET Socio-demographic Schedule (see Chapter 6, Instruments) and collected data on three areas:
-
‘self and home’
-
‘clinical history’
-
‘legal history’.
-
Clinical and social characteristics
-
Symptom severity: The BPRS, a researcher-rated instrument, was used to assess symptom severity over the two weeks prior to interview (see Chapter 6, Instruments). Only 18 items were utilised here in order to replicate the US study. 7
-
Insight: The ITAQ is an 11-item questionnaire assessing patient awareness of illness and need for treatment, with two subscales: the Awareness of Illness Scale and the Attitude to Treatment Scale (see Chapter 6, Instruments).
-
Substance misuse: The CAGE is a screening questionnaire for alcohol and drug misuse (see Chapter 6, Instruments).
-
Social functioning: The GAF, a researcher-rated, single-item scale, was used to assess impairment in functioning over the previous 2 weeks (see Chapter 6, Instruments).
Medication
-
Type of medication: We collected data on prescribed psychotropic medication from medical records.
-
Attitudes and adherence to medication: The DAI-10 assesses experiences of and attitudes towards medication (see OCTET Trial: instruments).
Experiences of services
-
Therapeutic relationships: The STAR-P assesses community patients’ relationships with their care co-ordinators (see Chapter 6, Instruments). The STAR–Clinician Version (STAR-C) was also administered with patients’ care co-ordinators (see below).
-
Satisfaction with services: The CSQ-8 assesses satisfaction with health services on eight items (see Chapter 6, Instruments).
-
Preference for joint decision-making and information-seeking: The API measures preferred autonomy in two subscales: the Decision Making Preference Scale and the Information Seeking Preference Scale (see Chapter 6, Instruments).
Experience of leverage and perceived coercion
-
Leverage: The MacArthur Leverage Interview ascertains experience of leverage. Leverage was defined as making support to obtain housing, money and child custody conditional on treatment adherence or reducing or dropping criminal charges if patients adhered. We report only lifetime experience here. Any positive response within a specific leverage area counts as ‘reported’. (See Chapter 6, Instruments and Box 2.)
-
Perceived coercion: The AES has three subscales. The Perceived Coercion Scale assesses perception of influence and control in treatment decisions (range 5–25, with a high score indicating a high level of perceived coercion); the Negative Pressures Scale (rated differently from in the OCTET Trial) assesses experienced threats and force (range 6–30, with a high score indicating lower negative pressure); and the Procedural Justice Scale assesses experience of having a say in one’s care (range 3–15, with a high score indicating feeling less involved in one’s care). In the ULTIMA study, each subscale was scored by calculating a mean value across all the items. No total score for the AES was utilised.
-
Fairness and effectiveness of pressure: The Index of Fairness assesses patient agreement with statements on the fairness of any experienced treatment pressure, and the Index of Effectiveness assesses their views of how effective this pressure has been in making them stay in treatment and gain control (see Chapter 6, Instruments).
-
Types of pressure: For each type of leverage reported, we asked the patient to identify the type of pressure they considered this to be according to Szmukler and Appelbaum’s185 five levels: persuasion, interpersonal leverage, inducement, threats or compulsion.
Service usage
-
The CSRI measures the number and duration of contacts the patient has had with a range of professionals during the 6 months prior to interview and the location of these meetings (24 items). Findings from this scale are not reported as a whole but its use provided data on details of care received, such as ‘number of outpatient visits’.
We also administered the STAR-C with each patient’s care coordinator about their relationship with the patient. The STAR-C has the same structure as the STAR-P, but its three subscales are Positive Collaboration (range 0–24), Emotional Difficulties (range 0–12, reverse scored) and Positive Clinician Input (range 0–12).
(The full Schedule of Procedures and the instruments listed here are available from the authors on request.)
Sample size and statistical analysis
Sample size
We designed this study primarily to describe leverage across the four patient groups by presenting descriptive statistics on the types of leverage in the whole sample and by group.
We therefore determined the sample size in order to provide sufficient power to detect clinically relevant differences between the four English groups and also between the English and US samples. We considered a 20% difference in any form of leverage to be clinically relevant. The US study7 reported on 1011 community mental health-care patients in five sites. The proportion of their cohort experiencing leverage ranged from 44% to 59% across the five sites (i.e. an average of approximately 50%). To detect a difference of 20% (from this baseline of 50%) at the 5% level of significance, and with 80% power, we calculated that a sample size of 100 patients in each of the study groups would be required, making a total sample size of 400 patients. This sample size calculation assumed equal groups (with no weights or stratification used).
Comparisons
We compared the four groups to each other with respect to patients’ sociodemographic characteristics, time-invariant clinical characteristics and legal history and current clinical characteristics and also with respect to the rates of reported leverage. Because the substance misuse group was significantly different from the combined groups of those with mental illness (see Results), we compared the three mental illness groups combined to the substance misuse group and also to each other without including the substance misuse group.
We carried out comparisons of rates of reported leverage across three or more groups using Kruskal–Wallis non-parametric tests. We used a variety of tests when only two groups were compared. These were Mann–Whitney U-tests for non-normally distributed continuous variables, chi-squared tests for binary variables and analysis of variance (ANOVA) for categorical variables. To compare our outcomes with the US sample,7 we calculated overall percentages and pooled means and SDs for the latter. We used a Student’s t-test when comparing means and a two-proportion Z-test when comparing percentages. We ran analyses in SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
For comparisons of patients’ characteristics and rates of reported leverage, we applied Bonferroni’s correction to any statistically significant results to verify that their statistical significance was maintained. (We present unadjusted p-values in all tables; all statistically significant findings maintained their significance unless otherwise stated.)
Factors associated with leverage
We explored possible associations between sample characteristics and types of leverage using univariate and multivariate multilevel logistic regressions.
As the sample comprised patients from four different groups, we treated it as a stratified sample with two levels or strata, the four groups (AOT, CMHT-psychosis, CMHT-non-psychosis, substance misuse) occupying the upper level and the patients forming the lower level. We expected that patients in the same group would be more similar to each other, thus breaking the independence assumption needed for standard statistical methods. We used multilevel models to analyse variables measured at different levels simultaneously, using a statistical model that included the various dependencies. 258 Variables that were univariately associated with the leverage at the level of statistical significance of p = 0.05 were included in the multivariate analyses.
For each type of leverage, we conducted the analysis using information only on liable patients unless otherwise stated. The analyses for ‘any type of leverage’ and ‘more than one type of leverage’ used data from patients who had children aged < 18 years, had someone managing their money or were arrested or under parole. For continuous variables, those scoring above the median were compared with those scoring below it. The Stata 9.0 command xtlogit on Windows was used for this analysis.
For each set of analyses, we treated reporting the four types of leverage, reporting any leverage and reporting more than one type of leverage as the outcome variables in turn. First, we examined associations between sample characteristics and leverages using all of the sociodemographic variables, psychiatric and legal history variables, and clinical and social characteristics variables as possible explanatory variables.
Second, we conducted a range of exploratory analyses. In order to replicate precisely the analyses conducted in the US study, we repeated our multivariate analyses using the variables utilised by Monahan et al. 7 in their multivariate analyses, regardless of whether or not these variables had reached the threshold for inclusion when we analysed them univariately (described below as ‘replication analyses’). For completeness, we included child access leverage in these analyses, although that was not collected in the US study. 7
Next, we repeated these multivariate analyses using all the variables used in the US study7 along with any other variables that our univariate analyses suggested were eligible for inclusion (described below as ‘combined analyses’). These analyses included the experience of service variables, which were not collected by Monahan et al. 7
Finally, because of the significant differences between the substance misuse group and the three mental illness groups, we also repeated our univariate and multivariate analyses for the mental illness group alone.
Perceived coercion
This analysis used six measures in total:
-
three specific measures of perceived coercion: Perceived Coercion Scale, Negative Pressures Scale, Procedural Justice Scale (i.e. the three AES subscales)
-
the patients’ rating of each type of leverage that they reported as one of five types of pressure (persuasion, interpersonal leverage, inducement, threats or compulsion);
-
patients’ ratings of the fairness and effectiveness of the pressure they had experienced: the Index of Fairness and Index of Effectiveness.
For some analyses, the patients’ identification of the type of leverage that they had reported was dichotomised into ‘less coercive’ pressures (persuasion, interpersonal leverage and inducement) and ‘more coercive’ pressures (threat and compulsion). We restricted these analyses, and the descriptive statistics for these measures, to the subsamples of patients liable to experience leverage (e.g. patients with children aged < 18 years being liable to experience child access leverage). We report mean and standard error (SE) for the AES subscales and Fairness and Effectiveness Indices, calculated over observed values only. We report the proportions for the types of pressure categorisation for each reported leverage, including missing values, whereas the histograms of these variables are based only on valid values.
We first examined associations between patient characteristics and the perceived coercion measures and the Fairness and Effectiveness Indices. To do so, we selected an initial set of possible predictor variables. We fitted univariate mixed-effects models with random intercept of the scales/indexes on each sample characteristic, adjusting for reported leverage (the US study7 variables) and grouping by sample (AOT, CMHT-psychosis, CMHT-non-psychosis, substance misuse). For those models with a likelihood-ratio test p-value of > 0.05, we fitted an ordinary linear regression model instead. We reduced the set of explicative variables to those significant in their corresponding model and further reduced it by keeping only uncorrelated explicative variables. We fitted a multivariate model for each scale or index on this set of explanatory variables using the likelihood ratio test once again to choose between a mixed-effects model with random intercept and an ordinary linear regression model. Forward stepwise analysis returned the final set of explanatory variables that were strongly associated with each scale. To investigate the association between sample characteristics and the dichotomous types of pressure categorisation, we used logistic regression restricted to those reporting leverage. The selection of explanatory variables followed a similar process as for the AES subscales and the Indices described above.
We then examined associations between the perceived coercion (AES) measures, Fairness and Effectiveness Indices and patients’ reporting of leverage. We plotted mean (SE) scores for each AES subscale and the Fairness and Effectiveness Indices by type of leverage for those patients who reported leverage and those who did not. Given that patients could report one or more types of leverage, we evaluated relationships between the AES subscales and the Indices and the types of leverage using independent mixed-effects models with random intercept, grouping by patient. In order to explore differences between the AES scales and the indices in the group of patients who reported leverage and in the group of those who did not, we added a variable indicating leverage experience to the above models. Similarly, we plotted mean (SE) scores for each subscale and index against the types of pressure categorisation for each type of leverage (for those patients who were liable to both experience the leverage and also report experiencing it). We further investigated the association between the scales or indices and the types of pressure categorisation by fitting an independent linear regression model for each AES subscale or Index on the types of pressure categorisation (again restricted to the subsample of patients liable to experience the respective leverage).
For each type of leverage, we drew histograms of the proportion of patients rating the leverage as each type of pressure (persuasion, interpersonal leverage, inducement, threat and compulsion). We then utilised the dichotomised types of pressure variable and tested the difference between the proportions rating the leverage as ‘more coercive’ and ‘less coercive’ using the Stata command bitest.
We assumed a two-tailed significance level of 5% throughout the analysis. We performed the analysis mainly using Stata version 12. (The statistical package R 2.13.2 was used to create Figures 21 and 22).
Data management
The research team recorded data by hand into the clinical research forms and two different researchers double-entered the data into SPSS. Once recruitment had been completed, we obtained additional required data from medical records. Recruitment from medical records proved time-consuming, as it often required reading consultant psychiatrists’ letters and other medical documents.
Three research assistants devoted 6 weeks’ full-time work to data checking, coding of collected data on medication and criminal records, and obtaining and entering data from medical records. We checked all data manually for accuracy. We then used special software to compare databases and check all of the data to ensure accuracy. We compared the double-entered data against each other, and discussed and corrected discrepancies. The statistician responsible for the analysis conducted additional data quality evaluations. These included range checks and logical and consistency checks that might not be picked up by checks at the individual patient level by the research staff who collected and entered the data. We froze the final cleaned data before the analysis commenced.
Results
Sample
We recruited 417 patients: 102 in the AOT group, 101 in the CMHT-psychosis group, 113 in the CMHT-non-psychosis group and 101 in the substance misuse group. Of 912 patients on the teams’ caseloads, 308 were uncontactable, had been discharged or were ineligible when further investigated. Of the 604 approached, 187 refused to participate.
Sample characteristics and leverage
Sample characteristics: the English sample compared with the US sample
Tables 35 and 36 detail the sociodemographic characteristics and psychiatric and legal history of the ULTIMA total sample and the four groups, compared with the US sample, using the same presentation format and variables as in the Monahan et al. 7 study, where available, for ease of comparison. Table 37 shows their clinical characteristics, also compared with the US sample. All references to ‘the US study’ in these tables, and those subsequent, relate to the Monahan et al. 7 study. Table 38 shows their experiences of services and perceived coercion.
| Characteristics | AOT (N = 102) | CMHT-P (N = 101) | CMHT-NP (N = 113) | SM (N = 101) | Total (N = 417) | US sample (N = 1011) | ||
|---|---|---|---|---|---|---|---|---|
| n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | p-valueb | n (%)/mean {SD} | p-valuec | |
| Age (years) | 40.1 {10.37} | 42.2 {10.67} | 43.7 {10.69} | 34.7 {8.56} | 40.3 {10.65} | < 0.001 | 43.4 {10.00} | < 0.001 |
| Male | 77 (76) | 55 (55) | 43 (38) | 77 (76) | 252 (60) | < 0.001 | 509 (50) | < 0.001 |
| General education, years | 12.1 {1.58} | 11.6 {1.66} | 11.6 {1.55} | 10.8 {1.21} | 11.5 {1.57} | < 0.001 | d | – |
| Ethnicity | < 0.001 | |||||||
| Whitee | 80 (78) | 86 (85) | 108 (95) | 98 (97) | 372 (89) | 341 (34) | – | |
| Otherf | 22 (22) | 15 (15) | 5 (5) | 3 (3) | 45 (11) | 662 (65) | – | |
| Born in UK | 88 (86) | 87 (86) | 99 (88) | 97 (96) | 371 (89) | 0.075 | d | – |
| Employed | 5 (5) | 17 (17) | 23 (20) | 23 (20) | 70 (17) | < 0.001 | d | – |
| Marital status | < 0.001 | d | – | |||||
| Single | 81 (79) | 63 (62) | 51 (45) | 55 (55) | 250 (60) | |||
| Married/cohabiting | 6 (6) | 23 (23) | 34 (30) | 31 (31) | 94 (23) | |||
| Separated/divorced | 14 (14) | 14 (14) | 25 (22) | 12 (12) | 65 (16) | |||
| Widowed and other | 0 (0) | 1 (1) | 3 (3) | 3 (3) | 7 (2) | |||
| Have children aged < 18 years | 20 (20) | 24 (24) | 37 (33) | 49 (49) | 130 (31) | < 0.001 | d | – |
| Children living | N = 20 | N = 24 | N = 37 | N = 49 | N = 130 | < 0.001 | d | – |
| With patient | 3 (15) | 13 (54) | 24 (65) | 17 (35) | 57 (44) | |||
| With separated partner | 10 (50) | 8 (33) | 9 (24) | 20 (41) | 47 (36) | |||
| With others | 7 (35) | 3 (13) | 3 (8) | 12 (25) | 25 (19) | |||
| Contact frequency | N = 17 | N = 11 | N = 12 | N = 32 | N = 72 | 0.429 | d | – |
| Regular | 6 (35) | 5 (50) | 7 (58) | 19 (59) | 37 (51) | |||
| Accommodation | N = 102 | N = 101 | N = 113 | N = 101 | N = 417 | 0.193 | d | – |
| Independent | 79 (77) | 86 (85) | 99 (88) | 81 (80) | 345 (83) | |||
| Supported | 22 (22) | 13 (13) | 13 (11) | 12 (12) | 60 (14) | |||
| Homeless | 1 (1) | 2 (2) | 1 (1) | 8 (8) | 12 (3) | |||
| If independent, lives | N = 79 | N = 86 | N = 99 | N = 81 | N = 345 | < 0.001 | d | – |
| Alone | 53 (67) | 41 (48) | 33 (33) | 27 (33) | 154 (45) | |||
| Characteristics | AOT (N = 102) | CMHT-P (N = 101) | CMHT-NP (N = 113) | SM (N = 101) | Total (N = 417) | US sample (N = 1011) | ||
|---|---|---|---|---|---|---|---|---|
| n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | p-valueb | n (%)/mean {SD} | p-valuec | |
| Diagnosis | < 0.001 | |||||||
| Schizophrenia | 93 (91) | 75 (74) | 0 (0) | 0 (0) | 168 (40) | 457 (45) | – | |
| Bipolar disorder | 3 (3) | 26 (26) | 0 (0) | 0 (0) | 29 (7) | 166 (16) | < 0.001 | |
| Major depression | 6 (6) | 0 (0) | 82 (73) | 0 (0) | 88 (21) | 299 (30) | < 0.001 | |
| Substance abuse | 0 (0) | 0 (0) | 1 (1) | 101 (100) | 102 (25) | 250 (25) | – | |
| Anxiety | d | d | d | d | d | 34 (3) | d | |
| Other diagnosis | 0 (0) | 0 (0) | 30 (26) | 0 (0) | 30 (7) | – | 40 (4) | – |
| Age at first contact with psychiatric services | 23.1 {7.58} | 25.5 {9.14} | 29.0 {11.72} | 23.3 {7.91} | 25.3 {9.57} | < 0.001 | d | d |
| Number of hospitalisations | 6.5 {5.34} | 3.2 {2.90} | 2.4 {3.62} | 0.2 {0.68} | 3.1 {4.20} | < 0.001 | d | d |
| More than two hospitalisations | 84 (82) | 50 (50) | 38 (34) | 2 (2) | 174 (42) | < 0.001 | 624 (62) | < 0.001 |
| Any involuntary hospital admission | 79 (78) | 56 (55) | 29 (26) | 4 (4) | 168 (40) | < 0.001 | d | d |
| Duration of illness, years | 17.0 {9.26} | 16.7 {10.78} | 14.6 {11.86} | 11.5 {8.63} | 15.0 {10.45} | < 0.001 | 21 {11.6} | < 0.001 |
| Number of outpatient contacts in last month | 6.3 {7.85} | 1.3 {1.73} | 1.1 {1.66} | 2.2 {1.34} | 2.7 {4.58} | < 0.001 | 4.4 {4.8} | < 0.001 |
| Any criminal conviction | 34 (33) | 24 (24) | 25 (22) | 83 (82) | 166 (40) | < 0.001 | d | d |
| Any imprisonment | 25 (25) | 12 (12) | 8 (7) | 48 (48) | 93 (22) | < 0.001 | d | d |
| Characteristics | AOT (N = 102) | CMHT-P (N = 101) | CMHT-NP (N = 113) | SM (N = 101) | Total (N = 417) | US sample (N = 1011) | ||
|---|---|---|---|---|---|---|---|---|
| n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | p-valueb | n (%)/mean {SD} | p-valuec | |
| CAGE: positive for drug or alcohol | 18 (18) | 20 (20) | 17 (15) | 76 (75) | 131 (31) | < 0.001 | 214 (21) | < 0.001 |
| BPRS | 34.2 {7.50} | 32.9 {9.74} | 35.8 {8.29} | 29.1 {7.04} | 33.0 {8.45} | < 0.001 | 32.4 {8.4} | < 0.050 |
| GAF | 56.0 {11.69} | 57.1 {14.54} | 55.2 {14.53} | 59.6 {11.13} | 56.9 {13.18} | 0.078 | 47.8 {9.4} | < 0.001 |
| ITAQ total score | 15.5 {5.61} | 17.7 {3.70} | 17.6 {3.38} | 16.5 {2.98} | 16.9 {4.11} | < 0.001 | 18.4 {3.8} | < 0.001 |
| ITAQ Awareness of Illness | 6.6 {2.66} | 7.2 {2.39} | 7.9 {1.68} | 6.6 {2.25} | 7.1 {2.31} | < 0.001 | d | d |
| ITAQ Attitude to Treatment | 8.9 (3.45) | 10.5 {2.08} | 9.8 {2.25} | 9.9 {1.68} | 9.8 {2.50} | < 0.001 | d | d |
| Factors | AOT (N = 102) | CMHT-P (N = 101) | CMHT-NP (N = 113) | SM (N = 101) | Total sample (N = 417) | p-valuea |
|---|---|---|---|---|---|---|
| Mean {SD} | Mean {SD} | Mean {SD} | Mean {SD} | Mean {SD} | ||
| API Decision Making | 48.8 {16.70} | 45.7 {14.68} | 52.9 {14.68} | 44.4 {15.17} | 48.1 {15.61} | < 0.001 |
| API Information Seeking | 73.1 {11.49} | 77.4 {13.13} | 79.9 {11.20} | 79.4 {8.18} | 77.5 {11.40} | < 0.001 |
| STAR-P | ||||||
| Total score | 33.9 {7.55} | 36.1 {8.54} | 37.6 {9.31} | 38.4 {6.13} | 36.6 {8.16} | < 0.00 |
| Positive Collaboration | 17.7 {4.29} | 18.5 {5.46} | 19.2 {5.21} | 19.8 {3.79} | 18.8 {4.80} | 0.001 |
| Positive Clinician Input | 7.5 {2.61} | 7.9 {2.70} | 8.9 {2.65} | 9.1 {2.16} | 8.4 {2.61} | < 0.001 |
| Non-Supportive Clinician Input | 9.0 {2.48} | 9.7 {2.40} | 9.7 {2.40} | 9.6 {1.91} | 9.5 {2.32} | 0.087 |
| STAR-C | ||||||
| Total score | 40.5 {5.58} | 38.9 {5.52} | 37.5 {6.51} | 37.6 {6.45} | 38.5 {6.16} | 0.009 |
| Positive Collaboration | 19.4 {3.33} | 18.7 {3.27} | 17.9 {4.11} | 17.6 {4.21} | 18.3 {3.84} | 0.034 |
| Emotional Difficulties | 10.2 {1.55} | 9.9 {1.48} | 9.6 {1.74} | 10.1 {1.46} | 9.9 {1.58} | 0.059 |
| Positive Clinician Input | 10.8 {1.35} | 10.4 {1.59} | 10.0 {1.50} | 9.9 {1.61} | 10.2 {1.56} | < 0.001 |
| CSQ-8 | 23.8 {5.58} | 25.4 {4.56} | 24.6 {5.12} | 27.3 {3.72} | 25.2 {4.95} | < 0.001 |
| DAI-10 | 3.0 {5.03} | 5.0 {3.90} | 4.2 {4.37} | 5.6 {2.92} | 4.4 {4.22} | 0.004 |
| AES Perceived Coercion | 2.6 {0.68} | 2.4 {0.63} | 2.4 {0.68} | 2.2 {0.57} | 2.4 {0.65} | < 0.001 |
| AES Negative Pressures | 4.0 {0.54} | 4.2 {0.54} | 4.4 {0.52} | 4.3 {0.40} | 4.2 {0.52} | < 0.001 |
| AES Procedural Justice | 2.4 {0.73} | 2.3 {0.63} | 2.3 {0.78} | 2.2 {0.60} | 2.3 {0.70} | – |
As Table 35 shows, the overall sample was predominantly male (n = 252, 60%), white (n = 372, 89%) and born in the UK (n = 371, 89%). Minority ethnic groups mostly consisted of black African, black Caribbean and South Asian patients. Employment rates were low (n = 70, 17%). Most patients were single (n = 250, 60%). Most (n = 345, 83%) lived in independent accommodation, although there were eight in the substance misuse group who were homeless. Of those in independent accommodation, just under half (n = 154, 45%) lived alone. The sample was comparable to the US sample7 in age (3 years younger, on average). Patients were more likely to be male than in the US sample (50% of the US sample being male).
As Table 36 shows, this was a sample of very long-term patients, with a mean of 15 years’ service contact and a young age of first mental health contact (mean 25.3 years), as well as repeated hospitalisations (mean 3.1). They were less likely than the US sample to have bipolar disorder or major depression [n = 29 (7%) and n = 88 (21%) of our sample, compared with n = 166 (16%) and n = 299 (30%) of the US sample]. They were less likely to have experienced more than two hospitalisations [n = 174 (42%) compared with n = 624 (62%)] and had a longer duration of psychiatric history (15 vs. 21 years). They had made fewer outpatient visits in the month prior to interview than their US counterparts (2.7 vs. 4.4 visits).
As Table 37 shows, severity of symptoms (BPRS, mean 33.0) and functioning (GAF, mean 56.9) indicated a relatively disabled group. Our sample was very similar to the US sample in symptom severity (the less than one-point difference being statistically significant but not clinically meaningful), but our sample had rather higher overall functioning (US sample mean 47.8). Our sample was more likely to screen positively for drug or alcohol misuse than the US sample [n = 131 (31%) vs. n = 214 (21%)], which was of course driven by our substance misuse group. They were slightly less insightful (ITAQ, mean 16.9 vs. 18.4) although the magnitude of this difference was very small.
As Table 38 shows, patients rated their therapeutic relationships fairly positively (STAR-P, mean 36.6, with similar subscale scores). Care co-ordinators also rated these therapeutic relationships fairly positively (STAR-C, mean 38.5 with similar subscale scores). Patients reported fairly high satisfaction with services (CSQ-8, mean 25.2). Their attitudes to medication and adherence were fairly positive (DAI, mean 4). They were fairly neutral about being involved in decision-making (Decision Making Preference, mean 48.1), but had stronger preferences for being given information about their care (Information Giving Preference, mean 77.5). They regarded their care as fairly coercive (Perceived Coercion, mean 2.4) and reported that they were only moderately involved in their care (Procedural Justice, mean 2.3), although they reported having experienced only a small number of negative pressures (Negative Pressures, mean: 4.2). (The US study7 did not report these variables.)
Our sample was clearly one of long-term patients who had experienced repeated hospitalisations. The majority of them were unemployed. Despite the differences mentioned, they were broadly comparable to the US sample. Data on experiences of services and perceived coercion, which we collected but the US study7 did not, indicated that our sample was fairly satisfied with several aspects of their care, but they also perceived it to be fairly coercive.
Sample characteristics: differences between the four groups
As Table 35 shows, general education was shorter in the substance misuse group (10.8 years) compared with the three mental illness groups. Non-white patients constituted 18.3% of the two psychosis groups compared with 5% and 3% of the CMHT-non-psychosis and substance misuse groups, respectively. Employment was markedly lower in the AOT group [n = 5 (5%) vs. n = 23 (20%) in the CMHT-non-psychosis and substance misuse groups]. The AOT group members were also much less likely to be married [n = 6 (6%) married vs. n = 31 (31%) in the substance misuse group, n = 34, 30% in the CMHT-non-psychosis group]. In fact, the majority (n = 144, 58%) of all of the single patients came from the two psychosis groups.
The number of patients with children aged < 18 years was far greater in the substance misuse group (n = 49, 49%) than in the AOT group (n = 20, 20%) and CMHT-psychosis group (n = 24, 24%). Of those with children aged < 18 years, proportionately fewer of the AOT group were living with them [n = 3 (15%) vs. n = 24 (65%) in the CMHT-non-psychosis group]. Of those patients who were living independently, proportionately more of the AOT group were living alone [n = 53 (67%) vs. n = 41 (48%) in the CMHT-psychosis group, n = 27 (33%) in the substance misuse group and n = 33 (33%) in the CMHT-non-psychosis group].
Diagnosis varied significantly between the four groups, as would be expected. All of the psychiatric history variables also varied significantly between the groups. The age at which patients first had contact with psychiatric services was significantly lower in the AOT and substance misuse groups (mean 23 years vs. 29 years in the CMHT-non-psychosis group). Similarly, the AOT group had been in contact with services for longer (mean 17 years vs. 11.5 for the substance misuse group). The AOT group had had more past hospitalisations (mean 6.5), which was uncommon in the substance misuse group (mean 0.2), and the vast majority of the AOT group had experienced any psychiatric hospitalisations in their lifetime [n = 79 (78%) vs. n = 29 (26%) of the CMHT-non-psychosis group and n = 4 (4%) of the substance misuse group]. The proportion who had experienced more than two hospitalisations followed the same pattern. In terms of legal history, far more of the substance misuse group had received criminal convictions [n = 83 (82%) vs. n = 25 (22%) and n = 24 (24%) in the CMHT-non-psychosis and -psychosis groups, respectively]. The proportion of patients with past imprisonment followed the same trend [n = 48 (48%) of the substance misuse group vs. n = 8 (7%) and n = 12 (12%) in the CMHT-non-psychosis and -psychosis groups, respectively] (see Table 36).
Severity of symptoms showed little variation between the groups in magnitude, although these differences were statistically significant. There was no difference in functioning. Far more of the substance misuse group screened as positive for drugs or alcohol, as would be expected. Insight varied significantly, with the CMHT groups being more insightful, although the differences were of small magnitude (see Table 37).
Patients’ ratings of their therapeutic relationships with care co-ordinators varied significantly between the four groups (see Table 38). The substance misuse group was the most positive about these relationships (STAR-P, mean: 38.4), whereas the AOT group was most negative (mean 33.9). The same pattern was observed for Positive Collaboration and Positive Clinician Input (STAR-P subscales) but the magnitude of the differences was very small and the Positive Collaboration finding was non-significant once multiple testing had been corrected for. Care co-ordinators’ ratings also differed significantly, but reflected the opposite pattern, being higher for the AOT group (STAR-C, mean 40.5) than for the substance misuse group (mean 37.6), although only Positive Clinician Input remained significant once multiple testing had been corrected for. Patients’ satisfaction was highest in the substance misuse group (CSQ-8, mean 27.3) and lowest in the AOT group (mean 23.8). Patients’ attitudes and adherence to medication were higher in the substance misuse group than in the CMHT groups and lowest in the AOT groups, but this was not significant once multiple testing had been adjusted for.
Patients in the CMHT-non-psychosis group were the most likely to prefer to be involved in decisions about their care (Decision Making Preference, mean 52.9), with those in the substance misuse group least likely to prefer this (mean 44.4). They were also most likely to prefer to have information about their care shared with them (Information Seeking Preference, mean 79.9), with the AOT group the least likely to prefer this (mean 73.1). Perceived coercion was highest in the AOT group (Perceived Coercion, mean 2.6) and lowest in the substance misuse group (mean 2.2). Patients in the AOT group reported experiencing slightly more threats (low Negative Pressures, mean 4.0 vs. 4.4 and 4.3 for the CMHT-non-psychosis and substance misuse groups, respectively). There was no statistically significant difference in reporting having a say in their care.
Patients in the AOT group were thus more severely and chronically ill, and more socially isolated, whereas the substance misuse group had more criminal convictions and past imprisonments. Patients in the AOT group reported having more negative therapeutic relationships and were less satisfied with their care. They were more likely to perceive coercion in their care, although they also cared less about being involved in decision-making and about having information shared with them.
Sample characteristics: differences between the mental illness and substance misuse groups
The substance misuse group contributed most to the variation in sample characteristics and so it was compared individually to the three mental illness groups (AOT and two CMHT groups) combined.
As Table 39 shows, patients in the substance misuse group were significantly younger than those in the whole mental illness group (mean 34.7 vs. 42.0 years), and included more men [n = 77 (76%) vs. n = 175 (55%)] and fewer patients from ethnic minorities [n = 3 (3%) vs. n = 42 (13%)], although the latter finding was not significant when multiple testing was corrected for. General education was slightly lower (mean 10.8 years vs. 11.8 years) and employment higher [n = 23 (20%) vs. n = 45 (14%)], although the employment finding was not significant when multiple testing was corrected for. The substance misuse group had more children aged < 18 years [n = 49 (49%) vs. n = 81 (26%)] and fewer of them were living alone in independent accommodation [n = 27 (33%) vs. n = 127 (48%)].
| Characteristics | Mental illness (N = 316) | SM (N = 101) | ||
|---|---|---|---|---|
| n (%)/mean {SD} | p-valueb | n (%)/mean {SD} | p-valuec | |
| Age (years) | 42.0 {10.65} | 0.034 | 34.7 {8.56} | < 0.001 |
| Male | 175 (55) | < 0.001 | 77 (76) | < 0.001 |
| General education (years) | 11.8 {1.60} | 0.062 | 10.8 {1.21} | < 0.001 |
| Ethnicity | 0.001 | 0.006 | ||
| White | 274 (87) | – | 98 (97) | – |
| Others | 42 (13) | – | 3 (3) | – |
| Employed | 45 (14) | 0.003 | 23 (20) | 0.023 |
| Marital status | < 0.001 | 0.225 | ||
| Single | 195 (62) | – | 55 (55) | – |
| Married/cohabiting | 63 (20) | – | 31 (31) | – |
| Separated/divorced | 53 (17) | – | 12 (12) | – |
| Widowed and other | 4 (1) | – | 3 (3) | – |
| Have children aged < 18 years | 81 (26) | 0.096 | 49 (49) | < 0.001 |
| Children live | N = 81 | 0.001 | N = 49 | 0.211 |
| With patient | 40 (49) | – | 17 (35) | – |
| With separated partner | 27 (33) | – | 20 (41) | – |
| With others | 13 (16) | – | 12 (25) | – |
| If independent, lives | N = 264 | < 0.001 | N = 81 | 0.025 |
| Alone | 127 (48) | – | 27 (33) | – |
As Table 40 shows, significant differences were found between the mental illness group and the substance misuse group for diagnosis (as would be expected) and for the psychiatric history variables. The substance misuse group had had fewer psychiatric hospitalisations (mean 0.2 vs. 4.0) and involuntary hospitalisations [n = 4 (4%) vs. n = 164 (52%)]. Age at first contact with psychiatric services was significantly lower for the substance misuse group (mean 23.3 vs. 25.9; p < 0.05), but this was not significant once multiple testing had been corrected for. The number of outpatient visits in the past month was also not significant once multiple testing had been corrected for. The substance misuse group had had more criminal convictions [n = 83 (82%) vs. n = 83 (26%)] and previous imprisonments [n = 48 (48%) vs. n = 45 (14%)].
| Characteristics | Mental illness (N = 316) | SM (N = 101) | ||
|---|---|---|---|---|
| n (%)/mean {SD} | p-valueb | n (%)/mean {SD} | p-valuec | |
| Diagnosis | < 0.001 | < 0.001 | ||
| Schizophrenia | 168 (53) | 0 (0) | ||
| Bipolar disorder | 29 (9) | 0 (0) | ||
| Major depression | 88 (28) | 0 (0) | ||
| Substance abuse | 1 (0) | 101 (100) | ||
| Other diagnosis | 30 (9) | 0 (0) | ||
| Age at first contact with psychiatric services | 25.9 {9.97} | < 0.001 | 23.3 {7.91} | 0.034 |
| Number of hospitalisations | 4.0 {4.43} | < 0.001 | 0.2 {0.68} | < 0.001 |
| More than two hospitalisations | 172 (54) | < 0.001 | 2 (2) | < 0.001 |
| Any involuntary hospitalisation | 164 (52) | < 0.001 | 4 (4) | < 0.001 |
| Duration of illness (years) | 16.1 {10.74} | 0.044 | 11.5 {8.63} | < 0.001 |
| Number of outpatient contacts in last month | 2.8 {5.21} | < 0.001 | 2.2 {1.34} | 0.004 |
| Any criminal conviction | 83 (26) | 0.077 | 83 (82) | < 0.001 |
| Any imprisonment | 45 (14) | 0.001 | 48 (48) | < 0.001 |
| CAGE: positive for drug or alcohol | 55 (17) | 0.656 | 76 (75) | < 0.001 |
| BPRS | 34.4 {8.61} | 0.043 | 29.1 {7.04} | < 0.001 |
| GAF | 56.1 {13.69} | 0.450 | 59.6 {11.13} | 0.025 |
| ITAQ Total score | 17.0 {4.40} | 0.008 | 16.5 {2.98} | 0.002 |
Not surprisingly, far more of the substance misuse group screened positively for drug or alcohol misuse [n = 76 (75%) vs. n = 55 (17%) for the mental illness group]. Patients in the mental illness group had more severe symptoms than the substance misuse group (BPRS, mean 34.4 vs. 29.1), as would be expected. The differences in insight and functioning (with the mental illness group scoring slightly higher for insight and lower for functioning) were statistically significant but not clinically meaningful and these differences ceased to be statistically significant once multiple testing had been adjusted for.
This analysis thus confirmed the broad findings reported in the previous section that the substance misuse group had much less psychiatric history but more criminal history.
Sample characteristics: differences between the three mental illness groups
The three mental illness groups were also compared independently of the substance misuse sample. As Table 39 shows, the homogeneity within this group and its contrast with the substance misuse group were confirmed by the fact that several sociodemographic characteristics which were significantly different between the four groups – years of general education, proportion of those with children aged < 18 years – were no longer statistically significant when the three mental illness groups were being compared with each other, and differences in age, ethnicity, employment and where their children lived ceased to be significant when multiple testing was corrected for. Differences in gender, marital status and living alone were still statistically significant when only the three mental illness groups were compared, with the AOT group being slightly younger on average, and far more of them being single and fewer of them living independently.
As Table 40 shows, diagnosis differed significantly between the three mental illness groups, as would be expected. All of the psychiatric and legal history variables continued to differ significantly between the three groups, apart from duration of psychiatric history and the proportion with criminal convictions. The AOT group had been younger, on average, at first contact with psychiatric services, had undergone more hospitalisations, and were more likely to have experienced involuntary hospitalisation; they were also more likely to have been imprisoned. The three groups differed significantly on insight, with the AOT group being slightly less insightful, but symptom scores, functioning and screening positive for drug or alcohol problems no longer reached statistical significance.
As Table 41 shows, differences between the three mental illness groups remained statistically significant for attitudes and adherence to medication, decision-making and information-seeking preferences, and therapeutic relationship. The AOT group had more negative attitudes to medication and adherence, and were less likely to prefer to have information shared with them; they were more likely to prefer to be involved in decision-making than the CMHT-psychosis group but less likely than the CMHT-non-psychosis group. Differences in how clinicians rated the therapeutic relationships remained statistically significant for only the Positive Collaboration subscale once multiple testing had been corrected for, with the AOT group reporting the lowest degree of positive collaboration.
| Factors | AOT (N = 102) | CMHT-P (N = 101) | CMHT-NP (N = 113) | p-valuea |
|---|---|---|---|---|
| Mean {SD} | Mean {SD} | Mean {SD} | ||
| DAI-10 | 3.03 {5.03} | 5.0 {3.90} | 4.7 {4.37} | 0.031 |
| API Decision Making | 48.8 {16.70} | 45.7 {14.68} | 52.9 {14.68} | 0.002 |
| API Information Seeking | 73.1 {11.49} | 77.4 {13.13} | 79.9 {11.20} | < 0.001 |
| STAR-P | ||||
| Total score | 33.9 {7.55} | 36.1 {8.54} | 37.6 {9.31} | < 0.001 |
| Positive Collaboration | 17.6 {4.29} | 18.5 {5.46} | 19.2 {5.21} | 0.002 |
| Positive Clinician Input | 7.5 {2.61} | 7.9 {2.70} | 8.9 {2.65} | < 0.001 |
| Non-supportive Clinician | 9.0 {2.48} | 9.7 {2.40} | 9.7 {2.40} | 0.046 |
| STAR-C | ||||
| Total score | 40.5 {5.58} | 38.9 {5.52} | 37.5 {6.51} | 0.009 |
| Positive Collaboration | 19.4 {3.33} | 18.7 {3.27} | 17.9 {4.11} | 0.083 |
| Emotional Difficulties | 10.2 {1.55} | 9.9 {1.48} | 9.6 {1.74} | 0.046 |
| Positive Clinician Input | 10.8 {1.35} | 10.4 {1.59} | 10.0 {1.50} | < 0.001 |
This analysis thus confirmed that many of the differences between the four groups were driven by the difference between the mental illness groups and the substance misuse group. Despite this, there were statistically significant differences between the three mental illness groups in several aspects of psychiatric and legal history, experiences of service and preferences, with the AOT group tending to be the more severe and chronic group, and the group with less-positive therapeutic relationships.
Leverage: the English sample and a comparison with the US sample
Table 42 displays the rates of lifetime experience of the four types of reported leverage for the total ULTIMA sample, the four groups and the US study7 sample. Overall, 145 patients (35%) reported any type of leverage, of whom 51 (12% of the sample) reported more than one type and seven reported more than two types. Leverage related to housing was by far the most common type (n = 98, 24%). Overall, n = 62 (15%) reported leverage through the criminal justice system. Only 10 patients (2%) reported financial leverage, but 34 patients (8%) reported leverage relating to child access, which represented 26% of the 130 patients with children aged < 18 years of age.
| Type of leverage | AOT (N = 102) | CMHT-P (N = 101) | CMHT-NP (N = 113) | SM (N = 101) | Total (N = 417) | USA (N = 1011) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size | n (%) | Sample size | n (%) | Sample size | n (%) | Sample size | n (%) | p-valuea | Sample size | n (%) | Sample size | n (%) | p-valueb | |
| Housing leverage | ||||||||||||||
| All | 102 | 19 (19) | 101 | 22 (22) | 113 | 13 (12) | 101 | 44 (44) | < 0.001 | 417 | 98 (24) | 1011 | 325 (32) | < 0.010 |
| Financial leverage | ||||||||||||||
| All | 102 | 3 (3) | 101 | 2 (2) | 113 | 0 (0) | 101 | 5 (5) | 0.083 | 417 | 10 (2) | 1011 | 121 (12) | < 0.001 |
| For whom applicablec | 48 | 3 (6) | 46 | 2 (4) | 42 | 0 (0) | 29 | 5 (17) | 0.083 | 165 | 10 (6) | 519 | 121 (32) | < 0.001 |
| Criminal justice leverage | ||||||||||||||
| All | 102 | 13 (13) | 101 | 7 (7) | 113 | 3 (4) | 101 | 37 (37) | 0.214 | 417 | 62 (15) | 1011 | 230 (23) | < 0.001 |
| For whom applicablec | 63 | 13 (21) | 38 | 7 (18) | 39 | 5 (13) | 92 | 37 (40) | 0.214 | 232 | 62 (26) | 512 | 230 (45) | < 0.001 |
| Child access leverage | ||||||||||||||
| All | 102 | 6 (6) | 101 | 6 (6) | 113 | 6 (5) | 101 | 16 (16) | 0.558 | 417 | 34 (8) | d | d | d |
| For whom applicablec | 20 | 6 (30) | 24 | 6 (25) | 37 | 6 (16) | 49 | 16 (33) | 0.412 | 130 | 34 (26) | d | d | d |
| Any type | 102 | 34 (33) | 101 | 30 (30) | 113 | 17 (15) | 101 | 64 (63) | < 0.001 | 417 | 145 (35) | 1011 | 519 (51) | < 0.001 |
| More than one type | 102 | 7 (7) | 101 | 5 (5) | 113 | 6 (5) | 101 | 33 (33) | < 0.001 | 417 | 51 (12) | d | d | d |
The level of leverage reported by our sample was lower than that reported by the US sample (51%). This was also the case for each of the three types of leverage included in both studies (housing, financial and criminal justice leverage), with the difference in leverage relating to finance being particularly striking (12% reporting this in the US sample vs. 2% in our sample).
Leverage: differences between the four groups
As Table 42 shows, the highest rates of leverage were reported by the substance misuse group. The majority of this group (n = 64, 63%) reported having experienced leverage in their lifetime (vs. 33% and 30% for the psychosis groups and 15% for the CMHT-non-psychosis group). They were also much more likely to report multiple types of leverage, with one-third of them (n = 33, 33%) doing so (vs. 7% in the AOT group and 5% in each CMHT group). The substance misuse and AOT groups accounted for almost all of the criminal justice system leverage. The substance misuse group both had more children aged < 18 years (n = 49, 49%) (see Table 38) and reported higher rates of this type of leverage [n = 16 (33%) vs. n = 6 (16%) for the CMHT-non-psychosis group].
The substance misuse group was, thus, much more likely to have experienced leverage, including multiple types of leverage.
Leverage: the mental illness groups compared with the substance misuse group
There were statistically significant differences between the mental illness groups combined and the substance misuse group in their reporting of leverage. Far more of the substance misuse group proportionately reported experiencing any type of leverage [n = 64 (63.4%) vs. n = 88 (27.8%); p < 0.001] and more than one type [n = 33 (32.7%) vs. n = 21 (6.6%); p < 0.001], as well as leverage in relation to housing [n = 44 (44%) vs. n = 54 (17%); p < 0.001]. This analysis thus confirmed the previous analysis comparing all four groups.
Factors associated with leverage
Primary analysis
Tables 43 and 44 show the univariate associations between sample characteristics and reporting each of the four individual types of leverage. In the univariate analyses, leverage in relation to housing was more likely to be reported by patients who were single, had children living with a separated partner, had an indication of current drug or alcohol misuse and were younger at first contact with psychiatric services. Criminal justice leverage was more commonly associated with having an ethnic minority background, not living alone and having little outpatient contact. In the multivariate analysis shown in Table 45, no variables retained their significance apart from ethnicity. Being white was associated with lower criminal justice leverage (with white patients being only 0.1 times as likely to report this).
| Characteristics | Leverage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Housing | Financial | Criminal justice | Child access | |||||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Age greater than median | 0.8 | a | 0.5 to 1.3 | 0.3 | a | 0.1 to 2.1 | 0.5 | a | 0.2 to 1.3 | 0.5 | a | 0.2 to 1.2 |
| White vs. other ethnicities | 0.8 | a | 0.3 to 1.8 | –b | – | – | 0.1 | < 0.010 | 0.03 to 0.5 | 0.3 | < 0.100 | 0.1 to 1.2 |
| Female vs. male | 1.6 | < 0.100 | 1.0 to 2.8 | 0.7 | a | 0.1 to 5.8 | 0.3 | a | 0.04 to 2.8 | 0.5 | a | 0.2 to 1.2 |
| Born in UK vs. in other countries | 1.2 | a | 0.5 to 2.8 | – | – | – | 3.6 | < 0.10 | 0.8 to 16.1 | – | – | – |
| General education (years) | 1.5 | a | 0.9 to 2.5 | 0.6 | a | 0.1 to 4.0 | 1.2 | a | 0.3 to 4.6 | 1.2 | a | 0.5 to 3.1 |
| Employed vs. unemployed/sheltered | 0.6 | a | 0.3 to 1.1 | 5.2 × 1013 | a | 0 to Inf | 3.6 | a | 0.4 to 31.6 | 0.7 | a | 0.2 to 1.8 |
| Single vs. married/cohabiting | 1.8 | < 0.050 | 1.1 to 3.1 | 5.7 | a | 0.3 to 114.8 | 0.8 | a | 0.2 to 2.5 | 1.6 | a | 0.7 to 3.5 |
| Have children aged < 18 years | 1.2 | a | 0.7 to 2.0 | 0.5 | a | 0.02 to 16.4 | 0.5 | a | 0.2 to 1.6 | – | – | – |
| Children live with patient vs. | ||||||||||||
| Living with separated partner | 2.6 | < 0.050 | 1.0 to 6.4 | –c | – | – | 0.2 | a | 0.02 to 2.0 | 1.9 | a | 0.8 to 4.6 |
| Living with others | 1.9 | a | 0.6 to 5.8 | – | – | – | 8.8 × 1011 | a | 0 to Inf | 1.9 | a | 0.6 to 5.5 |
| Contact frequency with children | ||||||||||||
| Infrequent/none (vs. regular, ≥ monthly) | 0.7 | a | 0.2 to 1.8 | – | – | – | 0.2 | a | 0.03 to 1.8 | 0.5 | a | 0.2 to 1.4 |
| Independent accommodation (vs. supported/homeless) | 0.3 | < 0.001 | 0.2 to 0.6 | 1.2 | a | 0.2 to 8.7 | 1.4 | a | 0.5 to 4.2 | 0.9 | a | 0.3 to 2.3 |
| If independent accommodation, living alone vs. living with others | 1.2 | a | 0.7 to 2.1 | 3.1 | a | 0.1 to 125.3 | 0.1 | < 0.050 | 0.03 to 0.7 | 1.3 | a | 0.5 to 3.4 |
| Diagnosis (schizophrenia vs.) | ||||||||||||
| Bipolar disorder | 0.4 | a | 0.1 to 1.4 | 4.9 × 10–13 | a | 0 to Inf | 1.1 | a | 0.1 to 13.8 | 1.9 | a | 0.4 to 10.3 |
| Major depression | 0.5 | < 0.100 | 0.2 to 1.1 | 4.3 × 10–13 | a | 0 to Inf | 2.1 × 1012 | a | 0 to Inf | 0.6 | a | 0.2 to 1.9 |
| Substance abuse | 2.7 | < 0.001 | 1.5 to 4.6 | 9.0 | < 0.1 | 0.8 to 100.2 | 2.3 | a | 0.8 to 6.6 | 1.2 | a | 0.5 to 3.3 |
| Other diagnosis | 0.4 | a | 0.1 to 1.4 | 4.3 × 10–13 | a | 0 to Inf | 2.1 × 1012 | a | 0 to Inf | 2.4 × 10–13 | a | 0 to Inf |
| Characteristics | Leverage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Housing | Financial | Criminal justice | Child access | |||||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Age at first contact with psychiatric services | 0.5 | < 0.050 | 0.3 to 0.9 | 0.6 | a | 0.1 to 3.5 | 0.8 | a | 0.3 to 2.2 | 0.5 | < 0.100 | 0.2 to 1.1 |
| Number of hospitalisations | 1.8 | < 0.100 | 0.9 to 3.5 | 0.3 | a | 0.1 to 1.5 | 0.5 | a | 0.2 to 1.4 | 2.5 | a | 0.8 to 8.1 |
| More than two hospitalisations | 1.8 | < 0.100 | 0.9 to 3.5 | 0.3 | a | 0.1 to 1.5 | 0.5 | a | 0.2 to 1.4 | 2.6 | a | 0.8 to 8.1 |
| Any involuntary hospitalisation | 1.4 | a | 0.7 to 2.6 | 6.4 | a | 0.2 to 232.2 | 0.9 | a | 0.1 to 9.1 | 1.2 | a | 0.5 to 2.9 |
| Duration of illness (years) | 1.4 | a | 0.8 to 2.2 | 0.3 | a | 0.03 to 2.2 | 0.7 | a | 0.2 to 1.9 | 1.2 | a | 0.6 to 2.7 |
| Number of outpatient contacts in last month | 1.1 | a | 0.7 to 2.0 | 1.2 | a | 0.2 to 10.0 | 0.2 | < 0.050 | 0.0 to 0.9 | 1.3 | a | 0.6 to 2.9 |
| Any criminal conviction | 1.5 | a | 0.9 to 2.7 | 0.8 | a | 0.1 to 7.4 | 1.2 | a | 0.2 to 6.3 | 1.2 | a | 0.5 to 2.7 |
| Any imprisonment | 1.7 | < 0.100 | 0.9 to 3.0 | 2.7 | a | 0.4 to 18.1 | 0.7 | a | 0.2 to 2.1 | 1.3 | a | 0.6 to 3.1 |
| CAGE: positive for drug or alcohol | 1.8 | < 0.050 | 1.0 to 3.2 | 2.5 | a | 0.5 to 13.7 | 1.0 | a | 0.3 to 3.9 | 1.5 | a | 0.7 to 3.4 |
| Characteristics | Leverage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Housing | Financial | Criminal justice | Child access | |||||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | |
| White (vs. other ethnicities) | – | – | – | – | – | – | 0.1 | < 0.050 | 0.0 to 0.7 | – | – | – |
| Single (vs. married/cohabiting) | 2.4 | b | 0.98 to 6.1 | – | – | – | – | – | – | – | – | – |
| Children living with patient vs. | ||||||||||||
| Living with a separated partner | 1.6 | b | 0.5 to 4.5 | – | – | – | – | – | – | – | – | – |
| Living with others | 1.4 | b | 0.4 to 4.7 | – | – | – | – | – | – | – | – | – |
| Independent accommodation (vs. supported/homeless) | 0.7 | b | 0.3 to 2.2 | – | – | – | – | – | – | – | – | – |
| If independent: | ||||||||||||
| Living alone (vs. living with others) | – | – | – | – | – | – | 0.2 | b | 0.0 to 1.0 | – | – | – |
| Diagnosis (schizophrenia vs.) | ||||||||||||
| Bipolar disorder | 2.2 | b | 0.3 to 15.1 | – | – | – | – | – | – | – | – | – |
| Major depression | 1.1 | b | 0.3 to 3.9 | – | – | – | – | – | – | – | – | – |
| Substance abuse | 2.3 | b | 0.8 to 6.6 | – | – | – | – | – | – | – | – | – |
| Other diagnosis | – | – | – | – | – | – | – | – | – | – | – | – |
| Age at first contact with psychiatric services | 0.9 | b | 0.4 to 2.3 | – | – | – | – | – | – | – | – | – |
| Number of outpatient contacts in last month | – | – | – | – | – | – | – | – | – | – | – | – |
| CAGE: positive for drug or alcohol | 0.9 | b | 0.3 to 2.5 | – | – | – | – | – | – | – | – | – |
Table 46 shows the univariate associations between both reporting any type of leverage and reporting more than one type and sociodemographic, clinical and social characteristics, whereas Table 47 shows the multivariate models. Reporting any form of leverage was associated in the univariate analysis with not living independently, major depression and substance misuse diagnoses, age of first contact with psychiatric services, having more than two hospitalisations, having ever experienced involuntary hospitalisation, duration of psychiatric history, having ever had a criminal conviction, having ever been imprisoned and insight. Multivariate analysis showed that reporting any form of leverage was associated with having a diagnosis of substance misuse (patients with substance misuse being 5.7 times as likely to report this), more than two hospitalisations (2.8 times as likely) and better insight (twice as likely).
| Characteristics | Leverage | |||||
|---|---|---|---|---|---|---|
| Any type | More than one type | |||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Age (years) | 0.7 | a | 0.5 to 1.2 | 0.9 | a | 0.5 to 1.7 |
| Male vs. female | 1.4 | a | 0.9 to 2.3 | 1.2 | a | 0.6 to 2.3 |
| General education (years) | 1.0 | a | 0.6 to 1.6 | 1.0 | a | 0.5 to 2.0 |
| White (vs. other ethnicities) | 0.6 | a | 0.3 to 1.3 | 0.7 | a | 0.2 to 2.5 |
| Born in UK (vs. other countries) | 1.8 | a | 0.9 to 3.9 | 1.1 | a | 0.4 to 3.3 |
| Employed (vs. unemployed/sheltered) | 0.6 | a | 0.3 to 1.1 | 0.9 | a | 0.4 to 1.9 |
| Single (vs. married/cohabiting) | 1.3 | a | 0.9 to 2.1 | 1.2 | a | 0.6 to 2.3 |
| Have children aged < 18 years | 1.4 | a | 0.9 to 2.2 | 1.9 | < 0.050 | 1.0 to 3.5 |
| Children live with patient vs. | ||||||
| A separated partner | 1.7 | a | 0.7 to 3.9 | 1.9 | a | 0.7 to 5.2 |
| Others | 2.3 | a | 0.8 to 6.4 | 1.2 | a | 0.3 to 4.2 |
| Contact frequency with children | ||||||
| Infrequent/none (vs. regular, ≥ monthly) | 0.5 | a | 0.2 to 1.3 | 0.6 | a | 0.2 to 2.0 |
| Independent accommodation (vs. supported/homeless) | 0.4 | < 0.010 | 0.2 to 0.7 | 0.4 | < 0.010 | 0.2 to 0.8 |
| If independent | ||||||
| Living alone (vs. living with others) | 0.9 | a | 0.5 to 1.5 | 0.9 | a | 0.4 to 1.9 |
| Diagnosis (schizophrenia vs.) | ||||||
| Bipolar disorder | 0.5 | a | 0.2 to 1.2 | 1.0 | a | 0.2 to 4.5 |
| Major depression | 0.4 | < 0.010 | 0.2 to 0.7 | 1.0 | a | 0.3 to 2.6 |
| Substance misuse | 3.0 | < 0.001 | 1.8 to 5.1 | 6.2 | < 0.001 | 3.0 to 12.8 |
| Other diagnosis | 0.5 | a | 0.2 to 1.4 | 0.4 | a | 0.1 to 3.6 |
| Age at first contact with psychiatric services | 0.5 | < 0.010 | 0.3 to 0.8 | 0.5 | a | 0.3 to 1.0 |
| More than two hospitalisations | 3.3 | < 0.001 | 1.8 to 6.0 | 2.6 | a | 0.9 to 6.9 |
| Any involuntary hospitalisation | 1.8 | < 0.050 | 1.1 to 3.0 | 1.5 | a | 0.6 to 3.5 |
| Duration of illness (years) | 1.9 | < 0.010 | 1.2 to 2.9 | 1.9 | a | 0.98 to 3.5 |
| Number of outpatient contacts in last month | 1.0 | a | 0.7 to 1.7 | 1.0 | a | 0.5 to 2.1 |
| Any criminal conviction | 2.5 | < 0.001 | 1.6 to 4.1 | 3.2 | < 0.010 | 1.5 to 6.8 |
| Any imprisonment | 2.7 | < 0.001 | 1.6 to 4.6 | 3.4 | < 0.001 | 1.7 to 6.7 |
| ITAQ total score | 2.0 | < 0.010 | 1.2 to 3.1 | 0.9 | a | 0.5 to 1.8 |
| CAGE: positive for drugs or alcohol | 1.6 | a | 0.96 to 2.7 | 2.6 | < 0.050 | 1.2 to 5.4 |
| Characteristics | Leverage | |||||
|---|---|---|---|---|---|---|
| Any type | More than one type | |||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Have children aged < 18 years | – | – | – | 1.5 | a | 0.7 to 2.8 |
| Independent accommodation (vs. supported/homeless) | 0.5 | a | 0.3 to 1.0 | 0.5 | < 0.050 | 0.2 to 0.9 |
| Diagnosis (schizophrenia vs.) | ||||||
| Bipolar disorder | 0.8 | a | 0.3 to 2.5 | 1.4 | a | 0.3 to 6.8 |
| Major depression | 0.6 | a | 0.3 to 1.3 | 1.2 | a | 0.4 to 3.5 |
| Substance misuse | 5.7 | < 0.001 | 2.2 to 15.1 | 3.0 | < 0.050 | 1.3 to 7.2 |
| Other diagnosis | 0.7 | a | 0.2 to 2.3 | 0.5 | a | 0.1 to 4.3 |
| Age at first contact with psychiatric services | 0.6 | a | 0.4 to 1.0 | – | – | – |
| More than two previous hospitalisations | 2.8 | < 0.010 | 1.4 to 5.6 | – | – | – |
| Any previous hospitalisation | 1.1 | a | 0.6 to 2.3 | – | – | – |
| Duration of illness (years) | 1.3 | a | 0.8 to 2.2 | – | – | – |
| Any criminal conviction | 1.4 | a | 0.7 to 2.6 | 1.4 | a | 0.6 to 3.4 |
| Any imprisonment | 1.8 | a | 0.9 to 3.7 | 2.4 | < 0.050 | 1.1 to 5.2 |
| ITAQ total score | 2.0 | < 0.050 | 1.1 to 3.4 | – | – | – |
| CAGE: positive for drugs or alcohol | – | – | – | 1.6 | a | 0.8 to 3.4 |
Reporting more than one type of leverage was associated in the univariate analysis with having children aged < 18 years of age, not living independently, substance misuse, having had a criminal conviction, having been imprisoned and screening as positive for drug or alcohol misuse. Multivariate analysis showed that reporting more than one type of leverage was associated with not living independently (patients who were living independently were half as likely to report this), substance misuse (three times as likely) and having a history of imprisonment (2.5 times as likely).
Patients were thus more likely to experience any type of leverage if they were from the substance misuse group, had been hospitalised more than twice and had better insight, whereas experiencing more than one type was associated with not living independently, substance misuse and a history of imprisonment. Criminal justice leverage was more likely to be reported by patients who were not white.
Exploratory analyses
Table 48 shows the ‘replication analysis’, that is, the multivariate analyses conducted as exact replications of the US study7 against the four leverages. As Table 48 shows, in these multivariate analyses, a higher likelihood of reporting housing leverage was associated with having a substance misuse diagnosis (those with substance misuse diagnosis being 4.4 times as likely to report this type of leverage as those without). Criminal justice leverage was associated with ethnicity (with white patients being only 0.2 times as likely to report this type of leverage). Child access leverage was associated with being older and having had more than two previous psychiatric hospitalisations (with younger patients being 0.4 times as likely to report this type and those with more than two hospitalisations being seven times as likely to report it).
| Characteristics | Leverage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Housing | Financial | Criminal justice | Child access | |||||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Age greater than median | 0.7 | a | 0.4 to 1.3 | 0.5 | a | 0.0 to 36.7 | 1.2 | a | 0.3 to 5.4 | 0.4 | < 0.050 | 0.2 to 1.0 |
| White (vs. other ethnicities) | 0.8 | a | 0.3 to 2.0 | – | – | – | 0.2 | < 0.050 | 0.0 to 1.0 | 0.3 | a | 0.1 to 1.4 |
| Male (vs. female) | 1.4 | a | 0.8 to 2.4 | 0.4 | a | 0.0 to 21.0 | 0.7 | a | 0.1 to 7.5 | 0.5 | a | 0.2 to 1.0 |
| Diagnosis (schizophrenia vs.) | ||||||||||||
| Bipolar disorder | 0.6 | a | 0.2 to 2.2 | – | – | – | 0.9 | a | 0.0 to 31.0 | 1.1 | a | 0.2 to 6.0 |
| Major depression | 0.7 | a | 90.3 to 1.5 | – | – | – | – | – | – | 0.7 | a | 0.2 to 2.6 |
| Substance abuse | 4.4 | < 0.001 | 1.9 to 10.4 | 11.5 | a | 0.1 to 1057.6 | 0.3 | a | 0.0 to 5.1 | 3.9 | a | 1.0 to 16.8 |
| Other diagnosis | 0.5 | a | 0.1 to 1.7 | – | – | – | – | – | – | 1.4 | a | 0.2 to 9.0 |
| More than two hospitalisations | 1.7 | a | 0.9 to 3.3 | 0.9 | a | 0.0 to 62.2 | 0.1 | a | 0.0 to 2.1 | 7.0 | < 0.001 | 2.2 to 21.7 |
| Duration of illness | 1.5 | a | 0.8 to 2.6 | 0.2 | a | 0.0 to 9.0 | 0.6 | a | 0.2 to 2.6 | 1.3 | a | 0.6 to 2.9 |
| Number of outpatient contacts in last month | 0.8 | a | 0.5 to 1.4 | 1.0 | a | 0.0 to 27.0 | 0.2 | a | 0.0 to 1.2 | 0.7 | a | 0.3 to 1.6 |
| ITAQ total score | 1.4 | a | 0.8 to 2.3 | 2.8 | a | 0.1 to 65.6 | 1.1 | a | 0.3 to 4.3 | 1.0 | a | 0.4 to 2.5 |
| BPRS | 1.2 | a | 0.7 to 2.2 | 3.1 | a | 0.1 to 150.1 | 1.5 | a | 0.3 to 6.9 | 1.3 | a | 0.5 to 3.4 |
| GAF | 0.6 | a | 0.4 to 1.1 | 1.6 | a | 0.1 to 35.5 | 1.3 | a | 0.3 to 5.1 | 0.5 | a | 0.2 to 1.2 |
| CAGE: positive for drug or alcohol | 1.3 | a | 0.7 to 2.4 | – | – | – | 0.8 | a | 0.2 to 3.9 | 1.0 | a | 0.4 to 2.8 |
Reporting any type of leverage was associated with having a substance misuse diagnosis (OR 8.3, 95% CI 3.5 to 19.7; p < 0.0001), more than two previous hospitalisations (OR 3.2, 95% CI 1.7 to 6.1; p < 0.0001), a longer duration of psychiatric history (OR 1.9, 95% CI 1.1 to 3.4; p < 0.050) and better insight (OR 1.9, 95% CI 1.1 to 3.2; p < 0.050). Reporting more than one type of leverage was only associated with substance misuse diagnosis (OR 12.5, 95% CI 3.4 to 45.8; p < 0.0001).
We next conducted our ‘combined’ analyses, repeating our analyses to include all the variables found significant in the US study analyses,7 as well as all the possible explanatory variables that had reached the threshold significance level in our univariate analyses. For these analyses, we included any clinical variables (including experience of services and perceived coercion) that were eligible based on univariate analysis. As Table 49 shows, univariate analysis suggested that, among these variables, none was associated with housing leverage or child access leverage; finance leverage was associated only with therapeutic relationship rated by the care co-ordinator; and criminal justice leverage was associated only with Positive Clinician Input as rated by the care co-ordinator.
| Characteristics | Leverage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Housing | Financial | Criminal justice | Child access | |||||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
| DAI-10 | 1.3 | 0.8 to 2.2 | a | 0.7 | 0.1 to 6.2 | a | 0.8 | 0.3 to 2.5 | a | 1.0 | 0.4 to 2.5 | a |
| API Decision Making | 0.8 | 0.5 to 1.3 | a | 0.6 | 0.1 to 6.3 | a | 1.3 | 0.4 to 3.8 | a | 1.3 | 0.6 to 2.9 | a |
| API Information Seeking | 1.2 | 0.8 to 2.0 | a | 7.5 | 0.6 to 97.3 | a | 1.1 | 0.4 to 3.2 | a | 1.2 | 0.5 to 2.6 | a |
| ITAQ | ||||||||||||
| Total score | 1.4 | 0.9 to 2.3 | a | 3.4 | 0.3 to 34.1 | a | 1.4 | 0.4 to 4.6 | a | 0.8 | 0.3 to 1.8 | a |
| Awareness of Illness | 1.4 | 0.8 to 2.3 | a | 3.2 | 0.4 to 25.3 | a | 2.4 | 0.6 to 9.4 | a | 0.9 | 0.3 to 2.2 | a |
| Attitude to Treatment | 1.3 | 0.8 to 2.2 | a | 6.1 | 0.2 to 164.6 | a | 0.7 | 0.2 to 2.2 | a | 1.1 | 0.5 to 2.5 | a |
| STAR-P | ||||||||||||
| Total score | 0.9 | 0.6 to 1.5 | a | 1.5 | 0.2 to 9.5 | a | 1.6 | 0.5 to 4.9 | a | 0.8 | 0.3 to 1.7 | a |
| Positive Collaboration | 1.1 | 0.7 to 1.8 | a | 1.3 | 0.2 to 7.9 | a | 1.7 | 0.6 to 5.0 | a | 0.7 | 0.3 to 1.5 | a |
| Positive Clinician Input | 0.8 | 0.5 to 1.3 | a | 1.1 | 0.2 to 7.1 | a | 2.1 | 0.6 to 6.9 | a | 0.6 | 0.3 to 1.4 | a |
| Non-supportive Clinician | 0.7 | 0.4 to 1.2 | a | 0.9 | 0.1 to 9.4 | a | 1.1 | 0.4 to 3.4 | a | 0.8 | 0.3 to 1.7 | a |
| STAR-C | ||||||||||||
| Total score | 1.1 | 0.6 to 1.8 | a | 36.2 | 1.4 to 918.0 | < 0.050 | 0.6 | 0.2 to 2.0 | a | 1.4 | 0.6 to 3.3 | a |
| Positive Collaboration | 1.1 | 0.7 to 1.9 | a | 42.2 | 1.2 to 1515.9 | < 0.050 | 0.8 | 0.3 to 2.5 | a | 1.4 | 0.6 to 3.3 | a |
| Emotional Difficulties | 1.3 | 0.8 to 2.2 | a | 130.8 | 2.2 to 7939.4 | < 0.050 | 1.0 | 0.3 to 3.2 | a | 1.1 | 0.4 to 2.6 | a |
| Positive Clinician Input | 0.8 | 0.5 to 1.3 | a | 3.4 | 0.4 to 31.3 | a | 0.3 | 0.1 to 1.1 | < 0.100 | 0.5 | 0.2 to 1.2 | a |
| BPRS | 1.5 | 0.91 to 2.55 | a | 1.9 | 0.2 to 15.4 | a | 0.8 | 0.2 to 2.4 | a | 1.0 | 0.5 to 2.3 | a |
| GAF | 0.6 | 0.4 to 1.03 | a | 4.0 | 0.6 to 26.0 | a | 1.5 | 0.5 to 4.3 | a | 0.7 | 0.3 to 1.5 | a |
As Table 50 shows, multivariate analysis indicated that housing leverage was associated with not living independently (with those living independently being 0.4 times as likely to report this type of leverage) and substance misuse diagnosis (4.5 times as likely to report this leverage compared with those with schizophrenia). No variable was associated with finance leverage. Criminal justice leverage was associated with ethnicity (with white patients being 0.02 times as likely to report this type of leverage) and, for those living independently, whether or not they lived alone (0.02 times as likely). Child access leverage was associated with having had more than two hospitalisations (6.9 times as likely).
| Characteristics | Leverage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Housing | Financial | Criminal justice | Child access | |||||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Age greater than median | 1.1 | a | 0.5 to 2.3 | – | – | – | 2.4 | a | 0.1 to 39.0 | 0.5 | a | 0.2 to 1.3 |
| White (vs. other ethnicities) | 0.9 | a | 0.4 to 2.3 | – | – | – | 0.02 | < 0.050 | 0.0 to 0.6 | 0.3 | a | 0.1 to 1.2 |
| Male (vs. female) | 1.2 | a | 0.7 to 2.2 | – | – | – | 1.3 | a | 0.0 to 32.0 | 0.5 | a | 0.2 to 1.1 |
| Born in UK (vs. other countries) | a | – | – | – | – | 3.7 | a | 2.2 to 59.5 | – | – | – | |
| Single (vs. married/cohabiting) | 1.6 | a | 0.9 to 3.0 | – | – | – | – | – | – | – | – | – |
| Independent accommodation (vs. supported/homeless) | 0.4 | < 0.010 | 0.2 to 0.7 | – | – | – | – | – | – | – | – | – |
| If independent: | ||||||||||||
| Living alone (vs. living with others) | – | – | – | – | – | – | 0.02 | < 0.050 | 0.0 to 0.7 | – | – | – |
| Diagnosis (schizophrenia vs.) | ||||||||||||
| Bipolar disorder | 0.7 | a | 0.2 to 2.6 | – | – | – | 1.3 | a | 0.0 to 358.8 | 1.0 | a | 0.2 to 5.8 |
| Major depression | 0.8 | a | 0.3 to 1.9 | – | – | – | – | – | – | 0.7 | a | 0.2 to 2.6 |
| Substance abuse | 4.5 | < 0.010 | 1.8 to 11.1 | – | – | – | 0.4 | a | 0.0 to 71.2 | 3.3 | a | 0.7 to 14.3 |
| Other diagnosis | 0.4 | a | 0.1 to 1.6 | – | – | – | – | – | – | 1.3 | a | 0.2 to 8.5 |
| Age at first contact with services | 0.7 | a | 0.4 to 1.2 | a | – | – | – | – | – | 0.5 | a | 0.2 to 1.3 |
| More than two hospitalisations | 1.5 | a | 0.8 to 3.1 | 0.0 | a | 0.0 to 29.5 | 0.4 | a | 0.0 to 35.4 | 6.9 | < 0.010 | 2.2 to 21.6 |
| Duration of illness | 1.0 | a | 0.5 to 2.0 | – | – | – | 0.7 | a | 0.1 to 8.4 | 0.9 | a | 0.4 to 2.4 |
| Number of outpatient contacts in last month | 0.7 | a | 0.4 to 1.2 | – | – | – | 0.4 | a | 0.0 to 5.9 | 0.7 | a | 0.3 to 1.7 |
| Any imprisonment | 1.2 | a | 0.6 to 2.3 | – | – | – | – | – | – | – | – | – |
| ITAQ total score | 1.4 | a | 0.8 to 2.5 | 20.4 | a | 0.1 to 4890.3 | 1.4 | a | 0.1 to 16.7 | 1.0 | a | 0.4 to 2.5 |
| STAR-C | ||||||||||||
| Total score | – | – | – | 511.9 | a | 0.3 to 80,5796.8 | – | – | – | – | – | – |
| BPRS | 1.2 | a | 0.6 to 2.1 | 19.9 | a | 0.1 to 5295.8 | 9.7 | a | 0.6 to 165.3 | 1.3 | a | 0.5 to 3.3 |
| GAF | 0.7 | a | 0.4 to 1.1 | – | – | – | 0.3 | a | 0.0 to 6.2 | 0.5 | a | 0.2 to 1.2 |
| CAGE: positive for drug or alcohol | 1.3 | a | 0.7 to 2.4 | – | – | – | 0.1 | a | 0.0 to 2.1 | 0.9 | a | 0.3 to 2.5 |
Univariate associations between the clinical characteristics variables and reporting any leverage or more than one type of leverage are shown in Table 51. Reporting any leverage was associated with better insight (ITAQ total score and Awareness of Illness subscale). Reporting more than one leverage was associated with screening positive for drugs or alcohol.
| Factors | Leverage | |||||
|---|---|---|---|---|---|---|
| Any type | More than one type | |||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | |
| DAI-10 total score | 1.1 | a | 0.7 to 1.8 | 0.7 | a | 0.3 to 1.3 |
| API Decision Making | 1.0 | a | 0.6 to 1.5 | 1.3 | a | 0.7 to 2.4 |
| API Information Seeking | 1.2 | a | 0.8 to 1.9 | 1.7 | a | 0.9 to 3.1 |
| ITAQ | ||||||
| Total score | 2.0 | < 0.010 | 1.2 to 3.1 | 0.9 | a | 0.5 to 1.8 |
| Awareness of Illness | 1.9 | < 0.010 | 1.2 to 3.1 | 1.0 | a | 0.5 to 2.1 |
| Attitude to Treatment | 1.5 | a | 0.98 to 2.4 | 1.0 | a | 0.5 to 1.9 |
| STAR-P | ||||||
| Total score | 0.7 | a | 0.4 to 1.1 | 1.4 | a | 0.8 to 2.6 |
| Positive Collaboration | 0.7 | a | 0.5 to 1.1 | 1.7 | a | 0.9 to 3.1 |
| Positive Clinician Input | 0.8 | a | 0.5 to 1.2 | 1.3 | a | 0.7 to 2.4 |
| Non-Supportive Clinician | 0.8 | a | 0.5 to 1.2 | 0.7 | a | 0.3 to 1.3 |
| STAR-C | ||||||
| Total score | 1.0 | a | 0.7 to 1.7 | 1.2 | a | 0.6 to 2.3 |
| Positive collaboration | 1.1 | a | 0.7 to 1.7 | 1.2 | a | 0.6 to 2.3 |
| Emotional Difficulties | 1.2 | a | 0.8 to 1.9 | 1.5 | a | 0.8 to 2.9 |
| Positive Clinician Input | 0.9 | a | 0.6 to 1.5 | 0.7 | a | 0.4 to 1.4 |
| BPRS | 1.6 | a | 0.99 to 2.6 | 1.6 | a | 0.8 to 3.3 |
| GAF | 0.6 | a | 0.4 to 1.0 | 0.9 | a | 0.5 to 1.6 |
| CAGE: positive for drug or alcohol | 1.6 | a | 0.96 to 2.7 | 2.6 | < 0.050 | 1.2 to 5.4 |
Reporting any leverage was associated with substance misuse diagnosis (compared with having schizophrenia: OR 6.0, 95% CI 2.2 to 16.5; p < 0.001) and having had more than two hospitalisations (OR 3.1, 95% CI 1.5 to 6.3; p < 0.01). Reporting more than one type of leverage was also associated with substance misuse diagnosis (compared with those with schizophrenia: OR 9.0, 95% CI 2.2 to 36.4; p < 0.01) and a history of imprisonment (OR 3.0, 95% CI 1.2 to 7.2; p < 0.05).
In the ‘replication’ analyses, patients were thus more likely to report any type of leverage if they had a substance misuse diagnosis, had more psychiatric history and better insight, whereas they were more likely to report more than one type if they had a substance misuse diagnosis. Reporting housing leverage was also associated with substance misuse, whereas criminal justice leverage was associated with ethnicity, and child access leverage with being older and having had more hospitalisations. In the ‘combined’ analyses, patients were more likely to report any type of leverage if they had a substance misuse diagnosis and had experienced more hospitalisations, whereas they were more likely to report multiple types if they had a substance misuse diagnosis and had been imprisoned.
Mental illness groups alone
We repeated our analyses for the three mental illness groups alone, as they were so different from the substance misuse groups in some of their key psychiatric history characteristics and their experiences of leverage. As Table 52 shows, univariate analysis suggested that a number of characteristics were associated with housing leverage: number of years in education, not living independently, lower age at first contact with psychiatric services, number of past psychiatric hospitalisations, involuntary hospitalisations and better functioning. No sociodemographic, clinical or social characteristic was univariately associated with financial leverage. Criminal justice leverage was, again, associated with ethnicity. Child access leverage was univariately associated with contact frequency with children (with those who had infrequent or no contact less likely to report this kind of leverage than those who had regular contact, among those not living with their children), as was the number of past psychiatric hospitalisations.
| Characteristics | Leverage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Housing | Financial | Criminal justice | Child access | |||||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | |
| White (vs. other ethnicities) | 0.7 | b | 0.3 to 1.9 | – | – | – | 0.1 | < 0.010 | 0.01 to 0.5 | 0.3 | b | 0.0 to 1.4 |
| General education (years) | 1.9 | < 0.050 | 1.0 to 3.4 | 0.6 | b | 0.1 to 4.6 | 1.3 | 0.3 to 5.6 | 2.1 | b | 0.7 to 6.6 | |
| If not living with children, contact frequency | ||||||||||||
| Infrequent/none (vs. regular, ≥ monthly) | 0.6 | b | 0.1 to 2.7 | – | – | – | – | – | – | 0.2 | < 0.050 | 0.0 to 0.9 |
| Independent accommodation (vs. supported/homeless) | 0.3 | < 0.001 | 0.2 to 0.6 | 0.8 | b | 0.1 to 6.3 | 1.1 | b | 0.2 to 4.6 | 0.8 | b | 0.2 to 3.5 |
| Age at first contact with services | 0.5 | < 0.050 | 0.3 to 0.9 | 0.3 | b | 0.0 to 3.4 | 0.9 | b | 0.2 to 3.8 | 0.8 | b | 0.3 to 2.4 |
| Number of past hospitalisationsc | 2.4 | < 0.010 | 1.3 to 4.7 | 1.2 | b | 0.1 to 15.3 | 1.1 | b | 0.2 to 6.7 | 4.0 | < 0.050 | 1.3 to 12.9 |
| Any involuntary hospitalisation | 2.0 | < 0.050 | 1.1 to 3.7 | – | – | – | 1.4 | b | 0.2 to 10.5 | 1.4 | b | 0.5 to 4.1 |
| GAF | 0.5 | < 0.050 | 0.3 to 0.97 | 1.4 | b | 0.1 to 13.6 | 1.2 | b | 0.3 to 5.1 | 0.7 | b | 0.2 to 2.1 |
As Table 53 shows, in the multivariate analyses, housing leverage was associated with general education (those with more years of education being 2.4 times as likely to report this leverage), not being in independent accommodation (those who were being 0.3 times as likely to report this type) and poorer functioning (0.4 times as likely). Criminal justice leverage was associated with ethnicity (with white patients being 0.1 times as likely to report it) and child access leverage was associated with lower contact frequency (those having infrequent contact being 0.2 times as likely to report it).
| Characteristics | Leverage | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Housing | Financial | Criminal justice | Child access | |||||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | |
| White (vs. other ethnicities) | – | – | – | – | – | – | 0.1 | < 0.010 | 0.0 to 0.5 | – | – | – |
| General education | 2.4 | < 0.050 | 1.2 to 4.7 | – | – | – | – | – | – | – | – | – |
| If not living with children, contact frequency | ||||||||||||
| Infrequent/none (vs. regular, ≥ monthly) | – | – | – | – | – | – | – | – | – | 0.2 | < 0.050 | 0.0 to 0.9 |
| Independent accommodation (vs. supported/homeless) | 0.3 | < 0.010 | 0.1 to 0.7 | – | – | – | – | – | – | – | – | – |
| Age at first contact with services | 0.6 | a | 0.3 to 1.2 | – | – | – | – | – | – | – | – | – |
| Number of past hospitalisationsb | 1.7 | a | 0.8 to 3.8 | – | – | – | – | – | – | 2.6 | a | 0.5 to 13.0 |
| Any involuntary hospitalisations | 1.5 | a | 0.7 to 3.2 | – | – | – | – | – | – | – | – | – |
| GAF | 0.4 | < 0.050 | 0.2 to 0.9 | – | – | – | – | – | – | – | – | – |
Table 54 reports the univariate associations between any type of leverage and more than one type of leverage and sociodemographic, clinical and social characteristics, for the mental illness groups alone, along with their multivariate models. Univariate analysis suggested that reporting any type of leverage was associated with having children aged < 18 years, accommodation, having schizophrenia compared with major depression, age at first contact with psychiatric services, number of previous psychiatric hospitalisations, having ever experienced involuntary psychiatric hospitalisation, duration of psychiatric history, having had a criminal conviction, having been imprisoned and insight. In the multivariate analysis, reporting any type of leverage was associated with having children aged < 18 years (3.1 times as likely), not living independently (those who did being 0.4 times as likely), having schizophrenia rather than major depression (those with major depression being 0.4 times as likely as those with schizophrenia), having had more psychiatric admissions (three times as likely) and better insight (three times as likely).
| Characteristics | Univariate | Multivariate | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any type of leverage | More than one type | Any type of leverage | More than one type | |||||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Have children aged < 18 years | 1.8 | < 0.050 | 1.0 to 3.1 | 2.8 | < 0.050 | 1.2 to 6.9 | 3.1 | < 0.010 | 1.5 to 6.1 | 3.6 | < 0.010 | 1.4 to 9.5 |
| Independent accommodation (vs. supported/homeless) | 0.4 | < 0.010 | 0.2 to 0.7 | 0.4 | < 0.050 | 0.1 to 0.9 | 0.4 | < 0.050 | 0.2 to 0.9 | 0.4 | b | 0.2 to 1.2 |
| Diagnosis (schizophrenia vs.) | ||||||||||||
| Bipolar disorder | 0.5 | b | 0.2 to 1.2 | 1.0 | b | 0.2 to 4.5 | 0.5 | b | 0.2 to 1.4 | – | – | – |
| Major depression | 0.4 | < 0.010 | 0.2 to 0.7 | 1.0 | b | 0.3 to 2.6 | 0.4 | < 0.050 | 0.3 to 0.8 | – | – | – |
| Substance misuse | 7.9 × 10–10 | b | 0 to Inf | – | – | – | 1.2 × 10–10 | b | 0 to Inf | – | – | – |
| Other diagnosis | 0.5 | b | 0.2 to 1.4 | 0.4 | b | 0.1 to 3.6 | 0.7 | b | 0.2 to 2.0 | – | – | – |
| Age at first contact with services | 0.6 | < 0.050 | 0.3 to 0.96 | 0.7 | b | 0.6 to 1.7 | 0.8 | b | 0.4 to 1.4 | – | – | – |
| Number of past hospitalisationsc | 3.7 | < 0.001 | 2.1 to 6.4 | 3.8 | < 0.050 | 1.2 to 11.5 | 3.0 | < 0.010 | 1.5 to 6.0 | 3.0 | b | 0.9 to 9.6 |
| Any involuntary hospitalisations | 2.6 | < 0.001 | 1.6 to 4.5 | 1.5 | b | 0.6 to 3.7 | 1.1 | b | 0.6 to 2.2 | – | – | – |
| Duration of illness | 1.8 | < 0.050 | 1.1 to 3.0 | 2.9 | < 0.050 | 1.0 to 8.1 | 1.6 | b | 0.9 to 2.9 | 2.6 | b | 0.9 to 7.7 |
| Any criminal convictions | 1.9 | < 0.050 | 1.1 to 3.3 | 2.2 | b | 0.9 to 5.3 | 1.0 | 0.5 to 2.2 | – | – | – | |
| Any imprisonment | 2.3 | < 0.050 | 1.2 to 4.4 | 3.4 | < 0.050 | 1.3 to 8.9 | 1.5 | b | 0.6 to 4.0 | 2.3 | b | 0.8 to 6.4 |
| ITAQ total score | 2.5 | < 0.010 | 1.5 to 4.1 | 1.2 | b | 0.5 to 3.0 | 3.0 | < 0.001 | 1.6 to 5.6 | – | – | – |
Reporting more than one type of leverage, for the mental illness groups alone, was univariately associated with having children aged < 18 years, not living independently, the number of previous psychiatric hospitalisations, duration of psychiatric history and having been imprisoned. In the multivariate analysis, reporting more than one type of leverage was associated only with having children aged < 18 years (with those who did being 3.6 times as likely to report this).
Perceived coercion
Associations between sample characteristics and perceived coercion
Sample sociodemographic characteristics univariately associated with the three AES subscales (Perceived Coercion, Negative Pressures and Procedural Justice) and the Fairness and Effectiveness Indices are shown in Table 55, whereas clinical characteristics and experiences of service variables univariately associated with these scales and indices are shown in Table 56.
| Characteristics | AES Perceived Coercion | AES Procedural Justice | Negative Pressures | Fairness index | Effectiveness index | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | 95% CI, p-value | Regression coefficient | 95% CI, p-value | Regression coefficient | 95% CI, p-value | Regression coefficient | 95% CI, p-value | Regression coefficient | 95% CI, p-value | |
| Age greater than median | ||||||||||
| White (vs. other ethnicities) | –0.26 | –0.47 to –0.05, < 0.010 | –0.29 | –0.52 to –0.07, < 0.05 | 0.22 | 0.05 to 0.39, < 0.050 | ||||
| Born in UK (vs. other countries) | ||||||||||
| Male (vs. female) | –0.13 | –0.24 to –0.03, < 0.01 | ||||||||
| Have children aged < 18 years | ||||||||||
| Independent accommodation (vs. supported/homeless) | 0.17 | 0.04 to 0.31, < 0.010 | ||||||||
| Living alone (vs. living with others) | –0.20 | –0.33 to –0.05, < 0.050 | ||||||||
| General education (years) | 0.05 | 0.02 to 0.09, < 0.01 | ||||||||
| Employed (vs. unemployed/sheltered) | –0.26 | –0.43 to –0.09, < 0.010 | 0.26 | 0.12 to 0.39, < 0.001 | ||||||
| Duration of illness | –0.00 | –0.01 to –0.00, < 0.001 | –0.00 | –0.02 to –0.00, < 0.050 | ||||||
| Number of past psychiatric hospitalisations | 0.02 | 0.01 to 0.04, < 0.010 | –0.02 | –0.03 to –0.00, < 0.010 | –0.04 | –0.06 to –0.03, < 0.001 | –0.03 | –0.05 to –0.02, < 0.001 | ||
| Have involuntary hospitalisations (vs. no involuntary hospitalisations) | 0.24 | 0.11 to 0.37, < 0.001 | –0.21 | –0.31 to –0.11, < 0.001 | –0.23 | –0.38 to –0.08, < 0.010 | –0.22 | –0.37 to –0.07, < 0.010 | ||
| Number of outpatient contacts in last month | –0.02 | –0.03 to –0.00, < 0.001 | –0.02 | –0.04 to –0.00, < 0.010 | ||||||
| Number of imprisonments | ||||||||||
| Have convictions (vs. no previous convictions) | –0.11 | –0.21 to 0.00, < 0.050 | ||||||||
| Have imprisonments (vs. no previous imprisonments) | –0.14 | –0.26 to –0.18, < 0.05 | ||||||||
| Factors | AES Perceived Coercion | AES Procedural Justice | AES Negative Pressures | Fairness index | Effectiveness index | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | 95% CI, p-value | Regression coefficient | 95% CI, p-value | Regression coefficient | 95% CI, p-value | Regression coefficient | 95% CI, p-value | Regression coefficient | 95% CI, p-value | |
| Study group (AOT group vs.) | ||||||||||
| SM | –0.41 | –0.59 to –0.22, < 0.001 | 0.29 | 0.15 to 0.43, < 0.001 | 0.38 | 0.18 to 0.59, < 0.001 | 0.42 | 0.21 to 0.62, < 0.001 | ||
| CMHT-NP | –0.23 | –0.41 to –0.05, < 0.010 | 0.36 | 0.23 to 0.51, < 0.001 | 0.26 | 0.05 to 0.47, < 0.050 | ||||
| CMHT-P | 0.22 | 0.08 to 0.37, < 0.010 | 0.33 | 0.12 to 0.54, < 0.010 | 0.30 | 0.10 to 0.51, < 0.010 | ||||
| Diagnosis (psychosis vs.) | ||||||||||
| Substance abuse | –0.31 | –0.47 to –0.15, < 0.001 | 0.18 | 0.05 to 0.30, < 0.010 | 0.22 | 0.04 to 0.40, < 0.050 | 0.27 | 0.09 to 0.44, < 0.010 | ||
| Affective | 0.23 | 0.11 to 0.36, < 0.001 | ||||||||
| Personality disorder | 0.36 | 0.1 to 0.64, < 0.010 | ||||||||
| GAF | 0.00 | 0.00 to 0.00, < 0.010 | 0.01 | 0.00 to 0.02, < 0.010 | 0.00 | 0.00 to 0.02, < 0.010 | ||||
| ITAQ total score | –0.03 | –0.04 to –0.01, < 0.001 | –0.04 | –0.05 to –0.02, < 0.001 | 0.02 | 0.00 to 0.03, < 0.010 | 0.05 | 0.04 to 0.07, < 0.010 | 0.04 | 0.03 to 0.06, < 0.001 |
| STAR-P total score | –0.03 | –0.04 to –0.02, < 0.001 | –0.03 | –0.04 to –0.02, < 0.001 | 0.02 | 0.01 to 0.02, < 0.001 | 0.04 | 0.03 to 0.04, < 0.001 | 0.003 | 0.002 to 0.04, < 0.001 |
| STAR-C total score | –0.02 | –0.04 to –0.01, < 0.001 | 0.01 | 0.00 to 0.02, < 0.010 | 0.02 | 0.00 to 0.03, < 0.001 | 0.02 | 0.01 to 0.04, < 0.001 | ||
| CSQ-8 | –0.05 | –0.06 to –0.04, < 0.001 | –0.06 | –0.07 to –0.05, < 0.001 | 0.02 | 0.01 to 0.03, < 0.001 | 0.07 | 0.06 to 0.09, < 0.001 | 0.07 | 0.06 to 0.09, < 0.001 |
| DAI-10 | –0.04 | –0.06 to –0.03, < 0.001 | –0.05 | –0.06 to –0.03, < 0.001 | 0.03 | 0.01 to 0.04, < 0.001 | 0.05 | 0.03 to 0.07, < 0.001 | 0.05 | 0.03 to 0.07, < 0.001 |
| BPRS | 0.00 | 0.00 to 0.02, < 0.010 | –0.01 | –0.02 to –0.00, < 0.001 | –0.01 | –0.02 to –0.00, < 0.010 | ||||
| API Information Seeking | –0.01 | –0.02 to –0.004, < 0.010 | 0.00 | 0.00 to 0.01, < 0.001 | –0.01 | 0.00 to 0.02, < 0.001 | 0.01 | 0.00 to 0.02, < 0.010 | ||
| API Decision Making | –0.01 | –0.02 to –0.00, < 0.001 | –0.02 | –0.02 to –0.01, < 0.001 | ||||||
| CAGE: positive for drugs or alcohol | 0.16 | 0.00 to 0.32, < 0.050 | 0.21 | 0.05 to 0.36, < 0.010 | ||||||
As Tables 57 and 58 show, in the multivariate analysis, the following associations were identified between sample characteristics and these scales and indices.
| Characteristics | AES Perceived Coercion (N = 359) | AES Procedural Justice (N = 304) | AES Negative Pressures (N = 285) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | p-value | 95% CI | Regression coefficient | p-value | 95% CI | Regression coefficient | p-value | 95% CI | |
| Male (vs. female) | – | – | – | – | – | – | – | – | – |
| White (vs. other ethnicities) | – | – | – | – | – | – | 0.19 | < 0.05 | 0.01 to 0.38 |
| General education (years) | – | – | – | – | – | – | 0.04 | –0.00 to 0.07 | |
| Independent accommodation (vs. supported/homeless) | – | – | – | – | – | – | 0.21 | < 0.01 | 0.06 to 0.36 |
| Number of past hospitalisations | – | – | – | – | – | – | – | – | – |
| Any involuntary hospitalisations (vs. no previous involuntary hospitalisations) | 0.16 | < 0.05 | 0.03 to 0.29 | – | – | – | – | – | – |
| Number of outpatient contacts | – | – | – | – | – | – | – | – | – |
| Have imprisonment (vs. no previous imprisonment) | – | – | – | – | – | – | – | – | – |
| Diagnosis (psychosis vs.) | |||||||||
| Other | 0.74 | < 0.05 | 0.07 to 1.4 | – | – | – | – | – | – |
| Substance abuse | – | – | – | – | – | – | – | – | – |
| Affective | – | – | – | – | – | – | – | – | – |
| Study group (AOT vs.) | |||||||||
| CMHT-NP | – | – | – | – | – | – | 0.13 | < 0.05 | 0.00 to 0.25 |
| CMHT-P | – | – | – | – | – | – | – | – | – |
| STAR-P total score | –0.02 | < 0.001 | –0.03 to –0.01 | –0.02 | < 0.001 | –0.03 to –0.01 | 0.01 | < 0.05 | 0.00 to 0.02 |
| STAR-C total score | – | – | – | –0.01 | < 0.05 | –0.03 to –0.00 | – | – | – |
| CSQ-8 | –0.02 | < 0.05 | –0.04 to –0.00 | –0.04 | < 0.001 | –0.06 to –0.02 | 0.02 | < 0.01 | 0.00 to 0.03 |
| ITAQ total score | – | – | – | – | – | – | – | – | – |
| DAI-10 | –0.02 | < 0.05 | –0.04 to –0.00 | – | – | – | – | – | – |
| API Decision Making | –0.00 | < 0.05 | –0.12 to –0.00 | – | – | – | – | – | – |
| API Information Seeking | – | – | – | – | – | – | 0.01 | < 0.01 | 0.00 to 0.13 |
| Characteristics | Fairness index (N = 237) | Effectiveness index (N = 198) | ||||
|---|---|---|---|---|---|---|
| Regression coefficient | p-value | 95% CI | Regression coefficient | p-value | 95% CI | |
| Male (vs. female) | – | – | – | – | – | – |
| White (vs. other ethnicities) | – | – | – | – | – | – |
| General education (years) | – | – | – | – | – | – |
| Living alone (vs. living with others) | – | – | – | – | – | – |
| Number of past hospitalisations | –0.02 | < 0.01 | –0.04 to –0.00 | –0.02 | < 0.01 | –0.04 to –0.00 |
| Have involuntary hospitalisations (vs. no previous involuntary hospitalisations) | – | – | – | – | – | – |
| Number of outpatient contacts | –0.02 | < 0.001 | –0.03 to –0.00 | – | – | – |
| Have imprisonment (vs. no previous imprisonment) | – | – | – | – | – | – |
| STAR-P total score | 0.01 | < 0.05 | 0.00 to 0.02 | – | – | – |
| STAR-C total score | – | – | – | – | – | – |
| CSQ-8 | 0.05 | < 0.001 | 0.03 to 0.07 | 0.07 | < 0.001 | 0.05 to 0.08 |
| ITAQ total score | 0.03 | < 0.01 | 0.01 to 0.05 | – | – | – |
| DAI-10 | – | – | – | – | – | – |
| Diagnosis (psychosis vs.) | ||||||
| Affective | – | – | – | – | – | – |
| Substance abuse | – | – | – | – | – | – |
| Other diagnosis | – | – | – | – | – | – |
| Study group (AOT vs.) | ||||||
| CMHT-NP | – | – | – | – | – | – |
| CMHT-P | – | – | – | 0.17 | < 0.001 | 0.00 to 0.32 |
| API Decision Making | 0.00 | < 0.01 | –0.01 to –0.00 | –0.007 | < 0.01 | –0.01 to –0.00 |
| API Information Seeking | 0.00 | < 0.05 | 0.00 to 0.02 | – | – | – |
Patients reported higher perceived coercion (higher Perceived Coercion scores) when they had poorer therapeutic relationships; were less satisfied with services; had more negative attitudes to, and compliance with, medication; and less of a preference for being involved with decision-making about their care. They also reported higher perceived coercion when they had experienced any involuntary hospitalisations and received an ‘other’ diagnosis (compared with psychosis). Patients reported having less of a say in their care (higher Procedural Justice scores) when they had poorer therapeutic relationships (rated both by them and by their care co-ordinator) and were less satisfied. They reported having experienced more negative pressures (lower Negative Pressures scores) when they had poorer therapeutic relationships and lower satisfaction and when they had had fewer years of education, lived in supported accommodation or were homeless, were in the AOT group (compared with the CMHT-non-psychosis group), were of non-white ethnicity and preferred not to have information shared with them (see Table 57).
Patients rated the treatment pressures that they had experienced as more fair when they reported better therapeutic relationships, higher satisfaction and better insight; had experienced fewer past hospitalisations and fewer outpatient visits; preferred not to be included in decision-making; and preferred to have information shared with them. They rated these treatment pressures as having been more effective when they had higher satisfaction, had experienced fewer past hospitalisations and were from the CMHT-psychosis group (compared with the AOT group) and preferred not to be involved in decision-making (see Table 58).
Table 59 shows the independent associations between sample characteristics and rating the reported leverage as ‘more coercive’, presented for each type of leverage. Among patients reporting housing leverage, they were more likely to rate the leverage as more coercive (as constituting a threat or compulsion) if they were older, were less satisfied and preferred to be involved in decision-making. Among those reporting criminal justice leverage, they were more likely to rate the leverage as more coercive if they had had a higher number of outpatient visits.
| Characteristic | Leverage | |||||
|---|---|---|---|---|---|---|
| Housing | Criminal justice | |||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Age | 1.06 | 1.01 to 1.11 | 0.018 | – | – | – |
| CSQ-8 | 0.89 | 0.80 to 0.98 | 0.024 | – | – | – |
| API Decision Making | 1.03 | 1.00 to 1.06 | 0.031 | – | – | – |
| Number of outpatient visits in last month | – | – | – | 1.71 | 1.09 to 2.68 | 0.020 |
Overall, patients who perceived their care to be more coercive (according to any or all of the three subscales) were thus less satisfied with services, with their therapeutic relationships and with taking medication. They were more likely to have had involuntary hospitalisations, to live in supported accommodation or be homeless and to be non-white, and to prefer not to be involved in decision-making or have information about their treatment shared with them. Conversely, those who thought that the treatment pressure they had experienced was fairer tended to be those who had better therapeutic relationships and satisfaction and also those who had had fewer past hospitalisations and fewer outpatient visits, as well as those who had better insight. When asked to identify the leverages that they had reported as more or less coercive, it was also those who were less satisfied who were likely to rate the leverages as more coercive, and they were also more likely to do so if they had experienced more outpatient visits and preferred to be involved in decision-making.
Associations between perceived coercion and reporting leverage
Table 60 presents the sample distribution of the three AES subscales, the Fairness and Effective Indices, and the types of pressure categorisation for patients who did, and patients who did not, experience the four types of leverages. Table 61 presents the same variables for patients who did, and patients who did not, experience any leverage and more than one leverage. Figure 21 is a graphical representation of the relationship between the type of reported leverage and the AES subscales and Fairness/Effectiveness Indices for those who did, and those who did not, report leverage. Statistical analysis indicated that whether patients reported a particular type of leverage or not, or reported any leverage or not, or more than one leverage or not, made no statistically significant difference to their perceptions about coercion in their care or its fairness or effectiveness. The only statistically significant findings were for the Index of Effectiveness: the mixed-effects model returned a significant (p ≤ 0.001) positive association with type of leverage, and the Negative Pressures rating also differed significantly depending on whether or not the patient reported any leverage, but the magnitude of these differences was negligible.
| Factors | Leverage | |||||||
|---|---|---|---|---|---|---|---|---|
| Housing (N = 417) (100%) | Finance (N = 165) (40%) | Criminal (N = 232) (56%) | Child access (N = 130) (31%) | |||||
| Yes | No | Yes | No | Yes | No | Yes | No | |
| n (%)/mean {SE} | n (%)/mean {SE} | n (%)/mean {SE} | n (%)/mean {SE} | n (%)/mean {SE} | n (%)/mean {SE) | n (%)/mean {SE} | n (%)/mean {SE} | |
| Leverage experienced | 98 (24) | 317 (76) | 10 (6) | 14 (8) | 62 (27) | 18 (8) | 34 (26) | 87 (67) |
| AES Perceived Coercion | 2.4 {0.07} | 2.4 {0.04} | 2.5 {0.19} | 2.3 {0.18} | 2.4 {0.10} | 2.3 {0.13} | 2.4 {0.11} | 2.4 {0.07} |
| AES Procedural Justice | 2.3 {0.07} | 2.3 {0.04} | 2.2 {0.34} | 2.2 {0.17} | 2.2 {0.09} | 2.4 {0.13} | 2.3 {0.11} | 2.2 {0.08} |
| AES Negative Pressures | 4.2 {0.06} | 4.3 {0.03} | 4.1 {0.29} | 4.1 {0.10} | 4.1 {0.07} | 4.2 {0.11} | 4.2 {0.09} | 4.3 {0.05} |
| Index of Fairness | 3.7 {0.07} | 3.8 {0.04} | 4.3 {0.22} | 3.7 {0.19} | 3.8 {0.09} | 3.9 {0.22} | 3.7 {0.14} | 3.9 {0.08} |
| Index of Effectiveness | 3.7 {0.08} | 3.8 {0.04} | 4.2 {0.30} | 3.8 {0.23} | 3.8 {0.09} | 4.1 {0.15} | 3.6 {0.15} | 3.8 {0.08} |
| Types of pressureb | ||||||||
| Persuasion | 19 (19) | – | 0 (40) | – | 6 (10) | – | 3 (9) | – |
| Interpersonal leverage | 23 (23) | – | 4 (0) | – | 5 (8) | – | 6 (18) | – |
| Inducement | 8 (8) | – | 0 (0) | – | 13 (21) | – | 3 (9) | – |
| Threat | 26 (27) | – | 5 (50) | – | 3 (5) | – | 17 (50) | – |
| Compulsion | 11 (11) | – | 0 (0) | – | 24 (39) | – | 3 (9) | – |
| Factors | Leverage | |||
|---|---|---|---|---|
| Any (N = 417) (100%) | More than one (N = 417) (100%) | |||
| Yes | No | Yes | No | |
| n (%)/mean {SE} | n (%)/mean {SE} | n (%)/mean {SE} | n (%)/mean {SE} | |
| Leverage experienced | 146 (35) | 271 (65) | 51 (12) | 366 (88) |
| AES Perceived Coercion | 2.4 {0.06} | 2.4 {0.04} | 2.3 {0.10} | 2.4 {0.04} |
| AES Procedural Justice | 2.3 {0.06} | 2.3 {0.04} | 2.2 {0.10} | 2.3 {0.04} |
| AES Negative Pressures | 4.2 {0.05} | 4.3 {0.03} | 4.1 {0.09} | 4.3 {0.03} |
| Fairness Index | 3.8 {0.04} | 3.8 {0.06} | 3.9 {0.11} | 3.8 {0.04} |
| Effectiveness Index | 3.8 {0.06} | 3.8 {0.05} | 3.8 {0.12} | 3.8 {0.04} |
FIGURE 21.
Associations between AES subscales and Fairness and Effectiveness scales and type of leverage. Plots include 1-SE bars. In (a) those liable and experiencing leverage; and (b) those liable and not experiencing leverage. Leverage type: 1, housing; 2, money; 3, criminal justice; 4, child care.
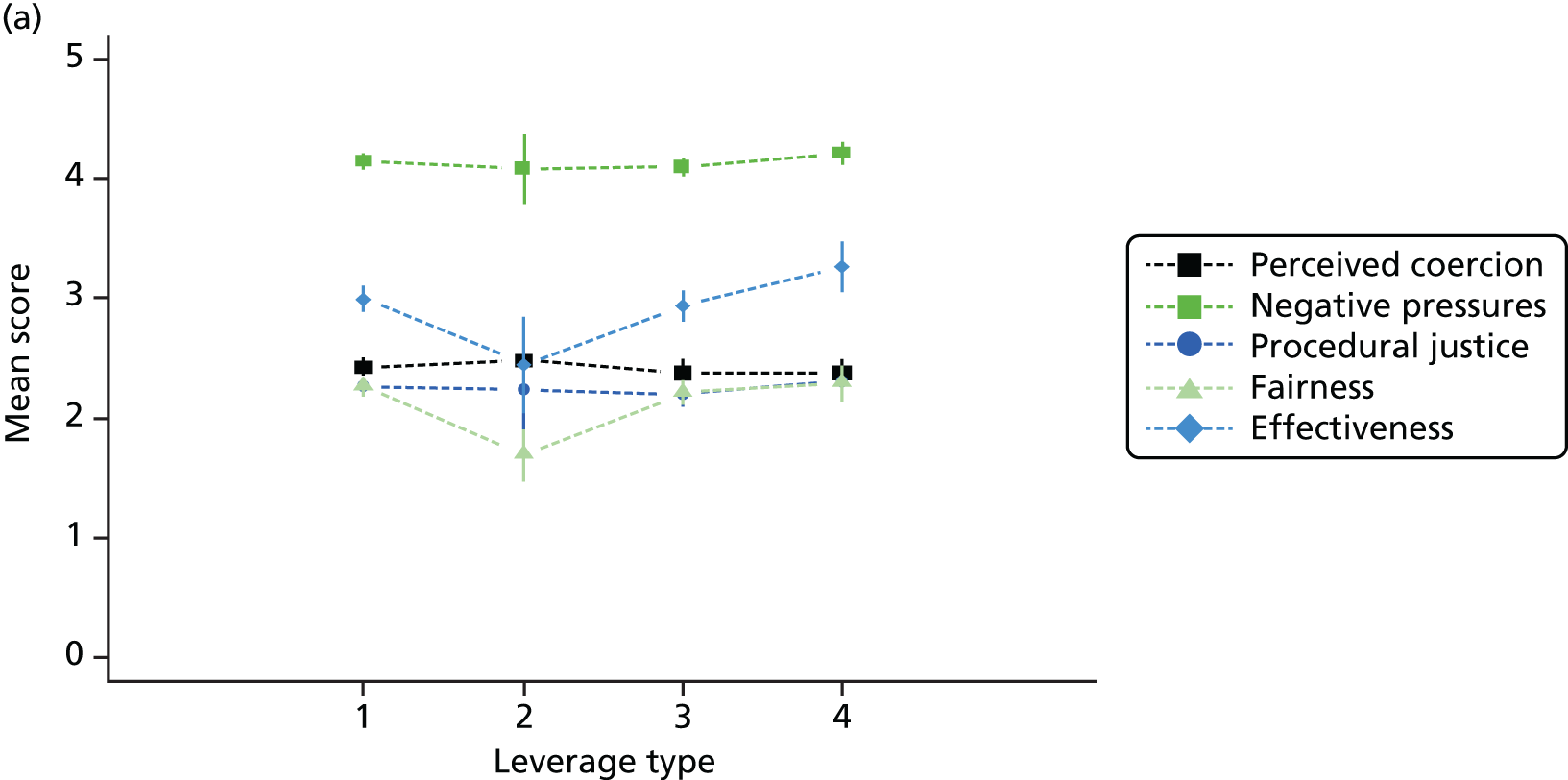
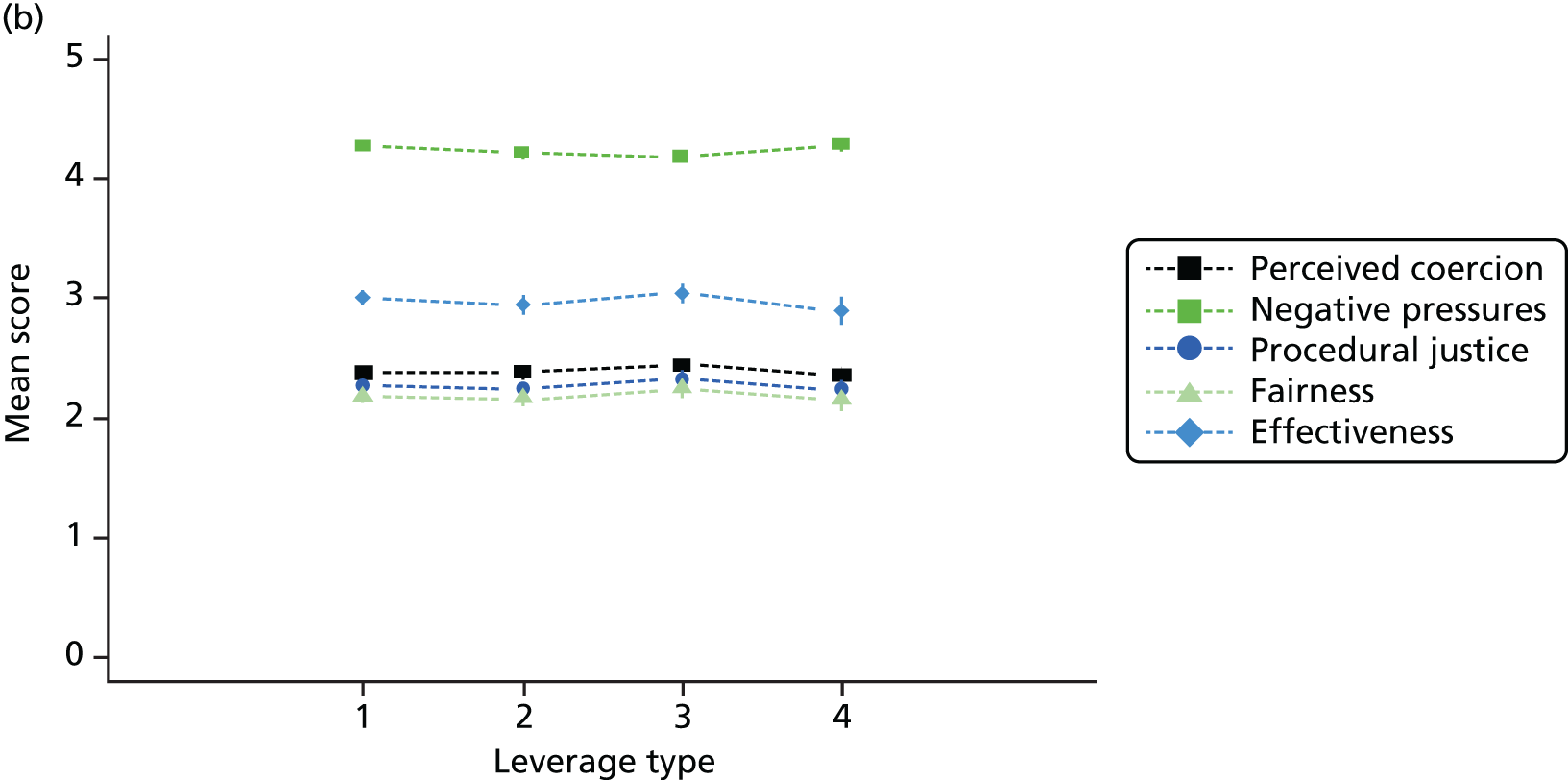
Figure 22 shows the relationship between the types of pressure categorisation and the AES subscales and Fairness/Effectiveness Indices. The only statistically significant finding was for child access leverage, for which the Effectiveness Index presented a significantly increasing trend. This indicated that for those liable to experience child access leverage and reporting it, the more coercive they perceived the leverage to be, the more effective they perceived it to be. Compared with those rating the leverage as ‘persuasion’ (at the least coercive end of the spectrum), those rating the leverage as ‘inducement’ had an effectiveness score 0.9 points higher (p = 0.278), those rating it as ‘threat’ had an effectiveness score 1.4 points higher (p = 0.043) and those rating it as ‘compulsion’ had an effectiveness score 2.7 points higher (p = 0.003).
FIGURE 22.
Associations between types of pressure and AES subscales and Fairness and Effectiveness indexes, for each type of leverage. (a) Housing leverage; (b) money leverage; (c) criminal justice leverage; and (d) child care leverage. Patients liable to and reporting the leverage only. Plots include 1-SE bars. 1, Persuasion; 2, interpersonal leverage; 3, inducement; 4, threat; 5, compulsion.
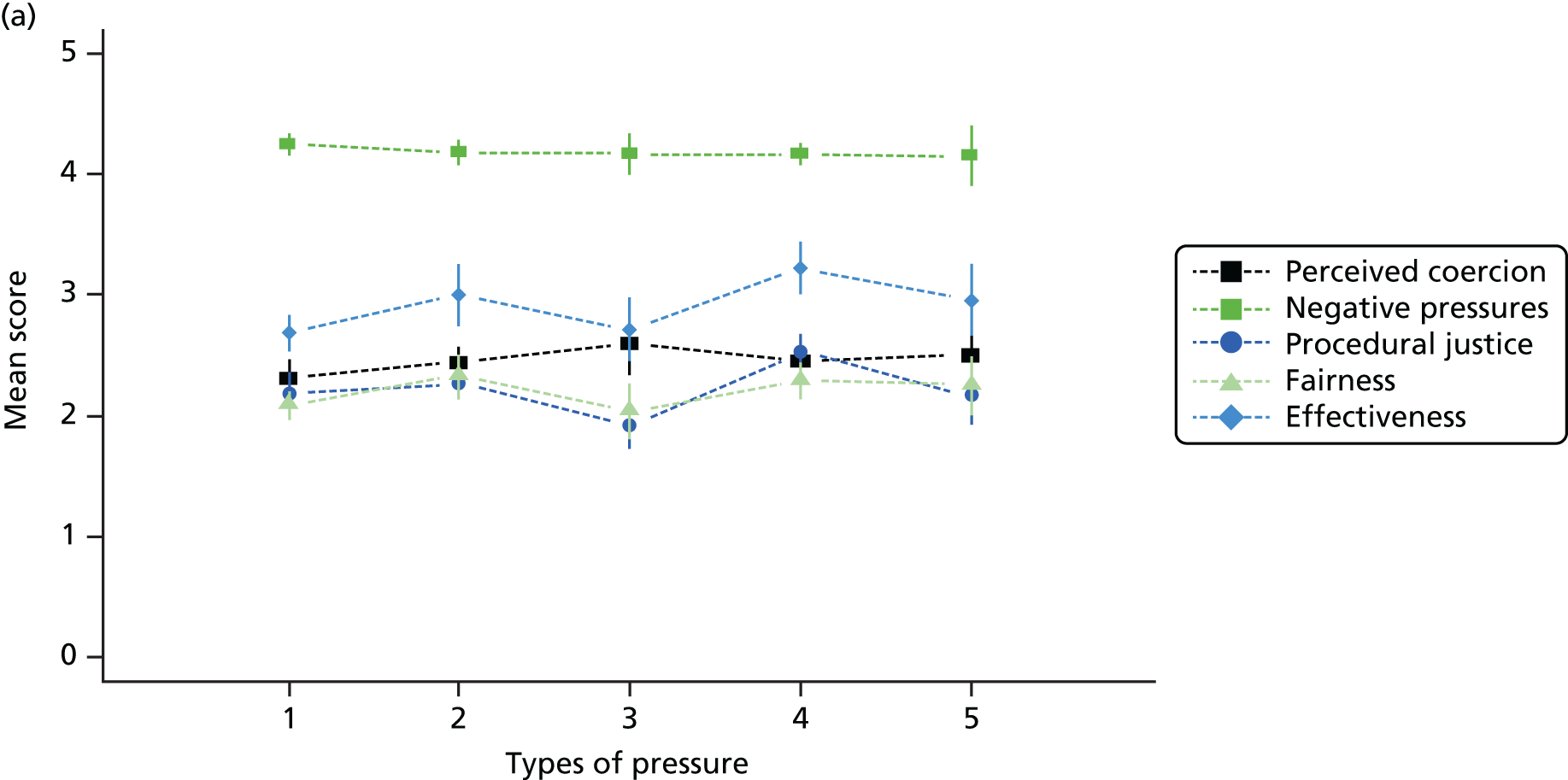
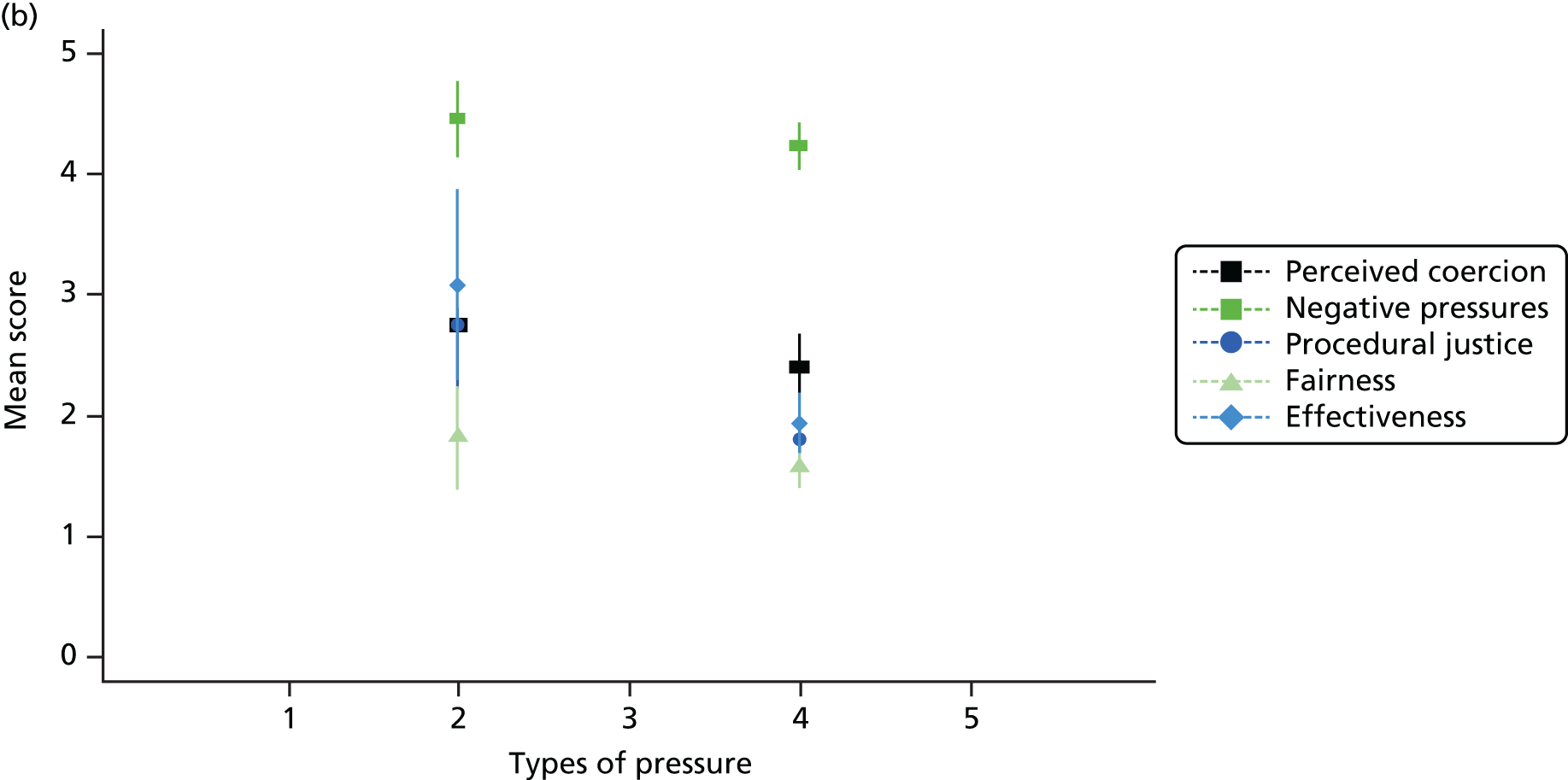

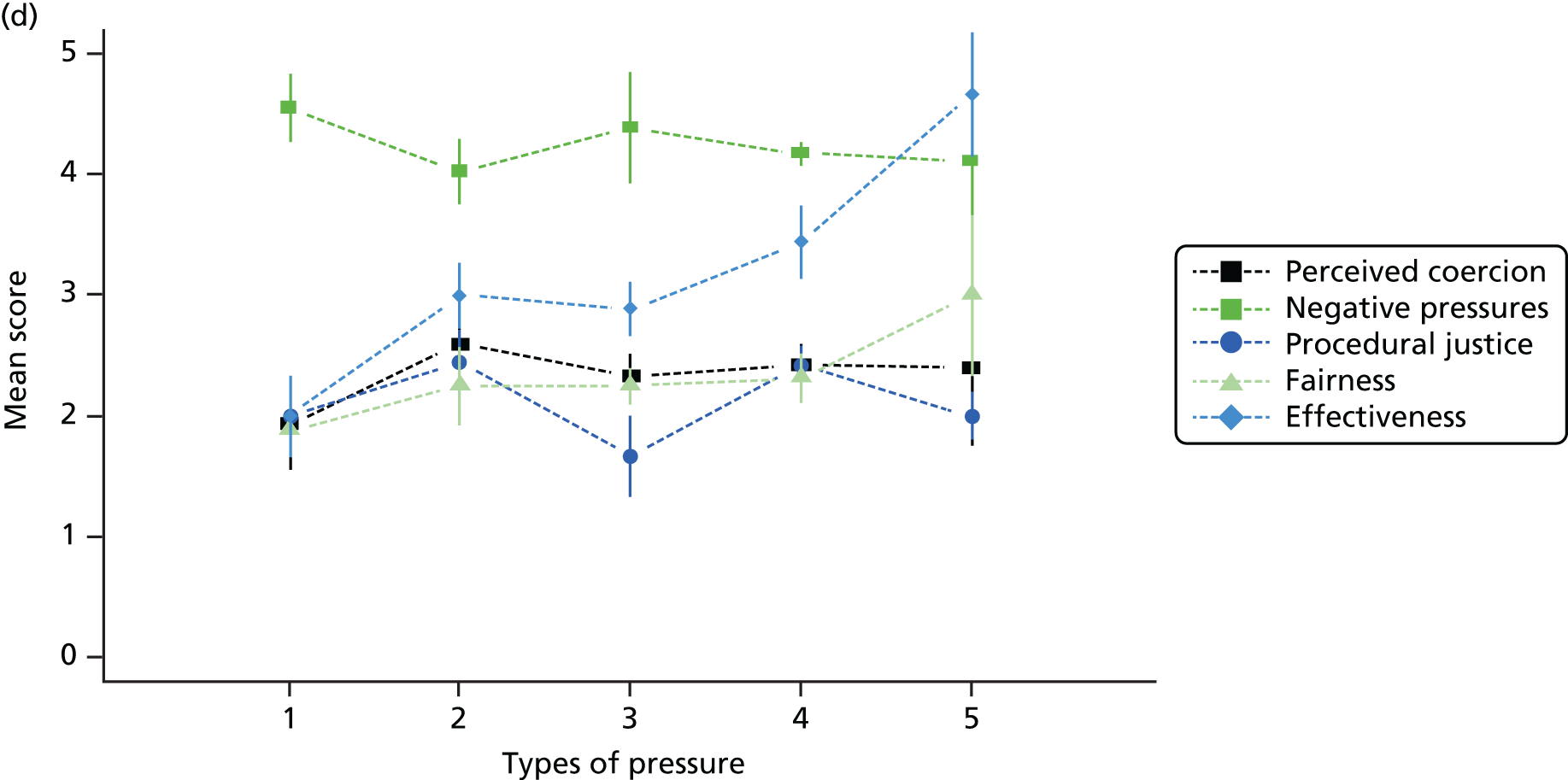
Figures 23 and 24 present the empirical distribution of the types of pressure categorisation (dichotomised as ‘more coercive’ and ‘less coercive’ and in the five categories, respectively) given by those reporting leverage (the same information taking into account missing values is reported in the two tables). None of the proportions was significantly different from 50%, indicating that there was no statistically significant difference between the proportions of patients rating their reported leverage experiences as more coercive rather than less coercive.
FIGURE 23.
Four types of reported leverage identified as ‘less coercive’ or ‘more coercive’ pressure. Patients liable to and reporting the leverage only. p = p-value testing proportion = 0.5; +, ’Less coercive’ pressures; –, ’Less coercive’ pressures.
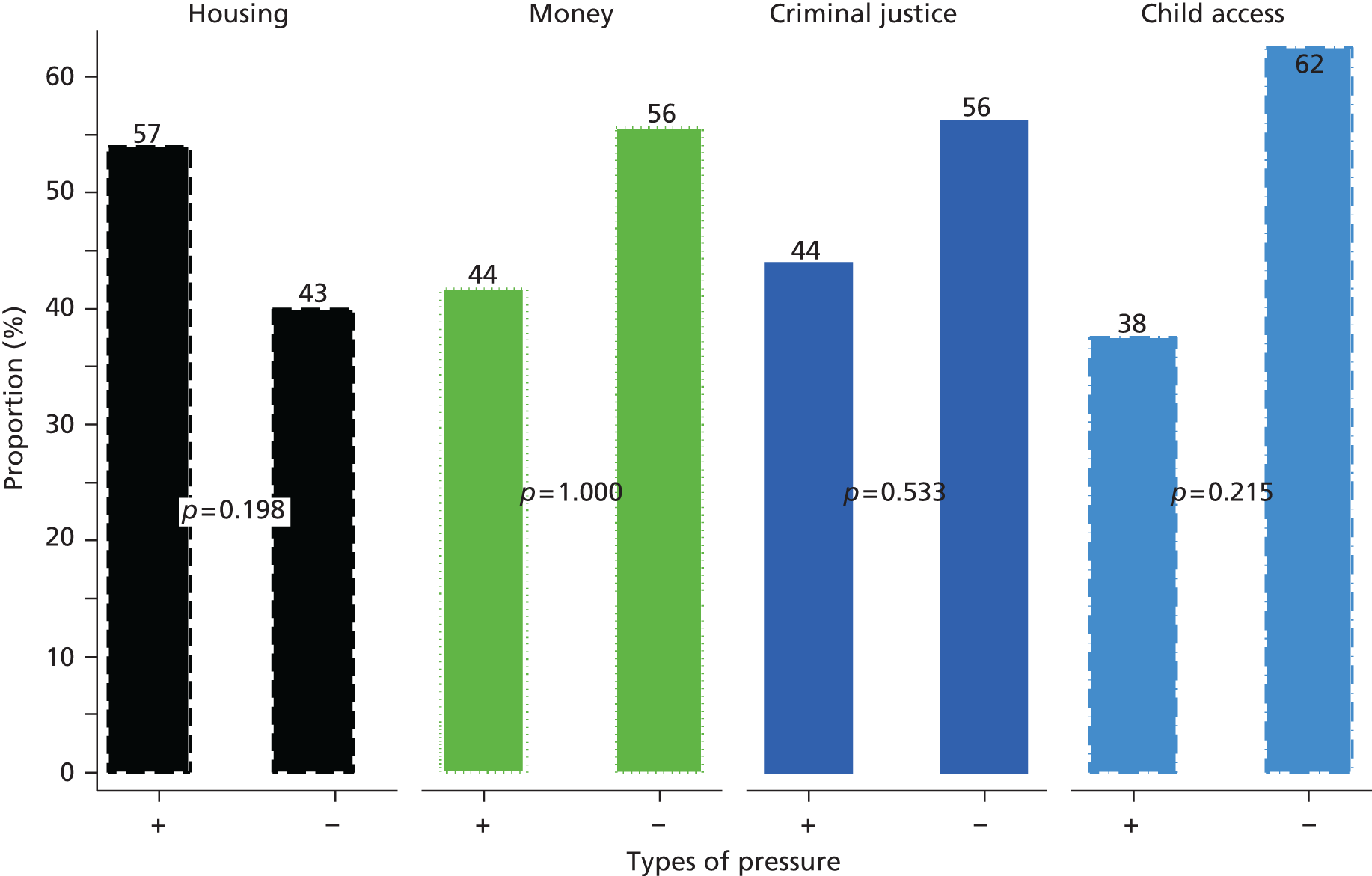
FIGURE 24.
Four types of reported leverage identified as type of pressure. Patients liable to and reporting the leverage only. 1, Persuasion; 2, interpersonal leverage; 3, inducement; 4, threat; 5, compulsion.
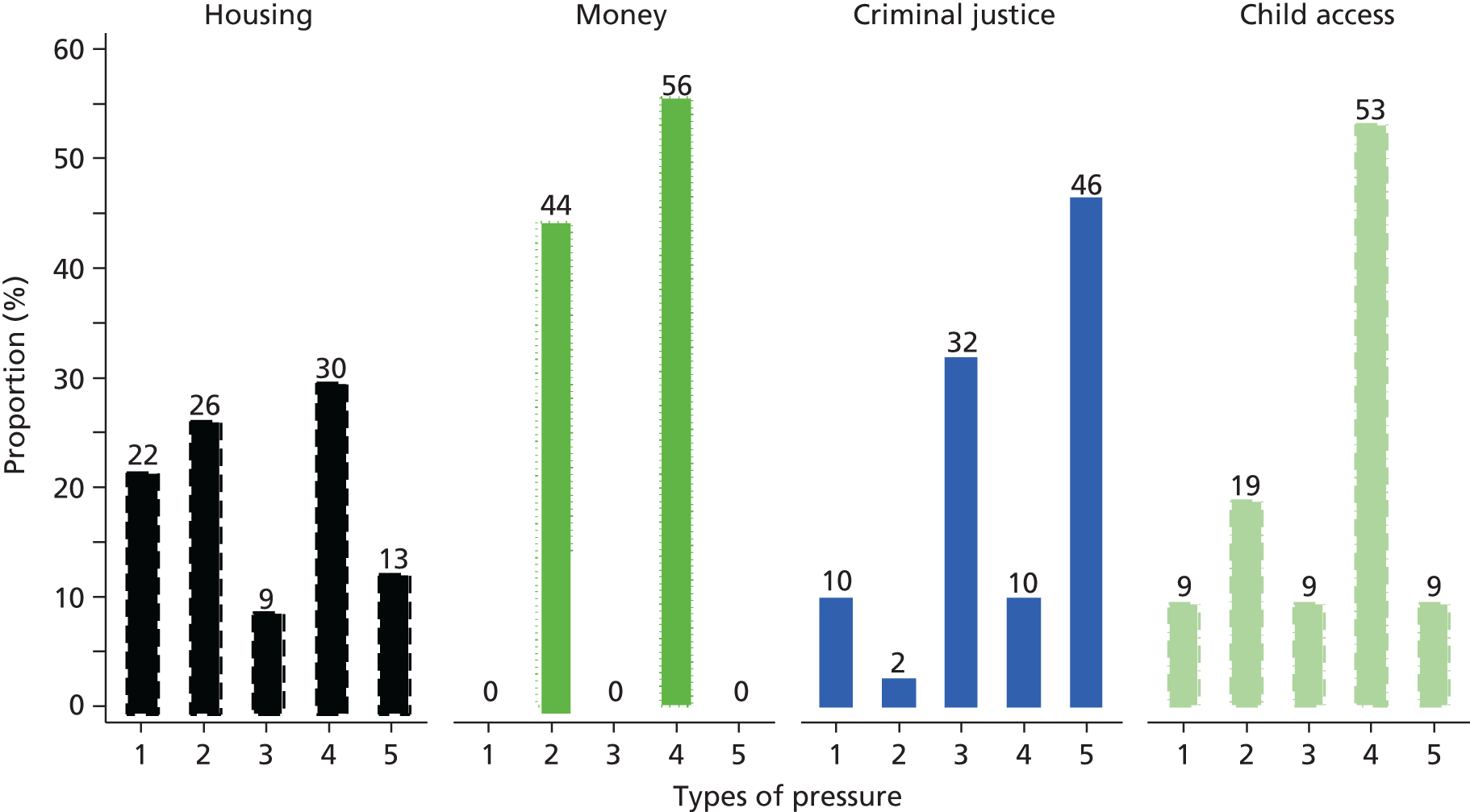
Reporting different sorts of leverage, or reporting it at all, thus generally made no significant difference to patients’ assessments of the coerciveness of their care, or their perceptions of the fairness and effectiveness and treatment pressures they had experienced. In the case of child access leverage, however, more coercive applications of the leverage (in the view of those reporting it) were perceived as being more effective.
Conclusions
-
One-third (35%) of our sample reported lifetime experiences of leverage.
-
This was much lower than the level reported in the USA (51%).
-
Housing leverage was the most frequently reported type (24%).
-
Rates of most leverages among patients with substance misuse diagnosis (63% reporting any leverage) were higher than those in the US and our other subgroups (AOT, CMHT-psychosis and CMHT-non-psychosis).
-
Patients were more likely to report leverage if they:
-
had experienced repeated hospitalisations
-
had a substance misuse diagnosis
-
were more insightful.
-
-
They were more likely to report multiple types of leverage if they:
-
had a substance misuse diagnosis
-
did not live independently
-
had a history of imprisonment.
-
-
Patients in the mental illness groups were more likely to report leverage if they:
-
had children aged under 18 years
-
had a diagnosis of schizophrenia
-
did not live in independent accommodation.
-
-
They were more likely to report multiple types of leverage if they had children aged < 18 years.
-
Reporting leverage made little difference to patients’ assessments of the coerciveness of their care and its fairness and effectiveness.
Chapter 19 ULTIMA Qualitative Study
Introduction
Although the ULTIMA Quantitative Study established the levels of experienced leverage in the four identified areas, the ULTIMA Qualitative Study sought to understand some of the underlying mechanisms involved in informal coercion and leverage by investigating it as part of social interactions in community mental health service delivery. The objective was ‘to conduct a detailed qualitative assessment of the experiences of patients, staff and carers’. Given the gaps identified in the current literature, the aims of this study were broad and included:
-
how informal coercion and leverage are perceived and experienced
-
how and when they are used
-
how they are perceived to take effect
-
ethical issues arising from their use (for use in the Ethical Analysis, see Chapter 20).
These aims were operationalised in two qualitative substudies: (1) patients’ perspectives on, and experiences of, informal coercion, and (2) community mental health professionals’ views on, and experiences of, using informal coercion.
This chapter draws substantially on papers244,259 published by members of the OCTET Coercion Programme Group: Canvin et al. ,259 with permission from Elsevier, and Rugkåsa et al. ,244 with permission from Springer Publishing Company.
Methods
In-depth interview study with patients
Design and data collection strategy
Given the sensitive nature of the topics under study, we selected individual interviews with patients as the method for data collection to ensure anonymity and confidentiality. One-to-one, semistructured interviews are well placed to generate data on personal experiences. 260 They allow for significant time and attention to be devoted to a single account and to explore the setting in which personal experiences are situated. 261
A topic guide was designed using Szmukler and Appelbaum’s204 typology of ‘treatment pressures’ and Neale and Rosenheck’s208 continuum of restrictiveness (see Chapter 17). The wider literature and the ULTIMA Quantitative Study protocol and instruments also informed the topic guide. As the terms informal coercion and leverage were unlikely to be meaningful to patients, we designed our questions around different ‘pressures’ they had experienced and asked all patients about such experiences in relation to housing, finances, children, the criminal justice system, drug and alcohol treatment and employment. We finalised the topic guide in collaboration with an experienced service user consultant.
The researcher (KC) opened each interview by inviting patients to talk about their mental health and service use history and reiterating the interest in any related pressures they might have experienced. Patients talked for as long as they wished before the researcher sought clarification and explored topics from the guide that had not been spontaneously raised. This approach had a number of inter-related advantages. First, it permitted patients to feel in control of the interview, which can facilitate openness and rich data; second, it allowed them to construct a narrative that reflected their priorities and the experiences that were significant for them; third, it allowed the researcher to explore the meaning patients attributed to phenomena via their experiential accounts which in turn allowed us to explore the use of informal coercion in context and, fifth, it permitted us to identify examples of informal coercion and leverage beyond those contained in the existing questionnaires and scales. We offered patients £25 for the interview as compensation for their time. The researcher was Krysia Canvin (KC, PhD in Law, white British, late 30s).
Sampling procedure
The sampling pool consisted of the 393 patients who had participated in the ULTIMA Quantitative Study and consented to be contacted again for a qualitative interview (23 declined to be contacted; two were deceased). We undertook purposive sampling with a view to achieving a maximum variation sample. 139 This took into account characteristics such as ethnicity, gender, time since first contact with mental health system, hospitalisations, team and diagnosis, as well as experiences and perceptions of pressure reported in the Quantitative Study. We aimed to sample an equal amount of patients from each of the four Quantitative Study patient groups: CMHT-psychosis, CMHT-non-psychosis, substance misuse, and AOT.
Data collection
We collected data in three waves to facilitate cycles of analysis and data collection and to allow periodic review of our subsample characteristics and experiences. We subsequently sampled new recruits to fill any gaps and reach saturation. 262 We adapted the interview schedule as analysis progressed to focus on emerging themes and test ideas. 141 We digitally audio-recorded the interviews, which lasted 70 minutes on average (range 20–100 minutes) and transcribed the files ad verbatim. We used the Atlas.ti qualitative data analysis software for data storage, retrieval and management.
Analysis
The study employed modified Grounded Theory analysis procedures. 140,141,263 This involved close examination of the data for experienced informal coercion, using a combination of codes emerging from the data and predetermined ‘sensitising concepts’ from the literature. 264 Using the constant comparison technique,265 we identified similarities and differences within and between accounts and sorted the data into analytical categories. We derived a set of criteria from the data in an inductive–deductive cycle,263 which we continually refined until all of the data was coded and categorised. Each different strand of analysis (see below) also involved topic specific and focused coding. Furthermore, the interview transcripts were examined to identify ethical issues arising (reported separately; see Chapter 20) (Box 6).
-
Systematic, detailed line-by-line open coding of interview transcripts.
-
Systematic coding incident by incident.
-
Memos (or notes) written about emerging themes and ideas.
-
Writing short summaries of individual interviews and important themes arising therein.
-
Expansion of memos and focused searching for data extracts (selective coding).
-
Further reading (relevant literature).
-
Selection of transcripts read and annotated by colleague.
-
Discussion of emerging themes amongst colleagues.
-
Exploration of links between themes.
-
Detailed interim analysis conducted, prior to final data collection.
-
Final analysis of entire data set.
This box has been reproduced from Canvin K, Rugkåsa J, Sinclair J, Burns T. Leverage and other informal pressures in community psychiatry in England. Int J Law Psychiatry 2013;36:100–6,259 with permission from Elsevier.
Focus group study with mental health professionals
Design and data collection strategy
Focus group discussions facilitate collection of data of an intersubjective nature. 260 In this study we sampled ‘naturalistic’ groups (i.e. existing groups, in this case outpatient teams, rather than people brought together for the purpose of research) to encourage professionals to express their own views and comment on those of others through discussion of real clinical cases as opposed to hypothetical or abstract situations. 266 Our aim was to capture the multidisciplinary dimension of current service delivery. We designed a topic guide based on a review of the literature and the qualitative interviews with the patient subsample. The guide was designed to investigate professionals’ experiences of using informal coercion (see Chapter 17, Background), other types of influencing behaviours and general interactions with reluctant patients and their families. To facilitate discussion about their own practice, we asked each group two opening questions:
-
What are the things you want patients to do?
-
What do you do to get them to do those things?
The researcher recorded responses to these two questions on a flip chart to act as prompts in the discussions that followed, and probed for case examples throughout. The groups were moderated to obtain reflection more than consensus, and, because we were investigating current service delivery, attention was primarily directed towards team approaches rather than individual ones. The sessions were led by one member of the research team (AS), with another member (either JR, KY or JS) observing and taking notes. We again digitally audio-recorded all focus groups, which ranged from 50 to 80 minutes in duration (average 60 minutes), transcribed them ad verbatim and imported the transcripts into the qualitative software package Atlas.ti for data storage, retrieval and management. The researchers were Anna Sulman (AS, social science graduate, white British female, early 30s), Jorun Rugkåsa (JR, PhD in sociology, white Norwegian, early 40s), Ksenija Yeeles (KY, BSc Psychology, white Croatian, late 40s) or Julia Sinclair (JS, DPhil/MRCPsy, white British, early 40s).
Sampling procedure
We constructed a purposive sample of six of the community teams from which the patient subsample described above was drawn. Sampling criteria included type of service and location.
Analysis
Each member of the qualitative research team read the transcripts and made a draft coding plan. We discussed these in detail before reaching consensus on a coding framework. Some codes corresponded to the themes included in the topic guide or derived from theoretical interests, whereas others emerged from the data. Any adjustments to the agreed framework were discussed among the researchers before they were implemented. The findings reported below are based on thematic analyses of the coding reports, using the constant comparison method. 142,267 The focus group transcripts were also examined closely to identify ethical issues arising (reported separately; see Chapter 20).
Results
Sample
Patients
The final sample (N = 39) is outlined in Table 62. Within the four groups, we achieved variation in the type of leverage reported and the number of types of leverage originally reported. The overall Qualitative Study sample comprised mainly white (n = 35), male patients (n = 24). They were living in independent housing (n = 30) and receiving social security benefits (n = 26); half were single (n = 20) and the majority had no children aged < 18 years (n = 30). Patients had a range of diagnoses, although four diagnoses in particular [schizophrenia (n = 12), depression (n = 8), bipolar disorder (n = 7) and opioid addiction (n = 10)] were the most common. The age of first contact with services ranged from 13 to 43 years (mean 20 years), whereas the number of hospital admissions reported ranged from 0 to 29 (mean: 4.7). This Qualitative Study sample had a higher proportion of patients with a diagnosis of bipolar disorder and multiple hospitalisations, respectively, than did the ULTIMA Quantitative Study sample.
| Characteristics | Mental health (N = 29) | SM (N = 10) | Total (N = 39) |
|---|---|---|---|
| n (%)/mean {SD} | n (%)/mean {SD} | n (%)/mean {SD} | |
| Age (years) | 43.4 {10.3} | 33.4 {8.54} | 40.9 {10.70} |
| Ethnicity | |||
| White | 26 (90) | 9 (90) | 35 (90) |
| Others | 3 (10) | 1 (1) | 4 (10) |
| Male | 16 (55) | 8 (80) | 24 (62) |
| Diagnosis (ICD-10) | |||
| Schizophrenia | 12 (41) | 0 (0) | 12 (31) |
| Bipolar disorder | 7 (24) | 0 (0) | 7 (18) |
| Major depression | 6 (21) | 0 (0) | 8 (21) |
| Substance abuse/opioid addiction | 0 (0) | 10 (100) | 10 (26) |
| Anxiety | 0 (0) | 0 (0) | 0 (0) |
| Other diagnosis | 4 (14) | 0 (0) | 7 (18) |
| More than two hospitalisations | 23 (79) | 0 (0) | 23 (59) |
| GAF | 57.5 {9.8} | 61.8 {7.31} | 58.6 {9.32} |
Mental health professionals
Between three and 13 professionals attended the six groups, and in total 48 patients (16 men, 32 women) took part, from a range of professions (Table 63).
| Profession | Number of participants |
|---|---|
| Nurse | 23 |
| Psychiatrist | 7 |
| Social worker | 5 |
| Community support worker | 5 |
| Occupational therapist | 1 |
| Student | 6 |
| Office manager | 1 |
| Total group | 48 |
Analyses conducted
Unlike quantitative, hypothesis-testing research, exploratory qualitative studies usually address the research questions in staged analyses. This is, in part, because of the inductive aspects of qualitative studies, which mean that some themes and categories emerge as data are collected and analysed, and analysis thus cannot be prespecified. Furthermore, the richness of large qualitative data sets means that there usually are several strands of analysis (most likely closely linked) that may be followed and the researchers must decide which ones to pursue and in what order. Based on the data collected and the overall research agenda of the OCTET Coercion Programme, we decided to focus on the following themes:
-
the notion of leverage from a patient perspective
-
how informal coercion is situated in the context of patients’ whole lives
-
professionals’ conceptualisations of how they influence patients in the treatment setting.
The findings reported below are accompanied by quotations from the transcripts to illustrate and validate our interpretations. 143 Quotations are attributed to patients identified by a unique patient ID number and team, and to professionals identified by discipline, unique ID number and focus group (FG) number. Where this is a dialogue with the interviewer, speakers are identified in full where first mentioned and by P (patient), C (carer) or I (interviewer) subsequently.
The notion of leverage from a patient perspective
This analysis draws on the 29 interviews with patients with a primary diagnosis of mental illness (see Table 62) and draws substantially on the sudy by Canvin et al. 259 This included those patients from AOT teams (AOT group) and CMHTs (CMHT-psychosis group) and patients with non-psychosis diagnoses from CMHTs (CMHT-non-psychosis group). The aim was to identify and clarify the pressure experienced by patients, and particularly the experience of leverage.
‘Treatment’ pressures compared with ‘stay well’ pressures
The pressures perceived by patients could be categorised as pressures to adhere to treatment and pressures to maintain their well-being. Treatment pressures were any pressures directly (but broadly) related to treatment. This included accepting prescribed medication as well as other therapeutic activities, often set out in individual patients’ treatment plans, such as attending meetings and accessing and engaging with services. Patients also described stay well pressures in the context of their mental illness. This included pressure to cease particular behaviours such as self-harm or alcohol use, for example, and this pressure, like treatment pressure, could come from mental health services or others. Stay well pressures could also involve meeting perceived sociocultural obligations or expectations, such as being a good parent or a good tenant, avoiding letting down oneself and others, staying ‘out of trouble’ or out of debt and avoiding homelessness.
Leveraged versus non-leveraged pressures
Pressures described by patients could be further differentiated on the basis of the presence or absence of certain features. On the basis of their descriptions, we classified as leveraged the pressures that possessed the following three features:
-
consequences contingent upon a specified response (conditionality)
-
a lever
-
direct communication by someone perceived to have the power to bring about the specified consequences (Box 7).
-
An element of conditionality, whereby different consequences will arise depending on the patient’s response to the pressure applied.
-
Some form of lever augments the pressure, improving the chances of influencing the patient.
-
Direct communication by an agent with the perceived power to follow through with the action perceived by the patient as intended to influence their behaviour.
A second group of pressures, non-leveraged pressures, lacked one or more of these features. Both treatment pressures and stay well pressures could be leveraged or non-leveraged (Figure 25). Examples of these four types of pressure can be seen in Table 64.
FIGURE 25.
Pressures experienced by patients. Reproduced from Canvin K, Rugkåsa J, Sinclair J, Burns T. Leverage and other informal pressures in community psychiatry in England. Int J Law Psychiatry 2013;36:100–6,259 with permission from Elsevier.
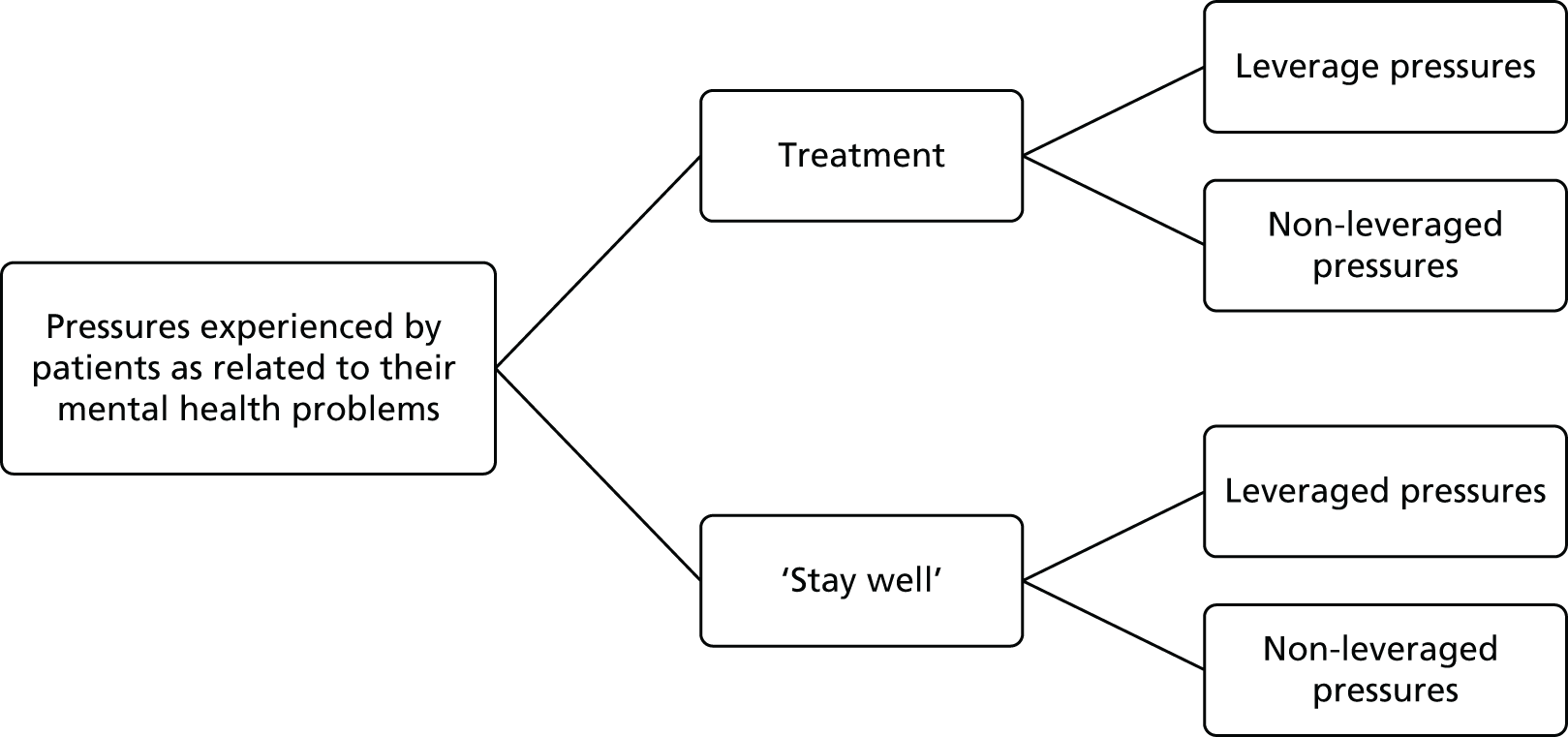
| Pressure | Treatment | Stay well |
|---|---|---|
| Leveraged | The CPN said that I had to take medicine all the time no matter what but if I didn’t take it for a long time I couldn’t function and I’d lose my place [in supported housing]36 AOT | The other slight pressure that was put on me was people saying things like, ‘Well of course if you’re going to be self-harming you won’t be allowed to have your daughter with you.’ [. . .] This open threat really38 CMHT-NP |
| Non-leveraged | If I don’t get treated I’m not going to be well enough to see [my daughter] and to be able to get anything out of it. [. . .] That was just coming from me5 CMHT-NP | I:‘So what kind of things do they say or do to encourage you to [avoid alcohol]?’P:[. . .] [Staff member] dropped by and he’s a star, he said to me, ‘I’ve been telling you to give up drinking but I’m drinking myself,’ so he’s actually stopped drinking so that he can support meCMHT-NP |
Leveraged pressures
The first two features of leveraged pressures, that is, conditionality and the use of a lever, both appeared to serve to augment the pressure applied. Patients often perceived that consequences were contingent upon their behaviour. They described situations in which, for example, they had perceived that remaining at home or qualifying for help with housing was contingent upon medication adherence or agreement to seeing the mental health team:
[The mental health team] said you can’t live in your house if you don’t take your medicine, you’ll have to live in hospital.
Patient 8, CMHT-psychosis
Patients also perceived that access to their children was dependent upon fulfilment of certain conditions:
Well [my CPN and psychiatrist] keep saying to me, ‘It will change. You will have [daughter] on your own one day.’ So this ‘one day’ is never happening. I say to them, ‘Well can’t I have another assessment to show that I can have [daughter] on my own?’ and they say, ‘It’s going to happen’ but it never does.
Have they said that you have to achieve something before that can happen?
Yes I have to stop cutting myself and stop taking overdoses. [. . .]
Do you feel you have enough control to be able to stop cutting?
No I don’t. I mean I can’t force myself to stop. I know I have to stop because of [daughter] and then when I think of [daughter] it just makes everything else worse and all the bad things come back up again.
A lever thus adds potency to pressure to co-operate with treatment (take medication or engage with the mental health team) or to stay well (stop self-harming). Patients perceived a wide range of levers being used to augment pressure in this way, including access to or discharge from services, access to social security benefits, hospital admission, depot injections and diversion from criminal charges or imprisonment. The third feature of leveraged pressure was that it was relayed via direct interpersonal interaction. Patients reported such pressure from various people, including mental health professionals, representatives from other health and social welfare agencies, courts, employers and police, and also from friends and family:
My wife threatened me, said at one point that unless I went to the local doctor she would take the children away from me.
Patient 11, AOT
An idea about the perceived power of the agent, or the person applying the pressure, to follow through with the proposed consequences, was clearly implicit in patients’ accounts.
Non-leveraged pressures
Patients described various pressures that missed one or more of the features of leveraged pressure. These were less tangible manifestations of pressure compared with the leveraged examples, but were nonetheless experienced as pressure. This included examples of non-conditional pressures, that is, where patients perceived a lack of consequences for not succumbing to the pressure they experienced:
[The social worker] said, ‘Do you want money management?’ And I said, ‘No,’ and they said, ‘Fine’. But yeah it was getting pressed on me a couple of times and I did actually agree to it but then I backed out.
Patient 9, CMHT-non-psychosis
Some also described feeling pressured as a result of professionals making predictions about future events:
[The social worker said] it was very likely that I would lose custody of the children [. . .]. And it was on the basis that I would end up getting ill and going into hospital again.
Patient 8, CMHT-psychosis
For some, pressure arose as a result of what they heard about or observed happening to other patients:
I have a friend who is a service user and he resents taking medication but he’s in a group home and he says that if he doesn’t take his medication they’ll kick him out. I mean that sounds awful to me. I mean, I am fortunate having independent living arrangements. [. . .] My nightmare is becoming a tramp, [. . .] so it keeps me on the straight and narrow I suppose.
Patient 22, AOT
Patients also described self-imposed pressures:
I was evicted from that housing association because of one of my drug-addict friends. [. . .] I hardly let anyone in [my new] flat at all because I don’t want to misuse the landlady by having people in smoking cannabis. I think I’d be betraying [her] trust.
Patient 30, CMHT-psychosis
Much of this non-leveraged pressure, therefore, originated from patients’ desire to avoid undesirable situations such as homelessness or debt, or to satisfy sociocultural expectations. Feelings of responsibility, especially towards their children, were often described as motivating both ‘stay well’ behaviour and the taking of medication:
It is only probably since I’ve had my children, [names removed], that I’ve realised how important it is to keep well. [. . .] When it was just me it didn’t matter so much [. . .]. That’s what keeps you going: having responsibilities.
Patient 4, CMHT-psychosis
How informal coercion is situated in the context of patients’ whole lives
This analysis included the same 29 interviews. It involved focused coding of patients’ accounts of their medication practices, particularly regarding their reasons for taking medication.
Situatedness is a concept used to account for the contribution to social phenomena of broader circumstances, whether social, political, economic or cultural. 268 We identified two key dimensions of the situatedness of patients’ medication practices in our analysis: first, personal, familial and social circumstances and, second, contact with the mental health system and those working within it.
Personal, familial and social circumstances
Patients’ accounts of their medication practices were often embedded in descriptions of their everyday lives. Many presented their reasons for taking medication in a way that suggested these reasons were inseparable from their home, family and work circumstances. The sociocultural, self-imposed pressures described above were often present in descriptions of how they negotiated with self and others about taking medication:
Medication was always a negotiation until I, you know, lost my marriage, lost that regular access to my children, lost properties, lost money, lost my job and found myself on disability living allowance.
Patient 2, CMHT-psychosis
To some extent, patients presented their reasons for taking medication not as a choice but as essential in order to maintain various aspects of their personal lives. Some explained this as a result of leverage, such as taking medication being a precondition to gaining access to or retain a housing place and/or social security benefits:
[With this housing provider] I have to be on the medication as well yeah. Although now, because it’s been 2.5 years I’ve obviously earned a good reputation with [the housing provider], I’ve had no trouble and no-one’s complained about me or nothing like that so now I do believe I could now, if I wanted to turn round and say to my doctor: ‘Well, I’d like to try and have less of the injection’. Or maybe even stop the injection but to be honest with you, just with how my – the last few years have been I’d rather stay on it for another few years until I feel more confident [about my recovery].
Patient 29, AOT
Contact with the mental health system and those working within it
Patients also alluded to how aspects of their contact with the mental health system led them to feel that they had ‘no choice’ about taking medication. For example, patients described how their choices and opportunities for decision-making were reduced by structured, routine practices by mental health professionals, such as observation of the use of oral medication and/or regular depot injections:
In [the AOT] I suppose they try to ensure that I take the medication and I get injections and so there’s no chance of not complying. [. . .] I don’t think they trust me to take ordinary pills.
Patient 22, AOT
Patients also described their medication practices as influenced by their concerns about the possibility of involuntarily hospitalisation under the MHA (being ‘sectioned’). Concern about involuntary hospitalisation was so powerful that it was described by one patient as, ‘probably mine and my friends’ biggest fear’ (patient 8, CMHT-psychosis). Mostly, these concerns were derived from personal experience of restraint and/or forced injections as an inpatient. Moreover, it was perceived as a threat that most patients reported as perpetually ‘hanging over’ them:
I agree to the things that I agree to now because the threat of sectioning you is a draconian power hanging over you and the reason I take medication and turn up to all the appointments is that I don’t want to go back [to hospital]. You’ve got to be seen to be cooperating to a point to stay out.
Patient 11, AOT
Patients also mentioned the role of their relationship with their mental health team, emphasising the benefits of encouragement over threats:
They do encourage you obviously to keep your appointments and things like that but because they don’t use threatening techniques I feel that I can trust them enough to keep my appointments. If they were threatening me or something I probably wouldn’t bother turning up!
Patient 8, CMHT-psychosis
Regular contact with the mental health team and the social interaction and relationships that this afforded were highly valued. One patient described them as ‘like family’. Some patients said they would be disappointed if contact were reduced or withdrawn. Others described how they continued to take medication out of concern about being refused services or other types of medication. Many also wanted to preserve their good relationship with mental health professionals.
There was a tendency for patients to describe changes in attitude and practice in response to different circumstances such as personal, familial and social circumstances and their relationships and interactions with their mental health team. For many patients, shifts in their medication practices and attitudes did not occur in a vacuum but could be linked to other (changes in) attitudes and perceptions, events and opportunities. Our findings suggest that patients’ medication practices are highly situated social processes, changeable in response to changing conditions.
Professionals’ conceptualisations of how they influence patients in the treatment setting
This analysis used all six focus groups and draws substantially on Rugkåsa et al. 244 When asked, ‘what are the things you want patients to do?’, mental health professionals’ replies broadly included wanting patients to take medication as prescribed, to engage with the team and keep appointments, and to take responsibility for leading more stable, healthy lives. When we asked professionals how they tried to achieve these goals, they provided rich, contextual accounts of how, and in what circumstances, they sought to exert influence over patients. We identified three categories of influencing behaviours:
-
building trusting relationships
-
negotiating agreements
-
asserting authority.
Building trusting relationships
The quality of their relationships emerged as the central way of attempting to influence patients to achieve treatment aims. Achieving good, trusting relationships required the professionals to be ‘honest’, ‘interested’, ‘fair’, ‘empathetic’, ‘reliable’ and ‘consistent’, all of which might, of course, be perceived as an ideal for any social relationship. Trust, often built up over time, was seen as fostering continued contact with services:
‘Cause we work with some of our patients for quite a long time – to work with somebody that they like and they trust and they can talk to – that often retains people in treatment, actually. When things are tough they will come and see you.
Nurse, 16, FG 3
Professionals described ‘good’ relationships as providing a platform for achieving ‘engagement’ and for educating, encouraging or reminding patients to take treatment, such as when the professional could reflect on past experiences with the patient:
‘Last September, this is what you were doing. You were in employment; you were much more active, seeing the family. That was obviously a good place to be. Let’s try and get back to that again’. So it’s reminding them that they were well and there was a reason for them being well and, again, ‘At that time you were taking 150 mg of Clozapine. [Now] you’re only taking 50. Do you think there’s something relating to that?’.
Nurse, 25, FG 4
They also perceived that being attuned to the patients’ situation, and taking their concerns and priorities into account, was crucial to get patients to ‘work with’ professionals. They perceived that focusing on patients’ priorities and perspectives not only provided necessary information about the patient (including why he or she might be reluctant to take treatment), but also could facilitate longer-term aims. Professionals described, for example, how they assisted patients who neglected themselves in keeping their homes clean and tidy, attending to their diet and personal hygiene and taking exercise. They also encouraged and supported educational activities and employment. Professionals assisted with paperwork and other forms of communication with other agencies and sometimes helped patients to ‘fight off’ eviction through extensive liaison with housing providers. Some professionals explained that they occasionally needed to apply assertive approaches to ensure that patients received the support to which they were entitled.
Several professionals indicated how offering something outside patients’ expectations, such as going out for coffee or meals or doing practical tasks, helped to pave the way for constructive interactions:
So I took [the plant] to him and said, ‘This is from [the gardening project], come and have a look’. And he later on came and thanked me for it ‘cause he was obviously quite touched by that. And a few weeks later he was down at the project digging and gardening. And he did that for quite a few months until he decided he’d had enough of it. But that was, I suppose, a slightly creative way of getting him to do what I wanted him to do.
Social worker, 9, FG 2
Negotiating agreements
Professionals frequently described negotiations with patients to find mutually acceptable solutions:
There was a female patient, Mary, who refused to have – she was on leave [from hospital] – refused to have her depot [injection]. Came to see me, I had a bit of a chat with her and I said ‘oh why don’t you have it every three weeks then’ [i.e. less frequently]. And she said ‘oh great, yes that’s fine’ and off she went and had it.
Psychiatrist, 27, FG 4
The descriptions of negotiations often focused on striking ‘deals’ or agreeing ‘contracts’, alluding to a relationship’s reciprocal dimensions. Negotiation also occurred when professionals and patients held radically different views about their respective rights and responsibilities. For example, professionals portrayed some patients as holding unrealistic expectations: thinking professionals possessed a ‘magic wand’ with which they could solve ‘any’ problem. They perceived that extensive assistance with practical issues in some cases undermined efforts to increase patients’ independence. If patients were unwilling to take on responsibilities of which they might be capable, professionals sometimes tried to renegotiate the relationship, which, at times, could be frustrating:
I find the most frustrating ones the ones that do want you to be their mother. And trying to get them to accept the fact that you’re not going to do that and that they do have to take responsibility for themselves. And that you’ll be there to help with bits.
Nurse, 24, FG 4
Although professionals emphasised an ambition to let patients’ views influence agreements, balancing a patient-centred approach with their responsibility for patients’ safety could occasionally limit room for negotiation:
It’s kind of compromise, isn’t it? Anne would perhaps prefer not to take any medication at all but in terms of the deals we might strike with her they’re a bit stacked on our side ‘cause we’ve got the Mental Health Act, but within that then there’s some compromise offered. [. . .] So it’s not all, ‘No, you will do exactly what I say’. That as far as you can, you give back but not to the extent that you make somebody ill again. So that would be the balance but that’s the kind of balance you’re trying to get in the deal.
Nurse, 24, FG 4
Asserting authority
Professionals presented building trusting relationships that facilitated negotiation of mutual agreements as the ideal way to achieve therapeutic aims. Nevertheless, when encouragement and education failed, ‘deals’ were broken or professionals believed patients were unable to act in their own best interests, they sometimes deemed more authoritative or assertive approaches to be necessary, such as counting pills, using depot injections or observing consumption (as also described by patients above) or more frequent visits. The ultimate assertion of authority was applying the MHA. Although professionals saw the appropriate use of the Act as part of their duty of care, it was portrayed as an inferior tool to what could be achieved by other means. Moreover, applying the Act was considered potentially to undermine relationships:
I think the next time I hear that things are bad I might insist [under the MHA] to be let in. But it’s a pretty heavy handed way of dealing with things, when they are a family who are in family therapy and you’re trying to work together. It’s [a] pretty sort of sledgehammer approach.
Social worker, 5, FG 2
They described previous experience of legal compulsion as alerting some patients to ‘early signs’ that an involuntary admission to hospital was being considered:
For example, someone’s starting to relapse and – [or] we think they are – and we may decide to do joint visits. Some of the patients are so experienced they say: ‘Oh, you’re doing joint visits. You must think I’m relapsing’.
Community support worker, 29, FG 4
The authority of the professional role (including the use of the MHA) therefore simultaneously represented a useful tool to ensure patient safety during relapse and yet also a threat to relationships.
Conclusions
-
Patients’ experiences of pressure were wide-ranging and pervasive.
-
These experiences related to many aspects of their lives.
-
They perceived pressures to come from family and friends and themselves as well as professionals.
-
We identified a patient-derived concept of leverage, based on the presence of: conditionality, a lever and the perceived power of the agent to bring about the stated consequences.
-
Pressure was linked to the proper execution of social roles.
-
We found additional types of pressure to those measured in the Quantitative Study.
-
These pressures were embedded in the context of people’s lives.
-
Patients’ medication practices were highly situated social processes.
-
Professionals were committed to patient-centred approaches and attempted to establish trusting relationships that enabled negotiated agreements.
-
Professionals felt obliged to assert their authority when patients relapsed but refused services and this was seen as a potential threat to therapeutic relationships.
Chapter 20 ULTIMA Ethical Analysis
Introduction
The objective of the ULTIMA Ethical Analysis was ‘to conduct a detailed qualitative assessment of the ethical dilemmas of patients, staff and carers’ participating in the study, using data from the ULTIMA Qualitative Study.
Our Ethical Analysis comprised two parts. First, we conducted a detailed conceptual and ethical analysis of threats and offers made to patients by professionals for the purpose of improving adherence to treatment in the context of community mental health care and produced a framework for judging the ethical status of an offer. Second, we conducted an examination of whether professionals act ethically when they use leverage in a variety of ways using interview and focus group transcripts from the Qualitative Study.
Framework for judging the ethical status of an offer
This section is summarised from a paper by members of the OCTET Coercion Programme Group – Dunn et al. 255
Informal coercion may take the form of threats or offers. Although threats are never justifiable, the ethical position on offers is more complex. Here we offer a five-step process that may be used to ascertain the ethical status of an offer in mental health care.
Examples of the proposals we examined here included proposals to enable or remove access to community services, visiting rights for children, access to supported housing placements, specialist help with welfare payments, access to hobbies and social activities, and providing financial rewards. Evidence suggests that professionals and patients consider such threats and offers to be ethically problematic because they are experienced as coercive, or involve treating patients unfairly. 217,241,242,269 The framework we lay out below for making ethical judgements about such proposals posits professional duties of care, rather than leverage, as the primary consideration. We intend this framework to be of practical guidance in deciding whether a specific proposal is, or is not, ethically acceptable.
Step 1: to decide whether the proposal is a threat or an offer
In distinguishing a threat from an offer, it is necessary to clarify – independently of the proposal – what duties the service owes the particular patient. Establishing such duties is a general responsibility of mental health professionals, teams and services. The duties will depend on how ethical values are interpreted and applied in practice, and will vary between different mental health-care systems, between services within a system and between different patients in a service.
Having established the duties of care, the key question is whether or not the proposal, if accepted or not, will lead to an outcome consistent with the professional having failed to act in line with these duties. If this is the case then the proposal is a threat and should not be made. If this is not the case then the proposal is an offer. If the proposal is an offer then further issues need to be considered before an ethical judgement is made (steps 2–5).
Step 2: to decide whether or not the offer is likely to be unwise
This question focuses particularly on consequences, both for the specific patient and for others. Although the offer might be of value to the patient in the short term, it may have longer-term detrimental effects for that patient, or detrimental effects on other patients.
Step 3: to decide whether or not the offer exploits the patient
The key consideration here is whether or not there are benefits to the mental health professionals, or system, if the patient accepts the offer. In making the final judgement about the ethical status of the offer, it will be important to separate benefits to the patient from benefits to the professionals and system.
Step 4: to decide whether or not the offer raises broader questions of fairness
At the micro level, the question is whether or not the offer treats other patients in the relevant service fairly. At the macro level, the question is whether or not the offer represents a good use of health-care resources.
Step 5: to decide whether or not the offer compromises the voluntariness of the patient’s decision-making
The main issue here is to ascertain if there is any way that the patient’s psychopathology impacts upon his or her agency such that the decision to accept the offer would not be a voluntary decision. The attractiveness of the offer per se (we have argued) does not affect voluntariness.
Having taken steps 2–5, the ethical issues relevant to the decision of ‘whether or not it is right to make the offer’ should have been identified. The fact that there might be ethical problems with the offer would not necessarily mean that it was unethical. In the case of offers (as opposed to threats), the overall anticipated benefits of making the offer would need to be balanced against the ethical problems identified, and both would need to be understood in the context of the individual patient at that particular time.
Ethical guidance for mental health professionals
This section draws substantially on a paper published by members of the OCTET Coercion Programme Group: Dunn et al. ,270 with permission from Sage Publications.
The three-fold definition of leverage proposed in Chapter 19 – the presence of conditionality, a lever and the perceived power of the agent to bring about the stated consequences – does not require the proposal to influence a patient’s choices successfully. Thus we can define a proposal as leverage without it having an actual effect on the patient’s behaviour. The ethical acceptability of the proposal will, however, depend on an assessment of the consequences that might result by imposing conditions on patients’ choices. The three case studies in Box 8 illustrate how leverage might be used in practice. These cases were developed from the data collected as part of the ULTIMA Qualitative Study (see Chapter 19). They cover a range of different community mental health service settings and illustrate the potential dilemmas and alternative interpretations that can arise when leverage is used in practice.
Jack, 24 years, lives at home with his parents. Jack has a diagnosis of schizophrenia, but has consistently refused to accept that he has a mental disorder. When unwell, Jack increases his cannabis use, which exacerbates his symptoms. Jack’s parents find it difficult to cope with his aggressive and threatening behaviour. They have sought advice from a support group and have told services that they want more support for themselves and their son. The AOT’s main concern is Jack’s well-being and his parents’ safety. Members of the team have suggested to Jack that if he stops using cannabis, they will help facilitate an unsupported housing placement for him. Jack’s parents support this proposal.
Case 2Ann, 35 years, is a single mother of three children. Ann has recurrent severe depression, which has involved several serious suicide attempts. Ann repeatedly stops taking the medication, asserting that she feels well enough to manage without it. When she does so, her mental state and ability to care for herself and her children gradually deteriorates, resulting in long periods of hospitalisation. Ann’s situation generates multiple practical and financial support needs. The CMHT have concerns about the well-being of Ann’s children in this unstable environment, and have encouraged her to consider what might happen to her children if she is hospitalised again. They have told her that next time she has a severe depressive episode it is likely that social services will conduct an assessment, potentially leading to her children being placed on the at-risk register. Ann is extremely worried that she may lose custody of her children.
Case 3Craig is 28 years old. He has misused various substances since his teens and is unable to hold down a job. He currently receives a daily supervised dose of methadone as part of a Drug Treatment Order imposed by the court in lieu of imprisonment. The order stipulates that he must reside with his parents, and is enforced with an electronic tag. Craig continues to take heroin on top of his methadone and has been told by his drug worker that if he wants to pick up his methadone on a daily basis to take unsupervised, he will have to return heroin-free urine tests.
The complex nature of therapeutic encounters in community mental health services means that there are no straightforward answers to the question of whether or not professionals act ethically when they use leverage. Indeed, as the three cases in Box 8 illustrate, it can also be difficult to ascertain whether or not leverage is actually being used, especially in clinical encounters in which professionals are required to provide information or when requirements for treatment adherence are enforced using legal frameworks. In the face of such complexity, we show how different duties can guide professionals’ judgements about whether or not, and when, it is acceptable to influence patients’ treatment adherence using leverage in a given situation. The four duties that we discuss below are those that can guide ethical practice in community mental health, irrespective of social and cultural context. 271 These duties are to:
-
benefit the individual patient
-
benefit other individuals (particularly carers, dependents and the wider public)
-
treat patients fairly
-
respect patients’ autonomy.
Duty to benefit the individual patient
That mental health professionals have a duty to benefit their patients is not contestable. How they should act to uphold this duty in practice ought to be determined by the unique needs of each patient. For this reason, enacting the duty to benefit the patient (and therefore acting ethically) depends on context-specific factors. It ought to be obvious, for example, that professionals should provide different services to a patient experiencing the acute phase of a psychotic illness compared with a patient receiving long-term support to manage an enduring psychotic illness. For the acutely ill patient, the scope of the duty to benefit him or her is likely to be focused – at least in the short term – on providing immediate psychiatric input to manage distressing symptoms and keep him or her safe. For the chronically ill patient, the scope of the duty will extend to include the facilitation of social activities, employment opportunities and contact with family.
Commonly, interpreting the duty to benefit a patient will need to take into account more nuanced differences between the needs of comparable patients within a service. How this duty ought to be interpreted in decisions about antipsychotic medications, for instance, will be shaped on a case-by-case basis by the associated side-effects for each drug and a patient’s views about weight gain, opportunity for exercise or the risk of developing a metabolic syndrome.
The duty to benefit the patient may manifest itself differently depending on the therapeutic model adopted by a service. In case 3, the duty to reduce harm caused to Craig by his illicit drug use through prescribing substitute medication will be judged to take primacy over meeting a duty to assist him in meeting additional social goals,272 particularly when taking methadone under supervision is a requirement of a Drug Treatment Order. In contrast, professionals working in the CMHT in case 2 are likely to interpret their duties to benefit Ann in terms of prioritising a broader set of obligations concerning positive social, employment or educational outcomes.
How the duty to benefit the patient is understood in light of the patient’s individual needs and the therapeutic culture of the service has implications for judging whether or not a specific act of leverage for a patient is ethically permissible. Moreover, because the application of this duty is context dependent, the same proposal might be ethical when presented to one patient, but unethical when presented to another patient. It is also conceivable that the same proposal might be ethical when presented to the same patient depending on circumstances at particular points in time. In case 1, Jack’s team proposed to provide him with a housing placement if he stops using cannabis. It is arguable that the team has a duty to benefit Jack by facilitating his access to a housing placement, because of their concerns about his well-being and his parents’ safety, irrespective of his use of illicit substances. If so, making this proposal would not be ethically acceptable: they should facilitate his housing placement anyway. Alternatively, if it were the case that Jack posed no risk to his parents, and he had not expressed any preference about his housing situation, the team might claim that their duty to benefit Jack does not extend to making alternative housing available to him. As such, they should conclude – from the standpoint of this duty – that they have no reason to make this proposal to Jack.
The duty to benefit the patient extends to ensuring that the patient is not harmed, or left worse off, by the provision of care. There are two ways that leverage might lead to negative outcomes for the patient. First, leverage might lead the patient to become increasingly dependent on the service, and unlikely to obtain control over – or take responsibility for – his or her own recovery. In case 1, the concern might be that leveraging Jack with the offer of a housing placement might create the expectation that such things will be provided for him, undermining his responsibility for making major life decisions in the future. Consequently, evidence about short-term risks and benefits will need to be balanced against foreseen long-term harms. Second, patients might perceive themselves to be worse off if an instance of leverage were to place conditions on a course of action that they would value. In case 2, for example, Ann’s quality of life may decrease when the proposal is made to have a children’s services assessment if she becomes unwell. Judgements about the acceptability of leverage here will depend on how patient benefit is conceptualised, and from whose perspective.
Duty to benefit other individuals
Mental health professionals have duties to other people in addition to the patient at whom leverage is directed, primarily other patients in the service, the patient’s carers, children and members of the public.
Other patients in the service
If, for example, other patients supported by the AOT in case 1 learn that the team is prepared to facilitate a housing placement for Jack if he stops using cannabis, it is conceivable that they might expect to be made a similar offer, and that failure to do so would impede their engagement with the team and adherence to treatment. Such actions could lead to deterioration in their mental state. Alternatively, as evidence from studies of financial inducements in mental health suggests, compliance among all patients might be enhanced by the use of such inducements. 273
Obligations to a patient’s carers and dependents
An act of leverage by a professional may result in significant burdens for a patient’s carers, such that leverage equates with the professional acting inconsistently with this duty. In case 1, the proposal to offer Jack a housing placement on condition that he stops using cannabis is aligned with the team’s identified duty to reduce the risk of harm to Jack’s parents. Such a proposal – if accepted – would also meet Jack’s parents’ request for additional services for their son. Moreover, it could be argued that the effect of Jack’s behaviour on his parents is such that it would be ethically unacceptable not to make this proposal.
Additionally, leveraging a patient by making an offer to him or her might reduce the stress experienced by carers who are required to support the patient. In case 3, Craig’s parents are supportive of the proposal to allow unsupervised access to methadone treatment if Craig returns drug-free urine tests, and have also agreed to increase his weekly allowance if he remains drug free. Here, leverage would be consistent with the drug worker’s duty towards Jack’s family carers.
Professional duties also extend to children and vulnerable adults who are dependent upon the patient. In case 2, Ann has significant caring responsibilities as a single mother of three children. The CMHT are aware that a failure to take her medication leads Ann to become unwell and unable to provide care for her children. It would be important here to assess whether or not using Ann’s children as a lever would itself increase the risk of Ann’s condition deteriorating such that her children are harmed or neglected. Equally, if the CMHT decide that they have an obligation to take immediate steps to safeguard Ann’s children, this duty ought to be enacted, and making this course of action conditional on Ann’s choices would be unacceptable.
Obligations to members of the public
In case 1, the behavioural problems that Jack has displayed towards his parents might be evidence of heightened risk to the public if the proposal to provide him with an unsupported housing placement is made. Alternatively, this risk may be no greater than if the proposal were not made, or the heightened level of risk can be managed such that the proposal would not impinge upon this duty.
There may also be limited obligations towards potential or future patients that fall within the scope of the duty to benefit other individuals. Such patients would include those individuals with mental health problems who have not sought help (or whose mental health problems have not yet developed), but who meet (or will meet) the criteria for treatment in the service. It is possible that professionals’ actions could undermine the delivery of sustainable and beneficial services to all patients. There is evidence, for example, that people from black and ethnic minority groups perceive mental health services to be unresponsive to their cultural norms and values274–277 and that these perceptions have resulted in individuals not seeking help from mainstream services. 278
Similarly, in cases of leverage, public perceptions of professionals making conditional proposals to patients could give rise to the view that such proposals involve manipulating disempowered, vulnerable patients into treatment to which they would not otherwise agree. This perception might, in turn, lead potential patients to turn away from mental health services, potentially with negative consequences for their mental health and well-being. Alternatively, widespread understanding that community mental health professionals offer inducements to patients might encourage more individuals to make contact with services.
Boundaries of the duty to benefit
The scope of professionals’ duties to provide a beneficial service to the patient and other individuals is broad, but not unlimited. It should be recognised that professionals may act in ways that are designed to bring about additional benefits for themselves, their colleagues or others. A professional might use leverage to meet targets for reducing involuntary hospital admissions, for example, or increasing the number of patients discharged to GPs, set by the employing organisation. Alternatively, a professional might justify an act of leverage on the grounds that she wishes to avoid the reputational damage that might result from a non-compliant patient harming him- or herself or others: so-called defensive practice.
Such actions can be justified only if they are also judged as being likely to benefit the patient or the other relevant individuals to whom this duty applies. There will be situations in which the benefits accrued through the use of leverage will extend beyond the patient and other individuals to include benefits to the professional issuing the proposal. In such situations, these additional benefits should be seen as positive by-products from any duty-based justification for leverage, but should not motivate professionals’ decisions to use leverage.
Duty to treat patients fairly
In addition to the obligation to deliver services that provide benefits to patients and other individuals, community mental health professionals are obliged to treat all patients fairly. This is a well-established ethical principle, endorsed across all health-care settings. If leverage is restricted to those patients who are not treatment adherent, patients will be managed in ways that are not equivalent. In particular, when an offer is made to influence a patient’s choice to accept treatment, those patients who have adhered to their treatment regimes lose out on an option. Does this, as Szmukler212 suggests, imply that patients are being treated unfairly?
Most arguments concerning the fair distribution of resources require people to be treated equitably, but not necessarily equally. Considerations relating to need and responsibility will be relevant here, but ethical arguments about the allocation of health resources start from facts about comparable cost-effectiveness of the interventions in question. 279,280 All acts of leverage have an opportunity cost associated with them, and community professionals need to be attuned to the fact that different acts of leverage will lead to outcomes for patients at markedly different costs to the service.
The cost-effectiveness of a specific act of leverage should be compared against other acts of leverage, other interventions provided by the service and the costs of not using leverage, such as those associated with medication wasted as a result of non-adherence or increased hospitalisation. In case 1, the team is proposing to facilitate Jack’s access to an unsupported housing placement on the condition that he agrees to stop using cannabis. The opportunity costs associated with Jack’s acceptance of this proposal should be determined. This placement will involve considerable expenditure and will require a substantial amount of the team’s time to arrange. The expected clinical benefit associated with the patient meeting the conditions of the proposal, and the likelihood of this benefit accruing, would also need to be assessed. Imagine instead that the team had proposed to improve Jack’s well-being by expanding his social circle by arranging a package of social activities for him. This alternative proposal would cost less and may involve a less substantial time commitment. Both proposals would also need to be compared against other ways of using resources within the service.
Duty to respect the patient’s autonomy
Another well-recognised ethical duty in health-care settings is the duty to respect patients’ autonomy. Specific concerns relating to autonomy have been identified as central to making ethical judgements about treatment in mental health. 281 Szmukler and Appelbaum,204 for example, argue that the coercive force applied in leveraging patients’ decisions about treatment undermines the voluntariness of those patients’ ability to act autonomously.
This argument is problematic. Leverage involves attempting to influence a patient’s behaviour. The patient is not acting on the basis of the decision he or she would have made had no conditions been placed upon his or her decision-making. Crucially, however, the patient remains able to decide between the (conditional) choices he or she is presented with (as discussed in the previous section). Importantly, it is precisely when a patient’s choices are manipulated in this way that he or she is forced to evaluate his or her values and commitments in life. In case 2, proposing to Ann that her children may be placed on the at-risk register if she does not engage with services requires her to assess the importance of having continual access to her children against the value she places on living her life without the involvement of support. In this sense, leveraging Ann requires her to be proactive in ascertaining what it is that she wants, what she values and what is important to her. Such considerations are those that are typically seen to be relevant to the exercise of personal autonomy.
To see the imposition of conditions on decision-making as a problem of voluntariness is to conflate autonomy and liberty. Although autonomy concerns the value of a person being able to exercise their free will, liberty concerns the value of a person being free to act without third-party interference. 282 Leverage involves manipulating the range of options from which a patient can choose, and therefore raises concerns about whether this action involves an unjustified infringement on the patient’s liberty. The imposition of such constraints does not, however, raise concerns about patient autonomy because leverage does not impact on the exercise of free will. A competent patient is able to make a decision, one way or the other, regardless of what conditions are placed upon his or her decision-making.
There will, of course, be acts of leverage that are problematic on the grounds that that they interfere with the patient’s ability to exercise his or her right to basic freedoms. Instead of the case as it is presented, imagine that a professional sought to leverage Ann by proposing to place her children in local authority care if she failed to adhere to keep taking her medication. Such a proposal would impinge upon Ann’s right to be free to raise her children and to forge a family. Teasing out whether leverage involves justified or unjustified infringements on liberty can be ascertained, we believe, by examining whether or not the proposal under consideration would lead to the mental health professional acting in a way that is proportionate to the benefit that is likely to be accrued in making the proposal. Thus, it would be ethically justified to leverage Ann in this way if the expected consequences of doing so were positive for either her or her children. This way of articulating the justification for threatening to restrict patients’ freedoms is, of course, the same justification that underpins other ways of justifying restrictions of personal liberty in the mental health context, most notably the use of compulsory powers of detention and treatment.
In community mental health services, patient autonomy is respected by adopting models of shared decision-making for treatment planning with a view to achieving a therapeutic alliance283 or through the use of mechanisms for advanced treatment decision-making. 191,284,285 In circumstances in which a patient has previously agreed to a comprehensive treatment plan, the use of leverage in a way that has not been endorsed by the patient in the development of this plan would be ethically problematic on autonomy grounds.
The manipulation involved in imposing conditions on patients’ choices also means that it is important to ensure that the patient is aware of exactly what will happen if he or she decides or refuses to accept the proposal. As discussed above (see Chapter 19), there is evidence to suggest that patients experience leverage (i.e. think that their choices are conditional) even when professionals have left open how they will act if the patient does – or does not – act in a particular way. Given the complexity in how treatment relationships and patients’ attitudes vary over time, there may often be uncertainty in how patients interpret the management of their care, particularly with regards to coercive interventions. In case 2, Ann is told that the next time she becomes unwell and requires hospitalisation, ‘it is likely’ that social services will become involved and assess her children’s welfare. This may be an act of leverage, or, if no conditions are being placed on Ann’s behaviour, it may be an instance of attempted persuasion by the team, or a ‘simple prediction’ (see Chapter 19) outlining what will happen to Ann’s children if she continues to act in the way she has previously. It is equally important, therefore, that professionals are able to recognise when they are using leverage and that this is made clear to patients.
Conclusions
-
We propose a five-step framework for the determination of the ethical status of offers by mental health professionals, designed to be a practical tool for decision-making.
-
We have given detailed guidance for professionals about how to exercise leverage, based on four duties:
-
to benefit the individual patient
-
to benefit other individuals (particularly carers, dependents and the wider public)
-
to treat patients fairly
-
to respect patients’ autonomy.
-
Chapter 21 ULTIMA discussion and conclusions
The key findings of the ULTIMA Study are shown in Box 9.
-
One-third (35%) of our sample reported lifetime experiences of leverage.
-
This was lower than the level reported in the USA (51%).
-
Housing leverage was the most frequently reported type (24%).
-
Rates of most leverages among patients with substance misuse diagnosis (63% reporting any leverage) were higher than those in the USA and our other subgroups (AOT, CMHT-psychosis, CMHT-non-psychosis).
-
Patients were more likely to report leverage if they:
-
had experienced repeated hospitalisations
-
had a substance misuse diagnosis
-
were more insightful.
-
-
They were more likely to report multiple types of leverage if they:
-
had a substance misuse diagnosis
-
did not live independently
-
had a history of imprisonment.
-
-
Patients in the mental illness groups were more likely to report leverage if they:
-
had children aged under 18 years
-
had a diagnosis of schizophrenia
-
did not live in independent accommodation.
-
-
They were more likely to report multiple types of leverage if they had children under 18 years.
-
Reporting leverage made little difference to patients’ assessments of the coerciveness of their care and its fairness and effectiveness.
-
We identified a patient-derived concept of leverage, based on the presence of conditionality, a lever and the perceived power of the agent to bring about the stated consequences.
-
Patients’ experiences of pressure were wide-ranging and pervasive, related to many aspects of their lives.
-
They perceived pressures to come from family and friends and themselves as well as professionals.
-
Pressure was seen as linked to the proper execution of social roles.
-
We found additional types of pressure to those measured in the Quantitative Study.
-
These pressures were embedded in the context of people’s lives.
-
Patients’ medication practices were highly situated social processes.
-
Professionals were committed to patient-centred approaches but felt obliged to assert their authority when patients deteriorated after refusing services.
-
We propose a five-step framework for the determination of the ethical status of offers by mental health professionals, designed to be a practical tool for decision-making.
-
We have given detailed guidance for professionals about how to exercise leverage, based on four duties.
This discussion chapter draws substantially on papers published by members of the OCTET Coercion Programme Group: Burns et al. ,110 with permission from the Royal College of Psychiatrists; Canvin et al. ,259 with permission from Elsevier; and Rugkåsa et al. ,244 with permission from Springer Publishing Company.
This was the first study of informal coercion in England. It demonstrates that informal coercion in general and leverage specifically are common in public mental health services here when they are dealing with individuals with significant levels of symptoms and disability. We examined patients’ experiences of leverage according to predefined measures but also examined the degree to which they perceived their care to be coercive, fair and effective. The Qualitative Study also considerably extends our understanding of informal coercion and its scope, based on the perceptions of both patients and mental health professionals.
A substantial proportion (one-third) of our whole sample of 417 patients reported the experience of leverage (feeling pressured to adhere to treatment) at some point in their lives, when asked about the predefined types of leverage (finance, housing, criminal justice and child access). The highest rate recorded was for housing leverage: one-quarter of the sample reported having been told that their access to housing was contingent on cooperating with treatment. There was little evidence that lifetime experiences of leverage made a difference to patients’ perceptions of the coerciveness of their recent care in general. They were equally balanced between rating their experiences of leverage as more coercive or as less.
From our qualitative work with patients, a distinction emerged between leveraged and non-leveraged pressures. We produced a patient-derived concept of leverage, based on the presence of: conditionality, a lever and the perceived power of the agent to bring about the stated consequences. Studies of community mental health patients rarely consider how the broader context of patients’ lives influences their medication practices or how they perceive mental health professionals’ attempts to influence these practices. The sociocultural environment in which patients’ attitudes develop and characteristics come into play is also often overlooked. Our analyses extend the understanding of leveraged and non-leveraged pressures in relation not only to treatment adherence, but also to other aspects of patients’ mental health and well-being. We also identified that patients may experience pressure related not only to their medication but also to wider aspects of their well-being and social roles. These pressures were situated in the complex sociocultural contexts of individuals’ lives and were placed upon them by health professionals and family friends but also by themselves.
For professionals, an ideal model of the therapeutic relationship in which courses of action might be negotiated with the patient was shown to come into conflict with a model of professional authority drawn on when acutely unwell patients refuse services. There were remarkable similarities between the kinds of informal coercion described by patients and mental health professionals. Albeit presented and evaluated in different ways by the two samples, the types of pressures reported concurred. Both groups described pressures to engage in treatment as well and to stay well more generally, with the aim of achieving long-term stability. Both groups also emphasised how patients’ previous experiences may lead them to perceive influence as coercive.
On the basis of the qualitative work conducted here, we also undertook a conceptual and ethical analysis of informal coercion in community mental health care, and from this analysis produced ethical guidance for professionals. This emphasised, above all, the degree to which using informal coercion ethically is a nuanced process, contingent on patients’ individual circumstances and the context in which both parties operate.
Levels of leverage and clinical groups
Leverage in our Quantitative Study relating to the four predefined categories (finance, housing, criminal justice and child access) varied considerably across the four groups within the whole ULTIMA sample.
Although individual mental illness diagnoses did not demonstrate significant associations with rates of leverage in the multivariate analyses, the broad clinical samples certainly did: the younger substance misuse group reported the highest level of leverage, even higher than in the whole US sample (63% compared with 51%). Levels of leverage were lower in the psychosis groups but lowest in the CMHT-non-psychosis group, reflecting the relative severity of illness in these groups.
Housing leverage, reported by one-quarter of our sample, was substantially higher in the substance misuse group (44%), presumably reflecting the practice of many landlords (both private and public sector) of demanding attendance at drug programmes as a condition of tenancy. The 20% rate found in patients with psychosis represents the treatment requirement for access to hostel and supervised accommodation.
International differences in leverage
The level of leverage reported here, although significant, was substantially lower than that reported in the USA (35% vs. 51%7), even for the most commonly reported leverage in our study, related to housing (24% in our sample vs. 32% in the US sample). The difference between the two would have been even greater if we had removed child access leverage, which was not reported in the US study7 (although it has been reported subsequently from the same sample213). This would have reduced the overall leverage of the English cohort to 31%. This level was very close to that found by a study of the same types of leverage conducted in Switzerland (29%). 241
Compulsion in the community was available in the USA during the Monahan study (‘mandated outpatient commitment’, equivalent to CTOs in England) and was experienced by 12–20% across the US sites. 7,286 Community compulsion was not available in the English context at the time of the ULTIMA Study and thus was not studied here; the US data on compulsion were not included in our comparison. Although it had no direct impact on the leverage figures reported, this does alert us to important differences in service context between the two jurisdictions at the time of the ULTIMA Study.
The most striking difference between the two national samples was in the use of money as a form of leverage. Over half of the US sample (n = 519) had a financial guardian or someone unofficially managing their money. Of these, 121 (32%) patients reported that receiving it had been made dependent upon their accepting treatment. In the English sample, 165 (40%) reported that they had someone managing their money but only 10 (6%) reported financial leverage. Money management remains a controversial issue in England and few teams use it or feel comfortable with it. Half (n = 5) of those reporting it as a form of leverage were in the substance misuse group and this may have been perceived as coming from families, as the clinical teams did not use it. Some AOTs in England are experimenting with its use. 28
The US has a highly developed system of ‘drug courts’ and, more recently, ‘mental health courts’220 dedicated to trying and sentencing individuals with behavioural and mental health problems. England does not have such a system but utilises a range of court diversion schemes whereby individuals are identified pre-trial and diverted into the health-care system. There is a risk with the English patients that they may not fully have registered that they were being diverted. In the USA, by contrast, the coercion is explicit in the sentencing procedure: ‘choose treatment or punishment’. In England, the patient is more often encouraged to seek treatment and the diversion nurse or psychiatrist then advises the court, which may agree to drop the case. In many cases (especially where the patient is acutely unwell), the patient may never even enter the court and face the judge or magistrate. It is thus possible that there were patients in the English sample who were subject to the equivalent of US criminal justice leverage in this less formal way, but failed to register it.
The differences we found between the English and US samples seem to reflect the very different approaches to social supports and welfare benefits in the two countries (as an international symposium on coercion involving the Monahan group and some of the OCTET Coercion Programme Group repeatedly highlighted). The European perspective is one characterised by a pervasive belief in the so-called entitlement of disabled individuals to a wide range of social benefits (e.g. housing, financial support). In the USA this is less likely to be an automatic entitlement and targeted where it is likely to do most good. The patients in the US study7 were, however, generally in receipt of these benefits and it is possible that higher rates of leverage in that study may reflect the more widespread sense of entitlement in the English sample rather than any higher actual leverage in the US sample.
Such contrasts may mean that some leveraged pressures may be viable in one context and not in another. In England, for example, it is unlawful under the Welfare Reform Act 2009287 for social security benefits to be made contingent upon acceptance of treatment. English and other European citizens have welfare entitlements independent of their mental health status241,288 in contrast with Canadian citizens,289 for example. In the USA, meanwhile, the use of leverage is described without question. 34,290 Furthermore, to threaten detention to induce patients to consent to hospital admission or treatment is prohibited by the English MHA Code of Practice. 48 Nevertheless, although prohibited, both patients and clinicians will be aware that statutory powers can be invoked, with subsequent consequences for patients’ legal status, rights and freedoms. This awareness feeds into a ‘coercion context’,250,291 an idea we discuss further below (see Informal coercion in the context of patient–professional relationships). According to the criteria emerging from the ULTIMA Qualitative Study (also discussed below; see A patient-derived concept of leveraged and non-leveraged pressure), this would amount to a form of non-leveraged pressure, on account of its unspoken and indirect nature.
Leverage and patient characteristics
Table 65 summarises the findings of our primary and exploratory analyses.
| Leverage | Main analysisb | Replication analysis | Combination | US study7 |
|---|---|---|---|---|
| Housing | None | Substance misuse (4.4) | Independent accommodation (0.4)c Substance misuse (4.5) |
Male (1.59) Substance misuse (0.64)c BPRS (1.43) GAF (0.66)c Hospitalisations (2.93) Outpatient visits (1.49) |
| Financial | None | None | None | Age (older less likely, 0.61) Psychotic disorder (1.62) Substance misuse (1.97) Insight (above median less likely, 0.55) Hospitalisations (1.97) |
| Criminal Justice | White ethnicity (0.1)c | White ethnicity (0.2)c | White ethnicity (0.02)c Living alone (0.02)c |
Age (0.53)c Male (1.59) Substance misuse (1.93) Psychiatric hospitalisations (1.85) Years in treatment (1.65) |
| Child access | None | Age (0.4)c More than two hospitalisations (7.0) |
More than two hospitalisations (6.9) | NA |
| Any leverage | Substance misuse (5.7) More than two hospitalisations (2.8) Insight (2.0) |
Substance misuse (8.3) More than two hospitalisations (3.2) Duration of psychiatric history Insight (1.9) |
Substance misuse (6.0) More than two hospitalisations (3.1) |
Age (0.65)c GAF (0.62)c Hospitalisations (2.89) Time in treatment (1.43) |
| More than one | Independent accommodation (0.5)c Substance misuse (3.0) Imprisonment (2.4) |
Substance misuse (12.5) | Substance misuse (9.0) Imprisonment (3.0) |
NA |
The only patient characteristics significantly associated with reporting any type of leverage according to our primary analysis were having a substance misuse diagnosis, having experienced more than two hospitalisations and better insight. Our exploratory analyses also suggested an association between reporting any leverage and having a longer duration of psychiatric history and more previous hospitalisations. In the US study,7 reporting any type of leverage was found to be associated with more factors, possibly because of their larger sample and greater clinical variation: being younger, having poorer functioning, having had more hospitalisations and having spent longer in treatment. This was a similar picture in terms of a broad definition of long-term illness and poor functioning. When examining variables associated with reporting more than one type of leverage (not tested in the US study7), we found this to be associated with not living in independent accommodation, substance misuse and having ever been imprisoned. The exploratory analyses also suggested associations with substance misuse and imprisonment.
When examining variables associated with each of the four types of leverage, our primary analysis found no variables to be associated with housing, financial or child access leverage. The exploratory analyses suggested associations between housing leverage and substance misuse diagnosis and not living in independent accommodation – and between child access leverage and age and having had more than two previous hospitalisations. The primary analysis found only ethnicity to be associated with criminal justice leverage, whereas the exploratory analyses supported this and also suggested an association with not living alone.
Overall, then, leverage was most likely to be associated with factors linked to poorer functioning and longer history of illness (such as substance misuse, previous hospitalisations, poor social functioning or not living independently). Having ever been imprisoned more than doubled the likelihood of reporting more than one type of leverage, although having had a criminal conviction did not. A history of imprisonment was not associated with criminal justice leverage, as might be expected, but ethnicity was: those who were non-white were 10 times as likely to report criminal justice leverage. This striking finding may reflect the realities of the criminal justice system. Having children aged < 18 years, particularly if in regular contact or living with them, made patients more likely to experience leverage overall. Having better insight into and attitudes towards illness also made reporting any leverage more likely: a somewhat surprising finding, which was in contrast with the US study. 7
Leverage within the mental illness groups
Because the substance misuse group was so different from the three mental illness groups in our study, we repeated our analyses for the mental illness groups combined (something not done by the US study7). The homogeneity of this mental illness group allowed for more patient characteristics to emerge as significantly associated with different leverages; although our findings for financial and criminal justice leverage did not change when only the mental illness group was included, housing leverage and child access leverage were associated with different variables in these analyses. Some of these findings are not easily interpretable and would need to be pursued further through theoretical work and a priori testing.
Patients in the mental illness group were more likely to report any type of leverage if they had children aged under 18 years, were not living in independent accommodation, had schizophrenia (compared with major depression), had had more previous hospitalisations and had better insight. They were also more likely to report more than one type if they had children aged under 18 years. For those who had children aged under 18 years, having contact with the children less frequently made them less likely to report child access leverage. Those who did not live in independent accommodation and had poorer functioning were much more likely to report housing leverage: this is to be expected as poorer functioning is likely to be associated with a need for supported housing. The same was true for those who had spent more years in education, a finding that is less easy to interpret.
Perceived coercion
There was little evidence that patients’ experience of the four types of leverage investigated here had much bearing on their perceptions of the coerciveness of their care in general, as experienced in the 6 months prior to interview, or on their perceptions of the fairness or effectiveness of the treatment pressures they had experienced. Our focus was on lifetime experience of leverage and on perceived coercion, fairness and effectiveness in the previous 6 months. This is unlikely to have accounted for the lack of association, however, as when patients were asked to identify the specific leverage or leverages they reported against a continuum of coerciveness from persuasion to compulsion, they were equally likely to identify these experiences as being at the more benign, less coercive, end of the spectrum than the more coercive end. These findings contrast with those of the Swiss study241 that perceived coercion was associated with leverage experience, although the authors also noted that ‘the relation between perceived coercion, fairness and effectiveness appears to be more complex’ than this finding suggests. Our results seem to bear out those of our Ethical Analysis: that distinguishing between a threat and an offer, or judging the degree of coercion involved in an offer, is a complex matter – as much for patients as for mental health professionals – and owes a great deal to individual circumstances and context.
There were, however, some indications of which groups of patients were more likely to rate their care as more coercive, although the magnitude of most of the associations found was small. Patients tended to perceive their care as more coercive (with higher perceived coercion, more negative pressures and feeling that they had less of a say in their care) if they were less satisfied with services, had poorer therapeutic relationships and were more negative about taking medication. They also perceived their care as more coercive if they had had involuntary hospitalisations, lived in supported accommodation or were homeless and were non-white; they tended to prefer not to be involved in decision-making or have information about their treatment shared with them. By contrast, patients tended to regard any treatment pressures that they had experienced as more fair and more effective if they had better therapeutic relationships and satisfaction, and were more insightful, and also if they had had fewer past hospitalisations and fewer outpatient visits.
A clear picture thus emerged of patients regarding their care as less coercive, fairer and more effective when they were more satisfied with services and were more positive about the relationship with their care coordinator, although no direction of effect can be inferred from our findings. Similarly, patients who experienced housing leverage were also likely to regard the housing leverage as more coercive if they were less satisfied with services. They were also likely to regard it as more coercive if they preferred to be involved in decision-making and were older. By contrast, those experiencing criminal justice leverage were more likely to regard it as more coercive if they had had a higher number of outpatient visits, suggesting that for this group, more contact with the outpatient service was perceived as more coercive.
A patient-derived concept of leveraged and non-leveraged pressure
The use of conditional proposals among mental health professionals has been described as the provision of ‘contingent support’. 208 The empirical literature, however, either describes different types of pressure in isolation from one another or conflates them without an overarching conceptual framework that would capture the distinctions between them. For example, the work of Monahan et al. 7 deals exclusively with ‘leveraged treatment pressures’; the study by Angell et al. 206 includes only ‘treatment pressures’ and does not distinguish clearly between leveraged and non-leveraged pressures. Neale and Rosenheck’s208 description of ‘therapeutic limit setting activities’ captures what we call leveraged and non-leveraged treatment pressures and stay well pressures, but is limited to mental health professionals in the USA.
The ULTIMA Qualitative Study suggested that leveraged pressures can be distinguished from other types of pressure on the basis of three particular characteristics (see Box 7): conditionality, a lever and the perceived power of the agent to bring about the consequences. This definition significantly extends the scope identified in the literature.
Our definition of leveraged pressure includes the pressure to adhere to treatment and to stay well. Although the goals of leverage have been described as including adherence to broader social acts,234 only leveraged treatment pressures have thus far been studied. Our analysis has shown that patients experience leveraged and non-leveraged pressure in relation to other aspects of their mental health and well-being, not just treatment adherence. Moreover, pressure is applied by a wide range of individuals from within but also beyond the mental health team. With one exception,292 the literature to date only focuses on pressure applied by mental health professionals.
Our definition of leveraged pressure also captures pressures described in the literature that are not identified as leverage. Our analysis suggests that these pressures, such as ‘positive pressure’ (e.g. emotional bonds, reciprocity, information provision), rewards or incentives, freedoms (e.g. taking medication unsupervised),206 ‘contingent support’ (e.g. the offer of help finding employment contingent on medication adherence) and ‘informal coercion’ (e.g. threat of involuntary hospitalisation)208 have the potential to be classified as leveraged pressures. Although only provisions related to housing, child access, finances or criminal justice have been described as levers in the literature, we thus identified a much wider variety of levers in patients’ accounts, including, for example, access to, or discharge from, services or reinstatement of a driving licence.
We also identified various non-leveraged pressures. Our analysis of patient experiences suggested that non-leveraged pressures arise not only via interpersonal interactions, but also from social expectations (patients’ understanding of ‘how things ought to be’) or transmitted through the experience of fellow patients. They include non-conditional pressure (pressure without consequences) and simple predictions of consequences. Our findings are thus in line with Szmukler and Appelbaum’s204 view that the element of conditionality adds another (potentially coercive) dimension to the kinds of proposals made to patients by clinicians. Szmukler and Appelbaum204 suggest that without conditionality such proposals simply amount to what they term ‘unwelcome predictions’ (e.g. where a clinician predicts that by ceasing to take medication, a patient will jeopardise their accommodation). In the absence of conditionality, such unwelcome predictions may be experienced as non-leveraged pressure.
The conceptualisation of the various types of pressure experienced by patients is important because it gives professionals and researchers a more rounded picture of what drives patients’ behaviour. Although we have paid close attention here to patient–professional relationships, our analysis of patients’ medication practices suggested that these are also situated in the wider social context of their family, employment, financial and housing circumstances; the mental health system and their team; their observations of others; and their past experiences and future expectations and concerns. We conclude that taking the situatedness of patients’ medication practices into account may offer fresh insights into why patients do or do not take their medication as prescribed.
Informal coercion in the context of patient-professional relationships
Current mental health policy is focused on community care and encourages patient-centred approaches. 147 Relationships are envisaged as mechanisms for mental health service delivery. 146,203 To the extent that mental health professionals are involved today, more than previously, in the private spheres of patients’ lives, deinstitutionalisation might be viewed as having changed not only the locus of care, but also, arguably, the relationships and interactions between mental health professionals and patients. 30,204 Our study of community mental health professionals highlights some aspects of how they conceptualise these interactions, which, in turn, help us gain a better understanding of their practice.
Mental health professionals’ emphasis on the importance of their relationships with patients was a recurrent theme in the focus groups. This has also been, as described above (see Part 4, Chapter 17), a central feature in the discourse on mental health services. 30,147,245–248 The focus group participants clearly stated that they wanted patients to adhere to treatment and look after their social, physical and mental well-being (i.e. to stay well). To facilitate this, the professionals attempted to build good, trusting relationships, which were perceived as a prerequisite to establishing reciprocal agreements and, through that, patient-centred care. This resonates with patients’ descriptions of pressure from professionals to stay well, as well as to adhere to treatment.
In practice, however, professionals suggest that they may need to assert their professional authority in these interactions when acutely unwell patients refuse services, presenting this as a necessary tool, albeit one with the potential to threaten relationships. In this context, they presented themselves as having a unique overview over what constituted patients’ best interests and, occasionally, an obligation to act against patients’ wishes. As a consequence, they described interactions occurring in a context that might evoke perceptions of coercion that would affect, and sometimes threaten, the very relationship that was considered a prerequisite for patient-centred care. This represents two overarching – and potentially conflicting – processes by which professionals sought to influence patients: one based on engagement facilitated by reciprocal relationships and one based on professional authority.
The first process of reciprocal relationships touches on a central feature of sociological theory, which is rarely applied to the study of community mental health services. This involves the understanding that the giving of gifts (material or symbolic) creates obligations in recipients to accept and reciprocate. Such universal reciprocal mechanisms are thought to constitute the foundation of relationships, feelings of community and trust. 293–295 Øye249 suggests that creating bonds and alliances with patients has always been a central feature of psychiatry, and applies this notion of reciprocity to an analysis of interactions on an inpatient ward. She describes how hospital ward staff sometimes provide services or favours that extend beyond their professional duties, such as giving patients cigarettes or staying on after their shift to provide support. These ‘gifts’ create expectations, she argues – among staff and patients alike – that patients will participate in the therapeutic activities offered. Many of the influencing behaviours identified in the literature (see Part 2, Chapter 5: Box 4) and in our data rely on similar reciprocal expectations.
Forming relationships that create reciprocal obligations in patients who are reluctant to take treatment might, on the face of it, appear manipulative. If, however, reciprocal obligations are inherent in all social relationships, this might simply tell us that the relationships between mental health professionals and patients rely on the same social mechanisms as most others. The context of deinstitutionalised services means that traditional boundaries between professional relationships and friendships become blurred (e.g. when giving practical assistance in the home205). The deinstitutionalised nature of the services provided by mental health professionals participating in our study thus arguably provides wider scope for initiating reciprocal obligations than the hospital setting because interactions occur across a broader range of arenas in patients’ lives, including those that are private, domestic, social and familial.
The second process relates to how reciprocity works in a context where one party ultimately holds authority to compel the other. This makes them unlike many other social relationships and, arguably, ones where reciprocal exchange cannot be balanced. 249 Although professionals in our study emphasised their efforts to negotiate ‘fair’ solutions, the reciprocal dimension to relationships between professionals and patients with severe mental illness differs from many other social relationships with regard to at least two inherent power dimensions. First, one party is employed to create a professional (i.e. not personal) relationship with the other (whether or not the other wants this) which, as shown, extends into the private sphere of the other’s life. Second, one party may compel the other if needed. Sjöström250 describes how the latter power differential forms part of the context surrounding these relationships. In an analysis of interactions in a psychiatric ward, he shows how clinicians might (consciously or not) evoke a coercion context on the basis of patients’ previous experiences. A patient who has been under compulsion a number of times, for example, might interpret a statement of how he or she ‘must’ or ‘ought to’ do something differently from patients without this experience, even at times when treatment is voluntary (i.e. not legally mandated). As we have argued above, in community care, simple predictions of how compulsion might become necessary might similarly evoke perceptions of a coercive environment.
Our data indicate that mental health professionals perceived that these power dimensions in some cases permeated their interactions with patients. Their professional authority was acknowledged as giving them an ‘advantage’ in negotiations and stood in contrast to their expressions of an ideal, more balanced, professional–patient relationship. According to mental health professionals, the awareness of the possibility of compulsion could therefore be enough to undermine trust, and subsequently threaten patient-centred care and recovery. This has also been reported by patients receiving community care. 296 Perceptions of services as coercive might be a barrier to people seeking care, as suggested by recent studies of CTOs. 210,297 Our analysis has shown that this coercion context, in addition to the effect on patient experiences as reported by others, forms part of how professionals conceptualise their role and produces potential conflicts between the inherent care and control aspects of that role.
This dual focus on patient-centred approaches and professional authority is accepted as a core part of service delivery. It is, however, understood by professionals as having the potential to undermine their interactions with reluctant patients. Our findings highlight how subjective experiences are central to understanding the micro-level dynamics of clinical encounters and how they impact on, and are influenced by, the implementation of policy. Given that current mental health policy gives a central role to therapeutic relationships, the conceptualisation of these relationships by professionals found here – namely, their awareness of a profound tension between a patient-centred, reciprocal model and the authority context in which they operate – highlights the very real difficulties they face in implementing such policy.
Ethical implications of informal coercion
Our study has also shed light on the range of positions in which professionals find themselves, ethically, in their relationships with patients, particularly when patients refuse their intervention. We have set out a framework for judging the ethical status of an offer. This framework does not provide an algorithm, but it does provide mental health professionals with a practical tool for making decisions. Because the normative considerations that are salient within this framework are generally those with which professionals are familiar (professional duties of care, foreseeable consequences and decision-making capacity), such a framework is likely to be useful for the practice of community mental health care. The judgements that need to be made require considerable understanding of the patient and they will often best be made after integrating information from several sources. The case conference might be an appropriate setting within which this framework is applied. It is important to recognise, however, that this framework will need to be applied pragmatically in view of the available evidence and must be subject to continual reassessment as the contextual factors relevant to making judgements about each step within the framework change.
We have also outlined four ethical duties underpinning community mental health care, which are relevant to making ethical judgements about the use of informal coercion: to benefit the individual patient; to benefit other individuals; to treat patients fairly; and to respect patients’ autonomy. The practical requirements that follow from these duties for the acceptability of specific acts of informal coercion have also been considered. Professionals must determine whether or not the use of informal coercion will involve care being provided in ways that are consistent with the requirements of these duties, regardless of whether the patient accepts or rejects the terms of the proposal. Although informal coercion is widely used within community mental health care, the complexity of clinical practice means that a judgement about whether a particular instance of informal coercion is right or wrong will not be straightforward. Instead, informal coercion, as a mechanism for attempting to influence patients’ behaviour, can be considered to be ethical only once the professionals have reasoned through the four duties (see Chapter 20), in view of the patient’s individual circumstances.
None of these four duties can be determined a priori as overriding, and all ought to be given due consideration. As with the framework for judging the ethical status of an offer, it is helpful to conceive of this process of making ethical judgements not as an algorithm for decision-making, but as a process akin to that of conducting risk assessments. Although informal coercion could be used unethically, because these decisions are in clear violation of one or more of the relevant duties, it is also possible that more than one course of action may be ethically defensible.
Notwithstanding this observation, a number of difficulties associated with translating the four duties into the decision to use informal coercion remain. First, professionals will need to ascertain how the specific requirements of each duty relate to each decision about informal coercion that they make. This is particularly challenging because we have identified competing accounts of the relevant considerations required to act in line with each duty. We have shown how the ethical duty to benefit a patient, for instance, differs depending on how patient benefit is conceptualised. Mental health professionals also need to consider the weight they give different kinds of outcomes. In particular, the comparative importance of subjective quality-of-life outcomes and objective social and biomedical outcomes (such as expected reductions in symptoms and increased involvement in employment or community activities) will need to be weighed up in the decision-making process.
Second, mental health professionals will have to make judgements between duties when these pull in opposing directions. It is possible that an ethical assessment of a particular instance of informal coercion concludes that it will probably lead to significant improvements in the patient’s health and well-being, but also result in other patients receiving fewer resources and an extra burden being imposed on the patient’s carers. Alternatively, the identified clash might be between clinical evidence, suggesting that informal coercion will bring benefits to the patient and others, and such an action failing to respect the patient’s autonomy. Should informal coercion be used in such situations? There are no straightforward answers to such questions and professionals will need to weigh up the comparative importance of particular duties in their professional setting, given the specific details of the situation in question.
Finally, there is a tension between conceiving of informal coercion as a single, isolated proposal for the purpose of ethical assessment and the fact that such a proposal will most often be part of a multifaceted and ever-evolving package of care. Although we do not advocate dissecting every care management decision made for patients within practice settings, it is important for mental health professionals to be attuned to how changes to patients’ care and treatment plans might amount to attempts to leverage patients in ways that are not ethically justified. Ethical analyses of acts of informal coercion may be undertaken beforehand, or as part of a post hoc review of a case.
Clearly, the process of making ethical judgements that we have outlined here should be done in a flexible and pragmatic manner, as a patient’s circumstances change or new evidence about the wider consequences of the use of leverage comes to light. Careful thought must be given as to how the assessment of informal coercion will take place in practice and how this assessment can be incorporated into service audit. We believe that, again, the case conference or team meeting is an appropriate setting in which such judgements can be made productively by professionals.
Intervening with severely ill groups
In the mental illness groups in the Quantitative Study, leverage rates were associated with increasing severity of illness. Mental health professionals are likely to intervene more robustly when faced with patients who are more severely ill. Similarly, mental health professionals reported in the Qualitative Study that they felt obliged to draw on a more authoritarian model when dealing with patients who were relapsing but refusing their services. The high levels of leverage in substance misusers may reflect a tougher negotiating approach to individuals generally perceived to have more control over their behaviour.
Both patients’ and professionals’ perceptions about and experiences of informal coercion may have implications for the therapeutic alliance. 210 We have highlighted the broad range of treatment pressures experienced by patients as additional, potentially competing demands. Professionals’ exploration of these with patients might help strengthen the therapeutic alliance. We found in our Quantitative Study that patients were likely to perceive their relationships with care coordinators and services as a whole as being poorer when they also felt more coerced; our Qualitative Study findings also showed that interactions not intended to be pressurising by health professionals may be perceived as such by patients, an observation also made elsewhere. 204,208 This is borne out by the finding of the Ethical Analysis that for an act of leverage to be ethical will depend on a range of individual and contextual factors in each situation.
This reiterates the importance of ensuring that information is understood correctly in therapeutic interactions. 298 An improved understanding of these different pressures could also contribute to the development of guidelines and safeguards to ensure that pressure is not applied inappropriately or unlawfully. Mental health professionals also highlighted a fundamental conflict, however, in that the perceived need to draw on their professional authority when faced with patients refusing treatment may be at odds with the notion of a trusting therapeutic and patient-centred relationship.
Limitations
ULTIMA Quantitative Study
The ULTIMA Quantitative Study had several limitations. In collecting types and levels of leverage from patients, it reported experience of leverage without third-party corroboration. Some of the leverages reported would probably have been disputed by the clinicians. Many mental health professionals may strive to recast leverage as persuasion, that is, to move it towards the less coercive end of Szmukler and Appelbaum’s continuum. 204 Leverage may also sometimes have been applied (particularly in court diversion schemes) but not recognised as such.
We were obliged to use differing sampling strategies for the different teams in the Quantitative Study, but it is unclear what effects this may have exerted. Our refusal rate was more than twice that in the US study sample7 (31% compared with 2–15%). The reasons for this are unclear. Although the direction of any potential bias is not obvious, it cannot be discounted that patients with higher levels of leverage may have been more likely to refuse, thereby reducing the reported English levels.
Higher levels of leverage were demonstrated to be associated with acts of violence (18–21% in the preceding 6 months) in the US sample. 299 In the absence of comparable violence data in the English sample, we cannot estimate whether or not it might have accounted for the reported leverage differences.
We did not collect data about patients’ actual treatment adherence, and are therefore unable to comment on whether or not this was affected by the pressures they perceived. To make any claims as to the efficacy or effectiveness of the informal coercion we describe here is beyond the scope of this study. Our aim, however, was to understand the range of pressures experienced by patients and how these relate to the narrower concept of leverage already defined from the professional viewpoint in the international literature.
ULTIMA Qualitative Study
The use of patients’ recollections and interpretations of complex interventions in the ULTIMA Qualitative Study might be seen as a potential limitation. Nevertheless, it has enabled us to see that from a patient perspective, the pressure from mental health services to engage with treatment is only one of a number of pressures that they face. This approach has also permitted insight into the range of pressures experienced from within and beyond mental health services, all of which may shape patients’ interactions with mental health professionals.
The ULTIMA Qualitative Study was based on relatively small samples and limited to one NHS trust; patients and professionals from other areas might have different experiences. The pressures reported here are, however, similar to those identified elsewhere (see Part 4, Chapter 19: Box 4). A strength of the focus group study was the multidisciplinary nature of the sample, which facilitated analysis of team-based service delivery, in line with current practice. Although individual participants’ professions meant that their practical interactions with patients differed, we found no systematic differences between professional groups as to how they conceptualised their relationships with patients. Given our design, however, we cannot conclude that these do not exist, and because varying levels of authority are vested in different professions, we recommend that this be a focus for future studies. A strength of the interview study with patients was how it used the ULTIMA Quantitative Study sample as a sampling frame, which ensured that patients in the Qualitative Study had experienced a range of experiences of leverage and different types of services.
Data collection for patients was undertaken before CTOs had been introduced in England and Wales, and the focus groups with mental health professionals were held when they had been in existence for only a few months. This would account for why the use of community compulsion was largely absent from the data.
As explained above, the nature of qualitative work means that many strands are available for analysis. In the analyses presented here, we deliberately focused on experiences of informal coercion, although the patient narratives also included examples of supportive and non-pressurising service delivery. Similarly, our focus on reasons for medication adherence excluded perspectives on non-adherence and the focus on relationships, negotiations and authority from the professional perspective did not include the strong concern with promoting independence that was also a common theme in the group discussions. These further analytical strands will be pursued after the programme grant period.
Conclusions and implications
The patterns of reported leverage in the English and US samples were, despite some differences of interest, more similar than different. Our findings, as well as the US ones, clearly indicate that a substantial proportion of individuals in public mental health care do not feel entirely free in their interactions with services. Although some pressure comes from family and friends, many experience mental health professionals as coercing them. These findings may also have implications for the concept of consent to treatment, as the MHA Code of Practice states that permission given by patients ‘under any unfair or undue pressure’ does not amount to consent.
It cannot be simply assumed from our data, however, that our patients disapproved of informal coercion. The literature indicates that patients may judge their coercion, whether formal or informal, to be either wrong or right in hindsight, and even that they can judge it as ‘wrong’ but helpful. 300 This may be seen as being borne out by the lack of evidence in our study that experiences of leverage made much difference to patients’ perceived coercion. Indeed, there was some suggestion that for those reporting child access leverage, the more coercive they regarded the leverage to be, the more effective they also believed it to be. Although not analysed yet, there was also a suggestion in the qualitative data that some patients did find some pressure helpful in some circumstances. (The analysis of these data will be presented in future publications.)
Many of the types of pressure explored in the ULTIMA Qualitative Study are worthy of close inspection, given that they are unmonitored and unregulated, potentially leaving patients without legal recourse regarding their human and social welfare rights; and that European human rights legislation ‘fails to capture much of the coercion experienced by patients in practice’. 301
Part 5 OCTET Coercion Programme: impact and dissemination, discussion, conclusions and recommendations
Chapter 22 Impact of the OCTET Trial
From the outset there was considerable interest in the OCTET Trial. We presented the trial design and hypotheses at close to 100 conferences and seminars during the preparation and recruitment period (see Chapter 23 and Acknowledgements, Dissemination of the OCTET Programme). Although some questioned the need for a trial (either because they were convinced that CTOs would have clear benefits or because they had no faith in them), most of these audiences were supportive of the need to test CTOs. All responses underlined the need for conducting a trial. The participation in our annual CTO conferences (see Chapter 23 and Appendix 4) showed a demand for obtaining information about how CTOs work and for sharing experiences in how they were used in the period shortly after their introduction.
Since the Trial results were published in The Lancet in March 2013,16 there has been considerable interest in the UK and internationally. The Trial has been reported in more than 20 newspapers, magazines, websites and newsletters either based on that publication or on interviews with the Principal Investigator, Professor Tom Burns. We have been invited to present our findings to practitioners, policy-makers, service users and academics. So far, we have given 67 presentations on the findings from OCTET (the Trial and the Qualitative and Capabilities Project substudies) in 22 different countries, and we have been invited to write several expert reviews of the CTO literature. 18,66,302,303 We have met with the Department of Health to discuss the implications of the research in the UK, and, recently, the report on the post-legislative scrutiny of the MHA 2007, published by the House of Commons, recommended that current use of CTO should be reviewed in view of the OCTET Trial results. 304
The OCTET Trial findings have also created some controversy. So far, we have been made aware of eight published letters to the editors of academic journals305–311 (including four in The Lancet) and three published articles312–314 that have sought to criticise the trial on methodological grounds. These criticisms usually revolve around the representativeness of the sample and the effect of protocol violations, and there has also been some misunderstanding of the nature of the control condition (leaving hospital via Section 17 Leave). We believe that we have given robust answers to these criticisms315–318 as we discuss below (see Chapter 24). The OCTET Trial publications are also, however, being cited as representing a rigorous study of CTO effectiveness. The article in The Lancet was recently listed as second of its top 10 psychiatry papers in 2013, and also awarded the prize for the best article in 2013 by the Norwegian Network on Acute Psychiatry.
Chapter 23 Dissemination, wider impact and capacity building
Publications and presentations
The OCTET Coercion Programme has to date produced 26 published papers and others are in preparation. It has also given rise to an edited book,319 reflecting international perspectives on community coercion. We have presented studies from the Programme, particularly the OCTET Trial, 109 times to date, including at nearly 100 conferences (see Appendix 4).
Organised events
We organised a series of OCTET conferences, held annually. These were attended by interested clinicians, including those involved in the trial, and were attended by up to 90 people each time (see Appendix 4). One member of the OCTET Coercion Programme Group (Dr Andrew Molodynski) is chairperson of an international working group on coercion for the World Association of Social Psychiatry, in which two other members of the group (Dr Jorun Rugkåsa and Professor Tom Burns) are also involved. The group has its own web page, and aims to promote education and awareness and provide links for researchers, clinicians and users of services.
Replication studies
The ULTIMA study is currently being replicated in New Zealand, India, The Netherlands, Hong Kong and Italy, with a further study being developed in Norway. One replication study, in Switzerland, has already reported its findings. 241
Commentaries and discussion
The OCTET Trial in particular has been the subject of a number of commentaries and letters to journals; we detail this below (see Chapter 24).
Parliamentary discussions
The OCTET Trial was cited in a parliamentary discussion of supervised community treatment in the UK parliament. 320
Associated studies
The OCTET Coercion Programme has also generated a number of associated studies:
-
Three studies conducted for the award of the degree of Doctor of Philosophy at Oxford University:
-
‘Continuity of Care and Patient Outcomes in Community Mental Health’ (Stephen Puntis):321 The primary question of this thesis utilises the OCTET Trial sample to investigate, over a 36-month time period, the association between coercion, continuity of care and patient outcomes.
-
‘The associations of informal coercion with legal compulsion, clinical outcomes and the therapeutic relationship in community mental health care’ (Ksenija Yeeles):322 This study investigates the relationship of informal coercion with formal compulsion and with clinical outcomes. It also tests whether the therapeutic relationship acts as a moderator of the relationship between treatment under different duration of legal compulsion and patients’ perceived coercion.
-
‘Psychiatric compulsion and long-term social outcomes for patients with psychosis: is there an association?’ (Francis Vergunst):323 This study tests associations between the duration of compulsion and 48-month social outcomes measured, using social network size, social inclusion and capabilities.
-
-
An updated systematic review of CTOs. 67
-
A survey of psychiatrists’ views of CTOs in 201069 and a follow-up survey under way.
Chapter 24 Criticisms of the OCTET Trial findings
As mentioned above, the OCTET Trial has provoked a vigorous international debate with several published letters305–310 and even articles devoted entirely to critiquing it. 312–314 These critiques mostly revolve around the nature of the control arm, protocol violations, sample selection and the choice of primary outcome measure. These publications have offered an opportunity to clarify inevitable confusions arising from presenting such a complex trial in the condensed form required by The Lancet, and we have responded to most of these critiques in print. 18,315–318 The same concerns were presented in differing forms by several of the respondents and can be summarised as follows.
The use of Section 17 Leave as the vehicle for randomisation to the non-CTO arm was misunderstood as ‘an alternative community provision’, particularly by international readers. 305,306,308 As we have indicated above (see Part 2, Chapter 6), clinicians in the trial used Section 17 Leave as envisaged, for a median of 8 days. A number of correspondents305,308,314 confused the ‘total time under compulsion’ (which included both the randomised compulsion and the duration of compulsion in readmissions, i.e. both intervention and outcome) with the time under the initial compulsion of randomisation. Naudet and El Sanharawi307 questioned the appropriateness of an intention-to-treat analysis when there is a significant proportion of protocol violators. Others too have commented that the number of protocol violations was high. Our per-protocol sensitivity analysis removing protocol violations, the standard method for addressing protocol violations, did not alter the study findings. Naudet and El Sanharawi307 requested, and received, data on our violators to conduct an equivalence meta-analysis with data from all three RCTs, but the US triallists have not been able to provide these to date.
The sample selection and its generalisability have also been questioned, suggesting that it could have excluded the ‘clear’ CTO candidates who would benefit the most. 308–310,313,314 Because of our study structure, we are unable to comment on how our sample related to the total number of patients considered for CTOs within the collaborating trusts. We were, however, able to confirm that their clinical characteristics matched closely those in other published CTO studies and thus that they were not, as suggested, a highly selected low-risk group. 308,313 No patients were included who were not clear candidates for a CTO. 313
Following the first publication of our findings, two criticisms were regularly raised, particularly when OCTET was presented to clinicians. The first was a need for a wider range of outcomes beyond hospitalisation. The second was a concern that beneficial effects in some subgroups of patients might be masked by an absence of effect (or even a negative effect) in other subgroups. We have since examined both of these questions by analysing our tertiary outcomes and conducting a prespecified subgroup analysis, neither of which found any benefits from CTOs (see Part 2, Chapter 6, Results). Nor did the OCTET Economic Evaluation find any beneficial effect of CTOs on patient-reported outcome measures of well-being, such as health-related quality of life or capabilities.
Chapter 25 OCTET Coercion Programme overall discussion
The 2007 amendment of the 1983 MHA for England and Wales, and in particular the introduction of CTOs, provided a stimulus for examining the nature and effects of coercion in mental health. Most earlier studies had confined themselves to the extent and determinants of involuntary admission. This work, however, had demonstrated that the patient experience was far from clear-cut, and many voluntary patients experienced their care as coerced. Moreover, our preparatory review of the evidence found that the effect of CTOs on patient outcomes had not been demonstrated: indeed, the only two RCTs had failed to find a positive impact. We therefore undertook a programme of work to explore aspects of the extent and experience of community coercion, both formal and informal, in England, and to undertake the most rigorous possible RCT of the effects of the newly introduced CTOs.
ULTIMA Study
This study of informal coercion was conducted before CTOs were available to clinicians in England and Wales. It confirmed that leverage was extensively used in community mental health services. Over one-third of patients had experienced that aspects of their life (accommodation, benefits, legal consequences) had been made conditional on their cooperating with treatment, despite being in treatment voluntarily. We concluded that informal coercion is common and influential, but it is effectively invisible. Although it was not something we examined systematically, there was no anecdotal evidence of any consistent attempt to include knowledge about leverage, and how patients may experience it, in the training of mental health staff or in guidelines. We found that some patients had mixed feelings about informal coercion: many did not like it, but some did appreciate it in some circumstances and thought it probably helped them.
Our exploration in qualitative studies of staff and patient opinions indicated that the ethical debate was undeveloped. Individuals often had strong feelings about the issues but little shared framework with which to discuss them and come to any consensus about practice.
-
Further qualitative work is urgently needed to strengthen ethical and clinical understanding of informal coercion.
-
This qualitative work should investigate differences between different professional groups.
-
Investigations into variations in the extent and effects of informal coercion are needed. Has it been reduced now that CTOs are available? Does it have an association with outcomes such as hospitalisation or patient satisfaction with services?
OCTET Study
We were able to demonstrate that a trial of CTOs could be conducted lawfully and ethically, and, in practice, clinicians did not consider the structure of the trial to be problematical. The requirement to randomise through Section 17 Leave, however, did lead to confusion, particularly in our readers from outside the UK. It was often taken to imply that only a very narrow range of CTO candidates was included (which was not the case). To avoid this complication, we believe that approaches such as the staged introduction of legislation, which have been used in the USA, should be considered by jurisdictions introducing such legislation to allow for rigorous testing. 60
Our trial of CTOs found a resounding absence of effect in all outcome measures. This finding is fully in line with the two previous RCTs, although their authors have often sought to emphasise possible benefits from non-randomised secondary analyses. Not only was there no benefit in the primary and secondary outcomes (hospitalisation data), but also there was no evidence of subgroup responses or tertiary benefits in social, clinical and satisfaction outcomes, and there was no evidence that CTOs were cost-effective. Our analysis of the ethics of CTO use indicated that there was no general ethical justification for this. These very stark findings must put the continued high use of CTOs into question.
Not surprisingly, these very robust conclusions have resulted in widespread criticisms of the study. These have been of varying substance. No RCT is perfect but most of the substantive criticisms have been answered reasonably comprehensively. The strongest, persisting criticism is from clinicians who insist that their clinical experience or before-and-after audits should be given precedence. We have, however, noticed in our public presentations that the strength of this criticism is fading, as clinicians have now been using the CTO regime for more than 5 years.
Given the mixed results from before-and-after studies (controlled and uncontrolled), we do not believe that anything other than further RCTs, more robustly designed, can advance this field. Further trials would need to address three limitations in the OCTET Trial if they are to advance our understanding, as well as conduct extensive follow-up:
-
generalisability – all potential CTO patients in a recruiting site would need to be randomised
-
violations – some form of control would have to be introduced to prohibit crossovers
-
any further studies in the UK should restrict Section 17 Leave to the recommended 1 week
-
follow-up should be of at least 2 years.
Qualitative interviews with mental health professionals, patients and family carers failed to find a consensus view on the experience of CTOs. The range of opinions demonstrated confusion about the scope and power of CTOs. They also vividly confirmed the need for careful, structured research to assess outcome in such complex interventions: several clinicians commented on the ‘obvious dramatic improvements’ that they were seeing in their patients in the Trial, despite the objective evidence that there was no difference.
Community treatment orders impose a significant burden on clinical teams, with their complex bureaucracy and review process. This was set up deliberately to ensure that they were not simply resorted to for clinicians’ convenience. Our detailed cost analysis found no advantage of CTOs in hospitalisation costs and significant disadvantages in the increased costs of informal care and legal procedures, such as manager hearings and tribunals. In a trial with equal outcomes, the lack of significant cost differences would normally be considered a clear advantage to the intervention group. In the OCTET Trial, however, patients paid a significant ‘cost’ in their loss of liberty.
-
Mechanisms need to be developed to include consideration of such costs (such as loss of liberty) into future cost–benefit analysis.
The use of the new capabilities instrument, the OxCAP-MH, for measuring the broader well-being of mental health patients is a particularly fruitful outcome of the OCTET Study. Coercion, by its nature, constricts the individual’s range of choices and so a well-being assessment that pays attention to those aspects of their lives that patients value is clearly extremely relevant.
-
Further extensive testing and use of the OxCAP-MH would enrich research in this field and is currently ongoing.
OCTET Follow-up Study
In the lead up to the introduction of CTOs, patient advocacy groups expressed a grave concern that the emphasis on coercion would undermine trust and drive patients away from services, resulting in increased disengagement. We tested this in our 3-year follow-up study with two measures of disengagement: disengagement from services altogether and periods of interruption in care. This also provided us with an opportunity to test whether or not the randomisation to CTO or Section 17 Leave had any enduring effects on hospitalisation. It did not. Nor was there any strong evidence of disengagement in either group. At 3 years after inclusion in the study, well over 90% were still in contact with services and only 20 patients had gone through more than one period of disengagement. Analysis of the association of duration of community compulsion in the whole sample suggested a small increase in engagement with longer periods under compulsion.
NHS research and development processes
OCTET coincided with the establishment of individual NHS trust R&D offices. The overwhelming burden of inefficiency that these structures imposed on our multisite trial cannot be ignored. Despite the trial having been peer reviewed for funding, and having been subjected to a full research ethics committee approval process and a legal opinion, it was subject to a further round of scrutiny in most trusts. This took from 2 days in one trust to 11 months in another. Twelve of the trusts we approached either never completed the process or refused to allow us to approach clinicians. Despite our research assistants having research passports (which were introduced in order to reduce paperwork) issued by the host trust, many trusts insisted on them gaining equivalent approval and CRB clearance again. The figures speak for themselves: 607 letters of access, 56 honorary contracts and 51 CRB checks. There was no consistency in practice between trusts; each interpreted the regulations in their own idiosyncratic manner.
Even when we were granted access, the practices of local departments were highly variable, from the enormously helpful to the frankly obstructive. Some trusts, for example, insisted that our research assistants could not extract data from notes or computer systems but must sit next to their own R&D worker and have the data dictated to them; one trust insisted that we must approach the relatives of deceased patients to obtain information about their treatment. We believe that this represents an indefensible waste of public money, both in the duplication of unnecessary checks but also in the inefficiency it imposes on researchers. Such unnecessary procedures may have added up to a year to the process of completing our study. We are even more concerned that such frustration will deter researchers from undertaking multisite trials in the future. We believe that these procedures are in urgent need of clarification and simplification, with a clear understanding that peer-reviewed, funded and ethically approved research does not need further scrutiny at the trust level other than to determine whether or not the trust has the resources to engage with it. The assumption needs to be explicit that research is good for patient care rather than something patients should be protected from, which is an attitude we regularly encountered.
Where does the evidence stand?
The OCTET Coercion Programme has confirmed a growing body of evidence3,67 that both compulsion and informal coercion are widespread in modern mental health care. We have also shown that patients, psychiatrists and family carers do not experience a clear distinction between compulsion and informal coercion. Even patients who are notionally entirely voluntary often consider their real choices limited, so research in this area needs to consider the coercion contexts250 in which care takes place. A significant minority of voluntary patients experience their cooperation with services as being explicitly pressurised in one way or another, as the ULTIMA Quantitative Study demonstrated, although in some situations this may not be considered entirely negative, as our qualitative work indicated. The perceived benefits of community compulsion vary considerably between and among patients, family and clinicians, as the OCTET Qualitative Study made clear.
The majority of published research on CTOs is descriptive and unable to address whether or not CTOs are effective. 3 More recently there have been a number of cohort studies of CTO outcomes. These give strikingly contradictory results on whether CTOs reduce hospitalisation or affect other outcomes,67 and most suffer from serious, but differing, methodological limitations. 18
We have reaffirmed that it is possible to conduct an RCT that is both lawful and ethical. The OCTET Trial confirmed the findings of the only two previously published RCTs, which found no advantage in terms of any hospitalisation outcomes for CTOs, despite significantly limiting patients’ freedom. Moreover, no clinical, subgroup or cost benefits have been demonstrated in any of these trials. The current state of CTO research thus provides no evidence of any beneficial effects of CTOs. The absence of any ongoing RCTs with superior methodology and extended follow-up makes it difficult to justify their continued use.
Chapter 26 Conclusions
Our research programme has provided many new and valuable insights into the use of coercion in modern community mental health care and the impact of CTOs. We have explored and discussed its findings extensively in the discussion chapter of each study, as well as in the previous chapter (see Chapter 25). We have also discussed and addressed the various controversies to which the programme gave rise (see Chapter 22).
We now draw out four main conclusions with indications for further research.
-
CTOs do not deliver clinical, social functioning or well-being benefits for patients and the evidence is now sufficiently strong that in the absence of further trials, moves should be made to restrict or stop their use.
-
Informal coercion is widespread and takes different forms.
-
OxCAP-MH represents an important innovation in patient-centred research in this ethically very delicate area and we would recommend further use and testing.
-
NHS Trust R&D procedures require urgent attention and simplification if multisite clinical trials are to play a central role in answering difficult clinical questions.
Chapter 27 Recommendations
We are fully satisfied, from both the results of our own trial and the combined international research literature, that CTOs do not confer any benefits. It is clear, however, from the range of reactions to our programme of research described above, that not everyone accepts this and CTOs continue to be imposed regularly. We therefore suggest the most rigorous form of further testing, as indicated below. Further studies will either confirm the current position and strengthen the case for the abandonment of CTOs or provide sufficiently strong evidence to overturn the current understanding.
-
Given that all of the three RCTs and both systematic reviews and the meta-analysis find no benefits for CTOs, there is a case for clinicians to review their practice urgently and exercise extreme restraint in their use.
-
There is a case for further research into both the extent and the forms of informal coercion and leverage.
-
There is a case for further qualitative work to strengthen ethical and clinical understanding of informal coercion.
-
This qualitative work should investigate differences between different professional groups.
-
Further trials of CTO are needed, which should:
-
randomise all potential CTO patients in a recruiting site to increase generalisability
-
introduce some form of control to prohibit crossovers
-
conduct follow-up of at least 2 years.
-
-
Mechanisms need to be developed to include consideration of such costs as loss of liberty into future cost–benefit analysis.
-
Further extensive testing and use of the OxCAP-MH should be conducted to enrich research into broader well-being for those with severe mental health problems.
Acknowledgements
Acknowledgements
This project was funded by the NIHR Programme Grants for Applied Research (RP-PG-0606–1006) and will be published in full in Programme Grants for Applied Research Journal. The OCTET Trial was adopted into the UKCRN and Mental Health Research Network (MHRN) portfolios and registered with ISRCTN (ISRCTN73110773). Oxford Health NHS Foundation Trust, the programme’s sponsor, had no role in study design, data collection, data analysis, interpretation or writing of the report. The lead author had full access to all of the data and had the final responsibility for the report.
Thanks are due to the 853 patients, family carers and mental health professionals who were interviewed as part of the research programme; the many clinical teams and NHS trusts who were involved; and the Mental Health Research Network, who provided invaluable assistance during recruitment and follow-up for the OCTET Trial.
Above all, thanks are due to the Oxford Mental Health Coercion (OCTET) Programme Group, as follows, whose contributions are detailed below (see Contributions of the OCTET Programme Group).
Main group (from Department of Psychiatry, University of Oxford, except where indicated)
Caroline Bennett, Kiki Burns, Tom Burns, Kathryn Davies, Alexandra Forrest, Montserrat De La Huerta, Lindsey Johnston, Naomi Lewis, Sarah Masson, Amy Mitchell, Andrew Molodynski (Department of Psychiatry, University of Oxford and Oxford Health NHS Foundation Trust), Lucy Murray, Helen Nightingale, Riti Patel, Stefan Priebe (Unit for Social and Community Psychiatry, Queen Mary, University of London), Stephen Puntis, Jorun Rugkåsa (Department of Psychiatry, University of Oxford and Health Services Research Unit, Akershus University Hospital, Norway), Lisa Russell, Aonghus Ryan, Tanya Smith, Lucinda Turnpenny, Francis Vergunst, Claire Visser, Sue Woods-Ganz and Ksenija Yeeles.
Qualitative studies
Krysia Canvin (Department of Psychiatry, University of Oxford), Julia Sinclair (Department of Psychiatry, University of Southampton) and Anna Sulman (Department of Psychiatry, University of Oxford).
Economic Evaluation and Capabilities Project:
Alastair Gray (Health Economics Research Centre, Department of Public Health, University of Oxford), Judit Simon (Health Economics Research Centre, Department of Public Health, University of Oxford and Department of Health Economics, Centre for Public Health, Medical University of Vienna, Austria).
Ethical analyses
Michael Dunn (The Ethox Centre, Nuffield Department of Population Health, University of Oxford) and Tony Hope (The Ethox Centre, Nuffield Department of Population Health, University of Oxford).
Legal analysis
John Dawson (Faculty of Law, University of Otago, New Zealand).
Statistics
Maria Vazquez Montes (Nuffield Department of Primary Care Health Sciences, University of Oxford), Constantinos Koshiaris (Nuffield Department of Primary Care Health Sciences, University of Oxford), Merryn Voysey (Centre for Statistics in Medicine, University of Oxford) and Louise Linsell (Department of Public Health and Primary Care, University of Oxford).
Contributions of the OCTET Programme Group
The following members of the OCTET Programme Group supported the OCTET Trial and the ULTIMA Quantitative Study through recruitment of study participants, data collection, data entry, data cleaning and analysis: Caroline Bennett (Research Assistant), Kiki Burns (Research Assistant), Kathryn Davies (Research Assistant), Alexandra Forrest (Research Assistant), Montserrat De La Huerta (Research Assistant), Lindsey Johnston (Research Assistant), Naomi Lewis (Research Assistant), Sarah Masson (Research Assistant), Amy Mitchell (Research Assistant), Lucy Murray (Research Assistant), Helen Nightingale (Research Assistant), Riti Patel (Research Assistant), Stephen Puntis (Research Assistant), Lisa Russell (Research Assistant), Aonghus Ryan (Research Assistant), Tanya Smith (Research Administrator and Data Manager), Lucinda Turnpenny (Research Assistant), Francis Vergunst (Research Assistant), Claire Visser (Research Assistant) and Sue Woods-Ganz (Research Administrator).
Andrew Molodynski (Consultant Psychiatrist and Honorary Clinical Senior Lecturer) contributed to study design, recruiting of psychiatrists by liaising with teams and trusts, researcher training and the interpretation of findings.
Stefan Priebe (Professor of Social and Community Psychiatry) contributed to study design.
Krysia Canvin (Research Fellow, ULTIMA study and OCTET Qualitative Study Lead), Anna Sulman (Research Assistant) and Jorun Rugkåsa were responsible for data collection for the OCTET and ULTIMA Qualitative Studies, and for the analysis and interpretation of the resulting data in collaboration with Julia Sinclair (Senior Lecturer in Psychiatry and Honorary Consultant Psychiatrist), who also participated in study design.
Alastair Gray (Professor of Health Economics) and Judit Simon (Senior Researcher then Professor of Health Economics) designed and were responsible for the OCTET Economic Evaluation and the Capabilities Project.
Michael Dunn (Lecturer and Research Associate) and Tony Hope (Professor of Medical Ethics and Honorary Consultant Psychiatrist) were responsible for the Ethical Analyses.
John Dawson (Professor of Law) conducted the OCTET Legal Analysis.
Responsibility for statistical analyses was held by Maria Vazquez Montes (Medical Statistician, OCTET and ULTIMA Studies Statistical Lead). She also designed the statistical analysis for all three studies. For the OCTET Trial, this was done in collaboration with Merryn Voysey (Senior Trial Statistician) and for the OCTET Follow-up Study it was done in collaboration with Constantinos Koshiaris (Statistical/Epidemiological Modeller). Constantinos Koshiaris also contributed to the statistical analysis of the ULTIMA Quantitative Study and conducted the statistical analysis for the OCTET Follow-up Study.
Louise Linsell (Senior Medical Statistician) contributed to the randomisation procedure for the OCTET Trial and the ULTIMA Quantitative Study.
Contributions of authors
Tom Burns (Professor of Social Psychiatry, Principal Investigator), Jorun Rugkåsa (Research Fellow, OCTET Trial and OCTET Follow-up Study manager), Ksenija Yeeles (Research Fellow, ULTIMA Study and OCTET Follow-up Study manager) and Jocelyn Catty (Research Consultant) drafted and revised the report and approved the final submitted version, on behalf of the OCTET Coercion Programme Group. Tom Burns, Jorun Rugkåsa and Ksenija Yeeles were also responsible for the overall design and management of the programme, oversaw recruitment and data collection for all three studies and held responsibility for data analysis, interpreting and writing up the results. Jocelyn Catty also contributed to the interpretation and writing up of the results.
Dissemination of the OCTET Programme
Presentations
International
2014
Burns T. Compulsion: Less Straight Forward Than it Looks. Psychiatry Seminar, Gothenburg University, Gothenburg, Sweden, 15 January 2014.
Burns T. Community Care of Severely Mentally Ill Individuals – What Works and What Does Not. Grand Rounds Lecture at Essex County Hospital Center, Cedar Grove, New Jersey, USA, 1 May 2014.
Burns T. Mandatory Outpatient Treatment in England: An RCT. Grand Rounds Lectures at the Duke University and Butner Central Regional Hospital, Butner, North Carolina, USA, 8 May 2014.
Burns T. Strengths and Weaknesses of the OCTET Trial. 17th EPA Section Epidemiology and Social Psychiatry Meeting, Ulm, Germany, 22 May 2014.
Puntis S. Is the Duration of Legal Compulsion Associated with Difference in Continuity of Care? 17th EPA Section Epidemiology and Social Psychiatry Meeting, Ulm, Germany, 22 May 2014.
Rugkåsa J. A Qualitative Study of Patient, Psychiatrist and Family Carer Experiences of Community Treatment Orders in England. 17th EPA Section Epidemiology and Social Psychiatry Meeting, Ulm, Germany, 22 May 2014.
Vergunst F. Does Coercion Affect Social Outcomes for Patients with Psychosis? 17th EPA Section Epidemiology and Social Psychiatry Meeting, Ulm, Germany, 22 May 2014.
Molodynski A. Use of Coercion in Mental Health Services in the UK. 17th EPA Section Epidemiology and Social Psychiatry Meeting, Ulm, Germany, 23 May 2014.
Molodynski A. International Themes on Coercion in Psychiatry and the Work of the WASP Coercion Group. 17th EPA Section Epidemiology and Social Psychiatry Meeting, Ulm, Germany, 23 May 2014.
Yeeles K. Are Informal Coercion and Formal Compulsion Related? 17th EPA Section Epidemiology and Social Psychiatry Meeting, Ulm, Germany, 23 May 2014.
Simon J. Measuring the Capability Sets of People with Severe Mental Health Disorders Using a Novel Multi-dimensional Instrument: The OxCAP-MH. International Health Economics Association, Dublin, Ireland, 13–16 July 2014.
Simon J. The OxCAP-MH: A Novel, Multi-dimensional, Patient-Reported Capabilities Instrument for Mental Health Research and Policy. For 2nd Meeting on Patient Reported Outcomes and Person Centred Care in Mental Health, American Association for the Advancement of Science (AAAs), Washington, USA, 26–28 September 2014.
Rugkåsa J. Family Carers and Coercion in the Community. 5th Qualitative Research on Mental Health Conference, Chania, Greece, 2–4 September 2014.
Rugkåsa J. Community Treatment Orders. Do they work? Invited presentation, Plenary Meeting, Akershus University Hospital, Lørenskog, Norway, 8 November 2014.
2013
Burns T. Informal Coercion in Mental Health Care: Acceptable or Not? Orygen Youth Health Seminar, Melbourne, VIC, Australia, 8 February 2013.
Burns T. Coercion in Mental Health. The International Growth of CTOs and the Different Origins of this Development. The Need for a Rigorous Testing of the Effect of CTOs and Our Current Study (OCTET). Clinical observations of the implementation of CTOs for Central Commissioned Psychiatry Training. Hong Kong, 1–2 February 2013.
Burns T. The Essential Ingredients in Psychiatric Community Care. 11th Scandinavian Network for Community Mental Health Conference. Lund, Sweden, 3–4 June 2013.
Rugkåsa J. What Patients and Family Carers Think About Community Treatment Orders: A Qualitative Study from England. 33rd International Congress of the International Academy of Law and Mental Health. Amsterdam, The Netherlands, 14–19 July 2013.
Rugkåsa J. Family Experiences of Community Coercion. 21st World Congress for Social Psychiatry, Lisbon, 29 June to 3 July 2013.
Rugkåsa J. International Developments Regarding CTOs. II European Congress on Assertive Outreach. Avilés, Spain, 26–28 June 2013.
Molodynski A. Community Treatment Orders in England: The Results of an RCT. International Academy of Law and Mental Health, Amsterdam, July 2013.
Molodynski A. Coercion and Compulsion, International Perspectives. 21st World Congress for Social Psychiatry, Lisbon, 29 June to 3 July 2013.
Molodynski A. Community Treatment Orders. 21st World Congress for Social Psychiatry, Lisbon, 29 June to 3 July 2013.
Yeeles K, Burns T, Molodynski A, Vazguez Montes M. Use of Informal Coercion in Community Mental Health Care. 33rd International Congress of the International Academy of Law and Mental Health. Amsterdam, The Netherlands, 14–19 July 2013.
Yeeles K, Vazquez-Montes M, Mitchell A, Burns T. Coercion, Therapeutic Relationship and Continuity of Care. Xth European Network for Mental Health Service Evaluation (ENMESH) International Conference, Verona, Italy, 3–5 October 2013.
Canvin, K. Predicting the Unpredictable? Findings from a Qualitative Study of Psychiatrists’ and Patients’ Experiences of CTOs in England. Paper presented at the 33rd Congress of the International Academy of Law and Mental Health, Amsterdam, The Netherlands, 14–19 July 2013.
Canvin, K. Service User Perspectives on Coercion in Psychiatry (Symposium on Community-based Compulsory Treatment: Emerging Findings From the United Kingdom and International Perspectives). Paper presented at the 33rd Congress of the International Academy of Law and Mental Health, Amsterdam, The Netherlands, 14–19 July 2013.
Canvin, K. Service User Perspectives on Coercion in Psychiatry (Symposium on Service User, Family, and Advocacy Perspectives on Coercion in Psychiatry). Paper presented at the 21st World Congress on Social Psychiatry, Lisbon, Portugal, 29 June to 3 July 2013.
Simon J. How do Severe Mental Illness and Community Coercion Affect People’s Capabilities? Annual conference of the Human Development and Capability Association, Managua, Nicaragua, 9–12 September 2013.
2012
Burns T, Rugkåsa J. Developments in Coercion in the Community for Schizophrenia Days 2012 – Mental Health Take-away. Stavanger, Norway, 5–9 November 2012.
Burns T. An RCT of Supervised Community Treatment (CTO) Use in England. RC Psych International Congress. Liverpool, UK, 10 July 2012.
Burns T. Community Treatment Orders in England & Wales: What Have We Learnt So Far? ECSP 1st European Congress for Social Psychiatry. Geneva, Switzerland, 4–6 July 2012.
Rugkåsa J. Carer Experiences with Community Treatment Orders in England. Seminar on carer experiences with chronic illness. University of Oslo, Oslo, 26 November 2012.
Rugkåsa J. Coercion in the Community – An Overview of Legal Regimes and Current Evidence. Invited workshop, Schizopfrenidagene, Stavanger, Norway, 7–9 November 2012.
Rugkåsa J. The Oxford Community Treatment Order Evaluation Trial. Tvangsforskningsnettverkets forskningsgruppe, Kringler, Norway, 22–23 September 2012.
Rugkåsa J. Community Treatment Orders: What Do We Know about How They Work? National Network on Research in Coercion in Psychiatry, Norway, 22–23 September 2012.
Rugkåsa, J. Current Evidence for Community Treatment Orders. Annual Conference, European Congress of Social Psychiatry, Geneva, 4–6 July 2012.
2011
Burns T. How Should the Effectiveness of Compulsory Outpatient Treatment Be Tested? The OCTET Trial. 15th World Congress of Psychiatry, World Psychiatric Association. Buenos Aires, Argentina, 18–21 September 2011.
Burns T. Understanding Research on Complex Interventions. Psychiatric Summer School, Department of Psychiatry, Ulm University, Gunzburg, Germany, 8–9 September 2011.
Burns T. CTOs: Finding the Evidence. International Congress of the Royal College of Psychiatrists. Brighton, UK, 29 June 2011.
Burns T. Evaluation of CTOs in the UK. Royal College of Psychiatrists Faculty of Forensic Psychiatry Annual Meeting, Berlin, Germany, 3 February 2011.
Rugkåsa J. Community treatment orders: a qualitative investigation of patient experiences in England. Paper presented at the IXth International Conference of the European Network for Mental Health Service Evaluation (ENMESH), Ulm, Germany, 23–25 June. Psychiatrische Praxis 2011;38.
Molodynski A, Manning C, Russell L, Rugkåsa J. UK psychiatrists’ opinions and experiences of Community Treatment Orders. Paper presented at the IXth International Conference of the European Network for Mental Health Service Evaluation (ENMESH), Ulm, Germany, 23–25 June. Psychiatrische Praxis 2011;38.
Yeeles K, Burns T, Molodynski A, M Montes-Vasquez. Use of informal coercion in community mental health care. IXth International Conference of the European Network for Mental Health Service Evaluation (ENMESH), Ulm, Germany, 23–25 June. Psychiatrische Praxis 2011;38.
Canvin K, Rugkåsa J. Patient experiences of leverage (informal coercion) in England: findings from a Qualitative Study. IXth International Conference of the European Network for Mental Health Service Evaluation (ENMESH), Ulm, Germany, 23–25 June. Psychiatrische Praxis 2011;38.
Simon J. Operationalising the Capabilities Approach for Mental Health Studies (OxCAP-MH). New Directions in Welfare Conference (OECD). Paris, France, 6 July 2011 – oral, opening plenary.
Ryan A, Patel R, Russell L, Turnpenny L, Visser C. Community treatment orders on trial: The OCTET RCT. IXth International Conference of the European Network for Mental Health Service Evaluation (ENMESH), Ulm, Germany, 23–25 June. Psychiatrische Praxis 2011;38.
Visser C, Patel R, Russell L, Ryan A, Turnpenny L. Legal and clinical dimensions to experimental research in social psychiatry: The case of the OCTET trial. IXth International Conference of the European Network for Mental Health Service Evaluation (ENMESH), Ulm, Germany, 23–25 June. Psychiatrische Praxis 2011;38.
2010
Burns T. Learning from Our Mistakes: How the ‘Wrong’ Result Can Set You ‘Right’ in Community Psychiatry Research. 2nd Joint International Conference of the Hong Kong College of Psychiatrists and the Royal College of Psychiatrist UK, Hong Kong, China, December 2010.
Burns T. The OCTET Trial. International meeting on mandated community treatment, Bellagio, Italy, 13–15 October 2010.
Burns T. Assertive Community Treatment and Difficult Patients: What We Have to Learn from the English Experience? 1st National Congress of the Italian Association of Young Psychiatrists, Riccione, Italy, 14–16 October 2010.
Burns T. How Should the Effectiveness of Compulsory Outpatient Treatment Be Tested? The OCTET Trial. 20th World Congress of Social Psychiatry, Marrakech, Morocco, 24–27 October 2010.
Burns T. What Do We Know about the Use of Community Treatment Orders, and What is the Need for Further Research? 2nd National Conference on research on coercion in psychiatric services. Arranged by the University of Tromsø, Oslo, Norway, 22–23 March 2010.
Rugkåsa J. Why Use Qualitative Methods in the Study of CTOs? Annual National Conference on Coercion in the Community, Oslo, Norway, 2010.
Vazquez-Montes M. [Use of Leverage Tools for Mental Treatment Compliance: A Statistics Application Example.] Medical application examples on statistics and introduction to Research Conference, Facultad de Matemáticas, Universidad de Yucatán, Yucatán, México, 2010.
2008
Davies K, Nightingale H, Burns T. What is the Nature and Extent of Informal Coercion (IC) in Mental Health Care? VIIIth International Conference of the European Network for Mental Health Service Evaluation (ENMESH), Krakow, Poland, 2008.
Yeeles K, Burns T. Community Treatment Orders: Challenges in Conducting an RCT. VIIIth International Conference of the European Network for Mental Health Service Evaluation (ENMESH), Krakow, Poland, 2008.
National (selected)
2014
Burns T. Evaluating Social Interventions: The Need for Rigour. Social Psychiatry MSc Module, IoP, London, 23rd January 2014.
Burns T. CTOs. Janssen Edinburgh Academic Journal Club, Royal Edinburgh Hospital, Edinburgh, 30 January 2014.
Rugkåsa J. Community Treatment Orders. Do they work? Norwegian Research Council conference Trondheim, Norway, 3–5 February 2014.
Burns T. CTO and the Finding of the OCTET Study. Northamptonshire Healthcare NHS Foundation Trust (NHFT) Seminar, Berrywood Hospital, York, 10 February 2014.
Rugkåsa J, Canvin K, Vergunst F. Findings and Research in Progress Examining the Effectiveness of CTOs in the UK. ICMHSR Seminar, University of York, 12 February 2014.
Rugkåsa, J. (2014). Community Treatment Orders: Effectiveness, Understanding and Impact. International Centre for Mental Health Social Research, University of York, UK, 12 February 2014.
Burns T. CTOs. Royal College of Psychiatrists Forensic Faculty Annual Conference, Belfast, 5 March 2014.
Molodynski A. OCTET: An RCT of CTOs. Northern and Yorkshire Spring Conference 2014, York, 21 March 2014.
Dawson J. The Results of the Randomised Trial of Community Treatment Orders for England and Wales. The Faculty of Law, University of Cardiff, Cardiff, March 2014.
Burns T. OCTET Study Findings. Springfield Hospital Academic Programme, South West London and St George’s Mental Health NHS Trust, London, 27 March 2014.
Burns T. CTOs and the OCTET Study. Judicial College Specialist Medical Members Course, Royal College of Psychiatrists, London, 1 July 2014.
Dawson J. The Results of the Randomised Trial of Community Treatment Orders for England and Wales. Ashburn Clinic, Dunedin, New Zealand, August 2014.
Burns T. Effectiveness of CTOs. Yorkshire Approved Mental Health Professionals Conference, Leeds, 12th September 2014.
Burns T. The Role of Compulsory Treatment in Psychiatry: What Works and for Whom? Royal College of Psychiatrists Faculty of General Adult Psychiatry Meeting, Brighton, 16 October 2014.
Burns T. Do CTOs Work? What the Evidence Shows. Mental Health Review Tribunal for Wales Training Day, Cardiff, 24 October 2014.
Dawson J. Randomised Controlled Trials of Community Treatment Order Regimes. Faculty of Law, University of Toronto, Toronto, ON, October 2014.
Dawson J. Can We tell if Community Treatment Orders Work? Dalhousie University, Halifax, Nova Scotia, October 2014.
Burns T. The OCTET Trial. Barnet, Enfield and Haringey Mental Health NHS Trust’s annual Mental Health Law Conference, Enfield, 6 November 2014.
Rugkåsa J. Personal Experiences of CTOs from Service User, Carer and Clinicians’ Perspectives. World Association of Social Psychiatry 50th Congress, London, UK, 13–15 November 2014.
2013
Burns T. OCTET: The Results. North East London NHS Foundation Trust workshop in London, 2 December 2013.
Burns T. OCTET: The Results. Institute of Psychiatry Friday Morning Teaching Session in London, 15 November 2013.
Burns T. CTOs in England: An RCT and Do CTOs work? – A Review of the Evidence. Janssen Meeting in Edinburgh, 31 October 2013.
Burns T. Community Treatment Orders. RCPsych London Division Mental Health Care in the Community Meeting, London, 24 October 2013.
Burns T. OCTET: The Results. Mental Health Act Network Meeting, Central and North West London NHS Foundation Trust, London 10 October 2013.
Burns T. Does Mandatory Outpatient Committal Stabilise Patients and Reduce Admissions? The OCTET RCT in England. Dartmouth-Hitchcock Medical Center Department of Psychiatry, Dartmouth, USA, 10 September 2013.
Burns T. Do CTOs Reduce the Readmission Rate in Psychosis Patients Discharged from Section 3 Over the Subsequent 12 months? Shaping the future for patient outcomes in schizophrenia conference organised by Janssen in London, 10 July 2013.
Burns T. Community Treatment Orders in England: An RCT. Otuska OCTET Lectures in Wolverhampton and Birmingham, 14 June 2013.
Burns T. OCTET: The Results. Institute of Psychiatry Maudsley Journal Club in London, 19 June 2013.
Burns T. OCTET: The Results. OCTET Study Conference, Social Psychiatry Group University of Oxford in London, 21 March 2013.
Rugkåsa J. Do CTOs Work? An Up to Date Review of the Evidence, Including the OCTET RCT. Sussex Partnership NHS Foundation Trust, Mental Health Law & Practice Conference, Brighton, 22 November 2013.
Rugkåsa J. New Evidence on CTOs: Results from the OCTET RCT. SUNLOW Seminars for Service User in London, London, UK, 26 April.
Canvin, K. A Qualitative Study of Patient, Psychiatrists and Family Carer Experiences of Community Treatment Orders. Sussex Partnership NHS Foundation Trust, Mental Health Law & Practice Conference, Brighton, 22 November 2013.
Canvin, K. Coercion in the Community: Mental Health Service User and Professional Experiences. BSA Medical Sociology 45th Annual Conference, York, UK, 11–13 September 2013.
2012
Burns T. Is Any Worthwhile Relationship Ever Free? RCPsych in Wales and the Welsh Psychiatric Society Joint Meeting: social factors–social inequality, Wales, 7 December 2012.
Burns T. Community Treatment Orders in England: An RCT. South West London & St George’s Mental Health NHS Trust academic programme, Tolworth, London, 20 September 2012.
Burns T. OCTET: Is it Possible to Conduct Rigorous Research on a Legal Condition? Research and Innovation Workshop organised by Birmingham and Solihull Mental Health NHS Foundation Trust, Birmingham, UK, 28 March 2012.
Burns T. Evaluating Social Interventions: The Need for Rigour. IoP Social Psychiatry course, London, 6 February 2012.
Rugkåsa J. Community Treatment Orders: What Have We Learnt so Far? 2012 National Scientific Meeting of the Mental Health Research Network, Birmingham, 25–27 April 2012.
Rugkåsa J. OCTET: An RCT of Community Treatment Orders. Forensic Mental Health Teaching Session, Institute of Psychiatry, King’s College London, 20 January 2012.
2011
Burns T. CTOs – How Will We know if They Work? South Eastern Division Autumn Academic Meeting. The Royal College of Psychiatrists, Kent, UK, 3 November 2012.
Rugkåsa J. Patient Experiences of Involuntary Psychiatric Treatment in the Community. 43rd Annual Conference of the British Sociological Association’s Medical Sociology Group, Chester, UK, 14–16 September 2012.
Rugkåsa J. Oxford Community Treatment Order Evaluation Trial (OCTET): Background and Early Findings from Qualitative Patient Interviews. 6th North East Mental Health Law Conference, Newcastle, UK, 10 June 2012.
Rugkåsa J. Assessing the Appropriateness of Community Treatment Orders and Patient Involvement and Understanding. Care Quality Commission’s conference ‘Improving the Care and Experience for Patients Detained Under the Mental Health Act’, London, UK, 24 March 2012.
Rugkåsa J. OCTET: Studying the Effectiveness of Community Treatment Orders. SUNLOW Seminars for Service User in London, London, UK, 25 February 2012.
Simon J. Capability Measurement in the OCTET Study: Developing the OxCAP-MH. ICECAP workshop, Birmingham, UK, 25–27 June 2012.
2010
Burns T. OCTET Audit on CTOs. Bi-Polar Conference arranged by Otsuka Pharmaceuticals, Birmingham, UK, 29 October 2010.
Burns T. Do Community Orders Work? London Mental Health Research Network – Showcase Conference, London, 8 February 2010.
Rugkåsa J. The Oxford Community Treatment Order Evaluation Trial. Poster presentation, Mental Health Research Network Annual Scientific Meeting, Nottingham, UK, 2010.
Rugkåsa J. Researching Community Treatment Orders. Poster presentation, Annual Conference of the National Forum for Assertive Outreach, Hatfield, UK, 2010.
Rugkåsa J, Molodynski A. Community Treatment Orders: Refresher Training. Oxfordshire and Buckinghamshire NHS Mental Health Foundation Trust, Buckingham, 29 September 2010.
Rugkåsa J, Molodynski A. CTOs: The Story so Far. Annual Meeting of the Faculty of Rehabilitation and Social Psychiatry, Leeds, UK, 2010.
Nightingale H. The Oxford Community Treatment Order Evaluation Trial. 9th Annual Research and Development Open Day. Arranged by North East London NHS Foundation Trust, London, UK, 25 March 2010.
Vazquez-Montes M, Yeeles K. Use of Leverage Tools in UK Community Mental Health Care. Poster, RSS2010 Conference, Brighton, UK, 13–17 September 2010.
2009
Burns T. OCTET Community Treatment Order Evaluation Trial (OCTET). Berkshire R&D Conference, University of Reading, 16 December 2009.
Burns T. OCTET: Conducting an RCT of the New Community Treatment Orders. Conference on Making a Difference with Evidence Based Research arranged by Surrey & Borders Partnership NHS Foundation Trust, Leatherhead, 26 November 2009.
Burns T. Evidence for CTOS: The OCTET Trial. Springfield University Hospital Academic Programme, London, 8 October 2009.
Burns T. Community Treatment Orders, the Evidence and Outcomes. Current Issues in Mental Health, conference arranged by Otsuka Pharmaceuticals. Stansted, 22 September 2009.
Burns T. Research into New Community Models: Must Try Harder. MHRN National Scientific Conference, Nottingham, 21 May 2009.
Burns T. Community Treatment Orders. BEH Acute Care Services Awayday arranged by Astra Zeneca, London Colney, 3 March 2009.
Molodynski A. Coercion and Compulsion in Community Mental Health Care. Annual conference of the general adult Faculty of the Royal College of Psychiatrists, Cardiff, 16 October 2009.
Molodynski A. The Oxford Study of Informal Coercion. Annual Conference of the Royal College of Psychiatrists, Liverpool, 4 June 2009.
Yeeles K, Molodynski A. Use of Leverage Tools to Improve Mental Health Care Adherence. 2nd Annual Ridgeway Partnership Research and Development Day, Oxford Learning Disability NHS Trust, Oxford, 21 January 2009.
Publications
Burns T, Yeeles K, Koshiaris C, Vazquez-Montes M, Molodynski A, Puntis S, et al. Effect of increased compulsion on readmission to hospital or disengagement from community services for patients with psychosis: follow-up of a cohort from the OCTET trial. Lancet Psychiatry 2015;2:881–90.
Rugkåsa J, Molodynski A, Yeeles K, Vazquez Montes M, Visser C, Burns T. Community treatment orders: clinical and social outcomes, and a sub-group analysis from the OCTET RCT. Acta Psychiatr Scand 2015;131:321–9.
Puntis S, Rugkåsa J, Forrest A, Mitchell A, Burns T. Associations between continuity of care and patient outcomes in mental health care: a systematic review. Psychiatr Serv 2015;66:354–63.
Vergunst F, Jenkinson C, Burns T, Simon J. Application of Sen’s capability approach to outcome measurement in mental health research: psychometric validation of a novel multi-dimensional instrument (OxCAP-MH). Human Welfare 2014;3:1–4.
Rugkåsa J, Dawson J, Burns T. The OCTET RCT – a reply to Dr Mustafa. Med Sci Law 2014;54:118–19.
Canvin K, Rugkåsa J, Sinclair J, Burns T. Patient, psychiatrist and family carer experiences of community treatment orders: qualitative study. Soc Psychiatry Psychiatr Epidemiol 2014;9:1873–82.
Molodynski A, Turnpenny L, Rugkåsa J, Burns T, Moussaouid D. Coercion and compulsion in mental healthcare: an international perspective. Asian J Psychiatr 2014;8:2–6.
Rugkåsa J, Dawson J, Burns T. CTOs: what is the state of the evidence? Soc Psychiatry Psychiatr Epidemiol 2014;49:1861–71.
Dunn M, Sinclair JM, Canvin KJ, Rugkåsa J, Burns T. The use of leverage in community mental health: ethical guidance for practitioners. Int J Soc Psychiatry 2014;60:759–65.
Burns T, Molodynski A. Community treatment orders: background and implications of the OCTET trial. Psychiatr Bull 2014;38:3–5.
Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet 2013;381:1627–33.
Burns T. Community treatment orders: state of the evidence. East Asian Arch Psychiatry 2013;23:35–6.
Burns T, Rugkåsa J, Molodynski A. Community treatment orders for patients with psychosis – authors’ reply. Lancet 2013;382:502–3.
Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187–96.
Maughan D, Molodynski A, Rugkåsa J, Burns T. A systematic review of the effect of community treatment orders on service use. Soc Psychiatry Psychiatr Epidemiol 2014;49:651–63.
Canvin K, Rugkåsa J, Sinclair J, Burns T. Leverage and other informal pressures in community psychiatry in England. Int J Law Psychiatry 2013;36:100–6.
Dunn M, Sinclair JM, Canvin KJ, Rugkåsa J, Burns T. The use of leverage in community mental health: ethical guidance for practitioners. Int J Soc Psychiatry 2014;60:759–65.
Dunn M, Maughan D, Hope T, Canvin K, Rugkåsa J, Sinclair J, et al. Threats and offers in community mental healthcare. J Med Ethics 2012;38:204–9.
Burns T, Yeeles K, Molodynski A, Nightingale H, Vazquez-Montes M, Sheehan K, et al. Pressures to adhere to treatment (‘leverage’) in English mental healthcare. Br J Psychiatry 2011;199:145–50.
Dawson J, Burns T, Rugkåsa J. Lawfulness of a randomised trial of the new community treatment order regime for England and Wales. Med Law Rev 2011;19:1–26.
Manning C, Molodynski A, Rugkåsa J, Dawson J, Burns T. Community treatment orders in England and Wales: national survey of clinicians’ views and use. Psychiatrist 2011;35:328–33.
Burns T. The dog that failed to bark. Psychiatrist 2010;34:361–3.
Rugkåsa J, Burns T. Community Treatment Orders. Psychiatry 2009;8:493–5.
Burns T, Dawson J. Community treatment orders: how ethical without experimental evidence? Psychol Med 2009;39:1583–6.
Burns T, Rugkåsa J, Molodynski A. The Oxford Community Treatment order Evaluation Trial (OCTET). Psychiatr Bull 2008;32:400.
Lawton-Smith S, Dawson J, Burns T. Community treatment orders are not a good thing. Br J Psychiatry 2008;193:96–100.
Press coverage (selected)
The Lancet. Top 10 Psychiatry Articles of 2012/13. URL: http://preview.smartfocusdigital.com/go.asp?/.2013.thelancet.psychiatry/bELA001 (accessed 1 October 2014).
Compulsory Community Treatment For Mentally Ill Patients Does Not Reduce Rates Of Hospitalisation. 13 May 2013. URL: http://informationonhealthonline.blogspot.co.uk/2013/05/compulsory-community-treatment-for.html (accessed 1 October 2014).
Manning S. ‘Psychiatric Asbos’ were an error says key advisor. The Independent on Sunday, 13 April 2013.
Recovery Network: Toronto. Compulsory Treatment does not reduce hospital re-admission. 1 April 2013. URL: http://recoverynetworktoronto.wordpress.com/2013/04/01/6495/ (accessed 11 August 2016).
Barchester Healthcare. CTO’s Don’t Work Says Man Who Championed Them. 16 April 2013. URL: www.barchester.com/Media/News/2013/4/ctos-dont-work-says-man-who-championed-them.htm (accessed 1 October 2014).
News Medical. Compulsory Community Treatment Not Found to Reduce Hospitalisation Rates of Mentally Ill Patients. 26 March 2013. URL: www.news-medical.net/news/20130326/Compulsory-community-treatment-not-found-to-reduce-hospitalisation-rates-of-mentally-ill-patients.aspx (accessed 3 August 2016).
Healio Psychiatric Annals. Compulsory Supervision Failed to Reduce Readmission Rates in Psychotic Patients. 28 March 2013. URL: www.healio.com/psychiatry/schizophrenia/news/online/%7B91364c34–9290–4cc9-bef8–5153235868a9%7D/compulsory-supervision-failed-to-reduce-readmission-rates-in-psychotic-patients (accessed 11 August 2016).
Medical Xpress. Compulsory Treatment Orders for Mental Illness Need Reviewing. 27 March 2013. URL: http://medicalxpress.com/news/2013–03-compulsory-treatment-mental-illness.html (accessed 11 August 2016).
Johnson S. Can we reverse the rising tide of compulsory admissions? Lancet 2013;381:1603–4.
Thornicroft G, Farrelly S, Szmukler G, Birchwood M, Waheed W, Flach C, et al. Clinical outcomes of Joint Crisis Plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial. Lancet 2013;381;1634–41.
McNicoll A. Community Treatment Orders Fail to Cut Mental Health Hospital Readmissions, Major Study Finds. Community Care, 26 March 2013. URL: www.communitycare.co.uk/articles/26/03/2013/119036/community-treatment-orders-fail-to-cut-mental-health-hospital-readmissions-major-study-finds.htm (accessed 11 August 2016).
NetDoctor. Study Casts Doubt on Effectiveness of Community Treatment Orders. 25 March 2013. URL: www.netdoctor.co.uk/interactive/news/theme_news_detail.php?id=801562108 (accessed 1 October 2014).
Cole K. Compulsory Supervision Does Not Reduce Hospital Re-Admissions. Mad in America Foundation, 26 March 2013. URL: www.madinamerica.com/2013/03/compulsory-supervision-does-not-reduce-readmission/ (accessed 11 August 2016).
Webber M. Community Treatment Orders Don’t Work. 26 March 2013. URL: http://martinwebber.net/?p=1019 (accessed 1 October 2016).
Walsh N. Outpatient Psych Programs Fail to Cut Readmission. MedPageToday, 26 March 2013. URL: www.medpagetoday.com/Psychiatry/Schizophrenia/38087 (accessed 11 August 2016).
Barrow M. Mental health orders ‘need urgent review’. The Times, 26 March 2013. URL: www.thetimes.co.uk/tto/health/mental-health/article3722930.ece (accessed 11 August 2016).
University of Oxford. Compulsory Treatment Orders for Mental Illness need Reviewing. 26 March 2013. URL: www.ox.ac.uk/media/news_stories/2013/130326.html (accessed 11 August 2016).
Dyer C. Community treatment orders have not reduced admissions, study shows. BMJ 2013;346:f1993. URL: www.bmj.com/content/346/bmj.f1993?tab = citation (accessed 11 August 2016).
Harris L. Don’t coerce the mentally ill into treatment. Pittsburgh Post-Gazette, 10 September 2014. URL: www.post-gazette.com/opinion/2014/09/10/Don-t-coerce-the-mentally-ill-into-treatment/stories/201409100044 (accessed 11 August 2016).
Awards and distinctions
Listed number two of the top 10 Lancet psychiatry papers of 2013: Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community Treatment Orders for patients with psychosis: a randomised controlled trial (OCTET). Lancet 2013;381:1627–33.
Award for best research article 2013–2013, Norwegian National Forum for Acute Psychiatry, Oslo, 14 February. Nasjonalt forum for akuttpsykiatri. Utdelt 14 Februar 2014 for artikkelen: Burns T, Rugkåsa J, Molodynksi A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community Treatment Orders for patients with psychosis: a randomised controlled trial (OCTET). Lancet 2013;381:1627–33.
Award for Excellent Research 2014 Akershus University Hospital, Lørenskog, 20 June. For artikkelen: Rugkåsa J, Dawson J. Community Treatment Orders: current evidence and its implications. Br J Psychiatry 2013;203:406–8.
Data sharing statement
Data from the OCTET Programme may be obtained by permission of the corresponding author from the UK Data Service ReShare (www.ukdataservice.ac.uk).
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- BBC News . Transcript of Sir Ian Blair’s Speech: The Dimbleby Lecture 2005. http://news.bbc.co.uk/1/hi/uk/4443386.stm (accessed 11 August 2016).
- Linklater M. Too dangerous to ignore?. The Times 2006.
- Churchill R, Owen G, Singh S, Hotopf M. International Experiences of Using Community Treatment Orders. London: Institute of Psychiatry; 2007.
- Dawson J. Community Treatment Orders: International Comparisons. Dunedin: Otago University; 2005.
- McDonnell E, Bartholomew T. Community treatment orders in Victoria: emergent issues and anomalies. Psychiatr Psychol Law 1997;4:25-36. http://dx.doi.org/10.1080/13218719709524893.
- Munetz MR, Galon PA, Frese FJ. The ethics of mandatory community treatment. J Am Acad Psychiatry Law 2003;31:173-83.
- Monahan J, Redlich AD, Swanson J, Robbins PC, Appelbaum PS, Petrila J, et al. Use of leverage to improve adherence to psychiatric treatment in the community. Psychiatr Serv 2005;56:37-44. http://dx.doi.org/10.1176/appi.ps.56.1.37.
- Green J, Britten N. Qualitative research and evidence based medicine. BMJ 1998;316:1230-2. http://dx.doi.org/10.1136/bmj.316.7139.1230.
- Black N. Why we need qualitative research. J Epidemiol Community Health 1994;48:425-6. http://dx.doi.org/10.1136/jech.48.5.425-a.
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694-6. http://dx.doi.org/10.1136/bmj.321.7262.694.
- Bressi Nath S, Alexander LB, Solomon PL. Case managers’ perspectives on the therapeutic alliance: a qualitative study. Soc Psychiatry Psychiatr Epidemiol 2012;47:1815-26. http://dx.doi.org/10.1007/s00127-012-0483-z.
- Mental Health Act. London: The Stationery Office; 2007.
- Anand P, Hunter G, Smith R. Capabilities and well-being: evidence based on the Sen-Nussbaum approach to welfare. Soc Indic Res 2005;74:9-55. http://dx.doi.org/10.1007/s11205-005-6518-z.
- Nussbaum MC, Sen A, Nussbaum MC, Sen A. The Quality of Life. Oxford: Clarendon Press; 1993.
- Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects. Ferney-Voltaire, France: World Medical Association; 2013.
- Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet 2013;381:1627-33. http://dx.doi.org/10.1016/S0140-6736(13)60107-5.
- Molodynski A, Rugkåsa J, Burns T. Coercion and compulsion in community mental health care. Br Med Bull 2010;95:105-19. http://dx.doi.org/10.1093/bmb/ldq015.
- Rugkåsa J, Dawson J, Burns T. CTOs: what is the state of the evidence?. Soc Psychiatry Psychiatr Epidemiol 2014;49:1861-71. http://dx.doi.org/10.1007/s00127-014-0839-7.
- Mental Health Atlas 2011. Geneva: WHO; 2011.
- Saving Lives: Our Healthier Nation. London: The Stationery Office; 1999.
- Incapacity Benefit and Severe Disablement Allowance Quarterly Summary Statistics: February. London: DWP; 2005.
- Mathers C, Lopez AD. Updated Projections of Global Mortality and Burden of Disease, 2002–2030: Data Sources, Methods and Results. Geneva: WHO; 2005.
- Kjellin L, Høyer G, Engberg M, Kaltiala-Heino R, Sigurjónsdóttir M. Differences in perceived coercion at admission to psychiatric hospitals in the Nordic countries. Soc Psychiatry Psychiatr Epidemiol 2006;41:241-7. http://dx.doi.org/10.1007/s00127-005-0024-0.
- Torrey EF, Entsminger K, Geller J, Stanley J, Jaffe DJ. The Shortage of Public Hospital Beds for Mentally Ill Persons. Arlington, VA: Treatment Advocacy Center; 2008.
- Gledhill K. Community Treatment Orders. J Mental Health Law 2007;16:149-69.
- Geller JL, Fisher WH, Grudzinskas AJ, Clayfield JC, Lawlor T. Involuntary outpatient treatment as ‘desinstitutionalized coercion’: the net-widening concerns. Int J Law Psychiatry 2006;29:551-62. http://dx.doi.org/10.1016/j.ijlp.2006.08.003.
- Eastman N. Reforming mental health law in England and Wales. BMJ 2006;332:737-8. http://dx.doi.org/10.1136/bmj.332.7544.737.
- Burns T, Firn M. Assertive Outreach in Mental Health: A Manual for Practitioners. Oxford: Oxford University Press; 2002.
- Moser LL. Coercion in Assertive Community Treatment: Examining Client, Staff, and Program Predictors. Ann Arbor, MI: ProQuest LLC; 2007.
- Davis S. Autonomy versus coercion: reconciling competing perspectives in community mental health. Community Ment Health J 2002;38:239-50. http://dx.doi.org/10.1023/A:1015267707856.
- Burns T. Community Mental Health Teams, A Guide to Current Practices. Oxford: Oxford University Press; 2004.
- Stanhope V, Matejkowski J. Understanding the role of individual consumer-provider relationships within assertive community treatment. Community Ment Health J 2010;46:309-18. http://dx.doi.org/10.1007/s10597-009-9219-2.
- Stein LI, Test MA. Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Arch Gen Psychiatry 1980;37:392-7. http://dx.doi.org/10.1001/archpsyc.1980.01780170034003.
- Bonnie RJ, Monahan J. From coercion to contract: reframing the debate on mandated community treatment for people with mental disorders. Law Hum Behav 2005;29:485-503. http://dx.doi.org/10.1007/s10979-005-5522-9.
- Sjöström S, Zetterberg L, Markström U. Why community compulsion became the solution - Reforming mental health law in Sweden. Int J Law Psychiatry 2011;34:419-28. http://dx.doi.org/10.1016/j.ijlp.2011.10.007.
- Burns T. The dog that failed to bark. Psychiatrist 2010;34:361-3. http://dx.doi.org/10.1192/pb.bp.110.030254.
- Caring for People: Community Care in the Next Decade and Beyond: Policy Guidance. London: Her Majesty’s Stationary Office; 1990.
- Knapp M, Beecham J, Anderson J, Dayson D, Leff J, Margolius O, et al. The TAPS project. 3: Predicting the community costs of closing psychiatric hospitals. Br J Psychiatry 1990;157:661-70. http://dx.doi.org/10.1192/bjp.157.5.661.
- Appelbaum PS. Thinking carefully about outpatient commitment. Psychiatr Serv 2001;52:347-50. http://dx.doi.org/10.1176/appi.ps.52.3.347.
- Priebe S, Badesconyi A, Fioritti A, Hansson L, Kilian R, Torres-Gonzales F, et al. Reinstitutionalisation in mental health care: comparison of data on service provision from six European countries. BMJ 2005;330:123-6. http://dx.doi.org/10.1136/bmj.38296.611215.AE.
- Ritchie JH. The Report of the Enquiry into the Care and Treatment of Christopher Clunis Presented to the Chairman of the North East Thames and South East Thames Regional Health Authorities. London: Her Majesty’s Stationary Office; 1994.
- Sensky T, Hughes T, Hirsch S. Compulsory psychiatric treatment in the community. II. A controlled study of patients whom psychiatrists would recommend for compulsory treatment in the community. Br J Psychiatry 1991;158:799-804. http://dx.doi.org/10.1192/bjp.158.6.799.
- Bindman J, Beck A, Thornicroft G, Knapp M, Szmukler G. Psychiatric patients at greatest risk and in greatest need. Impact of the Supervision Register Policy. Br J Psychiatry 2000;177:33-7. http://dx.doi.org/10.1192/bjp.177.1.33.
- Burns T. Supervised discharge orders. Psychiatr Bull 2000;24:401-2. http://dx.doi.org/10.1192/pb.24.11.401.
- Mental Health Act 2007: Patients on After Care Under Supervision (ACUS) Transitional Arrangement. London: Department of Health; 2008.
- Community Supervision Orders. Council Report CR18. London: Royal College of Psychiatrists; 1993.
- Toward a Better Mental Health Act. London: The Mental Health Alliance; 2005.
- Code of Practice: Mental Health Act 1983. London: The Stationery Office; 2008.
- Sheehan KA, Molodynski A. Compulsion and freedom in community mental healthcare. Psychiatry 2007;6:393-8. http://dx.doi.org/10.1016/j.mppsy.2007.07.009.
- Health and Social Care Act, Section 299. London: The Stationery Office; 2012.
- Monitoring the Mental Health Act in 2010/11. The Care Quality Commission’s Annual Report on the Exercise of its Function in Keeping Under Review the Operation the Mental Health Act 1983. London: CQC; 2011.
- Lepping P, Malik M. Community treatment orders: current practice and a framework to aid clinicians. Psychiatrist 2013;37:54-7. http://dx.doi.org/10.1192/pb.bp.111.037705.
- Smith M, Branton T, Cardno A. Is the bark worse than the bite? Additional conditions used within community treatment orders. Psychiatr Bull 2014;38:9-12. http://dx.doi.org/10.1192/pb.bp.113.043422.
- O’Reilly R. Why are community treatment orders controversial?. Can J Psychiatry 2004;49:579-84.
- Allen M, Smith VF. Opening Pandora’s box: the practical and legal dangers of involuntary outpatient commitment. Psychiatr Serv 2001;52:342-6. http://dx.doi.org/10.1176/appi.ps.52.3.342.
- Pinfold V, Bindman J. Is compulsory community treatment ever justified?. Psychiatr Bull 2001;25:268-70. http://dx.doi.org/10.1192/pb.25.7.268.
- Eastman N. Mental health law: civil liberties and the principle of reciprocity. BMJ 1994;308:43-5. http://dx.doi.org/10.1136/bmj.308.6920.43.
- Buchanan A. Risk of violence by psychiatric patients: beyond the “actuarial versus clinical” assessment debate. Psychiatr Serv 2008;59:184-90. http://dx.doi.org/10.1176/ps.2008.59.2.184.
- New Directions . Report on the Review of the Mental Health (Scotland) Act 1984 2001. www.mhtscotland.gov.uk/mhts/files/Millan_Report_New_Directions.pdf (accessed 11 August 2016).
- Burns T, Dawson J. Community treatment orders: how ethical without experimental evidence?. Psychol Med 2009;39:1583-6. http://dx.doi.org/10.1017/S0033291709005352.
- Kisely S, Campbell LA, Preston N. Compulsory community and involuntary outpatient treatment for people with severe mental disorders. Cochrane Database Syst Rev 2005;3. http://dx.doi.org/10.1002/14651858.cd004408.pub2.
- Preston NJ, Kisely S, Xiao J. Assessing the outcome of compulsory psychiatric treatment in the community: epidemiological study in Western Australia. BMJ 2002;324. http://dx.doi.org/10.1136/bmj.324.7348.1244.
- Steadman HJ, Gounis K, Dennis D, Hopper K, Roche B, Swartz M, et al. Assessing the New York City involuntary outpatient commitment pilot program. Psychiatr Serv 2001;52:330-6. http://dx.doi.org/10.1176/appi.ps.52.3.330.
- Swartz MS, Swanson JW, Wagner HR, Burns BJ, Hiday VA, Borum R. Can involuntary outpatient commitment reduce hospital recidivism? Findings from a randomized trial with severely mentally ill individuals. Am J Psychiatry 1999;156:1968-75.
- Swartz MS, Swanson JW. Involuntary outpatient commitment, community treatment orders, and assisted outpatient treatment: what’s in the data?. Can J Psychiatry 2004;49:585-91.
- Rugkåsa J, Dawson J. Community treatment orders: current evidence and the implications. Br J Psychiatry 2013;203:406-8. http://dx.doi.org/10.1192/bjp.bp.113.133900.
- Maughan D, Molodynski A, Rugkåsa J, Burns T. A systematic review of the effect of community treatment orders on service use. Soc Psychiatry Psychiatr Epidemiol 2014;49:651-63. http://dx.doi.org/10.1007/s00127-013-0781-0.
- Romans S, Dawson J, Mullen R, Gibbs A. How mental health clinicians view community treatment orders: a national New Zealand survey. Aust N Z J Psychiatry 2004;38:836-41. http://dx.doi.org/10.1080/j.1440-1614.2004.01470.x.
- Manning C, Molodynski A, Rugkåsa J, Dawson J, Burns T. Community treatment orders in England and Wales: national survey of clinicians’ views and use. Psychiatrist 2011;35:328-33. http://dx.doi.org/10.1192/pb.bp.110.032631.
- Mullen R, Dawson J, Gibbs A. Dilemmas for clinicians in use of Community Treatment Orders. Int J Law Psychiatry 2006;29:535-50. http://dx.doi.org/10.1016/j.ijlp.2006.09.002.
- Dawson J, Mullen R. Insight and use of community treatment orders. J Ment Health 2008;17:269-80. http://dx.doi.org/10.1080/09638230802052187.
- Dawson J, Romans S, Gibbs A, Ratter N. Ambivalence about community treatment orders. Int J Law Psychiatry 2003;26:243-55. http://dx.doi.org/10.1016/S0160-2527(03)00035-9.
- Gibbs A, Dawson J, Ansley C, Mullen R. How patients in New Zealand view community treatment orders. J Ment Health 2005;14:357-68. http://dx.doi.org/10.1080/09638230500229541.
- Canvin K, Bartlett A, Pinfold V. A ‘bittersweet pill to swallow’: learning from mental health service users’ responses to compulsory community care in England. Health Soc Care Community 2002;10:361-9. http://dx.doi.org/10.1046/j.1365-2524.2002.00375.x.
- Gibbs A, Dawson J, Forsyth H, Mullen R. Maori experience of community treatment orders in Otago, New Zealand. Aust N Z J Psychiatry 2004;38:830-5. http://dx.doi.org/10.1080/j.1440-1614.2004.01468.x.
- Gibbs A. Coping with compulsion: women’s views of being on a Community Treatment Order. Aust Soc Work 2010;63:223-33. http://dx.doi.org/10.1080/03124070903265740.
- O’Reilly RL, Keegan DL, Corring D, Shrikhande S, Natarajan D. A qualitative analysis of the use of community treatment orders in Saskatchewan. Int J Law Psychiatry 2006;29:516-24. http://dx.doi.org/10.1016/j.ijlp.2006.06.001.
- Gibbs A, Dawson J, Mullen R. Community treatment orders for people with serious mental illness: a New Zealand study. Br J Soc Work 2006;36:1085-100. http://dx.doi.org/10.1093/bjsw/bch392.
- Mullen R, Gibbs A, Dawson J. Family perspective on community treatment orders: a New Zealand study. Int J Soc Psychiatry 2006;52:469-78. http://dx.doi.org/10.1177/0020764006066836.
- Swartz MS, Swanson JW, Wagner HR, Hannon MJ, Burns BJ, Shumway M. Assessment of four stakeholder groups’ preferences concerning outpatient commitment for persons with schizophrenia. Am J Psychiatry 2003;160:1139-46. http://dx.doi.org/10.1176/appi.ajp.160.6.1139.
- Kisely S, Campbell LA. Methodological issues in assessing the evidence for compulsory community treatment. Curr Psychiatry Rev 2007;3:51-6. http://dx.doi.org/10.2174/157340007779815664.
- Szmukler G, Hotopf M. Effectiveness of involuntary outpatient commitment. Am J Psychiatry 2001;158:653-4. http://dx.doi.org/10.1176/appi.ajp.158.4.653-a.
- Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005;353:1209-23. http://dx.doi.org/10.1056/NEJMoa051688.
- Kisely S, Campbell LA. Community treatment orders for psychiatric patients: the emperor with no clothes. Can J Psychiatry 2006;51:683-5.
- Burns T. Hospitalisation as an outcome measure in schizophrenia. Br J Psychiatr Suppl 2007;191:37-41. http://dx.doi.org/10.1192/bjp.191.50.s37.
- Segal SP, Preston N, Kisely S, Xiao J. Conditional release in Western Australia: effect on hospital length of stay. Psychiatr Serv 2009;60:94-9. http://dx.doi.org/10.1176/ps.2009.60.1.94.
- Swartz MS, Wilder CM, Swanson JW, Van Dorn RA, Robbins PC, Steadman HJ, et al. Assessing outcomes for consumers in New York’s assisted outpatient treatment program. Psychiatr Serv 2010;61:976-81. http://dx.doi.org/10.1176/ps.2010.61.10.976.
- Lawton-Smith . Community Treatment Orders are not a good thing: for. Br J Psychiatry 2008;193:96-100. http://dx.doi.org/10.1192/bjp.bp.107.049072.
- Snow N, Austin WJ. Community treatment orders: the ethical balancing act in community mental health. J Psychiatr Ment Health Nurs 2009;16:177-86. http://dx.doi.org/10.1111/j.1365-2850.2008.01363.x.
- Dawson J, Burns T. Community Treatment Orders are not a good thing: against. Br J Psychiatry 2008;193:96-100. http://dx.doi.org/10.1192/bjp.bp.107.049072.
- Dale E. Is supervised community treatment ethically justifiable?. J Med Ethics 2010;36:271-4. http://dx.doi.org/10.1136/jme.2009.033720.
- Light EM, Robertson MD, Boyce P, Carney T, Rosen A, Cleary M, et al. The lived experience of involuntary community treatment: a qualitative study of mental health consumers and carers. Australas Psychiatry 2014;22:345-51. http://dx.doi.org/10.1177/1039856214540759.
- Burns T, Rugkåsa J, Dawson J, Doll H, Molodynski A, Priebe S, et al. Protocol 10PRT/0496: Oxford Community Treatment Order Evaluation Trial (OCTET): A Single-Outcome Randomised Controlled Trial of Compulsory Outpatient Treatment in Psychosis (ISRCTN73110773). London: The Lancet; 2011.
- Rugkåsa J, Molodynski A, Yeeles K, Vazquez Montes M, Visser C, Burns T. Community treatment orders: clinical and social outcomes, and a subgroup analysis from the OCTET RCT. Acta Psychiatr Scand 2015;131:321-9. http://dx.doi.org/10.1111/acps.12373.
- R (Munjaz) v Ashworth Hospital Authority (2005) UKHL 58. Mental Health Law Online; 2005.
- Convention for the Protection of Human Rights and Fundamental Freedoms . Council of Europe 1950.
- Lukoff D, Nuechterlein K, Ventura J. Manual for expanded brief psychiatric rating scale (BPRS). Schizophr Bull 1986;12:594-602.
- McEvoy JP, Freter S, Everett G, Geller JL, Appelbaum P, Apperson LJ, et al. Insight and the clinical outcome of schizophrenic patients. J Nerv Ment Dis 1989;177:48-51. http://dx.doi.org/10.1097/00005053-198901000-00008.
- Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry 1974;131:1121-3.
- Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J 1995;94:135-40.
- Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry 1992;149:1148-56. http://dx.doi.org/10.1176/ajp.149.9.1148.
- Priebe S, Watzke S, Hansson L, Burns T. Objective social outcomes index (SIX): a method to summarise objective indicators of social outcomes in mental health care. Acta Psychiatr Scand 2008;118:57-63. http://dx.doi.org/10.1111/j.1600-0447.2008.01217.x.
- Glick HA, Polsky D, Willke RJ, Schulman KA. A comparison of preference assessment instruments used in a clinical trial responses to the Visual Analog Scale from the EuroQol EQ-5D and the Health Utilities Index. Med Decis Making 1999;19:265-75. http://dx.doi.org/10.1177/0272989X9901900305.
- Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med 1983;13:177-83. http://dx.doi.org/10.1017/S0033291700050182.
- Awad AG. Subjective response to neuroleptics in schizophrenia. Schizophr Bull 1993;19:609-18. http://dx.doi.org/10.1093/schbul/19.3.609.
- McGuire-Snieckus R, McCabe R, Catty J, Hansson L, Priebe S. A new scale to assess the therapeutic relationship in community mental health care: STAR. Psychol Med 2007;37:85-9. http://dx.doi.org/10.1017/S0033291706009299.
- Attkisson C, Greenfield T, Marush M. The Use of Psychological Testing for Treatment Planning and Outcome Assessment. Mahwah, NJ: Lawrence Erlbaum Associates; 2004.
- Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients’ desire for autonomy: decision making and information-seeking preferences among medical patients. J Gen Intern Med 1989;4:23-30. http://dx.doi.org/10.1007/BF02596485.
- Hill SA, Laugharne R. Decision making and information seeking preferences among psychiatric patients. J Ment Health 2006;15:75-84. http://dx.doi.org/10.1080/09638230500512250.
- Burns T, Yeeles K, Molodynski A, Nightingale H, Vazquez-Montes M, Sheehan K, et al. Pressures to adhere to treatment (‘leverage’) in English mental health care. Br J Psychiatry 2011;199:145-50. http://dx.doi.org/10.1192/bjp.bp.110.086827.
- Gardner W, Hoge S, Bennett N, Roth L, Lidz C. Two scales for measuring patients’ perceptions of coercion during hospital admission. Behav Sci Law 1993;20:307-21. http://dx.doi.org/10.1002/bsl.2370110308.
- Swartz MS, Wagner HR, Swanson JW, Hiday VA, Burns BJ. The perceived coerciveness of involuntary outpatient commitment: findings from an experimental study. J Am Acad Psychiatry Law 2002;30:207-17.
- The MacArthur Coercion Study. Admission Experience Survey: Short Form. Chicago, IL: MacArthur Foundation; 2001.
- Swartz MS, Wagner HR, Swanson JW, Elbogen EB. Consumers’ perceptions of the fairness and effectiveness of mandated community treatment and related pressures. Psychiatr Serv 2004;55:780-5. http://dx.doi.org/10.1176/appi.ps.55.7.780.
- Van Dorn RA, Swartz M, Elbogen EB, Swanson JW. Perceived fairness and effectiveness of leveraged community treatment among public mental health consumers in five US cities. Int J Forensic Ment Health 2005;4:119-33. http://dx.doi.org/10.1080/14999013.2005.10471218.
- Beecham J. Collecting information: The Client Service Receipt interview. Ment Health Res Rev 1994;1:6-8.
- Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev Sci 2007;8:206-13. http://dx.doi.org/10.1007/s11121-007-0070-9.
- Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM. Statistics in medicine–reporting of subgroup analyses in clinical trials. N Engl J Med 2007;357:2189-94. http://dx.doi.org/10.1056/NEJMsr077003.
- Drummond MF, O’Brien B, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- The EuroQoL Group . EuroQoL – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. http://dx.doi.org/10.1097/00005650-199711000-00002.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2012.
- Tarricone R. Cost-of-illness analysis. What room in health economics?. Health Policy 2006;77:51-63. http://dx.doi.org/10.1016/j.healthpol.2005.07.016.
- Managing Long Term Sickness Absence and Incapacity for Work. London: NICE; 2009.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: Personal Social Services Research Unit, University of Kent; 2012.
- NHS Reference Costs 2012–13. London: DH; 2013.
- Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: Personal Social Services Research Unit, University of Kent; 2011.
- Unit Costs. London: CASH; 2008.
- Private Healthcare Tariff for Self-Pay Patients. n.d.
- Scottish National Tariff 2012/2013. Edinburgh: ISD Scotland; 2013.
- Annual Survey of Hours and Earnings 2012. London: ONS; 2013.
- Little RJ, Rubin DB. Statistical Analysis with Missing Data. Hoboken, NJ: Wiley; 2002.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med 2011;30:377-99. http://dx.doi.org/10.1002/sim.4067.
- Efron B, Tibshirani RJ. An Introduction to the Bootstrap. New York, NY: Chapman Hall; 1993.
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8. http://dx.doi.org/10.1192/bjp.187.2.106.
- Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making 1998;18:68-80. http://dx.doi.org/10.1177/0272989X98018002S09.
- Canvin K, Rugkåsa J, Sinclair J, Burns T. Patient, psychiatrist and family carer experiences of community treatment orders: qualitative study. Soc Psychiatry Psychiatr Epidemiol 2014;49:1873-82. http://dx.doi.org/10.1007/s00127-014-0906-0.
- Patton MQ. Qualitative Evaluation and Research Methods. Thousand Oaks, CA: Sage Publications; 1990.
- Cutcliffe JR. Adapt or adopt: developing and transgressing the methodological boundaries of grounded theory. J Adv Nurs 2005;51:421-8. http://dx.doi.org/10.1111/j.1365-2648.2005.03514.x.
- Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Research. Thousand Oaks, CA: Sage; 2006.
- Glaser BG. The constant comparative method of qualitative analysis. Soc Probl 1965;12:436-45. http://dx.doi.org/10.2307/798843.
- Smart C. Personal Life: New Directions in Sociological Thinking. London: Polity Press; 2007.
- Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187-96. http://dx.doi.org/10.1016/j.socscimed.2013.09.019.
- Vergunst F, Jenkinson C, Burns T, Simon J. Application of Sen’s capability approach to outcome measurement in mental health research: psychometric validation of a novel multi-dimensional instrument (OxCAP-MH). Hum Welf 2014;3:1-4.
- New Horizons: A Shared Vision for Mental Health. London: DH; 2009.
- No Health without Mental Health: A Cross-government Mental Health Outcomes Strategy for People of all Ages. London: DH; 2011.
- Social Value Judgements: Principles for the Development of NICE Guidance. London: NICE; 2008.
- Francis J, Byford S. SCIE’s Approach to Economic Evaluation in Social Care. London: Social Care Institute for Excellence; 2011.
- Brazier J. Is the EQ-5D fit for purpose in mental health?. Br J Psychiatry 2010;197:348-9. http://dx.doi.org/10.1192/bjp.bp.110.082453.
- Sen AK. Choice, Welfare and Measurement. Oxford: Blackwell; 1982.
- Human Development Report 1990. Oxford: Oxford University Press; 1990.
- Stiglitz JE, Sen A, Fitoussi J. Report by the Commission on the Measurement of Economic Performance and Social Progress. Commission on the Measurement of Economic Performance and Social Progress (CMEPSP); 2009.
- Cookson R. QALYs and the capability approach. Health Econ 2005;14:817-29. http://dx.doi.org/10.1002/hec.975.
- Ruger JP. Health and Social Justice. Oxford: Oxford University Press; 2009.
- Venkatapuram S. Health Justice: An Argument from the Capabilities Approach. Cambridge: Polity Press; 2012.
- Anand P. Capabilities and health. J Med Ethics 2005;31:299-303. http://dx.doi.org/10.1136/jme.2004.008706.
- Anand P. QALYs and capabilities: a comment on Cookson. Health Econ 2005;14:1283-6. http://dx.doi.org/10.1002/hec.1002.
- Coast J, Smith R, Lorgelly P. Should the capability approach be applied in health economics?. Health Econ 2008;17:667-70. http://dx.doi.org/10.1002/hec.1359.
- Lorgelly PK, Lawson KD, Fenwick EA, Briggs AH. Outcome measurement in economic evaluations of public health interventions: a role for the capability approach?. Int J Environ Res Public Health 2010;7:2274-89. http://dx.doi.org/10.3390/ijerph7052274.
- Brouwer WB, Culyer AJ, van Exel NJ, Rutten FF. Welfarism vs. extra-welfarism. J Health Econ 2008;27:325-38. http://dx.doi.org/10.1016/j.jhealeco.2007.07.003.
- Sen A. Personal utilities and public judgements: or what’s wrong with welfare economics. Econ J 1979;89:537-58. http://dx.doi.org/10.2307/2231867.
- Sen A. Utilitarianism and welfarism. J Phil 1979;76:463-89. http://dx.doi.org/10.2307/2025934.
- Coast J, Smith RD, Lorgelly P. Welfarism, extra-welfarism and capability: the spread of ideas in health economics. Soc Sci Med 2008;67:1190-8. http://dx.doi.org/10.1016/j.socscimed.2008.06.027.
- Sen A. Why health equity?. Health Econ 2002;11:659-66. http://dx.doi.org/10.1002/hec.762.
- Anand P, Hunter G, Carter I, Dowding K, Guala F, Van Hees M. The development of capability indicators. J Hum Dev Capabil 2009;10:125-52. http://dx.doi.org/10.1080/14649880802675366.
- Nussbaum M. Capabilities as fundamental entitlements: Sen and social justice. Fem Econ 2003;9:33-59. http://dx.doi.org/10.1080/1354570022000077926.
- Alkire S. Valuing Freedoms: Sen’s Capability Approach and Poverty Reduction. Oxford: Oxford University Press; 2005.
- Lorgelly P, Lorimer K, Fenwick E, Briggs A. The Capability Approach: Developing an Instrument for Evaluating Public Health Interventions (Final Report). Glasgow: Section of Public Health and Health Policy, University of Glasgow; 2008.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: Centre for Health Economics, University of York; 1999.
- Trauer T. Outcome Measurement in Mental Health. Cambridge: Cambridge University Press; 2010.
- Dawson J. Randomised controlled trials of mental health legislation. Med Law Rev 2002;10:308-21. http://dx.doi.org/10.1093/medlaw/10.3.308.
- Dawson J, Burns T, Rugkåsa J. Lawfulness of a randomised trial of the new community treatment order regime for England and Wales. Med Law Rev 2011;19:1-26. http://dx.doi.org/10.1093/medlaw/fwq030.
- Pinfold V, Bindman J, Thornicroft G, Franklin D, Hatfield B. Persuading the persuadable: evaluating compulsory treatment in England using Supervised Discharge Orders. Soc Psychiatry Psychiatr Epidemiol 2001;36:260-6. http://dx.doi.org/10.1007/s001270170058.
- Clayton R, Tomlinson H. The Law of Human Rights. Oxford: Oxford University Press; 2009.
- Dawson J, Gostin L, Bartlett P, Fennell P, McHale J, McKay R. The Principles of Mental Health Law and Policy. Oxford: Oxford University Press; 2010.
- Monitoring the Use of the Mental Health Act in 2012/13. London: CQC; 2014.
- Monitoring the Use of the Mental Health Act in 2009/10. London: CQC; 2010.
- Rawala M, Gupta S. Use of community treatment orders in an inner-London assertive outreach service. Psychiatr Bull 2014;38:13-8. http://dx.doi.org/10.1192/pb.bp.112.042184.
- Evans R, Makala J, Humphreys M, Mohan CRN. Supervised community treatment in Birmingham and Solihull: first 6 months. Psychiatrist 2010;34:330-3. http://dx.doi.org/10.1192/pb.bp.109.027482.
- Sun X, Briel M, Busse JW, You JJ, Akl EA, Mejza F, et al. Credibility of claims of subgroup effects in randomised controlled trials: systematic review. BMJ 2012;344.
- Patel MX, Matonhodze J, Baig MK, Gilleen J, Boydell J, Holloway F, et al. Increased use of antipsychotic long-acting injections with community treatment orders. Ther Adv Psychopharmacol 2011;1:37-45. http://dx.doi.org/10.1177/2045125311407960.
- Patel MX, Matonhodze J, Baig MK, Taylor D, Szmukler G, David AS. Naturalistic outcomes of community treatment orders: antipsychotic long-acting injections versus oral medication. J Psychopharmacol 2013;27:629-37. http://dx.doi.org/10.1177/0269881113486717.
- Lambert TJ, Singh BS, Patel MX. Community treatment orders and antipsychotic long-acting injections. Br J Psychiatry 2009;52:S57-62. http://dx.doi.org/10.1192/bjp.195.52.s57.
- Szmukler G, Appelbaum PS, Thornicroft G, Szmukler G. Textbook of Community Psychiatry. Oxford: Oxford University Press; 2001.
- Report of the Expert Committee: Review of the Mental Health Act 1983. London: DH; 1999.
- Liégeois A, Van Audenhove C. Ethical dilemmas in community mental health care. J Med Ethics 2005;31:452-6. http://dx.doi.org/10.1136/jme.2003.006999.
- Thornicroft G, Farrelly S, Szmukler G, Birchwood M, Waheed W, Flach C, et al. Clinical outcomes of Joint Crisis Plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial. Lancet 2013;381:1634-41. http://dx.doi.org/10.1016/S0140-6736(13)60105-1.
- Brock DW. A proposal for the use of advance directives in the treatment of incompetent mentally ill persons. Bioethics 1993;7:247-56. http://dx.doi.org/10.1111/j.1467-8519.1993.tb00291.x.
- Savulescu J, Dickenson D. The time frame of preferences, dispositions, and the validity of advance directives for the mentally ill. Philos Psychiatr Psychol 1998;5:225-46.
- Srebnik DS, La Fond JQ. Advance directives for mental health treatment. Psychiatr Serv 1999;50:919-25. http://dx.doi.org/10.1176/ps.50.7.919.
- Netten A, Burge P, Malley J, Potoglou D, Towers AM, Brazier J, et al. Outcomes of social care for adults: developing a preference-weighted measure. Health Technol Assess 2012;16. http://dx.doi.org/10.3310/hta16160.
- Grewal I, Lewis J, Flynn T, Brown J, Bond J, Coast J. Developing attributes for a generic quality of life measure for older people: preferences or capabilities?. Soc Sci Med 2006;62:1891-901. http://dx.doi.org/10.1016/j.socscimed.2005.08.023.
- Flynn TN, Louviere JJ, Peters TJ, Coast J. Best–worst scaling: what it can do for health care research and how to do it. J Health Econ 2007;26:171-89. http://dx.doi.org/10.1016/j.jhealeco.2006.04.002.
- Sweetman EA, Doig GS. Failure to report protocol violations in clinical trials: a threat to internal validity?. Trials 2011;12. http://dx.doi.org/10.1186/1745-6215-12-214.
- Al-Janabi H, Coast J, Flynn TN. What do people value when they provide unpaid care for an older person? A meta-ethnography with interview follow-up. Soc Sci Med 2008;67:111-21. http://dx.doi.org/10.1016/j.socscimed.2008.03.032.
- Sen A. Well-being, agency and freedom: the Dewey lectures 1984. J Phil 1985;82:169-221. http://dx.doi.org/10.2307/2026184.
- Burns T, Yeeles K, Koshiaris C, Vazquez-Montes M, Molodynski A, Puntis S, et al. Effect of increased compulsion on readmission to hospital or disengagement from community services for patients with psychosis: follow-up of a cohort from the OCTET Trial. Lancet Psychiatry 2015;2:881-90. http://dx.doi.org/10.1016/S2215-0366(15)00231-X.
- Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702-6. http://dx.doi.org/10.1093/aje/kwh090.
- Stettin B, Lamb R, Frese F. Elements of an ideal statutory scheme for mental health civil commitment. Psychiatr Ann 2014;44:102-8. http://dx.doi.org/10.3928/00485713-20140205-09.
- Catty J, Cowan N, Poole Z, Clement S, Ellis G, Geyer C, et al. Continuity of care for people with non-psychotic disorders. Int J Soc Psychiatry 2013;59:18-27. http://dx.doi.org/10.1177/0020764011421442.
- Priebe S, Yeeles K, Bremner S, Lauber C, Eldridge S, Ashby D, et al. Effectiveness of financial incentives to improve adherence to maintenance treatment with antipsychotics: cluster randomised controlled trial. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f5847.
- Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosoc Rehabil J 1993;16. http://dx.doi.org/10.1037/h0095655.
- Szmukler G, Appelbaum PS. Treatment pressures, leverage, coercion, and compulsion in mental health care. J Ment Health 2008;17:233-44. http://dx.doi.org/10.1080/09638230802052203.
- Angell B, Mahoney C. Reconceptualizing the case management relationship in intensive treatment: a study of staff perceptions and experiences. Adm Policy Ment Health 2007;34:172-88. http://dx.doi.org/10.1007/s10488-006-0094-7.
- Angell B, Mahoney CA, Martinez NI. Promoting treatment adherence in assertive community treatment. Soc Serv Rev 2006;80:485-526. http://dx.doi.org/10.1086/505287.
- Appelbaum PS, Le Melle S. Techniques used by assertive community treatment (ACT) teams to encourage adherence: patient and staff perceptions. Community Ment Health J 2008;44:459-64. http://dx.doi.org/10.1007/s10597-008-9149-4.
- Neale MS, Rosenheck RA. Therapeutic limit setting in an assertive community treatment program. Psychiatr Serv 2000;51:499-505. http://dx.doi.org/10.1176/appi.ps.51.4.499.
- Watts J, Priebe S. A phenomenological account of users’ experiences of assertive community treatment. Bioethics 2002;16:439-54. http://dx.doi.org/10.1111/1467-8519.00301.
- Van Dorn RA, Elbogen EB, Redlich AD, Swanson JW, Swartz MS, Mustillo S. The relationship between mandated community treatment and perceived barriers to care in persons with severe mental illness. Int J Law Psychiatry 2006;29:495-506. http://dx.doi.org/10.1016/j.ijlp.2006.08.002.
- Szmukler G, Daw R, Dawson J. A model law fusing incapacity and mental health legislation. J Ment Health Law 2010;20:11-24.
- Szmukler G. Financial incentives for patients in the treatment of psychosis. J Med Ethics 2009;35:224-8. http://dx.doi.org/10.1136/jme.2008.027151.
- Busch A, Redlich AD. Patients’ perception of possible child custody or visitation loss for nonadherence to psychiatric treatment. Psychiatr Serv 2007;58:999-1002. http://dx.doi.org/10.1176/ps.2007.58.7.999.
- Robbins PC, Petrila J, LeMelle S, Monahan J. The use of housing as leverage to increase adherence to psychiatric treatment in the community. Adm Policy Ment Health 2006;33:226-36. http://dx.doi.org/10.1007/s10488-006-0037-3.
- Elbogen EB, Soriano C, Van Dorn R, Swartz MS, Swanson JW. Consumer views of representative payee use of disability funds to leverage treatment adherence. Psychiatr Serv 2005;56:45-9. http://dx.doi.org/10.1176/appi.ps.56.1.45.
- Redlich AD, Steadman HJ, Robbins PC, Swanson JW. Use of the criminal justice system to leverage mental health treatment: effects on treatment adherence and satisfaction. J Am Acad Psychiatry Law 2006;34:292-9.
- Appelbaum PS, Redlich A. Use of leverage over patients’ money to promote adherence to psychiatric treatment. J Nerv Ment Dis 2006;194:294-302. http://dx.doi.org/10.1097/01.nmd.0000207368.14133.0c.
- Hoge SK, Lidz C, Mulvey E, Roth L, Bennett N, Siminoff L, et al. Patient, family, and staff perceptions of coercion in mental hospital admission: an exploratory study. Behav Sci Law 1993;11:281-93. http://dx.doi.org/10.1002/bsl.2370110306.
- Hoge SK, Lidz CW, Eisenberg M, Gardner W, Monahan J, Mulvey E, et al. Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. Int J Law Psychiatry 1997;20:167-81. http://dx.doi.org/10.1016/S0160-2527(97)00001-0.
- Redlich AD, Steadman HJ, Monahan J, Robbins PC, Petrila J. Patterns of practice in mental health courts: A national survey. Law Hum Behav 2006;30:347-62. http://dx.doi.org/10.1007/s10979-006-9036-x.
- Kirsh B, Tate E. Developing a comprehensive understanding of the working alliance in community mental health. Qual Health Res 2006;16:1054-74. http://dx.doi.org/10.1177/1049732306292100.
- Lingam R, Scott J. Treatment non-adherence in affective disorders. Acta Psychiatr Scand 2002;105:164-72. http://dx.doi.org/10.1034/j.1600-0447.2002.1r084.x.
- Seale C, Chaplin R, Lelliott P, Quirk A. Sharing decisions in consultations involving anti-psychotic medication: a qualitative study of psychiatrists’ experiences. Soc Sci Med 2006;62:2861-73. http://dx.doi.org/10.1016/j.socscimed.2005.11.002.
- Magnusson A, Högberg T, Lützén K, Severinsson E. Swedish mental health nurses’ responsibility in supervised community care of persons with long-term mental illness. Nurs Health Sci 2004;6:19-27. http://dx.doi.org/10.1111/j.1442-2018.2003.00171.x.
- Angell B. Measuring strategies used by mental health providers to encourage medication adherence. J Behav Health Serv Res 2006;33:53-72. http://dx.doi.org/10.1007/s11414-005-9000-4.
- Olofsson B, Norberg A, Jacobsson L. Nurses’ experience with using force in institutional care of psychiatric patients. Nord J Psychiatry 1995;49:325-30. http://dx.doi.org/10.3109/08039489509011924.
- Olofsson B, Norberg A. Experiences of coercion in psychiatric care as narrated by patients, nurses and physicians. J Adv Nurs 2001;33:89-97. http://dx.doi.org/10.1046/j.1365-2648.2001.01641.x.
- Gardner W, Lidz C. Gratitude and coercion between physicians and patients. Psychiatr Ann 2001;31:125-9. http://dx.doi.org/10.3928/0048-5713-20010201-10.
- Solomon P, Dennis DL, Monahan J. Coercion and Aggressive Community Treatment: A New Frontier in Mental Health Law. New York: Plenum Press; 1996.
- Lützén K. Subtle coercion in psychiatric practice. J Psychiatr Ment Health Nurs 1998;5:101-7. http://dx.doi.org/10.1046/j.1365-2850.1998.00104.x.
- Stanhope V, Marcus S, Solomon P. The impact of coercion on services from the perspective of mental health care consumers with co-occurring disorders. Psychiatr Serv 2009;60:183-8. http://dx.doi.org/10.1176/ps.2009.60.2.183.
- Gray R, Wykes T, Gournay K. From compliance to concordance: a review of the literature on interventions to enhance compliance with antipsychotic medication. J Psychiatr Ment Health Nurs 2002;9:277-84. http://dx.doi.org/10.1046/j.1365-2850.2002.00474.x.
- Zygmunt A, Olfson M, Boyer CA, Mechanic D. Interventions to improve medication adherence in schizophrenia. Am J Psychiatry 2002;159:1653-64. http://dx.doi.org/10.1176/appi.ajp.159.10.1653.
- Susser E, Roche B, Dennis DL, Monahan J. Coercion and Aggressive Community Treatment: A New Frontier in Mental Health Law. New York: Plenum Press; 1996.
- Lopez M, Dennis DL, Monahan J. Coercion and Aggressive Community Treatment: A New Frontier in Mental Health Law. New York: Plenum Press; 1996.
- Claassen D, Fakhoury WK, Ford R, Priebe S. Money for medication: financial incentives to improve medication adherence in assertive outreach. Psychiatr Bull 2007;31:4-7. http://dx.doi.org/10.1192/pb.31.1.4.
- Moser LL, Bond GR. Scope of agency control: assertive community treatment teams’ supervision of consumers. Psychiatr Serv 2009;60:922-8. http://dx.doi.org/10.1176/ps.2009.60.7.922.
- Korman H, Engster D, Milstein BM, Dennis DL, Monahan J. Coercion and Aggressive Community Treatment: A New Frontier in Mental Health Law. New York: Plenum Press; 1996.
- Anderson E, Levine M, Sharma A, Ferretti L, Steinberg K, Wallach L. Coercive uses of mandatory reporting in therapeutic relationships. Behav Sci Law 1993;11:335-45. http://dx.doi.org/10.1002/bsl.2370110310.
- Nicholson J. Use of child custody as leverage to improve treatment adherence. Psychiatr Serv 2005;56:357-8. http://dx.doi.org/10.1176/appi.ps.56.3.357-a.
- Jaeger M, Rossler W. Enhancement of outpatient treatment adherence: patients’ perceptions of coercion, fairness and effectiveness. Psychiatry Res 2010;180:48-53. http://dx.doi.org/10.1016/j.psychres.2009.09.011.
- Elbogen EB, Swanson JW, Swartz MS. Psychiatric disability, the use of financial leverage, and perceived coercion in mental health services. Int J Forensic Ment Health 2003;2:119-27. http://dx.doi.org/10.1080/14999013.2003.10471183.
- Swartz M, Swanson J. Outpatient commitment: when it improves patient outcomes. Curr Psychol 2008;7:25-3.
- Rugkåsa J, Canvin K, Sinclair J, Sulman A, Burns T. Trust, deals and authority: community mental health professionals’ experiences of influencing reluctant patients. Community Ment Health J 2014;50:886-95. http://dx.doi.org/10.1007/s10597-014-9720-0.
- Life and Times of a Supermodel. The Recovery Paradigm for Mental Health. London: Mind; 2008.
- Shepherd G, Boardman J, Slade M. Making Recovery a Reality. London: Sainsbury Centre for Mental Health; 2008.
- Gillard S, Simons L, Turner K, Lucock M, Edwards C. Patient and public involvement in the coproduction of knowledge: reflection on the analysis of qualitative data in a mental health study. Qual Health Res 2012;22:1126-37. http://dx.doi.org/10.1177/1049732312448541.
- Curtis LC, Hodge M. Ethics and boundaries in community support services: new challenges. New Dir Ment Health Serv 1995;66:43-60. http://dx.doi.org/10.1002/yd.23319950206.
- Øye C. The conditions of care: on the use of gifts and services as part of relationship building in inpatient psychiatry when user involvement is emphasised. Michael 2010;2:218-33.
- Sjöström S. Invocation of coercion context in compliance communication – power dynamics in psychiatric care. Int J Law Psychiatry 2006;29:36-47. http://dx.doi.org/10.1016/j.ijlp.2005.06.001.
- Wertheimer A. Coercion. Princeton, NJ: Princeton University Press; 1987.
- Feinberg J. The Moral Limits of the Criminal Law. Vol. 3: Harm to Self. New York, NY: Oxford University Press; 1986.
- Ryan CC. The normative concept of coercion. Mind Oxford 1980;89:481-98. http://dx.doi.org/10.1093/mind/LXXXIX.356.481.
- Murphy JG. Consent, Coercion, and Hard Choices. Virginia Law Review n.d.;67:79-95. http://dx.doi.org/10.1007/978-94-015-7922-3_7.
- Dunn M, Maughan D, Hope T, Canvin K, Rugkåsa J, Sinclair J, et al. Threats and offers in community mental healthcare. J Med Ethics 2012;38:204-9. http://dx.doi.org/10.1136/medethics-2011-100158.
- Newton-Howes G, Mullen R. Coercion in psychiatric care: systematic review of correlates and themes. Psychiatr Serv 2011;62:465-70. http://dx.doi.org/10.1176/ps.62.5.pss6205_0465.
- McNiel DE, Gormley B, Binder RL. Leverage, the treatment relationship, and treatment participation. Psychiatr Serv 2013;64:431-6. http://dx.doi.org/10.1176/appi.ps.201200368.
- Hox J. Applied Multilevel Analysis. Amsterdam: TT-Publikaties; 1995.
- Canvin K, Rugkåsa J, Sinclair J, Burns T. Leverage and other informal pressures in community psychiatry in England. Int J Law Psychiatry 2013;36:100-6. http://dx.doi.org/10.1016/j.ijlp.2013.01.002.
- Lewis A. Group child interviews as a research tool. Brit Educ Res J 1992;18:413-21. http://dx.doi.org/10.1080/0141192920180407.
- Lewis J, Ritchie J, Lewis J. Qualitative Research Practice. A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Meadows LM, Morse JM, Morse JM, Swanson J, Kuzel A. The Nature Of Evidence In Qualitative Inquiry. Thousand Oaks, CA: Sage; 2001.
- Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Thousand Oaks, CA: Sage; 1990.
- Blumer H. Symbolic Interactionism. Englewood Cliffs, NJ: Prentice-Hall; 1969.
- Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York, NY: Aldine; 1967.
- Kitzinger J, Holloway I. Qualitative Research In Health Care. Maidenhead: Open University Press; 2005.
- Denzin NK, Lincoln YS. Handbook of Qualitative Research. Thousand Oaks: Sage; 1995.
- Clarke A, Morse J, Stern P, Corbin J, Bowers B, Charmaz K, et al. Developing Grounded Theory: The Second Generation. Walnut Creek, CA: Left Coast Press; 2009.
- Priebe S, Sinclair J, Burton A, Marougka S, Larsen J, Firn M, et al. Acceptability of offering financial incentives to achieve medication adherence in patients with severe mental illness: a focus group study. J Med Ethics 2010;36:463-8. http://dx.doi.org/10.1136/jme.2009.035071.
- Dunn M, Sinclair JM, Canvin KJ, Rugkåsa J, Burns T. The use of leverage in community mental health: ethical guidance for practitioners. Int J Soc Psychiatry 2014;60:759-65. http://dx.doi.org/10.1177/0020764013519083.
- Beauchamp T, Bloch S, Green SA. Psychiatric Ethics. Oxford, UK: Oxford University Press; 2009.
- Drug Misuse: Psychosocial Interventions. London, England: NICE; 2007.
- Giuffrida A, Torgerson DJ. Should we pay the patient? Review of financial incentives to enhance patient compliance. BMJ 1997;315:703-7. http://dx.doi.org/10.1136/bmj.315.7110.703.
- Leong FT, Lau AS. Barriers to providing effective mental health services to Asian Americans. Ment Health Serv Res 2001;3:201-14. http://dx.doi.org/10.1023/A:1013177014788.
- Snowden LR. Barriers to effective mental health services for African Americans. Ment Health Serv Res 2001;3:181-7. http://dx.doi.org/10.1023/A:1013172913880.
- Keating F, Robertson D. Fear, black people and mental illness: a vicious circle?. Health Soc Care Community 2004;12:439-47. http://dx.doi.org/10.1111/j.1365-2524.2004.00506.x.
- Moffat J, Sass B, McKenzie K, Bhui K. Improving pathways into mental health care for black and ethnic minority groups: a systematic review of the grey literature. Int Rev Psychiatry 2009;21:439-49. http://dx.doi.org/10.1080/09540260802204105.
- Morgan C, Hutchinson G. The social determinants of psychosis in migrant and ethnic minority populations: a public health tragedy. Psychol Med 2010;40:705-9. http://dx.doi.org/10.1017/S0033291709005546.
- Williams A. Cost-effectiveness analysis: is it ethical?. J Med Ethics 1992;18:7-11. http://dx.doi.org/10.1136/jme.18.1.7.
- Sheehan M, Hope T, Rhodes R, Battin M, Silvers A. Medicine and Social Justice: Essays on the Distribution of Health Care. New York, NY: Oxford University Press; 2012.
- Radoilska L, Radoilska L. Autonomy and Mental Disorder. Oxford: Oxford University Press; 2012.
- Coggon J, Miola J. Autonomy, liberty, and medical decision-making. Camb Law J 2011;70:523-47. http://dx.doi.org/10.1017/S0008197311000845.
- McCabe R, Priebe S. The therapeutic relationship in the treatment of severe mental illness: a review of methods and findings. Int J Soc Psychiatry 2004;50:115-28. http://dx.doi.org/10.1177/0020764004040959.
- Dresser R. Bound to treatment: the Ulysses contract. Hastings Cent Rep 1984;14:13-6. http://dx.doi.org/10.2307/3561181.
- Rosenson MK, Kasten AM. Another view of autonomy: arranging for consent in advance. Schizophr Bull 1991;17:1-7. http://dx.doi.org/10.1093/schbul/17.1.1.
- Swartz MS, Swanson JW, Kim M, Petrila J. Use of outpatient commitment or related civil court treatment orders in five U.S. communities. Psychiatr Serv 2006;57:343-9. http://dx.doi.org/10.1176/appi.ps.57.3.343.
- Zigmond T. Pressures to adhere to treatment: observations on ‘leverage’ in English mental healthcare. Br J Psychiatry 2011;199:90-1. http://dx.doi.org/10.1192/bjp.bp.111.091876.
- Wadham J, Robinson A, Ruebain D, Uppal S. Blackstone’s Guide to the Equality Act 2010. Oxford: Oxford University Press; 2010.
- Weisstub DN, Arboleda-Flórez J. Canadian mental health rights in an international perspective. Sante Ment Que 2006;31:19-46. http://dx.doi.org/10.7202/013683ar.
- Wong Y-LI, Lee S, Solomon PL. Structural leverage in housing programs for people with severe mental illness and its relationship to discontinuance of program participation. Am J Psychiatr Rehabil 2010;13:276-94. http://dx.doi.org/10.1080/15487768.2010.523361.
- Fennell P, McSherry B, Weller P. Rethinking Rights-Based Mental Health Laws. Oxford: Hart Publishing; 2010.
- Redlich AD, Monahan J. General pressures to adhere to psychiatric treatment in the community. Int J Forensic Ment Health 2006;5:125-31. http://dx.doi.org/10.1080/14999013.2006.10471237.
- Mauss M. The Gift: Forms and Functions of Exchange in Archaic Societies. London: Routledge; 1990.
- Malinowski B. Argonauts of the Western Pacific: An Account of Native Enterprise and Adventure in the Archipelagoes of Melanesian New Guinea. London: Routledge; 1978.
- Wolff KH. The Sociology of Georg Simmel. New York, NY: The Free Press; 1950.
- Laugharne R, Priebe S, McCabe R, Garland N, Clifford D. Trust, choice and power in mental health care: experiences of patients with psychosis. Int J Soc Psychiatry 2012;58:496-504. http://dx.doi.org/10.1177/0020764011408658.
- Swartz MS, Swanson JW, Hannon MJ. Does fear of coercion keep people away from mental health treatment? Evidence from a survey of persons with schizophrenia and mental health professionals. Behav Sci Law 2003;21:459-72. http://dx.doi.org/10.1002/bsl.539.
- Kleinman A, Kleinman J. Suffering and its professional transformation: toward an ethnography of interpersonal experience. Cult Med Psychiatry 1991;15:275-301. http://dx.doi.org/10.1007/BF00046540.
- Swanson JW, Van Dorn RA, Monahan J, Swartz MS. Violence and leveraged community treatment for persons with mental disorders. Am J Psychiatry 2006;163:1404-11. http://dx.doi.org/10.1176/ajp.2006.163.8.1404.
- Priebe S, Katsakou C, Amos T, Leese M, Morriss R, Rose D, et al. Patients’ views and readmissions 1 year after involuntary hospitalisation. Br J Psychiatry 2009;194:49-54. http://dx.doi.org/10.1192/bjp.bp.108.052266.
- Richardson G. Coercion and human rights: a European perspective. J Ment Health 2008;17:245-54. http://dx.doi.org/10.1080/09638230802052211.
- Burns T. Community treatment orders: state of the evidence. East Asian Arch Psychiatry 2013;23:35-6.
- Burns T, Molodynski A. Community treatment orders: background and implications of the OCTET trial. Psychiatr Bull 2014;38:3-5. http://dx.doi.org/10.1192/pb.bp.113.044628.
- Post-legislative Scrutiny of the Mental Health Act 2007-HC 584: First report of Session 2013–14, Report, Together with Formal Minutes, Oral and Written Evidence. London: The Stationery Office; 2013.
- Nakhost A, Perry JC, Simpson AI. Community treatment orders for patients with psychosis. Lancet 2013;382. http://dx.doi.org/10.1016/S0140-6736(13)61703-1.
- McCutcheon R. Community treatment orders for patients with psychosis. Lancet 2013;382. http://dx.doi.org/10.1016/S0140-6736(13)61704-3.
- Naudet F, El Sanharawi M. Community treatment orders for patients with psychosis. Lancet 2013;382:501-2. http://dx.doi.org/10.1016/S0140-6736(13)61705-5.
- Geller J. Community treatment orders for patients with psychosis. Lancet 2013;382. http://dx.doi.org/10.1016/S0140-6736(13)61706-7.
- Mustafa FA. On the OCTET and supervised community treatment orders. Med Sci Law 2014;54:116-17. http://dx.doi.org/10.1177/0025802413506898.
- Mustafa FA. The OCTET trial, community treatment orders and evidence-based practice. Psychiatr Bull 2014;38. http://dx.doi.org/10.1192/pb.38.4.197.
- Owen AJ, Mirok D, Sood L. OCTET Study: flawed by type 2 error. Psychiatr Bull 2014;38:196-7. http://dx.doi.org/10.1192/pb.38.4.196b.
- Light E. The epistemic challenges of CTOs: commentary on . . . community treatment orders. Psychiatr Bull 2014;38:6-8. http://dx.doi.org/10.1192/pb.bp.113.045732.
- Curtis D. OCTET does not demonstrate a lack of effectiveness for community treatment orders. Psychiatr Bull 2014;38:36-9. http://dx.doi.org/10.1192/pb.bp.113.044800.
- Segal SP. Community treatment orders do not reduce hospital readmission in people with psychosis. Evid Based Ment Health 2013;16. http://dx.doi.org/10.1136/eb-2013-101438.
- Burns T. Letter in response to Dr Segal’s commentary. Evid Based Ment Health 2013;16. http://dx.doi.org/10.1136/eb-2013-101579.
- Burns T, Rugkåsa J, Molodynski A. Community treatment orders for patients with psychosis: authors’ reply. Lancet 2013;382:502-3. http://dx.doi.org/10.1016/S0140-6736(13)61707-9.
- Rugkåsa J, Dawson J, Burns T. The OCTET RCT: a reply to Dr Mustafa. Med Sci Law 2014;54:118-19. http://dx.doi.org/10.1177/0025802413518528.
- Molodynski A, Burns T. Author reply. Psychiatr Bull 2014;38:197-8. http://dx.doi.org/10.1192/pb.38.4.197a.
- Molodynski A, Rugkåsa J, Burns T. Coercion in Community Mental Health Care: International Perspectives. Oxford: Oxford University Press; 2016.
- Post-legislative scrutiny of the Mental Health Act 2007: Health Committee Contents. London: The Stationery Office; 2013.
- Puntis S. Continuity of Care and Patient Outcomes in Community Mental Health. Oxford: University of Oxford; 2015.
- Yeeles K. Associations of Informal Coercion with Legal Compulsion, Clinical Outcomes and Therapeutic Relationship in Community Mental Health Care. Oxford: University of Oxford; 2016.
- Vergunst F. Psychiatric Compulsion and Long-term Social Outcomes for Patients with Psychosis: Is there an Association?. Oxford: University of Oxford; 2015.
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51. http://dx.doi.org/10.1037/0022-3514.51.6.1173.
Appendix 1 Ethics amendments
OCTET ethics amendments
Amendment 1, approved April 2009
-
The inclusion of capabilities questions in the research instrument (see Chapter 10). Although these formed part of the original plan, they had not been available at the time that ethics approval was given.
-
The inclusion of a visual aid to help patients understand the study better in the consent process.
Amendment 2, approved June 2009
-
To reflect the changing nature of service configuration, the protocol was amended so as to recruit patients via inpatient services and not exclusively, as initially envisaged, through outpatient services.
Amendment 3, approved January 2011
-
To better capture the variation in views of clinicians and carers, with regard to the sensitive and contentious issue of CTOs, the planned focus group studies with these two groups was changed to individual in-depth interview studies.
-
To ensure that we had sufficient statistical power for the analysis set out in the protocol, the sample was enlarged by 10% to reach up to 330 patients by the end of the recruitment period.
Amendment 4, approved July 2011
-
To investigate the long-term effect of CTO on outcomes and on engagement with services in the OCTET Follow-up Study, an additional point of data collection at 36 months after randomisation was added.
ULTIMA ethics amendments
Amendment 1, approved June 2007:
-
Change of principal investigator following initial pilot.
Amendment 2, approved October 2007
-
To employ two more research assistants after receiving the NIHR funding grant.
-
To modify power calculation based on the newly published study7 and consequently change the sample size to 400.
-
In order to cover the range of patients who were likely to be subject to leverage, and to distinguish patients with long-term psychosis from disabled patients with long-term non-psychosis by adding a non-psychosis CMHT group.
-
To extend the study until 1 April 2010 because of the expanded samples, funding and the slow recruitment at the beginning of the study.
Amendment 3, approved December 2007
-
The study protocol was amended by adding semistructured, in-depth interviews with patients and with staff groups to better understand the mechanisms and functions of leverage in community mental health care, and better capture the variations in views of clinicians and patients.
Amendment 4, approved February 2008
-
The inclusion of the Psychiatric Autonomy Preference Index questionnaire to associate use of leverage and perceived coercion with patients’ autonomy preferences in psychiatric services.
Amendment 5, approved March 2008
-
The inclusion of eight questions on patients’ understanding of maintenance antipsychotic medication for the subgroup of study patients with a diagnosis of schizophrenia to investigate whether or not the level of informal coercion partly reflects differences between clinicians and patients in their understanding of the need for such continuation.
Appendix 2 Statistical analysis plans
OCTET statistical analysis plan
OCTET Follow-up Study statistical analysis plan
Appendix 3 Development of the Oxford Capabilities Questionnaire–Mental Health
| OCAP (2005 English version) | OCAP-18 | OxCAP-MH |
|---|---|---|
| C1. Does your health in any way limit your daily activities compared with most people of your age? (two-point scale: yes/no) |
5. Does your health in any way limit your daily activities, compared with most people your age? (two-point scale: yes/no) |
1. Does your health in any way limit your daily activities, compared to most people your age? (two-point scale: yes/no) |
| C63. Do you normally meet up with friends or family for a drink or a meal at least once a month? and C64–7. In general, why do you not meet friends or family for a drink or meal more often? (Please tick all that apply – Lack of money/ do not have time/Choose not to/Some other reason) |
6. Are you able to meet socially with friends, relatives or work colleagues? (two-point scale: yes/no) |
2. Are you able to meet socially with friends or relatives? (two-point scale: yes/no) |
| C31. Have you recently lost much sleep over worry? | 8. In the past 4 weeks, how often have you lost sleep over worry? (five-point scale: Always to Never) |
3. In the past 4 weeks, how often have you lost sleep over worry? (five-point scale: Always to Never) |
| C36. Have you recently been enjoying your recreational activities? | 9. In the past 4 weeks how often have you been able to enjoy your recreational activities? (five-point scale: Always to Never) |
4. In the past 4 weeks how often have you been able to enjoy your recreational activities? (five-point scale: Always to Never) |
| 13. Which of these applies to your home? (5 potential answers, one of them being ‘I own my own home outright/or on a mortgage.) |
5. Do you own your home (outright/or on a mortgage)? | |
| C43. Is your current accommodation adequate or inadequate for your current needs? | 15. How suitable or unsuitable is your accommodation for your current needs? (five-point scale: Very suitable to Very unsuitable) |
6. How suitable or unsuitable is your accommodation for your current needs? (five-point scale: Very suitable to Very unsuitable) |
| C46. Please indicate how safe you feel walking alone in the area near your home DURING THE DAY time C47. Please indicate how safe you feel walking along in the area near your home AFTER DARK (five-point scale: Very safe to Very unsafe) |
16. Please indicate how safe you feel walking alone in the area near your home: (five-point scale: Very safe to Very unsafe) |
7. Please indicate how safe you feel walking alone in the area near your home: (five-point scale: Very safe to Very unsafe) |
| C51. Please indicate how vulnerable you feel to domestic violence in the future – using a scale of 1–7 where 1 means ‘Not at all vulnerable’ and 7 means ‘Very vulnerable’ | 17. Please indicate how likely you believe it to be that you will be assaulted in the future (including sexual and domestic assault): (five-point scale: Very likely to Very unlikely) |
8. Please indicate how likely you believe it to be that you will be assaulted in the future (including sexual and domestic assault): (five-point scale: Very likely to Very unlikely) |
| C76–80. When seeking work in future how likely do you think it is that you will experience discrimination because of your . . . Race, Sexual Orientation, Gender, Religion, Age, and C86–90. Outside of any work or employment situation. How likely do you think it is that in the future you will be discriminated against because of your age? (5-point scale: Very likely to Very unlikely) |
18. In your current or any future employment, how likely do you think it is that you will experience discrimination (e.g. because of your race, gender, religion, sexual orientation, age, or health)? (five-point scale: Very likely to Very unlikely) 19. Outside of any employment, in your everyday life, how likely do you think it is that you will experience discrimination (e.g. because of your race, gender, religion, sexual orientation, age, or health)? (five-point scale: Very likely to Very unlikely) |
9a. How likely do you think it is that you will experience discrimination?
(five-point scale: Very likely to Very unlikely) 9b.On what grounds do you think it is likely that you will be discriminated against? Race/ethnicity, Gender, Religion, Sexual orientation, Age, Health or disability (including mental health) |
| 11. Please indicate how strongly you agree or disagree with the following statements: (five-point scale: Strongly agree to Strongly disagree) |
10. Please indicate how strongly you agree or disagree with the following statements: (five-point scale: Strongly agree to Strongly disagree) |
|
| C21. I am able to participate in the political activities that affect my life if I want to (five-point scale: Strongly agree to Strongly disagree) | a. I am able to influence decisions affecting my local area | a. I am able to influence decisions affecting my local area |
| C20. I am free to express my political views C22. I am free to practice my religion as I want to (five-point scale: Strongly agree to Strongly disagree) |
b. I am free to express my views including political and religious views | b. I am free to express my views including political and religious views |
| c. I am able to appreciate and value plants, animals and the world of nature | c. I am able to appreciate and value plants, animals and the world of nature | |
| C24. I respect value and appreciate other people (five-point scale: Strongly agree to Strongly disagree) |
d. I respect, value and appreciate people around me | d. I respect, value and appreciate people around me |
| C27. At present, how easy or difficult do you find it to enjoy the love care and support of your immediate family? (five-point scale: Very easy to Very difficult) |
7. At present, how easy or difficult do you find it to enjoy the love, care and support of your family and friends? (five-point scale: Very easy to Very difficult) |
e. I find it easy to enjoy the love, care and support of my family and friends |
| C23. My idea of a good life is based on my own judgement, and C56. I have a clear plan of how I would like my life to be (five-point scale: Strongly agree to Strongly disagree) |
e. I am free to decide for myself how to live my life | f. I am free to decide for myself how to live my life |
| C55. How often do you use your imagination and/or reasoning in your day to day life? (seven-point scale: All the time to Never) To what extent does your work make use of your skills and talents? Given you family history, dietary habits, lifestyle and health status until what age do expect to live? (Age in years) |
f. I am free to use my imagination and to express myself creatively (e.g. through art, literature, music, etc.) | g. I am free to use my imagination and to express myself creatively (e.g. through art, literature, music, etc.) |
| h. I have access to interesting forms of activity (or employment) | ||
| 10. Until what age do you expect to live, given your family history, dietary habits, lifestyle and health status? (Age in years) |
11. The next question asks you to think about your life expectancy: The average life expectancy in the UK is 77 years for men and 81 years for women. Some people think they are going to live longer than the average person whilst other people believe they are going to live shorter than the average person. 11a Given your family history, dietary habits, lifestyle and health status, do you expect to live . . .? (three-point scale: Longer/Same/Shorter than average) 11b. Until what age do you believe you are going to live? (Age in years) |
Appendix 4 OCTET conference
Appendix 5 Steering group and data monitoring committee composition
OCTET steering group
-
Independent clinician: Professor George Szmukler, Institute of Psychiatry, London.
-
Service user: Ms Alice Hicks, independent researcher, Oxford.
-
Service user organisation representatives: Jayasree Kalathil (Afiya Trust), 2009–10; Sophie Corlett (Director of External Relations, Mind).
-
Carer representative: Mrs Pat Ross, Oxfordshire Mind Oxford Health NHS Foundation Trust carer representative.
-
Lawyer: Ms Belinda Cheney.
OCTET data monitoring committee
-
Professor John Geddes, Professor of Psychiatry and Head of Oxford Clinical Trials Unit for Mental Illness, University of Oxford.
-
Professor Peter Bartlett, Professor of Mental Health Law, University of Nottingham.
-
Dr Helen Doll, Senior Departmental Statistician, Health Services Research Unit, Department of Public Health, University of Oxford.
List of abbreviations
- ACT
- Assertive Community Treatment
- AES
- MacArthur Admission Experience Survey
- AMHP
- approved mental health professional
- ANOVA
- analysis of variance
- AOT
- Assertive Outreach Team
- API
- Autonomy Preference Index
- BMI
- body mass index
- BPRS
- Brief Psychiatric Rating Scale
- CAGE
- ‘Cutting down’, ‘Annoyance by criticism’, ‘Guilty feeling’ and ‘Eye-openers’ screening questionnaire for alcohol and drug misuse
- CAPINDEX16
- 16-question capability index
- CBA
- controlled before-and-after [study]
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CMHT
- Community Mental Health Team
- CPN
- community psychiatric nurse
- CRB
- Criminal Records Bureau
- CSQ-8
- Client Satisfaction Questionnaire
- CSRI
- Client Service Receipt Inventory
- CTO
- community treatment order
- DAI-10
- Drug Attitude Inventory, 10-item version
- DMC
- data monitoring committee
- EIS
- Early Intervention Services
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D VAS
- EuroQol-5 Dimensions visual analogue scale
- FG
- focus group
- GAF
- Global Assessment of Functioning
- GP
- general practitioner
- HR
- hazard ratio
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- ID
- identification
- IDR
- incidence–density ratio
- ITAQ
- Insight and Treatment Attitudes Questionnaire
- MHA
- Mental Health Act
- MHRT
- Mental Health Review Tribunal
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute of Health Research
- OCAP
- Oxford Capabilities
- OCTET
- Oxford Community Treatment Order Evaluation Trial
- OR
- odds ratio
- OxCAP-MH
- Oxford Capabilities Questionnaire – Mental Health
- QALY
- quality-adjusted life-year
- R&D
- research and development
- RC
- responsible clinician
- RCT
- randomised controlled trial
- SD
- standard deviation
- SE
- standard error
- SIX
- Objective Social Outcomes Index
- SOAD
- second opinion appointed doctor
- STAR-C
- Scale To Assess Therapeutic Relationship–Clinician Version
- STAR-P
- Scale To Assess Therapeutic Relationship–Patient Version
- UBA
- uncontrolled before-and-after [study]
- ULTIMA
- Use of Leverage Tools to Improve Adherence in community Mental Health care