Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0407-10231. The contractual start date was in April 2009. The final report began editorial review in November 2014 and was accepted for publication in February 2016. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Elaine McColl is a subpanel member for the National Institute for Health Research (NIHR) Programme Grants for Applied Research (PGfAR) journal, but in that capacity has already declared a conflict of interest in respect of this grant and has not been involved in any discussions or decisions thereon. Elaine McColl was a NIHR journal editor for the NIHR PGfAR journal at the time that this report was written and has a declared conflict of interest in respect of this report and will not participate in any discussions, work or decisions thereon. The Keeping Children Safe programme received Flexibility and Sustainability Funding from Nottinghamshire County Teaching Primary Care Trust, University Hospitals Bristol NHS Foundation Trust and Norfolk and Suffolk Comprehensive Local Research Network and Research Capability Funding from Nottinghamshire County Teaching Primary Care Trust and Nottinghamshire Healthcare NHS Foundation Trust to support NIHR Faculty members’ salaries.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Kendrick et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction to the Keeping Children Safe programme of research
Why are child injuries important?
Unintentional injuries are a major public health challenge facing children in England today. Injuries are a particular problem in young children, with death and hospital admission rates being higher in the under-fives than at other ages in childhood. Unintentional injuries resulted in 311 deaths in the under-fives in England between 2008 and 2012, making injuries the most common cause of death in the 1–4 years age group. 1 More than 45,000 children aged < 5 years were admitted to hospital in England in 2012/13,2 and approximately 450,000 under-fives attended an emergency department (ED) in the UK following an unintentional injury in 20023 (the latest year for which detailed national data on unintentional injuries were collected in the UK). Childhood injuries, especially severe injuries, can also have long-term health, educational, social and occupational consequences. These include physical disability,4–6 psychological morbidity,7,8 cognitive or social impairment,9 lower educational achievement9,10 and poorer employment prospects. 9 In addition, injuries also impact psychologically on those caring for children. 7
Unintentional injuries do not just result in death and injury. They also place burdens on the NHS and other care agencies and on injured children and their families. The Chief Medical Officer (CMO)’s report for England in 2012 highlighted the high cost of injuries to the NHS and the potential for prevention. 11 The annual cost of ED attendances was estimated to be £9M, and the cost of hospital admissions was estimated to be £16–87M, depending on injury mechanism.
Unintentional injuries disproportionately affect children living in socioeconomic disadvantage. The socioeconomic gradient in unintentional injury deaths is steeper than for any other cause of death in childhood,12 with children living in the most disadvantaged households having a death rate that is 13 times higher than that for children living in the most advantaged households. 13
Child injury prevention policy in England
Child injury prevention has had varying prominence in government policy in England over the past 25 years. The Health of the Nation White Paper14 formed the central health policy in England between 1992 and 1997. It was the first attempt by a government in England to strategically improve the health of the population. Reduction in accidental injury was identified as one of five national targets for health improvement.
This was replaced by Saving Lives: Our Healthier Nation (1999)15 under the Labour administration’s health policy, which included accidental injury as one of its four key public health priorities. It set a target to reduce death rates from accidents by at least one-fifth and to reduce the rate of serious injury from accidents by at least one-tenth by 2010, describing this as a ‘tough but attainable target’. It also recognised that injury was a leading cause of childhood admissions to hospital. The White Paper announced that an interdepartmental and expert task force would be set up to advise on how the targets should be achieved.
The Accidental Injury Task Force published a report for the CMO in 2002 to identify steps that would have the greatest impact on injury prevention. 16 One working group focused on child injury. Recommendations included cross-governmental co-ordination of initiatives, data collection and integration, developing the workforce for delivery and leadership, and research and dissemination of evidence. It highlighted the significance of deprivation in childhood injury. The task force recommended that a series of headline interventions should form the core of local implementation plans, giving focus and clarity to the somewhat fragmented approach to injury prevention at the time. It also advised targeting of interventions at areas of health inequality.
The Every Child Matters17 policy arose with the Children Act 2004. 18 There were five outcomes that the policy sought to achieve for all children, one of which was ‘stay safe’, which included safety from unintentional injury.
A joint study by the Audit Commission and the Healthcare Commission, Better Safe Than Sorry, in 200719 examined the deployment of resources, arrangements for working in partnership and activities to prevent unintentional injury to children, especially the under-fives. The report contained a series of recommendations for the government, including re-emphasising the recommendations and strategy from the Accidental Injury Task Force and encouraging local organisations to take up and follow the evidence-based guidance contained within the report and commissioning the National Institute for Health and Care Excellence (NICE) to develop guidance on the prevention of unintentional injury for children aged < 15 years.
The Staying Safe: Action Plan was launched in 2008,20 setting out the government’s priorities for the period 2008–11. These included establishing the National Home Safety Equipment Scheme Safe at Home. 21 A review examining prevention practice at the time and making recommendations also arose from the action plan and led to the publication of Accident Prevention Amongst Children and Young People: a Priority Review. 22 The government also set a Public Service Agreement target (PSA 13) to improve children’s and young people’s safety that included four indicators, including one on a reduction in hospital admissions caused by unintentional and deliberate harm.
In 2010, the coalition government published the Healthy Lives, Healthy People White Paper,23 setting out plans for a comprehensive reform of the public health system. The plans revolved around decentralising public health and giving local authorities more power over public health budgets in their area. The new system took effect from April 2013, when Public Health England was established and public health services formally transferred from the NHS to local authorities. The new system focuses on outcomes rather than targets, which are set out in the Public Health Outcomes Framework,24 including one indicator to reduce hospital admissions from unintentional and deliberate injuries for the 0–4 years age group, with support from other partners in the public health system. Other indicators relate to reducing health inequalities.
In 2013, the CMO for England highlighted the issue of child accident prevention and has made a powerful economic case for preventing childhood injuries. 11
Other major national health-related initiatives included the development by NICE of a series of guidance documents on the prevention of unintentional injuries in children aged < 15 years. NICE published public health guidance, Strategies to Prevent Unintentional Injuries among Children and Young People Aged under 15 [public health guidance (PH) 29] in 2010. 25 Evidence published since the development of PH29 was reviewed in 2013 but did not result in any changes to the recommendations. 26 A further document, Preventing Unintentional Injuries in the Home among Children and Young People Aged under 15 (PH30) was also published in 2010. 27 PH29 recommends that local and national plans and strategies for children and young people’s health and well-being include a commitment to preventing unintentional injuries. Emphasis is also given to targeting injury prevention towards the most vulnerable groups to reduce inequalities in health.
Despite the policies described above, Better Safe Than Sorry also highlighted that there was little evidence of a systematic strategic approach to develop, implement and monitor programmes to prevent unintentional injuries in children within the NHS. 19 A report in 2012 from the European Child Safety Alliance and EuroSafe, the European Association for Injury Prevention and Safety Promotion, assessed evidence-based national-level child injury prevention policy measures in 31 European Union (EU) member states. 28 The report concluded that there was much scope for improvement in implementing child injury prevention measures in England, stating that if England had the unintentional injury death rate in 2010 of the EU country with the lowest rate (the Netherlands), 198 deaths in children and young people would have been avoided. It identified some progress in addressing the issue of child injury, but also that stronger government leadership was needed to produce and implement a national evidence-based child injury prevention strategy including funding for injury prevention measures, co-ordination of child injury prevention activities, infrastructure and capacity building. Recommendations included the integration of evidence-based good practice strategies into national public health programmes, the adoption and implementation of evidence-based injury prevention strategies at national and local levels and capacity building for stakeholders working at all levels. 29
The report also highlighted unintentional injuries as the leading cause of inequality in childhood deaths and acknowledged that the English government had supported studies examining inequities and provided time-limited funding for a home safety equipment scheme targeting disadvantaged families. However, it concluded that ‘vacillating government support for the injury issue and related programmes has not resulted in a comprehensive coordinated approach that would ensure equitable coverage of children on safety issues’ (p. 3). 29
The Keeping Children Safe (KCS) programme of research was, therefore, undertaken over a period of time in which there was an increasing acceptance of the need for evidence-based injury prevention, development of national guidelines to facilitate this and the use of indicators to reduce admissions for injuries in children and young people. However, during this period of time there was no national strategy or widespread adoption and implementation of co-ordinated evidence-based child injury prevention.
The most important injuries to focus on
The KCS programme of research focused on the prevention of thermal injuries, falls and poisonings. In terms of injury-related deaths in the under-fives in England, deaths from falls are the third most common, deaths from smoke, fire and flames are the fourth most common and deaths from poisoning are the sixth most common. 1 Thermal injuries, falls and poisonings are three of the four most common types of injury resulting in hospital admission in the under-fives in England. 2 In 2012/13, > 18,300 under-fives were admitted to hospital in England following a fall, > 5100 were admitted with poisoning and > 2210 were admitted following a thermal injury, 1420 of which were scalds. Emergency admissions for falls, poisonings and scalds in the under-fives cost the NHS in England £19.1M in 2012/13. 30 There are no recent data available on ED attendances, but data from 2002 show that approximately 280,000 under-fives attended an ED following a thermal injury, fall or poisoning in the UK. 3 The cost of these visits to the NHS converted to 2012/13 prices is nearly £32M. 31 In total, 80% of all admissions in children aged 0–14 years for thermal injuries occur in the under-fives, as do 73% of all poisonings and 45% of all scalds, highlighting the importance of focusing on this age group. The majority of injuries in the under-fives occur at home,32 hence the KCS programme focused on thermal injuries, falls and poisonings occurring at home in the under-fives.
The need to develop the evidence base for preventing thermal injuries, falls and poisonings
The NHS needs to be able to make evidence-based decisions about which interventions to fund to prevent home injury in childhood, but the lack of evidence on effectiveness and cost-effectiveness of interventions hampers decision-making. Systematic reviews and meta-analyses33–42 show that home safety interventions increase safety behaviours and use of safety equipment, but also highlight the lack of evidence about whether these interventions reduce injury occurrence or are cost-effective. In addition, there is a lack of data on the cost of injuries to children, families and the NHS and on how to implement effective child injury prevention interventions within the NHS. The KCS programme, therefore, aimed to increase evidence-based thermal injury, falls and poisoning prevention by assessing risk and protective factors for these injuries, evaluating the effectiveness and cost-effectiveness of interventions to prevent these injuries, developing injury prevention briefings (IPBs) for effective and cost-effective interventions and evaluating the implementation of one IPB in children’s centres. We have considered thermal injuries in two categories in this research programme – scalds and fire-related burns – because although the tissue injury and pathophysiology are similar, the mechanisms and potential safety measures are very different. Some work streams (e.g. work streams 1, 2 and 6) focus on specific types of thermal injuries (e.g. scalds or fire-related injuries) whereas others focus on all thermal injuries, depending on the existing evidence base. The programme of work to achieve the aims is outlined below.
The Keeping Children Safe programme of research
Research questions
The research questions addressed within six work streams in the KCS programme are outlined in the following sections and shown in Figure 1.
FIGURE 1.
The Keeping Children Safe programme of research.

Work stream 1
This work stream addressed the question, ‘What are the associations between modifiable risk and protective factors and medically attended injuries resulting from five common injury mechanisms in children under the age of 5 years?’ This question was answered by a series of five case–control studies exploring risk and protective factors for each of the three most common types of medically attended falls (falls from furniture, stair falls and falls on one level), poisonings and scalds. These five studies are collectively referred to as study A. In addition, a study to validate the self-reported exposures was nested within the case–control studies in study A, and this is referred to as study B.
Work stream 2
This work stream addressed the question, ‘What are the NHS and child and family costs of falls, poisonings and scalds?’ This was answered by a cohort study measuring costs and injury outcomes nested within the case–control studies in study A. In addition, as there were no validated tools to measure health-related quality of life (HRQL) in the short term following a range of injuries in the under-fives, this study also validated the toddler version of the Pediatric Quality of Life Inventory (PedsQL™)43 for this purpose. These two studies are referred to as study C, with the costs study referred to as the study C costs substudy and the validation of the PedsQL study referred to as the study C HRQL substudy.
Work stream 3
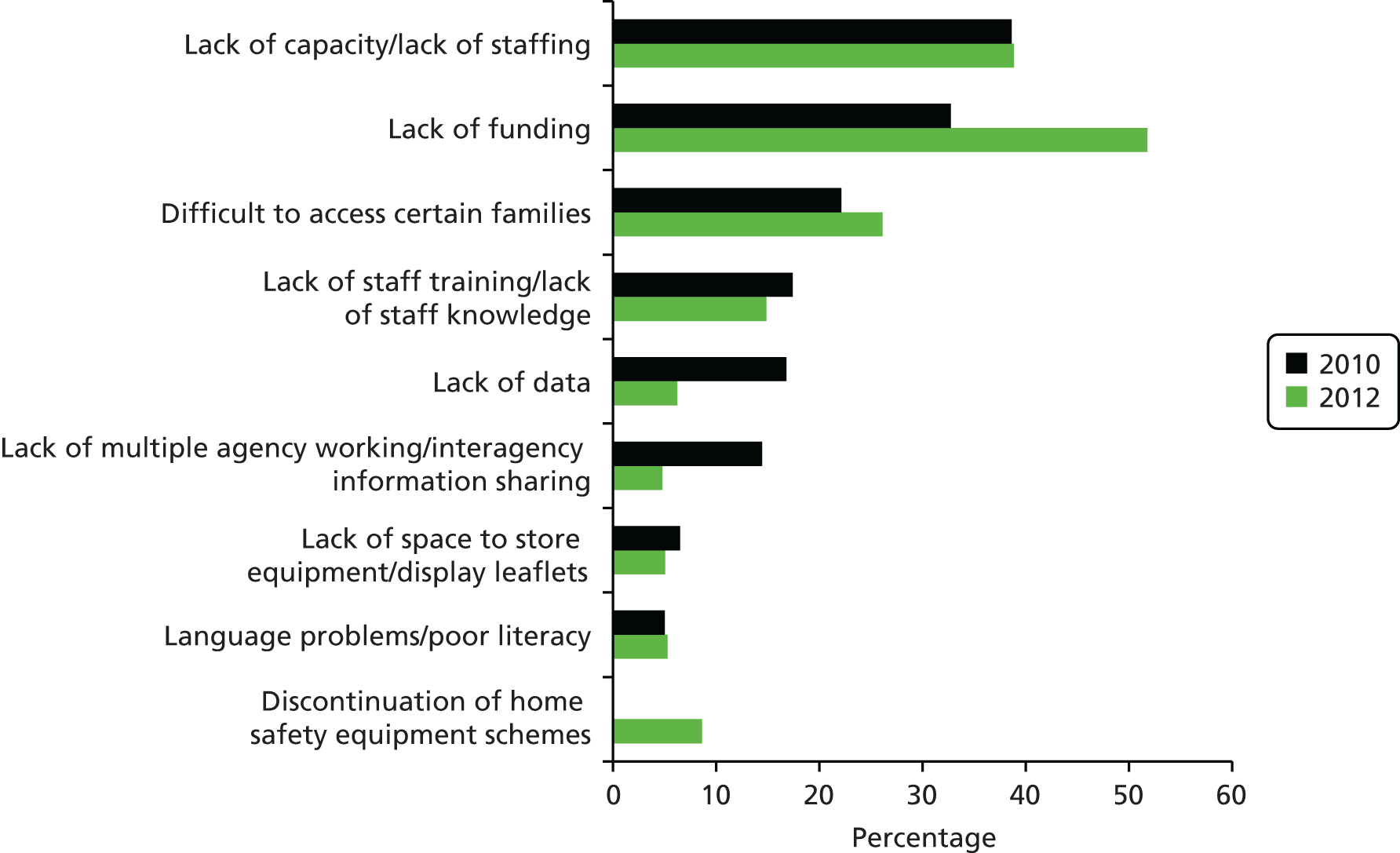
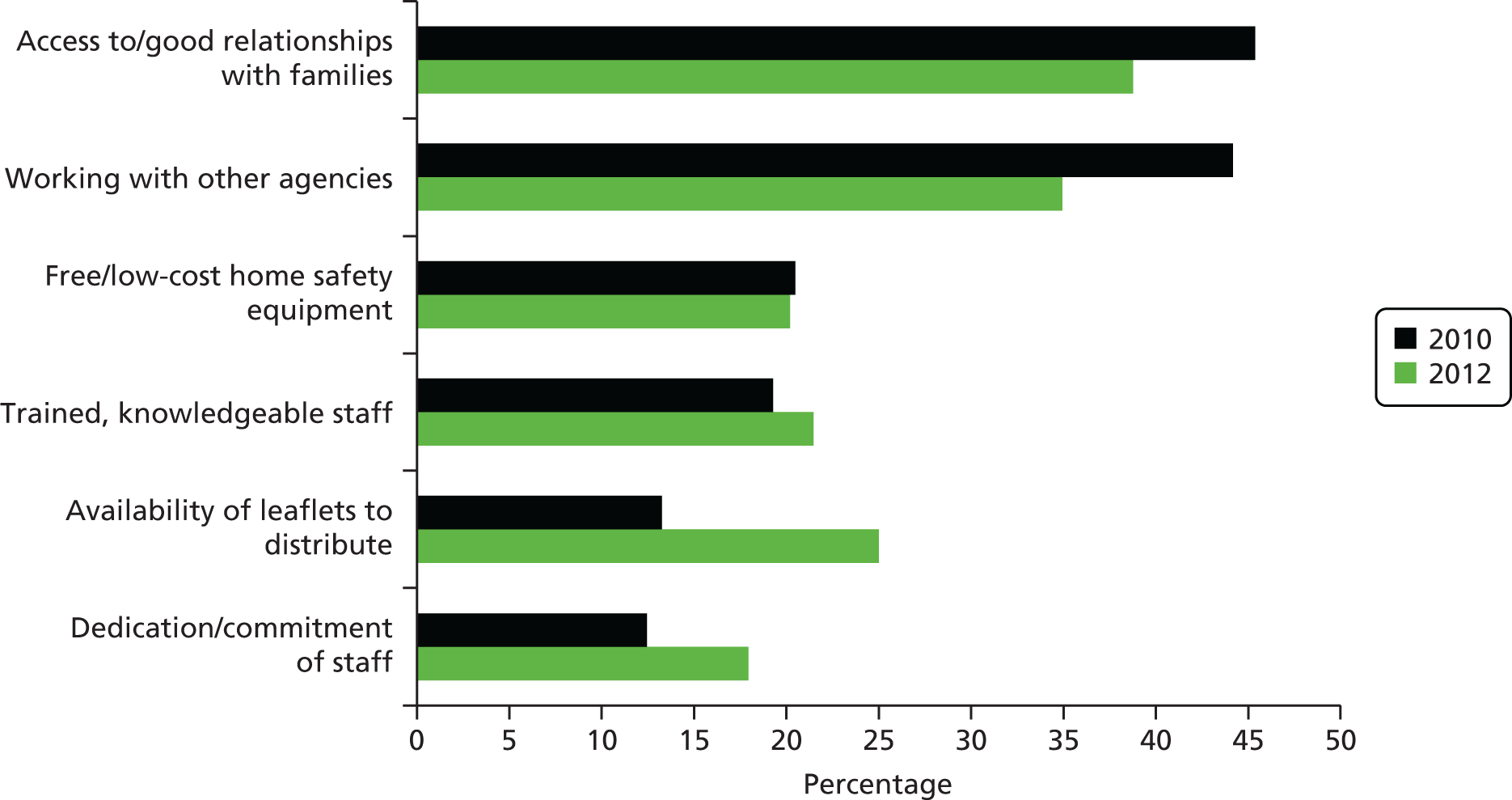
This work stream addressed the question, ‘What interventions are being undertaken by children’s centres to prevent thermal injuries, falls and poisonings?’. This question was answered by two national surveys of children’s centre managers and staff. These studies are referred to as study D.
Work stream 4
This work stream addressed the question, ‘What are the barriers to, and facilitators of, implementing thermal injuries, falls and poisoning prevention interventions among children’s’ centres, professionals and community members?’. This question was answered by three studies: first, a systematic review of the quantitative and qualitative evidence on barriers to, and facilitators of, injury prevention (study E); second, a qualitative study consisting of interviews with children’s centres managers and staff to explore their views on barriers to, and facilitators of, implementing injury prevention interventions in children’s centres (study F); and, third, a qualitative study of parents of injured and uninjured children to explore views on barriers to, and facilitators of, implementing home injury prevention nested in the case–control studies in study A (study G).
Work stream 5
This work stream addressed the question, ‘How cost-effective are strategies for preventing thermal injuries, falls and poisonings?’. This question was answered by systematic overviews and systematic reviews of the literature on preventing falls, poisonings, fire-related injuries and scalds (study H), a systematic review and pairwise meta-analysis (PMA) of home safety interventions (study I), network meta-analyses (NMAs) of interventions to promote smoke alarm use and promote falls prevention practices, poison prevention practices and scalds prevention practices (study J) and decision analyses of interventions found to be effective in the NMAs (study K).
Work stream 6
This work stream addressed the question, ‘How effective and cost-effective is implementing an IPB for one exemplar injury prevention intervention?’. This question was answered by a randomised controlled trial (RCT), set in children’s centres, which evaluated the effectiveness and cost-effectiveness of an IPB for the prevention of fire-related injury (study M). The trial was preceded by a review of the literature on the implementation and facilitation of health promotion interventions (study L) to inform the design of the intervention. Evidence from the trial was then incorporated into the development of a second IPB. This covered the prevention of fire-related injury, falls, poisonings and scalds, based on findings from studies A and D–M.
Structure of this report
Each work stream is reported in a separate chapter in the report. Each of these chapters includes the following sections: abstract, introduction, methods, results and discussion. This is followed by a chapter reporting the contribution of the lay research adviser who collaborated with the KCS programme from its inception to its completion. The report ends with three chapters drawing together the conclusions, implications and recommendations for research from the programme.
Chapter 2 What are the associations between modifiable risk and protective factors and medically attended injuries resulting from five common injury mechanisms in children under the age of 5 years? (Work stream 1)
Abstract
Research question
What are the associations between modifiable risk and protective factors and medically attended injuries resulting from five common injury mechanisms in children under the age of 5 years?
Methods
Five multicentre case–control studies were undertaken (study A). Cases were children aged < 5 years attending secondary care with a fall (three types: fall from furniture, fall on one level or a stair fall), poisoning or a scald. Control subjects (controls) were matched to cases on age, sex and calendar time, and were recruited from the register of the cases’ general practice (or neighbouring general practice). Exposures (safety equipment use, safety behaviours and hazards) were measured using parent-completed questionnaires and were validated by home observations in a sample of cases and controls (study B). Odds ratios (ORs) were estimated using conditional logistic regression adjusted for confounding factors.
Results
Validation of exposures
In total, 162 home observations were conducted. Sensitivities of ≥ 70% were found for eight out of 12 exposures for falls, for eight out of 15 exposures for poisoning and for three out of three exposures for scalds. Specificities of ≥ 70% were found for 10 out of 12 exposures for falls, for eight out of 15 exposures for poisoning and for two out of three exposures for scalds.
Falls from furniture
In total, 672 cases and 2648 controls participated. Parents of cases were more likely not to use a safety gate [adjusted odds ratio (AOR) 1.65, 95% confidence interval (CI) 1.29 to 2.12], to leave children on raised surfaces (AOR 1.66, 95% CI 1.34 to 2.06) and not to have taught their children rules about climbing on objects in the kitchen (AOR 1.58, 95% CI 1.16 to 2.15), and their children were less likely to climb or play on garden furniture (AOR 0.74, 95% CI 0.56 to 0.97)*. For children aged 0–12 months, parents of cases were more likely to leave children on raised surfaces (AOR 5.62, 95% CI 3.62 to 8.72), change nappies on raised surfaces (AOR 1.89, 95% CI 1.24 to 2.88) and put children in car/bouncing seats on raised surfaces (AOR 2.05, 95% CI 1.29 to 3.27) than parents of controls. In the 13–36 months age group, parents of cases were less likely to put car or bouncing seats on raised surfaces than parents of controls (AOR 0.22, 95% CI 0.05 to 0.94)*. In children aged > 36 months, cases were more likely to climb or play on furniture (AOR 9.25, 95% CI 1.22 to 70.07) than controls.
Falls on one level
In total, 582 cases and 2460 controls participated. Parents of cases were less likely not to use furniture corner covers (AOR 0.72, 95% CI 0.54 to 0.94)* and not to have rugs/carpets firmly fixed to the floor (AOR 0.77, 95% CI 0.59 to 0.99)* than parents of controls.
Stair falls
In total, 610 cases and 2658 controls participated. Compared with controls, parents of cases were more likely not to use safety gates on their stairs (AOR 2.50, 95% CI 1.90 to 3.29) or to leave them open (AOR 3.09, 95% CI 2.39 to 4.00) than to keep gates closed. Parents of cases were more likely not to have carpeted stairs (AOR 1.52, 95% CI 1.09 to 2.10) or not to have a landing part-way up their stairs (AOR 1.34, 95% CI 1.08 to 1.65). They were also more likely to consider their stairs not safe to use (AOR 1.46, 95% CI 1.07 to 1.99) or in need of repair (AOR 1.71, 95% CI 1.16 to 2.50). Case households were less likely than control households to have tripping hazards on their stairs (AOR 0.77, 95% CI 0.62 to 0.97)* or to not have handrails on all stairs (AOR 0.69, 95% CI 0.56 to 0.86)*.
Poisonings
In total, 567 cases and 2320 controls participated. Parents of cases were more likely not to store all medicines at adult eye level or above (AOR 1.59, 95% CI 1.21 to 2.09) and not to store all medicines safely (locked away or at adult eye level or above) (AOR 1.83, 95% CI 1.38 to 2.42). They were more likely not to put medicines (AOR 2.11, 95% CI 1.54 to 2.90) or household products (AOR 1.79, 95% CI 1.29 to 2.48) away immediately. Parents of cases were less likely not to store all household products safely (AOR 0.77, 95% CI 0.59 to 0.99)* and not to have taught children rules about what to do if medicines were left on the worktop (AOR 0.66, 95% CI 0.45 to 0.96)*.
Scalds
In total, 338 cases and 1438 controls participated. Parents of cases were more likely than parents of controls not to have taught their child rules about not climbing on things in the kitchen (AOR 1.66, 95% CI 1.12, 2.47), what to do or not do when parents are cooking on the cooker top (AOR 1.95, 95% CI 1.33, 2.85) or about hot things in the kitchen (AOR 1.89, 95% CI 1.30 to 2.75). They were also more likely than control parents to have left hot drinks within reach of their child (AOR 2.33, 95% CI 1.63 to 3.31). Cases were less likely than controls to have played or climbed on furniture (AOR 0.62, 95% CI 0.40 to 0.96)* or to have been left alone in the bath (AOR 0.47, 95% CI 0.30 to 0.75)*.
Conclusions
Despite a small number of apparently counterintuitive findings (indicated with an asterisk), a range of modifiable risk factors were associated with falls from furniture, falls on stairs, poisonings and scalds in children aged 0–4 years. These results provide evidence on which to base safety advice and recommendations.
Work stream 1 consisted of five case–control studies (study A) quantifying associations between modifiable risk factors and falls from furniture, falls on one level, falls on steps or stairs, poisonings and scalds. Work stream 1 also included a study to validate self-reported exposures in the case–control studies (study B). The findings from work stream 1 informed:
-
the decision analyses undertaken in work stream 5
-
the development of an IPB for the prevention of fire-related injuries, falls, poisonings and scalds undertaken in work stream 6 (see Chapter 7).
Introduction
The case–control studies focused on falls, poisonings and scalds as these are among the most common types of injury resulting in hospital admission and ED attendance in children aged 0–4 years in England and the UK. In 2012/13, > 26,000 children aged 0–4 years were admitted to hospital in England following a fall, poisoning or scald,2 as described in more detail below. There are no recent data available on ED attendances, but data from 2002 show that approximately 280,000 children aged 0–4 years attended an ED following a fall, poisoning or thermal injury (burns and scalds) in the UK. 3
Falls resulted in 19,569 hospital admissions in children aged 0–4 years in England in 2012/13. Of these, 18% were falls from furniture, 11% were falls down stairs or steps and 23% were falls on one level. 2 Falls also result in a large number of ED attendances in the UK; in 2002, there were 229,600 attendances in children aged 0–4 years following a fall. Of these, 18% were falls down stairs or steps and 31% were falls on one level. 3 Falls from furniture most commonly involve beds, chairs,2,44 baby walkers, bouncers, changing tables and high chairs. 45,46
Poisonings resulted in 5286 hospital admissions in children aged 0–4 years in England in 2012/3. The majority (74%) were medicinal poisonings, with 26% being non-medicinal poisonings. 2 Poisonings also result in a substantial number of ED attendances in the UK; in 2002, there were 24,887 attendances in children aged 0–4 years following a poisoning. 3
Scalds accounted for 1811 hospital admissions in children aged 0–4 years in England in 2012/13. 2 Most (61%) were caused by drinks, food, fats and cooking oils, 13% were caused by hot tap water and 26% were caused by other hot fluids. The number of ED attendances for scalds is not routinely available, but there were 26,015 attendances for all thermal injuries in children aged 0–4 years in the UK in 2002. 3 A recent UK study found that 67% of thermal injuries in children aged 0–4 years attending six hospitals in the UK and Ireland resulted from scalds;47 hence, it can be estimated that approximately 17,000 ED attendances occurred as a result of a scald in the UK in 2002.
Systematic overviews (study H)48 and a systematic review and PMA (study I)49 undertaken as part of the KCS programme of research found that home safety interventions providing education, some of which also provided safety equipment, can increase safety gate use and reduce baby walker use, increase safe storage of medicines and household products and availability of poison control centre (PCC) numbers and increase the proportion of families with a safe hot tap water temperature. However, little evidence was found showing whether such interventions reduced fall-related injuries, poisonings or scalds. These reviews highlighted the lack of adequately powered RCTs of interventions to prevent falls, poisoning or scalds that measured injury outcomes. One of the challenges is that, although on a population level injuries are a major public health problem, for individual children, specific injuries are relatively rare events. Hence, trials frequently require prohibitively large sample sizes and are extremely expensive and logistically difficult. Therefore, the best available evidence for effective interventions in the field of injury prevention often comes from rigorous case–control studies, for example those for smoke alarms50 and cycle helmets. 51 Such evidence has had a major impact on policy and legislation. The NHS, local authorities and other organisations need to be able to make decisions about which home safety interventions to commission or provide, but at present such decisions lack an evidence base. We have therefore undertaken these case–control studies to quantify associations between modifiable risk factors and falls, poisonings and scalds in young children.
Methods
The methods for these studies are described in full in the published protocols. 52–54
Objectives
The primary objectives of study A were to estimate associations between modifiable risk and protective factors and medically attended injuries resulting from five injury mechanisms in children aged < 5 years:
-
falls from furniture
-
falls on one level
-
stair falls
-
poisoning
-
scalds.
Our secondary objectives were to explore whether or not associations between risk and protective factors and injuries varied by child age, sex, ethnicity, single parenthood, housing tenure and unemployment and injury severity. 49
Study design
We used five multicentre matched case–control studies [one for each of the injury mechanisms (a)–(e)].
Setting
We recruited participants from EDs, minor injury units (MIUs) and hospital wards from acute NHS trusts in Nottingham, Bristol, Newcastle upon Tyne, Norwich, Gateshead, Derby, Great Yarmouth and Lincoln, UK. Recruitment of cases commenced on 14 June 2010 for all studies and finished on (a) 15 November 2011 for the falls from furniture study, (b) 15 November 2011 for the falls on one level study, (c) 30 September 2012 for the stair falls study, (d) 18 January 2013 for the poisoning study and (e) 18 January 2013 for the scalds study. Recruitment of controls commenced with recruitment of the first case to each study and controls were recruited within 4 months of recruitment of cases.
Participants
Cases were children aged 0–4 years with:
-
a fall from furniture
-
a fall on one level
-
a stair fall
-
a poisoning or suspected poisoning from a medicinal or other household product or
-
a scald, resulting in hospital admission or ED or MIU attendance.
Injuries had to have occurred at the address at which the child was registered with a general practitioner (GP) (hereafter referred to as the child’s home). Intentional and fatal injuries were excluded, as were children living in residential care. Cases were eligible to be recruited only once to the study.
We used two sources of controls; community controls and hospital controls. For clarity and simplicity the findings relating to community controls (hereafter referred to as controls) are presented in the main text of the report. Findings relating to hospital controls are summarised in Appendix 1. Children living in residential care were excluded. Controls were children aged 0–4 years without a medically attended injury of the same mechanism as the case on the date of the case’s injury. Controls were eligible to be recruited as a case or as a further control if their second recruitment occurred at least 12 months after their first recruitment. They were not eligible to be recruited more than twice to the study. We aimed to recruit an average of four controls per case, individually matched on age (within 4 months of age of case), sex and calendar time (within 4 months of case injury). To increase the study power and make the most efficient use of controls, when we recruited more than four controls per case (or when cases were later excluded), the extra controls were eligible to be matched to other cases who did not have four matched controls. These were matched on age (within 4 months of age of case), sex and calendar time (within 4 months of the case injury) and study centre, and were eligible to be used only once as an extra matched control.
The eligibility of putative cases to take part in the study was assessed from medical records by clinical staff prior to study invitations being issued. Research staff also assessed eligibility on receipt of completed study questionnaires. Potentially eligible cases were approached by clinical staff face to face during their medical attendance or by telephone or post within 72 hours of their attendance. Controls were recruited by post by general practice or primary care trust (PCT) staff, from the practice register of the case’s GP or, when the case’s practice was unable to participate, from that of a neighbouring practice. To minimise age differences between cases and controls resulting from the time taken to recruit practices and then recruit controls, study invites were sent to children born up to 4 months before and 2 months after the case’s date of birth. Ten children were invited to participate for each case. One reminder was sent to case and control non-respondents 2 weeks after the original mailing.
Variables
Data on injuries
We collected data from parents of cases and hospital controls on the type of injury sustained and the treatment received. We did not seek consent to access medical records to assess injury severity as we considered that this might discourage study participation. We therefore used parent-reported data on treatment as a proxy for injury severity. This is described in more detail below.
Definition of exposures
The exposures of interest were safety equipment use and home hazards measured for the 24 hours prior to the injury for cases and for the 24 hours prior to completing the questionnaire for controls. Safety behaviours were measured over the week prior to the injury for cases and the week prior to completing the questionnaire for controls.
The exposures measured for each study were:
-
falls from furniture – use of baby walkers, playpens (or travel cots while child awake) or stationary activity centres; use of safety gates anywhere in the house; use of harnesses in high chairs; changing nappies on a raised surface; leaving child unattended on a raised surface; placing car seats or bouncing cradles on a raised surface; having objects that children could climb on to reach high surfaces; frequency of children climbing or playing on furniture; and teaching children safety rules about falls
-
falls on one level – use of baby walkers, playpens (or travel cots while child awake) or stationary activity centres; use of safety gates anywhere in the house; rugs/carpets firmly fixed to the floor; electric wires or cables trailing across floors; floors clear of tripping hazards; use of furniture corner covers; locking back doors to prevent access to the garden; unsupervised playing in the garden; and teaching children safety rules about falls
-
stair falls – use of any safety gates; use of safety gates on stairs; leaving safety gate on stairs open; use of baby walkers, playpens (or travel cots while child awake) or stationary activity centres; presence of banisters and width of banister gaps; presence of handrails and tripping hazards on stairs; stairway characteristics (carpeted steps, lighting, steepness, width, landing part-way, winding stairs and steps, stair covering or handrails/banisters in need of repair); and teaching children safety rules about stairs
-
poisonings – storage of medicinal and household products (analgesics, iron/vitamins, cough medicine, antidepressants/hypnotics and any other medicines, bleach, dishwasher products, oven cleaner, toilet cleaner, turpentine/white spirit and rat/ant killer, garden chemicals and other household products)55,56 at adult eye level or above; storage of products in locked cupboards, drawers, fridges or cabinets; frequency of returning products to usual storage place immediately after use; use of child-resistant caps (CRCs) or blister packs on products; storage of medicines in a locked medicine box; not transferring products to other containers; use of a safety gate to prevent access to the kitchen; presence of things that child may climb on to reach high surfaces; use of baby walkers; and teaching children safety rules about poisonings.
-
Scalds – use of safety gates; presence of things that child may climb on to reach high surfaces; drinking hot drinks while holding a child; holding child while using cooker; passing hot drinks over a child; keeping hot drinks out of reach of children; use of curly/short kettle flexes; storing kettles at back of worksurface; use of back rings on cooker; turning saucepan handles away from edge of cooker; use of tablecloths; hot tap water/thermostat temperature; using cold water first when running a bath; measuring bathwater temperature; checking bath water temperature with elbow/hand; leaving child without an adult in the bath or bathroom; children running baths; frequency of child climbing or playing on furniture; use of baby walkers, playpens (or travel cots while child awake) or stationary activity centres; and teaching children safety rules about hot liquids in the kitchen and bathroom.
Definition of potential confounding variables
The potential confounding variables that were measured consisted of sociodemographic and economic characteristics, out-of-home child care and validated measures of child behaviour and temperament [Infant Behaviour Questionnaire (IBQ),57 Early Child Behaviour Questionnaire (ECBQ)58 and Child Behaviour Questionnaire (CBQ)59 activity and high-intensity pleasure subscales], safety rules,60 Parenting Daily Hassles (PDH) scale (parenting tasks subscale),61,62 parental mental health [Hospital Anxiety and Depression Scale (HADS)63] and proxy-reported child’s HRQL [PedsQL and a general health visual analogue scale (VAS)64]. Eight questions, each with three-point Likert scale responses from ‘not likely’ to ‘very likely’, assessed perceptions of children’s ability to climb; these were analysed as a categorical variable grouping responses into (1) all not likely, (2) at least one quite likely but none very likely and (3) at least one very likely. In addition, where plausible, some of the exposures listed above were also considered as potential confounders, for example use of a playpen may confound the relationship between use of a safety gate on stairs (as parents may be less likely to use a safety gate if they have a playpen) and the occurrence of a stair fall (as children may have less exposure to stairs if they spend time in a playpen).
As we were not able to recruit all controls from the same general practice as cases, area-level deprivation and distance from hopsital were included in all models as a priori confounders. Deprivation was measured using the 2010 version of the Index of Multiple Deprivation (IMD). 65 IMD scores for lower super output areas were matched to postcode using GeoConvert. 66 Distance from hospital was calculated based on postcodes and calculating straight line distances between two postcodes. 67 For cases we used the postcodes of the home address and the hospital that they attended. For controls we used the postcode of the home address and that of the hospital that the matched case attended. The choice of other confounders to include in multivariable models was determined through the use of causal directed acyclic graphs (DAGs), as described in Statistical methods.
Measurement of exposures and confounding variables
We developed age-specific questionnaires (0–12 months, 13–36 months and 37–59 months) for completion by parents or guardians using previously validated measures of exposure when possible68 (see Appendix 1, Case–control questionnaires). Questionnaires, study information leaflets and study invitation letters were pre-piloted on families from local children’s centres to assess face validity, comprehension, ease of completion and time taken to complete and were then piloted on 11 families of children who had attended EDs at participating NHS trusts and on 29 families from children’s centres in study centres.
Validation of exposure measurement (study B)
We assessed the agreement between exposures reported by parents on study questionnaires and those observed on home observations in a sample of cases and controls. Parents of participants in all case–control studies were asked to express interest in other child safety research projects (studies B, C and G) nested within study A. Home observations were undertaken as soon as possible after parents agreed to participate to miminise the time between questionnaire completion and home observation. Observations were undertaken by trained researchers, blind to parents’ responses on the study questionnaire, using a checklist of observations (see Appendix 1, Home observation checklist for study B). To assess whether or not recent changes to the home may account for differences between reported and observed exposures, participants were asked if changes to safety behaviours, safety equipment use or home hazards had been made in the preceeding 3 months and what the changes were, if any. We chose 3 months as the time period to allow for the time taken to recruit cases and controls to the home observation study (time between receipt of questionnaire and date of home visit: median 29 days, range 1–92 days). Participants were provided with a £5 gift voucher for use in local stores to thank them for their time.
Bias
We used several strategies to try to minimise bias. We aimed to minimise recall bias by inviting cases to participate in the study within 72 hours of the injury attendance and measured exposures over a short time period prior to the injury attendance (ranging from 24 hours to 1 week); for controls we measured exposures over the same time period prior to completing the study questionnaire. When possible, we validated the accuracy of self-reported exposures in cases and controls by home observations. To minimise non-response bias, we used methods shown in systematic reviews to increase response rates, including providing a small monetary incentive (£5) for the return of completed questionnaires, using personalised letters, sending mail by first class post, providing Freepost reply envelopes, using reminders including the provision of further questionnaires, keeping the questionnaire as short as possible and using university logos on study documentation. 69,70
Study size
Validation of exposures
For a sensitivity of 80%, assuming that a minimum of 20% of participants displayed the safety behaviour, used the safety equipment or had the hazard of interest, and a CI of ± 20%, 80 home visits were required. As it was plausible that sensitivity could vary between cases and controls, we aimed to recruit 80 cases and 80 controls.
Case–control studies
For the case–control studies, all sample size estimations were based on 80% power, a 5% significance level and a correlation between exposures in cases and controls of 0.1. Sample sizes were estimated to detect protective associations [i.e. an odds ratio (OR) of 0.7 for the falls studies and an OR of 0.63 for the poisoning and scalds studies]. These reductions were chosen as they were considered to be clinically important and required sample sizes that were feasible to achieve. For ease of interpretation of our results, we have presented ORs for risk factors for injury (i.e. not using safety equipment, not having a safety behaviour or having a hazard). The sample size estimations in the following sections therefore use the inverse of the protective ORs given above.
Falls
To detect an OR of 1.43, each case–control study would require 496 cases and 1984 controls for each type of fall (falls from furniture, falls on one level and stair falls), based on the exposure prevalence from previous studies71,72 [not using safety gates on stairs (55%) or across doorways (70%), not using a playpen (58%), not using a stationary activity centre (76%), rugs not firmly fixed to floors (46%), floors not clear of tripping hazards (57%%), using a baby walker (36%) and leaving a child unattended on raised surfaces (35%)]. We chose the exposure prevalence from this list that required the largest sample size.
Poisoning
To detect an OR of 1.59, 266 cases and 1064 controls would be required. This is based on the exposure prevalence estimated from the first 428 controls recruited to the study, taking account of missing data on exposures and choosing the exposure prevalence that required the largest sample size from not storing all medicines safely (27%), all cleaning products safely (55%) or all products safely (65%), not putting medicines away immediately after use (23%), not putting cleaning products away immediately after use (21%) or not putting all products away immediately after use (29%).
Scalds
To detect an OR of 1.59, 259 cases and 1036 controls would be required. This is based on the exposure prevalance estimated from the first 428 controls recruited to the study, taking account of missing data on exposures and choosing the exposure prevalence that required the largest sample size from drinking hot drinks while holding a child (27%) and not using kettles with curly/short flexes (22%).
Quantitative variables
All exposures were categorical variables. For confounders measured on a continuous scale, we assessed the linearity of their relationship with outcome measures by adding higher-order terms to regression models and tested significance using likelihood ratio tests with a p-value of < 0.05 taken as significant. When the relationship between age and the outcome of interest was non-linear we grouped age into the three age groups consistent with the age groups for which we had developed age-specific questionnaires (0–12 months, 13–36 months, ≥ 37 months). When other relationships were non-linear, we examined distributions of the confounders and grouped values based on cut-off points that separated the distribution into groups of similar values while ensuring sufficient numbers in each group for analysis. When standard groupings had been used in previous research, for example quintiles of deprivation scores, we grouped values similarly to allow comparisons with previous research. The cut-off points for groupings are given in the results tables.
We devised a score representing parents’ perceptions of their child’s ability to climb by combining responses across eight questions asking about perceptions of ability to climb or reach a range of hazards. Each question had a three-point Likert scale response from ‘not likely’ to ‘very likely’, with a ‘don’t know’ option. The score was created by categorising responses into (1) all not likely, (2) at least one quite likely but none very likely and (3) at least one very likely. Those with missing or ‘don’t know’ responses to individual items were categorised as missing an overall score unless respondents had at least one ‘very likely’ response. We also devised a composite categorical variable describing parents’ perceptions of their stair characteristics by combining responses across seven questions with a three-point Likert response from ‘agree’ to ‘disagree’ (stairs too steep, stairs too narrow, stairs poorly lit, steps in need of repair, banister/handrail in need of repair, stair covering in need of repair and stairs being safe to use). The categories of the composite variable were ‘unsafe’ (answered agree to any of the first six questions or disagree to last question), ‘moderately safe’ (answered combinations of agree, disagree and neither agree nor disagree) and ‘safe’ (answered disagree to all first six questions and agree to last question). Those with missing responses to individual items were categorised as missing a response on the composite variable unless they agreed with any of the first six questions or disagreed with the last question.
When the relationship between distance from hospital and the outcome of interest was non-linear, distance was grouped into quintiles. When the relationship between IMD and the outcome of interest was non-linear IMD was grouped into quintiles.
We used the treatment received as a proxy for injury severity. We created two categories: those who were seen and examined but who did not require any treatment and those requiring treatment in the ED, admitted to hospital or discharged with outpatient or primary care follow-up. We chose these groupings based on the number of cases in each group and combined hospital admissions, those treated in the ED and those discharged with outpatient or primary care follow-up as the numbers admitted to hospital and discharged with outpatient or primary care follow-up were small.
Statistical methods
We calculated kappa coefficients, sensitivities, specificities and predictive values (and 95% CIs) comparing each reported exposure with the observed exposure, with observations used as the ‘gold standard’.
Characteristics of cases and controls have been described using frequencies and percentages for categorical variables and means [standard deviations (SDs)] or medians [interquartile ranges (IQRs)] for continuous variables dependent on their distributions. Conditional logistic regression was used to estimate unadjusted ORs and AORs and 95% CIs for the matched analysis. Analyses were adjusted for area-level deprivation65 and distance from hospital and for confounders identified from DAGs. We developed separate DAGs for each exposure–outcome analysis. All variables that we considered as potential confounders were included in the DAG, and we used Dagitty software [see www.dagitty.net/ (accessed 2 October 2016)] to create a causal diagram for each exposure–outcome analysis and to identify the minimum adjustment set of variables. The regression model for each analysis was adjusted for the variables belonging to the minimum adjustment set for that exposure–outcome analysis by entering them on one step into the model. They were retained in the model regardless of statistical significance or effect on the OR for the exposure. Potential differential effects by child age, sex, ethnicity, single parenthood, housing tenure and unemployment were assessed by adding interaction terms to models. Significance was assessed using likelihood ratio tests with a p-value of < 0.01 taken as significant. When significant interactions were found, the results are presented stratified by socioeconomic variables. Differential effects by injury severity were assessed by stratifying analyses into those who were seen and examined but who did not require any further treatment and those who received treatment or who were admitted to hospital. For the unmatched analyses using hospital controls, unconditional logistic regression was used to estimate unadjusted ORs and AORs and 95% CIs. Analyses were adjusted for age, sex, area-level deprivation65 and distance from hospital, in addition to other confounders identified from DAGs. The population attributable fraction (PAF) per cent was calculated for exposures with statistically significantly raised AORs using a published formula. 73
We followed standard guidance on missing data for the PedsQL score and did not compute mean scale scores when > 50% of the individual scale score responses were missing. When > 50% of questions were answered, mean scale scores were generated with imputation of missing values using the mean of the answered questions. 74 For the HADS score we imputed single missing item values for each subscale using the mean of the remaining six items. When more than one item was missing, subscale scores were not computed. 75 The IBQ, ECBQ and CBQ allowed missing values and were scored as the total score divided by the number of questions answered. 76 We were unable to find guidance for dealing with missing values for the PDH scale so we used the same approach as for the HADS. The main analyses are complete-case analyses, excluding cases and controls with missing data for the exposure or confounding variables. Complete-case analysis gives unbiased estimates when people with missing data are a completely random subset of the individuals in a particular study; the missing data are then called missing completely at random. If, however, missingness is related to other observed or participant data, for example age or sex, this is called missing at random. We undertook multiple imputation, which assumes that missing data are missing at random, to create 20 imputed data sets. These were combined using Rubin’s rules. 77 The multiple imputation models included all sociodemographic characteristics, exposures and confounding variables considered in the analysis models, along with case–control status. The imputation models included interaction terms identified in the complete-case analyses when possible, but in some cases the imputation models would not converge when interaction terms were included so these were omitted. When exposures had > 5% of ‘not applicable’ responses, analyses were repeated coding these as a separate category.
For the validation of exposure measures, to assess whether differences between reported and observed practices may have arisen because of changes made to the home by families after completing questionnaires, we incorporated any changes made in the last 3 months as reported at the home visit to derive a modified value for each exposure. For any cell within the tables comparing reported and observed values, when the percentage of people reporting a change in the previous 3 months was > 20%, the numbers were adjusted to accommodate an assumed change from ‘yes’ to ‘no’ and vice versa, and positive predictive values (PPVs) and negative predictive values (NPVs) were recalculated.
Ethics
Approval for the case–control studies and the validation of exposures study was granted by Nottingham Research Ethics Committee 1 (reference number 09/H0407/14).
Results
Validation of exposures study (study B)
The process of recruitment to study B is shown in Figure 2. In total, 113 cases and 119 controls were contacted by the research team, of whom 81 (72%) and 81 (68%), respectively, received a home visit. This represents 3% of cases and 1% of controls eligible for study A. The period of time between receipt of questionnaire and the visit being carried out varied between 1 and 92 days, with a median of 29 days.
FIGURE 2.
Recruitment to the validation of exposures study (study B). a, Includes eight cases subsequently found not to be eligible for study A (study C, n = 7; study G, n = 1). These eight were not used to compare characteristics of participants in study B. b, Includes 37 controls subsequently found not to be eligible for study A.
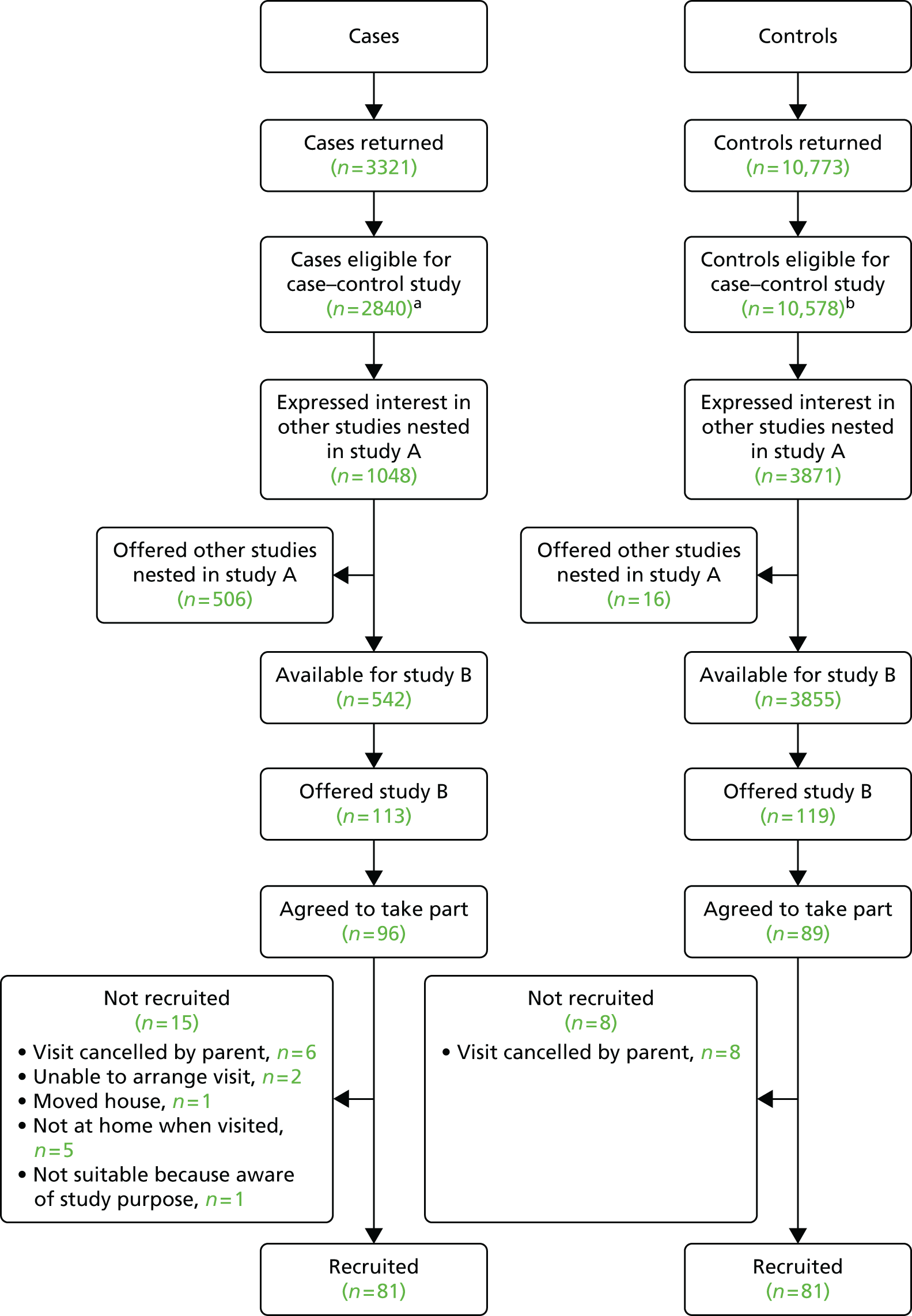
Table 1 shows the characteristics of families participating in the home observations and those returning completed questionnaires who were eligible to participate in any of the five case–control studies but who did not have a home observation. For most characteristics, there was no significant difference between families who participated and those who did not. Families for whom the questionnaire respondent was female or the participating child was male were more likely to participate; this was also the case for single-parent families or households with more adults out of work.
| Characteristic | Home observation (n = 162) | Cases/controls not observed at home (n = 13,248) | p-value |
|---|---|---|---|
| Age of child (months) | 0.15 | ||
| 0–12 | 20 (12.3) | 2329 (17.6) | |
| 13–36 | 107 (66.0) | 7883 (59.5) | |
| 37–62 | 35 (21.6) | 3036 (22.9) | |
| Sex of child: male | 103 (63.6) | 7232 (54.6) | 0.022 |
| Ethnic origin: white | 150 (92.6) | 11,860 (91.1) [225] | 0.50 |
| Number of children aged < 5 years in family | [204] | 0.81 | |
| 0 | 0 | 122 (0.9) | |
| 1 | 91 (56.2) | 7843 (60.1) | |
| 2 | 64 (39.5) | 4571 (35.0) | |
| ≥ 3 | 7 (4.3) | 508 (3.9) | |
| Case or control is first child | 67 (43.2) [7] | 5317 (43.9) [1136] | 0.87 |
| Sex of respondent: female | 156 (96.3) | 12,189 (92.0) | 0.045 |
| Maternal age ≤ 19 years at birth of first childa | 21 (13.6) [1] | 1328 (11.0) [112] | 0.31 |
| Single adult household | 29 (17.9) | 1505 (11.6) [313] | 0.014 |
| Adults out of work | [240] | < 0.001 | |
| 0 | 77 (47.5) | 7193 (55.3) | |
| 1 | 44 (27.2) | 4132 (31.8) | |
| ≥ 2 | 41 (25.3) | 1683 (12.9) | |
| Receipt of state benefits | 63 (39.4) [2] | 4754 (36.8) [331] | 0.50 |
| Overcrowding (more than one person per room) | 10 (6.4) [6] | 1004 (8.0) [775] | 0.45 |
| Non-owner occupier | 64 (39.5) | 4565 (35.2) [261] | 0.25 |
| Household has no car | 26 (16.0) | 1479 (11.3) [207] | 0.061 |
| Median IMD score (IQR) | 17.1 (9.5–34.0) [1] | 15.6 (9.3–27.6) [160] | 0.18 |
Table 2 shows the sensitivities, specificities and predictive values for exposures related to falls. NPVs were high (≥ 70%) for all 12 exposures relating to risk of falls. However, the PPV was ≥ 70% for only five of the fall exposures: safety gates at the top of the stairs; safety gates at the bottom of the stairs; use of safety gates elsewhere in the house; carpeted stairs; and the presence of a landing half-way up the stairs. The sensitivity for eight of the exposures was ≥ 70%. Exposures for which the sensitivity was < 70% were the presence of safety gates other than on the stairs and use of baby walkers, use of stationary play centres and use of travel cots as play pens. The specificity was ≥ 70% for 10 of the 12 exposures, being below this for banisters on stairs and handrails on stairs. Kappa coefficients ranged from 0.2 for use of baby walkers (slight agreement)79 to 0.74 for carpeted stairs (substantial agreement). 79 There was no significant difference [t = 1.77, degrees of freedom (df) = 1.42, p = 0.08] in measured stair steepness (stair height-to-depth ratio) between those reporting that their stairs were too steep (n = 23; mean 0.87, SD 0.21) and those not reporting that their stairs were too steep (n = 121; mean 0.82, SD 0.09). Observed banister gaps were significantly larger than reported gaps (n = 55; Z = 3.12, p = 0.002). The median reported gap was 3.0 inches (IQR 2.0–4.0 inches) whereas the median observed gap was 3.8 inches (IQR 3.5–4.3 inches).
| Practice | Number (%) observed to have practice | Sensitivity (95% CI) (%) | Specificity (95% CI) (%) | PPV (95% CI) (%) | NPV (95% CI) (%) | Kappa coefficienta (95% CI) |
|---|---|---|---|---|---|---|
| Has stair gate at top of stairsb [3] | 83 (52.2) | 90.4 (81.9 to 95.7) | 73.8 (61.5 to 84.0) | 81.5 (72.1 to 88.9) | 85.7 (73.8 to 93.6) | 0.65 (0.53 to 0.78) |
| Has stair gate at bottom of stairsb [6] | 59 (37.8) | 91.5 (81.3 to 97.2) | 82.6 (72.9 to 89.9) | 78.3 (66.7 to 87.3) | 93.4 (85.3 to 97.8) | 0.72 (0.61 to 0.83) |
| Has other safety gates in the houseb [0] | 57 (35.2) | 42.1 (29.1 to 55.9) | 95.7 (89.5 to 98.8) | 85.7 (67.3 to 96.0) | 73.2 (64.4 to 80.8) | 0.42 (0.28 to 0.56) |
| Stairs are carpetedb [1] | 142 (88.2) | 98.6 (95.0 to 99.8) | 75.0 (34.9 to 96.8) | 98.6 (95.0 to 99.8) | 75.0 (34.9 to 96.8) | 0.74 (0.49 to 0.98) |
| Presence of landing part-way up stairsb [2] | 75 (46.9) | 73.3 (61.9 to 82.9) | 85.1 (75.0 to 92.3) | 83.3 (72.1 to 91.4) | 75.9 (65.3 to 84.6) | 0.58 (0.46 to 0.71) |
| Presence of banisters on all stairsb [8] | 78 (50.6) | 91.0 (82.4 to 96.3) | 36.9 (25.3 to 49.8) | 63.4 (53.8 to 72.3) | 77.4 (58.9 to 90.4) | 0.29 (0.15 to 0.43) |
| Presence of handrails on all stairsb [6] | 57 (36.5) | 87.7 (76.3 to 94.9) | 51.1 (40.2 to 61.9) | 53.8 (43.1 to 64.2) | 86.5 (74.2 to 94.4) | 0.35 (0.22 to 0.48) |
| Use of corner covers on any furniture [0] | 17 (10.5) | 70.6 (44.0 to 89.7) | 85.5 (78.7 to 90.8) | 36.4 (20.4 to 54.9) | 96.1 (91.2 to 98.7) | 0.40 (0.21 to 0.58) |
| Use of baby walkerc [1] | 14 (8.7) | 57.1 (28.9 to 82.3) | 76.3 (67.4 to 83.8) | 22.9 (10.4 to 40.1) | 93.5 (86.5 to 97.6) | 0.20 (0.03 to 0.38) |
| Use of stationary play centrec [2] | 15 (9.4) | 60.0 (32.3 to 83.7) | 82.1 (73.8 to 88.7) | 31.0 (15.3 to 50.8) | 93.9 (87.1 to 97.7) | 0.30 (0.10 to 0.50) |
| Use of play penc [2] | 5 (3.1) | 80.0 (28.4 to 99.5) | 95.9 (90.7 to 98.7) | 44.4 (13.7 to 78.8) | 99.2 (95.4 to 100) | 0.55 (0.23 to 0.87) |
| Use of travel cot instead of a playpenc [1] | 10 (6.2) | 50.0 (18.7 to 81.3) | 93.2 (87.1 to 97.0) | 38.5 (13.9 to 68.4) | 95.7 (90.1 to 98.6) | 0.38 (0.11 to 0.65) |
Table 3 shows the sensitivities, specificities, predictive values and percentage agreement for 16 exposures relating to poisoning. All PPVs were low, the highest being 68% for all medicines having CRCs or blister packs. For 11 of the exposures, the NPV was > 70%, whereas sensitivity was > 70% for eight exposures. Kappa coefficients varied from –0.03 for all medicines stored in locked cupboard, cabinet, drawer or fridge (poor agreement)79 to 0.54 for medicines kept in fridge (moderate agreement). 79
| Practice | Number (%) observed to have practice | Sensitivity (95% CI) (%) | Specificity (95% CI) (%) | PPV (95% CI) (%) | NPV (95% CI) (%) | Kappa coefficienta (95% CI) |
|---|---|---|---|---|---|---|
| All medicines stored safelyb [23] | 68 (48.9) | 83.8 (72.9 to 91.6) | 31.0 (20.5 to 43.1) | 53.8 (43.8 to 63.5) | 66.7 (48.2 to 82.0) | 0.15 (0.01 to 0.28) |
| All household products stored safelyb [18] | 29 (20.1) | 75.9 (56.5 to 89.7) | 60.9 (51.3 to 69.8) | 32.8 (21.8 to 45.4) | 90.9 (82.2 to 96.3) | 0.25 (0.11 to 0.38) |
| All medicines and household products stored safelyb [22] | 16 (11.4) | 68.8 (41.3 to 89.0) | 68.5 (59.6 to 76.6) | 22.0 (11.5 to 36.0) | 94.4 (87.5 to 98.2) | 0.19 (0.05 to 0.34) |
| All medicines stored in locked cupboard, cabinet, drawer or fridge [5] | 3 (1.9) | 0 (0.0 to 70.8) | 87.7 (81.4 to 92.4) | 0 (0.0 to 17.6) | 97.8 (93.8 to 99.5) | –0.03 (–0.07 to 0.00) |
| All household products stored in locked cupboard, cabinet, drawer or fridge [8] | 11 (7.1) | 54.5 (23.4 to 83.3) | 79.0 (71.4 to 85.4) | 16.7 (6.4 to 32.8) | 95.8 (90.4 to 98.6) | 0.16 (0.00 to 0.33) |
| All medicines and household products stored in locked cupboard, cabinet, drawer or fridge [3] | 0 (0.0) | Unable to calculate because of frequencies of 0 in some cells | ||||
| All medicines stored at adult eye level or above [27] | 64 (47.4) | 78.1 (66.0 to 87.5) | 42.3 (30.6 to 54.6) | 54.9 (44.2 to 65.4) | 68.2 (52.4 to 81.4) | 0.20 (0.05 to 0.35) |
| All household products stored at adult eye level or above [22] | 10 (7.1) | 90.0 (55.5 to 99.7) | 88.5 (81.7 to 93.4) | 37.5 (18.8 to 59.4) | 99.1 (95.3 to 100) | 0.48 (0.27 to 0.69) |
| All medicines and household products stored at adult eye level or above [18] | 5 (3.5) | 80.0 (28.4 to 99.5) | 87.1 (80.3 to 92.1) | 18.2 (5.2 to 40.3) | 99.2 (95.5 to 100) | 0.25 (0.04 to 0.47) |
| All medicines have CRCs or blister packs [1] | 105 (65.2) | 93.3 (86.7 to 97.3) | 17.9 (8.9 to 30.4) | 68.1 (59.8 to 75.6) | 58.8 (32.9 to 81.6) | 0.13 (0.00 to 0.27) |
| Any medicines put in a container different from the one they came in [1] | 9 (5.6) | 33.3 (7.5 to 70.1) | 98.0 (94.3 to 99.6) | 50.0 (11.8 to 88.2) | 96.1 (91.8 to 98.6) | 0.37 (0.05 to 0.69) |
| All medicines kept in a locked medicine box [1] | 4 (2.5) | 50.0 (6.8 to 93.2) | 82.8 (76.0 to 88.4) | 6.9 (0.8 to 22.8) | 98.5 (94.6 to 99.8) | 0.08 (–0.06 to 0.22) |
| Medicines kept in the fridge [1] | 36 (22.4) | 61.1 (43.5 to 76.9) | 91.2 (84.8 to 95.5) | 66.7 (48.2 to 82.0) | 89.1 (82.3 to 93.9) | 0.54 (0.38 to 0.70) |
| All household products have CRCs [1] | 57 (35.4) | 71.9 (58.5 to 83.0) | 35.6 (26.4 to 45.6) | 38.0 (28.8 to 47.8) | 69.8 (55.7 to 81.7) | 0.06 (–0.06 to 0.19) |
| Any household products put in a container different from the one they came in [0] | 16 (9.9) | 6.3 (0.2 to 30.2) | 97.9 (94.1 to 99.6) | 25.0 (0.6 to 80.6) | 90.5 (84.8 to 94.6) | 0.06 (–0.12 to 0.24) |
| Safety catch/lock on fridgec [1] | 1 (0.6) | 100 (2.5 to 100) | 67.7 (48.6 to 83.3) | 9.1 (0.2 to 41.3) | 100 (83.9 to 100) | 0.12 (–0.10 to 0.33) |
Table 4 shows the sensitivities, specificities, predictive values and percentage agreement for exposures relating to scalds. Sensitivity was > 70% for all three scald-related exposures. The PPV was high for two exposures (a kettle with a curly flex and kettle kept at the back of the kitchen surface), whereas the NPV was high for having a safety gate across the kitchen doorway and for having a kettle kept at the back of the kitchen surface. Kappa coefficients ranged from 0.13 (slight agreement) to 0.57 (moderate agreement). 79
| Practice | Number (%) observed to have practice | Sensitivity (95% CI) (%) | Specificity (95% CI) (%) | PPV (95% CI) (%) | NPV (95% CI) (%) | Kappa coefficienta (95% CI) |
|---|---|---|---|---|---|---|
| Has cordless kettle or curly flex [2] | 156 (97.5) | 82.1 (75.1 to 87.7) | 75.0 (19.4 to 99.4) | 99.2 (95.8 to 100) | 9.7 (2.0 to 25.8) | 0.13 (– 0.02 to 0.28) |
| Kettle kept at back of kitchen surface [1] | 121 (75.2) | 94.2 (88.4 to 97.6) | 42.5 (27.0 to 59.1) | 83.2 (75.9 to 89.0) | 70.8 (48.9 to 87.4) | 0.42 (0.26 to 0.59) |
| Safety gate across kitchen doorway [0] | 34 (21.0) | 79.4 (62.1 to 91.3) | 85.2 (77.8 to 90.8) | 58.7 (43.2 to 73.0) | 94.0 (88.0 to 97.5) | 0.57 (0.43 to 0.72) |
Over-reporting of safety practices was more common than under-reporting. We were able to calculate predictive values for 30 safety practices and found that, for 24 of these, more families over-reported than under-reported (NPV exceeds PPV) and, for the remaining six practices, more families under-reported than over-reported (PPV exceeds NPV).
We explored whether or not differences between reported and observed safety practices could be accounted for by families changing safety practices between completing the questionnaire and the home observation. This did not appear to explain the differences between reported and observed practices, as the findings were similar to those from the main analysis when using the adjusted figures. 78 The results are available from the authors on request.
Associations between observations and self-reports differed significantly between cases and controls for only one exposure, which was storage of household products in containers that were different from the ones in which they came (χ2 = 4.91, p = 0.03). The results are available from the authors on request.
Case–control study of risk and protective factors for falls from furniture (study A)
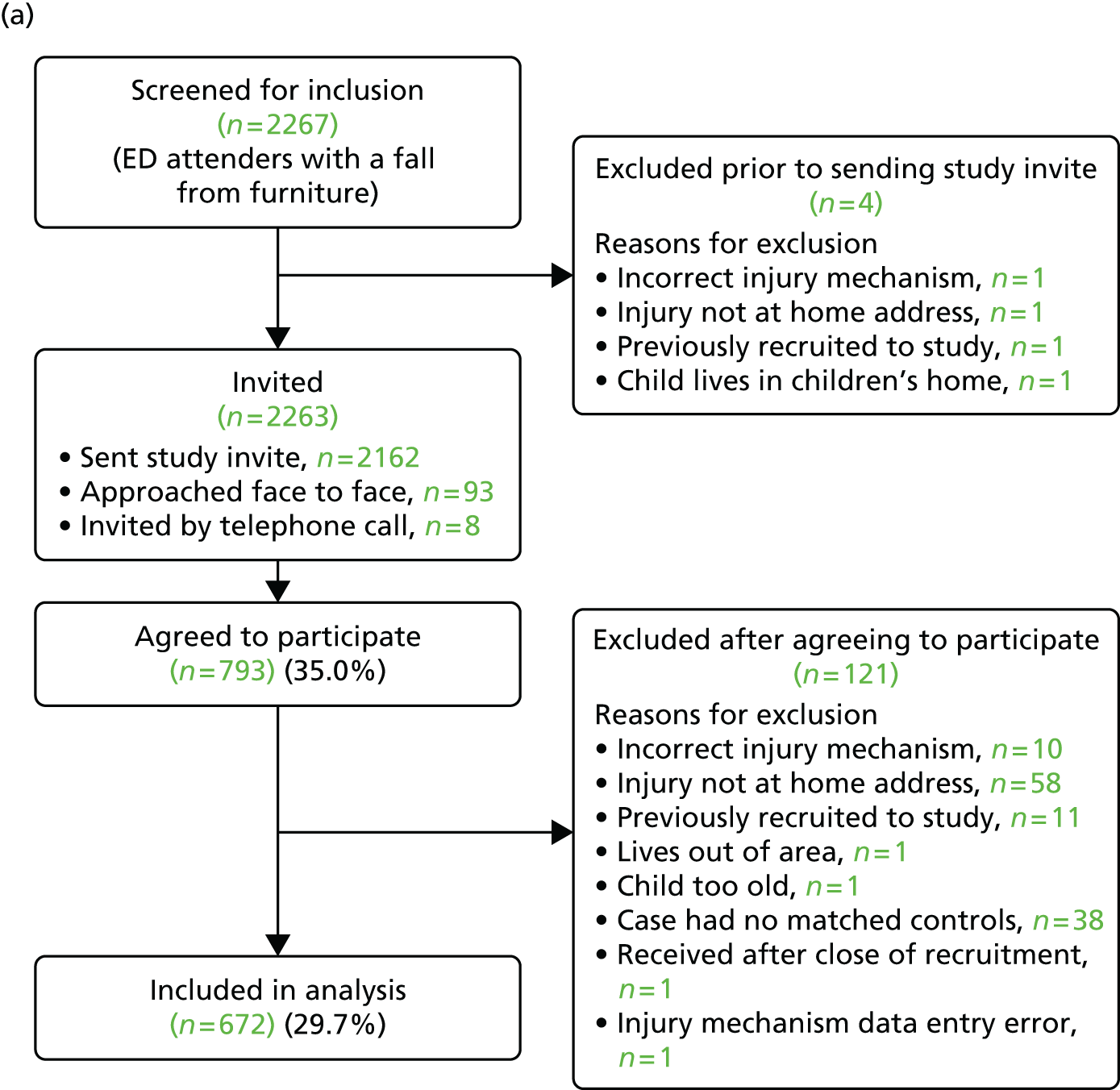
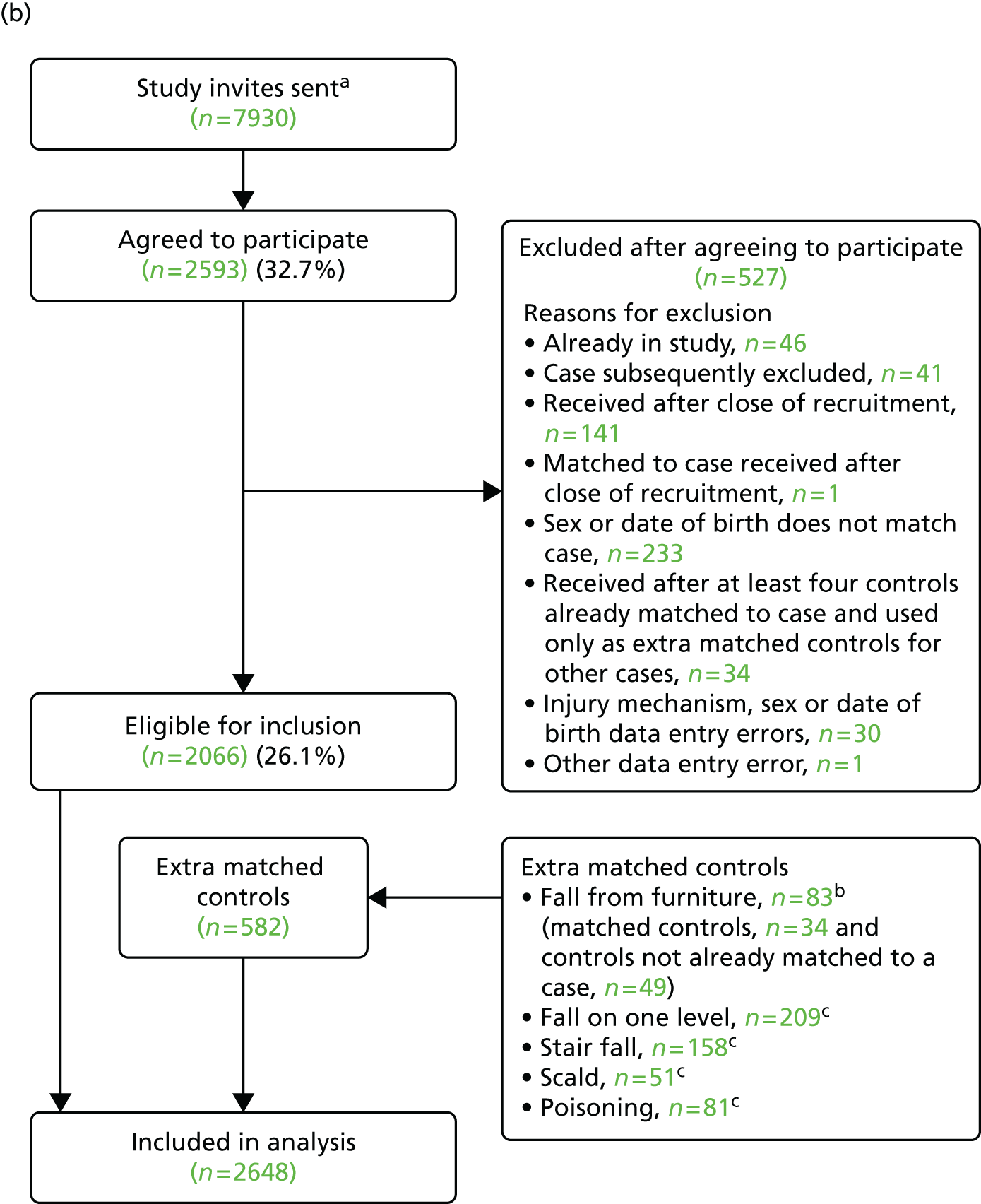
A total of 672 cases and 2648 controls participated in the study. The process of recruitment to the study is shown in Figure 3. In total, 35% of cases and 33% of controls agreed to participate. The age and sex of participants and non-participants in the falls from furniture study were similar, as shown in Table 5.
FIGURE 3.
Flow of cases and controls through the falls from furniture study: (a) recruitment of cases; and (b) recruitment of controls. a, Assumed to be 10 times the number of cases as practices were asked to invite 10 controls for each case; b, controls for cases from the falls from furniture study for whom there were more than four controls and controls for fall from furniture cases who were not matched to the case (e.g. because the case was excluded); c, controls for cases from the other four ongoing case–control studies. Reproduced with permission of JAMA Pediatrics 2015;169(2):145–153. 80 Copyright 2015 American Medical Association.
| Characteristic | Participants (N = 672), n (%) | Non-participants (N = 1470), n (%) | Significance |
|---|---|---|---|
| Age group (months) | |||
| 0–12 | 223 (33.2) | 451 (30.7) | χ2(2) = 4.05, p = 0.13 |
| 13–36 | 296 (44.0) | 716 (48.7) | |
| ≥ 37 | 153 (22.8) | 303 (20.6) | |
| Sex | |||
| Male | 365 (54.3) | 788 (53.6) | χ2(1) = 0.09, p = 0.76 |
| Female | 307 (45.7) | 682 (46.4) | |
The mean number of controls per case was 3.94. The median time from date of injury to date of questionnaire completion for cases was 10 days (IQR 6–20 days).
Most cases sustained single injuries (86%), most commonly a bang on the head (59%), cuts/grazes not requiring stitches (19%) and fractures (14%). Most cases (60%) were seen and examined but did not require treatment, with 29% treated in the ED, 4% were admitted to hospital and 7% treated and discharged with a follow-up appointment.
Table 6 shows the sociodemographic characteristics of cases and controls. As expected, because controls were recruited after the matched cases, they were slightly older than cases (median age 1.91 vs. 1.74 years). Cases were slightly more likely than controls to live in a household with no adults in paid work (17.7% vs. 12.6%), in a household receiving state benefits (43.0% vs. 35.9%) and in non-owner-occupied housing (39.5% vs. 32.2%).
| Characteristic | Cases (n = 672) | Controls (n = 2648) |
|---|---|---|
| Study centre | ||
| Nottingham | 246 (36.6) | 966 (36.5) |
| Bristol | 215 (32.0) | 832 (31.4) |
| Norwich | 146 (21.7) | 644 (24.3) |
| Newcastle | 65 (9.7) | 206 (7.8) |
| Age (years), median (IQR)a | 1.74 (0.84–2.86) | 1.91 (1.00–3.01) |
| Age group (months) | ||
| 0–12 | 223 (33.2) | 741 (28.0) |
| 13–36 | 296 (44.0) | 1270 (48.0) |
| 37–62 | 153 (22.8) | 637 (24.1) |
| Male | 365 (54.3) | 1478 (55.8) |
| Ethnic origin: white | 583 (88.9) [16] | 2403 (92.2) [41] |
| Children aged 0–4 years in family | [6] | [40] |
| 0 | 9 (1.4) | 20 (0.8) |
| 1 | 391 (58.7) | 1563 (59.9) |
| 2 | 231 (34.7) | 927 (35.5) |
| ≥ 3 | 35 (5.3) | 98 (3.8) |
| First child | 285 (45.4) [44] | 1093 (44.9) [212] |
| Maternal age ≤ 19 years at birth of first childb | 77 (12.5) [4] | 219 (9.0) [19] |
| Single adult household | 95 (14.5) [15] | 263 (10.2) [61] |
| Weekly out-of-home child care (hours), median (IQR) | 7.5 (0.0–18.0) [46] | 12.0 (1.0–22.0) [179] |
| Adults in paid employment | [16] | [45] |
| ≥ 2 | 319 (48.6) | 1481 (56.9) |
| 1 | 221 (33.7) | 795 (30.5) |
| 0 | 116 (17.7) | 327 (12.6) |
| Household receives state benefits | 280 (43.0) [21] | 928 (35.9) [65] |
| Overcrowding (more than one person per room) | 56 (8.8) [32] | 173 (6.9) [146] |
| Non-owner occupier | 262 (39.5) [9] | 838 (32.2) [49] |
| Household has no car | 95 (14.4) [10] | 288 (11.0) [40] |
| IMD score, median (IQR)c | 16.8 (10.0–31.9) | 14.9 (9.0–26.8) [28] |
| Distance from hospital (km), median (IQR) | 3.4 (1.9 to 5.4) | 3.9 (2.4 to 7.4) [29] |
| CBQ score, mean (SD)c | 4.68 (0.92) [45] | 4.67 (0.88) [234] |
| Long-term health condition | 60 (9.0) [5] | 185 (7.0) [14] |
| Child health VAS score (range 0–10), median (IQR)c | 9.9 (9.3–10.0) [6] | 9.7 (8.5–10.0) [22] |
| HRQL in children aged ≥ 2 years (PedsQL score), median (IQR)c,d | 93.1 (86.9 to 97.6), n = 287 [4] | 90.0 (82.9 to 94.4), n = 1270 [21] |
| Parental assessment of child’s ability to climb | [18] | [57] |
| All scenarios ‘not likely’ | 166 (25.4) | 536 (20.7) |
| One or more scenarios ‘quite likely’ and none ‘very likely’ | 85 (13.0) | 235 (9.1) |
| One or more scenarios ‘very likely’ | 403 (61.6) | 1820 (70.2) |
| PDH tasks subscale score, median (IQR)c,e | 13 (10 to 17) [65] | 14 (11 to 18) [168] |
| HADS score, mean (SD)c,e | 10.7 (6.0) [8] | 10.8 (6.0) [39] |
Table 7 shows the frequency of exposures among cases and controls and unadjusted ORs, and Table 8 shows ORs adjusted for a range of confounding variables. Adjusting for confounders had relatively little impact on most ORs; only one out of 13 ORs changed by > 10% after adjustment (had things child could climb on to reach high surfaces – OR 0.85, AOR 0.94). Compared with parents of controls, in the adjusted analyses parents of cases were more likely not to use a safety gate (AOR 1.65, 95% CI 1.29 to 2.12; PAF 15%), more likely to leave children on raised surfaces (AOR 1.66, 95% CI 1.34 to 2.06, PAF 23%) and more likely not to have taught their children rules about climbing on objects in the kitchen (AOR 1.58, 95% CI 1.16 to 2.15, PAF 16%) and their children were less likely to climb or play on garden furniture (AOR 0.74, 95% CI 0.56 to 0.97). Most of the ORs for the remaining nine exposures were close to 1, with seven being > 1 (ranging from 1.01 to 1.35) and two being < 1 (0.77 and 0.94). All had CIs indicating that associations could have occurred by chance.
| Exposure | Cases (n = 672) | Controls (n = 2648) | Unadjusted OR (95% CI) |
|---|---|---|---|
| Did not use any safety gatesa | 227 (36.9) [56] | 688 (27.7) [160] | 1.68 (1.36 to 2.07) |
| Used high chair without harness at least some daysb,c | 118 (26.3) [11] ((213)) | 522 (29.6) [34] ((853)) | 0.82 (0.65 to 1.05) |
| Had things child could climb on to reach high surfacesa | 248 (37.6) [12] | 1075 (40.9) [22] | 0.85 (0.70 to 1.04) |
| Left child on a raised surface at least some daysb,c | 357 (57.7) [13] ((40)) | 1221 (49.0) [33] ((121)) | 1.56 (1.29 to 1.88) |
| Changed nappy on raised surface at least some daysb,c | 297 (56.0) [10] ((132)) | 1106 (53.9) [30] ((565)) | 1.09 (0.89 to 1.33) |
| Put child in car/bouncing seat on raised surface at least some daysb,c | 59 (11.4) [11] ((142)) | 176 (8.8) [30] ((626)) | 1.33 (0.95 to 1.87) |
| Child climbed or played on furniture at least some daysb,c | 472 (78.1) [7] ((61)) | 1909 (77.9) [27] ((169)) | 0.95 (0.73 to 1.26) |
| Child climbed or played on garden furniture at least some daysb,c | 181 (34.4) [10] ((136)) | 816 (39.1) [28] ((532)) | 0.74 (0.62 to 0.98) |
| Had not taught child rules about climbing in kitchen | 282 (44.5) [39] | 1026 (40.0) [82] | 1.52 (1.15 to 2.00) |
| Had not taught child rules about jumping on bed/furniture | 283 (44.5) [36] | 1079 (42.0) [80] | 1.30 (0.97 to 1.73) |
| Cases (n = 519) | Controls (n = 2011) | Unadjusted OR (95% CI) | |
| Exposures measured only in children aged 0–36 months | |||
| Did not use baby walkera | 372 (73.5) [13] | 1359 (68.8) [36] | 1.27 (1.01 to 1.60) |
| Did not use playpen or travel cota | 411 (81.9) [17] | 1628 (82.6) [41] | 0.95 (0.73 to 1.23) |
| Did not use stationary activity centrea | 375 (74.6) [16] | 1469 (74.5) [39] | 0.98 (0.78 to 1.24) |
| Exposure | AOR (95% CI) | Confounders adjusted fora |
|---|---|---|
| Did not use any safety gatesb | 1.65 (1.29 to 2.12) | PDH score, HADS score, hours of out-of-home care, ability to climb, first child |
| Used high chair without harness at least some daysc | 0.77 (0.57 to 1.03) | CBQ score, hours of out-of-home care |
| Had things child could climb on to reach high surfacesb | 0.94 (0.75 to 1.24) | Hours of out-of-home care, ability to climb, first child, safety gate, safety rules on climbing in kitchen and jumping on furniture |
| Left child on a raised surface at least some daysc | 1.66 (1.34 to 2.06)d | CBQ score, hours of out-of-home care |
| Changed nappy on raised surface at least some daysc | 1.10 (0.87 to 1.40)d | CBQ score, hours of out-of-home care |
| Put child in car/bouncing seat on raised surface at least some daysc | 1.35 (0.91 to 2.01)d | CBQ score, hours of out-of-home care |
| Child climbed or played on furniture at least some daysc | 1.03 (0.73 to 1.44)d | CBQ score, hours of out-of-home care, things child could climb on to reach high surfaces |
| Child climbed or played on garden furniture at least some daysc | 0.74 (0.56 to 0.97) | CBQ score, hours of out-of-home care, things child could climb on to reach high surfaces |
| Had not taught child rules about climbing in kitchen | 1.58 (1.16 to 2.15) | HADS score, PDH score, first child, things child could climb on to reach high surfaces |
| Had not taught child rules about jumping on bed/furniture | 1.21 (0.87 to 1.68) | HADS score, PDH score, first child, things child could climb on to reach high surfaces |
| Did not use baby walkerb | 1.22 (0.90 to 1.65) | HADS score, PDH score, hours of out-of-home care, ability to climb, first child, uses safety gate, uses playpen/travel cot, uses activity centre |
| Did not use playpen or travel cotb | 1.01 (0.71 to 1.46) | HADS score, PDH score, hours of out-of-home care, ability to climb, first child, uses baby walker, uses safety gate, uses activity centre |
| Did not use stationary activity centreb | 0.94 (0.69 to 1.27) | HADS score, PDH score, hours of out-of-home care, ability to climb, first child, uses baby walker, uses playpen/travel cot, uses safety gate |
There were significant interactions with child age. ORs for each age group are shown in Table 9. Comparing cases to controls, for children aged 0–12 months, parents of cases were more likely to leave children on raised surfaces (AOR 5.62, 95% CI 3.62 to 8.72; PAF 50%), change nappies on raised surfaces (AOR 1.89, 95% CI 1.24 to 2.88; PAF 34%) and put children in car/bouncing seats on raised surfaces (AOR 2.05, 95% CI 1.29 to 3.27; PAF 12%) than parents of controls. In the 13–36 month age group, parents of cases were less likely to put car or bouncing seats on raised surfaces than controls (AOR 0.22, 95% CI 0.05 to 0.94). The effect for children climbing or playing on furniture was only significant in children aged 3 years and older, with cases being more likely to climb or play on furniture (AOR 9.25, 95% CI 1.22 to 70.07; PAF 88%) than controls.
| Exposure | AORa (95% CI) by age group | p-value from test for interaction | ||
|---|---|---|---|---|
| 0–12 months | 13–36 months | ≥ 37 months | ||
| Left child on raised surface at least some daysb | 5.62 (3.62 to 8.72) | 1.05 (0.77 to 1.44) | 1.00 (0.64 to 1.57) | < 0.001 |
| Nappy changed on raised surface at least some daysb | 1.89 (1.24 to 2.88) | 0.81 (0.59 to 1.11) | 0.76 (0.31 to 1.92) | 0.004 |
| Put child in car/bouncing seat on raised surface at least some daysb | 2.05 (1.29 to 3.27) | 0.22 (0.05 to 0.94) | 0.72 (0.13 to 3.87) | 0.001 |
| Climbed or played on furniture at least some daysb | 0.96 (0.60 to 1.52) | 0.75 (0.41 to 1.34) | 9.25 (1.22 to 70.07) | 0.007 |
Tables showing the results of the following sensitivity analyses are available from the authors on request. None of the AORs using the multiply imputed data differed by > 10% from those using the complete-case data for the main analysis. Five of the AORs for the interaction analyses differed by > 10% between the analysis using the multiply imputed data and the analysis using the complete-case data. All six exposures with a ‘not applicable’ response option had > 5% of ‘not applicable’ responses. Analyses were undertaken incorporating a separate category for ‘not applicable’ responses. None of the AORs for the six exposures differed by > 10% between the analyses with and the analyses without the ‘not applicable’ category.
Stratifying analyses by the treatment received (as a proxy for injury severity) resulted in AORs with fairly broad and overlapping 95% CIs for those seen and examined in the ED and those admitted/treated in the ED/discharged with follow-up for all exposures. The results from these analyses are available from the authors on request.
Case–control study of risk and protective factors for falls on one level (study A)
A total of 582 cases and 2460 controls participated in the falls on one level study. The process of recruitment to the study is shown in Figure 4. In total, 24% of cases and 24% of controls agreed to participate and were included in the analysis. Table 10 shows that participants and non-participants were similar in terms of sex and age.
FIGURE 4.
Flow of cases and controls through the falls on one level study: (a) recruitment of cases; and (b) recruitment of controls. a, Assumed to be 10 times the number of cases as practices were asked to invite 10 controls for each case; b, controls for cases from the other four ongoing case–control studies; c, controls for cases from the falls on one level study who had more than four controls and controls for falls on one level cases who were not matched to the case (e.g. because the case was excluded). Reproduced with permission from Benford P, Young B, Coupland C, Watson M, Hindmarch P, Hayes M, Goodenough T, Majsak-Newman G, Kendrick D. Risk and protective factors for falls on one level in young children: multicentre case–control study. Injury Prevention 2015;21:381–8. 81 Copyright © 2015 BMJ Publishing Group Ltd and Royal College of Paediatrics and Child Health. All rights reserved.
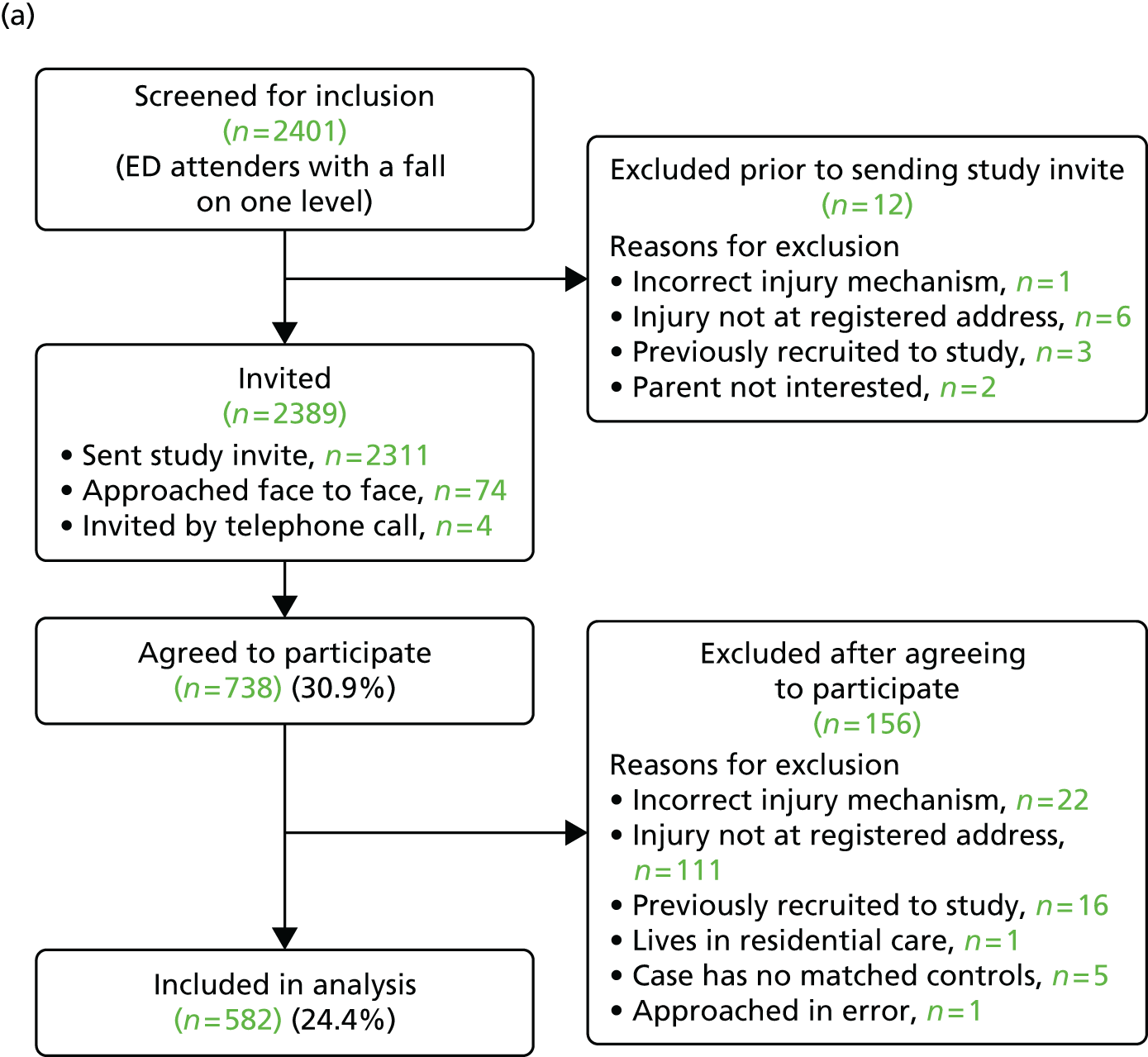
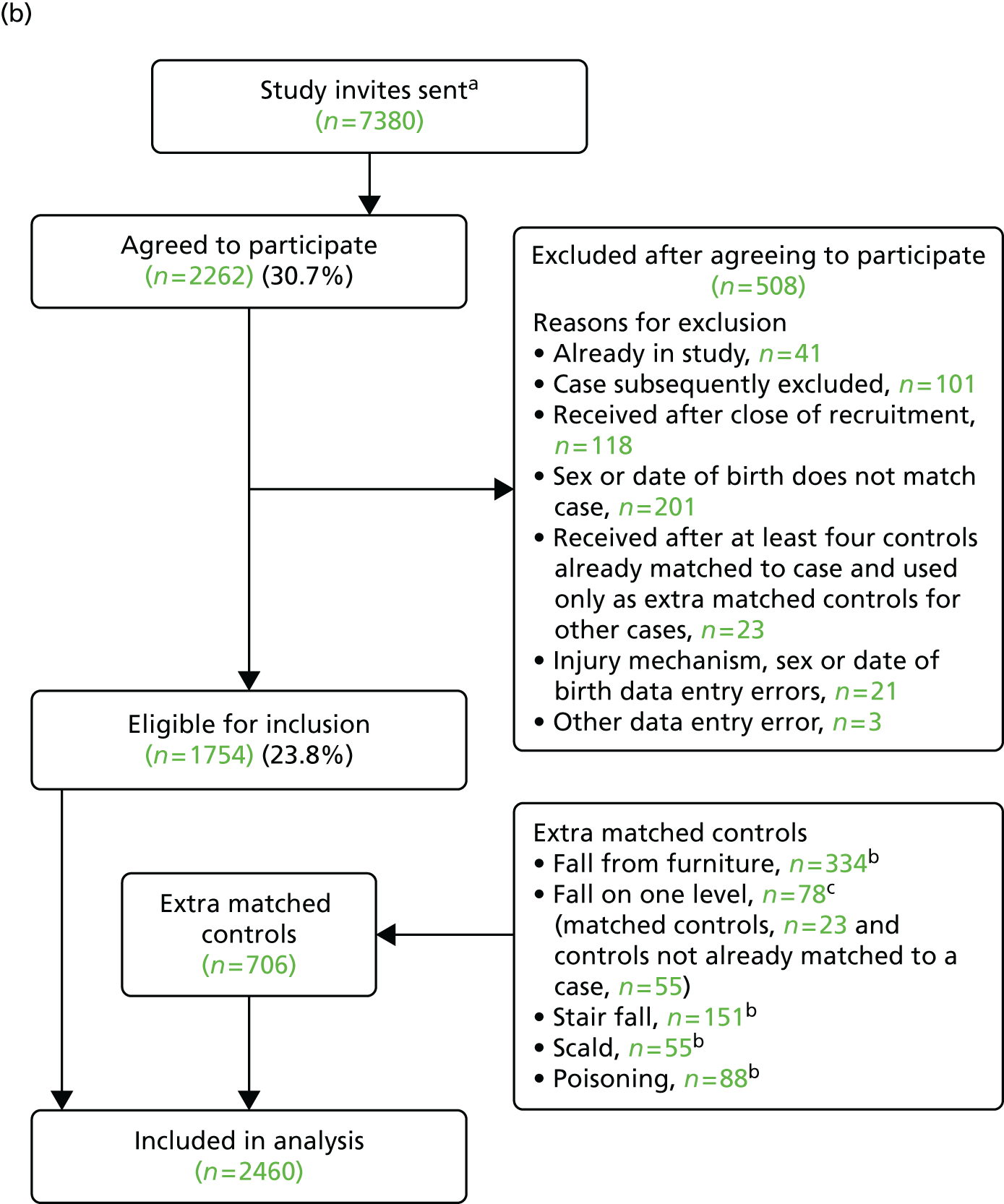
| Characteristic | Participants (N = 582), n (%) | Non-participants (N = 1653), n (%) | Total (N = 2235), n (%) | Significance |
|---|---|---|---|---|
| Age group (months) | ||||
| 0–12 | 72 (12.4) | 198 (12.0) | 270 (12.1) | χ2(2) = 0.06; p = 0.97 |
| 13–36 | 363 (62.4) | 1036 (62. 7) | 1399 (62.6) | |
| ≥ 37 | 147 (25.3) | 419 (25.3) | 566 (25.3) | |
| Sex | ||||
| Male | 360 (61.9) | 1008 (61.0) | 1368 (61.2) | χ2(1) = 0.14; p = 0.71 |
| Female | 222 (38.1) | 645 (39.0) | 867 (38.8) | |
The mean number of controls per case was 4.23. The median time from date of injury to date of questionnaire completion for cases was 10 days (IQR 6–20 days).
The majority of cases had sustained single injuries (80%), most commonly a bang on the head (52%), cuts/grazes not requiring stitches (29%) and cuts needing stitches (17%). In total, 47% of cases were seen and examined but did not require treatment, 46% were treated in the ED, 3% were admitted to hospital and 4% were treated and discharged with a follow-up appointment.
Table 11 shows the sociodemographic characteristics of cases and controls. Controls were slightly older than cases (median age 2.16 vs. 2.08 years). Cases were slightly more likely than controls to have a mother who was aged ≤ 19 years when she had her first child (16.5% vs. 10.8%), to live in a household with no adults in paid work (19.1% vs. 12.4%), to live in a household receiving state benefits (44.3% vs. 37.0%) and to live in non-owner-occupied housing (42.5% vs. 32.7%).
| Characteristic | Cases (n = 582) | Controls (n = 2460) |
|---|---|---|
| Study centre | ||
| Nottingham | 192 (33.0) | 765 (31.1) |
| Bristol | 180 (30.9) | 817 (33.2) |
| Norwich | 137 (23.5) | 614 (25.0) |
| Newcastle | 73 (12.5) | 264 (10.7) |
| Age (years), median (IQR)a | 2.08 (1.42–3.13) | 2.16 (1.53–3.22) |
| Age group (months) | ||
| 0–12 | 73 (12.5) | 206 (8.4) |
| 13–36 | 355 (61.0) | 1591 (64.7) |
| 37–62 | 154 (26.5) | 663 (27.0) |
| Male | 355 (61.0) | 1507 (61.3) |
| Ethnic origin: white | 512 (89.8) [12] | 2232 (91.9) [32] |
| Number of children aged 0–4 years in family | [11] | [34] |
| 0 | 2 (0.4) | 20 (0.8) |
| 1 | 365 (63.9) | 1438 (59.3) |
| 2 | 180 (31.5) | 867 (35.7) |
| ≥ 3 | 24 (4.2) | 101 (4.2) |
| First child | 244 (44.5) [34] | 959 (42.5) [206] |
| Maternal age ≤ 19 years at birth of first childb | 86 (16.5) [9] | 244 (10.8) [15] |
| Single adult household | 80 (14.0) [12] | 263 (10.9) [49] |
| Weekly out-of-home child care (hours), median (IQR) | 10 (0–20.0) [45] | 15 (2.5–24.0) [132] |
| Adults in paid work | [12] | [33] |
| ≥ 2 | 263 (46.1) | 1381 (56.9) |
| 1 | 198 (34.7) | 745 (30.7) |
| 0 | 109 (19.1) | 301 (12.4) |
| Household receives state benefits | 252 (44.3) [13] | 893 (37.0) [48] |
| Overcrowding (more than one person per room) | 51 (9.3) [32] | 173 (7.4) [127] |
| Non-owner occupier | 242 (42.5) [13] | 792 (32.7) [38] |
| Household has no car | 71 (12.3) [7] | 252 (10.4) [29] |
| IMD score, median (IQR)c | 17.1 (8.8–31.8) | 15.1 (9.3–26.8) [26] |
| Distance from hospital (km), median (IQR) | 3.3 (2.0–5.0) | 3.7 (2.4–6.4) [25] |
| CBQ score, mean (SD)c | 4.66 (0.98) [40] | 4.60 (0.87) [213] |
| Long-term health condition | 55 (9.7) [13] | 187 (7.6) [14] |
| Child health VAS score (range 0–10), median (IQR)c | 10 (9.3–10) [5] | 9.6 (8.5–10) [23] |
| HRQL (PedsQL score), median (IQR)c,d | 93.1 (86.1–97.6), n = 308 [12] | 89.3 (82.1–94.0), n = 1413 [29] |
| PDH tasks subscale score, median (IQR)c,e | 13.0 (9.0–16.0) [63] | 13.7 (10.0–17.1) [132] |
| HADS score, mean (SD)c,e | 10.7 (6.3) [14] | 11.0 (6.2) [35] |
Table 12 shows the frequency of exposures among cases and controls and unadjusted ORs, and Table 13 shows ORs adjusted for a range of confounding variables. Adjusting for confounders had relatively little impact on most ORs. Four out of 13 ORs changed by > 10% on adjustment (having tripping hazards on floors: OR 0.88, AOR 1.07; not using safety gate to prevent access to garden: OR 0.58, AOR 1.01; unsupervised playing in garden: OR 0.76, AOR 0.89; not using a playpen/travel cot: OR 0.76, AOR 0.90). Compared with parents of controls, in the adjusted analyses parents of cases were less likely not to use furniture corner covers (AOR 0.72, 95% CI 0.54 to 0.94) and less likely to have rugs/carpets not firmly fixed to the floor (AOR 0.77, 95% CI 0.59 to 0.99). ORs for most of the remaining 11 exposures were close to 1, with five being > 1 (ranging from 1.01 to 1.37) and six being < 1 (ranging from 0.73 to 0.97). All had CIs indicating that associations could have occurred by chance.
| Exposure | Cases (n = 582) | Controls (n = 2460) | Unadjusted OR (95% CI) |
|---|---|---|---|
| Did not use any safety gatesa | 134 (24.5) [36] | 524 (22.8) [157] | 1.10 (0.87 to 1.40) |
| No use of furniture corner coversa | 443 (76.6) [4] | 1982 (81.2) [20] | 0.76 (0.61 to 0.95) |
| Rugs/carpets not firmly fixed to the floora | 151 (26.4) [11] | 808 (33.1) [18] | 0.72 (0.59 to 0.89) |
| Electric wires or cables trailing across the floor at least some daysb,c | 86 (15.6) [14] ((18)) | 475 (19.9) [16] ((63)) | 0.72 (0.56 to 0.93) |
| Things on floor that could be tripped over at least some daysb,c | 371 (66.8) [14] ((13)) | 1698 (70.1) [16] ((21)) | 0.88 (0.72 to 1.07) |
| Not locking back doors to prevent access to the garden at least some daysb,c | 193 (38.8) [17] ((68)) | 851 (41.8) [23] ((259)) | 0.98 (0.79 to 1.22) |
| Not using safety gate to prevent access to the garden at least some daysb,c | 364 (89.7) [16] ((160)) | 1631 (93.6) [36] ((682)) | 0.58 (0.38 to 0.88) |
| Unsupervised playing in the garden at least some daysb,c | 154 (29.6) [13] ((48)) | 770 (34.6) [27] ((207)) | 0.76 (0.61 to 0.96) |
| Had not taught child rules about slippery floors | 218 (39.4) [28] | 910 (38.0) [66] | 1.07 (0.85 to 1.36) |
| Had not taught child rules about running in the house | 198 (36.0) [32] | 939 (39.2) [67] | 0.77 (0.60 to 0.98) |
| Safety practices measured only in children aged 0–36 months | |||
| Used baby walkera | 117 (27.7) [5] | 530 (29.9) [24] | 0.90 (0.71 to 1.15) |
| Did not use playpen or travel cota | 345 (82.1) [8] | 1521 (85.8) [24] | 0.76 (0.57 to 1.02) |
| Did not use stationary activity centrea | 350 (83.1) [7] | 1391 (78.5) [25] | 1.40 (1.05 to 1.86) |
| Exposure | AOR (95% CI) | Confounders adjusted fora |
|---|---|---|
| Did not use any safety gatesb | 1.12 (0.83 to 1.49) | HADS score, hours of out-of-home child care, PDH score, first child |
| Did not use furniture corner coversb | 0.72 (0.54 to 0.94) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Rugs/carpets not firmly fixed to the floorb | 0.77 (0.59 to 0.99)c | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Electric wires or cables trailing across the floor at least some daysd | 0.75 (0.55 to 1.02) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Things on floor that could be tripped over at least some daysd | 1.07 (0.82 to 1.38) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Did not lock back doors to prevent access to the garden at least some daysd | 0.97 (0.75 to 1.27) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Did not use safety gate to prevent access to the garden at least some daysd | 1.01 (0.58 to 1.74) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Unsupervised playing in the garden at least some daysd | 0.89 (0.68 to 1.17) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Had not taught child rules about slippery floors | 1.13 (0.83 to 1.52) | HADS score, PDH score, first child, uses safety gate |
| Had not taught child rules about running in the house | 0.73 (0.54 to 1.00) | HADS score, PDH score, first child, uses safety gate |
| Used baby walkerb | 0.83 (0.59 to 1.16) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate, uses playpen/travel cot, uses activity centre |
| Did not use playpen or travel cotb | 0.90 (0.61 to 1.33) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate, uses baby walker, uses activity centre |
| Did not use stationary activity centreb | 1.37 (0.95 to 1.97) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate, uses baby walker, uses playpen/travel cot |
There was a significant interaction between the number of adults living with the child and rugs/carpets not being firmly fixed to the floor. ORs for each category are shown in Table 14. In households where the child lived with one parent, rugs/carpets were more likely not to be fixed firmly to the floor in cases than in controls (AOR 2.54, 95% CI 1.16 to 5.54, PAF 18%), whereas in households where the child lived with more than one adult they were less likely not to be fixed firmly to the floor in cases than in controls (AOR 0.69, 95% CI 0.52 to 0.90).
| Exposure | AORa (95% CI) by number of adults living with child | p-value from test for interaction | |
|---|---|---|---|
| One | More than one | ||
| Rugs/carpets not firmly fixed to the floorb | 2.54 (1.16 to 5.54) | 0.69 (0.52 to 0.90) | p = 0.002 |
Tables showing the results of the following sensitivity analyses are available from the authors on request. Two of the AORs using the multiply imputed data differed by > 10% from those using the complete-case data for the main analysis (did not use safety gate to prevent access to garden: multiply imputed AOR 0.78, 95% CI 0.50 to 1.21; complete case AOR 1.01, 95% CI 0.58 to 1.74; not taught rules about running in the house: multiply imputed AOR 0.82, 95% CI 0.64 to 1.06; complete case AOR 0.73, 95% CI 0.54 to 1.00). One of the AORs for the interaction analyses differed by > 10% between analyses using the multiply imputed data and analyses using the complete-case data.
Three exposures with a ‘not applicable’ response option had > 5% of ‘not applicable’ responses. Analyses were undertaken incorporating a separate category for ‘not applicable’ responses. One of the AORs for the three exposures differed by > 10% between the analyses with and the analyses without the ‘not applicable’ category (did not use safety gate to prevent access to the garden: AOR with ‘not applicable’ category 1.01, 95% CI 0.58 to 1.74; AOR without ‘not applicable’ category 0.89, 95% CI 0.54 to 1.48).
Stratifying analyses by the treatment received (as a proxy for injury severity) resulted in AORs with fairly broad and overlapping 95% CIs for those seen and examined in the ED and those admitted/treated in the ED/discharged with follow-up for all exposures. The results from these analyses are available from the authors on request.
Case–control study of risk and protective factors for stair falls (study A)
A total of 610 cases and 2658 controls participated in the stair falls study. The process of recruitment to the study is shown in Figure 5. In total, 33% of cases and 29% of controls agreed to participate and were included in the analysis. Table 15 shows that participants and non-participants were similar in terms of sex, but a higher proportion of participants than non-participants were aged 0–12 months (19.0% vs. 12.3%).
FIGURE 5.
Flow of cases and controls through the stair falls study: (a) recruitment of cases; and (b) recruitment of controls. a, Assumed to be 10 times the number of cases as practices were asked to invite 10 controls for each case; b, controls for cases from the fall from stair falls study who had more than four controls and controls for stair falls cases who were not matched to the case (e.g. because the case was excluded); c, controls for cases from the other four ongoing case–control studies. Kendrick D, Zou K, Ablewhite J, Watson M, Coupland C, Bryony K, Hawkins A, Reading R. Risk and protective factors for falls on stairs in young children: multicentre case–control study. Archives of Disease in Childhood 2016;101:909–16. 82 Copyright © 2016 BMJ Publishing Group Ltd and Royal College of Paediatrics and Child Health. All rights reserved.
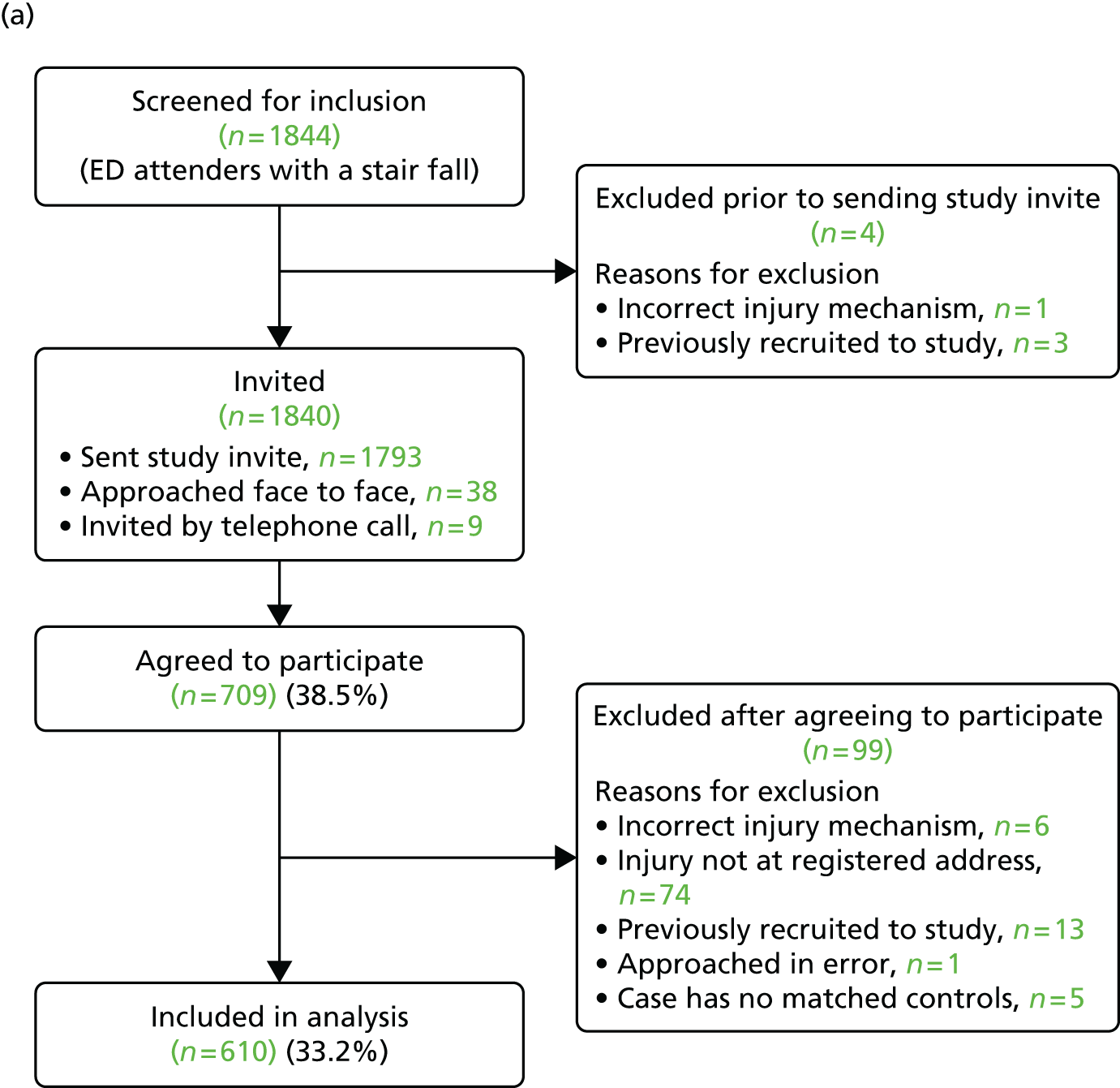
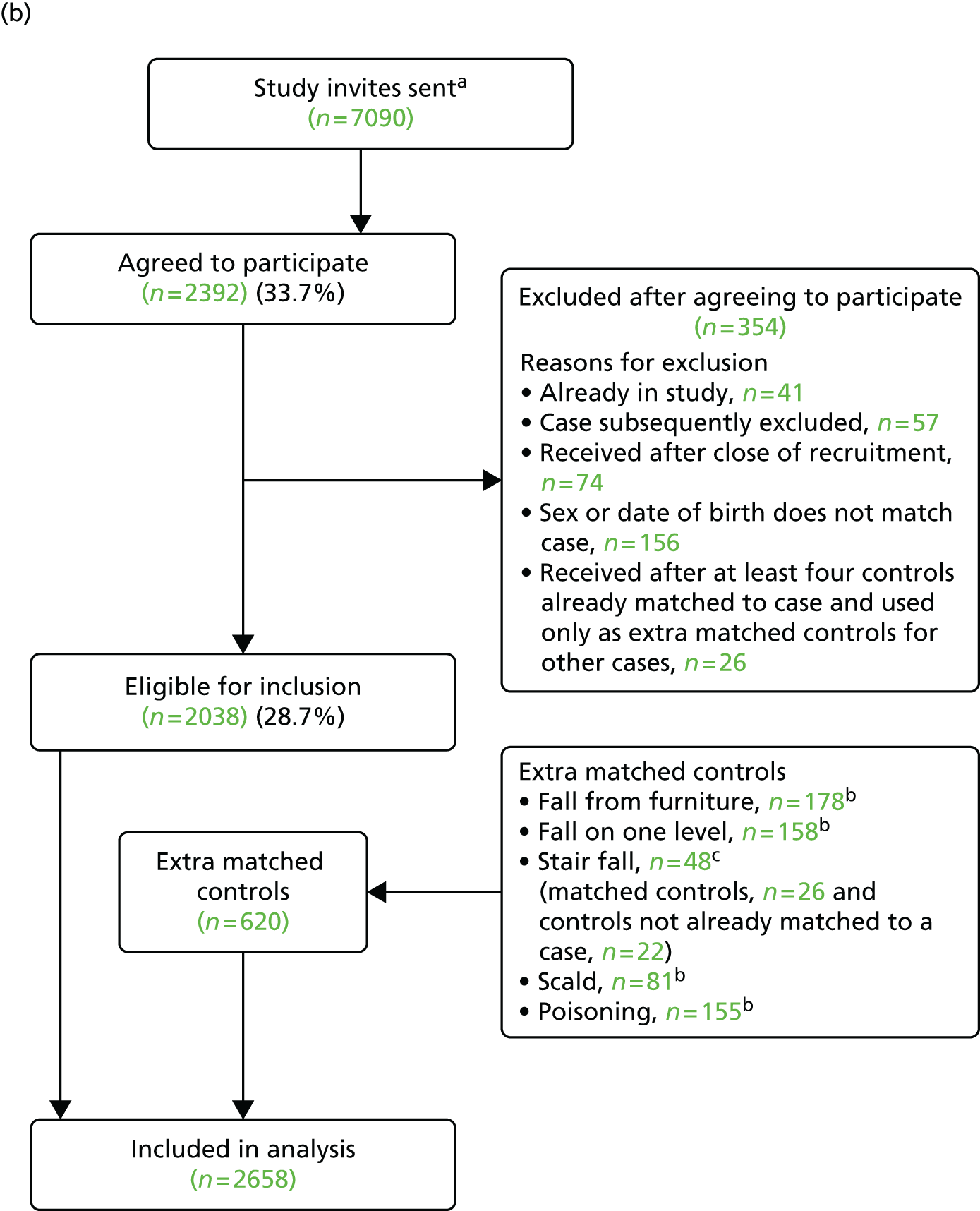
| Characteristic | Participants (N = 610), n (%) | Non-participants (N = 1131), n (%) | Total (N = 1741), n (%) | Significance |
|---|---|---|---|---|
| Age group (months) | ||||
| 0–12 | 116 (19.0) | 139 (12.3) | 255 (14.6) | χ2(2) = 15.5; p < 0.001 |
| 13–36 | 364 (59.7) | 704 (62.2) | 1068 (61.3) | |
| ≥ 37 | 130 (21.3) | 288 (25.5) | 418 (24.0) | |
| Sex | ||||
| Male | 303 (49.7) | 600 (53.1) | 903 (51.9) | χ2(1) = 1.81; p = 0.18 |
| Female | 307 (50.3) | 531 (46.9) | 838 (48.1) | |
The mean number of controls per case was 4.36. The median time from date of injury to date of questionnaire completion for cases was 11 days (IQR 7–21 days).
The majority of cases had sustained single injuries (85%), most commonly a bang on the head (66%), cuts/grazes not requiring stitches (14%) and broken bones (12%). Most cases (64%) were seen and examined but did not require treatment, 25% were treated in the ED, 5% were admitted to hospital and 6% were treated and discharged with a follow-up appointment.
Table 16 shows the sociodemographic characteristics of cases and controls. Compared with controls, cases were less likely to live in a household with more than one adult in paid work (50.0% vs. 59.0%). They also lived in areas with higher levels of deprivation (median IMD score 18.7 vs. 15.2), were more likely to have a mother who had had her first child aged ≤ 19 years (18.5% vs. 9.1%) and were more likely to live in a single adult household (14.6% vs. 10.5%), a household in receipt of state benefits (40.9% vs. 32.4%), in non-owner-occupied housing (40.4% vs. 32.2%) or in a household without a car (14.7% vs. 9.7%).
| Characteristic | Cases (n = 610) | Controls (n = 2658) |
|---|---|---|
| Study centre | ||
| Nottingham | 252 (41.3) | 1055 (39.7) |
| Bristol | 178 (29.2) | 796 (29.9) |
| Norwich | 97 (15.9) | 457 (17.2) |
| Newcastle | 83 (13.6) | 350 (13.2) |
| Age (years), median (IQR)a | 2.0 (1.2–2.9) | 2.0 (1.3–3.1) |
| Age group (months) | ||
| 0–12 | 113 (18.5) | 315 (11.9) |
| 13–36 | 362 (59.3) | 1694 (63.7) |
| 37–62 | 135 (22.1) | 649 (24.4) |
| Male | 299 (49.0) | 1320 (49.7) |
| Ethnic origin: white | 547 (91.5) [12] | 2371 (91.0) [52] |
| Children aged < 5 years in family | [8] | [44] |
| 0 | 7 (1.2) | 28 (1.1) |
| 1 | 358 (59.5) | 1566 (59.9) |
| 2 | 212 (35.2) | 911 (34.9) |
| ≥ 3 | 25 (4.2) | 109 (4.2) |
| First child | 242 (43.3) [51] | 1067 (44.5) [260] |
| Maternal age ≤ 19 years at birth of first childb | 100 (18.5) [7] | 219 (9.1) [15] |
| Single adult household | 87 (14.6) [15] | 272 (10.5) [76] |
| Weekly out-of-home child care (hours), median (IQR) | 13.5 (1.0–22.5) [43] | 15 (3.0–24.0) [165] |
| Adults in paid work | [16] | [56] |
| ≥ 2 | 297 (50.0) | 1534 (59.0) |
| 1 | 209 (35.2) | 784 (30.1) |
| 0 | 88 (14.8) | 284 (10.9) |
| Household receives state benefits | 241 (40.9) [21] | 838 (32.4) [68] |
| Overcrowding (more than one person per room) | 52 (9.1) [40] | 187 (7.5) [152] |
| Non-owner occupier | 241 (40.4) [14] | 836 (32.2) [65] |
| Household has no car | 88 (14.7) [12] | 254 (9.7) [50] |
| IMD score, median (IQR)c | 18.7 (10.1–32.7) | 15.2 (9.0–27.1) [35] |
| Distance from hospital (km), median (IQR) | 3.4 (2.2–5.4) | 3.9 (2.4–7.6) [34] |
| CBQ score, mean (SD)c | 4.7 (0.9) [43] | 4.6 (0.9) [293] |
| Long-term health condition | 63 (10.4) [6] | 202 (7.7) [19] |
| Child health VAS score (range 0–10), median (IQR)c | 9.9 (9.0–10.0) [9] | 9.7 (8.4–10.0) [19] |
| HRQL (PedsQL), median (IQR)c,d | 91.7 (83.3–97.6), n = 303 [6] | 89.3 (82.1–94.0), n = 1342 [18] |
| Parental assessment of child’s ability to open safety gate | [19] | [97] |
| Not likely | 423 (73.1) | 1808 (76.0) |
| Very or quite likely | 156 (26.9) | 571 (24.0) |
| PDH tasks subscale score, median (IQR)c,e | 14.0 (10.0–18.0) [61] | 14.0 (11.0–18.0) [152] |
| HADS score, mean (SD)c,e | 10.4 (6.2) [14] | 10.7 (5.9) [36] |
Table 17 shows the frequency of exposures among cases and controls and unadjusted ORs and Table 18 shows ORs adjusted for a range of confounding variables. Ten of the 24 ORs changed by > 10% on adjustment, with all reducing in magnitude (no carpet on stairs: OR 1.91, AOR 1.52; stairs too steep: OR 1.35, AOR 1.21; stairs too narrow: OR 1.35, AOR 1.28; stairs need repair: OR 1.97, AOR 1.71; stair covering needs repair: OR 1.74, AOR 1.41; stairs not safe: OR 1.71, AOR 1.46; no banisters: OR 1.44, AOR 1.27; not taught child rules about going downstairs: OR 1.60, AOR 1.36; not taught child rules about leaving things on stairs: OR 1.00, AOR 0.85; banister width 2.5–3.75 inches: OR 0.84, AOR 0.75).
| Exposure | Cases (n = 610) | Controls (n = 2658) | Unadjusted OR (95% CI) |
|---|---|---|---|
| Did not use any safety gatesa | 142 (23.7) [12] | 521 (20.6) [124] | 1.22 (0.97 to 1.53) |
| Exposures measured only for households with stairs | n = 598 | n = 2476 | |
| Gate closed | 174 (29.7) | 1245 (51.1) | 1.00 |
| Gate open | 210 (35.9) | 555 (22.8) | 2.93 (2.32 to 3.72) |
| No gatea | 201 (34.4) [13] | 636 (26.1)) [40] | 2.52 (1.97 to 3.22) |
| Did not have carpeted stairsa | 83 (14.1) [8] | 200 (8.2) [28] | 1.91 (1.44 to 2.53) |
| Did not have landing part-way up stairsa | 413 (69.6) [5] | 1556 (63.6) [28] | 1.35 (1.11 to 1.65) |
| Had spiral or winding stairsa | 96 (16.2) [7] | 402 (16.4) [30] | 1.04 (0.81 to 1.33) |
| Had tripping hazards on stairs at least some daysb,c | 183 (31.6) [4] ((14)) | 932 (38.4) [16] ((35)) | 0.73 (0.60 to 0.89) |
| Stairs too steepa | 218 (37.6) [18] | 743 (31.0) [80] | 1.35 (1.11 to 1.64) |
| Stairs too narrowa | 154 (26.8) [23] | 484 (20.4) [98] | 1.45 (1.17 to 1.80) |
| Stairs poorly lita | 103 (18.0) [26] | 329 (13.8) [94] | 1.37 (1.07 to 1.76) |
| Steps in need of repaira | 67 (11.7) [25] | 147 (6.2) [96] | 1.97 (1.45 to 2.70) |
| Banister/handrail on stairs in need of repaira | 68 (12.0) [32] | 203 (8.5) [98] | 1.46 (1.09 to 1.97) |
| Stair covering in need of repaira | 71 (12.4) [26] | 175 (7.4) [96] | 1.74 (1.28 to 2.36) |
| Stairs not safe to usea | 101 (17.2) [10] | 271 (11.1) [25] | 1.71 (1.33 to 2.21) |
| Did not have handrails on all stairsa | 215 (36.0) [1] | 1063 (43.3) [20] | 0.72 (0.60 to 0.88) |
| Did not have banisters or railings on all stairsa | 152 (26.4) [22] | 486 (20.1) [60] | 1.44 (1.17 to 1.79) |
| Not taught child rules about going downstairs | 173 (29.9) [20] | 624 (25.9) [70] | 1.60 (1.19 to 2.17) |
| Not taught child rules about carrying big/heavy things while going downstairs | 291 (50.3) [20] | 1134 (47.1) [68] | 1.33 (1.01 to 1.74) |
| Not taught child rules about leaving things on stairs | 320 (55.6) [22] | 1339 (55.5) [64] | 1.00 (0.77 to 1.30) |
| Exposure measured only for households with banisters | n = 424 | n = 1930 | |
| Banister width (inches) (IQR)a | 3 (2–4) [190] | 3 (2–4) [803] | |
| Up to 2.5 | 94 (40.2) | 400 (35.5) | 1 |
| > 2.5 to ≤ 3.75 | 67 (28.6) | 363 (32.2) | 0.88 (0.59 to 1.32) |
| > 3.75 | 73 (31.2) | 364 (32.3) | 0.84 (0.55 to 1.26) |
| Exposures measured only in children aged 0–36 months | n = 475 | n = 2009 | |
| Used baby walkera | 135 (29.3) [14] | 675 (34.1) [32] | 0.80 (0.63 to 1.00) |
| Did not use playpen or travel cota | 384 (83.3) [14] | 1645 (83.1) [30] | 1.03 (0.78 to 1.36) |
| Did not use stationary activity centrea | 348 (75.8) [16] | 1486 (75.2) [33] | 1.01 (0.79 to 1.29) |
| Exposure | AOR (95% CI) | Confounders adjusted fora |
|---|---|---|
| Did not use any safety gatesb | 1.22 (0.92 to 1.62) | HADS, PDH, first child, stair safety, hours of out-of-home child care |
| Gate closed | 1 | Child’s ability to open gate, taught child rules about going downstairs, carrying things downstairs and leaving things on stairs, stair safety |
| Gate open | 3.09 (2.39 to 4.00) | |
| No gateb | 2.50 (1.90 to 3.29)c | |
| Did not have carpeted stairsb | 1.52 (1.09 to 2.10)c | HADS, PDH, stair safety |
| Did not have landing part-way up stairsb | 1.34 (1.08 to 1.65) | Stair safety |
| Had spiral or winding stairsb | 0.97 (0.75 to 1.27) | Stair safety |
| Had tripping hazards on stairs at least some daysd | 0.77 (0.62 to 0.97) | HADS, PDH, stair safety |
| Stairs too steepb,e | 1.21 (0.94 to 1.56) | Stair safety |
| Stairs too narrowb,e | 1.28 (0.96 to 1.70) | Stair safety |
| Stairs poorly litb.e | 1.32 (0.97 to 1.79) | HADS, PDH, stair safety |
| Steps in need of repairb.e | 1.71 (1.16 to 2.50) | HADS, PDH, stair safety |
| Banister/handrail on stairs in need of repairb,e | 1.32 (0.92 to 1.88) | HADS, PDH, stair safety |
| Stair covering in need of repairb,e | 1.41 (0.99 to 2.02) | HADS, PDH, stair safety |
| Stairs not safe to useb,e | 1.46 (1.07 to 1.99) | HADS, PDH, stair safety |
| Did not have handrails on all stairsb,e | 0.69 (0.56 to 0.86) | HADS, PDH, stair safety |
| Did not have banisters or railings on all stairsb,e | 1.27 (0.99 to 1.63) | HADS, PDH, stair safety |
| Not taught child rules about going downstairs | 1.36 (0.92 to 2.02) | HADS, PDH, first child, child’s ability to open safety gate, safety gate, stair safety |
| Not taught child rules about carrying big/heavy things while going downstairs | 1.21 (0.83 to 1.75)c | HADS, PDH, first child, child’s ability to open safety gate, safety gate, stair safety |
| Not taught child rules about leaving things on stairs | 0.85 (0.60 to 1.22c | HADS, PDH, first child, child’s ability to open safety gate, safety gate, stair safety |
| Banister width (inches)a | Stair safety | |
| Up to 2.5 | 1 | |
| > 2.5 to ≤ 3.75 | 0.83 (0.53 to 1.29) | |
| > 3.75 | 0.75 (0.48 to 1.18) | |
| Used baby walkerb | 0.83 (0.63 to 1.10) | HADS, PDH, first child, hours of out-of-home child care |
| Did not use playpen or travel cotb | 1.07 (0.75 to 1.53) | HADS, PDH, uses baby walker, first child, hours of out-of-home child care |
| Did not use stationary activity centreb | 1.08 (0.80 to 1.46) | HADS, PDH, uses baby walker, first child, hours of out-of-home child care |
Compared with parents of controls, in the adjusted analysis parents of cases were more likely not to use safety gates on their stairs (AOR 2.50, 95% CI 1.90 to 3.29; PAF 21%) or to leave the gates open (AOR 3.09, 95% CI 2.39 to 4.00; PAF 24%), not to have carpeted stairs (AOR 1.52, 95% CI 1.09 to 2.10; PAF 5%) and not to have a landing part-way up their stairs (AOR 1.34, 95% CI 1.08 to 1.65; PAF 18%). They were also more likely to consider their stairs not safe to use (AOR 1.46, 95% CI 1.07 to 1.99; PAF 5%) or their steps in need of repair (AOR 1.71, 95% CI 1.16 to 2.50; PAF 5%). Case households were less likely than control households to have tripping hazards on their stairs (AOR 0.77, 95% CI 0.62 to 0.97) or to not have handrails on all stairs (AOR 0.69, 95% CI 0.56 to 0.86). ORs for most of the remaining 16 exposures were close to 1, with 11 being > 1 (ranging from 1.07 to 1.41) and five being < 1 (ranging from 0.69 to 0.97). All had CIs indicating that associations could have occurred by chance.
Table 19 shows significant interactions in the adjusted analysis. Comparing cases with controls, parents of cases aged 0–12 months and 13–36 months were more likely to have left safety gates on stairs open than closed, with a particularly high OR in parents with infants (AOR 0–12 months 8.64, 95% CI 3.99 to 18.68, PAF 46%; AOR 13–36 months 2.64, 95% CI 1.92 to 3.64, PAF 24%). Parents of cases in all age groups were more likely not to have a safety gate on stairs than to have a closed gate and the OR was again higher in parents with infants (AOR 0–12 months 3.27, 95% CI 1.48 to 7.20, PAF 18%; AOR 13–36 months 2.33, 95% CI 1.60 to 3.39, PAF 15%; AOR ≥ 37 months 2.08, 95% CI 1.23 to 3.51, PAF 32%). The association between safety gates and stair falls varied by baby walker use, with a particularly high OR for leaving a safety gate open compared with having a closed gate in walker users (AOR walker users 7.37, 95% CI 4.36 to 12.45, PAF 44%). Parents of cases in households in which no adults were in paid work were less likely not to have taught children rules about carrying things downstairs (AOR 0.44, 95% CI 0.20 to 0.96) or not to have taught children rules about leaving things on stairs (AOR 0.27, 95% CI 0.12 to 0.60). Parents of cases in single adult households were more likely not to have carpeted stairs (AOR 11.07, 95% CI 3.89 to 31.53, PAF 26%) and were less likely not to have taught children rules about leaving things on stairs (AOR 0.33, 95% CI 0.15 to 0.75).
| Exposure | AORa (95% CI) by age group | Test for interaction | ||
|---|---|---|---|---|
| 0–12 months | 13–36 months | ≥ 37 months | ||
| Stair gate left openb | 8.64 (3.99 to 18.68) | 2.64 (1.92 to 3.64) | 1.52 (0.76 to 3.03) | 0.008 |
| No stair gateb | 3.27 (1.48 to 7.20) | 2.33 (1.60 to 3.39) | 2.08 (1.23 to 3.51) | |
| AORa (95% CI) by use of baby walker | ||||
| Used walker | Did not use walker | |||
| Stair gate left openb | 7.37 (4.36 to 12.45) | 2.65 (1.87 to 3.76) | 0.002 | |
| No stair gateb | 2.54 (1.33 to 4.87) | 2.42 (1.63 to 3.59) | ||
| AORa (95% CI) by adults in paid work | ||||
| Two or more | One | None | ||
| Not taught child rules about carrying things downstairs | 1.45 (0.94 to 2.24) | 1.26 (0.76 to 2.09) | 0.44 (0.20 to 0.96) | 0.009 |
| Not taught child rules about leaving things on stairs | 1.01 (0.66 to 1.56) | 0.88 (0.54 to 1.42) | 0.27 (0.12 to 0.60) | 0.004 |
| AORa (95% CI) by number of adults living with child | ||||
| One adult | More than one adult | |||
| Not taught children rules about leaving things on stairs | 0.33 (0.15 to 0.75) | 0.95 (0.66 to 1.38) | 0.01 | |
| Stairs not carpetedb | 11.07 (3.89 to 31.53) | 1.15 (0.79 to 1.66) | < 0.001 | |
Tables showing the results of the following sensitivity analyses are available from the authors on request. In the analysis using community controls, the AORs for four exposures using the multiply imputed data differed by > 10% from those using the complete-case data for the main analysis. These were not having carpeted stairs (multiply imputed AOR 1.68, 95% CI 1.25 to 2.25; complete case AOR 1.52, 95% CI 1.09 to 2.10), having a stair carpet in need of repair (multiply imputed AOR 1.57, 95% CI 1.13 to 2.18; complete case AOR 1.41, 95% CI 0.99 to 2.03), not using a stationary activity centre (multiply imputed AOR 0.96, 95% CI 0.75 to 1.24; complete case AOR 1.08, 95% CI 0.80 to 1.46) and banister width (2.5–3.75 inches: multiply imputed AOR 0.85, 95% CI 0.61 to 1.20; complete case AOR 0.83, 95% CI 0.53 to 1.29; > 3.75 inches: multiply imputed AOR 0.90, 95% CI 0.65 to 1.25; complete case AOR 0.75, 95% CI 0.48 to 1.18). Four of the interactions from the complete-case analysis remained significant at the 1% level in the multiply imputed analysis and two [interactions between (1) teaching children rules about leaving things on stairs and single parent households and (2) teaching children rules about carrying things on stairs and parental unemployment] had p-values of 0.011 in the multiply imputed analysis. Patterns of risk were similar for the multiply imputed and complete-case analyses, but AORs differed by > 10% between the complete-case analyses and the multiply imputed analyses for 12 out of 20 AORs. Stratifying analyses by the treatment received (as a proxy for injury severity) resulted in AORs with fairly broad and overlapping 95% CIs for the seen and examined in the ED and the admitted/treated in the ED/discharged with follow-up groups for all exposures. The results from these analyses are available from the authors on request.
Case–control study of risk and protective factors for poisonings (study A)
A total of 567 cases and 2320 controls participated in the poisonings study. The process of recruitment to the study is shown in Figure 6. In total, 28% of cases and 28% of controls agreed to participate and were included in the analysis. The age and sex of participants and non-participants in the poisonings study were similar, as shown in Table 20.
FIGURE 6.
Flow of cases and controls through the poisonings study: (a) recruitment of cases; and (b) recruitment of controls. a, The study the participant had previously been recruited to was not recorded; b, includes eight participants previously recruited to one of the other ongoing CC studies as a case and five previously recruited to this study as a control > 12 months previously; c, assumed to be ten times the number of cases as practices were asked to invite 10 controls for each case; d, community controls for cases from the other four ongoing case–control studies; e, controls for cases from poisoning study that had more than four controls; f, includes nine participants previously recruited to one of the other ongoing CC studies as a control and one participant previously recruited to this study as a control > 12 months previously. Reproduced with permission from Kendrick D, Majsak-Newman G, Benford P, Coupland C, Timblin C, Hayes M, et al. Poison prevention practices and medically attended poisoning in young children: multicentre case–control study. Injury Prevention 2016; in press. 83 © 2017 by the BMJ Publishing group Ltd. All rights reserved.
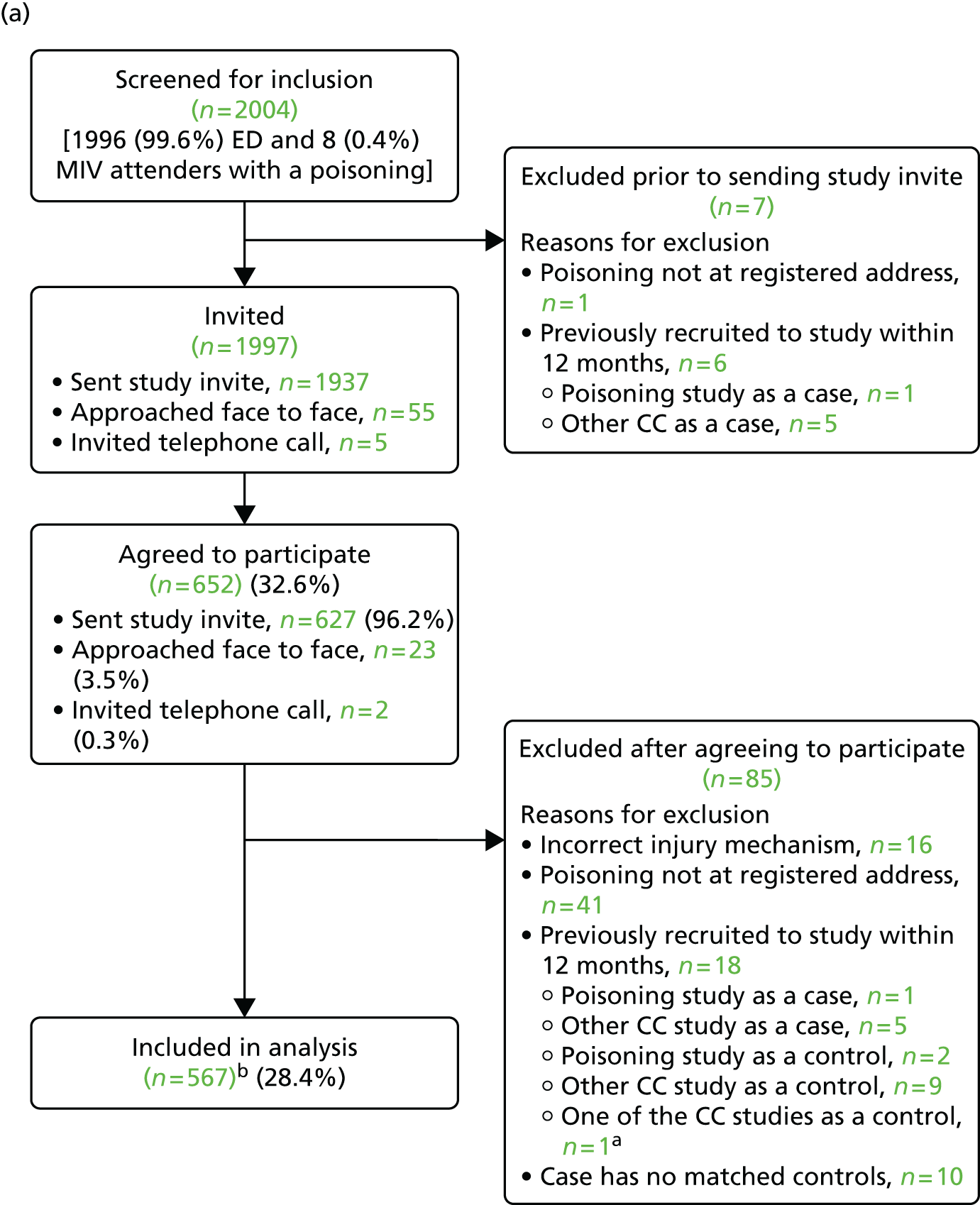
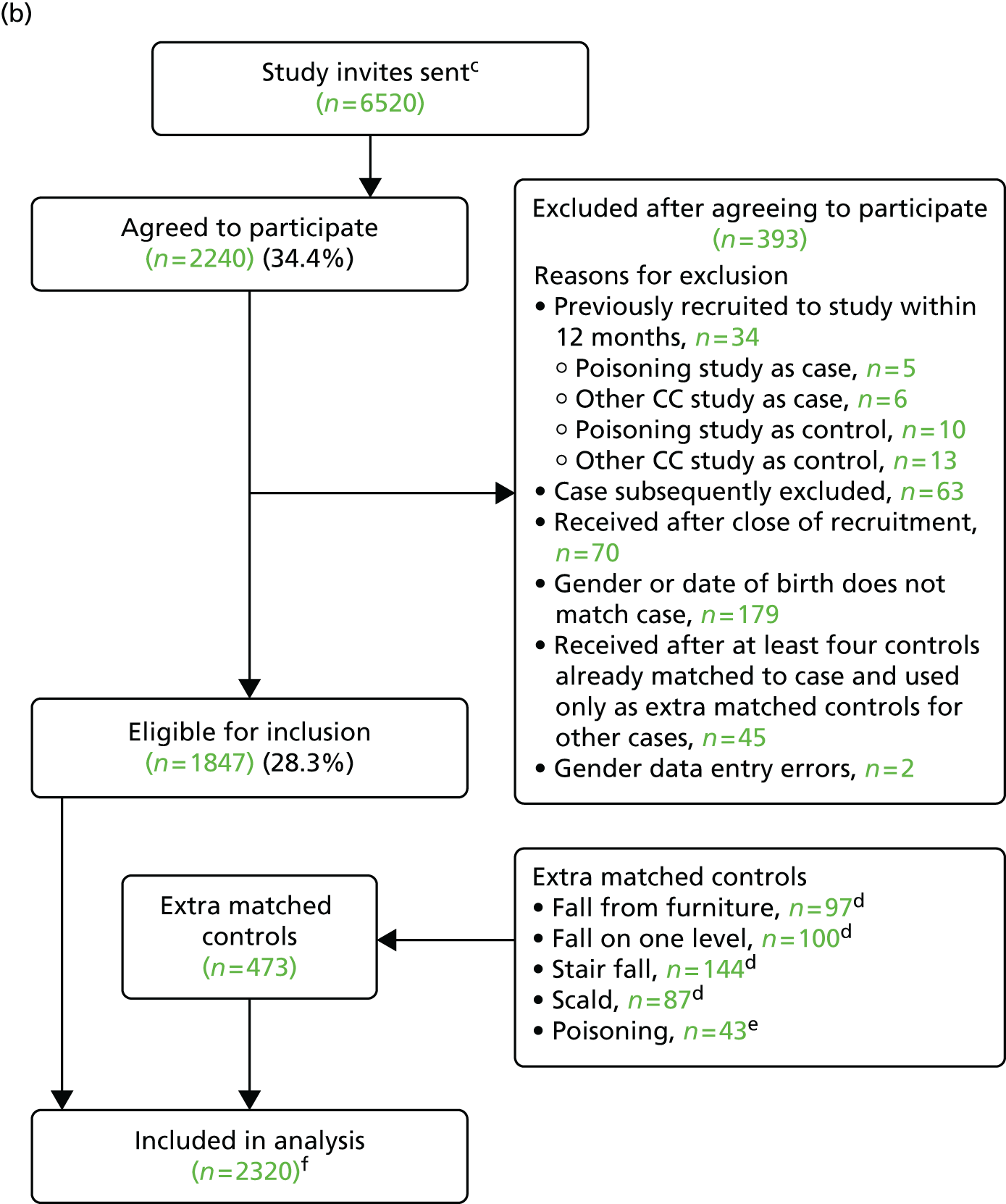
| Characteristic | Participants (N = 567), n (%) | Non-participants (N = 1345), n (%) | Total (N = 1912), n (%) | Significance |
|---|---|---|---|---|
| Age group (months) | ||||
| 0–12 | 65 (11.5) | 129 (9.6) | 194 (10.2) | χ2(2) = 1.67, p = 0.43 |
| 13–36 | 378 (66.7) | 926 (68.9) | 1304 (68.2) | |
| ≥ 37 | 124 (21.9) | 290 (21.6) | 414 (21.7) | |
| Sex | ||||
| Male | 280 (49.4) | 711 (52.9) | 991 (51.8) | χ2(1) = 1.93, p = 0.16 |
| Female | 287 (50.6) | 634 (47.1) | 921 (48.2) | |
The mean number of controls per case was 4.09. The median time from date of injury to date of questionnaire completion for cases was 12 days (IQR 6–22 days).
The majority of cases had sustained single injuries. Parents of seven cases reported injuries in addition to poisonings. Most cases (84%) were seen and examined but did not require treatment, 6% were treated in the ED, 8% were admitted to hospital and 2% were treated and discharged with a follow-up appointment.
Table 21 shows the sociodemographic characteristics of cases and controls.
| Characteristic | Cases (n = 567) | Controls (n = 2320) |
|---|---|---|
| Study centre | ||
| Nottingham | 193 (34.0) | 738 (31.8) |
| Bristol | 179 (31.6) | 794 (34.2) |
| Norwich | 106 (18.7) | 467 (20.1) |
| Newcastle | 89 (15.7) | 321 (13.8) |
| Age (years), median (IQR)a | 2.18 (1.49–2.92) | 2.24 (1.54–3.02) |
| Age group (months) | ||
| 0–12 | 65 (11.5) | 204 (8.8) |
| 13–36 | 378 (66.7) | 1575 (67.9) |
| 37–62 | 124 (21.9) | 541 (23.3) |
| Male | 280 (49.4) | 1210 (52.2) |
| Ethnic origin: white | 514 (92.1) [9] | 2115 (92.6) [36] |
| Children aged 0–4 years in family | [11] | [29] |
| 0 | 6 (1.1) | 16 (0.7) |
| 1 | 299 (53.8) | 1379 (60.2) |
| 2 | 229 (41.2) | 810 (35.4) |
| ≥ 3 | 22 (4.0) | 86 (3.8) |
| First child | 210 (41.7) [64] | 895 (42.7) [222] |
| Maternal age ≤ 19 years at birth of first childb | 84 (16.5) [8] | 208 (9.7) [14] |
| Single adult household | 92 (16.6) [13] | 262 (11.5) [43] |
| Weekly out-of-home child care (hours), median (IQR) | 12 (0.5–22.0) [31] | 15 (2.5–24.0) [112] |
| Adults in paid work | [11] | [35] |
| ≥ 2 | 263 (47.3) | 1281 (56.1) |
| 1 | 184 (33.1) | 742 (32.5) |
| 0 | 109 (19.6) | 262 (11.5) |
| Household receives state benefits | 228 (41.7) [20] | 795 (35.1) [54] |
| Overcrowding (more than one person per room) | 46 (8.8) [42] | 163 (7.4) [128] |
| Non-owner occupier | 241 (43.5) [13] | 771 (33.8) [41] |
| Household has no car | 81 (14.6) [11] | 219 (9.6) [28] |
| IMD score, median (IQR)c | 17.6 (10.3–31.7) | 15.1 (9.3–26.5) [24] |
| Distance from hospital (km), median (IQR) | 3.5 (2.2–5.9) | 4.0 (2.4–7.6) [24] |
| CBQ score, mean (SD)c | 4.75 (0.91) [24] | 4.61 (0.86) [186] |
| Long-term health condition | 53 (9.4) [5] | 187 (8.1) [21] |
| Child health VAS score (range 0–10), median (IQR)c | 9.8 (8.8–10) [2] | 9.6 (8.4–10) [14] |
| HRQL (PedsQL), median (IQR)c,d | 91.7 (85.7 to 97.2), n = 326 [3] | 89.3 (82.1 to 95.2), n = 1354 [24] |
| Parental assessment of child’s ability to access poisons | [21] | [96] |
| All scenarios ‘not likely’ | 22 (4.0) | 112 (5.0) |
| One or more scenarios ‘quite likely’ and none ‘very likely’ | 100 (18.3) | 513 (23.1) |
| One or more scenarios scenario ‘very likely’ | 424 (77.7) | 1599 (71.9) |
| PDH tasks subscale score, median (IQR)c,e | 14.0 (10.3 to 18.0) [50] | 14.0 (11.0 to 18.0) [113] |
| HADS score, mean (SD)c,e | 10.9 (6.1) [15] | 10.8 (6.2) [25] |
Table 22 shows the frequency of exposures among cases and controls and unadjusted ORs, and Table 23 shows ORs adjusted for a range of confounding variables. Four of the eighteen ORs changed by > 10% on adjustment (medicines transferred into different container: OR 1.15, AOR 0.96; household products not stored at adult eye level or above: OR 0.84, AOR 0.95; household products transferred into different containers: OR 1.74, AOR 1.20; no safety gate to stop access to kitchen: OR 0.91, AOR 1.05).
| Exposure | Cases (n = 567) | Controls (n = 2320) | Unadjusted OR (95% CI) |
|---|---|---|---|
| Did not have CRCs or blister packs for all medicinesa | 102 (18.2) [6] | 321 (13.9) [8] | 1.39 (1.09 to 1.78) |
| Did not have all medicines in locked medicines boxa | 447 (79.5) [5] | 1914 (82.8) [9] | 0.84 (0.66 to 1.06) |
| Not all medicines were locked awaya,b | 454 (83.6) [24] ((0)) | 1897 (85.4) [92] ((6)) | 0.87 (0.67 to 1.14) |
| Not all medicines were stored at adult level or abovea,b | 189 (40.7) [101] ((2)) | 612 (30.8) [324] ((10)) | 1.68 (1.35 to 2.09) |
| Not all medicines stored safelya | 165 (34.4) [87] | 506 (24.9) [287] | 1.73 (1.38 to 2.17) |
| Any medicines transferred into a different containera | 28 (5.0) [6] | 104 (4.5) [10] | 1.15 (0.74 to 1.77) |
| Did not put all or some medicines away immediately after useb,c | 213 (41.7) [16] ((40)) | 522 (26.2) [57] ((274)) | 2.00 (1.62 to 2.45) |
| Did not have CRCs for all cleaning productsa | 154 (27.5) [8] | 686 (29.7) [14] | 0.90 (0.73 to 1.11) |
| Not all household/cleaning products locked awaya,b | 353 (69.4) [54] ((4)) | 1590 (72.1) [106] ((10)) | 0.85 (0.68 to 1.05) |
| Not all household/cleaning products stored at adult level or abovea,b | 409 (83.5) [73] ((4)) | 1823 (86.0) [191] ((10)) | 0.84 (0.64 to 1.12) |
| Not all household/cleaning products stored safelya | 239 (49.9) [88] | 1138 (54.6) [234] | 0.82 (0.67 to 1.01) |
| Any cleaning products transferred into a different containera | 17 (3.0) [5] | 38 (1.6) [10] | 1.74 (0.97 to 3.12) |
| Did not use safety gate to stop child accessing kitchena | 411 (73.3) [6] | 1735 (75.1) [10] | 0.91 (0.73 to 1.13) |
| Had things child could climb on to reach high surfacesa | 281 (50.0) [5] | 1056 (45.7) [8] | 1.18 (0.96 to 1.44) |
| Did not put all or some household/cleaning products away immediately after useb,c | 131 (25.0) [30] ((14)) | 378 (17.1) [74] ((34)) | 1.62 (1.28 to 2.05) |
| Had not taught child rules about what to do or not do when sees cleaning products | 194 (36.1) [30] | 899 (40.0) [72] | 0.88 (0.70 to 1.10) |
| Had not taught child rules about what to do or not do if medicine on worktop | 239 (44.0) [24] | 1138 (50.7) [74] | 0.73 (0.58 to 0.93) |
| Cases (n = 443) | Controls (n = 1779) | ||
| Exposures measured only in children aged 0–36 months | |||
| Used baby walkera | 103 (24.3) [19] | 539 (30.6) [15] | 0.76 (0.59 to 0.98) |
| Exposure | AOR (95% CI) | Confounders adjusted fora |
|---|---|---|
| Did not have CRCs or blister packs for all medicinesb | 1.25 (0.95 to 1.65) | First child, ability to access poisons |
| Did not have all medicines in locked medicines boxb | 0.82 (0.47 to 1.43) | CRCs, HADS score, PDH score, ability to access poisons, hours of out-of-home care, first child, medicines locked, medicines put away immediately after use, uses kitchen safety gate, medicines stored high, things child could climb on to reach high surfaces |
| Not all medicines locked awayb | 0.91 (0.64 to 1.31)c | CRCs, HADS score, PDH score, uses kitchen safety gate, medicines stored high, things child could climb on to reach high surfaces, hours of out-of-home care |
| Not all medicines stored at adult level or aboveb | 1.59 (1.21 to 2.09) | CRCs, HADS score, PDH score, ability to access poisons, uses kitchen safety gate, first child, things child could climb on to reach high surfaces, hours of out-of-home care |
| Not all medicines stored safelyb | 1.83 (1.38 to 2.42) | CRCs, HADS score, PDH score, ability to access poisons, first child, uses kitchen safety gate, things child could climb on to reach high surfaces, hours of out-of-home care |
| Any medicines transferred into a different containerb | 0.96 (0.52 to 1.76) | CRCs, HADS score, PDH score, locked medicines box, medicines locked, medicines stored high |
| Did not put all or some medicines away immediately after used | 2.11 (1.54 to 2.90) | HADS score, PDH score, ability to access poisons, first child, medicines locked, medicines stored high, things child could climb on to reach high surfaces |
| Did not have CRCs for all cleaning productsb | 0.87 (0.69 to 1.10) | First child, ability to access poisons |
| Not all household/cleaning products locked awayb | 0.90 (0.69 to 1.17) | CRCs, HADS score, PDH score, uses kitchen safety gate, products stored high, things child could climb on to reach high surfaces, hours of out-of-home care |
| Not all household/cleaning products stored at adult level or aboveb | 0.95 (0.67 to 1.35)c | CRCs, HADS score, PDH score, ability to access poisons, uses kitchen safety gate, things child could climb on to reach high surfaces, hours of out-of-home care |
| Not all household/cleaning products stored safelyb | 0.77 (0.59 to 0.99) | CRCs, HADS score, PDH score, ability to access poisons, first child, uses kitchen safety gate, things child could climb on to reach high surfaces, hours of out-of-home care |
| Any cleaning products transferred into a different containerb | 1.20 (0.54 to 2.65) | CRCs, HADS score, PDH score, products locked, products stored high |
| Did not use safety gate to stop child accessing kitchenb | 1.05 (0. 80 to 1.37) | HADS score, PDH score, first child, hours of out-of-home care |
| Had things child could climb on to reach high surfacesb | 1.20 (0.93 to 1.54) | CRCs, HADS score, PDH score, ability to access poisons, first child |
| Did not put all or some household/cleaning products away immediately after used | 1.79 (1.29 to 2.48) | HADS score, PDH score, ability to access poisons, first child, products locked, products stored high, things child could climb on to reach high surfaces |
| Had not taught child rules about what to do or not do when see cleaning products | 0.81 (0.59 to 1.12) | CRCs, HADS score, PDH score, ability to access poisons, first child, products locked, products put away immediately after use, uses kitchen safety gate, products stored high, products transferred to different container |
| Had not taught child rules about what to do or not do if medicine on worktop | 0.66 (0.45 to 0.96) | CRCs, HADS score, PDH score, ability to access poisons, first child, locked medicines box, medicines locked, medicines put away immediately after use, uses kitchen safety gate, medicines stored high, medicines transferred to different container |
| Used baby walkerb | 0.82 (0.61 to 1.10) | HADS score, PDH score, first child, hours of out-of-home care |
Compared with parents of controls, in the adjusted analyses parents of cases were more likely not to store all medicines at adult eye level or above (AOR 1.59, 95% CI 1.21 to 2.09; PAF 15%) and were more likely not to store all medicines safely (locked away or at adult eye level or above) (AOR 1.83, 95% CI 1.38 to 2.42; PAF 16%). Parents of cases were less likely than parents of controls not to store all household products safely (locked away or at adult eye level or above) (AOR 0.77, 95% CI 0.59 to 0.99). They were also more likely not to put medicines away immediately after use (AOR 2.11, 95% CI 1.54 to 2.90; PAF 20%) or to put household products away immediately (AOR 1.79, 95% CI 1.29 to 2.48;, PAF 11%) and less likely not to have taught their children what to do or not do if medicines were left on the worktop (AOR 0.66, 95% CI 0.45 to 0.96). ORs for the remaining 12 exposures were close to 1, with four being > 1 (ranging from 1.05 to 1.25), and eight being < 1 (ranging from 0.81 to 0.96). All had CIs indicating that associations could have occurred by chance.
Table 24 shows significant interactions in the adjusted analysis comparing cases with controls. Parents of cases living in single adult households were more likely not to store all household products at adult eye level or above (AOR 2.43, 95% CI 1.09 to 5.43; PAF 50%). Parents of female cases were less likely not to keep all medicines locked away (AOR 0.59, 95% CI 0.37 to 0.94).
| Exposure | AORa (95% CI) by number of adults living with child | p-value from test for interaction | |
|---|---|---|---|
| One adult | More than one adult | ||
| Not all household/cleaning products were stored at adult eye level or aboveb | 2.43 (1.09 to 5.43) | 0.76 (0.52 to 1.11) | 0.007 |
| AORa (95% CI) by sex of child | |||
| Male | Female | ||
| Not all medicines were locked awayb | 1.48 (0.85 to 2.58) | 0.59 (0.37 to 0.94) | 0.009 |
Tables showing the results of the following sensitivity analyses are available from the authors on request. In the analysis using community controls, four of the AORs using the multiply imputed data differed by > 10% from those using the complete-case data for the main analysis. These were medicines not stored safely (multiply imputed AOR 1.62, 95% CI 1.29 to 2.05; complete case AOR 1.83, 95% CI 1.38 to 2.42), household/cleaning products not stored safety (multiply imputed AOR 0.91, 95% CI 0.73 to 1.13; complete case AOR 0.77, 95% CI 0.59 to 0.99), transferring cleaning products to different containers (multiply imputed AOR 1.47, 95% CI 0.80 to 2.69; complete case AOR 1.20, 95% CI 0.54 to 2.65) and not putting household/cleaning products away immediately after use (multiply imputed AOR 1.61, 95% CI 1.26 to 2.05; complete case AOR 1.79, 95% CI 1.29 to 2.48). Two of the AORs differed by > 10% between the multiply imputed and the complete-case interaction analyses.
One exposure with a ‘not applicable’ response option had > 5% of ‘not applicable’ responses. Analyses were undertaken incorporating a separate category for ‘not applicable’ responses. The AORs did not differ by > 10% between analyses with and analyses without the ‘not applicable’ category. The results from these analyses are available from the authors on request. Stratifying analyses by the treatment received (as a proxy for injury severity) resulted in AORs with fairly broad and overlapping 95% CIs for those seen and examined in the ED and those admitted/treated in the ED/discharged with follow-up for all exposures. The results from these analyses are available from the authors on request.
Case–control study of risk and protective factors for scalds (study A)
A total of 338 cases and 1438 controls participated in the scalds study. The process of recruitment to the study is shown in Figure 7. In total, 32% of cases and 29% of controls agreed to participate and were included in the analysis. The age and sex of participants and non-participants in the scalds study were similar, as shown in Table 25.
FIGURE 7.
Flow of cases and controls through the scalds study: (a) recruitment of cases; and (b) recruitment of controls. a, Assumed to be ten times the number of cases as practices were asked to invite 10 controls for each case; b, controls for cases from the other four ongoing case–control studies; c, controls for cases from scald study that had more than four controls and controls for scald cases that were not matched to the case (e.g. because case was excluded).
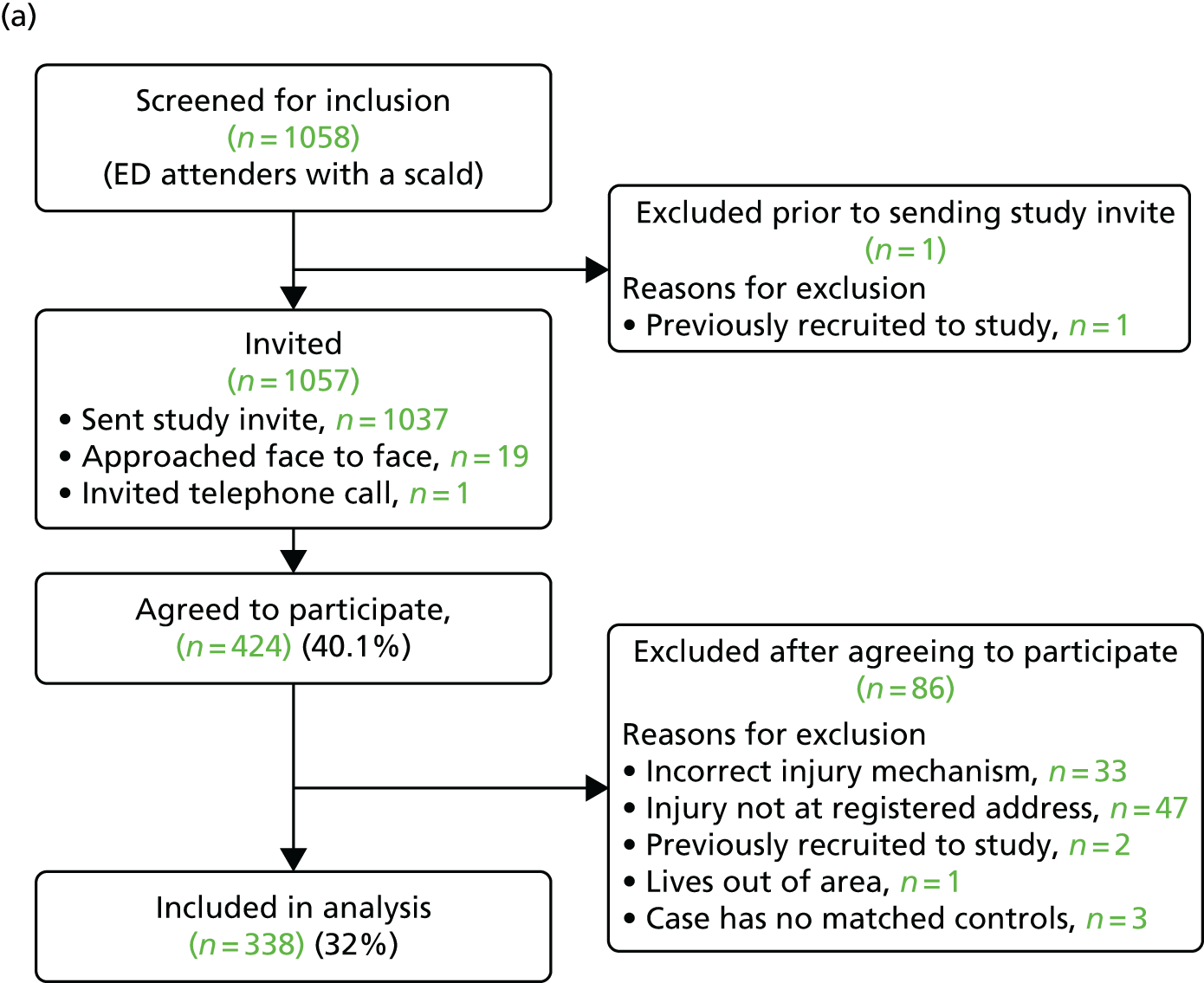
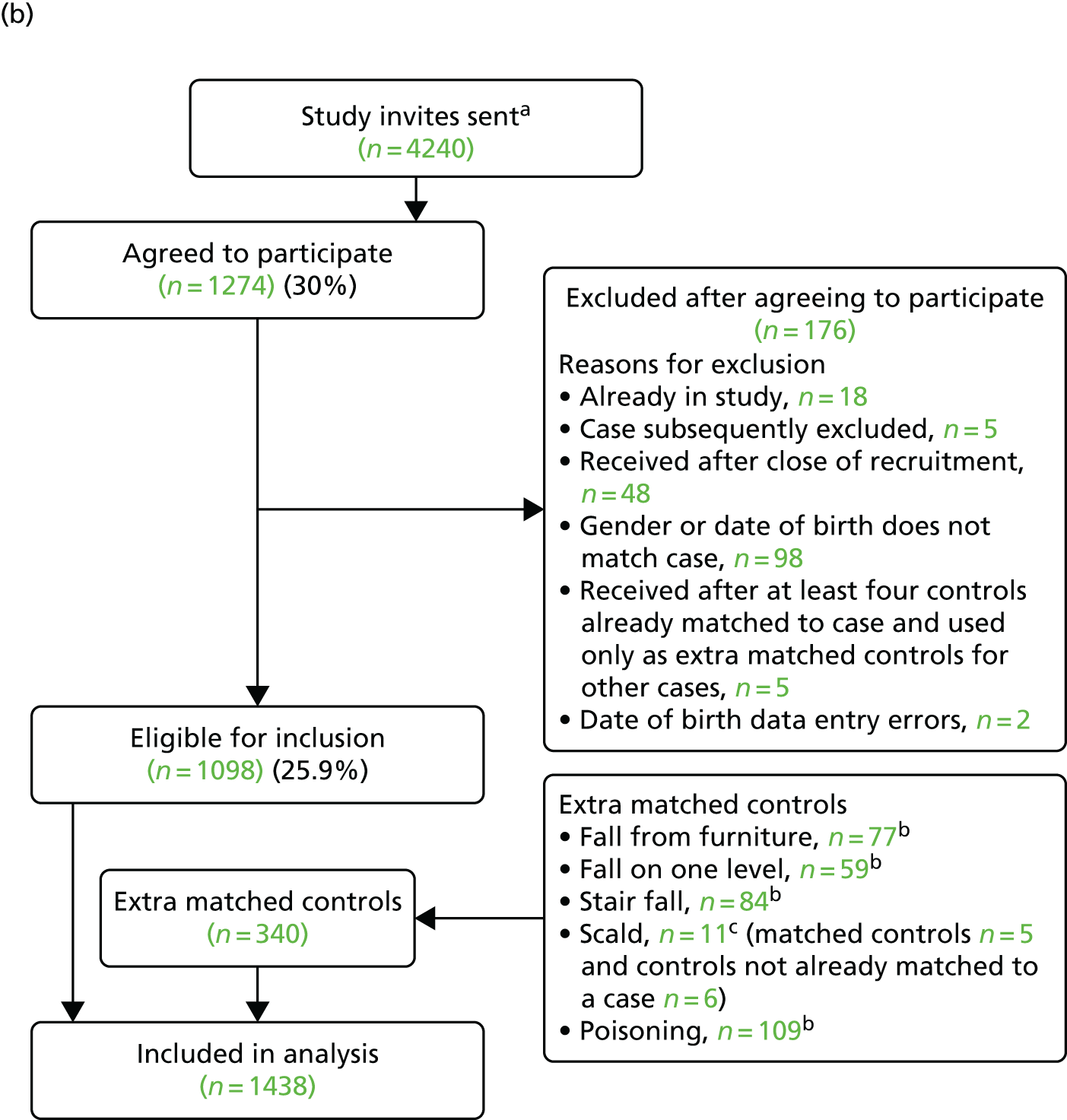
| Characteristic | Participants (N = 338), n (%) | Non-participants (N = 633), n (%) | Total (N = 971), n (%) | Significance |
|---|---|---|---|---|
| Age group (months) | ||||
| 0–12 | 97 (28.7) | 163 (25.8) | 260 (26.8) | χ2(2) = 4.60, p = 0.10 |
| 13–36 | 210 (62.1) | 383 (60.5) | 593 (61.0) | |
| ≥ 37 | 31 (9.2) | 87 (13.7) | 118 (12.2) | |
| Sex | ||||
| Male | 186 (55.0) | 364 (57.5) | 550 (56.6) | χ2(1) = 0.55, p = 0.46 |
| Female | 152 (45.0) | 269 (42.5) | 421 (43.4) | |
The mean number of controls per case was 4.25. The median time from date of injury to date of questionnaire completion for cases was 11 days (IQR 6–21 days).
All cases had sustained a scald and no other injury in addition to the scald. In total, 31% received treatment at the ED, 24% were seen and examined but did not require treatment, 18% were admitted to hospital and 27% were treated and discharged with a follow-up appointment.
Table 26 shows the sociodemographic characteristics of cases and controls. Controls were slightly older than cases (median age 1.56 vs. 1.47 years). Cases were less likely to be of white ethnic origin (81.8% vs. 91.3%) and more likely to have only one child under the age of 5 years (67.5% vs. 62.3%), live in an overcrowded household (15.2% vs. 8.6%) or live in a rented home (49.6% vs. 37.1%). Case households were more likely to receive state benefits than control households (46.0% vs. 35.0%). Cases lived in areas of higher social deprivation (median IMD score 20.6 vs. 15.7) and typically spent less time being cared for outside the home (median number of hours per week 5.5 vs. 12). Parental perception of their child’s ability to climb was lower for cases: 78.6% of case parents thought that it was very likely that their child could climb to at least one of the eight places described on the questionnaire compared with 82.8% of control parents.
| Characteristic | Cases (n = 338) | Controls (n = 1438) |
|---|---|---|
| Study centre | ||
| Nottingham | 123 (36.4) | 521 (36.2) |
| Bristol | 112 (33.1) | 490 (34.1) |
| Norwich | 54 (16.0) | 235 (16.3) |
| Newcastle | 49 (14.5) | 192 (13.4) |
| Age (years), median (IQR)a | 1.47 (1.03–1.96) | 1.56 (1.15–2.07) |
| Age group (months) | ||
| 0–12 | 91 (26.9) | 316 (22.0) |
| 13–36 | 216 (63.9) | 984 (68.4) |
| 37–62 | 31 (9.2) | 138 (9.6) |
| Male | 183 (54.1) | 808 (56.2) |
| Ethnic origin: white | 269 (81.8) [9] | 1295 (91.3) [19] |
| Number of children aged 0–4 years in family | [6] | [21] |
| 1 | 224 (67.5) | 883 (62.3) |
| 2 | 95 (28.6) | 476 (33.6) |
| ≥ 3 | 13 (3.9) | 58 (4.1) |
| First child | 140 (44.4) [23] | 581 (43.8) [111] |
| Maternal age ≤ 19 years at birth of first childb | 43 (14.6) [3] | 156 (11.8) [9] |
| Single adult household | 52 (15.9) [10] | 171 (12.2) [34] |
| Weekly out of home child care (hours), median (IQR) | 5.5 (0–18) [32] | 12 (0–24) [77] |
| Adults in paid work | [6] | [19] |
| ≥ 2 | 150 (45.2) | 802 (56.5) |
| 1 | 129 (38.9) | 433 (30.5) |
| 0 | 53 (16.0) | 184 (13.0) |
| Household receives state benefits | 151 (46.0) [10] | 491 (35.0) [35] |
| Overcrowding (more than one person per room) | 47 (15.2) [28] | 116 (8.6) [83] |
| Non-owner-occupier | 164 (49.5) [7] | 521 (37.1) [33] |
| Household has no car | 55 (16.5) [5] | 174 (12.3) [18] |
| IMD score, median (IQR)c | 20.6 (10.1–35.6) | 15.7 (9.5–28.8) [18] |
| Distance from hospital (km), median (IQR) | 3.9 (2.1–8.1) | 4.6 (2.6–10.3) [16] |
| CBQ score, mean (IQR)c | 4.7 (4.0–5.3) [18] | 4.6 (4.1–5.2) [155] |
| Long-term health condition | 22 (6.6) [7] | 77 (5.4) [13] |
| Child health VAS score (range 0–10), median (IQR)c | 9.9 (9.2–10) [4] | 9.6 (8.3–10) [4] |
| HRQL (PedsQL score), median (IQR)c,d | 94.8 (88.2–98.8), n = 79 [3] | 89.3 (88.1–94.1), n = 401 [3] |
| Parental assessment of child’s ability to climb | [6] | [12] |
| All scenarios ‘not likely’ | 24 (7.2) | 80 (5.6) |
| One or more scenarios ‘quite likely’ and none ‘very likely’ | 47 (14.2) | 165 (11.6) |
| One or more scenarios ‘very likely’ | 261 (78.6) | 1181 (82.8) |
| PDH tasks subscale score, median (IQR)c,e | 13 (10.0–16.0) [34] | 14 (11.0–18.0) [99] |
| HADS score, mean (IQR)c,e | 9 (6.0–13.0) [11] | 10 (6.0–14.0) [20] |
Table 27 shows the frequency of exposures among cases and controls and unadjusted ORs and Table 28 shows ORs adjusted for a range of confounding variables. Fifteen of the 28 ORs changed by > 10% after adjustment (no safety gate: OR 1.79, AOR 1.46; things that could be climbed on to reach high surfaces: OR 1.07, AOR 1.24; kettle not at back of worktop/cooker: OR 1.46, AOR 1.20; water temperature too hot: OR 0.67, AOR 0.96; water temperature not known or > 54°C: OR 1.29, AOR 0.99; played/climbed on furniture: OR 0.54, AOR 0.62; held by someone holding hot drink: OR 0.95, AOR 0.83; hot drinks in reach of child: OR 1.99, AOR 2.33; pan handles not turned to back of cooker: OR 1.26, AOR 0.91; child left alone in bathroom: OR 0.53, AOR 0.70; bath run by older child: OR 1.13, AOR 0.74; older child supervised child in bath: OR 0.82, AOR 1.10; not taught rules about bathtubs: OR 2.16, AOR 1.42; not using playpen/travel cot: OR 1.16, AOR 1.33; not using stationary activity centre: OR 1.62, AOR 1.22).
| Exposure | Cases (n = 338) | Controls (n = 1438) | Unadjusted OR (95% CI) |
|---|---|---|---|
| Did not use any safety gatesa | 82 (26.3) [26] | 242 (17.6) [65] | 1.79 (1.29 to 2.48) |
| Had things child could climb on to reach high surfacesa | 115 (34.7) [7] | 475 (33.2) [6] | 1.07 (0.81 to 1.42) |
| Did not have curly flex or cordless kettlea | 96 (29.3) [10] | 417 (29.5) [25] | 1.00 (0.76 to 1.31) |
| Kettle not at back of worktop/table or back ring of cookera | 41 (12.6) [12] | 135 (9.5) [17] | 1.46 (1.00 to 2.14) |
| Hot tap water too hota | 270 (82.8) [12] | 1249 (88.0) [18] | 0.67 (0.48 to 0.94) |
| Temperature of hot tap water not known or known to be ≥ 54 °Ca | 289 (88.7) [12] | 1212 (85.5) [21] | 1.29 (0.88 to 1.87) |
| Child climbed or played on furniture at least some daysb,c | 233 (74.4) [7] ((18)) | 1098 (80.6) [6] ((70)) | 0.54 (0.37 to 0.77) |
| Child held by someone holding a hot drink at least some daysb,c | 89 (28.2) [7] ((15)) | 395 (28.6) [6] ((50)) | 0.95 (0.72 to 1.26) |
| Child held by someone using a cooker at least some daysb,c | 77 (24.1) [7] ((11)) | 357 (25.7) [6] ((44)) | 0.91 (0.68 to 1.21) |
| Hot drinks passed over child’s head at least some daysb,c | 42 (12.9) [6] ((7)) | 147 (10.5) [9] ((28)) | 1.24 (0.85 to 1.80) |
| Hot drinks left within reach of child at least some daysb,c | 171 (53.9) [12] ((9)) | 534 (38.0) [12] ((21)) | 1.99 (1.54 to 2.57) |
| Hot drinks or hot liquids put on a table with a tablecloth at least some daysb,c | 57 (17.8) [8] ((10)) | 178 (12.9) [9] ((47)) | 1.47 (1.05 to 2.05) |
| Front rings of cooker used at least some daysb,c | 236 (75.2) [13] ((11)) | 1152 (82.2) [18] ((19)) | 0.67 (0.49 to 0.90) |
| Pan handles never turned towards the back of the cooker while cookingb,c | 104 (32.2) [9] ((6)) | 380 (27.2) [16] ((23)) | 1.26 (0.96 to 1.65) |
| Child left in bathroom without adult even for a moment at least some daysb,c | 55 (17.0) [6] ((8)) | 384 (27.2) [11] ((17)) | 0.53 (0.39 to 0.74) |
| Child left in bath without adult even for a moment at least some daysb,c | 40 (12.5) [9] ((8) | 314 (22.2) [12] ((13)) | 0.47 (0.32 to 0.68) |
| Bath run for child by an older child at least some daysb,c | 15 (5.6) [11] ((60)) | 65 (5.6) [19] ((252)) | 1.13 (0.61 to 2.11) |
| Older child looked after child in the bath at least some daysb,c | 29 (11.0) [10] ((64)) | 164 (14.2) [10] ((273)) | 0.82 (0.53 to 1.27) |
| Bath never run using cold water firstb,c | 246 (78.8) [8] ((18)) | 1125 (82.7) [22] ((56)) | 0.83 (0.61 to 1.13) |
| Temperature of bathwater never checked using thermometer or other gadgetb,c | 228 (74.5) [10] ((22)) | 1045 (75.5) [9] ((45)) | 0.95 (0.71 to 1.29) |
| Temperature of bathwater never checked using hand or elbowb,c | 90 (27.6) [7] ((5)) | 327 (23.4) [10] ((30)) | 1.23 (0.94 to 1.62) |
| Child not taught rules about things not to climb on in the kitchen | 160 (49.8) [17] | 609 (43.3) [32] | 1.52 (1.11 to 2.07) |
| Child not taught rules about what to do or not do when parents are cooking using the top of the cooker | 175 (53.2) [9] | 636 (45.1) [27] | 1.78 (1.29 to 2.44) |
| Child not taught rules about hot things in the kitchen | 181 (55.9) [14] | 655 (46.6) [32] | 1.79 (1.31 to 2.43) |
| Child not taught rules about what to do or not do when in the bathtub | 141 (44.2) [19] | 471 (33.7) [39] | 2.16 (1.56 to 2.98) |
| Safety practices measured only in children aged 0-36 months | |||
| n = 307 | n = 1300 | ||
| Used baby walkera | 81 (27.0) [7] | 446 (34.7) [15] | 0.71 (0.53 to 0.94) |
| Did not use playpen or travel cota | 252 (84.3) [8] | 1060 (82.5) [16] | 1.16 (0.82 to 1.65) |
| Did not use stationary activity centrea | 246 (82.0) [7] | 951 (74.0) [15] | 1.62 (1.17 to 2.25) |
| Exposure | AOR (95% CI) | Confounders adjusted fora |
|---|---|---|
| Did not use any safety gatesb | 1.46 (0.98 to 2.16) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care |
| Had things child could climb on to reach high surfacesb | 1.24 (0.89 to 1.72) | HADS score, PDH score, ability to climb, uses safety gate |
| Did not have curly flex or cordless kettleb | 0.93 (0.65 to 1.33) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Kettle not at back of worktop/table or back ring of cookerb | 1.20 (0.67 to 2.15) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Hot tap water too hotb | 0.96 (0.57 to 1.64) | HADS score, PDH score, ability to climb, first child, bath access |
| Temperature of hot tap water not known or known to be ≥ 54 °Cb | 0.99 (0.57 to 1.70)c | HADS score, PDH score, ability to climb, first child, bath access |
| Child climbed or played on furniture at least some daysd | 0.62 (0.40 to 0.96) | HADS score, PDH score, ability to climb, uses safety gate |
| Child held by someone holding a hot drink at least some daysd | 0.83 (0.57 to 1.21) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Child held by someone while using a cooker at least some daysd | 0.97 (0.67 to 1.41) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Hot drinks passed over child’s head at least some daysd | 1.18 (0.71 to 1.98) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Hot drinks left within reach of child at least some daysd | 2.33 (1.63 to 3.31) | HADS score PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Hot drinks or hot liquids put on a table with a tablecloth at least some daysd | 1.33 (0.85 to 2.08) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| The front rings of the cooker used at least some daysd | 0.70 (0.46 to 1.05) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Pan handles never turned towards the back of the cooker while cookingd | 0.91 (0.63 to 1.32) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Child left in bathroom without adult even for a moment at least some daysd | 0.70 (0.48 to 1.01) | HADS score, PDH score, ability to climb, first child, number of adults living with child, overcrowding |
| Child left in bath without adult even for a moment at least some daysd | 0.47 (0.30 to 0.75) | HADS score, PDH score, ability to climb, first child, number of adults living with child, overcrowding |
| Bath run for child by an older child at least some daysd | 0.74 (0.31 to 1.82) | HADS score, PDH score, ability to climb, first child, number of adults living with child, overcrowding |
| Older child looked after child in the bath at least some daysd | 1.10 (0.63 to 1.93) | HADS score, PDH score, ability to climb, first child, number of adults living with child, overcrowding |
| Bath never run using cold water firstd | 0.85 (0.60 to 1.22) | HADS score, PDH score, ability to climb, first child, hot water temperature |
| Temperature of bathwater never checked using thermometer or other gadgetd | 1.00 (0.70 to 1.43)c | HADS score, PDH score, ability to climb, first child, hot water temperature |
| Temperature of bathwater never checked using hand or elbowd | 1.19 (0.86 to 1.64) | HADS score, PDH score, ability to climb, first child, hot water temperature |
| Child not taught rules about things not to climb on in the kitchen | 1.66 (1.12 to 2.47) | HADS score, PDH score, ability to climb, first child, uses safety gate |
| Child not taught rules about what to do or not do when parents are cooking using the top of the cooker | 1.95 (1.33 to 2.85) | HADS score, PDH score, ability to climb, first child, uses safety gate |
| Child not taught rules about hot things in the kitchen | 1.89 (1.30 to 2.75) | HADS score, PDH score, ability to climb, first child, uses safety gate |
| Child not taught rules about what to do or not do when in the bathtub | 1.42 (0.85 to 2.37)c | HADS score, PDH score, ability to climb, first child, uses safety gate, bath access, hot water temperature, bath run with cold water first, bath temperature checked |
| Used baby walkerb | 0.74 (0.52 to 1.03) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care |
| Did not use playpen or travel cotb | 1.33 (0.86 to 2.06) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care, uses baby walker |
| Did not use stationary activity centreb | 1.22 (0.83 to 1.79) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care, uses baby walker |
Compared with parents of controls, in the adjusted analysis parents of cases were more likely to have not taught their child rules about things not to climb on in the kitchen (AOR 1.66, 95% CI 1.12 to 2.47; PAF 20%), what to do or not do when parents are cooking using the top of the cooker (AOR 1.95, 95% CI 1.33 to 2.85; PAF 26%) and about hot things in the kitchen (AOR 1.89, 95% CI 1.30 to 2.75; PAF 26%). They were also more likely than control parents to have left hot drinks within reach of their child (AOR 2.33, 95% CI 1.63 to 3.31; PAF 31%). Cases were less likely than controls to have played or climbed on furniture (AOR 0.62, 95% CI 0.40 to 0.96) or to have been left alone in the bath (AOR 0.47, 95% CI 0.30 to 0.75). ORs for most of the remaining 22 exposures were close to 1, with 10 being > 1 (ranging from 1.10 to 1.46) and 12 being ≤ 1 (ranging from 0.70 to 1.00). All had CIs indicating that associations could have occurred by chance.
As shown in Table 29, there were three exposures for which there was a significant interaction with one of the sociodemographic variables. Comparing cases with controls, parents in households with two or more adults in paid work were more likely not to have taught their child rules about what to do or not do when in the bathtub (AOR 2.81, 95% CI 1.43 to 5.53; PAF 33%). Compared with parents of controls, in single adult households parents of cases were less likely to have a hot water temperature of ≥ 54 °C (or not know the water temperature) (AOR 0.42, 95% CI 0.07 to 2.72), whereas, in households with two or more adults, parents of cases were more likely to have a hot water temperature of ≥ 54 °C (or not know the water temperature) (AOR 1.47, 95% CI 0.85 to 2.56). Compared with control parents, case parents living in rented accommodation were more likely never to check their child’s bathwater temperature using a thermometer or other gadget (AOR 1.84, 95% CI 1.03 to 3.28, PAF 36%), whereas parents of cases in owner-occupied housing were less likely to never check the bathwater temperature using a thermometer or other gadget (AOR 0.65, 95% CI 0.42 to 1.03).
| Exposure | AORa (95% CI) by number of adults in paid work | p-value from test for interaction | ||
|---|---|---|---|---|
| Two or more | One | None | ||
| Child not taught rules about what to do or not do when in the bathtub | 2.81 (1.43 to 5.53) | 0.61 (0.28 to 1.32) | 1.12 (0.37 to 3.39) | 0.006 |
| AORa (95% CI) by number of adults living with child | ||||
| One adult | More than one adult | |||
| Temperature of hot tap water not known or known to be ≥ 54 °Cb | 0.42 (0.07 to 2.72) | 1.47 (0.85 to 2.56) | 0.009 | |
| AORa (95% CI) by housing tenure | ||||
| Rented | Owner-occupied | |||
| Temperature of bathwater never checked using thermometer or other gadgetc | 1.84 (1.03 to 3.28) | 0.65 (0.42 to 1.03) | 0.005 | |
Tables showing the complete set of results of the following sensitivity analyses are available from the authors on request. Seventeen of the AORs using the multiply imputed data differed by > 10% from those using the complete-case data for the main analysis and these are shown in Table 30. Three of the AORs differed by > 10% between the multiply imputed and the complete-case interaction analyses.
| Exposure | Complete-case analysis | Multiple imputation analysis | % Difference | Difference |
|---|---|---|---|---|
| AORa (95% CI) | AORa (95% CI) | |||
| Did not use any safety gatesb | 1.46 (0.98 to 2.16) | 1.69 (1.21 to 2.34) | 15.5 | 0.25 |
| Hot tap water too hotb | 0.96 (0.57 to 1.64) | 0.76 (0.54 to 1.08) | –20.7 | –0.20 |
| Temperature of hot tap water not known or known to be ≥ 54 °Cb | 0.99 (0.57 to 1.70) | 1.39 (0.95 to 2.05) | 40.8 | 0.40 |
| Child climbed or played on furniture at least some daysc | 0.62 (0.40 to 0.96) | 0.73 (0.50 to 1.05) | 17.0 | 0.11 |
| Child held by someone holding a hot drink at least some daysc | 0.83 (0.57 to 1.21) | 1.05 (0.78 to 1.42) | 27.1 | 0.22 |
| Hot drinks passed over child’s head at least some daysc | 1.18 (0.71 to 1.98) | 1.40 (0.95 to 2.07) | 18.5 | 0.22 |
| Hot drinks or hot liquids put on a table with a tablecloth at least some daysc | 1.33 (0.85 to 2.08) | 1.48 (1.05 to 2.10) | 11.6 | 0.15 |
| Pan handles never turned towards the back of the cooker while cookingc | 0.91 (0.63 to 1.32) | 1.10 (0.83 to 1.46) | 21.0 | 0.19 |
| Child left in bathroom without adult even for a moment at least some daysc | 0.70 (0.48 to 1.01) | 0.61 (0.44 to 0.86) | –12.3 | –0.09 |
| Child left in bath without adult even for a moment at least some daysc | 0.47 (0.30 to 0.75) | 0.55 (0.38 to 0.80) | 17.1 | 0.08 |
| Bath run for child by an older child at least some daysc | 0.74 (0.31 to 1.82) | 0.92 (0.50 to 1.68) | 23.9 | 0.18 |
| Older child looked after child in the bath at least some daysc | 1.10 (0.63 to 1.93) | 0.75 (0.48 to 1.18) | –31.5 | –0.35 |
| Child not taught rules about things not to climb on in the kitchen | 1.66 (1.12 to 2.47) | 1.41 (1.02 to 1.93) | –15.3 | –0.25 |
| Child not taught rules about what to do or not do when parents are cooking using the top of the cooker | 1.95 (1.33 to 2.85) | 1.68 (1.21 to 2.32) | –14.0 | –0.27 |
| Child not taught rules about hot things in the kitchen | 1.89 (1.30 to 2.75) | 1.61 (1.18 to 2.19) | –14.9 | –0.28 |
| Child not taught rules about what to do or not do when in the bathtub | 1.42 (0.85 to 2.37) | 1.84 (1.32 to 2.58) | 29.9 | 0.42 |
| Did not use stationary activity centreb | 1.22 (0.83 to 1.79) | 1.45 (1.03 to 2.04) | 18.5 | 0.23 |
For five exposures, the proportion of ‘not applicable’ responses was > 5%. Analyses were undertaken incorporating a separate category for ‘not applicable’ responses. The AOR differed by > 10% in the analyses comparing cases with controls with and without a ‘not applicable’ category for the bath being run by an older child (AOR with ‘not applicable’ category 0.62, 95% CI 0.28 to 1.34; AOR without ‘not applicable’ category 0.74, 95% CI 0.31 to 1.82) and for older children looking after a younger child in the bath (AOR with ‘not applicable’ category 0.95, 95% CI 0.56 to 1.00; AOR without ‘not applicable’ category 1.10, 95% CI 0.63 to 1.93). The results from these analyses are available from the authors on request.
Stratifying analyses by the treatment received (as a proxy for injury severity) resulted in AORs with fairly broad and overlapping 95% CIs for the seen and examined in the ED and the admitted/treated in the ED/discharged with follow-up groups for almost all exposures. However, the AORs differed between those admitted/treated in the ED/followed up post discharge and those seen and examined in the ED for putting hot drinks or liquids on tables with tablecloths on. Parents of cases who were seen and examined in the ED were less likely than parents of controls to put hot drinks on tables with cloths (AOR 0.11, 95% CI 0.02 to 0.63), but parents of cases admitted to hospital/treated in the ED/followed up post discharge were more likely to put hot drinks on tables with tablecloths than parents of controls (AOR 2.02, 95% CI 1.22 to 3.36). The results from these analyses are available from the authors on request.
Discussion
Main findings
We found that a range of modifiable risk factors were associated with secondary care-attended falls from furniture, falls on stairs or steps, poisonings and scalds in children aged 0–4 years. Only two modifiable risk factors were associated with secondary care-attended falls on one level in children aged 0–4 years.
Compared with control parents, parents of children who had a fall from furniture were more likely not to use safety gates anywhere in the home (PAF 15%) and, for those with children aged 0–12 months, were more likely to have left them on raised surfaces (PAF 50%), changed nappies on raised surfaces (PAF 34%) and put them in car/bouncing seats on raised surfaces (PAF 12%). Parents of children who had fallen from furniture were less likely to put children aged 13–36 months in car/bouncing seats on raised surfaces (78% reduction in odds). They were more likely not to have taught children rules about things they should not climb on in the kitchen (PAF 16%) and, for those with children aged ≥ 37 months, their children played or climbed on furniture more often (PAF 88%) than control children. Case children who had had a fall from furniture played or climbed on garden furniture less often than control children (26% reduction in odds).
Compared with parents of controls, parents of children who had had a fall on one level were less likely not to use furniture corner covers (28% reduction in odds) and less likely not to have rugs/carpets firmly fixed to the floor (23% reduction in odds). The association with rugs/carpets firmly fixed to the floor varied with the number of adults in the household. Households with one adult in which children had had a fall on one level were more likely not to have rugs/carpets fixed to floors than control households (PAF 18%), whereas households with two adults in which children had had a fall on one level were less likely not to have rugs/carpets fixed to floors than control households (31% reduction in odds).
Compared with parents who kept safety gates closed, parents of children who had fallen down stairs or steps were more likely not to use safety gates on stairs (PAF 21%) or to leave safety gates on stairs open (PAF 24%) than parents of controls. Compared with control households, the odds of not using a safety gate on stairs and of leaving the gate open appeared to be particularly high in families with children aged 0–12 months (PAF 18% and 46%, respectively) and the odds of leaving safety gates open appeared to be high in families who used baby walkers (PAF 44%). Families with children who had fallen down stairs or steps were more likely than controls not to have carpeted stairs (PAF 5%) or not to have a landing part-way up their stairs (PAF 18%). They were also more likely to consider their stairs not safe to use (PAF 5%) or in need of repair (PAF 5%). They were less likely than controls to have tripping hazards on their stairs (23% reduction in odds) or not to have handrails on all stairs (31% reduction in odds). Compared with controls, families with no adults in paid work whose children had fallen down stairs or steps were more likely to have taught children rules about carrying things down stairs and leaving things on stairs (56% and 73% reduction in odds of not teaching rules, respectively). Compared with controls, single adult families whose children had fallen down stairs or steps were more likely to have taught children rules about leaving things on stairs (67% reduction in odds of not teaching rules) and to not have carpeted stairs (PAF 26%).
Compared with parents of controls, parents of children who had had a poisoning were more likely not to store medicines at adult eye level or above (PAF 15%), not to store medicines safely (locked away or at adult eye level or above) (PAF 16%) and not to put medicines (PAF 20%) or household products (PAF 11%) away immediately after use. They were also less likely not to store household products safely (23% reduction in odds) and not to have taught children rules about what to do if medicines are left on the worktop (34% reduction in odds). Parents of children who had had a poisoning in single adult households were more likely than control parents not to store household products at adult eye level or above (PAF 50%). Parents of girls who had had a poisoning were less likely than parents of controls not to lock medicines away (41% reduction in odds).
Compared with parents of controls, parents of children who had had a scald were more likely to have left hot drinks in reach of children (PAF 31%) and more likely not to have taught children rules about climbing in the kitchen (PAF 20%), about what to do or not to do when adults are using the top of the cooker (PAF 26%) or about hot things in the kitchen (PAF 26%). Parents of children who had had a scald were less likely than control parents to have left a child alone in the bath (53% reduction in odds) and their children climbed or played on furniture less often (38% reduction in odds). Compared with controls, families with at least two adults in paid work whose children had had a scald were more likely not to have taught children rules about what to do or not to do when in the bathtub (PAF 33%). Single adult families with children who had had a scald were less likely than controls to report an unsafe or unknown hot water temperature (58% reduction in odds). Compared with parents of controls, parents of children with a scald living in rented accommodation were more likely not to check the bathwater temperature with a thermometer (PAF 36%).
Most exposures were study specific. Not using safety gates (other than on stairs) was an exposure in all five case–control studies and ORs were > 1 for all studies (ranging from 1.05, 95% CI 0.80 to 1.37 for poisonings to 1.65, 95% CI 1.29 to 2.12 for falls from furniture). All case–control studies included exposures related to teaching children safety rules, but only teaching rules about climbing in the kitchen was measured in more than one study, with both studies finding ORs > 1 (falls from furniture OR 1.58, 95% CI 1.16 to 2.15; scalds OR 1.66, 95% CI 1.12 to 2.47). Across all studies, nine of the 13 ORs related to teaching safety rules were > 1 (ranging from 1.13, 95% CI 0.83 to 1.52 for rules about slippery floors and falls on one level to 1.95, 95% CI 1.33 to 2.85 for rules about what to do or not do when parents are using the top of the cooker and scalds).
Strengths and limitations
We report the largest case–control studies to date examining associations between a range of modifiable risk factors for falls, poisoning and scalds. These studies were conducted in NHS hospitals across England, including urban and rural areas. Adjustment was made for a wide range of potential confounding factors using DAGs. For four of our five studies, the majority of ORs using multiply imputed data for the main analysis did not differ by > 10% from those in the complete-case analysis. However, in most studies, a larger number of ORs in the interaction analyses differed by > 10% between the multiple imputation and the complete-case analyses.
Case–control studies have limitations arising from their observational nature. These include, but are not limited to, measurement error, a range of different types of bias and confounding. Each of these are discussed below. We validated measures for exposures when possible and found high (> 70%) sensitivities and specificities for six out of 12 falls exposures, for two out of 15 poisoning exposures and for two out of three scalds exposures. We used home observations as the ‘gold standard’, but it is possible that families may have made changes to their homes either as a result of the injury or in anticipation of the home observation. In addition, there may have been some social desirability bias, with parents reporting responses that they judged to be ‘more acceptable’. These may potentially explain some of the lack of agreement that we found between parent-reported and observed exposures. It is likely that some misclassification of exposures occurred. Misclassification is likely to be lowest when sensitivity and specificity are both high. Sensitivity and specificity were both > 70% for having safety gates on stairs or across kitchen doorways, having carpeted stairs and landings part-way up stairs, having playpens, furniture corner covers and cordless or curly-flexed kettles and storing household products at adult eye level or above. For other exposures, when misclassification is higher it is more likely that ORs are biased towards the null (although this does not always occur86) and this may partly explain our failure to find associations between some exposures and falls, poisonings and scalds. We did explore whether or not the differences between self-reported and observed exposures varied between cases and controls, and we found similar levels of under- and over-reporting for both groups for most exposures. This suggests that differential misclassification is unlikely to have occurred to a large extent. Our analyses did not take misclassification of exposures into account, and for this reason our findings should be interpreted with caution. Future studies should consider adjusting for exposure misclassification.
The participation rates for cases and controls were similar, but were low for all studies, ranging from 24% to 35% for cases and from 24% to 33% for controls across the five studies. If reasons for participation are associated with the exposure or outcome of interest, selection bias may have occurred. Our participation rates do not show large differences by case/control status, age and sex, but we were not able to assess the prevalence of exposures in participants and non-participants, and caution should be exercised in interpreting our findings. In addition to social desirability bias discussed above, recall bias may have occurred. These two types of bias could potentially impact on our ORs in different directions. As most injuries were relatively minor, it is possible that a small number of controls may have had similar injuries to cases and on the same date as the case injury but did not seek medical attention for those injuries. This could lead to misclassification of cases and controls. However, this is likely to apply to only a small number of controls; hence, we would expect this to have at most only a minor impact on our results. If seeking medical attention is associated with exposures of interest, this may lead to overestimation of ORs, but the extent to which this may have introduced bias is difficult to assess.
Most ORs for not teaching children various safety rules were > 1 across the five case–control studies and were significantly raised for rules about climbing in the kitchen for falls from furniture and scalds and for rules about what to do or not do when parents were using the cooker top and about not touching hot things for scalds. It is possible that parents who use safety rules supervise their children differently from parents who do not use rules and, as we were not able to adjust for this, residual confounding may partly explain these findings.
In all five case–control studies, cases were more disadvantaged than controls. Socioeconomic disadvantage is likely to be associated with some of the exposures of interest in our studies and, although we adjusted for a range of confounders, it is possible that some residual confounding remained. It is also possible that families belonging to black and minority ethnic (BME) groups were under-represented in our studies and that for some studies (scalds in particular) a higher proportion of cases than controls belonged to a BME group. The proportion of the population reported as white in the 2011 UK census was 86%,87 whereas the proportion of cases and controls from a BME group ranged from 8% to 18% and from 7% to 9%, respectively, across our five studies. The generalisability of our findings to BME groups may therefore be limited.
Overall, there were few significant interactions found, but our interaction analyses should be interpreted with caution for several reasons. First, a large number of tests for interactions were performed and, although we used a significance level of 1% for these tests, one in every 100 tests will be significant by chance alone. Second, subgroup numbers were small for many comparisons, leading to insufficient power to detect anything other than large differences in associations. Third, differences in estimates of associations between complete-case and multiple imputation analyses suggest that the findings of some of our interaction analyses were not robust to missing data. Consequently, these analyses should be considered as generating rather than testing hypotheses. The significant interactions that were found need confirmation from further research.
Our findings in relation to age are, in general, in keeping with what would be expected based on child development. For example, the increased odds of falls from furniture only in 0- to 12-month-olds who were left on, had nappies changed on or who were put in car/bouncing seats on raised surfaces is to be expected given that these are activities likely to be undertaken by parents whose children are not independently mobile. We found only a small number of exposures with significant interactions with sex, with the exposure more strongly associated with an injury in boys than in girls. The majority of these were in the poisonings case–control study. Boys have higher mortality rates for poisoning than girls88 and have been found to have higher hospital admission rates for poisonings than girls,55,89 although some studies including poisonings not requiring hospital admissions have failed to find significant differences by child sex. 90,91 As our cases mainly included minor injuries, this would be consistent with finding only a few exposures more strongly associated with poisonings in boys than in girls.
There were significant interactions for several exposures related to teaching safety rules with either the number of adults in the household or the number in paid work in the stair falls and scalds studies. Previous research suggests that parents start teaching safety rules between the ages of 2 and 4 years and at this point they move from mainly using strategies based on supervision and changing the home environment to teaching- and rule-based strategies to prevent injury. 92,93 Previous research also suggests that teaching safety rules can increase the risk of injury93,94 and that teaching needs to increase children’s understanding of the safety issue to reduce the extent to which they interact with hazards. 94 Our findings suggest that cases in single adult households and in households without adults in paid work are more likely to have been taught safety rules than controls. It is possible that families in which supervision may be more challenging (e.g. single adult households) or with fewer material resources (e.g. those without adults in paid work) rely more on teaching safety rules than on other injury prevention strategies, but this may not be an effective strategy in these circumstances. Further work is required to explore these hypotheses.
The many exposures in our studies resulted in multiple significance testing; hence, some associations may have been significant by chance alone. Our estimates of associations for some exposures were imprecise because of the low prevalence of some exposures such as use of playpens or stationary activity centres, use of safety gates to prevent access to gardens, transferring household products or medicines to other containers or baths being run by older children. Some exposures were not measured in our studies because they were known to be rare, and our studies were underpowered to detect anything other than implausibly large associations. For example, bunk bed falls account for only 10% of falls from beds and have an annual incidence rate of 0.3 per 1000 children-years. 45,95–98
Comparisons with existing literature
Comparing our findings with those of previously published studies has been limited by differences in the exposures measured, similar exposures measured in different ways or inadequately detailed descriptions of exposure measures. We have not compared our findings to studies in which cases represent a wide range of injury mechanisms99 because of the difficulty in interpreting findings that are not specific to single injury mechanisms. We found only one Australian case–control study of infants with head or face trauma100 matched on age to controls with which to compare the findings from our falls studies. The findings of the Australian study were consistent with our findings for changing nappies on high surfaces (OR 1.77, 95% CI 1.07 to 2.92) and use of high chairs without harnesses (OR 1.47, 95% CI 0.73 to 2.98). We found slightly raised odds of a fall from furniture for children who had not used a baby walker (OR 1.22, 95% CI 0.90 to 1.65) but slightly reduced odds of a fall on one level (0.83, 95% CI 0.58 to 1.10) and for a fall on stairs or steps (AOR 0.83, 95% CI 0.62 to 1.09), which was consistent with the results from the Australian study (OR for ever using a baby walker 0.83, 95% CI 0.50 to 1.38). However, this was inconsistent with the increased odds of a head injury in those using a baby walker most days (OR 2.47, 95% CI 0.97 to 6.48) found by the same study.
There are several case–control studies that we can compare the findings from our poisonings study with. A study from Greece including children predominantly aged 2–4 years attending hospital emergency clinics following a poisoning and non-injured age-, sex- and hospital-matched controls attending other outpatient clinics found no significant association between mother’s use of safely packaged products, mainly for detergents, and poisoning attendance (OR not presented). 101 An Australian study of 1- to 3-year-olds attending an ED following a poisoning and three different types of controls (community, ED attenders with another type of injury and ED non-injured attenders) found that a 1% increase in the percentage of medicinal substances stored in accessible locations in bathrooms increased the odds of poisoning by 3% (OR 1.03, 95% CI 1.002 to 1.080). 102
A case–control study from Thailand of children aged < 5 years attending hospitals following a poisoning matched with controls on age, sex and area of residence found no association between toxic substances in the home, storage practices, frequency of use, packaging or disposal practices and poisoning (ORs not presented). 103 A case–control study from Brazil of children aged < 5 years treated in hospital, matched with children seeking emergency care for other reasons on age, sex, hospital and presence in the home of the same toxic substances found in the case home, found an increased odds of poisoning in families storing toxic substances in boxes/cabinets (OR 3.80, 95% CI 1.15 to 12.49) and an increased odds of poisoning in families storing toxic substances < 150 cm from the floor (OR 16.59, 95% CI 2.86 to 96.20). 104
Comparing the findings from these studies with our control findings shows some consistency in terms of our higher odds of a poisoning in families not storing medicines at adult eye level or above and in families not storing poisons safely (at adult eye level or above or locked). The previous studies have not measured associations between putting medicines or household products away immediately and poisoning, and so we cannot compare our findings in this respect.
There are several case–control studies that we can compare our scalds study with. A Greek study of children predominantly aged 0–4 years attending an ED following a burn injury, of which 61% were scalds, matched on age and sex with non-injured ED attenders, found that a 1-unit increase in a burn avoidance index was associated with a 40% reduction in the odds of a burn (OR 0.6, 95% CI 0.5 to 0.8). 105 The burn avoidance index was a composite measure consisting of direction of handles of cooking utensils on the cooker while cooking, use of front/rear hotplates during cooking, keeping hot objects, foods and liquids in places inaccessible to children and avoidance of tablecloths on kitchen tables.
A study from Iraq of children aged 0–5 years admitted to a burns centre following a burn occurring at home, of which 79% were scalds, matched on age and sex to children admitted to hospital for other reasons, found that a 1-unit increase in a burns hazard score increased the odds of a burn by 32% (OR 1.32, 95% CI 1.02 to 1.71). 106 The burns hazard score included use of kerosene cookers, kerosene heaters, samovars for tea, home generators and non-electric heaters for bathwater, not knowing the boiler temperature, storing petrol at home, having no fire extinguisher and having no smoke alarm. A Dutch study of children aged 0–4 years attending an ED with burn injuries, 62% of which were scalds, matched on age with controls, found that storage of hot drinks in their original containers instead of in vacuum flasks increased the odds of a burn (OR 2.0, 90% CI 1.2 to 3.1). 107 A study in Bangladesh of children aged 0–12 years admitted to a burns unit and controls matched on age, sex and area of residence found that significantly more case households than control households had cooking equipment within reach of children (p < 0.001; OR not reported). 108
All of these case–control studies that we can compare our scalds study findings to studied children with burns and, although most of the burns were caused by scalds in these studies, some of the differences between these studies and our findings may reflect differing case definitions. In addition, there were few common exposures between these studies and our study, which may in part reflect differences between heating and cooking practices between countries. Our findings that families who had hot drinks in reach of children, drank hot drinks while holding children or passed hot drinks over children’s heads had an increased odds of a scald are in keeping with the findings from the Greek case–control study. 105 However, as that study used a composite measure of exposure, it is difficult to know the contribution made by keeping hot foods and liquids in inaccessible places to the odds of a scald. Similarly, we did not find significant associations between cooking practices such as use of the front rings of the cooker and turning pan handles towards the back of the cooker and, although these were included in the composite exposure measure in the Greek study, the contribution of these items to the odds of a scald in that study is unknown. 105
How these findings inform other research within the Keeping Children Safe programme
The findings from study A have been used to inform the decision analyses (study K) undertaken in work stream 5 assessing the cost-effectiveness of interventions to prevent falls and poisoning. They have also been used to inform recommendations on scalds, falls and poison prevention practices in the IPB for the prevention of fire-related injuries, scalds, falls and poisoning (study M).
Chapter 3 What are the NHS, child and family costs of falls, poisonings and scalds? (Work stream 2)
Abstract
Research question
What are the NHS, child and family costs of falls, poisonings and scalds? Is the PedsQL an acceptable and psychometrically sound measure of HRQL in children aged ≥ 2 years in an emergency medicine setting?
Methods
Study C consisted of two substudies. In the HRQL substudy, the toddler version of the PedsQL was used to obtain proxy reports of children’s pre-injury HRQL, with questionnaires completed immediately post injury and 2 weeks and 1, 3 and 12 months post injury. Instrument acceptability, internal consistency reliability, construct validity and responsiveness to change were measured. In the costs of injury substudy, resource use and expenditure questions were included in the HRQL questionnaire. Resource use data were combined with unit costs to calculate health-care and non-health-care costs.
Results
Health-related quality-of-life substudy
Internal consistency reliability was adequate (Cronbach’s α > 0.70). Retrospectively reported pre-injury scale, summary and total scores were (with the exception of the nursery/school subscale) higher than previously reported in healthy UK toddlers and in community controls in the current study. Children with a long-term health condition had poorer pre-injury PedsQL scores than those without, and hypotheses regarding post-injury physical functioning scores for groups defined by injury severity were supported. There were reductions in physical functioning from pre injury to post injury for children with more severe injuries, with most observed effect sizes being large (≥ 0.8).
Costs of injury substudy
In total, 344 parents completed resource use questionnaires, with > 95% of children recovering within 2 weeks of injury and almost 99% recovering within 1 month. Mean NHS costs ranged from £2588 to £2989 across injury mechanisms for children admitted for ≥ 2 days, from £719 to £1011 for those admitted for 0–1 days and from £97 to £178 for those attending an ED but not admitted. Scalds incurred the highest NHS costs for admissions for 0–1 days and for ED attendances. Comparisons between injury mechanisms were not possible for admissions for ≥ 2 days because of small numbers. Mean costs to families ranged from £99 to £399 across injury mechanisms for those admitted for ≥ 2 days, from £38 to £200 for those admitted for 0–1 days and from £18 to £68 for those attending an ED but not admitted. Family costs were highest for scalds for admissions for 0–1 days and for falls from furniture for ED attendances. Family costs mainly consisted of the costs of informal child care and the costs of taking time off work.
Conclusions
Health-related quality-of-life substudy
The PedsQL was a feasible and acceptable measure of HRQL in this population, with adequate internal consistency reliability, discrimination between varying levels of injury severity and sequelae and responsiveness to change. Findings in respect of construct validity were equivocal.
The costs of injury substudy
The NHS incurs high costs for admissions to hospital lasting ≥ 2 days following injuries, but these injuries are uncommon. More common injuries requiring shorter inpatient stays incur moderate costs, whereas the most common injuries requiring only ED attendance incur small costs. Costs to families can be substantial, especially for injuries requiring hospital admission.
Chapter summary
This chapter presents an overview of the costs and consequences of unintentional injuries to health services and to children and their families, including the economic and HRQL aspects. It describes the methods used to recruit participants to the study and the analyses undertaken. It presents data to validate the PedsQL for a range of injuries in preschool children and to measure the costs of injury to the NHS and families and discusses the key findings of each study. Finally, it outlines its strengths and weaknesses and considers the implications of the results.
Introduction
To date, there has been little information on the cost of unintentional injuries to the NHS, to children and to families, without which the NHS cannot make informed choices about which interventions to fund to prevent home injuries in childhood.
Measuring HRQL is an integral part of measuring the cost of children’s injuries, yet tools for doing this have not been validated for a wide range of injury types and severities in preschool children. 64,109–112 We therefore undertook a longitudinal study, nested within the case–control study described in work stream 1 (see Chapter 2). The primary objective of the study was to quantify children’s HRQL post injury and the costs to the NHS and families of such injuries and to assess the feasibility, acceptability and psychometric properties of the acute version of the PedsQL109 in a paediatric population with injuries. HRQL and cost data were analysed separately, with no attempt made to assign a monetary value to children’s HRQL for incorporation into the cost analysis. An alternative approach to assessing the costs of injuries would have been to estimate the burden of childhood injuries by measuring what society would be prepared to pay to avoid childhood injuries using willingness-to-pay methodology. Although the concept is appealing, practical difficulties have been well documented, relating mainly to the formulation of the questions asked and the interpretation of the responses given. 113 Information on costs and HRQL was used to inform decision analyses (study K) estimating the cost-effectiveness of a range of strategies to prevent childhood falls, poisoning and scalds undertaken in work stream 5 (see Figure 1 for a diagram of the component parts of the programme grant).
Unintentional injuries from falls, poisonings and scalds do not just result in death and injury. They also place burdens on the NHS and other care agencies and on injured children and their families. At a personal level, these burdens can, for example:
-
be financial (e.g. from loss of income if there is a need to take time off work, costs associated with travel to and from hospital or with making adaptations to the home)
-
impact on a child’s education
-
reduce a child’s ability to develop physically because of loss of mobility or reduction of fine motor skills
-
affect employment prospects
-
influence social interactions and life chances, for example as a result of severe scarring
-
affect HRQL, at least in the short term.
The costs of injury
In the UK, there is very limited evidence on the costs of unintentional childhood injuries. However, such information is important for prioritising spending on prevention, treatment and rehabilitation services and for economic evaluations of interventions. 114–116 Several studies have attempted to quantify the economic costs associated with unintentional injuries. 30,117–122 These have been undertaken from a variety of perspectives including medical care costs,117,119,120 medical and social care costs30 or medical care, social care and societal costs. 118,121,122 However, the estimates are not always specific to children30,118,121,122 or, when they do focus on children, studies do not always present data on the under-fives. 11 Some costs are estimated based on other types of injuries, for example transposed from data on road traffic crashes. 123
Although there are some data from other countries, estimates of the economic burden of injury cannot easily be compared between countries and across time because of differences in health-care systems, the absence of standardised methodologies, the different approaches used and a lack of epidemiological and cost data. 124 It should be noted that many previous cost and HRQL studies have used populations that were likely to have sustained more serious injuries.
The costs of injury can be categorised as direct costs resulting from the injury (e.g. costs to the health-care system such as ambulance transport, ED visits, admissions, primary care attendances, rehabilitation and drug costs), indirect costs, which represent the value of lost output because of reduced productivity caused by injury and any resultant disability and losses because of premature death (e.g. costs to the child, family or society such as loss of income from carers taking time off work or lost productivity in later life by the injured or disabled child) and intangible costs (e.g. costs of pain, grief, suffering, etc.). Some studies and sources provide estimates of direct costs and some of direct and indirect costs combined, as described below, but intangible costs, which are difficult to measure in monetary terms, have not been quantified to date.
In England, unintentional injuries occurring in or around the home are a leading cause of preventable death and disability for children aged < 5 years. 1 Falls, poisonings (including suspected poisonings) and thermal injuries are the most common causes of ED attendances3 and hospital admissions. 2 Although the majority of those injuries are not severe, the disproportionately large numbers of minor injuries are likely to account for the greater costs125 compared with the costs of relatively rare serious injuries (which individually would incur substantially higher lifetime costs). 1
Each year in England, > 280,000 children aged < 5 years visit an ED as a result of falls, thermal injuries or poisoning incidents. 3 These visits cost the NHS nearly £32M, based on the average cost of an ED attendance of £114. 31 These figures do not include children treated by GPs or treated at home. 126
In 2012/13 in England, > 18,300 falls, 5100 poisonings and 1420 scalds among under-fives resulted in emergency admissions. 2 About 90% of admissions were for < 2 days but almost 16% of scalds, 4% of falls and 2% of poisonings were more serious, requiring admission for > 3 days [data available from www.chimat.org.uk/earlyyears/injuries (accessed 4 October 2016)]. In total, the admissions cost the NHS £19.1M (at £586 per short-stay case and £2461 per long-stay case). 30 The most severe childhood injuries, such as severe scalds and traumatic brain injuries (TBIs) from falls, disproportionally contribute to costs to the NHS and other care agencies because of the longer length of hospital stay, cost of treatments in intensive care units, repeated operations and long-term rehabilitation.
Falls constitute almost half of all injury-related admissions to children aged < 5 years, with a rate of between 500 and 600 admissions per 100,000 children annually between 2008/9 and 2012/13 in England. 1 A population-based study of TBIs in north Staffordshire in the 1990s reported that, among under-fives, 62% of TBI cases (of all severities) resulted from falls, rising to > 70% if children who were dropped were included. 127 A study of children admitted with a TBI to intensive care units throughout England and Wales reported that the admission rate among under-fives was 5.3 per 100,000 children annually, with falls constituting 38% of the 136 cases in the sample. 128 These injuries can impose short- or long-term problems including post-traumatic stress,129 disability and cognitive and social impairment, impact negatively on learning ability and reduce chances of future employment and productivity. They also place significant financial130 and psychological distress120,131 on children and families, and are a major economic burden to society. 132
Estimates of short- and long-term costs of injuries, predominantly based on UK data, have been highlighted in the Chief Medical Officer’s Annual Report 201211 (Table 31) and a recent report and data analysis published by Public Health England. 1 The CMO’s report estimates the costs of severe injuries for the under 15s,11 as data are more readily available for injuries in this age group, whereas the Public Health England report breaks down the data into age categories, separating the < 5 years age group, and focuses on the most common childhood injuries, including falls, poisonings and scalds. 1 Both reports highlight the high financial costs, with the short-term health-care cost per case, that is, costs related to the hospital and other health service costs immediately after the injury, ranging from £2494 for the average cost of an injury to £14,000 for a serious road traffic injury. 118 The CMO’s report notes that the lifetime cost of a childhood TBI can be up to £4.95M per case at 2012 prices. 137,138
| Cost | Value updated to 2012 prices | Base values | Incidence (if applicable) | Population base | Unit | Source |
|---|---|---|---|---|---|---|
| Average cost of ED treatment leading to admission | £146 per patient | £146 per patient | NA | Number of cases: 135,131 (HES 20122) | Average cost for the UK (all types, all ages) | Curtis30 |
| Average cost for minor injury services leading to admission | £66 per patient | £66 per patient | NA | Number of cases: 135,131 (HES 20122) | Average cost for the UK (all types, all ages) | Curtis30 |
| Short-term costs, healthcare, RTI | £14,000 | £13,500 | 0–4 years: 82.5 per 100,000; 5–14 years: 55.75 per 100,000133 | Population estimates: 0–4 years: 3,393,400; 5–14 years: 6,091,500134 Total seriously injured (at least 3-day hospital stay): 6196 |
Average cost of a serious RTI (all ages) | Department for Transport135 |
| Short-term costs, health care, RTI | £14,000 | £13,500 | NA | 2272 seriously injured or killed on the road136 minus about 40 killed (HES 2010) = 2232 | Average cost of a serious RTI (all ages) | Department for Transport135 |
| Short-term costs, health care | £2494 | €2769 | 0–4 years: 82.5 per 100,000; 5–14 years: 55.75 per 100,000133 | Population estimates: 0–4 years: 3,393,400; 5–14 years: 6,091,500134 Total seriously injured (at least 3-day hospital stay): 6196 |
Average cost of an injury (all types, all ages) | Polinder et al.118 |
| Cost of a serious burn, short-term, health care | £65,788 | £63,157 | NA | NA | Average cost of inpatient treatment for a major burn, including high-dependency unit care | Pellatt et al.119 |
| Lifetime cost of a paediatric TBI (medical costs) | £271,805 | £268,000 | 5.6128 | 448128 | Indication of the lifelong medical cost for a child who suffers a severe TBI at age 3 years | Adapted from Wright (2011)137 by the Child Accident Prevention Trust138 |
| Lifetime cost of a paediatric TBI (all costs) | £4.95M | £4.89M | 5.6128 | 448128 | Indication of the lifelong medical cost, educational cost, productivity loss, benefits and tax loss for a child who suffers a severe TBI at age 3 years | Adapted from Wright et al.137 by the Child Accident Prevention Trust138 |
| Short- and long-term costs of TBI health care and non-health care | £1.43M | AUS$ 2.1M | 5.6128 | 448 (n = 47 for cyclists)128 | Lifetime average cost of a TBI (all ages) including all health-care costs plus social care costs, productivity losses, carer costs, etc. | Access Economics Pty Limited122 |
Calculating long-term costs can be complex, as this needs to take account of the long-term consequences of sustaining a severe injury such as educational costs (e.g. special needs for a disabled child), lost productivity costs and social care costs, which are not always well documented. 1 The potential total lifetime health-care, social care and social security costs of TBI in childhood, based on the number of cases in 2003, was estimated to be between £640M and £2.24B. 11
Using the methodology developed to cost road traffic accidents, the cost of a serious home accident (one requiring admission to hospital and including medical and support costs for the acute event, lost output over the period of recovery and the value of the avoidance of injury) to a child aged < 5 years has been estimated to be £33,200 in June 2009 prices using data for Great Britain. 123 (In this study, ‘serious’ was defined in the same way as the term is used in the reporting of road casualties; namely, the injury required admission to hospital at least overnight and involved concussion, crushing, laceration of > 5 cm, suspected or actual fracture, multiple injuries or other internal injuries and the outcome of which was inpatient treatment or admission or transfer to a specialist, long-stay or other hospital.)
Several UK studies have estimated the costs of childhood scalds. An average cost of acute inpatient treatment for a minor, uncomplicated paediatric scald [one involving < 10% of the total body surface area (TBSA)] has been estimated to be £1850 in 2002/3 prices,139 whereas the average cost of acute inpatient treatment of a ‘major scald’ (30–40% TBSA) in 2007–9 in a paediatric burns unit was as high as £55,000. 119 For a bathwater scald, NHS treatment costs were £25,226 and the wider societal costs were £71,902 at 2010 prices. 140
Health-related quality of life following childhood injury
The resource and productivity costs do not fully capture the burden of childhood injuries125 as they do not take account of the quality of life of, or psychological impact on, the child and family. The most commonly used generic measure of HRQL is the European Quality of Life-5 Dimensions (EQ-5D). 141 The EQ-5D measures health using five domains to produce 243 health states to which societal preference weights are assigned to generate a single ‘utility index’ value, captured on a scale ranging from 0 [for death (or negative values for states worse than death)] to 1 (perfect health) and which depend on the severity of the health problem. 125,142 The utility index is multiplied by the time lived within a health state to calculate quality-adjusted life-years (QALYs). Thus, 1 year lived in perfect health equates to 1 QALY and a year of life lived in less than perfect health equates to < 1 QALY. The EQ-5D has previously been used to measure HRQL following injury,125,133 but at the time of initiating our study it had not been used in injured children aged < 5 years. 143 The Child Health Utility 9D is a child-specific measure of HRQL but at the time of our study it had been validated only for use in children age 7–11 years (Katherine Stevens, University of Sheffield, April 2010, personal communication).
There is a dearth of research data in the UK on the estimation of QALYs for childhood injuries. The Long Term Health and Healthcare Outcomes of Accidental Injury (HALO) study followed a cohort of serious accident casualties aged ≥ 16 years (assembled from six previous cohort studies conducted by the same research group). Health state utilities were estimated using the EQ-5D. This study reported that the average QALY loss was between 0.1 and 0.2 QALYs per year, resulting in an average loss of 1.7 QALYs (primarily because of loss of quality rather than length of life) over the following 10 years for those who survived to 6 months after injury compared with a general population, after adjusting for mortality in that general population. The study did not measure QALY loss by injury type or in children aged < 5 years. In the constituent cohorts there were 65 cases of injury victims aged < 16 years at the time of the accident but only those aged ≥ 16 years were included in the HALO follow-up cohort (HALO study final report 2009, J Nicholl, University of Sheffield, April 2010, personal communication).
In the absence of UK data measuring utility decrements associated with injury, data from other countries may be useful in estimating QALY losses. Phillips et al. 140 estimate that a bathwater scald in a young child results in a loss of 9.1 QALYs, based on a utility decrement of 0.13 ascertained from a Spanish study of burn injuries in children and adults,144 in which utilities were ascertained using the EQ-5D, multiplied by 70 additional expected life-years.
Two studies in the USA quantified QALY losses for other types of injuries (poisonings and falls). 125,145 The first of these studies did not use a validated measure of health state utilities. 125 Rather, diagnosis- and age-specific estimates of QALY losses combined physician ratings of the longitudinal impact of injuries on pain and functioning146,147 with diagnosis-specific data on the likelihood that the injury would permanently impact on the ability to work or earnings potential. 148 The physician rating scales were not specific to children, but raters were asked to rate the likelihood of impairment and duration thereof separately for children and adults. Survey data, weighting the relative importance placed by respondents on different dimensions of impact, were used to translate the estimated impairment impacts into QALYs; most of these weights were specific to children and adolescents. The utility decrements for a fall ranged from 0.1 to 0.13 and for poisoning ranged from 0.03 to 0.046. 125 The second study145 was of children aged 5–17 years following a TBI resulting from a fall and reported an average utility index, based on the Quality of Well-being Index,149,150 of 0.687 at 3 months and 0.675 at 6 months. HRQL varied widely in this study, with the utility index ranging from 0.093 to 1.0 at the 3- and 6-month interview points. 145 QALY losses have also been described by injury severity (in those aged < 20 years) in a US study for all types of childhood injuries (including poisoning and medically treated child neglect) and the values per injured case were 28.2 for fatal injury, 1.6 for an admitted case and 0.04 for a non-admitted case. 151 In this study, QALYs were computed on the basis of lives lost to fatal injuries and years of life spent in a disabled state, weighted by physician ratings of the functional loss arising from the severity of the disability; QALY losses in future years were discounted to present values at a 3% annual rate. Physician ratings were based on those routinely used by the US National Highway Traffic Safety Administration;146 the author acknowledges that these are not fully validated ratings and that they were > 20 years old at the time of writing (2006).
Methodological issues in the measurement of HRQL in children aged < 5 years are attributed to a shortage of appropriately validated instruments that are sensitive to rapid developmental stages,152 lack of health state utility classification instruments for under 5s and use of proxies in the assessment of a child’s health state. 153,154 However, proxy reporting is justified by the lack of cognitive and language comprehension skills necessary for self-completion in children aged < 5 years. 155 Parental perceptions of a child’s HRQL are also important as the principal determinant of utilisation of health-care services. 64
Studies evaluating parent–child agreement for HRQL measures found some disagreements across the domains measured, with parents of sick children tending to underestimate child HRQL and parents of healthy children tending to overestimate child HRQL. 155
The PedsQL109 has been found to be a reliable instrument for the measurement of HRQL in children, and is widely applicable in research, clinical practice and community populations. 64,109 The advantages of the PedsQL include its brevity, age-appropriate versions and parallel forms for child and parent reporting. The UK-English version has been developed and validated in children with chronic health conditions and in healthy children,156,157 and has been recommended for the assessment of HRQL in the UK.
The PedsQL has been administered in trauma injuries to under-fives158 and older children,111,158,159 including children treated for limb fractures, where it has demonstrated good responsiveness in detecting statistically significant changes in the condition of patients over time. 111,159,160 The instrument has also been used extensively for paediatric TBIs112,131,158,161,162 and spinal cord injuries. 163,164 The studies have shown a substantial long-term reduction in children’s HRQL after moderate to severe injury, particularly with regard to participation in activities, the ability to communicate and the ability to care for themselves. In addition, severe TBIs may add a considerable burden on carers and families, as reported in one study. 131
More recently, the PedsQL has been evaluated for measuring short-term outcomes for paediatric minor injuries in the ED setting, where it was found to be responsive to changes in health status over 1–2 weeks post injury. 165,166 One of the limitations of the PedsQL, however, is that it does not allow for estimation of health utilities, necessary for the estimation of QALYs. One recent study has demonstrated the feasibility of mapping the PedsQL core scales into EQ-5D utilities; however, to date this has been carried out only for older children (aged 11–15 years). 167
Methods relating to the health-related quality-of-life and costs substudies
The multicentre longitudinal study (study C) reported here was carried out in four centres (Nottingham, Bristol, Norwich and Newcastle) to:
-
validate the PedsQL in a range of medically attended injuries in preschool children (HRQL substudy)
-
measure the costs of injury to the NHS and families (costs substudy).
Participants (children aged < 5 years attending an ED or MIU or admitted to hospital in four centres in the UK) were recruited to the case–control study (study A) investigating the relationship between a range of safety behaviours, safety equipment use and exposure to home hazards and the occurrence of falls,52 poisonings53 and scalds,54 as described in work stream 1 (see Chapter 2).
Participants in study A were asked to express interest (either during face-to-face recruitment or by post following postal recruitment) in participating in one of three nested studies (study B – validation of the tools used to collect exposure data for study A; study C – measurement of the costs of injury and validation of the PedsQL; and study G – parents’ perceptions of barriers to, and facilitators of, injury prevention). Parents recruited face to face had the nested studies explained to them and, if they expressed an interest in study C, they were given the 2-week and the 1-month questionnaires to complete at home. If they were interested in study B or G they were given at least 24 hours to decide whether to participate before being contacted again by the research team. When participants were recruited by post, and if their study A questionnaire had been returned within 2 weeks of the injury date (and with an expression of interest in the nested studies), they were allocated to study C in preference to the other two nested studies (except for a short period of time when recruitment to study B became a priority because of the completion deadline or when participants were recruited to study G if they fulfilled the sampling frame criteria).
As noted above, participants agreeing to take part in study C were initially given or were posted both the 2-week and the 1-month questionnaires at the same time, with clear instructions on how and when to complete them, that is, it was explained that there was no need to complete the 1-month questionnaire (and subsequent follow-up questionnaires) if their child had recovered by the previous time point measured. However, the strategy of posting the two questionnaires together was dropped as it became apparent that the majority of cases were minor injuries who had recovered by 2 weeks and therefore the 1-month and subsequent follow-up questionnaires were posted only to those who did not recover at previous time points.
Recruitment continued until approximately 400 cases had been recruited, stratified into five strata by injury mechanism (i.e. stair falls, falls on one level, falls from furniture, poisonings and scalds). HRQL data were also collected for study A community controls at baseline.
The questionnaires, which collected data on resource use, costs and HRQL, were self-completed by parents, either while in the ED/MIU or hospital ward or (more usually) on their return home, and were returned in person or by post to the research team.
Follow-up questionnaires (see Appendix 2, Follow-up questionnaires) were administered by post at up to four time points post injury (2 weeks and 1, 3 and 12 months), with the number of administrations depending on whether or not the child had recovered at the time of completion of the most recent questionnaire (Figure 8). We anticipated that most injuries would be relatively minor, with potentially short-lived impacts on children’s HRQL. The PedsQL has previously been shown to be responsive to changes in health status over 1–2 weeks post injury in children attending an ED following a minor injury. 165,166 For this reason, the first administration of the PedsQL in study C was at 2 weeks post injury. A maximum of three reminders were sent at each time point to non-respondents. This included an initial postal reminder containing the questionnaire followed by a telephone reminder and, if there was still no response, a mini-questionnaire (see Appendix 2, Mini questionnaire) was sent asking whether or not the child had fully recovered from their injury to ensure that no further follow-up questionnaires were sent. All follow-up questionnaires asked for the date of completion so that time since injury could be calculated. Participants were sent a £5 gift voucher for use in local stores for each completed questionnaire returned.
FIGURE 8.
Recruitment and questionnaire administration flow chart. a, Includes eight cases subsequently found not to be eligible for the case–control study (costs study, n = 7; other nested study, n = 1); b, includes nine invitations sent to cases subsequently found to be not eligible for study C and who did not return the 2-week questionnaire.
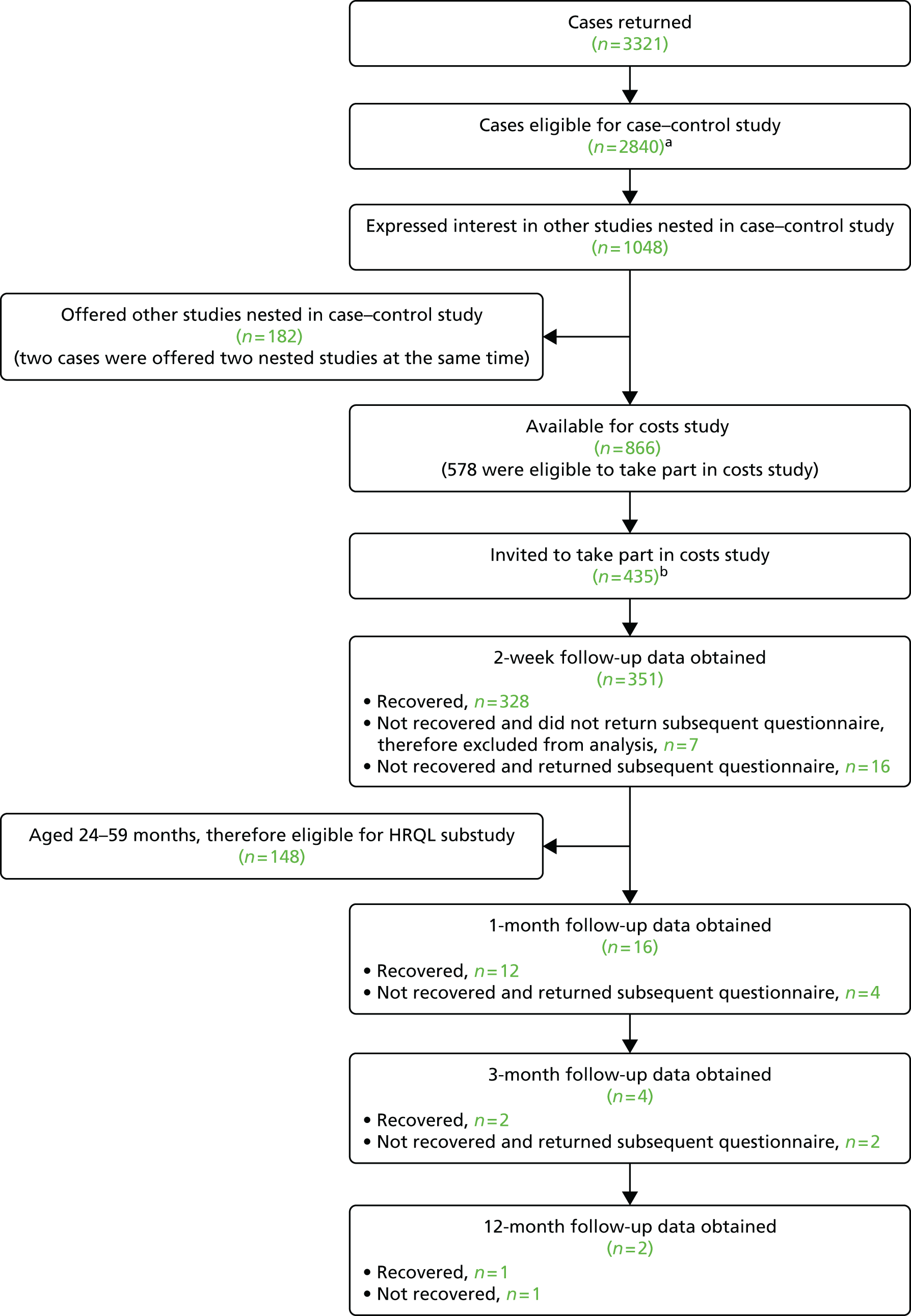
Ethics approval
Ethics approval was obtained from Nottingham Research Ethics Committee 1 (reference number 09/H0407/14).
Validation of the Pediatric Quality of Life Inventory (health-related quality-of-life substudy)
Methods
Describing the Pediatric Quality of Life Inventory
The PedsQL measurement model64,110 consists of generic core scales and disease-specific modules (not used in this study). The PedsQL 4.0 generic core scales in the parent proxy report version for toddlers (aged 2–4 years) include 21 items tapping four dimensions: physical functioning (eight items), emotional functioning (five items), social functioning (five items) and nursery/school functioning (three items).
Each item has a 5-point response scale (0 = never a problem; 1 = almost never a problem; 2 = sometimes a problem; 3 = often a problem; 4 = almost always a problem). In analysis, items are reverse scored and linearly transformed to a 0–100 scale (0 = 100, 1 = 75, 2 = 50, 3 = 25, 4 = 0). Scale scores are computed as the sum of the items answered divided by the number of items answered in that scale (to account for missing data), with higher scores denoting better HRQL. If > 50% of items in a given scale are missing, the scale score is not computed and is treated as missing. 64
Summary scores for physical health (eight items) and psychosocial health (13 items) and a total HRQL score (21 items) can be computed. The physical health summary score is equal to the physical functioning scale score. The psychosocial health summary score is calculated as the sum of the items in the emotional, social and nursery/school functioning scales divided by the number of items answered across these three scales. Similarly, the total HRQL score is computed as the sum of the items across all four scales divided by the total number of items answered. 64
The standard PedsQL generic core scales have a reference period of the past month and the acute version has a reference period of the past week. Following personal correspondence with the instrument’s developer (J Varni, Texas A&M University, 11 October 2007), we adapted the instrument to have a reference period of the past 2 weeks. This period was chosen because we considered that most children’s injuries would be relatively minor and, although many might resolve within 1 week post injury, a 1-week reference period might be too short to capture changes in HRQL, particularly for sprains, fractures and scalds. Although guidelines for measuring HRQL post injury168 recommend carrying out the first data collection post injury at 1 month, this is based primarily on studies of injured adults. There are few studies reporting HRQL in populations of children with a range of injuries. 8,169 Most children attending an ED or a MIU will have been previously healthy and will have suffered a minor injury, and hence impacts on HRQL may be short-lived. As participants for study C were recruited from among those already participating in study A, we considered the time taken to recruit participants would prevent measurement of HRQL at 1 week post injury. We therefore chose a 2-week reference period.
Administration of PedsQL validation questions
The general data collection methods used are described above. However, it should be noted that, at baseline and the follow-up time points, PedsQL items were asked only of parents of children aged ≥ 24 months; we refer to this subset of participants as the study C HRQL sample. This was necessary because the infant version of the PedsQL instrument170 was not available when the study was initiated. Although all children were aged ≤ 59 months at the time of the injury, four were aged 60 months by the time of questionnaire completion, but these were retained in the analyses reported in this chapter. The reference period for the PedsQL items at baseline was the 2 weeks prior to the injury that had led to attendance at the ED/MIU or admission to hospital for cases and the 2 weeks prior to questionnaire completion for community controls. In addition to the PedsQL, participants completed the baseline questionnaire for study A, which contained a 10-cm VAS of general health171 and a question about long-term health conditions.
Analysis
Only the 2-week follow-up data are reported here because of the very small number of children for whom responses at the later time points were requested and received (see Figure 8).
Analysis reflected that reported in previous papers on the reliability, validity and responsiveness to change of the PedsQL in general populations64,157 and in the ED setting. 166,172 Analysis was conducted using Mplus (version 6; Muthén & Muthén, Los Angeles, CA, USA).
Demographic and injury characteristic variables for participants and non-participants (i.e. study A participants eligible for but not agreeing to participate in the study C HRQL substudy) in the study C HRQL sample were compared using chi-squared tests and independent sample t-tests.
Item-level analysis
Item-level analysis was carried out separately on pre-injury data for all study A ‘cases’ aged ≥ 24 months (i.e. children attending an ED or a MIU or admitted to hospital with an injury; these results are reported in Tables 33–39 as the largest and therefore most robust sample) and in respect of pre- and post-injury data for the participants in the study C HRQL sample.
Following Varni et al. ,64 the rates of missing data per item and the distribution across the five response categories were examined as indicators of the feasibility and acceptability of the measure. Item means, item SDs and item–scale correlations, corrected for overlap, were calculated: item–scale correlations of ≥ 0.40 were considered adequate. 173 Item scaling success was calculated for each item, defined as the number of times that an item correlated higher, by ≥ 2 standard errors (SEs), with its hypothesised scale (with correction for overlap) than it did with each of the other three scales. 174 We then calculated the percentage of item scaling successes (relative to the total number of comparisons) for each scale.
Scale-level analysis
Analyses of missing scale scores, floor and ceiling effects, internal consistency and interscale correlations were carried out separately for pre-injury data for all study A ‘cases’ aged ≥ 24 months (these results are reported in Tables 33–39 as the largest and therefore most robust sample) and in respect of pre- and post-injury data for the participants in the study C HRQL sample. Confirmatory factor analysis was conducted solely on the study A ‘case’ pre-injury data as the number of participants in the study C HRQL sample was too small. Analyses addressing known-groups validity were conducted on the study A ‘cases’ in respect of groups defined by the presence of a long-term health condition and on the study C HRQL sample for groups defined by the nature and severity of the injury; analysis of responsiveness to change was confined to the study C HRQL sample.
Scale distributions
Also following Varni et al. ,64 we examined ceiling and floor effects [i.e. the percentage of responses with the maximum possible (100) and minimum possible (0) scores] for each scale and summary score and the percentage of children for whom a scale or summary score could not be computed (because > 50% of the constituent items were missing). Marked floor effects, particularly at baseline, would mean that deterioration in HRQL could not be detected, whereas marked ceiling effects would mean that there was no scope to detect improvement in HRQL.
Scale and summary mean scores were compared, using independent sample t-tests, with those from a previous study validating the PedsQL in a sample of healthy toddlers in the UK. 157 Scale and summary mean scores at baseline for study A ‘cases’ were also compared, using independent sample t-tests, with the corresponding mean scores for the age- and sex-matched community controls in study A who had not attended an ED or a MIU or been admitted to hospital on the date of the case injury.
Internal consistency reliability
Scale internal consistency reliability was examined through Cronbach’s alpha coefficient;175 alpha values of ≥ 0.70 are considered adequate for comparisons of patient groups with a higher criterion (α = 0.90) for analysis of individual patient scores. 173
Construct validity
Correlations between scale scores and with parents’ rating of their child’s overall health on a 10-cm VAS were examined as part of our analysis of construct validity. Following Varni et al. ,64 medium to large (≥ 0.40) correlations176 between the PedsQL scale scores were expected, given that the instrument was developed to measure the integrated multidimensional construct of paediatric HRQL and shared method variance.
Construct validity was examined through confirmatory factor analysis. In exploratory factor analysis, using principal components analysis with oblique rotation, Varni et al. 64 have previously identified a five-factor model; school functioning split into two factors but the other three factors that emerged were largely consistent with the a priori hypothesised structure (i.e. the other items loaded onto factors broadly corresponding to their hypothesised scales of physical functioning, emotional functioning and social functioning). Subsequent publications by the PedsQL development team confirmed an equivalent five-factor structure: across age subgroups (5–16 years);177,178 with respect to socioeconomic status;179 between healthy children and those with a chronic health condition;180 across race/ethnicity groups;181 over a period of 1 year;182 and across different modes of administration. 183 However, all of these studies were conducted in children aged ≥ 5 years. In personal communication with the research team, the instrument’s developer (J Varni, 12 November 2013) recommended testing a four-factor solution (physical functioning, emotional functioning, social functioning and nursery/school functioning) as there are only three items measuring nursery/school functioning in the PedsQL toddler version. We therefore tested a first-order four-factor model (in which each of the factors was correlated with each other) and an alternative second-order model in which three of the first-order factors (emotional functioning, social functioning and nursery/school functioning) were assumed to load onto a second-order factor (psychological health), which was in turn assumed to correlate with the physical function factor (Table 32). Model adequacy in our confirmatory factor analysis was initially tested by the chi-square test; criterion values of p ≥ 0.05 were considered indicative of acceptable fit. 184 However, the chi-square statistic is dependent on the sample size. 185 If the sample size is too small, one is more likely to find that an ‘inappropriate model’ fits the data; conversely, if the sample size is too large an appropriate model may well be rejected on the basis of a highly significant p-value. 186 We therefore also examined other goodness-of-fit statistics: the Tucker–Lewis Index (TLI), the comparative fit index (CFI), the standardised root-mean-square residual (SRMR) and the root-mean-square error of approximation (RMSEA). Values of TLI and CFI of > 0.90 and > 0.95, respectively, are considered indicative of good and excellent fit; for SRMR and RMSEA, values of ≤ 0.08 are desirable. 187 In addition, the Akaike and Bayesian information criteria (AIC and BIC) were used to assess the relative quality of alternative models.
| Item | Label | First order | Second order | |
|---|---|---|---|---|
| 1 | Walking score | PF1 | PF | PHa |
| 2 | Running score | PF2 | ||
| 3 | Active play/exercise score | PF3 | ||
| 4 | Lifting score | PF4 | ||
| 5 | Bathing score | PF5 | ||
| 6 | Picking up toys score | PF6 | ||
| 7 | Having hurts/aches score | PF7 | ||
| 8 | Energy level score | PF8 | ||
| 9 | Feeling afraid score | EF1 | EF | P-SH |
| 10 | Feeling sad score | EF2 | ||
| 11 | Feeling angry score | EF3 | ||
| 12 | Sleeping score | EF4 | ||
| 13 | Worrying score | EF5 | ||
| 14 | Playing with other children score | SF1 | SF | |
| 15 | Other kids wanting to play score | SF2 | ||
| 16 | Being teased score | SF3 | ||
| 17 | Ability to do the same as peers (social) score | SF4 | ||
| 18 | Keeping up with other children at play score | SF5 | ||
| 19 | Ability to do the same as peers (school/nursery) score | SC1 | SC | |
| 20 | Miss nursery/school – unwell | SC2 | ||
| 21 | Miss nursery/school – doctor’s appointment | SC3 | ||
Construct validity was further analysed through known-groups validity. For study A ‘cases’, pre-injury HRQL scores for children with and without a long-term health condition were compared using an independent sample t-test; previous studies (e.g. Varni et al. 188) have shown poorer HRQL in children with a chronic health problem than in healthy peers. More detailed known-groups analysis was carried out on data for the study C HRQL sample. We hypothesised that there would be no differences in baseline (i.e. pre-injury) PedsQL scores for any of the comparator groups described below, but that lower PedsQL scores (indicative of poorer HRQL) post injury, particularly in respect of physical functioning, would be observed in:
-
children whose parents reported that they were not fully recovered from the injury compared with those reported to be fully recovered
-
children treated for their injury in an ED/a MIU compared with those who were just examined
-
children who underwent radiography compared with those who did not undergo radiography
-
children admitted for observation or to a hospital ward compared with those who were discharged following examination
-
children who received medication for their injury compared with those who did not receive medication.
We further hypothesised a positive dose–response relationship for:
-
Children who had two or more procedures carried out compared with those who had one procedure only compared with those who had no procedures. [Procedures (and number of children undergoing each; total n = 148) consisted of blood test (n = 12), urine test (n = 2), radiography (n = 33), ultrasound, magnetic resonance imaging or computerised tomography scan (n = 1), medicine given by mouth (n = 54), medicine given by injection (n = 3), medicine applied to skin (n = 11), medicine provided to take home (n = 6), dressing applied to wound or burn (n = 11), stitches (n = 5), wound closure strips or wound glue (n = 28), bandage, sling or support (n = 15), splint (n = 0), manipulation of fracture or broken bone (n = 2), manipulation of dislocated joint (n = 1), operation to fix broken or fractured bone (n = 1), cast applied to broken or fractured bone (n = 8), physiotherapy (n = 0), stomach washout (n = 0), general anaesthetic (n = 4), local anaesthetic (n = 1), tetanus injection (n = 0), drip (n = 2), blood transfusion (n = 0), chest drain (n = 0), oxygen (n = 1), ventilation tube (n = 0), resuscitation (n = 0).]
-
Children who sustained a broken bone compared with those who sustained a cut needing stitches compared with those who sustained a cut or graze not needing stitches.
Previous studies143,166 have shown poorer quality of life among children with more severe injuries; we did not include a formal assessment of injury severity but comparisons (b)–(g) were designed as proxy measures of injury severity. Known-groups validity was examined through independent sample t-tests for comparisons (a)–(e) and through one-way analysis of variance (ANOVA), with post hoc Bonferroni tests for pairwise contrasts, for comparisons (f) and (g).
Responsiveness to change
Responsiveness to change was also examined following Stevens et al. 166 We examined change in PedsQL scores from baseline (i.e. pre injury) to follow-up in respect of the groups defined in (a)–(g). Separate paired-sample t-tests were carried out for each of the subgroups as defined, and for each comparison we then computed the effect size as the mean change from baseline divided by the SD of the score in that group at baseline. We hypothesised that the differences, particularly in respect of physical functioning, would be positive (i.e. indicating a reduction in HRQL from pre injury to post injury) in those who had not fully recovered, who had been treated for their injury, who had undergone radiography, who were admitted for observation or to a hospital ward, who had received medication or who had one or more procedures, and that effect sizes would be larger in magnitude than for their respective comparators, as described in the previous section.
In previous PedsQL studies, a minimally important difference (MID) of 4.5 points for the PedsQL total score for parent proxy report has been proposed,188 calculated as the sample’s standard error of measurement [SEM; defined as the product of the (baseline) SD and the square root of 1 minus Cronbach’s alpha]; MIDs for scale scores ranged from 6.92 for physical health to 9.67 for nursery/school health, with a MID of 5.49 for psychosocial summary. However, it has also been recommended by HRQL researchers189 that several estimates of the MID should be calculated and used to determine a range for the MID. Following Stevens et al. 166 we therefore estimated the MID in two ways: as the SEM and as half the baseline SD. 189–191
Results
Study participants
Completed study A questionnaires were received from 1334 parents of children aged ≥ 24 months, with completion dates ranging from 18 June 2010 to 28 February 2013. A total of 351 parents also returned a study C 2-week post-injury questionnaire but only 148 (42%) of these were for children aged 24–59 months and therefore eligible for the study C HRQL substudy. Of these 148, 134 (91%) answered one or more items on the PedsQL at both baseline and follow-up, 10 did not complete any items on the PedsQL at baseline (in five cases because the child was aged < 24 months at the time of completion of the baseline questionnaire) and six did not complete any items on the PedsQL at follow-up (two of whom had also left the PedsQL items blank at baseline). In this sample, dates of completion of the baseline and follow-up questionnaires ranged from 18 August 2010 to 23 January 2013 and from 29 August 2010 to 26 January 2013, respectively.
The time from injury to completion of the baseline questionnaire for the full study A sample ranged from 0 to 243 days, with a median of 11 days (IQR 6–21 days); 89.4% of questionnaires were completed within 28 days of the injury. In the study C HRQL sample, the time from injury to completion of the baseline questionnaire ranged from 0 to 79 days, with a median of 6 days (IQR 5–9 days). The time from injury to completion of the 2 week follow-up questionnaire ranged from 9 to 87 days, with a median of 22 days (IQR 17–30 days); only 7.4% responded within 14 days of the injury. The interval between completion of the baseline questionnaire and completion of the follow-up questionnaire ranged from 2 to 77 days, with a median of 13 days (IQR 9–22 days).
Demographic and injury mechanism variables for the full baseline study A sample and for those who did and did not participate in the study C HRQL substudy are shown in Tables 33 and 34.
| Characteristic | Study A cases (N = 1334), n (%) | Study C HRQL substudy participants (N = 148), n (%) | Study C HRQL substudy non-participants (N = 1186), n (%) |
|---|---|---|---|
| Male | 712 (53.4) | 75 (51.4) | 636 (53.6) |
| Ethnic origin: white | 1178 (90.1) | 136 (93.8) | 1042 (89.7) |
| Child has long-term condition | 180 (13.7) | 18 (12.6) | 162 (13.9) |
| First child | 458 (38.6) | 52 (35.5) | 406 (38.7) |
| Single parent household | 222 (17.1) | 29 (20.0) | 193 (16.7) |
| Household does not own accommodation | 539 (41.3) | 55 (37.9) | 484 (41.8) |
| Household does not own car | 180 (13.8) | 24 (13.3) | 156 (13.4) |
| Household receives social welfare benefits | 570 (44.2) | 70 (48.6) | 500 (43.6) |
| Mother < 20 years old at first birth | 179 (15.0) | 23 (16.5) | 156 (14.8) |
| Overcrowded accommodation | 115 (9.2) | 12 (8.6) | 103 (9.2) |
| Study centre | |||
| Nottingham | 507 (38.0) | 45 (30.4) | 462 (39.0) |
| Bristol | 385 (28.9) | 42 (28.4) | 343 (28.9) |
| Norwich | 279 (20.9) | 52 (35.1) | 227 (19.1) |
| Newcastle | 163 (12.2) | 9 (6.1) | 154 (13.0) |
| Age (months), mean (SD) | 36.88 (9.54) | 35.74 (9.16) | 37.03 (9.58) |
| IMD score, mean (SD) | 22.27 (16.23) | 19.27 (14.74) | 22.65 (16.37) |
| Injury details | Study A cases (N = 1334), n (%) | Study C HRQL substudy participants (N = 148), n (%) | Study C HRQL substudy non-participants (N = 1186), n (%) |
|---|---|---|---|
| Injury mechanism | |||
| Fall down stairs or steps | 307 (23.0) | 31 (20.9) | 276 (23.3) |
| Fall on one level | 313 (23.5) | 39 (26.4) | 274 (23.1) |
| Fall from furniture | 303 (22.7) | 39 (26.4) | 264 (22.3) |
| Poisoning | 331 (24.8) | 34 (23.0) | 297 (25.0) |
| Scald | 80 (6.0) | 5 (3.4) | 75 (6.3) |
| Total number of injuries sustained | |||
| One | 1142 (86.6) | 122 (83.0) | 1020 (87.1) |
| Two | 174 (13.2) | 25 (17.0) | 149 (12.7) |
| Three | 2 (0.2) | 0 (0.0) | 2 (0.2) |
| Nature of injury | |||
| Lost consciousness | 20 (1.5) | 4 (2.7) | 16 (1.3) |
| Bang on head | 437 (32.8) | 56 (37.8) | 381 (32.1) |
| Broken bone | 147 (11.0) | 15 (10.1) | 132 (11.1) |
| Cut needing stitches | 121 (9.1) | 13 (8.8) | 108 (9.1) |
| Cut or graze not needing stitches | 222 (16.6) | 21 (14.2) | 201 (16.9) |
| Other injury | 193 (14.5) | 20 (20.3) | 163 (13.7) |
The only statistically significant differences between participants and non-participants were in respect of study centre, IMD score and injury type. Of the four centres in which the study was taking place, children from the Norwich centre were over-represented and those from the Nottingham and Newcastle centres were under-represented among participants in the study C HRQL sample. Participants in the study C HRQL substudy had, on average, lower IMD scores than non-participants, denoting residence in less deprived areas. Finally, those who had sustained ‘other’ injuries were somewhat over-represented among participants in the study C HRQL substudy.
Item-level analyses
Item-level missing data, distribution of responses across the five response categories, means and SDs are shown in Table 35.
| Question | Missing data (%) | 0 | 25 | 50 | 75 | 100 | Mean | SD | |
|---|---|---|---|---|---|---|---|---|---|
| Physical | |||||||||
| 1 | Walking | 2.7 | 1.6 | 0.4 | 1.5 | 3.6 | 90.1 | 96.26 | 15.60 |
| 2 | Running | 2.6 | 2.2 | 0.7 | 3.3 | 5.0 | 86.1 | 94.21 | 18.71 |
| 3 | Active play | 2.8 | 1.5 | 0.7 | 2.0 | 5.5 | 87.6 | 95.49 | 16.13 |
| 4 | Lifting | 3.4 | 1.3 | 2.0 | 9.8 | 14.0 | 69.3 | 88.32 | 21.60 |
| 5 | Bathing | 2.8 | 1.0 | 0.7 | 2.2 | 4.9 | 88.2 | 95.91 | 14.99 |
| 6 | Picking up toys | 2.6 | 1.9 | 1.9 | 5.5 | 7.6 | 80.4 | 91.78 | 20.71 |
| 7 | Having hurts/aches | 3.1 | 0.3 | 1.9 | 10.8 | 16.9 | 66.9 | 88.25 | 19.85 |
| 8 | Energy level | 2.9 | 0.3 | 1.0 | 5.6 | 12.9 | 77.3 | 82.72 | 16.20 |
| Emotional | |||||||||
| 9 | Feeling afraid | 3.1 | 0.3 | 1.3 | 19.7 | 29.4 | 46.2 | 80.90 | 21.03 |
| 10 | Feeling sad | 2.8 | 0.0 | 0.5 | 12.1 | 26.8 | 57.6 | 86.44 | 18.21 |
| 11 | Feeling angry | 2.9 | 0.2 | 4.0 | 28.4 | 26.2 | 38.3 | 75.33 | 23.35 |
| 12 | Sleeping | 2.8 | 2.2 | 5.1 | 16.9 | 22.9 | 50.1 | 79.26 | 25.89 |
| 13 | Worrying | 3.2 | 0.2 | 0.9 | 6.7 | 18.3 | 70.6 | 90.86 | 16.87 |
| Social | |||||||||
| 14 | Playing with other kids | 2.6 | 1.4 | 1.9 | 7.2 | 18.0 | 68.8 | 88.72 | 20.79 |
| 15 | Other kids wanting to play | 2.7 | 0.2 | 0.4 | 5.1 | 18.3 | 73.3 | 92.16 | 15.23 |
| 16 | Being teased | 3.1 | 0.1 | 0.2 | 2.4 | 10.3 | 84.0 | 95.86 | 11.48 |
| 17 | Do same as peers | 2.8 | 1.3 | 1.3 | 4.6 | 10.4 | 79.5 | 92.59 | 18.51 |
| 18 | Keep up at play | 3.0 | 2.5 | 1.1 | 4.0 | 9.1 | 80.4 | 92.19 | 20.51 |
| Nursery/school | |||||||||
| 19 | Ability to do the same as peers (school/nursery) | 35.8 | 2.7 | 1.6 | 2.5 | 4.6 | 52.7 | 90.16 | 24.63 |
| 20 | Miss nursery/school – unwell | 35.3 | 0.1 | 0.4 | 7.7 | 17.5 | 39.0 | 86.65 | 18.44 |
| 21 | Miss nursery/school – doctor’s appointment | 35.2 | 0.0 | 0.6 | 4.7 | 12.0 | 47.5 | 91.03 | 16.43 |
Across all 1334 respondents, a total of 2116 PedsQL items were missing out of the 28,014 items (1334 × 21) administered, an item missing rate of 7.6%. At the level of individual items, rates of missing data were generally low (ranging from 2.6% to 3.4%) for items in the physical, emotional and social scales; however, higher rates (35.2–35.8%) were observed for the three items in the nursery/school scale, reflecting the fact that many of these children did not attend nursery and hence these questions were not applicable. Adjusting for non-attendance at nursery or school, rates of missing data for the three nursery/school items ranged from 3.8% (item 21) to 4.4% (item 19).
For all but two items (items 10 and 21), the entire response range of 0–100 was used. Item mean scores ranged from 75.33 to 96.26, with SDs ranging from 11.48 to 25.89. For 17 out of the 21 items (81%), item means were within a 10-point range of each other.
Item–own scale correlations (corrected for overlap) exceeded the criterion value of 0.4 for all but three items (items 8, 19 and 20). Item scaling success rates [defined as the number of times that an item correlated higher, by ≥ 2 SEs, with its hypothesised scale (with correction for overlap) than it did with each of the other three scales] were 22 out of 24 (92%), 15 out of 15 (100%), 15 out of 15 (100%) and 6 out of 9 (67%) for the physical functioning, emotional functioning, social functioning and nursery functioning scales, respectively, an overall item scaling success rate of 58 out of 63 (92%).
Similar patterns of item response were observed for baseline (pre-injury) and follow-up (post-injury) PedsQL responses in the study C HRQL sample (data not shown but available on request). As expected, in this sample, ceiling effects were less marked and item mean scores were lower post injury, indicative of poorer HRQL at this time.
Scale-level analyses
Scale distributions
Scale and summary scores could be computed for > 97% of participants for all but the nursery/school subscale, reflecting the patterns of item non-response reported in the previous section. Adjusting for those who did attend nursery, nursery/school scale scores were missing for 3.7% of children.
Floor effects were negligible but ceiling effects for the four scales ranged from 26.8% (emotional functioning) to 57.4% (social functioning). Ceiling effects were less marked for the psychosocial summary and total PedsQL scores (Table 36).
| Scale | Missing data (%) | Floor effects (%) | Ceiling effects (%) | Min. | Max. | Mean | SD | Cronbach’s α |
|---|---|---|---|---|---|---|---|---|
| Physical functioning | 2.7 | 0.0 | 50.3 | 9.38 | 100 | 92.87 | 12.78 | 0.852 |
| Emotional functioning | 2.7 | 0.0 | 26.8 | 5 | 100 | 82.53 | 15.83 | 0.794 |
| Social functioning | 2.6 | 0.1 | 57.4 | 0 | 100 | 92.24 | 13.13 | 0.780 |
| Nursery/school functioning | 35.2 | 0.0 | 50.3 | 25 | 100 | 89.33 | 14.65 | 0.537 |
| Psychosocial summary score | 2.7 | 0.0 | 18.4 | 12.5 | 100 | 87.77 | 11.81 | 0.839 |
| Total PedsQL score | 2.6 | 0.0 | 16.2 | 23.61 | 100 | 89.8 | 10.88 | 0.889 |
For two out of the four scale scores, the psychosocial summary score and the total PedsQL score, the reported mean pre-injury scores were statistically significantly higher (Table 37) than for a previously reported sample of healthy UK toddlers,157 but none of these mean differences exceeded the previously established MIDs for the corresponding scales. 188 For the nursery/school functioning scale, the reported mean pre-injury scores were statistically significantly lower than the previously reported values for healthy UK toddlers, but the observed difference was less than the previously established MID.
| Scale | Study A cases | Buck157 | Mean difference | 95% CI for difference | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |||
| Physical functioning | 1298 | 92.87 | 12.78 | 256 | 92.60 | 9.10 | 0.27 | –1.37 to 1.91 |
| Emotional functioning | 1298 | 82.53 | 15.83 | 255 | 76.00 | 14.60 | 6.53 | 4.43 to 8.63 |
| Social functioning | 1299 | 92.24 | 13.13 | 256 | 89.90 | 12.10 | 2.34 | 0.60 to 4.08 |
| Nursery/school functioning | 865 | 89.33 | 14.65 | 189 | 92.30 | 11.60 | –2.97 | –5.20 to –0.74 |
| Psychosocial summary score | 1298 | 87.77 | 11.81 | 256 | 84.60 | 10.50 | 3.17 | 1.61 to 4.73 |
| Total PedsQL score | 1299 | 89.80 | 10.88 | 256 | 87.80 | 8.70 | 2.00 | 0.58 to 3.42 |
For the physical, social and emotional functioning scale scores, the psychosocial summary score and the total PedsQL score, the reported mean pre-injury scores were also statistically significantly higher than the corresponding reported mean scores for the preceding 2 weeks for age- and sex-matched community controls from study A (data not shown but available on request). A statistically significant difference for the nursery/school scale was also observed, with lower scores for injured children than for controls. Mean differences (controls – cases) were, for the most part, small (ranging from 1.18 for the nursery/school scale to –6.21 for the emotional functioning scale), with only one exceeding the MID of 4.5. Mean scores for community controls, with the exception of physical functioning, were not statistically significantly different from those reported by Buck157 for a healthy toddler sample in the UK.
The reported pre-injury physical functioning and total PedsQL scores in cases in this study were also statistically significantly higher than the retrospectively reported pre-injury scores reported by Stevens et al. 166 in a US sample, but the differences were small in magnitude (2.87 for physical functioning and 1.80 for total PedsQL scores).
Internal consistency reliability
Internal consistency reliability was generally adequate, with Cronbach’s alpha coefficients in excess of the criterion of 0.70 for group comparisons for all but the nursery/school functioning scale and Cronbach’s alpha coefficients for total PedsQL scores almost reaching the higher criterion of 0.9 for individual-level data comparisons.
Construct validity
Interscale correlations of PedsQL scores ranged from 0.27 (emotional functioning with nursery functioning) to 0.62 (physical functioning with social functioning), with three out of six correlation coefficients exceeding the threshold for ‘moderate’ of 0.4. Correlations with the 10-cm VAS for parents’ rating of their child’s health in the 24 hours prior to the injury were low, ranging from 0.12 for social functioning to 0.25 for the psychosocial summary and total PedsQL scores.
Goodness-of-fit statistics from the confirmatory factor analysis for the first- and second-order models are shown in Table 38. Neither model suggests a good fit; p-values for the chi-square statistic are not ≥ 0.05, TLI and CFI statistics fall short of the criterion values of 0.90 and 0.95, respectively, whereas SRMR and RMSEA values exceed the threshold of 0.08. For the four-factor solution, items 7 and 8 have fairly low loadings onto the first factor (physical functioning). The highest correlations between factors are between physical functioning and social functioning (r = 0.65), physical functioning and nursery/school functioning (r = 0.72) and social functioning and nursery/school functioning (r = 0.91). These observations are consistent with patterns of observed inter-item correlations (data not shown but available on request), which show that items 7 (hurt or ache) and 8 (low energy) do not appear to be strongly correlated with the other physical functioning items and that item 19 [ability to do the same as peers (school/nursery)] does not correlate strongly with the other two nursery/school functioning items but does correlate moderately strongly with a number of social functioning items. Given the high correlation between physical functioning and the other three first-order factors, it is not surprising that the second-order factor structure (two-factor model) is not supported.
| Statistic | First-order model | Second-order model |
|---|---|---|
| Chi-square (df), p-value | 2477 (183), < 0.0001 | 2508 (185), < 0.0001 |
| TLI | 0.775 | 0.774 |
| CFI | 0.804 | 0.801 |
| SRMR | 0.084 | 0.083 |
| RMSEA | 0.098 | 0.098 |
| AIC | 214,540.127 | 214,567.001 |
| BIC | 214,896.706 | 214,913.244 |
In the known-groups validity analyses, as hypothesised in the full study A baseline sample, children with a long-term health condition had poorer pre-injury PedsQL scores than those without such a condition; observed differences for all but emotional functioning exceeded the corresponding established MIDs188 (Table 39).
| Scale | Child does not have long-term condition | Child has long-term condition | Mean difference (95% CI) | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |||
| Physical functioning | 1107 | 93.98 | 11.10 | 175 | 86.34 | 18.72 | 7.64a (5.66 to 9.62) | < 0.001 |
| Emotional functioning | 1107 | 83.26 | 15.24 | 175 | 78.17 | 18.69 | 5.09 (2.58 to 7.61) | < 0.001 |
| Social functioning | 1108 | 93.71 | 10.76 | 174 | 83.84 | 20.38 | 9.87a (7.87 to 11.87) | < 0.001 |
| Nursery/school functioning | 717 | 91.20 | 12.71 | 138 | 79.53 | 19.21 | 11.67a (9.12 to 14.21) | < 0.001 |
| Psychosocial summary score | 1108 | 88.96 | 10.48 | 174 | 80.68 | 16.33 | 8.28a (6.44 to 10.10) | < 0.001 |
| Total PedsQL score | 1108 | 90.99 | 9.29 | 175 | 82.79 | 16.00 | 8.20a (6.53 to 9.87) | < 0.001 |
Among the study C HRQL sample, the majority of our known-groups validity hypotheses were borne out (Tables 40 and 41). There were no significant differences in pre-injury scores for any of the comparator groups (a)–(g), as defined previously. Post-injury physical functioning scores were statistically significantly lower (indicative of poorer HRQL) relative to their respective comparators in:
-
children who were reported as not being fully recovered
-
children who were treated for their injury
-
children who had undergone radiography
-
children who received medication following their injury.
| Scale | (a) Child fully recovered (n = 124, 88%) (n = 81 for nursery) | (a) Child not fully recovered (n = 17, 12%) (n = 11 for nursery) | Difference (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Physical functioning | 89.46 | 15.92 | 66.54 | 24.92 | 22.92a (14.12 to 31.71) | < 0.001 |
| Emotional functioning | 86.41 | 15.30 | 78.53 | 12.34 | 7.88a (0.21 to 15.56) | 0.044 |
| Social functioning | 95.11 | 9.53 | 92.50 | 14.02 | 2.61 (–2.70 to 7.92) | 0.333 |
| Nursery/school functioning | 92.70 | 13.65 | 78.79 | 25.38 | 13.91a (4.07 to 23.74) | 0.006 |
| Psychosocial summary score | 90.99 | 10.37 | 85.43 | 12.60 | 5.56a (–0.03 to 11.14) | 0.051 |
| Total PedsQL score | 90.33 | 11.44 | 76.99 | 15.00 | 13.34a (1.71 to 13.94) | < 0.001 |
| (b) Examined only (n = 74, 52%) (n = 48 for nursery) | (b) Treated (n = 67, 48%) (n = 44 for nursery) | |||||
| Physical functioning | 90.41 | 16.36 | 82.59 | 20.33 | 7.82a (1.71 to 13.94) | 0.013 |
| Emotional functioning | 85.27 | 16.57 | 85.67 | 13.57 | –0.40 (–5.48 to 4.67) | 0.876 |
| Social functioning | 93.84 | 11.98 | 95.87 | 7.54 | –2.04 (–5.42 to 1.34) | 0.234 |
| Nursery/school functioning | 93.06 | 15.97 | 88.83 | 15.87 | 4.23 (–2.37 to 10.83) | 0.206 |
| Psychosocial summary score | 90.25 | 12.402 | 90.47 | 8.69 | –0.23 (–3.83 to 3.38) | 0.901 |
| Total PedsQL score | 90.16 | 13.09 | 87.13 | 12.01 | 3.02 (–1.18 to 7.22) | 0.157 |
| (c) Child underwent radiography (n = 96, 74%) (n = 62 for nursery) | (c) Child did not undergo radiography (n = 33, 26%) (n = 22 for nursery) | |||||
| Physical functioning | 92.19 | 12.81 | 68.94 | 23.86 | 23.26a (16.87 to 29.64) | < 0.001 |
| Emotional functioning | 86.41 | 15.57 | 81.52 | 13.89 | 4.90 (–1.11 to 10.90) | 0.110 |
| Social functioning | 96.36 | 8.21 | 86.70 | 13.92 | 9.66a (2.75 to 10.58) | 0.001 |
| Nursery/school functioning | 93.48 | 13.01 | 82.95 | 21.59 | 10.53a (3.00 to 18.05) | 0.007 |
| Psychosocial summary score | 91.74 | 10.07 | 85.45 | 11.86 | 6.29a (2.12 to 10.46) | 0.003 |
| Total PedsQL score | 91.75 | 10.30 | 78.60 | 14.82 | 13.15a (7.55 to 18.74) | < 0.001 |
| (d) Child not admitted for observation or to ward (n = 67, 56%) (n = 47 for nursery) | (d) Child admitted for observation or to ward (n = 53, 44%) (n = 32 for nursery) | |||||
| Physical functioning | 87.84 | 16.70 | 87.91 | 18.50 | –0.07 (–6.31 to 6.17) | 0.982 |
| Emotional functioning | 85.34 | 14.82 | 84.63 | 15.00 | 0.71 (–4.60 to 6.04) | 0.789 |
| Social functioning | 95.47 | 9.24 | 94.72 | 9.17 | 0.75 (–2.55 to 4.05) | 0.653 |
| Nursery/school functioning | 89.10 | 17.74 | 93.23 | 13.63 | –4.13 (–11.42 to 3.16) | 0.263 |
| Psychosocial summary score | 90.34 | 10.16 | 90.28 | 9.93 | 0.06 (–3.55 to 3.66) | 0.974 |
| Total PedsQL score | 89.13 | 11.40 | 89.24 | 11.98 | –0.11 (–4.28 to 4.04) | 0.956 |
| (e) Child did not receive medication (n = 53, 38%) (n = 33 for nursery) | (e) Child received medication (n = 88, 62%) (n = 59 for nursery) | |||||
| Physical functioning | 94.26 | 10.47 | 82.14 | 21.01 | 12.12a (6.00 to 18.25) | < 0.001 |
| Emotional functioning | 86.23 | 16.61 | 85.00 | 14.31 | 1.23 (–4.00 to 6.45) | 0.643 |
| Social functioning | 96.73 | 7.06 | 93.67 | 11.43 | 3.05 (–0.42 to 6.52) | 0.085 |
| Nursery/school functioning | 95.20 | 9.55 | 88.70 | 18.29 | 6.50 (–0.30 to 13.30) | 0.061 |
| Psychosocial summary score | 92.27 | 9.42 | 89.25 | 11.37 | 2.98 (–0.72 to 6.68) | 0.113 |
| Total PedsQL score | 92.73 | 8.78 | 86.30 | 13.97 | 6.42a (2.20 to 10.65) | 0.003 |
| Scale | (f) 0 procedures (n = 41, 29%) (n = 24 for nursery) | (f) 1 procedure (n = 47, 33%) (n = 31 for nursery) | (f) 2+ procedures (n = 53, 38%) (n = 37 for nursery) | p-value | Bonferroni post hoc tests, mean difference (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Difference 0 vs. 1 | Difference 0 vs. 2+ | Difference 1 vs. 2+ | ||
| Physical functioning | 94.82 | 10.79 | 85.95 | 18.75 | 81.07 | 21.37 | 0.001 | 8.86a (–0.44 to 18.17) | 13.74a,b (4.69 to 22.81) | 4.88 (–3.85 to 13.61) |
| Emotional functioning | 84.02 | 18.38 | 89.36 | 13.05 | 83.11 | 13.70 | 0.092 | –5.34 (–13.11 to 2.44) | 0.91 (–6.66 to 8.48) | 6.25 (–13.54 to 1.04) |
| Social functioning | 96.00 | 9.14 | 94.23 | 11.66 | 94.44 | 9.44 | 0.679 | 1.77 (–3.53 to 7.07) | 1.57 (–3.59 to 6.72) | –0.21 (–5.14 to 4.73) |
| Nursery/school functioning | 95.14 | 10.40 | 90.32 | 16.40 | 88.96 | 18.33 | 0.325 | 4.82 (–14.48 to 2.13) | 6.17 (–4.03 to 16.38) | 1.36 (–8.12 to 10.84) |
| Psychosocial summary score | 90.97 | 11.86 | 91.50 | 10.40 | 88.88 | 10.19 | 0.439 | –0.53 (–6.14 to 5.08) | 2.09 (–3.38 to 7.55) | 2.62 (–2.61 to 7.84) |
| Total PedsQL score | 92.15 | 10.99 | 89.18 | 13.32 | 85.66 | 12.69 | 0.044 | 2.97 (–3.48 to 9.41) | 6.49a,b (0.22 to 12.76) | 3.52 (–2.52 to 9.57) |
| (g) Cut without stitches (1) (n = 19, 42%) (n = 12 for nursery) | (g) Cut with stitches (2) (n = 11, 24%) (n = 11 for nursery) | (g) Fracture (3) (n = 15, 33%) (n = 8 for nursery) | p-value | Difference (1) vs. (2) | Difference (1) vs. (3) | Difference (2) vs. (3) | ||||
| Physical functioning | 85.19 | 19.23 | 88.84 | 11.35 | 58.33 | 23.29 | < 0.001 | –3.64 (–21.81 to 14.52) | 26.86a,b (10.30 to 43.43) | 30.51a,b (11.47 to 49.54) |
| Emotional functioning | 91.05 | 12.54 | 86.82 | 14.19 | 78.33 | 11.75 | 0.021 | 4.23 (–7.77 to 16.23) | 12.72a,b (1.78 to 23.66) | 8.48a (–4.09 to 21.06) |
| Social functioning | 96.25 | 7.25 | 95.45 | 8.20 | 88.67 | 14.94 | 0.106 | 0.80 (–9.24 to 10.84) | 7.58 (–1.57 to 16.74) | 6.79 (–3.73 to 17.31) |
| Nursery/school functioning | 97.22 | 7.40 | 87.88 | 17.23 | 70.83 | 26.73 | 0.010 | 9.34 (–9.25 to 27.94) | 26.39a,b (6.06 to 46.72) | 17.05a (–3.65 to 37.74) |
| Psychosocial summary score | 94.00 | 8.74 | 90.38 | 8.29 | 82.56 | 12.01 | 0.006 | 3.61 (–5.70 to 12.93) | 11.43a,b (2.94 to 19.93) | 7.82a (–1.94 to 17.58) |
| Total PedsQL score | 90.27 | 12.91 | 89.82 | 6.66 | 72.39 | 13.69 | < 0.001 | 0.46 (–10.90 to 11.82) | 17.88a,b (7.53 to 28.23) | 17.42a,b (5.52 to 29.32) |
Analysis of variance showed a statistically significant positive relationship between the number of procedures carried out and physical functioning [comparison (f); see Table 41], but post hoc tests indicated that the only significant contrast was between children who had undergone two or more procedures and children who had undergone none. Similarly, ANOVA showed an overall significant effect for comparison (g), but post hoc tests showed that the only significant contrast was between those who sustained a broken bone and those who sustained a cut or graze not requiring stitches. For comparator groups (a), (b), (c) and (e), the observed differences in physical functioning scores exceeded the previously established MID of 6.92,188 as did differences between those who had undergone two procedures and those who had undergone none for comparison (f), and between those who had sustained a fracture and those who had sustained any type of cut or graze for comparison (g).
Statistically significant differences in the direction expected were also observed for:
-
emotional functioning between children who were reported as not being fully recovered and those who had recovered
-
social functioning between those who had undergone radiography and those who had not
-
nursery/school functioning between:
-
those who had not fully recovered and those who had recovered
-
those who had undergone radiography and those who had not
-
those who had sustained a fracture and those who had sustained a cut not requiring stitches
-
-
the psychosocial summary score between those who had sustained a fracture and those who had sustained a cut not needing stitches, with the difference between those who had and those who had not fully recovered bordering on statistical significance
-
total PedsQL score between:
-
those who had not fully recovered and those who had recovered
-
those who had undergone radiography and those who had not
-
those who received medication and those who did not
-
those who underwent two or more procedures and those who underwent no procedures
-
those who had sustained a fracture and those who had sustained a cut requiring stitches or a cut not requiring stitches.
-
All statistically significant differences reached the previously reported MID for the corresponding scale. 188
Only for comparison (d) (those admitted for observation or to a ward vs. those not admitted) were there no statistically significant differences between the groups.
Responsiveness to change
As hypothesised, there were statistically significant reductions in physical functioning from pre-injury to post-injury for those who were not fully recovered, those who had been treated for their injury, those who had undergone radiography, those who had been admitted for observation or to a ward, those who had received medication and those who had undergone one or more procedures (Tables 42 and 43). These effect sizes ranged from 0.32 (for those who had one procedure carried out) to 1.54 (for those who had not fully recovered), with most being ‘large’ (≥ 0.8) by reference to Cohen’s criteria. 176 The observed mean differences ranged from 4.76 for children who had one procedure carried out to 27.08 for those who were not fully recovered, with most exceeding the previously established MID of 6.92 for this scale.
| Scale | (a) Child fully recovered (n = 118, 89%) (n = 73 for nursery) | (a) Child not fully recovered (n = 15, 11%) (n = 11 for nursery) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-injury | Post-injury | Differencea | ES | p-value | Pre-injury | Post-injury | Differencea | ES | p-value | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||||
| Physical functioning | 92.87 | 12.29 | 89.58 | 15.51 | 3.29 | 0.27 | 0.039 | 91.04 | 17.55 | 63.96 | 25.41 | 27.08b | 1.54 | 0.001 |
| Emotional functioning | 79.72 | 15.08 | 85.97 | 15.36 | –6.25 | –0.41 | < 0.001 | 80.00 | 13.36 | 79.67 | 12.17 | 0.33 | 0.02 | 0.892 |
| Social functioning | 93.90 | 10.40 | 94.99 | 9.67 | –1.09 | –0.10 | 0.344 | 93.00 | 16.99 | 92.00 | 14.37 | 1.00 | 0.06 | 0.670 |
| Nursery/school functioning | 87.39 | 14.99 | 92.69 | 13.60 | –5.30 | –0.35 | 0.005 | 91.67 | 17.48 | 78.79 | 25.38 | 12.88b | 0.74 | 0.171 |
| Psychosocial summary score | 86.97 | 9.81 | 90.80 | 10.43 | –3.83 | –0.39 | < 0.001 | 87.94 | 12.96 | 85.13 | 12.98 | 2.81 | 0.22 | 0.362 |
| Total PedsQL score | 89.37 | 9.39 | 90.29 | 11.28 | –0.92 | –0.10 | 0.410 | 89.19 | 14.33 | 76.36 | 15.59 | 12.83b | 0.90 | 0.005 |
| (b) Examined only (n = 71, 53%) (n = 45 for nursery) | (b) Treated (n = 62, 47%) (n = 39 for nursery) | |||||||||||||
| Pre-injury | Post-injury | Differencea | ES | p-value | Pre-injury | Post-injury | Differencea | ES | p-value | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||||
| Physical functioning | 92.65 | 13.97 | 90.41 | 16.63 | 2.24 | 0.16 | 0.303 | 92.68 | 11.72 | 82.45 | 20.02 | 10.23b | 0.87 | < 0.001 |
| Emotional functioning | 79.47 | 15.88 | 85.49 | 16.54 | –6.02 | –0.38 | 0.005 | 80.08 | 13.71 | 85.00 | 13.46 | –4.92 | –0.36 | 0.011 |
| Social functioning | 92.67 | 13.06 | 93.66 | 12.10 | –0.99 | –0.08 | 0.564 | 95.08 | 8.66 | 95.79 | 7.64 | –0.71 | –0.08 | 0.540 |
| Nursery/school functioning | 87.50 | 15.08 | 92.59 | 16.40 | –5.09 | –0.34 | 0.070 | 88.46 | 15.72 | 88.89 | 15.81 | –0.43 | –0.03 | 0.888 |
| Psychosocial summary score | 86.46 | 11.36 | 90.11 | 12.52 | –3.65 | –0.32 | 0.018 | 87.79 | 8.62 | 90.22 | 8.62 | –2.43 | –0.28 | 0.051 |
| Total PedsQL score | 88.96 | 11.33 | 90.26 | 13.16 | –1.30 | –0.11 | 0.426 | 89.79 | 8.30 | 86.95 | 11.72 | 2.84 | 0.34 | 0.071 |
| (c) Child did not undergo radiography (n = 96, 75%) (n = 62 for nursery) | (c) Child underwent radiography (n = 32, 25%) (n = 21 for nursery) | |||||||||||||
| Pre-injury | Post-injury | Differencea | ES | p-value | Pre-injury | Post-injury | Differencea | ES | p-value | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||||
| Physical functioning | 93.12 | 12.04 | 92.08 | 13.14 | 1.04 | 0.09 | 0.486 | 91.61 | 15.22 | 69.92 | 23.56 | 21.69b | 1.43 | < 0.001 |
| Emotional functioning | 77.89 | 14.79 | 86.04 | 15.58 | –8.15b | –0.55 | < 0.001 | 84.06 | 14.50 | 81.87 | 13.96 | 2.19 | 0.15 | 0.356 |
| Social functioning | 93.96 | 9.97 | 96.13 | 8.42 | –2.17 | –0.22 | 0.056 | 92.50 | 15.08 | 89.84 | 14.11 | 2.66 | 0.18 | 0.327 |
| Nursery/school functioning | 88.84 | 14.07 | 93.68 | 12.78 | –4.84 | –0.34 | 0.012 | 87.10 | 17.07 | 82.14 | 21.78 | 4.96 | 0.29 | 0.360 |
| Psychosocial summary score | 86.38 | 9.48 | 91.43 | 10.24 | –5.05 | –0.53 | < 0.001 | 88.53 | 12.41 | 85.70 | 11.96 | 2.83 | 0.23 | 0.193 |
| Total PedsQL score | 89.11 | 9.26 | 91.66 | 10.40 | –2.55 | –0.28 | 0.023 | 89.75 | 12.37 | 79.19 | 14.66 | 10.56b | 0.85 | < 0.001 |
| (d) Child not admitted (n = 67, 56%) (n = 47 for nursery) | (d) Child admitted (n = 52, 44%) (n = 30 for nursery) | |||||||||||||
| Pre-injury | Post-injury | Differencea | ES | p-value | Pre-injury | Post-injury | Differencea | ES | p-value | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||||
| Physical functioning | 93.04 | 10.36 | 87.41 | 17.26 | 5.63 | 0.54 | 0.007 | 93.45 | 13.41 | 88.88 | 17.27 | 4.57 | 0.34 | 0.126 |
| Emotional functioning | 77.95 | 15.80 | 84.92 | 14.71 | –6.97 | –0.44 | < 0.001 | 80.67 | 13.79 | 84.90 | 15.00 | –4.23 | –0.31 | 0.069 |
| Social functioning | 94.78 | 8.32 | 95.13 | 9.50 | –0.35 | –0.04 | 0.795 | 92.31 | 12.58 | 94.90 | 9.16 | –2.59 | –0.21 | 0.154 |
| Nursery/school functioning | 88.92 | 14.28 | 88.83 | 17.82 | 0.09 | 0.01 | 0.976 | 87.78 | 14.31 | 93.33 | 13.91 | –5.55 | –0.39 | 0.046 |
| Psychosocial summary score | 87.02 | 9.75 | 89.91 | 10.32 | –2.89 | –0.30 | 0.032 | 86.70 | 9.92 | 90.53 | 9.87 | –3.83 | –0.39 | 0.013 |
| Total PedsQL score | 89.43 | 8.65 | 88.89 | 11.58 | 0.54 | 0.06 | 0.703 | 89.45 | 10.07 | 89.81 | 11.35 | –0.36 | –0.04 | 0.843 |
| (e) No medication given (n = 49, 37%) (n = 29 for nursery) | (e) Medication given (n = 84, 63%) (n = 55 for nursery) | |||||||||||||
| Pre-injury | Post-injury | Differencea | ES | p-value | Pre-injury | Post-injury | Differencea | ES | p-value | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||||
| Physical functioning | 92.78 | 11.42 | 94.37 | 10.66 | –1.59 | –0.14 | 0.124 | 92.60 | 13.79 | 82.22 | 20.80 | 10.38b | 0.75 | < 0.001 |
| Emotional functioning | 78.21 | 15.94 | 85.92 | 16.51 | –7.71 | –0.48 | 0.002 | 80.65 | 14.21 | 84.88 | 14.35 | –4.23 | –0.30 | 0.016 |
| Social functioning | 95.20 | 8.90 | 96.53 | 7.23 | –1.33 | –0.15 | 0.304 | 92.98 | 12.40 | 93.56 | 11.60 | –0.58 | –0.05 | 0.698 |
| Nursery/school functioning | 89.37 | 13.16 | 94.54 | 10.03 | –5.17 | –0.39 | 0.050 | 87.20 | 16.37 | 88.94 | 18.36 | –1.74 | –0.11 | 0.537 |
| Psychosocial summary score | 87.23 | 9.31 | 91.75 | 9.50 | –4.52 | –0.49 | 0.001 | 87.00 | 10.68 | 89.24 | 11.50 | –2.24 | –0.21 | 0.110 |
| Total PedsQL score | 89.50 | 8.98 | 92.77 | 8.55 | –3.27 | –0.36 | 0.002 | 89.26 | 10.60 | 86.35 | 13.92 | 2.91 | 0.27 | 0.083 |
| Scale | (f) 0 procedures (n = 39, 29%) (n = 22 for nursery) | (f) 1 procedure (n = 42, 32%) (n = 28 for nursery) | (f) 2 procedures (n = 52, 39%) (n = 34 for nursery) | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-injury | Post-injury | Differencea | ES | p-value | Pre-injury | Post-injury | Differencea | ES | p-value | Pre-injury | Post-injury | Differencea | ES | p-value | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||||||||
| Physical functioning | 94.63 | 7.55 | 95.03 | 10.82 | –0.4 | –0.05 | 0.841 | 90.9 | 14.78 | 86.14 | 18.04 | 4.76 | 0.32 | 0.015 | 92.61 | 14.43 | 80.89 | 21.53 | 11.72b | 0.81 | 0.002 |
| Emotional functioning | 77.37 | 15.1 | 84.23 | 18.26 | –6.86 | –0.45 | 0.025 | 81.19 | 15.73 | 89.29 | 13.09 | –8.10b | –0.51 | 0.002 | 80.38 | 14 | 82.79 | 13.36 | –2.41 | –0.17 | 0.221 |
| Social functioning | 95.26 | 7.94 | 95.9 | 9.24 | –0.64 | –0.08 | 0.69 | 92.26 | 14.19 | 93.9 | 12.13 | –1.64 | –0.12 | 0.44 | 93.94 | 10.73 | 94.33 | 9.5 | –0.39 | –0.04 | 0.825 |
| Nursery/school functioning | 87.88 | 13.79 | 94.7 | 10.77 | –6.82 | –0.49 | 0.03 | 87.5 | 16.59 | 90.77 | 15.93 | –3.27 | –0.2 | 0.586 | 88.36 | 15.55 | 88.48 | 18.92 | –0.12 | –0.01 | 0.975 |
| Psychosocial summary score | 86.91 | 8.2 | 90.73 | 11.93 | –3.82 | –0.47 | 0.037 | 86.85 | 12.39 | 91.49 | 10.62 | –4.64 | –0.37 | 0.008 | 87.41 | 9.67 | 88.66 | 10.17 | –1.25 | –0.13 | 0.45 |
| Total PedsQL score | 90.01 | 7.15 | 92.43 | 10.77 | –2.42 | –0.34 | 0.173 | 88.51 | 12.04 | 89.29 | 13.15 | –0.78 | –0.06 | 0.599 | 89.53 | 10.16 | 85.46 | 12.74 | 4.07 | 0.4 | 0.074 |
Reductions in PedsQL scores from pre-injury to post-injury were also observed: for emotional, social and nursery functioning; for the psychosocial summary score; and for the total PedsQL score in those who had not fully recovered and those who had undergone radiography; and for total PedsQL score in those who were treated in the ED/MIU or on a ward, those who had received medication and those who had undergone two or more procedures. For the most part, these observed effect sizes were small to moderate (according to Cohen’s criteria of 0.2 for small and 0.5 for moderate) and few differences reached statistical significance or exceeded the corresponding previously established MIDs. 188
Contrary to expectations, improvements from pre-injury to post-injury with, in some instances, substantial effect sizes were observed for the emotional, social and nursery functioning scales, the psychosocial summary score and the total PedsQL score for children who had:
-
fully recovered
-
only been examined in the ED/MIU
-
not undergone radiography
-
not received medication
-
undergone no procedures.
The majority of these differences reached statistical significance.
Improvements from pre-injury to post-injury were also observed in respect of emotional, social and nursery functioning and the psychosocial summary score in those:
-
treated in the ED/MIU
-
admitted for observation or to a ward
-
receiving medication
-
who had undergone one or more procedures.
However, few of these differences reached statistical significance.
Using the full baseline study A sample, computed MIDs for the four domains of the PedsQL ranged from 4.92 for physical functioning to 9.97 for nursery functioning using the SEM method and from 6.39 for physical functioning to 7.92 for emotional functioning using the half of the baseline SD method. Computed MIDs using these two methods were 4.74 and 5.91, respectively, for the psychosocial summary score and 3.62 and 5.44, respectively, for the total PedsQL score.
Discussion
Main findings
In general, the PedsQL proved to be a feasible and acceptable measure of HRQL in this population, with adequate internal consistency reliability, the ability to discriminate between varying levels of injury severity and sequelae and evidence of responsiveness to change. Findings in respect of construct validity were, however, equivocal.
Strengths and limitations
A comprehensive classic psychometric analysis was conducted, mirroring previous analyses by the developers of the PedsQL and by others using the instrument in post-injury and ED populations, thereby facilitating comparisons with previous findings. The sample size using the baseline study A questionnaires was 1334, an adequate number for all of the analyses conducted.
However, the recall period of 2 weeks used in this study corresponded neither to the 4-week reference period of the standard PedsQL nor to the 1-week reference period of the acute version, which was used in the previously reported study of minor injuries by Stevens et al. 165,166 This therefore limits comparison of the findings with these studies.
The sample size for the study C HRQL substudy was relatively small (n = 148), and so it was not possible to conduct confirmatory factor analysis on post-injury HRQL scores; this has implications for the precision of other test statistics.
Pre-injury HRQL scores were of necessity retrospectively reported. Of some note is the finding from this research that retrospectively reported pre-injury scale, summary and total scores in the full study A sample were (with the exception of nursery/school functioning) statistically significantly higher than those reported by Buck157 in an earlier study of healthy UK toddlers and than those for community controls in the current study. A similar pattern of better HRQL pre-injury by comparison to US population norms188 is evident in the ED study by Stevens et al. ,166 although that group do not explicitly analyse or comment on this. Previous studies of HRQL in injured adults192,193 have also found pre-injury HRQL as recalled post-injury to be higher than population norms. Two potential explanations for this phenomenon have been put forward. The first is that those who sustain injuries are healthier, fitter, more active and more energetic than the general population of a similar age, with this better health status leading them into situations in which they are more likely to sustain an injury. The second explanation is that ‘response shift’191,194 may be present, in other words, that patients, or in this case parents acting as proxies, may be recalibrating the internal standards by which they evaluate HRQL in light of the experience of a traumatic event. Further research is needed to elucidate which of these explanations is the more plausible. Nonetheless, Watson et al. 192 and Wilson et al. 193 both conclude that retrospective recall of pre-injury HRQL provides a better baseline than do population norms for measuring post-injury impact.
Comparison with other studies
The overall rate of missing data of 7.6% was higher than the rates of 1.95% reported by Varni et al. 64 for proxy report for children aged 2–18 years and of 2.4% reported by Varni et al. 188 for children aged 2–16 years, but the average age of children in those samples was 9.3 years and 7.9 years, respectively. Higher rates of missing data are to be expected in samples of younger children as the nursery/school items do not apply to many toddlers. Varni et al. 188 reported an overall percentage of missing values on the nursery/school functioning scale for toddlers (aged 2–4 years) of 52%, a higher rate than that observed in the current study, with an inverse relationship between the age of the child and the level of missing data.
Findings in respect of item response distributions generally reflect those of Varni et al. ,64 with the full range of scores being used for all items in Varni et al. ’s sample and for all but two items in the study A pre-injury sample. Item distributions tended to be skewed towards higher HRQL in our sample and in Varni et al. ’s sample. 64 In their sample of 2- to 18-year-olds, Varni et al. 64 reported item means for proxy report ranging from 65.9 to 88.4, with means for 16 out of the 23 items falling within a 10-point range and item SDs ranging from 23.3 to 35.2; for the 15 items in the psychosocial summary score, proxy report item means ranged from 85.9 to 86.8, with SDs ranging from 24.1 to 34.2. They indicate that computing scale scores by simple linear averaging is possible when the means and SDs of items within a given scale or summary are roughly equivalent. 174 In the current study, for pre-injury data, a range similar to that reported by Varni et al. 64 was observed in respect of item means (75.33–96.26 for all items, 75.33–95.86 for the 13 items in the psychosocial summary score) and SDs (11.48–25.89 for all items and for those in the psychosocial summary score), suggesting that the calculation of scale scores according to the PedsQL algorithm was appropriate. Item–own scale correlations exceeded the criterion of ≥ 0.4 for 18 out of the 21 items in our sample, compared with all items for proxy report as reported by Varni et al. 64
In scale-level analyses, Varni et al. 64,195 reported a lack of floor effects for both healthy and ill children, with no more than 2.3% of children scoring the minimum possible value for any of the scale or summary scores, a finding reflected here. For proxy report, they reported ceiling effects among healthy children ranging from 10.3% for the total PedsQL score to 58.1% for social functioning. Ceiling effects for pre-injury scores in our sample were comparable to those reported by Varni et al. 195 in respect of 2- to 4-year-olds for emotional functioning and psychosocial summary scores, but were more pronounced in our sample for physical, social and nursery/school functioning and total PedsQL scores. Ceiling effects for pre-injury scores in our sample were also more marked than those reported by Buck157 in healthy UK toddlers for all but nursery/school functioning. In a comparable study to ours of retrospectively reported pre-injury PedsQL scores, Stevens et al. 166 also report high levels of ceiling effects (56.2% for physical functioning, 21.9% for psychosocial summary score and 18.6% for total PedsQL score).
Our findings in respect of item internal consistency reliability and interscale correlations in the current study largely reflect previous reports by Varni et al. 64 and by Buck,157 the latter in a population of healthy toddlers in the UK.
Findings from the confirmatory factor analysis in the current study did not support either the first- or the second-order solutions. Previous reports by the developers of the PedsQL suggest a stable factor structure across a range of disease and demographic subgroups and modes of administration;177–183,196 between healthy children and those with a chronic health condition;180 across race/ethnicity groups;181 over a period of 1 year;182 and across different modes of administration. 183 Amiri et al. 197 reported acceptable fit to a five-factor model in Iranian adolescents whereas Viira and Koka198 reported that goodness-of-fit statistics approached criteria for acceptable fit when the error covariance was set to be free between certain items in the physical, social and emotional functioning scales. However, poor factorial validity has been reported in adaptations of the PedsQL for Catalan199 and Serbian200 populations, despite adequate internal consistency, reliability and convergent validity against psychological constructs in the latter study. Hao et al. 201 also report poor fit against some of the goodness-of-fit indices for a five-factor model in confirmatory factor analysis of the Chinese version of the PedsQL, whereas Petersen et al. 202 report problems with fit to a four-factor model for parent proxy report in the Swedish adaptation. None of the previous reported studies used the toddler version of the PedsQL (although under-fives were included in some of the studies by the PedsQL development team, the reported findings on factor structure relate only to children aged ≥ 5 years).
However, findings from known-groups validity analyses do provide evidence of construct validity, with the majority of our hypotheses being borne out. Varni et al. 64 included a comparison between healthy, acutely ill and chronically ill children as part of their consideration of construct validity, and found significant overall differences and between all pairs of subgroups, for all PedsQL scale and summary scores; in a subsequent study,188 they again showed that healthy children had significantly higher scores on the PedsQL than those with a chronic condition. Upton et al. ,156 in the initial adaptation of the PedsQL for use in the UK, also reported significant differences in scores between healthy children and those with chronic health problems. These observations reflect our own findings in respect of pre-injury scores for children without and with a long-term health condition. Stevens et al. 166 found that the PedsQL, in particular the physical functioning scale, discriminated between injury types and good compared with poor clinical outcomes. Although our analyses are not directly comparable, as injury types and outcomes were recorded in different ways in the two studies, our results also show that PedsQL physical functioning scores were lower in children who were reported as not being fully recovered and those with more serious injuries. The main exception to our hypothesised associations was that there were no significant differences in PedsQL scores at follow-up between those admitted for observation or to a ward and those not admitted. We conjecture that this question may have been variably interpreted by parents, with some whose child stayed in the ED or MIU for a period of time for examination responding to the effect that their child had been ‘admitted for observation’ and others answering ‘not admitted’ in identical circumstances. Availability of a hospital bed rather than medical need may also have influenced admission patterns.
Reflecting the findings of Stevens et al. ,166 we also found the PedsQL to be responsive to change from pre-injury to post-injury, particularly in respect of physical functioning. Varni et al. 188 reported MIDs calculated according to the SEM method, defined as the product of the (baseline) SD and the square root of 1 minus Cronbach’s alpha; they report a MID for proxy report of 4.50 for the total PedsQL score, with scale score MIDs ranging from 6.92 for physical functioning to 9.67 for nursery/school functioning. In the current study, the MIDs for emotional and nursery/school functioning were similar to those previously reported, but those for physical and social functioning, psychosocial summary and total PedsQL scores were smaller. Stevens et al. 166 reported SEMs ranging from 4.0 to 6.5 and the half-SD index ranging from 6 to 9.
Resource use study (costs substudy)
Methods
The purpose of this multicentre longitudinal costs of injury study was to itemise, value and sum the costs of unintentional childhood injuries. 113 The study focused on the costs resulting from the injury borne by (1) the NHS and (2) the child and his or her family. The study did not attempt to quantify, in monetary terms, the impact on quality of life.
Administration of resource use questions
General data collection methods are described in Methods relating to the health-related quality-of-life and costs substudies. To obtain an estimate of NHS costs and child and family costs related to each child’s injury, resource use and expenditure questions were developed and included in the study C questionnaires. Parents were also asked to give informed consent for access to their child’s medical records to collect data to validate parent-reported resource use. Parents who did not provide consent were still eligible to participate in study C, but data were not extracted from their child’s records. The resource use questions collected parent self-reported information on the following:
-
NHS costs:
-
ED or MIU attendance – investigations and treatment received
-
inpatient stays – number of inpatient stays, length of stay, specialty, reason (e.g. operation type)
-
outpatient visits – health professional(s) visited, number of visits, average length of appointment
-
GP visits – number of visits, average length of appointment
-
nurse visits – number of visits, average length of appointment
-
other health professional visits (e.g. physiotherapist, health visitor)
-
prescribed medication
-
aids and appliances (e.g. crutches)
-
-
child and family costs:
-
visits to health professionals – mode of transport and associated costs, average travel time, average waiting time, average length of appointment
-
hospital outpatient visits – mode of transport and associated costs, average waiting time, average length of appointment
-
time off from usual activities [work (parent), nursery/preschool/playgroup (child)]
-
carers – informal (family members, e.g. time off work), formal (paid help) – for injured child and/or other dependents.
-
over-the-counter medication.
-
To validate the NHS resource use and expenditure data collected from parent-completed questionnaires, responses were compared with routine data from secondary care records for a subsample of 10% of the study participants. The aim was to extract data from two randomly sampled cases from each study centre for each of the five relevant injury mechanisms who had given consent to access their medical records, plus data from all cases at all centres who had been admitted to hospital and gave consent to access their medical records. However, not all centres had two cases with each type of injury. Consequently, the final sample included 42 cases, 14 from Norwich, 13 from Bristol, nine from Nottingham and six from Newcastle. Of the 42 cases, 10 had incurred a fall on one level, nine a fall on the stairs, 10 a fall from furniture, 10 a poisoning and three a scald. Six cases were admitted to hospital for their injury. Data were extracted from the medical records by researchers on whether or not the child was admitted, length of stay, investigations carried out, treatment received and outpatient visits.
Details of resource use were sought for the time since injury in the 2-week questionnaire and the time intervals between questionnaires for subsequent questionnaires (e.g. 2 weeks for the 1-month questionnaire, 2 months for the 3-month questionnaire).
Analysis
To obtain the average cost per case, the resource use data collected longitudinally using the self-completion questionnaires at 1, 3 and 12 months or until the child had completely recovered, whichever was sooner, were combined with unit cost data obtained from various sources, including NHS reference costs31 and the Personal Social Services Research Unit (PSSRU)30 (see Appendix 2, Table 146), and summed together. All costs were inflated to 2012 UK pounds. Data from individuals were included in all cost categories for which they reported resource use information. As not all individuals reported information for all categories (i.e. incomplete responses), average costs for each category were derived using variable numbers of responders. Additionally, total average costs (with associated uncertainty) were obtained using data from only individuals who responded to all cost categories.
Average costs were estimated for each type of injury (i.e. stair falls, falls on one level and falls from furniture, poisonings and scalds). An analysis was undertaken to investigate the sensitivity of the average cost estimates to variations in the unit costs assigned, that is, the impact of varying the unit costs of ED treatments and investigations as well as inpatient stays (known to vary widely across hospitals) within the IQR reported in the NHS reference costs on the results was investigated.
To validate the accuracy of parents’ responses to questions about their children’s use of health service resources, responses from a sample of parents were compared with the information contained in the medical records of their children. Kappa statistics were calculated to provide a quantitative measure of the magnitude of agreement between parents’ reporting and the medical records.
The main analysis was a complete-case analysis. Sensitivity analyses were undertaken for the primary cost outcomes – NHS costs, non-NHS costs and total costs – to check the robustness of the findings to missing data. Multiple imputation was undertaken assuming that data were missing at random. The imputation model included all cost component variables that sum together to produce the total overall cost. Because of non-normality of the cost component variables, predictive mean matching was used for the imputation. The imputation model also included the socioeconomic and injury characteristics listed later in Table 59. Fifty data sets were imputed, and were combined using Rubin’s rules. 77
Results
This section presents data on the costs to the NHS, such as costs relating to ED attendance, investigations and treatments, and costs relating to hospital admission. It also includes data on other health-care resource use, for example GP visits and attendance at outpatient departments, and data on non-health-care costs incurred by the family, for example costs of over-the-counter medication, travel and child care. Results describing the characteristics of study participants who were not fully recovered at 2 weeks and who were subsequently lost to follow-up are presented elsewhere. 203
The NHS and other costs are sensitive to the proportions of injured children who are admitted to hospital and lengths of stay in hospital for different types of injuries. In this study, because the recruitment regime invited the parents of all children who were admitted to hospital to participate, the proportion admitted is substantially higher than for home accidents as a whole. Over one-third of injured children in this sample were admitted to hospital (see Table 45), although most of these were admitted for observation, not for an overnight stay. Only 4.3% of our sample were admitted overnight, which is comparable with the percentage of children in this age group attending an ED who are admitted overnight following an injury (5%). 3
Table 44 shows the numbers of questionnaires administered by injury mechanism and administration date and the numbers actually returned (see also Figure 8). It includes only those participants with complete data over the 12-month follow-up period (i.e. all questionnaires returned until complete recovery). Of the 383 2-week questionnaires returned, 32 were mini-questionnaires (see Appendix 2, Mini questionnaire) that did not contain data on resource use and these are excluded from Table 44. In addition, seven cases were lost to follow-up (1 month, n = 5; 3 months, n = 2) and their recovery status was unknown; these have also been excluded from Table 44.
| Follow-up point (post injury) | Falls on one level | Stair falls | Falls from Furniture | Poisonings | Scalds | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | R | A | R | A | R | A | R | A | R | A | R | Cumulative % recovered | |
| 2 weeks | 76 | 76 | 86 | 82 | 96 | 88 | 63 | 63 | 23 | 19 | 344 | 328 | 95.3 |
| 1 month | 0 | 0 | 4 | 2 | 8 | 7 | 0 | 0 | 4 | 3 | 16 | 12 | 98.8 |
| 3 months | 0 | 0 | 2 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 4 | 2 | 99.4 |
| 12 months | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 1 | 99.7 |
To validate the accuracy of parents’ responses to questions about their children’s use of health service resources, responses from 42 parents were compared with the information contained in the medical records of their children. The results, including the kappa values illustrating interobserver agreement, are shown in Table 45. Landis and Koch79 provide a commonly used framework for interpreting kappa values:
-
0.81–1.00 – almost perfect agreement
-
0.61–0.80 – substantial agreement
-
0.41–0.60 – moderate agreement
-
0.21–0.40 – fair agreement
-
0.00–0.20 – slight agreement
-
< 0.00 – poor agreement.
| Variable | n | V = yes, Q = yes | % | V = no, Q = no | % | V = yes, Q = no | % | V = no, Q = yes | % | P (observed agreement) | P (expected agreement) | Kappa coefficient | 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Admitted to hospital | 42 | 2 | 5 | 34 | 81 | 4 | 10 | 2 | 5 | 0.86 | 0.79 | 0.32 | –0.09 to 0.74 |
| Overnight stay in hospital | 32 | 1 | 3 | 29 | 91 | 1 | 3 | 1 | 3 | 0.94 | 0.88 | 0.47 | –0.16 to 1.00 |
| Blood test in ED | 40 | 5 | 13 | 32 | 80 | 2 | 5 | 1 | 3 | 0.93 | 0.73 | 0.72 | 0.43 to 1.00 |
| Urine test in EDa | 39 | 0 | 0 | 36 | 92 | 3 | 8 | 0 | 0 | 0.92 | 0.92 | 0.00 | Undefined to 1.00 |
| Radiography in ED | 39 | 5 | 13 | 33 | 85 | 1 | 3 | 0 | 0 | 0.97 | 0.76 | 0.89 | 0.69 to 1.00 |
| Observation in ED | 35 | 11 | 31 | 11 | 31 | 7 | 20 | 6 | 17 | 0.63 | 0.50 | 0.26 | –0.06 to 0.58 |
| Advice in ED | 39 | 28 | 72 | 1 | 3 | 7 | 18 | 3 | 8 | 0.74 | 0.73 | 0.03 | –0.27 to 0.34 |
| Medicine by mouth in ED | 40 | 6 | 15 | 26 | 65 | 2 | 5 | 6 | 15 | 0.80 | 0.62 | 0.47 | 0.17 to 0.78 |
| Medicine by injection in EDa | 38 | 0 | 0 | 36 | 95 | 2 | 5 | 0 | 0 | 0.95 | 0.95 | 0.00 | Undefined to 1.00 |
| Cream on skin in ED | 38 | 4 | 11 | 31 | 82 | 1 | 3 | 2 | 5 | 0.92 | 0.75 | 0.68 | 0.35 to 1.00 |
| Medicine to take home from ED | 38 | 1 | 3 | 32 | 84 | 3 | 8 | 2 | 5 | 0.87 | 0.83 | 0.21 | –0.25 to 0.68 |
| Dressing for wounds in ED | 40 | 2 | 5 | 36 | 90 | 0 | 0 | 2 | 5 | 0.95 | 0.86 | 0.64 | 0.19 to 1.00 |
| Stitches in ED | 38 | 1 | 3 | 36 | 95 | 1 | 3 | 0 | 0 | 0.97 | 0.92 | 0.65 | 0.03 to 1.00 |
| Bandage/sling/support in ED | 38 | 1 | 3 | 35 | 92 | 0 | 0 | 2 | 5 | 0.95 | 0.90 | 0.48 | –0.12 to 1.00 |
| Manipulation of broken/fractured bone in ED | 39 | 1 | 3 | 38 | 97 | 0 | 0 | 0 | 0 | 1.00 | 0.95 | 1.00 | 1.00 to 1.00 |
| Cast to hold fracture/broken bone in EDa | 39 | 0 | 0 | 38 | 97 | 0 | 0 | 1 | 3 | 0.97 | 0.97 | 0.00 | Undefined to 1.00 |
| General anaesthetic in ED | 40 | 4 | 10 | 35 | 88 | 1 | 3 | 0 | 0 | 0.98 | 0.80 | 0.88 | 0.64 to 1.00 |
| Local anaesthetic in EDa | 39 | 0 | 0 | 36 | 92 | 2 | 5 | 1 | 3 | 0.92 | 0.93 | –0.04 | –0.11 to 0.04 |
| Drip in EDa | 38 | 0 | 0 | 37 | 97 | 1 | 3 | 0 | 0 | 0.97 | 0.97 | 0.00 | Undefined to 1.00 |
| Oxygen therapy in EDa | 39 | 0 | 0 | 36 | 92 | 2 | 5 | 1 | 3 | 0.92 | 0.93 | –0.04 | –0.11 to 0.04 |
| Intubation in EDa | 39 | 0 | 0 | 38 | 97 | 1 | 3 | 0 | 0 | 0.97 | 0.97 | 0.00 | Undefined to 1.00 |
| Day-case visit(s)a | 43 | 0 | 0 | 39 | 91 | 4 | 9 | 0 | 0 | 0.91 | 0.91 | 0.00 | Undefined to 1.00 |
| Consultant visit(s)a | 42 | 0 | 0 | 38 | 90 | 4 | 10 | 0 | 0 | 0.90 | 0.90 | 0.00 | Undefined to 1.00 |
Care is needed in interpreting the results. Kappa values are strongly influenced by the prevalence of the outcome and there are extremes of prevalences in many of the variables, as noted in Table 45. For example, a urine test in the ED had a low prevalence of three out of 39 (8%), and all three had been misreported in the parent questionnaire, giving a kappa of 0.00, although the probability of observed agreement is 0.92. As noted, for example by Feinstein and Cicchetti,204 kappa is difficult to interpret in these circumstances [i.e. a low kappa value despite high agreement (for the prevalent category)]. There is poor agreement for observation in the ED, and advice in the ED resulting in probabilities of observed agreement of 0.63 and 0.74, respectively, resulting in kappa values of 0.26 and 0.03, respectively. This may be because the ‘medical’ interpretation of these categories differed from the parents’ interpretation.
The following procedures and visits have been omitted from Table 45 because, in the validation sample, no parents reported and/or no children had a particular procedure/visit recorded in their medical records. The omitted variables are:
-
scan in the ED
-
splint in the ED
-
manipulation of dislocated joint in the ED
-
operation to fix fracture in the ED
-
physiotherapy in the ED
-
stomach wash in the ED
-
tetanus injection in the ED
-
blood transfusion in the ED
-
chest drain in the ED
-
resuscitation in the ED
-
hospital nurse visit(s)
-
physiotherapist visits(s).
Note that because of the very small number of inpatient stays (i.e. four reported by parents and six reported in medical records, with agreement of only two) it was not possible to assess the agreement for length of stay in hospital.
Table 45 illustrates that > 95% of children were reported to have recovered from their injuries within 2 weeks of their accident and almost 99% within 1 month. However, there was variation in the proportions recovered within 2 weeks by injury mechanism, ranging from 100% for falls on one level and poisonings to 95.3% for stair falls, 91.7% for falls from furniture and 82.7% for scalds.
Parents of 435 children who reported seeking medical attention at an ED, a MIU or a walk-in centre were invited to participate, of whom 351 (81%) agreed and from whom NHS resource use information was collected via the return of the 2-week follow-up questionnaire (Table 46). Of these, 129 children (39% of those for whom admission status was known) were reported by parents to have been admitted for observation or treatment.
| Variable | n (%) |
|---|---|
| Type of NHS unit for initial contact | |
| ED | 341 (97) |
| MIU | 0 (0) |
| Walk-in centre | 10 (3) |
| Admitted | |
| Admitted for observation | 114 (32) |
| Admitted for overnight stay | 15 (4) |
| Not admitted | 202 (58) |
| Not known whether or not admitted | 23 (7) |
Based on parental questionnaires, and therefore with limited reliability, Table 47 shows that two-thirds of cases required only the lowest levels of investigation and treatment, with a further 16% of cases requiring category 2 investigations (e.g. radiography) and either category 1 or category 2 treatment. Definitions of investigations and treatment categories are provided in Table 47.
| Resource | Injury mechanism | ||||
|---|---|---|---|---|---|
| Falls on one level, n (%) | Falls on stairs, n (%) | Falls from furniture, n (%) | Poisonings, n (%) | Scalds, n (%) | |
| Number of responders | 64 | 77 | 75 | 57 | 15 |
| ED treatment and investigationa | |||||
| VB03Z emergency medicine, category 3 investigation with category 1–3 treatment | 0 (0) | 1 (1) | 2 (3) | 0 (0) | 0 (0) |
| VB04Z emergency medicine, category 2 investigation with category 4 treatment | 1 (2) | 2 (3) | 1 (1) | 0 (0) | 0 (0) |
| VB05Z emergency medicine, category 2 investigation with category 3 treatment | 1 (2) | 0 (0) | 0 (0) | 1 (2) | 0 (0) |
| VB06Z emergency medicine, category 1 investigation with category 3–4 treatment | 5 (8) | 1 (1) | 1 (1) | 0 (0) | 0 (0) |
| VB07Z emergency medicine, category 2 investigation with category 2 treatment | 3 (5) | 5 (6) | 10 (13) | 1 (2) | 0 (0) |
| VB08Z emergency medicine, category 2 investigation with category 1 treatment | 9 (14) | 2 (3) | 4 (5) | 9 (16) | 0 (0) |
| VB09Z emergency medicine, category 1 investigation with category 1–2 treatment | 45 (70) | 63 (82) | 53 (71) | 43 (75) | 15 (100) |
| VB11Z emergency medicine, no investigation with no significant treatment | 0 (0) | 3 (4) | 4 (5) | 3 (5) | 0 (0) |
| Hospital admission at initial ED visit | |||||
| ≥ 2 days | 1 (2) | 2 (3) | 3 (4) | 3 (5) | 1 (7) |
| ≤ 1 day | 17 (27) | 26 (34) | 19 (25) | 34 (60) | 6 (40) |
| GP surgery | |||||
| 1 visit | 5 (8) | 5 (6) | 3 (4) | 2 (4) | 2 (13) |
| ≥ 2 visits | 0 (0) | 2 (3) | 1 (1) | 0 (0) | 0 (0) |
| Outpatient department | |||||
| 1 visit | 3 (5) | 2 (3) | 7 (9) | 0 (0) | 2 (13) |
| ≥ 2 visits | 0 (0) | 4 (5) | 0 (0) | 0 (0) | 4 (27) |
| Health visitor | |||||
| 1 visit | 3 (5) | 2 (3) | 1 (1) | 4 (7) | 3 (20) |
| ≥ 2 visits | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Subsequent inpatient daysb | |||||
| 1 day | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 0 (0) |
| ≥ 2 days | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (7) |
| Prescribed medication | |||||
| Number prescribed medication | 6 (9) | 6 (8) | 3 (4) | 1 (2) | 5 (33) |
As described earlier, 344 out of 351 (98%) parents who agreed to participate provided data on recovery from injury and were included in the analysis. Seven participants who completed the 2-week questionnaire and were known not to have fully recovered at 2 weeks were subsequently lost to follow-up. These participants were similar in terms of age, sex, injury mechanism, admission status and NHS costs to those not lost to follow-up (Table 48).
| Age (months) | Sex | Injury mechanism | IMD score | Admittance status | HRG code for ED treatment | NHS cost in the first 2 weeks post injury (£) |
|---|---|---|---|---|---|---|
| 28 | Male | Fall from furniture | 27.2 | Admitted for 0–1 days | VB09Z | 700.01 |
| 32 | Male | Fall on one level | 42.5 | Not admitted | VB07Z | 142.92 |
| 38 | Female | Fall on stairs | 8.8 | Missing | Missing | Missing |
| 43 | Female | Fall from furniture | 10.8 | Admitted for 0–1 days | VB09Z | 741.11 |
| 10 | Male | Scald | 41.5 | Admitted for 0–1 days | VB08Z | 700.01 |
| 49 | Female | Fall on one level | 11.8 | Not admitted | VB08Z | 130.76 |
| 25 | Female | Fall from furniture | 35.5 | Not admitted | VB09Z | 91.47 |
Complete data were available for 288 (84%), 314 (91%) and 268 (78%) participants for NHS costs, non-NHS costs and combined NHS and non-NHS costs, respectively. In total, 95% of children were reported by parents to be fully recovered within 2 weeks of injury and 99% (n = 340) were reported to be fully recovered within 1 month of injury. Table 49 reports the characteristics of the study participants. Falls injuries were reported most frequently (75%), with 18% of injuries being poisonings and 7% being scalds. The mean age of participants was 23 months and 49% were male. Participants were relatively disadvantaged, with 43% of households receiving state benefits, 37% living in non-owner-occupied accommodation and 15% of households not having any adults in paid work. Few children (8%) had a long-term health condition prior to the injury.
| Characteristic | Participants (n = 344), n (%) |
|---|---|
| Study centre | |
| Nottingham | 103 (29.9) |
| Bristol | 126 (36.6) |
| Norwich | 96 (27.9) |
| Newcastle | 19 (5.5) |
| Injury mechanism | |
| Fall on one level | 76 (22.1) |
| Fall from furniture | 96 (27.9) |
| Fall on stairs or steps | 86 (25.0) |
| Poisoning | 63 (18.3) |
| Scald | 23 (6.7) |
| Age (months), mean (SD) | 22.9 (13.0) |
| Male | 169 (49.1) |
| Ethnic origin: white | 312 (94.0) [12] |
| Number of children aged < 5 years in family | [12] |
| 1 | 200 (60.2) |
| 2 | 115 (34.6) |
| ≥ 3 | 17 (5.1) |
| First child | 143 (45.1) [27] |
| Maternal age ≤ 19 years at birth of first child | 48 (14.8) [19] |
| Single adult household | 46 (13.9) [14] |
| Weekly out-of-home child care (hours), median (IQR) | 6 (0.0–20.0) [23] |
| Adults in paid work | [12] |
| ≥ 2 | 168 (50.6) |
| 1 | 114 (34.3) |
| 0 | 50 (15.1) |
| Household receives state benefits | 143 (43.2) [13] |
| Overcrowding (more than one person per room) | 26 (8.1) [23] |
| Non-owner occupier | 124 (37.3) [12] |
| Household has no car | 45 (13.5) [10] |
| IMD score, mean (SD) | 19.6 (14.4) |
| Distance from hospital (km), median (IQR) | 3.7 (2.2–6.5) |
| Long-term health condition | 25 (7.6) [13] |
| Child health VAS score (range 0–10), median (IQR) | 9.9 (9.0–10.0) [11] |
Health-care resource use and costs are presented in Tables 50–54 by injury mechanism, and non-health-care resource use and costs are presented in Tables 55–57 by injury mechanism. The total health-care and non-health-care costs per child are presented in Table 58. (The sources of the costs used are shown in Appendix 2, Tables 145 and 146. )
| Not admitted at initial ED visit | Admitted overnight at initial ED visit | Admitted for observation at initial ED visit | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | Falls | Poisonings | Scalds | Falls | Poisonings | Scalds | |||||||
| On one level | On stairs | From furniture | On one level | On stairs | From furniture | On one level | On stairs | From furniture | |||||||
| Number of children in each emergency medicine treatment and investigation category (see definitions in Table 47) | |||||||||||||||
| n | 46 | 49 | 53 | 20 | 8 | 1 | 2 | 3 | 3 | 1 | 17 | 26 | 19 | 34 | 6 |
| VB01Z | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| VB02Z | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| VB03Z | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| VB04Z | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| VB05Z | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| VB06Z | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 |
| VB07Z | 1 | 2 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 3 | 2 | 1 | 0 |
| VB08Z | 6 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 2 | 8 | 0 |
| VB09Z | 35 | 42 | 39 | 16 | 8 | 0 | 0 | 0 | 2 | 1 | 10 | 21 | 14 | 25 | 6 |
| VB11Z | 0 | 3 | 4 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mean | 98.97 | 94.48 | 96.66 | 87.03 | 82.98 | 210.42 | 227.58 | 233.30 | 137.06 | 114.01 | 132.35 | 122.03 | 124.62 | 124.43 | 114.01 |
| SE | 2.46 | 2.81 | 2.97 | 3.50 | 5.56 | – | 17.16 | 11.44 | 23.04 | – | 5.84 | 3.39 | 4.33 | 3.36 | 0.00 |
| Median | 91.47 | 91.47 | 91.47 | 91.47 | 91.47 | 210.42 | 227.58 | 244.74 | 114.01 | 114.01 | 114.01 | 114.01 | 114.01 | 114.01 | 114.01 |
| Min. | 57.52 | 57.52 | 57.52 | 57.52 | 57.52 | 210.42 | 210.42 | 210.42 | 114.01 | 114.01 | 114.01 | 114.01 | 114.01 | 91.47 | 114.01 |
| Max. | 142.92 | 190.71 | 142.92 | 130.76 | 91.47 | 210.42 | 244.74 | 244.74 | 183.14 | 114.01 | 183.14 | 162.06 | 162.06 | 162.06 | 114.01 |
| ED treatment and investigation costs (£): sensitivity analysis using lower interquartile limit for ED treatments and investigations | |||||||||||||||
| Mean | 84.55 | 80.47 | 83.32 | 73.67 | 69.39 | 180.67 | 182.78 | 183.48 | 119.87 | 101.09 | 114.67 | 107.04 | 108.77 | 108.29 | 101.09 |
| SE | 2.17 | 2.27 | 2.73 | 3.42 | 5.93 | – | 2.11 | 1.40 | 18.78 | – | 4.50 | 2.58 | 3.22 | 2.46 | 0.00 |
| Median | 78.45 | 78.45 | 78.45 | 78.45 | 78.45 | 180.67 | 182.78 | 183.48 | 119.87 | 101.09 | 114.67 | 107.04 | 108.77 | 108.29 | 101.09 |
| Min. | 42.21 | 42.21 | 42.21 | 42.21 | 42.21 | 180.67 | 180.67 | 180.67 | 101.09 | 101.09 | 101.09 | 101.09 | 101.09 | 78.45 | 101.09 |
| Max. | 123.29 | 147.28 | 123.29 | 112.61 | 78.45 | 180.67 | 184.88 | 184.88 | 157.43 | 114.19 | 157.43 | 138.73 | 138.73 | 138.73 | 101.09 |
| ED treatment and investigation costs (£): sensitivity analysis using upper interquartile limit for ED treatments and investigations | |||||||||||||||
| Mean | 111.15 | 105.76 | 108.29 | 97.76 | 92.78 | 227.19 | 251.67 | 259.83 | 148.10 | 119.00 | 142.84 | 129.20 | 132.77 | 133.50 | 119.00 |
| SW | 2.76 | 2.94 | 3.17 | 3.92 | 6.49 | – | 24.48 | 16.32 | 29.10 | – | 7.54 | 4.30 | 5.61 | 4.22 | 0.00 |
| Median | 102.69 | 102.69 | 102.69 | 102.69 | 102.69 | 227.19 | 251.67 | 276.15 | 119.00 | 119.00 | 119.00 | 119.00 | 119.00 | 119.00 | 119.00 |
| Min. | 63.03 | 63.03 | 63.03 | 63.03 | 63.03 | 227.19 | 227.19 | 119.00 | 119.00 | 119.00 | 119.00 | 119.00 | 119.00 | 102.69 | 119.00 |
| Max. | 156.99 | 203.33 | 156.99 | 145.94 | 102.69 | 227.19 | 276.15 | 278.68 | 206.29 | 148.91 | 206.29 | 178.68 | 178.68 | 178.68 | 119.00 |
| Variable | Falls | Poisonings | Scalds | ||
|---|---|---|---|---|---|
| On one level | On stairs | From furniture | |||
| Admissions | |||||
| Number of cases | 1 | 3 | 3 | 3 | 3 |
| Admission for 1–2 days | 0 | 3 | 3 | 3 | 2 |
| Admission for > 2 days | 1 | 0 | 0 | 0 | 1 |
| Costs (£) | |||||
| Mean | 2461 | 586 | 586 | 586 | 1211 |
| SE | – | – | – | – | 625 |
| Median | 2461 | 586 | 586 | 586 | 586 |
| Min. | 2461 | 586 | 586 | 586 | 586 |
| Max. | 2461 | 586 | 586 | 586 | 2461 |
| Variable | Cost per child by injury mechanism (£) | ||||
|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | |||
| On one level | On stairs | From furniture | |||
| Number of responders | 64 | 77 | 75 | 57 | 15 |
| Admission for 0–1 day | |||||
| Mean | 586 | 586 | 586 | 586 | 586 |
| SE | 0 | 0 | 0 | 0 | 0 |
| Median | 586 | 586 | 586 | 586 | 586 |
| Min. | 586 | 586 | 586 | 586 | 586 |
| Max. | 586 | 586 | 586 | 586 | 586 |
| Admission for ≥ 2 days | |||||
| Mean | 2461 | 2461 | 2461 | 2461 | 2461 |
| SE | – | – | – | – | – |
| Median | 2461 | 2461 | 2461 | 2461 | 2461 |
| Min. | 2461 | 2461 | 2461 | 2461 | 2461 |
| Max. | 2461 | 2461 | 2461 | 2461 | 2461 |
| GP visits | |||||
| Mean | 2.75 | 2.06 | 0 | 0.2 | 2.33 |
| SE | 2.75 | 1.27 | 0 | 0.2 | 1.68 |
| Median | 0 | 0 | 0 | 0 | 0 |
| Min. | 0 | 0 | 0 | 0 | 0 |
| Max. | 176 | 88 | 0 | 11.63 | 23.25 |
| Outpatient visits | |||||
| Mean | 6.52 | 16.82 | 16.68 | 0 | 70.93 |
| SE | 3.70 | 6.93 | 5.88 | 0 | 32.52 |
| Median | 0 | 0 | 0 | 0 | 0 |
| Min. | 0 | 0 | 0 | 0 | 0 |
| Max. | 139 | 278 | 278 | 0 | 417 |
| Health visitor | |||||
| Mean | 0.74 | 0.13 | 0.28 | 1.19 | 1.40 |
| SE | 0.47 | 0.09 | 0.28 | 0.63 | 1.40 |
| Median | 0 | 0 | 0 | 0 | 0 |
| Min. | 0 | 0 | 0 | 0 | 0 |
| Max. | 21 | 5.09 | 21 | 21 | 21 |
| Subsequent inpatient daysa | |||||
| Mean | 0 | 0 | 7.81 | 0 | 78.13 |
| SE | 0 | 0 | 7.81 | 0 | 78.13 |
| Median | 0 | 0 | 0 | 0 | 0 |
| Min. | 0 | 0 | 0 | 0 | 0 |
| Max. | 0 | 0 | 586 | 0 | 1172 |
| Prescribed medication | |||||
| Mean | 0.16 | 0.1 | 0.05 | 0.03 | 2.39 |
| SE | 0.08 | 0.05 | 0.03 | 0.03 | 1.18 |
| Median | 0 | 0 | 0 | 0 | 0 |
| Min. | 0 | 0 | 0 | 0 | 0 |
| Max. | 3.64 | 2.23 | 2.23 | 1.75 | 13.12 |
| Variable: total health-care costs | Cost per child by injury mechanism (£) | ||||
|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | |||
| On one level | On stairs | From furniture | |||
| Admitted overnight | |||||
| Number of responders | 1 | 2 | 3 | 3 | 1 |
| Mean | 2810.42 | 2688.96 | 2988.67 | 2598.05 | 2588.13 |
| SE | – | 16.80 | 227.60 | 23.04 | – |
| Median | 2810.42 | 2688.94 | 2861.61 | 2575.01 | 2588.13 |
| Min. | 2810.42 | 2672.14 | 2673.65 | 2575.01 | 2588.13 |
| Max. | 2810.42 | 2705.74 | 3430.74 | 2644.14 | 2588.13 |
| Admitted for observation | |||||
| Number of responders | 17 | 26 | 19 | 34 | 6 |
| Mean | 719.59 | 746.55 | 735.48 | 725.47 | 1010.92 |
| SE | 5.73 | 17.33 | 13.73 | 7.99 | 231.22 |
| Median | 700.01 | 700.73 | 700.01 | 677.47 | 781.14 |
| Min. | 700.01 | 700.01 | 700.01 | 677.47 | 702.24 |
| Max. | 769.14 | 1026.06 | 850.11 | 855.88 | 2150.01 |
| Not admitted | |||||
| Number of responders | 46 | 49 | 53 | 20 | 8 |
| Mean | 119.91 | 114.99 | 126.80 | 96.71 | 178.10 |
| SE | 9.93 | 10.37 | 11.12 | 7.81 | 52.00 |
| Median | 91.47 | 91.47 | 91.47 | 91.47 | 114.35 |
| Min. | 57.52 | 57.52 | 57.52 | 57.52 | 57.52 |
| Max. | 437.79 | 474.69 | 437.79 | 227.27 | 508.47 |
| Sensitivity analysis | Cost per child by injury mechanism (£) | ||||
|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | |||
| On one level | On stairs | From furniture | |||
| Sensitivity analysis using lower limit | |||||
| Admitted overnight | |||||
| Number of responders | 1 | 2 | 3 | 3 | 1 |
| Mean | 2090.67 | 1954.14 | 2169.19 | 1890.87 | 1885.21 |
| SE | – | 1.74 | 159.58 | 18.78 | – |
| Median | 2090.67 | 1954.14 | 2072.78 | 1872.09 | 1885.21 |
| Min. | 2090.67 | 1952.39 | 1958.9 | 1872.09 | 1885.21 |
| Max. | 2090.67 | 1955.88 | 2480.88 | 1928.43 | 1885.21 |
| Admitted for observation | |||||
| Number of responders | 17 | 26 | 19 | 34 | 6 |
| Mean | 501.91 | 526.57 | 515.53 | 505.89 | 724.84 |
| SE | 4.44 | 16.40 | 11.40 | 6.04 | 166.02 |
| Median | 487.09 | 487.09 | 487.09 | 487.09 | 568.22 |
| Min. | 487.09 | 487.09 | 487.09 | 464.45 | 489.32 |
| Max. | 543.43 | 802.73 | 654.82 | 603.99 | 1537.09 |
| Not admitted | |||||
| Number of responders | 46 | 49 | 53 | 20 | 8 |
| Mean | 102.83 | 99.65 | 109.52 | 81.40 | 159.63 |
| SE | 8.73 | 9.65 | 10.06 | 6.18 | 51.37 |
| Median | 78.45 | 78.45 | 78.45 | 78.45 | 101.33 |
| Min. | 42.21 | 42.21 | 42.21 | 42.21 | 42.21 |
| Max. | 379.19 | 435.42 | 379.19 | 176.23 | 495.45 |
| Sensitivity analysis using upper limit | |||||
| Admitted overnight | |||||
| Number of responders | 1 | 2 | 3 | 3 | 1 |
| Mean | 3231.19 | 3117.03 | 3461.05 | 3013.1 | 2997.12 |
| SE | – | 24.12 | 261.82 | 29.10 | – |
| Median | 3231.19 | 3117.03 | 3320.58 | 2984 | 2997.12 |
| Min. | 3231.19 | 3092.91 | 3094.42 | 2984 | 2997.12 |
| Max. | 3231.29 | 3141.15 | 3968.15 | 3071.29 | 2997.12 |
| Admitted for observation | |||||
| Number of responders | 17 | 26 | 19 | 34 | 6 |
| Mean | 832.07 | 857.53 | 848.12 | 838.62 | 1155.84 |
| SE | 7.39 | 18.12 | 15.49 | 9.32 | 264.52 |
| Median | 807.00 | 807.72 | 807.00 | 807.00 | 888.13 |
| Min. | 807.00 | 807.00 | 807.00 | 790.69 | 809.23 |
| Max. | 894.29 | 1144.68 | 1002.21 | 986.43 | 2461.00 |
| Not admitted | |||||
| Number of responders | 43 | 49 | 53 | 20 | 8 |
| Mean | 133.56 | 126.86 | 140.21 | 108.62 | 190.83 |
| SE | 10.70 | 10.64 | 11.77 | 9.02 | 52.85 |
| Median | 102.69 | 102.69 | 102.69 | 102.69 | 102.69 |
| Min. | 63.03 | 63.03 | 63.03 | 63.03 | 63.03 |
| Max. | 475.42 | 491.35 | 475.42 | 261.28 | 519.69 |
| Non-health-care resource use categories | Resource use by injury mechanism, n (%) | ||||
|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | |||
| On one level | On stairs | From furniture | |||
| Number of responders | 70 | 77 | 87 | 59 | 21 |
| Taking over-the-counter medication | 31 (44) | 31 (40) | 29 (33) | 3 (5) | 11 (52) |
| Purchased aids or equipmenta | 9 (13) | 19 (25) | 12 (14) | 12 (20) | 4 (19) |
| Incurred travel costs | 6 (9) | 7 (9) | 7 (8) | 5 (8) | 3 (14) |
| Incurred time off work | 7 (10) | 15 (19) | 13 (15) | 9 (15) | 6 (29) |
| Injured child | |||||
| In formal child care | 0 (0) | 1 (0) | 1 (1) | 0 (0) | 0 (0) |
| In informal child care | 12 (17) | 17 (22) | 13 (15) | 7 (12) | 6 (29) |
| Other children | |||||
| In formal child care | 19 (27) | 22 (29) | 29 (33) | 25 (42) | 10 (47) |
| In informal child care | 0 (0) | 2 (3) | 1 (1) | 0 (0) | 1 (5) |
| Non-health-care cost categories | Cost per child by injury mechanism (£) | ||||
|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | |||
| On one level | On stairs | From furniture | |||
| Number of responders | 70 | 77 | 87 | 59 | 21 |
| Over-the-counter medication | |||||
| Mean | 2.29 | 2.2 | 2.32 | 0.17 | 5.49 |
| SE | 0.32 | 0.33 | 0.38 | 0.12 | 2.25 |
| Median | 0.00 | 0.00 | 0.00 | 0.00 | 3.99 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 8.88 | 9.78 | 17.76 | 4.89 | 47.01 |
| Aids | |||||
| Mean | 0.07 | 3.47 | 0.62 | 1.83 | 1.14 |
| SE | 0.07 | 1.48 | 0.33 | 1.31 | 0.96 |
| Median | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 4.80 | 100.00 | 20.00 | 75.88 | 20.00 |
| Formal child care | |||||
| Mean | 0.00 | 5.47 | 4.10 | 0.00 | 0.77 |
| SE | 0.00 | 4.26 | 3.96 | 0.00 | 0.77 |
| Median | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 0.00 | 320.08 | 344.39 | 0.00 | 16.21 |
| Informal child care | |||||
| Mean | 17.40 | 20.88 | 44.15 | 27.80 | 91.01 |
| SE | 5.95 | 5.63 | 11.71 | 9.01 | 36.42 |
| Median | 0.00 | 0.00 | 0.00 | 0.00 | 22.84 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 363.32 | 228.40 | 589.73 | 498.44 | 671.40 |
| Time off work | |||||
| Mean | 8.90 | 22.79 | 19.73 | 22.2 | 78.36 |
| SE | 3.40 | 6.96 | 5.63 | 7.67 | 33.21 |
| Median | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 111.44 | 334.32 | 229.04 | 222.88 | 572.60 |
| Travel | |||||
| Mean | 0.52 | 0.70 | 0.61 | 0.92 | 0.95 |
| SE | 0.29 | 0.27 | 0.26 | 0.68 | 0.55 |
| Median | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 17.40 | 12.58 | 14.47 | 39.40 | 8.40 |
| Total | |||||
| Mean | 29.18 | 57.52 | 71.42 | 52.92 | 177.73 |
| SE | 6.69 | 10.62 | 13.48 | 11.78 | 50.03 |
| Median | 4.89 | 12.58 | 14.47 | 17.13 | 33.44 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 367.31 | 412.14 | 605.30 | 498.44 | 699.55 |
| Non-health-care cost categories | Cost per child by injury mechanism (£) | ||||
|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | |||
| On one level | On stairs | From furniture | |||
| Admitted overnight | |||||
| Number of responders | 2 | 3 | 4 | 3 | 3 |
| Mean | 213.17 | 177.68 | 99.16 | 284.77 | 399.17 |
| SE | 154.14 | 112.44 | 31.27 | 122.01 | 161.77 |
| Median | 213.17 | 68.52 | 108.69 | 279.98 | 397.32 |
| Min. | 59.03 | 61.99 | 14.47 | 75.88 | 119.91 |
| Max. | 367.31 | 402.54 | 164.8 | 498.44 | 680.29 |
| Admitted for observation | |||||
| Number of responders | 16 | 24 | 21 | 37 | 7 |
| Mean | 38.14 | 73.73 | 65.41 | 52.76 | 199.51 |
| SE | 12.74 | 17.15 | 20.71 | 11.63 | 74.45 |
| Median | 4.89 | 30.81 | 8.88 | 22.84 | 4.89 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 145.70 | 228.40 | 266.84 | 277.84 | 474.43 |
| Not admitted | |||||
| Number of responders | 46 | 46 | 57 | 17 | 9 |
| Mean | 17.58 | 37.45 | 68.26 | 17.91 | 48.21 |
| SE | 4.67 | 11.15 | 18.10 | 8.34 | 28.36 |
| Median | 4.89 | 6.89 | 8.88 | 0.00 | 4.89 |
| Min. | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Max. | 116.33 | 412.14 | 605.30 | 123.05 | 239.38 |
| Total health-care and non-health-care cost categories | Cost per child by injury mechanism (£) | ||||
|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | |||
| On one level | On stairs | From furniture | |||
| Admitted overnight | |||||
| Number of responders | 1 | 2 | 3 | 3 | 1 |
| Mean | 3177.73 | 2921.21 | 3065.95 | 2882.82 | 2708.04 |
| SE | – | 153.48 | 252.61 | 142.62 | – |
| Median | 3177.73 | 2921.21 | 2964.39 | 2854.99 | 2708.04 |
| Min. | 3177.73 | 2767.73 | 2688.12 | 2,650.89 | 2708.04 |
| Max. | 3177.73 | 3074.68 | 3545.33 | 3142.58 | 2708.04 |
| Admitted for observation | |||||
| Number of responders | 14 | 24 | 19 | 34 | 6 |
| Mean | 754.14 | 817.57 | 800.97 | 780.70 | 1191.90 |
| SE | 17.77 | 27.64 | 28.15 | 16.90 | 249.19 |
| Median | 732.23 | 731.58 | 725.90 | 731.42 | 971.52 |
| Min. | 704.00 | 700.01 | 700.01 | 700.01 | 734.68 |
| Max. | 914.84 | 1126.32 | 1097.58 | 1133.72 | 2314.81 |
| Not admitted | |||||
| Number of responders | 44 | 44 | 49 | 17 | 7 |
| Mean | 135.95 | 154.62 | 197.07 | 115.55 | 224.59 |
| SE | 12.08 | 17.87 | 26.49 | 12.20 | 70.34 |
| Median | 102.77 | 98.36 | 107.78 | 96.36 | 212.72 |
| Min. | 57.52 | 71.40 | 71.40 | 57.52 | 57.52 |
| Max. | 498.33 | 555.06 | 1043.08 | 227.27 | 513.36 |
The results in Tables 50–57 show that the burden of injury, especially on families (i.e. non-health-care costs), can be considerable, even for injuries that were treated in the ED and did not require admission. Table 57 shows that for non-admitted children, non-health-care costs can be as high as £600, although the median values across injury mechanisms were all < £10.
For children admitted for treatment (as opposed to observation), costs to families (i.e. non-health-care costs) are much higher, with scalds being the most ‘expensive’ injuries – the median cost is almost £400 and the maximum is £680 (see Table 57). It should be noted that these costs are based on responses from only three parents.
By far the largest components of the non-health-care costs were informal child care and time off work, ranging up to £670 for child care and £570 for time off work (see Table 56). However, the median costs of these components were zero in both cases, except for informal care for scalds (£22.84).
The total non-health-care costs were highest for scalds (mean £177), with a maximum of almost £700 (see Table 56). Falls from furniture were the most expensive falls (mean £71, maximum £605).
Falls can also be high-cost injuries (see Table 53) for the health sector, with total health-care costs per child ranging up to £2989 for falls from furniture. Note that in Table 52 one child incurred an inpatient stay of 15 days costing £2461 following a fall from furniture; however, because of missing responses on the self-completion questionnaire, it was not possible to obtain a total health-care cost for this child (i.e. they do not contribute a cost to Table 53). Similarly, a child who incurred a high inpatient cost of £2720 following a scald (see Table 51) was subsequently excluded from the total health-care cost calculations (see Table 53). Repeated outpatient visits and the costs associated with readmissions contribute to high health-sector costs for scalds (see Table 52).
Among children not admitted after their initial visit to the ED, health-care costs are typically between £100 and £200 (see Table 53), with scalds being slightly more expensive than other injuries.
NHS and non-NHS costs were not found to be correlated with deprivation (Figure 9), although there was some evidence that participants on benefits on average had lower non-NHS costs than those not on benefits (Figure 10). NHS and non-NHS costs by injury mechanism were similar across study centres, except for Newcastle, which was difficult to compare because of the low number of participants recruited (n = 19) (Figure 11).
FIGURE 9.
Scatterplots of costs against IMD score: (a) health-care costs; and (b) non-health-care costs. Reproduced with permission from Cooper NJ, Kendrick D, Timblin C, Hayes M, Majsak-Newman G, Meteyard K, Hawkins A, Kay B. The short-term cost of falls, poisonings and scalds occurring at home in children under 5 years old in England: multicentre longitudinal study. Injury Prevention 2016; [published online first 29 January 2016] http://dx.doi.org/10.1136/injuryprev-2015-041808. 203 Copyright © 2015 by the BMJ Publishing Group Ltd. All rights reserved.


FIGURE 10.
Box plots of health-care and non-health-care costs by benefit status. Reproduced with permission from Cooper NJ, Kendrick D, Timblin C, Hayes M, Majsak-Newman G, Meteyard K, Hawkins A, Kay B. The short-term cost of falls, poisonings and scalds occurring at home in children under 5 years old in England: multicentre longitudinal study. Injury Prevention 2016; [published online first 29 January 2016] http://dx.doi.org/10.1136/injuryprev-2015-041808. 203 Copyright © 2015 by the BMJ Publishing Group Ltd. All rights reserved.
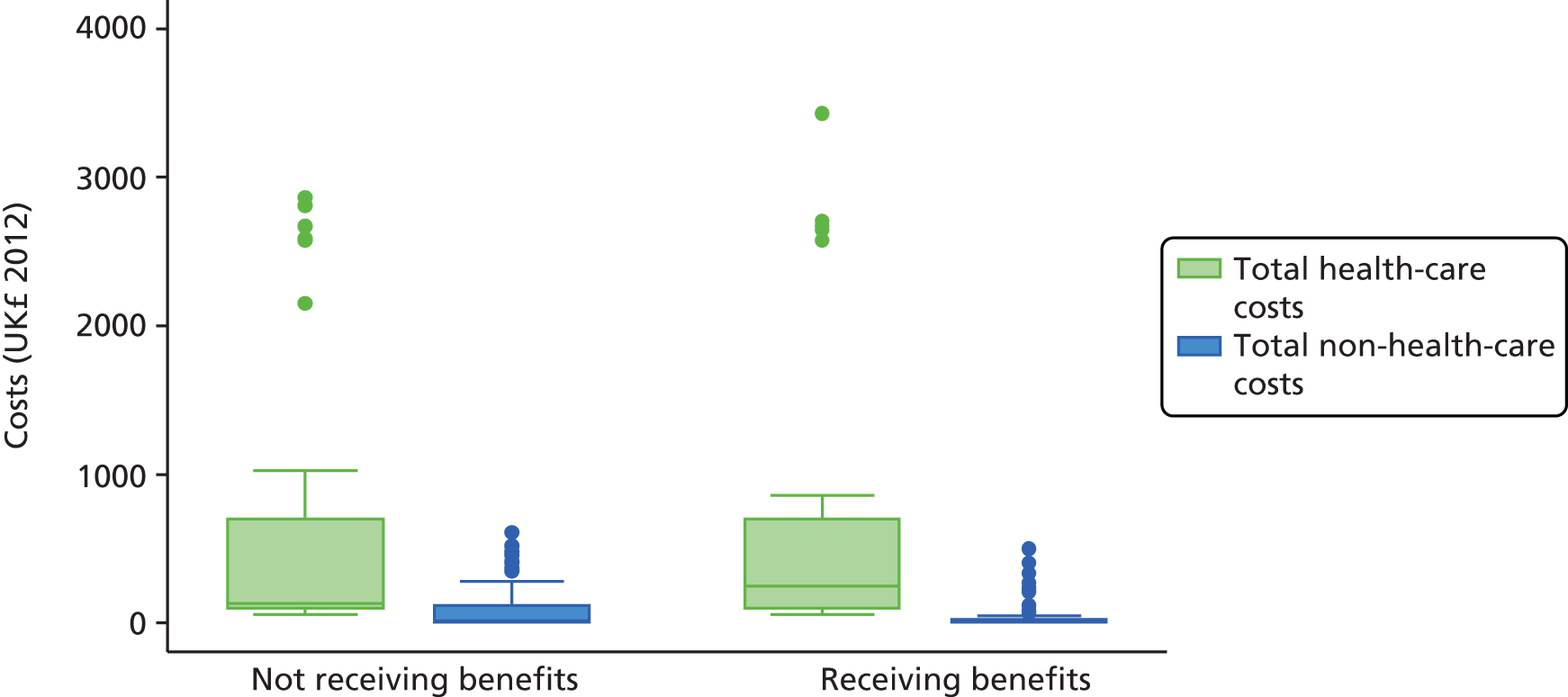
FIGURE 11.
Box plots of health-care and non-health-care costs by study centre. Reproduced with permission from Cooper NJ, Kendrick D, Timblin C, Hayes M, Majsak-Newman G, Meteyard K, Hawkins A, Kay B. The short-term cost of falls, poisonings and scalds occurring at home in children under 5 years old in England: multicentre longitudinal study. Injury Prevention 2016; [published online first 29 January 2016] http://dx.doi.org/10.1136/injuryprev-2015-041808. 203 Copyright © 2015 by the BMJ Publishing Group Ltd. All rights reserved.

The multiple imputation model used the cost component-level data together with socioeconomic and injury data to estimate the total NHS and non-NHS costs for all participants. Table 59 shows the number of households with complete and missing cost data as well as socioeconomic and injury characteristics. The imputed results (Table 60) are comparable to the complete-case analysis with the exception of the mean cost of falls on one level (£2022, SE £1177) and falls from furniture (£2448, SE £651) for those children admitted overnight. This is likely because of the small number of children in all admitted overnight injury categories, resulting in substantial uncertainty in the mean cost estimates, portrayed by the large SEs.
| Variable | Number of households | |
|---|---|---|
| Complete data | Missing | |
| Cost component | ||
| A&E treatments and investigations | 312 | 32 |
| Inpatient stay (admitted to A&E) | 339 | 5 |
| Other A&E costs | 344 | 0 |
| Outpatient stay | 319 | 25 |
| Inpatient stay | 344 | 0 |
| Health visitor visits | 326 | 18 |
| GP visits | 331 | 13 |
| Prescribed medication | 341 | 3 |
| Dental care | 344 | 0 |
| Over-the-counter medication | 338 | 6 |
| Aids | 338 | 6 |
| Professional care | 344 | 0 |
| Care provided by relatives | 340 | 4 |
| Time off usual activities | 329 | 15 |
| Time off work | 339 | 5 |
| Travel to A&E | 344 | 0 |
| Travel to hospital | 319 | 25 |
| Travel to general practice | 331 | 13 |
| Travel to other appointments | 325 | 19 |
| Socioeconomic and injury characteristics | ||
| Age | 344 | 0 |
| Sex | 344 | 0 |
| IMD score | 344 | 0 |
| Injury mechanism | 344 | 0 |
| Distance from hospital | 344 | 0 |
| VAS score | 333 | 11 |
| Hours cared for out of home | 321 | 23 |
| Mean behaviour score | 321 | 23 |
| Total HADS score | 331 | 13 |
| Single parent household | 330 | 14 |
| Mother aged ≤ 19 years at first birth | 325 | 19 |
| Ethnicity | 332 | 12 |
| Study centre | 344 | 0 |
| Total health-care and non-health-care cost categories | Cost per child by injury mechanism (£), mean (SE) | ||||
|---|---|---|---|---|---|
| Falls | Poisonings | Scalds | |||
| On one level | On stairs | From furniture | |||
| Admitted overnight | |||||
| Number of responders | 2 | 3 | 4 | 3 | 3 |
| NHS costs | 1808.79 (1021.58) | 2681.52 (22.65) | 2349.11 (667.69) | 2598.06 (23.04) | 2612.66 (47.96) |
| Non-NHS costs | 213.17 (154.14) | 177.68 (112.44) | 99.16 (31.27) | 284.77 (122.01) | 400.54 (162.84) |
| Total costs | 2021.96 (1173.10) | 2859.21 (109.81) | 2448.27 (651.39) | 2882.82 (142.62) | 3013.20 (181.21) |
| Admitted for observation | |||||
| Number of responders | 19 | 26 | 21 | 37 | 8 |
| NHS costs | 737.49 (16.37) | 746.55 (17.32) | 755.43 (21.26) | 724.94 (7.63) | 945.74 (176.03) |
| Non-NHS costs | 42.92 (14.88) | 72.32 (16.07) | 65.42 (20.71) | 52.78 (11.63) | 190.11 (71.74) |
| Total costs | 780.41 (24.82) | 818.87 (26.07) | 820.85 (32.38) | 777.71 (15.83) | 1135.85 (190.93) |
| Not admitted | |||||
| Number of responders | 50 | 52 | 66 | 21 | 10 |
| NHS costs | 131.29 (15.71) | 124.65 (9.82) | 124.65 (9.59) | 97.49 (8.62) | 164.32 (42.21) |
| Non-NHS costs | 21.25 (5.67) | 35.59 (10.08) | 64.51 (15.97) | 16.96 (8.03) | 44.48 (25.70) |
| Total costs | 152.55 (18.12) | 150.25 (15.49) | 189.02 (20.85) | 114.44 (11.67) | 208.80 (51.69) |
Discussion
Main findings
This study sought to expand on current knowledge about the burden on the health service and families of unintentional injuries to children aged < 5 years in the home.
Of those who responded to the initial resource use questionnaire, > 95% of their children were reported to have recovered from their injuries within 2 weeks and almost 99% within 1 month. As expected, children admitted overnight incurred the highest health-care costs as well as the highest family (non-health-care) costs including child care, travel and time off work, although these accounted for < 5% of the children in the sample. Hence, the distribution of health-care and non-health-care costs was highly skewed, with the majority of participants incurring only small to moderate costs but a few children incurring more substantial costs.
Specifically, the study provides data showing that, even for the families of children treated in the ED and not admitted to hospital for observation or treatment, there are significant costs, notably for child care and time off work. The study also showed that these costs vary by injury mechanism.
Strengths and limitations
As we expected children admitted to hospital to have higher health-care costs than those not admitted, we oversampled admissions to increase the precision of cost estimates in this group. Although 40% of our sample was admitted, most children were admitted only for observation, with only 4.3% admitted overnight. This is very similar to the proportion of under-fives attending an ED following an injury at home who were admitted to hospital in 2002 when the last national data were collected from the Home Accident Surveillance System (HASS) in UK EDs. 3 The proportion of children admitted for < 1 day in 2002 according to the HASS was only 0.6%,3 a figure much smaller than in our study. This difference may partly reflect the development of short-stay paediatric assessment units (SSPAUs), which provide assessment, investigation, observation and treatment for children with acute illnesses or injuries. 205 These are becoming increasingly common but are not yet provided by all hospitals. 206 The most common injuries admitted to SSPAUs are head injuries and ingestions. 207 The changing pattern of emergency paediatric service provision over recent years and the lack of national data on the proportion of ED attenders aged < 5 years who are admitted to inpatient wards or SSPAUs after an injury at home makes it difficult to assess the representativeness of our sample. However, it is likely that children admitted as inpatients or to SSPAUs are over-represented in our study. To our knowledge, there are no recent data available for the UK on the proportions of children admitted to hospital, admitted for observation or attending an ED but not admitted by injury type that we could use to weight our cost data to estimate total costs for each injury type. We have therefore analysed costs for admitted and non-admitted children separately. In addition, as we studied only five injury mechanisms, our findings are not generalisable beyond those injury mechanisms.
Our study population included children participating in the case–control studies in work stream 1 (see Chapter 2). They are likely to be children whose parents are more interested in child safety than the general population of parents of injured children. Furthermore, as this substudy focused on the costs of injuries, it is possible that parents who considered that they had incurred greater costs may have been more motivated to participate than those who considered that they incurred fewer costs. This may have resulted in an overestimation of the costs of injury in our study.
The numbers of participants in our study, especially when disaggregated by injury mechanism and admission status, could be very small. As a result of this, some cost estimates are imprecise.
Comparisons of treatments reported by parents with those recorded in medical records showed only fair or poor agreement for most questions asking parents about what treatments their children had received in the ED (assuming that medical record data are the ‘gold standard’). This may possibly be because of the ways in which information is understood by parents or because of the nature of the questions asked in this study. Even apparently straightforward questions relating to whether the parent received advice in the ED had low kappa values, as did the question about whether the child was observed in the ED. With the advent of SSPAUs, it is understandable that parents may find it hard to distinguish between admission to an inpatient ward and admission to a SSPAU. Further refinement of questions to measure resource use in this area is needed. For the 42 individuals with complete data in the validation sample, the mean ED treatment and investigation costs were estimated to be £137 based on medical record data and £111 based on parents’ responses to the self-completion questionnaire. This suggests that using parent-reported health-care costs may lead to a relatively small underestimation of actual costs to the NHS, assuming that medical record data are the ‘gold standard’.
Comparison with other studies
It is difficult to compare the findings of this study with the results of other studies for a number of reasons: differences in study populations or health-care services or the tendency to look solely at health-care costs, specific types of (usually) more severe injuries or those with long-term consequences or other age ranges. 11,119,122,124,125,138,140 However, one study, that by Griffiths et al. ,139 noted that an uncomplicated hot drink scald can result in health-care costs of £1850, a figure not dissimilar to our finding for the maximum cost of an admission for observation for a scald. We have been unable to find any studies reporting the costs to families of home injuries in the under-fives with which to compare our findings. Our study, and the lack of other published studies, highlights the importance of measuring the cost of both major and minor childhood injuries, caused by a variety of mechanisms, to inform evidence-based policy making for injury prevention.
Chapter 4 What injury prevention interventions are being undertaken by children’s centres to prevent thermal injuries, falls and poisonings? Children’s centres’ use of injury prevention interventions: two cross-sectional national surveys (work stream 3)
Abstract
Research question
What interventions are being undertaken by children’s centres to prevent thermal injuries, falls and poisonings?
Methods
Two national postal surveys of children’s centre managers selected from all children’s centres in 30 PCTs across England were undertaken (study D). The surveys covered injury prevention activity, knowledge and attitudes towards injuries and their prevention, barriers to, and facilitators of, injury prevention and partnership working. The 2010 survey focused on fire-related injuries. The 2012 survey focused on falls, poisonings and scalds.
Results
The response rate was 56% (384/688) in the 2010 survey and 61% (517/843) in the 2012 survey. In both surveys, around 60% of children’s centres identified unintentional injuries as one of their three main priorities, although fewer than half had a written injury prevention strategy. Managers held positive attitudes towards injury prevention, but reported gaps in their knowledge. Two-thirds of centres had access to local home safety equipment schemes in 2010, but only 42% had access in 2012. Common barriers to injury prevention were lack of staff capacity, lack of funding and working with ‘hard-to-reach’ groups. Common facilitators were good relationships with families, working with other agencies, low-cost/free safety equipment schemes and trained and knowledgeable staff.
Conclusions
Most children’s centres do not have an evidence-based strategic approach to child injury prevention. To ensure effective injury prevention, children’s centres need support to plan, deliver and evaluate their activities.
Chapter summary
This work stream consisted of two national cross-sectional surveys of children’s centres. They were used to inform the development of an injury prevention intervention (an IPB) for delivery by children’s centres, which was evaluated using a RCT (study M in work stream 6) (see Chapter 7). So that information on the prevention of fire-related injuries was obtained in time to inform the design of the intervention, two surveys were undertaken. The first was conducted early in the KCS programme and covered fire-related injury. The second was conducted later in the KCS programme to inform the design of the second IPB for preventing thermal injuries, falls, poisonings and scalds. The relationship between the component studies in the KCS programme is shown in Figure 1.
Introduction
In 2007 the Audit Commission/Health Care Commission report Better Safe Than Sorry19 highlighted that unintentional injuries are a major public health threat for preschool children in England, but that many of those charged with developing and implementing local strategies to prevent unintentional injury found it difficult to do so, and that there was little evidence of a systematic approach to develop, implement and monitor programmes to prevent unintentional injuries in children.
To improve the health of children in England, centres providing children and families with a range of co-ordinated services from a variety of professionals were set up under the Sure Start scheme between 2004 and 2010. 208,209 These centres have the potential to improve home safety for children through the evidence-based Healthy Child Programme and the provision of advice on accident and injury prevention that forms part of their statutory guidance. 210 However, despite recent evaluations of the Sure Start programme, we currently know little about the extent to which children’s centres are fulfilling this role. 211–216 Study D describes and quantifies the injury prevention activities being undertaken by children’s centres across England.
Methods
The objective of the surveys undertaken in this study was to explore the activities being undertaken by children’s centres to prevent thermal injuries, falls and poisonings in children aged < 5 years. Two cross-sectional national surveys of children’s centres in England were undertaken. A survey of fire-related injury prevention took place in 2010,217 whereas the focus of the 2012 survey was the prevention of falls, poisonings and scalds. The 2010 study population consisted of managers of children’s centres in 30 PCTs [three in each of 10 strategic health authority (SHA) areas] across England. Two of the 30 PCTs had merged by 2012, so the 2012 study population consisted of managers of all children’s centres in 29 PCTs. When managers managed more than one centre, they were asked to complete a questionnaire for each centre.
The questionnaires included questions about the management and organisation of children’s centres, child health priority areas and injury prevention activities. We used questions from previous surveys when possible. 218–220 We assessed face validity by asking members of the Faculty of Medicine and Health Sciences at the University of Nottingham who were not injury prevention researchers to review the questionnaires. We checked content validity by asking injury prevention experts and the lay research adviser within the study group to review the questionnaire. 221 We used a variety of methods to enhance the reliability of questions, including adhering to the ‘principles of questionnaire design’,222 expert advice and piloting. 222,223 We piloted the questionnaires using managers from four children’s centres from PCTs across the country who were not part of the final sample. Minor changes were made to the questionnaires following piloting. Copies of the questionnaires are provided in Appendix 3.
Methods that have previously been shown in systematic reviews to increase response rates were used. These included using reminders, providing further questionnaires, keeping the questionnaires as short as possible, providing Freepost reply envelopes, providing an assurance of confidentiality, using the NHS logo on the envelope and questionnaire to try and influence saliency and using university logos on study documentation. 69,70 Questionnaires were sent out in March 2010 (fire-related injury prevention) and January 2012 (fall, poisoning and scald prevention). Three reminders were used to improve the response rate. 69,70 For the first survey, a random one in 10 sample of questionnaires was double entered and discrepancies identified and corrected. The data entry error rate was 0.19%. For the second survey, all data were double entered by an external data entry company and discrepancies identified and corrected. Data were analysed using Stata/SE 11.0 (StataCorp LP, College Station, TX, USA).
Sample size estimations, based on the prevalance of responses to questions on injury activity in primary care groups (PCGs),219 indicated that for an unclustered design, 196 responses would allow the prevalance of the following to be estimated with a maximum 95% CI of ±7%: unintentional injuries ranked as least important of a range of health topics (66%), taking action to prevent injuries (34%), having a written injury prevention strategy (29%) or believing that the organisation can be effective in preventing injuries (58%).
In 2010 there were 2918 children’s centres in England and 147 PCTs, giving an average of 20 children’s centres per PCT. Assuming a 65% response rate from children’s centres, based on health professionals’ response rates in previous similar surveys218–220 gave an average cluster size of 13 responses per PCT. The design effect to account for cluster sampling assuming an intraclass correlation coefficient (ICC) of 0.05 and an average cluster size of 13 is 1.6. Therefore, 314 responses were required from a total of 25 PCTs (n = 314/13). To ensure a national spread of children’s centres, PCTs were stratified by SHA (n = 10) and three PCTs were sampled at random within each SHA to give 30 PCTs in total. Questionnaires were sent to all children’s centres in those 30 PCTs. By the time of the 2012 survey, more children’s centres had been established and two PCTs had merged, so questionnaires were sent to all children’s centres in the 29 PCTs.
The majority of attitudinal questions required responses on a five-point Likert scale. For the purposes of analysis we combined the ‘strongly agree’ and ‘agree’ responses into an ‘agree’ category and the ‘disagree’ and ‘strongly disagree’ responses into a ‘disagree’ category. Responses to open questions were categorised by generating a coding list and assigning responses to categories. This was undertaken by two researchers working independently and any disagreements were handled by consensus-forming discussions. Categorical variables are described using frequencies and percentages. No adjustment for clustering has been made as these are purely descriptive statistics. Approval for the study was granted by North Nottinghamshire Research Ethics Committee (reference number 09/H0407/44).
Results
In the 2010 survey, 694 questionnaires were posted, five were returned undelivered and one recipient was no longer a children’s centre. The response rate was 56% (384/688). In the 2012 survey, 851 questionnaires were posted, eight were returned undelivered and, of the 526 returned, nine were blank, giving a response rate of 61% (517/843). The denominators vary for responses to individual questions presented in the following sections as not all respondents answered all questions.
Characteristics of children’s centres
Table 61 shows the characteristics of the children’s centres that participated in the 2010 and 2012 surveys. The percentage of respondents from phase 3 children’s centres increased between the 2010 and 2012 surveys, with a concomitant reduction in the percentages of respondents from phase 1 and phase 2 centres. Most centres were led (i.e. managed) by local authorities or education departments at both time points, with very few having a NHS lead. Responses were fairly evenly distributed across SHA areas in both the 2010 survey and the 2012 survey. In both surveys, a larger proportion of responses came from the South East Coast SHA (20% in 2010 and 19% in 2012).
| Characteristic | 2010 survey, n (%) | 2012 survey, n (%) |
|---|---|---|
| Phase | [6] | [31] |
| 1 (2004–6) | 148 (39) | 144 (30) |
| 2 (2006–8) | 203 (54) | 197 (41) |
| 3 (2008–10) | 24 (6) | 141 (29) |
| Lead agency | [28] | [54] |
| Local authority/education | 268 (75) | 334 (72) |
| Charity | 24 (7) | 59 (13) |
| NHS | 10 (3) | 10 (2) |
| SHA | ||
| East Midlands | 28 (7) | 58 (11) |
| East of England | 41 (11) | 69 (13) |
| London | 29 (8) | 43 (8) |
| North East | 32 (8) | 37 (7) |
| North West | 35 (9) | 36 (7) |
| South Central | 35 (9) | 43 (8) |
| South East Coast | 75 (20) | 98 (19) |
| South West | 39 (10) | 54 (10) |
| West Midlands | 25 (7) | 34 (7) |
| Yorkshire and the Humber | 45 (12) | 45 (9) |
Children’s centre priority areas and injury prevention strategies
Table 62 shows the priority afforded to injury prevention by children’s centres in 2010 and 2012. A similar percentage of respondents considered injury prevention to be among their three main child health priorities in 2010 (58%) and 2012 (60%). In 2010, 16% (59/374, 10 missing) placed injury prevention first whereas in 2012, 16% (80/485, 32 missing) placed injury prevention first. Fewer than half the respondents in 2010 (47%) and 2012 (42%) stated that their children’s centre had an injury prevention strategy, and most did not know if their PCT/local authority had an injury prevention strategy at each time point (61% for PCTs/local authorities in 2010, 65% for local authorities in 2012 and 74% for PCTs in 2012), as shown in Table 63.
| Priority areas | 2010, n (%) | 2012, n (%) |
|---|---|---|
| Unintentional injury prevention | 221 (58) | 308 (60) |
| Healthy diet/healthy lifestyle | 309 (81) | 410 (79) |
| Breastfeeding | 93 (24) | 189 (37) |
| Mental health/emotional well-being | 57 (15) | 91 (18) |
| Child protection | 42 (11) | 93 (18) |
| Dental health | 41 (11) | 36 (7) |
| Ante-/postnatal support | 39 (10) | 40 (8) |
| Smoking cessation support | 31 (8) | 25 (5) |
| Speech/language/literacy/communication support | – | 61 (12) |
| Immunisation | – | 30 (6) |
| Response | Your children’s centre, n (%) | Your PCT/local authority, n (%) | Your PCT, n (%) | Local authority, n (%) | |
|---|---|---|---|---|---|
| 2010 [32] | 2012 [49] | 2010 [30] | 2012 [62] | 2012 [42] | |
| Yes | 164 (47) | 198 (42) | 129 (36) | 100 (22) | 156 (33) |
| No | 153 (43) | 222 (47) | 11 (3) | 18 (4) | 11 (2) |
| Don’t know | 35 (10) | 48 (10) | 214 (60) | 337 (74) | 308 (65) |
Knowledge and attitudes
In the 2010 survey, the potential for improving knowledge was demonstrated as few (11%, 38/348) knew that the most common cause of death was choking and suffocation or that falls are the most common non-fatal injury (33%, 115/350). Respondents’ attitudes towards injury prevention from the 2010 survey are shown in Figure 12. Attitudes towards injury prevention were positive, with the majority believing that most child accidents were preventable (94%, 358/379) and that children’s centres could effectively prevent accidents (99%, 377/381) and most disagreeing that other agencies had greater responsibilities for preventing child accidents than children’s centres (64%, 244/379).
FIGURE 12.
Attitudes towards injury prevention among respondents. From Watson et al. 217 under the Creative Commons Attribution Non-Commercial 3.0 Unported License (see https://creativecommons.org/licenses/by-nc/3.0/).
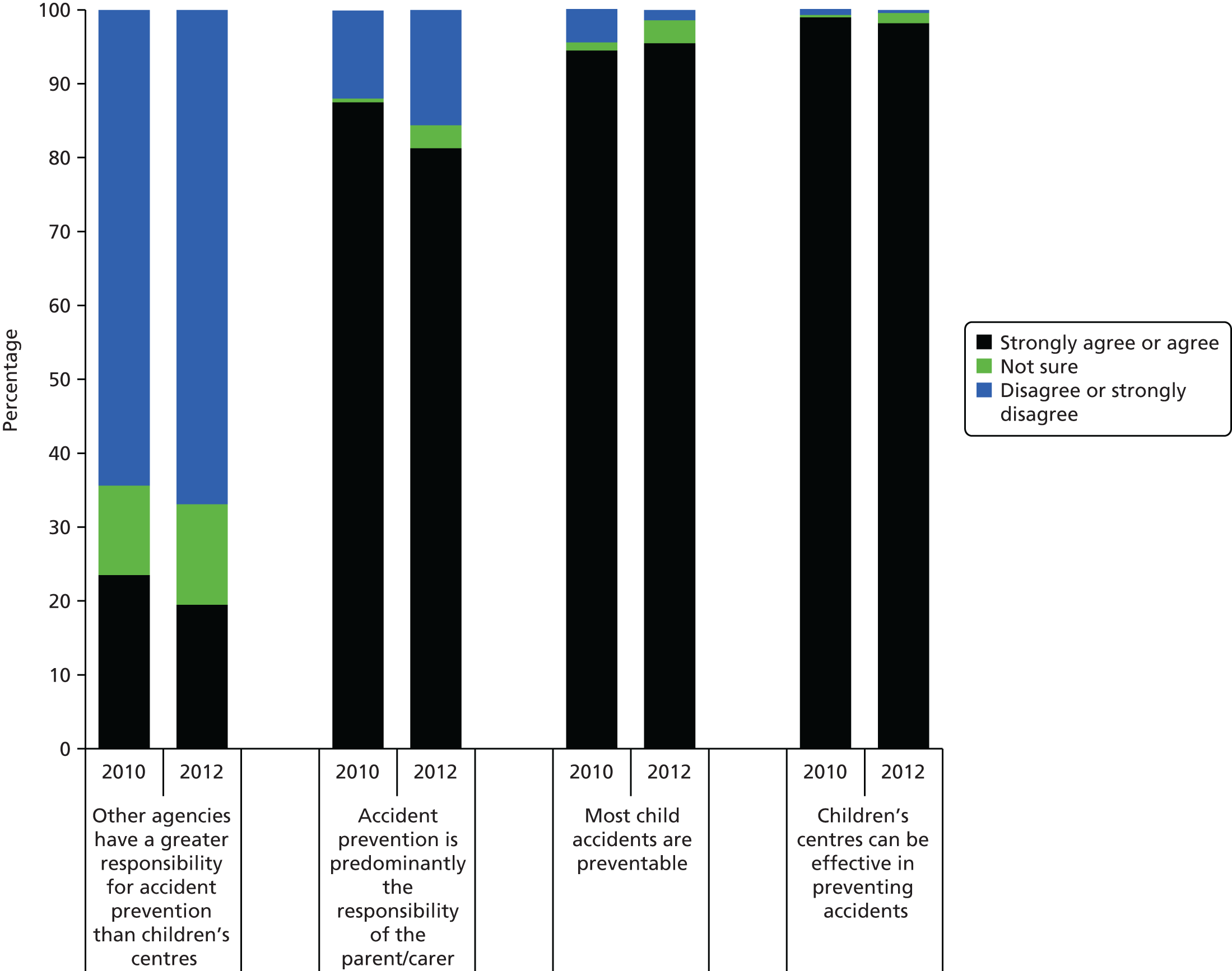
Respondent attitudes towards injury prevention from the 2012 survey are also shown in Figure 12 and are very similar to the findings from 2010. In the 2012 survey, knowledge of the main cause of child injury deaths in the under-fives in the home remained poor, with only 12% (51/435) knowing that most child injury deaths resulted from choking and suffocation and 47% (211/445) knowing that falls were the most common non-fatal injuries.
In the 2010 survey, respondents were more likely to think that providing home safety equipment (89%, 330/372), providing one-to-one (88%, 329/372) or group home safety advice (86%, 316/368) or media campaigns on home safety (69%, 256/371) would be more effective than providing leaflets without additional advice (40%, 150/376). The questions on the effectiveness of prevention activities were not asked in the 2012 survey.
Injury prevention activities
Injury prevention activities in 2010 and 2012 are shown in Figure 13. In the 2010 survey, 97% (364/376) of centres were involved in some form of injury prevention including displaying posters on child safety (97%, 371/382), participating in Child Safety Week (93%, 348/376), inviting outside speakers to talk to parents (78%, 293/378), collecting data on child accidents (56%, 205/365), lobbying or campaigning on child safety issues (34%, 122/364), working with local media (17%, 63/372) or issuing first aid kits (15%, 55/375). The involvement in injury prevention in 2012 was very similar to that in 2010.
FIGURE 13.
Injury prevention activities undertaken by children’s centres.
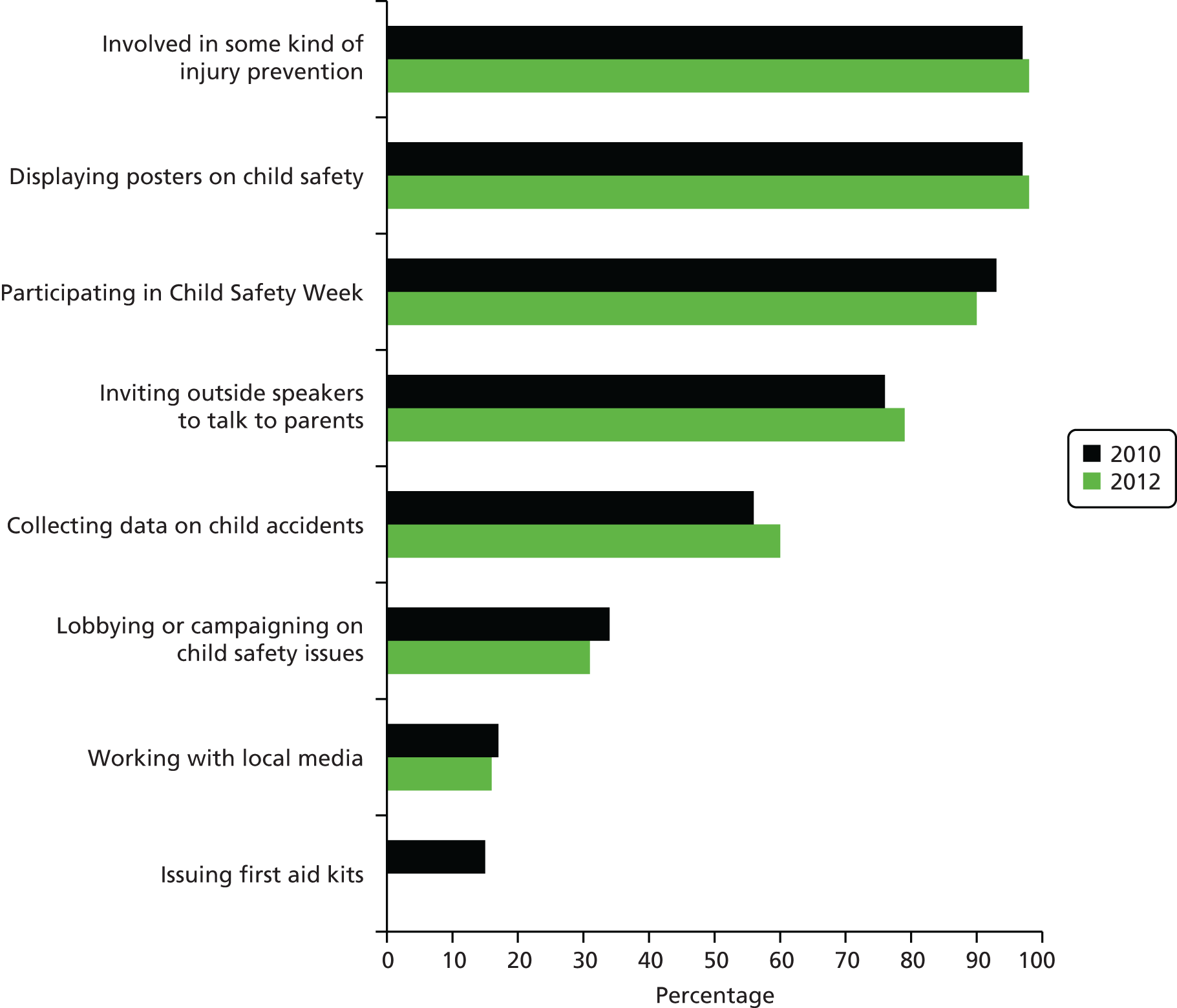
Centres provided advice on a range of fire-related injury prevention topics (Figure 14). Advice was most commonly provided on general fire safety, smoking cessation and bonfire and firework safety and least commonly on barbecue safety, candle safety, handling hot irons and making fire escape plans. Providing leaflets was the approach most commonly used to address most of these topics.
FIGURE 14.
Advice provided by children’s centres on fire prevention (2010 survey). From Watson et al. 217 under the Creative Commons Attribution Non-Commercial 3.0 Unported License (see https://creativecommons.org/licenses/by-nc/3.0/).
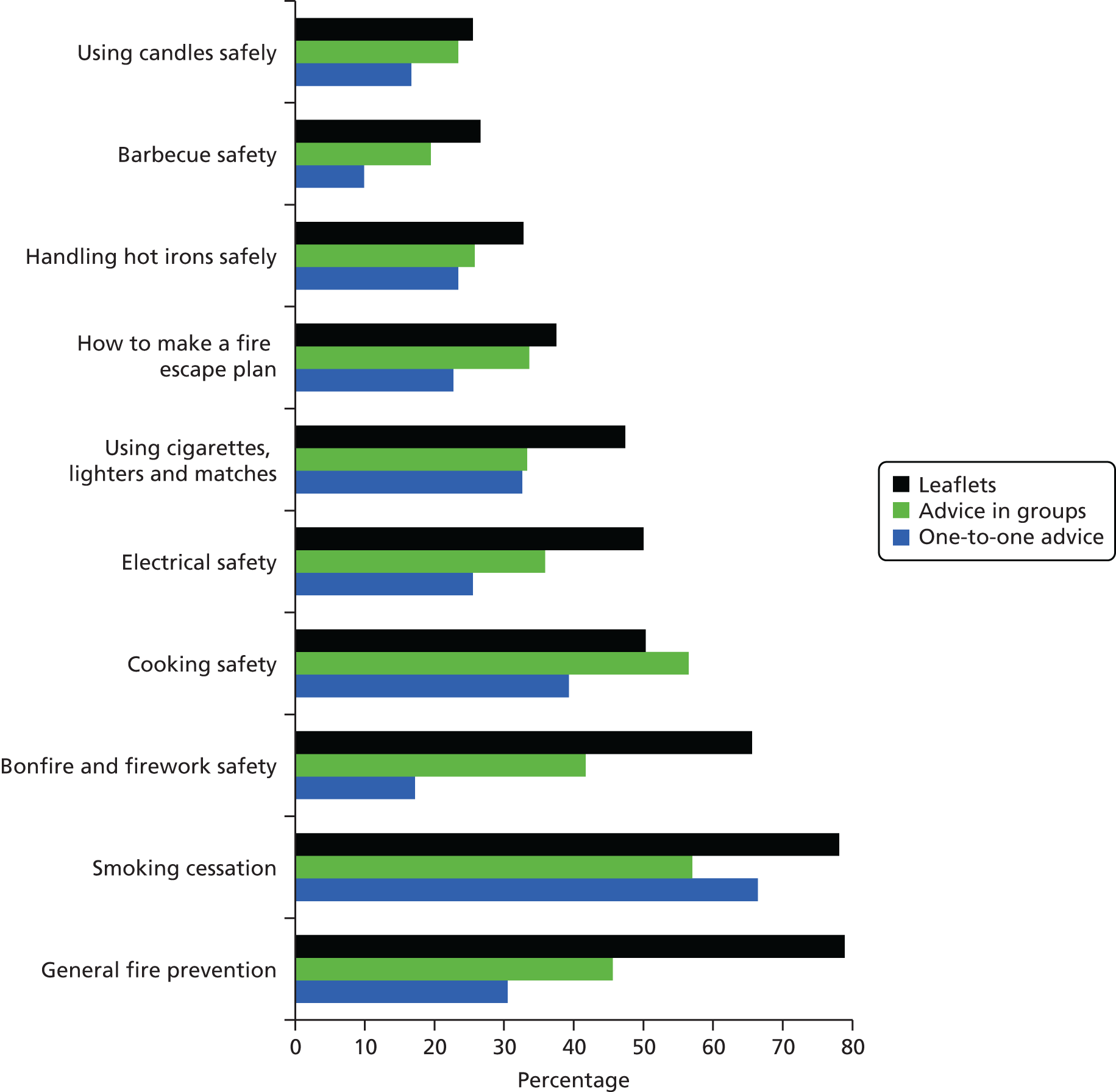
Centres provided advice on a range of falls, poisonings and scalds prevention topics (Figures 15–17). For falls prevention, advice was most commonly provided on stair safety, not leaving children on high surfaces, what to do if a child has a head injury and general falls prevention and was least commonly provided on non-slip bath mats, baby walker safety and high chair and pushchair safety. For poisoning prevention, advice was most commonly provided on safe storage of hazardous substances such as medicines and household chemicals and general poisoning prevention and least commonly provided on poisonous plants and disposal of unwanted medicines. For scalds prevention, advice was most commonly provided on handling hot drinks, general scald prevention and cooking safety and least commonly provided on thermostatic mixer valves (TMVs). It appears that advice in groups and one-to-one advice was being used more commonly for falls, poisonings and scalds prevention in 2012 than for fire-related injury prevention in 2010.
FIGURE 15.
Advice provided by children’s centres on falls prevention (2012 survey). From Watson MC, Mulvaney C, Timblin C, Stewart J, Coupland CA, Deave T, Hayes M, Kendrick D. Missed opportunities to keep children safe? National Survey of injury prevention activities of children’s centres. Health Education Journal 2016;75:833–42. 224 http://dx.doi.org/10.1177/0017896916629816. Published with kind permission from SAGE Publishing.
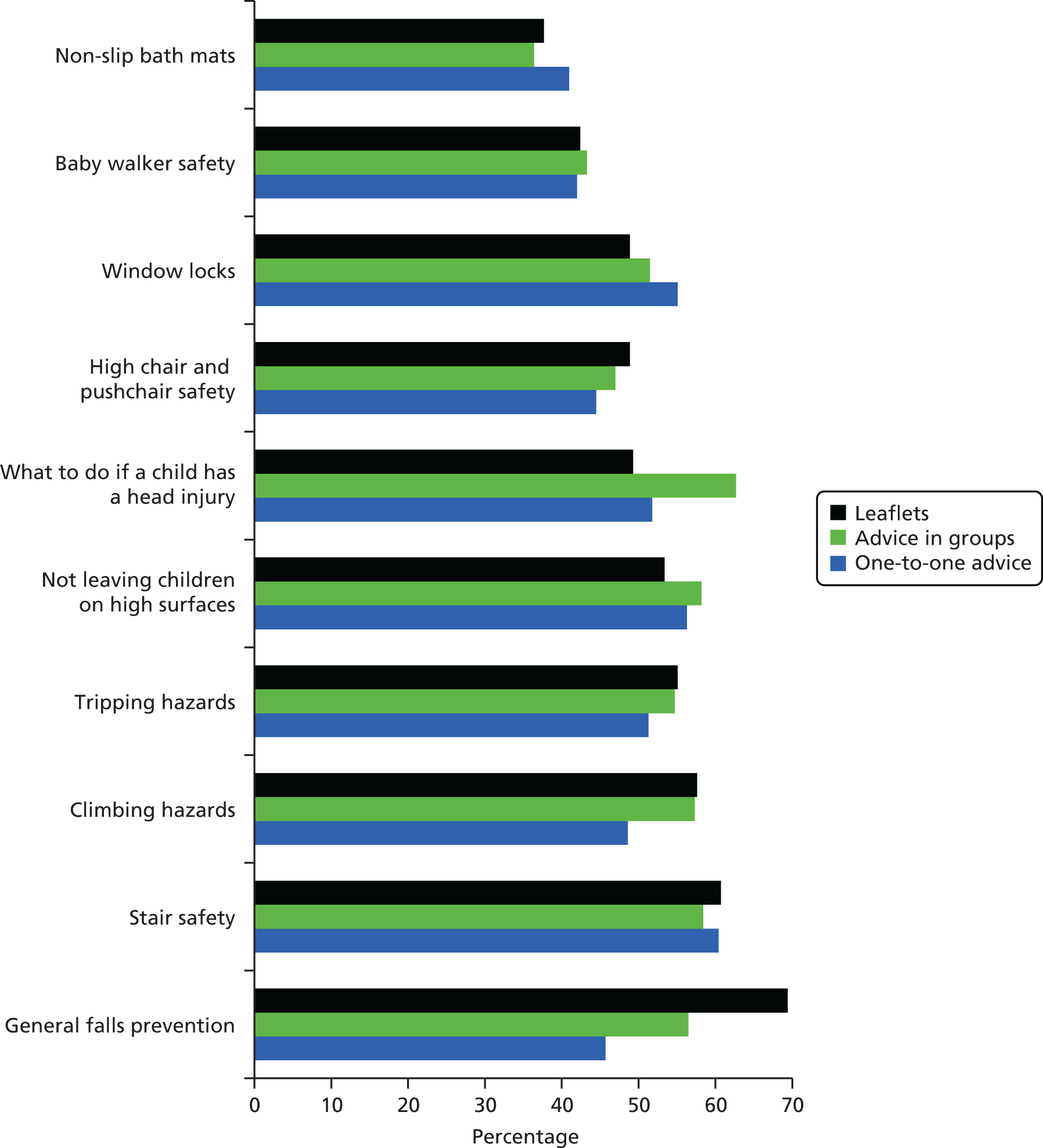
FIGURE 16.
Advice provided by children’s centres on poisoning prevention (2012 survey). From Watson MC, Mulvaney C, Timblin C, Stewart J, Coupland CA, Deave T, Hayes M, Kendrick D. Missed opportunities to keep children safe? National Survey of injury prevention activities of children’s centres. Health Education Journal 2016;75:833–42. 224 http://dx.doi.org/10.1177/0017896916629816. Published with kind permission from SAGE Publishing.
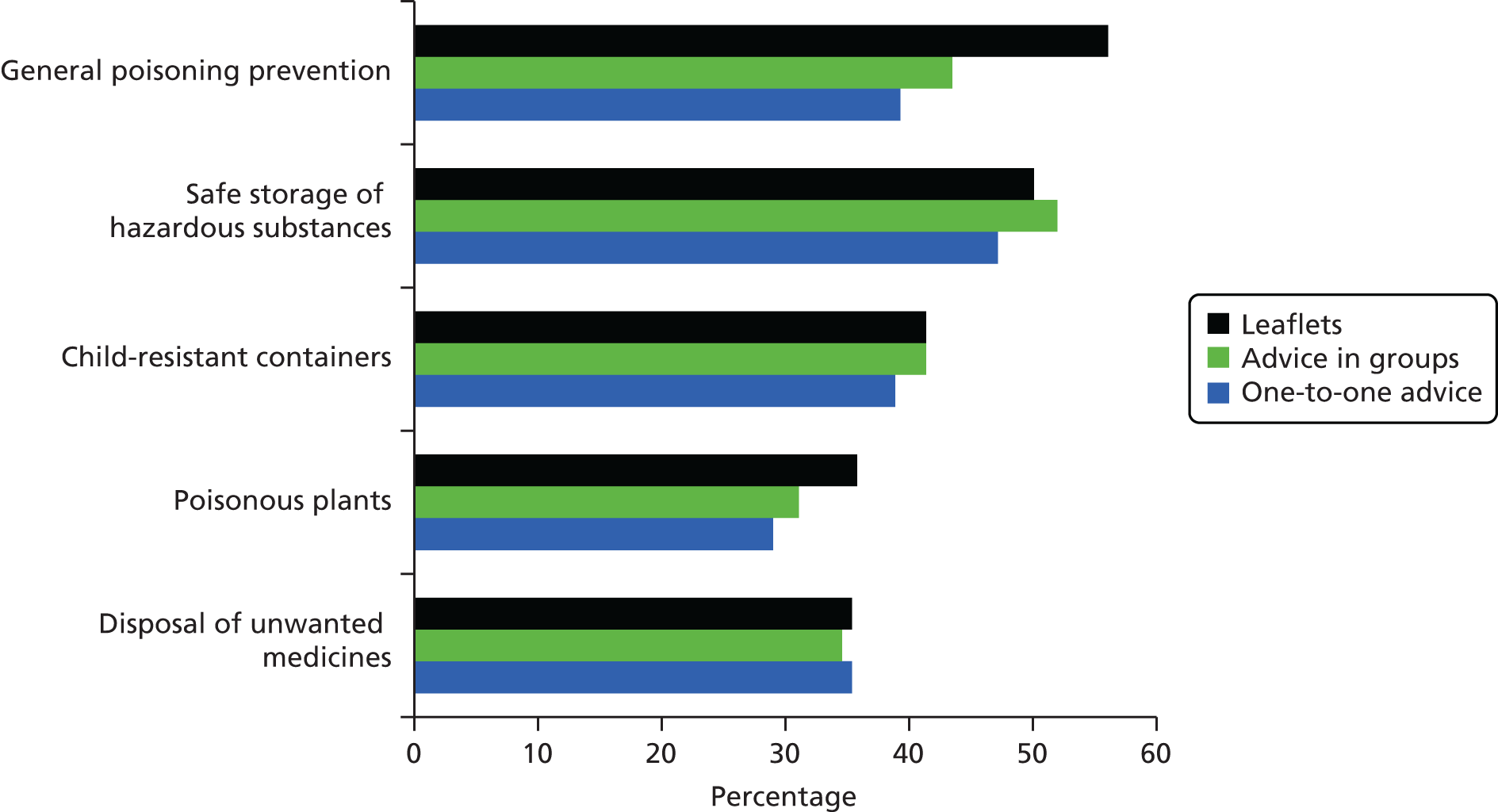
FIGURE 17.
Advice provided by children’s centres on scald prevention (2012 survey). From Watson MC, Mulvaney C, Timblin C, Stewart J, Coupland CA, Deave T, Hayes M, Kendrick D. Missed opportunities to keep children safe? National Survey of injury prevention activities of children’s centres. Health Education Journal 2016;75:833–42. 224 http://dx.doi.org/10.1177/0017896916629816. Published with kind permission from SAGE Publishing.

In the 2010 survey, two-thirds (64%, 245/384) of centres were aware of a home safety equipment scheme in their locality, whereas one in five (21%, 79/384) did not know if their area had a scheme. One-quarter of those with schemes (26%, 60/233) had schemes provided through the Royal Society for the Prevention of Accidents (RoSPA) national Safe At Home scheme and just over half the schemes (58%, 135/234) were based within children’s centres. Many schemes were fairly new, with 50% (122/245) being established within the preceding 18 months. Schemes provided, and in most cases fitted (78%, 186/238), a varying range of items of safety equipment, most commonly free (68%, 165/241) or at low cost (18%, 43/241). Equipment provided included stair gates, fireguards, cupboard locks, window catches and furniture corner covers. Stair gates were the most commonly provided (91%, 220/242) and furniture corner covers the least commonly provided (42%, 102/242).
In the 2012 survey, fewer centres (42%, 217/517) reported a home safety equipment scheme in their area and one-fifth (22%, 112/517) did not know if there was such a scheme. Of those that had a scheme, 7% (17/248) were part of the Safe At Home national scheme organised by RoSPA. Similar to the 2010 findings, almost half (47%, 101/217) the schemes had been in operation for < 18 months and 9% (19/217) had been in operation for > 4.5 years. Over half the schemes (53%, 111/211) operated from children’s centres. Schemes provided corner covers (68%, 104/154), devices to measure bathwater temperature (51%, 76/149), first aid kits (29%, 42/143), fridge locks (52%, 78/149), lockable medicine cupboards (10%, 15/143), safety catches for cupboards and drawers (74%, 111/150), safety gates (63%, 95/150), TMVs (4%, 5/140) and window locks (47%, 69/148). Most provided free (60%, 128/214) or low-cost equipment (34%, 73/214) and a smaller number loaned the equipment (5%, 10/214). Most (69%, 140/202) delivered equipment to homes and fitted it (55% 114/206).
Joint working
In the 2010 survey, few respondents (15%, 56/375) were aware of a local child accident prevention group. There was evidence of joint injury prevention work being undertaken with a range of organisations, most commonly community nursing services (86%, 331/384), fire and rescue services (69%, 266/384) and road safety organisations (61%, 233/384). There was also evidence of referral to other services such as NHS smoking cessation services (95%, 360/377) and fire and rescue services for smoke alarms (86%, 321/375) and fire safety risk assessments (85%, 309/362).
In the 2012 survey, 14% (68/503) of respondents knew of a child accident prevention group in their area and 59% (296/503) stated that they did not know whether or not there was such a group. In 2012, centres were not asked if they worked with other organisations on injury prevention. Some centres referred families to safety equipment schemes (47%, 221/466), to pharmacists for the safe disposal of unwanted medicines (49%, 230/472) and to organisations for home safety checks (53%, 251/473), most of which referred to fire and rescue services (62%, 122/198). Very few referred families to an organisation for TMVs (3%, 13/461).
Barriers to, and enabling factors for, injury prevention work
The main barriers to, and enabling factors for, injury prevention activities in the 2010 and 2012 surveys are shown in Figures 18 and 19, respectively. Lack of capacity in terms of staff time (39%, 131/339 in 2010; 39%, 162/417 in 2012) and lack of funding (33%, 111/339 in 2010; 52%, 216/417 in 2012) were the most frequently mentioned barriers. The most frequently mentioned enabling factors were access to families (45%, 113/249 in 2010; 39%, 121/312 in 2012) and working with other agencies (44%, 110/249 in 2010; 35%, 109/312 in 2012).
Support for injury prevention activities
In the 2010 survey, most respondents stated that training (97%, 362/373), provision of educational materials (95%, 351/369), examples of good practice (94%, 341/363), help with planning injury prevention (94%, 343/366), support for working with partners (89%, 320/358) and communities (88%, 311/354) and help with evaluating activities (85%, 303/356) would be useful for their centre.
Discussion
Main findings
In both surveys we found that around 60% of children’s centres identified unintentional injuries as one of their three main priorities but fewer than half had a written injury prevention strategy. Providing leaflets to parents was the most common approach for delivering injury prevention information in 2010 and it remained a common method in 2012, despite this being perceived as less effective than other methods. Although managers held positive attitudes towards injury prevention, they had gaps in their knowledge about injury prevention and about important local initiatives. Two-thirds of centres had access to a local home safety equipment scheme in 2010 but this had fallen to 42% in 2012, with fewer schemes in 2012 providing and fitting free equipment. Our findings suggest that most centres do not have an evidence-based strategic approach, that child injury prevention appears to be a neglected area within children’s centres given the scale of the problem and that most centres would welcome help and support in planning, delivering and evaluating child injury prevention. The findings suggest the considerable scope for improving the provision of child injury prevention activities in children’s centres, which is the focus of the RCT (study M) undertaken in work stream 6 of this programme (see Chapter 7).
Strengths and limitations of the study
Our response rates are similar to those of surveys of other professional groups225 but, as in many surveys, non-response bias may have occurred whereby respondents may have been more interested and active in injury prevention than non-respondents. If this is the case the findings may overestimate injury prevention activity within children’s centres. Similarly, as we collected self-reported activity data, social desirability bias may have led to overestimation of ‘true’ activity levels. If either type of bias has occurred, given the scope for increasing injury prevention that we have demonstrated, this would strengthen our conclusions.
Our surveys provided a broad overview of the injury prevention activity taking places in children’s centres. The survey was not able to explore injury prevention activity in detail or the motivations for choosing particular ways of working or undertaking particular activities. Such information is important for designing interventions for delivery in children’s centres and for understanding and developing the role that children’s centres play in child injury prevention.
Data from the national database of children’s centres (Leila Allsopp, Department for Children, Schools and Families, 1 July 2009, personal communication), which we used as our sampling frame in 2010, indicated that 37% of centres were established in phase 1 (2004–6), 59% in phase 2 (2006–8) and 4% in phase 3 (2008–10). The database that we used as our sampling frame in 2012 (Shirley Best, Department for Education, 29 November 2011, personal communication) indicated that 31% of centres were set up in phase 1 (2004–6), 49% in phase 2 (2006–8) and 21% in phase 3 (2008–10). The phase of the centres responding to our 2010 and 2012 surveys was similar to that in the national sample, suggesting that our findings should be broadly generalisable to children’s centres across England. One-fifth of responses came from children’s centres located within the South East Coast SHA in the 2010 and 2012 surveys. This reflected the existence of a larger number of children’s centres in this area compared with other SHAs in the national database of children’s centres.
Comparisons with existing research
We were not able to find any other published studies exploring children’s centre injury prevention activities for comparison with our study. Previous surveys of injury prevention activities by health authorities218 and PCGs219 report findings similar to ours in terms of lack of capacity, lack of useful data and lack of prioritisation of injury prevention work. 218,219
Despite national publications highlighting the importance of child injury prevention and the priority it should be afforded,1,19,22,25 child injury prevention was not among the top three child health priorities for two-fifths of children’s centres that responded to our survey. We also found lack of a strategic approach to injury prevention, with many centres not having a written injury prevention strategy and reliance on less effective methods of behaviour change such as providing leaflets,226 suggesting that better use could be made of the current evidence base, consistent with the conclusions in the Better Safe Than Sorry report. 19 As most managers held positive attitudes to injury prevention, believed that children’s centres could be effective in preventing injuries and were keen to receive support, there is scope for further developing the injury prevention activities being delivered by children’s centres.
Although we found evidence of joint working with individual organisations, most respondents did not know of the existence of local injury prevention groups or strategies, suggesting suboptimal partnership working227–230 despite recent recommendations. 1,19,22,25 Working effectively in partnership across agencies and organisations can be a complex process231–233 and it is likely that children’s centres will need support to do this. There have been numerous recommendations for the creation of local injury prevention co-ordinator posts19,22,234,235 and, if such posts are established, these could support children’s centres in their injury prevention work.
How these findings inform other research within the Keeping Children Safe programme
Our surveys confirm the scope for improving the provision of child injury prevention activities in children’s centres. The findings from study D have been used to inform the development of guides for interviews with children’s centre managers and staff to explore barriers to, and facilitators of, injury prevention (study G in work stream 4; see Figure 1 and Chapter 4). The findings have also been used to develop an injury prevention intervention (an IPB) for delivery by children’s centres, which was evaluated using a RCT (study M in work stream 6; see Chapter 7). Finally, the findings were used to develop a second IPB incorporating the findings from all of the studies in the KCS programme.
Chapter 5 What are the barriers to, and facilitators of, implementing thermal injury, falls and poisoning prevention interventions among children’s centres, professionals and community members? (Work stream 4)
Abstract
Research question
What are the barriers to, and facilitators of, implementing thermal injury, falls and poisoning prevention interventions among children’s centres, professionals and community members?
Methods
This work stream included three studies exploring barriers to, and facilitators of, injury prevention: a systematic review (study E), a qualitative study of children’s centre managers and staff (study F) and a qualitative study of parents of injured and uninjured children (study G).
Study E
Quantitative papers were identified from a systematic review undertaken in work stream 5 (study I), which was supplemented with a systematic review of qualitative evidence. Bibliographic databases and other sources were searched up to May 2009 for quantitative papers and up to March 2010 for qualitative papers. Data were explored using framework analysis and synthesised narratively.
Study F
Semistructured interviews were conducted with managers and staff from children’s centres across four study sites. Interview topics included health and safety promotion programmes, barriers to, and facilitators of, delivering health promotion, engaging parents and development of staff capacity and child injury prevention. Data were analysed using framework analysis.
Study G
Semistructured interviews were conducted with parents of injured and uninjured children (cases and controls from study A). Maximum variation sampling was used to ensure a range of child ages, injury types and deprivation levels. Interview topics included beliefs about injury prevention, injury prevention strategies, control over injury prevention actions and barriers to, and facilitators of, injury prevention actions. Data were analysed using thematic analysis.
Results
In total, 64 papers (quantitative, n = 57; qualitative, n = 7) were included in the systematic review. Thirty-three interviews were conducted with staff from 16 children’s centres and 64 parents were interviewed, 16 whose children had had a fall, 16 whose children had had a poisoning, 16 whose children had had a scald and 16 whose children had not had an injury. The review found that many studies did not explicitly explore barriers and facilitators and, when they were explored, this was most often from the perspective of those delivering the intervention. A range of barriers and facilitators was found consistently across studies E–G. These included the need for interventions to be delivered by staff with trusted relationships with families, tailoring interventions to the needs of families and stage of development of the child, focusing on specific injury prevention topics and providing simple and reinforced messages. Parents identified that ‘real-life’ stories of how injuries had happened may help to raise awareness.
Conclusions
Facilitators for children’s centres and parents to undertake injury prevention were identified as were modifiable barriers. The effect of addressing these barriers and facilitators within interventions aimed at children’s centres and families requires evaluation.
Chapter summary
This work stream consisted of a systematic review of facilitators of and barriers to home injury prevention interventions for preschool children (study E), a qualitative study exploring the views of children’s centre managers and staff regarding facilitators of and barriers to injury prevention (study F) and a qualitative study exploring parents’ views of facilitators of and barriers to implementing injury prevention within the home (study G). Findings from this work stream were used to inform the design of an injury prevention intervention for delivery in children’s centres. The design and evaluation of this intervention is reported in work stream 6 (see Chapter 7).
Introduction
Over the last 20 years, numerous studies of injury prevention activity among front-line health professionals, public health professionals and health-care organisations in the UK have consistently demonstrated that child injury prevention is given a low priority and is inadequately resourced, that professionals have unmet training needs to deliver injury prevention and that systematic implementation of evidence-based practice is lacking. 19,218–220,236–244 More recently, in 2010, NICE produced two guidelines on preventing unintentional injuries in children and young people (PH2925 and PH3027), which clearly defined the evidence-based interventions that should be provided and the responsibilities for professionals and organisations in implementing those interventions. The impact of the NICE guidelines on child injury prevention practice awaits assessment.
Among parents, professionals and organisations, a range of barriers to, and facilitators of, injury prevention has been found. A systematic review of qualitative literature undertaken in 2011 reported on barriers to, and facilitators of, interventions that supply or install home safety equipment or provide home safety risk assessments. 245 Barriers and facilitators covering 15 areas were found. Legal and policy barriers included the short-term nature of many programmes, lack of co-ordination and weak legislation or regulation. Information provision was a barrier, with parents reporting a lack of information and service providers reporting difficulties in providing information to families in accommodation with a rapid turnover of tenants. Living in homes that people were not free to modify, homes in which people lacked autonomy to make household decisions or rented homes with high tenant turnover were major barriers to installing safety equipment and childproofing a home, as were equipment costs, poor-quality or malfunctioning equipment and a lack of skills to fit equipment. Difficulty in understanding child development and anticipating injury risk, having fatalistic attitudes towards injuries, being suspicious of strangers entering the home to assess or install equipment, being suspicious of ‘free’ equipment and parental perceptions of officials blaming or accusing them of neglect or abuse all acted as barriers. A lack of experience of specific risks in a new environment and lack of understanding by health workers of child safety norms and expectations in immigrants’ cultures were also cited as barriers. 245
Facilitators included legislation that required action when children were resident in the home (e.g. fire and Rescue Services Act 2004246), providing timely information (e.g. safety information provided in the community after birth was more likely to be retained than that provided in hospital at the time of birth), using ‘real-life’ incidents, partnerships and collaborations between service providers, having landlords with the ability and motivation to repair properties, training for landlords, councils and parents in installing, replacing and using equipment and providing ongoing support and maintenance for safety equipment. Parental supervision was acknowledged as a major facilitator but, as this was resource intensive, the need to supplement it with other forms of injury prevention was emphasised. 245
At the level of professionals, a systematic review of the global literature identified six barriers to professionals undertaking injury prevention activities. 247 These were inadequate knowledge and training, lack of time, lack of resources, lack of confidence in counselling parents about injury prevention or in their ability to influence parents’ behaviour, the setting in which professionals worked and personal injury prevention behaviour. 247 Surveys of English health organisations, including health authorities and PCTs, identified the low priority given to unintentional injuries,218,219 lack of strategic planning,218,219 lack of capacity and resources, in particular injury prevention co-ordinator posts,218 lack of useful local data,218 inadequately developed multiagency working219 and a lack of knowledge about the burden of injuries and the effectiveness of interventions. 219
At an organisational level, it is vital to understand the context within which interventions are set. Despite this, details on context, methods and implementation of interventions are rarely reported in the literature. Several systematic reviews conclude that the characteristics of innovations, communities, individuals and the delivery of the intervention are all important in determining the effectiveness of implementation. 248–251 In terms of providers, recognition of the need for a specific intervention, belief in its beneficial effects, confidence in ability and having the necessary skills to deliver the intervention have consistently been found to be associated with successful implementation. 248 At an organisational level, important aspects for achieving implementation are a culture conducive to change, effective leadership and programme champions and providing training that includes active learning delivered in a supportive atmosphere with ongoing technical assistance, resources and support. 248
As described in work stream 3 (see Chapter 4), children’s centres have a key role in promoting child and family safety. It is therefore important to understand how home safety interventions can be most effectively implemented within the context of children’s centres. The findings from study D described in work stream 3 demonstrate considerable interest in and motivation for undertaking child injury prevention work within children’s centres. However, this is coupled with a lack of prioritisation of the topic, gaps in knowledge about child injuries, lack of a strategic evidence-based approach to injury prevention and a range of barriers to undertaking injury prevention, most commonly lack of funding and lack of staff capacity. This work stream aimed to gain a greater understanding of the barriers to, and facilitators of, injury prevention for children’s centres and parents. The findings from work stream 4 were used to inform the design of a child injury prevention intervention (an IPB plus a training and facilitation package to support its implementation), which was evaluated as part of work stream 6 (see Chapter 7). The methods and results for studies E–G are reported in this chapter along with an overarching discussion covering all three studies.
Systematic review using quantitative and qualitative studies of barriers to, and facilitators of, implementing home safety interventions among families with young children (study E)
Methods
The objective was to systematically review quantitative [RCTs, non-RCTs (including quasi-randomised studies) and controlled before-and-after studies (CBAs)] and qualitative (all designs) studies on barriers to, and facilitators of, implementing home safety interventions to prevent unintentional injuries in children aged 0–4 years. The systematic review was conducted in parallel with an update of a Cochrane systematic review of the effectiveness of home safety interventions,49 undertaken as part of the KCS programme of research and reported in Chapter 6 (work stream 5). We used the quantitative papers identified from the Cochrane systematic review and supplemented these with a systematic review of qualitative evidence. Full details of the methods used are reported elsewhere. 49,252
Studies were eligible if they included children aged ≤ 5 years and their families, provided home safety education with or without the provision of safety equipment for the prevention of falls, poisonings or thermal injuries and reported barriers to, or facilitators of, success of the intervention. Community injury prevention programmes (e.g. World Health Organization Safe Community-type interventions) were included only if it was clear that they provided home safety education for the prevention of falls, poisonings or thermal injuries to individual parents or groups of parents. Studies reporting fire setting were excluded because of the difficulty of attributing intent. The sources searched and search strategies for the Cochrane review are described in work stream 5 (see Chapter 6). Searches were conducted from the date of inception of the bibliographic databases up to 31 May 2009. We searched MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Applied Social Sciences Index and Abstracts (ASSIA), PsycINFO and Web of Science for qualitative evidence from the date of database inception to March 2010 as well as a range of other electronic sources. The search strategy for qualitative papers is provided in Appendix 4, Search strategy for identification of qualitative studies for the systematic review of barriers to, and facilitators of, injury prevention (study E).
All papers included in the Cochrane review were assessed for inclusion by two reviewers searching the full-text articles for mention of reported barriers and facilitators. Assessment of risk of bias was undertaken as described in work stream 5. Titles and abstracts of qualitative papers were assessed for inclusion independently by two reviewers. We did not appraise qualitative papers for quality because there is considerable debate about (1) whether qualitative studies should be appraised for quality, (2) which methods should be used and (3) the degree of agreement between different appraisers and different methods. 253–255 Data were extracted from eligible articles by two reviewers independently using a standard data extraction form. Disagreements between reviewers in study selection or data extraction were handled by consensus-forming discussions. Data were synthesised using an iterative process to develop themes, which were explored using framework analysis. 256
Results
The process of the selection of studies is shown in Figure 20. Sixty-four studies were included in the review, 57 sourced from the Cochrane review72,257–312 and seven from the searches for qualitative studies. 92,313–318 Tables of excluded studies are available from the authors on request. The risk of bias in the included quantitative studies is shown later in Table 72, which demonstrates that many studies were at risk of bias, most commonly from inadequate allocation concealment or lack of blinding of outcome assessment.
FIGURE 20.
Process of the selection of quantitative and qualitative studies for the review. Reproduced from Ingram JC, Deave T, Towner E, Errington G, Kay B, Kendrick D. Identifying facilitators and barriers for home injury prevention interventions for pre-school children: a systematic review of the quantitative literature. Health Education Research 2012;27(2):258–68,252 by permission of Oxford University Press.

Seven key facilitators and six key barriers were identified from the included studies. Table 64 shows the key facilitators and Table 65 shows the key barriers. These key facilitators and barriers are summarised in the following sections.
| Study | Facilitators | ||||||
|---|---|---|---|---|---|---|---|
| Intervention approach | Focused message | Minimal changes | Role of the deliverer | Safety equipment accessibility | Behaviour change models | Incentives | |
| Quantitative studies | |||||||
| Babul 2007257 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Carman 2006258 | ✓ | ✓ | ✓ | ✓ | |||
| Coggan 2000259 | ✓ | ✓ | ✓ | ||||
| Colver 1982260 | ✓ | ✓ | ✓ | ✓ | |||
| DiGuiseppi 2002261 | ✓ | ✓ | ✓ | ✓ | |||
| Emond 2002262 | ✓ | ✓ | |||||
| Fergusson 1982263 | ✓ | ✓ | ✓ | ||||
| Georgieff 2004264 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Gielen 2002265 | ✓ | ✓ | |||||
| Gielen 2007266 | ✓ | ✓ | ✓ | ✓ | |||
| Guyer 1989267 | ✓ | ✓ | |||||
| Harvey 2004268 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Hendrickson 2005269 | ✓ | ✓ | |||||
| Jenkins 1996270 | ✓ | ✓ | ✓ | ✓ | |||
| Johnston 2000271 | ✓ | ✓ | ✓ | ✓ | |||
| Katcher 1989272 | ✓ | ✓ | ✓ | ✓ | |||
| Kelly 1987273 | ✓ | ✓ | |||||
| Kelly 2003274 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Kendrick 1999275 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Kendrick 2011276 | ✓ | ✓ | ✓ | ✓ | |||
| King 2001277 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Krug 1994278 | ✓ | ✓ | |||||
| LeBailly 1990279 | ✓ | ✓ | |||||
| Llewellyn 2003280 | ✓ | ✓ | |||||
| Mallonee 2000281 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| McDonald 2005282 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| McLoughlin 1982283 | ✓ | ||||||
| Miller 1982284 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Mock 2003285 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Mueller 2008286 | ✓ | ✓ | ✓ | ✓ | |||
| Nansel 2002287 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Nansel 2008288 | ✓ | ✓ | ✓ | ✓ | |||
| Odendaal 2009289 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Olds 1994290 | ✓ | ✓ | ✓ | ||||
| Ozanne-Smith 2002291 | ✓ | ✓ | ✓ | ||||
| Paul 1994292 | ✓ | ✓ | ✓ | ||||
| Petridou 1997293 | ✓ | ✓ | ✓ | ||||
| Pless 2007294 | ✓ | ✓ | |||||
| Posner 2004295 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Rey 1993296 | ✓ | ||||||
| Sangvai 2007297 | ✓ | ✓ | ✓ | ✓ | |||
| Schelp 1987298 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Schlesinger 1996299 | ✓ | ||||||
| Schwarz 1993300 | ✓ | ✓ | ✓ | ||||
| Schwebel 2009301 | ✓ | ✓ | ✓ | ||||
| Svanström 1995302 | ✓ | ||||||
| Swart 2008303 | ✓ | ✓ | ✓ | ✓ | |||
| Sznajder 2003304 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Thomas 1984305 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Vineis 1994306 | ✓ | ✓ | ✓ | ||||
| Waller 1993307 | ✓ | ✓ | ✓ | ||||
| Watson 200572 | ✓ | ✓ | ✓ | ✓ | |||
| Woolf 1987308 | ✓ | ✓ | ✓ | ✓ | |||
| Woolf 1992309 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Yang 2008310 | ✓ | ✓ | ✓ | ||||
| Ytterstad 1995311 | ✓ | ✓ | ✓ | ✓ | |||
| Zhao 2006312 | ✓ | ✓ | ✓ | ✓ | |||
| Qualitative studies | |||||||
| Carr 2005313 | ✓ | ✓ | ✓ | ||||
| Gibbs 2005314 | ✓ | ||||||
| Morrongiello 200492 | ✓ | ✓ | ✓ | ||||
| Morrongiello 2004315 | ✓ | ✓ | ✓ | ✓ | |||
| Morrongiello 2009316 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Pollack-Nelson 2002317 | ✓ | ||||||
| Van Niekerk 2010318 | ✓ | ✓ | ✓ | ✓ | |||
| Author | Barriers | |||||
|---|---|---|---|---|---|---|
| Cultural | Socioeconomic | Complex interventions | Deliverer constraints | Physical barriers | Behavioural barriers | |
| Quantitative studies | ||||||
| Babul 2007257 | ✓ | ✓ | ||||
| Carman 2006258 | ✓ | ✓ | ✓ | |||
| Coggan 2000259 | ✓ | |||||
| Colver 1982260 | ✓ | ✓ | ||||
| DiGuiseppi 2002261 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Emond 2002262 | ✓ | |||||
| Fergusson 1982263 | ✓ | |||||
| Georgieff 2004264 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Gielen 2002265 | ✓ | ✓ | ✓ | ✓ | ||
| Gielen 2007266 | ||||||
| Guyer 1989267 | ✓ | ✓ | ||||
| Harvey 2004268 | ✓ | ✓ | ||||
| Hendrickson 2005269 | ✓ | ✓ | ||||
| Jenkins 1996270 | ✓ | ✓ | ||||
| Johnston 2000271 | ✓ | |||||
| Katcher 1989272 | ✓ | ✓ | ||||
| Kelly 1987273 | ✓ | ✓ | ||||
| Kelly 2003274 | ✓ | |||||
| Kendrick 1999275 | ✓ | |||||
| Kendrick 2011276 | ✓ | ✓ | ✓ | ✓ | ||
| King 2001277 | ✓ | ✓ | ||||
| Krug 1994278 | ✓ | ✓ | ✓ | |||
| LeBailly 1990279 | ✓ | ✓ | ✓ | ✓ | ||
| Llewellyn 2003280 | ✓ | ✓ | ||||
| Mallonee 2000281 | ✓ | |||||
| McDonald 2005282 | ✓ | ✓ | ||||
| McLoughlin 1982283 | ✓ | ✓ | ✓ | |||
| Miller 1982284 | ✓ | ✓ | ✓ | |||
| Mock 2003285 | ✓ | ✓ | ||||
| Mueller 2008286 | ✓ | ✓ | ||||
| Nansel 2002287 | ✓ | ✓ | ||||
| Nansel 2008288 | ✓ | ✓ | ✓ | |||
| Odendaal 2009289 | ✓ | ✓ | ✓ | |||
| Olds 1994290 | ✓ | ✓ | ||||
| Ozanne-Smith 2002291 | ✓ | ✓ | ||||
| Paul 1994292 | ✓ | ✓ | ✓ | |||
| Petridou 1997293 | ✓ | ✓ | ||||
| Pless 2007294 | ✓ | ✓ | ||||
| Posner 2004295 | ✓ | |||||
| Rey 1993296 | ✓ | ✓ | ||||
| Sangvai 2007297 | ✓ | ✓ | ||||
| Schelp 1987298 | ✓ | ✓ | ||||
| Schlesinger 1996299 | ✓ | |||||
| Schwarz 1993300 | ✓ | ✓ | ||||
| Schwebel 2009301 | ✓ | ✓ | ||||
| Svanström 1995302 | ||||||
| Swart 2008303 | ✓ | ✓ | ||||
| Sznajder 2003304 | ✓ | ✓ | ✓ | |||
| Thomas 1984305 | ✓ | ✓ | ||||
| Vineis 1994306 | ✓ | |||||
| Waller 1993307 | ✓ | ✓ | ✓ | |||
| Watson 200572 | ✓ | ✓ | ✓ | |||
| Woolf 1987308 | ✓ | |||||
| Woolf 1992309 | ✓ | ✓ | ✓ | |||
| Yang 2008310 | ✓ | ✓ | ||||
| Ytterstad 1995311 | ✓ | |||||
| Zhao 2006312 | ✓ | ✓ | ||||
| Qualitative studies | ||||||
| Carr 2005313 | ✓ | ✓ | ✓ | |||
| Gibbs 2005314 | ✓ | ✓ | ||||
| Morrongiello 200492 | ✓ | ✓ | ||||
| Morrongiello 2004315 | ✓ | ✓ | ✓ | |||
| Morrongiello 2009316 | ✓ | ✓ | ✓ | |||
| Pollack-Nelson 2002317 | ✓ | ✓ | ✓ | ✓ | ||
| Van Niekerk 2010318 | ✓ | ✓ | ||||
Facilitators
Features of successful interventions were prearranged home safety visits, at which free safety equipment was provided and fitted with easy-to-use instructions, particularly for low-income families; tailoring methods for different groups or individuals and combining with environmental measures (active and passive interventions); community involvement and awareness raising to understand community perceptions and values and address these and to reduce stigma, normalise safety practices and reach high-risk groups; and partnership working with a range of organisations. For some types of injury (e.g. scald prevention through reducing hot tap water temperature), focusing on a single type of injury was helpful, as was providing short and simple home safety messages. Simple methods for reinforcing advice, such as continued contact with health professionals, group sessions in clinics, poster displays, mailed reminders and stickers to display in the home, were described as helpful. Interventions requiring minimal, simple, non-repetitive action to implement (such as lowering the hot water temperature) were more likely to be successful than those requiring more complex or repeated actions. Interventions providing and fitting safety equipment had greater effects than those providing discount vouchers for equipment purchase or those providing advice about equipment and local suppliers or facilitating access to equipment in other ways. Studies using behaviour change models for influencing parental safety behaviour and techniques to increase self-efficacy found these to be beneficial. The use of techniques to achieve organisational change in terms of delivering home safety interventions was also considered important. A range of incentives was used successfully to encourage participation in studies and uptake of interventions such as providing free interventions (safety equipment or first aid training), small monetary incentives for completing outcome measurement tools or crèche facilities for group sessions.
Using professionals who had established a relationship with families to deliver safety messages had many benefits, as they were trusted familiar figures and were accepted in the home. Trained lay community volunteers were more acceptable to some communities, and it was appreciated when they were able to deliver messages in the primary language of participants or were of the same ethnic origin. The credibility of home safety messages was enhanced in some studies by being delivered in clinical settings, such as child health clinics or EDs. Those delivering the interventions gained both home safety knowledge and skills in delivering home safety interventions, and this helped to sustain interventions.
Barriers
Parents in some studies, particularly in disadvantaged areas, were suspicious of unannounced home visits because of mistrust of the health system, child protection fears, immigration issues and/or fear of strangers in the home. Transient populations, with frequent house moves, were difficult to deliver interventions to and those moving house sometimes removed safety equipment. Living in rented accommodation prevented equipment being fitted because families worried that landlords might object or equipment might inconvenience other tenants (e.g. smoke alarms going off) or families could not afford to make changes to a property they did not own. Language barriers and low literacy hampered the delivery of interventions in some studies and using interpreting services and translators proved difficult. Families living with economic constraints would often choose food and daily living items over the purchase of safety equipment. In addition, installing equipment required time, tools and skills. When safety equipment broke, was faulty or was perceived as inconvenient or annoying by families (e.g. smoke alarms), this contributed to poor compliance.
Families’ beliefs, traditions and supervisory behaviours influenced whether or not they were likely to take part in studies and the extent to which they were willing to change their home safety and supervisory practices. Short intervention periods and brief educational interventions including single home visits or well-child contacts or awareness raising campaigns were viewed as insufficient to change beliefs and behaviours.
Complex interventions were not always successful if they addressed too many home safety topics in one intervention or used multiple methods that required several concurrent behaviour changes. Often they also required more highly skilled practitioners, which made them less sustainable. Interventions that needed large numbers of staff or volunteer training or large amounts of time to deliver were sometimes unsuccessful because of time constraints, and were often unsustainable.
Identifying barriers to, and facilitators of, injury prevention among children’s centre managers and staff (study F)
Methods
The objective of this study was to explore perceptions of barriers to, and facilitators of, implementing health promotion and injury prevention interventions among children’s centre staff.
Semistructured interviews were conducted with staff members from children’s centres, which were sampled purposively to include a range of characteristics: phase of establishment of children’s centre, PCT area, lead agency and catchment population size. For each study site we identified phase 1 and phase 2 centres in the most deprived 30% of super output areas, as assessed by 2007 Indices of Multiple Deprivation for each region,319,320 and located in the two PCT areas closest to each study site. Children’s centre managers were approached by researchers by letter, followed by a telephone call to discuss the study and answer any questions managers might have.
Researchers from the four study sites, Nottingham, Norwich, Newcastle and Bristol, undertook interviews lasting for 30–45 minutes at the children’s centre, university or local NHS premises, at a time convenient to participants. Participation was voluntary and participants were free to withdraw at any time. Participants completed a consent form prior to interview. Interview topics included details about health and safety promotion programmes, focusing on aspects of the barriers to, and facilitators of, holding health promotion sessions, the best ways to engage with parents and the development of staff capacity and child safety work. An interview topic guide was developed using the findings from study D described in work stream 3 (see Chapter 4) and is shown in Appendix 4, Interview guide for interviews with children’s centre managers and staff (study G). Interviews were digitally recorded and transcribed verbatim. Quotations are presented using a code giving the study centre name, a number for the children’s centre and a letter for the interviewee.
Analysis was undertaken using framework analysis321,322 and completed with software package NVivo 9.2 (QSR International, Warrington, UK). The initial framework was developed by researchers in Nottingham coding six randomly selected transcripts and reviewed by researchers in Bristol who developed the final thematic framework after analysing data from the 33 interviews. Emerging themes were reviewed by researchers from the four study sites and the qualitative consultant to the KCS research programme at each stage of the analysis. Coding consistency was checked by independent coding of two interviews by two researchers during development of the initial framework and of four interviews once coding was complete for all 33 interviews. Disagreements were handled by consensus-forming discussions. The coding frame was reviewed by researchers in all study sites, the qualitative consultant and the lay research adviser. Ethics approval was granted by North Nottinghamshire Research Ethics Committee (reference number 09/H0408/113).
Results
Semistructured interviews were conducted with 33 staff members (17 managers and 16 staff nominated by managers with face-to-face contact with parents and responsibility for organising health promotion activities) from 16 children’s centres across the four study areas. The characteristics of participating children’s centres are shown in Table 66. This indicates that a wide range of children’s centres across the four study sites took part in the study in terms of lead agency, rural/urban setting, phase and length of operation.
| Characteristic | Number of centres | |||
|---|---|---|---|---|
| Study centre | ||||
| Nottingham | 4 | |||
| Newcastle | 4 | |||
| Bristol | 4 | |||
| Norwich | 4 | |||
| Organisational setting | ||||
| NHS | 4 | |||
| LA | 11 | |||
| Charity | 1 | |||
| Rural/urban setting | ||||
| Urban | 10 | |||
| Urban/inner city | 1 | |||
| Urban and outer urban | 1 | |||
| Urban and phase 3 added rural population | 1 | |||
| City suburb | 3 | |||
| Phase | ||||
| 1 | 7 | |||
| 2 | 9 | |||
| Length of time children’s centre in operation (years) | ||||
| ≤ 2 | 1 | |||
| 3–4 | 6 | |||
| 5–6 | 2 | |||
| ≥ 7 | 5 | |||
| No information | 2 | |||
| Study centre | Organisational setting | Rural/urban | ||
| NHS = 4 LA = 11 Charity = 1 |
Urban = 10 Urban/inner city = 1 Urban and outer urban = 1 Urban and phase 3 added rural population = 1 City suburb = 3 |
1 = 7 2 = 9 |
≤ 2 years = 1 3–4 years = 6 5–6 years = 2 ≥ 7 years = 5 No information = 2 |
|
Seven key facilitators and six key barriers were identified. These are shown in Boxes 1 and 2, illustrated by participants’ quotations.
Our policies are formed from the Children’s Act um and Working Together to Safeguard Children and the staying safe element and the being healthy element of Every Child Matters that overrides everything . . . all policies with the children’s centres alongside the priorities highlighted in the Children and Young people’s plan which then provides us with um information for our self-evaluation and our service improvement plans which highlights specific national indicators.
Nottingham3a
Access to local data on injuries
This year we’re focussing on erm the, the accident and emergency . . . the numbers of visits to accident and emergency departments . . . in hospitals and we’ve identified particularly this area that I work, it has one of the highest levels erm of, of accidents, tragic accidents. So we’re working on how, how to prevent . . . [and] how to equip parents with the skills.
Nottingham1a
We got all of the data, the health data from accident and emergency for example which was really, really powerful and that provides us with an education programme not just for the centre but actually for children as well . . . I think [it] is possibly the most powerful data you’ll ever have really and broken down into specific ages as well.
Newcastle2b
Aligning with local needs
Because we’ve got a parent’s forum, and I’m sure D has spoken about this, is that we consult with them about what sort of things that they want, erm, thinking about health promotion, thinking about things that which, you know top of our agenda really. So they’ve been very successful.
Nottingham1b
Whether it’s specific parents meeting when we invite them in for their opinions and things they’d like but then also . . . because some people won’t come to that kind of forum . . . so we encourage staff to chat with parents in a session where it’s very relaxed and ask them about their feedback things that they’d like to see things that they don’t like things that they’d like help on and that and we try and then respond to that as best we can. So it’s not the fact that we’re just asking their opinions and doing nothing about it we then can signpost on all . . . we can say ‘well actually people are really interested in that area we’ll try and get somebody in to come and discuss that with them’.
Nottingham2b
Working in partnership with other organisations
It brings to us an overview of what’s happening city wide because we want to link with all the other children’s centres, it brings an overview of statistics that they get about hospital attendances and concerns and sort of what type of accidents are happening in the home. So it gives us the information for us to then work with. It also because it’s a partnership gives opportunities to do joint funded things and things such as promoting the booklets that we’ve had from the Child Safety Forum.
Newcastle1b
Yeah, well obviously we’ve got the five outcomes, so we’ve got ‘Be healthy, staying safe’, which is one of our, our five outcome groups and, erm, we, in this, this area here we have one local ‘Be healthy, staying safe’ group, which has health visitors, midwives, specialist family support team, nutritionists, those key people, that come to those meetings and, we do an improvement plan for the children’s centre, which looks at those elements of health promotion and everything and how other agencies can support that.
Nottingham1b
Funding to provide interventions/programmes
Norwich1b: Erm, we worked in conjunction with preschools in the area and made safety calendars. We worked alongside the fire service who installed smoke alarms . . .
Interviewer: And what’s the reason mainly for that sort of stopping?
Norwich1b: A lot of the stuff was the funding, so the First Aid, all the courses . . . the First Aid, the safety packs, the food hygiene, all of those were funding issues.
And Safety Crackers again it was a voluntary, a small voluntary organisation, they had a paid worker who’d overseen the programme and obviously looked at bids and funding and what have you but they also had an employed fitter who could go out to parents’ homes and fit things like smoke alarms, fit safety gates and it was a one-stop shop but they lost their funding.
Newcastle3a
Engagement with parents and families
Understanding community needs and strong trust-based relationships with parents and families
Relationships . . . and relationship building. You’ve got to get the trust of people who, they will be here for the accident bit, they’ll be here for the healthy eating, they’ll be here for absolutely every aspect of it so you’ve got to build those relationships up.
Newcastle2b
If you want to really get the most disadvantaged families when it comes to erm these things, I think you have got to be really creative and a lot of it does come down to the staff and how it is promoted and word of mouth in this area is really, really vital. So if it is run by somebody who is already known in the community or is trusted then it is ‘oh is it so and so doing it? Fine okay I will come’. So I think that is quite important.
Bristol1a
Facilities appropriate to the varied needs of parents and providing support to access children’s centres
It’s a massive step sometimes just to come through the door of the children’s centre. And . . . some people might be feeling quite isolated. They may not want to come in on their own, erm, they might not think it’s for them, they might not think it’s for everybody.
Newcastle4a
If we want parents to come along then we need to look at things like crèche and making sure that whatever the parents are learning the crèche workers are doing with the children. So if they’re doing something around healthy eating maybe in the crèche, you know the crèche workers are cutting up an apple and talking to the children about it so the parents and the children are learning together.
Newcastle3a
For vulnerable families, they need to be able to see someone that they recognise, know what they’re going for, so as much information that you can show, talk to them and say ‘look this is what we’re going to be doing, if you come along, I’m going to be there and so and so is going to be there and we’re all going to do it together’. I think that’s what you need for some of them . . . and the time that they actually do it and yeah just giving them as much information . . . with our groups we’re so, although they’re very structured, if a child doesn’t want to sing, it doesn’t matter I know that things have got to be structured but I think it needs to have a little bit of leeway. And then after, you’ll probably find if you’re running a programme for 5 weeks in the third week it was no problem at all it’s just getting them through the door.
Bristol1b
Effective communication
So I think there needs to be that level of passion because it’s got to be a continuous thing you’re not going to sell it to every single parent so you’ve got to be prepared to 25 parents in order to get the five that actually would like to do it so you’ve got to have that strong momentum I think to carry on going for it and believing in it.
Nottingham2b
I think it is . . . it’s the practical they enjoy the practical side and actually . . . and having . . . small groups but being engaged with their children the . . . on reflection when I was looking at this before, if you target a health initiative at a parent themselves initially that’s where we get the resistance. Because we are engaging with their children parents tend to want the best for their children and parents will engage in things for their children.
Nottingham3a
Practical support to promote safety messages
If it was something about safety in the home environment, and we managed to get them plug sockets and things like that, just saying to them have you got your plug sockets in . . . Have you got your stair gate up, have you . . . so make, have you used that new mattress that we’ve been able to get for you so that we’ve got that follow on. So it is not that they just come to a programme and away you go, it is about that follow-up really.
Newcastle3a
But what we offer advice, we will offer to go into the home and give advice to people at any time, we will use what we get from the Child Prevention Forum, also we do have a checklist that we do ourselves in the home. Particularly when we engage with people we do the 8-week visits and we try to cover that with people, you know we’ll take in the bags that we give, we do give plug covers and things like cupboard locks and drawer locks so we give them and they are easy to put in place, so we do go through that. We also offer a home visit at any time, we’d include all the information about what the fire service does and actually if there was anything else that we could do we would do that.
Newcastle1b
Using parent feedback to improve interventions
We do ongoing evaluations so if we find that something is not going well, you know at the end of each term we would ask parents to give us evaluation about you know the best things of the group and how we can improve it and then we will change things according to the feedback that we have had.
Bristol1a
Evaluating interventions/programmes
We did have a big evaluation last year um with the mental health team to look at how we can make it work better, which is why we agreed to try a different take on it this time but again it’s not working. What is working well is the individual referrals, so parents who want to go and speak to somebody individually um and individual counselling whereas I think opening up about your own stress, your own mental health within the group setting a lot of parents find very difficult.
Nottingham3a
High-quality training that can be cascaded to team members
I suppose, some training is – not is only as good, but is only as successful as the person you send on it, and how competent they are at coming back. So, some of our team are competent enough to go on training . . . and come back, and then talk to the whole staff as a team at a staff meeting, and suggest running a workshop on it . . . when training is delivered . . . and put together, . . . you need to think about how you can train someone on something, and empower them to take it back.
Norwich4a
What we try and do is send staff that have got that ‘oh yes I’d really like to go and see that’ and encourage them to go and then to come back and share and then to put it in practice . . . lead it and champion . . . we find that works quite well rather than everybody learning a little bit we’ve got some people that know an awful lot that can then share the information.
Nottingham2b
We used to get data from A&E that said, this is the amount of accidents you’ve had with under-fives from your area. We saw a significant dip. I don’t think it was the safety packs, I think it was the increased contact that workers were having with families, and the safety packs were the sort of sweetener to get through the door, because they loved them. But we don’t get that data now, so we don’t know what we do, whether what we are doing is working.
Norwich1a
Bristol1a: Well back when we were Sure Start local programme, I think that we were provided with some data around accidents within the home and number of admissions.
Interviewer: So do you have those figures?
Bristol1a: I don’t know, I haven’t got those figures any more. We used to get a lot more reporting from health when we were Sure Start Local Programme but as a children’s centre have dried up.
Lack of prioritisation of injuries as a key issue
I mean, accident prevention in the first Sure Start targets were about reducing hospital admissions, so that’s where the Home Safety Scheme came. That isn’t a target for us any more.
Norwich3a
Erm so it is like trying to join up what is already working in the area, where are the gaps that sort of thing. So we identified four areas that we felt were the biggest health issues for [this local area] of which home safety isn’t one of them.
Bristol1a
Unsustainability of interventions because of limited time or resources
My worry is that the health promotion practitioner has now left and hasn’t been replaced and it really did need that one person because we used to have meetings every month or so to arrange that. If you lose that one person that is going to co-ordinate that we would probably still do our own thing around safety week but would it be the big event that it is?
Nottingham4b
You know, because the point was made, once it’s gone, it’s gone. And are we sure we’re getting to the most vulnerable? But you do have to have, you know, benefits and various other criteria, and that’s the majority of our families. Erm, so it’s like do you have a hierarchy of need, or is it just you fit that criteria and then it works? You know, you get the equipment, but when 600 units have gone out, that’s it. Because I’ve got over 2000 children in my catchment area.
Norwich3a
Lack of funding or facilities to provide health promotion
[Parents response was] ’Wow – really waiting to see that’ and . . . sort of . . . giving out healthy food and stuff but when it came to signing up for course we found there weren’t enough places for all of them so it kind of put them off and they thought what was the point of that that was kind of their reaction the parents . . . so I thought I’m not sure if they should have done that unless there were lots of places for all of them
Bristol2b
We worked with a local organisation called Health First, who had reduced price, er, safety equipment as well, so we would point people in their direction if they wanted some additional things. And we had a much bigger budget to be able to do that . . . so we stopped doing that when we ran out of money to do it.
Norwich1a
There used to be, erm, something quite good, which was locally, called Safety Crackers. But they haven’t got the . . . funding for that, so sadly, that was quite a good service as well.
Newcastle4a
Difficulty engaging ‘hard-to-reach’ groups
. . . a very multicultural community um I think there’s over 50 different ethnicities within our particular area, it’s also very transient which means that we have constantly got a lot of moving so within a space of a year you could have upwards of 15 families living in one particular accommodation where they come in, they are there for a short period of time and then they move on and another family comes in . . . isolation is a big issue within the local area, the cultural mix is generally quite good . . . but where you have an asylum seeker that is placed in accommodation in a road which is not within their cultural mix they do become very isolated and it takes a lot of support to get them out of the house [and] some of the accommodation um isn’t particularly suitable for young families.
Nottingham3a
The government would love it yes the government would love it if we could put our hands on and actively encourage to get through the door teenage parents . . . you know what I mean . . . under age mums . . . that kind of thing and actually they’re probably out there but they’re very, very hard to reach and they don’t always engage and that so . . . we never stop trying and we’re always looking at different ways of trying to encourage people in.
Nottingham2b
Poor communication between other community professionals and children’s centres
I felt irritated in the past where staff at children’s centres have been expected to pick up what I felt were very much health issues so they you know we have been told oh who is your link member of staff for smoking cessation and I am thinking well yeah I could have someone on paper but actually that doesn’t mean very much and they don’t have that knowledge and expertise. Um at times it’s been quite hard to get from health practitioners the support that you want.
Bristol3b
The fire service we do send referrals in for them to do a home safety assessment for smoke alarms as need be. One thing we don’t get back from that is any feedback . . . we don’t know if it’s happened and we don’t know the numbers.
Nottingham4b
Identifying barriers to, and facilitators of, injury prevention among parents and caregivers (study G)
Methods
The objective of this study was to identify key facilitators and barriers for parents in terms of keeping their children safe from unintentional injury within the home. Participants recruited to the case–control studies undertaken in work stream 1 (see Chapter 2) were eligible to participate in this or two other studies nested within the case–control studies (studies B and C). Participants were eligible to participate in only one nested study, so those participating in study B or C were excluded from taking part in this study.
A sampling frame was devised to aid maximum variation sampling. This grouped parents by injury type (falls, poisonings, scalds or no injury) and deprivation, based on the IMD65 (less than the median IMD rank and greater than or equal to the median IMD rank). Before inviting parents to participate, researchers checked the sampling frame to ensure that participants would add to the variation within the sample. 323 Sixty-five parents across four centres (Nottingham, Bristol, Norwich and Newcastle) consented to participate and were recruited: 49 parents whose child had attended an ED or a MIU or had been admitted to hospital with an unintentional injury and 16 parents whose child had not experienced an unintentional injury requiring secondary care attendance when recruited to the study (as defined for recruiting controls for the case–control studies in work stream 1).
Data were collected using semistructured interviews. The interview topic guide was developed using findings from the systematic review of barriers to, and facilitators of, injury prevention252 described earlier in this chapter (study E). Four pilot interviews were undertaken across two study centres. Following piloting, the interview guide was adapted with minor word changes and additional prompts. Data from pilot interviews were not included in the analysis. Two versions of the interview guide were developed: one for use when interviewing parents whose child had experienced an injury and one for use with parents with an uninjured child. The guide covered five main topics: parental beliefs about injury prevention, strategies that can help to prevent injuries, parent or carer control over injury prevention actions, barriers to injury prevention actions and facilitators of injury prevention actions (see Appendix 4 for the interview guides).
Interviews lasted between 30 and 60 minutes and were conducted in the parents’ home. They were digitally recorded, anonymised prior to transcription and transcribed verbatim. Initially, data were explored for emerging themes by one researcher reading and rereading transcripts. Four transcripts were also read by a group of researchers consisting of an independent research consultant, a lay research advisor who was also a parent and two researchers from different study sites and an agreed coding structure was produced. This was applied to subsequent interview transcripts. Other emerging themes were discussed and agreed until a final set of themes was applied to all remaining interview transcripts. The coding process included identifying both confirming and disconfirming cases. 324 Data analysis was facilitated using NVivo 9.
Ethics approval was granted by Nottingham Research Ethics Committee 1 (reference number 09/H0407/14).
Results
The process of selection of participants is shown in Figure 21. The characteristics of the 65 children whose parents participated in the study are shown in Table 67. There illustrates wide variation in terms of child age and deprivation and good representation of both male and female children, with roughly equal numbers of children recruited across the four study sites. One interview was inaudible and was excluded from the analyses.
FIGURE 21.
Recruitment to the study identifying barriers to, and facilitators of, injury prevention among parents and caregivers (study G). a, Includes eight cases subsequently found not to be eligible for study A (study C, n = 7; study G, n = 1). These eight were not used to compare characteristics of participants in study B. b, Includes 37 controls subsequently found not to be eligible for study A.

| Centre | Injury mechanism | |||
|---|---|---|---|---|
| Fall | Poisoning | Scald | No injury | |
| Nottingham | Female; age 3 years; IMD rank 13,476 | Female; age 2 years; IMD rank 1399 | Female; age < 1 year; IMD rank 13,692 | Male; age 3 years; IMD rank 10,967 |
| Male; age 2 years; IMD rank 11,759 | Male; age 3 years; IMD rank 6244 | Female; age 1 year; IMD rank 31,559 | Male; age 2 years; IMD rank 5291 | |
| Male; age 2 years; IMD rank 30,973 | Male; age 2 years; IMD rank 21,774 | Male; age 1 year; IMD rank 26,413 | Male; age 2 years; IMD rank 27,268 | |
| Female; age 3 years; IMD rank 17,970 | Female; age 2 years; IMD rank 15,537 | Male; age 2 years; IMD rank 28,812 | Female; age 1 year; IMD rank 25,571 | |
| Bristol | Female; age 1 year; IMD rank 30,256 | Male; age 2 years; IMD rank 25,659 | Female; age 1 year; IMD rank 25,613 | Male; age 3 years; IMD rank 28,758 |
| Male; age 2 years; IMD rank 12,414 | Male; age 1 year; IMD rank 8833 | Female; age < 1 year; IMD rank 28,416 | Female; age 2 years; IMD rank 27,694 | |
| Male; age < 1 year; IMD rank 31,697 | Male; age 1 year; IMD rank 22,767 | Female; age 2 years; IMD rank 18,495 | Male; age 2 years; IMD rank 3028 | |
| Male; age 2 years; IMD rank 2895 | Male; age 1 year; IMD rank 7849 | Male; age 1 year; IMD rank 12,787 | Male; age 1 year; IMD rank 7462 | |
| Female; age > 1 year; IMD rank 19,014 | ||||
| Male; age 2 years; IMD rank 2829 | ||||
| Norwich | Female; age 3 years; IMD rank 21,939 | Male; age 3 years; IMD rank 18,121 | Female; age < 1 year; IMD rank 21,219 | Male; age 1 year; IMD rank 10,072 |
| Male; age 1 year; IMD rank 3721 | Male; age 2 years; IMD rank 7803 | Female; age 2 years; IMD rank 17,202 | Male; age 3 years; IMD rank 21,939 | |
| Female; age 4 years; IMD rank 6014 | Female; age 3 years; IMD rank 17,202 | Female; age 4 years; IMD rank 8628 | ||
| Male; age 1 year; IMD rank 18,121 | Male; age 3 years; IMD rank 21,313 | Female; age 2 years; IMD rank 7914 | ||
| Newcastle | Female; age 1 year; IMD rank 4126 | Female; age 3 years; IMD rank 15,067 | Male; age 1 year; IMD rank 7131 | Female; age 4 years; IMD rank 13,335 |
| Male; age 1 year; IMD rank 10,213 | Male; age 4 years; IMD rank 18,700 | Male; age 1 year; IMD rank 6562 | Male; age 1 year; IMD rank 29,509 | |
| Female; age 1 year; IMD rank 6815 | Female; age 2 years; IMD rank 25,678 | Male; age 3 years; IMD rank 8391 | Female; age 2 years; IMD rank 14,770 | |
| Male; age < 1 year; IMD rank 3979 | Female; age 2 years; IMD rank 11,964 | Female; age 2 years; IMD rank 4454 | Male; age 2 years; IMD rank 29,273 | |
| Male; age 1 year; IMD rank 7967 | ||||
Barriers for parents undertaking injury prevention within the home
Five main themes, each with subthemes, emerged relating to barriers to injury prevention. All parents described multiple barriers. The five main themes and related subthemes were:
-
lack of anticipation by parents of injury-producing events and/or their consequences:
-
lack of anticipation that injury-producing event would occur because of child’s age and/or stage of development
-
anticipation of injury-producing event but lack of anticipation of the severity of injury that may occur during the event
-
anticipation of injury-producing events but no translation into preventative action
-
-
fatalism:
-
inevitable events that were impossible to prevent
-
falls were more likely to be viewed as inevitable than poisonings or scalds
-
-
interrupted supervision:
-
distractions and multitasking
-
maternal fatigue
-
number of children in the household and the presence of older siblings
-
difficulties of parenting alone
-
-
environmental constraints:
-
safety equipment cannot be relied on to prevent injury
-
safety equipment was not relevant for the family
-
cost of safety equipment
-
difficulties in having or using safety equipment when the property is not owned by parents
-
-
timing/targeting of safety information in relation to ages and stages of child development:
-
information arriving too late in relation to the ages and stages of child development
-
lack of safety information
-
feeling bombarded by safety information.
-
Quotations illustrating these themes and subthemes are provided in Box 3.
I was surprised because for one I’d never known him go on the worktop, like go to reach for anything on the worktop, I didn’t think he’d be able to reach, erm, because of having two children before we know not to leave things on the edge of the worktop you know so it wasn’t and [B] said it wasn’t right on the edge it was kind of halfway back. But you know he was obviously determined and he was stretching as far as he possibly could. So yeah, it was a case of not realising how much he’d grown and – and erm, yeah – so I was surprised.
Scald, Nottingham, male, age 2 years, ≥ median IMD
Fatalism
I don’t think anyone can stop anyone from doing anything to be fair. If someone thought that they could stop a child from having an accident then they are quite delusional cos then you’re going down the route of you can stop rape from happening you can stop violence and all that stuff you can’t. Some things are just going to happen.
Fall, Newcastle, female, age 1 year, < median IMD
Interrupted supervision
It’s difficult to try and get on with just daily tasks . . . You know like cooking and cleaning it’s hard to do those kinds of things and watch [M] at the same time.
Poisoning, Newcastle, male, age 4 years,< median IMD
Erm time I think busy I mean I work full-time I work evenings I am all over the place so I’ve always got so much to do erm so maybe like when you haven’t had enough sleep she is not a good sleeper at night so I mean the night before last we got about 2 and a half hours of sleep. So it’s easy to overlook something or forget something you have got a lot on your mind . . . and it’s just trying and I keep on top of everything so I think that is like my biggest worry or potentially when things can go wrong I mean that’s how the accident happened.
Fall, Newcastle, female, age 1 year, < median IMD
And yeah its just a juggling act three kids you have always got to have eyes in the back of your head . . . He is little yeah and you you forget that as well like when you have got a 5-year-old and you got a baby . . . 2 is still only a baby he is only young himself so you have got to be careful not to expect too much of them so erm cos he looks so much bigger as well than a baby you know.
Poisoning, Bristol, male, age 2 years, ≥ median IMD
Environmental constraints
We don’t own the property we rent privately rent and err our landlord just has done hardly anything to the house . . . so that’s frustrating as its out of our hands . . . and I think you do you do tend to put off buying the safety gear because you have already spent a ton of money.
Fall, Newcastle, female, age 1 year, < median IMD
Especially with it not being my because its a rented house. I can’t put shelving across here. So I am just sort of following him around pretty much. I mean ideally I would put shelves up so I can move everything up a height and erm yeah put door catches on things you can’t drill, erm the taps [bath taps] are quite hard yeah cos they are not mixers and it’s really like I am sure no matter how tight I tie them he can undo them.
Fall, Nottingham, male, age 2 years,< median IMD
Timing of safety information
I think there should be some leaflets given out or something cos you get lots of leaflets when you are pregnant or when you first have a child and I think it is may be something that needs to be sort of pushed onto parents just to make you more aware because I wasn’t aware, I didn’t think about it I’ll admit it, you just don’t you know.
Poisoning, Nottingham, female, age 2 years, < median IMD
The trouble is I do think when you have got kids you get bombarded with so many leaflets from so many different places it could be about this that and everything that you tend to maybe either put them in a pile and not look at them anyway.
Fall, Bristol, male, age 2 years,< median IMD
Facilitators for parents undertaking injury prevention within the home
Five main themes, most of which had subthemes, emerged relating to facilitators of injury prevention. All parents described a combination of these strategies and the way that they combined these strategies altered with child age and development. The five main themes were:
-
anticipating and responding to injury risk:
-
anticipating injury risk and reducing risk through supervision
-
anticipating injury risk and reducing risk through separation of child and hazard
-
-
parental supervision:
-
never leaving the child alone
-
knowing where the child is and listening for silence as a cue for parental intervention
-
parents changed from never leaving the child alone to listening as children got older
-
-
teaching children about hazards and safety rules:
-
use of controlled risk as a teaching tool
-
explaining risk and consequences of injury
-
creating and adhering to safety rules
-
-
adapting the home:
-
minimising access to rooms perceived as particularly hazardous
-
placing items perceived as hazardous out of the child’s reach
-
installing and using safety equipment
-
-
learning from other parents’ ‘real-life’ stories:
-
real-life stories raise awareness and help parents anticipate injury risk.
-
Quotations illustrating these themes and subthemes are provided in Box 4.
So we are kind of pre-empting it a bit . . . . Yeah and just seeing what he’s trying to do and thinking right how can we protect him from that? . . . I think it’s just common sense more so than anything isn’t it?
Poisoning, Bristol, male, age 1 year, < median IMD
One is to keep her away from all sort of dangers especially in the kitchen from knife, bottles, medicine, all sharps, steps and any other things that we perceived to be dangerous to her really but what we try to do is to keep a constant eye on her. I mean that’s the main thing that we always do. We try to keep an eye on her, anything that looks dangerous we try to remove it.
Scald, Bristol, female, age 2 years, ≥ median IMD
Parental supervision
Its just being on your guard at all times it don’t matter if you think like you’re cleaning stuff and that is in a safe place out of his reach cos he they will still get to it. It’s knowing where they are. Listen out for the silence when it goes silent you know they are up to something.
Fall, Bristol, male, age 2 years, < median IMD
The stair gates are helpful of course they are helpful they are a tool that we do use and they can keep so you can you can go away or you can leave them unsupervised for a time but I think the most important thing is the supervision.
Control, Newcastle, male, age 2 years, < median IMD
Teaching children about hazards and safety rules
Because they learn from what’s right from wrong from an early age. They learn that no you can’t touch the kettle that that it’s going to be hot and if you touch it it is going to burn you. Same with the cooker you can’t reach and get grab something off the cooker and things like that they need to still know what is right from wrong that if they touch something it is going to hurt them and if something is hot.
Control, Nottingham, male, age 3 years, ≥ median IMD
Like with the radiator that is hot, we let him touch it, just the once, just to see so he knows that it’s hot so he doesn’t go back we did that with the taps as well so it’s just sort of letting them experiment with things to see that they can hurt and that they are a danger and stuff.
Fall, Norwich, male, age 1 year, < median IMD
Adapting the home
When they are younger obviously the safety equipment because you can’t teach them rules but you try as well but you need the equipment as well.
Control, Nottingham, male, age 2 years, < median IMD
We got two baby gates on the ground floor we got one upstairs just to prevent falling on the stairs we got these corner I don’t know how you call them covering the corners not to bump in to them er what else do we do . . . we got locks in the kitchen on every single cupboard we are planning to put them on the drawers as well because now she is interested in the drawers . . . we keep all doors or the gates closed all the time because she is wandering off and doing things that you wouldn’t want her to do . . . what else We did . . . we lowered the cot as she grew level by level so its on the ground level at the moment preventing her falling out.
Poisoning, Nottingham, female, age 2 years, < median IMD
Erm no chemicals are kept in there medicines are kept high up in an enclosed shelf it’s not locked but you need two hands and to be an adult to get it out so it is not easy for the children the children couldn’t reach it even with their steps they couldn’t reach it.
Control, Norwich, male, age 3 years, ≥ median IMD
Learning from other parents ‘real-life’ stories
. . . actual case studies of what’s happened to people’s children so that they know that yes this can happen and it’s true life and to be aware.
Poisoning, Nottingham, female, age 2 years, < median IMD
The iron I am really aware of because again that was an experience with someone that I knew had an iron dropped on himself when he was a baby and you know had brain damage from it so, so I am always really careful to think about that very much.
Fall, Nottingham, female, age 3 years, < median IMD
Discussion
Main findings
The systematic review and interviews with children’s centre managers, staff and parents have enabled identification of key barriers to, and facilitators of, implementing injury prevention by children’s centres and parents. Many of these were of direct relevance to, the design of, the intervention evaluated in work stream 6 (see Chapter 7). Some were contradictory, for example the provision of high-quality training was seen as an important facilitator by children’s centre managers and staff but the systematic review found that the requirement for a large amount of training for an intervention could also be a barrier. The systematic review also found that interventions needed to have a sufficiently long intervention period and multiple contacts to be successful in changing behaviour, but these interventions were also less likely to be implemented successfully or be sustainable because of resource requirements. It was therefore clear that there were trade-offs between some facilitators and barriers, which required compromises in the design of the intervention in work stream 6.
The key findings from studies E–G relevant for the design of the intervention in work stream 6 and the sources of the findings are shown in Table 68. This illustrates the similarities and differences between the findings arising from the different sources and the value of using findings from multiple sources.
| Intervention should | Source of recommendation | ||
|---|---|---|---|
| Systematic review | Interviews with children’s centre managers and staff | Interviews with parents | |
| Be based on a behaviour change model | |||
| Be delivered by professionals with an established trusted relationship with parents | |||
| Be delivered by enthusiastic and motivated staff | |||
| Be tailored to family needs and take account of the complexity of real-life situations | |||
| Be tailored to the child’s stage of development, addressing anticipation of injury risk and appropriate use of reasoning and safety rules | |||
| Challenge parents’ preconceived ideas when necessary | |||
| Address a small number of injury prevention topics, using short and simple messages with reinforcement, and not require multiple, concurrent behaviour changes | |||
| Provide required facilities (e.g. crèche/interpreter) | |||
| Provide incentives for behavioural change and/or for completion of outcome measurement tools | |||
| Be of sufficient duration and intensity to achieve behavioural change, but not so resource intensive that it is unfeasible to deliver | |||
| Address local/national priorities | |||
| Use local/national injury data | |||
| Be based on effective partnership working | |||
| Be adequately resourced | |||
| Provide high-quality training but not require unsustainable amounts of training | |||
| Provide opportunities to learn from parents’ real-life injury experiences | |||
Strengths and limitations of these studies
The use of three different studies to explore barriers to, and facilitators of, implementing home safety interventions from the perspectives of parents and professionals has allowed us to identify themes that are important to the deliverers of injury prevention interventions and to those receiving interventions. The use of different methodologies to explore the same phenomenon provided diversity of views and allowed triangulation of data and verification across studies, enhancing the credibility of the findings. Each study also had its strengths. To our knowledge, our systematic review is the first to combine data from quantitative and qualitative studies of barriers to, and facilitators of, child home safety interventions. Likewise, to our knowledge, the study of the views of children’s centre managers and staff is the first qualitative study in its field. The wide range of roles and experiences of participants provided breadth and depth to the interview responses. The children’s centres were situated in rural, suburban and urban settings across wide geographical areas, and barriers and facilitators were broadly similar across all study centres and are likely to be generalisable to other children’s centres in England. The qualitative study of parents’ views about barriers to, and facilitators of, the prevention of children’s injuries at home is the largest to date, adding considerably to the small amount of existing qualitative evidence in this area. It includes parents of children of varying ages and socioeconomic circumstances, including both parents whose children had been injured and parents whose children had not been injured, providing a range of parental perspectives within the data. The size of this study and the inclusion of parents whose children have experienced a variety of injury mechanisms has allowed, for the first time, comparison of barriers and facilitators across injury mechanisms.
Qualitative research is increasingly being used in multicentre research programmes to help answer complex research questions. 327 However, little has been written about the potential applications and limitations of the approach. Both interview studies undertaken as part of work stream 4 were conducted by a team of researchers from the four study sites. One of the main advantages of multicentre qualitative research is the additional capacity and expertise to execute the research, allowing a wide range of different perspectives to be captured. 328 This can also be advantageous when recruitment is challenging, and we were able to recruit additional participants at two study centres when recruitment was lower than expected at another centre. Sharing of expertise also extended to the data analysis, whereby multiple researchers were involved in the analytical process, helping to improve the rigour of the findings. 329 There are also potential limitations to undertaking qualitative research across multiple study sites. As the researcher plays a central role in eliciting information by creating ‘unique conversational spaces’,330 it is important to ensure that consistent methods are used across the research sites. 328 This was achieved in the KCS programme by the use of multicentre training, the development of standard operating procedures, sharing and reading the first four transcripts between researchers coding the data and regular teleconferences, face-to-face meetings and e-mail contact.
Our review was limited, as all reviews are, by the quality of the included studies and the quality of their reporting. Our review focused on barriers and facilitators identified by authors of included studies. As these were not the primary outcome measures for most included studies, it is possible that some outcome reporting bias occurred in authors’ reports of these. Details about how authors became aware of barriers to and facilitators of the delivery of the interventions within their studies were sparse, and explicit attempts by authors to study barriers and facilitators were rare. Most studies reported on barriers and facilitators from the perspective of those delivering interventions, not from the perspective of those receiving interventions.
Our interviews with children’s centre managers and staff took place during a time of reorganisation for many children’s centres, making it difficult at times to find staff who were willing and able to participate, and a small number of interviews were curtailed because of other work pressures. Managers nominated staff members to participate in interviews, hence a selection bias may have occurred whereby particular views are under- or over-represented. The wide range of responses provided by participants would suggest that this may not have occurred to an important extent. Nominated staff tended to be more hesitant and unsure about their children’s centre’s role in injury prevention than managers, but they were able to provide information about the practical experience of delivering interventions, which was very valuable.
It is possible that the parents and children’s centre staff who agreed to take part in the interviews had a particular interest in or were motivated by the aims of the study or child safety in general and that their views may reflect this. As for other qualitative research, given its context-specific nature, it is not appropriate to generalise our findings to the wider population of parents or children’s centres. However, the maximum variation sampling, the large number of interviews conducted and the multicentre nature of both of our interview studies will have helped to obtain a wide representation of views and experiences, which should be broadly transferable to parents of young children and children’s centre staff in other disadvantaged areas of the country.
Comparisons with the published literature
Our review extends the findings of the systematic review of qualitative studies by Smithson et al. ,245 who explored barriers to, and facilitators of, interventions supplying and/or installing home safety equipment and home safety risk assessments. The key facilitators, in common with those we found, were partnership working, training, policy drivers, providing culturally sensitive information and advice, providing interventions appropriate to the family’s needs and living conditions, having trusting relationships with professionals, providing education relevant to a child’s developmental stage and acknowledging mothers’ ongoing safety efforts. 245 In contrast to the Smithson et al. review,245 we found that the use of behaviour change models to guide the design of interventions and focusing on fewer types of injury also acted as facilitators. Both our review and that of Smithson et al. 245 identified many similar barriers including socioeconomic, cultural and language barriers, lack of control over housing and poor housing conditions and mistrust of professionals and their motives. Our review also highlighted the difficulty of providing interventions to transient populations and of achieving behavioural change with one-off educational interventions, short-lived interventions or complex interventions that require multiple concurrent behavioural changes in the face of long-held beliefs and practices and the unsustainability of interventions requiring large investments of resources or staff time. In contrast, Smithson et al. 245 highlighted social isolation and poor relationships between mothers and their partners or with the household decision makers as barriers to injury prevention. Making physical changes to the home or allowing an outside agency into the home (e.g. to fit safety equipment or undertake a home safety assessment) is likely to need agreement from all adults living in the household. This may have emerged as a barrier in the Smithson et al. review,245 as it included only studies supplying or installing safety equipment or providing home safety assessments, whereas our review included studies with a much broader range of interventions.
The facilitators identified in the interviews with children’s centre managers and staff are consistent with those from our systematic review252 and Smithson et al. ’s review245 regarding partnership working and engagement of families. In terms of barriers, our findings are consistent with the review findings245,252 regarding absence of local injury data, low prioritisation of injuries, short-term interventions, low literacy levels, low income levels, problems with communication between professionals and inadequate funding, resources or time. In addition, our findings are consistent with the barriers to, and facilitators of, injury prevention identified by children’s centre mangers in our national survey of children’s centres in England undertaken as part of work stream 3217 (see Chapter 4).
The findings from interviews with parents regarding barriers to injury prevention are also consistent with those from our systematic review252 and Smithson et al. ’s review245 in terms of constraints from economics or living conditions, difficulties in understanding child development and anticipating injury risk, fatalistic attitudes towards injuries and mistrust of professionals, and a lack of information on child safety for parents. In terms of facilitators, our findings are consistent with those of the Smithson et al. review245 in terms of the use of ‘real-life’ injury experiences as learning opportunities for parents, the importance of supervision and the importance of timely safety information.
The findings from our review and qualitative studies are also consistent with recommendations from NICE on interventions to support changing health-related behaviours. 226 Recommendations include providing interventions based on partnership working that are evidence based, tailored to individuals’ needs and developed with the target population, that enhance self-efficacy and that are based on theories or models of behaviour change.
How these findings inform other research within the Keeping Children Safe programme
The findings from studies E–G were used to inform the development of an injury prevention intervention (an IPB) for delivery by children’s centres, which was evaluated using a RCT (study M in work stream 6; see Chapter 7). Finally, the findings were used to develop a second IPB incorporating the findings from all studies in the KCS programme (see Figure 1).
Chapter 6 How effective and cost-effective are a range of strategies for preventing falls, poisoning and scalds based on decision-analysis models incorporating data generated from research questions 1–3 and systematic reviews of the published literature? (Work stream 5)
Abstract
Research question
How cost-effective are strategies for preventing thermal injuries, falls and poisonings?
Methods
This work stream consisted of four studies:
-
Study H. Systematic overviews were carried out, with bibliographic databases and other sources searched (fires, March 2009; falls, October 2010; poisonings, January 2012; scalds, October 2012). Data were synthesised narratively.
-
Study I. A systematic review was carried out, with bibliographic databases and other sources searched to May 2009. Random-effects PMAs were used to estimate pooled ORs and incidence rate ratios (IRRs).
-
Study J. Random-effects NMAs were used to estimate pooled effect sizes for all combinations of interventions.
-
Study K. Decision analyses were used to estimate incremental cost-effectiveness ratios (ICERs) and probabilities of interventions being cost-effective.
Results
There was little evidence on the impact of home safety interventions on risk of injury or death from fires, scalds, falls or poisonings.
Fire prevention
Most evidence related to smoke alarms. Several case–control studies found that smoke alarm ownership was associated with a lower risk of house fire death and injury. PMA showed that interventions increased functional alarm ownership (OR 1.81, 95% CI 1.30 to 2.52). NMA found that education plus home safety inspection plus providing and fitting low-cost/free equipment was most effective in increasing functional alarm ownership [OR 7.15, 95% credible interval (CrI) 2.40 to 22.73; p best = 0.66]. Education plus providing and fitting low-cost/free equipment was the most cost-effective intervention (£34,200 per QALY, reducing to £4500 per QALY assuming that there were 1.8 children aged < 5 years per household).
Scald prevention
Most evidence related to ‘safe’ bathwater temperatures. Narrative reviews and PMA found that interventions promoted ‘safe’ temperatures (OR 1.41, 95% CI 1.07 to 1.86). NMA found that education plus providing and fitting low-cost/free equipment (TMVs) was the most effective intervention (OR 38.82, 95% CrI 3.58 to 599.10; p best = 0.97). However, this was the most cost-effective intervention only if TMVs were fitted during major refurbishment or in new builds for families in social housing, in which case money was saved.
Falls prevention
Most evidence related to safety gates and baby walker use. Narrative reviews and PMA found that interventions increased safety gate use (OR 1.61, 95% CI 1.19 to 2.17). NMA found that education plus home safety inspection plus providing and fitting low-cost/free equipment was the most effective intervention (OR 7.80, 95% CrI 3.18 to 21.3; p best = 0.97). Usual care (p best = 0.999) had the highest probability of being cost-effective (at £30,000 per QALY) and education had the lowest ICER (£284,068 per QALY). Narrative reviews and PMA found that interventions reduced baby walker use (OR 1.57, 95% CI 1.18 to 2.09). NMA found that education was most effective (OR for walker use 0.48, 95% CrI 0.31 to 0.84).
Poisoning prevention
Most evidence related to safe storage of medicines and household products. Narrative reviews and PMA found that interventions increased the safe storage of medicines (OR 1.53, 95% CI 1.27 to 1.84) and household products (OR 1.55, 95% CI 1.22 to 1.96). NMA found that education plus providing and fitting low-cost/free equipment was the most effective intervention for medicines (OR 2.51, 95% CrI 1.01 to 6.00; p best = 0.39) and education plus home safety inspection plus providing and fitting low-cost/free equipment was the most effective intervention for household products (OR 2.59, 95% CrI 0.59 to 15.16; p best = 0.37). Usual care (p best = 0.83) had the highest probability of being cost-effective (at £30,000 per QALY) for the safe storage of medicines. Education had the lowest ICER compared with usual care at £41,330 per QALY, reducing to £19,315 per QALY if education was targeted at families in the most disadvantaged areas where injury rates were higher. For safe storage of cleaning products, all interventions were more costly and less effective than usual care.
Conclusions
In general, more intensive interventions (e.g. education plus providing and fitting low-cost/free equipment and in some cases home safety inspection) were more effective than less intensive interventions, but the most effective interventions were not necessarily the most cost-effective.
Chapter summary
All studies in this work stream relate to evidence on the prevention of fire-related injuries, scalds, falls and poisonings. The work stream consists of study H (overviews of reviews and systematic reviews of primary studies), study I (update of a Cochrane systematic review of home safety interventions and PMAs of interventions), study J (NMAs of interventions) and study K (decision analyses of interventions). This chapter commences with an overall introduction and then describes the methods for studies H–K in turn. The results are then presented for fire prevention, scalds prevention, falls prevention and, finally, poisonings prevention interventions. As many studies are included in more than one of our overviews of reviews, systematic reviews or meta-analyses, to avoid repetition we present one table describing the characteristics of the reviews included in all overviews and a second describing the characteristics of the primary studies included in all overviews, systematic reviews and meta-analyses. Within each injury mechanism, the results from studies H–K are described in turn. The chapter ends with an overarching discussion.
Introduction
Over the last 25 years, and prior to the KCS programme, a series of systematic reviews have been undertaken evaluating the effect of a wide range of home safety interventions in childhood for the prevention of thermal injuries, falls and poisoning,33–42,331–337 including four by members of the KCS study group. 33–36 Only three of these reviews included meta-analyses,33,37,40 with the remainder being narrative reviews. Both the narrative reviews and meta-analyses provided evidence that home safety interventions were effective in promoting some safety behaviours (e.g. storage of medicines and household products out of reach, having a ‘safe’ hot tap water temperature) and possession and use of some items of safety equipment (e.g. possession of a functional smoke alarm and of a fitted and used stair gate). The reviews also demonstrated a lack of evidence about whether or not home safety interventions reduced injury rates. However, there was considerable variation in the findings of the reviews because of differences in the populations, settings, interventions and outcomes of studies included in the reviews. The reviews also varied widely in scope and quality. Since commencing the KCS programme, a small number of further relevant reviews have been published. 338–340 Multiple systematic reviews, especially when their findings are not consistent, generate uncertainty for policy makers and practitioners, making evidence-based decision making difficult. 341 There is therefore a need to consolidate evidence across existing reviews and, as many reviews were undertaken > 10 years ago, a need to update the evidence with more recently published studies.
Overviews are useful when there are multiple interventions for the same condition or problem reported in separate systematic reviews. 342 Study H therefore reports the findings from four systematic overviews and systematic reviews of more recently published studies covering the prevention of fire-related injuries, scalds, falls and poisonings in childhood. Study I presents the findings from an update of a Cochrane systematic review and meta-analysis of home safety interventions for the prevention of fire-related injuries, scalds, falls and poisonings in childhood. 33
The interventions evaluated in these systematic reviews and meta-analysis were heterogeneous and included various combinations of education, home safety inspection, provision of free or low-cost safety equipment and fitting of equipment. Some aimed only to prevent single types of injury (e.g. fire-related injuries), whereas others aimed to prevent a range of injuries. The treatment of control arms also varied across studies; they most often received ‘usual care’, but some control arms received generic safety advice or elements of the intervention, for example home safety inspection but not home safety equipment. Decision-makers have to make decisions about the ‘best’ intervention to commission or provide to prevent child injuries and analyses ‘lumping’ varying intervention treatments together or varying control treatments together are of limited use for these decisions. NMA methods343–345 extend standard (pairwise) meta-analysis to allow all interventions to be compared with one another, including comparisons not evaluated within any of the primary studies. Health technology assessment is making increasing use of NMA to inform decisions about optimal intervention strategies for medical conditions. 346 In injury prevention, in which interventions are frequently complex and multifaceted but the number of studies evaluating each intervention is only small, NMA is particularly relevant. At the time of commencing the programme grant there were no published NMAs in the field of child home injury prevention. Study J presents the findings from the first NMAs to evaluate child home safety interventions for fire-related injuries, scalds, falls and poisonings.
Knowing which interventions are most effective for preventing injuries is important, but cost-effectiveness is an essential part of any decision-making process. At the time of commencing the KCS programme there were few economic evaluations of interventions to prevent fire-related injuries, scalds, falls or poisonings in the UK. 347,348 One economic evaluation of a RCT of a smoke alarm giveaway programme in disadvantaged wards in London found higher costs and higher injury and fatality rates in intervention wards than in control wards; the study concluded that the programme, as delivered in the trial, was unlikely to be a cost-effective use of resources. 347 Since commencing the KCS programme, a systematic review and quality assessment of economic evaluations of 48 injury prevention studies was published in 2012,349 with searches run up to the end of 2009, which included only the economic evaluation of a smoke alarm giveaway programme cited above. A systematic review of published economic evaluations of legislation, regulations and standards and/or their enforcement and promotion by mass media to prevent unintentional injuries in children undertaken to support NICE guidance PH2925 found no UK studies. 116 An economic modelling exercise undertaken to support NICE guidance PH29,25 PH3027 and PH31350 explored the cost-effectiveness of regulations for and the enforcement, promotion and monitoring of the installation of TMVs in social housing where there are children aged < 5 years. 351 This concluded that the cost per QALY gained ranged from £67,000 to £144,600 depending on uptake in eligible households over a 15-year period (assumed to be 70% and 30%, respectively). An economic evaluation of a RCT designed to fit TMVs in social housing households with children aged < 5 years concluded that, if fitted as part of a major refurbishment or rebuild of social housing, the public purse saved £1.41 for every £1 spent and it was likely that installing TMVs represented value for money. 140 The KCS programme aimed to increase the evidence base in this area by undertaking a series of decision analyses (study K) of interventions to prevent fire-related injuries, scalds, falls and poisonings found to be effective in the NMA undertaken earlier in the programme (study J). The findings from studies H–K informed the development of the intervention (the IPB for preventing fire-related injuries), which was tested using a RCT in work stream 6 (see Chapter 7). The findings from work stream 5 were subsequently used, in conjunction with the findings from all other work streams in the programme, to develop an IPB for the prevention of fire-related injuries, scalds, falls and poisonings (see Chapter 7).
Methods
The methods for the overviews of reviews and systematic reviews (study H), the PMAs (study I), the NMAs (study J) and the decision analyses (study K) are described in turn in the following sections.
Overviews of reviews and systematic review of primary studies published subsequent to the reviews (study H)
Objectives
The objectives of the overviews and systematic reviews were to:
-
summarise the evidence from systematic (narrative) reviews or meta-analyses of non-legislative home safety interventions for preventing thermal injuries (fire-related injuries and scalds), falls and poisonings within the home in children aged 0–19 years that report injuries, safety equipment possession or use or injury prevention practices
-
update the evidence from systematic reviews by systematically reviewing more recently published primary studies (RCTs, non-RCTs, CBAs, cohort studies and case–control studies), appraising study quality and extracting data or, when necessary, obtaining data from authors
-
identify primary studies and data for inclusion in NMAs (study J) and identify plausible effect sizes for interventions to inform decision analyses.
Methods
Eligibility criteria
Overviews of reviews, systematic reviews and meta-analyses of experimental (RCTs, non-RCTs and CBAs) and controlled observational (cohort and case–control) studies were eligible for inclusion. Systematic reviews were defined using the Cochrane reviewer’s handbook definition. 342 Reviews were eligible if they reported:
-
Non-legislative interventions aimed at the prevention of fire-related injuries, scalds, falls or poisonings among children aged 0–19 years.
-
The use of home safety equipment or other injury prevention practices for the primary, secondary or tertiary prevention of fire-related injuries, scalds, falls or poisonings. Primary prevention referred to preventing the injury-producing events (e.g. fires), secondary prevention referred to preventing an injury occurring during the event (e.g. a smoke alarm does not prevent the fire but can prevent an injury by alerting people and enabling escape from the fire) and tertiary prevention referred to minimising the impact of the injury through the provision of first aid.
-
Interventions within the scope of activities undertaken by children’s centres in England. The remit of children’s centres included the provision of ‘advice on accident and injury prevention’ (p. 12)210 (contains public sector information licensed under the Open Government Licence v3.0); interventions beyond this remit, such as legislative interventions, World Health Organization Safe Community programmes or complex home visiting programmes, were excluded.
Primary studies, of the designs described above and published following the date of the most recent comprehensive systematic review, were eligible for inclusion. We searched from the date of the most recent review that included all study designs, interventions and outcomes eligible for our reviews. For fire prevention, these were the reviews published by Towner et al. in 1996352 and Warda et al. in 1999. 353,354 For the prevention of scalds, falls and poisoning we chose the most recent review, which was the 2001 review by Towner et al. 36 For first aid interventions only one systematic review was found, which included only four studies;355 hence, searches for primary studies for first aid interventions were run from the date of inception of the databases.
Information sources
We searched MEDLINE, EMBASE, CINAHL, ASSIA, PsycINFO and Web of Science. The dates for which searches were run for each overview are shown in Table 69.
| Interventions | Searches for reviews | Searches for primary studies |
|---|---|---|
| Fire prevention | Date of inception to March 2009 | January 1996 to March 2009 |
| Scald prevention | Date of inception to October 2012 | January 2001 to October 2012 |
| Falls prevention | Date of inception to October 2010 | January 2001 to October 2010 |
| Poisoning prevention | Date of inception to January 2012 | January 2001 to January 2012 |
| First aid interventions | Date of inception to October 2010 | Date of inception to October 2010 |
Searches
Search terms for MEDLINE are provided in Appendix 5, Search terms for the overviews of reviews and primary studies for study H for each overview and systematic review, with strategies adapted as necessary for the other databases. Other sources searched are listed in Appendix 5, Other sources searched for overviews of reviews and primary studies for study H. Searches were not restricted by language or publication status. Articles were translated when necessary.
Study selection
Titles and abstracts of articles were scanned independently by two reviewers to identify articles to retrieve in full. When articles appeared eligible but no abstract was available, full articles were retrieved. Disagreements between reviewers were dealt with by consensus-forming discussions and referral to a third reviewer.
Data collection process
Data were extracted on study design, participants, interventions, comparator groups and outcomes independently by two reviewers using a standardised data extraction form. Disagreements between reviewers were dealt with by consensus-forming discussions and referral to a third reviewer.
Assessment of risk of bias
Assessments of risk of bias were carried out independently by two reviewers. Disagreements between reviewers were dealt with by consensus-forming discussions and referral to a third reviewer.
The risk of bias for reviews was assessed using the Overview Quality Assessment Questionnaire (OQAQ). 356 The risk of bias for primary studies was assessed using adequacy of allocation concealment, blinding of outcome assessment and follow-up of at least 80% of participants for RCTs and blinding of outcome assessment, follow-up of at least 80% of participants and balance of confounders between treatment groups for non-RCTs and CBAs. For overviews conducted later in the programme of research (scalds, poisonings and first aid interventions) we assessed risk of bias for primary studies using the criteria specified in the Cochrane reviewers handbook. 342 The risk of bias for cohort and case–control studies was assessed using the Newcastle–Ottawa Scale. 357
Data synthesis
Data were synthesised narratively. We tabulated the characteristics of included reviews and included primary studies. For each primary study included in a review, we tabulated which reviews it was included in and the outcomes that it reported.
Pairwise meta-analyses of the effectiveness of home safety interventions (study I)
Objective
The objective of the systematic review and meta-analyses was to synthesise evidence from RCTs, non-RCTS and CBAs on the effectiveness of home safety education provided to children (or families with children) aged 0–19 years, with or without the provision of low-cost, discounted or free equipment (hereafter referred to as home safety interventions), in reducing injury rates or increasing home safety equipment possession or use or injury prevention practices.
Methods
We updated a Cochrane systematic review and PMAs previously published by members of the KCS programme team. 33 This included PMAs for outcomes for which NMA was not possible (study J).
Eligibility criteria
Randomised controlled trials, non-RCTs and CBAs whose participants were children and young people (aged ≤ 19 years) and their families and which evaluated home safety interventions provided by health or social care professionals, school teachers, lay workers or voluntary or other organisations aimed at reducing home injuries or increasing home safety practices were included. To be included, studies had to report injuries, possession and use of home safety equipment or injury prevention practices among their outcome measures. The outcomes of interest for the KCS programme were:
-
fire prevention – possession of a smoke alarm, possession of a functional smoke alarm, checking or changing smoke alarm batteries, possession of fireguards, storage of matches out of reach, possession of a fire extinguisher, possession of a fire escape plan
-
scald prevention – having a safe hot tap water temperature, keeping hot drinks/foods out of reach
-
falls prevention – possession of a fitted safety gate, possession or use of a baby walker, possession of a non-slip bath mat or decals, possession of window safety devices (locks, screens or opening width restrictors, hereafter referred to as window locks), never leaving a child alone on a high surface
-
poisoning prevention – storing medicines out of reach, storing other household products out of reach, storing poisons out of reach, storing plants out of reach, possession of the PCC number.
Information sources
We searched the Cochrane Central Register of Controlled Trials, MEDLINE, EMBASE, PsycINFO, Web of Science, CINAHL, Database of Abstracts and Reviews of Effects, NHS Economic Evaluation Database and Health Technology Assessment database from date of inception to end of May 2009. In addition, a range of websites was searched (to June 2009) and hand searching was carried out of abstracts from the 1st to the 9th World Conferences on Injury Prevention and Control, the journal Injury Prevention (to March 2009) and reference lists of articles included in the review and published systematic reviews. The sources searched are shown in Appendix 5, Other sources searched for study I. Authors of published and unpublished studies were contacted as described in the published review. 49
Search
The MEDLINE search strategy is provided in Appendix 5, Search strategy for study I. This was adapted as necessary for other databases. Searches were not restricted by language or publication status. Articles were translated when necessary.
Study selection
Titles and abstracts of articles were scanned independently by two reviewers to identify articles to retrieve in full. When articles appeared eligible but no abstract was available, full articles were retrieved. Disagreements between reviewers were dealt with by consensus-forming discussions and referral to a third reviewer.
Data collection processes
Data were extracted independently by two reviewers using a standardised data extraction form. Disagreements between reviewers were dealt with by consensus-forming discussions and referral to a third reviewer. Authors of studies were contacted to supply unpublished data, including individual participant data when this allowed studies to be included in our meta-analyses (e.g. when papers reported composite outcomes such as safety scores but individual items of the composite measure were outcomes in our meta-analyses). When individual participant data were obtained, we formatted these in a standard format.
Assessment of risk of bias
Assessments of risk of bias were made independently by two reviewers. Disagreements between reviewers were dealt with by consensus-forming discussions and referral to a third reviewer.
Data synthesis
Meta-analyses were undertaken when three or more studies reported the same outcome. For injury rates, pooled IRRs were estimated using random-effects models. For CBAs, we estimated follow-up injury rates adjusted for baseline rates. For binary outcome measures (safety equipment possession or use, injury prevention practices), pooled ORs were estimated using random-effect models. Studies were adjusted for clustering as necessary and management of studies with more than one intervention or control arm is described in the published review. 49 Cases with missing values were excluded from all analyses.
Heterogeneity between effect sizes was described using forest plots, chi-square tests and the I2 statistic. Potential explanations for heterogeneity were explored by a priori subgroup analyses, which included whether or not safety equipment was provided, study setting and study quality. Publication and related biases for binary outcomes were investigated using the approach recommended in recent guidelines. 358 For meta-analyses of injury rates, when there were ≥ 10 studies we assessed publication bias using Egger’s test. The individual contribution of each study to the pooled result was assessed graphically, and sensitivity analyses were undertaken to assess the effect of removing each study from each analysis. The robustness of the findings with respect to study quality was assessed using subgroup analyses by comparing treatment effects between randomised and non-randomised studies and between RCTs with and without adequate allocation concealment, blinded outcome assessment and follow-up of at least 80% of participants in each study arm.
Network meta-analyses (study J)
Objective
The objective of the NMAs was to evaluate the effectiveness of home safety interventions for the prevention of fires, scalds, falls and poisonings using an extension of PMA that enables comparison of all evaluated interventions simultaneously within a single coherent analysis.
Methods
Study identification
Data were extracted from primary studies identified from the overviews of reviews and systematic reviews of more recently published primary studies undertaken in study H. When individual participant data were used in the PMA for study I, the same data were used in study J.
Statistical methods
Network meta-analyses were undertaken for the following binary outcomes:
-
fire prevention – possession of a smoke alarm, possession of a functional smoke alarm, possession of different types of battery-powered alarms, possession of fireguards, storage of matches out of reach, possession of a fire extinguisher, possession of a fire escape plan
-
scald prevention – having a safe hot tap water temperature, keeping hot drinks/foods out of reach
-
falls prevention – possession of a fitted safety gate, possession or use of a baby walker, possession of a non-slip bath mat or decals, possession of window locks, never leaving a child alone on a high surface
-
poisoning prevention – storing medicines out of reach, storing other household products out of reach, storing poisons out of reach, storing plants out of reach, possession of the PCC number.
Pairwise meta-analyses are usually restricted to calculating a pooled estimate of effectiveness comparing two groups, often an intervention group with a control group. Home safety interventions are often complex and multifaceted interventions, consisting of various combinations of safety education, the provision of free or low-cost safety equipment, fitting of safety equipment and home safety assessments. The control arms used in studies of home safety interventions may include usual care (which can vary between studies), generic safety advice (as opposed to specific or tailored advice) or some, but not all, of the elements of the intervention. Consequently, PMA often involves some ‘lumping’ together of interventions (and control conditions). For example, in PMAs of interventions to promote functional smoke alarms,33,37,40 interventions that provided education were grouped together with interventions that provided smoke alarms. This included interventions fitting low-cost/free smoke alarms, providing but not fitting low-cost/free smoke alarms, providing home safety inspections and referring to child safety centres. In addition, the educational component of these interventions included very brief face-to-face advice, providing leaflets and videos, providing generic or tailored safety advice or classes or lectures on parenting/child safety. The control conditions included unspecified usual care, well child visits, standard/generic safety advice, leaflets, videos, information about or referral to child safety centres and home safety inspections.
However, commissioners, service providers and parents, among others, need to decide on the ‘best’ intervention for preventing a particular injury. NMA enables comparison of all evaluated interventions simultaneously within a single coherent analysis. 343–345 Suppose we have studies providing effect estimates for a control compared with intervention A and for intervention A compared with intervention B. NMA allows estimation not only of the pooled effects when pairwise evidence exists (direct comparison between control and intervention A and between intervention A and intervention B) but also of effects when interventions are not directly compared but are linked through a connected network of studies (indirect comparison between control and intervention B). Interventions can also be ranked in order of effectiveness. This approach is increasingly being used in health technology assessment when deciding on the optimal intervention strategy for a particular condition. 346,359
Network meta-analysis was used to compare all interventions with one another, using all available data in a connected network of studies and a standard NMA random-effects model with a binary outcome. 344,345 Pooled estimates of intervention effects for all combinations of pairwise comparisons were obtained. Intervention effectiveness was ranked based on absolute intervention effects (derived using an underlying rate based on the usual-care arms) and the probability that each intervention was best for a particular outcome was calculated. 344
The between-study SD parameter was used to assess the variability in effect sizes within pairwise comparisons above that expected by chance. 360–362 We assessed and tested the consistency between evidence from studies that directly compared the two treatments under consideration (‘direct’ evidence) and evidence from the remaining studies in the network (‘indirect’ evidence). We also assessed goodness of fit of the model. Analyses were conducted using a Markov chain Monte Carlo (MCMC) method344 and fitted using WinBUGS software [version 1.4.3; Medical Research Council (MRC) Biostatistics Unit, Cambridge, UK]. 363 Further technical details of the analysis together with the WinBUGS code are available from the authors on request.
In addition, we have already taken steps to start to address some of the research recommendations arising from the KCS programme to allow for more detailed analysis of the evidence by extending methods for NMAs. These include methods for adjusting for baseline risk, simultaneously incorporating aggregate and individual participant data, exploring effect modifiers and extrapolating evidence across different networks for multiple outcomes. These are not described in this report and the reader is referred to the publications. 364–367
Decision analyses (study K)
Objective
The objective of the decision analyses was to determine the cost-effectiveness of interventions shown to be effective (defined as those for which the 95% CI or the 95% CrI did not include the value of 1) in the NMA undertaken in study J. This included interventions to:
-
increase the prevalence of functioning smoke alarms
-
increase the prevalence of TMVs
-
increase the prevalence of safety gate use
-
increase the prevalence of the safe storage of medicines and household products.
Methods
We evaluated the impact on overall lifetime costs and quality of life of living in a household with or without the item of safety equipment or safety practice of interest (functioning smoke alarm, a TMV, a safety gate and safe storage of poisons and household products) in hypothetical populations of newborn infants, from birth to 4 years of age. We used three-stage mathematical models to estimate lifetime QALYs and intervention costs from a public sector perspective [UK NHS costs, Personal Social Services (PSS) costs and other public sector costs], discounted at the standard annual rate of 3.5%. 114 ICERs and the principle of dominance368 were applied based on calculating the ICER of each intervention compared with the next most effective intervention. That is, an intervention was dominated by an alternative intervention if the alternative was both less costly and more effective and extendedly dominated if an alternative intervention was both more costly and more effective but had a lower ICER (i.e. provided better value for money). Cost-effectiveness acceptability curves presenting the probabilities of interventions being cost-effective at different decision-makers’ cost per additional QALY thresholds114 were estimated from the models.
Decision models
Our decision modelling was guided by published principles for good modelling practice and design369 and NICE public health methods guidance. 370,371 We used the software package R (version 2.15.1; R Foundation for Statistical Computing, Vienna, Austria) to construct models and these were assessed using Monte Carlo simulation in R or MCMC simulation in WinBUGS 1.4.3. 372 Figure 22 illustrates the three-stage decision model using the example of interventions to promote the prevalence of functional smoke alarms and Figure 23 illustrates the decision model structure within each yearly cycle of the stage 2 (preschool) model.
FIGURE 22.
Schematic diagram illustrating the three-stage process for decision modelling using the example of interventions to promote the prevalence of functional smoke alarms. Note: shaded box is an intermediate state that may occur within any one yearly cycle. Adapted from Saramago et al. 373 under the Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).

FIGURE 23.
Decision model structure within each yearly cycle of the stage 2 (preschool model) model. Note: the oval nodes match to the oval nodes in the schematic diagram in Figure 22.
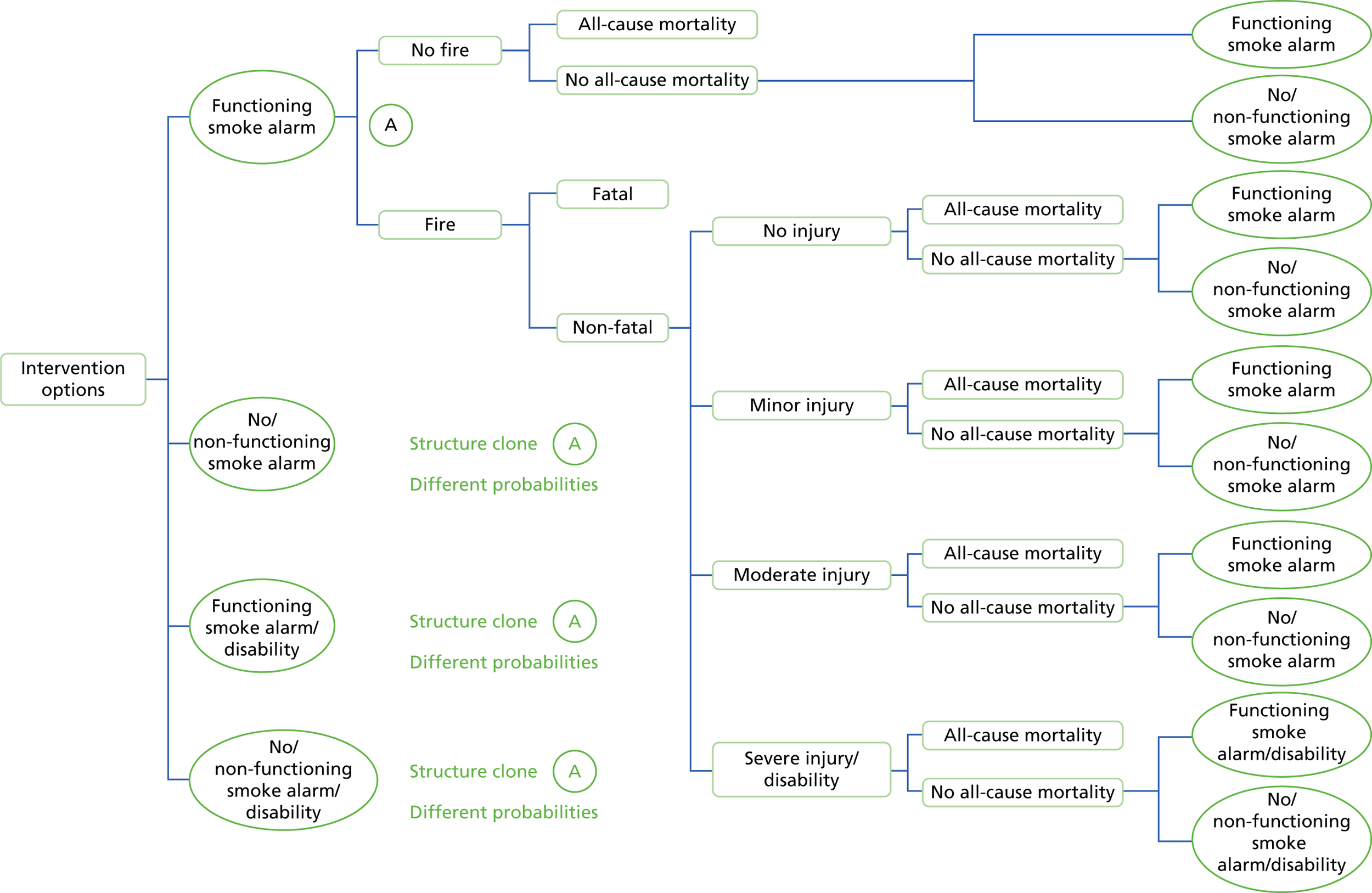
The first stage of the model, referred to as the intervention model, consisted of a decision tree analysing the effectiveness of interventions to increase the prevalence of functional smoke alarms (informed by NMA undertaken in study J374) and the costs of these interventions. The second stage of the model, referred to as the pre-school model, used outputs of the intervention model as its primary inputs and modelled fire-related injuries (i.e. minor, moderate and severe) and fatalities of children during the preschool period (aged 0–4 years) using a Markov state-transition structure incorporating a decay/repair factor to allow smoke alarms to cease functioning and to be repaired. The third stage of the model, referred to as the long-term model, modelled over an individual’s lifetime, includes costs and health effects of fire-related injuries occurring from birth to 4 years of age, using a Markov state-transition structure. For the Markov models in the second and third stages of the analysis, a yearly cycle duration was used and models were run for 100 years (5 years in stage 2 and 95 years in stage 3). Total costs and QALYs were established for each intervention by attributing costs (inflated to 2012 prices) and quality-of-life weights to each state.
Evidence used to inform the base-case model, together with distribution information when applicable, is presented in Appendix 5, Base-case model inputs for the decision analysis for smoke alarms for study K for smoke alarm interventions, Appendix 5, Base-case model inputs for the decision analysis for safe hot tap water temperatures for study K for safe hot tap water temperature interventions, Appendix 5, Base-case model inputs for the decision analysis for safety gates to prevent stairway falls for study K for safety gate interventions, Appendix 5, Base-case model inputs for the decision analysis for safe storage of medicines for study K for safe storage of medicines and Appendix 5, Base-case model inputs for the decision analysis for safe storage of household products for study K for safe storage of household products. When possible, input parameters were informed by UK-based data. When possible we tried to ensure that input parameters that were common across decision models were consistent but as the models were developed at different times across the project this was not always possible (see Appendix 5). A summary of the base-case methodological assumptions is outlined in Table 70.
| Element of assessment | Base case |
|---|---|
| Type of economic evaluation | Cost–utility analysis |
| Perspective on costs | Public sector |
| Perspective on outcomes | All health effects on individuals |
| Evidence on outcomes | Simultaneous synthesis of evidence on multiple interventions |
| Measure of health effects | QALYs |
| Main source of data for measurement of HRQL | Reported directly by patients (J Nicholl, personal communication)a |
| Source of preference data for valuation of changes in HRQL | Representative sample of the public (UK population norms)375 |
| Discount rate | An annual rate of 3.5% for costs and health effects |
| Equity weighting | An additional QALY has the same weight, regardless of the characteristics of the individuals who gain the health benefit |
| Size of the cohort simulated | 100,000 |
| Time horizon | 100 years – until population all dead to account for all outcomes |
Main modelling assumptions
We made a series of assumptions during the modelling:
-
The possession of ‘functioning’ smoke alarms was a surrogate/intermediate outcome for household risk of fire-related injury/death. We used previously published evidence to support this assumption. 37,376,377 The evidence used for the decision-analysis models for other interventions is given in the base-case evidence tables in Appendix 5.
-
The probability of a household accepting an intervention was assumed to be the same across all interventions because of a lack of information on the acceptance of different smoke alarm promotion interventions. When this information was available for decision-analysis models for other interventions it was used and is described in the base-case evidence tables in Appendix 5.
-
The benefit of a household having a functioning smoke alarm accrues to a single child aged 0–4 years of age. This ignored the potential benefits for other household members and is therefore a conservative assumption. This assumption also applies to models for interventions for TMVs, safety gates and the safe storage of medicines and household products.
-
As with most Markov models, we assumed that the probability of future fire-related injuries was independent of previous fires or fire-related injuries and remained constant throughout the model time frame (i.e. 5 years for part 2 of the model). This assumption also applies to models for interventions for TMVs, safety gates and the safe storage of medicines and household products.
-
The model allows for only one fire or fire-related injury in a single cycle (i.e. 1 year). This assumption also applies to models for interventions for TMVs, safety gates and the safe storage of medicines and household products.
Uncertainty
Modelling took account of uncertainty around input parameter point estimates through the use of posterior probability distributions from 5000 MCMC simulations for estimates of the effectiveness of interventions from the NMAs and the use of probability distributions based on point estimates and SEs (see Appendix 5) for other model parameters obtained from the literature. The decision model was evaluated by performing 5000 MCMC simulations. Mean costs and mean QALYs were averaged across all 5000 MCMC simulations.
We assessed the robustness of our findings to the assumptions that we made during modelling and to the data that we used to populate models through a series of one-way sensitivity analyses. For interventions to promote functional smoke alarms these included reducing the prevalence of smoke alarms in households prior to interventions from 80% to 50%;347 reducing the probability of accepting the intervention from 90% to 50%;347 reducing the probability of the decay of safety equipment from 0.1 to 0; and increasing the number of children per household from 1 to 1.8 (i.e. the national average). 378
For the decision analyses for interventions to promote a safe hot tap water temperature, sensitivity analyses included increasing the probability of accepting non-TMV interventions from 0.74 to 0.9 (as used in the functional smoke alarm model); reducing the probability to 0 of a child incurring a scald when safe hot water is practised, as for the TMV interventions; removing the fixed costs associated with setting up a scheme to promote safe hot water as promotion of safe hot water is likely to be part of a wider home safety scheme; increasing the number of scalds per year to 653 from 582,700 households140 to reflect the probability of a scald in children in social housing/deprived areas; and including the costs of TMVs and fitting separately (i.e. not part of a refurbishment or rebuild scheme). 140
For the decision analyses for interventions to increase the possession of a fitted safety gate, analyses included reducing the number of safety gates fitted to 1; reducing the cost of education by using the cost of providing a leaflet only; providing low-cost (£5) rather than free safety gates; reducing the fixed costs of the intervention to £40,000; increasing the number of children per household from 1 to 1.8; reducing the probability of possessing a fitted safety gate from 0.56 to 0.45 to reflect the baseline possession of a fitted and used stair gate in families in deprived areas of Nottingham;72 and changing the utility deficits by assuming no uncertainty from 0.05, 0.1 and 0.2 for mild, moderate and severe injuries, respectively, to 0.07, 0.19 and 0.34, respectively. 143
For the decision analysis for interventions to promote the safe storage of medicines, the sensitivity analyses included changing the baseline probability of safe storage from 75% (ascertained from the results of study A) to 93%56 or to 50% (assumption); changing the probability that the intervention is accepted from 90% to 50% (assumption); changing the proportion admitted from 63%379 to 83.3% (Philip Miller, ED nurse, Nottingham University Hospitals NHS Trust, 7 April 2014, personal communication); changing the incidence of unintentional poisoning from 18.07 per 10,000 person-years to 44.9 and 48.5 per 10,000 person-years, reflecting the injury rates among those aged < 5 years living in the two most disadvantaged quintiles based on the Townsend deprivation index;91 changing the number of cupboard locks from one Pop-It™ lock (costing £2.65) (Kid Rapt, Usk, UK) and one magnetic lock (costing £4.80) to two Pop-It locks (costing £5.30) and two magnetic locks (costing £9.60); increasing the number of children in a household from 1 to 1.8;378 and increasing the uncertainty associated with the utility decrements for poisoning injuries from 10% of the utility decrement value to, first, 20% and, second, 50%.
Finally, for the decision analyses for interventions to promote the safe storage of household products, sensitivity analyses included changing the baseline probability of safe storage from 45% (ascertained from the results of study A) to 93%;56 changing the probability that the intervention is accepted from 90% to 50% (assumption); changing the proportion admitted from 33.2%2 to 83.3% (Philip Miller, personal communication); increasing the incidence of unintentional poisoning from 12.04 per 10,000 person-years to 44.9 and 48.5 per 10,000 person-years, reflecting the injury rates among those aged < 5 years living in the two most disadvantaged quintiles based on the Townsend deprivation index;91 and increasing the number of children in a household from 1 to 1.8. 378
Results
During the period in which the KCS programme was being undertaken, the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme commissioned a feasibility study of the effectiveness of a children’s centre-based parenting intervention that included first aid. 380 It was therefore decided that the intervention being developed within the KCS programme would not include first aid. The overview of reviews of first aid interventions was completed but did not therefore inform the development of the intervention. The published paper describes the methods and results of that overview381 but they are not described further in this report.
Fire prevention
Figure 24 shows the process of identification and selection of reviews and primary studies to be included in the overview and in the NMAs for fire prevention interventions (studies H and J). Ten narrative systematic reviews, four meta-analyses (which also included narrative systematic reviews of outcomes not included in meta-analyses) and 63 primary studies were included in the overview. Thirty of the 63 primary studies were included in at least one NMA for fire prevention outcomes. For the overview of fire prevention interventions, search results from bibliographic databases were combined for reviews and primary studies, and so the flow chart for the process of study selection for fire prevention interventions is less detailed than that for the other overviews.
FIGURE 24.
Process of study identification and selection for the overview of reviews and NMAs for fire prevention outcomes (studies H and J). Created using data from Cooper et al. 374

Figure 25 shows the process and selection of primary studies included in the systematic review and PMAs of home safety education and safety equipment for fire, scalds, falls and poisoning prevention outcomes (study I). Thirty-three studies were included in at least one meta-analysis for the fire prevention outcomes.
FIGURE 25.
Identification and selection of studies for inclusion in the PMAs for fire, scalds, falls and poisoning prevention (study I). IPD, individual participant data. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
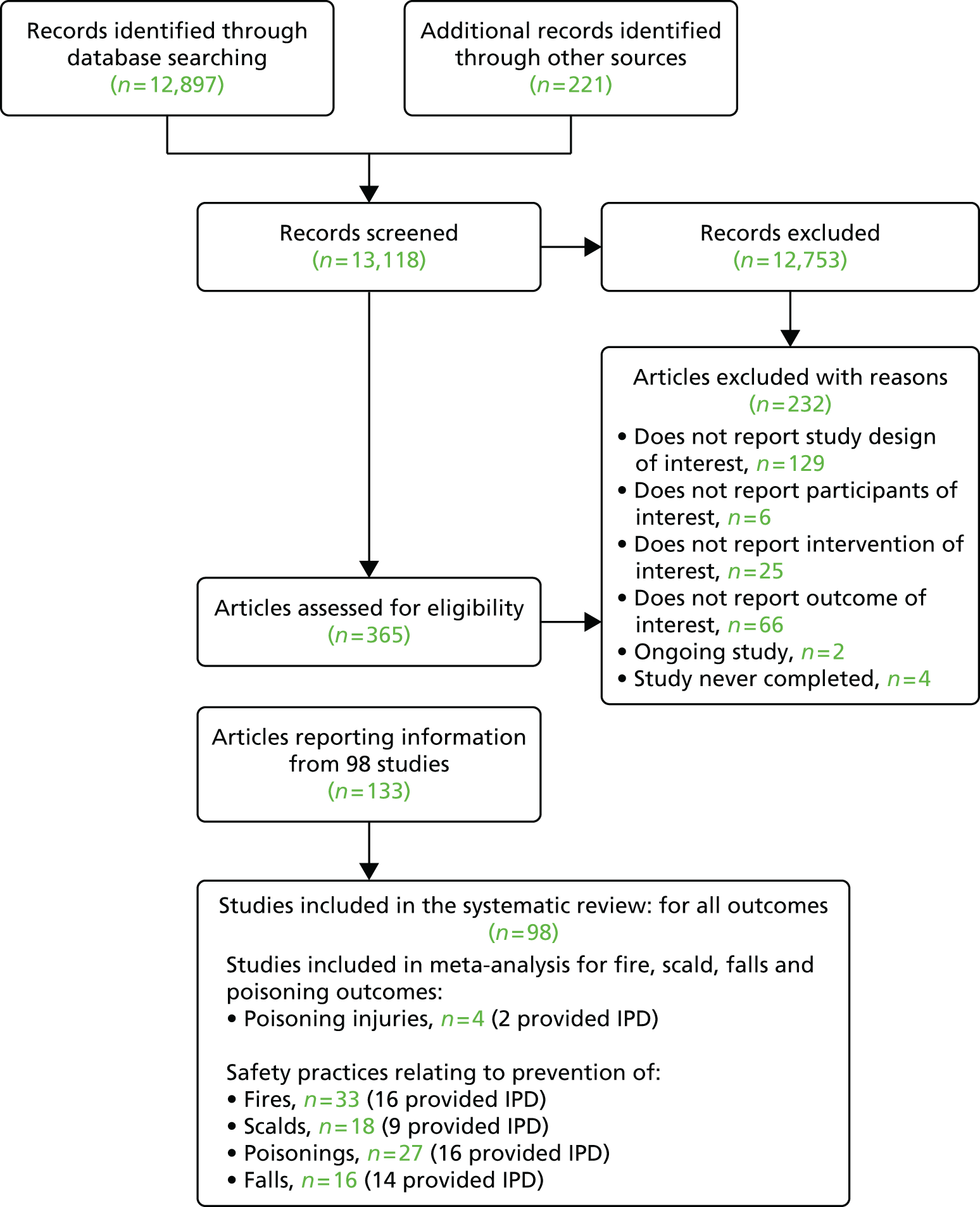
Characteristics of reviews and primary studies
The characteristics and quality assessment of the reviews included in the fire prevention overview (study H) are shown in Table 71. Four reviews focused specifically on fire prevention interventions,37,353,354,391 with the remainder including interventions addressing a range of injury mechanisms. The risk of bias in included reviews was variable, with OQAQ scores ranging from 2 to 7 (median 5) out of a maximum possible score of 7.
| Study | Design | Interventions | OQAQ score | Included in overview | |||
|---|---|---|---|---|---|---|---|
| Fi | S | Fa | P | ||||
| Bass 1993382 | Narrative review of RCTs and non-RCTs | Injury prevention counselling in primary care settings | 4 | ||||
| DiGuiseppi 200040 | Narrative review and meta-analysis of RCTs | Individual-level interventions delivered in clinical settings, including primary care and acute care | 6 | ||||
| DiGuiseppi 200137 | Narrative review and meta-analysis of RCTs and non-RCTs | Mass media, counselling, home safety checks, provision of equipment and legislation delivered in clinical settings, homes and schools | 6 | ||||
| Elkan 2000383 | Narrative review and meta-analysis of RCTs, non-RCTs and CBAs | Home visiting by British health visitors or personnel with responsibilities within the remit of British health visitors | 5 | ||||
| Guyer 2009338 | Narrative review of experimental and quasi-experimental designs | Counselling, safety equipment and home visits delivered by GPs, community health workers and paediatricians | 4 | ||||
| Kendrick 1994384 | Narrative review of studies of all designs | Education, counselling, provision of safety equipment, home visits and legislation | 2 | ||||
| Kendrick 2007385 | Narrative review and meta-analysis of RCTs, non-RCTs and CBAs | Individual and group-based parenting interventions | 7 | ||||
| Kendrick 200733/201249 | Narrative review and meta-analysis of RCTs, non-RCTs and CBAs | Home safety education and provision of safety equipment delivered by health or social care professionals, school teachers, lay workers or voluntary or other organisations in health-care settings, schools and homes | 7 | ||||
| Lyons 2003332 | Narrative review of RCTs, non-RCTs, CBAs and ITS | Reduction of physical hazards in the home by community health workers, trained researchers/volunteers, GPs and paediatricians | 7 | ||||
| Lyons 200642/Turner 2011340 | Narrative review of RCTs | Education, safety equipment and reduction of hazards delivered by community nurses, trained researchers, project assistants, occupational therapists and health visitors in home, health-care and clinical settings | 5 | ||||
| McClure 2005333 | Narrative review of CBAs and BAs | Injury counselling and household injury hazard identification delivered by paediatricians and health staff in community settings | 4 | ||||
| Nilsen 2004334 | Narrative review of CBAs | Education, home safety inspection and environmental improvements delivered by paediatricians, local health staff and school staff in community settings | 3 | ||||
| Nixon 2004336 | Narrative review of CBAs and RCTs | Targeted education, household hazard identification and control, promotion of poison control telephone information service delivered by paediatricians and local health staff in community settings | 3 | ||||
| Parbhoo 2010386 | Narrative review of studies of all designs | Any strategy to reduce paediatric burns | 3 | ||||
| Pearson 2009387 | Narrative review of RCTs, non-RCTs, CBAs and BAs | Supply and/or installation of home safety equipment and/or home risk assessments delivered by GPs, doctors, nurses, research assistants, paediatricians, community health workers and health visitors in various settings | 5 | ||||
| Speller 199541 | Narrative review of studies of all designs | Education by paediatricians, GPs and trained interviewers in any setting | 4 | ||||
| Spinks 2004335 | Narrative review of CBAs and RCTs | Counselling and hazard identification by paediatricians and health staff in community settings | 4 | ||||
| Ta 2006391 | Narrative review of studies of all designs | Counselling, education, safety equipment provision, home safety checks, safety centre referrals and arson prevention campaigns delivered by fire service professionals, physicians, teachers, community health workers and volunteers in all settings | 4 | ||||
| Towner 1996352 | Narrative review of RCTs, non-RCTs, CBAs and ITS | Education, safety equipment and home visits delivered by paediatricians, local health staff and school staff in any setting | 4 | ||||
| Towner 200136 | Narrative review of RCTs, non-RCTs, CBAs and BAs | Home safety inspection, modification and education delivered by paediatricians, local health staff, school staff and community outreach workers in any setting | 2 | ||||
| Turner 2004337 | Narrative review of non-RCTs and CBAs | Community-based interventions to reduce burns and scalds in children | 7 | ||||
| US Preventive Services Task Force 1996388 | Narrative review of RCTs, non-RCTs and CBAs | Counselling in clinical settings to prevent household and recreational injuries | 2 | ||||
| Warda 1999353 | Narrative review of studies of all designs | Modifiable risk factors for fires – smoke alarms, smoking, alcohol use and drug use (did not directly evaluate interventions) | 5 | ||||
| Warda 1999354 | Narrative review of studies of all designs | Education, counselling, safety equipment provision, home safety checks and legislation delivered in all settings | 5 | ||||
| Waters 2001331 | Narrative review of studies of all designs | Education and environment modification targeted to individuals and communities and applicable to the Australian situation | 3 | ||||
The characteristics of the primary studies included in the fire prevention overview (study H), the systematic review and PMA (study I) and the NMAs (study J) are shown in Table 72. Most (n = 42, 67%) primary studies were RCTs, seven (11%) were non-RCTs, 10 (16%) were CBAs and three (5%) were case–control studies. The design of one (2%) study was insufficiently described to distinguish whether it was a non-RCT or a CBA. Tables of excluded reviews and primary studies are available on request from the authors. The risk of bias in the included primary studies was also variable; 43% of RCTs had adequate allocation concealment, 53% followed up at least 80% of participants in each arm and 31% had blinded outcome assessment. Of the non-RCTs and CBAs, 12% had blinded outcome assessment, 47% followed up at least 80% of participants in each arm and 29% had a balanced distribution of confounders between treatment arms. The case–control studies scored 7, 7 and 8 (out of a maximum of 9) on the Newcastle–Ottawa Scale, indicating that they were of high quality.
| Study | Design and risk of bias | Participants | Intervention | Included in overview (study H) | Included in PMA (study I) | Included in NMA (study J) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fi | S | Fa | P | Fi | S | Fa | P | Fi | S | Fa | P | ||||
| Adler 1994392 | RCT A = Y; B = N; F = N |
Children aged 5–16 years with a history of fire setting or fire play (n = 138) | I1 = educational material, two home visits by firefighters to provide education, behaviour modification, parental instruction in use of negative consequences in the event of fire setting, plotting events leading up to an incident and discussing alternative ways of responding to incidents in future I2 = as I1 plus offer of psychiatric referral C1 = fire safety educational material C2 = fire safety educational material plus offer of psychiatric referral |
||||||||||||
| Azeredo 2003393 | CBA B = N; F = U; BC = U |
Children attending kindergarten classes (grades 1–5) in 12 schools (n = approx. 6300) | I = multifaceted injury prevention curriculum in schools, including fire safety education and smoke alarm giveaway and installation C = opportunity to have a smoke alarm installed |
||||||||||||
| Babul 2007257 | RCT A = Y; B = N; F = N |
Parents of newborn infants at a general hospital serving mainly urban or suburban communities (n = 600) | I1 = home visit from community health nurse to identify hazards and teach parents how to remove or modify the hazards; free safety kit (smoke alarm, safety gate 50% discount coupon, table corner cushions, cabinet locks, blind cord wind-ups, water temperature card, doorstoppers, electrical outlet covers, poison control sticker); instructional brochure targeting falls, burns, poisoning and choking; risk assessment checklist I2 = free safety kit (see I1) C = usual care |
||||||||||||
| Ballard 1992394 | Case–control study NOS score: 7 |
Households with fatal or non-fatal residential fire injury (n = 372) | Exposures = smoking and alcohol drinking behaviour | ||||||||||||
| Barone 1988395 | RCT A = N; B = N; F = N |
Five parenting classes (n = 108 parents of toddlers) | I = slides, handouts on burn prevention, bathwater thermometer, hot water gauge, usual safety education C = usual safety education |
||||||||||||
| Baudier 1998396 | RCT A = U; B = U; F = N |
Infant schoolchildren from 42 schools and their parents (n = 494 parents) | Exploratory phase in two schools: I = use of safety teaching kit by teachers in schools, cartoon book and sticker given to children to take home, weekly posters displayed on classroom doors to inform parents, exhibition in school hall, leaflets distributed, meeting held with parents about the risk of accidents discussed in school C = none of the above. Operational phase in 40 schools: I = provision to schools of safety teaching kit with user guide, leaflets, stickers, posters, suggestion of a mini exhibition, meeting with parents (six took place in 20 schools with parent participation at meetings ranging from 0% to 20%) C = none of the above |
||||||||||||
| Blake 1993397 | NRCT/CBA B = U; F = N; BC = U |
Parents in two inner-city health clinics (n = 171) | I = educational video to increase awareness of accident prevention C = no video |
||||||||||||
| Bulzacchelli 2009398 | NRCT B = N; F = N; BC = N |
Parents of children aged 1 month to 7 years attending a well-child clinic in low-income urban communities (n = 294) | I1 = prescribed visit to mobile safety centre for safety advice, interactive safety exhibits and provision of safety devices at reduced cost (safety gates, cabinet locks, referral to fire department for free smoke alarm installation) I2 = encouraged to visit mobile safety centre C = told about purpose of mobile safety centre and given more information on request but not referred to centre |
||||||||||||
| Campbell 2001399 | RCT A = U; B = Y; F = N |
Hispanic migrant youths aged 11–16 years, low income (n = 660) | I = eight sessions of multimedia first aid and home safety training presented by bilingual and bicultural college students C = eight sessions of multimedia tobacco and alcohol prevention education presented by bilingual and bicultural college students |
||||||||||||
| Carlsson 2011400 | NRCT B = U; F = N; BC = N |
Mothers with low educational level with 4- to 7-month-old babies attending two child health-care centres (n = 99) | I = 30- to 60-minute workshop discussing burn and scald prevention and a 1-hour home visit with researcher covering child injury prevention C = usual care |
||||||||||||
| Chan 2004401 | RCT A = U; B = U; F = U |
Families in two districts of Hong Kong with children aged < 3 years admitted to hospital with an unintentional injury (n = 76) | I = four quarterly home visits and monthly telephone follow-ups from lay home visitors focusing on practical solutions to injury prevention and standard educational material on injury prevention C = standard educational material on injury prevention |
||||||||||||
| Christakis 2006402 | RCT A = Y; B = Y; F = Y |
Parents of children aged < 11 years attending clinics in the previous 3 years (n = 887) | I1 = web-based safety information for parents plus notification to health-care provider of safety topics that parents had expressed an interest in online and information on those topics I2 = notification to health-care provider of safety topics that parents had expressed an interest in online and information on those topics I3 = web-based safety information for parents C = usual care |
||||||||||||
| Clamp 199871 | RCT A = Y; B = N; F = Y |
Families with children aged < 5 years registered at one GP surgery (n = 165) | I = GP safety advice, leaflets and low-cost safety equipment (smoke alarms, window locks, cupboard and drawer catches, socket covers, door slam devices, fireguards, stair gates). Discounted items offered to families in receipt of means-tested state benefits (36.1%) C = usual care |
||||||||||||
| Colver 1982260 | RCT A = U; B = U; F = N |
Families with children aged < 5 years attending child health clinics, day nurseries, nursery classes and a toddler group in a deprived area (n = 80) | I = encouraged to watch television safety campaign, home visit, advice on benefits to obtain safety equipment and local availability of safety equipment C = encouraged to watch television safety campaign |
||||||||||||
| Davis 1987403 | RCT A = U; B = N; F = N |
41 grade 4–6 classes (n = 857) | I = six 1-hour fire safety lessons with workbook, demonstrations, teacher training, materials and take-home materials for parents C = usual lessons |
||||||||||||
| Dershewitz 1977404/1979405 | RCT A = U; B = Y; F = N |
Mothers of children attending a medical clinic enrolled in prepaid medical plan (n = 308) | I = safety advice, safety booklet and free safety equipment provided by researcher C = free safety equipment provided by researcher |
||||||||||||
| DiGuiseppi 2002261 | RCT A = Y; B = Y; F = N |
Households in council rented accommodation (n = 2145) | I = free smoke alarm with offer of free fitting and reminder to change batteries C = no smoke alarm |
||||||||||||
| Fergusson 1982263 | NRCT B = U; F = Y; BC = Y |
Families of children aged 2–3 years participating in the Christchurch Child Development Study (n = 1126) | I = ‘Mr Yuk’ stickers for poisonous substances, list of substances to which stickers should be attached and educational leaflet provided by researcher C = none of the above |
||||||||||||
| Franklin 2002406 | CBA B = U; F = U; BC = N |
Children and young people aged 4–17 years referred from the county court system, fire departments, schools and parents after fire-setting behaviour (n = 252) | I = 1-day multidisciplinary programme with interactive content focusing on impact of fire-setting behaviour including peer counselling approach C = no programme |
||||||||||||
| Gaffney 1996407 | CBA B = U; F = U; BC = U |
Populations of unspecified control and intervention areas (n not reported) | I = multifaceted community campaign to reduce risk factors and the rate of hot water scalds in children aged 0–4 years C = no campaign |
||||||||||||
| Garcia 1996408 | CBA (C) B = U; F = U; BC = U |
Fourth-grade elementary schoolchildren and their parents (n = 3904) | I = safety fair at schools, which included interactive safety stations on poisons, fires and home injuries C = no safety fairs |
||||||||||||
| Georgieff 2004264 | CBA B = U; F = N; BC = N |
Children aged < 3 years from five deprived wards (n = 92) | I1 = awareness-raising campaign including leaflets, logo, radio advert campaign, bus advertising campaign, burns and scalds road shows (advice) – free bathwater thermometers and hot tap water temperature testing by researchers I2 = I1 + free TMV for baths C = none of the above |
||||||||||||
| Gielen 2001409 | RCT A = Y; B = Y; F = N |
Paediatric residents in a hospital-based clinic serving a low-income community (n = 31) | I = 1-hour injury prevention seminar plus 5 hours of injury prevention training C = 1-hour injury prevention seminar |
||||||||||||
| Gielen 2002265 | RCT A = U; B = U; F = U |
First- and second-year paediatric residents and their patient–parent dyads, low-income population of parents of children aged 0–6 months (n = 187) | I = safety counselling by professional health educator, discounted home safety equipment during visit to Children’s Safety Centre, home visit involving hazard assessment (targeting falls, burns and poisonings) and safety recommendations C = safety counselling by professional health educator, discounted home safety equipment during visit to Children’s Safety Centre |
||||||||||||
| Gielen 2007266 | RCT A = Y; B = ; F = Y |
Parents of children aged 4–66 months attending an urban paediatric ED (n = 901) | I = personalised report containing tailored, stage-based messages based on the precaution adoption process model C = report on other child health topics |
||||||||||||
| Gomez-Tromp 2011410 | CBA B = U; F = U; BC = U |
Children aged 9–13 years in 35 schools (n = 1260) | I = scalds prevention programme consisting of seven lessons, a DVD, a workbook for each pupil and a downloadable teacher’s manual C = waiting list for the above |
||||||||||||
| Guyer 1989267 | CBA B = U; F = Y; BC = N |
Population of 14 cities and towns in Massachusetts (n = 286,676) | I = community injury prevention programme including injury counselling by paediatricians to parents of young children and home safety inspections C = no community injury prevention programme |
||||||||||||
| Harvey 2004268 | RCT A = U; B = N; F = N |
Households without smoke alarms in areas with a high prevalence of residential fire deaths and a low prevalence of functional smoke alarms; primarily low-income residents and/or high proportion of rented housing (n = 4455) | I = smoke alarm installation C = voucher for free smoke alarm |
||||||||||||
| Hendrickson 2005269 | RCT A = N; B = N; F = Y |
Mothers with children aged 1–4 years, predominantly Mexican/Mexican American (n = 82) | I = safety counselling from researchers, identification of home hazards, provision of safety equipment (doorknob covers, smoke detectors or new batteries if smoke alarm already in situ, fire extinguisher, cabinet latches and outlet covers) C = none of the above |
||||||||||||
| Hillman 1986411 | RCT A = U; B = U; F = Y |
Second-, third- and fourth-grade school students (n = 60) | I1 = fire response training provided by undergraduate and postgraduate students including rationale for responses and behavioural practice I2 = fire response training provided by undergraduate and postgraduate students including rationale for responses and verbal practice I3 = fire response training provided by undergraduate and postgraduate students without rationale for responses and behavioural practice I4 = fire response training provided by undergraduate and postgraduate students without rationale for responses and verbal practice |
||||||||||||
| Hwang 2006412 | CBA B = N; F = U; BC = Y |
Third- and fourth-grade students in two elementary schools in an urban, poor community (n = 150) | I = home visit from fire service personnel and installation of free smoke alarm with 10-year battery plus provision of fire escape plan C = usual care |
||||||||||||
| Jenkins 1996270 | RCT A = Y; B = Y; F = Y |
Families with children aged 0–17 years admitted to a paediatric burns unit (n = 141) | I = education pre discharge from nurses, physiotherapists or occupational therapists about burn care and prevention using specially designed booklet C = routine discharge teaching without booklet |
||||||||||||
| Johnston 2000271 | RCT A = N; B = N; F = Y |
Families of children aged 4–5 years enrolled in Head Start programme provided to socioeconomically disadvantaged children (n = 418) | I = home safety inspections by educational paraprofessionals followed by provision of educational materials and syrup of ipecaca and smoke alarms and batteries as appropriate C = home safety inspection and written information only |
||||||||||||
| Johnston 2006413 | NRCT (I1 +I2 vs. C) with nested RCT (I1 vs. I2) B = U; F = N; BC = N |
Pregnant women at < 22 weeks’ gestation (n = 343) | I1 = three home visits during pregnancy including home safety information; well-child visits enhanced by the addition of a ‘Healthy Steps’ professional I2 = well-child visits enhanced by the addition of a ‘Healthy Steps’ professional C = usual care |
||||||||||||
| Jones 1983414 | RCT A = U; B = U; F = Y |
Third-grade students (n = 47) | I1 = external instruction (children trained in fire responses) I2 = self-instruction (children trained in fire responses plus trained to verbalise, monitor, evaluate and reinforce their behaviour) |
||||||||||||
| Jones 1989415 | RCT A = U; B = U; F = Y |
Third-grade students (n = 46) | I1 = training in fire response skills including provision of rationale for why responses are appropriate I2 = training in fire response skills |
||||||||||||
| Jordan 1993416 | Cohort NOS score: 9 |
Pregnant/parenting mothers aged < 18 years at birth of child who gave birth in Baltimore in 1983 (n = 529) | Exposure = receipt of home safety information from any source | ||||||||||||
| Katcher 1989272 | RCT A = U; B = U; F = N |
Consecutive paediatric clinic clients randomised to two groups (n = 697) | I = counselling by paediatrician plus tap water thermometer and tap water safety literature C = counselling by paediatrician and tap water safety literature |
||||||||||||
| Kelly 1987273 | RCT A = U; B = Y; F = N |
Parents of 6-month-old children attending primary care centre for well child care (n = 129) | I = three-part individualised safety course at well-child care visits C = routine safety education |
||||||||||||
| Kelly 2003274 | RCT (C) A = U; B = Y; F = Y |
Parents of children aged 15 months to 6 years attending women, infants and children clinics (n = 289) | I = videotape and PCC pamphlet and PCC stickers C = usual care |
||||||||||||
| Kendrick 1999275 | NRCT B = N; F = N; BC = Y |
Children aged 3–12 months registered at 36 general practices (n = 2119) | I = health visitor safety advice at child health surveillance consultations, provision of low-cost equipment (stair gates, fireguards, cupboard and drawer locks, smoke alarms), home safety checks and first aid training C = usual care |
||||||||||||
| Kendrick 2005417 | RCT A = Y; B = N; F = Y |
Women at ≥ 28 weeks’ gestation registered at 64 general practices (n = 1174) | I = discussion and advice from midwife and health visitor on walker use, checklist, anonymised parental accounts of walker injuries, postcard, fridge magnet, birthday card, signing of a plan of action C = usual care |
||||||||||||
| Kendrick 2007418 | RCT A = Y; B = Y; F = Y |
Children aged 7–10 years in state-funded primary schools (n = 459) | I = injury prevention curriculum targeting falls, poisonings, fires and burns delivered by school teachers trained by fire service personnel C = usual care |
||||||||||||
| Kendrick 2011276 | RCT A = Y; B = Y; F = Y |
Households with children aged < 5 years in social housing in disadvantaged communities (n = 124) | I = TMV fitted by qualified plumber and educational leaflets prior to and at the time of fitting C = usual care |
||||||||||||
| King 2001277 | RCT A = Y; B = Y; F = Y |
Children aged < 8 years attending an ED for injury or medical complaint (n = 1172) | I = home safety inspection, information on correcting any deficiencies, discount vouchers for safety equipment, demonstrations of use of safety devices and information on preventing specific injuries provided by researcher C = home safety inspection and safety pamphlet |
||||||||||||
| Kolko 2001419 | NRCT B = N; F = Y; BC = N |
Boys referred for services by the City of Pittsburgh Bureau of Fire (n = 54) | I1 = cognitive–behavioural therapy designed to encourage behaviours other than fire setting I2 = fire safety education including instruction in fire safety skills, prevention practices, fire protection and evacuation C = home visit by firefighter providing information about the danger of fires and the function of firefighters and asking children to promise not to get involved in unsanctioned fire play |
||||||||||||
| Lacouture 1978420 | CBA (C) B = N; F = U; BC = Y |
Schoolchildren aged 6–14 years in Wilmington (intervention) and Scituate (control), Massachusetts (n = 400) | I = community poison prevention education programme directed at schoolchildren C = no community poison prevention education programme |
||||||||||||
| Lamb 2006421 | CBA B = Y; F = U; BC = U |
Children from primary schools in four education authorities aged 10–11 years (n = 145, with follow-up study to assess changes over time in 671 children) | I = one 2-hour visit to ‘Lifeskills’ experiential learning centre C = no visit to centre |
||||||||||||
| LeBailly 1990279 | NRCT B = U; F = N; BC = U |
Families attending two paediatric group practices, one in urban area, other in suburban area (n = 407) | I1 = well child visit and safety equipment I2 = well child visit, safety equipment and safety counselling by physician I3 = well child visit and safety counselling by physician C = well child visit |
||||||||||||
| LeBlanc 200699 | Case–control NOS score: 7 |
Children aged ≤ 7 years presenting to an ED with injuries from falls, burns or scalds, ingestions or choking matched to children who presented during the same period with acute non-injury-related conditions (n = 692) | Exposures = tap water temperature > 54°C, kettle or appliances with dangling cords, no stove guard | ||||||||||||
| Macarthur 2003422 | Cohort NOS score: 6 |
Parents or guardians of children aged < 9 years (n = 504) | Exposed group = campaign (media, retail and community partners) emphasising lowering hot water tap temperature, child safety in the kitchen, keeping hot drinks away from child and checking smoke alarms regularly Unexposed group = none of the above |
||||||||||||
| Mallonee 1996423/2000281 | CBA B = N; F = Y; BC = N |
Population of a 24-square mile area of Oklahoma City (intervention area) and population of the rest of Oklahoma (control area) (n = 213,607 dwellings) | I = distribution of smoke alarms door to door by volunteers and community agencies to homes without a smoke alarm C = no smoke alarm distribution |
||||||||||||
| Margolis 2001424 | Cohort NOS score: 7 |
Low-income pregnant mothers and their infants aged < 2 years in Durham, North Carolina (n = 317) | Exposed group = two to four home safety checks per month through the infant’s first year of life providing parental education on child health and development and injury prevention Unexposed group = usual care (women who had sought prenatal care during the 9 months before the programme’s initiation) |
||||||||||||
| Marshall 1998425 | Case–control NOS score: 7 |
All fatal residential fires in North Carolina over a 1-year period (n = 155) | Exposures = presence of one or more potential rescuers, presence of a functioning smoke detector | ||||||||||||
| Matthews 1988426 | NRCT B = U; F = Y; BC = U |
Mothers of toddlers recruited from clinics, day care centres (n = 26) | I = home safety inspection, video, handouts, modelling regarding safety and managing dangerous child behaviour, hot water thermometers, choke tube C = home visit with video, handouts, modelling on language simulation |
||||||||||||
| McDonald 2005282 | RCT A = Y; B = ; F = N |
Parents of children aged 6 weeks to 24 months attending well child clinic (n = 144) | I = tailored safety advice in kiosk in well child clinic, feedback report to paediatrician to encourage safety counselling, information on safety equipment savings at child safety centre C = usual care |
||||||||||||
| Miller 1982284 | NRCT B = U; F = Y; BC = Y |
Children attending for routine paediatrician health care (n = 240) | I = pamphlet and a 1-minute educational message from paediatrician plus low-cost smoke detector C = usual care |
||||||||||||
| Minkovitz 2003427 | RCT A = N; B = Y; F = N |
Children aged ≤ 3 years (n = 2235) | I = Healthy Steps programme for the first 3 years of life including extended well-child office visits to address questions and concerns about child development and behaviour and to promote positive parent–child interactions, home visits to promote intellectual and emotional development, child development telephone line, parent support groups and written health promotion information including safety advice. Programme delivered by paediatricians and Healthy Steps specialists (nurses, nurse practitioners, social workers and early childhood educators) C = usual care |
||||||||||||
| Minkovitz 2003427 | NRCT B = N; F = Y; BC = N |
Children aged ≤ 3 years (n = 3330) | As previous entry | ||||||||||||
| Mock 2003285 | CBA B = N; F = N; BC = N |
Families attending private, low-fee and subsidised child health clinics in Mexico (n = 1124) | I1 (private clinics) = lectures and demonstrations lasting for 6 hours. Use of audio visual material including the Injury Prevention Program I2 (low-fee clinics) = I1 + some participants also received clinic-based counselling I3 (subsidised clinics) = half-hour household visits by nurses + audio visual materials used C = standard injury prevention counselling |
||||||||||||
| Mori 1986428 | RCT A = U; B = Y; F = U |
Preschool children aged 3–5 years (n = 30) | I1 = children instructed by preschool teachers who had received home safety manual and professional supervision I2 = children instructed by preschool teachers who had received home safety manual |
||||||||||||
| Mueller 2008286 | RCT A = N; B = N; F = Y |
Households with low to mid-level income (n = 750) | I1 = installation of ionisation alarm, maintenance instructions given and fire extinguisher provided I2 = installation of photoelectric alarm, maintenance instructions given and fire extinguisher provided |
||||||||||||
| Nansel 2002287 | RCT A = Y; B = U; F = Y |
Parents of children aged 6–20 months attending well child check (n = 213) | I = tailored computer-generated safety advice in well child clinic C = generic computer-generated safety advice in well child clinic |
||||||||||||
| Nansel 2008288 | NRCT B = N; F = N; BC = N |
Parents of children aged ≤ 4 years attending well child visits at three paediatric clinics with mainly low- to middle-income patients (n = 305) | I1 = tailored injury prevention advice I2 = tailored injury prevention advice and feedback to health-care provider C = generic injury prevention advice |
||||||||||||
| Odendaal 2009289 | RCT A = N; B = Y; F = Y |
Households with children aged ≤ 10 years living in low-income communities (n = 211) | I = home safety check, safety advice, free safety devices (insulation tape for connecting electrical cords, safety nails for attaching electrical cords to walls or floors, paraffin storage container with CRC and warning label and bag and hook for safe storage of poisonous substances) C = usual care |
||||||||||||
| Paul 1994292 | RCT A = U; B = U; F = N |
Families with children aged 10 months to 2 years born at a local rural hospital (n = 198) | I = home safety check, tailored education booklet, local safety equipment retail outlets identified, mail order addresses provided or equipment ordered through research team and made available at local hospital C = none of the above |
||||||||||||
| Peterson 1984429 | CBA B = Y; F = Y; assessment of balance of confounders not possible because of small numbers |
Children who were occasionally left without parental supervision (n = 8) | I1 = training on a range of emergency situations I2 = training on a range of emergency situations as in I1 but timed so that I2 could act as control for I1 |
||||||||||||
| Petridou 1997293 | CBA B = N; F = Y; BC = Y |
Random sample of households containing children or adolescents from towns on two Greek islands (n = 349) | I = community intervention including safety seminars for parents, courses with primary and secondary schoolchildren on safety and resuscitation and leaflets; focused intense intervention including lay home visitors and weekly visits to discuss home safety in households with children or older people C = none of the above |
||||||||||||
| Phelan 2009430/2011431 | RCT A = Y; B = N; F = Y |
Pregnant women, aged ≥ 18 years, < 19 weeks’ gestation, attending prenatal practices (n = 355) | I = home safety inspection, provision and fitting of free safety equipment (stair gates, non-slip matting under rugs, window guards, repair of stair handrails, cupboard/drawer locks, doorknob covers, storage bins, socket covers, smoke detectors, carbon monoxide detectors, stove guards, stove locks) and safety advice handout C = safety advice handout |
||||||||||||
| Posner 2004295 | RCT A = Y; B = Y; F = N |
Caregivers of children aged < 5 years attending an ED for a home injury (n = 96) | I = home safety counselling by trained lay personnel, home safety kit (cupboard and drawer locks, socket covers, bathtub spout covers, non-slip bath decals, bathwater thermometer, PCC number stickers, free small parts tester) and home safety literature C = home safety literature |
||||||||||||
| Reich 2011432 | RCT A = Y; B = Y; F = Y |
Low-income primiparous women (n = 198) | I = educational book containing information on home safety C1 = book with non-educational text C2 = no book |
||||||||||||
| Rowland 2002433 | RCT A = Y; B = N; F = Y |
Households from a local authority housing estate (n = 2145) | I1 = ionisation smoke alarm with a zinc battery I2 = ionisation smoke alarm with a zinc battery and pause button I3 = ionisation smoke alarm with a lithium battery and pause button I4 = optical smoke alarm with a lithium battery I5 = optical smoke alarm with a zinc battery |
||||||||||||
| Runyan 199250 | Case–control study NOS score: 8 |
Fatal and non-fatal residential fires in predominantly rural areas (n = 434 fires) | Exposures = smoke detector and other characteristics of house, characteristics of people in house, fire response system and characteristics of fire | ||||||||||||
| Sangvai 2007297 | RCT A = Y; B = N; F = N |
Parents of children aged 0–5 years enrolled at three paediatric practices (n = 319) | I = safety counselling from physician and researcher, free safety equipment (smoke detectors, gun locks, cabinet locks and water temperature cards) and brief educational handout for parents C = usual care |
||||||||||||
| Scherz 1968434 | CBA (C) B = U; F = U; BC = U |
Families of army personnel (n not reported) | I = free CRC attached to boxes of children’s aspirin, sold at Post Exchanges C = children’s aspirin sold at other sites without CRC attached |
||||||||||||
| Schwarz 1993300 | CBA B = N; F = N; BC = Y |
Population of nine census tracts, predominantly low income, urban, African American (n = 34,203) | I = home safety inspection, modification and education in homes and at block and community meetings; provision of syrup of ipecac, smoke alarms and batteries, bathwater thermometers, night lights, emergency centre number sticker and fridge sticker with information on preventing injury C = none of the above |
||||||||||||
| Schwebel 2009301 | RCT A = U; B = U; F = Y |
Female heads of household in two low-income housing districts (n = 238) | I = basic education and materials on safe use of kerosene and kerosene-powered appliances and treatment of kerosene-related injuries provided by trained paraprofessionals C = usual care |
||||||||||||
| Shapiro 1987435 | RCT A = U; B = U; F = Y |
Women admitted to the maternity wards of three hospitals (n = 604) | I = pamphlet about tap water scalds and thermometer for testing plus a 1-minute educational message summarising the pamphlet C = pamphlet and thermometer |
||||||||||||
| Smith 2006436 | RCT A = U; B = N; F = U |
Children aged 6–12 years (n = 24) | I1 = parent voice smoke alarm I2 = conventional smoke alarm |
||||||||||||
| Steele 1985437 | CBA (C) B = U; F = U; BC = U |
Populations of Escondido (intervention, n = 62,000) and Chula Vista (control, n = 75,000), California | I = community poison prevention programme including mass media, training of health-care personnel to provide poison prevention education to clients, safety fairs C = no community poison prevention programme |
||||||||||||
| Steele 1985437 | RCT A = U; B = U; F = U |
Parents of children aged 6 months to 4 years attending well baby clinics, primary caretakers aged ≥ 18 years, English speaking with a telephone available (n not reported) | I1 = one-to-one poisoning education with reinforcement by physician I2 = I1 + burns education I3 = one-to-one burns education with reinforcement by physician C = no education |
||||||||||||
| Swart 2008303 | RCT A = N; B = Y; F = Y |
Households with children aged < 10 years in low-income communities (n = 410) | I = home visits with safety advice on the prevention of burns, poisoning and falls; free safety devices (childproof locks and paraffin container safety caps) C = usual care |
||||||||||||
| Sznajder 2003304 | RCT A = Y; B = N; F = Y |
Socioeconomically disadvantaged families with medical or psychological difficulties that place them at high risk (n = 100) | I = free home safety kit (cupboard and drawer locks, door handle covers, furniture corner protectors, socket covers, non-slip bath mat, smoke alarms, PCC number stickers), home safety counselling by health professionals and safety leaflets C = home safety counselling by health professionals and safety leaflets |
||||||||||||
| Tan 2004438 | NRCT B = U; F = Y; BC = Y |
Caregivers and infants aged 4–5 months attending three health clinics (n = 708) | I = structured nurse counselling, leaflets aimed at discouraging baby walker use C = none of the above |
||||||||||||
| Thomas 1984305 | RCT A = N; B = U; F = Y |
Parents attending well-baby classes (n = 55) | I = standard information and literature plus a lecture on burn prevention provided by nurse practitioners, leaflets on protecting the home against fire, adjusting hot water settings and costs of smoke alarms at local stores and discount coupon for smoke alarms C = standard information and literature |
||||||||||||
| Vineis 1994306 | NRCT B = N; F = N; BC = U |
Parents of newborn babies (n = 1015) | I = 15 minutes of counselling by nurse and distribution of three educational booklets – one on prevention of home injuries in childhood, one on smoking and one on passive smoking C = None of the above |
||||||||||||
| Waller 1993307 | RCT A = U; B = U; F = Y |
A random sample of Dunedin-area children aged ≤ 3 years taken from birth records (n = 121) | I = free plumbing advice and home visit to measure tap water temperature and discuss dangers of hot water in the home and how to reduce tap water temperature provided by nurses C1 = no home visit C2 = no home visit and no baseline data collection |
||||||||||||
| Watson 200572 | RCT A = Y; B = N; F = N |
Families with children aged < 5 years on caseloads of health visitors in deprived areas (n = 3428) | I = health visitor safety consultation, free fitted safety equipment (stair gates, fireguards, cupboard and drawer locks, smoke alarms, window locks); free items supplied and fitted for families in receipt of benefits (50.0%), with free delivery for others (50.0%) C = usual care |
||||||||||||
| Williams 1988439 | RCT A = U; B = N; F = U |
Pregnant women attending prenatal classes (n = 74) | I = 1-hour lecture, handouts on burns prevention, usual safety education C = usual safety education |
||||||||||||
| Williams 1989440 | RCT A = U; B = U; F = Y |
Children in the second and third grade at a school in Virginia (n = 48) | I1 = fire safety and fear reduction education and teaching of behavioural skills I2 = fire safety education and teaching of behavioural skills I3 = discussion of fire safety |
||||||||||||
| Wissow 1989441 | RCT A = U; B = Y; F = N |
Families with children aged < 6 years attending a paediatric ED or clinic following injury (n = 62) | I = home hazard inspection, education and free safety equipment provided at home (smoke alarm battery, poison control sticker, syrup of ipecac, safety latches, outlet plugs) C = free safety equipment provided at hospital |
||||||||||||
| Woolf 1987308 | RCT (C) A = U; B = Y; F = N |
Families attending a medical ED with a child aged < 5 years, urban poor population (n = 202) | I = counselling by medical staff on poisoning treatment methods, leaflet on poisoning prevention, PCC number sticker and syrup of ipecac C = none of the above |
||||||||||||
| Woolf 1992309 | RCT (C) A = U; B = Y; F = Y |
Families of children aged ≤ 5 years with a poisoning who contacted the PCC and did not have syrup of ipecac (n = 301) | I = mailed $1 coupon for syrup of ipecac, one cupboard lock, checklist for poison proofing the home, leaflets C = none of the above |
||||||||||||
| Yang 2008310 | RCT A = U; B = N; F = Y |
Rural households participating in a cohort study examining multiple health outcomes (n = 654) | I1 = ionisation alarm and carbon zinc battery I2 = ionisation alarm and lithium battery I3 = photoelectric alarm and carbon zinc battery I4 = photoelectric alarm and lithium battery |
||||||||||||
| Ytterstad 1998442 | CBA B = U; F = Y; BC = N |
Children aged ≤ 5 years in Harstad (intervention) and Trondheim (control), Norway (n = 14,573 person-years) | I = promotion of tap water thermostat setting to 55 °C and of increased parental vigilance in putative burn risk situations C = none of the above |
||||||||||||
| Zhao 2006312 | RCT A = N; B = Y; F = Y |
Primary schoolchildren aged 7–13 years (year 2000, n = 5872; year 2001, n = 5880) | I = health education on injury prevention including scalds prevention, safe storage of pots of hot water C = health education on prevention of other common childhood diseases |
||||||||||||
Reducing fire-related injuries
Study H
The overview included nine systematic reviews reporting interventions to prevent fire-related injuries,33,36,37,41,353,354,384,387,391 which, between them, drew on data from only four primary studies. No meta-analyses that reported the effect of interventions on fire-related injuries were found. The reviews found two case–control studies reporting the risk of injury or death in homes with and without smoke alarms. Both found a two- to threefold increase in the odds of a fatal house fire compared with a non-fatal house fire in households with smoke alarms. 50,425 The reviews found inconsistent or insufficient evidence about whether or not interventions promoting smoke alarms were associated with a reduction in fire-related injuries, from one RCT261 and one CBA. 423 The CBA reported an increased prevalence of smoke alarm use, which was also associated with a reduction in fire-related injuries. 423 This finding was not confirmed by the RCT, but this may be explained by the ineffectiveness of the intervention in the trial, as there was no significant increase in the prevalence of smoke alarm use. 261
Two case–control studies explored the odds of fatal house fires related to smoking and alcohol use. 50,394 The first found significant increases in the risk of a fatal house fire when smoking was the source of ignition of the fire and when household members were impaired by drugs or alcohol. 50 The second found a significantly greater risk of a fatal household fire among households with smokers than among those with non-smokers, a dose–response relationship with the number of smokers in the household and an increased risk with smoking 10–19 cigarettes per day or ≥ 20 cigarettes per day compared with non-smokers. The same study found no significant association between the number of alcoholic drinks consumed per household member and risk of fatal house fire. 394
There were insufficient studies to undertake PMA or NMA for the effect of home safety interventions on fire-related injuries in studies I and J.
Promoting smoke alarm ownership and function and other smoke alarm outcomes
Study H
The overview included three systematic reviews and meta-analyses33,37,40 and nine systematic reviews36,41,42,331,353,382,383,387,391 reporting the effect of interventions on a range of smoke alarm outcomes. Evidence from the meta-analyses indicates that interventions to promote smoke alarm ownership and function are effective. The first meta-analysis combined effect sizes on smoke alarm ownership from five studies (OR 1.74, 95% CI 1.03 to 2.96),40 the second meta-analysis combined effect sizes on smoke alarm ownership from 10 studies (OR 1.21, 95% CI 0.89 to 1.64)37 and the third meta-analysis combined effect sizes on having a functional smoke alarm from 13 studies (OR 1.85, 95% CI 1.24 to 2.75). 33 Subgroup analyses indicate that interventions provided in the clinical setting40 or as part of routine child health surveillance37 are effective, whereas those delivered in other settings may be less effective.
The majority of systematic narrative reviews concluded that a diverse range of interventions to promote smoke alarm ownership and function were effective. 36,353,382,383,387,391 One systematic review confined to examining the effect of home safety equipment and risk assessment schemes387 concluded that there is inconsistent evidence from six robust studies, using observed outcomes and a control group, about the presence of functional alarms. Four suggested that the intervention increased functioning smoke alarm presence and two suggested no significant impact on smoke alarms.
A total of 39 primary studies reporting smoke alarm ownership or functioning were identified (29 from reviews71,72,257,261,265,267–271,273,275,277,279,281,282,284,285,287,295,297,300,304,305,393,395,403,409,423,426 and 10 from additional searches for primary studies;266,286,288,310,397,398,412,418,431,433). The studies not included in a review suggest that there is conflicting evidence about the effect of type of smoke alarm on smoke alarm functioning. 286,310,433 Two RCTs found that alarms with lithium batteries were more likely to remain functional than those with carbon zinc batteries. 310,433
Seven primary studies reporting the effectiveness of interventions in promoting other smoke alarm outcomes were included in the overview. The outcomes reported include checking or changing smoke alarm batteries, false alarms, reasons for non-functional alarms, redeeming vouchers for free alarms, awakening to alarms and time to awaken or escape. There appears to be inconsistent evidence about the effect of interventions on checking or changing smoke alarm batteries. 282,287,288,295 One RCT found that photoelectric alarms were significantly less likely to cause false alarms than ionising alarms. 310 One RCT found that installing smoke alarms was more effective at increasing the prevalence of functional smoke alarms than providing vouchers for families to redeem against alarm purchase, with 47% of vouchers not redeemed. 268 Finally, one RCT found that children are significantly more likely to awaken to a parent-voice alarm than to a standard smoke alarm and that time to awaken and time to escape were significantly shortened with parent-voice compared with standard alarms. 436
Study I
Pairwise meta-analysis of 17 studies evaluating home safety interventions (education plus provision of smoke alarms and home safety inspections in some studies),71,72,261,265,266,269,271,275,277,284,285,297,304,395,398,426,431 which updated the meta-analysis by Kendrick et al. 33 described in the previous section, found that interventions significantly increased functional smoke alarm ownership (OR 1.81, 95% CI 1.30 to 2.52) (Figure 26). Interventions that provided smoke alarms appeared to be more effective (OR 2.49, 95% CI 1.53 to 4.06) than those that did not (OR 1.12, 95% CI 0.87 to 1.45). Seventeen studies reported ownership of alarms (as opposed to functional status)71,261,266,267,269,270,273,277,282,287,288,295,305,395,403,418,426 and meta-analysis showed that interventions may be associated with a small increase in smoke alarm ownership (OR 1.17, 95% CI 0.97 to 1.42). Publication bias may have occurred in the functional smoke alarm ownership analysis (p-value for the tests of asymmetry = 0.063 and inspection of the funnel plot indicated the possibility of missing studies with non-significant findings), but findings remained significant after application of the regression bias adjustment method (OR 1.44, 95% CI 1.07 to 1.92).
FIGURE 26.
Forest plot of effect sizes for possession of a functional smoke alarm from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
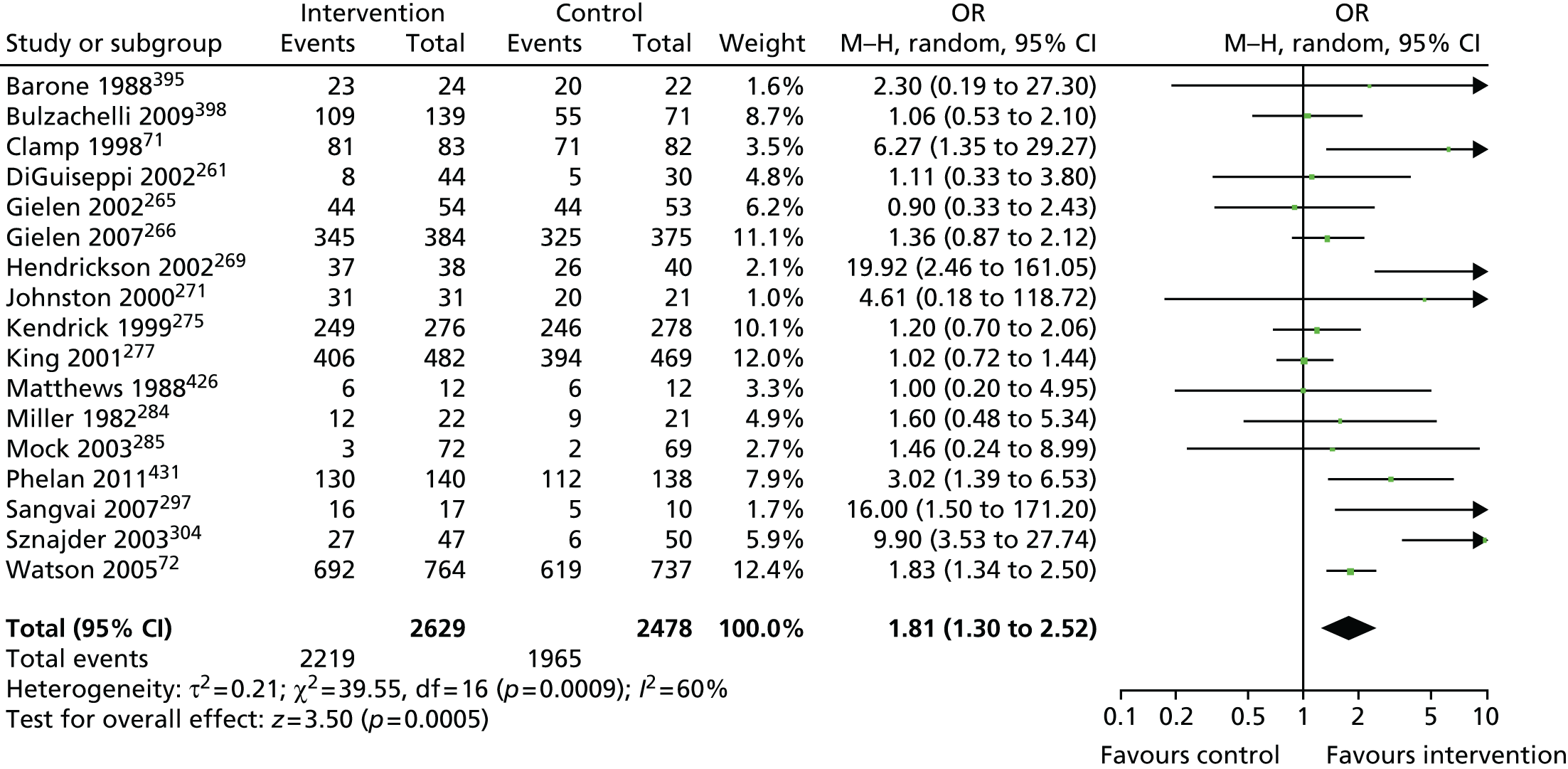
Four studies that reported checking or changing smoke alarm batteries in the last 6 months were included in a meta-analysis as part of study I. 282,287,288,295 There was no evidence that home safety interventions were effective in increasing the proportion of families who had checked or changed smoke alarm batteries in the preceding 6 months (OR 1.15, 95% CI 0.63 to 2.08) (Figure 27).
FIGURE 27.
Forest plot of effect sizes for smoke alarm batteries being checked or changed from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
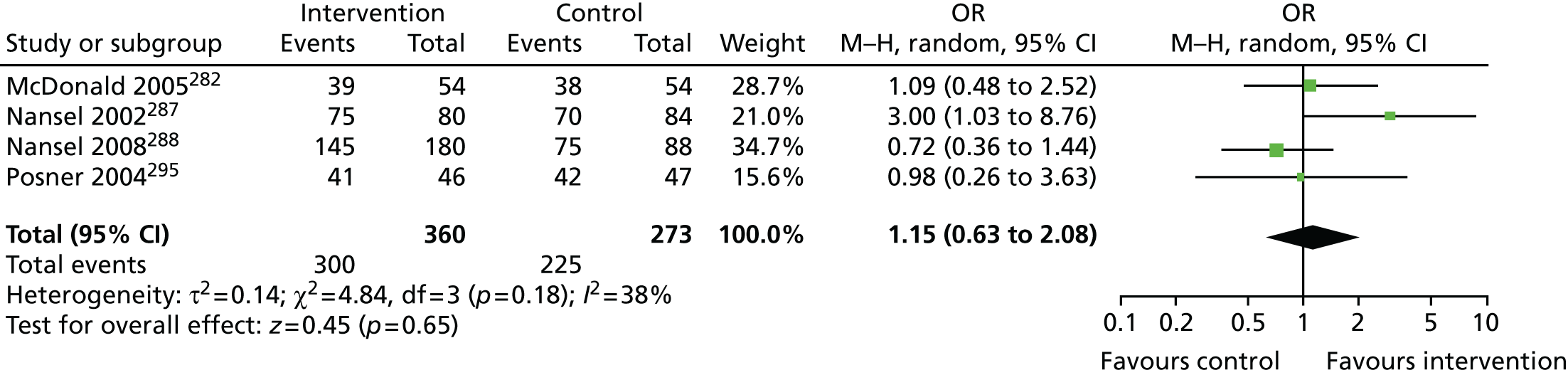
Study J
Network meta-analysis was used to determine the effect of component elements of home safety interventions on having a functional smoke alarm in 20 of the studies identified from the overview. 71,72,261,265,266,268,269,271,275,277,284,285,297,300,304,395,398,409,426,431 Interventions used in these studies were categorised into seven distinct groupings and the NMA estimated the 21 possible pairwise comparisons between the seven interventions reported in the 20 studies. The data used in the NMA from each study for fire prevention outcomes are shown in Table 73. The pooled estimates, 95% CrIs and, when available, direct within-trial estimates are reported in Table 74. The most intensive intervention (home safety education plus equipment provision plus fitting of safety equipment plus home safety assessment) was the most likely to be the most effective (probability = 0.66), with an OR compared with usual care of 7.15 (95% CrI 2.40 to 22.73).
| Comparison (intervention number) | Study | Study design | Follow-up (number of months) | Intervention | Study quality | Has functional smoke alarm (numbers adjusted for clustering) | |
|---|---|---|---|---|---|---|---|
| Number of smoke alarms | Total number of households | ||||||
| Usual care (1) vs. education (2) | Gielen 2001409 | RCT | 12 | 1 | A = Y, B = Y, F = N | 54 (52.02)a | 56 (53.95)a |
| 2 | 77 (74.18)a | 80 (77.07)a | |||||
| Mock 2003285 | CBA | 6 | 1 | B = N, F = N, C = N | 10 (2.33)b | 297 (69.18)b | |
| 2 | 18 (3.03)b | 308 (71.74)b | |||||
| Gielen 2007266 | RCT | 0.5–1 | 1 | A = Y, B = N, F = Y | 325 | 375 | |
| 2 | 345 | 384 | |||||
| Bulzacchelli 2009398 | NRCT | 0.5 | 1 | B = N, F = N, C = N | 55 | 71 | |
| 2 | 109 | 139 | |||||
| Usual care (1) vs. education + low-cost/free equipment (3) | Miller 1982284 | NRCT | 1.5 | 1 | B = U, F = Y, C = Y | 46 (9.34)b | 105 (21.31)b |
| 3 | 61 (12.38)b | 108 (21.92)b | |||||
| Clamp 199871 | RCT | 1.5 | 1 | A = Y, B = N, F = Y | 71 | 82 | |
| 3 | 81 | 83 | |||||
| Usual care (1) vs. education + low-cost/free equipment + home safety inspection (4) | Kendrick 1999275 | NRCT | 25 | 1 | B = N, F = N, C = Y | 321 (245.62)b | 363 (277.76)b |
| 4 | 325 (248.68)b | 361 (276.23)b | |||||
| Hendrickson 2005269 | RCT | 1.5 | 1 | A = N, B = N, F = Y | 26 | 40 | |
| 4 | 37 | 38 | |||||
| Sangvai 2007297 | RCT | 6 | 1 | A = Y, B = N, F = N | 5 | 10 | |
| 4 | 16 | 17 | |||||
| Usual care (1) vs. education + low-cost/free equipment + fitting (5) | DiGuiseppi 2002261 | RCT | 12–18 | 1 | A = Y, B = Y, F = N | 5 (5)c | 30 (30)c |
| 5 | 8 (8)c | 44 (44)c | |||||
| Watson 200572 | RCT | 12 | 1 | A = Y, B = N, F = N | 619 | 737 | |
| 5 | 692 | 764 | |||||
| Usual care (1) vs. education + low-cost/free equipment + fitting + home safety inspection (7) | Schwarz 1993300 | CBA | 12 | 1 | B = N, F = N, C = Y | 816 | 1060 |
| 7 | 866 | 902 | |||||
| Phelan 2011431 | RCT | 12 | 1 | A = Y, B = N, F = Y | 112 | 138 | |
| 7 | 130 | 140 | |||||
| Education (2) vs. education + low-cost/free equipment (3) | Barone 1988395 | RCT | 6 | 2 | A = N, B = N, F = N | 34 (20.08)b | 38 (22.45)b |
| 3 | 39 (23.04)b | 41 (24.22)b | |||||
| Education (2) vs. education + low-cost/free equipment + fitting (5) | Sznajder 2003304 | RCT | 1.5–2 | 2 | A = Y, B = N, F = Y | 6 | 50 |
| 5 | 27 | 47 | |||||
| Education + low-cost/free equipment (3) vs. education + low-cost/free equipment + home safety inspection (4) | Gielen 2002265 | RCT | 12 | 3 | A = U, B = U, F = N | 47 (44.20)b | 56 (52.66)b |
| 4 | 47 (44.20)b | 58 (54.54)b | |||||
| Education + low-cost/free equipment + home safety inspection (4) vs. education + home safety inspection (6) | Matthews 1988426 | NRCT | 0.5 | 4 | B = U, F = Y, C = U | 6 | 12 |
| 6 | 6 | 12 | |||||
| Johnston 2000271 | RCT | 3 | 4 | A = N, B = N, F = Y | 211 (20.05)b | 211 (21.15)b | |
| 6 | 136 (31.07)b | 143 (31.14)b | |||||
| King 2001277 | RCT | 12 | 4 | A = Y, B = Y, F = Y | 394 | 469 | |
| 6 | 406 | 482 | |||||
| Education + low-cost/free equipment + home safety inspection (4) vs. education + low-cost/free equipment + fitting + home safety inspection (7) | Harvey 2004268 | RCT | 9 | 4 | A = U, B = N, F = N | 997 (781.59)d | 1545 (1211.19)d |
| 7 | 1421 (1113.99)d | 1583 (1240.98)d | |||||
| Intervention | Usual care (1) | Education (2) | Education + equipment (3) | Education + equipment + home inspection (4) | Education + equipment + fitting (5) | Education + home inspection (6) | Education + equipment + fitting + home inspection (7) |
|---|---|---|---|---|---|---|---|
| Usual care (1) | 0.99 (0.39 to 2.33) | 3.18 (0.98 to 11.18) | 2.82b (1.13 to 8.93) | 2.71 (0.85 to 8.88) | 3.48 (0.75 to 26.53) | 7.15b (2.40 to 22.73) | |
| Education (2) | 1.34 (0.66 to 2.65) | 3.52 (0.84 to 14.46) | 2.87 (0.84 to 13.19) | 2.76 (0.80 to 10.27) | 3.56 (0.64 to 34.50) | 7.25b (1.87 to 30.33) | |
| Education + equipment (3) | 3.25 (0.49 to 22.95) | 2.29 (0.23 to 22.61) | 0.89 (0.24 to 3.57) | 0.86 (0.16 to 4.51) | 1.10 (0.19 to 9.00) | 2.26 (0.46 to 10.55) | |
| Education + equipment + home inspection (4) | 5.94 (0.96 to 48.79) | 0.82 (0.30 to 2.22) | 0.98 (0.17 to, 4.49) | 1.24 (0.35 to 5.55) | 2.59 (0.64 to 8.13) | ||
| Education + equipment + fitting (5) | 1.65 (0.30 to 7.61) | 9.90b (3.53 to 27.74) | 1.27 (0.19 to 13.37) | 2.61 (0.52 to 13.26) | |||
| Education + home inspection (6) | 1.17 (0.34 to 6.98) | 2.09 (0.24 to 10.52) | |||||
| Education + equipment + fitting + home inspection (7) | 5.24 (0.84 to 26.41) | 4.82b (3.88 to 6.00) |
Three studies evaluated the effect of alarm type and battery type on alarm function. 286,310,433 The data used in the NMA from each study are shown in Table 75 and the pooled estimates, 95% CrIs and, when available, direct within-trial estimates are reported in Table 76. Ionisation smoke alarms with lithium batteries were most likely to be the best type for increasing possession of a functioning alarm (p best = 0.69), although there was considerable uncertainty in these estimates as shown by the wide 95% CrIs in Table 76.
| Study | Study design | Follow-up (number of months) | Intervention | Study quality | Has functional smoke alarm | |
|---|---|---|---|---|---|---|
| Number of smoke alarms | Total number of households | |||||
| Rowland 2002433 | RCT | 15 | Ionisation zinc | A = Y, B = N, F = Y | 142 | 257 |
| Ionisation lithium | 44 | 63 | ||||
| Optical lithium | 24 | 79 | ||||
| Optical zinc | 40 | 57 | ||||
| Mueller 2008286 | RCT | 9 | Ionisation zinc | A = N, B = N, F = Y | 264 | 332 |
| Optical zinc | 322 | 340 | ||||
| Yang 2008310 | RCT | 12 | Ionisation zinc | A = U, B = N, F = Y | 154 | 157 |
| Ionisation lithium | 154 | 154 | ||||
| Optical lithium | 178 | 180 | ||||
| Optical zinc | 149 | 152 | ||||
| Ionisation zinc | Ionisation lithium | Optical lithium | Optical zinc | |
|---|---|---|---|---|
| Ionisation zinc | 4.56 (0.45 to 247.70) | 0.75 (0.06 to 15.70) | 2.40 (0.21 to 21.83) | |
| Ionisation lithium | 3.02 (0.52 to 51.10) | 0.17 (0.00 to 2.52) | 0.52 (0.00 to 5.05) | |
| Optical lithium | 0.55 (0.10 to 4.95) | 0.15 (0.01 to 1.00) | 3.14 (0.14 to 38.04) | |
| Optical zinc | 2.53 (0.56 to 9.00) | 0.47 (0.03 to 3.20) | 2.50 (0.25 to 16.39) |
Study K
The findings from the decision analysis evaluating the cost-effectiveness of different interventions for promoting possession of functional smoke alarms are described below. Four of the seven interventions evaluated in the base-case analysis had higher costs or higher ICERs than more effective interventions (namely education plus free safety equipment and education plus free safety equipment and fitting of equipment plus home safety inspection) and were therefore excluded from further consideration (Table 77). Of the remaining three interventions, education plus free safety equipment had the lowest estimated ICER compared with usual care, at £34,200 per QALY gained.
| Intervention | Expected QALYs (95% CrI)a | Expected costs (95% CrI) (£)a | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained)b | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| Usual care (1) | 25,056 (25,039 to 25,074) | 19,317 (7850 to 40,561) | – | – | – | 0.62 | 0.31 |
| Education (2) | 25,056 (25,039 to 25,074) | 20,055 (8750 to 41,093) | – | – | Extendedly dominated | < 0.001 | 0.001 |
| Education + equipment (3) | 25,056 (25,039 to 25,074) | 20,094 (9193 to 40,546) | 0.02 | 777 | 34,200 | 0.38 | 0.69 |
| Education + equipment + home safety inspection (4) | 25,056 (25,039 to 25,074) | 22,091 (11047 to 42,710) | – | – | Dominated | < 0.001 | < 0.001 |
| Education + equipment + fitting (5) | 25,056 (25,039 to 25,074) | 21,638 (10654 to 42,219) | – | – | Dominated | < 0.001 | < 0.001 |
| Education + home safety inspection (6) | 25,056 (25,039 to 25,074) | 21,991 (10673 to 43,168) | – | – | Dominated | < 0.001 | < 0.001 |
| Education + equipment + fitting + home safety inspection (7) | 25,056 (25,039 to 25,074) | 23,596 (12,021 to 44,319) | 0.001 | 3502 | 3,466,635 | < 0.001 | < 0.001 |
Figure 28 shows the probability of the alternative interventions being cost-effective. At a threshold value of £30,000 per QALY gained, usual care has the highest probability of being cost-effective (0.62). However, when this threshold value is increased to £50,000, education plus low-cost/free equipment has the highest probability of being cost-effective (0.69), demonstrating that there is considerable uncertainty in decisions within the £30,000–50,000 threshold range.
FIGURE 28.
Cost-effectiveness acceptability curves for interventions promoting possession of functional smoke alarms. E, education; F, fitting; FE, low-cost/free equipment; HSI, home safety inspection; UC, usual care. Adapted from Saramago et al. 373 under the Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).
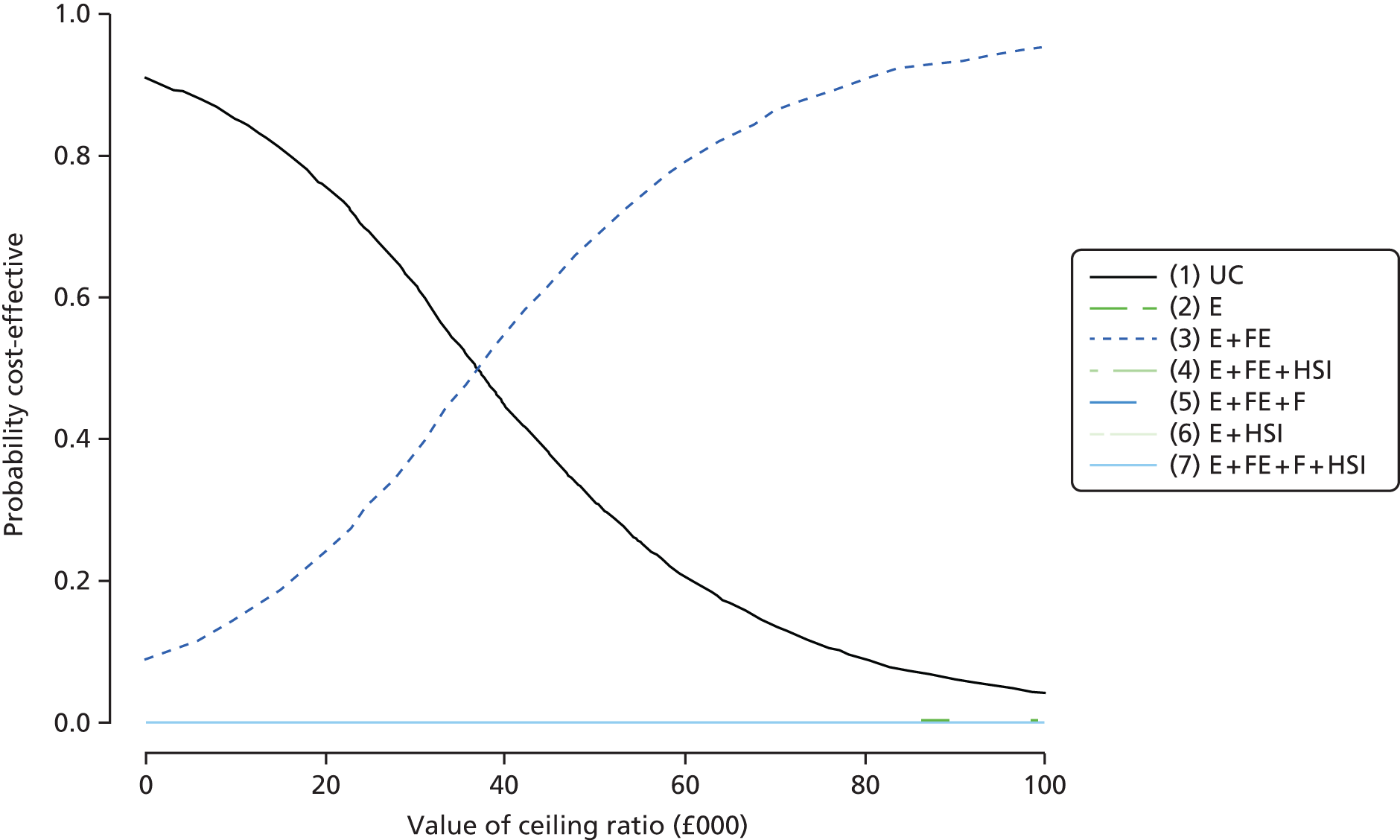
We undertook a series of sensitivity analyses assessing the robustness of the findings to modelling assumptions and data used in the modelling, as described in the methods section (Table 78). Dominated and extendedly dominated interventions have been removed from Table 78. All sensitivity analyses assessed the probability of interventions being cost-effective at a threshold of £30,000. Reducing the prevalence of smoke alarms in UK households from 80% to 50% resulted in ICERs that increased as the intensity of the intervention increased from education to education plus free equipment and fitting plus home safety inspection; however, for any of these interventions to be adopted, decision makers needed to be willing to pay or displace large amounts of funds (i.e. ICERs were ≥ £180,000 per additional QALY).
| Intervention | Expected QALYs (95% CrI)a | Expected costs (95% CrI) (£)a | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained) | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| SA1: prevalence of smoke alarms in households of 50% | |||||||
| Usual care (1) | 25,056.054 (25,038.86 to 25,073.69) | 20,813 (8337 to 43,726) | – | – | – | 0.99 | 0.98 |
| Education (2) | 25,056.070 (25,038.88 to 25,073.71) | 23,732 (11,327 to 46,646) | 0.020 | 2919 | 180,400 | < 0.001 | < 0.001 |
| Education + equipment (3) | 25,056.079 (25038.88 to 25073.72) | 25,715 (13029 to 48245) | 0.009 | 1983 | 225,545 | 0.01 | 0.02 |
| Education + equipment + fitting + home safety inspection (7) | 25,056.081 (25,038.89 to 25,073.72) | 37,863 (18,872 to 61,155) | 0.002 | 12,148 | 5,955,269 | < 0.001 | < 0.001 |
| SA2: probability of accepting the intervention of 50% | |||||||
| Usual care (1) | 25,056.159 (25,038.67 to 25,074.24) | 19,470 (7948 to 40,486) | – | – | – | 0.24 | 0.09 |
| Education + equipment (3) | 25,056.177 (25,038.69 to 25,074.26) | 19,695 (8618 to 39,932) | 0.020 | 225 | 12,701 | 0.76 | 0.91 |
| Education + equipment + fitting + home safety inspection (7) | 25,056.177 (25,038.70 to 25,074.26) | 21,656 (10,383 to 42,046) | 0.000 | 1961 | 3,502,138 | < 0.001 | < 0.001 |
| SA3: null decay of safety equipment | |||||||
| Usual care (1) | 25,056.404 (25,039.07 to 25,074.24) | 18,839 (7684 to 39,507) | – | – | – | 0.96 | 0.82 |
| Education (2) | 25,056.413 (25039.07 to 25,073.81) | 19,530 (8558 to 39,944) | 0.009 | 691 | 80,117 | 0.04 | 0.17 |
| Education + equipment (3) | 25,056.416 (25039.08 to 25,073.82) | 20,094 (9193 to 40,546) | 0.003 | 564 | 209,061 | 0.001 | 0.01 |
| Education + equipment + fitting + home safety inspection (7) | 25,056.417 (25,039.09 to 25073.82) | 23,596 (12,021 to 44319) | 0.001 | 3,502 | 3,466,635 | < 0.001 | < 0.001 |
| SA4: considering 1.8 children per household | |||||||
| Usual care (1) | 44,349.503 (44,318.77 to 44,380.10) | 32,867 (12,272 to 71,150) | – | – | – | 0.11 | 0.03 |
| Education + equipment (3) | 44,349.544 (44,318.82 to 44,380.14) | 33,050 (13,428 to 69,595) | 0.040 | 183 | 4456 | 0.89 | 0.97 |
| Education + equipment + fitting + home safety inspection (7) | 44,349.546 (44,318.83 to 44,380.14) | 36,531 (16,836 to 73,296) | 0.002 | 3481 | 1,923,416 | < 0.001 | < 0.001 |
| SA5: same probability of injury for households with functioning and non-functioning smoke alarms | |||||||
| Usual care (1) | 25,057.511 (25,039.23 to 25,073.87) | 15,279 (6611 to 31,524) | – | – | – | 0.96 | 0.94 |
| Education + equipment (3) | 25,057.519 (25,039.24 to 25,073.88) | 16,562 (7924 to 32,584) | 0.008 | 1283 | 154,513 | 0.04 | 0.06 |
| Education + equipment + fitting + home safety inspection (7) | 25,057.520 (25,039.23 to 25,073.88) | 20,080 (10,842 to 35,798) | 0.001 | 3518 | 9,772,579 | < 0.001 | < 0.001 |
As the probability of accepting interventions varied considerably between the trials that informed the effectiveness model input parameters, the effect of reducing the acceptance rate from 90% to 50% was assessed. This resulted in a reduction in the ICER from £34,200 in the base case to £12,701 for education plus low-cost/free equipment compared with usual care. Reducing the probability of decay/repair of the safety equipment from 0.1 to 0 resulted in all interventions being dominated by education, which had an ICER of £80,117 compared with usual care. An increase in the number of children aged < 5 years per household from 1 to 1.8378 resulted in a reduction in the ICER from £34,200 to £4456 for education plus low-cost/free equipment compared with usual care.
Promoting fireguard possession and use
Study H
The overview included one systematic review and meta-analysis33 and three systematic reviews36,42,387 reporting the effect of interventions on the possession and use of fireguards. The meta-analysis reported some evidence that home safety education was effective in increasing the use of fire guards based on the combined effect sizes from four studies (OR 1.40, 95% CI 1.00 to 1.95), all of which included interventions that provided fireguards. 33 Of the four narrative reviews, one reported weak evidence that a free or discounted supply of fireguards, in conjunction with safety education, increased the use of fireguards and weak evidence that free home safety equipment and installation with safety education had no impact on the fitting and use of fireguards. 387 One review reported no significant increase in the use of fireguards33 and the remaining two reviews did not draw any specific conclusions about the effect of interventions on the use of fireguards. 36,42
Six primary studies reported the effect of interventions on the possession and use of fireguards (all from reviews71,72,275,292,295,417). One study reported a significant increase in the use of fireguards following the provision of safety advice, leaflets and low-cost equipment including fireguards. 71 Five studies reported no significant effect of interventions, all of which included home safety education and four of which also provided free or discounted safety equipment, with two of these including the provision of fireguards72,275 and two not providing fireguards. 292,295 The one study not providing equipment involved information cards, fridge magnets and checklists in addition to safety education. 417
Study I
The updated searches for study H did not find any additional studies evaluating home safety education, which also included the provision of fireguards. Therefore, the PMA includes the same four studies71,72,275,417 reported in Kendrick et al. 33 There was some evidence that home safety interventions were effective in increasing the use of fire guards (OR 1.40, 95% CI 1.00 to 1.95) (Figure 29).
FIGURE 29.
Forest plot of effect sizes for use of fire guards from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
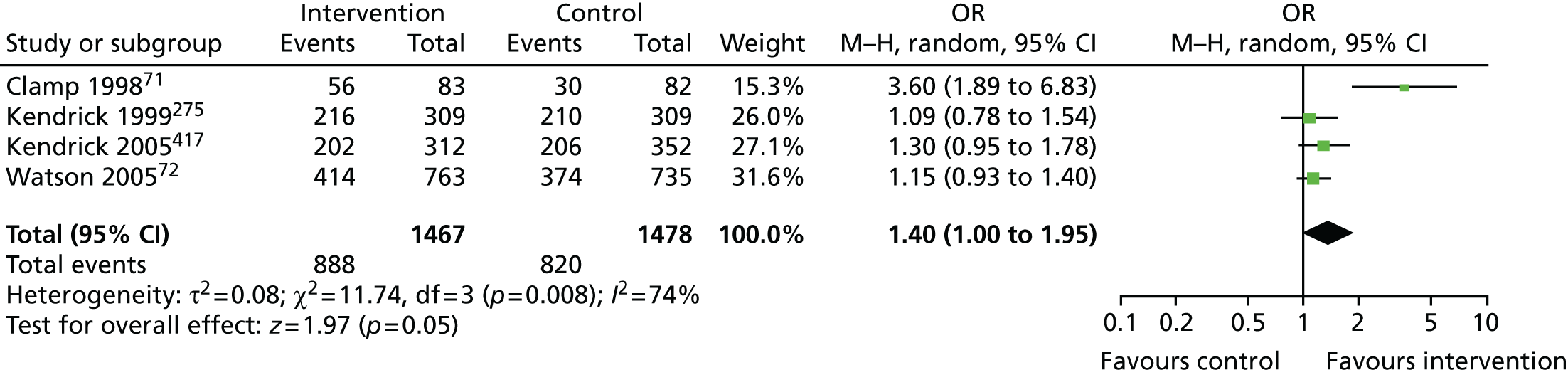
Study J
Network meta-analysis was used to determine the effect of component elements of home safety interventions on use of fireguards in four studies identified from the overview. 71,72,275,417 These studies included five interventions and the NMA estimated the 10 possible pairwise comparisons between the five interventions reported in the four studies. The data used in the NMA from each study are shown in Table 79. The pooled estimates, 95% CrIs and, when available, direct within-trial estimates are reported in Table 80. None of the interventions differed significantly from each other. The intervention with the highest probability of being the most effective was education plus equipment plus home safety inspection (p best = 0.28), but the probabilities were very similar for all interventions (range 0.20–0.28) except for education plus low-cost/free equipment (p best = 0.05).
| Study | Study design | Follow-up (months) | Intervention | Study qualitya | Has fireguard | |
|---|---|---|---|---|---|---|
| Number of fireguards | Total number of households | |||||
| Kendrick 2005417 | RCT | 9 | Usual care (1) | A = Y, B = N, F = Y | 205.91b | 351.55b |
| Education (2) | 201.72b | 312.21b | ||||
| Clamp 199871 | RCT | 1.5 | Usual care (1) | A = Y, B = N, F = Y | 30 | 82 |
| Education + equipment (3) | 56 | 83 | ||||
| Kendrick 1999275 | N-RCT | 25 | Usual care (1) | B = N, F = N, C = Y | 210.54b | 309.01b |
| Education + equipment + home safety inspection (4) | 216.48b | 309.01b | ||||
| Watson 200572 | RCT | 12 | Usual care (1) | A = Y, B = N, F = N | 374 | 735 |
| Education + equipment + fitting (5) | 414 | 763 | ||||
| Intervention | Usual care (1) | Education (2) | Education + equipment (3) | Education + equipment + home safety inspection (4) | Education + equipment + fitting (5) |
|---|---|---|---|---|---|
| Usual care (1) | 0.77 (0.06 to 9.20) | 0.28 (0.02 to 3.56) | 0.91 (0.07 to 11.22) | 0.87 (0.07 to 10.42) | |
| Education (2) | 0.77 (0.56 to 1.06) | 0.36 (0.01 to 13.15) | 1.17 (0.04 to 43.19) | 1.13 (0.03 to 40.96) | |
| Education + equipment (3) | 0.28 (0.15 to 0.53) | 3.28 (0.09 to 119.70) | 3.15 (0.09 to 110.70) | ||
| Education + equipment + home safety inspection (4) | 0.91 (0.65 to 1.29) | 0.97 (0.02 to 36.89) | |||
| Education + equipment + fitting (5) | 0.87 (0.71 to 1.07) |
Study K
Decision analyses were not undertaken for interventions to promote fireguard use as no interventions were found to be effective in NMAs.
Promoting fire extinguisher possession
Study H
The overview included one systematic review and meta-analysis33 and one systematic review42 reporting the effect of interventions on the possession of fire extinguishers. The meta-analysis, which combined effect sizes from four studies, reported that home safety education interventions, one of which included the provision of fire extinguishers, were not effective in increasing the possession of fire extinguishers (OR 0.95, 95% CI 0.40 to 2.23). 33 One systematic review33 reported mixed findings from studies not included in the meta-analysis, but effect sizes were not reported. The other review42 included one relevant primary study but did not draw any conclusions specific to the possession of fire extinguishers.
Nine primary studies reported the effect of interventions to promote the possession of fire extinguishers; seven of these studies were identified from reviews269,277,279,293,304,399,441 and two from additional searches for primary studies. 257,412 One study found a significant effect on the possession of fire extinguishers of an intervention involving home safety education, home hazard assessment and the provision of items of equipment including fire extinguishers. 269 Other studies delivering home safety education, hazard identification and assistance with obtaining safety equipment did not report a significant effect on the possession of fire extinguishers. 257,277,279,304,441 Two studies involving a community injury prevention programme including seminars, workshops, courses and home visits293 and an intervention involving a home visit from fire service personnel focusing on smoke alarms and fire escape plans412 both reported no increase in the possession of fire extinguishers. One study did not report the effect of the intervention on the possession of fire extinguishers. 399
Study I
Pairwise meta-analysis of five studies evaluating home safety education257,269,277,293,304 found a lack of evidence that interventions were effective in increasing the possession of fire extinguishers (OR 0.90, 95% CI 0.53 to 1.51) (Figure 30).
FIGURE 30.
Forest plot of effect sizes for possession of a fire extinguisher from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49

Study J
Network meta-analysis was used to determine the effect of the component elements of home safety interventions on the possession of fire extinguishers in four studies identified from the overview. 257,269,277,293 These studies included six interventions and the NMA estimated the 15 possible pairwise comparisons between the six interventions reported in the four studies. The data used in the NMA from each study are shown in Table 81. The pooled estimates, 95% CrIs and, when available, direct within-trial estimates are reported in Table 82. None of the interventions differed significantly from each other. The intervention with the highest probability of being the most effective was community campaign plus education plus home visit (p best = 0.63).
| Study | Study design | Follow-up (months) | Intervention | Study qualitya | Has fire extinguisher | |
|---|---|---|---|---|---|---|
| Number of fire extinguishers | Total number of households | |||||
| Hendrickson 2002269 | RCT | 1.5 | Usual care (1) | A = N, B = N, F = Y | 15 | 40 |
| Education + equipment + home safety inspection (3) | 28 | 38 | ||||
| Babul 2007257 | RCT | 12 | Usual care (1) | A = Y, B = N, F = N | 98 | 148 |
| Education + equipment (2) | 110 | 172 | ||||
| Education + home safety inspection (5) | 94 | 162 | ||||
| Petridou 1997293 | CBA | 20 | Usual care (1) | B = N, F = Y, C = Y | 12.99b | 100.12b |
| Community campaign + education + home visits (6) | 5.35b | 97.83b | ||||
| King 2001277 | RCT | 12 | Education + equipment (not fire extinguishers) + home safety inspection (4) | A = Y, B = Y, F = Y | 232 | 469 |
| Education + home safety inspection (5) | 213 | 482 | ||||
| Intervention | Usual care (1) | Education + equipment (2) | Education + equipment + home safety inspection (3) | Education + equipment (not fire extinguishers) + home safety inspection (4) | Education + home safety inspection (5) | Community campaign + education + home visits (6) |
|---|---|---|---|---|---|---|
| Usual care (1) | 1.11 (0.09 to 14.21) | 0.21 (0.01 to 2.91) | 0.64 (0.02 to 23.48) | 0.78 (0.06 to 10.32) | 2.64 (0.18 to 37.76) | |
| Education + equipment (2) | 1.10 (0.08 to 0.56) | 0.19 (0.00 to 6.96) | 0.58 (0.02 to 20.76) | 0.70 (0.05 to 9.37) | 2.34 (0.06 to 91.83) | |
| Education + equipment + home safety inspection (3) | 0.21 (0.70 to 1.75) | 3.12 (0.04 to 285.70) | 3.81 (0.09 to 161.2) | 13.07 (0.26 to 582.30) | ||
| Education + equipment (not fire extinguishers) + home safety inspection (4) | 1.22 (0.10 to 15.16) | 4.06 (0.05 to 334.50) | ||||
| Education + home safety inspection (5) | 0.78 (0.50 to 1.21) | 0.71 (0.44 to 1.12) | 1.24 (0.96 to 1.60) | 3.34 (0.08 to 138.10) | ||
| Community campaign + education + home visits (6) | 2.58 (0.90 to 1.60) |
Study K
Decision analyses were not undertaken for interventions to promote the possession of fire extinguishers, as none of the interventions was found to be effective in NMA.
Safe storage of matches and other matches-related outcomes
Study H
Two meta-analyses33,40 and one systematic review354 reporting the effect of interventions on the storage of matches out of reach of children were included in the overview. One meta-analysis40 reported that there was a modest but non-significant effect on safe storage of matches based on the findings of two studies reporting this outcome (no effect size reported). The second meta-analysis33 pooled the findings of five studies and found a lack of evidence that home safety inspection was effective in increasing the safe storage of matches (OR 1.23, 95% CI 0.56 to 2.68). The systematic review354 identified only one relevant study, which did not find a significant effect of the intervention on the safe storage of matches.
Six primary studies reporting the effect of interventions on the safe storage of matches were identified from reviews. 269,273,275,277,304,404 No further studies were identified from additional searches for primary studies. All six studies found no significant effect on the safe storage of matches of interventions involving safety education,273,404 provision of a safety kit304 and safety education combined with home hazard checks and provision of equipment or assistance with obtaining equipment. 269,275,277
Study I
Pairwise meta-analysis of six studies reporting the effect of interventions on the storage of matches out of reach of children269,273,275,277,304,404 found a lack of evidence that home safety education was effective (OR 1.03, 95% CI 0.63 to 1.68) (Figure 31).
FIGURE 31.
Forest plot of effect sizes for storing matches out of reach of children from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
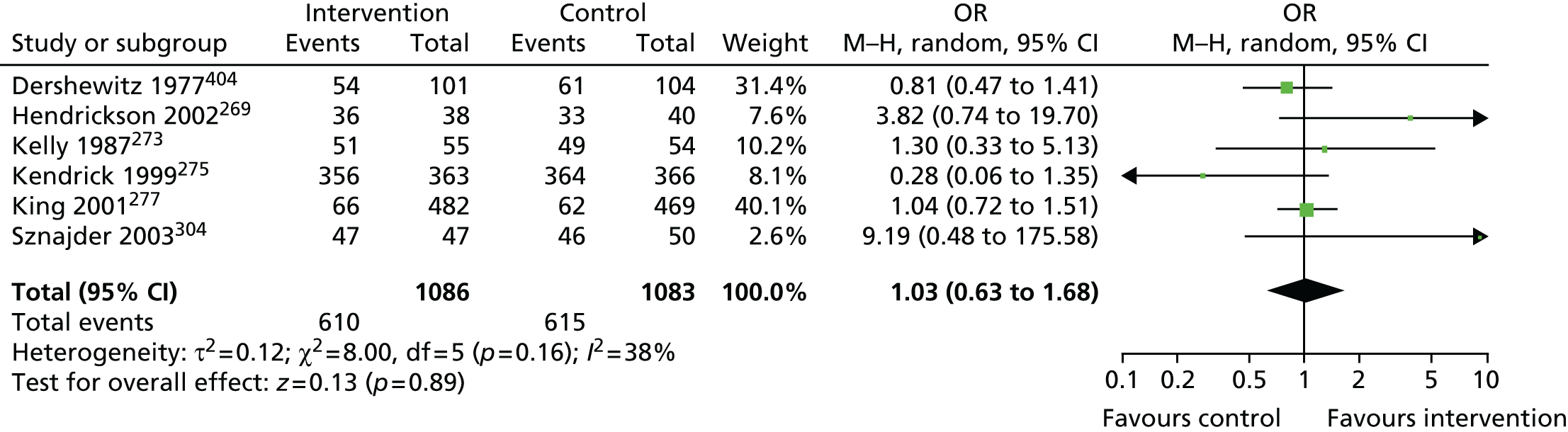
Two primary studies reported other matches-related outcomes, neither of which was included in a systematic review. One study provided training and teaching resources to teachers of children and reported a significant improvement in the number of children never using matches. 418 The other study provided a home visit from fire service personnel and did not report any reduction in the rate of lighting of matches or lighters. 412
Study J
Network meta-analysis was used to determine the effect of component elements of home safety interventions on the safe storage of matches in five studies identified from the overview. 269,273,275,304,404 These studies included four interventions and the NMA estimated the six possible pairwise comparisons between the four interventions reported in the five studies. The data used in the NMA from each study are shown in Table 83. The pooled estimates, 95% CrIs and, when available, direct within-trial estimates are reported in Table 84. None of the interventions differed significantly from each other. The intervention with the highest probability of being the most effective was education + equipment + home safety inspection (p best = 0.40).
| Study | Study design | Follow-up (months) | Intervention | Study qualitya | Safe storage of matches | |
|---|---|---|---|---|---|---|
| Number of households with safe storage of matches | Total number of households | |||||
| Kelly 1987273 | RCT | 7 | Usual care (1) | A = U, B = Y, F = N | 49 | 54 |
| Education (2) | 51 | 55 | ||||
| Hendrickson 2002269 | RCT | 1.5 | Usual care (1) | A = N, B = N, F = Y | 33 | 40 |
| Education + equipment + home safety inspection (3) | 36 | 38 | ||||
| Kendrick 1999275 | RCT | 25 | Usual care (1) | B = N, F = N, C = Y | 364 | 366 |
| Education + equipment + home safety inspection (3) | 356 | 363 | ||||
| Dershewitz 1977404 | RCT | 2 | Usual care (1) | A = U, B = Y, F = N | 61 | 104 |
| Education + equipment + home safety inspection (3) | 54 | 101 | ||||
| Sznajder 2003304 | RCT | 2 | Education (2) | A = Y, B = N, F = Y | 46 | 50 |
| Education + equipment + fitting (4) | 47 | 47 | ||||
| Intervention | Usual care (1) | Education (2) | Education + equipment (3) | Education + equipment + home safety inspection (4) |
|---|---|---|---|---|
| Usual care (1) | 0.78 (0.04 to 11.95) | 1.09 (0.21 to 5.26) | 0.04 (0.00 to 4.24) | |
| Education (2) | 0.77 (0.19 to 3.03) | 1.40 (0.06 to 36.58) | 0.06 (0.00 to 2.12) | |
| Education + equipment + home safety inspection (3) | 1.08 (0.21 to 5.29) | 0.04 (0.00 to 5.37) | ||
| Education + equipment + fitting (4) | 0.11 (0.01 to 2.08) |
Study K
Decision analyses were not undertaken for interventions to promote the storage of matches out of reach of children, as none of the interventions was found to be effective in NMA.
Having or practising a fire escape plan
Study H
Two systematic narrative reviews reported outcomes related to having or practising a fire escape plan. 33,387 The first review33 found four studies reporting this outcome, two of which reported a significant difference that favoured the intervention group. The second review387 included one relevant study and reported that home risk assessment and free/discounted supply and installation of safety equipment had a positive effect on having a fire escape plan.
A total of six primary studies reporting fire escape plan outcomes were identified, five from systematic reviews293,295,300,399,441 and one from additional searches for primary studies. 412 Interventions that were effective included multimedia first aid and home safety training,399 a home visit from fire service personnel,412 a community programme including safety seminars for parents, workshops with teachers, courses for schoolchildren and weekly home visits293 and a home visit involving safety education, modification and provision of safety items. 300 Two studies that did not demonstrate an effect of interventions on having or practising a fire escape plan both involved home safety education that targeted a range of injuries, one with a safety kit295 and one with hazard identification and free safety equipment. 441
Study I
Pairwise meta-analysis of four studies reporting on having or practising a fire escape plan293,295,399,412 found that home safety interventions increased the proportion of families with a fire escape plan (OR 2.01, 95% CI 1.45 to 2.77) (Figure 32).
FIGURE 32.
Forest plot of effect sizes for having a fire escape plan from studies evaluating home safety educational interventions. IV, inverse variance. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
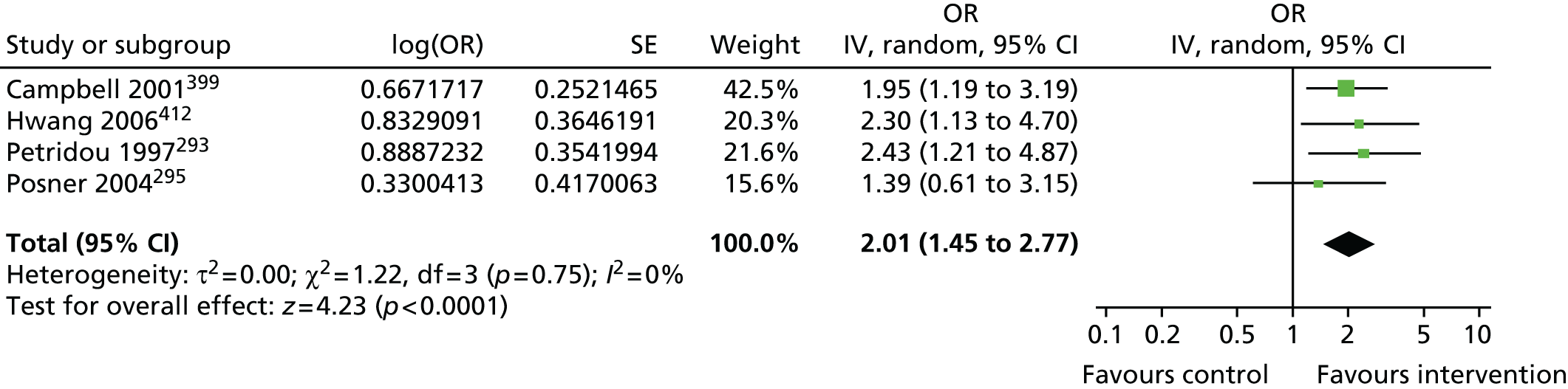
Study J
Network meta-analysis was used to determine the effect of component elements of home safety interventions on the possession of a fire escape plan in three studies identified from the overview. 293,295,399 These studies included four interventions and the NMA estimated the six possible pairwise comparisons between the four interventions reported in the three studies. The data used in the NMA from each study are shown in Table 85. The pooled estimates, 95% CrIs and, when available, direct within-trial estimates are reported in Table 86. None of the interventions differed significantly from each other. The intervention with the highest probability of being the most effective was usual care (p best = 0.53).
| Study | Study design | Follow-up (months) | Intervention | Study qualitya | Has fire escape plan | |
|---|---|---|---|---|---|---|
| Number of households with plan | Total number of households | |||||
| Petridou 1997293 | CBA | 20 | Usual care (1) | B = N, F = Y, C = Y | 15.29b | 100.12b |
| Community campaign + education + home visits (4) | 29.81b | 97.83b | ||||
| Posner 2004295 | RCT | 2.5 | Education (2) | A = Y, B = Y, F = N | 26 | 47 |
| Education + equipment (3) | 31 | 49 | ||||
| Campbell 2001399 | RCT | 12 | Usual care (1) | A = U, B = Y, F = N | 52.51c | 168.19c |
| Education (2) | 52.51c | 111.87c | ||||
| Intervention | Usual care (1) | Education (2) | Education + equipment (3) | Community campaign + education + home visits (4) |
|---|---|---|---|---|
| Usual care (1) | 0.71 (0.05 to 9.86) | 0.07 (0.00 to 2.90) | 0.40 (0.03 to 5.47) | |
| Education (2) | 0.51 (0.31 to 0.84) | 0.10 (0.01 to 1.39) | 0.56 (0.01 to 23.41) | |
| Education + equipment (3) | 0.72 (0.32 to 1.62) | 5.70 (0.06 to 503.10) | ||
| Community campaign + education + home visits (4) | 0.41 (0.21 to 0.82) |
Study K
Decision analyses were not undertaken for interventions to promote the possession of fire escape plans, as none of the interventions was found to be effective in NMAs.
Interventions to promote other fire prevention practices
Study H
No meta-analyses were found for other outcomes related to fire prevention practices. One narrative review354 reported interventions to teach safer fire responses, based on six primary studies. 411,414,415,428,429,440 It concluded that school-based programmes using active participation of children in learning fire responses were more effective than programmes using passive methods. It also concluded that skill retention was poor but was improved by periodic repetition and by the addition of fear reduction techniques and teaching the rationale behind behaviours. Two primary studies reporting this outcome were identified from further searches. One of these studies found a significant improvement in the demonstration of the correct action to take in a clothing fire and in knowledge of the correct actions to take in a house fire following delivery of a school-based injury prevention curriculum. 418 The other study reported that a significantly higher proportion of children who visited a learning centre performed the correct response and displayed the correct knowledge about a fire escape routine. 421
The overview included one review reporting the effectiveness of interventions to prevent fire setting or match play,33 which included three primary studies. 392,406,419 Two of these studies reported significant reductions in the incidence of fire setting or match play behaviour that favoured the intervention group. 406,419
The overview included one systematic review33 and six primary studies288,292,295,401,412,418 reporting outcomes related to cooking safety. One study found that significantly more intervention arm parents childproofed their boiler and rice cooker. 401 No significant differences were found between treatment arms for other cooking safety outcomes, including children cooking on the stove412 or without an adult present,418 for keeping children away from the stove,288 for turning pan handles away from the room288,295 or for using cooker guards. 292
Three studies reported outcomes related to the safe use of paraffin appliances. 289,301,303 All reported composite scores of paraffin safety practices, with two failing to find a significant difference between intervention arms289,303 and the third finding significantly safer scores in intervention arm families. 301 Two studies also reported the individual items that constituted the paraffin safety scores. 301,303 These included a range of safety practices, none of which was found to differ significantly between treatment arms in either study.
Two studies reported candle safety,295,303 with neither finding a significant difference between treatment groups for leaving burning candles in an empty room,295 leaving candles on unstable surfaces303 or using candles < 30 cm from flammable materials. 303
Two studies reported electrical safety outcomes. 289,295 One of the studies reported no significant difference between intervention arms in the proportion of families with overloaded electrical sockets295 and the other reported a composite electrical safety score, failing to find a significant difference between intervention arms. 289
One study reported two outcomes related to safe smoking practices, finding no significant difference between intervention arms with respect to smoking in bed or safe disposal of ashes. 295 The same study also found no significant difference between intervention arms in the proportion of families using an oven to heat the kitchen. 295 Finally, one study reported no significant difference between intervention arms in the safe storage of irons. 275
It was not possible to undertake pairwise meta-analyses (study I), NMA (study J) or decision analyses (study K) for any of these other fire prevention outcomes because of the small number of studies reporting each outcome.
Scalds prevention
Figure 33 shows the process of identification and selection of reviews and primary studies included in the overview and in the NMA for scalds prevention interventions (studies H and J). Ten narrative systematic reviews, four meta-analyses including a narrative systematic review and 39 primary studies were included in the overview and 22 primary studies in the NMA for scalds outcomes.
FIGURE 33.
Process of study identification and selection for the overview of reviews and NMAs for scalds prevention. NRCT, non-RCT. From Zou et al. 389 under the Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).
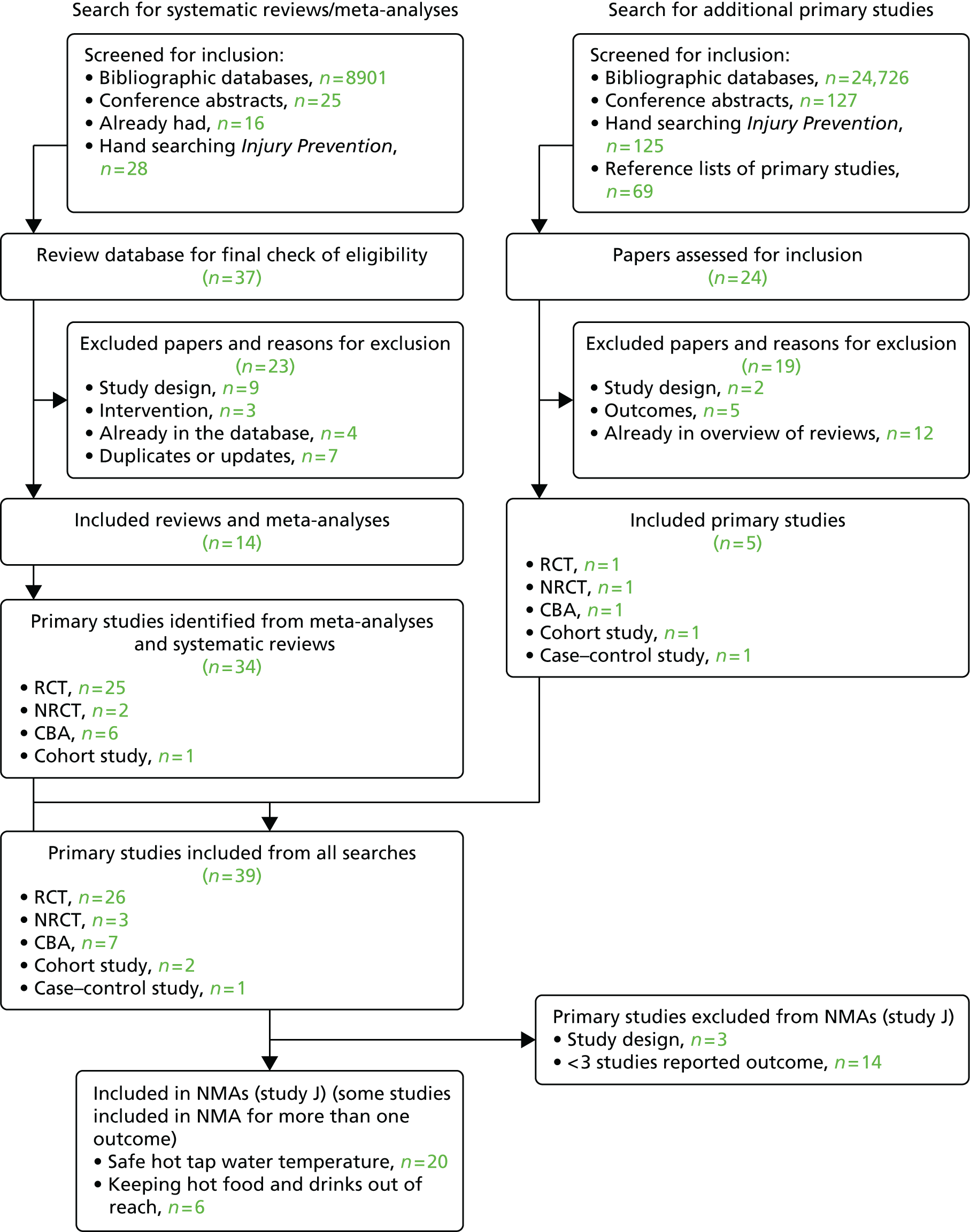
Characteristics of included reviews and primary studies
The characteristics and quality assessment of the reviews included in the scalds prevention overview (study H) are shown in Table 71. One review evaluated community-based scald prevention interventions337 and stated that there was a lack of studies from which to draw conclusions about the effectiveness of community-based programmes to prevent burns and scalds. The other reviews examined a number of different injury mechanisms, including scalds, but did not draw any conclusions specific to scalds prevention interventions. The risk of bias in included reviews was variable, with OQAQ scores ranging from 2 to 7 (median 5) out of a maximum possible of 7.
The characteristics of the primary studies included in the scalds prevention overview (study H), the systematic review and PMA (study I) and the NMAs (study J) are shown in Table 72. Twenty-six (67%) primary studies were RCTs, four (10%) were non-RCTs, six (15%) were CBAs, two (5%) were cohort studies and one (3%) was a case–control study. Tables of excluded reviews and primary studies are available on request from the authors. The risk of bias in included primary studies was also variable; 42% of RCTs had adequate allocation concealment, 58% followed up at least 80% of participants in each arm and 38% demonstrated blinded outcome assessment. None of the 10 non-RCTs and CBAs demonstrated blinded outcome assessment, three followed up at least 80% of participants in each arm and two had a balanced distribution of confounders between intervention arms. The two cohort studies scored 6 and 7 (out of a maximum of 9) on the Newcastle–Ottawa scale, indicating that they were of high quality. The case–control study scored 7 on the same scale.
Preventing scald injuries
Study H
Four narrative reviews36,49,337,385 reported the effectiveness of interventions for the prevention of scald injuries based on two primary studies. 312,442 One review of home safety interventions concluded that there was a lack of evidence that home safety interventions were effective in reducing rates of thermal (fire and scald) injuries. 49 One review concluded that there is little evidence that educational approaches alone have achieved any reductions in rates of burn and scald injuries. 36 One review concluded that there was a paucity of studies of the effectiveness of community-based injury prevention programmes for preventing burns and scalds in children. 337 The final review drew no conclusions specific to scald injury prevention. 385 No meta-analyses reported the effect of interventions on scald injuries. The first primary study was a CBA study and reported a reduction in the number of scalds and the severity of scald injuries following a community campaign and education from public health nurses at home visits and at childhood immunisations promoting lowering of tap water thermostat temperature. 442 However, the statistical significance of these findings was not reported. The second study, a RCT, found a significant reduction in the occurrence of scalds and burns in an intervention group receiving school-based health education delivered to children and parents. 312
It was not possible to undertake PMA, NMA or decision analyses for interventions to prevent scalds because of the small number of studies.
Safe hot tap water temperature
Study H
All 14 reviews reported the effect of interventions on safe hot water temperature,36,40,49,331,332,337,338,340,382,383,385–388 two of which included meta-analyses combining effect sizes for having a safe hot tap water temperature. 40,49 Both meta-analyses showed a significant effect favouring the intervention group, with pooled ORs of 2.32 (95% CI 1.46 to 3.68) based on combining effect sizes from four studies40 and 1.41 (95% CI 1.07 to 1.86) based on combining effect sizes from 16 studies,49 four of which were the same studies as in the DiGuiseppi and Roberts review. 40 Three reviews concluded that interventions had a positive effect on safe hot tap water temperature. 36,331,382 One review recommended periodic counselling of parents on measures to reduce the risk of unintentional injuries from hot tap water. 388
Twenty-nine primary studies reported the effect of interventions promoting safe hot water temperature, 26 of which were identified from reviews257,264,265,272,273,275–277,285,287,288,292,295,297,300,304,305,307,395,422,427,431,432,435,439 and three of which were identified from additional searches for primary studies. 99,402,424 Eighteen of the studies gave an explicit definition of safe water temperature, ranging from ≤ 46 °C276 to ≤ 60 °C. 307
Interventions were effective at promoting safe hot tap water temperature in six studies. 257,276,277,287,431,439 In three of these studies, interventions combined safety education, a home safety assessment and items of equipment that targeted a number of hazards. 257,277,431 Of these, one study reported the provision of an item relating to hot tap water temperature (water temperature card). 257 The other interventions demonstrating a significant effect included an educational leaflet on bathwater scalds plus the fitting of a TMV276 and a handout targeting burn and scald prevention combined with a 10-minute287 or 1-hour439 safety lecture.
Families in the intervention groups in five studies were significantly more likely to check or test hot tap water temperature compared with control group families. 257,272,295,422,435 Of these studies, one provided safety education, a home safety assessment and safety items including a water temperature card257 and one delivered safety counselling to prevent a range of injuries and a free home safety kit, which included a bathwater thermometer and bath tap spout covers among other items. 295 The other studies reporting a significant effect evaluated interventions providing a bathwater thermometer during paediatric clinic consultations,272 a 1-minute educational message about tap water scalds delivered in maternity wards435 and a national 1-week safety campaign delivered via the media, community partners and retail stores, where free water temperature testing cards were available. 422
The studies described above also reported that significantly more intervention families lowered their hot water temperature422 and significantly more intervention families used spout covers for bath taps. 295
Nineteen studies reported no significant effect of interventions on a range of outcomes related to safe hot water temperature. 99,264,265,273,275,285,287,288,292,297,300,304,307,395,402,424,427,432 They evaluated integrated or individual interventions including home visits, safety checks, safety education, counselling and safety devices.
Study I
The PMA evaluating home safety interventions (education plus provision of home safety inspections and safety equipment in some studies) included the same 16 studies as the meta-analysis by Kendrick et al. 49 described in study H. Intervention group families were more likely to have a safe hot tap water temperature than control group families (OR 1.41, 95% CI 1.07 to 1.86) (Figure 34).
FIGURE 34.
Forest plot of effect sizes for safe hot tap water temperature from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
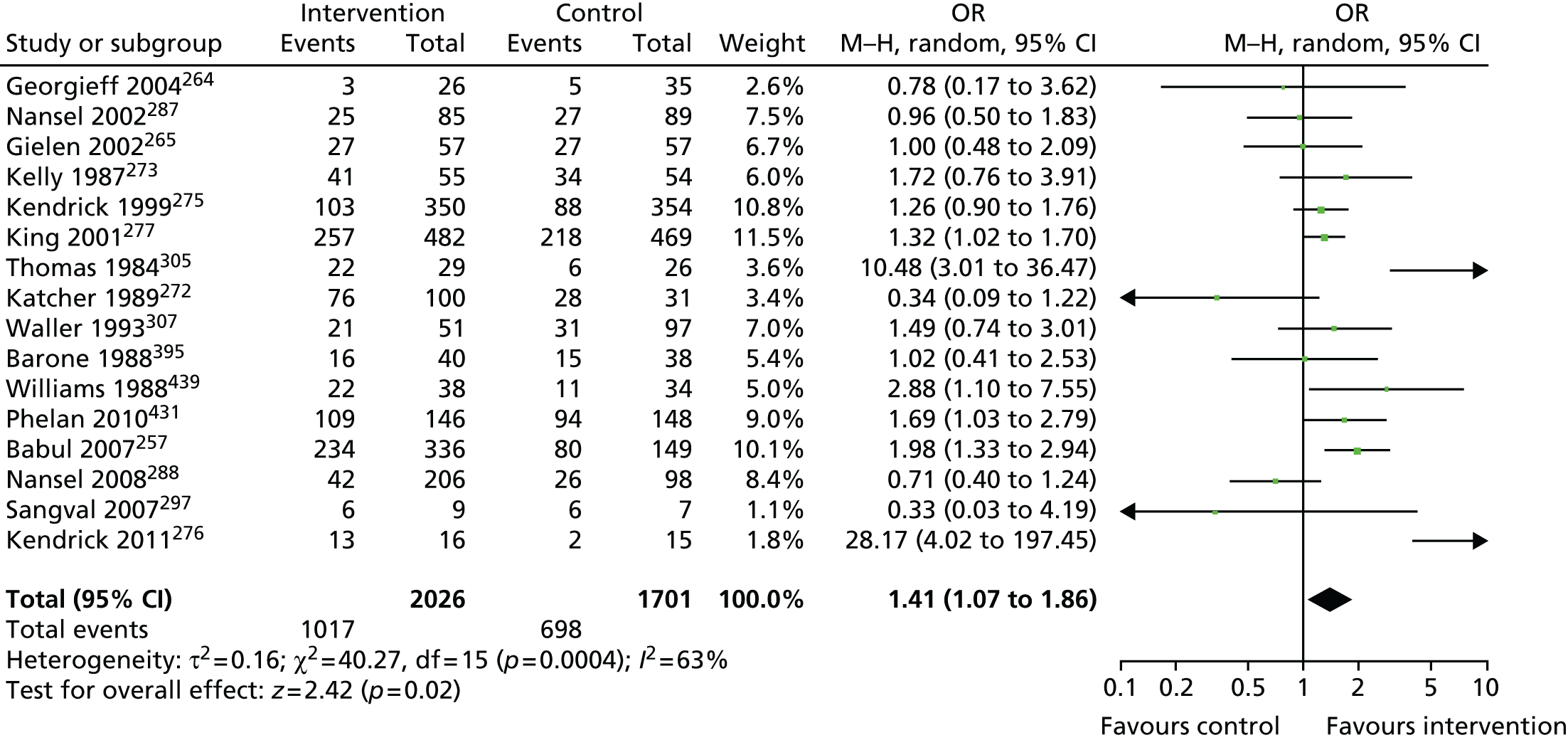
Study J
Network meta-analysis explored the effects of component elements of the interventions on safe hot water temperature among 20 studies. 257,264,265,272,273,275–277,287,288,297,300,304,305,307,395,402,431,432,439 The data used in the NMA from each study are shown in Table 87. Table 88 reports the pooled estimates, 95% CrIs and, when available, direct within-trial estimates. The NMA estimated the 36 possible pairwise comparisons between the nine included interventions. Home safety education plus free or low-cost provision and fitting of TMVs was most likely to be effective (p best = 0.97) with an OR compared with usual care of 38.82 (95% CrI 3.58 to 599.10).
| Pairwise comparisona | Study | Study design | Follow-up (months) | Interventiona | Number of households with safe water (adjusted for clustering) | Total number of households |
|---|---|---|---|---|---|---|
| 2 vs. 1 | Williams 1988439 | RCT | 1 | 1 | 10.78b | 34.30b |
| 2 | 21.56b | 38.23b | ||||
| Nansel 2002287 | RCT | 0.75 | 1 | 27 | 89 | |
| 2 | 25 | 85 | ||||
| Kelly 1987273 | RCT | 7 | 1 | 34 | 54 | |
| 2 | 41 | 55 | ||||
| Thomas 1984305 | RCT | 1.5 | 1 | 6 | 26 | |
| 2 | 22 | 29 | ||||
| Nansel 2008288 | Non-RCT | 1 | 1 | 26 | 98 | |
| 2 | 42 | 206 | ||||
| Christakis 2006402 | RCT | 0.5–1 | 1 | 14 | 200 | |
| 2 | 48 | 384 | ||||
| Reich 2011432 | RCT | 2–18 | 1 vs. 2 | OR 1.44 (SE 0.44) | ||
| 3 vs. 1 | Babul 2007257 | RCT | 10 | 1 | 80 | 149 |
| 3 | 113 | 163 | ||||
| Barone 1988395 | RCT | 6 | 1 | 14.52b | 36.79b | |
| 3 | 16.46b | 39.70b | ||||
| Sangvai 2007297 | RCT | 6 | 1 | 6 | 7 | |
| 3 | 6 | 9 | ||||
| 4 vs. 1 | Kendrick, 1999275 | Non-RCT | 25 | 1 | 87.72c | 353.82c |
| 4 | 103.49c | 349.88c | ||||
| King 2001277 | RCT | 12 | 1 | 218 | 469 | |
| 4 | 257 | 482 | ||||
| 5 vs. 1 | Babul 2007257 | RCT | 10 | 1 | 80 | 149 |
| 5 | 121 | 173 | ||||
| Schwarz 1993300 | CBA | 12 | 1 | 770.9b | 1053b | |
| 5 | 566b | 896b | ||||
| Georgieff 2004264 | CBA | Unknown | 1 | 4.99b | 34.95b | |
| 5 | 4.99b | 30.96b | ||||
| 6 vs. 1 | Kendrick 2011276 | RCT | 12 | 1 | 2 | 15 |
| 6 | 13 | 16 | ||||
| 7 vs. 1 | Georgieff 2004264 | CBA | Unknown | 1 | 4.99b | 34.95b |
| 7 | 3.00b | 25.97b | ||||
| 8 vs. 1 | Waller 1993307 | RCT | 4 | 1 | 31 | 97 |
| 8 | 21 | 51 | ||||
| 3 vs. 2 | Katcher, 1989272 | RCT | 1 | 2 | 28 | 31 |
| 3 | 76 | 100 | ||||
| 5 vs. 3 | Babul 2007257 | RCT | 10 | 3 | 113 | 163 |
| 5 | 121 | 173 | ||||
| Gielen 2002265 | RCT | 12 | 3 | 26.92b | 56.83b | |
| 5 | 26.92b | 56.83b | ||||
| 7 vs. 5 | Georgieff 2004264 | CBA | Unknown | 5 | 4.99b | 30.96b |
| 7 | 3.00b | 25.97b | ||||
| 9 vs. 2 | Phelan 2011431 | RCT | 12 | 2 | 94 | 148 |
| 9 | 109 | 146 | ||||
| Sznajder 2003304 | RCT | 2 | 2 | 3 | 47 | |
| 9 | 0 | 42 |
| Intervention | Usual care (1) | Education (2) | Education + equipment (thermometer) (3) | Education + equipment (not scald related) + home safety inspection (4) | Education + equipment (thermometer) + home safety inspection (5) | Education + TMV + fitting (6) | Education + TMV + fitting + home safety inspection (7) | Education + home safety inspection (8) | Education + equipment (not scald related) + fitting + home safety inspection (9) |
|---|---|---|---|---|---|---|---|---|---|
| Usual care (1) | 1.73 (0.98 to 3.20) | 0.97 (0.41 to 2.14) | 1.29 (0.46 to 3.56) | 0.99 (0.43 to 2.24) | 38.82 (3.58 to 599.10) | 0.67 (0.09 to 4.34) | 1.48 (0.30 to 7.03) | 1.77 (0.33 to 6.81) | |
| Education (2) | 1.64 (0.66 to 4.29) | 0.56 (0.21 to 1.38) | 0.75 (0.22 to 2.37) | 0.58 (0.20 to 1.52) | 22.58 (1.93 to 366.00) | 0.39 (0.04 to 2.79) | 0.86 (0.15 to 4.48) | 1.03 (0.21 to 3.42) | |
| Education + equipment (thermometer) (3) | 1.66 (1.11 to 2.50) | 0.34 (0.09 to 1.22) | 1.32 (0.38 to 5.19) | 1.02 (0.42 to 2.62) | 40.71 (2.21 to 706.40) | 0.69 (0.08 to 5.11) | 1.52 (0.26 to 9.34) | 1.81 (0.30 to 8.54) | |
| Education + equipment (not scald related) + home safety inspection (4) | 1.30 (1.01 to 1.59) | 0.77 (0.20 to 2.88) | 30.78 (2.23 to 553.90) | 0.52 (0.05 to 4.48) | 1.14 (0.17 to 7.53) | 1.37 (0.19 to 7.39) | |||
| Education + equipment (thermometer) + home safety inspection (5) | 0.75 (0.64 to 0.90) | 1.02 (069 to 1.52) | 39.47 (3.08 to 672.20) | 0.68 (0.09 to 4.40) | 1.49 (0.25 to 8.73) | 1.78 (0.28 to .38) | |||
| Education + TMV + fitting (6) | 28.17 (4.01 to 197.46) | 0.02 (0.00 to 0.37) | 0.04 (0.00 to 0.67) | 0.04 (0.00 to 0.68) | |||||
| Education + TMV + fitting + home safety inspection (7) | 0.78 (0.31 to 1.97) | 0.68 (0.13 to 3.46) | 2.22 (0.19 to 28.58) | 2.62 (0.21 to 29.37) | |||||
| Education + home safety inspection (8) | 1.49 (0.74 to 3.01) | 1.19 (0.12 to 9.28) | |||||||
| Education + equipment (not scald related) + fitting + home safety inspection (9) | 1.53 (0.94 to 2.47) |
Study K
This section reports the findings from the decision analysis evaluating the cost-effectiveness of different interventions promoting a safe hot tap water temperature. Seven of the nine interventions evaluated in the base-case analysis had higher costs than more effective interventions and were therefore excluded from further consideration (Table 89). Of the remaining two interventions, education had the lowest estimated ICER compared with usual care, at £40,271 per QALY gained.
| Intervention | Expected QALYs (95% CrI)a | Expected costs (95% CrI) (£)a | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained)b | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| Usual care (1) | 27,111 (27,092 to 27,130) | 9,246 (7390 to 11,133) | 0.75 | 0.26 | |||
| Education (2) | 27,111 (27,093 to 27,130) | 11,289 (9848 to 12,828) | 0.05 | 2042 | 40,271 | 0.25 | 0.54 |
| Education + equipment (thermometer) (3) | 27111 (27,092 to 27,130) | 12,507 (10,803 to 14,343) | Dominated | 0.006 | 0.02 | ||
| Education + equipment (not scald related) + home safety inspection (4) | 27,111 (27,092 to 27,130) | 21,273 (18,738 to 23,825) | Dominated | < 0.001 | < 0.001 | ||
| Education + equipment (thermometer) + home safety inspection (5) | 27,111 (27,092 to 27,130) | 21,407 (18,742 to 24,084) | Dominated | < 0.001 | < 0.001 | ||
| Education + TMV + fitting (6) | 27,111 (27,093 to 27,129) | 15,726 (14,246 to 17,702) | 0.07 | 4437 | 68,455 | 0.003 | 0.18 |
| Education + TMV + fitting + home safety inspection (7) | 27,111 (27,092 to 27,130) | 28,972 (25,081 to 32,961) | Dominated | < 0.001 | < 0.001 | ||
| Education + home safety inspection (8) | 27,111 (27,092 to 27,130) | 21,056 (18,359 to 23,876) | Dominated | < 0.001 | < 0.001 | ||
| Education + equipment (not scald related) + fitting + home safety inspection (9) | 27,111 (27,092 to 27,130) | 20,929 (18,295 to 23,776) | Dominated | < 0.001 | < 0.001 |
Figure 35 shows the probability of the alternative interventions being cost-effective. At a threshold value of £30,000 per QALY gained, usual care has the highest probability of being cost-effective (0.75). However, when this threshold value is increased to £50,000, education has the highest probability of being cost-effective (0.54), demonstrating considerable uncertainty in the decisions within the £30,000–50,000 threshold range.
FIGURE 35.
Cost-effectiveness acceptability curves for interventions to promote safe hot tap water temperature. E, education; F, fitting; FE, equipment (not scald related); HSI, home safety inspection; Th, equipment (thermometer); UC, usual care.
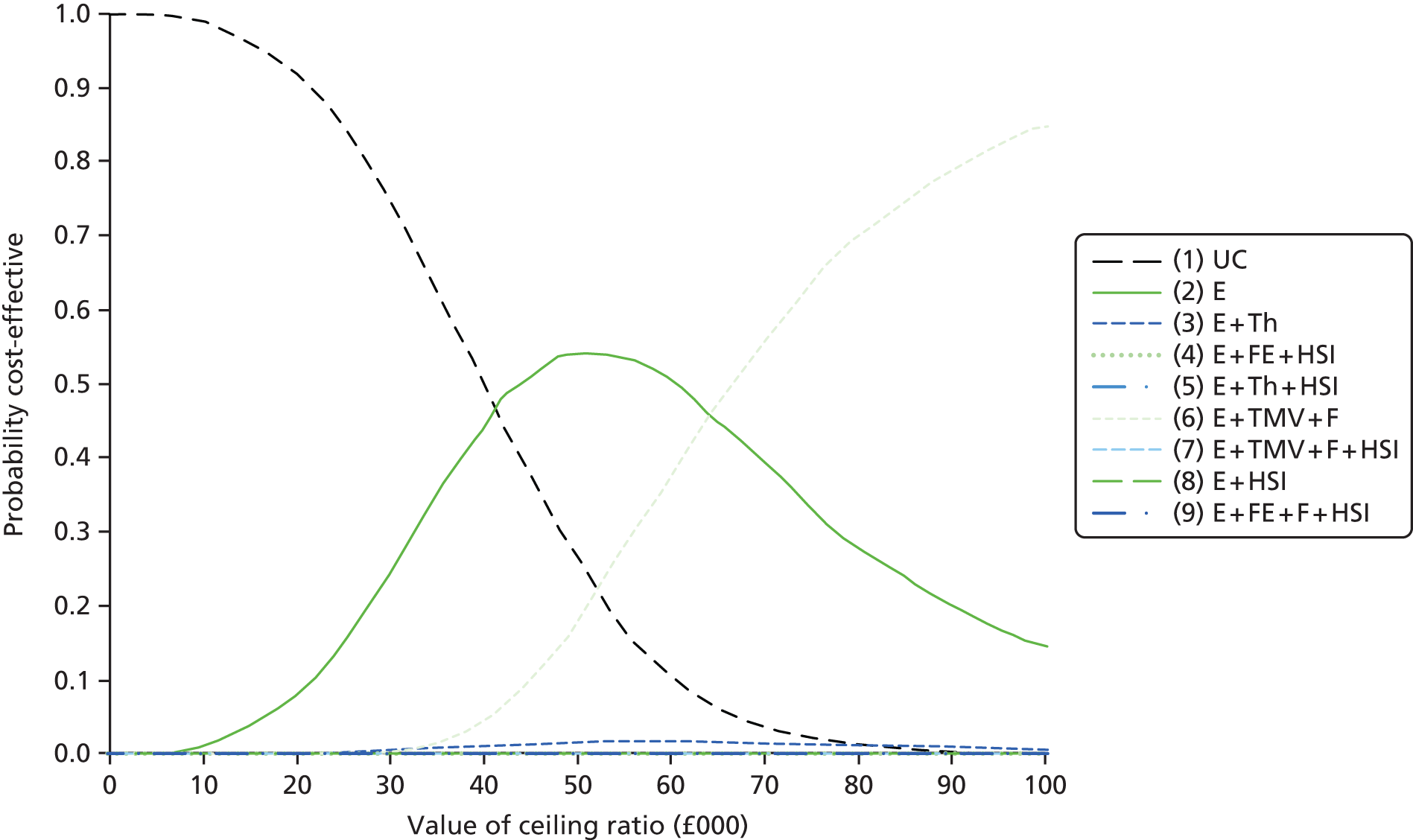
A range of sensitivity analyses varying the base-case assumptions and inputs, as outlined in the methods section, were implemented (Table 90). Reducing the probability of a scald to zero for households with a safe hot water temperature for all interventions (SA2), not just TMV interventions, and removing the fixed costs of setting up a safe hot water scheme (SA3) resulted in the ICER for education compared with usual care decreasing from £40,271 per QALY gained to £30,571 and £23,975. The cost-effectiveness results were found to be very sensitive to the probability of a scald. When this parameter was changed to the estimated probability of a scald among children living in social housing (653/582,700 from Phillips et al. 140) to reflect provision of the intervention to families living in social housing, the ICER for education plus TMV and fitting compared with usual care reduced from £68,455 to –£20,828 (i.e. cost saving).
| Intervention | Expected QALYs | Expected costs (£) | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained) | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| SA1: probability accept intervention assumed higher for non-TMV interventions, i.e. 0.9 (as in smoke alarm decision model) | |||||||
| Usual care (1) | 27,111 | 9278 | 0.70 | 0.23 | |||
| Education (2) | 27,111 | 11,593 | 0.06 | 2314 | 37,852 | 0.29 | 0.62 |
| Education + TMV + fitting (6) | 27,111 | 15,675 | 0.06 | 4081 | 74,075 | 0.002 | 0.14 |
| SA2: probability of scald set to 0 for all interventions not just TMV when safe hot water temperature | |||||||
| Usual care (1) | 27,111 | 8767 | 0.48 | 0.13 | |||
| Education (2) | 27,111 | 10,498 | 0.06 | 1730 | 30,571 | 0.50 | 0.80 |
| Education + TMV + fitting (6) | 27,111 | 15,702 | 0.05 | 5203 | 103,344 | < 0.001 | 0.03 |
| SA3: fixed costs removed (i.e. set to £0) as ‘safe hot water temperature’ likely to be part of a wider home safety scheme | |||||||
| Usual care (1) | 27,111 | 9,268 | 0.36 | 0.07 | |||
| Education (2) | 27,111 | 10,489 | 0.05 | 1221 | 23,975 | 0.62 | 0.71 |
| Education + TMV + fitting (6) | 27,111 | 14,906 | 0.07 | 4416 | 68,194 | 0.006 | 0.20 |
| SA4: number of scalds increased to 653 per year from 582,700 households140 to reflect providing intervention to families in social housinga | |||||||
| Usual care (1) | 27,111 | 30,631 | < 0.001 | < 0.001 | |||
| Education + TMV + fitting (6) | 27,111 | 22,072 | 0.41 | –8559 | –20,828 | 0.98 | 0.98 |
| SA5: assumed TMVs fitted separately (i.e. not part of a refurbishment or rebuild scheme) – cost for TMVs increased to £150 (SE £55) based on range £40 for TMV to £260 for complex fitting140 | |||||||
| Usual care (1) | 27,111 | 9,299,220 | 0.74 | 0.30 | |||
| Education (2) | 27,111 | 11,321,380 | 0.05 | 2022 | 39,756 | 0.25 | 0.67 |
| (Education + TMV + fitting (6) | 27,111 | 102,345,625 | 0.06 | 91,024 | 1,394,153 | 0.005 | 0.006 |
Safe handling of hot food and drinks
Study H
The overview included one systematic review and meta-analysis49 and three systematic reviews337,340,387 reporting the effect of interventions on the safe handling of hot food and drinks. The meta-analysis estimated the pooled OR for six studies for the effect of home safety education on keeping hot food and drinks out of the reach of children. 49 Families receiving home safety education were not significantly more likely to keep hot drinks out of the reach of children than control group families (OR 0.95, 95% CI 0.61 to 1.48). No reviews drew conclusions specific to the effectiveness of interventions for promoting the safe handling of hot food or drinks.
A total of 10 primary studies were identified for the overview, eight from reviews257,269,275,287,288,295,422,444 and two from additional searches for primary studies. 400,410
One study reported that significantly more families in the intervention group than control families tested the temperature of food prepared in a microwave oven. 444 The study delivered an intervention that included home visits with active guidance on injury prevention and regular monthly telephone follow-ups. The remaining eight studies evaluated a range of interventions including home safety education, tailored safety advice, home safety assessments, the provision of discounted or free home safety equipment and exposure to a child safety campaign and all reported no significant differences in the safe handling of hot food and drinks between the intervention group and the control group. 257,269,275,287,288,400,410,422
Study I
Pairwise meta-analysis of six studies evaluating home safety education, the same six studies as in the meta-analysis of Kendrick et al. 49 described in study H, found no effect of interventions promoting the safe handling of hot food and drinks (OR 0.95, 95% CI 0.61 to 1.48) (Figure 36).
FIGURE 36.
Forest plot of effect sizes for keeping hot food or drinks out of reach of children from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
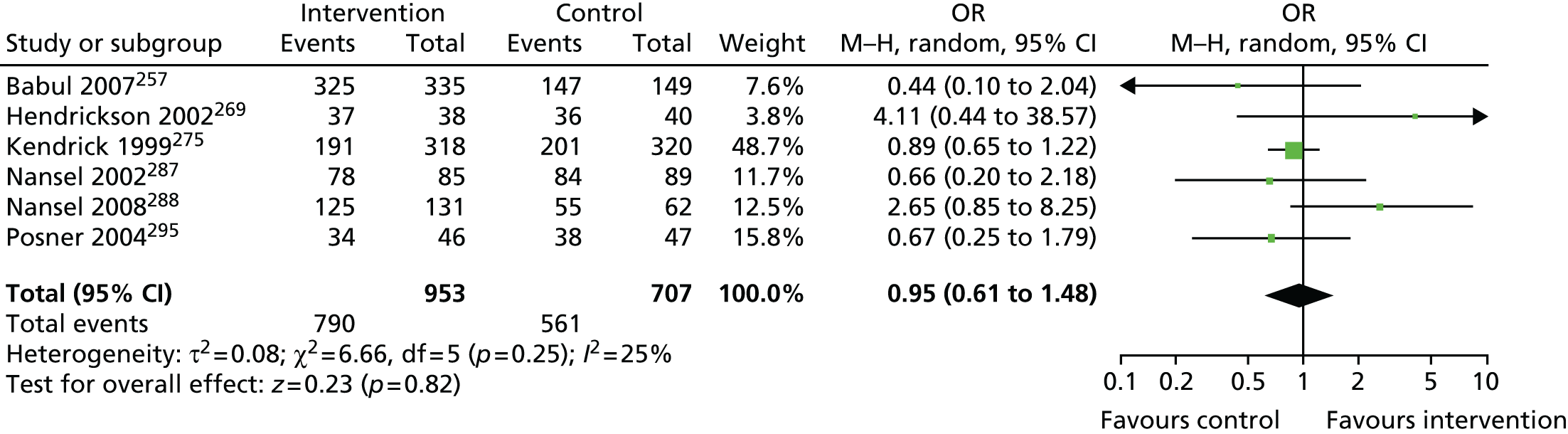
Study J
Network meta-analysis was used to determine the effect of component elements of home safety interventions explored in the six studies included in the PMA on keeping hot food and drinks out of the reach of children. 257,269,275,287,288,295 The NMA estimated the six possible pairwise comparisons between the four interventions reported in the six studies, finding no significant difference between any of the interventions. The data used from each study are shown in Table 91 and the pooled estimates and 95% CrIs are shown in Table 92.
| Pairwise comparison | Study | Study design | Follow-up (months) | Intervention | Number of households with hot food and/or drinks out of reach (nos adjusted for clustering) | Total number of households (nos adjusted for clustering) |
|---|---|---|---|---|---|---|
| Usual care (1) vs. education (2) | Nansel 2002287 | RCT | 0.75 | 1 | 84 | 89 |
| 2 | 78 | 85 | ||||
| Nansel 2008288 | Non-RCT | 1 | 1 | 55 | 62 | |
| 2 | 125 | 131 | ||||
| Usual care (1) vs. education + equipment (3) vs. education + equipment + home safety inspection (4) | aBabul 2007257 | RCT | 10 | 1 | 147 | 149 |
| 3 | 158 | 163 | ||||
| 4 | 167 | 172 | ||||
| Usual care (1) vs. education + equipment + home safety inspection (4) | Kendrick 1999275 | Non-RCT | 25 | 1 | 230 (200.91)b | 336 (319.70)b |
| 4 | 219 (191.30)b | 364 (317.96)b | ||||
| Hendrickson 2002269 | RCT | 1.5 | 1 | 36 | 40 | |
| 4 | 37 | 38 | ||||
| Education (2) vs. education + equipment (3) | Posner 2004295 | RCT | 2.5 | 2 | 38 | 47 |
| 3 | 34 | 46 |
| Intervention | Usual care (1) | Education (2) | Education + equipment (3) | Education + equipment + home safety inspection (4) |
|---|---|---|---|---|
| Usual care (1) | 1.29 (0.34 to 4.84) | 0.76 (0.17 to 3.66) | 0.98 (0.32 to 3.78) | |
| Education (2) | 0.59 (0.12 to 2.90) | 0.77 (0.15 to 4.80) | ||
| Education + equipment (3) | 1.29 (0.26 to 7.68) | |||
| Education + equipment + home safety inspection (4) |
Study K
As none of the interventions for promoting the safe handling of hot food and drinks was found to be effective in the NMA, decision analyses were not undertaken for this outcome.
Kitchen and cooking safety practices
Study H
The overview included nine systematic reviews reporting on the effectiveness of interventions to promote kitchen and cooking safety practices. 36,49,331,332,337,338,340,385,387 The reviews drew no conclusions specific to the effectiveness of interventions to promote kitchen and cooking safety practices and no meta-analyses were identified for these outcomes.
Eight primary studies reported kitchen and cooking safety practices, with six identified from the reviews260,288,295,418,422,444 and two identified from additional searches for primary studies. 99,400 One of the eight studies reported that intervention group families were significantly more likely to have childproofed electrical kitchen heating devices (e.g. boiler, rice cooker). 444 Intervention group families received a programme that involved four quarterly home visits and monthly telephone follow-ups targeting a range of injuries including scalds. Another study found that intervention group homes were significantly more likely to have a ‘child-protected’ cooker (not defined) and to have removed objects that could allow a child to climb and reach the sink following a group scald and burn prevention workshop and a home visit delivering tailored child injury prevention information. 400 No significant differences between intervention and control groups with regard to kitchen and cooking safety practices were reported in the remaining studies. These included evaluations of the effectiveness of a school-based injury prevention programme for improving practices of children when cooking without an adult,418 home safety assessments, education plus discount vouchers for safety, equipment on use of cooker guards and on keeping heating devices out of the reach of children,277 an ED-based home safety intervention to promote cooking on the back burners of cookers or turning pan handles towards the back of the cooker,295 tailored home safety education about keeping children away from the cooker or oven or turning pan handles away from the edge of the cooker288 and a scald and burn prevention media campaign to promote using the back burners of cookers, keeping children out of the kitchen when cooking, turning pot handles to the back of the cooker and removing dangling cords of heating devices. 422 Finally, there were no significant differences between cases (children who presented with injuries from falls, burns, scalds, ingestions or choking) and controls with regard to having a cooker guard or dangling cords of heating devices. 99
Pairwise meta-analysis and NMA were not undertaken for interventions promoting kitchen and cooking safety practices as the number of studies reporting each outcome was small.
Other scald prevention practices
Study H
Eight reviews were included in the overview evaluating the effect of interventions on other scald-related outcomes. 36,49,331,332,338,340,385,387 The reviews drew no conclusions specific to the effectiveness of interventions for other scald prevention practices and no meta-analyses were identified for these outcomes. Four primary studies identified from the reviews reported other scald-related outcomes,260,295,303,407 with no further studies identified from subsequent searches for primary studies. Of these four studies, two observed significant effects on burn safety scores (representing safer burn prevention practices) of interventions involving home safety education, home safety assessments and free home safety equipment. 295,303 In another study, significantly more families in the intervention group made their home safer after a television campaign, home safety advice, a home safety assessment check and advice on welfare benefits available to purchase safety equipment and the local availability of equipment. 260 A multifaceted campaign aimed at reducing the occurrence of scalds in children aged 0–4 years reported no significant effect of the intervention on scald prevention behaviours. 407
Pairwise meta-analysis and NMA were not undertaken for interventions promoting other scald prevention practices as the number of studies reporting each outcome was small.
Falls prevention
Figure 37 shows the process of identification and selection of reviews and primary studies included in the overview and NMAs for falls prevention outcomes. Twelve narrative systematic reviews, one meta-analysis including a narrative systematic review and 29 primary studies were included in the overview, and 16 primary studies were included in the NMAs for falls prevention outcomes.
Characteristics of included reviews and primary studies
The characteristics and quality assessment of reviews included in the overview are shown in Table 71. One review focused specifically on falls prevention interventions,333 with the remainder including interventions addressing a range of injury mechanisms. The risk of bias in included reviews was variable, with OQAQ scores ranging from 2 to 7 (median 4) out of a maximum possible score of 7.
The characteristics of the primary studies included in the overview, the systematic review and PMA and the NMAs are shown in Table 72. Most (n = 20, 69%) primary studies were RCTs, five (17%) were non-RCTs, three (10%) were CBAs and one (3%) was a cohort study. Tables of excluded reviews and primary studies are available on request from the authors. The risk of bias in included primary studies was also variable; at least half of the RCTs had adequate allocation concealment (55%) and follow-up of at least 80% of participants in each arm (50%). One-third of RCTs carried out blinded outcome assessments (35%). None of the non-RCTs and CBAs carried out blinded outcome assessments, one-third (38%) followed up at least 80% of participants in each arm and half (50%) had a balanced distribution of confounders between intervention arms. The cohort study scored 9 (out of a maximum of 9) on the Newcastle–Ottawa scale, indicating that it was of high quality.
Preventing falls or fall-related injuries
Study H
The overview included nine systematic reviews reporting interventions to prevent falls or fall-related injuries,33,36,41,331,333–335,383,445 drawing on data from only three primary studies. 267,416,438 Two reviews drew conclusions about the effectiveness of interventions to prevent falls or fall-related injuries, with both concluding that there was a paucity of evidence in this area. 33,333 The three primary studies included in the reviews consisted of one non-RCT,438 one CBA study267 and one cohort study. 416 The cohort study found fewer self-reported fall-related injuries among those receiving home safety information, but the statistical significance was not reported. 416 The CBA study found some evidence of a reduction in fall-related injuries (OR 0.78, 95% CI 0.61 to 1.00) from a community-based injury prevention programme. 267 The non-RCT found no significant effect on falls or fall-related injuries of nurse counselling to reduce baby walker use. 438 It was not possible to combine effect sizes from these last two studies in PMA or NMA as the numerators and denominators were not published and individual participant data, from which they could be calculated, was provided by only one study. 438
Pairwise meta-analyses and NMAs were not undertaken for interventions to reduce falls or fall-related injuries, as the number of studies reporting these outcomes was small.
Promoting safety gate possession and use
Study H
The overview included one systematic review and meta-analysis33 and five reviews42,332,338,383,387 reporting the effect of interventions on the possession and use of safety gates. The meta-analysis, which combined effect sizes from 10 studies, reported that home safety education interventions, some of which included the provision of safety gates, were effective in increasing safety gate possession and use (OR 1.26, 95% CI 1.05 to 1.51). There was some evidence that interventions that provided safety gates may have slightly larger effect sizes (OR 1.37, 95% CI 1.15 to 1.62) than those that did not (OR 1.24, 95% CI 0.94 to 1.64). 33 Of the six reviews, that by Lyons et al. 332 and a subsequent update that utilised different eligibility criteria42 found no increase in the possession or use of safety gates. The other reviews reported conflicting or unclear evidence on the effect of interventions to increase safety gate possession and use. 33,338,383,387 Three of these reviews each found only single studies reporting a significant effect of the intervention. 33,338,387 The other review383 reported that intervention families obtained and fitted safety gates but did not report the significance of this finding.
A total of 16 primary studies reporting safety gate possession and use were identified (14 from reviews71,72,257,260,265,275,277,282,287,295,304,413,417,441 and two from additional searches for primary studies288,431). Three studies reported a significant increase in the possession and use of safety gates on stairs,72,413,431 two of which provided home safety education and fitted free or low-cost safety gates,72,431 with the third providing only home safety education. 413 The remaining 13 studies reported no significant effect of the interventions, only three of which provided low-cost safety gates71,275 or discount vouchers,277 with none fitting safety gates.
Study I
Pairwise meta-analysis of 12 studies evaluating home safety education, which in some studies also included the provision of safety gates and home safety inspections,71,72,265,275,277,282,287,288,295,304,417,431 found that interventions significantly increased the possession of a fitted safety gate (OR 1.61, 95% CI 1.19 to 2.17) (Figure 38). Interventions providing safety gates appeared to be more effective (OR 2.05, 95% CI 1.08 to 3.89) than those that did not (OR 1.26, 95% CI 0.96 to 1.64).
FIGURE 38.
Forest plot of effect sizes for having a fitted safety gate from studies evaluating home safety educational interventions (some of which included the provision of safety gates). M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
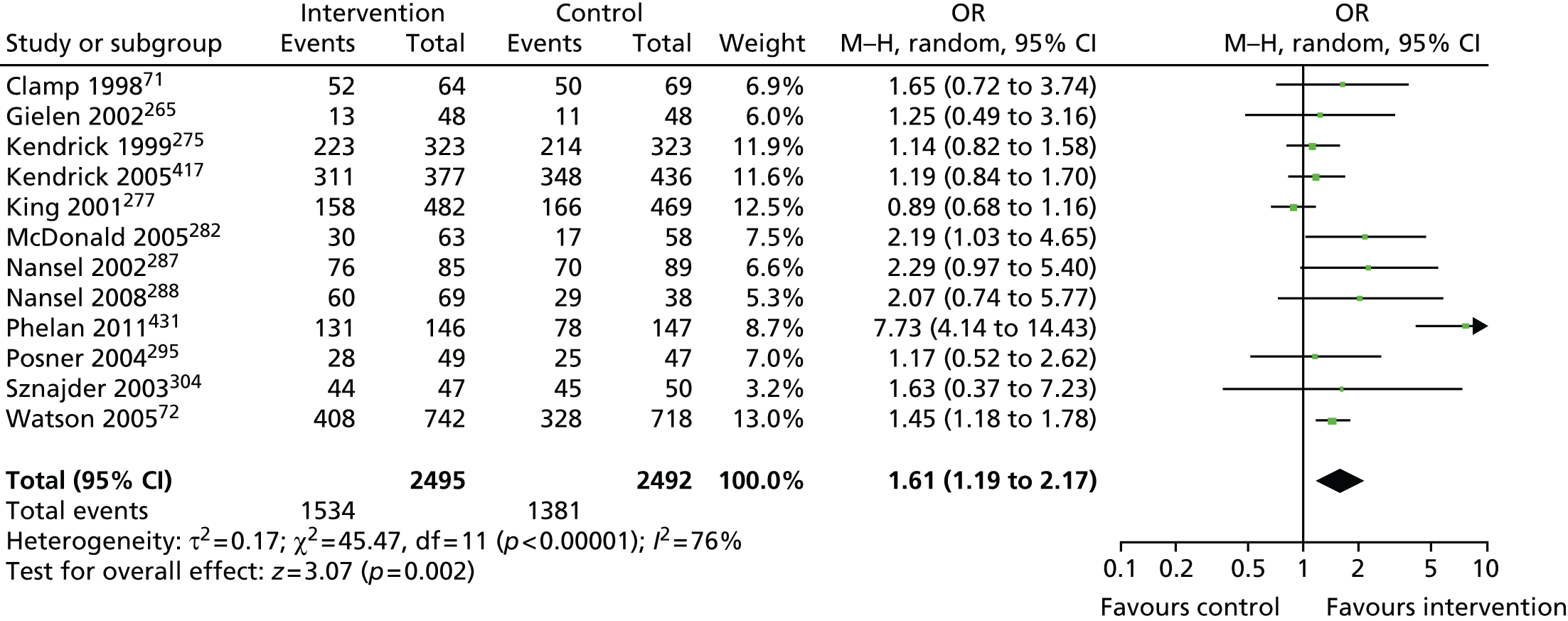
Study J
Network meta-analysis was used to determine the effect of component elements of home safety interventions explored in the 12 studies included in the PMAs for safety gate possession and use. 71,72,265,275,277,282,287,288,295,304,417,431 These studies included seven interventions and the NMA estimated the 21 possible pairwise comparisons between the seven interventions reported in the 12 studies. The data used in the NMA from each study for each of the falls prevention outcomes are shown in Table 93. The pooled estimates, 95% CrIs and, when available, direct within-trial estimates are reported in Table 94. The most intensive intervention (home safety education plus equipment provision plus fitting of safety equipment plus home safety inspection) was the most likely to be the most effective (p best = 0.97), with an OR compared with usual care of 7.80 (95% CrI 3.18 to 21.30). This combination of interventions resulted in significantly more households having fitted safety gates than any of the other combinations of interventions, with effect sizes being between five and eight times greater with the most intensive intervention.
| Pairwise comparison | Study | Study design | Follow-up (months) | Study qualityb | Intervention | Safety gate (n/N) | Baby walker (n/N) | Window locks (n/N) | High surfaces (n/N) | Bath mat (n/N) |
|---|---|---|---|---|---|---|---|---|---|---|
| Usual care (1) vs. education (2) | cNansel 2002287 | RCT | 0.75 | A = Y, B = Y, F = Y | 1 | 70/89 | 30/89 | |||
| 2 | 76/85 | 19/85 | ||||||||
| Kendrick 2005417 | RCT | 9 | A = Y, B = N, F = Y | 1 | 418/524 (348.4/436.8)d | 230/543 (105.3/248.5)d | ||||
| 2 | 373/452 (310.9/376.8)d | 131/463 (60.0/211.9)d | ||||||||
| eNansel 2008288 | NRCT | 1 | B = N, F = N, C = N | 1 | 29/38 | 12/38 | 21/24 | |||
| 2 | 60/69 | 13/69 | 55/62 | |||||||
| fTan 2004438 | NRCT | 5 | B = U, F = Y, C = Y | 1 | 393/480 | |||||
| 2 | 143/228 | |||||||||
| Usual care (1) vs. education + equipment (3) | gBabul 2007257 | RCT | 10 | A = Y, B = N, F = N | 1 | 31/148 | 69/148 | |||
| 3 | 22/162 | 89/161 | ||||||||
| Clamp 199871 | RCT | 1.5 | A = Y, B = N, F = Y | 1 | 50/69 | 72/82 | ||||
| 3 | 52/64 | 80/83 | ||||||||
| McDonald 2005282 | RCT | 1 | A = Y, B = U, F = N | 1 | 10/41 | |||||
| 3 | 23/54 | |||||||||
| Usual care (1) vs. education + equipment + home safety inspection (4) | gBabul 2007257 | RCT | 10 | A = Y, B = N, F = N | 1 | 31/148 | 69/148 | |||
| 4 | 26/173 | 84/170 | ||||||||
| Kendrick 1999275 | NRCT | 25 | B = N, F = N, C = Y | 1 | 241/364 (214.3/323.6)h | 339/336 | ||||
| 4 | 251/364 (223.2/323.6)h | 323/362 | ||||||||
| Hendrickson 2002269 | RCT | 1.5 | A = N, B = N, F = Y | 1 | 21/39 | |||||
| 4 | 24/34 | |||||||||
| Usual care (1) vs. education + equipment + fitting (5) | Watson 200572 | RCT | 12 | A = Y, B = N, F = N | 1 | 328/718 | 493/741 | |||
| 5 | 408/742 | 550/767 | ||||||||
| Usual care (1) vs. education + home safety inspection (6) | Petridou 1997293 | CBA | 20 | B = N, F = Y, C = Y | 1 | 64/128 (50.4/100.1)i | ||||
| 6 | 66/131 (48.9/97.8)i | |||||||||
| Usual care (1) vs. education + equipment + fitting + home safety inspection (7) | Phelan 2011431 | RCT | 12 | A = Y, B = N, F = Y | 1 | 78/147 | 29/138 | 145/150 | 59/149 | |
| 7 | 131/146 | 24/140 | 146/149 | 56/150 | ||||||
| Education (2) vs. education + equipment (3) | Posner 2004295 | RCT | 2.5 | A = Y, B = Y, F = N | 2 | 25/47 | 4/8 | 44/50 | 34/47 | |
| 3 | 28/49 | 4/7 | 12/17 | 44/49 | ||||||
| Education (2) vs. education + equipment + fitting (5) | Sznajder 2003304 | RCT | 1.5 to 2 | A = Y, B = N, F = Y | 2 | 45/50 | 14/50 | 37/49 | ||
| 5 | 44/47 | 19/47 | 31/48 | |||||||
| Education + equipment (3) vs. education + equipment + home safety inspection (4) | Gielen 2002265 | RCT | 12 | A = U, B = U, F = N | 3 | 11/48 (12.9/47.4)j | ||||
| 4 | 13/48 (10.9/47.4)j | |||||||||
| Babul 2007257g | RCT | 10 | A = Y, B = N, F = N | 3 | 22/162 | 89/161 | ||||
| 4 | 26/173 | 84/170 | ||||||||
| Education + equipment + home safety inspection (4) vs. education + home safety inspection (6) | King 2001277 | RCT | 12 | A = Y, B = Y, F = Y | 4 | 158/482 | 29/482 | 285/469 | ||
| 6 | 166/469 | 33/469 | 299/482 |
| Intervention | Usual care (1) | Education (2) | Education + equipment (3) | Education + equipment + home safety inspection (4) | Education + equipment + fitting (5) | Education + home safety inspection (6) | Education + equipment + fitting + home safety inspection (7) |
|---|---|---|---|---|---|---|---|
| Usual care (1) | 1.43 (0.90 to 2.49) | 1.63 (0.93 to 3.03) | 1.28 (0.69 to 2.79) | 1.52 (0.84 to 3.38) | 1.43 (0.56 to 4.42) | 7.80a (3.08 to 21.3) | |
| Education (2) | 1.48 (0.97 to 2.25) | 1.14 (0.56 to 2.23) | 0.90 (0.41 to 2.07) | 1.07 (0.51 to 2.41) | 1.01 (0.33 to 3.25) | 5.46a (1.75 to 16.1) | |
| Education + equipment (3) | 1.92 (1.05 to 3.51)a | 1.17 (0.52 to 2.63) | 0.78 (0.38 to 1.77) | 0.94 (0.42 to 2.41) | 0.88 (0.32 to 2.80) | 4.77 (1.56 to 15.2)a | |
| Education + equipment + home safety inspection (4) | 1.13 (0.82 to 1.58) | 1.25 (0.49 to 3.17) | 1.20 (0.45 to 3.25) | 1.12 (0.52 to 2.49) | 6.13 (1.75 to 18.7)a | ||
| Education + equipment + fitting (5) | 1.45 (1.18 to 1.79)a | 1.63 (0.37 to 7.23) | 0.94 (0.27 to 3.28) | 5.07 (1.47 to 15.9)a | |||
| Education + home safety inspection (6) | 1.12 (0.86 to 1.47) | 5.48 (1.23 to 20.7)a | |||||
| Education + equipment + fitting + home safety inspection (7) | 7.73 (4.14 to 14.4)a |
Study K
This section describes the findings from the decision analysis evaluating the cost-effectiveness of different interventions to increase possession of fitted safety gates to prevent stairway falls. In the base-case analysis, seven interventions were evaluated (Table 95), of which four were found to have higher costs or a higher ICER than more effective interventions (namely education plus free or low-cost safety equipment, education plus free or low-cost safety equipment plus home safety inspection, education plus free or low-cost safety equipment plus fitting of the equipment and education plus home safety inspection). Of the remaining three interventions, education had the lowest estimated ICER compared with usual care, at £284,068 per QALY gained. Figure 39 shows the probability of the alternative interventions being cost-effective. At a threshold value of £30,000 per QALY gained, usual care had the highest probability of being cost-effective (0.999).
| Intervention | Expected QALYs (95% CrI)a | Expected costs (95% CrI) (£)a | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained)b | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| Usual care (1) | 25,056.326 (25,039.202 to 25,073.452) | 3431 (2446 to 4826) | 0.999 | 0.999 | |||
| Education (2) | 25,056.334 (25,039.207 to 25,073.460) | 5529 (4543 to 6859) | 0.007 | 2089 | 284,068 | < 0.001 | 0.001 |
| Education + equipment (3) | 25,056.334 (25,039.209 to 25,073.462) | 18,358 (13,338 to 23,472) | Extendedly dominated | < 0.001 | < 0.001 | ||
| Education + equipment + home safety inspection (4) | 25,056.334 (25,039.211 to 25,073.458) | 21,252 (15,203 to 27,432) | Dominated | < 0.001 | < 0.001 | ||
| Education + equipment + fitting (5) | 25,056.334 (25,039.207 to 25,073.462) | 25,017 (17,621 to 32,589) | Dominated | < 0.001 | < 0.001 | ||
| Education + home safety inspection (6) | 25,056.334 (25,039.209 to 25,073.458) | 8454 (6803 to 10240) | Dominated | < 0.001 | < 0.001 | ||
| Education + equipment + fitting + home safety inspection (7) | 25,056.335 (25,039.212 to 25,073.462) | 26,227 (18,409 to 34,246) | 0.009 | 22,745 | 2,405,800 | < 0.001 | < 0.001 |
FIGURE 39.
Cost-effectiveness acceptability curves for the base-case analysis indicating the probability that each intervention is the most cost-effective for a range of willingness–to-pay ratios. E, education; F, fitting; FE, low-cost/free equipment; HSI, home safety inspection; UC, usual care.
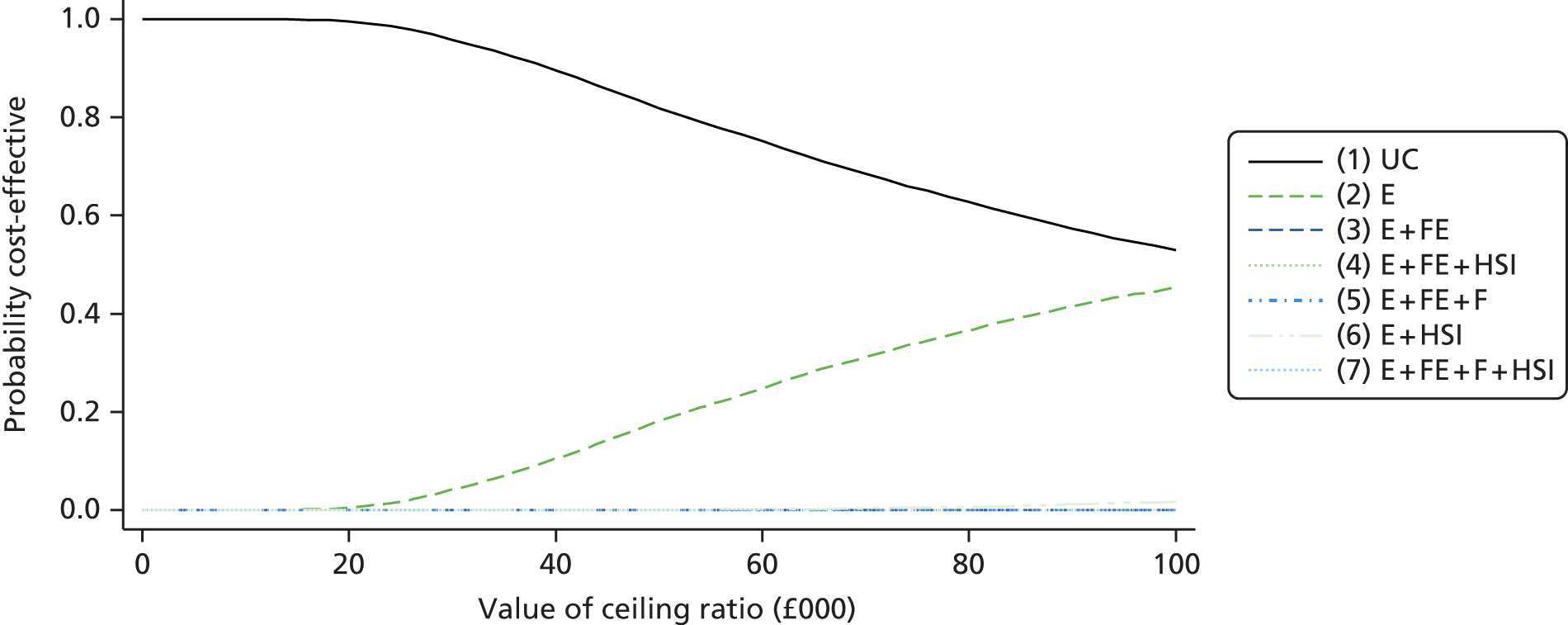
A range of sensitivity analyses varying the base-case assumptions and inputs was carried out (Table 96). All assessed the probability of interventions being cost-effective at thresholds of £30,000 and £50,000. The sensitivity analyses carried out involved reducing the number of safety gates fitted to one; reducing the cost of education by using the cost of providing a leaflet only; providing low-cost (£5) rather than free safety gates; halving the fixed cost of an intervention programme; changing the number of children per household from 1 to 1.8;378 reducing the probability of possessing a fitted safety gate from 0.56 to 0.45 to reflect the baseline possession of a fitted and used stair gate by families in deprived areas of Nottingham;72 and changing the utility deficits from 0.05, 0.1 and 0.2 for mild, moderate and severe injuries, respectively, to 0.07, 0.19 and 0.34. 143
| Intervention | Expected QALYs (95% CrI)a | Expected costs (£) (95% CrI)a | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained) | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| SA1: number of safety gates reduced from two to one | |||||||
| Usual care (1) | 25,056 (25,039 to 25,073) | 3427 (2446 to 4847) | 0.999 | 0.999 | |||
| Education (2) | 25,056 (25,039 to 25,073) | 5529 (4543 to 6883) | 0.007 | 2090 | 283,228 | < 0.001 | 0.001 |
| Education + equipment + fitting + home safety inspection (7) | 25,056 (25,039 to 25,073) | 17,361 (12,683 to 22,083) | 0.009 | 13,860 | 1,466,433 | < 0.001 | < 0.001 |
| SA2: reducing the cost of education by using the cost of providing a leaflet only | |||||||
| Usual care (1) | 25,056 (25,039 to 25,073) | 3428 (2446 to 4847) | 0.996 | 0.961 | |||
| Education (2) | 25,056 (25,039 to 25,073) | 4,482 (3537 to 5854) | 0.007 | 1053 | 143,846 | 0.0 | 0.039 |
| Education + equipment + fitting + home safety inspection (7) | 25,056 (25,039 to 25,073) | 25,217 (17,712 to 32842) | 0.009 | 21,714 | 2,296,038 | < 0.001 | < 0.001 |
| SA3: providing low-cost (£5) rather than free safety gates | |||||||
| Usual care (1) | 25,056 (25,039 to 25,073) | 3428 (2446 to 4847) | 0.999 | 0.999 | |||
| Education (2) | 25,056 (25,039 to 25,073) | 5529 (4543 to 6883) | 0.007 | 2090 | 283,228 | < 0.001 | < 0.001 |
| Education + equipment + fitting + home safety inspection (7) | 25,056 (25,039 to 25,073) | 22,919 (16,233 to 29,678) | 0.009 | 19,411 | 2,053,078 | < 0.001 | < 0.001 |
| SA4: fixed costs of intervention reduced to £40,000 | |||||||
| Usual care (1) | 25,056 (25,040 to 25,073) | 3428 (2446 to 4847) | 0.999 | 0.999 | |||
| Education (2) | 25,056 (25,040 to 25,073) | 5529 (4543 to 6884) | 0.007 | 2090 | 157,348 | < 0.001 | 0.001 |
| Education + equipment + fitting + home safety inspection (7) | 25,056 (25,040 to 25,073) | 26,252 (18,372 to 34,271) | 0.009 | 22,752 | 1,336,429 | < 0.001 | < 0.001 |
| SA5: increased number of children per household from 1 to 1.8378 | |||||||
| Usual care (1) | 25,056 (25,039 to 25,073) | 3236 (2229 to 4685) | 0.999 | 0.999 | |||
| Education (2) | 25,056 (25,039 to 25,074) | 5572 (4582 to 6866) | 0.008 | 2319 | 292,258 | < 0.001 | 0.001 |
| Education + equipment + fitting + home safety inspection (7) | 25,056 (25,039 to 25,074) | 29,867 (18,141 to 41,807) | 0.01 | 26,566 | 2,585,853 | < 0.001 | < 0.001 |
| SA6: changing the baseline probability of possession of a fitted safety gate from 0.56 to 0.45 to reflect a deprived area72 | |||||||
| Usual care (1) | 25,056 (25,039 to 25,074) | 3141 (2258 to 4428) | 1 | 0.999 | |||
| Education (2) | 25,056 (25,039 to 25,074) | 5569 (4591 to 6866) | 0.008 | 2436 | 291,812 | < 0.001 | 0.001 |
| Education + equipment + fitting + home safety inspection (7) | 25,056 (25,039 to 25,074) | 31,690 (23,318 to 36,884) | 0.011 | 28,522 | 2,612,847 | < 0.001 | < 0.001 |
| SA7: changing utility deficits to 0.07, 0.19 and 0.34 for mild, moderate and severe injuries, respectively, to reflect Brussoni et al.143 | |||||||
| Usual care (1) | 25,056 (25,039 to 25,073) | 3424 (2450 to 4819) | 1 | 0.999 | |||
| Education (2) | 25,056 (25,039 to 25,073) | 5524 (4538 to 6847) | 0.008 | 2086 | 267,482 | < 0.001 | 0.001 |
| Education + equipment + fitting + home safety inspection (7) | 25,056 (25,039 to 25,073) | 26,195 (18,262 to 34,310) | 0.01 | 22,686 | 2,257,270 | < 0.001 | < 0.001 |
The results were not particularly sensitive to any of the changes.
Promoting the possession and use of non-slip bathroom items
Study H
The overview included one systematic review and meta-analysis33 and three reviews332,338,387 reporting the effect of interventions on the possession and use of non-slip bathroom items. The meta-analysis, which combined effect sizes from three studies, reported that home safety education interventions, some of which included the provision of bath mats or decals, were not effective in increasing the possession of non-slip bathroom items (OR 1.16, 95% CI 0.51 to 2.63). 33 Of the three reviews, one332 found a significant increase in the possession of non-slip bath mats and two338,387 reported no significant increase in possession of non-slip bathroom items.
Five primary studies reported the effect of interventions to promote the possession and use of non-slip bathroom items (four from reviews293,295,304,441 and one from additional searches for primary studies431). One study reported a significant increase in the use of non-slip bath decals following home safety education and the provision of a home safety kit that included bath decals. 295 The other four studies reported no significant effect of the interventions. All included home safety education, with two including a home safety assessment431,441 and one providing non-slip bath mats. 304
Study I
Pairwise meta-analysis of four studies evaluating home safety education,293,295,304,431 which in some studies included the provision of non-slip bathroom items and home safety inspections, found that interventions were not effective in increasing the possession of non-slip bathroom items (OR 1.10, 95% CI 0.68 to 1.79) (Figure 40).
FIGURE 40.
Forest plot of effect sizes for possession of non-slip bathroom items from studies evaluating home safety educational interventions (some of which included provision of non-slip bathroom items). M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49

Study J
Network meta-analysis was not possible for possession of non-slip bathroom items as there were only two unconnected networks of three interventions.
Promoting the possession and use of window safety devices
Study H
The overview included one systematic review and meta-analysis33 and five reviews42,332,338,383,387 reporting the effect of interventions on the possession and use of window safety devices (locks, restrictors or screens). The meta-analysis, which combined effect sizes from five studies, found that home safety education interventions, some of which included the provision of window locks or restrictors, were not effective in increasing the possession of window safety devices (OR 1.16, 95% CI 0.84 to 1.59). 33 Of the reviews, two reported significant improvements in the use, frequency of use and location of window locks,42,338 and one reported a significant increase in the use of window locks. 387 Two reviews reported conflicting findings33,332 and one review reported findings in which the significance level was not reported. 383
Ten primary studies, nine identified from reviews71,72,260,269,275,277,292,304,444 and one identified from additional searches for primary studies,431 reported the effect of interventions to promote the possession and use of window safety devices. Two studies reported a significant effect, one on fitted window locks72 and one on childproofed window frames. 444 One of these studies provided home safety education and supplied and fitted window locks for free to low-income families, with free delivery of low-cost window locks to other families. 72 The second study provided only home safety education. 444 Eight studies did not report a significant increase in the possession and use of window safety devices. All included home safety education and five included the identification or provision of free or low-cost window safety devices.
Study I
Pairwise meta-analysis of six studies evaluating home safety education,71,72,269,275,277,431 which in some studies included the provision of window safety devices and home safety inspections, found that interventions were not effective in increasing the possession of window safety devices (OR 1.10, 95% CI 0.68 to 1.79) (Figure 41).
FIGURE 41.
Forest plot of effect sizes for possession of window safety devices from studies evaluating home safety educational interventions (some of which included the provision of window safety devices). M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49

Study J
Network meta-analysis explored the effects of component elements of the interventions among the six studies included in the PMA for possession of window safety devices. 71,72,269,275,277,431 These included six interventions as listed in Table 97 (see also Table 93) The NMA estimated the 15 possible pairwise comparisons between these interventions. Education plus home safety inspection was most likely to be effective (p best = 0.26), but there was very little difference between any of the interventions.
| Intervention | Usual care (1) | Education + equipment (3) | Education + equipment + home safety inspection (4) | Education + equipment + fitting (5) | Education + home safety inspection (6) | Education + equipment + fitting + home safety inspection (7) |
|---|---|---|---|---|---|---|
| Usual care (1) | 4.09 (0.27 to 67.9) | 1.05 (0.19 to 6.89) | 1.28 (0.11 to 14.2) | 1.10 (0.057 to 25.2) | 1.74 (0.11 to 30.5) | |
| Education + equipment (3) | 0.27 (0.46 to 1.11) | 0.26 (0.01 to 7.29) | 0.31 (0.007 to 11.4) | 0.27 (0.004 to 17.1) | 0.42 (0.008 to 21.0) | |
| Education + equipment + home safety inspection (4) | 0.93 (0.31 to 2.80) | 1.24 (0.054 to 22.1) | 1.06 (0.092 to 12.6) | 1.65 (0.055 to 44.1) | ||
| Education + equipment + fitting (5) | 0.78 (0.63 to 0.98) | 0.85 (0.020 to 44.8) | 1.38 (0.034 to 57.2) | |||
| Education + home safety inspection (6) | 0.95 (0.72 to 1.24) | 1.56 (0.024 to 89.8) | ||||
| Education + equipment + fitting + home safety inspection (7) | 0.60 (0.09 to 3.13) |
Study K
Decision analyses were not undertaken for interventions to promote the possession of window locks as none of the interventions was significantly better than any other in the NMA.
Promoting the possession and use of furniture corner covers
Study H
The overview included five systematic reviews33,332,338,383,387 reporting the effect of interventions promoting the possession and use of furniture corner covers. No meta-analyses were found for this outcome. Two reviews reported interventions associated with significant reductions in sharp-edged bench tops,332,383 two reviews reported conflicting evidence of the effect of interventions on furniture corner cover use33,387 and one review included a study reported elsewhere as significantly increasing the use of furniture corner covers although the review did not specifically report this finding. 338
Four studies reported the effect of interventions to promote the possession and use of furniture corner covers. 257,273,292,304 Two studies found a significant effect of the intervention on use of protective devices on table corners or bench tops. 292,304 One of these studies provided the item to intervention families as part of a free home safety kit304 and the other study provided assistance with identifying retail outlets selling the item in addition to a home safety assessment and home safety education. 292 Two studies found no significant effect of the intervention, with one study delivering home safety education, which included the provision of furniture corner covers,257 and the other study providing only home safety education. 273
It was not possible to undertake a PMA or NMA for possession and use of furniture corner covers as only two studies reported numerators and denominators in all arms of the study. 273,304
Promoting the possession and use of high-chair harnesses
Study H
The overview included three systematic narrative reviews33,332,338 reporting the effect of interventions on the possession and use of high-chair harnesses. No meta-analyses were found for this outcome. All three reviews found no evidence that interventions were effective in increasing the use of high-chair harnesses.
Two studies reported interventions to promote the use of high-chair harnesses, neither of which found evidence that interventions were effective at increasing use of this item. The interventions involved home safety education, a home safety assessment and advice on where to purchase equipment,292 and home safety education plus a free home safety kit that did not include a high-chair harness. 304 It was not possible to undertake PMA or NMA for this outcome because of the small number of studies included.
Reducing baby walker possession or use
Study H
The overview included one meta-analysis33 and three reviews332,338,387 reporting the effect of interventions on baby walker possession or use. The meta-analysis, which combined effect sizes from six studies, found some evidence that interventions were effective in reducing baby walker possession or use (OR for having or using a walker 0.66, 95% CI 0.43 to 1.00). One review338 reported conflicting evidence on the effect of interventions to prevent baby walker use and two reviews found no evidence of a reduction in baby walker use. 332,387
Nine studies reported interventions to reduce baby walker use. 257,277,287,288,295,304,417,431,438 Two studies, focusing solely on preventing baby walker-associated injuries, reported a significant reduction in ownership and use of baby walkers. 417,438 The first study provided education to reduce walker use from nurses during child visits for immunisation438 and the second provided an educational package delivered by health visitors and midwives before and after childbirth. 417 The remaining studies all provided education about baby walkers as part of interventions aimed at preventing a range of childhood injuries.
Study I
Pairwise meta-analysis of the nine studies of home safety education for the reduction of baby walker use257,277,287,288,295,304,417,431,438 found that interventions were effective in increasing the proportion of families who did not have or use a walker (OR 1.57, 95% CI 1.18 to 2.09) (Figure 42).
FIGURE 42.
Forest plot of effect sizes for not having or using a baby walker from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
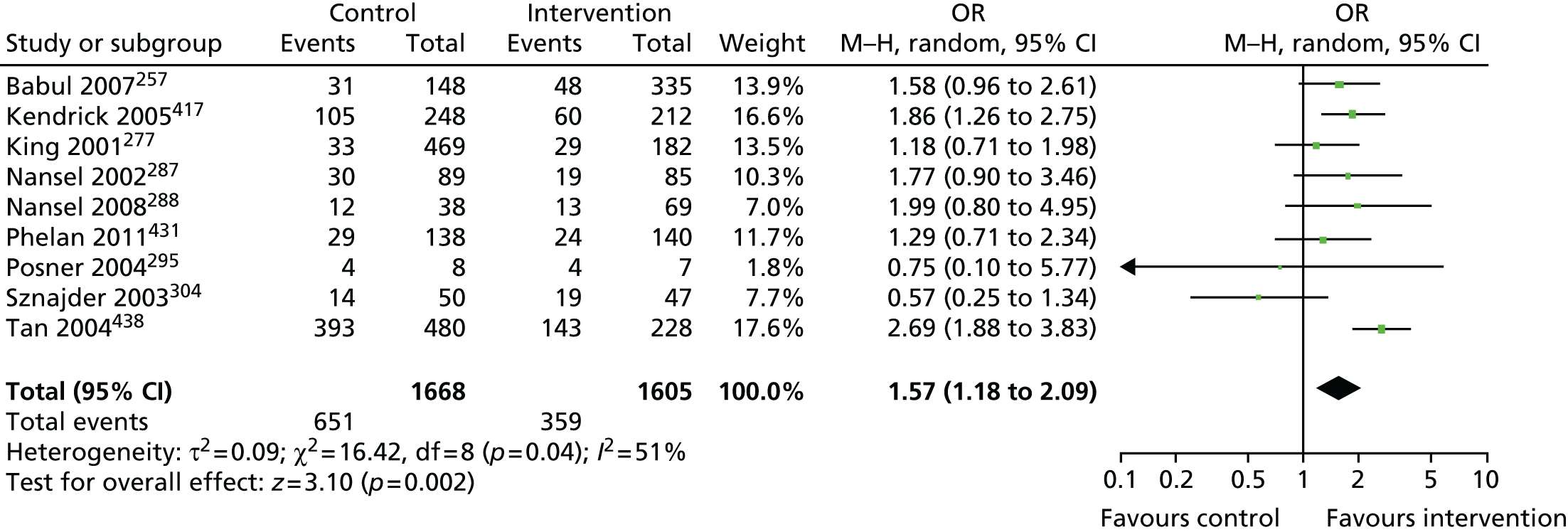
Study J
Network meta-analysis explored the effects of component elements of the interventions from the nine studies included in the PMA for baby walker possession or use. 257,277,287,288,295,304,417,431,438 The data for these studies are provided in Table 93. The studies included seven interventions, which are listed in Table 98. The NMA estimated the 21 possible pairwise comparisons between the seven interventions. The education-only intervention was the most effective (p best = 0.65), with families in the education-only intervention group being less likely to possess or use a baby walker than those in the usual-care group (OR 0.48, 95% CrI 0.31 to 0.84).
| Intervention | Usual care (1) | Education (2) | Education + equipment (3) | Education + equipment + home safety inspection (4) | Education + equipment + fitting (5) | Education + home safety inspection (6) | Education + equipment + fitting + home safety inspection (7) |
|---|---|---|---|---|---|---|---|
| Usual care (1) | 0.48 (0.31 to 0.84)a | 1.51 (0.56 to 3.65) | 1.07 (0.37 to 2.89) | 0.85 (0.29 to 3.35) | 1.28 (0.29 to 5.06) | 0.78 (0.27 to 2.22) | |
| Education (2) | 0.46 (0.36 to 0.58)a | 3.15 (1.02 to 8.38)a | 2.25 (0.66 to 6.24) | 1.80 (0.53 to 6.24) | 2.68 (0.55 to 10.93) | 1.63 (0.47 to 4.96) | |
| Education + equipment (3) | 0.59 (0.33 to 1.08) | 1.33 (0.17 to 10.3) | 0.70 (0.26 to 2.02) | 0.56 (0.13 to 2.97) | 0.84 (0.21 to 3.52) | 0.52 (0.13 to 2.22) | |
| Education + equipment + home safety inspection (4) | 0.67 (0.38 to 1.19) | 0.89 (0.48 to 1.64) | 0.79 (0.16 to 4.71) | 1.20 (0.43 to 3.26) | 0.73 (0.17 to 3.24) | ||
| Education + equipment + fitting (5) | 1.75 (0.75 to 4.08) | 1.51 (0.20 to 9.30) | 0.91 (0.16 to 4.47) | ||||
| Education + home safety inspection (6) | 0.85 (0.51 to 1.42) | 0.61 (0.10 to 3.69) | |||||
| Education + equipment + fitting + home safety inspection (7) | 0.78 (0.43 to 1.42) |
Study K
Baby walker use may impact differentially on different mechanisms of falls. 447 For example, using baby walkers has been associated with an increased risk of head injuries from stair falls and their use may also increase the risk of falls on one level from tipping over. However, baby walkers may reduce the risk of falls from furniture if they prevent infants from reaching furniture to climb on or reduce the risk of falls on one level if infants spend less time walking and more time in the baby walker. Using baby walkers has been identified as a risk factor for poisonings and burns as they can allow infants to reach hazards that they would not be able to reach if they not using a baby walker. Furthermore, since these risks were described, some countries, for example Canada, have banned the sale of baby walkers447 and design changes introduced by the 2005 European standard448 may have altered the risk of walker-associated injuries. More complex decision analyses are therefore required to evaluate the cost-effectiveness of interventions to reduce baby walker use and this is included in the recommendations for research resulting from the KCS programme.
Preventing children being left unattended on high surfaces
Study H
The overview included two systematic narrative reviews33,387 reporting the effect of interventions on preventing children being left unattended on high surfaces. No meta-analyses were found for this outcome. Neither review reported a significant effect of interventions.
Three primary studies included in the systematic reviews reported this outcome. There was no evidence of the effectiveness of interventions to prevent children being left unattended on a high surface. The studies delivered interventions involving home safety education and a free safety kit257,295 and home safety education alone. 288
Study I
Pairwise meta-analysis of three studies of home safety education for preventing children being left unattended on high surfaces257,288,295 found no evidence that education was effective (OR for does not leave child alone on high surfaces 0.84, 95% CI 0.58 to 1.20) (Figure 43).
FIGURE 43.
Forest plot of effect sizes for preventing children being left unattended on high surfaces from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
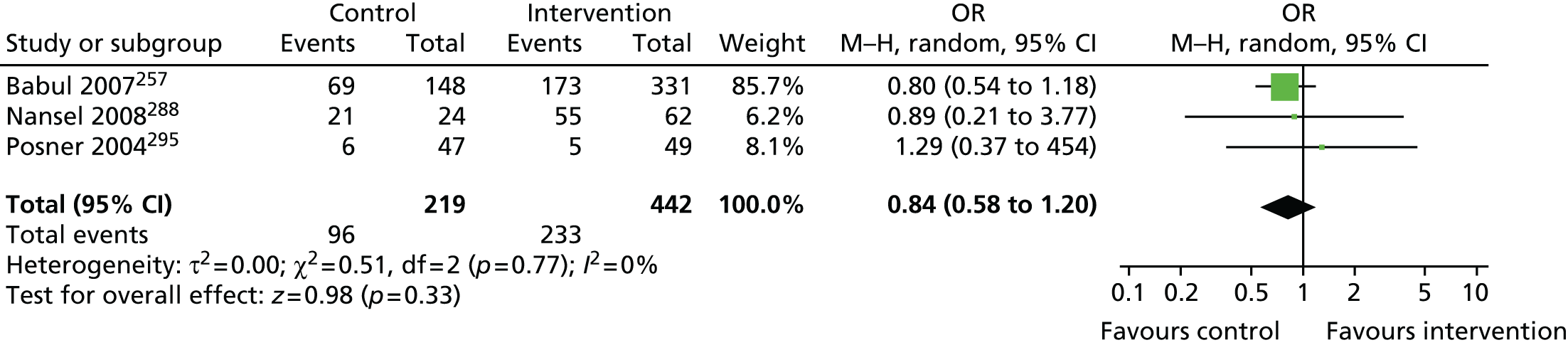
Study J
Network meta-analysis estimated the six possible pairwise comparisons between the four interventions listed in Table 99 (data for these studies are shown in Table 93). There was very little difference between the interventions, but education only was the least likely to be effective in preventing children being left on high surfaces (p best = 0.10), with an OR of 0.56 (95% CrI 0.06 to 4.65) compared with education plus low-cost/free equipment and an OR of 0.50 (95% CrI 0.03 to 8.76) compared with education plus low-cost/free equipment plus home safety inspection.
| Intervention | Usual care (1) | Education (2) | Education + equipment (3) | Education + equipment + home safety inspection (4) |
|---|---|---|---|---|
| Usual care (1) | 1.94 (0.20 to 14.4) | 1.13 (0.12 to 6.75) | 1.01 (0.089 to 9.18) | |
| Education (2) | 0.89 (0.18 to 5.84) | 0.56 (0.064 to 4.65) | 0.50 (0.032 to 8.76) | |
| Education + equipment (3) | 0.71 (0.44 to 1.13) | 3.06 (0.61 to 14.3) | 0.89 (0.099 to 9.67) | |
| Education + equipment + home safety inspection (4) | 0.89 (0.56 to 1.42) | 1.27 (0.80 to 2.00) |
Study K
Decision analyses were not undertaken for interventions to prevent children being left unattended on high surfaces, as none of the interventions was significantly better than any other in the NMA.
Interventions to promote stairway safety
Study H
The overview included four systematic narrative reviews33,36,332,383 reporting the effect of interventions on stairway safety. No meta-analyses were found for this outcome. The reviews all found no evidence that interventions were effective in promoting safe indoor stairways. One review reported mixed findings regarding the effect of interventions on outdoor stair safety. 33
Six primary studies reported interventions to promote stairway safety practices, five identified from reviews269,277,292,293,300 and one identified from additional searches for primary studies. 418 The interventions in these studies included home safety education plus home safety assessments269,277,292 and an injury prevention curriculum including falls prevention education delivered to children in a school setting. 418 There was no evidence that these interventions were effective in preventing children playing on stairs or in promoting safe indoor stairways, including the presence of handrails, railings or adequate lighting on stairs, a reduction in the number of railings or stairs in disrepair, a reduction in the ease of opening doors to cellars or basements and stairs properly designed in terms of safety features. There was a significant improvement observed in the modification of safety features of outdoor stairs293 following a multifaceted community intervention and a significant reduction in missing or loose porch railings after home safety education, a home safety assessment and modification of hazards. 300 It was not possible to undertake PMA or NMA or decision analyses for these stairway safety outcomes because of the small number of studies.
Interventions to reduce tripping hazards
Study H
The overview included five systematic narrative reviews33,36,332,338,383 reporting the effect of interventions on tripping hazards. No meta-analyses were found for this outcome. Four reviews reported the effect of interventions on the fixing of rugs or carpets. 33,36,338,383 One review found a significant reduction in tripping hazards from rugs or floor coverings. 383 Another review included the same primary study but did not report the relevant outcome. 36 Two reviews did not find a significant effect of interventions on the fixing of rugs or carpets. 33,338 Four reviews reported the effect of interventions on other tripping hazards. 33,36,332,338 Two reviews36,332 found a reduction in tripping hazards from electrical cords but not tripping hazards from floors in need of repair, although the reviews did not specifically report these outcomes. One review33 reported conflicting evidence regarding interventions to reduce tripping hazards from floors in disrepair and cables or leads likely to cause falls. One review338 found no evidence that interventions were effective in reducing other tripping hazards.
Four primary studies, all included in the reviews described above, reported on the effect of interventions on tripping hazards. 269,275,300,304 One study included home safety education, a home safety assessment and modification of hazards and found a significant reduction in tripping hazards from loose floor coverings. 300 Other outcomes related to tripping hazards reported by this and the other studies did not differ significantly between treatment groups, including tripping hazards posed by electrical cables, floors in disrepair and unsafe rugs and carpets. The interventions in the other studies included home safety education and home safety assessment269,275 and a free safety kit. 304 It was not possible to undertake PMA or NMA or decision analyses for tripping hazard outcomes because of the small number of studies.
Interventions to promote other falls prevention practices
Study H
The overview included two systematic narrative reviews33,332 reporting the effect of interventions on other falls prevention practices. No meta-analyses were found for this outcome. Both reviews reported on interventions to reduce the accessibility of roofs,33,332 with both including evidence demonstrating a significant effect favouring the intervention group. Both reviews also reported on the effect of interventions on balcony safety,33,332 with both finding no evidence that interventions were effective in promoting balcony safety. One review33 reported the effect of interventions on safe furniture layout, reporting that significantly more intervention group families rearranged furniture to avoid staggering the layout. One review332 reported an intervention that demonstrated a significant improvement in lighting in corridors. Both reviews33,332 reported an intervention to reduce the amount of climbable fencing, with neither review reporting a significant effect.
One primary study demonstrated a significant effect of an intervention to reduce the accessibility of roofs,292 one study reported that significantly more intervention group families rearranged furniture to avoid staggering the layout401 and one study293 demonstrated a significant improvement in lighting in corridors. Other studies found no significant effects of interventions with regard to balcony safety or climbable fencing or gates.
It was not possible to undertake PMA or NMA as the number of studies reporting each outcome was small.
Poisoning prevention
Figure 44 shows the process of identification and selection of reviews and primary studies included in the overview and in the NMA for poisoning prevention interventions. Thirteen narrative systematic reviews, two meta-analyses including a narrative systematic review and 47 primary studies were included in the overview, 28 of which were included in the NMA for poisoning outcomes.
Characteristics of included reviews and primary studies
The characteristics and quality assessment of the reviews included in the overview are shown in Table 71. One review focused specifically on community-based poisoning prevention interventions336 and the others evaluated interventions to prevent a range of injury mechanisms. The risk-of-bias assessment of included reviews produced OQAQ scores ranging from 2 to 7 (median 4) out of a maximum possible score of 7.
The characteristics of the primary studies included in the overview, systematic review, PMA and NMA are shown in Table 72. Thirty-one (66%) of the 47 primary studies in the overview were RCTs, eight (17%) were non-RCTs, seven (15%) were CBAs and one (2%) was a case–control study. Tables of excluded reviews and primary studies are available on request from the authors. The risk-of-bias assessment of included primary studies indicated that just under half the RCTs reported adequate allocation concealment (42%), follow-up of at least 80% of participants in each arm (48%) and blinded outcome assessment (48%). None of the non-RCTs and CBAs demonstrated blinded outcome assessment, five (33%) followed up at least 80% of participants in each arm and five (33%) had a balanced distribution of confounders between treatment arms. The case–control study scored 7 (out of a maximum of 9) on the Newcastle–Ottawa scale, indicating that it was of good quality.
Preventing poisoning-related injuries
Study H
The overview included nine systematic reviews reporting interventions to prevent poisoning-related injuries. 33,36,334–336,383,387,388,445 The reviews included a total of seven different primary studies reporting this outcome. 263,267,275,309,434,437 In addition, one study did not report poisoning rates72 but did provide individual participant data for inclusion in a meta-analysis33 combining poisoning rates from three studies. The meta-analysis found a lack of evidence that interventions reduced poisoning rates (rate ratio 1.03, 95% CI 0.78 to 1.36). The seven primary studies reporting poisoning-related injuries included in the reviews consisted of two RCTs,309,437 two non-RCTs263,275 and three CBA studies. 267,434,437 The study that did not report poisoning rates but that did provide IPD was a RCT. 72 One further primary study, a RCT reporting poisoning rates, was identified by systematic review searches. 312
Two of the eight primary studies reported significantly lower rates of medically attended or self-reported poisonings in the intervention groups. The studies evaluated child-resistant aspirin containers,434 reporting a reduction in the proportion of medically attended aspirin poisonings in the intervention area, and a school-based educational intervention targeting a range of injuries and involving teachers, parents and pupils. 312
The remaining six studies reported no significant effect of interventions on medically attended poisonings. These interventions included the provision of ‘Mr Yuk’ stickers (depicting a green-faced grimacing man with a protruding tongue) for alerting children to poisoning hazards,263 the provision of safety items [telephone stickers, coupon for syrup of ipecac (emetic agent), cabinet lock, checklist for ‘poison proofing’ the home and pamphlets],309 safety education and safety equipment provision covering a range of injuries275,437 and community injury prevention programmes. 267,437 The study not reporting poisoning rates but providing IPD did not find a significant effect of education and the provision and fitting of free safety equipment. 72
Study I
Meta-analysis of four studies evaluating home safety interventions (education plus in some studies the provision of home safety inspections and safety equipment)72,263,275,312 found a lack of evidence that interventions reduced the rate of poisoning (IRR 0.93, 95% CI 0.65 to 1.32) (Figure 45).
FIGURE 45.
Forest plot of effect sizes for poisoning injury rates from studies evaluating home safety educational interventions. IV, inverse variance. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49

It was not possible to undertake NMA for interventions to prevent poisonings because of the small number of studies.
Promoting the safe storage of medicines
Study H
The overview included one meta-analysis33 and 10 systematic reviews33,40,42,332,338,383,385,387,388,445 reporting the effect of interventions on the safe storage of medicines. The meta-analysis found evidence that education, with or without the provision of safety equipment, was effective in increasing the safe storage of medicines (OR 1.57, 95% CI 1.22 to 2.02). 33
A total of 25 primary studies reporting on interventions promoting the safe storage of medicines were identified, 18 from reviews71,72,257,260,273,282,287,292,295,297,300,304,306,396,399,405,427 and seven from additional searches for primary studies. 99,266,288,303,398,431,432 Of the 25 studies, seven reported that significantly more intervention than control group families stored medicines safely,71,72,260,266,292,300,396 all of which evaluated interventions targeting multiple injury mechanisms. The interventions in these studies consisted of GP safety advice with access to low-cost safety equipment (including cupboard locks) for families receiving means-tested state benefits,71 a home visit with safety checks and tailored safety advice including assistance in obtaining home safety devices,72,260,292, a home safety inspection, education and modification,300 a standardised safety consultation and the provision and fitting of safety equipment (including cupboard locks) free to low-income families,292 a personalised safety report (including the promotion of the safe storage of poisons) printed at a computer kiosk in an ED266 and prevention lessons delivered by teachers to children in schools with take-home materials and posters displayed for parents. 396
The remaining 18 studies, evaluating a range of interventions including safety education, tailored safety education, or safety education plus equipment, demonstrated no significant difference between treatment groups in the safe storage of medicines.
Study I
Meta-analysis of 13 studies evaluating home safety interventions (education plus the provision of home safety assessments and safety equipment in some studies),71,72,257,266,273,282,287,288,295,300,303,304,404 which updated the meta-analysis described in study H,33 found that interventions were effective in increasing the storage of medicines out of reach (OR 1.53, 95% CI 1.27 to 1.84) (Figure 46). Storing medicines out of reach was defined as stored in locked cupboards, drawers or cabinets; stored at or above adult waist level; or stored so that they are inaccessible to a child.
FIGURE 46.
Forest plot of effect sizes for storage of medicines out of reach from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
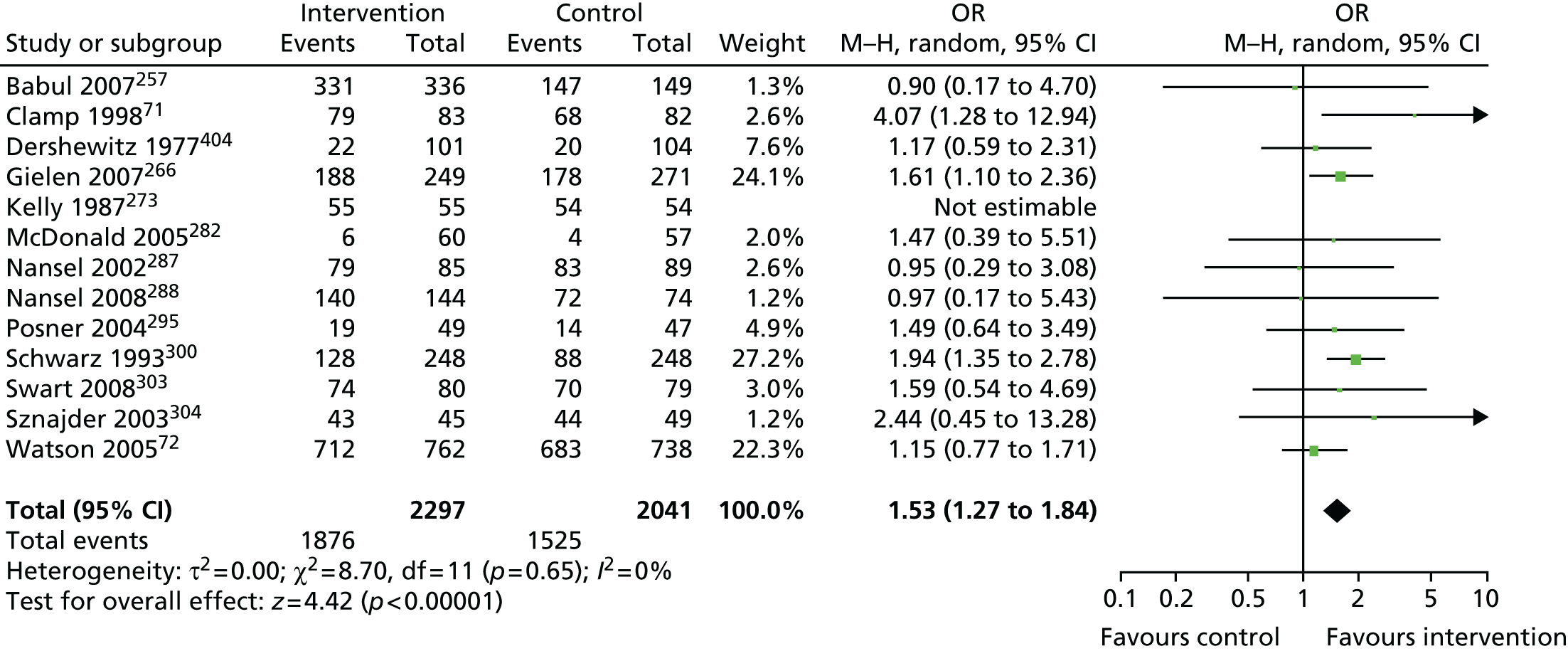
Study J
Data from studies included in the NMAs of poisoning outcomes are shown in Table 100. NMA was used to estimate the 21 possible pairwise comparisons between seven interventions to promote the safe storage of medicines from 13 studies (Figure 47). Home safety interventions with education and low-cost or free equipment were the most likely to be effective (p best = 0.39), with an estimated OR compared with usual care of 2.51 (95% CrI 1.01 to 6.00).
| Pairwise comparison | Study | Study qualitya | Intervention | Safe storage of medicines | Safe storage of other household products | Safe storage of poisons | Possession of PCC telephone number | Safe storage of poisonous plants |
|---|---|---|---|---|---|---|---|---|
| Usual care (1) vs. education (2) | Kelly 1987,273 RCT, USAb | A = U, B = Y, F = N | 1 | 54/54 | 43/54 | |||
| 2 | 55/55 | 49/55 | ||||||
| Nansel 2002,287 RCT, USAc | A = Y, B = U, F = Y | 1 | 83/89 | 65/89 | 59/89 | |||
| 2 | 79/85 | 66/85 | 63/85 | |||||
| Kelly 2003,274 cluster RCT, USAd | A = U, B = Y, F = Y | 1 | 45.56/136.68d | |||||
| 2 | 112.95/137.63d | |||||||
| McDonald 2005,282 RCT, USA | A = Y, B = U, F = N | 1 | 6/60 | 3/57 | ||||
| 2 | 4/57 | 6/61 | ||||||
| Gielen 2007,266 RCT, USA | A = Y, B = N, F = Y | 1 | 178/271 | 44/62 | 222/333 | |||
| 2 | 188/249 | 57/73 | 245/322 | |||||
| Nansel 2008,288 non-RCT, USA | A = U, B = N, F = N | 1 | 72/74 | 59/73 | 50/59 | |||
| 2 | 140/144 | 117/144 | 90/119 | |||||
| Reich 2011,432 RCT, USAd | A = Y, B = Y, F = Y | 1 | Log-OR (SE) = –0.192 (0.2863)e | |||||
| 2 | ||||||||
| Equipment only (1) vs. education + equipment (3) | Woolf 1987,308 cluster RCT, USA | A = U, B = Y, F = N | 1 | 29/143 | ||||
| 3 | 47/119 | |||||||
| Woolf 1992,309 cluster RCT, USA | A = U, B = Y, F = N | 1 | 60/151 | 59/151 | ||||
| 3 | 89/150 | 117/150 | ||||||
| Clamp 1998,71 RCT, UK | A = U, B = N, F = Y | 1 | 68/82 | 49/82 | ||||
| 3 | 79/83 | 59/83 | ||||||
| Usual care (1) vs. education + equipment (3) vs. education + equipment + home safety inspection (4) | Babul 2007,257 RCT, Canada | A = Y, B = N, F = N | 1 | 147/149 | 112/147 | |||
| 3 | 171/173 | 136/172 | ||||||
| 4 | 160/163 | 123/160 | ||||||
| Usual care (1) vs. education + equipment + home safety inspection (4) | Kendrick 1999,275 cluster non-RCT, UK | B = N, F = N, C = Y | 1 | 317/367 | ||||
| 4 | 322/363 | |||||||
| Sangvai 2007,297 RCT, USA | A = Y, B = Y, F = N | 1 | 3/10 | |||||
| 4 | 13/16 | |||||||
| Swart 2008,303 non-RCT, South Africa | A = U, B = Y, F = Y | 1 | 70.26/79.58c | 46.86/57.96d | ||||
| 4 | 74.07/80c | 50.87/58.27d | ||||||
| Hendrickson 2002,269 USA, RCT | A = N, B = N, F = Y | 1 | 14/40 | 8/40 | ||||
| 4 | 34/38 | 34/38 | ||||||
| Usual care (1) vs. education + equipment (3) | Watson 2005,72 cluster RCT, UK | A = Y, B = N, F = Y | 1 | 683/738 | 327/669 | |||
| 3 | 712/762 | 368/693 | ||||||
| Usual care (1) vs. education + home safety inspection (6) | Petridou 1997,293 cluster non-RCT, Greece | B = N, F = Y, C = Y | 1 | 67.26/100.12d | ||||
| 6 | 71.08/97.83d | |||||||
| Usual care (1) vs. education + equipment + home safety inspection + fitting (7) | Schwarz 1993,300 cluster non-RCT, USA | B = N, F = N, C = Y | 1 | 88.42/248.37d | ||||
| 7 | 128.16/248.37d | |||||||
| Phelan 2011,431 RCT, USA | A = Y, B = N, F = Y | 1 | 17/149 | 16/138 | ||||
| 7 | 2/150 | 71/139 | ||||||
| Usual care (1) vs. education + home visit (8) | Minkovitz 2003,427 RCT, USAf | A = Y, B = N, F = Y | 1 | 463/761 | ||||
| 8 | 523/832 | |||||||
| Minkovitz 2003,427 cluster non-RCT, USAf | B = N, F = Y, C = Y | 1 | 596/955 | |||||
| 8 | 754/1189 | |||||||
| Johnston 2006,413 non-RCT, USA | B = N, F = Y, C = Y | 1 | 155/232 | 82/91 | ||||
| 8 | 71/91 | 222/232 | ||||||
| Education (2) vs. education + equipment (3) | Posner 2004,295 RCT, USA | A = Y, B = Y, F = N | 2 | 14/47 | 22/47 | 27/47 | 9/16 | |
| 3 | 19/49 | 34/49 | 35/49 | 11/16 | ||||
| Bulzacchelli 2009,398 non-RCT, USA | A = U, B = N, F = N | 2 | 5/49 | |||||
| 3 | 10/105 | |||||||
| Education (2) vs. education + equipment + fitting (5) | Sznajder 2003,304 RCT, France | A = Y, B = N, F = Y | 2 | 44/49 | 32/41 | 48/49 | ||
| 5 | 43/45 | 40/48 | 41/48 | |||||
| Education + equipment (3) vs. education + equipment + home safety inspection (4) | Gielen 2002,265 cluster RCT, USAd | A = U, B = U, F = N | 3 | 6.87/56.93d | ||||
| 4 | 5.89/58.89d | |||||||
| Education + equipment (3) vs. equipment only (9) | Dershewitz 1977,404 non-RCT, USA | A = U, B = Y, F = N | 3 | 22/102 | 1/101 | |||
| 9 | 20/104 | 0/104 | ||||||
| Education + equipment + home safety inspection (4) vs. education + equipment + home safety inspection + fitting (7) | King 2001,277 RCT, USA | A = Y, B = Y, F = Y | 4 | 261/469 | ||||
| 7 | 273/482 |
FIGURE 47.
Network meta-analysis and PMA results for the safe storage of medicines. Heterogeneity: between-study variance = 0.06 (95% CrI 0.000 to 1.087). Key: NMA results in black; PMA results in green. Interventions are displayed in the order that they were entered in the analysis. E, education; F, fitting; FE, low-cost/free equipment; H–H, head to head; HSI, home safety inspection; HV, home visit; NA, not applicable; Pbest, probability that intervention is the best; UC, usual care. From Achana et al. 449 under Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).
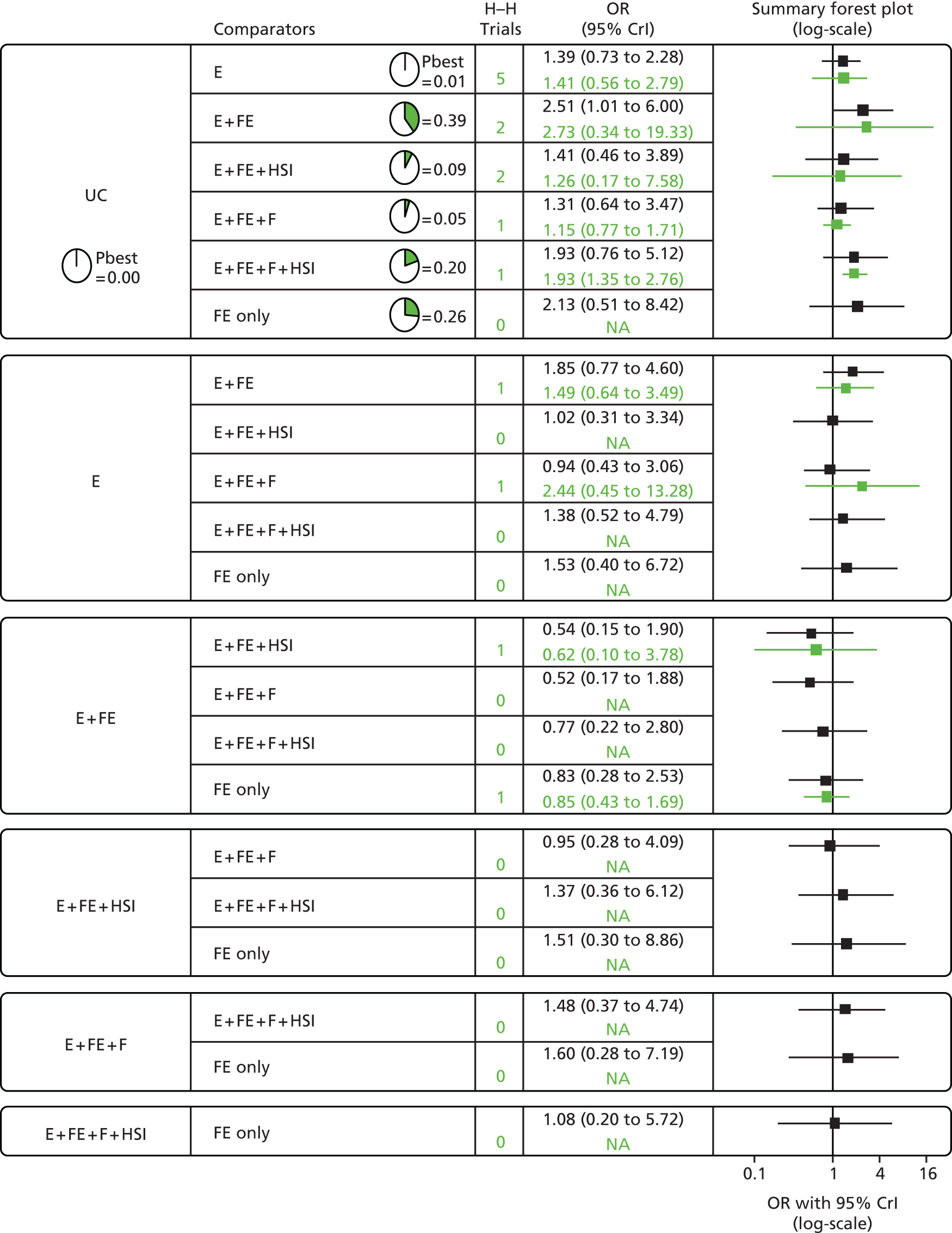
Study K
Seven interventions were evaluated, of which three were excluded from further consideration because they had higher costs than more effective interventions (Table 101). Home safety education had the lowest estimated ICER compared with usual care, at £41,330 per QALY gained, followed by education and the provision of free equipment, with an ICER of £90,615 compared with usual care. Figure 48 shows the probability of the alternative interventions being cost-effective. At a threshold value of £30,000 per QALY gained, usual care had the highest probability of being cost-effective (0.83) followed by education (0.17).
| Intervention | Expected QALYs (95% CrI)a | Expected costs (95% CrI) (£)a | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained) | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| Usual care (1) | 25,056.559 (25,039.293 to 25,073.828) | 4169 (2872 to 6045) | 0.828 | 0.301 | |||
| Education (2) | 25,056.578 (25,039.328 to 25,073.855) | 5435 (4197 to 7271) | 0.031 | 1273 | 41,330 | 0.172 | 0.698 |
| Education + equipment (3) | 25,056.578 (25,039.328 to 25,073.857) | 7089 (5829 to 8,921) | 0.032 | 2927 | 90,615 | 0.000 | 0.000 |
| Education + equipment + home safety inspection (4) | 25,056.578 (25,039.326 to 25,073.857) | 9051 (7737 to 10,930) | 0.030 | 4881 | Dominated | 0.000 | 0.000 |
| Education + equipment + fitting (5) | 25,056.578 (25,039.326 to 25,073.855) | 8695 (7392 to 10,570) | 0.030 | 4522 | Dominated | 0.000 | 0.000 |
| Education + equipment + home safety inspection + fitting (6) | 25,056.580 (25,039.328 to 25,073.857) | 9506 (8166 to 11,410) | 0.031 | 5338 | Dominated | 0.000 | 0.000 |
| Equipment (7) | 25,056.578 (25,039.322 to 25,073.855) | 6270 (5027 to 8099) | 0.031 | 2111 | Dominated | 0.000 | 0.002 |
FIGURE 48.
Cost-effectiveness acceptability curves for interventions to promote safe storage of medicines. E, education; FE, low-cost/free equipment; pCE, probability cost-effective; UC, usual care.
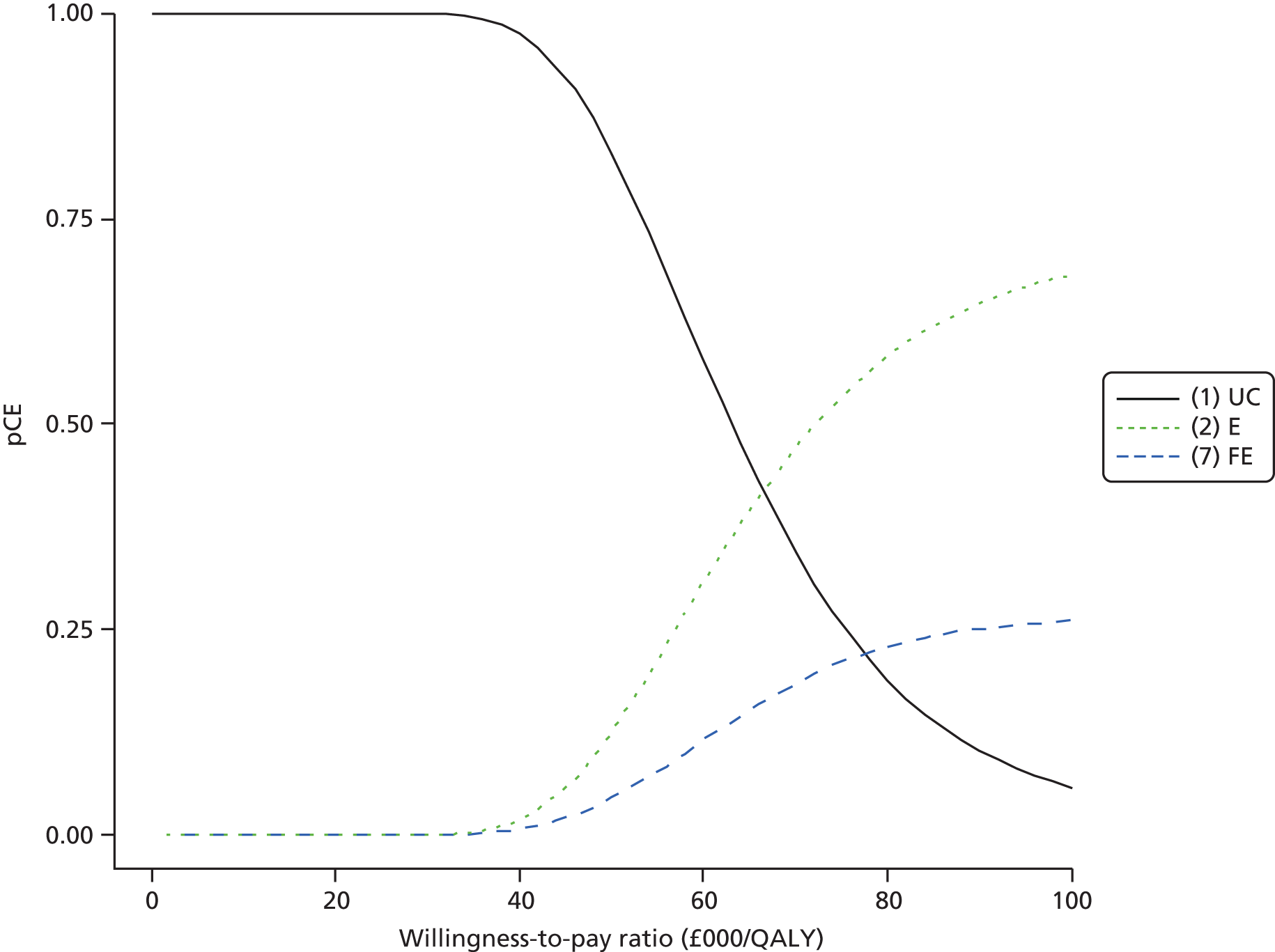
A range of sensitivity analyses varying the base-case assumptions and inputs, as outlined in the methods section, was implemented (Table 102). All assessed the probability of interventions being cost-effective at a threshold of £30,000 and £50,000. The results were mainly sensitive to the baseline incidence of unintentional injuries; when this was increased to reflect a higher incidence rate among children aged < 5 years living in the two most disadvantaged quintiles (SA9 and SA10), the ICER for education compared with usual care reduced from £41,330 to < £20,000 per QALY gained.
| Intervention | Expected QALYs (95% CrI)a | Expected costs (95% CrI) (£)a | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained) | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| SA1: probability that intervention is effective changed from posterior to predictive distribution of intervention effects and baseline rate | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 4169 (2872 to 6045) | 0.850 | 0.453 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 5463 (4221 to 7319) | 0.027 | 1298 | 47,160 | 0.150 | 0.540 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 6300 (5032 to 8163) | 0.028 | 2140 | 74,625 | 0.000 | 0.006 |
| SA2: baseline probability of safe storage changed from 75% (KCS community controls) to 93%56 | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 3158 (2030 to 4720) | 0.998 | 0.867 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 4056 (2938 to 5599) | 0.013 | 898 | 71,065 | 0.002 | 0.133 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 4302 (3184 to 5850) | 0.013 | 1139 | 87,285 | 0.000 | 0.000 |
| SA3: baseline probability of safe storage changed from 75% (KCS community controls) to 50% (assumption) | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 4903 (3542 to 7022) | 0.942 | 0.59 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 6885 (5585 to 8921) | 0.037 | 1985 | 53,970 | 0.058 | 0.41 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 8567 (7273 to 10,620) | 0.036 | 3671 | 101,700 | 0.000 | 0.000 |
| SA4: probability intervention is accepted changed from 90% to 50% (assumption) | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 4169 (2,872 to 6045) | 0.979 | 0.745 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 5227 (3,965 to 7059) | 0.017 | 1061 | 62,195 | 0.02 | 0.254 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 5693 (4429 to 7527) | 0.017 | 1526 | 87,356 | 0.000 | 0.001 |
| SA5: proportion admitted changed from 63%450 to 83.3% (Phil Miller, Nottingham University Hospitals NHS Trust, January 2014, personal communication) | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 5140 (3430 to 7606) | 0.625 | 0.146 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 6358 (4711 to 8776) | 0.036 | 1214 | 33,630 | 0.374 | 0.852 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 7202 (5548 to 9627) | 0.036 | 2043 | 55,495 | 0.000 | 0.002 |
| SA6: provided with two Pop-It locks costing £2.65 per lock | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 4169 (2872 to 6045) | 0.828 | 0.298 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 5435 (4197 to 7271) | 0.031 | 1273 | 41,330 | 0.17 | 0.677 |
| Equipment | 25,060 (25,040 to 25,070) | 5787 (4548 to 7596) | 0.031 | 1629 | 51,685 | 0.002 | 0.026 |
| SA7: provided with two magnetic locks costing £4.80 per lock | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 4169 (2872 to 6045) | 0.828 | 0.301 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 5435 (4197 to 7271) | 0.031 | 1273 | 41,330 | 0.172 | 0.698 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 6751 (5491 to 8585) | 0.031 | 2592 | 82,570 | 0.000 | 0.000 |
| SA8: increased number of children per household from 1 to 1.8378 | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 4169 (2872 to 6045) | 0.242 | 0.026 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 5435 (4197 to 7271) | 0.031 | 1273 | 22,960 | 0.755 | 0.962 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 6270 (5027 to 8099) | 0.031 | 2111 | 37,210 | 0.003 | 0.012 |
| SA9: change incidence of medically reported poisonings from 30.1 to 44.9 per 10,000 person-years (rate of unintentional poisonings among children aged < 5 years in the fourth most deprived quintile451) | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 5963 (3814 to 8986) | 0.226 | 0.040 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 7110 (5119 to 10,070) | 0.06 | 1171 | 19,315 | 0.764 | 0.929 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 7958 (5944 to 10,882) | 0.062 | 2002 | 32,025 | 0.010 | 0.030 |
| SA10: change incidence of medically reported poisonings from 30.1 to 48.5 per 10,000 person-years (rate of unintentional poisonings among children aged < 5 years in the fifth most deprived quintile451) | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 6380 (4239 to 9731) | 0.172 | 0.031 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 7539 (5451 to 10,751) | 0.062 | 1149 | 18,275 | 0.818 | 0.938 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 8375 (6296 to 11,590) | 0.063 | 1983 | 30,760 | 0.010 | 0.030 |
| SA11: change estimate of SE of utility decrements from 10% to 20% of mean utility decrement value (assumption) | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 4131 (2842 to 6011) | 0.800 | 0.800 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 5409 (4187 to 7176) | 0.031 | 1289 | 40,770 | 0.200 | 0.200 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 6283 (5038 to 8041) | 0.032 | 2152 | 66,850 | 0.000 | 0.000 |
| SA12: change estimate of SE of utility decrements from 10% to 50% of mean utility decrement value (assumption) | |||||||
| Usual care (1) | 25,060 (25,040 to 25,070) | 4095 (2899 to 6038) | 0.794 | 0.304 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 5382 (4238 to 7217) | 0.031 | 1290 | 41,265 | 0.206 | 0.696 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 6257 (5082 to 8100) | 0.032 | 2155 | 66,825 | 0.000 | 0.000 |
Promoting the safe storage of household and other products
Study H
The overview included two systematic reviews and meta-analyses33,40 and nine narrative reviews36,42,332,338,383,385,387,388,445 reporting the effect of interventions on the safe storage of household and other products (defined as the use of safety catches or locks on cupboards/drawers, the use of CRCs and storage out of the reach of children). One meta-analysis reported evidence that education, with or without the provision of safety equipment, was effective in increasing the safe storage of household products (OR 1.63, 95% CI 1.22 to 2.17). 33 The other meta-analysis of similar interventions delivered in a clinical setting reported that intervention families were 1.8 times more likely to store cleaning agents safely. 40
A total of 31 primary studies reporting the safe storage of household and other products were identified (24 from reviews71,72,257,260,263,265,269,273,275,277,282,287,292,295,297,304,306,309,396,399,405,413,427 and seven from additional searches for primary studies99,266,288,303,398,431,432). Six studies reported that significantly more intervention group families stored household and other products safely. 72,260,269,292,295,309 One of these studies provided safety education plus equipment,309 four provided safety education, equipment and home safety inspections,72,260,269,292 and one delivered home safety counselling and safety equipment with specific injury-focused instructions. 295 The remaining 25 studies found no significant differences between groups in the safe storage of household and other products, evaluating a range of interventions including general or tailored safety education, home safety equipment and home safety inspections.
Study I
Pairwise meta-analysis of 15 studies,71,72,266,269,273,275,277,282,287,288,295,303,304,309,404 which updated the meta-analysis described in study H,33 found that home safety interventions (education plus the provision of home safety inspections and home safety equipment in some studies) increased the safe storage of cleaning products (defined as for the safe storage of medicines) (OR 1.55, 95% CI 1.22 to 1.96) but there was significant heterogeneity between effect sizes (Figure 49). Interventions providing locks appeared to be more effective (OR 1.87, 95% CI 1.28 to 2.72) than those providing education without locks (OR 1.13, 95% CI 0.92 to 1.40). Interventions delivered at home also appeared to be more effective (OR 2.14, 95% CI 1.06 to 4.32) than those provided in clinical settings (OR 1.29, 95% CI 1.10 to 1.51).
FIGURE 49.
Forest plot of effect sizes for storage of household products out of reach from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
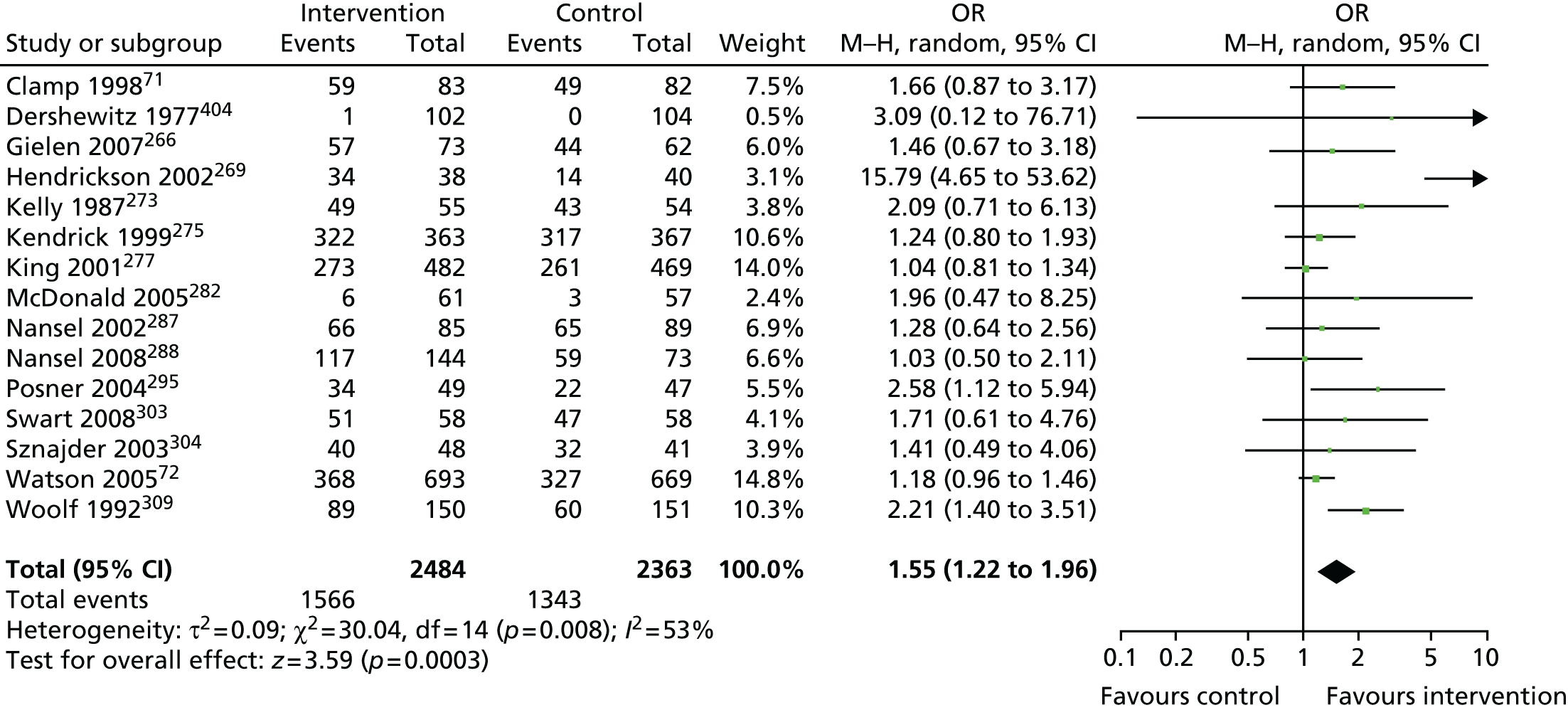
Study J
Network meta-analysis estimated the 21 possible pairwise comparisons between the seven interventions promoting the safe storage of household products other than medicines in the 15 studies listed in Table 100. The most intensive home safety intervention (education plus low-cost/free equipment and fitting plus home safety inspection) was most likely to be effective (p best = 0.37), with an estimated OR compared with usual care of 2.59 (95% CrI 0.59 to 15.16), but no interventions were significantly more effective than usual care (Figure 50).
FIGURE 50.
Network meta-analysis and PMA results for the safe storage of household products. Heterogeneity: between-study variance = 0.3 (95% CrI 0.018 to 1.562). Key: NMA results in black; PMA results in green. Interventions are displayed in the order that they were entered in the analysis. E, education; F, fitting; FE, low-cost/free equipment; H–H, head to head; HSI, home safety inspection; NA, not applicable; Pbest, probability that intervention is the best; UC, usual care. From Achana et al. 449 under Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).
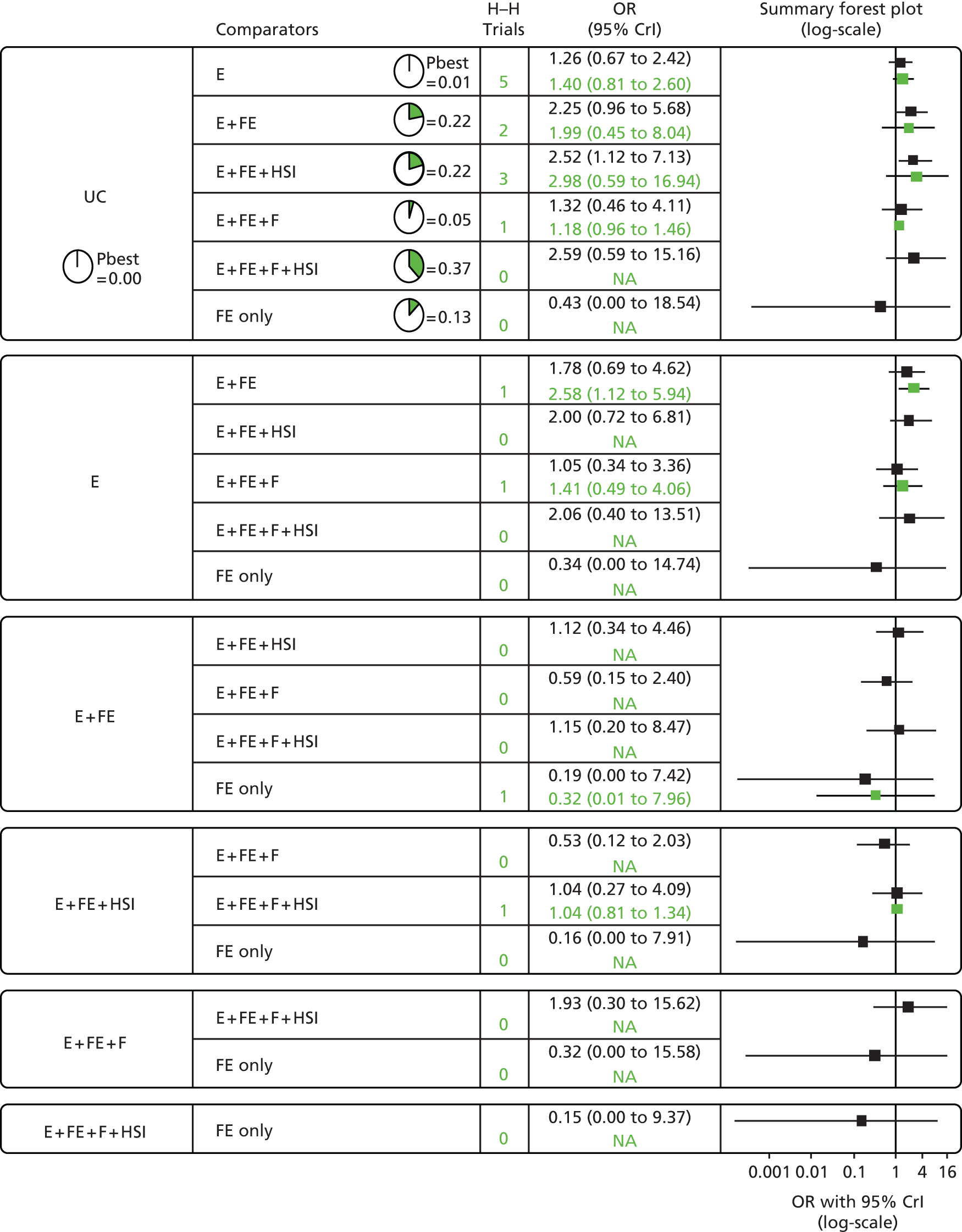
Study K
Seven interventions were evaluated (Table 103) but all interventions were more costly and less effective than usual care. This is likely to reflect the OR being < 1.0 for the safe storage of household products comparing children with a poisoning to community controls in study A (i.e. OR 0.77, 95% CI 0.59 to 0.99). In sensitivity analyses, all interventions remained more costly and less effective than usual care (results available from the authors on request).
| Intervention | Expected QALYs (95% CrI)a | Expected costs (95% CrI) (£)a | Incremental QALYs | Incremental costs (£) | ICER (£/QALY gained) | Probability CE (at £30,000 threshold) | Probability CE (at £50,000 threshold) |
|---|---|---|---|---|---|---|---|
| Usual care (1) | 25,060 (25,040 to 25,070) | 2504 (1770 to 3623) | 1 | 1 | |||
| Education (2) | 25,060 (25,040 to 25,070) | 3813 (3057 to 4969) | –0.0063 | 1308 | –199,600 | 0 | 0 |
| Education + equipment (3) | 25,060 (25,040 to 25,070) | 6249 (5361 to 7415) | –0.0073 | 3731 | –489,250 | 0 | 0 |
| Education + equipment + home safety inspection (4) | 25,060 (25,040 to 25,070) | 6013 (5136 to 7170) | –0.0076 | 3495 | –438,600 | 0 | 0 |
| Education + equipment + fitting (5) | 25,060 (25,040 to 25,070) | 6553 (5655 to 7722) | –0.0063 | 4035 | –615,350 | 0 | 0 |
| Education + equipment + fitting + home safety inspection (6) | 25,060 (25,040 to 25,070) | 4374 (3591 to 5494) | –0.000042 | 1863 | –1,729,000 | 0 | 0 |
| Equipment (7) | 25,060 (25,040 to 25,070) | 4924 (4123 to 6053) | –0.000042 | 2416 | –2,233,000 | 0 | 0 |
Promoting the safe storage of poisons
Study H
Interventions promoting the safe storage of poisons (i.e. when the type of poisonous product was not specified) are reported with those promoting the safe storage of medicines and the safe storage of household products.
Study I
Studies reporting the safe storage of unspecified poisons were analysed separately from those reporting the safe storage of medicines or household products in study I. PMA of five studies reporting interventions promoting the safe storage of poisons265,266,297,398,431 found some evidence that home safety education (plus the provision of locks and home safety inspections in some studies) was associated with poisons being stored more safely (OR 2.07, 95% CI 0.92 to 4.66) (Figure 51).
FIGURE 51.
Forest plot of effect sizes for the storage of poisons out of reach from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
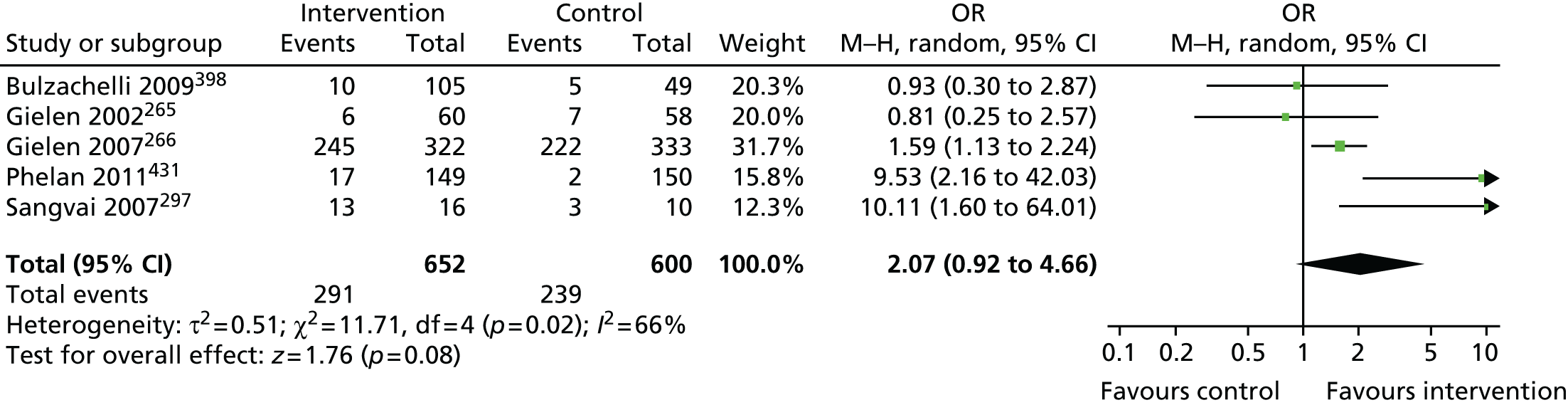
Study J
Network meta-analysis estimated the 10 possible pairwise comparisons between five interventions promoting the safe storage of poisons in the nine studies listed in Table 100. The most intensive home safety intervention (education plus low-cost/free equipment and fitting plus home safety inspection) was most likely to be effective (p best = 0.78), with an estimated OR compared with usual care of 11.10 (95% CrI 1.60 to 141.50) (Figure 52).
FIGURE 52.
Network meta-analysis and PMA results for interventions promoting the safe storage of poisons. Heterogeneity: between-study variance = 0.24 (95% CrI 0.005 to 2.647). Key: NMA results in black; PMA results in green. Interventions are displayed in the order that they were entered in the analysis. E, education; F, fitting; FE, low-cost/free equipment; H–H, head to head; HSI, home safety inspection; HV, home visit; NA, not applicable; Pbest, probability that intervention is the best; UC, usual care. From Achana et al. 449 under Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).

Study K
A decision analysis for the safe storage of poisons was not conducted as the exposures studied in study A were specific types of medicine or household products as opposed to non-specific ‘poisonous substances’. Consequently, data were not available for decision analyses for this outcome.
Promoting the use of child-resistant caps
Study H
Six systematic narrative reviews reporting the use of CRCs were included in the overview. 33,42,332,383,387,445 No meta-analyses reporting this outcome were found.
Four primary studies reported use of CRCs, two identified from the included reviews277,300 and two identified from additional searches for primary studies. 99,303 Of the four studies, one reported that significantly more intervention group families stored paraffin in containers with CRCs. 303 This study evaluated the effect of four home visits providing safety education on several injury mechanisms, with home safety inspections and provision of safety devices including childproof locks and CRCs. The remaining three studies evaluated interventions including safety education, safety equipment and home safety inspections, but no significant effects were reported for this outcome. 277,300
It was not possible to undertake PMA or NMA as the number of studies was small.
Promoting the possession and use of syrup of ipecac
Study H
The overview included one systematic review and meta-analysis33 and eight systematic narrative reviews36,40,332,338,383,387,388,445 reporting the effect of interventions on the possession and use of syrup of ipecac. The meta-analysis33 found evidence that education, with or without the provision of safety equipment, was effective in increasing possession of syrup of ipecac (OR 3.34, 95% CI 1.50 to 7.41).
Fifteen primary studies reporting possession or use of syrup of ipecac were identified from the included reviews. 265,271,273,274,279,282,287,292,293,300,308,309,420,437,441 Searches for additional primary studies identified no further eligible studies reporting this outcome. Eight of the 15 studies reported that significantly more families in the intervention group possessed or used syrup of ipecac. 271,279,282,292,293,300,308,420 Of the eight studies, two focused specifically on poisoning prevention. One evaluated the provision of counselling about poisoning treatment methods, a leaflet on poison prevention, a PCC number sticker and free syrup of ipecac with instructions delivered to parents during consultations at a children’s hospital emergency clinic. 308 The other assessed the impact of a community education programme aimed predominantly at school pupils and involving information on the risks of products, methods of poison prevention and the correct use of a poison centre. 420 The other six studies reporting a positive effect evaluated a home visit, safety inspection, educational materials and safety equipment including syrup of ipecac,271 safety equipment and safety counselling by a physician,279 home safety checks and a tailored education booklet plus assistance in locating and obtaining home safety devices,292 a tailored safety report generated by an interactive computer kiosk in a well-child clinic, information on safety equipment savings at a child safety centre and a feedback report for the paediatrician to encourage safety counselling,282 and multifaceted community programmes providing home safety inspections and education with the provision of safety items including syrup of ipecac300 or home safety inspections with the discussion of specific home safety issues. 293
The remaining seven studies evaluated interventions involving safety education, tailored safety education, the provision of syrup of ipecac and community programmes providing safety education, but reported no significant difference in the possession or use of syrup of ipecac favouring the intervention group.
Study I
Pairwise meta-analysis of 10 studies evaluating home safety education (including the provision of syrup of ipecac in some studies)265,271,273,274,282,287,293,300,308,309 found that interventions were effective in increasing syrup of ipecac possession (OR 3.34, 95% CI 1.50 to 7.44) (Figure 53). Interventions providing syrup of ipecac appeared to be more effective (OR 10.41, 95% CI 2.40 to 45.09) than those not providing it (OR 1.77, 95% CI 1.08 to 2.91). Interventions provided at home appeared to be more effective (OR 5.45, 95% CI 1.22 to 24.32) than those provided in clinical settings (OR 2.02, 95% CI 1.08 to 3.75).
FIGURE 53.
Forest plot of effect sizes for the possession of syrup of ipecac from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
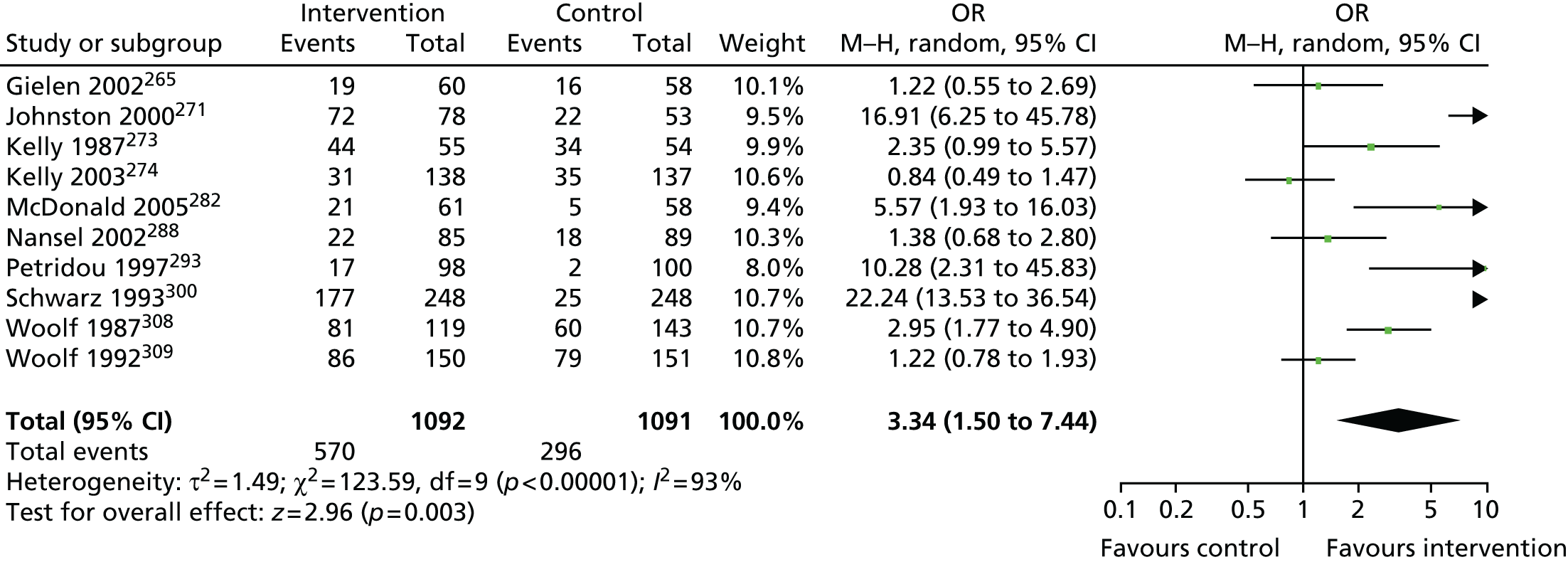
Network meta-analysis or decision analyses were not carried out for interventions to promote the possession of syrup of ipecac, as the use of syrup of ipecac by lay people has never been recommended in the UK and is no longer recommended for managing poisoning in children in the USA. 452
Promoting the use of poison control centre stickers and telephone numbers
Study H
The overview included one systematic review and meta-analysis33 and seven systematic narrative reviews36,40,42,338,387,388,445 reporting the effect of interventions on the use of PCC stickers and telephone numbers. The meta-analysis33 found evidence that education, with or without the provision of safety equipment, was effective in increasing the availability of PCC telephone numbers (OR 3.67, 95% CI 1.84 to 7.33).
Thirteen primary studies (11 identified from reviews257,263,269,274,287,293,295,308,309,413,441 and two identified from additional searches for primary studies288,431) reported the effect of interventions promoting the use of PCC stickers and/or telephone numbers. Six of the 13 studies reported a significant effect favouring the intervention group. 269,274,308,309,413,431 These studies evaluated safety education, the provision of PCC stickers and telephone numbers, home safety inspections and the Healthy Steps child development and behaviour programme, in which one intervention group received the Healthy Steps programme and another intervention group received the programme and antenatal home visits. The study found a significant effect only for the Healthy Steps programme compared with usual care. 413 The remaining seven studies did not report a significant improvement in the use of PCC stickers and telephone numbers in the intervention groups, having evaluated a range of interventions including education, tailored safety education, the provision of PCC stickers and home safety inspections.
Study I
Pairwise meta-analysis of nine studies evaluating home safety education (including the provision of PCC number stickers in some studies),269,274,287,288,293,295,308,309,431 which updated the meta-analysis reported in study H,33 found that interventions were effective in increasing the proportion of families who had the PCC number accessible (OR 3.30, 95% CI 1.70 to 6.39) (Figure 54). Interventions providing PCC stickers may be more effective (OR 4.44, 95% CI 2.08 to 9.49) than those not providing stickers (OR 2.66, 95% CI 0.93 to 7.67). Interventions delivered at home (OR 5.99, 95% CI 2.08 to 17.26) may be more effective than those delivered in clinical settings (OR 2.10, 95% CI 0.85 to 5.15).
FIGURE 54.
Forest plot of effect sizes for having a PCC sticker available from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
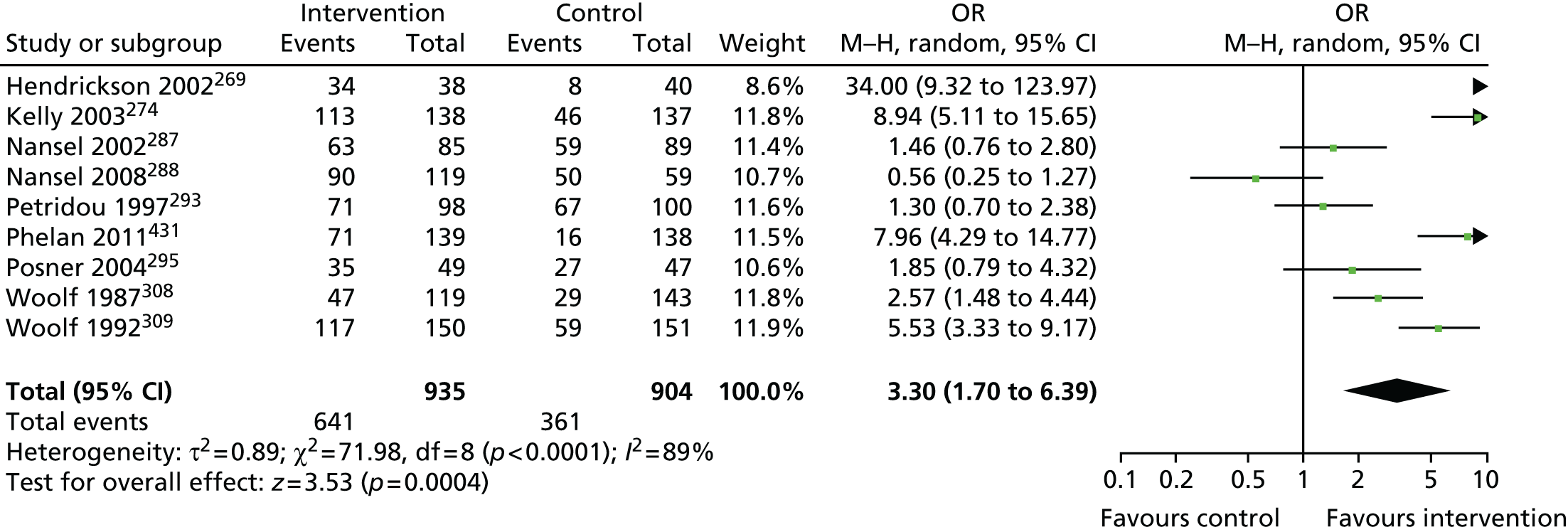
Study J
Network meta-analysis estimated the 21 possible pairwise comparisons between six interventions to promote having a PCC number available in 10 of the studies included in the PMA, as listed in Table 100. Interventions delivering education, low-cost or free equipment and home safety inspection were more likely to be effective in increasing possession of a PCC number (p best = 0.76; OR 38.82, 95% CrI 2.19 to 687.10) (Figure 55).
FIGURE 55.
Network meta-analysis and PMA results for interventions to promote having a PCC number available. Heterogeneity: between-study variance = 1.35 (95% CrI 0.328 to 3.709). Key: NMA results in black; PMA results in green. Interventions are displayed in the order that they were entered in the analysis. E, education; F, fitting; FE, low-cost/free equipment; H–H, head to head; HSI, home safety inspection; HV, home visit; NA, not applicable; Pbest, probability that intervention is the best; UC, usual care. From Achana et al. 449 under Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).
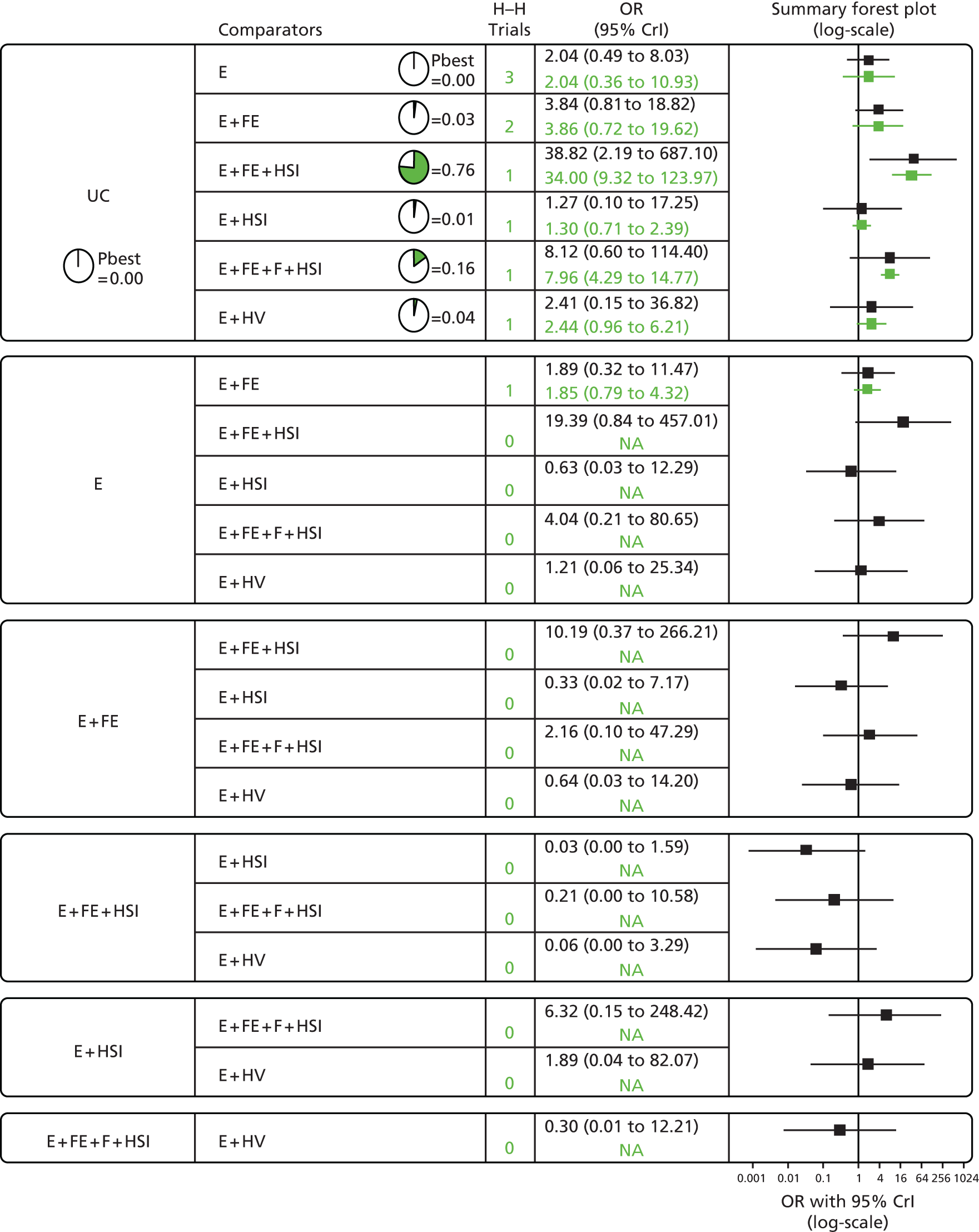
Study K
Decision analyses were not undertaken for interventions to promote having a PCC number available because the exposures studied in study A did not include having a PCC number available as PCCs are not provided for public use in the UK. Consequently, data were not available for decision analyses for this outcome.
Promoting other poisoning prevention practices
Study H
Twelve reviews33,36,42,332,334–336,338,383,387,388,445 reporting other poisoning prevention outcomes were included in the overview.
A total of 13 primary studies reporting other poisoning prevention practices were identified, nine from the reviews257,263,267,271,295,304,408,437 and four from additional searches for primary studies. 289,303,418,432 Of the 13 studies, two evaluated the effect of education, provision of safety equipment and home safety inspections on poisoning hazards scores, with both finding significant effects favouring the intervention group. 289,303 One reported a significant improvement in intervention group poison safety scores after a school safety fair408 and one observed significantly safer storage of beauty products and paraffin properly labelled and stored in tightly closed non-glass containers. 303 The remaining studies evaluated a range of interventions including community injury prevention programmes, safety education, tailored safety education and the provision of safety equipment, but reported no significant effects favouring the intervention groups.
Study I
Meta-analysis of three studies reporting storing plants out of reach,257 plants not being accessible295 or not having any toxic plants in the home304 found a lack of evidence that home safety education was effective in promoting the safe storage of plants (OR 1.18, 95% CI 0.40 to 3.48) (Figure 56).
FIGURE 56.
Forest plot of effect sizes for storage of plants out of reach from studies evaluating home safety educational interventions. M–H, Mantel-Haenszel. Originally published in Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, Hubbard SJ, Sutton AJ, Smith S, Wynn P, Mulvaney CA, Watson MC, Coupland C. Home safety education and provision of safety equipment for injury prevention. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD005014. http://dx.doi.org/10.1002/14651858.CD005014.pub3. 49
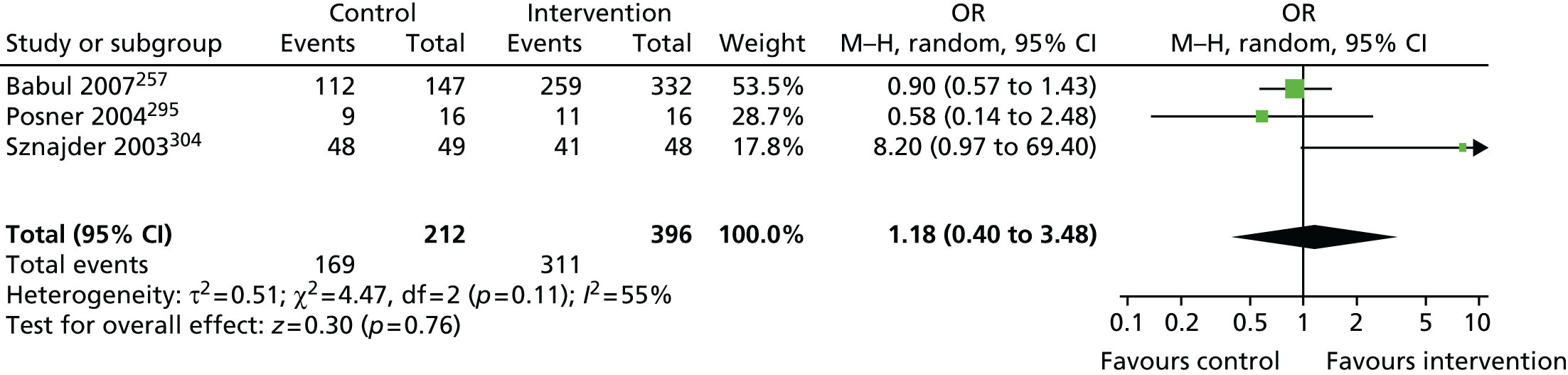
Study J
Network meta-analysis estimated the 10 possible pairwise comparisons between five interventions to promote the safe storage of poisonous plants in three studies as listed in Table 100. There was no evidence that any one of the interventions was more likely to be effective than the others in promoting safe storage of poisonous plants (Figure 57).
FIGURE 57.
Network meta-analysis and PMA results for the safe storage of poisonous plants. Heterogeneity: between-study variance = 1.00 (95% CrI 0.003 to 3.818). Key: NMA results in black; PMA results in green. Interventions are displayed in the order that they were entered in the analysis. E, education; FE, low-cost/free equipment; H–H, head to head; HSI, home safety inspection; NA, not applicable; Pbest, probability that intervention is the best; UC, usual care. From Achana et al. 449 under Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).

Study K
Decision analysis was not undertaken for interventions to promote the safe storage of plants, as none of the interventions in the NMA was any more effective than any other.
Discussion
Main findings
Fire-related injury prevention
There was a paucity of evidence relating to the impact of home safety interventions on the risk of fire-related injury or death. Most evidence related to the promotion of smoke alarms. A small number of case–control studies have demonstrated that households with smoke alarms have a lower risk of death and injury from house fires than households without smoke alarms. Narrative review- and PMA-level evidence demonstrated that interventions to promote smoke alarm ownership significantly increase the proportion of homes with a functional alarm, but there is a lack of evidence about whether or not these interventions reduce the risk of injury or death from house fires. NMA demonstrated that more intensive interventions [i.e. those including components that provided equipment (with or without fitting), home safety inspection or both in addition to education] were the most effective. The most effective intervention included education, the provision of low-cost/free equipment, fitting and home safety inspection. Ionisation smoke alarms with lithium batteries were most likely to be the best type of alarm for increasing possession of a functioning alarm. Data from the case–control studies identified in study H were used in the decision analysis for smoke alarms. The most effective intervention was not the most cost-effective. Decision analyses demonstrated that providing education and low-cost/free equipment was the most cost-effective intervention (£34,200 per QALY gained). The cost per QALY gained reduced to £4500 when it was assumed that there were 1.8 children aged < 5 years per household.
Evidence relating to the effect of other fire-prevention interventions was very limited. There was narrative review-level evidence and evidence from PMA of four studies that home safety interventions were effective in increasing the proportion of families having or practising a fire escape plan; however, NMA found no significant difference between interventions consisting of various combinations of education, home safety inspection, community campaigns and provision of safety equipment, and so the most effective type of home safety intervention remains unclear. There was some evidence from narrative reviews and PMA that home safety interventions may be effective in increasing the possession of fireguards, but, again, NMA found no significant difference between interventions including various combinations of education, home safety inspection and the provision and fitting of safety equipment, and so the most effective intervention remains unclear. There was no consistent review-, PMA- or NMA-level evidence that home safety interventions were effective in promoting the possession of fire extinguishers, the safe storage of matches or the checking or changing of smoke alarm batteries. There was review-level evidence from one narrative review that school-based education was effective in improving fire responses among children, and there was review-level evidence from one narrative review that two very different interventions (one multidisciplinary single-day programme and one course of cognitive–behavioural therapy) may be effective in reducing fire setting or match play.
Scalds prevention
There was a paucity of evidence relating to the impact of home safety interventions on the risk of scald-related injury or death. Most evidence related to the effect of interventions promoting having a ‘safe’ hot tap water temperature. Most, but not all studies, gave an explicit definition of a ‘safe’ temperature, but there was no consensus, with the criterion values ranging from ≤ 46 °C to ≤ 60 °C. There was evidence from narrative reviews and PMA that home safety interventions were effective in promoting having a safe hot water temperature. NMA demonstrated that education plus free or low-cost provision and fitting of TMVs was most likely to be effective. Decision analyses indicated that this was the most cost-effective intervention only if TMVs were provided as part of major refurbishment or new builds and to families living in social housing; otherwise, usual care or education was most cost-effective but with considerable uncertainty in the threshold range of £30,000–50,000 per QALY gained.
There was very limited evidence relating to the effect of interventions on promoting the safe handling of hot food or drinks. Narrative reviews and PMA did not demonstrate that home safety interventions were effective in promoting the safe handling of food or drinks. NMA found no significant difference between groups for interventions consisting of education, home safety inspections and the provision of safety equipment. There was no consistent narrative review-level evidence of the effectiveness of home safety interventions for promoting a range of other cooking safety practices or other scald prevention practices.
Falls prevention
There was a paucity of evidence relating to the impact of home safety interventions on the risk of fall-related injury or death. Most evidence related to the promotion of safety gate use and the reduction of baby walker use. Narrative review and PMA demonstrated that home safety interventions were effective in promoting safety gate use. NMA demonstrated that the most intensive intervention (education, equipment provision, fitting of safety equipment and home safety inspection) was most likely to be the most effective intervention. Decision analyses demonstrated that, at a threshold of £30,000 per QALY gained, usual care had the highest probability of being cost-effective. Findings were sensitive to the cost of the education package; when this was reduced to reflect a less intensive education package (e.g. a leaflet) while assuming that effectiveness was the same, usual care and education had similar probabilities (0.56 and 0.44, respectively) of being cost-effective at a threshold of £30,000 per QALY gained. Narrative review and PMA demonstrated that home safety interventions were effective in reducing baby walker use and NMA demonstrated that interventions that consisted of education only were the most effective. Decision analyses were not undertaken for interventions to reduce baby walker use as more complex analyses are required to take account of the potential protective effect of walkers on some types of falls, changes in risk of walker-related falls from changes to EU standards for baby walkers and some countries banning baby walker sales.
There was very limited evidence about the effect of other falls prevention interventions. Narrative reviews, PMAs and NMAs did not demonstrate that interventions to promote the use of window safety devices (locks, guards or devices to limit opening width) or those to prevent children being left on high surfaces were effective. Narrative reviews and PMA did not demonstrate that interventions to promote the use of non-slip bathroom products (mats, decals) were effective. There was no consistent narrative review-level evidence that interventions to promote the use of furniture corner covers or high-chair harnesses were effective, nor that other interventions to promote stairway safety or balcony safety or to reduce tripping hazards were effective.
Poisoning prevention
There was a paucity of evidence relating to the impact of home safety interventions on the risk of poisoning-related injury or death. PMA did not demonstrate that home safety interventions were effective in reducing poisoning rates based on the findings from four studies. Most evidence related to the effect of interventions on promoting the safe storage of medicines or household products. Narrative reviews and PMA demonstrated that home safety interventions were effective in promoting the storage of medicines out of reach of children. NMA demonstrated that education with the provision of low-cost or free equipment was the intervention most likely to be effective. Decision analyses demonstrated that, at a threshold of £30,000 per QALY gained, usual care had the highest probability of being cost-effective. Findings were very sensitive to the cost of the education package; when this was reduced to reflect a less intensive education package (e.g. a leaflet) while assuming that effectiveness was the same, education had the highest probability of being cost-effective at a threshold of £30,000 per QALY gained. Narrative reviews and PMA demonstrated that home safety interventions were effective in promoting the storage of household products out of reach. NMA demonstrated that, although the most intensive home safety intervention (education, low cost or free equipment, home safety inspection and fitting) was most likely to be effective, none of the interventions was significantly more effective than usual care. Decision analysis demonstrated that all interventions were more costly and less effective than usual care.
There was evidence from narrative reviews and PMA that home safety interventions were effective in increasing the proportion of families with a PCC number available. NMA demonstrated that interventions consisting of education, the provision of safety equipment and home safety inspections were more effective than other interventions. Decision analysis was not undertaken for this outcome as publicly available PCCs are not available in the UK. There was evidence from narrative reviews and PMA that home safety interventions were effective in promoting the possession of syrup of ipecac but, as the use of syrup of ipecac by lay people has never been recommended in the UK and is no longer recommended for managing poisoning in children in the USA,452 NMA and decision analyses for this outcome were not undertaken.
There was very limited evidence relating to interventions to promote other poison prevention practices. Narrative reviews and PMA did not demonstrate that home safety interventions were effective in promoting the safe storage of unspecified poisons, but NMA demonstrated that education plus low-cost or free equipment plus home safety inspections was more effective than other interventions in promoting this outcome. Narrative reviews, PMA and NMA did not demonstrate that home safety interventions were effective at promoting the safe storage of poisonous plants out of reach. There was no consistent narrative review-level evidence that home safety interventions were effective in promoting the use of CRCs or other poisoning prevention practices.
Strengths and limitations of the studies
Study H
Our series of overviews are the first to address the prevention of fire-related injuries, scalds, falls and poisonings in childhood. Our inclusion of primary studies published since the most recent comprehensive systematic review ensured that our overviews included the most up-to-date evidence. As we identified and examined all primary studies from the reviews included in the overview, this should limit bias arising from selective reporting of findings in reviews. Although our overviews focused on interventions that could be implemented in children’s centres in England and Wales, the findings should be more broadly generalisable to providers of community health and social care in other high-income countries.
There are several limitations to our overviews. The quality of the included studies was variable and for most outcomes there was a limited number of available studies. Studies showed wide variation in terms of the content of the intervention, population size, socioeconomic background, delivery method of the intervention and follow-up period. Many studies had small sample sizes and limited power. For multifaceted interventions it was not possible to determine which components were responsible for the observed effects. The interventions included in all overviews came almost exclusively from higher-income countries, therefore the findings are unlikely to be generalisable to low- and middle-income counties. The overview included non-legislative interventions, but legislative or regulatory interventions have been effective in preventing some injuries453 and it is possible that adding a legislative component to the education or engineering interventions that we reviewed may further enhance their effectiveness. Outcome reporting bias may have occurred because some primary studies reported insufficient data for relevant outcomes.
Study I
The update49 to the Cochrane review of home safety interventions33 is the largest and most comprehensive published review of home safety interventions to prevent a range of childhood injuries to date. It is the only published review in the field of child home injury prevention to obtain and use individual participant data. This has allowed inclusion of unpublished data from a number of studies in meta-analyses, helping to minimise outcome reporting bias and increase the power of meta-analyses. The small number of studies included in some of our analyses led to a lack of precision in effect size estimates. As discussed in the published review, the quality of included studies was very variable, and sensitivity analyses restricting analyses to RCTs indicated that most findings were robust to this. 49 However, some analyses were not robust to restricting analyses to studies with adequate allocation concealment, blinded outcome assessment or follow-up of at least 80% of participants, with smaller effect sizes seen in higher-quality studies. However, caution must be exercised in interpretation of these subgroup analyses because of the small number of studies in the subgroups. Many of our PMAs were found to have significant heterogeneity between effect sizes. This may have been partly because interventions providing safety equipment were more effective than those not providing safety equipment and interventions provided in the home or community were more effective than those provided in clinical settings. Significant heterogeneity often remained within subgroup analyses, highlighting the importance of the NMAs undertaken in study J, which allowed for much finer categorisation of interventions. As study I included a subset of studies included in the overviews, many of the limitations of the primary studies included in the overviews were also relevant to study I.
Study J
To our knowledge, study J represents the first NMA of interventions to prevent fire-related injuries, scalds, falls or poisonings at home in childhood. We have demonstrated the usefulness of NMA for comparing multiple injury prevention interventions and for teasing out the relative effectiveness of each, even when the number of studies evaluating the same comparison is small. NMA will also become increasingly useful as more studies are completed, as some of our effect size estimates lacked precision because of the small numbers of studies. As our NMAs characterise interventions more finely than previous PMAs, our findings are likely to be more useful for policy makers, service commissioners and providers when choosing between interventions.
As discussed in the published papers from study J, there was some inconsistency between direct and indirect evidence between studies comparing education with education plus the provision and fitting of equipment in the NMA for smoke alarms,374 but not in the other NMAs that we undertook. 446,449 We removed the single study that provided direct evidence comparing education with education and the provision and fitting of safety equipment to assess if this contributed to the inconsistency, but the ranking of which intervention was most effective remained unchanged. We also found considerable heterogeneity between studies in the NMAs for smoke alarms, window locks, not leaving children on high surfaces, having a PCC number available and the safe storage of poisonous plants and, because the numbers of studies were small, there was considerable uncertainty surrounding these estimates. Despite being able to more finely categorise interventions than in previous PMAs,33,37,40 some ‘lumping’ of interventions (and of control treatments) will still remain within categories. For example, some education-only interventions provide only leaflets, whereas others provide intensive face-to-face teaching sessions on home safety), but a lack of detail in the primary study reports about the interventions precluded further subcategorisation. In addition, the low-cost/free safety equipment provided in some studies may not have been relevant to the outcome concerned (i.e. equipment may have included socket covers and smoke alarms, which would not prevent fall injuries). We were able to explore this for the NMA for stair gates by splitting the equipment provision into relevant/not relevant or not stated, with findings similar to those of the main analysis.
As discussed for studies H and I, the quality of studies included in our analyses was variable. Restricting NMAs to RCTs only (as described in published papers374,446,449) produced similar findings to those reported above. We were unable to explore the effect of restricting analyses by other quality markers such as allocation concealment, blinding of outcome assessments or completeness of follow-up, as the number of studies included was too small. The other limitations of the studies included in studies H and I, as discussed above, are also relevant to study J.
Study K
The decision analyses undertaken for study K for interventions to prevent falls and poisonings are, to our knowledge, the first studies of this type to evaluate home safety interventions for the prevention of these injuries in the UK. Our decision analyses for interventions promoting the possession and use of smoke alarms and for interventions promoting a safe hot tap water temperature add to the very limited data in these two areas. There are a range of limitations to our decision analyses. Difficulties in categorising interventions and control conditions, as described in the previous section, also apply to the decision analyses. A range of assumptions was made in each decision analysis and, although we used sensitivity analyses to assess the impact of varying these assumptions, not all assumptions were able to be investigated. For example, there is some evidence that a child admitted to hospital with a burn or a poisoning is more likely to be admitted in the future with the same type of injury than with another injury,454 but our analyses did not take this into account. Social inequalities exist in the possession of items of safety equipment such as smoke alarms and safety gates455 in families with children aged < 5 years in the UK, and some interventions may be more cost-effective if targeted at particular groups, but our analysis did not take this into account. Throughout the decision analyses it was assumed that the probability of accepting an intervention by households was the same; however, lack of evidence meant that it was not possible to investigate the validity of this assumption. It is plausible that different interventions may have different probabilities of acceptance by households. For example, householders may be less likely to accept interventions that require house inspections as this may be seen as an intrusion on family life. Finally, data on injury treatment costs are country specific and hence our findings may not be generalisable to other countries with different health-care systems.
Economic evaluation has only recently been applied to public health interventions. 255,370,456,457 There are specific challenges to evaluating public health interventions including attributing the effects (intended and unintended) of the intervention on the target population, deciding which costs and consequences should be included, the acceptability of the intervention to a range of stakeholders and maintaining a balance between efficiency and equity of resource allocation. 458,459 In addition, particularly for public health interventions, a key issue relates to ‘who pays and who benefits’, as cost savings will vary when a wider societal perspective is taken. 140 The analyses presented here were conducted from a public sector perspective and included costs incurred by different stakeholders including the NHS, social services and the fire and rescue service, who are often responsible for home safety checks and the supply of smoke alarms. However, these analyses were limited to HRQL outcomes expressed in terms of QALYs. Future studies may want to consider both welfare and quality of life more broadly by adopting a cost–consequence approach371 or a multi-criteria decision-making approach. 459 Such an endeavour would need to consider thresholds carefully because it is unclear whether or not the same threshold (i.e. £30,000 per QALY gained) is relevant to different sectors of the economy beyond health care.
In terms of our analyses, estimates of the effectiveness of interventions have been based on data from the NMAs from RCTs, non-RCTs and CBA studies. These studies usually reported the effect of the intervention on intermediate outcomes such as the possession of safety equipment rather than on injury occurrence. The associations between intermediate outcomes and injury occurrence were therefore obtained from observational studies, including the case–control studies undertaken in study A. We acknowledge that there is greater potential for bias in observational studies than in RCTs and effect sizes obtained from RCTs may vary from those obtained from observational studies. We also attempted to minimise bias in the NMAs by restricting analyses to RCTs and findings were robust to these sensitivity analyses. There are several factors that our analyses did not take account of, which, had we done so, would be likely to increase the cost-effectiveness of the interventions. First, we did not take account of the lost productivity of more severely injured children, who will have many years to live with reduced productivity. Second, some interventions, such as smoke alarms and TMVs, will benefit all household members not just children aged < 5 years. Third, we did not take account of the long-term costs of care for disabled children, for example the costs of residential care. Fourth, we did not take account of the personal costs of caring for disabled children or the lost productivity of parents and other carers. Finally, our decision analyses assumed that interventions were aimed at preventing only one type of injury. However, in practice, interventions such as home safety equipment schemes provide education and fit equipment aimed at preventing a range of injuries. This means that costs such as set-up costs, travel costs and the cost of safety equipment fitters’ time used in our models will overestimate costs if interventions to prevent more than one type of injury are provided simultaneously. More complex decision analyses are required to incorporate costs and benefits across multiple interventions and injury types.
Comparisons with existing literature
Study H
In terms of the overviews, our findings are consistent with those of previous systematic reviews. 33–42,331–337 Our findings extend those of previous systematic reviews by including more recently published studies but, despite this, there is still a paucity of evidence that home safety interventions to prevent fire-related injuries, scalds, falls or poisonings in children aged < 5 years are effective in reducing injury rates, with only a small number of studies reporting these outcomes. Our overviews demonstrate that the body of evidence on the effectiveness of interventions to promote the possession and use of functional smoke alarms, safe hot tap water temperatures, the possession and use of safety gates and the safe storage of medicines and household cleaners out of reach and to reduce baby walker use is becoming stronger as more studies are published.
Study I
The findings of the PMAs build on the findings from the three previously published relevant reviews containing meta-analyses33,37,40 but are more positive than these in terms of the effect of home safety interventions on safety practices. The review and meta-analysis by DiGuiseppi and Roberts40 found that interventions delivered in a clinical setting were effective in promoting a safe hot tap water temperature, in increasing smoke alarm ownership and in increasing the safe storage of cleaning products. It concluded that clinical counselling had little effect on most home safety practices designed to childproof the home and there was limited evidence about the impact of counselling on childhood injuries. The review and meta-analysis by DiGuiseppi and Higgins37 found that interventions were effective in increasing functional smoke alarm ownership only when these interventions were delivered in clinical settings and there was a smaller effect size than we found. Our findings are likely to be more positive as we included a larger number of studies and obtained and used individual participant data, which allowed for analysis of previously unpublished data. In addition, some studies not included in the DiGuiseppi and Higgins37 review had large sample sizes312,460,461 and some studies for which we had individual participant data and which were not included in the DiGuiseppi and Higgins review demonstrated very positive effects for some outcomes. 269,295,304,312,431,462 As expected, our findings are consistent with the review and meta-analysis by Kendrick et al. ,33 as study I was an update of that review. The publication of new studies since the original review allowed meta-analyses to be undertaken for additional outcomes (e.g. fire escape plans) and strengthened the evidence for the effect of interventions to promote safety gate use and prevent baby walker use.
Study J
To our knowledge, there are no published NMAs comparing different interventions to prevent fire-related injuries, scalds, falls and poisonings in childhood with which to compare our findings. By categorising interventions more finely in our NMAs, we have been able to demonstrate the important elements of interventions that contribute to their effectiveness. Our NMA finding that more intensive interventions, all of which included the provision of free or low-cost safety equipment, were more effective than interventions consisting of education alone for the promotion of smoke alarms, safe hot water temperatures, safety gates and the storage of medicines and household products out of reach strengthens the evidence from previous meta-analyses suggesting that interventions providing free or low-cost safety equipment may be more effective than those not providing free or low-cost safety equipment. 37,418
Study K
We have only been able to find economic analyses of interventions to promote functional smoke alarm ownership347,463 and TMVs140 in a UK setting with which to compare our findings. The two smoke alarm studies evaluated the provision and installation of free smoke alarms compared with ‘no intervention’, based on the findings of one trial261 of a smoke alarm giveaway programme in disadvantaged areas in London, UK. The first found a higher number of injuries and deaths and higher costs in intervention areas and concluded that a smoke alarm programme as delivered in the trial was unlikely to be cost-effective. 347 The second, a decision analysis, was based on the findings from the first study but used an estimate of the relative risk of suffering injury from a fire at home for households without a smoke alarm compared with those with a functioning alarm from other studies (this was not estimated as part of the trial). The ICER was £23,046, suggesting that smoke alarm giveaway programmes were likely to be cost-effective at the threshold used by NICE of £30,000 per QALY. Our analyses of smoke alarms have extended those of the previous studies by assessing the cost-effectiveness of a range of interventions. We were able to do this by using effect size estimates for a range of interventions (i.e. ranging from usual care to multifaceted interventions including a combination of education, free or low-cost safety equipment, equipment fitting and home safety inspections) obtained from our NMAs. This has enabled us to establish the most cost-effective intervention and to show that, when analyses take account of the average number of children in households with children, education plus providing low-cost/free equipment is highly cost-effective with a cost per QALY gained of £4500.
In terms of TMVs, the previous economic evaluation was based on a trial that evaluated the provision of an educational leaflet with free fitting of a TMV in households with children aged < 5 years living in social housing in Glasgow, UK. This analysis assumed that TMVs were fitted as part of refurbishment or new builds as opposed to stand-alone interventions. The study found that TMVs were associated with a saving to the public purse of £1.41 for every £1 spent and concluded that fitting TMVs for families with young children in social housing as part of major refurbishment or new builds was very likely to represent good value for money. 140 Our decision analyses, which used some of the data from the same economic evaluation,140 also found that TMVs were very likely to be cost-effective if fitted in households with young children living in social housing as part of major refurbishment or new builds. The decision analyses extended the previous analyses by demonstrating that TMVs were very unlikely to be cost-effective if fitted under different circumstances.
How these findings inform other research within the Keeping Children Safe programme
The findings from studies H–K have been used to produce two IPBs as part of the KCS programme. These resources incorporate evidence on the effectiveness and cost-effectiveness of home safety interventions with best practice obtained from those running injury prevention programmes. The first IPB covered the prevention of fire-related injury. The provision of the IPB and a package to support its use was evaluated using a RCT (study M) described in work stream 6 of the KCS programme (see Chapter 7). The second IPB was produced at the end of the KCS programme of work and covered fire-related injuries, scalds, falls and poisonings. 464
Chapter 7 Multicentre cluster randomised controlled trial evaluating implementation of a fire-prevention injury prevention briefing in children’s centres (work stream 6)
Abstract
Research question
How effective and cost-effective is implementing an IPB for one exemplar injury prevention intervention?
Methods
Work stream 6 consisted of a review of reviews on implementation and facilitation of health promotion interventions (study L) and a RCT evaluating the effectiveness and cost-effectiveness of an IPB for the prevention of fire-related injuries (study M) with a nested economic analysis and qualitative study. The findings were incorporated into the development of a second IPB covering fire-related injuries, falls, poisonings and scalds.
Study M was a three-arm multicentre cluster RCT set in 36 children’s centres in Nottingham, Bristol, Norwich and Newcastle. Families with a child aged < 3 years were eligible to participate. Children’s centres were randomly allocated to one of three arms: IPB plus support (training and facilitation) (IPB+ arm), IPB without support (IPB-only arm) and control (usual care). IPB+ arm children’s centres were provided with training as well as facilitation contacts at 1, 3, 5 and 8 months. The intervention period was 12 months. The primary outcome measure was the proportion of families with a fire escape plan. Secondary outcomes included other fire safety behaviours and measures of IPB implementation, resource use and expenditure. Random-effects modelling was used to compare outcomes between treatment arms and for the economic analysis. Qualitative data were subject to thematic analysis.
Results
In study L, 10 reviews were identified. A number of common themes emerged about factors affecting the implementation of community prevention programmes. The review identified the Promoting Action on Research in Health Services (PARIHS) framework and Carroll et al. ’s fidelity framework, which informed intervention design and the measurement of fidelity and implementation.
Thirty-six children’s centres and 1112 families participated in study M. Follow-up data were obtained from all children’s centres and from 751 (68%) families.
The IPB was implemented by children’s centres in both intervention arms, with greater implementation in the IPB+ arm. Compared with control arm families, more IPB+ arm families received advice on key safety messages and more families in each intervention arm attended fire safety sessions. The intervention did not increase fire escape plan prevalence (AOR IPB only vs. control 0.93, 95% CI 0.58 to 1.49; AOR IPB+ vs. control 1.41, 95% CI 0.91 to 2.20) but did increase the proportion of families reporting more fire escape behaviours (AOR IPB only vs. control 2.56, 95% CI 1.38 to 4.76; AOR IPB+ vs. control 1.78, 95% CI 1.01 to 3.15). IPB-only arm families were less likely to report children playing with matches or lighters (AOR 0.27, 95% CI 0.08 to 0.94) and reported more bedtime fire safety routines (AOR for a 1-unit increase in the number of routines 1.59, 95% CI 1.09 to 2.31) than control arm families. The IPB-only intervention was less costly and marginally more effective than usual care, whereas the IPB+ intervention was both more costly and marginally more effective than usual care.
Conclusions
Neither intervention was effective at increasing the proportion of families with a fire escape plan, but both IPB+ and IPB increased the delivery of fire safety messages by children’s centres and improved some fire prevention behaviours by families.
Chapter summary
Work stream 6 consisted of a review of the literature on the implementation and facilitation of health promotion interventions (study L) and a RCT set in children’s centres that evaluated the effectiveness of an IPB for the prevention of fire-related injuries (study M). The RCT also contained a nested cost-effectiveness analysis and a qualitative study evaluating the implementation of the IPB. Work stream 6 also contained the final phase of the KCS programme of research, in which the findings from studies A and studies D–M were used to inform the development of a second IPB for the prevention of fire-related injuries, falls, poisonings and scalds.
Introduction
Fires are an important cause of morbidity and mortality in childhood. The UK has one of the highest mortality rates among high-income countries for deaths from fire and flames in children aged 0–14 years. 465 In 2011–12, English fire and rescue services attended > 44,000 house fires, which resulted in 21 child deaths, with a further 35 children injured for each fatality. 377 Deaths from fire and flames show the steepest social gradient of all injuries. 13 In England and Wales, children whose parents have never worked or are long-term unemployed have death rates from exposure to smoke, fire and flames that are 38 times higher than those of children whose parents have managerial/professional occupations. 13
Some interventions are effective at reducing the risk of fire-related injuries and promoting fire prevention practices. Use of smoke alarms reduces the risk of death in house fires. 50,425 Education, with or without safety equipment being provided, is effective at increasing the prevalence of functioning smoke alarms37,49 and home safety education increases the prevalence of fire escape planning. 49 Despite this, there is little evidence of systematic implementation of such injury prevention in the NHS,19 and it is unlikely that this is any different in the social care or the voluntary sectors. A national survey of children’s centres undertaken in work stream 3 (study D) of the KCS programme (see Chapter 4) and a systematic review (study E) undertaken in work stream 4 (see Chapter 5) identified the main barriers to, and facilitators of, implementing injury prevention interventions. These included the type of approach used (one-to-one, group work, partnership working, tailored methods), the characteristics of the deliverer, complexity of the intervention, resources, accessibility to safety equipment and importance of achieving behavioural change. 217,252 It is therefore important that interventions to promote injury prevention take these barriers and facilitators into account.
As described in work stream 4, children’s centres provide community-based integrated services, information and support for families with young children. They aim to improve outcomes for young children and their families, with a particular focus on the most disadvantaged, to reduce inequalities in health. 210,466 They have a remit to promote child safety and the potential to reach a population at particular risk of fire-related injury. We therefore developed a fire prevention intervention for use in children’s centres. This was based on evidence gathered in previous work streams in the KCS programme and consisted of an IPB for children’s centres and a training and facilitation package to support implementation of the IPB. The IPB combined evidence on the effectiveness of fire safety interventions with best practice from those who had experience of running injury prevention programmes. The five key messages in the IPB were:
-
the importance of smoke alarm use and maintenance
-
having a family fire escape plan
-
identifying potential causes of house fires
-
the safe storage of matches and lighters
-
having a bedtime fire safety routine.
Methods
The methods are described in full in the published protocol467 and summarised in the following sections.
Objective
The objective was to evaluate the effectiveness and cost-effectiveness of an educationally based intervention (IPB) with or without facilitation as a means of changing the behaviours of families and children’s centre staff to improve fire safety in the home.
Design
We undertook a three-arm multicentre cluster RCT with an economic analysis and a nested qualitative study set in children’s centres in four trial sites in England (Nottingham, Bristol, Norwich and Newcastle). A cluster RCT was appropriate because the intervention was delivered at the level of the children’s centres and individual allocation of families living in close proximity could lead to contamination.
Participants
Children’s centres
Children’s centres were established in phases. Phase 1 (2004–6) targeted the 20% most deprived wards in England and phase 2 (2006–8) included the 30% most deprived wards and expanded into some of the 70% less deprived communities. Phase 3 (2008–10) extended to all remaining areas. 468 Phase 1 and phase 2 children’s centres were eligible to participate, with priority given to phase 1 centres. Children’s centres were recruited by postal invitation, followed by a telephone call and introductory recruitment visit. Children’s centres provided written informed consent to participate.
Families
Families living in the catchment areas of children’s centres with a child aged < 3 years who had attended the children’s centre in the preceding 3 months were eligible to participate. Families in which a parent was aged < 16 years were excluded.
Families were recruited using a range of strategies including postal invitation and face-to-face invitation by children’s centre staff or researchers. They provided written informed consent and were considered recruited to the trial on receipt of a completed consent form and baseline questionnaire.
Intervention
The intervention consisted of an IPB and a training and support package to facilitate its implementation. The intervention was developed using the UK MRC guidance for the development and evaluation of complex interventions469 and included the following stages:
-
Identifying the evidence base. Evidence about the effectiveness of interventions was ascertained from preceding work in the KCS programme. This included systematic reviews of interventions to prevent injuries from house fires (study H) in work stream 549,374 (see Chapter 6) and a systematic review of facilitators of and barriers to home injury prevention interventions for preschool children (study E)252 in work stream 4 (see Chapter 5). Evidence about the design, content and delivery of the intervention came from several sources. These included the Health Development Agency’s Effective Action Briefing for putting evidence into practice for the promotion of domestic smoke alarms470 and a review of reviews of the literature on the implementation and facilitation of health promotion interventions undertaken as preliminary work for this trial (study L). The objectives of the literature review were to determine factors affecting implementation of health promotion programmes, identify frameworks to assist in the measurement of the implementation process and consider the application of this information to the design of the intervention for work stream 6. Ten key reviews were identified. 248,249,251,471–477 The reviews found that careful implementation of programmes enhanced outcomes and the level of implementation achieved was an important determinant of programme outcomes. A number of common themes emerged about factors affecting the implementation of community prevention programmes. Four reviews had convergent findings for 11 explanatory factors, including funding, a positive work climate, shared decision making, co-ordination with other agencies, formulation of tasks, leadership, programme champions, administrative support, providers’ skill proficiency, training and technical assistance. 248,251,475,476 One framework identified, the PARIHS framework,478 was used to guide the design and evaluation of the facilitation package and another, Carroll et al. ’s472 fidelity framework, was used to measure the fidelity of the intervention. The PARIHS framework provides three interacting core elements of evidence, context and facilitation and Carroll et al. ’s472 framework informs the measurement of fidelity in terms of adherence to an intervention, exposure or dose, quality of delivery, participant responsiveness and programme differentiation.
-
Identifying appropriate theory. The intervention was developed based on five behavioural change theories (health belief model, social cognitive theory, theory of reasoned action, theory of self-regulation and self-control, and theory of subjective culture and interpersonal relations) identified from a review of behaviour change theories for injury prevention. 479 Our intervention aimed to address the three factors described as necessary and sufficient for producing a behaviour change by helping participants (both children’s centre staff and families) to form intentions to change behaviour and remove environmental barriers, and providing participants with the knowledge and skills to perform the behaviour.
-
Modelling processes and outcomes. We undertook stakeholder interviews with people who had a national insight into both the policy framework within which children’s centres operated and the overarching operational issues to provide an understanding of the context within which the trial was set. We undertook four workshops, one in each trial site, which provided a mix of large and medium-sized urban locations as well as more rural settings. Workshop delegates included local practitioners and policy makers, including children’s centre managers and staff, fire and rescue services, NHS staff and commissioners of children’s services. Workshops ensured that the IPB and the training and facilitation package complemented and recognised existing fire-prevention initiatives, built on existing knowledge about implementation in children’s centres and how to reach families in the community, and provided input from potential end users and those with specialist expertise in implementation. A postal survey from study D in work stream 3 (see Chapter 4)217 and interviews with children’s centre managers and staff (study F) in work stream 4 (see Chapter 5) gave information about current injury prevention activity, barriers to, and facilitators of, injury prevention activity and the context within which children’s centres operated. Interviews with parents of injured and uninjured children (study G) in work stream 4 (see Chapter 5) provided us with information about parents’ barriers to, and facilitators of, home injury prevention. In addition, we undertook structured interviews with 200 parents from children’s centres in the four study centres to understand their current injury prevention activity, determine their understanding and use of fire escape plans and estimate the prevalence of fire escape plans and the ICC for fire escape plans. The questionnaire is shown in Appendix 6, Parents’ survey for measuring the prevalence of fire protection practices and the methods for this are described in full in the associated publication. 480 As a result of the findings in relation to the prevalence of working smoke alarms, the proposed primary outcome measure for the trial was changed to having a fire escape plan, as described in Definition of primary and secondary outcome measures. A composite secondary outcome measure describing five key component elements of a fire escape plan using latent variable analysis was also developed.
Allocation to the intervention and delivery of the intervention
Once the required number of families for each children’s centre had been recruited, children’s centres were stratified by trial site (four strata: Nottingham, Bristol, Norwich and Newcastle) and randomly allocated within strata to one of three arms using permuted block randomisation with a block size of 3. The allocation schedule was produced by an independent statistician using the randomisation algorithm in Stata/SE version 11 and was provided to an independent administrator who prepared sequentially numbered sealed opaque envelopes (one set for each of the four trial co-ordinating centres) containing allocations. Children’s centres were randomised in trios; once each stratum contained three children’s centres, the administrator opened envelopes for each block of three children’s centres.
The three trial arms consisted of:
-
IPB plus facilitation (IPB+ arm)
-
IPB without facilitation (IPB-only arm)
-
usual care (control arm).
The intervention was delivered over a period of 12 months. Children’s centres in the IPB+ arm were provided with the IPB, a training session (immediately before the start of the 12-month intervention period) and a facilitation package, described later in this section.
The IPB contained information:
-
for managers on why preventing fire-related injuries is important, who the target group is, what effective interventions can be provided, creative ways of reaching the target group and how to evaluate use of the IPB
-
for staff on why preventing fire-related injuries is important, who is at greatest risk, the main causes of house fires, what staff can do to help, what works to prevent house fires, where to get specialist advice and help and activities for use with parents, including session plans and resources covering five key messages (use of smoke alarms, fire escape plans, causes of house fires, children’s development and risk of house fires and bedtime safety routines).
Children’s centres were asked to deliver the fire prevention messages to participating families using the format that they considered most appropriate to their target audience. If they were unable to deliver all five messages, they were asked to focus on use of smoke alarms and fire escape plans, as these have the strongest evidence base. The IPB is provided in Appendix 6, Injury prevention briefing 1.
Children’s centres were provided with a training session prior to commencing delivery of the intervention. The aims of the training were to ensure that key staff:
-
were familiar with the IPB and confident about its authority, reflecting how it had been developed
-
understood the information that it contained
-
felt confident about delivering the key safety messages to parents
-
were aware of the support that the local fire and rescue service was able to offer to staff and parents
-
understood their obligations as part of the trial and the support that the local research teams would be providing.
The training was participative in nature and started with injury epidemiology and why children are at risk of injuries and progressed to the content of the IPB and how to use the IPB. The training allowed people to try out an exercise from the IPB and to ask for further information. Training was led by the same person from the Child Accident Prevention Trust in conjunction with local research teams and the local fire and rescue services. When the detailed content of the IPB was introduced to participants, it was stressed that it was the key messages that they needed to present to parents. The exercises in the IPB were seen as one means of doing this, but centres were given the freedom to choose how best to deliver the key messages, having regard for the way that they interact with parents (e.g. group sessions, outreach, one-to-one opportunities, displays). The final part of the training programme (‘Using the IPB as effectively as possible’) was key to ensuring that children’s centres developed and implemented a plan for delivering the IPB. A draft implementation plan was provided, and this was incorporated into the facilitation package to enable researchers to assess progress with implementing the IPB.
The training session was piloted with nine staff covering a range of roles and seniorities from two children’s centres that were not participating in the trial. Piloting led to several small changes in the programme. Training was provided at venues away from children’s centres. To ensure consistency of training, the content of the presentations and discussions was monitored and recorded by the research teams. The training was evaluated by a questionnaire (shown in Appendix 6, Injury prevention briefing training evaluation questionnaire) completed by delegates at the end of the session.
The facilitation package consisted of the training plus contacts at months 1, 3 and 8. These used a two-stage approach with a postal or electronic questionnaire followed by a face-to-face or telephone interview, depending on progress with implementing the IPB. A fourth contact was made at months 4–5 if there was no progress with implementation of the IPB at month 3. The facilitation contacts collected information on progress with implementing the IPB, addressed children’s centre staff questions and discussed barriers to implementation, gave advice and examples of good practice from other centres and provided a resource list and list of contacts for other organisations. The facilitation package was designed to be similar to the advice and support that might be provided by an injury prevention co-ordinator (as recommended in the NICE guidance on injury prevention25).
Children’s centres in the IPB-only arm were mailed the IPB and covering letter encouraging them to use the IPB. They were not provided with any training or facilitation. Children’s centres in the usual-care arm were asked to continue to provide their usual information on home safety. The IPB was posted to usual care arm children’s centres after collection of post-intervention data.
Outcome measures
Outcome measures were ascertained at 12 months’ follow-up, defined as 12 months post commencement of the intervention in the IPB+ and IPB-only arms and 12 months post randomisation in the usual-care arm.
Definition of primary and secondary outcome measures
The primary outcome was the proportion of families reporting having a fire escape plan. The primary outcome measure for the trial described in the original proposal was possession of a functional smoke alarm. However, the findings from the structured interviews with parents attending children’s centres as part of the preliminary work for the trial indicated that the reported prevalence of functional smoke alarms was high (91%; see Table 108), thus precluding the use of this as the primary outcome measure. This was therefore changed to families having a fire escape plan because the systematic reviews (studies H and I) in work stream 5 indicated that there was more evidence that interventions could be effective at increasing fire escape planning than evidence for other fire safety behaviours.
Secondary outcome measures included:
-
family participants:
-
the proportions of families with more and fewer fire escape behaviours using a binary measure derived from five component items shown in Table 110
-
the proportion of families with smoke alarms fitted and working on every level of their home
-
the proportion of families reporting fire setting or match play by their children
-
a bedtime fire safety routine score consisting of 10 items (see Table 116)
-
the proportion of families accessing smoking cessation services
-
the number of correct responses to fire safety knowledge questions
-
the proportion of families satisfied with the home safety information provided by children’s centres
-
implementation of the IPB assessed by:
-
the proportion of families receiving advice on each of the five key messages
-
the proportion of families attending a fire safety session
-
the number of fire safety sessions attended
-
the proportion of families attending a fire safety session at a children’s centre
-
the proportion of families attending sessions about each of the five key messages
-
-
families’ resource use and expenditure in relation to fire safety practices
-
-
children’s centres as participants:
-
the proportion of children’s centres providing information and advice on the topics of the five key messages
-
resource use and expenditure incurred in relation to fire safety practices
-
implementation of the IPB assessed by:
-
the proportion of children’s centres with an implementation plan (IPB+ and IPB-only arms)
-
the month at which the implementation plan was finalised (IPB+ arm only)
-
the proportion of children’s centres using each of the five exercises in the IPB (IPB+ and IPB-only arm)
-
the proportion of children’s centres using methods other than the IPB sessions to deliver the five key messages (IPB+ and IPB-only arms)
-
the number of fire safety sessions provided (all three arms)
-
the number of parents exposed to IPB sessions (IPB+ and IPB-only arms).
-
-
barriers to, and facilitators of, children’s centres implementing the IPB (IPB+ and IPB-only arms) and barriers to, and facilitators of, injury prevention work (all three arms).
-
Ascertainment of outcomes
Outcomes were ascertained using a range of tools as summarised in Table 104 and described in the following sections.
| Data collection toola | IPB+ arm | IPB-only arm | Usual-care arm |
|---|---|---|---|
| Data collected from families | |||
| Baseline self-completion questionnaire | |||
| Follow-up self-completion questionnaire | |||
| Data collected from children’s centres | |||
| Baseline manager/staff questionnaire | |||
| Follow-up manager/staff questionnaire | |||
| Facilitation contacts questionnaire at 1, 3, 4/5 and 8 months | |||
| Facilitation contacts interview at 1, 3, 4/5 and 8 months | |||
| Activity logs | |||
| Follow-up facilitation and implementation fidelity questionnaire | |||
| Follow-up facilitation and implementation fidelity interview | |||
Ascertaining family outcomes
The baseline self-completion questionnaire included questions on sociodemographic and economic characteristics, household information, previous fire-related injuries, fire safety behaviours and fire safety equipment, knowledge and understanding of what causes fires, home safety information provided by children’s centres and satisfaction with this information (see Appendix 6, Baseline self-completion questionnaire for parents). Questions on fire safety behaviours and fire safety equipment were developed from the structured interviews of parents undertaken to inform the trial. 480 The questionnaire was piloted on families attending children’s centres that were not taking part in the trial.
The baseline questionnaire was adapted for follow-up by adding questions on resource use and expenditure incurred (see Appendix 6, Follow-up self-completion questionnaire for parents). A shorter version of the questionnaire was used for reminders, with up to two reminders used. Questionnaires were administered by post, telephone or face to face. Families who completed a questionnaire were provided with a £5 gift voucher. 69,70
Ascertaining children’s centre outcomes
Postal questionnaires were used to collect information from children’s centre managers or staff on the promotion of fire prevention activity (see Appendix 6, Baseline manager/staff questionnaire). Questions were based on those used in the national survey of injury prevention activity among children’s centres in England undertaken in work stream 3 (study D)217 (see Chapter 4). Questions on resource use were added to follow-up questionnaires (see Appendix 6, Follow-up manager/staff questionnaire). The baseline questionnaire was piloted on 10 children’s centres across England that were not taking part in the trial.
Data for assessing implementation of the IPB were obtained from facilitation contacts questionnaires and interviews (e.g. time at which an implementation plan was finalised) in the IPB+ arm, from the 12-month follow-up implementation fidelity questionnaires and interviews (e.g. having an implementation plan, providing sessions on the five key messages, barriers to and facilitators of implementing the IPB) in the IPB+ and IPB-only arms and from activity logs (data on parents’ attendance at sessions) from all arms. The questionnaires and interview schedules for facilitation contacts are given in Appendix 6, Facilitation contacts questionnaires and Facilitation contacts interview, respectively.
The implementation fidelity questionnaire and interview schedule were based on Carroll et al. ’s472 framework, the review of the literature on the implementation and facilitation of health promotion interventions (study L), the systematic review of barriers to and facilitators of home injury prevention undertaken in work stream 4 (study E),252 findings from the national survey of children’s centre managers and staff undertaken in work stream 3 (study D)217 and interviews with children’s centre managers and staff undertaken in work stream 4 (study G). Questionnaires were administered to, and interviews undertaken with, managers and/or staff responsible for the delivery of the IPB in the IPB+ and the IPB-only arms. Interviews covered the topics outlined in Carroll et al. ’s472 implementation fidelity framework: adherence to the intervention; exposure or dose (whether or not the frequency and content of the fire safety messages were delivered as planned); quality of delivery (how staff perceived the quality of the fire safety messages that were delivered); participant responsiveness (whether or not families were fully engaged with the intervention); and programme differentiation (elements of the intervention that were considered essential for fire safety). They also contained questions about children’s centre staff experiences of IPB implementation, including barriers and facilitators and suggested improvements to the IPB. The 12-month follow-up facilitation and implementation fidelity questionnaire and interview schedule are shown in Appendix 6, 12-month follow-up facilitation and implementation fidelity questionnaires and 12-month follow-up facilitation and implementation fidelity interview schedules, respectively.
Sample size
Eleven children’s centres per arm were required to detect an absolute difference in the percentage of families with a fire escape plan of 20% in either of the two intervention arms compared with the usual-care arm. This was based on 80% power and a 5% significance level (two sided), and assumed a usual-care arm prevalence of 42% and an ICC of 0.05 (ascertained from structured interviews with families attending children’s centres in the four trial sites480) and that outcomes were assessed on 20 families per children’s centre. In total, 33 children’s centres were required, which was increased to 36 to allow for potential dropouts. Allowing for 33% loss to follow-up among families, 30 families per children’s centre (total 1080) were required.
Blinding
It was not possible to blind children’s centre managers and staff, researchers providing the facilitation package or families to treatment arm allocation. When parents required support from a researcher to complete the follow-up questionnaire, or when questionnaires were completed by telephone, researchers were not blinded to treatment arm allocation. Quantitative analyses were undertaken blind to treatment arm allocation for the primary and secondary outcomes but not for the economic analysis.
Withdrawals
Participants were free to withdraw from the trial at any stage, but their data were included up to the date of withdrawal.
Analysis
This section describes the quantitative analysis for the primary and secondary outcomes followed by the health economic analysis and the qualitative analysis.
Baseline characteristics are described informally by treatment arm. All analyses of primary and secondary outcomes were conducted on an intention-to-treat basis in that families and children’s centres were analysed in the arm to which they were randomised. Quantitative analyses for the primary and secondary outcomes were undertaken using Stata versions 11 and 13.
Primary outcome measure
The proportion of families reporting a fire escape plan was compared between treatment arms (IPB+ vs. usual care and IPB only vs. usual care, with a significance level of 0.05 for each comparison) using random-effects logistic regression, including children’s centre as a random effect. The model included randomisation stratum as a fixed effect and adjusted for two cluster-level variables (lead agency of the children’s centre and Office for Standards in Education (Ofsted) report scores for overall effectiveness) and two family-level variables (having a fire escape plan at baseline and IMD 2010 score65). Subgroup analyses explored differential effects of the intervention by IMD score by adding interaction terms to the regression model. The ICC was estimated using one-way ANOVA.
Secondary outcome measures
Family-level outcome measures
Binary outcomes were compared between treatment arms (IPB+ vs. usual care and IPB only vs. usual care) using random-effects logistic regression, and ordinal outcomes were compared between treatment arms using random-effects ordinal regression, with regression models including children’s centre as a random effect. Models included randomisation stratum as a fixed effect and adjusted for lead agency of the children’s centre, Ofsted report scores for overall effectiveness, baseline value of the secondary outcome measure and IMD score.
Children’s centre-level outcome measures
The provision of information and advice on the five key IPB messages, provision of fire prevention sessions for families and use of methods other than the IPB were described by treatment arm. Quantitative comparisons were not made because of the small numbers.
Barriers to and facilitators of children’s centres implementing the IPB were coded and categorised and described for the IPB+ and IPB-only arms.
Missing data
The main analysis was a complete-case analysis. Sensitivity analyses were undertaken for the primary outcome and included multiple imputation assuming that data were missing at random and analyses assuming no change in the primary outcome compared with the baseline value in families lost to follow-up. 481 Fifty data sets were imputed and combined using Rubin’s rules. 77 The imputation model included all variables in the model for the main analysis plus baseline variables, which were age of youngest child, number of children in the family, maternal age, accommodation type, housing tenure, ethnic group, number of adults in the household, number of smokers and whether or not there is a heavy drinker in the household. English as a first language was not included as a variable in the multiple imputation model because of problems with perfect prediction. Cluster number (as a categorical variable) was not included as a variable in the imputation model as the imputation model would not converge when it was included, but the multilevel logistic model run on the imputed data set took clustering into account.
Health economic analysis
The cost-effectiveness analysis of the trial utilised the primary effectiveness end point – whether a family reported having a fire escape plan – and the economic end point of total cost of the intervention. A summary of the base-case analysis is provided in Table 105 and includes the items recommended by the Consolidated Health Economic Evaluation Reporting Standards (CHEERS)482 when reporting economic evaluations of health interventions.
| Description | Base-case analysis |
|---|---|
| Type of evaluation | Prospective cost–utility analysis alongside a cluster RCT |
| Time horizon | 1 year |
| Perspective | Societal |
| Comparators | Usual care, IPB only and IPB+ |
| Cost categories | Children’s centre; fire and rescue service; other agencies including local councils; family |
| Base year for calculating costs/prices | 2012 UK£ |
| Analytical methods | Hierarchical model allowing for clustering and adjusting for the baseline covariates included in the primary effectiveness analysis |
| Outcome | Cost per additional fire escape plan |
Data on the effectiveness end point – whether a family reported having a fire escape plan – were extracted from the parent 12-month follow-up questionnaires.
Resource use and cost data were obtained from three different sources:
-
trial site (i.e. Nottingham, Norwich, Newcastle and Bristol) researchers’ logbooks, which were used to record all of the activities relating to IPB implementation and, when applicable, facilitation
-
children’s centre follow-up questionnaires detailing their fire safety activities
-
parent 12-month follow-up questionnaires, which provided information about the resources and costs related to fire safety sessions that they attended and home safety inspections undertaken at their homes.
The cost-effectiveness analysis was conducted from a societal perspective and included costs incurred by children’s centres, fire and rescue services and other agencies that provide home safety advice/inspections such as local councils and family costs. Costs were analysed at the family level. To achieve this, the trial site and children’s centre-level costs were averaged equally across families randomised within each trial site and cluster, respectively, and then combined with the family-level costs to give a total cost per family.
As the inverse of the difference in probabilities of having a fire escape plan, say between IPB only and usual care, is equal to the number needed to treat (NNT), the cost-effectiveness ratio can be interpreted as the cost per additional fire escape plan under the intervention. The cost per additional fire escape plan (i.e. the primary outcome) was estimated for the IPB-only and IPB+ facilitation arms of the trial compared with the usual-care arm. In addition, the cost of developing the IPB was estimated from developers’ logbooks, but was not incorporated into the cost-effectiveness analysis as this is a fixed one-off cost that would not be encountered again if this intervention was implemented in practice.
The economic analysis was carried out with the family as the unit of analysis, and had to take account of the clustered nature of the trial design (i.e. randomisation was at the children’s centre level),483 adjusting for the baseline covariates included in the primary effectiveness analysis. Additionally, the clinical and economic end points may themselves be correlated within families as well as within children’s centre clusters, thus the analysis needed to simultaneously allow for this. Methods for such an analysis have recently been reviewed and compared484 (although they have rarely been used in practice), and guidance for good practice has been written. We adopted a random-effects modelling approach485 that extended the random-effects model used to analyse the effectiveness data on their own, as described above. A further complicating factor was that our effectiveness outcome (proportion of families reporting having a fire escape plan) was dichotomous, unlike many cost-effectiveness analyses for which both effectiveness and cost outcomes are continuous and often assumed to be multivariate normal. 485 Multivariate methods for analysing a mixture of continuous and dichotomous outcomes have been developed486 including approaches that allow for clustering. 487 We approached this complication by a factorisation of the model likelihood for costs and effects into the product of a marginal and conditional likelihood (continuous for costs and logistic for effects). 486,488 Such a factorisation also allowed the specification of distributions other than normal for the costs and, following a preliminary examination of the cost data, which were heavily (right) skewed, it was decided to model total costs at the family level using a gamma distribution (which has been advocated in the literature). 489 This required adding £1 to each family cost for the analysis and then subtracting £1 from the results.
To construct an appropriate but somewhat ‘non-standard’ model we used WinBUGS488 software, which allows great flexibility in model specification and estimates model parameters using MCMC methods. 488 An algebraic outline of the model is provided in Appendix 6, Statistical appendix and the associated WinBUGS code is available from the authors on request.
For the estimated model parameters, we report means, SEs and 95% CrIs, taken as the medians, SDs and 2.5–97.5% centiles from the samples of the posterior distributions. Cost-effectiveness acceptability curves were calculated by estimating the probability that the intervention was cost-effective for each value of the ceiling ratio (this is the value of the willingness to pay per additional fire escape plan) from the posterior distributions. The results tables present IPB only and IPB+ compared with usual care (but not compared with each other) to be consistent with the effectiveness analysis presented. However, the cost-effectiveness acceptability curves give the probability of each comparator being the most cost-effective for a range of willingness-to-pay thresholds and intrinsically compare all comparators simultaneously, which facilitates identification of the optimal intervention.
As a sensitivity analysis to check the robustness of the findings to missing data, a multiple imputation analysis was conducted. Following the same method as for the effectiveness imputation analysis described earlier, we extended the imputation model to include the four cost components (listed in Table 127), which sum together with the intervention costs (excluded from the imputation model because of no missing data) to produce the total overall cost per family. Because of non-normality of the cost component variables, predictive mean matching was used for imputation as well as for IMD score (as opposed to regression-based estimates for the other variables). As data analysis was carried out using MCMC in WinBUGS, it was not practical to perform 50 imputations (as performed for effectiveness); instead, 10 imputations were conducted and combined using Rubin’s rules77 as before.
Qualitative analysis
Data from the facilitation contacts were analysed manually using content analysis after categorisation into main subheadings256 followed by a thematic analysis. Data from the implementation fidelity interviews were subject to framework analysis490 using the NVivo 10 software package (QSR International, Warrington, UK). A priori themes were identified that reflected the structure of questions within the 12-month follow-up facilitation and implementation fidelity interview schedules.
Initial analysis was carried out by two researchers who identified levels of implementation and emergent major and minor themes through cycles of coding. Levels of implementation were described based on recommendations for use contained in the IPB and the four elements of ‘adherence’ in the ‘implementation fidelity framework’ (content, coverage, frequency and duration of delivery). The initial coding framework was reviewed by the principal investigator and two senior researchers. Further cycles of coding enabled researchers to identify, develop and refine more detailed themes within the data and to classify them within the framework. 472 Discrepancies and disagreements were identified and addressed. The final classification was reviewed by researchers from all four trial sites based on their more detailed local knowledge of their children’s centres, IPB implementation and the 12-month interview data. When necessary, the categorisation was also verified against facilitation interviews at earlier time points and study activity logs. This was particularly important in cases in which there had been staff changes between RCT inception and completion. Adjustments were made in three cases following this process.
Incorporating findings from the trial into the development of a second injury prevention briefing
Following completion of the trial, we incorporated evidence from the trial into the development of a second IPB. This covered the prevention of fire-related injuries, falls, poisonings and scalds, based on findings from studies A and D–M in the KCS programme of research. We undertook four workshops, one in each trial site, with users of the fire prevention IPB in the trial and with potential future users of a future IPB to inform decisions about the content of the second IPB, the preferred structure and how to make the IPB more user-friendly.
Ethics and organisational review
Ethics approval was provided by Derbyshire Research Ethics Committee (reference number 11/EM/0011) and the University of the West of England Bristol Research Ethics Committee (reference number HSC/11/06/61). The trial received NHS organisational approval from PCTs when staff who worked in children’s centres were employed by PCTs.
Trial registration
This trial was registered as ClinicalTrials.gov NCT01452191 (13 October 2011) and ISRCTN65067450 (6 December 2012).
Results
Developing the injury prevention briefing
Stakeholder interviews
Two interviews were conducted, one with a children’s centre leaders’ network co-ordinator, at the time part of Together for Children, an organisation working in partnership with the Department for Education to support local authorities in their delivery of Sure Start children’s centres, and the second with a regional programme lead with Together for Children.
The key points from the interviews were:
-
There was uncertainty with regard to the policy framework for children’s centres resulting from the change of government in May 2010.
-
There was little national guidance on how children’s centres should operate. The autonomy afforded to children’s centres was reducing as was input from parents into how centres operated. There was a target for reducing hospital attendances for accidents but this was (unhelpfully) combined with other conditions. Local priorities were often decided on the basis of interests of centre staff members.
-
Children’s centre staff who work with families were considered the most appropriate to involve in accident prevention, but centres tended not to have subject specialist staff.
-
Parents did not raise accident prevention as a topic although they were interested in first aid. Centres often had difficulty engaging ‘hard-to-reach’ groups.
Workshops
A total of 162 delegates were invited to the four workshops and 83 (51%) attended, with the number of delegates per workshop ranging from 19 (Bristol and Newcastle) to 24 (Nottingham). The four most common occupational groups attending were children’s centre managers and staff (n = 32, 39%), health visiting team staff (n = 16, 19%), fire and rescue service staff (n = 15, 18%) and other health sector personnel (n = 8, 10%). Other delegates included directors/managers of children’s or community services, safeguarding managers or board members, commissioning managers, health promotion specialists, unintentional injury co-ordinators/public health nurses, a youth engagement manager, a director of a child safety project, a home safety equipment scheme manager/co-ordinator, a consumer advisor and a child accident prevention consultant.
The key points to emerge from the workshops were:
-
The IPB needed to be directed at three audiences – commissioners, managers and practitioners – with varying content for each audience.
-
Decisions on activities undertaken by children’s centres varied between centres and localities.
-
Local data were needed to assist in making the case for action but were difficult to obtain.
-
Injury prevention was not embedded in the everyday work of a children’s centre and was in competition with other topics during home visits.
-
The importance of ensuring that all staff with the opportunity to deliver safety messages delivered the same message.
-
Messages for parents should be kept simple.
-
Injury prevention may be challenging because of parental apathy, an attitude that their own homes are not at risk, a lack of awareness of the consequences of injuries, low levels of education and literacy among parents or cultural differences.
-
Group sessions in children’s centres were not always well attended. Families at highest risk often did not attend children’s centres. Home visits might be more effective.
Drafting the injury prevention briefing
The drafting of the IPB was undertaken by the researchers who led the workshops. Drafts were reviewed and commented on by all members of the research team, several of whom were in regular contact with children’s centres. In response to the workshops, the IPB was divided into three sections that were capable of being read independently:
-
advice for commissioners
-
advice for children’s centre managers
-
advice for practitioners.
The IPB is shown in Appendix 6, Injury prevention briefing 1. The main part of the document focused on providing children’s centre staff with information and tools to enable them to provide appropriate and consistent safety advice to families using key safety messages for five fire prevention topics. Exercises for use with groups of families were provided for each of the five topics, with recognition that these would not be suitable in all circumstances, for example when outreach workers were visiting families’ homes.
The five key safety topics included in the practitioners’ section were:
-
the importance of having working smoke alarms
-
understanding the potential causes of fires
-
understanding children’s development and its association with the need to store matches and lighters safely
-
the need for a bedtime safety routine
-
the need for and components of a family fire escape plan.
Research evidence from studies H and I in work stream 5 (see Chapter 6) was strongest for the first and last of these topics and, therefore, if time did not permit all topics to be addressed, the importance of covering these issues was emphasised.
Developing the facilitation package
The facilitation package consisted of a combination of face-to-face and telephone contacts at 1, 3, 4/5 and 8 months using structured electronic questionnaires and interviews. The questionnaires and interview schedules are provided in Appendix 6. They were intended to address the barriers to undertaking injury prevention identified in earlier work in the KCS programme (studies D–F) and the key issues that emerged from the workshops. In addition, they were also designed to raise the profile of fire prevention within children’s centres and ensure that it was kept on their agenda throughout the intervention period, allow assessment of progress with IPB implementation, identify difficulties and solutions to these, identify examples of good practice to share with other centres, provide information (e.g. a resources list, contact details for other agencies who could contribute to delivering fire prevention safety messages) and provide support to help implement the IPB.
The injury prevention briefing training sessions
A total of 31 children’s centre staff from the IPB+ arm attended training sessions at four locations. Their roles are presented in Table 106. Twenty-eight attenders completed the evaluation questionnaire wholly or in part. The responses to the questions are shown in Figures 58 and 59. Attenders were generally very positive about the training and stated that the training achieved its aims. One possible exception to this was that only 71% of attenders agreed or strongly agreed that they felt confident about presenting the key fire safety messages to parents at their children’s centre.
| Role | Bristol | Newcastle | Norwich | Nottingham |
|---|---|---|---|---|
| Community health support worker | 1 | |||
| Community health assistant practitioner | 2 | |||
| Children’s centre manager | 1 | 3 | 1 | |
| Children’s centre nursery nurse | 1 | |||
| Children’s centre programme co-ordinator | 1 | |||
| Children’s centre safeguarding and family support manager | 1 | |||
| Children’s centre senior family support worker | 1 | |||
| Children’s centre session worker | 1 | 2 | ||
| Children’s worker manager | 1 | |||
| Community support manager | 1 | |||
| Deputy children’s centre leader | 1 | |||
| Family support worker | 2 | 1 | 3 | 2 |
| Health and family support worker | 1 | |||
| Health visitor (attached to a children’s centre; conducts health and safety training) | 1 | |||
| Play workers | 2 | |||
| Special needs co-ordinator | 1 | |||
| Total | 7 | 8 | 6 | 10 |
FIGURE 58.
Responses to positively worded statements about the IPB training in IPB+ arm training session attenders.

FIGURE 59.
Responses to negatively worded statements about the IPB training in IPB+ arm training session attenders.
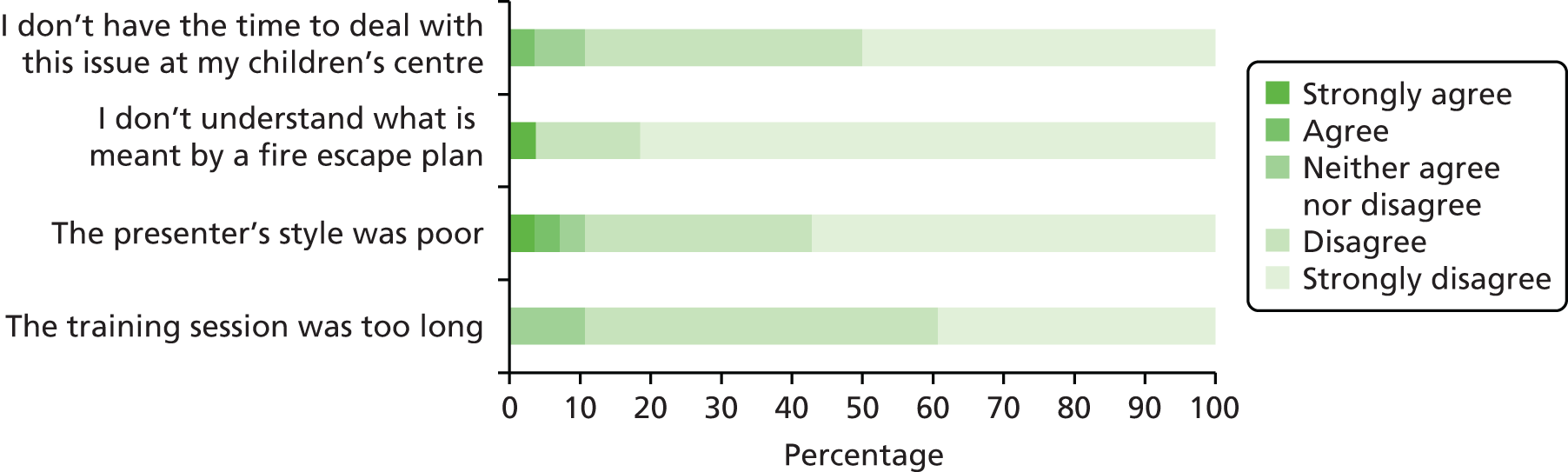
Structured interviews with parents to ascertain fire safety practices and fire escape behaviours
Twenty-one children’s centres were invited to participate and all agreed to participate. This included five centres each from Nottingham, Newcastle and Norwich and six from Bristol. Interviews were conducted with a total of 200 parents across the four centres, representing an 84% response rate. The characteristics of participants are shown in Table 107. Most respondents (92%) were mothers and described themselves as being white British (83%), 50% lived in rented accommodation and 19% lived in single parent households, with 45% of households having only one child.
| Characteristic | n (%)a |
|---|---|
| Age group (years) of parent | |
| < 20 | 17 (9) |
| 21–30 | 90 (45) |
| 31–40 | 75 (38) |
| 41–50 | 15 (8) |
| > 50 | 3 (2) |
| Ethnicity | [1] |
| White British | 166 (83) |
| Black Caribbean/African | 9 (5) |
| Asian | 5 (3) |
| Chinese | 4 (2) |
| Other | 15 (8) |
| Sex of respondent | [2] |
| Female | 182 (92) |
| Male | 16 (8) |
| Accommodation type | |
| Private rented | 58 (29) |
| Social housing | 42 (21) |
| Owner-occupied | 94 (47) |
| Temporary/living with parents | 6 (3) |
| Number of adults in household | [2] |
| 1 | 38 (19) |
| 2 | 148 (75) |
| ≥ 3 | 12 (6) |
| Number of children in household | |
| 1 | 89 (45) |
| 2 | 69 (35) |
| ≥ 3 | 42 (21) |
| Age (years) of children in household | |
| < 1 | 23 (12) |
| 1 | 55 (28) |
| 2 | 30 (15) |
| 3 | 26 (13) |
| ≥ 4 | 66 (33) |
Table 108 shows that smoke alarms were reported in the vast majority of homes (96%), of which virtually all (95% of those reporting a smoke alarm) were reported to be functional. Just over two-thirds (71%) of parents reported having functional smoke alarms on at least two levels of their home. Just over half of the respondents (54%) reported having a bedtime safety routine, but most described only one element of this routine (median 1, IQR 0–1, range 0–3). Eighty-one parents (42% of the 191 respondents answering that question) reported having a fire escape plan. The ICC for having a fire escape plan was 0.049 (95% CI 0.004 to 0.259). Only nine parents (11%) had practised their plan.
| Fire safety practices | n (%)a |
|---|---|
| Smoke alarms | |
| At least one smoke alarm in residence | 191 (96) |
| First alarm reported to be working | 182 (95) |
| Alarm working on at least two levels of residence | 136 (71) |
| Have bedtime routine | [5] |
| No | 90 (46) |
| Yes | 105 (54) |
| Descriptive elements of bedtime routine (n = 228 elements) | |
| Turn off all electric items | 87 (38) |
| Indoor doors closed | 60 (26) |
| Turn oven/cooker off | 21 (9) |
| Fire turned off | 15 (7) |
| Keys accessible | 12 (5) |
| Outside door closed | 11 (5) |
| Windows closed | 7 (3) |
| Lights off | 6 (3) |
| Ensure cigarettes/candles extinguished | 5 (2) |
| Turn appliances off | 4 (2) |
| Other | 9 (4) |
| Has a fire escape plan | [9] |
| Yes | 81 (42) |
| Those with a plan who have practised it | |
| Yes | 9 (11) |
When asked to describe their fire escape plan, most respondents described one element (median 1, IQR 0–1, range 0–4). The elements described by families are shown in Table 109. The descriptions given were insufficiently detailed to allow for assessment of the comprehensiveness or adequacy of the plan.
| Elements of fire escape plans (n = 168 elements) | n (%) |
|---|---|
| Escaping from main exit | 44 (26) |
| Jump out onto balcony/extension roof | 41 (24) |
| Exit from window higher than ground floor | 27 (16) |
| Exit from downstairs window | 27 (16) |
| Lower from window on to mattress | 9 (5) |
| Just have one door/exit so have to use that | 9 (5) |
| Keys are near windows/door | 5 (3) |
| Ring 999 | 3 (2) |
| Blanket/fire extinguisher | 1 (1) |
| Make sure exits are clear | 1 (1) |
| Have ladder upstairs | 1 (1) |
Findings from these interviews illustrated that it was not feasible to use functional smoke alarms as a trial outcome measure because of its high prevalence. The lower prevalence of having a fire escape plan would enable this to be used as an outcome measure but the open-ended question did not produce sufficiently detailed responses to enable understanding of what parents meant when they reported having a fire escape plan. It was therefore decided that separate closed questions about component elements of a fire escape plan would be used to assess the contents of fire escape plans. These questions covered five key components of fire escape plans that were included in the IPB, namely having a smoke alarm and knowing what it sounded like, having door keys accessible, having window keys accessible, keeping exits clear and having a torch next to the bed. To reduce type 1 error arising from multiple significance testing, it was decided that a composite measure would be developed describing behaviour across these five components for use as a secondary outcome measure. Latent variable analysis was undertaken for this purpose and the results of this are outlined in the following section. Similarly, an open question about bedtime safety routines produced a limited number and type of responses, with most parents describing only one element. Closed questions covering the elements of a bedtime safety routine used in the IPB were therefore included in the trial questionnaires.
Developing a composite fire escape behaviour variable
Data from the baseline trial questionnaire completed by 1112 parents were used to develop the composite fire escape behaviour variable. The frequency of reporting of each of the five component elements is shown in Table 110.
| Elements of a fire escape plan | n (%)a |
|---|---|
| Has torch | [24] |
| Yes | 347 (31.9) |
| No | 741 (68.1) |
| Knows sound of alarm | [82] |
| Yes | 1006 (97.7) |
| No | 24 (2.3) |
| External door keys accessible (days per week) | [31] |
| Never | 67 (6.2) |
| ≤ 1 | 47 (4.3) |
| 2–3 | 25 (2.3) |
| 4–5 | 16 (1.5) |
| 6–7 | 926 (85.7) |
| Window keys accessible (days per week) | [56] |
| Never | 145 (13.7) |
| ≤ 1 | 75 (7.1) |
| 2–3 | 26 (2.5) |
| 4–5 | 14 (1.3) |
| 6–7 | 796 (75.4) |
| Exits clear (days per week) | [53] |
| Never | 86 (8.1) |
| ≤ 1 | 51 (4.8) |
| 2–3 | 44 (4.2) |
| 4–5 | 40 (3.8) |
| 6–7 | 838 (79.1) |
A two-class model provided the best fit to the data, categorising participants into ‘more fire escape behaviours’ (87% of participants) and ‘fewer fire escape behaviours’ (13% of participants). Table 111 presents the posterior probabilities for each component element for the two groups.
| Elements of fire escape plan | Class 1: more fire escape behaviours | Class 2: fewer fire escape behaviours |
|---|---|---|
| Has torch | ||
| Yes | 0.334 | 0.223 |
| No | 0.666 | 0.777 |
| Knows sound of alarm | ||
| Yes | 0.982 | 0.944 |
| No | 0.018 | 0.056 |
| External door keys accessible (days per week) | ||
| Never | 0.037 | 0.225 |
| ≤ 1 | 0.009 | 0.265 |
| 2–3 | 0.005 | 0.143 |
| 4–5 | 0.008 | 0.059 |
| 6–7 | 0.942 | 0.308 |
| Window keys accessible (days per week) | ||
| Never | 0.095 | 0.403 |
| ≤ 1 | 0.033 | 0.31 |
| 2–3 | 0.01 | 0.114 |
| 4–5 | 0.011 | 0.028 |
| 6–7 | 0.85 | 0.144 |
| Exits clear (days per week) | ||
| Never | 0.051 | 0.276 |
| ≤ 1 | 0.005 | 0.328 |
| 2–3 | 0.021 | 0.177 |
| 4–5 | 0.034 | 0.061 |
| 6–7 | 0.889 | 0.158 |
A typical member of the ‘more fire escape behaviours group’ had a torch, was aware of how their smoke alarm sounded, had door and window keys accessible for > 2–3 days per week and had exits clear for > 4–5 days per week. A typical member of the ‘fewer fire escape behaviours’ group did not have a torch, was not aware of how their smoke alarm sounded, had door and window keys accessible on ≤ 1 day per week and had exits clear on ≤ 1 day per week. The question about whether participants had a fire escape plan was used as an external validation criterion for the new composite measure. A multivariable logistic regression model estimated the association between parents reporting that they had a fire escape plan and the binary composite measure. After adjusting for potential confounders, participants allocated to the ‘more fire escape behaviours’ group had a 2.5 times higher odds of reporting having an escape plan (OR 2.48, 95% CI 1.59 to 3.86).
Trial results
Recruitment and retention
Thirty-eight children’s centres were recruited to the trial. This included two pairs of children’s centres that shared the same management team. Each pair was therefore treated as one children’s centre for trial purposes, giving a total of 36 children’s centres. A total of 1112 parents were recruited to the trial from the 36 children’s centres. Recruitment commenced in June 2011 and was completed in May 2012. The flow of children’s centres and parents through the trial is shown in Figures 60 and 61, respectively.
FIGURE 60.
Recruitment of children’s centres and flow of children’s centres through the trial. a, When there were more children’s centres than were required we randomly sampled those to participate; b, sample size fulfilled in study centre with phase 1 children’s centres; c, no facilitation contact necessary at month 5; d, data not used in analysis because of poor quality of data provided by some children’s centres. CC, children’s centre.
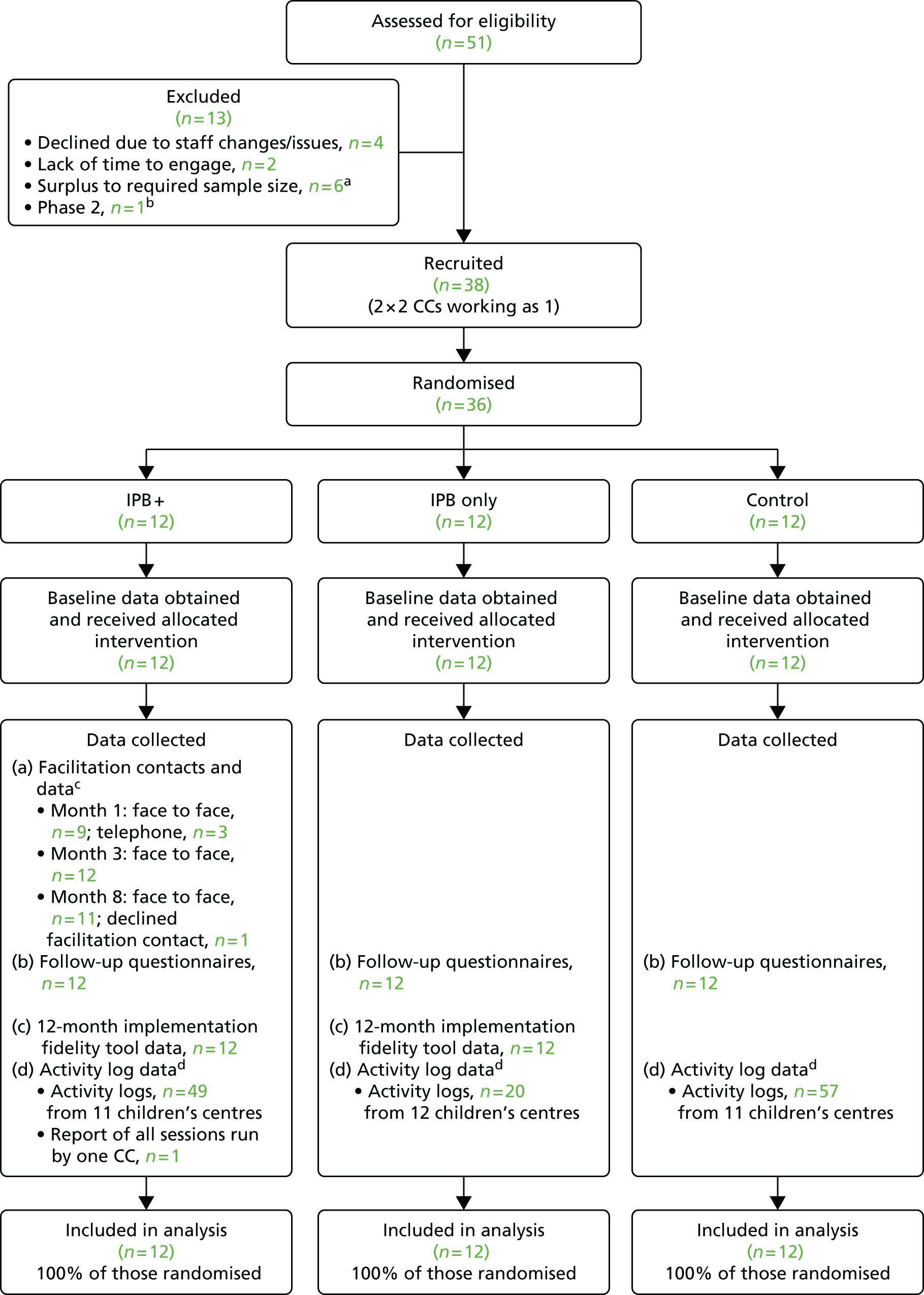
FIGURE 61.
Recruitment of parents and flow of parents through the trial. CC, children’s centre. From Hindmarch et al. 491 under the Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).
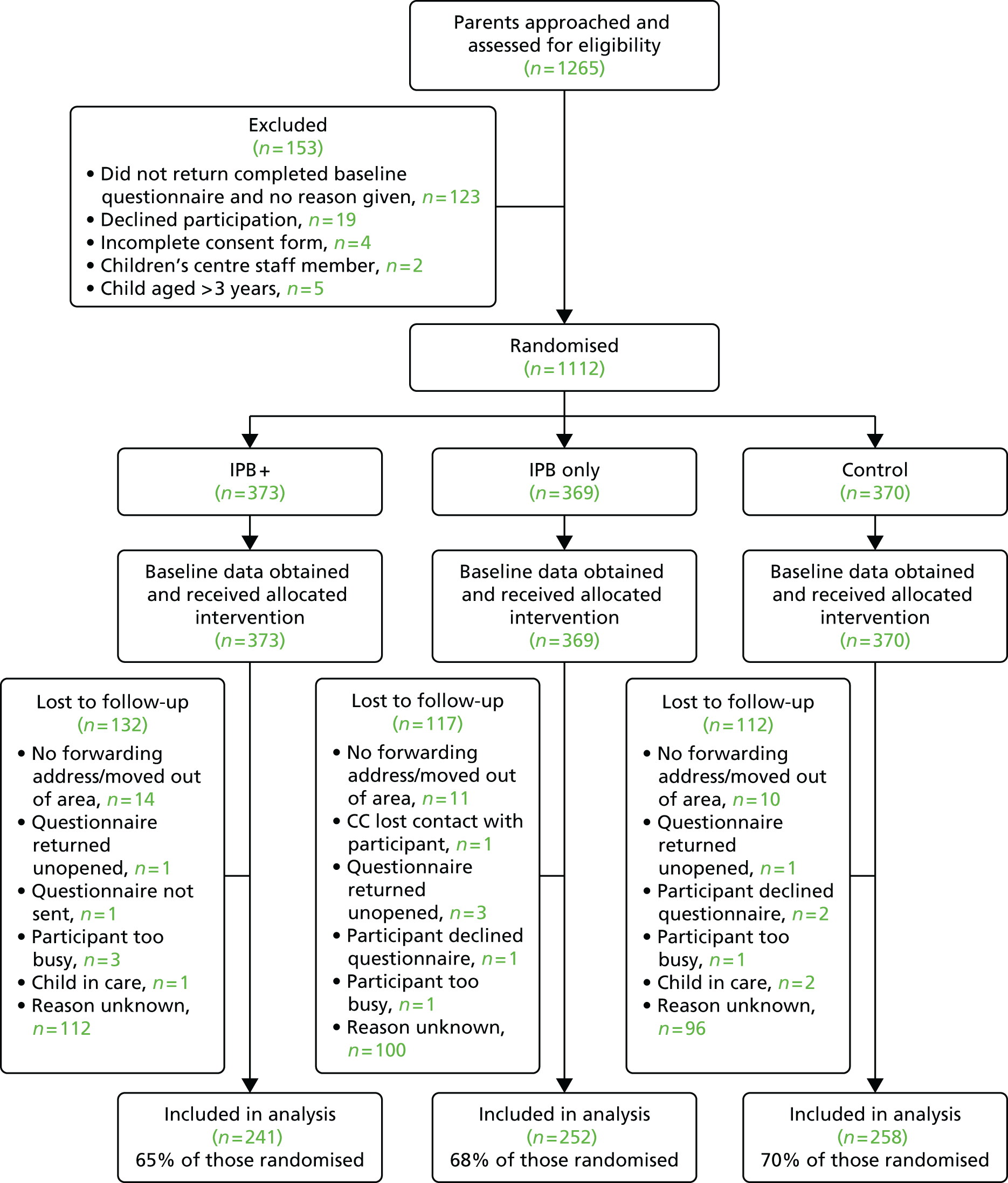
Outcome data were collected from all 36 children’s centres and from 751 (68%) parents. Follow-up rates did not differ significantly between treatment arms (IPB+ 65%, IPB only 68%, usual care 70%; OR for IPB+ vs. usual care 0.79, 95% CI 0.49 to 1.27; OR for IPB only vs. usual care 0.96, 95% CI 0.59 to 1.55). Follow-up rates did differ by baseline characteristics as shown in Table 112. Families with mothers aged 16–20 years (AOR 0.44, 95% CI 0.24 to 0.81 vs. families with older mothers), those in non-owner-occupied accommodation (AOR 0.48, 95% CI 0.35 to 0.66 vs. those in owner-occupied accommodation) and those living in more disadvantaged areas (AOR 0.47, 95% CI 0.29 to 0.78 comparing the most disadvantaged quintile of the IMD with the least disadvantaged quintile65) were significantly less likely to be retained in the trial.
| Characteristica | Retained, n (%) | Lost to follow-up, n (%) | Univariate OR (95% CI) | AOR (95% CI): model with factors significant at p ≤ 0.02 on univariate analysis | AOR (95% CI): final model |
|---|---|---|---|---|---|
| Youngest child aged [25] | |||||
| 0–1 years | 333 (69) | 151 (31) | 1.00 | ||
| 1–2 years | 405 (67) | 198 (33) | 0.94 (0.72 to 1.23) | ||
| Number of children in family [41] | |||||
| 1 | 383 (71) | 159 (29) | 1.00 | ||
| 2 | 238 (68) | 113 (32) | 0.88 (0.65 to 1.19) | 0.93 (0.67 to 1.29) | |
| 3 | 71 (59) | 50 (41) | 0.59 (0.39 to 0.90) | 0.75 (0.46 to 1.21) | |
| ≥ 4 | 37 (65) | 20 (35) | 0.77 (0.43 to 1.40) | 1.00 (0.52 to 1.93) | |
| Mother aged [52] | |||||
| > 20 years | 701 (70) | 305 (30) | 1.00 | ||
| 16–20 years | 25 (46) | 29 (54) | 0.34 (0.19 to 0.61) | 0.48 (0.24 to 0.94) | 0.44 (0.24 to 0.81) |
| Lives in [17] | |||||
| House | 616 (70) | 265 (30) | 1.00 | ||
| Flat or other | 126 (59) | 88 (41) | 0.62 (0.45 to 0.86) | 0.89 (0.60 to 1.31) | |
| Tenure [25] | |||||
| Owner-occupied | 368 (79) | 96 (21) | 1.00 | ||
| Non-owner-occupied | 369 (59) | 254 (41) | 0.39 (0.30 to 0.52) | 0.60 (0.42 to 0.85) | 0.48 (0.35 to 0.66) |
| Ethnic group [50] | |||||
| White British | 685 (68) | 323 (32) | 1.00 | ||
| Other | 32 (59) | 22 (41) | 0.76 (0.41 to 1.40) | ||
| English is first language [12] | |||||
| No | 57 (59) | 39 (41) | 1.00 | ||
| Yes | 688 (69) | 316 (31) | 1.49 (0.95 to 2.34) | 1.33 (0.80 to 2.22) | |
| Single adult household [43] | |||||
| No | 622 (71) | 255 (29) | 1.00 | ||
| Yes | 109 (57) | 83 (43) | 0.56 (0.40 to 0.78) | 0.71 (0.49 to 1.03) | |
| Any smoker in household [30] | |||||
| No | 534 (70) | 225 (30) | 1.00 | ||
| Yes | 199 (62) | 124 (38) | 0.72 (0.54 to 0.96) | 0.88 (0.63 to 1.21) | |
| Household member drinks six or more drinks on one occasion [110] | |||||
| No | 292 (70) | 128 (30) | 1.00 | ||
| Yes | 401 (68) | 191 (32) | 0.94 (0.71 to 1.25) | ||
| IMD quintile (range) [4] | |||||
| 1 (2.4–15.6) | 176 (79) | 46 (21) | 1.00 | ||
| 2 (15.7–25.7) | 171 (75) | 58 (25) | 0.76 (0.48 to 1.20) | 0.81 (0.49 to 1.35) | 0.83 (0.50 to 1.35) |
| 3 (25.8–34.6) | 147 (67) | 71 (33) | 0.55 (0.35 to 0.86) | 0.70 (0.42 to 1.18) | 0.65 (0.40 to 1.06) |
| 4 (34.7–46.6) | 134 (61) | 84 (39) | 0.44 (0.28 to 0.69) | 0.53 (0.32 to 0.87) | 0.56 (0.34 to 0.91) |
| 5 (46.7–74.8) | 123 (56) | 98 (44) | 0.35 (0.23 to 0.56) | 0.50 (0.30 to 0.86) | 0.47 (0.29 to 0.78) |
| Had fire escape plan [19] | |||||
| No | 436 (69) | 196 (31) | 1.00 | ||
| Yes | 304 (66) | 157 (34) | 0.90 (0.69 to 1.17) | ||
Characteristics of participants
The characteristics of the children’s centres that participated in the trial are shown in Table 113, and the fire safety advice that they provided at baseline is shown in Table 114. The characteristics of parents at baseline are shown in Table 115 and the fire safety practices reported by parents at baseline are shown in Table 116. The characteristics of children’s centres and parents appeared well balanced between treatment arms. Most children’s centres (72%) were managed by the local authority and were phase 1 centres (89%), one-quarter (26%) were rated by Ofsted as outstanding for overall effectiveness and the median catchment population was 811 (IQR 574–998). Most children’s centres reported providing advice on each of the key messages from the IPB. More than 75% provided advice on fire escape planning, > 80% provided advice on smoke alarms and keeping cigarettes/matches/lighters out of reach and > 90% provided advice on other causes of house fires and bedtime safety routines.
| Characteristic | Trial arma | ||
|---|---|---|---|
| Usual care (n = 12), n (%) | IPB only (n = 12), n (%) | IPB+ (n = 12), n (%) | |
| Lead agency | |||
| Local authority | 10 (83.3) | 7 (58.3) | 9 (75.0) |
| NHS | 2 (16.7) | 0 (0.0) | 1 (8.3) |
| Voluntary sector led | 0 (0.0) | 5 (41.7) | 2 (16.7) |
| Phase of children’s centre | |||
| 1 | 10 (83.3) | 11 (91.7) | 11 (91.7) |
| 2 | 2 (16.7) | 1 (8.3) | 1 (8.3) |
| 3 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Number of children in catchment area, median (IQR) | 754 (529–999) | 776 (565–905) | 854 (608–1076) |
| Characteristics from Ofsted reports | |||
| Overall effectiveness | [1] | ||
| Outstanding | 3 (25.0) | 2 (16.7) | 4 (36.4) |
| Good | 5 (41.7) | 10 (83.3) | 6 (54.5) |
| Satisfactory | 4 (33.3) | 0 (0.0) | 1 (9.1) |
| Capacity for sustained improvement | [1] | [5] | [4] |
| Outstanding | 3 (27.3) | 1 (14.3) | 2 (25.0) |
| Good | 4 (36.4) | 6 (85.7) | 6 (75.0) |
| Satisfactory | 4 (36.4) | 0 (0.0) | 0 (0.0) |
| Topics that children’s centre provides advice on | Trial arm | ||
|---|---|---|---|
| Usual care (N = 12), n (%) | IPB only (N = 12), n (%) | IPB+ (N = 12), n (%) | |
| Smoke alarms | |||
| No advice/don’t know | 0 (0.0) | 2 (16.7) | 0 (0.0) |
| Advice provideda | 12 (100.0) | 10 (83.3) | 12 (100.0) |
| How to make a fire escape plan | [1] | ||
| No advice/don’t know | 3 (25.0) | 2 (18.2) | 3 (25.0) |
| Advice provideda | 9 (75.0) | 9 (81.8) | 9 (75.0) |
| Other causes of house fires (cooking safety, electrical safety or handling hot irons safely) | |||
| No advice/don’t know | 0 (0.0) | 1 (8.3) | 0 (0.0) |
| Advice provideda | 12 (100.0) | 11 (91.7) | 12 (100.0) |
| Child behaviour and fire prevention (use and storage of cigarettes, lighters and matches) | [1] | ||
| No advice/don’t know | 2 (16.7) | 2 (16.7) | 2 (18.2) |
| Advice provideda | 10 (83.3) | 10 (83.3) | 9 (81.8) |
| Bedtime routines to prevent fires | |||
| No advice/don’t know | 0 (0.0) | 1 (8.3) | 0 (0.0) |
| Advice provideda | 12 (100.0) | 11 (91.7) | 12 (100.0) |
| Characteristic | Trial arma | ||
|---|---|---|---|
| Usual care (N = 370), n (%) | IPB only (N = 369), n (%) | IPB+ (N = 373), n (%) | |
| Study centre | |||
| Nottingham | 89 (24.1) | 98 (26.6) | 91 (24.4) |
| Newcastle | 86 (23.2) | 88 (23.8) | 87 (23.3) |
| Norwich | 95 (25.7) | 82 (22.2) | 93 (24.9) |
| Bristol | 100 (27.0) | 101 (27.4) | 102 (27.3) |
| Adults in household (aged ≥ 18 years) | [13] | [15] | [15] |
| 1 | 61 (17.1) | 72 (20.3) | 59 (16.5) |
| 2 | 276 (77.3) | 254 (71.8) | 280 (78.2) |
| ≥ 3 | 20 (5.6) | 28 (7.9) | 19 (5.3) |
| Children in household (aged < 18 years) | [12] | [13] | [16] |
| 1 | 169 (47.2) | 173 (48.6) | 200 (56.0) |
| 2 | 132 (36.9) | 115 (32.3) | 104 (29.1) |
| ≥ 3 | 57 (15.9) | 68 (19.1) | 53 (14.8) |
| Number of other families living in the same household | |||
| 0 | 341 (92.2) | 332 (90.0) | 336 (90.1) |
| 1 | 16 (4.3) | 23 (6.2) | 20 (5.4) |
| ≥ 2 | 13 (3.5) | 14 (3.8) | 17 (4.6) |
| Number of families with children aged | [10] | [6] | [9] |
| < 1 year | 163 (45.3) | 143 (39.4) | 178 (48.9) |
| 1–2 years | 197 (54.7) | 220 (60.6) | 186 (51.1) |
| Mother’s age group 16–20 years | [16] | [19] | [17] |
| Yes | 17 (4.8) | 17 (4.9) | 20 (5.6) |
| No | 337 (95.2) | 333 (95.1) | 336 (94.4) |
| Father’s age group 16–20 years | [57] | [67] | [59] |
| Yes | 6 (1.9) | 6 (2.0) | 8 (2.5) |
| No | 307 (98.1) | 296 (98.0) | 306 (97.5) |
| Family ethnicity | [20] | [18] | [12] |
| White British | 337 (96.3) | 323 (92.0) | 348 (96.4) |
| Asian/Asian British | 5 (1.4) | 13 (3.7) | 6 (1.7) |
| Black/black British | 5 (1.4) | 15 (4.3) | 2 (0.6) |
| Mixed | 3 (0.9) | 0 (0.0) | 5 (1.4) |
| English as first language | 336 (92.1) [5] | 319 (87.6) [5] | 349 (94.1) [2] |
| Household type | [13] | [6] | [6] |
| Rented | 193 (54.1) | 203 (55.9) | 193 (52.6) |
| Owner-occupied | 154 (43.1) | 148 (40.8) | 162 (44.1) |
| Lives with parents | 9 (2.5) | 12 (3.3) | 12 (3.3) |
| Shared ownership | 1 (0.3) | 0 (0.0) | 0 (0.0) |
| Lives above ground floor (if lives in a flat) | [29] | [17] | [23] |
| Yes | 50 (14.7) | 39 (11.1) | 50 (14.3) |
| No | 5 (1.5) | 10 (2.8) | 8 (2.3) |
| NA (i.e. does not live in a flat) | 286 (83.9) | 303 (86.1) | 292 (83.4) |
| Deprivation (IMD score of household) | [2] | [1] | [1] |
| Mean (SD) | 31.0 (16.9) | 34.7 (16.5) | 29.6 (16.1) |
| Smokers in household | [11] | [9] | [10] |
| None | 245 (68.2) | 251 (69.7) | 263 (72.5) |
| 1 | 76 (21.2) | 81 (22.5) | 69 (19.0) |
| 2 | 31 (8.6) | 27 (7.5) | 27 (7.4) |
| ≥ 3 | 7 (1.9) | 1 (0.3) | 4 (1.1) |
| Total cigarettes smoked per day in households with at least one smoker, median (IQR) | 10 (10–20) [3] | 10 (6–20) [7] | 10 (10–20) [7] |
| At least one person in household drinks four or more times a week | 21 (5.8) [10] | 19 (5.3) [8] | 24 (6.6) [12] |
| At least one person in household drinks six or more drinks on one occasion | 208 (61.7) [33] | 173 (52.3) [38] | 211 (61.3) [29] |
| Safety practices | Trial arma | ||
|---|---|---|---|
| Usual care (N = 370), n (%) | IPB only (N = 369), n (%) | IPB+ (N = 373), n (%) | |
| Family have a fire escape plan | [7] | [5] | [7] |
| No | 204 (56.2) | 211 (58.0) | 217 (59.3) |
| Yes | 159 (43.8) | 153 (42.0) | 149 (40.7) |
| Component elements of fire escape plan | |||
| Torch next to bed | [6] | [8] | [10] |
| No | 246 (67.6) | 253 (70.1) | 242 (66.7) |
| Yes | 118 (32.4) | 108 (29.9) | 121 (33.3) |
| Knows sound of smoke alarm | [27] | [23] | [32] |
| No | 9 (2.6) | 10 (2.9) | 5 (1.5) |
| Yes | 334 (97.4) | 336 (97.1) | 336 (98.5) |
| Front door key accessible | [10] | [16] | [5] |
| ≥ 4 days per week | 317 (88.1) | 304 (86.1) | 321 (87.2) |
| Never/< 4 days per week | 43 (11.9) | 49 (13.9) | 47 (12.8) |
| Window keys accessible | [18] | [24] | [14] |
| ≥ 4 days per week | 278 (79.0) | 267 (77.4) | 265 (73.8) |
| Never/< 4 days per week | 74 (21.0) | 78 (22.6) | 94 (26.2) |
| Exits clear | [18] | [24] | [11] |
| ≥ 4 days per week | 297 (84.4) | 284 (82.3) | 297 (82.0) |
| Never/< 4 days per week | 55 (15.6) | 61 (17.7) | 65 (18.0) |
| Fire escape behaviours composite variable | |||
| More fire escape behaviours | 329 (88.9) | 319 (86.4) | 320 (85.8) |
| Fewer fire escape behaviours | 41 (11.1) | 50 (13.6) | 53 (14.2) |
| Those with fire escape plan who have discussed it with adults in the house | [1] | [3] | [2] |
| No | 16 (10.1) | 17 (11.3) | 18 (12.2) |
| Yes | 142 (89.9) | 133 (88.7) | 129 (87.8) |
| Those with fire escape plan who have practised it | [2] | [1] | |
| No | 110 (70.1) | 104 (68.0) | 116 (78.4) |
| Yes | 47 (29.9) | 49 (32.0) | 32 (21.6) |
| Those with fire escape plan who have a second fire escape plan | [6] | [2] | [3] |
| No | 100 (65.4) | 110 (72.8) | 114 (78.1) |
| Yes | 53 (34.6) | 41 (27.2) | 32 (21.9) |
| Smoke alarms fitted and working on every level | [17] | [20] | [24] |
| No | 89 (25.2) | 89 (25.5) | 89 (25.5) |
| Yes | 264 (74.8) | 260 (74.5) | 260 (74.5) |
| Child(ren) found playing with matches/lighters | [2] | [8] | |
| No | 353 (95.9) | 354 (95.9) | 352 (96.4) |
| Yes | 15 (4.1) | 15 (4.1) | 13 (3.6) |
| Fire safety routines when going to bed | |||
| Closes all internal doors | [22] | [15] | [13] |
| ≥ 4 days per week | 203 (58.3) | 223 (63.0) | 199 (55.3) |
| Never/< 4 days per week | 145 (41.7) | 131 (37.0) | 161 (44.7) |
| Checks front door locked | [4] | [14] | [4] |
| ≥ 4 days per week | 345 (94.3) | 326 (91.8) | 334 (90.5) |
| Never/< 4 days per week | 21 (5.7) | 29 (8.2) | 35 (9.5) |
| Turns off lights | [5] | [11] | [8] |
| ≥ 4 days per week | 343 (94.0) | 332 (92.7) | 337 (92.3) |
| Never/< 4 days per week | 22 (6.0) | 26 (7.3) | 28 (7.7) |
| Turns electrical appliances off at the sockets | [7] | [11] | [7] |
| ≥ 4 days per week | 193 (53.2) | 214 (59.8) | 197 (53.8) |
| Never/< 4 days per week | 170 (46.8) | 144 (40.2) | 169 (46.2) |
| Turns off electric/gas fires | [15] | [22] | [8] |
| ≥ 4 days per week | 333 (93.8) | 329 (94.8) | 345 (94.5) |
| Never/< 4 days per week | 22 (6.2) | 18 (5.2) | 20 (5.5) |
| Makes sure a fireguard/spark guard is in place | [34] | [35] | [25] |
| ≥ 4 days per week | 302 (89.9) | 293 (87.7) | 303 (87.1) |
| Never/< 4 days per week | 34 (10.1) | 41 (12.3) | 45 (12.9) |
| Checks that the oven and all the rings on the cooker are turned off | [7] | [7] | [5] |
| ≥ 4 days per week | 333 (91.7) | 320 (88.4) | 318 (86.4) |
| Never/< 4 days per week | 30 (8.3) | 42 (11.6) | 50 (13.6) |
| Makes sure cigarettes are put out | [29] | [23] | [20] |
| ≥ 4 days per week | 331 (97.1) | 328 (94.8) | 341 (96.6) |
| Never/< 4 days per week | 10 (2.9) | 18 (5.2) | 12 (3.4) |
| Puts matches/lighters out of reach of children | [18] | [19] | [13] |
| ≥ 4 days per week | 328 (93.2) | 328 (93.7) | 337 (93.6) |
| Never/< 4 days per week | 24 (6.8) | 22 (6.3) | 23 (6.4) |
| Blows out candles | [16] | [17] | [18] |
| ≥ 4 days per week | 319 (90.1) | 320 (90.9) | 325 (91.5) |
| Never/< 4 days per week | 35 (9.9) | 32 (9.1) | 30 (8.5) |
| Bedtime fire safety routine score, median (IQR) | 9 (8–10) [36] | 9 (8–10) [39] | 9 (8–10) [23] |
| Families’ knowledge of the causes of fires in the homeb | |||
| 0 | 48 (13.0) | 49 (13.3) | 38 (10.2) |
| 1 | 198 (53.5) | 198 (53.7) | 201 (53.9) |
| 2 | 119 (32.2) | 113 (30.6) | 130 (34.9) |
| 3 | 5 (1.4) | 9 (2.4) | 4 (1.1) |
| Satisfaction with home safety advice received from children’s centre staff | [9] | [12] | [14] |
| Very/fairly satisfied | 221 (61.2) | 199 (55.7) | 206 (57.4) |
| Less than very/fairly satisfied | 36 (10.0) | 45 (12.6) | 41 (11.4) |
| Haven’t received information | 104 (28.8) | 113 (31.7) | 112 (31.2) |
| Have spoken to FRS about fire safety | [3] | [3] | [6] |
| No | 250 (68.1) | 263 (71.9) | 280 (76.3) |
| Yes | 117 (31.9) | 103 (28.1) | 87 (23.7) |
| Of those who had spoken to FRS, had a home safety check from FRS | [3] | [1] | [2] |
| No | 59 (51.8) | 35 (34.3) | 38 (44.7) |
| Yes | 55 (48.2) | 67 (65.7) | 47 (55.3) |
| Have received advice about preventing fires | [12] | [10] | [8] |
| No | 165 (46.1) | 191 (53.2) | 209 (57.3) |
| Yes | 193 (53.9) | 168 (46.8) | 156 (42.7) |
One-fifth of parents (18%) lived in single adult households, 51% had only one child, 57% did not own their accommodation, 95% classed themselves as white British and 92% spoke English as their first language. The mean IMD score was 31.7 (SD 16.6).
Two-fifths (42%) of parents had a fire escape plan, of whom 89% had discussed the plan with other adults in the house and 28% had practised the plan. Four of the five component elements of the fire escape plan were reported by > 75% of parents, with only 32% reporting having a torch next to the bed. Most parents (87%) were in the ‘more fire escape behaviours’ group for the composite fire escape behaviours variable. Most parents (75%) reported that they had a smoke alarm fitted and working on every level of their home. Only 4% of parents had found their children playing with matches or lighters. Most parents undertook most bedtime safety practices on at least 4 days per week, with 41% of parents not closing all internal doors and 44% not turning electrical appliances off at the sockets on at least 4 days per week.
Implementation of the injury prevention briefing
Analysis of data from the implementation fidelity interviews suggested that there were four levels of IPB implementation, which were associated with different levels of delivery. A description of the criteria for each level of implementation is given in Table 117. Most children’s centres achieved extended implementation, followed by essential implementation. Only six (25%) children’s centres achieved minimal or non-implementation. It appeared that more IPB+ children’s centres than IPB-only children’s centres achieved extended levels of implementation.
| Criteria | Level | |||
|---|---|---|---|---|
| Extended – diverse delivery methods, wide coverage and additional content | Essential – minimum delivery methods and key content | Minimal – considered implementation but little evidence of successful engagement or delivery | Non-implementation – did not actively engage with the study specifications or implement any aspect of the IPB | |
|
|
|
|
|
| Arm | n (%) | n (%) | n (%) | n (%) |
| IPB+ | 8 (66.7) | 3 (25.0) | 1 (8.3) | 0 (0.0) |
| IPB only | 2 (16.7) | 5 (41.7) | 4 (33.3) | 1 (8.3) |
Quotations from the implementation fidelity interviews for children’s centres in each of the levels of implementation are provided in Boxes 5–8 to illustrate the varying degrees of implementation.
We had boards and things up and children centre reception and after the fire engine had been there were photographs of the fire engine and all the children and the fire safety in the home booklet pages photocopied out of books and stuck up again . . . we try to encourage people to come along to the workshops as well.
Used additional information or content (beyond injury prevention briefing)
We’ve tried to do it in a couple of different ways so we set up the large training room sort of in a comedy fashion . . . We have clothes all over a heater that wasn’t turned on to try and make it a bit more interactive.
We watched the fancy a cuppa DVD which is from the child accident prevention people as well. So we tried doing a lot of different things to make it a bit more interesting, but it’s actually pinning people down to come along to a session so the community fire officers came in and spoke to everybody within the group.
Used more than two messages
We did cover the IPB and that’s what we used to get the information out to the parents. We used the IPB in the safety workshops and then we took information to talk to the parents in groups about smoke alarms and particular age-appropriate behaviour with children making sure that your lighters and your candles and your matches were out of reach . . . I think over the course of the year, we probably covered every exercise with parents where everybody is being given pretty much all the information out of the booklet.
Every few weeks after the fire safety message we’d put up a display with pictures around what we‘ve just done to back up information that would be given out in the groups. So we had a display around Christmas safety and not leaving your Christmas tree light on and candles . . . so, we were trying to link quite a lot of things back to fire safety.
Active engagement with wide population of parents
The feedback from parents has been really positive . . . very sort of like oh yes! I went home and we talked about the safety plan and we checked the smoke alarm, so actually the parents who I’ve spoken to have been picking up the safety messages.
Delivered to more than one group
We did the sessions and included everybody but knowing that it was important to get the people who were part of the survey involved as much as possible . . . each parent who was part of the study received either in the hand or through the post the fire safety booklet and then the information that you sent out, everybody got a copy of that, and everybody was invited to take part in the safety workshops, the event days with the fire engine, and the chip pans.
Provided usual non-injury prevention briefing-related fire safety activities
We’ve had community fire people to come into the groups and fill in questionnaires about having fire service come out to your home and have a wander round so we had a few parents have had those home visits.
The event was just lots of different activities. It was held in the hall as well as outside so it was kind of quite spread out. So there was just different types of activities to get parents and children involved in different kind of key fire messages.
Delivered two messages
We had smoke alarms and we were getting children used to like the sounds of smoke alarm and just talking to parents.
The children made a big fire engine from junk and we talked about the fire and rescue services. I can’t think what else but yes it was just lots of different activities, just getting different messages across really in a fun way.
Discrete delivery or limited integration into other children’s centre sessions
We had the one big event and then within . . . other activities like home visits where we have done home safety checks or talks.
Study recruited parents and/or passive involvement of wider community
Yes, the leaflet that we sent out and . . . yes, obviously with those that have had home visits.
Attendance at groups and things is so hit and miss that I don’t think it’s a reflection on what the activity was at all because obviously other families came, I just think it’s . . . the nature of the game really. Like I said we don’t tend to have . . . I don’t know . . . you don’t have static attendance at stuff.
Injury prevention briefing information only
Only IBP information described in the interviews.
May or may not have provided additional non-injury prevention briefing-related fire safety activitiesNo other fire safety activities mentioned in the interviews.
The fire safety stuff has not been a priority . . .
And the next question was around had anything gone particularly well in relation to using the IPB? You responded no to that. You only delivered it with a couple of parents didn’t you?
Yes, I did a couple of things . . . I mean it was helpful in terms of kind of doing ‘walkarounds’ and things in peoples’ homes and going through that side of things but no we’ve not really done much more.
May or may not have provided additional non-injury prevention briefing-related fire safety activities
That’s not to say that fire safety isn’t a massive priority in a family home but if you walk into a home and they’ve not got any money, the bank account has been shut or they’ve not got any food . . . I don’t know, they’ve had a letter from children’s services or something like that, you need to deal with that on that day. You know and yes, if there’s a lighter on the table you’ll deal with that at the same time but your biggest kind of issue is what you’re faced with.
Initially we didn’t know anything about the injury prevention briefing, E [the manager of the children’s centre] and one of the team leaders arranged that. But I didn’t realise the extent to which we never had the injury prevention briefing book so we were just thinking that you wanted to talk to parents so I think right from the beginning we have been at a misunderstanding. Also our manager at that time, two of the staff that set it up have left, our strategic manager has also been on long-term sick, the manager of our team has retired and we are going through a management of change so we have been short-staffed.
I thought I don’t really know what IPB is . . . I am thinking we must have got something somewhere so I went and got it.
Adapted from Beckett et al. 492 under the Creative Commons Attribution License 4.0 (see https://creativecommons.org/licenses/by/4.0/legalcode).
All (n = 12, 100%) of the IPB+ arm children’s centres and 58% (n = 7) of the IPB-only arm children’s centres developed a plan for implementing the IPB. Two-thirds (n = 7/11, 64%) of the IPB+ arm children’s centres had developed their plan by the 3-month facilitation contact. Figures 62 and 63 show the percentage of children’s centres that reported giving advice on each of the five key IPB messages and reported the use of the IPB exercises, respectively. The numbers were too small to compare these quantitatively. Fire-safety promotion activities reported by children’s centres on the follow-up questionnaire, by treatment arm, are shown in Table 118. From Table 118 and Figures 61 and 62 it appears that more of the IPB+ arm children’s centres than IPB-only arm children’s centres gave advice on each of the key safety messages and used each of the exercises. In addition, 92% (n = 11) of the IPB+ arm children’s centres and 50% (n = 6) of the IPB-only arm children’s centres reported using methods other than the IPB to deliver fire safety messages.
FIGURE 62.
Provision of advice on each of the five key IPB messages by children’s centres in the IPB-only and IPB+ arms reported in the implementation fidelity interviews at follow-up.
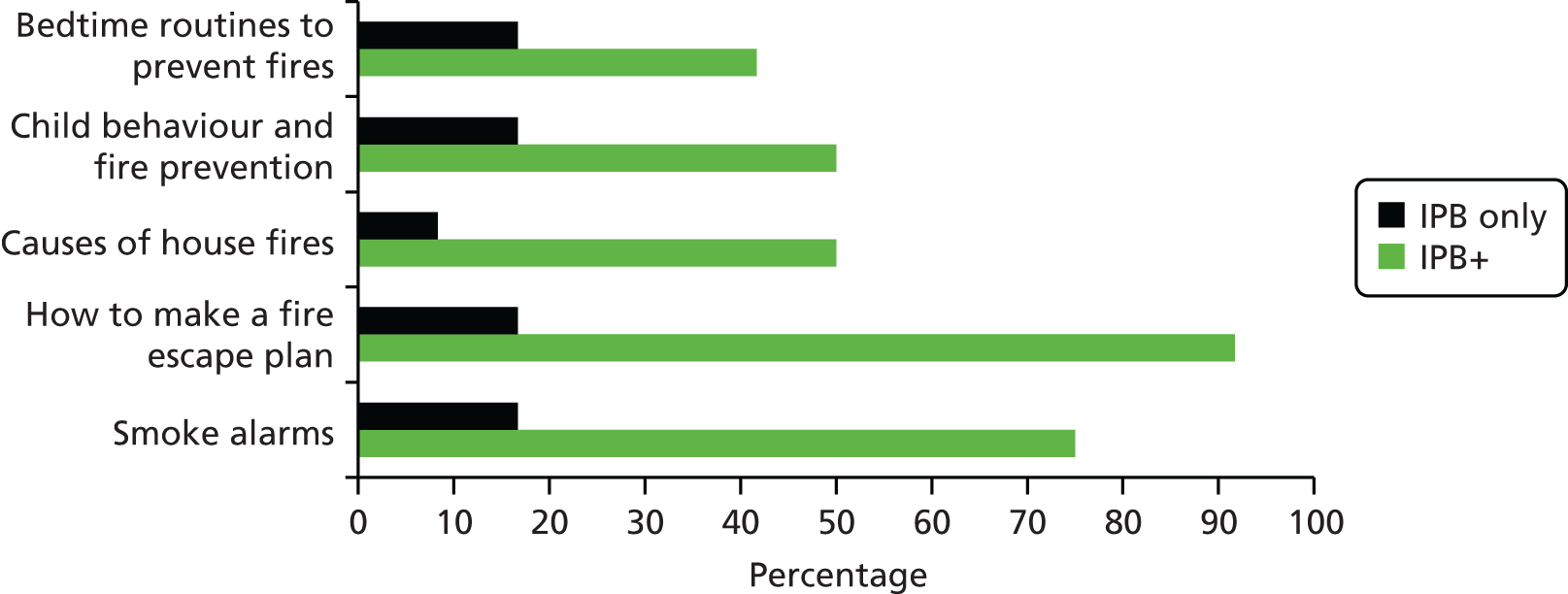
FIGURE 63.
Use of the IPB exercises by children’s centres in the IPB-only and IPB+ arms reported in the implementation fidelity interviews at follow-up.
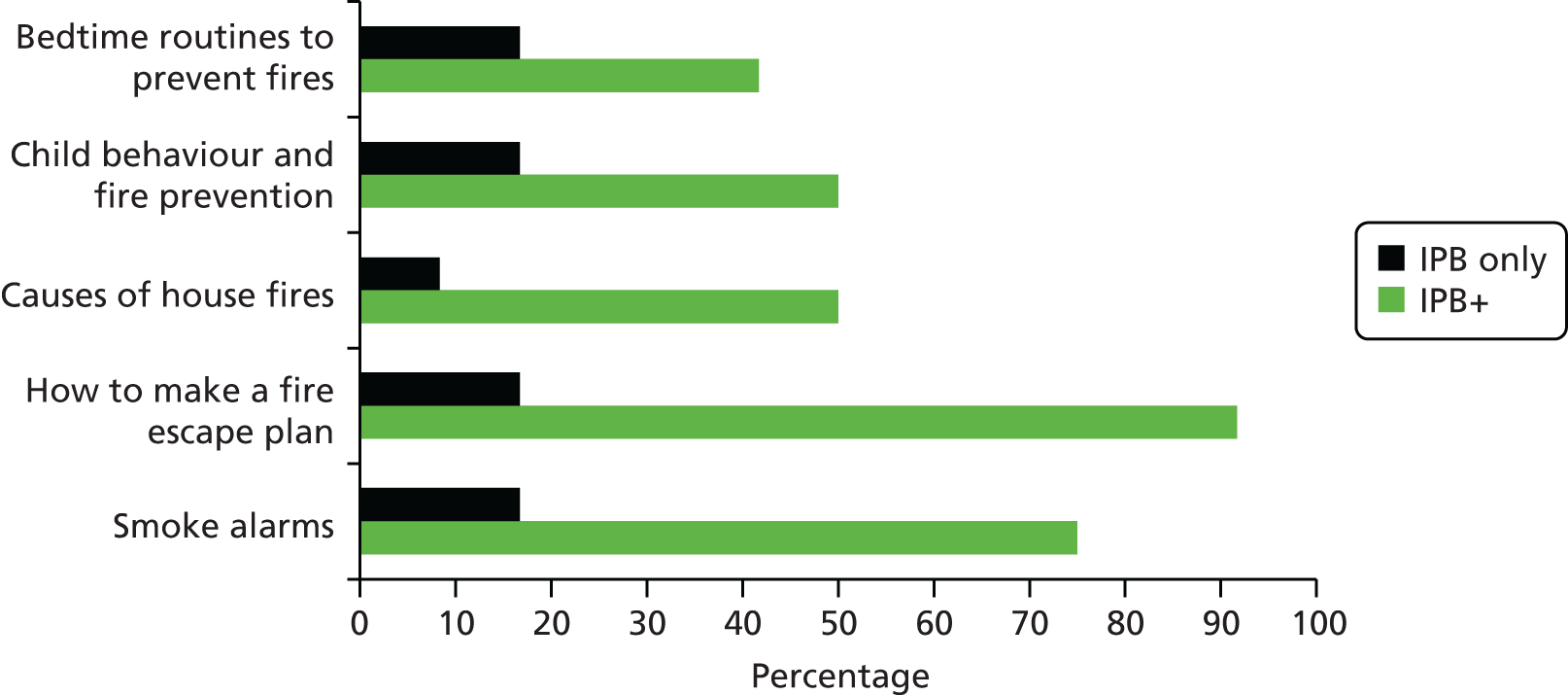
| Secondary outcome measures | Trial arma | ||
|---|---|---|---|
| Usual care (N = 12), n (%) | IPB only (N = 12), n (%) | IPB+ (N = 12), n (%) | |
| Advice provided on | |||
| Smoke alarms | [1] | ||
| No advice/don’t know | 1 (8.3) | 0 (0.0) | 1 (8.3) |
| Advice provided (one to one, in groups or leaflets) | 11 (91.7) | 11 (100.0) | 11 (91.7) |
| How to make a fire escape plan | [1] | ||
| No advice/don’t know | 3 (27.3) | 3 (25.0) | 0 (0.0) |
| Advice provided (one to one, in groups or leaflets) | 8 (72.7) | 9 (75.0) | 12 (100.0) |
| Causes of house fires (advice provided on one or more of cooking safety, electrical safety, handling hot irons safely) | |||
| No advice/don’t know | 1 (8.3) | 0 (0.0) | 0 (0.0) |
| Advice provided (one to one, in groups or leaflets) | 11 (91.7) | 12 (100.0) | 12 (100.0) |
| Child behaviour and fire prevention (safe use and storage of cigarettes, lighters and matches) | |||
| No advice/don’t know | 4 (33.3) | 1 (8.3) | 0 (0.0) |
| Advice provided (one to one, in groups or leaflets) | 8 (66.7) | 11 (91.7) | 12 (100.0) |
| Bedtime routines to prevent fires | [1] | [1] | |
| No advice/don’t know | 6 (54.5) | 4 (33.3) | 0 (0.0) |
| Advice provided (one to one, in groups or leaflets) | 5 (45.5) | 8 (66.7) | 11 (100.0) |
| Ran fire safety sessions | |||
| Yes | 5 (41.7) | 7 (58.3) | 11 (91.7) |
| No/don’t know | 7 (58.3) | 5 (41.7) | 1 (8.3) |
| Number of sessions runb | [2] | ||
| 0 | 7 (58.3) | 5 (41.7) | 1 (10.0) |
| 1 | 4 (33.3) | 1 (8.3) | 2 (20.0) |
| 2 | 1 (8.3) | 5 (41.7) | 2 (20.0) |
| 3 | 0 (0.0) | 0 (0.0) | 3 (30.0) |
| 4 | 0 (0.0) | 1 (8.3) | 0 (0.0) |
| 5 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 6 | 0 (0.0) | 0 (0.0) | 1 (10.0) |
| 7 | 0 (0.0) | 0 (0.0) | 1 (10.0) |
| Number of sessions runb | [2] | ||
| 0 or 1 | 11 (91.7) | 6 (50.0) | 3 (30.0) |
| ≥ 2 | 1 (8.3) | 6 (50.0) | 7 (70.0) |
| FRS attended to help provide any sessions | [1] | [1] | |
| No | 8 (72.7) | 6 (50.0) | 4 (36.4) |
| Yes | 3 (27.3) | 6 (50.0) | 7 (63.6) |
Table 119 shows parent-reported receipt of advice and other fire prevention promotion. These data are consistent with the findings above regarding implementation of the IPB and suggest that the IPB+ arm achieved significantly greater implementation of the IPB than the usual-care arm. The IPB-only arm achieved a lesser degree of implementation, with significant differences between the IPB-only arm and the usual-care arm only in terms of parents attending fire safety sessions. Significantly more parents in the IPB+ arm than in the usual-care arm reported receiving advice on each of the five key IPB messages, with ORs ranging from 2.21 (95% CI 1.18 to 4.12) (bedtime safety routines) to 3.35 (95% CI 1.98 to 5.68) (causes of fires). There were no significant differences in the proportion of parents who reported receiving advice for each of the five key IPB messages between the IPB-only arm and the usual-care arm. The proportion of parents who received advice ranged from 10% to 24% in the usual-care arm, from 12% to 34% in the IPB-only arm and from 21% to 43% in the IPB+ arm. In total, 28% of the IPB+ arm, 13% of the IPB-only arm and 14% of the usual-care arm parents received advice about fire escape planning. Significantly more IPB+ arm parents than usual-care arm parents received advice on more than two safety messages (30% vs. 12%; AOR 3.06, 95% CI 1.72 to 5.43), but there was no significant difference in this item between IPB-only and usual-care arm parents (15% vs. 12%; AOR 1.09, 95% CI 0.57 to 2.10).
| Receipt of fire safety advice and promotion | Trial arma | IPB only vs. usual care | IPB+ vs. usual care | ||||
|---|---|---|---|---|---|---|---|
| Usual care (N = 258), n (%) | IPB only (N = 252), n (%) | IPB+ (N = 241), n (%) | AOR (95% CI)b | p-value | AOR (95% CI)b | p-value | |
| Received advice on the five key IPB messages | |||||||
| Smoke alarmsc | [54] | [52] | [54] | ||||
| No | 155 (76.0) | 132 (66.0) | 107 (57.2) | 1.00 | 1.00 | ||
| Yes | 49 (24.0) | 68 (34.0) | 80 (42.8) | 1.36 (0.82 to 2.26) | 0.23 | 2.27 (1.40 to 3.67) | < 0.01 |
| Matchesc | [56] | [57] | [58] | ||||
| No | 177 (87.6) | 167 (85.6) | 133 (72.7) | 1.00 | 1.00 | ||
| Yes | 25 (12.4) | 28 (14.4) | 50 (27.3) | 1.05 (0.54 to 2.04) | 0.89 | 2.74 (1.51 to 4.96) | < 0.01 |
| Fire escape plans | [55] | [58] | [57] | ||||
| No | 175 (86.2) | 168 (86.6) | 133 (72.3) | 1.00 | 1.00 | ||
| Yes | 28 (13.8) | 26 (13.4) | 51 (27.7) | 0.79 (0.40 to 1.55) | 0.50 | 2.38 (1.35 to 4.21) | < 0.01 |
| Bedtime safety routines | [54] | [56] | [56] | ||||
| No | 183 (89.7) | 173 (88.3) | 147 (79.5) | 1.00 | 1.00 | ||
| Yes | 21 (10.3) | 23 (11.7) | 38 (20.5) | 0.89 (0.44 to 1.82) | 0.76 | 2.21 (1.18 to 4.12) | 0.01 |
| Causes of fires | [57] | [56] | [57] | ||||
| No | 169 (84.1) | 149 (76.0) | 113 (61.4) | 1.00 | 1.00 | ||
| Yes | 32 (15.9) | 47 (24.0) | 71 (38.6) | 1.50 (0.85 to 2.65) | 0.17 | 3.35 (1.98 to 5.68) | < 0.01 |
| Number of key safety messages had advice on | [53] | [52] | [52] | ||||
| ≤ 2 | 180 (87.8) | 170 (85.0) | 132 (69.8) | 1.00 | 1.00 | ||
| 3–5 | 25 (12.2) | 30 (15.0) | 57 (30.2) | 1.09 (0.57 to 2.10) | 0.80 | 3.06 (1.72 to 5.43) | < 0.01 |
| Attended a fire safety session in the last year | [53] | [50] | [49] | ||||
| No | 197 (96.1) | 178 (88.1) | 155 (80.7) | 1.00 | 1.00 | ||
| Attended one or more | 8 (3.9) | 24 (11.9) | 37 (19.3) | 3.20 (1.27 to 8.06) | 0.01 | 7.07 (3.05 to 16.38) | < 0.01 |
| Attended a fire safety session at children’s centre | [53] | [50] | [49] | ||||
| No | 197 (96.1) | 185 (91.6) | 163 (84.9) | 1.00 | 1.00 | ||
| Attended one or more | 8 (3.9) | 17 (8.4) | 29 (15.1) | 2.18 (0.85 to 5.63) | 0.11 | 5.14 (2.20 to 12.03) | < 0.01 |
| Attended fire safety session about each of the five key messages in the IPB in the last yeard | [53] | [50] | [49] | ||||
| Smoke alarms | |||||||
| No | 198 (96.6) | 180 (89.1) | 158 (82.3) | 1.00 | 1.00 | ||
| Yes | 7 (3.4) | 22 (10.9) | 34 (17.7) | 3.34 (1.30 to 8.58) | 0.01 | 6.71 (2.80 to 16.04) | < 0.01 |
| Matches | |||||||
| No | 201 (98.0) | 189 (93.6) | 169 (88.0) | 1.00 | 1.00 | ||
| Yes | 4 (2.0) | 13 (6.4) | 23 (12.0) | 2.80 (0.85 to 9.29) | 0.09 | 6.78 (2.24 to 20.55) | < 0.01 |
| Fire escape plans | |||||||
| No | 201 (98.0) | 188 (93.1) | 162 (84.4) | 1.00 | 1.00 | ||
| Yes | 4 (2.0) | 13 (6.9) | 30 (15.6) | 3.48 (1.06 to 11.44) | 0.04 | 9.88 (3.31 to 29.43) | < 0.01 |
| Bedtime safety routines | |||||||
| No | 202 (98.5) | 189 (93.6) | 172 (89.6) | 1.00 | 1.00 | ||
| Yes | 3 (1.5) | 13 (6.4) | 20 (10.4) | 3.93 (1.04 to 14.93) | 0.04 | 7.83 (2.23 to 27.55) | < 0.01 |
| Causes of fires | |||||||
| No | 198 (96.6) | 184 (91.1) | 162 (84.4) | 1.00 | 1.00 | ||
| Yes | 7 (3.4) | 18 (8.9) | 30 (15.6) | 0.56 (0.0 to 11.9) | 0.06 | 5.52 (2.29 to 13.30) | < 0.01 |
Significantly more families in the IPB+ and IPB-only arms than usual-care arm parents had attended one or more fire safety sessions in the last year (19%, 12% and 4%, respectively; AOR IPB+ vs. usual care 7.07, 95% CI 3.05 to 16.38; AOR IPB only vs. usual care 3.20, 95% CI 1.27 to 8.06) and significantly more IPB+ and IPB-only parents than usual-care arm parents had attended a fire safety session at a children’s centre (15%, 8% and 4%, respectively; AOR IPB+ vs. usual care 5.14, 95% CI 2.20 to 12.03; AOR IPB only vs. usual care 2.18, 95% CI 0.85 to 5.63). Significantly more parents in the IPB+ arm than usual-care arm parents had attended a fire safety session on each of the key IPB messages, with AORs ranging from 5.52 (95% CI 2.29 to 13.30) (session on causes of fires) to 9.88 (95% CI 3.31 to 29.43) (session on fire escape planning). Significantly more parents in the IPB-only arm than usual-care arm parents had attended a fire safety session on three of the key IPB messages [session on smoke alarms: AOR 3.34, 95% CI 1.30 to 8.58; session on fire escape planning: AOR 3.48, 95% CI 1.06 to 11.44; session on bedtime safety routines: AOR 3.93, 95% CI 1.04 to 14.93).
Primary and secondary outcome measures
Table 120 shows the primary and secondary outcome measures by treatment arm. There was no significant difference between treatment arms in the proportion of families who reported having a fire escape plan (AOR IPB only vs. usual care 0.93, 95% CI 0.58 to 1.49; AOR IPB+ vs. usual care 1.41, 95% CI 0.91 to 2.20) and this did not vary by family-level deprivation measured using the IMD 2010 score (p-value for interaction 0.86). Significantly more IPB-only families (AOR 2.56, 95% CI 1.38 to 4.76) and IPB+ families (AOR 1.78, 95% CI 1.01 to 3.15) were in the ‘more fire escape planning behaviours’ group than usual-care arm families. Parents in the IPB-only arm were significantly less likely to have found their children playing with matches or lighters than usual-care arm parents (AOR 0.27, 95% CI 0.08 to 0.94) and they also reported significantly more bedtime fire safety routines than usual-care arm parents (AOR for a 1-unit increase in the number of bedtime fire safety routines 1.59, 95% CI 1.09 to 2.31). There were no other significant differences in other secondary outcome measures. The ICC for the primary outcome measure was 0.00261 (95% CI 0.00000 to 0.02737).
| Outcome measures | Trial arma | IPB only vs. usual care | IPB+ vs. usual care | ||||
|---|---|---|---|---|---|---|---|
| Usual care (N = 258), n (%) | IPB-only (N = 252), n (%) | IPB+ (N = 241), n (%) | AOR (95% CI) | p-value | AOR (95% CI) | p-value | |
| Primary outcome measureb | |||||||
| Family have fire escape plan | [4] | [9] | [5] | ||||
| No | 135 (53.2) | 135 (55.6) | 116 (49.2) | 1.00 | 1.00 | ||
| Yes | 119 (46.9) | 108 (44.4) | 120 (50.8) | 0.93 (0.58 to 1.49) | 0.76 | 1.41 (0.91 to 2.20) | 0.13 |
| Secondary outcome measuresc | |||||||
| Fire escape behaviours composite variable | |||||||
| Fewer fire escape behaviours | 45 (17.4) | 29 (11.5) | 32 (13.3) | 1.00 | 1.00 | ||
| More fire escape behaviours | 213 (82.6) | 223 (88.5) | 209 (86.7) | 2.56 (1.38 to 4.76) | < 0.01 | 1.78 (1.01 to 3.15) | 0.05 |
| Component elements of fire escape plan (presented for descriptive purposes only) | |||||||
| Torch next to bed | [38] | [40] | [34] | ||||
| No | 130 (59.1) | 133 (62.7) | 121 (58.5) | ||||
| Yes | 90 (40.9) | 79 (37.3) | 86 (41.5) | ||||
| Knows sound of smoke alarm | [8] | [14] | [8] | ||||
| No | 7 (2.8) | 6 (2.5) | 9 (3.9) | ||||
| Yes | 243 (97.2) | 232 (97.5) | 224 (96.1) | ||||
| Front door key accessible | [4] | [5] | [1] | ||||
| Never/< 4 days | 31 (12.2) | 28 (11.3) | 18 (7.5) | ||||
| ≥ 4 days per week | 223 (87.8) | 219 (88.7) | 222 (92.5) | ||||
| Window keys accessible | [7] | [14] | [8] | ||||
| Never/< 4 days | 71 (28.3) | 45 (18.9) | 51 (21.9) | ||||
| ≥ 4 days per week | 180 (71.7) | 193 (81.1) | 182 (78.1) | ||||
| Exits clear | [8] | [5] | [5] | ||||
| Never/< 4 days | 35 (14.0) | 31 (12.6) | 35 (14.8) | ||||
| ≥ 4 days per week | 215 (86.0) | 216 (87.4) | 201 (85.2) | ||||
| Smoke alarms fitted and working on every level | [7] | [12] | [8] | ||||
| No | 22 (8.8) | 14 (5.8) | 13 (5.6) | 1.00 | 1.00 | ||
| Yes | 229 (91.2) | 226 (94.2) | 220 (94.4) | 1.61 (0.71 to 3.66) | 0.25 | 1.56 (0.71 to 3.42) | 0.27 |
| Fire setting or match play by children | [52] | [49] | [49] | ||||
| No | 197 (95.6) | 198 (97.5) | 181 (94.3) | 1.00 | 1.00 | ||
| Yes | 9 (4.4) | 5 (2.5) | 11 (5.7) | 0.27 (0.08 to 0.94) | 0.04 | 1.2 (0.43 to 3.08) | 0.77 |
| Bedtime fire safety routine score, median (IQR)d | 8 (8–9) [9] | 9 (8–10) [16] | 8.5 (8–9) [11] | 1.59 (1.09 to 2.31) | 0.02 | 1.22 (0.85 to 1.76) | 0.28 |
| Took part in smoking cessation courses/support | [60] | [43] | [43] | ||||
| No | 5 (19.2) | 8 (33.3) | 5 (23.8) | 1.00 | 1.00 | ||
| Yes | 21 (80.8) | 16 (66.7) | 16 (76.2) | 0.23 (0.04 to 1.43) | 0.12 | 0.61 (0.11 to 3.40) | 0.57 |
| Families’ knowledge of the causes of fires in the homed | |||||||
| 0 | 78 (30.2) | 81 (32.1) | 70 (29.1) | 1.10 (0.77 to 1.57) | 0.61 | 1.22 (0.86 to 1.73) | 0.26 |
| 1 | 93 (36.1) | 86 (34.1) | 76 (31.5) | ||||
| 2 | 80 (31.0) | 81 (32.1) | 85 (35.3) | ||||
| 3 | 7 (2.7) | 4 (1.6) | 10 (4.2) | ||||
| Home safety information provided by children’s centree | [57] | [55] | [53] | ||||
| Neither satisfied nor dissatisfied, fairly dissatisfied, very dissatisfied | 16 (8.0) | 22 (11.2) | 23 (12.2) | 1.00 | 1.00 | ||
| Very satisfied, fairly satisfied | 31 (15.4) | 46 (23.4) | 73 (38.8) | 1.08 (0.4 to 2.8) | 0.87 | 1.79 (0.7 to 4.4) | 0.20 |
| Haven’t received information | 154 (76.6) | 129 (65.5) | 92 (48.9) | ||||
Adjusted ORs for the primary outcome measure from the complete-case analysis (AOR IPB only vs. usual care 0.93, 95% CI 0.58 to 1.49; AOR IPB+ vs. usual care 1.41, 95% CI 0.91 to 2.20) differed from those in the analysis using multiply imputed data by only 1% for the IPB only arm compared with the usual-care arm (AOR 0.92, 95% CI 0.58 to 1.46) and by < 1% for the IPB+ arm compared with the usual-care arm (AOR 1.40, 95% CI 0.89 to 2.21).
Assuming that participants with missing data at follow-up had a baseline value for having a fire escape plan, there were similar results for the IPB-only arm compared with the usual-care arm (AOR 0.95, 95% CI 0.60 to 1.51; 2% difference in AORs between the complete-case analysis and the analysis assuming no change from baseline) and for the IPB+ arm compared with the usual-care arm (AOR 1.39, 95% CI 0.91 to 2.12; 1% difference in AORs between the complete-case analysis and the analysis assuming no change from baseline).
Cost-effectiveness
The cost of developing the IPB was estimated from researchers’ logbooks to be £15,860. Table 121 presents the unit costs applied to the resource use data that were obtained from the questionnaires and logbooks to obtain the overall costs. The cost of implementing the IPB with or without facilitation is presented in Table 122. The costs are reported as both a cost per children’s centre (i.e. cluster) and a cost per family randomised; the latter is used in the cost-effectiveness analysis. It can be observed that the costs associated with facilitation of the IPB varied across study centres (range £84.74–327.84).
| Resource | Value | Source |
|---|---|---|
| Parental costs | ||
| Time costs | £45.70 per hour | Department for Transport493 |
| Travel costs by car | £0.18 per km | Department for Transport493 |
| IPB implementation costs | ||
| Researcher’s time | £19.04 per hour | University of Nottingham pay scale |
| Administrator’s time | £11.24 per hour | University of Nottingham pay scale |
| Children’s centre, FRS and other agency costs | ||
| FRS staff time | £36.00 per hour | Adam Shaw, Cheshire fire and Rescue Service, 20 September 2012, personal communication |
| Children’s centre staff time | £18.00 per hour | Curtis, 201230 (assumed same as home care worker) |
| Home safety inspection | £15.33 | Based on 40-minute visit by children’s centre, FRS or other agency (as in decision models) |
| Arm | Study centre | Number of families randomised | Number of children’s centres | IPB printing and distribution cost (£) | IPB training session cost (£) | IPB facilitation cost (£) | Total cost per study centre (£) | Total cost per children’s centre (£) | Total cost per family randomised (£) |
|---|---|---|---|---|---|---|---|---|---|
| Usual care | Bristol | 100 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Newcastle | 86 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Norwich | 95 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Nottingham | 89 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| IPB only | Bristol | 101 | 3 | 152.50 | 0.00 | 0.00 | 152.50 | 50.83 | 1.51 |
| Newcastle | 88 | 3 | 152.50 | 0.00 | 0.00 | 152.50 | 50.83 | 1.73 | |
| Norwich | 82 | 3 | 152.50 | 0.00 | 0.00 | 152.50 | 50.83 | 1.86 | |
| Nottingham | 98 | 3 | 152.50 | 0.00 | 0.00 | 152.50 | 50.83 | 1.56 | |
| IPB+ | Bristol | 102 | 3 | 152.50 | 1328.95 | 327.84 | 1809.29 | 603.10 | 17.74 |
| Newcastle | 87 | 3 | 152.50 | 1408.84 | 220.57 | 1781.91 | 593.97 | 20.48 | |
| Norwich | 93 | 3 | 152.50 | 1488.74 | 127.90 | 1769.14 | 589.71 | 19.02 | |
| Nottingham | 91 | 3 | 152.50 | 1568.63 | 84.74 | 1805.87 | 601.96 | 19.84 |
Tables 123 and 124 present details about the fire safety activities, including home safety inspections, undertaken by the different agencies (i.e. children’s centres, fire and rescue service, parents, etc.). This information was combined with the unit costs presented in Table 121 to obtain the cost estimates incurred by the different agencies by treatment arm (Table 125). When these ‘other intervention costs’ were aggregated across agencies, costs in the usual-care arm were estimated to be highest.
| Fire safety activity summary | Trial arm | ||
|---|---|---|---|
| Usual care | IPB only | IPB+ | |
| Proportion of children’s centres that ran fire safety sessions | 5/11a | 7/12 | 11/12 |
| Of those that ran fire safety sessions | |||
| Mean number of fire safety sessions (min. to max.) | 1.2 (1 to 2) | 2.1 (1 to 4) | 3.1 (1 to 7) |
| Mean session length (min. to max.) | 116.25 (90 to 120) | 90.25 (30 to 120) | 89 (30 to 130) |
| Mean number of children’s centre staff providing fire safety session (min. to max.) | 4.25 (2 to 20) | 2.03 (0 to 2) | 3.34 (1 to 5) |
| Mean number of fire and Rescue Service staff providing fire safety session (min. to max.) | 1.85 (1 to 5) | 0.6 (0 to 2) | 0.78 (0 to 6) |
| Proportion of children’s centres that received other help from FRS staff | 5/12 | 3/12 | 8/12 |
| Proportion of children’s centres that received visits from FRS staff | 4/12 | 1/12 | 3/12 |
| Proportion of children’s centre staff attending fire safety training | 6/11a | 10/10a | 3/12 |
| Fire safety activity and home safety inspection summary | Trial arm | ||
|---|---|---|---|
| Usual care, n/N (%) | IPB only, n/N (%) | IPB+, n/N (%) | |
| Parents attending fire safety sessions | 8/205 (4) | 24/178 (13) | 34/189 (18) |
| Parents who had a home safety inspection | 23/202 (11) | 34/201 (17) | 45/146 (31) |
| Home safety inspection bya | |||
| Children’s centre | 3/23 | 4/34 | 6/45 |
| Fire and rescue service | 10/23 | 16/34 | 24/45 |
| Other agency (e.g. council) | 10/23 | 19/34 | 16/45 |
| Cost components | Usual care, mean (min. to max.) | IPB only, mean (min. to max.) | IPB+, mean (min. to max.) | |||
|---|---|---|---|---|---|---|
| Per cluster | Per family | Per cluster | Per family | Per cluster | Per family | |
| Number of clusters/families | 9 | 151 | 9 | 140 | 9 | 123 |
| Fire safety sessions (£) | ||||||
| Children’s centre costs | 421.00 (0.00 to 1800a) | 13.72 (0.00 to 62.07) | 63.00 (0.00 to 198.00) | 2.06 (0.00 to 7.07) | 222.00 (0.00 to 900.00) | 7.63 (0.00 to 32.14) |
| FRS costs | 74.38 (0.00 to 378.00) | 2.57 (0.00 to 13.03) | 68.66 (0.00 to 288.00) | 2.20 (0.00 to 9.60) | 136.49 (0.00 to 372.00) | 4.38 (0.00 to 11.63) |
| Parental costs to attend sessions | 2.59 (0.00 to 22.85) | 0.15 (0.00 to 22.85) | 9.15 (0.00 to 22.85) | 0.59 (0.00 to 17.14) | 14.83 (0.00 to 62.32) | 1.09 (0.00 to 35.18) |
| Home safety inspections (£) | ||||||
| Children’s centre costs | 3.41 (0.00 to 15.33) | 0.20 (0.00 to 15.33) | 6.81 (0.00 to 30.66) | 0.44 (0.00 to 15.33) | 8.52 (0.00 to 30.66) | 0.62 (0.00 to 15.33) |
| FRS costs | 13.63 (0.00 to 30.66) | 0.76 (0.00 to 15.33) | 13.63 (0.00 to 30.66) | 1.07 (0.00 to 15.33) | 22.14 (0.00 to 76.65) | 1.62 (0.00 to 15.33) |
| Other agency costs | 10.22 (0.00 to 45.99) | 0.61 (0.00 to 15.33) | 22.14 (0.00 to 45.99) | 1.42 (0.00 to 45.99) | 15.33 (0.00 to 45.99) | 1.12 (0.00 to 15.33) |
| Total (£) | ||||||
| Other intervention costs | 303.01 (30.66 to 1367.67) | 18.06 (0.00 to 90.43) | 117.87 (45.89 to 210.58) | 7.58 (0.00 to 45.06) | 224.97 (110.66 to 497.62) | 16.46 (2.70 to 51.33) |
| IPB provision, training and facilitation costs plus other intervention costs | 303.01 (30.66 to 1367.67) | 18.06 (0.00 to 90.43) | 143.68 (62.51 to 240.22) | 9.24 (1.51 to 46.79) | 507.81 (290.26 to 859.92) | 37.16 (21.18 to 79.20) |
One children’s centre was identified as a potential outlier with maximum costs incurred by the centre estimated at £1800. However, when this centre was removed, costs in the usual-care arm still remained higher than in the IPB-only or IPB+ arms (mean £254.25 with a maximum per cluster of £792.00) because of the fire safety sessions run by children’s centres being, on average, longer in duration and more staff intensive Table 119. The distribution of costs by cluster within a trial site is presented separately in Figure 64 for each of the intervention arms.
FIGURE 64.
Plot of total costs per family (2010 UK£) by cluster (i.e. children’s centre): (a) usual care; (b) IPB only; and (c) IPB+. Boxes represent the lower and upper quartiles around the median, lines represent the lower and higher extremes, and dots represent outliers.
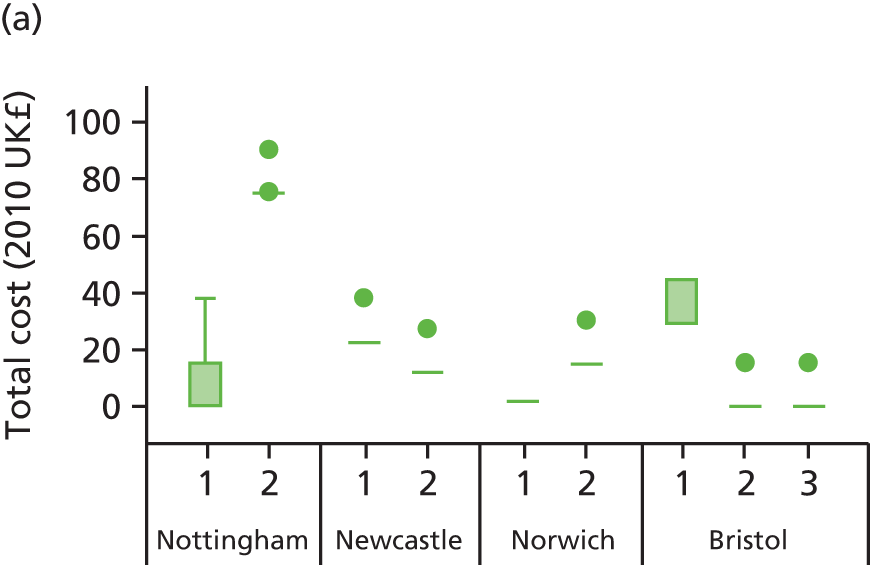
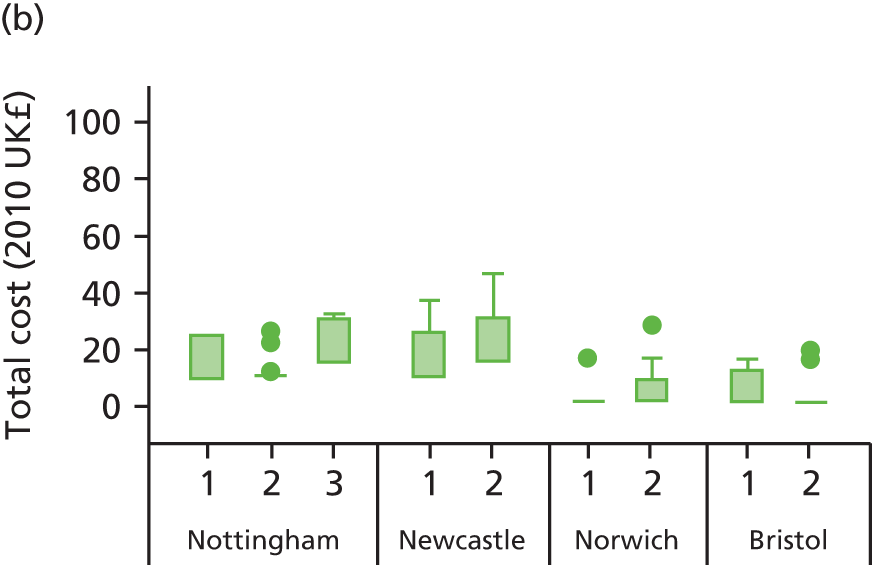
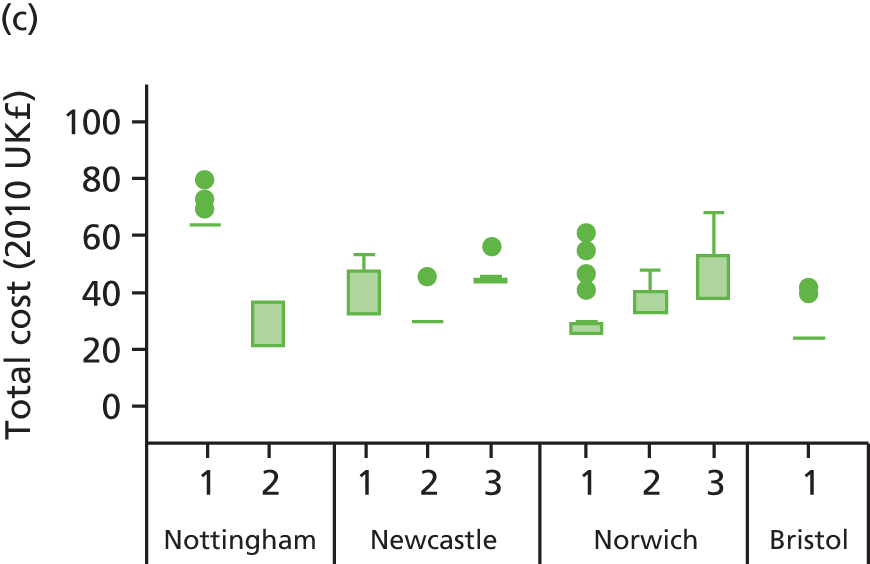
Table 126 presents the results of the cost-effectiveness analysis comparing the IPB-only and IPB+ arms with usual care. As stated in the methods section, the inverse of the difference in the probabilities of having a fire escape plan, say between IPB only and usual care, is equal to the NNT and therefore the cost-effectiveness ratio can be interpreted as the cost per additional fire escape plan under the intervention. The results of the analysis ignoring the effect of clustering, covariates and correlation between costs and effects show that IPB only is less costly and only marginally more effective than usual care, resulting in an ICER of –£1260 per additional fire escape plan, whereas IPB+ is more costly and only marginally more effective than usual care, resulting in an ICER of £616.13 per additional fire escape plan. It can be observed that, when allowing for the effect of clustering and correlation between costs and effects, the uncertainty is reduced.
| Description | Trial arm | IPB only vs. usual care | IPB+ vs. usual care | ||
|---|---|---|---|---|---|
| Usual care | IPB only | IPB+ | |||
| Number of families | 151 | 140 | 123 | ||
| Number of children’s centres | 9 | 9 | 9 | ||
| ‘Naive analysis’ (ignoring clustering, covariates and correlation between costs and effects) | |||||
| Mean cost per family (95% CrI) (£) | 18.06 (0.00 to 75.10) | 9.24 (1.51 to 29.84) | 37.16 (21.18 to 63.87) | –8.82 | 19.10 |
| Probability of having a fire escape plan | 0.46 (r = 69/151) | 0.46 (r = 65/140) | 0.49 (r = 60/123) | 0.007 | 0.031 |
| ICER (£) | –1260.00 | 616.13 | |||
| Analysis incorporating effect of clustering, covariates and correlation between costs and effects | |||||
| Mean cost per family (95% CrI) (£) | 21.15 (3.95 to 38.31) | 12.65 (4.66 to 20.03) | 41.41 (31.58 to 52.41) | –8.49 | 20.26 |
| Probability of having a fire escape plan (95% CrI) | 0.48 (0.35 to 0.56) | 0.49 (0.38 to 0.58) | 0.48 (0.37 to 0.58) | 0.03 | 0.02 |
| ICER (£) | –275.31 | 1007.96 | |||
| Sensitivity analysis omitting outlying cluster 6 in the usual-care arm (incorporating effect of clustering and correlation between costs and effects) | |||||
| Mean cost per family (95% CrI) (£) | 14.99 (6.16 to 24.11) | 13.26 (4.52 to 22.24) | 39.97 (31.25 to 48.41) | –1.74 | 24.98 |
| Probability of having a fire escape plan (95% CrI) | 0.47 (0.34 to 0.51) | 0.50 (0.37 to 0.64) | 0.48 (0.34 to 0.62) | 0.03 | 0.01 |
| ICER (£) | –53.01 | 3778.55 | |||
In a sensitivity analysis, the children’s centre with the potentially outlying cost (as noted above) was removed from the analysis (see Table 126). The resulting ICERs were –£53.01 for the IPB-only group compared with usual care and £3778.55 for the IPB+ group compared with usual care. Cost-effectiveness acceptability curves for the base-case analysis and the sensitivity analysis removing the outlying children’s centre are presented in Figure 65.
FIGURE 65.
Cost-effectiveness acceptability curves: base-case (complete-case) analysis and complete-case analysis omitting the outlier.
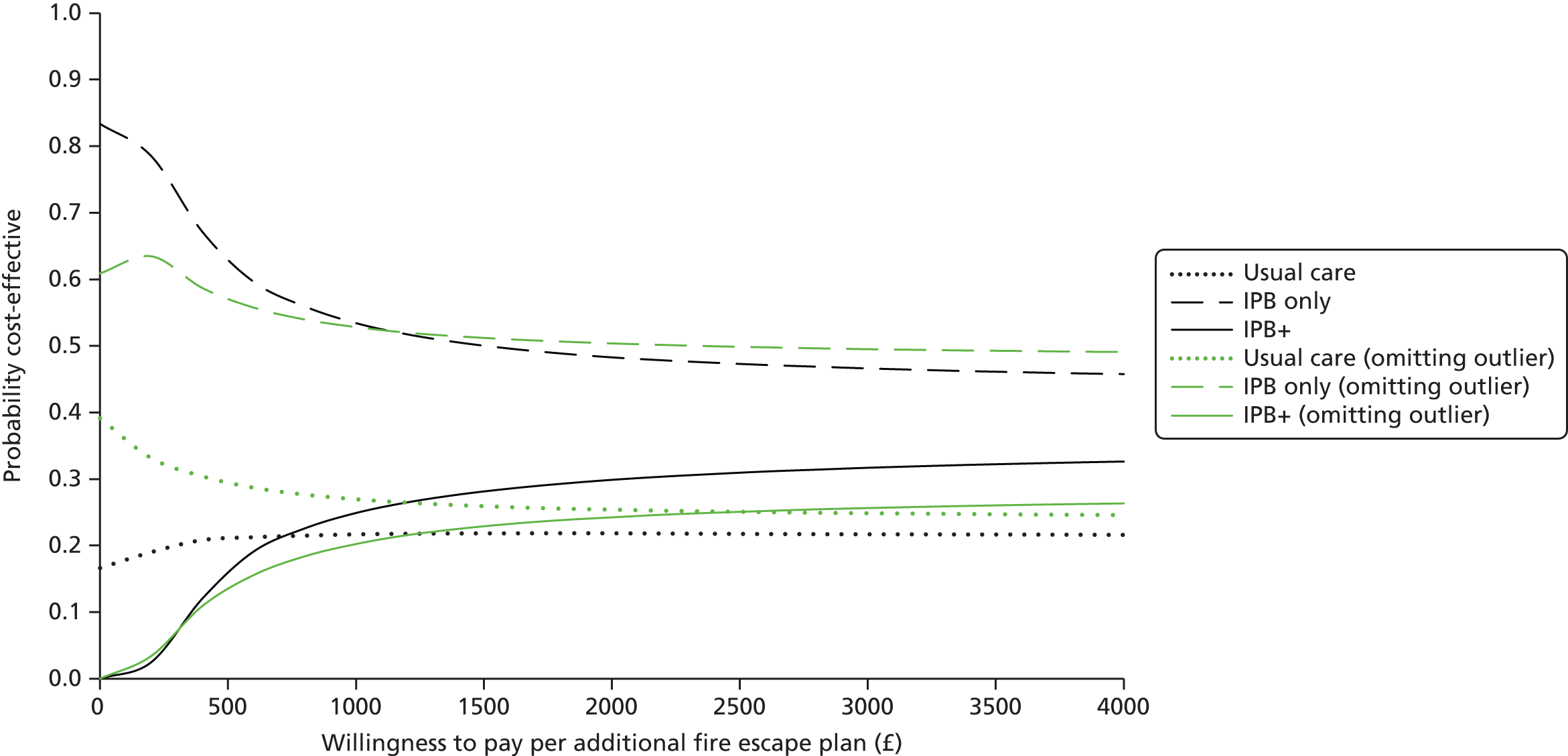
Table 127 shows the extent of the missing data within the cost components, which ranged from just under 50% (parental costs) to nearly 60% (children’s centre costs). Because of the extent of the missing values, the results of the imputation analysis should be interpreted with caution.
| Cost components | Complete (£) | Incomplete (imputed) (£) | Total (£) |
|---|---|---|---|
| Parental costs | 563 | 549 | 1112 |
| Fire and rescue service costs including HSI | 510 | 602 | 1112 |
| Children’s centre costs including HSI | 451 | 661 | 1112 |
| Other agency costs including HSI | 594 | 518 | 1112 |
Table 128 displays the results of the cost-effectiveness analysis based on the imputed data set. It can be observed that the average total costs per family and thus the differences between the arms are broadly similar to those in the primary (non-imputed) analysis reported in Table 126. For example, in the imputed data set the mean cost difference between the IPB-only arm and the usual-care arm is –£8.60, whereas in the complete-case data set it is –£8.49; similarly, in the imputed data set the mean cost difference between the IPB+ arm and the usual-care arm is £23.80, whereas in the complete-case data set it is £20.26. The probability of a fire escape plan was similar to that in the primary analysis for the usual-care arm, but it decreased from 0.49 to 0.44 for the IPB-only arm and increased from 0.48 to 0.58 for the IPB+ arm. These changes mean that the point estimate for the difference in effectiveness between the IPB-only arm and the usual-care arm is now fractionally negative, which makes the ICER positive. Note that these results should be interpreted with caution because of the large proportion of missing data imputed, ranging from just under 50% for parental costs to nearly 60% for children’s centre costs.
| Description | Trial arm | IPB only vs. usual care | IPB+ vs. usual care | ||
|---|---|---|---|---|---|
| Usual care | IPB only | IPB+ | |||
| Number of families | 370 | 369 | 373 | ||
| Number of clusters | 12 | 12 | 12 | ||
| Cost per family (95% CI) (£) | 19.21 (14.64 to 23.77) | 10.80 (6.48 to 14.73) | 43.01 (38.71 to 47.33) | –8.60 | 23.80 |
| Probability of fire escape plan (95% CI) | 0.44 (0.37 to 0.52) | 0.44 (0.37 to 0.52) | 0.58 (0.50 to 0.65) | –0.00 | 0.13 |
| ICER | 6447.53 | 177.61 | |||
| Probability cost-effective at a WTP of £1000 | 0.02 | 0.02 | 0.96 | ||
| Probability cost-effective at a WTP of £2000 | 0.01 | 0.01 | 0.98 | ||
Incorporating findings from the trial into the development of a second injury prevention briefing
Four workshops were held with users of the fire prevention IPB and potential users of a future IPB. The numbers that were invited and who attended each workshop are shown in Table 129.
| Location | Number invited | Number attending |
|---|---|---|
| Bristol | 10 | 6 |
| Newcastle | 38 | 15 |
| Nottingham | 25 | 7 |
| Norwich | 27 | 8 |
| Total | 100 | 36 |
The key findings from the workshops were:
-
activities need to be designed in ways that help parents think about their situations and possible solutions, rather than just telling them what to do
-
activities need to be flexible and adaptable by users of the briefing to accommodate their opportunities and the capabilities of their client groups
-
separate information for managers is not needed
-
advice on how to obtain local data is needed
-
information on the non-financial consequences of injury and, when known, the cost-effectiveness of interventions should be included
-
a short section highlighting the needs of parents and children with disabilities would be helpful
-
all injury topics should be covered in one document, with a front section on child development, anticipatory guidance, common risk factors, etc., followed by self-contained activities and, finally, detailed information on each type of injury.
These findings were incorporated into the design of the IPB covering the prevention of fire-related injuries, falls, poisonings and scalds. The IPB is shown in Appendix 6, Injury prevention briefing 2 and is available to download from www.nottingham.ac.uk/research/groups/injuryresearch/projects/kcs/index.aspx (accessed 1 November 2016).
Discussion
Main findings
A complex intervention to change behaviours to improve fire safety in the home was developed using the MRC complex interventions framework. 469 Data from a series of studies undertaken earlier in the KCS programme, interviews with stakeholders and workshops with practitioners were used to develop an IPB for the prevention of fire-related injuries and a training and facilitation package to support its implementation in children’s centres. The implementation of the IPB was tested using a RCT (study M) with an economic evaluation and nested qualitative study. A further IPB covering the prevention of fire-related injuries, scalds, falls and poisonings was subsequently developed using data from all component elements of the KCS programme.
The three-arm trial, which compared IPB+, IPB only and usual care, found that families in either intervention arm were not significantly more likely to report having a fire escape plan than usual-care arm families (AOR IPB vs. usual care 0.93, 95% CI 0.58 to 1.49; AOR IPB+ vs. usual care 1.41, 95% CI 0.91 to 2.20). However, families in both intervention arms reported significantly more behaviours that were component elements of fire escape planning (AOR IPB vs. usual care 2.56, 95% CI 1.38 to 4.76; AOR IPB+ vs. usual-care 1.78, 95% CI 1.01 to 3.15). Families in the IPB-only arm reported significantly more bedtime fire safety practices (AOR for a 1-unit increase in the number of bedtime fire safety routines 1.59, 95% CI 1.09 to 2.31) and were significantly less likely to report that their children had been found playing with matches or lighters (AOR 0.27, 95% CI 0.08 to 0.94) than families in the usual-care arm.
Families in the IPB+ arm were significantly more likely than usual-care arm families to report receiving advice on each of the five key safety messages in the IPB, whereas, although the proportion who reported receiving advice was higher in the IPB-only arm than in the usual-care arm for most messages, it was not significantly higher. The proportion receiving advice on the five key messages ranged from 21% in the IPB+ arm, 12% in the IPB-only arm and 10% in the usual-care arm for advice on bedtime safety routines to 43%, 34% and 24% for advice on smoke alarms, respectively. Families in both intervention arms were significantly more likely to report attending a fire safety session than usual-care arm families; most of these sessions were delivered at children’s centres.
All children’s centres in the IPB+ arm and 58% of children’s centres in the IPB-only arm developed a plan for implementing the IPB. More children’s centres in the IPB+ arm provided advice on each of the five key messages and ran sessions on each of the five key messages than IPB-only children’s centres, but the numbers were too small to allow for statistical analysis. Data from the qualitative study supported the finding that IPB+ children’s centres showed greater implementation of the IPB than IPB-only children’s centres and that children’s centres found the IPB and the facilitation package relevant and useful.
The economic analysis, which was conducted from a societal perspective including costs incurred by the family, children’s centre, fire and rescue service and other agencies that provided home safety inspections, showed that the IPB-only intervention dominates usual care as it is both less costly and marginally more effective, whereas the IPB+ intervention is more costly but only marginally more effective than usual care.
Strengths and limitations
The intervention that we developed was theoretically based and used the MRC complex intervention framework and evidence generated from numerous studies within the KCS programme. Our evaluation included a thorough assessment of the implementation of the intervention, used mixed methods and incorporated an economic evaluation. The treatment arms appeared well balanced at baseline, recruitment exceeded our required sample size, losses to follow-up were as estimated in our sample size calculation and the retention rate was similar across treatment arms. Findings from the multiply imputed data set were very similar to those in the complete-case analysis for the main analysis and the economic analysis.
Although we found evidence of implementation of the IPB, it is clear that the five key safety messages did not reach all families in either intervention arm (67%, 59% and 47% of families did not receive information on any of the messages in the usual-care arm, IPB-only arm and IPB+ arm, respectively). It is possible that greater implementation of the intervention may have achieved greater behavioural change. The qualitative study provided insight into possible explanations for the limited implementation. All children’s centres described major current, imminent or recent restructuring, which made it hard to deliver services and implement health promotion messages, including the IPB. Staff changes, budget constraints and staff capacity to take on additional tasks also limited implementation. Some centres found it difficult to prioritise fire safety over other health promotion topics because of a lack of local statistics to demonstrate local need. Centres had difficulty in delivering specific fire safety ‘sessions’, with poor parental attendance because of competing or more urgent issues or life changes for parents, frequent moves or children’s illnesses. Some centres found engaging parents in fire safety education difficult because of a perceived lack of relevance, perceptions that the information was already known, fear of being patronised or peer pressure. However, once parents were ‘through the door’, staff were frequently surprised by the depth of their engagement. Implementation was more effective when integrated into existing sessions. Trial procedures introduced additional demands for the children’s centre staff around data collection.
The finding that a significantly higher proportion of families in both intervention arms than in the usual care arm belonged to the ‘more fire escape behaviours’ group, without a significant difference in the proportions reporting having a fire escape plan, requires further exploration. The study questionnaire defined a fire escape plan as ‘. . . a plan of what you would do to escape from the house if a fire broke out or the smoke alarm went off’. As a result of structured parent interviews earlier in the programme we added questions covering some of the elements of a fire escape plan, which the IPB provided advice on (knowing the sound of a smoke alarm, having a torch beside the bed, having door and window keys accessible, having clear exit routes). These were combined into a composite secondary outcome measure categorised as ‘more fire escape behaviours’ or ‘fewer fire escape behaviours’. Our trial findings suggest that it may not be useful to use a single-item question to measure possession of a fire escape plan. Further work will explore responses to open questions about actions that families would take if they could smell smoke and/or the smoke alarm was sounding and how these relate to the single-item question on having a fire escape plan. Our primary and most of our secondary outcome measures were self-reported by parents or children’s centre staff. Participants (parents or children’s centre staff) could not be blinded to treatment arm and hence there was the potential for outcome detection bias.
Our finding that providing the IPB without facilitation cost less than usual care appears counterintuitive. A potential explanation is that session plans provided in the IPB allowed children’s centres to deliver more focused sessions that required fewer staff. We found that the intervention arms provided sessions of a similar length using a similar number of staff for delivery, and that both intervention arms provided shorter sessions using fewer staff than the usual-care arm. It is acknowledged that the intervention cost component of the cost-effectiveness analysis is subject to the size of the target population (i.e. the number of children’s centres). Although we excluded IPB developmental costs from the cost-effectiveness analysis, we did include printing and distribution costs for the IPB and facilitator training costs. However, we would expect the latter costs to decrease as the target population increased because of economies of scale for printing and training, etc., which would potentially make the IPB+ intervention more cost-effective.
Our trial had three arms and multiple secondary outcome measures, leading to multiple significance testing and the potential for type 1 errors. Many of the effect estimates for the secondary outcome measures, especially at the level of children’s centres, were imprecise because of small numbers. We were unable to fit the imputation model without getting error messages if we included cluster as a categorical variable, and so clustering has not been taken into account in the imputation model, although cluster was accounted for in the analysis. There is some evidence that multiple imputation with a classical logistic regression (not accounting for clustering) can provide unbiased estimates of the intervention effect. 494 In addition, our use of multiple imputation assumes that data are missing at random, which may not be the case, in particular for participants who did not respond at 12 months, as discussed in the following paragraph. In addition, there were a large number of missing cost data in the economic analysis and, although the results using multiple imputation were similar to those from the complete-case analysis, caution must be taken in interpreting these findings.
We used strategies to minimise losses to follow-up and retained sufficient participants to meet our sample size requirements, but there was some evidence that families retained in the trial were less disadvantaged than those lost to follow-up. Following up participants was challenging and resource intensive because of household moves, families no longer using the children’s centre and changes in mobile phone numbers. The ongoing national evaluation of children’s centres has found that most children’s centre services were used by families for < 1 year. 495 Under these conditions, it is difficult to achieve high levels of penetration of the intervention, to deliver multiple safety messages or to reinforce the same message and to achieve high follow-up rates. Higher follow-up rates may have been achieved through the use of a repeated outcome measurement, but this has to be weighed against the burden that this places on participants, particularly those from disadvantaged communities. Despite differential loss to follow-up, those retained in our trial still represented a population experiencing substantial disadvantage.
All children’s centres were retained in the trial. Most (89%) children’s centres participating in the trial were phase 1 centres in the most disadvantaged areas, so our findings should be generalisable to other children’s centres in similar areas. Participants (children’s centres or parents) may differ from non-participants in terms of interest in fire prevention and this may limit generalisability. Attenders at children’s centres are likely to differ from non-attenders and few participants came from a black or ethnic minority group or had English as a second language. Our findings are therefore likely to be generalisable to the predominantly white British, English-speaking population of children’s centre attenders.
Comparisons with existing research
We were unable to find any published evaluations of injury prevention interventions delivered by children’s centres. Sure Start Local Programmes (SSLPs) were the forerunners to children’s centres, aiming to improve health and well-being of families and young children. They provided integrated early education, child care, health care and family support services in disadvantaged areas. The National Evaluation of Sure Start (NESS)214 followed up > 9000 families and children in 150 SSLPs, comparing outcomes with those in families and children in the Millennium Cohort Study (MCS) living in similarly disadvantaged areas without SSLPs. At the age of 3 years, children in SSLP areas had a significantly lower accidental injury rate than those in the non-SSLP areas. SSLP area families used more child and family-related services than those in non-SSLP areas. The authors note that differences in injury rates may reflect temporal trends because of non-equivalent data collection periods for SSLP and MCS families. A further evaluation when children reached the age of 5 years included > 7000 randomly selected families (from the 9000 used in the 3-year evaluation) and found no significant difference in the injury rate between families in SSLP areas and MCS families in non-SSLP areas. 496
Children’s centres are currently being evaluated nationally in a multicomponent 6-year study [Evaluation of Children’s Centres in England (ECCE)], which has yet to report its main findings. The first strand of the ECCE surveyed children’s centre leaders from approximately 500 centres to characterise children’s centres and the services that they provide. 212 The proportion of children’s centres in the most deprived areas led by local authority staff was similar to that found in our trial (72% vs. 81%, respectively). Findings from the most deprived areas in the ECCE were similar to those from our trial in terms of lone parent families (19% vs. 18%, respectively), families with only one child (47% vs. 51%, respectively) and families living in rented accommodation (48% vs. 54%, respectively). The proportion of white British families in the ECCE was lower than in the trial (70% vs. 95%, respectively). Fewer parents in the ECCE reported having received home safety advice than at baseline in our trial (15% vs. 69%, respectively), but this may reflect differences in the questions asked in the two studies. The proportion of families reporting having a smoke alarm on every floor of their home was similar in the ECCE and in the trial at baseline (79% vs. 74%, respectively), but more ECCE families had tested their smoke alarms in the last 6 months than families in the trial (69% vs. 40%, respectively). 495 Our trial population was therefore broadly similar to families using children’s centres in the most disadvantaged areas of the country with the exception of the trial population being more likely to be white British, more likely to have received home safety advice at baseline and possibly displaying fewer fire safety behaviours.
The ECCE survey212 also found that children’s centres were operating in a changing environment, with 40% experiencing recent cuts in services or staffing and many leaders managing two or more centres. This echoes the findings from our interviews with children’s centre staff, who frequently reported difficulties with implementing the IPB because of reorganisations, staff changes and loss of staff members. The second strand of the ECCE, a survey of 5700 parents,495 showed varied patterns of children’s centre use by parents. Some families were only limited users of services (19%), some used many children’s centre services and activities (38%) and some showed no clear pattern of service use (43%). Our finding that children’s centre staff reported low levels of parental attendance at fire safety sessions may reflect the ECCE findings that most parents are not frequent users of children’s centre services. In addition, the ECCE found that only 8% of parents had used home safety advice or courses provided by children’s centres. This may indicate a lack of prioritisation and provision of injury prevention by children’s centres [as found in our national surveys (study D) in work stream 3; see Chapter 4], coupled with less parental interest in home safety compared with other children’s centre services. 495 Consistent with these findings, children’s centres in our trial reported difficulties in prioritising injury prevention and a lack of parental interest in the subject. We found in work stream 4 (study G; see Chapter 5) that some parents failed to anticipate injury-producing events or the injuries that they could result in. Previous research suggests that perceived susceptibility to injury is important for safety behaviour change. 479 Although the activities in the IPB were aimed at raising parents’ perceptions of susceptibility, this will have required parents to perceive their families as sufficiently susceptible to have participated in fire safety activities provided by children’s centres. Future studies and injury prevention programmes may achieve greater changes in safety behaviour if they incorporate activities aimed at enhancing parents’ perceived susceptibility to injury prior to commencement of the study or programme, as well as during the programme.
The challenges of delivering evidence-based programmes within children’s centres were explored in questionnaires and interviews with staff in 121 children’s centres in the ECCE evaluation. The evaluation found widespread use of evidence-based programmes, particularly parenting programmes, but children’s centre staff ‘appeared to struggle with the concept of evidence-based practice. Some gave equal weight to research evidence and personal experience’ (p. 56). 211 Tension was also reported between maintaining programme fidelity and offering potentially less demanding programmes for families. 211 In addition, only a small number of families were reached by the best-evidenced programmes. 211 These findings share some similarities with those from our trial. Fewer than 50% of families received each of the key safety messages in the IPB and < 20% attended fire safety sessions. Children’s centres reported that it was easier to incorporate fire safety messages into existing activities than run specific fire safety sessions. As in the ECCE, this may have resulted in a reduction in intervention fidelity, as activities are likely to have been adapted and shortened. Our implementation fidelity interviews showed that most children’s centres, particularly those receiving training and facilitation, undertook a range of activities to implement the IPB. This suggests that children’s centres can provide evidence-based injury prevention if provided with the resources and support to do so. However, greater behavioural changes may be achieved if intervention penetration could be increased and if intervention fidelity could be enhanced.
Chapter 8 Patient and public involvement
Patient and public involvement (PPI) underpinned the KCS programme from its inception to its conclusion. The main contributor to PPI was an experienced lay researcher who had worked with members of the KCS programme team on previous child safety projects. In addition, other parents with young children advised the project on the design of some of our data collection tools. This chapter describes the extensive PPI involvement provided by the lay research adviser over the 7 years from when the project was designed to its completion.
Our lay research adviser attended multicentre 3-monthly project management group meetings and 6- to 8-weekly KCS programme meetings with the Nottingham team. Each of these meetings had a specific PPI agenda item to which the lay research adviser spoke. In addition, she contributed to all other discussions at these meetings and provided a lay perspective to the decision-making process. Over time, she contributed increasingly to the evolution of the KCS programme, finding her work enjoyable and a useful learning experience. She feels that she was able to add a personal perspective, looking at processes from a parent’s point of view. As one member of the research team commented:
She brought a much needed different perspective and voice to the team . . . she was very good at challenging and questioning – this brought greater understanding.
During the design of the project, the lay research adviser advised on study design, particularly in relation to strategies for participation recruitment and retention. She contributed to drafting the grant proposal, particularly to the sections on PPI involvement and dissemination, but also by commenting on other sections of the application. Early in the KCS programme the PPI input involved commenting on protocols, advising on detailed recruitment and retention strategies and working on invitation letters and information leaflets, questionnaires and a lay summary of the programme for the KCS programme website. She was able to assess the tone, readability, font and content of the documents, making sure that they were written in plain English. This was of great value to the team, as this quotation from one team member illustrates:
It was really helpful to have the involvement of someone who was able to translate our jargon into plain language.
The lay research adviser attended NIHR training on patient information for parents and children, in-house training on research methods and on undertaking home observations for study B and the training for children’s centres for using the IPB for the RCT in study M. She also drafted reports on PPI input for interim reports and drafted this section of the final report. She received payment for her time and involvement in the project in line with local and INVOLVE policies on consumer/lay involvement (www.invo.org.uk/posttypepublication/involve-policy-on-payments-and-expenses-for-members-of-the-public-including-involve-group-members-february-2016/).
The lay research adviser made substantial and important contributions to studies A, B, G and M in the KCS programme. She has described her input in the following sections.
Study A (piloting of case–control questionnaires)
I visited a local Nottingham children’s centre with a researcher for the purpose of piloting questionnaires with parents. I established a good bond with parents and when the questionnaires were returned, they were all from parents that I had spoken to. One of the parents was particularly interested in being involved further with the study. With my support, she went on to provide feedback on a follow-up questionnaire at a later stage in the study. She was able to represent the views of a significant ethnic minority in the area and also had two young children.
As the researcher who accompanied her on this occasion commented:
She was able to engage participants in the community to take part piloting study tools and had a better response than the researcher present at the same session.
Study B (validation of tools used to collect data)
After some initial study specific training, checking my ‘letter of access’ with the Human Resources department and of course contributing to and becoming familiar with the questionnaire, I embarked on a series of some 25 joint home visits with a researcher. The roles of leader and recorder were shared over the course of visiting. I was keen to make sure that we had a good sample of parents from ethnic minorities and kept this firmly on the agenda. I was able to share views about what it would be like to have a researcher coming into your home and what was required to help set up visits in a way that would encourage parents to engage openly with the research team.
The first contact was very important in order to gain a rapport with the parent – to have a friendly disposition and understand that the parent may be having a bad day. The parent may need to be reassured that it was fine if their child woke up and their attention was diverted. Sometimes participants were nervous about our visit, but I was able to reassure them. Joint visiting diffused the tension, avoiding the intensity of a one-to-one and, as a lay research advisor, I was able to put parents at their ease with friendly remarks and by taking an interest in them. I reassured them that they were not being ‘checked up on’. Some parents seemed embarrassed because the house was untidy and I empathised with them about this. If their child had previously had an accident, for example had fallen downstairs, they were understandably sensitive. I was able to empathise without giving direct advice.
The data sheet completed, we left the parent after giving them a safety leaflet. We parked some distance from the home and double checked the data (for example on the issue of storing things at adult eye level, which can be difficult with people of different heights, but deciding that the participant’s eye level was the correct marker). We documented any additional field material and I received positive feedback on the legibility of my writing!
The researcher who undertook these home observations with our lay research advisor commented that:
She was involved extensively in study B. Her attendance at the home visits was valuable not only for the process of data collection, but also in diffusing the tension around asking participants to show us, for example, where they stored medicines and other potentially harmful substances, and other aspects related to home safety about which they could feel uncomfortable. Having been initially daunted at the thought of conducting such visits I am impressed at how smoothly they went, and our lay research advisor’s sensitivity helped in their successful facilitation.
Study G (interview study of parents to identify barriers to, and facilitators of, injury prevention)
I contributed by reading and commenting on transcripts of interviews and themes using experience I had acquired being part of a previous qualitative study. I felt that I was able to add another dimension to the analysis.
This quotation from one of the research team indicates the lay research advisor’s contribution to the analytical process:
Her feedback helped to ensure an objective approach was taken to the data analysis.
Study M (interview study of parents in children’s centres about safety practices)
I interviewed parents at children’s centres in several areas of Nottingham, exploring fire safety practices of the parent/carer of 0–4 year olds. I felt that the parents responded well, and I allowed them time to explain fully about related issues that were on their mind (for example one parent had experience of a fire).
Her contribution is summarised by one researcher as follows:
She was able to make members of the public comfortable so that they felt at ease at asking questions about the study.
Study M (randomised controlled trial of the injury prevention briefing)
I was involved in the development of written material, information and consent forms, recruitment of parents for questionnaires at several children’s centres. Further on in the study I supported a parent from a different ethnic background to contribute to the development of a follow-up questionnaire. More recently I made many phone calls and sent extra follow-up questionnaires to parents, noting any changes of address. I felt that this encouraged the favourable response rate achieved.
Regarding involvement in study M one researcher commented:
Our lay research advisor was able to assist with recruitment to the study, making potential study participants feel comfortable by explaining the study in a straightforward and understandable way.
Our lay research advisor has also played a major role in the dissemination of study findings. She contributed to Child Safety Week activities at the local hospital to raise awareness of the KCS programme to potential participants. She had a poster presented at the 11th World Conference on Injury Prevention and Safety Promotion in October 2012 and at the Society for Academic Primary Care conference in July 2013. The highly visual poster, entitled ‘Improving injury prevention research through PPI – towards working in partnership’, highlighted the importance of PPI involvement in the KCS programme, with photographs showing her in different roles, for example visiting a children’s centre, looking at a medicine cupboard, reading a report and attending a team meeting (Figure 66).
FIGURE 66.
Improving injury prevention research through PPI poster.
In addition, she was a valued member of the Nottingham KCS programme team during Mayfest, an annual free open day for the community and alumni and friends of Nottingham University. She helped to staff the presentation stand, which involved parents and children in ‘hands-on’ activities promoting the home safety messages arising from the KCS programme. The lay research advisor was pivotal in producing a leaflet to provide participants with feedback on the findings from studies A and G (Figure 67). This involved framing the messages that we wanted to put across in a parent-/carer-friendly way to help encourage participants to read and absorb the information. She was also active in producing a dedicated website providing fuller participant result information [available at www.nottingham.ac.uk/go/safe (accessed 2 November 2016)]. Feedback from the research team indicates that:
Her involvement is fundamental in disseminating research findings to the public, ensuring that whilst they should be communicated in an accessible way, we should be wary of dumbing down.
FIGURE 67.
Leaflet containing findings from studies A and G.
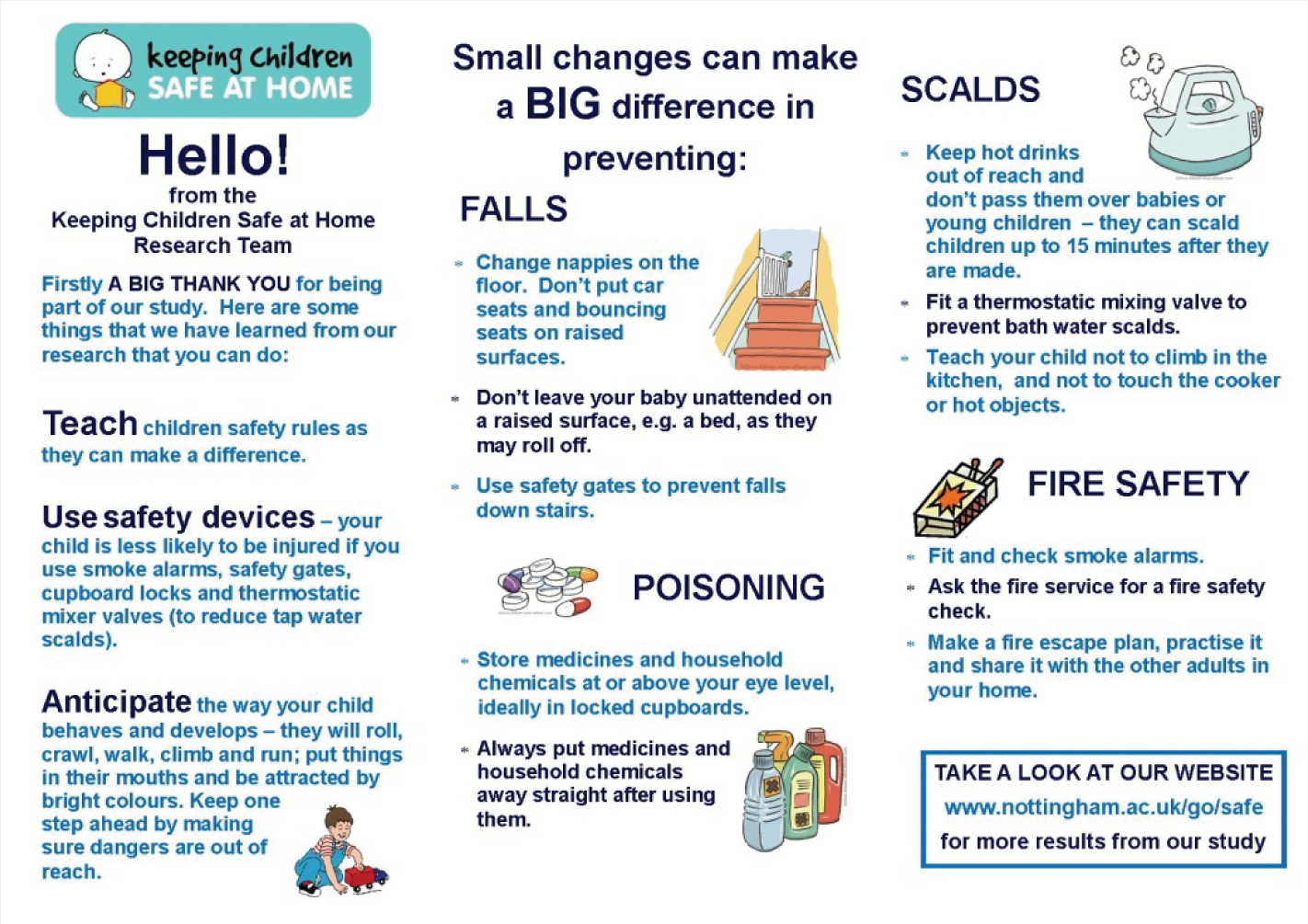
To summarise, PPI has played a major role in the KCS programme and the impact of this can be seen in a number of areas including the recruitment of participants, the achievement of high follow-up rates, the formulation of parent-friendly study material and the dissemination process.
Chapter 9 Overall conclusion
The KCS programme addressed the issue of childhood injuries occurring in the home through 13 interlinked studies, involving both quantitative and qualitative methods and including the perspectives of families, children’s centre staff, health professionals and other stakeholders with an injury prevention role. The studies took place in four sites throughout England, including both urban and rural locations and a diverse range of social areas. PPI has underpinned this research.
The research undertaken within the KCS programme generated new evidence about what works to prevent home injuries in children and the cost of such injuries, explored injury prevention practices by parents and children’s centres, reviewed and narratively synthesised and meta-analysed existing data, assessed the cost-effectiveness of a range of interventions and developed and tested an injury prevention intervention (an IPB for the prevention of fire-related injuries and training and support to implement the IPB) using a RCT. Finally, the findings from all work streams were used to develop a further IPB covering the prevention of fire-related injuries, scalds, falls and poisonings.
The KCS programme also advanced methodological approaches in the field of child home injury prevention, which will have applications in evaluating other public health interventions. This included a range of developments to NMA to simultaneously incorporate aggregate and individual participant data, adjust for baseline risk, explore effect modifiers and evaluate evidence on multiple outcomes across different networks. The IPB was developed using innovative methods to bring together evidence of effectiveness with practitioner experience of implementing interventions. The RCT evaluating the IPB incorporated a comprehensive assessment of implementation of the intervention rarely seen in child injury research, adding to our understanding of factors aiding successful implementation.
Patient and public involvement
Throughout the programme, from its design and original funding application to producing the final report and undertaking dissemination activities, we have worked collaboratively with an experienced lay research adviser (see Chapter 8). Her role developed over the course of the programme, with increasing involvement in developing and piloting study documentation and tools, undertaking data collection, participation in analysis, presenting her work at conferences, writing for publication, producing written feedback and website information for families who participated in the programme, drafting the lay summary of the final report and participating in dissemination events. We also had additional input from other lay advisers on the development and piloting of study tools.
Synergies
The KCS programme was much more than the sum of its parts. The synergies between the 13 component studies, with all studies informing at least one and often many other studies within the programme, allowed a very large body of work to be produced more quickly than would have been possible with individually funded research projects. It enabled the use of consistent approaches and the sharing of skills, resources and data between component projects. There are many examples of this within the programme and several are given here to illustrate this point. Conducting multiple overviews of reviews and systematic reviews simultaneously (studies E, H and I) allowed, when appropriate, studies identified in one review to be included in other reviews and simultaneous data extraction and risk-of-bias assessment. The collection of individual participant data for PMAs (study I) allowed the development of methods to incorporate individual participant data into NMAs (study J). Conducting five large case–control studies (study A) allowed the sharing of analysis plans and syntax files between studies, enabling consistency of analyses and reducing duplication of work. In addition, the KCS programme used simultaneous identification of participants for multiple studies (studies A–C and G), enhancing research efficiency and reducing costs. Importantly, the programme enabled learning from earlier parts to be efficiently incorporated into later parts. For example, the experiences of developing and evaluating the implementation of the IPB for the prevention of fire-related injuries (study M) allowed for the rapid development of a more comprehensive IPB, which also addressed the limitations of the first IPB.
Conclusions
The KCS programme aimed to increase evidence-based NHS thermal injury, falls and poisoning prevention by assessing risk and protective factors for these injuries, evaluating the effectiveness and cost-effectiveness of interventions to prevent these injuries, developing IPBs for effective and cost-effective interventions and evaluating the implementation of one IPB in children’s centres.
Work stream 1 found that a range of risk factors were significantly associated with secondary care-attended falls from furniture, falls on stairs or steps, poisonings and scalds in children aged 0–4 years. Only two modifiable risk factors were significantly associated with secondary care-attended falls on one level in children aged 0–4 years.
Work stream 2 found that the PedsQL was a feasible and acceptable measure of HRQL in young children following injury, with adequate internal consistency reliability, the ability to discriminate between varying levels of injury severity and sequelae and evidence of responsiveness to change. Findings in respect of construct validity were equivocal. In terms of the health-care costs of injury, scalds had the highest mean total cost for ED attendances and admissions for observation. Poisonings had the lowest mean total cost for ED attendances and falls on one level had the lowest mean total cost for admissions for observation. The number of admissions requiring at least one overnight stay was too small to reliably estimate health-care costs. In terms of non-health-care costs, informal child care and time off work were the major contributors and could be considerable. Scalds had the highest mean non-health-care costs and falls on one level had the lowest mean non-health-care costs.
Work stream 3 found that most children’s centres did not use an evidence-based strategic approach and child injury prevention appeared to be a neglected area within children’s centres given the scale of the problem. To ensure effective injury prevention children’s centres need support to plan, deliver and evaluate their activities, and centres would welcome such support.
Work stream 4 found a range of barriers to and facilitators of parents preventing child injuries in the home and those delivering injury prevention programmes. Many of these barriers and facilitators are addressable during the design of injury prevention interventions. The effect of addressing these barriers and facilitators on the degree of implementation of injury prevention programmes and on the outcomes of such programmes requires evaluation.
Work stream 5 found that some interventions were effective and some were both effective and cost-effective in promoting home safety and preventing fire-related injuries, scalds, falls and poisonings. More intensive interventions (e.g. those providing education and free or low-cost safety equipment and in some cases fitting equipment and providing home safety inspections) were more likely to be effective than less intensive interventions for promoting functional smoke alarms, having a safe hot water temperature, use of safety gates on stairs and the safe storage of medicines and household products. The most effective interventions were not necessarily the most cost-effective. Decision analyses were conducted from a public sector perspective and included costs incurred by different stakeholders including NHS and non-NHS organisations. However, analyses were limited to HRQL outcomes expressed in terms of QALYs and future studies may want to consider both welfare and quality of life more broadly (e.g. a cost–consequence analysis or a multicriteria decision-making approach), but thresholds would need careful consideration as it is unclear whether or not a threshold of £30,000 per QALY gained is relevant to different sectors of the economy beyond health care.
Work stream 6 identified factors associated with successful implementation of health promotion interventions and incorporated this evidence, along with that from earlier work streams, into the development of an IPB for the prevention of fire-related injuries and a package of training and support to facilitate its implementation in children’s centres. Providing children’s centres with the IPB and a training and facilitation package to support its implementation, designed to address barriers to and facilitators of injury prevention, was effective in increasing some safety behaviours. Providing children’s centres with the IPB alone was marginally more effective and cost less than usual care, whereas providing the IPB with support (IPB+) was marginally more effective but more costly than usual care. Findings from all work streams were used to develop a more comprehensive IPB for the prevention of fire-related injuries, scalds, falls and poisonings.
Dissemination and impact
The extensive programme of research undertaken within the KCS programme has synthesised existing evidence and generated new evidence about preventing fire-related injuries, scalds, falls and poisonings. It has developed and tested evidence-based resources for preventing child injury. Evidence generated by the KCS programme has already informed the evidence update for the NICE guidelines on strategies to prevent unintentional injuries in children and young people aged < 15 years,26 Public Health England guidance for local authorities on reducing unintentional injuries in and around the home in children aged < 5 years1 and the CMO’s annual report for 2012. 11 In addition, it has informed local injury prevention strategies497 and successful bids for home safety equipment schemes. 497,498
We developed a standard operating procedure for communications and publications and a plan for dissemination of the KCS programme findings. These identified target audiences including:
-
child health policy-makers
-
child health commissioners
-
child health and child care practitioners
-
injury prevention practitioners
-
voluntary sector, charitable and partner organisations such as the fire and rescue services
-
study participants and the wider population of families with young children
-
researchers.
We will use a wide range of methods to reach these audiences including:
-
targeted audience-specific feedback for strategic bodies (e.g. Department of Health, Department for Education, Public Health England, strategic directors/directors of public health in local authorities, strategic directors in commissioning bodies), professional bodies (e.g. Faculty of Public Health, Royal College of Paediatrics and Child Health, British Association for Community Child Health, British Association for Child and Adolescent Public Health, Community Practitioners and Health Visitors Association) and other organisations (e.g. Local Government Association, Royal Society for Public Health, Association of Directors of Public Health, Association of Public Health Observatories, Injury Observatory for Britain and Ireland)
-
articles in practitioner publications targeting local authorities, health commissioners and providers, voluntary organisations and the charity sector
-
presentations at conferences for practitioner audiences
-
articles for and newsletters to local authorities, health commissioners and providers, injury prevention practitioners and participants
-
peer-reviewed publications in academic journals in the fields of injury epidemiology and prevention, child health, public health, health promotion and research methods
-
presentations at academic conferences
-
existing distribution networks (Child Accident Prevention Trust, RoSPA, Kid Rapt, Injury Prevention News, etc.).
Dissemination activities to date include 37 peer-reviewed papers from the KCS programme, with a further one in press, 42 presentations at national conferences and nine at international conferences. There have been seven press releases about the KCS programme and its publications and 11 newspaper articles. Four dissemination events were held, one in each study centre, for children’s centre staff and other groups with a child health or injury prevention role (e.g. health visiting team staff, fire and rescue service staff, local authority public health staff) to provide information on the findings form the KCS programme. A total of 166 people attended these events.
The IPB for the prevention of fire-related injuries, scalds, falls and poisonings is one of the key outputs of the KCS programme. It has been made freely available on the KCS programme website (see www.nottingham.ac.uk/research/groups/injuryresearch/projects/kcs/index.aspx) and will be widely disseminated to relevant audiences electronically. The IPB has also been provided (with training in how to use it) to the children’s centres that participated in the RCT in the KCS programme. In addition, the KCS programme team secured external funding to provide the IPB (with training) for up to 180 health and child care staff in Nottinghamshire and 190 health and child care staff, fire and rescue service staff, voluntary sector organisations, early years professionals and health visiting students in Bristol. Furthermore, the Nottingham KCS programme team have secured funding for the injury prevention component of Nottingham CityCare Partnership’s successful Big Lottery bid (Small Steps Big Changes programme) (www.nottinghamcitycare.nhs.uk/ssbc/). This project aims to provide systematic evidence-based injury prevention appropriate to the age and stage of development for all families with children aged 0–3 years in the most disadvantaged areas of the city. The IPB will form part of the intervention and will be provided with training to 200 health and child care professionals, voluntary organisations, peer supporters and graduates from the Family Nurse Partnership programme who will deliver the injury prevention programme. The project evaluation will be undertaken by a team of researchers, including some from the KCS programme.
The lay research advisor for the KCS programme has drafted web pages reporting the main findings from the KCS programme for the KCS programme website and leaflets describing the main findings and giving the address for those web pages. Leaflets are being mailed to > 9600 families who participated in the KCS programme. The Nottingham and Bristol KCS programme teams have participated in university open days for the public, providing information on findings from the KCS programme.
A guide for commissioners of child health services on preventing unintentional injuries to the under-fives has been produced in collaboration with the Child Accident Prevention Trust and disseminated to all directors of public health in England. The guide is available online (www.nottingham.ac.uk/research/groups/injuryresearch/documents/kcs-guide-for-commissioners.pdf).
Chapter 10 Implications for practice
This chapter brings together the implications for preventing home injuries in the under-fives arising from each of the work streams.
Work stream 1
If the associations estimated in our case–control studies represent causal relationships, some falls from furniture, falls on stairs or steps, poisonings and scalds may be prevented by incorporating home safety advice based on our findings into child health contacts. Such contacts could include child surveillance programme contacts (i.e. well-child visits in primary care), contacts following injuries in primary, secondary and tertiary care and injury prevention contacts such as home safety assessments or at referral for or fitting of home safety equipment. Similar advice could also be incorporated into personal child health records and other health promotion materials for parents of young children.
Work stream 2
There are no implications for practice from work stream 2.
Work stream 3
Our findings indicate that there is considerable potential for the development of the delivery of injury prevention activities by children’s centres. Children’s centre managers and staff are interested in preventing injuries and are motivated to deliver injury prevention activities. However, they need further support to develop injury prevention strategies and plan and implement prevention programmes and training and resources to deliver effective injury prevention activities.
Work stream 4
Those implementing injury prevention interventions need to take account of potential barriers and facilitators relevant to their specific context, intervention and population. Implementing interventions without addressing such factors is likely to lead to suboptimal outcomes.
Interventions designed for delivery by children’s centre staff need to address children’s centre priorities, be adequately resourced, include high-quality training and ongoing support for staff, be delivered by staff with effective communication skills, provide local injury data and encourage sharing of good practice, evaluation and reflective practice. Interventions need to be built on trusting relationships with families. They should be engaging for families, tailored to their needs and their child’s stage of development, address socioeconomic barriers and be culturally sensitive. They should be based on models of behaviour change, provide clear and simple messages, limit the number of behaviours that they attempt to change and provide incentives for behaviour change.
Work stream 5
Injury prevention strategies and guidelines, and commissioners and providers of injury prevention services, can be informed by our findings, specifically that providing education plus free/low-cost smoke alarms is cost-effective for reducing house fire-related injuries; that education coupled with fitting free TMVs for families with young children living in social housing is cost-effective in reducing scalds; and that providing low-intensity education (e.g. leaflets) is cost-effective in reducing poisonings from medicines.
Work stream 6
Children’s centres can effectively deliver injury prevention activities to families with young children living in disadvantaged communities if provided with evidence-based resources for this purpose (an IPB for the prevention of fire-related injuries). Providing children’s centres with training and facilitation to implement the IPB can result in greater delivery of injury prevention activities than providing resources without training and facilitation.
Through using the IPB, children’s centres can enhance some safety behaviours in families with young children living in disadvantaged communities. An IPB can be effective in increasing fire escape planning behaviours, reducing match play and increasing the number of bedtime fire safety practices. Providing training and facilitation to help implement the IPB can achieve greater implementation, but this approach may be less cost-effective than providing the IPB without facilitation.
The findings from all work streams in the KCS programme are summarised in a further evidence-based IPB for practitioners covering the prevention of fire-related injuries, falls, poisonings and scalds in the under-fives. This provides the evidence on effective interventions to prevent injuries and activities for use with parents addressing the key safety messages. The IPB is freely available from www.nottingham.ac.uk/research/groups/injuryresearch/projects/kcs/index.aspx.
The key messages from the KCS programme for commissioners of injury prevention programmes to consider and for practitioners to deliver to families for the prevention of fire-related injuries, scalds, falls and poisonings are shown in the following sections. These messages could be delivered as part of the Healthy Child Programme and be incorporated into the Personal Child Health Record and health promotion material for parents of young children. They could also be provided by health and child care practitioners during contacts following injuries and during injury prevention contacts such as home safety assessments or at referral for or fitting of home safety equipment.
General safety advice
-
Children are less likely to be injured in households that use safety devices such as smoke alarms, safety gates, cupboard locks and TMVs (to reduce tap water scalds).
-
Teaching children safety rules can reduce the risk of injury.
Preventing fire-related injury
-
Fit and check smoke alarms.
-
Home safety checks can help families to make homes safer. Ask the fire service for a fire safety check.
-
Make a fire escape plan, practise it and share it with the other adults in the home.
Preventing scalds
-
Keep hot drinks out of reach and do not pass them over babies or young children.
-
Fit a TMV to prevent bathwater scalds.
-
Teach children not to climb in the kitchen and not to touch the cooker or hot objects.
Preventing falls
-
Change nappies on the floor and do not put car seats and bouncing seats on raised surfaces.
-
Do not leave babies unattended on a raised surface, for example a bed, as they may roll off.
-
Use safety gates to prevent falls downstairs and always close them after use.
-
Cover stairs with carpet to reduce the risk of falls.
-
Teach children rules about not climbing on objects from which they could fall.
Preventing poisoning
-
Fit cupboard locks to cupboards where medicines and household chemicals are stored.
-
Store medicines and household chemicals in locked cupboards or locked medicines boxes that are at or above adult eye level.
-
Always put medicines and household chemicals away straight after using them.
Chapter 11 Recommendations for research
The KCS programme makes the following recommendations for research.
Important recommendations for research
-
Further intervention studies, preferably RCTs, to evaluate the effectiveness and cost-effectiveness of home safety interventions. These need to provide detailed descriptions of intervention and control arm treatments, and measure and report injury outcomes, home safety equipment use and safety behaviours. Studies should explicitly report how they addressed potential barriers and facilitators in the design of their intervention and explore barriers to and facilitators of implementing interventions from a range of perspectives.
-
Further intervention studies, preferably RCTs, to explore the effectiveness and cost-effectiveness of delivering other injury prevention interventions within children’s centres and of IPBs implemented by different professional groups and in different settings.
-
Further meta-analyses, particularly of studies measuring injury outcomes and safety behaviours, as the number of primary studies increases.
-
Pairwise meta-analyses and NMAs incorporating covariate information to evaluate whether or not targeting interventions at specific population groups is more effective than providing non-targeted interventions.
-
Further economic evaluations to enhance the evidence base for the prevention of fire-related injuries, scalds, falls and poisonings in childhood. Economic evaluations should measure the NHS, family and societal costs of a wide range of injuries, using large representative samples of injured children. Studies measuring utility decrements for a wide range of childhood injuries requiring different levels of health-care resource use would be particularly useful. Economic evaluations are needed that evaluate within a single analytical model complex multicomponent interventions such as home safety schemes providing education and safety equipment to prevent a range of injuries. Future studies may want to consider both welfare and quality of life more broadly (e.g. a cost–consequence analysis or a multicriteria decision-making approach), but thresholds would need careful consideration as it is unclear whether or not a threshold of £30,000 per QALY gained is relevant to different sectors of the economy beyond health care.
Recommendations for research of interest but of lesser importance
-
UK studies that explore the effect on the estimation of costs of using parent-reported data compared with health-care resource use data obtained from medical records.
-
Studies to explore why retrospectively reported pre-injury HRQL scores tend to be higher than those for the general population from whom the injured sample is drawn.
-
Further investigation of the psychometric properties of the PedsQL in a large sample of healthy UK toddlers (a general population sample) using modern psychometric methods such as item response theory.
-
Further surveys of injury prevention activity to assess the extent to which children’s centres are fulfilling their remit to deliver injury prevention activities as they continue to develop and evolve.
-
Qualitative and quantitative studies to evaluate the use of ‘real-life’ injury experiences as learning opportunities for parents within injury prevention interventions.
Acknowledgements
Nottinghamshire County Teaching PCT hosted the programme until March 2012. Nottinghamshire Healthcare NHS Trust hosted the programme from April 2012.
Contributions of others
We would like to thank the following people for their invaluable help with undertaking components of this programme of work.
Work stream 1
Dr Asiya Maula (University of Nottingham) who assisted with recruitment and data analysis; Dr Paula Sealey (University of Nottingham) who assisted with recruitment; Clare Ferns (Norfolk and Norwich University Hospitals NHS Foundation Trust), Nathalie Horncastle (Norfolk and Norwich University Hospitals NHS Foundation Trust), Pilar Muñoz (University of the West of England), Benita Laird-Hopkins (University of the West of England), Emma Davison (Newcastle upon Tyne Hospitals NHS Foundation Trust) and Laura Simms (Newcastle upon Tyne Hospitals NHS Foundation Trust) who assisted with data entry and data management; study participants who completed questionnaires and allowed us to visit them in their homes; liaison health visitors, research nurses and staff from EDs, MIUs and inpatient wards who assisted with recruitment from Nottingham University Hospitals NHS Trust, Derby Teaching Hospitals NHS Foundation Trust, Norfolk and Norwich University Hospitals NHS Foundation Trust, United Lincolnshire Hospitals NHS Trust, James Paget University Hospitals NHS Foundation Trust, University Hospitals Bristol NHS Foundation Trust, North Bristol Healthcare Trust, Newcastle Upon Tyne Hospitals NHS Foundation Trust, Gateshead NHS Foundation Trust and Northumbria Healthcare NHS Foundation Trust; Primary Care Research Networks for East Midlands and South Yorkshire, Leicestershire, Northamptonshire and Rutland, East of England, Northern and Yorkshire and South West who assisted with recruitment and Trent, Norfolk and Suffolk, Northumberland Tyne and Wear and Western Comprehensive Local Research Networks who provided support for recruitment.
Work stream 2
Study participants who completed questionnaires.
Work stream 3
Children’s centre managers who participated in the surveys.
Work stream 4
Dr Jenny C Ingram (University of Bristol) and Gail Errington (University of Nottingham) who assisted with the review of barriers to and facilitators of injury prevention; Dr Paula Sealey (University of Nottingham) who assisted with interviews of children’s centre staff; and parents and children’s centre staff who participated in the interviews.
Work stream 5
Professor Andrea Manca (University of York) who provided PhD supervision (during a NIHR Career Development Fellowship) and advised on decision modelling and Mr Ken Dunn (University Hospital of South Manchester) who advised on model structure and supplied data to inform the model parameters for assessing the cost-effectiveness of smoke alarms and the promotion of safe hot water temperatures; Dr Sofia Dias and Guobing Lu (University of Bristol) and Stephen JC Rice (University of York) who advised on methods for adjusting NMAs for baseline risk; Dr Sylwia Bujkiewicz (University of Leicester) who advised on NMA with multiple outcomes; Professor David Jones (University of Leicester) who provided PhD supervision in relation to undertaking NMAs and decision modelling for poisoning and falls outcomes; Paula Dhiman (University of Leicester) who assisted with the NMA for smoke alarms; Dr Ilyas Nohaid, Dr Zhimin He, Dr Elodie Le Cozannet, Jayne Simpson and Jacqueline Mhizha-Murira (University of Nottingham) who assisted with systematic reviewing; and Professor Jon Nicholl (University of Sheffield) for providing data from the HALO study.
Work stream 6
Dr Paula Sealey (University of Nottingham) who assisted with data collection; Benita Laird-Hopkins (University of the West of England) who assisted with data collection and data management; families and children’s centre staff who participated in work stream 6; and Trial Steering Committee members: Professor Alison Kemp (chairperson; Cardiff University), Mrs Sally Kerry (Queen Mary University of London), Dr Phil Edwards (London School of Hygiene and Tropical Medicine), Ian Evans (Child Accident Prevention Trust), Sally Jaeckle (Strategic Lead for Early Childhood Services, Bristol City Council), Liz Jenkins (St Werburgh’s Park Nursery School and Children’s Centre, Bristol), Andy Townsend (Lifeskills Safety Centre, Bristol) and Sue Webster (Children’s Centre Leaders’ Network).
Contributions of authors
Denise Kendrick (Professor of Primary Care Research) was Chief Investigator for the study. She was a lead applicant and Principal Investigator for the Nottingham study centre, was responsible for oversight of the programme, study co-ordination and management of staff and contributed to study design, study implementation, analysis and interpretation (all work streams) and to writing the manuscript.
Joanne Ablewhite (Research Fellow) contributed to study co-ordination, participant recruitment and data collection (work streams 1, 2, 4 and 6), qualitative analysis and interpretation (work stream 4) and to writing the manuscript.
Felix Achana (PhD Student) undertook the evidence synthesis and economic analysis for poisoning outcomes and interpretation of the results (work stream 5) and contributed to writing the manuscript.
Penny Benford (Research Fellow) contributed to participant recruitment and data collection (work streams 1, 2 and 6), analysis (work stream 1) and to writing the manuscript.
Rose Clacy (Lay Consumer Adviser) was the PPI representative for this study and contributed to study design, development of data collection tools, participant recruitment and data collection (work streams 1 and 6) and to writing the manuscript.
Frank Coffey (Associate Professor and Consultant in Emergency Medicine) was a co-applicant and emergency medicine lead for the study. He contributed to the study design, participant recruitment, data collection (work stream 1) and writing the manuscript.
Nicola Cooper (Professor of Healthcare Evaluation Research) was a co-applicant, led the economic evaluation (work streams 2, 5 and 6) and co-led the evidence synthesis components of the programme (work stream 5) and contributed to study design, analysis and interpretation and to writing the manuscript.
Carol Coupland (Associate Professor and Reader in Medical Statistics) was a co-applicant, contributed to the study design, provided statistical and data analytical guidance and contributed to the interpretation and analysis of data (work streams 1, 3 and 6) and to writing the manuscript.
Toity Deave (Associate Professor for Family and Child Health) was a researcher on the KCS programme of work and became Principal Investigator for the Bristol centre in November 2011. She co-ordinated the RCT (work stream 6) and contributed to participant recruitment and data collection (work streams 1, 2, 4 and 6), analysis (work streams 4 and 6) and literature reviewing (work stream 5) and to writing the manuscript.
Trudy Goodenough (Research Fellow) contributed to participant recruitment and data collection (work streams 1, 2, 4 and 6) and analysis (work streams 4 and 6) and to writing of the manuscript.
Adrian Hawkins (Clinical Trials Officer) contributed to participant recruitment and data collection (work streams 1, 2, 4 and 6), analysis and interpretation (work streams 4 and 6) and literature reviewing (work stream 5) and to writing the manuscript.
Mike Hayes (Principal Consultant) was a co-applicant, contributed to study design, designed and led the training used in the RCT, co-authored the IPB that was used in the RCT and the later edition that was a practitioner-focused output from the project (work stream 6), provided expert input to the economic analysis (work stream 2) and contributed to writing the manuscript.
Paul Hindmarch (Clinical Trials Officer) contributed to participant recruitment and data collection (work streams 1, 2, 4 and 6), analysis and interpretation (work stream 6) and literature reviewing (work stream 5) and to writing the manuscript.
Stephanie Hubbard (Lecturer in Medical Statistics) undertook the evidence synthesis and economic analysis for the falls outcomes and interpretation of the results (work stream 5) and contributed to writing the manuscript.
Bryony Kay (Research Nurse) contributed to participant recruitment and data collection (work streams 1, 2 and 6), analysis (work stream 4) and literature reviewing (work stream 5) and to writing the manuscript.
Arun Kumar (Research Fellow, University of Nottingham) contributed to data analysis (work stream 6) and to writing the manuscript.
Gosia Majsak-Newman (Research Fellow) contributed to data collection and analysis (work streams 1, 2, 4 and 6) and literature reviewing (work stream 5) and to writing the manuscript.
Elaine McColl (Professor of Health Services Research and Director of Newcastle Clinical Trials Unit) was a co-applicant and Principal Investigator for the Newcastle centre and contributed to study design, study implementation, analysis and interpretation of the data, particularly validation of the PedsQL (work stream 2), and to writing the manuscript.
Lisa McDaid (Research Associate) contributed to data collection (work streams 1, 2, 4 and 6) and analysis (work streams 4 and 6) and to writing the manuscript.
Phil Miller (Senior Research Nurse) contributed to participant recruitment and data collection (work streams 1 and 2) and reviewing the literature (work stream 5) and to writing the manuscript.
Caroline Mulvaney (Senior Research Fellow) contributed to data analysis and interpretation of the findings (work stream 3) and to writing the manuscript.
Isabel Peel (Research Nurse) contributed to participant recruitment and data collection (work streams 1 and 2) and data analysis (work stream 4) and to writing the manuscript.
Emma Pitchforth [RAND (Europe)] was the independent research consultant for this study and contributed to the development of qualitative data collection tools and qualitative data analysis (work stream 4) and to writing the manuscript.
Richard Reading (Consultant Community Paediatrician) was a co-applicant and Principal Investigator for the Norwich study centre and contributed to study design, study implementation (work streams 1, 2 and 4–6) and analysis and to writing the manuscript.
Pedro Saramago (Research Fellow) undertook the evidence synthesis and economic analysis for fire-related outcomes and the interpretation of results (work stream 5) and contributed to writing the manuscript.
Jane Stewart (Senior Research Fellow) contributed to the research programme and study co-ordination, data collection (work streams 1, 2, 4 and 6), analysis and interpretation (work streams 1, 3, 4 and 6) and to writing the manuscript.
Alex Sutton (Professor of Medical Statistics) was a co-applicant, co-led the evidence synthesis components of the programme (work stream 5) and contributed to study design, analysis and interpretation (work streams 5 and 6) and to writing the manuscript.
Clare Timblin (Research Assistant) led the data management (all work streams) and contributed to data collection (work stream 3) and analysis (work stream 1) and to writing the manuscript.
Elizabeth Towner (Emeritus Professor of Child Health) was a co-applicant and Principal Investigator for the Bristol centre until 2011. She contributed to the study design, co-authored the IPB that was used in the RCT (work stream 6) and contributed to analysis and literature reviewing (work stream 4) and to writing the manuscript.
Michael C Watson (Associate Professor in Public Health) was a co-applicant, contributed to the study design, led work stream 3 and contributed to data interpretation and to writing the manuscript.
Persephone Wynn (Research Fellow) contributed to participant recruitment and data collection (work stream 1), analysis (work streams 1 and 6) and literature reviewing (work stream 5) and to writing the manuscript.
Ben Young (Research Assistant) contributed to literature reviewing (work stream 5), data collection (work stream 2) and analysis (work streams 1 and 6) and to writing the manuscript.
Kun Zou (Research Assistant) contributed to literature reviewing (work stream 5) and analysis (work stream 1) and to writing the manuscript.
Publications
Achana FA, Cooper NJ, Dias S, Lu G, Rice SJ, Kendrick D, Sutton AJ. Extending methods for investigating the relationship between treatment effect and baseline risk from pairwise meta-analysis to network meta-analysis. Stat Med 2012;32:752–71.
Cooper NJ, Kendrick D, Achana F, Dhiman P, He Z, Wynn P, et al. Network meta-analyses to evaluate the effectiveness of interventions to increase the uptake of smoke alarms. Epidemiol Rev 2012;34:32–45.
Ingram JC, Deave T, Towner E, Errington G, Kay B, Kendrick D. Identifying facilitators and barriers for home injury prevention interventions for pre-school children: a systematic review of the quantitative literature. Health Educ Res 2012;27:258–68.
Kendrick D, Maula A, Stewart J, Clacy R, Coffey F, Cooper N, et al. Keeping children safe at home: protocol for three matched case–control studies of modifiable risk factors for falls. Inj Prev 2012;18:e3.
Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev 2012;9:CD005014.
Saramago P, Sutton AJ, Cooper NJ, Manca A. Mixed treatment comparisons using aggregate and individual participant level data. Stat Med 2012;31:3516–36.
Watson MC, Mulvaney C, Kendrick D, Stewart J, Coupland C, Hayes M, et al. National survey of the injury prevention activities of Sure Start children’s centres. Inj Prev 2012;18:A103.
Deave T, Goodenough T, Stewart J, Towner E, Majsak-Newman G, Hawkins A, et al. Contemporary hazards in the home: keeping children safe from thermal injuries. Arch Dis Child 2013;98:485–9.
Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, et al. Home safety education and provision of safety equipment for injury prevention. Evid Based Child Health 2013;8:761–939.
Young B, Wynn PM, He Z, Kendrick, D. Preventing childhood falls within the home: overview of systematic reviews and a systematic review of primary studies. Accid Anal Prev 2013;60:158–71.
Achana FA, Cooper NJ, Bujkiewicz S, Hubbard SJ, Kendrick D, Jones DR, Sutton AJ. Network meta-analysis of multiple outcome measures accounting for borrowing of information across outcomes. BMC Med Res Methodol 2014;14:92.
Achana F, Hubbard S, Sutton A, Kendrick D, Cooper N. An exploration of synthesis methods in public health evaluations of interventions concludes that the use of modern statistical methods would be beneficial. J Clin Epidemiol 2014;67:376–90.
Beckett K, Goodenough T, Deave T, Jaeckle S, McDaid L, Benford P, et al. Implementing an injury prevention briefing to aid delivery of key fire safety messages in UK children’s centres: qualitative study nested within a multi-centre randomised controlled trial. BMC Public Health 2014;14:1256.
Deave T, Hawkins A, Kumar A, Cooper N, Goodenough T, Watson M, et al. Implementation of a fire-prevention injury prevention briefing in children’s centres: a multicentre cluster-randomised controlled trial. Lancet 2014;384:S6.
Deave T, Towner E, McColl E, Reading R, Sutton A, Coupland C, et al. Multicentre cluster randomised controlled trial evaluating implementation of a fire prevention injury prevention briefing in children’s centres: study protocol. BMC Public Health 2014;14:69.
Deave T, Hawkins A, Kumar A, Hayes M, Cooper N, Watson M, et al. Evaluating implementation of a fire-prevention injury prevention briefing in children's centres: cluster randomised controlled trial. PLOS ONE 2017;12:e0172584. https://doi.org/10.1371/journal.pone.0172584
He Z, Wynn P, Kendrick D. Non-resuscitative first-aid training for children and lay people: a systematic review. J Emerg Med 2014;31:763–8.
Hubbard S, Cooper N, Kendrick D, Young B, Wynn PM, He Z, et al. Network meta-analysis to evaluate the effectiveness of interventions to prevent falls in children under age 5 years. Inj Prev 2014;67:376–90.
Majsak-Newman G, Benford P, Ablewhite J, Clacy R, Coffey F, Cooper N, et al. Keeping children safe at home: protocol for a matched case–control study of modifiable risk factors for poisoning. Inj Prev 2014;20:e10.
Saramago P, Cooper N, Sutton A, Hayes M, Dunn K, Manca A, Kendrick D. Cost-effectiveness of interventions for increasing the possession of functioning smoke alarms in households with pre-school children: a modelling study. BMC Public Health 2014;14:459.
Watson M, Benford P, Coupland C, Clacy R, Hindmarch P, Majsak-Newman G, et al. Validation of a home safety questionnaire used in a series of case–control studies. Inj Prev 2014;20:336–42.
Watson MC, Mulvaney C, Kendrick D, Stewart J, Coupland C, Hayes M, et al. National survey of the injury prevention activities of children’s centres. Health Soc Care Community 2014;22:40–6.
Wynn P, Stewart J, Kumar A, Clacy R, Coffey F, Cooper N, et al. Keeping children safe at home: protocol for a case–control study of modifiable risk factors for scalds. Inj Prev 2014;20:e11.
Zou K, Wynn P, Miller P, Hindmarch P, Majsak-Newman G, Young B, et al. Preventing childhood scalds within the home: overview of systematic reviews and a systematic review of primary studies. Burns 2014;41:907–24.
Ablewhite J, McDaid L, Hawkins A, Peel I, Goodenough T, Deave T, et al. Approaches used by parents to keep their children safe at home: a qualitative study to explore the perspectives of parents with children aged under five years. BMC Public Health 2015;15:983.
Ablewhite J, Peel I, McDaid L, Hawkins A, Goodenough T, Deave T, et al. Parental perceptions of barriers and facilitators to preventing child unintentional injuries within the home: a qualitative study. BMC Public Health 2015;15:280.
Achana F, Sutton A, Kendrick D, Wynn P, Young B, Jones D, et al. The effectiveness of different interventions to promote poison prevention behaviours in households with children: network meta-analysis. PLOS ONE 2015;10:e0121122.
Benford P, Young B, Coupland C, Watson M, Hindmarch P, Hayes M, et al. Risk and protective factors for falls on one level in young children: multicentre case–control study. Inj Prev 2015. http://dx.doi.org/10.1136/injuryprev-2015–041581
Kendrick, D, Maula A, Reading R, Hindmarch P, Coupland C, Watson M, et al. Risk and protective factors for falls from furniture in young children: multicentre case–control study. JAMA Pediatrics 2015;169:145–53.
Kendrick D, Zou K, Ablewhite J, Watson M, Coupland C, Kay B, et al. Risk and protective factors for falls on stairs in young children: multicentre case–control study. Arch Dis Child 2016;101:909–16.
Cooper N, Kendrick D, Timblin C, Hayes M, Majsak-Newman G, Meteyard K, et al. The short-term cost of falls, poisonings and scalds occurring at home in children under 5 years old in England: multicentre longitudinal study. Inj Prev 2016. doi:10.1136/injuryprev-2015–041808
Goodenough T, Kay B, Deave T, Towner E, Stewart J, Ablewhite J, et al. Barriers and facilitators to delivering injury prevention interventions in English children’s centres. Int J Health Prom Educ 2016;54:60–71.
Kendrick D, Majsak-Newman G, Benford P, Coupland C, Timblin C, Hayes M, et al. Poison prevention practices and medically attended poisoning in young children: multicentre case–control study [published online ahead of print 4 November 2016]. Injury Prev 2016.
Ploubidis G, Edwards P, Kendrick D. Measuring behaviours for escaping from house fires: use of latent variable models to summarise multiple behaviours. BMC Res Notes 2015;8:789.
Watson M, Mulvaney C, Timblin C, Stewart J, Coupland C, Deave T, et al. Missed opportunities to keep children safe? National survey of injury prevention activities of children’s centres [published online ahead of print 25 February 2016]. Health Educ J 2016. http://dx.doi.org/10.1177/0017896916629816
Wynn P, Zou K, Young B, Majsak-Newman G, Hawkins A, Kay B, et al. Prevention of childhood poisoning in the home: overview of systematic reviews and a systematic review of primary studies. Int J Inj Contr Saf Promot 2016;23:3–28.
Data sharing statement
Study participants were recruited prior to the period when data sharing became common practice. Participants were therefore not asked on consent forms to provide consent to data sharing; hence, only the data within the report and appendices are available.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- Reducing Unintentional Injuries In and around the Home among Children under Five Years. London: Public Health England; 2014.
- Health and Social Care Information Centre . Hospital Episode Statistics, Admitted Patient Care, England – 2012–13: External Causes n.d. www.hscic.gov.uk/catalogue/PUB12566 (accessed 27 January 2014).
- 24th (Final) Report of the Home and Leisure Accident Surveillance System. 2000, 2001 and 2002 Data. London: Department for Trade and Industry; 2003.
- Valadka S, Poenaru D, Dueck A. Long-term disability after trauma in children. J Pediatr Surg 2000;35:684-7. https://doi.org/10.1053/jpsu.2000.5943.
- Polinder S, Meerding WJ, Toet H, Mulder S, Essink-Bot ML, van Beeck EF. Prevalence and prognostic factors of disability after childhood injury. Pediatrics 2005;116:e810-7. https://doi.org/10.1542/peds.2005-1035.
- Winthrop AL, Brasel KJ, Stahovic L, Paulson J, Schneeberger B, Kuhn EM. Quality of life and functional outcome after pediatric trauma. J Trauma 2005;58:468-73. https://doi.org/10.1097/01.TA.0000153940.23471.B7.
- Sturms LM, van der Sluis CK, Stewart RE, Groothoff JW, ten Duis HJ, Eisma WH. A prospective study on paediatric traffic injuries: health-related quality of life and post-traumatic stress. Clin Rehabil 2005;19:312-22. https://doi.org/10.1191/0269215505cr867oa.
- Martin-Herz SP, Zatzick DF, McMahon RJ. Health-related quality of life in children and adolescents following traumatic injury: a review. Clin Child Fam Psychol Rev 2012;15:192-214. https://doi.org/10.1007/s10567-012-0115-x.
- Anderson V, Brown S, Newitt H, Hoile H. Educational, vocational, psychosocial, and quality-of-life outcomes for adult survivors of childhood traumatic brain injury. J Head Trauma Rehabil 2009;24:303-12. https://doi.org/10.1097/HTR.0b013e3181ada830.
- Gabbe BJ, Brooks C, Demmler JC, Macey S, Hyatt MA, Lyons RA. The association between hospitalisation for childhood head injury and academic performance: evidence from a population e-cohort study. J Epidemiol Community Health 2014;68:466-70. https://doi.org/10.1136/jech-2013-203427.
- CMO Annual Report 2012. Our Children Deserve Better: Prevention Pays. London: Department of Health; 2013.
- Marmot M. Fair Society, Healthy Lives: A Strategic Review of Inequalities in England. London: University College London; 2010.
- Edwards P, Roberts I, Green J, Lutchmun S. Deaths from injury in children and employment status in family: analysis of trends in class specific death rates. BMJ 2006;333:119-21. https://doi.org/10.1136/bmj.38875.757488.4F.
- The Health of the Nation: A Strategy for Health in England. London: HMSO; 1992.
- Saving Lives: Our Healthier Nation. London: The Stationery Office; 1999.
- Preventing Accidental Injury – Priorities for Action. Report to the Chief Medical Officer from the Accidental Injury Task Force. London: Department of Health; 2002.
- Every Child Matters: Change for Children. Nottingham: Department for Education and Skills; 2004.
- Children Act 2000. London: The Stationery Office; 2000.
- Better Safe than Sorry: Preventing Unintentional Injury to Children. London: Audit Commission; 2007.
- Staying Safe: Action Plan. Nottingham: Department for Children, Schools and Families; 2008.
- Royal Society for the Prevention of Accidents . Safe At Home – The National Home Safety Equipment Scheme n.d. www.rospa.com/home-safety/advice/child-safety/safe-at-home/ (accessed 8 January 2017).
- Accident Prevention amongst Children and Young People: A Priority Review. London: Department of Health; 2009.
- Healthy Lives, Healthy People: Our Strategy for Public Health in England. London: The Stationery Office; 2010.
- Public Health England . Public Health Outcomes Framework n.d. www.phoutcomes.info/ (accessed 7 January 2017).
- Strategies to Prevent Unintentional Injuries among Under-15s. London: NICE; 2010.
- Strategies to Prevent Unintentional Injuries among Children and Young People Aged under 15: Evidence Update February 2013. Manchester: NICE; 2013.
- Preventing Unintentional Injuries in the Home among Children and Young People Aged under 15: Home Safety Assessments and Providing Safety Equipment. London: NICE; 2010.
- How Safety Conscious are European Countries towards Children?. Birmingham: EuroSafe; 2012.
- European Child Safety Alliance and EuroSafe . Child Safety Report Card: England, 2012 n.d. www.childsafetyeurope.org/reportcards/info/england-report-card.pdf (accessed 3 November 2016).
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: Personal Social Services Research Unit, University of Kent; 2012.
- NHS Reference Costs 2012–13. London: Department of Health; 2013.
- Morrison A, Stone DH, Doraiswamy N, Ramsay L. Injury surveillance in an accident and emergency department: a year in the life of CHIRPP. Arch Dis Child 1999;80:533-6. https://doi.org/10.1136/adc.80.6.533.
- Kendrick D, Coupland C, Mulvaney C, Simpson J, Smith SJ, Sutton A, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev 2007;1. https://doi.org/10.1002/14651858.cd005014.pub2.
- Dowswell T, Towner EM, Simpson G, Jarvis SN. Preventing childhood unintentional injuries – what works? A literature review. Inj Prev 1996;2:140-9. https://doi.org/10.1136/ip.2.2.140.
- Towner E, Dowswell T, Jarvis S. Reducing Childhood Accidents. The Effectiveness of Health Promotion Interventions: A Literature Review. London: Health Education Authority; 1993.
- Towner E, Dowswell T, Mackereth C, Jarvis S. What Works in Preventing Unintentional Injuries in Children and Young Adolescents? An Updated Systematic Review. London: Health Development Agency; 2001.
- DiGuiseppi C, Higgins JP. Interventions for promoting smoke alarm ownership and function. Cochrane Database Syst Rev 2001;2. https://doi.org/10.1002/14651858.cd002246.
- Pless IB. The Scientific Basis of Childhood Injury Prevention. A Review of the Medical Literature. London: Child Accident Prevention Trust; 1993.
- Prevention and Reduction of Accidental Injury in Children and Older People. London: Health Development Agency; 2003.
- DiGuiseppi C, Roberts IG. Individual-level injury prevention strategies in the clinical setting. Future Child 2000;10:53-82. https://doi.org/10.2307/1602825.
- Speller V, Mulligan J, Law C, Foot B. Preventing Injury in Children and Young People: A Review of the Literature and Current Practice. Southampton: Wessex Institute of Public Health Medicine; 1995.
- Lyons RA, John A, Brophy S, Jones SJ, Johansen A, Kemp A, et al. Modification of the home environment for the reduction of injuries. Cochrane Database Syst Rev 2006;4.
- Varni JW. The PedsQL™ Measurement Model for the Pediatric Quality of Life Inventory n.d. www.pedsql.org/ (accessed 6 January 2017).
- Pitone ML, Attia MW. Patterns of injury associated with routine childhood falls. Pediatr Emerg Care 2006;22:470-4. https://doi.org/10.1097/01.pec.0000226869.41803.50.
- Watson W, Ozanne-Smith J, Begg S, Imberger A, Ashby K, Stathakis V. Injuries Associated with Nursery Furniture and Bunk Beds. Clayton, VIC: Monash University Accident Research Centre; 1997.
- Dedoukou X, Spyridopoulos T, Kedikoglou S, Alexe DM, Dessypris N, Petridou E. Incidence and risk factors of fall injuries among infants: a study in Greece. Arch Pediatr Adolesc Med 2004;158:1002-6. https://doi.org/10.1001/archpedi.158.10.1002.
- Kemp AM, Jones S, Lawson Z, Maguire SA. Patterns of burns and scalds in children. Arch Dis Child 2014;99:316-21. https://doi.org/10.1136/archdischild-2013-304991.
- Young B, Wynn PM, He Z, Kendrick D. Preventing childhood falls within the home: overview of systematic reviews and a systematic review of primary studies. Accid Anal Prev 2013;60:158-71. https://doi.org/10.1016/j.aap.2013.08.001.
- Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev 2012;9. https://doi.org/10.1002/14651858.cd005014.pub3.
- Runyan CW, Bangdiwala SI, Linzer MA, Sacks JJ, Butts J. Risk factors for fatal residential fires. N Engl J Med 1992;327:859-63. https://doi.org/10.1056/NEJM199209173271207.
- Thompson DC, Rivara FP, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst Rev 1999;4. https://doi.org/10.1002/14651858.cd001855.
- Kendrick D, Maula A, Stewart J, Clacy R, Coffey F, Cooper N, et al. Keeping children safe at home: protocol for three matched case–control studies of modifiable risk factors for falls. Inj Prev 2012;18. https://doi.org/10.1136/injuryprev-2012-040394.
- Majsak-Newman G, Benford P, Ablewhite J, Clacy R, Coffey F, Cooper N, et al. Keeping children safe at home: protocol for a matched case–control study of modifiable risk factors for poisoning. Inj Prev 2014;20. https://doi.org/10.1136/injuryprev-2014-041234.
- Wynn P, Stewart J, Kumar A, Clacy R, Coffey F, Cooper N, et al. Keeping children safe at home: protocol for a case–control study of modifiable risk factors for scalds. Inj Prev 2014;20. https://doi.org/10.1136/injuryprev-2014-041255.
- Groom L, Kendrick D, Coupland C, Patel B, Hippisley-Cox J. Inequalities in hospital admission rates for unintentional poisoning in young children. Inj Prev 2006;12:166-70. https://doi.org/10.1136/ip.2005.011254.
- Patel B, Groom L, Prasad V, Kendrick D. Parental poison prevention practices and their relationship with perceived toxicity: cross-sectional study. Inj Prev 2008;14:389-95. https://doi.org/10.1136/ip.2008.019604.
- Gartstein MA, Rothbart MK. Studying infant temperament via the Revised Infant Behavior Questionnaire. Infant Behav Dev 2003;26:64-86. https://doi.org/10.1016/S0163-6383(02)00169-8.
- Putnam SP, Gartstein MA, Rothbart MK. Measurement of fine-grained aspects of toddler temperament: the early childhood behavior questionnaire. Infant Behav Dev 2006;29:386-401. https://doi.org/10.1016/j.infbeh.2006.01.004.
- Putnam SP, Rothbart MK. Development of short and very short forms of the Children’s Behavior Questionnaire. J Pers Assess 2006;87:102-12. https://doi.org/10.1207/s15327752jpa8701_09.
- Morrongiello BA, Midgett C, Shields R. Don’t run with scissors: young children’s knowledge of home safety rules. J Pediatr Psychol 2001;26:105-15. https://doi.org/10.1093/jpepsy/26.2.105.
- Crnic KA, Greenberg MT. Minor parenting stresses with young children. Child Dev 1990;61:1628-37. https://doi.org/10.2307/1130770.
- Crnic KA, Booth CL. Mothers’ and fathers’ perceptions of daily hassles of parenting across early childhood. J Marriage Fam 1991;53:1043-50. https://doi.org/10.2307/353007.
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69-77. https://doi.org/10.1016/S0022-3999(01)00296-3.
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800-12. https://doi.org/10.1097/00005650-200108000-00006.
- Department for Communities and Local Government . English Indices of Deprivation 2010 n.d. www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 29 October 2014).
- UK Data Service Census Support . GeoConvert n.d. http://geoconvert.mimas.ac.uk/ (accessed 22 December 2014).
- Department for Education . Education and Skills in Your Area. Postcode Distances n.d. www.education.gov.uk/cgi-bin/inyourarea/distance.pl (accessed 29 October 2014).
- Watson M, Kendrick D, Coupland C. Validation of a home safety questionnaire used in a randomised controlled trial. Inj Prev 2003;9:180-3. https://doi.org/10.1136/ip.9.2.180.
- Edwards PJ, Roberts I, Clarke MJ, DiGuiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009;3. https://doi.org/10.1002/14651858.mr000008.pub4.
- McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al. Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients. Health Technol Assess 2001;5. https://doi.org/10.3310/hta5310.
- Clamp M, Kendrick D. A randomised controlled trial of general practitioner safety advice for families with children under 5 years. BMJ 1998;316:1576-9. https://doi.org/10.1136/bmj.316.7144.1576.
- Watson M, Kendrick D, Coupland C, Woods A, Futers D, Robinson J. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330:178-81. https://doi.org/10.1136/bmj.38309.664444.8F.
- Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health 1998;88:15-9. https://doi.org/10.2105/AJPH.88.1.15.
- Varni JW. The PedsQL Scoring Algorithm n.d. www.pedsql.org/score.html (accessed 27 February 2015).
- GL Assessment . The Hospital Anxiety and Depression Scale. Frequently Asked Questions. How Should Missing Data Be Treated n.d. www.gl-assessment.co.uk/products/hospital-anxiety-and-depression-scale/hospital-anxiety-and-depression-scale-faqs (accessed 27 February 2015).
- Rothbart M. Mary Rothbart’s Temperament Questionnaires. Frequently Asked Questions n.d. www.bowdoin.edu/~sputnam/rothbart-temperament-questionnaires/faq/ (accessed 27 February 2015).
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley; 1987.
- Watson M, Benford P, Coupland C, Clacy R, Hindmarch P, Majsak-Newman G, et al. Validation of a home safety questionnaire used in a series of case–control studies. Inj Prev 2014;20:336-42. https://doi.org/10.1136/injuryprev-2013-041006.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. https://doi.org/10.2307/2529310.
- Kendrick D, Maula A, Reading R, Hindmarch P, Coupland C, Watson M, et al. Risk and protective factors for falls from furniture in young children: multicentre case–control study. JAMA Pediatrics 2015;169:145-53. https://doi.org/10.1001/jamapediatrics.2014.2374.
- Benford P, Young B, Coupland C, Watson M, Hindmarch P, Hayes M, et al. Risk and protective factors for falls on one level in young children: multicentre case–control study. Inj Prev 2015;21:381-8. https://doi.org/10.1136/injuryprev-2015-041581.
- Kendrick D, Zou K, Ablewhite J, Watson M, Coupland C, Bryony K, et al. Risk and protective factors for falls on stairs in young children: multicentre case–control study. Arch Dis Child 2016;101:909-16.
- Kendrick D, Majsak-Newman G, Benford P, Coupland C, Timblin C, Hayes M, et al. Poison prevention practices and medically attended poisoning in young children: multicentre case–control study. Inj Prevent 2016. http://dx.doi.org/10.1136/injuryprev-2016-042156.400.
- Ploubidis G, Edwards P, Kendrick D. Measuring behaviours for escaping from house fires: use of latent variable models to summarise multiple behaviours. BMC Res Notes 2015;8. https://doi.org/10.1186/s13104-015-1769-5.
- Stewart J, Benford P, Wynn P, Watson MC, Coupland C, Deave T, et al. Modifiable risk factors for scald injury in children under 5 years of age: a multi-centre case–control study. Burns 2016;42:1831-43. https://doi.org/10.1016/j.burns.2016.06.027.
- Jurek AM, Greenland S, Maldonado G, Church TR. Proper interpretation of non-differential misclassification effects: expectations vs. observations. Int J Epidemiol 2005;34:680-7. https://doi.org/10.1093/ije/dyi060.
- Office for National Statistics . Ethnicity and National Identity in England and Wales 2011 n.d. www.ons.gov.uk/ons/rel/census/2011-census/key-statistics-for-local-authorities-in-england-and-wales/rpt-ethnicity.html#tab-conclusions (accessed 16 November 2015).
- Peden M, Oyegbite K, Ozanne-Smith J, Hyder A, Branche C, Rahman A, et al. World Report on Child Injury Prevention. Geneva: World Health Organization, UNICEF; 2008.
- Schmertmann M, Williamson A, Black D. Stable age pattern supports role of development in unintentional childhood poisoning. Inj Prev 2008;14:30-3. https://doi.org/10.1136/ip.2007.016253.
- Tyrrell EG, Orton E, Tata LJ, Kendrick D. Children at risk of medicinal and non-medicinal poisoning: a population-based case–control study in general practice. Br J Gen Pract 2012;62:e827-33. https://doi.org/10.3399/bjgp12X659303.
- Orton E, Kendrick D, West J, Tata LJ. Independent risk factors for injury in pre-school children: three population-based nested case–control studies using routine primary care data. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0035193.
- Morrongiello BA, Ondejko L, Littlejohn A. Understanding toddlers’ in-home injuries: I. Context, correlates, and determinants. J Pediatr Psychol 2004;29:415-31. https://doi.org/10.1093/jpepsy/jsh046.
- Morrongiello BA, Ondejko L, Littlejohn A. Understanding toddlers’ in-home injuries: II. Examining parental strategies, and their efficacy, for managing child injury risk. J Pediatr Psychol 2004;29:433-46. https://doi.org/10.1093/jpepsy/jsh047.
- Morrongiello BA, McArthur BA, Bell M. Managing children’s risk of injury in the home: does parental teaching about home safety reduce young children’s hazard interactions?. Accid Anal Prev 2014;71:194-200. https://doi.org/10.1016/j.aap.2014.04.016.
- Belechri M, Petridou E, Trichopoulos D. Bunk versus conventional beds: a comparative assessment of fall injury risk. J Epidemiol Community Health 2002;56:413-17. https://doi.org/10.1136/jech.56.6.413.
- D’Souza AL, Smith GA, McKenzie LB. Bunk bed-related injuries among children and adolescents treated in emergency departments in the United States, 1990–2005. Pediatrics 2008;121:e1696-702. https://doi.org/10.1542/peds.2007-2555.
- Macgregor DM. Injuries associated with falls from beds. Inj Prev 2000;6:291-2. https://doi.org/10.1136/ip.6.4.291.
- Selbst SM, Baker MD, Shames M. Bunk bed injuries. Am J Dis Child 1990;144:721-3. https://doi.org/10.1001/archpedi.1990.02150300121031.
- LeBlanc JC, Pless IB, King WJ, Bawden H, Bernard-Bonnin A-C, Klassen T, et al. Home safety measures and the risk of unintentional injury among young children: a multicentre case–control study. CMAJ 2006;175:883-7. https://doi.org/10.1503/cmaj.050592.
- Elkington J, Blogg S, Kelly J, Carey V. Head injuries in infants: a closer look at baby-walkers, stairs and nursery furniture. N S W Public Health Bull 1999;10:82-3. https://doi.org/10.1071/NB99037.
- Petridou E, Kouri N, Polychronopoulou A, Siafas K, Stoikidou M, Trichopoulos D. Risk factors for childhood poisoning: a case-control study in Greece. Inj Prev 1996;2:208-11. https://doi.org/10.1136/ip.2.3.208.
- Schmertmann M, Williamson A, Black D, Wilson L. Risk factors for unintentional poisoning in children aged 1–3 years in NSW Australia: a case–control study. BMC Pediatr 2013;13. https://doi.org/10.1186/1471-2431-13-88.
- Chatsantiprapa K, Chokkanapitak J, Pinpradit N. Host and environment factors for exposure to poisons: a case–control study of preschool children in Thailand. Inj Prev 2001;7:214-17. https://doi.org/10.1136/ip.7.3.214.
- Ramos CL, Barros HM, Stein AT, Costa JS. Risk factors contributing to childhood poisoning. J Pediatr 2010;86:435-40. https://doi.org/10.2223/jped.2033.
- Petridou E, Trichopoulos D, Mera E, Papadatos Y, Papazoglou K, Marantos A, et al. Risk factors for childhood burn injuries: a case–control study from Greece. Burns 1998;24:123-8. https://doi.org/10.1016/S0305-4179(97)00095-8.
- Othman N, Kendrick D. Risk factors for burns at home in Kurdish preschool children: a case–control study. Inj Prev 2013;19:184-90. https://doi.org/10.1136/injuryprev-2012-040412.
- van Rijn OJ, Bouter LM, Kester AD, Knipschild PG, Meertens RM. Aetiology of burn injuries among children aged 0–4 years: results of a case–control study. Burns 1991;17:213-19. https://doi.org/10.1016/0305-4179(91)90107-R.
- Daisy S, Mostaque AK, Bari TS, Khan AR, Karim S, Quamruzzaman Q. Socioeconomic and cultural influence in the causation of burns in the urban children of Bangladesh. J Burn Care Rehabil 2001;22:269-73. https://doi.org/10.1097/00004630-200107000-00004.
- Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P. The PedsQL in pediatric cancer: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales, Multidimensional Fatigue Scale, and Cancer Module. Cancer 2002;94:2090-106. https://doi.org/10.1002/cncr.10428.
- Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126-39. https://doi.org/10.1097/00005650-199902000-00003.
- Ding R, McCarthy ML, Houseknecht E, Ziegfeld S, Knight VM, Korehbandi P, et al. The health-related quality of life of children with an extremity fracture: a one-year follow-up study. J Pediatr Orthop 2006;26:157-63. https://doi.org/10.1097/01.bpo.0000218521.98244.7e.
- McCarthy ML, MacKenzie EJ, Durbin DR, Aitken ME, Jaffe KM, Paidas CN, et al. The Pediatric Quality of Life Inventory: an evaluation of its reliability and validity for children with traumatic brain injury. Arch Phys Med Rehabil 2005;86:1901-9. https://doi.org/10.1016/j.apmr.2005.03.026.
- Sheldon TA, Jefferson T, Demicheli V, Mugford M. Elementary Economic Evaluation in Health Care. London: BMJ Books; 2000.
- Guide to the Methods of Technology Appraisal. London: NICE; 2008.
- Judging Whether Public Health Interventions Offer Value for Money. London: NICE; 2013.
- Anderson R, Moxham T. Preventing Unintentional Injuries in Children: Systematic Review to Provide an Overview of Published Economic Evaluations of Relevant Legislation, Regulations, Standards, and Or Their Enforcement and Promotion by Mass Media. Final Report (Updated) 2010 n.d. www.nice.org.uk/Guidance/PH29/Evidence (accessed 21 July 2014).
- Malek M, Chang BH, Gallagher SS, Guyer B. The cost of medical care for injuries to children. Ann Emerg Med 1991;20:997-1005. https://doi.org/10.1016/S0196-0644(05)82979-8.
- Polinder S, Toet H, Mulder S, van Beeck E. APOLLO: The Economic Consequences of Injury – Final Report. Amsterdam: Consumer Safety Institute; 2008.
- Pellatt RA, Williams A, Wright H, Young AE. The cost of a major paediatric burn. Burns 2010;36:1208-14. https://doi.org/10.1016/j.burns.2010.04.008.
- Rockhill CM, Fann JR, Fan MY, Hollingworth W, Katon WJ. Healthcare costs associated with mild traumatic brain injury and psychological distress in children and adolescents. Brain Inj 2010;24:1051-60. https://doi.org/10.3109/02699052.2010.494586.
- The Economic Burden of Unintentional Injury in Canada. Toronto, ON: Ministry of Health; 1998.
- Access Economics Pty Limited . The Economic Cost of Spinal Cord Injury and Traumatic Brain Injury in Australia 2009. www.tac.vic.gov.au/about-the-tac/our-organisation/research/tac-neurotrauma-research (accessed 19 August 2015).
- Walter LK. Re-valuation of Home Accidents. Published project report PPR483. Wokingham: Transport Research Laboratory; 2010.
- Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev 2006;12:212-18. https://doi.org/10.1136/ip.2005.010983.
- Miller TR, Romano EO, Spicer RS. The cost of childhood unintentional injuries and the value of prevention. Future Child 2000;10:137-63. https://doi.org/10.2307/1602828.
- Preventing Unintentional Injuries among Under-15s. Costing Report. Implementing NICE Guidance. London: NICE; 2010.
- Hawley CA, Ward AB, Long J, Owen DW, Magnay AR. Prevalence of traumatic brain injury amongst children admitted to hospital in one health district: a population-based study. Injury 2003;34:256-60. https://doi.org/10.1016/S0020-1383(02)00193-6.
- Parslow RC, Morris KP, Tasker RC, Forsyth RJ, Hawley CA. UK Paediatric Traumatic Brain Injury Study Steering Group . Epidemiology of traumatic brain injury in children receiving intensive care in the UK. Arch Dis Child 2005;90:1182-7. https://doi.org/10.1136/adc.2005.072405.
- Odenbach J, Newton A, Gokiert R, Falconer C, Courchesne C, Campbell S, et al. Screening for post-traumatic stress disorder after injury in the pediatric emergency department – a systematic review protocol. Syst Rev 2014;3. https://doi.org/10.1186/2046-4053-3-19.
- Osberg JS, Kahn P, Rowe K, Brooke MM. Pediatric trauma: impact on work and family finances. Pediatrics 1996;98:890-7.
- Aitken ME, McCarthy ML, Slomine BS, Ding R, Durbin DR, Jaffe KM, et al. Family burden after traumatic brain injury in children. Pediatrics 2009;123:199-206. https://doi.org/10.1542/peds.2008-0607.
- Polinder S, Haagsma JA, Toet H, van Beeck EF. Epidemiological burden of minor, major and fatal trauma in a national injury pyramid. Br J Surg 2012;99:114-21. https://doi.org/10.1002/bjs.7708.
- Hospital Episode Statistics, Admitted Patient Care, England 2008–9. Newport: Health and Social Care Information Centre; 2011.
- Office for National Statistics . Annual Mid-Year Population Estimates for England and Wales n.d. www.ons.gov.uk/ons/rel/popestimate/population-estimates-for-england-and-wales/mid-2012/mid-2012-population-estimates-for-england-and-wales.html (accessed 15 December 2015).
- Reported Road Casualties in Great Britain: 2011 Annual Report – a Valuation of Road Accidents and Casualties in Great Britain in 2011. London: Department for Transport; 2011.
- Reported Road Casualties in Great Britain: Main Results 2012. London: Department for Transport; 2013.
- Wright C, Wordsworth R, Glennie L. Counting the Cost of Meningitis: A Severe Case of Bacterial Meningitis n.d. www.meningitis.org/assets/x/53379 (accessed 15 December 2015).
- Child Accident Prevention Trust . The Costs of Head Injuries n.d. www.makingthelink.net/costs-head-injuries (accessed 15 December 2015).
- Griffiths HR, Thornton KL, Clements CM, Burge TS, Kay AR, Young AE. The cost of a hot drink scald. Burns 2006;32:372-4. https://doi.org/10.1016/j.burns.2005.10.025.
- Phillips CJ, Humphreys I, Kendrick D, Stewart J, Hayes M, Nish L, et al. Preventing bath water scalds: a cost-effectiveness analysis of introducing bath thermostatic mixer valves in social housing. Inj Prev 2011;17:238-43. https://doi.org/10.1136/ip.2010.031393.
- EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Gold MR, Stevenson D, Fryback DG. HALYS and QALYS and DALYS, oh my: similarities and differences in summary measures of population health. Annu Rev Public Health 2002;23:115-34. https://doi.org/10.1146/annurev.publhealth.23.100901.140513.
- Brussoni M, Kruse S, Walker K. Validity and reliability of the EQ-5D-3L™ among a paediatric injury population. Health Qual Life Outcomes 2013;11. https://doi.org/10.1186/1477-7525-11-157.
- Sánchez JL, Perepérez SB, Bastida JL, Martínez MM. Cost–utility analysis applied to the treatment of burn patients in a specialized center. Arch Surg 2007;142:50-7. https://doi.org/10.1001/archsurg.142.1.50.
- Tilford JM, Aitken ME, Goodman AC, Fiser DH, Killingsworth JB, Green JW, et al. Child health-related quality of life following neurocritical care for traumatic brain injury: an analysis of preference-weighted outcomes. Neurocrit Care 2007;7:64-75. https://doi.org/10.1007/s12028-007-0037-5.
- Hirsch AE, Eppinger RH, Shame T. Impairment Scaling from the Abbreviated Injury Scale. Washington, DC: National Highway Traffic Safety Administration; 1983.
- Miller TR, Pindus NM, Douglass JB, Rossman SB. Nonfatal Injury Costs and Consequences: A Data Book. Washington, DC: Urban Institute Press; 1995.
- Detailed Claims Information Special Tabulation. Boca Raton, FL: NCCI; 1998.
- Kaplan RM, Anderson JP, Spiker B. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia, PA: Lippincott-Raven; 1996.
- Kaplan RM, Anderson JP. A general health policy model: update and applications. Health Serv Res 1988;23:203-35.
- Liller KD. Injury Prevention for Children and Adolescents: Research, Practice and Advocacy. Washington, DC: American Public Health Association; 2006.
- Solans M, Pane S, Estrada MD, Serra-Sutton V, Berra S, Herdman M, et al. Health-related quality of life measurement in children and adolescents: a systematic review of generic and disease-specific instruments. Value Health 2008;11:742-64. https://doi.org/10.1111/j.1524-4733.2007.00293.x.
- Griebsch I, Coast J, Brown J. Quality-adjusted life-years lack quality in pediatric care: a critical review of published cost–utility studies in child health. Pediatrics 2005;115:e600-14. https://doi.org/10.1542/peds.2004-2127.
- Polinder S, Haagsma JA, Lyons RA, Gabbe BJ, Ameratunga S, Cryer C, et al. Measuring the population burden of fatal and nonfatal injury. Epidemiol Rev 2012;34:17-31. https://doi.org/10.1093/epirev/mxr022.
- Upton P, Lawford J, Eiser C. Parent–child agreement across child health-related quality of life instruments: a review of the literature. Qual Life Res 2008;17:895-913. https://doi.org/10.1007/s11136-008-9350-5.
- Upton P, Eiser C, Cheung I, Hutchings HA, Jenney M, Maddocks A, et al. Measurement properties of the UK-English version of the Pediatric Quality of Life Inventory 4.0 (PedsQL) generic core scales. Health Qual Life Outcomes 2005;3. https://doi.org/10.1186/1477-7525-3-22.
- Buck D. The PedsQL™ as a measure of parent-rated quality of life in healthy UK toddlers: psychometric properties and cross-cultural comparisons. J Child Health Care 2012;16:331-8. https://doi.org/10.1177/1367493512448127.
- Willis CD, Gabbe BJ, Butt W, Cameron PA. Assessing outcomes in paediatric trauma populations. Injury 2006;37:1185-96. https://doi.org/10.1016/j.injury.2006.07.011.
- Janssens L, Gorter JW, Ketelaar M, Kramer WL, Holtslag HR. Health-related quality-of-life measures for long-term follow-up in children after major trauma. Qual Life Res 2008;17:701-13. https://doi.org/10.1007/s11136-008-9339-0.
- Varni JW, Seid M, Knight TS, Uzark K, Szer IS. The PedsQL 4.0 Generic Core Scales: sensitivity, responsiveness, and impact on clinical decision-making. J Behav Med 2002;25:175-93. https://doi.org/10.1023/A:1014836921812.
- Erickson SJ, Montague EQ, Gerstle MA. Health-related quality of life in children with moderate-to-severe traumatic brain injury. Dev Neurorehabil 2010;13:175-81. https://doi.org/10.3109/17518420903479867.
- Rivara FP, Koepsell TD, Wang J, Temkin N, Dorsch A, Vavilala MS, et al. Disability 3, 12, and 24 months after traumatic brain injury among children and adolescents. Pediatrics 2011;128:e1129-38. https://doi.org/10.1542/peds.2011-0840.
- Garma SI, Kelly EH, Daharsh EZ, Vogel LC. Health-related quality of life after pediatric spinal cord injury. J Pediatr Psychol 2011;36:226-36. https://doi.org/10.1093/jpepsy/jsq037.
- Oladeji O, Johnston TE, Smith BT, Mulcahey MJ, Betz RR, Lauer RT. Quality of life in children with spinal cord injury. Pediatr Phys Ther 2007;19:296-300. https://doi.org/10.1097/PEP.0b013e31815a12ef.
- Stevens MW, Drendel AL, Hainsworth KR. Pediatric minor injury outcomes: an initial report. Pediatr Emerg Care 2011;27:371-3. https://doi.org/10.1097/PEC.0b013e318216b0e7.
- Stevens MW, Hainsworth KR, Weisman SJ, Layde PM. Health-related quality of life in pediatric minor injury: reliability, validity, and responsiveness of the Pediatric Quality of Life Inventory in the emergency department. Arch Pediatr Adolesc Med 2012;166:74-81. https://doi.org/10.1001/archpediatrics.2011.694.
- Khan KA, Petrou S, Rivero-Arias O, Walters SJ, Boyle SE. Mapping EQ-5D utility scores from the PedsQL™ generic core scales. Pharmacoeconomics 2014;32:693-706. https://doi.org/10.1007/s40273-014-0153-y.
- Van Beeck EF, Larsen CF, Lyons RA, Meerding WJ, Mulder S, Essink-Bot ML. Guidelines for the conduction of follow-up studies measuring injury-related disability. J Trauma 2007;62:534-50. https://doi.org/10.1097/TA.0b013e31802e70c7.
- Polinder S, Haagsma JA, Belt E, Lyons RA, Erasmus V, Lund J, et al. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-783.
- Varni JW, Limbers CA, Neighbors K, Schulz K, Lieu JE, Heffer RW, et al. The PedsQL™ Infant Scales: feasibility, internal consistency reliability, and validity in healthy and ill infants. Qual Life Res 2011;20:45-5. https://doi.org/10.1007/s11136-010-9730-5.
- Brunner HI, Maker D, Grundland B, Young NL, Blanchette V, Stain AM, et al. Preference-based measurement of health-related quality of life (HRQL) in children with chronic musculoskeletal disorders (MSKDs). Med Decis Making 2003;23:314-22. https://doi.org/10.1177/0272989X03256008.
- Mistry RD, Stevens MW, Gorelick MH. Health-related quality of life for pediatric emergency department febrile illnesses: an evaluation of the Pediatric Quality of Life Inventory 4.0 Generic Core Scales. Health Qual Life Outcomes 2009;7. https://doi.org/10.1186/1477-7525-7-5.
- Nunnally JC, Bernstein IH. Psychometric Theory. New York: McGraw–Hill; 1994.
- McHorney CA, Ware JE, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 1994;32:40-66. https://doi.org/10.1097/00005650-199401000-00004.
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297-334. https://doi.org/10.1007/BF02310555.
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. London: Lawrence Erlbaum Associates; 1977.
- Limbers CA, Newman DA, Varni JW. Factorial invariance of child self-report across age subgroups: a confirmatory factor analysis of ages 5 to 16 years utilizing the PedsQL 4.0 Generic Core Scales. Value Health 2008;11:659-68. https://doi.org/10.1111/j.1524-4733.2007.00289.x.
- Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-1.
- Limbers CA, Newman DA, Varni JW. Factorial invariance of child self-report across socioeconomic status groups: a multigroup confirmatory factor analysis utilizing the PedsQL 4.0 Generic Core Scales. J Behav Med 2008;31:401-11. https://doi.org/10.1007/s10865-008-9166-3.
- Limbers CA, Newman DA, Varni JW. Factorial invariance of child self-report across healthy and chronic health condition groups: a confirmatory factor analysis utilizing the PedsQLTM 4.0 Generic Core Scales. J Pediatr Psychol 2008;33:630-9. https://doi.org/10.1093/jpepsy/jsm131.
- Limbers CA, Newman DA, Varni JW. Factorial invariance of child self-report across race/ethnicity groups: a multigroup confirmatory factor analysis approach utilizing the PedsQL 4.0 Generic Core Scales. Ann Epidemiol 2009;19:575-81. https://doi.org/10.1016/j.annepidem.2009.04.004.
- Varni J, Limbers CA, Newman D, Seid M. Longitudinal factorial invariance of the PedsQL™ 4.0 Generic Core Scales child self-report version: one year prospective evidence from the California State Children’s Health Insurance Program (SCHIP). Qual Life Res 2008;17:1153-62. https://doi.org/10.1007/s11136-008-9389-3.
- Varni JW, Limbers CA, Newman DA. Using factor analysis to confirm the validity of children’s self-reported health-related quality of life across different modes of administration. Clin Trials 2009;6:185-95. https://doi.org/10.1177/1740774509102309.
- Hu L-T, Bentler PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods 1998;3:424-53. https://doi.org/10.1037/1082-989X.3.4.424.
- Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor analysis: the effect of sample size. Psychol Bull 1988;103:391-410. https://doi.org/10.1037/0033-2909.103.3.391.
- Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equation Model 2002;9:233-55. https://doi.org/10.1207/S15328007SEM0902_5.
- Marsh HW, Hau K-T, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Struct Equ Modeling 2004;11:3320-41. https://doi.org/10.1207/s15328007sem1103_2.
- Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003;3:329-41. https://doi.org/10.1367/1539-4409(2003)003<0329:TPAAPP>2.0.CO;2.
- Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol 2008;61:102-9. https://doi.org/10.1016/j.jclinepi.2007.03.012.
- Wyrwich KW, Nienaber NA, Tierney WM, Wolinsky FD. Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care 1999;37:469-78. https://doi.org/10.1097/00005650-199905000-00006.
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003;41:582-92. https://doi.org/10.1097/01.MLR.0000062554.74615.4C.
- Watson WL, Ozanne-Smith J, Richardson J. Retrospective baseline measurement of self-reported health status and health-related quality of life versus population norms in the evaluation of post-injury losses. Inj Prev 2007;13:45-50. https://doi.org/10.1136/ip.2005.010157.
- Wilson R, Derrett S, Hansen P, Langley J. Retrospective evaluation versus population norms for the measurement of baseline health status. Health Qual Life Outcomes 2012;10. https://doi.org/10.1186/1477-7525-10-68.
- Sprangers MA, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med 1999;48:1507-15. https://doi.org/10.1016/S0277-9536(99)00045-3.
- Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-2.
- Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-43.
- Amiri P, Eslamian G, Mirmiran P, Shiva N, Jafarabadi MA, Azizi F. Validity and reliability of the Iranian version of the Pediatric Quality of Life Inventory™ 4.0 (PedsQL™) Generic Core Scales in children. Health Qual Life Outcomes 2012;10. https://doi.org/10.1186/1477-7525-10-3.
- Viira R, Koka A. Health-related quality of life of Estonian adolescents: reliability and validity of the PedsQL™ 4.0 Generic Core Scales in Estonia. Acta Paediatr 2011;100:1043-7. https://doi.org/10.1111/j.1651-2227.2011.02193.x.
- Huguet A, Miró J. Development and psychometric evaluation of a Catalan self- and interviewer-administered version of the Pediatric Quality of Life Inventory version 4.0. J Pediatr Psychol 2008;33:63-79. https://doi.org/10.1093/jpepsy/jsm040.
- Stevanović D, Lakić A, Damnjanović M. Some psychometric properties of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales (PedsQL™) in the general Serbian population. Qual Life Res 2011;20:945-9. https://doi.org/10.1007/s11136-010-9833-z.
- Hao Y, Tian Q, Lu Y, Chai Y, Rao S. Psychometric properties of the Chinese version of the Pediatric Quality of Life Inventory 4.0 generic core scales. Qual Life Res 2010;19:1229-33. https://doi.org/10.1007/s11136-010-9672-y.
- Petersen S, Hägglöf B, Stenlund H, Bergström E. Psychometric properties of the Swedish PedsQL, Pediatric Quality of Life Inventory 4.0 generic core scales. Acta Paediatr 2009;98:1504-12. https://doi.org/10.1111/j.1651-2227.2009.01360.x.
- Cooper NJ, Kendrick D, Timblin C, Hayes M, Majsak-Newman G, Meteyard K, et al. The short-term cost of falls, poisonings and scalds occurring at home in children under 5 years old in England: multicentre longitudinal study. Inj Prev 2016;22:41-334. https://doi.org/10.1136/injuryprev-2015-041808.
- Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol 1990;43:543-9. https://doi.org/10.1016/0895-4356(90)90158-L.
- Short Stay Paediatric Assessment Units – Advice for Commissioners and Providers. London: Royal College of Paediatrics and Child Health; 2009.
- Quality and Safety Programme Paediatric Emergency Services – Case for Change. London: NHS London Health Programmes; 2013.
- Levett I, Berry K, Wacogne I. Review of a paediatric emergency department observation unit. Emerg Med J 2006;23:612-13. https://doi.org/10.1136/emj.2005.029470.
- Fifth Report of Session 2009–10, Sure Start Children’s Centres. London: The Stationery Office; 2010.
- Choice for Parents, the Best Start for Children: A Ten Year Strategy for Childcare. London: HMSO; 2004.
- Sure Start Children’s Centres Statutory Guidance. London: Department for Education; 2010.
- Goff J, Hall J, Sylva K, Smith T, Smith G, Eisenstadt N, et al. Evaluation of Children’s Centres in England (ECCE) Strand 3: Delivery of Family Services by Children’s Centres. Oxford: Department for Education; 2013.
- Tanner E, Agur M, Hussey D, Hall J, Sammons P, Sylva K, et al. Evaluation of Children’s Centres in England (ECCE) Strand 1: First Survey of Children’s Centre Leaders in the Most Deprived Areas 2012.
- Melhuish E, Belsky J, Barnes J. Evaluation and value of Sure Start. Arch Dis Child 2010;95:159-61. https://doi.org/10.1136/adc.2009.161018.
- The Impact of Sure Start Local Programmes on Three Year Olds and their Families. London: DCSF; 2008.
- Melhuish E, Belsky J, Leyland AH, Barnes J. National Evaluation of Sure Start Research Team . Effects of fully-established Sure Start Local Programmes on 3-year-old children and their families living in England: a quasi-experimental observational study. Lancet 2008;372:1641-7. https://doi.org/10.1016/S0140-6736(08)61687-6.
- Hutchings J, Gardner F, Bywater T, Daley D, Whitaker C, Jones K, et al. Parenting intervention in Sure Start services for children at risk of developing conduct disorder: pragmatic randomised controlled trial. BMJ 2007;334. https://doi.org/10.1136/bmj.39126.620799.55.
- Watson MC, Mulvaney CA, Kendrick D, Stewart J, Coupland C, Hayes M, et al. Keeping Children Safe programme team . National survey of the injury prevention activities of children’s centres. Health Soc Care Community 2014;22:40-6. https://doi.org/10.1111/hsc.12059.
- Watson M, White J. Accident prevention activities: a national survey of health authorities. Health Educ J 2001;60:275-83. https://doi.org/10.1177/001789690106000309.
- Kendrick D, Groom L, Hippisley-Cox J, Savelyich BS, Webber E, Coupland C. Accidental injury: a neglected area within primary care groups and trusts?. Health Educ Res 2003;18:380-8. https://doi.org/10.1093/her/cyf028.
- Watson M, Kendrick D, Coupland C, Futers D. Childhood injury prevention: the views of health visitors and nursery nurses working in deprived areas. Int J Health Promot Educ 2007;45:4-10. https://doi.org/10.1080/14635240.2007.10708091.
- Litwin M. How to Measure Survey Reliability and Validity. Los Angeles, CA: Sage Publications; 1995.
- Belson W. Validity in Survey Research. Aldershot: Gower; 1986.
- Oppenheim A. Questionnaire Design, Interviewing and Attitude Measurement. London: Continuum; 1992.
- Watson MC, Mulvaney C, Timblin C, Stewart J, Coupland CA, Deave T, et al. Missed opportunities to keep children safe? National Survey of injury prevention activities of children’s centres. Health Educ J 2016;75:833-42.
- Cook JV, Dickinson HO, Eccles MP. Response rates in postal surveys of healthcare professionals between 1996 and 2005: an observational study. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-160.
- Behaviour Change: The Principles for Effective Interventions. London: NICE; 2007.
- Declaration of Alma-Ata. Geneva: World Health Organization; 1978.
- Ottawa Charter for Health Promotion. Copenhagen: World Health Organization; 1986.
- The Health of the Nation. Key Area Handbooks: Accidents. London: HMSO; 1993.
- Preventing Childhood Accidents: Guidance on Effective Action. London: Child Accident Prevention Trust; 2003.
- Working Together for Better Health. London: Department of Health; 1993.
- Watson M. Alliances against accidents. Pract Nurs 1994;5.
- Scriven A. Alliances in Health Promotion. London: Macmillan; 1998.
- Hogg C. Preventing Children’s Accidents: A Guide for Health Authorities and Boards. London: Child Accident Prevention Trust; 1996.
- Towner E, Carter Y, Hayes M. Implementation of injury prevention for children and young people. Inj Prev 1998;4:26-33. https://doi.org/10.1136/ip.4.2008.S26.
- Carter YH, Jones PW. General practitioners’ beliefs about their role in the prevention and treatment of accidents involving children. Br J Gen Pract 1993;43:463-5.
- Carter YH, Morgan PS, Lancashire RJ. General practitioners’ attitudes to child injury prevention in the UK: a national postal questionnaire. Inj Prev 1995;1:164-8. https://doi.org/10.1136/ip.1.3.164.
- Kendrick D, Marsh P, Williams EI. How do practice nurses see their role in childhood injury prevention?. Inj Prev 1995;1:159-63. https://doi.org/10.1136/ip.1.3.159.
- Kendrick D, Marsh P, Williams EI. General practitioners: child accident prevention and ‘the health of the nation’. Health Educ Res 1995;10:345-53. https://doi.org/10.1093/her/10.3.345.
- Marsh P, Kendrick D, Williams EI. Health visitors’ knowledge, attitudes and practices in childhood accident prevention. J Public Health Med 1995;17:193-9. https://doi.org/10.1093/oxfordjournals.pubmed.a043092.
- Kendrick D, Illingworth R, Hapgood R, Woods AJ, Collier J. Baby walkers – health visitors’ current practice, attitudes and knowledge. J Adv Nurs 2003;43:488-95. https://doi.org/10.1046/j.1365-2648.2003.02746.x.
- Rhodes K, Kendrick D, Collier J. Baby walkers: paediatricians’ knowledge, attitudes, and health promotion. Arch Dis Child 2003;88:1084-5. https://doi.org/10.1136/adc.88.12.1084.
- Woods AJ, Hapgood R, Colier J, Kendrick D, Watts K, Illinworth R. Midwives’ knowledge of, attitudes to and practice with baby walkers. Midwifery 2003;19:63-71. https://doi.org/10.1054/midw.2002.0332.
- Tomlinson R, Sainsbury C. Childhood injury prevention advice: a survey of health professionals responses to common scenarios. Child Care Health Dev 2004;30:301-5. https://doi.org/10.1111/j.1365-2214.2004.00436.x.
- Smithson J, Garside R, Pearson M. Barriers to, and facilitators of, the prevention of unintentional injury in children in the home: a systematic review and synthesis of qualitative research. Inj Prev 2011;17:119-26. https://doi.org/10.1136/ip.2010.026989.
- Fire and Rescue Services Act 2004. London: the Stationery Office; 2004.
- Woods AJ. The role of health professionals in childhood injury prevention: a systematic review of the literature. Patient Educ Couns 2006;64:35-42. https://doi.org/10.1016/j.pec.2005.12.011.
- Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol 2008;41:327-50. https://doi.org/10.1007/s10464-008-9165-0.
- Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature. Tampa, FL: University of South Florida; 2005.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O, Peacock R. Storylines of research in diffusion of innovation: a meta-narrative approach to systematic review. Soc Sci Med 2005;61:417-30. https://doi.org/10.1016/j.socscimed.2004.12.001.
- Stith S, Pruitt I, Dees JE, Fronce M, Green N, Som A, et al. Implementing community-based prevention programming: a review of the literature. J Prim Prev 2006;27:599-617. https://doi.org/10.1007/s10935-006-0062-8.
- Ingram JC, Deave T, Towner E, Errington G, Kay B, Kendrick D. Identifying facilitators and barriers for home injury prevention interventions for pre-school children: a systematic review of the quantitative literature. Health Educ Res 2012;27:258-68. https://doi.org/10.1093/her/cyr066.
- Harden A, Gough D, Gough D, Oliver S, Thomas J. An Introduction to Systematic Reviews. London: Sage Publications; 2012.
- Pope C, Mays N, Popay J. Synthesising Qualitative and Quantitative Health Evidence: A Guide to Methods. Maidenhead: Open University Press; 2007.
- Systematic Reviews. York: University of York; 2009.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114-16. https://doi.org/10.1136/bmj.320.7227.114.
- Babul S, Olsen L, Janssen P, McIntee P, Raina P. A randomized trial to assess the effectiveness of an infant home safety programme. Int J Inj Contr Saf Promot 2007;14:109-17. https://doi.org/10.1080/17457300701272474.
- Carman J, Friedman E, Lamb D, Lennon K. Evaluating the impact of a child injury prevention project. Community Pract 2006;79:188-92.
- Coggan C, Patterson P, Brewin M, Hooper R, Robinson E. Evaluation of the Waitakere Community Injury Prevention Project. Inj Prev 2000;6:130-4. https://doi.org/10.1136/ip.6.2.130.
- Colver AF, Hutchinson PJ, Judson EC. Promoting children’s home safety. Br Med J 1982;285:1177-80. https://doi.org/10.1136/bmj.285.6349.1177.
- DiGuiseppi C, Roberts I, Wade A, Sculpher M, Edwards P, Godward C, et al. Incidence of fires and related injuries after giving out free smoke alarms: cluster randomised controlled trial. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7371.995.
- Emond A, Pollock J, Deave T, Bonnell S, Peters TJ, Harvey I. An evaluation of the First Parent Health Visitor Scheme. Arch Dis Child 2002;86:150-7. https://doi.org/10.1136/adc.86.3.150.
- Fergusson DM, Horwood LJ, Beautrais AL, Shannon FT. A controlled field trial of a poisoning prevention method. Pediatrics 1982;69:515-20.
- Georgieff K, Maw C. The Wakefield District Burns & Scalds Prevention Project. Wakefield: Wakefield MDC, Health Development Unit; 2004.
- Gielen AC, McDonald EM, Wilson ME, Hwang WT, Serwint JR, Andrews JS, et al. Effects of improved access to safety counseling, products, and home visits on parents’ safety practices: results of a randomized trial. Arch Pediatr Adolesc Med 2002;156:33-40. https://doi.org/10.1001/archpedi.156.1.33.
- Gielen AC, McKenzie LB, McDonald EM, Shields WC, Wang M-C, Cheng Y-J, et al. Using a computer kiosk to promote child safety: results of a randomized, controlled trial in an urban pediatric emergency department. Pediatr 2007;120:330-9. https://doi.org/10.1542/peds.2006-2703.
- Guyer B, Gallagher SS, Chang BH, Azzara CV, Cupples LA, Colton T. Prevention of childhood injuries: evaluation of the Statewide Childhood Injury Prevention Program (SCIPP). Am J Public Health 1989;79:1521-7. https://doi.org/10.2105/AJPH.79.11.1521.
- Harvey PA, Aitken M, Ryan GW, Demeter LA, Givens J, Sundararaman R, et al. Strategies to increase smoke alarm use in high-risk households. J Community Health 2004;29:375-85. https://doi.org/10.1023/B:JOHE.0000038653.59255.57.
- Hendrickson SG. Reaching an underserved population with a randomly assigned home safety intervention. Inj Prev 2005;11:313-17. https://doi.org/10.1136/ip.2004.007229.
- Jenkins HM, Blank V, Miller K, Turner J, Stanwick RS. A randomized single-blind evaluation of a discharge teaching book for pediatric patients with burns. J Burn Care Rehabil 1996;17:49-61. https://doi.org/10.1097/00004630-199601000-00012.
- Johnston BD, Britt J, D’Ambrosio L, Mueller BA, Rivara FP. A preschool program for safety and injury prevention delivered by home visitors. Inj Prev 2000;6:305-9. https://doi.org/10.1136/ip.6.4.305.
- Katcher ML, Landry GL, Shapiro MM. Liquid-crystal thermometer use in pediatric office counseling about tap water burn prevention. Pediatrics 1989;83:766-71.
- Kelly B, Sein C, McCarthy PL. Safety education in a pediatric primary care setting. Pediatrics 1987;79:818-24.
- Kelly NR, Huffman LC, Mendoza FS, Robinson TN. Effects of a videotape to increase use of poison control centers by low-income and Spanish-speaking families: a randomized, controlled trial. Pediatrics 2003;111:21-6. https://doi.org/10.1542/peds.111.1.21.
- Kendrick D, Marsh P, Fielding K, Miller P. Preventing injuries in children: cluster randomised controlled trial in primary care. BMJ 1999;318:980-3. https://doi.org/10.1136/bmj.318.7189.980.
- Kendrick D, Stewart J, Smith S, Coupland C, Hopkins N, Groom L, et al. Randomised controlled trial of thermostatic mixer valves in reducing bath hot tap water temperature in families with young children in social housing. Arch Dis Child 2011;96:232-9. https://doi.org/10.1136/adc.2009.175059.
- King WJ, Klassen TP, LeBlanc J, Bernard-Bonnin AC, Robitaille Y, Pham B, et al. The effectiveness of a home visit to prevent childhood injury. Pediatrics 2001;108:382-8. https://doi.org/10.1542/peds.108.2.382.
- Krug A, Ellis JB, Hay IT, Mokgabudi NF, Robertson J. The impact of child-resistant containers on the incidence of paraffin (kerosene) ingestion in children. S Afr Med J 1994;84:730-4.
- LeBailly SA, Freel K, Hicks-Bartlett S, Kirschenman J, Ritts-Benally K, Sasicki J. The Children’s Safety Research Project. Elk Grove Village, IL: American Academy of Pediatrics; 1990.
- Llewellyn G, McConnell D, Honey A, Mayes R, Russo D. Promoting health and home safety for children of parents with intellectual disability: a randomized controlled trial. Res Dev Disabil 2003;24:405-31. https://doi.org/10.1016/j.ridd.2003.06.001.
- Mallonee S. Evaluating injury prevention programs: the Oklahoma City Smoke Alarm Project. Future Child 2000;10:164-74. https://doi.org/10.2307/1602829.
- McDonald EM, Solomon B, Shields W, Serwint JR, Jacobsen H, Weaver NL, et al. Evaluation of kiosk-based tailoring to promote household safety behaviors in an urban pediatric primary care practice. Patient Educ Couns 2005;58:168-81. https://doi.org/10.1016/j.pec.2004.08.015.
- McLoughlin E, Vince CJ, Lee AM, Crawford JD. Project Burn Prevention: outcome and implications. Am J Public Health 1982;72:241-7. https://doi.org/10.2105/AJPH.72.3.241.
- Miller RE, Reisinger KS, Blatter MM, Wucher F. Pediatric counseling and subsequent use of smoke detectors. Am J Public Health 1982;72:392-3. https://doi.org/10.2105/AJPH.72.4.392.
- Mock C, Arreola-Risa C, Trevino-Perez R, Almazan-Saavedra V, Zozaya-Paz JE, Gonzalez-Solis R, et al. Injury prevention counselling to improve safety practices by parents in Mexico. Bull World Health Organ 2003;81:591-8.
- Mueller BA, Sidman EA, Alter H, Perkins R, Grossman DC. Randomized controlled trial of ionization and photoelectric smoke alarm functionality. Inj Prev 2008;14:80-6. https://doi.org/10.1136/ip.2007.016725.
- Nansel T, Weaver N, Donlin M, Jacobsen H, Kreuter MW, Simons-Morton B. Baby, be safe: the effect of tailored communications for pediatric injury prevention provided in a primary care setting. Parent Educ Couns 2002;46:175-90. https://doi.org/10.1016/S0738-3991(01)00211-7.
- Nansel TR, Weaver NL, Jacobsen HA, Glasheen C, Kreuter MW. Preventing unintentional pediatric injuries: a tailored intervention for parents and providers. Health Educ Res 2008;23:656-69. https://doi.org/10.1093/her/cym041.
- Odendaal W, van Niekerk A, Jordaan E, Seedat M. The impact of a home visitation programme on household hazards associated with unintentional childhood injuries: a randomised controlled trial. Accid Anal Prev 2009;41:183-90. https://doi.org/10.1016/j.aap.2008.10.009.
- Olds DL, Henderson CR, Kitzman H. Does prenatal and infancy nurse home visitation have enduring effects on qualities of parental caregiving and child health at 25 to 50 months of life?. Pediatrics 1994;93:89-98.
- Ozanne-Smith J, Day L, Stathakis V, Sherrard J. Controlled evaluation of a community based injury prevention program in Australia. Inj Prev 2002;8:18-22. https://doi.org/10.1136/ip.8.1.18.
- Paul CL, Sanson-Fisher RW, Redman S, Carter S. Preventing accidental injury to young children in the home using volunteers. Health Promot Int 1994;9:241-8. https://doi.org/10.1093/heapro/9.4.241.
- Petridou E, Tolma E, Dessypris N, Trichopoulos D. A controlled evaluation of a community injury prevention project in two Greek islands. Int J Epidemiol 1997;26:173-9. https://doi.org/10.1093/ije/26.1.173.
- Pless IB, Hagel BE, Patel H, Leduc D, Magdalinos H. Preventing product related injuries. A randomised controlled trial of poster alerts. Can J Public Health 2007;98:271-5.
- Posner JC, Hawkins LA, Garcia-Espana F, Durbin DR. A randomized, clinical trial of a home safety intervention based in an emergency department setting. Pediatrics 2004;113:1603-8. https://doi.org/10.1542/peds.113.6.1603.
- Rey S, Courtois X, Zmirou D, François M, Oberle D, Navet J. Evaluation of an educational action on accident prevention in children. Pediatrie 1993;48:727-33.
- Sangvai S, Cipriani L, Colborn DK, Wald ER. Studying injury prevention: practices, problems, and pitfalls in implementation. Clin Pediatr 2007;46:228-35. https://doi.org/10.1177/0009922806293861.
- Schelp L. Community intervention and changes in accident pattern in a rural Swedish municipality. Health Promot 1987;2:109-25. https://doi.org/10.1093/heapro/2.2.109.
- Schlesinger ER, Dickson DG, Westaby J, Lowen L, Logrillo VM, Maiwald AA. A controlled study of health education in accident prevention. Am J Dis Child 1996;111:490-6. https://doi.org/10.1001/archpedi.1966.02090080068004.
- Schwarz DF, Grisso JA, Miles C, Holmes JH, Sutton RL. An injury prevention program in an urban African-American community. Am J Public Health 1993;83:675-80. https://doi.org/10.2105/AJPH.83.5.675.
- Schwebel DC, Swart D, Simpson J, Hobe P, Hui SK. An intervention to reduce kerosene-related burns and poisonings in low-income South African communities. Health Psychol 2009;28:493-500. https://doi.org/10.1037/a0014531.
- Svanström L, Ekman R, Schelp L, Lindström A. The Lidköping Accident Prevention Programme – a community approach to preventing childhood injuries in Sweden. Inj Prev 1995;1:169-72. https://doi.org/10.1136/ip.1.3.169.
- Swart L, van Niekerk A, Seedat M, Jordaan E. Paraprofessional home visitation program to prevent childhood unintentional injuries in low-income communities: a cluster randomized controlled trial. Inj Prev 2008;14:164-9. https://doi.org/10.1136/ip.2007.016832.
- Sznajder M, Leduc S, Janvrin MP, Bonnin MH, Aegerter P, Baudier F, et al. Home delivery of an injury prevention kit for children in four French cities: a controlled randomized trial. Inj Prev 2003;9:261-5. https://doi.org/10.1136/ip.9.3.261.
- Thomas KA, Hassanein RS, Christophersen ER. Evaluation of group well-child care for improving burn prevention practices in the home. Pediatrics 1984;74:879-82.
- Vineis P, Ronco G, Ciccone G, Gogliani F. Home injuries in children: a population-based intervention trial. Epidemiology 1994;5:349-51. https://doi.org/10.1097/00001648-199405000-00016.
- Waller AE, Clarke JA, Langley JD. An evaluation of a program to reduce home hot tap water temperatures. Aust J Public Health 1993;17:116-23. https://doi.org/10.1111/j.1753-6405.1993.tb00118.x.
- Woolf A, Lewander W, Filippone G, Lovejoy F. Prevention of childhood poisoning: efficacy of an educational program carried out in an emergency clinic. Pediatrics 1987;80:359-63.
- Woolf AD, Saperstein A, Forjuoh S. Poisoning prevention knowledge and practices of parents after a childhood poisoning incident. Pediatrics 1992;90:867-70.
- Yang J, Peek-Asa C, Jones MP, Nordstrom DL, Taylor C, Young TL, et al. Smoke alarms by type and battery life in rural households: a randomized controlled trial. Am J Prev Med 2008;35:20-4. https://doi.org/10.1016/j.amepre.2008.03.020.
- Ytterstad B, Wasmuth HH. The Harstad Injury Prevention Study: evaluation of hospital-based injury recording and community-based intervention for traffic injury prevention. Accid Anal Prev 1995;27:111-23. https://doi.org/10.1016/0001-4575(94)00036-L.
- Zhao CH, Qiu HS, Qiu HX. Interventions to prevent accidental injuries in children between 7 and 13 years of age. Zhongguo Dang Dai Er Ke Za Zhi 2006;8:331-3.
- Carr S. Peer educators – contributing to child accident prevention. Community Pract 2005;78:174-7.
- Gibbs L, Waters E, Sherrard J, Ozanne-Smith J, Robinson J, Young S, et al. Understanding parental motivators and barriers to uptake of child poison safety strategies: a qualitative study. Inj Prev 2005;11:373-7. https://doi.org/10.1136/ip.2004.007211.
- Morrongiello BA, Kiriakou S. Mothers’ home-safety practices for preventing six types of childhood injuries: what do they do, and why?. J Pediatr Psychol 2004;29:285-97. https://doi.org/10.1093/jpepsy/jsh030.
- Morrongiello BA, Zdzieborski D, Sandomierski M, Lasenby-Lessard J. Video messaging: what works to persuade mothers to supervise young children more closely in order to reduce injury risk?. Soc Sci Med 2009;68:1030-7. https://doi.org/10.1016/j.socscimed.2008.12.019.
- Pollack-Nelson C, Drago DA. Supervision of children aged two through six years. Inj Control Saf Promot 2002;9:121-6. https://doi.org/10.1076/icsp.9.2.121.8696.
- Van Niekerk A, Menckel E, Laflamme L. Barriers and enablers to the use of measures to prevent pediatric scalding in Cape Town, South Africa. Public Health Nurs 2010;27:203-20. https://doi.org/10.1111/j.1525-1446.2010.00846.x.
- Office for National Statistics . Index of Multiple Deprivation 2007 n.d. http://data.gov.uk/dataset/index_of_multiple_deprivation_imd_2007 (accessed 9 October 2014).
- Department for Communities and Local Government . Indices of Deprivation 2007 n.d. http://webarchive.nationalarchives.gov.uk/+/http:/www.communities.gov.uk/communities/neighbourhoodrenewal/deprivation/deprivation07/ (accessed 29 October 2014).
- Ritchie J, Spencer L, Huberman M, Matthew M. The Qualitative Researcher’s Companion. London: Sage Publications; 2002.
- Ritchie J, Spencer E, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice. London: Sage Publications; 2003.
- Patton M. Qualitative Evaluation and Research Methods. Newbury Park, CA: Sage Publications; 1990.
- Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technol Assess 1998;2.
- Ablewhite J, McDaid L, Hawkins A, Peel I, Goodenough T, Deave T, et al. Approaches used by parents to keep their children safe at home: a qualitative study to explore the perspectives of parents with children aged under five years. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2252-x.
- Ablewhite J, Peel I, McDaid L, Hawkins A, Goodenough T, Deave T, et al. Parental perceptions of barriers and facilitators to preventing child unintentional injuries within the home: a qualitative study. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1547-2.
- Pope C, Mays N. Qualitative Research in Health Care. Oxford: Blackwell Publishing; 2006.
- Johnson JK, Barach P, Vernooij-Dassen M. HANDOVER Research Collaborative . Conducting a multicentre and multinational qualitative study on patient transitions. BMJ Qual Saf 2012;21:i22-8. https://doi.org/10.1136/bmjqs-2012-001197.
- Mays N, Pope C. Rigour and qualitative research. BMJ 1995;311:109-12. https://doi.org/10.1136/bmj.311.6997.109.
- Pezalla AE, Pettigrew J, Miller-Day M. Researching the researcher-as-instrument: an exercise in interviewer self-reflexivity. Qual Res 2012;12:165-85. https://doi.org/10.1177/1468794111422107.
- Waters E, Shield J, Nolan T, Green J, Elkington J, Moller J, et al. Evidence-Based Health Promotion: No. 4 Child Injury Prevention. Melbourne, VIC: Victorian Government Department of Human Services; 2001.
- Lyons RA, Sander LV, Weightman AL, Patterson J, Jones SALS, Rolfe B, et al. Modification of the home environment for the reduction of injuries. Cochrane Database Syst Rev 2003;4. https://doi.org/10.1002/14651858.cd003600.
- McClure R, Nixon J, Spinks A, Turner C. Community-based programmes to prevent falls in children: a systematic review. J Paediatr Child Health 2005;41:465-70. https://doi.org/10.1111/j.1440-1754.2005.00685.x.
- Nilsen P. What makes community based injury prevention work? In search of evidence of effectiveness. Inj Prev 2004;10:268-74. https://doi.org/10.1136/ip.2004.005744.
- Spinks A, Turner C, McClure R, Nixon J. Community based prevention programs targeting all injuries for children. Inj Prev 2004;10:180-5. https://doi.org/10.1136/ip.2003.004903.
- Nixon J, Spinks A, Turner C, McClure R. Community based programs to prevent poisoning in children 0–15 years. Inj Prev 2004;10:43-6. https://doi.org/10.1136/ip.2003.003822.
- Turner C, Spinks A, McClure R, Nixon J. Community-based interventions for the prevention of burns and scalds in children. Cochrane Database Syst Rev 2004;3. https://doi.org/10.1002/14651858.cd004335.pub2.
- Guyer B, Ma S, Grason H, Frick KD, Perry DF, Sharkey A, et al. Early childhood health promotion and its life course health consequences. Acad Pediatr 2009;9:142-9.e1.
- Pearson M, Garside R, Moxham T, Anderson R. Preventing unintentional injuries to children in the home: a systematic review of the effectiveness of programmes supplying and/or installing home safety equipment. Health Promot Int 2011;26:376-92. https://doi.org/10.1093/heapro/daq074.
- Turner S, Arthur G, Lyons RA, Weightman AL, Mann MK, Jones SJ, et al. Modification of the home environment for the reduction of injuries. Cochrane Database Syst Rev 2011;2. https://doi.org/10.1002/14651858.cd003600.pub3.
- Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-15.
- Higgins J, Green S. The Cochrane Handbook for Systematic Reviews of Interventions n.d. www.cochrane-handbook.org (accessed 17 July 2014).
- Lumley T. Network meta-analysis for indirect treatment comparisons. Stat Med 2002;21:2313-24. https://doi.org/10.1002/sim.1201.
- Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 2005;331:897-900. https://doi.org/10.1136/bmj.331.7521.897.
- Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med 2004;23:3105-24. https://doi.org/10.1002/sim.1875.
- Cooper NJ, Peters J, Lai MC, Juni P, Wandel S, Palmer S, et al. How valuable are multiple treatment comparison methods in evidence-based health-care evaluation?. Value Health 2011;14:371-80. https://doi.org/10.1016/j.jval.2010.09.001.
- Ginnelly L, Sculpher M, Bojke C, Roberts I, Wade A, Diguiseppi C. Determining the cost effectiveness of a smoke alarm give-away program using data from a randomized controlled trial. Eur J Public Health 2005;15:448-53. https://doi.org/10.1093/eurpub/cki146.
- McDaid D, Park A. Making the economic case for injury prevention and safety promotion: a systematic review of the literature. Inj Prev 2010;16. https://doi.org/10.1136/ip.2010.029215.876.
- Polinder S, Segui-Gomez M, Toet H, Belt E, Sethi D, Racioppi F, et al. Systematic review and quality assessment of economic evaluation studies of injury prevention. Accid Anal Prev 2012;45:211-21. https://doi.org/10.1016/j.aap.2011.07.004.
- Preventing Unintentional Road Injuries among Under-15s. London: NICE; 2010.
- Anderson R, Moxham T. Strategies to Prevent Unintentional Injury in Children. Economic Modelling of Legislation Regulations and Related National Strategies to Promote the Wider Use of 20 Mph Zones in Residential Areas, and TMVs in Social Housing for Families n.d. www.nice.org.uk/Guidance/PH29/Evidence (accessed 21 July 2014).
- Towner E, Dowswell T, Jarvis S, Simpson G. Preventing Unintentional Injuries in Children and Young Adolescents. York: NHS Centre for Reviews and Dissemination; 1996.
- Warda L, Tenenbein M, Moffatt ME. House fire injury prevention update. Part I. A review of risk factors for fatal and non-fatal house fire injury. Inj Prev 1999;5:145-50. https://doi.org/10.1136/ip.5.2.145.
- Warda L, Tenenbein M, Moffatt ME. House fire injury prevention update. Part II. A review of the effectiveness of preventive interventions. Inj Prev 1999;5:217-25. https://doi.org/10.1136/ip.5.3.217.
- Van de Velde S, Heselmans A, Roex A, Vandekerckhove P, Ramaekers D, Aertgeerts B. Effectiveness of nonresuscitative first aid training in laypersons: a systematic review. Ann Emerg Med 2009;54:447-57. https://doi.org/10.1016/j.annemergmed.2008.11.005.
- Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol 1991;44:1271-8. https://doi.org/10.1016/0895-4356(91)90160-B.
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses n.d. www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 24 October 2014).
- Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d4002.
- Cooper NJ, Spiegelhalter D, Bujkiewicz S, Dequen P, Sutton AJ. Use of implicit and explicit Bayesian methods in health technology assessment. Int J Technol Assess Health Care 2013;29:336-42. https://doi.org/10.1017/S0266462313000354.
- Borenstein M, Hedges LJPTH, Rothstein HR. Introduction to Meta-Analysis. Chichester: Wiley; 2009.
- Cooper NJ, Sutton AJ, Lu G, Khunti K. Mixed comparison of stroke prevention treatments in individuals with nonrheumatic atrial fibrillation. Arch Intern Med 2006;166:1269-75. https://doi.org/10.1001/archinte.166.12.1269.
- Cooper NJ, Sutton AJ, Morris D, Ades AE, Welton NJ. Addressing between-study heterogeneity and inconsistency in mixed treatment comparisons: application to stroke prevention treatments in individuals with non-rheumatic atrial fibrillation. Stat Med 2009;28:1861-81. https://doi.org/10.1002/sim.3594.
- Spiegelhalter DJ, Thomas A, Best N, Lunn D. WinBUGS User Manual Version 1.4. Cambridge: MRC Biostatistics Unit; 2003.
- Saramago P, Sutton AJ, Cooper NJ, Manca A. Mixed treatment comparisons using aggregate and individual participant level data. Stat Med 2012;31:3516-36. https://doi.org/10.1002/sim.5442.
- Achana FA, Cooper NJ, Dias S, Lu G, Rice SJ, Kendrick D, et al. Extending methods for investigating the relationship between treatment effect and baseline risk from pairwise meta-analysis to network meta-analysis. Stat Med 2013;32:752-71. https://doi.org/10.1002/sim.5539.
- Achana F, Hubbard S, Sutton A, Kendrick D, Cooper N. An exploration of synthesis methods in public health evaluations of interventions concludes that the use of modern statistical methods would be beneficial. J Clin Epidemiol 2014;67:376-90. https://doi.org/10.1016/j.jclinepi.2013.09.018.
- Achana FA, Cooper NJ, Bujkiewicz S, Hubbard SJ, Kendrick D, Jones DR, et al. Network meta-analysis of multiple outcome measures accounting for borrowing of information across outcomes. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-92.
- Weinstein MC. Principles of cost-effective resource allocation in health care organizations. Int J Technol Assess Health Care 1990;6:93-103. https://doi.org/10.1017/S0266462300008953.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of Guidelines for Good Practice in Decision-Analytic Modelling in Health Technology Assessment. Southampton: NIHR Evaluation, Trials and Studies Coordinating Centre; 2006.
- Methods for the Development of NICE Public Health Guidance. London: NICE; 2009.
- National Institute for Health and Care Excellence . Methods for the Development of NICE Public Health Guidance n.d. http://publications.nice.org.uk/methods-for-the-development-of-nice-public-health-guidance-third-edition-pmg4 (accessed 15 December 2015).
- Lunn D, Thomas A, Best N, Spiegelhalter D. WinBUGS – a Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput 2000;10:325-37. https://doi.org/10.1023/A:1008929526011.
- Saramago P, Cooper NJ, Sutton AJ, Hayes M, Dunn K, Manca A, et al. Keeping Children Safe at Home study . Cost-effectiveness of interventions for increasing the possession of functioning smoke alarms in households with pre-school children: a modelling study. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-459.
- Cooper NJ, Kendrick D, Achana F, Dhiman P, He Z, Wynn P, et al. Network meta-analysis to evaluate the effectiveness of interventions to increase the uptake of smoke alarms. Epidemiol Rev 2012;34:32-45. https://doi.org/10.1093/epirev/mxr015.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: University of York; 1999.
- Fires in the Home: Findings from the 2004/05 Survey of English Housing. London: Office of the Deputy Prime Minister; 2006.
- Fire Statistics Great Britain 2011 to 2012. London: Department for Communities and Local Government; 2012.
- Families and Households in the UK, 2001 to 2010. London: ONS; 2010.
- HES Online . Hospital Episode Statistics for England. Inpatient Statistics 2012–13 n.d. www.hscic.gov.uk/hes (accessed 5 May 2014).
- Mytton J, Ingram J, Manns S, Stevens T, Mulvaney C, Blair P, et al. The feasibility of using a parenting programme for the prevention of unintentional home injuries in the under-fives: a cluster randomised controlled trial. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18030.
- He Z, Wynn P, Kendrick D. Non-resuscitative first-aid training for children and laypeople: a systematic review. Emerg Med J 2014;31.
- Bass JL, Christoffel KK, Widome M, Boyle W, Scheidt P, Stanwick R, et al. Childhood injury prevention counseling in primary care settings: a critical review of the literature. Pediatrics 1993;92:544-50.
- Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al. The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature. Health Technol Assess 2000;4.
- Kendrick D, Marsh P. The Effectiveness of Intervention Programmes in Reducing Accidental Injuries to Children and Young People: A Literature Review. Sheffield: Trent Regional Health Authority; 1994.
- Kendrick D, Barlow J, Hampshire A, Polnay L, Stewart-Brown S. Parenting interventions for the prevention of unintentional injuries in childhood. Cochrane Database Syst Rev 2007;4. https://doi.org/10.1002/14651858.cd006020.pub2.
- Parbhoo A, Louw QA, Grimmer-Somers K. Burn prevention programs for children in developing countries require urgent attention: a targeted literature review. Burns 2010;36:164-75. https://doi.org/10.1016/j.burns.2009.06.215.
- Pearson M, Garside R, Moxham T, Anderson R. Preventing Unintentional Injuries among Under-15s in the Home. Systematic Reviews of Effectiveness and Cost-Effectiveness of Home Safety Equipment and Risk Assessment Schemes. Exeter: Peninsula Technology Assessment Group, Peninsula Medical School, Universities of Exeter and Plymouth; 2009.
- Guide to Clinical Preventive Services. Baltimore, MD: US Preventive Services Task Force; 1996.
- Zou K, Wynn P, Miller P, Hindmarch P, Majsak-Newman G, Young B, et al. Preventing childhood scalds within the home: overview of systematic reviews and a systematic review of primary studies. Burns 2014;41:907-24. https://doi.org/10.1016/j.burns.2014.11.002.
- Wynn P, Zou K, Young B, Majsak-Newman G, Hawkins A, Kay B, et al. Prevention of childhood poisoning in the home: overview of systematic reviews and a systematic review of primary studies. Int J Inj Contr Saf Promot 2016;23:2-28. https://doi.org/10.1080/17457300.2015.1032978.
- Ta VM, Frattaroli S, Bergen G, Gielen AC. Evaluated community fire safety interventions in the United States: a review of current literature. J Community Health 2006;31:176-97. https://doi.org/10.1007/s10900-005-9007-z.
- Adler R, Nunn R, Northam E, Lebnan V, Ross R. Secondary prevention of childhood firesetting. J Am Acad Child Adolesc Psychiatry 1994;33:1194-202. https://doi.org/10.1097/00004583-199410000-00015.
- Azeredo R, Stephens-Stidham S. Design and implementation of injury prevention curricula for elementary schools: lessons learned. Inj Prev 2003;9:274-8. https://doi.org/10.1136/ip.9.3.274.
- Ballard JE, Koepsell TD, Rivara F. Association of smoking and alcohol drinking with residential fire injuries. Am J Epidemiol 1992;135:26-34. https://doi.org/10.1093/oxfordjournals.aje.a116198.
- Barone VJ. An Analysis of Well Child Parenting Classes: The Extent of Parent Compliance with Health-Care Recommendations to Decrease Potential Injury of their Toddlers. Kansas City, MO: University of Kansas; 1988.
- Baudier F, Marchais M, Ferry B, Bourderont D, Pinochet C, Blum D. A cooperative program for the prevention of domestic accidents in children at the department of the Doubs. II. Educative aspects and evaluation. Arch Fr Pediatr 1988;45:499-503.
- Blake KD, Griffioen A, Taylor BW. Impact of a Child Accident Prevention Video on Parents of Preschool Children n.d.
- Bulzacchelli MT, Gielen AC, Shields WC, McDonald EM, Frattaroli S. Parental safety-related knowledge and practices associated with visiting a mobile safety center in a low-income urban population. Fam Community Health 2009;32:147-58. https://doi.org/10.1097/FCH.0b013e31819947a6.
- Campbell NR, Ayala GX, Litrownik AJ, Slymen DJ, Zavala F, Elder JP. Evaluation of a first aid and home safety program for Hispanic migrant adolescents. Am J Prev Med 2001;20:258-65. https://doi.org/10.1016/S0749-3797(01)00300-2.
- Carlsson A, Bramhagen AC, Jansson A, Dykes AK. Precautions taken by mothers to prevent burn and scald injuries to young children at home: an intervention study. Scand J Public Health 2011;39:471-8. https://doi.org/10.1177/1403494811405094.
- Chan CC. Promoting a Safer Household Environment: A Volunteer Based Home Visit Program n.d.
- Christakis DA, Zimmerman FJ, Rivara FP, Ebel B. Improving pediatric prevention via the internet: a randomized, controlled trial. Pediatrics 2006;118:1157-66. https://doi.org/10.1542/peds.2006-0209.
- Davis JW. Get fired Up: A Model for Developing Inschool Four-H Programs (Safety). Clemson, SC: Clemson University; 1987.
- Dershewitz RA, Williamson JW. Prevention of childhood household injuries: a controlled clinical trial. Am J Public Health 1977;67:1148-53. https://doi.org/10.2105/AJPH.67.12.1148.
- Dershewitz RA. Will mothers use free household safety devices?. Am J Dis Child 1979;133:61-4. https://doi.org/10.1001/archpedi.1979.02130010067011.
- Franklin GA, Pucci PS, Arbabi S, Brandt MM, Wahl WL, Taheri PA. Decreased juvenile arson and firesetting recidivism after implementation of a multidisciplinary prevention program. J Trauma 2002;53:260-4. https://doi.org/10.1097/00005373-200208000-00012.
- Gaffney D. Preventing Hot Water Scalds Among Young Children in New South Wales n.d.
- Garcia V. Safety Fairs: Evaluation of a School-Based Injury Prevention Program n.d.
- Gielen AC, Wilson ME, McDonald EM, Serwint JR, Andrews JS, Hwang WT, et al. Randomized trial of enhanced anticipatory guidance for injury prevention. Arch Pediatr Adolesc Med 2001;155:42-9. https://doi.org/10.1001/archpedi.155.1.42.
- Gomez-Tromp M, Ben Meftah J, Gebhardt W, Prinsenberg T. Effect evaluation of a school based burn and scalds prevention programme in the Netherlands. Burns 2011;37. https://doi.org/10.1016/S0305-4179(11)70040-7.
- Hillman HS, Jones RT, Farmer L. The acquisition and maintenance of fire emergency skills: effects of rationale and behavioral practice. J Pediatr Psychol 1986;11:247-58. https://doi.org/10.1093/jpepsy/11.2.247.
- Hwang V, Duchossois GP, Garcia-Espana JF, Durbin DR. Impact of a community based fire prevention intervention on fire safety knowledge and behavior in elementary school children. Inj Prev 2006;12:344-6. https://doi.org/10.1136/ip.2005.011197.
- Johnston BD, Huebner CE, Anderson ML, Tyll LT, Thompson RS. Healthy steps in an integrated delivery system: child and parent outcomes at 30 months. Arch Pediatr Adolesc Med 2006;160:793-800. https://doi.org/10.1001/archpedi.160.8.793.
- Jones R, Haney J. Refinement of a Primary Preventive Approach to Fire Emergencies: A Comparison of External and Self-Instruction Strategies for Training and Maintaining Fire Emergency Responding. Pittsburgh, PA: University of Pittsburgh; 1983.
- Jones RT, Ollendick TH, McLaughlin KJ, Williams CE. Elaborative and behavioral rehearsal in the acquisition of fire emergency skills and the reduction of fear of fire. Behav Ther 1989;20:93-101. https://doi.org/10.1016/S0005-7894(89)80120-0.
- Jordan EA, Duggan AK, Hardy JB. Injuries in children of adolescent mothers: home safety education associated with decreased injury risk. Pediatrics 1993;91:481-7. https://doi.org/10.1097/01241398-199307000-00067.
- Kendrick D, Illingworth R, Woods A, Watts K, Collier J, Dewey M, et al. Promoting child safety in primary care: a cluster randomised controlled trial to reduce baby walker use. Br J Gen Pract 2005;55:582-8.
- Kendrick D, Groom L, Stewart J, Watson M, Mulvaney C, Casterton R. ‘Risk Watch’: cluster randomised controlled trial evaluating an injury prevention program. Inj Prev 2007;13:93-8. https://doi.org/10.1136/ip.2006.013862.
- Kolko DJ. Efficacy of cognitive-behavioral treatment and fire safety education for children who set fires: initial and follow-up outcomes. J Child Psychol Psychiatry 2001;42:359-69. https://doi.org/10.1111/1469-7610.00729.
- Lacouture P, Minisci M, Gouveia WA, Lovejoy FH. Evaluation of a community-based poison education program. Clin Toxicol 1978;13:623-9. https://doi.org/10.3109/15563657808988267.
- Lamb R, Joshi MS, Carter W, Cowburn G, Matthews A. Children’s acquisition and retention of safety skills: the Lifeskills program. Inj Prev 2006;12:161-5. https://doi.org/10.1136/ip.2005.010769.
- Macarthur C. Evaluation of Safe Kids Week 2001: prevention of scald and burn injuries in young children. Inj Prev 2003;9:112-16. https://doi.org/10.1136/ip.9.2.112.
- Mallonee S, Istre GR, Rosenberg M, Reddish-Douglas M, Jordan F, Silverstein P, et al. Surveillance and prevention of residential-fire injuries. N Engl J Med 1996;335:27-31. https://doi.org/10.1056/NEJM199607043350106.
- Margolis PA, Stevens R, Bordley WC, Stuart J, Harlan C, Keyes-Elstein L, et al. From concept to application: the impact of a community-wide intervention to improve the delivery of preventive services to children. Pediatrics 2001;108. https://doi.org/10.1542/peds.108.3.e42.
- Marshall SW, Runyan CW, Bangdiwala SI, Linzer MA, Sacks JJ, Butts JD. Fatal residential fires: who dies and who survives?. JAMA 1998;279:1633-7. https://doi.org/10.1001/jama.279.20.1633.
- Matthews J. An Analysis of Dangerous Behaviour in Toddlers. Kansas City, MO: University of Kansas; 1988.
- Minkovitz CS, Hughart N, Strobino D, Scharfstein D, Grason H, Hou W, et al. A practice-based intervention to enhance quality of care in the first 3 years of life: the Healthy Steps for Young Children Program. JAMA 2003;290:3081-91. https://doi.org/10.1001/jama.290.23.3081.
- Mori L, Peterson L. Training preschoolers in home safety skills to prevent inadvertent injury. Clinical J Child Psychol 1986;15:106-14. https://doi.org/10.1207/s15374424jccp1502_1.
- Peterson L. The ‘safe at home’ game. Training comprehensive prevention skills in latchkey children. Behav Modif 1984;8:474-94. https://doi.org/10.1177/01454455840084002.
- Phelan KJ, Khoury J, Xu Y, Lanphear B. Validation of a HOME Injury Survey. Inj Prev 2009;15:300-6. https://doi.org/10.1136/ip.2008.020958.
- Phelan KJ, Khoury J, Xu Y, Liddy S, Hornung R, Lanphear BP. A randomized controlled trial of home injury hazard reduction: the HOME injury study. Arch Pediatr Adolesc Med 2011;165:339-45. https://doi.org/10.1001/archpediatrics.2011.29.
- Reich SM, Penner EK, Duncan GJ. Using baby books to increase new mothers’ safety practices. Acad Pediatr 2011;11:34-43. https://doi.org/10.1016/j.acap.2010.12.006.
- Rowland D, DiGuiseppi C, Roberts I, Curtis K, Roberts H, Ginnelly L, et al. Prevalence of working smoke alarms in local authority inner city housing: randomised controlled trial. BMJ 2002;325:998-1001. https://doi.org/10.1136/bmj.325.7371.998.
- Scherz RG. Childhood poisonings from medications: three prevention programs that worked. Mil Med 1968;133:911-13.
- Shapiro MM, Katcher ML. Injury-prevention education during postpartum hospitalisation. Am J Dis Child 1987;141.
- Smith GA, Splaingard M, Hayes JR, Xiang H. Comparison of a personalized parent voice smoke alarm with a conventional residential tone smoke alarm for awakening children. Pediatrics 2006;118:1623-32. https://doi.org/10.1542/peds.2006-0125.
- Steele PS, Spyker DA. Symposium on injuries and injury prevention: poisonings. Pediatr Clin North Am 1985;32:77-86. https://doi.org/10.1016/S0031-3955(16)34757-5.
- Tan NC, Lim NM, Gu K. Effectiveness of nurse counselling in discouraging the use of the infant walkers. Asia Pac J Public Health 2004;16:104-8. https://doi.org/10.1177/101053950401600205.
- Williams GE. An Analysis of Prenatal Education Classes: An Early Start to Injury Prevention. Kansas City, MO: University of Kansas; 1988.
- Williams CE, Jones RT. Impact of self-instructions on response maintenance and children’s fear of fire. J Clin Child Psychol 1989;18:84-9. https://doi.org/10.1207/s15374424jccp1801_10.
- Wissow L. Home Injury Hazards in the Inner City n.d.
- Ytterstad B, Smith GS, Coggan CA. Harstad injury prevention study: prevention of burns in young children by community based intervention. Inj Prev 1998;4:176-80. https://doi.org/10.1136/ip.4.3.176.
- Murray DM, Catellier DJ, Hannan PJ, Treuth MS, Stevens J, Schmitz KH, et al. School-level intraclass correlation for physical activity in adolescent girls. Med Sci Sports Exerc 2004;36:876-82. https://doi.org/10.1249/01.MSS.0000126806.72453.1C.
- Chow CB, Chan CC, Cheung WL, Chan YC, Cheng JCY, Luis PK. Promoting a Safer Household Environment: a Volunteer-Based Home Visit Program. Hong Kong: Hong Kong Childhood Injury Prevention and Research Association; 2006.
- Preventing Unintentional Injuries in Children and Young Adolescents. York: Centre for Reviews and Discrimination; 1996.
- Hubbard S, Cooper N, Kendrick D, Young B, Wynn PM, He Z, et al. Network meta-analysis to evaluate the effectiveness of interventions to prevent falls in children under age 5 years. Inj Prev 2015;21:98-108.
- European Child Safety Alliance . European Child Safety Alliance and ANEC Joint Position Statement: Baby Walkers n.d. www.childsafetyeurope.org/publications/positionstatements/info/baby-walkers-position-statement.pdf (accessed 2 October 2014).
- Child Use and Care Articles. Baby Walking Frames. Safety Requirements and Test Methods. London: BSI; 2005.
- Achana FA, Sutton AJ, Kendrick D, Wynn P, Young B, Jones DR, et al. The effectiveness of different interventions to promote poison prevention behaviours in households with children: a network meta-analysis. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0121122.
- Health and Social Care Information Centre . Hospital Episode Statistics, Admitted Patient Care, England – 2012–13: External Causes n.d. www.hscic.gov.uk/catalogue/PUB12566 (accessed 27 January 2014).
- Orton E, Kendrick D, West J, Tata LJ. Persistence of health inequalities in childhood injury in the UK: a population-based cohort study of children under 5. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0111631.
- American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention . Poison treatment in the home. American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Pediatrics 2003;112:1182-5.
- Garside R, Moxham T. Preventing Unintentional Injury in Children Review 4: Strategic and Regulatory Frameworks for Guiding, Enforcing or Promoting Activities to Prevent Unintentional Injury in Children and Young People in the Home Environment. Exeter: Peninsula Technology Assessment Group, Peninsula Medical School, Universities of Exeter and Plymouth; 2009.
- Sellar C, Ferguson JA, Goldacre MJ. Occurrence and repetition of hospital admissions for accidents in preschool children. BMJ 1991;302:16-9. https://doi.org/10.1136/bmj.302.6767.16.
- Kendrick D, Mulvaney C, Watson M. Does targeting injury prevention towards families in disadvantaged areas reduce inequalities in safety practices?. Health Educ Res 2009;24:32-41. https://doi.org/10.1093/her/cym083.
- Armstrong R, Waters E, Moore L, Riggs E, Cuervo LG, Lumbiganon P, et al. Improving the reporting of public health intervention research: advancing TREND and CONSORT. J Public Health 2008;30:103-9. https://doi.org/10.1093/pubmed/fdm082.
- Kelly M, McDaid D, Ludbrook A, Powell J. Economic Appraisal of Public Health Interventions. London: NHS Health Development Agency; 2005.
- Morestin F, Gauvin F-P, Hogue M-CN, Benoit F. Methods for Synthesizing Knowledge about Public Policies. Quebec, QC: Institut National de Santé Publique Quebec; 2010.
- Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy 2009;93:85-92. https://doi.org/10.1016/j.healthpol.2009.07.012.
- Bentzen I. Does Intervention Prevent Injuries in Children? An Evaluation of the Safety for Active Children Programme in Odense, Denmark, 1989–93. Tromso: University of Tromso; 1997.
- Yorkston E, Turner C, Schluter PJ, McClure R. Quantifying the effect of a community-based injury prevention program in Queensland using a generalized estimating equation approach. Inj Prev 2007;13:191-6. https://doi.org/10.1136/ip.2006.014225.
- Hendrickson S. Reaching an underserved population with a randomly assigned home safety intervention. Inj Prevent 2005;11:313-17.
- Pitt M, Anderson R, Moxham T. Cost-Effectiveness Modelling of Home Based Interventions Aimed at Reducing Unintentional Injuries in Children. Exeter: Peninsula Medical School, Universities of Exeter and Plymouth; 2009.
- Hayes M, Kendrick D. behalf of the Keeping Children Safe study team . A Guide for Commissioners of Child Health Services on Preventing Unintentional Injuries Among the under Fives 2016. www.nottingham.ac.uk/research/groups/injuryresearch/projects/kcs/index.aspx (accessed 5 December 2016).
- Sethi D, Towner E, Vincenten J. European Report on Child Injury Prevention. Geneva: World Health Organization; 2008.
- The Core Purpose of Sure Start Children’s Centres: Government Vision. London: Department for Education; 2012.
- Deave T, Towner E, McColl E, Reading R, Sutton A, Coupland C, et al. Multicentre cluster randomised controlled trial evaluating implementation of a fire prevention injury prevention briefing in children’s centres: study protocol. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-69.
- Sure Start Children’s Centres: Memorandum for the Children, Schools and Families Committee. London: National Audit Office; 2009.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Brussoni M, Towner E, Hayes M. Evidence into practice: combining the art and science of injury prevention. Inj Prev 2006;12:373-7. https://doi.org/10.1136/ip.2005.011403.
- Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2010;3. https://doi.org/10.1002/14651858.cd005470.pub2.
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci 2007;2. https://doi.org/10.1186/1748-5908-2-40.
- Davis DA, Taylor-Vaisey A. Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ 1997;157:408-16.
- Dusenbury L, Brannigan R, Falco M, Hansen WB. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Educ Res 2003;18:237-56. https://doi.org/10.1093/her/18.2.237.
- Fleuren M, Wiefferink K, Paulussen T. Determinants of innovation within health care organizations: literature review and Delphi study. Int J Qual Health Care 2004;16:107-23. https://doi.org/10.1093/intqhc/mzh030.
- Greenhalgh T, Robert G, Bate P, Kyriakidou O, Macfarlane F, Peacock R. How to Spread Good Ideas: A Systematic Review of the Literature on Diffusion, Dissemination and Sustainability of Innovations in Health Service Delivery and Organisation 2004. www.nets.nihr.ac.uk/__data/assets/pdf_file/0017/64340/FR-08–1201-038.pdf (accessed 10 December 2015).
- Helfrich CD, Damschroder LJ, Hagedom HJ, Daggett GS, Sahay A, Ritchie M, et al. A critical synthesis of literature on the promoting action on research implementation in health services (PARIHS) framework. Implementation Sci 2010;5:1-20. https://doi.org/10.1186/1748-5908-5-82.
- Rycroft-Malone J. The PARIHS framework – a framework for guiding the implementation of evidence-based practice. J Nurs Care Qual 2004;19:297-304. https://doi.org/10.1097/00001786-200410000-00002.
- Gielen A, Sleet Da, DiClemente R. Injury and Violence Prevention: Behavioral Science Theories, Methods and Applications. San Francisco, CA: Jossey-Bass; 2006.
- Deave T, Goodenough T, Stewart J, Towner E, Majsak-Newman G, Hawkins A, et al. Contemporary hazards in the home: keeping children safe from thermal injuries. Arch Dis Child 2013;98:485-9. https://doi.org/10.1136/archdischild-2012-302901.
- White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ 2011;342. https://doi.org/10.1136/bmj.d40.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reportings Standards (CHEERS) – explanation and elaboration: a report on the ISPOR health economic evaluations publication guidelines good reporting practices task force. Value Health 2013;16:231-50. https://doi.org/10.1016/j.jval.2013.02.002.
- Gomes M, Ng ES, Grieve R, Nixon R, Carpenter J, Thompson SG. Developing appropriate methods for cost-effectiveness analysis of cluster randomized trials. Med Decis Making 2012;32:350-61. https://doi.org/10.1177/0272989X11418372.
- Gomes M, Grieve R, Nixon R, Edmunds W. Statistical methods for cost-effectiveness analyses that use data from cluster randomized trials: a systematic review and checklist for critical appraisal. Med Decis Making 2012;32:209-20. https://doi.org/10.1177/0272989X11407341.
- Grieve R, Nixon R, Thompson SG. Bayesian hierarchical models for cost-effectiveness analyses that use data from cluster randomized trials. Med Decis Making 2010;30:163-75. https://doi.org/10.1177/0272989X09341752.
- Teixeira-Pinto A, Normand SL. Correlated bivariate continuous and binary outcomes: issues and applications. Stat Med 2009;28:1753-73. https://doi.org/10.1002/sim.3588.
- Fitzmaurice G, Laird NM. Regression models for a bivariate discrete and continuous outcome with clustering. J Am Stat Assoc 1995;90:845-52. https://doi.org/10.1080/01621459.1995.10476583.
- Lunn D, Jackson C, Best N, Thomas A, Spiegelhalter D. The BUGS Book – A Practical Introduction to Bayesian Analysis. Boca Raton, FL: Chapman & Hall/CRC; 2012.
- Thompson SG, Nixon RM. How sensitive are cost-effectiveness analyses to choice of parametric distributions?. Med Decis Making 2005;25:416-23. https://doi.org/10.1177/0272989X05276862.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analyzing Qualitative Data. Oxford: Routledge; 1994.
- Hindmarch P, Hawkins A, McColl E, Hayes M, Majsak-Newman G, Ablewhite J, et al. Recruitment and retention strategies and the examination of attrition bias in a randomised controlled trial in children’s centres serving families in disadvantaged areas of England. Trials 2015;16. https://doi.org/10.1186/s13063-015-0578-4.
- Beckett K, Goodenough T, Deave T, Jaeckle S, McDaid L, Benford P, et al. Implementing an Injury Prevention Briefing to aid delivery of key fire safety messages in UK children’s centres: qualitative study nested within a multi-centre randomised controlled trial. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-1256.
- Department for Transport . TAG Unit 3.5.6: Values of Time and Vehicle Operating Costs. Transport Analysis Guidance (TAG) 2014. www.gov.uk/transport-analysis-guidance-webtag (accessed 19 August 2015).
- Caille A, Leyrat C, Giraudeau B. A comparison of imputation strategies in cluster randomized trials with missing binary outcomes [published online ahead of print 7 April 2014]. Stat Methods Med Res 2014.
- Maisey R, Speight S, Haywood S, Hall J, Sammons P, Hussey D, et al. Evaluation of Children’s Centres in England (ECCE). Strand 2: Baseline Survey of Families Using Children’s Centres in the Most Disadvantaged Areas. Darlington: Department for Education; 2013.
- The Impact of Sure Start Local Programmes on Five Year Olds and their Families. London: Department for Education; 2010.
- Blackburn With Darwen Accident Prevention Strategy 2014–2017 2014. www.blackburn.gov.uk/Lists/DownloadableDocuments/BwDAccidentPreventionStrategy2014-2017.pdf (accessed 10 December 2015).
- Child Accident Prevention Trust . The Nottingham and Nottinghamshire Avoidable Injuries Strategy for Children and Young People n.d. www.makingthelink.net/case-study/nottingham-and-nottinghamshire-avoidable-injuries-strategy-children-and-young-people (accessed 22 October 2016).
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2012.
- Family and Childcare Trust . Childcare Costs Survey n.d. http://fct.bigmallet.co.uk/sites/default/files/files/Childcare_Costs_Survey_FCT_2013_FINAL.pdf#overlay-context=annual-childcare-costs-surveys (accessed 19 August 2015).
- Office for National Statistics . Annual Survey of Hours and Earnings 2012. www.ons.gov.uk/ons/rel/ashe/annual-survey-of-hours-and-earnings/2012-provisional-results/index.html (accessed 19 August 2015).
- Office for National Statistics . Population and Household Estimates for the United Kingdom 2011. www.ons.gov.uk/ons/rel/census/2011-census/population-estimates-by-five-year-age-bands-and-household-estimates--for-local-authorities-in-the-united-kingdom/stb-population-and-household-estimates-for-the-united-kingdom-march-2011.html (accessed 10 December 2015).
- Istre GR, McCoy M, Carlin DK, McClain J. Residential fire related deaths and injuries among children: fireplay, smoke alarms, and prevention. Inj Prev 2002;8:128-32. https://doi.org/10.1136/ip.8.2.128.
- Hemington-Gorse SJ, Potokar TS, Drew PJ, Dickson WA. Burn care costing: the Welsh experience. Burns 2009;35:378-82. https://doi.org/10.1016/j.burns.2008.08.012.
- Communities and Local Government . Fire Statistics, United Kingdom 2007 2007. http://webarchive.nationalarchives.gov.uk/20120919132719/www.communities.gov.uk/publications/corporate/statistics/firestatisticsuk2007 (accessed 28 February 2017).
- Office for National Statistics . Interim Life Tables England and Wales 2006–08 2009. www.ons.gov.uk/ons/search/index.html?newquery=interim+life+tables (accessed 15 December 2015).
- DiGuiseppi C, Slater S, Roberts I, Adams L, Sculpher M, Wade A, et al. The ‘Let’s Get Alarmed!’ initiative: a smoke alarm giveaway programme. Inj Prev 1999;5:177-82. https://doi.org/10.1136/ip.5.3.177.
- Curtis L. Unit Costs of Health and Social Care 2008. Canterbury: Personal Social Services Research Unit, University of Kent; 2008.
- NHS Reference Costs 2008–9. London: Department of Health; 2010.
- Fires in the Home: Findings from the 2002/3 British Crime Survey. London: ONS; 2004.
- The Economic Cost of Fire: Estimates for 2004. London: Office of the Deputy Prime Minister; 2006.
- Sanchez JL, Bastida JL, Martínez MM, Moreno JM, Chamorro JJ. Socio-economic cost and health-related quality of life of burn victims in Spain. Burns 2008;34:975-81. https://doi.org/10.1016/j.burns.2007.12.011.
- Office for National Statistics . Death Registration Summary Tables England and Wales 2012. www.ons.gov.uk/ons (accessed 5 May 2014).
- Office for National Statistics . ONS Census 2001: First Results on Population for England and Wales n.d. www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-225134 (accessed 17 July 2014).
- Office for National Statistics . Deaths Registered in England and Wales 2005–12 n.d. www.ons.gov.uk (accessed 17 July 2014).
- Morrongiello BA, Schwebel DC. Gaps in childhood injury research and prevention: what can developmental scientists contribute?. Child Dev Perspect 2008;2:78-84. https://doi.org/10.1111/j.1750-8606.2008.00046.x.
- Miller TR, Finkelstein AE, Zaloshnja E, Hendrie D, Liller KD. Injury Prevention for Children and Adolescents: Research, Practice and Advocacy. Washington, DC: American Public Health Association; 2012.
- Health and Social Care Information Centre . Hospital Episode Statistics for England. Inpatient Statistics, 2012–13 2013. www.hscic.gov.uk/hes (accessed 5 May 2014).
- Office for National Statistics . Statistical Bulletin: Annual Mid-Year Population Estimates, 2011 and 2012 2013. www.ons.gov.uk/ons/dcp171778_320900.pdf (accessed 5 May 2014).
- Mowry JB, Spyker DA, Cantilena LR, Bailey JE, Ford M. 2012 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th Annual Report. Clin Toxicol 2013;51:949-1229. https://doi.org/10.3109/15563650.2013.863906.
- Anokye NK, Trueman P, Green C, Pavey TG, Hillsdon M, Taylor RS. The cost-effectiveness of exercise referral schemes. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-954.
- Pavey TG, Anokye N, Taylor AH, Trueman P, Moxham T, Fox KR, et al. The clinical effectiveness and cost-effectiveness of exercise referral schemes: a systematic review and economic evaluation. Health Technol Assess 2011;15. https://doi.org/10.3310/hta15440.
- Browne W. An illustration of the use of reparameterisation methods for improving MCMC efficiency in crossed random effect models. Multilevel Model Newsl 2004;16:13-25.
Appendix 1 Case–control questionnaires, home observation checklist for study B and summary of analyses using hospital controls for study A
Summary tables of analyses using hospital controls for study A
| Characteristic | Cases (n = 672) | Community controls (n = 2648) | Hospital controls (n = 1334) |
|---|---|---|---|
| Study centre | |||
| Nottingham | 246 (36.6) | 966 (36.5) | 468 (35.1) |
| Bristol | 215 (32.0) | 832 (31.4) | 441 (33.1) |
| Norwich | 146 (21.7) | 644 (24.3) | 289 (21.7) |
| Newcastle | 65 (9.7) | 206 (7.8) | 136 (10.2) |
| Age (years), median (IQR)a | 1.74 (0.84–2.86) | 1.91 (1.00–3.01) | 1.98 (1.29–2.95) |
| Age group (months) | |||
| 0–12 | 223 (33.2) | 741 (28.0) | 211 (15.8) |
| 13–36 | 296 (44.0) | 1270 (48.0) | 815 (61.1) |
| 37–62 | 153 (22.8) | 637 (24.1) | 308 (23.1) |
| Male | 365 (54.3) | 1478 (55.8) | 723 (54.2) |
| Ethnic origin: white | 583 (88.9) [16] | 2403 (92.2) [41] | 1164 (89.3) [30] |
| Children aged 0–4 years in family | [6] | [40] | [27] |
| 0 | 9 (1.4) | 20 (0.8) | 15 (1.1) |
| 1 | 391 (58.7) | 1563 (59.9) | 771 (59.0) |
| 2 | 231 (34.7) | 927 (35.5) | 460 (35.2) |
| ≥ 3 | 35 (5.3) | 98 (3.8) | 61 (4.7) |
| First child | 285 (45.4) [44] | 1093 (44.9) [212] | 540 (43.8) [102] |
| Maternal age ≤ 19 years at birth of first childb | 77 (12.5) [4] | 219 (9.0) [19] | 214 (18.0) [15] |
| Single adult household | 95 (14.5) [15] | 263 (10.2) [61] | 189 (14.6) [36] |
| Weekly out-of-home child care (hours), median (IQR) | 7.5 (0–18.0) [46] | 12.0 (1.0–22.0) [179] | 10.0 (0–20.0) [113] |
| Adults out of work | [16] | [45] | [34] |
| 0 | 319 (48.6) | 1481 (56.9) | 590 (45.4) |
| 1 | 221 (33.7) | 795 (30.5) | 480 (36.9) |
| 2 | 116 (17.7) | 327 (12.6) | 230 (17.7) |
| Receives state benefits | 280 (43.0) [21] | 928 (35.9) [65] | 592 (45.8) [42] |
| Overcrowding (more than one person per room) | 56 (8.8) [32] | 173 (6.9) [146] | 135 (10.9) [98] |
| Non-owner occupier | 262 (39.5) [9] | 838 (32.2) [49] | 560 (43.1) [34] |
| Household has no car | 95 (14.4) [10] | 288 (11.0) [40] | 184 (14.1) [27] |
| IMD score, median (IQR)c | 16.8 (10.0–31.9) | 14.9 (9.0–6.8) [28] | 18.0 (9.7–32.6) [1] |
| Distance (km) from hospital, median (IQR) | 3.4 (1.9–5.4) | 3.9 (2.4–7.4) [29] | 3.5 (2.2–5.5) [1] |
| CBQ score, mean (SD)c | 4.68 (0.92) [45] | 4.67 (0.88) [234] | 4.68 (0.97) [96] |
| Long-term health condition | 60 (9.0) [5] | 185 (7.0) [14] | 117 (8.9) [24] |
| Child health VAS score (range 0–10), median (IQR)c | 9.9 (9.3–10.0) [6] | 9.7 (8.5–10.0) [22] | 10.0 (9.0–10.0) [17] |
| HRQL (PedsQL), median (IQR)c,d | n = 287, 93.1 (86.9–97.6) [4] | n = 1270, 90.0 (82.9–94.4) [21] | n = 658, 92.9 (84.5–97.6) [22] |
| Parental assessment of child’s ability to climb | [18] | [57] | [39] |
| All scenarios ‘not likely’ | 166 (25.4) | 536 (20.7) | 120 (9.3) |
| One or more scenario ‘quite likely’ and none ‘very likely’ | 85 (13.0) | 235 (9.1) | 179 (13.8) |
| One or more scenario ‘very likely’ | 403 (61.6) | 1820 (70.2) | 996 (76.9) |
| PDH tasks subscale score, median (IQR)c,e | 13 (10–17) [65] | 14 (11–18) [168] | 14 (10–17) [144] |
| HADS score, mean (SD)c,e | 10.7 (6.0) [8] | 10.8 (6.0) [39] | 10.7 (6.2) [37] |
| Exposure | Cases (n = 672) | Community controls (n = 2648) | Hospital controls (n = 1334) | Community controls, unadjusted OR (95% CI) | Hospital controls, unadjusted OR (95% CI) |
|---|---|---|---|---|---|
| Did not use any safety gatesa | 227 (36.9) [56] | 688 (27.7) [160] | 293 (23.3) [77] | 1.68 (1.36 to 2.07) | 1.92 (1.56 to 2.37) |
| Used high chair without harness at least some daysb,c | 118 (26.3) [11] ((213)) | 522 (29.6) [34] ((853)) | 235 (24.8) [32] ((356)) | 0.82 (0.65 to 1.05) | 1.08 (0.84 to 1.40) |
| Had things child could climb on to reach high surfacesa | 248 (37.6) [12] | 1075 (40.9) [22] | 503 (38.1) [13] | 0.85 (0.70 to 1.04) | 0.98 (0.81 to 1.19) |
| Left child on a raised surface at least some daysb,c | 357 (57.7) [13] ((40)) | 1221 (49.0) [33] ((121)) | 478 (38.5) [31] ((60)) | 1.56 (1.29 to 1.88) | 2.18 (1.79 to 2.65) |
| Changed nappy on raised surface at least some daysb,c | 297 (56.0) [10] ((132)) | 1106 (53.9) [30] ((565)) | 493 (46.2) [27] ((239)) | 1.09 (0.89 to 1.33) | 1.49 (1.21 to 1.83) |
| Put child in car/bouncing seat on raised surface at least some daysb,c | 59 (11.4) [11] ((142)) | 176 (8.8) [30] ((626)) | 52 (5.0) [34] ((251)) | 1.33 (0.95 to 1.87) | 2.46 (1.67 to 3.63) |
| Child climbed or played on furniture at least some daysb,c | 472 (78.1) [7] ((61)) | 1909 (77.9) [27] ((169)) | 1016 (80.2) [26] ((41)) | 0.95 (0.73 to 1.26) | 0.88 (0.70 to 1.12) |
| Child climbed or played on garden furniture at least some daysb,c | 181 (34.4) [10] ((136)) | 816 (39.1) [28] ((532)) | 441 (40.2) [30] ((206)) | 0.78 (0.62 to 0.98) | 0.78 (0.63 to 0.97) |
| Had not taught child rules about climbing in kitchen | 282 (44.5) [39] | 1026 (40.0) [82] | 427 (33.8) [71] | 1.52 (1.15 to 2.00) | 1.57 (1.29 to 1.91) |
| Had not taught child rules about jumping on bed/furniture | 283 (44.5) [36] | 1079 (42.0) [80] | 434 (34.5) [75] | 1.30 (0.97 to 1.73) | 1.52 (1.25 to 1.85) |
| Exposures measured only in children aged 0–36 months | Cases (n = 519) | Community controls (n = 2011) | Hospital controls (n = 1026) | Community controls, unadjusted OR (95% CI) | Hospital controls, unadjusted OR (95% CI) |
| Did not use baby walkera | 372 (73.5) [13] | 1359 (68.8) [36] | 713 (71.3) [26] | 1.27 (1.01 to 1.60) | 1.12 (0.88 to 1.42) |
| Did not use playpen or travel cota | 411 (81.9) [17] | 1628 (82.6) [41] | 827 (83.0) [30] | 0.95 (0.73 to 1.23) | 0.92 (0.70 to 1.22) |
| Did not use stationary activity centrea | 375 (74.6) [16] | 1469 (74.5) [39] | 805 (80.7) [29] | 0.98 (0.78 to 1.24) | 0.70 (0.54 to 0.90) |
| Exposure | Community controls, AOR (95% CI) | Hospital controls, AOR (95% CI) | Confounders adjusted fora |
|---|---|---|---|
| Did not use any safety gatesb | 1.65 (1.29 to 2.12) | 1.78 (1.38 to 2.30) | PDH score, HADS score, hours of out-of-home care, ability to climb, first child |
| Used high chair without harness at least some daysc | 0.77 (0.57 to 1.03) | 1.06 (0.80 to 1.41) | CBQ score, hours of out-of-home care |
| Had things child could climb on to reach high surfacesb | 0.96 (0.75 to 1.24) | 1.21 (0.94 to 1.57) | Hours of out-of-home care, ability to climb, first child, uses safety gate, safety rules on climbing in kitchen and jumping on furniture |
| Left child on a raised surface at least some daysc | 1.66 (1.34 to 2.06) | 2.38 (1.91 to 2.97) | CBQ score, hours out-of-home care |
| Changed nappy on raised surface at least some daysc | 1.10 (0.87 to 1.40) | 1.19 (0.93 to 1.51) | CBQ score, hours of out-of-home care |
| Put child in car/bouncing seat on raised surface at least some daysc | 1.35 (0.91 to 2.01) | 1.79 (1.16 to 2.78) | CBQ score, hours of out-of-home care |
| Child climbed or played on furniture at least some daysc | 1.03 (0.73 to 1.44) | 1.48 (1.06 to 2.07) | CBQ score, hours of out-of-home care, things child could climb on to reach high surfaces |
| Child climbed or played on garden furniture at least some daysc | 0.74 (0.56 to 0.97) | 0.90 (0.69 to 1.17) | CBQ score, hours of out-of-home care, things child could climb on to reach high surfaces |
| Had not taught child rules about climbing in kitchen | 1.58 (1.16 to 2.15) | 1.16 (0.87 to 1.55) | HADS score, PDH score, first child, things child could climb on to reach high surfaces |
| Had not taught child rules about jumping on bed/furniture | 1.21 (0.87 to 1.68) | 0.94 (0.69 to 1.27) | HADS score, PDH score, first child, things child could climb on to reach high surfaces |
| Did not use baby walkerb | 1.22 (0.90 to 1.65) | 1.30 (0.94 to 1.78) | HADS score, PDH score, hours of out-of-home care, ability to climb, first child, uses safety gate, uses playpen/travel cot, uses activity centre |
| Did not use playpen or travel cotb | 1.01 (0.71 to 1.46) | 0.83 (0.57 to 1.08) | HADS score, PDH score, hours of out-of-home care, ability to climb, first child, uses baby walker, uses safety gate, uses activity centre |
| Did not use stationary activity centreb | 0.94 (0.69 to 1.27) | 0.78 (0.56 to 1.08) | HADS score, PDH score, hours of out-of-home care, ability to climb, first child, uses baby walker, uses playpen/travel cot, uses safety gate |
| Characteristic | Cases (n = 582) | Community controls (n = 2460) | Hospital controls (n = 1525) |
|---|---|---|---|
| Study centre | |||
| Nottingham | 192 (33.0) | 765 (31.1) | 556 (36.5) |
| Bristol | 180 (30.9) | 817 (33.2) | 515 (33.8) |
| Norwich | 137 (23.5) | 614 (25.0) | 307 (20.1) |
| Newcastle | 73 (12.5) | 264 (10.7) | 147 (9.6) |
| Age (years), median (IQR)a | 2.08 (1.42–3.13) | 2.16 (1.53–3.22) | 1.81 (1.08–2.84) |
| Age group (months) | |||
| 0–12 | 73 (12.5) | 206 (8.4) | 384 (25.2) |
| 13–36 | 355 (61.0) | 1591 (64.7) | 819 (53.7) |
| 37–62 | 154 (26.5) | 663 (27.0) | 322 (21.1) |
| Male | 355 (61.0) | 1507 (61.3) | 779 (51.0) |
| Ethnic origin: white | 512 (89.8) [12] | 2232 (91.9) [32] | 1324 (88.7) [33] |
| Number of children aged 0–4 years in family | [11] | [34] | [23] |
| 0 | 2 (0.4) | 20 (0.8) | 23 (1.5) |
| 1 | 365 (63.9) | 1438 (59.3) | 858 (57.1) |
| 2 | 180 (31.5) | 867 (35.7) | 543 (36.2) |
| ≥ 3 | 24 (4.2) | 101 (4.2) | 78 (5.2) |
| First child | 244 (44.5) [34] | 959 (42.5) [206] | 620 (44.1) [119] |
| Maternal age ≤ 19 years at birth of first childb | 86 (16.5) [9] | 244 (10.8) [15] | 215 (15.8) [24] |
| Single adult household | 80 (14.0) [12] | 263 (10.9) [49] | 215 (14.5) [40] |
| Weekly out of home child care (hours), median (IQR) | 10 (0–20.0) [45] | 15 (2.5–24.0) [132] | 8 (0–20.0) [119] |
| Adults in paid work | [12] | [33] | [39] |
| ≥ 2 | 263 (46.1) | 1381 (56.9) | 684 (46.0) |
| 1 | 198 (34.7) | 745 (30.7) | 554 (37.3) |
| 0 | 109 (19.1) | 301 (12.4) | 248 (16.7) |
| Receives state benefits | 252 (44.3) [13] | 893 (37.0) [48] | 663 (44.9) [50] |
| Overcrowding (more than one person per room) | 51 (9.3) [32] | 173 (7.4) [127] | 151 (10.6) [103] |
| Non-owner occupier | 242 (42.5) [13] | 792 (32.7) [38] | 618 (41.3) [30] |
| Household has no car | 71 (12.3) [7] | 252 (10.4) [29] | 223 (14.9) [30] |
| IMD score, median (IQR)c | 17.1 (8.8–31.8) | 15.1 (9.3–26.8) [26] | 17.6 (10.1–33.1) |
| Distance (km) from hospital, median (IQR) | 3.3 (2.0–5.0) | 3.7 (2.4–6.4) [25] | 3.5 (2.1–5.6) |
| CBQ score, mean (SD)c | 4.66 (0.98) [40] | 4.60 (0.87) [213] | 4.68 (0.93) [109] |
| Long-term health condition | 55 (9.7) [13] | 187 (7.6) [14] | 130 (8.6) [15] |
| Child health VAS score (range 0–10), median (IQR)c | 10 (9.3–10) [5] | 9.6 (8.5–10) [23] | 9.9 (9.0–10) [18] |
| HRQL (PedsQL), median (IQR)c,d | n = 308, 93.1 (86.1–97.6) [12] | n = 1413, 89.3 (82.1–94.0) [29] | n = 678, 92.9 (85.7–97.6) [13] |
| PDH tasks subscale score, median (IQR)c,e | 13.0 (9.0–16.0) [63] | 13.7 (10.0–17.1) [132] | 13.0 (9.0–17.0) [139] |
| HADS score, mean (SD)c,e | 10.7 (6.3) [14] | 11.0 (6.2) [35] | 10.7 (6.1) [33] |
| Exposure | Cases (n = 582) | Community controls (n = 2460) | Hospital controls (n = 1525) | Community controls, unadjusted OR (95% CI) | Hospital controls, unadjusted OR (95% CI) |
|---|---|---|---|---|---|
| Did not use any safety gatesa | 134 (24.5) [36] | 524 (22.8) [157] | 416 (29.3) [105] | 1.10 (0.87 to 1.40) | 0.78 (0.63 to 0.98) |
| No use of furniture corner coversa | 443 (76.6) [4] | 1982 (81.2) [20] | 1203 (79.9) [20] | 0.76 (0.61 to 0.95) | 0.82 (0.65 to 1.04) |
| Rugs/carpets not firmly fixed to the floora | 151 (26.4) [11] | 808 (33.1) [18] | 415 (27.9) [38] | 0.72 (0.59 to 0.89) | 0.93 (O.75 to 1.15) |
| Electric wires or cables trailing across the floor at least some daysb,c | 86 (15.6) [14] ((18)) | 475 (19.9) [16] ((63)) | 249 (17.2) [19] ((62)) | 0.72 (0.56 to 0.93) | 0.89 (0.68 to 1.16) |
| Things on floor that could be tripped over at least some daysb,c | 371 (66.8) [14] ((13)) | 1698 (70.1) [16] ((21)) | 1012 (69.3) [29] ((36)) | 0.88 (0.72 to 1.07) | 0.89 (0.72 to 1.10) |
| Not locking back doors to prevent access to the garden at least some daysb,c | 193 (38.8) [17] ((68)) | 851 (41.8) [23] ((259)) | 485 (37.9) [27] ((218)) | 0.98 (0.79 to 1.22) | 1.04 (0.84 to 1.29) |
| Not using safety gate to prevent access to the garden at least some daysb,c | 364 (89.7) [16] ((160)) | 1631 (93.6) [36] ((682)) | 899 (91.3) [38] ((502)) | 0.58 (0.38 to 0.88) | 0.83 (0.56 to 1.22) |
| Unsupervised playing in the garden at least some daysb,c | 154 (29.6) [13] ((48)) | 770 (34.6) [27] ((207)) | 327 (24.9) [27] ((186)) | 0.76 (0.61 to 0.96) | 1.26 (1.01 to 1.58) |
| Not taught child rules about slippery floors | 218 (39.4) [28] | 910 (38.0) [66] | 745 (51.1) [67] | 1.07 (0.85 to 1.36) | 0.62 (0.51 to 0.76) |
| Not taught child rules about running in the house | 198 (36.0) [32] | 939 (39.2) [67] | 703 (48.3) [71] | 0.77 (0.60 to 0.98) | 0.60 (0.49 to 0.74) |
| Exposures measured only in children aged 0–36 months | |||||
| n = 428 | n = 1797 | n = 1203 | |||
| Used baby walkera | 117 (27.7) [5] | 530 (29.9) [24] | 319 (27.4) [40] | 0.90 (0.71 to 1.15) | 1.01 (0.79 to 1.30) |
| Did not use playpen or travel cota | 345 (82.1) [8] | 1521 (85.8) [24] | 963 (83.2) [45] | 0.76 (0.57 to 1.02) | 0.93 (0.69 to 1.25) |
| Did not use stationary activity centrea | 350 (83.1) [7] | 1391 (78.5) [25] | 893 (77.0) [44] | 1.40 (1.05 to 1.86) | 1.47 (1.10 to 1.96) |
| Exposure | Community controls, AOR (95% CI) | Hospital controls, AOR (95% CI) | Confounders adjusted fora |
|---|---|---|---|
| Did not use any safety gatesb | 1.12 (0.83 to 1.49) | 0.80 (0.61 to 1.05) | HADS score, hours of out-of-home child care, PDH score, first child |
| Did not use furniture corner coversb | 0.72 (0.54 to 0.94) | 0.81 (0.61 to 1.06) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Rugs/carpets not firmly fixed to the floorb | 0.77 (0.59 to 0.99) | 0.97 (0.75 to 1.25) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Electric wires or cables trailing across the floorc | 0.75 (0.55 to 1.02) | 1.00 (0.73 to 1.36) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Things on floor that could be tripped overc | 1.07 (0.82 to 1.38) | 0.97 (0.74 to 1.26) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Did not lock back doors to prevent access to the gardenc | 0.97 (0.75 to 1.27) | 1.14 (0.89 to 1.46) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Did not use safety gate to prevent access to the gardenc | 1.01 (0.58 to 1.74) | 1.00 (0.61 to 1.64) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Unsupervised playing in the gardenc | 0.89 (0.68 to 1.17) | 1.24 (0.93 to 1.64) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate |
| Had not taught child rules about slippery floors | 1.13 (0.83 to 1.52) | 0.80 (0.61 to 1.05) | HADS score, PDH score, first child, uses safety gate |
| Had not taught child rules about running in the house | 0.73 (0.54 to 1.00) | 0.78 (0.58 to 1.03) | HADS score, PDH score, first child, uses safety gate |
| Used baby walkera | 0.83 (0.59 to 1.16) | 0.97 (0.70 to 1.34) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate, uses playpen/travel cot, uses activity centre |
| Did not use playpen or travel cota | 0.90 (0.61 to 1.33) | 0.92 (0.63 to 1.36) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate, uses baby walker, uses activity centre |
| Did not use stationary activity centrea | 1.37 (0.95 to 1.97) | 1.36 (0.95 to 1.96) | HADS score, hours of out-of-home child care, PDH score, first child, uses safety gate, uses baby walker, uses playpen/travel cot |
| Characteristic | Cases (n = 610) | Community controls (n = 2658) | Hospital controls (n = 2087) |
|---|---|---|---|
| Study centre | |||
| Nottingham | 252 (41.3) | 1055 (39.7) | 740 (35.5) |
| Bristol | 178 (29.2) | 796 (29.9) | 666 (31.9) |
| Norwich | 97 (15.9) | 457 (17.2) | 424 (20.3) |
| Newcastle | 83 (13.6) | 350 (13.2) | 257 (12.3) |
| Age (years), median (IQR)a | 2.0 (1.2–2.9) | 2.0 (1.3–3.1) | 1.9 (1.2–2.9) |
| Age group (months) | |||
| 0–12 | 113 (18.5) | 315 (11.9) | 443 (21.2) |
| 13–36 | 362 (59.3) | 1694 (63.7) | 1188 (56.9) |
| 37–62 | 135 (22.1) | 649 (24.4) | 456 (21.8) |
| Male | 299 (49.0) | 1320 (49.7) | 1140 (54.6) |
| Ethnic origin: white | 547 (91.5) [12] | 2371 (91.0) [52] | 1811 (88.7) [46] |
| Children aged < 5 years in family | [8] | [44] | [35] |
| 0 | 7 (1.2) | 28 (1.1) | 24 (1.2) |
| 1 | 358 (59.5) | 1566 (59.9) | 1232 (60.0) |
| 2 | 212 (35.2) | 911 (34.9) | 702 (34.2) |
| ≥ 3 | 25 (4.2) | 109 (4.2) | 94 (4.6) |
| First child | 242 (43.3) [51] | 1067 (44.5) [260] | 858 (44.5) [158] |
| Maternal age ≤ 19 years at birth of first childb | 100 (18.5) [7] | 219 (9.1) [15] | 286 (15.3) [25] |
| Single adult household | 87 (14.6) [15] | 272 (10.5) [76] | 305 (15.0) [47] |
| Weekly out-of-home child care (hours), median (IQR) | 13.5 (1.0–22.5) [43] | 15 (3.0–24.0) [165] | 8.0 (0.0–20.0) [154] |
| Adults in the family in paid work | [16] | [56] | [45] |
| > 1 | 297 (50.0) | 1534 (59.0) | 946 (46.3) |
| 1 | 209 (35.2) | 784 (30.1) | 719 (35.2) |
| 0 | 88 (14.8) | 284 (10.9) | 377 (18.5) |
| Receives state benefits | 241 (40.9) [21] | 838 (32.4) [68] | 900 (44.4) [62] |
| Overcrowding (more than one person per room) | 52 (9.1) [40] | 187 (7.5) [152] | 205 (10.5) [131] |
| Non-owner occupier | 241 (40.4) [14] | 836 (32.2) [65] | 886 (43.3) [40] |
| Household has no car | 88 (14.7) [12] | 254 (9.7) [50] | 308 (15.0) [33] |
| IMD score, median (IQR)c | 18.7 (10.1–32.7) | 15.2 (9.0–27.1) [35] | 18.0 (10.0–33.0) |
| Distance (km) from hospital, median (IQR) | 3.4 (2.2–5.4) | 3.9 (2.4–7.6) [34] | 3.5 (2.2–5.5) [1] |
| CBQ score, mean (SD)c | 4.7 (0.9) [43] | 4.6 (0.9) [293] | 4.7 (1.0) [137] |
| Long-term health condition | 63 (10.4) [6] | 202 (7.7) [19] | 185 (9.0) [29] |
| Child health VAS score (range 0–10), median (IQR)c | 9.9 (9.0–10.0) [9] | 9.7 (8.4–10.0) [19] | 9.9 (9.2–10.0) [19] |
| HRQL (PedsQL), median (IQR)c,d | n = 303, 91.7 (83.3, 97.6) [6] | n = 1342, 89.3 (82.1, 94.0) [18] | n = 961, 92.9 (86.9, 97.6) [24] |
| Parental assessment of child’s ability to open safety gate | [19] | [97] | [55] |
| Not likely | 423 (73.1) | 1808 (76.0) | 1356 (76.0) |
| Very or quite likely | 156 (26.9) | 571 (24.0) | 429 (24.0) |
| PDH tasks subscale score, median (IQR)c,e | 14.0 (10.0–18.0) [61] | 14.0 (11.0–18.0) [152] | 13.7 (10.0–17.0) [214] |
| HADS score, mean (SD)c,e | 10.4 (6.2) [14] | 10.7 (5.9) [36] | 10.7 (6.1) [48] |
| Exposure | Cases (n = 610) | Community controls (n = 2658) | Hospital controls (n = 2087) | Community controls, unadjusted OR (95% CI) | Hospital controls. unadjusted OR (95% CI) |
|---|---|---|---|---|---|
| Did not use any safety gatesa | 142 (23.7) [12] | 521 (20.6) [124] | 540 (28.0) [159] | 1.22 (0.97 to 1.53) | 0.80 (0.65 to 0.99) |
| Exposures measured only for households with stairs | |||||
| n = 598 | n = 2476 | n = 1840 | |||
| Gate closed | 174 (29.7) | 1245 (51.1) | 975 (54.3) | 1 | 1 |
| Gate open | 210 (35.9) | 555 (22.8) | 159 (8.9) | 2.93 (2.32 to 3.72) | 7.40 (5.70 to 9.61) |
| No gatea | 201 (34.4) [13] | 636 (26.1) [40] | 662 (36.9) [44] | 2.52 (1.97 to 3.22) | 1.70 (1.36 to 2.13) |
| Did not have carpeted stairsa | 83 (14.1) [8] | 200 (8.2) [28] | 162 (9.0) [36] | 1.91 (1.44 to 2.53) | 1.66 (1.25 to 2.20) |
| Did not have landing part-way up stairsa | 413 (69.6) [5] | 1556 (63.6) [28] | 1152 (63.7) [32] | 1.35 (1.11 to 1.65) | 1.31 (1.07 to 1.60) |
| Had spiral or winding stairsa | 96 (16.2) [7] | 402 (16.4) [30] | 308 (17.1) [39] | 1.04 (0.81 to 1.33) | 0.94 (0.73 to 1.21) |
| Had tripping hazards on stairsb,c | 183 (31.6) [4] ((14)) | 932 (38.4) [16] ((35)) | 584 (34.0) [68] ((54)) | 0.73 (0.60 to 0.89) | 0.94 (0.77 to 1.15) |
| Stairs too steepa | 218 (37.6) [18] | 743 (31.0) [80] | 571 (32.5) [82] | 1.35 (1.11 to 1.64) | 1.25 (1.03 to 1.52) |
| Stairs too narrowa | 154 (26.8) [23] | 484 (20.4) [98] | 417 (23.9) [94] | 1.45 (1.17 to 1.80) | 1.17 (0.94 to 1.45) |
| Stairs poorly lita | 103 (18.0) [26] | 329 (13.8) [94] | 261 (15.0) [99] | 1.37 (1.07 to 1.76) | 1.25 (0.97 to 1.60) |
| Steps in need of repaira | 67 (11.7) [25] | 147 (6.2) [96] | 133 (7.6) [97] | 1.97 (1.45 to 2.70) | 1.60 (1.18 to 2.19) |
| Banister/handrail on stairs in need of repaira | 68 (12.0) [32] | 203 (8.5) [98] | 188 (10.8) [99] | 1.46 (1.09 to 1.97) | 1.13 (0.84 to 1.52) |
| Stair covering in need of repaira | 71 (12.4) [26] | 175 (7.4) [96] | 157 (9.0) [98] | 1.74 (1.28 to 2.36) | 1.43 (1.06 to 1.93) |
| Stairs not safe to usea | 101 (17.2) [10] | 271 (11.1) [25] | 217 (12.1) [41] | 1.71 (1.33 to 2.21) | 1.51 (1.17 to 1.96) |
| Did not have handrails on all stairsa | 215 (36.0) [1] | 1063 (43.3) [20] | 670 (37.0) [30] | 0.72 (0.60 to 0.88) | 0.96 (0.79 to 1.16) |
| Did not have banisters or railings on all stairsa | 152 (26.4) [22] | 486 (20.1) [60] | 394 (22.2) [67] | 1.44 (1.17 to 1.79) | 1.25 (1.01 to 1.58) |
| Had not taught child rules about going downstairs | 173 (29.9) [20] | 624 (25.9) [70] | 584 (33.3) [86] | 1.60 (1.19 to 2.17) | 0.86 (0.70 to 1.05) |
| Had not taught child rules about carrying big/heavy things while going downstairs | 291 (50.3) [20] | 1134 (47.1) [68] | 921 (52.5) [86] | 1.33 (1.01 to 1.74) | 0.92 (0.76 to 1.11) |
| Had not taught child rules about leaving things on stairs | 320 (55.6) [22] | 1339 (55.5) [64] | 1031 (58.6) [80] | 1.00 (0.77 to 1.30) | 0.88 (0.73 to 1.07) |
| Exposure measured only for households with banisters | |||||
| n = 424 | n = 1930 | n = 1379 | |||
| Banister width (inches), median (IQR)a,d | 3 (2–4) [190] | 3 (2–4) [803] | 3 (2–4) [673] | ||
| Up to ≤ 2.5 | 94 (40.2) | 400 (35.5) | 290 (41.1) | 1 | 1 |
| > 2.5 to ≤ 3.75 | 67 (28.6) | 363 (32.2) | 204 (28.9) | 0.88 (0.59 to 1.32) | 1.01 (0.71 to 1.45) |
| > 3.75 | 73 (31.2) | 364 (32.3) | 212 (30.3) | 0.84 (0.55 to 1.26) | 1.06 (0.75 to 1.51) |
| Exposures measured only in children aged 0–36 months | |||||
| n = 475 | n = 2009 | n = 1631 | |||
| Used baby walkera | 135 (29.3) [14] | 675 (34.1) [32] | 418 (26.4) [47] | 0.80 (0.63 to 1.00) | 1.16 (0.92 to 1.45) |
| Did not use playpen or travel cota | 384 (83.3) [14] | 1645 (83.1) [30] | 1319 (83.7) [55] | 1.03 (0.78 to 1.36) | 0.97 (0.74 to 1.28) |
| Did not use stationary activity centrea | 348 (75.8) [16] | 1486 (75.2) [33] | 1263 (80.0) [52] | 1.01 (0.79 to 1.29) | 0.78 (0.61 to 1.00) |
| Exposure | Community controls, AOR (95% CI) | Hospital controls, AOR (95% CI) | Confounders adjusted fora |
|---|---|---|---|
| Did not use any safety gatesb | 1.22 (0.92 to 1.62) | 0.77 (0.59 to 1.00) | HADS score, PDH score, first child, stair safety, hours of out-of-home child care |
| Gate closed | 1 | 1 | Child’s ability to open safety gate, taught child rules about going down the stairs, carrying things down the stairs, leaving things on the stairs, stair safety |
| Gate open | 3.09 (2.39 to 4.00) | 7.60 (5.60 to 10.32) | |
| No gate | 2.50 (1.90 to 3.29) | 1.91 (1.45 to 2.52) | |
| Did not have carpeted stairsb | 1.52 (1.09 to 2.10) | 1.46 (1.07 to 2.00) | HADS score, PDH score, stair safety |
| Did not have landing part-way up stairsb | 1.34 (1.08 to 1.65) | 1.29 (1.05 to 1.59) | Stair safety |
| Had spiral or winding stairsb | 0.97 (0.75 to 1.27) | 0.92 (0.71 to 1.19) | Stair safety |
| Had tripping hazards on stairsc | 0.77 (0.62 to 0.97) | 0.90 (0.72 to 1.12) | HADS score, PDH score, stair safety |
| Stairs too steepb,d | 1.21 (0.94 to 1.56) | 1.34 (1.03 to 1.74) | Stair safety |
| Stairs too narrowb,d | 1.28 (0.96 to 1.70) | 1.09 (0.82 to 1.44) | Stair safety |
| Stairs poorly litb,d | 1.32 (0.97 to 1.79) | 1.23 (0.91 to 1.07) | HADS score, PDH score, stair safety |
| Steps in need of repairb,d | 1.71 (1.16 to 2.50) | 1.45 (1.00 to 2.11) | HADS score, PDH score, stair safety |
| Banister/handrail on stairs in need of repairb,d | 1.32 (0.92 to 1.88) | 1.10 (0.78 to 1.54) | HADS score, PDH score, stair safety |
| Stair covering in need of repairb,d | 1.41 (0.99 to 2.03) | 1.38 (0.97 to 1.97) | HADS score, PDH score, stair safety |
| Stairs not safe to useb,d | 1.46 (1.07 to 1.99) | 1.40 (1.04 to 1.90) | HADS score, PDH score, stair safety |
| Did not have handrails on all stairsb,d | 0.69 (0.56 to 0.86) | 0.94 (0.76 to 1.16) | HADS score, PDH score, stair safety |
| Did not have banisters or railings on all stairsb,d | 1.27 (0.99 to 1.63) | 1.17 (0.92 to 1.50) | HADS score, PDH score, stair safety |
| Had not taught child rules about going downstairs | 1.36 (0.92 to 2.02) | 0.82 (0.58 to 1.17) | HADS score, PDH score, first child, child’s ability to open safety gate, safety gate, stair safety |
| Had not taught child rules about carrying big/heavy things while going downstairs | 1.21 (0.83 to 1.75) | 0.84 (0.63 to 1.13) | HADS score, PDH score, first child, child’s ability to open safety gate, safety gate, stair safety |
| Had not taught child rules about leaving things on stairs | 0.85 (0.60 to 1.22) | 0.80 (0.60 to 1.08) | HADS score, PDH score, first child, child’s ability to open safety gate, safety gate, stair safety |
| Banister width (inches)b | Stair safety | ||
| Up to ≤ 2.5 | 1 | 1 | |
| > 2.5 to ≤ 3.75 | 0.83 (0.53 to 1.29) | 1.03 (0.71 to 1.49) | |
| > 3.75 | 0.75 (0.48 to 1.18) | 1.05 (0.72 to 1.52) | |
| Used baby walkerb | 0.83 (0.63 to 1.10) | 1.25 (0.96 to 1.63) | HADS score, PDH score, first child, hours of out-of-home child care |
| Did not use playpen or travel cotb | 1.07 (0.75 to 1.53) | 1.13 (0.80 to 1.61) | HADS score, PDH score, uses baby walker, first child, hours of out-of-home child care |
| Did not use stationary activity centreb | 1.08 (0.80 to 1.46) | 0.91 (0.67 to 1.22) | HADS score, PDH score, uses baby walker, first child, hours of out-of-home child care |
| Characteristic | Cases (n = 567) | Community controls (n = 2320) | Hospital controls (n = 2253) |
|---|---|---|---|
| Study centre | |||
| Nottingham | 193 (34.0) | 738 (31.8) | 842 (37.4) |
| Bristol | 179 (31.6) | 794 (34.2) | 699 (31.0) |
| Norwich | 106 (18.7) | 467 (20.1) | 435 (19.3) |
| Newcastle | 89 (15.7) | 321 (13.8) | 277 (12.3) |
| Age (years), median (IQR)a | 2.18 (1.49–2.92) | 2.24 (1.54–3.02) | 1.82 (1.15–2.85) |
| Age group (months) | |||
| 0–12 | 65 (11.5) | 204 (8.8) | 517 (22.9) |
| 13–36 | 378 (66.7) | 1575 (67.9) | 1253 (55.6) |
| 37–62 | 124 (21.9) | 541 (23.3) | 483 (21.4) |
| Male | 280 (49.4) | 1210 (52.2) | 1240 (55.0) |
| Ethnic origin: white | 514 (92.1) [9] | 2115 (92.6) [36] | 1954 (88.7) [50] |
| Children aged 0–4 years in family | [11] | [29] | [32] |
| 0 | 6 (1.1) | 16 (0.7) | 25 (1.1) |
| 1 | 299 (53.8) | 1379 (60.2) | 1362 (61.3) |
| 2 | 229 (41.2) | 810 (35.4) | 735 (33.1) |
| ≥ 3 | 22 (4.0) | 86 (3.8) | 99 (4.5) |
| First child | 210 (41.7) [64] | 895 (42.7) [222] | 934 (44.6) [158] |
| Maternal age ≤ 19 years at birth of first childb | 84 (16.5) [8] | 208 (9.7) [14] | 312 (15.5) [24] |
| Single adult household | 92 (16.6) [13] | 262 (11.5) [43] | 318 (14.4) [52] |
| Weekly out-of-home child care (hours), median (IQR) | 12 (0.5–22.0) [31] | 15 (2.5–24.0) [112] | 9 (0–20) [170] |
| Adults in paid work | [11] | [35] | [51] |
| ≥ 2 | 263 (47.3) | 1281 (56.1) | 1047 (47.4) |
| 1 | 184 (33.1) | 742 (32.5) | 781 (35.5) |
| 0 | 109 (19.6) | 262 (11.5) | 374 (17.0) |
| Receives state benefits | 228 (41.7) [20] | 795 (35.1) [54] | 951 (43.5) [65] |
| Overcrowding (more than one person per room) | 46 (8.8) [42] | 163 (7.4) [128] | 213 (10.1) [137] |
| Non-owner occupier | 241 (43.5) [13] | 771 (33.8) [41] | 928 (42.0) [44] |
| Household has no car | 81 (14.6) [11] | 219 (9.6) [28] | 319 (14.4) [34] |
| IMD score, median (IQR)c | 17.5 (10.3–31.7) | 15.1 (9.3–26.5) [24] | 18.2 (9.9–33.3) [1] |
| Distance (km) from hospital, median (IQR) | 3.5 (2.2–5.9) | 4.0 (2.4–7.6) [24] | 3.4 (2.0–5.6) |
| CBQ score, mean (SD)c | 4.75 (0.91) [24] | 4.61 (0.86) [186] | 4.6 (0.95) [149] |
| Long-term health condition | 53 (9.4) [5] | 187 (8.1) [21] | 204 (9.2) [32] |
| Child health VAS score (range 0–10), median (IQR)c | 9.8 (8.8–10) [2] | 9.6 (8.4–10) [14] | 9.9 (9.2–10) [26] |
| HRQL (PedsQL), median (IQR)c,d | n = 326, 91.7 (85.7–97.2) [3] | n = 1354, 89.3 (82.1–95.2) [24] | n = 995, 92.9 (86.1–97.6) [26] |
| Parental assessment of child’s ability to access poisons | [21] | [96] | [111] |
| All scenarios ‘not likely’ | 22 (4.0) | 112 (5.0) | 253 (11.8) |
| One or more scenarios ‘quite likely’ and none ‘very likely’ | 100 (18.3) | 513 (23.1) | 552 (25.8) |
| One or more scenarios ‘very likely’ | 424 (77.7) | 1599 (71.9) | 1337 (62.4) |
| PDH tasks subscale score, median (IQR)c,e | 14.0 (10.3–18.0) [50] | 14.0 (11.0–18.0) [113] | 13 (10.0–17.0) [233] |
| HADS score, mean (SD)c,e | 10.9 (6.1) [15] | 10.8 (6.2) [25] | 10.6 (6.1) [49] |
| Exposure | Cases (n = 567) | Community controls (n = 2320) | Hospital controls (n = 2253) | Community controls, unadjusted OR (95% CI) | Hospital controls, unadjusted OR (95% CI) |
|---|---|---|---|---|---|
| Did not have CRCs or blister packs for all medicinesa | 102 (18.2) [6] | 321 (13.9) [8] | 207 (9.3) [26] | 1.39 (1.09 to 1.78) | 2.17 (1.68 to 2.81) |
| Did not have all medicines in locked medicines boxa | 447 (79.5) [5] | 1914 (82.8) [9] | 1561 (70.2) [30] | 0.84 (0.66 to 1.06) | 1.65 (1.32 to 2.06) |
| Not all medicines were locked awaya,b | 454 (83.6) [24] ((0)) | 1897 (85.4) [92] ((6)) | 1582 (76.3) [164] ((15)) | 0.87 (0.67 to 1.14) | 1.59 (1.24 to 2.03) |
| Not all medicines were stored at adult eye level or abovea,b | 189 (40.7) [101] ((2)) | 612 (30.8) [324] ((10)) | 478 (25.7) [372] ((22)) | 1.68 (1.35 to 2.09) | 1.99 (1.61 to 2.46) |
| Not all medicines were stored safelya | 165 (34.4) [87] | 506 (24.9) [287] | 360 (18.6) [315] | 1.73 (1.38 to 2.17) | 2.30 (1.84 to 2.86) |
| Any medicines transferred into a different containera | 28 (5.0) [6] | 104 (4.5) [10] | 93 (4.2) [26] | 1.15 (0.74 to 1.77) | 1.21 (0.78 to 1.86) |
| Did not put all medicines away immediately after useb,c | 213 (41.7) [16] ((40)) | 522 (26.2) [57] ((274)) | 455 (24.4) [96] ((289)) | 2.00 (1.62 to 2.45) | 2.22 (1.81 to 2.73) |
| Did not have CRCs for all cleaning productsa | 154 (27.5) [8] | 686 (29.7) [14] | 465 (20.9) [26] | 0.90 (0.73 to 1.11) | 1.44 (1.17 to 1.78) |
| Not all household/cleaning products were locked awaya,b | 353 (69.4) [54] ((4)) | 1590 (72.1) [106] ((10)) | 1425 (68.7) [160] ((19)) | 0.85 (0.68 to 1.05) | 1.03 (0.84 to 1.27) |
| Not all household/cleaning products were stored at adult eye level or abovea,b | 409 (83.5) [73] ((4)) | 1823 (86.0) [191] ((10)) | 1507 (78.0) [303] ((19)) | 0.84 (0.64 to 1.12) | 1.42 (1.09 to 1.85) |
| Not all household/cleaning products were stored safelya | 239 (49.9) [88] | 1138 (54.6) [234] | 891 (46.0) [317] | 0.82 (0.67 to 1.01) | 1.17 (0.96 to 1.43) |
| Any cleaning products transferred into a different containera | 17 (3.0) [5] | 38 (1.6) [10] | 40 (1.8) [27] | 1.74 (0.97 to 3.12) | 1.70 (0.96 to 3.03) |
| Did not use safety gate to stop child accessing kitchena | 411 (73.3) [6] | 1735 (75.1) [10] | 1597 (71.9) [33] | 0.91 (0.73 to 1.13) | 1.07 (0.87 to 1.32) |
| Had things child could climb on to reach high surfacesa | 281 (50.0) [5] | 1056 (45.7) [8] | 796 (35.8) [29] | 1.18 (0.96 to 1.44) | 1.79 (1.49 to 2.16) |
| Did not put all household/cleaning products away immediately after useb,c | 131 (25.0) [30] ((14)) | 378 (17.1) [74] ((34)) | 372 (18.5) [159] ((87)) | 1.62 (1.28 to 2.05) | 1.47 (1.17 to 1.84) |
| Had not taught child rules about what to do or not do when sees cleaning products | 194 (36.1) [30] | 899 (40.0) [72] | 1082 (50.3) [100] | 0.88 (0.70 to 1.10) | 0.56 (0.46 to 0.68) |
| Had not taught child rules about what to do or not do if medicine on worktop | 239 (44.0) [24] | 1138 (50.7) [74] | 1246 (58.1) [110] | 0. 73 (0.58 to 0.93) | 0.57 (0.47 to 0.68) |
| Exposures measured only in children aged 0–36 months | |||||
| n = 443 | n = 1779 | n = 1770 | |||
| Used baby walkera | 103 (24.3) [19] | 539 (30.6) [15] | 472 (27.3) [43] | 0.76 (0.59 to 0.98) | 0.85 (0.67 to 1.09) |
| Exposure | Community controls, AOR (95% CI) | Hospital controls, AOR (95% CI) | Confounders adjusted fora |
|---|---|---|---|
| Did not have CRCs or blister packs on all medicinesb | 1.25 (0.95 to 1.65) | 2.31 (1.74 to 3.07) | First child, ability to access poisons |
| Did not have all medicines in locked medicines boxb | 0.82 (0.47 to 1.43) | 1.30 (0.83 to 2.04) | CRCs, HADS score, PDH score, ability to access poisons, hours of out-of-home care, first child, medicines locked, medicines put away immediately after use, uses kitchen safety gate, medicines stored high, things child could climb on to reach high surfaces |
| Not all medicines were locked awayb | 0.91 (0.64 to 1.31) | 1.43 (1.04 to 1.98) | CRCs, HADS score, PDH score, uses kitchen safety gate, medicines stored high, things child could climb on to reach high surfaces, hours of out-of-home care |
| Not all medicines were stored at adult level or aboveb | 1.59 (1.21 to 2.09) | 1.95 (1.51 to 2.51) | CRCs, HADS score, PDH score, ability to access poisons, uses kitchen safety gate, first child, things child could climb on to reach high surfaces, hours of out-of-home care |
| Not all medicines stored safely | 1.83 (1.38 to 2.42) | 2.28 (1.75 to 2.97) | CRCs, HADS score, PDH score, able to access poisons, first child, uses kitchen safety gate, things child could climb on to reach high surfaces, hours of out-of-home care |
| Any medicines transferred into a different containerb | 0.96 (0.52 to 1.76) | 0.96 (0.54 to 1.73) | CRCs, HADS score, PDH score, locked medicines box, medicines locked away, medicines stored high |
| Did not put all medicines away immediately after usec | 2.11 (1.54 to 2.90) | 2.22 (1.68 to 2.93) | HADS score, PDH score, ability to access poisons, first child, medicines locked, medicines stored high, things child could climb on to reach high surfaces |
| Did not have CRCs for all cleaning productsb | 0.87 (0.69 to 1.10) | 1.44 (1.14 to 1.81) | First child, ability to access poisons |
| Not all household/cleaning products were locked awayb | 0.90 (0.69 to 1.17) | 1.07 (0.83 to 1.37) | CRCs, HADS score, PDH score, uses kitchen safety gate, products stored high, things child could climb on to reach high surfaces, hours of out-of-home care |
| Not all household/cleaning products were stored at adult level or aboveb | 0.95 (0.67 to 1.35) | 1.34 (0.97 to 1.85) | CRCs, HADS score, PDH score, ability to access poisons, uses kitchen safety gate, things child could climb on to reach high surfaces, hours of out-of-home care |
| Not all household/cleaning products stored safelyb | 0.77 (0.59 to 0.99) | 1.16 (0.92 to 1.48) | CRCs, HADS score, PDH score, ability to access poisons, first child, uses kitchen safety gate, things child could climb on to reach high surfaces, hours of out-of-home care |
| Any cleaning products transferred into a different containerb | 1.20 (0.54 to 2.65) | 1.82 (0.84 to 3.93) | CRCs, HADS score, PDH score, products locked, products stored high |
| Did not use safety gate to stop child access the kitchenb | 1.05 (0.80 to 1.37) | 1.08 (0.84 to 1.39) | HADS score, PDH score, first child, hours of out-of-home care |
| Had things child could climb on to reach high surfacesb | 1.20 (0.93 to 1.54) | 1.47 (1.16 to 1.87) | CRCs, HADS score, PDH score, ability to access poisons, first child |
| Did not put all household/cleaning products away immediately after usec | 1.79 (1.29 to 2.48) | 1.56 (1.16 to 2.09) | HADS score, PDH score, ability to access poisons, first child, products locked, products stored high, things child could climb on to reach high surfaces |
| Had not taught child rules about what to do or not do when see cleaning products | 0.81 (0.59 to 1.12) | 0.63 (0.47 to 0.83) | CRCs, HADS score, PDH score, ability to access poisons, first child, products locked, products put away immediately after use, uses kitchen safety gate, products stored high, products transferred to different container |
| Had not taught child rules about what to do or not do if medicine on worktop | 0.66 (0.45 to 0.96) | 0.54 (0.40 to 0.73) | CRCs, HADS score, PDH score, ability to access poisons, first child, locked medicines box, medicines locked away, medicines put away immediately after use, uses kitchen safety gate, medicines stored high, medicines transferred to different container |
| Used baby walkerb | 0.82 (0.61 to 1.10) | 0.98 (0.74 to 1.30) | HADS score, PDH score, first child, hours of out-of-home care |
| Characteristic | Cases (n = 338) | Community controls (n = 1438) | Hospital controls (n = 2490) |
|---|---|---|---|
| Study centre | |||
| Nottingham | 123 (36.4) | 521 (36.2) | 917 (36.8) |
| Bristol | 112 (33.1) | 490 (34.1) | 768 (30.8) |
| Norwich | 54 (16.0) | 235 (16.3) | 488 (19.6) |
| Newcastle | 49 (14.5) | 192 (13.4) | 317 (12.7) |
| Age (years), median (IQR)a | 1.47 (1.03–1.96) | 1.56 (1.15–2.07) | 2.00 (1.24–2.96) |
| Age group (months) | |||
| 0–12 | 91 (26.9) | 316 (22.0) | 491 (19.7) |
| 13–36 | 216 (63.9) | 984 (68.4) | 1419 (57.0) |
| 37–62 | 31 (9.2) | 138 (9.6) | 580 (23.3) |
| Male | 183 (54.1) | 808 (56.2) | 1324 (53.2) |
| Ethnic origin: white | 269 (81.8) [9] | 1295 (91.3) [19] | 2206 (90.4) [51] |
| Number of children aged 0–4 years in family | [6] | [21] | [37] |
| 1 | 224 (67.5) | 883 (62.3) | 1473 (60.0) |
| 2 | 95 (28.6) | 476 (33.6) | 871 (35.5) |
| ≥ 3 | 13 (3.9) | 58 (4.1) | 109 (4.4) |
| First child | 140 (44.4) [23] | 581 (43.8) [111] | 1008 (44.0) [200] |
| Maternal age ≤ 19 years at birth of first childb | 43 (14.6) [3] | 156 (11.8) [9] | 354 (15.8) [29] |
| Single adult household | 52 (15.9) [10] | 171 (12.2) [34] | 360 (14.8) [56] |
| Weekly out of home child care (hours), median (IQR) | 5.5 (0–18) [32] | 12 (0–24) [77] | 10.0 (0–20) [170] |
| Adults in paid work | [6] | [19] | [57] |
| ≥ 2 | 150 (45.2) | 802 (56.5) | 1165 (47.9) |
| 1 | 129 (38.9) | 433 (30.5) | 835 (34.3) |
| 0 | 53 (16.0) | 184 (13.0) | 433 (17.8) |
| Receives state benefits | 151 (46.0) [10] | 491 (35.0) [35] | 1386 (57.4) [76] |
| Overcrowding (more than one person per room) | 47 (15.2) [28] | 116 (8.6) [83] | 213 (9.1) [151] |
| Non-owner occupier | 164 (49.5) [7] | 521 (37.1) [33] | 1010 (41.4) [51] |
| Household has no car | 55 (16.5) [5] | 174 (12.3) [18] | 350 (14.3) [41] |
| IMD score, median (IQR)c | 20.6 (10.1–35.6) | 15.7 (9.5–28.8) [18] | 17.8 (9.9–32.1) |
| Distance (km) from hospital, median (IQR) | 3.9 (2.1–8.1) | 4.6 (2.6–10.3) [16] | 3.4 (2.1–5.4) |
| CBQ score, mean (IQR)c | 4.7 (4.0–5.3) [18] | 4.6 (4.1–5.2) [155] | 4.7 (4.0–5.3) [168] |
| Long-term health condition | 22 (6.6) [7] | 77 (5.4) [13] | 236 (9.6) [30] |
| Child health VAS (range 0–10), median (IQR)c | 9.9 (9.2–10) [4] | 9.6 (8.3–10) [4] | 9.9 (9.1–10) [24] |
| HRQL (PedsQL), median (IQR)c,d | n = 79, 94.8 (88.2–98.8) [3] | n = 40, 89.3 (88.1–94.1) [3] | n = 124, 92.9 (85.7–97.6) [26] |
| Parental assessment of child’s ability to climb | [6] | [12] | [43] |
| All scenarios ‘not likely’ | 24 (7.2) | 80 (5.6) | 130 (5.3) |
| One or more scenarios ‘quite likely’ and none ‘very likely’ | 47 (14.2) | 165 (11.6) | 314 (12.8) |
| One or more scenarios ‘very likely’ | 261 (78.6) | 1181 (82.8) | 2003 (81.9) |
| PDH tasks subscale, median (IQR)c,e | 13 (10.0–16.0) [34] | 14 (11.0–18.0) [99] | 13.7 (10.0–17.0) [248] |
| HADS score, mean (IQR)c,e | 9 (6.0–13.0) [11] | 10 (6.0–14.0) [20] | 10 (6.0–14.0) [54] |
| Exposure | Cases (n = 338) | Community controls (n = 1438) | Hospital controls (n = 2490) | Community controls, unadjusted OR (95% CI) | Hospital controls, unadjusted OR (95% CI) |
|---|---|---|---|---|---|
| Did not use any safety gatesa | 82 (26.3) [26] | 242 (17.6) [65] | 626 (26.7) [149] | 1.79 (1.29 to 2.48) | 0.98 (0.75 to 1.28) |
| Had things child could climb on to reach high surfacesa | 115 (34.7) [7] | 475 (33.2) [6] | 966 (39.2) [28] | 1.07 (0.81 to 1.42) | 0.82 (0.65 to 1.05) |
| Does not have curly flex or cordless kettlea | 96 (29.3) [10] | 417 (29.5) [25] | 761 (31.3) [62] | 1.00 (0.76 to 1.31) | 0.91 (0.70 to 1.17) |
| Kettle not at back of worktop/table or back ring of cookera | 41 (12.6) [12] | 135 (9.5) [17] | 234 (9.6) [54] | 1.46 (1.00 to 2.14) | 1.35 (0.95 to 1.93) |
| Hot tap water too hota | 270 (82.8) [12] | 1249 (88.0) [18] | 1940 (80.0) [64] | 0.67 (0.48 to 0.94) | 1.21 (0.89 to 1.64) |
| Temperature of hot tap water not known or known to be > 54 °Ca | 289 (88.7) [12] | 1212 (85.5) [21] | 2058 (84.6) [56] | 1.29 (0.88 to 1.87) | 1.43 (1.00 to 2.04) |
| Child climbed or played on furniture at least some daysb,c | 233 (74.4) [7] ((18)) | 1098 (80.6) [6] ((70)) | 1890 (81.3) [41] ((125)) | 0.54 (0.37 to 0.77) | 0.67 (0.51 to 0.88) |
| Child held by someone holding a hot drink at least some daysb,c | 89 (28.2) [7] ((15)) | 395 (28.6) [6] ((50)) | 420 (18.3) [47] ((148)) | 0.95 (0.72 to 1.26) | 1.75 (1.34 to 2.29) |
| Child held by someone while using a cooker at least some daysb,c | 77 (24.1) [7] ((11)) | 357 (25.7) [6] ((44)) | 445 (19.2) [42] ((132)) | 0.91 (0.68 to 1.21) | 1.33 (1.01 to 1.76) |
| Hot drinks passed over child’s head at least some daysb,c | 42 (12.9) [6] ((7)) | 147 (10.5) [9] ((28)) | 184 (7.8) [44] ((99)) | 1.24 (0.85 to 1.80) | 1.74 (1.22 to 2.49) |
| Hot drinks left within reach of child at least some daysb,c | 171 (53.9) [12] ((9)) | 534 (38.0) [12] ((21)) | 899 (37.9) [37] ((80)) | 1.99 (1.54 to 2.57) | 1.92 (1.52 to 2.43) |
| Hot drinks or hot liquids put on a table with a tablecloth at least some daysb,c | 57 (17.8) [8] ((10)) | 178 (12.9) [9] ((47)) | 303 (13.1) [46] ((126)) | 1.47 (1.05 to 2.05) | 1.44 (1.06 to 1.97) |
| The front rings of the cooker used at least some daysb,c | 236 (75.2) [13] ((11)) | 1152 (82.2) [18] ((19)) | 1870 (79.4) [43] ((93)) | 0.67 (0.49 to 0.90) | 0.78 (0.59 to 1.03) |
| Pan handles never turned towards the back of the cooker while cookingb,c | 104 (32.2) [9] ((6)) | 380 (27.2) [16] ((23)) | 649 (27.5) [57] ((75)) | 1.26 (0.96 to 1.65) | 1.25 (0.97 to 1.61) |
| Child left in bathroom, without adult, even for a moment at least some daysb,c | 55 (17.0) [6] ((8)) | 384 (27.2) [11] ((17)) | 600 (25.1) [40] ((63)) | 0.53 (0.39 to 0.74) | 0.61 (0.45 to 0.83) |
| Child left in bath, without adult, even for a moment at least some daysb,c | 40 (12.5) [9] ((8)) | 314 (22.2) [12] ((13)) | 512 (21.5) [44] ((63)) | 0.47 (0.32 to 0.68) | 0.52 (0.37 to 0.73) |
| Bath run for child by an older child at least some daysb,c | 15 (5.6) [11] ((60)) | 65 (5.6) [19] ((252)) | 111 (5.5) [54] ((421)) | 1.13 (0.61 to 2.11) | 1.02 (0.59 to 1.78) |
| Older child looked after child in the bath at least some daysb,c | 29 (11.0) [10] ((64)) | 164 (14.2) [10] ((273)) | 265 (13.4) [54] ((463)) | 0.82 (0.53 to 1.27) | 0.80 (0.53 to 1.19) |
| Bath never run using cold water firstb,c | 246 (78.8) [8] ((18)) | 1125 (82.7) [22] ((56)) | 1760 (77.5) [65] ((155)) | 0.83 (0.61 to 1.13) | 1.08 (0.81 to 1.44) |
| Temperature of bathwater never checked using thermometer or other gadgetb,c | 228 (74.5) [10] ((22)) | 1045 (75.5) [9] ((45)) | 1688 (73.7) [60] ((141)) | 0.95 (0.71 to 1.29) | 1.04 (0.79 to 1.37) |
| Temperature of bathwater never checked using hand or elbowb,c | 90 (27.6) [7] ((5)) | 327 (23.4) [10] ((30)) | 561 (23.9) [48] ((91)) | 1.23 (0.94 to 1.62) | 1.21 (0.94 to 1.58) |
| Child not taught rules about things not to climb on in the kitchen | 160 (49.8) [17] | 609 (43.3) [32] | 824 (34.9) [129] | 1.52 (1.11 to 2.07) | 1.85 (1.47 to 2.34) |
| Child not taught rules about what to do or not do when parents are cooking using the top of the cooker | 175 (53.2) [9] | 636 (45.1) [27] | 873 (36.6) [107] | 1.78 (1.29 to 2.44) | 1.97 (1.56 to 2.48) |
| Child not taught rules about hot things in the kitchen | 181 (55.9) [14] | 655 (46.6) [32] | 920 (38.6) [105] | 1.79 (1.31 to 2.43) | 2.02 (1.59 to 2.55) |
| Child not taught rules about what to do or not do when in the bathtub | 141 (44.2) [19] | 471 (33.7) [39] | 653 (27.6) [123] | 2.16 (1.56 to 2.98) | 2.08 (1.64 to 2.64) |
| Exposures measured only in children aged 0–36 months | |||||
| n = 307 | n = 1300 | n = 1910 | |||
| Used baby walkera | 81 (27.0) [7] | 446 (34.7) [15] | 494 (26.6) [56] | 0.71 (0.53 to 0.94) | 1.01 (0.77 to 1.34) |
| Did not use playpen or travel cota | 252 (84.3) [8] | 1060 (82.6) [16] | 1543 (83.5) [61] | 1.16 (0.82 to 1.65) | 1.06 (0.76 to 1.48) |
| Did not use stationary activity centrea | 246 (82.0) [7] | 951 (74.0) [15] | 1458 (78.9) [63] | 1.62 (1.17 to 2.25) | 1.22 (0.89 to 1.67) |
| Exposure | Community controls, AOR (95% CI) | Hospital controls, AOR (95% CI) | Confounders adjusted fora |
|---|---|---|---|
| Did not use any safety gatesb | 1.46 (0.98 to 2.16) | 1.15 (0.83 to 1.61) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care |
| Had things child could climb on to reach high surfacesb | 1.24 (0.89 to 1.72) | 0.99 (0.73 to 1.34) | HADS score, PDH score, ability to climb, uses safety gate |
| Does not have curly flex or cordless kettleb | 0.93 (0.65 to 1.33) | 0.82 (0.59 to 1.12) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Kettle not at back of worktop/table or back ring of cookerb | 1.20 (0.67 to 2.15) | 1.11 (0.69 to 1.79) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Hot tap water too hotb | 0.96 (0.57 to 1.64) | 1.24 (0.81 to 1.89) | HADS score, PDH score, ability to climb, first child, bath access |
| Temperature of hot tap water not known or known to be > 54 °Cb | 0.99 (0.57 to 1.70) | 1.50 (0.93 to 2.40) | HADS score, PDH score, ability to climb, first child, bath access |
| Child climbed or played on furniture at least some daysc | 0.62 (0.40 to 0.96) | 0.74 (0.50 to 1.08) | HADS score, PDH score, ability to climb, safety gate |
| Child held by someone holding a hot drink at least some daysc | 0.83 (0.57 to 1.21) | 1.51 (1.05 to 2.15) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Child held by someone while using a cooker at least some daysc | 0.97 (0.67 to 1.41) | 1.39 (0.99 to 1.96) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Hot drinks passed over child’s head at least some daysc | 1.18 (0.71 to 1.98) | 1.70 (1.06 to 2.73) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Hot drinks left within reach of child at least some daysc | 2.33 (1.63 to 3.31) | 2.76 (2.00 to 3.80) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Hot drinks or hot liquids put on a table with a tablecloth at least some daysc | 1.33 (0.85 to 2.08) | 1.45 (0.97 to 2.17) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| The front rings of the cooker used at least some daysc | 0.70 (0.46 to 1.05) | 0.95 (0.66 to 1.36) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Pan handles never turned towards the back of the cooker while cookingc | 0.91 (0.63 to 1.32) | 1.01 (0.73 to 1.40) | HADS score, PDH score, ability to climb, first child, uses safety gate, climbable objects, playing/climbing on furniture, safety rules about climbing in kitchen |
| Child left in bathroom, without adult, even for a moment at least some daysc | 0.70 (0.48 to 1.01) | 0.88 (0.62 to 1.24) | HADS score, PDH score, ability to climb, first child, number of adults living with child, overcrowding |
| Child left in bath, without adult, even for a moment at least some daysc | 0.47 (0.30 to 0.75) | 0.65 (0.43 to 0.98) | HADS score, PDH score, ability to climb, first child, number of adults living with child, overcrowding |
| Bath run for child by an older child at least some daysc | 0.74 (0.31 to 1.82) | 0.89 (0.41 to 1.90) | HADS score, PDH score, ability to climb, first child, number of adults living with child, overcrowding |
| Older child looked after child in the bath at least some daysc | 1.10 (0.63 to 1.93) | 0.95 (0.58 to 1.55) | HADS score, PDH score, ability to climb, first child, number of adults living with child, overcrowding |
| Bath never run using cold water firstc | 0.85 (0.60 to 1.22) | 1.04 (0.75 to 1.44) | HADS score, PDH score, ability to climb, first child, hot water temperature |
| Temperature of bathwater never checked using thermometer or other gadgetc | 1.00 (0.70 to 1.43) | 1.26 (0.90 to 1.75) | HADS score, PDH score, ability to climb, first child, hot water temperature |
| Temperature of bathwater never checked using hand or elbowc | 1.19 (0.86 to 1.64) | 1.15 (0.85 to 1.56) | HADS score, PDH score, ability to climb, first child, hot water temperature |
| Child not taught rules about things not to climb on in the kitchen | 1.66 (1.12 to 2.47) | 1.68 (1.20 to 2.35) | HADS score, PDH score, ability to climb, first child, uses safety gate |
| Child not taught rules about what to do or not do when parents are cooking using the top of the cooker | 1.95 (1.33 to 2.85) | 1.76 (1.27 to 2.45) | HADS score, PDH score, ability to climb, first child, uses safety gate |
| Child not taught rules about hot things in the kitchen | 1.89 (1.30 to 2.75) | 1.65 (1.19 to 2.29) | HADS score, PDH score, ability to climb, first child, uses safety gate |
| Child not taught rules about what to do or not do when in the bathtub | 1.42 (0.85 to 2.37) | 1.57 (1.03 to 2.40) | HADS score, PDH score, ability to climb, first child, uses safety gate, bath access, hot water temperature, bath run with cold first, bath temperature checked |
| Used baby walkerb | 0.74 (0.52 to 1.03) | 1.16 (0.85 to 1.60) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care |
| Did not use playpen or travel cotb | 1.33 (0.86 to 2.06) | 1.14 (0.75 to 1.73) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care, baby walker |
| Did not use stationary activity centreb | 1.22 (0.83 to 1.79) | 1.09 (0.76 to 1.58) | HADS score, PDH score, ability to climb, first child, hours of out-of-home care, baby walker |
Case–control questionnaires
Case 0–12 months questionnaire
Case 13–36 months questionnaire
Case 37–59 months questionnaire
Control 0–12 months questionnaire
Control 13–36 months questionnaire
Control 37–59 months questionnaire
Home observation checklist for study B
Appendix 2 Follow-up questionnaires and mini questionnaire, medical record data extraction form and unit cost tables for study C
Mini questionnaire
Unit cost tables
| HRG code | Descriptiona,b | ED: not leading to admitted | ED: leading to admittedc | MIU: not leading to admitted | MIU: leading to admittedc | Walk-in centre: not leading to admitted | Walk-in centre: leading to admittedc |
|---|---|---|---|---|---|---|---|
| VB01Z | Emergency Medicine, Any Investigation with Category 5 Treatment | 264 (132–319) | 359 (241–502) | 63 (29–29) | 175 (113–130) | 58 (58–58) | |
| VB02Z | Emergency Medicine, Category 3 Investigation with Category 4 Treatment | 257 (173–328) | 319 (267–375) | 167 (57–248) | 123 (105–107) | 49 (49–49) | |
| VB03Z | Emergency Medicine, Category 3 Investigation with Category 1–3 Treatment | 220 (184–245) | 245 (185–276) | 149 (67–177) | 111 (78–123) | 85 (45–74) | |
| VB04Z | Emergency Medicine, Category 2 Investigation with Category 4 Treatment | 191 (147–203) | 210 (181–227) | 86 (55–94) | 136 (77–151) | 66 (45–58) | |
| VB05Z | Emergency Medicine, Category 2 Investigation with Category 3 Treatment | 164 (140–187) | 183 (157–206) | 88 (44–128) | 103 (71–90) | 63 (45–48) | |
| VB06Z | Emergency Medicine, Category 1 Investigation with Category 3–4 Treatment | 114 (95–131) | 137 (114–149) | 84 (57–106) | 69 (43–107) | 40 (39–39) | 36 (36–36) |
| VB07Z | Emergency Medicine, Category 2 Investigation with Category 2 Treatment | 143 (123–157) | 162 (139–179) | 76 (50–96) | 83 (55–92) | 40 (39–39) | |
| VB08Z | Emergency Medicine, Category 2 Investigation with Category 1 Treatment | 131 (113–146) | 155 (130–175) | 94 (56–130) | 106 (50–139) | 58 (51–51) | |
| VB09Z | Emergency Medicine, Category 1 Investigation with Category 1–2 Treatment | 91 (78–103) | 114 (101–119) | 58 (42–63) | 46 (36–42) | 58 (46–79) | 35 (35–35) |
| VB10Z | Emergency Medicine, Dental Care | 68 (78–103) | 152 (151–157) | 95 (26–126) | 89 (47–110) | 43 (24–62) | |
| VB11Z | Emergency Medicine, No Investigation with No Significant Treatment | 71 (59–82) | 94 (151–98) | 51 (43–58) | 49 (21–92) | 38 (32–41) | 42 (38–42) |
| Resource | Unit cost (IQR) (£) | Source |
|---|---|---|
| Health-care resources | ||
| Long inpatient stay ≥ 2 days (average cost per episode) | 2461.00 (1771–2865) | Curtis30 |
| Short inpatient stay 0–1 day (average cost per episode) | 586.00 (386–688) | Curtis30 |
| Day case | 680.00 (460–837) | Curtis30 |
| GP visit (average length of visit 11.7 minutes) | 36.00 | Curtis30 |
| GP-based nurse visit (average length of visit 15.5 minutes) | 11.63 | Curtis30 |
| Health visitor – home visit (average length of visit 20 minutesa) | 21.00 | Curtis30 |
| Health visitor – telephone (average length of call 7.1 minutesb) | 5.08 | Curtis30 |
| Consultant outpatient visit | 139.00 | Curtis30 |
| Hospital-based nurse visit | 22.00 | Curtis30 |
| Physiotherapist | 17.00 | Curtis30 |
| Subsequent visit to ED | 155.87 | Department of Health31 |
| Prescribed medication | ||
| Fucidin cream | 3.64 | BNF499 |
| Paracetamol | 0.72 | |
| Ibuprofen | 1.51 | |
| Eye drops | 1.75 | |
| Penicillin | 1.90 | |
| Flucloxacillin | 13.12 | |
| Yellow paraffin cream | 3.28 | |
| Aqueous cream | 1.72 | |
| Oilatum | 4.65 | |
| Hydrocortisone | 1.71 | |
| Siligel | 19.00 | |
| Pressure garment | 2.86 | |
| Silicon patch | 7.50 | |
| Non-health-care resources | ||
| Over-the-counter medication | ||
| Paracetamol | 4.89 | Chemist Direct [www.chemistdirect.co.uk/ (accessed 2 November 2016)] |
| Ibuprofen | 3.99 | |
| Sensodyne toothpaste | 3.89 | |
| Sudocrem | 3.49 | |
| Bio-Oil | 20.37 | |
| Professional child care (per hour) | 4.05 | Family and Childcare Trust500 |
| Time off paid work (per day) | ||
| 16–17 years | 32.00 | Office for National Statistics501 |
| 18–21 years | 55.90 | |
| 22–29 years | 82.40 | |
| 30–39 years | 111.40 | |
| 40–49 years | 114.50 | |
| 50–59 years | 107.20 | |
| 60+ years | 95.60 | |
| Time off other activities, i.e. non-work (per day) | 45.70 | Department for Transport493 |
| Travel (per km assuming average speed of 56 km/h) | 0.11 | Department for Transport493 |
Medical record data extraction form
Unique identity code:
Q1.1 Was child admitted to hospital for their original injury?
Q1.2 Number of nights?
Q1.3 Tests carried out in ED/ward.
-
Blood tests.
-
Urine tests.
-
Radiography.
-
Scan (computerised tomography, ultrasound, magnetic resonance imaging).
-
Other.
Q1.4 Treatments carried out in ED/ward
-
Observations.
-
Advice.
-
Medications by mouth.
-
Medications by injection.
-
Cream on skin.
-
Medications to take home.
-
Dressing to wound/burn.
-
Stitches.
-
Wound closure strips or glue.
-
Bandage/sling/support.
-
Splint.
-
Manipulation of fractured bone.
-
Dislocated joint.
-
Operation to fix fracture.
-
Cast/plaster of Paris.
-
Physiotherapy.
-
Stomach washout.
-
General anaesthetic.
-
Local anaesthetic.
-
Tetanus injection.
-
Drip.
-
Blood transfusion.
-
Chest drain.
-
Oxygen therapy.
-
Intubation.
-
Resuscitation.
-
Other.
Q1.5 Admissions since accident.
-
Number of overnight admissions.
-
Number of day-case admissions.
Q1.6 Other health professional contacts.
-
Doctor/consultant outpatients.
-
Nurse-led clinic.
-
Physiotherapist.
-
Other.
Appendix 3 The 2010 and 2012 questionnaires for study D
The 2010 questionnaire for study D
The 2012 questionnaire for study D
Appendix 4 Search strategy for study E and interview guides for studies F and G
Search strategy for identification of qualitative studies for the systematic review of barriers to, and facilitators of, injury prevention (study E)
The following search strategy was used to search MEDLINE. The search strategy was adapted as necessary for other databases.
-
comparative stud$.mp.
-
intervention stud$.mp.
-
evaluation stud$.mp.
-
feasibility.mp
-
qualitative.mp
-
1 or 2 or 3 or 4 or 5
-
human.sh.
-
exp CHILD/
-
exp INFANT/
-
MINORS/
-
(child$ or infan$ or young$ or minor$ or toddl$ or bab$).mp.
-
6 or 7 or 8 or 9 or 10 or 11
-
“EARLY INTERVENTION (EDUCATION)”/
-
exp EDUCATION/
-
exp PATIENT EDUCATION/ or exp HEALTH EDUCATION/ or exp EDUCATION/
-
exp Public Health/ed
-
exp PARENTING/
-
exp COUNSELING/
-
training.mp.
-
(educat$ or train$ or teach$ or parent$ or counsel$).mp. [mp=title, original title,
-
abstract, name of substance, mesh subject heading]
-
13 or 14 or 15 or 16 or 17 or 18 or 19 or 20
-
exp Accident Prevention/
-
SAFETY/
-
exp Safety Management/
-
safety practice$.mp.
-
exp Drug storage/
-
Hazardous Substances/ae, po [Adverse Effects, Poisoning]
-
22 or 23 or 24 or 25 or 26 or 27
-
safety equipment.mp. or Equipment Safety/
-
exp Infant Equipment/
-
protective devices.mp. or exp Protective Devices/
-
(fire-guard$ or fireguard$).mp.
-
(stair$ adj3 gate$).mp.
-
(protect$ adj3 device$).mp.
-
(kettle$ adj3 (flex$ or cable$ or wire$)).mp.
-
(cook$ adj3 guard$).mp.
-
(smok$ adj3 alarm$ or smok$ adj3 detect$).mp.
-
29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37
-
21 or 38
-
exp ACCIDENTS/ or exp ACCIDENTS, HOME/
-
exp EYE BURNS/ or exp BURNS, CHEMICAL/ or exp BURNS, INHALATION/ or exp
-
BURNS/ or exp BURNS, ELECTRIC/
-
SMOKE INHALATION INJURY/ or SMOKE/
-
exp POISONING/
-
CARBON MONOXIDE POISONING/ or exp POISONING/
-
exp “Wounds and Injuries”/
-
(accident$ or burn$ or scald$ or asphyx$ or chok$ or cut$ or suffocat$ or poison$ or
-
fracture$ or wound$ or injur$).mp.
-
exp FRACTURES/
-
suffocation.mp. or Asphyxia/
-
exp IPECAC/
-
NEAR DROWNING/ or exp DROWNING/ or drowning.mp.
-
40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50
-
barrier$.mp
-
facilitator$.mp
-
lever$.mp
-
motivator$.mp
-
implementation.mp
-
(process adj3 measure$).mp
-
52 or 53 or 54 or 55 or 56 or 57
-
(focus adj3 group$).mp
-
interview$.mp
-
59 or 60
-
(6 and 7 and 11) and (20 or 28 or 39) and 51
-
7 and 11 and (20 or 28 or 39) and 51
-
(6 and 7 and 11) and (20 or 28 or 39) and 51 and 61
Interview guide for interviews with children’s centre managers and staff (study G)
Interview guide for interviews with parents of injured children (study F)
Interview guide for interviews with parents with uninjured children (study G)
Appendix 5 Search terms and strategies for studies H and I and base-case model inputs for the decision analyses for study K
Search terms for the overviews of reviews and primary studies for study H
Reproduced from Cooper NJ, Kendrick D, Achana F, Dhiman P, He Z, Wynn P, Le Cozannet E, Saramago P, Sutton A. Network meta-analysis to evaluate the effectiveness of interventions to increase the uptake of smoke alarms. Epidemiologic Reviews 2012;34:32–45, by permission of Oxford University Press; Accident Analysis & Prevention 2013;60:158–171. Young B, Wynn PM, He Z, Kendrick D. Preventing childhood falls within the home: overview of systematic reviews and a systematic review of primary studies. 48 Copyright 2013, with permission from Elsevier; Wynn P, Zou K, Young B, Majsak-Newman G, Hawkins A, Kay B, Mhizha-Murira J, Kendrick D. Prevention of childhood poisoning in the home: overview of systematic reviews and a systematic review of primary studies. International Journal of Injury Control and Safety Promotion 2016;23:2–28;390 and Achana FA, Sutton AJ, Kendrick D, Wynn P, Young B, Jones DR, et al. (2015) The effectiveness of different interventions to promote poison prevention behaviours in households with children: a network meta-analysis. PLOS ONE 10(4): e0121122. 449 http://dx.doi.org/10.1371/journal.pone.0121122.
Fire-related injuries
The following search strategy was used to search MEDLINE for overviews of reviews, systematic reviews and meta-analyses. The search strategy was adapted as necessary for the other databases.
-
review.m_titl.
-
systematic.m_titl.
-
meta-analysis.m_titl.
-
review.pt.
-
meta-analysis.pt.
-
1 or 2 or 3 or 4 or 5
-
limit 6 to humans
-
exp CHILD/
-
exp INFANT/
-
1exp ADOLESCENT/
-
MINORS/
-
(child$ or adolesc$ or infan$ or young$ or minor$ or toddl$ or bab$).tw.
-
8 or 9 or 10 or 11 or 12
-
exp “early intervention (education)”/
-
exp EDUCATION/
-
exp Public Health/ed
-
exp PARENTING/
-
exp COUNSELING/
-
training.tw.
-
(educat$ or train$ or teach$ or parent$ or counsel$).tw.
-
14 or 15 or 16 or 17 or 18 or 19 or 20
-
exp Accident Prevention/ or injury prevention.tw.
-
SAFETY/
-
exp safety Management/
-
safety practice$.tw.
-
(firework or bonfire or barbecue).tw.
-
exp Cookery/
-
exp “Cooking and Eating Utensils”/
-
microwave.tw.
-
exp electricity/ or exp electric wiring/
-
(electrical appliance or electric blanket).tw.
-
candle.tw.
-
exp fire Extinguishing Systems/ or fire extinguisher.tw.
-
fire escape.tw.
-
exp firesetting Behavior/
-
thermostat$.tw.
-
hot iron.tw.
-
exp Heating/
-
22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38
-
safety equipment.tw. or exp Equipment Safety/
-
exp Infant Equipment/
-
exp protective devices/ or (protect$ adj3 device$).tw.
-
exp “interior design and furnishings”/
-
(fire-guard$ or fireguard$).tw.
-
(cook$ adj3 guard$).tw.
-
(((smok$ adj3 alarm$) or smok$) adj3 detect$).tw.
-
exp consumer product safety/
-
40 or 41 or 42 or 43 or 44 or 45 or 46 or 47
-
exp Smoking Cessation/
-
exp smoking/pc [prevention and control]
-
49 or 50
-
exp ACCIDENTS/ or exp ACCIDENTS, HOME/
-
exp burns/ or exp fires/
-
exp SMOKE INHALATION INJURY/ or SMOKE.tw.
-
exp “Wounds and Injuries”/
-
(accident$ or burn$ or wound$ or injur$).tw.
-
52 or 53 or 54 or 55 or 56
-
exp first aid/
-
(first adj3 aid).tw.
-
58 or 59
-
(7 and 13 and (21 or 39 or 48 or 51) and 57) or (7 and 60)
The above search was adapted to find primary studies published since the most comprehensive systematic review,352 substituting the terms below for study design terms in lines 1–6.
For experimental study designs
-
randomi?ed controlled trial.pt.
-
randomi?ed controlled trials.sh.
-
randomi?ed controlled trial$.mp. or Randomi?ed Controlled Trials/
-
random allocation.sh.
-
double blind method.sh.
-
single blind method.sh.
-
Random Allocation/
-
1 or 2 or 3 or 4 or 5 or 6 or 7
-
Clinical Trials/ or Placebos/
-
CONTROLLED CLINICAL TRIAL.pt.
-
comparative stud$.mp.
-
intervention stud$.mp.
-
control group$.mp. or Control Groups/
-
placebo$.mp. or PLACEBOS/
-
evaluation stud$.mp.
-
9 or 10 or 11 or 12 or 13 or 14 or 15
For case–control and cohort studies
-
exp Case-Control Studies/
-
exp Cohort Studies/
-
1 or 2
First aid
The following search strategy was used to search MEDLINE for overviews of reviews, systematic reviews and meta-analyses. The search strategy was adapted as necessary for the other databases.
-
review.m_titl.
-
systematic.m_titl.
-
meta-analysis.m_titl.
-
review.pt.
-
meta-analysis.pt.
-
1 or 2 or 3 or 4 or 5
-
limit 6 to humans
-
(lay people or lay-people or laypeople or layperson$ or lay-person$ or lay person$).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
(bystander or by-stander).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
parents/ or fathers/ or mothers/ or single parent/ or persons/
-
middle-aged.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
persons/ or legal guardians/
-
adolescen$.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
adult$.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
Child$.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
(caregiver$ or care giver$ or care-giver$).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
(child minder$ or childminder$ or child-minder$ or childminding or child minding).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
Population/
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
-
child health services/ or “early intervention (education)”/ or preventive health services/
-
child welfare.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
Learning/ed [Education]
-
educational measurement.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
exp public health/ed
-
train*.tw.
-
learn*.tw.
-
teach*.tw.
-
instruct*.tw.
-
counsel*.tw.
-
question$.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
(educat$ or train$ or teach$ or Parent$ or counsel$).tw.
-
20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31
-
accident$.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
emergencies.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
first aid/mt
-
(“pediatric first aid” or “paediatric first aid”).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
health education/st
-
(“first aid” or “first-aid” or First Aid or First-aid).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
basic life support.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
emergency treatment/ or first aid/ or resuscitation/
-
(emergency medicine or emergency nursing).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
first aid.tw.
-
first response.tw.
-
prehospital care.mp. or pre-hospital care.tw. [mp=title, abstract, heading word, table of contents, key concepts]
-
prehospital management.mp. or pre-hospital management.tw. [mp=title, abstract, heading word, table of contents, key concepts]
-
Life support*.tw.
-
bystander cardiopulmonary resuscitation.mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
(“layperson CPR” or “lay-person CPR” or “layperson cardiopulmonary resuscication” or “lay-person cardiopulmonary resuscitation”).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
lifesupport*.tw.
-
lifesaving.tw.
-
first response/
-
life support/
-
life saving/
-
life-saving/
-
(“CPR” or “Cardio Pulmonary Resuscitation”).mp. or “Cardiopulmonary Resuscitation”/ [mp=title, abstract, heading word, table of contents, key concepts]
-
Cardio-Pulmonary Resuscitation/
-
33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56
-
(First Aid cours$ or first-aid cours$).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
(First Aid Skill$ or first-aid skill$).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
(First Aid Training or First-Aid Training).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
Survival skill$.mp.
-
(life support cours$ or life-support cours$).mp. [mp=title, abstract, heading word, table of contents, key concepts]
-
58 or 59 or 60 or 61 or 62
-
7 and 19 and 32 and 57 and 63
The above search was adapted to find primary studies published since the most comprehensive systematic review,352 substituting the terms below for study design terms in lines 1–6.
For experimental study designs
-
randomi?ed controlled trial.pt.
-
randomi?ed controlled trials.sh.
-
randomi?ed controlled trial$.mp. or Randomi?ed Controlled Trials/
-
random allocation.sh.
-
double blind method.sh.
-
single blind method.sh.
-
Random allocation/
-
1 or 2 or 3 or 4 or 5 or 6 or 7
-
clinical trials/ or Placebos/
-
CONTROLLED CLINICAL TRIAL.pt.
-
Comparative stud$.mp.
-
intervention stud$.mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
-
control group$.mp. or Control Groups/
-
placebo$.mp. or PLACEBOS/ [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
-
evaluation stud$.mp.
-
9 or 10 or 11 or 12 or 13 or 14 or 15
For case–control and cohort studies
-
exp Case-Control Studies/
-
exp Cohort Studies/
-
1 or 2
Falls
The following search strategy was used to search MEDLINE for studies with experimental or observational designs, and adapted as necessary for the other databases.
-
exp Case-Control Studies/
-
exp Cohort Studies/
-
1 or 2
-
randomized controlled trial.pt.
-
randomized controlled trials.sh.
-
randomized controlled trial$.mp. or Randomized Controlled Trials/
-
random allocation.sh.
-
double blind method.sh.
-
single blind method.sh.
-
Random Allocation/
-
4 or 5 or 6 or 7 or 8 or 9 or 10
-
Clinical Trials/ or Placebos/
-
controlled clinical trial.pt.
-
comparative stud$.mp.
-
intervention stud$.mp.
-
control group$.mp. or Control Groups/
-
placebo$.mp. or Placebos/
-
evaluation stud$.mp.
-
12 or 13 or 14 or 15 or 16 or 17 or 18
-
exp child/
-
exp infant/
-
exp adolescent/
-
exp minors/
-
(child$ or adolesc$ or infan$ or young$ or toddl$ or bab$).tw.
-
20 or 21 or 22 or 23 or 24
-
exp “early intervention (education)”/
-
exp education/
-
exp public health/ed
-
exp parenting/
-
exp counseling/
-
(educat$ or train$ or teach$ or parent$ or counsel$ or supervis$).tw.
-
26 or 27 or 28 or 29 or 30 or 31
-
exp accident prevention/ or injury prevention.tw.
-
exp safety/
-
exp safety management/
-
safety practice$.tw.
-
33 or 34 or 35 or 36
-
safety equipment.tw. or exp equipment safety/
-
exp infant equipment/
-
exp protective devices/ or (protect$ adj3 device$).tw.
-
exp “interior design and furnishings”/
-
((stair$ or safety) adj3 gate$).tw.
-
((bab$ adj3 walk$) or (infant$ adj3 walk$)).tw.
-
((bab$ adj3 exercis$) or (bab$ adj3 bouncer$)).tw.
-
(playpen$ or activity cent$ or play cent$).tw.
-
(play$ adj3 equipment).tw.
-
(cot$ or crib$).tw.
-
(furniture adj3 corner adj3 cover$).tw.
-
(trip adj3 (flex$ or cable$ or wire$ or lead$)).tw.
-
((high adj3 chair$) or highchair or (changing adj3 table$) or cradle$).tw.
-
(pushchair$ or pram$ or stroller$).tw.
-
((child adj3 safety adj3 restraint$) or (safety adj3 harness$)).tw.
-
((((high or raised) and surface$) or bed$) adj3 (fall$ or drop$ or push$ or roll$)).tw.
-
(window$ adj3 (safety or lock$ or guard$ or bar$ or catch$ or screen$ or restrict$ or limit$ or opening$)).tw.
-
(child-proof or child proof or childproof).tw.
-
(glass adj3 (safety or film)).tw.
-
(garden$ adj3 (lock$ or restrict$ or access$)).tw.
-
((roof$ or rooves) adj3 (lock$ or restrict or access$)).tw.
-
(bath$ adj3 (mat$ or decal$ or $slip$)).tw.
-
(wet adj3 floor).tw.
-
((trip$ adj3 hazard$) or stumble$ or (lose adj3 balance)).tw.
-
((carpet$ or rug$) adj3 (fix$ or loose or trip$)).tw.
-
((floor$ or stair$ or step$) and $repair$).tw.
-
(stair$ adj3 (light$ or safe$ or play$ or climb$ or trip$ or fall$)).tw.
-
(banister$ or handrail$ or stair$ or railing$).tw.
-
(furniture adj3 (climb$ or jump$ or play$ or fall$ or layout)).tw.
-
(balcon$ adj3 fall$).tw.
-
exp consumer product safety/
-
or/38-68
-
exp accidents/ or exp accidents, home/
-
exp accidental falls/
-
exp “wounds and injuries”/
-
(accident$ or cut or cuts or bruis$ or fracture$ or wound$ or laceration$ or injur$).tw.
-
or/70-73
-
(3 or 11 or 19) and 25 and (32 or 37 or 69) and 74
Search terms for systematic reviews and meta-analyses were as above but with terms 1–19 replaced with:
-
review.m_titl.
-
systematic.m_titl.
-
meta-analysis.m_titl.
-
review.pt.
-
meta-analysis.pt.
-
1 or 2 or 3 or 4 or 5
Poisoning
The following search strategy was used to search MEDLINE for overviews of reviews, systematic reviews and meta-analyses. The search strategy was adapted as necessary for the other databases.
-
review.m_titl.
-
systematic.m_titl.
-
meta-analysis.m_titl.
-
review.pt.
-
meta-analysis.pt.
-
1 or 2 or 3 or 4 or 5
-
limit 6 to humans
-
exp child/
-
exp infant/
-
exp adolescent/
-
exp minors/
-
(child$ or adolesc$ or infan$ or young$ or toddl$ or bab$).tw.
-
or/8-12
-
exp “early intervention (education)”/
-
exp education/
-
exp public health/ed
-
exp parenting/
-
exp counseling/
-
(educat$ or train$ or teach$ or parent$ or counsel$ or supervis$).tw.
-
exp accident prevention/ or injury prevention.tw.
-
exp safety/
-
exp safety management/
-
safety practice$.tw.
-
safety equipment.tw. or exp equipment safety/
-
exp infant equipment/
-
exp protective devices/ or (protect$ adj3 device$).tw.
-
exp “interior design and furnishings”/
-
exp consumer product safety/
-
exp drug storage/
-
((medicine$ or drug$) adj3 storage).tw.
-
exp hazardous substances/ae, po or (hazardous adj3 substance$ adj3 storage).tw.
-
exp household products/ae, po or (household adj3 product$ adj3 storage).tw.
-
(((child adj3 resistant) or childproof) adj3 (closure$ or cap$ or container$)).tw.
-
((cupboard$ or cabinet$ or drawer$ or box$) adj3 ($lock$ or latch$)).tw.
-
(medicine$ or cosmetics or ((clean$ or beauty or make-up or household or hazardous or industrial) adj3 (supplies or products or materials))).tw.
-
((toiletries or vitamin$ or cigarette$) adj3 (storage or cupboard$ or cabinet$ or drawer$ or box$ or reach or label$)).tw.
-
((toxi$ or pollutant$ or gas$) adj3 prevent$).tw.
-
((toxic or poison$) adj3 plant$ adj3 prevent$).tw.
-
exp ipecac/
-
(poison$ adj3 (control or sticker$ or telephone or number or emergenc$)).tw.
-
or/14-40
-
exp accidents/ or exp accidents, home/
-
exp poisoning/
-
exp “wounds and injuries”/
-
(accident$ or poison$ or injur$ or ingest$ or swallow$ or inhal$).tw.
-
or/42-45
-
7 and 13 and 41 and 46
The above search was adapted to find primary studies published since the most comprehensive systematic review,352 substituting the terms below for study design terms in lines 1–6.
For experimental study designs
-
randomi?ed controlled trial.pt.
-
randomi?ed controlled trials.sh.
-
randomi?ed controlled trial$.mp. or Randomi?ed Controlled Trials/
-
random allocation.sh.
-
double blind method.sh.
-
single blind method.sh.
-
Random Allocation/
-
1 or 2 or 3 or 4 or 5 or 6 or 7
-
Clinical Trials/ or Placebos/
-
CONTROLLED CLINICAL TRIAL.pt.
-
comparative stud$.mp.
-
intervention stud$.mp.
-
control group$.mp. or Control Groups/
-
placebo$.mp. or PLACEBOS/
-
evaluation stud$.mp.
-
9 or 10 or 11 or 12 or 13 or 14 or 15
For case–control and cohort studies
-
exp Case-Control Studies/
-
exp Cohort Studies/
-
1 or 2
Scalds
The following search strategy was used to search MEDLINE for overviews of reviews, systematic reviews and meta-analyses. The search strategy was adapted as necessary for the other databases.
-
review.m_titl.
-
systematic.m_titl.
-
meta-analysis.m_titl.
-
review.pt.
-
meta-analysis.pt.
-
4 or 1 or 3 or 2 or 5
-
limit 6 to humans
-
exp child/
-
exp infant/
-
exp adolescent/
-
exp minors/
-
(child$ or adolesc$ or infan$ or young$ or minor$ or toddl$ or bab$).tw.
-
8 or 11 or 10 or 9 or 12
-
exp “early intervention (education)”/
-
exp education/
-
exp public health/ed
-
exp parenting/
-
expcounseling/
-
training.tw.
-
(edcat$ or train$ or teach$ or parent$ or counsel$).tw.
-
18 or 19 or 16 or 17 or 20 or 15 or 14
-
exp accident prevention/ or injury prevention.tw.
-
exp safety/
-
exp safety management/
-
safety practice$.tw.
-
exp cookery/
-
exp “cooking and eating utensils”/
-
microwave.tw.
-
hot water.tw.
-
hot liquid.tw.
-
hot drink$.tw.
-
hot food.tw.
-
(thermo$ or thermostat$).mp. or TMV.tw.
-
safety equipment.tw. or exp equipment safety/
-
exp infant equipment/
-
exp protective devices/ or (protect$ adj3 device$).tw.
-
(kettle* or teapot* or samovar* or coffee pot* or jug*).tw.
-
(kettle$ adj3 (flex$ or cable$ or wire$)).tw.
-
(cook$ adj3 guard$).tw.
-
(oven$ or stove$ or grill$ or hob$).mp.
-
(“saucepan$” or “sauce pan$” or “sauce-pan$”).tw.
-
kettle.tw.
-
(water adj3 temperature).mp.
-
hot tap water.tw.
-
bath$.tw.
-
steam$.tw.
-
hotfa*cet water.tw.
-
water temperature.tw.
-
cooker safety.tw.
-
(“table cloth$” or “table-cloth$”).tw.
-
exp heat/
-
exp hot temperature/ae
-
or/22-52
-
exp bath/ae
-
exp accidents/ or exp accidents, home/
-
exp burns/
-
exp “wounds and injuries”/
-
(accident$ or burn$ or scald$ or wound$ or injur$).tw.
-
or/54-58
-
7 and 13 and (21 or 53) and 59
The above search was adapted to find primary studies published since the most comprehensive systematic review,352 substituting the terms below for study design terms in lines 1–6.
For experimental study designs
-
randomi?ed controlled trial.pt.
-
randomi?ed controlled trials.sh.
-
randomi?ed controlled trial$.mp. or Randomi?ed Controlled Trials/
-
random allocation.sh.
-
double blind method.sh.
-
single blind method.sh.
-
Random Allocation/
-
1 or 2 or 3 or 4 or 5 or 6 or 7
-
Clinical Trials/ or Placebos/
-
CONTROLLED CLINICAL TRIAL.pt.
-
comparative stud$.mp.
-
intervention stud$.mp.
-
control group$.mp. or Control Groups/
-
placebo$.mp. or PLACEBOS/
-
evaluation stud$.mp.
-
9 or 10 or 11 or 12 or 13 or 14 or 15
For case–control and cohort studies
-
exp Case-Control Studies/
-
exp Cohort Studies/
-
1 or 2
Other sources searched for overviews of reviews and primary studies for study H
From Wynn P, Zou K, Young B, Majsak-Newman G, Hawkins A, Kay B, Mhizha-Murira J, Kendrick D. Prevention of childhood poisoning in the home: overview of systematic reviews and a systematic review of primary studies. International Journal of Injury Control and Safety Promotion 2016;23:2–28390 and Achana FA, Sutton AJ, Kendrick D, Wynn P, Young B, Jones DR, et al. (2015) The effectiveness of different interventions to promote poison prevention behaviours in households with children: a network meta-analysis. PLOS ONE 10(4): e0121122. 449 http://dx.doi.org/10.1371/journal.pone.0121122
| Other electronic sources | Hand searching |
|---|---|
| Cochrane Database of Systematic Reviews | Injury Prevention (journal) |
| Database of Abstracts of Reviews of Effects | Abstracts from World Conferences on Injury Prevention and Controla |
| NHS Economic Evaluation Database and Health Technology Assessment database | Reference lists of included overviews of reviews, systematic reviews, meta-analyses and primary studies |
| Injury Prevention Research Centers at the Centers for Disease Control (USA) | |
| NICE (UK) | |
| Children’s Safety Network (USA) | |
| International Society for Child and Adolescent Injury Prevention (international) | |
| Child Accident Prevention Trust (UK) | |
| RoSPA (UK) | |
| Injury Control Resource Information Network (USA) | |
| National Injury Surveillance Unit (Australia) | |
| SafetyLit (USA) | |
| National Research Register (UK) (up to September 2007) | |
| UK Clinical Research Network Portfolio |
Other sources searched for study I
| Other electronic sources | Hand searching (to June 2009) |
|---|---|
| Injury Prevention Research Centers at the Centers for Disease Control (USA) | Abstracts from the First to Ninth World Conferences on Injury Prevention and Control |
| Health Development Agency (UK) (up to March 2005) | Injury Prevention (journal) (to March 2009) |
| NICE (UK) | Reference lists of articles included in the review and of published systematic reviews |
| Children’s Safety Network (USA) | |
| International Society for Child and Adolescent Injury Prevention (international) | |
| Child Accident Prevention Trust (UK) | |
| Injury Control Resource Information Network (USA) | |
| National Injury Surveillance Unit (Australia) | |
| SafetyLit (USA) | |
| National Research Register (UK) (up to September 2007) | |
| UK Clinical Research Network Portfolio | |
| metaRegister of Current Controlled Trials | |
| Index to Theses |
Search strategy for study I
The following search strategy was used to search MEDLINE. The search strategy was adapted as necessary for the other databases.
-
randomized controlled trial.pt.
-
exp Randomized Controlled Trial/
-
randomi?ed controlled trial*.mp.
-
exp Random Allocation/
-
exp Double-Blind Method/
-
exp Single-Blind Method/
-
exp Clinical Trial/
-
controlled clinical trial.pt.
-
comparative stud*.mp.
-
intervention stud*.mp.
-
control group*.mp.
-
placebo*.mp.
-
evaluation stud*.mp.
-
placebo*.mp.
-
exp Placebos/
-
exp control groups/
-
random allocation.mp.
-
or/1-17
-
Humans/
-
18 and 19
-
exp Child/
-
exp Infant/
-
exp Adolescent/
-
exp Minors/
-
(child* or adolesc* or infan* or young* or minor* or toddl* or baby or babies).mp.
-
or/21-25
-
exp “Early Intervention (Education)”/
-
exp Education/
-
exp Patient Education as Topic/
-
exp Health Education/
-
public health/ed
-
exp Parenting/
-
exp Counseling/
-
training.mp.
-
(educat* or train* or teach* or parent* or counsel*).mp.
-
or/27-35
-
exp Accident Prevention/
-
exp Safety/
-
exp Safety Management/
-
safety practice*.mp.
-
exp Drug Storage/
-
exp Hazardous Substances/po, ae [Poisoning, Adverse Effects]
-
or/37-42
-
exp Equipment Safety/
-
(safety adj3 equipment).mp.
-
exp Infant Equipment/
-
exp Protective Devices/
-
(fireguard* or fire-guard*).mp.
-
(stair* adj3 gate*).mp.
-
(bab* adj3 walk*).mp.
-
(protect* adj3 device*).mp.
-
(kettle* adj3 (flex* or cable* or wire*)).mp.
-
(cook* adj3 guard*).mp.
-
(smok* adj3 (alarm* or detect*)).mp.
-
or/44-54
-
exp Accidents/
-
exp Accidents, Home/
-
exp Burns, Chemical/
-
exp Eye Burns/
-
exp Burns/
-
exp Burns, Inhalation/
-
exp Burns, Electric/
-
exp Smoke/
-
exp Smoke Inhalation Injury/
-
exp Poisoning/
-
exp Carbon Monoxide Poisoning/
-
exp “Wounds and Injuries”/
-
(accident* or burn* or scald* or asphyx* or chok* or cut* or suffocat* or poison* or fracture* or wound* or injur*).mp.
-
exp Fractures, Bone/
-
exp Asphyxia/
-
suffocat*.mp.
-
exp Ipecac/
-
exp Drowning/
-
exp Near Drowning/
-
or/56-74
-
20 and 26
-
36 or 43 or 55
-
75 and 76 and 77
-
(2004* or 2005* or 2006* or 2007* or 2008* or 2009*).ed.
-
78 and 79
Base-case model inputs for the decision analysis for smoke alarms for study K
General base-case model inputs
| Parameter description | Point estimate (95% CrI) | Parameter distribution | Source |
|---|---|---|---|
| Stage 1: Intervention model | |||
| Cohort settings | |||
| Total number of households in the UK | 26,442,100 | Office for National Statistics502 | |
| Probabilities of possessing a functioning smoke alarms following each intervention | |||
| (1) Usual care | 0.695 (0.647 to 0.740) | Posterior distribution inputted directly from NMA | NMA by Cooper et al.374 |
| (2) Education | 0.671 (0.207 to 0.942) | As above | As above |
| (3) Education + free/low-cost equipment | 0.876 (0.459 to 0.986) | As above | As above |
| (4) Education + free/low-cost equipment + home safety inspection | 0.852 (0.448 to 0.983) | As above | As above |
| (5) Education + free/low-cost equipment + fitting | 0.859 (0.400 to 0.982) | As above | As above |
| (6) Education + home safety inspection | 0.880 (0.413 to 0.991) | As above | As above |
| (7) Education + free/low-cost equipment + fitting + home safety inspection | 0.941 (0.651 to 0.993) | As above | As above |
| Smoke alarm | |||
| Probability of accepting intervention (assumed same for all interventions) | 0.9 | Fixed | Assumption based on studies included in NMA374 |
| Probability of a household having a functioning smoke alarm (baseline) | 0.860 | Beta (n = 18,386) | Department for Communities and Local Government377 (Table 2.3) |
| Probability of owning a smoke alarm with a battery life of 1 year | 0.750 | Beta (n = 15,850) | Office of the Deputy Prime Minister376 (Table 5.3) |
| Probability of testing smoke alarm at least once a year | 0.850 | Beta (n = 18,372) | Office of the Deputy Prime Minister376 (Figure 5.1) |
| Probability of testing smoke alarm less than once a year | 0.02 | Beta (n = 18,372) | Office of the Deputy Prime Minister376 (Figure 5.1) |
| Stages 2 and 3: Preschool and long-term model | |||
| Probability of a fire | |||
| Probability of a fire when functioning smoke alarms present | Fires when smoke alarm was present, operated and raised or not the alarm = 20,706 (out of 43,451 fires); assuming that fires occurred in different dwellings: 20,706/26,442,100 = 0.000783 | Beta (n = 26,442,100) | Department for Communities and Local Government377 (Table 2.4) |
| Probability of a fire when non-functioning smoke alarms present | Fires when smoke alarm was present but did not operate = 7854 (out of 43,451 fires); assuming that fires occurred in different dwellings: 7854/26,442,100 = 0.000297 | Beta (n = 26,442,100) | Department for Communities and Local Government377 (Table 2.4) |
| Probability of a fire when no smoke alarms present or unspecified | Fires when smoke alarm was absent or unspecified = 14,891 (out of 43,451 fires); assuming that fires occurred in different dwellings: 14,891/26,442,100 = 0.000563 | Beta (n = 26,442,100) | Department for Communities and Local Government377 (Table 2.4) |
| Probability of inside household fire being attended by the fire and rescue service | 0.15 | Beta (n = 272) | Office of the Deputy Prime Minister376 (Table 3.4) |
| Probability of injury or fatality | |||
| Probability of a fatality following a fire when functioning smoke alarm present | Fires when smoke alarm was present, operated and raised or not the alarm and there were fatal casualties = 122 (out of 287 casualties); 122/20,706 = 0.005892 | Beta (n = 20,706) | Department for Communities and Local Government377 (Table 2.4) |
| Probability of a fatality following a fire when non-functioning or no smoke alarm | Fires when smoke alarm was present but did not operate or was absent and there were fatal casualties = 165 (out of 287 casualties); 165/(7854 + 14,891) = 0.007254 | Beta (n = 22,745) | Department for Communities and Local Government377 (Table 2.4) |
| Probability of no injury following a house fire with ‘functioning’ and ‘no/non-functioning’ smoke alarms | Probability of injury when functional smoke alarm present = 0.11; therefore, the probability of no injury with ‘functioning’ smoke alarm = 1 – 0.11 = 0.89 Probability of injury when functional smoke alarm absent = 0.125; therefore, the probability of no injury without ‘functioning’ smoke alarm = 1 – 0.125 = 0.875 |
Beta (n = 43,451) | Istre et al.503 (Table 2) |
| Probability that a child aged 0–4 years incurs a minor, moderate or severe injury given a burn injury, following a house fire | Minor injury 0.368; moderate injury 0.158; severe injury (requires inpatient stay in an intensive care unit of > 5 days) 0.474 | Multinomial (n = 19) | Mr Kenn Dunn, University Hospital of South Manchester, 8 September 2010, personal communication |
| Additional proportion of burn unit costs incurred in an intensive therapy unit | 0.4 (assumption SE = 0.1) | Beta (alpha = 9.2, beta = 13.8) | Assumption based on analysis in Hemington-Gorse et al.504 |
| Probability of having a precautionary check-up following a fire | 0.437 | Beta (n = 12,935) | Department for Communities and Local Government505 (Table 8) |
| Probability of all-cause mortality for a UK citizen aged from 0 to 100 years (for use in each decision model cycle) | Age dependent | Office for National Statistics 2009506 | |
Base-case model inputs for quality-of-life weights and costs (updated to 2012 prices)
| Model input | Point estimate (SE) | Parameter distribution | Source |
|---|---|---|---|
| Stage 1: Intervention model | |||
| Intervention costs | |||
| Cost of home safety inspection based on cost of local authority home care worker for 40 minutes of their time including travel | £23 per hour, thus 40 minutes = £15.33 | Fixed | Curtis30 |
| Cost of smoke alarm giveaway | £4.89 | Fixed | Jane Zdanowska, Nottinghamshire County Council, 28 September 2010, personal communication |
| Cost of providing education programme per household accepting the intervention – based on cost of home care worker for 20 minutes of their time including travel | Assume £20 per hour, thus 20 minutes = £6.66 | Fixed | Assumption |
| Fixed cost of an intervention scheme – programme co-ordination | Considering a simulated cohort of 100,000 households = £79,529 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Additional administrative cost incurred for each household that accepts the intervention | Distribution costs divided by the number of households in the cohort and updated to 2012 prices = £0.40 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Cost of having the smoke alarm installed | Installation costs divided by the number of smoke alarms installed and updated to 2012 prices = £11.83 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Stages 2 and 3: Preschool and long-term model | |||
| Health-care costs/resource use | |||
| Mean number of minutes of paramedic unit – assumed only attends when severe injuries | 49.5 | Normal [variance = 26.32 (assumption)] | Curtis508 |
| Mean number of minutes of emergency ambulance – assumed only attends when moderate injuries | 38.6 | Normal [variance = 26.32 (assumption)] | Curtis508 |
| Mean cost per minute of a paramedic unit | £8.00 | Fixed | Curtis508 – updated to 2012 prices |
| Mean cost per minute of an emergency ambulance | £7.89 | Fixed | Curtis508 – updated to 2012 prices |
| Mean cost of a minor injury | £1206 (£209) | Log-normal | Mr Kenn Dunn, University Hospital of South Manchester, 8 September 2010, personal communication |
| Mean cost of a moderate injury | £2855 (£1415) | Log-normal | As above |
| Mean cost of a severe injury | £64,939 (£32,019) | Log-normal | As above |
| Mean incurred NHS costs of disability per year | £379.50 (£85.50) | Gamma (alpha = 16, beta = 0.047) | Medical Care Research Unit (J Nicholl, personal communication) – updated to 2012 prices |
| Mean cost of precautionary check-up | £68.80 (£21.50) | Normal | Department of Health509 |
| Out-of-pocket/private costs | |||
| Cost of smoke alarm 1-year battery to individual | £1.54 | Fixed | www.safelincs.co.uk (accessed 3 November 2016) |
| Total cost of damage caused by the fire | £1298 (£245) | Gamma (alpha = 16, beta = 0.016) | Office of the Deputy Prime Minister510 (Table 3.8) – updated to 2012 prices |
| Cost of a fatality following a household fire – includes coroner and autopsy costs | £205.50 | Fixed | Ginnelly et al.347 (Table 1) – updated to 2012 prices |
| Law enforcement and rescue service costs | |||
| Cost of police attending – assumed only attend when severe injuries | £173.90 | Fixed | Ginnelly et al.347 (Table 1) – updated to 2012 prices |
| Cost of fire and rescue service attending a domestic fire | £3386 | Fixed | Office of the Deputy Prime Minister511 (Table 3.6) – updated to 2012 prices |
| Utility parameters per cycle | |||
| Deficit in utilities for minor injury (DRG 460 + 459) | 0.049 | Fixed | Sanchez et al.512 |
| Deficit in utilities for moderate injury (DRG 458 + 457) | 0.069 | Fixed | Sanchez et al.512 |
| Deficit in utilities for severe injury (DRG 472) | 0.107 | Fixed | Sanchez et al.512 |
| Deficit in utilities following a disability | 0.1 (0.025) | Beta (alpha = 14.3, beta = 128.7) | Medical Care Research Unit (J Nicholl, personal communication) |
| General background utilities for non-injured population | < 25 years 0.94 (SD 0.12); 25–34 years 0.93 (SD 0.15); 35–44 years 0.91 (SD 0.16); 45–54 years 0.85 (SD 0.25); 55–64 years 0.80 (SD 0.26); 65–74 years 0.78 (SD 0.26); > 75 years 0.73 (SD 0.27) | Normal | Kind et al.375 |
Base-case model inputs for the decision analysis for safe hot tap water temperatures for study K
General base-case model inputs
| Model input | Point estimate (95% CrI) | Parameter distribution | Source |
|---|---|---|---|
| Stage 1: Intervention model | |||
| Cohort settings | |||
| Total number of households in the UK | 26,442,100 | Office for National Statistics502 | |
| Probabilities of safe hot water following each intervention | |||
| (1) Usual care | 0.35 (0.30 to 0.40) | Posterior distribution inputted directly from NMA | From NMA of safe hot water interventions |
| (2) Education | 0.48 (0.34 to 0.63) | As above | As above |
| (3) Education + thermometer | 0.35 (0.19 to 0.54) | As above | As above |
| (4) Education + free/low-cost not scald equipment + home safety inspection | 0.41 (0.20 to 0.66) | As above | As above |
| (5) Education + thermometer + home safety inspection | 0.35 (0.19 to 0.55) | As above | As above |
| (6) Education + TMV + fitting | 0.95 (0.66 to 1.00) | As above | As above |
| (7) Education + TMV + fitting + home safety inspection | 0.27 (0.04 to 0.79) | As above | As above |
| (8) Education + home safety inspection | 0.45 (0.15 to 0.79) | As above | As above |
| (9) Education + free/low-cost not scald equipment + fitting + home safety inspection | 0.49 (0.16 to 0.78) | As above | As above |
| Safe hot water | |||
| Probability of accepting intervention (assumed same for all interventions) | 0.74 | Beta (n = 62) | Kendrick et al.276 |
| Probability that a household has safe hot water baseline | 0.15 (0.12 to 0.19) | Meta-analysis of trials | |
| Number of children per household | 1.8 | ||
| Stages 2 and 3: Preschool and long-term model | |||
| Probability of a scald | |||
| Probability of a scald when safe hot water using TMV | 0 | Assumption | |
| Probability of a scald when safe hot water using ‘other’ interventions | 0.000057 | 10% of probability of scald when no safe hot water | Assumption |
| Probability of a scald when no safe hot water | 0.00057 | Beta (n = 3,486,469) assumes 1.8 children per household | Phillips et al.140 and Office for National Statistics378 |
| Probability move from safe hot water to no safe hot water at the end of a cycle | 0 | Assumption | |
| Probability move from no safe hot water to safe hot water at the end of a cycle | 0.13 | Beta (n = 62) | Kendrick et al.276 |
| Probability of an injury or a fatality | |||
| Probability of a fatality following a scald | 0 | NA | Office for National Statistics513 |
| Probability of a child aged 0–4 years attending an ED with a scald but not admitted to hospital | 0.23 | Beta (n = 653) | Philips et al. 2011140 |
| Probability of a child aged 0–4 years incurring a minor, moderate or severe injury given a scald injury | Minor injury 0.21; moderate injury 0.68; severe injury (requires inpatient stay in an intensive care unit of > 5 days) 0.11 | Multinomial (n = 1107) | Mr Ken Dunn, South Manchester University Hospital, 8 September 2010, personal communication |
| Probability of all-cause mortality for a UK citizen aged from 0 to 100 years (for use in each decision model cycle) | Age dependent | Office for National Statistics506 | |
Base-case model inputs for quality-of-life weights and costs (updated to 2012 prices) for interventions to promote safe hot tap water temperatures
| Model input | Point estimate (SE) | Parameter distribution | Source |
|---|---|---|---|
| Stage 1: Intervention model | |||
| Intervention costs | |||
| Cost of home safety inspection based on cost of local authority home care worker for 40 minutes of their time including travel | £23 per hour, thus 40 minutes = £15.33 | Fixed | Curtis30 |
| Cost of thermometer giveaway | £0.83 | Fixed | Katcher et al.272 |
| Cost of TMV including fitting | £12.37 (assuming part of housing association or local authority new build or refurbishment) | Fixed | Phillips et al.140 |
| Cost of providing education programme per household accepting the intervention – based on cost of home care worker for 20 minutes of their time including travel | Assuming £20 per hour, thus 20 minutes = £6.66 | Fixed | Assumption |
| Fixed cost of an intervention scheme – programme co-ordination | Considering a simulated cohort of 100,000 households = £79,529 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Additional administrative cost incurred for each household that accepts the intervention | Distribution costs divided by the number of households in the cohort and updated to 2012 prices = £0.40 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Stages 2 and 3: Preschool and long-term model | |||
| Health-care costs/resource use | |||
| Mean cost of attending an ED but discharged without admission | £183 (£18.25) | Log-normal | Department of Health31 |
| Mean cost of minor scald – no inpatient stay | £1086 (£8) | Log-normal | Mr Ken Dunn, South Manchester University Hospital, 8 September 2010, personal communication |
| Mean cost of moderate scald – inpatient stay ≤ 5 days | £14,940 (£102) | Log-normal | Mr Ken Dunn, South Manchester University Hospital, 8 September 2010, personal communication |
| Mean cost of severe scald – inpatient stay > 5 days | £41,157 (£2518) | Log-normal | Mr Ken Dunn, South Manchester University Hospital, 8 September 2010, personal communication |
| Mean incurred NHS costs of disability per year | £379.50 (£85.50) | Gamma (alpha = 16, beta = 0.047) | Medical Care Research Unit (J Nicholl, personal communication)367 – updated to 2012 prices |
| Utility parameters per cycle | |||
| Deficit in utilities for minor injury/no inpatient stay (DRG 460) | 0.060 | Fixed | Sanchez et al.512 |
| Deficit in utilities for minor injury/inpatient stay (DRG 459) | 0.090 | Fixed | Sanchez et al.512 |
| Deficit in utilities for moderate injury (DRG 458 + 457) | 0.093 | Fixed | Sanchez et al.512 |
| Deficit in utilities for severe injury (DRG 472) | 0.137 | Fixed | Sanchez et al.512 |
| Deficit in utilities following a disability per year | 0.1 (0.025) | Beta (alpha = 14.3, beta = 128.7) | Medical Care Research Unit (J Nicholl, personal communication) |
| General background utilities for non-injured population | < 25 years 0.94 (SD 0.12); 25–34 years 0.93 (SD 0.15); 35–44 years 0.91 (SD 0.16); 45–54 years 0.85 (SD 0.25); 55–64 years 0.80 (SD 0.26); 65–74 years 0.78 (SD 0.26); > 75 years 0.73 (SD 0.27) | Normal | Kind et al.71 |
Base-case model inputs for the decision analysis for safety gates to prevent stairway falls for study K
General base-case model inputs
| Model input | Point estimate (95% CrI) | Parameter distribution | Source | |
|---|---|---|---|---|
| Stage 1: Intervention model | ||||
| Probabilities of possessing a fitted safety gate following each intervention | ||||
| (1) Usual care | 0.64 (0.60 to 0.68) | Posterior distribution is inputted directly from NMA | Hubbard et al.446 | |
| (2) Education | 0.73 (0.56 to 0.86) | As above | As above | |
| (3) Education + free/low-cost equipment | 0.75 (0.56 to 0.88) | As above | As above | |
| (4) Education + free/low-cost equipment + home safety inspection | 0.72 (0.46 to 0.89) | As above | As above | |
| (5) Education + free/low-cost equipment + fitting | 0.75 (0.49 to 0.91) | As above | As above | |
| (6) Education + home safety inspection | 0.74 (0.33 to 0.95) | As above | As above | |
| (7) Education + free/low-cost equipment + fitting + home safety inspection | 0.93 (0.75 to 0.98) | As above | As above | |
| Safety gate | ||||
| Baseline probability that a household has a fitted safety gate | 0.56 | Normal on logit scale | Meta-analysis of baseline data and control groups from NMA studies with usual care in control arm | |
| Probability of accepting the intervention | 0.76 | Normal on logit scale | Meta-analysis of participation rates recorded in NMA studies | |
| No of children per household | 1 | Assumption | ||
| Stages 2 and 3: Preschool and long-term model | ||||
| Number of falls in children aged 0–4 years | Mean 41,246 (SE 84.28) | Normal | HASS 2002 (extracts from the Department of Trade and Industry’s Home and Leisure Accident Surveillance System (HASS/LASS), Helen Shaw, RoSPA, 1 May 2014, personal communication). Stairway falls 2002 – lower limit 41,081 and upper limit 41,411 for number of falls | |
| Probability of a fall | Number of falls/3,486,469 | Office for National Statistics514 | ||
| Relative risk of a fall downstairs when safety gate is in use vs. no safety gate | Ln(OR) = 0.916, SE[Ln(OR)] = 0.14 | Normal | Data from KCS study A: cases compared with community controls adjusted analysis OR (for did not use safety gate vs. closed safety gate) = 2.50 (95% CI 1.90 to 3.29) | |
| Probability of using an emergency ambulance | 0.242 | Fixed | Hospital Episode Statistics (2012)2 – 24.2% of all cases arrived by emergency transfer (ambulance/helicopter); used for all severities of injuries | |
| Probability of a mild fall injury (attends ED but not admitted) | 2604/2724 = 0.9560 | HASS 2002 (extracts from the Department of Trade and Industry’s Home and Leisure Accident Surveillance System (HASS/LASS), Helen Shaw, RoSPA, 1 May 2014, personal communication) | ||
| Probability of a moderate fall injury (attends ED and admitted for < 2 days) | 88/2724 = 0.0323 | Multinomial | ||
| Probability of a severe fall injury (attends ED and admitted for ≥ 2 days) but not long-term disability | (32 – 2)/2724 = 0.0110 | Severe injuries with estimated number with long-term disability subtracted, i.e. 0.000652 × 2724 = 1.78 ≈ 2 | ||
| Probability of a severe fall injury (attends ED and admitted for ≥ 2 days) and a long-term disability | 0.000652 | SMARTRISK121 | ||
| Probability of a fatal fall injury | 0.000000163 | Office for National Statistics – England and Wales mortality statistics: four stairway deaths in those aged 0–4 years in 2002–12, average of 0.57 per year;515 n = 3,496,750 children aged 0–4 year olds in 2011 census489 | ||
| Probability that after a fall the household keeps the safety gate already in place | 0.95 | Uniform(0.9,1) | Assumption | |
| Probability that after a fall the household remains in the no safety gate arm | 0.56 | Uniform(0.5,0.62) | Based on Morrongiello and Schwebel516 | |
Base-case model inputs for quality-of-life weights and costs (updated to 2012 prices)
| Model input | Point estimate (SE) | Parameter distribution | Source |
|---|---|---|---|
| Stage 1: Intervention model | |||
| Intervention costs | |||
| Cost of home safety inspection based on cost of health visitor for 5 minutes of their time | £44 per hour, thus 5 minutes = £3.67 | Fixed | Curtis30 |
| Cost of safety equipment (safety gates × 2) | £38.30 | Fixed | NICE PH30 costing template27 (£18 per safety gate) updated to 2012 prices |
| Cost of installation | 18 minutes to fit a safety gate at a cost of £24.93 per hour = £7.48 | Fixed | Gary Smith, Groundwork Creswell, 29 September 2014, personal communication |
| Cost of providing education programme per household accepting the intervention – based on cost of home care worker for 5 minutes of their time during a routine visit | Assuming £44 per hour, thus 5 minutes = £3.67 | Fixed | Assumption (based on Curtis30) |
| Fixed cost of an intervention scheme – programme co-ordination | Considering a simulated cohort of 100,000 households = £79,529 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Cost of travel (time and travel) when intervention is provided in the home | £5 | Fixed | Nottingham home safety scheme hourly rate including on-costs and vehicle costs = £25 (estimated through Gary Smith, Ground work Creswell, 29 September 2014, personal communication) to install five items of safety equipment; one-fifth of hourly rate was allocated to safety gates |
| Additional administrative cost incurred for each household that accepts the intervention | Distribution costs divided by the number of households in the cohort and updated to 2012 prices = £0.40 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Stages 2 and 3: Preschool and long-term model | |||
| Cost of emergency transfers included for 25.4% of all falls injuries | £263 (£21.48) | Gamma | Curtis30 |
| Cost of ED treatment of cases not leading to hospital inpatient stay (minor injury) | £112 (£27.46) | Gamma | Curtis30 |
| Cost of ED treatment for cases leading to hospital inpatient stay (moderate or severe injury) | £146 (£42.22) | Gamma | Curtis30 |
| Cost of a non-elective short (< 2 days) inpatient admission | £586 (£223.70) | Gamma | Curtis30 |
| Cost of a non-elective long (≥ 2 days) inpatient admission | £2461 (£810.37) | Gamma | Curtis30 |
| Annual cost of chronic ill health | £380.30 (£98.44) | Gamma | Medical Care Research Unit (J Nicholl, personal communication) – updated to 2012 prices |
| Cost of fatal injury | £205.50 | Fixed | Ginelly et al.347 – reported in functional smoke alarm model373 |
| Utility parameters per cycle | |||
| Utility deficit for minor injury | 0.05 | Uniform(0,0.1) | Assumption – half moderate utility deficit |
| Utility deficit for moderate injury | 0.10 | Fixed | Utility decrement 0.10 for falls injury in children aged 0–4 years.517 Brussoni et al.143 looked at all injuries for ages 0–16 years using 1-month change in EQ-5D-3L |
| Utility deficit for severe injury | 0.20 | Uniform(0.1,0.3) | Assumption – double moderate and long-term disability |
| Utility deficit associated with disability per year | 0.10 (0.025) | Beta | Medical Care Research Unit (J Nicholl, personal communication) |
| General background utilities for non-injured population | < 25 years 0.94 (SD 0.12); 25–34 years 0.93 (SD 0.15); 35–44 years 0.91 (SD 0.16); 45–54 years 0.85 (SD 0.25); 55–64 years 0.80 (SD 0.26); 65–74 years 0.78 (SD 0.26); > 75 years 0.73 (SD 0.27) | Normal | Kind et al.375 |
Base-case model inputs for the decision analysis for safe storage of medicines for study K
General base-case model inputs
| Model input | Point estimate (95% CrI) | Parameter distribution | Source |
|---|---|---|---|
| Stage 1: Intervention model | |||
| Probabilities of safe storage of medicines following each intervention | |||
| (1) Usual care | 0.90 (0.84 to 0.94) | Posterior distribution inputted directly from NMA analysis | NMA449 |
| (2) Education | 0.87 (0.83 to 0.91) | As above | As above |
| (3) Education + free/low-cost equipment | 0.95 (0.89 to 0.98) | As above | As above |
| (4) Education + free/low-cost equipment + home safety inspection | 0.90 (0.76 to 0.96) | As above | As above |
| (5) Education + free/low-cost equipment + fitting | 0.90 (0.81 to 0.96) | As above | As above |
| (6) Education + free/low-cost equipment + fitting + home safety inspection | 0.93 (0.83 to 0.97) | As above | As above |
| (7) Free/low-cost equipment | 0.94 (0.78 to 0.98) | As above | As above |
| Safe storage of medicine | |||
| Baseline prevalence of safe storage of medicines | 0.75 | Beta (n = 2033) | Prevalence rate among community controls |
| Probability of accepting the intervention | 0.90 | Fixed | Assumption based on value in functional smoke alarm model |
| Stages 2 and 3: Preschool and long-term model | |||
| Probability of accidental exposure/ingestion | 0.00181 | Beta (n = 3,599,180) | Poisoning cases in preschool children = 10,837, UK preschool population in 2005–9 = 3,599,180.451 The numerator (n = 10,837 × 0.6 = 6502) was derived based on information90 suggesting that 1316 (60%) of the 2193 medically reported poisonings identified in the THIN database were due to ingestion of a medicinal substance |
| Relative risk of exposure to a medicinal substance | Ln(OR) = –0.60 (SE 0.14) | Normal | From KCS study A: OR 1.83 (95% CI 1.38 to 2.42) |
| Probability of using emergency ambulance | 0.242 | Fixed | Hospital Episode Statistics518 – 24.2% of all cases arrived by emergency transfer (ambulance/helicopter) |
| Probability of inpatient admission following a medicinal poisoning injury (ICD-10: X40–X44) | 0.6992 | Beta (n = 6502) | Hospital Episode Statistics518 – number of poisoning cases (X40–X44) admitted in 0- to 4-year-olds (period 2012–13) in England = 3909. Scaled up by a factor of 1.163 (i.e. 3909 × 1.163 = 4546 cases for the whole of the UK) based on mid-2012 population estimates for UK and England519 |
| Probability of severe injury | 0.00191 | Beta (n = 4546) | Mowry et al.520 (Table 13) – 1.91% of major poisoning cases (across all age groups) resulted in a permanent health condition; numerator = 0.019 × 4546 = 86 |
| Probability of fatal injury | 0.00116 | Beta (n = 87) | UK mortality statistics513 – one fatality from medicinal poisonings in 0- to 4-year-olds (assumed fatality occurred after a long inpatient stay) |
| UK mortality statistics | Normal | Office for National Statistics506 | |
Base-case model inputs for quality-of-life weights and costs (updated to 2012 prices)
| Model input | Point estimate (SE) | Parameter distribution | Source |
|---|---|---|---|
| Stage 1: Intervention model | |||
| Intervention costs | |||
| Cost of home safety inspection based on cost of local authority home care worker for 40 minutes of their time including travel | £23 per hour, thus 40 minutes = £15.33 | Fixed | Curtis30 |
| Cost of safety equipment (cupboard locks ×2) updated to 2012 prices | £6.80 (range £4.54–13.62) | Fixed | NICE PH30 costing template27 |
| Cost of installation | £11.83 | Fixed | Same as smoke alarms |
| Cost of providing education programme per household accepting the intervention – based on cost of home care worker for 20 minutes of their time including travel | Assume £20 per hour, thus 20 minutes = £11.33 | Fixed | Assumption |
| Fixed cost of an intervention scheme – programme co-ordination | Considering a simulated cohort of 100,000 households = £79,529 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Additional administrative cost incurred for each household that accepts the intervention | Distribution costs divided by the number of households in the cohort and updated to 2012 prices = £0.40 | Fixed | DiGuiseppi et al.507 – updated to 2012 prices |
| Stages 2 and 3: Preschool and long-term model | |||
| Cost of emergency transfers | £263 (£21.48) | Gamma | Curtis30 |
| Cost of ED treatment of cases not leading to hospital inpatient stay (minor injury) | £112 (£27.41) | Gamma | Curtis30 |
| Cost of ED treatment of cases leading to hospital inpatient stay (major injury) | £146 (£42.22) | Gamma | Curtis30 |
| Cost of a non-elective short (< 2 days) inpatient admission | £586 (£223.70) | Gamma | Curtis30 |
| Cost of a non-elective long (≥ 2 days) inpatient admission | £2461 (£810.37) | Gamma | Curtis30 |
| Annual cost of chronic ill health | £386.42 (£96.72) | Gamma | Medical Care Research Unit (J Nicholl, personal communication) |
| Cost of fatal injury | £205.50 | Fixed | Ginelly et al.347 – reported in functional smoke alarm model |
| Cost of 11.7-minute GP consultation | £43 | Fixed | Curtis30 |
| Cost of a health visitor visit lasting 40 minutes for severe poisonings (i.e. those that result in a permanent injury) | £44 (£15.56) | Gamma | Curtis30 |
| Utility parameters per cycle | |||
| Utility deficit for minor injury | 0.03 (0.003) | Beta | Utility decrement of 0.03 for poisoning injury;125 assumed SE is 10% of the mean521,522 |
| Utility deficit for moderate injury | 0.046 (0.0046) | Beta | Utility decrement of 0.046 for poisoning injury;517 assumed SE is 10% of the mean521,522 |
| Utility deficit for severe injury | 0.146 (0.0146) | Beta | Utility decrement of 0.046 for poisoning injury517 and decrement associated with disability of 0.1 from the HALO study (J Nicholl, personal communication); assumed SE is 10% of mean521,522 |
| Utility deficit associated with disability per year | 0.10 (0.025) | Beta | Medical Care Research Unit (J Nicholl, personal communication) |
| General background utilities for non-injured population | < 25 years 0.94 (SD 0.12); 25–34 years 0.93 (SD 0.15); 35–44 years 0.91 (SD 0.16); 45–54 years 0.85 (SD 0.25); 55–64 years 0.80 (SD 0.26); 65–74 years 0.78 (SD 0.26); > 75 years 0.73 (SD 0.27) | Normal | Kind et al.375 |
Base-case model inputs for the decision analysis for safe storage of household products for study K
Note that the base-case model inputs for quality-of-life weights and costs are the same as those used for the safe storage of medicines in Base-case model inputs for the decision analysis for safe storage of medicines for study K.
General base-case model inputs
| Model input | Point estimate (95% CrI) | Parameter distribution | Source of information |
|---|---|---|---|
| Stage 1: Intervention model | |||
| All parameters are the same as for medicinal poisoning except for those below | |||
| Probabilities of safe storage of non-medicinal poisons | |||
| (1) Usual care | 0.608 (0.566 to 0.649) | Posterior distribution inputted directly from NMA | NMA449 |
| (2) Education | 0.660 (0.518 to 0.789) | As above | As above |
| (3) Education + free/low-cost equipment | 0.779 (0.584 to 0.895) | As above | As above |
| (4) Education + free/low-cost equipment + home safety inspection | 0.799 (0.640 to 0.915) | As above | As above |
| (5) Education + free/low-cost equipment + fitting | 0.676 (0.430 to 0.868) | As above | As above |
| (6) Education + free/low-cost equipment + fitting + home safety inspection | 0.803 (0.453 to 0.960) | As above | As above |
| (7) Free/low-cost equipment | 0.403 (0.003 to 0.961) | As above | As above |
| Stages 2 and 3: Preschool and long-term model | |||
| Probability of safe storage of non-medicines | 0.454 | Beta (n = 2320) | Prevalence rate among community controls from study A |
| Relative risk of exposure to a non-medicinal substance comparing children with a poisoning with community controls | OR 0.77 (95% CI 0.59 to 0.99) | Normal on log odds scale | Study A: community controls adjusted analysis |
| Probability of accidental exposure/ingestion | 0.0012 | Beta (n = 3,599,180) | Orton et al.,451 Tyrrell et al.90 |
| Probability of inpatient admission following a non-medicinal poisoning injury (ICD-10: X45–X49) | 1377 poisoning cases (X45–X49) admitted in 0- to 4-year-olds in England. Scaled up by 1.163 based on mid-2012 population for the UK: (1377 × 1.16)/4335.8 = 0.368 | Beta | Health and Social Care Information Centre,518 Office for National Statistics519 |
Appendix 6 Statistical appendix, interview schedules and questionnaires for study M, and injury prevention briefings
Parents’ survey for measuring the prevalence of fire protection practices
Injury prevention briefing 1
Injury prevention briefing training evaluation questionnaire
Baseline self-completion questionnaire for parents
Follow-up self-completion questionnaire for parents
Baseline manager/staff questionnaire
Follow-up manager/staff questionnaire
Facilitation contacts questionnaires
Facilitation contacts interview
12-month follow-up facilitation and implementation fidelity questionnaires
12-month follow-up facilitation and implementation fidelity interview schedules
Statistical appendix
Below is an algebraic outline of the hierarchical model applied in the economic analysis conducted alongside the multicentre cluster RCT reported in Chapter 7.
where eijk and cijk are the effects (e = 0 no fire escape plan; e = 1 fire escape plan exists) and costs in the ith family of the jth cluster allocated to the kth intervention arm (k = 1, usual care; k = 2, IPB only; k = 3, IPB+); pijk is the underlying probability of a fire escape plan at the family level; ηk is the shape parameter of the gamma distribution and is intervention arm specific and λijk is the rate parameter of the gamma distribution at the family level; φijk is the underlying mean of the costs (and is a function of λijk and ηk) at the family level; μje is the underlying mean effect on the logit scale for the jth cluster and μjc is the intercept of the linear predictor for the cost for the kth cluster; βj is the regression coefficient that links the cost and effect equations at the family level and is treatment arm specific; θje (defined further down as μke. clus) and θjc are the underlying cluster-specific means, which, within a intervention arm, are assumed to be exchangeable and normally distributed with variance τ.e2 and τ.c2, respectively; μkc. clus is the intercept of the linear predictor for the cost for the underlying mean effect; and βkc. clus is the regression coefficient that links the cost and effect equations at the cluster level. The model was extended to include covariates. These were incorporated, as for any regression model, by adding them to the linear predictor.
WinBUGS uses the Bayesian statistical approach to inference and as such requires prior distributions to be placed on all unknown model parameters. For all parameters, vague prior distributions were specified, allowing the data to dominate the analysis. Preliminary analyses indicated that the mixing of the MCMC chains was poor because of high autocorrelation between consecutive samples, even when re-parameterising the model to incorporate hierarchical centring523 (an approach aimed at reducing this problem). This means that the MCMC estimation is very inefficient and it was necessary to run the MCMC chains for a very large number of iterations to guarantee an accurate estimation of model parameters. Thus, the model was ‘burnt in’ for 20,000 iterations followed by a further 130,000 iterations on which parameter estimation and inference were based. Convergence of the MCMC sampler was assessed using the Gelman–Rubin diagnostic by running multiple chains with different starting values. 488
Injury prevention briefing 2
List of abbreviations
- AIC
- Akaike information criterion
- ANOVA
- analysis of variance
- AOR
- adjusted odds ratio
- ASSIA
- Applied Social Sciences Index and Abstracts
- BIC
- Bayesian information criterion
- BME
- black and minority ethnic
- CBA
- controlled before-and-after study
- CBQ
- Child Behaviour Questionnaire
- CFI
- comparative fit index
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMO
- Chief Medical Officer
- CRC
- child-resistant cap
- CrI
- credible interval
- DAG
- directed acyclic graph
- df
- degree of freedom
- ECBQ
- Early Child Behaviour Questionnaire
- ECCE
- Evaluation of Children’s Centres in England
- ED
- emergency department
- EQ-5D
- EuroQol-5 Dimensions
- EU
- European Union
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- HALO
- Long Term Health and Healthcare Outcomes of Accidental Injury
- HASS
- Home Accident Surveillance System
- HRQL
- health-related quality of life
- IBQ
- Infant Behaviour Questionnaire
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- IMD
- Index of Multiple Deprivation
- IPB
- injury prevention briefing
- IQR
- interquartile range
- IRR
- incidence rate ratio
- KCS
- Keeping Children Safe
- MCMC
- Markov chain Monte Carlo
- MCS
- Millennium Cohort Study
- MID
- minimally important difference
- MIU
- minor injury unit
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NMA
- network meta-analysis
- NNT
- number needed to treat
- NPV
- negative predictive value
- Ofsted
- Office for Standards in Education
- OQAQ
- Overview Quality Assessment Questionnaire
- OR
- odds ratio
- PAF
- population attributable fraction
- PARIHS
- Promoting Action on Research in Health Services
- PCC
- poison control centre
- PCG
- primary care group
- PCT
- primary care trust
- PDH
- Parenting Daily Hassles
- PedsQL
- Pediatric Quality of Life Inventory
- PH
- public health guidance
- PMA
- pairwise meta-analysis
- PPI
- patient and public involvement
- PPV
- positive predictive value
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RMSEA
- root-mean-square error of approximation
- RoSPA
- Royal Society for the Prevention of Accidents
- SD
- standard deviation
- SE
- standard error
- SEM
- standard error of measurement
- SHA
- strategic health authority
- SRMR
- standardised root-mean-square residual
- SSLP
- Sure Start Local Programme
- SSPAU
- short-stay paediatric assessment unit
- TBI
- traumatic brain injury
- TBSA
- total body surface area
- TLI
- Tucker–Lewis Index
- TMV
- thermostatic mixer valve
- VAS
- visual analogue scale