Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0109-10078. The contractual start date was in January 2011. The final report began editorial review in July 2017 and was accepted for publication in July 2018. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
The following authors had clinical/professional involvement in crisis teams during the course of the Crisis resolution team Optimisation and RElapse prevention (CORE) programme of research: David Osborn, Claire Henderson, Stephen Pilling, Fiona Nolan, Kathleen Kelly, Nicky Goater, Alyssa Milton and Ellie Brown. The following authors declare multiple research grants as chief investigator or co-applicant from the National Institute for Health Research during the course of the CORE programme of research: Brynmor Lloyd-Evans, David Osborn, Gareth Ambler, Louise Marston, Oliver Mason, Nicola Morant, Claire Henderson, Stephen Pilling, Fiona Nolan, Richard Gray, Tim Weaver and Sonia Johnson.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Lloyd-Evans et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
SYNOPSIS
Background
Crisis resolution teams (CRTs) were mandated in the UK in 2000 under The NHS Plan: A Plan for Investment. A Plan for Reform. 1 They remained mandatory for almost a decade and, subsequently, have continued to be the preferred model of community crisis response in most mental health catchment areas. There has been a large workforce movement into these teams: several thousand mental health professionals now work in them. 2 Sometimes called home treatment or crisis assessment teams, CRTs provide rapid assessment in mental health crises and, if feasible, offer intensive home treatment as an alternative to hospital admission. 3 CRTs typically aim to offer 24-hour access and a ‘gatekeeping’ function, controlling access to inpatient beds and assessing suitability for home treatment before admission. 4 CRTs’ primary purpose is to reduce the use of hospital beds to manage crises. Reasons for this include the high cost of hospital admissions and the unpopularity of psychiatric hospitals with many service users. 5 Pioneers have also suggested that community management of crises can result in opportunities for service users to develop, in their normal living context, skills and insights, which will help them to cope better with future crises. 6,7 In addition, home treatment potentially offers more scope for working with social networks and addressing the social antecedents of crises in the community. 8,9 Therapeutic alliances between CRT staff and patients are based more on negotiation and equal partnerships than relationships between staff and patients in hospital are. 10 Therefore, a patient who has experienced effective home management of a crisis may subsequently be more able to manage their own health effectively, remain engaged with services and seek help at an early stage when warning signs of another crisis emerge. 11
Although the evidence base for CRTs was criticised as scant when they first became national policy,12,13 some positive findings had already been reported at the time this study was conceived. A national investigation14 into the early stages of CRT policy implementation indicated a mean reduction of 10% in admissions in areas where CRTs were available, rising to 20% when they operated for 24 hours a day. Moreover, naturalistic investigations of CRT introduction to catchment areas,15–17 as well as a randomised trial,18 suggest that CRTs can reduce hospital admissions. Two health economic assessments have shown lower health-care costs when CRTs are available. 19,20 There is also some evidence that service user satisfaction with acute care is higher when CRTs are available. 15,18 Little is known about the views of carers regarding the current UK model of CRTs. Outcomes, such as symptoms and social functioning, appear similar with or without CRT care. 15,18 A survey of London CRT staff was reassuring regarding workforce impact, suggesting fairly good satisfaction and low burnout. 21
Despite indications of the CRT model’s potential clinical effectiveness, there have been considerable reservations about its delivery in routine settings. 22,23 A national survey24 of CRTs found that only 40% of teams described themselves as fully established, with one-third of teams not involved in gatekeeping, as in some areas many hospital admissions take place without CRT assessment. The same survey24 showed that only just over half of teams offered a 24-hour, 7-day home-visiting service. Ward managers and CRT leaders still view a significant minority of hospital admissions as unnecessary. 25 Impact on bed use also varies between trusts26,27 and reductions in bed-days tend to be less marked than those in the number of hospital admissions. 13,17 Moreover, a reanalysis of the data from the national investigation of CRT implementation reported above13 suggested that the impact of CRT implementation on admissions cannot be disentangled from that of concomitant cuts in available inpatient beds, leading to uncertainty about the extent to which the new CRTs may be responsible for reduced admissions. 14 The Royal College of Psychiatrists and the Mental Health Act Commission have highlighted continuing difficulties with bed overoccupancy in a number of hospitals, and reports from both bodies express doubt as to whether or not CRTs have achieved their intended effects throughout the country. 27,28 Furthermore, any impact of CRTs seems thus far to be on voluntary admissions, and some evidence suggests that use of the Mental Health Act29 may even increase with CRTs in place. 13,30 There is a need to develop and implement well-integrated pathways through the acute care system that are clearly understood by CRT staff, managers and primary and secondary care referrers. 23
Service users and carers, although positive overall about receiving care in their own homes, report some dissatisfaction with CRTs,22,31 especially regarding continuity of care and relationships with staff. Specifically, they are concerned about having too many staff involved in each episode of care, with contacts often being fleeting and superficial. Information and planning of care are not sufficiently shared between staff and services. Discharge is often abrupt, with support for recovery falling off rapidly after the immediate crisis period. Some also report that the range of interventions offered is too narrow and focused on short-term symptom control. Other types of support, such as help in addressing practical and social problems that are often antecedents of crises32,33 and in developing better strategies for maintaining well-being and avoiding future crises, are highly valued, but insufficiently available.
Thus, CRTs appear to be potentially effective in meeting their goals of reducing inpatient admissions and improving service user experiences, but their implementation and the outcomes achieved seem to be very variable in practice. The difficulties in implementing new forms of treatment with demonstrated efficacy in trials in routine settings have been extensively described. 34,35 Facilitators of implementation include leadership in teams and from senior managers within organisations, financial and other incentives, systems for monitoring fidelity, a consistent set of local policies and guidelines that support the practice, and practitioner training. Interventions involving a single facilitating factor, such as training, rarely achieve change; packages with multiple measures and continuing measures to sustain change are usually required.
A potential barrier to effective implementation of the CRT model, alongside resource constraints, is the loosely specified nature of the model. There is only limited evidence available on critical ingredients and specific interventions associated with good outcomes. 6 The underdeveloped nature of the CRT model is apparent when comparing it with other complex service-level interventions, which have been the focus of programmes aimed at establishing and disseminating models of good practice. Most prominent in mental health is the US National evidence-based practices (EBP) project,36 which offers a model for evaluating whether or not complex service-level interventions operate as intended for achieving quality improvement in mental health settings. The EBP project has been applied to practices including assertive community treatment and individual placement and support.
Key stages in the EBP project are the development of a fidelity measure specific to the practice and the development of implementation resource kits designed to enable services to achieve high fidelity, followed by testing of whether or not they succeed. 37 Fidelity scales measure how far a service adheres to a model based on the best evidence about the most effective practice. 38 Once a fidelity scale has been established, further research can be conducted to test whether or not model adherence does indeed result in better outcomes, so that fidelity scale development and outcome measurement may be an iterative process as such evidence accumulates. The Supported Employment Fidelity Scale, for example, assesses 15 items relating to employment services’ staffing, organisation and service provision. 39 Evaluations have repeatedly found positive associations between model fidelity and employment outcomes. 40–44
Crisis resolution teams are comparable with models in the EBP project in that there is some evidence for their efficacy in the right conditions. However, an evidence-based and tested method of assessing and improving fidelity to a model of good practice is lacking, as the tools needed for widespread implementation of an optimal model of CRT practice are still lacking. Developing and testing such tools for CRTs, using a strategy based on the EBP project, is therefore of high interest for policy-makers and service planners.
As mentioned previously, service users have criticised the lack of continuity of care between services during and following a period of CRT care. 31 There is a documented gap in mental health care post discharge, with service users feeling that they are suddenly left to deal with their recovery without any support. 45 This is likely to be one of the factors contributing to the relatively high rates of re-admission to acute care found in CRTs, a limiting factor regarding their capacity to reduce overall admission numbers and acute care costs. Recent work on self-management interventions provides promising evidence for the clinical effectiveness of such programmes and their potential to bridge this gap. In chronic physical illnesses, supporting patients to learn to manage their own health has resulted in some benefits to quality of care and, in some cases, health outcomes. 46 In mental health, this approach has produced a new generation of interventions aimed at helping service users to better manage their condition and achieve their individual goals. Some examples are the Wellness Recovery Action Plan,47 the Recovery Workbook48 and the Pathways to Recovery: Workbook. 49 These programmes differ in structure and degree of clinician involvement but share an emphasis on peer facilitation and support and a focus on people’s own strengths, goals and resources. Most of these approaches incorporate relapse prevention work, aimed at helping service users and their carers to recognise and respond to early warning signs of deterioration in their mental health. 50
According to the recovery model,51 hope, social inclusion, meaningful activity and supportive relationships often matter more to service users than managing symptoms. Reflecting this, self-management interventions include not only relapse prevention work but also plans for maintaining general well-being and achieving personal recovery goals. Self-management approaches, both simple relapse prevention planning and broader recovery-focused interventions, are widely advocated in mental health, supporters including the Royal College of Psychiatrists,52 the NHS’s The Mental Health Policy Implementation Guide3 and the charity Rethink Mental Illness. 53 A limited number of small US studies demonstrate successful recruitment to studies of such interventions and some positive changes. 48,54 However, there is not enough evidence to establish whether or not self-management interventions achieve their intended goals with people with serious mental health problems.
The CORE programme
The CORE (Crisis resolution team Optimisation and RElapse prevention) study is a 6-year programme comprising two workstreams. Workstream 1 aims to deliver a means of optimising CRTs at a team level, through investigating what constitutes best practice in CRTs and developing and testing a fidelity measure and a service improvement programme for achieving high fidelity.
Workstream 1 focuses on team-level change, whereas workstream 2 addresses limitations in CRT care at an individual level by developing and testing an intervention for service users leaving CRT care. As described previously (see Background), pioneers of the CRT model argue that crises present an opportunity to work towards change in service users’ and their networks’ abilities to manage their mental health and respond to crises. 8 This fits with the priorities of service users, who report that episodes of CRT care currently seem to end without adequate support for longer-term recovery in place. 45 We thus aimed to investigate whether or not extending CRT management through the addition of a peer-supported self-management intervention can prevent future crises and improve service user experiences and outcomes.
The main substantial UK studies of the last decade regarding CRTs involved members of the CORE programme team, including a naturalistic investigation of the intervention’s impact on a range of social and clinical outcomes,15 the only randomised trial,18 health economic studies,19,20 an investigation of patient factors associated with being admitted rather than treated at home,55 a workforce study21 and the CRT national survey. 24 Thus, the current project is the next step in a continuing programme of investigation of community acute alternatives to hospital admission.
Aims and objectives
The aim of the CORE study was to establish evidence at both the team and individual service user level as to how CRT functioning may be optimised to reduce reliance on inpatient care and to enhance recovery.
The objectives of the CORE study were to:
-
define best practice in CRTs, drawing on empirical evidence when possible, and on the views of service users, carers, professionals and experts when such empirical evidence is not available
-
formulate a model for achieving best practice in CRT organisation and operation, and a fidelity measure to assess whether or not this is achieved
-
develop a service improvement programme for achieving high-fidelity care and conduct a mixed-methods investigation of its impact
-
develop, pilot and assess the clinical effectiveness and cost-effectiveness of a peer-supported self-management intervention, designed to reduce relapse and enhance progress towards personal recovery goals among CRT service users.
Workstream 1 addresses objectives 1–3, aiming to develop and test a means of optimising CRT functioning. Evidence was investigated regarding the critical ingredients of CRT care and the perspectives of CRT stakeholders on good practice. This informed the formulation of a model of best practice in CRT care. Based on this, a CRT fidelity scale and a strategy for improving fidelity based on a service improvement programme were developed. Higher team fidelity was then explored to establish whether or not it is associated with better individual outcomes, and a preliminary investigation of the programme’s impact was conducted.
Workstream 2 addresses objective 4, aiming to test whether or not a self-management intervention, initiated at the point of discharge, can reduce relapse and use of acute services and enhance service user experiences and outcomes. The three stages of workstream 2 are the selection of the intervention and adaptation to a CRT context, testing its feasibility and acceptability, and investigation of its clinical effectiveness and cost-effectiveness in a randomised controlled trial (RCT).
Overview of the programme
The research was conducted between April 2011 and April 2017.
Figure 1 provides an overview of the CORE programme and the components of each workstream. The studies in the two workstreams were conducted in parallel and comprised six modules, providing within each workstream progression from pre-clinical/theoretical stages to development of each programme and then evaluation in RCTs. The only direct inter-relationship between the two workstreams was between module 1 and module 4, as some of the feedback obtained from qualitative interviews with CRT service users informed the development of the peer-supported intervention. Thus, methods and results for the two workstreams are reported separately.
FIGURE 1.
Overview of the CORE programme. SMI, severe mental illness.

Patient and public involvement structures in the CORE study
The high priority that service users and carers attach to crisis care and their reservations regarding CRT implementation were the main drivers for the CORE programme. Public involvement was an integral part of planning and conducting the research throughout the CORE project.
In this section, the structures through which patient and public involvement (PPI) was facilitated during the CORE study are summarised, including the types of PPI activity undertaken. The impacts of public involvement on the study are briefly discussed in Public involvement activities. In addition, interviews with members of the CORE study service user and carer working groups on the experience and impact of PPI in the study were conducted by an independent researcher. A report summarising feedback from these interviews is also provided at the end of the synopsis (see Impact of public involvement on the study).
Patient and public involvement structures in the CORE study
-
A service user researcher co-applicant. An experienced service user consultant advised the study pre funding and was a co-applicant. Her contributions to the study included (1) overall planning and design, (2) leading training in interviewing skills for service user and carer working group members, (3) contributing to the selection and modification of the self-management recovery plan used in the workstream 2 trial, and (4) supporting and supervising the study public involvement co-ordinator. She elected not to remain fully involved in the study in years 4–6 of the project, although she continued to support the study public involvement co-ordinator until the end of his employment in the study.
-
A public involvement co-ordinator. A public involvement co-ordinator was funded for 1 day a week for the duration of the study. Key functions of the post were to manage and support the work of the working groups and front the public involvement in the study. Although funded from the start of the research, the appointment did not start until 1 year into the study because of the difficulties getting the innovative job matched to an appropriate NHS pay band.
-
Study service user and carer working groups. In the first year of the study, people with lived experience of using mental health services or caring for people using services were recruited to two working groups: one for service users and one for carers. These opportunities were advertised through the (former) Mental Health Research Network (MHRN), the National Service User Survivors Network, Rethink Mental Illness, and local service user groups Service User Research Forum (SURF), South Essex Service User Research Group and Service User and Carer Advisory Group Advising on Research (SUGAR). Twenty-three service users and 13 carers applied. Interviews were offered to 14 service users and 13 were appointed. Twelve carers were interviewed and seven were appointed. Two additional carers were recruited in 2013 (to replace two group members who left the study.) Priority was given to applicants with direct experience of CRTs and some previous involvement in research. Although some working group members contributed to only parts of the study, nine service users and six carers remained involved as working group members throughout.
Working groups were conducted separately for service users, and for carers, on five occasions. In addition, 12 joint meetings, two interviewer training days and three interviewer supervision sessions have been held. Additional consultations on specific topics were carried out via e-mail. About 2 years into the study, the two working groups elected to merge and hold joint meetings (having worked together as peer interviewers and in developing the CRT fidelity scale).
Working group meetings were used for members to contribute advice on the planning and conduct of the research in general. They also allowed planning and reflection on the specific study PPI activities listed later in this report. All working group meetings were attended by the programme manager who, along with the study public involvement co-ordinator, ensured that advice and suggestions from the working group were shared with others in the study team and fed into planning the study.
-
Service user and carer representation on the study steering committee. One service user and one carer with previous research experience were recruited to the CORE study steering committee [via SURF, the University College London (UCL) service user research group and SUGAR]. They participated in annual steering committee meetings that provided independent oversight and guidance for the study.
-
Research assistants with lived experience. During the course of the study, three research assistants with significant lived experience of mental health problems and two more with significant caring experience were recruited. This was not a deliberate strategy, although personal experience of mental health problems and mental health services was listed as a desirable criterion on research assistant person specifications, and adverts stated that applications from people with personal experience of mental health problems were welcome. These researchers were, however, able to bring their relevant lived experience to the role, for instance acting as peer interviewers or peer fidelity reviewers when necessary, and helping to support the working group and public involvement co-ordinator.
-
CRT staff involvement in the study. A working group of eight CRT clinicians was recruited from the 10 NHS trusts participating in module 1 interviews. This group met four times in 2011/12 and contributed to selecting a self-management resource for use in workstream 2 and the development of the CRT fidelity scale in module 2. A virtual working group of 11 CRT developers – international experts with experience of planning or managing CRT services – were recruited and contributed to the development of the CRT fidelity scale in modules 1 and 2. Further input from mental health staff with experience of working in or with CRTs was provided by clinical academic study applicants, and two CRT clinicians from participating NHS trusts who attended study meetings throughout the project. Extra input from clinicians from the lead NHS trust was sought for specific activities (e.g. the concept mapping process used to develop the CRT fidelity scale in module 2).
A budget for public involvement in the study was included in the grant awarded by the funders. The study public involvement co-ordinator post was funded as a NHS band 5 role. Working group members were offered paid involvement at a rate of £15 per hour (time to review study documents prior to meetings was included in payments). Working group members’ travel costs to meetings were also reimbursed.
The service users in the research group (led by Thomas Kabir) from the now-disbanded MHRN were a valuable source of advice with PPI arrangements on the study, regarding recruitment and payment arrangements and facilitating access to free benefits advice for working group members. The MHRN also helped set up two consultation meetings with service users and carers during preparation of the research grant, allowing service user and carer involvement with initial study planning.
Workstream 1
The CRT model has not been highly specified in the literature, as its critical ingredients are not yet established. 6 There is limited evidence about how best to implement CRTs and what type of interventions to deliver within them. 4 Workstream 1 developed the CRT model by investigating what constitutes best practice in CRTs and how difficulties in CRT model implementation identified in recent reports may be addressed.
The approach that was adopted in workstream 1 was based on the US EBP programme. 36 Central to the EBP method is the development of a fidelity scale, based, when available, on empirical evidence on components of the model associated with clinical effectiveness, and on stakeholder qualitative evidence and expert consultation when this is unavailable. Development of fidelity measures for complex interventions in mental health has been advocated not only as a means to define an intervention and measure services’ adherence to the model specified, but also to support service improvement. 56 Following fidelity scale development, a service improvement programme including manuals, training materials and guidance on implementation was designed to help teams achieve high fidelity and hence best practice.
The first part (module 1) of workstream 1 focused on investigating and defining best practice in CRTs. First, we reviewed current evidence regarding critical ingredients of CRT care and of relevant guidance. Second, we conducted a national survey of CRT managers in order to examine current service organisation and delivery and any initiatives to improve CRT practice. Third, we explored the perspective of service users, carers, professionals and experts on best CRT practice and their suggestions for service improvement. Findings from these studies were used to inform the emerging development of a model of CRT practice.
In module 2,we aimed to develop and test a CRT fidelity scale, designed to assess how far best practice as defined following module 1 is achieved. The fidelity scale was developed through a rigorous and systematic process, using stakeholders’ views to prioritise potential fidelity items drawn from the available evidence. The CRT fidelity scale was subsequently tested in a national survey of CRT model fidelity. We then developed a service improvement programme (SIP) for CRTs, with the fidelity programme as the central framework. The CORE SIP was modelled on the EBP project’s implementation resource kits,57 with content derived from the fidelity scale and provision of good-practice examples from the national survey.
The final stage in workstream 1 (module 3) involved a mixed-methods assessment of the impact of the SIP for achieving high fidelity to the CORE-defined model of good practice. Methods for this evaluation were finalised in the previous modules to ensure that it corresponded to key goals embodied in the CRT fidelity scale and SIP. Twenty-five CRTs were recruited to participate in a cluster randomised trial, with teams as the unit of randomisation: 15 of these were randomly allocated to the experimental intervention and 10 were randomly allocated to the control intervention. The aims were to establish (1) whether or not fidelity scores increase following the SIP, (2) whether or not teams receiving the SIP (the experimental intervention) achieve better service user experiences and better performance on key indicators of service use and (3) whether or not higher fidelity scores are associated with better outcomes at a team level. In addition, qualitative methods were used to explore participant experiences of the SIP.
Module 1.1: implementation of the crisis resolution team model in adult mental health settings – a systematic review
See Appendix 1 for the published report of this work. 58 The report is accessible at the following URL: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-015-0441-x (accessed 28 March 2019).
The review is registered with PROSPERO as CRD42013006415.
Aim
The aim of this review was to systematically acquire and synthesise evidence regarding critical components and key organisational principles of CRT services. In the review, quantitative evidence on associations between specific CRT characteristics and outcomes was prioritised. However, initial searches confirmed the belief that clear empirical evidence was likely to be limited. Literature on the views of stakeholders, including service users, carers, clinicians and service leaders, about best practice in CRTs was reviewed. In addition, the recommendations that government and expert organisations make about CRT service delivery and organisation were examined.
Methods for data collection
A systematic review was conducted. The databases MEDLINE, EMBASE, PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Web of Science were searched to November 2013, without time limit or geographical restrictions. Studies were included from anywhere in the world and in any language. A further web-based search was conducted for published government and expert guidelines on CRT services; this was restricted to England. Full search terms are provided in the published report. 58
The following types of study were included:
-
quantitative studies comparing outcomes between CRTs with different characteristics, or between CRTs and other service models
-
national or regional surveys reporting associations between CRT characteristics and outcomes
-
qualitative studies exploring the views of stakeholders, including service users, carers and clinicians, of what makes a good CRT service
-
published guidelines from statutory and non-statutory bodies making recommendations for effective, good-quality CRT care in the NHS in England.
Analysis
A narrative synthesis was conducted, based on guidance from the Centre for Reviews and Dissemination. 59 Each of the above types of study was separately investigated. Statistical meta-analysis was not feasible because of the heterogeneity of included studies with regard to study aims and design, outcomes assessed, service settings and characteristics. The mixed-methods appraisal tool (MMAT),60 a tool that allows quality rating of a variety of types of study, was used to assess the quality of individual studies.
Key findings
Sixty-nine studies and documents were included in the review. The composition and activities of CRTs varied substantially across studies. Studies also varied in quality, with the total mean score on the MMAT scale60 indicating moderately high quality.
Overall, quantitative comparison studies and CRT surveys provide relatively little evidence regarding the specific characteristics of CRTs that are associated with positive outcomes. Many studies of CRT outcomes give relatively little detail regarding the characteristics of the CRTs, making it very difficult to draw conclusions about associations between service elements and outcomes. One comparison of two CRT models found the presence of a psychiatrist within the team to be associated with reduced admissions, and a national survey suggested an association between 24-hour opening and lower admissions. Little other relevant evidence was obtained.
Qualitative studies and government and expert guidelines provide more detailed specification of best practice in CRTs. Stakeholders emphasised accessibility, integration with other local mental health services, provision of time to talk and practical help, treatment at home when possible and continuity of care. CRT guidelines prioritised the provision of a 24-hour, 7 days per week multidisciplinary service, including a psychiatrist and medical prescriber, relapse prevention planning on discharge from the CRT and a gatekeeping role for CRTs in controlling inpatient admissions. The need for adequate staffing to meet service demands and high quality of staff training were also frequently emphasised.
Strengths and limitations
In order to establish the critical ingredients of CRTs, this review used a systematic search strategy to identify all available types of evidence. The multidatabase search for relevant research studies was supplemented with hand-searching of reference lists and contacting authors about conference abstracts. Although this search included international literature regarding CRT services and closely related models, the search for government and expert guidelines was confined to England because of resource limitations and challenges in identifying and accessing such sources.
Another limitation was the fact that because of the wide variation among studies and incomplete reporting of CRT characteristics, it was not feasible to conduct quantitative synthesis of results or compare the clinical effectiveness of CRTs across studies. Furthermore, the MMAT60 is a relatively unsophisticated means of assessing quality, even though it is probably the best available single measure for synthesising the quality of studies using a mixture of methods. The tool treats different methodologies as equivalent and merges different components of quality into a single score, which is potentially reductive and misleading. 61
The review did not exclude any papers on the basis of quality, as it was wished to fully assess the current evidence base regarding CRT services. As a result, some studies with lower quality scores were included, which may potentially compromise the strength of the conclusions. However, steps were taken to take account of the variability in the quality of included studies in our synthesis of the evidence.
Recommendations for future research
This extent to which empirically based critical ingredients of CRT good practice can be identified is constrained by the fact that only a very small number of studies address this question. Interpretation and synthesis of the studies that have been conducted are impeded by wide variations in models and outcomes investigated and lack of detailed information on service characteristics. Future studies of CRTs should provide a more comprehensive description of the CRT and comparison services, as recommended by the Consolidated Standards of Reporting Trials (CONSORT) guidelines. 62 Although there was relatively little quantitative evidence regarding the critical ingredients associated with good CRT outcomes, there was a high degree of consensus from stakeholders and policy guidance about an optimal CRT model, broadly corroborating initial government guidance accompanying the national mandate to introduce CRTs. 3 This provides a basis for development of a more highly specified CRT model and of a means to assess adherence to this model: a priority for CRT research. It would now be valuable to conduct further research into the characteristics of CRTs associated with good outcomes and good patient experiences.
Module 1.2: national implementation of a mental health service model – a survey of crisis resolution teams in England
See Appendix 2 for the published report of this work. 63 The report is accessible at the following URL: http://onlinelibrary.wiley.com/doi/10.1111/inm.12311/abstract (accessed 28 March 2019).
Aims
A national survey of CRT managers was conducted in 2011/12. The aims of the survey were to map the provision of all CRTs in England and describe CRT organisation and service delivery, explore the teams’ adherence to key policy recommendations3 and compare CRT managers’ views on actual and desirable CRT characteristics.
Methods for data collection
Between November 2011 and July 2012, the manager of every crisis resolution/home treatment team (or equivalent) in England was invited to complete an electronic survey. If a team manager could not be reached or wished to delegate the survey, another senior member of the team was invited to participate. The survey consisted of a 90-item questionnaire, which was based on previous national surveys of crisis services24,64 and was further refined after a pilot in four CRTs. The questionnaire covered a range of aspects of CRT organisation and service delivery, including exploring which interventions are available from CRTs. In addition, reports were elicited on local initiatives and priorities for service improvement, and views regarding ideal characteristics of CRTs. The survey could be completed online or as a telephone interview with a researcher. Data from the questionnaire were entered directly into a secure online system and were downloaded into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet and transferred to IBM SPSS Statistics (IBM Corporation, Armonk, NY, USA) for analysis.
Analysis
There were three stages of data analysis:
-
Data regarding CRTs’ organisation and service delivery were summarised using descriptive statistics. Any free-text responses were coded to allow quantitative description of the most frequent responses.
-
When data directly related to recommendations from the original CRT guidance,3 questionnaire variables were recoded or combined in order to examine the degree to which CRTs were adhering to guidance in three domains – referral criteria and access, interventions and staffing. The extent to which CRTs adhered to guidance in each domain was reported.
-
In order to investigate any discrepancies between actual and perceived desirable CRT practice, the proportion of CRTs in which a service characteristic was present was compared with the proportion in which a service characteristic was rated by managers as fairly or very useful.
Key findings
Through service mapping, we identified a total of 218 CRTs, with some CRT provision in all 65 mental health NHS trusts in England. One hundred and ninety-two CRTs (88%) took part in the survey and 184 respondents (84%) completed at least two-thirds of the questionnaire.
Table 1 shows the composition of CRTs: nurses and psychiatrists were employed in almost all teams, but representation of other professions varied greatly from team to team.
| Staff professional group/type | CRTs teams employing, or with dedicated time from, staff of this type, n/N (%) |
|---|---|
| Consultant psychiatrist | 148/171 (87) |
| Psychiatrist (other grade) | 129/171 (75) |
| Nurse | 171/171 (100) |
| Social worker | 122/171 (71) |
| Occupational therapist | 72/171 (42) |
| Psychologist | 50/171 (29) |
| Pharmacist | 29/171 (17) |
| Graduate mental health worker | 10/171 (6) |
| Other support worker/staff without a mental health professional qualification | 145/171 (85) |
| Approved mental health professional | 109/173 (63) |
| Non-medical prescriber | 79/168 (47) |
| Number of clinical staff in CRT team (full-time equivalent) (n = 171) | Mean 20.8 (SD 8.7; range 4.4–53.6) |
The survey also enquired about delivered interventions (Table 2). These were most often focused on prescription and delivery of medication, rather than on psychological, social or practical interventions.
| Type of intervention | Number of CRTs reporting providing this intervention to most or all service users who need it, n/N (%) |
|---|---|
| During CRT care | |
| Prescribing medication | 164/181 (91) |
| Delivering medication | 139/181 (77) |
| Supervising service users taking medication | 147/181 (81) |
| Going shopping with/for service users | 74/181 (41) |
| Preparing food with service users | 35/181 (19) |
| Helping service users to clean their home | 23/181 (12) |
| Helping with problems with welfare benefits | 106/181 (59) |
| Helping with debt problems | 94/181 (52) |
| Accompanying service users to the police station or court | 30/181 (17) |
| Accompanying service users to GP appointments | 58/181 (32) |
| Physical health checks | 118/181 (65) |
| Staying with service users for extended periods to ensure safety or mitigate isolation | 64/181 (35) |
| Discharge support | |
| Formulating written relapse prevention plans with service users | 116/184 (63) |
| Using advance directives or crisis cards | 68/184 (37) |
| Using self-management programmes (e.g. a Wellness Recovery Action Plan) | 68/184 (37) |
| Offering follow-up telephone calls or visits post discharge | 83/184 (45) |
Only one-third of CRTs (62/187, 33%) reported always acting as gatekeepers to inpatient beds, as stipulated in the original policy implementation guidance. 3 An even smaller proportion of CRTs (35/187, 19%) reported always attending formal assessments for compulsary admission under the Mental Health Act. 29 Most CRTs (186/188, 99%) were also engaged in early discharge work, identifying inpatients who could go home earlier with support from the CRT.
Team managers were asked to rate whether or not a number of aspects of service delivery were important, and to report whether or not they were actually able to provide these at present. Table 3 shows the results and indicates many discrepancies between actual and desired provision, for example in being able to provide practical support of various types to service users and in being able to spend extended periods of time with them. Thus, from the perspective of our work, the important overarching theme is that, although there are many gaps in areas such as psychological and social interventions and capacity to spend extended time with service users, such gaps do not result from these aspects of provision being seen as low priority. Rather, it appears that managers who were surveyed would have liked to deliver a much richer service than was possible in practice.
| CRT characteristic | Percentage of CRTs providing this (to most or all service users where needed) | Percentage of respondents rating this as very or fairly important for CRTs to provide | Discrepancy (%) |
|---|---|---|---|
| Accompanying service users to GP appointments | 32 | 85 | 53 |
| Staying with service users for extended periods to ensure safety or mitigate isolation | 36 | 85 | 49 |
| Helping service users to clean their home | 12 | 59 | 47 |
| Preparing food with service users | 19 | 69 | 40 |
| Accompanying service users to the police station or court | 17 | 67 | 40 |
| Employing carers as staff | 16 | 55 | 39 |
| Employing service users as staff | 26 | 64 | 38 |
| Helping service users with debt problems | 52 | 89 | 37 |
| Going shopping with/for service users | 41 | 78 | 37 |
| Client-held records | 43 | 79 | 36 |
| Minimum duration for staff visits | 13 | 48 | 35 |
| Minimum frequency for staff visits | 37 | 72 | 35 |
| Helping with problems with welfare benefits | 59 | 91 | 32 |
| Accepting self-referrals from service users not previously known to services | 21 | 44 | 23 |
| Providing physical health checks | 65 | 88 | 23 |
| Attending Mental Health Act29 assessments | 48 | 70 | 22 |
| Working with people with learning difficulties | 58 | 36 | −22 |
| Working with people with a personality disorder | 79 | 52 | −27 |
Strengths and limitations
This survey had a high response rate (88%), which gives confidence that the sample of respondents is representative of senior CRT staff in England. However, there are two main limitations. First, the use of self-reporting may have resulted in an over-reporting of CRT implementation because of social desirability bias. Second, the survey was cross-sectional in nature, thus shedding no light on changes over time.
Recommendations for future research
The survey suggested that the original policy mandate and guidance were not sufficient to achieve nationwide CRT implementation as intended. This supports conclusions from the US EBP programme36 that high fidelity to good practice is unlikely to be achieved without regular structured assessment of implementation. A need was thus identified for future research to develop and test tools to support implementation and monitoring of CRTs. CRT stakeholders’ views and priorities, including those of service users and carers, should also be investigated and taken into account in developing an empirically based optimum model of CRT care. Tracking service delivery nationwide by repeated surveys over time will also be important to achieving and sustaining implementation of a CRT model matching perceived needs.
Module 1.3: a qualitative study of stakeholders’ views on critical ingredients of crisis resolution teams and their implementation
See Appendix 3 for a link to the full report of this work. 65 The report is also accessible at https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1421-0/open-peer-review (accessed 28 March 2019).
Aim
Previous research has shown that there is insufficient empirical evidence regarding the critical ingredients of CRTs (see Module 1.1) and that CRTs are not fully implemented as intended (see Module 1.2). The EBP programme36 recommends drawing on a broad range of stakeholder views in which empirical evidence linking service content to outcome is limited. Therefore, in this qualitative study, the aim was to examine stakeholders’ experiences of CRTs and their views regarding best practice.
Methods of data collection
Semistructured interviews and focus groups were conducted with different groups of CRT stakeholders: service users (n = 41 individual interviews), carers (n = 20 interviews) and practitioners (n = 147, comprising CRT staff, managers and referrers; nine individual interviews and 26 focus groups were conducted). The referrers group included clinicians from community mental health services, inpatient wards, liaison psychiatry services and general practitioners, thus representing a range of common referrers to CRT services. Participants were drawn from 10 mental health catchment areas across England. In addition, key experts (n = 11), involved in the development of CRTs internationally, were interviewed in order to provide a broad perspective on the history and theoretical origins of CRTs and on their intended aims and characteristics.
Topic guides were developed in collaboration with project advisory groups of service users, carers and clinicians, representing CRT stakeholders, to make sure that priority issues and the concerns of each group regarding CRT practice were covered. The overall aim was to explore views from all perspectives about what constitutes best practice in CRTs. Aspects of CRT care identified by previous research as problematic were included. Interviews with service users and carers were conducted by trained peer researchers (service users and/or carers) whenever available; the rest were conducted by non-peer study researchers. Data from practitioners were collected via focus groups, when feasible, or via individual interviews if it proved too difficult to convene focus groups. All interviews were audio-recorded and transcribed.
Analysis
Data were analysed using thematic analysis66 supported by NVivo 9 software (QSR International, Warrington, UK). Using this analytical strategy, aspects of CRT work were explored that were perceived to be important, successful and unsuccessful, using both inductive and deductive approaches. Owing to the large corpus of data, a staged approach was used. An initial basic set of themes was developed, based on a small subsample of transcripts, in order to capture broad areas and organise the data. This set of themes was progressively elaborated through group discussions and an iterative process of reading and coding further transcripts. Later stages of analysis were focused on developing a nuanced understanding of parts of the data corpus relevant to our aims. Peer researchers, as well as members of project advisory groups representing all stakeholder groups, were involved in all the stages of the analysis. These collective processes can enhance validity by promoting reflexivity67 and ensuring that the perspectives of all stakeholder groups are considered in the analysis. 68
Key findings
There was a high level of agreement between stakeholder groups, with 11 features of CRT work identified as important across the groups. These were organised into three broad domains: (1) organisation of care, (2) the content of CRT work and (3) the role of CRTs within the acute and continuing care systems. For each feature, similarities and variations in stakeholders’ views on successful and unsuccessful aspects of current CRT practice and implementation were considered. Findings are summarised below.
-
Organisation of care:
-
Ease of access and speed of response were identified as being among the most important aspects of initial CRT contact for service users and carers. The need for 24-hour, 7-day access was emphasised, although the resource challenges of this were acknowledged. All stakeholder groups recognised the benefits of self-referral for known clients. Accident and emergency departments were viewed as the least satisfactory referral pathway.
-
Regularity, reliability and clarity were valued by stakeholders as these facilitate trust, emotional support and monitoring of risk and change. A few service users reported poor communication and infrequent visits from staff as the least helpful aspect of their care, whereas a small minority of service users and carers described large negative impacts when staff were not reliable.
-
Flexibility for referrals, timing of visits, forms of support and duration of contact were advocated by all stakeholder groups, with service users particularly valuing flexible timing of visits and involvement in their planning. Implementation issues identified include resource limitations and difficulties with predicting workloads.
-
Staff continuity was greatly valued by service users and carers as it can facilitate trust and relationship building, whereas the lack of it was one of the least helpful aspects of CRT contact. Practitioners and CRT developers were aware of the importance of staff continuity and the need to improve it. Several strategies to prioritise continuity within a shift-working system were discussed.
-
Staff mix and experience – service users and carers valued staff experienced in crisis work and CRT-specific staff training was viewed as essential by practitioners. CRT staff and developers identified multidisciplinary staff mix as one of the most important aspects of good practice. However, only a minority of CRT staff groups described their own teams as multidisciplinary. Practitioners often described overall staffing levels as stretched or inadequate because of resource limitations.
-
-
The content of CRT work:
-
Involving the whole family – CRT developers and practitioners described family involvement at initial assessments as valuable in helping them to develop a holistic view of the crisis and to decide on the suitability of home treatment and CRT interventions. Although family involvement was valued by carers, many often felt excluded from decisions about treatment and support.
-
Emotional support was extremely important for service users and many described this as the most helpful aspect of their CRT contact. Staff with excellent basic emotional skills, such as kindness and empathy, and staffing continuity, with opportunities to develop therapeutic relationships, were identified as facilitating provision of high-quality emotional support. A few service users and carers said that they had not received any emotional support, as their contacts with CRT staff were brief and focused on organising care or medication.
-
CRT interventions – medication supervision was identified as the principal intervention, although stakeholders agreed that CRTs were often too narrowly focused on this at the expense of other forms of support. Practical interventions were valued, but their availability was often limited by time and resources. Psychological input, self-management and physical health checks were also valued but not frequently provided.
-
-
The role of CRTs within the acute and continuing care systems:
-
Gatekeeping hospital admissions was seen as the most important function of CRTs by developers, with CRT capacity to prevent admissions under threat when this did not take place.
-
Providing home-based treatment was valued across stakeholders for preserving freedom, social contacts and daily routines, and allowing greater privacy and safety for service users. Stakeholders from all groups were concerned about whether or not home treatment decisions were based on clinical need or a requirement to reduce hospital admissions.
-
Continuity and communication with other services around discharge were seen as particularly important by stakeholders. However, all stakeholder groups reported problems in continuity of care and effective interservice communication. Almost all practitioners and developers reported misunderstandings and lack of knowledge about CRTs among referrers. A number of strategies were suggested to help improve working relationships and continuity with other services.
-
Strengths and limitations
To our knowledge, this was the first study to provide an in-depth, multiperspective qualitative exploration of the successes and failures of CRTs across a wide range of contexts, covering trusts in urban, suburban and rural areas of England. The perspectives and experiences of all relevant stakeholder groups were explored and compared. The large number of qualitative data and the diverse demographic, clinical, service use and professional characteristics of the study’s sample help ensure that the common themes identified generally reflect the views of these stakeholder groups.
Given that service users were recruited through CRT clinicians, it is likely that the study’s sample under-represents service users who were not very engaged with services or who had generally negative experiences of CRTs. Because of the challenges of reporting concisely on such a large data corpus, the study focused on common themes and prevailing views within each stakeholder group. Thus, some less common concerns or views have not been thoroughly explored in depth, and the approach in this initial analysis of a very large number of interviews is necessarily broad rather than in-depth.
Recommendations for future research
Many of the findings from this study had direct implications for the development of a more highly specified CRT model, especially in relation to improving service user and carer experiences. Priority areas for service improvement and for further research in optimising team function and outcomes include continuity of care, provision of emotional and practical support, carer involvement, and the quantity and quality of contact with CRT staff. Findings also highlight challenges to CRT implementation in contexts of stringent resource limitations and complex service configurations. Most previous UK CRT research has been conducted in urban areas; some stakeholders in our interviews raised challenges to implementing the CRT model fully in more rural areas (e.g. in achieving a rapid response service and providing frequent home visits). Further research is needed to understand and assess barriers of, and facilitators to, successful implementation of good CRT care in different contexts. In relation to initiatives for CRT improvement, qualitative research including multiple stakeholder perspectives is a rich source for understanding the impact of initiatives and barriers of, and facilitators to, achieving intended improvements. Use of implementation science methodologies in understanding how to overcome barriers and achieve change is a priority for future research.
Module 2.1: development and piloting of a crisis resolution team fidelity scale
See Appendix 4 for the published report of this work. 69 The report is accessible at the following URL: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-016-1139-4 (accessed 28 March 2019).
Aims
Fidelity scales are measures of the extent to which services adhere to a model of high-quality care, based on evidence and on stakeholder consensus. They are designed as tools to support quality improvement. 56 There is evidence for some fidelity scales of an association between higher fidelity and superior service outcomes. 70 Fidelity scales have been developed for use in some mental health service models,71 especially in the USA, but none exist for CRTs.
The aim of this study was to develop a highly defined and validated fidelity scale for CRTs. The study aimed to (1) systemically develop a CRT fidelity scale, (2) test its feasibility and utility in practice and (3) conduct an initial investigation of its psychometric properties.
Methods
Concept mapping72 was used to construct the CRT fidelity scale. This is a method used in the development of measures to identify and group into relevant domains a set of priority items based on stakeholder consensus. Potential service model characteristics were identified from module 1 (the literature review),58 the national survey of CRT managers63 and a qualitative investigation of CRT stakeholder perspectives. All yielded potential items for inclusion in a longlist of characteristics of high-quality CRT delivery. Next, this longlist of characteristics, identified as associated with good practice in CRTs, was condensed and combined into a list of fidelity scale statements by a group of academic, service user and clinician stakeholders by, for example, removing duplicates and combining closely related items. Following this, a series of concept mapping meetings involving stakeholders with different perspectives was held. Participants were asked to prioritise statements in terms of their importance for CRT best practice and to sort statements into groups of conceptually related statements. Specialist Ariadne concept mapping software (version 1.0; Talcott, Amsterdam, the Netherlands) was then used to analyse participants’ grouping of statements, using a form of cluster analysis, to generate a series of ‘cluster solutions’, which distinguished domains of CRT fidelity to reflect how participants grouped statements. The software also generated a mean importance rating for each statement from participants’ prioritisation of statements, which allowed the fidelity statements considered most important by stakeholders within each conceptual domain to be identified. Cluster solutions generated by the software were then reviewed by a small group of stakeholders, who selected the cluster solution that produced the most conceptually coherent set of domains of CRT fidelity, and named each domain, reaching consensus through discussion. The chosen cluster solution, that is, the final concept map, was then used to develop the CRT fidelity scale. Statements representing each fidelity domain were selected for inclusion in the fidelity scale. Statements of higher importance within each domain were selected for inclusion. Operational definitions were developed for each statement and anchor points specified for scoring, with reference to the development work carried out in module 1. Adherence to fidelity items is measured on a five-point scale. In common with other fidelity scales,70 a score of 5 on each item was taken to represent excellent model fidelity, that is, a service was adherent to best practice standards for this item. A score of 3 was taken to represent moderate fidelity, that is, a service was adhering to some essential requirements for best practice in this area, but not achieving all desirable elements of best practice for this item. The measure was thus able to distinguish services with ‘good’ overall model fidelity (i.e. a mean score of ≥ 4 per item) and services with ‘fair’ model fidelity (i.e. a mean score of 3–4 per item). At each stage of development, further stakeholder consultation was sought.
A fidelity review process was developed and piloted for collection of fidelity scale data. Reviews took place over 1 full day and were carried out by three reviewers: one clinician, one service user/carer and one researcher. CRT managers were contacted before the review to identify required documents and to establish the schedule. The review day involved interviews with managers, staff, liaising service staff, service users and carers; reviewing 10 anonymised case records; and reviewing service policies and records. Reviewers collected data using checklists and interview schedules, and scored fidelity items together at the end of the review. A draft fidelity review report was sent to team managers for clarifications before a final report and fidelity score were provided. Pilot reviews were initially conducted in four CRTs, followed by a 75-team review with CRTs from different parts of England, Scotland and Wales (see Crisis resolution team fidelity survey). Following reviews, researchers sought feedback from managers regarding the acceptability of the fidelity review and the validity and clarity of the fidelity scale.
Three psychometric properties of the fidelity scale were investigated:
-
Face validity was assessed through feedback from managers of CRTs participating in the pilot.
-
The presence of floor or ceiling effects and the ability of items to discriminate between higher and lower fidelity teams were investigated by assessing the range of scores from the 75-team review.
-
Inter-rater reliability was investigated using an extended vignette designed by researchers using mock fidelity review records.
Results
To construct the scale, an initial list of 232 identified service model characteristics was condensed to 72 fidelity scale statements by examining them for duplication and overlap. Sixty-eight participants were then involved in concept mapping, including representatives from all stakeholder groups (including service users, carers, CRT clinicians and managers, and CRT researchers). A four-cluster solution was chosen as the most coherent concept map. The clusters were named as (1) referrals and access, (2) content and delivery of care, (3) staffing and team procedures and (4) location and timing of care. Thirty-nine statements receiving a high level of endorsement were included in the final fidelity scale, representing each of the four clusters.
The three broad stakeholder groups in the process were service users and carers, CRT clinicians and others (including CRT researchers). All statements that were rated as very important (i.e. a mean score of > 4) by any of the three groups or as moderately important (i.e. a mean score of > 2.5) by more than one stakeholder group were included in the scale, either as a distinct item or among item-scoring criteria. Table 4 summarises the four clusters of items (subscales) defined through the process and the mean importance score for the items in each.
| Cluster | Number of statements from concept mapping (N = 72), n (%) | Mean of mean importance scores for statements in this cluster | Number of statements in the CRT fidelity scale (N = 39), n (%) |
|---|---|---|---|
| 1. Referrals and access | 14 (19) | 3.41 | 10 (26) |
| 2. Content and delivery of care | 26 (36) | 2.84 | 16 (41) |
| 3. Staffing and team organisation | 25 (35) | 2.98 | 10 (26) |
| 4. Location and timing of care | 7 (10) | 3.15 | 3 (8) |
The first version of the fidelity scale was piloted in 75 teams in a range of urban and rural locations and catchment sizes. Feedback indicated that fidelity reviews and reports received afterwards were perceived as acceptable and helpful, although reviews were time-consuming. The first version of the fidelity scale was reviewed after 50 reviews. All 39 items were retained, with minor changes made to 19 items in creating version 2 of the fidelity scale. Version 2 was piloted alongside the original version in nine CRTs.
Seventeen reviewers participated in the inter-rater reliability exercise, using version 2 of the fidelity scale. An estimated kappa correlation of 0.65 [95% confidence interval (CI) 0.54 to 0.76] between ratings was identified, indicating moderately high similarity between ratings within an item. The estimated intraclass correlation (ICC) averaged over the 16 raters was very high, at a value of 0.97 (95% CI 0.95 to 0.98). Consistency of agreement ICCs produced nearly identical values (i.e. an ICC of 0.97), equivalent to Cronbach’s alpha.
Results indicate that the fidelity scale distinguished between higher- and lower-fidelity CRTs, with a wide range of scores obtained on each item. Piloting version 2 of the scale generated modest changes to fidelity scores compared with version 1 piloting, but increased scale clarity.
Strengths and limitations
Using concept mapping, the study systematically developed the first CRT fidelity scale, based on best available evidence and stakeholder input. The so-far inconsistent implementation of CRTs has limited the potential benefits of providing this service model. 24 The CORE fidelity scale has potential to support CRT model implementation and aid quality improvement work by providing a clear specification of this service model. This addresses the study’s overarching aim of improving the care provided to service users experiencing an acute mental health crisis.
There were two limitations of the study’s CRT fidelity scale development: the scope of stakeholder consultation and the degree of testing of psychometric properties conducted.
It was aimed to include stakeholder views at all stages of development. However, during concept mapping, clinicians outnumbered service users and carers in terms of input, and some stakeholder groups (e.g. primary care referrers to CRTs and emergency services) were not represented. Stakeholder input was largely from the UK, so it is not known how far the fidelity scale represents views of international stakeholders and how appropriate it is for use outside the UK.
Research implications
The content and criterion validity of the study’s fidelity scale require investigation to demonstrate the legitimacy of the scale as a measure of service quality, and further testing of the scale’s inter-rater and test–retest reliability is also a priority. A clinical need to develop and evaluate a resource manual to help CRTs achieve service standards and aid quality improvement38 has been addressed in the (module 3) CORE SIP trial. 73 There is also a need to explore the feasibility and utility of the fidelity scale in international contexts where the model is used, such as in Norway and the Netherlands.
The development of the CRT fidelity scale has demonstrated concept mapping to be a feasible method in developing and defining the CRT service model. The development and piloting of the study’s CRT fidelity scale provides a model of PPI in research and audit. 74
Crisis resolution team fidelity survey
As well as serving to pilot the CORE CRT fidelity scale, the 75-team survey provided useful information about implementation of the CRT model nationally in England. See Appendix 4 for a reference to the published results of this work. 69
Forty-seven NHS trusts were approached, with 149 CRTs within their catchment areas. Of these, 75 CRTs from 27 trusts took part in the survey. The study sample of 75 teams comprised 70 teams in England, one team in Scotland and four teams in Wales.
In the 75 teams surveyed, the total scores ranged from 73 to 151 (possible range 39–195). The median score was 122 and the interquartile range (IQR) was 111–132 (these two findings were not reported in the published paper69 on the development of the scale; see Appendix 4). Higher scores indicate higher model fidelity.
The median scores per item across all 75 teams for each subscale within the CRT fidelity scale are provided in Table 5. The low score for the ‘location and timing of help’ subscale reflects the fact that many CRT teams had no access to residential crisis houses or acute day units, and typically provide a less intensive service (i.e. less frequent visits to service users) than recommended in the CORE scale and in the original CRT guidance.
| CRT fidelity scale subscale | Median score | Interquartile range |
|---|---|---|
| Referrals and access (10 items) | 3.40 | 2.73–3.71 |
| Content and delivery of care (16 items) | 2.86 | 2.22–3.50 |
| Staffing and team procedures (10 items) | 3.25 | 1.49–2.48 |
| Location and timing of help (3 items) | 1.85 | 2.36–3.94 |
The fidelity items for which teams typically showed poor fidelity to the CORE CRT model (median score of 1 or 2) and the items for which teams typically showed good model fidelity (median score of 4 or 5) are presented in Table 6.
| CRT fidelity scale items with | |
|---|---|
| Low fidelity in most CRT teams (median score of 1–2) | High fidelity in most CRT teams (median score of 4–5) |
| 1. The CRT responds quickly to new referrals | 2. The CRT is easily accessible to all eligible referrers |
| 14. The CRT assesses carers’ needs and offers carers emotional and practical support | 4. The CRT will consider working with anyone who would otherwise be admitted to an adult acute psychiatric hospital |
| 16. The CRT promotes service users’ and carers’ understanding of illness and medication and addresses concerns about medication | 5. The CRT provides a 24-hour, 7-day service |
| 17. The CRT provides psychological interventions | 6. The CRT has a fully implemented ‘gatekeeping’ role |
| 18. The CRT considers and addresses service users’ physical health needs | 8. The CRT provides explanation and direction to other services for service users, carers and referrers regarding referrals that are not accepted |
| 22. The CRT prioritises good therapeutic relationships between staff and service users and carers | 10. The CRT is a distinct service that only provides crisis assessment and brief home treatment |
| 24. The CRT helps plan service users’ and service’s responses to future crises | 11. The CRT assertively engages and comprehensively assesses all service users accepted for CRT support |
| 29. The CRT is a full multidisciplinary staff team | 15. The CRT reviews, prescribes and delivers medication for all service users when needed |
| 31. The CRT has comprehensive risk assessment and risk management procedures | 19. The CRT helps service users with social and practical problems |
| 36. The CRT has systems to provide consistency of staff and support to a service user during a period of CRT care | 23. The CRT offers service users choice regarding location, timing and types of support |
| 37. The CRT can access a range of crisis services to help provide an alternative to hospital admission | 27. The CRT has adequate staffing levels |
| 38. The CRT provides frequent visits to service users | 28. The CRT has a psychiatrist or psychiatrists in the CRT team, with adequate staffing levels |
| 32. The CRT has systems to ensure the safety of CRT staff members | |
| 33. The CRT has effective record keeping and communication procedures to promote teamwork and information sharing between CRT staff | |
| 35. The CRT takes account of equality and diversity in all aspects of service provision | |
| 39. The CRT mostly assesses and supports service users in their home | |
There are three main findings from this survey regarding implementation of the CRT model in practice in England. First, CRTs typically achieve only moderate fidelity in adhering to an optimal CRT model: teams’ scores ranged from low to moderately high fidelity; no team achieved an average item score of > 4, which would indicate very good model fidelity. Second, the range of scores achieved for each item suggests that the CRT fidelity scale is not unrealistically rigorous: all items were being delivered with high fidelity in some CRTs and, therefore, are achievable in routine care. Third, although areas of strength and limitations regarding CRT model adherence varied from team to team, the study’s survey shows that CRT teams typically struggled to provide core elements of the CRT model specified in government guidance,3 such as rapid response, a range of care from a multidisciplinary team and help with planning recovery and future crisis response.
This study thus corroborates the findings of previous surveys that relied on CRT managers’ reports of their teams’ organisation and service delivery,24,63 and suggests that the CRT model has been inconsistently and only partially implemented in England. It suggests that a national mandate and policy guidance may in themselves be insufficient to ensure implementation of a complex service model as planned. It reinforces the need to develop effective resources to support implementation and service improvement in CRTs.
Module 2.2: development of the service improvement programme
A CRT SIP was developed to support teams in improving adherence to the CRT model, as defined in the CORE CRT fidelity scale.
See Appendix 5 for the published report of this work. 73 The report is also accessible at the following URL: https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-016-1283-7 (accessed 28 March 2019).
The CORE CRT SIP was designed to support CRT teams in identifying target areas for service improvement and in developing and implementing plans to improve current practice. It was modelled on the US EBP programme’s implementation resource kits,57 with content informed by module 1 and by the content of the fidelity scale. Development of the SIP was led by a co-applicant (Steve Onyett), who brought expertise in promoting leadership and change management in health settings, and the study principal research associate (Elaine Johnston), who brought experience of working as a clinical psychologist in CRT teams. The SIP’s content was developed and refined iteratively, with input from the study team and consultants, and advice from senior clinicians with relevant CRT experience from local NHS trusts.
Structures and resources included in the SIP are available in the online CRT resource pack and are accessible at the following URL: www.ucl.ac.uk/core-resource-pack (accessed 7 March 2019). The structures and resources include:
-
Assessment of adherence to current CRT best practice measured by the CORE CRT fidelity scale. The stipulated time points for fidelity reviews were at baseline, 6 months and at the end of the 12-month study period, with detailed feedback provided to teams on their strengths, areas of low fidelity and changes in team fidelity since previous reviews. This was designed to help identify targets for service improvement, to inform planning for how to achieve them and to provide positive reinforcement for any implementation successes achieved during the previous 6 months.
-
Structures to guide service improvement work. A number of structures based on the EBP framework were adopted to guide service improvement. These included a 1-day, whole-team-scoping event for each CRT to kick-start the SIP feedback on the fidelity review, service improvement groups of managers and clinical leaders within each CRT meeting regularly to develop service improvement plans, and collaboration between CRT managers and staff in teams receiving the intervention, which will be promoted by the research team. Collaboration activities will include an online forum, regular bulletins from the research team about implementation progress at study sites and at least two meetings/events during the study period to promote sharing of experience, knowledge and best practice. Evidence suggests that these types of collaborative learning events have the potential to support improvements in the quality of services. 75
-
Access to a CRT facilitator (0.1 full-time equivalent for each team) to help teams develop and implement their service improvement plans. Facilitators were managers or senior clinicians with experience of working in or with CRTs, but not necessarily with experience within the team in which they had this role. Facilitators were provided with initial and follow-up group training and individual coaching; they were invited to regular implementation meetings with the study team to feedback how on the intervention was progressing and discuss ways of overcoming barriers to service improvement. Facilitators were encouraged to adopt a solution-focused approach76 in working with teams, building on teams’ existing strengths and focusing on achievable goals, rather than dwelling on the development and consequences of potentially intractable problems.
-
Access to a web-based resource pack manual (i.e. the CORE CRT resource pack), including practical resources, guidance and training materials to support implementation; case studies from high-fidelity CRT services outlining strategies for achieving high fidelity; relevant reading; useful links; and video and audio clips of service users, carers and staff involved in clinical CRT work and service improvement research, providing rationale for fidelity scale items and ideas for improving support. Resources that were linked to each of the items on the fidelity scale were provided.
The CORE CRT SIP, with implementation support from facilitators during the year of the intervention, was thus designed to provide ongoing help to teams during the course of the project. The nature of this support could be individualised to be appropriate to the team context and to address specific local barriers to implementation of the CRT model, as specified in the CORE fidelity scale. This could include support with securing leadership support, structuring team workflows to support implementation or providing expert technical assistance with implementing the CRT model when required, in line with EBP implementation theory. 77
Module 2.3: preparing for the CORE crisis resolution team service improvement programme trial
During the development and piloting of the CRT fidelity scale (modules 2.1 and 2.2), plans for the CORE CRT SIP trial (module 3) were refined. Consultation on the trial design, outcome measures and intervention content were achieved by the following:
-
a symposium event, held in May 2014, to which managers and clinicians from CRT teams participating in the study, policy-makers and service planners, and service users from the CORE working group and local service user groups were invited
-
a 4-day visit in 2013 by the CRT programme manager (BL-E) to US implementation experts, including study consultant Professor Gary Bond and his colleagues from the Dartmouth Psychiatric Research Center, and Professor Kim Mueser and colleagues from the University of Boston
-
consultation with the study team, the study service user and carer working group, and senior CRT clinicians from NHS trusts (but not the CRT teams) participating in the trial.
Twenty-five CRTs from eight NHS trusts were recruited to participate in the trial. These were selected to include inner- and outer-London sites, other large urban areas in southern England and more mixed suburban and rural areas. A full nationwide spread of sites was not feasible within the study’s resources.
The feasibility and acceptability of proposed outcome measures for the trial were confirmed. Measures of service user experience and assessing satisfaction with, and perceived continuity of, care had been used in the pilot trial of the CORE peer-supported self-management programme (module 5), so were known to be suitable for use with a CRT population. Measures of staff well-being had been previously used successfully in a multisite study of staff morale in acute services, including CRTs, which was also led by the CORE study chief investigator. 78 The CRT fidelity scale was thoroughly piloted in the 75-team survey.
The research and development and information technology (IT) departments of participating NHS trusts were contacted to check the availability of anonymised acute service use data for cohorts of service users for the trial. Similar data had also been collected for participants in the module 5 pilot trial for the peer-supported self-management programme. Epidemiologists at UCL were consulted about how best to collect data about the catchment area populations of CRTs participating in the trial, from which to assess teams’ admission rates. Population data for 18- to 64-year-olds were available from the Office for National Statistics via ‘nomisweb’ at a broad (borough) or detailed (lower super output area) level as required to allow accurate estimation of the population served by each CRT team (www.nomisweb.co.uk/; accessed 7 March 2019).
Meanwhile, the content and format of the online CRT resource pack (designed to support service improvement in the CRT trial) was iteratively improved. Senior CRT clinicians from teams not participating in the trial gave feedback on early versions of the online resource. The staggered start date for CRT teams participating in the trial allowed further early feedback and refinement of the resource in response to teams’ early experience. Developments made through this process included (1) the addition of a ‘news’ section and access to the UCL crisis care Twitter feed (www.twitter.com; Twitter, Inc., San Francisco, CA, USA), to increase the feel of the resource pack as a living, evolving aid for CRTs, (2) standardisation of the way guidance for each fidelity item was presented to aid clarity (the subheadings were target, why this is important, ways of doing this well and examples of good practice), and (3) addition of more case study examples and video testimonies to reinforce the importance of each fidelity item to service users’ experience and to show that they currently are being achieved in UK teams.
Module 3: a cluster randomised controlled trial evaluating the CORE service improvement programme for mental health crisis resolution teams
The full protocol for this trial has been published73 (see Appendix 5). The report is also accessible at the following URL: https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-016-1283-7 (accessed 28 March 2019).
Aims
A cluster randomised trial was conducted in order to evaluate the impact of the CORE CRT SIP. CRTs allocated to the intervention arm received the SIP over a 1-year period; control CRTs did not receive the intervention. The trial tested the hypotheses that a CRT SIP can improve service users’ experiences of CRT care (primary hypothesis), reduce acute service use and improve CRT staff well-being. The trial also aimed to investigate whether or not fidelity scores increase in CRTs receiving the intervention, and to explore the associations between CRT fidelity scores and service outcomes. Through a qualitative evaluation, the trial sought to understand stakeholders’ experience of the SIP and barriers to, and facilitators of, its implementation.
Methods of data collection
Twenty-five CRTs were recruited from eight NHS trusts across southern England and the Midlands, covering urban, suburban and rural areas. CRTs identified by the earlier CORE fidelity survey as already achieving good model fidelity were excluded, as were CRTs anticipating any major service reorganisation during the trial period. At least two participating CRTs from each NHS trust were required, to allow randomisation of CRTs within trusts. Fifteen teams were randomised to receive the SIP, which involved support from a CRT facilitator, access to online implementation resources and feedback from regular service audits (for further information regarding the intervention, see Module 2.2). Ten teams were allocated to the control group. The primary outcome was service users’ satisfaction with CRT service, as measured by the Client Satisfaction Questionnaire (CSQ). 79
Service user satisfaction was chosen as the primary outcome because of the evidence from previous qualitative studies and surveys that the implementation of CRTs has not clearly improved service users’ experiences of mental health crisis care to the extent hoped for, and which trials indicate is possible. 58 The specific choice of the CSQ as the primary outcome measure was because it was brief and widely used, and has proved sensitive to differences between service models in other studies in acute care settings. 79 The calculated sample size for the trial provided 95% power to detect half of 1 standard deviation (SD) difference between groups in mean satisfaction measured by the CSQ (3.5 points assuming a typical SD of 7.0 points) using a two-sided test, allowing for within-team clustering (ICC 0.05 for clusters of size 15) and unequal 3 : 2 (intervention-to-control) randomisation.
Randomisation was stratified by NHS trust to ensure that within each trust some CRTs received the intervention, and some acted as control teams. A statistician, independent of the study, generated allocation sequence lists and conducted randomisations for all participating teams within each NHS trust at the same time, once baseline fidelity reviews had been completed at all sites within the trust. There were no blinding arrangements, as study researchers and CRT staff were aware of teams’ allocation status. Service user participants providing data for the trial’s primary outcome and trusts’ informatics teams providing service use data are unlikely to have known whether or not teams were receiving the SIP.
The trial comprised the following components:
-
Quantitative evaluations of service user experience – from each CRT, the trial aimed to sequentially recruit 15 eligible service users at baseline and another sample of 15 service users at follow-up (months 10–12 of the trial intervention period), providing a total sample of 375 at each time point. CRT staff were asked to screen then contact all eligible CRT service users during this period to ask about their willingness to speak to a researcher, and researchers then sought to contact all potential participants until the target of 15 per team was achieved. Eligibility criteria were that participants had used the CRT service for at least 7 days, were able to read and understand English, had the capacity to provide informed consent and did not pose too high a risk to others to participate. At each time point, researchers administered two structured questionnaires (i.e. the CSQ79 and Continu-um80), which measured perceived continuity of care.
-
Quantitative evaluations of staff well-being – all clinical CRT staff were invited to complete online self-report questionnaires on staff morale (as measured by the Maslach Burnout Inventory81), job satisfaction (as measured by the Work Engagement Scale82) and psychological health (as measured by the General Health Questionnaire83) at baseline and follow-up (months 10–12 of the trial intervention period).
-
Quantitative evaluations of service use – anonymised demographic and service use data were collected from electronic patient records at baseline and follow-up. The data were collected for two cohorts: service users admitted to CRT care during a 1-month period ending 6 months prior to the study start date (baseline) and service users admitted in month 7 of the study intervention year (follow-up). These data were used to assess rates of re-admission to acute services following CRT care. All service users admitted to acute services over a 6-month period up to the study baseline date and during months 7–12 of the intervention year; these data were used to assess total hospital admission rates in the catchment area of each CRT. Study researchers provided a pro forma to appropriate administrators or informatics team specifying what type of data needed to be collected and for which time period. The study outcomes were then calculated from this raw data. Data were collected only for patients aged 18–64 years, that is, the age range included by all CRTs to ensure comparability of data across sites. Details of how patient records data were defined and operationalised are provided in the published results paper84 for the workstream 1 trial (see Appendix 6).
-
Participating teams’ CRT model fidelity was assessed at the 1-day ‘fidelity review’ audit, to be conducted at baseline and at the 1-year follow-up using the CORE CRT fidelity scale. 69
-
Qualitative evaluation – the CRT service improvement facilitators were interviewed each month throughout the intervention year in order to record implementation activities the teams had undertaken. Six case study sites were purposively selected following the 12-month fidelity reviews. At each study site, individual interviews were conducted with CRT managers, CRT facilitators and their clinical supervisor, and a focus group with CRT staff in order to explore their experience of the SIP.
Teams were recruited to the study between September and December 2014, with a 1-year trial intervention period. All baseline fidelity reviews were conducted before teams were randomised. Baseline data from service users and staff were collected following each team’s fidelity review; for some teams, baseline data collection was completed after randomisation.
Analysis
Statistical analyses were conducted using Stata® (StataCorp LP, College Station, TX, USA) and qualitative data were analysed using NVivo 9 software. For each of the trial components, the analysis was as follows:
-
Service user experience – in order to test whether or not participants’ satisfaction with the CRT was greater in the teams that received the intervention than in the control teams (our primary hypothesis), linear random-effects modelling was used with a random effect for CRT, controlling for mean baseline client satisfaction score by CRT. Perceived continuity of care was also compared between control and intervention teams using a similar linear random-effects model. ICCs were calculated for both outcomes, with CRT as the clustering variable.
-
Staff well-being linear random-effects models were used to compare mean staff psychological well-being, mean staff involvement and mean staff burnout scores between the intervention group and control arm. ICCs are shown for all outcomes using CRT as the clustering variable.
-
Service use – routine data were used on admissions to acute services, bed use and population size to compare service use patterns between intervention and control teams. Whether or not there were any significant differences between intervention and control teams in rates of re-admissions within 6 months of an initial admission to acute care were investigated. Poisson random-effects modelling was used with bed use, admission rate or rate of re-admission to acute care set as the exposure variable, as appropriate, and using trust as the random effect. Two analyses were conducted for inpatient admission and bed use outcomes. The first analysis compared intervention and control group teams at follow-up, adjusting for baseline score on the outcome measure. This provides the more valid comparison of change in outcome during the study period. The second analysis adjusted for catchment area population, thus providing an alternative absolute comparison of inpatient admissions and bed use in the two groups. ICCs are shown using trust as the clustering variable.
-
CRT model fidelity – the relationship at team level was explored between the change in team fidelity scores from baseline to the 1-year follow-up and changes in five study outcomes: service user satisfaction, staff job satisfaction, inpatient admissions, inpatient bed use and re-admission following CRT care. The relationship between fidelity change and outcomes was analysed using linear regression.
-
Qualitative evaluation – descriptive data were reported on implementation activities and service initiatives that took place during the study intervention year. The time spent by staff on the online resource kit was captured by Google Analytics (Google Inc., Mountain View, CA, USA). Qualitative data from interviews and focus groups on barriers to, and facilitators of, achieving change, based on the SIP, were analysed using thematic analysis. 66
Results
All 25 CRTs were successfully recruited and retained in the trial. Sixty-two per cent of the eligible service users, who expressed willingness to CRT staff to participate in the study, gave informed consent to researchers to complete measures of satisfaction and continuity (353/567 at baseline and 371/594 at follow-up). The mean age of service user participants was 43 years (SD 15 years) at baseline and 42 years (SD 14 years) at follow-up; the majority were female (59% at baseline and 61% at follow-up) and most identified as white (86% at baseline and 81% at follow-up). At each time point, 79% of clinical staff then working in the participating CRTs completed the survey (441/560 at baseline and 432/544 at follow-up). The mean age of staff participants was 43 years (SD 10 years) at baseline and follow-up; the majority identified as female (66% at baseline and 63% at follow-up) and white (68% at baseline and 65% at follow-up). (For further information about recruitment rates and service user and staff participants’ characteristics, see the paper84 referred to in Appendix 6.) No serious adverse events (SAEs) were identified during participant recruitment and data collection, and no study-related harms were reported by participating CRTs during the trial intervention.
The key findings are summarised in Table 7. There was no statistically significant difference in service user satisfaction (primary outcome) or service user-rated continuity of care between the intervention and control group teams. There were no significant differences between the two groups in three of the four staff self-rated well-being measures; better general psychological health outcomes for intervention group staff just achieved significance. There were significantly fewer inpatient admissions and inpatient bed-days (including both voluntary and compulsory admissions) at follow-up in the intervention group than in the control group, with adjustment for baseline rates. There were no significant differences between the two groups in the rates of compulsory admissions or rates of re-admission to acute care for people who had already experienced an episode of CRT care.
| Measure | Trial arm | Adjusted analysis estimate (95% CI)a | ICC (95% CI) | |
|---|---|---|---|---|
| Control (N = 10 CRTs) | Intervention (N = 15 CRTs) | |||
| Service user outcomes | ||||
| CSQ (satisfaction with CRT service: primary outcome), median (IQR) | 28 (23–31) | 28 (24–32) | 0.97 (–1.02 to 2.97) | 0.15 (0.04 to 0.25) |
| Continuum (perceived continuity of care), mean (SD) | 40 (9) | 40 (10) | –0.06 (–2.78 to 2.66) | 0.07 (0.00 to 0.14) |
| Staff outcomes, mean (SD) | ||||
| MBI (emotional exhaustion) coefficient | 20 (10) | 18 (11) | –1.92 (–4.30 to 0.46) | 0.07 (0.00 to 0.15) |
| MBI (personal accomplishment) coefficient | 36 (8) | 37 (8) | 0.19 (–1.39 to 1.78) | 0.02 (0.00 to 0.07) |
| UWES (job satisfaction) coefficient | 38 (9) | 40 (8) | 1.07 (–0.81 to 2.96) | 0.07 (0.00 to 0.13) |
| GHQ coefficient | 12 (6) | 11 (5) | –1.29 (–2.39 to –0.20) | 0.05 (0.00 to 0.11) |
| Service use outcomes IRRs, n (median, IQR) | ||||
| Inpatient admissions | Baseline: 170 (129–245) | Baseline: 152 (60–219) | 0.09 (0.00 to 0.19) | |
| Follow-up: 170 (121–236) | Follow-up: 119 (42–179) | |||
| Compulsory admissionsd | Baseline: 70 (26–77) | Baseline: 54 (19–77) | 0.02 (0.00 to 0.04) | |
| Follow-up: 56 (32–72) | Follow-up: 42 (23–42) | |||
| Inpatient bed-days | Baseline: 6061 (4331–6683) | Baseline: 4294 (2614–5703) | 0.04 (0.00 to 0.08) | |
| Follow-up: 4685 (2846–9296) | Follow-up: 3830 (2356–6161) | |||
| Re-admissions following CRT care | Baseline: 16 (10–22) | Baseline: 12 (7–16) |
|
0.49 (0.05 to 0.92) |
| Follow-up: 22 (–31) | Follow-up: 12 (3–25) | |||
There was a weak correlation between an increase in team fidelity scores over the intervention period and improved patient satisfaction, with a correlation coefficient of 0.34 (p = 0.10). This can be interpreted so that a change of 10 fidelity points corresponds to a change of 0.65 CSQ points. There was a weak correlation between an increase in fidelity scores and a reduction in re-admissions following CRT care (correlation coefficient 0.38; p = 0.06). No significant association was found between the change in fidelity scores and changes in hospital admission rates, inpatient bed-days or staff well-being. For a breakdown of CRTs’ fidelity scores and relationships with outcomes, see the paper84 referred to in Appendix 6.
The qualitative evaluation established three broad domains capturing stakeholder views and experiences of the SIP (for a more detailed description, see Appendix 7):
-
Components of the SIP – stakeholders described support from the CORE team as well co-ordinated, with regular, ongoing help provided when needed. Some teams reported finding their facilitator easily contactable and approachable, whereas others felt that facilitators lacked presence within teams. Most teams and facilitators felt the role was more helpful when facilitators were internal and known to the team. Experiences of the scoping day were largely positive, and stakeholders felt that it promoted engagement and action planning. Fidelity reviews were seen as time-consuming, but some teams found them helpful in motivating staff and helping them reflect on their practice. Some stakeholders did not see the review as accurately measuring a team’s practice. The fidelity review report was considered valuable feedback, helping teams with quality improvement planning. The resource pack website was somewhat underutilised and was mainly accessed for browsing and fact-finding.
-
Process factors – lack of time to engage with the programme was the most frequently cited process factor, with the busy and overstretched nature of CRT work emphasised by all stakeholder groups. Several stakeholders stated that 12 months was not enough time for teams to implement service changes and see their effects. Staff motivation and morale was the second most frequently cited process factor, with the potential to influence programme implementation positively and negatively. The majority of stakeholders mentioned team ownership as an important factor affecting input and engagement with the study. The programme was described as increasing team ownership by increasing awareness of how staff should be practising. Many stakeholders viewed the programme as a structure to support service improvement and as a means of benchmarking their practice. Support from seniors in the trust was considered important as it could increase motivation and engagement. Service user involvement was also highlighted, although it was not achieved in all teams.
-
Impact of the programme – the majority of stakeholders described service innovations resulting from participation in the programme. Stakeholders also reported various ways in which service user experience improved following the programme. Team communication was seen as being improved, as the programme promoted a shared sense of purpose and understanding of the team’s tasks. Team purpose was enhanced as stakeholders were encouraged to address areas of practice that may previously have been neglected. Staff motivation was perceived as having improved at both individual clinician and team levels. Many stakeholders wished for quality improvement work to continue after the study end, seeing CORE as part of a bigger whole. However, two teams described a lack of impact of the programme. Lack of resources and staff turnover were cited as barriers to implementing SIPs.
Successes
Fairly good response rates of > 60% of service users referred by CRTs and nearly 80% of CRT staff were achieved. The primary outcome was negative, but our results did suggest that the implementation of the CORE SIP may have led to a reduction in hospital admission rates and inpatient bed use, when adjusting for baseline scores. Given the importance of reducing hospital admissions as an aim of CRTs, and to patient experience, it was believed that this positive finding provides an encouraging indication that the CORE CRT SIP is a worthwhile intervention. Although no significant differences were found in other outcomes, there were non-significant trends in favour of the intervention group teams regarding patient satisfaction, re-admission to acute services following CRT care and all staff well-being outcomes. The majority of intervention teams improved model fidelity over the study period, whereas none of the control teams did, which suggests that our programme was successful to some extent. There was also some evidence across all teams of a small positive association between increase in fidelity and improvement in outcomes for patient satisfaction and re-admission following CRT care.
The inclusion of 25 CRTs in varied geographical and sociodemographic contexts suggests that the trial findings may have general applicability to CRTs in England; however, generalisability to other national contexts is uncertain.
The qualitative interviews show that, overall, stakeholders had positive experiences of the SIP. The majority of stakeholders were able to describe ways in which the programme had a positive impact in their team, resulting in service innovations and improved staff motivation and service user experience.
Limitations and challenges
Several limitations arose from the study design. CRT service delivery and outcomes may have been affected by local policy directives and service initiatives that were independent of the trial intervention; the extent of these, and whether or not some teams were affected more than others, is unclear. As stakeholders pointed out, the 1-year follow-up period may have been too short for teams to implement their service improvement plans and to capture all the effects of the intervention.
Two limitations regarding the data collected for the primary outcome of service user satisfaction create uncertainty about whether the lack of a positive result on the primary outcome reflects a real lack of impact from the SIP on patient experience or methodological limitations of the study. First, the ICC for the primary analysis (ICC 0.12) was somewhat larger than anticipated (i.e. ICC 0.05), suggesting that the power of the main study was lower than planned (83%). However, the observed reduction in CSQ of 0.97 units was also far lower than the anticipated reduction of 3.5 units, and too small to be very meaningful in terms of patient experience, so this reduced power is unlikely to have substantially influenced the study findings. Second, and more importantly, the study participants may have been unrepresentative. It was not possible to establish from CRT teams how many service users were eligible and how many were approached by staff about taking part in the survey of satisfaction to measure the primary outcome for the study. Therefore, it cannot be determined whether recruited participants were representative of the CRTs’ service users in general or whether they over-represent those who are best engaged with CRT staff. This might also relate to the ceiling effect that was observed with the trial primary outcome measure (i.e. the CSQ). Service user participants were highly satisfied with care compared with previous studies. 15,18 In addition, the brief study measure might have not been sensitive enough to capture differences in service user satisfaction with CRTs.
Neither CRT staff nor fidelity reviewers were blind to teams’ allocation status during follow-up CRT fidelity reviews. Teams in the intervention group might have been more motivated to demonstrate fidelity gains than those in the control group. Reviewers may have also been subconsciously biased in favour of the intervention group. These phenomena may have served to exaggerate the difference found between intervention and control teams’ fidelity scores.
Study researchers were unable to independently verify that all relevant records were provided from NHS patient records, as they were anonymised. One trust was unable to provide information about whether inpatient admissions were compulsory or voluntary at follow-up. Researchers could not determine from the information provided whether service users were physically present on the ward during the whole of their inpatient admissions or whether they were on leave.
Recommendations for future research
Outcomes from the SIP that were trialled showed some promise in relation to effects on inpatient admission, but the primary study hypothesis was not confirmed. This suggests that the SIP and the fidelity scale are a potential basis for quality improvement in CRTs, but that further refinement is still needed.
Only a weak relationship was found between changes in overall fidelity scores and changes in outcome, and not for all key CRT outcomes. Therefore, the criterion validity of the fidelity scale and its utility as a marker of CRT service quality should be further explored. More robust testing of inter-rater reliability of the scale is needed in vivo.
It is possible that the critical components of CRT services lie within the CORE fidelity scale, but are not sufficiently weighted for teams’ overall fidelity scores to relate closely to service outcomes. Future research could further investigate the relationship between team outcomes and specific fidelity scale item or subscale scores.
A future economic evaluation could explore the cost-effectiveness of the intervention as delivered in this trial. A process evaluation could helpfully examine which aspects of service provision were addressed in service improvement plans and where additional support may have been needed to enhance the impact of the programme. The types of activity undertaken by CRT facilitators to support teams’ service improvement could be explored from facilitators’ monthly reports to help identify any gaps in support.
Conclusions and reflections for workstream 1
Workstream 1 of the CORE programme has produced several outputs of practical usefulness to clinical services and service planners in supporting service improvement in CRTs. These include:
-
a systematic review that synthesises current evidence about the critical components of CRTs and their implementation
-
benchmarking data about CRT service organisation and delivery from a national survey with an excellent response rate in 2014 and objective assessment from a 75-team fidelity survey in 2014
-
a comprehensive qualitative survey of stakeholders’ views about, and priorities for, high-quality care in CRT services
-
a clearly defined, highly specified model for CRT care, based on best available evidence, and a rigorous, road-tested audit process to assess teams’ adherence to this model
-
a set of resources to support service improvement with some evidence of effectiveness in reducing number of inpatient admissions and service use.
The value of these resources to service planners and policy-makers is demonstrated by their use by expert bodies and policy-making organisations nationally in the UK. Data from the module 1 national CRT survey were shared pre publication with Mind, NHS England, Health Education England and the Care Quality Commission (the body responsible for quality inspections of health and social care services in England), and informed publications including Mind’s acute care campaign report ‘Listening to Experience’85 and NHS England’s London Mental Health Crisis Commissioning Guide. 86 The CRT fidelity scale is advertised as a ‘national inspiration’ in the Crisis Care Concordat campaign led by NHS England. 87 Benchmarking data from our 75-team fidelity survey have been used by the Care Quality Commission88 and the Royal College of Psychiatrists89 in recent reports presenting recommendations for CRT care. Resources from the online CRT resource pack have been shared with the Royal College of Psychiatrists’ Home Treatment Accreditation Scheme to support service improvement among CRTs in the Home Treatment Accreditation Scheme network.
The CORE SIP trial (module 3) did not achieve all its aims, but showed promise in helping to reduce inpatient service use. Two major challenges for future research remain. First, there were limited relationships found between CRT teams’ fidelity gains and improvement in outcomes in the trial: there were weak to moderate associations between fidelity gains and improved patient experiences and reduced re-admissions following CRT care, but not with inpatient admission rates or bed use. Perhaps the lack of clearer associations is understandable; teams’ fidelity changes were typically modest in the trial, and most teams were of moderate fidelity at both trial time points. Experience from other fidelity scales suggests that even when a well-established fidelity measure is paired with a robust, relevant outcome measure, the correlations are in the moderate range at best. 70,90 However, for CRTs, further research is needed to establish which aspects of CRT model fidelity might relate most closely to specific outcomes. The study did not find empirical confirmation that the total score on the CRT fidelity scale is a wholly valid indicator of service quality.
Second, further research is required about how best to support service improvement in CRTs. The results from the CORE trial offer mixed messages about the impact of the CORE SIP. The trial’s primary outcome was not significant, suggesting that the programme did not improve patient experience in CRTs. The proximal goal of fidelity gain was achieved for most teams (and in none of the control services); some important secondary outcomes (inpatient admission rates and bed use) did yield significant, positive results. Further evaluation of a set of service improvement resources is desirable, which address the implementation challenges identified in the qualitative evaluation of our trial (e.g. leadership support, underuse of the online support, ensuring available time for the CRT facilitator). Evaluation of the impact of such a set of resources on patient experience in a patient population that is more clearly representative (and probably less satisfied) than the service user participants recruited to our trial is also desirable. The CORE CRT SIP does provide useful resources for future studies to build on, and which are of immediate practical use to support CRTs in developing their own quality improvement plans.
Workstream 2
It was the aim within workstream 2 to develop and evaluate a peer-supported self-management programme to address the gap between CRT support and continuing care, promote recovery and reduce relapse. An audit provided to the research team by one CRT participating in workstream 1 (see Module 2) found a 50% rate of re-admission to acute care following a period of CRT support. This high rate of relapse following CRT care has since been confirmed by a multisite study. 91 In addition, it was found in workstream 1 that interventions to prevent relapse and re-admission to acute care are generally not part of CRT service delivery. Mental health self-management programmes have the potential to address these limitations by supporting service users to learn skills to manage their psychological well-being and avoid future crises. 92 Self-management programmes can be supported by health professionals, health para-professionals and peer-support workers (PSWs) who have themselves experienced mental ill health, or a combination of these groups.
Government health policy and guidelines93–95 promote the use of PSWs to provide support and some specific interventions to mental health service users. Support provided by PSWs has been advocated as a way to improve outcomes for people following a mental health crisis. 96 Guidelines and consultation with advocacy groups suggest that peers may be appropriate supporters for the delivery of self-management programmes, whereas the employment of PSWs to deliver self-management support is becoming increasing common within the NHS. 97,98 However, existing evidence for the clinical effectiveness and cost-effectiveness of peer-support programmes is still inconclusive, and further trials of clearly defined interventions are needed. 99 To our knowledge, there have been no evaluations of peer-facilitated, self-management interventions for people leaving CRT care. In the study’s initial consultations with service users and carers, clinicians and trial methodologists in preparation of this proposal, PSWs emerged as the preferred choice for delivery of the self-management intervention.
Thus, the CORE research group set out to develop and evaluate a peer-supported, self-management intervention. The main goals of the intervention were to (1) reduce relapse, re-admission and bed use rates by enhancing service users’ and their networks’ abilities to respond to early signs of crises; (2) enhance continuity by bridging the perceived gap between crises and continuing care; and (3) enhance service users’ abilities to manage their illnesses and progress towards recovery goals.
Workstream 2 reports the iterative development of a peer-supported, self-management intervention for people leaving CRT care, following Medical Research Council (MRC)’s guidelines100 for developing and evaluating complex interventions. This comprises:
-
development and feasibility testing phases (module 4) – systematic reviews of self-management and peer-support interventions for severe mental illnesses (SMIs), stakeholder consultation and feasibility testing of a programme of support
-
an internal pilot RCT of a peer-supported, self-management programme (module 5)
-
a definitive evaluation of the trial intervention in a multisite RCT (module 6).
Module 4.1: self-management for people with serious mental illness – a meta-analytic review
A report based on this review was published by the National Institute for Health and Care Excellence (NICE) as guidelines,95 which were subsequently updated. See Appendix 8 for a link to the published paper. 101 The report is also accessible at the following URL: www.nice.org.uk/guidance/cg178 (accessed 7 March 2019). The review is registered with PROSPERO as CRD42017043048.
Aims
The study aimed to review the evidence of short-, medium- and long-term clinical effectiveness of self-management programmes for SMIs through a systematic meta-analytic review compared with other comparable therapies or standard care. Quantitative synthesis of results from different studies was also conducted.
Methods of data collection
Studies were included if participants were adults, aged ≥ 18 years and diagnosed with a SMI, that is, with a clinical diagnosis of schizophrenia spectrum disorders (schizoaffective disorder, delusional disorder and psychosis), bipolar disorder or major depression. Studies with mixed populations (including personality disorder) using secondary care mental health services were also included. Participants at any stage of their illness, that is, as part of early intervention or more chronic/later stages, were included in this review. Further details and full search terms are provided in the paper101 referred to in Appendix 8; searches were conducted without time limit or geographical restrictions.
The types of self-management programmes included were those that aimed to help service users develop their own mental health self-management strategies and coping skills in order to achieve better clinical and/or social outcomes. The outcomes of the included studies were grouped as symptom-focused outcomes, service use outcomes, functioning outcomes and recovery-related outcomes.
Characteristics of the study design, the intervention, participants and outcomes for all available data at all provided time points were extracted. Authors were contacted and asked to provide any missing data.
Analysis
Studies were reviewed for bias using the Cochrane risk-of-bias tool,102 which was used to assess the quality of evidence by evaluating the risk of bias, inconsistency, indirectness, imprecision and publication bias. Extracted quantitative data were meta-analysed using appropriate random-effects models for dichotomous data (relative risk and 95% CIs) and continuous data [standardised mean differences (SMD)]. Outcomes were analysed at the end of treatment, post intervention (short term), up to 1 year post intervention (medium term) and over and including 1 year post intervention (long term). When more than one self-management intervention was evaluated in a study, these arms were combined for comparison with the control group. Review Manager software (RevMan 5.2; The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark) was used to conduct the meta-analyses. When outcome data were reported for more than one follow-up point, the time point closest to 1 year post intervention was used.
Key findings
Thirty-two RCTs with 4961 randomised individuals met the eligibility criteria for this review. The types of interventions included typically offered guided self-management, supported by a clinician or peer worker. There was wide variation in the duration of programmes, and in the number, duration and frequency of sessions within programmes. The majority of studies were conducted in Western countries, with a smaller but significant proportion in Asian and developing countries (κ = 7). The majority of studies included participants who were currently living in the community, with eight studies recruited from inpatient settings. In relation to clinical diagnosis, 16 studies included participants with only schizophrenia spectrum disorder and seven included only those with a diagnosis of bipolar disorder. The remaining nine included mixed populations of participants with schizophrenia, psychosis, bipolar, major depressive disorder and personality disorder.
The meta-analysis found some evidence of short- and long-term positive impacts, albeit relatively small ones, of self-management programmes on total symptoms (SMD experimental vs. control at follow-up: –0.81, 95% CI –1.18 to –0.44; p < 0.00001), social functioning (SMD –0.55, 95% CI –0.92 to 0.17; p < 0.0000), self-rated recovery (SMD –0.24, 95% CI –0.36 to –0.11; p = 0.0003) and quality of life (SMD –0.26, 95% CI –0.39 to –0.13; p < 0.0001). Initial analyses found no clear effect on number of relapses or length of time in hospital; although heterogeneity was high in these meta-analyses, numbers were small and there was some evidence of an effect on relapse, with one study moved to reduce heterogeneity.
Strengths and limitations
Using a broad inclusion criterion for SMI in this review, and including studies of mixed populations of secondary mental health service users, has ensured that the findings of the review are relevant to the CRT context of the workstream 2 CORE study trial. All studies included in this review were RCTs, but there was variation in the reporting of sequence generation and allocation concealment and, as is common in complex interventions, the blinding of participants and personnel was not always consistent. The greatest cause for concern was the selective reporting of outcomes, which was noted or not clearly reported in over half of the studies reviewed. Furthermore, the small number of studies and small number of participants in the studies meant that it was difficult to discern any evident publication bias.
Other limitations were high heterogeneity in many of the meta-analyses conducted, and relatively infrequent inclusion of re-admission and other service use outcomes. Comparisons of self-management with treatment as usual and those with active controls were pooled together. This potentially makes interpretation of results more challenging, although, in fact, we found no evident differences in results relating to type of comparator. There were also variations in the timing of the follow-up comparison.
Recommendations for future research
The review does not determine the relative clinical effectiveness of different types of self-management programme; further research and an established typology of self-management programmes are needed to achieve this. Importantly, future research needs to be of higher quality. Additional design features should also be considered, for example collecting longer-term follow-up data and applying consistency to the spread of outcome measures, with relapse and service use outcomes consistently measured. Future studies should also examine whether or not any variations in delivery could have an impact on service user outcomes and costs. Establishing whether or not guided self-management programmes (e.g. supported by clinicians or peer workers) are more effective than self-guided programmes is clearly relevant to determining the most cost-effective types of intervention. There is also scope for researching the application of computer-based programmes or applications (‘apps’), as this is a growing area of health research because of the potential for wider reach and reduced costs.
Module 4.2: systematic review of peer-support interventions
See Appendix 9 for the published report of this work. 103 The report is also accessible at the following URL: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-14-39 (accessed 28 March 2019).
Research aims
Comprehensive evidence has not previously been available about how effective peer-support programmes are and whether or not they improve outcomes for people with severe mental health problems. Although some systematic reviews of peer support are available, these are limited to subtypes of peer support or for people with depression only. This study aimed to review trials of community-based, peer-provided support for people with SMI.
Methods of data collection
The effects of peer-provided interventions were examined via objective outcomes, such as employment and re-admission to hospital and psychiatric symptoms, as well as self-reported outcomes, such as quality of life, recovery, empowerment, hope and satisfaction with services. Eligibility criteria were established. Published and unpublished RCTs, including cluster RCTs and factorial RCTs, were included.
Types of participants
Studies were included if participants were adults with SMI, specifically bipolar or schizophrenia spectrum disorder, or mixed populations of people using secondary mental health services. Studies were excluded if participants were diagnosed with unipolar depression or personality disorder. Peers either were currently using or had previously used secondary mental health services.
Types of interventions
The review included interventions that involved community-based peer support designed specifically to facilitate recovery from SMI. Residential and inpatient peer-run programmes were excluded, as well as peer-support programmes focusing on outcomes other than mental health recovery. Peer-support programmes were categorised into three types based on previous literature: mutual support groups, peer-support services (additional or separate from standard mental health care) or peer-provided mental health care (see the paper103 referred to in Appendix 9 for further details).
Search strategy
The study searched the Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, EMBASE, MEDLINE, preMEDLINE and PsycINFO from inception to January 2013, with no geographical restrictions, combining synonyms for SMI, peer support and RCT using the AND command. Data were extracted independently by two reviewers. Full search terms are provided in the paper103 referred to in Appendix 9.
Analysis
The SMD and Hedges’ g were calculated for continuous outcomes, and studies were weighted using the inverse of variance. For dichotomous outcomes, risk ratios were calculated and studies were combined using the Mantel–Haenszel method. All outcomes were reported with 95% CIs using random-effects models. Statistical heterogeneity was assessed by inspecting forest plots, conducting the chi-squared test and calculating the I2-statistic. Meta-analysis was conducted using RevMan, and the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system was used to rate confidence in the evidence from each analysis of pooled data.
Key findings
Eighteen trials (including 13 from the USA), with a total of 5597 participants, were included. Programme content and participants’ characteristics varied substantially, and outcomes were incompletely reported. Independent reviewers found a high risk of bias. It was only possible to synthesise a small number of studies. The quantitative data synthesis showed some evidence that peer support was associated with positive effects on empowerment from mutual support (SMD –1.44, 95% CI –2.79 to –0.09), and on recovery (SMD –0.24, 95% CI –0.39 to –0.09) and hope (SMD –0.14, 95% CI –0.27 to –0.02) from peer-support interventions post treatment and at follow-up. However, these effects varied across different types of peer support and confidence and this evidence was graded very low. There was very little or no evidence to suggest that peer support was associated with positive effects on satisfaction with services, overall symptoms or hospitalisation.
Strengths and limitations
Through using a broad inclusion criterion for SMI in this review, and including studies of mixed populations of secondary mental health service users, it was ensured that the findings of the review are relevant to the CRT context of the workstream 2 CORE study trial. Searches were highly sensitive, and the review provides a comprehensive synthesis of outcomes that were considered important by triallists and service users. The main outcomes were identified a priori, although hope and empowerment were added post hoc. Only randomised trials were included, as they provide the best evidence of efficacy, in line with best practice guidelines for systematic reviews. 102
Nevertheless, the conclusions were limited by the small number of eligible studies, which did not allow the conduct of subgroup analyses. Another limitation was the substantial variation in programme content and trial populations, which may have contributed to observed heterogeneity. Confidence in existing evidence was low because of poor study design and incomplete reporting of included studies. Peer support was categorised based on previous typologies, as there were no clearly defined models or fidelity criteria. Overall, there was not enough current evidence to conclude that peer-support interventions are either effective or ineffective for people with severe mental health problems.
Recommendations for future research
This review highlighted the need for high-quality research to accurately evaluate the clinical effectiveness and cost-effectiveness of peer-support interventions for people with severe mental health problems. Further research is needed to develop, clearly describe and test theory-based interventions. It was difficult to distinguish different types of peer support using an existing typology as programmes varied in many factors. A distinction between structured self-management-focused programmes and longer-term, less structured ones could be considered in future typologies. Future research should develop and describe clear models of peer support in order to facilitate future trials and help future reviewers synthesise the data more effectively. Trials including a process evaluation could help understand whether or not the peer-support programme is implemented as intended and mechanisms by which any treatment effects are achieved. 104 Future research should also examine critical ingredients that might contribute to programme success and appropriate target populations.
Most of the studies included in this review were poorly reported and failed to adhere to the CONSORT guidelines for conducting and reporting trials. 105 This review further highlights the need to improve standards for reporting trials of social and psychological interventions. Future trials of peer-support programmes must be registered in advance,106 publish their protocols, clearly state all outcomes and time points to be assessed, and describe interventions in full.
Module 4.3: development of a peer-support intervention
See Appendix 10 for the published report107 of this work. The report is also accessible at the following URL: https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-017-2900-6 (accessed 28 March 2019).
Research aims
Although self-management peer-support programmes have shown promising evidence of effectiveness, the empirical evidence for their effectiveness is still limited, as shown by the systematic reviews we conducted (see Module 4.1 and Module 4.2). Following on from these reviews, it was aimed to identify or develop a peer-supported, self-management programme appropriate for people discharged from CRT care.
Methods
The intervention was selected and developed through consultation with expert reference groups of CRT staff, as well as service users and carers. Multistage qualitative interview and focus group consultations were held to examine programme acceptability and feasibility and determine programme content. At each stage, consultations were conducted by a combination of service users, carers, clinicians and academic researchers. Focus groups and interviews were audio-recorded and then transcribed to be analysed.
Initial semistructured interviews explored service users’ views on peer support and priorities for support following CRT care. Semistructured interviews were conducted, usually by service user or carer researchers, with 41 service users recruited from CRTs in 10 NHS trusts in England. A self-management intervention (i.e. the Personal Recovery Plan)108 was then identified by the CORE service user, carer and clinician advisory groups as the best potential fit for the study’s objectives and to address the priorities of interviewed peer supporters. The Personal Recovery Plan108 structure was aligned to the themes reported in our systematic review findings (see Module 4). Focus groups of the key stakeholders were conducted to address the design of the proposed peer-facilitated self-management programme. Further modifications were identified through a feedback session with the newly recruited PSWs, as well as reviews by members of the study team, including CRT senior clinicians.
For modelling purposes, a pre-pilot of the intervention was facilitated by four trained PSWs, recruited from within the CORE service user advisory group, with 11 CRT service users post discharge. A psychologist supported weekly group supervision with the PSWs and was available if additional support was needed. Following completion of the one-on-one pre-pilot intervention, qualitative feedback was obtained through a focus group with the PSWs (n = 4) and individual interviews with the service users (n = 9). Both groups provided qualitative feedback on their experiences of the programme and suggestions about how it might be improved.
Further qualitative feedback was gathered from participants in the treatment arm of a pilot RCT embedded in the crisis resolution team service (see Module 5). Through these stages of consultations and feedback, a manualised peer-supported intervention for recovery and relapse prevention following a mental health crisis was developed and refined.
Analysis
Qualitative data from interviews were analysed by a team of researchers using thematic analysis. NVivo 9 software was used to code and analyse the data into different themes. The analytic strategy combined inductive and deductive approaches in order to explore initial research questions, as well as themes that characterised participants’ own experiences. A collaborative and iterative approach was adopted: a research team lead by a principal analyst read transcripts, developed a coding frame and regularly discussed emerging themes. This process was repeated at all qualitative phases. In addition, the feedback obtained from the stakeholders and pilot participants was later incorporated into the design of the intervention.
Results
Data from initial qualitative interviews and focus groups with CRT staff, service users and carers indicated support for the overall purpose and content of the programme, and for PSWs as providers of the intervention. Service users’ expressed needs were in line with the self-management approach. They endorsed sessions on relapse prevention, crisis planning, signposting and goal-setting as potentially useful. A small number of negative views, mainly concerns raised by carers and clinicians regarding peer support, highlighted the need for adequate PSW training, protocols, supervision and recruitment procedures.
Feedback regarding the concerns raised about the programme guided the development of training and procedures for the pre-pilot. Participant feedback after testing in the pre-pilot was largely positive regarding the facilitation of the programme by PSWs. Nearly all participants stated that they benefited from the peer-support experience. Some reported that the relationship itself was more useful than the structured section of self-management workbook, which was underutilised. The workbook was modified based on qualitative feedback from both participants and PSWs in order to improve usability. Minor changes to the language in the workbook were made in discussion with the PSWs and the study service user and carer expert reference groups. By replacing a definition of recovery in the original plan, space was created in the study version for participants to record their personal meaning of recovery, following discussion with their PSW. More blank space was included throughout the plan to allow participants space to include information, potentially using a range of media, relevant to their personal recovery plans. Moreover, additional training for PSWs was provided to facilitate workbook use.
Strengths and limitations
In some cases, the peer-support programme could not be adapted to accommodate service users’ views and requests during feasibility testing and piloting. A few participants wanted more than 10 sessions with the PSWs; however, this could not be changed because of funding and requirements for a consistently delivered trial intervention. One service user expressed a wish for a more closely ‘matched’ peer, but it was not feasible to provide this given the small PSW teams at each site.
Overall, however, the study has employed a process of systematically and iteratively obtaining stakeholder feedback at the different stages of intervention development. This has helped develop an intervention that matches on the needs and priorities of the target client group. The resulting trial intervention is clearly defined and manualised to enable consistent implementation and replicability. The different stages of consultations were important to strengthen the robustness and usability of our programme. The consultations allowed us to gauge stakeholder acceptability, but they were also useful in identifying gaps and areas of key importance when training PSWs and integrating the programme into a crisis team setting.
As Lovell et al. 109 pointed out, there are both advantages and disadvantages in using an approach that develops theory and models before conducting an exploratory trial. Developing complex interventions is a time-consuming and resource-heavy process, and incorporating and balancing the viewpoints of different stakeholder groups can be labour intensive. Nevertheless, this process is essential as it systematically incorporates the evidence base with current viewpoints while iteratively testing and refining the intervention design as it develops. The effectiveness of this peer-supported intervention in terms of its impact on service user outcomes and the economic impact remains to be piloted (module 5) and then evaluated in a full-scale definitive RCT (module 6).
Module 5: peer-supported self-management programme pilot trial
Aims
The pilot trial was used to test out trial procedures regarding recruitment, randomisation, data collection and storage, the study outcome measures and analysis plans. Qualitative feedback from study participants and PSWs was also sought to identify any further changes needed to the self-management workbook or arrangements for training, supervising and supporting the PSWs. This would allow amendments to the protocol to be made, if necessary, before the main trial to optimise the intervention provided to participants and its evaluation.
Methods
Forty participants were recruited from one CRT in an inner-London NHS trust and randomised to a treatment or control group. Twenty-one participants in the treatment group were offered up to 10 sessions with a PSW who supported them in using a self-management workbook. Nineteen participants in the control group were sent the self-management workbook but no additional guidance or peer support to help them use it. Patient-reported outcome measures were collected at baseline and 4-month follow-up interviews. Data regarding service use, including the primary outcome of re-admission to acute care, were collected from electronic patient records for the year before trial entry and the 1 year of follow-up.
Brief qualitative interviews were conducted with participants in the treatment group at the end of the trial intervention to explore their experience of the programme of support. A focus group was conducted with the PSW providers of the intervention about their views on content and implementation of the programme.
The few changes made to the trial protocol between the module 5 pilot trial and the module 6 main trial are reported in Module 6, Methods. Otherwise, the trial methods were retained as described in the section below on the main trial (see Module 6) and in the paper110 referred to in Appendix 11.
Results
Recruitment and retention
Of the 234 patients screened, 151 met the trial eligibility criteria. Of these 151, 40 (26%) were recruited to the trial. Fifteen could not be contacted, 42 declined and no decision was elicited from 54 participants before 1 month following CRT discharge had elapsed and they became ineligible. Of the 21 participants randomised to the treatment group, 17 received the trial intervention as per protocol (minimum of three sessions), one declined to meet their PSW and three were allocated to a PSW late following administrative oversights in the study or clinical teams. The 4-month follow-up interviews were completed with 34 out of 40 participants (85%). Primary outcome data regarding re-admission to acute care were obtained for all participants.
Qualitative interviews
Follow-up interviews were completed with 18 out of the 21 participants (86%) who were randomised to receive PSW support. The other three participants declined a follow-up interview. A focus group was conducted with PSWs (n = 4).
Most feedback about the programme was positive. Participants commented on the usefulness of PSWs providing information about mental health problems and treatment, and of having additional support. Eight participants commented on the helpfulness of meeting someone with similar symptoms or experiences, and 11 out of 16 participants (69%) who met with a PSW described the relationship as good:
We became friends and we spoke the same language.
Pilot participant 30
It was nice to meet somebody who’s just not a professional . . . somebody who actually suffers from it on a day-to-day basis.
Pilot participant 22
Help with practical activities was also valued, such as looking for local services, coping strategies for tinnitus, financial help and help with housing.
Positive comments about the recovery plan were that it is useful to have goals and that it was useful for recovery and thinking about triggers or keeping well:
I wouldn’t say, like, it’s changed my life. Like, it has opened my eyes to a few things, you know, just from doing the book. I write down a lot more stuff now.
Pilot participant 22
One participant liked the blank pages for ‘paintings’, but another did not like having blank pages. Four participants did not find all the sections ‘relevant,’ did not find it useful or were not ready to think about recovery. The PSWs (n = 4) suggested no further changes to the recovery plan in their focus group.
Participants reported that sessions typically lasted for 1 hour and that this seemed a good length. The meetings were in various locations including participants’ homes, community settings and a crisis house.
Four participants found the sessions unhelpful: one did not like weekly meetings, one did not get on with her PSW or like working to a timetable, one was made homeless and was disappointed that his PSW could not help with this, and one felt ‘let down’ by her PSW having one session and then becoming unwell. Two other participants found the programme helpful overall, but did not like particular aspects. One participant found recovery-focused work unhelpful when they had not yet met with a psychiatrist. The other participant found PSW advice unhelpful.
The most common suggestion for improvements to the programme was to have more sessions (i.e. from four participants). Other suggestions were a participant meet-up group or website, PSWs contacting participants at set times, clarifying whether or not PSWs can meet with participants after the programme, more support with housing problems and recruiting PSWs who are likely to stay well.
Discussion
The pilot trial demonstrated that recruiting and retaining participants in a trial and to the trial intervention were feasible, and confirmed the acceptability of the trial intervention.
From the experience of the pilot trial, the following changes were made to the trial procedures and outcome measures for the main trial:
-
Participants were categorised by screening clinicians as having psychosis or bipolar disorder or not, with the aim of recruiting at least half of the trial participants with psychosis/bipolar disorder to ensure that they were broadly representative of CRT service users in general.
-
Procedures were improved for informing clinical services that participants in the treatment group were ready to be allocated to a PSW, and for checking that this allocation had been done. (The trial data officer logged this information, which was checked by the trial manager.) This was to ensure that prompt access to a PSW was provided for participants in the treatment group.
-
A measure of perceived continuity of care80 was dropped following the pilot and replaced by briefer measures of loneliness,111 social network112 and neighbourhood social capital. 113 These measures were thought to be more likely to change directly as a result of the trial intervention, while omitting the continuity-of-care measure avoided extending the length of the interview schedule unduly.
-
A measure of the participant-rated recovery orientation of the PSW114 was added as an additional measure for participants in the treatment group, completed as a telephone interview by the non-blinded study data officer once a 4-month follow-up interview had been completed. This was part of a planned process evaluation for the trial.
-
The PSWs’ training programme was refined in response to PSW feedback about challenges that were encountered. Changes resulted in more discussion and guidance in training on ways of using the recovery plan collaboratively, and managing role boundaries and endings of support.
Because primary outcome data were obtained for all participants and no major changes were made to the trial intervention, a decision was taken (with approval from the independent Trial Steering Committee, the Trial Data Monitoring and Ethics Committee and the funders) to incorporate the pilot trial into the main trial. This turned the pilot trial in to an internal pilot: for this reason, outcomes data from the pilot trial are not reported separately, but included in the module 6 main trial results.
Module 6: a randomised controlled trial of the clinical effectiveness of a peer-delivered self-management intervention to prevent relapse in crisis resolution team users
See Appendix 11 for referral to the protocol of this trial. 110 The report is also accessible at the following URL: http://bmjopen.bmj.com/content/7/10/e015665 (accessed 28 March 2019).
For a full report of this work, see the paper115 referred to in Appendix 12.
Aims and objectives
The aim of the study was to test the peer-facilitated self-management intervention that was developed (see Module 4.3) to bridge the gap between crisis and continuing care, reducing relapse and promoting recovery. This trial compares the clinical effectiveness and cost-effectiveness of this intervention, delivered by trained PSWs to people just discharged from the CRT, with treatment as usual, supplemented by distribution of the recovery plan booklet by post without any specific support in engaging with it and using it.
The primary hypothesis was that service users receiving the experimental intervention would be less likely to relapse within 1 year of discharge from the CRT (indicated by re-admission to any mental health acute care service) than those receiving the control intervention.
The secondary hypothesis tested whether or not being in the experimental rather than the control condition is associated with a longer time to first admission to acute care and fewer days in acute care over 1 year. In addition, the study tested the hypotheses that at the 4- and 18-month follow-ups the experimental intervention would result in better perceived recovery, greater self-management skills, greater satisfaction with services, fewer symptoms, less loneliness and better social networks than the control intervention.
The study also evaluated the cost-effectiveness of the peer-facilitated self-management intervention compared with the treatment-as-usual intervention at 18 months.
Methods
This trial was a rater-blind RCT with two parallel arms (with an allocation ratio of 1 : 1) powered on the primary outcome, with adjustment for clustering by PSWs. Participants were identified from the caseload of CRTs in six NHS trusts (four in London, one in South East England and one in the South West of England).
Participant inclusion and exclusion criteria
Service users were eligible if they were on the caseload of one of the participating CRTs for at least 1 week because of a mental health crisis, and if they had the capacity and willingness to give informed consent to enter the trial and did so within 1 month of CRT discharge. CRT clinicians initially identified potentially eligible participants. The CRT clinicians passed on details to the research team of those who appeared to have capacity to enter the trial and who were willing to be contacted by a researcher. People presenting too high a risk to others to be seen alone even on NHS premises, those discharged to addresses outside the CRT’s catchment area and those who could not understand the intervention when delivered in English were excluded. Any service users who were aged < 18 years were also excluded. The aim was for study conclusions to be generalisable to the whole population of people discharged from CRT and, therefore, restricting sample entry on variables such as age and diagnosis was avoided. At the pilot stage, people with psychosis and bipolar disorder had proved harder to recruit than people with non-psychotic disorders. Therefore, to ensure representativeness, a threshold was set of at least 50% of participants in total to be identified at screening as having schizophrenia, other psychosis or bipolar disorder.
A sample size of 440 participants was required to detect a difference in admission rates during the follow-up period of 50% in the control group versus 35% in the intervention group, with 80% power, 5% significance and 1 : 1 allocation. This calculation allowed for clustering by PSW in only the intervention arm, assuming an ICC of 0.03 and a cluster size of 11.
Interventions
The peer-facilitated self-management intervention was delivered in a series of up to 10 sessions with a PSW. The intervention was structured around the completion of a self-management workbook with the following structured components: personal recovery goals, plans to re-establish community functioning and support networks following a crisis, identifying early warning signs and creating a relapse prevention plan, and strategies and coping resources to maintain well-being.
In the control condition, participants were sent the self-management workbook to complete by themselves or with others if they wished.
Outcomes
The primary outcome was whether or not, in the 1 year of follow-up from study entry, participants were re-admitted to an acute care setting, including acute inpatient wards, CRTs, crisis houses and acute day care.
Secondary outcomes included service use measures over a 1-year period (days in acute care and time to first relapse) and outcomes measured at baseline and at the 4- and 18-month follow-ups: self-rated recovery (as measured by the Questionnaire about the Process of Recovery116), self-management skills (as measured by the Illness Management and Recovery Scale92), overall satisfaction with mental health services (as measured by the CSQ79), symptom severity (as measured by the Brief Psychiatric Rating Scale117), loneliness (as measured by the University of California’s, Los Angeles Loneliness Scale111); and social network size (as measured by the Lubben Social Network Scale112).
Further demographic and clinical measures were used to characterise the sample and adjust for variables known to be associated with the primary outcome. These include clinical diagnosis as recorded on electronic records, a measure of social circumstances (as measured by the Social Outcomes Index118), a measure of neighbourhood social capital (as measured by the Health and Lifestyles Survey Social Capital Questionnaire113) and self-reported screening measures of alcohol use [as measured by the Alcohol Use Disorders Identification Test – Consumption (AUDIT-C119)] and drug use [as measured by the Drug Abuse Screening Test – 10 items (DAST-10120)].
The EuroQol-5 Dimensions, three-level version (EQ-5D-3L) data were also collected at baseline and at 4 and 18 months to calculate quality-adjusted life-years (QALYs). QALYs were calculated as the area under the curve adjusting for baseline using linear regression.
Procedures
Once written consent was obtained, a study researcher completed baseline measures with all participants as a structured interview. Participants were then block randomised into treatment and control groups, stratified by site. At the 4- and 18-month follow-ups, researchers again sought written informed consent from participants before completing the follow-up research interviews. Researchers completing the assessments were blinded to participants’ allocation status. If for any reason a face-to-face interview was not feasible, a telephone interview was offered, although in that case symptom severity could not be measured as the measure depends on observer ratings.
Once all participants from a participating NHS trust were recruited into the study, a study researcher contacted the appropriate administrators or informatics team within the trust to collect data from electronic patient records, using a standardised schedule of the information required for each patient. This procedure was repeated 1 year after recruitment to collect data for primary and secondary outcomes. The NHS IT and administrator staff collecting the data, as well as study researchers cleaning the data and calculating the study outcomes, were blinded to participant group allocation status.
All data were entered using a web-based system. Data from electronic patient records were first checked, cleaned and calculated in Microsoft Excel.
Analysis
All analyses were on an intention-to-treat basis and were conducted using Stata.
For the primary outcome (re-admission to acute care during the study period), data were analysed using logistic regression with random intercepts, adjusted for clustering by PSW. Diagnosis (psychosis or bipolar disorder vs. no psychosis/bipolar disorder) and centre were entered into the model as fixed effects.
For secondary outcomes, linear- or zero-inflated negative binomial regression with random intercepts was utilised when appropriate, with PSW as the random effect, controlling for the baseline value of the outcome, condition and centre. Random-effects Poisson regression was planned to assess the total number of days spent in acute care and Cox regression frailty model for time to first re-admission. However, on seeing the structure of the data, zero-inflated negative binomial with robust standard errors was more appropriate, given that more than half of participants had not spent any days in acute care since baseline. For number of days in acute care, the centre was entered into the model as a fixed effect.
Supportive analyses using analogous statistical methods to the primary analyses were conducted on the primary outcome, adjusting for any significant baseline differences between randomised groups and the amount of improvement for both groups between baseline and follow-up. Predictors of missingness were also explored and controlled for in supportive analysis (see Report Supplementary Material 2).
The primary cost-effectiveness analysis is a complete-case analysis of the incremental cost per QALY gained of the peer-facilitated self-management intervention compared with treatment as usual. Costs include the cost of the peer-facilitated intervention including cost of training and supervision as well as unit costs applied to mental health service use collected from mental health trust files. Costs are from baseline until 12 months, adjusting for costs 12 months prior to baseline. QALYs between 12 and 18 months were discounted at a rate of 3.5%. All analyses include clustering by PSW. Cost-effectiveness acceptability curves (CEACs) and 95% CIs were calculated using bootstrapping. Further details of the methods and results of the trial economic analysis are provided in Appendix 13.
Results
From the 3288 service users screened, 1848 were assessed as eligible and a total of 441 participants were recruited, including participants recruited for the pilot trial. The CONSORT flow diagram (Figure 2) shows participant flow through the study.
FIGURE 2.
The CONSORT flow diagram for study recruitment and retention.
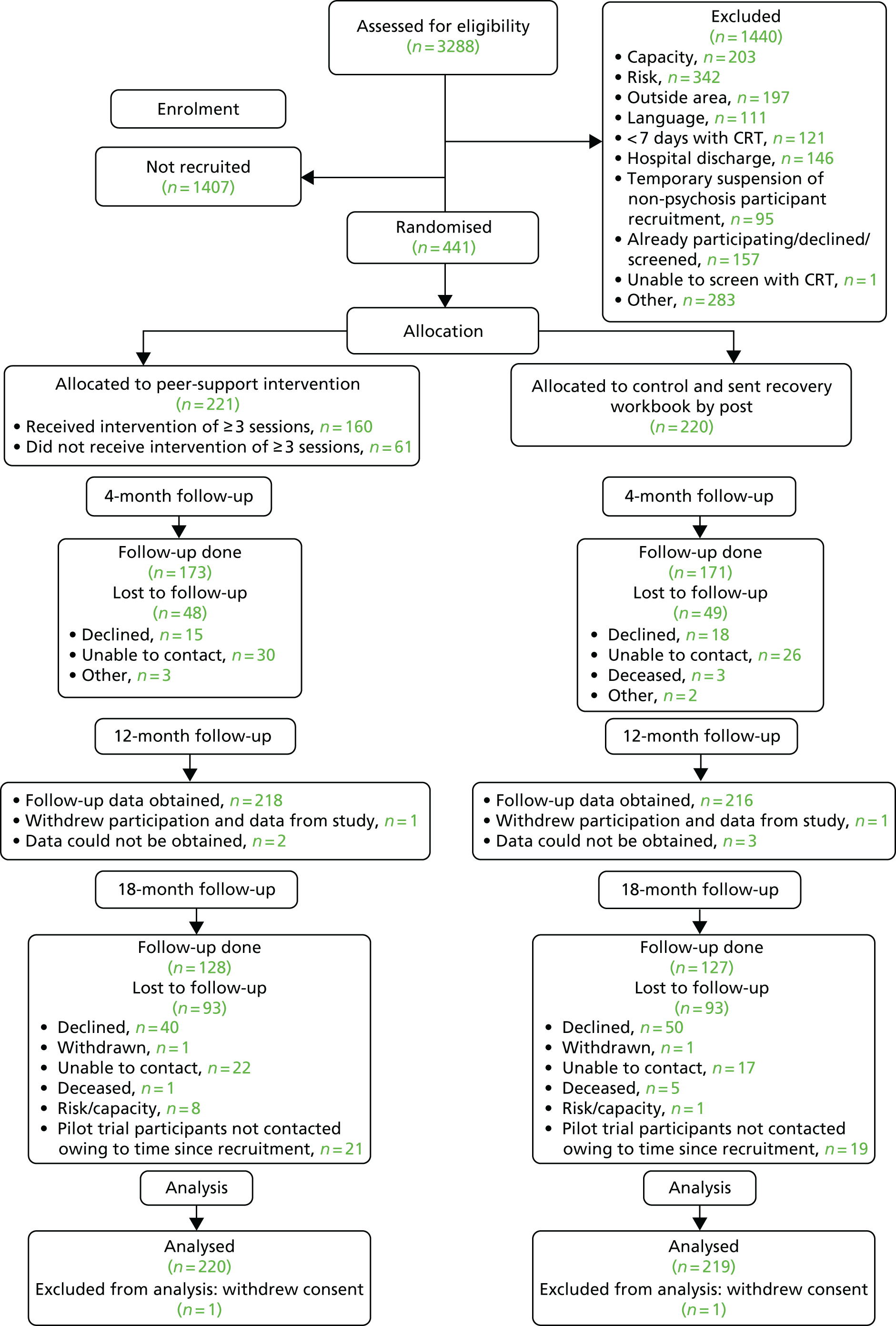
Forty participants were recruited in the internal pilot trial between 14 May 2013 and 12 November 2013. The remaining 401 participants were recruited between 12 March 2014 and 3 July 2015. Follow-up interviews were arranged as soon as possible after 4 and 18 months from the date of recruitment. The final follow-up interview took place on 23 February 2017. Participants had a mean age of 40 years (SD 13 years), 40% of those who gave information about their gender were male (175/438) and 65% identified as being white (285/438). At the 4-month follow-up, 344 participants completed the interview assessment (completion rate 78%); 255 participants completed the 18-month interview assessment (completion rate 58%). For a breakdown of participant recruitment numbers and further details on participant characteristics (see Report Supplementary Material 1).
Findings on the primary outcome favoured the intervention group: 29% of intervention group participants were re-admitted to acute care within 1 year compared with 38% of control group participants [odds ratio (OR) 0.66, 95% CI 0.43 to 0.99; p = 0.0438] (Table 8). This persisted with planned adjustments.
| Outcome | Trial arm | Difference/ratio between groups (95% CI) | p-value | ICC (95% CI) | |
|---|---|---|---|---|---|
| Control (N = 216) | Intervention (N = 218) | ||||
| Primary | |||||
| Re-admission to acute care over 1 year, n (%) | 83 (38) | 64 (29) | OR 0.66 (0.43 to 0.99)a | 0.0438 | 0.08 (0.00 to 0.24) |
| Secondary | |||||
| Satisfaction with mental health services, median (IQR) | |||||
| At 4 months | 26 (20–29) | 26 (23–30) | 1.96 (1.03 to 2.89)b | < 0.0001 | 0.25 (0.08 to 0.24) |
| At 18 months | 26 (21–30) | 27 (22–31) | 0.98 (–0.50 to 2.46)b | 0.1945 | 0.13 (0.00 to 0.42) |
| Time (days) to first re-admission to acute care during 1-year follow-up, median (IQR) | 86 (43–180) | 112 (42–242) | HR 0.71 (0.52 to 0.97) | 0.0291 | 0.14 (0.00 to 0.29) |
| Time (days) spent in acute care during 1-year follow-up, median (IQR) | 0 (0–24) | 0 (0–26) | IRR 1.01 (0.76 to 1.36) | 0.9208 | 0.20 (0.05 to 0.35) |
| Self-management skills, mean (SD) | |||||
| At 4 months | 50 (8) | 51 (8) | 1.06 (–0.49 to 2.61)b | 0.1807 | 0.00 (0.00 to 0.19) |
| At 18 months | 52 (8) | 53 (9) | 1.24 (–0.77 to 3.26)b | 0.2270 | 0.02 (0.00 to 0.25) |
| Self-rated recovery, mean (SD) | |||||
| At 4 months | 55 (16) | 57 (16) | 2.90 (0.08 to 5.72)b | 0.0441 | 0.04 (0.00 to 0.22) |
| At 18 months | 58 (70) | 60 (13) | 0.48 (–3.32 to 4.29)b | 0.8032 | 0.23 (0.02 to 0.44) |
| Symptom severity, mean (SD) | |||||
| At 4 months | 41 (12) | 39 (12) | –1.08 (–3.17 to 1.01)b | 0.3115 | 0.02 (0.00 to 0.21) |
| At 18 months | 40 (13) | 39 (12) | –0.71 (–3.58 to 2.17)b | 0.6306 | 0.14 (0.00 to 0.36) |
| Loneliness, median (IQR) | |||||
| At 4 months | 22 (20–24) | 22 (19–24) | 0.03 (–0.66 to 0.73)b | 0.9254 | 0.12 (0.00 to 0.30) |
| At 18 months | 22 (19–25) | 22 (19–24) | –0.01 (–0.89 to 0.86)b | 0.9805 | 0.00 (0.00 to 0.23) |
| Social network size, mean (SD) | |||||
| At 4 months | 12 (6) | 12 (5) | –0.06 (–1.02 to 0.90)b | 0.9005 | 0.17 (0.00 to 0.35) |
| At 18 months | 12 (6) | 13 (6) | 1.05 (–0.02 to 2.12)b | 0.0549 | 0.02 (0.00 to 0.24) |
| Service use | |||||
| Number of community mental health team contacts at 12 months, mean (SD) | 7.60 (14) | 7.00 (13) | 0.16 (–2.28 to 2.61)b | ||
Regarding secondary outcomes, time to re-admission was longer in the intervention group than in the control group. However, the numbers of days in acute care were not significantly different. Initial descriptive analyses found an unexpected difference between groups in the number of days between randomisation and discharge from the index acute care admission. In view of this, a post hoc sensitivity analysis was conducted excluding these days and including only days that were part of acute care re-admissions. The intervention group participants had fewer acute care days than control group participants, but not at a statistically significant level [experimental vs. control group: median number of days in acute care 0 vs. 0 (IQR 0–10 vs. 0–22); mean number of days in acute care 13 vs. 19 (SD 31 vs. 40); incidence rate ratio (IRR) 0.90, 95% CI 0.66 to 1.23; p = 0.515]. There was no evidence of a difference between groups in the number of contacts with the community mental health teams, which were the main secondary care providers after CRT discharge.
At the 4-month follow-up, overall satisfaction with mental health care received was greater in the intervention group than in the control group. This was because there was a difference in mean satisfaction scores between the randomised groups at 4 months [experimental vs. control: mean 26 (SD 5) vs. mean 24 (SD 6)], which is not shown in Table 8 because of the median (IQR) being more appropriate for skewed data. In addition, there was a significant difference in self-rated recovery favouring the intervention, but this just failed to reach statistical significance in the sensitivity analysis with adjustment for predictors of missingness (IRR 2.18, 95% CI –0.72 to 5.08). There were no other significant differences at 4 months. At 18 months, there was little evidence of any effect, except that the difference in social network size favoured the intervention approached, but did not reach, statistical significance.
Similar numbers of participants in each group reported that they had read the workbook at the 4-month interview [i.e. 133 (84%) out of 158 participants in the control group vs. 142 (88%) out of 162 in the intervention group]. However, more participants in the intervention group reported using it to make written plans. Using the workbook to make written plans was reported by between 28% (38/138 participants for the section ‘Managing your ups and downs’) and 44% (61/138 participants for the section ‘Moving on after a crisis’) of participants in the control group, compared with between 58% (83/144 participants for the section ‘Your goals and dreams’) and 64% (92/144 participants for the section ‘Keeping well’) of the intervention group.
Adverse events
Serious adverse events were actively monitored for both trial groups until the completion of the 4-month follow-up interview. PSWs and supervisors were asked to report any SAEs directly to the trial manager or data officer and record them on participant contact logs. The trial data officer also contacted the PSWs’ supervisor and CRT manager or principal investigator at each site monthly, who screened for SAEs among participants with reference to patient records. Additional adverse events reported to the study team were also recorded for participants at any stage of participation in the study.
Seventy-one SAEs were identified in the pilot and main trial (29 in the treatment group and 42 in the control group):
-
55 re-admissions to acute care, all in the context of relapse of an episodic mental illness and/or interpersonal problems
-
11 attempted suicides
-
one participant charged with attempted murder (of a police officer)
-
four deaths – two by suicide and two in unclear circumstances (control group).
All SAEs were assessed by involved clinicians, the trial clinical reviewer (the chief investigator) and the independent clinical reviewer (Trial Steering Committee chairperson). Participant deaths and the attempted murder were additionally reviewed by the Data Monitoring and Ethics Committee chairperson. No SAEs were judged to be related to the study.
Cost-effectiveness analysis
The total cost per PSW for training and supervision was £2548, or £292 per patient. Patients had an average of 6 appointments (95% CI 5.5 to 6.5 appointments), with a total cost of the peer-support intervention of £132 (95% CI £118 to £145). Including mental health acute care and community costs calculated from patient files, the total cost over 12 months adjusting for baseline was £6459 (95% CI £4766 to £8151) for the peer-facilitated self-management intervention and £6720 (95% CI £5329 to £8112) for the control group, with a mean incremental cost difference of –£261 (95% CI –£2450 to £1928). Patients in the peer-facilitated self-management group had an average of 0.991 (95% CI 0.931 to 1.051) QALYs over 18 months, baseline adjusted, compared with 0.968 (95% CI 0.907 to 1.03) QALYs for the treatment-as-usual group, with mean incremental QALYs per patient of 0.023 (95% CI –0.062 to 0.107). Drawing a straight line between 4- and 18-month QALYs, the mean QALYs at 12 months are 0.651 (95% CI 0.612 to 0.689) for the PSW group and 0.640 (95% CI 0.600 to 0.679) for the workbook-only group, with a mean difference of 0.011 (95% CI –0.043 to 0.065).
The intervention dominates treatment as usual (more QALYs for a lower cost), with a 64% probability that the intervention is cost-effective compared with treatment as usual at 12 months and at £20,000 willingness to pay for a QALY gained. For a full report of the health economic analysis, see Appendix 13.
Strengths and limitations
This was a rigorously conducted RCT with blinding of researchers and data analysts, although blinding of participants was not possible. Data for the primary outcome were collected from patient records from blinded NHS staff, although clinicians working with the participants could not be blinded. A power calculation determined sample size. As anticipated when planning the project, an excellent follow-up rate was obtained for the primary outcome when data were collected from patient records, and good follow-up rates of nearly 80% were obtained at 4 months, although they fell below 60% at 18 months.
There is a 64% probability that the intervention is cost-effective compared with treatment as usual, resulting in more QALYs for lower costs, even after the cost of the intervention was taken into account. The difference in costs and QALYs is not statistically significant though, with wide CIs for the costs. This is the main reason that the probability that the intervention is cost-effective is lower than expected, given that the intervention dominates treatment as usual.
One limitation of the study could arise from the way participants were recruited. CRT staff identified potentially eligible service users from their caseload; therefore, it was possible that those recruited were service users who were well engaged with, and easy to contact by, CRT staff. Patient data for five participants at baseline and five participants at follow-up could not be retrieved by NHS IT teams and, thus, had to be treated as missing. A completion rate of > 60% was not achieved for the 18-month follow-up interview because of difficulty in contacting and consenting participants. This was despite efforts to maximise the response rate by offering participants shorter telephone interviews as an alternative to face-to-face interviews. The 18-month follow-up was planned once participant recruitment had been completed, with the agreement and additional funds from the study funder. Another limitation with potential to introduce bias and limit generalisability is that only 24% of those eligible were recruited to the trial.
Recommendations for future research
Research is required to further investigate the critical ingredients and underlying mechanisms of change of this successful intervention. A planned process analysis using data from this study can help with this, exploring the relationship with outcomes of completion of the recovery plan, therapeutic alliance with the PSW and the PSW’s perceived recovery orientation, and the degree of match between PSW and service users on demographic and clinical variables.
Replication studies to corroborate the findings from this trial are desirable. However, the intervention appears successful as a means of reducing relapse in people following discharge from a CRT after home treatment, a result that coheres with the success of other self-management interventions in people with mental health problems. 95,121 The reduction in relapse also translates to a potential reduction in the average cost per patient, compensating the cost of the intervention. There is thus a good case for wider dissemination of such interventions in routine NHS settings, and for research to investigate the best methods of supporting their implementation.
Conclusions and reflections for workstream 2
Development work for workstream 2 confirmed the acceptability to people using CRTs of additional post-crisis support from a PSW, and of support with relapse prevention. Given the findings from workstream 1, about how infrequently relapse prevention work is provided as part of CRT support,63 such support can address an unmet need for CRT service users. Our preliminary testing established that it is feasible for PSWs to deliver a structured self-management programme in this post-crisis context. An established framework for developing complex interventions was followed:100 evidence review, stakeholder consultation, modelling and feasibility testing, then piloting. This ensured that before evaluation in a trial, the peer-supported, self-management programme and the operating procedures for delivering it had been developed and refined to maximise utility, acceptability and feasibility. The development time, funded as part of the CORE programme, therefore gave the intervention the best chance of demonstrating effectiveness.
The primary hypothesis was confirmed, suggesting that this intervention is a potentially useful one in crisis populations in mental health service settings. The result persisted with adjustment for whether or not participants were in a SMI psychosis/bipolar disorder group, suggesting that the intervention may be helpful for people with a wide range of mental health conditions following CRT support. The absolute reduction in admissions in the trial (i.e. 29% in the intervention group compared with 38% in the control group) was smaller than the 15% reduction that was anticipated when planning the trial. However, rates of re-admission to acute care were lower than originally anticipated in both groups. (The sample size calculation was based on a reduction in re-admissions from 50% to 35% of participants.) These relatively low admission rates to acute care could be explained by the most unwell CRT service users not being recruited to the trial, or it may be that using the recovery plan without support from a PSW had some effect in reducing admissions for control group participants. Therefore, the absolute risk difference between groups was understandably smaller than anticipated (i.e. 9% rather than 15%), but the relative risk difference between groups in the actual results was broadly similar to what had originally been anticipated. Given the importance of acute admission as an outcome, the intervention effect is considered, with a number needed to treat of about 11 to avoid a re-admission, to be potentially meaningful as well as statistically significant, although the limited impact on secondary outcomes at each time point is also noted.
This finding should be seen in the context of an already promising evidence base for self-management interventions for SMI (see review in Appendix 8). 95 Given these prior positive findings, it is suggested that the evidence base for the clinical effectiveness of self-management interventions for SMI is now notably strong. However, although the study has found an effect on relapse that had not clearly been demonstrated previously, findings on some secondary outcomes were disappointing in comparison with other self-management studies, in which effects have been found on measures such as symptoms, hope and empowerment. This makes mechanisms of effect relatively difficult to explain in the study. The secondary measures tended to be summary scores encompassing a large number of domains; it may be that more specific measures of potential intervention targets would have shown more effect.
The findings from the workstream 2 trial substantially augment the evidence base for peer-support interventions for SMI, providing the most robust evidence yet for the clinical effectiveness and cost-effectiveness of any peer-provided intervention in a UK secondary mental health setting. It adds to evidence from recent US trials that structured, peer-delivered recovery-focused interventions, including a relapse prevention component – such as a wellness and recovery action plan121 or recovery workbook48 – can improve outcomes for mental health service users. It helps address the evidence gap for peer support in mental health, whereby peer support is increasingly commonly provided in mental health settings97 in the absence previously of strong evidence for its clinical effectiveness and cost-effectiveness. 103
The design and procedures for the workstream 2 trial were robust, with oversight from a clinical trials unit regarding trial procedures and management. The primary outcome of re-admission to acute care was objectively measured, and outcome data were provided for 98% of participants. This can give a high level of confidence about the validity of the positive trial finding. An acceptable response rate of nearly 80% was also achieved for the end-of-treatment secondary outcomes. The lower response rate for secondary outcomes at the 18-month follow-up of just below 60% is a limitation of the study.
The randomised trial context in which the intervention was delivered had some impact on how it was implemented and how trial results may be reflected in routine care. About one in seven CRT service users screened and one in four of those eligible took part in the trial. However, it is unclear to what extent this reflects the proportion of CRT service users who might accept this intervention if offered as part of routine care. Take-up rate may have been affected by the need to consent to participate in a trial. Not all eligible service users could be contacted to ask about interest in the programme; more might have been contacted by involved clinicians during CRT support if the intervention were part of routine care.
Peer-support workers delivering the intervention were only employed to work with trial participants, so the timing and amount of work on offer were not wholly predictable. PSWs at most sites were therefore employed on zero-hours contracts and at times faced challenges to fit meetings with participants around other commitments. Many PSWs were delivering an intervention of exactly this nature for the first time in the trial; their confidence and familiarity with the recovery plan are likely to have improved during the course of the trial. Integration and lines of communication with CRT teams and supervisors also needed to be developed during the course of the trial. The extent of any negative impact of these factors on the quality of the study intervention delivered or its effectiveness are unclear; however, these difficulties are likely to be mitigated if the intervention was embedded as a routine part of CRT services. There are therefore some grounds for optimism that the intervention could be more effective in routine care than in this trial context.
The positive trial result generates a number of fruitful avenues for future research. First, replication of the findings from this trial in future studies is desirable. Second, a better understanding of the critical components and mechanisms of effect of the intervention is needed. This is particularly pertinent, given the negative results for secondary outcomes that may have been expected to result in reduced rates of relapse (reduced symptoms, better personal recovery, more social support). A planned process evaluation from the CORE trial data will attempt to identify whether or not there are independent effects on outcomes from the relationship with the PSW and completion of the recovery plan. Adaptations to the study intervention are also of interest in understanding its critical components. Whether the self-management plan support could be provided equally well by non-PSWs or whether other forms of peer support might be as effective in supporting people post crisis are potential directions for future research. Third, there is a need to understand why some CRT users declined the intervention or discontinued it (i.e. nearly 30% of those participants in the intervention group), and how their needs might best be addressed. The qualitative interviews with participants in the piloting phases of our study indicated that a minority of service users were ambivalent or unenthusiastic about making a written recovery plan, but the extent to which this dissuaded people from taking up the intervention or continuing with it is unclear. Future qualitative studies could helpfully explore this.
Last, the utility of the trial intervention in other mental health service settings is of interest, for instance for service users following other types of acute care, or in community services providing longer-term support.
The main clinical implication of this work is that our findings support the wider use of the CORE peer-provided self-management programme as a means to reduce relapse and increase satisfaction with care for people discharged from CRT services.
Public involvement activities
As well as PPI contributions to overall study design and planning, the CORE study included PPI involvement through members of the study working groups in the following activities.
Development of interview guides and information sheets (modules 1, 4 and 5)
Topic guides for qualitative interviews with service users and carers in module 1 (CRT stakeholder interviews) and modules 4 and 5 (peer-supported self-management programme; interviews with participants in preliminary testing and piloting) were developed in collaboration with the study working group. A draft version of the information sheet for the workstream 2 trial was also reviewed by peer researchers through the MHRN’s Feasibility And Support to Timely recruitment for Research (FAST-R) reviewing service. 122
Qualitative interviewing (workstream 1, module 1)
Twelve working group members, the public involvement co-ordinator and two research assistants with relevant lived experience conducted interviews in module 1 (CRT stakeholder interviews). This ensured that 54 of 61 interviews (89%) with service user and carer participants were conducted by peer interviewers. The peers from the working groups were being paid £60 per interview.
Working group interviewers were provided with 2 days’ training in interviewing skills. Support was also given through three group supervision meetings and feedback from the programme manager who listened to interviews.
Qualitative interview analysis (workstream 1, module 1)
The CRT stakeholder interviews were analysed using thematic analysis. An initial coding frame was drawn up by the programme manager. Fifteen of the peer researchers (including 11 who did interviews) then reviewed at least one transcript and gave advice on any necessary revisions to the coding frame (in addition to similar input from other members of the study team). A 2-hour basic training session was provided to help with this task, and there was also a follow-up reflection meeting. An opportunity was also subsequently given to advise on a draft write-up of a paper relating to the analysis.
Focus group facilitation (workstream 1, module 1, and workstream 2, module 4)
Seven focus groups were conducted with service users (n = 5) and carers (n = 2) to seek feedback on initial plans for a peer-supported self-management programme for use in workstream 2. Six of these focus groups were facilitated by peer interviewers. In addition, a black and minority ethnic (BME) focus group about views on CRT care was convened and conducted by a member of the working group to address a concern that BME service users’ views may have been under-represented in CRT stakeholder interviews in module 1.
Fidelity measure development (workstream 1, module 2)
Peer researchers were involved throughout the development of the fidelity measure. Two research assistants with lived experience contributed to reducing a longlist of 330 statements about CRTs down to 72 statements. These 72 statements were grouped and prioritised by stakeholders in a concept mapping process, which involved 16 service users and six carers, and generated the 39-item scale. Peers from the working groups had opportunities to give input to eight iterations of the fidelity measure as it was refined. Peer researchers also inputted into the development of the questions for service users and carers in the fidelity reviews. Six out of 18 of those taking part in the inter-rater reliability testing exercise for the fidelity scale were peers from the study working group.
Fidelity reviews (workstream 1, modules 2 and 3)
Nine of the working group members, the public involvement co-ordinator and five research assistants with lived experience acted as reviewers in the CRT fidelity reviews on the study. All 140 reviews (75 in the module 2 CRT survey, 65 during the module 3 trial) were thus able to include a service user or carer reviewer. Half a day’s training, plus e-training, was provided to reviewers.
Crisis resolution team resource kit development (workstream 1, module 2)
The content of the online CRT resource kit was discussed in two working group meetings and members contributed material relevant to enhancing users’ experience in CRTs. Four members of the working group and the public involvement co-ordinator provided video testimonials that were included in the resource kit of the SIP.
Peer-support work (workstream 2, modules 4–6)
The working group provided advice on refining workbook content and procedures for the peer-support programme. In addition, all four peers who delivered the peer support at the pre-pilot stage (module 4) and three of five at pilot stage (module 5) were from the CORE working group (including the public involvement co-ordinator). This enabled further refinement of the intervention processes and workbook content, including through a focus group.
In the main peer-supported self-management programme trial (module 6), training for the PSWs in all six study sites was co-facilitated by a peer trainer, one of three members of the CORE working group who had worked as a PSW in the piloting stages. A 5-day training course was provided (reduced for smaller groups of trainees). Two ‘top-up’ training meetings were also provided for all PSWs on the trial, which were co-facilitated by two PSWs from the working group. The public involvement co-ordinator also visited four of the sites where no peer supervisor was available to provide peer supervision, and was available for added support if wanted.
Dissemination
Three members of the study working group presented on study PPI and the peer-support project at two study symposium events. The study public involvement co-ordinator has contributed to a number of study publications as a co-author. The study working group members are acknowledged on three published and planned papers in which they have had significant involvement regarding the development of the CRT fidelity scale, CRT stakeholders’ views on CRTs and the development of the peer-supported, self-management programme.
Following publication of the workstream 1 and 2 trial results, there is an opportunity for working group members to lead on writing a blog or report on each trial aimed at service user and carer readers.
Other involvement
Other public involvement on the study has included (1) interview panels for researcher posts have included a peer interviewer approximately 50% of the time, (2) 12 members of the working group contributed to informal interviews about their experience and reflections on PPI in the study and (3) a research assistant with relevant lived experience has led on conducting qualitative interviews with PSW teams (n = 6) as an addition to the funded study.
Impact of public involvement on the study
Working group members’ and researchers’ reflections on the experience and impact of PPI on the CORE study is reported in the following section. Advice from the study working groups contributed to all aspects of study planning. It is not always possible to unpick which or to what extent decisions were influenced by working group involvement. However, five examples of decisions about study plans that originated from the working group and were adopted directly following PPI advice are as follows:
-
A decision was made to offer carer participants in the study (modules 1 and 4) a £20 gift of cash to acknowledge their time and help. This was not originally costed in the budget, but was recommended by the working group as important to recognise their contribution equally to that of service users.
-
A suggestion to audio-record PSW sessions with participants in the module 6 trial to facilitate the process recording was rejected on the advice of the working group as potentially off-putting to participants and damaging to the therapeutic relationship with the PSW.
-
The coding frame for CRT stakeholder interviews (module 1) was substantially revised following feedback from peer involvement in the analysis. Themes had previously mainly described different functions of the CRTs’ work – the revised coding frame focused much more on participants’ experience of CRT care. The relationship between service users and staff in CRTs was added as a new theme in analysis.
-
The working group advocated including a peer reviewer in each CRT fidelity review team (modules 2 and 3), advising that this would help make service user and carer participants in reviews feel more comfortable and might elicit more candid feedback about services. This suggestion was adopted in study plans and achieved in 100% of the 140 fidelity reviews conducted during the study.
-
The working group, and the working group members who worked as PSWs in the preliminary testing phase of the project, recommended that supervision from a peer supervisor should be available to all PSW teams in the CORE trial (modules 5 and 6). When peer supervision could not be arranged within the participating NHS trust, the study public involvement co-ordinator visited PSW teams and offered peer supervision.
An independent consultant (SP) collaborated with a study co-applicant (TW) to explore user experiences of involvement in the programme. The following brief report outlines this.
User involvement in the CORE programme: the views and experience of the CORE study service use and carer working group
Authors: Sue Patterson, Principal Research Fellow – Mental Health, Metro North Hospital and Health Service (MNHHS), QLD, Australia and Associate Professor, Department of Applied Psychology, Griffith University, Mount Gravatt, QLD, Australia; and Tim Weaver, Associate Professor of Mental Health Services Research, Middlesex University, London, UK.
Introduction
Policies internationally endorse the active participation of non-professional stakeholders in the design and delivery of health and social care. The UK policy commitment to PPI in research is supported by investment in infrastructure designed to enable involvement. Funders, governance and support bodies commonly require evidence that people potentially affected by the research are involved in various ways. 123,124 However, it remains for researchers to determine the purpose and methods of involvement. Consequently, the involvement of service users has been enacted in diverse ways at different stages of the research process. Researchers have been called on to examine user involvement in studies they lead. 125 This report represents one such examination.
Patient and public involvement within the CORE programme
Service users and carers have been variously involved in the CORE programme:
-
a service user consultant/researcher was a study co-applicant
-
employed as a PPI co-ordinator
-
participated in working groups performing advisory functions
-
conducted of a range of programme activities:
-
peer support
-
resource kit development
-
fidelity measure development
-
fidelity reviews
-
qualitative interviews
-
focus group facilitation
-
interview analysis.
-
Method
The CORE programme management group sought to examine the clinical ‘effectiveness’ and acceptability of the PPI model employed in the CORE programme, with reference to experience of involvement and views about what worked well and areas for improvement.
The aims of the study were therefore to:
-
describe the process and methods of involvement in the CORE programme
-
‘evaluate’ PPI from the perspectives of contributors.
A qualitative approach was adopted and was underpinned by an interpretive social paradigm. 126
This qualitative study received ethics approval from the Middlesex University Health and Education Ethics Committee on 22 June 2015 (reference number MH19). Participation in the evaluation was open to all people involved in CORE programme PPI activities. Potential participants were approached by a CORE programme manager seeking permission to provide their contact details to Sue Patterson. Contributors were provided with an information sheet and (if they agreed to an interview) this interview was conducted at the participant’s convenience. Interviews were conducted by Sue Patterson during July and August 2015. Interviews were semistructured, audio-recorded and transcribed verbatim. Participants received a £20 honorarium.
Analysis involved developing summary accounts of each participant’s views, coding and labelling content in accordance with study objectives. An initial analysis was presented to the PPI working group and feedback informed further analysis and interpretation.
Findings
The contributors
Interviews were completed with 12 contributors aged between 30 and 76 years. Most were women (n = 9). Although contributors had in common ‘lived experiences’ with mental illness and mental health services, contributors reported varied life histories. The majority reported substantial experience of PPI. Involvement in the CORE programme covered the activities listed in Introduction but varied in duration. Some (n = 7) reported continuous involvement from ‘the beginning’, and a minority had become involved subsequently (n = 2) or withdrew (n = 3).
Contributors shared the view that PPI in research generally aimed to improve processes and outcomes by ‘grounding’ research, enhancing its ethical status and improving feasibility, acceptability, relevance and credibility.
Contributors commonly linked their involvement in the CORE programme’s PPI to personal well-being, the intrinsic rewards associated with making a contribution and an aspiration to improve mental health services.
Patient and public involvement in the CORE programme: the process and practicalities
Organisation and communication
The study found broad consensus that the ‘process’ of involvement was professionally, respectfully and efficiently managed. Continuity of management throughout was considered particularly important in this regard. Most contributors reported that opportunities for involvement had been clearly explained and often made favourable comparisons with other involvement experiences. A minority, however, reported an initial uncertainty about expectations and expressed concern about lack of communication between working group meetings.
Payments
The CORE programme team was commended by interview respondents for the management of payments to enable participation of people receiving income support.
Relationships with study team
Contributors reported that their contact was primarily with the programme manager and PPI co-ordinator. The consensus was that the research team collectively and individually were accepting, friendly, caring and approachable. Many contributors described instances when they felt that they had been treated sensitively and respectfully. Most contributors thought that their input was valued. Some contributors mentioned other researchers on the team but said that they did not know the chief investigator or understand the role of the service user co-applicant.
Patient and public involvement activities
Working groups
Working groups were described by the majority of collaborators as cohesive and functional. Generally, contributors considered the discussion at working groups on topic, appropriate and constructive. Although reporting that debate was sometimes robust, most contributors considered this appropriate and respectful. Many spoke of ‘learning’ about and deepening understanding of the research and workings of CRTs. Divergent opinions were expressed by a minority, with concern expressed about:
-
the structure, frequency, facilitation and shifting membership of groups hindering establishment of group identity and function
-
domination of discussion by ‘strong personalities’ expressing personal concerns of marginal relevance or regarded as ‘radical’
-
combination of carers’ and service users’ working groups given differing perspectives on mental illness and ‘recovery’
-
under-representation of minority groups including people from BME backgrounds.
Development of the fidelity measure
Contributors found the development of the CRT fidelity measure intellectually and philosophically challenging. Although some contributors said that they understood the methodology and the process, others reported confusion. The process was described as particularly difficult, with some contributors struggling to prioritise the elements of a ‘good’ crisis service. Concern was expressed by some that their views in relation to the appropriateness or number of items were not given sufficient weight.
Qualitative interviews
Contributors who had conducted qualitative interviews typically viewed this as appropriate and reported enjoying and learning from the process. While acknowledging that assumptions of shared understanding or language could be problematic, the contributors spoke of observing interview participants relaxing when their status as a ‘peer’ was disclosed; most expressed the view that peer interviewers generated better (‘more honest’) data. Some contributors, however, reported that hearing others recount distressing experiences could ‘be close to home’ and that they struggled to maintain boundaries and the interviewer role at times.
Qualitative data analysis
Few of the interviewed contributors reported involvement in analysis of qualitative data. Although this limits our ability to draw conclusions about participants’ experience of this aspect, those who were involved in analysis did report some discomfort with the task and uncertainty about how feedback provided was incorporated into the final analysis.
Fidelity reviews
Contributors reported participating in up to 20 fidelity reviews. Some endorsed the review process enthusiastically and considered their input valued both by the service being reviewed and the research team. Several reported difficulties adhering to the interview schedule and wanted to explore issues that seemed important to themselves or the person being interviewed. Some contibutors were concerned about the use of a standardised measure in vastly different contexts and questioned the appropriateness of evaluating quality quantitatively.
Influence and impact of patient and public involvement on CORE
Most contributors welcomed the opportunity to express views and, although wanting these heard, were aware and accepting of the constraints within which a programme of research, such as CORE, operated.
Some contributors, however, felt constrained, noting that because some working group meetings were convened after the ethics review of the relevant CORE substudy was complete, the scope for amending study procedures was limited by the willingness of the investigators to submit amendments to the Research Ethics Committee (and tolerate any consequent delays).
Although noting that impact was difficult to assess, contributors were typically confident that PPI had shaped or influenced the process of the CORE programme in various ways:
-
influencing the CRT best practice model
-
making activities more ‘user-friendly’ or respectful (e.g. restructuring focus groups)
-
design of the resource kit
-
design of the peer-based self-management intervention
-
design of study documents (e.g. participant information sheets)
-
enhancing the credibility of fidelity reviews
-
qualitative data collection.
The experience of involvement
The majority of contributors described their participation as developing interpersonal and practical skills they considered valuable. Many spoke of ‘learning’ about research or the ways health services ‘work’. Contributors commonly spoke of being affected emotionally or psychologically. Sometimes experiences were transient (e.g. ‘being upset’ listening to service users’ accounts), sometimes lasting – contributors spoke of deepening sense of self-esteem and respect, of coming to develop a new (and preferred) sense of self. Some contributors reported that involvement with the CORE programme had facilitated further involvement opportunities.
The majority of contributors described PPI in the CORE programme as robust, meaningful and worthwhile, and generally experienced it as a rewarding and intellectually stimulating activity. Contributors linked the maintenance of their involvement to feeling respected and trusting that their input was valued. However, some (including two who discontinued participation) expressed the view that they and their input were marginalised and reported dissatisfaction with the process and the level of involvement achieved in relation to aspects of research design.
Summary points
Study limitations
Several factors require caution in interpreting these findings. The timing of the interviews some 4 years into the CORE programme may have affected recall. Moreover, not all PPI contributors participated, and it is entirely possible that those who did not take part in interviews had different experiences and views.
What worked well?
-
The PPI co-ordinator role was considered important and the management of PPI generally was commended.
-
Relationships and interaction with team members were respectful. The CORE programme team were commended by interview respondents for creating an enabling environment, in which most contributors felt respected and valued.
-
‘Flexibility’ to ‘drop in and out’ of activities that allowed contributors to fit the type and extent of involvement with capacity, interest, capabilities and motivation.
-
Organisation and communication were considered efficient.
-
Payments were managed appropriately.
-
For the majority of contributors, the working group provided a sound ‘base’ for involvement, supporting a sense of shared identity and purpose. Meetings were generally seen as productive and the different perspectives represented were seen to generate robust but respectful discussion.
What could be improved?
-
For some, the meetings were too infrequent, too large (and/or diverse) and overly tolerant of the behaviour of some members whose ‘off-topic’ input and recourse to personal experience were seen to disrupt the process.
-
Reference to constraints on the influence and ability to ‘change things’ was recurrent in contributors’ accounts. Although most were pragmatic and understanding of the constraints research operated within, many cited that ethics review and the research timetables limited the extent to which any major influence could be exerted on study design and implementation.
Acknowledgements and declarations
The evaluation was undertaken by Dr Sue Patterson as part of the programme of work supported by the MNHHS Chairman’s Scholarship award with in-kind support of the MNHHS. Dr Tim Weaver is a co-investigator on the original CORE programme funding application. His involvement has been advisory, and he had no formal responsibility or involvement in the major workstreams to which the service user and carer working groups contributed.
No payment was made for the evaluation. Expenses for Dr Patterson to travel to interviews, transcription costs and honoraria for participants were paid from the CORE programme research project budget.
Thanks go to members of the CORE programme team for their administrative and logistical support. Sincere thanks go to the PPI contributors and research team members who generously shared their views.
Overall conclusions
The national implementation of CRTs in England was proposed as a means of resolving the ‘acute care crisis’,127 and trial evidence indeed suggests that CRTs can reduce the number of inpatient admissions and increase satisfaction with acute care. 18 However, it is less clear if all the aspirations of stakeholders for CRTs are met by CRTs as implemented in practice in England. When scaled up to a national level, CRTs’ impact on reducing bed use and costs is uncertain. 13,14 Rates of re-admission to acute care following support from a CRT may be as high as 50% over 1 year. 91 A number of recent reports by government and expert bodies have been highly critical of CRTs and acute care generally. 28,85,86,88 A recent report by the Care Quality Commission88 found that only 14% of service users felt that they had received the right care from mental health services during a mental health crisis. Recurrently identified problems include a lack of continuity of care and responsiveness, an unduly limited range of interventions, fragmented therapeutic relationships and a lack of support at (and following) the point of discharge. 58
In this context, the twin aims of the CORE study – of developing evidence about how to implement high-quality CRT services and reduce relapse for people who have used CRT services – are of high importance for policy-makers and people who work in or with CRTs or who use CRT services.
The development work for workstream 1 established the following key points. First, the model of CRT care endorsed in The NHS Plan1 and accompanying policy guidance3 when CRTs were mandated nationally retains broad support. An easily accessible CRT service that provides rapid-response, brief, intensive support to people who would otherwise be admitted to hospital, which offers medical psychological and social support to service users, and involves their families and other social supporters was endorsed across all stakeholder groups with a high degree of consensus. Second, this model of CRT care is feasible: the national fidelity review conducted for the CORE study found that all aspects of a specified good practice model for CRTs were achieved by some teams. Third, CRT implementation nationally is highly variable;63 CRTs are working in varying acute and community service contexts, and few teams are achieving consistently high-quality care. A national mandate and policy directives have proved insufficient to achieve consistent implementation as planned among CRTs nationally. Two outputs from the CORE study, the CRT fidelity scale69 and the CRT SIP,73 sought to meet this need for more successful implementation of a CRT best practice model.
The CRT fidelity scale encapsulates a highly specified model of CRT good practice and provides a means to assess how far CRT teams are achieving such good practice. Its thorough development process, including a large stakeholder concept mapping exercise, ensures that it reflects the best available evidence and the priorities of all stakeholder groups for CRTs. There was a good level of consensus between stakeholder groups, including service users and carers and clinicians, on the key ingredients of high-quality CRT care. An encouraging conclusion from the study is that the CRT fidelity review audit process developed in the CORE study was experienced as helpful by teams. Seventy-five CRTs were recruited as planned for the study’s fidelity survey; all 75 CRTs were retained in the CORE trial, which involved, for many teams, four reviews over a 2-year period. Qualitative feedback from CRT teams and managers about the fidelity scale was positive. Promising evidence for the reliability of scores from fidelity reviews has been established. However, the limited extent of associations between total fidelity scores and outcomes established in the CORE trial indicates that there is further work needed to confirm or improve the psychometric robustness of the CRT fidelity scale, or to identify the most critical components of service quality within it or which components are most associated with which aspects of CRT model fidelity.
The CRT SIP was also well received by teams. The national fidelity survey found that access to supervision, mentoring or CRT-specific training is very limited for many CRT staff. The SIP’s team scoping day to plan service priorities, receive support from an experienced CRT facilitator and enable access to practical resources to support good practice offered welcome resources to equip teams to deliver service improvement. The CORE SIP trial results suggest that it did not meet all its aims. In particular, the study found no significant difference in service user satisfaction between teams receiving the SIP and controls (although it is possible that the lack of a positive finding was because of the unrepresentative, highly satisfied service user participant group recruited to the trial). Promisingly, however, the SIP did prove able to increase teams’ fidelity scores, and there was evidence of reductions in admission rates and inpatient bed use compared with a control group of teams not receiving this. These promising results suggest that the SIP has value in itself to support service improvements in teams, and provides a useful resource from which to develop and evaluate refined implementation resources in future. The barriers to full take up of the SIP in teams, identified by the study’s qualitative evaluation, can help direct future efforts. In particular, the online resource pack appears to have been underused, and ensuring staff time for SIP activities and buy-ins from senior management was challenging. Current plans for more assertive use of policy levers to monitor and promote quality improvement in CRTs in line with CORE fidelity specifications may also be of value to focus service improvement efforts and achieve management and commissioners’ active support. The Achieving Better Access Programme128 exemplifies these attempts: it provides a 5-year programme to clarify quality standards and audit delivery of these more rigorously, in order to improve access to services and evidence-based treatments within them across mental health care. The CORE fidelity standards have fed into the Achieving Better Access Programme standards128 for mental health acute care.
Workstream 2 of the CORE programme focused on providing effective post-crisis support, aiming to ameliorate the often-abrupt transition from intensive CRT support to follow-on care45 and to reduce the known high rates of relapse (as measured by re-admission to acute care)91 following CRT service use. Thus, reduction in relapse (as measured by re-admission to acute care) was selected as the primary aim of the intervention and the primary trial outcome, being highly relevant to both service users’ experience and recovery and service costs. Development work for workstream 2 established the promising evidence base for self-management interventions in mental health95 and the acceptability, in principle, to CRT users of peer-provided support focusing on relapse prevention. It allowed a careful process of developing, testing and refining a peer-provided self-management intervention for testing in a trial. The study was greatly helped by being able to draw on existing high-quality resources. First, the study produced an adapted version of the Personal Recovery Plan,129 a mental health self-management resource developed by Rachel Perkins and Julie Repper in co-production with service users. Second, the training team from the Nottingham Institute for Mental Health helped the study team develop and deliver a bespoke, adapted and abbreviated version of its accredited peer-support training for the PSWs delivering the trial intervention. A pre-pilot phase allowed refinement of the intervention content and procedures before the main trial. The benefits of this staged, development and piloting process, drawing on best available resources and evidence as recommended in the MRC guidelines for evaluating complex interventions,100 are confirmed by the positive trial results.
The CORE trial of a peer-provided, self-management programme for people leaving CRT services produced a positive result on its primary outcome in a robust RCT: rates of re-admission to acute care were significantly lower for those in the intervention group than in the control group (29% vs. 38%). The positive result for satisfaction with care suggests that the intervention enhanced service users’ experience of care too. Not all the trial outcomes had positive results. The intervention appears to have no effect on residual symptom levels or social outcomes (i.e. employment, social network, loneliness); different types of support may be required to address these needs. No benefits were apparent on secondary outcomes at the 18-month follow-up: the effects of the intervention may dissipate over time. Nevertheless, the positive outcomes that were achieved were of high importance to service users’ experience, clinical recovery and service costs, and constitute an effective intervention.
This positive trial result generates further questions of interest. It is not known, for example, whether or not other types of service provider could deliver the self-management programme as effectively as the PSWs in this trial. It is equally unknown whether or not other types of peer support (e.g. less structured programmes) for people following a mental health crisis could produce similarly positive results. In the light of the trial’s positive findings, these are fruitful lines of research. A current trial of a peer-support programme for people leaving acute inpatient care68 will provide a useful addition to the developing evidence base regarding peer-provided support in NHS acute settings.
Two conclusions can be drawn from the CORE workstream 2 trial. First, it adds to the promising evidence base95 for self-management interventions in mental health as a means to promote recovery and reduce relapse. The CORE fidelity survey69 highlighted that recovery plans or collaborative relapse prevention plans are seldom offered routinely in CRTs. Our study illustrates a mechanism through which this type of support can be provided effectively to people following a period of CRT support. Further research about optimal means and settings in which to deliver self-management interventions in mental health is a high priority given the low costs and high feasibility of implementing self-management programmes compared with many other types of support.
Second, the trial adds significantly to the current evidence regarding peer support for SMI (i.e. people using secondary mental health services, including a substantial proportion with psychosis and bipolar disorder) in particular. The employment of PSWs has proliferated in the NHS in the last decade,98 ahead of a corresponding evidence base. Although there is some existing evidence that peer support can help reduce symptoms for people with depression,130 the evidence regarding peer support for people with SMI is less robust. 103 The trial found reduced levels of re-admission to acute care (29% in the intervention group compared with 38% in the control group: a reduction that is statistically significant and is believed to be clinically meaningful) for a participant group including people with common mental disorders and almost 50% of participants with bipolar disorder or psychosis. The primary trial outcome remained statistically significant even with adjustment for whether or not participants were in this bipolar/psychosis group. Based on two recent systematic reviews,103,131 it is believed that this study is the first UK multisite randomised trial of a peer-provided intervention for people with SMI, and the first trial anywhere to demonstrate an objectively measured reduction in acute service use for this group in a peer-provided intervention.
Overall, the CORE programme has produced a set of resources that help to specify and assess optimal CRT care, and can help CRT teams with achieving quality improvement. It has also trialled an effective peer-provided self-management programme to prevent relapse for people following CRT care. These outputs can help achieve the overarching goal of improving care for people experiencing a mental health crisis.
Summary of main research recommendations
-
Empirical evidence is needed regarding the characteristics of CRTs that are associated with outcomes (module 1.1). It would also be desirable if possible to explore whether or not impact varies between clinical and social subgroups. The fidelity measure has potential to be used in such a study.
-
The costs and cost-effectiveness of the CORE CRT SIP will be assessed in planned future work using data from the workstream 1 trial.
-
Implementation of the SIP proved highly variable despite a multipronged approach involving training, coaching, a framework for priority-setting and monitoring, and electronic resources. Research on how to achieve more consistent implementation in NHS mental health services would be helpful to inform future initiatives to improve quality in CRTs and other types of team.
-
The findings from the peer-supported self-management trial, especially in relation to the positive primary outcome, are promising and warrant further replication and exploration. An implementation–evaluation study would be a helpful design, with concurrent investigation of methods for implementing such interventions in routine settings and of their effect on outcomes suggested.
-
There is a need for better-designed and better-reported trials to evaluate the effects from well-developed peer-support interventions. Our trial partially addresses this need, but other forms of peer support are also in use and have potential to improve outcomes; evidence is needed on whether or not they are clinically effective and cost-effective. Non-trial designs also have potential to contribute to understanding of the ways in which such interventions may be helpful and effective from service user and peer-support perspectives, and of variations in what works for whom with such interventions.
-
In addition, regarding the peer-supported self-management intervention, a better understanding is needed of critical components and mechanisms of effect of the intervention. This is particularly pertinent, given the negative results for secondary outcomes. A planned process evaluation of data from the CORE peer-support trial, which explores associations between process factors and the positive outcomes that were achieved in the trial, will contribute to this goal.
Acknowledgements
Contributions of authors
Sonia Johnson (Professor of Social and Community Psychiatry) was chief investigator and led the study.
Brynmor Lloyd-Evans (Senior Lecturer, Mental Health Research), Danielle Lamb (Research Associate) and Melanie Lean (Research Associate) managed the study.
Brynmor Lloyd-Evans, David Osborn (Professor of Psychiatric Epidemiology), Gareth Ambler (Senior Lecturer, Statistics), Louise Marston (Senior Research Associate, Statistics), Oliver Mason (Reader in Clinical Psychology, Mental Health Research), Nicola Morant (Lecturer, Qualitative Research), Claire Henderson (Clinical Senior Lecturer, Mental Health Research), Rachael Hunter (Principal Research Associate, Health Economics), Stephen Pilling (Professor of Clinical Psychology and Clinical Effectiveness), Fiona Nolan (Professor of Clinical Mental Health Nursing Practice Research), Richard Gray (Professor of Clinical Nursing), Tim Weaver (Associate Professor in Mental Health Research) and Sonia Johnson designed the study.
Brynmor Lloyd-Evans, David Osborn, Gareth Ambler, Louise Marston, Oliver Mason, Rachael Hunter, Stephen Pilling and Sonia Johnson formed the study management group that oversaw the conduct of the study.
Oliver Mason, Sarah Sullivan (Research Fellow, Mental Health Research), Claire Henderson, Richard Gray, Kathleen Kelly (Consultant Psychiatrist, CRT Expertise) and Nicky Goater (Consultant Psychiatrist, CRT Expertise) acted as site leads during the study.
Gareth Ambler and Louise Marston led the development of statistical analysis plans and conducted statistical analyses for the study.
Rachael Hunter led the development of health economic analysis plans and conducted economic analyses for the study.
Nicola Morant led the development of qualitative analysis plans and oversaw qualitative analyses for the study.
David Hindle (Public Involvement Co-ordinator, PPI) co-ordinated public involvement in the study.
Elaine Johnston (Principal Research Associate, CRT Practice Expertise) led the development and delivery of the CORE SIP for the workstream 1 trial (with Steve Onyett; see Contributions of others).
Oliver Mason and Alyssa Milton (Principal Research Associate, Peer-supported Self-management Practice Expertise) led the adaptation and development of the recovery plan workbook for the workstream 2 peer-supported, self-management intervention trial.
Alyssa Milton led the development of supervision structures and development and delivery of training for the workstream 2 peer-supported, self-management intervention trial.
Marina Christoforou (Research Assistant), Kate Fullarton (Research Assistant), Beth Paterson (Research Assistant), Jonathan Piotrowski (Research Assistant), Michael Davidson (Research Assistant), Rebecca Forsyth (Research Assistant), Liberty Mosse (Research Assistant), Monica Leverton, Puffin O’Hanlon (Research Assistant), Edward Mundy (Research Assistant), Tom Mundy (Research Assistant), Ellie Brown (Research Assistant), Sarah Fahmy (Research Assistant), Emma Burgess (Research Assistant) Alasdair Churchard (Research Assistant), Claire Wheeler (Research Assistant) and Hannah Istead (Research Assistant) contributed to running the study, data collection and data management.
Brynmor Lloyd-Evans, Marina Christoforou and Sonia Johnson drafted this report.
Overall study management and sponsorship of the study was provided by Camden and Islington NHS Foundation Trust.
Contributions of others
Lottie Millett assisted with responses to editors and reviewers. All authors contributed to and approved the report.
Our colleague, Steve Onyett, died suddenly in September 2015. Steve led the design and development of the workstream 1 CRT SIP and contributed to the design and conduct of the whole CORE study research programme. His contribution to the study and his warmth and generosity as a colleague are greatly missed.
We are grateful to Professor Gary Bond, who acted as a consultant for the study. His advice and experience contributed substantially to development of the CRT fidelity scale and SIP in workstream 1 of the study.
We are grateful to the members of the CORE Service User and Carer Advisory Group who contributed to the planning and conduct of the whole study. (CORE Advisory Group members: Mary Clarke, Stephanie Driver, Pauline Edwards, Kathleen Fraser-Jackson, Jackie Hardy, Kate Holmes, Lyn Kent, Jacqui Lynskey, Brendan Macken, Mary Plant, Tony Rivett, Jo Shenton, Geoff Stone, Janice Skinner, Jules Tennick and Gen Wallace.)
We are grateful for the time and help of all the service users and their families, and clinical staff and managers from NHS trusts that participated in the study.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health and Social Care.
References
- The NHS Plan: A Plan for Investment. A Plan for Reform. London: DHSC; 2000.
- Glover G, Johnson S, Johnson S, Needle J, Bindman J, Thornicroft G. Crisis Resolution and Home Treatment in Mental Health. Cambridge: Cambridge University Press; 2008.
- The Mental Health Policy Implementation Guide. London: Department of Health; 2001.
- Johnson S. Crisis resolution and home treatment teams: an evolving model. Adv Psychiatr Treat 2013;19:115-23. https://doi.org/10.1192/apt.bp.107.004192.
- Rose D. Users’ Voices: The Perspectives of Mental Health Service Users on Community and Hospital Care. London: Sainsbury Centre for Mental Health; 2001.
- Johnson S, Needle J, Johnson S, Needle J, Bindman J, Thornicroft G. Crisis Resolution and Home Treatment in Mental Health. Cambridge: Cambridge University Press; 2008.
- Stein LI, Test MA. Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Arch Gen Psychiatry 1980;37:392-7. https://doi.org/10.1001/archpsyc.1980.01780170034003.
- Bridgett C, Polak P. Social systems intervention and crisis resolution. Part 1: assessment. Adv Psychiatr Treat 2003;9:424-31. https://doi.org/10.1192/apt.9.6.424.
- Bridgett C, Polak P. Social systems intervention and crisis resolution. Part 2: treatment. Adv Psychiatr Treat 2003;9:432-8.
- Smyth MG, Hoult J. The home treatment enigma. BMJ 2000;320:305-8. https://doi.org/10.1136/bmj.320.7230.305.
- Pelosi AJ, Jackson GA. Home treatment – enigmas and fantasies. BMJ 2000;320:308-9.
- Johnson S, Thornicroft G, Johnson S, Needle J, Bindman J, Thornicroft G. Crisis Resolution and Home Treatment in Mental Health. Cambridge: Cambridge University Press; 2008.
- Glover G, Arts G, Babu KS. Crisis resolution/home treatment teams and psychiatric admission rates in England. Br J Psychiatry 2006;189:441-5. https://doi.org/10.1192/bjp.bp.105.020362.
- Jacobs R, Barrenho E. Impact of crisis resolution and home treatment teams on psychiatric admissions in England. Br J Psychiatry 2011;199:71-6. https://doi.org/10.1192/bjp.bp.110.079830.
- Johnson S, Nolan F, Hoult J, White IR, Bebbington P, Sandor A, et al. Outcomes of crises before and after introduction of a crisis resolution team. Br J Psychiatry 2005;187:68-75. https://doi.org/10.1192/bjp.187.1.68.
- Keown P, Tacchi MJ, Niemiec S, Hughes J. Changes to mental healthcare for working age adults: impact of a crisis team and an assertive outreach team. Psychiatrist 2007;31:288-92. https://doi.org/10.1192/pb.bp.106.012054.
- Jethwa K, Galappathie N, Hewson P. Effects of a crisis resolution and home treatment team on in-patient admissions. Psychiatrist 2007;31:170-2. https://doi.org/10.1192/pb.bp.106.010389.
- Johnson S, Nolan F, Pilling S, Sandor A, Hoult J, McKenzie N, et al. Randomised controlled trial of acute mental health care by a crisis resolution team: the North Islington crisis study. BMJ 2005;331. https://doi.org/10.1136/bmj.38519.678148.8F.
- McCrone P, Johnson S, Nolan F, Pilling S, Sandor A, Hoult J, et al. Economic evaluation of a crisis resolution service: a randomised controlled trial. Epidemiol Psychiatr Soc 2009;18:54-8. https://doi.org/10.1017/S1121189X00001469.
- McCrone P, Johnson S, Nolan F, Pilling S, Sandor A, Hoult J, et al. Impact of a crisis resolution team on service costs in the UK. Psychiatrist 2009;33:17-9. https://doi.org/10.1192/pb.bp.107.018648.
- Nelson T, Johnson S, Bebbington P. Satisfaction and burnout among staff of crisis resolution, assertive outreach and community mental health teams. A multicentre cross-sectional survey. Soc Psychiatry Psychiatr Epidemiol 2009;44:541-9. https://doi.org/10.1007/s00127-008-0480-4.
- Helping People Through Mental Health Crisis: The Role of Crisis Resolution and Home Treatment Services. London: NAO; 2007.
- The Pathway to Recovery: A Review of NHS Acute Inpatient Mental Health Services. London: Commission for Healthcare Audit and Inspection; 2008.
- Onyett S, Linde K, Glover G, Floyd S, Bradley S, Middleton H. Implementation of crisis resolution/home treatment teams in England: national survey 2005–6. Psychiatrist 2008;32:374-7.
- Morgan S. Are Crisis Resolution & Home Treatment Teams Seeing the Patients They Are Supposed to See?. London: National Audit Office; 2008.
- Desai S, Kinton M. Who’s Been Sleeping in my Bed? The Incidence and Impact of Bed Over-occupancy in the Mental Health Acute Sector. Findings of the Mental Health Act Commission’s Bed Occupancy Survey. London: Mental Health Act Commission; 2006.
- The Mental Health Act Commission: Rights, Risk, Recovery Twelfth Biennial Report 2005–7. London: The Stationary Office; 2008.
- Royal College of Psychiatrists . Old Problems, New Solutions: Improving Acute Psychiatric Care for Adults in England 2016. http://media.wix.com/ugd/0e662e_aaca63ae4737410e9e2873dfde849841.pdf (accessed 12 October 2016).
- Mental Health Act 1983. London: The Stationery Office; 1983.
- Furminger E, Webber M. The effect of crisis resolution and home treatment on assessments under the 1983 Mental Health Act: an increased workload for approved social workers?. Br J Soc Work 2009;39:901-17. https://doi.org/10.1093/bjsw/bcm171.
- Clark F, Khattak S, Nahal J, Linde K. Crisis Resolution and Home Treatment: The Service User and Carer Experience. London: National Audit Office; 2008.
- Polak PR. The crisis of admission. Soc Psychiatry Psychiatr Epidemiol 1967;2:150-7. https://doi.org/10.1007/BF00578050.
- Jones M, Polak P. Crisis and confrontation. Br J Psychiatry 1968;114:169-74. https://doi.org/10.1192/bjp.114.507.169.
- Drake RE, Bond GR, Essock SM. Implementing evidence-based practices for people with schizophrenia. Schizophr Bull 2009;35:704-13. https://doi.org/10.1093/schbul/sbp041.
- Tansella M, Thornicroft G. Implementation science: understanding the translation of evidence into practice. Br J Psychiatry 2009;195:283-5. https://doi.org/10.1192/bjp.bp.109.065565.
- Torrey WC, Drake RE, Dixon L, Burns BJ, Flynn L, Rush AJ, et al. Implementing evidence-based practices for persons with severe mental illnesses. Psychiatr Serv 2001;52:45-50. https://doi.org/10.1176/appi.ps.52.1.45.
- Mueser KT, Torrey WC, Lynde D, Singer P, Drake RE. Implementing evidence-based practices for people with severe mental illness. Behav Modif 2003;27:387-411. https://doi.org/10.1177/0145445503027003007.
- Mowbray CT, Holter MC, Teague GB, Bybee D. Fidelity criteria: development, measurement, and validation. Am J Eval 2003;24:315-40. https://doi.org/10.1177/109821400302400303.
- Bond GR, Becker DR, Drake RE, Vogler KM. A fidelity scale for the individual placement and support model of supported employment. Rehabil Couns Bull 1997;40:265-84.
- Drake RE, McHugo GJ, Becker DR, Anthony WA, Clark RE. The New Hampshire study of supported employment for people with severe mental illness. J Consult Clin Psychol 1996;64:391-9. https://doi.org/10.1037/0022-006X.64.2.391.
- Becker DR, Smith J, Tanzman B, Drake RE, Tremblay T. Fidelity of supported employment programs and employment outcomes. Psychiatr Serv 2001;52:834-6. https://doi.org/10.1176/appi.ps.52.6.834.
- Gowdy EL, Carlson LS, Rapp CA. Practices differentiating high-performing from low-performing supported employment programs. Psychiatr Rehabil J 2003;26:232-9. https://doi.org/10.2975/26.2003.232.239.
- Becker DR, Xie H, McHugo GJ, Halliday J, Martinez RA. What predicts supported employment program outcomes?. Community Ment Health J 2006;42:303-13. https://doi.org/10.1007/s10597-006-9037-8.
- McGrew JH, Griss ME. Concurrent and predictive validity of two scales to assess the fidelity of implementation of supported employment. Psychiatr Rehabil J 2005;29:41-7. https://doi.org/10.2975/29.2005.41.47.
- Hopkins C, Niemiec S. Mental health crisis at home: service user perspectives on what helps and what hinders. J Psychiatr Ment Health Nurs 2007;14:310-18. https://doi.org/10.1111/j.1365-2850.2007.01083.x.
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff 2001;20:64-78. https://doi.org/10.1377/hlthaff.20.6.64.
- Copeland ME. Wellness recovery action plan: a system for monitoring, reducing and eliminating uncomfortable or dangerous physical symptoms and emotional feelings. Occup Ther Ment Health 2002;17:127-50. https://doi.org/10.1300/J004v17n03_09.
- Barbic S, Krupa T, Armstrong I. A randomized controlled trial of the effectiveness of a modified recovery workbook program: preliminary findings. Psychiatr Serv 2009;60:491-7. https://doi.org/10.1176/appi.ps.60.4.491.
- Ridgway P, McDiarmid D, Davidson L, Bayes J, Ratzliff S. Pathways to Recovery: A Strengths Recovery Self-help Workbook. Lawrence, KS: University of Kansas; 2010.
- Birchwood M, Spencer E. Early intervention in psychotic relapse. Clin Psychol Rev 2001;21:1211-26. https://doi.org/10.1016/S0272-7358(01)00105-2.
- Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychiatr Rehabil J 1993;16:11-23. https://doi.org/10.1037/h0095655.
- A Common Purpose: Recovery in Future Mental Health Services. London: SCIE, CSIP and RCPsych; 2007.
- Rethink Mental Illness . Recovery and Self-Management n.d. www.rethink.org/living_with_mental_illness/recovery_and_self_management/index.html (accessed 30 September 2009).
- Cook JA, Copeland ME, Hamilton MM, Jonikas JA, Razzano LA, Floyd CB, et al. Initial outcomes of a mental illness self-management program based on wellness recovery action planning. Psychiatr Serv 2009;60:246-9. https://doi.org/10.1176/ps.2009.60.2.246.
- Cotton MA, Johnson S, Bindman J, Sandor A, White IR, Thornicroft G, et al. An investigation of factors associated with psychiatric hospital admission despite the presence of crisis resolution teams. BMC Psychiatry 2007;7. https://doi.org/10.1186/1471-244X-7-52.
- Bond GR, Evans L, Salyers MP, Williams J, Kim HW. Measurement of fidelity in psychiatric rehabilitation. Ment Health Serv Res 2000;2:75-87. https://doi.org/10.1023/A:1010153020697.
- McHugo GJ, Drake RE, Whitley R, Bond GR, Campbell K, Rapp CA, et al. Fidelity outcomes in the National Implementing Evidence-Based Practices Project. Psychiatr Serv 2007;58:1279-84. https://doi.org/10.1176/ps.2007.58.10.1279.
- Wheeler C, Lloyd-Evans B, Churchard A, Fitzgerald C, Fullarton K, Mosse L, et al. Implementation of the Crisis Resolution Team model in adult mental health settings: a systematic review. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0441-x.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. A Product from the ESRC Methods Programme. Version 1. Lancaster: Lancaster University; 2006.
- Pluye P, Robert E, Cargo M, Bartlett G, O’Cathain A, Griffiths F, et al. Proposal: A Mixed Methods Appraisal Tool for Systematic Mixed Studies Reviews. Montréal, QC: McGill University; 2011.
- Greenland S. Invited commentary: a critical look at some popular meta-analytic methods. Am J Epidemiol 1994;140:290-6. https://doi.org/10.1093/oxfordjournals.aje.a117248.
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-18.
- Lloyd-Evans B, Paterson B, Onyett S, Brown E, Istead H, Gray R, et al. National implementation of a mental health service model: a survey of Crisis Resolution Teams in England. Int J Ment Health Nurs 2018;27:214-26. https://doi.org/10.1111/inm.12311.
- Johnson S, Gilburt H, Lloyd-Evans B, Boardman H, Leese M, Osborn D, et al. Alternatives to hospital admission: emerging models and populations served. Br J Psychiatry 2009;194:456-63. https://doi.org/10.1192/bjp.bp.108.051698.
- Morant N, Lloyd-Evans B, Fullarton K, Brown E, Paterson B, . Crisis resolution and home treatment: stakeholders’ views on critical ingredients and implementation in England. BMC Psychiatry 2017;17. https://doi.org/10.1186/s12888-017-1421-0.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Barry CA, Britten N, Barber N, Bradley C, Stevenson F. Using reflexivity to optimize teamwork in qualitative research. Qual Health Res 1999;9:26-44. https://doi.org/10.1177/104973299129121677.
- Gillard S, Simons L, Turner K, Lucock M, Edwards C. Patient and public involvement in the coproduction of knowledge: reflection on the analysis of qualitative data in a mental health study. Qual Health Res 2012;22:1126-37. https://doi.org/10.1177/1049732312448541.
- Lloyd-Evans B, Bond GR, Ruud T, Ivanecka A, Gray R, Osborn D, et al. Development of a measure of model fidelity for mental health Crisis Resolution Teams. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1139-4.
- Bond GR, Peterson AE, Becker DR, Drake RE. Validation of the revised Individual Placement and Support fidelity scale (IPS-25). Psychiatr Serv 2012;63:758-63. https://doi.org/10.1176/appi.ps.201100476.
- Monroe-DeVita M, Teague GB, Moser LL. The TMACT: a new tool for measuring fidelity to assertive community treatment. J Am Psychiatr Nurses Assoc 2011;17:17-29. https://doi.org/10.1177/1078390310394658.
- Trochim WMK. An introduction to concept mapping for planning and evaluation. Eval Program Plann 1989;12:1-16. https://doi.org/10.1016/0149-7189(89)90016-5.
- Lloyd-Evans B, Fullarton K, Lamb D, Johnston E, Onyett S, Osborn D, et al. The CORE Service Improvement Programme for mental health crisis resolution teams: study protocol for a cluster-randomised controlled trial. Trials 2016;17. https://doi.org/10.1186/s13063-016-1283-7.
- Hayes H, Buckland S, Tarpey M. INVOLVE Briefing Notes for Researchers: Public Involvement In NHS, Public Health and Social Care Research. Southampton: National Institute for Health Research; 2012.
- Schouten LM, Hulscher ME, van Everdingen JJ, Huijsman R, Grol RP. Evidence for the impact of quality improvement collaboratives: systematic review. BMJ 2008;336:1491-4. https://doi.org/10.1136/bmj.39570.749884.BE.
- McKergow M, Clarke J. Solutions Focus Working: 80 Real Life Lessons for Successful Organisational Change. Edinburgh: Solutions Books; 2007.
- Torrey WC, Bond GR, McHugo GJ, Swain K. Evidence-based practice implementation in community mental health settings: the relative importance of key domains of implementation activity. Adm Policy Ment Health 2012;39:353-64. https://doi.org/10.1007/s10488-011-0357-9.
- Johnson S, Osborn DP, Araya R, Wearn E, Paul M, Stafford M, et al. Morale in the English mental health workforce: questionnaire survey. Br J Psychiatry 2012;201:239-46. https://doi.org/10.1192/bjp.bp.111.098970.
- Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann 1982;5:233-7. https://doi.org/10.1016/0149-7189(82)90074-X.
- Rose D, Sweeney A, Leese M, Clement S, Jones IR, Burns T, et al. Developing a user-generated measure of continuity of care: brief report. Acta Psychiatr Scand 2009;119:320-4. https://doi.org/10.1111/j.1600-0447.2008.01296.x.
- Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav 1981;2:99-113. https://doi.org/10.1002/job.4030020205.
- Schaufeli WB, Bakker AB, Salanova M. The measurement of work engagement with a short questionnaire: a cross-national study. Educ Psychol Meas 2006;66:701-16. https://doi.org/10.1177/0013164405282471.
- Goldberg D, Williams P. A User’s Guide to the General Health Questionnaire. Windsor: NFER-Nelson; 1988.
- Lloyd-Evans B, Osborn D, Marston L, Lamb D, Ambler G, Hunter R, et al. The CORE service improvement programme for mental health crisis resolution teams: results from a cluster-randomised trial [published online ahead of print February 14 2019]. Br J Psychiatry 2019. https://doi.org/10.1192/bjp.2019.21.
- Listening to Experience: An Independent Inquiry into Acute and Crisis Mental Healthcare. London: Mind; 2011.
- London Mental Health Crisis Commissioning Guide. London: NHS England; 2014.
- NHS England . Mental Health Crisis Care Concordat: Improving Outcomes for People Experiencing a Mental Health Crisis 2014. www.crisiscareconcordat.org.uk/ (accessed 20 November 2015).
- Care Quality Commission . Right Here Right Now: People’s Experiences of Help, Care and Support During a Mental Health Crisis 2015. www.cqc.org.uk/sites/default/files/20150630_righthere_mhcrisiscare_full.pdf (accessed 23 May 2016).
- Crisp N, Smith G, Nicholson K. Old Problems, New Solutions – Improving Acute Psychiatric Care for Adults in England. London: The Commission on Acute Adult Psychiatric Care; 2016.
- Kim SJ, Bond GR, Becker DR, Swanson SJ, Langfitt-Reese S. Predictive validity of the individual placement and support fidelity scale (IPS-25): a replication study. J Vocat Rehabil 2015;43:209-16. https://doi.org/10.3233/JVR-150770.
- Werbeloff N, Chang CK, Broadbent M, Hayes JF, Stewart R, Osborn DPJ. Admission to acute mental health services after contact with crisis resolution and home treatment teams: an investigation in two large mental health-care providers. Lancet Psychiatry 2017;4:49-56. https://doi.org/10.1016/S2215-0366(16)30416-3.
- Mueser K, Gingerich S, Campbell-Orde T, Carpenter J, Leff H. Measuring the Promise: A Compendium of Recovery Measures. Cambridge, MA: Human Services Research Institute; 2005.
- No Health Without Mental Health: Implementation Framework. London: DHSC; 2012.
- Service User Experience in Adult Mental Health. Improving the Experience of Care for People Using Adult NHS Mental Health Services. London: British Psychological Society; 2012.
- Psychosis and Schizophrenia in Adults: Prevention and Management. Manchester: NICE; 2014.
- Bowers L, Whittington R, Nolan P, Parkin D, Curtis S, Bhui K, et al. The City 128 Study of Observation and Outcomes on Acute Psychiatric Wards. London: The Stationery Office; 2006.
- Repper J, Aldridge B, Gilfoyle S, Gillard S, Perkins R, Rennison J. Peer Support Workers: Theory and Practice. London: Centre for Mental Health and Mental Health Network, NHS Confederation; 2013.
- Repper J, Aldridge B, Gilfoyle S, Gillard S, Perkins R, Rennison J. Peer Support Workers: A Practical Guide to Implementation. Implementing Recovery Through Organizational Change Briefing Paper. London: Centre for Mental Health and Mental Health Network NHS Confederation; 2013.
- Chien W, Lui S, Clifton A. Peer support for schizophrenia. Cochrane Database Syst Rev 2013;12. https://doi.org/10.1002/14651858.CD010880.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Lean M, Fornells-Ambrojo M, Milton A, Lloyd-Evans B, Harrison-Stewart B, Yesufu-Udechuku A, et al. Self-management interventions for people with severe mental illness: systematic review and meta-analysis [published online ahead of print March 22 2019]. Br J Psychiatry 2019. https://doi.org/10.1192/bjp.2019.54.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. London: The Cochrane Collaboration; 2011.
- Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry 2014;14. https://doi.org/10.1186/1471-244X-14-39.
- Oakley A, Strange V, Bonell C, Allen E, Stephenson J. RIPPLE Study Team . Process evaluation in randomised controlled trials of complex interventions. BMJ 2006;332:413-16. https://doi.org/10.1136/bmj.332.7538.413.
- Altman DG. Better reporting of randomised controlled trials: the CONSORT statement. BMJ 1996;313:570-1. https://doi.org/10.1136/bmj.313.7057.570.
- Harrison BA, Mayo-Wilson E. Trial registration: understanding and preventing reporting bias in social work research. Res Soc Work Pract 2014;24:372-6. https://doi.org/10.1177/1049731513512374.
- Milton A, Lloyd-Evans B, Fullarton K, Morant N, Paterson B, Hindle D, et al. Development of a peer-supported, self-management intervention for people following mental health crisis. BMC Research Notes 2017;10. https://doi.org/10.1186/s13104-017-2900-6.
- Repper J, Perkins R. My Personal Recovery Plan. Nottingham: Nottinghamshire Healthcare NHS Trust; 2008.
- Lovell K, Bower P, Richards D, Barkham M, Sibbald B, Roberts C, et al. Developing guided self-help for depression using the Medical Research Council complex interventions framework: a description of the modelling phase and results of an exploratory randomised controlled trial. BMC Psychiatry 2008;8. https://doi.org/10.1186/1471-244X-8-91.
- Johnson S, Mason O, Osborn D, Milton A, Henderson C, Marston L, et al. Randomised controlled trial of the clinical and cost-effectiveness of a peer-delivered self-management intervention to prevent relapse in crisis resolution team users: study protocol. BMJ Open 2017;7. https://10.1136/bmjopen-2016-015665.
- Hays RD, DiMatteo MR. A short-form measure of loneliness. J Pers Assess 1987;51:69-81. https://doi.org/10.1207/s15327752jpa5101_6.
- Lubben J, Blozik E, Gillmann G, Iliffe S, von Renteln Kruse W, Beck JC, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist 2006;46:503-13. https://doi.org/10.1093/geront/46.4.503.
- Health and Lifestyles: A Survey of the UK Population – Part 1. London: Health Education Authority; 1995.
- Russinova Z, Rogers ES, Cook KF, Ellison ML, Lyass A. Conceptualization and measurement of mental health providers’ recovery-promoting competence: the recovery promoting relationships scale (RPRS). Psychiatr Rehabil J 2013;36:7-14. https://doi.org/10.1037/h0094741.
- Johnson S, Lamb D, Marston L, Osborn D, Mason O, Henderson C, et al. Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet 2018;392:409-18. https://doi.org/10.1016/S0140-6736(18)31470-3.
- Neil ST, Kilbride M, Pitt L, Nothard S, Welford M, Sellwood W, et al. The questionnaire about the process of recovery (QPR): a measurement tool developed in collaboration with service users. Psychosis 2009;1:145-55. https://doi.org/10.1080/17522430902913450.
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep 1962;10:799-812. https://doi.org/10.2466/pr0.1962.10.3.799.
- Priebe S, Watzke S, Hansson L, Burns T. Objective social outcomes index (SIX): a method to summarise objective indicators of social outcomes in mental health care. Acta Psychiatr Scand 2008;118:57-63. https://doi.org/10.1111/j.1600-0447.2008.01217.x.
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 1998;158:1789-95. https://doi.org/10.1001/archinte.158.16.1789.
- Skinner HA. The drug abuse screening test. Addict Behav 1982;7:363-71. https://doi.org/10.1016/0306-4603(82)90005-3.
- Cook JA, Copeland ME, Floyd CB, Jonikas JA, Hamilton MM, Razzano L, et al. A randomized controlled trial of effects of Wellness Recovery Action Planning on depression, anxiety, and recovery. Psychiatr Serv 2012;63:541-7. https://doi.org/10.1176/appi.ps.201100125.
- Staley K, Ashcroft J, Doughty L, Szmukler G. Making it clear and relevant: patients and carers add value to studies through research document reviews. Ment Health Soc Inclusion 2016;20:36-43.
- Research Governance Framework for Health and Social Care. London: DHSC; 2005.
- BRC Guidance: Involving Users in the Research Process. (Version 1). London: BRC; 2010.
- Staniszewska S, Brett J, Mockford C, Barber R. The GRIPP checklist: strengthening the quality of patient and public involvement reporting in research. Int J Technol Assess Health Care 2011;27:391-9. https://doi.org/10.1017/S0266462311000481.
- Neuman WL. Social Research Methods: Qualitative and Quantitative Approaches. Boston, MA: Pearson Education; 2010.
- Appleby L. So, are things getting better?. Psychiatr Bull 2003;27:441-2. https://doi.org/10.1017/S0955603600003585.
- Achieving Better Access to Mental Health Services by 2020. London: DHSC; 2016.
- Taking Back Control: A Guide to Planning Your Own Recovery. London: South West London and St George’s Mental Health NHS Trust; 2007.
- Pfeiffer PN, Heisler M, Piette JD, Rogers MA, Valenstein M. Efficacy of peer support interventions for depression: a meta-analysis. Gen Hosp Psychiatry 2011;33:29-36. https://doi.org/10.1016/j.genhosppsych.2010.10.002.
- Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev 2013;3. https://doi.org/10.1002/14651858.CD004807.pub2.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- National Schedule of Reference Costs 2015–16. London: DHSC; 2017.
- Dolan P. Modelling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Hunter RM, Baio G, Butt T, Morris S, Round J, Freemantle N. An educational review of the statistical issues in analysing utility data for cost-utility analysis. PharmacoEconomics 2015;33:355-66. https://doi.org/10.1007/s40273-014-0247-6.
- Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ 1997;6:327-40. https://doi.org/10.1002/(SICI)1099-1050(199707)6:4<327::AID-HEC282>3.0.CO;2-W.
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. Hoboken, NJ: Wiley Online Library; 2002.
Appendix 1 Systematic review paper
Module 1.1
Link to published paper ‘Implementation of the Crisis Resolution Team model in adult mental health settings: a systematic review’: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-015-0441-x (accessed 28 March 2019).
Full reference: Wheeler C, Lloyd-Evans B, Churchard A, Fitzgerald C, Fullarton K, Mosse L, et al. Implementation of the crisis resolution team model in adult mental health settings: a systematic review. BMC Psychiatry 2015;15:74. 58
Appendix 2 National survey of crisis resolution teams
Module 1.2
Link to published paper ‘National implementation of a mental health service model: a survey of Crisis Resolution Teams in England’: http://onlinelibrary.wiley.com/doi/10.1111/inm.12311/abstract (accessed 28 March 2019).
Full reference: Lloyd-Evans B, Paterson B, Onyett S, Brown E, Istead H, Gray R, et al. National implementation of a mental health service model: a survey of crisis resolution teams in England. Int J Ment Heal Nurs 2018;27:214–26. 63
Appendix 3 Qualitative study
Module 1.3
The full report of the qualitative study ‘Crisis resolution and home treatment: stakeholders’ views on critical ingredients and implementation in England’ has been published with open access and is available here: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1421-0/open-peer-review (accessed 28 March 2019).
Full reference: Morant N, Lloyd-Evans B, Lamb D, Fullarton K, Brown E, Paterson B, et al. Crisis resolution and home treatment: stakeholders’ views on critical ingredients and implementation in England. BMC Psychiatry 2017;17:254. 65
Appendix 4 Development of fidelity scale
Module 2.1
Link to published open-access paper ‘Development of a measure of model fidelity for mental health Crisis Resolution Teams’: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-016-1139-4 (accessed 28 March 2019).
Full reference: Lloyd-Evans B, Bond GR, Ruud T, Ivanecka A, Gray R, Osborn D, et al. Development of a measure of model fidelity for mental health Crisis Resolution Teams. BMC Psychiatry 2016;16:427. 69
Appendix 5 Trial protocol
Module 2.2
Link to open-access protocol ‘The CORE Service Improvement Programme for mental health crisis resolution teams: study protocol for a cluster-randomised controlled trial’: https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-016-1283-7 (accessed 28 March 2019).
Full reference: Lloyd-Evans B, Fullarton K, Lamb D, Johnston E, Onyett S, Osborn D, et al. The CORE Service Improvement Programme for mental health crisis resolution teams: study protocol for a cluster-randomised controlled trial. Trials 2016;17:158. 73
Appendix 6 A cluster randomised trial of the CORE service improvement programme
Module 3
Link to published open-access paper: www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/core-service-improvement-programme-for-mental-health-crisis-resolution-teams-results-from-a-clusterrandomised-trial/672F8C10123B6D0C63CBC20329024E16 (accessed 28 March 2019).
Full reference: Lloyd-Evans B, Osborn D, Marston L, Lamb D, Ambler G, Hunter R, et al. The CORE service improvement programme for mental health crisis resolution teams: results from a cluster-randomised trial [published online ahead of print February 14 2019]. Br J Psychiatry 2019. 84
Appendix 7 Qualitative findings
Module 3: qualitative findings from stakeholder interviews
Three broad domains were established that capture stakeholder views and experiences of the CORE SIP. These were (1) components of the programme, (2) process factors that shaped implementation of the programme and (3) the impact of the programme on teams and their practice.
Components of the service improvement programme
Support from the CORE programme team was described as being well co-ordinated, with regular, ongoing help being appreciated by stakeholders. The study team was perceived as being available as teams needed. However, one manager felt that the study team had a lack of insight into the nature of busy clinical practice, which might have limited the usefulness of support offered. Some frontline staff reported that study team contact had been mostly with management, and they were less aware of the support that had been available. Support to facilitators from the CORE team was described as taking place regularly and as needed, and facilitators appreciated that support was on hand whenever requested. Some facilitators took advantage of support available more than others. Coaching was useful in enabling facilitators to reflect and gain perspective on their teams, and feel that any hurdles that they were experiencing were not unique to them.
Experience of support from facilitators to teams was mixed. Some teams reported finding their facilitator easily contactable and approachable. When facilitator contact with teams was regular, this was perceived as helpful and increased focus on quality improvement work. Some teams and facilitators found that the lack of protected time for the facilitator role resulted in facilitators being thinly spread and lacking presence within teams, making the role slightly ineffectual. Most teams and facilitators felt that the role was more helpful when facilitators were internal and known to the team and trust. It was felt that this promoted engagement and trust, and pre-existing knowledge of teams and their practice enabled quality improvement planning, giving more credibility to the role. However, one person reported that being an internal facilitator might have resulted in being more tolerant and forgiving when CORE programme work waned.
Experiences of the scoping day were largely positive. In some teams, there was a delay in holding the scoping day from the beginning of the study, and this time lost within the year hindered opportunities for progress. Teams reported that the scoping day was helpful in promoting engagement and for action planning, providing a dedicated time and place for discussion.
Fidelity reviews were frequently described as being a rather time-consuming process, requiring a lot of preparation from teams. When the fidelity review process was considered positively, teams described that reviews helped with staff motivation and promoted reflection. Some stakeholders identified a lack of sensitivity in the review’s ability to accurately measure a team’s practice and changes made. Given the short-term duration of contact with service users, it was difficult for teams to gather required feedback. Some stakeholders questioned the usefulness of the interim review, and sometimes felt that this distracted from quality improvement work during the year.
The fidelity review report was considered valuable feedback, especially coming from an external source. Reports helped teams with quality improvement planning and reflecting on their current practice more.
Despite good intentions reported by many stakeholders, the resource pack website was somewhat underutilised. When stakeholders did access the website, it was often reported as being used more for browsing and fact-finding than being used proactively with service planning. Resources for some fidelity items on the website were quite sparse, which someone reported finding disappointing, particularly at the beginning of the year.
Process factors
A lack of time to engage with the CORE SIP was the most frequently cited process factor identified. The busy and overstretched nature of providing crisis home treatment was mentioned repeatedly across all stakeholder groups. This included a lack of time to prepare for fidelity reviews, to engage with the facilitator, to meet as a team and plan quality improvement work, to use the resource pack website, to implement quality improvement work and to reflect on practice. Several stakeholders also stated that 12 months does not give teams enough time to implement service changes and see this take effect.
Related to this, a lack of staff availability had an effect on the programme. This included instability within teams and staff vacancies, as well as practical difficulties in arranging meetings as a team because of the busy shift-work nature of clinical work. Changes in team leadership were also an important factor influencing implementation of the programme.
Team ownership was discussed positively and negatively as a process factor, and was mentioned by a majority of stakeholders. When teams did not have ownership over the programme, this arose from a lack of insight into the study and its rationale, which had a negative effect on engagement with and input to the study. One facilitator reported being met with significant resistance and hostility from a team. When teams demonstrated greater ownership over the programme, input and service improvement work was much greater. One facilitator found that openness and honesty from teams promoted their ownership and engagement. Several stakeholders spoke of the crucial need to promote engagement at the beginning of the year to ensure engagement and meaningful work throughout the programme. Stakeholders discussed the need to involve all staff members as a cohesive team to promote ownership and engagement, and identified a crucial role for the team leader in supporting this. The model of best practice provided by the programme was described as increasing team ownership by increasing awareness of how they should be practising.
Staff motivation and morale was the second most frequently cited process factor, influencing implementation of the programme positively and negatively. A willingness and openness to change and new ideas were associated with greater motivation and team morale, whereas resistance to research and a feeling that participation has been imposed from above hindered engagement. Pre-existing team dynamics were cited as important factors influencing motivation and implementation of the programme.
The programme was seen by many stakeholders as an important structure to support improvement. Some stakeholders reported that CORE formalised existing plans for service improvement work, and provided the time and opportunity to implement this. The model increased awareness of model best practice, and enabled teams to reflect on their practice and challenge and revise existing processes.
Related to this, stakeholders viewed the CORE programme as a means of benchmarking their practice. Several stakeholders reported seeing the value of the CORE programme in providing a quantifiable measure of practice, and the utility of this in enabling teams to compare their practice nationally, and evaluate how their practice changes over time.
Support from senior staff in the trust was established as another important process factor. Motivation was increased in teams that felt supported by their trust. This gave a sense of credibility to the programme. Engagement was promoted when this filtered down from management. When teams did not feel supported by the trust, this was demotivating and resulted in teams feeling that they were acting alone, making it difficult to affect change.
When it took place, service user involvement was an important process factor. Stakeholders mentioned how it was important to have their input, and the programme provided a platform for service user voices to be heard. Service user involvement was not achieved in all teams, and when it took place it largely involved service users speaking at away days, being involved in SIP working groups and providing feedback to inform fidelity reviews.
Impact of the programme
A majority of stakeholders identified specific service innovations resulting from CORE programme participation. These included improved provision of psychological interventions, more systematic and detailed documentation processes, improved resources and handouts provided to service users, more time spent working with carers and more work addressing physical health-care needs. One facilitator described that beyond specific changes made, staff confidence in their ways of working following the CORE programme had increased significantly.
Related to this, several stakeholders mentioned ways in which service user experience has improved following the CORE programme. Stakeholders described that interventions provided are now more structured in nature, with improved quality of time spent with service users. Some stakeholders described that a more holistic ethos to care had been adopted, and communication with service users (e.g. notifying on what time to expect a home visit) had also improved.
The CORE programme was found to have improved team communication among many stakeholders, with new systems and processes adopted that enabled staff to think and operate along the same lines. Several stakeholders also noted that CRT communication with community and inpatient teams was also improved. Stakeholders also identified that the CORE programme improved team purpose, provided an opportunity to refocus and addressed areas of practice that had previously been neglected (related to structure to support improvement). Staff motivation was also improved, with stakeholders stating that the CORE programme promoted a ‘can do’ attitude within teams. A positive impact on motivation was described at individual clinician and team levels. However, one stakeholder described that when their team did not improve on their fidelity score as much as they had anticipated at follow-up, motivation was negatively affected.
A majority of stakeholders highlighted that they saw the CORE programme as being part of a bigger whole. Stakeholders wished for quality improvement work to remain ongoing after the study end, attempting to fully embed changes made and seek further feedback to ensure that standards continued to improve.
Despite this, two teams described a lack of effect from the programme. One manager said that the support received did not make much difference to the way the team functioned, citing resource limitations as an explanation of this. Another team highlighted that a high rate of staff turnover had made it difficult to implement changes they desired to make. Numerous stakeholders expressed the view that it would take longer than the 1-year study period to see results of new changes implemented by the programme.
Appendix 8 Systematic review of self-management
Module 4.1
Link to published paper ‘Self-management interventions for people with severe mental illness: systematic review and meta-analysis’: www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/selfmanagement-interventions-for-people-with-severe-mental-illness-systematic-review-and-metaanalysis/5E9AF3AA73A83EA1128E8414F1233795 (accessed 28 March 2019).
Full reference: Lean M, Fornells-Ambrojo M, Milton A, Lloyd-Evans B, Harrison-Stewart B, Yesufu-Udechuku A, et al. Self-management interventions for people with severe mental illness: systematic review and meta-analysis [published online ahead of print March 22 2019]. Br J Psychiatry 2019. 101
Appendix 9 Systematic review of peer support
Module 4.2
Link to published open-access paper ‘A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness’: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-14-39 (accessed 28 March 2019).
Full reference: Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry 2014;14:39. 103
Appendix 10 Development of peer-supported self-management intervention
Module 4.3
Link to published open-access paper ‘Development of a peer-supported, self-management intervention for people following mental health crisis’: www.ncbi.nlm.nih.gov/pmc/articles/PMC5680762/ (accessed 28 March 2019).
Full reference: Milton A, Lloyd-Evans B, Fullarton K, Morant N, Paterson B, Hindle D, et al. Development of a peer-supported, self-management intervention for people following mental health crisis. BMC Res Notes 2017;10:588. 107
Appendix 11 Trial protocol
Module 6
The study protocol for this trial can be found online at the following URL: www.ucl.ac.uk/core-study/workstream-02/core-phase3-protocol (accessed 28 March 2019).
The study protocol has been published in BMJ Open and is available at the following URL: https://bmjopen.bmj.com/content/7/10/e015665.info (accessed 28 March 2019).
Full reference: Johnson S, Mason O, Osborn D, Milton A, Henderson C, Marston L, et al. Randomised controlled trial of the clinical and cost-effectiveness of a peer-delivered self-management intervention to prevent relapse in crisis resolution team users: study protocol. BMJ Open 2017;7:e015665. 110
Appendix 12 Full report of peer-support trial
Link to published open-access paper: www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31470-3/fulltext (accessed 28 March 2019).
Full reference: Johnson S, Lamb D, Marston L, Osborn D, Mason O, Henderson C, et al. Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet 2018;392:409–18. 115
Appendix 13 The CORE workstream 2 health economic evaluation
This appendix reports the economic analysis that accompanied the workstream 2, module 6 trial of the peer-supported self-management programme for people leaving CRTs.
The aim of the economic evaluation was to calculate the probability that peer-provided self-management is cost-effective compared with a control for a range of values of willingness to pay for 1 QALY gained over 12 months.
Method
Mental health service use (community and acute services) data for the trial 12-month follow-up period were collected from patient files. Health-related quality-of-life data were collected as part of participant interviews, using the EQ-5D-3L at baseline and at 4 and 18 months.
Analyses
The primary analysis for the economic evaluation is a complete-case analysis to maintain consistency with the statistical analysis and assume the same missing data mechanism. A sensitivity analysis accounting for loss to follow-up and missing data using multiple imputation was also conducted (see Supportive analysis).
Cost of the intervention
The cost of the intervention includes the cost of training PSWs and supervision by clinical staff. The cost of PSWs is calculated as the cost of an Agenda for Change band 3 member of staff, using hourly costs from the Personal Social Services Research Unit (PSSRU). 132 Data on supervision of PSWs by other clinical staff were collected from each trust as part of the trial.
Cost of 12-month mental health service use
Acute and community mental health service use, for the intervention and control groups, was collected from electronic patient records held by mental health trusts at baseline and at 12 months for the previous 12 months. Unit costs from published sources132 and Department of Health and Social Care reference costs133 were applied to mental health service use over 12 months. The cost of mental health clusters was estimated based on diagnosis.
Ordinary least squares regression including covariates for randomisation to PSW or workbook, baseline service use and clustering for PSW with 5000 bootstrap replications was used to calculate the mean difference in costs between PSW plus workbook and workbook and 95% CIs.
There was no discounting of costs given that they were reported over 12 months only. All costs are reported in 2015/16 Great British pounds.
Quality-adjusted life-years
The mean cost per QALY gained of PSW plus workbook compared with workbook over 4 months and 18 months was calculated. QALYs were calculated using the EQ-5D-3L and the formula developed by Dolan134 and as the area under the curve for each group from baseline to 4 and 18 months, controlling for any baseline differences using regression analysis. 135 Patients who died during the study were included as a zero at the date of death and assuming a straight line from their last completed EQ-5D-3L until death. Linear regression including covariates for randomisation to PSW or workbook, baseline utility score and clustering for PSW with 5000 bootstrap replications was used to calculate the mean difference in QALYs between PSW plus workbook and workbook and 95% CIs. QALYs from 12 to 18 months are discounted at a rate of 3.5%.
An additional analysis was also conducted to calculate QALYs over 12 months to have a follow-up duration consistent with data collected from clinical records. To obtain a 12-month value to calculate QALYs, a straight line was assumed between 4 and 18 months’ follow-up and the utility value calculated that would occur at 12 months on that line.
Incremental cost-effectiveness ratio
The mean incremental cost per QALY gained was calculated by dividing the covariate for randomisation to PSW or workbook in the 12-month costs regression analysis above (see Cost of 12-month mental health service use) by the randomisation covariate in the QALY regression analysis at 12 months. This was achieved by using the methodology set out in Briggs et al. 136
Cost-effectiveness plane and cost-effectiveness acceptability curve
The results of the bootstrap for the 12-month QALYs and 12-month costs have been reported on a cost-effectiveness plane. To report the probability that PSW is cost-effective compared with workbook only for a range of values of willingness to pay for 1 QALY gained, the results of the bootstrap analysis will also be used to generate a CEAC. CEACs and the probability that PSW is cost-effective compared with workbook alone at a £20,000 willingness to pay for 1 QALY will be reported for (1) 12-month costs and 18-month QALYs, (2) 12-month costs and 4-month QALYs and (3) 12-month costs and estimated 12-month QALYs.
Supportive analyses
The following supportive analyses were conducted and the new incremental cost-effectiness ratio and CEAC reported:
-
Cost of PSWs including supervision and training using costs provided by mental health trusts.
-
Weekly supervision and training for PSWs using PSSRU costs.
-
The utility decrement associated with a mental health inpatient admission will be calculated using linear regression and the difference calculated in utility for patients that are mental health inpatients at 4 months versus those living in the community. The utility decrement will be divided by 365 to calculate the daily utility decrement of being an inpatient. To calculate QALYs, all patients will have the constant from the linear regression with a decrement applied for each day they are an inpatient.
-
Multiple imputation using chained equations to impute missing QALYs. The study did not impute missing data for mental health resource-use data as it is difficult to identify missing data from the mental health resource-use data. For example, it was assumed that the patient had an inpatient admission when one was recorded. For patients with no subsequent inpatient admissions recorded it was assumed that this was because they did not have an admission, not that the data were missing. Bootstrapping was applied to the imputed data sets using the three-step procedure set out in Little and Rubin. 137
All analyses were conducted in Stata version 13.
Results
Cost of the intervention
The cost per PSW for training and supervision is reported in Table 9. There was a range of models for peer-support supervision, including frequency of supervision and grade of clinical staff responsible for supervision, with the most common model being fortnightly supervision with a grade 8 supervisor. Including costs of overheads and assuming that supervision was on a fortnightly basis (the most common model), the cost per PSW for supervision and training and weighting for different seniorities of supervision was £2548. Each PSW had an average caseload of 6.5 patients allocated to them, including patients who never used the intervention. This translates to a cost per patient randomised to the PSW arm of £392 for the cost of training and supervision.
| Activity | Description | Number of PSWs | Cost (£) | |
|---|---|---|---|---|
| Total | Per PSW | |||
| UCL training costs | 7 days training plus 4 days preparation | 30 | 1560 | 52 |
| PSWs attending training | 67.5 hours (9 days) per PSW | 30 | 50,625 | 1688 |
| Attending supervision: once per week | 24 meetings (2 hours per meeting) | 30 | 36,000 | 1200 |
| Attending supervision: once per fortnight | 12 meetings (2 hours per meeting) | 30 | 18,000 | 600 |
| Providing weekly group supervision (24 meetings, 2 hours per meeting) | 2 band 8a clinicians (£62/hour) | 15 | 5952 | 397 |
| 1 band 7 CRT manager (£52/hour) | 5 | 2496 | 499 | |
| 2 band 6 nurses (£42/hour) | 10 | 4032 | 403 | |
| Total weighted cost per PSW | 416 | |||
| Providing fortnightly group supervision (12 meetings, 2 hours per meeting) | 2 band 8a clinicians (£62/hour) | 15 | 2976 | 198 |
| 1 band 7 CRT manager (£52/hour) | 5 | 1248 | 250 | |
| 2 band 6 nurses (£42/hour) | 10 | 2016 | 201 | |
| Total weighteda cost per PSW | 208 | |||
The average number of appointments per patient was 6 (95% CI 5.5 to 6.5 appointments). Assuming that each meeting between the patient and PSW was 1 hour in duration, the average cost per patient was £132 (95% CI £118 to £145). Including supervision and training, the total average cost per patient of the PSW plus workbook was £524 (95% CI £509 to £537).
Cost of 12-month mental health service use
The mean cost of mental health services use at baseline and 12 months is reported in Table 10. Data on resource use is reported in Report Supplementary Material 2 – secondary analyses.
| Health-care resource | Cost, mean (95% CI) | |||
|---|---|---|---|---|
| PSW plus workbook (n = 221) | Workbook only (n = 220) | |||
| Baseline | 12 months | Baseline | 12 months | |
| Acute care | £6008 (£4631 to £7385) | £3673 (£2156 to £5220) | £5351 (£3846 to £6855) | £4023 (£2525 to £5522) |
| Communitya | £1740 (£1362 to £2119) | £2390 (£1954 to £2825) | £1941 (£1478 to £2405) | £2581 (£2076 to £3086) |
Including the cost of supervision and training and the PSW intervention and adjusting for baseline differences, the total cost of mental health services for the PSW group at 12 months was £6459 (95% CI £4766 to £8151). The total cost for the workbook-only group at 12 months with baseline adjusted was £6720 (95% CI £5329 to £8112). The mean incremental cost difference of the PSW group minus the workbook group at 12 months adjusting for baseline and including the cost of the PSW was –£261 (95% CI –£2450 to £1928).
Quality-adjusted life-years
Utility scores for patients who completed the EQ-5D-3L are reported in Table 11. The results include data from the four patients who died. At 18 months, adjusting for baseline and discounting at 3.5%, the mean QALYs for the PSW plus workbook group was 0.991 (95% CI 0.931 to 1.051) and 0.968 (95% CI 0.907 to 1.03) for the workbook-only group, with a mean difference of 0.023 (95% CI –0.062 to 0.107). Drawing a straight line between the 4- and 18-month QALYs, the mean QALYs at 12 months was 0.651 (95% CI 0.612 to 0.689) for the PSW group and 0.640 (95% CI 0.600 to 0.679) for the workbook-only group, with a mean difference of 0.011 (95% CI –0.043 to 0.065).
| Intervention | Utility scores by time point, n, mean (SD) | QALYs (18 months), n, mean (SD) | ||
|---|---|---|---|---|
| Baseline | 4 months | 18 months | ||
| Workbook | ||||
| EQ-5D-3L | 220, 0.595 (0.331) | 169, 0.658 (0.328) | 124, 0.675 (0.322) | 116, 0.950 (0.450) |
| PSW plus workbook | ||||
| EQ-5D-3L | 217, 0.613 (0.323) | 173, 0.671 (0.310) | 122, 0.698 (0.331) | 107, 1.011 (0.403) |
Incremental cost-effectiveness ratio, cost-effectiveness plane and cost-effectiveness acceptability curves
Peer-support worker plus workbook results in more QALYs and lower costs for all analyses and, hence, dominates the workbook-only intervention. The cost-effectiveness plane is reported in Figure 3 and the CEAC in Figure 4. At 12 months and a £20,000 willingness to pay for 1 QALY gained, there is a 70% chance that the PSW plus workbook intervention is cost-effective compared with workbook only. The lower percentage probability for a dominant incremental cost-effectiveness ratio is because of the wide CI for costs and the overlapping CIs for QALYs. A total of 48% of values on the cost-effectiveness plane fall in the north-east quadrant, where the intervention has a greater cost and more QALYs than the control arm. A total of 20% of values on the cost-effectiveness plane correspond with the intervention being cost-saving and more QALYs (the south-east quadrant). A total of 16% and 15% fall in the south-west and north-west quadrants, respectively, where the intervention results in fewer QALYs, but in the north-west quadrant it also results in a greater cost. The probability that PSW plus workbook is cost-effective increases at each additional follow-up time point. This is due to more QALYs being available for longer follow-ups (i.e. there is a maximum of 1 QALY at 12 months’ follow-up and 1.5 QALYs at 18 months’ follow-up) and the difference in utilities between the two groups being maintained over time. There is a 60% probability that that PSW plus workbook is cost-effective compared with workbook alone at 4 months and a 70% probability at 18 months at a willingness to pay for a QALY gained of £20,000.
FIGURE 3.
Cost-effectiveness plane for 12-month QALYs and costs based on bootstrap results.
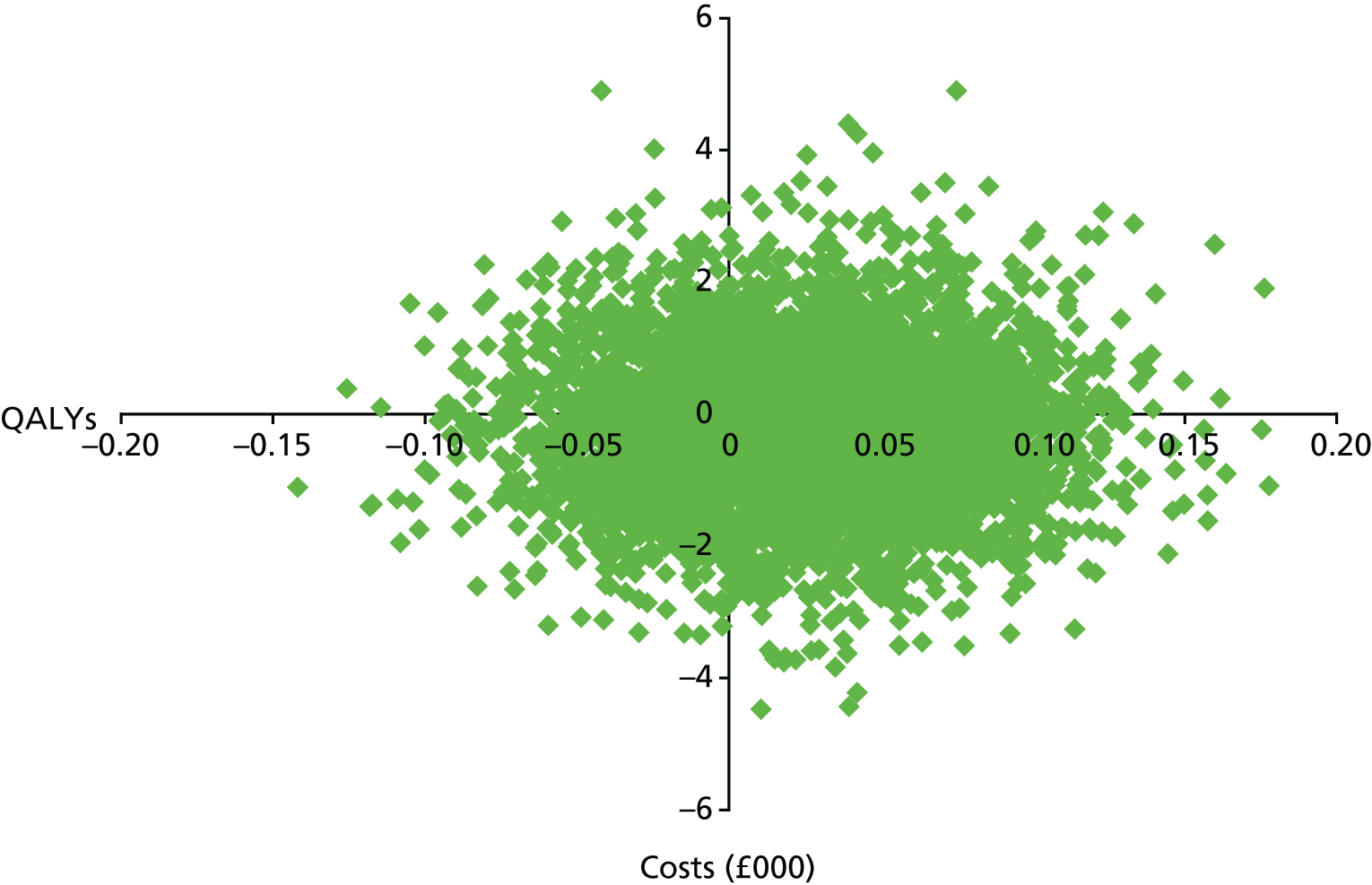
FIGURE 4.
Cost-effectiveness acceptability curve for 18-, 12- and 4-month QALYs and 12-month costs based on bootstrap results.
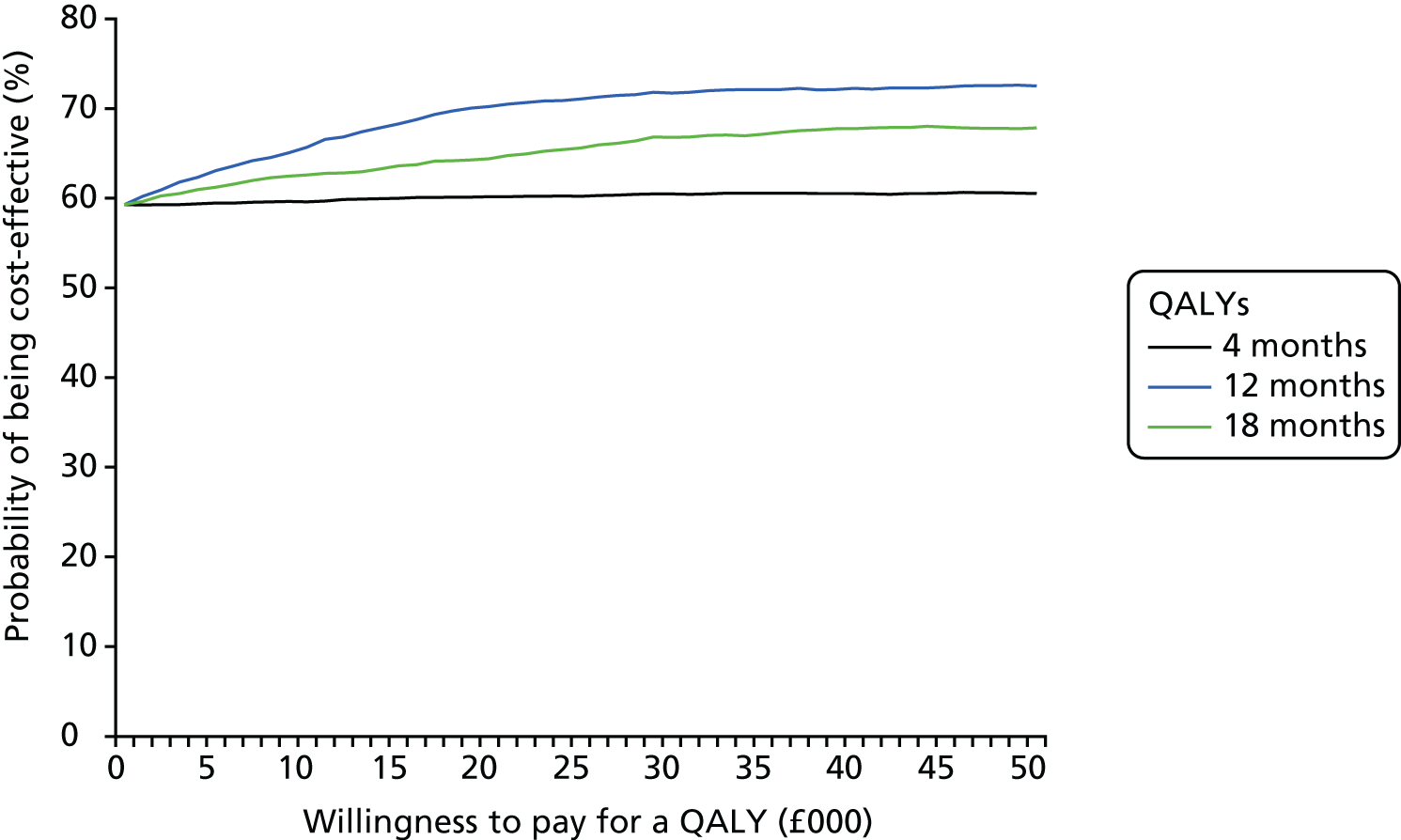
Supportive analyses
-
Mental health trust costs and fortnightly supervision: the costs provided by mental health trusts for the cost per hour of PSWs and clinical supervision staff were lower than those reported in the PSSRU. This is because the PPSRU uses the specific pay point for staff and includes less cost for overheads. The cost per hour for a PSW, as provided by the mental health trust, was £13 per hour. For clinical supervision it was £31 per hour for a band 8a clinician, £25 per hour for a band 7 CRT manager and £20 per hour for a band 6 nurse. As a result, the total cost of supervision and training assuming mental health trust costs is £1343 per PSW or £207 per patient.
Applying these costs to the data and running the bootstrap regression, patients randomised to PSW cost £437 less than the workbook group (95% CI –£2492 to £1618). Using mental health trust costs, there is a 75% probability that PSW is cost-effective compared with workbook only with 18-month QALYs and 12-month costs.
-
The other model of supervision used was weekly supervision of PSWs by clinical staff. The total cost of the supervision and training with weekly supervision and PSSRU costs is £3356 per PSW and £516 per patient.
Applying these costs to the data and running the bootstrap regression, patients randomised to PSW cost £65 less than the workbook group (95% CI –£2119 to £1989). Using mental health trust costs, there is a 66% probability that PSW is cost-effective compared with workbook only with 18-month QALYs and 12-month costs.
-
Being an inpatient in acute care at 4 months was associated with a utility decrement of 0.130 (95% CI –0.27 to 0.010). Applying this to inpatient days with a constant of 0.668, both groups had a mean utility of 0.661 (95% CI 0.658 to 0.663).
-
Level of educational attainment and whether or not patients were in open employment were both predictors of missing 18-month EQ-5D-3L scores and QALYs, with patients with higher levels of educational attainment and those in open employment less likely to be missing data. The exact question for these variables changed between the pilot and main trials, so this analysis was conducted for the main trial data only.
Using multiple imputation with chained equations and imputing QALYs for 44 data sets given 44% of missing data for QALYs in the main trial, the mean incremental QALYs for the PSW compared with control was 0.019 (95% CI –0.081 to 0.120). There is a 57% probability that PSW is cost-effective compared with workbook only using the imputed QALYs and bootstrapping.
Discussion
The PSW intervention dominated the workbook in that it cost less than the workbook when cost savings from prevented acute care were taken into account and resulted in more QALYs, although the differences were not statistically significant. There is a 64% probability that PSW is cost-effective compared with the workbook only at a £20,000 willingness to pay for 1 QALY gain at 12 months. This varies between 57% and 75% depending on the duration of the analysis and assumptions made about the intensity of the supervision.
Strengths and weaknesses
The analysis includes resource use from mental health services only. This had the strength of providing a high level of follow-up for resource use. It restricts the perspective of the analysis to mental health costs only though, and insufficient information was available to include other costs in the analysis. The potential benefits to the PSWs themselves also was not captured. These are likely to increase the economic benefit of the intervention further given the positive impact on employment and skills acquisition of the intervention for the PSWs.
A key weakness of the analysis is that the follow-up periods for costs and outcomes are not the same. In the original protocol, self-completed follow-up to collect EQ-5D-3L and calculate QALYs was to occur at 4 months only, with resource-use data for 12 months from randomisation. To address this, applying a utility decrement was initially proposed, calculated using baseline and 4-month EQ-5D-3L data, to inpatient admissions. Part way through the study, an extension was given to collect self-completed questionnaires, such as the EQ-5D-3L, at 18 months. Although this 18-month follow-up did not match up with the resource-use collection from patient files, the self-completed longer duration was preferable to assumptions regarding re-admission and utility decrements and the utility decrements analysis became supportive analysis 3, which showed no difference between the two groups in the number of QALYs. Further work is required to model the costs and QALYs over different time horizons.
There was poor follow-up for the EQ-5D-3L, with only 50% of patients having complete QALYs. Multiple imputation of the results increases the total QALY impact, but also increases the CIs, reducing the probability that the intervention is cost-effective.
List of abbreviations
- BME
- black and minority ethnic
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CINAHL
- Cumulative Index of Nursing and Allied Health Literature
- CONSORT
- Consolidated Standards of Reporting Trials
- CORE
- Crisis resolution team Optimisation and RElapse prevention
- CRT
- crisis resolution team
- CSQ
- Client Satisfaction Questionnaire
- EBP
- evidence-based practices
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- ICC
- intraclass correlation
- IQR
- interquartile range
- IRR
- incidence rate ratio
- IT
- information technology
- MHRN
- Mental Health Research Network
- MMAT
- mixed-methods appraisal tool
- MNHHS
- Metro North Hospital and Health Service
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- OR
- odds ratio
- PPI
- patient and public involvement
- PSSRU
- Personal Social Services Research Unit
- PSW
- peer-support worker
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RR
- risk ratio
- SAE
- serious adverse event
- SD
- standard deviation
- SIP
- service improvement programme
- SMD
- standardised mean difference
- SMI
- severe mental illness
- SUGAR
- Service User and Carer Advisory Group Advising on Research
- SURF
- Service User Research Forum
- UCL
- University College London
