Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0610-10097. The contractual start date was in April 2012. The final report began editorial review in April 2018 and was accepted for publication in February 2019. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None of the authors has any professional interests in the services studied in this research programme that could constitute a conflict of interest. Sandra Eldridge reports membership of the Health Technology Assessment (HTA) Clinical Trials Board and the National Institute for Health Research Clinical Trials Unit Standing Advisory Committee. Stefan Priebe reports previous membership of the HTA Mental, Psychological and Occupational Health Panel (2013–2018).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Killaspy et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
SYNOPSIS
Introduction
We report on results from the QuEST (Quality and Effectiveness of Supported Tenancies for people with mental health problems) study, a national programme of research into mental health supported accommodation services in England. Many of those who use these services have a diagnosis of schizophrenia or other psychosis, with associated difficulties in managing everyday activities. Specialist mental health supported accommodation services are a key component of the ‘whole-system care pathway’ for people with complex and longer-term mental health problems, often providing support to people on discharge to the community after lengthy or recurrent hospital admissions. We estimate that around 60,000 people in England live in supported accommodation at considerable cost to the tax payer. 1,2 Despite this, there has been little research to guide practitioners and commissioners in the most effective models and the support that should be provided. This research aimed to address this gap by providing evidence on the current provision, quality, cost and effectiveness of supported accommodation for people with mental health problems in England.
Background
The NHS Hospital Plan of 19623 heralded the process of deinstitutionalisation in England and Wales and the development of community-based mental health care, a key component of which is supported accommodation. In England, around one-third of working-age adults with severe mental health problems reside in supported accommodation provided by health and social services, voluntary organisations, housing associations and other independent providers. These include nursing and residential care homes, group homes, hostels, blocks of individual or shared tenancies with staff on site, and independent tenancies with ‘floating’ or outreach support from staff. Local statutory community mental health services provide care co-ordination and clinical expertise to the residents and staff of supported accommodation projects through the Care Programme Approach. 4 In 2006, around 12,500 people with mental health problems in England were in a nursing or residential care home1 and around 40,000 were receiving floating outreach. 2
The majority of those who require these services have complex mental health needs and functional impairments that have an impact on their ability to manage activities of daily living. Despite medication, many experience ongoing symptoms of their illness and impairments in cognition associated with long-term severe psychosis, reducing their motivation and organisational skills. 5 They may require assistance to manage their medication, bills, personal care, shopping, cooking, cleaning and laundry. However, the majority have been shown to be able to sustain community tenure with support and many gain skills and can manage with less support over time. 6,7 Nevertheless, most are unemployed and socially isolated. 8 In short, despite the move towards community-based care, this group remains one of the most socially excluded in society. 9 Supported accommodation services have a very important role in assisting people with complex mental health problems to live in the community, but despite this and the large resources dedicated to these services, there has been very little research to investigate their effectiveness. 10
The only survey of mental health supported accommodation to be carried out in England (led by co-investigator SP) found few differences in the characteristics of service users in different types of setting or in the support offered. 11 This survey sampled 12 nationally representative regions and identified a total of 481 projects, of which 250 were randomly sampled. Of these, 153 responded to a postal survey; 57 were nursing/residential care homes (with a mean of 16 residents), 61 were individual or shared flats with on-site staff support (with a mean of 13 service users) and 30 provided floating outreach to a mean of 34 service users in their own flats, usually rented from the local authority or a housing association. The majority were male, 80% had a diagnosis of a psychotic disorder and 48% also had a history of substance misuse. There were no differences in service user characteristics between service types. Around 40% of those in supported housing or receiving floating outreach were participating in some form of community activity (compared with 25% of those in residential care) but similar numbers of hours were spent by service users across all settings in education or work (mean 13 hours per week) and only 3% were in open employment. Staff made contact with users an average of 6 days per week in supported housing and 4 days per week in floating outreach services. Between four and six service users (18–25%) moved on from each service annually. Almost all service users were prescribed medication and all services provided support with activities of daily living. The costs of services appeared to be driven by the local tradition of provision rather than clinical need. Shepherd and Macpherson12 have also commented that the development of local supported accommodation provision appears to be largely determined by history, the sociodemographic context of the area and the support available from primary care and secondary mental health services.
Although the previous survey did not find major differences between the content of care provided in supported housing and floating outreach services, many areas of the UK operate supported accommodation pathways where service users move from higher- to lower-staffed settings as their skills improve. This allows for graduated ‘testing’ but necessitates repeated moves. A number of studies have identified discrepancies between stakeholder views on the level of support required, with service users tending to prefer more independent accommodation and staff and family members tending to prefer the person to live in a staffed environment. 13–15 An important criticism of more highly staffed settings is the use of institutional regimes and impaired facilitation of service users’ autonomy through over-support and a poor rehabilitative culture. 16 Conversely, some service users have reported that independent tenancies are lonely. 16,17
At the time that we developed the QuEST programme, there had been no trials investigating the effectiveness of supported accommodation services for people with mental health problems18 and few good-quality studies investigating the effectiveness of these services. 10 The paucity of research reflects the logistic difficulties in researching this area. Randomisation to different types of housing support may be resisted by clinicians who feel that service users require a staged process, moving from higher- to lower-supported settings as their skills and confidence increase, and by service users with clear preferences for particular services. It also seems that the availability of supported housing stock is more influential than clinical need in determining accommodation allocation. The lack of evidence means that we do not know whether or not individuals are following the most clinically effective and cost-effective routes to independence. Recently, the results of a major trial in Canada comparing usual care with ‘Housing First’ (a floating outreach model that targets individuals with mental health problems who are homeless) found that Housing First was associated with greater housing stability, but other gains in clinical and social outcomes were less clear. 19 The QuEST programme aimed to address this gap in the evidence.
Objectives of the QuEST programme
-
To adapt the Quality Indicator for Rehabilitative Care (QuIRC) and an existing patient-reported outcome measure, the Client Assessment of Treatment (CAT) scale, for use in mental health supported accommodation.
-
To assess quality and costs of supported accommodation services in England and the proportion of people who successfully move on to more independent settings.
-
To identify service and service user factors (including costs) associated with greater quality of life, autonomy, satisfaction with care and move-on.
-
To assess the feasibility, required sample size and appropriate outcomes and costs for a randomised evaluation of two models of supported accommodation. One provides a constant level of staff support on-site (supported housing) and the other provides outreach support of flexible intensity to people in independent tenancies (floating outreach).
Figure 1 illustrates the interconnecting work packages (WPs) and timelines.
FIGURE 1.
Flow chart showing relationships between WPs. CAT-SA, Client Assessment of Treatment for Supported Accomodation; FO, floating outreach; QuIRC-SA, Quality Indicator for Rehabilitative Care: Supported Accommodation; SH, supported housing; WP, work package.
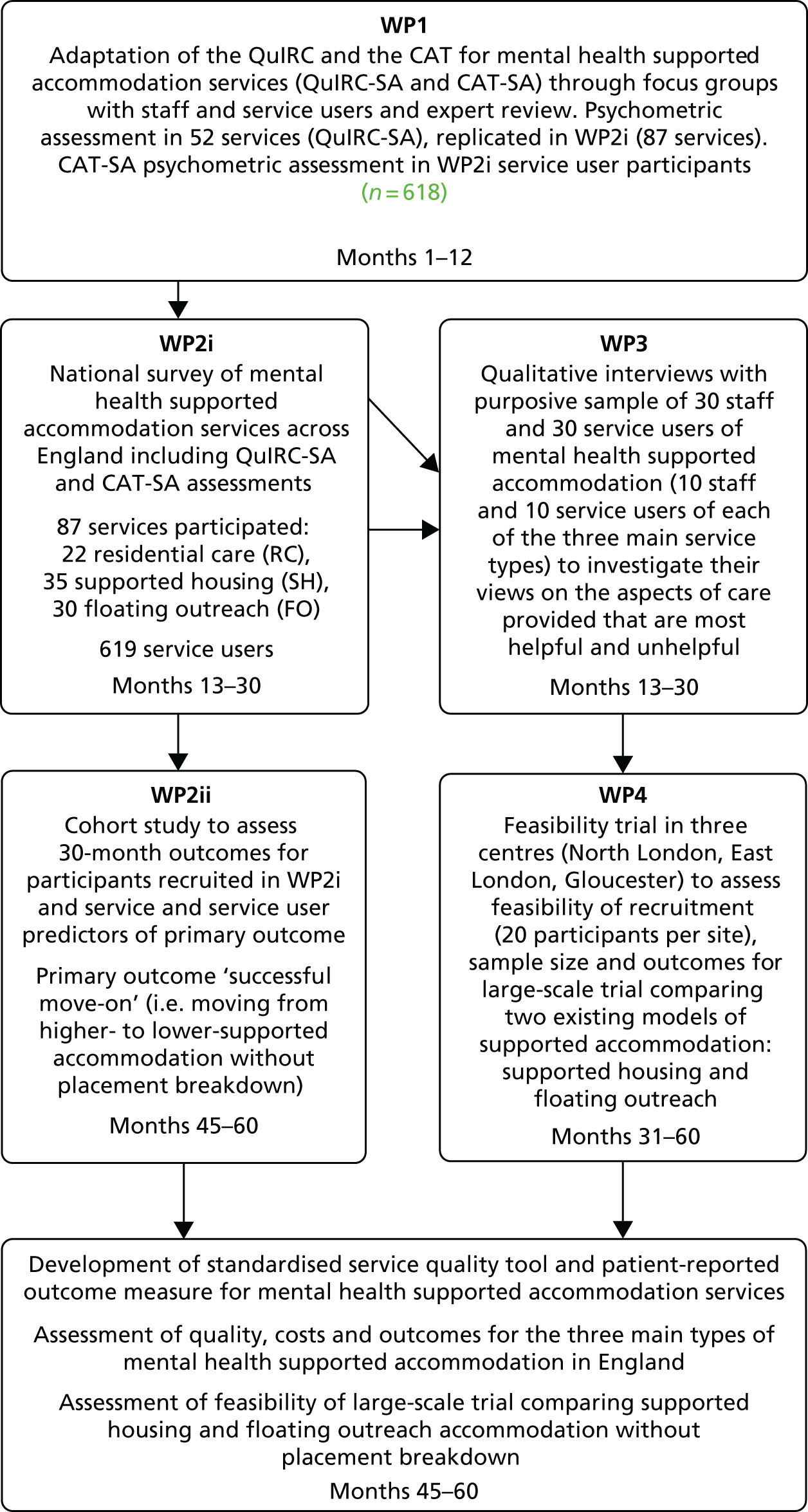
Objective 1 was addressed in the first WP (WP1) of the programme: adaptation of an existing standardised quality assessment tool used in longer-term mental health units, and an existing patient-report outcome measure, for use in mental health supported accommodation settings.
Objectives 2 and 3 were addressed through WP2 and WP3.
WP2 comprised two components:
-
survey of a nationally representative sample of supported accommodation services across England that used the standardised tools adapted in WP1, together with additional descriptive data collected from staff and a random sample of service users to describe and compare the content and costs of care delivered in the three main types of supported accommodation service provided in England (residential care, supported housing and floating outreach)
-
Longitudinal follow-up of the random sample of service users recruited in WP2i over 30 months to identify service and service user factors associated with our primary outcome – move-on to less supported accommodation.
Work package 3 comprised in-depth qualitative evaluation of staff and service user perspectives on the aspects of care considered most beneficial in supporting recovery and the barriers to providing these.
Objective 4 was addressed in WP4: an evaluation of the feasibility of a randomised trial to compare two existing models of supported accommodation (supported housing and floating outreach).
Study preparation
Recruitment of research team
-
Ms Sarah Dowling: Project Manager, University College London – started 18 September 2012.
-
Dr Sima Sandhu: Researcher, Queen Mary University of London – started 1 September 2012.
-
Dr Rose McGranahan: Researcher, Queen Mary University of London – started 1 January 2016.
-
Dr Peter McPherson: Research Associate, University College London – started 4 October 2012.
-
Dr Joanna Krotofil: Research Associate, University College London – started 1 January 2013.
-
Ms Isobel Harrison: Research Associate, University College London – provided maternity cover for Joanna Krotofil from January to July 2014 and remained involved with the project through North Thames Clinical Research Network funding.
No-cost extension
The National Institute for Health Research kindly agreed a 6-month no-cost extension to our contract to acknowledge the time lag between the official contract start date and the date when the relevant subcontracts were agreed that enabled recruitment of the research team.
Ethics approval
Application for ethics approval for WP1–3 of the programme was made in November 2012 and approval was received on 4 February 2013 from the Harrow Research Ethics Committee (reference 12/LO/2009). Ethics approval for WP4 was sought on 12 March 2015 and approval was received on 7 April 2015 from Liverpool Central Research Ethics Committee (reference 15/NW/0252).
Research governance
The research was conducted in keeping with usual research governance guidance and processes. The chief investigator and researchers prepared appropriate standard operating procedures for all WPs. The researchers were trained in the use of the study materials by Helen Killaspy and piloted these prior to use. In 2014, the research was audited by North London Central Research Consortium and no concerns were identified.
Programme management
The chief investigator and programme manager managed the day-to-day running of the programme, overseen by the Programme Management Group (PMG), which met quarterly to review study progress and address managerial and scientific issues as they arose. The Programme Steering Group (PSG) provided an objective ‘quality assurance’ process, reviewing progress and advising the PMG if problems arose that might have an impact on the successful completion of the research. We also recruited a Service User Reference Group to provide an independent view on aspects of the research that were of particular relevance to users of supported accommodation services. The PMG also consulted with an independent group of clinical and policy experts in the field of supported accommodation at relevant stages of the programme, particularly in relation to the adaptations to the service quality tool in WP1 and recruitment in WP4. In addition, a dissemination event and stakeholder roundtable event were held at the end of the programme, attended by members of this expert group, to discuss the implications of the programme findings for future practice and policy.
Patient and public involvement
We recognised that the involvement of service user expertise was key to the success of the programme and included PPI throughout, from design to dissemination. The co-investigator Gerard Leavey co-ordinated these activities. We consulted with the North London Service User Research Forum (SURF) about the focus and design of the study prior to submitting the proposal for funding and incorporated suggestions into the application (e.g. having an independent service user reference group to consult throughout). We further consulted the SURF in relation to the adaptation of the tools in WP1, the interpretation of the results in WP2, the development of the topic guides in WP3 and WP4 and addressing recruitment issues in WP4.
One of our co-applicants (MA) has lived experienced of severe mental illness and of living in supported accommodation. He has worked closely with our group on previous studies in the field of complex psychosis and contributed to our lay summary at the design/application stage and throughout the programme as a member of the PMG. He was also the service user expert on our PSG. After funding for our programme was agreed, we recruited a second service user expert to join Maurice Arbuthnott on the PMG. Service user representatives in the PMG were actively involved in commenting on the delivery of the research programme, reviewing progress and assisting in the development of plans to disseminate the research findings.
We also recruited three lay members with experience of severe mental health problems and supported accommodation services to our Service User Reference Group. This group was facilitated by Gerard Leavey and met every 6 months to provide an independent view on all aspects of the research that were of particular relevance to users of supported accommodation services.
The PSG meetings were held every 6 months to provide oversight to the research programme, reviewing its progress and advising the PMG if problems arose that might have an impact on its successful completion. The service user representative on this group contributed to these discussions.
All service user experts were paid £50 per meeting plus travel expenses.
Study progress (start date: 1 October 2012)
Work package 1: project months 1–12
Data collection in WP1 was completed on time. However, it was decided that further analysis of the psychometric properties of the adapted QuIRC using the larger sample of service managers and service users recruited in WP2 was indicated. The results were published in April 2016 in BMC Psychiatry. 20 Adaptation of the CAT scale was completed on time and the results were published in March 2016 in BMC Psychiatry. 21
Work package 2i: project months 13–30
The first component of WP2 (national survey) was completed on time and the main quantitative results comparing the three main types of supported accommodation were published in November 2016 in Lancet Psychiatry. 22
Work package 2ii: project months 45–60
The second component (30-month follow-up of service users’ progress) commenced in June 2016 and data collection was completed in August 2017. Researchers tracked service users through 3-monthly contact with their supported accommodation service manager to minimise loss to follow-up. The results were published in The British Journal of Psychiatry. 23,24
Work package 3: project months 13–24
Work package 3 was completed on time and the results were published in July 2017 in BMC Health Services Research. 25
Work package 1: adaptation of the Quality Indicator for Rehabilitative Care and Client Assessment of Treatment scale for use in supported accommodation services
The aim of WP1 was to adapt an existing quality assessment tool and an existing patient-rated outcome measure for use in supported accommodation services. The QuIRC26 is an international, standardised tool that assesses quality of care in longer-term mental health facilities. It is completed by the service manager and provides descriptive data and quality ratings, expressed as percentages, for seven domains of care (living environment, therapeutic environment, treatments and interventions, self-management and autonomy, social interface, human rights, and recovery-based practice). It has excellent inter-rater reliability and domain ratings are positively associated with standardised measures of service users’ autonomy and experiences of care. 26,27 Therefore, it can provide a proxy assessment of service users’ views of a facility even though it is completed by the unit manager. It is freely available as a web-based resource (www.quirc.eu). Table 1 provides a summary of the tool content and structure.
| Domain | Number of items scoring domain | Examples of areas covered | Example of item |
|---|---|---|---|
| Living environment | 22 | Privacy, décor, cleanliness, meals, mobility access, access to laundry facilities, access to outside space | Is there a private room for patients/residents to meet with their visitors? |
| Therapeutic environment | 35 | Staffing, aims of service, therapeutic optimism, service user involvement in decisions about the service, staff supervision | How hopeful are you that the majority of your current patients/residents will show improvement in their general functioning over the next 2 years? |
| Treatments and interventions | 27 | Staff training, facilitating access to evidence-based interventions, managing challenging behaviour, processes for review of treatment and care | How often are therapeutic effects and side effects of psychiatric medication reviewed? |
| Self-management and autonomy | 27 | Facilitating service user involvement in decisions about own care, supporting service users to gain skills for more independent living, avoidance of ‘blanket restrictions’ | Is there a process for supporting patients to manage their own medication? |
| Social interface | 10 | Facilitating access to community resources, engaging with family, supporting service users’ friendships, providing support to vote in elections | How many of your patients/residents regularly take part in activities in the community? |
| Human rights | 24 | Access to advocacy and legal representation, formal complaints process in place, case notes kept securely and confidentially | Is a welfare/benefits advice service available to your patients/residents? |
| Recovery-based practice | 19 | Individualised and collaborative care planning, ex-service users employed in the service, working towards successful move-on to more independent accommodation | Please estimate the number of your patients/residents who have moved on from your unit to more independent accommodation in the last 2 years? |
The CAT scale is a seven-item, international, standardised, patient-reported outcome measure with good psychometric properties28 that was originally developed for inpatient mental health care (see Appendix 1). Each item is rated from 0 (not at all satisfied) to 10 (entirely satisfied).
Methods
Tool content review and adaptations
The content of the QuIRC was first reviewed by the research team to identify obviously problematic items (e.g. irrelevant items or those requiring rephrasing). Three focus groups with staff and service users recruited from North London were held, one of each focus group from each of the three main types of supported accommodation in England (residential care, supported housing and floating outreach) to gain participants’ views on the relevance of individual QuIRC (staff) and CAT (service user) items. Focus groups were facilitated by the researchers under the supervision of Gerard Leavey. The relevant QuIRC items (staff focus groups) and all seven CAT items (service user focus groups) were used to structure and focus the discussion, which aimed to identify items that required amendment/deletion and additional items. The focus groups were recorded and transcribed and the researchers collated responses.
The findings were supplemented by the advice of three panels of experts who also reviewed the QuIRC and CAT. The first panel comprised five members with expertise in supported accommodation (two senior clinicians, a service manager, a senior policy advisor and a Care Quality Commission senior adviser). The second expert panel was our QuEST study service user reference group, which comprised three members with lived experience of specialist mental health supported accommodation and services. The third expert panel was the North London SURF, which comprised 12 members with lived experience of mental health problems and expertise in mental health services research. All three expert panels were sent the original QuIRC and CAT and a document summarising the comments from the focus groups. They were asked for their opinion about the suggested amendments and any additional amendments. The researchers collated all responses from the focus groups and expert panels, identifying items where there was consensus for adaptation, deletion or a new item. These were reviewed by the QuEST PMG to gain final agreement on changes. The revised QuIRC was then piloted with three service managers (one of each of the three types of supported accommodation) in North London and final amendments to wording were made.
Psychometric property assessment of the adapted Quality Indicator for Rehabilitative Care
To assess the psychometric properties (item response spread, internal consistency, inter-rater reliability, sampling adequacy) of the adapted QuIRC, supported accommodation services were randomly selected from a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) database of all supported accommodation services (residential care, supported housing and floating outreach) in each of 14 nationally representative areas of England (see Work package 2 for further details of area selection and scoping of services). Two services of each of the three types were randomly selected from each of the 14 areas with the aim of recruiting 20 managers from each type of service (60 in total). The researchers contacted service managers to gain their informed consent for participation. Two researchers attended a face-to-face interview with participating service managers. One researcher led the interview and both researchers independently rated the adapted QuIRC from the answers given by the unit manager.
Data analyses were conducted by Sarah White, statistician from St George’s University London, who was involved in the development of the original QuIRC. Items were considered to have inadequate response spread if > 90% of service managers gave the same response. Internal consistency of domain scores was assessed using Cronbach’s alpha and considered acceptable if > 0.6. Inter-rater reliability was assessed using kappa coefficients for categorical data (weighted kappa if more than two categories) and intraclass correlation coefficients (ICCs) for normally distributed, continuous data, and considered acceptable if > 0.7.
Psychometric property assessment of the adapted Client Assessment of Treatment
The psychometric properties of the adapted CAT were assessed in the 618 service users who participated in the national survey of supported accommodation services in WP2 (see Work package 2 for full details of the approach to sampling and recruitment). Internal consistency was assessed using Cronbach’s alpha. Convergent validity was assessed through correlation with ratings of participants’ subjective quality of life using the Manchester Short Assessment of Quality of Life (MANSA),29 which has a total maximum mean score between 1 and 7.
Results
Each staff focus group comprised four members (the service manager plus three support workers). The three service user focus groups had five or six members (residential care, n = 6; supported housing, n = 5; floating outreach, n = 5).
Adapted Quality Indicator for Rehabilitative Care
A total of 28 QuIRC items were rephrased, 20 items were deleted and 10 items were added. For example, item 77 from the original QuIRC was adapted to better reflect the nature of support within these settings (original item: ‘How many of your staff are trained in control and restraint techniques?’; amended item: ‘How many of your staff are trained in breakaway techniques?’), whereas item 116 was simply omitted (‘Are patients/residents free to send and receive uncensored mail or email?’). The final version had 143 items. It was also agreed that because floating outreach services are not ‘building based’ but provide support to people living in an independent tenancy, the items relating to the living environment of the service were not relevant and, therefore, the adapted QuIRC would not be able to provide a rating on this domain for these services.
Inter-rater reliability of the QuIRC was carried out with managers of 14 residential care homes, 21 supported housing services and 17 floating outreach services (52 services in total).
Only 16 out of the 143 items showed a poor response spread. Internal consistency was inadequate for all domains except therapeutic environment and treatments and interventions. However, the analysis was limited by a relatively small sample size and the lack of variability in response to some items. With regard to inter-rater reliability, 70 ICC analyses were conducted and only one item was found to be unreliable. A total of 186 kappa coefficient analyses were conducted and four items were found to be unreliable (κ < 0.7). In addition, there were 14 items where analyses could not be conducted because there were too few cases (five items), zero variance (two items) or where variables were constants (seven items). The full results of these assessments are available in Killaspy et al. 20
The PMG agreed amendments to the adapted QuIRC in response to the results. It was decided to keep items with inadequate variance because (1) to drop them would have disrupted the logical flow of the tool content and (2) greater variance might be achieved in future development of the tool for use in settings outside the UK. Additional explanatory information was added to improve the reliability of one item, one item was dropped completely and unreliable response options were dropped for three items.
It was also agreed that internal consistency would be reassessed using the larger sample of 87 services participating in WP2 along with an assessment of sampling adequacy (the proportion of variance among the variables that might be common variance) using the Kaiser–Meyer–Olkin (KMO) statistic. Hair30 suggested a KMO value of ≥ 0.5 to evaluate whether or not a sample of data has sufficient common variance to make exploratory factor analysis appropriate.
Internal consistency improved on all domains with the larger sample (Table 2). All domains met the KMO > 0.5 criterion of sampling adequacy. It should be noted however that both Cronbach’s alpha and the KMO statistic are influenced by sample size and in this analysis the sample size was still smaller than desirable for robust estimates of both properties (generally 300 observations). However, we were able to investigate whether or not there was adequate common variance within the domain items to assume that the domain had coherence. We replicated the approach taken in the original development of the QuIRC, where items were considered to load onto a factor (domain) if they scored > ± 0.3. As some items had zero variance, they were removed before analysis (living environment: two items; self-management and autonomy: three items; human rights: four items). All items loaded onto a factor within that domain at the > ± 0.3 level (i.e. each item was contributing to the common variance within the domain).
| Domain | Number of items scoring domain | WP1 services (n = 52) | WP2 services (n = 87) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) domain score | Range | Cronbach’s alpha | Mean (SD) domain score | Range | Cronbach’s alpha | KMO | ||
| Living environment | 20 | 81.0 (7.1) | 62.3–94.3 | 0.39 | 81.2 (8.7) | 53.9–96.2 | 0.56 | 0.58 |
| Therapeutic environment | 33 | 62.2 (7.3) | 48.5–78.9 | 0.66 | 61.4 (6.9) | 38.2–75.4 | 0.66 | 0.51 |
| Treatments and interventions | 27 | 55.1 (8.4) | 36.7–76.3 | 0.66 | 54.2 (8.1) | 35.1–73.2 | 0.64 | 0.61 |
| Self-management and autonomy | 33 | 69.0 (5.8) | 53.7–81.8 | 0.40 | 68.0 (6.9) | 39.3–83.8 | 0.62 | 0.58 |
| Social interface | 7 | 59.0 (10.8) | 33.9–89.7 | 0.27 | 58.9 (12.1) | 37.6–85.6 | 0.49 | 0.56 |
| Human rights | 21 | 86.7 (5.0) | 71.4–96.7 | 0.09 | 85.5 (6.9) | 66.1–97.5 | 0.37 | 0.53 |
| Recovery-based practice | 18 | 71.7 (8.2) | 51.9–91.4 | 0.53 | 69.2 (9.9) | 31.8–90.5 | 0.67 | 0.57 |
We engaged the same information technology specialist who developed the web-based version of QuIRC to develop a similar application for the adapted QuIRC for supported accommodation services. This increases its accessibility, reduces the time required to complete it compared with a face-to-face interview, and provides a built-in scoring algorithm. It has a similar facility to the original QuIRC application in producing a printable report for the service manager about the performance of their service on the adapted QuIRC domains, comparison benchmarking data for similar services and suggestions for how to improve performance. The final version of the adapted QuIRC was named the Quality Indicator for Rehabilitative Care: Supported Accomodation (QuIRC-SA).
Adapted Client Assessment of Treatment
All seven CAT items were considered relevant by the focus group participants and expert reference group members, with only slight modification of the wording required (e.g. ‘treatment/care’ was changed to ‘support/care’). No items were deleted or added. Cronbach’s alpha was 0.89. With regard to convergent validity, scores on the adapted CAT were positively correlated with the mean total MANSA (quality of life) score (rs = 0.35; p < 0.001). Full results are available in Sandhu et al. 21
Links to other work packages
The QuIRC-SA and CAT-SA were used to assess service quality and service user experience in the national survey of supported accommodation services (WP2i), the prospective cohort study (WP2ii) and the feasibility trial comparing supported housing and floating outreach (WP4).
Limitations
Quality Indicator for Rehabilitative Care: Supported Accommodation
One of the limitations of the QuIRC-SA was the inadequate internal consistency. Although the domains were coherent [as measured by sampling variance (KMO statistic)], it is possible that the estimates of internal consistency (Cronbach’s alpha) may have been influenced by our sample size; a sample size of 300 to 400 is desirable in order to obtain robust estimates of internal consistency. The decision to retain items with inadequate response variance may be considered a limitation of the tool. Although it could be argued that the retention of these items unnecessarily increases the size and administration time of the QuIRC-SA, omitting them would have disrupted the logical flow of the tool. We were not intervening to improve service quality during the QuEST programme and we therefore did not assess the tool’s sensitivity to change. Test–retest reliability was not assessed as we felt that this was too onerous for busy service managers (as the tool takes 1 hour to complete). Both should be assessed in future studies, but their omission had no influence on the findings of later phases of the QuEST programme as we used only baseline QuIRC-SA assessments.
Client Assessment of Treatment for Supported Accommodation
Although the development and testing procedures for the CAT-SA were rigorous, a number of limitations must be acknowledged. First, we did not collect data on symptoms or clinical profile when assessing the psychometric properties of the measure, which negates the possibility of investigating potential relationships between CAT-SA ratings and symptomology. Second, owing to the nature of our investigations, test–retest reliability and sensitivity to change have not been assessed. Third, additional validation procedures are needed to establish its validity in countries outside England. Finally, service user experience/appraisals on the CAT-SA may be influenced by support received outside the supported accommodation setting.
Key findings
Quality Indicator for Rehabilitative Care: Supported Accommodation
-
The QuIRC-SA is the first standardised tool for quality assessment of specialist mental health supported accommodation services.
-
Of 143 items, only 18 showed a narrow response range, and five had poor inter-rater reliability.
-
The QuIRC-SA had excellent inter-rater reliability and exploratory factor analysis showed that items loaded onto the domains to which they had been allocated.
-
The QuIRC-SA can be recommended as a self-report quality assessment tool for supported accommodation services.
-
A digital version is available, free to use, at www.quirc.eu.
Client Assessment of Treatment for Supported Accommodation
-
All items of the CAT were considered relevant to mental health supported accommodation services; slight changes to wording were made.
-
The CAT-SA demonstrated good internal consistency and convergent validity.
-
The CAT-SA can be recommended as a ‘patient-reported outcome measure’ for use in mental health supported accommodation services.
Work package 2: national survey of supported accommodation services across England (work package 2i) and cohort study to investigate service user outcomes (work package 2ii)
The aim of this WP was to describe supported accommodation in England and factors associated with positive outcomes and costs.
The main objective of the national cross-sectional survey (WP2i) was to describe the provision and quality of supported accommodation for people with mental health problems in England and to investigate service and service user factors associated with service users’ quality of life, autonomy and satisfaction with care. Specifically, we investigated the following research questions:
-
Is there a difference in service users’ quality of life, autonomy, ratings of the therapeutic milieu of services and satisfaction with care between the three main types of supported accommodation (i.e. residential care, supported housing and floating outreach services)?
-
Can any variation in these be explained by service and service user characteristics?
Work package 2i: national survey of supported accommodation services
Methods
Our sample size was estimated to assess the difference in proportion of people moving on from each of the three types of supported accommodation 30 months after recruitment (assessed in the second component of WP2 – the cohort study). Our original estimate was that we needed to recruit 90 services (30 of each type) and 450 service users (five from each service) from 14 nationally representative areas based on an intraservice cluster correlation coefficient of 0.07 and a mean cluster size of five. We selected the 14 areas using an index developed by Priebe et al. 11 for their postal survey of supported accommodation, which ranks local authority areas on the basis of mental health morbidity, social deprivation, urbanicity, provision of community mental health care, supported accommodation, local authority mental health-care spend and housing demand. Recruitment was carried out between 1 October 2013 and 31 October 2014.
The researchers contacted key personnel working in housing departments in each of the 14 areas to first scope the local provision of mental health supported accommodation services and the number of places available in each. Residential care homes for adults with mental health problems in each area were also identified from the Care Quality Commission (the registration authority for care homes in England and Wales) website to ensure that none was missed (www.cqc.org). Services that were unusually large (> 80 service users) or small (< 6 service users) were excluded to increase generalisability of the sample. Five areas were replaced with another area closest on the sampling index: three because the area had no residential care services and two because the researchers were unable to clarify local supported accommodation provision (see Appendix 2, Table 5).
After 15 services of each of the three types were recruited, we reviewed our sampling strategy. We recalculated our intraservice correlation coefficient using responses to one item of the managers’ research interview [their estimate of the proportion of service users who had moved to more independent accommodation (residential care and supported housing) or required less support (floating outreach) in the last 12 months] and found it to be 0.18. A larger service user sample (624 rather than 450) was thus required. Owing to the relatively small number of residential care services identified, the number of services needed was adjusted to 21 residential care, 35 supported housing and 35 floating outreach, and the number of service user participants per service was increased to a maximum of 10.
The researchers randomly ordered the services in each area and within each of the three service types and contacted service managers sequentially to invite their participation. Service managers were given up to 4 weeks to reply. When the target number of services of each type had been recruited or the list exhausted for each area, the researchers moved on to the next area (see flow chart in Killaspy et al. 22).
Where service managers responded to the initial contact, the researchers arranged a time to discuss the study further by telephone. If the manager was willing for their service to participate, the researchers arranged a face-to-face meeting to explain the study to staff. A list of potentially eligible service users was then obtained from the service manager (excluding those they considered to be unable to give informed consent to participate and those absent from the accommodation for any reason). Each potentially eligible service user was allocated a unique identifier code. The service user list for each service was randomly ordered by the researchers in blocks of six. Service users in the first block were approached in any order by the researchers to seek their participation and subsequent blocks were generated until five service users had been recruited or the list was exhausted for each service. All potential participants received a participant information sheet about the study and had at least 2 days to read it and address queries to the researchers before giving their informed consent to participate.
Data collection
The researchers completed face-to-face interviews with the service manager, keyworkers and service users at which the following data were collected.
Service manager: description of the service
-
Service quality was assessed using the QuIRC-SA. 20
-
A proforma was used to gather details of the annual budget, referral processes and input from local mental health services.
Keyworker staff: service user assessments
-
A pro forma was used to collect service user participants’ clinical and risk history.
-
A Likert-type scale assessed the staff member’s expectation of the service user moving on (residential care/supported housing clients) or managing with less support (floating outreach clients) in the next 12 months.
-
Challenging behaviours were assessed with the Special Problems Rating Scale (SPRS),31 which records the presence and severity of 14 challenging behaviours, giving a total mean score of 0 to 2.
-
Needs were assessed with the Camberwell Assessment of Needs Short Assessment Scale (CANSAS),32 which rates 22 domains of care on a 3-point scale (0 = no need, 1 = met need, 2 = unmet need).
-
Use of substances was rated with the Clinician Alcohol and Drugs Scale (CADS),33 from which a dichotomous problematic/non-problematic score can be derived.
-
Social functioning was assessed with the Life Skills Profile (LSP). 34 The 39 items rate various aspects of the service user’s social and everyday functioning from 1 to 4. Higher scores denote better functioning. A total score (from 39 to 156) and five subdomain scores can be derived.
-
The adapted version of the Client Service Receipt Inventory (CSRI)35 was used to collect contacts with professionals/services within and outside the supported accommodation service, details of any medical and/or psychiatric admissions and contacts with family members over the past 3 months. These data were used in the health economic assessment.
Service users
-
A pro forma was used to collect sociodemographic details and details of any incidents of abuse (verbal, physical or sexual abuse), self-harm or exploitation by others from within or outside the service over the last 12 months.
-
Quality of life was assessed with the MANSA;29 the service user rates 12 life domains on a scale from 1 (could not be worse) to 7 (could not be better). A total mean score between 1 and 7 is generated.
-
Social inclusion was assessed with the Social Outcome Index (SIX),36 which gives a rating from 0 to 6 from four social domains [i.e. employment, housing, living alone or with family/partner, and contact with friend(s)].
-
Service users rated their autonomy using the Resident Choice Scale (RCS). 37 The degree to which they have choice over 22 aspects of daily activities is rated on a four-point scale, giving a maximum possible score of 88.
-
Users of residential care and supported housing services rated the therapeutic milieu of the service with the Good Milieu Index (GMI). 38 General satisfaction with the service and the degree to which it facilitates confidence and abilities are rated on a scale of 1 to 5, with higher scores denoting greater satisfaction.
-
Satisfaction with care was assessed with the CAT-SA. 21
Data analysis
Data were entered into a purpose designed database by the researchers. After data cleaning, data were transferred to Stata® (StataCorp LP, College Station, TX, USA) statistical software for analysis. Differences between services, including the adapted QuIRC domain scores, service user characteristics and ratings of standardised assessments were investigated using simple descriptive statistics and regression analyses. Multilevel regression was used to investigate the association between service factors (adapted QuIRC domain ratings and contextual factors) and service user factors (sociodemographic characteristics, clinical history, social functioning, needs, substance misuse and challenging behaviours) with service user ratings of quality of life, autonomy, good milieu of the service and satisfaction with care (see www.ucl.ac.uk/psychiatry/research/epidemiology-and-applied-clinical-research-depa/projects/quest-project for full details of the analysis plan). We assumed the convention that in any regression analysis at least 10–20 participants for each predictor should be entered into the model.
Results
A total of 22 residential care, 35 supported housing and 30 floating outreach services were recruited. From these 87 services, 619 users were recruited (residential care, n = 159; supported housing, n = 251; floating outreach, n = 209). A total of 193 keyworkers completed ratings on service users.
The full characteristics of the three types of service and their users are shown in tables 1 and 2 of Killaspy et al. 22
In summary, floating outreach provided more places than the other two types of service. Both floating outreach and supported housing services expected to work with their users for a median of 2 years, whereas for residential care this was 5 years. All three types of service used similar processes to assess new referrals. Almost all services had clinical input from a community mental health team or community rehabilitation team, despite the fact that only one-third of floating outreach clients were subject to the Care Programme Approach (vs. almost all residential care and supported housing clients). Supported housing services scored highest on six of the seven domains of the QuIRC (floating outreach scored slightly higher for human rights).
Most service users were male (66%), single (66%) and unemployed (82%). Users of residential care services were older and had been known to mental health services longer than users of the other two types of service. Most (68%) had a primary diagnosis of psychosis but one-third of floating outreach service users had depression/anxiety. The proportion of service users with substance misuse problems was relatively small (16% alcohol, 12% drugs), with the lowest prevalence among residential care service users. Users of residential care and supported housing had slightly more previous admissions than users of floating outreach and more were subject to a community treatment/restriction order. Overall, 40% of service users had committed an act of violence at some time, but there were few serious incidents of risk to others in the last 2 years. More users of supported housing (26%) and floating outreach (21%) had self-harmed within the last 2 years than users of residential care (4%). Risk of serious self-neglect was reported for 57% overall (72% for users of residential care services and at least 50% for users of the other two types of services). Vulnerability to exploitation was reported for around one-third of users in supported housing and floating outreach services and for 41% of those in residential care. Overall, 67% to 78% of service users across the three types of accommodation were considered a risk to themself or others.
There were few differences in social function and challenging behaviours between service users in the three types of accommodation, but those in residential care, unsurprisingly, had more needs than those in supported housing or floating outreach. However, there were few unmet needs across the three types of accommodation. Users of supported housing and floating outreach were more likely to report having been a victim of crime in the last 12 months than those in residential care (residential care 8%, supported housing 25%, floating outreach 22%) and around half of these incidents involved physical assault. Residential care service users had higher ratings of satisfaction with their safety than users of the other two types of service.
Regression analyses that took account of clustering by area and service showed lower quality-of-life scores for those in floating outreach and supported housing than for those in residential care services, but higher levels of autonomy in both supported housing and floating outreach than in residential care (see table 3 in Killaspy et al. 22). In these analyses, the therapeutic milieu (which could not be assessed in floating outreach services) was rated higher by users of supported housing than by users of residential care [mean difference 0.973, 95% confidence interval (CI) 0.126 to 1.821; p = 0.024], yet there were no statistically significant differences between the three service types in terms of satisfaction with the care received.
Appendix 2, Tables 6 and 7, show the results of the regression analyses that investigated service and service user characteristics associated with service users’ quality of life, autonomy, ratings of the therapeutic milieu (residential care and supported housing only) and satisfaction with care. The QuIRC domains therapeutic environment and recovery-based practice were found to be highly correlated. It was decided to keep recovery-based practice in the models as this domain had been found to be a predictor of successful discharge from inpatient mental health rehabilitation units in a previous study. 39 As data could not be collected for living environment domain scores for floating outreach services, this domain was also dropped from the regression models. The 19 variables included (see Appendix 2, Tables 6 and 7) were agreed by the PMG on the basis of those where differences were found in the summary statistics and where there was clinical justification.
In these analyses, which accounted for differences in service user characteristics, service users’ quality of life (MANSA) did not differ between supported housing and residential care but remained lower for those in floating outreach than for those in residential care. Supported housing was still predictive of higher autonomy (RCS) than residential care but floating outreach was not. In addition, positive associations were found between service users’ quality of life and the mental health morbidity/housing index of the local area, service user age, primary diagnosis (psychosis vs. non-psychosis) and problematic drug use. Negative associations were found with the number of places occupied per service, the adapted QuIRC recovery-based practice domain score and the number of unmet needs. However, the small size of the coefficients suggests that these associations had very little clinical impact. Service users’ autonomy was negatively associated with the QuIRC-SA domain treatments and interventions score and unmet needs, but, again, small coefficients suggest that these associations were of limited clinical significance. For each additional occupied place per service, there was a small reduction in service users’ ratings of satisfaction with care (CAT-SA) and the therapeutic milieu (GMI). The GMI ratings were positively associated with the QuIRC-SA human rights domain score, service users’ age, staff ratings of their social function (LSP) and risk history. Once again, small coefficients limit the clinical relevance of these findings.
Health economic component
Methods
The use of services was estimated from staff and service user interviews using an adapted version of the CSRI. 35 Both health-care and social care costs were included in the analyses. Services included those provided externally as well as contacts with staff of the supported accommodation service. Participants provided information on whether or not specific professionals had been seen in the previous 3 months, how often they had been seen and whether or not this was in a group setting. Information relating to the previous 3 months was obtained on contacts with care co-ordinators, psychiatrists, other doctors, psychologists, community mental health nurses, occupational therapists, social workers, counsellors and art therapists. Contacts with staff of the supported accommodation service were broken down into face-to-face contacts, group sessions and personal care. It was assumed that group sessions consisted of four participants. In addition, details of admissions to hospital in the previous 12 months for mental health or physical health reasons were provided. Service costs were calculated by combining the service use data with appropriate unit cost information. 40 Total costs of services used in the previous 3 months were calculated, as were total inpatient costs for the previous 12 months. An overall total for the previous year was calculated by multiplying the 3-month costs by 4 and adding to the inpatient costs. Comparisons in terms of service use and costs were made between the three groups (i.e. residential care, supported housing, floating outreach). Total cost differences were assessed using a mixed-effects multilevel regression model, controlling for clinical and demographic factors. To generate cost-effectiveness, planes we used a bootstrapped linear regression model for both the cost and the MANSA score, and controlled for area. One thousand cost-outcome differences between (1) residential care and supported housing and (2) residential care and floating outreach were generated and plotted.
Results
There were clear differences in the proportion of each group using specific services (see tables 4 and 5 and the appendix of Killaspy et al. 22). Those in residential care were most likely to receive input from the supported accommodation staff through group sessions and to be in receipt of personal care. Those in supported housing and floating outreach had similar levels of face-to-face and group contacts with supported accommodation staff. Users of supported housing had the highest input from community team care co-ordinators (79% vs. 64% of residential care and 45% of floating outreach service users) and the highest rate of psychiatric admission (24% vs. 11% of residential care and 9% of floating outreach service users). Floating outreach service users generally had lower levels of service use than those in the other two groups. Of those who used specific services, the intensity of use did not differ markedly between the groups for most services. However, those in residential care had more nurse contacts, face-to-face sessions and personal care contacts than users of the other two services. They also had longer stays in hospital for mental health reasons, although this was influenced by some outliers.
The services with the highest costs were inpatient care and face-to-face contact with supported accommodation staff. Excluding inpatient care, the costs of service use during the previous 3 months were highest for users of residential care, followed by those receiving floating outreach. Inpatient costs were lowest in the floating outreach group and similar in the other two groups. This was also reflected in the total costs pertaining to a 1-year period such that total costs were highest for residential care service users and lowest for floating outreach service users.
The multilevel models showed that after making adjustment for demographic and clinical characteristics, the residential care group had costs that were, on average, £1483 more than for supported housing and £5381 more than for floating outreach. The average costs for supported housing were £3898 more than for floating outreach. We found that residential care service users had a quality-of-life (MANSA) score that was 0.274 points higher than users of supported housing and 0.722 higher than users of floating outreach, and those in supported housing had a score that was 0.449 points higher than for those in floating outreach (see table 3 in Killaspy et al. 22). These figures suggest that it costs £5412 to achieve an extra 1-point improvement on the MANSA (representing a clinical improvement of > 14%) if residential care is chosen rather supported housing, £7453 if residential care is chosen rather than floating outreach and £8682 if supported housing is chosen rather than floating outreach. Appendix 2, Figure 4, shows the uncertainty around these point estimates and indicates that although residential care is most likely to generate higher costs and better outcomes (quality of life) than supported housing, there is still a reasonable probability of lower costs and better outcomes for supported housing. Appendix 2, Figures 5 and 6, show that residential care and supported housing are both highly likely to produce better outcomes but higher costs than floating outreach.
With regard to service users’ autonomy, both supported housing and floating outreach produced better outcomes than residential care and were less expensive. That is to say that they were ‘dominant’. Supported housing was more expensive than floating outreach but it was associated with greater autonomy, with a cost of £46,405 for every extra unit improvement in autonomy achieved.
Links to other work packages
The QuIRC-SA and CAT-SA, developed in WP1, were used to assess service quality and service user experiences in WP2i. Service users in supported housing and floating outreach had similar levels of risk, social functioning, challenging behaviours and autonomy, and received similar levels of input from their supported accommodation support workers, suggesting equipoise between the two service types, which supported the rationale for a comparison of these two service models in the feasibility trial (WP4).
Limitations
A number of limitations must be acknowledged. In spite of using a sampling strategy explicitly designed to minimise bias and produce a nationally representative sample, service users who declined to participate or who lacked capacity to consent may have introduced a sampling bias. In addition, our findings cannot be generalised to supported accommodation services and systems outside England. Finally, the cross-sectional nature of WP2i means that we cannot infer causality from our findings.
Key findings
-
Compared with floating outreach, service users in residential care and supported housing had more severe mental health problems.
-
Over half of all service users were at risk of serious self-neglect and over one-third had been vulnerable to exploitation over the previous 2 years.
-
One-quarter of those in supported housing and one-fifth of those receiving floating outreach services had been the victim of crime in the last year, compared with 8% of those in residential care.
-
Residential care was the most expensive service and floating outreach was the cheapest. Residential care and supported housing were both highly likely to produce better outcomes but had higher costs than floating outreach.
-
As assessed by the QuIRC-SA, supported housing demonstrated the best quality of care compared with the other two service types.
-
After adjusting for clinical differences between service users, quality of life was similar for those in residential care and supported housing, but lower for those in floating outreach. Autonomy was greater for those in supported housing than in residential care and floating outreach. Satisfaction with care was similar across service types.
Work package 2ii: cohort study
The aim of WP2ii was to assess the proportion of people in supported accommodation who successfully moved on to more independent accommodation over 30 months and to identify service and service user factors (including costs) associated with move-on.
The primary outcome, ‘successful move-on’, was defined as the proportion of participants in each service type who moved to more independent accommodation successfully without placement breakdown over the 30-month follow-up period. Because floating outreach is provided to people living in a permanent tenancy, for this service type, the primary outcome was defined as managing with fewer hours of support per week rather than moving home.
Our specific research questions were:
-
What proportion moved on to more independent accommodation overall and by service type?
-
What proportion moved on to more independent accommodation and sustained it for the 30-month follow-up (i.e. did not move back to more supported accommodation)?
-
How much of the variation in outcome was due to service type and service quality (measured by the QuIRC-SA domains), before and after accounting for service user characteristics (age, sex, diagnosis, length of stay, morbidity)?
We also investigated a secondary outcome, defined as the proportion of participants who moved on to more independent accommodation and sustained it for 30 months (i.e. without placement breakdown, any move back to more supported accommodation or any hospital admission) overall and by service type.
To minimise the influence of time in service and clinical differences between service users in different types of supported accommodation, we planned to undertake further investigation of service user level outcomes for the subgroup of individuals in the main cohort who had been living in supported accommodation for < 9 months at recruitment. Nine months was chosen as a pragmatic balance between being relatively new to the service and being there long enough for staff and service users to be able to rate the various outcome measures. For this subgroup, we aimed to investigate the following research questions:
-
Is there a difference in service users’ quality of life, autonomy and staff-rated social function at the30-month follow-up between users of different types of service, after adjusting for the baseline score of each outcome?
-
Is there a difference in service users’ quality of life, autonomy and staff-rated social function at the30-month follow-up between users of different types of service after adjusting for baseline score, service quality and service user characteristics?
-
How much of the variation in these outcomes is due to service type and quality, after accounting for service user characteristics?
-
Are there differences in service use and costs at the 30-month follow-up?
Methods
Data collection
After participants were recruited in WP2i, the researchers maintained contact with the relevant service manager every 3 months to monitor whether or not the service user had moved on to less supported accommodation, moved to more supported accommodation or had any admission(s) to hospital. For those who had moved, details of the new supported accommodation service were obtained and contact was made with the new service staff. If the service user moved on to a fully independent accommodation, with no supported accommodation staff involvement, their care co-ordinator (when applicable) was contacted to provide ongoing monitoring of their accommodation status. This process was continued over the 30-month follow-up period.
At the 30-month follow-up point, the researchers completed telephone interviews with supported accommodation staff or care co-ordinators and confirmed details of any moves to alternative supported or independent accommodation during the 30-month period and the length of time in each accommodation. From these data, an overall assessment of whether or not the person had progressed successfully was made [i.e. moved to less supported accommodation (for those in floating outreach services, this was operationalised as having fewer hours of support per week) without placement breakdown].
If a relevant staff member could not be identified (e.g. if the service user had moved to a fully independent tenancy without floating outreach support and been discharged from mental health services), NHS case records were accessed to collect primary outcome data on move-on. For all participants who were reported to have had a hospital admission, case notes were also checked to clarify this. The researchers also completed the adapted version of the CSRI35 with the staff member, corroborating the length of any admissions from the case notes for the health economic analysis where possible.
For the cohort of participants who had been in their accommodation for < 9 months at recruitment, researchers conducted additional face-to-face interviews with service users and their support workers or care co-ordinators. If the service user had moved on to fully independent accommodation and had no contact with supported accommodation or mental health staff, only the service user interview could be completed. These interviews comprised the same measures completed at recruitment, assessing, (1) from staff interviews, social functioning (LSP),34 substance use (CADS),33 challenging behaviours (SPRS)31 and needs (CANSAS),32 and, (2) from service user interviews, quality of life (MANSA),29 social outcomes (SIX),36 autonomy (RCS),37 therapeutic milieu (GMI)38 and satisfaction with care (CAT-SA). 21
Data analysis
Data were entered into a purpose designed database by the researchers. Data checks were completed on all records, comparing the recorded data with the data entered into the database. After cleaning, data were transferred to Stata statistical software for analysis. Descriptive analyses were conducted for all variables.
Primary outcome
For the primary outcome, a logistic mixed-effects model was fitted using xtmelogit, with a random intercept for service and a fixed effect for area as this was used in the sampling frame as a design variable. Univariate analysis was used to identify service and service user variables with a significant association (p < 10%) with the primary outcome for inclusion in multilevel models investigating predictors of the primary outcome. As the analysis of baseline data showed that the QuIRC-SA domains therapeutic environment and recovery-based practice were very highly correlated (Spearman’s rho = 0.87) and the variance inflation factor exceeded 10, it was decided to dispense with the therapeutic environment domain score as the recovery-based practice domain score had previously been shown to predict successful discharge from inpatient rehabilitation services. 39 The QuIRC-SA domains included in the univariable analysis were therefore restricted to treatments and interventions, self-management and autonomy, social interface, human rights, and recovery-based practice. Living environment was excluded as it does not apply to floating outreach services.
Service user variables included in the univariate analysis included sociodemographic and clinical characteristics [age, sex, clinical history, diagnosis (non-psychotic vs. psychotic disorder), length of stay with service], social functioning (LSP), total unmet needs (CANSAS), substance misuse (CADS), challenging behaviours (SPRS), risk of self-neglect and/or vulnerability to exploitation, risk to others and risk of self-harm. Variables were examined for collinearity. Those that did not allow discrimination between service users because the counts were too high or too low were excluded.
Selected variables were included separately in the univariable model to ascertain whether or not there was a difference in successful move-on between service types after adjusting for these variables. Those that showed a significant association (p = 10%) were included in the multivariable model. In our multivariable models, we assumed the convention that at least 10–20 participants for each predictor should be entered.
Sensitivity analyses
To address factors that may have influenced our primary outcome (clinical profile of service users, geographical location of service, definition of primary outcome for floating outreach, service user time in service), the following sensitivity analyses were conducted on the primary outcome by service type:
-
a propensity score analysis that collated an average treatment effect from the following variables: social function – LSP score,34 age, diagnosis of psychosis/no psychosis and a composite risk variable (vulnerability to risk of exploitation with or without risk to others, with or without self-harm in the last 2 years)
-
excluding participants who did not have a diagnosis of psychosis
-
replacing the geographical area variable with the geographic area sampling index score
-
only categorising floating outreach service users as having a positive outcome if the number of hours per week of support had reduced by at least 50% since recruitment
-
comparing service users who had been in the supported accommodation for < 9 months at recruitment with those who had been there for ≥ 9 months.
Secondary outcome
A logistic mixed-effects model was fitted using xtmelogit, with a random intercept for service and a fixed effect for area to assess the secondary outcome by service type.
Subgroup analysis
We planned to use multilevel models to investigate factors associated with service user ratings of quality of life, autonomy and satisfaction with care in the subcohort of participants who had been living in their accommodation for < 9 months at recruitment. However, the sample for whom data were available was too small and thus only descriptive data are presented.
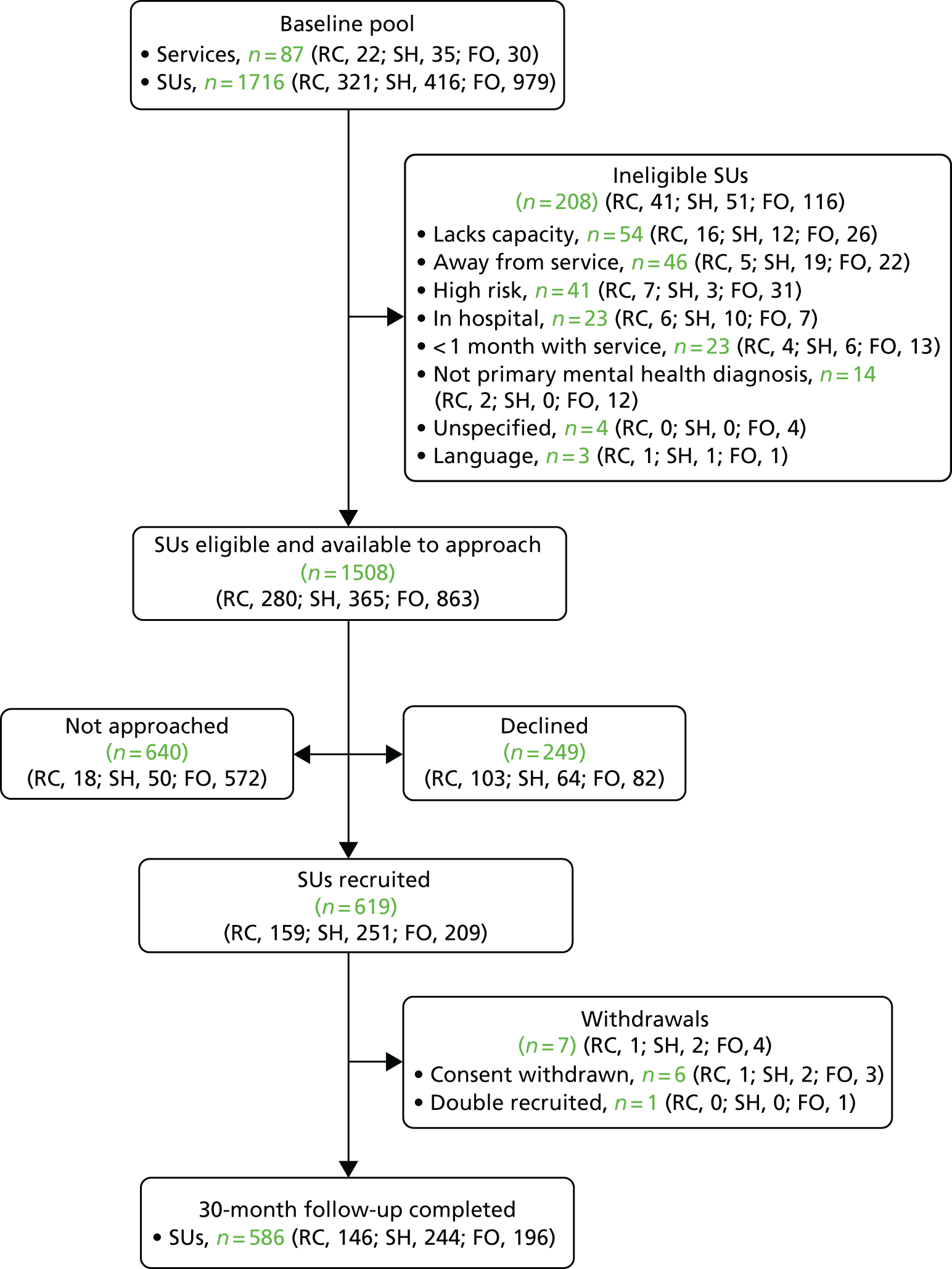
Results
Participant flows in the cohort are shown in Figure 2. After accounting for withdrawals (n = 7) and deaths (n = 26), we followed up 586 out of 619 (95%) participants over 30 months (residential care n = 146; supported housing n = 244; floating outreach n = 196).
FIGURE 2.
Participant flow during the prospective study. FO, floating outreach; RC, residential care; SH, supported housing; SU, service user.
Descriptive data
Descriptive data for participants at follow-up by service type are shown in Appendix 3, Table 8. Overall, 110 out of 586 participants (18.8%) had a hospital admission during the 30-month period. Incidents of risk to others were highest among users of residential care (14% vs. 11.5% for users of supported housing and 4.1% for those in receipt of floating outreach). Episodes of self-harm were highest among users of supported housing (17.3% vs. 14.8% receiving floating outreach and 4.2% in residential care). Around one-third (30.5%) of supported housing service users who had not moved on were considered by staff as ready for move-on, compared with 8.5% of those in residential care and 6.9% of those receiving floating outreach.
Missing data
Overall, there were very little missing primary or secondary outcome data (see Appendix 3, Table 8).
Primary outcome
In total, 243 out of 586 participants (41.5%) achieved the primary outcome of successful move-on to less supported accommodation. The proportions achieving the primary outcome in residential care, supported housing and floating outreach were 15 out of 146 (10.3%), 96 out of 244 (39.3%) and 132 out of 196 (67.3%) participants, respectively. The unadjusted odds ratio (OR) of achieving the primary outcome for users of floating outreach compared with residential care was 28.81 (95% CI 11.53 to 72.02; p < 0.001). For floating outreach compared with supported housing service users, the OR was 5.11 (95% CI 2.47 to 10.57; p < 0.001). The unadjusted OR of achieving the primary outcome for users of supported housing versus residential care was 5.64 (95% CI 2.30 to 13.84; p < 0.001) (see Appendix 3, Table 9).
The univariable analysis identified positive associations with the primary outcome for the QuIRC-SA service quality domain scores for human rights (OR 1.09, 95% CI 1.02 to 1.16; p = 0.007) and recovery-based practice (OR 1.04, 95% CI 1.00 to 1.08; p = 0.054), as assessed at recruitment. The QuIRC-SA social interface domain score was negatively associated with the primary outcome (OR 0.95, 95% CI 0.91 to 0.98; p = 0.001). Service user total unmet needs, length of time in the supported accommodation service and a composite risk variable (risk of vulnerability to exploitation with or without risk of self-harm) at recruitment were also negatively associated with the primary outcome (see Appendix 3, Table 9).
After adjusting for these variables in the multilevel model, users of floating outreach services were almost eight times more likely to be managing with less support at follow-up than users of residential care (OR 7.96, 95% CI 2.92 to 21.69; p < 0.001) and almost three times more likely than supported housing service users (OR 2.74, 95% CI 1.01 to 7.41; p < 0.001). Users of supported housing were almost three times more likely to have moved on to less supported accommodation than those in residential care (OR 2.90, 95% CI 1.05 to 8.04; p = 0.04).
Sensitivity analyses
The results of the sensitivity analyses are shown in Appendix 3, Tables 10 and 11. All analyses showed a similar pattern of results to the main adjusted and unadjusted models, with higher odds of floating outreach service users achieving the primary outcome than users of supported housing and residential care, and higher odds of supported housing service users achieving the primary outcome than those in residential care.
Secondary outcome
Few (17/243, 7%) individuals who moved on had an admission after they had moved. This was most likely among supported housing service users, among whom 12 out of the 96 (12.5%) who moved on had a subsequent hospital admission [vs. none of the 15 who moved on from residential care and 5/132 (3.8%) of those who moved on from floating outreach]. The results of the analysis of our secondary outcome multivariable model are shown in Appendix 3, Table 12.
Subgroup analyses
The subgroup analyses results are shown in Appendix 3, Tables 13 and 14. The mean satisfaction with care (CAT-SA) scores were highest in residential care [mean 8.2, standard deviation (SD) 2.0]. There was little difference in mean quality-of-life (MANSA) and autonomy (RCS) scores between users of the three service types. Social function (LSP) was lowest in residential care (mean 118.3, SD 19.4) and highest in floating outreach (mean 127.2, SD 12.1).
Health economic component
Methods
Data on services used by residents were collected from staff at the 30-month follow-up with a short version of the CSRI. For the subcohort of participants who had been in the service for < 9 months at baseline, data were also collected from service users directly. Costs were calculated as described in Work package 2, Health economic component, and a similar multilevel model was used for analysing cost differences for the full sample. Information on inpatient use during the whole 30-month follow-up was available. We did not extrapolate the 3-month non-inpatient costs across the 30-month period.
The association between the primary outcome measure and costs was investigated in two ways. First, costs were compared for each group among those who achieved the outcome and those who did not. Second, the primary outcome variable was entered into the multilevel models to investigate the overall relationship with cost. We do need to be cautious in interpreting the results though because it is to be expected that those who do move to a lower level of care will have correspondingly lower costs. Adjusting for participant characteristics does allow us to quantify the impact more precisely.
Results
From the staff-reported service use information in Appendix 3, Table 15, it can be seen that supported housing service users were more likely to have had care co-ordinator contacts in the 3-month period up to the 30-month follow-up than users of residential care. Only one-quarter of floating outreach service users had these contacts. Contacts with psychiatrists and other doctors were relatively common, although less so for the floating outreach service users. Face-to-face and group contacts with supported accommodation staff were both most likely for the residential care participants, followed by those from supported housing and then those in the floating outreach. During the whole 30-month follow-up period, the supported housing service users were twice as likely as floating outreach service users to have had psychiatric inpatient episodes. There was little difference in the proportions having inpatient stays because of physical health problems between the three service types. Appendix 3, Table 16, reveals little difference in the intensity of service use among those actually in contact with services. The average number of face-to-face staff contacts with supported accommodation staff was higher for users of floating outreach. For those with admissions to hospital for psychiatric reasons, the number of days over the 30-month period was highest for the residential care service users. Excluding inpatient days, care costs were highest for personal care in residential care service users, followed by face-to-face contacts with supported accommodation staff and other doctor contacts (see Appendix 3, Table 17). Among supported housing service users, face-to-face contacts with supported accommodation staff had the highest costs followed by care co-ordinator costs. Face-to-face contacts with supported accommodation staff also had the highest costs for floating outreach service users. Total non-inpatient costs were, on average, around twice as high for residential care service users (£1434) compared with supported housing (£718) and floating outreach (£640) service users. After controlling for demographic and clinical variables in the multilevel regression model, users of residential care had costs that were, on average, £440 (95% CI –£245 to £1124) more than those for supported housing service users and £601 (95% CI –£54 to £1257) more than those for floating outreach service users. These CIs indicate that the cost differences were not statistically significant. Psychiatric inpatient costs were similar for users of residential care and supported housing, both about twice the cost of floating outreach service users. After controlling for demographic and clinical variables, residential care users had inpatient costs that were, on average, £5214 (95% CI –£2844 to £13,272) more than for supported housing and £7481 (95% CI –£210 to £15,172) more than for floating outreach service users.
Appendix 3, Table 18, shows the self-reported use of services at follow-up for those who had been living in their accommodation for < 9 months at baseline. Around two-thirds of residential care and supported housing service users had contacts with their care co-ordinators at some point in the previous 3 months, whereas only around one-quarter of floating outreach service users had such contacts. Most participants had contacts with psychiatrists, with a slightly higher proportion among floating outreach service users. About two-thirds of residential care and supported accommodation service users had face-to-face contacts with supported accommodation staff; far fewer in the floating outreach group had these. Around half and one-third of the residential care and supported housing service users, respectively, had group contacts, whereas none in the floating outreach group did. The average numbers of contacts for those with them show relatively similar numbers for the groups for most services (see Appendix 3, Table 19). There were noticeable differences for community mental health nurses and for personal care but the numbers receiving such care were very low. The highest service costs (excluding inpatient care) were for face-to-face contacts with supported accommodation staff, contacts with care co-ordinators and contacts with doctors other than psychiatrists (see Appendix 3, Table 20). Total mean non-inpatient costs were highest for supported housing service users (£649), followed by users of residential care (£512) and floating outreach (£398). We did not test these differences for statistical significance because of the small numbers in each group in this subcohort. Psychiatric inpatient costs were far higher among residential care service users than among the supported housing and floating outreach groups. Costs for inpatient care related to physical health problems were similar between the groups.
Across the full sample, those who achieved the primary outcome had mean (SD) costs at 30-month follow-up of £388 (£700), whereas those who did not achieve this had costs of £1214 (£2594). After adjustment, those who moved on to lower levels of care had costs that were, on average, £427 lower than those who did not – a difference that was statistically significant (95% CI £43 to £811). The mean (SD) inpatient costs for those who achieved the primary outcome were £2713 (£10,062) and for those who did not they were £15,142 (£40,463). The multilevel model revealed that inpatient costs for those who moved on were £14,608 (95% CI £8593 to £20,624) less than for those who did not. For the subcohort, the mean (SD) non-inpatient costs were £456 (£751) for those achieving the primary outcome and £626 (£573) for those who did not. The respective figures for inpatient costs were £2517 (£4705) and £10,732 (£41,776).
Appendix 3, Table 21, shows the costs for each of the three participant groups. In each case, there were cost savings for those who had moved to lower levels of support with the exception of inpatient care for the subcohort in the supported housing group.
Links to other work packages
WP2ii followed the cohort of participants recruited in WP2i and our analyses to identify predictors of our primary outcome used the data gathered at WP2i recruitment.
Limitations
Findings from WP2ii must be viewed in the light of a number of limitations. First, successful move-on (the primary outcome) for floating outreach service users was operationalised as having fewer hours of support per week than at baseline. Arguably, this is a lower threshold for ‘success’ than that applied to service users of residential care and supported housing and thus the higher ‘move-on’ we found for floating outreach service users may have been overestimated. Nevertheless, our sensitivity analysis that reclassified floating outreach service users as having a successful outcome only if the number of hours of support they were receiving had reduced by more than half found similar results. Second, as we were unable to monitor service users directly, it is possible that participants who moved on to full independence (discharged from floating outreach services) may have returned to some form of supported accommodation without the research team knowing. However, we attempted to address this through case note reviews of all participants at the 30-month follow-up. Third, follow-up data for some service users was collected through case notes only; although this allowed us to assess both the primary and secondary outcomes (a strength of our design), some other data, such as contact with family for our health economic analysis, could not be collected. Fourth, service use data provided by staff and participants may have be prone to recall error. However, the period of interest was 3 months and it is assumed that this is short enough to mitigate against this possibility. Fifth, it is possible that in some cases there may have been confusion over service definitions and double counting between care co-ordinator and support staff contacts. However, if this occurred it is unlikely to have been a major issue because care co-ordinator contacts were far less frequent than support staff contacts. Finally, owing to the small sample size for the < 9-month subcohort, we were unable to conduct inferential analyses for this group.
Key findings
-
We achieved a high follow-up rate, collecting primary outcome data on 95% of participants at 30-month follow-up.
-
Successful move-on was achieved by 15 out of 146 service users (10.3%) in residential care, 96 out of 244 service users (39.3%) in supported housing and 132 out of 196 service users (67.3%) from floating outreach.
-
Successful move-on was associated with the service’s quality scores at recruitment; QuIRC-SA domain scores for human rights and recovery-based practice were positively associated with the primary outcome and QuIRC-SA social interface domain score was negatively associated with it.
-
More unmet needs, greater risks and longer length of time in the service were negatively associated with participants moving on successfully.
-
After adjusting for these variables, floating outreach service users were more likely than those in residential care (OR 7.96, 95% CI 2.92 to 21.69; p < 0.001) and supported housing (OR 2.74, 95% CI 1.01 to 7.41, p < 0.001) to achieve successful move-on. The adjusted OR of achieving successful move-on for supported housing service users compared with those in residential care was 2.90 (95% CI 1.05 to 8.04; p < 0.001).
-
Very few service users had an admission after moving on.
-
For service users who had been in their accommodation for < 9 months at recruitment, satisfaction with care (CAT-SA) was highest among those in residential care. This group also had the lowest social functioning. There was little difference in quality-of-life (MANSA) and autonomy (RCS) scores between users of the three service types in this subgroup.
-
Service costs for those who had moved on were significantly lower than for those who did not.
Work package 3: qualitative investigation of staff and service user experiences of supported accommodation
The aim of WP3 was to complement the quantitative findings of WP2i by exploring staff and service user experiences of supported accommodation to understand in greater depth the support provided in the three types of supported accommodation services across England and the aspects of care considered most helpful and unhelpful.
Methods
A purposive sample of 30 staff and 30 service users was recruited from the three types of supported accommodation recruited from across England in WP2 (i.e. residential care, supported housing and floating outreach), taking account of gender, age, length of stay (service users) and seniority and experience (staff). The researchers approached potential participants after completing data collection for WP2 and invited them to take part in an interview about their experiences of living or working in supported accommodation services. They were given an information sheet about the study and the researcher explained its purpose and answered any questions. Written informed consent was gained before the interview. Separate topic guides for the staff and service user interviews were developed by the PMG with the researchers, and reviewed and amended after discussion with the Service User Reference Group and North London SURF (see study website for copies of the topic guides: www.ucl.ac.uk/quest). Both had a similar structure and addressed four main areas:
-
Staff –
-
Views on the goals and purpose of supported accommodation.
-
Views on the most effective aspects of the support/care provided in the service.
-
Areas where they experience challenges to providing effective support/care.
-
How the service promotes independence/move-on?
-
-
Service users –
-
Purpose of being in supported accommodation.
-
Experiences and aspects of the support or service they find helpful.
-
Experiences and aspects of the support or service they find unhelpful.
-
Barriers to gaining more independence and move-on.
-
Prompts were used to elicit specific examples from participants’ own experience, when possible, to illustrate issues that could have a bearing on the success or breakdown of a placement. In preparation for WP4, participants’ views about comparing the effectiveness of two models of supported accommodation (supported housing and floating outreach) through a randomised controlled trial (RCT) were explored and they were asked to suggest appropriate outcomes for such a study.
Data analysis
Interviews were recorded digitally, transcribed and anonymised before being entered into NVivo 10 (QSR International, Warrington, UK) software for coding. Transcripts were subjected to inductive semantic thematic analysis41 with the main research questions forming the basis for the initial coding frame. Further analysis sought to identify differences in the experiences of staff and users of different service types and the aspects of care considered particularly helpful/unhelpful. Coding was based on the search for patterns in terms of things occurring in a similar way, things occurring in different ways, if things occur in a sequential way, frequency of occurrence and any ascribed causation. A second coder checked for consistency and validity of interpretations in a randomly selected 20% of the coded interviews. Once this verification procedure was complete, the categorisation and theme generation process commenced. Conceptually similar codes were grouped to form subthemes, which were then grouped to form larger, candidate main themes. The thematic structure was agreed through discussion between the researcher (Sima Sandhu) and the leads for WP3 (SP and GL). Further details of the approach to data analysis are available in Sandhu et al. 25
Results
Participants
The length of time that service user participants had lived in the current supported accommodation service ranged from 3 months to > 11 years, with a mean of 3.3 years. Staff had worked in the current service for between 3 months and 20 years, with a mean of 6.5 years, and they had worked in mental health services from 1 to 31 years, with a mean of 12.75 years. Participants’ demographic characteristics are shown in Table 3.
| Participant | Residential care | Supported housing | Floating outreach |
|---|---|---|---|
| Staff (n = 30) | |||
| Gender | 5 male, 5 female | 2 male, 8 female | 5 male, 5 female |
| Mean age (years) (range) | 51 (28–65) | 41 (21–59) | 48 (32–59) |
| Seniority | 5 managers; 5 support workers | 3 managers; 7 support workers | 4 managers; 6 support workers |
| Service users (n = 30) | |||
| Gender | 6 male; 4 female | 5 male; 5 female | 5 male; 5 female |
| Mean age (years) (range) | 45 (20–68) | 34 (25–52) | 40 (22–61) |
Main themes
Purpose/goals of the service
There was consensus between service users and staff about the main purpose of supported accommodation, which was most frequently cited as being to provide support for users to attain and sustain greater independence. Four related subthemes emerged: supporting people with their mental health; providing safety and stability; building confidence; and building independence:
I think the purpose is to support people that um, generally obviously have a mental health problem, support them from being at crisis stage, back into independence, and to um, bring about positive outcomes, so that they can become independent.
Staff: 116. Support worker – floating outreach. Female
To achieve this, services needed to provide practical support for users to gain confidence in managing activities of daily living, encouraging them to build on their existing capabilities, and to provide living environments that were safe, secure and stable:
And most of the people that come here have struggled to live independently on their own without any ongoing support. So um, so they’ve found it a lot safer and a lot securer.
Staff: 070. Manager – supported housing. Female
Staff, in particular, emphasised their role in supporting service users with their financial affairs (budgeting, paying bills, accessing appropriate benefits and managing debt) and in advocating for service users:
We would look at income and expenditure – particularly if they were worried about money, or found themselves in debt. If they found themselves in debt I would, and I have done, encouraged them to make the call to the debtor and explain their circumstances, and maybe a little bit of their own personal background, so that there’s an element of understanding, and try if necessary to come to an arrangement whereby, you know they are making repayments on a lower, at a lower rate.
Staff: 089. Support worker – floating outreach. Female
Service users reported that staff gave them the encouragement and help they needed to achieve the things that they wanted to do. Across service types, this included gaining independence with activities of daily living, and in floating outreach services, users valued being supported to work towards employment:
Well it’s confidence-building, helping you to deal with things that you need to know about, like it’s how to pay rent and your bills and how to keep yourself clean and . . . and where you should go.
Service user: 141. Supported housing. Male
I wish to one day you know become like that so I could live independently; I’d really love that – you know?
Service user: 065. Floating outreach. Male
Effective/helpful aspects of the service
Six interrelated themes reflected staff views about how to work effectively towards the goals: incremental steps to progress; knowing the individual well; the support of other service users; working together to avoid de-skilling and dependency; tailoring support for social and community engagement; and good liaison with other services.
Services that supported their users to gain skills incrementally were regarded as effective and helpful by staff and users alike. These services tended to ‘support with’ rather than ‘do for’ people:
. . . and that progress report is looking at what they achieved last month and what new things have been introduced this month. So the idea is to keep introducing new things, and to step away from the things they no longer need support with. So, you know, we have service users where we would be going to the cinema with them two or three times a week, who now go to the cinema by themselves. So what we would then do is introduce an activity that maybe they will need support with – and then they go and do that by themselves, and that’s the progress.
Staff: 033. Support worker – floating outreach. Female
Services were more likely to be considered effective when staff understood their clients well and formed trusting relationships:
Well . . . they’re there to support you, they’re there to support you and um, you can trust them. I mean they’re sincere, genuine, um, they have a proper attitude.
Service user: 025. Residential care. Male
Staff noted that service users also appeared to benefit from feeling supported by other clients living in the accommodation:
I think you can see them support . . . like especially [Name] and [Name]. They’re particularly supportive of each other, so . . . I feel with a lot of them they do come together and they will support each other. They’ll always ask the other one ‘oh are you OK’ and ‘how are you doing?’, and you know it’s nice.
Staff: 095. Support worker–supported housing. Female
There was an awareness from both staff and service users that individuals needed to be encouraged and supported to do things to encourage them to gain/regain skills:
I got a little bit of support with it yeah. Kind of . . . you know, a bit from me and a bit from the staff really . . . They’re . . . it’s not like they force you to do things but you’ve got to put, you know, you’ve got to input yourselves . . . because it does take, primarily it does take yourselves to do it, yeah.
Service user: 035. Residential care. Male
Staff were mindful that social and community-based activities needed to be tailored to the individual to maximise their appeal, with the aim of creating wider social networks as part of the person’s rehabilitation:
Well I think what we’ve done initially is we’ve actually took the time to sit down with people and actually talk to ‘em about what their interests are; so what they actually would like to do. Like we found out that one of the residents apparently was a keen cook, many years ago, so we got him engaged with a local mental health charity who do cooking lessons and bakery lessons, so he goes every week . . . he’s absolutely delighted with that.
Manager: 083. Residential care. Female
Um, we do . . . we run activities here, we do the gardening clubs, walking clubs to get people socialising sort of with other customers in the area and to get people active as well. Um, we’ll organise things; we organise trips for them to go out from here as well so that they, you know they’re not socially isolated.
Staff: 052. Support worker – supported housing. Female
Staff also noted the importance of appropriate training, regular supervision and being flexible in their approach. Joint working with community mental health services and other agencies was seen as crucial for an effective service, as was awareness of when involvement from other services was needed:
Yes, because if something’s not working, then at least it’s more than one head thinking right well, what else can we try, where else can we go with this?
Staff: 089. Support worker – floating outreach. Female
Service users noted that the practical and emotional support given when attending appointments with external agencies was particularly helpful:
So . . . I, I went for um, a scan . . . and ECG [electrocardiogram], and [Name] came with me to see the consultant for the results. And I’m so glad she did . . . So you see I have got very little faith in the medical profession. Um, and as I say, [Name] supported me through that . . . she helped me through it.
Service user: 076. Supported housing. Male
Challenges/unhelpful aspects of the service
Poor communication with other agencies was seen as a particular challenge by staff, as well as a lack of suitable training and supervision. In addition, staff and service users felt that staff were pressured and did not always have adequate time available to support service users with their activities (inside the accommodation and in the community), which limited their progress:
Well just . . . or . . . just mainly that it’s getting tied, where there’s only one staff and you can’t leave the building – for me that’s the . . . the major stumbling block.
Staff: 009. Support worker – residential care. Male
And I asked to go to Asda [www.asda.com] in the day, with [Name], because we were getting . . . I wanted a few things from there. He said, ‘oh, no you can’t go . . .’. Then I ended up not going . . . we, we ended up not going – couldn’t go . . . because it, because there wasn’t other people going . . . There’s not always enough staff on here to go out.
Service user: 019. Residential care. Male
Both staff and service users also reported that conflicts between service users were particularly unhelpful and stressful:
But then you’ll get somebody say like [Name] who will come into the room and just start like throwing things, um, and then obviously tensions mount or you’ve got two people that wanna get in the lift at the same time together and neither of them will back down so they’ll just try and get in there together and then have a fight.
Manager: 083. Residential care. Female
Sometimes I think . . . the only sort of criticism if you wanna call it that, is that sometimes, you know another resident might be annoying you or there’s something going on . . . You know I’m not talking massive things, I’m just like, you know um . . . I dunno, say upstairs messing our kitchen up or something say. Just, you know nothing . . . um, or someone’s behaviour . . . you know . . . that you know is outside of the rules if you like.
Service user: 098. Supported housing. Female
Service users reported that a lack of choice and involvement in decisions about things that concerned them was unhelpful. Related to this, some staff also expressed a particular concern about creating dependency among service users:
I think that um, still . . . the relationship I think is very much a dependency relationship from the resident’s point of view; I think that the residents um, still look to the staff as . . . or do look to the staff as kind of their nursemaids and their housemaids and their [in-breath] um, you know everything to do with that really.
Manager: 083. Residential care. Female
Others noted the particular difficulties that arose when users did not engage with services:
The only thing that gets in the way is the client engagement side of things. I would say we . . . we can offer across . . . we can either offer the support or signpost to the support that that service user needs . . . The support services are there, the support that we can provide are there, the only barriers sometimes to clients being successful is their engagement.
Manager: 094. Floating outreach. Female
Facilitators of and barriers to moving on to greater independence
As noted earlier, staff felt that preparing for greater independence could be achieved by working incrementally on specific skills to help service users gain confidence. Staff emphasised the importance of planning for move-on a long time ahead. This included ensuring that there was good communication and close working with staff from the relevant community mental health team throughout the process to ensure that adequate support would be provided after the move. Staff also highlighted the need to have open conversations with service users throughout their time with the service about move-on, but without forcing the issue with them:
So it’s discussed at every support plan meeting – they happen monthly, 2-monthly, 3-monthly, depending on what the client’s needs are, um, so we just, we discuss about moving on, if it’s moving on from accommodation based, or whether it’s to another accommodation setting that they require, [in-breath] but was also discuss about the steps towards independent living and what services, or support needs to take place to achieve that.
Staff: 099. Manager – floating outreach. Female
Aside from a lack of suitable accommodation to move on to, staff reported that the biggest barrier to service users’ progress was anxiety about move-on (both the process and the likelihood of success), which could manifest in resistance from service users and staff. Service users expressed appropriate concerns about the location of any future home, if they would have enough support and if they would feel lonely if they moved to more independent accommodation:
Yeah I do yeah, because um, what’s in the back of my mind is that, you know, what I’ve been through, I don’t want to, I don’t want a repeat of that again. So, you know, if you take that support away – you know moving on from here to another place – you know, in the back of my mind, I don’t wanna, I don’t wanna go through again what I’ve been through ‘cos I don’t think I could come back from another one.
Service user: 085. Floating outreach. Male
Views on comparing the effectiveness of two models of supported accommodation through a randomised controlled trial
The majority of staff and service users felt that a study to compare the two models of supported accommodation would be useful and should go ahead but there was concern about the use of random allocation in such a study:
I can understand that it would be useful. The . . . the problem I’ve got really is that if I’m quite sure that if I was to go er, back to head office and say well we’ve got . . . we’re discharging someone, we’re just gonna flip a coin and say well you’re going here and you’re . . . that they would say well, it’s not person-centred and you’re not, you’re not addressing the needs of the individual.
Manager: 034. Residential care. Male
No I think they should really leave it down to the person, individual to say, d’you know what, I’ll give that a go or I’ll give that a go. And then they can . . . then they decide which they think is gonna be better for them – you know – and how they coped in both those situations.
Service user: 076. Supported housing. Male
However, many participants stated that as long as service users’ needs and preferences, and the views of the referring clinicians, were taken into account, randomisation could be possible in some cases. Participants suggested the following outcomes for assessment in the trial: mental health (including hospitalisations); physical health; quality of life; social inclusion; managing the tenancy; level of independence; substance misuse; incidents of risk; medication adherence; ability to manage activities of daily living/social functioning; and engagement and satisfaction with services.
Links to other work packages
Although some concerns were raised regarding randomisation, service user and staff participants were supportive of the planned feasibility trial (WP4).
Limitations
A number of limitations are acknowledged. Although we attempted to maximise the generalisability of our findings through purposive sampling, we cannot be certain that the views and experiences reported here fully capture, or reflect, those of all staff and service users in these settings. It is possible that participants were unwilling to report particular events or behaviours, such as poor working practices, in case they would be perceived in a negative way. In addition, the inclusion of diverse models of supported accommodation may have led to overly inclusive conclusions, but the high levels of thematic convergence suggest that this was not a significant issue.
Key findings
-
Staff and service users, across all supported accommodation types, shared an understanding of the purposes of these services to build skills and confidence for more independent living.
-
Staff described how they worked with service users to achieve this in an incremental, tailored way that built on their strengths and interests and incorporated a rehabilitative and recovery-orientated approach.
-
Conflicts between service users were noted by staff and service users as unhelpful. Both staff and service users expressed anxieties about managing with less support after move-on.
Work package 4: feasibility of a trial to compare the effectiveness of supported housing and floating outreach services
In WP4, we aimed to assess the feasibility, sample size and outcomes for a large-scale trial to compare the clinical effectiveness and cost-effectiveness of two commonly used models of mental health supported accommodation: supported housing and floating outreach. Our aim was to establish whether or not participant recruitment and randomisation to different types of supported accommodation was possible, including the acceptability to service users, clinicians and service providers, and the feasibility given the complex logistics involved. Our evaluation included a qualitative component to assess service user and staff experiences of the trial, including the process of randomisation and their views on the usefulness and feasibility of a larger-scale trial.
Methods
Trial design
This was an individually randomised, parallel-group trial.
Sample size
As this was a feasibility study, a formal sample size calculation was not conducted. The original target was to recruit and randomise 60 participants from across the three study sites.
Setting
The feasibility trial was conducted in three sites that provided both types of supported accommodation and where the study team had good links (i.e. North London – Camden and Islington; East London – Tower Hamlets, Newham and Hackney; Gloucester and Cheltenham).
Inclusion/exclusion criteria
All service users in the three study sites referred to either supported housing or floating outreach services who had housing rights in the local area and were subject to the Care Programme Approach were eligible for inclusion. Those who lacked capacity to give informed consent were excluded.
Recruitment process
Each of the three sites had a system for referral of service users to local supported accommodation services. All those referred to supported housing or floating outreach were considered for potential participation in the study. The research team first met with the relevant staff at each site to explain the purposes of the study and clarified the local referral processes. A researcher who liaised with the key personnel involved in co-ordinating the referrals system and the local clinicians making referrals was based at each study site. They gained details of any new referrals and contacted the referring clinicians to discuss whether or not the individual might be appropriate for participation in the study and, if so, the researcher contacted them to gain informed consent for participation. When the clinical team felt that it was not appropriate for the person to be approached about the study, that individual was not contacted by the researcher. Recruitment took place over 12 months from June 2015.
After 6 months, we decided to adjust our approach to try to increase recruitment. In addition to the processes described above, researchers met with the managers of acute inpatient wards and community mental teams operating across the three sites to identify any individuals being considered for referral to supported housing who had not yet been referred. Service users who did not consent to randomisation were offered to participate in a naturalistic cohort whereby they gave informed consent to complete the same research interviews as trial participants but their supported accommodation was not allocated randomly.
Allocation of participants to trial arms
Participants in the trial were randomly allocated on an equal basis to receive either a local supported housing or a floating outreach service. Computer-generated randomisation was conducted independently of the research team by a statistician from the Pragmatic Clinical Trials Unit based at Queen Mary University of London and stratified by site. The outcome of randomisation was communicated to the QuEST project manager who then communicated it to the local referrals co-ordinator, and referrer, to process the participant’s supported accommodation allocation accordingly.
Comparison services
Supported housing services provided a constant level of staffing on-site to a number of service users living in individual or shared tenancies with the expectation of move-on within 2 years. Floating outreach services provided visiting support of flexible intensity to service users living in a permanent (non-time-limited) independent tenancy.
Content of care was assessed using the QuIRC-SA,20 completed with the service manager once for each service, 6 months after the participant was randomised (assuming that they had moved to the service). This was completed only once per service.
Data collection
We collected the following metrics to inform the feasibility of a larger trial: number of referrals to the trial; number recruited; attrition (i.e. number who withdrew consent to continue with the research, declined to move to the allocated service or could not be located at follow-up); and time from recruitment to moving into either type of supported accommodation. We assessed the feasibility of potential outcome measures through collection of data from service users, support staff and service managers, at recruitment and 6 and 12 months after recruitment (Table 4).
| Scale | Assessment of | Gathered from |
|---|---|---|
| Baseline | ||
| Pro forma | Sociodemographic details | Service user (+ case notes) |
| Brief Psychiatric Rating Scale42 | Symptoms | Service user |
| MANSA29 | Quality of life | Service user |
| Time Use Survey43 | Activities | Service user |
| SIX36 | Social outcomes | Service user |
| LSP34 | Social function | Staff |
| Compliance scale | Medication adherence | Staff |
| Health of the Nation Outcome Scale44 | Clinical status | Staff |
| Time Use Survey43 | Activities | Staff |
| CADS33 | Substance misuse | Staff |
| 6-month follow-up | ||
| Time Use Survey43 | Activities | Service user |
| Scale To Assess Therapeutic Relationship – Service user45 | Engagement | Service user |
| Time Use Survey43 | Activities | Staff |
| Scale To Assess Therapeutic Relationship – Clinician45 | Engagement | Staff |
| 12-month follow-up | ||
| Brief Psychiatric Rating Scale42 | Symptoms | Service user |
| MANSA29 | Quality of life | Service user |
| Time Use Survey43 | Activities | Service user |
| SIX36 | Social outcomes | Service user |
| CAT-SA21 | Satisfaction with care | Service user |
| Scale To Assess Therapeutic Relationship – Service user45 | Engagement | Service user |
| LSP34 | Social function | Staff |
| Compliance scale | Medication adherence | Staff |
| Health of the Nation Outcome Scale44 | Clinical status | Staff |
| Time Use Survey43 | Activities | Staff |
| CADS33 | Substance misuse | Staff |
| Scale To Assess Therapeutic Relationship – Clinician45 | Engagement | Staff |
Masking of researchers
The feasibility of using a telephone interview to collect follow-up data from service users was also explored. At the 12-month follow-up, the researcher met with the service user participant, took informed consent, then telephoned a second researcher (blind to the participant’s supported accommodation allocation) who completed one instrument from the interview battery (MANSA) with the participant. This measure was selected as all others would have invalidated the blinding by revealing the participant’s allocation.
Qualitative evaluation
We aimed to recruit five participants who had agreed to randomisation and five who had not but who had agreed to be followed up naturalistically, along with their respective referrers, to assess their experiences of the trial, the process of randomisation and their views on the usefulness and feasibility of a larger-scale trial. The aim was to elicit and detail common themes systematically that could inform the feasibility of a larger trial. lnterviews were recorded, independently transcribed and anonymised. The text data were entered into a software package (NVivo 10) to assist management and coding. The interviews were analysed using thematic content analysis; a coding frame was developed by one of the researchers (Rose McGranahan), with supervision from Stefan Priebe and Gerard Leavey, which was expanded and modified to include further codes as new themes and subthemes emerged in the course of interviews and analysis.
Data analysis
We followed Consolidated Standards of Reporting Trials (CONSORT) guidelines on the analysis of feasibility trials for the presentation of our results. 46 However, our analysis was mainly descriptive and focused on the recruitment rate, acceptability of randomisation to participants and staff, ease of collection of data, characteristics of participants, other baseline and outcome variables, the feasibility of masking outcome assessments, loss to follow-up and any adverse events.
Cost-effectiveness
Service use in the period before follow-up was measured using the CSRI35 and combined with unit costs. The service costs were derived from expenditure data. Cost-effectiveness of the two types of service was to be assessed by combining service costs with the composite outcomes described above. We also planned to use the Short Form questionnaire-12 items47 and the EuroQol-5 Dimensions (EQ-5D)48 to derive quality-adjusted life-years. The use of both is appropriate because there are concerns about using the EQ-5D in this population. 49 Uncertainty around the cost-effectiveness estimate was to be assessed using cost-effectiveness planes and cost-effectiveness acceptability curves.
Results
Feasibility metrics
We screened 1432 potential participants, of whom 87 were ineligible (not on a Care Programme Approach, n = 63; no recourse to public funds/housing, n = 24), 456 were deemed inappropriate for participation by the research team (no plans for move-on/new admission, n = 194; already housed, n = 99; no response from clinical team, n = 60; own accommodation, n = 51; referral withdrawn, n = 22; previously screened, n = 13; eviction in process, n = 8; moved out of area, n = 5; and clinician refused access, n = 4) and 851 were deemed inappropriate for participation by the clinical team. The most common reasons were that the individual had a high level of support needs and was felt to be inappropriate for floating outreach (n = 524) or that they had low support needs and were thus inappropriate for supported housing (n = 137). In total, 17 service users consented to participate, with eight service users randomised and nine participating in the naturalistic arm. The CONSORT flow diagram is presented in Figure 3.
FIGURE 3.
The WP4 CONSORT flow diagram. CMHT, community mental health team; DNA, did not attend; FO, floating outreach; SH, supported housing.
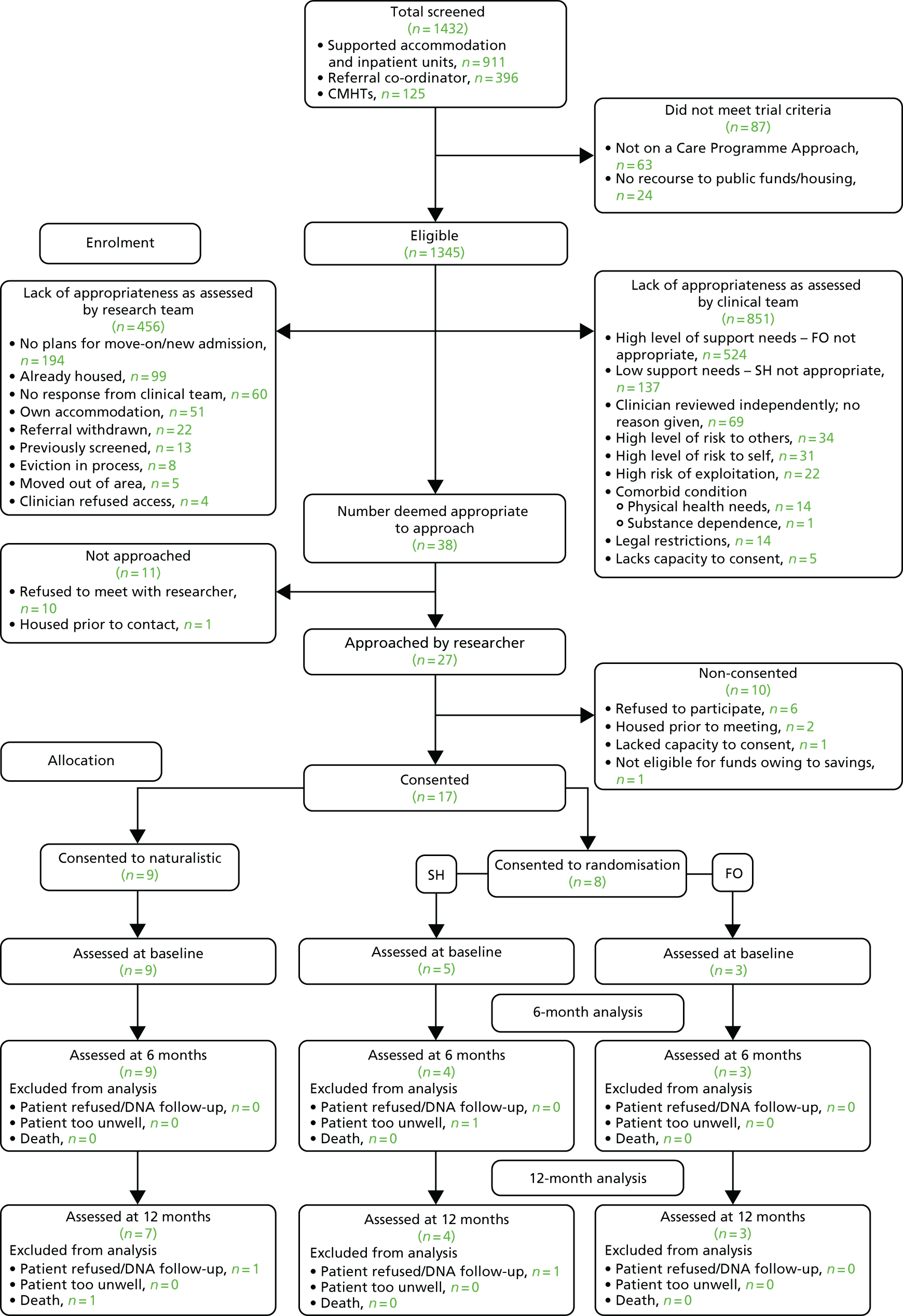
Attrition
Of the 17 recruited participants, three were lost to follow-up [one randomised (one refused follow-up); two naturalistic (one death; one refused follow-up)].
Time from recruitment to moving
Of those randomised, three out of eight participants (38%) moved to their allocated accommodation. The median time from recruitment to moving was 4 months [interquartile range (IQR) 1.5–5.5 months].
Collection of outcome data
Demographic data for the naturalistic and randomised cohort are presented in Appendix 4, Table 22. A high level of data collection was achieved for each outcome, with completion ranging from 76% to 100% across all follow-up periods. At baseline, 100% of measures were completed, but completion rates dropped as the study progressed, primarily because of participant attrition (n = 3) described above. Of the measures, the Time Use Survey and the Scale to Assess Therapeutic Relationship (STAR) had the lowest completion rates. The completeness of data collection, organised by time point, is presented in Appendix 4, Table 22.
Our blinding procedures, tested at the 12-month follow-up, were successful. Telephone administration of the MANSA, by a researcher who was unaware of the participants’ allocation (supported housing/floating outreach), was completed without revealing the participants’ experimental condition.
Harms/unintended consequences
No harms or unintended consequences occurred during the course of WP4.
Economic evaluation
The CSRI and EQ-5D data were collected at baseline and 12-month follow-up. Owing to the very small numbers, it was not feasible to conduct the health economic analyses.
Qualitative findings
We carried out in-depth qualitative interviews with 11 service user participants and 10 staff [including care co-ordinators who referred participants to the study (n = 6), and those who knew of the study but did not refer participants (n = 4)]. Four main themes emerged from the service user and staff interviews that shed light on the impediments to recruitment: preference for a certain type of supported accommodation, rejection of randomisation, complexity of randomisation and value of the trial.
Preference for a certain type of supported accommodation
Staff interviews revealed a strong belief that supported housing and floating outreach offered quite different support to individuals and they therefore struggled to consider an individual as potentially suitable for either service. They voiced concerns that service users would be insufficiently or inappropriately supported in floating outreach and might be vulnerable to exploitation or at risk of relapse:
I suppose ultimately, when a decision is made to move someone into a . . . to allow them to go into an independent council flat with floating support, clinically we’ve already made the decision that you don’t think . . . it’s going to be a waste of resources for . . . Because there’s clinical reasons why you’d refer someone to a 9 to 5 project. I’d be slightly worried about medication compliance or maybe slightly worried about safeguarding issues.
Staff: 2998. Referrer (unsuccessful). Male
They held a clear conviction that the two models operated as sequential components of a ‘step-down model’, whereby service users move from more highly supported to less supported accommodation as they gain the skills to live more independently. They spoke of how this system provided the opportunity for staff and service users to be confident that the person would be able to manage in an independent tenancy by the time they reached the point of referral to floating outreach:
. . . the structure we’ve got does work quite well because they are in [supported accommodation provider], they stay with the staff, they are tested in the 24 hour, they are tested in the low, and then off to their own flat. It’s not a bad programme really.
Staff: 0020. Referrer (unsuccessful). Female
Although some service users had a clear preference for either floating outreach or supported housing, others appeared to see advantages and disadvantages for both types. This observation applied to participants who agreed to randomisation and those who joined the naturalistic group. Service users who expressed a preference for floating outreach felt that this model would allow them to be more independent and maintain control over their lives:
I’m [forties] years of age, I’m fed up of being monitored. I’m quite able, I can cook. I can clean. I can look after myself. I can wash my clothes. I can have a bath. I can do everything on my own.
Service user: 5010. Naturalistic follow-up (fully independent). Female
Some consented to randomisation simply to increase their chance of being allocated to this form of support. For others, the preference for floating outreach was based on having more control over where they would live as they would be able to ‘bid’ for a tenancy in their preferred area. Sometimes this was in order to be close to friends and family, and sometimes it was part of their ‘risk-management strategy’, to avoid areas with known individuals who might exploit them or offer them illicit substances:
I like to be close to my family, you know, my daughter round, you know, my grandchildren, things like that. I thought [borough] or somewhere like that I’d like to live, if it was like that.
Service user: 4014. Naturalistic follow-up (supported housing). Female
Well I was worried that I would end up in a bad area of town . . . I might get involved in drugs again.
Service user: 5050. Naturalistic follow-up (fully independent). Male
Some service users acknowledged being influenced in their preference by family and staff and some reported previous negative experiences of other forms of supported accommodation and a lack information about supported housing that made them feel more positive about floating outreach as the preferred option.
Service users who expressed a preference for supported housing reported feeling concerned about the risks associated with more independent settings. Often they felt underprepared and expressed anxiety about relapse and ‘moving backwards’ if they were to move to a tenancy with floating outreach support:
I’m not ready for my flat yet, but everyone is saying I’m ready for it, but I’m not ready. I’m ready for it, but I’m ready for it now, but I just want that extra 6 months to make sure that I’m stable. I don’t want to get my flat and become unwell again. It costs the government so much money.
Service user: 2049. Randomised (supported housing). Male
Many seemed influenced by their family’s or support workers’ views that they were not ready for floating outreach and some had previous negative experiences of floating outreach services. Some held a clear preference for a particular supported housing service in a specific location, close to family or friends. Others felt that the lack of available tenancies would mean that they would wait longer for a floating outreach option that supported housing. Some expressed a preference to live among others rather than alone:
I think supported housing is better for some people . . . I prefer supported because you’re surrounded with people.
Service user: 0033. Randomised (supported housing). Male
Service user preferences, a lack of availability of independent tenancies leading to delays in individuals moving to floating outreach services and a perceived lack of staff resources to facilitate service users taking part in the feasibility trial were also cited by staff as impediments to recruitment into the study.
Rejection of randomisation
A number of service users and staff voiced ethics concerns about having accommodation decided by randomisation. Many service users suggested that housing was too important to decide by chance, and staff often reflected that a (perceived) lack of equipoise between supported housing and floating outreach services made random allocation inappropriate:
It’s a bit . . . We’re talking about someone’s home here, do you know what I mean? It’s a base need. It seems like something quite serious to flip a coin about, if you know what I mean?
Service user: 0033. Randomised (supported housing). Male
So, yes I understand the randomisation process, but I would hate to think that it was to the detriment of the well-being of a client in a sense. There must be some clinical judgement based on where that client goes.
Staff: 5010. Referrer (successful). Female
Specifically, staff suggested that the level of support and oversight in supported housing may be oppressive for an individual with relatively limited support needs, whereas a person with higher support needs may not receive the level of support necessary to facilitate recovery if they were randomised to their own tenancy with floating outreach. Service users also indicated that the individual and clinician should have the final say over housing and support arrangements. Similarly, staff voiced concerns about the randomisation aspect of the trial that was felt to negate the need for clinical judgement in deciding on supported accommodation options. Staff also felt that randomisation inappropriately excluded the service user from the process of decision-making about their accommodation.
Complexity of randomisation
Despite providing informed consent for participation at recruitment, one or two service users found it difficult to recall the processes relating to the process of randomisation when undertaking the qualitative interviews some weeks later. Some staff felt that the process of randomisation was too complicated for service users to understand and that this could lead to confusion or disappointment if they were allocated to a service they did not wish to move to. However, some staff also seemed to struggle with understanding the process and acknowledged this difficulty when they had tried to explain the study to potential participants:
The first time I heard about [the trial] I thought maybe it was a platform to find a way of how our clients can get accommodation easily. That’s what I initially thought, but obviously, as you indicated, it’s not about them, it’s about basically the support they can get once they get that accommodation. Yeah. That’s what I thought.
Staff: 0033. Referrer (successful). Male
Value of a trial
Despite the many obstacles to recruitment we encountered, all those who participated in the qualitative interviews felt that it would be worthwhile to carry out a larger trial. Several service users felt that the results from such a study would be of use in understanding which models of supported accommodation worked best and many appeared to gain some satisfaction from feeling that they had contributed to this cause:
It’s helpful; you need to find out things about people who are unwell and to better things in the future to come through us who are unwell. I don’t mind helping that.
Service user: 2017. Naturalistic (supported housing). Male
The majority of service users spoke positively about their experience of taking part in the trial, saying that they had enjoyed it. Staff also indicated that further research had potential to benefit service users, but were vague about how this might happen.
Links to other work packages
The QuIRC-SA and CAT-SA, developed in WP1, were used to assess service quality and service user experience in this WP. Findings from WP2i and WP3 indicated equipoise between supported housing and floating outreach, and service user and staff support for WP4.
Limitations
The main limitation was the major challenges we faced to recruitment, although, arguably, this was more of an outcome than a limitation. Although we made changes to our original recruitment strategy after 6 months, seeking referrals from inpatient units and community mental health teams directly, the delay in making this decision may have reduced access to potential participants. However, recruitment did not increase significantly after this point. We made extensive efforts to engage potential referrers but it is possible that we failed to make contact with some who were simply not known to us.
Key findings
-
Our feasibility trial was successful in showing that a large-scale trial is not feasible.
-
We screened 1432 potential participants, but only consented 17 to participate: eight service users were randomised and nine participated in the naturalistic group.
-
The majority of potential participants were not approached as they were deemed to be clinically inappropriate for the study by their clinical team (n = 851).
-
Of the 17 recruited participants, three were lost to follow-up (one randomised and two naturalistic).
-
Of those randomised, three out of eight participants (38%) moved to their allocated accommodation.
-
The median time from recruitment to moving was 4 months (IQR 1.5–5.5 months).
-
Qualitative interviews indicated that participation was impeded by service user preferences for certain types of supported accommodation and staff views that individuals needed to graduate through the existing step-down pathway. There were concerns regarding whether or not it was appropriate for supported accommodation type to be decided through randomisation. In spite of this, participants broadly agreed that a larger trial would be valuable.
Summary of QuEST study findings
Work package 1
We adapted an existing quality assessment tool for longer-term mental health facilities (the QuIRC) and an existing patient-reported outcome measure (the CAT) for use in supported accommodation services. This process comprised (1) review of the content by focus groups of staff and service users of the three types of supported accommodation services in England and three expert panels; (2) agreement of suggested amendments by the PMG; (3) assessment of the psychometric properties (item response variance, internal consistency and inter-rater reliability) of the adapted QuIRC; and (4) assessment of the psychometric properties (internal consistency and convergent validity) of the adapted CAT.
Amendments to the wording of 28 QuIRC items were made, 20 items were deleted and 10 new items were added. Only five adapted QuIRC items were found to be unreliable but further amendments to four of these were possible and only one item was dropped completely. The psychometric properties of the adapted QuIRC were acceptable. An online application has been developed to provide web-based access for supported accommodation service managers to use the tool, the ‘QuIRC-SA’, to assess the quality of their services directly.
Minor amendments to the wording of all seven CAT items were made. The adapted version, the CAT-SA, demonstrated good internal consistency and satisfactory convergent validity.
Both measures can be recommended for routine use in mental health supported accommodation services.
Work package 2i
A sample of 87 supported accommodation services were recruited from 14 nationally representative areas of England (residential care, n = 22; supported housing, n = 35; floating outreach, n = 30). Interviews with each service manager and 619 randomly selected service users and their support staff were carried out to collect descriptive and quantitative data. Around two-thirds of service users across all three types of accommodation were male and the majority were single and unemployed. Around one-third of floating outreach service users had a primary diagnosis of depression or anxiety whereas the majority of those in residential care and supported housing had a primary diagnosis of psychosis. This suggests a slightly more varied diagnostic profile than was identified by Priebe et al. ’s11 telephone survey. We also identified greater variability in support provided between service types than Priebe et al. 11
Staff rated those in residential care as having the highest needs and a greater requirement for assistance with personal care than the other two types of supported accommodation; across all three types of service, most needs were met. The three types of service had similar referral and assessment processes and most service users were subject to the Care Programme Approach and, therefore, received additional input from a local statutory community mental health service. Around one-fifth of participants had a recent history of significant self-harm, but this was much higher among those in supported housing and floating outreach than among those in residential care. Around one-third were vulnerable to exploitation and over half were at risk of self-neglect, with the highest proportion among those in residential care (almost three-quarters). Users of supported housing and floating outreach services were more likely to have been a victim of crime in the last year than users of residential care.
Supported housing and floating outreach services worked to the same time frame, with an expectation that service users would move on to less supported accommodation or manage with less support within 2 years of being taken on. In regression analyses that accounted for differences in service user characteristics, service users’ quality of life did not differ between supported housing and residential care but was lower for those in floating outreach than for those in residential care. Supported housing was associated with higher autonomy than residential care but floating outreach was not.
Floating outreach services provided more places per service than the other two types of supported accommodation and costs of care were lowest (and highest for residential care). However, with regard to cost-effectiveness, there was a reasonable probability that supported housing provided better value for money with regard to quality of life than the other two types of service. Supported housing also produced better outcomes than residential care with regard to autonomy and was less expensive.
Work package 2ii
We followed 586 out of the 619 participants recruited in WP2i over 30 months, representing a 95% follow-up rate, to assess the proportion who successfully moved on to more independence and identify service and service user factors associated with this. We also planned to collect more comprehensive follow-up data on a subcohort of those who had been in their supported accommodation for < 9 months at recruitment, to compare quality of life, autonomy and social function between service types. Unfortunately we were only able unable to recruit half (73/147) of this group, which precluded statistical comparisons.
Two-thirds of those in floating outreach achieved the primary outcome of managing with less support at the 30-month follow-up. One-third of those in supported housing and 1 in 10 of those in residential care successfully moved on to less supported accommodation. Successful move-on was positively associated with service quality, specifically the degree to which the service promoted human rights and recovery-based practice (as assessed by the QuIRC-SA). Service users with more unmet needs, more risk and longer length of stay in the service (all of which are markers of greater morbidity) were associated with lower odds of successful move-on. We also identified a paradoxical finding that higher scores on the social interface QuIRC-SA domain at recruitment were associated with lower odds of successful move-on. This domain reflects the degree to which family members are involved in service users’ care and the degree to which the service engages service users with local community resources. It is possible that services that achieve greater family engagement may find greater resistance from family members for service users to move to more independent accommodation, an issue identified in previous studies. 50 In addition, it may be that service users who were more integrated into local community activities may have been reluctant to move to alternative accommodation in a different locality.
Work package 3
In our qualitative investigation, we found considerable agreement between staff and service user views on the goals and purposes of supported accommodation services. Participants’ narratives consistently returned to themes of building individuals’ skills and confidence for more independence incrementally and avoiding inadvertently creating dependency on services. Staff understanding of the facilitators of effective practice included many elements that can be conceptualised within rehabilitative and recovery-orientated practice. However, the time-limited nature of services provoked anxiety among service users and staff about how the person would manage when they moved to a less intensive service. Staff and service user participants agreed that a trial comparing the effectiveness of two models of supported accommodation, supported housing and floating outreach, would be valuable.
Work package 4
We conducted a feasibility trial to assess the viability, required sample size and potential outcomes for a randomised evaluation of two supported accommodation models: supported housing and floating outreach. This component of the programme was conducted in three sites: North London, East London and Gloucestershire. We aimed to recruit at least 60 service users referred to supported accommodation services and randomise them to receive either supported housing or floating outreach.
We collaborated with local supported accommodation referral co-ordinators, inpatient ward managers and care co-ordinators to identify eligible service users. We used the findings from WP3 in our recruitment approach. When we identified a potential participant, we contacted the referring clinician to explain the rationale for the study and enquire whether or not it was clinically appropriate for the service user to be considered for recruitment (i.e. whether or not they could potentially manage in either supported housing or an independent tenancy with floating outreach support). If the clinician agreed, we approached the service user to explain the purpose of the study and gain their informed consent for participation. Participants were randomised on an equal basis to move to supported housing or an independent tenancy with floating outreach support and the outcome of randomisation was communicated to the local referrals co-ordinator to process accordingly. If the individual declined to be randomised, they were given the opportunity to participate in the naturalistic arm of the study, whereby we followed them over the course of 12 months but had no influence on their supported accommodation allocation. For all participants, randomised or naturalistic, we conducted baseline interviews and 6-month and 12-month follow-up interviews with both the individual and a member of staff involved in their support.
Recruitment was challenging. We screened 1432 potential participants, but only consented 17 to participate: eight service users were randomised and nine participated in the naturalistic arm. The majority of potential participants were not approached as they were deemed to be clinically inappropriate for the study by their clinical team (n = 851).
We also conducted qualitative interviews with staff and service users involved to gain a fuller understanding of their views regarding the feasibility of a larger trial. We interviewed 11 service users (six who were randomised and five from the naturalistic arm) and 10 staff members (six who had referred service users to the trial and four who had refused) and analysed our data using thematic content analysis.
Four main themes emerged from the service user and staff interviews: preference for a certain type of supported accommodation, rejection of randomisation, complexity of randomisation and the value of a trial. Service users voiced concern about their housing situation being decided at random, mainly because they had a preference for either supported housing or floating outreach, or because they perceived differences between the two models. In spite of this, they were in support of a larger trial, citing the value of further research and the potential benefits for others. Staff often held a strong belief in the need for the existing ‘step-down’ model, revealing a lack of perceived equipoise between supported housing and floating outreach services. They also cited a lack of availability of supported accommodation and housing as a potential recruitment barrier. Some clinicians felt that it was unethical to use randomisation in relation to a person’s accommodation but most felt that a larger trial would be valuable.
Successes and challenges
The QuEST project achieved all four of its original objectives, on time and within budget. We delivered the first specialist quality assessment tool for supported accommodation services, which is now also available as a free online self-assessment tool. We also delivered the first specialist ‘patient-reported outcome measure’ for these services, which is also freely available for use. These tools have the potential to help drive up the quality of existing services through benchmarking and monitoring of quality improvement initiatives at the local or national level. They can also be used in future research studies in this field.
We completed the first, detailed national survey of the provision, quality and effectiveness of mental health supported accommodation services in England. Our results provide important data to assist our understanding of the similarities and differences between supported accommodation service types and the users of these services. Our cohort study was characterised by low attrition and identified service characteristics that contribute to successful move-on for service users that can help to focus future skills training for the staff working in these settings. It has also helped to clarify the characteristics of service users who require longer-term support.
However, a number of challenges were encountered. Most striking was the low recruitment rate in WP4. Despite adapting our recruitment strategy, we failed to recruit an adequate sample to justify investment in a full-scale trial. Nevertheless, this is an important and useful finding that helps to inform the direction of future research in this area. Similarly, our attempts to follow-up in person a subcohort of participants in WP2ii who had been in their supported accommodation service for < 9 months at recruitment proved very difficult, and we were unable to carry out the data analyses that we had hoped might inform the comparative effectiveness of different service types because of the small sample size.
Summary of findings from the whole QuEST programme
The QuEST research programme allowed us to adapt a standardised measure to assess the quality of care provided and a patient-reported outcome measure for specialist mental health supported accommodation services. These were used, along with other tools, to survey a nationally representative sample of the three main types of supported accommodation in England (i.e. residential care, supported housing and floating outreach). This represents the first, detailed description of these services and their users in England.
Although our findings indicate that most people residing in mental health supported accommodation are single men with a diagnosis of a psychotic illness, one-third of those receiving floating outreach have depression or anxiety. Although people residing in residential care have the highest needs and require most support, the majority of users of all three types of service were subject to the Care Programme Approach (the statutory framework for mental health services in England) and, therefore, received additional clinical input from a local statutory community mental health service. This is appropriate given our finding that around two-thirds of participants had a significant risk history, with the most prevalent risks being self-neglect and vulnerability to exploitation. Users of supported housing and floating outreach services were more likely to have been a victim of crime in the last year than users of residential care.
A number of similarities were found between supported housing and floating outreach services and both worked to the same time frame, with an expectation that service users would move on to less supported accommodation or manage with less support within 2 years of being taken on. Service user ratings of satisfaction with care were similar across services but, in our regression models that adjusted for differences in clinical characteristics, we found that quality of life for those in residential care and supported housing was similar and higher than for those receiving floating outreach, and autonomy was higher for those in supported housing. This has important implications for commissioners and service planners, because, although floating outreach services are the cheapest form of supported accommodation, there was a reasonable probability that supported housing provided better value for money with regard to quality of life and autonomy.
In our cohort study, we found that 41% of people progressed to a lower level of supported accommodation over 30 months but there were large differences in this outcome between service types. After adjusting for clinical differences, individuals receiving floating outreach were almost eight times more likely to be able to manage with less support than those in residential care and almost three times more likely than those in supported housing. Similarly, those in supported housing were almost three times more likely to move on to less supported accommodation than those in residential care. Successful progression to less supported accommodation was associated with the degree to which the service promoted human rights (including access to advocacy, privacy and a complaints process) and adopted a recovery orientation (which includes involving and empowering service users as much as possible in decisions about their own care and holding hope for their progress). Service users with greater morbidity were less likely to achieve successful move-on. Unsurprisingly, successful progression to less supported accommodation was associated with lower costs of care.
Our qualitative investigation of staff and service user experiences of supported accommodation suggested that staff were adopting a rehabilitative and recovery-orientated approach in their work with service users. However, the time-limited nature of services provoked anxiety among service users and staff about how the person would manage when they moved to a less intensive service.
Staff and service users were supportive of our plans for a feasibility trial to compare the effectiveness of supported housing and floating outreach services. Concerns about the process of randomisation were addressed in our approach to recruitment to ensure that referring clinicians’ and service users’ preferences were taken into account; participants were only randomised to one of the services where they had capacity to give informed consent and where there was clinical equipoise about the most appropriate service. We also included individuals who did not consent to be randomised but who agreed to complete research interviews. We included outcomes suggested by staff and service users in WP3 and a qualitative component to ensure that we captured participants’ experiences and views about the feasibility trial. Nevertheless, the feasibility trial struggled to recruit. Although we identified > 1400 potentially eligible participants, we randomised only eight. Clinical teams often declined for us to approach service users as they felt clear about which supported accommodation the individual required. Our qualitative investigation of the impediments to recruitment identified that the current ‘step-down’ pathway is ingrained in the culture of mental health services and clinicians perceived a lack of equipoise between the two models of supported accommodation we hoped to compare. Ultimately, the feasibility trial was successful in clarifying that it is not feasible to assess different models of supported accommodation in England through means of a RCT.
Implications for practice
Our results highlight the need for a range of supported accommodation services to be provided at the local level that can respond to the differing levels of individuals’ needs and we identified the pros and cons of different models. This will, we hope, facilitate a more thoughtful discussion about future service investment; during the course of the programme we were aware of ongoing cuts to the more intensive, higher-supported settings in favour of cheaper, floating outreach services. Our results suggest that all three types of supported accommodation are of value and that service planning should certainly not only respond to financial drivers. In particular, our health economic findings suggested that supported housing provided good value for money when outcomes such as quality of life and autonomy are considered. Nevertheless, we found through our cohort study that floating outreach services were able to support the highest proportion of individuals to manage with less support over time. Facilitating successful move-on is the key aim of supported accommodation services and this is, therefore, an important finding. We note that in our survey both supported housing and floating outreach service managers reported that they expected to work with individuals for around 2 years. This rather arbitrary time frame has been adopted by commissioners across the country in response to non-evidence-based parameters set, historically, by the Supporting People programme. Our results show that most people in supported accommodation do not move on within this time frame. The concrete interpretation of this 2-year expectation can pose significant risks to individuals who require longer-term supported accommodation, putting them and staff under unnecessary pressure to move on to more independent accommodation prematurely. Indeed, our findings highlight the tension for supported accommodation services between promoting service user autonomy and providing care; more supported environments were associated with higher levels of quality of life, and the promotion of greater independence seemed to place individuals at greater risk of being a victim of crime. Our qualitative findings suggested that staff and service users experienced appropriate anxiety about how the person/ they would manage with less support after move-on. It was extremely encouraging that, despite their non-professional training, staff in supported accommodation appear to have adopted many aspects of a rehabilitative and recovery orientation in their work. As we found that this approach, along with the promotion of human rights, facilitated successful progression to more independent accommodation, this should be encouraged through training and supervision.
Conclusions
The QuEST programme delivered two standardised outcome measures to assess the quality and user experiences of supported accommodation services. Our findings suggested that the current ‘step-down’ pathway, whereby individuals move from higher- to lower-supported accommodation over time, is deeply ingrained in the system without clear evidence for this approach. The two more intensive models (residential care and supported housing) were associated with better quality of life than floating outreach, and supported housing was associated with greater autonomy. Overall, supported housing represented good value for money. Services that promoted human rights and recovery were more successful in supporting service users to move on (or, for floating outreach, to manage with less support). This outcome was more likely for users of floating outreach services than supported housing and least likely for users of residential care. Users with the greatest morbidity were less likely to move on successfully.
Our feasibility trial showed that the effectiveness of different models of supported accommodation cannot be assessed through randomised trials in this country.
Our findings cannot provide clear guidance on the most effective model(s) of mental health supported accommodation. It seems likely that a range of options will continue to be required to provide appropriate support to assist the recovery of individuals with differing needs. Future investment in this area should be guided by assessment of the mental health needs of the local population and the pros and cons of the different services that our study identified, rather than being based on purely financial drivers.
Recommendations for future research
Research in the field of mental health supported accommodation is underdeveloped and there is huge scope for further studies to inform and build on the evidence base about what works and for whom. Given our finding that trials comparing the effectiveness of existing models of supported accommodation appear unfeasible, future research will need to adopt alternative methods. International surveys of supported accommodation are needed to map and compare the different models in operation. However, these need to be detailed surveys that take account of contextual factors (e.g. the morbidity of the local population and the availability of other components of the mental health system). Service mapping technology has been developing over recent years, allowing the assessment of ‘relative technical efficiency’ of specific components of health systems using Monte Carlo Data Envelopement Analysis. 51 This has been applied to mental health systems and is beginning to incorporate social care system components. 52 It allows information about local service provision to be understood in the context of the particular needs of the locality, providing useful intelligence for service planners. This field is growing and may prove particularly useful in enhancing understanding of the relative merits of different types of mental health supported accommodation.
Our programme included a national cohort study comparing outcomes in the three main types of mental health supported accommodation in England. Future prospective cohort studies could compare different subtypes of the three main models to inform their relative effectiveness. However, cohort studies are time consuming and expensive to conduct and it may be that developments in ‘big data’ technology will ultimately prove fruitful in harnessing comparable outcome data on a national scale. This area is currently underdeveloped.
In the meantime, more qualitative studies are needed to gain a deeper understanding of the specific components of care delivered by different subtypes of supported accommodation services that are most useful to service users. Although we concluded that it is not feasible to compare existing models of supported accommodation through randomised trials, it may well be feasible to develop and test through randomised trial interventions that aim to improve delivery of specific aspects of care, for example those interventions that we found to be associated with better outcomes in our cohort study, such as promotion of human rights and recovery-orientated practice. Qualitative methods would also help in the development of these kinds of interventions, in the process evaluation of trials evaluating them and in studies designed to inform their successful implementation.
Finally, although there is a growing international evidence base pertaining to supported accommodation, interpretation of the literature53 is hampered by a lack of comparable description of different supported accommodation services. This could be addressed by encouraging researchers and journals to adopt a consistent taxonomy, such as the one that one of our research team members (PM) developed alongside the QuEST programme,54 so that results can be compared and collated.
Research priorities
-
Assessment of the sensitivity to change and test–retest reliability of the QuIRC-SA.
-
International surveys of mental health supported accommodation services and service user characteristics to provide comparative data on the different models in operation in different settings and their target service user group(s).
-
Cohort studies to identify the aspects of care and support associated with better outcomes to assist our understanding of how best to focus staff training and resources.
-
Qualitative research to complement the findings from surveys and cohort studies to further enhance our understanding of the specific approaches and components of care that constitute ‘best practice’ in supported accommodation from staff and service user perspectives.
-
Results from these studies will inform the development of complex interventions to enhance the quality of care delivered in mental health supported accommodation services. These should then be evaluated in terms of their clinical effectiveness and cost-effectiveness through RCTs.
Dissemination activities
Publications by work package
Work package 1
Killaspy H, White S, Dowling S, Krotofil J, McPherson P, Sandhu S, et al. Adaptation of the Quality Indicator for Rehabilitative Care (QuIRC) for use in mental health supported accommodation services (QuIRC-SA). BMC Psychiatry 2016;16:101. https://doi.org/10.1186/s12888-016-0799-4
Sandhu S, Killaspy H, Krotofil J, McPherson P, Harrison I, Dowling S, et al. Development and psychometric properties of the Client’s Assessment of Treatment Scale for Supported Accommodation (CAT-SA). BMC Psychiatry 2016;16:43. https://doi.org/10.1186/s12888-016-0755-3
Work package 2i
Killaspy H, Priebe S, Bremner S, Dowling S, Harrison I, Krotofil J, et al. Quality of life, autonomy, satisfaction, and costs associated with mental health supported accommodation services in England: a national survey. Lancet Psychiatry 2016;3:1129–37. https://doi.org/10.1016/S2215-0366(16)30327-3
Work package 2ii
Killaspy H, Priebe S, McPherson P, Zenasni Z, Greenberg L, McCrone P, et al. Predictors of moving on from mental health supported accommodation in England: national cohort study. British J Psychiatr 2019;10:1–7. https://doi.org/10.1192/bjp.2019.101
Work package 3
Sandhu S, Priebe S, Leavey G, Harrison I, Krotofil J, McPherson P, et al. Intentions and experiences of effective practice in mental health specific supported accommodation services: a qualitative interview study. BMC Health Serv Res 2017;17:471. https://doi.org/10.1186/s12913-017-2411-0
Work package 4
Killaspy H, Priebe S, McPherson P, Zenasni Z, McCrone P, Dowling S, et al. Feasibility Randomised trial comparing two forms of mental health supported accommodation (supported housing and floating outreach); a component of the QuEST (Quality and Effectiveness of Supported Tenancies) study. Frontiers in Psychiatry 2019;10:258. https://doi.org/10.3389/fpsyt.2019.00258
Additional publications
Killaspy H. Supported accommodation for people with mental health problems. World Psychiatry 2016;15:74–5. https://doi.org/10.1002/wps.20278
Dalton-Locke C, Attard R, Killaspy H, White S. Predictors of quality of care in mental health supported accommodation services in England: a multiple regression modelling study. BMC Psychiatry 2018;18:344. https://doi.org/10.1186/s12888-018-1912-7
Krotofil J, McPherson P, Killaspy H. Service user experiences of specialist mental health supported accommodation: a systematic review of qualitative studies and narrative synthesis. Health Soc Care Community 2018;26:787–800. https://doi.org/10.1111/hsc.12570
McPherson P, Krotofil J, Killaspy, H. Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry 2018;18:128. https://doi.org/10.1186/s12888-018-1725-8
McPherson P, Krotofil J, Killaspy H. What works? Towards a new classification system for mental health supported accommodation services: the simple taxonomy for supported accommodation (STAX-SA). [Feature paper – special issue: ‘mental health and social care and social interventions’]. Int J Environ Res Public Health 2018;15:190. https://doi.org/10.3390/ijerph15020190
Conference presentations
-
European Network for Mental Health Services Research (ENMESH) conference, Verona, October 2013.
-
Professor Helen Killaspy. The QuEST Study: Quality and Effectiveness of Supported Tenancies for people with mental health problems.
-
-
European Psychiatric Association Social Psychiatry Section meeting, Ulm, May 2014.
-
Professor Helen Killaspy. Quality and Effectiveness of Services for People with Complex Psychosis.
-
-
World Psychiatric Association, Madrid, September 2014.
-
Professor Helen Killaspy. The QuEST Study: Quality and Effectiveness of Supported Tenancies for people with mental health problems.
-
-
World Association for Social Psychiatry (WASP) conference, London, October 2014.
-
Dr Sima Sandhu. Integration in Practice: Experience and Views of those Working in Specialist Mental Health Supported Accommodation in England.
-
-
Housing Associations’ Charitable Trust (HACT) seminar, London, November 2014.
-
Professor Helen Killaspy. The QuEST Study: Quality and Effectiveness of Supported Tenancies for people with mental health problems.
-
-
St Martin of Tours, annual staff conference, London, December 2014.
-
Professor Helen Killaspy. The QuEST Study: Quality and Effectiveness of Supported Tenancies for people with mental health problems.
-
-
Implementing Recovery through Organisational Change (ImROC) national conference, Nottingham, February 2015.
-
Professor Helen Killaspy. The QuEST Study: Quality and Effectiveness of Supported Tenancies for people with mental health problems.
-
-
National Conference on Mental Health Supported Housing, Royal College of Psychiatrists and Mental Health Providers’ Forum, London, March 2015.
-
Professor Helen Killaspy. The QuEST Study: Quality and Effectiveness of Supported Tenancies for people with mental health problems.
-
-
ENMESH conference, Malaga, October 2015.
-
Professor Helen Killaspy. Overview of the QuEST programme.
-
Dr Joanna Krotofil. Systematic literature review of the evidence for different models of supported accommodation for people with mental health problems.
-
Dr Peter McPherson. Adaptation of the Quality Indicator for Rehabilitative Care for supported accommodation services.
-
Ms Isobel Harrison. Results from the national survey of supported accommodation services in England.
-
Sarah Dowling. Staff morale in supported accommodation in England.
-
-
Royal College of Psychiatrists Rehabilitation and Social Psychiatry Faculty Conference, Nottingham, November 2015.
-
Professor Helen Killaspy. Overview of the QuEST programme.
-
Dr Peter McPherson and Dr Joanna Krotofil. A systematic literature review of the evidence on mental health supported accommodation.
-
Dr Sima Sandhu. Staff and service user experiences of supported accommodation in England.
-
-
Royal College of Psychiatrists’ International Congress, London, July 2016.
-
Professor Helen Killaspy. Evidence for the whole system approach for people with complex psychosis.
-
Sarah Dowling. Integration of statutory and non-statutory provision in mental health supported accommodation.
-
-
World Association for Social Psychiatry (WASP) conference, Delhi, December 2016.
-
Professor Helen Killaspy. Quality and effectiveness of mental health supported accommodation in England.
-
-
ENMESH conference, Groningen, October 2017.
-
Professor Helen Killaspy. Overview of the QuEST programme and main results.
-
Peter McPherson. What works? Towards a new classification system for mental health supported accommodation services: the simple taxonomy for supported accommodation (STAX-SA).
-
Dr Rose McGranahan. Results of a qualitative investigation of staff and service user experiences of a feasibility trial of supported accommodation in England.
-
Ms Sarah Dowling. Results of a study of staff morale in mental health supported accommodation in England.
-
Mr Christian Dalton-Locke and Ms Rose Tierney. Predictors of quality of supported accommodation services in England.
-
-
World Psychiatric Association International Congress, Berlin, October 2017.
-
Professor Helen Killaspy. Results from the QuEST Study – Quality and Effectiveness of Supported Tenancies for people with mental health problems – a National Programme of Research in England.
-
-
Royal College of Psychiatrists Faculty of Social and Rehabilitation Psychiatry, Bournemouth, November, 2017.
-
Professor Helen Killaspy. Results from the QuEST Study – Quality and Effectiveness of Supported Tenancies for people with mental health problems – a National Programme of Research in England.
-
-
Australian National University, Canberra, Australian Capital Territory. Invited lecture, academic programme, March 2018.
-
Professor Helen Killaspy. Where Now for Mental Health Supported Accommodation Policy and Research? Implications of Findings from the Quality and Effectiveness of Supported Tenancies Study.
-
-
Housing Associations’ Charitable Trust (HACT) symposium on mental health supported accommodation; improving quality and demonstrating value. Invited keynote speaker, Leeds, October 2018.
-
Professor Helen Killaspy. Findings from the Quality and Effectiveness of Supported Tenancies (QuEST) Study.
-
Additional dissemination activities
-
Annual newsletter sent to all participating services.
-
QuEST website (www.ucl.ac.uk/quest).
-
Dissemination event (10 January 2018):
-
A dissemination event was held at Woburn House, Tavistock Square, London, to share our main findings. The event was attended by over 80 stakeholders, including service users with lived experience of mental health supported accommodation, service managers, commissioners, policy-makers, clinicians and supported accommodation providers. Organisations that were represented included Camden Clinical Commissioning Group, Leicestershire County Council, Reading Borough Council, St Mungo’s, One Housing, Mind, Single Homeless Project, St Martin of Tours, Family Mosaic, Rethink, Look Ahead, Camden and Islington NHS Foundation Trust, South West London and St George’s Mental Health NHS Trust, South London and Maudsley NHS Foundation Trust, Gloucestershire Hospitals NHS Foundation Trust, The McPin Foundation, Mental Health Providers Forum (MHPF), HACT, North London Central Research Consortium, North London SURF and Integra Community Living Options. The event was covered on Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) by The Mental Elf (@MentalElf) using the hashtag #QuESTproject; The Mental Elf has over 55,000 followers on Twitter alone and this approach to augmenting our dissemination event proved highly successful. It resulted in 566 tweets from 174 participants, with over 8 million Twitter impressions in January 2018. This saw an increase in enquiries and website traffic during and following our final dissemination event. Interviews with Helen Killaspy, Peter McPherson and Michael Sheppard, Chief Executive of Warrington Community Living, have been made available on The Mental Elf’s SoundCloud page (www.soundcloud.com/national-elf-service; accessed 19 August 2019).
-
-
Stakeholder roundtable (7 February 2018):
-
A roundtable event was held on 7 February 2018, with key policy-makers and supported accommodation experts, in order to discuss findings from the QuEST study and consider their potential implications for policy, practice and future research. Attendees included: Steve Appleton (Contact Consulting), Andy Bell (Centre for Mental Health), Jed Boardman (The WHO Mental Health Atlas), Andrew van Doorn (HACT), Sarah Dowling (University College London), Sean Duggan (NHS Confederation), Sridevi Kalidindi (South London and Maudsley NHS Foundation Trust), Helen Killaspy (University College London), Paul McCrone (King’s College London), Tim Miller (Haringey Clinical Commisioning Group and Haringey Council), Peter Molyneux (South West London and St George’s Mental Health Trust), Jonathan Moore (Rethink), Stefan Priebe (Queen Mary University of London) and Kathy Roberts (Mental Health Providers Forum).
-
Acknowledgements
We thank the National Institute for Health Research for funding the study and Camden and Islington NHS Foundation Trust, the fundholder.
We wish to acknowledge the valuable contribution of the QuEST study researcher team (Dr Peter McPherson, Dr Joanna Krotofil, Dr Sima Sandhu, Mr Christian Dalton-Locke, Ms Isobel Harrison and Dr Rose McGranahan) in preparing the study questionnaires, participant recruitment, data collection and data entry. Dr Sima Sandhu conducted the qualitative data analysis in WP3 and Dr Rose McGranahan conducted the qualitative data analysis in WP4, supervised by Stefan Priebe and Gerard Leavey. We thank Dr Sarah White for conducting part of the data analysis in WP1, and Dr Steven Bremner and Dr Zohra Zenasni for conducting the data analysis in WP2 under the supervision of Sandra Eldridge.
We would also like to thank the members of our Expert Panel (Mr Dave Fearon, Dr Patrick Gillespie, Dr Geraldine Strathdee and Mr Andrew Van Doorn) and our Service User Reference Group (Ms Katherine Barrett, Mr James Bennett and Mr Gavin McCabe) for their input throughout the programme.
We are also very grateful to our PSG for their valuable advice and oversight (Professor Tom Craig, Chairperson, King’s College London; Dr Lee Shepstone, Senior Statistician, University of East Anglia; Ms Alison Tingle, Mental Health Policy Advisor, Department of Health and Social Care; and Mr Maurice Arbuthnott, Service User Expert, North London SURF).
Finally, we warmly thank all of the participants at each site who agreed to be involved in this research programme.
Contributions of authors
Helen Killaspy (Chief Investigator, Professor of Rehabilitation Psychiatry and Honorary Consultant in Rehabilitation Psychiatry) conceived and designed the programme. She also managed the day-to-day running of the programme, which was overseen by the PMG [chaired by Helen Killaspy and this comprised all co-investigators, researchers, the programme manager and two service user experts (one of whom was also a co-investigator – Maurice Arbuthnott)]. The PMG met quarterly to review study progress and addressed managerial and scientific issues as they arose. She also drafted the report.
Stefan Priebe (Professor of Social and Community Psychiatry and Honorary Consultant Psychiatrist) conceived and designed the programme.
Michael King (Professor of Primary Care Psychiatry) conceived and designed the programme.
Sandra Eldridge (Professor of Biostatistics) conceived and designed the programme, and oversaw the statistical analysis.
Paul McCrone (Professor of Health Economics) conducted the health economics analyses in WP2 and WP4, and drafted the report.
Geoff Shepherd (Senior Consultant) conceived and designed the programme.
Maurice Arbuthnott (Service User Representative) conceived and designed the programme.
Gerard Leavey (Professor of Mental Health and Wellbeing) conceived and designed the programme.
Sarah Curtis (Professor of Health and Risk) conceived and designed the programme.
Peter McPherson (Research Associate) conceived and designed the programme, and drafted the report.
Sarah Dowling (Programme Manager) managed the day-to-day running of the programme, which was overseen by the PMG. She also drafted the report.
All authors were involved in the interpretation of the data and reviewed and revised the report.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health and Social Care.
References
- National Statistics . Community Care Statistics, Supported Residents (Adults) – England, 2006 2006.
- Department of Communities and Local Government . Research into the Effectiveness of Floating Support Services for the Supporting People Programme. Final Report 2006.
- Ministry of Health . Hospital Plan for England and Wales 1962.
- Department of Health and Social Care . The Care Programme Approach for People With a Mental Illness Referred to the Specialist Psychiatric Services. 1990.
- Holloway F. The Forgotten Need for Rehabilitation in Contemporary Mental Health Services: A Position Statement from the Executive Committee of the Faculty of Rehabilitation and Social Psychiatry. London: Royal College of Psychiatrists; 2005.
- Leff J, Trieman N. Long-stay patients discharged from psychiatric hospitals. Social and clinical outcomes after five years in the community. The TAPS Project 46. Br J Psychiatry 2000;176:217-23. https://doi.org/10.1192/bjp.176.3.217.
- Trieman N, Leff J. Long-term outcome of long-stay psychiatric in-patients considered unsuitable to live in the community. TAPS Project 44. Br J Psychiatry 2002;181:428-32. https://doi.org/10.1192/bjp.181.5.428.
- Boardman J, Currie A, Killaspy H, Mezey G. Social Inclusion and Mental Health. London: Royal College of Psychiatrists; 2010.
- Social Exclusion Unit . Mental Health and Social Exclusion 2004.
- Fakhoury WK, Murray A, Shepherd G, Priebe S. Research in supported housing. Soc Psychiatry Psychiatr Epidemiol 2002;37:301-15. https://doi.org/10.1007/s00127-002-0549-4.
- Priebe S, Saidi M, Want A, Mangalore R, Knapp M. Housing services for people with mental disorders in England: patient characteristics, care provision and costs. Soc Psychiatry Psychiatr Epidemiol 2009;44:805-14. https://doi.org/10.1007/s00127-009-0001-0.
- Shepherd G, Macpherson R, Thornicroft G, Szmukler G, Mueser KT, Drake R. Oxford Textbook of Community Mental Health. Oxford: Oxford University Press; 2011.
- Friedrich RM, Hollingsworth B, Hradek E, Friedrich HB, Culp KR. Family and client perspectives on alternative residential settings for persons with severe mental illness. Psychiatr Serv 1999;50:509-14. https://doi.org/10.1176/ps.50.4.509.
- Minsky S, Riesser GG, Duffy M. The eye of the beholder: housing preferences of inpatients and their treatment teams. Psychiatr Serv 1995;46:173-6. https://doi.org/10.1176/ps.46.2.173.
- Piat M, Lesage A, Boyer R, Dorvil H, Couture A, Grenier G, et al. Housing for persons with serious mental illness: consumer and service provider preferences. Psychiatr Serv 2008;59:1011-17. https://doi.org/10.1176/appi.ps.59.9.1011.
- Ryan T, Pearsall A, Hatfield B, Poole R. Long term care for serious mental illness outside the NHS: A study of out of area placements. J Ment Heal 2004;13:425-9. https://doi.org/10.1080/09638230410001729861.
- Walker R, Seasons M. Supported housing for people with serious mental illness: resident perspectives on housing. Can J Commun Ment Health 2002;21:137-51. https://doi.org/10.7870/cjcmh-2002-0010.
- Chilvers R, Macdonald GM, Hayes AA. Supported housing for people with severe mental disorders. Cochrane Database Syst Rev 2002;2. https://doi.org/10.1002/14651858.CD000453.
- Aubry T, Goering P, Veldhuizen S, Adair CE, Bourque J, Distasio J, et al. A multiple-city RCT of housing first with assertive community treatment for homeless Canadians with serious mental illness. Psychiatr Serv 2016;67:275-81. https://doi.org/10.1176/appi.ps.201400587.
- Killaspy H, White S, Dowling S, Krotofil J, McPherson P, Sandhu S, et al. Adaptation of the Quality Indicator for Rehabilitative Care (QuIRC) for use in mental health supported accommodation services (QuIRC-SA). BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0799-4.
- Sandhu S, Killaspy H, Krotofil J, McPherson P, Harrison I, Dowling S, et al. Development and psychometric properties of the client’s assessment of treatment scale for supported accommodation (CAT-SA). BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0755-3.
- Killaspy H, Priebe S, Bremner S, McCrone P, Dowling S, Harrison I, et al. Quality of life, autonomy, satisfaction, and costs associated with mental health supported accommodation services in England: a national survey. Lancet Psychiatry 2016;3:1129-37. https://doi.org/10.1016/S2215-0366(16)30327-3.
- Killaspy H, Priebe S, McPherson P, Zenasni Z, Greenberg L, McCrone P, et al. Predictors of moving on from mental health supported accommodation in England: national cohort study. British J Psychiatr 2019;10:1-7. https://doi.org/10.1192/bjp.2019.101.
- Killaspy H, Priebe S, McPherson P, Zenasni Z, McCrone P, Dowling S, et al. Feasibility Randomised trial comparing two forms of mental health supported accommodation (supported housing and floating outreach); a component of the QuEST (Quality and Effectiveness of Supported Tenancies) study. Frontiers in Psychiatry 2019;10.
- Sandhu S, Priebe S, Leavey G, Harrison I, Krotofil J, McPherson P, et al. Intentions and experiences of effective practice in mental health specific supported accommodation services: a qualitative interview study. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2411-0.
- Killaspy H, White S, Wright C, Taylor TL, Turton P, Schützwohl M, et al. The development of the Quality Indicator for Rehabilitative Care (QuIRC): a measure of best practice for facilities for people with longer term mental health problems. BMC Psychiatry 2011;11. https://doi.org/10.1186/1471-244X-11-35.
- Killaspy H, White S, Wright C, Taylor TL, Turton P, Kallert T, et al. Quality of longer term mental health facilities in Europe: validation of the quality indicator for rehabilitative care against service users’ views. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0038070.
- Richardson M, Katsakou C, Torres-González F, Onchev G, Kallert T, Priebe S. Factorial validity and measurement equivalence of the Client Assessment of Treatment Scale for psychiatric inpatient care – a study in three European countries. Psychiatry Res 2011;188:156-60. https://doi.org/10.1016/j.psychres.2011.01.020.
- Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester Short Assessment of Quality of Life (MANSA). Int J Soc Psychiatry 1999;45:7-12. https://doi.org/10.1177/002076409904500102.
- Hair JF. Multivariate Data Analysis. Upper Saddle River, NJ: Pearson Prentice Hall; 2006.
- Leff J, Szmidla A. Evaluation of a special rehabilitation programme for patients who are difficult to place. Soc Psychiatry Psychiatr Epidemiol 2002;37:532-6. https://doi.org/10.1007/s00127-002-0578-z.
- Slade M, Phelan M, Thornicroft G, Parkman S. The Camberwell Assessment of Need (CAN): comparison of assessments by staff and patients of the needs of the severely mentally ill. Soc Psychiatry Psychiatr Epidemiol 1996;31:109-13. https://doi.org/10.1007/BF00785756.
- Drake RE, Mueser KT, McHugo GJ, Sederer LI, Dickey B. Outcomes Assessment in Clinical Practice. Baltimore, MD: Williams & Wilkins; 1996.
- Parker G, Rosen A, Emdur N, Hadzi-Pavlov D. The Life Skills Profile: psychometric properties of a measure assessing function and disability in schizophrenia. Acta Psychiatr Scand 1991;83:145-52. https://doi.org/10.1111/j.1600-0447.1991.tb07381.x.
- Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- Priebe S, Watzke S, Hansson L, Burns T. Objective social outcomes index (SIX): a method to summarise objective indicators of social outcomes in mental health care. Acta Psychiatr Scand 2008;118:57-63. https://doi.org/10.1111/j.1600-0447.2008.01217.x.
- Hatton C, Emerson E, Robertson J, Gregory N, Kessissoglou S, Walsh PN. The Resident Choice Scale: a measure to assess opportunities for self-determination in residential settings. J Intellect Disabil Res 2004;48:103-13. https://doi.org/10.1111/j.1365-2788.2004.00499.x.
- Røssberg JI, Friis S. A suggested revision of the Ward Atmosphere Scale. Acta Psychiatr Scand 2003;108:374-80. https://doi.org/10.1034/j.1600-0447.2003.00191.x.
- Killaspy H, Marston L, Green N, Harrison I, Lean M, Holloway F, et al. Clinical outcomes and costs for people with complex psychosis; a naturalistic prospective cohort study of mental health rehabilitation service users in England. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0797-6.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: PSSRU, University of Kent; 2013.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep 1962;10:799-812. https://doi.org/10.2466/pr0.1962.10.3.799.
- Jolley S, Garety PA, Ellett L, Kuipers E, Freeman D, Bebbington PE, et al. A validation of a new measure of activity in psychosis. Schizophr Res 2006;85:288-95. https://doi.org/10.1016/j.schres.2006.03.012.
- Wing JK, Beevor AS, Curtis RH, Park SB, Hadden S, Burns A. Health of the Nation Outcome Scales (HoNOS). Research and development. Br J Psychiatry 1998;172:11-8. https://doi.org/10.1192/bjp.172.1.11.
- McGuire-Snieckus R, McCabe R, Catty J, Hansson L, Priebe S. A new scale to assess the therapeutic relationship in community mental health care: STAR. Psychol Med 2007;37:85-9. https://doi.org/10.1017/S0033291706009299.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. PAFS consensus group . CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. https://doi.org/10.1097/00005650-199603000-00003.
- Williams A. The Role of the EuroQoL Instrument in QALY Calculations. York: Centre for Health Economics, University of York; 1995.
- McCrone P, Patel A, Knapp M, Schene A, Koeter M, Amaddeo F, et al. A comparison of SF-6D and EQ-5D utility scores in a study of patients with schizophrenia. J Ment Health Policy Econ 2009;12:27-31.
- Tanzman B. An overview of surveys of mental health consumers’ preferences for housing and support services. Hosp Community Psychiatry 1993;44:450-5. https://doi.org/10.1176/ps.44.5.450.
- Torres-Jiménez M, García-Alonso CR, Salvador-Carulla L, Fernández-Rodríguez V. Evaluation of system efficiency using the Monte Carlo DEA: the case of small health areas. Eur J Oper Res 2015;242:525-35. https://doi.org/10.1016/j.ejor.2014.10.019.
- Salvador-Carulla L, García-Alonso C, Gonzalez-Caballero JL, Garrido-Cumbrera M. Use of an operational model of community care to assess technical efficiency and benchmarking of small mental health areas in Spain. J Ment Health Policy Econ 2007;10:87-100.
- McPherson P, Krotofil J, Killaspy H. Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1725-8.
- McPherson P, Krotofil J, Killaspy H. What works? Toward a new classification system for mental health supported accommodation services: the Simple Taxonomy for Supported Accommodation (STAX-SA). Int J Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15020190.
Appendix 1 The Client Assessment of Treatment scale and Client Assessment of Treatment Scale for Supported Accommodation
Reproduced from Sandhu et al. 21 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Appendix 2 Tables of results from work package 2i
| Area | Index score | Residential care | Supported housing | Floating outreach | Total services | Total SUs | |||
|---|---|---|---|---|---|---|---|---|---|
| Services | SUs | Services | SUs | Services | SUs | ||||
| Telford | –0.755 | 1 | 7 | 2 | 15 | 1 | 50 | 4 | 72 |
| Cheshire East | –0.645 | 3 | 34 | 8 | 106 | 5 | 128 | 16 | 268 |
| Subtotal | 4 | 41 | 10 | 121 | 6 | 178 | 20 | 340 | |
| Bath and North East Somerset | –0.540 | 1 | 8 | 4 | 32 | 6 | 154 | 11 | 194 |
| Doncaster | –0.427 | 0 | 0 | 2 | 23 | 1 | 12 | 3 | 35 |
| Subtotal | 1 | 8 | 6 | 55 | 7 | 166 | 14 | 229 | |
| Warrington | –0.236 | 3 | 56 | 5 | 56 | 7 | 132 | 15 | 244 |
| Stockton | –0.082 | 3 | 48 | 1 | 13 | 4 | 35 | 8 | 96 |
| Subtotal | 6 | 104 | 6 | 69 | 11 | 167 | 23 | 340 | |
| Wirral | 0.034 | 10 | 173 | 7 | 119 | 5 | 143 | 22 | 435 |
| Reading | 0.168 | 2 | 23 | 2 | 27 | 7 | 107 | 11 | 157 |
| Subtotal | 12 | 196 | 9 | 146 | 12 | 250 | 33 | 592 | |
| Coventry | 0.313 | 2 | 32 | 4 | 49 | 3 | 144 | 9 | 225 |
| Hull | 0.501 | 7 | 163 | 5 | 55 | 5 | 104 | 17 | 322 |
| Subtotal | 9 | 195 | 9 | 104 | 8 | 248 | 26 | 547 | |
| Brent | 1.056 | 4 | 41 | 10 | 92 | 6 | 170 | 20 | 303 |
| Tower Hamlets | 1.570 | 2 | 29 | 10 | 155 | 3 | 86 | 15 | 270 |
| Subtotal | 6 | 70 | 20 | 247 | 9 | 256 | 35 | 573 | |
| Camden | 1.767 | 3 | 53 | 19 | 247 | 7 | 203 | 29 | 503 |
| Islington | 1.776 | 4 | 81 | 16 | 175 | 2 | 63 | 22 | 319 |
| Subtotal | 7 | 134 | 35 | 422 | 9 | 266 | 51 | 822 | |
| Totals | 45 | 748 | 95 | 1164 | 62 | 1531 | 202 | 3443 | |
| Variable | MANSA (n = 599) | RCS (n = 618) | ||||
|---|---|---|---|---|---|---|
| Mean difference | 95% CI | p-value | Mean difference | 95% CI | p-value | |
| Type of service | ||||||
| Supported vs. residential | –0.138 | –0.402 to 0.126 | 0.306 | 0.145 | 0.010 to 0.279 | 0.035 |
| Floating vs. residential | –0.424 | –0.734 to –0.114 | 0.007 | 0.011 | –0.122 to 0.144 | 0.873 |
| Mental health morbidity of local area (Mental Illness Needs Index score) | 0.178 | 0.024 to 0.332 | 0.023 | 0.033 | –0.043 to 0.110 | 0.397 |
| Number of spaces occupied | –0.006 | –0.010 to –0.002 | 0.001 | 0.001 | –0.001 to 0.002 | 0.581 |
| QuIRC-SA domain | ||||||
| Treatments and interventions | 0.007 | –0.005 to 0.020 | 0.256 | –0.007 | –0.014 to –0.001 | 0.020 |
| Self-management and autonomy | 0.004 | –0.024 to 0.032 | 0.780 | 0.008 | –0.004 to 0.021 | 0.189 |
| Social interface | 0.001 | –0.006 to 0.009 | 0.722 | 0.000 | –0.004 to 0.003 | 0.861 |
| Human rights | 0.001 | –0.018 to 0.020 | 0.882 | 0.008 | 0.000 to 0.016 | 0.051 |
| Recovery-based practice | –0.015 | –0.030 to 0.000 | 0.049 | –0.002 | –0.009 to 0.005 | 0.647 |
| Sociodemographic/clinical characteristics | ||||||
| Age (years) | 0.007 | 0.001 to 0.012 | 0.015 | –0.001 | –0.003 to 0.001 | 0.406 |
| Female vs. male | –0.026 | –0.156 to 0.104 | 0.699 | –0.042 | –0.097 to 0.013 | 0.135 |
| Non-white vs. white ethnicity | –0.072 | –0.298 to 0.154 | 0.530 | 0.000 | –0.085 to 0.086 | 0.991 |
| Psychotic vs. non-psychotic illness | 0.199 | 0.019 to 0.379 | 0.031 | –0.026 | –0.082 to 0.029 | 0.353 |
| LSP | 0.004 | –0.001 to 0.009 | 0.106 | 0.003 | 0.001 to 0.005 | 0.001 |
| SPRS | –0.008 | –0.048 to 0.032 | 0.703 | 0.009 | –0.003 to 0.021 | 0.150 |
| CANSAS number of unmet needs | –0.053 | –0.090 to –0.016 | 0.005 | –0.017 | –0.035 to 0.000 | 0.048 |
| Problematic drug use (yes vs. no) | 0.221 | 0.006 to 0.437 | 0.044 | 0.040 | –0.025 to 0.105 | 0.228 |
| Problematic alcohol use (yes vs. no) | 0.002 | –0.151 to 0.156 | 0.978 | 0.047 | –0.016 to 0.111 | 0.146 |
| Risk to self/others in past 2 years (yes vs. no) | 0.059 | –0.085 to 0.204 | 0.421 | –0.011 | –0.069 to 0.047 | 0.716 |
| Grand mean | 3.915 | 2.512 to 5.318 | < 0.001 | 2.349 | 1.676 to 3.021 | < 0.001 |
| Variable | GMI (n = 396) | CAT-SA (n = 595) | ||||
|---|---|---|---|---|---|---|
| Mean difference | 95% CI | p-value | Mean difference | 95% CI | p-value | |
| Type of service | ||||||
| Supported vs. residential | 0.219 | –0.871 to 1.309 | 0.694 | –0.194 | –0.753 to 0.365 | 0.496 |
| Floating vs. residential | –0.095 | –0.705 to 0.516 | 0.761 | |||
| Mental health morbidity of local area (Mental Illness Needs Index score) | 0.060 | –0.032 to 0.153 | 0.202 | 0.006 | –0.001 to 0.014 | 0.112 |
| Number of spaces occupied | –0.946 | –1.841 to –0.052 | 0.038 | –0.279 | –0.544 to –0.014 | 0.039 |
| QuIRC-SA domain | ||||||
| Treatments and interventions | 0.081 | –0.008 to 0.169 | 0.073 | 0.009 | –0.020 to 0.038 | 0.544 |
| Self-management and autonomy | 0.020 | –0.084 to 0.124 | 0.703 | 0.002 | –0.050 to 0.054 | 0.944 |
| Social interface | –0.009 | –0.051 to 0.032 | 0.657 | –0.002 | –0.020 to 0.017 | 0.848 |
| Human rights | 0.089 | 0.017 to 0.160 | 0.015 | 0.028 | –0.009 to 0.065 | 0.135 |
| Recovery-based practice | –0.048 | –0.117 to 0.021 | 0.175 | –0.012 | –0.042 to 0.017 | 0.406 |
| Sociodemographic/clinical characteristics | ||||||
| Age (years) | 0.044 | 0.015 to 0.074 | 0.003 | 0.014 | 0.002 to 0.025 | 0.017 |
| Female vs. male | 0.286 | –0.607 to 1.179 | 0.530 | –0.123 | –0.452 to 0.206 | 0.463 |
| Non-white vs. white ethnicity | –0.024 | –1.370 to 1.321 | 0.972 | –0.273 | –0.755 to 0.209 | 0.266 |
| Psychotic vs. non-psychotic illness | –0.099 | –1.005 to 0.808 | 0.831 | –0.112 | –0.487 to 0.263 | 0.560 |
| LSP | 0.071 | 0.036 to 0.107 | < 0.001 | 0.033 | 0.021 to 0.045 | < 0.001 |
| SPRS | 0.058 | –0.199 to 0.315 | 0.657 | –0.025 | –0.114 to 0.064 | 0.581 |
| CANSAS number of unmet needs | –0.028 | –0.306 to 0.250 | 0.843 | –0.009 | –0.107 to 0.089 | 0.863 |
| Problematic drug use (yes vs. no) | 1.053 | 0.020 to 2.087 | 0.046 | 0.163 | –0.274 to 0.600 | 0.464 |
| Problematic alcohol use (yes vs. no) | 0.411 | –0.596 to 1.419 | 0.424 | 0.322 | –0.060 to 0.704 | 0.098 |
| Risk to self/others in past 2 years (yes vs. no) | 1.174 | 0.235 to 2.113 | 0.014 | 0.414 | 0.060 to 0.768 | 0.022 |
| Grand mean | –2.889 | –12.272 to 6.494 | 0.546 | 1.054 | –1.885 to 3.993 | 0.482 |
FIGURE 4.
Cost-effectiveness plane comparing residential care and supported housing.
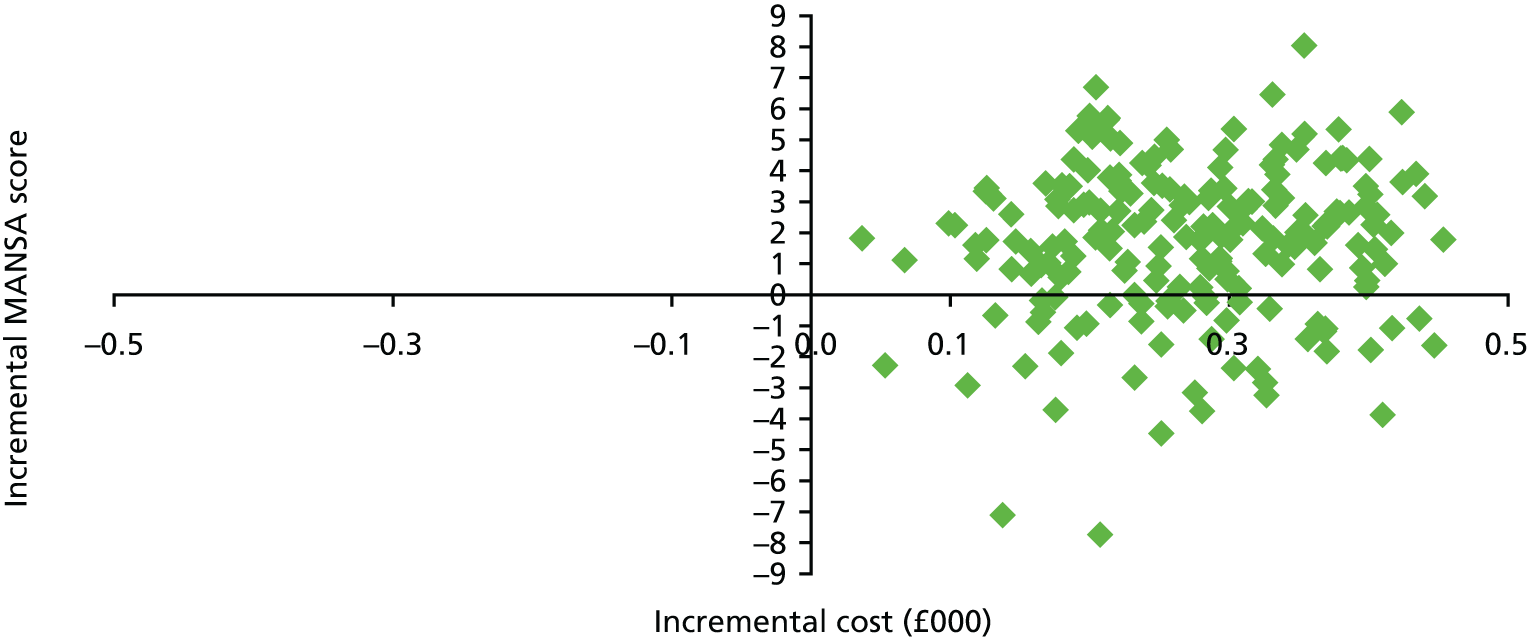
FIGURE 5.
Cost-effectiveness plane comparing residential care and floating outreach.
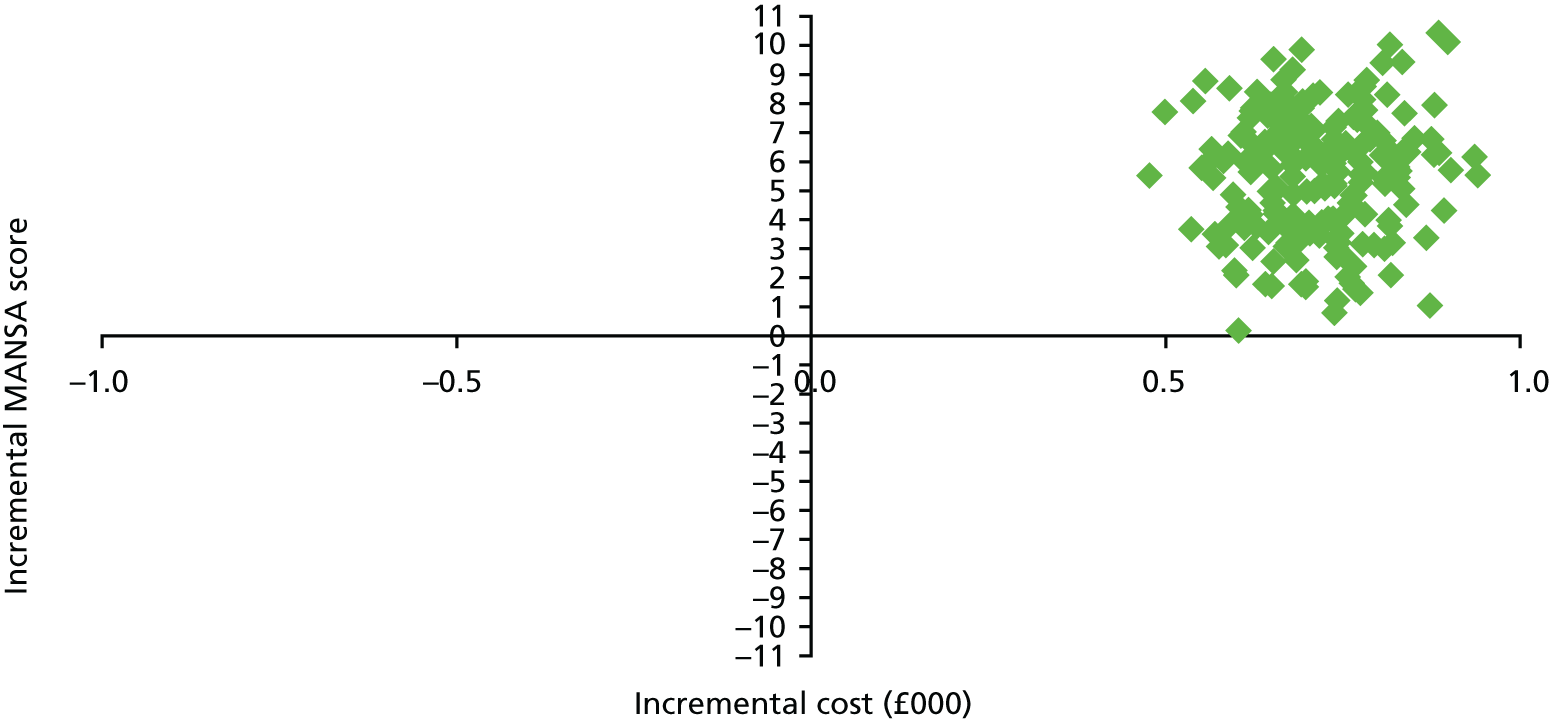
FIGURE 6.
Cost-effectiveness plane comparing supported housing and floating outreach.
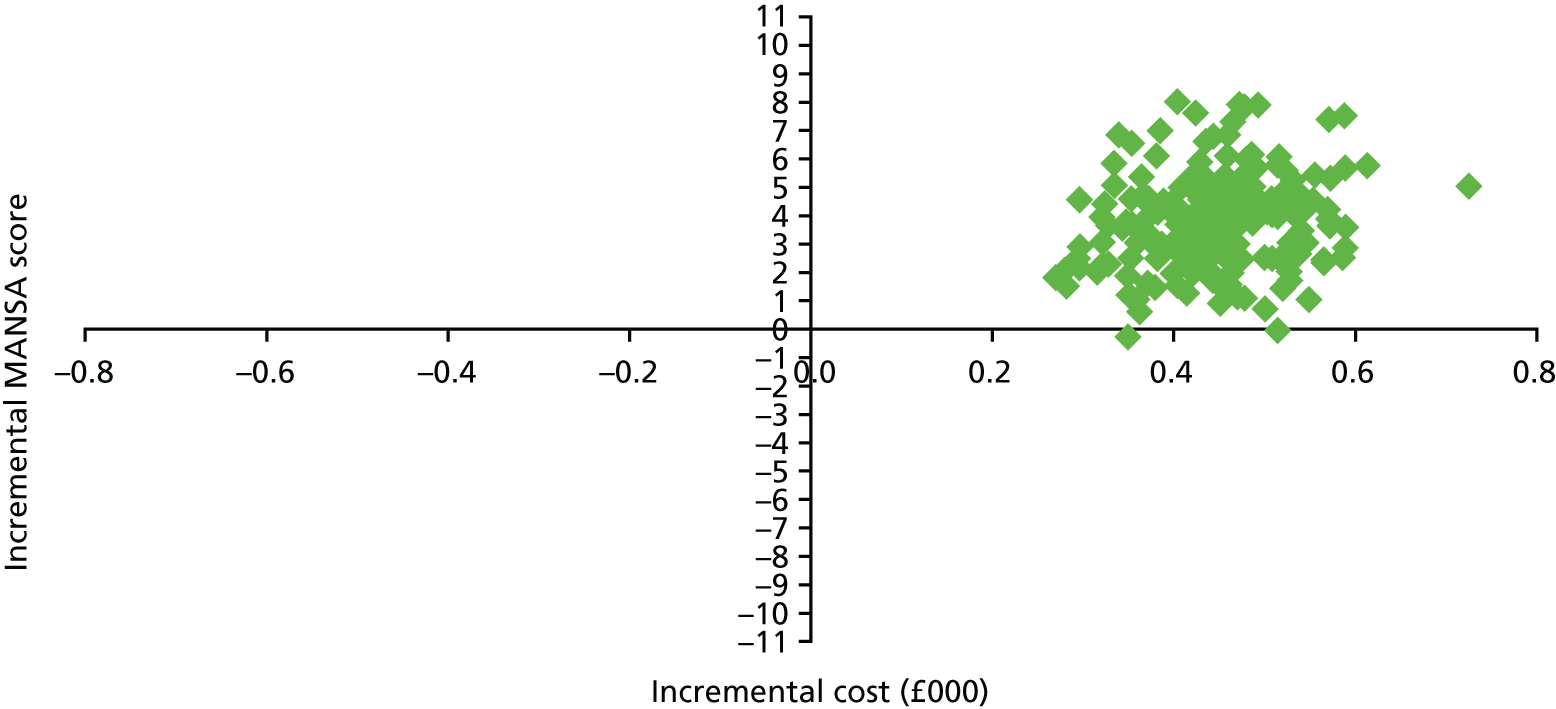
Appendix 3 Results from work package 2ii
| Residential care, n = 146 (%) | Supported housing, n = 244 (%) | Floating outreach, n = 196 (%) | Total, n = 586 (%) | |
|---|---|---|---|---|
| Number of psychiatric admissions | n = 144 | n = 243 | n = 196 | n = 583 |
| 0 | 117 (81.3) | 183 (75.3) | 173 (88.3) | 473 (81.1) |
| 1 | 16 (11.1) | 31 (12.8) | 11 (5.6) | 58 (9.9) |
| > 1 | 11 (7.6) | 29 (11.9) | 12 (6.1) | 52 (8.9) |
| Number of involuntary psychiatric admissions | n = 144 | n = 243 | n = 196 | n = 583 |
| 0 | 125 (86.8) | 201 (82.7) | 182 (92.9) | 508 (87.1) |
| 1 | 11 (7.6) | 27 (11.1) | 8 (4.1) | 46 (7.9) |
| > 1 | 8 (5.6) | 15 (6.2) | 6 (3.1) | 29 (5.0) |
| Any episodes of being in prison? | n = 143 | n = 243 | n = 196 | n = 582 |
| 5 (3.5) | 9 (3.7) | 2 (1.0) | 16 (2.7) | |
| Any incidents of violence? | n = 143 | n = 243 | n = 196 | n = 582 |
| 20 (14.0) | 28 (11.5) | 8 (4.1) | 56 (9.6) | |
| Any episodes of self-harm? | n = 143 | n = 243 | n = 196 | n = 582 |
| 6 (4.2) | 42 (17.3) | 29 (14.8) | 77 (13.3) | |
| Any incidents of fire-setting? | n = 142 | n = 242 | n = 196 | n = 580 |
| 1 (0.7) | 4 (1.7) | 1 (0.5) | 6 (1.0) | |
| Any incidents of sexual offending? | n = 141 | n = 243 | n = 195 | n = 579 |
| 4 (2.8) | 4 (1.6) | 0 (0.0) | 8 (1.4) | |
| For participants who have not moved on, are they considered ready to move on? | 8/94 (8.5) | 29/95 (30.5) | 5/72 (6.9) | 42/261 (16.1) |
| Variable | OR | 95% CI | p-value |
|---|---|---|---|
| Primary analysis: unadjusted | |||
| Supported housing vs. residential care | 5.64 | 2.30 to 13.84 | < 0.001 |
| Floating outreach vs. residential care | 28.81 | 11.53 to 72.02 | < 0.001 |
| Floating outreach vs. supported housing | 5.11 | 2.47 to 10.57 | < 0.001 |
| Primary analysis: adjusteda | |||
| Supported housing vs. residential care | 2.90 | 1.05 to 8.04 | 0.04 |
| Floating outreach vs. residential care | 7.96 | 2.92 to 21.69 | < 0.001 |
| Floating outreach vs. supported housing | 2.74 | 1.01 to 7.41 | < 0.001 |
| Service user variables at recruitment | |||
| Age | 0.99 | 0.97 to 1.01 | 0.373 |
| Psychosis | 0.63 | 0.36 to 1.09 | 0.101 |
| Length of stay with service in months | 0.99 | 0.98 to 0.99 | < 0.001 |
| Social function (LSP total) | 1.01 | 0.99 to 1.03 | 0.498 |
| Unmet needs (CANSAS total unmet) | 0.81 | 0.70 to 0.94 | 0.006 |
| Challenging behaviours (SPRS total) | 0.98 | 0.84 to 1.13 | 0.739 |
| Drug use (CADS problematic use) | 0.83 | 0.39 to 1.79 | 0.642 |
| Self-neglect and/or vulnerable to exploitation | 0.58 | 0.35 to 0.98 | 0.040 |
| Service variables at recruitment | |||
| QuIRC-SA social interface domain score | 0.95 | 0.91 to 0.98 | 0.001 |
| QuIRC-SA human rights domain score | 1.09 | 1.02 to 1.16 | 0.007 |
| QuIRC-SA recovery-based practice domain score | 1.04 | 1.00 to 1.08 | 0.054 |
| Variable | Effect estimate | 95% CI | p-value |
|---|---|---|---|
| Propensity score analysis: ATEa | |||
| Supported housing vs. residential care | 0.23 | 0.09 to 0.38 | 0.002 |
| Floating outreach vs. residential care | 0.51 | 0.29 to 0.72 | < 0.001 |
| Floating outreach vs. supported housing | 0.27 | 0.05 to 0.46 | 0.018 |
| Variable | OR | 95% CI | p-value |
| Sensitivity analysis: including only participants with psychosisb | |||
| Supported housing vs. residential care | 4.22 | 1.56 to 11.42 | 0.005 |
| Floating outreach vs. residential care | 15.08 | 5.31 to 42.78 | < 0.001 |
| Floating outreach vs. supported housing | 3.57 | 1.51 to 8.43 | 0.004 |
| Sensitivity analysis: replacing area with mental health index score | |||
| Supported housing vs. residential care | 6.97 | 2.74 to 17.72 | < 0.001 |
| Floating outreach vs. residential care | 31.00 | 11.41 to 84.27 | < 0.001 |
| Floating outreach vs. supported housing | 4.45 | 2.09 to 9.46 | < 0.001 |
| Sensitivity analysis: reclassifying primary outcome for floating outreach to include only those with 50% reduction in hours of supportb | |||
| Supported housing vs. residential care | 5.94 | 2.21 to 15.98 | < 0.001 |
| Floating outreach vs. residential care | 21.74 | 8.05 to 58.69 | < 0.001 |
| Floating outreach vs. supported housing | 3.66 | 1.64 to 8.15 | 0.001 |
| Variable | < 9 months (n = 147) | ≥ 9 months (n = 439) | p-value for interaction | ||
|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||
| Supported housing vs. residential care | 5.85 | 2.20 to 15.56 | 5.66 | 1.13 to 38.37 | 0.99 |
| Floating outreach vs. residential care | 31.10 | 11.32 to 85.48 | 27.60 | 5.16 to 147.46 | |
| Variable | OR | 95% CI | p-value |
|---|---|---|---|
| Supported housing vs. residential care | 1.50 | 0.64 to 2.35 | < 0.001 |
| Floating outreach vs. residential care | 3.15 | 2.28 to 4.02 | < 0.001 |
| Floating outreach vs. supported housing | 1.65 | 0.97 to 2.33 | < 0.001 |
| Scale | Service type | Number of observations | Number missing | Mean | SD | Median | IQR |
|---|---|---|---|---|---|---|---|
| Quality of life (MANSA) | Overall | 73 | 74 | 4.5 | 1.1 | 4.5 | 4.0–5.1 |
| Residential Care | 15 | 8 | 4.7 | 0.7 | 4.7 | 4.2–5.4 | |
| Supported Housing | 40 | 33 | 4.5 | 1.0 | 4.4 | 4.0–5.2 | |
| Floating Outreach | 18 | 33 | 4.4 | 1.3 | 4.8 | 3.7–5.1 | |
| Autonomy (RCS) | Overall | 71 | 76 | 3.4 | 0.5 | 3.5 | 3.2–3.7 |
| Residential Care | 15 | 8 | 3.2 | 0.6 | 3.3 | 2.9–3.6 | |
| Supported Housing | 41 | 32 | 3.4 | 0.4 | 3.5 | 3.3–3.7 | |
| Floating Outreach | 15 | 36 | 3.4 | 0.8 | 3.6 | 3.2–3.9 | |
| Satisfaction with care (CAT-SA) | Overall | 47 | 100 | 7.5 | 2.5 | 8.3 | 5.6–9.7 |
| Residential Care | 13 | 10 | 8.2 | 2.0 | 9.3 | 6.9–9.7 | |
| Supported Housing | 30 | 43 | 7.4 | 2.4 | 7.9 | 5.4–9.7 | |
| Floating Outreach | 4 | 47 | 6.3 | 4.2 | 8.0 | 3.9–8.7 | |
| Social function (LSP) | Overall | 63 | 84 | 122.1 | 16.0 | 123.0 | 112.0–135.0 |
| Residential Care | 15 | 8 | 118.3 | 19.4 | 113.0 | 104.0–140.0 | |
| Supported Housing | 39 | 34 | 122.5 | 15.4 | 124.0 | 113.0–135.0 | |
| Floating Outreach | 9 | 42 | 127.2 | 12.1 | 131.0 | 121.0–134.0 |
| Number of participants | Mean difference | 95% CI | |
|---|---|---|---|
| Quality of life (MANSA) | 73 | ||
| Supported housing vs. residential care | 0.17 | –0.38 to 0.71 | |
| Floating outreach vs. residential care | 0.02 | –0.58 to 0.62 | |
| Autonomy (RCS) | 71 | ||
| Supported housing vs. residential care | 0.20 | –0.09 to 0.50 | |
| Floating outreach vs. residential care | 0.12 | –0.22 to 0.46 | |
| Satisfaction with care (CAT-SA) | 47 | ||
| Supported housing vs. residential care | –1.40 | –2.72 to –0.08 | |
| Floating outreach vs. residential care | –3.71 | –5.85 to –1.57 | |
| Social function (LSP) | 63 | ||
| Supported housing vs. residential care | 3.33 | –6.41 to 13.07 | |
| Floating outreach vs. residential care | 5.14 | –7.86 to 18.14 |
| Service | Accommodation type, n (%) | ||
|---|---|---|---|
| Residential care (N = 141) | Supported housing (N = 242) | Floating outreach (N = 193) | |
| External staff | |||
| Care co-ordinator | 65 (46) | 144 (60) | 48 (25) |
| Psychiatrist | 55 (39) | 101 (42) | 42 (22) |
| Other doctor | 92 (65) | 124 (51) | 84 (44) |
| Psychologist | 7 (5) | 8 (3) | 6 (3) |
| CMHN | 23 (16) | 43 (18) | 21 (11) |
| OT | 5 (4) | 14 (6) | 17 (9) |
| Social worker | 14 (10) | 18 (7) | 10 (5) |
| Counsellor | 2 (1) | 3 (1) | 5 (3) |
| Art therapist | 7 (5) | 5 (2) | 5 (3) |
| Contact with supported accommodation staff | |||
| Face to face | 98 (70) | 144 (60) | 81 (42) |
| Group | 93 (66) | 96 (40) | 15 (8) |
| Personal care | 41 (29) | 5 (2) | 0 (0) |
| Inpatient care | |||
| Psychiatric inpatient | 27 (18) | 60 (25) | 23 (12) |
| Physical inpatient | 20 (14) | 41 (17) | 23 (12) |
| Service | Residential care (n = 141) | Supported housing (n = 242) | Floating outreach (n = 193) |
|---|---|---|---|
| External staff | |||
| Care co-ordinator | 3.2 (3.4) | 4.0 (3.6) | 4.2 (4.7) |
| Psychiatrist | 1.2 (0.4) | 1.2 (0.5) | 1.3 (0.7) |
| Other doctor | 3.1 (2.6) | 2.7 (2.9) | 3.0 (3.1) |
| Psychologist | 2.3 (1.9) | 1.8 (0.5) | 3.3 (2.2) |
| CMHN | 2.7 (1.9) | 5.1 (4.6) | 3.9 (2.5) |
| OT | 3.0 (1.9) | 2.3 (2.9) | 1.5 (0.6) |
| Social worker | 1.9 (1.4) | 2.4 (1.8) | 3.9 (7.1) |
| Counsellor | 7.0 (4.2) | 6.7 (4.7) | 8.8 (6.9) |
| Art therapy | 6.7 (5.5) | 11.0 (8.6) | 6.6 (4.5) |
| Contact with supported accommodation staff | |||
| Face to face | 12.2 (11.4) | 16.6 (16.1) | 22.8 (34.6) |
| Group | 9.5 (11.4) | 11.4 (11.4) | 4.6 (6.8) |
| Personal care | 70.1 (49.8) | 97.4 (51.6) | – |
| Inpatient care | |||
| Psychiatric inpatient | 176.3 (211.1) | 126.0 (149.1) | 122.3 (175.5) |
| Physical inpatient | 8.4 (7.3) | 13.8 (27.0) | 10.7 (23.2) |
| Service | Residential care (n = 141) | Supported housing (n = 242) | Floating outreach (n = 193) |
|---|---|---|---|
| External staff | |||
| Care co-ordinator | 55 (106) | 91 (131) | 40 (113) |
| Psychiatrist | 49 (67) | 55 (76) | 30 (67) |
| Other doctor | 91 (131) | 59 (105) | 57 (108) |
| Psychologist | 16 (87) | 6 (37) | 14 (93) |
| CMHN | 16 (46) | 32 (99) | 15 (53) |
| OT | 2 (14) | 3 (19) | 3 (10) |
| Social worker | 7 (27) | 7 (31) | 8 (70) |
| Counsellor | 2 (21) | 2 (20) | 3 (21) |
| Art therapy | 20 (148) | 10 (84) | 8 (51) |
| Contact with supported accommodation staff | |||
| Face to face | 240 (417) | 344 (683) | 445 (1470) |
| Group | 63 (91) | 62 (172) | 4 (24) |
| Personal care | 849 (3356) | 46 (395) | 0 (0) |
| Total non-inpatient costs | 1434 (3501) | 718 (906) | 640 (1584) |
| Inpatient care | |||
| Psychiatric inpatient | 11,376 (39,336) | 10,816 (31,900) | 5011 (24,763) |
| Physical inpatient | 671 (2286) | 1352 (7068) | 729 (4963) |
| Total inpatient costs | 12,046 (39,356) | 12,169 (32,281) | 5739 (25,144) |
| Service | Accommodation type, n (%) | ||
|---|---|---|---|
| Residential care (N = 15) | Supported housing (N = 41) | Floating outreach (N = 18) | |
| External staff | |||
| Care co-ordinator | 9 (60) | 27 (66) | 5 (28) |
| Psychiatrist | 5 (33) | 22 (54) | 2 (11) |
| Other doctor | 9 (60) | 28 (68) | 13 (72) |
| Psychologist | 1 (7) | 0 (0) | 0 (0) |
| CMHN | 1 (7) | 6 (15) | 2 (11) |
| OT | 1 (7) | 1 (2) | 3 (17) |
| Social worker | 1 (7) | 3 (7) | 0 (0) |
| Counsellor | 0 (0) | 3 (7) | 1 (6) |
| Art therapist | 0 (0) | 0 (0) | 1 (6) |
| Contact with supported accommodation staff | |||
| Face to face | 10 (67) | 26 (65) | 3 (17) |
| Group | 7 (47) | 14 (34) | 0 (0) |
| Personal care | 2 (13) | 1 (2) | 0 (0) |
| Inpatient care | |||
| Psychiatric inpatient | 3 (20) | 9 (23) | 1 (6) |
| Physical inpatient | 3 (20) | 6 (15) | 6 (33) |
| Service | Accommodation type, mean (SD) | ||
|---|---|---|---|
| Residential care (n = 15) | Supported housing (n = 41) | Floating outreach (n = 18) | |
| External staff | |||
| Care co-ordinator | 4.1 (3.4) | 6.0 (5.7) | 4.0 (3.0) |
| Psychiatrist | 1.6 (0.9) | 1.3 (0.6) | 1.0 (0.0) |
| Other doctor | 2.3 (1.7) | 3.9 (4.9) | 2.7 (2.3) |
| Psychologist | 1.0 (–) | – | – |
| CMHN | 12.0 (–) | 8.5 (6.3) | 3.5 (0.7) |
| OT | 1.0 (–) | 1.0 (–) | 1.0 (0.0) |
| Social worker | 1.0 (–) | 2.0 (1.0) | – |
| Counsellor | – | 4.3 (1.5) | 11.0 (–) |
| Art therapist | – | – | 3.0 (–) |
| Contact with supported accommodation staff | |||
| Face to face | 9.4 (8.1) | 8.4 (4.6) | 45.3 (64.8) |
| Group | 6.6 (7.9) | 6.6 (7.3) | – |
| Personal care | 45.5 (62.9) | 90.0 (–) | – |
| Inpatient care | |||
| Psychiatric inpatient | 258.3 (412.8) | 30.6 (28.2) | 296.0 (–) |
| Physical inpatient | 8.0 (10.4) | 9.3 (6.0) | 5.2 (4.4) |
| Service | Accommodation type, mean (SD) | ||
|---|---|---|---|
| Residential care (n = 15) | Supported housing (n = 41) | Floating outreach (n = 18) | |
| External staff | |||
| Care co-ordinator | 94 (126) | 152 (209) | 43 (90) |
| Psychiatrist | 58 (100) | 74 (82) | 12 (35) |
| Other doctor | 59 (72) | 112 (187) | 89 (112) |
| Psychologist | 9 (36) | 0 (0) | 0 (0) |
| CMHN | 30 (115) | 46 (139) | 14 (42) |
| OT | 2 (6) | 1 (4) | 4 (9) |
| Social worker | 3 (10) | 6 (23) | 0 (0) |
| Counsellor | 0 (0) | 7 (27) | 3 (15) |
| Art therapist | 0 (0) | 0 (0) | 23 (98) |
| Contact with supported accommodation staff | |||
| Face to face | 149 (232) | 191 (447) | 209 (818) |
| Group | 21 (45) | 20 (44) | 0 (0) |
| Personal care | 88 (337) | 32 (204) | 0 (0) |
| Total non-inpatient costs | 512 (424) | 649 (626) | 398 (835) |
| Inpatient care | |||
| Psychiatric inpatient | 18,032 (66,024) | 2461 (6417) | 5739 (24,349) |
| Physical inpatient | 933 (2996) | 837 (2362) | 1004 (2008) |
| Total inpatient costs | 18,964 (65,934) | 3298 (6522) | 6743 (24,181) |
| Variable | Accommodation type, mean (SD) | |||||
|---|---|---|---|---|---|---|
| Residential care | Supported housing | Floating outreach | ||||
| Yes | No | Yes | No | Yes | No | |
| Full cohort | ||||||
| Non-inpatient care | 398 (317) | 1552 (3676) | 590 (713) | 801 (1005) | 240 (687) | 1517 (2432) |
| Inpatient care | 0 (0) | 13,426 (41,339) | 4754 (12,955) | 16,978 (39,433) | 1537 (7747) | 14,407 (41,458) |
| Subcohort | ||||||
| Non-inpatient care | 155 (–) | 537 (427) | 557 (568) | 707 (665) | 363 (953) | 488 (475) |
| Inpatient care | 0 (–) | 20,319 (68,206) | 3817 (5988) | 2973 (6939) | 1211 (2313) | 21,127 (45,944) |
Appendix 4 Tables of results from work package 4
| Demographic data | Naturalistic (n = 9) | Randomised (n = 8) | Overall (n = 17) |
|---|---|---|---|
| Age (years), mean (SD) | 38.8 (10.7) | 38.9 (10.1) | 38.8 (10.1) |
| Male, n (%) | 6 (66.7) | 6 (75.0) | 12 (70.6) |
| Ethnicity – white, n (%) | 4 (44.4) | 4 (50.0) | 8 (47.1) |
| Diagnosis, n (%) | |||
| Schizophrenia | 8 (88.9) | 6 (75.0) | 14 (82.4) |
| Bipolar affective disorder | 1 (11.1) | 1 (12.5) | 2 (11.8) |
| Other | 0 (0.0) | 1 (12.5) | 1 (5.9) |
| Mean (SD) years of contact with services | 12.6 (9.6) | 8.3 (6.3) | 10.5 (8.3) |
| Previous type of accommodation, n (%) | |||
| House/flat (owner occupied) | 2 (22.2) | 1 (12.5) | 3 (17.6) |
| House/flat (housing association/council) | 0 (0.0) | 1 (12.5) | 1 (5.9) |
| House/flat (private rent) | 2 (22.2) | 2 (25.0) | 4 (23.5) |
| Hostel/group home | 0 (0.0) | 4 (50.0) | 4 (23.5) |
| Sheltered housing | 3 (33.3) | 0 (0.0) | 3 (17.6) |
| Residential home | 1 (11.1) | 0 (0.0) | 1 (5.9) |
| Hospital ward | 1 (11.1) | 0 (0.0) | 1 (5.9) |
| Scale | Interview | Participants providing data, n (%) (N = 17) | Mean % of scale completed |
|---|---|---|---|
| Baseline | |||
| Brief Psychiatric Rating Scale | Service user | 17 (100) | 100 |
| MANSA | Service user | 17 (100) | 90 |
| Time Use Survey | Service user | 17 (100) | 100 |
| Social Inclusion Scale | Service user | 17 (100) | 99 |
| EQ-5D | Service user | 17 (100) | 100 |
| CSRI | Service user | 17 (100) | – |
| LSP | Staff | 17 (100) | 98 |
| Compliance scale | Staff | 17 (100) | 100 |
| Health of the Nation Outcome Scale | Staff | 17 (100) | 98 |
| Time Use Survey | Staff | 17 (100) | 100 |
| CADS | Staff | 17 (100) | 100 |
| 6-month follow-up | |||
| Time Use Survey | Service user | 16 (94) | 94 |
| STAR – Client | Service user | 15 (88) | 88 |
| Time Use Survey | Staff | 14 (82) | 78 |
| STAR – Clinician | Staff | 17 (100) | 100 |
| 12-month follow-up | |||
| Brief Psychiatric Rating Scale | Service user | 14 (82) | 82 |
| MANSA | Service user | 14 (82) | 75 |
| Time Use Survey | Service user | 14 (82) | 82 |
| Social Inclusion Scale | Service user | 14 (82) | 82 |
| CAT scale | Service user | 13 (76) | 74 |
| STAR – Client | Service user | 13 (76) | 76 |
| EQ-5D | Service user | 14 (82) | 100 |
| CSRI | Service user | 14 (82) | – |
| LSP | Staff | 15 (88) | 88 |
| Compliance | Staff | 13 (76) | 76 |
| Health of the Nation Outcome Scale | Staff | 15 (88) | 85 |
| Time Use Survey | Staff | 11 (65) | 65 |
| CADS | Staff | 15 (88) | 88 |
| STAR – Clinician | Staff | 14 (82) | 82 |
List of abbreviations
- CADS
- Clinician Alcohol and Drugs Scale
- CANSAS
- Camberwell Assessment of Needs Short Assessment Scale
- CAT
- Client Assessment of Treatment
- CAT-SA
- Client Assessment of Treatment for Supported Accommodation
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CSRI
- Client Service Receipt Inventory
- ENMESH
- European Network for Mental Health Services Research
- EQ-5D
- EuroQol-5 Dimensions
- GMI
- Good Milieu Index
- HACT
- Housing Associations Charitable Trust
- ICC
- intraclass correlation coefficient
- IQR
- interquartile range
- KMO
- Kaiser–Meyer–Olkin
- LSP
- Life Skills Profile
- MANSA
- Manchester Short Assessment of Quality of Life
- OR
- odds ratio
- PMG
- Programme Management Group
- PSG
- Programme Steering Group
- QuEST
- Quality and Effectiveness of Supported Tenancies for people with mental health problems
- QuIRC
- Quality Indicator for Rehabilitative Care
- QuIRC-SA
- Quality Indicator for Rehabilitative Care: Supported Accommodation
- RCS
- Resident Choice Scale
- RCT
- randomised controlled trial
- SD
- standard deviation
- SIX
- Social Outcome Index
- SPRS
- Special Problems Rating Scale
- STAR
- Scale to Assess Therapeutic Relationship
- SURF
- Service User Research Forum
- WP
- work package
