Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number rp-pg-1210-12007. The contractual start date was in December 2012. The final report began editorial review in January 2018 and was accepted for publication in December 2018. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Karina Lovell, Peter Bower, Penny Bee, Richard Drake, Patrick Callaghan, Andrew Grundy, Anne Rogers, Helen Brooks and Linda Davies report holding other grants from the National Institute for Health Research during the conduct of this study.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Lovell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
SYNOPSIS
The problem we set out to address
For the last two decades, mental health policy and ethos have placed increasing emphasis on involving services users, and their carers, in their own care. This vision is in part driven by a strong moral argument that health-care delivery should be shaped and informed by the very people whom it aims to affect. Service users and carers, by virtue of their lived experience, can bring a wealth of experiential knowledge and expertise to mental health-care management.
Research evidence is accumulating to confirm that increased service user and carer involvement can lead to positive outcomes for both health-care systems and their users. 1–5 Service user involvement has been shown to enhance service quality and care engagement, reduce rates of enforced treatment and readmission and lessen social isolation and stigma. 6–8
Care planning is one area of contemporary practice that is conducive to service user involvement. 5–12 Mental health-care planning has been defined as ‘the process through which services in relation to an individual’s care are “assessed, planned, co-ordinated and reviewed“’13 (contains public sector information licensed under the Open Government Licence v3.0). The National Institute for Health and Care Excellence (NICE) states that people using mental health services should develop a care plan with mental health and social care professionals, and be given a copy of this care plan with an agreed date for review. 14 The Five Year Forward View for Mental Health15 upholds collaborative care planning as a priority goal for mental health services, and an essential Care Quality Commission (CQC) standard. 16
Although principles of service user and carer involvement are embedded in policy ideologies, evidence suggests that they have been suboptimally translated in practice. Service users and carers consistently report feeling unsupported by care planning processes and continue to request greater involvement in their care. 7,16,17 Dissatisfaction is evident across a variety of service settings and with a range of professional roles. 18,19 A recent CQC review of care involvement has highlighted ‘longstanding concerns’ with care planning involvement, concluding that routine practice can diverge quite substantially from policy recommendations for ‘person-centred care’20 (contains public sector information licensed under the Open Government Licence v3.0).
Identified barriers to service user and carer involvement in mental health services include poor information exchange,5 ritualised practices that limit opportunities for involvement,5,17 inhibitions or misconceptions regarding patient confidentiality and/or professional resistance to sharing decision-making power. Importantly, our recent systematic review5 found conceptual differences in the interpretation and meaning of involvement between service users and professionals. Although professionals tended to focus on objective evidence of service user involvement, such as ensuring that care plans were shared with and signed by service users, service users and carers tended to prioritise the qualitative experience of their involvement, specifically the consistency and quality of their care planning relationships.
If meaningful service user and carer involvement in care planning is to be achieved, then there is a pressing need to agree and foster a system-wide, user-centred model of collaboration and involvement. 21,22 Our research programme aimed to address the gap between policy and practice by addressing this need.
Aims of the programme
The Enhancing the Quality of User and Carer Involvement in Care Planning (EQUIP) programme was led by the University of Manchester and Manchester Mental Health and Social Care NHS Trust (now Greater Manchester Mental Health NHS Foundation Trust) in collaboration with the University of Nottingham and Nottinghamshire Healthcare NHS Trust. Prior to the programme grant award, we were awarded a Programme Development Grant (RP-DG-1209-10020) to undertake preparatory work, including a literature review, delivering a research methods course for service users and carers to increase service user and carer capacity to engage with the proposed research (see Appendix 1). In our programme of work, we aimed to develop, evaluate, implement and disseminate a co-produced and co-delivered training intervention for mental health professionals to improve service user and carer involvement in care planning.
This work was divided into four separate but inter-related workstreams (Figure 1).
FIGURE 1.
The EQUIP programme. Blue arrows denote service user and carer advisory group involvement. Dark blue boxes denote direct service user and carer advisory group input/output. Green arrows and boxes indicate significant input from service user and carer co-applicants/researchers. AMA, Ask Me Anything; RCT, randomised controlled trial.
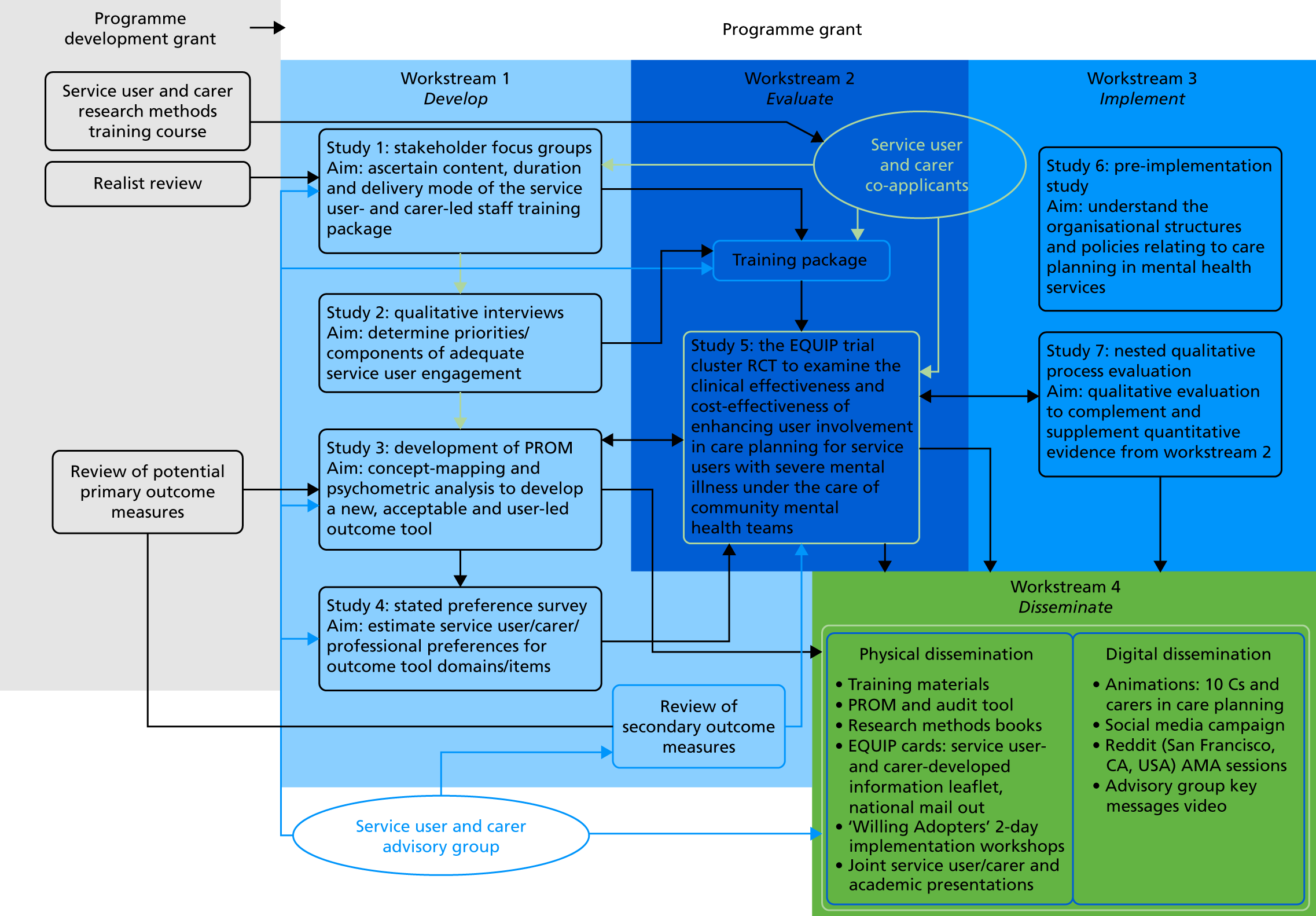
Workstream 1
-
Develop a co-produced training intervention to improve service user and carer involvement in care planning for mental health professionals.
-
Develop and validate a patient-reported outcome measure (PROM) of service user involvement in care planning, develop an audit tool and assess individual preferences for key aspects of care planning involvement.
Workstream 2
-
Evaluate the clinical effectiveness and cost-effectiveness of a co-delivered training package to enhance service user and carer involvement in care planning in secondary care mental health services.
Workstream 3
-
Understand the contextual, individual and organisational barriers and facilitators, and examine the processes involved in the development and use of service user- and carer-involved care planning.
Workstream 4
-
Disseminate our findings, training intervention materials and patient-mediated resources produced during the programme to all relevant stakeholders using multiple methods.
Programme management
The programme was sponsored by Manchester Mental Health and Social Care Trust, and the EQUIP multidisciplinary team was based across two sites (University of Manchester and University of Nottingham) and collectively formed the Programme Management Group, which met quarterly to monitor programme progression. The chief investigator was responsible for the overall leadership, management and output from the programme, and there was a designated lead for each workstream. Each site had a principal investigator, who led monthly team meetings with all programme site staff. A full risk assessment of the programme was conducted by the chief investigator and the trial manager, and a risk register was developed. The risk register was managed and monitored by the trial manager and the chief investigator, and was a standing agenda item at each Programme Management Group meeting. A Programme Steering Committee was established, comprising an independent chairperson with expertise in programme grants and care planning, and three other independent members including a service user and a clinician with experience of working in community teams. The Programme Steering Committee met biannually throughout the duration of the programme.
Ethics
The programme received a favourable ethics opinion from the National Research Ethics Service on 8 August 2014 (National Research Ethics Service Committee North West Lancaster, Research Ethics Committee reference 14/NW/0297; Integrated Research Application System project ID 125899).
Patient and public involvement
In our programme development grant (RP-DG-1209-10020), we developed and delivered a 6-day interactive training course on research methods for service users and carers to facilitate active engagement in the research programme. From this cohort, two service users and a carer became co-applicants on the programme grant, and others formed the service user and carer advisory group (SUCAG). Two service users were appointed (0.5 whole-time equivalent) for the duration of the programme and the carer (through personal choice) was appointed on a casual basis.
The service user and carer co-applicants have been integral to the research design, data collection, analysis and dissemination in workstreams 1 and 3, co-developing and delivering the training in workstream 2 and disseminating in workstream 4. The co-applicants have been supported to lead on writing papers and presenting at conferences, and to facilitate this process each service user and carer co-applicant was paired with a writing mentor. Three of the EQUIP papers16,17,23 have been led by co-applicants and all have developed considerable research skills; Andrew Grundy has completed the first year of a PhD (Doctor of Philosophy) qualification.
The service user co-applicants have also been fundamental in the provision of the research methods training, which we continued to deliver throughout the programme. A research methods book based on the training with significant contribution from service users and carers has been developed.
A SUCAG was convened at the start of the programme grant and held 11 meetings between March 2013 and April 2017. Members of the SUCAG were recruited from the first two cohorts of the service user and carer research methods training course, and those with similar experience from the Nottingham area. An independent chairperson of the group was recruited via expression of interest from the pool of trained service users and carers.
Members of the SUCAG (14 in total) have had a primary role in advising the study team throughout the grant. Activities have included confirming outcome measures for the trial across a range of domains that were identified by service users and carers as part of the programme development work; informing development of the PROM through identification of key questions of ‘quality in care planning’; co-developing a definition of care planning; contributing to the methodological development of workstream 3, particularly in relation to the use of diaries and observations of care planning meetings; contributing to the development of the trial outcome measure packs (advice on presentation and ordering of measures to reduce participant fatigue); contributing case studies for intervention training; and reviewing all the participant trial documentation, for example by providing reviews of the participant information sheets and covering letters prior to submission for ethics review.
The SUCAG meetings have also provided a regular opportunity for the research team to provide feedback on the programme progress and to explain the funder reporting requirements, for example the 24-month checkpoint reporting process.
Members of the SUCAG were invited to apply to become trainers to co-deliver the training intervention for health professionals in workstream 2. The rationale for running a ‘train the trainers’ course was that few had any experience in training and expressed fears and concerns about training mental health professionals. Nine people applied and all were offered places on a ‘train the trainers’ course (with the view that six would co-deliver the training and three would be held in reserve in case of sickness/absence).
Throughout the programme grant, we have used the EQUIP website (http://research.bmh.manchester.ac.uk/equip), Twitter (https://twitter.com/Care_Plan) (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) and regular study newsletters to engage with interested parties and to keep them up to date with the programme. We have also sought to use online and innovative media platforms to actively engage with service users, carers and health professionals via our patient-mediated materials (e.g. the service user 10Cs16 animation of care planning and accompanying EQUIP cards, http://research.bmh.manchester.ac.uk/equip/10Cs, and the award-winning carers animation, http://research.bmh.manchester.ac.uk/equip/mentalhealthcareplanning). With the SUCAG, we have developed a video dissemination of patient and public involvement (PPI) in the study to ensure that it is accessible to a wider public audience beyond our research participants and colleagues in health and academia.
The strength of PPI throughout the programme grant has been underpinned by having a nominated lead for PPI in place to co-ordinate PPI activities across the four workstreams, to liaise with the SUCAG and to provide support to co-applicants with lived experience of mental health difficulties. We were awarded the Mental Health Research Network award for outstanding carer involvement in March 2014. In 2018, we were awarded the National Institute for Health Research (NIHR) Clinical Research Network (CRN) McPin MQ Service User & Carer Involvement in Mental Health Research Award. Notably, all of our SUCAG members have taken up advisory group roles in other studies.
We have all benefited and feel privileged to have worked with service users and carers. There is little doubt that the quality of the programme has been much enhanced by our co-development, delivery, production and dissemination activities.
Workstream 1: development
The aims of workstream 1 were to develop a:
-
training intervention to enhance service user and carer involvement in care planning in secondary care mental health services
-
PROM that better meets user and carer requirements for quantifying the extent of their care planning involvement in UK mental health services.
Key findings from a systematic review conducted as part of the programme development grant (RP-DG-1209-10020; see Appendix 1) created a foundation on which to build up evidence through the workstream using focus groups (study 1) and interviews (study 2) with service users, carers and mental health professionals. Following data collection, findings were synthesised by the whole research team during a ‘synthesis day’ and key material was generated with which to develop training material for a course for health professionals. The data collected were also used to inform the content for a PROM and the audit tool (study 3) and a stated preference survey (study 4) to measure service user and carer involvement in care planning.
Outputs
The findings of the systematic review are published in Bee et al. 24 (see Appendix 2).
Study 1
The aim of study 1 was to develop the content, delivery mode and length of a user- and carer-led training intervention for health professionals, and to improve user and carer involvement in care planning.
Methods
Focus groups were conducted with a range of stakeholders (service users, carers and mental health professionals). Focus group interview schedules were informed by the systematic review5 and developed by the research team, with input from academics, clinicians and service users and carers from the research programme and the SUCAG. Schedules covered current perspectives on user involvement in care planning, the process and outcomes of care planning, prior experiences of service user and carer involvement and potential training requirements. Focus groups lasted approximately 60–90 minutes and were undertaken at a range of locations to support participation: at university campuses, trust sites and community locations (e.g. at carers’ centres and participants’ homes). Participants received high-street gift vouchers worth £25 for taking part.
Participants were recruited purposively from Manchester Mental Health and Social Care Trust using a range of methods (trust intranet advertisements, press releases, posters in trust premises and information distributed through carer and service user networks and forums). An initial target to conduct six focus groups was exceeded, with a total of nine focus groups taking place, involving 61 participants across the groups. Four focus groups were conducted with service users and carers (n = 34), four were with health professionals (n = 18) and there was one mixed group with users, carers and professionals (n = 9).
Focus groups were recorded, transcribed and anonymised, then analysed using a qualitative framework approach,25 an acknowledged method of analysing primary qualitative data pertaining to health-care practices with policy relevance. 26 Data from the focus groups were synthesised with further data from individual interviews (study 2) and key findings are reported in study 2.
Study 2
The aim of study 2 was to determine the priorities and core concepts underpinning service user and carer engagement and involvement in care planning in mental health services.
Methods
Individual qualitative interviews were conducted with service users, carers and mental health professionals.
Data from individual interviews were collected with the intention to combine with study 1 data to prevent missing any issues that participants might be reluctant to raise in a focus group situation. 27 Participants were recruited as per study 1, with further recruitment from Nottinghamshire Healthcare NHS Trust via poster displays, trust newsletters and the intranet, university press releases, oral presentations at service user and carer groups and via service user and carer news bulletins and websites. Interviews lasted approximately 60–90 minutes and were undertaken at a range of locations to support participation: at university campuses, trust sites and community locations (e.g. at carers’ centres and participants’ homes). Participants received high-street gift vouchers worth £25 for taking part. A total of 74 interviews across Manchester (n = 43) and Nottingham (n = 31) were completed (22 service users, 21 carers, 3 user/carers and 28 professionals). A number of interview participants also took part in the focus groups in study 1 (n = 22).
Interviews were recorded, transcribed and anonymised, and analysed in combination with data from study 1 using framework analysis. Framework analysis is commonly used within qualitative health research and allows for both inductive and deductive coding to be incorporated into the analysis process, which means that codes emerging from the data can be combined with important codes that were identified prior to the study. The analysis team comprised service user and carer co-applicants working alongside experienced qualitative researchers for independent coding purposes. The team read their transcripts on multiple occasions to familiarise themselves with the data before starting to code the transcripts. The data and analysis were managed using a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) database comprising participant characteristics, along with a Microsoft Word (Microsoft Corporation, Redmond, WA, USA) document containing emerging themes from each transcript, to provide a data trail. The team met regularly to discuss their own emergent codes, to develop a provisional coding framework, to discuss alternative explanations of interpretations and to ensure that the emerging codes remained grounded in the original data for purposes of validity. This approach to analysis meant that during the constant comparison of new data, the provisional framework was amended and re-shaped to enable the introduction of new codes, and allowed for the removal of other codes that became superfluous over the course of the analysis. The resultant framework contained only those codes agreed on by the whole analysis team. Previous iterations of the coding framework were stored for purposes of transparency and the research team agreed as a whole when data saturation had occurred and no new themes were emerging from the data. In order to further strengthen the validity of the qualitative findings, the final coding framework was presented to the wider study team, which was asked to comment on whether the framework seemed grounded in the data, on any omissions in the framework or any ambiguities.
Key findings
The combined data from studies 1 and 2 were divided into separate categories for user and carer data and health professional data.
Health professionals
A clear training need was identified by health professionals, with strong support for the idea of user and carer involvement in that training, and for whole-team training for greater impact. A range of barriers to service user involvement were identified, including individual barriers, such as skills deficits and staff understanding of user-involved care planning, and organisational barriers, including workload/resource pressures, the current key performance indicator/target culture of the NHS and difficulties balancing involvement with risk management.
Service users and carers
In accordance with the professional data, users and carers identified a need for training for all mental health staff, but there was a feeling that senior clinicians might benefit most. There were suggestions that training should prioritise skills in active listening and communication, assertiveness and time for reflection. Participants believed that the training should be mandatory, accredited and updated regularly, and should be co-delivered in order to value the expertise of service users and carers. Potential barriers to effective training were also raised, including staff workload and attitude, lack of accountability and reluctance among service users and carers to be involved as trainers. Issues around care plans also emerged, where care plans were seen as meaningless, not tailored to individuals and not taking into account service users’ and carers’ wishes, experiences or needs. Participants felt that good involvement is facilitated by good relationships with and between staff, effective communication, partnership working and allowing sufficient time during care planning. Barriers to involvement were highlighted as frequent staff changes, workload, lack of knowledge about services by all parties, unhelpful staff attitudes and episodes of severe illness.
Outputs
A full description of the methods, analysis and results have been published in Bee et al. ,24 Cree et al. 17 and Grundy et al. 16 (see Appendix 2).
Strengths and limitations
We examined care planning issues with contemporary mental health services in depth across a large sample and from multiple stakeholder perspectives, maximising the transferability of our findings. We included service users and carers in analysis (independent coders) and presented our coding manuals to the SUCAG to optimise the rigour of our analysis. It is likely that the health professionals who took part in these studies were those who were motivated to achieve ‘good’ care planning and/or were open to organisational and individual change. The data also reflect only the views of health professionals within only two NHS trusts and may not be generalisable to other individuals, settings or localities. In terms of service user and carer data, we interviewed a self-selected sample of participants, many of whom had particularly strong views on the shortcomings of the care planning process. Despite efforts to recruit directly from black, Asian and minority ethnic (BAME) third-sector organisations, there was only a small minority of participants from BAME groups.
What the studies add
Health professional data show that a combination of individual and organisational factors currently hinder successful service user and carer involvement in care planning, and highlight a clear need to deliver training to increase the quality and consistency of care planning procedures. The studies also draw attention tothe fact that service users and carers are concerned about the way in which care plans are created and implemented, and that there is a shared perception between service users and carers of a reluctance among health professionals to involve them in the care planning process.
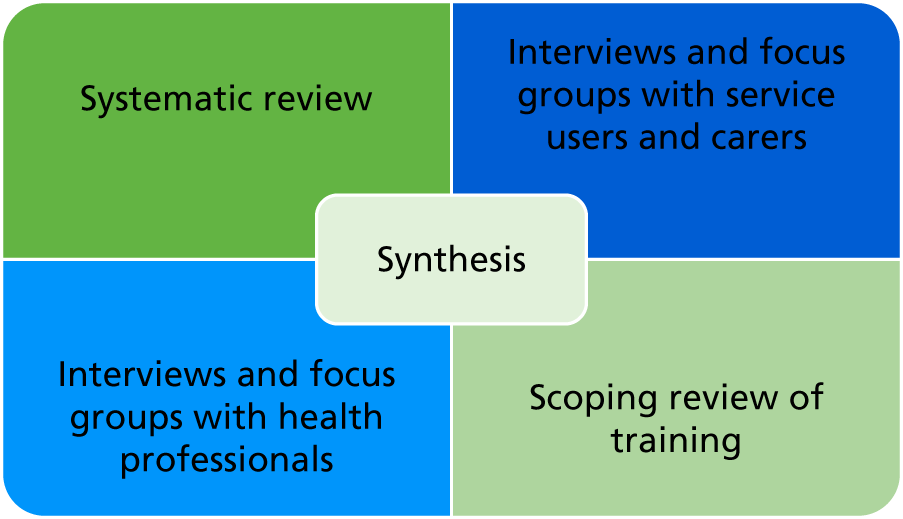
Scoping review of training
Building on the evidence gathered for training content, a scoping review was conducted to identify relevant work that could inform the development, delivery and implementation of the training courses. Three key reviews were identified. 28–30 The exercise produced a number of key findings relevant to the development of the training programme, including that small interactive groups are more effective than large didactic groups; educational outreach (supervision) is effective; improving collaboration between health professionals might be helpful; multifaceted interventions are likely to be better than single-strand intervention; and providing patient materials may help implementation.
Data synthesis
A synthesis day was held with all study applicants and researchers in November 2013.
The two key aims of the synthesis day were to:
-
synthesise the evidence from workstream 1 to develop the training intervention for health professionals
-
develop a ‘train the trainers’ course for service users and carers to co-deliver the training intervention.
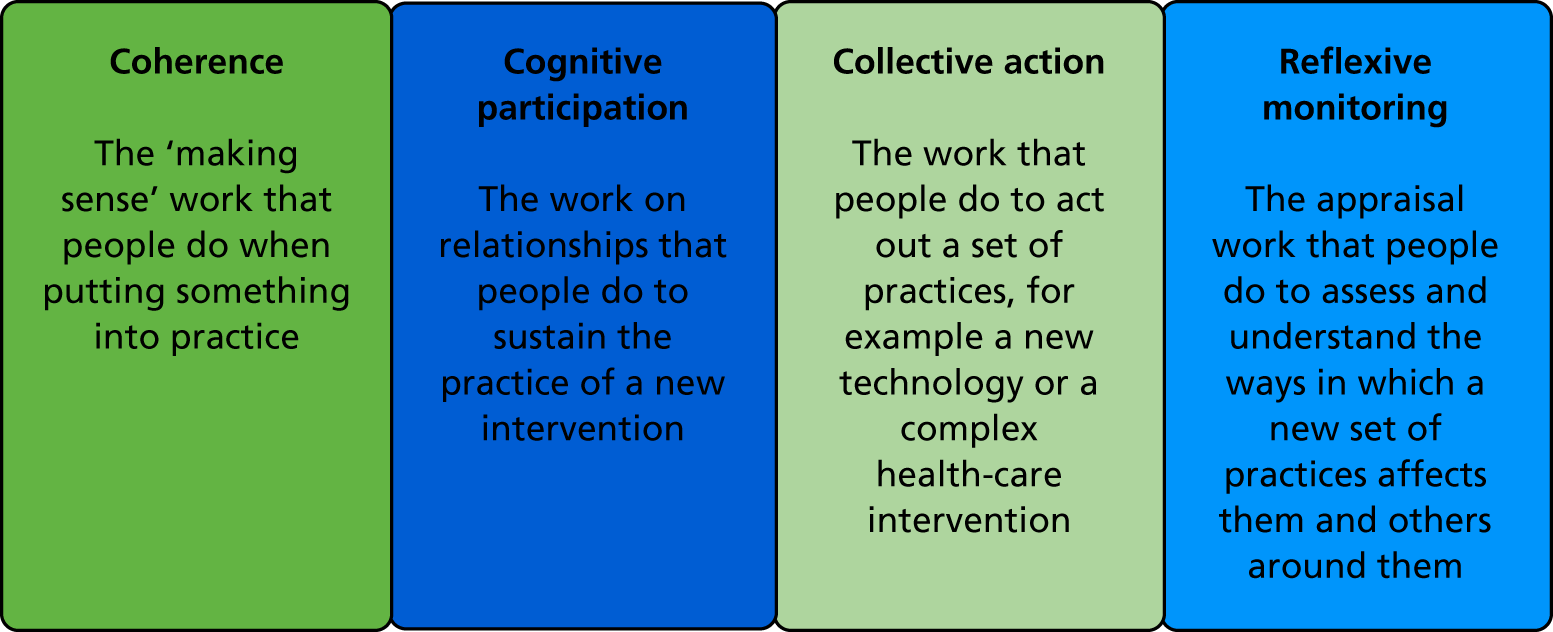
Structured summaries of key findings from the systematic review, focus groups and interviews with service users, carers and health professionals, and from the scoping review of training interventions, were distributed by study leads to the group (see Appendix 2). Our synthesis (Figure 2) followed a similar format to formats of previous studies, where we successfully synthesised a variety of data sources. 31–33 A group discussion involved tabulating key evidence statements within a matrix where each row referred to the results from each dataset and each column represented one of the core training components for both the training intervention and the ‘train the trainers’ course (see Appendix 2).
FIGURE 2.
Synthesis of multiple data sources.
Training intervention for health professionals
The core training components included the content, attendance, duration, delivery mode, resources needed and system requirements that we wished to address. The matrix provided the platform for a structured discussion between the programme team to derive the final training intervention and ‘train the trainers’ course. Those components that did not provide evidence or were ambiguous were discussed by applicants in small teams until a consensus was reached.
The training intervention is detailed in accordance with the Template for Intervention Description and Replication (TIDieR) guidelines in Box 1. 34
Why: our aim was to co-develop, co-produce and co-deliver (with service users/carers) a best-evidence, acceptable and feasible training programme for mental health professionals to enhance user and carer involvement in care planning. Two reviews were conducted, including a narrative synthesis (Bee et al. 5), which examined how user-involved care planning is operationalised within mental health services and to establish where, how and why challenges to user involvement occur; and a scoping review of training reviews and interventions that change clinician behaviour. In addition, focus groups and individual interviews with service users, carers and health professionals were conducted to ascertain training content and delivery requirements and to determine the priorities and components of adequate user and carer involvement in care planning. The evidence from the reviews and qualitative data were synthesised to develop and design the training.
What: a range of training materials have been developed for the training, including Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) slides, case scenarios, audio-recordings from health professionals, service users and carers and a trainer’s manual.
Who: the synthesis identified that the training should be multidisciplinary, including all health professionals and psychiatrists. Team training was seen as optimal and, as far as possible, teams will be trained together. The training will be delivered by two of the co-applicants (both academics with teaching experience) and three or four service users and carers who have attended a 4-day ‘train the trainers’ course.
How: the synthesis indicated that training should include a range of formats: face to face, self-directed learning and follow-up supervision. The consensus exercise indicated a minimum of 15 hours and maximum of 30 hours. The course will run for 2 days (12 hours) plus 6 hours’ follow-up supervision and 8 hours’ self-directed learning (optional). Hence, each health professional will receive 18 hours of facilitated training and an additional optional 8 hours’ self-directed learning.
Where: consensus was reached that the training venue should be outside the clinical area, geographically convenient, provide good catering and in a venue with appropriate training resources.
When and how: the training will be delivered to each cluster randomised to the training intervention over 2 days. In recruiting teams, we ask that 80% of the care co-ordinators within each team attend the training. The training will be delivered within 6 weeks of service users being recruited into the trial.
Tailoring: the intervention has been tailored for health professionals.
Modifications: only minor modifications will be made in the light of feedback during the trial. If the trial is successful and we implement the training across other NHS trusts, modifications will be made in the light of feedback collected from the process evaluation.
How well: fidelity of the training has been ensured by the careful development and synthesis work described earlier, the ‘train the trainers’ course, the development of a detailed manual and the delivery of training by the same groups of trainers.
The core components of the training were a training package including a training manual, training materials, presentations, and group exercise materials consisting of 2 days’ face-to-face training (12 hours in total), an 8-hour optional self-directed learning package and 6 hours’ supervision per team in the 6 months post training.
The 2-day training intervention included interactive presentations, audio-visual clips, small group exercises, skills practice exercises (including role play), live demonstrations of good practice, and working with anonymised care plans or anonymised examples from professionals’ caseloads. We wanted to move away from the ‘sharing personal stories’ model of user/carer ‘involvement’ in delivering training; thus, although the academic researcher was the lead facilitator, the service users and the carers facilitated group work, shared both positive and negative experiences of care planning and shared ideas around good and poor practice with the wider group throughout the 2 days.
The training team consisted of two academic researchers, six service users and one carer. We delivered the initial training as a whole team to ensure consistency; subsequent training sessions comprised one academic researcher and two or three service users and carers. Over the duration of the study, some of the service users and carers took leading roles in the training. The training was designed to be a co-produced and co-delivered training resource.
‘Train the trainers’ course
The synthesis contributed to the development of the ‘train the trainers’ course. A 4-day course was designed to train service users and carers to deliver the training course to health professionals. The underlying philosophy of the programme was participatory learning and andragogy (adult learning) and aimed to enable participants to understand the principles of training and identify the attributes and values of an effective trainer. The training focused on core educational principles of delivering high-quality training, including facilitating small and large groups, engaging and empowering trainees and maximising the use of training materials. The fourth day of training included a review of the EQUIP professional training intervention for health professionals and an opportunity to practice presentation and facilitation skills.
In addition to our three service user and carer co-applicants, we recruited six service users and carers from our SUCAG with the aim of having a core team of six trainers and three reserves in case of sickness/absence. The course was delivered by the study team in June 2014 and incorporated 2 days of educational principles, 1 day of micro-teaching with peer feedback and a final day focusing on delivering the training intervention for health professionals. (Training materials are available on request from the authors.)
Evaluation of the ‘train the trainers’ course
The aim of the study was to obtain views from service users and carers who attended the ‘train the trainers’ course 1 year following completion of the course, when participants had had exposure of delivering the training. In particular, the team wanted to elicit feedback on training facilitation, content and preparedness for undertaking a trainer role on the EQUIP care planning training intervention for mental health professionals.
Methods
Individual semistructured interviews to explore participants’ views on training acceptability were used. Letters of invitation to take part in the evaluation were sent to all nine trainees approximately 7 months after the completion of training. Participants had to opt in (by e-mailing or phoning). All nine trainees agreed to take part and provided written informed consent. Interviews were digitally recorded and transcribed verbatim. Of the nine participants, there were six service users (four female, two male) and three carers (two female, one male). Transcripts were analysed independently by two members of the trial team using thematic inductive coding of themes emerging to uncover meaning in participants’ accounts of their involvement in the training process. 35 The team met to review themes and reach agreement on the coding of the data and the overarching themes.
Key findings
Course content was rated highly but may benefit from review and/or extension to allow the range of topics and resulting professional training programme to be covered in more depth. Trainees who delivered the training intervention to health professionals were positive about their support experiences, preparedness and personal impacts. Service users and carers wanted to gain new skills and confidence in presentation/facilitation as well as to make a difference to health-care practice. We also found that service users desired different levels of involvement in training facilitation – some wanted to take a more active role than others.
Outputs
A full description of the methods, analysis and results has been published in Fraser et al. 36 (see Appendix 2).
Study 3
The aim of study 3 was to co-develop, with service users and carers, a PROM to assess user/carer involvement in mental health-care planning and an audit tool for mental health services.
Patient-reported outcome measure
We undertook a systematic review reporting the use, development and/or validation of user- and/or carer-reported outcome measures of involvement in mental health-care planning. 37 The review revealed a lack of care planning measures that are able to meet service user nominated acceptability criteria alongside published standards for psychometric quality. Our aim was to co-develop a PROM to assess user and carer involvement in care planning and the SUCAG suggested that the measure should include the following attributes: suitable for use in the UK; developed via service user and carer collaboration; available in a self-report format for both service users and carers; rated by both service users and carers; based on a social and recovery model; continuous rather than a dichotomous scale; and between 12 and 15 items long.
Audit tool
We developed an audit tool to inform clinicians, services, auditors and researchers who want to quantify levels of user and carer involvement in care planning.
Methods
Potential PROM items were generated from data collected in workstream 1 (studies 1 and 2); 70 candidate items were developed. Face validity was examined with a mixed sample of 16 members of the SUCAG using cognitive interviewing. Nine items were removed because the SUCAG found their language or wording unclear or hard to understand.
The remaining 61 items constituted the nascent scale. Members of the SUCAG were also asked to comment on potential response formats. Consensus was reached for a five-point Likert scale with named anchors of ‘strongly disagree’ and ‘strongly agree’ and a middle neutral value with the label ‘neither agree nor disagree’.
We recruited self-identified service users with severe and enduring mental health problems and carers to complete the emerging PROM, using multiple recruitment strategies (including advertising on NHS trust intranets, newsletter and press releases; posters displayed on trust premises, local trust-based and third-sector study advocates, via Twitter and re-tweeted by local and national mental health charities across the UK and local and national service user and carer forums). Data were collected using online (SelectSurvey version 4.5; ClassApps, Kansas City, MO, USA), postal and face-to-face modalities.
In total, 402 participants completed the 61-item PROM. A randomly selected sample of the 402 were approached to undertake a second completion 4 weeks after baseline, to assess test–retest validity, and 59 test–retest PROMs were completed.
For Rasch analysis, a minimum sample size of 250 allows for > 99% confidence that item calibrations are stable to within ± 0.5 logits, irrespective of scale targeting. This minimum sample size was also deemed sufficient. Prior to statistical analysis, data were double entered and a 5% accuracy check was made. Less than 0.1% errors were detected during the double-entry procedure.
Psychometric and statistical analysis of the data were conducted, involving exploratory factor analysis, Mokken analysis,38 Rasch analysis,39 category threshold analysis, differential item functioning, local dependency, scale reliability, unidimensionality and test–retest reliability. An iterative process of item removal reduced the remaining 61 items to a final 14-item scale (Table 1). The final scale has acceptable scalability (H0 = 0.69), reliability (α = 0.92), fit to the Rasch model [χ2(70) = 97.25, p = 0.02], and no differential item functioning or locally dependent items. Scores remained stable over the 4-week follow-up period, indicating good test–retest reliability.
| Item | Completely disagree | Neither agree nor disagree | Completely agree | ||
|---|---|---|---|---|---|
| 1. The care plan has a clear objective | 0 | 1 | 2 | 3 | 4 |
| 2. I am satisfied with the care plan | 0 | 1 | 2 | 3 | 4 |
| 3. I am happy with all of the information on the care plan | 0 | 1 | 2 | 3 | 4 |
| 4. The contents of the care plan were agreed on | 0 | 1 | 2 | 3 | 4 |
| 5. Care is received as it is described in the care plan | 0 | 1 | 2 | 3 | 4 |
| 6. The care plan is helpful | 0 | 1 | 2 | 3 | 4 |
| 7. My preferences for care are included in the care plan | 0 | 1 | 2 | 3 | 4 |
| 8. The care plan is personalised | 0 | 1 | 2 | 3 | 4 |
| 9. The care plan addresses important issues | 0 | 1 | 2 | 3 | 4 |
| 10. The care plan helps me to manage risk | 0 | 1 | 2 | 3 | 4 |
| 11. The information provided in the care plan is complete | 0 | 1 | 2 | 3 | 4 |
| 12. The care plan is worded in a respectful way | 0 | 1 | 2 | 3 | 4 |
| 13. Important decisions are explained to me | 0 | 1 | 2 | 3 | 4 |
| 14. The care plan caters for all the important aspects of my life | 0 | 1 | 2 | 3 | 4 |
For the audit tool (Table 2), we completed a three-round consensus exercise with our SUCAG (n = 16) and reduced the 61 candidate PROM items to form a shorter six-item audit tool. In round 1, items were presented to the SUCAG members (n = 16), who were each asked to select the top 10 PROM items that they felt were most important to include in an audit tool. A total of 27 items were identified by the group. In round 2, these 27 items were discussed, with individuals providing verbal reasoning for their choices. The 27 items were then re-rated for importance based on the group discussion, reducing the pool down to 10 items. In round 3, these 10 items were identified and discussed further until consensus was reached on six audit tool priorities. Psychometric assessment assessed the performance of the six items identified by the SUCAG using a combination of classical test, Mokken and Rasch analyses. Test–retest reliability was calculated using t-tests of interval level scores between baseline and 2- and 4-week follow-up.
| Item | Completely disagree | Neither agree nor disagree | Completely agree | ||
|---|---|---|---|---|---|
| 1. I am satisfied with the care plan | 0 | 1 | 2 | 3 | 4 |
| 2. My preferences for care are included in the care plan | 0 | 1 | 2 | 3 | 4 |
| 3. The care plan helps me to manage risk | 0 | 1 | 2 | 3 | 4 |
| 4. The information provided in the care plan is complete | 0 | 1 | 2 | 3 | 4 |
| 5. Important decisions are explained to me | 0 | 1 | 2 | 3 | 4 |
| 6. The care plan caters for all the important aspects of my life | 0 | 1 | 2 | 3 | 4 |
Key findings
The 14-item PROM ‘Enhancing the Quality of User and Carer Involvement in Care Planning (EQUIP)’ scale displays excellent psychometric properties and is capable of unidimensional linear measurement. The scale is short, user- and carer-centred and will be of direct benefit to clinicians, services, auditors and researchers wishing to quantify levels of user and carer involvement in care planning (see Table 1). A six-item audit tool was also developed for NHS trusts (see Table 2).
Strengths and limitations
We undertook a stringent, methodological process leading to an initial PROM measure of 61 items, developed in conjunction with service users and carers, and reduced to a 14-item psychometrically validated PROM. Measure length and ease of completion were identified as key user-nominated attributes for PROM acceptability. However, the utility of any measure depends on its validity, reliability, sensitivity and feasibility of completion and a trade-off between these criteria is often necessary. It is possible that some concepts that were originally conceived as important to service users during item generation were not adequately represented by the items retained in the final measure. This accepted, the final measure encompassed a breadth of items that represented a multiplicity of user responses. The attributes selected as most important for the audit tool were chosen by our SUCAG and may lack a diverse or representative sample of individuals using secondary care mental health services.
What this study adds
Current measures, such as those used by the UK CQC, focus on objective indicators of care planning administration rather than those aspects of care planning that service users value most. Our 14-item PROM ‘Enhancing the Quality of User and Carer Involvement in Care Planning (EQUIP)’ addresses this gap. The scale is short, user- and carer-centred and will be of direct benefit to clinicians, services, auditors and researchers wishing to quantify levels of user and carer involvement in care planning.
Outputs
The systematic review reporting the outcome measures of involvement in mental health-care planning has been published in Gibbons et al. 37 (see Appendix 2).
The description of analysis, methods and results of the PROM has been published in Bee et al. 40 (see Appendix 2).
Study 4
The aim of study 4 was to use a stated preference survey to estimate the strength of user/carer preferences and weights for key items included in the audit tool.
Methods
We used a binary discrete choice experiment with five attributes (i.e. whether or not preferences for care are included in the care plan; whether or not the care plan helps me manage risk; completeness of the information in the care plan; whether or not important decisions are explained to me; and whether or not all important aspects of my life are catered for) and an additional attribute describing the time per person spent on care planning related activities. Each attribute had five levels. Each level described how the service might be described by service users, from completely disagree (the reference level) to completely agree. Table 3 shows an example choice question; 13 choice questions were designed, with each choice question describing two alternative care planning approaches for participants to choose their preferred option.
| Which care plan do you prefer? (tick one) | Care plan A | Care plan B |
|---|---|---|
| My preferences for care are included in the care plan | Completely disagree | Completely agree |
| The care plan helps me to manage risk | Neither agree nor disagree | Disagree |
| The information provided in the care plan is complete | Completely agree | Agree |
| Important decisions are explained to me | Neither agree nor disagree | Disagree |
| The care plan caters for all the important aspects of my life | Agree | Neither agree nor disagree |
| The average time you spend each month to prepare for, attend or follow up on care planning meetings is . . . | 2 hours | 4 hours |
Service user and carer participants were recruited from adult secondary care mental health services in two NHS trusts, and online via social media. Participant characteristics were summarised with descriptive statistics. The analyses included all participants who completed one or more choice set. For the analysis, the completely disagree level of each attribute was used as the reference level for each of the audit tool attributes. This gives an indication of the value to participants of moving from the worst to an improved level of involvement in the care planning process.
This first step was to summarise and describe the data and inform further analysis. Accordingly, it was hypothesised that higher levels for the audit tool attributes (e.g. agree or completely agree) would be preferred to lower levels (e.g. disagree or completely disagree). In contrast, it was thought that participants would prefer to spend less rather than more time per month on care planning activities. A conditional logit regression using maximum likelihood estimation was used as the starting point for the analysis. 41,42 However, participants’ preferences may vary because of factors that are observed, such as sociodemographic characteristics, type of respondent (service user or carer), design factors (e.g. postal vs. online survey), or because of unobserved factors. To account for this, a random-effects, mixed logistic regression model was used for the main analysis. 43 The analysis treated all attributes as random.
A marginal rate of substitution was calculated using the time spent per month on care planning related activities to estimate the amount of time each person is willing to trade to gain their preferred levels of each audit tool attribute.
Stata® version 15 (Stata Corp LP, College Station, TX, USA) was used for all the analyses reported here. The mixed logistic regression used the published mixlogit and wtp (delta) user commands developed for Stata. 44,45
Key findings
We recruited 232 participants, of whom 89% completed all choice questions. Most responses were from service users (n = 132/215, 61%), carers (n = 49/215, 23%) and people identifying themselves as both service users and carers (n = 34/215, 16%). Seventeen participants did not report if they were services users or carers. The mixed logit regression results are summarised in Table 4.
| Attribute | Coefficient (SE) | p-value | MRS (95% CI) |
|---|---|---|---|
| My preferences for care are included in the care plan | |||
| Completely disagree | Reference level | ||
| Disagree | –0.539 (0.080) | < 0.001 | –4.6 (–7.9 to –1.4) |
| Neither agree nor disagree | 0.102 (0.069) | 0.141 | 0.9 (–0.4 to 2.2) |
| Agree | 0.567 (0.083) | < 0.001 | 4.9 (1.4 to 8.3) |
| Completely agree | 0.797 (0.103) | < 0.001 | 6.8 (2.1 to 11.5) |
| The care plan helps me to manage risk | |||
| Completely disagree | Reference level | ||
| Disagree | –0.508 (0.076) | < 0.001 | –4.4 (–7.7 to –1.0) |
| Neither agree nor disagree | 0.209 (0.082) | 0.011 | 1.8 (0.2 to 3.4) |
| Agree | 0.532 (0.083) | < 0.001 | 4.6 (1.3 to 7.9) |
| Completely agree | 0.484 (0.099) | < 0.001 | 4.2 (0.4 to 7.9) |
| The information provided in the care plan is complete | |||
| Completely disagree | Reference level | ||
| Disagree | –0.116 (0.071) | 0.102 | –1.0 (–2.3 to 0.3) |
| Neither agree nor disagree | –0.002 (0.077) | 0.979 | 0.0 (–1.3 to 1.3) |
| Agree | 0.115 (0.083) | 0.165 | 1.0 (0.0 to 2.5) |
| Completely agree | 0.188 (0.077) | 0.015 | 1.6 (0.1 to 3.1) |
| Important decisions are explained to me | |||
| Completely disagree | Reference level | ||
| Disagree | –0.230 (0.070) | 0.001 | –2.0 (–3.7 to –0.2) |
| Neither agree nor disagree | 0.077 (0.064) | 0.227 | 0.7 (–0.5 to 1.8) |
| Agree/completely agree | 0.577 (0.076) | < 0.001 | 4.9 (1.6 to 8.3) |
| The care plan caters for all the important aspects of my life | |||
| Completely disagree | Reference level | ||
| Disagree | –0.216 (0.070) | 0.002 | –1.9 (–3.6 to –0.1) |
| Neither agree nor disagree | 0.049 (0.063) | 0.436 | 0.4 (–0.7 to 1.5) |
| Agree/completely agree | 0.519 (0.079) | < 0.001 | 4.5 (1.2 to 7.7) |
| Average time you spend each month to prepare for, attend or follow up on care planning meetings | |||
| Time | –0.002 (0.001) | 0.005 | Not applicable |
The data suggested that preferences were strongest for the attribute ‘my preferences for care are included in the care plan’, with service users prepared to spend 5 hours [95% confidence interval (CI) 1 to 8 hours] and 7 hours (95% CI 2 to 12 hours) per month for improvements compared with the reference level. The least preferred attribute was whether or not the information included in the care plan was complete, with participants willing to spend 1.5 hours (95% CI 0.1 to 3.0 hours) for improvements, compared with the reference level.
Strengths and limitations
Service users and carers were involved in the design of the discrete choice experiment, survey materials and recruitment. Our recruitment methods increased the chance of self-selection into the study and may reduce the representativeness of participants and we used analysis methods to help account for variation in participants’ preferences because of unobserved factors or individual characteristics. In addition, survey respondents were based in the UK and were predominantly female and white British. Thus, the results may not be generalisable within and outside the UK. We used a main effects design that means that important interactions between the study attributes were not accounted for, reducing the robustness of the results.
What this study adds
To our knowledge, this is one of the first large, full-profile, discrete choice experiments conducted with people with serious mental illness. The study results demonstrated that participants preferred care plans that emphasised their involvement by including their preferences, helping them to manage risk, catering for all of the important aspects of their life and by having important decisions explained to them. The completeness of information included in the care plan was the least preferred attribute. The marginal rates of substitution suggested that service users are willing to spend time for improvements to the way in which they are involved in their care planning. Our findings could be used to help services target improvements in care planning to the aspects most important to service users.
Outputs
The full results of the stated preference survey are reported in Appendix 2.
Workstream 2: evaluation
Study 5
The aim of workstream 2 (study 5) was to evaluate the clinical effectiveness and cost-effectiveness of a training intervention to enhance service user and carer involvement in care planning in secondary care mental health services.
Methods
We conducted a pragmatic cluster trial of the clinical effectiveness and cost-effectiveness of the training intervention to enhance service user- and carer-involved care planning compared with controls in UK NHS community mental health services. The trial used cohort and cross-sectional samples to reduce risks to recruitment and retention. The cluster cohort was recruited at baseline and followed over the 6 months of the trial, whereas the cluster cross-section was recruited at the end of the trial. Consenting service users cared for by each community mental health team (CMHT) were recruited and carers were recruited from consenting service users. Each CMHT was randomised to either intervention (training in care planning) or control (usual-care planning). The CMHTs randomised to intervention received the training package.
We recruited service users and carers from CMHTs between July 2014 and December 2015 from 10 NHS trusts across the UK. Service users were aged ≥ 18 years with a severe mental illness under the care of participating CMHTs. CMHTs screened lists and excluded patients who were not deemed to have capacity to provide fully informed consent or who were too unwell at the time of recruitment. The primary outcome was patient self-reported ‘autonomy support’ measured using the Health Care Climate Questionnaire (HCCQ-10). 46 The HCCQ-10 is a self-report scale based on self-determination theory and measures ‘autonomy support’, defined as patient perceptions of the degree to which they experience their health professionals as supporting choice and ensuring that their behaviour (and behaviour change) is congruent with their values. The scale has 10 items, examples of which include ‘I feel that my mental health-care provider team has provided me with choices and options’ and ‘My mental health-care provider team has worked with me to develop a mental health-care plan’. Items are scored on a seven-point scale from ‘strongly disagree’ to ‘strongly agree’. An overall score is calculated as the mean of the items (expressed out of 100), with a higher score indicating greater ‘autonomy support’.
Secondary outcomes included patient self-reported involvement in decisions (EQUIP PROM);40 satisfaction with services [Verona Service Satisfaction Scale (VSS54)];47 side effects of antipsychotic medication [Glasgow Antipsychotic Side Effects Scale (GASS)];48,49 well-being [Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS)];48 recovery and hope [Developing Recovery Enhancing Environment Measure (DREEM)];50 anxiety and depression [Hospital Anxiety and Depression Scale (HADS)];51 alliance and engagement [California Psychotherapy Alliance Scale (CALPAS)];52 quality of life [World Health Organization Quality of Life (WHOQOL) questionnaire];53 carer satisfaction [Carer and User Expectations of Services (CUES)];54 quality-adjusted life-years (QALYs); and use of services. Measures were completed at baseline (pre training) and at 6 months post training (cohort sample), and at 6 months post training only (cross-sectional sample).
Outcomes for the cross-sectional sample included the HCCQ-1046 and the PROM. 40 Carer measures included the EQUIP PROM40 and WHOQOL53 and carer satisfaction was measured using the Carers’ and Users’ Expectations of Services – Carer version (CUES-C). 54 A summary of outcome measures, including scoring ranges, can be found in Table 5.
| Outcome measures | Baseline | 6-month follow-up | |
|---|---|---|---|
| Cohort design | Cross-sectional sample | ||
| Primary outcome measure | Autonomy support | HCCQ-1046
|
HCCQ-10 |
| Secondary outcome measures | User and carer involvement | EQUIP PROM40
|
EQUIP PROM (short version)
|
| Satisfaction | VSSS-5447
|
||
| Medication side effects | GASS48
|
||
| Well-being | WEMWBS49
|
||
| Recovery and hope | DREEM50
|
||
| Mental health symptoms | HADS51
|
||
| Alliance/engagement | CALPAS-1252
|
||
| Quality of life | WHOQOL-BREF53
|
||
To recruit service users into the cluster cohort, clinical studies officers (CSOs) sent out an introductory letter, participant information sheet and consent to contact form. On receipt of the consent to contact form, service users were invited to interview to complete baseline measures. Consenting service users were asked to nominate a carer to be included in the study who, if nominated, was provided with a questionnaire pack (including introductory letter, information sheet, questionnaire, prepaid envelope and consent to contact at 6-month follow-up form).
Service users were recruited to the cluster cross-section by a postal survey, distributed by CSOs to all service users in CMHTs (excluding those already in the cluster trial) recruited to the cluster cohort 6 months following randomisation.
Following recruitment of service users and carers, clusters were allocated randomly to either intervention or usual-care by the clinical trials unit of the Manchester Academic Health Science Centre.
The trial protocol was published55 (the original trial protocol and a summary of amendments can be found in Appendix 3).
Intervention
All consenting CMHTs allocated to the intervention received the training intervention. We asked that at least 80% of staff designated as ‘care co-ordinators’ (i.e. those with a caseload) committed to attending the training. Training was delivered within 6 weeks of service users being recruited into the trial. Clusters allocated to the control condition of ‘usual practice in care planning’ did not have access to the training intervention training.
Sample size and statistical methods
The original sample size calculation was for 24 clusters and 480 patients. Recruitment issues identified early in the trial meant that a decision was made to increase the number of clusters to 36 to ensure sufficient power. The recruitment methods used in EQUIP meant that the proportions of patients responding to the study was variable within sites (from 5% to 30%) and difficult to predict. Therefore, increasing the numbers of clusters to 18 meant that recruitment of more patients than the planned 480 was likely, unless specific measures were taken to reduce the numbers of patients per site (e.g. sampling patients within clusters, or limiting the numbers of patients per cluster). Such additional measures would have proven difficult in practice. Therefore, the decision to increase the number of clusters to 36 led to recruitment of 609 patients. The low-risk and non-invasive nature of the intervention and because the cluster design meant that all patients were exposed whether or not they formally participated in the trial means that it is unlikely that any participants had faced additional risk of harm because of the decision to increase cluster numbers and the subsequent increase in the total sample size.
We wrote to the Research Ethics Committee outlining the recruitment numbers at the end of the trial and the committee raised no issues, but we accept that this issue should have been stated explicitly to the Research Ethics Committee when we raised the cluster numbers.
The Research Ethics Committee’s response was as follows:
The Committee has reviewed your letter regarding the over recruitment into this study. Although they acknowledged that nothing could be done since the study has been declared closed, they pointed out that it was not clear from your letter why the cluster was increased. They stated that whilst the design meant that the numbers in each cluster were difficult to control, the CI [chief investigator] had overall responsibility of the study and should have been aware of the overall recruitment and when a possibility of over recruitment became apparent, the REC [Research Ethics Committee] should have been notified immediately. They concluded that although no actual harm had occurred at this time, they strongly advised that if this happens in the future, you must notify the REC immediately the participant numbers are likely above what had been approved by the REC and submit an amendment.
National Research Ethics Service Committee Northwest Preston (Health Research Authority), 2019, personal communication.
The primary outcome was the HCCQ-10,46 but data on the use of this scale by people with severe mental illness were limited, so we used a standardised effect to calculate sample size for the cluster trial. Twelve clusters per arm and a mean of 20 service users per cluster (total sample size of 480 participants) would have > 80% power to detect a standardised effect size of 0.4. This assumes an intracluster correlation coefficient (ICC) of 0.05 and an 80% follow-up rate, providing 384 participants with complete data in the analysis. For the cross-sectional study, we required the same number of patients in each cluster.
Analysis was completed using Stata version 13 and followed a statistical analysis plan prepared prior to analysis and approved by the independent Programme Steering Committee. The plan identified the cluster trial as the primary analysis, with the cluster cross-section and combined analyses to be presented as secondary analyses. For the cluster trial, intervention effects were estimated using a linear mixed model with a random intercept for teams. Analysis of outcomes followed intention-to-treat principles with outcome data included for all patients irrespective of receipt of the intervention or completion of care planning during the time scale of the trial. The pattern of missing data was assessed in terms of baseline characteristics of service users to check for differential non-response. Predictors of non-response were included as covariates in each model to satisfy the missing at random assumption of maximum likelihood used in estimating linear mixed models. Missing baseline data for the cohort sample were cluster mean imputed.
Participant flow
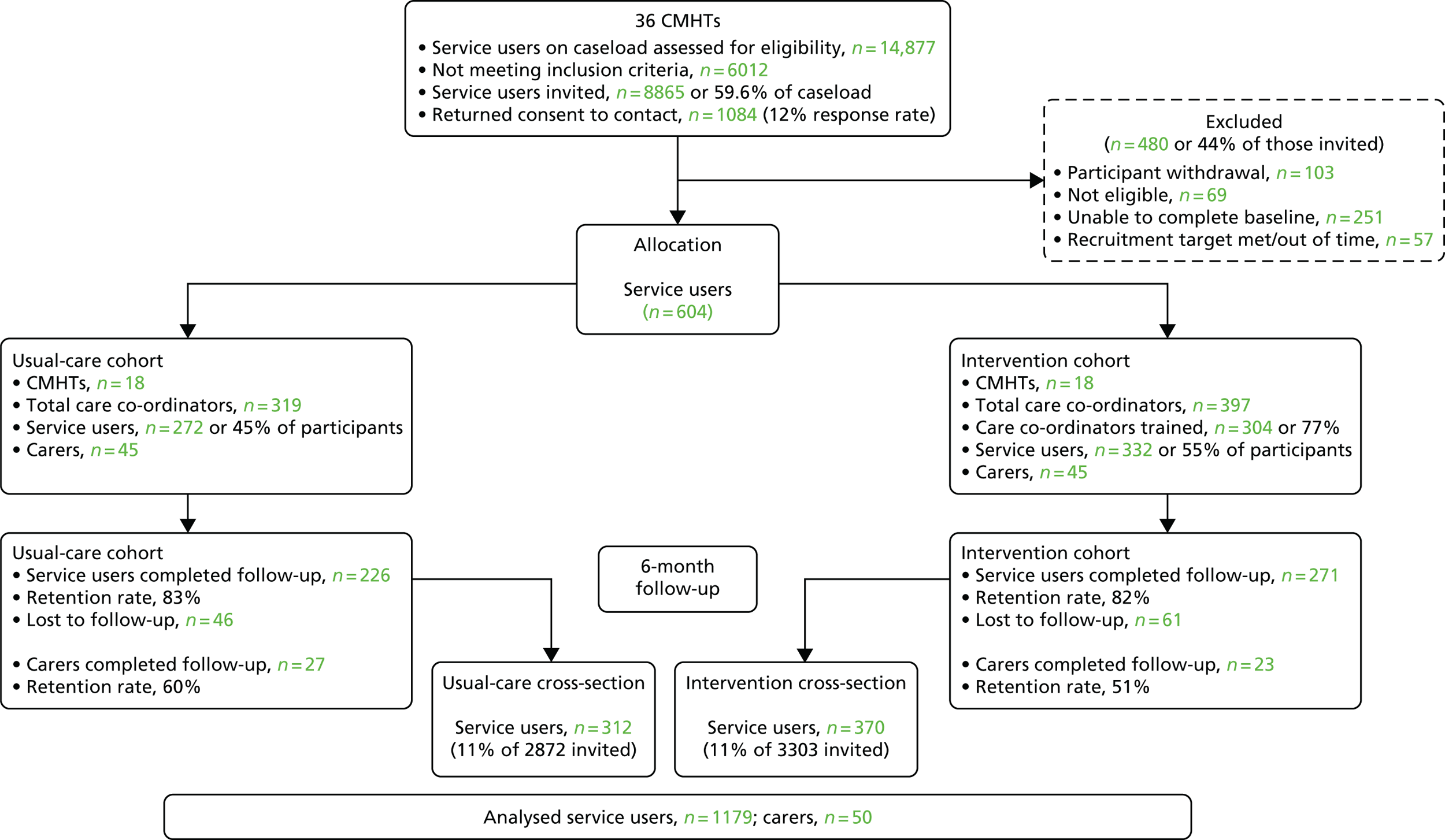
Participant flow for the cluster trial and cross-sectional sample is shown in Figure 3. During recruitment, the number of service users per cluster was smaller than estimated in the sample size calculation. We increased the number of clusters from 12 to 18 per arm to ensure sufficient power, and 36 teams were randomised to either the intervention (n = 18) or the usual-care (n = 18) group. There was appreciable uncertainty regarding the effect size for the outcome, which is indicated by the use of a standardised rather than absolute effect size and also the adoption of an ICC of 0.05. Given that there was minimal cost to continuation, it seemed appropriate to continue recruitment of centres rather than termination to protect the power of the trial against the ICC being larger than expected. The Programme Steering Committee, Research Ethics Committee and NIHR approved continued recruitment beyond the target size. In total, 604 service users and 90 carers were recruited to the cluster cohort. Ten out of the 18 CMHTs demonstrated ≥ 80% attendance of care co-ordinators at the training (range 48–100%). Retention at the 6-month follow-up for service users in each CMHT ranged from 76% to 93%, with an overall mean of 82% (n = 497). Retention of carers was limited, ranging from 0% to 100% between clusters, with an overall mean of 56% (n = 50). For the cross-sectional study, 682 service users were recruited [mean number per CMHT was 19.5 service users, standard deviation (SD) 14.0 service users].
FIGURE 3.
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram for cluster randomised controlled trial and cluster cross-section.
Demographics
Combining the cluster trial and cross-sectional samples (n = 1286), 58% of service users were female, 48% were aged between 45 and 64 years, 38% were aged between 25 and 44 years, 87% described themselves as white and only 13% were employed (Table 6). Demographics were broadly similar between the cluster cohort and cross-sectional samples and between intervention and usual care (Tables 6 and 7). Of the 90 carers in the cluster trial, just over half were female and most were white (Table 8).
| Demographic variable | Cohort | ||||
|---|---|---|---|---|---|
| Usual care (N = 271) | Intervention (N = 333) | ||||
| n | % | n | % | ||
| Gender | Female | 156 | 58 | 199 | 60 |
| Non-female | 107 | 39 | 128 | 38 | |
| Missing | 8 | 3 | 6 | 2 | |
| Ethnic group | White | 232 | 86 | 295 | 89 |
| Non-white | 33 | 12 | 32 | 10 | |
| Missing | 6 | 2. | 6 | 2 | |
| Education | Secondary school | 108 | 40 | 129 | 39 |
| Higher education | 153 | 56 | 182 | 55 | |
| Missing | 10 | 4 | 22 | 7 | |
| Accommodation | Owner-occupier | 85 | 31 | 97 | 29 |
| Other | 176 | 65 | 227 | 68 | |
| Missing | 10 | 4 | 10 | 3 | |
| Living arrangements | Alone or with a pet | 191 | 70 | 225 | 68 |
| With someone else | 75 | 28 | 102 | 30.63 | |
| Missing | 5 | 2 | 6 | 2 | |
| Employment | Employed | 37 | 14 | 45 | 14 |
| Other | 230 | 85 | 281 | 84 | |
| Missing | 4 | 1 | 7 | 2 | |
| Demographic variable | Cross-sectional | ||||
|---|---|---|---|---|---|
| Usual care (N = 309) | Intervention (N = 373) | ||||
| n | % | n | % | ||
| Gender | Female | 172 | 56 | 225 | 60 |
| Non-female | 131 | 42 | 141 | 38 | |
| Missing | 6 | 2 | 7 | 2 | |
| Ethnic group | White | 275 | 89 | 314 | 84 |
| Non-white | 28 | 9 | 45 | 12 | |
| Missing | 6 | 2 | 14 | 4 | |
| Education | Secondary school | 147 | 48 | 167 | 45 |
| Higher education | 112 | 36 | 151 | 40 | |
| Missing | 50 | 16 | 55 | 15 | |
| Accommodation | Owner-occupier | 84 | 27 | 113 | 30 |
| Other | 217 | 70 | 246 | 66 | |
| Missing | 8 | 3 | 14 | 4 | |
| Living arrangements | Alone or with a pet | 164 | 53 | 197 | 53 |
| With someone else | 142 | 46 | 170 | 46 | |
| Missing | 3 | 1 | 6 | 2 | |
| Employment | Employed | 40 | 13 | 55 | 15 |
| Other | 265 | 86 | 306 | 84 | |
| Missing | 4 | 1 | 12 | 3 | |
| Demographic variable | Cohort | ||||
|---|---|---|---|---|---|
| Usual care (N = 44) | Intervention (N = 46) | ||||
| n | % | n | % | ||
| Gender | Female | 22 | 50 | 25 | 54.35 |
| Non-female | 22 | 50 | 20 | 43.48 | |
| Missing | 0 | 0 | 1 | 2.17 | |
| Ethnic group | White | 39 | 89 | 40 | 87 |
| Non-white | 5 | 11 | 6 | 13 | |
| Missing | 0 | 0 | 0 | 0 | |
| Education | Secondary school | 17 | 39 | 20 | 43 |
| Higher education | 22 | 50 | 23 | 50 | |
| Missing | 5 | 11 | 3 | 7 | |
| Accommodation | Owner-occupier | 25 | 57 | 32 | 70 |
| Other | 19 | 43 | 14 | 30 | |
| Missing | 0 | 0 | 0 | 0 | |
| Living arrangements | Alone or with a pet | 13 | 30 | 14 | 30 |
| With someone else | 31 | 70 | 31 | 67 | |
| Missing | 0 | 0 | 1 | 2 | |
| Employment | Employed | 15 | 34 | 23 | 50 |
| Other | 29 | 66 | 22 | 48 | |
| Missing | 31 | 70 | 1 | 2 | |
Cluster trial (service users)
Primary outcome Health Care Climate Questionnaire (cluster cohort)
The HCCQ-1046 was the primary outcome measure. High scores represent higher appraisals of care. The mean and SD in the intervention and usual-care group are given in Table 9 with the adjusted mean difference and 95% CI. Results show no difference in HCCQ-10 scores between intervention and usual care at 6 months. The ICC indicates that approximately 2% of the variation of HCCQ-10 at 6 months is between teams, showing little difference in HCCQ-10 scores between teams.
| Time point | Usual care | Intervention | Adjusteda mean difference (intervention – usual care) | 95% CI | p-value | ICC | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | |||||
| Baseline | 5.06 | 1.66 | 271 | 5.27 | 1.48 | 334 | ||||
| 6 months | 4.93 | 1.78 | 226 | 5.01 | 1.70 | 270 | –0.064 | –0.343 to 0.215 | 0.653 | 0.02 |
Secondary outcomes (cluster trial)
The results of the secondary outcomes (Table 10) in the cluster trial showed no significant difference between the intervention and usual care at 6 months, except for VSSS-54. The adjusted mean difference indicates that the intervention group had higher (meaning more satisfied) VSSS-54 scores than the usual-care group, which showed a small, statistically significant difference at the 5% level. The 95% CIs are wide and, therefore, the true effect is potentially negligible. With all secondary outcomes, the ICC demonstrates very little variation between CMHTs.
| Outcome | Time point | Usual care | Intervention | Adjusteda mean difference (intervention – usual care) | 95% CI | p-value | ICC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | ||||||
| PROMa | Baseline | 22.81 | 8.78 | 271 | 22.07 | 8.58 | 334 | ||||
| 6 months | 21.64 | 11.18 | 152 | 21.32 | 9.62 | 193 | 0.396 | –1.817 to 2.609 | 0.726 | 0.05 | |
| HADS-A (anxiety)a,b | Baseline | 11.37 | 5.36 | 271 | 12.23 | 5.18 | 334 | ||||
| 6 months | 10.85 | 5.86 | 171 | 12.10 | 5.37 | 209 | 0.430 | –0.334 to 1.194 | 0.270 | 0.00 | |
| HADS-D (depression)a,b | Baseline | 9.19 | 5.31 | 271 | 10.03 | 5.18 | 334 | ||||
| 6 months | 8.91 | 5.83 | 171 | 9.81 | 5.49 | 209 | –0.001 | –0.861 to 0.858 | 0.998 | 0.00 | |
| VSSS-54a,b | Baseline | 3.58 | 0.62 | 271 | 3.53 | 0.61 | 331 | ||||
| 6 months | 3.53 | 0.80 | 155 | 3.51 | 0.72 | 192 | 0.120 | 0.001 to 0.239 | 0.049 | 0.01 | |
| CALPASa,b | Baseline | 4.98 | 1.27 | 271 | 5.06 | 1.19 | 334 | ||||
| 6 months | 4.87 | 1.45 | 151 | 4.81 | 1.38 | 192 | –0.010 | –0.259 to 0.239 | 0.935 | 0.01 | |
| GASS | Baseline | 17.73 | 10.37 | 271 | 18.30 | 8.93 | 334 | ||||
| 6 months | 17.80 | 11.57 | 114 | 19.80 | 10.28 | 144 | 1.316 | –1.075 to 3.708 | 0.281 | 0.05 | |
| WHOQOLa | Baseline | 3.03 | 1.02 | 271 | 3.04 | 1.05 | 334 | ||||
| 6 months | 3.20 | 1.19 | 157 | 3.16 | 1.11 | 201 | 0.024 | –0.170 to 0.218 | 0.808 | 0.00 | |
| DREEMa | Baseline | 39.20 | 12.32 | 271 | 38.81 | 11.86 | 334 | ||||
| 6 months | 41.07 | 13.78 | 161 | 38.83 | 13.29 | 204 | –0.661 | –2.600 to 1.278 | 0.504 | 0.002 | |
Cluster trial (carers)
The three outcomes completed by carers were the 14-item EQUIP PROM, WHOQOL and CUES-C. The results showed no significant difference in PROM or CUES-C scores between intervention and usual care at 6 months. There was a slight difference in WHOQOL scores, indicating that the intervention improves quality of life by approximately half a unit on the 1–5 scale (0.484), but the CI for this estimate is wide, suggesting potentially negligible difference. Controlling for baseline variables, the between-cluster variation in all three measures is negligible and so the ICC is effectively zero, showing no difference between CMHTs (Table 11).
| Outcome | Time point | Usual care | Intervention | Adjusteda mean difference (intervention – usual care) | 95% CI | p-value | ICC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | ||||||
| PROM | Baseline | 19.48 | 10.96 | 44 | 20.97 | 12.64 | 20 | ||||
| 6 months | 16.45 | 10.86 | 46 | 20.10 | 8.00 | 22 | 0.392 | –5.676 to 6.460 | 0.899 | 0.00 | |
| WHOQOL | Baseline | 3.45 | 0.90 | 44 | 3.69 | 0.81 | 46 | ||||
| 6 months | 3.27 | 1.15 | 26 | 3.91 | 1.00 | 23 | 0.484 | 0.009 to 0.959 | 0.046 | 0.00 | |
| CUES-C | Baseline | 24.68 | 8.02 | 44 | 24.67 | 8.28 | 46 | ||||
| 6 months | 24.12 | 9.97 | 26 | 22.71 | 9.08 | 24 | –0.972 | –4.4383 to 2.440 | 0.577 | 0.00 | |
Outcomes for cross-sectional study
The two outcomes completed by service users and carers were the HCCQ-10 and the PROM. Results show no significant difference in the HCCQ-10 and the PROM between intervention and usual care at 6 months. The mean and SD in the intervention and usual-care group are given in Table 12 with the adjusted mean difference and 95% CI. Controlling for baseline variables, the between-cluster variation in all three measures is negligible and so the ICC is effectively zero, showing no variation between CMHTs.
| Outcome | Time point | Usual care | Intervention | Adjusteda mean difference (intervention – usual care) | 95% CI | p-value | ICC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | ||||||
| HCCQ-10 | 6 months | 5.10 | 1.72 | 284 | 5.08 | 1.72 | 344 | –0.132 | –0.511 to 0.247 | 0.495 | 0.05 |
| PROM | 6 months | 25.25 | 13.60 | 242 | 25.62 | 13.46 | 309 | –0.691 | –4.068 to 2.686 | 0.688 | 0.07 |
Key findings
The results showed no statistically significant difference in HCCQ-10 scores between the intervention and usual care at 6 months. The ICC indicates that only 2% of the variation of HCCQ-10 at 6 months was between teams.
The results of the ‘cluster cross-section’ and combined analyses were similar to the primary analysis, with no statistically significant difference on the primary outcome between the intervention and usual care at6 months. Analyses of secondary outcomes in the ‘cluster cohort’ found a significant effect on a single outcome of service satisfaction. However, the 95% CIs are wide and, therefore, the true effect is potentially negligible. In terms of opportunities to use the training in routine contacts with patients, data from patient self-report suggested that 79% of patients providing data saw their CMHT during the 6-month follow-up, with a mean of 12.3 contacts. Our intervention to improve user- and carer-involved care planning in community mental health services was well attended and acceptable to staff, but had no significant effects on patient perceptions of autonomy support, or other outcomes.
Cost-effectiveness
An economic evaluation was integrated into the clinical trial to assess whether or not the EQUIP training intervention was cost-effective at each of the different levels that decision-makers may be willing to pay in order to gain 1 unit of health benefit.
Methods
Service use data were collected at baseline and the 6-month follow-up for all service users who participated in the cluster trial, as were health status data [EuroQol-5 Dimensions, five-level version (EQ-5D-5L)]. The service use data were collected using a survey adapted for the EQUIP trial. The service use data were combined with published national unit costs to estimate costs. 56,57 The costs of delivering the intervention were estimated from the costs incurred in the trial and the number of people trained. They included the costs of health-care professionals’ time to attend the training and the costs of trainers’ time to deliver the training. The costs of consumables and room hire were also included. The QALYs were estimated by combining the EQ-5D-5L data with UK-specific utility weights using the crosswalk methodology recommended by NICE at the time of the evaluation. 58,59 The analysis used the perspective of the NHS and social care (costs) and service users (QALYs). The time horizon for the primary analysis was the 6-month follow-up point of the trial. Analysis of the economic data was based on intention-to-treat principles, and missing data (owing to incomplete observations and missing follow-up) were imputed using multiple imputation. Regression analyses were used to estimate the net costs and outcomes of the EQUIP training intervention, adjusting for participant sociodemographic characteristics and team cluster (baseline covariates) that may influence costs and QALYs. A generalised linear regression model, with a gamma distribution and log-link, was used to account for the skewed nature of the cost data. An ordinary least squares regression model was used to estimate net QALYs. This required the assumption that the QALY data were normally distributed, which was tested in the sensitivity analysis. The net cost and QALY were bootstrapped to estimate the probability that the EQUIP training intervention was cost-effective at different hypothetical amounts decision-makers may be willing to pay to gain an additional QALY. Sensitivity analysis explored the relative cost-effectiveness of the training intervention if different choices were made about the study methods. These included using different measures of benefit, alternative estimates of the unit cost of the intervention, complete-case analysis and the use of a beta distribution to estimate net QALYs.
Key findings
Eighty-two per cent of service users completed follow-up (497/604). A total of 581 service users (581/604; 96%) completed the EQ-5D-5L at baseline and 537 (89%) had sufficient service use data to estimate baseline costs. At the 6-month follow-up, 442 service users (73%) had complete EQ-5D-5L data and 334 (55%) had complete service use data. Overall, 322 service users (53%) had complete baseline and 6-month follow-up cost, utility and QALY data (see Appendix 3 for further detail). There were no differences between participants with complete and missing data on all but two of the sociodemographic variables. These were whether or not the service user had one or more than one diagnosis (chi-squared test; p = 0.033) and whether or not the participants lived in accommodation that they owned (chi-squared test; p < 0.001). The rate of missing data did not appear to differ between the intervention and usual-care groups. Tables 13 and 14 summarise the EuroQol-5 Dimensions (EQ-5D) data and costs of services used.
| Outcome | Usual care (n = 146) | EQUIP (n = 176) | ||
|---|---|---|---|---|
| Frequency | % | Frequency | % | |
| No problems with mobility | ||||
| Baseline | 91 | 62 | 100 | 57 |
| Follow-up | 85 | 58 | 97 | 55 |
| No problems with self-care | ||||
| Baseline | 99 | 68 | 117 | 67 |
| Follow-up | 101 | 69 | 108 | 61 |
| No problems with usual activity | ||||
| Baseline | 66 | 45 | 68 | 39 |
| Follow-up | 66 | 45 | 62 | 35 |
| No problems with pain or discomfort | ||||
| Baseline | 70 | 48 | 69 | 39 |
| Follow-up | 69 | 47 | 74 | 42 |
| No problem with anxiety or depression | ||||
| Baseline | 38 | 26 | 50 | 28 |
| Follow-up | 52 | 36 | 33 | 19 |
| Cost category | Cohort, mean (95% CI) | |
|---|---|---|
| Usual care | EQUIP | |
| Primary care services | ||
| Baseline | £164 (£131 to £196) | £157 (£131 to £182) |
| Follow-up | £140 (£113 to £168) | £158 (£128 to £188) |
| Community-based services | ||
| Baseline | £692 (£590 to £794) | £601 (£504 to £698) |
| Follow-up | £559 (£456 to £661) | £523 (£425 to £621) |
| Social care services | ||
| Baseline | £28 (£10 to £45) | £71 (£40 to £103) |
| Follow-up | £42 (£16 to £68) | £41 (£19 to £64) |
| Accident and emergency | ||
| Baseline | £73 (£15 to £132) | £30 (£17 to £44) |
| Follow-up | £49 (£20 to £78) | £30 (£14 to £47) |
| Hospital outpatient services | ||
| Baseline | £241 (£184 to £297) | £314 (£243 to £385) |
| Follow-up | £247 (£181 to £313) | £216 (£157 to £276) |
| Hospital day services | ||
| Baseline | £240 (< £1 to £563) | £612 (£17 to £1207) |
| Follow-up | £5 (< £1 to £16) | £18 (< £1 to £43) |
| Hospital inpatient stay (≥ 1 night) | ||
| Baseline | £154 (£83 to £225) | £86 (£44 to £128) |
| Follow-up | £128 (£38 to £218) | £73 (£30 to £117) |
| EQUIP training intervention | £0.00 (£0.00) | £23 (not applicable) |
There was no indication that the number of people using a service and the average cost per person differed between groups at baseline or follow-up. Wide 95% CIs indicated a high level of variation in the average costs per person.
The net costs and QALYs are shown in Table 15 (primary analysis and sensitivity analyses using the QALY as the measure of health benefit). There was no evidence that the costs or health benefit differed between the training intervention and usual care. The primary analysis, using a willingness-to-pay threshold of £15,000 per QALY, indicated that there was a net saving of £3600 per QALY lost associated with training. Whether or not the savings offset the QALY loss depends on the decision-makers’ willingness to pay to gain 1 QALY. If decision-makers are willing to pay £5000–15,000 to gain 1 QALY then the probability that the training intervention was cost-effective was between 0.29 and 0.49. The probability ranged between 0.09 and 0.75 in the sensitivity analyses using the QALY.
| Analysis | Net costa,b (5th percentile; 97.5th percentile) | Net QALYsa (5th percentile; 97.5th percentile) | ICER (£/QALY) | Probability that EQUIP is cost-effective if WTPT = | |
|---|---|---|---|---|---|
| £5000/QALY | £15,000/QALY | ||||
| Primary | –£54 (–£193; £84) | –0.014 (–0.034; 0.005) | £3600 saving per QALY lost | 0.16 | 0.41 |
| Complete case | –£96 (–£310; £117) | 0.004 (–0.021; 0.029) | EQUIP dominates | 0.80 | 0.75 |
| Costs of EQUIP intervention | |||||
| £0 | –£79 (–£217; £60) | –0.014 | £5643 saving per QALY lost | 0.52 | 0.20 |
| £29 | –£35 (–£176; £106) | (–0.034; 0.005) | £2500 saving per QALY lost | 0.32 | 0.13 |
| £57 | –£5 (–£146; £136) | –0.014 | £357 saving per QALY lost | 0.21 | 0.09 |
| Beta distribution for QALYS | –£54 (–£193; £84) | –0.041 (–0.10; 0.014) | £1317 saving per QALY lost | 0.56 | 0.17 |
| New value set for EQ-5D-5L | –£54 (–£193; £84) | –0.003 (–0.020; 0.013) | £18,000 saving per QALY lost | 0.75 | 0.65 |
Outputs
A full description of the protocol has been published in Bower et al. 55 (see Appendix 3).
A full description of the methods, analysis and results of the cluster randomised controlled trial (RCT) has been published in Lovell et al. 60 (see Appendix 3).
A full description of the methods, analysis and results of the cost-effectiveness has been submitted.
Delivery and acceptability of the training intervention
Training was delivered to 18 CMHTs in 10 NHS trusts. Owing to service need and the logistics of taking an entire team out of usual work for 2 days, most teams were divided and the training was delivered twice. In total, 350 health professionals (249 female, 101 male) attended the training, ranging from 4 to 39 trainees (mean 19.44 trainees) at each 2-day session. CMHTs teams consisted of 304 care co-ordinators (mainly nurses, occupational therapists and social workers); the remaining 46 were students, support workers and clinical managers. Although psychiatrists were invited, none attended.
We used the Training Acceptability Rating Scale (TARS-161 and TARS-262) to evaluate the acceptability of the training, with six self-report items assessing general acceptability, perceived effectiveness, negative side effects, appropriateness, consistency and social validity. Items were rated on a six-point Likert scale, from ‘strongly disagree’ (score 1) to ‘strongly agree’ (score 6). TARS-2 assesses attendees’ overall impressions of the impact of the teaching process and its outcomes and consists of nine items, rated on a four-point scale from ‘not at all’ (score 0) to ‘a great deal’ (score 3). TARS-2 also includes three open-ended questions asking about the ‘most helpful’ part of the training, any ‘recommended changes’ and ‘any other comments’. Questions 1–6 were summed to calculate an overall acceptability score (range 6–36), and questions 7–15 were summed to calculate a perceived impact score (range 0–27). The overall TARS score was calculated by summing the responses to questions 1–15 (possible range 6–63). 63,64
Analysis
Descriptive statistics were used for the TARS results and open-ended comments were analysed using content analysis. 65
Findings
The results demonstrated high levels of satisfaction/acceptability of the training, with the median overall TARS score as 56 out of 63, median ‘acceptability’ score as 34 out of 36 and median ‘perceived impact’ score as 22 out of 27 (Table 16). Open-ended comments reflected six qualitative themes: the value of the co-production model, time to reflect on practice, delivery preferences, comprehensiveness of content, need to consider organisational context and emotional response (with six people commenting that they did not find the training helpful). The co-production model was key to the training intervention, and 102 participants commented on the value of the service user and carer contribution to the training, in terms of the value of their shared experiences, perspectives and insights, and appreciating them as facilitators. Participants appreciated the opportunity to take ‘time out’ to reflect on practice (n = 50).
| Outcome | n | Median | Interquartile range | Range |
|---|---|---|---|---|
| Total ‘acceptability’ questions 1–6 (score 1–36) | 289 | 34 | 31–36 | 6–36 |
| Total ‘perceived impact’ questions 7–15 (score 0–27) | 301 | 22 | 19–25 | 4–27 |
| Total TARS questions 1–15 (score 6–63) | 283 | 56 | 51–61 | 24–63 |
All teams were provided with supervision: 2 half-days of 3 hours in the 6 months following the training. Overall, supervision was poorly attended, with < 50% of the original professionals attending. Supervision for those who did attend focused on practice changes that they had made (e.g. including carers in the care plan and writing the service user’s perspective into the care plan) and difficulties encountered when they tried to include some service users in their care plan. Although all of the health professionals were sent the 8-hour optional self-directed learning package, only one individual reported looking at this. Reasons for not looking at the self-directed learning included ‘being too busy’, ‘wanted to look at it but dropped off to do list’, ‘forgot’ and ‘don’t like e-learning’.
Outputs
A full description of methods, analysis and results has been published in Grundy et al. 23 (see Appendix 3).
Strengths and limitations
The study achieved the required sample size in both the cluster trial and the cross-sectional sample and we achieved a high follow-up rate (82%). Our comprehensive outcome assessment increases confidence that our observed lack of effect is robust. Our pragmatic design was intended to improve service user and carer involvement in routine mental health services. Our intervention was delivered in 18 CMHTs across 10 NHS trusts with over 300 care co-ordinators. However, our volunteer sites may not be fully representative of the wider population, and we lacked data by which to compare our participants with the eligible population. A known risk to cluster trial validity is professionals recruiting differently depending on allocation. To reduce risk, we selected patients via existing registers and invited patients before revealing allocation to teams. Practitioners could potentially exclude patients after invitation, although this involved a small proportion of service users and did not differ between arms. Measures of service use and contact with professionals were based on self-report, and such measures may not always agree with other sources, such as service records. Limitations that are specific to the economic evaluation suggest additional uncertainty about the relative cost-effectiveness of the training intervention. Changes in care planning reflect a change in process, which may in turn lead to changes in health and other resource use. However, the 6-month follow-up of the study may be too short for the training to feed through to changing either use of services and costs or overall health and QALYs. There was insufficient evidence to support modelling work to extrapolate from the trial to longer time periods.
The measure of health benefit for the primary analysis was the QALY, which is widely used in mental health trials comparing different types of treatment or patient management. However, it may not be an appropriate measure to detect changes in care planning processes and any indirect impact on subsequent health.
What this study adds
Despite a high level of attendance and satisfaction with the training intervention, no significant effect was found on the primary outcome (perceptions of autonomy support) or other outcomes. There was no evidence that the costs or health benefit differed between the training intervention and usual care. The primary and sensitivity analyses suggested that the probability that the intervention was cost-effective was between 9% and 75% for those analyses using the QALY as the measure of health benefit. Embedding service user and carer involvement in care planning may require considerably greater investment of resources. Benefits for service users may be apparent only over the longer term.
Workstream 3: implementation
The aim of workstream 3 (studies 6 and 7) was to understand the contextual, individual and organisational barriers and facilitators and examine the processes involved in the development and use of service user- and carer-involved care planning.
This work package consisted of two studies (6 and 7), which were designed to:
-
understand the perspectives of professionals, service users and carers about the influences that inhibit or promote user involvement and integration of care planning into clinical settings
-
explore and assist with explaining the impact of the novel training intervention in enhancing user involvement in care planning in mental health settings.
An exploration of the existing operationalisation of care planning and potential barriers to the implementation of the training intervention was undertaken prior to the development of the intervention. This was done so that views and arrangements related to existing practices could create the foundation on which to build an intervention likely to fit best with the work and organisation of pre-existing day-to-day practice.
Theoretical framework
Both studies in the workstream were carried out sensitised by implementation theory concepts informed by normalisation process theory (NPT) (Figure 4).
Investigations of successful implementation require an approach that understands both complex interventions and their contexts prior to the development of trials to test effectiveness. 67,68 Implementation theory allows researchers to identify factors that ‘promote and inhibit the routine incorporation of complex interventions into everyday life’. 67 It focuses on the work that people do to ensure that interventions become adopted, normalised and embedded. NPT is one of a range of theories that offer a heuristic framework within which to optimise the development of a trial intervention applicable to three stages:66
-
designing an intervention
-
describing the context within which an intervention is located and implemented
-
supporting the retrospective interpretation of the implementation of an intervention.
Other implementation theories were used at the explanatory analysis point; these included Concepts from the Consolidated Framework for Implementation Research (CFIR), which were useful in exploring outer setting and contextual variables relevant to a rapidly changing mental health context. Of most relevance were theories relating to how social networks and relational work explained the personal care options and management leveraged by users, which lay outside the care planning arrangements and ethos of formal clinical settings. 69 The notions of navigation, negotiation and collective efficacy were relevant to understanding the nature of management work undertaken in users’ own personal communities. 70
Study 6
Pre-implementation exploration of the environmental influences
To explore the distal political, economic, policy and clinical environments, we conducted semistructured interviews with key informants involved locally and nationally in mental health policy, practice and research. This was designed to elicit key informants’ perspectives on the state and progress of user involvement in mental health planning and practice. We also carried out a mapping exercise of the contemporary organisational structures and care planning policies. This broader picture was intended to complement analysis undertaken in workstream 1, which was designed to explore current care planning with service users, carers and health professionals with direct involvement in care planning. This was predicated on the notion that key informants would have access to insider policy and practice information, relationships and opinions likely to be relevant in the development and evaluation of the trial being undertaken in workstream 2 to test the effectiveness of a training intervention for mental health professionals (see Brooks et al. 66). We referred to the NPT toolkit framed as a set of propositions to guide the stakeholder interviews (www.normalizationprocess.org/npt-toolkit.aspx; accessed 15 June 2015). We then used NPT as a coding frame67 adapted from the RESTORE71 and EUWISE72 projects to conduct analysis.
Mapping exercise
Aim
To understand the pre-existing organisational structures and care planning related policies in place at all levels within the organisation.
Objectives
To understand the operationalised pre-existing arrangements and views of care planning by undertaking a mapping exercise through:
-
analysing trust documents relevant to care planning
-
exploring audits related to care planning
-
identifying how care planning activities are recorded (e.g. Amigos in Manchester and Rio in Nottingham – patient record systems)
-
reviewing service user experience from surveys and committee and audit minutes.
Method and analysis
Two reports of findings were produced from documentary analysis of the above sources (see Appendix 4). Additionally, EQUIP team members met to discuss and interpret policies, procedures, documentation and information technology systems used for care planning. Additional mapping exercises were undertaken for a number of additional sites as the number of recruitment sites included in the trial increased over the course of the trial (see Appendix 4).
Stakeholder interviews
Aim
To explore stakeholder views of care planning and expectations of individual and organisational ‘barriers’ to and ‘facilitators’ of service user- and carer-involved care planning prior to the development of the training (herein referred to as stakeholder interviews).
Objectives
To identify stakeholder understandings of contemporary arrangements for care planning through interviews with key informants exploring the:
-
potential facilitators of and barriers to the implementation of service user- and carer-led planning within mental health services
-
feasibility of a social network mapping method for tracking the processes of change associated with service user- and carer-involved care planning.
Methods and analysis
Prior to the commencement of the trial (study 5, workstream 2), we worked with investigators in workstream 1 to develop the content of the training. We analysed interview transcripts of participants (health professionals, service users and carers) to identify potential ‘barriers’ to and ‘facilitators’ of service user-/carer-involved care planning.
Additional interviews allowed for the incorporation of the views of key informants not included in workstream 1 (stakeholders outside the trusts and high-level managers within the trusts). A focus of these interviews was the feasibility of delivering a user- and carer-led training package to improve service user and carer involvement in care planning. 66 This feasibility related specifically to their experience of:
-
understanding user involvement and participation
-
multidisciplinary perspectives
-
knowledge and experience of care planning
-
resource allocation
-
official policy catalysts
-
organisational cultural acceptance
-
organisation resistance and facilitation.
Interviews were carried out face to face or via the telephone. Interviews were digitally recorded and transcribed verbatim. Participants were recruited from prominent knowledge positions, including high-level NHS managers, subject-relevant academics and policy-makers, and were selected on the basis that they were likely to be immersed in critical understanding of contemporary care planning and user involvement in mental health care. Participants were identified through purposive and snowballing sampling starting from a list of national key contacts developed by the applicants. We asked the respondents interviewed for names of other potential interviewees. Sampling continued until theme saturation occurred. Saturation was considered sufficient after 13 interviewees were recruited.
The starting focus of analysis was the summative perspectives of key stakeholders collected as part of workstream 1. Data were analysed using framework analysis. The transcripts were coded independently by two researchers using adaptive theorising and sensitising concepts from NPT. Analysis of interview data and snowball sampling were conducted in accordance with the constant comparative method. Analysis was carried out concurrently with data collection and sampling in line with iterative constant comparison.
The data collected and findings produced were designed to complement the mapping exercise described in aim 1 (to understand the pre-existing organisational structures) and data collected in workstream 1 as well as feeding into the development of the trial to be undertaken within workstream 2. Themes that arose in interviews were later compared with those in study 7 of the actual barriers and facilitators encountered during the roll-out, implementation and embedding of the new care planning practices at baseline and 6 and 12 months post training.
Key findings
The framework analysis undertaken in workstream 1 illuminated the likely barriers to and facilitators of implementing the proposed training from the point of views of professionals, service users and carers immediately involved within care planning. The stakeholder findings sensitised by and interpreted with reference to implementation theory incorporated wider environmental views of key informants with broader knowledge, which further expanded on the list of potential barriers and facilitators that were likely to have an impact on the implementation of the intervention.
All stakeholders supported the need for training to improve involvement in care planning and considered such a view to be normative. Any potential problems that were likely to arise were predicted to be related to the implementation at meso and organisational levels. The preoccupation with recording processes and lack of ability to do this in a minimally disruptive manner were viewed as potentially taking precedence over the competing imperatives to ensure patient centeredness.
Interview data from workstream 1 highlighted the importance of interpersonal relationships between health professionals and service users while concomitantly acknowledging that current resource and workload challenges make developing these relationships difficult and seemingly less of a priority. Interviews with key informants further supported the centrality of relationships and relational work and flagged how this could be downplayed through attempts at practice standardisation in a climate of limited resources.
The identification of outer setting factors (the economic, political and social context in which an organisation resides) was less prominent in accounts from workstream 1 than a focus on inner setting features that needed to be changed. The structural, political and cultural contexts were not seen as a primary concern. By contrast, interviews with key informants illuminated the relevance of these contexts and described the impact of the historical legacy of care planning and, given their distance from services, these stakeholders seemed more able to comment critically on cultural impediments to change within services.
Outputs
A full discussion of findings from the mapping exercise and key stakeholder interviews has been published in Brooks et al. 66 (see Appendix 4).
What this study adds
This study added to existing data by highlighting the potential impact of organisational bureaucracy and the cultural history of mental health services in the implementation of the proposed intervention.
Study 7
Process evaluation
A process evaluation of the training programme delivered as part of the trial was considered appropriate because successful implementation of the training intervention implicated a range of explanatory factors, including the integrity of the intervention and the acceptability of the intervention to both clinicians and service users, which is absent from the traditional outcomes of trials. 73
The process evaluation was designed to explore how far the training intervention had been taken up and implemented into the daily work of the health professionals who attended training and what the consequences of this uptake had been. It aimed to complement and supplement the evidence provided by the cluster trial as recommended by the Medical Research Council (MRC) framework for evaluation of complex interventions. 74
The objectives were to examine how:
-
the training for service user- and carer-involved care planning and its principles had an impact on, and was incorporated into, existing routine clinical practices
-
care planning training influenced the way in which professionals related to, communicated with and negotiated therapeutic options with users
-
care planning training and arrangements had an impact on existing methods of coping, self-care and the development of service user expertise and how it shaped and transformed relationships between service users and professionals
-
the impact of training on service users’ perceptions of networks, a sense of control, security and identity compared with previous care planning practices
-
service users perceived preparation and support arrangements for engaging with the form and content of the new system of care planning.
Methods and analysis
Semistructured interviews were undertaken with service users (n = 29), carers (n = 4) and mental health professionals (n = 21) from both the usual-care and intervention arms of the RCT at three time points (baseline, 6 months and 12 months post intervention). Participants were eligible for the study if they were service users, carers or professionals from the CMHTs included in the RCT sites. Service users were invited to take part via written invitation including an information sheet and consent to contact form. Eligible staff members were approached by e-mail. Included service users were asked to identify eligible carer participants. Interviews aimed to obtain in-depth data on the experience of utilising and receiving the EQUIP intervention and identify changes to practice over time. Service users involved in the study also completed ‘ego’ network mapping at the beginning of baseline interviews to develop an understanding of the impact of social networks in the management of mental health and to examine the role of care planning over time within those networks (Figure 5).
Service users included in the process evaluation were invited to have a care planning meeting observed and to complete a diary over the 12-month follow-up period. Two service users returned completed diaries and one consented to have a care planning meeting observed. The main reason for these low levels of uptake was that most participants reported that insufficient care planning activity took place over the 12-month period to warrant participation in such activities.
Interviews and observations were digitally audio-recorded and transcribed verbatim before being analysed thematically using NVivo software (QSR International, Warrington, UK). Iterative modifications were made to the initial framework through the removal of duplicate codes, recategorisation and the addition of new codes.
Participants who took part in the study were:
-
29 service users from five trial sites – 55% (n = 16) were female and 62% (n = 18) were from the intervention arm of the trial
-
four carers from three trial sites – 50% were female (n = 2) and 75% (n = 3) were from the intervention arm of the trial
-
21 professionals from four trial sites – 86% (n = 18) were female and 90% (n = 19) were from the intervention arm of the trial.
Key findings
Baseline data
Despite a general awareness of the care planning process, most service users and carers had not seen their care plan or been involved in its development. Care plans and care planning were characterised by a failure to meet the complexity of mental health needs including the holistic and broader contextual and environmental influences having an impact on a person’s ability to manage their condition and against the backdrop of the potential coercive elements of mental health services.
Current definitions of care planning (e.g. NICE guidelines14) focus on the inclusion of patient experience in the delivery of mental health care. However, current organisational imperatives relating to quality assessment failed to address this sufficiently, which meant that current care planning processes were interpreted as fulfilling one organisational need (e.g. measuring organisational targets) at the expense of undertaking the purported aim of care planning relating to choice, need and the everyday means of managing mental health.
The personal network analysis of users revealed a range of imaginative and complex arrangements implicating a wide range of network members, organisations and valued personal activities, which provided the bases and resources for managing mental health. In general, these resources were invisible in accounts of the processes and outcomes of descriptions of care planning arrangements within services.
Care plans rarely featured in individuals’ specification of their networks of self-management support. All stakeholder groups felt that care plans were of most relevance to the professionals and health systems in which they were based. Care planning processes prioritised organisational and risk agendas, which further distanced care plans and care planning from the everyday lives of service users.
Potential strategies to reorient care plans to the priorities and everyday lives of service users included the use of evidence-based tools designed to prompt discussion about harnessing resources to self-manage and the separation of risk management and needs elicitation activities. Social network mapping interventions that reveal the everyday and preferred means of managing the relationships and resources likely to support people might be more a more appropriate means of planning for the management for mental health than current care planning processes.
Outputs
A full discussion of findings from baseline data has been published in Brooks et al. 75 (see Appendix 4) and Brooks et al. 76 (see Appendix 4).
Longitudinal process evaluation
The findings from the process evaluation were, on the whole, consistent with the lack of effect found in the parallel cluster trial and the potential barriers identified at baseline. Data from the concurrent process evaluation illuminated a lack of organisational readiness and support for implementation and insufficient consideration of the required type of range of relational work associated with the intervention. This was further reinforced by the context in which the intervention was implemented, which diminished the initial enthusiasm for training as reported by front-line professionals. These wider contextual factors were not the focus of intervention design or implementation.
The professionals included in the study were positive about the training intervention and particularly valued the service user and carer input into the training design and delivery. They described how the training initially strengthened moral values about the need to involve service users and carers in the care planning process and increased motivation for change. Through delivering training at a team level, cohesion within teams was also promoted. However, a lack of continuity of care and resource limitations both within and outside health services reduced the possibility of sustaining and acting on such motivations, which meant that service users were unlikely to benefit from the professional training.
The process evaluation also demonstrated that, given the subtle nature of the changes in professional behaviour that were identified over the 12-month period, they may have gone unnoticed by service users (which was also reflected in the service user data). Such minor behavioural shifts were unlikely to have been sufficient to challenge entrenched practices and negative perceptions from both sides of the service user/professional dyad relating to health service relationships and health services more generally, which were identified at baseline.
A full discussion of findings from the longitudinal process evaluation can be found in Appendix 4.
Strengths and limitations
The workstream draws its strengths from the in-depth qualitative approach combined with the longitudinal design and theoretical underpinnings. Such methods allowed for anticipated implementation barriers to be explored in real time. However, there were a number of limitations. Participants included in all of the studies within the workstream self-selected themselves to take part in the study. Therefore, any data produced may not be generalisable to other mental health service users, carers or professionals. Furthermore, in study 7, only those service users who were involved in the trial were eligible to take part. As a result, those service users who were acutely unwell or were considered by professionals to not be suitable for the trial were ineligible. Despite recruitment endeavours to recruit carers, only four were recruited to study 7 (initial target was up to 10) and although carers’ views coalesced with those of service users in the most part, their views may be under-represented in current reporting.
What this study adds
The training was a success in so far as it gained ideological buy-in from those charged with delivering user-centred care planning. However, there was a failure of training to become embedded and normalised in practice. This relates to a lack of organisational readiness to accept change together with an underestimation and lack of investment in the amount of relational work required to make it work. Even the changes that were observed over the 12-month period were too subtle to challenge the existing discontent with care planning as identified at baseline.
Care planning based on shared decision-making that is compatible with user and carer engagement and values is more likely to be achieved if delivered by peer support workers and occupational therapists whose values align more readily than those of existing care co-ordinators or nurses.
Care planning focused on managing mental health based on principles of connecting to others, and activities that are valued in people’s everyday life, is likely to be a more effective and acceptable replacement for traditional care planning than modifying through training professional attitudes to user participation.
Workstream 4: dissemination
The aim of workstream 4 was to disseminate our findings, training intervention materials and patient-mediated resources produced during the programme to all relevant stakeholders using multiple methods. We disseminated our findings throughout the programme.
Our implementation strategy utilised a number of known effective mechanisms for the dissemination of findings, and activities occurred at local, regional, national and international levels via professional, service user and carer organisations, in health, social care and third-sector services. We have completed the following dissemination activities and developed patient-mediated materials and resources.
Publications and conferences
To date, 16 manuscripts have been published open access, in peer-reviewed journals with impact factors ranging from 1.827 to 7.06. An additional manuscript has been submitted. We have supported service users and carers to first author three publications by adopting a ‘buddy system’. We have also presented findings from our programme at 22 local, 20 national and five international conferences.
Patient-reported outcome measure and audit tool
The EQUIP PROM and EQUIP audit tool were developed (see Tables 4 and 5) and have been made freely available for use via the University of Manchester Intellectual Property Click2Go portal. The audit tool is being used in three mental health NHS trusts.
Patient-mediated materials
We developed with service users and carers a range of information materials to facilitate service user- and carer-involved care planning including the following.
User and carer definition of care planning
A definition of care planning using a structured exercise was developed by the SUCAG:
A good care plan is one over which service users have a sense of ownership. It is interactive, person-centred and accessible in an understandable form. It provides recovery-focused individually relevant information, addresses current and future needs and sets out objectives that are achievable, time-bounded and regularly reviewed. All decisions are justifiable and health professionals are accountable for any identified support that is not received.
EQUIP Advisory Group, 2015.
This definition has been incorporated into the ‘Willing Adopters’ training and into the EQUIP cards.
Animations
Findings from the published work undertaken in workstream 1 were used to develop two animations to convey key messages to a lay audience. The two animations were created by a professional animator detailing the 10 Cs of care planning (http://research.bmh.manchester.ac.uk/equip/10Cs;16 accessed 31 August 2019) and carers’ perspectives on care planning (http://research.bmh.manchester.ac.uk/equip/mentalhealthcareplanning;17 accessed 31 August 2019).
Enhancing the Quality of User and Carer Involvement in Care Planning cards
Using a structured session with our SUCAG, we defined five key questions that service users and carers could ask their care team about their care plan. The SUCAG felt that the most effective way of presenting this material was to produce a small pocket-sized fold-out card that contained the five questions and the definition of care planning. The cards are intended to be handy tools for service users and carers to refer to before and during a care planning meeting. Cards were designed utilising the same illustrations as in the animations for continuity. Details of how cards were disseminated are given in Dissemination of materials. Images of the cards can be found in Appendix 5.
Research methods course for service users and carers
In our Programme Development Grant (RP-DG-1209-10020) we developed a 6-day interactive research methods course, delivered over 6 months, for service users and carers to facilitate increased engagement in the research process. During the programme, we delivered the course twice with service user co-applicants, and our course has been cited as an exemplar of good practice by the Mental Health Research Network and published in the NICE shared learning database. 77 We completed a 6-day course during the programme. A further 6-day course and four 2-day courses were commissioned by the Mental Health Research Network, which were delivered in 2013/14 in London, Nottingham and Manchester. The 2-day course has subsequently been adopted and embedded by the Recovery College in Nottingham Healthcare Trust, and has been delivered by members of our team 16 times from 2012 to 2017, averaging seven participants per course. More widely, the course has been incorporated as a model of good practice in a number of NIHR and other funded grants. For example, we have adapted the training course for a Horizon 2020 bid and have trained PPI leads in Europe, who have cascaded the training to service users and carers with cognitive and sensory impairment. We have delivered a shortened version of our course to PPI members of a NIHR Research for Patient Benefit that aimed to improve care for young people with communication difficulties. We will be repeating the 6-day course for two funded NIHR Programme Grants for Applied Research, which we are leading or co-applicants for [RP-PG-1016-2001; enhancing the quality of psychological interventions delivered by telephone (EQUITy) and RP-PG-0216-20009; improving access to psychological therapy on acute mental health wards]. The training will also be delivered in 2018 as part of a MRC-funded bid in Indonesia and in Kenya and Tanzania as part of a funded NIHR Global Health grant.
Research methods book
The drive to enhance PPI in research means that members of the public are increasingly and actively involved in research projects. Well-planned and -resourced and meaningful involvement necessitates that these representatives achieve sufficient confidence, knowledge and skills to navigate the research process in an often short time period. To complement our research methods course, we are currently developing a research methods book, which is intended to provide a short but detailed overview of the main methods and applications of health services research. During the development of our course, we undertook a scoping search and could not find an appropriate and relevant textbook that aimed to provide in-depth research methods training to patient and pubic representatives. Our book aims to enable patient and public representatives to share a common language with academic research colleagues, and participate meaningfully and collaboratively in research projects.
The research book has been written by course facilitators (EQUIP programme co-applicants and researchers), including our service user and carer co-applicants. We have worked closely with our SUCAG to ensure that the right content, language and pitch are used. The book contains chapters detailing the research process, PPI, evidence synthesis and critical appraisal, quantitative research, qualitative research, health economics, measurement scale design and evaluation, research governance and ethics, and dissemination. Our book ties in with the designs of our other products by utilising illustrations from our EQUIP cards and animations. The book has been published and is available in hard copy (via Manchester University Press; www.manchesteruniversitypress.co.uk/9781526136534/; accessed 31 August 2019) or as a free open-access download (www.manchesteropenhive.com/view/9781526136527/9781526136527.xml; accessed 31 August 2019).
‘Willing Adopters’
Our aim was to support the roll-out of the training intervention (including all our training materials and resources) by inviting 10 NHS mental health trusts to become ‘Willing Adopters’. We originally planned to provide up to 3 days (an initial 2 days with a 1-day follow-up meeting 6 months later) of consultation with the EQUIP training team via a dissemination/implementation workshop to trust staff and service user and carer co-facilitators. The ‘Willing Adopters’ intervention comprised:
-
a ‘train the trainers’ course for health professionals (ideally those who have previously attended the training intervention) and a ‘train the trainers’ course for users and carers (recruited by the trust) to facilitate the course (all training materials including Microsoft PowerPoint, scenarios, digital clips, training manual, etc.)
-
an interactive workshop with health professionals, managers and service users and carers focused on implementation and sharing of lessons learned from the training and workstream 3
-
provision of all patient-mediated materials co-produced during the programme including the service user and carer definition of care planning, two animations to demonstrate the key components of service user- and carer-involved care planning; a pocket-sized leaflet with five key questions that service users and carers could ask health professionals about their care plan
-
the EQUIP audit tool and guidance for use to measure the extent of user and carer involvement in care planning before and after training.
The EQUIP ‘Willing Adopters’ package was offered to all nine of the NHS mental health trusts that participated in the trial phase (two of the Manchester mental health trusts have merged). The package has been delivered at seven trusts, but the model of delivery has varied dependent on their needs. Owing to an underspend on the grant, we have secured an agreement with the NIHR for £50,000 to continue the implementation following the end of the programme.
Coventry and Warwickshire Partnership NHS Trust
There has been commitment from all levels including senior management since the training intervention was first delivered. The ‘Willing Adopters’ workshop was delivered to the trust in October 2016. Day 1 focused on orientation and implementation of the EQUIP programme for senior managers, health professionals and service user and carers. Days 2 and 3 delivered a hybrid of the training intervention and ‘train the trainers’ involving six service users and carers and six health professionals. However, neither health professionals nor service users and carers felt confident to deliver the training alone and we jointly delivered the 2-day training to two CMHTs. The trust training team has since delivered five training sessions to 82 staff working in CMHTs. The trust is using the EQUIP care planning audit tool to measure service user involvement in care planning. The trust planned to roll out the training to all older adults and learning disability teams in early 2018. To ensure further embedding, a session on enhanced user and carer involvement in care planning is to be incorporated into the trust staff induction programme. Ongoing support by the EQUIP team will continue to be provided via 2- to 3-monthly teleconferences.
South West Yorkshire Partnership Foundation Trust
A 2-day ‘Willing Adopters’ package was delivered to seven senior staff at the trust in March 2017. The trust was keen to embed the training via the Recovery College to maximise service user and carer input. The Recovery College involving nine health professionals and six service users received the 2-day training package in September 2017. A further implementation half-day was delivered in October 2017; plans are now afoot to roll out the training to both community and inpatient staff and intend to use the audit tool. The EQUIP team will provide continued support to the Recovery College.
Pennine Care NHS Foundation Trust
The ‘Willing Adopters’ package was delivered to the trust in July 2017. The trust requested that the training package be condensed to a 1-day version to minimise service disruption. Although committed, it was keen that the EQUIP team deliver the training, which has been delivered seven times to health professionals (with in excess of 250 staff attending) from a wide range of services, including community mental health, early intervention, inpatient, older people’s, learning disability and children and young people’s services. The trust has made significant progress with embedding service user- and carer-involved planning with considerable buy-in from senior management with away days with service users and carers focused on improving care planning. The trust developed and implemented a new care planning template.
Lincolnshire Partnership NHS Foundation Trust
The ‘Willing Adopters’ package was delivered to seven mental health staff, two service users and two carers at Lincolnshire Partnership NHS Foundation Trust. The trust adapted the training to include a local perspective including results from a community survey, and developed examples of good care plans and risk plans, which evidenced service user involvement. The trust has plans to roll out training to the CMHTs during 2018 and use peer workers to support care/safety planning within the teams.
Leicestershire Partnership NHS Trust
The ‘Willing Adopters’ package was delivered on 14 and 15 December 2017. The learning from EQUIP has been fed into a 1-year project on care planning and recovery, and this will result in a new approach for the trust, including training, care planning and tools for recovery.
Greater Manchester Mental Health NHS Foundation Trust
Manchester Mental Health Trust and Greater Manchester West NHS Foundation Trust merged, and are now the Greater Manchester Mental Health NHS Foundation Trust. We delivered the training to the usual-care group and two further CMHT teams, with a further training session delivered in February 2018. The trust distributed the EQUIP cards via the NIHR CRN CSOs and for a 1-month period in 2017 the trust included a card with every care planning appointment letter (n = 2100). Cards were also placed within clinic waiting rooms, handed out during appointments with service users by CSOs and made available to CMHT staff to hand out to their clients.
The trust has included ‘user-involved care planning’ in its quality account, incorporated it into its service user engagement plan, developed a new template for care planning, and are funding a band 4 role specifically designed for an individual with lived experience and to deliver and embed care planning training. We will deliver the training to this newly appointed person and clinical leads in October and will offer further bespoke training to the ‘trainer’.
2Gether NHS Foundation Trust
The 2Gether NHS Foundation Trust was not part of the trial but contacted us following our dissemination and intends to use our materials and training.
Dissemination of materials
We used a systematic approach to dissemination activities in order to ensure comprehensive and thorough communication of our key messages and materials.
Phase 1 dissemination (August 2017) entailed of a mail-out of 50,000 EQUIP cards with an accompanying letter detailing information and web addresses of the animations. A total of 225 recipients were included in the phase 1 mail-out, including 70 chief executive officers of mental health NHS trusts, 61 CMHT managers, 14 third-sector organisations and 80 recovery colleges.
Focused distribution of EQUIP cards with Greater Manchester Mental Health Trust was via the NIHR CRN CSOs. Over a period of 1 month (September 2017), cards were included with care planning appointment letters by CMHT administration staff across the trust. A total of 2100 cards were distributed over a 4-week period. Cards were also placed within clinic waiting rooms, handed out during appointments with service users by CSOs and made available to CMHT staff to hand out to their clients.
Posters detailing the 10 Cs of care planning were displayed in clinic waiting rooms, and also in meeting rooms used for care planning appointments, at the request of the Greater Manchester Mental Health NHS Foundation Trust research champions. Playback of the two animations was arranged to take place on available monitors and interactive touch screens in clinic waiting rooms. Links to the animations were shared via the trust website, newsletters and e-mail to staff and service users who had provided contact details for such communication.
Phase 2 dissemination (November/December 2017) was focused on sharing the findings from workstream 2, and involved a mail-out to all of the trial participants and mental health trusts involved in the trial. Trial participants who requested to be informed of the research findings each received a lay summary of the results, details of how to view the animations and an EQUIP card. Staff involved in the trial also received a copy of the results, links to the animations and EQUIP cards to pass on to their clients.
Digital dissemination
Considerable effort was focused on digitally disseminating our findings. The digital campaign was launched on 13 July 2017 following a live Reddit Ask Me Anything (AMA) session, hosted by the EQUIP team.
Reddit Ask Me Anything
The live session was focused on the findings from workstream 1 (Grundy et al. ,16 Cree et al. 17 and Bee et al. 40). The session generated a lot of interest, with an audience of 38,500 people and 7283 positive votes (i.e. people liked this work). The total reach of the AMA was 8.88 million people (data provided by Reddit). 78
The National Institute for Health Research ‘Let’s Get Digital’ competition
Both animations were submitted to the NIHR Let’s Get Digital competition, with the carers’ perspectives animation shortlisted and subsequently named as the winner of the video category. Following this success, the animation was presented to Google (Google Inc., Mountain View, CA, USA) at an event in London in November 2017.
Twitter and Facebook
A Twitter account (@Care_Plan) was created in 2013 and was used on an ad hoc basis to share work throughout the programme. Following the Reddit AMA and shortlisting for the NIHR award, a systematic approach to sharing the animations was employed to generate interest and increase the number of views.
Data from a search of keywords tweeted including ‘user involvement’, ‘carer involvement’, ‘mental health, ‘care planning’ and ‘service delivery’ were provided by the University of Manchester library team, which allowed key Twitter accounts to be identified. Accounts were systematically selected based on relevance and number of followers. Direct contact with identified accounts involved tweets from the EQUIP account containing the EQUIP definition and links to the animations.
With support from the University of Manchester Digital Marketing Team in August 2017, we advertised via Twitter and Facebook to increase exposure to the two animations. Viewing metrics were monitored throughout the digital campaign to gauge reach and success of activity. Subsequent adjustments were made to the advertising strategy in real time based on these metrics. The results showed that the combined number of views of both animations had exceeded 335,000, with viewer retention of 6.9%, which exceeds the current average duration of video viewing hosted on Facebook (5.5%). Final analytics revealed worldwide views in Europe, North America, Africa, Asia and Australasia, an audience age range between 13 and ≥ 65 years and a gender split, with female viewers accounting for > 75% of the total audience.
Key messages video
We consulted our SUCAG to determine how it would like to disseminate the key messages from the programme, and, following discussion, it was decided that a short animation would be the preferred method to communicate findings; it is available on YouTube (YouTube, LLC, San Bruno, CA, USA; www.youtube.com) and the EQUIP website: http://research.bmh.manchester.ac.uk/equip/mainfindings (accessed 31 August 2019).
Patient and public involvement video
In October 2017, a 2-day workshop was held with the production company Patient Voices (Landbeach, UK) to develop and film a short video about PPI involvement; this is available on the EQUIP website and YouTube (http://research.bmh.manchester.ac.uk/equip/resourcesandlinks/; accessed 31 August 2019).
Conference
We ran a joint service user and carer 1-day professional, national conference to disseminate our results to users, carers, mental health professionals and other key stakeholders on 13 April 2018. More than 70 people attended the conference [including NHS staff and research and development staff (n = 34), service user/carers (n = 19), academics (n = 15) and Katherine Horner (our NIHR programme manager)]. Five NHS trusts that had completed the ‘Willing Adopters’ training presented their progress towards good practice and implementation of service user- and carer-involved care planning. Evaluation of the conference found that 97.5% of respondents would attend/recommend the event to others if this kind of conference was available again. Aspects of the conference respondents enjoyed most were the sharing of good practice by the NHS trusts, opportunities to network and the animations (PPI, 10Cs and summary of findings).
Strengths and limitations of the programme
Key strengths of the overall programme (the strengths and limitations of individual studies are discussed in the relevant sections) include completing all aspects of the programme to time and target. We recruited to time and target with each individual study, recruiting in excess of 2135 service users, carers and health professionals over the 5 years of the programme. Our service user and carer involvement was integral from conception, delivery and dissemination of the programme. A further strength of the programme was our extensive dissemination outputs produced by service users and carers and subsequent outputs (in total we published 14 academic papers and presented at > 50 conferences). We also developed a PROM and audit tool that can be used by researchers and in routine clinical practice.
The most important limitation of our programme was our failure to work further on implementation earlier in the programme; although our implementation workstream ran throughout the 5 years, more intense organisational buy-in earlier on may have yielded different results. This is justified from the promising results of our ‘Willing Adopters’ programme.
Discussion
Our programme set out to improve the involvement of service users and carers in care planning in mental health services. Through four inter-related workstreams, we successfully achieved all of our objectives on time, and reached or exceeded all of our recruitment targets. We have successfully co-developed, co-delivered and evaluated a ‘best-evidence’ training intervention for mental health professionals. We have developed and validated a 14-item PROM, providing the first unidimensional measure of service user and carer involvement in mental health-care planning. We have developed a six-item audit tool to measure service user satisfaction with care planning involvement and assessed service user and carer preferences to weight its constituent items and help direct quality improvement in practice. In parallel to this work, we have co-produced patient-mediated materials, including animations and pocket-sized prompt cards for service-users and carers, and shared these extensively to reach a maximum audience.
Developing and evaluating our training intervention
Using evidence gathered from literature reviews and our own extensive work with stakeholders, we developed our training intervention in collaboration with service users, carers and NHS representatives. Our training embraced a bottom-up approach to professional behaviour change, and offered 18 hours of facilitated training to multidisciplinary teams (12 hours of direct learning, 6 hours of follow-up supervision), plus an additional 8 hours of optional self-directed learning. Our training was co-delivered, by service users and carers, to 350 mental health professionals (304 care co-ordinators) working in CMHTs in 10 NHS trusts in England. We evaluated the impact of the training on patient outcomes by recruiting 604 service users and 90 carers to a cluster trial, and 682 service users to a cross-sectional study. Our training was well attended and positively evaluated by staff but had no significant effect on our patient-rated primary outcome measure (the HCCQ-10) 6 months after training.
Our inability to demonstrate benefits from our training intervention demands exploration. We evaluated an intervention that was derived from published evidence and designed specifically to overcome known barriers to collaborative care planning. The recent Making Good Decisions in Collaboration (MAGIC) programme79 has identified many front-line challenges to embedding shared decision-making into UK NHS secondary health-care settings, including the misplaced confidence of staff, a perceived lack of support for shared decision-making and inaccurate assumptions about patients’ preferences. Importantly, the MAGIC study excludes mental health settings, but its findings resonate closely with those of our own systematic review, which has similarly identified barriers relating to the readiness, skills and confidence of mental health professionals to engage service users and carers in discussions about their care. 5 Extensive qualitative work undertaken in phase 1 of the EQUIP programme subsequently confirmed the need to train front-line staff in partnership working and identified this as a training priority upheld by all stakeholder groups.
Our training intervention was designed and delivered in line with stakeholder preferences and took account of current best evidence emphasising the importance of interprofessional learning, interactive group work and educational outreach. We set out to train whole teams and included exercises and role plays that challenged embedded attitudes, reviewed current practice, built a shared understanding of service user involvement and improved skills in sharing decision-making with patients. Training attendance was high, but there were important limits. We stipulated an attendance rate of 80% per team, and 10 out of 18 teams achieved this goal (range 48–100%). However, no psychiatrists attended, which may ultimately have limited the impact of our intervention.
Our training was evaluated extremely positively by attending professionals, with co-delivery by service users and carers being the most valued aspect of the intervention. The co-production and co-delivery of training in partnership with service users and carers is becoming increasingly common in mental health and presents a unique opportunity to promote the ethos of partnership working at all levels of a health-care system.
Although we sought qualitative feedback on the relevance and impact of our training from staff, we did not assess the ongoing enactment of enhanced beliefs and skills. Anecdotal feedback collected during supervisory sessions and data collected during the nested process evaluation suggested that pockets of practice improvement occurred, but direct observations and/or analysis of real-time care planning discussions are needed to independently verify this behaviour change. Professionals involved in the process evaluation also felt that such changes may be too subtle for services users to notice within the follow-up period. Without such data, we are unable to determine definitively whether our training failed to translate into practice change, or whether practice changes did occur but failed to demonstrably affect trial outcomes.
Identifying and quantifying outcomes
The notion that training may have instigated practice changes but did not have a significant impact on patient outcomes raises one of two possibilities: either the practice-based charges were not of sufficient depth or spread to enact an effect or the trial outcomes were not sufficiently sensitive to this change.
Previous programmes have identified a lack of suitable patient-reported measures for shared decision-making, and our team has successfully responded to this challenge by developing and validating a new patient-reported measure of mental health-care planning involvement. Importantly, however, the availability of this measure was not assured at the programme commencement and thus an alternative primary outcome measure was sought.
The primary outcome for our trial was the HCCQ-10, a self-report scale based on self-determination theory. 46 The HCCQ-10 measures ‘autonomy support’, defined as patient perceptions of the degree to which health professionals support patient choice and ensure that their behaviour (and behaviour change) is congruent with patient values. The HCCQ-10 has 10 items, an example of which is ‘My mental health-care provider team has worked with me to develop a mental health-care plan’, and is aligned with our aim to improve patient and carer involvement in the care planning process. Secondary outcomes assessing patient experience and benefit were chosen by a consensus exercise with our patient advisory group, and included our newly validated EQUIP PROM.
We used established tools and all outcome measures were validated for our patient population. Although concerns have been expressed about the suitability of some measures (e.g. the WEMWBS for people with psychosis), all measures retained acceptable levels of reliability and validity, raising confidence in our trial’s findings.
Challenges in the timing and concept of outcome measurement cannot be underestimated. Although outcome assessments occurred at the 6-month follow-up, it is not untypical for people under the Care Programme Approach (CPA) to have their care plan reviewed on an annual basis. Although most, if not all, of our participants were under the CPA, we took the view that care planning is a continuous process rather than a single event of activity. Opportunities to use the training in routine contacts thus extended beyond the CPA. Data from patient self-report suggested that 79% of patients saw their CMHT during the 6-month follow-up, with a mean of 12.3 contacts per person. Although these data are reassuring, we cannot exclude the possibility that patients’ appraisals of autonomy remained biased towards their experiences in more formal care planning meetings.
Longer follow-up has been possible in our ‘Wiling Adopter’ sites, and early evidence is emerging to suggest improvements in care planning assessed by Care Commission Quality (CQC) ratings. Whether these improvements can be directly attributed to our training intervention or to wider organisational strategy is unclear. Published literature on shared decision-making highlights a tension between the use of validated and reliable measures for research purposes, and the neglect of measures normally used to drive quality improvement. 80 Adopting recognised quality improvement measures can potentially strengthen team commitment to practice-based interventions and enhance the likelihood of positive behaviour change.
Locating training in the context of wider organisational change
Accepting that our trial measures were fit for purpose and sensitive to change places onus on philosophical and structural design of our intervention. Our decision to prioritise a bottom-up approach and deliver training to front-line staff was justified by the need to balance effective intervention with maximal reach. However, the lack of significant differences in outcomes between our trial arms suggests that short-term staff training is not an effective way to embed service involvement in care planning practice.
Significantly, our results concur with a growing body of evidence that highlights the challenges associated with embedding shared decision-making in routine services. 81–85 At present, evidence on how to encourage service user involvement in care planning decisions is limited86 and there is no proven method of implementing shared decision-making across routine mental health settings. A recent review of studies to enhance shared decision-making in psychosis has shown that the majority of trials have delivered and evaluated interventions to patients, with only one testing training for clinicians. 82 Our programme, and specifically our trial, thus provides some important learning.
Synthesis of findings across our workstreams suggests that it is unlikely, although not impossible, that our training intervention was suboptimally applied. A recent systematic review87 suggests that the majority of training interventions can improve staff skills, and qualitative evaluation within our programme provides confirmatory evidence of individual impact. Direct communication with participating trusts has enabled us to estimate < 5% turnover of staff from baseline to the 6-month follow-up, adding weight to our expectation of a proximal training effect. Rather, we argue that our training intervention most probably encountered its biggest challenges in initiating and sustaining routine behaviour change and having an impact on distal patient-centred outcomes.
Our inability to show an effect of the training may in part be explained by data from our qualitative process evaluation, which suggested that, despite ideological buy-in from trained staff, our training failed to become embedded and normalised in local provision. Supervision sessions were offered to staff post training but demonstrated very low uptake. This widespread failure to engage in supervision may in part reflect the fact that professionals’ work priorities, workload and availability were not conducive to incorporating new knowledge and skills from training into their existing role. Qualitative data collected at the 6- and 12-month follow-ups suggested that there was an absence of organisational readiness to accept change, and an underestimation and deficient investment in the amount of relational work required to make it successful. This combination of stretched staff and services, in the absence of organisational requirement and support to incorporate training into usual practice, most probably had an impact on the probability of eliciting measurable changes in service user and carer involvement.
Service users and professionals in the process evaluation identified alternative roles, such as recovery workers, support workers and occupational therapists, as being the most likely to have the time to undertake the required relational work to successfully enact user-centred care planning. A recent review supports the incorporation of such alternative forms of service provision within mental health care to improve outcomes for patients while reducing the pressure on the mental health system. 88
Lessons in change management for mental health services
Effective change management demands accurate analysis of the causes of the presenting problem. A particular strength of our programme lies in our two substudies that were informed and underpinned by implementation science (studies 6 and 7). Baseline data from our nested process evaluation suggested that the current operationalisation and utilisation of care planning within mental health services was likely to be a significant barrier to involving patients and carers in the care planning process,76 and pointed to a need to develop a successful strategy to optimise training implementation.
Our focus on developing and evaluating a relatively low-cost, bottom-up approach to behaviour change inevitably led to the prioritisation of our training intervention. In line with the change management literature, we designed a training intervention to enact developmental (skills-based) and transitional (cognitive-based) change. We included a director of nursing and the host trust’s director of patient experience as co-applicants with costed time for programme input and involved these high-level managers in evidence synthesis and intervention design. In response to baseline data that identified a need for high-level buy-in to facilitate training attendance, we also leveraged higher managerial support to make our training mandatory to front-line staff. These strategies were effective in promoting meaningful engagement in our intervention but did not fully extend to securing the levels of organisational support necessary to support the translation of training into everyday practice. Future work should consider adopting evidence-based, phase-specific implementation strategies to enhance training impacts and effects.
A key learning point derived from the recent MAGIC programme was that professional attitudes and understanding of shared decision-making constitute a core focus for practice change. 83 Importantly, however, although MAGIC examined a number of clinical contexts, it excluded mental health. Mental health services have a unique service history founded on concepts of containment and coercion89 and, as such, any initiative to enhance service user involvement and decision-making may face particular and additional challenges. Patients in mental health services often present with long-term and complex diagnoses, and can experience significant stigma. 90,91 These observations allude to potentially important differences between mental and physical health services that may require a somewhat different balance and mix of intervention components and evidence to effectively redress. Historically, the majority of patients and carers have felt marginalised in care planning decisions,5 and the potential for short-term training interventions to have an impact on these entrenched attitudes may be disproportionately constrained.
Of particular interest in the current programme was the readiness of our ‘Willing Adopter’ sites to accept our training intervention without clear evidence of clinical effect or cost-effect. Arguably, equipping professionals with the skills to effectively involve service user and cares in their care may be conceived as a value-based initiative, with potential for continuous rather than immediate improvement in health-care culture and outcomes, which is supported by data from the process evaluation. Strong moral and ethical reasons for involving people in care planning persist and the historical marginalisation and neglect of mental health services may be fostering an urgent need for innovation. The most successful ‘Willing Adopters’ in our programme have benefited from substantial high-level managerial support, supportive ‘middle managers’ and excellent staff who appear open to change. Thus, at a time when NHS redesign techniques are advocating bottom-up commitments from patient and professional stakeholders, our work has demonstrated an explicit need to continue to ensure that these are located within active spheres of organisational accountability and systems-level transformation. For example, the process evaluation identified the need to reconsider the structure and content of existing care planning documentation. All of the stakeholders felt that the current formulation of care plans served organisational agendas rather than the needs of service users,76 and this limited the relevance of including service users in such bureaucratic processes. Future work should consider ways to increase the relevance of care planning to the everyday lives of service users.
Macrolevel theories of health-care improvement have been previously criticised for their limited explanatory power and may not be appropriate for understanding fine-grained enablers of and barriers to the sustainability of change. Participation in our research trial required some institutional agreement from our host health organisations but did not require significant commitment beyond the promise of staff training time. It is therefore unclear if our training participants viewed our intervention as integral to service function, or merely as a research-based initiative competing with other demands. Effective interventions may ultimately require more comprehensive and enduring commitment, including explicit validation of time spent with patients, endorsement of partnership through clinical leadership and incentives, and fostering new ways to meet patient needs within the constraints of current resources. However, such comprehensive models raise significant challenges for implementation and assessment in a rigorous, controlled fashion. A further consideration is the extent to which a RCT was the correct vehicle to test our intervention. On reflection, it may have been more appropriate to focus on implementation outputs as demonstrated by our ‘Willing Adopters’. Further work is indicated to explore the enablers and outcomes of our training implementation in the context of everyday implementation.
Identifying alternative strategies for evaluation
Outside our cluster trial, our programme took a whole-systems approach to service improvement. This approach acknowledged the multifactorial issues involved in health care and recognises that successful implementation relies on a combination of interventions supporting the organisation, the clinicians and the patients. Long-standing deficits in mental health policy and practice have led to feelings of exclusion and passivity for many patients, and, therefore, parallel efforts to increasing patient agency, activation and health literacy are likely to become important. We have co-produced with service users and carers animations and prompt cards to increase the likelihood of mutually useful conversations between patients and clinicians and provide an alternative or additive strategy for evaluation. Our strategic use of social media to communicate our work has substantially enhanced the reach and impact of these outputs and set a precedent for future dissemination. The importance of accountability in care planning, and finding ways of eliciting needs from service users that are meaningful to them, which might fall outside conventional care planning practices, are essential to explore.
Recommendations for future research
-
There remains an urgent need to develop ways of improving service user and carer involvement in their care plans. More complex, comprehensive and enduring interventions may be required, such as the use of incentives, linkage to routine outcome monitoring and better integration into routine clinical systems. However, such comprehensive models raise significant challenges for their implementation (and their assessment in a rigorous, controlled fashion).
-
Research should focus on developing and evaluating new organisational initiatives to address contextual barriers to service and carer involvement in care planning. These initiatives should include the introduction of both ‘bottom-up’ and ‘top-down’ structural changes, such as accountability systems, as well as system-level strategies that encourage or facilitate shared access to care plans.
Implications for clinical practice
The evaluation of the training intervention was extremely positive. The co-production and co-delivery of training in partnership with service users and carers is increasingly common in mental health care. In this study, we have shown the possibilities and potential of this endeavour. When working with service users and carers in the development and delivery of training it is important that service users and carers are equipped to handle potential resistance from staff. The roles of service users and carers should be negotiated carefully and agreed at the outset. The involvement of service users and carers must be concomitant with ongoing support and supervision. In the end, mental health professionals’ involvement of service users and carers will be enhanced and further potential for shared decision-making is apparent.
Services we have been working with have recognised that service user and carer involvement requires improvement, but they need to acknowledge that, in addition to the training, new organisational initiatives to address contextual barriers to service and carer involvement in care planning are required. Such initiatives may include the introduction of ‘top-down’ structural changes, such as accountability systems, as well as system-level strategies that encourage or facilitate shared access to care plans. Initiatives may examine ways of incorporating mandatory requirements for staff to actively involve service users and carers in care planning (e.g. as part of clinical supervision, job role specifications and continuing professional development). This approach might affect changes in service user satisfaction in care planning involvement more effectively.
Acknowledgements
We would like to acknowledge the support we have received from the NIHR Clinical Research Network and CSOs, who contributed significant effort in recruitment for our trial and also supported dissemination at the end of our programme. We also give thanks to our Programme Steering Committee (Professor Alan Simpson, Dr Dean McMillan, Dr Michael Coffey and Bethan Edwards) and our SUCAG [Debbie Butler (chairperson), Donna More, Dawn Perry, Joe Keaney, Dave Waldram, Jo Bramley, Michael Osborne, Orla Judge and Kate Lurie], which shaped the EQUIP programme and gave such valuable insight into the lived experience of receiving care, and care planning in mental health services.
Service user and carer trainers received numeration for training delivery. This payment was solely for training course facilitation post trial, and was negotiated with ‘Willing Adopter’ sites after all the evaluative research was completed.
Contributions of authors
Professor Karina Lovell was the chief investigator for the programme and was co-lead of workstream 2.
Professor Penny Bee was a co-applicant and was the lead of workstream 1 and workstream 4.
Professor Peter Bower was a co-applicant and co-lead for workstream 2.
Dr Helen Brooks led workstream 3 and undertook participant recruitment and research interviews and assessments in workstream 3 and the trial.
Mr Patrick Cahoon was a co-applicant and offered critical clinical and organisational insights with delivery and implementation.
Professor Patrick Callaghan was a co-applicant.
Dr Lesley-Anne Carter led the statistical analysis.
Mrs Lindsey Cree was a co-applicant.
Professor Linda Davies was a co-applicant.
Dr Richard Drake was a co-applicant.
Mrs Claire Fraser was the programme manager.
Dr Chris Gibbons undertook psychometric testing and development of the PROM.
Mr Andrew Grundy was a co-applicant.
Dr Kathryn Hinsliff-Smith undertook participant recruitment and research assessments for the trial.
Dr Oonagh Meade undertook participant recruitment and research interviews.
Professor Chris Roberts was a co-applicant.
Professor Anne Rogers was a co-applicant.
Dr Kelly Rushton undertook participant recruitment and research assessments for the trial.
Dr Caroline Sanders was a co-applicant for workstream 3.
Ms Gemma Shields conducted the health economics analysis.
Ms Lauren Walker was a co-applicant.
All authors contributed to delivering the programme and to the drafting, revision and approval of the final report. All applicants were involved in the programme conception, design, methods, analysis and interpretation.
Publications
Gibbons CJ, Bee PE, Walker L, Price O, Lovell K. Service user- and carer-reported measures of involvement in mental health care planning: methodological quality and acceptability to users. Front Psychiatry 2014;5:178.
Bee P, Brooks H, Fraser C, Lovell K. Professional perspectives on service user and carer involvement in mental health care planning: a qualitative study. Int J Nurs Stud 2015;52:1834–45.
Bee P, Price O, Baker J, Lovell K. Systematic synthesis of barriers and facilitators to service user-led care planning. Br J Psychiatry 2015;207:104–14.
Bower P, Roberts C, O’Leary N, Callaghan P, Bee P, Fraser C, et al. A cluster randomised controlled trial and process evaluation of a training programme for mental health professionals to enhance user involvement in care planning in service users with severe mental health issues (EQUIP): study protocol for a randomised controlled trial. Trials 2015;16:348.
Brooks H, Sanders C, Lovell K, Fraser C, Rogers A. Re-inventing care planning in mental health: stakeholder accounts of the imagined implementation of a user/carer involved intervention. BMC Health Serv Res 2015;15:490.
Cree L, Brooks HL, Berzins K, Fraser C, Lovell K, Bee P. Carers’ experiences of involvement in care planning: a qualitative exploration of the facilitators and barriers to engagement with mental health services. BMC Psychiatry 2015;15:208.
Bee P, Gibbons C, Callaghan P, Fraser C, Lovell K. Evaluating and Quantifying User and Carer Involvement in Mental Health Care Planning (EQUIP): co-development of a new patient-reported outcome measure. PLOS ONE 2016;11:e0149973.
Brooks H, Rushton K, Walker S, Lovell K, Rogers A. Ontological security and connectivity provided by pets: a study in the self-management of the everyday lives of people diagnosed with a long-term mental health condition. BMC Psychiatry 2016;16:409.
Grundy AC, Bee P, Meade O, Callaghan P, Beatty S, Olleveant N, Lovell K. Bringing meaning to user involvement in mental health care planning: a qualitative exploration of service user perspectives. J Psychiatr Ment Health Nurs 2016;23:12–21.
Hughes-Morley A, Hann M, Fraser C, Meade O, Lovell K, Young B, et al. The impact of advertising patient and public involvement on trial recruitment: embedded cluster randomised recruitment trial. Trials 2016;17:586.
Brooks HL, Lovell K, Bee P, Sanders C, Rogers A. Is it time to abandon care planning in mental health services? A qualitative study exploring the views of professionals, service users and carers. Health Expectations 2017;21:597–605.
Fraser C, Grundy A, Meade O, Callaghan P, Lovell K. EQUIP training the trainers: an evaluation of a training programme for service users and carers involved in training mental health professionals in user-involved care planning. J Psychiatr Ment Health Nurs 2017;24:367–76.
Grundy AC, Walker L, Meade O, Fraser C, Cree L, Bee P, et al. Evaluation of a co-delivered training package for community mental health professionals on service user- and carer-involved care planning. J Psychiatr Ment Health Nurs 2017;24:358–66.
Brooks H, Lovell K, Bee P, Fraser C, Molloy C, Rogers A. Implementing an intervention designed to enhance service user involvement in mental health care planning: a qualitative process evaluation. Soc Psychiatr Epidemiol 2018;54:221–33.
Camacho EM, Shields G, Lovell K, Coventry PA, Morrison AP, Davies LM. A (five-)level playing field for mental health conditions?: exploratory analysis of EQ-5D-5L-derived utility values. Qual Life Res 2018;27:717–24.
Lovell K, Bee P, Brooks H, Cahoon P, Callaghan P, Carter LA, et al. Embedding shared decision-making in the care of patients with severe and enduring mental health problems: the EQUIP pragmatic cluster randomised trial. PLOS ONE 2018;13:e0201533.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health and Social Care.
References
- Department of Health and Social Care . Refocusing the Care Programme Approach. Policy and Positive Practice Guidance 2008.
- World Health Organization . Draft Mental Health Action Plan An Overview 2012.
- Commonwealth of Australia . Fourth National Mental Health Plan An Agenda for Collaborative Government Action in Mental Health 2009–2014 2009.
- Simpson EL, House AO. User and carer involvement in mental health services: from rhetoric to science. Br J Psychiatry 2003;183:89-91. https://doi.org/10.1192/bjp.183.2.89.
- Bee P, Price O, Baker J, Lovell K. Systematic synthesis of barriers and facilitators to service user-led care planning. Br J Psychiatry 2015;207:104-14. https://doi.org/10.1192/bjp.bp.114.152447.
- Thornicroft G, Tansella M. Growing recognition of the importance of service user involvement in mental health service planning and evaluation. Epidemiol Psichiatr Soc 2005;14:1-3. https://doi.org/10.1017/S1121189X00001858.
- Richards DA, Lankshear AJ, Fletcher J, Rogers A, Barkham M, Bower P, et al. Developing a U.K. protocol for collaborative care: a qualitative study. Gen Hosp Psychiatry 2006;28:296-305. https://doi.org/10.1016/j.genhosppsych.2006.03.005.
- Henderson C, Flood C, Leese M, Thornicroft G, Sutherby K, Szmukler G. Effect of joint crisis plans on use of compulsory treatment in psychiatry: single blind randomised controlled trial. BMJ 2004;329. https://doi.org/10.1136/bmj.38155.585046.63.
- Crawford MJ, Aldridge T, Bhui K, Rutter D, Manley C, Weaver T, et al. User involvement in the planning and delivery of mental health services: a cross-sectional survey of service users and providers. Acta Psychiatr Scand 2003;107:410-14. https://doi.org/10.1034/j.1600-0447.2003.00049.x.
- Gately C, Rogers A, Sanders C. Re-thinking the relationship between long-term condition self-management education and the utilisation of health services. Soc Sci Med 2007;65:934-45. https://doi.org/10.1016/j.socscimed.2007.04.018.
- Rogers A, Day J, Randall F, Bentall RP. Patients’ understanding and participation in a trial designed to improve the management of anti-psychotic medication: a qualitative study. Soc Psychiatry Psychiatr Epidemiol 2003;38:720-7. https://doi.org/10.1007/s00127-003-0693-5.
- Simpson A, Hannigan B, Coffey M, Barlow S, Cohen R, Jones A, et al. Recovery-focused care planning and coordination in England and Wales: a cross-national mixed methods comparative case study. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0858-x.
- NHS Choices . Care Programme Approach 2015. www.nhs.uk/conditions/social-care-and-support-guide/pages/care-programme-approach.aspx (accessed 20 November 2017).
- NICE . Service User Experience in Adult Mental Health: Improving the Experience of Care for People Using Adult NHS Mental Health Services. Guidance and Guidelines 2011. www.nice.org.uk/guidance/cg136 (accessed 11 November 2017).
- NHS England . Implementing the Five Year Forward View for Mental Health 2016. www.england.nhs.uk/wp-content/uploads/2016/07/fyfv-mh.pdf (accessed 31 August 2019).
- Grundy AC, Bee P, Meade O, Callaghan P, Beatty S, Olleveant N, et al. Bringing meaning to user involvement in mental health care planning: a qualitative exploration of service user perspectives. J Psychiatr Ment Health Nurs 2016;23:12-21. https://doi.org/10.1111/jpm.12275.
- Cree L, Brooks HL, Berzins K, Fraser C, Lovell K, Bee P. Carers’ experiences of involvement in care planning: a qualitative exploration of the facilitators and barriers to engagement with mental health services. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0590-y.
- Coffey M, Hannigan B, Simpson A. Care planning and coordination: imperfect solutions in a complex world. J Psychiatr Ment Health Nurs 2017;24:333-4. https://doi.org/10.1111/jpm.12393.
- Care Quality Commission . Survey of Mental Health Inpatient Services 2009.
- Care Quality Commission . Better Care In My Hands: A Review of How People Are Involved in Their Care 2016.
- Doody O, Butler MP, Lyons R, Newman D. Families’ experiences of involvement in care planning in mental health services: an integrative literature review. J Psychiatr Ment Health Nurs 2017;24:412-30. https://doi.org/10.1111/jpm.12369.
- Drummond C, Simpson A. ‘Who’s actually gonna read this?’ An evaluation of staff experiences of the value of information contained in written care plans in supporting care in three different dementia care settings. J Psychiatr Ment Health Nurs 2017;24:377-86. https://doi.org/10.1111/jpm.12380.
- Grundy AC, Walker L, Meade O, Fraser C, Cree L, Bee P, et al. Evaluation of a co-delivered training package for community mental health professionals on service user- and carer-involved care planning. J Psychiatr Ment Health Nurs 2017;24:358-66. https://doi.org/10.1111/jpm.12378.
- Bee P, Brooks H, Fraser C, Lovell K. Professional perspectives on service user and carer involvement in mental health care planning: a qualitative study. Int J Nurs Stud 2015;52:1834-45. https://doi.org/10.1016/j.ijnurstu.2015.07.008.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-39.
- Michell L, Barbour R, Kitzinger J. Developing Focus Group Research: Politics, Theory and Practice. Thousand Oaks, CA: Sage Publications Ltd; 1999.
- Robertson R, Jochleson K. Interventions that Change Clinician Behaviour: Mapping the Literature. London: NICE; 2007.
- Reeves S, Zwarenstein M, Goldman J, Barr H, Freeth D, Hammick M, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2008;1. https://doi.org/10.1002/14651858.CD002213.pub2.
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003;362:1225-30. https://doi.org/10.1016/S0140-6736(03)14546-1.
- Lovell K, Bower P, Richards D, Barkham M, Sibbald B, Roberts C, et al. Developing guided self-help for depression using the Medical Research Council complex interventions framework: a description of the modelling phase and results of an exploratory randomised controlled trial. BMC Psychiatry 2008;8. https://doi.org/10.1186/1471-244X-8-91.
- Dowrick C, Gask L, Edwards S, Aseem S, Bower P, Burroughs H, et al. Researching the mental health needs of hard-to-reach groups: managing multiple sources of evidence. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-226.
- Bradshaw T, Wearden A, Marshall M, Warburton J, Husain N, Pedley R, et al. Developing a healthy living intervention for people with early psychosis using the Medical Research Council’s guidelines on complex interventions: phase 1 of the HELPER - InterACT programme. Int J Nurs Stud 2012;49:398-406. https://doi.org/10.1016/j.ijnurstu.2011.10.008.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:80-92. https://doi.org/10.1177/160940690600500107.
- Fraser C, Grundy A, Meade O, Callaghan P, Lovell K. EQUIP training the trainers: an evaluation of a training programme for service users and carers involved in training mental health professionals in user-involved care planning. J Psychiatr Ment Health Nurs 2017;24:367-76. https://doi.org/10.1111/jpm.12361.
- Gibbons CJ, Bee PE, Walker L, Price O, Lovell K. Service user- and carer-reported measures of involvement in mental health care planning: methodological quality and acceptability to users. Front Psychiatry 2014;5. https://doi.org/10.3389/fpsyt.2014.00178.
- Mokken R. A theory and procedure of scale analysis: with applications in political research . Contemp Sociol 1971;2. https://doi.org/10.1515/9783110813203.
- Rasch G. Probabilistic Models for Some Intelligence and Attainment Tests. Copenhagen: Danish Institute for Educational Research; 1960.
- Bee P, Gibbons C, Callaghan P, Fraser C, Lovell K. Evaluating and Quantifying User and Carer Involvement in Mental Health Care Planning (EQUIP): co-development of a new patient-reported outcome measure. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0149973.
- Ryan M, Gerard K, Amaya-Amaya M. Using Discrete Choice Experiments to Value Health and Health Care. Berlin: Springer; 2008.
- Louviere J, Hensher D, Swait J. Stated Choice Methods. Cambridge: Cambridge University Press; 2000.
- Hess S, Train K. Correlation and scale in mixed logit models. J Choice Modelling 2017;23:1-8. https://doi.org/10.1016/j.jocm.2017.03.001.
- Hole AR. Fitting mixed logit models by using maximum simulated likelihood. Stata J 2007;7:388-401. https://doi.org/10.1177/1536867X0700700306.
- Hole AR. A comparison of approaches to estimating confidence intervals for willingness to pay measures. Health Econ 2007;16:827-40. https://doi.org/10.1002/hec.1197.
- Ludman EJ, Simon GE, Rutter CM, Bauer MS, Unützer J. A measure for assessing patient perception of provider support for self-management of bipolar disorder. Bipolar Disord 2002;4:249-53. https://doi.org/10.1034/j.1399-5618.2002.01200.x.
- Ruggeri M, Dall’Agnola R. The development and use of the Verona Expectations for Care Scale (VECS) and the Verona Service Satisfaction Scale (VSSS) for measuring expectations and satisfaction with community-based psychiatric services in patients, relatives and professionals. Psychol Med 1993;23:511-23. https://doi.org/10.1017/S0033291700028609.
- Waddell L, Taylor M. A new self-rating scale for detecting atypical or second-generation antipsychotic side effects. J Psychopharmacol 2008;22:238-43. https://doi.org/10.1177/0269881107087976.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Ridgway PA. Assessing the Recovery Commitment of Your Mental Health Services: A User’s Guide for the Developing Recovery Enhancing Environments Measure (DREEM). Rideford: Recovery Devon; 2004.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Gaston L. Reliability and criterion-related validity of the California Psychotherapy Alliance Scales (CALPAS) – patient version. Psychol Assess 1991;3:68-74. https://doi.org/10.1037/1040-3590.3.1.68.
- Group TW. The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc Sci Med 1998;46:1569-85. https://doi.org/10.1016/S0277-9536(98)00009-4.
- Lelliott P, Beevor A, Hogman G, Hyslop J, Lathlean J, Ward M. Carers’ and users’ expectations of services – carer version (CUES-C): a new instrument to support the assessment of carers of people with a severe mental illness. J Ment Health 2003;12:143-52. https://doi.org/10.1080/0963823031000103452.
- Bower P, Roberts C, O’Leary N, Callaghan P, Bee P, Fraser C, et al. A cluster randomised controlled trial and process evaluation of a training programme for mental health professionals to enhance user involvement in care planning in service users with severe mental health issues (EQUIP): study protocol for a randomised controlled trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0896-6.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: Personal Social Services Research Unit, University of Kent; 2016.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2015 to 2016 2016. www.gov.uk/government/publications/nhs-reference-costs-2015-to-2016 (accessed 31 August 2019).
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- NICE . Position Statement on Use of the EQ-5D-5L Valuation Set 2017. www.nice.org.uk/Media/Default/About/what-we-do/NICE-guidance/NICE-technology-appraisal-guidance/eq5d5l_nice_position_statement.pdf (accessed 7 November 2017).
- Lovell K, Bee P, Brooks H, Cahoon P, Callaghan P, Carter LA, et al. Embedding shared desicion-making in the care of patients with severe and enduring mental health problems: the EQUIP pragmatic cluster randomised trial. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0201533.
- Davis J, Rawana E, Capponi D. Acceptability of behavioural staff management techniques. Behav Res Treat 1989;4:23-44. https://doi.org/10.1002/bin.2360040104.
- Milne D, Noone S. Teaching and Training for Non-Teachers. Hoboken, NJ: John Wiley & Sons, Inc.; 1996.
- Myles P, Milne D. Outcome evaluation of a brief shared learning programme in cognitive behavioural therapy. Behav Cogn Psychother 2004;32:177-88. https://doi.org/10.1017/S1352465804001183.
- Milne D. An empirical definition of clinical supervision. Br J Clin Psychol 2007;46:437-47. https://doi.org/10.1348/014466507X197415.
- Weber R. Basic Content Analysis. Thousand Oaks, CA: SAGE Publications Ltd; 1990.
- Brooks H, Sanders C, Lovell K, Fraser C, Rogers A. Re-inventing care planning in mental health: stakeholder accounts of the imagined implementation of a user/carer involved intervention. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1154-z.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Lau R, Stevenson F, Ong BN, Dziedzic K, Treweek S, Eldridge S, et al. Achieving change in primary care – causes of the evidence to practice gap: systematic reviews of reviews. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0396-4.
- Kennedy A, Vassilev I, James E, Rogers A. Implementing a social network intervention designed to enhance and diversify support for people with long-term conditions. A qualitative study. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0384-8.
- Vassilev I, Rogers A, Kennedy A, Koetsenruijter J. The influence of social networks on self-management support: a metasynthesis. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-719.
- Macfarlane A, O’Reilly-de Brún M. Using a theory-driven conceptual framework in qualitative health research. Qual Health Res 2012;22:607-18. https://doi.org/10.1177/1049732311431898.
- EU-WISE . EU-WISE Final Project Report n.d. https://cordis.europa.eu/docs/results/279/279081/final1-eu-wise-final-report.pdf (accessed 31 August 2019).
- Greenhalgh A, Kryiakidou O, Peacock R. How to Spread Good Ideas. A Systematic Review of the Literature on Diffusion, Dissemination and Sustainability on Innovations in Health Service Delivery and Organisation n.d. www.netscc.ac.uk/netscc/hsdr/files/project/SDO_FR_08-1201-038_V01.pdf (accessed 31 August 2019).
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694-6. https://doi.org/10.1136/bmj.321.7262.694.
- Brooks H, Rushton K, Walker S, Lovell K, Rogers A. Ontological security and connectivity provided by pets: a study in the self-management of the everyday lives of people diagnosed with a long-term mental health condition. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1111-3.
- Brooks HL, Lovell K, Bee P, Sanders C, Rogers A. Is it time to abandon care planning in mental health services? A qualitative study exploring the views of professionals, service users and carers. Health Expect 2017;21:597-605. https://doi.org/10.1111/hex.12650.
- NICE . Enhancing the Quality of Service User Involved Care Planning in Mental Health Services (EQUIP) n.d. www.nice.org.uk/sharedlearning/enhancing-the-quality-of-service-user-involved-care-planning-in-mental-health-services-equip (accessed August 2019).
- MentalHealthService . Science Ama Series: We Are a Team of Researchers from the Universities of Manchester and Nottingham, UK, Working on a 5 Year Program to Enhance the Quality of Care Planning in Mental Health Services. AMA 2017. https://thewinnower.com/papers/7228-science-ama-series-we-are-a-team-of-researchers-from-the-universities-of-manchester-and-nottingham-uk-working-on-a-5-year-program-to-enhance-the-quality-of-care-planning-in-mental-health-services-ama (accessed 31 August 2019).
- The Health Foundation . The MAGIC Programme: Evaluation 2013. www.health.org.uk/publications/the-magic-programme-evaluation (accessed 31 August 2019).
- Kasper J, Heesen C, Köpke S, Fulcher G, Geiger F. Patients’ and observers’ perceptions of involvement differ. Validation study on inter-relating measures for shared decision making. PLOS ONE 2011;6.
- Elwyn G, Laitner S, Coulter A, Walker E, Watson P, Thomson R. Implementing shared decision making in the NHS. BMJ 2010;341. https://doi.org/10.1136/bmj.c5146.
- Stovell D, Morrison AP, Panayiotou M, Hutton P. Shared treatment decision-making and empowerment-related outcomes in psychosis: systematic review and meta-analysis. Br J Psychiatry 2016;209:23-8. https://doi.org/10.1192/bjp.bp.114.158931.
- Joseph-Williams N, Lloyd A, Edwards A, Stobbart L, Tomson D, Macphail S, et al. Implementing shared decision making in the NHS: lessons from the MAGIC programme. BMJ 2017;357. https://doi.org/10.1136/bmj.j1744.
- Iles V, Sutherland K. Organisational Change: A Review for Healthcare Managers, Professionals and Researchers. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2001.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-37.
- Duncan E, Best C, Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database Syst Rev 2010;1. https://doi.org/10.1002/14651858.CD007297.pub2.
- McEwan D, Ruissen GR, Eys MA, Zumbo BD, Beauchamp MR. The effectiveness of teamwork training on teamwork behaviors and team performance: a systematic review and meta-analysis of controlled interventions. PLOS ONE 2017;12.
- Johnson S, Lamb D, Marston L, Osborn D, Mason O, Henderson C, et al. Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet 2018;392:409-18. https://doi.org/10.1016/S0140-6736(18)31470-3.
- Rogers A, Day JC, Williams B, Randall F, Wood P, Healy D, et al. The meaning and management of neuroleptic medication: a study of patients with a diagnosis of schizophrenia. Soc Sci Med 1998;47:1313-23. https://doi.org/10.1016/S0277-9536(98)00209-3.
- Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry 2002;1:16-20.
- Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health 2013;103:777-80. https://doi.org/10.2105/AJPH.2012.301056.
- Department of Health and Social Care . The NHS Plan: A Plan for Investment, A Plan for Reform 2000.
- Blenkiron P, Mo KH, Cuzen J, Hammill AC. Involving service users in their mental health care: the CUES Project. Psychiatric Bull 2018;27:334-8. https://doi.org/10.1017/S095560360000297X.
- Bramesfeld A, Wedegärtner F, Elgeti H, Bisson S. How does mental health care perform in respect to service users’ expectations? Evaluating inpatient and outpatient care in Germany with the WHO responsiveness concept. BMC Health Serv Res 2007;7. https://doi.org/10.1186/1472-6963-7-99.
- Torgerson DJ. Contamination in trials: is cluster randomisation the answer?. BMJ 2001;322:355-7. https://doi.org/10.1136/bmj.322.7282.355.
- Hutton JL. Are distinctive ethical principles required for cluster randomized controlled trials?. Stat Med 2001;20:473-88. https://doi.org/10.1002/1097-0258(20010215)20:3<473::AID-SIM805>3.0.CO;2-D.
- Edwards SJ, Braunholtz DA, Lilford RJ, Stevens AJ. Ethical issues in the design and conduct of cluster randomised controlled trials. BMJ 1999;318:1407-9. https://doi.org/10.1136/bmj.318.7195.1407.
- Richards DA, Hill JJ, Gask L, Lovell K, Chew-Graham C, Bower P, et al. Clinical effectiveness of collaborative care for depression in UK primary care (CADET): cluster randomised controlled trial. BMJ 2013;347. https://doi.org/10.1136/bmj.f4913.
- Kennedy A, Bower P, Reeves D, Blakeman T, Bowen R, Chew-Graham C, et al. Implementation of self management support for long term conditions in routine primary care settings: cluster randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.f2882.
- Eldridge SM, Ashby D, Feder GS. Informed patient consent to participation in cluster randomized trials: an empirical exploration of trials in primary care. Clin Trials 2005;2:91-8. https://doi.org/10.1191/1740774505cn070oa.
- Conrad P. Qualitative research on chronic illness: a commentary on method and conceptual development. Soc Sci Med 1990;30:1257-63. https://doi.org/10.1016/0277-9536(90)90266-U.
- Gately C, Rogers A, Kirk S, McNally R. Integration of devices into long-term condition management: a synthesis of qualitative studies. Chronic Illn 2008;4:135-48. https://doi.org/10.1177/1742395308092484.
- Rogers A, Kirk S, Gately C, May CR, Finch T. Established users and the making of telecare work in long term condition management: implications for health policy. Soc Sci Med 2011;72:1077-84. https://doi.org/10.1016/j.socscimed.2011.01.031.
- Pahl R, Spencer L, Phillipson C, Allan G, Morgan D. Social Networks and Social Exclusion: Sociological and Policy Perspectives. Aldershot: Ashgate; 2004.
- Mair FS, Hiscock J, Beaton SC. Understanding factors that inhibit or promote the utilization of telecare in chronic lung disease. Chronic Illn 2008;4:110-17. https://doi.org/10.1177/1742395308092482.
- Allen D, Griffiths L, Lyne P. Understanding complex trajectories in health and social care provision. Sociol Health Illn 2004;26:1008-30. https://doi.org/10.1111/j.0141-9889.2004.00426.x.
- Dinniss S, Roberts G, Hubbard C, Hounsell J, Webb R. User-led assessment of a recovery service using DREEM. Psychiatric Bull 2018;31:124-7. https://doi.org/10.1192/pb.bp.106.010025.
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69-77. https://doi.org/10.1016/S0022-3999(01)00296-3.
- Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 2013;22:1717-27. https://doi.org/10.1007/s11136-012-0322-4.
- Herdman M, Gudex C, Lloyd A, . Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- Davies LM, Lewis S, Jones PB, Barnes TR, Gaughran F, Hayhurst K, et al. Cost-effectiveness of first- v. second-generation antipsychotic drugs: results from a randomised controlled trial in schizophrenia responding poorly to previous therapy. Br J Psychiatry 2007;191:14-22. https://doi.org/10.1192/bjp.bp.106.028654.
- Davies LM, Barnes TR, Jones PB, Lewis S, Gaughran F, Hayhurst K, et al. A randomized controlled trial of the cost-utility of second-generation antipsychotics in people with psychosis and eligible for clozapine. Value Health 2008;11:549-62. https://doi.org/10.1111/j.1524-4733.2007.00280.x.
- Rawlins MD, Culyer AJ. National Institute for Clinical Excellence and its value judgments. BMJ 2004;329:224-7. https://doi.org/10.1136/bmj.329.7459.224.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. https://doi.org/10.1002/hec.635.
- Sendi PP, Briggs AH. Affordability and cost-effectiveness: decision-making on the cost-effectiveness plane. Health Econ 2001;10:675-80. https://doi.org/10.1002/hec.639.
- Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ 2002;11:415-30. https://doi.org/10.1002/hec.678.
- Briggs AH, O’Brien BJ. The death of cost-minimization analysis?. Health Econ 2001;10:179-84. https://doi.org/10.1002/hec.584.
- Normalisation Process Theory n.d. www.normalizationprocess.org/npt-toolkit.aspx (accessed 12 November 2017).
- Charmaz K, Smith JA, Harre R, Van Lagenhave L. Rethinking Methods in Psychology. London: Sage; 1995.
- Glaser BG, Strauss AL. The Discovery Of Grounded Theory: Strategies For Qualitative Research. Chicago, IL: Aldine Publishing Company; 1967.
- Coffey A, Atkinson P. Making Sense of Qualitative Data: Complementary Research Strategies. Thousand Oaks, CA: SAGE Publications Ltd; 1996.
- Brooks H, Lovell K, Bee P, Fraser C, Molloy C, Rogers A. Implementing an intervention designed to enhance service user involvement in mental health care planning: a qualitative process evaluation. Soc Psychiatr Epidemiol 2018;54:221-33.
Appendix 1 The National Institute for Health Research Programme Development Grants final report form
Appendix 2 Workstream 1
Published manuscripts
See Bee et al. ,5,24,40 Cree et al. ,17 Fraser et al. ,36 Gibbons et al. ,37 and Grundy et al. 16
The EQUIP synthesis day
Appendix 3 Workstream 2
Enhancing the Quality of User and Carer Involvement in Care Planning in mental health services: clinical cluster randomised controlled trial and process evaluation
Appendix 5 Workstream 4
Enhancing the Quality of User and Carer Involvement in Care Planning card
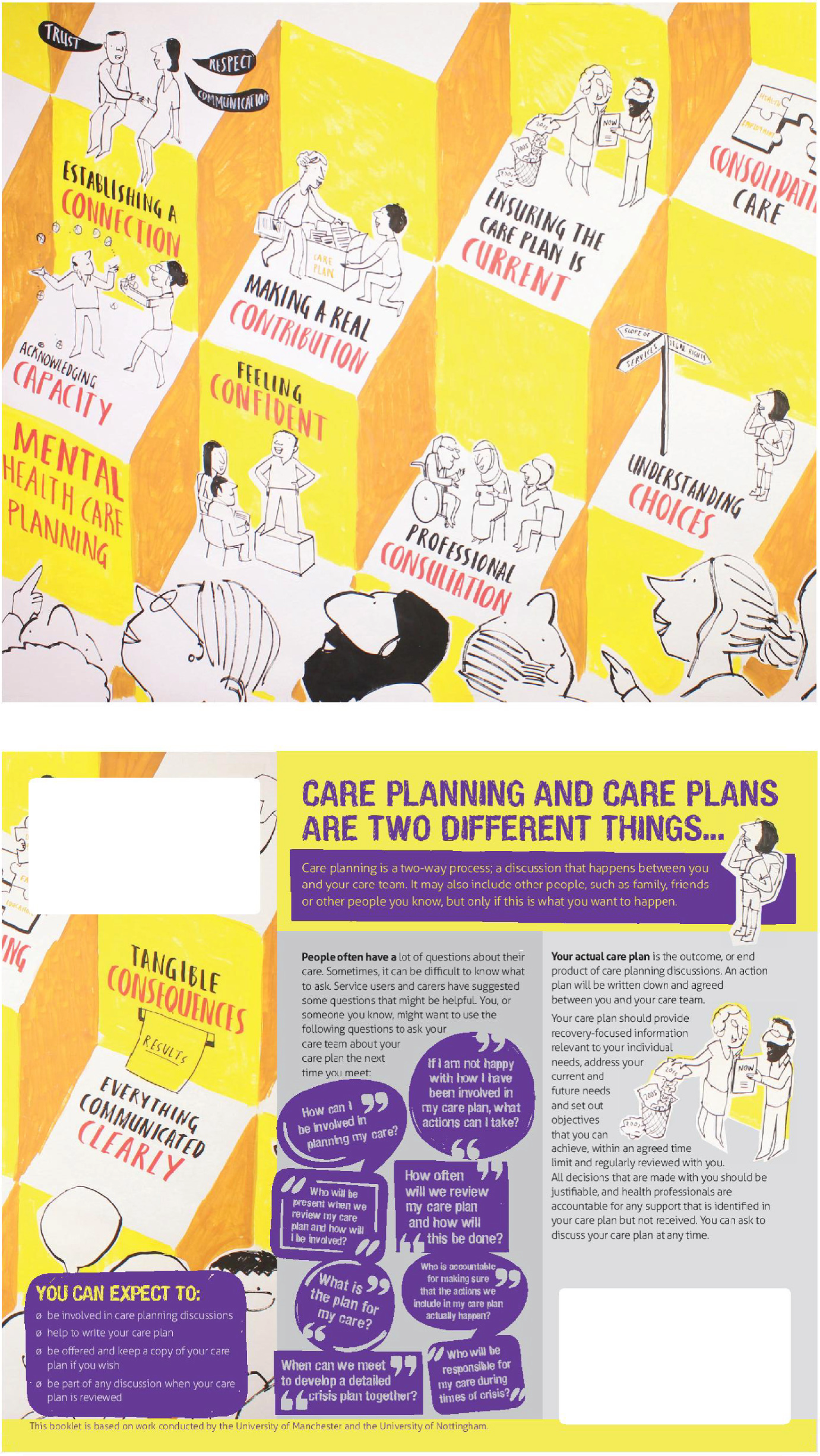
Summary Training Acceptability Rating Scale analysis
| Variable | Trial | Control group | ‘Willing Adopters’ |
|---|---|---|---|
| Training participants | 350 | 102 | 192 |
| TARS completed | 310 | 98 | 154 |
| Overall TARS score (possible range: 6–63) | Mean 4.48, median 6 | Mean 53.97, median 56 | Mean 52.18, median 54 |
| Acceptability score (possible range: 6–36) | Mean 32.99, median 34 | Mean 32.09, median 2 | Mean 1.27, median 32 |
| Perceived impact score (possible range: 0–27) | Mean 21.48, median 22 | Mean 21.64, median 23 | Mean 20.88, median 21 |
List of abbreviations
- AMA
- Ask Me Anything
- BAME
- black, Asian and minority ethnic
- CALPAS
- California Psychotherapy Alliance Scale
- CI
- confidence interval
- CMHT
- community mental health team
- CPA
- Care Programme Approach
- CQC
- Care Quality Commission
- CRN
- Clinical Research Network
- CSO
- clinical studies officer
- CUES
- Carers’ and Users’ Expectations of Services
- CUES-C
- Carers’ and Users’ Expectations of Services – carer version
- DREEM
- Developing Recovery Enhancing Environment Measure
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQUIP
- Enhancing the Quality of User and Carer Involvement in Care Planning
- GASS
- Glasgow Antipsychotic Side Effect Scale
- HADS
- Hospital Anxiety and Depression Scale
- HCCQ-10
- Health Care Climate Questionnaire
- ICC
- intracluster correlation coefficient
- MAGIC
- Making Good Decisions in Collaboration
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- PPI
- patient and public involvement
- PROM
- patient-reported outcome measure
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SUCAG
- service user and carer advisory group
- TARS
- Training Acceptability Rating Scale
- TIDieR
- Template for Intervention Description and Replication
- WEMWBS
- Warwick–Edinburgh Mental Wellbeing Scale
- WHOQOL
- World Health Organization Quality of Life