Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-1209-10013. The contractual start date was in December 2011. The final report began editorial review in February 2020 and was accepted for publication in June 2021. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2021 Taylor et al. This work was produced by Taylor et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Taylor et al.
SYNOPSIS
Setting the scene
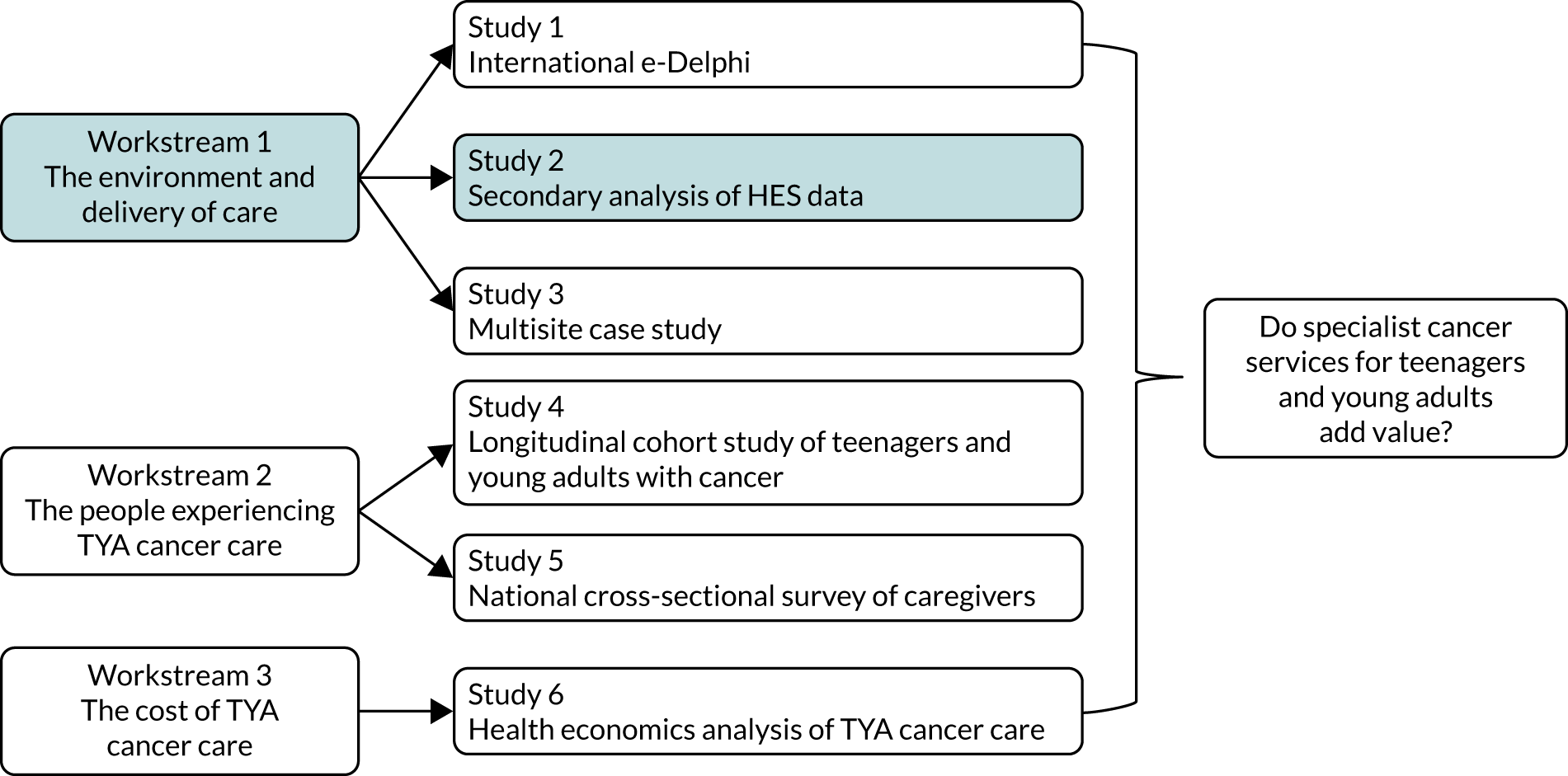
Young people have unique needs that differ from those of children or older adults, yet traditional policy and services serve children and young people as a single population. Consequently, teenagers and young adults can find themselves being treated in a children’s service or can become lost within adult health services. 1–3 The impact of this was identified in teenagers and young adults, who account for just 1% of all cancer diagnoses, but in whom cancer is the highest non-accidental cause of death. 4,5 Outcomes for young people are also documented to be poorer than for children and older adults. 6 The reason for this is multifactorial, including the range of cancer types (Figure 1); prolonged time to diagnosis; unfavourable tumour biology, as increasing age within this range is associated with worsening survival in certain cancers; inconsistent use of molecular diagnostics that may be central to optimal care;7 limited access to clinical trials;6,8,9 lack of concordance with treatment protocols;10 and a lack of specialist supportive care. 6,11 In addition, young people themselves have described unsatisfactory experiences of care, which include lack of recognition of their autonomy, failure to maintain their need to continue to meet normal life goals during treatment, lack of peer support, care by staff with little experience of young people, and inappropriate care environments. 12,13 The additional unique psychosocial and health-care needs of this specific population are also being increasingly highlighted in the international literature. 14–17 Place of treatment and cancer care, in terms of both disease and age-appropriate specialist settings, is increasingly acknowledged as significant to the outcome for teenagers and young adults with cancer. 17–19
FIGURE 1.
The distribution of tumour types in young people is unique and not replicated in other age groups (adapted with permission from Lorna A Fern, University College London Hospitals NHS Foundation Trust, 2021, personal communication, based on the data from Birch et al. 4). CNS, central nervous system.
Provision of teenage and young adult cancer care in England
Specialised teenage and young adult (TYA) cancer services in the UK have evolved over the past 30 years, with much input from the charity Teenage Cancer Trust. 20,21 Since the 1960s, a model of delivering cancer care to children has been established,11 and in 2001 adult cancer services were reconfigured into cancer networks, resulting in improvements in both patient experience and outcomes. 22 The first teenage cancer unit opened in the Middlesex Hospital in 1990, but it was not until 2005 that national policy was published that formalised the configuration of services specifically for teenagers and young adults. 23
The release of the National Institute for Health and Care Excellence (NICE) improving outcomes guidance (IOG) for children and young people with cancer in 200523 was a significant landmark on the landscape of English TYA cancer service development. This outlined detail about the provision of services for teenagers and young adults, such as clinical organisation, facilities, and diagnostic and therapeutic modalities. 23 Although this guidance supported subsequent service delivery, the evidence review that underpinned it was a collation of evidence on child and adult cancer services, some of which was assessed to be of fair to poor quality. Of the 15 pieces of evidence reviewed, only two were specific to teenagers and young adults. 24
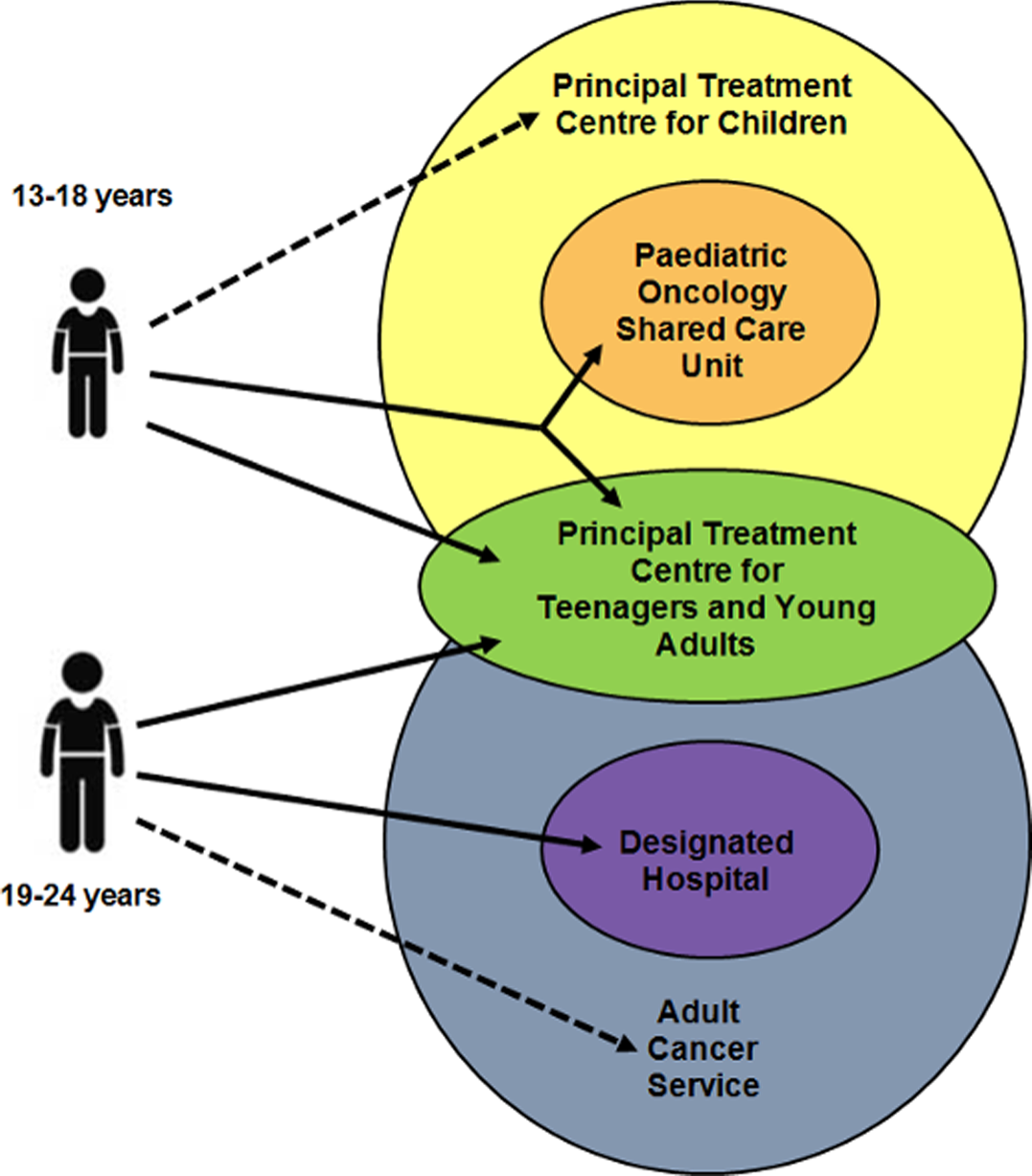
Despite the evolution and development of UK cancer services for young people, there continued to be variation regarding where young people with cancer received their care. 25 Even with government recommendations advocating ‘young person-friendly’ health services,26 many young people in the UK were cared for on adult wards27 or in children’s services28 (Figure 2). It was suggested that it was ‘inappropriate’ to deliver care to young people in either child or adult environments of care,30,31 or in settings not equipped to meet their needs. 32
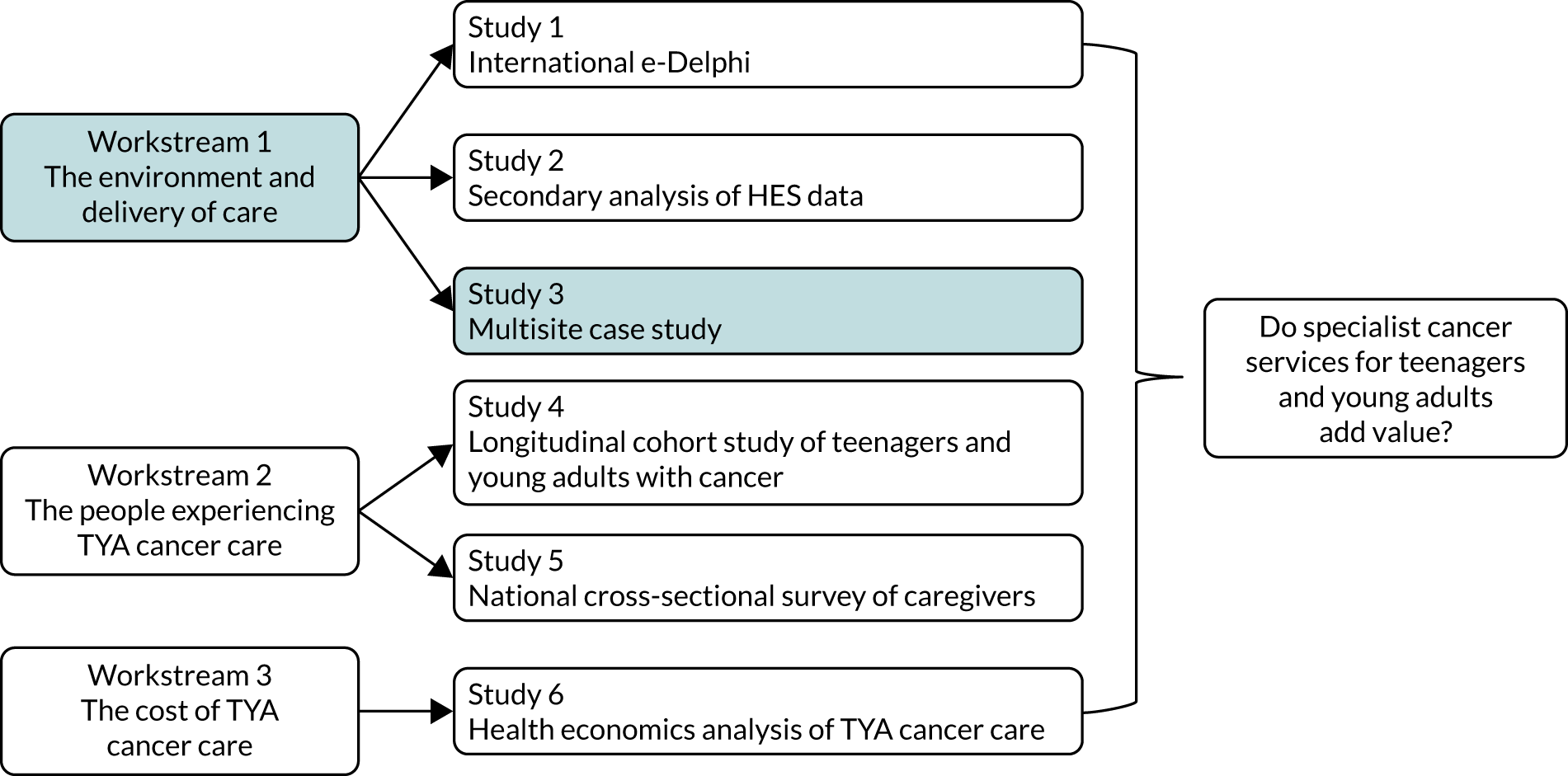
FIGURE 2.
An illustration of the three types of health service where young people with cancer may be cared for. Reproduced with permission from Sarah Lea. 29 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure below includes minor additions and formatting changes to the original figure. Images reproduced from Nottingham University Hospitals NHS Trust, 2017 with permission (Nottingham University Hospitals NHS Trust, 2021, personal communication).

Prior to the release and implementation of the IOG, approximately 52% of young people in England had been receiving care in a hospital that became a principal treatment centre (PTC). This group mainly comprised teenagers (aged 15–18 years) rather than young adults (aged 19–24 years). The place of care was a key focus within the IOG,23 which stated young people should be treated in an ‘age-appropriate environment’ and have access to ‘age-appropriate’ facilities. What made an environment or facility age-appropriate was not defined. However, specialist services could not be mandated without sufficient evidence to underpin them. This led to the process of designation (i.e. cancer services for young people in England were structured into networks of care with a central TYA-PTC as a ‘hub’ of expertise and hospitals with adult cancer services surrounding the TYA-PTC could apply to be ‘designated’ to provide cancer care to young people aged 19–24 years).
The model of service delivery for young people with cancer in England in 2012, when this programme of work began, consisted of 13 TYA networks of care with a TYA-PTC and varying numbers of associated designated hospitals (Figure 3). The TYA-PTC provided treatment expertise across the range of cancers common in young people, supported by a dedicated TYA multidisciplinary team (MDT) to meet the psychosocial needs of this population, within an environment that was tailored to the developmental and social needs of young people. 21 Young people aged up to 16 years could receive care in a children’s PTC or a paediatric oncology shared care unit that was authorised to provide certain aspects of supportive care, such as administration of blood products or simple chemotherapy drugs. Young people aged 19–24 years were to have ‘unhindered access’ to age-appropriate care and had the choice of being referred to a TYA-PTC or to stay in an adult cancer unit in a designated hospital within the network (Figure 4).
FIGURE 3.
Map of the location of the 13 TYA cancer networks in England. (1) Cambridge, (2) Bristol, (3) Oxford, (4) Liverpool, (5) Newcastle, (6) East Midlands, (7) Birmingham, (8) Southampton, (9) Leeds, (10) Manchester, (11) South Thames, (12) North Thames and (13) Sheffield.

FIGURE 4.
The range of places where a young person with cancer may receive their care, dependent on whether they are aged 13–18 or 19–24 years. Young people may receive access to specialist TYA cancer care (highlighted by the solid arrows), but young people may still be cared for in either child or adult cancer services (highlighted by the dashed arrows). Reproduced with permission from Sarah Lea. 29 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure below includes minor additions and formatting changes to the original figure.
There was a requirement that designated hospitals would notify the TYA-PTC of young people newly diagnosed with cancer so that there was ‘sharing of responsibility for patient management’ between the tumour site-specific clinical team at the designated hospital and the experts at the TYA-PTC. 33 Moreover, young people at designated hospitals should have ‘unhindered access’ to the support of the wider MDT via outreach work performed by the specialist professionals from the TYA-PTC (e.g. young people’s social workers). 23 Within each network there were also hospitals that were not allocated to provide care to TYA (non-designated hospitals). A proportion of teenagers and young adults continued to be cared for in these non-designated hospitals without access to the age-specific expertise of the TYA MDT at the PTC or access to age-appropriate care throughout their entire cancer journey. 34
Although there was a variety of services in which a young person may receive their cancer care, dependent on their disease, age, location and availability of services, there was variation in how this was translated and implemented across England. Of the 76 hospitals that were designated to deliver TYA cancer care, in 2013 approximately one-third were unable to deliver ≥ 50% of the standards that had been specified for being designated. 35 There were no consequences of this, and these hospitals have remained designated for teenagers and young adults, despite lacking many elements of a young adult-friendly cancer service. 36
BRIGHTLIGHT
The guidance and policy directing TYA cancer services in England in 2010 was not based on evidence and there was a lack of research evaluating how well these TYA cancer care networks operated. BRIGHTLIGHT is the applied health research programme providing this evaluation, which evolved from feasibility work in the Essence of Care study in 2009/10 that informed the methods for BRIGHTLIGHT. 37–41 During the Essence of Care study, we identified wide variation in the delivery of care across England, which informed the need for all the studies within the programme to be multicentre as well as containing longitudinal aspects. Although we have achieved this, we have been challenged by recruitment to the cohort and changes in regulatory processes throughout the study period, resulting in delays and preventing the detailed analysis of the cohort data necessary to fully understand the results. As a result, we provide a tentative conclusion in the knowledge that further work may be required to further inform answers to the overarching question: do specialist cancer services for teenagers and young adults add value?
Objectives
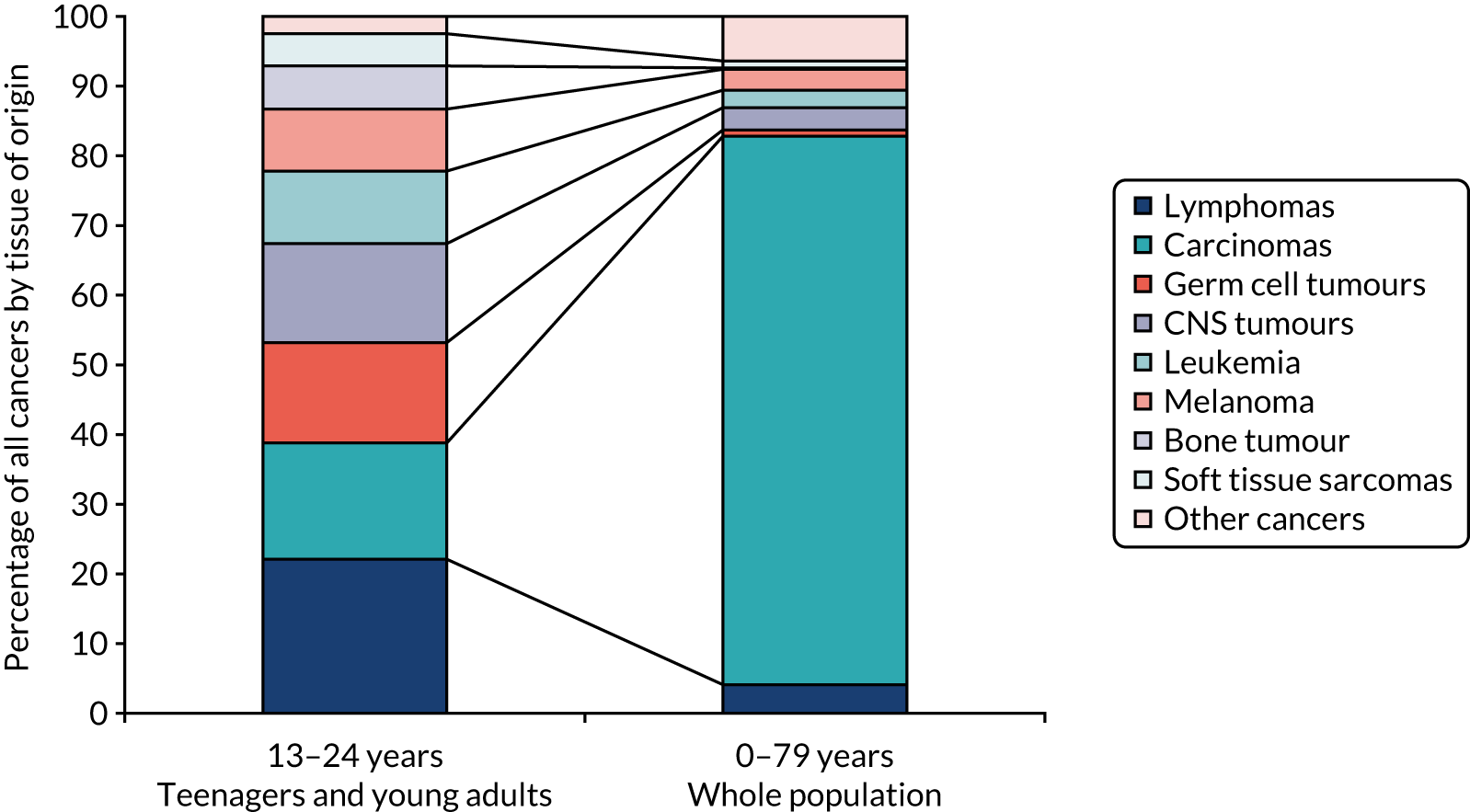
The programme of research was divided into three workstreams (Figure 5).
FIGURE 5.
Flow diagram depicting the inter-relationships between the workstreams. HES, Hospital Episode Statistics.
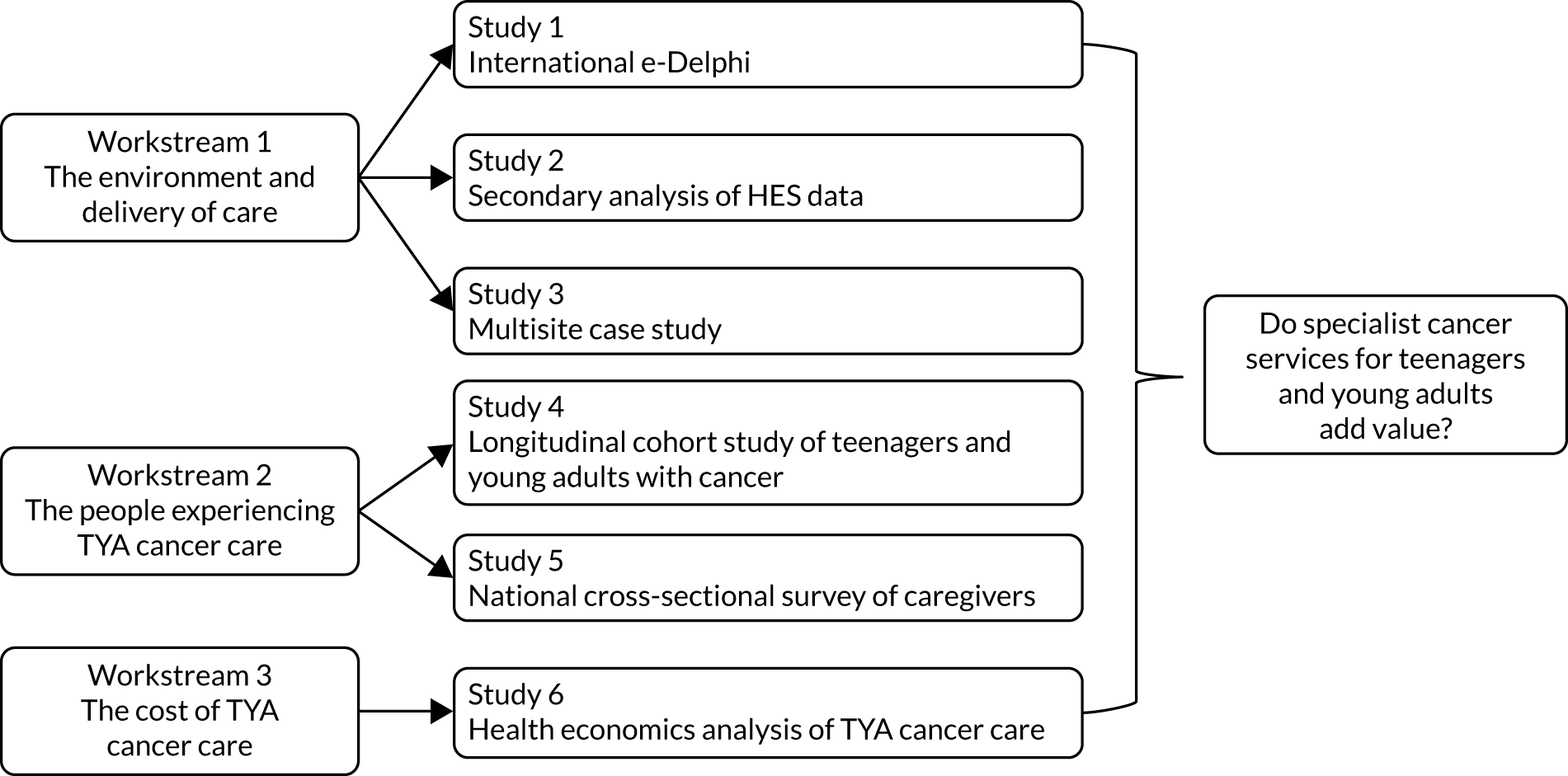
Workstream 1: establishes the description of teenage and young adult cancer care including specialist care
-
1.1. Explore the culture of care through non-participant observation, semistructured interviews and analysis of departmental documents.
-
1.2. Identify the specialist competencies and added value of specialist health professionals through an international Delphi survey.
-
1.3. Develop the TYA Cancer Specialism Scale to categorise three levels of TYA care and apply to individual patient-level data.
Workstream 2: examines care of young people with cancer in a cohort study
-
2.1. Relate the level of cancer care received by teenagers and young adults to quality of life (QoL), satisfaction with care, clinical processes and clinical outcomes (overall, by age group and by tumour type).
-
2.2. Examine young people’s experience of cancer care through a longitudinal descriptive survey.
-
2.3. Compare social and educational milestones among young people receiving different levels of TYA cancer care.
-
2.4. Examine geographic and sociodemographic inequalities in access to TYA cancer care.
Workstream 3: examines the economics of the levels of teenage and young adult cancer care
-
3.1. Calculate detailed costs to the NHS and Personal Social Services of teenagers and young adults receiving different levels of cancer care.
-
3.2. Estimate the cost incurred by teenagers and young adults and families receiving different levels of cancer care.
-
3.3. Calculate the cost-effectiveness of different levels of cancer care.
Programme management
A core group was responsible for the day-to-day management of the programme, including the chief investigator (Jeremy Whelan), programme lead (Rachel Taylor), lead for patient and public involvement (PPI) (Lorna Fern) and representation from each workstream (Faith Gibson, Sarah Lea and Nishma Patel). The core team met on a monthly basis to discuss study progress and address issues that needed attention, such as recruitment into the cohort. A wider executive team comprised the co-applicants of the programme who provided methodological expertise as required (Julie Barber, Stephen Morris, Richard Feltbower, Dan Stark, Louise Hooker and Rosalind Raine). The executive team had an annual meeting to discuss study progress, review results and discuss future study conduct. BRIGHTLIGHT was developed with young people and the young advisory panel (YAP), comprising 23 young people, who met yearly for a face-to-face workshop and were consulted on all impending changes through a closed Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) page. Additional meetings with YAP members involved in specific projects were held either face to face or by teleconference (see Acknowledgements). Finally, we had a steering committee, chaired by William Van’t Hoff (Great Ormond Street Hospital for Children NHS Foundation Trust), which comprised experts in QoL (Meriel Jenney, Children’s Hospital for Wales, Cardiff), longitudinal research (Lisa Calderwood, Centre for Longitudinal Studies), TYA cancer care (Laura Clark, Teenage Cancer Trust) and research delivery (Zoe Coombe and Jocelyn Walters, Comprehensive Research Network managers).
A summary of the alterations to the programme
Two additional studies were added to the programme at no additional cost. One of these was a mosaic study, mapping TYA-PTC services, which was used to inform the selection of cases in study 3. Data from caregivers (study 5) were made possible through a mechanism used by the contract research company to reduce family interference during the face-to-face interviews in study 4.
Four contract variations have been approved by the National Institute for Health Research (NIHR) Central Commissioning Facility, including three extensions to the grant. As a result, rather than ending in December 2016, the grant ended in December 2019. This was to accommodate the unanticipated difficulty in recruiting to the cohort (study 4) and to ensure that we had enough time for longitudinal data collection and for the required analyses. The third variation in contract allowed for removal of workstream 4, which had been directed towards implementation of changes within the duration of the grant. Because of the delays described above, the methods suggested in the grant application could not be implemented. However, we had developed additional studies and secured funding for a number of these early in the process (see Work arising from the grant).
The fourth variation in contract provided funding for support for analysis for objectives 2.3 (study 4), and secondary data analysis. There have been challenges beyond our control appointing to this post, so these analyses are not included in the report but are ongoing.
Alterations to the original plan also included analyses that we were not able to undertake in study 4 (the cohort study). We were not able to explore geographic and sociodemographic inequalities in access to TYA care as we reduced our sample size and recruited a fifth of the total population diagnosed with cancer. We were also unable to conduct the planned granular analysis of age and cancer type for this reason.
Patient, public and carer involvement in BRIGHTLIGHT
Involvement prior to submission of the research proposal
The initial idea to evaluate specialist cancer care for young people was professionally driven. However, recognising the unique challenges that this group faces, we felt that a successful programme grant would hinge on involving young people throughout the process. BRIGHTLIGHT is a study about young people with cancer, designed and driven by young people with cancer. Five young people worked as co-researchers during the feasibility work, which was instrumental to the study design, the development of survey materials and the identification of suitable outcome measures. Young people were also integral to dissemination, including co-authoring papers. 37,39
With such an extensive programme we began making links with communities involved in young people’s care and research delivery prior to protocol submission. Our PPI partners also included parents, siblings, professionals caring for young people, charitable organisations and research networks. We worked with partner groups to optimise the acceptability of study design, delivery, research question and outcomes.
Our experience of PPI prior to submission prepared us well for the commitment and resources required for a successful PPI strategy. In addition to the PPI lead, we employed a cohort manager to manage PPI activities. One young person joined us as a co-applicant. However, as is often the case with young people who finish treatment and move on to full time employment, she had other day-to-day commitments. Thirteen years had passed since her diagnosis and her role came to a natural end.
We recently published our 10-year PPI experience. 42
Establishing our patient, public involvement group and networks
Young people
Young people working as co-researchers during the feasibility work lent itself well to this short intensive piece of work. However, we felt that the sustainability of this model was not viable given the life-stage commitments of young people and the length of the proposed programme. Our application stated:
An initial workshop will be held with the Young Persons Reference Group; thereafter they will be consulted using options such as email discussion rather than face-to-face meetings, recognising the range of life stage commitments of TYA [teenagers and young adults].
Discussions with young people between December 2011 and August 2012 revealed that e-mail would not be an appropriate or responsive method of involvement, as e-mail was no longer ‘vogue’ (YAP workshop participant) and had been replaced by Facebook. Young people also advocated some face-to-face contact to foster relationships between themselves and the research team. We opted for a closed Facebook page, which took 14 months to be approved by our NHS trust and opened in October 2013, 13 months after the 2012 workshop. This delay was unfortunate, as it meant that many young people who attended the 2011/12 groups had moved on/changed contact details in this time.
We accessed young people through the conference ‘Find Your Sense of Tumour (FYSOT)’. 43 Annually between 2008 and 2017, we consulted around 200 young people aged 13–24 years on study design, suitability of research questions, outcome, recruitment approach and dissemination. 42,44,45 Young people gave their opinions individually and anonymously through handheld device surveys. We also recruited four young people from FYSOT to perform in our dissemination event ‘There is a Light’.
Parents and siblings
We planned to include parents and siblings and, following notification of funding, we visited existing groups of young people (Leeds/Birmingham) and family events (Cambridge). The Cambridge event involved focus groups with young people and parents/siblings. In our original plan, we stated our intention to report back to parents annually. In response to recruitment problems we focused efforts on understanding the barriers to recruitment from young people and professionals. Additionally, we added a further strand of data collection in response to our PPI work to more fully understand the experiences of carers.
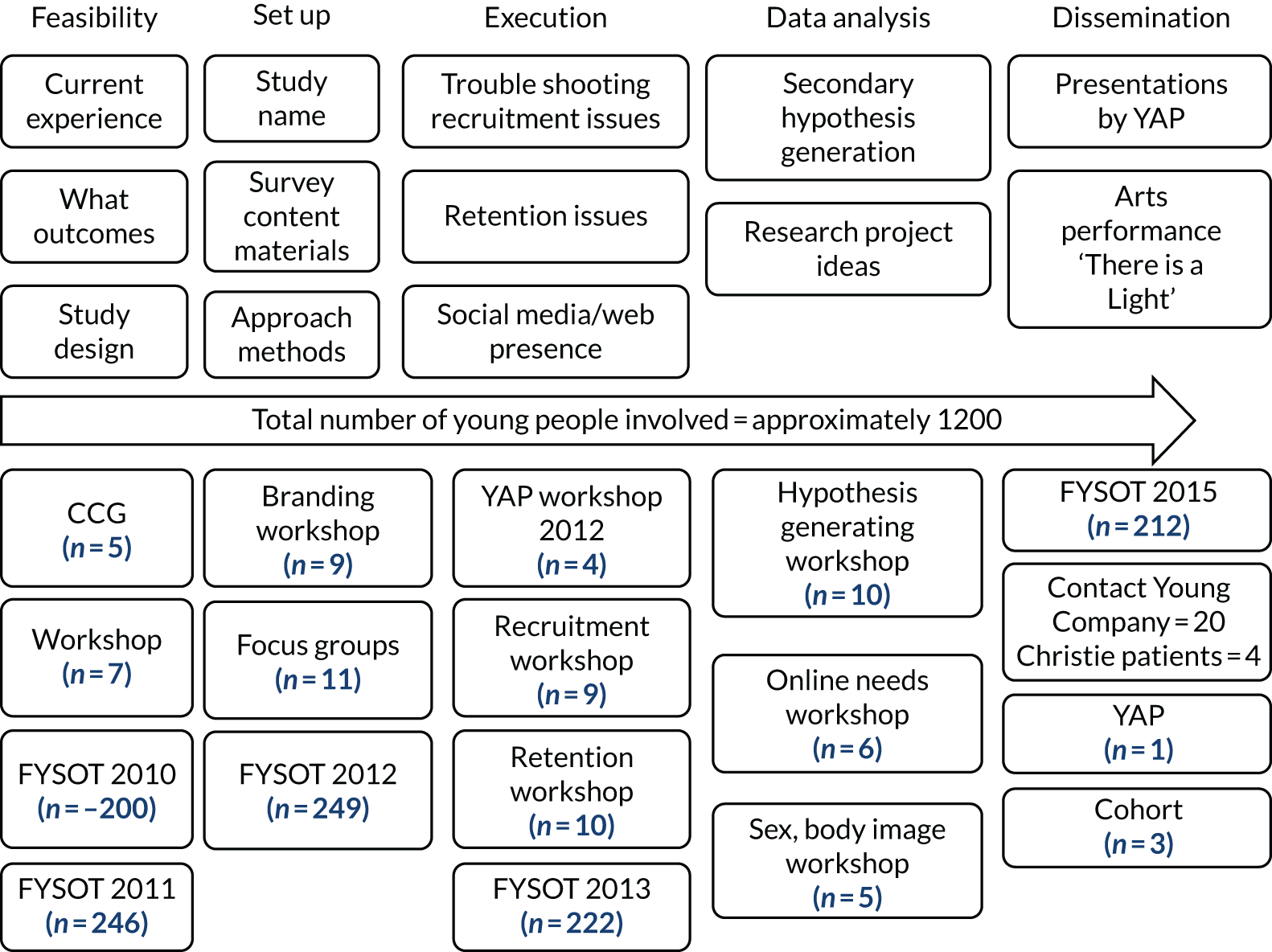
We have involved around 1200 people in our PPI strategy (not including professionals) (Figure 6).
FIGURE 6.
A schematic diagram of BRIGHTLIGHT PPI involvement.
Networks
The care of young people is complex with low incidence rates, multiple cancer types and care delivered across children, TYA and adult services in over 100 NHS trusts; consequently, project delivery was always going to be challenging. In anticipation of this we developed a third PPI group of ‘networks’. These included clinical/non-clinical staff delivering care, research network staff, adult PPI groups and charitable organisations.
Patient and public involvement aims
The aim is that PPI would contribute to developing all aspects of the research programme and contributing to the evidence supporting PPI through publishing our experiences and evaluations.
Methods
Patient and public involvement was undertaken through group work in participatory workshops.
The YAP remains connected through the closed Facebook page, which was monitored daily by the lead for PPI or a delegated team member. Contact was predominantly via group messenger to advertise workshops, post questions and advertise relevant activities and opportunities to participate in other projects. On only one occasion did the lead for PPI have to intervene because of inappropriate postings.
Workshops
Workshops have evolved in response to feedback from young people. 46 Changes included sending out the full aims, objectives and agenda prior to the workshop, allowing more time for young people to network, trying to engage a wider group of young people, varying the times, days and location of workshops and playing quiet music during activities and breaks. The typical workshop structure can be seen in Appendix 1:
The staff were amazing, very informative. Made me feel included throughout. It was a relaxed informal atmosphere which didn’t make the goal of the day seem to [sic] strenuous or daunting. Also thanks for the voucher MERRY CHRISTMAS [drawing of love heart].
The research team were actively involved in workshops, taking part in role play to illustrate some of the issues around recruitment. We piloted this in 2013 as an alternative to updating young people on the progress of the study through a presentation using PowerPoint® (Microsoft Corporation, Redmond, WA, USA), and it received favourable feedback. In 2014, we re-enacted a meeting held with the NIHR to illustrate further points about recruitment/retention. Workshops were followed up within 48 hours with an e-mail from the PPI lead to enquire about any distress/upset. No distress was reported, with young people reporting that they felt that the workshops were therapeutic and enjoyed the opportunity to contribute to the research agenda and meet with other young people.
The role of the young advisory panel in programme management
Review of documents and development of survey materials
The YAP contributed to survey development and approach materials through focus groups and telephone cognitive interviewing. 47 During the set-up of study 4, comments from young people included amending the approach period, wording on the patient information leaflet and formatting of the consent forms allowing young people to tick boxes rather than initialling, and we have now introduced this to all our consent forms. Parents also commented on survey materials during set-up and appeared more sensitive to questions than young people. Questions that parents felt were insensitive were double-checked with young people who had no problem with them.
Branding
The YAP were responsible for rebranding the study from the ‘2012 TYA Cancer Cohort Study’ to BRIGHTLIGHT in response to young people noting that the study name needed to be memorable. 44
Interventions for recruitment
Recruitment to BRIGHTLIGHT began in July 2012, with early signs of lower than anticipated recruitment. Despite this, our acceptance rate by patients approached to participate was 80% and we believe this high level of acceptability was due to our extensive PPI strategy during study design and set-up. We turned to our PPI partners for recruitment advice. Young people suggested a more appealing patient information sheet, audiovisual information, advocating informed choice by publicising that professionals should facilitate young people’s awareness of all research studies available to them and recruitment by other members of the treatment team. In response to these suggestions, we designed a shorter patient information sheet, which was given out with the paper document, videos of the information sheet and a ‘meet the team’ section on the website. Recognising that the YAP are an engaged group, we sought validation of suggestions around approach and recruitment with participants of FYSOT in 2013. 45 We also trained a group of social workers/youth support workers to gain consent. Lastly, we held a workshop with youth support co-ordinators and enrolled our networkers to contribute to a weekly Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) recruitment campaign. However, this was not as successful as Twitter recruitment had proved for research on other diseases. 48–50
Interventions for retention
Uptake to participate in the BRIGHTLIGHT cohort among those approached was higher than anticipated, as was retention at wave 2 (i.e. 12 months after diagnosis). However, we noted falling retention rates at wave 3 (i.e. 18 months after diagnosis) to around 30%. In response, we focused our 2014 workshop on strategies to improve retention and introduced interventions including personalised letters to participants and feedback of results using info graphics. After implementation of these measures, retention rates increased to 60%. 51
Dissemination and publicity
The YAP have contributed to our dissemination and publicity programme, including presentation of emerging results by two YAP members at FYSOT (link to FYSOT presentation52); chairing the BRIGHTLIGHT/TYAC (Teenage and Young Adult with Cancer professional organisation) conference in July 2017; and an interview on BBC Radio 5 Live (BBC, London, UK). National dissemination by a novel route was achieved through collaboration with Dr Brian Lobel, Contact Young Company and four young people with a previous cancer diagnosis. 53 The collaboration involved a series of workshops with the research team, young people and theatre group to create an artistic interpretation of emerging BRIGHTLIGHT results. Additional funding was secured from the Wellcome Trust and Macmillan Cancer Support, which allowed the performance to tour professional and patient conferences, including FYSOT in 2017. The performance received great reviews in terms of content, artistic talent and accessibility of results. 54 The young people participating also expressed benefit from being part of the team. 55
New studies
The YAP have contributed to new study development, which addressed online information needs,56 end-of-treatment concerns57 and the development of a sarcoma-specific patient-reported outcome measure. 58,59 Additionally, the YAP commented that the impact of cancer on sex, body image and relationships was poorly addressed; thus, we held two workshops with a view to new study development. 60 This has resulted in a patient-initiated study examining sexual health in young people with cancer, which was unsuccessful in the first grant submission but further applications for funding are planned. YAP members who wish to pursue a research career are co-applicants on new studies.
We do not have any negative effects to report from our PPI strategy. However, we do recognise the commitment and resource required from the research team to ensure that young people are included effectively in the study.
Discussion and conclusions
BRIGHTLIGHT was designed by young people with cancer for young people with cancer. Their involvement has been integral to study success and we will continue to engage with them as we interpret and disseminate the results and create new projects. Over 10 years we have optimised our engagement strategies in response to young people and changing technology,42 especially social media. Despite this, there are some areas where we feel we did not quite achieve complete success.
Diversity
The gender balance of the YAP was predominantly female, a phenomenon not unique to BRIGHTLIGHT. Although we had some ethnic variation within the group (around 20% of the YAP were ethnic minorities), it did not always reflect this diversity due to the variability of workshop attendance. Attendance at workshops was generally in the region of 9–10 young people, which was around half of our YAP. We sought feedback and were given multiple reasons including ‘too rainy to attend’, ‘hottest day of year, too hot to attend’, ‘would be better in summer holidays’, ‘would be better if not in summer holidays’. After several attempts of varying the times, calendar month and location, we felt that there was no real preference and workshops are now held on a Friday/Saturday in London (all expenses are paid and a voucher is given for attendance).
Bereavement
There is always a risk when bringing young people with cancer together over time that bereavements may occur within the group. Three deaths occurred within our group. We arranged for the local Macmillan Support and Information Service to offer bereavement support; however, this was not taken up (to our knowledge) and because of patient confidentiality, we would not be told of any young people who had approached the service.
Unanticipated events
Several unexpected events occurred. First, the lengthy and bureaucratic NHS processes meant that some of the suggestions that young people wanted could not be implemented or took considerable amounts of time: for example, shortening the patient information sheets, implementation of the Facebook page and utilising social workers/youth support co-ordinators for recruitment. Meeting expectations of the YAP, particularly around the use of emerging technology and social media, was constrained by resources and internal governance issues. After the Facebook page was established, young people requested Twitter, then Instagram (Facebook, Inc., Menlo Park, CA, USA; www.instagram.com), then Snapchat (Snap Inc., Santa Monica, CA; www.snapchat.com), curation of which would have required a dedicated communications team. Therefore, we did not implement a Snapchat account and our Instagram account did not really flourish.
Following our feasibility work, policies were put in place for codes of conduct (e.g. alcohol, smoking, drug use) and expenses. Further to this, several policies were implemented in response to events. An ‘out-of-hours’ policy was introduced in response to a young person having to make an emergency trip home late at night following sickness of her child during a 2-day workshop. Second, a ‘sickness policy’ was implemented after a young person (> 16 years) was admitted to hospital via accident and emergency (A&E) during a workshop and refused to give a next of kin contact. Finally, although no distress has been reported after the workshops, in response to an e-mail follow-up after a workshop, we had one incident of significant distress during dinner after a workshop. This young person was referred to their treatment team for support.
Reflections/critical perspective
We feel that we have successfully integrated the contributions of young people into our programme of research. This has been dependent on several things but mainly commitment and dedication from the research team to the principle that involving young people is worthwhile. Budgeting adequate funding within the grant has also been pivotal to our PPI success, with dedicated personnel to deal with some of the administration behind user involvement. We have shown that given appropriate support, young people can make a valuable contribution to research and we hope that our experience inspires other research teams to reach out to ‘hard-to-reach’ groups and involve them in research.
We would like to extend our thanks to the young people and PPI partners who have contributed to BRIGHTLIGHT since 2008.
Defining the competence of health-care professionals caring for teenagers and young adults with cancer
Aims
The relationship of study 1 to the rest of the programme is shown in Figure 7. We aimed to identify the specialist competencies and added value of specialist TYA health-care professionals through an international Delphi survey.
FIGURE 7.
Flow diagram highlighting the study referred to in Defining the competence of health-care professionals caring for teenagers and young adults with cancer. HES, Hospital Episode Statistics.
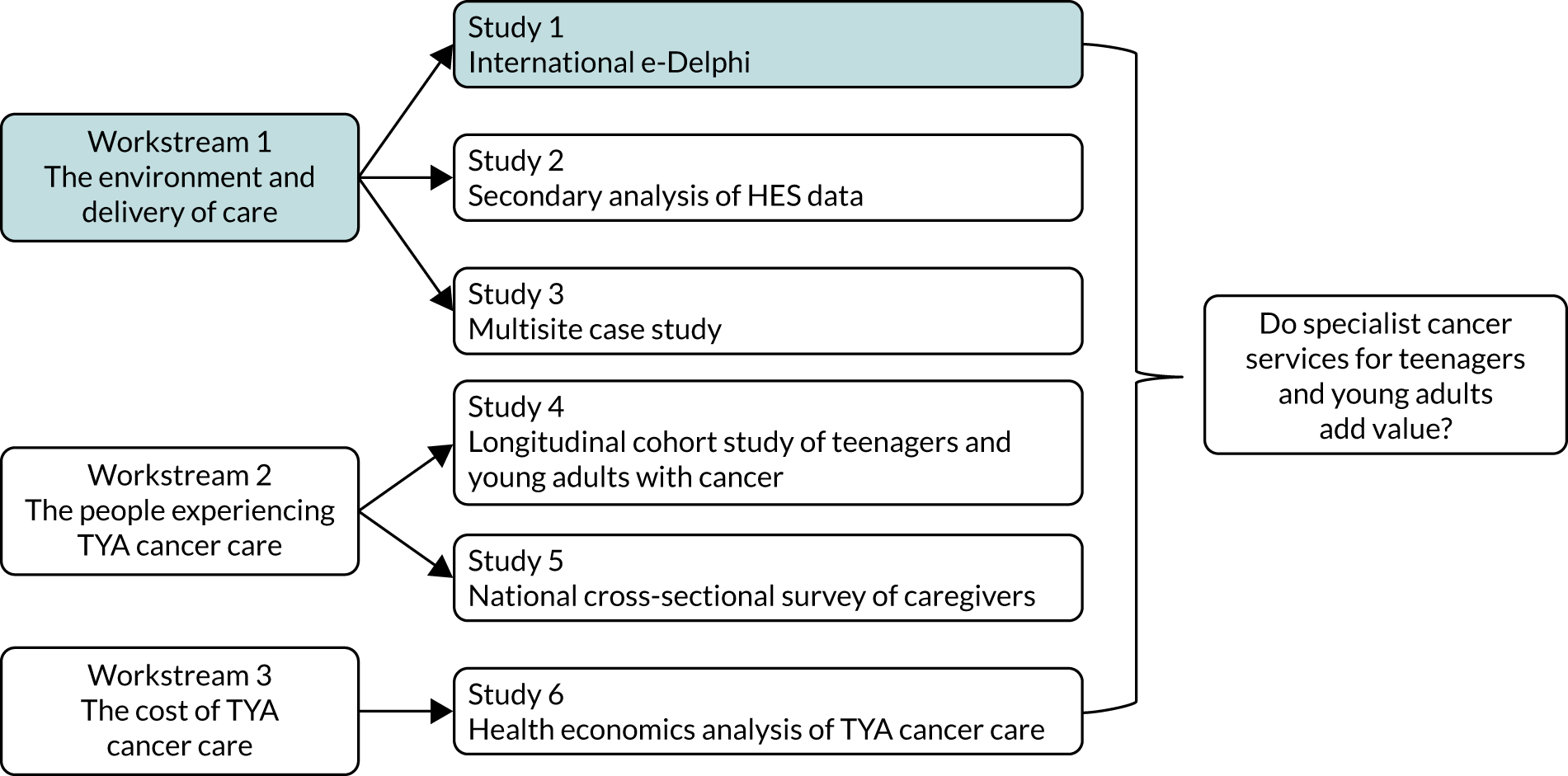
Methods
We sought to use a consensus approach and selected a Delphi technique, which normally involves two or more rounds of postal or online questionnaires. The Delphi technique employs ‘experts’ as panel members. There is little consensus as what defines an ‘expert’61 and, therefore, ‘expert’ for the Delphi study reported here was defined as any health professional working in TYA cancer care for a minimum of 12 months.
Round 1 questionnaire
A comprehensive list of competencies was generated from our preliminary study,38 and this formed the content for the first round of this Delphi survey. These were subdivided into skills, knowledge, attitudes and communication. All the questions had closed-ended responses using 9-point Likert scales (i.e. strongly agree to strongly disagree). However, as the competency list was initially generated by health-care professionals based in the UK, several open-ended questions were included to ensure that the survey would accommodate the opinions of professionals in other countries. The questionnaire was administered through a web-based survey programme.
Round 2 questionnaire
Only items for which there was no agreement were included in the round 2 questionnaire. Qualitative content analysis was used to analyse responses to open-ended questions. Panel members were also requested to identify five skills, areas of knowledge, and attitudes that they considered the most important.
Data analysis
Items were ranked and reported according to medians. Medians of 7–9 were defined as strong support, 4–6.5 as moderate support and 1–3.5 as weak support. The mean absolute deviation from the median was calculated and the level of agreement was categorised according to thirds of the mean absolute deviation from the median (low > 1.41, moderate 1.08–1.41, high < 1.08). These summaries were also calculated according to profession (medical doctor, nurse, other health-care professional) and differences determined using chi-squared tests to compare the number of respondents who had strong agreement (consensus).
Key findings
Study 1 is reported in full. 62 In summary, a total of 179 health-care professionals registered to be members of the expert panel, of whom 159 (89%) returned the round 1 questionnaire. Valid responses were available from 158 (88%) professionals, and 136 (86%) of these 158 responded to round 2. The majority of these professionals were nurses or medical doctors from Europe and North America. In round 1, consistent high levels of agreement were reached on all statements related to skills (n = 27), knowledge (n = 18), attitudes (n = 24) and communication (n = 19). In round 2, there was highest consensus on being able to discuss sensitive subjects; knowing about current therapies; knowing normal TYA physical and psychological development; knowing about the impact of cancer on psychological development; knowing about the side effects of treatment and how this differs from children and older adults; and knowing about fertility preservation.
There were aspects that all professional groups agreed were important. Most agreement was in the attitudes required for caring for young people with cancer: being friendly and approachable, being honest, being respectful and being committed to caring for young people with cancer. Other areas of agreement included being able to identify the impact of disease on young people’s life and working in partnership with young people; knowing how to provide age appropriate care; and knowing the side effects of treatment and how this was different for children or older adults. There was agreement that key aspects of communication were being able to listen to young people’s concerns, talking about difficult issues and being able to speak to young people using familiar language while retaining a professional boundary.
Limitations
A limitation was that the composition of the expert panel was predominantly experts working in Europe or North America; therefore, our results may reflect a Western perspective. ‘Expert’ was defined as working with teenagers and young adults for a minimum of 12 months, but we did not specify the age of the TYA population. As international variation exists, this could have influenced the importance assigned to areas of competence. In addition, the process used to create our expert panel may have excluded those who were not members of professional organisations or had published in this area.
A further limitation was that the survey was available in English only. Finally, we did not ask participants about their training background and, therefore, we could not examine the differences between those who were child trained and those who were adult trained.
Inter-relationship with the rest of the programme
This provided the context for understanding the complex elements of the multiprofessional role for study 3.
Quantifying specialist care
Aims
The relationship of study 2 to the rest of the programme is shown in Figure 8. We aimed to develop a TYA Cancer Specialism Scale to quantify and categorise the levels of TYA cancer care and then apply this to individual patient-level data.
Methods
Details of the development of the metric to quantify specialist care have been reported as supplemental file 2 in Taylor et al. 63 In summary, this metric was developed from Hospital Episode Statistics (HES) admitted patient care (APC) data. NHS trusts containing a TYA-PTC were defined and the trust code was identified from NHS Digital HES records. For all the patients in the cohort study (study 4), every APC spell was assigned to be either specialist TYA-PTC care (based on the trust code) or care elsewhere. A proportion of TYA care was calculated for each member of the cohort at 6 and 12 months after diagnosis.
Key findings
The inpatient HES data were successfully linked to 1074 out of 1114 young people recruited. The distribution of the proportion of care by 6 and 12 months after diagnosis suggested that there were three natural groups occurring within the data. Categories of care were calculated based on the proportion of specialist care received: all care received in a TYA-PTC (ALL-TYA-PTC), some care in a TYA-PTC and some care in either a children’s or adult cancer centre (SOME-TYA-PTC), or no care received in a TYA-PTC (NONE-TYA-PTC).
Limitations
Assigning ‘specialist’ care to the whole trust code rather than the hospital within the trust, we assumed that the young person would receive care from the TYA MDT wherever they were cared for within the trust. The metric was developed using APC data only, which did not account for any care delivered in outpatient units. There was a further assumption that all TYA-PTCs were the same, and we did not account for the difference in TYA-specific services each provided. For example, some were better developed with a TYA environment, employed TYA-specific staff (e.g. youth support co-ordinators) and had established relationships with the designated hospitals in their network, whereas others did not have any of this in place at the time of study. Finally, there was a large variation in the proportion of TYA-PTC care in the SOME-TYA-PTC group, ranging from 3% to 99%. If a young person, for example, was admitted to a local hospital for febrile neutropenia but had all their remaining care in ALL or NONE-TYA-PTC, then they were assigned to the SOME group.
Inter-relationship with the rest of the programme
This metric was the exposure variable for studies 4–6 (see Identifying the outcomes associated with specialist teenage and young adult cancer care to Calculating the cost of specialist teenage and young adult cancer care).
Understanding the culture of care
Aims
The relationship of study 3 to the rest of the programme is shown in Figure 9. We aimed to explore the culture of TYA cancer care to answer three specific research questions:
-
How does the context of each TYA-PTC and its network shape young people’s individual experience of care?
-
What is different and what is common across the culture of TYA cancer care in the four TYA-PTCs and networks of care?
-
What are the perceptions of care of young people and professionals in each TYA-PTC and its network?
Methods
This was a multiple case study conducted across four TYA cancer networks in England. The cases were informed from our feasibility work describing the unique history of the TYA-PTC, the environment and patient population that shaped care delivery. 41 In addition to the four TYA-PTCs, 20 hospitals linked to these were also included and young people were recruited in 17. Young people were aged 13–24 years with a confirmed cancer diagnosis and undergoing treatment. Health-care professionals delivering care to young people were also included and purposively sampled to represent the range of professions in the MDT. Data were collected through semistructured interviews, tours and shadowing with health-care professionals, and participant observation. Thematic analysis was used to identify themes between, within and across the four cases – deconstructing and reconstructing the components of the culture of care that emerged, thereby enabling synthesis and contextualisation of data.
Key findings
The results for study 3 are available in full. 29,64,65 Twenty-nine young people and 41 health-care professionals were interviewed, and there were 120 hours of observation. Young people were predominantly in the TYA-PTC group (n = 22; 76%); and health-care professionals included ward-based nurses (n = 9), clinical nurse specialists (n = 8), nurse leaders/managers (n = 9), youth support co-ordinators (n = 4), social workers (n = 3), medical doctors (n = 3), non-nurse service managers (n = 2), education roles (n = 2) and allied health professionals (n = 1).
An initial analysis was undertaken of the interviews with young people and health-care professionals, which were synthesised with existing literature to develop a definition of age-appropriate care. 64 It was not possible to provide a simple definition as age-appropriate care was identified as a more complex entity comprising seven core components: best treatment; health-care professional knowledge; communication, interactions and relationships; recognising individuality; empowering young people; promoting normality; and the environment. These formed a conceptual model with each core component comprising a number of subthemes, with the relationships between the components being interlinked. Defining age-appropriate care highlighted the aspects that have the potential to enhance care. These are potentially the components to focus on to improve the delivery of care. For example, providing the best treatment relies on having access to clinical trials.
The study findings brought together data from all sources and settings to explore the culture of care for young people with cancer. They were broadly divided into three categories: the physical and social environments of care; communication and core values; and the development of health-care professional holistic competence and the culture of care.
The physical and social environments of care
The décor, structure, function and facilities of a physical environment tailored specifically to the needs of young people were highlighted as important. Health-care professionals and teenagers and young adults agreed on similar aesthetic features, for example colourful décor that created a less clinical atmosphere. Professionals described how wards in the TYA-PTC provided modern, colourful and well-resourced environments, and these settings facilitated health-care professionals to enjoy interactions with their patients and colleagues. Health-care professionals identified that the physical surroundings in which they interacted with their patients had an impact on the conversations that they had. Young people described the atmosphere on these wards as calm, relaxed and homely, which promoted normality.
There was a relationship between the physical environments in which young people were cared for, their experiences of care and the social relationships that they built with those around them. The dedicated social spaces provided in the TYA-PTC enabled youth support co-ordinators to better fulfil their role, where the environment provided the space and facilities to bring young people together.
Communication and core values
Communication was the major visible process of care that occurred between young people and professionals, both at an individual level and within groups. Three types of communication emerged:
-
Interpersonal – young people recognised effective communication, and they identified and valued the relationships they built with health-care professionals. Young people recognised and valued the meaningful interactions that they had with health-care professionals, both within TYA-PTCs and designated hospitals. Young people described continuity and consistency with health-care professionals as advantageous, enabling them to build relationships with those caring for them. Likewise, health-care professionals acknowledged that continuity of care was important. Youth support co-ordinators described an essential part of their role was being a ‘constant’ for patients. Continuity of staff and the implementation of routine communication processes, such as effective handovers between professionals, meetings and discussion groups provided opportunities for a united and knowledgeable health-care team to form and to flourish.
-
Intra-hospital – there were multiple and separate circles of intraprofessional communication about care within a hospital, involving all members of the direct care team and others. Processes described by health-care professionals were more complex where multiple teams were involved. Young people spoke specifically about the role of the clinical nurse specialist and their part in ensuring care was not disjointed.
-
Hospital to hospital – communication was back and forth between the teams at the designated hospitals, shared care hospitals and the TYA-PTC, ensuring that both the young person’s clinical and their psychosocial needs were being met. There was variation in processes that affected overall experience.
Three core values emerged: recognising individuality, promoting normality and empowering young people. These core values were an essential part of the less visible ‘below the surface’ culture, and were values that underpinned TYA cancer care across all settings. Delivery of care tailored to the individual patient’s needs and effective provision of information were highlighted as important by young people and professionals. Health-care professionals sought to encourage those young people who were cognitively able to have some control over their care and the decisions made about it.
The development of health-care professional holistic competence and the culture of care
The formation and sharing of a culture where care was responsive to the unique needs of the teenagers and young adults was influenced by four factors: a consistent volume of young people using services, effective leadership, an appropriate and accepting attitude, and patience.
Consistency and a large number of young people using a service was important in the formation of an age-appropriate, young person-centred culture of care. The TYA-PTCs hosted a consistent, concentrated volume of young people, compared with many of the children’s and adult cancer settings. In all contexts, leadership was essential to shape and perpetuate the culture of care. Leaders were vital in bringing together the whole team, creating a culture in which all health-care professionals communicated with each other effectively. Leaders were important in assisting the formation of trusting relationships between all members of the team. Shared beliefs and ‘buy-in’ of health-care professionals into what was different and special about caring for young people with cancer were core to the culture of care. It took considerable time for such connections and knowledge about caring for young people to develop on both a network and a local level, particularly as these networks could span a variety of specialties: adult, child and a wide range of tumour site-specific teams.
The importance of the core values that underpin care, and the need for education, effective leadership and multidisciplinary teamworking was described as essential. These should be prioritised when developing and evaluating interventions that contribute to the delivery of care. Care delivered in an environment that promotes normality through facilitating socialisation with peers was described as essential to the delivery of optimal holistic and young person-centred care. Growing and nurturing a culture of care that meets the unique needs of young people with cancer and improves their experiences of care takes time and commitment.
Limitations
Although purposeful sampling was planned and employed where possible, the willingness and availability of study participants affected the final sample. For these reasons, younger teenagers, those with a brain tumour and those with melanoma are all examples of under-represented patient groups.
A limitation was that eligibility for participation included being able to speak English. In addition, health-care professionals were frequently time-limited and busy with their clinical and support roles, which was particularly so for medical staff. Furthermore, some methods of data collection proved challenging, such as walking interviews, and the observations undertaken did not provide opportunity for complete research immersion into the sites visited, as would have been possible with traditional ethnographic techniques.
Inter-relationship with the rest of the programme
Study 3 provided the qualitative evaluation of the delivery of care in which the quantitative data gathered in study 4 could be compared and contextualised.
Identifying the outcomes associated with specialist teenage and young adult cancer care
Aims
The relationship of study 4 to the rest of the programme is shown in Figure 10. Our aim for study 4 was to establish a cohort of teenagers and young adults who were newly diagnosed with cancer to determine the outcomes associated with category of care. This included:
-
relating the category of cancer care to QoL, satisfaction with care, and clinical processes and clinical outcomes
-
examining young people’s experience of care.
FIGURE 10.
Flow diagram highlighting the study referred to in Identifying the outcomes associated with specialist teenage and young adult cancer care.

Methods
Details of recruitment into the cohort and a description of the cohort are reported. 63,66,67 In summary, the cohort study was conducted across England, recruiting in 109 NHS trusts, of which 97 recruited at least one young person. Young people were eligible to participate if they were aged 13–24 years and had a new diagnosis of cancer.
Data were collected from young people using a bespoke questionnaire, the BRIGHTLIGHT survey, which contained five validated patient-reported outcome measures, and 169 patient experience questions related to pre-diagnosis experience, diagnostic experience, place of care, contact with health-care professionals, treatment experience, fertility, involvement in clinical trials, adherence, communication and co-ordination of care, education, employment, well-being, and relationships. 37,47 The BRIGHTLIGHT surveys are freely available under licences detailed in the following links: [https://xip.uclb.com/product/brightlight_wave1; https://xip.uclb.com/product/brightlight_waves2-4; and https://xip.uclb.com/product/brightlight_wave5 (accessed 1 June 2021)]. The survey was administered five times in 3 years by an independent research organisation through face-to-face interviews in young people’s homes during wave 1 (i.e. 4–7 months after diagnosis) then either online or through a telephone interview at waves 2–5 (i.e. 12, 18, 24 and 36 months after diagnosis). Data about young people’s cancer and clinical care were obtained from their medical records and the National Cancer Registration and Analysis Service. Comparisons were made between young people treated in NONE-TYA-PTC, SOME-TYA-PTC or ALL-TYA-PTC.
Key findings
The results for study 4 are reported in full68,69 and additional results are reported in Appendix 2. A total of 1126 young people were recruited, and valid consents were available for 1114. A description of the cohort is reported in full. 63 The group mean total QoL improved for all patients, but was 5.63 points higher (95% CI 2.77 to 8.49 points) for young people receiving SOME-TYA-PTC care, and 4.17 points higher (95% CI 1.07 to 7.28 points) compared with ALL-TYA-PTC care. These differences were greatest 6 months after diagnosis, but reduced over time and did not meet the 8-point level that is clinically significant. The rate of improvement was significantly greater in the ALL-TYA-PTC and SOME-TYA-PTC groups so there was minimal difference between the ALL-TYA-PTC and NONE-TYA-PTC by 3 years after diagnosis. Young people receiving NONE-TYA-PTC care were more likely to have been offered a choice of place of care, be older, be from more deprived areas, be in work and have less severe disease. However, multivariable analyses of measured confounding factors did not explain the differences observed.
Young people who had NONE-TYA-PTC care had the highest survival, followed by those who received ALL-TYA-PTC and SOME-TYA-PTC care. Adjusted analyses showed no significant difference according to the category of care. Clinical records linked to levels of care were available in 1009 young people receiving NONE-TYA-PTC care and indicated they were less likely to have a molecular diagnosis (where relevant), be reviewed by a children’s or TYA MDT, have an assessment by supportive care services or discuss fertility than those treated in SOME-TYA-PTC or ALL-TYA-PTC.
There was no difference in perceived social support anxiety or depression between the three groups, but young people in the SOME-TYA-PTC and ALL-TYA-PTC groups had higher illness perception than those in the NONE-TYA-PTC group (i.e. they were more likely to perceive themselves as ill). Finally, there were no differences in young people’s experience of care, and the majority were satisfied irrespective of where they were treated.
Limitations
Young people in the cohort had significantly lower survival than those not recruited, which suggested that there was recruitment bias. 63 Potentially, these patients were in hospital longer, thus facilitating more opportunities for recruitment. Only one-fifth of the population was recruited, so the results of the cohort do not necessarily reflect those of the rest of the population. The limitations of the TYA Cancer Specialism Scale were discussed in Quantifying specialist care, which includes the limitations of the results from the cohort. The BRIGHTLIGHT survey was administered face to face at the first wave, as this increase’s retention into longitudinal research47 and at waves 2–5 there was the option of a telephone interview or online completion. This may have introduced response and/or social desirability bias. 70 Finally, we used the only measure of QoL that was available in 2011 that had been validated across the ages 13–24 years. Although the PedsQL is well established for measuring outcome, as a generic measure of QoL this may not have been sensitive enough to detect differences according to the place of care. Age is one of the key factors determining where young people are treated, but the PedsQL does not have significant changes across the various age versions to reflect the developmental differences [i.e. there is little difference in the wording between the child (8–12 years), teen (13–18 years) version and young adult versions].
Inter-relationship with the rest of the programme
Patient experience is a central tenet of health-care policy and is important to how quality of care is measured. Establishing the cohort and study 4 were therefore central to evaluating specialist cancer services. Study 4 also enabled study 5 to be conducted (caregivers were identified and nominated by young people) and data for study 6 were collected from the cohort at the time as the survey was administered.
Determining if specialist teenage and young adult services support caregiver’s information and support needs
Aims
The relationship of study 5 to the rest of the programme is shown in Figure 11. The aim of study 5 was to evaluate whether or not caregivers of teenagers and young adults with cancer had unmet information and support needs, and if this varies by level of care category.
FIGURE 11.
Flow diagram highlighting the study referred to in Determining if specialist teenage and young adult services support caregiver’s information and support needs.

Caregivers play an important role in providing support for young people when they have a cancer diagnosis. 71 In our development work underpinning the programme grant, we showed one of the skills in caring for this population is the unique pattern of communication, which is unlike children’s or adult cancer care. Communication with children is focused mainly on parents, whereas communication with adults is directed at the person affected with cancer. However, with young people, professionals need to involve those caring for young people, whether it be parents, partners or friends, while also being cognisant of the young person’s right to confidentiality. 38
In our original application, the lack of caregiver perspective was a criticism from one of the reviewers, but was an aspect of TYA cancer care that we were unable to evaluate because of limited resources. However, during the set-up of study 4, the contract research company administering the BRIGHTLIGHT survey suggested that a paper questionnaire could be administered at the time of the first wave of data collection (this is a method used to limit involvement of other members of the household during face-to-face survey administration). A scoping review of the literature identified no study on caregivers of teenagers and young adults with cancer. Much of the early literature examining caregivers of children and older adults focused on unmet needs. This was therefore the focus of study 5.
Methods
The methods for study 5 have been reported in full. 72
The BRIGHTLIGHT Carer Questionnaire (BCQ) was developed based on caregiver unmet need questionnaires and was developed for caregivers of children and older adults. The BCQ has 15 multi-item questions covering four domains: information needs; experience of the cancer treatment centre and contact with health-care professionals; emotional well-being and relationship with the young person; and support for completing practice tasks. Responses are on a range of 3-, 4- and 5-point Likert scales. The BCQ is freely available under the following licence: https://xip.uclb.com/i/healthcare_tools/brightlight_carer.html (accessed 1 June 2021). The BCQ was administered as a paper questionnaire to the person who young people nominated as being their main caregiver. If this person was not in the property at the time of the young person’s interview, it was left for the young person to administer. The BCQ was returned in a free-post envelope; no reminders were given.
Principal component analysis was used to reduce 22 items from the BCQ into five domains: (1) the support that caregivers received, (2) satisfaction with support, (3) information provided, (4) opportunities to make decisions about treatment (5) and services provided for caregivers. Caregiver data were linked to young person data though a unique study code so that comparisons could be made between the three categories of care: NONE-TYA-PTC, SOME-TYA-PTC and ALL-TYA-PTC.
Analysis
Comparisons between the three categories of care described in study 4 (i.e. ALL-TYA-PTC, SOME-TYA-PTC and NONE-TYA-PTC) were made using cross-tabulation and chi-squared tests.
Key findings
A total of 518 caregivers returned the BCQ, and 514 of these could be linked to young people’s data in the cohort. Study 5 is reported in full in Martins et al. 72 The majority were white (90%), mothers (81%) aged between 35 and 54 years (71%). Regression analysis, adjusting for caregiver and young person characteristics, indicated that there was no difference in the support that caregivers received depending on where the young person was treated. Caregivers of patients in ALL-TYA-PTC care had greater satisfaction with the support. Where care was delivered in SOME-TYA-PTC care, caregivers received the most amount of information; however, they had fewer opportunities to make decisions. Finally, satisfaction in services provided specifically for caregivers were reported mostly by caregivers who had ALL-TYA-PTC care.
Limitations
Participants were predominantly female, white and mothers, so their needs may not represent those of fathers, partners and members of other ethnic groups. There was no validated questionnaire available for caregivers of teenagers and young adults, so a measure was developed based on existing literature. Although content validity was confirmed, and later analysis confirmed construct validity, the BCQ may not include all of the issues that caring for a young person with cancer could entail. Analysis of the BCQ was limited to 22 items that were selected on the basis that they had the potential to be influenced by specialist care; other aspects of unmet needs, such as emotional well-being, were not included but could be an important aspect of care delivered in a TYA-PTC.
Inter-relationship with the rest of the programme
Study 5 enabled us to evaluate the value of specialist care on caregivers who are an important source of support for young people.
Calculating the cost of specialist teenage and young adult cancer care
Aims
The relationship of study 6 to the rest of the programme is shown in Figure 12. The aim of study 6 was to examine the economics of the categories of TYA cancer care. Specific objectives were to:
-
calculate detailed costs to the NHS and personal social services of teenagers and young adults
-
estimate the cost incurred by teenagers and young adults, and families
-
calculate the cost-effectiveness of the different categories of care.
FIGURE 12.
Flow diagram highlighting the study referred to in Calculating the cost of specialist teenage and young adult cancer care.
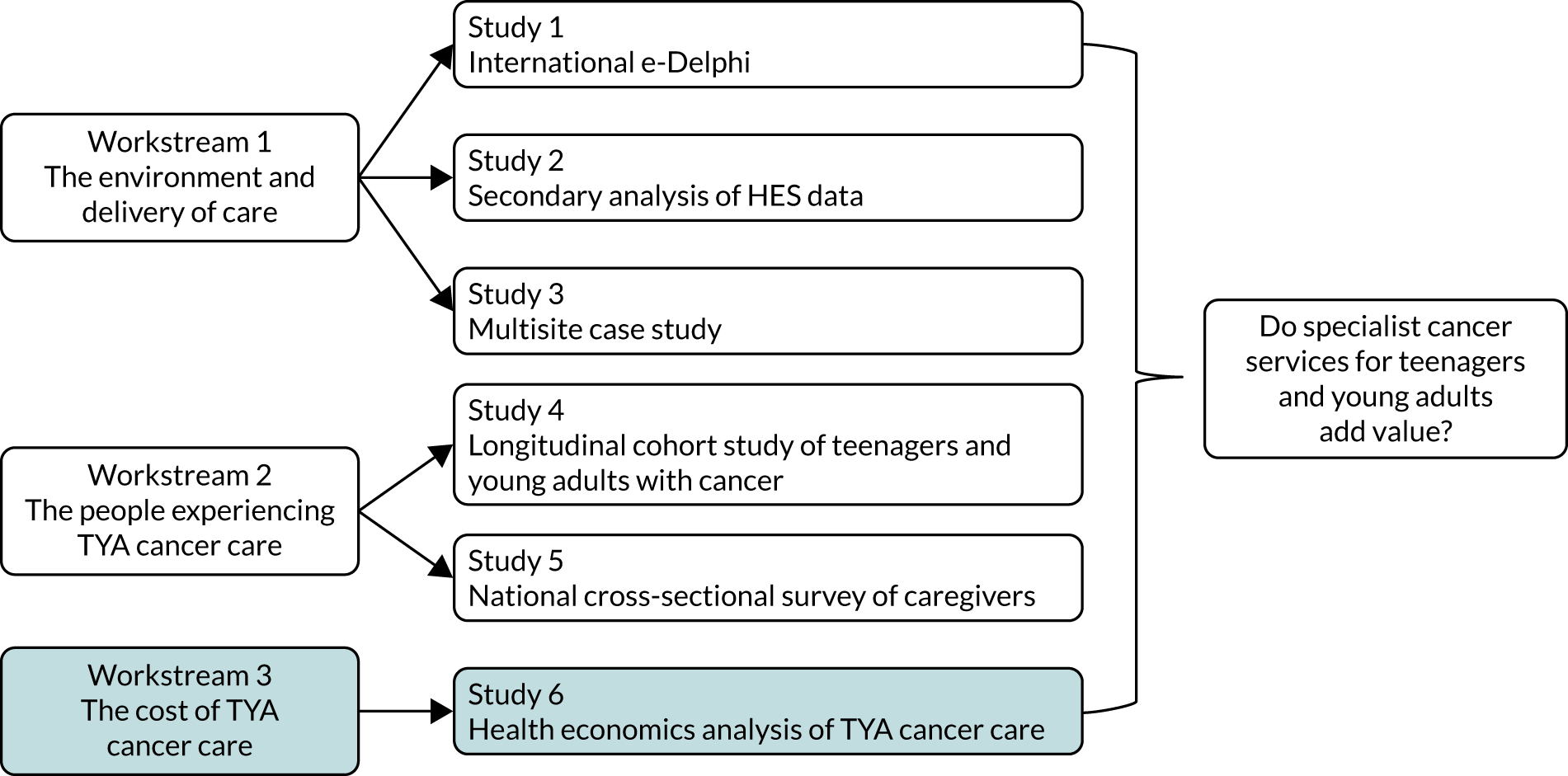
Methods
Details of study 6 are included in Appendix 3. In summary, data for the health economics analysis were collected from the cohort in study 4. Young people completed a Cost of Care Questionnaire (CoCQ) at the time of interview that comprised nine multi-item questions on additional costs incurred as a result of a cancer diagnosis. This asked respondents to reflect on the time from diagnosis to the interview. Young people were also asked to complete a cost record, which contained the same information but recorded weekly in 3-monthly cycles at 9 and 12 months after diagnosis. These questionnaires were paper self-report versions returned in a freepost envelope. No reminders were sent. The CoCQ and cost record are freely available to download under the following licence: https://xip.uclb.com/i/healthcare_tools/brightlight_healtheconomics.html (accessed 1 June 2021). Analysis of HES data was undertaken to calculate hospital costs and to calculate young people’s travel costs in the first 12 months after diagnosis (see Appendix 3 for details of the methods).
Key findings
The results are presented in detail in Appendix 3. HES data were available for 1044 young people. The mean hospital costs in the first 12 months after diagnosis were highest among patients receiving SOME-TYA-PTC care (mean £43,000, 95% confidence interval £39,831 to £46,169); there were no significant differences in costs between the NONE-TYA-PTC and SOME-TYA-PTC groups. Findings in the adjusted analysis showed that the highest cost was incurred by the SOME-TYA-PTC group, followed by the ALL-TYA-PTC group, with the lowest cost incurred by the NONE-TYA-PTC group. These differences were statistically significant.
In the fully adjusted analysis for calculating travel costs, the sample size was 733 and the SOME-TYA-PTC group continued to incur the highest cost, followed by the ALL-TYA-PTC and NONE-TYA-PTC groups. The mean of out-of-pocket expenses for patients receiving NONE-TYA-PTC care, SOME-TYA-PTC care and ALL-TYA-PTC care for the first 6 months from diagnosis were £284.77, £743.83 and £976.46, respectively. Similarly, out-of-pocket expenses for patients receiving NONE-TYA-PTC care, SOME-TYA-PTC care and ALL-TYA-PTC care at 6–9 months were £58.52, £280.58 and £122.14, respectively. At 10–12 months, these out-of-pocket expenses were £398.66, £98.17 and £179.40, respectively. Food purchased as a result of hospitalisation was the highest cost item. The mean number of quality-adjusted life-years (QALYs) gained per patient was 2.45 (95% CI 2.28 to 2.62) for patients receiving NONE-TYA-PTC care, 2.15 (95% CI 1.74 to 2.14) for those receiving SOME-TYA-PTC care and 2.20 (95% CI 1.94 to 2.28) for ALL-TYA-PTC care, which were not significant.
Limitations
Only a proportion of the cohort completed the CoCQ and there was a low response rate to the cost record; therefore, out-of-pocket expenses could be under- or overestimates of the true costs to patients. The health economics assessment utilised data collected in study 4 only, so no assessment of the cost of the environment of care or staffing specialised units was undertaken. Much of the infrastructure and staffing in the TYA-PTCs is provided through charitable funding, which the hospital cost analysis does not account for. The hospital costs were higher in the SOME-TYA-PTC and ALL-TYA-PTC groups, but these may not be higher to the NHS if they were to some degree offset by charitable funding.
Inter-relationship with the rest of the programme
Study 6 provided the health economic analysis for the whole programme.
Work arising from the grant
As referred to in Setting the scene, a planned fourth workstream included in the original grant application was changed to reflect the gradual inclusion of several linked projects. A summary of these and progress throughout the programme are summarised in Table 1.
| Theme | Project description | Progress |
|---|---|---|
| Diagnostic pathways |
REFER_ME Perceived poor diagnostic timeliness is a consistently reported and significant concern for young people, which they themselves have highlighted as a research priority. 73 Young people wanted questions on the pre-diagnostic experience included in the BRIGHTLIGHT survey, but these did not relate to the main objectives of the study. However, inclusion afforded us the opportunity to explore in detail in a large sample, routes to diagnosis |
Collaboration with Epidemiology of Cancer Healthcare and Outcomes group at University College London Two publications accepted74,75 Funding from CRUK_EDAG received in 2019 to undertake additional analysis (Lorna A Fern, personal communication) |
| Access to research |
RECRUIT_ME Recruitment to the cohort study was more challenging than we had anticipated. Fern et al. 76 have previously developed a model to support strategies to improve recruitment of teenagers and young adults to clinical trials. We have now expanded on this work to look at access to all research, especially the barrier and facilitators. 45,66,77 This also links to the NHS long-term plan, which specifies a target to recruit 50% of young people to clinical trials by 202578 |
Collaboration with the NIHR TYA cancer lead and multiple sites across England The YAP co-hosted a NIHR TYA research summit in 2018 to set the agenda for increasing access to research A NIHR RfPB application was rejected in 2019 and a NIHR programme development grant was rejected in 2021 An application will be submitted to UKRI in 2021 |
| Cancer care in specific populations |
RELEASE_ME Young people in prison were excluded from participation in the BRIGHTLIGHT cohort because of the extreme challenges of access, consent and data collection. However, health-care professionals informally reported the inequality of access to care, the impact of a prisoner-patient population on service delivery, the negative impact on care experience and also the concern about whether or not outcomes for this population were as good as the outcomes for those not in prison |
Led by Dr Elizabeth Davis at King’s College London NIHR HSDR funding was received in 2018 to explore this through analysis of NHS data, in-depth interviews with patient-prisoners, and workshops to develop a strategy to change practice (grant reference 16/52/53)79 |
|
Developing a SAM Sarcoma is a common cancer type in young people and is well represented in the cohort. There are QoL measures available specifically for many types of cancer, but not for sarcoma, which may be due to the heterogeneity of sarcoma (affecting soft tissue and bone, across all areas of the body). A disease-specific QoL measure is often recommended to capture the issues specific to a defined population. Without knowing the patient-report experience, it is not possible develop a measure of QoL that accurate reflects patients QoL. QoL is an important outcome for patients; if we are developing interventions to improve young people’s psychosocial outcomes, it would be helpful to have a measure available to use as an outcome |
Collaboration with members of the Psychosocial and survivorships, and sarcoma clinical studies group at the NCRI Funding was awarded from Sarcoma UK in 2016 (grant reference SUK102.2016LG). Data collection is now complete, and analysis is anticipated to be complete in 2021. 58,80,81 Additional funding from Sarcoma UK was awarded in 2019 to undertake secondary analysis of the qualitative data to understand the route to diagnosis (grant reference SUK203.018), and in 2020 for a study to develop an intervention for fear of recurrence (grant reference SUK201.2019), also using secondary analysis of SAM data |
|
| Supporting psychosocial outcomes |
INFORM_ME Imparting information through the internet is commonplace and is often deemed more acceptable to young people. However, reviews82,83 have shown that interventions used to support psychological well-being, mostly utilising technology, and technology interventions used to support various outcomes have mostly shown no benefit, for reasons including no involvement of patients in the development of the intervention and interventions being developed independent of theory. We anticipate that many interventions we will be developing in the future will be delivered online or will embrace digital technology. Therefore, we wanted to understand more about how young people use the internet |
Collaboration with nurse consultants from Leeds and Bristol Funding was awarded from Teenage Cancer Trust in 2016 and is completed56,84 |
|
End of treatment The end of treatment is known to be a transition point generating high anxiety for young people and was identified by the YAP and in our early feasibility work as a priority for further understanding and support |
Collaboration with nurse consultants from Leeds and London, and principal lecturers from Coventry University Funding was awarded from Teenage Cancer Trust in 2018 and is completed57,85,86 |
|
|
Social reintegration In addition to the end-of-treatment study outline above, a more detailed investigation into social reintegration is being undertaken. This project is using education, employment and social engagement data from the British Household Panel Survey and the UK Household Longitudinal Study databases to provide the non-cancer controls for the same secondary analysis that will be undertaken with BRIGHTLIGHT data. A cohort of 400 young people aged 16–39 years will also be established |
Led by Professor Dan Stark at the University of Leeds Funding was awarded by the Economic and Social Research Council in 2019 (grant reference ES/S00565X/1) and the study commenced in 2020 |
|
|
Sexuality and intimacy This was a subject the YAP identified as an issue that was under-researched and not adequately addressed by clinical teams |
Led by Professor Brian Lobel at Rose Bruford and the Royal Central School of Speech and Drama A grant application was rejected by the British Academy in 2020 |
|
|
Caregiver information and support needs The unmet needs have been described, but additional analysis is planned to understand more of emotional needs and factors that could predict caregiver needs that could inform an intervention to support caregivers |
Led by Nicky Pettitt, Nurse Consultant at University Hospitals Birmingham NHS Trust. A proposal was submitted as part of a MRES. Support is being provided for the analysis and submission to a NIHR HEE/ICA CDRF | |
| Delivery of health care |
When cure is not likely We undertook a study to understand the needs of young adults in the last year of life. This study collected a data set from patients, their nominated carer and health-care professional, linking this through workshops to the reflections of other patients, families and health-care professionals. This has expanded our understanding of the challenges specific to the delivery of excellent end-of-life-care to young adults with cancer |
Collaboration with teams in Leeds and Southampton Funding was awarded from Marie Curie in 2013 (grant reference 15722). The study is complete87,88 |
|
BRIGHTLIGHT extension study The results of BRIGHTLIGHT are all about the delivery of specialist TYA cancer care. There have been changes to the way services are delivered for young people in England so the TYA-PTC links to hospitals designated in the region to deliver care |
A NIHR post-doctoral fellowship was rejected in 2018. An application for a similar project was awarded in 2020 through the NIHR Policy Research Programme (grant reference NIHR201438) to commence in 2021 | |
| Patient and public involvement and engagement |
Using the arts to inform health-care research BRIGHTLIGHT was developed with young people and they have been integral in study management. As noted above, they have also identified issues that need further exploration. They have also played a role in dissemination where we have been exploring more novel ways of disseminating our results, so they are more meaningful to people who do not necessarily understand graphs and the scientific way results are traditionally presented |
Led by Professor Brian Lobel at Rose Bruford and the Royal Central School of Speech and Drama Funding was awarded by the Wellcome Trust in 2016 to develop a theatrical performance (grant reference 204162/Z/16/Z). There is a Light: BRIGHTLIGHT played for 11 nights in seven cities across the UK in 2017. The evaluation was accepted for publication in 202089 A NIHR programme development grant was rejected in 2020 to extend dissemination of BRIGHTLIGHT through enhanced engagement. This was resubmitted in May 2021 |
Do specialist cancer services for teenagers and young adults add value?
The question that subtitles the BRIGHTLIGHT programme of research, ‘Do specialist cancer services for teenagers and young adults add value?’, was initially posed in response to concerns raised by opposing groups and individuals. These included professionals and advocates who were directly involved in the early development of cancer services that were specifically aimed to address the needs of teenagers and young adults, and also concerns raised by others, who, in these early stages, questioned the appropriateness or necessity of such services. The motives were both intellectually inquisitorial and, perhaps especially in the context of constrained health-care resources, practical.
The first TYA services to emerge did so largely through local initiatives, usually with the support of a charity that was focused on funding provision of dedicated inpatient facilities: Teenage Cancer Trust. This did not follow a model of preconceived health-care planning, but rather sought and exploited opportunities when local champions could promote such developments in a permissive institution. There was no blueprint or coherent strategy and, consequently, the services that were housed by the new Teenage Cancer Trust units arose sporadically and varied one from another in many aspects of structure and provision. Such initiatives were undoubtedly popular, receiving support from professionals, patients, and charities supporting young people and their families, as well as opinion leaders. The evolution of a more comprehensive approach to the care of young people with cancer, based on multidisciplinary working that took account of the recognised developmental issues of teenagers and young adults, was stimulated by, and then developed further around, these first local services. At the same time, some professional resistance was also evident, most clearly demonstrated through, and indeed measured by, a reluctance to refer teenagers and young adults to these new services.
We therefore set out to conduct an evaluation of TYA cancer services to generate evidence that would be informative from the level of individual patient care up to developing future health policy and its associated resource allocation. Health policy also provided a starting point as the publication in 2005 of the NICE IOG on children and young people’s cancer services included an endorsement of dedicated TYA cancer services,23 despite a slender evidence base. The need for complex methodological approaches was immediately apparent, given that ‘specialist services’ were ill-defined and there was a lack of both pre-agreed meaningful outcome measures and a controllable intervention. Our preliminary work, which included young people from the outset, sought to address these methodological challenges, and thus there emerged both a study primary end point, QoL, and an approach to measuring exposure to specialist care.
The BRIGHTLIGHT programme of research adopted a multiple-methods approach to capture the complexities of delivering health care as well as measuring the impact. We have come to the end of the programme in the unforeseen position that the results of one workstream do not concur with those of the other. Results from the cohort showed that young people who had no access to specialist care had the highest QoL, but they had the slowest rate of improvement in QoL. They had the lowest reported processes reflecting quality of care and the lowest travel costs. Young people who received all their care in a specialist unit had the fastest improvement of QoL, but the highest household expenditure. Finally, young people who received care in a specialist unit but also a children’s or adult cancer unit had the lowest QoL, highest NHS cost and incurred the most costs for food while in hospital. However, there was no difference in survival or satisfaction with care wherever young people were treated. Furthermore, caregivers of young people who had all or some access to specialist care had the fewest unmet needs.
Although the cohort study may not have shown value for specialist services for young people, the case study provided a more detailed understanding of specialist care through conceptualising the phrase ‘age-appropriate’ care and demonstrating the core components of the culture. This required a service to have a critical mass of young people, which would enable health-care professionals to develop competence not just in cancer-related care but also in young person-related care (e.g. how to promote normality and empowerment). There needed to be effective leadership to facilitate ‘buy-in’ from the health-care team, so the wider organisation, and not just the specialist unit, became TYA orientated. Importantly, through inclusion of sites that had been established for decades as well as those that were newer, we were able to show that this culture took time to develop.
The NICE IOG was published in 2005,23 but the guidance was not officially implemented until 2010, and this was not an instantaneous process at every TYA-PTC. The established TYA-PTCs were able to implement many recommendations relatively promptly, whereas others who had limited facilities and personnel had more challenges to navigate to implement an embedded TYA service. When the cohort was recruited in 2012–15, the TYA MDT was not well established in every TYA-PTC and relationships between the TYA-PTCs and networked hospitals were often embryonic. At the time that recruitment to the cohort ended, data collection for the case study had begun, which highlighted the importance of time – evolution of services required time to become established, for the relationships between organisations to develop and for the TYA MDT to mature. It could be surmised that, when the cohort were recruited, this was the start of the evolution, whereas the case study reflects a time where culture was becoming more established.
Since 2015, there have been a myriad of changes nationally in TYA cancer services. These include:
-
The availability of TYA-specific university education at level 5, 6 and 7. 90
-
Increased numbers of TYA-specific professionals, notably nurses and youth workers, who are able to provide care over and above standard cancer care. Many of these positions are funded through the third sector, which also funds twice-yearly meetings so that these professionals have the opportunity to come together to share best practice.
-
Publication of evidence-based guidance on the delivery of TYA cancer care that was freely available to support best practice. 91
-
Publication of TYA cancer competency frameworks for nurses92 and youth workers.
-
Roll-out of a nurse support network so nurses employed by the TYA-PTC link to the designated hospitals to provide young people with the TYA aspect of their care. This ensures that they have access to the same resources that they would have if they were in the TYA-PTC (e.g. support to remain in education, awareness of available psychological support).
-
Increased awareness of the challenges that young people have at the end of treatment have led to national initiatives to provide transition support going from having treatment to being off treatment.
-
The development and implementation of a TYA-specific holistic needs assessment.
-
Launch of the Adolescent and Young Adult Global Cancer Congress, an annual international conference rotating between the UK, USA and Australia. This has expanded the network for TYA health-care professionals with the potential benefit of improving patient care through greater sharing of best practice.
The TYA services in England have now been established for over a decade. We can speculate that all the changes that have been implemented focusing on developing services nationally rather than locally, promoting the sharing of best practice and increasing the co-ordination of care, would have a positive impact on patient-reported outcome. There has been additional progress with national cancer policies including TYA-specific targets (e.g. 50% of young people recruited into a clinical trial by 2025) and a service specification drafted that promotes joint care. The question we would now ask is ‘Would we show the same results in 2021 as we did in the 2012 cohort?’.
Recommendations for research
Research methods
Over the period of the programme grant we have learnt much about conducting research involving young people with cancer. The evaluation from the perspective of young people utilised a longitudinal cohort design on the basis that it was not possible to manipulate where young people received care but we needed to capture how the care received at diagnosis influenced perceived outcomes in the short and medium terms. Although this afforded us the opportunity to gather a wealth of valuable data, this has taken many years to be completed. For this reason, we were unable to capture the influence of the dynamic changes in services. The complexities of researching health care have become recognised in recent years with the emergence of methods specifically designed to capture this, such as rapid ethnography93 and applied systems thinking. 94 We would therefore recommend using these or similar methods to capture the complexities of the relationships between stakeholders and the environment.
We have published extensively on involving young people in research, the barriers to this and the potential mechanisms to overcome these barriers. 45,66,67 However, we found that, even with proactive changes to the protocol, these mechanisms did not always have the desired benefit of improving recruitment; yet the rate of refusal of young people to join the cohort was low,63 and our experience with the NIHR TYA stakeholder meeting and National Cancer Research Institute (NCRI) TYA research groups has been that there is much enthusiasm from young people for supporting initiatives to increase TYA opportunities to have access to research. It may be that a single change in research process is not sufficient to affect improvements in study accrual, and a multipronged approach is required. We would recommend that this is guided by a conceptual framework, such as the 5As model proposed by Fern et al. 76 The 5As are availability (cancer trials are not always available for teenagers and young adults because of the rare cancer types they present with), appropriateness (studies often have inappropriate age eligibility criteria applied, which is based on whether the study has originated from children’s or adult oncology/haematology), accessibility (studies are often not open where young people are being treated), awareness (increased awareness among health-care professionals and teenagers and young adults about the importance of trial entry is required) and acceptability (the study question and trial design must be acceptable to both the professional and young person). 76 These 5As can help to identify where the barriers lie and guide where interventions and changes in service delivery may be of benefit.
Research arising from the programme
A priority for further research has emerged that links results from workstreams 1 and 2 and is immediately relevant to the definition of TYA services currently envisaged in draft NHS England service specifications for both TYA-PTCs and designated hospitals. A study that reproduces the methodology used by BRIGHTLIGHT but updated with data from TYA diagnosed in 2021 would determine whether or not the results seen at the first wave of data collection in the cohort are being reproduced with a similar differential of outcomes between NONE, SOME and ALL groups. If this was so, there would be a strong argument for urgent exploration of those poorly defined factors that determine ‘membership’ of these groups. Alternatively, there may no longer be separation between these groups, a result that might be consequent on an improved access to the key elements of specialist care as described here, including outside the TYA-PTC. Simultaneously, rapid evaluation of cancer services for teenagers and young adults should be conducted to determine whether or not the culture of TYA care has, in fact, evolved. Through the use of rapid methods it would be possible to explore interactions and co-ordination of care in most, if not all, TYA-PTCs. This would capture the variation in service delivery and the potential to link patient-reported outcome and experience to the care they receive.
We have reported in detail the limitations of the TYA Cancer Specialism Scale and how we defined the categories of care. 68 This could be refined through including outpatient data, not just APC data, and categorising ‘specialist’ based on the hospital where young people received care, not just the trust. The SOME group warrants further investigation to determine if there is an optimum proportion of care in a TYA-PTC that has benefit rather than the crude classification of 0%, 100% and 1–99%.
We defined ‘specialist’ as care delivered in a TYA-PTC; however, these are all different and there are non-TYA-PTCs that have more TYA-specific facilities than a TYA-PTC does. As we now have a definition of age-appropriate care, we are in a unique position to be able to use survey data from the cohort to ‘test’ the conceptual model. This will enable us to objectively identify which of the components of the model define age-appropriate care and which of these are associated with better outcomes. This would guide commissioners and hospital administrators/managers on what aspects of care to invest in, that would most likely be beneficial to young people.
Although we showed that the NONE-TYA-PTC group cost the least to the NHS, this cost was calculated based on the assumption that the NHS was incurring all the cost. However, much of the infrastructure of the TYA-PTCs and some of the designated hospitals is funded through the third sector (Teenage Cancer Trust 2019 annual report notes that they supported 28 specialist units across the UK). 95 A total of 122 members of the TYA health-care team in the UK are also funded through third-sector funding: nurses (n = 76), youth workers (n = 36) and MDT co-ordinators (n = 10). These are costs that would have been included in the ALL and SOME groups in this analysis. Taking these into consideration would enable the actual cost to the NHS to be calculated.
Finally, data collection from the cohort continued for 3 years; at this time we saw that QoL was comparable in all three groups, with those receiving ALL-TYA-PTC and SOME-TYA-PTC care having an improvement in QoL more rapidly to being a mean of 1–5 points different from the NONE-TYA-PTC group. What would be important to establish is whether the rate of improvement continued, in which case by 5–10 years after diagnosis, QoL could potentially be superior for the ALL and SOME groups in comparison with the NONE group. The philosophy of TYA cancer care is that support is provided to enable young people to continue their lives to achieve the milestones that they would have had they not had cancer. Three years may not have been sufficient time to be able to capture this benefit. A follow-up survey when the cohort is 10 years post diagnosis would enable this benefit to be determined. This would also afford the opportunity to explore outcomes other than QoL and survival that could have benefited from specialist care.
Acknowledgements
Project website: www.brightlightstudy.com.
Steering group
William Van’t Hoff, Great Ormond Street Hospital for Children NHS Foundation Trust (chairperson).
Lisa Calderwood, Institute of Education, UCL.
Zoe Coombe, Greater Manchester and Cheshire Cancer Research Network.
Laura Clark, Teenage Cancer Trust, London.
Meriel Jenney, Children’s Hospital for Wales, Cardiff.
Jocelyn Walters, Central South Coast Cancer Research Network.
Young advisory panel
Zeena Beale, Mathew Cook, Ciaran Fenton, Emily Freemantle, Laura Haddad, Steph Hammersley, Amy Lang, Joshua Lerner, Tanya Loughlin, Jason Jin Loo, Yaajan Govindia, Kelly Pilgrim, Jennifer Helen Miller, Arif Nasir, Poppy Richards, Mariia Onasanya, Stephen Sutton, Amy Riley, Paris Tompkins, Freya Voss, Antonia Young, Max Williamson, JJ Wheeler and Lara Veitch
Principal investigators for study 4
Only principal investigators who consented to being named in publications have been included.
Claire Hemmaway, Barking, Havering and Redbridge Hospitals NHS Trust.
Anita Amadi, Barnet and Chase Farm Hospitals NHS Trust.
Keith Elliott, Barnsley Hospital NHS Foundation Trust.
Leanne Smith, Blackpool, Fylde and Wyre Hospitals NHS Trust.
Shirley Cocks, Bolton NHS Foundation Trust.
Victoria Drew, Bradford Teaching Hospitals NHS Foundation Trust.
Elizabeth Pask, Central Manchester University Hospitals NHS Foundation Trust.
Anne Littley, Central Manchester University Hospitals NHS Foundation Trust.
Mark Bower, Chelsea and Westminster Hospital NHS Trust.
Scott Marshall, City Hospitals Sunderland NHS Foundation Trust.
Lorna Dewar, Colchester Hospital University NHS Trust.
Nnenna Osuji, Croydon Health Services NHS Trust.
David Allotey, Derby Hospitals NHS Foundation Trust.
Karen Jewers, East Lancashire Hospitals NHS Trust.
Asha Johny, Gloucestershire Hospitals NHS Foundation Trust.
Nicola Knightly, Great Western Hospitals NHS Foundation Trust.
Robert Carr, Guy’s and St Thomas’ Hospital NHS Foundation Trust.
Alison Milne, Hampshire Hospitals NHS Foundation Trust.
Claire Hall, Harrogate and District NHS Foundation Trust.
James Bailey, Hull and East Yorkshire Hospitals NHS Trust.
Christine Garlick, Ipswich Hospital NHS Foundation Trust.
Alison Brown, Isle of Wight Healthcare NHS Trust.
Carolyn Hatch, Lancashire Teaching Hospitals NHS Foundation Trust.
Vivienne E. Andrews, Medway NHS Foundation Trust.
Sara Greig, Milton Keynes Hospital NHS Foundation Trust.
Jennifer Wimperis, Norfolk and Norwich University Hospital NHS Trust.
Suriya Kirkpatrick, North Bristol NHS Trust.
Jonathan Nicoll, North Cumbria University Hospitals NHS Trust.
Ivo Hennig, Nottingham University Hospitals NHS Trust.
Karen Sherbourne, Oxford Radcliffe Hospital NHS Trust.
Clare Turner, Plymouth Hospitals NHS Trust.
Claire Palles-Clark, Royal Surrey County Hospital NHS Trust.
Christine Cox, Royal United Hospital Bath NHS Trust.
Yeng Ang, Salford Royal NHS Foundation Trust.
Jonathan Cullis, Salisbury NHS Foundation Trust.
Daniel Yeomanson, Sheffield Children’s NHS Foundation Trust.
Ruth Logan, Sheffield Teaching Hospitals NHS Foundation Trust.
Deborah Turner, South Devon Healthcare NHS Trust.
Dianne Plews, South Tees Hospitals NHS Trust.
Juliah Jonasi, Southend University Hospital NHS Foundation Trust.
Ruth Pettengell, St George’s Healthcare NHS Trust.
Kamal Khoobarry, Surrey and Sussex Healthcare NHS Trust.
Angela Watts, The Dudley Group of Hospitals NHS Foundation Trust.
Louise Soanes, The Royal Marsden NHS Foundation Trust.
Claudette Jones, The Royal Orthopaedic Hospital NHS Trust.
Michael Jenkinson, The Walton Centre for Neurology and Neurosurgery NHS Trust.
Nicky Pettitt, University Hospital Birmingham NHS Foundation Trust.
Vijay Agarwal, University Hospital Birmingham NHS Foundation Trust.
Beth Harrison, University Hospitals Coventry and Warwickshire NHS Trust.
Fiona Miall, University Hospitals of Leicester NHS Trust.
Gail Wiley, University Hospitals of Morecambe Bay NHS Trust.
Lynda Wagstaff, Walsall Hospitals NHS Trust.
Fiona Smith, West Hertfordshire Hospitals NHS Trust.
Sarah Janes, Western Sussex NHS Trust.
Serena Hillman, Weston Area Health NHS Trust.
Christopher Zaborowski, Yeovil District Hospital NHS Foundation Trust.
Contributions of authors
Rachel M Taylor (https://orcid.org/0000-0002-0853-0925) (Director of the CNMAR, Honorary Associate Professor) led the management of the programme, including submission of all the regulatory applications for each workstream; conducted the Delphi survey (study 1); wrote the look-up tables for defining specialist care for the analysis of HES data for the TYA Cancer Specialism Scale (study 2); co-supervised the PhD student conducting the case study (study 3); led the conduct the cohort study (study 4) and caregiver study (study 5); provided data management for the health economic analysis (study 6); and provided support for Lorna A Fern for PPI.
Lorna A Fern (https://orcid.org/0000-0003-4821-8466) (NCRI TYA Researcher and Patient/Public Involvement Lead) led PPI and supported the conduct of the cohort study (study 4) and caregiver study (study 5).
Julie Barber (https://orcid.org/0000-0001-5762-762X) (Associate Professor in Medical Statistics) conducted the analysis for the cohort study (study 4), and provided statistical oversight for the analysis of the TYA Cancer Specialism Scale (study 2) and caregiver study (study 5).
Faith Gibson (https://orcid.org/0000-0002-8125-4584) (Professor of Child Health and Cancer Care) was the workstream 1 lead and primary supervisor for the PhD student conducting the case study (study 3).
Sarah Lea (https://orcid.org/0000-0001-9054-6055) (Research Facilitator) conducted the case study (study 3).
Nishma Patel (https://orcid.org/0000-0002-2652-5185) (Research Fellow) conducted the health economics analysis (study 6).
Stephen Morris (https://orcid.org/0000-0002-5828-3563) (Professor of Health Economics) was the workstream 3 lead and supervised the health economics study (study 6).
Javier Alvarez-Galvez (https://orcid.org/0000-0001-9512-7853) (Research Fellow) conducted the analysis for the TYA Cancer Specialism Scale (study 2) and caregiver study (study 5).
Richard Feltbower (https://orcid.org/0000-0002-1728-9408) (Senior Lecturer in Epidemiology) conducted the directed acyclic graph (DAG) analysis to identify the confounding variables for the cohort study (study 4).
Louise Hooker (https://orcid.org/0000-0002-5641-2325) (Teenage Cancer Trust Lead Nurse) contributed to the design of the programme and revised the content of the BRIGHTLIGHT survey (study 4).
Ana Martins (https://orcid.org/0000-0002-5036-4959) (Research Associate) prepared the caregiver data, contributed to analysis and wrote the manuscript (study 5).
Dan Stark (https://orcid.org/0000-0002-6172-733X) (Professor of Teenage and Young Adult Cancer Research) contributed to the design of the programme and interpretation of QoL data (study 4).
Rosalind Raine (https://orcid.org/0000-0003-0904-749X) (Head of Department of Applied Health Research, Director, NIHR ARC North Thames, NIHR Senior Investigator) contributed to the design of the programme and interpretation of results.
Jeremy S Whelan (https://orcid.org/0000-0001-6793-5722) (Professor of Cancer Medicine) was the chief investigator of the programme. He conceived the study, led the preliminary work and the applications for funding. He led and supported the research team throughout the programme and also provided essential clinical knowledge on TYA cancer and its management.
Publications
Peer-reviewed publications
Fern LA, Taylor RM, Barber JA, Alvarez-Galvez J, Feltbower R, Lea S, et al. Processes of care and survival associated with treatment in specialist teenage and young adult cancer centres: results from the BRIGHTLIGHT cohort study. BMJ Open 2021;11:e044854. https://doi.org/10.1136/bmjopen-2020-044854
Fern L, Taylor RM, Millington H, Ashton J, Grew T, Brooman K, et al. The art of age-appropriate care: reflecting on a conceptual model of the cancer experience for teenagers and young adults. Cancer Nurs 2013,36:E27–38. https://doi.org/10.1097/NCC.0b013e318288d3ce
Herbert A, Lyratzopolous G, Whelan J, Taylor RM, Barber J, Gibson F, Fern LA. Diagnostic timeliness in teenagers and young adults with cancer: cross-sectional findings from the BRIGHTLIGHT Cohort. Lancet Child Adolesc Health 2018;2:180–90. https://doi.org/10.1016/S2352-4642(18)30004-X
Kenten C, Martins A, Fern LA, Gibson F, Lea S, Ngwenya N, et al. Qualitative study to understand the barriers to recruiting young people with cancer to BRIGHTLIGHT: a national cohort study in England. BMJ Open 2017;7:e018291. https://doi.org/10.1136/bmjopen-2017-018291
Koo MM, Lyratzopoulos G, Herbert A, Abel GA, Taylor RM, Barber J, et al. Association of self-reported presenting symptoms with timeliness of help-seeking among adolescents and young adults with cancer in the BRIGHTLIGHT study. JAMA Netw Open 2020;3:e2015437. https://doi.org/10.1001/jamanetworkopen.2020.15437
Lea S, Gibson F, Taylor RM. ‘Holistic competence’: how is it developed and shared by nurses caring for adolescents and young adults with cancer? [published online ahead of print.] J Adolesc Young Adult Oncol 2021. https://doi.org/10.1089/jayao.2020.0120
Lea S, Gibson F, Taylor RM. The culture of young people’s cancer care in the UK: a narrative review and synthesis of the literature. Eur J Cancer Care 2019;28:e13099. https://doi.org/10.1111/ecc.13099
Lea S, Taylor RM, Martins A, Fern LA, Whelan JS, Gibson F. Conceptualizing age-appropriate care for teenagers and young adults with cancer: a qualitative mixed-methods study. Adolesc Health Med Therapeutics 2018;9:149–66. https://doi.org/10.2147/AHMT.S182176
Lea S. Perspectives: a newly qualified nurse’s experience of starting a clinical academic career. J Res Nurs 2015;20:252–5. https://doi.org/10.1177/1744987115580896
Martins A, Alvarez-Galvez J, Fern LA, Vindrola C, Gibson F, Whelan JS, Taylor RM. The BRIGHTLIGHT national survey of the impact of specialist teenage and young adult cancer care on caregivers’ information and support needs. Cancer Nurs 2021;44:235–43. https://doi.org/10.1097/NCC.0000000000000771
Stark D, Fern LA, Gibson F, Hawkins M, Hough R, McCabe MG, Taylor R. Transitioning adolescent and young adult cancer care research out of its adolescence. Eur J Cancer Care 2018;27:e12962. https://doi.org/10.1111/ecc.12962
Taylor RM, Fern LA, Barber JA, Alvarez-Galvez J, Feltbower R, Lea S, et al. Specialist age-appropriate care and quality of life outcomes in a longitudinal cohort of teenagers and young adults: the BRIGHTLIGHT study. BMJ Open 2020;10:e038471. https://doi.org/10.1136/bmjopen-2020-038471
Taylor RM, Lobel B, Thompson K, Onshila A, Croasdale M, Whelan JS, Fern LA. BRIGHTLIGHT researchers as ‘dramaturgs’: creating There is a Light from complex research data. Res Involv Engagem 2020;6:48. https://doi.org/10.1186/s40900-020-00222-5
Taylor RM, Fern LA, Barber JA, Alvarez Galvez J, Stark DP, Feltbower R, et al. Description of the BRIGHTLIGHT Cohort: the evaluation of teenagers and young adult cancer services in England. BMJ Open 2019;9:e027797. https://doi.org/10.1136/bmjopen-2018-027797
Taylor RM, Aslam N, Lea S, Whelan JS, Fern LA. Optimizing a retention strategy with young people for BRIGHTLIGHT, a longitudinal cohort study examining the value of specialist cancer care for young people. J Adolesc Young Adult Oncol 2017;6:459–69. https://doi.org/10.1089/jayao.2016.0085
Taylor RM, Fern LA, Aslam N, Whelan JS. Direct access to potential research participants for a cohort study using a confidentiality waiver included in UK National Health Service legal statutes. BMJ Open 2016;6:e011847. https://doi.org/10.1136/bmjopen-2016-011847
Taylor RM, Solanki A, Aslam N, Whelan JS, Fern LA. A participatory study of teenagers and young adults’ views on access and participation in cancer research. Eur J Oncol Nurs 2016;20:156–64. https://doi.org/10.1016/j.ejon.2015.07.007
Taylor RM, Feltbower RG, Aslam N, Raine R, Whelan JS, Gibson F. Modified international e-Delphi survey to define healthcare professional competencies for working with teenagers and young adults with cancer. BMJ Open 2016;6:e011361. https://doi.org/10.1136/bmjopen-2016-011361
Taylor RM, Fern L, Solanki A, Hooker L, Carluccio A, Pye J, et al. Development and validation of the BRIGHTLIGHT Survey, a patient-reported experience measure for young people with cancer. Health Qual Life Outcomes 2015;13:107. https://doi.org/10.1186/s12955-015-0312-7
Taylor RM, Pearce S, Gibson F, Fern L, Whelan J. Developing a conceptual model of teenage and young adult experiences of cancer through meta-synthesis. Int J Nurs Stud 2013;50:832–46. https://doi.org/10.1016/j.ijnurstu.2012.09.011
Vindrola-Padros C, Taylor RM, Lea S, Hooker L, Pearce S, Whelan J, Gibson F. Mapping adolescent cancer services: how do young people, their families, and staff describe specialized cancer care in England? Cancer Nurs 2016;39:358–66. https://doi.org/10.1097/NCC.0000000000000315
Conference presentations
Anazodo A, Fern L. What Can We Learn From Cross Country Comparisons of Cancer Care for Adolescents and Young Adults (AYAs) to Improve Cancer Outcomes? Paris: UICC World Cancer Congress; 4 November 2016 (invited).
Aslam N, Gibson F, Taylor RM, Whelan J, Raine R, Feltbower R. Professional Competence for Working with Teenagers and Young Adults with Cancer: Consensus and Dissension Revealed in the BRIGHTLIGHT Delphi Survey. Abstract O188 (Oral Presentation). Cape Town: International Society of Paediatric Oncology SIOP Congress; October 2015.
Aslam N, Gibson F, Taylor RM, Whelan J, Raine R, Feltbower R. Professional competence for working with teenagers and young adults with cancer: consensus and dissension revealed in the BRIGHTLIGHT study. Pediatr Blood Cancer 2015;62:S194.
Fern L, Taylor R, Barber J, Alvarez-Galvez J, Feltbower R, Gibson F, et al. How Well are Clinical Processes of Care Documented for Teenagers and Young Adults with Cancer Treated in Specialist and Non-Specialist Centres: BRIGHTLIGHT Study Findings. Lyon: 51st Congress of the International Society of Paediatric Oncology (SIOP); October 2019.
Fern L, Taylor R, Barber J, Alvarez-Galvez J, Feltbower R, Gibson F, et al. How well are clinical processes of care documented for teenagers and young adults with cancer treated in specialist and non-specialist centres: Brightlight study findings. Pediatr Blood Cancer 66:V104 SIOP19-0304.
Kenten C, Martins A, Fern LA, Gibson F, Lea S, Ngwenya N, et al. A Qualitative Study to Understand the Barriers to Recruiting Adolescents and Young Adults with Cancer to BRIGHTLIGHT, a National Cohort Study (Poster Presentation). Atlanta, GA: 2nd Global AYA Cancer Congress; 5–7 December 2017.
Kenten C, Fern LA, Taylor RM, Martins A, Lea S, Ngwenya N, Whelan JS, Gibson F. A Qualitative Study to Understand the Barriers to Recruiting Adolescents and Young Adults with Cancer to BRIGHTLIGHT, a National Cohort Study. Liverpool: NCRI Annual Conference; 5–8 November 2017.
Lea S, Taylor RM, Gibson F. Developing and Sustaining a Shared Culture of Care for Young People with Cancer. Lyon: 51st Congress of the International Society of Paediatric Oncology (SIOP); October 2019. Pediatr Blood Cancer 66:N19 SIOP19-0721.
Lea S, Taylor R, Gibson F. The Importance of the Physical Environment in Creating a Social Environment for Adolescents and Young Adults in Hospital (Poster). Ascot: RCPCH/SAHM Adolescent Health 2019 Coming of Age Conference; 18–19 September 2019.
Lea S, Taylor R, Gibson F. ‘It’s a Very Good Vehicle to Create Your Relationship’: Importance of the Physical Environment When Creating a Social Hospital Environment (Oral). Sheffield: 2019 RCN International Research Society Conference; September 2019.
Lea S, Gibson F, Martins A, Fern LA, Whelan JS, Taylor RM. The Five ‘Es’ of Holistic Care for Adolescents and Young Adults With Cancer (Oral). London: Qualitative Health Research Network Conference; 21–22 March 2019.
Lea S, Taylor RM, Martins A, Fern LA, Whelan JS, Gibson F. ‘No Peppa Pig!’: Conceptualising Age-appropriate Care for Teenagers and Young Adults with Cancer (Oral). Birmingham: 2018 RCN International Research Society Conference; 16–18 April 2018.
Lea S, Taylor RM, Martins A, Fern L, Whelan JS, Gibson F. Conceptualising Age-appropriate Care For Teenagers and Young Adults With Cancer: A BRIGHTLIGHT Study (Poster Presentation). Atlanta, GA: 2nd Global AYA Cancer Congress; 5–7 December 2017.
Lea S, Taylor R, Martins A, Fern L, Whelan J, Gibson F. ‘It Was Like Having a Big Sleepover with Our Chemo Bags On’: Exploring the Relationship Between Physical and Social Hospital Environments (Oral Presentation). Edinburgh: 1st Global AYA Cancer Congress; 5–7 December 2016.
Martins A, Fern LA, Whelan JS, Taylor RM. A National Survey of Carers of Teenagers and Young Adults with Cancer Unmet Information and Support Needs (Poster). Southampton: British Psychosocial Oncology Society Conference; 8–9 March 2018.
Martins A, Fern L, Whelan JS, Taylor RM. Carers of Teenagers and Young Adults with Cancer Have Unmet Information and Support Needs (Poster). Liverpool: NCRI Annual Conference; November 2017.
Taylor RM, Fern LA, Barber JA, Alvarez-Galvez J, Feltbower RG, Lea S, et al. BRIGHTLIGHT: Do Specialist Services for Teenagers and Young Adults with Cancer Add Value? (Oral) Toronto: AYA Survivorship Symposium: Caring for the Future; 8 April 2021 (virtual).
Taylor RM. A Canadian Vision for AYA Care: Insights and Ideas from England and Australia (Plenary). Toronto: Pediatric Oncology Group of Ontario (POGO) Annual Conference; November 2019.
Taylor RM, Martins A, Alvarez-Galvez J, Fern LA, Vindrola-Padros C, Barber JA, et al. The BRIGHTLIGHT National Survey of the impact of Specialist Teenage and Young Adult Cancer Care on Caregivers’ Information and Support Needs. Barcelona: 44th ESMO Congress (ESMO 2019); 27 September–1 October 2019.
Taylor RM, Martins A, Alvarez-Galvez J, Fern LA, Vindrola-Padros C, Barber JA, et al. The BRIGHTLIGHT national survey of the impact of specialist teenage and young adult cancer care on caregivers’ information and support needs. Annals Oncol 2019;30(Suppl. 5):mdz275.008.
Taylor RM, Fern LA, Whelan JS on behalf of the BRIGHTLIGHT Team. The Challenge of Measuring Teenage and Young Adult Experience of Cancer in a Longitudinal Survey (Symposium Presentation). Birmingham: 2018 RCN International Research Society Conference; 16–18 April 2018.
Taylor RM, Fern LA, Gibson F, Whelan JS. What are the Barriers to Recruiting Young People With Cancer to Research? (Poster Presentation). Edinburgh: 1st Global AYA Cancer Congress; 5–7 December 2016.
Taylor RM, Aslam N, Feltbower R, Raine R, Whelan JS, Gibson F. G405 Defining Healthcare Professional Competence for Working with Teenagers And Young Adults With Cancer – A BRIGHTLIGHT Study (Oral Presentation). Birmingham: Royal College of Paediatrics and Child Health Annual Conference; 2015.
Taylor RM, Aslam N, Feltbower R, Raine R, Whelan JS, Gibson F. G405 Defining healthcare professional competence for working with teenagers and young adults wiith cancer – a BRIGHTLIGHT study. Arch Dis Childhood 2015;100(Suppl. 3):A166.
Taylor RM on behalf of the BRIGHTLIGHT Team. BRIGHTLIGHT: Emerging Results (Invited Presentation). Leeds TYAC Winter Education Day; 28 November 2013.
Taylor R, Fern L, Gibson F, Whelan J. Steps in the Development of a Patient-reported Outcome Measure for Teenage and Young Adults With Cancer: The BRIGHTLIGHT Survey. Abstract 0148 (Oral Presentation). London: International Society of Paediatric Oncology SIOP XXXXIV Congress; October 2012.
Taylor R, Fern L, Gibson F, Whelan J. Steps in the development of a patient-reported outcome measure for teenage and young adults with cancer; the BRIGHTLIGHT survey. Pediatr Blood Cancer 2012;59:1009.
Taylor RM, Fern L, Gibson G, Pye J, Whelan J. Development of a Patient-reported Outcome Measure for TYA With Cancer: The BRIGHTLIGHT Survey (Oral Presentation). Nottingham: TYAC Spring Education Day; 20 January 2012.
Vindrola C, Finlayson S, Hooker L, Pearce S, Taylor R, Whelan J, Gibson F. Creating a Taxonomy of Teenage and Young Adult Cancer Care in England Through a Mapping Study. Abstract O179 (Oral Presentation). Toronto: International Society of Paediatric Oncology SIOP XXXXVI Congress; October 2014.
Vindrola C, Finlayson S, Hooker L, Pearce S, Taylor R, Whelan J, Gibson F. Creating a taxonomy of teenage and young adult cancer care in England through a mapping study. Pediatr Blood Cancer 2014;61:S152.
Presentations linked to BRIGHTLIGHT outside the programme objectives
Fern LA, Taylor RM, Gibson F, Millington H, Whelan J. ‘It’s All in the Name’, Branding a Longitudinal Cohort Study with Young People: BRIGHTLIGHT (Poster Presentation). Liverpool: NCIN Annual Conference; 4–7 November 2012.
Fern LA, Taylor RM, Gibson F, Millington H, Whelan J. ‘It’s All in the Name’, Branding a Longitudinal Cohort Study with Young People: BRIGHTLIGHT (Poster Presentation). Nottingham: TYAC Spring Education Day; 20 January 2012.
Koo M, Lyratzopoulos G, Herbert A, Taylor R, Barber J, Gibson F, et al. Self-Reported Presenting Symptoms and Timeliness of Help-Seeking Among Teenagers and Young Adults with Cancer: Findings from the BRIGHTLIGHT Cohort. 51st Lyon: Congress of the International Society of Paediatric Oncology (SIOP); October 2019. Pediatr Blood Cancer 66:V105 SIOP19-1019.
Koo M, Lyratzopolous G, Taylor R, Herbet A, Barber J, Gibson F, et al. Presenting Cancer Symptoms and Diagnostic Timeliness Among Teenagers and Young Adults: Findings from the BRIGHTLIGHT Cohort (Poster). Sydney, NSW: 3rd Global AYA Cancer Congress; 4–6 December 2018.
Lea S, Taylor R, Gibson F. Starting Out on a Clinical-academic Pathway: The Experience of a Newly Qualified Nurse. Abstract G227 (Poster Presentation). Birmingham: Royal College of Paediatrics and Child Health Annual Conference; 2015.
Lea S, Taylor R, Gibson F. G227(P) Starting out on a clinical academic pathway: the experience of a newly-qualified nurse. Arch Dis Childhood 100(Suppl. 3):A96.
Martins A, Taylor R, Lobel B, McCann B, Soanes L, Whelan J, Fern L. ‘Does that Mean that Cancer Patients Can’t Have Sex?’ – Adolescent and Young Adults’ Support and Information Preferences (Poster) . Sydney, NSW: 3rd Global AYA Cancer Congress; 4–6 December 2018.
Ngwenya N, Kenten C, Jones L, Gibson F, Pearce S, Stirling C, et al. ‘Hospice Scares the Life Out of Me’: Breaking Down Barriers to Communication with Young Adults with Terminal Cancer (Oral Presentation). Montreal: 21st International Congress on Palliative Care; 18–21 October 2016.
Solanki A, Taylor R, Aslam N, Gibson F, Whelan J, Fern L. The Challenges and Reality of Patient and Public Involvement (PPI) with Teenagers and Young Adults (Poster Presentation). Nottingham: 2015 RCN International Research Society Conference; 21st April 2015.
Taylor RM, Lobel B, Thompson K, Whelan JS, Fern LA. Working with Young People to Creatively Disseminate a National PROMS Study – Developing ‘There is a Light: BRIGHTLIGHT’. Leeds: PROMS Annual UK Research Conference; 13 June 2019 (won the award for Innovation in PPI).
Taylor RM. Measuring Quality of Life in Young People with Cancer (Invited Presentation). Birmingham: TYAC Annual Conference; 11–12 September 2018.
Taylor RM, Lobel B, Thompson K, Croasdale M, Onashile A, McInally W, et al. There is a Light: BRIGHTLIGHT – Working with Young People to Create Impactful Dissemination (Oral). Birmingham: TYAC Annual Conference; 11–12 September 2018.
Taylor RM, Martins A, Lea S, Whelan JS, Fern LA. Participatory Research: Using Board Games to Guide Secondary Analysis of Big Data (Oral Presentation). Oxford: 2017 RCN International Research Society Conference; 6 April 2017.
Taylor R, Martins A, Lea S, Whelan J, Fern L. 003 PP: collaborating with young people to set the agenda for secondary analysis of the BRIGHTLIGHT dataset. BMJ Open 2017;7(Suppl. 2). https://doi.org/10.1136/bmjopen-2017-016492.21
Taylor RM on behalf of the BRIGHTLIGHT Team. What is BRIGHTLIGHT? (Oral Presentation). Liverpool: NCRI Annual Conference; 5–8 November 2017.
Taylor RM, Whelan JS. BRIGHTLIGHT: AYA programmes Adding Value (Invited Speakers). Atlanta, GA: 2nd Global AYA Cancer Congress; 5–7 December 2017.
Taylor RM, Martins A, Lea S, Whelan JS, Fern LA. Let’s Play Twister! Novel Methods to Facilitate Understanding of Complex Research Methods and Generate Secondary Research Hypotheses with Young People. Atlanta, GA: 2nd Global AYA Cancer Congress; 5–7 December 2017.
Taylor RM, Whelan J, Solanki A, Aslam N, Fern LA. ‘Okay to Ask’: Young People’s Views About Access to and Participation in Research (Oral Presentation). Sydney, NSW: Inaugural International Adolescent and Young Adult Oncology Congress; 3rd December 2015.
Taylor RM [symposium lead]. Teenagers, Young Adults and Access to Research: Perspectives from Policy, Participants and Researchers (Symposium Presentation). Glasgow: 2014 RCN International Research Society Conference; 4 April 2014.
Taylor RM [symposium lead]. BRIGHTLIGHT: A Lesson in Collaboration (Symposium Presentation). Glasgow: 2014 RCN International Research Society Conference; 3rd April 2014.
Taylor RM, Whelan J, Solanki A, Aslam N, Fern LA. Empowering Young People to Participate in Research: Young People’s Views About Research Access and Participation (Poster Presentation). Birmingham: NCIN Annual Conference; 9 June 2014 (received the patient choice award).
Taylor RM, Whelan J, Solanki A, Aslam N, Fern LA. ‘Okay to Ask’: Young People’s Views About Access to and Participation in Research (Poster Presentation). Liverpool: NCRI Cancer Conference; 4 November 2014.
Taylor RM, Fern L, O’Hara C, Solanki A, Whelan J on behalf of the BRIGHTLIGHT Team. A Multi-faceted Approach to Collaboration: The BRIGHTLIGHT Experience (Oral Presentation). London: Accepted Centre for Nursing and Midwifery Led Research: Research in Clinical Practice Conference 2013; 18 February 2013.
Taylor RM on behalf of the BRIGHTLIGHT Team. BRIGHTLIGHT: Do Specialist Services for TYA With Cancer Add Value? (Invited Presentation). Birmingham: TYA with Haematological Malignancy Conference; 28 March 2013.
Taylor RM, Whelan J, Solanki A, Aslam N, Fern L. The 7TH ‘D’: Don’t Decide For Me. (Poster Presentation). Leeds: TYAC Winter Education Day; 28 November 2013.
Whelan J, Pearce S, Jones L, Stirling C, Hough R, Riley V, et al. An introduction to BRIGHTLIGHT on end of life care for young adults: what do young adults with cancer and their families need and how can it best be delivered? BMJ Support Palliat Care 2013;3:133–4. https://doi.org/10.1136/bmjspcare-2013-000453b.25
Whelan J, Taylor R, Fern L. BRIGHTLIGHT: The 2012 TYA Cancer Cohort Study (Invited Presentation). Exeter, University of Exeter: South West TYA Conference; September 2012.
Data-sharing statement
Study 3 was a qualitative study and, therefore, the data generated is not suitable for sharing beyond that contained within the report. Owing to regulatory approvals and data held under licence, there are no data from study 2, 5 and 6 that can be shared. Data for studies 1 and 4 are available from the corresponding authors of the publications. Further information about data sharing can be obtained from the corresponding author of this report.
Patient Data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health and Social Care.
References
- Ministry of Health . The Welfare of Children in Hospital, Platt Report 1959.
- Royal College of Physicians . On the Margins of Medical Care. Why Young Adults and Adolescents Need Better Healthcare 2015.
- Stevens MC. The ‘Lost Tribe’ and the need for a promised land: the challenge of cancer in teenagers and young adults. Eur J Cancer 2006;42:280-1. https://doi.org/10.1016/j.ejca.2005.11.007.
- Birch JM, Pang D, Alston RD, Rowan S, Geraci M, Moran A, et al. Survival from cancer in teenagers and young adults in England, 1979–2003. Br J Cancer 2008;99:830-5. https://doi.org/10.1038/sj.bjc.6604460.
- Whelan J, Fern L, Kelly D, Gibson F. Cancer Care for Adolescents and Young Adults. Oxford: Blackwell; 2008.
- Pollock BH. Where adolescents and young adults with cancer receive their care: does it matter?. J Clin Oncol 2007;25:4522-3. https://doi.org/10.1200/JCO.2007.12.1715.
- Ferrari A, Montello M, Budd T, Bleyer A. The challenges of clinical trials for adolescents and young adults with cancer. Pediatr Blood Cancer 2008;50:1101-4. https://doi.org/10.1002/pbc.21459.
- Albritton KH, Eden T. Access to care. Pediatr Blood Cancer 2008;50:1094-8. https://doi.org/10.1002/pbc.21461.
- Fern L, Davies S, Eden T, Feltbower R, Grant R, Hawkins M, et al. Rates of inclusion of teenagers and young adults in England into National Cancer Research Network clinical trials: report from the National Cancer Research Institute (NCRI) Teenage and Young Adult Clinical Studies Development Group. Br J Cancer 2008;99:1967-74. https://doi.org/10.1038/sj.bjc.6604751.
- Butow P, Palmer S, Pai A, Goodenough B, Luckett T, King M. Review of adherence-related issues in adolescents and young adults with cancer. J Clin Oncol 2010;28:4800-9. https://doi.org/10.1200/JCO.2009.22.2802.
- Whelan J. Where should teenagers with cancer be treated?. Eur J Cancer 2003;39:2573-8. https://doi.org/10.1016/j.ejca.2003.09.014.
- Cassano J, Nagel K, O’Mara L. Talking with others who ‘just know’: perceptions of adolescents with cancer who participate in a teen group. J Pediatr Oncol Nurs 2008;25:193-9. https://doi.org/10.1177/1043454208319972.
- Hedström M, Skolin I, von Essen L. Distressing and positive experiences and important aspects of care for adolescents treated for cancer. Adolescent and nurse perceptions. Eur J Oncol Nurs 2004;8:6-17. https://doi.org/10.1016/j.ejon.2003.09.001.
- Barr RD, Ferrari A, Ries L, Whelan J, Bleyer WA. Cancer in adolescents and young adults: a narrative review of the current status and a view of the future. JAMA Pediatr 2016;170:495-501. https://doi.org/10.1001/jamapediatrics.2015.4689.
- Bleyer A. The adolescent and young adult gap in cancer care and outcome. Curr Probl In Pediatr Adolesc Health Care 2005;35:182-217. https://doi.org/10.1016/j.cppeds.2005.02.001.
- Fernandez C, Fraser GA, Freeman C, Grunfeld E, Gupta A, Mery LS, et al. Principles and recommendations for the provision of healthcare in Canada to adolescent and young adult-aged cancer patients and survivors. J Adolesc Young Adult Oncol 2011;1:53-9. https://doi.org/10.1089/jayao.2010.0008.
- Osborn M, Little C, Bowering S, Orme L. Youth Cancer Services in Australia: development and implementation. International perspectives on AYAO, part 3. J Adolesc Young Adult Oncol 2013;2:118-24. https://doi.org/10.1089/jayao.2012.0032.
- Fardell JE, Patterson P, Wakefield CE, Signorelli C, Cohn RJ, Anazodo A, et al. A narrative review of models of care for adolescents and young adults with cancer: barriers and recommendations. J Adolesc Young Adult Oncol 2018;7:148-52. https://doi.org/10.1089/jayao.2017.0100.
- Rae CS, Pole JD, Gupta S, Digout C, Szwajcer D, Flanders A, et al. Development of system performance indicators for adolescent and young adult cancer care and control in Canada. Value Health 2020;23:74-88. https://doi.org/10.1016/j.jval.2019.08.004.
- Whiteson M. The Teenage Cancer Trust – advocating a model for teenage cancer services. Eur J Cancer 2003;39:2688-93. https://doi.org/10.1016/j.ejca.2003.08.023.
- Carr R, Whiteson M, Edwards M, Morgan S. Young adult cancer services in the UK: the journey to a national network. Clin Med 2013;13:258-62. https://doi.org/10.7861/clinmedicine.13-3-258.
- Macmillan Cancer Support . The Role of Cancer Networks in the New NHS 2012.
- National Institute for Health and Care Excellence . Guidance on Cancer Services: Improving Outcomes in Children and Young People With Cancer 2005. www.nice.org.uk/guidance/csg7/resources/improving-outcomes-in-children-and-young-people-with-cancer-update-773378893 (accessed 9 September 2016).
- National Institute for Health and Care Excellence . Improving Outcomes in Children and Young People With Cancer: The Evidence Review 2005.
- Kennedy I. Getting it Right for Children and Young People Overcoming Cultural Barriers in the NHS so as to Meet their Needs. London: Department of Health and Social Care; 2010.
- NHS England and the Department of Health and Social Care . You’re Welcome Pilot 2017: Refreshed Standards for Piloting 2017.
- Dean L, Black S. Exploring the experiences of young people nursed on adult wards. Br J Nurs 2015;24:229-36. https://doi.org/10.12968/bjon.2015.24.4.229.
- Jones LJ, Pini SA, Morgan SJ, Birk GK, Stark DP. How do teenagers and young adults with cancer experience their care? A European survey. J Adolesc Young Adult Oncol 2017;6:102-10. https://doi.org/10.1089/jayao.2016.0011.
- Lea S. The Culture of Teenage and Young Adult Cancer Care in England: A Multiple-Case Study Across Four Networks of Care 2019. https://openresearch.lsbu.ac.uk/researcher/80898/mrs-sarah-lea (accessed 1 June 2021).
- Kelly D, Pearce S, Mulhall A. ‘Being in the same boat’: ethnographic insights into an adolescent cancer unit. Int J Nurs Stud 2004;41:847-57. https://doi.org/10.1016/j.ijnurstu.2004.03.011.
- Steinbeck K, Brodie L. Bringing in the voices: a transition forum for young people with chronic disability. Neonatal Paediatr Child Health Nurs 2006;9:22-6.
- McDonagh JE, Viner RM. Lost in transition? Between paediatric and adult services. BMJ 2006;332:435-6. https://doi.org/10.1136/bmj.332.7539.435.
- NHS England . NHS Standard Contract for Cancer: Teenagers and Young Adults 2013.
- O’Hara C, Khan M, McCabe M, Francis L, Moran T. Notifications of Teenagers and Young Adults with Cancer to a Principal Treatment Centre 2009–2010. National Cancer Intelligence Network; 2013.
- National Cancer Peer Review Programme . National Peer Review Report: Teenage and Young Adult Cancer Services Report 2012 2013 2013.
- National Cancer Action Team . Manual for Cancer Services: Teenagers and Young Adult Measures 2011.
- Fern LA, Taylor RM, Whelan J, Pearce S, Grew T, Brooman K, et al. The art of age-appropriate care: reflecting on a conceptual model of the cancer experience for teenagers and young adults. Cancer Nurs 2013;36:E27-38. https://doi.org/10.1097/NCC.0b013e318288d3ce.
- Gibson F, Fern L, Whelan J, Pearce S, Lewis IJ, Hobin D, et al. A scoping exercise of favourable characteristics of professionals working in teenage and young adult cancer care: ‘thinking outside of the box’. Eur J Cancer Care 2012;21:330-9. https://doi.org/10.1111/j.1365-2354.2011.01322.x.
- Taylor RM, Fern L, Whelan J, Pearce S, Grew T, Millington H, et al. ‘Your Place or Mine?’ Priorities for a specialist teenage and young adult (TYA) cancer unit: disparity between TYA and professional perceptions. J Adolesc Young Adult Oncol 2011;1:145-51. https://doi.org/10.1089/jayao.2011.0037.
- Taylor RM, Pearce S, Gibson F, Fern L, Whelan J. Developing a conceptual model of teenage and young adult experiences of cancer through meta-synthesis. Int J Nurs Stud 2013;50:832-46. https://doi.org/10.1016/j.ijnurstu.2012.09.011.
- Vindrola-Padros C, Taylor RM, Lea S, Hooker L, Pearce S, Whelan J, et al. Mapping adolescent cancer services: how do young people, their families, and staff describe specialized cancer care in England?. Cancer Nurs 2016;39:358-66. https://doi.org/10.1097/NCC.0000000000000315.
- Taylor RM, Whelan JS, Gibson F, Morgan S, Fern LA. BRIGHTLIGHT Team . Involving young people in BRIGHTLIGHT from study inception to secondary data analysis: insights from 10 years of user involvement. Res Involv Engagem 2018;4. https://doi.org/10.1186/s40900-018-0135-x.
- Teenage Cancer Trust . FYSOT Programme 2021. www.teenagecancertrust.org/find-your-sense-tumour-programme (accessed September 2021).
- Taylor RM, Mohain J, Gibson F, Solanki A, Whelan J, Fern LA. Novel participatory methods of involving patients in research: naming and branding a longitudinal cohort study, BRIGHTLIGHT. BMC Med Res Methodol 2015;15. https://doi.org/10.1186/s12874-015-0014-1.
- Taylor RM, Solanki A, Aslam N, Whelan JS, Fern LA. A participatory study of teenagers and young adults views on access and participation in cancer research. Eur J Oncol Nurs 2016;20:156-64. https://doi.org/10.1016/j.ejon.2015.07.007.
- BRIGHTLIGHT . User Involvement. 2021. www.brightlightstudy.com/user-involvement/ (accessed 1 June 2021).
- Taylor RM, Fern LA, Solanki A, Hooker L, Carluccio A, Pye J, et al. Development and validation of the BRIGHTLIGHT Survey, a patient-reported experience measure for young people with cancer. Health Qual Life Outcomes 2015;13. https://doi.org/10.1186/s12955-015-0312-7.
- Guillory J, Kim A, Murphy J, Bradfield B, Nonnemaker J, Hsieh Y. Comparing Twitter and online panels for survey recruitment of e-cigarette users and smokers. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.6326.
- Keaver L, McGough A, Du M, Chang W, Chomitz V, Allen JD, et al. Potential of using Twitter to recruit cancer survivors and their willingness to participate in nutrition research and web-based interventions: a cross-sectional study. JMIR Cancer 2019;5. https://doi.org/10.2196/cancer.7850.
- Wasilewski MB, Stinson JN, Webster F, Cameron JI. Using Twitter to recruit participants for health research: an example from a caregiving study. Health Inform J 2019;25:1485-97. https://doi.org/10.1177/1460458218775158.
- Taylor RM, Aslam N, Lea S, Whelan JS, Fern LA. Optimizing a retention strategy with young people for BRIGHTLIGHT, a longitudinal cohort study examining the value of specialist cancer care for young people. J Adolesc Young Adult Oncol 2017;6:459-69. https://doi.org/10.1089/jayao.2016.0085.
- BRIGHTLIGHT . The YAP Go To FYSOT. 2014. www.brightlightstudy.com/event/november-2014-brightlight-update-at-fysot/ (accessed 1 June 2021).
- Contact . CYC: There Is a Light n.d. https://contactmcr.com/development/there-is-a-light-brightlight/ (accessed 1 June 2021).
- The List . Chrysalis Festival: There Is a Light: Brightlight & How to Save the World. Ish 2017. www.list.co.uk/article/98012-chrysalis-festival-there-is-a-light-brightlight-and-how-to-save-the-world-ish/ (accessed 1 June 2021).
- Vimeo . Finding the Light. 2017. https://vimeo.com/238045094 (accessed 1 June 2021).
- Lea S, Martins A, Morgan S, Cargill J, Taylor RM, Fern LA. Online information and support needs of young people with cancer: a participatory action research study. Adolesc Health Med Ther 2018;9:121-35. https://doi.org/10.2147/AHMT.S173115.
- Lea S, Martins A, Bassett M, Cable M, Doig G, Fern LA, et al. Issues experienced and support provided to adolescents and young adults at the end of active treatment for cancer: a rapid review of the literature. Eur J Cancer Care 2018;27. https://doi.org/10.1111/ecc.12972.
- Martins A, Whelan JS, Bennister L, Fern LA, Gerrand C, Onasanya M, et al. Qualitative study exploring patients experiences of being diagnosed and living with primary bone cancer in the UK. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-028693.
- Storey L, Fern LA, Martins A, Wells M, Bennister L, Gerrand C, et al. A critical review of the impact of sarcoma on psychosocial wellbeing. Sarcoma 2019;2019. https://doi.org/10.1155/2019/9730867.
- Martins A, Taylor RM, Lobel B, McCann B, Soanes L, Fern LA. Sex, body image and relationships: a BRIGHTLIGHT workshop on information and support needs of adolescents and young adults. J Adolesc Young Adult Oncol 2018;7:572-8. https://doi.org/10.1089/jayao.2018.0025.
- Baker J, Lovell K, Harris N. How expert are the experts? An exploration of the concept of ‘expert’ within Delphi panel techniques. Nurse Res 2006;14:59-70. https://doi.org/10.7748/nr2006.10.14.1.59.c6010.
- Taylor RM, Feltbower RG, Aslam N, Raine R, Whelan JS, Gibson F. Modified international e-Delphi survey to define healthcare professional competencies for working with teenagers and young adults with cancer. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011361.
- Taylor RM, Fern LA, Barber JA, Alvarez-Galvez J, Feltbower R, Morris S, et al. Description of the BRIGHTLIGHT cohort: the evaluation of teenagers and young adult cancer services in England. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-027797.
- Lea S, Taylor RM, Martins A, Fern LA, Whelan JS, Gibson F. Conceptualising age-appropriate care for teenagers and young adults with cancer: a qualitative mixed methods study. Adolesc Health Med Therapeutics 2018;9:149-66. https://doi.org/10.2147/AHMT.S182176.
- Lea S, Gibson F, Taylor RM. ‘Holistic competence’: how is it developed and shared by nurses caring for adolescents and young adults with cancer? [published online ahead of print March 10 2021]. J Adolesc Young Adult Oncol 2021. https://doi.org/10.1089/jayao.2020.0120.
- Kenten C, Martins A, Fern LA, Gibson F, Lea S, Ngwenya N, et al. Qualitative study to understand the barriers to recruiting young people with cancer to BRIGHTLIGHT: a national cohort study in England. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-018291.
- Taylor RM, Fern LA, Aslam N, Whelan JS. Direct access to potential research participants for a cohort study using a confidentiality waiver included in UK National Health Service legal statutes. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011847.
- Taylor RM, Fern LA, Barber J, Alvarez-Galvez J, Feltbower R, Lea S, et al. Longitudinal cohort study of the impact of specialist cancer services for teenagers and young adults on quality of life: outcomes from the BRIGHTLIGHT study. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-038471.
- Fern LA, Taylor RM, Barber J, Alvarez-Galvez J, Feltbower R, Lea S, et al. Processes of care and survival associated with treatment in specialist teenage and young adult cancer centres: results from the BRIGHTLIGHT cohort study. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-044854.
- Kreuter F, Presser S, Tourangeau R. Social desirability bias in CATI, IVR, and web surveys: the effects of mode and question sensitivity. Public Opinion Q 2008;72:847-65. https://doi.org/10.1093/poq/nfn063.
- Deshields TL, Rihanek A, Potter P, Zhang Q, Kuhrik M, Kuhrik N, et al. Psychosocial aspects of caregiving: perceptions of cancer patients and family caregivers. Support Care Cancer 2012;20:349-56. https://doi.org/10.1007/s00520-011-1092-1.
- Martins A, Alvarez-Galvez J, Fern LA, Vindrola C, Gibson F, Whelan JS, et al. The BRIGHTLIGHT national survey of the impact of specialist teenage and young adult cancer care on caregivers’ information and support needs. Cancer Nurs 2021;44:235-43. https://doi.org/10.1097/NCC.0000000000000771.
- Aldiss S, Fern LA, Phillips RS, Callaghan A, Dyker K, Gravestock H, et al. Research priorities for young people with cancer: a UK priority setting partnership with the James Lind Alliance. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-028119.
- Herbert A, Lyratzopoulos G, Whelan J, Taylor RM, Barber J, Gibson F, et al. Diagnostic timeliness in adolescents and young adults with cancer: a cross-sectional analysis of the BRIGHTLIGHT cohort. Lancet Child Adolesc Health 2018;2:180-90. https://doi.org/10.1016/S2352-4642(18)30004-X.
- Koo MM, Lyratzopoulos G, Abel GA, Taylor RM, Barber J, Gibson F, et al. Association of self-reported presenting symptoms with timeliness of help-seeking among adolescents and young adults with cancer in the BRIGHTLIGHT study. JAMA Open 2020;3. https://doi.org/10.1001/jamanetworkopen.2020.15437.
- Fern LA, Lewandowski J, Coxon KM, Whelan J. National Cancer Research Institute Teenage and Young Adult Clinical Studies Group, UK . Available, accessible, aware, appropriate and acceptable: a strategy for improving participation of teenagers and young adults in cancer clinical trials. Lancet Oncol 2014;15:e341-50. https://doi.org/10.1016/S1470-2045(14)70113-5.
- Fern LA, Taylor RM. Enhancing accrual to clinical trials of adolescents and young adults with cancer. Pediatr Blood Cancer 2018;65. https://doi.org/10.1002/pbc.27233.
- National Health Service . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 1 October 2021).
- How is cancer care best provided to patients in English prisons? Assessing the disease burden in the prison population, experiences of diagnosis, treatment and support, and of receiving and providing cancer care. Health Serv Del Res 2021.
- Kosir U, Bowes L, Taylor RM, Gerrand C, Windsor R, Onasanya M, et al. Psychological adaptation and recovery in youth with sarcoma: a qualitative study with practical implications for clinical care and research. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-038799.
- Martins A, Bennister L, Fern LA, Gerrand C, Onasanya M, Storey L, et al. Development of a patient-reported experience questionnaire for patients with sarcoma: the Sarcoma Assessment Measure (SAM). Qual Life Res 2020;29:2287-97. https://doi.org/10.1007/s11136-020-02481-x.
- Aldiss S, Baggott C, Gibson F, Mobbs S, Taylor RM. A critical review of the use of technology to provide psychosocial support for children and young people with long-term conditions. J Pediatr Nurs 2015;30:87-101. https://doi.org/10.1016/j.pedn.2014.09.014.
- Walker E, Martins A, Aldiss S, Gibson F, Taylor RM. Psychosocial Interventions for adolescents and young adults diagnosed with cancer during adolescence: a critical review. J Adolesc Young Adult Oncol 2016;5:310-21. https://doi.org/10.1089/jayao.2016.0025.
- Lea S, Martins A, Morgan S, Cargill J, Taylor RM, Fern LA. Health care professional perceptions of online information and support for young people with cancer in the United Kingdom. Adolesc Health Med Ther 2019;10:103-16. https://doi.org/10.2147/AHMT.S211142.
- Lea S, Martins A, Bassett M, Cable M, Doig G, Fern LA, et al. Exploring young people’s experience of ending active cancer treatment: when the ‘little cancer treatment bubble’ pops. Cancer Nurs 2021;44:288-94. https://doi.org/10.1097/NCC.0000000000000798.
- Lea S, Martins A, Fern LA, Bassett M, Cable M, Doig G, et al. The support and information needs of adolescents and young adults with cancer when active treatment ends. BMC Cancer 2020;20. https://doi.org/10.1186/s12885-020-07197-2.
- Kenten C, Ngwenya N, Gibson F, Flatley M, Jones L, Pearce S, et al. Understanding care when cure is not likely for young adults who face cancer: a realist analysis of data from patients, families and healthcare professionals. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-024397.
- Ngwenya N, Kenten C, Jones L, Gibson F, Pearce S, Flatley M, et al. Experiences and preferences for end-of-life care for young adults with cancer and their informal carers: a narrative synthesis. J Adolesc Young Adult Oncol 2017;6:200-12. https://doi.org/10.1089/jayao.2016.0055.
- Taylor RM, Lobel B, Thompson K, Onshila A, Croasdale M, Whelan JS, et al. BRIGHTLIGHT researchers as ‘dramaturgs’: creating There is a Light from complex research data. Res Involve Engage 2020;6. https://doi.org/10.1186/s40900-020-00222-5.
- Coventry University . Teenager/Young/Adults/Cancer/Care. 2021. www.coventry.ac.uk/study-at-coventry/faculties-and-schools/health-and-life-sciences/nursing-midwifery-and-health/teenager-young-adults-cancer-care/ (accessed 1 June 2021).
- Smith S, Mooney S, Cable M, Taylor RM. The Blueprint of Care for Teenagers and Young Adults with Cancer. London: Teenage Cancer Trust; 2016.
- Teenage Cancer Trust endorsed by The Royal College of Nursing . Competencies: Caring for Teenagers and Young Adults With Cancer: A Competence and Career Framework for Nursing. 2014. www.teenagecancertrust.org/sites/default/files/Nursing-framework.pdf (accessed 1 June 2021).
- Vindrola-Padros C. Rapid Ethnographies: A Practical Guide. Cambridge: University of Cambridge Press; 2020.
- De Savigny D, Blanchet K, Adam T. Applied Systems Thinking for Health Systems Research: A Methodological Handbook. London: Open University Press; 2017.
- Teenage Cancer Trust . Annual Report And Accounts 2019 2019. www.teenagecancertrust.org/sites/default/files/Annual%20Report%202019-web.pdf (accessed 1 June 2021).
- World Health Organisation . International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) Version for 2010 2010. https://icd.who.int/browse10/2010/en#!C00-C97 (accessed 1 October 2021).
- Greenberg M, Klassen A, Gafni A, McBride ML, Albritton K. Outcomes and metrics: measuring the impact of a comprehensive adolescent and young adult cancer program. Cancer 2011;117:2342-50. https://doi.org/10.1002/cncr.26040.
- Sironi G, Barr RD, Ferrari A. Models of care-there is more than one way to deliver. Cancer J 2018;24:315-20. https://doi.org/10.1097/PPO.0000000000000338.
- Zebrack B, Mathews-Bradshaw B, Siegel S. LIVESTRONG Young Adult Alliance . Quality cancer care for adolescents and young adults: a position statement. J Clin Oncol 2010;28:4862-7. https://doi.org/10.1200/JCO.2010.30.5417.
- Department of Health . Reference Costs 2015–16 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/577083/Reference_Costs_2015-16.pdf (accessed 1 October 2021).
- Department of Health and Social Care . NHS Patient, Visitor and Staff Car Parking Management 2021. https://www.gov.uk/government/publications/nhs-patient-visitor-and-staff-car-parking-principles (accessed 1 October 2021).
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
Appendix 1 Example of the structure of a patient and public involvement workshop
B RIGHTLIGHT
User involvement workshop 5 – Hypotheses Generating
Friday 18 September 2015
Venue:
Time 11–4pm (must be finished at 4pm)
Objective of workshop
-
To generate hypotheses to underpin secondary analysis from YP perspective.
-
Generate ideas about the content of the website.
-
Generate new ideas for social media use, newsletter content, retention card content.
Outputs
-
Output from hypotheses generating task/ideas for secondary analysis.
-
Journal article/editorial on young person’s input into secondary analysis, hypotheses generating.
-
Photos of the day.
ATTENDEES
BRIGHTLIGHT: Lorna Fern, Rachel Taylor, Anita Solanki, Sarah Lea, Ana Martins.
Delegates: 9 young people (collect demographic and consent forms).
FORMAT OF DAY
Set up projector or TV to play loop of videos and photos of previous workshops.
Attendees arrive and settle 10.30–11.00 in the café/canteen area
Welcome (11.00–11.15).
Rules: Lorna to do.
Anonymity.
Confidentiality.
Recording, photos and videos.
Fire alarms, toilets.
Down time.
Activity 1: ice breaker activity (11.15–11.45)
Using pipe cleaners ask young people to create object representing how they felt on their journey to workshop/current, followed by introductions of themselves starting with older members first, e.g. how long they’ve been involved, what kind of activities they have participated in.
Activity 2: presentation (11.45–12.00)
Introduce BRIGHTLIGHTs main aims (for those who have not attended before).
Update YAP on BRIGHTLIGHT progress made since last workshop.
Introduce objectives and purpose of the day followed by a programme of the day’s activities.
Ensure young people have a clear understanding of their purpose of the task/day.
Activity 3: website/social media/newsletter exercise (12.00–13.00)
New website look
AS to lead: Show new web.
Ask to think if they like, remind them of their ideas from last time – are these represented on new website?
Load existing page to show new members of how the page currently appears. Ways to improve the general look of page.
Break for lunch 13.00–13.45
13.45–14.00 Lorna will explain secondary analysis and hypotheses generating.
Activity 4: BRIGHTLIGHT Twister (14.00–15.45)
Introduce task using examples with the help of the team to demonstrate the Twister game.
SL Set up Dictaphone to record discussion.
BRIGHTLIGHT twister game (see separate instructions).
This will be reported on flip charts by RT.
LF: oversee.
RT: list combinations from spinner board.
Facilitators: AS/AM/SL (may not all be required so go upstairs for coffee).
Feedback and group discussion
Ask YP to regroup and discuss collectively the combinations from the Twister game.
Facilitator prompts.
Questions to ask/think about:
-
Why are the two related?
-
Can anyone give examples using their own experience?
Using the final list young people will be given three dots and asked to individually choose the three they think are the most important. This list will be presented to young people, who will be invited to work with the BRIGHTLIGHT team on the analysis and write up of these data.
Goodbyes 15.45–16.00.
If there’s time before lunch or at the end of the day
Newsletter
Content ideas.
What’s missing?
How often?
Post workshop meeting.
Questions to ask/think about:
-
What kind of updates about the study do you want to know?
-
How frequently should we upload study information?
-
What else would you like to see on the Facebook page?
Young people can compare to other Facebook groups they are part of to suggest ways of improving BRIGHTLIGHT.
Appendix 2 Report of workstream 2 (study 4) results
Objectives
To undertake a longitudinal cohort study of young people with cancer to:
-
2.1. relate the level of cancer care that teenagers and young adults received to QoL, satisfaction with care, clinical processes and clinical outcomes (overall, by age group and by tumour type)
-
2.2. examine young people’s experience of cancer care through a longitudinal descriptive survey.
Study design
Workstream 2 was an embedded longitudinal cohort study, obtaining data from young people through a bespoke survey. 47 The survey was administered at five time points during the first 3 years after diagnosis (i.e. 6, 12, 18, 24 and 36 months). A scale was developed (Quantifying specialist care) using HES inpatient data to measure episodes of care in different NHS trusts and was used to assign young people into groups depending on how much inpatient care they had delivered in a TYA-PTC in the first 12 months after diagnosis: all care delivered in a TYA-PTC (ALL-TYA-PTC), no care in a TYA-PTC (NONE-TYA-PTC) or some care delivered in a TYA-PTC with additional care in a children’s or adult cancer unit (SOME-TYA-PTC).
Participants and setting
BRIGHTLIGHT opened to recruitment between October 2012 and April 2015 in 109 English hospitals, of which 97 recruited at least one young person. Eligibility was defined as being aged 13–24 years, newly diagnosed with cancer [International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes C00-C9796] in an English hospital and recruited within 4 months of diagnosis. There was no eligibility exclusion for a language or sensory impairment affecting communication. The following groups were excluded: those serving a custodial sentence, those not anticipated to be alive at the first point of data collection (6 months after diagnosis), those with recurrence of a previous cancer, or those who were incapable of completing a survey. Details of the recruitment process are reported elsewhere. 63,66
Data collection
Data were collected from three sources: young people’s self-report, patient clinical records, and NHS and Public Health England databases. Details of data sources and the content of the BRIGHTLIGHT survey are reported elsewhere. 47,63
Objective 2.1: quality of life, clinical processes and outcomes of care
These are reported in full (see Identifying the outcomes associated with specialist teenage and young adult cancer care).
Objective 2.2: experience of care
Methods
Data presented for objective 2.2 have been chosen to reflect young people’s experience of the delivery of care (Table 2). Metrics have been proposed that are indicative of good TYA cancer care. 17–19,97–99 Metrics reflecting good TYA care at service and clinical record level are reported for objective 2.1 (e.g. considered for a clinical trial, discussed in a MDT), but a number of these service-level metrics were also reported through patient self-report, including fertility, access to members of the MDT and access to clinical trials. Questions were also included that related to the NICE guidance (choice of place of care) and reflecting age-appropriate care (involvement in treatment decisions, communication and co-ordination of care). 39,64 Some questions were asked at every wave of data collection and some were only asked at wave 1.
| Aspect of care delivery | Number of questions | Example response format | Time points |
|---|---|---|---|
| Choice of place of care | 3 | Yes/no | Wave 1 |
| Access to members of the MDT | 1 | Yes/no | All waves |
| Involvement in treatment decisions | 1 | 5-point scale (‘Yes definitely’ to ‘only one treatment available’) | Wave 1 |
| Fertility | 4 | Yes/no, descriptive outcome | Wave 1 (revisited at wave 5) |
| Participation in clinical trials | 3 | Yes/no, descriptive outcome | All waves |
| Communication with the health-care team | 16 | 5-point scale (‘Always’ to ‘never’) | Wave 1 |
| Coordination of care | 1 | 5-point scale (‘Very well’ to ‘very poorly’) | Wave 1 |
Results
Fewer young people who received ALL-TYA-PTC care were given the choice about where they could receive treatment and care, and fewer in the SOME-TYA-PTC group made a decision. The choice made by most of those in the NONE-TYA-PTC group was for care in the closest hospital, whereas more young people in the SOME-TYA-PTC group chose a hospital further away (Table 3). Irrespective of where young people were treated, the majority reported that health-care professionals had prepared them for treatment-related side effects (NONE-TYA-PTC, n = 256, 93%; SOME-TYA-PTC, n = 300, 96%; ALL-TYA-PTC, n = 187, 97%). Similarly, few young people reported that they would have liked to be more involved in their treatment decisions (NONE-TYA-PTC, n = 15, 5%; SOME-TYA-PTC, n = 15, 5%; ALL-TYA-PTC, n = 5, 3%). Young people in the NONE-TYA-PTC group had less access to members of the MDT representing specialist TYA services and supportive care than young people in the other two groups.
| Question | Level of TYA care at 12 months after diagnosis | ||
|---|---|---|---|
| NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | |
| Were you given a choice about where you could receive treatment and care, even if you decided not to make a choice? (N = 505),a n (%) | |||
| No | 100 (45) | 77 (47) | 72 (60) |
| Yes | 121 (55) | 87 (53) | 48 (40) |
| And did you decide to choose where to receive your treatment and care? (N = 255),b n (%) | |||
| No | 4 (3) | 11 (13) | 2 (4) |
| Yes | 116 (97) | 76 (87) | 46 (96) |
| Did you choose the closest hospital offered for your treatment and care, or a hospital further away? (N = 239), n (%) | |||
| Closest hospital | 102 (87) | 28 (37) | 26 (57) |
| A hospital further away | 15 (13) | 48 (63) | 20 (43) |
There were no differences in the number of young people who had spoken to someone about banking sperm or freezing eggs or embryos according to level of care; however, this occurred more often in males than females. Most young men were given the opportunity to bank sperm and mostly this was successful. More young women in the ALL-TYA-PTC group than the other two groups were given the opportunity to freeze eggs/embryos and took this opportunity (Table 4). Most young people felt the way their treatment team had handled the experience of fertility treatment was excellent/good (NONE-TYA-PTC, n = 93, 85%; SOME-TYA-PTC, n = 143, 88%; ALL-TYA-PTC, n = 91, 83%). Other reasons for deciding not to bank sperm or freeze eggs/embryos included receiving treatment that did not affect fertility, not yet reaching puberty and already pregnant when diagnosed. At every wave of data collection, fewer young people were offered entry into a clinical trial and fewer agreed to take part in the NONE-TYA-PTC group than the SOME-TYA-PTC and ALL-TYA-PTC groups (Table 5). Young people reported better communication from their nurse specialist than their cancer specialist (oncologist or haematologist) but there were no differences according to level of care (Table 6). The was also no difference in young people’s perceptions of the co-ordination of care (NONE-TYA-PTC, n = 246, 89%; SOME-TYA-PTC, n = 279, 90%; ALL-TYA-PTC, n = 183, 95%).
| Question | Level of TYA care at 12 months after diagnosis | |||||
|---|---|---|---|---|---|---|
| Male | Female | |||||
| NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | |
| Before you started treatment, did anyone talk to you about banking sperm/freezing eggs or embryos? n (%) | ||||||
| Yes | 108 (94) | 142 (97) | 89 (95) | 43 (57) | 58 (58) | 41 (58) |
| Were you given the opportunity to bank sperm/freeze eggs or embryos? n (%) | ||||||
| Yes | 98 (92) | 139 (99) | 82 (96) | 17 (41) | 33 (59) | 30 (75) |
| What did you decide to do? n (%) | ||||||
| Banked sperm/froze eggs or embryos successfully | 74 (76) | 115 (83) | 68 (83) | 5 (29) | 13 (39) | 12 (40) |
| Attempted to bank sperm/freeze eggs or embryos but it was not successful | 7 (7) | 15 (11) | 8 (10) | 0 (0) | 0 (0) | 0 (0) |
| Wanted to but did not want to delay the start of treatment | 1 (1) | 0 (0) | 0 (0) | 3 (18) | 4 (12) | 4 (13) |
| Did not want to bank/freeze | 11 (11) | 5 (4) | 6 (7) | 6 (35) | 14 (42) | 8 (27) |
| Other | 5 (5) | 3 (2) | 0 (0) | 3 (18) | 2 (6) | 6 (20) |
| Question | Level of TYA care at 12 months after diagnosis | ||
|---|---|---|---|
| NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | |
| Have you been offered entry into a clinical trial? n (%) | |||
| Wave | |||
| 1 | 71/271 (26) | 119/300 (40) | 74/188 (39) |
| 2 | 7/159 (4) | 22/191 (12) | 15/109 (14) |
| 3 | 6/116 (5) | 8/152 (5) | 10/88 (11) |
| 4 | 9/104 (9) | 20/106 (19) | 7/87 (8) |
| 5 | 8/89 (8) | 12/99 (12) | 7/66 (11) |
| Have you agreed to take part in a clinical trial? n (%) | |||
| Wave | |||
| 1 | 52/69 (75) | 98/116 (85) | 70/73 (96) |
| 2 | 7/9 (77) | 19/23 (83) | 15/15 (100) |
| 3 | 4/6 (67) | 6/8 (75) | 8/9 (89) |
| 4 | 8/9 (89) | 16/17 (94) | 4/6 (67) |
| 5 | 7/8 (88) | 10/12 (83) | 6/7 (86) |
| Question | Level of TYA care at 12 months after diagnosis | |||||
|---|---|---|---|---|---|---|
| Cancer specialista | Nurse specialist | |||||
| NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | |
| When I want them to, the cancer specialist/nurse specialist explains things to me directly rather than to someone else (e.g. parent, partner), n (%) | ||||||
| Always/usually | 257 (96) | 292 (96) | 180 (94) | 103 (99) | 145 (99) | 94 (99) |
| Total | 269 | 303 | 192 | 104 | 146 | 95 |
| I can speak privately with the cancer specialist/nurse specialist when I want to, n (%) | ||||||
| Always/usually | 234 (91) | 271 (90) | 173 (91) | 103 (99) | 142 (96) | 92 (97) |
| Total | 259 | 302 | 189 | 104 | 148 | 95 |
| The cancer specialist/nurse specialist treats me with dignity and respect, n (%) | ||||||
| Always/usually | 266 (98) | 286 (94) | 180 (94) | 105 (100) | 147 (99) | 94 (99) |
| Total | 271 | 305 | 192 | 105 | 148 | 95 |
| The cancer specialist/nurse specialist listens to what I have to say, n (%) | ||||||
| Always/usually | 264 (97) | 296 (97) | 188 (98) | 105 (100) | 146 (99) | 94 (99) |
| Total | 271 | 304 | 191 | 105 | 148 | 95 |
| Information is provided in a way that I can understand, n (%) | ||||||
| Always/usually | 250 (92) | 286 (94) | 177 (92) | 102 (97) | 132 (96) | 93 (98) |
| Total | 271 | 305 | 192 | 105 | 147 | 95 |
| The cancer specialist/nurse specialist uses terms that I do not understand, n (%) | ||||||
| Rarely/never | 153 (57) | 184 (60) | 112 (59) | 77 (74) | 117 (79) | 75 (79) |
| Total | 271 | 305 | 192 | 104 | 148 | 95 |
| The cancer specialist/nurse specialist explains any terms that I do not understand, n (%) | ||||||
| Always/usually | 230 (85) | 258 (85) | 175 (91) | 94 (91) | 131 (89) | 83 (88) |
| Total | 269 | 304 | 192 | 103 | 147 | 95 |
| The cancer specialist/nurse specialist is upfront if there is bad news, n (%) | ||||||
| Always/usually | 251 (96) | 290 (97) | 180 (95) | 97 (99) | 140 (96) | 87 (95) |
| Total | 261 | 300 | 189 | 98 | 145 | 92 |
Appendix 3 Report of workstream 3 (study 6) results
Objectives
-
3.1. Compare costs to the NHS and personal social services between teenagers and young adults receiving different categories of cancer care.
-
3.2. Estimate and compare the cost to young people and families of different categories of cancer care.
-
3.3. Calculate the cost-effectiveness of different categories of TYA care.
The analyses to meet objectives 3.1 and 3.2 are described below. For objective 3.3, which was designed to include long-term cost-effectiveness modelling, our separate analyses of survival, health-related QoL and costs showed higher costs and worse health among patients receiving SOME-TYA-PTC or ALL-TYA-PTC care than those receiving NONE-TYA-PTC care; therefore, long-term economic modelling was not warranted.
Objective 3.1: NHS and personal social services costs
Methods
The BRIGHTLIGHT cohort included 1114 young people aged 13–24 years, who were newly diagnosed with cancer (ICD-10 codes C00–C97) in an English hospital and recruited within 4 months of diagnosis. Participants were identified through the national cancer waiting times data set and via tumour-specific MDTs at 97 NHS hospitals in England. Data from the HES database were used to calculate the costs associated with hospital care among study participants, including data for APC and outpatient visits (including chemotherapy and radiotherapy) and A&E attendances. Data for every person in the BRIGHTLIGHT cohort were sent to NHS Digital for linkage to the HES database covering all use of services over the period April 2012–March 2016. Linked HES data were then returned to the researchers for analysis.
To calculate hospital costs, we included all hospital contacts by participants in the BRIGHTLIGHT cohort, irrespective of cause, including chemotherapy and radiotherapy. For APC and outpatient visits we applied the relevant Healthcare Resource Group to each of our four financial years of HES data (i.e. 2012/13–2015/16) to produce a Healthcare Resource Group code for every admitted patient spell and outpatient attendance in that year. We then applied National Reference Costs from each financial year to calculate the cost of each spell and attendance at current prices. All costs were inflated to 2015/16 constant prices using the NHS Pay and Prices Index. 100 For A&E visits, we applied a single unit cost to every visit (£147.80), computed as the weighted average across all A&E visits in the National Reference Costs database. Data were recorded for every BRIGHTLIGHT patient on date of diagnosis, which was linked with the HES data based on the BRIGHTLIGHT study identifier. All APC spells, outpatient visits and A&E visits outside the first 12 months of diagnosis were dropped. For APC, this resulted in a data set of 20,215 costed spells across 1023 patients [mean cost per spell £1681, standard deviation (SD) £2994, median £681; interquartile range £368–2027]. For outpatients, there were 35,730 attendances across 1078 patients (mean cost per attendance £187, SD £180, median £160, interquartile range £129–220). For A&E attendances, there were 1221 costed visits across 574 patients. Patients with no costs for a specific type of contact (e.g. admitted care, outpatient, A&E) were assigned a zero cost for that type of contact.
Our main exposure variable was the categories of TYA specialist care (TYA-PTC) described in Quantifying specialist care. 63 We calculated mean 12-month combined hospital costs by categories of TYA specialist care and tested for significant differences using regression analyses. To account for skewness of the cost data, we used a generalised linear model with gamma family and log-link, running adjusted and unadjusted models. We also considered using log-normal, Gaussian, inverse Gaussian and negative binomial distributions, but the gamma model gave the best fit in terms of residual plots and the Akaike information criterion. In adjusted models we controlled for the same covariates used to analyse the primary outcome (see Identifying the outcomes associated with specialist teenage and young adult cancer care). 47 There were missing data for some of these covariates, so we reran the regression models including variables with no missing data only (i.e. disease severity,63 age at diagnosis, city/area, cancer type). We predicted hospital costs by categories of specialist TYA care controlling for the covariates (predictive margins).
Results
A total of 1044 patients were linked to the HES database with data on the categories of TYA specialist care (93% of the BRIGHTLIGHT cohort). Mean (SD) and median (interquartile range) costs of APC for the whole sample for the first 12 months from diagnosis were £30,473 (£36,599) and £15,528 (£6731–42,453), respectively (Table 7). For outpatient visits and A&E visits, the figures were £5472 (£5802) and £3649 (£1985–£6717), and £149 (£229) and £0 (£0–148), respectively. Costs were highly skewed (Figure 13). The combined mean and median costs were £36,094 (£38,835) and £20,365 (£9861–51,455); APC costs accounted for 84% of the mean combined cost, outpatient visits accounted for 15% and A&E visits accounted for < 1%. Of the 1044 patients in the sample, 359 (34%) had NONE-TYA-PTC care, 415 (40%) had SOME-TYA-PTC care and 270 (26%) had ALL-TYA-PTC care. For all four types of contact, unadjusted mean and median costs were highest among patients who received SOME-TYA-PTC care.
| Categories of TYA specialist care | Mean (% combined) | SD | Median | 25th percentile | 75th percentile | Observations |
|---|---|---|---|---|---|---|
| APC | ||||||
| NONE-TYA-PTC | 15,769 (78) | 24,786 | 7665 | 2118 | 16,293 | 359 |
| SOME-TYA-PTC | 44,896 (87) | 41,303 | 29,272 | 13,058 | 65,198 | 415 |
| ALL-TYA-PTC | 27,856 (84) | 33,679 | 14,779 | 7264 | 35,004 | 270 |
| Whole sample | 30,473 (84) | 36,599 | 15,528 | 6731 | 42,453 | 1044 |
| Outpatient visits | ||||||
| NONE-TYA-PTC | 4236 (21) | 5393 | 2450 | 1357 | 4703 | 359 |
| SOME-TYA-PTC | 6609 (13) | 6605 | 4782 | 2618 | 8683 | 415 |
| ALL-TYA-PTC | 5367 (16) | 4539 | 3812 | 2268 | 7092 | 270 |
| Whole sample | 5472 (15) | 5802 | 3649 | 1985 | 6717 | 1044 |
| A&E visits | ||||||
| NONE-TYA-PTC | 143 (1) | 229 | 0 | 0 | 148 | 359 |
| SOME-TYA-PTC | 197 (< 1) | 261 | 148 | 0 | 296 | 415 |
| ALL-TYA-PTC | 82 (< 1) | 147 | 0 | 0 | 148 | 270 |
| Whole sample | 149 (< 1) | 229 | 0 | 0 | 148 | 1044 |
| Combined | ||||||
| NONE-TYA-PTC | 20,147 (100) | 28,043 | 10,676 | 4829 | 21,162 | 359 |
| OME-TYA-PTC | 51,703 (100) | 42,863 | 36,407 | 17,907 | 72,570 | 415 |
| ALL-TYA-PTC | 33,305 (100) | 35,362 | 20,090 | 10,640 | 43,461 | 270 |
| Whole sample | 36,094 (100) | 38,835 | 20,365 | 9861 | 51,455 | 1044 |
FIGURE 13.
Distribution of costs by type of hospital contact. (a) APC; (b) outpatient visits; (c) A&E visits; and (d) combined.


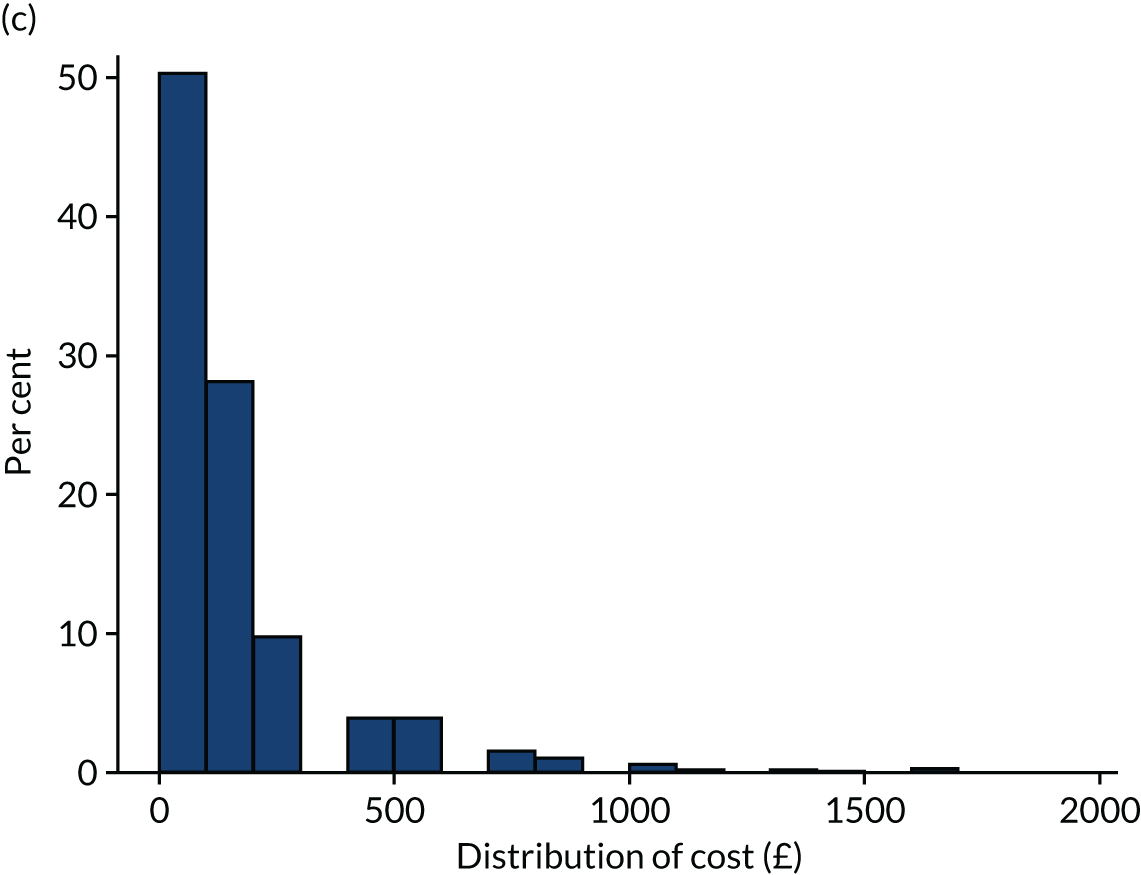
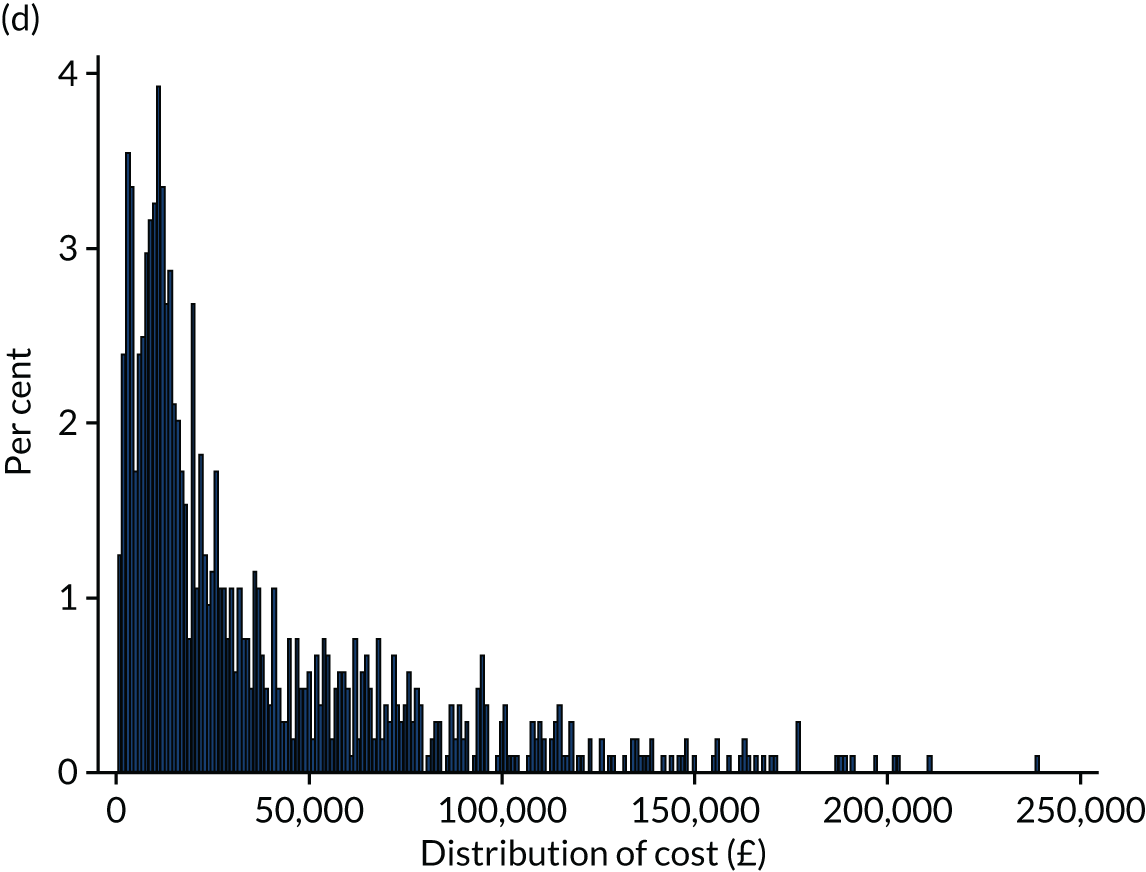
The covariates used in the regression analyses are described in Table 8. When adjusting only for covariates with no missing data (i.e. age at diagnosis, cancer type, severity group, city/area), mean hospital costs were highest among the patients receiving SOME-TYA-PTC care (mean £43,000, 95% CI £39,831 to £46,169) (Table 9 and Figure 14). There were no significant differences in costs between the NONE-TYA-PTC and SOME-TYA-PTC groups. The findings were broadly similar for the model including all covariates, with the highest cost incurred by the SOME-TYA-PTC group and then the ALL-TYA-PTC group, and lowest costs in the NONE TYA-PTC group. These differences were statistically significant.
| Categories of TYA specialist care | Whole sample | |||
|---|---|---|---|---|
| NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | ||
| Age at diagnosis (years)a | ||||
| Mean | 21 | 19 | 20 | 20 |
| SD | 3 | 3 | 3 | 3 |
| Observations | 359 | 415 | 270 | 1044 |
| Ethnic group (n) | ||||
| White | 89 | 84 | 85 | 86 |
| Other | 11 | 16 | 15 | 14 |
| Observations | 351 | 408 | 259 | 1018 |
| IMD quintile (n) | ||||
| 1 (most deprived) | 24 | 25 | 19 | 23 |
| 2 | 19 | 17 | 18 | 18 |
| 3 | 19 | 21 | 19 | 20 |
| 4 | 23 | 19 | 19 | 20 |
| 5 (least deprived) | 15 | 19 | 24 | 19 |
| Observations | 354 | 404 | 263 | 1021 |
| Cancer type (n)a | ||||
| Leukaemia | 8 | 14 | 20 | 13 |
| Lymphoma | 39 | 24 | 35 | 32 |
| CNS | 3 | 3 | 6 | 4 |
| Bone | 3 | 20 | 3 | 9 |
| Sarcomas | 3 | 10 | 6 | 7 |
| Germ cell | 20 | 18 | 17 | 18 |
| Skin | 9 | 0 | 2 | 4 |
| Carcinomas (not skin) | 14 | 10 | 10 | 11 |
| Other | 2 | 1 | 1 | 1 |
| Observations | 359 | 415 | 270 | 1044 |
| Severity group (n)a | ||||
| Least | 70 | 43 | 49 | 54 |
| Intermediate | 19 | 24 | 30 | 24 |
| Most | 11 | 33 | 22 | 23 |
| Observations | 359 | 415 | 270 | 1044 |
| Days from first symptoms to diagnosis | ||||
| Mean | 135 | 125 | 116 | 127 |
| SD | 193 | 165 | 157 | 174 |
| Observations | 264 | 304 | 188 | 777 |
| Number of GP visits | ||||
| Mean | 2 | 2 | 2 | 2 |
| SD | 3 | 3 | 4 | 3 |
| Observations | 274 | 311 | 193 | 800 |
| Given a choice about where to receive treatment? (n) | ||||
| No or aged < 19 years | 58 | 76 | 79 | 71 |
| Yes | 42 | 24 | 21 | 29 |
| Observations | 288 | 356 | 233 | 877 |
| Long-term condition (n) | ||||
| No | 93 | 89 | 91 | 91 |
| Yes | 7 | 11 | 9 | 9 |
| Observations | 277 | 311 | 193 | 781 |
| Location (n)a | ||||
| Birmingham | 15 | 18 | 7 | 14 |
| Bristol | 18 | 9 | 3 | 11 |
| Cambridge | 4 | 2 | 1 | 2 |
| Manchester | 9 | 11 | 7 | 9 |
| Merseyside | 4 | 3 | 4 | 4 |
| East Midlands | 5 | 8 | 27 | 12 |
| Leeds | 7 | 9 | 14 | 10 |
| Newcastle | 4 | 2 | 12 | 5 |
| Oxford | 2 | 1 | 3 | 2 |
| London | 23 | 28 | 5 | 21 |
| Sheffield | 2 | 3 | 5 | 3 |
| Southampton | 7 | 5 | 11 | 7 |
| Observations | 359 | 415 | 270 | 1044 |
| Percentage of contacts in TYA care | ||||
| Mean | 0 | 72 | 100 | 55 |
| SD | 0 | 24 | 100 | 44 |
| Minimum | 0 | 3 | 100 | 0 |
| Maximum | 0 | 99 | 100 | 100 |
| Observations | 359 | 415 | 270 | 1044 |
| Category of TYA specialist care | Predictive margin | SE | p-value | 95% CI |
|---|---|---|---|---|
| Unadjusted (1044 observations) | ||||
| NONE-TYA-PTC | 20,147 | 1180 | < 0.001 | 17,835 to 22,460 |
| SOME-TYA-PTC | 51,703 | 2816 | < 0.001 | 46,184 to 57,222 |
| ALL-TYA-PTC | 33,305 | 2249 | < 0.001 | 28,898 to 37,713 |
| Adjusted (only covariates with no missing data;a 1044 observations) | ||||
| NONE-TYA-PTC | 26,671 | 1294 | < 0.001 | 24,135 to 29,207 |
| SOME-TYA-PTC | 43,000 | 1617 | < 0.001 | 39,831 to 46,169 |
| ALL-TYA-PTC | 31,904 | 1601 | < 0.001 | 28,765 to 35,042 |
| Adjusted (all covariates; 733 observations) | ||||
| NONE-TYA-PTC | 24,931 | 1415 | < 0.001 | 22,159 to 27,703 |
| SOME-TYA-PTC | 41,227 | 1781 | < 0.001 | 37,737 to 44,717 |
| ALL-TYA-PTC | 31,985 | 1987 | < 0.001 | 28,092 to 35,879 |
FIGURE 14.
Predictive margins: (a) APC; (b) outpatient visits; (c) A&E visits; and (d) combined.
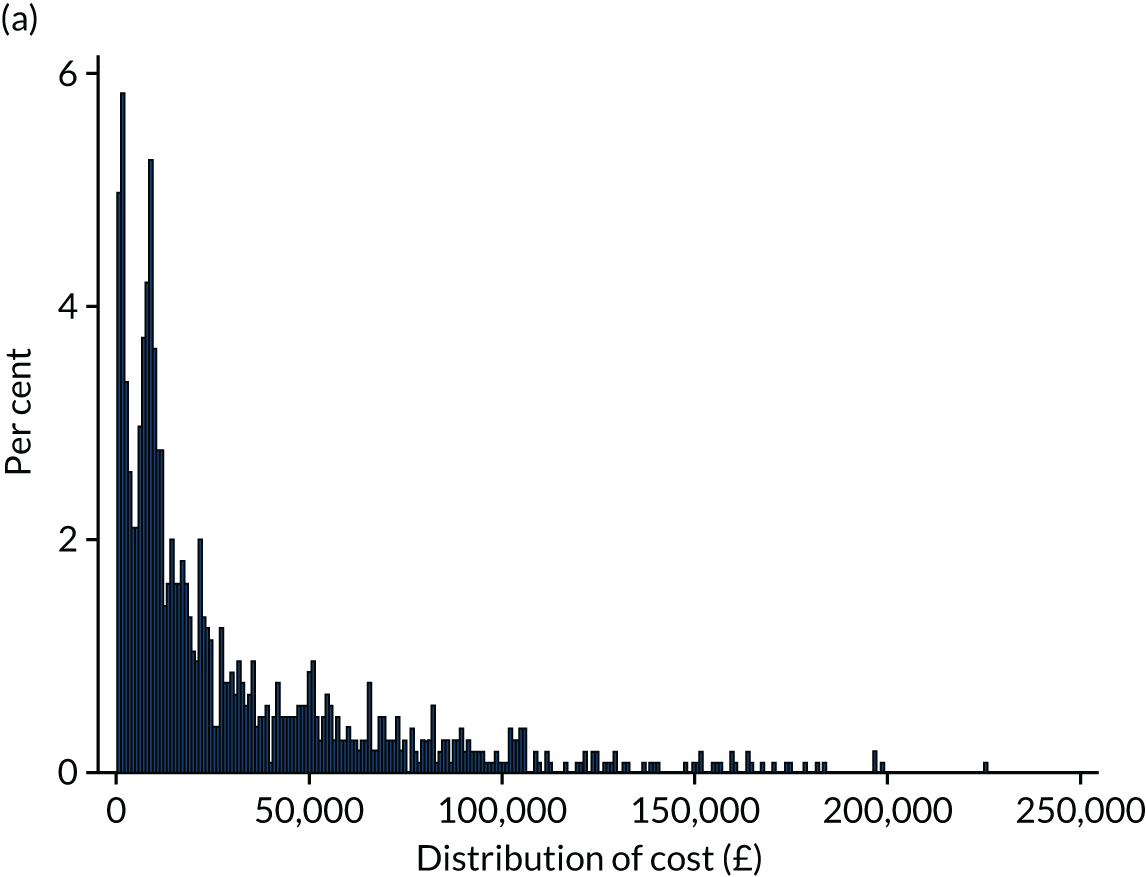
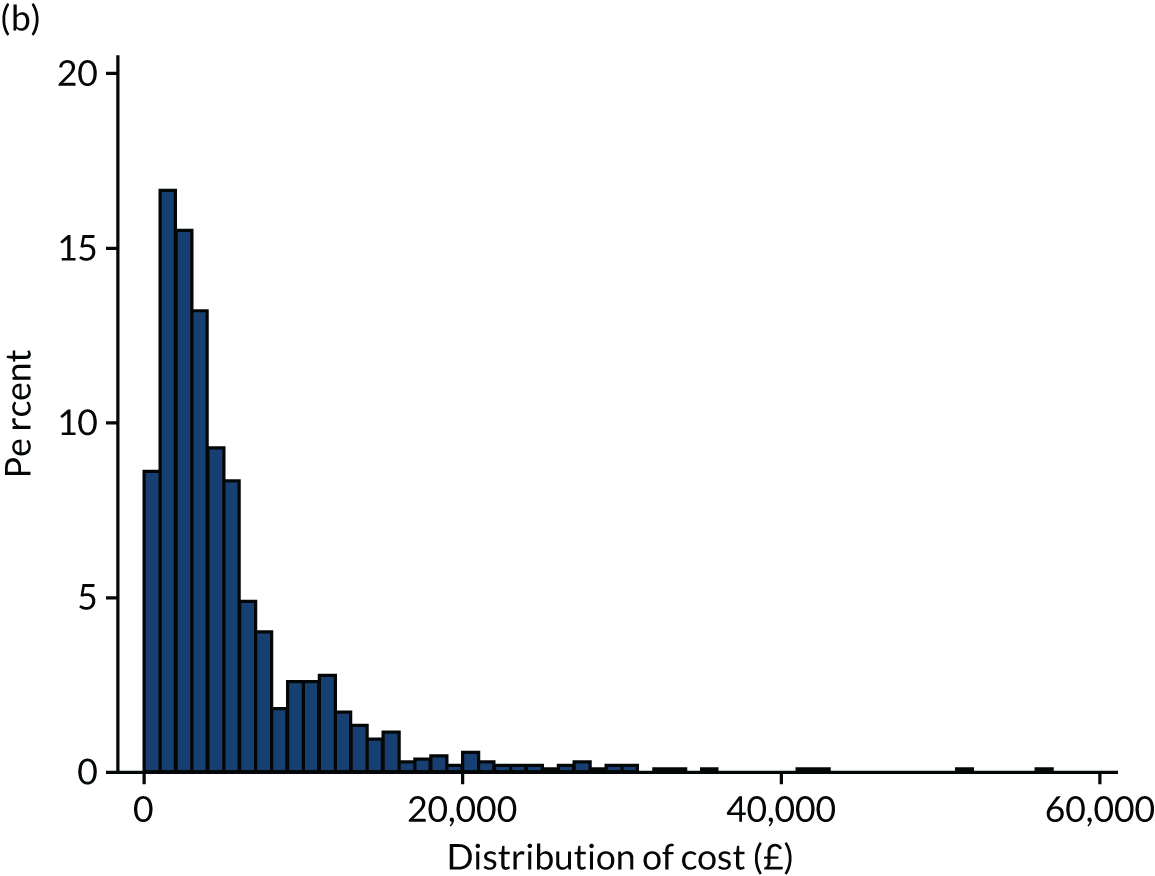
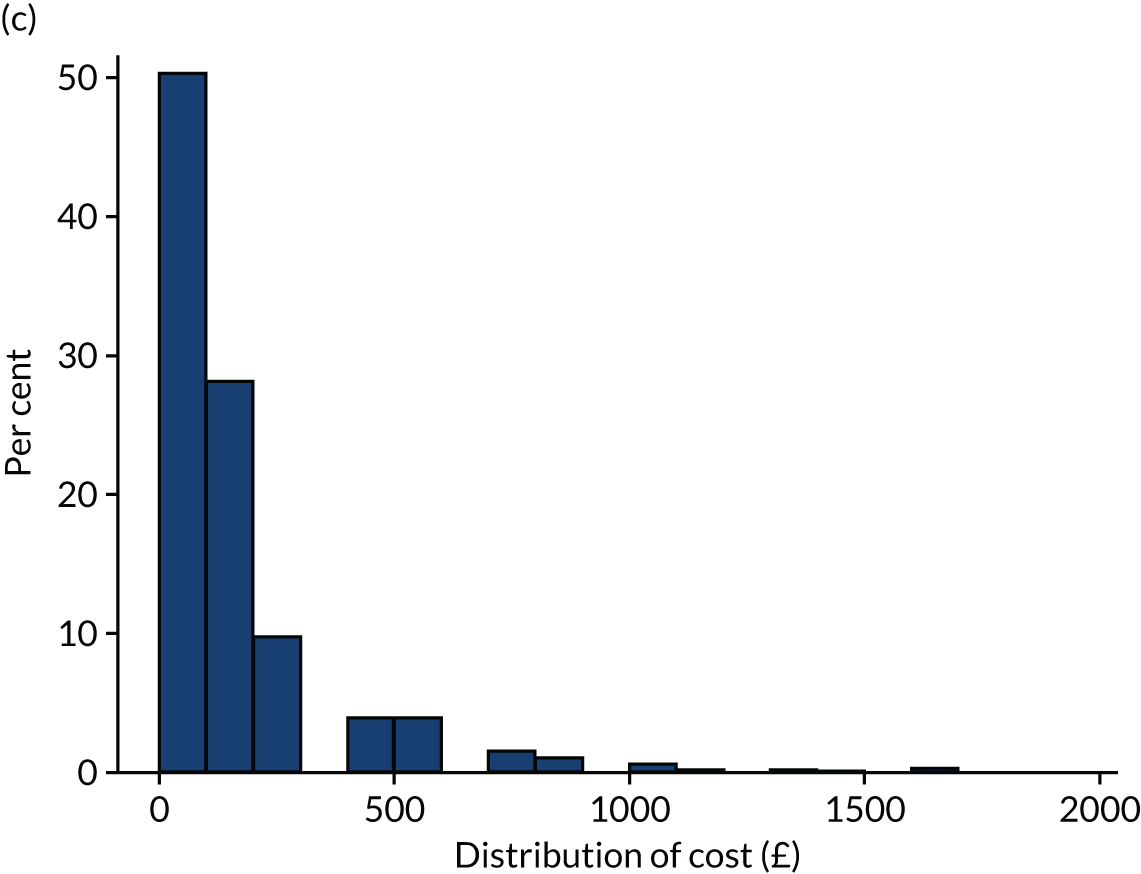

Objective 3.2: costs to young people and families
Methods
Participants were asked to complete a CoCQ retrospectively at 6 months after diagnosis, and cost records were completed prospectively at 6 months and 9 months for the following 3 months. Respondents were asked to record information relating to their travel costs and other out-of-pocket expenses related to the cancer and its treatment. The return rate for the questionnaires was 7–24% (Table 10). In terms of travel costs, participants were asked to record the names of up to five hospitals that they had visited since they were diagnosed with cancer and their usual method of transport to the hospital. The responses to the questionnaires were merged with the patient’s postcode of residence. The postcode of each hospital was found from online searches. The distance between the postcode of residence at diagnosis and hospital was computed using www.theaa.com, and travel costs were estimated according to the stated main method of transport. A total of 317 patients reported data for 966 trips (Table 11).
| n | % | |
|---|---|---|
| CoCQ, 0–6 months | 297 | 24 |
| Cost record, 6–9 months | 136 | 12 |
| Cost record, 9–12 months | 80 | 7 |
| Mode of transport | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Car | 815 | 25.40 | 34.29 | 0.27 | 264.60 |
| Taxi/cab | 32 | 125.45 | 164.35 | 2.34 | 640.00 |
| Bus | 16 | 6.00 | 0.00 | 6.00 | 6.00 |
| Tube/train within London | 32 | 44.98 | 3.84 | 24.00 | 47.20 |
| Train | 41 | 114.55 | 128.92 | 13.60 | 676.00 |
| Cycling | 3 | 0.00 | 0.00 | 0.00 | 0.00 |
| Walking | 15 | 0.00 | 0.00 | 0.00 | 0.00 |
| NHS transport | 12 | 0.00 | 0.00 | 0.00 | 0.00 |
| Total | 966 |
Methods of transport were car (84%), train (4%), taxi (3%), tube (3%), bus (2%,) on foot (2%), NHS transport (1%) and cycling (< 1%) (see Table 11). The last three of these were assigned zero cost to the patient/family. For car journeys, a cost per mile was applied from www.theaa.com; for taxis a cost per mile was applied from Uber (Uber Technologies, Inc., San Francisco, CA, USA); and for train journeys a cost per mile was applied from www.trainline.com. For buses and tube journeys, costs per trip were taken from www.tfl.gov.uk. All trips were costed as return journeys. Mean costs per trip by mode of transport are in Table 11. All car journeys were assumed to incur parking charges. The cost record recorded mean parking costs per week, which were applied to every APC stay. Parking costs for outpatient visits were based on national hospital parking costs per hour from the House of Commons, assuming a 3-hour stay. 101 Of the 966 trips, 494 were to a hospital with a TYA-PTC (mean travel cost £36.13), and 472 trips were to a hospital without a TYA-PTC (£27.77) (Table 12). We assumed that these were the mean travel costs incurred by patients and families to visit an ALL-TYA-PTC and NONE-TYA-PTC, respectively. These two mean costs were then applied to every outpatient visit and APC stay in the HES data over the 1-year period, differentiating between trips to a TYA-PTC or not. We included zero travel costs for A&E visits, assuming travel would usually be by NHS ambulance. Travel costs for APC trips were assumed to be incurred every day of the stay. Total travel costs were summed across all visits and stays per patient. These costs were analysed using the same statistical methods as for NHS costs.
| Type of hospital | n | Mean | SE | 95% CI |
|---|---|---|---|---|
| NONE-TYA-PTC | 472 | 27.77 | 2.53 | 22.8 to 32.74 |
| ALL-TYA-PTC | 494 | 36.13 | 2.61 | 31.0 to 41.27 |
| All | 966 | 32.04 | 1.82 | 56.70 to 35.63 |
For the other out-of-pocket expenses, patients and families were asked to record directly in Great British pounds the costs incurred under several headings over each time period: telephone calls, food, childcare, respite care, pet sitting/kennel fees, delivery/errand charges, cleaning services, domestic help, adaptations to the home, clothing, wigs, medical equipment, private medical fees, counselling and physiotherapy. Owing to small numbers, we only report mean values by categories of care.
Results
Unadjusted travel costs for SOME-TYA-PTC care were higher (£4168 per year, 95% CI £3836 to £4500) than those for ALL-TYA-PTC care (£2945, 95% CI £2654 to £3236) and NONE-TYA-PTC care (£1876, 95% CI £1708 to £2027). In the fully adjusted analysis, the sample size was 733 and the SOME-TYA-PTC group continued to incur the highest cost, followed by the ALL-TYA-PTC and NONE-TYA-PTC groups (Table 13). For the adjusted for covariates with no missing data, the trend was the same.
| Category of TYA specialist care | n | Mean | SE | 95% CI |
|---|---|---|---|---|
| Unadjusted | ||||
| NONE-TYA-PTC | 1044 | 1867 | 81 | 1708 to 2027 |
| SOME-TYA-PTC | 1044 | 4168 | 169 | 3836 to 4500 |
| ALL-TYA-PTC | 1044 | 2945 | 148 | 2654 to 3236 |
| Adjusted travel costs (all covariates) | ||||
| NONE-TYA-PTC | 733 | 2204 | 100 | 2008 to 2400 |
| SOME-TYA-PTC | 733 | 3510 | 125 | 3264 to 3755 |
| ALL-TYA-PTC | 733 | 2950 | 150 | 2656 to 3245 |
| Adjusted (only for variables with no missing dataa) | ||||
| NONE-TYA-PTC | 1044 | 2277 | 86 | 2107 to 2447 |
| SOME-TYA-PTC | 1044 | 3660 | 111 | 3442 to 3878 |
| ALL-TYA-PTC | 1044 | 2884 | 116 | 2655 to 3113 |
The mean total costs of out-of-pocket expenses for patients receiving NONE-TYA-PTC care, SOME-TYA-PTC care and ALL-TYA-PTC care for the first 6 months from diagnosis were £284.77, £743.83 and £976.46, respectively (Table 14). Similarly, out-of-pocket expenses for patients receiving NONE-TYA-PTC care, SOME-TYA-PTC care and ALL-TYA-PTC care at 6–9 months were £58.52, £280.58 and £122.14, respectively, and at 9–12 months were £398.66, 98.17 and 179.40, respectively. Food was the highest-cost item. Note that the low response rates decreased over time.
| Category | Out-of-pocket expenses, 0–6 months | Out-of-pocket expenses, 6–9 months | Out-of-pocket expenses, 9–12 months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| NONE-TYA-PTC, £ (n) | SOME-TYA-PTC, £ (n) | ALL-TYA-PTC, £ (n) | NONE-TYA-PTC, £ (n) | SOME-TYA-PTC, £ (n) | ALL-TYA-PTC, £ (n) | NONE-TYA-PTC, £ (n) | SOME-TYA-PTC, £ (n) | ALL-TYA-PTC, £ (n) | |
| Calls | 26.56 (86) | 64.26 (97) | 49.09 (59) | 4.04 (41) | 18.37 (49) | 9.62 (34) | 0 (3) | 3 (7) | 34 (14) |
| Food | 101.76 (88) | 480.39 (105) | 293.33 (66) | 25.06 (41) | 123.30 (49) | 50.47 (34) | 45.33 (3) | 35.89 (7) | 35.75 (14) |
| Childcare | 2.37 (95) | 1.85 (108) | 85.98 (61) | 0 (41) | 1.53 (49) | 2.35 (34) | 0 (3) | 0 (7) | 4.29 (14) |
| Respite care | 0 (95) | 19.12 (113) | 0 (66) | 0 (41) | 0 (49) | 0 (34) | 0 (3) | 0 (7) | 0 (14) |
| Pet sitting/kennel fees | 1.07 (94) | 10.51 (110) | 15.82 (67) | 2.68 (41) | 0.20 (49) | 0.88 (34) | 33.33 (3) | 4.29 (7) | 9.29 (14) |
| Delivery/errand charges | 16.67 (95) | 32.63 (107) | 84.70 (66) | 2.41 (41) | 7.26 (49) | 8.67 (34) | 0 (3) | 0 (7) | 0 (14) |
| Cleaning service | 27.58 (95) | 21.35 (111) | 94.12 (68) | 9.39 (41) | 0 (49) | 0.74 (34) | 280 (3) | 0 (7) | 60 (14) |
| Domestic help | 2.87 (94) | 14.44 (108) | 58.15 (65) | 2.07 (41) | 1.63 (49) | 3.68 (34) | 40 (3) | 0 (7) | 8.57 (14) |
| Adaptations to home | 1.03 (97) | 32.15 (107) | 134.40 (67) | 0 (41) | 16.43 (49) | 0.44 (34) | 0 (3) | 0 (7) | 0 (14) |
| Clothing | 41.15 (96) | 83.12 (106) | 69.55 (67) | 12.74 (41) | 26.90 (49) | 38.04 (34) | 0 (3) | 55 (7) | 0 (14) |
| Wig | 13.46 (95) | 48.60 (111) | 14.78 (67) | 0 (41) | 4.94 (49) | 3.12 (34) | 0 (3) | 0 (7) | 0 (14) |
| Medical equipment | 3.02 (96) | 8.95 (112) | 5.30 (67) | 0 (41) | 0.61 (49) | 1.82 (34) | 0 (3) | 0 (7) | 0 (14) |
| Private medical fees | 38.54 (96) | 36.62 (111) | 37.06 (68) | 0 (41) | 73.06 (49) | 0.56 (34) | 0 (3) | 0 (7) | 0 (14) |
| Counselling | 2.08 (96) | 5.95 (111) | 0 (67) | 0.21 (41) | 4.55 (49) | 0 (34) | 0 (3) | 0 (7) | 0 (14) |
| Physiotherapy | 0 (96) | 1.40 (114) | 0 (68) | 0 (41) | 1.80 (34) | 1.74 (34) | 0 (3) | 0 (7) | 0 (14) |
| Total | 284.77 (73) | 743.83 (76) | 976.46 (48) | 58.52 (41) | 280.58 (49) | 122.14 (34) | 398.66 (3) | 98.17 (7) | 179.40 (14) |
Objective 3.3: cost-effectiveness of different categories of teenage and young adult care
Methods
EuroQol-5 Dimensions, three-level version (EQ-5D-3L), questionnaires were completed at 6 months (wave 1), 12 months (wave 2), 18 months (wave 3), 24 months (wave 4) and 36 months (wave 5) post diagnosis and converted into utility scores using a UK value set. 102 Questionnaires were not completed at diagnosis as patients were not identified until up to 4 months after diagnosis. The QALYs were calculated for each respondent as the area under the curve up to 36 months. The values at wave 1 were assumed to have persisted since diagnosis. Response rates at each wave were 75%, 66%, 54%, 48%, 46% (Table 15), and QALYs were available for 18% of respondents, who completed all five waves, with no missing data. Utility scores at each time point and QALYs were analysed using the same statistical methods as for NHS costs. Given the extent of missing data, no imputation was undertaken, and in adjusted analyses we controlled for variables with no missing data only.
| Wave | Mean (n) | SE | 95% CI | Minimum | Maximum | Dead (n) | Negative health state |
|---|---|---|---|---|---|---|---|
| 1: 6 months | 0.76 (830) | 0.01 | 0.75 to 0.78 | –0.24 | 1 | 0 | 13 |
| 2: 12 months | 0.82 (546) | 0.01 | 0.81 to 0.84 | –0.22 | 1 | 6 | 2 |
| 13: 8 months | 0.79 (446) | 0.01 | 0.76 to 0.82 | –0.08 | 1 | 24 | 4 |
| 4: 24 months | 0.75 (402) | 0.02 | 0.72 to 0.78 | –0.18 | 1 | 45 | 7 |
| 5: 36 months | 0.7 (385) | 0.02 | 0.66 to 0.74 | –0.17 | 1 | 73 | 1 |
| QALYs | 2.27 (151) | 0.06 | 2.17 to 2.37 | 0.43 | 2.9 | – | – |
Results
The unadjusted mean QALYs per patient were 2.45 (95% CI 2.28 to 2.62) for patients receiving NONE-TYA-PTC care, 1.94 (95% CI 1.74 to 2.14) for those receiving SOME-TYA-PTC care and 2.20 (95% CI 1.94 to 2.28) for those receiving ALL-TYA-PTC care (Table 16). Trends were similar in adjusted analyses (Table 17), with overlapping 95% CIs between each group.
| Utility score | NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (n) | SE | 95% CI | Mean (n) | SE | 95% CI | Mean (n) | SE | 95% CI | |
| At 6 months | 0.81 (277) | 0.01 | 0.79 to 0.84 | 0.70 (312) | 0.01 | 0.67 to 0.72 | 0.78 (193) | 0.02 | 0.75 to 0.82 |
| At 12 months | 0.85 (175) | 0.02 | 0.82 to 0.89 | 0.78 (209) | 0.02 | 0.73 to 0.80 | 0.83 (126) | 0.02 | 0.79 to 0.87 |
| At 18 months | 0.85 (129) | 0.02 | 0.80 to 0.89 | 0.74 (177) | 0.02 | 0.66 to 0.76 | 0.78 (106) | 0.03 | 0.72 to 0.84 |
| At 24 months | 0.80 (126) | 0.03 | 0.74 to 0.85 | 0.69 (142) | 0.03 | 0.60 to 0.72 | 0.75 (109) | 0.03 | 0.69 to 0.82 |
| At 36 months | 0.79 (110) | 0.03 | 0.74 to 0.85 | 0.60 (157) | 0.03 | 0.54 to 0.67 | 0.71 (92) | 0.04 | 0.63 to 0.78 |
| QALYs | 2.45 (40) | 0.08 | 2.28 to 2.62 | 1.94 (66) | 0.10 | 1.74 to 2.14 | 2.2 (40) | 0.11 | 1.94 to 2.28 |
| Utility score | n | NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | 95% CI | Mean | SE | 95% CI | Mean | SE | 95% CI | ||
| At 6 months | 733 | 0.81 | 0.02 | 0.77 to 0.84 | 0.71 | 0.01 | 0.68 to 0.74 | 0.78 | 0.02 | 0.74 to 0.82 |
| At 12 months | 480 | 0.85 | 0.02 | 0.81 to 0.89 | 0.79 | 0.02 | 0.75 to 0.82 | 0.84 | 0.03 | 0.79 to 0.89 |
| At 18 months | 387 | 0.84 | 0.04 | 0.77 to 0.91 | 0.74 | 0.03 | 0.69 to 0.78 | 0.80 | 0.04 | 0.72 to 0.88 |
| At 24 months | 353 | 0.77 | 0.04 | 0.69 to 0.86 | 0.70 | 0.04 | 0.63 to 0.77 | 0.79 | 0.05 | 0.69 to 0.89 |
| At 36 months | 340 | 0.79 | 0.07 | 0.66 to 0.92 | 0.61 | 0.04 | 0.53 to 0.69 | 0.77 | 0.08 | 0.62 to 0.92 |
| QALYs | 133 | 2.45 | 0.15 | 2.15 to 2.75 | 2.08 | 0.1 | 1.89 to 2.27 | 2.34 | 0.17 | 2.00 to 2.68 |
Cost-effectiveness of specialist care
The results for each separate analysis by category of care are summarised in Table 18. Bearing in mind the limitations of the analyses in terms of missing data and small numbers of responses, especially for the out-of-pocket expenses and QALYs, the NONE-TYA-PTC group persistently had the lowest NHS and travel costs of the three groups, and the highest QALYs. Notwithstanding the limitations of the data, taken at face value this suggests that SOME-TYA-PTC and ALL-TYA-PTC care are dominated by NONE-TYA-PTC care (i.e. are more costly and less effective). Given these findings, further long-term economic modelling was not undertaken.
| NONE-TYA-PTC | SOME-TYA-PTC | ALL-TYA-PTC | |
|---|---|---|---|
| NHS costs | Best | Worst | Middle |
| Travel costs | Best | Worst | Middle |
| Other out-of-pocket expenses, 0–6 months | Best | Middle | Worst |
| Other out-of-pocket expenses, 6–9 months | Best | Worst | Middle |
| Other out-of-pocket expenses, 9–12 months | Worst | Best | Middle |
| Survivala | Best | Worst | Middle |
| Utility score at 6 months | Best | Worst | Middle |
| Utility score at 12 months | Middle | Worst | Best |
| Utility score at 18 months | Best | Worst | Middle |
| Utility score at 24 months | Middle | Worst | Best |
| Utility score at 36 months | Best | Worst | Middle |
| QALYs | Best | Worst | Middle |
Glossary
- Specialist care
- This term is used throughout this report to describe care delivered in the teenage and young adult principal treatment centre, as described in the National Institute for Health and Care Excellence improving outcomes guidance for children and young people with cancer in 2005 [National Institute for Health and Care Excellence. Guidance on Cancer Services: Improving Outcomes in Children and Young People With Cancer. 2005. URL: www.nice.org.uk/guidance/csg7/resources/improving-outcomes-in-children-and-young-people-with-cancer-update-773378893 (accessed 28 September 2021)]. This was translated as 13 principal treatment centres for teenagers and young adults across England in Newcastle, Leeds, Manchester, Liverpool, Sheffield, Nottingham/Leicester (joint East Midlands service), Birmingham, Oxford, Cambridge, Bristol, Southampton, University College London Hospital and the Royal Marsden in London.
List of abbreviations
- A&E
- accident and emergency
- APC
- admitted patient care
- BCQ
- BRIGHTLIGHT Carer Questionnaire
- CoCQ
- Cost of Care Questionnaire
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- FYSOT
- Find Your Sense of Tumour
- HES
- Hospital Episode Statistics
- HSDR
- Health Services and Delivery Research
- HTA
- Health Technology Assessment
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- IOG
- Improving Outcomes Guidance
- MDT
- multidisciplinary team
- NCRI
- National Cancer Research Institute
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PPI
- patient and public involvement
- PTC
- principal treatment centre
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- SD
- standard deviation
- TYA
- teenage and young adult
- TYA-PTC
- teenage and young adult principal treatment centre
- YAP
- young advisory panel