Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0109-10061. The contractual start date was in January 2011. The final report began editorial review in February 2019 and was accepted for publication in February 2020. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Adab et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
SYNOPSIS
Background
Chronic obstructive pulmonary disease (COPD) is a chronic progressive respiratory condition with an estimated worldwide prevalence of 9.21–11.7%2 in adults aged ≥ 30 years. However, at least half of all people with COPD (depending on the diagnostic criteria) remain undiagnosed, representing a large number with potentially unmet need. 3,4 COPD is defined by the presence of airflow obstruction among those with relevant risk factors but there is increasing recognition that the disease is heterogeneous, with different causative factors, phenotypic characteristics and varying prognosis. 5,6 A substantial proportion of those with COPD are of working age, and there is some evidence that they have poorer employment history,7 higher rates of sickness absence8 and poorer work performance [because of presenteeism (working while unwell)]9 compared with the general population. In the UK, COPD is estimated to cost the NHS around £1.5B (2011 costs),10,11 with total costs (including societal and intangible costs) nearing £48.5B (2014 costs)12 per year. This compares with estimates of around US$49.9B in the USA (2010 prices)13 and €48.4B in the European Union (2011 prices). 14
At the time of developing this proposal in 2009/10, there was much uncertainty about the natural history of COPD,5,15 how to approach early identification of patients16,17 and what interventions were effective for early-stage disease. During the conduct of the programme, both the UK National Screening Committee and the US Preventive Services Task Force (USPSTF) highlighted the lack of randomised controlled trial (RCT) evidence that showed that screening for COPD is beneficial. We therefore sought a variation to our contract to undertake additional work to that proposed in the original funded application: to follow up trial participants to examine the impact of screening on clinical outcomes. There was also little information on the impact that having COPD has on work performance and occupation. Furthermore, most of the previous research to explore prognosis and natural history of COPD were based on people with COPD recruited through secondary care and specialised settings, rather than within primary care. 18–20 The overall aim of this programme was therefore to recruit a unique UK primary care COPD cohort to address some of these uncertainties and, as a platform for future research, to test novel health service interventions.
Overview of research programme
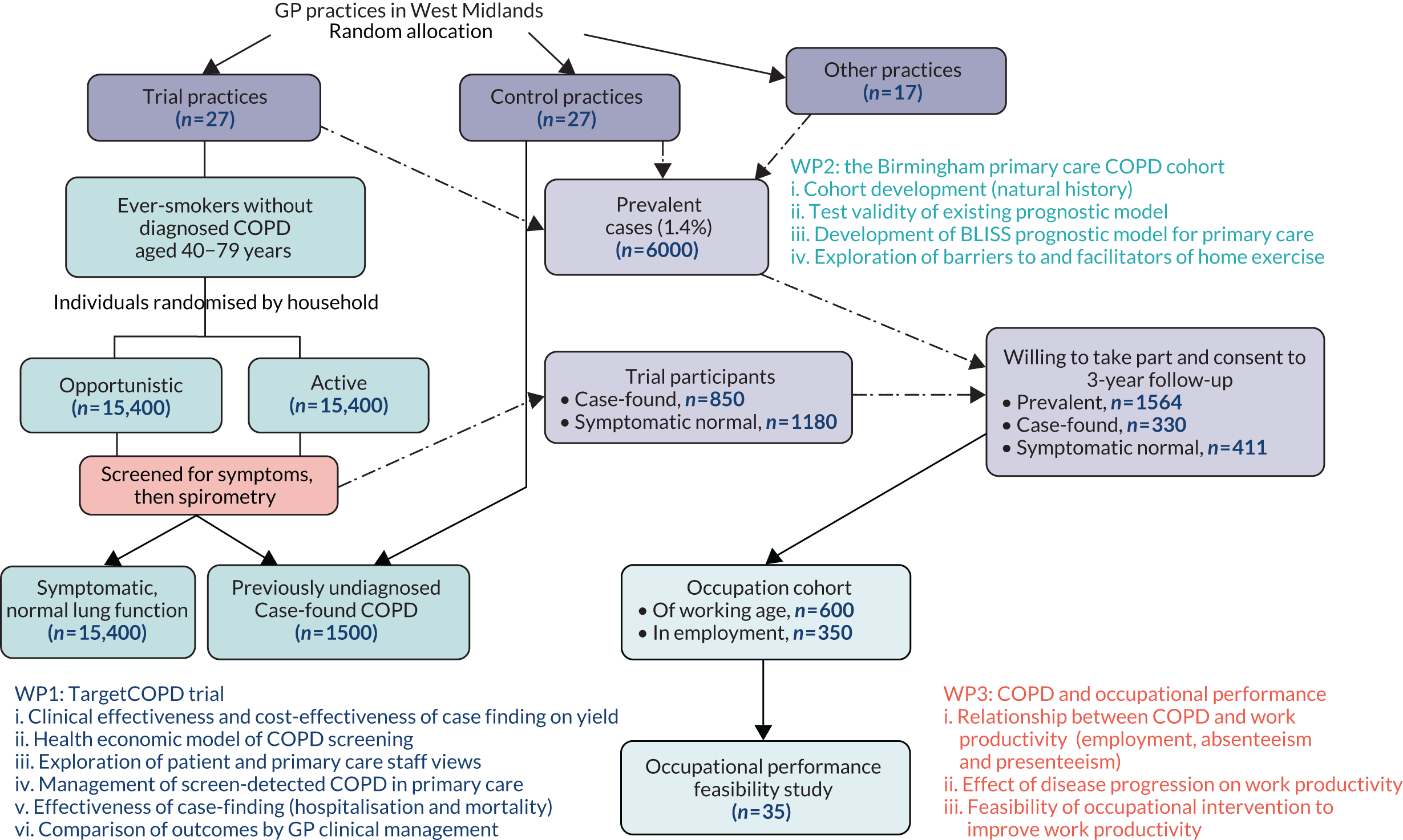
The programme consisted of three inter-related work packages (WPs), each addressing several research questions. Figure 1 provides an overview of the linked WPs in the programme, which are briefly described below. Each WP is then described in more detail, outlining the rationale, the research questions addressed and a summary of the findings and outputs linked to the original programme objectives. A full list of publications arising from our programme is available in Appendix 1.
FIGURE 1.
Overview of the programme of work. BLISS, Birmingham Lung Improvement StudieS.
Work package 1: clinical trial to evaluate case-finding; TargetCOPD trial
The aim of this WP was to ascertain the most clinically effective and cost-effective approach to identifying undiagnosed COPD. Initially, this was considered in terms of yield (WP1i), but with additional follow-up (in a variation to the contract) in terms of clinical outcomes (WP1v and vi). A Markov model was also developed to estimate the long-term cost-effectiveness of a systematic screening programme for undiagnosed COPD. Finally, we explored the views of patients on the process and outcomes of case-finding and the perspective of staff in primary care on the concept of case-finding and percieved implications for their practice.
The objectives were to:
-
ascertain the clinical effectiveness and cost-effectiveness of targeted case-finding (opportunistic or active) compared with routine care
-
develop a Markov model to compare the cost-effectiveness of systematic case-finding with current practice
-
explore the views of patients and primary care staff on COPD case-finding
-
describe the clinical management of screen-detected COPD patients in primary care
-
assess the long-term effectiveness of COPD case-finding on respiratory hospitalisations and mortality
-
compare outcomes among screen-detected COPD patients who were adequately managed by their general practitioner (GP) with those among patients who were not.
Work package 2: Birmingham primary care chronic obstructive pulmonary disease cohort
The aim of this WP was to develop a cohort of more than 2000 people with COPD who would be representative of those in a primary care setting, including more people with mild/moderate disease than included in previous cohorts. Participants were recruited from COPD registers in general practices as well as from participants in the TargetCOPD trial in WP1. This included those who were identified through case-finding and those who took part in the case-finding trial and reported respiratory symptoms but did not have COPD based on spirometry.
The participants were followed up every 6 months for around 3 years (2012–16) and their data were linked to routine data on hospitalisation and mortality obtained from NHS Digital. We used these data to externally validate an established prognostic model [the age, dyspnoea, airflow obstruction (ADO) prognostic score] in predicting mortality. In addition, we developed a new prognostic model [the Birmingham Lung Improvement StudieS (BLISS) index] to predict the risk of respiratory hospitalisation in this primary care population.
A sample of 26 cohort participants were also invited to attend focus groups to explore barriers to and facilitators of undertaking physical activity (PA), which is one of the most important components of treatment for people with COPD.
The establishment of the cohort also provides an opportunity for testing novel interventions in future.
The objectives were to:
-
recruit a primary care cohort of 2000 new and existing COPD patients
-
test the validity of existing COPD prognostic models in a primary care COPD population
-
develop a prognostic model (BLISS index) to predict respiratory hospitalisations suitable for a primary care population
-
explore barriers to and facilitators of PA participation among people with COPD.
Work package 3: chronic obstructive pulmonary disease and occupational performance
The aims of this WP were to (1) examine the relationship between clinical characteristics and severity of COPD and occupational outcomes, including employment, work absenteeism and presenteeism (working while unwell); (2) examine whether or not disease progression over time is associated with occupational outcomes; and (3) assess the feasibility and benefits of offering formal occupational health (OH) assessment and subsequent recommendations aimed at improving work-based indices. Participants in this WP were a subsample of the larger cohort recruited in WP2.
The objectives were to:
-
examine factors associated with occupational performance (employment, absenteeism and presenteeism) among COPD patients of working age
-
examine how disease progression (lung function decline, exacerbation) over time is associated with occupational performance (employment, absenteeism and presenteeism) among COPD patients in employment
-
assess the feasibility of offering OH assessment with recommendations to people with COPD.
Work package 1: clinical trial to evaluate case-finding – TargetCOPD trial
Objective (i): to ascertain the clinical effectiveness and cost-effectiveness of targeted case-finding (opportunistic or active) compared with routine primary care (work package 1i, published trial report)21
Parts of this section are based on Jordan et al. 21 Reprinted from The Lancet Respiratory Medicine, Vol. 4, Rachel E Jordan, Peymané Adab, Alice Sitch, Alexandra Enocson, Deirdre Blissett, Sue Jowett, et al. , Targeted case finding for chronic obstructive pulmonary disease versus routine practice in primary care (TargetCOPD): a cluster-randomised controlled trial, pp. 720–30, Copyright 2016, with permission from Elsevier.
Rationale
Several reports from the UK government and health charities22,23 have highlighted the burden of COPD, the extent of underdiagnosis and the variation in access to and participation in relevant services. The Department of Health and Social Care published an outcomes strategy for people with COPD in 2011 that recommended opportunist and the systematic case-finding to minimise late diagnosis. 22 However, the most clinically effective and cost-effective approach for identifying undiagnosed cases was not known. Although some published studies reported the yield from either active24–26 or opportunistic27–29 approaches to case-finding using spirometry, these were limited because of a lack of comparison groups, the restricted number and range of participants, a lack of follow-up and different target populations (e.g. specific age groups; all current smokers or people who have smoked; whether or not symptoms were considered prior to spirometry). Furthermore, general population screening using spirometry was not recommended16 because it would identify many people without clinically important disease, for whom there is little evidence of effective interventions. 30 We therefore sought to evaluate different approaches to case-finding for undiagnosed COPD, focusing on yield and cost-effectiveness (from a health-care perspective). To our knowledge, this was the first major trial to compare different targeted recruitment approaches with case-finding with routine care.
What we did
We recruited 54 GP practices across the West Midlands (10 August 2012–22 June 2013) to take part in the 12-month trial and randomised these clusters to case-finding or to continue with routine care. All patients on the practice registers aged 40–79 years who had no existing diagnosis of COPD and had ever smoked (based on GP electronic records) were eligible for and included in the trial. Using a computer-generated randomisation sequence, we randomised practices (balanced on practice characteristics) and in the intervention case-finding arm we randomised individual households of patients to receive one of two approaches to case-finding: opportunistic (offered screening opportunistically when they visited the practice for any reason) or active (additionally offered screening through a postal invitation). Screening was carried out in two stages, with an initial questionnaire (see Appendix 2) followed by an invitation to attend for diagnostic spirometry for those who reported relevant chronic respiratory symptoms. Our study case definition of 1-year incident COPD was either (1) a new diagnosis of COPD by the GP (based on new entry on practice COPD register) or (2) the presence of airflow obstruction on screening [defined as forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) < 0.7 post bronchodilator, in line with recommendations from the guidelines31 produced by the National Institute for Health and Care Excellence (NICE)] in patients with chronic respiratory symptoms. Sample sizes were based on estimates from our published model (see published paper21 for full details) and required 27,768 patients per group. Primary outcomes were analysed using appropriate regression analyses adjusted for practice-level deprivation, ethnicity and age. The active versus opportunistic comparison required logistic regression with fixed effects and the targeted versus routine comparison required multilevel models with random effects. We undertook a within-trial cost-effectiveness analysis to calculate the cost per additional case detected of both strategies versus routine care, and we undertook a detailed cost analysis of the screening processes using standard NHS32,33 and trial-specific costs34 (2013 prices), including set-up costs and training costs. Equipment and training costs were amortised over 3–5 years using a discount rate of 3.5%. Sensitivity analyses considered patient costs, alternative case-finding scenarios and models of care (GP, community or secondary care led).
What we found
A flow diagram of participants is available in the published paper. 21 We found that very few new cases of COPD were diagnosed in the routine care practices (n = 337; 0.8%). The odds of finding new cases were seven times higher using the targeted approach than with routine care [n = 1278 (4%); adjusted odds ratio (OR) 7.45, 95% confidence interval (CI) 4.80 to 11.55; p < 0.0001], and active case-finding (combining opportunistic and active postal invitation to screening) was twice as effective as opportunistic-only [n = 822 (5%) vs. n = 370 (2%); adjusted OR 2.34, 95% CI 2.06 to 2.66; p < 0.0001]. Active case-finding may also be more cost-effective than the opportunistic approach (£333 vs. £376 per additional case detected, respectively). The incremental cost-effectiveness ratio (ICER) for active case-finding was £573 per additional case detected compared with opportunistic case-finding. Sensitivity analyses made little difference, although a secondary care-led service was more expensive.
Strengths and limitations
To our knowledge, this was the first RCT to compare yield of undiagnosed COPD from a comparison of different screening approaches with routine practice and to estimate their cost-effectiveness. However, the efficiency of screening could have been improved by using different screening tests, or pre-screening algorithms applied to electronic health records (EHRs) to target screening invitations to those at highest risk. Even with the most intensive screening approach, only 38% of those invited for screening responded, and not all those who responded and had symptoms attended for diagnostic spirometry. Further research should focus on how to maximise screening coverage and uptake and improve the efficiency of the screening process.
Objective (ii): to develop a model (using Markov decision analysis) to compare the cost-effectiveness of a systematic case-finding programme with current practice (work package 1ii, published)35
Rationale
The TargetCOPD trial confirmed that active approaches to screening result in a higher proportion of undiagnosed COPD patients being identified compared with routine care. People with screen-detected COPD are expected to benefit from treatment resulting in improved quality of life, increased survival and reduction in hospital admissions. To provide data for policy-makers to consider the longer term benefits of screening for COPD in relation to investment in other health services, a cost-utility model is needed. Published economic evaluations in COPD have primarily considered interventions for the disease rather than for those who are screen detected,36 and others have concentrated on the costs of COPD in burden of illness studies. 37 No trial-based economic evaluation had considered case-finding. NICE guidelines38 included a simple decision tree-based modelling to determine the cost-effectiveness of opportunistic case-finding among people aged > 35 years who have smoked and have a chronic cough. However, the model was simplistic and included many assumptions for which evidence was limited. We developed a model-based economic evaluation of the long-term costs and benefits of screening for undiagnosed COPD.
What we did
We used costs (using 2015 prices39) and outcome data from the TargetCOPD trial, in combination with the best available published data, and additional information from our linked Birmingham COPD cohort study (WP2) to develop a Markov decision-analytic model to address this objective. The model compared the cost-effectiveness of a 3-yearly systematic case-finding programme aimed at people aged > 50 years who have smoked with current practice because the yield of new cases was very small in younger age groups. The model had a time cycle of 3 months, which was short enough to capture important COPD-related events, and a time horizon of 50 years, assuming a maximum age of 100 years. Patient-level data on case-finding pathways were obtained from our TargetCOPD RCT. The model outcome was cost per quality-adjusted life-year (QALY) gained, from a health service perspective. Discounting was applied to costs and outcomes at 3.5%. Multiple one-way sensitivity analyses assessed what impact modification of key parameters had on the results. We considered varying the starting age, screening interval and time horizon as well as the screening processes (questionnaire response, spirometry attendance rate), treatment initiation rates and effectiveness of treatments.
What we found
We estimated the ICER of systematic case-finding compared with routine care to be £16,596 per additional QALY gained. Using the commonly used willingness-to-pay threshold in the UK (£20,000 per QALY), we estimated there was 78% probability of cost-effectiveness. The estimate was robust to sensitivity analyses, with the main cost-driver being uptake of screening. The most cost-effective age to begin screening was around 60 years. Better ascertainment of treatment effectiveness will help improve precision but, using the best current estimates from the literature,40,41 screening is likely to be cost-effective provided that at least 12% respond to a screening questionnaire, > 26% attend spirometry and > 8% of screen-detected patients are adequately treated and managed.
Strengths and limitations
To our knowledge, this is the first economic model to evaluate the long-term cost-effectiveness of a COPD case-finding strategy, using contemporaneous data sources to inform estimates and using multiple sensitivity analyses to test the robustness of the model. However, the validity of some of the assumptions underlying the model is unknown. In particular, there is uncertainty around the effect of treatment on progression and the natural history of COPD. Future research should refine the model based on data from studies that provide more accurate estimates of effectiveness and consider additional costs, such as those to the health service, of pathways to deal with a larger number of identified cases.
Objective (iii): to explore the views of (a) patients invited to take part in case-finding, in terms of the process and outcomes (work package 1iii, published),42 and (b) primary care staff, in relation to case-finding (work package 1iii, published)43
Rationale
Although there has been much research examining the yield from different case-finding activities, few previous studies have examined other aspects related to the development of a screening programme. One important aspect is the acceptability of screening and understanding the perspective of both patients and those who provide screening. We undertook two studies: one to explore the views of patients who had been invited for screening as part of the TargetCOPD trial, about the screening process and outcomes, and another to understand the process from the perspective of primary care staff who would manage those who are case-found.
What we did
For the patient perspective, we invited for interview people who had been invited for screening in either the active or opportunistic arm as part of the TargetCOPD trial (i.e. adults aged ≥ 40 years with a smoking history who had been considered eligible for the trial by their GP). We invited four groups of patients: those who (1) were invited and consented to take part in screening, (2) were invited and declined, (3) attended screening but did not have COPD and (4) attended and had abnormal lung function suggesting COPD. We sought their views on the screening process and their reflections on the outcomes of screening.
For the primary care staff perspective, we invited 20 staff, including GPs, nurses and managers in practices that had taken part in the TargetCOPD trial. Participants were invited to share their views on COPD case-finding, including their perceptions of the benefits, harms, and barriers to and facilitators of implementing a screening programme in primary care.
For both studies, interviews were transcribed and analysed using the framework approach.
What we found
Forty-three patients and 20 health-care staff were interviewed. Patients generally considered screening to be a good thing, and the presence of symptoms on prompting facilitated their attendance. The importance of ensuring that the screening process is convenient was highlighted, and patients worried that GPs did not have the time to follow up after screening.
Barriers to attending screening included psychological and practical factors. The former related to denial and failure to recognise symptoms, fear of the ‘test’ and perceiving lung disease as less important within the hierarchy of their health problems. Practical barriers included lack of time, inability to access GP appointments and having caring and other responsibilities that were considered more important.
Among primary care staff, although they also generally supported screening for undiagnosed COPD, they also commented on concerns around potential negative consequences, including an increase in workload for GPs and overdiagnosis in patients. Some commented that, currently, diagnosed patients were not being adequately treated. Perceived barriers to implementing screening included lack of resources and limited access to diagnostic services. However, potential solutions, including better support from secondary care, an increase in specialist COPD nurses and better community respiratory service provision, were also discussed. Poor knowledge of COPD in terms of recognising symptoms and how to manage those with the disease was also highlighted as a problem that needs to be addressed.
For a screening programme to be implemented and have high uptake, it is important to raise patient awareness of COPD risk factors and symptoms and provide training and additional resources for primary care. In particular, it is important to ensure that management pathways for diagnosed COPD patients are optimised before further cases are identified.
Strengths and limitations
To our knowledge, this was the first study to explore perceptions of patients and health-care providers on different stages of case-finding. However, we did not explore experiences of the approach to recruitment for screening (questionnaire at GP surgery or by post) and no participant commented on this. In addition, we did not invite and have not captured the views of people who reported no chronic respiratory symptoms as part of screening. Furthermore, inviting patients in the context of research may not reflect views on screening in practice. For health-care staff, those who participated are likely to be more engaged in case-finding and their views may represent those who are more proactive in management of case-found COPD.
Objective (iv): to describe the clinical management of screen-detected chronic obstructive pulmonary disease patients in primary care and compare management in those who were versus those who were not on the practice chronic obstructive pulmonary disease registers (work package 1iv, manuscript submitted)
Rationale
From a public health perspective, screening is more than a screening test. To have an impact on clinical outcomes, a number of criteria need to be fulfilled and, in the UK, the National Screening Committee considers these carefully before recommending commencement of a population screening programme. The criteria relate to the condition, the screening test, the treatments available for those who are screen detected and the characteristics of the programme and its implementation. In relation to the programme implementation, it is important to ensure that resources are available and pathways are in place to manage screen-detected individuals. In the UK, NICE has set out a pathway for the diagnosis and management of people with COPD. 31 As part of the TargetCOPD trial, patients with chronic respiratory symptoms who attended spirometry screening had their results fed back to their GP, with a note for them to follow NICE guidelines for further management. However, there are few studies that have examined how patients diagnosed with COPD are subsequently managed and whether or not primary care staff follow recommended pathways for managing these patients. We therefore obtained data from GP EHRs and self-reported data from case-found patients (those with airflow obstruction on spirometry who fulfil the NICE recommended criteria for diagnosing COPD) to describe the clinical management of case-found COPD patients (identified through the TargetCOPD trial) and compare this with that of patients newly diagnosed with COPD through routine care. In addition, we compared characteristics and management for those who were or were not entered on to the practice COPD register.
What we did
We identified patients who had been newly diagnosed with COPD (case-finding, n = 857; routinely diagnosed, n = 764) during the period August 2012 to June 2014 in the 54 GP practices that took part in the TargetCOPD trial. Data on demographic and clinical characteristics, as well as a range of clinical assessments and interventions recommended by NICE for people with COPD, were extracted from EHRs for a subset of patients covering the period April 2011 to September 2017. In addition, patients who had been identified through case-finding were invited to complete a health questionnaire around 5 years after their first diagnosis, in March 2018, with a reminder 2 months later.
For all patients, we determined whether or not they had been added to the practice COPD register used in reporting for the Quality and Outcomes Framework (QOF) by the end of the TargetCOPD trial period. The number of COPD-related clinical assessments and interventions were summed to form a clinical management score. Multilevel logistic regression was used to assess for associations between participant characteristics and the likelihood of being added to a disease register, comparing those who were identified through case-finding with those routinely diagnosed. Multilevel linear regression was used to assess associations between participant characteristics, COPD disease registration and the clinical management score.
What we found
Figure 2 shows a summary of participants included in these analyses. The primary analysis showed that just over one-fifth (182/857; 21.2%) of case-found patients, but almost all of the routinely diagnosed patients (708/764; 92.7%), had been added to the QOF COPD register within 12 months of assessment [median time from trial spirometry assessment to COPD registration 152 days, interquartile range (IQR) 72–258]. Factors associated with a higher likelihood of COPD registration among case-found patients were current and former smoking (adjusted OR 8.68, 95% CI 2.53 to 29.82, vs. OR 6.32, 95% CI 1.88 to 21.29, respectively) and lower percentage of predicted FEV1 (OR 0.96, 95% CI 0.95 to 0.98).
FIGURE 2.
Flow of participants contributing to analyses for this study. a, Included in current study.

Electronic health record data were available for 532 out of 1629 patients (identified through case-finding, n = 344; identified through usual care, n = 188) (Table 1). The characteristics of participants with and without EHR data were broadly similar. Factors associated with a higher clinical management score were being on the COPD register (adjusted β 5.06, 95% CI 4.36 to 5.75, which means that the score was on average 5 units higher for those on the COPD register than for those not on the register) and a higher number of comorbidities (adjusted β 0.38, 95% CI 0.11 to 0.65, which means that the score increased by 0.38 units for each additional comorbidity). Although of only borderline statistical significance, there was also a negative association with being case-found rather than routinely diagnosed (adjusted β –0.69, 95% CI –1.44 to 0.07).
| Diagnosis | ||||
|---|---|---|---|---|
| Case-finding (N = 344) | Usual care (N = 188) | |||
| n a | % | n a | % | |
| Clinical assessment | ||||
| MRC dyspnoea score recorded | 98 | 28.5 | 171 | 91.0 |
| CAT score recorded | 36 | 10.5 | 94 | 50.0 |
| Spirometry undertaken | 48 | 14.0 | 79 | 42.0 |
| COPD severity recorded | 33 | 9.6 | 96 | 51.1 |
| BMI recorded | 244 | 70.9 | 168 | 89.4 |
| Oxygen saturations recorded | 41 | 11.9 | 55 | 29.3 |
| Chest X-ray undertaken | 13 | 3.8 | 9 | 4.8 |
| Depression screen undertaken | 54 | 15.7 | 55 | 29.3 |
| Clinical intervention | ||||
| Listed on COPD register | 78 | 22.7 | 175 | 93.1 |
| Care plan recorded | 38 | 11.0 | 97 | 51.6 |
| Annual review undertaken | 91 | 26.5 | 170 | 90.4 |
| Smoking cessation counselling provided | 157 | 45.6 | 139 | 73.9 |
| Nicotine replacement therapy | 27 | 7.8 | 17 | 9.0 |
| Influenza vaccination provided | 240 | 69.8 | 138 | 73.4 |
| Pneumococcal vaccine provided | 19 | 5.6 | 23 | 12.2 |
| Pulmonary rehabilitation provided | 17 | 4.9 | 42 | 22.3 |
| Inhaler technique assessed | 56 | 16.3 | 116 | 61.7 |
| Inhaler prescribed | ||||
| Salbutamol | 128 | 37.2 | 152 | 80.9 |
| Ipratropium | 5 | 1.5 | 10 | 5.3 |
| Salmeterol | 3 | 0.9 | 10 | 5.3 |
| Fluticasone | 3 | 0.9 | 1 | 0.5 |
| Budesonide | 0 | 0.0 | 0 | 0.0 |
| Beclometasone | 20 | 5.8 | 13 | 6.9 |
| Fluticasone/salmeterol | 33 | 9.7 | 70 | 37.2 |
| Budesonide/formoterol | 12 | 3.5 | 23 | 12.2 |
| Any of the above inhalers | 134 | 39.0 | 163 | 86.7 |
| Antibiotic rescue pack | 10 | 2.9 | 43 | 22.9 |
| Prednisolone | 51 | 14.8 | 96 | 51.1 |
| Clinical management score | ||||
| < 5 | 225 | 65.4 | 17 | 9.0 |
| 5 to 9 | 83 | 24.1 | 73 | 38.8 |
| ≥ 10 | 33 | 9.6 | 98 | 52.1 |
| Median (IQR) | 3 | 2–5 | 10 | 7–12 |
Self-reported questionnaire data were available for 375 out of 857 case-found patients. Only one-fifth of these patients were on the COPD register and, overall, one-third were aware of their diagnosis through their GP (88.5% of those on the COPD register vs. 17.5% of those not on the register). Around 45% had attended a COPD annual review, with the proportion being higher for those on the COPD register (83.3% vs. 34.7%). Factors associated with a higher clinical management score in this group were having a larger number of comorbidities (adjusted β 0.38,95% CI 0.10 to 0.65), higher COPD Assessment Test (CAT) score (adjusted β 0.05, 95% CI 0.01 to 0.08) and lower percentage of predicted FEV1 (adjusted β –0.03, 95% CI –0.04 to –0.01). Being on the COPD register was also significantly associated with a higher management score (adjusted β 3.48, 95% CI 2.81 to 4.15).
A proportionately high number of case-found patients with COPD were not added to practice COPD registers and these patients were less likely to receive recommended effective treatments for their condition. Overall, even those who were on the COPD register did not receive all recommended interventions, including smoking cessation advice or referral to pulmonary rehabilitation.
Strengths and limitations
This is one of the largest studies to evaluate the clinical management of screen-detected COPD patients in primary care. The lack of availability of EHR data on all trial participants was a limitation, and the validity of the EHR data is dependent on the clinical coding practices used. Nevertheless, the missing data are likely to be random, based on similarity of characteristics between those with and without data. Furthermore, the self-reported data from those who responded to questionnaires broadly verified the findings from health records.
Objective (v): to assess the long-term effectiveness of case-finding for chronic obstructive pulmonary disease on respiratory hospitalisations and mortality (work package 1v, manuscript in preparation) and objective (vi): to compare outcomes (including health-related quality of life) among screen-detected chronic obstructive pulmonary disease patients in primary care who were managed adequately by their general practitioner (based on the practice chronic obstructive pulmonary disease registers) with those who were not
Rationale
Since starting our programme of work, the UK National Screening Committee undertook a review to consider screening for COPD44,45 and the USPSTF updated their review. 46 Both recommended against screening for the time being, citing the need to establish evidence on clinical effectiveness of early identification before recommending systematic programmes for screening. The benefits of case-finding in improving health-related quality of life (HRQoL) and QALY gains has also not been previously studied.
Through our original trial, the infrastructure was in place to assess whether or not screening and early detection of COPD benefited patients in the longer term. We therefore sought a variation to the contract to extend follow-up and to link data on all patients who were part of the original trial with routinely available data. We obtained data on all eligible participants from NHS Digital on hospitalisations [through Hospital Episode Statistics (HES) data] and mortality, from the start of the trial until the last date available. We also sought approval from the National Research Ethics Committee and legal approval from the Confidentiality Advisory Group to obtain relevant patient identifiable data from GP practice records through an opt-out process and hold these temporarily to allow data linkage with the data obtained from NHS Digital. We were then able to compare outcomes among those who were in practices where active screening took place with those in the routine care arm practices (WP1v).
Additionally, to improve the input into the health economic model developed previously, we sought to obtain additional data on quality of life among screen-detected COPD patients some years after diagnosis and to compare outcomes among those who were managed in accordance with NICE guidelines with outcomes among those who were not.
What we did
Data on mortality and hospitalisations (all-cause and respiratory) were obtained for all eligible patients (who were alive at the start of the intervention, n = 74,693) from 54 participating practices in the TargetCOPD trial. Patient demographic data and information on whether or not the patient was on the practice QOF COPD register within 12 months of the trial were obtained from GP records. We also administered a questionnaire in 2017/18 to all case-found patients identified through the TargetCOPD trial to invite them to respond to questions on quality of life as well as their health and treatments received for COPD. Cox proportional hazard models, using random effects to account for clusters and adjusted for potential confounding factors, were used to model the time to event outcomes (death, first all-cause hospital admission and first respiratory hospital admission) in the intervention (active or targeted) and routine care arms. The time to event was censored at the death (for admission outcomes) or data extraction (30 September 2017 for hospital admissions and 13 October 2017 for deaths) if no event occurred. We also compared outcomes for the two intervention arms (active and opportunistic). Finally, for screen-detected cases, we compared mortality and hospitalisation as well as HRQoL measures [EuroQol-5 Dimensions (EQ-5D) and CAT scores] among those who were or were not added to the practice QOF register. Based on data from objective v, we used addition to the practice COPD register as a proxy measure for being better managed and treated for COPD. Analyses were adjusted for baseline values as well as for a range of potential confounders, including age, sex, ethnicity and baseline values for lung function, comorbidities and smoking status.
What we found
Among the 32,743 participants in the case-finding arms, 1557 had a respiratory hospitalisation compared with 1899 among the 41,950 participants in the routine arm over a mean follow-up period of 4.3 years [adjusted hazard ratio (HR) 1.04, 95% CI 0.73 to 1.47]. The corresponding HR for all-cause hospitalisation and mortality were 1.06 (95% CI 0.66 to 1.71) and 1.15 (95% CI 0.82 to 1.61), respectively, suggesting that, overall, there was no significant difference in risk of first hospitalisation and mortality between those who were in the screening arm compared with those in the routine care arm of the trial.
Within the two intervention groups in the case-finding arm there was no statistically significant difference between groups in terms of overall hospitalisations and mortality (adjusted HR 1.01, 95% CI 0.98 to 1.04, and adjusted HR 1.08, 95% CI 0.96 to 1.20, respectively). The adjusted HR for respiratory hospitalisation in the active group compared with the opportunistic group was 1.14 (95% CI 1.02 to 1.27), indicating an increased hazard of respiratory admissions in the former group (where yield from screening was higher).
Comparison of outcomes for screen-detected patients who were on the QOF COPD register with those who were not also showed no statistically significant difference in relation to all-cause hospitalisation (adjusted HR 0.86, 95% CI 0.66 to 1.11), respiratory hospitalisation (adjusted HR 0.95, 95% CI 0.52 to 1.73) and mortality (adjusted HR 1.06, 95% CI 0.53 to 2.12).
Thus, despite screening resulting in a higher yield of undiagnosed cases of COPD, there was no difference between those who were in practices with or without screening in terms of clinical outcomes at 4 years. The poor clinical management of COPD generally, and very low addition of case-found patients (particularly those with less severe disease) to the practice COPD register, may be an explanation for the findings. Given these results, we did not undertake a health economic analysis to examine cost per hospital admission avoided or cost per life-year saved.
In the adjusted analyses examining HRQoL, there was no statistically significant difference in EQ-5D scores between the two groups (adjusted mean difference –0.006, 95% CI –0.048 to 0.036). The adjusted mean CAT score was statistically significantly and clinically higher in those who were on the COPD register than in those who were not (mean difference 2.317, 95% CI 0.481 to 4.153), indicating a greater impact of COPD on their life and poorer quality of life. This difference is likely to reflect the more severe disease and characteristics of those who are added to the COPD register compared with those who are not, rather than being a result of how they were managed.
Strengths and limitations
To our knowledge, this is the first trial to report clinical outcomes from a large trial of screening for undiagnosed COPD. The trial was not powered to detect clinical outcomes because that was not the primary aim, but, nevertheless, it has provided reasonable effect estimates. The poor clinical management of people with screen-detected COPD limits the ability of detecting any potential benefits and thus the interpretation of findings. The low proportion of screen-detected patients being entered on the COPD register may explain the observed lack of effectiveness of screening.
Additional outputs and published analyses related to work package 1
The main TargetCOPD trial paper was disseminated more widely at respiratory conferences internationally and won the following awards:
-
Royal College of General Practitioners (RCGP) award for ‘best paper of the year 2016’ in Category 2 (CVD, Renal, Respiratory, Oral, ENT & Ophthalmology).
-
European Respiratory Society (ERS) best abstract in primary care 2015.
-
American Thoracic Society (ATS) best abstract Clinical Problems Assembly 2015.
-
Society for Academic Primary Care nomination for best abstract 2015.
Additional related papers include the following.
Jordan et al.47
This was the protocol for the TargetCOPD trial, outlining the rationale, methods and analysis plan.
Miller et al.48
In this analysis we used data from the TargetCOPD trial and compared how the application of two different definitions of airflow obstruction would impact on the clinical characteristics of the population who would be labelled as having COPD. The definition used in the trial was based on the ratio of FEV1/FVC < 0.7 [the fixed ratio (FR)], which is recommended by NICE. The second definition was based on using the lower limit of normal (LLN) that is increasingly being recommended. We found that, among 2607 people who attended for spirometry, around one-third had airflow obstruction using the FR definition compared with 20% using the LLN definition. There was overlap between the two groups. However, those identified by the FR and not the LLN definition were older, had better lung function and fewer respiratory symptoms, but had a higher rate of heart disease. Overall, we demonstrated that using the FR rather than LLN identifies a greater proportion of individuals with cardiac, rather than respiratory, clinical characteristics.
Haroon et al.49
This analysis used data from the TargetCOPD trial to develop a validated algorithm and risk score to target case-finding on those at highest risk of undiagnosed COPD and thus improve the efficiency of any future case-finding process. Although other COPD risk scores have been developed, this was the first that was based on identifying case-found COPD (rather than incident clinical COPD diagnosed through routine care) and is therefore more useful in the context of case-finding in primary care.
Haroon et al.50
In this analysis we used a case–control study design to match incident COPD cases from 340 GP practice registers (using the UK Clinical Practice Research Datalink) to two controls (based on age, sex and practice). Predictive risk factors for COPD were identified from practice records and used to develop a clinical risk score. The risk score was validated using a sample from a further 20 practices. The model, including smoking status, history of asthma and lower respiratory tract infections, and prescription of salbutamol in the previous 3 years, resulted in reasonable prediction (c-statistic 0.85, 95% CI 0.83 to 0.86).
Haroon et al.51
This systematic review (based on studies from 1997 to 2013) summarised the uptake and yield from different approaches to screening for undiagnosed COPD in primary care. Data from three RCTs, one non-randomised trial and 35 uncontrolled studies showed that all approaches result in identification of new undiagnosed cases. The review suggested that targeting higher-risk individuals (e.g. smokers) and using questionnaires or handheld flow meters prior to diagnostic screening was likely to increase yield. However, it also highlighted the need for well-conducted RCTs.
Haroon et al.52
This review compared the diagnostic accuracy of different COPD screening tests in primary care. A total of 10 studies were identified from 1997 to 2013 and included use of screening questionnaires [mainly the COPD Diagnostic Questionnaire (CDQ)], handheld flow meters [e.g. the copd-6 (Vitalograph Ltd, Buckingham, UK)] or a combination. Handheld flow meters demonstrated higher test accuracy than questionnaires but the review highlighted the need for high-quality evaluation of comparative screening strategies.
Work package 2: the Birmingham primary care chronic obstructive pulmonary disease cohort
Objective (i): to recruit a cohort of 2000 new and existing chronic obstructive pulmonary disease patients from general practices in the West Midlands (work package 2, linked to work package 1, published)53
Rationale
The natural history of COPD is still not understood, and several expert reviews have highlighted a need to further investigate both old and new longitudinal data. 5,15 Prior to this programme, a number of relevant COPD disease cohorts had been established,54–56 but these included patients with more advanced disease from secondary care settings, with short duration of follow-up, and were mainly of small size. Other large population cohorts have also been used to address questions relevant to COPD. 57–60 However, because these were not specifically set up to address COPD, not all relevant measures were undertaken and the quality of lung function was not always prioritised. There were no UK primary care COPD cohorts with patients representing the range of disease severity, particularly including people with mild/moderate disease, or a diverse socioeconomic mix. Furthermore, existing cohort studies included neither people with COPD who were identified through case-finding nor patients reporting respiratory symptoms but who had normal lung function [former Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 0]. 61 The evidence on progression to COPD in the latter group is limited and contradictory,62–64 and methods for assessing symptoms are inconsistent. 62,65 The clinical relevance and natural history for this patient group and screen-detected cases are unclear.
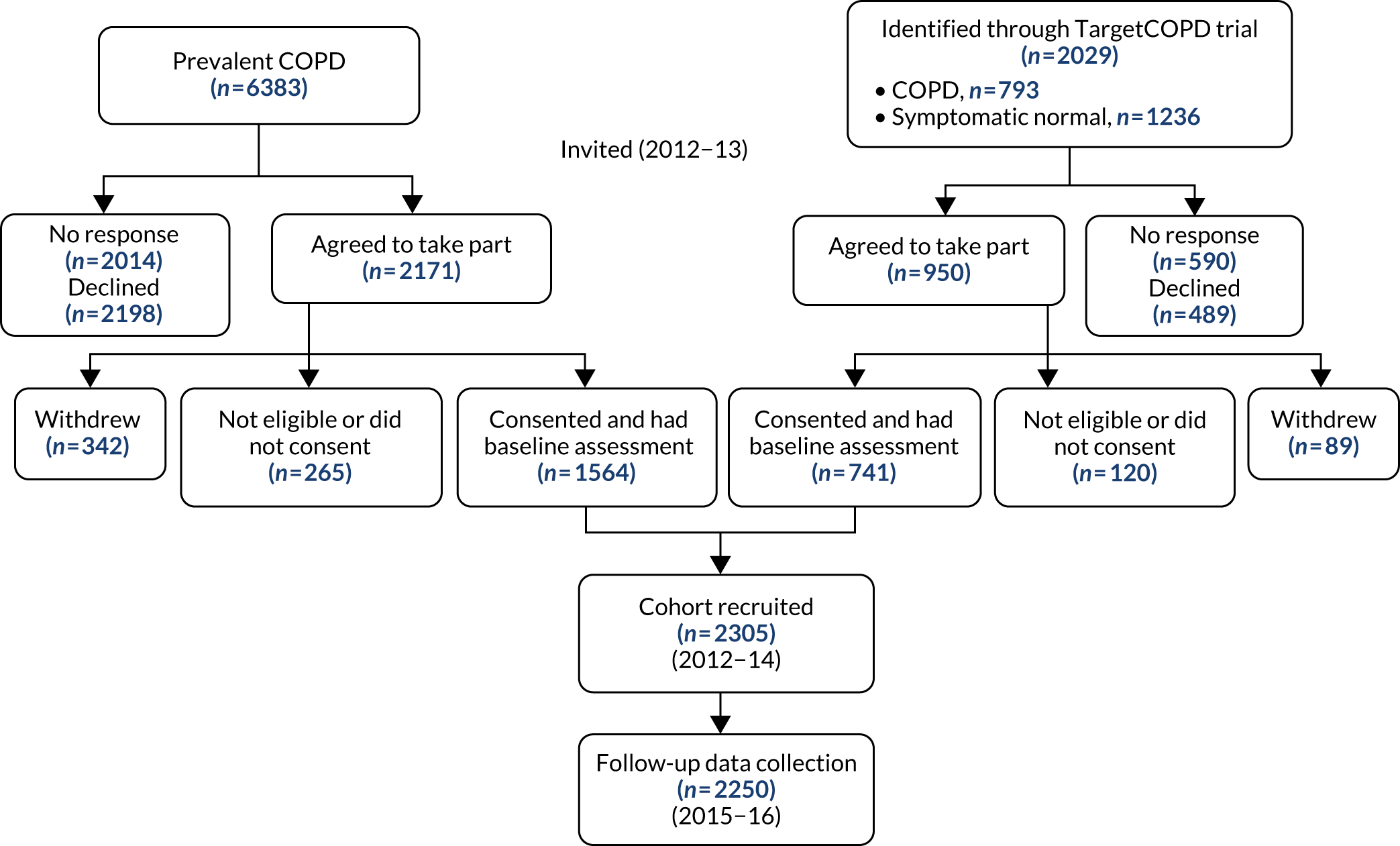
What we did
We recruited 2305 patients aged ≥ 40 years from 71 practices across the West Midlands (Figure 3), comprising 1564 patients with previously diagnosed COPD, 330 previously undiagnosed patients with respiratory symptoms and airflow obstruction confirmed by spirometry (case-found COPD) and 411 symptomatic patients with normal lung function confirmed by spirometry. 53
FIGURE 3.
Flow chart of patient recruitment and assessment for the Birmingham COPD cohort study.
Baseline assessments were undertaken by trained researchers using standardised protocols between 2012 and 2014 (Figure 4). Assessments included high-quality pre- and post-bronchodilator spirometry using an ndd EasyOne® spirometer (ndd Medizintechnik AG, Zurich, Switzerland). Other measurements included height and weight, body fat percentage estimation using the Tanita BC-420SMA Body Composition Analyser (Tanita Europe BV, Amsterdam, the Netherlands), assessment of grip strength using a Saehan Hydraulic Hand Dynamometer (Saehan Corp., Masan, Republic of Korea) and assessment of exercise capacity using the sit-to-stand test. In addition, trained researchers used face-to-face interviews to obtain occupational history. Information on skill content of occupations was used to assign a four-digit standard occupational classification (SOC2010)66 code for current or main occupation using the CASCOT (computer assisted structured coding tool) software (online version, Office for National Statistics, Newport, UK).
FIGURE 4.
Cumulative number of cohort participants recruited and having baseline assessments by month.

Participants were also asked to complete questionnaires that sought data on demographic characteristics, lifestyle (smoking history and exercise habits), symptoms, exacerbation history, general health, diagnosed medical conditions, health-care usage and the home environment (see Appendix 3). HRQoL was assessed using disease-specific (CAT)67 and generic (EQ5D)68 instruments, and the Patient Health Questionnaire-9 (PHQ-9)69 instrument was used to screen for depression. Work productivity was assessed through questions on work absence and presenteeism using the Stanford Presenteeism Scale (SPS-6)70 and the Work Productivity and Activity Impairment questionnaire (WPAI). 71
At 6-monthly intervals, patients were sent follow-up questionnaires by post. All follow-up questionnaires included items on employment, general health, lung health, exacerbations, new diagnoses, attendance at pulmonary rehabilitation, health-care utilisation, smoking history, medications, depression and HRQoL. Some questionnaires included additional items, which are summarised in Table 2.
| Questionnaire | Special items in questionnaire | Response rate (%) |
|---|---|---|
| 6 months | Self-management, exercise, COPD knowledge, major events | 73.0 |
| 12 months | Major events | 67.6 |
| 18 months | Handwashing, diet | 69.2 |
| 24 months | Self-management, handwashing, exercise, self-efficacy | 66.1 |
| 30 months | Pain symptoms, fatigue | 62.8 |
| Follow-up assessment | Exercise, smoking cessation, e-cigarette use, major events, sleep, vitamin use | 88.3 |
| Supplementary | Anxiety, illness perception, self-perception | 78.8 |
Patients were invited for a final assessment visit around 3 years after baseline (2015–16). In addition to post-bronchodilator spirometry, other baseline assessment measures and questionnaires were repeated. Cohort participants’ routine data on comorbidities and medications were extracted from GP records. Linked data on hospital episodes and mortality were also obtained from NHS Digital for the period 1 April 2012 to 31 March 2016.
Establishment of this cohort allowed important questions of relevance to patient benefit to be addressed (WP2i).
What we found
Follow-up data were available for 2250 patients (97.6%), and almost two-thirds (1469, 63.7%) returned for face-to-face follow-up assessment. Six-monthly questionnaires were completed by around two-thirds of patients (62.8–73.0%; see Table 2). In the initial 2 years of follow-up, 267 (12%) patients had at least one respiratory-related hospital admission, based on HES data. Over the entire period of follow-up (minimum 1.8 years, maximum 3.8 years), 382 patients (17%) had at least one respiratory hospital admission and 170 (7%) had died at the time data were obtained from NHS Digital.
Strengths and limitations
We established one of the largest primary care COPD cohorts, which is novel in that it includes case-found patients. A limitation was that fewer than one-third of case-found patients agreed to join the cohort. Our recruitment strategy resulted in an over-representation of patients with less severe disease because patients had to be ambulatory. Despite attempts to include patients from diverse ethnic backgrounds, the majority were white.
Objective (ii): to test the validity of existing chronic obstructive pulmonary disease prognostic models in a primary care chronic obstructive pulmonary disease population (work package 2, published);72 and objective (iii): to develop a prognostic model (BLISS index) to predict respiratory hospitalisations suitable for a primary care population (work package 2, drafted, see Appendix 4)
Rationale
A better understanding of factors predicting prognosis and the development of a prognostic model can facilitate doctor–patient consultations and inform management decisions and health service planning. For COPD, a simple measure of lung function, FEV1, has historically been used to grade severity. However, there is increasing recognition that this measure is not a good predictor of clinical outcomes. Alternative measures of lung function may improve diagnostic73 and prognostic ability. 74,75
A number of studies have also described a range of factors other than lung function that are associated with COPD progression, deriving prognostic indices. The first [BODE (body mass index, airflow obstruction, dyspnoea, and exercise) index] was developed to predict mortality risk in those with COPD. 56 However, the method of development was not clear, its validity has not always been confirmed and not all measures are practical in non-specialist settings. 76 Since then, several other prognostic models have been developed and, since we started the programme, a number of systematic reviews have been undertaken to summarise these. 77–79 The reviews show that existing prognostic models are heterogeneous in terms of the number and type of predictors, the prognostic outcome, time horizon and statistical approach. Most focus on predicting mortality risk,56,76,80–82 although others were developed to predict additional outcomes such as exacerbations,83,84 COPD-related hospitalisation,85 respiratory hospital attendance/admission86 and exacerbation or hospitalisation. 87,88 Only three indices84,87,88 were derived from primary care populations, despite this being where most COPD patients are managed, and most included patients with more severe established disease. No models were developed in populations that included case-found patients. Few studies were validated or used recommended statistical approaches for deriving the model.
The most recent review showed that the ADO index was most discriminatory in predicting mortality. 78 For a prognostic model to be used by clinicians, it needs to be simple and capture the required patient data with minimum resource;89 the ADO index fulfils these criteria. We therefore undertook validation of the ADO index for mortality within our cohort (WP2, objective ii).
However, in relation to predicting respiratory hospitalisation, which is an important outcome to consider, current models have moderate discriminative ability. This suggests that other relevant predictors are missing from these prognostic models. We therefore derived a new COPD prognostic model, the BLISS index, for use in a primary care population (with 2-year respiratory hospitalisation as primary outcome and all-cause hospitalisation, exacerbations, primary care consultations and mortality as secondary outcomes), using recommended statistical techniques (WP2, objective iii, draft paper; see Appendix 4).
What we did (objective ii)
We validated the ADO index using data from 1701 patients from the Birmingham COPD cohort study (case-found or on the practice COPD register) who had complete data for the variables required for this study. We externally validated the ADO index for predicting 3-year mortality, with 1- and 2-year mortality as secondary end points. Discrimination was calculated using area under the curve (AUC), also known as the c-statistic, and calibration was assessed using a calibration plot with locally weighted scatterplot smoothing (LOWESS) and measures such as the calibration slope. In sensitivity analyses, we included only patients with existing COPD and those with complete data.
What we found (objective ii)
The ADO index was discriminatory for predicting 3-year mortality (c-statistic 0.74, 95% CI 0.69 to 0.79), with similar discriminatory ability for 1- and 2-year mortality (c-statistic 0.73, 95% CI 0.66 to 0.80, and c-statistic 0.72, 95% CI 0.67 to 0.76, respectively). The ADO index overpredicted mortality at each time point, which was more pronounced at 1- and 2-year mortality time points (calibration slopes 0.95, 0.79 and 0.79 for 3-, 2- and 1-year mortality, respectively) and in those with higher baseline ADO scores. Thus, although the ADO index shows promising discrimination in a primary care population, the model may need to be recalibrated if the ADO index is used to provide well-calibrated risk predictions for 1- or 2-year mortality. Discrimination and calibration were similar in sensitivity analyses.
What we did (objective iii)
To develop and internally validate a new prognostic model in primary care to predict respiratory hospital admissions within 2 years, we linked self-reported and clinical data for all patients with COPD from the Birmingham COPD cohort (331 case-found and 1558 previously diagnosed) with routine HES obtained through NHS Digital. The primary outcome for the prognostic model was the occurrence of a respiratory-related hospital admission (using primary diagnostic codes) from entry to the cohort study up to 2 years (May 2012 to June 2014). Secondary analysis considered outcomes during the full period until the NHS Digital data were obtained (1 April 2016). The maximum follow-up time was around 4 years.
A list of 23 candidate variables was drawn up based on those included in other models for COPD, along with other variables identified by a consensus panel comprising study investigators, clinicians and patients. The degree of airflow obstruction was deemed clinically important but, owing to the documented statistical problems with the commonly used FEV1% predicted (FEV1 as a percentage of what would be predicted as normal),75 the best variable to be included in the model was not clear. We therefore tested three variables as candidate predictors in the model [FEV1% predicted, forced expiratory volume in 1 second quotient (FEV1Q), and FEV1/height2]. With 267 events for the primary outcome, up to 26 candidate variables could be used, based on the rule of thumb of 10 events per candidate variable. 90
The model was developed using backward elimination with p < 0.157 for retention. Fractional polynomials were considered and multiple imputation using chained equations was used for missing data. Discrimination was assessed using the c-statistic and calibration was also assessed. Bootstrapping was used for internal validation and the optimum-adjusted performance statistics were presented. A sensitivity analysis was conducted using only those with previously diagnosed COPD.
What we found (objective iii)
Over a median follow-up of 2.9 years (range 1.8 to 3.8 years), 382 participants (16%) had a respiratory admission and 267 (12%) had a respiratory admission in the primary 2-year period. Participants with hospitalisations were more likely to be older (70.3 vs. 67.0 years; p < 0.001), be male (66% vs. 59%; p = 0.017), be more deprived [median Index of Multiple Deprivation (IMD) score of 30.3 vs. 24.4; p = 0.0025], have a lower body mass index (BMI) (mean 28.2 vs. 28.8 kg/m2; p = 0.108), have more severe airflow obstruction (mean FEV1% predicted 56.5% vs. 75.2%), have worse dyspnoea [Medical Research Council (MRC) dyspnoea grade 3 57.5% vs. 51%; p < 0.001] and have worse quality-of-life scores (median CAT score 24 vs. 17; p < 0.001). They were more likely to report previous exacerbations based on the use of antibiotics or steroids (60% vs. 43%; p < 0.001) and to report previous hospitalisations in the previous 12 months (18.4% vs. 2.6%; p < 0.001). Participants with hospitalisations were also more likely to report a higher rate of vapours, gases, dusts or fumes (VGDF) (71% vs. 62%; p = 0.004), to report exposure to smoking (31% vs. 27% current smokers; p = 0.019) and to have diabetes (24% vs. 15%; p = 0.001) and cardiovascular disease (20% vs. 15% with coronary heart disease; p = 0.049).
Using a pragmatic approach to model development, and including only variables that are widely available or feasible to obtain in primary care, six variables were retained in the final developed model: age, CAT score, respiratory admissions in the previous 12 months, BMI, diabetes and FEV1% predicted. After adjustment for optimism, the primary model performed well in discriminating between those who will and those who will not have 2-year respiratory admissions (c-statistic 0.75, 95% CI 0.72 to 0.79). Four further variables were included in the secondary analysis but had similar score performance. Sensitivity analysis with prevalent COPD cases resulted in an identical apparent c-statistic but included smoking status in addition to the six variables in the primary model. Overall, the BLISS score may perform better in predicting respiratory admissions than the scores currently available, but further research is required to compare this model with existing ones in other data sets. Important next steps are external validation, proposing and evaluating a model of use to guide patient management, and exploration of the best ways to implement such a score in primary care practice.
Strengths and limitations
We used recommended and up-to-date approaches for our validation study and model development, overcoming limitations of previous studies. Using data from a research cohort (the Birmingham primary care COPD cohort) meant that measurements were of high quality and undertaken at prescribed time points. However, the cohort population may not be fully generalisable to primary care because patients with more severe disease who were housebound were excluded. Including screen-detected patients was a strength and limitation but sensitivity analyses excluding these patients did not substantially alter the findings. For model development, although the variable components for the score are relatively simple, these may not be routinely collected or available, and calculation of the score requires software.
Objective (iv): to explore barriers to and enablers of participation in physical activity among people with chronic obstructive pulmonary disease in primary care (work package 2, published)91
Rationale
Although the majority of people with COPD who are likely to be detected through case-finding could be offered evidence-based interventions, there are few effective interventions for those with milder disease. One intervention that has received increasing interest is exercise. Observational studies have reported an association between higher PA levels and lower morbidity92–94 across the full range of COPD severity. Exercise is the cornerstone of pulmonary rehabilitation programmes (PRPs), which have been shown to have a positive impact on COPD symptoms and prognosis. 95 However, PRP provision is limited and uptake is low. 96 To better understand the motivation for PA engagement among people with COPD in the community, we explored perceived barriers and facilitators among people with COPD using the framework from social cognitive theory.
What we did
A purposive sample of 26 patients (age range 50–89 years; men, n = 15) from the Birmingham COPD cohort study, with a range of COPD severity, was recruited to participate in one of four focus groups. Thematic analysis was undertaken to identify key concepts related to their self-efficacy beliefs.
What we found
Several barriers to and enablers of PA closely related to self-efficacy beliefs and symptom severity were identified. The main barriers were health-related (fatigue, mobility problems, breathing issues caused by the weather), psychological (embarrassment, fear, frustration/disappointment), attitudinal (lack of feeling in control of their condition, disregard of PA benefits, older age perception) and motivational. The main enabling factors were related to motivation (PA as part of caring duties, deriving enjoyment from activity or the social aspects), attitudes (positive view of PA), self-regulation (e.g. keeping to a routine) and performance accomplishments (sense of achievement in fulfilling personal goals). This information can help to tailor management of people with COPD.
Strengths and limitations
The use of social cognitive theory in this study was novel, and allowed the identification of personal barriers related to perceptions, motivation and attitudes towards physical activity, which went beyond the external barriers identified in previous studies. This understanding can inform interventions that have the potential to improve attendance and adherence. Furthermore, by including distinct subgroups of patients, we identified context-specific factors, such as barriers specific to those who are in paid employment, thereby informing the tailoring of future interventions.
However, the study participants predominantly had mild to moderate COPD and so the findings may not reflect the views of those with more severe disease. Furthermore, the voluntary nature of participation may have meant that the views of some who were less interested in PA were not included. The emergence of themes may also have been influenced by the use of social cognitive theory, and potentially different themes might have dominated had a different theoretical framework been used.
Other collaborations and analyses of cohort data
One of the aims of establishing a cohort was to allow it to become a platform for testing other hypotheses and interventions. As a result, several groups, including postgraduate students and other collaborators, worked with us to introduce discrete questions in some of the follow-up questionnaires or undertook analyses from the data collected for the cohort study. The main substudies are described below.
Cohort data used for analyses leading to a PhD thesis: Buni97
Rationale
There has long been uncertainty about the nature and prognosis of people with chronic respiratory symptoms who do not yet meet the accepted airflow obstruction criteria for COPD. 98 In 2001, the GOLD committee included an additional ‘at-risk’ stage in the description of COPD patients with a view to considering early interventions. Patients in this stage (known as GOLD stage 0) were thought to be ‘at risk’ of developing COPD in the future. 61 However, in 2006, GOLD stage 0 was removed from the classification owing to a lack of supporting evidence regarding progression to diagnosed COPD. Nevertheless, there remain many patients (particularly smokers) in the population with such symptoms; some patients even carry a formal diagnosis of COPD and are therefore potentially ‘overdiagnosed’. It is debated whether these patients represent a group with ‘pre-clinical’ COPD or if they have other conditions that explain their symptoms. We undertook a range of primary and secondary data analyses to help answer these questions.
What we did
We undertook three linked systematic reviews to identify and assess published studies that (1) examined the risk of developing COPD among GOLD stage 0 patients compared with the normal population, (2) examined the prognosis of GOLD 0 patients compared with established COPD patients and/or (3) evaluated factors that affected the prognosis of GOLD 0 patients. The primary studies included analysis of (a) data from the 2010 Health Survey for England (HSE)99 to evaluate the independent effect of respiratory symptoms by airflow obstruction on quality of life, (b) cross-sectional data from the Birmingham COPD cohort study to compare the characteristics and health outcomes of GOLD 0 patients with newly diagnosed (case-found) COPD patients who had airflow obstruction and (c) cross-sectional data from the Birmingham COPD cohort study to compare the characteristics and health outcomes of people on the GP COPD register who did not have airflow obstruction (overdiagnosed) with those of people who had spirometric obstruction.
What we found
The systematic reviews revealed very few published studies evaluating the prognosis of people with GOLD 0 symptoms, and the studies that were found were heterogeneous in design, populations and outcomes. A tentative conclusion was that those with GOLD 0 symptoms may show faster decline in FEV1 than the normal population, but the risk of developing COPD was not consistent. Persistent GOLD 0 symptoms may be an important predictor of development of COPD and FEV1 decline. Persistent symptoms were associated with continued smoking and, in some studies, the presence of metabolic syndrome. GOLD 0 patients had similar risks of mortality to GOLD 1 patients, and those who were current smokers had similar risks to GOLD 2 patients. GOLD 0 patients often had similar health-care use to established COPD patients.
The HSE analyses revealed a gradient of effect on quality of life from ‘normal’ to those with COPD. Asymptomatic patients with airflow obstruction only were much more similar to ‘normals’, and those with GOLD 0 were more similar to those with both symptoms and airflow obstruction (i.e. defined as COPD). Dyspnoea and wheeze were more strongly associated with poor quality of life than chronic productive cough.
Analyses of the Birmingham COPD cohort showed that GOLD 0 patients had similar consumption of health-care resources to those newly identified with COPD, additionally indicating similar quality of life, exercise capacity and exacerbation-like events in these two groups. GOLD 0 patients were more likely to be female, to be obese and to have multiple comorbidities (e.g. cardiovascular disease, hypertension, diabetes and depression) than diagnosed COPD patients, but they were not more likely to have either diagnosed or undiagnosed asthma (assessed using GOLD/ATS definition of bronchodilator reversibility; a change of > 12% of baseline FEV1 if this exceeds 200 ml). Overall, 10% had reversible airflow obstruction suggestive of asthma.
Overdiagnosed COPD patients (≈14% on UK COPD registers) were also more likely to be female, to have never smoked and to be obese (19% had restrictive pattern disease) and were slightly more likely to have multiple comorbidities. Around 20% of these patients had spirometric abnormalities consistent with restrictive lung disease. Their quality of life, exacerbation history, exercise capacity and health-care utilisation were very similar to those of GOLD 0 patients.
In conclusion, the presence of respiratory symptoms is epidemiologically and clinically relevant. GOLD 0 patients have similar poor quality of life and health-care consumption to those with mild COPD. It is still uncertain whether this group will develop COPD or if they are ill because they have other conditions. It is also possible that spirometric criteria for defining COPD need to be reconsidered. Future longitudinal studies are needed to further investigate GOLD stage 0 and to inform management guidelines that may include earlier interventions. This is important to help improve patients’ quality of life, reduce the risk of misdiagnosis and reduce inappropriate health-care resource use.
Collaboration with Professor Mike Thomas from the University of Southampton: Brien et al.100
This analysis explored demographic factors, lung function/COPD-related symptoms and psychosocial/behavioural factors associated with quality-of-life impairment (using COPD CAT scores) in people with COPD. In a multivariable model, we showed that dyspnoea, illness perception, dysfunctional breathing symptoms and depression explained most of the impairment in quality of life. Thus, interventions targeting psychological factors could improve outcomes in people with COPD.
Linked trial funded through the NIHR National School of Primary Care Research: Jolly et al.101
This trial was a modification of a WP in the original programme grant, with additional funding. Overall, 577 people with earlier-stage COPD (MRC dyspnoea grade 1 or 2) were recruited from general practices (2014–15). Participants were randomised to a nurse-delivered telephone health coaching intervention (smoking cessation, increasing PA, medication management and action-planning) or usual care. Compared with usual care, participants in the intervention group reported significantly greater PA at 6 months.
Dickens et al.102
We obtained additional funding from the National Institute for Health Research (NIHR) School of Primary Care Research to undertake a linked study to assess the accuracy of microspirometry as a screening tool for undiagnosed COPD. The relevant measurements were undertaken during cohort participants’ visits. We compared lung function measures obtained from the Vitalograph® (Vitalograph Ltd, Buckingham, UK) lung monitor with post-bronchodilator confirmatory spirometry. We found that the optimal cut-off point for the lung monitor was a FEV1/FEV6 of < 0.78, resulting in sensitivity of 82.8% (95% CI 78.3% to 86.7%) and specificity of 85.0% (95% CI 79.4% to 89.6%).
Cohort data used by Master of Public Health students: Khan et al.103
In this analysis, the extent of self-management behaviour and support reported by cohort participants was described. The majority of 1078 responders reported taking medications as instructed and receiving annual influenza vaccinations. However, only 40% had self-management plans and half reported never having received advice on diet/exercise. Fewer than half of current smokers had been offered help to quit in the previous year. Having a self-management plan was associated with better medication adherence and better disease knowledge.
Cohort data used as part of a PhD thesis: Kosteli104
One chapter is dedicated to the focus groups exploring the views of COPD patients on PA.
Work package 3: chronic obstructive pulmonary disease and occupational performance
Objective (i): to examine factors associated with employment (published), absenteeism and presenteeism (published) among COPD patients of working age (work package 3)105,106
Rationale
Among those with COPD in the UK, approximately 40% are below retirement age; of these, 25% are not able to work. 107 Among those who continue to work, COPD is likely to affect work capability through sickness absence (9% of all certified absences) and working while unwell (presenteeism). 108 Data from other countries suggest that people with COPD (including undiagnosed109 and mild disease110) have a poorer employment history and retire earlier than people with normal lung function,111 but there were no data quantifying this in the UK, and no studies to examine presenteeism or productivity among working adults with COPD. Indirect societal costs attributable to COPD (largely owing to absenteeism) are high. Studies based on other conditions suggest that presenteeism costs may exceed those associated with absenteeism. 112 Few studies have examined which factors among people with COPD are associated with lower employment and work productivity. This information could inform future interventions, which could, in turn, improve patients’ work experience, thereby reducing the burden and societal costs related to COPD.
What we did
We undertook cross-sectional analysis of baseline data of patients from the Birmingham COPD cohort who were of working age. We compared the characteristics of those who were in paid employment with those who were not. Logistic regression analysis was used to assess the effects of sociodemographic, clinical and occupational characteristics on the likelihood of being employed. Using the subsample in paid employment, we examined characteristics associated with absenteeism (defined by self-report over the previous 12 months) and presenteeism (assessed using the Stanford Presenteeism Scale).
What we found
Among the 1889 people in the cohort who had COPD, 608 were of working age, of whom 248 (40.8%) were in work. Older age (60–64 years vs. 30–49 years: OR 0.28, 95% CI 0.12 to 0.65), lower educational level (no formal qualification vs. degree/higher level: OR 0.43, 95% CI 0.19 to 0.97), poorer prognostic score [highest vs. lowest quartile of modified BODE score: OR 0.10, 95% CI 0.03 to 0.33] and history of high occupational exposure to VGDF (high VGDF vs. no VGDF exposure: OR 0.32, 95% CI 0.12 to 0.85) were associated with a lower probability of being employed. Only the degree of breathlessness component within the BODE score was significantly associated with employment. Among those who were in paid employment, degree of breathlessness was the only factor associated with both absenteeism (high absenteeism in severe vs. mild dyspnoea: OR 1.84, 95% CI 0.54 to 6.27; p < 0.01) and presenteeism (working while unwell in severe vs. mild dyspnoea: OR 18.11, 95% CI 2.93 to 112.21; p < 0.01). Additionally, increasing history of occupational exposure to VGDF was independently associated with presenteeism (poor presenteeism in medium/high exposure vs. no exposure: OR 4.34, 95% CI 1.26 to 14.93; p < 0.01).
Based on these findings, future interventions should focus on managing breathlessness and reducing occupational exposures to VGDF to improve work capability among those with COPD.
Strengths and limitations
The inclusion of a wide range of patients with COPD from primary care, including case-found patients, was novel. The assessment of occupation in detail and linking with a job exposure matrix to estimate VGDF exposure was a strength. However, overall, the sample of participants in paid employment was small and the wide CIs for several estimates suggest that there was insufficient power to clarify associations. We did not have objective measures of absenteeism and some other measures were also based on self-report, which may introduce errors.
Objective (ii): to examine how disease progression (lung function decline, exacerbation) over time is associated with occupational performance (employment, absenteeism and presenteeism) among chronic obstructive pulmonary disease patients in employment (work package 3, manuscript in preparation)
Rationale
The burden of COPD on the working population is high. The relationship between sickness and disability and unemployment is poorly understood and could be better informed by longitudinal follow-up. A number of factors, including sociodemographic characteristics, the general economic environment and the severity of chronic disease, have an impact on employment and an individual’s ability to work. We undertook longitudinal analysis to examine how disease progression is associated with occupational outcomes, adjusting for clinical, sociodemographic, occupational and labour market factors.
What we did
We used data collected during the follow-up period for those with COPD in the Birmingham COPD cohort study. Participants completed a series of questionnaires at baseline, providing information on their demographics, socioeconomic circumstances, health, lifestyle and occupation. At 6-monthly intervals they completed further questionnaires, reporting on changes in employment and, for those in paid employment, completed questions on presenteeism and absenteeism. Trained research assistants collected clinical information at two face-to-face assessments (baseline and the final follow-up), which included spirometry. We undertook longitudinal analyses, including participants who were in paid employment at baseline.
Four markers of disease progression were assessed: FEV1 (no or limited decline vs. greater decline), number of respiratory-related hospital admissions, breathlessness (no increase vs. increase in MRC score) and symptom impact (no increase vs. increase in CAT score).
For the primary analyses, decline in FEV1 was based on the following thresholds (comparing baseline spirometry values with those at the final follow-up): > 113.3 ml per year in men and > 90.1 ml per year in women. These were based on the upper limit of normal decline rates in FEV1 described in healthy adults. 113 Respiratory-related hospital admissions was calculated as the number of admissions during the study follow-up (continuous data). The minimal clinically important difference (MCID) for the MRC respiratory questionnaire (1-point increase)114 was used to define worsening breathlessness, where MRC scores were compared at two time points (baseline and final follow-up for each outcome measure). Additionally, the MCID value for the CAT score was used to define worsening symptom impact. However, because this varies in the current literature,115 two analyses were conducted. The primary analysis was based on an increase of < 2 or ≥ 2 points at the final follow-up.
Multivariable regression analyses were conducted to examine the effects of disease progression on each of the outcomes, adjusting for age, sex, educational attainment, social deprivation (using the IMD derived from participant home postcode), MRC score, GOLD staging, occupational exposure to VGDF in current job at baseline visit (paid employment and presenteeism analyses) and number of hours worked at baseline (absenteeism analysis).
What we found
Among the 248 participants with COPD who were in paid employment at baseline, follow-up data were available for 174 (70.2%). Among those who were followed up, 144 (82.8%) remained in paid employment and 30 (17.2%) who had initially been in paid employment became unemployed. The mean length of follow-up was 25.8 months [standard deviation (SD) 5.8 months].
Our point estimates were suggestive of an association between increasing number of respiratory-related hospital admissions (OR 0.32, 95% CI 0.09 to 1.14; p = 0.08), decline in FEV1 (OR 0.64, 95% CI 0.11 to 3.71; p = 0.62) and worsening MRC dyspnoea score (OR 0.62, 95% CI 0.19 to 2.06; p = 0.44) and reduced probability of remaining in paid employment, but CIs were very wide and no firm conclusions were possible. We found no associations between worsening symptom impact (CAT score) and reduced probability of remaining in paid employment.
Prospective absenteeism data were available for 113 (59.8%) participants, with a mean length of follow-up of 19.5 months (SD 5.3 months). Among this group, 63 (55.8%) reported taking > 1 day off over the follow-up period. Absenteeism ranged from 0.5 to 180.0 days per year [mean 16.3 days off per year (SD 28.9 days off per year); median 6.0 days off per year (IQR 2.7–5.5 days off per year)]. In the total cohort population, the mean and median days off per year were 9.0 (SD 23.0) and 1.5 (IQR 0.0–7.0), respectively.
Worsening breathlessness [incidence rate ratio (IRR) 3.06, 95% CI 1.29 to 7.26; p = 0.01] and respiratory hospital admissions (IRR 2.01, 95% CI 1.09 to 3.69; p = 0.03) were associated with an increased risk of sickness absence duration, and point estimates suggested that worsening symptom impact (CAT score) might also have an effect, although CIs were wide. Associations between FEV1 decline and sickness absence duration were not observed.
Follow-up data on presenteeism were available for 163 (86.2%) participants, among whom 43 (26.4%) had worsening presenteeism. Worsening presenteeism was significantly associated with worsening CAT score (OR 5.74, 95% CI 1.18 to 27.83; p = 0.03) and may be associated with worsening MRC dyspnoea score (OR 2.25, 95% CI 0.76 to 6.68; p = 0.14). No strong evidence of any patterns were observed between FEV1 decline or respiratory-related admissions and worsening presenteeism.
In summary, disease progression, characterised by a greater number of respiratory hospital admissions (proxy for severe exacerbations) and worsening symptoms, may be associated with poorer work productivity. We did not find any associations between physiological decline, measured by increase in airflow obstruction, and occupational outcomes. Given the wide CIs, further research is needed to increase power to detect genuine associations.
Strengths and limitations
Although participants were drawn from a population with a wide range of sociodemographic, clinical and occupational characteristics, the analyses were based on a small sample size, resulting in low power and lack of precision for many estimates. The observed associations raise hypotheses for future research and have to be interpreted with caution. The length of follow-up (2.5 years on average) may be insufficient for observing a decline in lung function, and cut-off points for abnormal decline are not agreed. The study included an older working population and, therefore, a healthy worker survivor effect might apply.
Objective (iii): to assess the feasibility and benefits of offering formal occupational health assessment and subsequent recommendations aimed at improving work-based indices to people with chronic obstructive pulmonary disease in employment (work package 3, published PhD thesis)116
Rationale
A UK government report focused on the need to support individuals of working age to remain in or to return to employment from sickness absence. 117 The report made a number of recommendations, including the need for early workplace interventions, improved access to OH services and changes in sickness certification from ‘sick’ to ‘fit’ notes. 118 The feasibility and effectiveness of early workplace interventions to support people with COPD with poor work performance has not been assessed.
What we did
Within the Birmingham COPD cohort, we invited all those who were in paid employment at baseline to a tailored assessment with an OH practitioner to explore and identify workplace factors that might negatively affect their work performance or exacerbate their condition, and to recommend appropriate modifications. Participants’ self-management practices were also assessed. Recommendations were sent to the participant and, with their permission, to their GP and their employer. We examined acceptability (uptake of intervention and recommendations and exploration of participant views) and feasibility (proportion with recommendations and uptake) of the intervention.
What we found
Only 35 (11.3%) eligible patients agreed to take part; 109 (35.3%) declined and 153 (49.5%) did not respond. The main reasons for declining to take part included perceived lack of need (n = 54; 49.5%), had already made workplace adjustments (n = 8; 7.3%) and concern about employer involvement (n = 5; 4.6%). Most of those who took part (n = 28; 80.0%) required at least one OH recommendation and all required and received self-management recommendations. The most common OH recommendations were to modify working practices and to seek advice from the workplace OH department (or GP for those with limited access to OH services) about their respiratory symptoms in the work environment. However, only 28 out of 75 (37.3%) recommendations were reported as implementable by the interviewed participants.
Overall, the very low uptake rates for the intervention and low implementation of recommendations suggest that, in its current format, this is not a worthwhile intervention. In particular, participants were hesitant about employer involvement. Nevertheless, the finding that modifiable workplace adaptations and self-management actions were identified for almost all participants suggests that there may be benefit from such assessments to be undertaken in a different context.
Strengths and limitations
Although this was a novel intervention, the main limitation was the small sample size. Therefore, any patterns assessed among those who received recommendations should be interpreted with caution. Although the absence of randomisation and a control group makes it difficult to draw conclusions about the impact of the intervention on patients, the purpose was to explore feasibility. It was not possible to involve any employers in the study. Therefore, uptake of recommendations from the employer’s perspective is unknown.
Additional outputs and published analyses related to work package objectives
-
Rai,116 shortlisted for the British Thoracic Society Early Career Investigator of the Year award (2013), with a ‘highly commended’ prize award.
-
Rai et al. 119 This systematic review (based on 44 studies published from 1937 to 2017) summarised the effects of COPD on employment and work productivity. The main findings were that people with COPD were less likely to be in paid employment than similar counterparts without COPD. There was also some evidence of poorer work productivity among people with COPD, although relatively few studies had examined the effect of disease on presenteeism. The limitations in the current evidence were highlighted, with recommendations for future research.
Patient and public involvement
Patient advisory group
Patient involvement has been a central part of this programme from the planning stage. From the start, we involved a patient with COPD (Michael Darby) who was the former chairperson of the Birmingham ‘Breathe Easy’ patient group and has advised on previous research studies. In discussion with him, we planned to set up a small panel of patients [the patient advisory group (PAG)] chaired by MD. MD was also invited to the external programme steering committee meetings and wider investigator meetings.
Prior to submission of the proposal, MD contributed to the programme plans by advising on the following aspects:
-
the need for clear and simple patient information leaflets, with a suggestion that these are read through and commented on by the PAG
-
the potential problem of incomplete response rates to mailed questionnaires and the suggestion of obtaining data through additional sources if possible (leading to us supplementing data collection by use of EHRs)
-
highlighting potential ill health among the PAG and suggesting a deputy chairperson to support the role.
The PAG was formed once the programme started and five individuals with COPD were appointed. Over the course of the programme, the group met five times, with additional support in between to comment on documents and meetings with other researchers to discuss new project ideas. Each meeting was attended by at least three PAG members and lasted for around 2 to 3 hours. A charter with terms of reference was drawn up and agreed, and PAG members were provided with some initial training at the first meeting.
The PAG provided input to the following aspects of the programme:
-
commenting on and modifying wording for the patient information leaflets
-
suggestions for improving the wording and flow of questionnaires and how these were grouped
-
piloting completion of questionnaires to provide an estimate of timing
-
piloting the patient assessment process and advising on how to organise the assessments
-
advising on practical issues that patients would face when attending assessments and how to support patient attendance
-
ensuring that we included an opt-out process for patients who may not want their data accessed through the practice as part of the TargetCOPD follow-up study.
At each meeting, PAG members received an update on the programme and the findings so far and had an opportunity to reflect and comment. Mostly, this resulted in general approval and support of the findings, with no modifications.
The PAG has been consulted about the dissemination of findings and has suggested that an opportunity to invite patients to an open evening with interesting speakers, reports on the findings and a social element (preferably in spring) would be welcome.
Multistory
During the course of the programme we were approached by an arts-based charity, Multistory (URL: https://multistory.org.uk; accessed 31 August), who had commissioned an artist to undertake a project (Black Country Lungs) to describe the story of people with COPD in the Black Country. 120 The charity approached us based on the BLISS research programme from a website search. They used a discussion on the various themes in the programme and our findings as a basis for exploring ideas with patients who took part in their project.
In addition to their main exhibition, a preview of artwork was displayed at the University of Birmingham Science and Art Exhibition, where members of the public and participants from our research study were invited. Our research group was involved in a panel discussion at which we summarised the findings from our programme. 121
Conclusions and research recommendations
Screening for undiagnosed chronic obstructive pulmonary disease
Underdiagnosis of COPD is well recognised worldwide, with at least half of patients thought to be undiagnosed. 122 Although there is some evidence that, overall, these individuals consume health services to an equivalent degree to those with diagnosed disease,123 there is insufficient evidence that screening for undiagnosed COPD is worthwhile. 46,124,125 One common uncertainty is the lack of trial evidence that the early identification of COPD leads to clinical benefits.
Our systematic reviews of studies of case-finding have shown that targeting screening to a higher-risk group is important126 and identified which of the currently tested screening strategies is/are most effective in increasing yield. 51 The TargetCOPD trial demonstrated that case-finding for undiagnosed COPD is a cost-effective process for increasing the number of new COPD cases identified with much higher yield than routine practice, particularly if using an active, targeted approach. 21 Furthermore, we have used data from the trial to develop alternative algorithms for case-finding that may improve the efficiency of the process further by reducing the number needed to screen. 49
The majority of newly identified cases in the TargetCOPD trial had potential to benefit from evidence-based recommended treatments. Using the best available evidence from the literature for our assumptions, our economic model demonstrated that a systematic, 3-yearly screening programme is likely to be cost-effective, with favourable cost/QALY gained in all scenarios (paper under review). We also found that case-finding was generally acceptable to patients42 and primary care staff,43 although a lack of awareness in relation to symptoms (among patients) and approaches to effective management of early disease (among health-care staff), as well as limited resources to deal with increasing numbers of people with COPD, were highlighted by both groups.
Longer-term follow-up of patients who were case-found through our trial demonstrated that just over one in five were added to the practice COPD register and, even among these patients, guideline-recommended management was rarely administered. This may be related to the concerns raised in our qualitative study around low awareness of management of early COPD, lack of resources and perceived lack of effective strategies.
After 4 years’ follow-up, we demonstrated no evidence that screening had an effect on clinical outcomes. Hospitalisation and mortality rates did not significantly differ between patients in the case-finding or routine care practices. Although respiratory hospitalisation rates were significantly higher in the active than in the opportunistic case-finding arm, there was no significant difference between groups in overall hospitalisation or mortality. This may be related to more hospitalisations being attributed to a respiratory cause in these patients who had a COPD diagnosis.
This finding may seem to contrast with the findings from our Markov model, which suggest that estimates of cost-effectiveness are robust as long as 8% of screen-detected patients are optimally treated. However, considering the small number of case-found patients added to the COPD register, the low levels of implementation of treatment and the probably reduced benefits of such treatment among more mildly affected patients could take the effective benefit of case-finding in our patient population below 8%.
Implications for screening
The lack of observed effects of case-finding on clinical outcomes in our trial could be related to a number of factors. First, we had a very low level of uptake of screening overall. Less than 40% of eligible patients responded to the initial screening questionnaire. Low levels of awareness of symptoms, lack of perceived susceptibility, fear of screening or greater importance being attached to competing comorbidities may explain this. Further research is needed to identify approaches for increasing uptake if a population screening programme is to be implemented.
Second, we found poor management of screen-detected COPD cases, with relatively few of them being added to the practice COPD register, with subsequent reviews and initiation of evidence-based interventions. Interviews with primary health-care staff around perceptions of screening highlighted fears around workload implications and overdiagnosis and the need for better training on how to manage screen-detected COPD. Further research should focus on the development and evaluation of pathways of care for screen-detected COPD cases. Furthermore, there is a need for prioritisation of resources to increase the capacity of primary care staff to deal with an influx of new COPD cases and the development of training programmes to support better management of people with COPD.
Third, we assumed that screen-detected COPD patients are the same as clinically diagnosed patients, with similar natural history of disease and with the same response to interventions. This assumption needs to be tested in future research. Follow-up of case-found patients is important to understand disease progression better over time. Furthermore, clinical trials should test the effectiveness of current therapies in case-found populations to assess whether or not they are as effective in these patients.
Overall, our findings are in keeping with the recommendations by the UK National Screening Committee43,44 and the USPSTF45 that screening for undiagnosed COPD should not currently be implemented. The research recommended above will help support future decision-making. Although in this report, and in common with many respiratory researchers, we frequently use the word ‘case-finding’, where case-finding is undertaken in a systematic way it is a form of screening and, therefore, should be subject to the same criteria before being implemented.
Multidimensional prognostic model for chronic obstructive pulmonary disease
People with COPD have high risk of respiratory infections resulting in hospitalisation and also a higher risk of premature mortality than those without COPD. However, COPD is heterogeneous and not all patients progress in the same way. Traditionally, lung function has been used to grade COPD severity, but there is increasing evidence that prognosis is determined by an inter-related set of factors, which has led to the development of multidimensional prognostic models. 127 Existing models have predominantly been developed in secondary care populations and are mainly developed to predict mortality risk; few have been developed using high-quality statistical approaches or been externally validated, and they often do not perform better than measures of lung function alone. 78,127,128 The most recent NICE guidelines31 highlight the need for prognostic tools that are validated in UK primary care COPD populations and that examine outcomes wider than just mortality.
We externally validated the ADO score, which was identified as the most discriminatory for 3-year mortality in a systematic review, in a UK primary care population. 78 Although we found that it has promising discrimination, the model needs to be recalibrated if used to predict risk of mortality within 1 to 2 years.
We also developed a new prognostic index to predict 2-year risk of hospitalisation for people with COPD in primary care. Our new BLISS model, which includes variables that are easily available in primary care settings, has promising discrimination and was adjusted for overfitting to help ensure calibration is more reliable in case-found individuals.
Further work is needed to externally validate the BLISS prognostic index. Further research is also needed to evaluate the use of the index to classify people with COPD into higher- and lower-risk groups to aid management decisions.
Occupational outcomes in chronic obstructive pulmonary disease
A high proportion of people with COPD are of working age, but they have poorer rates of employment and poor work productivity compared with those without COPD. To our knowledge, this was the first study to examine which factors are associated with occupational outcomes among people with COPD. We found that increasing breathlessness, disease progression (increasing number of respiratory hospital admissions rather than lung function decline) and greater occupational exposure to VGDF were associated with poorer work productivity. These disease-related factors were more likely to be associated with poor work productivity than sociodemographic and lifestyle factors. Our findings suggest that there may be a continuum from presenteeism to absenteeism to loss of employment.
Although our OH-focused intervention was not feasible, modifiable workplace adaptations and self-management actions were identified for almost all participants, suggesting possible benefit from such assessments in a different context.
Further research is needed to examine how presenteeism and absenteeism are related to better understand presenteeism in relation to health and to assess whether or not interventions to modify the course of COPD have an impact on occupational outcomes.
Summary of research recommendations
Screening
-
Development and evaluation of interventions to better implement effective treatments for COPD in primary care, including pathways to manage case-found COPD.
-
Evaluation of existing interventions in case-found COPD to determine if the interventions have similar effectiveness.
-
Long-term follow-up of TargetCOPD participants to establish whether or not clinical benefits might occur, given that people with case-found disease had milder symptoms and better lung function than those already on GP practice COPD registers. Development and evaluation of approaches for increasing uptake of invitation for screening for undiagnosed COPD.
-
Development of more efficient approaches to case-finding and identifying which screening test or strategy has the best performance (in terms of sensitivity and specificity).
-
Development and evaluation of different models for delivery of quality-assured diagnostic spirometry screening services, considering workforce implications and how this could be incorporated into the new early diagnostic hubs for primary care networks proposed in the long-term plan.
Prognosis
-
Description of natural history and prognosis of case-found patients and those with indicative symptoms but normal lung function, describing any heterogeneity, and establishing whether or not there are phenotypic characteristics that are associated with progression.
-
Exploration of how prognostic models might be used by primary care staff in managing COPD patients.
-
Evaluation of the BLISS prognostic model in directing patient management.
-
Validation of the BLISS case-finding algorithm.
-
External validation of the impact of the BLISS prognostic model.
-
Consideration of the development of new prognostic scores for primary care COPD patients that predict all-cause (rather than respiratory) hospitalisation, given the multimorbid nature of the condition.
Work-related impacts
-
Examination of the relationship between presenteeism and absenteeism and whether or not presenteeism has an impact on health-related outcomes.
-
Development and evaluation of interventions to reduce dyspnoea and VGDF exposure in occupational outcomes in people with COPD.
-
Codevelopment and evaluation of an OH intervention to improve work productivity among people with COPD who are in paid employment.
Acknowledgements
The BLISS programme research costs were funded by the NIHR Programme Grants for Applied Research programme. Recruitment for the TargetCOPD trial was supported by the Clinical Research Network.
The co-investigator team (Peymané Adab, Rachel Jordan, David Fitzmaurice, Jon Ayres, KK Cheng, Brendan Cooper, Amanda Daley, Sheila Greenfield, Kate Jolly, Sue Jowett, Martin Miller, Richard Riley, Stanley Siebert, Robert Stockley and Alice Turner) met 6-monthly to review progress and advise on aspects of the programme.
The programme management group (Peymané Adab, Rachel Jordan, David Fitzmaurice, Alexandra Enocson and Andrew Dickens) met weekly to oversee programme progress, with contributions from other co-investigators and researchers at different stages of the programme. In addition to specific contributions outlined below, all authors have contributed to drafting or revising sections of this report and have approved the final submitted version.
Contributions of authors
Peymané Adab (https://orcid.org/0000-0001-9087-3945) (Professor of Public Health and Chronic Disease Epidemiology) co-designed the programme, wrote the initial proposal with support from other co-investigators, co-led the programme, oversaw the cohort WP and wrote the first draft of the final report. She was a member of the programme management committee and the external steering committee.
Rachel E Jordan (https://orcid.org/0000-0002-0747-6883) (Reader in Epidemiology) co-designed the programme, supported leading the programme, led and oversaw the TargetCOPD trial and wrote sections of the final report. She was a member of the programme management committee and the external steering committee.
David Fitzmaurice (https://orcid.org/0000-0002-9104-6252) (Professor of General Practice) co-led the programme and advised on GP practice recruitment and clinical aspects of the TargetCOPD trial. He was a member of the programme management committee and contributed to the external steering committee.
Jon G Ayres (https://orcid.org/0000-0002-3163-3674) (Professor of Environmental and Respiratory Medicine) conceived WP3 and initially oversaw this WP.
KK Cheng (https://orcid.org/0000-0002-1516-1857) (Professor of Public Health and Primary Care) contributed to the programme design and to writing the initial proposal. He advised on epidemiological aspects of the programme.
Brendan G Cooper (https://orcid.org/0000-0003-0785-1038) (Consultant Clinical Scientist) provided advice on physiological measurements and oversaw the spirometry training and quality control for the programme.
Amanda Daley (https://orcid.org/0000-0002-4866-8726) (Professor of Behavioural Medicine) advised on aspects of questionnaire design and PA assessment.
Andrew Dickens (https://orcid.org/0000-0002-7591-8129) (Research Fellow) co-ordinated the cohort study and, in the final year, the overall programme. He sat on the management committee and contributed to all aspects of the programme.
Alexandra Enocson (https://orcid.org/0000-0002-4415-0989) (Programme Manager) co-ordinated the programme, ensuring all governance aspects were in place and managing the research team undertaking fieldwork. She managed the research team and led the analysis for the qualitative study to explore patients’ views of case-finding. She also sat on the programme management committee.
Sheila Greenfield (https://orcid.org/0000-0002-8796-4114) (Professor of Medical Sociology) advised on and oversaw the qualitative aspects of the programme.
Shamil Haroon (https://orcid.org/0000-0002-0096-1413) (Academic Clinical Lecturer in Public Health and GP trainee) undertook systematic reviews of case-finding, led the analysis and writing up of the audit of management of case-found COPD patients, undertook and analysed the qualitative study to explore the views of health professionals and undertook the analysis and writing up of the BLISS case-finding algorithm.
Kate Jolly (https://orcid.org/0000-0002-6224-2115) (Professor of Public Health and Primary Care) advised on all aspects of the programme and contributed to questionnaire design and interpretation of the findings. She also contributed to the design of the qualitative elements of the programme and PA assessment.
Sue Jowett (https://orcid.org/0000-0001-8936-3745) (Reader in Health Economics) oversaw the design, analysis and writing up of the health economic aspects of the programme. She mentored the health economists who undertook analysis.
Tosin Lambe (https://orcid.org/0000-0002-6229-2454) (Health Service Researcher and Health Economic Modeller) undertook the main analysis for the health economic model in WP1 and commented on the final report.
James Martin (https://orcid.org/0000-0002-0847-0985) (Lecturer in Medical Statistics) undertook statistical analysis for all WPs under the supervision of Alice Sitch and contributed to interpretation of the findings.
Martin R Miller (https://orcid.org/0000-0001-9971-5759) (Honorary Professor of Medicine) advised on clinical aspects of the programme, designed the programme for quality control of spirometry and advised on measures of lung function to be included in the prognostic model.
Kiran Rai (https://orcid.org/0000-0002-3250-0275) (Research Fellow) designed, contributed to data collection, analysed and wrote all elements of WP3, under the supervision of Jon Ayres, Rachel Jordan and Peymané Adab. She contributed to other aspects of the programme and, in the final years, was part of the programme management committee.
Richard D Riley (https://orcid.org/0000-0001-8699-0735) (Professor of Biostatistics) advised on the design and analysis of the trial in WP1 and the prognostic model in WP2.
Steve Sadhra (https://orcid.org/0000-0001-8829-0986) (Reader in Occupational Health) contributed to the occupational WP, delivering the intervention for the OH feasibility study.
Alice Sitch (https://orcid.org/0000-0001-7727-4497) (Lecturer in Medical Statistics) wrote the statistical analysis plans and oversaw statistical analyses undertaken, with interpretation for the programme.
Stanley Siebert (https://orcid.org/0000-0001-8959-3014) (Professor of Labour Economics) advised on questionnaires for WP3 and interpretation of data on factors contributing to unemployment among those with COPD.
Robert A Stockley (https://orcid.org/0000-0003-3726-1207) (Professor of Medicine) provided clinical expertise and advised on interpretation of findings in the programme.
Alice Turner (https://orcid.org/0000-0002-5947-3254) (Reader and Consultant in Respiratory Medicine) advised on clinical aspects of the programme, including the inputs for the health economics model. She advised on all aspects of the programme.
Contributions of others
The authors would like to express their heartfelt thanks to the following:
-
The patients and the general practices that participated in the programme and made the research possible.
-
Members of the PAG: Michael Darby (chairperson), Anne Yeomans, Maireade Bird, Raymond Burberry, Marie James, Jan Turner and Ian Black. Special thanks to Michael Darby, who also sat on the study management group and the external steering committee.
-
Programme administrators Ellen Sainsbury and Amanda Davies.
-
External members of the Steering Committee: Debbie Jarvis (chairperson and subject expert), Michael Darby (lay member), Jane Wolstenholme (Health Economics expertise) and Simon Gates (statistical expertise).
-
Jen Marsh, an original co-investigator who helped with statistical aspects when planning the programme.
-
All research assistants and the research team members who supported and co-ordinated aspects of the data collection, including Joanne O’ Beirne-Elliman. Those who supported aspects of the health economic evaluation, including Deirdre Blissett, who undertook the main trial-based health economic analysis for the TargetCOPD trial in WP1, and Zainab Abdali.
-
The PhD students who have contributed to data collection, processing and analyses, including Halima Buni, who undertook analyses of cohort data, Spencer Keene, who undertook initial analysis and writing up of the ADO validation study and Maria-Christina Kosteli, who undertook the qualitative study on barriers to and facilitators of exercise in people with COPD, with support from Nicola Heneghan.
Publications
Lambe T, Adab P, Jordan RE, Sitch A, Enocson A, Jolly K, et al. Model-based evaluation of the long-term cost-effectiveness of systematic case-finding for COPD in primary care. Thorax 2019;74:730–9.
Haroon S, Adab P, Dickens AP, Sitch AJ, Rai K, Enocson A, et al. Impact of COPD case finding on clinical care: a prospective analysis of the TargetCOPD trial. BMJ Open 2020;10:e038286.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health and Social Care.
References
- Ntritsos G, Franek J, Belbasis L, Christou MA, Markozannes G, Altman P, et al. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2018;13:1507-14. https://doi.org/10.2147/COPD.S146390.
- Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, et al. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Glob Health 2015;5. https://doi.org/10.7189/jogh.05-020415.
- Jordan RE, Lam KB, Cheng KK, Miller MR, Marsh JL, Ayres JG, et al. Case finding for chronic obstructive pulmonary disease: a model for optimising a targeted approach. Thorax 2010;65:492-8. https://doi.org/10.1136/thx.2009.129395.
- Martinez CH, Mannino DM, Jaimes FA, Curtis JL, Han MK, Hansel NN, et al. Undiagnosed obstructive lung disease in the United States. Associated factors and long-term mortality. Ann Am Thorac Soc 2015;12:1788-95. https://doi.org/10.1513/AnnalsATS.201506-388OC.
- Rennard SI, Vestbo J. Natural histories of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2008;5:878-83. https://doi.org/10.1513/pats.200804-035QC.
- Rennard SI, Vestbo J. The many ‘small COPDs’: COPD should be an orphan disease. Chest 2008;134:623-7. https://doi.org/10.1378/chest.07-3059.
- Roche N, Dalmay F, Perez T, Kuntz C, Vergnenègre A, Neukirch F, et al. Impact of chronic airflow obstruction in a working population. Eur Respir J 2008;31:1227-33. https://doi.org/10.1183/09031936.00089607.
- Britton M. The burden of COPD in the UK: results from the confronting COPD survey. Respir Med 2003;97:S71-9. https://doi.org/10.1016/S0954-6111(03)80027-6.
- Schultz AB, Edington DW. Employee health and presenteeism: a systematic review. J Occup Rehabil 2007;17:547-79. https://doi.org/10.1007/s10926-007-9096-x.
- Mahon B, Bartlett C, Isojärvi J, Edwards M, Glanville J. Literature Review: The Economic Costs of Lung Disease and the Cost Effectiveness of Policy and Service Interventions. York: York Health Economics Consortium on behalf of the British Lung Foundation (BLF) and the British Thoracic Society; 2017.
- McLean S, Hoogendoorn M, Hoogenveen RT, Feenstra TL, Wild S, Simpson CR, et al. Projecting the COPD population and costs in England and Scotland: 2011 to 2030. Sci Rep 2016;6. https://doi.org/10.1038/srep31893.
- Trueman D, Woodcock F, Hancock E. Estimating the Economic Burden of Respiratory Illness in the UK. London: British Lung Foundation; 2017.
- Ford ES, Murphy LB, Khavjou O, Giles WH, Bolt JB, Croft JB. Total and state-specific medical and absenteeism costs of COPD among adults aged 18 years in the United States for 2010 and projections through 2020. Chest 2015;147:31-45. https://doi.org/10.1378/chest.14-0972.
- Gibson GJ, Loddenkemper R, Lundbäck B, Sibille Y. Respiratory health and disease in Europe: the new European Lung White Book. Eur Respir J 2013;42:559-63. https://doi.org/10.1183/09031936.00105513.
- Kohansal R, Soriano JB, Agusti A. Investigating the natural history of lung function: facts, pitfalls, and opportunities. Chest 2009;135:1330-41. https://doi.org/10.1378/chest.08-1750.
- U.S Preventive Services Task Force . Screening for chronic obstructive pulmonary disease using spirometry: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2008;148:529-34. https://doi.org/10.7326/0003-4819-148-7-200804010-00212.
- Soriano JB, Zielinski J, Price D. Screening for and early detection of chronic obstructive pulmonary disease. Lancet 2009;374:721-32. https://doi.org/10.1016/S0140-6736(09)61290-3.
- Han MK, Quibrera PM, Carretta EE, Barr RG, Bleecker ER, Bowler RP, et al. Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med 2017;5:619-26. https://doi.org/10.1016/S2213-2600(17)30207-2.
- Alahmari AD, Kowlessar BS, Patel AR, Mackay AJ, Allinson JP, Wedzicha JA, et al. Physical activity and exercise capacity in patients with moderate COPD exacerbations. Eur Respir J 2016;48:340-9. https://doi.org/10.1183/13993003.01105-2015.
- Karch A, Vogelmeier C, Welte T, Bals R, Kauczor HU, Biederer J, et al. The German COPD cohort COSYCONET: aims, methods and descriptive analysis of the study population at baseline. Respir Med 2016;114:27-3. https://doi.org/10.1016/j.rmed.2016.03.008.
- Jordan RE, Adab P, Sitch A, Enocson A, Blissett D, Jowett S, et al. Targeted case finding for chronic obstructive pulmonary disease versus routine practice in primary care (TargetCOPD): a cluster-randomised controlled trial. Lancet Respir Med 2016;4:720-30. https://doi.org/10.1016/S2213-2600(16)30149-7.
- Department of Health and Social Care (DHSC) . An Outcomes Strategy for Chronic Obstructive Pulmonary Disease (COPD) and Asthma in England 2011.
- British Lung Foundation . Invisible Lives: Chronic Obstructive Pulmonary Disease (COPD) – Finding the Missing Millions 2007. https://lunguk.org/NR/rdonlyres/E027CA18-B5C6-49AB-96FA-C4AF55E6F484/0/InvisibleLivesreport.pdf (accessed 21 April 2021).
- Frank TL, Hazell ML, Linehan MF, Frank PI. The diagnostic accuracies of chronic obstructive pulmonary disease (COPD) in general practice: the results of the MAGIC (Manchester Airways Group Identifying COPD) study. Prim Care Respir J 2006;15:286-93. https://doi.org/10.1016/j.pcrj.2006.07.007.
- Tinkelman DG, Price DB, Nordyke RJ, Halbert RJ. COPD screening efforts in primary care: what is the yield?. Prim Care Respir J 2007;16:41-8. https://doi.org/10.3132/pcrj.2007.00009.
- Bednarek M, Maciejewski J, Wozniak M, Kuca P, Zielinski J. Prevalence, severity and underdiagnosis of COPD in the primary care setting. Thorax 2008;63:402-7. https://doi.org/10.1136/thx.2007.085456.
- Buffels J, Degryse J, Heyrman J, Decramer M. DIDASCO Study . Office spirometry significantly improves early detection of COPD in general practice: the DIDASCO Study. Chest 2004;125:1394-9. https://doi.org/10.1378/chest.125.4.1394.
- Van Schayck CP, Loozen JM, Wagena E, Akkermans RP, Wesseling GJ. Detecting patients at a high risk of developing chronic obstructive pulmonary disease in general practice: cross sectional case finding study. BMJ 2002;324. https://doi.org/10.1136/bmj.324.7350.1370.
- Vandevoorde J, Verbanck S, Gijssels L, Schuermans D, Devroey D, De Backer J, et al. Early detection of COPD: a case finding study in general practice. Respir Med 2007;101:525-30. https://doi.org/10.1016/j.rmed.2006.06.027.
- Wilt TJ, Niewoehner D, MacDonald R, Kane RL. Management of stable chronic obstructive pulmonary disease: a systematic review for a clinical practice guideline. Ann Intern Med 2007;147:639-53. https://doi.org/10.7326/0003-4819-147-9-200711060-00009.
- National Institute for Health and Care Excellence (NICE) . Chronic Obstructive Pulmonary Disease in Over 16s: Diagnosis and Management. NICE Guideline [NG115] 2010.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2013. Canterbury: Personal Social Services Research Unit, University of Kent; 2013.
- National Institute for Health Research . NIHR Costing Report n.d. www.crn.nihr.ac.uk/resources/resource-template/ (accessed 11 August 2015).
- Jordan RE, Adab P, Sitch A, Enocson A, Blissett D, Jowett S, et al. Supplementary appendix. Supplement to: Targeted case finding for chronic obstructive pulmonary disease versus routine practice in primary care (TargetCOPD): a cluster-randomised controlled trial. Lancet Respir Med 2016;4:P720-30.
- Lambe T, Adab P, Jordan RE, Sitch A, Enocson A, Jolly K, et al. Model-based evaluation of the long-term cost-effectiveness of systematic case-finding for COPD in primary care. Thorax 2019;74:730-9. https://doi.org/10.1136/thoraxjnl-2018-212148.
- Dretzke J, Blissett D, Dave C, Mukherjee R, Price M, Bayliss S, et al. The cost-effectiveness of domiciliary non-invasive ventilation in patients with end-stage chronic obstructive pulmonary disease: a systematic review and economic evaluation. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19810.
- Ramsey SD, Sullivan SD. The burden of illness and economic evaluation for COPD. Eur Respir J 2003;41:29s-35s. https://doi.org/10.1183/09031936.03.00078203.
- National Institute for Health and Care Excellence (NICE) . Chronic Obstructive Pulmonary Disease: Costing Report – Implementing NICE Guidance 2011.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit; 2015.
- Karner C, Chong J, Poole P. Tiotropium versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014;7. https://doi.org/10.1002/14651858.CD009285.pub3.
- Nannini LJ, Poole P, Milan SJ, Holmes R, Normansell R. Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2013;11. https://doi.org/10.1002/14651858.CD003794.pub4.
- Enocson A, Jolly K, Jordan RE, Fitzmaurice DA, Greenfield SM, Adab P. Case-finding for COPD in primary care: a qualitative study of patients’ perspectives. Int J Chron Obstruct Pulmon Dis 2018;13:1623-32. https://doi.org/10.2147/COPD.S147718.
- Haroon S, Jordan RE, Fitzmaurice DA, Adab P. Case finding for COPD in primary care: a qualitative study of the views of health professionals. Int J Chron Obstruct Pulmon Dis 2015;10:1711-18. https://doi.org/10.2147/COPD.S84247.
- UK National Screening Committee (UK NSC) . UK NSC Policy on Chronic Obstructive Pulmonary Disease 2013.
- Cartwright S. An Evaluation of Screening for COPD Against the National Screening Committee Criteria. London: Public Health England; 2012.
- Guirguis-Blake JM, Senger CA, Webber EM, Mularski RA, Whitlock EP. Screening for chronic obstructive pulmonary disease: evidence report and systematic review for the US Preventive Services Task Force. JAMA 2016;315:1378-93. https://doi.org/10.1001/jama.2016.2654.
- Jordan RE, Adab P, Jowett S, Marsh JL, Riley RD, Enocson A, et al. TargetCOPD: a pragmatic randomised controlled trial of targeted case finding for COPD versus routine practice in primary care: protocol. BMC Pulm Med 2014;14. https://doi.org/10.1186/1471-2466-14-157.
- Miller MR, Haroon S, Jordan RE, Sitch AJ, Dickens AP, Enocson A, et al. Clinical characteristics of patients newly diagnosed with COPD by the fixed ratio and lower limit of normal criteria: a cross-sectional analysis of the TargetCOPD trial. Int J Chron Obstruct Pulmon Dis 2018;13:1979-86. https://doi.org/10.2147/COPD.S146914.
- Haroon S, Adab P, Riley RD, Fitzmaurice D, Jordan RE. Predicting risk of undiagnosed COPD: development and validation of the TargetCOPD score. Eur Respir J 2017;49. https://doi.org/10.1183/13993003.02191-2016.
- Haroon S, Adab P, Riley RD, Marshall T, Lancashire R, Jordan RE. Predicting risk of COPD in primary care: development and validation of a clinical risk score. BMJ Open Respir Res 2015;2. https://doi.org/10.1136/bmjresp-2014-000060.
- Haroon SM, Jordan RE, O’Beirne-Elliman J, Adab P. Effectiveness of case finding strategies for COPD in primary care: a systematic review and meta-analysis. NPJ Prim Care Respir Med 2015;25. https://doi.org/10.1038/npjpcrm.2015.56.
- Haroon S, Jordan R, Takwoingi Y, Adab P. Diagnostic accuracy of screening tests for COPD: a systematic review and meta-analysis. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008133.
- Adab P, Fitzmaurice DA, Dickens AP, Ayres JG, Buni H, Cooper BG, et al. Cohort profile: the Birmingham Chronic Obstructive Pulmonary Disease (COPD) Cohort Study. Int J Epidemiol 2017;46. https://doi.org/10.1093/ije/dyv350.
- Donaldson GC, Seemungal TA, Patel IS, Bhowmik A, Wilkinson TM, Hurst JR, et al. Airway and systemic inflammation and decline in lung function in patients with COPD. Chest 2005;128:1995-2004. https://doi.org/10.1378/chest.128.4.1995.
- Vestbo J, Anderson W, Coxson HO, Crim C, Dawber F, Edwards L, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate End-points (ECLIPSE). Eur Respir J 2008;31:869-73. https://doi.org/10.1183/09031936.00111707.
- Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004;350:1005-12. https://doi.org/10.1056/NEJMoa021322.
- Kohansal R, Martinez-Camblor P, Agustí A, Buist AS, Mannino DM, Soriano JB. The natural history of chronic airflow obstruction revisited: an analysis of the Framingham offspring cohort. Am J Respir Crit Care Med 2009;180:3-10. https://doi.org/10.1164/rccm.200901-0047OC.
- Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999;160:1856-61. https://doi.org/10.1164/ajrccm.160.6.9902115.
- Prescott E, Bjerg AM, Andersen PK, Lange P, Vestbo J. Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. Eur Respir J 1997;10:822-7.
- Yin P, Jiang CQ, Cheng KK, Lam TH, Lam KH, Miller MR, et al. Passive smoking exposure and risk of COPD among adults in China: the Guangzhou Biobank Cohort Study. Lancet 2007;370:751-7. https://doi.org/10.1016/S0140-6736(07)61378-6.
- Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. GOLD Scientific Committee . Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001;163:1256-76. https://doi.org/10.1164/ajrccm.163.5.2101039.
- Vestbo J, Lange P. Can GOLD stage 0 provide information of prognostic value in chronic obstructive pulmonary disease?. Am J Respir Crit Care Med 2002;166:329-32. https://doi.org/10.1164/rccm.2112048.
- Mannino DM. GOLD stage 0 COPD: is it real? Does it matter?. Chest 2006;130:309-10. https://doi.org/10.1016/S0012-3692(15)51839-4.
- de Marco R, Accordini S, Cerveri I, Corsico A, Antó JM, Künzli N, et al. Incidence of chronic obstructive pulmonary disease in a cohort of young adults according to the presence of chronic cough and phlegm. Am J Respir Crit Care Med 2007;175:32-9. https://doi.org/10.1164/rccm.200603-381OC.
- Mannino DM, Doherty DE, Sonia Buist A. Global initiative on Obstructive Lung Disease (GOLD) classification of lung disease and mortality: findings from the Atherosclerosis Risk in Communities (ARIC) study. Respir Med 2006;100:115-22. https://doi.org/10.1016/j.rmed.2005.03.035.
- Office for National Statistics . Standard Occupational Classification 2010 n.d. www.ons.gov.uk/methodology/classificationsandstandards/standardoccupationalclassificationsoc/soc2010 (accessed 13 December 2019).
- Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J 2009;34:648-54. https://doi.org/10.1183/09031936.00102509.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Koopman C, Pelletier KR, Murray JF, Sharda CE, Berger ML, Turpin RS, et al. Stanford presenteeism scale: health status and employee productivity. J Occup Environ Med 2002;44:14-20. https://doi.org/10.1097/00043764-200201000-00004.
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics 1993;4:353-65. https://doi.org/10.2165/00019053-199304050-00006.
- Keene SJ, Jordan RE, Franssen FM, de Vries F, Martin J, Sitch A, et al. External validation of the updated ADO score in COPD patients from the Birmingham COPD Cohort. Int J Chron Obstruct Pulmon Dis 2019;14:2395-407. https://doi.org/10.2147/COPD.S212381.
- Miller MR, Pedersen OF, Pellegrino R, Brusasco V. Debating the definition of airflow obstruction: time to move on?. Eur Respir J 2009;34:527-8. https://doi.org/10.1183/09031936.00103309.
- Miller MR, Pedersen OF, Dirksen A. A new staging strategy for chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2007;2:657-63.
- Miller MR, Pedersen OF. New concepts for expressing forced expiratory volume in 1 s arising from survival analysis. Eur Respir J 2010;35:873-82. https://doi.org/10.1183/09031936.00025809.
- Puhan MA, Garcia-Aymerich J, Frey M, ter Riet G, Antó JM, Agustí AG, et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO index. Lancet 2009;374:704-11. https://doi.org/10.1016/S0140-6736(09)61301-5.
- Dijk WD, Bemt Lv, Haak-Rongen Sv, Bischoff E, Weel Cv, Veen JC, et al. Multidimensional prognostic indices for use in COPD patient care: a systematic review. Respir Res 2011;12. https://doi.org/10.1186/1465-9921-12-151.
- Guerra B, Haile SR, Lamprecht B, Ramírez AS, Martinez-Camblor P, Kaiser B, et al. Large-scale external validation and comparison of prognostic models: an application to chronic obstructive pulmonary disease. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1013-y.
- Smith LE, Moore E, Ali I, Smeeth L, Stone P, Quint JK. Prognostic variables and scores identifying the end of life in COPD: a systematic review. Int J Chron Obstruct Pulmon Dis 2017;12:2239-56. https://doi.org/10.2147/COPD.S137868.
- Soler-Cataluña JJ, Martínez-García MA, Sánchez LS, Tordera MP, Sánchez PR. Severe exacerbations and BODE index: two independent risk factors for death in male COPD patients. Respir Med 2009;103:692-9. https://doi.org/10.1016/j.rmed.2008.12.005.
- Esteban C, Quintana JM, Aburto M, Moraza J, Capelastegui A. A simple score for assessing stable chronic obstructive pulmonary disease. QJM 2006;99:751-9. https://doi.org/10.1093/qjmed/hcl110.
- Esteban C, Quintana JM, Aburto M, Moraza J, Arostegui I, España PP, et al. The health, activity, dyspnea, obstruction, age, and hospitalization: prognostic score for stable COPD patients. Respir Med 2011;105:1662-70. https://doi.org/10.1016/j.rmed.2011.05.005.
- Niewoehner DE, Lokhnygina Y, Rice K, Kuschner WG, Sharafkhaneh A, Sarosi GA, et al. Risk indexes for exacerbations and hospitalizations due to COPD. Chest 2007;131:20-8. https://doi.org/10.1378/chest.06-1316.
- Bertens LC, Reitsma JB, Moons KG, van Mourik Y, Lammers JW, Broekhuizen BD, et al. Development and validation of a model to predict the risk of exacerbations in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2013;8:493-9. https://doi.org/10.2147/COPD.S49609.
- Schembri S, Anderson W, Morant S, Winter J, Thompson P, Pettitt D, et al. A predictive model of hospitalisation and death from chronic obstructive pulmonary disease. Respir Med 2009;103:1461-7. https://doi.org/10.1016/j.rmed.2009.04.021.
- Miravitlles M, Llor C, de Castellar R, Izquierdo I, Baró E, Donado E. Validation of the COPD severity score for use in primary care: the NEREA study. Eur Respir J 2009;33:519-27. https://doi.org/10.1183/09031936.00087208.
- Briggs A, Spencer M, Wang H, Mannino D, Sin DD. Development and validation of a prognostic index for health outcomes in chronic obstructive pulmonary disease. Arch Intern Med 2008;168:71-9. https://doi.org/10.1001/archinternmed.2007.37.
- Jones RC, Donaldson GC, Chavannes NH, Kida K, Dickson-Spillmann M, Harding S, et al. Derivation and validation of a composite index of severity in chronic obstructive pulmonary disease: the DOSE Index. Am J Respir Crit Care Med 2009;180:1189-95. https://doi.org/10.1164/rccm.200902-0271OC.
- Wyatt JC, Altman DG. Commentary: Prognostic models: clinically useful or quickly forgotten?. BMJ 1995;311:1539-41. https://doi.org/10.1136/bmj.311.7019.1539.
- Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996;49:1373-9. https://doi.org/10.1016/S0895-4356(96)00236-3.
- Kosteli MC, Heneghan NR, Roskell C, Williams SE, Adab P, Dickens AP, et al. Barriers and enablers of physical activity engagement for patients with COPD in primary care. Int J Chron Obstruct Pulmon Dis 2017;12:1019-31. https://doi.org/10.2147/COPD.S119806.
- Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Antó JM. Regular physical activity modifies smoking-related lung function decline and reduces risk of chronic obstructive pulmonary disease: a population-based cohort study. Am J Respir Crit Care Med 2007;175:458-63. https://doi.org/10.1164/rccm.200607-896OC.
- Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Antó JM. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax 2006;61:772-8. https://doi.org/10.1136/thx.2006.060145.
- Maltais F, Bourbeau J, Shapiro S, Lacasse Y, Perrault H, Baltzan M, et al. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2008;149:869-78. https://doi.org/10.7326/0003-4819-149-12-200812160-00006.
- Bolton CE, Bevan-Smith EF, Blakey JD, Crowe P, Elkin SL, Garrod R, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013;68:ii1-30. https://doi.org/10.1136/thoraxjnl-2013-203808.
- Johnston K, Grimmer-Somers K. Pulmonary rehabilitation: overwhelming evidence but lost in translation?. Physiother Can 2010;62:368-73. https://doi.org/10.3138/physio.62.4.368.
- Buni H. The Relevance of Chronic Respiratory Symptoms Without Airflow Obstruction: Health-Related Characteristics and Impact on Patient Prognosis 2016. http://etheses.bham.ac.uk/6699/.
- Lopez-Campos JL, Alcazar B. Evaluation of symptomatic patients without airflow obstruction: back to the future. J Thorac Dis 2016;8:E1657-60. https://doi.org/10.21037/jtd.2016.12.103.
- NatCen Social Research and Royal Free and University College Medical School Department of Epidemiology and Public Health . Health Survey for England, 2010 2012.
- Brien SB, Stuart B, Dickens AP, Kendrick T, Jordan RE, Adab P, et al. Independent determinants of disease-related quality of life in COPD – scope for nonpharmacologic interventions?. Int J Chron Obstruct Pulmon Dis 2018;13:247-56. https://doi.org/10.2147/copd.s152955.
- Jolly K, Sidhu MS, Hewitt CA, Coventry PA, Daley A, Jordan R, et al. Self management of patients with mild COPD in primary care: randomised controlled trial. BMJ 2018;361. https://doi.org/10.1136/bmj.k2241.
- Dickens A, Fitzmaurice D, Adab P, Sitch A, Riley RD, Enocson A, et al. Accuracy of Vitalograph lung monitor as a screening test for COPD in primary care. NPJ Prim Care Respir Med 2020;30:1-8. https://doi.org/10.1038/s41533-019-0158-2.
- Khan A, Dickens AP, Adab P, Jordan RE. Self-management behaviour and support among primary care COPD patients: cross-sectional analysis of data from the Birmingham Chronic Obstructive Pulmonary Disease Cohort. NPJ Prim Care Respir Med 2017;27. https://doi.org/10.1038/s41533-017-0046-6.
- Kosteli MC. Imagery Use in Older Adults 2016. http://etheses.bham.ac.uk/6780/.
- Rai KK, Jordan RE, Siebert WS, Sadhra SS, Fitzmaurice DA, Sitch AJ, et al. Birmingham COPD Cohort: a cross-sectional analysis of the factors associated with the likelihood of being in paid employment among people with COPD. Int J Chron Obstruct Pulmon Dis 2017;12:233-42. https://doi.org/10.2147/COPD.S119467.
- Rai KK, Adab P, Ayres JG, Siebert WS, Sadhra SS, Sitch AJ, et al. Factors associated with work productivity among people with COPD: Birmingham COPD Cohort. Occup Environ Med 2017;74:859-67. https://doi.org/10.1136/oemed-2016-104014.
- Britton M. The burden of COPD in the UK: results from the Confronting COPD survey. Respir Med 2003;97:71-9. https://doi.org/10.1016/S0954-6111(03)80027-6.
- Schultz AB, Edington DW. Employee health and presenteeism: a systematic review. J Occup Rehabil 2007;17:547-79. https://doi.org/10.1007/s10926-007-9096-x.
- Roche N, Dalmay F, Perez T, Kuntz C, Vergnenègre A, Neukirch F, et al. Impact of chronic airflow obstruction in a working population. Eur Respir J 2008;31:1227-33. https://doi.org/10.1183/09031936.00089607.
- Sin DD, Stafinski T, Ng YC, Bell NR, Jacobs P. The impact of chronic obstructive pulmonary disease on work loss in the United States. Am J Respir Crit Care Med 2002;165:704-7. https://doi.org/10.1164/ajrccm.165.5.2104055.
- Yelin E, Katz P, Balmes J, Trupin L, Earnest G, Eisner M, et al. Work life of persons with asthma, rhinitis, and COPD: a study using a national, population-based sample. J Occup Med Toxicol 2006;1. https://doi.org/10.1186/1745-6673-1-2.
- Collins JJ, Baase CM, Sharda CE, Ozminkowski RJ, Nicholson S, Billotti GM, et al. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J Occup Environ Med 2005;47:547-57. https://doi.org/10.1097/01.jom.0000166864.58664.29.
- Kretschman D, Gao W, Dupuis J, Latourelle J, O’Connor G. Rate of FEV1 decline in healthy adults: defining the upper limit of normal in the Framingham Heart Study. Am J Respir Crit Care Med 2012;185. https://doi.org/10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A2056.
- Mahler DA, Witek TJ. The MCID of the transition dyspnea index is a total score of one unit. COPD 2005;2:99-103. https://doi.org/10.1081/copd-200050666.
- Alma H, de Jong C, Jelusic D, Wittmann M, Schuler M, Flokstra-de Blok B, et al. Health status instruments for patients with COPD in pulmonary rehabilitation: defining a minimal clinically important difference. NPJ Prim Care Respir Med 2016;26. https://doi.org/10.1038/npjpcrm.2016.41.
- Kalirai KK. The Effects of Chronic Obstructive Pulmonary Disease on Work Related Outcomes 2016. http://etheses.bham.ac.uk/6846/ (accessed 4 February 2020).
- Black C. Working for a Healthier Tomorrow: Work and Health in Britain. London: Department for Work and Pensions; 2008.
- Verbeek J, Madan I. From sick notes to fit notes. BMJ 2009;339. https://doi.org/10.1136/bmj.b3114.
- Rai KK, Adab P, Ayres JG, Jordan RE. Systematic review: chronic obstructive pulmonary disease and work-related outcomes. Occup Med 2018;68:99-108. https://doi.org/10.1093/occmed/kqy012.
- Multistory . Black Country Lungs 2017. https://multistory.org.uk/project/black-country-lungs/ (accessed 5 December 2018).
- University of Birmingham Arts & Science Festival . Black Country Lungs: In Conversation 2018. https://artsandsciencefestival.co.uk/festival-event/black-country-lungs-in-conversation/ (accessed 5 December 2018).
- Almagro P, Soriano JB. Underdiagnosis in COPD: a battle worth fighting. Lancet Respir Med 2017;5:367-8. https://doi.org/10.1016/S2213-2600(17)30133-9.
- Labonté LE, Tan WC, Li PZ, Mancino P, Aaron SD, Benedetti A, et al. Undiagnosed chronic obstructive pulmonary disease contributes to the burden of health care use. Data from the CanCOLD study. Am J Respir Crit Care Med 2016;194:285-98. https://doi.org/10.1164/rccm.201509-1795OC.
- UK National Screening Committee (UK NSC) . UK NSC Recommendation on Chronic Obstructive Pulmonary Disease 2018. https://legacyscreening.phe.org.uk/copd (accessed 19 October 2018).
- Lin K, Watkins B, Johnson T, Rodriguez JA, Barton MB. U.S. Preventive Services Task Force . Screening for chronic obstructive pulmonary disease using spirometry: summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2008;148:535-43. https://doi.org/10.7326/0003-4819-148-7-200804010-00213.
- Haroon SM, Adab PA, Jordan RE. Case finding for COPD in primary care: a systematic review. Prim Care Respir J 2012;21:354-7. https://doi.org/10.4104/pcrj.2012.00060.
- Bellou V, Belbasis L, Konstantinidis A, Tzoulaki I, Evangelou E. A systematic review of prognostic models in COPD. Eur Respir J 2017;50. https://doi.org/10.1183/1393003.congress-2017.PA1565.
- Guerra B, Gaveikaite V, Bianchi C, Puhan MA. Prediction models for exacerbations in patients with COPD. Eur Respir Rev 2017;26. https://doi.org/10.1183/16000617.0061-2016.
Appendix 1 List of publications arising from programme, with full-text links
Peer-reviewed papers (published)
| Title | Journal | Authors | Year | Full text link |
|---|---|---|---|---|
| Accuracy of Vitalograph lung monitor as a screening test for COPD in primary care | npj Primary Care Respiratory Medicine | Dickens AP, Fitzmaurice DA, Adab P, Sitch A, Riley RD, Enocson A, Jordan RE | 2019 | |
| External validation of the updated ADO score in COPD patients from the Birmingham COPD cohort. | International Journal of Chronic Obstructive Pulmonary Disease | SJ Keene, RE Jordan, FME Franssen, F de Vries, J Martin, A Sitch, A Turner, AP Dickens, D Fitzmaurice, P Adab | 2019 | www.ncbi.nlm.nih.gov/pmc/articles/PMC6818100/ |
| A model-based evaluation of the long-term cost-effectiveness of systematic case-finding for COPD in primary care | Thorax | Lambe T, Adab P, Jordan R, Sitch A, Enocson A, Jolly K, Marsh J, Riley RD, Miller MR, Cooper BG, Turner AM, Ayres J, Stockley R, Greenfield S, Siebert S, Daley A, Cheng KK, Fitzmaurice D, Jowett S | 2019 | http://doi.org/10.1136/thoraxjnl-2018-212148 |
| Case-finding for COPD in Primary Care: A qualitative study of patients’ perspectives | International Journal of Chronic Obstructive Pulmonary Disease | Enocson A, Jolly K, Jordan R, Fitzmaurice D, Greenfield S, Adab P, Cheng K, Cooper BG, Daley A, Dickens A, O’Beirne-Elliman J, Haroon S, Jowett S, Kalirai K, Marsh J, Miller MR, Riley R, Stockley R, Turner A | 2018 | https://doi.org/10.2147/COPD.S147718 |
| Clinical characteristics of patients newly diagnosed with chronic obstructive pulmonary disease by the fixed ratio and lower limit of normal criteria: a cross-sectional analysis of the TargetCOPD trial | International Journal of COPD | MR Miller, S Haroon, RE Jordan, A Sitch, AP Dickens, A Enocson, DA Fitzmaurice, P Adab | 2018 | https://doi.org/10.2147/COPD.S146914 |
| Systematic review: chronic obstructive pulmonary disease and work-related outcomes | Occupational Medicine | K K Rai, P Adab, J G Ayres, R E Jordan | 2018 | https://doi.org/10.1093/occmed/kqy012 |
| Independent determinants of disease-related quality of life in COPD – scope for non-pharmacological interventions? | International Journal of COPD | Brien SB, Stuart B, Dickens AP, Kendrick T, Jordan RE, Adab P, Thomas M | 2018 | https://doi.org/10.2147/COPD.S152955 |
| Factors associated with work productivity among people with COPD: Birmingham COPD Cohort | Occupational and Environmental Medicine | K Rai, R Jordan, JG Ayres, S Siebert, SS Sadhra, A Sitch, D Fitzmaurice, P Adab | 2017 | http://doi.org/10.1136/oemed-2016-104014 |
| Self-management behaviour and support among primary care COPD patients: Cross-sectional analysis of data from the Birmingham Chronic Obstructive Pulmonary Disease Cohort | npj Primary Care Respiratory Medicine | A Khan, AP Dickens, P Adab, RE Jordan | 2017 | https://doi.org/10.1038/s41533-017-0046-6 |
| Predicting risk of undiagnosed COPD in primary care: Development and validation of the TargetCOPD score | European Respiratory Journal | Haroon SMM, Adab P, Riley RD, Fitzmaurice D, Jordan RE | 2017 | https://doi.org/10.1183/13993003.02191-2016 |
| Barriers and enablers of physical activity engagement for patients with chronic obstructive pulmonary disease (COPD) in primary care | International Journal of COPD | M-C Kosteli, N Heneghan, C Roskell, SE Williams, P Adab, AP Dickens, A Enocson, D Fitzmaurice, K Jolly, R Jordan, S Greenfield, J Cumming | 2017 | https://doi.org/10.2147/COPD.S119806 |
| Birmingham COPD Cohort: a cross-sectional analysis of the factors associated with the likelihood of being in paid employment among people with COPD | International Journal of COPD | KK Kalirai, RE Jordan, WS Siebert, SS Sadhra, DA Fitzmaurice, AJ Sitch, JG Ayres, P Adab | 2016 | https://doi.org/10.2147/COPD.S119467 |
| Cohort Profile: The Birmingham Chronic Obstructive Pulmonary Disease (COPD) Cohort Study | International Journal of Epidemiology | P Adab, DA Fitzmaurice, AP Dickens, JG Ayres, H Buni, BG Cooper, AJ Daley, A Enocson, S Greenfield, K Jolly, S Jowett, K Kalirai, JL Marsh, MR Miller, RD Riley, WS Siebert, RA Stockley, AM Turner, KK Cheng, RE Jordan | 2016 | https://doi.org/10.1093/ije/dyv350 |
| Targeted case finding for chronic obstructive pulmonary disease versus routine practice in primary care (TargetCOPD): a cluster-randomised controlled trial | Lancet Respiratory | RE Jordan, P Adab, A Sitch, A Enocson, D Blissett, S Jowett, JL Marsh, RD Riley, MR Miller, BG Cooper, AM Turner, K Jolly, JG Ayres, S Haroon, RA Stockley, S Greenfield, S Siebert, A Daley, KK Cheng, D Fitzmaurice | 2016 | https://doi.org/10.1016/S2213-2600(16)30149-7 |
| Predicting risk of COPD in primary care: development and validation of a clinical risk score | BMJ Open Respiratory Research | Haroon SMM, Adab P, Riley RD, Marshall T, Lancashire R, Jordan RE | 2015 | www.ncbi.nlm.nih.gov/pmc/articles/PMC4379885/ |
| Case finding for COPD in primary care: a qualitative study of the views of health professionals | International Journal of COPD | Haroon S, Jordan RE, Fitzmaurice DA, Adab P | 2015 | https://doi.org/10.2147/COPD.S84247 |
| Diagnostic accuracy of screening tests for COPD: a systematic review and meta-analysis | BMJ Open Respiratory Research | Haroon S, Jordan R, Takwoingi Y, Adab P | 2015 | https://doi.org/10.1136/bmjopen-2015-008133 |
| Effectiveness of case finding strategies for COPD in primary care: a systematic review and meta-analysis | NPJ Primary Care Respiratory Medicine | Haroon SM, Jordan RE, O’Beirne-Elliman J, Adab P | 2015 | https://doi.org/10.1038/npjpcrm.2015.56 |
| TargetCOPD: a pragmatic randomised controlled trial of targeted case finding for COPD versus routine practice in primary care: protocol | BMC Pulmonary Medicine | RE Jordan, P Adab, S Jowett, JL Marsh, RD Riley, A Enocson, MR Miller, BG Cooper, AM Turner, JG Ayres, KK Cheng, K Jolly, RA Stockley, S Greenfield, S Siebert, A Daley, D Fitzmaurice | 2014 | https://doi.org/10.1186/1471-2466-14-157 |
| Case finding for chronic obstructive pulmonary disease in primary care: a pilot randomised controlled trial | British Journal of General Practice | Shamil Haroon, Peymane Adab, Carl Griffin, Rachel Jordan | 2013 | https://doi.org/10.3399/bjgp13x660788 |
| Case finding for chronic obstructive pulmonary disease: a model for optimising a targeted approach | Thorax | Jordan RE, Cheng KK, Miller M, Marsh J, Ayres J, Fitzmaurice D, Adab P, Lam KBH | 2012 | https://doi.org/10.1136/thx.2009.129395 |
| Case finding for COPD in primary care: a systematic review | Primary Care Respiratory Journal | Shamil M Haroon, Peymane A Adab, Rachel E Jordan | 2012 | https://doi.org/10.4104/pcrj.2012.00060 |
Conference proceedings
| Title | Journal | Conference | Authors | Year | Volume | Issue | Pages |
|---|---|---|---|---|---|---|---|
| A Comparison Of The ADO, BODE And DOSE Scores For Predicting Respiratory Hospitalisations In A Primary Care COPD Cohort | BMC Journal of Diagnostic & Prognostic Research | MEMTAB | A Dickens, R Jordan, A Enocson, D Fitzmaurice, A Sitch, P Adab | 2017 | 1 (Supp1):7. DOI: 10.1186/s41512–016–0001-y | ||
| Screening Test Accuracy Of Case Finding Interventions For Chronic Obstructive Pulmonary Disease In Primary Care: A Systematic Review | American Journal of Respiratory and Critical Care Medicine | ATS 2014 | Haroon SMM, Jordan RE, Adab P | 2014 | 189 | A2955 | |
| The Case Finding Yield For COPD In Primary Care: A Systematic Review And Meta-Analysis | American Journal of Respiratory and Critical Care Medicine | ATS 2014 | Haroon SMM, Jordan RE, O’Bierne-Elliman J, Adab P | 2014 | 189 | A2955 | |
| Detecting COPD Among Symptomatic Patients In Primary Care: A Comparison Of The COPD Assessment Test And The COPD Diagnostic Questionnaire | American Journal of Respiratory and Critical Care Medicine | ATS 2014 | Haroon SMM, Jordan RE, Enocson A, Fitzmaurice D, Adab P | 2014 | 189 | A2955 | |
| Over Diagnosis Of Chronic Obstructive Pulmonary Disease By GOLD Criteria Includes Older Male Subjects With Lower CAT Scores, More Heart Disease And Hypertension | American Journal of Respiratory and Critical Care Medicine | ATS 2014 | Haroon SMM, Miller MR, Fitzmaurice DA, Enocson A, Jordan RE, Adab P | 2014 | 189 | A2955 | |
| Forced Vital Capacity Definition Substantially Alters Prevalence Of Chronic Obstructive Pulmonary Disease | American Journal of Respiratory and Critical Care Medicine | ATS 2014 | Haroon SMM, Miller MR, Fitzmaurice DA, Enocson A, Jordan RE, Adab P | 2014 | 189 | A2955 | |
| Detecting undiagnosed COPD: Using routine primary care data to select and validate candidate variables for COPD risk prediction | European Respiratory Journal | ERS 2013 | Haroon SMM, Jordan RE, Riley R, Lancashire R, Marshall T, Adab P | 2013 | 42 | Suppl. 57 | 2399 |
Conference presentations/posters
| Date | Conference | Format | Title | Authors |
|---|---|---|---|---|
| 2019 | ERS | Oral presentation | Effect of screening for undiagnosed COPD on respiratory hospitalisation and mortality – 4-year follow-up of the TargetCOPD trial | Adab P, Fitzmaurice D, Martin J, Sitch A, Ayres JG, Cheng KK, Cooper BG, Daley A, Dickens AP, Enocson A, Greenfield S, Jolly K, Jowett S, Miller MR, Riley RD, Siebert S, Stockley RA, Turner A, Haroon S, Jordan RE |
| 2019 | ERS | Oral presentation | Development of the Birmingham Lung Improvement Studies (BLISS) prognostic score for COPD patients in primary care: data from the Birmingham COPD cohort | Jordan RE, Fitzmaurice D, Martin J, Sitch A, Ayres JG, Cheng KK, Cooper BG, Daley A, Dickens AP, Enocson A, Greenfield S, Jolly K, Jowett S, Miller MR, Riley RD, Siebert S, Stockley RA, Turner A, Haroon S, Adab P |
| 2019 | SAPC | Oral presentation | The impact of COPD case finding on clinical care: a prospective analysis of the TargetCOPD trial | Haroon S, Adab P, Dickens AP, Sitch A, Rai K, Enocson A, Fitzmaurice DA, Jordan RE |
| 2019 | RCGP Midland Faculty Research Symposium | Oral presentation | The impact of COPD case finding on clinical care: a prospective analysis of the TargetCOPD trial | Haroon S, Adab P, Dickens AP, Sitch A, Rai K, Enocson A, Fitzmaurice DA, Jordan RE |
| 2019 | ERS | Poster | External validation of the updated ADO score to predict mortality in patients from the Birmingham COPD cohort | Keene SJ, Jordan RE, de Vries F, Franssen FME, Martin J, Sitch A, Dickens A, Fitzmaurice DA, Adab P |
| 2019 | ERS | Oral presentation | Determinants of long-term changes in ADO prognostic score in UK COPD primary care patients: results from The Health Improvement Network | Keene |
| 2019 | ERS | Poster | The effects of COPD progression on work productivity: the Birmingham COPD Cohort | Kalirai R, Adab P, Ayres J, Fitzmaurice D, Jordan R on behalf of the BLISS investigators |
| 2019 | ERS | Oral presentation | Rai | |
| 2019 | British Thoracic Society | Oral presentation | Three million needles in a haystack | R Jordan |
| 2018 | Society for Research on Nicotine & Tobacco Europe conference | Poster | Prevalence, views and experience of e-cigarette use by COPD patients in The Birmingham COPD Cohort | A Farley, M Swallow, R Jordan, A Enocson, A Dickens, D Kotz, D Fitzmaurice, P Adab |
| 2018 | ERS | Poster | Prevalence, views, and experience of e-cigarette use by COPD patients in the Birmingham COPD Cohort | M Swallow, A Farley, R Jordan, A Enocson, A Dickens, D Fitzmaurice, P Adab |
| 2018 | ERS | Poster | Clinical management of patients newly diagnosed with COPD through targeted case finding and routine care: A longitudinal analysis of the TargetCOPD trial | S Haroon, A Dickens, P Adab, A Sitch, K Rai, A Enocson, D Fitzmaurice, R Jordan |
| 2017 | ERS | Poster | Evaluating a simple lung monitor as a screening test for COPD in primary care | A Dickens, P Adab, D Fitzmaurice, B Cooper, M Miller, A Sitch, R Riley, A Enocson, R Jordan |
| 2017 | SAPC | Elevator pitch presentation | Can a simple lung monitor be used as a screening test for COPD in primary care? | A Dickens, P Adab, D Fitzmaurice, B Cooper, M Miller, A Sitch, R Riley, A Enocson, R Jordan |
| 2017 | IPCRG World | Oral presentation | Evaluating a simple lung monitor as a screening test for COPD in primary care | R Jordan |
| 2016 | UHB Academic Grand Round | Invited speaker | Controversies in screening: the case of COPD | R Jordan |
| 2016 | IPCRG World | Oral presentation | Avoiding infections among patients with COPD: cross sectional analysis of the Birmingham COPD cohort | Jordan R, Woodall V, Sitch A, Khan A, Dickens A, Enocson A, Fitzmaurice D, Adab P |
| 2016 | COPD10 | Poster | Prevalence and characteristics of low oxygen saturation (SpO2) in a primary care COPD cohort | A Enocson, RE Jordan, P Adab, AP Dickens, D Fitzmaurice |
| 2016 | COPD10 | Poster | Delivering high quality spirometry in primary care: a report of spirometry quality in the BLISS programme | S Haroon, A Dickens, M Miller, B Cooper, A. Enocson, RE Jordan, D Fitzmaurice, P Adab |
| 2016 | COPD10 | Poster | A Comparison Of The ADO, BODE And DOSE Scores For Predicting Respiratory Hospitalisations In A Primary Care COPD Cohort | A Dickens, R Jordan, A Enocson, D Fitzmaurice, A Sitch, P Adab |
| 2016 | COPD10 | Poster | Prevalence Of Sleep Apnoea And Its Associated Impact On Quality Of Life In A Primary Care COPD Population | A Dickens, A Enocson, R Jordan, D Fitzmaurice, P Adab |
| 2016 | COPD10 | Oral presentation | Early diagnosis of COPD. Insights from BLISS: The Birmingham Lung Improvement Studies | R Jordan |
| 2016 | COPD10 | Oral presentation | Reflections on early identification of COPD | P Adab |
| 2016 | SAPC | Poster | A Comparison Of The ADO, BODE And DOSE Scores For Predicting Respiratory Hospitalisations In A Primary Care COPD Cohort | A Dickens, R Jordan, A Enocson, D Fitzmaurice, A Sitch, P Adab |
| 2016 | SAPC | Elevator pitch presentation | Prevalence of sleep apnoea and its associated impact on quality of life in a primary care COPD population | A Dickens, A Enocson, R Jordan, D Fitzmaurice, P Adab |
| 2016 | MEMTAB | Poster | A Comparison Of The ADO, BODE And DOSE Scores For Predicting Respiratory Hospitalisations In A Primary Care COPD Cohort | A Dickens, R Jordan, A Enocson, D Fitzmaurice, A Sitch, P Adab |
| 2016 | ERS | Poster | Prevalence and characteristics of low oxygen saturation (SpO2) in a primary care COPD cohort | A Enocson, RE Jordan, P Adab, AP Dickens, D Fitzmaurice |
| 2016 | ERS | Poster discussion | A Comparison Of The ADO, BODE And DOSE Scores For Predicting Respiratory Hospitalisations In A Primary Care COPD Cohort | A Dickens, R Jordan, A Enocson, D Fitzmaurice, A Sitch, P Adab |
| 2016 | ERS | Poster | Prevalence Of Sleep Apnoea And Its Associated Impact On Quality Of Life In A Primary Care COPD Population | A Dickens, A Enocson, R Jordan, D Fitzmaurice, P Adab |
| 2016 | ERS | Poster | Predicting risk of undiagnosed COPD in primary care: Development and validation of the TargetCOPD score | S Haroon, P Adab, A Dickens, R Riley, D Fitzmaurice, R Jordan |
| 2016 | ERS | Poster | Prevalence and predictors of electronic cigarette use by patients with COPD in the Birmingham COPD cohort | A Farley, K Kalirai, R Jordan, A Enocson, A Dickens, D Fitzmaurice, P Adab |
| 2016 | ERS | Poster discussion | Modelling the long-term effects of an active case finding programme for undiagnosed COPD | T Lambe, R Jordan, P Adab, D Fitzmaurice, A Enocson, S Jowett |
| 2016 | ERS | Oral presentation | Using the ADO score in primary care to target pulmonary rehabilitation to patients at high risk of hospital admission: model using primary care cohorts and published literature | R Jordan, A Dickens, A Enocson, D Fitzmaurice, R Ryan, T Marshall, P Adab |
| 2016 | ERS | Invited speaker | What is the most clinically and cost-effective approach for identifying undiagnosed COPD? | R Jordan |
| 2015 | IPCRG World | Oral presentation | Predicting risk of undiagnosed COPD in primary care: Development and validation of the TargetCOPD model | S Haroon, R Jordan, R Riley, D Fitzmaurice, P Adab |
| 2015 | IPCRG World | Oral presentation | Case finding for COPD in primary care: a qualitative study of the views of health professionals | S Haroon, R Jordan, P Adab |
| 2015 | ATS | Poster | TargetCOPD: A pragmatic randomised controlled trial of targeted case finding for COPD versus routine practice in primary care | Jordan RE, Adab P, Sitch AJ, Enocson A, Blissett D, Jowett S, Riley RD, Marsh J, Miller MR, Cooper B, Turner AM, Ayres JG, Jolly K, Stockley R, Greenfield S, Siebert S, Daley A, Cheng KK, Fitzmaurice DA |
| 2015 | ERS | Oral presentation | COPD over diagnosis in the UK | Halima Buni, Rachel Jordan, Peymane Adab, Alexandra Enocson, Kar Keung Cheng |
| 2015 | ERS | Oral presentation | TargetCOPD: A pragmatic randomised controlled trial of targeted case finding for COPD versus routine practice in primary care | RE Jordan, P Adab, A Sitch, A Enocson, D Blissett, S Jowett, J Marsh, R Riley, M Miller, B Cooper, A Turner, JG Ayres, KK Cheng, K Jolly, R Stockley, S Greenfield, S Siebert, A Daley, D Fitzmaurice |
| 2015 | SAPC | Oral presentation | TargetCOPD: A cluster RCT of targeted case finding for COPD vs routine practice in primary care | Jordan RE, Adab P, Sitch AJ, Enocson A, Blissett D, Jowett S, Riley RD, Marsh J, Miller MR, Cooper B, Turner AM, Ayres JG, Jolly K, Stockley R, Greenfield S, Siebert S, Daley A, Cheng KK, Fitzmaurice DA |
| 2014 | ATS | Poster | Screening Test Accuracy Of Case Finding Interventions For Chronic Obstructive Pulmonary Disease In Primary Care: A Systematic Review | Haroon S, Jordan R, Adab P, Takwoingi Y |
| 2014 | ATS | Poster | The Case Finding Yield For COPD In Primary Care: A Systematic Review And Meta-Analysis | Haroon S, Jordan R, Adab P, O’Beirne-Elliman J |
| 2014 | ATS | Poster | Over diagnosis of chronic obstructive pulmonary disease by GOLD criteria includes older male subjects with lower CAT scores, more heart disease and hypertension | Haroon S, Miller MR, Enocson A, Fitzmaurice DA, Jordan R, Adab P |
| 2014 | ATS | Poster | Forced vital capacity definition substantially alters prevalence of chronic obstructive pulmonary disease | Haroon S, Miller MR, Enocson A, Fitzmaurice DA, Jordan R, Adab P |
| 2014 | ATS | Poster | Detecting COPD among symptomatic patients in primary care: a comparison of the COPD Assessment Test and the COPD Diagnostic Questionnaire | Haroon S, Jordan R, Enocson A, Fitzmaurice D, and Adab P |
| 2014 | ATS | Poster | The Birmingham COPD Cohort Study: A Cross-sectional Comparison Of The Characteristics Of Ever-smokers And Never-smokers | Alexandra Enocson, Andy Dickens, Rachel Jordan, David Fitzmaurice, Peymane Adab |
| 2014 | IPCRG World | Oral presentation | The Birmingham COPD Cohort Study: A Cross-Sectional Comparison Of The Characteristics Of Ever-Smokers And Never-Smokers | R Jordan, A Enocson, A Dickens, D Fitzmaurice, P Adab |
| 2014 | IPCRG World | Oral presentation | Predicting the risk of COPD in Primary Care: Development and validation of a COPD risk score | S Haroon, R Riley, R Lancashire, T Marshall, R Jordan, P Adab |
| 2014 | IPCRG World | Invited speaker | Preventing COPD admissions: Strategies for risk prediction in Primary Care | R Jordan |
| 2014 | NIHR SPCR Primary Care Research Showcase | Poster | COPD Screener Study: Evaluation of a simple COPD screener as a novel screening test for case finding for COPD in primary care | Rachel Jordan, Nicola Adderley, Peymane Adab, Brendan Cooper, Alexandra Enocson, David Fitzmaurice, Martin Miller, Richard Riley |
| 2014 | ERS | Poster | Birmingham COPD Cohort: factors associated with absenteeism | Kiran Kalirai, Peymané Adab, Rachel Jordan, David Fitzmaurice, Jon Ayres |
| 2014 | Birmingham City Council in-house research meeting | Poster (not peer reviewed, MPH student) | The Birmingham COPD Cohort Study: A Cross-sectional Analysis of Self-Management Behaviours and Support in adults with COPD | Ainee Khan, Rachel Jordan, Andy Dickens, Alexandra Enocson, David Fitzmaurice, Peymane Adab |
| 2014 | ERS | Oral presentation | Comparison of characteristics of COPD patients with an established diagnosis, with those newly identified through case-finding – The Birmingham COPD Cohort Study | P Adab, A Dickens, A Enocson, D Fitzmaurice, R Jordan |
| 2014 | BTS | Poster | Feasibility of delivering an occupational health intervention aimed at improving work productivity among COPD working patients | K Kalirai, P Adab, RE Jordan, JG Ayres, S Sadhra |
| 2013 | ERS | Poster | Detecting undiagnosed COPD: Using routine primary care data to select and validate candidate variables for COPD risk prediction | S Haroon, R Jordan, R Riley, R Lancashire, T Marshall, P Adab |
| 2013 | ERS | Poster | Birmingham COPD cohort: Comparison of characteristics of employed with non-employed patients | K Kalirai, P Adab, R Jordan, D Fitzmaurice, J Ayres |
| 2013 | ERS | Poster | The Birmingham COPD Cohort Study – Associations between CAT, lung health and health care utilisation | AP Dickens, P Adab, R Jordan, A Enocson, J Ayres, D Fitzmaurice |
| 2013 | RCGP symposium | Poster | Birmingham COPD Cohort: comparison of characteristics of employed with non-employed patients | K Kalirai, P Adab, R Jordan, D Fitzmaurice, J Ayres |
| 2013 | BTS | Oral presentation | A cross-sectional analysis of the effect of COPD on work capability using the Birmingham COPD cohort | K Kalirai, P Adab, R Jordan, D Fitzmaurice, J Ayres |
| 2013 | ERS | Poster | Birmingham COPD Cohort: comparison of characteristics of employed with non-employed patients | Kiran Kalirai; Peymane Adab; Rachel Jordan, David Fitzmaurice, Jon Ayres |
| 2013 | BTS | Poster | The relationship between employment status, work productivity and quality of life among patients with COPD: Cross-sectional analysis of the Birmingham COPD Cohort | K Kalirai, P Adab, R Jordan, D Fitzmaurice, J Ayres |
| 2012 | COPD8 | Poster | The Birmingham COPD Cohort Study protocol: a primary care cohort of COPD patients | P Adab, A Dickens, R Backman, K Kalirai, A Enocson, D Fitzmaurice, J Ayres, KK Cheng, RE Jordan and the BLISS Investigators |
| 2012 | COPD8 | Poster | TargetCOPD: a pragmatic randomised controlled trial of targeted case finding for COPD versus routine practice in primary care: protocol | Rachel Jordan, Ruth Backman, Andrew Dickens, David Fitzmaurice, Alexandra Enocson, Peymane Adab and the BLISS Investigators |
Appendix 2 Screening questionnaire for TargetCOPD trial
Appendix 3 Baseline questionnaires for Birmingham chronic obstructive pulmonary disease cohort participants
Appendix 4 Development of the Birmingham Lung Improvement Studies prognostic score for chronic obstructive pulmonary disease patients in primary care: data from the Birmingham chronic obstructive pulmonary disease cohort
List of abbreviations
- ADO
- age, dyspnoea, airflow obstruction
- ATC
- American Thoracic Society BLISS Birmingham Lung Improvement StudieS
- BMI
- body mass index
- BODE
- body mass index, airflow obstruction, dyspnoea, and exercise
- CAT
- COPD Assessment Test
- CI
- confidence interval
- COPD
- chronic obstructive pulmonary disease
- EHR
- electronic health record
- EQ-5D
- EuroQol-5 dimensions
- ERS
- European Respiratory Society
- FEV1
- forced expiratory volume in 1 second
- FVC
- forced vital capacity
- HES
- Hospital Episode Statistics
- HR
- hazard ratio
- HRQoL
- health-related quality of life
- HSE
- Health Survey for England
- ICER
- incremental cost-effectiveness ratio
- IMD
- index of multiple deprivation
- IQR
- interquartile range
- IRR
- incidence rate ratio
- LLN
- lower limit of normal
- MCID
- minimal clinically important difference
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- OH
- occupational health
- OR
- odds ratio
- PA
- physical activity
- PAG
- patient advisory group
- PRP
- pulmonary rehabilitation programme
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- RCGP
- Royal College of General Practitioners
- RCT
- randomised controlled trial
- SD
- standard deviation
- USPSTF
- US Preventive Services Task Force
- VGDF
- vapours, gases, dusts or fumes
- WP
- work package
