Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0610-10108. The contractual start date was in January 2012. The final report began editorial review in February 2019 and was accepted for publication in April 2022. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Wenborn et al. This work was produced by Wenborn et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Wenborn et al.
Chapter 1 Introduction: setting the scene
Defining dementia
‘Dementia is a term used to describe a range of cognitive and behavioural symptoms that can include memory loss, problems with reasoning and communication and change in personality, and a reduction in a person’s ability to carry out daily activities, such as shopping, washing, dressing and cooking’ (© NICE 2018. Dementia: Assessment, Management and Support for People Living with Dementia and Their Carers. Available from www.nice.org.uk/guidance/ng97 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication). 1 There are a range of conditions that cause dementia, the most common in the UK being Alzheimer’s disease, as well as vascular dementia, mixed dementia, dementia with Lewy bodies and frontotemporal dementia amongst others. A person with dementia finds it increasingly difficult to remember, know where they are, know who other people are, keep track of time, organise themselves and their activities, understand what is being said, communicate with other people, make decisions, or learn new things. As a result, the person experiences increasing difficulty in carrying out activities of daily living (ADL) and other valued and meaningful activities; they progressively need more and more assistance from family and friends, as well as from professional carers. The way in which carers support a person with dementia to cope with their impairments can either optimise or decrease the individual’s performance and as a result can dictate the degree of disability and lack of agency or sense of control that is experienced. 2,3
The number of people living with dementia
It is estimated that 47 million people worldwide were living with dementia in 2015 and, although the number is still rising globally owing to an ageing population, the incidence is decreasing in some countries because of the take up of public health information to adopt healthier lifestyles. 4 The 2015 UK figure was estimated to be 850,000 people living with dementia, with almost two-thirds living in the community. 5
The impact of caring for a person living with dementia
The current financial cost to the NHS, local authorities and families in England is £26.3B per year, of which £11.6B is attributable to the support provided by unpaid carers (i.e. primarily family members). 5 Indeed, unpaid care accounts for three-quarters of the total cost for people living with dementia within the community. 5 The impact of caring for someone living with dementia is not only financial, but can also be both physically and psychologically demanding. As the person with dementia loses the ability to carry out everyday tasks and their former activities and roles, family carers often experience a feeling of increased burden and stress. About 40% of family carers of people with dementia have clinically significant depression or anxiety; carers can also have poorer physical health, more absences from work and lower quality of life than non-carers. 4 Carer stress predicts care home admission and elder abuse. 4
Living Well with Dementia: a policy priority
Several UK Government policies aim to improve health and social care service provision for people with dementia and their carers. A watershed point in England was the publication of Living Well with Dementia: A National Dementia Strategy,6 the first significant policy document to address these issues. This strategy had three main aims: (1) raise awareness and understanding, (2) provide earlier diagnosis and support, and (3) maximise living well with dementia. The strategy was underpinned by 17 objectives to be achieved over 5 years. The subsequent Prime Minister’s Challenges7,8 urged action to do more to achieve the strategy first by 2015, and then by 2020, and thus raised the profile of dementia as being a clinical and research priority. 7,8 The UK Government subsequently pledged to provide community-based programmes that aimed to improve quality of life for people with dementia and their carers. 9
Training and supporting carers and tailoring psychosocial interventions to meet the specific needs of individuals are key components to achieving the dementia strategy objectives. Personalised interventions can improve family carers’ well-being, delay admission to care homes and reduce the risk of institutionalisation by up to one-third. 10,11 More recently, and following on from the drive for earlier diagnosis,12 the importance of providing psychosocial interventions for people with dementia has been emphasised both internationally13 and nationally. 14
Psychosocial interventions
Psychosocial interventions, which include physical, cognitive or social activities, can have positive and cost-effective outcomes on cognition, quality of life and institutionalisation. 15,16 Since this research programme commenced (2012), funding for psychosocial dementia research has increased and a range of interventions have been, and are being, developed and evaluated through randomised controlled trials (RCTs) and other methodologies. UK-funded studies cover a range of interventions, for example Dementia And Physical Activity,17 brief interventions to promote independence18 and tailored activities. Furthermore, a multicentre RCT of goal-oriented cognitive rehabilitation (the GREAT trial) demonstrated good achievement of goals but no benefit to validated outcomes,19 and an implementation study is about to commence.
Defining occupational therapy
Humans have an innate need to engage in personally meaningful activities to maintain physical and mental health and well-being. People who have dementia increasingly need support to engage in such activities. 2 Occupational therapy is a complex, dynamic process that comprises multiple practices, the implementation of which is individualised, with the relationship between the person(s) and the therapist being fundamental because the process necessitates the active involvement of the person(s) and therapist working in partnership. 20 Occupational therapists utilise core skills to engage people in personally meaningful occupation. They collaborate with the client (often including the client’s family and/or carer as well) in assessment, enablement, problem-solving, environmental assessment and adaptation, and use activity as a therapeutic tool. 21 Hence, engaging in meaningful activity is both the means and the outcome of the occupational therapy process and intervention.
Community Occupational Therapy in Dementia
In the Netherlands, Graff et al. 22 developed the Community Occupational Therapy in Dementia (COTiD) programme. It comprises 10 1-hour sessions of home-based occupational therapy provided over 5 weeks by an occupational therapist who works in partnership with the person who has dementia and their family caregiver on individualised goals to improve skills in meaningful daily activities through the use of effective strategies, adaptation of the (physical and social) environment, and developing the caregivers’ abilities and sense of competence. A single-site RCT of 135 pairs of people with mild to moderate dementia and their family caregivers (n = 270) compared COTiD with treatment as usual (TAU), which did not include any occupational therapy provision. The study demonstrated improved ADL skills, quality of life and mood in people with dementia, and improved quality of life, mood and sense of competence in family caregivers. 23,24 COTiD was also found to be cost-effective. 25 A subsequent study in Germany found no difference between providing COTiD and providing a single consultation visit by an occupational therapist. 26 Although the comparator group in this latter trial was different, the integral process evaluation highlighted the need not only to translate but also to adapt complex interventions to the local context for evaluation and cross-national comparison to be effective. 27 COTiD is now being translated, adapted and evaluated in other European countries. A pilot study is under way in France, and a prospective cohort study in Italy has demonstrated positive effect on caregiver burden, as well as improved activities performance and satisfaction for people with dementia. 28
UK occupational therapy practice
Currently, people with dementia living in England may or may not see an occupational therapist at the point of diagnosis and, if they do, only briefly, primarily for assessment of risk and support needs. Traditionally, occupational therapy has been provided later on in the dementia pathway; however, this is changing as a result of implementation of the previously described policy that promotes earlier diagnosis and easy access to post-diagnostic support services. At whatever point the occupational therapy is provided, the focus is invariably on the person with dementia, with their family carers’ needs considered primarily in terms of their ability to support the person with dementia within their role as a carer. Occupational therapy is not often geared towards meeting the carer’s personal or occupational needs.
The Graff study23–25 demonstrated the potential value of the occupational therapy intervention being provided at an earlier point, with a focus not only on the person with dementia but also on enabling and skilling up their family carer, who will inevitably be required to provide increasing support for the person with dementia if they are to remain engaged in meaningful activities, while also meeting their own needs, including occupational balance. It therefore appeared that COTiD had great potential for adoption in the UK. However, the culture, health and social care service provision and context differs between the Netherlands and England. At the time of the Graff study, people in the Netherlands were diagnosed with dementia by either a neurologist or a geriatrician within an outpatient clinic. There was no community occupational therapy nor older people’s mental health service provision for people with dementia within the Dutch insurance-based model of health care. Within the UK, health care has long been provided free at the point of delivery through the NHS. At the point of designing this research programme, specialist older people’s mental health services were well established, with multiprofessional teams, including occupational therapists, providing assessment and intervention services within hospital and community settings, including people’s own homes. Memory Assessment Services were just being established to provide early diagnosis and access to a range of support for people with dementia and their family carers. The UK National Institute for Health and Care Excellence (NICE) recommends that occupational therapy should be considered to support functional ability in people living with mild to moderate dementia. 1 The current Memory Services National Accreditation Programme standard 6, ‘psychosocial interventions’, requires services to provide timely access to psychosocial interventions for occupational and functional aspects of dementia, including access to occupational therapy, and access to advice and support on assistive and telecare solutions designed to assist people with ADL: a core domain of occupational therapy practice. 29
Therefore, this applied research programme, Valuing Active Life in Dementia (VALID), was funded to translate, adapt, develop, evaluate and implement a community occupational therapy intervention for people with mild to moderate dementia and their family carers in England.
Chapter 2 The VALID applied research programme
Programme aim
The aim of the VALID programme was to translate, adapt, develop, evaluate and implement a community occupational therapy intervention that will promote independence, meaningful activity and quality of life for people with mild to moderate dementia and their family carers within England.
Programme objectives
The VALID programme objectives were to:
-
translate and adapt COTiD into the Community Occupational Therapy in Dementia – the UK version (COTiD-UK) intervention and training programme and optimise it for use in the UK
-
test the feasibility of implementing COTiD within UK health and social care services
-
field test the proposed outcome measures through an internal pilot trial of COTiD-UK compared with TAU
-
estimate the effectiveness of COTiD-UK in improving the functional independence of people with mild to moderate dementia through a multicentre, pragmatic, single-blind, RCT
-
evaluate the cost-effectiveness of COTiD-UK compared with TAU
-
assess the implementation of COTiD-UK through monitoring and budget impact analysis
-
disseminate the findings of the VALID research programme widely.
Programme structure
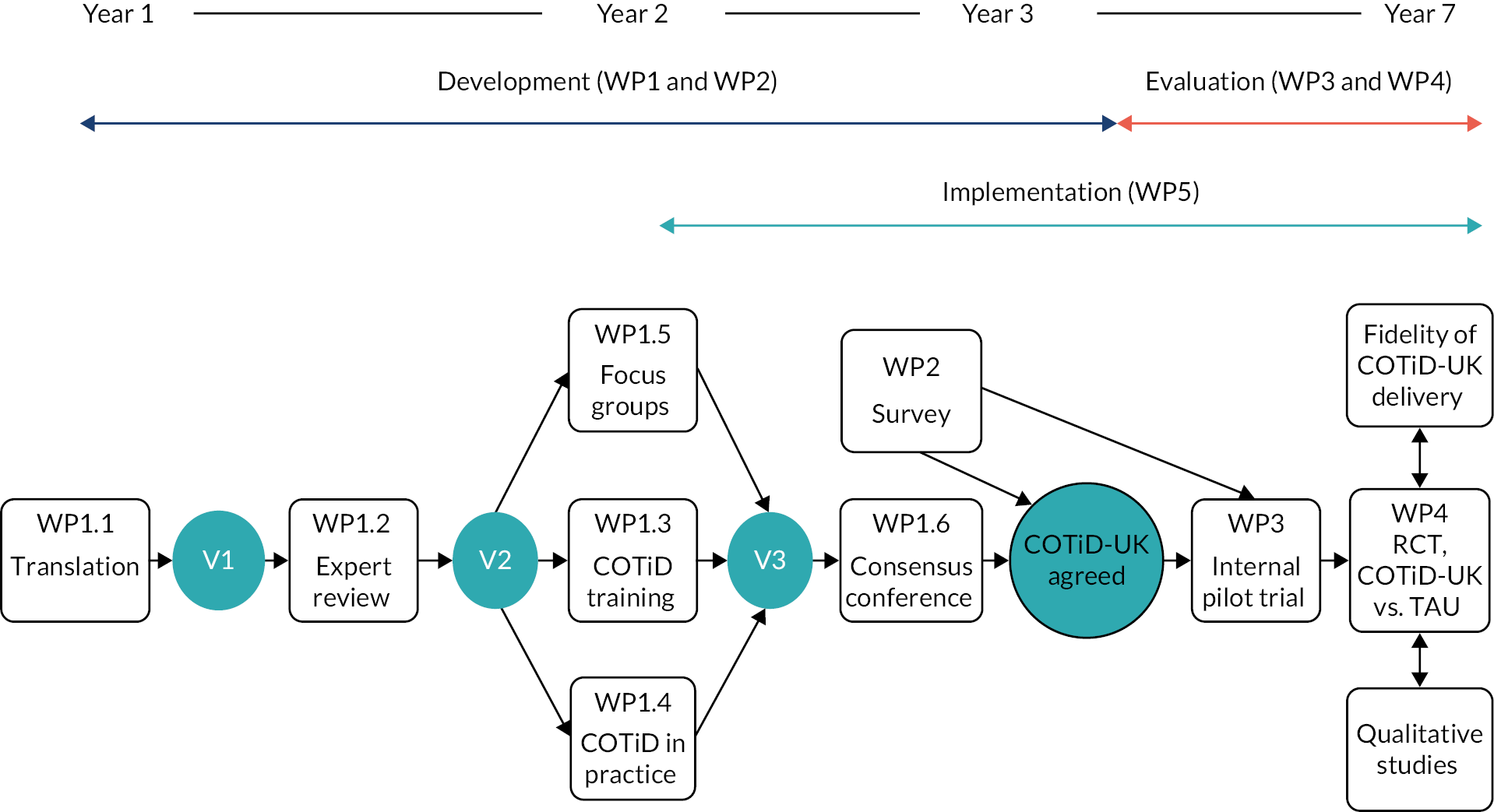
The VALID programme followed the Medical Research Council framework for developing and evaluating complex interventions30 and comprised three phases and five associated work packages (WPs): development (WP1 and WP2), piloting and evaluation (WP3 and WP4), and implementation (WP5). Figure 1 illustrates the sequence of WPs and activities across the programme. Table 1 summarises the WPs and their respective aims and activities.
FIGURE 1.
The VALID research pathway diagram.
| Phase (WP) aim | Activity | Data collected |
|---|---|---|
| Development phase (1/2) | ||
| To translate and adapt the COTiD guideline and training package to maximise its suitability for use within the UK, and to produce the COTiD-UK intervention in readiness for evaluation in WP3 and WP4 | WP1 | |
| 1.1 Translation of Dutch intervention manual and the training materials (including subtitling DVD) to produce version 1 of the manual | Comments from review of translation | |
| 1.2 Expert review and amendment of translated manual to produce version 2 of the manual | Expert opinion feedback sheets | |
| 1.3 COTiD training using version 2 of the manual and materials | COTiD training: | |
|
||
| 1.4 COTiD put into practice using version 2 of manual | COTiD in practice: | |
|
||
|
||
|
||
|
||
| 1.5 Focus groups conducted with people with dementia and with family carers who did not receive COTiD | Focus group transcripts and field notes | |
| 1.6 Consensus conference held to consider version 3 of the manual | Record of group discussions | |
| WP2 | ||
| 2.1 Online survey | Survey responses (quantitative and qualitative) | |
| Piloting phase (3) | ||
| To field test the outcome measures and trial procedures, and finalise the COTiD-UK intervention mode of delivery, training and supervision | Internal pilot trial of COTiD-UK compared with TAU across three research sites | ACCEPT review |
| Evaluation (4) | ||
| To determine the clinical effectiveness and cost-effectiveness of COTiD-UK compared with TAU | Multisite RCT | Outcome measures data including: |
|
||
|
||
| Qualitative studies | ||
| 1. Taking part in the COTiD-UK intervention | Semistructured interviews with dyads and occupational therapists who took part in COTiD-UK | |
| 2. Why people declined to take part in the trial | Semistructured interviews with family carers who had declined to take part in the VALID RCT | |
| Economic evaluation | COTiD-UK training and provision costs. Service receipt costs and quality-of-life measure | |
| Implementation (5) | ||
| To determine the feasibility and effectiveness of COTiD-UK in usual clinical practice | Assessing the fidelity of COTiD-UK delivery | COTiD-UK session transcripts |
| Review of data using the Theoretical Domains Framework | Evaluation phase: | |
|
||
|
||
|
||
|
||
|
||
|
||
| Piloting and evaluation phases | ||
|
||
|
||
|
||
|
||
|
Changes to the original research plan
The research aim and six out of the seven objectives remained the same; however, the timing and design of the programme were revised, as described in the following section.
Development phase
The time needed to translate the Dutch COTiD manual and training materials (including subtitling the training videos) was initially underestimated. Completion of the task was further delayed until the original Dutch author was available to check the translated materials for accuracy. Hence, the task took nearly 1 year, rather than 6 months, as originally scheduled. This, together with delays in agreeing occupational therapist capacity and funding to cover their time at the 10 participating research sites, delayed the start of the COTiD training by a further 6 months. Further delays in setting up research sites and obtaining the relevant local governance approvals then delayed the intervention being provided in practice: this was originally scheduled to start following the first training day in January 2013 but actually started at the first sites in April 2013. Further delays in gaining management agreement at some sites to release the occupational therapists meant that in some sites, the intervention did not start until July 2013. A series of information technology (IT) and information governance challenges and complicating issues delayed some of the occupational therapists’ video-recorded data being transferred to the research team. This subsequently delayed their analysis and provision of feedback to the occupational therapists on their performance. Other activities, therefore, had to be rescheduled; specifically, the occupational therapy focus groups, which were initially scheduled for the final training day in June 2013. These needed to be deferred by 3–4 months to ensure that participants had some experience of providing the intervention in practice so as to be able to discuss it. Hence, the consensus event could not run until after the intervention had been provided and, therefore, took place in September 2013. Completing the analysis of the development phase data to finalise the COTiD-UK intervention in readiness for the trial then took a further 6 months. Therefore, the development phase took twice as long as originally scheduled.
Piloting and evaluation phase
The delays outlined above, plus unexpected staff absence (May to July 2014), meant that the internal pilot trial (WP3) started nearly 2 years later than scheduled. Having moved from the internal pilot trial to the full RCT (WP4), a range of challenges hampered its completion to time and target. These included delays in recruiting research sites because of the complex nature of the trial, which required both researcher and occupational therapist capacity to deliver, then the recruitment of pairs rather than individual participants.
Several interested sites were not able to proceed because of lack of researcher and/or occupational therapist capacity. Research support required funding from the local Clinical Research Network (CRN), which was not always forthcoming, and not all NHS trusts agreed to free up occupational therapists’ time so that they could take part in the study. It should be noted that only 2 out of 15 sites managed to obtain excess treatment costs, namely the additional funding that is required within the UK to deliver the clinical intervention being evaluated, as this is not included in the research grant award. This was despite the initial award of subvention funding for the programme as a whole because no trust met the threshold needed to reclaim the costs. This inevitably reduced the capacity to deliver the intervention in a timely way in some sites because the occupational therapists’ availability was dependent on the goodwill of their service managers, who had to balance their support for the study with the need to provide the level of service commissioned. This restricted the occupational therapist capacity such that more research sites than originally planned had to be recruited to achieve the dyad recruitment target within the time frame agreed with the funder.
In addition to this, additional occupational therapists had to be trained throughout the trial period to deliver the intervention as new sites were recruited, and one-quarter of those originally recruited later dropped out as a result of changing jobs, service reconfiguration or sick leave. The complexity of liaising with clinical teams to recruit dyads in tandem with occupational therapists’ capacity to deliver the intervention within the protocol time scale, while maintaining researcher masking and in many cases with limited occupational therapist time being available, resulted in trial recruitment taking longer than expected. Therefore, the trial recruitment period was initially extended by 6 months and then a further 9 months to the end of June 2017, following a successful variation-to-contract application to the funders for an 18-month extension to the programme. The final data were collected towards the end of January 2018. Hence, the RCT took 40, rather than 36 months to complete, as originally planned.
The original plan was to collect follow-up data for all participants at 12, 26 and 52 weeks, and for the first 40% of those recruited at 78 weeks (n = 192). The 18-month variation-to-contract extension was calculated to enable the 26-week follow-up data to be collected for all participants, while the percentage of 52-week follow-ups had to be reduced from 100% (n = 480) to 77% (n = 368) to complete the RCT within the revised time scale.
Implementation phase
It was originally planned to complete the implementation phase (WP5) after the RCT had finished, to fulfil objective 6, but this structure and objective was changed because of a number of factors.
First, developments within the growing field of implementation science since the grant application was submitted recommended that implementation should be integrated throughout a programme of research such as this, rather than be left as a stand-alone package at the end. 31 Second, as the development phase had over-run as described, thus delaying the piloting and evaluation phases, it was not feasible to complete the implementation phase as planned.
However, the range and depth of data collected within the development, piloting and evaluation phases strongly contributed to this aspect of the programme, and the learning from these resulted in some of the activities originally and specifically planned for WP5 no longer being necessary. Therefore, the implementation phase was revised to consist of (1) a descriptive study to assess the fidelity of delivery of the COTiD-UK intervention within the RCT, and (2) an exploratory study to understand why the intervention was or was not delivered as planned by reviewing data collected during the development, pilot and evaluation phases using the Theoretical Domains Framework (TDF). 32 The revised plan is described in more detail in Chapter 7.
A budget impact analysis was not carried out because the statistical results indicated a low probability that the intervention would be cost-effective and, therefore, that the intervention was not likely to be implemented.
Programme management and governance
Programme Steering Committee
An independent Programme Steering Committee (PSC) acted as the oversight body on behalf of the Sponsor [North East London NHS Foundation Trust (NELFT)] and funder [National Institute for Health and Care Research (NIHR)]. The role of the PSC was to provide expert advice that was independent of the research team, monitor progress, advise on proposed changes to the programme’s plans in the light of new evidence or other unanticipated development, and provide written support for any requests for additional funding or time extensions. It comprised an independent chairperson, statistical and clinical advisors, a person living with dementia, a former spousal carer and, on occasion, a funder representative. Relevant members of the research team attended as requested to provide information and progress reports.
Programme Management Group
A Programme Management Group (PMG) had operational responsibility to deliver the programme of research. It was chaired by the chief investigator (MO) and comprised the majority of co-applicants, plus members of the research team and other collaborators as required and invited. The PMG met face to face or over the telephone at varying intervals depending on the stage of the research programme.
On some occasions, a smaller group (referred to as the Principal Investigators Group) involving the chief investigator (MO); Sheffield (GM) and Humber (EMC) research centre Principal Investigators; qualitative/patient and public involvement (PPI) lead (FP); and programme manager (JW) met, usually over the telephone, to consider research, recruitment and dissemination activities in more practical detail. They were also joined by other members of the team as and when relevant, for example, they were joined by the trial manager to discuss site and participant recruitment.
Occupational Therapy Reference Group
An Occupational Therapy Reference Group (OTRG) comprising UK occupational therapists with experience of working with people with dementia and their family carers provided independent specialist occupational therapy advice to the research team to ensure that the proposed research activities were relevant and feasible in terms of current UK occupational therapy service provision and practice. It was chaired by the clinical occupational therapist co-applicant (SR), supported by the programme manager and reported to the PSC.
Trial management and governance (work packages 3 and 4 only)
The RCT was run by the NIHR UK Clinical Research Collaboration (UKCRC)-registered Priment Clinical Trials Unit at University College London (UCL), which provides specialist expertise in the design, conduct and analyses of trials in primary care and mental health. The trial was set up and conducted in accordance with Priment quality management systems and standard operating procedures (SOPs) for non-Clinical Trials Of An Investigational Medicinal Product.
Trial Management Team
Day-to-day responsibility was delegated by the chief investigator to the programme manager and the trial manager and relevant members of the trial team. The Trial Management Team (TMT) ensured that the trial was conducted, recorded and reported in accordance with the protocol, good clinical practice, all regulatory requirements and other essential procedures for running trials, as documented by the SOPs developed by the Priment clinical trials unit and the sponsor.
Trial Management Group
A Trial Management Group (TMG) consisting of the chief investigator, members of the TMT and Priment met at regular intervals to monitor the conduct and progress of the trial, with the frequency of meeting depending on the stage of the study. The division of responsibilities was defined following clinical trials unit/sponsor SOPs and conducted accordingly.
Data Monitoring and Ethics Committee
An independent Data Monitoring and Ethics Committee (DMEC) was responsible for safeguarding the interests of trial participants, assessing the safety and efficacy of the interventions during the trial, and monitoring the overall conduct of the clinical trial. The DMEC reported to the PSC.
Chapter 3 Development phase: developing COTiD-UK (work packages 1 and 2)
Aims
The aims of the development phase were to translate and adapt the COTiD guidelines and training package to maximise its suitability and feasibility for use within the UK and to produce the COTiD-UK intervention in readiness for evaluation in a RCT.
There were two WPs:
-
WP1 – translation and adaptation of the COTiD intervention and training package
-
WP2 – online survey to scope current community occupational therapy service provision and practice for people with dementia and their family carers in the UK.
Ethics approval
Full ethics approval for WP1 and WP2 was gained from NRES Committee Yorkshire & the Humber – Leeds West on 28.11.12, Ref No 12/YH/0492. Five amendments (four substantial and one non-substantial) were approved to cover protocol and documentation updates, and new documents as needed. Local research and development governance approvals were obtained at each research site as appropriate. Informed consent was received from all participants.
The COTiD guideline and training package
As described earlier, the COTiD guideline and training package was developed in the Netherlands and published in Dutch,23 and subsequently in French33 and Italian. 34
The COTiD intervention
The aim of the COTiD intervention is to improve the person with dementia’s ability to carry out daily activities, improve the family carer’s sense of competence and, thereby, enhance the quality of life for both parties. COTiD consists of 10 1-hour sessions delivered over 5 weeks. The person with dementia and their carer are both clients and, for this reason, are both actively involved and work in partnership with the occupational therapist.
There are three phases.
Strengths, needs and case formulation phase (sessions 1–4)
Following an introductory session (number 1) to establish rapport and explain the format of the intervention, this phase comprises:
-
an occupational performance history interview35 with the person who has dementia
-
an ethnographic interview36 with the carer
-
recording the dyad’s daily routine/schedule using a diary sheet
-
skills observation to assess the person with dementia’s motor and process skills and the carer’s communication, interaction skills and coping skills
-
strategy observation to assess the person with dementia’s current strategies
-
environmental assessment
-
summarising and interpreting the information in readiness for the next phase (the occupational therapist does this in preparation for phase 2, it does not constitute one of the COTiD sessions).
Goal-setting phase (session 5)
In session 5, the occupational therapist summarises the information gained from the narrative interviews conducted with the person with dementia and with the family carer, plus the completed environmental assessment, activity and strategy observations. Then, together with the person who has dementia and their family carer, they list and prioritise the goals to be addressed during the intervention phase (shared decision-making). Goals may be joint or individual to either party.
Implementation of the intervention plan phase (sessions 6–10)
During sessions 6–10, the person with dementia and their carer work through the agreed intervention plan activities using either strategy training or external compensation to enable the person with dementia’s occupational performance. The occupational therapist also uses the consultation advice model to coach the carer in problem-solving skills. 37 The carer is encouraged to consider and implement effective strategies using the ‘how can you achieve that’ approach to best enable the person with dementia to carry out activities by effectively using their remaining strategies and adaptations made to the physical and social environment, while also reducing their care burden and meeting their own needs. The sessions primarily take place where the person with dementia lives. The ethnographic interview may take place in the carer’s home, and some implementation sessions may take place outside the home, that is within the local community, depending on the goals that have been set.
The COTiD training package
In the Netherlands, 4 training days are provided; the first 3 days each run 1 month apart, followed by a fourth day 3 months later. The first 3 days cover the three phases of the intervention, respectively. Content includes didactic teaching and practising some of the skills needed, for example the activity and strategy assessments. A case study is used, with participants role-playing the part of the occupational therapist, while actors simulate the role of the dyad. A carousel format is used, that is participants take it in turns to ask the actor(s) questions, with the actors providing feedback at the end regarding their experience. Participants practise their new skills in between the training days by providing sessions to dyads. These sessions are video-recorded and the recordings are brought to the next training day for trainer and peer feedback, during which discussion is framed by a checklist devised for evaluating the occupational therapist skills. The fourth day covers how to market the intervention and again features participants using role play to explain the purpose and value of COTiD to a range of potential stakeholders, for example a consultant psychiatrist, team manager and service commissioner. The COTiD knowledge questionnaire, COTiD vignettes and COTiD training evaluation are completed during this last training day.
Development of COTiD-UK
Introduction
A mixed-methods approach was used and included the following activities: translation and expert review of the manual and training materials; evaluation of the COTiD training for occupational therapists and COTiD delivery in practice; focus groups; semistructured interviews; a consensus conference; and an online survey. Quantitative and qualitative data were collected and analysed to develop COTiD-UK. Some of the data were further analysed within the implementation phase (WP5) and those results are, therefore, reported in Chapter 7.
Work package 1: translation and adaptation of the COTiD intervention and training package
Step 1.1: translation
The COTiD Dutch manual was translated into English by a commercial company,22 checked for accuracy by MG (original author) and then edited by JW to ensure that it contained commonly used UK language and occupational therapy terminology. This resulted in the first version of the manual.
Step 1.2: expert review and amendment
Method
Version 1 was reviewed by the VALID OTRG in terms of the content, language, occupational therapy terminology and intervention components. Comments were reviewed independently, discussed by JW, SH and SR, and then discussed with MG.
Results
All suggested amendments were agreed, including renaming some of the COTiD phases to better reflect UK occupational therapy terminology; substituting the Model of Human Occupation Screening Tool (MOHOST) assessment38 for the Assessment of Motor and Process Skills (AMPS) assessment39 as it is a more widely used assessment tool within UK occupational therapy practice; and the practical activity examples were made culturally relevant. This resulted in the second version of the manual, which was used in steps 1.3 and 1.4.
Step 1.3: COTiD training
Method
Three training days were held at monthly intervals in each of the three main study centres (Hull, London and Sheffield). MG delivered the training, supported by JW, using training materials and subtitled video clips translated from the original Dutch materials. In between training days, the occupational therapists started practising and video-recording their new skills (each were provided with a small digital video camera). The recordings were brought to the following training days for peer and trainer feedback. A fourth training day was held at each site 3 months later to discuss their progress.
The following data were collected from each occupational therapist participant:
-
COTiD Knowledge Questionnaire – translated from Dutch and comprising six multiple-choice questions aimed at checking the respondents’ knowledge of the COTiD intervention. It was completed during training day 4.
-
COTiD vignettes – two translated vignettes each describing a dyad taking part in COTiD were completed online following training day 4. The aim was to assess participants’ understanding of putting COTiD into practice by completing seven questions related to the COTiD process, using free text. The potential score ranged from 0 to 112, with higher scores reflecting higher understanding. JW and SH assessed the responses, using a translated checklist, based on a ‘model’ answer having achieved 100% inter-rater reliability.
COTiD training evaluation
A translated questionnaire was completed during training day 4 to collect participants’ views through quantitative and qualitative responses.
Results
Participants
Occupational therapists (n = 44) were recruited from across the three main study centres, covering 10 organisations, of whom 33 completed all four training days.
COTiD knowledge acquisition
Thirty-three participants completed the COTiD knowledge questionnaire. The number of correctly answered questions ranged from one to four, with just under one-fifth of respondents (n = 6, 18.2%) obtaining the higher mark and 15% obtaining the lower mark. Fourteen occupational therapists (42% of those who attended the final training day) completed the COTiD vignettes exercise with scores ranging from 20 to 79, with a mean score of 58 and median score of 59.
COTiD training evaluation
The majority felt that the course length was adequate, but nearly half felt that there was insufficient time between the training days to absorb the information provided. Half of the participants agreed/strongly agreed that the content was clear, whereas others would have liked more content focused on the less familiar aspects, for example conducting the occupational performance history interview and ethnographic interviews. The video feedback was valued in principle but considered to have become repetitive, taking up too high a proportion of the training days.
Step 1.4: delivering COTiD in practice
Method
Dyads comprising a person with dementia and a family carer were recruited at local sites to take part in the COTiD intervention. The aim was to identify how the intervention needed to be adapted in readiness for delivery within the piloting and evaluation phases. The following data were collected.
Video-recordings of COTiD sessions
The occupational therapists video-recorded two COTiD sessions with each dyad. The recordings were evaluated by one of four occupational therapist researchers familiar with the COTiD intervention (two in the UK and two in the Netherlands) to assess the occupational therapists’ COTiD skill development and level of competence using a translated checklist.
COTiD provision checklists
Data regarding the dyads’ demographic and clinical characteristics, as well as the duration and content of the COTiD sessions delivered, were collected via a checklist. A descriptive statistical analysis was completed to establish the participants’ demographic and clinical characteristics, and a thematic analysis of the intervention goals set and activities engaged in by the dyad with the occupational therapist during the sessions was conducted.
Semistructured interviews with dyads, managers and referrers
Semistructured interviews, using an Indicative Topic Guide, were conducted with dyads who had taken part in COTiD to explore dyads’ views of the COTiD intervention. These dyads were purposively sampled to represent as wide a range of experiences across the three sites, including: relationship between the dyad (i.e. spousal or non-spousal), gender, age. These interviews were conducted face to face at the person with dementia’s home.
Managers of occupational therapists who had taken part in the COTiD training and delivered the COTiD sessions were interviewed over the telephone, using an Indicative Topic Guide, to explore the organisational and managerial issues of delivering COTiD at the service level. People who had contributed by referring potential participants to the study team were interviewed in order to explore study recruitment issues, including the suitability of promotional materials and information provided and timing of the invitation. Referrers were purposively sampled to represent a range of professional background/role across the three sites.
All interviews were audio-recorded, transcribed verbatim, checked for accuracy and anonymised. The interview transcripts were coded and organised using NVivo version 10 (QSR International, Warrington, UK) by two researchers who developed a coding framework and completed a thematic analysis of (1) the dyad interview data set and (2) the manager and referrer interview data set.
Focus groups with occupational therapists
Focus groups were held with occupational therapists after the fourth training day to explore their views on the training provided, COTiD intervention and delivery requirements, and barriers to and facilitators of putting COTiD into practice within the UK. Four researchers were involved, with two facilitating each group and completing field notes and reflective accounts during and immediately after the groups to capture non-verbal communication observed and their own reflections and interpretations. The groups were audio-recorded and the recordings were independently transcribed. Transcripts were analysed using thematic analysis, with each researcher reading one or two transcripts, assigning codes, categories and then themes to the data. The team discussed and iteratively checked these against the transcripts to strengthen trustworthiness. Once there was overall agreement on codes, categories and themes, these were then applied to all the transcripts.
Results
Participants
In total, 130 people with dementia together with a family carer (n = 260) across 9 of the 10 sites consented to take part in the COTiD intervention. Nineteen dyads either withdrew before completing the sessions or did not receive the intervention owing to lack of occupational therapist availability to deliver it.
The age of people living with dementia ranged from 54 to 94 years, with a mean age of 79 years, and the age of family carers ranged from 22 to 95 years, with a mean age of 65 years. In total, 51% of people living with dementia were male and 61% of family carers were female. A total of 72.6% of the dyads were spousal couples and 22.2% were parent–adult child pairs, and 64% of the family carers co-habited with the person living with dementia. The majority of dyads were white British.
Video-recordings of COTiD sessions
In total, 28 of the 33 occupational therapists provided at least one video. The total number of recordings received was 196. Inter-rater reliability of at least 80% was achieved by the four assessors. In practice it proved impracticable to assess the strategy observation videos because the assessors did not have access to the strategy observation checklist that should have been completed by the occupational therapist. In addition, nearly 10% of the videos could not be categorised for assessment because the occupational therapists had not named the file correctly. The level of competence in delivering the intervention was originally set at 80%, but the mean scores ranged from 60% to 78%. However, the raters’ feedback suggested that certain checklist items were not well correlated with the total score and, therefore, did not truly reflect the therapists’ level of competence to deliver COTiD.
Using the video cameras was challenging to some, and many found the IT and information governance processes very difficult to adhere to, not least because at some of the sites the only available equipment was outdated.
COTiD provision checklists
Forty-one checklists were analysed. In total, 161 activities were listed, with the most utilised activities being (in order of the most frequently utilised) domestic, home-based leisure, memory/orientation, personal care, physical activity and social contact. Fifty-seven goal-setting forms (number of goals, n = 153) were analysed. The range of goals set included (in order of the most frequently cited) increasing enjoyable home-based activity, carer education, domestic activities, personal care, physical activity, increased time for carer, community-based leisure, increasing social contact and improving memory/orientation. The format used to write goals varied tremendously, ranging from using just one word, for example ‘Diary’, through to more detailed goals, for example ‘to be able to dress in appropriate clothing for occasion and time of year’. It was not always clear as to who the goal related to: the person with dementia, the family carer or the dyad. Some goals were worded in the negative, for example ‘X will stop doing Y’.
Semistructured interviews with dyads, managers and referrers
Nine dyads were interviewed; all but one dyad were spousal dyads who co-habited. Dyads reported often struggling to identify ‘valued’ activities that they might pursue separately or together. In addition, in relation to the balance between talking and actually carrying out activities during the sessions, dyads wanted more and earlier ‘doing’. Their views were mainly positive. Suggested improvements included providing more support and guidance for identification of goals and subsequent activities.
Five referrers and four managers were interviewed. Given that the themes relate primarily to implementation of COTiD in practice, they are reported within Chapter 7.
Focus groups with the occupational therapists who had delivered the COTiD intervention
Five focus groups were conducted, with between five and eight participants in each; a total of 28 occupational therapists from eight of the participating organisations took part. Three main themes were identified from the data, each with subthemes:
-
COTiD training – timing, content and practising skills
-
COTiD intervention – benefits, challenges, follow-up, occupational therapy support workers, manual and structure
-
participation in the research process.
The third theme, regarding participants’ experience of taking part in the research process, in terms of what enabled or challenged their input, has been reported elsewhere. 40
Occupational therapists felt that the training needed to be provided as near as possible to the actual delivery of the intervention and needed to include more UK-relevant examples and more complex case studies. The COTiD intervention was seen to be truly client centred, occupational therapy specific and involving carers in their own right, and was referred to as ‘being the bedrock of OT [occupational therapist] practice, almost giving us permission to be OTs again’. It was felt that session frequency and length needed to be much more flexible because it was usually not possible to provide the 10 sessions within the stipulated 5 weeks, as a result of either occupational therapist capacity and/or dyad availability. In addition, it was also felt that dyads needed longer between the latter COTiD sessions to actually put planned goals and activities into practice before reviewing progress at the next session with the occupational therapist.
Step 1.5: focus groups with people with dementia and family carers of people with dementia who had not received the COTiD intervention
The aim of these focus groups was to elicit views of the COTiD programme from people with dementia and family carers and the extent to which the programme might meet their needs and preferences, and identify any aspects that may require changes to make the programme suitable for use in the UK.
Method
Separate focus groups were conducted with people living with dementia and with family carers who were currently supporting people living with dementia or had done so in the previous 2 years. No one who participated had received the COTiD intervention. Each group was run by an experienced facilitator, supported by a scribe who observed, recorded non-verbal communication and made field notes. The groups were audio-recorded, and the recordings were then transcribed and an inductive, data-driven thematic analysis was completed.
Results
Six focus groups were conducted: three with people with dementia and three with family carers (n = 39). Three themes emerged, with positive, negative and ambivalent views of COTiD running across all three themes: loss and living with dementia, ‘what helped us’, and consistency and continuity.
In summary, participants suggested that COTiD delivery needed to be flexible in terms of timing and length of the intervention; fit into their existing demands; include the person living with dementia and their family carer as partners within the process; include a focus on previous occupations; and be provided at the appropriate (i.e. early) stage of their dementia pathway.
A more detailed description and discussion of these focus groups has been reported elsewhere. 41
In addition, the COTiD training and provision costs were identified and are reported in the economic evaluation section (see Chapter 6).
The manual was updated in light of the data collected above to produce version 3.
Step 1.6: consensus conference
Method
A consensus conference was held to agree the content of the COTiD-UK intervention. Participants included people with dementia and family carers, some of whom had taken part in the COTiD intervention and others who had not; occupational therapists who had attended the COTiD training, some of whom had subsequently delivered the COTiD intervention in practice; multidisciplinary team members, including those who had referred dyads to take part in the COTiD intervention; and managers of occupational therapists involved in the training and intervention delivery.
Version 3 of the COTiD manual was circulated in advance of the event, including an abbreviated version for people living with dementia that mainly comprised the information sheets to be provided to participants during the intervention. Following presentations from the research team, participants were asked to discuss three questions, in mixed groups of approximately eight participants each. The questions were (1) ‘How relevant do you think the COTiD manual is for addressing problems in daily living experienced by people living with dementia in the UK?’; (2) ‘How appropriate do you think the intervention is for people and how could it be improved?’; and (3) ‘How well do you think the structure of the intervention fits the UK context?’. Two researchers joined each group: one to facilitate the discussion and one to take notes. The discussion notes were transcribed and analysed thematically.
Results
Thirty-one participants attended the event. There was consensus that COTiD fits the UK context well and could be beneficial in reducing risks and preventing crises. There was a view that it ‘fills a significant gap’ that existed at that time, and that providing an evidence base for COTiD in the UK would ‘futureproof’ it. There was also discussion about the importance of ensuring that there is funding available for COTiD in the light of the ever-changing commissioning processes and priorities.
In summary, key messages related to the importance of the intervention being delivered in a timely and flexible manner; concern about what would happen in practice after the intervention finishes; the fact that COTiD ‘legitimises . . . spending time getting to know people before beginning intervention’ (occupational therapist participant), a practice that was felt to have been discouraged in recent years; the importance of considering the terminology used in the manual; and the potential benefit of COTiD to people with dementia.
Work package 2: online survey to scope current community occupational therapy service provision and practice for people with dementia and their family carers in the UK
The aims of the online survey were to identify current UK occupational therapy service provision and practice for people living with dementia and their family carers, and to explore the potential facilitators of and barriers to implementing COTiD in the UK.
Method
A questionnaire was developed through reviewing the literature, researcher knowledge and consultation with the VALID OTRG. It was piloted with the local occupational therapy service and subsequently amended. To identify current practice, participants were asked about their occupational therapist role, local service provision, referral routes, access to assistive technology and use of assessment tools, using open and closed questions and Likert scales. Descriptive statistics were calculated, including totals (n) and percentages, as well as the ranges, medians, means and standard deviations. To explore the potential implementation of COTiD in UK practice, respondents were asked to reply to four questions, using free text. A thematic analysis of the responses was conducted. An optional section invited participants to provide demographic and contact details, which would be entered into a gift voucher prize draw. The survey was conducted online over 4 months. Recruitment of occupational therapists working with people living with dementia was through direct invitation to community mental health teams listed on the Personal Social Services Research Unit database and via the Memory Services National Accreditation Programme, primarily by e-mail containing a link to the questionnaire. The questionnaire was also promoted via established local and national professional networks, relevant websites and newsletters.
Results
In total, 230 occupational therapists consented to take part, of whom 197 provided quantitative data and 138 also provided qualitative data. A detailed description and discussion of the quantitative data that related to current service provision at the time of the survey has been reported elsewhere. 42
In summary, the key findings were that over half of the respondents undertook primarily profession-specific work; occupational therapy-specific assessments were the most common profession-specific task – two-thirds of referrals for initial assessments were for people with mild to moderate dementia; the median time spent per person with dementia was 2.5 hours; and most respondents could prescribe equipment to support personal care activities, as well as telecare, but not for reminiscence or leisure activities. This information informed the revised intervention and training content. It also informed the development of the template document used to collect TAU information from the research sites that took part in the RCT.
Finalising the COTiD-UK intervention and training package in readiness for the evaluation phase
The COTiD-UK intervention
The UK intervention is designed to be delivered more flexibly in terms of timing (up to 10 hours over approximately 10 weeks) to maximise the availability of both occupational therapists and dyads, and to provide dyads with time to put their agreed activities and plans into practice in between sessions with the occupational therapist. The content is similar to the COTiD intervention, but its delivery is less prescriptive; for example, occupational therapists complete the physical and social environmental assessments and the activity and strategy analyses but use the assessment tools that they usually use in their own practice/service, rather than the translated COTiD checklists and tools. The one-to-one narrative interviews are conducted in the same way but follow on from the introductory session to start building rapport with the dyad and provide opportunity to discuss what is important to them as soon as possible. There is an emphasis on engaging in activity earlier and more frequently within the sessions. Goals are set in the same way, through discussion between the dyad and the occupational therapist, but can be evaluated and added to throughout the sessions if dyads’ views and/or circumstances change over time. The sessions usually take place where the person with dementia lives but, depending on the goals, may also take place in the local community, for example the sports club, local library or garden centre. During the final session, the dyad and occupational therapist evaluate the success in achieving the goals and plan ahead for the future.
The COTiD-UK training programme
The COTiD-UK training programme was restructured into 3 days because it was felt that the content could realistically be covered in this time; this also made it more affordable and feasible for services to release occupational therapists to attend. Days 1 and 2 ran consecutively, and day 3 took place after participants had put COTiD-UK into practice. The content was revised from the original to include more complex case examples, presented in the form of role plays with the occupational therapists taking on all roles, rather than incurring the cost of employing actors to perform the dyad roles. Time to practise the narrative interviews and goal-setting sessions, along with actually using the audio-recording equipment, was included, plus more time and emphasis on setting and writing specific, measurable, achievable, relevant, time-bound (SMART) goals,43 including a group exercise. The COTiD knowledge questionnaire was refined to make it more easily understood and more accurately reflect the revised COTiD-UK intervention. The online COTiD vignette task was dropped from the COTiD-UK training because of the low response rate and reported difficulty that participants had in understanding and completing it.
Audio-recordings were used instead of video-recordings, and updated IT and information governance guidance was provided to participants. Before delivering COTiD-UK in the RCT, occupational therapists were required to complete a ‘training dyad’, which incorporated audio-recording as many sessions as practicable. These recordings were then reviewed by a COTiD-UK trainer using a refined checklist to assess the occupational therapists’ competence. These checklists later became the basis from which fidelity measures for the RCT were developed (see Implementation phase). A supervision structure was put in place for the intervention providers, with supervision provided by either a COTiD-UK trainer or a local supervisor who had also completed the COTiD-UK training.
Development phase: conclusion
Analysis of the data collected through the sequence of activities described above resulted in the COTiD intervention being translated and adapted to maximise its suitability and feasibility for use within the UK context, specifically the health and social care sector, and hereafter is referred to as COTiD-UK. This version was then ready to be evaluated in an internal pilot and subsequent full RCT (i.e. WP3 and WP4), as reported in Piloting and evaluation phases: internal pilot and randomised controlled trial of COTiD-UK compared with treatment as usual (work packages 3 and 4).
The dyad recruitment materials and processes were also refined in readiness for the evaluation phase. For example, participant feedback indicated that some people were not comfortable with using the term ‘family carer’ at the post-diagnostic stage. As a result, the term ‘supporter’ was used on future participant recruitment documents, such as information sheets and consent forms, and when communicating with dyads. The term ‘family carer’ continued to be used within study protocols and published outputs.
This phase took twice as long to complete as originally planned but reflects the range of activities used and depth of data collected, which importantly included the perspectives of people with dementia and family carers, as well as occupational therapists and other professional groups. A number of logistical challenges arose, including delays in recruiting research sites, occupational therapists and dyads; IT and information governance difficulties experienced at some sites; and obtaining the necessary governance approvals at some sites to actually deliver the COTiD intervention. However, it was important that the intervention was not only translated but also adapted to maximise its suitability and feasibility for use within the UK culture, and health and social care provision.
Chapter 4 Piloting and evaluation phase: internal pilot and randomised controlled trial of COTiD-UK compared with treatment as usual (work packages 3 and 4)
Aim
The aim of this phase was to determine the clinical effectiveness and cost-effectiveness of the COTiD-UK intervention compared with TAU.
There were two WPs:
-
WP3 – internal pilot trial.
-
WP4 – full RCT.
Hypotheses
It was hypothesised that, compared with TAU, COTiD-UK would:
-
significantly improve ADL in people with dementia
-
significantly improve quality of life for the people with dementia and their family carers
-
demonstrate cost-effectiveness.
Ethics approval
NHS ethics approval for WP3 and WP4 was gained from the NRES Committee London – Camberwell St Giles on 14 July 2014 (reference number 14/LO/0736). Eighteen amendments (13 non-substantial and five substantial) were approved to cover protocol and trial documentation updates; the addition of new trial sites and participant identification centres, registration with Join Dementia Research and new trial documentation as required; and postgraduate student studies linked to the VALID programme (as outlined in Development of research capacity). The appropriate local research and development governance approvals were obtained at each research site.
Written informed consent was obtained from all participants.
Work package 3: internal pilot trial
The aim of WP3 was to conduct an internal pilot trial of COTiD-UK compared with TAU to:
-
field test the outcome measures to be used to measure the effectiveness of COTiD-UK
-
finalise the intervention modes of delivery and associated training and supervision of those delivering COTiD-UK
-
field test trial procedures.
Work package 4: full randomised controlled trial
The aim of WP4 was to conduct a RCT to:
-
determine the clinical effectiveness of COTiD-UK compared with TAU
-
determine the cost-effectiveness of COTiD-UK compared with TAU.
Work package 3 was designed as an internal pilot, with the intention of moving forward into WP4, the full RCT, if predefined success criteria based on the Acceptance Checklist for Clinical Effectiveness Pilot Trials (ACCEPT) model were met. 44 This checklist provides a systematic basis for assessing whether or not a pilot trial has adequately tested a study design, methods and procedures, and, therefore, whether or not the pilot data can be integrated into the full trial data set without compromising trial integrity. There are three potential outcomes:
-
Unequivocal acceptance of pilot data – the design and methods are confirmed as being feasible and appropriate except for minor details; therefore, pilot data can be carried forward to the main trial data set.
-
Conditional acceptance – the design and methods are found to be feasible and appropriate in principle but need refinement; therefore, a decision including the pilot data must be delayed until the variation in procedures for the full pragmatic trial is known.
-
Non-acceptance of pilot data – the need for substantial change is identified; therefore, the pilot data cannot be carried forward to the main trial data set.
Moving from internal pilot to the full randomised controlled trial
The internal pilot trial ran from September 2014 to April 2015 in the three main research sites (Hull, NELFT and Sheffield). The internal pilot trial procedures and data set were reviewed by the central research team against the predefined ACCEPT criteria,44 and were presented to the independent PSC in April 2015. The criteria assessed were trial design; sample size; intervention training and fidelity of delivery; participants’ recruitment strategy and eligibility criteria; consent procedures; randomisation process; blinding data collection, quality and management; research governance; and data analysis.
The research team reported that no significant changes had been made to the study design. Recruitment had initially been slower than expected, with 44 dyads (88% of the target of 50 dyads) having been consented by April 2015. However, the recruitment rate was picking up, and retention at the 12-week follow-up, at the first site, was 89%. It was agreed that more sites and occupational therapists than originally planned would need to be recruited to enable the recruitment of the target sample of 480 dyads to be achieved within time.
It was decided to omit the Canadian Occupational Performance Measure:45 partly because it was felt that the number of measures needed to be reduced to lessen the burden on participants and partly because of the feedback from research staff about the difficulties experienced in administering this assessment in a consistent, reliable way over time and between assessors. Some refinements were made to the web-based database, and a data entry handbook was written to maximise consistency of data collection and entry across time points and research sites.
The outcome of this review confirmed that the design and methods were feasible and appropriate except for minor details, and resulted in the PSC supporting the unequivocal acceptance of the internal pilot data within the full trial data set.
The methodology and results reported here, therefore, derive from the trial procedures used and the data set collected during the internal pilot and full RCT. This study is reported in accordance with the Consolidated Standards of Reporting Trials (CONSORT) statement. 46 The trial protocol and outcomes are reported elsewhere in detail47,48 and, therefore, are summarised here.
Method
Study design
The study design was a multicentre, pragmatic, two-arm, parallel-group, single-blind individually RCT with an internal pilot. People with mild to moderate dementia were recruited along with an identified family carer (a dyad or pair). Recruited dyads were individually randomised and allocated to receive either TAU or the COTiD-UK intervention in addition to TAU, which may or may not have included occupational therapy provision depending on usual practice at the recruiting sites. The intention was to recruit 50 dyads for the internal pilot and a further 430 dyads for the RCT. The study ran in NHS trusts across England, and participants were primarily recruited from older adult community mental health teams and memory services across inner city, urban and rural areas.
Recruitment
In March 2015, during the COTiD-UK evaluation phase, VALID joined the Join Dementia Research register, and 22% of the RCT participants were recruited via this route, although the percentage varied across research sites. This NIHR initiative, in partnership with the Alzheimer’s Society (London, UK), Alzheimer’s Scotland (Edinburgh, UK) and Alzheimer’s Research UK (Cambridge, UK), enables people to register their interest in taking part in dementia research and, thereby, be matched to relevant studies. 49
Recruitment of dyads to the RCT involved local participant-relevant organisations as appropriate at each research site. For example, within NELFT, dyads were recruited via the local Alzheimer’s Society and Age UK (London, UK) branches through attending events, such as dementia cafés, carer support groups, early intervention services and cognitive stimulation groups. However, the level and nature of this involvement varied from site to site, according to what community support services were provided locally and by whom, and the recruitment procedures usually utilised within the site.
Interventions
COTiD-UK
The COTiD-UK intervention consists of up to 10 hours of community occupational therapy delivered over 10 weeks to the dyad, primarily at the person with dementia’s home and in their local community. The content, as well as the training and supervision model, are described in detail at the end of Chapter 3, Development phase: developing COTiD-UK (work packages 1 and 2).
Adherence to the intervention was defined as dyads reaching the goal-setting phase, as agreed through discussion between the occupational therapist researchers and the COTiD-UK trainers, which indicated that the initial core elements of the intervention had been delivered.
Treatment as usual
The TAU group received standard clinical care, usually provided in the recruiting site, which may or may not have included standard occupational therapy. Given that usual service provision varied between and within the recruiting trusts, each site completed a template detailing the usual treatment offered.
Outcome measures
The outcome measures were selected to replicate the Dutch23–25 and German26 studies where possible, while also using tools more commonly used within UK studies. The primary outcome measure was the Bristol Activities of Daily Living Scale (BADLS),50 with the primary end point at 26 weeks. This retained the focus on the ability to perform ADL as the primary outcome, given that it was not feasible to use the AMPS as Graff and colleagues23 had because of the lack of AMPS-trained occupational therapists in the UK and the potential resource implications for using this across a much larger sample size with more follow-up data collection points. Secondary outcome measures for the person with dementia were selected to assess cognition (Mini Mental State Examination),51 ADL ability (Interview of Deterioration in Daily activities of Dementia),52 condition-specific quality of life [Dementia Quality of Life (DEMQOL) scale]53 and mood (Cornell Scale for Depression in Dementia). 54
Secondary outcome measures for the family carer assessed sense of competence (Sense of Competence Questionnaire)55 and mood [Hospital Anxiety and Depression Scale (HADS)]. 56
Social contacts, leisure activities and serious adverse events were recorded for all participants. Self-reported quality of life data [EuroQol-5 Dimensions, five-level version (EQ-5D-5L)] were collected for both the person with dementia and their carer,57 and resource use data [Client Service Receipt Inventory (CSRI)]58 were collected for all participants to facilitate the economic evaluation [reported in Chapter 6, Economic evaluation (work packages 1, 3 and 4)].
Therefore, the majority of the outcome measures replicated those used in the Dutch23–25 and German26 studies.
Procedure
Data were collected through a face-to-face interview with the dyad at the person with dementia’s home at baseline and at 12 and 26 weeks post randomisation. A reduced data set was collected through a telephone interview with the family carer at 52 and 78 weeks. This comprised, in the case of the person with dementia and the family carer, the BADLS total score, plus the occurrence of any serious adverse events, the CSRI score, information on social contacts and leisure activities, as reported by the family carer, plus, in the case of the family carer only, HADS and EQ-5D-5L scores. As explained previously (see Chapter 2, The VALID applied research programme), the original intention was to collect data for all dyads at 52 weeks and the first 40% of dyads recruited at 78 weeks (n = 192); however, as part of the variation to contract, this was revised to following up the first 77% of dyads recruited at 52 weeks, while the target sample at 78 weeks remained the same. Follow-up data collection was undertaken by site-based research staff masked to the dyad’s allocation.
The target sample size was based on a standardised mean difference of 0.35 in the BADLS total score between the COTiD-UK and the TAU groups, with the anticipated effect size determined using the clinical expertise of the applicant group and based on the DOMINO group consensus advice regarding the minimum clinically important difference using the BADLS. 59 To detect this difference using a two-sample t-test with 90% power and a significance level of 5%, and after adjusting for 15% attrition, 5% non-adherence in the TAU group and the clustering of dyads by occupational therapist in the COTiD-UK group [assumed intracluster correlation coefficient (ICC) with an average of 10 dyads per therapist], we planned to recruit 256 dyads to the COTiD-UK group and 224 dyads to the TAU group.
Statistical analysis followed a predefined statistical analysis plan with no interim analysis and used Stata® version 15 (StataCorp LP, College Station, TX, USA).
Occupational therapists delivering the COTiD-UK intervention completed a COTiD-UK checklist for each dyad to quantify the number, frequency, length and content of sessions provided, and audio-recorded all sessions where it was practicable. These data enabled the intervention costs to be calculated for the economic evaluation [see Economic evaluation (work packages 1, 3 and 4)], the intervention fidelity to be assessed (see Implementation phase) and the percentage of goals achieved, partially achieved and not achieved to be calculated (see Results section).
Results
Recruitment of sites, occupational therapists and dyads
Approximately 30 NHS trusts expressed interest in taking part in the study, 15 of which were set up as research sites between September 2014 and May 2017, although one did not proceed to recruiting dyads. Forty-four occupational therapists were trained to deliver COTiD-UK, 32 of whom proceeded to the RCT and were allocated at least one dyad each; however, one occupational therapist was subsequently unavailable to provide the intervention as planned owing to ill health. Reasons for dropout of occupational therapists included the employing organisation not being recruited as a site or the site’s failure to recruit participants, sickness, job turnover or not being made available because of service and organisational constraints. Dyad recruitment took place between September 2014 and July 2017, and the last follow-up assessment was completed in January 2018 when the study shut to recruitment in line with the revised funding agreement. The recruitment and retention rate varied across sites, with some sites exceeding their recruitment target whilst more sites did not achieve their initial target, a challenge that we have reported in more detail elsewhere. 60
Baseline data
In total, 468 dyads were randomised, with 249 dyads assigned to COTiD-UK and 219 assigned to TAU. The demographic and clinical characteristics of the two groups were very similar at baseline. The people with dementia ranged in age from 55 to 97 years, with a mean of 78.6 years, and family carers ranged in age from 29 to 94 years, with a mean of 69.1 years. The vast majority of participants were white British. Of the people with dementia, three-quarters were married and about one-quarter lived alone. In addition, half had a diagnosis of Alzheimer’s disease, one-fifth had vascular dementia and just over 10% had a mixed presentation. About 85% were categorised as having mild dementia. About three-quarters of the family carers were spouses, with most of the rest being adult children.
Outcomes at 26 weeks
At 26 weeks, 406 dyads remained in the trial (86.7%), giving an attrition rate of 13.3%. Outcome data were collected and analysed for 368 dyads (78.6% of the total sample; COTiD-UK, n = 207; TAU, n = 161), giving an attrition rate of 21.4%.
At 26 weeks, the BADLS total score did not differ at the 5% level when comparing the two groups, with an adjusted mean difference estimate of 0.35 [95% confidence interval (CI) –0.81 to 1.51; p = 0.55]. The adjusted (for baseline BADLS total score and randomised group) ICC estimate for the primary outcome at week 26 was 0.043. This reflects the level of correlation between the BADLS total scores for dyads treated by the same occupational therapist within the COTiD-UK group. When considering the within-dyad mean BADLS total score, to account for missing items, the mean difference estimate was 0.02 (95% CI –0.04 to 0.07). Predictors of missingness were identified as the ethnicity of the person with dementia and marital status of the family carer. When also adjusting for predictors of missing data, the mean difference estimate in BADLS total score was 0.34 (95% CI –0.82 to 1.49). The complier-average causal effect, which provides a measure of the effect of the COTiD-UK intervention in the population that took part and reached the goal-setting phase of the intervention, at week 26 was estimated as 0.42 (95% CI –0.77 to 1.60).
Secondary outcomes were similar between the two groups at week 26. For continuous outcomes, all effect estimates were close to zero. For the numbers of leisure and social contacts, intensity rate ratio estimates were close to 1.
At the 26-week follow-up, research staff collecting outcome data were reported as having been unmasked as to the dyad allocation for 45 of the 338 assessments (13.3%).
Adherence and goal achievement
Of the 249 dyads allocated to the COTiD-UK arm, 22 did not reach the goal-setting phase. Excluding the dyads where one partner died (n = 3) and the eight who withdrew from the trial, the non-adherence rate was 4.6%, compared with the estimated rate of 5%.
The number of goals set and achieved, as recorded on the COTiD-UK checklist, was analysed for the 227 dyads who reached this stage of the intervention. The number of goals set ranged from 1 to 13, with a mean of 4.09 goals. The number of goals set was 920, of which 729 (79.24%) were achieved, 107 (11.63%) were partially achieved and 84 (9.13%) were not achieved, meaning that 90.8% of goals were either fully or partially achieved. Three of the 227 dyads did not achieve any of their agreed goals, two of whom withdrew following goal-setting.
Serious adverse events
Between baseline and week 26, 131 serious adverse events had been recorded, and a further 108 had been recorded between week 26 and week 78, giving a total of 239 over the trial, with no causality attributed to taking part in the trial or the intervention.
Longer-term follow-up: 52 and 78 weeks
At 52 weeks, the BADLS total score was collected and analysed for 239 dyads (51.1% of the total sample; COTiD-UK, n = 137; TAU, n = 102).
At 78 weeks, the BADLS total score was collected and analysed for 113 dyads (24.1% of the total sample; COTiD-UK, n = 67; TAU, n = 46).
Exploratory analysis of BADLS scores, as well as of HADS scores and number of social contacts and leisure activities at 52 and 78 weeks, found no difference between the COTiD-UK and the TAU groups over these extended time periods.
Piloting and evaluation phase: conclusion
This was a well-run trial, which achieved 97.5% of the target recruitment sample; indeed, to the best of our knowledge, it is the largest trial of occupational therapy for people with dementia and their family carers to date in the UK. Recruitment of research sites took longer than planned owing to the complexity of the study, namely the need for both researcher and occupational therapist capacity to be in place. The former required CRN support, which varied across regions, and the latter was usually dependent on local service support, as only 2 out of the 15 sites were able to obtain excess treatment costs. The recruitment and retention rate varied across sites, with some sites exceeding their recruitment target, whilst more sites did not achieve their initial target.
Chapter 5 Qualitative studies (work package 4)
Two qualitative studies were embedded within the trial design:
-
taking part in the COTiD-UK intervention
-
why people declined to take part in the research trial.
Taking part in the COTiD-UK intervention
Aim
The aim of this study was to explore the experience of taking part in the COTiD-UK intervention from the perspective of people with dementia, family carers and occupational therapists.
Objectives
-
How were people with dementia, family carers and occupational therapists involved in the COTiD-UK intervention?
-
What meanings, beliefs, viewpoints, reasons and explanations did people attach to the intervention?
-
Did people with dementia, family carers and occupational therapists experience the COTiD-UK intervention in different ways? If so, how and why?
-
How did the accounts of people with dementia, family carers, and occupational therapists compare and contrast with the trial outcome data?
-
What factors may influence implementing COTiD-UK in practice?
Method
Semistructured interviews to explore views on the experiences of the intervention were conducted with a purposive sample of members of each group (i.e. people with dementia, family carers and occupational therapists) who had taken part in the intervention.
Telephone interviews were conducted with seven occupational therapists who had delivered the COTiD-UK intervention. A sampling framework was used to achieve maximum variation in terms of occupational therapist prior clinical experience, level of COTiD-UK experience and research site.
Face-to-face interviews were conducted with 22 dyads (people with dementia and their family carers) who had received the COTiD-UK intervention. Interviews took place in the person with dementia’s home within 2 weeks of their final COTiD-UK session. A sampling framework was used to achieve maximum variation in terms of dyad demographics (age, gender, relationship, cohabitating or not, and ethnicity) and the level of COTiD-UK experience of the occupational therapist delivering the intervention. Informed consent was obtained from all participants. Two occupational therapist researchers (JB and JW), who had experience of delivering the COTiD-UK intervention, carried out the interviews. Prompts were used to help maximise participants’ recall, such as a photograph of the occupational therapist who had delivered the COTiD-UK sessions and copies of the goal-setting and evaluation form.
All interviews were audio-recorded, transcribed verbatim, checked for accuracy and anonymised prior to analysis. Inductive thematic analysis was used. 61 JB and JW initially read the transcripts and generated coding categories independently, and then met to agree a coding framework. All transcripts were then coded using the agreed framework, with each researcher coding half the data set, and the framework being refined through further discussion as needed. Themes were then identified and refined through discussion with each other and a third researcher (FP). NVivo qualitative data analysis software, version 11, was used to organise and manage the data.
A selection of the indicative findings from the occupational therapist interviews were validated in terms of their meaningfulness, verisimilitude and wider transferability, through discussion with the VALID occupational therapist reference group. This group was asked if these findings ‘rang true’ (verisimilitude) and had resonance with issues within their experience (meaningfulness and wider transferability), whether anything unexpected was included or omitted, and whether or not they reflected their own practice experience. The reference group confirmed the resonance and relevance to their experience and practice of the findings that occupational therapists valued the opportunity to do ‘real OT [occupational therapist]’. They specified this in terms of the intervention focus as enabling engagement in personally meaningful occupations; including the time needed to really get to know, and to work equally with, the person with dementia and their family carer, and actually to carry out activities within the sessions.
Similarly, a selection of the indicative findings from the dyad interviews were discussed with the VALID PPI reference group to check if they ‘rang true’, and whether anything unexpected was included or omitted when they reflected on their personal caring experience. This group confirmed the resonance of and relevance to their lived experience and practice in caring of the findings that dyads valued the opportunity to tell their story; for this to be listened to (often for the first time); to work in partnership with the occupational therapist; and to participate in such sessions early in their dementia journey.
The themes and subthemes were then further refined and defined through discussion between the three researchers involved.
To achieve the fifth objective, regarding implementation of COTiD-UK in practice, a Framework Analysis was informed by the completed inductive analysis of the interview transcripts and the TDF. 32 The methodology and findings from this analysis are reported in Implementation phase.
Findings
Six themes were identified from the occupational therapist interview data: (1) valuing the occupational focus of COTiD-UK, (2) timing and relationships, (3) achieving SMART goals; (4) developing COTiD-UK knowledge and skills; (5) delivering COTiD-UK within current organisational models; and (6) delivering COTiD-UK in the future.
Four themes were identified from the dyad interview data: (1) achieving goals, (2) working together, (3) effect of dementia and (4) COTiD-UK outcomes.
Objectives 1 to 3: the experience of taking part in the COTiD-UK intervention
The first three themes from each data set primarily relate to the first three study objectives and are reported in detail elsewhere,62 so are summarised briefly here.
Occupational therapist interview themes
Valuing the occupational focus of COTiD-UK
The occupational therapists saw the COTiD-UK intervention, with its focus on enabling meaningful activity, as being ‘real OT’ and, therefore, valued the opportunity to put into practice what they had specifically trained to do. Subthemes related to utilising core occupational therapy skills, recognising the level of skill required to deliver a complex intervention, focusing on the carer as an occupational being in their own right, and developing the carer’s coping strategies.
Timing and relationships
The occupational therapists discussed how timing and relationships could affect the delivery of COTiD-UK. Subthemes related to the optimal timing of the intervention in relation to diagnosis, having the time to really get to know a dyad and actually engaging in activities within sessions, as well as acknowledging times when goals were not achieved within the 10 weeks if their success was dependent on other resources or services being available. The pre-existing relationship between people with dementia and carers can affect their engagement within COTiD-UK, and the relationship established between the occupational therapist and the dyad affects the quality of their communication and collaboration, as needed within COTiD-UK.
Achieving SMART goals
The occupational therapists discussed the range of factors that could affect dyads identifying, selecting, prioritising, writing and achieving SMART goals, describing practical examples of processes and strategies that they used to facilitate this process. In selecting goals, they emphasised the need to take account of factors such as dyad members’ physical health conditions, degree of insight into their capabilities, level of ability and motivation.
Dyad interview themes
Achieving goals
The people with dementia and their family carers stated that they had valued the opportunity to talk to and be listened to by the occupational therapist about what was important to them, and they felt that they had been enabled to identify goals meaningful to them. As for the occupational therapists, dyads discussed the factors that they saw as being taken into account to set realistic goals, including their physical health and the severity of their dementia symptoms. Dyads described how the occupational therapist’s support had contributed to them achieving their goals. Family carers talked about the occupational therapist providing useful information and signposting to resources, as well as taking an enabling and/or problem-solving approach, while people with dementia talked about the occupational therapist actually carrying out the activity alongside them.
Working together
Dyads reported valuing the occupational therapist’s approach, which was described as being flexible, open and honest, as well as motivating and enabling of the dyad’s to progression at their own pace. Dyads saw this as supporting them to be active participants in working alongside the occupational therapist and independently on their own initiative, as needed, throughout the process.
Effect of dementia
Primarily, family carers recounted how they had first recognised the signs that ‘all was not right’ with the person with dementia and described the pathway that led to the person receiving their diagnosis. Family carers also spoke about the level and quality of subsequent support that they had received from services. They went on to describe how the symptoms of dementia, as well as other physical and/or medical conditions, affect their ability and opportunity to engage in meaningful activities. Similar to the occupational therapists, dyads also discussed the optimal time to be offered the COTiD-UK intervention in relation to receiving their diagnosis.
Objective 4: COTiD-UK outcomes
The fourth theme identified from the dyad interviews was ‘COTiD-UK outcomes’, with dyads describing what they saw as the result of the COTiD-UK intervention. There were four subthemes: (1) meeting expectations, (2) engaging in activity, (3) looking ahead and (4) living well with dementia.
Meeting expectations
Generally, participants said that they had not known what to expect from the sessions, not least because they mostly had no previous experience of occupational therapy. However, some did have prior experience, either through their work, for example as a family carer who worked as a nurse, or because they, or someone they knew, had previously received occupational therapy for another medical condition such as stroke or a mental health condition such as depression. Although dyad members had little clear idea of what might be involved in or the result of occupational therapy, they had just decided to ‘give it a go’. Some dyads discussed what they expected, hoping that the sessions ‘may help them’ without being sure of how or in what way, while others saw that their contributing to the research ‘may help others in the future’.
Despite participants not knowing what to expect, all felt that it had exceeded what they had hoped to gain:
Carer: But I think yeah it certainly turned out kind of more productive than I thought.
Person with dementia: Yeah.
Dyads were not able to suggest how the intervention could be improved. The only concern that they voiced was that the intervention had to come to an end and that they would value the opportunity to see the occupational therapist again in the future:
Interviewer: Anything that you feel we could change?
Carer: No. Nothing, nothing. It was perfect.
Person with dementia: Definitely not.
Engaging in activity
Dyads identified the activities that they had taken up either during or as a result of the sessions. These were predominantly activities that they had not undertaken for a while, such as swimming, playing golf, running, ballroom dancing, playing bowls, gardening, painting, baking, listening to music, board games and card games, to name just a few. Some people had also taken up new activities that they had not undertaken before, including calligraphy, creative writing, developing computer skills and joining a walking group. Some people described strategies suggested by the occupational therapist that they had put into practice so as to enable the person with dementia to engage in an activity more independently. These included using noticeboards, diaries and checklists to organise their weekly and daily routines; using simpler or colour-contrasting equipment in the kitchen; and following and ticking off step-by-step recipes or instructions on a paper document to complete a task. Dyads also described strategies that they had used to enable the carer to feel more confident about leaving the person with dementia alone while they undertook their own activities, such as meeting friends and attending a sewing group. Such strategies included leaving prompt cards stating where the carer had gone and what time they expected to be back, or training the person with dementia to use a mobile telephone:
Illuminating and drew attention to perhaps you know what you could do. What sort of things you could do, so that – that was good wasn’t it? You know not just from the point of view of the research but for you to go forward and – and do things.
Carer
Looking ahead
Dyads reported that they felt informed through the activities and, thereby, more confident about looking and planning ahead to manage their situation in the future, in two specific aspects. First, both people with dementia and carers stated that they found strategies introduced by the occupational therapist that aimed to enable continued activity engagement to be very useful on a practical level. Second, the information that the occupational therapist had provided in terms of how to access relevant resources and services as and when needed gave family carers, in particular, confidence that they would, in future, know how and where to obtain the help that they may later need:
So I don’t think it’s going to be . . . it’s not going to be life-changing within the 10 weeks or whatever, it’s not going to be like wow this is you know. But it gradually it – it does help and I mean it certainly helped us to be able to plan ahead as well.
Carer
Living well with dementia
Dyads described how they felt that they would have to put their lives ‘on hold’ after they were first diagnosed because they would have to drop their usual routines and activities, having assumed that the condition would stop them from carrying on with them. However, the experience of still engaging in meaningful activities within and as a result of the COTiD-UK sessions had illustrated that much was still possible:
Carer: Oh yes, I think it’s been very valuable as I say. Hasn’t it?
Person with dementia: Mm definitely.
Carer: Yeah. And it – it makes you feel more that you want to go on and . . . not – not just give in to things.
Person with dementia: Mm [nodding head in agreement].
Carer: Go on and try and achieve a quality to life in that respect.
Objective 5: putting COTiD-UK into practice
The remaining three occupational therapist themes – developing COTiD-UK knowledge and skills, delivering COTiD-UK within current organisational models and delivering COTiD-UK in the future – are discussed in Implementation phase because these relate primarily to the implementation of COTiD-UK in practice.
Conclusion
These findings provide insights from the perspective of the people with dementia and carers who took part in the COTiD-UK sessions as to what they felt they had achieved. Both people with dementia and their carers provided positive examples of activities engaged in not only during, but also as a result of, the sessions and occupational therapist input. Dyads saw the intervention as demonstrating to them what they could still do and how they could plan ahead to continue with their valued activities.
Occupational therapists described COTiD-UK, with its focus on occupation, as being ‘real OT’ and valued the time that it provided to really get to know both the person with dementia and their family carer to learn what was important to them individually and together, and valued being able to engage in activities alongside the person with dementia and/or their family carer during the sessions.
There was no apparent divergence of views between the people with dementia and their family carers. In instances when the family carer spoke more, the interviewer ensured that the person with dementia was brought into the conversation and asked for their opinion as well, but in such a way that the person with dementia did not feel under pressure if they could not remember. In some cases, a family carer would express an opinion and then ask the person with dementia if they agreed or wanted to say something different, as it ‘was not just their opinion that mattered’. In many interviews, the person with dementia was seen to agree through non-verbal gestures, such as nodding their head, even if they did not articulate a response.
People with dementia, carers and occupational therapists spoke about how they had ‘worked together’ to achieve the goals, with occupational therapists providing examples of how they had facilitated the dyad to take the initiative and people with dementia and carers describing the occupational therapist’s approach that had enabled them to go at their own pace and feel in control.
However, these findings contrast with the statistical results reported in the previous section, which provided no evidence of clinical benefit from the COTiD-UK intervention. The qualitative data found dyads reporting a wide range of positive impacts on their lives, specifically relevant to the aims of the occupational therapy intervention, in terms of continuing with activities they valued and seeing ways forward to continuing these and planning ahead, so as to live well with dementia.
Why people declined to take part in the research trial
The methodology and findings of the qualitative interviews with family carers who declined to take part in the RCT are reported in detail elsewhere63 and, therefore, are summarised here.
Aim
The aim of this study was to explore reasons why family carers and people with dementia declined to take part in the VALID research trial.
Method
Four of the 15 trial sites took part in this study. This was a purposeful sample based on which sites were still recruiting to the RCT and had research staff available and willing to identify potential participants. ‘Decliners’ were identified locally during the screening process and were approached only if it was thought unlikely to cause distress. Verbal permission to share contact details with the trial manager who would conduct the interview was sought. Family carers who had been identified as meeting the inclusion criteria but who subsequently declined to take part in the RCT were interviewed over the telephone. An indicative topic guide was used to guide the semistructured interviews, which was designed to explore the reasons for declining participation in the VALID RCT and the decision-making processes involved. The interviews were audio-recorded and transcribed verbatim. Inductive thematic analysis was used, with two researchers independently reading and coding the transcripts and then meeting to agree a coding framework and to identify themes. 58
Findings
Ten family carers who were part of a dyad that had declined to take part in the RCT were interviewed (four wives, three husbands and three female adult child carers). The interviews were intentionally short to reduce impact and inconvenience. All interviewees expressed an interest in taking part in dementia research in general. The family carers judged the invitation to take part in the study and the level of information provided to be generally acceptable for themselves, but some described it as being overwhelming or confusing for the person with dementia they supported. The person-centred nature of the intervention made it difficult for family carers to understand how it may benefit themselves and also, specifically, the person with dementia. Family carers reported that the decision on whether or not to take part was made in the same way as all of their decisions; however, although most were carer-led decisions, two interviewees reported that their decision had been led by the person with dementia.
Two main themes were identified in relation to whether or not taking part in the study was considered to be ‘worth it’: (1) protectiveness and (2) ‘It’s not for us’.
First, family carers emphasised how they sought to protect the person with dementia, themselves as carers and the dyad’s current way of life. They regarded it as important to protect the person with dementia from any situation that could potentially cause distress, or expose them to embarrassment, frustration or shame. They also highlighted the wish to maintain their privacy and avoid the perceived stigma associated with having dementia. Some expressed acceptance of their situation, whereas others described themselves as ‘managing fine’ and, therefore, not needing any further intervention at that point.
Second, family carers highlighted the potential inconvenience and disruption to themselves as a result of the time that they would need to give to take part in the study and possibly also the intervention. They were hesitant to take on additional commitments because they were already busy. Some felt that the intervention would not provide benefit in their case because the person with dementia was either too early or too late in their dementia journey to gain anything from it.
Conclusion
These findings underline the importance of research being designed to accommodate participants’ preferences and commitments, as well as the stage of dementia reached. They can therefore usefully inform future study recruitment, communication strategies and intervention designs. They highlight that there is no ‘one-size-fits-all’ approach to facilitating people with dementia and their carer’s research participation. This study identified that study designs needed to better engage with or set up processes to accommodate the specific needs of people with dementia and their family carers, if they are to enable a wider range of people to take part in research that aims to develop and evaluate psychosocial interventions potentially relevant to them.
Chapter 6 Economic evaluation (work packages 1, 3 and 4)
The economic evaluation is summarised here and is reported elsewhere. 64
Work package 1: the cost of COTiD training and economic evaluation feasibility analysis
A preliminary analysis to assess the cost of providing the COTiD training and intervention in WP1 was carried out. These costs were updated after the trial and the results are reported in the following section. The main cost components associated with the training were venue hire, trainer costs, occupational therapist attendance, consumables and audio-feedback supervision. The main cost components associated with providing the COTiD intervention in practice were session time (including preparation and recording time) and occupational therapist travel time and cost.
Work packages 3 and 4: cost–utility analysis of COTiD-UK compared with treatment as usual
Aims and methods
The cost–utility of COTiD-UK compared with TAU in dementia was investigated using the data from the VALID trial.
For the base-case analysis, the perspective of the NHS and Personal Social Services (PSS) was adopted, including the costs for the person with dementia only and measuring health-related quality of life (HRQoL) in terms of quality-adjusted life-years (QALYs) using the DEMQOL scale. 53,65 Several additional analyses were also carried out, including different costs (NHS and PSS costs for the person with dementia and carer, societal cost for the person with dementia only and also including the carer) and using different HRQoL questionnaires to assess the person with dementia’s QALYs.
The cost of the COTiD-UK training and intervention was assessed using trial data on the number of sessions and occupational therapists’ time, travel time and cost. The cost of the occupational therapy training and start-up was not included in the main evaluation; this was assessed separately because it was a fixed cost that should not be included in the main analysis.
For every person with dementia and their carer, the NHS and PSS service use cost was estimated (including GP costs, practice and community nurse costs, inpatient, outpatient and day case visits for specialist care, occupational therapy and physiotherapy costs, social worker costs, nursing home costs, domestic home help costs, cost of meals on wheels and day care costs), as well as cost of medications, adaptations, equipment and continence products needed as a result of dementia and changes in accommodation (e.g. residential care). Where a societal perspective was adopted, additional costs for the people with dementia (productivity losses due to illness and out-of-pocket payments for health-care service, adaptations and equipment) and carers (productivity losses due to informal care time, transport costs and out-of-pocket payments for health-care services) were included. Resource use data were collected retrospectively using an adapted version of the CSRI at baseline (covering the previous 12 weeks) and at 12 and 26 weeks. 58 Unit costs were taken from published sources. 66–73 Costs were calculated in 2017 Great British pounds and inflated where necessary. 74
The time horizon was 26 weeks, reflecting the ‘within-trial’ period. Extrapolation beyond the end of the trial was not undertaken because the within-trial analysis found no significant clinical benefits or cost reductions. Given that the time horizon is shorter than one year, discounting was not applied to costs or outcomes.
The effectiveness of the intervention was measured in terms of QALYs, calculated based on HRQoL and mortality data collected during the trial. HRQoL was assessed using the DEMQOL scale53 and DEMQOL-Proxy75 (for people with dementia only) and EQ-5D-5L76,77 (for the person with dementia and carers) questionnaires. Each EQ-5D-5L and DEMQOL and DEMQOL-Proxy health state was converted into a single utility value, applying weights based on valuations of the general population. 65,78,79 Utility profiles were constructed assuming a straight-line relation between each of the scores at each follow-up point. The QALYs experienced from baseline to 26 weeks were calculated as the area underneath this profile. In the additional analyses, in which both the person with dementia and their carer’s QALYs were included, costs and QALYs were summed. Although cost-effectiveness results are reported for each instrument, including a QALY that combines the person with dementia and carer quality of life, the base-case results consider the DEMQOL scale as the instrument that describes quality of life in dementia more accurately.
Cost–utility was expressed in terms of incremental net monetary benefit (INMB), which was calculated as the difference in mean QALYs per person for COTiD-UK compared with TAU multiplied by the maximum willingness to pay for a QALY minus the difference in mean cost per person (NICE 2013). 80 Non-parametric methods for calculating CIs around the incremental cost-effectiveness ratio based on bootstrapped estimates of the mean cost and QALY differences were used to account for data skewness. The analysis was performed adjusting for baseline values and study sites. Multiple imputation by chained equations (m = 20) was used to estimate missing values, accounting for age, gender, study site and treatment group. 81
Extensive sensitivity analysis was performed, including probabilistic sensitivity analysis, to control for uncertainty in the parameter values used. Cost-effectiveness acceptability curves, showing the probability that COTiD-UK was cost-effective compared with TAU at a range of values for the maximum willingness to pay for a QALY (£20,000 and £30,000 per QALY), were generated based on the proportion of the bootstrap replications across all 20 imputed data sets, with positive INMBs. 82–84
Results
The cost of training the occupational therapists to deliver COTiD-UK was estimated at £96,469 (£3000 per occupational therapist), including venue hiring, trainers’ costs, occupational therapists’ and supervisors’ attendance, additional material and audio-feedback supervision.
The mean cost per dyad of providing the COTiD-UK intervention, including the session time and transport cost, was estimated to be £619.
Taking an NHS and PSS perspective, including costs and benefits to the person with dementia only, measuring HRQoL based on DEMQOL scale and accounting for missing data, the mean total NHS and PSS cost per person with dementia was £2689 (95% CI £2272 to £3105) in the COTiD-UK group and £1919 (95% CI £1488 to £2349) in the TAU group for the entire time horizon of 26 weeks. The mean total QALYs (calculated using the DEMQOL scale) per person with dementia was 0.320 (95% CI 0.311 to 0.328) in the COTiD-UK group and 0.310 (95% CI 0.302 to 0.317) in the TAU group.
In the base-case analysis, using the above results and adjusting for baseline values, there was a significant difference in costs between the two groups (mean incremental cost for COTiD-UK £784, 95% CI £233 to £1334), but no significant difference in outcomes (mean QALYs gained 0.00664, 95% CI –0.00404 to 0.01732). Therefore, we preferred not to report the incremental cost-effectiveness ratio. The INMB for COTiD-UK compared with TAU was negative at a maximum willingness-to-pay value for a QALY of £20,000 (mean –£651, 95% CI –£878 to –£424) or £30,000 (mean –£585, 95% CI –£824 to –£345).
At the maximum willingness-to-pay value for a QALY of £20,000 (£30,000) the probability that the COTiD-UK is cost-effective was 0.02% (0.04%). The results were not significantly different when re-running the analysis without adjustment and using complete cases.
Chapter 7 Implementation phase
Implementation of COTiD-UK in practice (work package 5)
The aim of this WP was to determine the feasibility and effectiveness of implementing COTiD-UK into day-to-day practice. At the grant application stage, it had been planned to complete this WP after the RCT; however, the range and depth of data collected during the development, piloting and evaluation phases had made some of the planned activities redundant by then, or impracticable to complete, as explained in the following sections. This amendment to the programme structure also reflects advances in the field of implementation science since the grant application, with the current recommendation being to integrate such activities throughout this type of programme. 31 Vernooij-Dassen and Moniz-Cook31 highlight the importance of avoiding the risk of ‘implementation error’ or low intervention fidelity that can occur when conducting pragmatic trials in real-life practice settings, as low fidelity can result in the degree of effectiveness of an intervention being poorly estimated. It is also important to examine the context within which the intervention was delivered so as to better understand what factors enabled or hindered its delivery within a real-life practice setting.
Changes made to the study design
Theoretical Domains Framework
It had been planned to evaluate the implementation of the intervention using the TDF. 85 The TDF was developed with the aim of simplifying and integrating the multitude of behaviour change theories into a single framework that could be used in implementation research, and originally comprised 12 domains. 86 As the result of a content validity study, the framework was later revised to consist of 14 domains, so this version was used instead. 32 Not all of the domains are relevant to every intervention study and there is overlap between some.
The TDF domains can be mapped onto the Capability, Opportunity, Motivation (COM-B), hub of the behaviour change wheel (BCW). 86 The COM-B system characterises behaviour change in terms of three essential conditions that interact for behaviour to occur: capability, opportunity and motivation. This provides an approach to understanding behaviour change in context and, therefore, is used here to structure the reporting of the results.
Surveillance phase
In the original plan, a surveillance phase had been planned to examine the implementation of the intervention in a routine service outside the context of a RCT. This would have required recruiting and training a further 30 occupational therapists from areas proximal to the three main research centres to deliver the COTiD-UK intervention to 10 dyads each, collecting basic pre- and post-clinical outcome data on the people with dementia and family carers (n = 600). These additional data would be analysed to identify for how long and for whom benefits of COTiD-UK persist. It was also planned to identify characteristics that may indicate barriers to and facilitators of implementing the intervention, evaluate the training provided and obtain the occupational therapists’ views of the intervention.
In terms of the rationale for change, the data collected in the COTiD-UK development, piloting and evaluation phases made some of the activities redundant; for example, occupational therapists’ views of the COTiD training and intervention had been collected in WP1 and used in the development of the COTiD-UK intervention, and further data were obtained through the qualitative interviews conducted with occupational therapists who delivered COTiD-UK within the RCT. In addition, it was not actually possible to complete a separate surveillance study within the programme timeline, given that previous phases had over run as a result of the challenges of recruiting sites and then dyads, as well as training and retaining occupational therapists during the RCT phase. It, therefore, became unrealistic and unnecessary to recruit additional sites, occupational therapists and dyads to obtain what would have been very few new data.
In the revised plan, it was, therefore, decided to study implementation of the intervention within the RCT, specifically the extent to which the intervention was delivered as specified (i.e. fidelity of the intervention delivery).
Process evaluation
In the original plan, the fidelity of intervention delivery was to be assessed by the occupational therapists completing checklists online after each session and by video-recording two sessions with each dyad seen, and then reviewing these 1 week later to complete a further online checklist.
In terms of the rationale for change, there had been a poor response rate for occupational therapists completing the COTiD vignettes online in WP1, and feedback from other studies suggested that this is not unusual; therefore, completing checklists online did not appear to be a viable option for data collection. Meanwhile, the response rate from occupational therapists completing the COTiD/COTiD-UK checklist and goal-setting forms was good overall; therefore, it was decided to continue with this format.
In the revised plan, the occupational therapists completed a COTiD-UK checklist for each dyad seen within the RCT and then either inputted it to the online database themselves or submitted it to the COTiD-UK trainer/supervisor to input on their behalf. This checklist was used to record the number, frequency, length and content of sessions provided. These data also enabled the intervention costs to be calculated for the economic evaluation, as reported in Chapter 6, Economic evaluation (work packages 1, 3 and 4). In addition, the occupational therapists audio-recorded all of the COTiD-UK sessions as practicable, as described in the Assessing intervention fidelity section.
Qualitative interviews
In the original plan, it was planned to conduct qualitative interviews with occupational therapists and family carers in cases where it had been identified as easier and more difficult to implement the intervention in practice, to go on and explore the factors that led to success or difficulties.
In terms of rationale for change, given the relatively large number of semistructured qualitative interviews completed with dyads, managers and referrers involved in the development phase [see Chapter 3, Development phase: developing COTiD-UK (work packages 1 and 2)], and then with occupational therapists and dyads participating in COTiD-UK during the RCT [see Chapter 5, Qualitative studies (work package 4)], it was judged to be unnecessary to conduct more implementation-specific interviews.
In the revised plan, the themes identified from the inductive thematic analysis of the earlier qualitative interviews were, therefore, further considered in relation to the TDF domains and COM-B. The added advantage of this approach was that the interviews were conducted with both dyad members together, thus enabling the voices of people with dementia to be heard, thus enabling us to gather information that we had not set out to acquire.
Revised work package 5: implementation phase plan
The implementation phase, therefore, was revised to consist of two aspects:
-
a descriptive study to assess intervention fidelity (i.e. to what degree was the COTiD-UK intervention delivered as planned within the RCT)?
-
an exploratory study to understand why the intervention was, or was not, delivered as planned.
Assessing intervention fidelity
Interpreting data about intervention effectiveness requires an assessment of which intervention components were delivered and whether or not they were delivered as planned (i.e. the fidelity of delivery). 87,88 Two fidelity studies were conducted alongside the RCT and are reported in detail elsewhere89 and, therefore, are summarised here.
Aim
The first study aimed to develop a reliable measure for assessing intervention fidelity and the second study aimed to assess the fidelity of delivery of the COTiD-UK intervention across sessions, sites and occupational therapists.
Method
The studies used a longitudinal observational design nested within the RCT. Where practicable, all COTiD-UK intervention sessions were audio-recorded. Fidelity checklists and coding guidelines were developed, piloted and refined until good agreement was achieved between two coders. Ten per cent of sessions were purposively sampled from 12 sites and 31 occupational therapists. Transcripts were coded using the checklists developed in the first study, of which 10% were double-coded to ensure that agreement was maintained. Percentages of the components delivered were calculated for each session, site and occupational therapist.
Results
A reliable measure of intervention fidelity was developed after several rounds of piloting and amendment. Application of this measure found that COTiD-UK was delivered with moderate fidelity across the six sessions, although the mean range varied across sites and occupational therapists.
Conclusion
A reliable, systematic method for measuring fidelity of the delivery of COTiD-UK, which can be adapted for use in similar interventions, was developed. This demonstrated that COTiD-UK was delivered with moderate fidelity across all key sessions. Overall, there can be a reasonable degree of confidence that intervention effects can be attributed to the intervention content, but this cannot be extended to all sites and occupational therapists.
Why was the intervention delivered or not delivered as planned?
It is important not only to measure the degree to which the intervention was delivered as planned, but also to understand the factors that enabled or hindered its delivery within a real-life practice setting. This requires understanding and reporting the context within which the intervention was delivered. 90 The context can be multilayered, that is at the individual, team, organisational and community levels. 31 This is particularly important to consider within a multisite trial, in which the context will inevitably differ between and within sites. A degree of variability is, therefore, to be expected owing to the range of occupational therapists, who have mixed levels of prior knowledge, expertise and motivation, as well as their degree of COTiD-UK specific experience, and who are delivering the intervention across a number of sites, geographical areas, clinical and service settings, to participants with differing characteristics and levels of engagement. The more complex the intervention, the more context dependent it becomes, particularly for interventions that depend on the active participation of those both delivering and receiving the intervention, which in the case of COTiD-UK is made more complex by the dyadic nature of the intervention.
Aim
To explore the factors that enable or hinder the provision of the COTiD-UK intervention in practice.
Method
Data collected during the earlier development, piloting and evaluation phases were reviewed using the 14 TDF domains: knowledge, skills, social/professional role and identity, beliefs about capabilities, optimism, beliefs about consequences, reinforcement, intentions, goals, memory, attention and decision processes, environmental context and resources, social influences, emotions, and behavioural regulation. 32
The following data were reviewed:
-
COTiD-UK development phase (Chapter 3) – focus groups with people with dementia and with family carers who did not receive the COTiD intervention; COTiD knowledge questionnaire and vignettes; COTiD training evaluation; focus groups with occupational therapists who had delivered COTiD; semistructured interviews with dyads who took part in COTiD; semistructured interviews with managers and referrers involved in the implementation of COTiD; consensus event; and survey of current occupational therapy practice
-
piloting and evaluation phases (Chapters 4 and 5) – COTiD-UK knowledge questionnaire; COTiD-UK training evaluation; COTiD-UK supervision records; COTiD-UK checklist/goal-setting forms; semistructured interviews with dyads and occupational therapists who took part in COTiD-UK.
Results
The results are reported using the COM-B system structure described earlier, that is the three components that interact for behaviour to occur: capability, opportunity and motivation. 86
Capability
‘Capability’ here refers to the individual’s capacity to engage in the activity, and is subdivided into psychological and physical aspects, and includes having the necessary knowledge and skills. 86
Knowledge
The results of the COTiD knowledge questionnaire and vignette activity completed in the development phase suggested that the occupational therapists had acquired limited knowledge of the COTiD intervention at that point. However, it is acknowledged that the knowledge questionnaire results may also have reflected the apparent difficulty that participants had in understanding some of the questions and instructions, which had been translated literally from the original Dutch materials but not amended to better reflect UK terminology, and that the method of scoring the six multiple-choice questions required all, and only, the correct options to be checked for the question to be marked as correct. The updated version of the COTiD-UK knowledge questionnaire used in the evaluation phase suggested that a higher level of knowledge about the intervention had been gained by the end of the first two training days. However, this apparent knowledge gain may have been partly accounted for by using a revised marking system that more accurately scored participants’ responses out of 20.
A theme of ‘COTiD training’ was identified from the focus groups conducted with occupational therapists in the development phase. This included both positive feedback (that the information provided about how to conduct the narrative interviews was in-depth and thorough), and as negative feedback (that some of the content was too basic and simply reiterated what people already knew). This reflects the level of experience and expertise that UK occupational therapists already had in working with people with dementia, their carers and in the community, as well-established areas of practice in the UK. 42 This contrasted with the Netherlands, where working specifically with people with dementia, in the community and with family carers was not common practice at the time when Graff first developed the COTiD intervention and training course. 22
One of the themes derived from the interviews conducted with the occupational therapists who delivered COTiD-UK within the RCT was ‘Developing COTiD-UK knowledge and skills’, from which two subthemes are relevant here: ‘building on prior knowledge and experience’ and ‘utilising the COTiD-UK training’. Occupational therapists reflected on how their existing knowledge, skills and previous experience influenced their COTiD-UK knowledge acquisition. Some reported feeling initially anxious that they did not ‘know enough’, while some said that they would have felt more confident if they had known more about specific standardised assessment tools that occupational therapists from other research sites were routinely using. In general, they described a growing realisation that they were drawing on existing knowledge and skills:
And I suppose realising, I think initially a lot of the, my anxiety was around thinking that it was something completely different to what I normally do as an OT [occupational therapist]. And then over time I’ve realised and I felt more comfortable and confident in just utilising my normal skills and what I do every day in my other, you know in my normal job.
Occupational therapist
Skills
The occupational therapists also described how ‘utilising the COTiD-UK training’ supported them to develop the skills needed to provide the intervention. This included the timing, that is two consecutive days followed by another day once they had put COTiD-UK into practice; content, which focused on the aspects of COTiD-UK that were less familiar, such as the narrative interviews; format, which included time to practise the skills needed by role-playing a case study, setting SMART goals in small groups and hands-on practice using the audio-recorders; and useful resources provided, such as sets of laminated interview prompt cards, which were frequently referred back to and used when delivering the sessions. However, although the training was described in positive terms, it was seen as being only the starting point to developing competence in delivering COTiD-UK:
We had 2 days’ training and – and as good as it was I still felt that there was still a lot more that I could learn.
Occupational therapist
The occupational therapists stated that they ultimately developed their COTiD-UK skills, competence and confidence through actually delivering it in practice and, therefore, ‘learning through experience’. Occupational therapists felt that completing the training dyad sessions and the one-to-one feedback that they received from the COTiD-UK trainer proved invaluable, alongside listening back to the audio-recordings, as recommended within the training. By delivering COTiD-UK in practice their confidence grew, particularly with specific aspects, such as conducting the narrative interviews and setting SMART goals with the dyad:
I would say the training, it was great but I think the real thing is just doing it, isn’t it?
Occupational therapist
This is also reflected in the occupational therapists’ accounts of gaining confidence in the process of delivering COTiD-UK, as with one practitioner describing how:
It’s obviously got fluent the more I’ve done it.
Occupational therapist
Memory, attention and decision processes
Occupational therapists also described how ‘utilising COTiD-UK supervision’ supported their knowledge and skill development. A range of models were outlined: individual, group or peer; face to face; or over the telephone. The support available from both local supervisors and peers was seen as being beneficial, especially to discuss specific cases or check on the availability of local resources if they were providing COTiD-UK outside their usual geographical area. Peer supervision also afforded opportunities to check on operational queries relating to the research process, for example completing the COTiD-UK checklist or entering data into the web-based database, without feeling ‘silly’.
Behavioural regulation
‘Utilising COTiD-UK supervision’ also contributed to behavioural regulation in that it enabled the occupational therapists to reflect on their practice and plan how to continue to develop their COTiD-UK experience.
Opportunity
Opportunity here refers to factors extrinsic to the individual that make the behaviour possible or prompt it, and is subdivided into social and physical aspects. 86
Environmental context and resources
Many occupational therapists completing the COTiD training evaluation during the development phase suggested that the training would have been more beneficial if it had been provided nearer to actually putting the intervention into practice with dyads; because of the organisational and governance delays at some sites, there had not been opportunity to put COTiD into practice alongside the first 3 training days, as originally planned.
Occupational therapists participating in the focus groups in the development phase described a range of challenges to providing COTiD, including the additional time needed compared with their usual input, working in a very different way to usual practice, especially for those who normally worked in a generic role, and the conflict of prioritising COTiD dyads over service users at greater risk. Several occupational therapists emphasised the need for active support from managers:
It is essential that your leader is very involved and very proactive.
Occupational therapist
A theme identified from the interviews with occupational therapists who had delivered COTiD-UK within WP4 concerned the degree to which it varied from their usual practice. This was primarily dependent on whether they currently worked within a generic or profession-specific role. Those working in a generic role described themselves as usually ‘fire-fighting’, as the focus was inevitably on risk assessment and crisis management. However, they described how they also used their occupational therapy values and skills to achieve this and, therefore, still very much identified as occupational therapists. Conversely, those who worked in profession-specific roles described themselves as being ‘lucky’ in terms of being able to focus on providing occupational therapy intervention; however, they discussed the tension that this could cause with colleagues who had to then deal with a crisis situation while they continued to prioritise delivering COTiD-UK. Ultimately, the occupational therapists strived to maintain their professional identity:
I’ve always been very occupational focused in mind.
Occupational therapist
Analysis of the qualitative data collected within the WP2 survey of current practice highlighted the need for top-down staff support, with support from managers, commissioners as well as the therapists themselves. Linked to this, the next common theme was resources and funding, the perception being that if managers and commissioners supported the intervention, then this would result in more funding, hence, more staff and, therefore, the additional time and resources needed to deliver COTiD. Other facilitators were identified as being occupational therapists playing a more profession-specific/less-generic role within clear care pathways that included the occupational therapy role, and early assessment, diagnosis and intervention, with effective relationships across relevant services.
Motivation
Motivation here refers to the brain processes that energise and direct behaviour, and is subdivided into reflective and automatic processes. 86
Beliefs about capabilities
The COTiD training evaluation forms completed on the fourth training day in the development phase asked the occupational therapists to rank their level of agreement with the following statement: ‘I have achieved the knowledge and experience I expected from the training’. Of the 32 responses, 21 (65.5%) strongly agreed or agreed, eight (25%) neither agreed nor disagreed and three (9.4%) disagreed or strongly disagreed. This would suggest that the occupational therapists’ subjective perception of their level of knowledge obtained was higher than suggested by the numerical results achieved on the COTiD knowledge questionnaire, which is discussed earlier under the Knowledge section.
A theme of ‘What helped’ was identified from the focus groups conducted in WP1 with people with dementia and family carers who had not received COTiD. 41 Some participants reported being more proactive than others in seeking out support. However, one participant actively avoided seeking help and support and expressed his preference to care for his wife alone, as he felt best placed to do this.
Optimism
A theme from the occupational therapists’ interviews concerned how COTiD-UK goals were achieved. Occupational therapists discussed how the dyads’ level of motivation and ownership regarding the goals affected their ultimate success. Alongside this, a theme from the dyad interviews related to how goal achievement was associated with the occupational therapist’s practical support, information provision, problem-solving and enabling approach.
This concurs with data collected on the COTiD-UK checklists regarding the number of goals achieved compared with the number of goals set. When goals were not achieved, this was often because the person with dementia lacked the motivation to engage.
Beliefs about consequences
During the WP1 focus groups, people with dementia and family carers who had not received the COTiD intervention expressed their preference for more support and signposting to relevant services to be provided post diagnosis. 41 There was some frustration over being given a diagnosis and then left for months to digest the information and cope alone, with no contact from services.
Based on participants’ previous experience of services, two related issues that featured in all group discussions were the need for continuity of support throughout the dementia pathway and the need for consistency of approach. Many people found the services they dealt with fragmentary and inconsistent in the support provided, and said that they had simply been left to deal with the diagnosis after seeing the specialist doctor. In dealing with health services to date, participants felt that they were repeatedly asked the same questions and got the impression that there was little or no communication between professionals. They thought that having the same therapist throughout the 10-week COTiD intervention would go some way to having some consistency of approach:
That is what they need, continuity. Different people coming in wouldn’t work.
Family carer
Both family careers and people with dementia emphasised the importance to them of services following up to see how people were managing in their daily lives. For COTiD, they suggested having some follow-up sessions at varying intervals after the last intervention session to ensure that people were implementing what was worked on and to see if further support was needed.
Conclusion
This exploratory study to understand why the intervention was, or was not, delivered as planned highlighted the multi-layered and complex context that affected COTiD-UK delivery across the sites. The TDF domains identified as being the most relevant to COTiD-UK implementation in practice were knowledge and skills (capability), environmental context and resources (opportunity), and beliefs about capabilities (motivation).
Chapter 8 Patient and public involvement
There has been a commitment throughout the VALID programme to involving people living with dementia, family carers of people with dementia and members of the public. This reflects the growing awareness that service user, carer and public involvement is central to NHS research activities to focus on relevant issues. It has been recognised that such involvement improves the quality, depth and utility of research. 91
Patient and public involvement is reported here using the Guidance for Reporting Involvement of Patients and the Public 2 (GRIPP2-SF) (short form) format: the first international evidence-based, consensus informed guidance for reporting PPI in research. 92
Aim
The aim of involving people living with dementia, family carers of people with dementia and the general public in the VALID research programme was to help ensure that the research design and activities were relevant to people with dementia and their family carers, and feasible in practice.
Methods
Valuing Active Life in Dementia patient and public involvement reference group
A PPI reference group was established, and terms of reference determined. The purpose of the group was agreed as being to ensure that patient, carer and public involvement was embedded within the VALID research programme. It reported to the PSC and provided updates to the PMG. It was chaired by the PPI lead co-applicant, an academic with extensive experience of working with service users and the voluntary sector. There were three members, all former spousal carers of people living with dementia, one of whom also belonged to the PSC and two who belonged to the PMG. The group met between two and four times per year, depending on the stage of the programme. PPI involvement and activity across the programme was reviewed at each meeting in terms of programme management and governance, research activities and research outputs. The VALID programme manager supported the group by providing progress updates for information; ensuring regular administrative support for resourcing and co-ordinating meetings, taking minutes at the meetings, and circulating information about relevant training opportunities, provided by either the sponsor or other relevant organisations.
Patient and public involvement strategic principles
At the beginning of the programme, the group agreed key strategic principles for effectively involving people living with dementia and family carers. A strategy document was drafted by the PPI co-applicant lead, which was then discussed and successively amended following each discussion with the VALID PPI reference group. The group then wrote an abbreviated version and both documents were circulated to research staff and co-applicants, as well as the PSC, PMG and DMEC chairpersons and members.
In summary, the finally agreed strategic principles were to:
-
Consider possibilities for the level and nature of service user and carer involvement to include–93,94
-
consultation: researchers consult service users and/or carers about the research design and activities
-
collaboration: researchers and service users and/or carers work in partnership to manage the research activities
-
user-led/user-controlled research: service users and/or carers lead the research (often through ongoing involvement with a community or voluntary organisation led by service users and/or carers).
-
-
Review the broader research processes to see where service users and/or carers can be involved in shaping them, to potentially include shaping research designs; ensuring that research designs incorporate relevant service user and/or carer experience; advising on the intervention process; joining research staff recruitment panels and/or research staff training; data collection, analysis and interpretation; and dissemination activities.
-
Consider what support service users and carers may need to be effectively involved. 95 There needs to be a balance between the strategic intent of the research and the personal commitment and interests of those involved. There needs to be clarity about the project, roles and time commitments, with effective communication channels, easy access to project materials and facilities and adequate resources to manage practicalities, such as access, payments and effects on benefits. All of these need to be negotiated in the working context of the project and those service user and carer volunteers involved in practice. Access and support should be actively enabled to ensure the involvement of ‘harder to reach’ and diverse populations. 96 To ensure equal opportunities in involvement, there should be active awareness and respect for diversity, including communication differences. Related ongoing support and training needs should be identified and actively managed. 97 Prepare research staff to work with service users and ensure a working handover in the event of staff changes. Avoid unnecessarily short deadlines for responses.
-
Review service user and carer experiences of being involved. 98,99 Service users and carers should be offered regular, supported opportunities to discuss their experiences of involvement over the course of the research, and these experiences should be monitored and reported; research designs need to appropriately incorporate service user and carer experience.
Results
Grant application stage
People living with dementia and family carers were consulted locally (north-east London/Essex) and nationally at the grant application stage to confirm the relevance of the topic and feasibility of the proposed research design and intervention. This was achieved by talking one to one with and with small groups of people living with dementia and family carers attending a local Alzheimer’s Society social group (20 people in total); e-mail consultation via the Uniting Carers branch of Dementia UK (London, UK) and discussion with the Dementias & Neurodegenerative Diseases Research Network (which is part of the NIHR CRN) produced a further 20 responses.
A lay co-applicant (JH) was recruited, and not only contributed her personal experience as a former spousal family carer, but also brought her writing skills to finalise the lay summary section of the application. She was subsequently provided with an honorary contract by the lead NHS organisation.
Patient and public involvement in the Valuing Active Life in Dementia research programme management and governance
JH was a member of the PMG and drew on her experience as a published writer to support the programme outputs. A second formal spousal carer (DP), with experience of holding a similar role within a previous dementia research programme, was also a PMG member. A former spousal carer and a person living with dementia were members of the PSC. The latter was enabled to attend meetings first by his wife accompanying him to and from the meetings, and then by a number of undergraduate psychology students who spent their intern placements supporting him to engage in a range of activities. Three lay members joined the DMEC; each had personal and/or professional experience of supporting someone to live with dementia.
All PPI members of the PSC and PMG were recruited via the former Uniting Carers branch within Dementia UK. PPI members of the DMEC were recruited via the chairperson’s existing networks. All PPI colleagues were ratified by the funder prior to them taking up their role. Travel and other relevant expenses, such as the costs of a supporter to accompany the person with dementia to meetings, were available, in line with published guidelines. 92 However, most PPI representatives declined to claim this funding. A letter of agreement was in place to provide funding to the lay co-applicant in recognition of her professional writing contribution to the programme, and a service-level agreement was in place between the sponsor and Dementia UK to fund their involvement in recruiting and supporting PPI members of the PSC and PMG, and recruiting participants to attend the consensus event held within the COTiD-UK development phase.
Patient and public reference group involvement in Valuing Active Life in Dementia research activities
Throughout the research programme, the PPI reference group was consulted regarding the content and format of study materials aimed at participants to ensure that they were understandable and fit for purpose. This included participant recruitment documents, such as participant information sheets, consent forms, promotional posters and fliers, and indicative topic guides for the qualitative interviews that were conducted with dyads who had taken part in the COTiD intervention within the development phase. Following PPI feedback, materials were amended as suggested in readiness for submission of the relevant ethics approval. Similar consultation also took place to support the production of participant recruitment documents needed for MSc and PhD studies linked to the VALID research programme (see Development of research capacity).
During the evaluation phase, two PPI reference group members attended the COTiD-UK training that was provided to the occupational therapists delivering the intervention within the RCT. Both reported finding this to be a valuable experience, and one which improved their understanding of the intervention being evaluated. The occupational therapist participants gave positive feedback on the additional dimension that these two former carers of people living with dementia brought to the training; therefore, ideally, similar input would be included in any future COTiD-UK training programme.
The PPI reference group contributed to the analysis of the qualitative data collected through semistructured interviews with dyads who had taken part in the COTiD-UK intervention within the RCT. Indicative findings with data excerpts were presented and discussed to validate and add observations to the researchers’ initial analysis. One member of the group also contributed to the qualitative analysis of data collected via a national online survey of family carers conducted for a PhD study linked to the VALID research programme and will co-author the subsequent peer-reviewed publication.
One PPI reference group member joined the interview panel to recruit an occupational therapist researcher at the beginning of the programme, and subsequently provided a PPI training session within the sponsor’s local research and development training programme.
Involvement of patient and carer organisations in Valuing Active Life in Dementia research activities
During the COTiD-UK development phase, people living with dementia and family carers were recruited through collaboration with relevant local user organisations to take part in focus groups, for example local branches of Alzheimer’s Society and Age UK. Current and former family carers of people with dementia were recruited via Uniting Carers to take part in a consensus event held to further develop the COTiD-UK intervention through interactive discussion. This early work in the evaluation phase took place before the VALID PPI reference group was established and, as a consequence, another group was involved in the scrutiny of participant recruitment documents for the focus groups and consensus event. The South Yorkshire Dementia Research Advisory Group was a pre-established group of people living with dementia in Sheffield who met on a regular basis to advise researchers. The Uniting Carers development lead was named as the independent person on the participant recruitment documents, although she did not receive any enquiries.
The head of research and evaluation at Dementia UK was the named independent person on the RCT participant information sheets. A 3-monthly reporting system was established with the VALID programme manager to monitor the frequency and nature of the enquiries received. Over the duration of the RCT, one enquiry (of a local operational nature) was received and this was redirected to the relevant research site by the VALID programme manager to provide a local response.
Patient and public involvement reference group involvement in Valuing Active Life in Dementia research outputs
It is vital to keep research participants, collaborators and the general public informed of research progress. The dissemination and impact strategy is discussed later (see Chapter 9, Dissemination and impact activities). The lay co-applicant collaborated with the research team to update the programme website and was involved in producing the regular newsletters circulated to research participants and other interested parties; she also contributed to writing the Plain language summary for this report. The VALID PPI reference group have a key ongoing role in ensuring that there is lay input into the planning and execution of the dissemination activities. These include producing a lay summary of project design and findings for circulation to all research participants, collaborators and other interested individuals and organisations.
Discussion and conclusions
Here, we will discuss how well the PPI strategic principles were achieved across the programme. First, in relation to the level and nature of service user and carer involvement, there was certainly systematic and interactive consultation and collaboration, all of which were planned, identified, recorded and reviewed. Consultation included developing the grant application and research design and reviewing participant recruitment materials. Collaboration included qualitative data analysis and producing key outputs, such as the VALID newsletter and website. Members expressed some frustration about the constraints imposed on the format and content needed in producing research documents if they were to meet the requirements for gaining ethics approval, which was not felt to be user-friendly for people with cognitive impairment. Opportunities for service users and/or carers to lead the research were not identified. However, two of the three PPI reference group members have gone on to work as peer researchers on a subsequent study led by the same chief investigator, encouraged by the experience and interest gained through their involvement with VALID.
Second, PPI reference group members were involved in research processes, such as joining research staff recruitment panels, contributing to the training provided to the occupational therapists delivering COTiD-UK during the RCT, qualitative data analysis and interpretation, and dissemination activities, such as producing the VALID newsletter and updating the website.
Third, the need to support lay members to contribute to meetings was recognised, and a number of strategies were co-produced through the PPI reference group to enable their participation, for example the PPI lead co-applicant circulated the ‘VALID PPI Strategic Principles’ document to the PMG, PSC and DMEC chairpersons to raise their awareness of the importance of enabling lay members to participate effectively in meetings, and offered some practical suggestions as to how this might be achieved. The PSC chairperson met with lay colleagues (either face to face or over the telephone) in advance of the meeting to provide an explanation of the reports provided and the topics likely to be discussed; they also offered to debrief PPI members following the meetings if they wished. An administrative standard practice was to provide all meeting documents 2 weeks beforehand, posting them in hard copy if preferred, as well as sending them electronically, together with an explanation as to the purpose of each. A glossary of general research and specific VALID terms was produced and constantly updated, and included in all meeting papers along with an organisational chart initiated and developed by a member of the PPI reference group, which was also made available on the VALID website.
Finally, the PPI reference group had planned to review the PPI experience across the trial research sites. A procedure for contacting sites to identify the relevant PPI contact locally was agreed. However, despite numerous follow-up attempts made by the group, the PPI lead and members of the wider support team, hardly any details were forthcoming, and only one locally active contact was identified. The proposed telephone or face-to-face interviews to explore the nature, level and quality of the PPI experience could, therefore, not be carried out. It may be that this contact was made at too late a stage in the trial, but the lack of responses more likely reflects the lack of PPI activity specifically linked to the VALID programme at local sites where groups often worked episodically on task-specific PPI activities.
Reflections/critical perspectives
The range of research activities to which PPI members can contribute is potentially extensive: from designing studies and developing grant applications to joining research management and governance committees, to reviewing research recruitment materials and process, to collecting and analysing data, and to disseminating research outcomes. It is important to recognise these opportunities as well as the diversity of PPI members in terms of their differing motivations to get involved, experiences and views, and time available to contribute. PPI members have knowledge and experience that is of value to the project at all stages and levels. It is, therefore, important to afford users the opportunity to feed into the project at all levels and stages throughout by providing the relevant introductions and opportunity to comment at all meetings. Despite awareness of this it can be hard to achieve, but ongoing review and dialogue did help improve this aspect of meetings organisation over time.
Reflecting on their experiences towards the end of the programme, PPI reference group members reported mixed experiences and views about their involvement. This variation appears to stem from the differing meetings and activities that they had each been involved in, not least working with different members of the research team, and perhaps from bringing different interests and motivations for becoming involved initially. Some felt better included, listened to and valued than others, and that their respective skills were utilised more than those of others. Researchers, therefore, need to be prepared to recognise that PPI colleagues will have varying experiences, perspectives and views to contribute, and so time needs to be given to enable these to be voiced, discussed and, where possible, considered. PPI members highlighted the need for the research team to provide clear information at the very start about the project, about what their role(s) within it would or could be and the time commitment required. It is especially important to bear in mind that some PPI colleagues are contributing in a voluntary capacity and often have other commitments for which sufficient time needs to factored in for them to respond. The research process itself was seen as being slow at points and so it was sometimes difficult to maintain momentum. The turnover of staff within the central research team was also seen to have hampered communication. Take-up of the various training opportunities offered, and the degree to which they were felt to have been useful, was experienced as mixed.
It was felt that much had been learned by PPI members and also by research team members over the course of the programme about current developments within the field of PPI, while also acknowledging that more contemporary PPI innovations might not have been fully incorporated, not least the changing terminology used to describe those involved. It is important that all those involved in the research recognise and respect the essential role that PPI members played and fully value the diversity of experience and views that this brings to the process.
There has clearly been an ongoing and active commitment to PPI demonstrated over the duration of the programme, starting at the grant application stage and planned to continue throughout the ongoing dissemination phase. This has primarily been achieved through the evaluative support of the VALID PPI reference group, which has consistently provided valued critical discussion and collaboration. The level and type of activity varied in response to the stage of the research programme, and as outlined above, other individuals and organisations have also contributed. We thank them all for their input.
Chapter 9 Dissemination and impact activities
It has been important to keep research participants, clinical and academic collaborators, professional colleagues and the general public informed about the progress of the programme.
Dissemination and impact strategy
A dissemination and impact strategy was developed and monitored by the principal investigators group and co-ordinated by the programme manager. Key objectives were to raise awareness of the programme among the general public, NHS and relevant organisations and research bodies, such as service commissioners, policy-makers, professional bodies and government bodies not only to secure the commitment of clinical services at the study sites, but also to establish relationships with relevant stakeholders and users of research. ‘Users’ of this research were identified as being people living with dementia and family carers, along with the organisations supporting and representing them, practitioners, service commissioners, and the academic community.
Peer-reviewed publications
For the full list of peer-reviewed publications arising from the programme, see Acknowledgements, Publications.
The professional impact to date of the peer-reviewed publications is demonstrated by the fact that one publication, by Swinson et al. 42 was one of the most frequently downloaded British Journal of Occupational Therapy papers in 2016 (and was available as open access for a limited time) and another, by Di Bona et al. ,40 was selected as the British Journal of Occupational Therapy ‘Editor’s Pick’ during the month of its publication, which meant that it was more actively promoted by the journal’s publisher.
Other dissemination activities
Additional dissemination activities are listed in Report Supplementary Material 1, including oral and poster presentations at international, national and local events for research, practitioner and lay audiences, as well as general media items.
Research outputs were submitted to the relevant NIHR programme manager for approval in line with the ‘28 day’ rule, reported as part of the annual reporting system, entered into ‘ResearchFish’ (research impact assessment platform),100 and circulated to research staff, collaborators and interested parties as relevant on publication.
Newsletter
A newsletter was produced twice per year with support from JH, and was circulated electronically to collaborators, academic and professional colleagues, interested individuals and organisations. It was sent electronically both in embedded e-mail format and as an attached PDF, with hard copies also available on request. A hard copy was sent to all research participants via their local research team.
Website
A website was set up to contain information about the programme for a professional and lay audience (www.ucl.ac.uk/valid), including research participants and collaborators, and was regularly updated by a research assistant within the central research team in conjunction with the lay co-applicant. The site included two secure sections – one for the occupational therapists involved in intervention delivery and one for research staff and collaborators – to facilitate access to the most up-to-date programme documents and materials. In reality, this latter aspect was not used as much as foreseen owing to numerous technological issues; for example, NHS staff were frequently dependent on different or outdated software provided within their organisations and were, therefore, not able to open or download the documents in the correct format. The website was hosted by UCL and, for this reason, needed to adhere to the UCL ‘house style’, not least to maintain the technical support required. For this reason, the site was sometimes seen as not being as ‘user-friendly’ in style as it could have been to more effectively engage a wide audience, including people with dementia and their supporters. However, the website has continued to be regularly accessed from across the world.
Social media
A Twitter account (@VALIDResearch) (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) was established and had 122 followers as of January 2019. Activity was sporadic, with posts primarily being made when key programme milestones were reached, such as RCT recruitment, or to advertise dissemination activities, such as conference presentations or new publications. Guidelines on the safe and professional use of social media produced by UCL and the Royal College of Occupational Therapists were followed. Given that the use of social media has grown exponentially over the course of the programme, it is acknowledged that future research studies and personnel could make more regular and productive use of these opportunities to disseminate research progress, as well as support the recruitment of research participants.
Future dissemination and impact activities
The VALID PPI reference group will have a key role to play in planning the dissemination activities following the end of the programme. These will include producing a lay summary of the programme design and findings for circulation to all research participants, collaborators and other interested individuals and organisations. The group will also contribute to the planning and content of future dissemination events, the details of which are yet to be decided.
Chapter 10 Development of research capacity
The VALID programme has provided opportunities to develop research capacity at postdoctoral, doctoral and postgraduate levels for a number of research staff, students and practitioners, many of whom are occupational therapists.
Post-doctoral research experience
The VALID programme provided postdoctoral experience for Jennifer Wenborn, a highly experienced occupational therapist, who used her combination of research and management skills to plan and co-ordinate a wide range of research activities in the role of programme manager. Sinéad Hughes, also an occupational therapist, gained postdoctoral research experience through completing a range of qualitative and quantitative activities during the development phase, and then of setting up a RCT, funded by the National Multiple Sclerosis Society (USA) before being appointed to a postdoctoral research fellowship based at the University of British Columbia, Canada. Nadia Crellin also gained trial management experience, before being appointed as programme manager for another NIHR-funded Programme Grants for Applied Research within the sponsor’s department.
Doctoral studies
Two research team members have been supported as part-time PhD students, both of whom have contributed to the VALID programme data collection, analysis and dissemination as part of their doctoral studies.
Becky Field, an occupational therapist and research associate at the Sheffield site, was registered as a part-time health services research PhD student in the School of Health and Related Research, University of Sheffield, and was awarded her PhD in summer 2020. Her study explored the take-up of psychosocial interventions by people with early-stage dementia and whether or not a readiness to engage in these interventions can be identified. The first phase included a secondary analysis of qualitative data collected through the semistructured interviews conducted with people with dementia and their family carers who had taken part in the COTiD intervention within the programme’s development phase (WP1). 101 Ethics approval for the above was obtained as a substantial and a non-substantial amendment to the VALID protocol. The second and main phase involved further empirical research, recruiting participants independently of VALID, and, therefore, has separate ethics and governance approval. In 2017, Becky Field was awarded the Early Researcher Award by the Royal College of Occupational Therapists for an oral presentation of her work at its annual conference, and in 2018 she received a Research Career Development Grant from the UK Occupational Therapy Research Foundation (UKOTRF) to continue her PhD studies.
Jacki Stansfeld, formerly a research assistant within the central research team (and now programme manager for another NIHR-funded Programme Grants for Applied Research multicentre RCT within the sponsor’s department), was registered as a part-time PhD student in the Division of Psychiatry, UCL, and was awarded her PhD in spring 2019. Her PhD study, ‘Sense of competence in family carers of people living with dementia: a positive psychology perspective’, seeks to understand the impact of positive aspects of caring on caregiver sense of competence in dementia. 102 Her study developed a new conceptual model of sense of competence in family caregivers of people living with dementia to advance the theoretical understanding of this construct to inform the development of appropriate clinical interventions to further support family carers in their role. This PhD used the VALID RCT baseline data (WP3 and WP4) alongside independently collected quantitative and qualitative data, and two systematic reviews, with three publications to date and more in preparation/planned. 103–105
There was also opportunity to collaborate with another doctoral research student, Holly Walton, a full-time PhD student registered at the Department of Clinical, Educational and Health Psychology at UCL, and funded by the UCL Economic and Social Research Council Doctoral Training Centre (Grant Reference: ES/J500185/1). Holly Walton completed her PhD at the end of 2018. As part of her work to develop a methodology and tools to assess the fidelity of an intervention being developed within another dementia research programme led by Martin Orrell, Holly Walton conducted two fidelity assessment studies embedded in the RCT (see Implementation phase). 89
Postgraduate studies
Two members of the central research team implemented aspects of the WP3 and WP4 protocol as part of their MSc courses. Jacqueline Mundy, trial manager and a registered nurse, carried out the qualitative study with family carers who had declined to participate in the RCT [see Chapter 5, Qualitative studies (work package 4)] for her part-time MSc in health service research at City, University of London, that was awarded with distinction in January 2018. 63 Jacqueline Mundy refined the indicative topic guide that had been previously been developed through a review of the literature, and obtained the relevant ethics and governance approvals needed for the additional recruitment documents required for this MSc project, as a substantial amendment to the RCT protocol.
Jane Burgess, an occupational therapist, joined the central research team on secondment from her substantive memory services clinical lead post as the COTiD-UK trainer and supervisor for WP3 and WP4. Jane Burgess completed a part-time MSc, in Dementia: Causes, Treatments and Research, at University College London in autumn 2019. She conducted six of the dyad qualitative interviews and led the thematic analysis of the dyad and occupational therapist interview data [see Chapter 5, Qualitative studies (work package 4)]. 62 She was subsequently recruited to a substantive research post, utilising her trial management and interventional research experience to contribute to or take on the role of local principal investigator for other portfolio studies within the sponsor’s department.
Laura Di Bona, an occupational therapist researcher at the Sheffield site, obtained funding to evaluate a care home pilot intergenerational scheme, which gained national interest, and more recently has been awarded research capacity funding to lead a project on peer support for her local NHS trust, as well as being the first occupational therapist to be accepted onto the School of Health and Related Research (ScHARR) clinical research academy.
Research experience for lay colleagues and occupational therapist participants
As noted above, two members of the PPI reference group (JH and DP) moved on to contributing as peer researchers for other dementia studies.
Alongside the more formal research student opportunities noted above, many practising occupational therapists have engaged in the research process through their participation in the development phase activities, such as recruiting and seeking informed consent from participants, collecting research data, delivering a manualised intervention, taking part in focus group and/or completing the online the survey, and/or delivering the COTiD-UK intervention within the RCT, thus increasing their research knowledge, skills and experience. Feedback from the occupational therapists has consistently been positive about the value of being able to contribute to the research to build the profession’s evidence base. There are several examples of these occupational therapist participants continuing their research involvement. For example, in Sheffield, some have since delivered the intervention within another RCT, and one has recently been seconded to the local research department through research capacity funding.
Jennifer Wenborn and another occupational therapist who took part in the development phase COTiD training and delivery were appointed as allied health professional research champions for their respective CRN areas. This collaboration between the NIHR and the Council for Allied Health Professions Research aims to build momentum and maximise the visibility and impact of allied health professionals in a research context, both locally and nationally. 106
Chapter 11 Conclusion and recommendations
Summary of the programme and outcomes
This applied research programme focused on the development and evaluation of a community occupational therapy intervention for people with mild to moderate dementia and their family carers. It built on the COTiD intervention that was developed and found to be clinically effective and cost-effective in the Netherlands. 23–25
The VALID research programme consisted of five WPs across three phases: (1) development of the UK version of the intervention, known as COTiD-UK (WP1 and WP2); (2) piloting and evaluation through an internal pilot and full RCT of COTiD-UK compared with TAU, along with an economic evaluation and two embedded qualitative studies (WP3 and WP4); and (3) implementation of COTiD-UK in practice (WP5), including assessment of the intervention delivery fidelity. In summary, the following outcomes were achieved.
A mixed-methods approach was taken in the development phase to translate, put into practice and adapt the COTiD intervention and training model and resources to maximise its suitability and feasibility for use within the UK culture and health and social care service context. This produced the UK version of the intervention, known as COTiD-UK.
The trial statistical results did not indicate any benefit of the COTiD-UK intervention compared with TAU for the outcomes selected. 48 The COTiD-UK intervention was assessed as being delivered within the RCT overall with moderate fidelity, albeit with variation between occupational therapists and sites. 89 Likewise, the economic evaluation did not find COTiD-UK to be cost-effective compared with TAU. This is in contrast to the qualitative study, with dyads describing the outcome of the intervention in very positive terms, and providing examples of how they had taken up activities they had not undertaken for a while and felt enabled to plan how they would continue their occupational participation in the future. 62 Over 90% of goals set by the dyads taking part in COTiD-UK were achieved. 48 The occupational therapists felt that COTiD-UK was ‘real OT’ and allowed them to utilise their unique core skills and expertise. 62
Inevitably, we encountered challenges while conducting this extensive research programme. The development phase took twice as long as originally scheduled. This was because of underestimating the time that the translation of the Dutch materials would take, and then a series of organisational challenges across the 10 sites at which occupational therapists were trained to put COTiD into practice. The piloting and evaluation phase was, therefore, delayed. The internal pilot was reviewed with the Independent PSC against the ACCEPT criteria, which agreed that the data collected to date could be carried forward into the main trial data set. 44 This pragmatic trial was conducted against a background of various organisational issues. Recruitment of sites took longer than scheduled, partly because it became necessary to recruit more sites than originally planned because the number of occupational therapists available at most sites was smaller and the dropout rate higher than expected. It was a complex study to conduct because it required sites to co-ordinate researcher capacity (researchers were often enlisted from local CRNs), and to recruit and collect data from dyads rather than individual participants, as well as ensure there was sufficient occupational therapist capacity to deliver the COTiD-UK intervention within the protocol time frame. This was particularly problematic because only 2 of the 12 trial sites managed to obtain excess treatment costs, which inevitably reduced the availability of occupational therapists at any point. This, therefore, led to delays in being able to recruit participants until therapists were available to provide the intervention within a timely manner following randomisation. The delivery of the intervention was, therefore, often dependent on the goodwill of the occupational therapists, their managers and their colleagues, who supported them to implement this alongside their usual practice and the need to continue delivering the usual commissioned services.
This was a well-run study and, to the best of our knowledge, is the largest RCT of occupational therapy for people with dementia and their family carers in the UK to date. The non-adherence rate of 4.6% and attrition rate of 13% at 26 weeks were both close to the 5% and 15% estimates, respectively, that we used to calculate the sample size, based on similar trials of other psychosocial interventions. 107,108
The ICC estimate is slightly higher than that used in the sample size calculation and the full sample size was not quite attained (97.5%). Despite this, the large p-value (0.55) obtained for a test of the null hypothesis of no difference in the BADLS total score between groups and a 95% CI (–0.85 to 1.51) covering zero from a large sample is not suggestive of an effect estimate that would have differed significantly from zero, had the intended sample size been attained.
It is recognised that in clinical trials there may be differences in the quantitative results and the qualitative findings. This may be more likely when psychosocial interventions deliver a rewarding and socially meaningful experience. It could, therefore, be suggested that the positive qualitative findings reflected the impact of receiving the face-to-face and personalised engagement, particularly if the local service provision did not usually include support for people at this stage of their dementia pathway. However, the outcomes that dyads reported were very occupationally focused, with reports of meaningful activities that had been dropped resuming and of new ones being established. It is unlikely that this would have happened purely through the social engagement within the COTiD-UK sessions.
The intervention fidelity was lower than that reported in the Graff study,23 which was a small trial involving only two occupational therapists, who were deeply committed and also closely monitored while delivering the intervention. This was a much larger trial, with 15 sites and 468 dyads, involving 32 occupational therapists with varying levels of prior clinical and COTiD-UK-specific expertise. However, the majority of the occupational therapists delivering the COTiD-UK intervention already had extensive experience of working with people living with dementia and family carers or working in the community.
Given the differences in the Dutch and English results, it is possible that the different settings in the Netherlands and the UK for the intervention delivery played a role. This is especially likely because usual care differed between the two countries. The Dutch control group did not receive any occupational therapy because occupational therapy was not provided in the community to people with dementia at that time.
By contrast, occupational therapy practice for people with dementia is well established within the UK. Over the course of this research programme, UK memory services became better established, and the policy impetus for earlier diagnosis and access to services means that more people receive some occupational therapy input at the mild to moderate stage of dementia. However, this is usually far less than the COTiD-UK intervention provides and is usually focused on just the person with dementia rather than being a dyadic intervention. 42 It primarily aims to inform the diagnostic process or assess/manage the person with dementia’s level of risk, and any input to family carers usually focuses on their ability to perform their role and tasks as a carer and not their own occupational needs, such as is the case with COTiD-UK. 42 Therefore, we acknowledge that the provision of occupational therapy within the TAU group inevitably varied between and within the participating research sites and, for this reason, was a variable that we could not control.
We feel that the difference with the Dutch results is unlikely to be accounted for by adapting the COTiD intervention or training programme. The COTiD-UK intervention retained the same core principles and components of the original COTiD intervention but is more flexible in its content and delivery; for example, the occupational therapists can use a wider range of assessment and intervention tools that are already in regular use within UK practice, and the time span for delivery is extended from 5 to 10 weeks to better meet the needs of pairs and be more feasible for service delivery. 42 We restructured the COTiD-UK training programme into 2 consecutive days followed by a third day once the therapists had put COTiD-UK into practice to be more cost-effective and feasible for services to release staff, and to better meet the needs of UK occupational therapists, many of whom already have extensive experience of working with people living with dementia or family carers or in the community.
Limitations
We collected data regarding social contact and leisure activities over the previous 12 weeks because we anticipated that these should increase as an outcome of the intervention. However, there were some problems with the quality of these data, partly because of dyads’ difficulty in recalling their activities accurately and partly owing to a lack of consistency in how this information was recorded by the researchers, despite training. This brings into question how accurate the results in this domain are.
We found that there was a very high rate of goal attainment; however, given the design, it was not feasible to ask people in the TAU group to set goals for comparison given that goal-setting is a key part of the intervention. The GREAT trial19 (Goal-orientated cognitive rehabilitation in early stage dementia) also found positive results for goal attainment, which was the primary outcome, but no difference between the treatment and the control groups on the validated secondary outcomes covering the conventional range of domains. Further complicating matters, the goals set with the GREAT participants at baseline were not shared with the therapist providing the intervention, who may then have worked on different goals altogether. We felt that asking people in the TAU group within this study to set goals may raise their expectations and optimism around success, and potentially lead to demoralisation when the goals are unfulfilled. Owing to the sample size and extended follow-up timescale, it was not feasible for us to offer the intervention to the TAU group on completion of all data collection as sometimes happens.
A further limitation is that the sample was not representative of the UK population in terms of ethnicity because most people included were white British. Nevertheless, this is not unusual in this kind of study, as it can be difficult to recruit other ethnic groups and fluency in English was part of the eligibility criteria. However, this was essential to enable data collection and the intervention to be provided on the basis of all providers and participants sharing similar levels of first language skills. It is possible that the nature of the dyadic relationship (spouse or parent-adult child) and living situation (living alone or together) may have impacted the intervention in terms of the type of goals set and how they were achieved. This study was not designed or powered to look at such individual differences, but from our experiences we had no reason to think there was any discernible impact from these factors. In addition, we did not collect data on social class, which may potentially have affected the dyads’ participation in the intervention, in that those with fewer resources available to them may find it more difficult to achieve their goals.
Implications for practice
The trial statistical results did not indicate any benefit of the COTiD-UK intervention, as delivered in this trial, compared with usual care for the outcomes measured. However, the qualitative findings indicated that the occupational therapists felt that COTiD-UK was ‘real OT’ and utilised their core unique skills, namely enhancing health and well-being through taking part in activity, and the dyads provided tangible examples of how they had resumed or taken up meaningful activities as a result of the sessions. There is no evidence to suggest that occupational therapy input in general does not continue to be a highly valued and important part of multiprofessional teamworking and service provision. The relatively well-developed occupational therapy practice for people with dementia in the UK provides a firm foundation for occupational therapists continuing to contribute to community teamwork and memory service provision for people with cognitive problems and their families.
Recommendations for future research
Traditionally, psychosocial intervention research has focused on measuring outcomes such as cognition, daily living abilities and quality of life because these are core domains potentially affected by dementia that these interventions seek to improve. The measures used were mostly developed for use within pharmacological studies and tended to focus on the level of deterioration and impairment. There are inherent difficulties in expecting improvements in ADL in someone with a progressive disorder such as dementia, despite conflicting findings in the Dutch study. In our study, we noted that, in the main, dyads set goals related to a wider range of activities than those covered by the BADLS, for example leisure, creative, social and community based.
Since the VALID programme started in 2012, there has been a growing focus on measuring outcomes in dementia research that are beyond simply the negative consequences, such as cognitive impairment and functional decline. For example, a number of positive psychology measures have been developed, which may help to better understand how people’s capabilities and self-management skills might be enhanced through training and goal-setting. 109 It is, therefore, important to develop tools and methods to measure outcomes of complex interventions, such as COTiD-UK, that truly reflect the occupational aim and nature of the intervention, as well as what is meaningful and prioritised by people with dementia and family carers rather than the traditional. Given that over 90% of goals set by the dyads taking part in COTiD-UK were fully or partially achieved and covered a much broader scope than traditional ADL activities, further analysis of the goals set and met could inform the future selection and development of more meaningful occupational outcome measures, tools and processes.
There is now a focus on developing patient-related outcomes in formats that make them suitable for self-report. This would enable data to be collected directly from people with dementia themselves rather than having to rely on proxy data from carers who can provide their own views only.
Conclusion
This study found no statistical evidence for the clinical effectiveness of COTiD-UK compared with the usual care provided, despite the perceived enthusiasm from the occupational therapists, people with dementia and family carers who took part. The programme of research was conducted to a very high standard of methodology with an independent PSC and a DMEC. The delivery of the COTiD-UK intervention achieved moderate fidelity, suggesting that people with dementia and family carers were receiving the sessions as planned and true to the goals and purpose of the intervention and study protocol. Having considered sources of bias, we found no particular reason to question the validity of our statistical results in relation to the clinical effectiveness and also the value for money of COTiD-UK.
We have shown that it is possible to conduct and effectively deliver a well-designed, high-quality, highly complex clinical trial of occupational therapy across 15 sites and requiring intervention delivery by experienced occupational therapists. This paved the way for demonstrating the potential feasibility of other large-scale trials in dementia.
Acknowledgements
This research would not have been possible without the support of the people with dementia, their family carers, and the local principal investigators, research teams, occupational therapists and clinical colleagues who took part in the development and evaluation phases of this programme. We thank the following organisations for their participation and co-operation:
-
Central and North West London NHS Foundation Trust
-
Cornwall Partnership NHS Foundation Trust
-
Devon Partnership NHS Trust
-
Dorset HealthCare University NHS Foundation Trust
-
East London NHS Foundation Trust
-
Essex Partnership University NHS Foundation Trust (formerly South Essex Partnership University NHS Foundation Trust)
-
Humber Teaching NHS Foundation Trust (formerly Humber NHS Foundation Trust)
-
NAViGO Health and Social Care Community Interest Company
-
Norfolk Community Health and Care/Norfolk and Suffolk NHS Foundation Trust
-
North East London NHS Foundation Trust
-
Oxleas NHS Foundation Trust
-
Rotherham, Doncaster and South Humber NHS Foundation Trust
-
Sheffield Health and Social Care NHS Foundation Trust
-
South London and Maudsley NHS Foundation Trust
-
South West London and St George’s Mental Health NHS Trust
-
Surrey and Borders Partnership NHS Foundation Trust
-
Sussex Partnership NHS Foundation Trust
-
2Gether NHS Foundation Trust
-
West London Mental Health NHS Trust.
We also thank the following groups, organisations and individuals who supported us throughout the programme:
-
Sandra Nolle, VALID Administrator and Office Manager, NELFT.
Programme Steering Committee members
-
Dr Claire Ballinger (chairperson), University of Southampton.
-
Dr Christian Bottomley, London School of Hygiene and Tropical Medicine.
-
Professor Stephen Curran, South West Yorkshire Partnership NHS Foundation Trust (June 2013 to November 2015).
-
Dr Jane Fleming, Institute of Public Health, University of Cambridge.
-
Professor Priscilla Harries, Brunel University London.
-
Mrs Kate Harwood, lay member.
-
Mr Keith Oliver, lay member.
Data Monitoring and Ethics Committee members
-
Professor Jill Manthorpe (chairperson), King’s College London.
-
Dr Stephanie Daley, Brighton and Sussex Medical School.
-
Ms Jenny Helier, King’s College London.
-
Dr Rekha Elaswarapu, lay member.
-
Ms Jane Hopkins, lay member.
-
Ms Shamime Lakda, lay member.
Occupational Therapy Reference Group members
-
Sally Rooks (chairperson), North East London NHS Foundation Trust (November 2012 to 2018).
-
Sarah Bains, Derbyshire Healthcare NHS Foundation Trust (November 2012 to May 2014).
-
Carol Duff, Lincolnshire Partnership NHS Foundation Trust (May 2015 to 2018).
-
Julie Edwards, Sheffield Health and Social Care NHS Foundation Trust (November 2012 to 2018).
-
Joan Hansen, Tees, Esk and Wear Valleys NHS Foundation Trust (September 2014 to 2018).
-
David Heasman, South West London and St George’s Mental Health NHS Trust (November 2012 to September 2014).
-
Andy Lucas, Humber Centre for Forensic Psychiatry (November 2012 to 2018).
-
Alice Moody, 2gether NHS Foundation Trust (November 2012 to 2018).
-
Caroline O’Haire, North East London NHS Foundation Trust (November 2012 to November 2013).
-
Karin Orman, Royal College of Occupational Therapists (November 2012 to 2018).
-
Shirley Pearce, Royal College of Occupational Therapists Specialist Section – Older People, Dementia Forum Lead (September 2014 to 2018).
-
Pasna Sallis, Royal College of Occupational Therapists Specialist Section – Older People, Dementia Forum Lead (November 2012 to January 2014).
-
Jane Tuxworth, Lincolnshire Partnership NHS Foundation Trust (November 2012 to January 2014).
We particularly thank Karin Orman and the Royal College of Occupational Therapists for supporting this group and providing a venue for their meetings.
Patient and Public Involvement Reference Group members
-
Professor Fiona Poland (chairperson), University of East Anglia, VALID co-applicant, PPI lead.
-
Kate Harwood, lay member.
-
Jane Hill, lay member, VALID co-applicant.
-
David Prothero, lay member.
We also thank Dr Karen Harrison-Dening, and Joy Watkins (deceased) at Dementia UK for their support in recruiting PPI representatives to join the PSC and PMG; recruiting participants to contribute to the consensus event conducted in WP1; and being named as the independent contact on the relevant research participant information sheets.
We also thank the South Yorkshire Dementia Research Advisory Group for their useful comments regarding the participant recruitment materials produced for the evaluation phase.
This programme of research was hosted and sponsored by NELFT. We, therefore, thank our NELFT colleagues within the research and development department and clinical services for their continued support of the programme and research team.
The VALID research team acknowledge the support of the NIHR CRN.
We thank the Priment Clinical Trials Unit at UCL for their support in conducting the RCT.
Elena Pizzo and Stephen Morris were (in part) supported by the National Institute for Health and Care Research (NIHR) Collaboration for Leadership in Applied Health Research and Care North Thames at Bart’s Health NHS Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, NIHR or Department of Health and Social Care.
We acknowledge the support of the UCLH NIHR Biomedical Research Centre.
Contributions of authors
Jennifer Wenborn (https://orcid.org/0000-0001-7311-8972) (Senior Clinical Research Associate – Occupational Therapist: Division of Psychiatry, University College London/Research & Development Department, North East London NHS Foundation Trust), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. As programme manager, she co-ordinated all aspects of the programme delivery and managed the central research team in NELFT. She co-ordinated and contributed to the COTiD-UK development activities (WP1); contributed to the design and analysis of the online survey of occupational therapy practice (WP2). In WP3 and WP4 she was a member of the TMG, collected and analysed the qualitative data, trained and supervised the occupational therapists delivering COTiD-UK, and contributed to the economic evaluation and fidelity studies; she supported the PPI and OTRGs; co-ordinated the dissemination of the programme; and prepared the final report in collaboration with other co-authors.
Gail Mountain (https://orcid.org/0000-0002-5417-7691) [Professor of Applied Dementia Research: Centre for Applied Dementia Studies, University of Bradford/School of Health and Related Research (ScHARR), University of Sheffield], as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. She managed the Sheffield research centre; contributed to the COTiD-UK development activities (WP1); supervised the occupational therapists delivering COTiD-UK, and contributed to the trial delivery, qualitative design, fidelity study and implementation activities (WP5); and led the publication strategy.
Esme Moniz-Cook (https://orcid.org/0000-0002-7232-4632) (Professor of Clinical Psychology of Ageing and Dementia Care Research: Faculty of Health Sciences, University of Hull), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. She managed the Humber research centre; contributed to the COTiD-UK development activities (WP1); trial recruitment and delivery (WP3 and WP4); and implementation activities (WP5).
Fiona Poland (https://orcid.org/0000-0003-0003-6911) (Professor of Social Research Methodology: School of Health Sciences, University of East Anglia), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. She was the qualitative and PPI lead, contributed to the COTiD-UK development activities (WP1) and supervised the qualitative design and analysis.
Michael King (https://orcid.org/0000-0003-4715-7171) (Professor of Primary Care Psychiatry: Division of Psychiatry, University College London) as a co-applicant contributed to the design and methodology of the research programme and was a member of the PMG and TMG. He supervised the conduct of the RCT (WP3 and WP4).
Rumana Omar (https://orcid.org/0000-0003-1483-1932) (Professor of Statistics: Department of Statistical Science, University College London) as a co-applicant contributed to the design and methodology of the research programme and was a member of the PMG and TMG. She designed, supervised and validated the RCT statistical analysis (WP3 and WP4).
Aidan O’Keeffe (https://orcid.org/0000-0002-0776-0868) (Associate Professor of Statistics: Department of Statistical Science, University College London) was a member of the TMG, conducted the RCT statistical analysis and prepared the trial statistical report and anonymised data set.
Stephen Morris (https://orcid.org/0000-0002-5828-3563) (Professor of Health Economics: Department of Applied Health Research, University College London), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. He designed and supervised the economic evaluation (WP1, WP3 and WP4). He is now RAND Professor of Health Services Research: Department of Public Health and Primary Care, University of Cambridge, UK.
Elena Pizzo (https://orcid.org/0000-0003-0790-7505) (Senior Research Associate – Health Economist: Department of Applied Health Research, University College London) conducted the economic evaluation (WP1, WP3 and WP4).
Susan Michie (https://orcid.org/0000-0003-0063-6378) (Professor of Health Psychology/Director: UCL Centre for Behaviour Change, Department of Clinical, Educational and Health Psychology, University College London), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. She supervised the COTiD-UK fidelity study and contributed to the implementation activities (WP5).
Myrra Vernooij-Dassen (https://orcid.org/0000-0002-9746-9897) (Professor of Psychosocial Care for Frail Older Persons: Radboud University Medical Centre, Nijmegen, the Netherlands), as a co-applicant, contributed to the design and methodology of the research programme. She was a PMG member and contributed to the COTiD-UK adaptation, RCT and implementation activities.
Maud Graff (https://orcid.org/0000-0003-4361-4291) (Professor of Occupational Therapy: Radboud University Medical Centre, Nijmegen, the Netherlands) developed the original COTiD intervention in the Netherlands. She contributed to the COTiD-UK adaptation, RCT and implementation activities.
Jane Hill (https://orcid.org/0000-0001-9045-8012) (Writer and Former Carer), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. She contributed her personal experience of caring for a person with dementia, and her professional writing skills to enhance the research participant recruitment materials and programme dissemination – website, newsletters and Plain language summary.
David Challis (https://orcid.org/0000-0002-6464-2286) (Professor of Community Care Research/Director: Personal Social Services Research Unit, University of Manchester), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. He provided specialist advice on the development and evaluation of complex community interventions and the RCT design and analysis. He is now Professor of Community Care Research, Institute of Mental Health, University of Nottingham.
Ian Russell (https://orcid.org/0000-0002-0069-479X) (Professor of Clinical Trials: Medical School, Swansea University), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. He provided specialist advice on the RCT design, methodology and analysis.
Catherine Sackley (https://orcid.org/0000-0002-8580-6622) (Professor of Physiotherapy/Head of Department: Public Health Sciences Research, King’s College London), as a co-applicant, contributed to the design and methodology of the research programme and was a PMG member. She provided specialist advice on the development and evaluation of complex community/occupational therapy interventions and the RCT design, methodology and analysis.
Sinéad Hynes (https://orcid.org/0000-0002-3199-7355) (Clinical Researcher – Occupational Therapist: North East London NHS Foundation Trust) contributed to the design, conduct and analysis of the COTiD-UK development activities (WP1); the design, conduct and analysis of the online survey (WP2), and was the trial manager July to October 2014. She is now Lecturer in Occupational Therapy: School of Health Sciences, National University of Ireland Galway, Ireland.
Nadia Crellin (https://orcid.org/0000-0002-9497-5874) (Postdoctoral Researcher: Research & Development Department, North East London NHS Foundation Trust/Division of Psychiatry, University College London) was the RCT trial manager October 2014 to January 2016. She is now research fellow at Nuffield Trust.
Jacqueline Mundy (https://orcid.org/0000-0001-7917-7041) (Research Nurse: Research & Development Department, North East London NHS Foundation Trust/MSc student: School of Health Sciences; City, University of London) was the trial manager from April 2016 to June 2018; designed and conducted the qualitative study that explored why people declined to take part in the RCT. She is now specialist stroke nurse at Essex Stroke Hub Team, North East London NHS Foundation Trust.
Jane Burgess (https://orcid.org/0000-0002-4626-6424) (Clinical Researcher – Occupational Therapist: Research & Development Department, North East London NHS Foundation Trust/MSc student: Division of Psychiatry, University College London) trained and supervised the occupational therapists delivering COTiD-UK; chaired the COTiD-UK supervisors group; oversaw the COTiD-UK delivery and COTiD-UK data collection and management; completed the COTiD-UK intervention data analysis; collected and analysed the qualitative data; and contributed to the fidelity study and implementation activities.
Tom Swinson (https://orcid.org/0000-0003-2314-9193) (Senior Research Assistant – Occupational Therapist: Research & Development Department, North East London NHS Foundation Trust) contributed to the COTiD-UK development activities (WP1); contributed to the design, conducted and analysed the online survey of occupational therapy practice (WP2); completed the COTiD-UK intervention data analysis (WP3 and WP4); contributed to the fidelity study; provided technical support to the occupational therapists delivering the occupational therapy intervention throughout the programme; and set up and edited the VALID website. He is now occupational therapist in Herts and Broxbourne Adult Disability Team, Hertfordshire County Council, Stevenage.
Laura Di Bona (https://orcid.org/0000-0002-5659-4368) (Research Associate – Occupational Therapist: School of Health and Related Research, University of Sheffield) contributed to the COTiD-UK development activities (WP1); trained and supervised the occupational therapists who delivered the COTiD-UK intervention; contributed to the qualitative data collection and analysis; and contributed to the implementation activities.
Becky Field (https://orcid.org/0000-0003-3502-2691) (Research Associate – Occupational Therapist/PhD student: School of Health and Related Research, University of Sheffield) contributed to the COTiD-UK development activities (WP1); managed trial recruitment at the Sheffield research site; and contributed to the implementation activities.
Cathryn Hart (https://orcid.org/0000-0003-3582-0685) (Assistant Director, Research & Development: Humber Teaching NHS Foundation Trust, Hull) managed the research team and RCT activities at the Humber site, and contributed to the multisite RCT conduct.
Jacki Stansfeld (https://orcid.org/0000-0002-4491-5523) (Senior Research Assistant: Research & Development Department, North East London NHS Foundation Trust/PhD student: Division of Psychiatry, University College London) contributed to the COTiD-UK development activities (WP1); contributed to the analysis of the online survey of occupational therapy practice (WP2); contributed to the RCT activities, including training research staff at other sites. She is now the RADAR (Research into Antipsychotic Discontinuation and Reduction) Programme Manager at North East London NHS Foundation Trust.
Holly Walton (https://orcid.org/0000-0002-8746-059X) (PhD student: Department of Clinical, Educational and Health Psychology, University College London) conducted the fidelity study. She is now research fellow in the Department of Applied Health Research, University College London.
Sally Rooks (https://orcid.org/0000-0002-5460-0146) (Clinical Lead Occupational Therapist: North East London NHS Foundation Trust), as a co-applicant, contributed to the design and methodology of the research programme, was a PMG member and chaired the independent OTRG. She contributed to the COTiD-UK development activities (WP1); the design, conduct and analysis of the online survey of occupational therapy practice (WP2); and the RCT trial conduct and occupational therapist qualitative data analysis.
Ritchard Ledgerd (https://orcid.org/0000-0001-5646-577X) (Dementia Clinical Lead: Research & Development Department, North East London NHS Foundation Trust) contributed to the COTiD-UK development activities (WP1); and contributed to the design, conduct and analysis of the online survey of occupational therapy practice (WP2).
Martin Orrell (https://orcid.org/0000-0002-1169-3530) (Director, Institute of Mental Health/Head, Division of Psychiatry and Applied Psychology, Faculty of Medicine & Health Sciences, University of Nottingham), as the lead applicant/chief investigator, supervised the design and methodology of all stages of the research programme, and chaired the PMG. He contributed to the development of COTiD-UK (WP1); supervised the design and analysis of the online survey of occupational therapy practice (WP2); chaired the TMG (WP3 and WP4); oversaw the revision of the implementation WP; contributed to programme dissemination in terms of publications and conference presentations; and oversaw the writing of the final report.
All authors contributed to dissemination of the programme. All authors provided a critical review and final approval of the report.
Publications
Burgess J, Wenborn J, Di Bona L, Orrell M, Poland F. Taking part in the community occupational therapy in dementia UK intervention from the perspective of people with dementia, family carers and occupational therapists: a qualitative study. Dementia (London) 2021;20:2057–76. https://doi.org/10.1177/1471301220981240
Di Bona L, Wenborn J, Field B, Hynes SM, Ledgerd R, Mountain G, Swinson T. Enablers and challenges to occupational therapists’ research engagement: a qualitative study. Br J Occup Ther 2017;80:642–50. https://doi.org/10.1177/0308022617719218
Field B, Mountain G, Burgess J, Di Bona L, Kelleher D, Mundy J, Wenborn J. Recruiting hard to reach populations to studies: breaking the silence: an example from a study that recruited people with dementia. BMJ Open 2019;9:e030829.
Hynes SM, Field B, Ledgerd R, Swinson T, Wenborn J, di Bona L, et al. Exploring the need for a new UK occupational therapy intervention for people with dementia and family carers: Community Occupational Therapy in Dementia (COTiD). A focus group study. Aging Ment Health 2016;20:762–9. https://doi.org/10.1080/13607863.2015.1037243
Mundy J, Stansfeld J, Orrell M, Cartwright M, Wenborn J. Reasons for nonparticipation in the Valuing Active Life in Dementia randomised controlled trial of a dyadic occupational therapy intervention: an interview study. SAGE Open Med 2020;8:1–12. https://doi.org/10.1177/2050312120958926
Pizzo E, Wenborn J, Burgess J, Mundy J, Orrell M, King M, Omar R, Morris S. Cost-utility analysis of community occupational therapy in dementia (COTiD-UK) versus usual care: results from VALID, a multi-site randomised controlled trial in the UK. PLOS ONE 2022;17:e0262828.
Swinson T, Wenborn J, Hynes S, Orrell M, Stansfeld J, Rooks S, et al. Community Occupational Therapy for People with Dementia and their family carers: a national survey of current occupational therapy practice. Br J Occup Ther 2016;79:85–91.
Walton H, Tombor I, Burgess J, Groake H, Swinson T, Wenborn J, et al. Measuring fidelity of delivery of the Community Occupational Therapy in Dementia-UK intervention. BMC Geriatrics 2019;19:364.
Wenborn J, Hynes S, Moniz-Cook E, Mountain G, Poland F, King M, et al. Community Occupational Therapy for people with dementia and family carers (COTiD-UK) versus treatment as usual (Valuing Active Life in Dementia [VALID] study): study protocol for a randomised controlled trial. Trials 2016;17:65.
Wenborn J, O’Keeffe AG, Mountain G, Moniz-Cook E, King M, et al. Community Occupational Therapy for people with dementia and family carers (COTiD-UK) versus treatment as usual (Valuing Active Life in Dementia [VALID]) study: a single-blind, randomised controlled trial. PLOS Med 2021;18:e1003433.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PGfAR programme or the Department of Health and Social Care.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
References
Glossary
- Community Occupational Therapy in Dementia – the UK version
- The adapted UK version of Community Occupational Therapy in Dementia comprising 10 hours delivered over approximately 10 weeks by an occupational therapist to the person with dementia and their family carer at home and in their local neighbourhood.
- Community Occupational Therapy in Dementia
- The original Dutch version of a programme of occupational therapy for people with dementia comprising 10 1-hour sessions delivered over 5 weeks by an occupational therapist to the person with dementia and their family carer at home.
- Dyad
- A person with mild to moderate dementia and their family carer/supporter recruited to take part in the research. See also pair.
- Excess treatment costs
- The difference between the cost of providing the existing standard treatment or intervention and the cost of the treatment/intervention being evaluated within the research trial. Service commissioners are responsible for paying excess treatment costs because they are not covered by research grant funding, and it should be noted that the process of claiming excess treatment costs changed during the course of this study.
- Intracluster correlation coefficient
- A measure of the correlation between observations within the same cluster. In this study, it refers to the correlation of the Bristol Activities of Daily Living Scale total scores for dyads/pairs who received Community Occupational Therapy in Dementia – UK version from the same occupational therapist.
- Pair
- A person with mild to moderate dementia and their family carer/supporter recruited to take part in the research together. See also dyad.
- Treatment as usual
- In this study, treatment as usual refers to the service(s) usually provided within the research recruitment site locality, and may or may not include standard occupational therapy.
List of abbreviations
- ACCEPT
- Acceptance Checklist for Clinical Effectiveness Pilot Trials
- ADL
- activities of daily living
- AMPs
- Assessment of Motor and Process Skills
- BADLS
- Bristol Activities of Daily Living Scale
- BCW
- Behaviour Change Wheel
- CI
- confidence interval
- COM-B
- Capability, Opportunity, Motivation – hub of the Behaviour Change Wheel
- COTiD
- Community Occupational Therapy in Dementia
- COTiD-UK
- Community Occupational Therapy in Dementia – the UK version
- CRN
- Clinical Research Network
- CSRI
- Client Service Receipt Inventory
- DEMQOL
- Dementia Quality of Life
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- HADS
- Hospital Anxiety and Depression Scale
- HRQoL
- health-related quality of life
- ICC
- intracluster correlation coefficient
- INMB
- incremental net monetary benefit
- IT
- information technology
- NELFT
- North East London NHS Foundation Trust
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- OTRG
- Occupational Therapy Reference Group
- PMG
- Programme Management Group
- PPI
- patient and public involvement
- PSC
- Programme Steering Committee
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SOP
- standard operating procedure
- TAU
- treatment as usual
- TDF
- Theoretical Domains Framework
- TMG
- Trial Management Group
- TMT
- Trial Management Team
- UCL
- University College London
- VALID
- Valuing Active Life in Dementia
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/RGTJ7429).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
