Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 15/126/11. The contractual start date was in January 2018. The final report began editorial review in June 2020 and was accepted for publication in December 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Coulman et al. This work was produced by Coulman et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Coulman et al.
Chapter 1 Background
Background to the research
Intellectual disability (often referred to as learning disability in UK health settings) is described in International Classification of Diseases, Eleventh Revision, as a disorder of intellectual development. 1 Consistent with contemporary definitions, intellectual disability emerges during the ‘developmental period’ (usually taken to mean before age 18 years) and is characterised by low cognitive ability (i.e. an intelligence quotient of < 70) and low levels of adaptive behaviour (such as communication, and social and independence skills, assessed using standardised tools). Prevalence studies internationally suggest that approximately 2–3% of children and adolescents have an intellectual disability. 2 Based on Department for Education data published from the National Pupil Database (NPD), there are approximately 300,000 children of school age with an intellectual disability in England. 3 Data from the Global Burden of Disease Study suggest that approximately 1.43% of children aged < 5 years in the UK have an intellectual disability. 4
Owing to challenges in intelligence quotient testing in younger children, especially for disabled children, the term global developmental delay is often used to refer to children who, when older than 5 years of age, are likely to attract a label of intellectual disability. 5 Global developmental delay is defined in terms of a delay in two or more developmental domains (from among the following five) in children aged < 5 years: (1) gross and/or fine motor skills, (2) speech and language, (3) cognition, (4) social and personal skills, and (5) daily living skills or activities. 5 Children with intellectual disability/global developmental delay may also have other diagnoses, including Down syndrome, other genetic syndromes (e.g. fragile X syndrome, Rett syndrome, Cornelia de Lange syndrome) or autism. For example, in the UK, children with an intellectual disability may be 33 times more likely than children without an intellectual disability to meet diagnostic criteria for autism. 6
Young children with an intellectual disability face, by definition, cognitive, learning, social and everyday living challenges. These children also experience a range of other social, health and educational inequalities. 7 For example, at aged 3 years, children with intellectual disability have lower levels of prosocial behaviours and higher levels of both internalising and externalising problems than children without intellectual disability, and these disparities generally increase throughout early and middle childhood. 8 In the physical health domain, children with intellectual disability are up to 70% more likely to be obese, which in turn increases the long-term risk of obesity-related health problems. 9 Children with an intellectual disability and their families are also more likely to be exposed to multiple social and economic risks, including poverty and negative life events. 6
Parents of children with intellectual disability also often have elevated levels of stress, mental and physical health problems themselves. Meta-analyses and results from higher-quality research designs (such as population-based national samples) have suggested, for example, that mothers of children with intellectual disability are about 1.5 times more likely than other mothers to experience depression10 and, similarly, 1.4 times more likely than other mothers to have high levels of psychological symptoms indicative of mental health problems. 11 Data from the UK Millennium Cohort Study (a population-representative birth cohort) also show that fathers of young children with intellectual disability are twice as likely to score above the cut-off point on a psychiatric disorder screen when compared with fathers of other young children. 12 The day-to-day burden of care for a child with intellectual disability is also high even when compared with other carers (e.g. dementia family carers). 13 Longitudinal research further suggests that the severity of the needs of children with intellectual disability can be associated with the well-being of their family members, especially parents. In particular, increased behavioural and emotional problems in children with intellectual disabilities also leads to deterioration in parental well-being over time, and typically vice versa. 14
Despite significant needs, access to supports and services for families of children with intellectual disability is fraught with negative experiences and is often described as ‘battling’ against the system. 15 Access to services and professionals is also limited. For example, < 30% of parents of children with an intellectual disability who also had a diagnosable mental health problem had access to mental health services in the preceding 12 months. 16 Therefore, children with intellectual disability and their parents face significant health inequalities and potential problems with accessing appropriate support.
Moving beyond parents’ well-being, there is also intellectual disability family research that applies family systems theory to examine putative effects on other family members and on family subsystems. 17,18 Siblings of children with an intellectual disability, for example, may be at a small, but elevated, risk for behavioural and emotional problems compared with other children who do not have a brother or sister with intellectual disability. 19 In addition, parental relationship problems, parent–child relationships, sibling relationships and overall family functioning may all be adversely affected in families of children with an intellectual disability. 14
Given this research evidence, interventions and supports are needed that target both parental or family well-being and developmental outcomes for the child with intellectual disability. Developmental challenges for children with an intellectual disability, and inequalities affecting their families, emerge early in life (certainly by ages 3–5 years), and so early intervention and support is important as both an individual family and larger policy priority. 20 In addition to parental well-being, what parents do with their child with intellectual disability and the relationships they build with them have been shown to be crucial for the development of children with intellectual disability (as they are for all children). The parent–child relationship quality at age 3 years, for example, predicted behaviour problems when children with intellectual disability were aged 5 years. 21 Negative dimensions of parenting in the early years period (i.e. aged 3–5 years) also mediated the effects of maternal well-being on the behaviour problems of children with an intellectual disability at aged 7 and 11 years. 22 Therefore, interventions that also target parenting practices/strategies and parent–child relationships could have significant potential to support families of young children with intellectual disability.
Rationale for the current study
The existing evidence base for early family/parent-based interventions for families of children with intellectual disability is significantly limited. There is some evidence relating to early intervention approaches that focus only on teaching new or extended skills to children with intellectual disability (e.g. Eldevik et al. 23), without any additional support for family members. 23 Similarly, there are some potentially effective intervention strategies from a psychological therapy perspective (such as cognitive–behavioural therapy and, more recently, mindfulness-based approaches) to reduce parental psychological distress in families of children with intellectual disabilities, where the interventions do not also focus on child outcomes. 24,25 Psychoeducation interventions may also be used in UK services, typically addressing one or more of three components: (1) information about disability, (2) information about services and supports available to families and (3) potentially a brief psychoeducational perspective on well-being. 26 Although such psychoeducation interventions have been evaluated with parents of pre-school children,27 parents of adolescents approaching transition28 and with parents of adults,29 the evaluations are small in size and rarely use randomised controlled trial (RCT) designs. 26 Other psychoeducation programmes have had a focus on services and improving access to services only,30 including by increasing parents’ confidence to access services. 31
Parenting interventions, which can focus on both child and parental outcomes, have recently been systematically reviewed by the National Institute for Health and Care Excellence (NICE) to inform the Mental Health Problems in People with Learning Disabilities: Prevention, Assessment, and Management clinical guideline. 32 The NICE guidance reviewed 15 RCTs of parenting programmes that involved parents of children with intellectual disability. These programmes were not developed for parents of children with intellectual disability [but were adapted from mainstream parenting programmes, e.g. Stepping Stones Triple P33 (Triple P International Pty Ltd, Brisbane, QLD, Australia)] and the programmes were not targeted at families of young children with intellectual disability. The single exception with an early intervention focus was a RCT of an individual family-delivered positive behavioural support intervention for young children with intellectual disability and severe behaviour problems. The RCT compared the intervention alone to a version that included a parent optimism component. 34 The parenting programmes reviewed by NICE also did not explicitly target parent well-being, but focused on a problem related to the child (e.g. behaviour problems). In terms of evidence gaps, NICE found no evidence relating to group parenting programmes designed specifically for parents of young children with intellectual disability, without a specific focus on a problem related to the child and with the explicit aim of improving parent psychosocial well-being. Therefore, there is a gap in both the availability of suitable group parenting programmes as well as an established gap in the evidence base.
A further limitation in the evidence base is the lack of approaches that have involved co-production with families35 or those including family members themselves as partners in supporting other families that have a child with an intellectual disability. This is despite evidence that parents’ lived experience can be beneficial in supports for families of disabled children more generally. For example, a recent systematic qualitative synthesis36 of research in which parents offer peer support to other parents of children with disabilities identified four themes describing the benefits of peer–peer support: (1) shared social contact with other parents, (2) learning from the experiences of other parents, (3) parent supporters gaining self-confidence and expertise, and (4) all participants valuing the opportunity to support others in group contexts. 36
Parenting programmes for families of children with intellectual disability are likely to remain a priority for UK services for several decades. In England, learning (intellectual) disability services across the NHS, local authorities and the for-profit and third sector are undergoing considerable change as a result of the government’s transforming care programme. The service model from the transforming care programme identifies early intervention/early support and support and skills training for parents as a part of a regional/community response to better services for families of children with intellectual disability. 37 In Scotland, parenting interventions are also a priority and are seen as a key way to improve the life chances of disadvantaged groups, including children with intellectual disability. The Scottish Government has proposed a co-ordinated parenting strategy across statutory and third-sector organisations, with partners from the third sector taking a lead in delivering parenting interventions. 38
In response to the identified needs and gaps in the existing evidence base, we previously co-produced (with family carers) the Early Positive Approaches to Support (E-PAtS) programme. The E-PAtS programme is designed as a group parenting programme that is suitable for all families of young children with intellectual disability, and addresses issues for parents and the child that may already be experienced or will be likely to emerge during the course of the child’s development. The E-PAtS programme is a bespoke parenting programme that is specifically informed by intellectual disability research. The programme is co-delivered by a trained family carer facilitator and a professional facilitator across eight group sessions. The primary focus is to enhance parental psychosocial well-being. A detailed description of the E-PAtS programme is provided in Chapter 2 and the logic model is presented in Appendix 1.
Aims and objectives
The aim of the E-PAtS feasibility RCT was to assess the feasibility of delivering the E-PAtS programme to family carers of children with an intellectual disability by community parenting support service provider organisations. The study will contribute to the evidence base on the well-being of families with a young child with intellectual disability. Importantly, the study will inform a potential, definitive RCT of the clinical effectiveness and cost-effectiveness of the E-PAtS programme.
The study primary objectives were to assess the following:
-
the feasibility of recruiting eligible participants to the study and the most effective recruitment pathways to identify families of young children with intellectual disability
-
the feasibility of recruiting suitable intervention providers and facilitators to deliver the E-PAtS intervention
-
recruitment rates and retention through the 3- and 12-month post-randomisation follow-up data collection
-
the acceptability of study processes, including randomisation, to service provider organisations, facilitators and family carers through qualitative interviews
-
the acceptability of intervention delivery to service provider organisations, facilitators and family carers through qualitative interviews
-
adherence to the intervention, reach and fidelity of implementation of the E-PAtS intervention through attendance records, evaluation of session recordings and participant/facilitator qualitative interviews
-
usual practice in this setting and use of services/support by intervention and control participants
-
acceptability of collecting and analysing routinely collected data within a definitive RCT
-
service provider organisation willingness to participate in a definitive trial
-
the feasibility and acceptability of the –
-
proposed primary outcome measure for a definitive trial as methods to measure the effectiveness of the intervention [i.e. the Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS) at 12 months post randomisation]
-
proposed secondary outcome measures for a definitive trial, including resource use and health-related quality of life data, as methods to measure effectiveness of the intervention and to conduct an embedded health economic evaluation within a definitive RCT.
-
Chapter 2 Intervention
The E-PAtS programme
The E-PAtS programme is a group parenting programme for parents/family carers of children with an intellectual disability. The E-PAtS programme has been developed in response to the contexts, research and theoretical assumptions discussed in Chapter 1 to provide timely, effective and sensitive support to families of children with an intellectual disability. The programme aims to bolster family resources and resilience to achieve positive outcomes for parents who attend, as well as for their children and other family members. The components of the intervention (i.e. the six key principles of the E-PAtS programme and the programme materials and curriculums) are described in the E-PAtS logic model (see Appendix 1) alongside the main mechanisms of impact, potential outcomes (used to inform the methods of the current research) and longer-term outcomes that could be examined in a later study.
The E-PAtS programme was developed by Nick Gore, starting in 2011/12, in collaboration with a patient and public involvement (PPI) partner [i.e. the Challenging Behaviour Foundation (CBF) (Chatham, UK)], parents of children with intellectual disability, and intellectual disability professionals and researchers (including research team members Richard Hastings and Jill Bradshaw). The original programme content and rationale for the E-PAtS intervention was informed by the development of a framework that summarised relevant research evidence in the intellectual disability field39 by early intervention theory, especially the developmental systems model,40 and by the principles of co-production, both in designing the programme and also in its delivery (i.e. using a family carer co-facilitator working jointly with a professional).
Development process for the E-PAtS intervention
Key topic areas for inclusion in the E-PAtS intervention curriculum were developed using a workshop model. An initial 1-day workshop was held in January 2013 and involved a total of 17 participants, all of whom had attended prior initial meetings with Nick Gore to discuss the programme development. Workshop participants were a mix of parents and professionals with expertise in the proposed curriculum topic area (e.g. sleep). The task of the initial workshop group was to design 2.5-hour sessions that would serve as an evidenced-based introduction to a topic area, including practical skills or tools that would be needed in the first group that families might attend after a diagnosis or soon after suspicions are first raised about a child’s development. The workshop group were also given context informed by the emerging intervention logic (e.g. the session content should help to prepare families for the future emergence of problems and how to engage with professionals and services to obtain support).
The workshop content was edited, revised and manualised by Nick Gore during 2013. In this period, the original workshop members provided commentary and editorship to multiple editions of the materials that were developed. Feedback to support development of the programme was also gained from a parent/family carer focus group (comprising six additional family carers) via presentation and discussion with several multiprofessional groups (who were additional to the original workshop group) and a series of six in-depth development meetings between Nick Gore and a parent/carer who participated in the first workshop and later became a programme facilitator. The E-PAtS programme was pilot tested three times over the following 4 years, with more than 94 families participating (once led by Nick Gore and a parent facilitator and twice with Nick Gore training new facilitators). Following the second pilot, and a subsequent focus group that comprised programme facilitators, the E-PAtS programme materials and manuals were refined further. Therefore, the programme tested in the current research had been robustly developed and pilot tested prior to this study.
E-PAtS programme content and structure
The E-PAtS programme is fully manualised (comprising a programme manual and a programme implementation manual) and is typically delivered over an 8-week period. The programme is delivered in a group format to up to 12 parents/family carers, representing a maximum of eight families. Two parents/family carers from each family are invited to attend, but typically both family members attend approximately one half of the same sessions. Programme facilitators are typically professionals who are employed by third-sector organisations, but have included a range of health and social care professionals (and could include education professionals). Each programme is also delivered with a parent/family carer co-facilitator employed by the organisation specifically to deliver the E-PAtS programme. Facilitators deliver the programme in pairs (one professional and one parent/family carer facilitator) after completing a 5-day training programme and a period of supervised practice. Supervised practice consists of between two and three supervision meetings with the E-PAtS programme trainer during the first facilitation of a programme.
Facilitators are typically required to have prior experience of supporting children with intellectual disability and/or their families, but are likely to have a variety of professional roles and qualifications. Family carer facilitators are the parent of a child with an intellectual disability. The E-PAtS programme may be delivered in a range of community settings, including child development centres, community centres and church halls. In the current research, host organisations met the costs of programme delivery that relate to the training of facilitators, employment of facilitators, use of facilities and reproduction of materials. All E-PAtS materials, manuals and workbooks (including any future updates or revisions) are provided to trained host organisations for their continued and sole use at no cost.
All participating families attend a programme preparation session/interview with facilitators (undertaken by telephone in the current study) or other professionals from the host organisation (either face to face or by telephone) prior to the delivery of the programme curriculum as a standard part of E-PAtS programme implementation. This session helps prepare parents for the programme, ensures that it fits with their current needs and expectations, and identifies and proactively resolves any barriers regarding attendance and engagement for both parents/family carers from the family who are expecting to attend the groups. Carers also have opportunities throughout the programme to highlight any other factors that facilitators could address to support their engagement in the programme.
The E-PAtS programme comprises eight 2.5-hour group sessions, delivered at times of day determined by the provider according to the needs and preferences of participating families. A summary of E-PAtS programme sessions is provided in Table 1. The first two sessions of the E-PAtS curriculum predominantly focus on the emotional and well-being needs of parents/family carers together with the development of a family system of support. Session 1 provides an introduction to the programme and establishes group processes (see Table 1), before providing advice and strategies to support access to professional services and financial supports for families and their children. The second session focuses on the emotional vulnerabilities and needs of parents/family carers of children with intellectual disability, supports service access in relation to these and empowers parents/family carers to develop self-management and social support systems to reduce these vulnerabilities and needs and build resilience over the long term. Further consideration and support in relation to both building systems of family support and safeguarding the emotional well-being of parents/family carers is also included as a component of each subsequent session, and is further expanded on in the final session of the programme (i.e. session 8), which brings together all learning and supports to allow this to be continually used in the future.
| Session | Content |
|---|---|
| Session 1 | |
| Working together |
|
| Session 2 | |
| Looking after you and your family |
|
| Session 3 | |
| Supporting sleep |
|
| Session 4 | |
| Interaction and communication |
|
| Session 5 | |
| Supporting active development |
|
| Session 6 | |
| Supporting challenges 1 |
|
| Session 7 | |
| Supporting challenges 2 |
|
| Session 8 | |
| Bringing it all together |
|
Sessions 3–7 focus predominantly on supporting parent/family carer knowledge and confidence in responding to child-focused areas of need that are also associated with poor outcomes for parents and families of young children with intellectual disability. Session 3 provides advice and support in relation to sleep. Session 4 provides information to help children acquire effective functional communication and session 5 provides information to help children develop a range of adaptive skills. Sessions 6 and 7 draw on all previous sessions and provide additional curriculum content to help carers prevent and address problem behaviour currently displayed by their child or problem behaviour that they may be at risk of developing in future.
Each programme session is based on best practice developed through co-production with a range of professional experts and family carers. Sessions provide an overview of each area, with theoretical and practical considerations, to empower family carers with knowledge and activate improved patterns of family interaction (following the developmental systems model for early intervention). 40 Each session also includes further resources and signposting to support future advice and professional input for families that require this. The E-PAtS programme is designed as a cohesive programme curriculum rather than a menu of choices, with the expectation that parents/family carers attend the majority of sessions whether or not they or their child has support needs in the topic area. This is based on a premise that families and their children who attend the programme are at increased risk of experiencing complex needs across topic areas at some point in the child’s development, but that this could be reduced through early intervention and proactive support. In addition, it is considered that participating family carers will contribute towards the group process mechanisms, with the potential to support other group members in relation to one or more of the curriculum areas. This group process and mutual support may have potential benefits for both the carer in question and other group members.
Although the E-PAtS programme encourages and aims to facilitate full programme attendance, it is recognised that the complexity of family life for family carers supporting a child with intellectual disability may result in occasional non-attendance. The programme therefore incorporates a range of strategies to support families in such an instance. First, the programme provides a workbook of resources that provides access to important information and prompts development of bespoke strategies for families (relevant sections of which are provided to families even if a session is missed). Second, facilitators aim to accommodate any missed sessions, should these occur, by allocating time for brief catch-up discussions with families at the start or end of a subsequent session. Finally, as previously described, several core curriculum areas (and those associated with carer well-being in particular) run throughout all sessions (rather than being prescribed to a specific session), and so can be accessed by family carers even if an individual session is missed.
All of the E-PAtS curriculum components are delivered via a combination of oral and video presentations, group discussion and in-group exercises. The E-PAtS programme group process aims to create an emotionally and socially supportive setting that encourages engagement and addresses the well-being needs of family carers. First, meeting and working with peers who are experiencing similar challenges and needs, as well as being supported by a facilitator who is also a family carer, provides emotional validation and inspiration to group members. Second, programme facilitators have received training and supervision to develop therapeutic competencies to be used in conjunction with delivery of all curriculum areas. These skills help ensure that the emotional needs of family carers are recognised and responded to sensitively and constructively, and that supportive relationships are fostered between group members.
Presentation of materials and exercises is also designed to support family carer engagement, identify their particular needs and strengths, and empower them to build on these. Prior to delivery of each programme, facilitators are required to make localised adaptions to programme materials (e.g. information provided about current and local financial and service supports). Facilitators are also trained to respond to the specific needs of individual group members during delivery of each session (e.g. citing examples and strategies that are aligned with the presenting needs and circumstances of family carers who are in attendance and their children).
Family carers are given opportunities to rehearse and develop strategies and skills within sessions, but are not assigned tasks to complete between sessions. This is based on the assumption that participants will likely present with a range of different needs and circumstances and are likely to need to develop family support systems and personal resources as a prerequisite to implementing self-management and child-focused strategies at home. Implementation outside of the group setting may be possible for some participants within the time frame of programme delivery, but more typically this is expected to occur following programme completion.
All family carers are provided with a workbook that accompanies the programme. The workbook contains additional materials, tools and signposting to relevant resources in relation to each content area. The workbook is built around a ‘person-centred profile’, detailing the specific support needs for each family’s child. By completing the workbook throughout the programme, families are empowered to create a resource based on their knowledge and experience, combined with evidence-based practices, to inform broader systems of family and child support in the future. The workbook also allows information and learning from the programme to be shared with other family members who are unable to attend sessions directly. This is intended to contribute towards engagement with fathers and other family carers, and the development of a shared and collaborative family approach for supporting children.
In addition to the programme manual (focused on the delivery of each session and the session content and materials), the implementation manual includes practical elements that the provider organisation and facilitators need to deliver the E-PAtS programme. The implementation manual’s content includes role profiles for facilitators, practical suggestions about location set-up and all additional resources required to deliver the programme. There is also a training programme and manual for training facilitators to deliver the programme. The 5 days of training are guided by a manualised curriculum, comprising 1.5 days of teaching in relation to the evidence base, theory and ways of working that underpin the E-PAtS programme; 1.5 days of teaching regarding the programme curriculum for the programme; and 2 days of tutoring practice-based demonstration regarding curriculum delivery, group process and co-production in the delivery of the programme. Facilitators are required to be able to demonstrate necessary skills and understanding of the E-PAtS programme during the final training session prior to implementation, and receive two or three supervision sessions from the trainer (in addition to any supervision with the host organisation) during their first delivery of the programme. To date, all training has been provided by Nick Gore and/or Jill Bradshaw, but work is under way with regard to a ‘train-the-trainers’ programme training.
E-PAtS programme adherence
An initial definition of adherence to the E-PAtS intervention was focused on attending a total of five out of the eight sessions, but specified a pattern of attendance at the level of an individual family carer (i.e. one from the first two sessions, three of sessions 3–7 and the final session 8). During the course of the research, this definition was revised in two main ways: (1) to reflect that adherence was better described at the level of the family (in keeping with assumptions in the logic model) and (2) to simplify the definition to count any five sessions attended from the eight as representing adherence. This revised definition is used in the results and is discussed in Chapter 6.
Chapter 3 Methods
Design
The study was a two-arm cluster (family carers in families) RCT with 1 : 1 randomisation using randomly permuted blocks, stratified by study site and choice of either study pathway. Primary participants selected one of two study pathways if they were randomised to the control arm: (1) pathway A families were offered the E-PAtS programme subsequent to the 12-month follow-up and (2) pathway B families were not offered the E-PAtS programme. Participants were recruited, asked to select study pathway A or B, and then randomised. Intervention participants were offered the E-PAtS programme immediately and all participants continued to have access to the usual support and advice services provided. The feasibility of using a range of established outcome measures proposed to test the intervention in a main trial was assessed. This study was not designed to test effectiveness. The acceptability of proposed outcome measures will inform the selection of outcome measures for a definitive trial.
Setting
The study was designed to take place in up to four study sites, defined as geographical areas where service provider organisations offer support services to parents.
Ethics
Ethics approval for this study was given by the University of Warwick Humanities and Social Sciences Research Ethics Committee on 14 December 2017 (reference number 30/17-18).
Usual practice
The comparator intervention was usual practice, with an optional waiting list for the E-PAtS programme. Usual practice includes any service (mainstream and specialised) provided to families and their children with intellectual disability as a part of an Education Health and Care Plan (or equivalent outside England) or via any other mechanism. Children with intellectual disability and their families could receive a wide variety of care and support from health, social and education sectors and the third sector, depending on their needs. Usual practice may vary by function (e.g. parent support, intervention for the child) and/or by the main recipient (e.g. the parent, the child with intellectual disability, the whole family). Usual practice may include parenting support or psychological therapy for psychosocial health, but we did not recruit primary family carers who were already receiving a recognisable parenting programme intervention or a psychological therapy for mental health problems at the time of baseline assessments (see Exclusion criteria). Participants were not asked to refrain from attending other interventions or therapies during the study. Usual practice was recorded through service use data. In addition, a question was included in an online UK survey of parents of young children with intellectual disability (n = 673), carried out by the research team at the University of Warwick (Coventry, UK), to record parents’ recent use of early years and early intervention services. These data enabled us to generally assess families’ level of access to interventions and describe the difference in content, delivery and value between usual practice and the E-PAtS programme. Usual-practice data will inform a later definitive trial and other future research.
Feasibility randomised controlled trial
Site selection
Service provider organisations were selected as sites for the E-PAtS feasibility study if they fulfilled the following selection criteria:
-
The site was prepared to refer a sufficient number of potential participants/families to the study team.
-
The site was prepared to deliver up to two E-PAtS courses at two periods throughout the study: (1) immediately following randomisation and (2) following data collection 12 months post randomisation for control participants.
Participant selection
Families were referred to the study team by service provider organisations in their local area following a flexible multipoint recruitment method, including established referral routes, local and national charitable support organisations, local authority services, special schools and nurseries, after school/weekend services for children with special educational needs and disabilities, parent/family support groups, social media, advertising in the media in local areas and self-referral.
The strategy was aimed to be flexible and collaborative. All potential participants confirmed interest in participating in the study either directly with the service provider organisation or by returning a completed reply slip to the study team. Potential participants were contacted by study team researchers to arrange a short screening/recruitment interview.
Participant screening
A screening interview was conducted either by telephone or face to face with a study team research assistant (see Eligibility criteria). Study processes, in particular the screening process, were fully explained and family carers were provided with a participant information sheet and given sufficient time to consider the information. Written consent or verbal consent was obtained in face-to-face or telephone screening interviews, respectively. Screening measures were taken to establish eligibility (see Eligibility criteria), including the Vineland Adaptive Behaviour Scales (VABS)42 and the Brief Family Distress Scale. 43 Scoring of the VABS was conducted following the screening visit by the research assistant and this was quality checked by an additional trained member of the study team. The family carer was informed of their eligibility status and, if applicable, a recruitment interview was arranged.
Eligibility criteria
Clusters were family units with at least one young child with intellectual disability. For each cluster, a main family carer was recruited to the study. Subsequently, a second family carer was recruited to the study, if applicable.
The identified child with intellectual disability had to meet the following criteria.
Inclusion criteria
-
Aged 1.5–5 years (up to the day before the child’s 6th birthday).
-
An administrative label of any severity of intellectual disability (learning disability/ learning difficulties in UK terminology), referring to identification of the child within the education, health or social care systems as having intellectual disability, or as eligible for receipt of specialist intellectual disability services, or diagnoses indicating the presence of intellectual disability for younger children (e.g. ‘global developmental delay’).
-
A VABS44 composite score of < 80 (i.e. allowing for measurement error but still indicating significant developmental delay) at the time of the screening interview.
Exclusion criteria
-
The child is placed in a 24-hour residential placement at baseline.
-
The child is placed in a foster placement that is due to end before the 12-month post-randomisation follow-up data collection point.
-
The child had current child protection concerns identified.
The family unit and participants/family carers had to meet the following criteria.
Inclusion criteria
-
A biological, step, adoptive or foster (if placement was planned to extend to 12 months’ follow-up) parent or adult family carer, including older siblings, grandparents or other family members who live in the family home.
-
Main family carer was available to attend the E-PAtS intervention.
-
Aged ≥ 18 years.
-
Sufficient level of English language ability, enabling (verbal) completion of proposed outcome measures.
Exclusion criteria
-
Enrolled in a group-delivered or individually delivered parenting programme outside the study at baseline (main family carer only).
-
Enrolled in a programme of personal psychological therapeutic support at baseline (given that the E-PAtS programme is focused on family carer well-being).
-
If any family carer in the family had already participated in an E-PAtS intervention.
-
The family was recognised to be in a state of current crisis and unable to cope, indicated by a score of 9 or 10 on the 10-point Brief Family Distress Scale45 (assessed by primary family carer report only). Families in a state of crisis presented with needs that could not be addressed in a proactive programme and required urgent case management. Alternative forms of support were recommended to families in crisis.
Recruitment and consent
A recruitment interview was conducted either by telephone or face to face with a study team research assistant. All study processes were explained in detail, including randomisation and burden for the participant. Written or verbal consent was obtained in face-to-face or telephone interviews, respectively. In addition, the following data collection forms were completed: a participant’s contacts form that included multiple methods of contact (i.e. address, telephone, e-mail address) to minimise loss to follow-up; preferences for follow-up data collection (i.e. face-to-face interview completion, telephone-based completion or postal questionnaires); preferences for choice of study pathway (participants randomised to the control group who choose pathway A were invited to attend the E-PAtS programme at 12 months post randomisation and participants who choose pathway B were invited to an E-PAtS programme course); and a baseline questionnaire, including baseline demographics and proposed outcome measures.
Sample size
A target of 64 families (32 families in the usual-practice arm and 32 families in the intervention arm) were to be recruited to the study. As this was a feasibility study and the purpose was to provide estimates of key parameters for a future trial rather than to have enough power to detect statistically significant differences, a formal a priori power calculation was not conducted. 46 However, recruiting 64 families was to provide a certain level of precision around a 95% confidence interval (CI). For example, this precision is ± 9.8% for a consent rate of 80%, if 64 families are recruited.
Randomisation and masking
The E-PAtS trial is a two-arm, cluster RCT. Clusters were families with a child with intellectual disability and up to two parents/family carers were recruited per family. Families were randomised following recruitment and completion of all baseline measures. Families were randomised using randomly permuted blocks of size four, stratified by study site and choice of study pathway (A or B), with an equal allocation 1 : 1 to E-PAtS in addition to usual practice or usual practice alone. The study manager/data manager, neither of whom were involved in recruitment or data collection, conducted randomisation and informed participants and the service provider organisation of their allocation by telephone. Research assistants at sites responsible for collecting follow-up data and all remaining study team members (including the trial statistician) remained blind to participants’ allocation. At follow-up data collection, participants were asked not to reveal their allocation to the research assistants. However, if the participant’s allocation was revealed it was noted.
Study primary objectives
The following primary objectives were measured and used to inform the decision to progress to a definitive trial:
-
recruitment rates and effectiveness of recruitment pathways
-
study retention rates
-
adherence to the E-PAtS programme
-
fidelity of E-PAtS programme delivery
-
service provider organisation recruitment rates and willingness to participate in feasibility and definitive trial
-
assessment of the barriers and facilitating factors for recruitment, engagement and intervention delivery from the perspective of all stakeholders
-
measurement of usual practice
-
acceptability of collecting and analysing routinely collected data within a definitive trial.
The feasibility of using a range of established outcome measures proposed to test the intervention in a main trial was assessed. This study was not designed to test effectiveness. The acceptability of individual proposed outcome measures (via completion rates, quality of completion and qualitative data) informed the selection of outcome measures for a definitive trial. The proposed outcome measures included those for individual family members, subsystem relationships and overall family functioning. Proposed outcomes were chosen based on outcome areas prompted by the E-PAtS logic model; experience in research with families of young children with intellectual disability, including the total measurement load family carers have been willing to bear; brevity but with good psychometric properties; and potential comparisons with national data sets (e.g. Millennium Cohort Study47) to provide context for the meaning of scores obtained. All proposed outcome measures were administered to family carers. Table 2 shows details and timings of all proposed outcome measures for a definitive trial [Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) figure].
| Time point | Target of outcome | Screening | Study period | ||||
|---|---|---|---|---|---|---|---|
| Baseline (up to 8 weeks prior to randomisation) | Randomisation (up to 5 weeks prior to intervention) | Follow-up | |||||
| 3 months post randomisation | 3–9 months post randomisation | 12 months post randomisation | |||||
| Enrolment | |||||||
| Consent for eligibility | F | ✗ | |||||
| Eligibility screening | F | ✗ | |||||
| VABS42 (full) | C | ✗ | |||||
| Brief Family Distress Scale | F | ✗ | |||||
| Informed consent | F | ✗ | |||||
| Contacts data | F | ||||||
| Randomisation allocation | N/A | ✗ | |||||
| Assessments | |||||||
| Demographic data | F | ||||||
| WEMWBS48 | F | ✗ | ✗ | ✗ | |||
| HADS49 | F | ✗ | ✗ | ✗ | |||
| EQ-5D-5L50 | F | ✗ | ✗ | ✗ | |||
| Brief COPE51 | F | ✗ | ✗ | ✗ | |||
| CBCL52 | C | ✗ | ✗ | ✗ | |||
| Paediatric Quality of Life Inventory™ version 4.0 generic core scales53 | C | ✗ | ✗ | ✗ | |||
| Relationship Happiness Scale47 | F | ✗ | ✗ | ✗ | |||
| Family APGAR Scale54 | F | ✗ | ✗ | ✗ | |||
| Strengths and Difficulties Questionnaire55 | F | ✗ | ✗ | ✗ | |||
| Sibling Relationship Questionnaire (revised) (where relevant)56 | C | ✗ | ✗ | ✗ | |||
| Family Support Scale57 | F | ✗ | ✗ | ✗ | |||
| FMSS58 | F and C | ✗ | ✗ | ✗ | |||
| Parenting Sense of Competence Scale (seven items)59 | F | ✗ | ✗ | ✗ | |||
| Positive Gains Scale60 | F | ✗ | ✗ | ✗ | |||
| Disagreement over issues related to child,47 co-parenting44 | F | ✗ | ✗ | ✗ | |||
| CPRS45 | F and C | ✗ | ✗ | ✗ | |||
| Parent activities/involvement index | F and C | ✗ | ✗ | ✗ | |||
| Group Cohesion Scale (eight items)61 | F | ✗ | |||||
| Client Service Receipt Inventory62 | F and C | ✗ | ✗ | ✗ | |||
| VABS42 (brief) | C | ✗ | |||||
| Participant views on use of routine collected data in future trial | F | ✗ | |||||
| Process evaluation: participant interviews | F | ✗ | |||||
| Process evaluation: facilitator interviews | N/A | ✗ | |||||
| Process evaluation: service provider organisation interviews | N/A | ✗ | |||||
Participants completed the VABS at baseline. A report consisting of the standard report generated by online VABS prefaced by an adapted two-page summary was provided to participants shortly following baseline completion. The two-page summary was designed by the research team, with PPI input provided by the advisory group. It consisted of an adapted description of the VABS, the method of collecting the data, and a description of current and next developmental level and ideas about how the child might be supported to achieve the next level. It also included information on the technical report, emphasising that it might be of use for professionals working with the child and noting that the report compared the child with typically developing children and that there can be many reasons why a child does not score high on a particular item.
Process evaluation
Medical Research Council guidance was used as a framework for the process evaluation to describe implementation processes, review the intervention logic model through examining intervention mechanisms, and consider the role of context in shaping intervention implementation and mechanisms. 63 The process evaluation employed a mixed-methods approach and focused on the study primary objectives. Qualitative interviews with facilitators, service provider organisations and family carers examined implementation processes, intervention mechanisms, the role of contextual factors and interrogate patterns in the quantitative data, as well as informing assessment of the feasibility of implementing the E-PAtS programme within a definitive trial.
Fidelity of intervention delivery was assessed by determining the proportion of key messages and activities that were completed as intended in each session in two ways. The primary measure of fidelity was completion of the E-PAtS programme observation checklist by a trained observer based on video-recorded or audio-recorded sessions delivered in the intervention arm. A separate observation checklist was available for each of the eight E-PAtS programme sessions. Checklists consisted of between 16 and 38 items (with an average of 29 items) that correspond to key activities, discussions and learning points that need to occur in a given session. Observers were required to rate whether or not an item was covered by the facilitator pair. The second measure of fidelity utilised self-completion checklists that are used as a standard part of the E-PAtS programme implementation by facilitators. A separate checklist was available for each of the eight sessions and was available for facilitators to complete after each session. Checklist items cover key activities and discussions (with some, but not complete, correspondence to the observations checklist) and were rated as either having been covered or not having been covered by facilitators.
Statistical methods/analysis plan
The study protocol follows SPIRIT guidelines and the analysis and reporting of this RCT is in accordance with the CONSORT (Consolidated Standards of Reporting Trials) extension for randomised pilot and feasibility trials guidelines. Significance tests are not reported as the E-PAtS feasibility RCT was not powered to test hypotheses. The majority of outcome analyses are descriptive in nature. Continuous data are reported as means and standard deviations (SDs), or medians and interquartile ranges (IQRs), as appropriate. Categorical data are reported as frequencies and proportions. Feasibility outcomes were estimated with their associated 95% CIs. The main preliminary analyses of outcome measures are intention to treat based, accounting for clustering (family carers in families) using multilevel models. Single-carer families are included as a cluster of size one.
The analysis of the proposed primary outcome for a definitive trial examined mean WEMWBS scores between arms at 12 months post randomisation, with baseline WEMWBS scores included as a covariate. The analysis also adjusted for randomisation factors. Remaining potential outcome measures for a definitive trial were analysed similarly, with appropriate multilevel regression models. Results from all regression models are reported using point estimates and 95% CIs. Outcomes were also explored in relation to the definition of adherence to the E-PAtS programme (see Chapter 2 for definition of completion/adherence) and to consider two additional perspectives on family session attendance as additional exploratory analyses:
-
the actual number of sessions attended by a family unit (i.e. at least one family member), with any instances where both family carers attended the same session counting as one and not two
-
the actual number of sessions attended by the main family carer.
Box plots were used to illustrate differences in baseline and 12-month follow-up WEMWBS scores (i.e. the candidate primary outcome measure for a definitive trial) by adherence and session attendance.
Exploratory complier-average causal effect (CACE) analyses were conducted for our main adherence definition and our two measures of session attendance by fitting two-stage least squares instrumental variables regression models. Models included baseline WEMWBS scores and site as covariates, and accounted for the correlated nature of participants within families by including cluster robust standard errors (SEs). The purpose of these analyses was to explore the impact of accounting for adherence and session attendance on the intervention effect estimates, and to test the robustness of these findings to different perspectives associated with adherence. Estimates are reported as adjusted mean differences and associated 95% CIs. For session attendance, model coefficients were multiplied by eight to estimate the maximum efficacy.
Economic evaluation
The overall objective of the health economic component of the E-PAtS feasibility study was to provide early evidence on economic aspects of the E-PAtS programme and an assessment of the best possible ways of expressing the cost-effectiveness of the programme within a larger subsequent trial. This included (1) an early assessment of the economic costs associated with the programme; (2) an assessment of the broader resource use and health-related quality outcomes associated with the programme; (3) identification of appropriate sources of unit costs for potential resource consequences and an assessment of how much primary costing research will be required for the main study; (4) identification of available routine health and social data sources that could be used to complement and validate self-reported resource utilisation data; and (5) an assessment of the best possible way of expressing the cost-effectiveness of the E-PAtS programme using future preference-based approaches.
Economic costs associated with the E-PAtS programme
A focus of the economic evaluation in a future trial is to estimate the cost of delivering the E-PAtS programme in community settings, including the costs of employing the programme facilitators and costs of delivering the group sessions. This information was collected by asking both professional facilitators and family carer facilitators for the E-PAtS programme to complete detailed weekly activity logs, outlining the cost of delivering each E-PAtS session [including costs associated with programme delivery time, indirect administrative activities (e.g. paperwork), planning for groups, telephone calls and E-PAtS programme supervision activities]. The weekly activity logs also recorded the mode, distance and time spent on travelling by each facilitator as part of E-PAtS programme-related activities. The hourly employer costs for the E-PAtS facilitators were obtained from the E-PAtS programme manager and included salaries, employer on-costs and revenue and capital overheads. Travel costs per mile were obtained from the website of HM Revenue and Customs of the UK Government. 64 Additional expenditures, such as refreshments, participant travel and child-care costs associated with the E-PAtS intervention, were valued in accordance with what was recorded in the weekly activity logs.
This information was collected from E-PAtS professional facilitators and family carer facilitators in two of the study sites (this information was collected for sites 1 and 3 only). Detailed weekly activity logs were used, outlining the cost of delivering each E-PAtS session.
Routine data analysis
In response to reviewer comments suggesting linkage to routine data was explored in this feasibility study, we aimed to do the following: (1) map out the relevant data providers, data sets available and associated timescales that could be linked to a future trial population, (2) explore participant acceptance of linking to these data sources, (3) explore the possibility of routine data access for a definitive trail and (4) describe the logistics of linking, transferring and storing data. The decision was made to not consent participants to linkage of data as part of this feasibility study, but to explore the acceptability of consent with current participants at 12 months. It was not intended for the data to be reported as part of the feasibility study outcomes and so data applications were not submitted.
Qualitative methods/analysis plan
Thematic analysis was used to analyse each group of interviews (with providers, facilitators and family carers) separately and independently, followed by qualitative synthesis across all interviews to provide an overarching synthesis of family carers’ experiences and perceptions related to the study objectives. 65 A triangulation exercise was conducted, combining qualitative and quantitative data analysis results.
A full statistical and health economics analysis plan and a qualitative analysis plan were written by the statistician, health economist and qualitative researcher, and approved by the Study Management Group (SMG) and Study Steering Committee (SSC) prior to analysis taking place.
Retention strategy
A number of strategies were used to encourage participant retention:
-
At baseline, participants selected their preferred follow-up method for the 3- and 12-month follow-ups (i.e. post, telephone or face to face). Throughout the study, participants could change their follow-up method at any point by informing the study team.
-
Participant incentives (£10 for each main family carer and £15 for each second family carer) were sent to participants prior to follow-up data collection.
-
A systematic procedure was used to contact participants for each follow-up, ensuring that a minimum of three telephone contacts, plus additional contacts by e-mail or additional telephone numbers provided, were attempted for each participant.
-
For non-responding participants, a minimum data set [consisting of three prioritised outcome measures of WEMWBS, EuroQol-5 Dimensions, five-level version (EQ-5D-5L) and the Parenting Sense of Competence Scale, aligning with the intervention logic model and taking into consideration participant burden] was offered to reduce participant burden and maximise follow-up rates.
Changes to the protocol
There was one amendment of note to the original protocol of the study. The exclusion criteria were updated to state that families would be excluded if they scored 9 or 10 (in crisis and unable to cope) on the 10-point Brief Family Distress Scale. The original exclusion criterion stated that the family were recognised to be in a state of current crisis with a score of ≥ 8. This change followed a SMG meeting where the team considered that families in crisis but able to cope could benefit from attending the E-PAtS groups and should therefore be included in the study. Any family considered at risk at any point in the study would be signposted to appropriate support services.
Chapter 4 Public and participant involvement
Public and participant involvement during this project focused on two main processes. First, a family carer was an independent member of the SSC appointed by the funder. Payment was offered to the family carer SSC member in addition to covering their expenses.
The second PPI process focused on a family carer advisory group that was managed by the PPI partner grant applicant organisation through the CBF. There were nine family carers in total recruited to the advisory group. They were recruited using a mixture of targeted recruitment (i.e. inviting family carers who had already been trained as E-PAtS facilitators, who would have insight into and experience of the intervention) and an open invitation for expressions of interest to the CBF network of families that were unlikely to have experience of the E-PAtS programme but who had relevant life experience (as they had children who might have benefited if the E-PAtS programme had been around when they were younger). Five members of the advisory group (four from Northern Ireland and one from England) were also E-PAtS facilitators, although they were not involved with E-PAtS delivery for this research. Four members of the group (from across England) were family carers with no experience of the E-PAtS programme. Two family carers were fathers and seven were mothers.
Once they had expressed an interest in joining the advisory group, family carers were contacted to arrange an initial telephone call or discussion in person by either the project manager from CBF or the family support manager from the Mencap in Northern Ireland (Belfast, UK). For those with no previous experience of the E-PAtS programme, the initial discussion involved:
-
an overview of the E-PAtS intervention
-
an overview of the feasibility study
-
a summary of the commitment involved in joining the advisory group
-
practical arrangements for the meetings.
For those who had been E-PAtS facilitators and were familiar with the intervention, the initial discussion covered the latter two areas. Family carers were invited to ask questions and share any particular interests they had relevant to the study. Telephone calls were followed up with a written summary of the information prepared by CBF, and carers were offered a subsequent telephone call if they wanted to discuss anything further once they had read the documents. Two family carers took up this offer of a subsequent telephone call. One group member had to step down from the group during the study (because of other demands) and two new members were recruited part-way through the project. Family carers were paid £50 in vouchers for each advisory group meeting, with additional payment for work on e-mail consultations between meetings.
Advisory group meetings were chaired by the PPI co-ordinator and attended by the lead researchers so that they could hear views of family carers and discuss with them directly. Meetings were on two sites – at the CBF offices (Chatham, UK) and the Mencap Children’s Centre (Belfast, UK) – and linked by Skype™ (Microsoft Corporation, Redmond, WA, USA). Family carers unable to attend either site in person were also able to attend using Skype. At the first meeting, carers were asked if the meeting arrangements worked for them. They were also asked if one of them would like to chair the meetings in future. All were happy with the original set-up and preferred to focus on the content rather than chairing the meeting.
The first meeting was on 7 February 2018 and covered:
-
a presentation from the study chief investigators explaining the study (which was also intended to be used in recruitment events for participants)
-
the terms of reference for the group to be discussed, edited and agreed
-
input to the online UK survey that was being carried out to inform an understanding of usual practice
-
the measures proposed to gather service receipt data.
The second meeting planned for May 2019 had to be postponed as material was not ready for discussion by the advisory group in time and some consultation was carried out electronically instead. The second meeting was on 19 September 2019 and focused on the initial findings from the process evaluation. The third and final planned meeting took place using Zoom (Zoom Video Communications, San Jose, CA, USA), due to the COVID-19 pandemic, in June 2020 to discuss materials intended to disseminate study findings to participants and facilitators. We also sought family carers’ views on priorities for dissemination and influencing policy/practice.
Advisory group members were asked to comment on a number of study documents by e-mail. Between two and four family carers responded to each of these requests, with often in-depth comments and suggestions. CBF staff members also commented on these study documents. All were offered the chance to discuss on the telephone with CBF if they wished. Requests for comments on study documents included:
-
comments on recruitment materials (January 2018)
-
comments on the wording of the VABS report (June 2018)
-
comments on sections of the questionnaire (September 2018)
-
comments on topic guides for interviews and the routine data questionnaire (January 2019)
-
comments on the 12-month follow-up questionnaire (May 2019)
-
feedback on the lay summary for the current report (June 2020).
When the May 2019 meeting was postponed, CBF staff requested that Nick Gore record a video, edited and shared by CBF, to update the advisory group members on study progress. Family carer advisors were invited to direct any questions to Nick Gore or to the CBF.
The PPI co-ordinator was a member of the SMG as a full participant and so was also to identify areas where family carer advisory group input may be helpful. Several of the e-mail consultations were agreed as a result of this involvement. The advisory group was a standing item on the SMG agenda and the involvement of the PPI co-ordinator was pivotal to ensuring that PPI was discussed at every meeting, both in terms of how to meaningfully engage the group and how to respond to the feedback from the advisory group. Feedback was also provided to the advisory group about recommendations that they had made and actions taken by the research team (or an explanation as to why a particular piece of advice was not actioned).
Key suggestions and feedback from the advisory group that directly affected the research included the following:
-
recommendations on how to explain the role of the study more effectively as part of the recruitment presentation (a new slide was added as a result)
-
changes to the structure, content and wording of the report on the VABS for parents
-
informing content for the online UK survey to assess usual practice and, in particular, the content and presentation of the service receipt questionnaire
-
informing content of interview topic guides, particularly about how to approach difficult topics with carers
-
clarity and suitability of terminology used in the study (e.g. main and second carer to be used)
-
identification of future research/development questions, such as whether a school-age version of the E-PAtS programme could be developed and how older siblings might be involved in E-PAtS groups
-
informing content for routine data questionnaire.
Routine data questionnaire at the 12-month follow-up
A questionnaire was developed with input from our PPI co-ordinator and the family carer advisory group, and this was one of the most detailed aspects of PPI involvement and advice. The questions aimed to explore the acceptability of linkage to different routine data sources, as well as linkage of their own data compared with their child’s data. An explanatory section at the start of the questionnaire introduced the concept of routine data followed by a number of questions.
Routine data questionnaire development
The questions and explanation for this questionnaire were redrafted twice. First, following feedback from our PPI co-ordinator to make the explanation clearer at the start of the questionnaire and second, following feedback from the advisory group. Feedback was collated from two members of the advisory group and some of the suggestions are shown below. All feedback was used to finalise the questionnaire and the SMG signed off the final version:
Don’t forget, a proportion of people filling out these questionnaires will have a learning disability themselves. Some may struggle with longer words/explanations. In addition to this, parents of children with disabilities usually hate paperwork as we are often inundated with it. The less parents feel they have to fill out, the more amenable they will be.
I think it’s also vital that whoever is presenting this information to the participants is well informed and explains it both in a non-threatening manner and consistently across the participants. Many parents will listen to what they’re being told as opposed to fully digesting the written information.
I think people may have some concern about why their information is needed – for example if someone has had mental health difficulties in the past they may be worried sharing this information could lead to involvement with social services – I know that you say the info is securely held and only used for the specific research project, but I wonder if this needs to be explained further to reassure people that this would not happen?
I particularly like the part about numbers and codes. I think this will reassure people. I also thought the part about having to prove the data is kept secure and not to be used for other purposes would reassure people.
Question 3 – this question may start to scare people off. Social services use the term ‘children’s services’ or ‘children’s social care’ for that reason. There’s a taboo around this area for sure. People don’t like to admit that their child is a CIN [Child in Need]. This is compounded by the fact that children who are under a CPO [Child Protection Order] or who are ‘at risk’ are also under the same umbrella term. Think about using another term or phrase here. Let’s be honest, if your child is a ‘looked after child’ or under CP [Child Protection], you’re hardly going to freely offer access to this information.
Much of the feedback was relevant to this specific patient population, which will be particularly useful for the development of the definitive trial participant information in relation to routine data.
Chapter 5 Results
Both quantitative and qualitative results are discussed in the context of the progression criteria and have been mapped on to the objectives of the study, as detailed in the study protocol. The results are reported in six main sections (Table 3).
| Objective | Results discussed |
|---|---|
| 1. Site and participant characteristics | |
|
|
| 2. The RCT | |
| The feasibility of recruiting eligible participants to the study and the most effective recruitment pathways to identify families of young children with intellectual disability |
|
| Recruitment rates and retention through 3-month and 12-month post-randomisation follow-up data collection |
|
| The acceptability of study processes, including randomisation, to service provider organisations, facilitators and family carers through qualitative interviews |
|
| 3. Piloted outcome measures proposed to test the effectiveness of the intervention in a main trial | |
| The feasibility and acceptability of the proposed outcome measures as methods to measure the effectiveness of the intervention and to conduct an embedded health economic evaluation within a definitive RCT |
|
| 4. Feasibility testing of the intervention | |
| The feasibility of recruiting suitable service provider organisations and facilitators to deliver the E-PAtS intervention |
|
| Adherence to the intervention, reach and fidelity of implementation of the E-PAtS intervention through attendance records, evaluation of session recordings and participant/facilitator qualitative interviews |
|
| The acceptability of intervention delivery to service provider organisations, facilitators and family carers through qualitative interviews |
|
| 5. Usual practice | |
| Usual practice in this setting and use of services/support by intervention and control participants |
|
| 6. Feasibility/recommendations for a future trial | |
| Service provider organisation willingness to participate in a definitive trial |
|
| The feasibility of conducting an embedded health economic analysis in a definitive trial |
|
| Acceptability of collecting and analysing routinely collected data within a definitive RCT |
|
| Progression criteria | |
Site and participant characteristics
Site/service provider organisations characteristics
Three sites were involved in the study to support recruitment of participants and deliver the E-PAtS intervention. Two sites were part of one service provider organisation, Mencap Northern Ireland, and one site was part of a second service provider organisation, an independent local Mencap group in England. The service provider organisations are third-sector organisations that support people with intellectual disabilities in an area of London and in Northern Ireland. Prior working relationships existed with two of the sites (Belfast and Derry) that supported recruitment to the study. The other site (Barnet) was recruited specifically for this study, with support from the Royal Mencap Society (London, UK). Two sites were characterised by urban contexts and one site was characterised by a mixture of urban and more rural contexts.
Belfast
Mencap Northern Ireland’s family support service has been running for 3.5 years. The focus of the work is to support families with children aged 0–7 years with intellectual disability, developmental delay and/or autism. The majority of the work with families takes place at the Mencap Children’s Centre in Belfast, where families can access a variety of supports. Prior to the current study, the E-PAtS programme had been delivered in Belfast on six occasions. A family support manager employed by Mencap Northern Ireland was available to support intervention implementation and research.
Barnet
Barnet Mencap (London, UK) provides a range of services and runs campaigns alongside people with intellectual disability, and people with autism and their families to secure good services and support in the borough. This includes provision of parenting programmes to families of children with intellectual disability. Barnet Mencap took part in piloting an early version of the E-PAtS programme, but had not otherwise delivered the programme (in its current form) prior to taking part in the study. A small degree of managerial support was available to support intervention implementation and research activities.
Derry
Family support services by Mencap Northern Ireland are also provided in Derry, largely with a community-based focus (and without a specific centre, as there is in Belfast). A family support worker operates within a wide range of local community, voluntary and statutory organisations to build links with relevant families. Prior to the current study, the E-PAtS programme had been delivered in Derry on one occasion. Support for the intervention implementation and research activities was available through the same manager employed by Mencap Northern Ireland, as in Belfast, and a manager based at Derry.
Participant characteristics
In total, 95 participants were recruited to the E-PAtS study. Table 4 details the characteristics of the study participants, which were broadly balanced between the control and intervention arms. The majority of participants were biological mothers (n = 65, 68%). Biological mothers accounted for 88% of main carers (n = 65). Of the 21 second carers, 86% were biological fathers (n = 18). Only four participants reported that their child with intellectual disability lived with them on a part-time basis. Overall, around three-quarters of participants classified themselves as being either white British or white Irish (n = 50). Twenty-three participants (41%) were educated to degree level or above. This compares with 27% of the UK population, according to the 2011 census. Overall, 45% of participants reported being employed or self-employed (n = 43), with 46% of main carers looking after the home and family (n = 34). Twelve participants (13%) were finding things difficult financially, with a further 25% ‘just about getting by’ (n = 24). There were some slight differences between arms in the financial question categories. For example, 11 intervention participants said that they could raise £2000 in a week for an emergency ‘easily’ and nine reported that they were ‘living comfortably’. This compares with three and two participants in the control group, respectively. By combining categories to avoid smaller numbers, however, 36% of both intervention and control participants said they could raise £2000 in a week (n = 34). The majority of participants considered themselves as being in ‘good’ or ‘very good’ health (n = 72, 76%).
| Characteristic | Main family carer | Second family carer | ||
|---|---|---|---|---|
| Control (N = 37), n (%) | Intervention (N = 37), n (%) | Control (N = 10), n (%) | Intervention (N = 11), n (%) | |
| Relationship to child | ||||
| Biological mother | 30 (81) | 35 (95) | 0 (0) | 0 (0) |
| Biological father | 4 (11) | 0 (0) | 9 (90) | 9 (82) |
| Adoptive mother | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
| Adoptive father | 0 (0) | 0 (0) | 1 (10) | 0 (0) |
| Foster mother | 0 (0) | 2 (5) | 0 (0) | 0 (0) |
| Grandmother | 0 (0) | 0 (0) | 0 (0) | 2 (18) |
| Missing | 2 (5) | 0 (0) | 0 (0) | 0 (0) |
| Living arrangements | ||||
| Child lives with family full time | 35 (95) | 34 (92) | 10 (100) | 7 (64) |
| Child lives with family part time | 0 (0) | 1 (3) | 0 (0) | 3 (27) |
| Missing | 2 (5) | 2 (5) | 0 (0) | 1 (9) |
| Ethnicity | ||||
| Black/African/black British: African | 2 (5) | 4 (11) | 0 (0) | 1 (9) |
| Black/African/black British: Caribbean | 0 (0) | 2 (5) | 0 (0) | 0 (0) |
| Black: other | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
| Mixed: other | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| Ethnic: other | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
| White: English/Welsh/Scottish/Northern Irish/British | 20 (54) | 17 (46) | 7 (70) | 6 (55) |
| White: Irish | 6 (16) | 8 (22) | 2 (20) | 4 (36) |
| White: other | 4 (11) | 1 (3) | 1 (10) | 0 (0) |
| Any other ethnic background | 1 (3) | 1 (3) | 0 (0) | 0 (0) |
| Prefer not to say | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| Missing | 2 (5) | 2 (5) | 0 (0) | 0 (0) |
| Qualifications | ||||
| No qualifications | 2 (5) | 0 (0) | 0 (0) | 1 (9) |
| Some GCSEs passes or equivalent | 5 (14) | 5 (14) | 2 (20) | 3 (27) |
| Five or more GCSEs at A*–C or equivalent | 3 (8) | 4 (11) | 1 (10) | 1 (9) |
| Five A/AS Levels or equivalent | 0 (0) | 2 (5) | 0 (0) | 0 (0) |
| Higher education but below degree level | 10 (27) | 7 (19) | 2 (20) | 2 (18) |
| Degree (e.g. BA, BSc, MA) | 14 (38) | 17 (46) | 5 (50) | 3 (27) |
| Do not know | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 2 (5) | 2 (5) | 0 (0) | 1 (9) |
| Employment | ||||
| In a job and currently working for an employer | 9 (24) | 14 (38) | 8 (80) | 5 (45) |
| On maternity/paternity/parental leave | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
| Self-employed | 1 (3) | 2 (5) | 1 (10) | 3 (27) |
| Full-time student | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
| Doing voluntary work | 0 (0) | 0 (0) | 1 (10) | 0 (0) |
| Looking after home and family | 17 (46) | 17 (46) | 0 (0) | 1 (9) |
| Unemployed | 3 (8) | 0 (0) | 0 (0) | 0 (0) |
| Do something else | 3 (8) | 2 (5) | 0 (0) | 1 (9) |
| Missing | 2 (5) | 2 (5) | 0 (0) | 1 (9) |
| Financial situation: total weekly household income | ||||
| ≤ £200 | 2 (5) | 5 (14) | 0 (0) | 2 (18) |
| Between £201 and £300 | 7 (19) | 4 (11) | 1 (10) | 0 (0) |
| Between £301 and £400 | 8 (22) | 6 (16) | 2 (20) | 1 (9) |
| Between £401 and £500 | 6 (16) | 3 (8) | 1 (10) | 1 (9) |
| Between £501 and £600 | 4 (11) | 6 (16) | 1 (10) | 2 (18) |
| Between £601 and £700 | 3 (8) | 4 (11) | 3 (30) | 1 (9) |
| Between £701 and £800 | 1 (3) | 2 (5) | 1 (10) | 1 (9) |
| Between £801 and £900 | 1 (3) | 2 (5) | 0 (0) | 2 (18) |
| Between £901 and £1000 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| > £1000 | 3 (8) | 2 (5) | 1 (10) | 1 (9) |
| Missing | 2 (5) | 3 (8) | 0 (0) | 0 (0) |
| Financial situation: how are you managing financially? | ||||
| Living comfortably | 2 (5) | 5 (14) | 0 (0) | 4 (36) |
| Doing all right | 16 (43) | 14 (38) | 5 (50) | 5 (45) |
| Just about getting by | 13 (35) | 8 (22) | 3 (30) | 0 (0) |
| Finding it quite difficult | 3 (8) | 2 (5) | 1 (10) | 1 (9) |
| Finding it very difficult | 1 (3) | 3 (8) | 1 (10) | 0 (0) |
| Missing | 2 (5) | 5 (14) | 0 (0) | 1 (9) |
| Financial situation: could you raise £2000 in a week for an emergency? | ||||
| I could easily raise the money | 3 (8) | 7 (19) | 0 (0) | 4 (36) |
| I could, but it would involve some sacrifices | 9 (24) | 4 (11) | 5 (50) | 2 (18) |
| I would have to do something drastic | 7 (19) | 5 (14) | 1 (10) | 1 (9) |
| I do not think I could raise the money | 14 (38) | 17 (46) | 4 (40) | 4 (36) |
| Missing | 4 (11) | 4 (11) | 0 (0) | 0 (0) |
| Health | ||||
| Very good | 14 (38) | 14 (38) | 2 (20) | 6 (55) |
| Good | 13 (35) | 16 (43) | 6 (60) | 1 (9) |
| Fair | 7 (19) | 5 (14) | 2 (20) | 2 (18) |
| Bad | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Very bad | 1 (3) | 0 (0) | 0 (0) | 1 (9) |
| Missing | 2 (5) | 2 (5) | 0 (0) | 1 (9) |
| Longstanding illness, disability or infirmity | ||||
| No | 28 (76) | 27 (73) | 7 (70) | 8 (72) |
| Yes | 7 (19) | 8 (22) | 3 (30) | 3 (27) |
| Missing | 2 (5) | 2 (5) | 0 (0) | 0 (0) |
As can be seen from Table 5, a higher proportion of the children with intellectual disability were boys (as reported by the main family carer). Of those children attending a school or nursery, 60% were in a specialist provision setting (n = 27). Of those who provided answers to the questions (n = 5 were missing), one-quarter reported that their child had a visual impairment (n = 17) and 14% reported that their child had a hearing impairment (n = 10). Around half of participants reported that their child had no physical health problems (n = 39). Sixty per cent of the children with intellectual disability had a sibling aged between 4 and 16 years (n = 47). The characteristics of the children were reasonably balanced between the two trial arms. For further information on participant and child characteristics see Appendices 2 and 3.
| Characteristic | Reported by main family carer, n (%) | |
|---|---|---|
| Control (N = 37) | Intervention (N = 37) | |
| Gender of child | ||
| Male | 23 (62) | 27 (73) |
| Female | 12 (32) | 10 (27) |
| Missing | 2 (5) | 0 (0) |
| School/nursery attendance | ||
| Not in school/nursery | 10 (27) | 14 (38) |
| Mainstream preschool/nursery | 9 (24) | 5 (14) |
| SRB in mainstream preschool/nursery | 4 (11) | 3 (8) |
| Mainstream school | 1 (3) | 3 (8) |
| Special school | 2 (5) | 1 (3) |
| Special preschool/nursery | 8 (22) | 9 (24) |
| Missing | 3 (8) | 2 (5) |
| Visual impairment | ||
| No | 26 (70) | 26 (70) |
| Yes | 9 (24) | 8 (22) |
| Missing | 2 (5) | 3 (8) |
| Hearing impairment | ||
| No | 29 (78) | 30 (81) |
| Yes | 6 (16) | 4 (11) |
| Missing | 2 (5) | 3 (8) |
| Physical health problems | ||
| No | 19 (51) | 20 (54) |
| Yes | 16 (43) | 13 (35) |
| Missing | 2 (5) | 4 (11) |
| Sibling aged 4–16 years | ||
| No | 10 (27) | 14 (38) |
| Yes | 25 (68) | 22 (59) |
| Missing | 2 (5) | 1 (3) |
Qualitative interview sample
Qualitative interviews were performed with participants, facilitators and service provider organisation staff. For participants, interviews were purposively sampled based on site, randomisation allocation, family carer status (main vs. second family carers) and intervention attendance levels (Table 6). All Facilitators and service provider organisations were invited to interview (Table 7).
| Protocol category | Interviews completed (n) | |||
|---|---|---|---|---|
| Site 1 | Site 2 | Site 3 | Total | |
| A: up to 10 main family carers from families receiving the E-PAtS intervention | 5 | 5 | 2 | 12 |
| B: up to 10 second family carers from families receiving the E-PAtS intervention | ||||
| 1: second family carers who took part in the E-PAtS programme themselves | 2 | 0 | 0 | 2 |
| 2: second family carers who did not attend group sessions, but the main family carer did | 1 | 0 | 0 | 1 |
| C: up to 10 family carers randomised to the intervention arm, but who either did not attend the intervention or dropped out after one or two sessions | 1 | 1 | 1 | 3 |
| D: up to 10 family carers randomised to the usual-practice arm of the feasibility trial | ||||
| 1: main family carers in control group who took part in the study | 4 | 6 | 0 | 10 |
| 2: second family carers in control group who took part in the study | 1 | 1 | 0 | 2 |
| 3: second family carers in control group who did not take part in the study | 0 | 0 | 0 | 0 |
| Site | Interviews completed (n) | |
|---|---|---|
| Facilitator | Service providers | |
| Site 1 | 3 | 1 |
| Site 2 | 4 | 1 |
| Site 3 | 1 | Same as site 1 |
| Total | 8 | 2 |
The randomised controlled trial
Objective: the feasibility of recruiting eligible participants to the study and the most effective recruitment pathways to identify families of young children with intellectual disability
The feasibility of recruiting eligible participants to the E-PAtS study was assessed by reporting the most effective method of identifying potentially eligible families (quantitatively and qualitatively) and the acceptability of recruitment strategies (qualitatively).
Method of family recruitment
Participants were referred to the study team either directly or indirectly by service provider organisations (Mencap Northern Ireland and Barnet Mencap, referred to hereafter as Mencap) that were instructed to use a multipoint recruitment strategy, including established referral routes, local and national charitable support organisations, local authority services, special schools and nurseries, after school/weekend services for children with special educational needs and disabilities, parent/family support groups, social media, advertising in the media in local areas and self-referral (Table 8).
| Site | Method of referral, n of families (%) | ||
|---|---|---|---|
| Indirect referral (advertising, word of mouth, etc.) | Directly by Mencap | Directly from Mencap-arranged parent sessions | |
| Site 1 | 8 (12.7) | 32 (50.8) | 23 (36.5) |
| Site 2a | 3 (4.4) | 65 (95.6) | 0 (0) |
| Site 3 | 0 (0) | 17 (89.5) | 2 (10.5) |
| Total | 11 (7.3) | 114 (76.0) | 25 (16.7) |
The majority (92.7%) of families were referred directly by Mencap, either through referrals or parent sessions arranged by Mencap. In sites 2 and 3, the majority of families were referred directly through referrals. In site 1, however, the parent sessions were a successful referral route. Only 7.3% of families were referred indirectly through advertising, word of mouth, etc. Most participants were described in qualitative interviews as being recruited through Mencap, either directly or at a parent session. Some participants stated that they were recruited by social media or word of mouth:
So I first heard about it from Mencap because they support us and so I was told about it and I was told about the information.
We were at a Mencap support group, kind of meeting and they mentioned it and they just thought that we would be good for it.
I think it was on the Mencap Facebook [Facebook, Inc., Menlo Park, CA, USA] page they had advertised it and then a few parents then had said ‘we are going to it’. So it was through word of mouth then that I sort of registered interest and came along.
Mencap was asked to complete logs for all potentially eligible families approached. However, these were not completed because of the time pressures during the recruitment period. Therefore, reporting of the number of families directly approached by Mencap or the proportion of approached families that were subsequently referred to the study team either directly or indirectly cannot be reported, and this is a limitation of this feasibility study.
Feasibility and acceptability of recruitment strategies
In qualitative interviews, both family carers and programme delivery staff highlighted two key recruitment pathways: (1) personal contact with a practitioner (most often a member of Mencap staff) or (2) through parents finding out about the programme from Mencap social media sites (e.g. Facebook). One practitioner (facilitator, site 1) suggested that recruitment needed to be done by charities embedded within the local community, but it would be important to identify and involve various groups and not just rely on one organisation, as there is a risk that recruitment might reach only those already attending support groups.
Facilitators did not identify significant challenges with recruiting family carers and the main methods described above appeared to be feasible to implement. Facilitators reported that randomisation (and therefore possible allocation to the control group) was seen as a barrier to participation when explaining the study to family carers, but not to the extent that it appeared to undermine the feasibility or acceptability of a full RCT.
Objective: recruitment rates and retention through 3- and 12-month post-randomisation follow-up data collection
The feasibility of recruiting and retaining participants at 3 and 12 months’ follow-up was assessed by reporting recruitment and follow-up rates (quantitative) and barriers to follow-up data collection (qualitative).
Recruitment rates and participant retention
Recruitment rates and retention at 3 and 12 months post-randomisation are reported quantitatively. Reflections from the study team, in addition to barriers to and facilitators of recruitment and retention, as detailed in qualitative interviews, are also described (Figure 1).
FIGURE 1.
The E-PAtS CONSORT flow diagram. a, A total of 150 families were contacted in the study. One of the sites recruited families in two rounds and some of the families (n = 16) referred from this site were referred for both the first and second round (if they were not recruited on the first round). Reproduced with permission from Coulman et al. 41 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original.
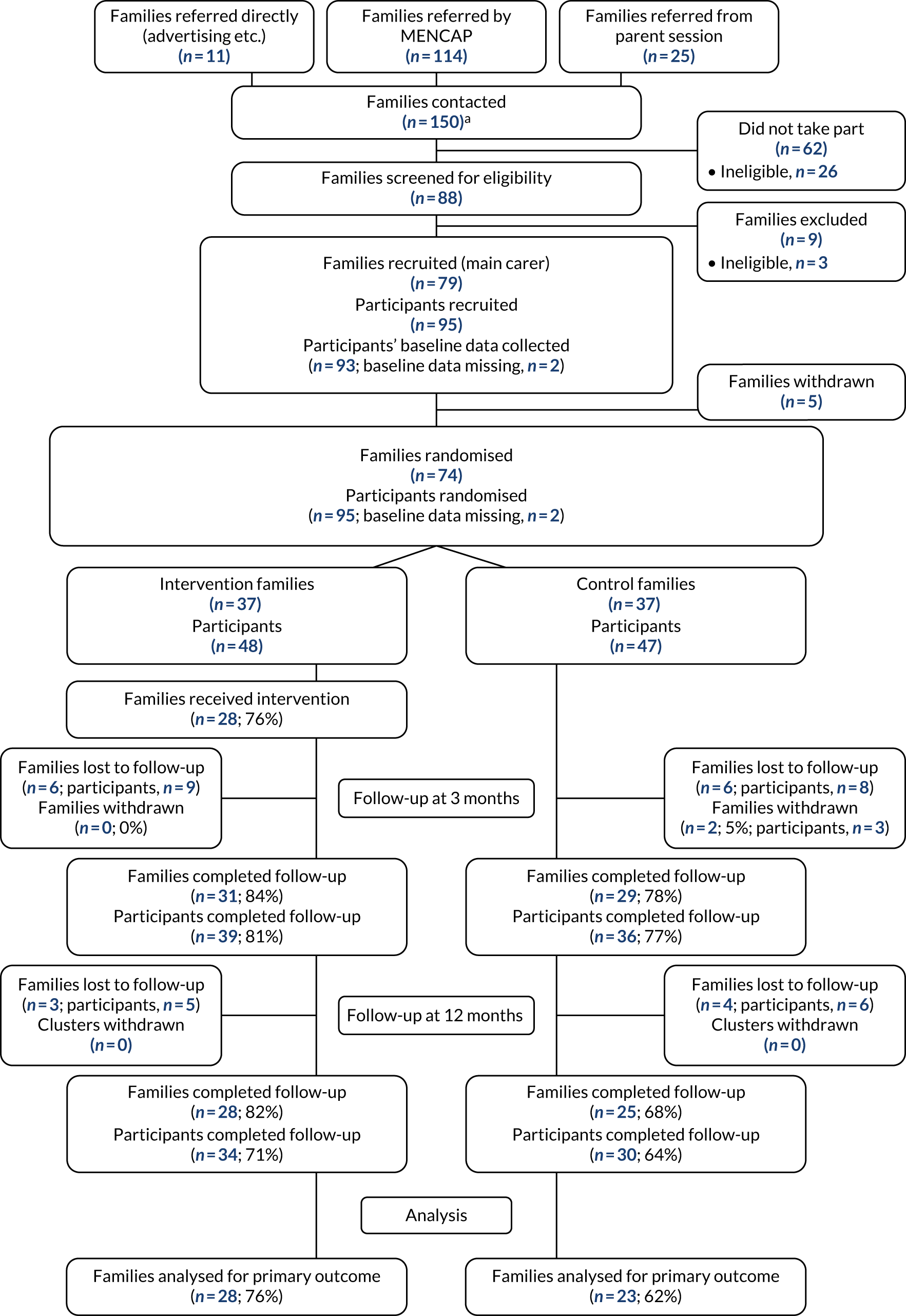
Recruitment of families
The study recruitment target was defined as recruitment of 64 families/clusters by two to four service provider organisations that deliver one or two intervention group sessions each. Initially, two service provider organisations (sites 1 and 2) were recruited to recruit 32 clusters/families and deliver two intervention group sessions each. The recruitment period was scheduled for the summer term of 2018, immediately prior to the intervention start dates, which, in turn, were timed to coincide with school term dates to maximise attendance at group sessions. However, because of unforeseen variations in school holiday dates in site 1, the recruitment period at site 1 was shortened to complete recruitment and deliver the intervention prior to the start of school summer holidays. To accomplish this, staff resource was reallocated between sites and recruitment periods were condensed. Despite this, recruitment targets were exceeded in site 1, with 38 clusters recruited in 6 weeks (26 March 2018–1 May 2018). However, recruitment targets were not met in site 2, with 15 clusters recruited in 5 weeks (18 April 2018–18 May 2018). Despite 41 referrals of interested families in site 2, 22.0% of these families were not recruited because they were unable to attend sessions. This was much higher than in site 1 (6.3%). Organisation of the intervention sessions differed in each site, which may have had an impact on recruitment rates. Although site 1 scheduled group sessions around the availability of recruited participants, there was limited flexibility in the timings of the intervention sessions in site 2 because of venue restrictions.
A second recruitment period in the summer of 2018 was approved by the SSC to meet the initial study recruitment target. Recruitment was paused in site 1, as it was considered that the potential study population could have been exhausted during the initial recruitment period. However, recruitment continued in site 2 to deliver to one intervention group and to assess recruitment feasibility. Amendments to the organisation of the intervention group sessions were introduced, including increased flexibility in the times/days of the intervention sessions, to improve participant availability. A third site (site 3) was recruited to deliver to one intervention group to further demonstrate recruitment feasibility.
In site 2, 16 families that were interested in taking part but who were not recruited in phase 1 were recontacted and 11 new families/clusters were referred to the study team (one indirectly and 10 directly by Mencap). Although the recruitment target was set at approximately 16 families, only seven families were recruited to the study in 11 weeks (15 June 2018–29 August 2018). In site 3, 14 families were recruited in 5 weeks (11 July 2018–13 August 2018) and recruitment was stopped because the recruitment target was met.
In total, 74 families and 95 participants were recruited and randomised in three sites, delivering between one and three intervention group sessions across two recruitment phases.
Participants’ barriers to and facilitators of taking part in the study
Overwhelmingly, participants stated that their motivation to take part in the study was to support their child with disabilities, including to educate themselves on how to deal with specific challenges that they were currently facing with their child. However, family carer facilitators also reported altruistic reasons to help similar families:
. . . because I really want to be there for my son, in terms of physically, emotionally and psychologically so I really want to know more in order to teach him so he can be better.
As I said before its things like toilet training and what have you. That will be one of our challenges and for that alone I would probably go and I would feel like I have this good opportunity and I wouldn’t want to miss it.
Do you know what, what really motivated me as well, was the fact that I felt like it was going to really make a difference, you know, not only to our life, but also like taking part in the study might help other people.
Participants described that they had experienced limited support for families of children with learning disabilities and that they were motivated to promote any additional support. Positive reviews from other family carers also encouraged participants to take part in the study:
I have heard very good things about it. I would be keen to do it.
I couldn’t have spoken about [name] without crying, my heart just broke for him because there was nothing available. He does attend . . . all the medical side of things, the therapies are fine and between the 45-minute sessions half the time he will not engage so I was just very fearful of the unknown and what am I going to do to help this child so I was very grateful for the E-PAtS course at that time.
Sometimes just for families with children with learning disabilities there’s little support, there is a bit of support, you know, you have to fight for quite a lot. I think it is good there are people out there proactively trying to make things easier. I’m very supportive of it in that regard.
Participant retention at 3 months
Eighty-four per cent (n = 31) and 78% (n = 29) of intervention and control families, respectively, provided follow-up data at 3 months, including either completion of the Five Minute Speech Sample (FMSS) by telephone interview or questionnaire completion by telephone, face to face or posting completed questionnaires (Table 9).
| Measure completed | Phase 1 | Phase 2 | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Site 1 | Site 2 | Site 2 | Site 3 | |||||||
| n | % | n | % | n | % | n | % | n | % | |
| Families: FMSS only | 5 | 62.5 | 1 | 12.5 | 0 | 0.0 | 2 | 25.0 | 8 | 13.3 |
| Participants: FMSS only | 7 | 63.6 | 2 | 18.2 | 0 | 0.0 | 2 | 18.2 | 11 | 14.7 |
| Families: questionnaire only | 6 | 46.2 | 5 | 38.5 | 1 | 7.7 | 1 | 7.7 | 13 | 21.7 |
| Participants: questionnaires only | 9 | 56.3 | 5 | 31.3 | 1 | 6.3 | 1 | 6.3 | 16 | 21.3 |
| Families: questionnaire and FMSS | 19 | 48.7 | 9 | 23.1 | 4 | 10.3 | 7 | 17.9 | 39 | 65.0 |
| Participants: questionnaires and FMSS | 25 | 52.1 | 10 | 20.8 | 4 | 8.3 | 9 | 18.8 | 48 | 64.0 |
Barriers specific to 3-month follow-up data collection
The FMSS was used at baseline and the 3-month follow-up for all study participants. This measure asked parents to ‘talk about their child for 5 minutes without interruption, about their thoughts and feelings about the subject and how they get along together’. Participants were generally apprehensive about completing the FMSS and thought that the experience would be difficult and uncomfortable. At the 3-month follow-up, some participants reported that they declined to complete the measure because of its demanding nature. The response rate for completion of the FMSS reduced from 100% at baseline to 62% at the 3-month follow-up. It is therefore possible that the FMSS deterred participants from completing the 3-month follow-up, affecting retention at this point. This also demonstrated that the FMSS was unacceptable to some study participants. Therefore, it was decided that the FMSS would not be repeated at the 12-month follow-up. Furthermore, an administrative error in the phase 1 3-month follow-up data collection affected up to 18 participants in site 1, in that participants may have been posted the researcher case report form. The case report form contained the scoring measures used by the researcher to score the FMSS and included terms such as ‘critical comments’ and ‘negative relationship’. It was considered that this may have caused distress and put participants off completing the FMSS. All participants were contacted by letter and by telephone to apologise. No participant stated at the time or in qualitative interviews subsequently that this affected their decision to complete the FMSS. However, the impact of this error on FMSS completion rates is unknown.
Participant retention at 12 months
Seventy-six per cent (n = 28) and 68% (n = 25) of intervention and control families, respectively, completed follow-up data collection at 12 months, including either completion of the VABS by telephone interview or questionnaire completion by telephone, face to face or posting completed questionnaires (Table 10).
| Measure completed | Phase 1 | Phase 2 | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Site 1 | Site 2 | Site 2 | Site 3 | |||||||
| n | % | n | % | n | % | n | % | n | % | |
| Families: VABS only | 7 | 53.8 | 3 | 23.1 | 0 | 0.0 | 3 | 23.1 | 13 | 25.0 |
| Participants: VABS only | 7 | 53.8 | 3 | 23.1 | 0 | 0.0 | 3 | 23.1 | 13 | 20.3 |
| Families: questionnaire only | 7 | 70.0 | 0 | 0.0 | 2 | 20.0 | 1 | 10.0 | 10 | 19.2 |
| Participants: questionnaires only | 10 | 76.9 | 0 | 0.0 | 2 | 15.4 | 1 | 7.7 | 13 | 20.3 |
| Families: questionnaire and VABS | 13 | 44.8 | 10 | 34.5 | 4 | 13.8 | 2 | 6.9 | 29 | 55.8 |
| Participants: questionnaires and VABS | 19 | 50.0 | 11 | 28.9 | 4 | 10.5 | 4 | 10.5 | 38 | 59.4 |
Barriers to all follow-up data collection
Participants described barriers to participation in the follow-up when they were contacted to arrange the relevant follow-up, including unavailability because of holidays, busy times of the year, such as Christmas, and family illness/hospitalisation.
Furthermore, the method of follow-up data collection was complicated by the type of proposed outcome measures and the requirement of blinding researchers to participant allocation. As a result, participants selecting postal data collection were still required to complete the FMSS (at the 3-month follow-up) or VABS (at the 12-month follow-up) by telephone and those participants selecting face-to-face or telephone data collection were required to complete the Group Cohesion Scale, a measure that identified the participant allocation (at the 3-month follow-up) with a different member of the team on a separate occasion. This increased participant burden, complicated the data collection procedure and may have had an impact on retention rates. However, this was not evidenced in qualitative interviews with participants.
Objective: the acceptability of study processes, including randomisation, to service provider organisations, facilitators and family carers through qualitative interviews
The acceptability of study processes was explored in qualitative interviews with participants, facilitators and service provider organisations.
Acceptability of participant recruitment
Overall, participants’ experience of being recruited was positive, including their interactions with the research team and the provision of information about the study. Participants appeared, almost universally, to have a clear idea of what they had ‘signed up to’ and what they would be expected to do as part of the research. Some participants were less clear on the specific tasks and timing (e.g. when and how many questionnaires would need to be completed). This was linked to the perceived complexity and extensive amount of information provided to participants:
There was a lot of information. Whatever we were told and whatever was happening at the time we were perfectly happy with, you know. If there was to be follow-ups or the questionnaires, to tell you the truth I can’t remember now how often the questionnaire lands on the mat, we fill it in but I couldn’t say to you we are due a questionnaire in November.
Main family carer, site 1
The experience of being recruited into the study contrasted with that of interactions with other professionals/services with whom participants had dealt. Participation in the study (and, for families in the intervention group, the E-PAtS programme) followed an explicit invitation to do so. Family carers contrasted this with their experience of trying to access services provided by other agencies/services, when they had often encountered numerous barriers (e.g. waiting lists, bureaucracy, needing to wait until a child had reached a certain age). Being approached and offered a service (or at the very least participation in a research study) therefore represented a different form of interaction that participants valued.
Acceptability of randomisation and the randomisation process
Participants were randomised on a 1 : 1 ratio to the intervention or control group. All control participants were offered the opportunity to attend the intervention subsequent to the 12-month follow-up data collection time point, if they had chosen to be offered the intervention in this way during recruitment. Participants generally understood the concept of randomisation and found the concept of randomisation in this setting acceptable. However, some participants spoke of their confusion and lack of clarity with regard to the process of study allocation (e.g. when control participants would be able to attend the course) and requested clearer information. Facilitators echoed this and felt that, as a result, randomisation was off-putting for participants. Although some participants described their happiness at being allocated to the intervention group and not having to wait 12 months to attend the E-PAtS group sessions, some control participants spoke of how disappointed they were not to be able to attend the group sessions immediately. Furthermore, participants spoke of practical issues if they were required to wait 12 months to attend the intervention sessions (e.g. changes in circumstances, such as the child starting school or alterations in the parents’ working situations, or changes in the child’s age may impact the participant’s ability to attend or eligibility to attend, respectively). However, follow-up rates at 3 months were comparable in intervention and control groups, and therefore the concerns raised may not have affected participants’ continued involvement in the study:
I think when I was initially putting my name down I just wanted to get the classes, but when it was explained I was happy enough. I mean, if everybody can’t do it then everybody can’t do it, and it was randomly selected.
I didn’t want to wait another year because you just don’t know what is going to happen in that year do you . . . I felt like I had won the lottery.
Yeah and I think the fact that it was the study with the control, that they might do it and they might not, I think that put people off.
. . .when I first heard of the E-PAtS study I thought ‘happy days’, this is finally something that can help us here and we need this help because we don’t have a lot of family support, we don’t have other services showing any interest in us’ and to then find out it was being put off for a year it was hard to accept.
I suppose I was like this was a bit of a misunderstanding for me because they were telling me yes and then they said I had to wait, so it wasn’t explained very well.
Because after finishing the study you have to wait 1 year which is probably the time that [name] is in full time school. Then I have to get a job and I have no idea.
Acceptability of method of data collection
Generally, participants described their experience of completing the questionnaires as ‘fine’. Participants were satisfied with the logistics of completing the questionnaires, which included telephone, face-to-face or postal options. Refer to Table 11 for completion rates of follow-up data. Over the course the study, three family carers changed their method of questionnaire completion (two from postal to telephone, and one from telephone to postal):
Sending the questionnaire was good, I had time for filling the form in, to send it back. The phone calls was not a problem at all.
| Method of data collection | Site 1 | Site 2 | Site 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Selected | Completed | Selected | Completed | Selected | Completed | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| 3 months | ||||||||||||
| Telephone | 5 | 9.6 | 4 | 7.7 | 4 | 16.0 | 0 | 0.0 | 2 | 11.8 | 2 | 11.8 |
| Face to face | 6 | 11.5 | 5 | 9.6 | 2 | 8.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Post | 41 | 78.9 | 32 | 61.5 | 19 | 76.0 | 22 | 88.0 | 15 | 88.2 | 8 | 47.1 |
| 12 months | ||||||||||||
| Telephone | 5 | 9.6 | 2 | 3.8 | 4 | 16.0 | 1 | 4.0 | 2 | 11.8 | 1 | 5.9 |
| Face to face | 6 | 11.5 | 4 | 7.6 | 2 | 8.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Post | 41 | 78.9 | 30 | 57.7 | 19 | 76.0 | 19 | 76.0 | 15 | 88.2 | 7 | 41.1 |
Acceptability of study pathway options
Primary participants selected one of two pathways, if randomised to the control arm. Families in pathway A were offered the E-PAtS programme subsequent to the 12-month follow-up and families in pathway B were not offered the E-PAtS programme. Only one carer selected pathway B, demonstrating that being offered the option of attending the E-PAtS programme on a waiting list basis was the most acceptable process to participants. When questioned regarding the acceptability of this study process, participants expressed confusion. Some participants did not differentiate between randomisation and choice of study path. However, participants did suggest that they chose pathway A to keep their options open and to allow them the choice to attend the E-PAtS programme on a waiting list basis if allocated to the control arm. Participants also implied that research assistants may have encouraged this choice. However, participants’ change in circumstances may have had an impact on their decision. Participants questioned the suitability of the waiting list E-PAtS course if their child would no longer be ‘eligible’ because of their age at the time of the 12-month follow-up. This concern was predicted by the study team and so all participants were offered the E-PAtS programme if they were randomised to the control arm and their child was just outside age range by the time of their E-PAtS intervention:
Well, they said it’s best to option like that so I made that option because it’s nothing otherwise.
I don’t know if there’s much point in doing this because my daughter would have been 5 practically by that stage. I know from a research point of view you have to go for a random group. From a personal perspective in terms of what I was going to get out of it I would have felt that having to wait would have taken away from the value of it for me.
Acceptability of study questionnaires
Participants expressed that completion of the questionnaires was time-consuming and this was off-putting. One participant said that, because of the demands of parenting a child with intellectual disability, more time may be needed to complete the questionnaires:
Long! Long! It was fine! The interviewer was very good and everything but it was long.
. . . giving people the time like 1 month because I mean normal people can do something in 1 week, whereas we can’t, we are kind of I would say busier than other mums, so we want to do something but we can’t, sometimes I even forget to eat lunch.
The impact of study questionnaires
Participants found questions examining parents’ well-being difficult to answer. However, being asked these questions also resulted in parents feeling acknowledged. Parents described directing all of their energy onto their child to the point that they neglect their own needs. Therefore, the questionnaires required the participants to consider the impact of parenting a child with intellectual disability on their own and their families’ lives. Participants stated that completing the questionnaires made them realise that caring for a child with intellectual disability has an impact on the whole family and not just the parents:
. . . reading that questionnaire actually made me realise how this affects everybody around us, us and [elder child] now I see that [study child] has a huge impact on [elder child], it’s a huge impact, and it’s not a good one as well so it was interesting.
. . . the first thing what you think of is about him, you worry about the child and everything, you never think how it is actually affecting the whole family and everything you do and how your life is changed, so it was very interesting.
To be asked those questions, how do you cope, and at the time when I filled in those questions I was in a really dark place, it was really difficult to cope with, but actually for somebody to reach out and say ‘how are you feeling’, was kind of a good acknowledgement, you know what I mean?
I suppose it’s always easier to answer questions about your daughter, than maybe, about yourself, and your own feelings, that side kind of, it wasn’t the question, it’s just, sometimes it’s harder to think about your own feelings about something. It’s quite a sensitive subject.
Participants described how answering measures about their child instigated reflection, both on how difficult their situation may be and on how delayed their child may be. For some parents who had not received a clinical diagnosis, the questionnaires provided a means to compare the development of their child to children without diagnoses of intellectual disability. Participants spoke about how ‘emotional’, ‘upsetting’ and ‘depressing’ completing the questionnaires was and how the self-examination required to answer the questions was difficult:
. . . when you sit down and fill a questionnaire in for a few days afterwards you’re a bit like ‘God our life is terrible’, things that we didn’t realise we had because you’re kind of putting it down on paper so you go over them again.
I almost felt . . . it’s hard to describe but it was just a wee bit depressing, to fill it in about your child what they could and couldn’t do and realising that how far behind she was. It was sort of a bit more of a wake-up call of the things she couldn’t do that she should have been able to do I suppose.
I remember feeling, yeah, I remember feeling really down afterwards, because suddenly I realised how little he spoke. There was a list of probably about a hundred words there and I think I ticked about seven and they weren’t clear words. That suddenly made me think ‘my god this is actually real’.
Participants described completion of the questionnaires individually, as a couple and with other family members as a positive thing:
It was emotional! You know it’s one thing living it but when you see things written down like some of the questions, it really made you think and stuff, but you know it was a bit of a roller coaster. When we did our first questionnaire, my husband and I, we set aside a time when we could both sit down at the table and he does his, I do mine and then we both kind of share experiences and stuff and we both kind of had a little cry. The thing is you carry on everything, you do the best you can and you’re so focused on stopping meltdowns and keeping them safe and all that you don’t realise really how hard your day is sometimes, so there was a lot of reflection on that.
I think when you get a huge questionnaire like that it does bring it home to you, it’s quite profound when you look at it in black and white and you see exactly the extent of the things you’re dealing with which is different from your other children, but I think that is a good idea, a really good idea.
Answering questions regarding their child’s development provided participants with an opportunity to consider their child’s development and realise areas of concern, resulting in participants feeling more confident and knowledgeable about their child’s needs. Participants also took comfort at follow-up data collection when their child had advanced/made progress in certain areas:
Well, they actually gave me more knowledge onto what I was actually doing because before then I was kind of clueless . . . Yeah, it gave me a kind of confidence to know that I’ve made progress in some certain areas.
Impact of the Vineland Adaptive Behaviour Scales report
Feedback on the VABS report was varied. Although some participants described regularly receiving similar documentation, others expressed that the language used in the report was too clinical and should be simplified for parents. One participant expressed disappointment, as they considered the report to be ‘compensation’ for taking part in the study:
I got it and it was like double Dutch to me; I didn’t understand what the report was trying to say. I looked at it, it was too difficult. It was very scientific . . . I really struggled to get anything worthwhile out of it and as I just said I was a bit disappointed.
That report is not good and that’s supposed to be . . . well for me in my head, rightly or wrongly, that was supposed to be, not compensation, but it was supposed to be . . . we didn’t get on the real thing so here is something in return for giving up some of your time and then that didn’t. I didn’t find it useful. I couldn’t really understand it.
There were conflicting views on the content of the report. Some families felt that the report was extremely accurate, whereas other questioned the accuracy. Some participants thought that the report was generic and that they would have preferred a more personalised report, whereas others stated that the report was personalised and specific to their child’s needs:
Incredible! I couldn’t believe how it felt like they really knew him.
No. I think it goes for any child, their mum knows them best and there’s a lot of jargon, a lot of words and it didn’t feel personal to him. It went off data that I provided, it wasn’t like a handwritten report from someone who knew him so no I didn’t make any use of that.
Participants described the practical advice provided in the report and how these recommendations had been applied at home. The report, for example, was utilised by some parents when communicating with education and child-care services to improve understanding of the child’s needs in these settings. The report was also circulated to health-care professionals and was used as evidence in Disability Living Allowance (UK social security benefit scheme) applications:
I thought it was useful to receive it and it gave us a bit of focus on things we could work on with her.
Even when my son wanted to go to school I showed them this report as well and it helped the school as well.
It also is useful for any other forms, like DLA [Disability Living Allowance] . . . the information was good because it really highlighted the additional needs that he has that sometimes you as parents forget about because you just get on with it.
As for the study questionnaires, the VABS report similarly highlighted the challenges parents experienced with their child, and parents described difficulty when faced with this information:
It kind of hit home as well. It was quite . . . I was a wee bit numb after. It was . . . what’s the word, it kind of highlighted it from there, the evenings that we talked about it. It was real. It kind of reaffirms everything that you know, they’d got our kids all down to a tee, but it was kind of a wee bit hard to read sometimes because you don’t really think about that, you’re just getting on with every day but no, it was definitely good.
Piloted outcome measures proposed to test the effectiveness of the intervention in a main trial
Objective: the feasibility and acceptability of the proposed outcome measures as methods to measure the effectiveness of the intervention and to conduct an embedded health economic evaluation within a definitive randomised controlled trial
The measures were summarised using descriptive statistics, with any preliminary evidence of differences between the intervention and control groups explored. The acceptability of outcome measures was assessed in qualitative interviews with participants.
Data completeness of proposed outcome measures
The parent-reported proposed outcome measures were well completed (Table 12). The progression criteria target was to reconsider a measure if < 70% of collected data were useable. When at least one item of a measure had been completed, all items were useable for the majority of measures. The Sibling Relationship Questionnaire (SRQ) was the most poorly completed, with 84% of the questionnaires being useable at 12 months post randomisation. The items most frequently left unanswered across time points were ‘how much do the sibling and the child tell each other everything?’, ‘how much do the sibling and the child share secrets and private feelings?’ and ‘how much do the sibling and child insult and call each other names?’ These items require a certain level of communication ability, which may not have been acquired because of the young the age of the child or their intellectual disability.
| Measure | Baseline | 3 months | 12 months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| At least one item of measure completed (n) | Completed to useable extent (n)a | Percentage useable | At least one item of measure completed (n) | Completed to useable extent (n)a | Percentage useable | At least one item of measure completed (n) | Completed to useable extent (n)a | Percentage useable | |
| WEMWBS | 90 | 90 | 100 | 63 | 62 | 98 | 50 | 50 | 100 |
| HADS | 92 | 92 | 100 | 59 | 59 | 100 | 51 | 51 | 100 |
| VABS: child-level variable | 72 | 72 | 100 | Not collected at the 3-month time point | 42 | 42 | 100 | ||
| Family APGAR Scale | 92 | 92 | 100 | 58 | 57 | 98 | 51 | 50 | 98 |
| Family Support Scale | 92 | 92 | 100 | 60 | 60 | 100 | 50 | 50 | 100 |
| Positive Gains Scale | 89 | 89 | 100 | 60 | 60 | 100 | 50 | 50 | 100 |
| CPRS | 93 | 91 | 98 | 60 | 60 | 100 | 51 | 51 | 100 |
| Child–Parent Activity Index | 93 | 93 | 100 | 60 | 60 | 100 | 51 | 51 | 100 |
| EQ-5D-5L | 92 | 92 | 100 | 63 | 63 | 100 | 51 | 51 | 100 |
| Child resource use | 58 | 58 | 100 | 47 | 47 | 100 | |||
| Parents resource use | 58 | 58 | 100 | 47 | 47 | 100 | |||
| Brief COPE | 92 | 91 | 99 | 60 | 60 | 100 | 51 | 51 | 100 |
| Happiness of Relationship Scale | 68 | 68 | 100 | 55 | 55 | 100 | 46 | 46 | 100 |
| Co-Parenting Agreement Scale | 69 | 69 | 100 | 49 | 49 | 100 | 40 | 40 | 100 |
| Conflict | 69 | 69 | 100 | 48 | 48 | 100 | 42 | 42 | 100 |
| CBCL | 93 | 88 | 95 | 59 | 53 | 90 | 48 | 43 | 90 |
| Paediatric Quality of Life Inventory | 91 | 91 | 100 | 57 | 57 | 100 | 48 | 48 | 100 |
| Group Cohesion Scale | Not collected at baseline | Not collected at the 3-month time point | 23 | 20 | 87 | ||||
| Strengths and Difficulties Questionnaire (for siblings) | 62 | 62 | 100 | 37 | 37 | 100 | 32 | 32 | 100 |
| SRQ | 63 | 58 | 92 | 36 | 33 | 92 | 32 | 27 | 84 |
Analysis of proposed outcome measures
Table 13 summarises information on the return of questionnaires and suitable summary statistics depending on the distribution of the data for each proposed outcome (i.e. family carer-reported outcome measures) measured at baseline, 3 months post randomisation and 12 months post randomisation by trial arm. The score range of the WEMWBS, the proposed primary outcome measure, is 14–70, with higher scores indicating higher levels of mental well-being. The mean UK population norm is 51. Ninety-five per cent of participants completed the measure at baseline, all to a useable extent (n = 90). Forty-nine per cent of control arm participants (n = 23) and 56% of intervention arm participants (n = 27) completed the measure at the 12-month time point. Again, the forms were well completed and all of those returned were useable. In the control group, the mean WEMWBS score was 43.2 (SD 8.9) at baseline and 43.4 (SD 11.0) 12 months post randomisation. In the intervention group, scores were 43.9 (SD 10.6) and 46.5 (SD 10.9) at baseline and 12 months post randomisation, respectively.
| Measure | Control arm | Intervention arm | ||||
|---|---|---|---|---|---|---|
| Baseline | 3 months | 12 months | Baseline | 3 months | 12 months | |
| WEMWBS: score range 14–70; higher scores indicate higher levels of mental well-being | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 28 (60) | 23 (49) | 45 (94) | 35 (73) | 27 (56) |
| Useable forms, n (%) of those returned | 45 (100) | 28 (100) | 23 (100) | 45 (100) | 34 (97) | 27 (100) |
| Mean score (SD) | 43.2 (8.9) | 42.7 (9.4) | 43.4 (11.0) | 43.9 (10.6) | 45.5 (9.2) | 46.5 (10.9) |
| Range | 23–62 | 21–60 | 21–65 | 19–66 | 23–61 | 25–68 |
| HADS anxiety: score range 0–21; higher scores indicate greater anxiety | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 33 (69) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 47 (100) | 33 (100) | 28 (100) |
| Mean score (SD) | 10.6 (3.7) | 11.4 (4.8) | 9.9 (4.4) | 10.1 (4.4) | 10.2 (4.9) | 8.0 (4.4) |
| Range | 0–19 | 4–20 | 3–19 | 1–21 | 1–19 | 1–20 |
| HADS depression: score range 0–21; higher scores indicate higher levels of depression | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (27) | 23 (49) | 47 (98) | 33 (69) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 47 (100) | 33 (100) | 28 (100) |
| Mean score (SD) | 7.9 (3.9) | 8.6 (4.1) | 8.9 (4.2) | 7.2 (4.0) | 7.1 (4.4) | 6.1 (4.4) |
| Range | 0–16 | 2–20 | 3–20 | 0–17 | 0–15 | 0–14 |
| HADS emotional distress: sum of anxiety and depression subscales – score range 0–42; higher scores indicate greater emotional distress | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 33 (69) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 47 (100) | 33 (100) | 28 (100) |
| Mean score (SD) | 18.4 (6.8) | 19.9 (7.7) | 18.8 (8.0) | 17.3 (7.8) | 17.2 (8.8) | 14.1 (8.2) |
| Range | 0–33 | 6–32 | 6–34 | 4–38 | 1–32 | 1–32 |
| VABS: child-level variable | Not collected at 3-month time point | Not collected at 3-month time point | ||||
| Composite score: standardised score, mean 100 | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 22 (59)a | 37 (100) | 20 (54)a | ||
| Useable forms, n (%) of those returned | 35 (100) | 22 (100) | 37 (100) | 20 (100) | ||
| Median score (IQR) | 55 (40–67) | 64.5 (58–69) | 58 (50–66) | 67.5 (58.5–70.5) | ||
| Range | 25–78 | 46–73 | 34–76 | 45–73 | ||
| Communication: standardised score, mean 100 | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 22 (59)a | 37 (100) | 20 (54)a | ||
| Useable forms, n (%) of those returned | 35 (100) | 22 (100) | 37 (100) | 20 (100) | ||
| Median score (IQR) | 44 (26–67) | 63 (52–70) | 55 (34–64) | 61 (52–70.5) | ||
| Range | 20–83 | 39–77 | 20–85 | 40–80 | ||
| Family APGAR Scale: five items, score range 0–10; higher scores indicate better family function | ||||||
| Forms returned, n (%) of those randomised | 44 (94) | 26 (55) | 23 (49) | 48 (100) | 32 (67) | 28 (58) |
| Useable forms, n (%) of those returned | 44 (100) | 25 (96) | 22 (96) | 48 (100) | 32 (100) | 28 (100) |
| Mean score (SD) | 7.3 (2.4) | 7.5 (2.7) | 6.5 (3.2) | 6.9 (2.9) | 7.1 (3.0) | 6.4 (2.8) |
| Range | 2–10 | 1–10 | 0–10 | 0–10 | 0–10 | 1–10 |
| Family Support Scale: number of informal sources of support available | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 22 (47) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 22 (100) | 47 (100) | 34 (100) | 28 (100) |
| Median score (IQR) | 10 (8–12) | 11 (9–12) | 11 (10–13) | 10 (7–12) | 8 (6–11) | 10 (7.5–11) |
| Range | 5–13 | 3–13 | 2–13 | 3–13 | 2–13 | 2–13 |
| Family Support Scale: number of formal sources of support available | ||||||
| Forms returned, n (%) of those randomised | 43 (91) | 26 (55) | 22 (47) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 43 (100) | 26 (100) | 22 (100) | 47 (100) | 34 (100) | 28 (100) |
| Median score (IQR) | 4 (3–5) | 4 (4–5) | 4 (4–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Range | 1–5 | 3–5 | 3–5 | 1–5 | 2–5 | 2–5 |
| Mean helpfulness of informal sources of support available: scored 0 (not at all helpful) to 4 (extremely helpful) | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 22 (47) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 22 (100) | 47 (100) | 34 (100) | 28 (100) |
| Mean score (SD) | 1.8 (0.8) | 1.8 (0.7) | 1.6 (0.6) | 2.0 (0.9) | 2.0 (0.8) | 2.0 (1.0) |
| Range | 0.5–3.5 | 0.7–3.0 | 0.5–3.0 | 0.5–4.0 | 0–3.8 | 0.6–4.0 |
| Mean helpfulness of formal sources of support available: scored 0 (not at all helpful) to 4 (extremely helpful) | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 22 (47) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 22 (100) | 47 (100) | 34 (100) | 28 (100) |
| Mean score (SD) | 2.4 (1.0) | 2.3 (0.8) | 2.0 (1.1) | 2.5 (1.0) | 2.5 (0.9) | 2.6 (1.0) |
| Range | 0.6–4.0 | 0.5–4.0 | 0.4–4.0 | 0.2–4.0 | 0.6–4.0 | 0.5–4.0 |
| Positive Gains Scale: seven items, score range 7–35; higher scores indicate higher positive gains | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 44 (92) | 34 (71) | 27 (56) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 44 (100) | 33 (97) | 27 (100) |
| Median score (IQR) | 13 (9–15) | 12.5 (10–15) | 12 (9–14) | 11 (8–15) | 12 (9–15) | 11 (8–14) |
| Range | 7–24 | 7–19 | 7–19 | 7–23 | 7–35 | 7–20 |
| CPRS 15 items: conflict – eight items, score range 8–40; higher scores indicate greater conflict | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 48 (100) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 46 (96) | 34 (100) | 28 (100) |
| Mean score (SD) | 18.9 (6.4) | 20.0 (6.1) | 20.3 (6.2) | 19.2 (6.8) | 18.5 (8.0) | 18.0 (7.3) |
| Range | 8–32 | 9–30 | 10–32 | 8–33 | 8–35 | 8–32 |
| CPRS 15 items: closeness – seven items, score range 7–35; lower scores indicate a less close relationship | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 48 (100) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 42 (93) | 24 (92) | 19 (83) | 45 (94) | 33 (97) | 28 (100) |
| Mean score (SD) | 25.9 (5.4) | 25.8 (5.5) | 27.6 (3.7) | 26.9 (4.7) | 28.1 (5.2) | 29.7 (3.8) |
| Range | 13–35 | 11–34 | 19–35 | 17–35 | 15–35 | 22–35 |
| Child–Parent Activity Index: five items, score range 5–25; higher scores indicate higher frequencies of activities shared with child | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 48 (100) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 48 (1000) | 34 (100) | 28 (100) |
| Mean score (SD) | 20.6 (3.4) | 20.4 (3.3) | 20.9 (3.1) | 20.4 (3.1) | 20.6 (3.4) | 20.6 (3.2) |
| Range | 13–24 | 13–25 | 14–25 | 12–25 | 12–25 | 13–25 |
| EQ-5D VAS: score range 0 (worst health) – 100 (best health) | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 28 (60) | 23 (49) | 47 (98) | 35 (73) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 28 (100) | 23 (100) | 47 (100) | 35 (100) | 28 (100) |
| EQ-5D-5L index value: score range 0.28–1 (perfect health) | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 28 (60) | 23 (49) | 48 (100) | 35 (73) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 28 (100) | 23 (100) | 48 (100) | 34 (97) | 27 (96) |
| Brief COPE: 17 items, three subscales – active avoidance coping, score range 6–24 | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 45 (96) | 33 (97) | 28 (100) |
| Mean score (SD) | 13.9 (3.1) | 12.1 (2.4) | 12.3 (2.7) | 13.2 (3.5) | 13.3 (3.4) | 12.8 (3.4) |
| Range | 8–20 | 8–18 | 7–18 | 6–21 | 8–20 | 7–21 |
| Brief COPE: 17 items, three subscales – problem focused coping, score range 5–20 | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 46 (98) | 34 (100) | 28 (100) |
| Mean score (SD) | 18.8 (3.4) | 18.2 (3.4) | 18.2 (3.6) | 18.0 (3.4) | 18.8 (3.0) | 19.2 (2.9) |
| Range | 11–24 | 10–23 | 11–24 | 10–24 | 11–24 | 14–24 |
| Happiness of Relationship Scale: one item scored 1–7; higher scores indicate greater happiness | ||||||
| Forms returned, n (%) of those randomised | 37 (79) | 25 (53) | 21 (45) | 31 (65) | 30 (63) | 25 (52) |
| Useable forms, n (%) of those returned | 37 (100) | 25 (100) | 21 (100) | 31 (100) | 30 (100) | 25 (100) |
| Answered ‘cannot say’, n | 2 | 2 | 1 | 2 | 2 | 2 |
| Median score (IQR), excluding those who answered ‘cannot say’ | 6 (5–7) | 7 (5–7) | 6.5 (5–7) | 7 (6–7) | 6 (4.5–7) | 6 (5–7) |
| Range | 1–7 | 1–7 | 1–7 | 1–7 | 1–7 | 1–7 |
| Co-Parenting Agreement Scale: four items, score range 0–6; higher scores indicate greater co-parenting agreement | ||||||
| Forms returned, n (%) of those randomised | 38 (81) | 22 (47) | 22 (47) | 31 (65) | 27 (56) | 18 (38) |
| Useable forms, n (%) of those returned | 38 (100) | 22 (100) | 21 (95) | 31 (100) | 27 (100) | 18 (100) |
| Median score (IQR) | 5.5 (4.3–6.0) | 5.6 (4.3–5.8) | 5.3 (4.8–5.8) | 4.8 (3.5–6.0) | 4.3 (3.5–6.0) | 5.0 (3.3–6.0) |
| Range | 1.0–6.0 | 0.5–6.0 | 0.3–6.0 | 0.5–6.0 | 0–6 | 2.3–6.0 |
| Conflict: one item scored 1–7; higher scores indicate greater exposure to conflict | ||||||
| Forms returned, n (%) of those randomised | 38 (81) | 22 (47) | 23 (49) | 31 (65) | 26 (54) | 19 (40) |
| Useable forms, n (%) of those returned | 38 (100) | 22 (100) | 23 (100) | 31 (100) | 26 (100) | 19 (100) |
| Answered ‘cannot say’, n | 3 | 1 | 2 | 1 | 1 | 2 |
| Median score (IQR), excluding those who answered ‘cannot say’ | 2 (1–3) | 2 (1–4) | 2 (1–3) | 2 (1–2) | 2 (1–4) | 2 (1–3) |
| Range | 1–6 | 1–6 | 1–6 | 1–4 | 1–6 | 1–4 |
| CBCL internalising score | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 25 (53) | 22 (47) | 48 (100) | 34 (71) | 26 (54) |
| Useable forms, n (%) of those returned | 43 (96) | 24 (96) | 19 (86) | 45 (94) | 29 (85) | 24 (92) |
| Mean score (SD) | 19.1 (9.0) | 19.5 (11.0) | 21.8 (11.6) | 19.8 (11.3) | 18.2 (12.8) | 18.2 (13.6) |
| Range | 3–37 | 3–40 | 9–46 | 2–51 | 3–49 | 1–42 |
| CBCL externalising score | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 25 (53) | 22 (47) | 48 (100) | 34 (71) | 26 (54) |
| Useable forms, n (%) of those returned | 43 (96) | 24 (96) | 19 (86) | 45 (94) | 29 (85) | 24 (92) |
| Mean score (SD) | 21.5 (9.7) | 22.6 (11.5) | 22.9 (10.3) | 19.0 (11.5) | 17.6 (13.8) | 16.6 (11.7) |
| Range | 3–42 | 2–43 | 4–41 | 2–44 | 0–46 | 1–46 |
| CBCL total problem score | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 25 (53) | 22 (47) | 48 (100) | 34 (71) | 26 (54) |
| Useable forms, n (%) of those returned | 43 (96) | 24 (96) | 19 (86) | 45 (94) | 29 (85) | 24 (92) |
| Mean score (SD) | 67.5 (26.4) | 70.6 (33.6) | 73.2 (27.5) | 63.3 (32.5) | 59.2 (38.9) | 56.8 (34.1) |
| Range | 13–120 | 7–129 | 16–120 | 10–142 | 9–140 | 3–115 |
| Paediatric Quality of Life Inventory total score: score range 0–100; higher scores indicate better health-related quality of life | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 24 (51) | 21 (45) | 46 (96) | 33 (69) | 27 (56) |
| Useable forms, n (%) of those returned | 45 (100) | 24 (100) | 21 (100) | 46 (100) | 33 (100) | 27 (100) |
| Mean score (SD) | 55.0 (16.9) | 57.0 (18.6) | 48.5 (21.2) | 61.6 (17.6) | 59.8 (17.7) | 61.2 (17.3) |
| Range | 26–94 | 17–89 | 0–85 | 24–85 | 26–89 | 19–87 |
| Group Cohesion Scale: score range 8–32; higher scores indicate better group cohesion | ||||||
| Forms returned, n (%) of those randomised | 23 (48) | |||||
| Useable forms, n (%) of those returned | 20 (87) | |||||
| Median score (IQR) | 29.5 (24.5–32.0) | |||||
| Range | 8–32 | |||||
| Strengths and Difficulties Questionnaire (for siblings): 25 items; higher scores indicate a higher degree of problems for each subscale | ||||||
| Number reporting a sibling aged 4–16 years | 25 | 25 | 25 | 22 | 22 | 22 |
| Prosocial: five items, score range 0–10 | ||||||
| Forms returned, n (%) of those randomised | 32 (97) | 17 (52) | 14 (42) | 30 (100) | 20 (67) | 18 (60) |
| Useable forms, n (%) of those returned | 32 (100) | 17 (100) | 14 (100) | 30 (100) | 20 (100) | 18 (100) |
| Median score (IQR) | 8.0 (7.5–9.5) | 8.0 (7.0–9.0) | 7.5 (7.0–9.0) | 8.5 (6.0–10.0) | 8.5 (5.0–10.0) | 8.0 (6.0–10.0) |
| Range | 1.2–10.0 | 5.0–10.0 | 1.0–10.0 | 1.0–10.0 | 0.0–10.0 | 5.0–10.0 |
| Internalising problems: sum of emotional and peer problems subscale, score range 0–20 | ||||||
| Forms returned, n (%) of those randomised | 32 (97) | 17 (52) | 14 (42) | 30 (100) | 20 (67) | 18 (60) |
| Useable forms, n (%) of those returned | 32 (100) | 17 (100) | 14 (100) | 30 (100) | 20 (100) | 18 (100) |
| Median score (IQR) | 4.5 (2.5–9.0) | 4.0 (3.0–7.0) | 5.5 (4.0–11.0) | 2.0 (1.0–9.0) | 5.5 (2.5–8.0) | 4.0 (3.0–6.0) |
| Range | 0.0–15.0 | 0.0–13.0 | 0.0–15.0 | 0.0–16.0 | 0.0–11.0 | 0.0–17.0 |
| Externalising problems: sum of hyperactivity and conduct, score range 0–20 | ||||||
| Forms returned, n (%) of those randomised | 32 (97) | 17 (52) | 14 (42) | 30 (100) | 20 (67) | 18 (60) |
| Useable forms, n (%) of those returned | 32 (100) | 17 (100) | 14 (100) | 30 (100) | 20 (100) | 18 (100) |
| Median score (IQR) | 7.0 (3.0–9.0) | 5.0 (4.0–9.0) | 8.0 (3.0–11.0) | 4.5 (2.0–7.0) | 6.8 (3.5–10.0) | 4.5 (3.0–7.0) |
| Range | 1.0–13.3 | 2.0–13.0 | 1.0–12.0 | 0.0–15.0 | 0.0–18.3 | 0.0–15.0 |
| SRQ warmth: score range 1–5; higher scores indicate higher levels of warmth in relationship | ||||||
| Forms returned, n (%) of those randomised | 33 (100) | 17 (52) | 14 (42) | 30 (100) | 19 (63) | 18 (60) |
| Useable forms, n (%) of those returned | 30 (91) | 14 (82) | 10 (71) | 24 (80) | 15 (79) | 15 (83) |
| Mean score (SD) | 3.1 (0.8) | 3.1 (0.6) | 3.1 (0.7) | 3.4 (0.5) | 3.4 (0.9) | 3.6 (0.7) |
| Range | 1.0–4.3 | 2.0–4.2 | 1.5–4.0 | 2.3–4.3 | 2.0–5.0 | 2.5–4.8 |
| SRQ conflict: score range 1–5; higher scores indicate higher levels of conflict in relationship | ||||||
| Forms returned, n (%) of those randomised | 33 (100) | 17 (52) | 14 (42) | 30 (100) | 19 (63) | 18 (60) |
| Useable forms, n (%) of those returned | 30 (91) | 15 (88) | 10 (71) | 28 (93) | 18 (95) | 17 (94) |
| Mean score (SD) | 2.0 (0.9) | 2.2 (0.9) | 2.4 (1.3) | 1.9 (0.7) | 2.1 (0.8) | 2.1 (0.7) |
| Range | 1.0–4.0 | 1.0–4.5 | 1.0–4.3 | 1.0–3.3 | 1.0–3.5 | 1.0–3.0 |
Higher scores on the anxiety and depression subscales of Hospital Anxiety and Depression Scale (HADS) indicate higher levels of anxiety and depression. The score range is 0–21 for both subscales. The mean baseline score of the anxiety component was 10.6 (SD 3.7) in the control group and 10.1 (SD 4.4) in the intervention group. This compares with the UK average of 6.14. At 12 months post randomisation, mean scores were 9.9 (SD 4.4) and 8.0 (SD 4.4) in the control and intervention groups, respectively. Similarly, depression scores in the participants were higher than the UK population norm (3.68) and some reduction in score was observed in the intervention group, which was not reflected in the control group. All completed questionnaires were of a useable standard. See Appendix 4 for further information on proposed secondary outcomes.
Multilevel regression analysis comparing intervention with control group, adjusting for baseline score and site
The results from the exploratory multilevel regression are given in Table 14 for each of the parent-reported secondary outcome measures. The mean WEMWBS score in the intervention group was 3.96 points higher than in the control group (95% CI –1.39 to 9.32) at 12 months post randomisation. As previously stated, this is a feasibility study and so it was not powered to detect an effect size of a given value. However, the authors of the measure indicate that, when comparing groups, half a standard difference is said to be meaningful (approximately 5 points in this instance) and in the case of individuals a ± 3-point change in score is said to be meaningful.
| Measure | n | Two-level model | |
|---|---|---|---|
| Estimate | 95% CI | ||
| WEMWBS | 47 | 3.96 | –1.39 to 9.32 |
| HADS | |||
| Anxiety | 50 | –1.62 | –3.39 to 0.15 |
| Depression | 50 | –1.30 | –2.89 to 0.28 |
| Total: emotional distress | 50 | –2.89 | –5.83 to 0.04 |
| VABSa | |||
| Composite | 42 | 0.42 | –3.03 to 3.88 |
| Communication | 42 | –1.17 | –6.83 to 4.50 |
| Family APGAR Scale | 50 | 0.49 | –0.90 to 1.88 |
| Family Support Scale | |||
| Count informal sources | 49 | –0.82 | –1.94 to 0.29 |
| Count formal sources | 49 | –0.60 | –1.04 to –0.16 |
| Mean helpfulness: informal | 49 | 0.15 | –0.24 to 0.55 |
| Mean helpfulness: formal | 49 | 0.40 | –0.22 to 1.02 |
| Positive Gains Scale | 47 | 0.18 | –2.06 to 2.41 |
| CPRS | |||
| Conflict | 50 | –0.78 | –3.89 to 2.32 |
| Closeness | 45 | 0.60 | –1.33 to 2.53 |
| Child–Parent Activity Index | 51 | 0.22 | –1.24 to 1.68 |
| Happiness of Relationship Scale | 42 | 0.33 | –0.51 to 1.17 |
| Co-Parenting Agreement Scale | 39 | 0.06 | –0.80 to 0.93 |
| Conflict | 41 | –0.12 | –1.13 to 0.89 |
| EQ-5D | |||
| VAS | 50 | 1.70 | –5.81 to 9.22 |
| Index value | 50 | 0.04 | –0.04 to 0.12 |
| Brief COPE | |||
| Active avoidance | 50 | 0.46 | –1.14 to 2.06 |
| Problem focused | 50 | 0.16 | –1.35 to 1.68 |
| Positive coping | 50 | 0.52 | –1.12 to 2.22 |
| CBCL | |||
| Internalising score | 41 | –2.80 | –7.60 to 2.00 |
| Externalising score | 41 | –1.86 | –5.55 to 1.82 |
| Total problems | 41 | –9.00 | –20.79 to 2.88 |
| Paediatric Quality of Life Inventory total score | 46 | 7.0 | –1.84 to 15.78 |
| SDQ: siblings | |||
| Prosocial | 32 | 0.5 | –1.07 to 2.17 |
| Internalising score | 32 | –1.6 | –4.32 to 1.12 |
| Externalising score | 32 | –0.6 | –3.47 to 2.37 |
| Sibling Relationship Questionnaire | |||
| Warmth | 19 | 0.1 | –0.63 to 0.84 |
| Conflict | 25 | –0.3 | –0.84 to 0.3 |
By further example, the anxiety score, as measured by the HADS, was 1.62 lower in the intervention group (95% CI 3.39 lower to 0.15 higher) and depression score was 1.30 lower (95% CI 2.89 lower to 0.28 higher). With the exception of the ‘count of formal sources’ section of the Family Support Scale, effect sizes in all secondary outcome measures are suggestive of positively favouring the intervention group. Even in this instance, however, despite the number of formal sources of help available being lower in the intervention arm than in the control arm at 12 months, the helpfulness rating [rated between 0 (not at all helpful) and 4 (extremely helpful)] of these sources when they existed was 0.40 higher in the intervention group (95% CI 0.22 lower to 1.02 higher).
Residual plots of the models were checked and the normality assumption was reasonably met; however, in a larger study where the estimates of between-group differences is of primary importance, variable transformation may be required.
Acceptability of proposed outcome measures
Participants described that questions sometimes required adoption of a best-fit approach; for example, some parents thought that questions were not applicable because of the age/developmental stage of the child:
. . . like it always is with questionnaires, the answers didn’t always fit. You felt that you were choosing the answer but really your answer needed a bit more nuance.
Participants described difficulty in recalling data required to answer the resource use/health economics questions:
. . . we did need to sit down and check both our diaries ‘did you take him to that doctor, that was a year ago’, or ‘there’s a speech and language that you took him to’, ‘oh and there’s one that you took him to an eye appointment’ so we would be relatively organised because we have to be because with so many appointments we don’t want to miss anything but I can imagine, I don’t know your demographics, but I would assume that if you were maybe a single mum or a different type of person than us it would have been quite hard to find all the information because it went quite far back.
Participants identified an error in the scale of the parenting sense of competence measure:
So the tend to agree or tend to disagree actually sounded more negative or more positive than the other one. So the scales weren’t great and some of the questions were a bit ‘what do you mean by that?’
Participants said that the language section of the Child Behaviour Checklist was difficult to complete because of the volume of words and difficulties in recall:
But in terms of the questions, I think none of the questions were particularly hard apart from maybe the number of words he had and what words he had.
One participant questioned the relevance of the finance questions in the study:
I didn’t know why it was relevant to ask about the financial things ‘could you find this X amount of money in this time?’ The purpose of the study it’s about the child and it’s about his needs and the family adapt and help manage the child so I don’t know why financial came into it, that would be one thing. Disability doesn’t really discriminate against class. Everything else was grand. Similar questions have been asked of me, by therapists, but I did find it a bit intrusive. Why do I need to go over . . . ? I don’t know what relevance it has. Maybe it’s about social background and how well the child comes on and maybe if people . . . I don’t know.
The FMSS was used at baseline with all study participants. Participants were generally apprehensive prior to completion of the FMSS. For example, some participants thought that the experience would be difficult and uncomfortable. However, there were contrasting views regarding the difficulty of completing the measure. Although some participants described the experience as ‘OK’ or ‘fine’ and less demanding than they expected, other participants described the experience as difficult and ‘emotional’. Some participants did not like the measure being unstructured and felt unnerved, as though they were being tested. At the 3-month follow-up, some participants described how they declined to complete the measure because it was so demanding:
Yeah. I think the second time I declined to do that bit just because I didn’t feel I had 2 minutes worth of talk in me.
I was thinking it was gonna be difficult and the first time when I done the recording I actually prepared little notes for myself but once I started talking and she told me ‘that’s it, finished’ and I was like ‘Oh, OK . . . it was fine. I was actually surprised at how a lot I had to say about [study child].
It is also possible that completing the measure over the telephone was not appropriate. One participant described the lack of body language/gestures from the researcher while completing the measure over the telephone intimidating:
But it is a wee bit unnerving because you are not doing it face to face so you don’t get any reaction you just have silence at the other end of the phone. So it can be a bit unnerving. You feel like you are being tested. Five minutes seems to be quite a long time when you’re talking about the child . . .
Feasibility testing of the intervention
Objective: the feasibility of recruiting suitable service provider organisations and facilitators to deliver the E-PAtS intervention
The feasibility of delivery of recruiting suitable service provider organisations is discussed and the acceptability of facilitator training, as detailed in qualitative interviews, is reported.
Recruitment of service provider organisations
Service providers for this study had been identified through the research team’s contacts and Mencap had provided a supporting letter for the funding application. Therefore, no process of service provider recruitment was required during the feasibility study.
Facilitators selected to deliver intervention
Although E-PAtS had been previously delivered in Northern Ireland, a new cohort of facilitators was recruited and trained to deliver the intervention at all three sites. In accordance with E-PAtS protocols (see Chapter 2), facilitators included both professionals and family carers. Facilitators were recruited by Mencap Northern Ireland and the local Mencap Barnet group, with support from the E-PAtS programme developers. Facilitator job descriptions were available that detailed desirable skills, attributes and experiences for facilitators. Professional facilitators were all pre-existing members of staff within the provider organisations. Family carer facilitators were parents of children or adults with a disability who were subsequently paid by provider organisations to attend training and deliver the intervention. As is standard for the E-PAtS programme, facilitator training was conducted in group format (with a combination of family carer facilitators and professional facilitators) over a 5-day period and was led by an E-PAtS programme trainer. One training group was co-ordinated in site 2 and another covered both sites 1 and 3. Training comprised theory and practical exercises and all facilitator pairs were supervised by an E-PAtS programme trainer during their first delivery of the programme (which included all interventions in the trial at sites 1 and 3 and the first intervention group at site 2).
Site 1
Two facilitator pairs delivered E-PAtS groups to families in the intervention arm at site 1. This comprised one male family carer facilitator and female professional facilitator dyad who delivered one group, and one female family carer and female professional dyad who delivered a second group.
Site 2
Five facilitators were involved in delivering E-PAtS groups to families in the intervention arm at site 2. A female family carer facilitator and female professional facilitator delivered all sessions for two of the groups together. A further female family carer facilitator, female professional facilitator, and a female facilitator who was both a family carer and professional worked in combination to deliver a third group (with a dyad that reflected a family carer and professional ensured in each case).
Site 3
Three facilitators were involved in delivering the E-PAtS programme to a group of families in the intervention arm in site 3. This comprised one male family carer facilitator who delivered all sessions for the group, one female professional facilitator who delivered three sessions and one female professional facilitator who delivered five sessions.
Acceptability of facilitator training
Facilitators reported having enjoyed the training. They commented positively on the quality and depth of the information and the fact that information provision took place alongside seeking the views/experiences of trainee facilitators. These aspects of the training had helped those participating to ‘make sense’ of the information provided and the rationale for the different activities that were delivered to family carers during the programme:
We learnt quite quick but it was quite in depth so we went into quite a lot of psychology and the basis behind what makes the training work, not what we were going to teach the parents particularly but to give that understanding of the background that formed it and the science behind it I suppose and that was very useful to draw on during our training . . .
Guidance on practising strategies to manage emotions (of the self and others) in the groups was seen as useful. Training covered (and emphasised) the creation of a suitable environment for running the groups (e.g. not judging people), which was valued. These positive assessments of the training course led participants to feel that they had received the training and information they needed to be able to deliver programme sessions to families.
Objective: adherence to the intervention, reach and fidelity of implementation of the E-PAtS intervention through attendance records, evaluation of session recordings and participant/facilitator qualitative interviews
Intervention adherence is discussed both in the context of attendance patterns and in barriers to and facilitators of attending, as discussed in qualitative interviews. Intervention fidelity is assessed through the evaluation of session recordings and self-completed checklist.
Intervention adherence
The E-PAtS intervention was attended by:
-
main family carers recruited to the study
-
second family carers recruited to the study
-
second family carers or family members not recruited to the study (i.e. non-study attendees).
Main family carers were eligible if they could attend the E-PAtS intervention. Eligibility for second family carers was not dependent on availability for intervention sessions. However, second family carers were invited to E-PAtS group sessions. In addition, some family members who did not take part in the study (for unknown reasons) later expressed an interest in attending the E-PAtS group sessions. These family members attended as non-study participants and, for these family members, only attendance data were collected.
Adherence to the E-PAtS programme was defined as at least one family carer from a family attending five of the eight E-PAtS sessions (see Chapter 2). According to this definition, 26 out of 37 families adhered to the intervention (70.3%). In terms of session attendance, four families attended zero sessions (10.8%) and seven families attended all eight sessions (18.9%). The modal number of sessions attended by a family was seven (11/37 families, 29.7%) (Table 15).
| Adherence and session attendance | Category | Intervention families (N = 37), n | % |
|---|---|---|---|
| Five or more sessions by at least one family member | Not adherent | 11 | 29.7 |
| Adherent | 26 | 70.3 | |
| Number of sessions attended by at least one family member | 0 | 4 | 10.8 |
| 1 | 0 | 0.0 | |
| 2 | 2 | 5.4 | |
| 3 | 0 | 0.0 | |
| 4 | 5 | 13.5 | |
| 5 | 6 | 16.2 | |
| 6 | 2 | 5.4 | |
| 7 | 11 | 29.7 | |
| 8 | 7 | 18.9 | |
| Number of sessions attended by main family carer | 0 | 4 | 10.8 |
| 1 | 1 | 2.7 | |
| 2 | 3 | 8.1 | |
| 3 | 2 | 5.4 | |
| 4 | 6 | 16.2 | |
| 5 | 5 | 13.5 | |
| 6 | 1 | 2.7 | |
| 7 | 9 | 24.3 | |
| 8 | 6 | 16.2 |
Warwick–Edinburgh Mental Wellbeing Scale scores at baseline and 12 months by adherence and attendance
Figures 2–7 illustrate WEMWBS scores by adherence and attendance. Descriptively, there is some evidence to suggest that average WEMWBS scores are higher with adherence and increasing attendance. However, higher average baseline scores for those with adherence or attendance was also observed.
FIGURE 2.
Warwick–Edinburgh Mental Wellbeing Scale scores at baseline and at 12 months post randomisation by adherence. Plot created for those participants with both baseline and 12-month WEMWBS data available.

FIGURE 3.
Warwick–Edinburgh Mental Wellbeing Scale scores at baseline and at 12 months post randomisation by family attendance. Plot created for those participants with both baseline and 12-month WEMWBS data available.
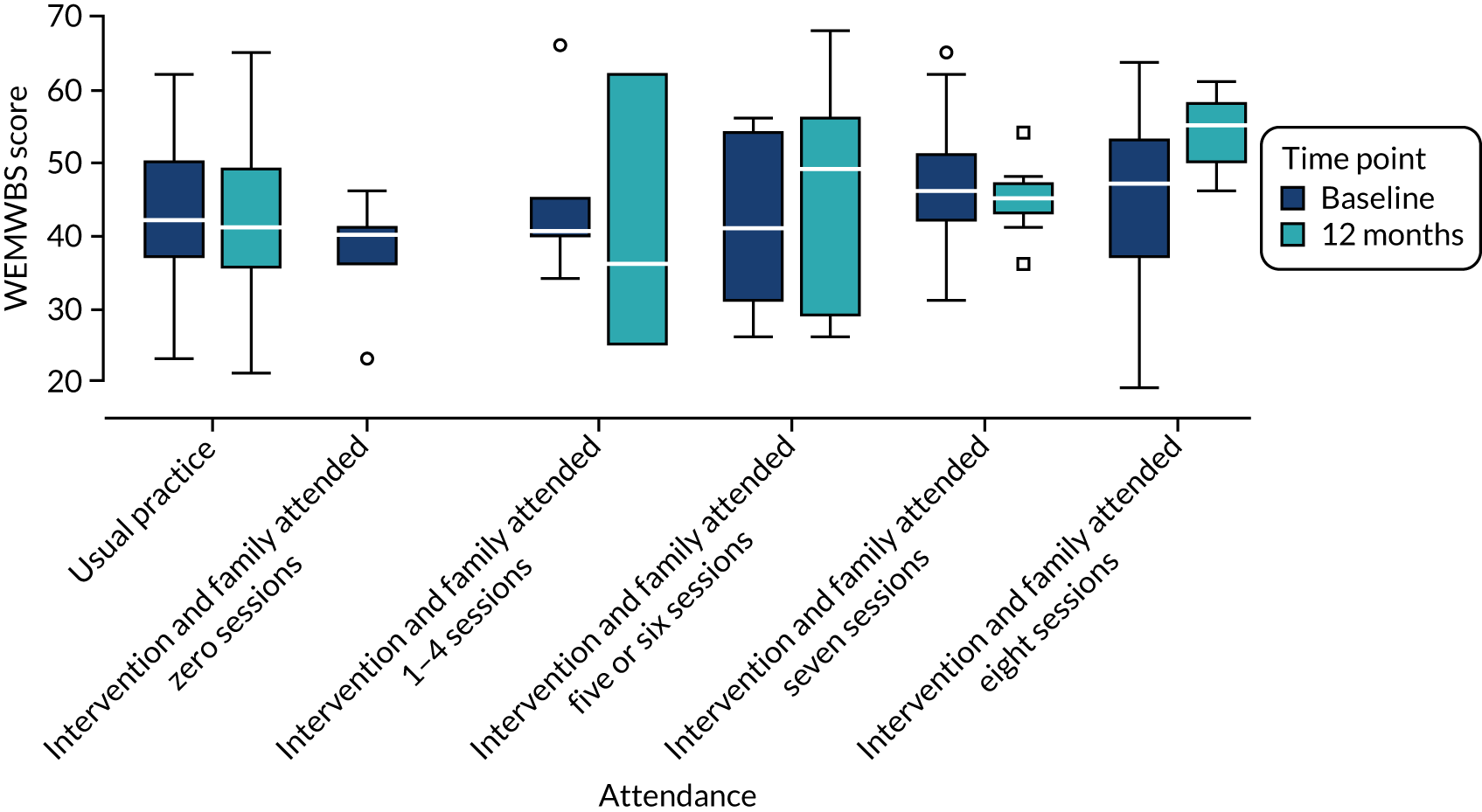
FIGURE 4.
Warwick–Edinburgh Mental Wellbeing Scale scores at baseline and at 12 months post-randomisation by main family carer attendance. Plot created for those participants with both baseline and 12-month WEMWBS data available.
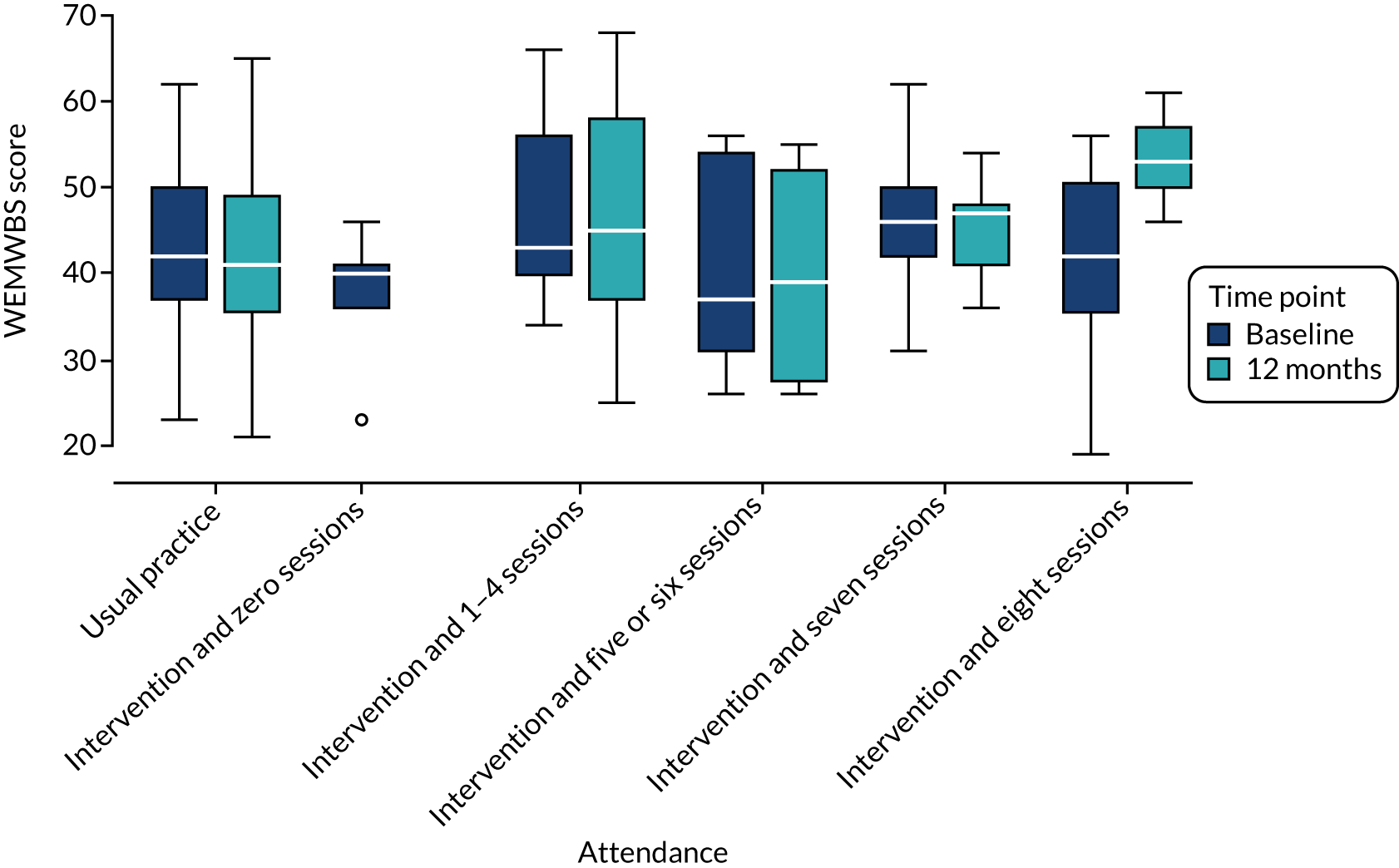
FIGURE 5.
Relationship between adherence group and availability of WEMWBS at 12 months.
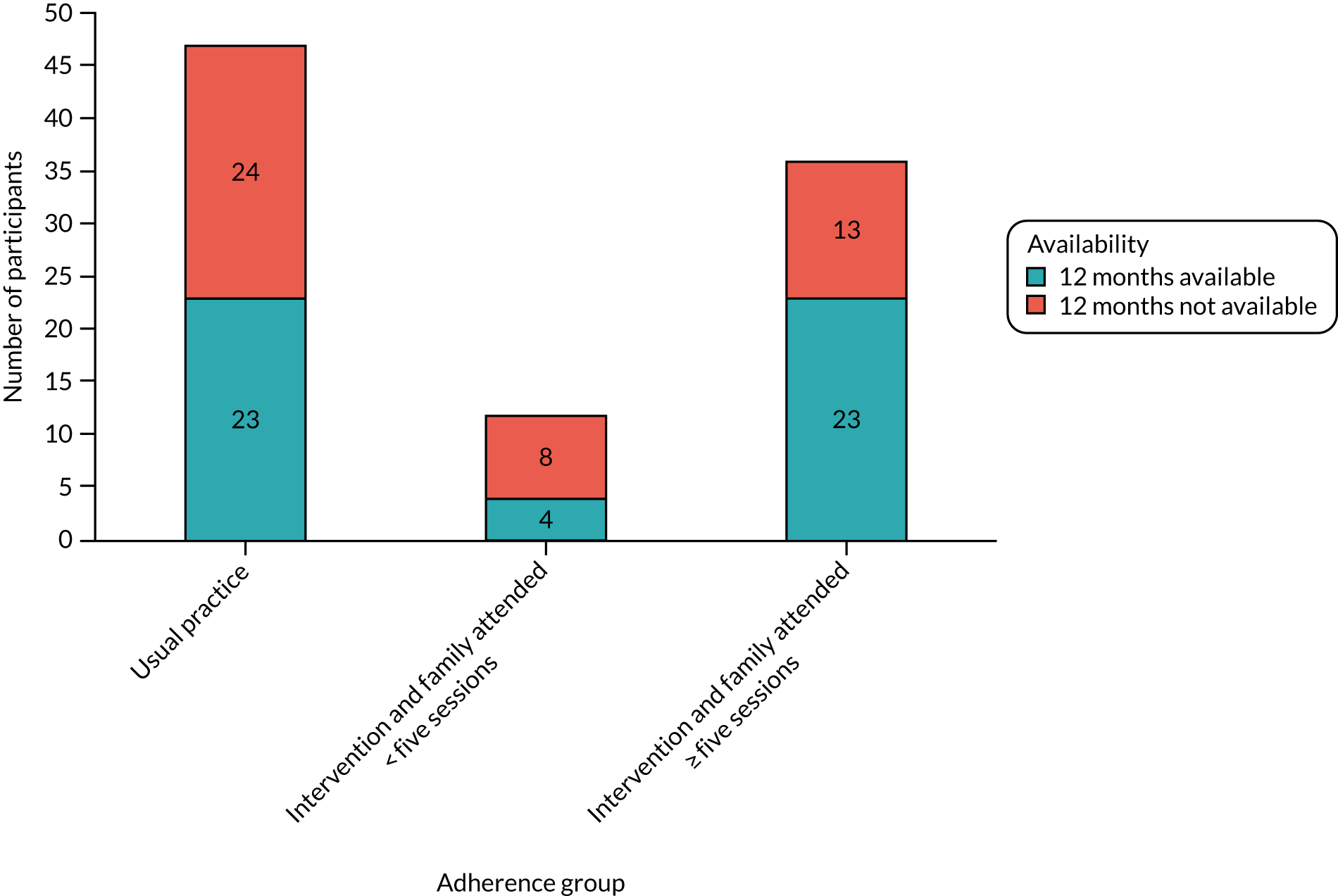
FIGURE 6.
Relationship between family attendance and availability of WEMWBS at 12 months.
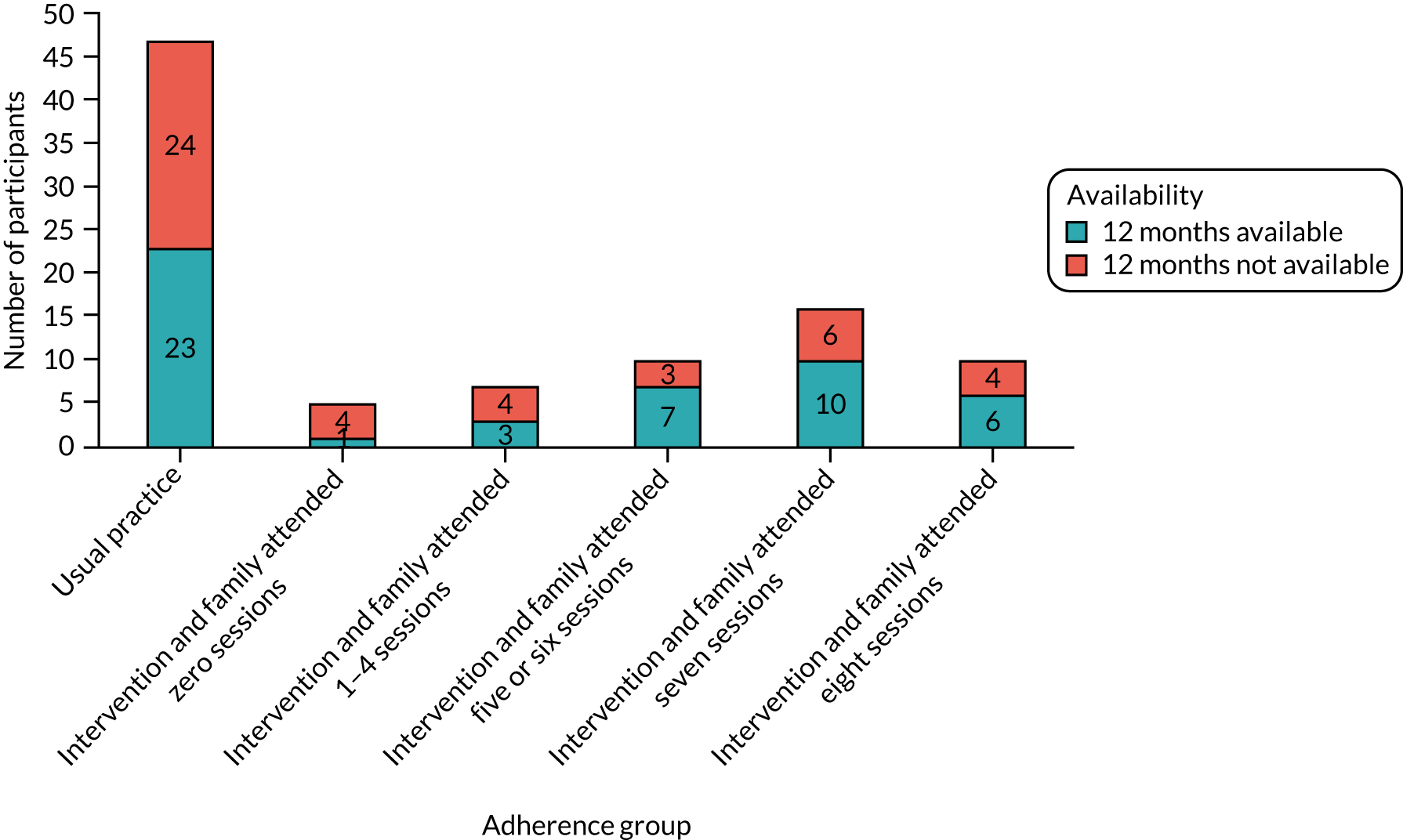
FIGURE 7.
Relationship between main family carer attendance and availability of WEMWBS at 12 months.
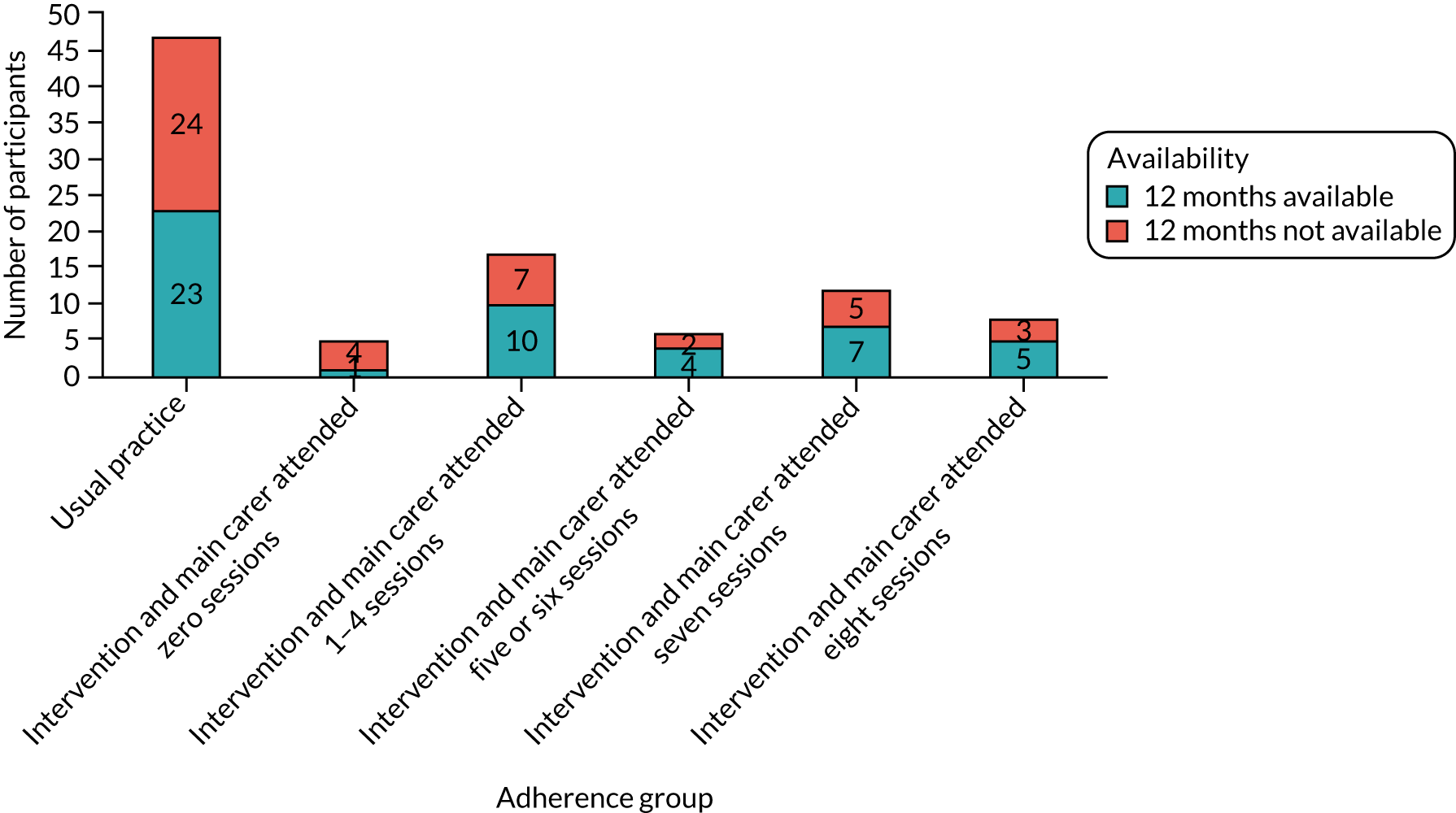
Relationship between adherence, attendance and availability of proposed outcome data
Figures 5–7 illustrate that adherence and attendance were associated with the availability of the WEMWBS at 12 months. This pattern was clearest for adherence, with availability of WEMWBS scores at 12 months being higher for participants with higher levels of adherence.
Exploratory complier-average causal effects analyses
Table 16 provides the original analysis of the proposed primary outcome for a definitive trial (i.e. WEMWBS at 12 months): an equivalent analysis using a single-level model with SEs inflated for clustering of participants within families and findings from the CACE analyses. The models imply that the effect of receiving the intervention (rather than just being randomised to it) either as adherence or as increasing attendance is associated with further gains in well-being at 12 months post randomisation.
| Model | Adjusted mean differencea | 95% CI |
|---|---|---|
| Two-level model | 3.96 | –1.39 to 9.32 |
| Single-level modelb | 4.38 | –1.02 to 9.78 |
| IV regression accounting for adherenceb | 5.05 | –0.70 to 10.79 |
| Maximum efficacy based on family session attendance | 5.84 | –0.80 to 12.40 |
| Maximum efficacy based on main family carer attendance | 6.84 | –0.84 to 14.53 |
| Maximum efficacy based on main family carer attendance, main family carer responses only (n = 36) | 4.85 | –3.71 to 13.41 |
Barriers to and facilitators of E-PAtS attendance
A number of barriers to participants attending sessions were discussed in qualitative interviews. Responsibilities at home, including child care, or if another family member had an event or illness/medical appointment, resulted in participants not attending sessions. In addition, work responsibilities, including working shift patterns or difficulties arranging time off with employers, were a barrier. These were also provided as reasons why partners did not attend the sessions, as one family carer may have been required to work or stay at home. Finally, the length of the journey to the venue and/or unreliable public transport affected attendance rates:
It was just getting somebody to look after [name] I suppose because he does have complex needs and I can’t just leave him with anybody. That was probably the biggest challenge.
. . . our older children do various after school activities and things like that, football Thursday nights or the night it was on . . .
The only thing for me would be the availability of it because of my shift pattern, I mean my shift pattern is a terrible shift pattern, but it just meant I didn’t get the full benefit out of it.
Fidelity: evaluation of session recordings
A total of seven observation recordings (two of which were video-recordings and the remainder were audio-recordings) were available for analysis. These covered sessions 4 (n = 1), 5 (n = 2), 6 (n = 2) and 8 (n = 2) and all intervention deliver sites (site 1, n = 4; site 2, n = 1; and site 3, n = 2). One of the recordings covered an entire session, with the majority capturing part of a session.
On average, 95.7% (range 88–100%) of checklist items were observed to occur in recordings, with 100% of items observed during four of these recordings (Table 17).
| Session | Percentage of checklist items completed |
|---|---|
| Site 1 | |
| Session 4 (video) | 94 |
| Session 5 | 100 |
| Session 6 | 100 |
| Session 8 | 100 |
| Site 2 | |
| Session 6 (video) | 100 |
| Site 3 | |
| Session 5 | 88 |
| Session 8 | 88 |
Five (27.8%) out of a total of 18 group sessions were not recorded because of technical issues or errors. Two (33.3%) out of six groups did not provide consent to record the group sessions. Evidence from qualitative interviews suggested that participants may not have felt comfortable with the recordings because of the sensitive nature of the group discussion:
I think maybe definitely not the videos, where you’re filming people but recording, that’s OK, but I think you need to take the video, because nobody wants their face in that, especially if they’re talking about something so important and close to them, they want people . . . their reaction and how they’re gonna speak, they want people to feel free to do it. If they’re being filmed that’s a big no, no to me. If it was me sitting there I wouldn’t want to be on camera talking about somebody like that.
Fidelity to curriculum components
Facilitators were asked to complete a session summary form at the end of each session to indicate what session components were completed. Per cent of components delivered ranged from 85% to 100% (97.1% overall) (Table 18).
| Group, site | n/N (%) complete |
|---|---|
| Group 1, site 1 | 189/199 (95 complete) (did not return session 8) |
| Group 2, site 1 | 195/199 (98) (did not return session 8) |
| Group 1, site 2 | 174/174 (100) (non-attendance meant that sessions 7 and 8 did not run) |
| Group 2, site 2 | 203/203 (100) |
| Group 3, site 2 | 200/203 (99) |
| Group 1, site 3 | 80/94 (85) (some sessions missing data) |
| Total | 961 components (97.1) |
Factors affecting implementation fidelity
Data from qualitative interviews with facilitators indicated that facilitators believed that they had succeeded in delivering most session activities with good fidelity. Facilitators appeared to be committed to delivering the programme as intended and felt confident in doing so. This was linked partly to receipt of the facilitator training, which had helped them to understand the purpose and ordering of activities:
I actually fully understood the aims and how to get those key messages across. I understood, along with my parent [facilitator], the function behind each session and how they all sort of linked in and carried through and we were able (from the feedback we got at the time) we were able to actually get those messages across.
Practitioner
The provision of a facilitator manual was also seen as helpful in enabling smooth progress through key activities. A number of facilitators described the importance of the time they spend preparing for each session in enabling them to deliver programme activities effectively:
I personally took a lot of time to prepare because that just is how I am, I’m not good at . . . I like to do a lot of preparation before, I’m not comfortable with ad hoc and just doing things. I much prefer to really prepare on things so it was fine. I think if I’d have had to do it without much preparation that would have worried me, but I had a chance every week to have a good think. I used to spend a day before planning what I was going to say and how that was going to go, that was always needed for me. I’ve never thought ‘we don’t need to sit down’. It always helps me.
Facilitator
The importance of creating effective partnerships between co-facilitators was also highlighted:
. . . with the first person that I facilitated with we just we worked really well together, I think. It was quite a natural partnership I think between me and [name of co-facilitator] and we were agreeable to keep to time and we did manage to get most the information that we wanted to from each session, I don’t think there was any week that we didn’t get through it all and we pretty much kept to time.
Facilitator
We had a great relationship with loads of preparation time together and everything went smoothly. We felt the same about how each session went and difficulties. We did have a couple of difficulties with one carer and we were able to come to an agreement on how to handle it and it was fine, it was all good.
Facilitator
Facilitators described being aware that some flexibility in the focus of group discussions, such as on an aspect of the material that had particular relevance for them, was permitted, as long as all intended intervention activities were covered:
I think [trainer] was happy enough if you were asked a direct question or you knew something yourself that could help a family or if you could explain something in a different way, I think he was more than happy for you to do that. As long as you cover the content and don’t leave great chunks of it out, as long as you get through all the content, the way you do it I think he led us to believe that was fine. There has to be room, you’re not just standing there like a robot reading it, you’re interacting with people and respond to how or what questions they’re asking you, I don’t think that would ever be an issue.
Facilitator
A key skill that facilitators described employing was deciding to what extent group discussions around a particular point (including those not directly related to the focus of the intervention session) should be allowed to continue before bringing participants back to the planned material:
Err well I mean we managed to cover everything that was in the course. As I said sometimes these digressions to other more pressing issues that were on people’s minds. So, someone would come along and say, ‘I visited such a such school yesterday and I’m getting this advice, and I’m getting this advice from people’ and then we’d go on to that topic for a bit, but I don’t think you can change the course of that it’s just you need to have a little bit of flexibility to allow people to offload, I guess, what’s really on their mind.
Facilitator
When children of participants were present in the session, this could make covering planned activities more difficult. Likewise, practical issues, such as problems with Wi-Fi connections (for access to programme videos), were also mentioned by facilitators.
Objective: the acceptability of intervention delivery to service provider organisations, facilitators and family carers through qualitative interviews
The acceptability of intervention delivery to participants and service provider organisations is reported in the context of intervention receipt and perceived impacts of the E-PAtS programme. Key mechanisms through which the E-PAtS programme works are discussed.
Intervention receipt
Parents were overwhelmingly positive about the group atmosphere. Participants enjoyed the informal and friendly environment:
I did expect when I went to be in a big huge board room and there would be lots of people there and it would be very formal and everything . . . but it was very intimate, everyone was very friendly, everyone was on first name terms – it was just appreciated.
Peer support was an important aspect of the group sessions. Participants described how the interactive nature of the group allowed participants to share valuable experiences with one another in a confidential manner. Participants attending the group with other parents who had experienced similar situations to themselves was considered an important aspect of the course.
Participants described how they appreciated that they did not feel judged and were supported by the facilitators and other members of the group. Facilitators spoke about how the group members were very supportive of one another, despite the sensitive content of the course:
I think everybody was prepared to open up and speak frankly and there was an understanding that what was said in the room stayed in the room and I think people did feel able to open up and kind of wanted to support each other.
We were openly talking about our problems without thinking that we were being judged or anything.
. . . there was a lot of emotion in every group that I had, there was a lot of different emotion and upset, and a lot of support.
Facilitator
However, in contrast, it was suggested that a lack of cohesion in one group may have been due to variations among group members in the current challenges being faced by parents and the child’s clinical diagnosis:
I thought it would have been better to be honest. I think it was because the children were so different. Again, in an ideal world if you were able to separate the group into children with autism and behavioural challenges, and children with complex needs and medical issues I think there would have been more cohesion between group members, but we were all so different.
The group sessions were described as informative, but interactive and not didactic. Participants described the programme content positively and found the handouts a useful reference tool at the time and subsequent to the course end. Participants were satisfied with facilitators’ knowledge and willingness to provide extra resource when requested or helpful. Practical activities seemed popular and beneficial among group members, particularly an activity in session 4 that was used to demonstrate the frustration children may experience when trying to communicate. Furthermore, participants appeared to appreciate the role-play exercises, despite initial apprehension:
. . . it’s fantastic that you’re able to have almost like a manual to go back to, to sort of just refer to.
. . . it was easy for us to ask any questions and they answered them. Sometimes they tried to find even much more information than was in the handouts.
. . . you had to try and communicate what is on this page for the other person to draw and it was virtually impossible and that really had us in tears, I was like ‘oh I feel so sorry for him!’ That was massive. That really . . . I found very, very hard but also a brilliant way of understanding where he was at.
The course was evidence based and this allowed parents to understand the reasons behind certain behaviours that their child showed:
I liked the grounding of the topic in research and evidence.
However, some parents described how the information provided was quite basic or that they were being provided with information of which they were already aware. There was conflicting feedback regarding the relevance of some of the programme content. Although some strategies (e.g. sleeping/eating) were considered irrelevant for children with certain medical conditions, other parents described how all of the topics were relevant:
. . . there was quite a lot of information I already knew from various things I’ve read a lot myself, been to various things.
. . . he’s physically sick and has to be up on suction so he wants to sleep but because of his medical interventions he can’t. So there’s no quick fix for that.
Participants were overwhelmingly positive about the E-PAtS programme facilitators. Participants praised facilitators’ professionalism and described how well the groups were facilitated, particularly when faced with difficult situations in the group or dominant personalities. Participants appreciated the preparation involved in organising the groups, such as the professional presentation of information and additional touches, such as refreshments. Additional information, often local information and not part of the course content, was also provided by facilitators if requested:
They were very friendly, very open, you know. They don’t judge anybody, so it was very OK. They did it very well, they handled it very, very well.
So yes, there’s a big dynamic but the course leaders handled it very well.
It was clear that the people who were delivering the course had spent ages getting the presentation set up and supplied biscuits and good coffee.
Facilitators were described as empathetic and genuine. Participants valued family carer facilitators sharing past experiences and ideas, and were comforted by the fact that facilitators had ‘walked the road themselves’:
. . . the way they talked about their own experiences, you were sitting there thinking ‘oh my goodness, they’ve been through this’ and it was lovely to hear, it made you warm inside (I know that sounds corny!) but it made you think ‘oh I can do this, they’ve been through this, they’re out the other side (I suppose) of this’ and it was really reassuring.
. . . very sympathetic to everyone and the stage that everyone was going through so that was nice rather than someone who had just been there and who basically didn’t have a clue what you were going through.
Participants also appreciated the additional effort facilitators made to source local and individual information:
What was interesting was that a lot of the stuff that we could get support with was based in Mencap and that London area, so I couldn’t access any of that support because I don’t live there, I live in Kent. So what was lovely the following week the lady came back with a list of all the stuff in my local area. She spent time looking for it in kind of Folkestone and Dover which is where I live, which is really lovely, you know.
Facilitators reported that most participants were receptive to the content of the group sessions; however, a minority of participants did not engage fully. Strategies taught in the group sessions were attempted at home and discussed subsequently in group sessions. Most participants appeared comfortable to share experiences in the group setting and facilitators described speaking to participants individually if they felt it was necessary:
. . . we had some who were really appreciative of the information we were feeding to them and then we had one or two that I felt like perhaps it was not necessary for them or it might have been various reasons that they felt we were not giving them anything new or they’d heard it all before.
I’ve always worried before I delivered that somebody would say ‘oh that’s not going to work for me’ or ‘that’s stupid that won’t work’ that kind of negative opinion but it never came up, people were always very receptive to things.
. . . that was important as well, to try and help them say what they needed to say but if they wanted to do it later on a 1 : 1 basis that was fine.
Perceived aims of the E-PAtS programme
Facilitators were questioned about what they considered the intervention aims to be. Empowering family carers in a person-centred course was considered a key aim to enable parents to ‘become experts’ on their child and not just to learn through didactic teaching. Peer support was considered an important mechanism by which the E-PAtS programme works. For example, facilitators spoke of the value of understanding other parents’ struggles and learning strategies from other parents. Additionally, facilitators recognised that family carers may have previously felt isolated prior to the course and that it was valuable to meet other family carers in similar situations. A key aim of the E-PAtS programme was to provide information and also signposting to support services currently available. Family carers were taught to understand their child’s more difficult behaviours and to have realistic expectations following the course. Finally, the importance of family carers looking after themselves was instilled throughout the course:
It wasn’t experts lecturing parents, because I think parent/carers have had enough of that. It was sharing their own experience and their own struggles and valuing the parents input which I think is quite strong in the ethos of E-PAtS.
. . . at the end of every module it was ‘you can only do so much, so look after yourself first’.
. . . the big thing is breaking the isolation for people who may have been the first experience they have of having conversations with other parents.
I suppose for me it was providing the information to people around the particular areas that were covered in the course. So, you know, the sleep, challenging behaviour, the communication, the life skills, looking after yourself.
They’re not unrealistic. There’s no magic wand at all . . . We wouldn’t say to someone ‘we’ve got a magic wand; we’re gonna cure these sleep problems’.
Key mechanisms through which the E-PAtS programme works
In qualitative interviews, family carers and facilitators described four main processes through which learning and potential impacts from the E-PAtS programme occurred: (1) peer support, (2) direct learning from intervention activities/materials, (3) the sharing of learning with other family members and (4) signposting to sources of further support. First, as noted above, peer support appeared to comprise multiple dimensions, including reducing isolation, creating a safe space in which to share experiences, the normalisation of these experiences and the opportunity to learn from others in a similar situation. Group dynamics and interaction therefore helped to generate learning and support, which, to some extent, transcended or cut across specific activities and developed during the course. When participants missed one weekly session, facilitators would often provide a recap or catch-up the following week, and some group discussions carried over from one week to the next:
. . . at the end we had one lady who came to probably the last two sessions so we had to try and catch up with her, put her up to speed on what we’d been discussing up to that point. So it was like, even though the other parents were happy for us to do that because then they could sit there and reflect on what they were talking about before and we didn’t make it long-winded, we just kept it short and brief, just so that one parent . . . and we said ‘do you mind?’ and they were ‘oh no, no, we don’t mind because we can’t remember some of it so we don’t mind hearing it again’.
Facilitator
The second process (i.e. direct learning from E-PAtS programme activities) comprised the learning of new insights and strategies that parents/carers were introduced to during the programme by the facilitators, including the importance of self-care, understanding their child’s behaviour and, more generally, reflecting on the way in which they interacted with their child:
I didn’t even know that brushing teeth had different steps. I thought it was just brushing teeth, I didn’t know it was like opening the toothpaste and then putting a little bit on it and putting it in the mouth, it has different levels. I didn’t know these things so they told us and we found out how difficult it might be for my child.
1B01A
Third, and linked to individual-level learning, many shared this learning from the programme with family members, including encouraging them to adopt strategies acquired during the E-PAtS sessions:
That was a nice feeling as a facilitator that people came back and people were saying ‘this is amazing you know’, people were emotional and saying we went home and shared this with grannys and grandads and they used it; for example, the challenging behaviour section I remember one mummy said ‘my parents just think he is being naughty’, her child was autistic, ‘but when I showed them this information and explained it to them they kind of got it for the first time’. That’s incredible that that was going to change her life and potentially her child’s life because it was just looking at things in a different way.
Practitioner
There appeared to be some variation, however, in the response of family members to the sharing of learning from the programme and the ease with which it could be integrated within everyday home environments:
I did discuss with him but by the time I got home everything I said to him was ‘we had 3 hours of sessions’ and everything I said to him was less than 15 minutes because when I was telling him about it ‘OK, this is what we should not do, this is what we should do’ observation and all that, ‘OK, OK, OK but you understand everything I’ve said to you, right?’ and he said ‘yes’, ‘OK carry on’, it’s just the way they are, ‘alright . . .’. He didn’t really show any interest to learn from me, so he didn’t encourage me to say more sadly.
I shared it with the dad because I’m telling him ‘he has [?]’ so I’ve been able to share some stuff with him which he understands very well now.
Fourth, signposting of services was an important way in which families were linked to additional support and resources:
The first session as well was lots of signposting to organisations so having that information and knowing where they can go. A lot of them were already plugged in to [site 2] Mencap services so I think they would have already known who they could go to to ask for support, but hopefully E-PAtS has just kind of reiterated that. But for a parent who perhaps hadn’t done anything with Mencap before then it would have provided them with a lot of information that signposting.
Facilitator
I think what I think generally what I think is good about E-PAtS has really done lots for parents like me because it has allowed me to see that I am not alone, and having other parents share their experiences and it has really helped me calm down, knowing that I’m not alone. If I need to, if I’m worried or feel down at any point in time, I can easily approach the pre-school team and that’s really helped.
As can be seen from the above quotation, the sense of being connected to others encompassed professional support services and also a broader feeling of being connected to others.
Perceived impacts of the E-PAtS programme
Participants described improved mental health and positivity as a result of attending the E-PAtS group sessions. Participants described learning to ‘take care of themselves’ by allocating time for their own well-being. Participants described increased confidence both when managing their child’s challenging behaviour and when advocating for their child to medical professionals. Understanding why their child may demonstrate challenging behaviour resulted in participants handling their child’s ‘meltdowns’ better through improved patience and an overall ability to cope:
I was suffering from depression but now I’ve stopped taking my medication.
One of the daddy’s said ‘I haven’t been out on my motorbike in years and I just took myself out on my motorbike for a while’.
Facilitator
I’m not intimidated by doctors; if I don’t feel my son is getting the care he needs I will say something.
I don’t worry so much about people judging me if he’s having a meltdown in the middle of TK Maxx [Watford, UK] because I won’t get him a dinosaur he’s holding.
I’ve been able to know certain behaviours that come with autism, so I’m not surprised any more when he acts in certain ways.
There are times I go on the internet just to see what can I do and everything in there is stories, stories, stories. I don’t know what to do, I was just confused. So I cried, ‘what do I do? A beautiful little boy, what do I do with you?’. So when I went to the sessions it was so helpful, you cannot imagine.
Peer and professional support resulted in participants feeling acknowledged and ‘not alone’. Attending the E-PAtS programme resulted in improved parent–child relationships with siblings of the child with intellectual disability. For example, participants described improvements in communication and increased duration of quality time spent with other children.
Participants described acting on specific information provided in E-PAtS group sessions. Strategies for assisting with living skills, including sleep, brushing teeth, eating and dressing, were introduced at home. Parents also described breaking down steps of individual tasks, such as brushing teeth, to make difficult tasks more manageable for the child. Participants described establishing routines to encourage positive behaviours and discourage challenging behaviours. Participants encouraged independence by allowing the child to attempt to dress, wash or feed themselves, and encouraged other family members to do the same. Furthermore, participants described actively involving siblings in the child’s care, which in turn has had a positive impact on the child’s behaviour and sibling relationships:
. . . it was kind of the living skills, and the idea of breaking them down into parts of the task . . . I’d have to do that [brush teeth] for him, but he can go in the downstairs toilet and get his toothbrush and toothpaste and bring it to me and afterwards he can put it back and after I’ve brushed his teeth I can let him brush his teeth after.
. . . with the likes of routine ‘and put this into place’ because now on her [Grandma] wall I have this chart that we can now go down and be like ‘no, this is what we’re gonna put into practice’.
But my mum would do everything . . . and I’d say ‘no no let him do it himself’ and there are things he can do even if you need to load the spoon for him it doesn’t mean he can’t put it in his mouth.
Facilitators and participants described how attending the E-PAtS programme sessions had a positive impact on communication, including using symbols, with their child and their child’s behaviour:
. . . this one family it made such a difference to them, it really, really did and to see the change in their child from one week to the next with a few simple strategies, one of which was remaining calm when the child is doing what he’s doing and you’re afraid of him hurting themselves, not running in there and being as excitable and anxious as the child but just bring it all down a notch, that was the main thing that she took away from that and it had such a big impact, that was brilliant.
. . . some of the people there had children who had ASD [autism spectrum disorder] who had presented with things that [study child] presented with, I was given tips and stuff, so I can’t pinpoint exactly what, but certainly it had a really positive impact at home.
Sharing of knowledge from the E-PAtS programme with others – which was identified as a key programme mechanism – enabled individuals and organisations to adopt new practices or to act as a support mechanism for parents:
And that was again highlighted so it’s OK to struggle at times but to reach out and get support and talk to other parents, that was a big thing that really helped, talking to other parents.
It was great because now my child’s school has now brought in that aspect of it. They’re using that a lot now at school. . . . to help with his communication and his choices and things throughout the day.
Yes. I shared it with the dad . . . which he understands very well now.
Usual practice
Objective: usual practice in this setting and use of services/support by intervention and control participants
Usual practice in this setting was assessed by (1) service use data collected at 3 and 12 months’ follow-ups (see Objective: the feasibility of conducting an embedded health economic analysis in a definitive trial), (2) an online UK survey of parents of young children with intellectual disability, and (3) perception of usual practice through interviews with family carer facilitators and service provider organisations.
Usual-practice survey of parents of young children with intellectual disability
Rather than survey parents of young children with intellectual disability nationally for the feasibility study only, we took the opportunity to include a question about usual practice in a separate online UK survey being carried out by the research team at the University of Warwick. The survey targeted a similar population to that for whom the E-PAtS programme was designed. In summary, 673 parental carers from across the UK participated in the survey. The majority of the children were male (n = 481, 75.0%) and the mean child age was 4.78 (SD 1.78) years. The sample included children with a variety of different disability diagnoses/labels that were suspected or diagnosed. The most common were autism (n = 524, 77.86%; 50.52% diagnosed, 12.04% in assessment, 15.30% awaiting assessment), special educational needs (n = 390, 57.95%; 43.98% diagnosed, 8.47% in assessment, 5.50% awaiting assessment), intellectual disability (n = 328, 48.74%; 33.43% diagnosed, 6.84% in assessment, 8.47% awaiting assessment), developmental delay (n = 317, 47.10%; 37.44% diagnosed, 5.65% in assessment, 4.01% awaiting assessment) and social communication disorder (n = 214, 31.80%; 17.09% diagnosed, 6.39% in assessment, 8.32% awaiting assessment). The majority of parental carer respondents were the child’s biological mother (n = 613, 91.1%), although a few were biological fathers (n = 28, 4.2%), adoptive mothers (n = 13, 1.9%), grandmothers (n = 10, 1.5%) or other carers (n = 5, 0.7%). The age range of parental carers was 22–72 years, with a mean of 36.54 (SD 2.29) years, and the majority of parental carers were female (n = 633, 94.1%).
Participants in the online UK survey were asked if, in the past 12 months, they had received an intervention or focused support for their child or for themselves. Less than one-third of participants (29.3%) reported that their child or themselves had received such an intervention or support. If participants reported that they had received intervention/support in the preceding 12 months, they were also asked to briefly describe this intervention/support. Analysis of these responses showed that 10.5% of survey participants clearly named a parent training/support intervention [including EarlyBird (National Autistic Society, London, UK), The Incredible Years parenting programmes, Stepping Stones Triple P or therapy/counselling for themselves]. Therefore, usual practice for families of young children with intellectual disability and related conditions in the UK rarely includes parenting group programmes.
Participant perceptions of usual practice
The E-PAtS course was described as unique to other courses available to family carers of children with intellectual disability. Facilitators and participants valued that the E-PAtS programme was designed and delivered specifically to parents of children with intellectual disability and was not a generic parenting course. Participants valued attending and sharing experiences and knowledge of local support available with other parents of children with intellectual disability. The co-delivery aspect was considered to differentiate the E-PAtS from other courses available (i.e. participants welcomed the interactive course delivery, compared with the ‘lecturing’ styles of other courses). Participants and facilitators described the E-PAtS programme as a positive course in the way the content was organised, the way the course was structured and the course’s child focus. The E-PAtS programme differed from other courses available because it was developed specifically for children aged < 5 years and dealt with addressing challenging behaviour:
. . . other programmes I’ve delivered and we’ve had a range of ages and the one that I can think of particularly, the ones with the older kids really scared the ones with the younger kids because they were saying ‘mine does this’ sort of thing but I think because they’re all of a similar age that’s a very positive thing as well.
. . . not many courses talk about challenging behaviour and I think it’s an area that is very . . . it can cause a lot of distress to parents and children and it’s very needed to be understood, to be able to deal with it really.
You get sent on courses or sent to groups where you might be the only parent there with a child with additional needs and that is really tough and generally people were saying we just don’t go, we just don’t do it, why would we because it just makes us feel worse than before we went.
. . . very much someone standing, a professional person standing and speaking in a lecture format and that’s fine. I think what E-PAtS brought that was really different was that opportunity for discussion around those sorts of things and to talk about personal experience and share that and learn from others, and, as I say, as much about getting advice and tips and that support generally, and understanding.
Feasibility/recommendations for a future trial
Objective: service provider organisation willingness to participate in a definitive trial
Service provider willingness to participate in a definitive trial was assessed using surveys provided to potential service provider organisations.
Service provider organisation survey results
The survey that was distributed to organisations that were representative of those likely to be invited to provide the E-PAtS programme within a future trial produced 15 responses. There was significant interest in running the E-PAtS programme, which was seen to have strong fit with the organisations’ roles and purpose. Although delivery of the intervention was broadly seen as feasible, much lower levels of perceived feasibility were reported for the provision of funds to train facilitators and, to some extent, other aspects of funding needed. There was significant variation (mainly linked to organisational structure/purpose) as to whether or not respondents thought fulfilling staff requirements would be difficult to achieve.
The majority of organisations (13/14 organisations that answered the relevant question) indicated that they were somewhat or very likely to participate in a future RCT. When respondents indicated uncertainty concerning participation in a future trial, this was linked to two main issues: (1) the feasibility of securing additional/external funding for training and programme delivery and (2) the need to consult with and gain approval from senior management. Although some respondents did raise concerns about the trial design (and randomisation of participants to a control condition), this did not appear to be a major obstacle to participation. The key barriers that would need to be addressed were the resources required to deliver the programme and the provision of sufficient time to address this prior to the start of programme implementation.
Suggested improvements to the E-PAtS programme
Parents and facilitators expressed different views on the age of the child for whom the E-PAtS programme may be suitable. Some parents/facilitators thought that parents of older children or children who had received a diagnosis would benefit from the course, whereas others suggested that the course was introductory and more suited to parents of younger children. Some participants also suggested that group members would benefit from groups that were focused on a specific disorder (e.g. different groups for autism, Down syndrome, etc).
Suggested improvements to the course content included improvements to the presentation of the handbook and the slides, which were considered to be too scientific and sometimes not appropriate, specifically the developmental table in the communication session 4. However, the developmental table in the session has since been removed from the E-PAtS programme content. Some participants suggested that the course sessions were too long and could be shortened without compromising the content. Some groups experienced a double session (structured to help fit all sessions into available time frames for families and organisations) during delivery and this was sometimes experienced as too long, and it was proposed that sessions should not be combined.
Facilitators and participants who facilitated/attended smaller groups expressed the view that larger groups would be preferable and emphasised the importance of local groups so that the course is accessible to more parents. Guest speakers who were experts in certain areas of child development, optional one-to-one sessions and follow-up group sessions were also suggested as desirable.
Objective: the feasibility of conducting an embedded health economic analysis in a definitive trial
The feasibility of conducting a health economic evaluation in a definitive trial was assessed in this feasibility study.
Cost estimation for delivery of the E-PAtS programme
The results of the cost estimation for delivery of the E-PAtS programme are provided for each study site in Table 19 (as of 17 April 2020). The cost components are aggregated into three categories: (1) staff costs, including supervision, planning, direct delivery, meetings with professionals, telephone calls and paper work; (2) travel costs, which were based on the distances reported by programme facilitators and modes of transport; and (3) other costs, such as costs of refreshments, reimbursed participant travel and child-care costs associated with delivering the programme sessions.
| Set-up cost | Site 1 | Site 3 |
|---|---|---|
| Initial training (£) | 3174.17 | 3426.67 |
| Mean costs per session (£) | ||
| Staff | 61.25 | 96.11 |
| Travel | 12.40 | 8.39 |
| Other | 17.72 | 5.04 |
| Total | 91.37 | 109.55 |
Table 19 shows the mean intervention costs per session delivered at each site. These varied from £91.37 (site 1) to £109.55 (site 3). The main driver of the intervention costs per session delivered was staff costs, which were valued at £61.25 in site 1 and £96.11 in site 3. Initial training costs (set-up) were £3426.67 in site 3 and £3174.17 in site 1 to prepare new E-PAtS programme facilitators.
Broader resource consequences associated with the E-PAtS programme
Data were collected about broader resource use associated with the E-PAtS programme at 3 and 12 months. These data included parents’ and children’s use of hospital care services (i.e. hospital inpatient stays, hospital day centres, hospital accident and emergency visits and hospital outpatient clinic appointments), children’s development centres and children’s day centres, community-based health care [i.e. general practitioner (GP) services, health visitors, paediatricians, ophthalmologists, audiologists, speech and language therapies, physiotherapists, psychologists, psychiatrists, dentists, child mental health services, private child care, nurseries and occupational therapists], community-based social care (i.e. counsellors, family or patient support, Women’s Aid, housing department services and Citizens Advice bureau services) and medicines. The resource use questionnaires were piloted to evaluate participants’ comprehension levels of the resource use questions.
Analyses of broader resource consequences
Resource use items were summarised by trial arm (intervention and control) and follow-up period. Means and SEs for resource use values by resource category were estimated by trial allocation group for each of the follow-up periods, namely months 1–3 and 4–12.
Tables 20 and 21 present resource use values for parents and their children, with complete data by trial allocation and study period. With respect to children, the resource values are presented for subcategories of resource item, including (1) health-care services, such as GP services, health visitors, paediatricians, ophthalmologists, audiologists, speech and language therapies, physiotherapists, psychologists, psychiatrists, dentists, child mental health services, private child care, nurseries, occupational therapists and other services, and (2) hospital services, such as hospital inpatient stays, hospital day centres, hospital accident and emergency, hospital outpatient clinics, children’s development centres and children’s day centres. With respect to parents, legal and social services, such as counsellors, family or patient support, Women’s Aid, housing department services and Citizens Advice bureau services, were incorporated in addition to health-care services.
| Resource use | Months 1–3 | Months 9–12 | ||
|---|---|---|---|---|
| Intervention (n = 32) | Control (n = 26) | Intervention (n = 25) | Control (n = 22) | |
| Health care, social care, voluntary or private service, mean number of contacts (SE) | ||||
| GP surgery | 1.50 (0.32) | 0.88 (0.20) | 1.20 (0.37) | 1.18 (0.32) |
| GP out of hours | 0.09 (0.05) | 0.19 (0.08) | 0.48 (0.19) | 0.23 (0.11) |
| GP home visits | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| General practice nurse | 0.16 (0.10) | 0.12 (0.08) | 0.12 (0.09) | 0.05 (0.05) |
| Calls to NHS Direct | 0.06 (0.06) | 0.85 (0.77) | 0.04 (0.04) | 0.05 (0.05) |
| District nurse | 1.22 (0.72) | 0.96 (0.77) | 0.60 (0.48) | 1.05 (0.69) |
| Health visitor | 0.19 (0.07) | 0.23 (0.08) | 0.12 (0.09) | 0.14 (0.14) |
| Paediatrician | 0.72 (0.23) | 0.50 (0.11) | 0.68 (0.14) | 0.86 (0.12) |
| Ophthalmology | 0.34 (0.10) | 0.50 (0.14) | 0.28 (0.14) | 0.64 (0.12) |
| Audiology | 0.59 (0.14) | 0.46 (0.13) | 0.40 (0.14) | 0.45 (0.14) |
| Speech and language | 4.19 (0.61) | 2.85 (0.62) | 4.68 (1.02) | 5.50 (1.76) |
| Physiotherapist | 1.72 (0.54) | 2.00 (0.83) | 1.36 (0.67) | 3.14 (1.83) |
| Psychologist | 0.25 (0.20) | 0.38 (0.14) | 0.16 (0.07) | 0.27 (0.10) |
| Psychiatrist | 0.00 (0.00) | 0.08 (0.05) | 0.00 (0.00) | 0.00 (0.00) |
| Dentist | 0.50 (0.13) | 0.38 (0.10) | 0.88 (0.16) | 0.55 (0.11) |
| Child and adolescent mental health service provider | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Private child care | 4.81 (1.81) | 2.96 (2.02) | 3.80 (2.42) | 3.27 (1.96) |
| Nursery | 6.56 (2.23) | 14.12 (4.08) | 17.68 (5.01) | 20.50 (6.12) |
| Occupational therapist | 2.31 (0.58) | 4.31 (2.32) | 3.24 (0.94) | 4.05 (1.77) |
| Other health | 1.34 (0.77) | 0.38 (0.24) | 0.12 (0.07) | 0.41 (0.32) |
| Other services | 0.44 (0.28) | 1.15 (0.71) | 0.04 (0.04) | 0.09 (0.09) |
| Hospital or day services, mean (SE) | ||||
| Hospital inpatient stay (days) | 0.34 (0.24) | 0.58 (0.54) | 0.16 (0.11) | 1.77 (1.19) |
| Hospital day centre (visits) | 0.00 (0.00) | 0.08 (0.05) | 0.12 (0.07) | 0.00 (0.00) |
| Hospital accident and emergency (visits) | 0.34 (0.15) | 0.23 (0.12) | 0.48 (0.18) | 0.27 (0.12) |
| Hospital outpatients clinic (visits) | 0.38 (0.21) | 0.65 (0.46) | 0.52 (0.16) | 0.45 (0.23) |
| Children’s development centre (visits) | 0.44 (0.30) | 0.00 (0.00) | 0.36 (0.21) | 0.23 (0.13) |
| Children’s day centre (visits) | 0.66 (0.44) | 0.08 (0.08) | 0.64 (0.64) | 0.05 (0.05) |
| Medication use, n (%) | 21 (65.63) | 12 (46.15) | 18 (72.00) | 16 (72.73) |
| Resource use | Months 1–3 | Months 9–12 | ||
|---|---|---|---|---|
| Intervention (n = 32) | Control (n = 26) | Intervention (n = 25) | Control (n = 22) | |
| Health care, social care, voluntary or private service, mean number of contacts (SE) | ||||
| GP surgery | 1.41 (0.39) | 0.85 (0.22) | 1.44 (0.56) | 0.50 (0.16) |
| GP out of hours | 0.06 (0.04) | 0.04 (0.04) | 0.08 (0.08) | 0.00 (0.00) |
| GP home visit | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| General practice nurse | 0.25 (0.10) | 0.12 (0.08) | 0.12 (0.07) | 0.00 (0.00) |
| Calls to NHS direct | 0.03 (0.03) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| District nurse | 0.13 (0.13) | 0.08 (0.08) | 0.00 (0.00) | 0.00 (0.00) |
| Health visitor | 0.09 (0.07) | 0.04 (0.04) | 0.00 (0.00) | 0.00 (0.00) |
| Social worker | 0.06 (0.06) | 0.08 (0.08) | 0.08 (0.06) | 0.00 (0.00) |
| Physiotherapist | 0.03 (0.03) | 0.46 (0.46) | 0.12 (0.09) | 0.18 (0.18) |
| Occupational therapist | 0.00 (0.00) | 0.08 (0.08) | 0.00 (0.00) | 0.00 (0.00) |
| Home help | 0.00 (0.00) | 10.38 (10.38) | 0.16 (0.16) | 0.73 (0.57) |
| Psychiatrist | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Psychologist | 0.28 (0.28) | 0.08 (0.08) | 0.40 (0.40) | 0.18 (0.18) |
| Dentist | 0.72 (0.22) | 0.38 (0.11) | 0.76 (0.17) | 0.55 (0.19) |
| Counsellor | 0.03 (0.03) | 0.35 (0.24) | 0.72 (0.53) | 0.32 (0.24) |
| Family or patient support | 0.16 (0.13) | 0.92 (0.64) | 0.36 (0.36) | 0.05 (0.05) |
| Women’s Aid | 0.09 (0.09) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Housing department services | 0.06 (0.06) | 0.04 (0.04) | 0.28 (0.28) | 0.00 (0.00) |
| Citizens Advice bureau | 0.06 (0.06) | 0.08 (0.08) | 0.04 (0.04) | 0.00 (0.00) |
| Other health-care services | 0.75 (0.39) | 0.00 (0.00) | 0.76 (0.41) | 0.36 (0.28) |
| Other social care services | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Other voluntary services | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Other private services | 0.06 (0.06) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Hospital or day services, mean (SE) | ||||
| Hospital inpatient stay (days) | 0.16 (0.16) | 0.00 (0.00) | 0.00 (0.00) | 0.05 (0.05) |
| Hospital day centre (visits) | 0.00 (0.00) | 0.00 (0.00) | 0.04 (0.04) | 0.00 (0.00) |
| Accident and emergency (visits) | 0.16 (0.10) | 0.08 (0.05) | 0.04 (0.04) | 0.00 (0.00) |
| Outpatient clinic (visits) | 0.06 (0.04) | 0.15 (0.09) | 0.28 (0.17) | 0.00 (0.00) |
| Day centre (visits) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Other hospital (visits) | 0.00 (0.00) | 0.46 (0.46) | 0.04 (0.04) | 0.00 (0.00) |
| Medication use, n (%) | 9 (28.13) | 2 (7.69) | 6 (24.00) | 2 (9.09) |
Nurseries and private child-care services were commonly used among children with complete data. Private child-care services were used an average of 4.81 times per child in the intervention group and 2.96 times per child in the control group over the first 3 months. Over months 1–4, nurseries were used 17.68 times in the intervention group and 20.50 times in the control group. Twenty-one children (65.63%) in the intervention arm used medications over months 1–3, compared with 12 children (46.15%) in the control arm. Use of hospital services, such as inpatient, day case and outpatient services, was relatively low in both trial arms. GP surgery use was the most common form of community health-care services for parents. Among parents, the mean number of GP surgery contacts was 1.44 in the intervention group compared with 0.50 in the control group over months 9–12.
Sources of unit costs for broader resource consequences
Resource inputs were valued using various secondary sources for unit costs. Sources of unit costs for inpatient hospital admissions over the study time horizon and other hospital services, such as day care, outpatient care and accident and emergency visits, were obtained from national tariffs (NHS reference costs trusts schedules). 66 Unit costs for community-based health and social services were derived from a range of national compendia, including the Personal Social Services Research Unit unit cost compendium67 and NHS reference costs trusts schedules. 66 The costs of using private child care and nurseries were obtained from the Childcare Costs Survey 2015. 68
Sources of medication costs per dose were largely obtained from the British National Formulary69 or the British National Formulary for Children. 70 Table 22 provides a compendium of unit costs for the broader resource consequences that were valued at 2018/19 prices (GBP) and inflated, where necessary, using the NHS Hospital and Community Health Services Pay and Prices Index. 67
| Resource item | Source | Unit cost (£, 2018/19) |
|---|---|---|
| Health care, social care voluntary or private services | ||
| GP surgery (contact) | PSSRU 201967 | 39.23 |
| GP per out of hours (contact) | PSSRU 201871 | 110.58 |
| GP per home visit (visit) | PSSRU 201871 | 46.65 |
| General practice nurse (hour) | PSSRU 201871 | 42.97 |
| Calls to NHS direct (contact) | UK Parliament 201372 | 8.11 |
| District nurse (hour) | PSSRU 201871 | 42.69 |
| Health visitor (hour) | PSSRU 201073 | 40.50 |
| Paediatrician (contact) | PSSRU 201674 | 214.98 |
| Ophthalmology (contact) | NHS reference costs 201975 | 98.00 |
| Audiology (contact) | NHS reference costs 201975 | 108.00 |
| Speech and language (contact) | PSSRU 201674 | 45.37 |
| Psychiatrist (hour) | PSSRU 201674 | 145.85 |
| Psychologist (hour) | PSSRU 201674 | 44.39 |
| Dentist (hour)a | PSSRU 201967 | 133.00 |
| Child and adolescent mental health service provider (contact) | PSSRU 201276 | 84.16 |
| Physiotherapist (hour) | PSSRU 201871 | 50.99 |
| Occupational therapist (hour) | PSSRU 201967 | 48.00 |
| Private child care (week) | Childcare Costs Survey 2015 68 | 214.72 |
| Nursery (week) | Childcare Costs Survey 2015 68 | 231.76 |
| Social worker (hour)b | PSSRU 201967 | 50.00 |
| Home help (hour) | PSSRU 201871 | 22.51 |
| Counsellor (hour) | PSSRU 201673 | 44.39 |
| Family or patient support (hour) | PSSRU 201674 | 31.71 |
| Women’s Aid (hour) | PSSRU 200677 | 116.79 |
| Housing department servicesc (week) | PSSRU 201178 | 189.01 |
| Citizens Advice bureau (contact) | PSSRU 200677 | 15.64 |
| Hospital services | ||
| Hospital inpatient stay (day) | NHS reference costs 201866 | 354.41 |
| Hospital day centre (visit) | NHS reference costs 201975 | 752.00 |
| Hospital accident and emergency (visit) | NHS reference costs 201975 | 166.00 |
| Hospital outpatients clinic (visit) | NHS reference costs 201975 | 148.00 |
| Children’s development centre (visit) | PSSRU 201379 | 36.79 |
| Children’s day centre (visit) | PSSRU 201871 | 368.32 |
Analysis of health-related quality-of-life outcomes
The health-related quality of life of the parents was assessed using the EQ-5D-5L obtained at 3 months’ and 12 months’ follow-up. The EQ-5D-5L has two measurement components. The first component is a descriptive system that categorises health-related quality of life into the following five dimensions: (1) ‘mobility’, (2) ‘self-care’, (3) ‘usual activities’, (4) ‘pain/discomfort’ and (5) ‘anxiety/depression’. Participants report their level of function for each dimension within one of the following five ordinal levels: (1) no problems, (2) slight problems, (3) moderate problems, (4) severe problems and (5) extreme problems/unable to perform. The crosswalk value set for the EQ-5D-5L was used to value responses to construct an EQ-5D-5L utility score for each respondent. 50 The utility scores are indexed at 0 or 1 (0 represents death, 1 represents full health and values below 0 indicate health states that are worse than death). The utility scores can be converted into quality-adjusted life-years (QALYs) using an area under the baseline-adjusted utility curve and can be calculated using linear interpolation between utility scores at baseline, 3 months and 12 months. The second part of the EuroQol-5 Dimensions (EQ-5D) is a visual analogue scale (VAS), which ranges from 100 (best health condition) to 0 (worst health condition) and describes the participant’s own assessment of their health status.
We report descriptive statistics for EQ-5D-5L utility scores and VAS scores at each time point. Similarly, we report descriptive statistics for levels of function for each of the five dimensions of the EQ-5D-5L, as well as suboptimal (less than optimal) levels of function (defined as some, moderate, severe or extreme problems) by trial arm and follow-up point.
Table 23 shows that health-related quality-of-life outcomes were marginally better for the intervention group than for the control group. The mean EQ-5D-5L score was marginally higher for the intervention group than for the control group at 3 months (0.803 vs. 0.746) and 12 months (0.838 vs. 0.812). In addition, the mean EQ-5D VAS score was marginally higher for the intervention group than for the control group at 3 months (74.22 vs. 74.00) and at 12 months (74.56 vs. 69.77). The table shows broadly similar patterns in less than optimal levels of function between the intervention and control groups for each of the five dimensions of the EQ-5D-5L, at 3 and 12 months, other than for self-care at 3 months.
| EQ-5D-5L dimension | Level | 3 months | 12 months | ||
|---|---|---|---|---|---|
| Intervention (N = 35), n (%) | Control (N = 28), n (%) | Intervention (N = 24), n (%) | Control (N = 22), n (%) | ||
| Mobility | No problem | 31 (88.57) | 20 (71.43) | 21 (84.00) | 18 (81.82) |
| Slight problem | 4 (11.43) | 5 (17.86) | 1 (4.00) | 4 (18.18) | |
| Moderate problem | 0 (0.00) | 1 (3.57) | 2 (8.00) | 0 (0.00) | |
| Severe problem | 0 (0.00) | 1 (3.57) | 0 (0.00) | 0 (0.00) | |
| Extreme problem | 0 (0.00) | 1 (3.57) | 0 (0.00) | 0 (0.00) | |
| Less than optimal | 4 (11.43) | 8 (28.57) | 3 (12.50) | 4 (18.18) | |
| Self-care | No problem | 35 (100.00) | 25 (89.29) | 23 (92.00) | 21 (95.45) |
| Slight problem | 0 (0.00) | 1 (3.57) | 2 (8.00) | 1 (4.55) | |
| Moderate problem | 0 (0.00) | 2 (7.14) | 0 (0.00) | 0 (0.00) | |
| Severe problem | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| Extreme problem | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| Less than optimal | 0 (0.00) | 3 (10.71) | 2 (8.00) | 1 (4.55) | |
| Usual activity | No problem | 26 (74.29) | 20 (71.43) | 19 (76.00) | 17 (77.27) |
| Slight problem | 5 (14.29) | 5 (17.86) | 6 (24.00) | 4 (18.18) | |
| Moderate problem | 2 (5.71) | 3 (10.71) | 0 (0.00) | 1 (4.55) | |
| Severe problem | 1 (2.86) | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| Extreme problem | 1 (2.86) | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| Less than optimal | 9 (25.71) | 8 (28.57) | 6 (24.00) | 5 (22.73) | |
| Pain | No pain | 20 (57.14) | 12 (42.86) | 15 (60.00) | 8 (36.36) |
| Slight pain | 8 (22.86) | 12 (42.86) | 6 (24.00) | 11 (50.00) | |
| Moderate pain | 5 (14.29) | 2 (7.14) | 3 (12.00) | 3 (13.64) | |
| Severe pain | 2 (5.71) | 1 (3.57) | 1 (4.00) | 0 (0.00) | |
| Extreme pain | 0 (0.00) | 1 (3.57) | 0 (0.00) | 0 (0.00) | |
| Less than optimal | 15 (42.86) | 16 (57.14) | 10 (40.00) | 14 (63.64) | |
| Anxiety | No anxiety | 13 (38.24) | 11 (39.29) | 11 (44.00) | 11 (50.00) |
| Slight anxiety | 13 (38.24) | 9 (32.14) | 10 (40.00) | 5 (22.73) | |
| Moderate anxiety | 5 (14.71) | 5 (17.86) | 3 (12.00) | 5 (22.73) | |
| Severe anxiety | 3 (8.82) | 3 (10.71) | 1 (4.00) | 1 (4.55) | |
| Extreme anxiety | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| Less than optimal | 21 (61.76) | 17 (60.71) | 14 (56.00) | 11 (50.00) | |
| EQ-5D-5L score, mean (SE) | 0.803 (0.03) | 0.746 (0.04) | 0.838 (0.03) | 0.812 (0.03) | |
| VAS score, mean (SE) | 74.22 (2.57) | 74.00 (3.13) | 74.56 (4.47) | 69.77 (3.16) | |
Expression of cost-effectiveness of the E-PAtS programme
The cost-effectiveness of health and social care programmes can be expressed in terms of incremental cost per unit change in a primary outcome measure, which is called the incremental cost-effectiveness ratio. Outcome measures within the feasibility study included the WEMWBS. However, this is not a preference-based measure that permits the estimation of QALYs amenable to cost-effectiveness decision-making. 80
Combining disparate outcomes for parents and children in a single preference-based outcome measure will be a challenge for a future economic evaluation of the E-PAtS programme. It is anticipated that QALY-based approaches will not be able to capture the disparate effects of the E-PAtS programme on both parents and children, partly because of an absence of a validated multiattribute utility measure for early childhood and partly because of methodological challenges surrounding aggregation of disparate benefits for both parents and children in a single metric.
Discrete choice experiments (DCEs) offer a preference-based approach for valuing the potentially disparate effects of the E-PAtS programme. DCEs are broadly used in health economics to address a wide range of health policy-related questions. For example, they can be used to improve adherence to public health programmes or to quantify the trade-offs that trial participants are willing to make between different features of health care. 81 The approach stemmed from random utility theory,82 which assumes that respondents behave with the aim of maximising the utility of given choices. Sustaining adherence to a social intervention programme, such as the E-PAtS programme, has been a main task for improving the implementation quality of the intervention. 83 The evidence revealed by a DCE can be used for policy-makers in delivering the E-PAtS programme. Given the results of a DCE revealing the preferences of trial participants, delivering a bespoke programme based on the DCE results will enhance the possibility of adherence to the programme.
One of the purposes of this feasibility study was to examine factors associated with the adherence to and reach of the intervention for a future trial. Various approaches have been recommended to identify attributes for DCEs, including literature reviews, expert opinion, qualitative research and evidence from other existing studies. On the basis of the qualitative interviews performed as part of the E-PAtS intervention and the preferences stated by the trial participants, four attributes relating to the adherence and reach of the E-PAtS programme were identified: (1) location, (2) timing of the intervention, (3) method and (4) frequency. In the same manner, two levels for each of the attributes can be delineated to explore factors associated with the adherence to the E-PAtS programme:
-
location (home or drop-in clinic)
-
acceptability of randomisation (i.e. timing, now or to be offered the E-PAtS programme at a later date)
-
method of data collection (face to face, telephone, alternate between face to face and telephone)
-
frequency (weekly or monthly).
It is anticipated that the utility function for the DCE in a future definitive trial-based economic evaluation of the E-PAtS programme will be expressed within a mixed logit model. 83 All attributes will also be coded as a dummy, with one level for each attribute coded as the reference group. If a cost attribute is additionally introduced into a DCE, a future evaluation can aim to estimate marginal rates of substitution between changes in the cost attribute and the remaining attributes. 84
It is crucial to structure an efficient design in constructing choice sets of a DCE questionnaire. D-efficiency, which is an indicator of statistical efficiency minimising the determinant of the covariance matrix, needs to be considered. 84,85 The information with regard to priors for coefficients can be obtained from the feasibility study. To list all possible choices (i.e. a full factorial design) would be impractical for future trial participants, as this would require too many choice sets. For example, four attributes with four levels would result in 256 possible scenarios (44 = 256). It is also important to arrive at a balanced design that allows for each level to be chosen equally (i.e. levels of attributes need to be chosen an equal number of times, thereby minimising the variance in the parameter estimates). Therefore, a fractional factorial design rather than full fractional design will be considered to reduce the number of selected scenarios.
A DCE can be incorporated into an economic evaluation of the E-PAtS programme with a view to informing a cost–benefit analysis. 86 Cost–benefit analysis is not widely used in health economic evaluations as it is cumbersome to put monetary values onto health outcomes. However, by comparing the costs between delivery options delineated by variations in facilitator, location and timing, method and frequency, the results of the economic evaluation can be expressed as a net monetary benefit (NMB) within the frame of a cost–benefit analysis.
The NMB can be constructed by use of difference in costs and effects, which is analogous to an incremental cost-effectiveness ratio in a cost-effectiveness analysis. The NMB can be expressed as:
where ΔE is the effectiveness difference between comparators, λ is the maximum willingness to pay and ΔC is the cost difference between trial arms. When incorporating a DCE into an economic evaluation, ΔE is the regression coefficient of the outcome measures, and λ can be obtained in the survey as a price proxy of salary or income,85 or by directly asking the willingness to pay for the chosen option. 86 In general, a positive NMB means that the chosen treatment option is cost-effective as the costs are outweighed by the benefits of the intervention. 87
In conclusion, a preference elicitation approach, such as a DCE, is likely to be required to supplement the economic evaluation of the E-PAtS programme. This will quantify participants’ preferences for the heterogeneous outcome measures used in the E-PAtS programme. By using a DCE, decision-makers should be able to compare the trade-offs between different outcomes. The DCE results can be helpful in developing the effective delivery of the E-PAtS programme.
Objective: acceptability of collecting and analysing routinely collected data within a definitive randomised controlled trial
Extraction of data from routine data sources is widely conducted as part of clinical trials, as it can provide a rich source of data for both resource use and clinical outcomes without requesting it from patients or study participants. 88 This section explores research and public considerations around the use of routine data collection for a definitive trial.
Using routine data for economic evaluations
There are several advantages of using routine data for a future economic evaluation of the E-PAtS programme. First, routine data can be used to validate and complement resource use data from the trial data collection instruments. In clinical trials, broader resource use data can be collected using health economic questionnaires completed by trial participants. The questionnaires request information about use of hospital services, community-based health and social care services, and medications. Use of routinely collected data enables researchers to track patients prospectively and retrospectively. 89 Linkage with routine data can also provide information about the medical history of patients. Therefore, researchers involved in future evaluations of the E-PAtS programme can refer to routine data when self-reported questionnaires provide insufficient information about participants. In addition, routine data can be used to inform long-term epidemiological models of disease or health status progression.
Second, routine data can supplement incomplete resource use information observed in trial-based economic evaluations. As the data offers information on past medical records, routine data can be used when designing an economic analysis that starts after patient or participant follow-up is completed. The routine data can be used for modelling parameters of costs in designing a study for which resource use data are not collected. Likewise, routinely collected data can be useful when baseline resource use data are needed but absent in a clinical trial that has already started. 90
However, existing routine data does not always provide information on social care. For an economic evaluation of the E-PAtS programme, collecting data on social care service use is essential, as children with intellectual disabilities commonly use various social care services in addition to hospital services. The State of Caring Survey and the Adult Social Care Survey offer information about social care, but they are limited in that the data are presented at an area level rather than an individual level. 91 Likewise, the NPD provides information about education and social care data in England, but the data are limited to children. As an example, in an end-of-life care trial, social care data that were obtained from local authorities were linked with routine data at an individual level to secondary health-care data. 91 Therefore, contrary to the aforementioned advantages of using routine data, it is likely that an element of prospective data collection will be required when conducting an economic evaluation that encompasses a social care element.
Based on the advantages of routine data, a future, trial-based economic evaluation of the E-PAtS programme may extract key resource use items from the Mental Health Minimum Data Set (MHMDS) and Hospital Episode Statistics. The MHMDS deals with children and young people’s access to psychological therapies, intellectual disabilities or autism services. This data set is based on mental health currencies and payments, formerly Payment by Results, and so the data can be helpful for mental health policy-makers and researchers who work on policy evaluations. The MHMDS also provides information regarding children and young people who access psychological therapies and other outpatient clinics for intellectual disabilities and services in the community.
Hospital Episode Statistics data cover a wide range of information about patients admitted to NHS hospitals in England (e.g. clinical information about diagnoses, patient age, gender, race and ethnicity, methods of admission and discharge, and geographical information of the admitted patients). In principle, Hospital Episode Statistics data cover all secondary care attendances in England.
Potential data providers and their data sets
Routine data sources can provide information regarding community care service use, such as use of GP services and hospital services (e.g. inpatient days).
Table 24 summarises potential data sources of interest for a future trial, both for resource outcomes and for longer-term follow-up. We have identified data providers in England that could be linked to on a national level. Other data providers that cover only one local area or only a percentage of the population have not been included, as a future trial would need to link all participants as efficiently as possible using the fewest number of data providers.
| Data provider | Data set | Brief summary of data | Real time? |
|---|---|---|---|
| NHS Digital: England | Community Services Data Set | Publicly funded community services for all ages, including health centres, schools, district nursing, health visiting and many more | No |
| HES | Details of all admissions, A&E attendances and outpatient appointments | No | |
| MHMDS | Children and young people’s access to psychological therapies, learning disabilities or autism | No | |
| NPD: England | Key stage attainment | A number of data sets that report the attainment at key stages 1–5 | No |
| Early years attendance | Details of the hours a child attended early years establishments before the mandatory age of attending school | No | |
| School attendance/absence/exclusions | A number of data sets that indicate if a child took any unapproved/approved absences during each term at a public school | No | |
| Child in need/child looked after | Information on children in need referred to children’s services and children looked after who are looked after by local authorities | No |
Timelines for accessing data
One of the main challenges of using routine data is the time it takes to apply and receive approval for access. 92 For example, the process for accessing hospital data from NHS Digital took more than 1 year for the Building Blocks Trial. 92 In addition, application approvals often rely on other parts of the research process, such as ethics approvals and other requirements (e.g. legal approvals), for data linkage. Therefore, the length of time to access routine data can often far exceed initial expectations.
Data providers do not make information on timelines generally available, as the time from submitting an application to receipt of data will depend on the complexity of the project as well as how much more detail is required in the application when submitted. Our recommendations for a faster approval process include the following:
-
talking to data providers as early as possible about the project
-
asking for documents (data flows, consent material) to be reviewed by data providers prior to other approvals being submitted (ethics)
-
reading the guidance available from data providers on completing the application
-
responding in a timely manner when contacted by the data provider.
‘Where access is of no additional cost an application will be made’
Originally, it was intended to apply for data from providers where there is no cost for data (e.g. the NPD). However, the decision was made to not consent participants to linkage of data as part of this feasibility study and, instead, to explore the acceptability of consent with current participants at 12 months. It was agreed that the time required to apply for data would outweigh anything that could be learnt by carrying out this process. Other projects in the Centre for Trials Research have applied for and accessed data from both NHS Digital and the NPD, and therefore nothing more could be learnt by doing this again for this project. 92–94 It was not intended for the data to be reported as part of the feasibility study-proposed outcomes (i.e. data on education outcomes) and so it would be an inefficient use of resource (both trial staff and public resource at the data provider end). Requests for data from data providers need to demonstrate the public benefit associated with the release of data and this could not be justified or demonstrated in this case.
Logistics of linking, transferring and storing routine data
For a future trial, the following logistical considerations will need to be incorporated into the final design.
Consent
Most data providers prefer an opt-in consent model. The NPD, in particular, mandate this. This would include consent from both parent/carers and the children. For health data, it is possible to use an opt-out model by applying for section 251 support95 from the Health Research Authority Confidentiality Advisory Group (applicable in England and Wales only). NHS ethics approval would also be required if applying for section 251 support.
Data matching
Identifiers (IDs) common to all data providers that could be used to match to their data sets are postcode, date of birth and name (first and surname). These would need to be collected in a future trial and provided to each data provider for linkage.
Data linkage
To enable the linkage of data sets from a number of data providers, a constant ID would also need to be provided when sending IDs for matching. This is likely to be the trial ID and would need to distinguish between parent/carer and child/children.
Data storage
To hold data from NPD, data can be accessed via the Secure Research Service only (hosted by the Office for National Statistics). A minimum data set of trial data would need to be transferred to this secure platform to enable analysis of the routine data (e.g. baseline data). Data from other data providers could either be transferred to the secure platform or held by the trial team. By utilising the secure platform, this will satisfy data security requirements placed on the trial team by data providers, as access is via a remote portal and data cannot be held locally by the trial team. Outputs from analysis will follow small numbers policy and will be reviewed before tables/figures are exported to ensure individuals cannot be identified.
Acceptability of routine data collection (quantitative)
Table 25 presents participants’ views on the acceptability of their routinely collected data being used in a future study. For further information, see Appendices 5 and 6. Forty-seven participants answered the questions surrounding routine data collection. Around one-third of participants were aware that researchers were able to request access to hospital data, with slightly fewer participants being aware that school and social care data can be requested. The intervention participants were less comfortable with the idea of agreeing to their/their child’s routine data being accessed. For example, 46% of intervention participants said that they would be ‘not at all comfortable’ or ‘not very comfortable’ with agreeing to their hospital data being accessed in a future study (compared with 9% of control participants). Thirty-eight per cent of the intervention group said they would have been less likely to take part in the E-PAtS programme if consent to access their routine hospital data had been requested. Only 9% of control participants answered that they would be less likely to take part in the study.
| Data collection | All participants, n (%) | |
|---|---|---|
| Control (N = 23) | Intervention (N = 24) | |
| Hospital data | ||
| Were you aware that researchers are able to request access to hospital data? | ||
| No | 13 (57) | 16 (67) |
| Yes | 9 (39) | 7 (29) |
| Missing | 1 (4) | 1 (4) |
| Would you be comfortable in agreeing to us accessing your data in a future study? | ||
| Not at all comfortable | 0 (0) | 6 (25) |
| Not very comfortable | 2 (9) | 5 (21) |
| No preference | 9 (39) | 4 (17) |
| Quite comfortable | 7 (30) | 7 (29) |
| Very comfortable | 4 (17) | 2 (8) |
| Missing | 1 (4) | 0 (0) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||
| Not at all comfortable | 0 (0) | 4 (17) |
| Not very comfortable | 1 (4) | 5 (21) |
| No preference | 10 (43) | 3 (13) |
| Quite comfortable | 7 (30) | 9 (38) |
| Very comfortable | 4 (17) | 3 (13) |
| Missing | 1 (4) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your data? | ||
| Definitely less likely to take part | 0 (0) | 4 (17) |
| Slightly less likely to take part | 2 (9) | 5 (21) |
| No difference | 18 (68) | 12 (50) |
| Slightly more likely to take part | 0 (0) | 1 (4) |
| Definitely more likely to take part | 2 (9) | 0 (0) |
| Missing | 1 (4) | 2 (8) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||
| Definitely less likely to take part | 0 (0) | 6 (25) |
| Slightly less likely to take part | 3 (13) | 4 (17) |
| No difference | 17 (74) | 12 (50) |
| Slightly more likely to take part | 1 (4) | 1 (4) |
| Definitely more likely to take part | 1 (4) | 1 (4) |
| Missing | 1 (4) | 0 (0) |
| School data | ||
| Were you aware that researchers are able to request access to school data? | ||
| No | 17 (74) | 17 (71) |
| Yes | 6 (26) | 7 (29) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||
| Not at all comfortable | 0 (0) | 4 (17) |
| Not very comfortable | 1 (4) | 2 (8) |
| No preference | 13 (57) | 7 (29) |
| Quite comfortable | 4 (17) | 8 (33) |
| Very comfortable | 4 (17) | 3 (13) |
| Missing | 1 (4) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||
| Definitely less likely to take part | 0 (0) | 3 (13) |
| Slightly less likely to take part | 2 (9) | 1 (4) |
| No difference | 17 (74) | 17 (71) |
| Slightly more likely to take part | 1 (4) | 1 (4) |
| Definitely more likely to take part | 2 (9) | 1 (4) |
| Missing | 1 (4) | 1 (4) |
| Social care data | ||
| Were you aware researchers are able to request access to social care data? | ||
| No | 16 (70) | 17 (71) |
| Yes | 7 (30) | 7 (29) |
| Missing | 0 (0) | 0 (0) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||
| Not at all comfortable | 0 (0) | 4 (17) |
| Not very comfortable | 1 (4) | 3 (13) |
| No preference | 14 (61) | 7 (29) |
| Quite comfortable | 2 (9) | 8 (33) |
| Very comfortable | 5 (22) | 2 (8) |
| Missing | 1 (4) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||
| Definitely less likely to take part | 0 (0) | 4 (17) |
| Slightly less likely to take part | 2 (9) | 3 (13) |
| No difference | 17 (74) | 15 (63) |
| Slightly more likely to take part | 1 (4) | 1 (4) |
| Definitely more likely to take part | 2 (9) | 1 (4) |
| Missing | 1 (4) | 0 (0) |
Acceptability of routine data collection (qualitative)
Questions were included in the interview schedule to explore the acceptability of a future trial linking to routine data sources. The questions on routine data collection/linkage appeared to be hard for some participants to understand, including what was intended by this activity, how data would be accessed, and the issue of whether or not some forms of data (e.g. GP visits, contact with social services) would be more or less sensitive.
There appeared to be considerable variation in the extent to which participants would be happy to take part in a study where routine data linkage would take place. Overall, although some people did have concerns about taking part in a trial of the E-PAtS programme, which included routine data collection, it was not a significant enough issue to mean that they would refuse to participate. Some participants understood and were in favour of the idea of routine data collection reducing the number of questions that they themselves had to answer. Several also expressed a desire to help contribute to research that would meet the needs of children and their families, which might therefore over-ride concerns about the use of their personal data.
There was also variation in the extent to which participants saw all routine data as similar (e.g. in terms of acceptability of researchers accessing it). In particular, some participants saw data on contact with social services as much more sensitive than number of GP visits, for instance. Similarly, there was a mix of views on the extent to which the acceptability and sensitivity of accessing data differed according to whether information related to the participant or to their child. For a number of participants, the decision to consent to data linkage would depend on knowing why the data were needed and how they would be kept secure. It was often difficult for participants to see the relevance of some of the data that might be collected during a future trial using data linkage. For example, some parents did not see why data on health service utilisation would be collected, as they are not immediately related to participation in the E-PAtS programme.
Overall, participants appeared to think that the researchers would access named files from the GP surgeries, etc, and that when they worked with the data researchers might know whose data they were using:
I didn’t really think that they would hand stuff out like that, is that not all supposed to be confidential?
Routine data: brief synthesis
The results from both the questionnaire and interviews indicate a mixture of views towards the acceptability of consenting and linking both participants’ and their child’s data. With this in mind, for a future trial we would recommend:
-
working very closely with parent groups/PPI groups to ensure that the explanations around the use of routine data are clear and provide justification for the linking of data
-
considering asking for consent as a separate process to consent to the trial to ensure that enrolment to trial is not biased (note that this will in turn bring about other bias in terms of outcomes that use routine data).
Progression criteria
Progression criteria are detailed in Tables 26–28.
| Progression criterion | Progress | Number (if applicable) | Percentage (95% CI) (if applicable) |
|---|---|---|---|
| Recruitment of families: 50% of families approached, and who are eligible, consent to the study (and thus are willing to be randomised) | Achieved | 79/121 | 65 (56 to 74) |
| Rate of recruitment: the target sample of 64 families is achieved within the study recruitment period | Partly achieved. Seventy-four families were recruited in two recruitment phases, but picture not consistent across all sites/rounds |
Site 1: 40 Site 2 (round 1): 17 Site 2 (round 2): 8 Site 3: 14 |
|
| Randomisation feasibility: 10–16 families are recruited in a local area of the E-PAtS provider to allow randomisation, with a maximum of eight families per E-PAtS group | Mostly achieved. One site in round 2 recruited fewer than 10 families and one E-PAtS group contained 10 families (although fewer second family carers attended groups than anticipated) |
Recruitment – Site 1: 38 families recruited Site 2 (round 1): 15 families recruited Site 2 (round 2): seven families recruited Site 3: 14 families recruited Group 1: 10 families Group 2: eight families Group 3: three families Group 4: four families Group 5: four families Group 6: eight families |
|
| Study retention: 75% of main family carers are retained for follow-up at the 12-month data collection point | Not achieved (70%) |
Total: 64/95 Main: 52/74 Second: 12/21 |
67 (56 to 77) 70 (59 to 80) 57 (34 to 78) |
| Adherence: 70% of main family carers and 40% of recruited second family carers adhere to the E-PAtS programme (i.e. ‘one of first two sessions, three from the remaining six sessions, and the final integrative session’) | Achieved (under updated definition of adherence). Family attendance of at least five sessions was 76% | ||
| Fidelity: 70% of the E-PAtS programme curriculum components are rated as partially or fully present in all recorded group sessions available for analysis | Achieved. Session summary forms (facilitator checklists following delivery of each session) reported that the percentage of components delivered ranged from 85% to 100% (97.1% overall) | ||
| Usual practice: between baseline and the 12-month follow-up, no more than 30% of main family carers in the usual-practice arm of the study receive a parenting programme [e.g. The Incredible Years® (Seattle, WA, USA) parenting programmes, Stepping Stones Triple P or similar] |
Achieved. Method revised, but 10% of family carers of young children with intellectual disability in an online UK survey reported receiving any of the named interventions for their child or themselves in the preceding 12 months We had originally planned to collect monthly diary data and include a usual-practice question in the parent advisory group, but this was replaced by the online UK survey data |
| Progression criterion | Progress |
|---|---|
| Provider willingness to participate in a definitive trial: a sufficient number of training providers indicate a willingness to take part in a new trial and to provide the number of E-PAtS groups needed for the definitive trial (numbers needed are to be informed by a sample size calculation for the definitive trial protocol) |
This criterion can be addressed fully only once the sample size and plan for a definitive trial are clear However, we gathered some relevant data: 9 out of 14 respondents to the survey of potential providers were unsure whether or not their organisation would be willing to deliver the E-PAtS programme within a RCT (question included reference to randomisation and use of control group). However, when asked how likely it was that their organisation would agree to deliver the E-PAtS programme within the specific RCT being planned by us, 13 out of 14 organisations indicated that it was somewhat/very likely We have also had discussions with one national provider willing to deliver the E-PAtS programme in four sites across the UK for a definitive trial |
| Progression criterion | Progress | Number (if applicable) | Percentage (95% CI)(if applicable) |
|---|---|---|---|
| The recruitment pathways leading to the largest numbers of families recruited and highest levels of consent, while not introducing important bias, will be identified and used to inform the protocol |
Seventy-three per cent of families were referred directly by Mencap Nineteen per cent of families were referred from Mencap-arranged parent information sessions Eight per cent of families were referred indirectly through advertising, word of mouth, etc. |
||
| Proposed primary outcome: will be confirmed as the WEMWBS if 90% of the collected measure are usable (data completeness) | At least 90% of collected WEMWBS were usable |
Baseline: 90/90 3 months: 62/63 12 months: 50/50 |
Baseline: 100 3 months: 98 112 months: 100 |
| Proposed secondary outcomes: any secondary outcome will be reconsidered if < 70% of collected data are usable for any measure | No secondary outcome measures have < 70% useable data | ||
| Usual-practice trial arm: if ≥ 70% of parents choose one of the study paths (A or B) then this study path will be used in the definitive trial | Over 70% of families chose pathway A (option to be offered the E-PAtS programme at 1 year) | 73/74 | 98 |
Chapter 6 Discussion and conclusions
In this chapter, we first summarise and interpret the main findings of the research in relation to the primary objectives, then consider PPI in the study and its impact, followed by a consideration of the strengths and limitations of the research and implications of the study findings for future delivery of the E-PAtS intervention, before summarising the progression criteria for a full trial.
Summary and interpretation of findings
Recruitment and retention
More than the planned 64 families were recruited during this research study. The target number was not quite achieved during the originally planned recruitment period. However, the research team had not anticipated that the main recruitment would be focused on a site in Northern Ireland, where school summer holidays begin at least 1 month before English schools. Therefore, our recruitment window was shorter than anticipated to make sure that the intervention would be completed by the end of May (so as not to get too close to school summer holidays). To further test recruitment, we added a second short phase of recruitment following the school summer holidays in 2018 and also added a second site in Northern Ireland. Adding this second phase of recruitment meant that we exceeded our initial recruitment target for the number of families in the research.
Although recruitment was successful overall, there was variation across sites, and a number of lessons from the research about recruitment pathways and factors to consider in selecting and preparing sites for recruitment in any future research. In particular, recruitment was relatively rapid in the Northern Ireland sites 1 and 3, compared with site 2. Overall, the recruitment pathways leading to the most success were (1) families already known to the provider organisations that were approached directly about the study and (2) information sessions that were run at a variety of times in each site to which families and also other local organisations and professionals were invited. These information sessions typically involved senior members of the research team attending, giving a standard presentation about the research (and what would be involved for families), which was carefully designed in advance, and answering questions. Both of these recruitment pathways worked best in Northern Ireland, where the provider organisation had a family support worker who was in contact with families, had previous experience of the E-PAtS intervention, and was also well-connected with other regional organisations that supported families of young children with intellectual disability. Although similar expertise was available in site 2, the existing relationships with families were not as extensive and the family support function was less well resourced. Additionally, set up for recruitment in site 2 was slower, partly because the initial focus on recruitment in Northern Ireland was to try to beat the earlier deadline imposed by the timing of the school summer holiday. However, recruitment was still slower during the second recruitment phase.
It is difficult to draw strong conclusions about the key facilitating factors for recruitment since by phase 2 there was a smaller pool of families left known to the provider in site 2. In site 2, families in the first phase of recruitment had not been recruited, for the most part, because they could not attend at the fixed time for the E-PAtS intervention group. However, changing this for the second recruitment phase did not seem to markedly improve recruitment (although, again, the pool of available families was by then potentially smaller).
In a larger potential future trial there would need to be a larger number of sites, and some variation between sites would be inevitable. Reaching the recruitment target overall would be the priority. There is, however, a secondary consideration. Smaller recruitment numbers in site 2 meant that E-PAtS groups were run with fewer families than is considered ideal. The qualitative data suggested that this did affect the experience of family carers receiving the intervention. For any future recruitment, it will be important to consider a balance of (1) the provider organisation’s existing resources for family support and the strength of their connections with other local organisations that might also be able to identify suitable families for the research, (2) the ability to be flexible in arranging intervention sessions’ times and locations to fit with families’ needs and (3) the size of the population of potentially suitable families with whom the provider already has contact. The latter is important in making sure that sufficient families are recruited to randomise sufficient numbers to the intervention arm of a trial.
Data summarised in the CONSORT flow diagram (see Figure 1) show that very few family carers did not take part or were excluded because they did not meet the study eligibility criteria. This suggests that the information about study eligibility was clear and could be used again with confidence in future research. From those initially contacted about the study (after expressing some interest), the largest group who ended up not taking part cited time commitment or the timing of intervention sessions as the reason for non-participation. To increase efficiency in recruitment for a larger study, it would be important (as already noted) to offer flexibility on the timing of intervention session delivery and also to carefully review study materials so that the time commitment required is clearer from the start.
Although the logic of the E-PAtS intervention focuses on families and therefore recruitment at the family level (as clusters) is the most important, second family carers were recruited in one-quarter of families. In a much larger study, this may be a sufficient proportion to gather some data about the potential impact of the intervention on fathers and other second family carers, and also the experiences of fathers and other carers involved with the intervention. Almost all second family carers recruited were fathers, as were a small proportion of main family carers. Despite collecting data on marital status, only 55% of participants answered these questions, meaning that the proportion of single parents supporting a child with intellectual disability could not be reliably reported.
Overall, recruited family carers were relatively well educated, with a majority having some higher education. There was a small amount of ethnic diversity (mainly in site 2) and there was evidence of socioeconomic deprivation in the sample, with relatively low levels of family weekly income. Approximately one half of family carers indicated that they were just managing or were struggling with finances and, again, almost one half of family carers suggested that they would not have the financial resources to raise funds in an emergency. Therefore, overall, the recruitment methods appeared to capture some diversity. Considering methods to increase ethnic diversity in the recruited sample, in particular, would be important for any future research and some focused PPI work on this issue would be useful. We address this point again later (see Strengths and limitations of the research).
Retention of families and individual carers in the study is most important at the 12-month post-randomisation follow-up point, as this would likely be the primary end point for any future larger trial. If a future study focuses on analysis at the level of the family then retention of families may be the primary consideration. In the current study, 81% of families in the intervention arm and 73% of families in the control arm completed at least one outcome at the 12-month follow-up. Seventy per cent of main family carers completed at least one outcome measure at follow-up and, focusing on the potential primary outcome for a future trial (i.e. the WEMWBS), 51% of main family carers completed the mental well-being questionnaire at the 12-month follow-up. These data show the potential for a good retention rate overall, given that some data collection with at least one family carer from a family was achieved at the 12-month follow-up with three-quarters of families. However, in any future research it will be important to maximise the completion of the primary outcome during successful data collection contacts. The qualitative data also suggested some improvements to a future study design and methods that might assist with retention. In particular, participants reflected on the number of data being collected (and that this could be reduced) and there was evidence of some confusion about when data would be collected. Improved communication with participants throughout the process may help in future.
The study team was successful in recruiting participants for qualitative interviews, suggesting that any process evaluation elements involving family carer interviews would be feasible in a future larger trial.
Intervention providers and E-PAtS facilitators
Sufficient providers and facilitators (i.e. professionals and family carers) were recruited to deliver the E-PAtS intervention in the feasibility study, delivering more E-PAtS groups than originally planned. New facilitators were also successfully trained and supervised through their first delivery of the E-PAtS intervention. Only one of the facilitators trained was subsequently deemed not suitable to deliver the intervention at this time, but this did not affect delivery as sufficient additional capacity had been built in at the training stage. Given the very low rate of unsuitable facilitators after training, the selection/recruitment process for facilitators appears to be fit for purpose.
Provider organisations and facilitators were positive about the E-PAtS intervention, valued the co-production/co-delivery approach, in particular, and have continued to deliver the intervention following the study. The provider organisations were all recruited from the same umbrella organisation that had an established relationship with the team members. However, a small survey of potential provider organisations without established relationships with the research team (12 non-Mencap organisations, one Mencap organisation and two unknown organisations) also confirmed interest in the focus of the intervention and the nature/logic of the intervention model, and, for a definitive RCT, a wider variety of provider organisations would need to be recruited to deliver the programme. The most significant barrier identified for future participation in a larger study was funding. Funding for the intervention would need to be secured as a part of the planning for a future trial, especially as providers in sites would probably need to deliver several E-PAtS groups. Therefore, the total funding commitment would probably be beyond the resources of many community-based organisations supporting families of young children with intellectual disability.
Provider organisations did express concern about the randomised nature of the design, but were persuaded by the perceived importance of the research for families of young children with intellectual disability. Provider organisations also recognised the significance of offering families a choice of study pathway (i.e. what they would be offered in the control arm of the study) and supported this as a way in the current study to gather direct data about the design of a future trial. Although contamination between trial arms is a potential risk, the chances of contamination appear minimal. First, although not specifically asked, there was no evidence of contamination in the qualitative interviews with participants or facilitators. Second, family carer facilitators would not have been in contact with any families in the control group during the trial period at all. Last, although we cannot say for sure, the likelihood that professional facilitators were specifically working with these families at this time is minimal.
Feasibility and acceptability of study processes and proposed outcome measures
Provider organisations (see Intervention providers and E-PAtS facilitators) found the randomisation to be acceptable. Family carers also found randomisation in the current study to be acceptable. It was not straightforward to clearly describe to them the choice of study pathway (i.e. their choice of being offered the E-PAtS programme if they were randomised to the control arm) and there was evidence from the qualitative interviews that parents may partly have chosen to be offered the E-PAtS programme later because they perceived that they had nothing to lose by doing so. Family carers also indicated in interviews that some research assistants may have encouraged carers to make this choice or reinforced participants’ observation that they would have nothing to lose by choosing to be offered the E-PAtS programme at the end of the study because they did not have to take up any offer later on. Nevertheless, all bar one family chose to be offered the E-PAtS programme at the end of the study period if they were to end up in the control arm, indicating that this would be an acceptable future comparator in a randomised study.
Family carers generally appreciated being given a choice about how they completed outcome measures (i.e. face to face, by questionnaire or over the telephone) and appreciated the opportunity to change the data completion method during the study (with three carers opting to make a change during the study). The vast majority of carers opted for non-face-to-face methods of data collection, and this also provided some flexibility for the research team, who were able to use a variety of strategies for following up participants to complete study measures.
One of our strategies to increase the acceptability of completing study measures was to provide a report based on the VABS standardised assessment, including some practical recommendations for families. The format and style of the report were finalised following PPI consultation. However, this report was met with a mixed response. Several participants valued the report and its format and style. However, some found it to be too ‘clinical’ in nature. Although this report seems unlikely to have helped to increase the acceptability of the data collection procedures, it might still be useful to include in a future study after a review of its style and content (perhaps after further PPI input). In particular, it would be helpful to consider if the second section of the report (i.e. the standard computer-generated report from the VABS software package) is needed.
In terms of the outcome measures themselves, the main comment in the qualitative interviews was that the outcome measures package was long. There is substantial potential to reduce the number of measures included in a future study and to prioritise outcomes using the logic model by considering possible overlap in the content of some measures. The FMSS was removed from the outcome measures after the 3-month follow-up, given the negative reactions from a number of participants and reflection from the SMG that this was not a crucial outcome. Some rapid coding of the speech samples (not reported here) also suggested that there was little variation in participants’ scores on this measure, and therefore there would be very little opportunity to demonstrate change. This combination of evidence suggests that the FMSS should not be included in a future trial. Otherwise, there were no particularly strong reactions to any other outcome measure. In addition, the data on completion of outcome measures support this conclusion. There were very high levels of data completion for all other measures in the study. Although we did not assess cost-effectiveness in this study, the feasibility of conducting an economic evaluation in a definitive trial was assessed. The health-related quality-of-life measure (i.e. EQ-5D) had a high degree of data completeness. The service receipt tool did attract some comments about the time it took to complete and the effort in recalling information, especially for families with multiple contacts and appointments with services and professionals. Overall, the results of the present research suggest that gathering data to enable a cost-effectiveness evaluation in a future trial would be feasible.
Data gathered during the interviews (including some survey questions) about the potential to include routine data collection in a future study suggested that this would, on the whole, be acceptable to family carers. An assessment of the availability of routine data sources suggested that some sources of routine data would also be feasible to collect. In the event that routine data collection is to be included in future research, data gathered in the current study suggest that it would be important to include clear educational messaging for participants about routine data and how such data can be provided to researchers. This should reduce any concerns that participants might have about routine data collection.
Although the current research was not designed to test the clinical effectiveness and cost-effectiveness of the E-PAtS intervention, there was preliminary evidence that the chosen proposed outcome measures (including the potential primary outcome for a later trial – the WEMWBS) reflected changes in the intervention arm of the study that are specified in the logic the model. Group differences at the 12-month follow-up were in the expected direction. However, the models fitted in this feasibility study adjusted for the clustered nature of carers within families only. In a definitive study, in addition to clustering of carers within a family, the clustering of families within E-PAtS groups may also require accounting for in statistical models. This is a form of partial nesting (i.e. clustering that would occur within one arm of the trial only), and similar to ignoring the clustering of carers within families, can lead to artificially narrow SEs and, hence, CIs that are artificially narrow and p-values that are artificially small. In line with the findings from Candlish et al. ,96 we would propose a heteroscedastic, partially nested mixed-effects model for handling this form of clustering. These analyses nonetheless suggest that it should be possible, in principle, to select from the outcomes tested in the current study to inform the outcome measures package for a future larger trial.
Intervention acceptability, adherence and fidelity
Qualitative interviews with participants showed that the E-PAtS intervention was positively perceived, and family carers reported positive outcomes for themselves and their family. As in other studies of interventions with an element of peer-to-peer support, parents valued the intervention beyond its specific content for shared contact with other families, learning from the experiences of other families and a process of mutual support among E-PAtS group members (note that the E-PAtS programme is not a wholly peer-support intervention as one facilitator is a professional). 36 Family carer facilitators also gained some additional expertise through the E-PAtS programme training and delivery, and gained in confidence. In terms of the safety of the intervention, it is also important to note that no potentially related adverse events were reported during the research.
Adherence to the E-PAtS intervention was assessed primarily at the level of family attendance at E-PAtS sessions. Seventy-six per cent of families in the intervention arm of the trial attended at least five of the eight E-PAtS sessions. A session was counted as attended by a family if at least one family carer from the family attended the session. This definition of adherence is a good fit with the E-PAtS logic model and E-PAtS programme practice. Therefore, second family carers are welcomed and encouraged to be involved in the intervention. However, it is left to families to decide how to manage their attendance. From the pattern of attendance and from qualitative data from participants and facilitators, it was clear that families typically focused on the main family carer attending E-PAtS sessions, with sometimes shared attendance responsibilities, but otherwise any second family carer attended when the main family carer could not.
Although the E-PAtS programme is designed to be delivered across eight sessions, there is recognition, as for most similar group-based parent interventions, that families are unlikely to be able to attend every single session. Families of children with an intellectual disability are also likely to face additional challenges relating to attendance at intervention sessions compared with families of non-disabled children. In particular, families may have limited financial capacity and the care demands of raising a child with an intellectual disability (especially for personal care) are higher than for other carers. 13 Therefore, the E-PAtS programme includes a number of mechanisms (see Chapter 2) to support family carers who have missed sessions (e.g. provision of handouts and other materials and catch-up contact with a facilitator before or after another session or between sessions). Facilitators also clearly communicated to families that the priority was for at least one carer from the family to attend as many E-PAtS sessions as possible and, ideally, for that to be the same family carer throughout.
Given all of these points, it became very clear that the initially proposed criteria for E-PAtS programme adherence were not a good match with the intervention logic and that they were unworkable for families. The initial criterion for adherence was to attend one of the first two sessions, three of the following five sessions and also the eighth integrative session. This attendance pattern was never communicated to families nor to E-PAtS programme facilitators. In addition, adherence for second family carers in a family was proposed to follow the same definition. Given how families managed attendance, and were encouraged to manage attendance, the application of such a definition for second family carers adherence was inappropriate. Given the mechanisms for repetition of content themes and catch-up for missed sessions, a more typical adherence definition relating to a total number of sessions (five) from those available (eight) was deemed a better match with the logic model and more pragmatic. In any future trial it would be helpful to gather more data about facilitators’ actions to catch up with individual families/carers for missed sessions and data on how family carers engage with materials provided for sessions that they missed. This would give a fuller picture of participants’ engagement with the intervention.
Fidelity of E-PAtS intervention delivery was assessed using a facilitator-completed checklist after each session and session recordings that were later rated by researchers. Facilitators reported that they had delivered almost all of the required content of the sessions (97%) and all eight E-PAtS sessions were delivered in all sites for all groups of family carers. Sometimes facilitators were not able to deliver a particular session (e.g. due to illness), but in every such case another local facilitator was able to take their place. This does reinforce the need for each site to have more than two facilitators trained and available. Research ratings of seven recorded E-PAtS sessions also showed that > 85% of expected content was delivered in all recorded sessions (and this was 100% for four out of the seven recorded sessions). These data suggest that the training and support process, and E-PAtS manual work well together to ensure a high degree of fidelity in delivery of the intervention.
Exploratory analyses also showed that WEMWBS scores at both baseline and 12 months were higher for participants whose families adhered to the intervention and as session attendance increased. Similarly, the availability of WEMWBS scores at 12 months was higher for those families with adherence and higher attendance levels at the family level. Finally, statistical models accounting for non-adherence or session attendance highlighted the potential for larger effect sizes for the WEMWBS at 12 months if adherence is increased.
For the definitive trial, analyses examining the impact of adherence on outcome will need to consider the following aspects:
-
How different conceptualisations of adherence/attendance map onto the logic model. The definition currently in use implies transferral of knowledge to a family carer absent from a session.
-
If session attendance adequately captures ‘adherence’ in the context of the E-PAtS programme, or if intervention fidelity and group dynamics should also be accounted for.
-
The plausibility of the key assumptions underlying the CACE analyses. For example, the adherence definition made the implicit assumption that participants in families that attended four or fewer sessions receive no benefit from being randomised to the E-PAtS programme (the ‘exclusion restriction’).
-
The extent to which clustering of adherence needs explicit accounting for.
-
Approaches to account for missing outcome data, which appeared to be related to whether or not a family adhered to the intervention.
Usual practice
Part of the expressed rationale for service providers to become involved in the study was their perception that families of young children with intellectual disability are not routinely offered an intervention like the E-PAtS programme. Therefore, provider organisation perceptions were that the E-PAtS programme was different from usual practice. Family carers in the qualitative research were of a similar view and suggested, in particular, that the bespoke nature of the E-PAtS programme (designed for families of young children with intellectual disability) and the co-production and co-delivery elements were different from usual practice. There was some evidence that not all of the content of the E-PAtS programme was new to the families, but the bringing together of the content and its delivery context were perceived as different from usual practice. Some parents had come across similar content to some of the E-PAtS programme content in their own research, especially on the internet.
Descriptive analysis of data from a question added into an online survey of young families of children with intellectual disability and related conditions in the UK showed that fewer than one-third of families had received any identifiable intervention for either their child or themselves as a family carer in the preceding 12 months. Just over 10% had received a clearly named intervention, and these included parent training approaches, such as Stepping Stones Triple P. However, this clearly represents a minority of families and suggests that a group for family carers, such as the E-PAtS groups, is quite distinct from usual practice in availability (in addition to in content). Family carer members of the advisory group also discussed the lack of support, similar to the E-PAtS programme, that had been available to them when their children were younger.
Patient and public involvement
A family carer member attended all SSC meetings and contributed to all discussions. They were also able to offer a particularly helpful perspective on strategies for follow-up of family carers, the potential importance of the intervention for family carers (in the context of a lack of similar support) and interpretation of the process evaluation findings. On reflection, although the family carer was very well informed and able to participate fully in the SSC, it would have been helpful for the research team to offer some preparation time before each meeting to be able to orientate the family carer to the topics to be discussed and any less familiar concepts (as well as answering any questions they may have had). Alternatively, or additionally, the family carer could have been put in contact with the PPI co-ordinator for support.
Overall, the family carer advisory group members were able to guide how materials and questions should be presented to carers more effectively. They were also able to give practical input to the wider usual-practice study questionnaire, based on their expertise of what services are available in England and Northern Ireland. Advisory group members helped to keep the research team focused on a family carer perspective, and their lived experience enabled them to identify issues that may not have occurred to the research team, but were potentially very important for participants.
Reflecting on the PPI process, the research team considered the aspects of PPI involvement through the advisory group that had worked well and less well. First, in terms of successful aspects of the advisory group, it was helpful to have a mixture of family carers (e.g. some with older children looking back, some with younger children, some familiar with the E-PAtS programme and some not). Second, meeting face to face was most valuable, including making sure that senior research team members attended the meetings in person. Although the meetings took time for all participants (family carers and research team), the time was well spent. Third, the process adopted at each meeting was to make sure that carers were well informed and updated before asking them to provide their input. This educational element was crucial and worked especially well when lead research team members explained aspects of the research process that were unfamiliar to carers (e.g. an accessible presentation on the role of process evaluation). Fourth, it was important to listen to the views of the family carers and to take the time to explain why we were not able to act on some suggestions. This communicated respect for the role of the family carer advisors. Finally, it was important to keep family carers updated about the study in between meetings and they were interested and keen to receive the updates.
In terms of lessons learned for PPI work in any future research, we did not plan as effectively as possible the timings of the advisory group meetings to tie in with key study milestones. For example, the first advisory group meeting was too late to discuss most recruitment materials and consultation had to be undertaken by e-mail. Engagement with the advisory group was always more effective the earlier it took place in the development of an aspect of the research. It was also not always clear that senior research team members had prioritised their involvement in attending the advisory group, but this is clearly an important marker of respect for the group. A small amount of turnover in family carer advisory group membership was experienced and this is important to plan for in any future study (e.g. the need to induct new members perhaps at several points during a longer study). Although the chairing of the advisory group was offered to the carers themselves, they did not want to take on the role. It would be useful in future to consider directly recruiting a family carer who would be willing to take on this role, as it may also give a different flavour to the meetings and help to give more control to the family carer advisors. Alternatively, a co-chairing arrangement with a co-applicant could be discussed.
Strengths and limitations of the research
A particular strength of the research was the ongoing partnership both with the provider organisations and PPI partner organisation, and with family carers themselves. PPI effectively ran throughout the whole project from the organisation of the E-PAtS programme delivery, the training of professional and family carer facilitators, the delivery of the E-PAtS programme, and the family carer roles on the advisory group and the SSC. Being closely connected to support organisations and to family carers throughout the study enhanced the quality and the practical value of the research. These partnerships probably also contributed to the achievement of the project objectives. Maintaining a strong co-productive stance in any future E-PAtS study is imperative. The research also benefited from dedicated, grant-funded time for a co-applicant working in the CBF, whose main role was to manage the PPI input from the advisory group and to keep PPI issues live in the SMG meetings.
An additional strength was the combination of subject expertise in the field of intellectual disability and methodology experts on the research team. This is a strength of many National Institute for Health Research research projects. However, in this case, the trials unit co-investigators also had considerable expertise in the field of intellectual disability, having completed a number of trials with this population group. The practical and methodological solutions to day-to-day challenges throughout the research study were much more sensitive to the needs of the population group and their families as a result of this added layer of shared interest and expertise. Again, it would be useful to capitalise on established intellectual disability expertise and positive working relationships between the teams involved in the current project in any future E-PAtS programme research. The success of the study was also boosted by extensive research expertise in the team, not just in the field of intellectual disability, but also working directly with families and on family members adjustment to living with a child with intellectual disability.
The main limitations of the research were the naive definition of adherence to the intervention proposed before the start of the project and a difficulty in obtaining recordings of the intervention sessions for independent fidelity ratings. In terms of adherence, before this research, there had not been a clear definition of adherence for the E-PAtS programme and the research team developed an overly complex conceptualisation of adherence as a starting point. This definition was not only far too restrictive but also not a good match for the intervention logic model. We were able to address this problem during the research and this means that any future research can begin with a much clearer adherence definition. In terms of recordings of intervention sessions, we were able to develop a fidelity rating tool and we demonstrated the feasibility of using this tool for rating both video- and audio-recordings. However, it was difficult to obtain recordings from the provider organisations because this process relied on facilitators setting up the recording equipment among their other preparation tasks for E-PAtS programme sessions. We had planned for receiving one or two video-recordings for each E-PAtS group delivered. However, we received seven session recordings in total, many of which were audio-recordings. Given that fidelity was possible to rate from audio-recordings, in any future research it would be worth considering planning from the beginning to use audio-recordings (for which the equipment set up is much simpler) and more attention needs to be given to practical steps to ensure that more recordings are available for independent fidelity ratings.
We considered one further issue that is both a potential strength and a limitation. In any future delivery of the E-PAtS programme, in practice, provider organisations would probably recruit families to groups that they would be organising. The recruitment process used in the current study closely reflects the likely future implementation model. However, as noted earlier, the recruited sample did appear to be relatively well educated and this may reflect families that the provider organisations were already in contact with and those they were able to attract using the adopted recruitment and advertising methods. In a future study, some revisions to the recruitment method would be useful. For example, the research team could develop some direct contacts with other non-provider organisations in each site and work with them on recruitment, perhaps especially for targeting less represented and vulnerable groups.
Implications for the E-PAtS intervention
The E-PAtS intervention itself has continued to evolve following feedback from delivery. A number of adjustments to the intervention were made throughout the research, in particular to address implementation and delivery issues that emerged. In addition, some of the current study findings have implications for future and especially larger-scale research on the E-PAtS programme.
First, there is a need to establish a network of supervisors/trainers for a multisite study. Online (rather than face-to-face) training for trainers has been successfully delivered in two sites, independent of the current study. This reduces costs for delivery, particularly as it becomes possible to train groups of facilitators from different geographical areas at the same time. It also eliminates the costs of travel for both facilitators and trainers and the costs of room bookings. Although the time for delivering the training remains the same, the removal of travel means that it is possible to divide the training over a greater number of days (e.g. delivery in halfdays), which can be advantageous for trainees and facilitators. This is likely to represent important flexibility for a larger study. Capacity to deliver the E-PAtS programme has been being built up in a number of sites across the UK to ensure a strong base in case of a larger-scale future research study.
Second, support for family carers who miss sessions has been an important element of the E-PAtS programme from the start, but the need to make this more transparent and to document this support has been highlighted through the feasibility study. There are a variety of methods by which family carers who have missed sessions may gain this missing information from facilitators, including receiving the information (in abbreviated form) during a telephone discussion (e.g. before the next session) or in person (e.g. by coming earlier to the start of the next session). In future research, the extent to which this happens should be more clearly documented and added to fidelity checklists.
Third, given the numbers of families where a second family carer was recruited, the low number of second family carers who attended the intervention and that there is now a clearer conceptualisation of adherence defined at the level of the family, it may be useful to review the E-PAtS programme focus on up to two carers in each family (see Chapter 2). Where families are more complex, it would be useful to be open to the potential for more than two carers in a family being recruited and to involve, through information-sharing and other mechanisms, more than one additional carer.
With the advent of COVID-19, the possibility of online delivery of the E-PAtS programme is also being explored across three sites (one in England, one in Wales and one in Canada). This may also be important for future and larger trials, particularly as it is unclear how and when restrictions will lift or if families of potentially vulnerable individuals will be willing to attend face-to-face group interventions. Although some costs may reduce (e.g. facilitator and family carer travel, room costs and refreshments) and families may find it easier to ‘attend’ (as there would be less need for child care), there would be challenges. Some of the intervention mechanisms may be difficult to replicate virtually. For example, group dynamics was considered a key mechanism through which the E-PAtS programme worked and may not be achievable virtually. In addition, participants valued the protected time and space while attending the E-PAtS programme and felt open to discuss personal challenges at the group sessions, something they may not feel while attending virtually from their home. Furthermore, disadvantaged families may not have access to suitable equipment or internet to attend online. These challenges would need to be addressed if online delivery of the E-PAtS programme is considered.
Progression criteria and potential for future trial
Following the presentation and discussion of the research findings, Tables 25–27 summarise the progression criteria prespecified in the study protocol and the data relating to each criterion. Also included in these tables are data relating to points that did not have specific criteria attached, but were designed to inform a future study. The progression criteria and associated data have been discussed in detail by the SMG and the SSC. The SSC recommended that the research progresses to a full trial. This was because all progression criteria were met fully, except for two points that require clarification. First, during the current study the research team realised that there was a need to fully review and revise the definition of E-PAtS programme adherence. Using the updated definition, the progression criterion was met. However, on the basis of the prespecified definition, the progression criterion was not met. Second, retention was above the progression target, with the focus on completion of at least one outcome measure by a carer from each recruited cluster (family). However, retention was slightly below target when one considers the proportion of main family carers retained at the 12-month follow-up.
If we had originally written the progression criteria using the now more usual traffic light system, then retention at 12 months would likely have been in an amber zone. 97 The SMG and SSC discussed retention in this context. As argued earlier, both the SMG and SSC concluded that there was good evidence to suggest that retention could be improved in a future trial. First, the research team by the end of the study had developed a series of clearer protocols for following up participants. Second, at the family level, the research team were successful in gathering at least one measure in a higher proportion of cases. Therefore, the task would be to ensure that contact and data completion becomes focused on the primary outcome in future research. Third, the SSC was supportive of the research team’s proposal to reduce the overall data collection load on carers in a future study (informed by participants’ comments in interviews that the questionnaire was long). Finally, data from the qualitative interviews also suggested that there could be clearer communication with participants in a future study about the need for follow-up data collection and the timing of follow-up.
Acknowledgements
We would like to thank all of the participants who took part in the E-PAtS feasibility study. Many thanks go to all E-PAtS facilitators involved in the study, family carers who contributed to the study through the SSC and advisory group, staff at the CBF and all independent members of the SSC.
Thanks to Diana Smith and Alison Baker at CEDAR (Centre for Educational Development Appraisal and Research) and the team at the Centre for Trials Research for providing administrative support. Particular thanks to the team at Mencap, including Joanne Sweeney, Margaret Kelly, Ranjan Sen and Valerie Lam.
Contributions of authors
Elinor Coulman (https://orcid.org/0000-0002-8854-2140) (Research Associate) managed the trial, conducted qualitative analysis and prepared the report for publication.
Nick Gore (https://orcid.org/0000-0003-1086-7647) (Senior Lecturer) co-led the study and contributed to report writing.
Gwenllian Moody (https://orcid.org/0000-0002-2000-4944) (Research Associate) managed the trial and contributed to report writing.
Melissa Wright (https://orcid.org/0000-0002-1011-4795) (Research Associate Statistician) carried out the statistical analysis and wrote up the results for publication.
Jeremy Segrott (https://orcid.org/0000-0001-6215-0870) (Senior Lecturer) led the process evaluation and wrote up the results for publication.
David Gillespie (https://orcid.org/0000-0002-6934-2928) (Senior Research Fellow) managed the statistical analysis and contributed to report writing.
Stavros Petrou (https://orcid.org/0000-0003-3121-6050) (Professor of Health Economics) managed the health economics analysis and contributed to report writing.
Fiona Lugg-Widger (https://orcid.org/0000-0003-0029-9703) (Research Fellow) managed the linkage with routine data aspect and contributed to report writing.
Sungwook Kim (https://orcid.org/0000-0002-1254-5038) (Researcher) carried out the health economics analysis and wrote up the results for publication.
Jill Bradshaw (https://orcid.org/0000-0002-0379-8877) (Senior Lecturer) provided expertise in qualitative design, the VABS analysis and contributed to the writing of the report.
Rachel McNamara (https://orcid.org/0000-0002-7280-1611) (Principal Research Fellow) supervised the Cardiff University team and provided expertise in trial management.
Andrew Jahoda (https://orcid.org/0000-0002-3985-6098) (Professor of Learning Disabilities) provided expertise in qualitative methods and analysis, and intellectual disability.
Geoff Lindsay (https://orcid.org/0000-0001-5253-3851) (Director of CEDAR) provided expertise in parenting research.
Jacqui Shurlock (https://orcid.org/0000-0003-4325-2833) led the PPI component of the trial.
Vaso Totsika (https://orcid.org/0000-0003-1702-2727) (Associate Professor) provided expertise in parent involvement.
Catherine Stanford (https://orcid.org/0000-0003-3920-0272) (Research Assistant) carried out quantitative and qualitative data collection, carried out qualitative data analysis and contributed to the writing of the report for publication.
Samantha Flynn (https://orcid.org/0000-0003-3466-9506) (Research Assistant) carried out quantitative and qualitative data collection, and carried out qualitative data analysis.
Annabel Carter (https://orcid.org/0000-0001-6879-9881) (Research Assistant) carried out quantitative and qualitative data collection, and carried out qualitative data analysis.
Christian Barlow (https://orcid.org/0000-0001-5759-0310) (Data Manager) carried out data management.
Richard Hastings (https://orcid.org/0000-0002-0495-8270) (Deputy Director of CEDAR) co-led the trial and prepared the report for publication.
Publication
Coulman E, Gore N, Moody G, Wright M, Segrott J, Gillespie D, et al. Early Positive Approaches to Support (E-PAtS) for families of young children with intellectual disability: a feasibility randomised controlled trial. Front Psychiatry 2021;12:729129.
Data-sharing statement
All available data can be obtained by contacting the corresponding author. The full trial protocol can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Salvador-Carulla L, Reed GM, Vaez-Azizi LM, Cooper SA, Martinez-Leal R, Bertelli M, et al. Intellectual developmental disorders: towards a new name, definition and framework for ‘mental retardation/intellectual disability’ in ICD-11. World Psychiatry 2011;10:175-80. https://doi.org/10.1002/j.2051-5545.2011.tb00045.x.
- Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res Dev Disabil 2011;32:419-36. https://doi.org/10.1016/j.ridd.2010.12.018.
- Public Health England . People With Learning Disabilities in England. Chapter 1. Education and Children’s Social Care n.d. www.gov.uk/government/publications/people-with-learning-disabilities-in-england/chapter-1-education-and-childrens-social-care-updates (accessed 14 March 2020).
- Global Research on Developmental Disabilities Collaborators . Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Glob Health 2018;6. https://doi.org/10.1016/S2214-109X(18)30309-7.
- Mithyantha R, Kneen R, McCann E, Gladstone M. Current evidence-based recommendations on investigating children with global developmental delay. Arch Dis Child 2017;102:1071-6. https://doi.org/10.1136/archdischild-2016-311271.
- Emerson E, Hatton C. Mental health of children and adolescents with intellectual disabilities in Britain. Br J Psychiatry 2007;191:493-9. https://doi.org/10.1192/bjp.bp.107.038729.
- Emerson E, Hatton C. Health Inequalities and People with Intellectual Disabilities. Cambridge, UK: Cambridge University Press; 2014.
- Bailey T, Totsika V, Hastings RP, Hatton C, Emerson E. Developmental trajectories of behaviour problems and prosocial behaviours of children with intellectual disabilities in a population-based cohort. J Child Psychol Psychiatry 2019;60:1210-18. https://doi.org/10.1111/jcpp.13080.
- Emerson E, Robertson J, Baines S, Hatton C. Obesity in British children with and without intellectual disability: cohort study. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3309-1.
- Singer GH. Meta-analysis of comparative studies of depression in mothers of children with and without developmental disabilities. Am J Ment Retard 2006;111:155-69. https://doi.org/10.1352/0895-8017(2006)111[155:MOCSOD]2.0.CO;2.
- Emerson E. Mothers of children and adolescents with intellectual disability: social and economic situation, mental health status, and the self assessed social and psychological impact of the child’s difficulties. J Intellect Disabil Res 2003;47:385-99. https://doi.org/10.1046/j.1365-2788.2003.00498.x.
- Emerson E, McCulloch A, Graham H, Blacher J, Llwellyn GM, Hatton C. Socioeconomic circumstances and risk of psychiatric disorders among parents of children with early cognitive delay. Am J Intellect Dev Disabil 2010;115:30-42. https://doi.org/10.1352/1944-7558-115.1.30.
- Totsika V, Hastings RP, Vagenas D. Informal caregivers of people with an intellectual disability in England: health, quality of life and impact of caring. Health Soc Care Community 2017;25:951-61. https://doi.org/10.1111/hsc.12393.
- Hastings RP. Do children with intellectual and developmental disabilities have a negative impact on other family members? The case for rejecting a negative narrative. Int Rev Res Dev Disabil 2016;50:165-94. https://doi.org/10.1016/bs.irrdd.2016.05.002.
- Griffith GM, Hastings RP. ‘He’s hard work, but he’s worth it’. The experience of caregivers of individuals with intellectual disabilities and challenging behaviour: a meta-synthesis of qualitative research. J Appl Res Intellect Disabil 2014;27:401-19. https://doi.org/10.1111/jar.12073.
- Toms G, Totsika V, Hastings R, Healy H. Access to services by children with intellectual disability and mental health problems: population-based evidence from the UK. J Intellect Dev Disabil 2015;40:239-47. https://doi.org/10.3109/13668250.2015.1045460.
- Cridland EK, Jones SC, Magee CA, Caputi P. Family-focused autism spectrum disorder research: a review of the utility of family systems approaches. Autism 2014;18:213-22. https://doi.org/10.1177/1362361312472261.
- Trivette CM, Dunst CJ, Hamby DW. Influences of family-systems intervention practices on parent–child interactions and child development. Topics Early Child Spec Educ 2010;30:3-19. https://doi.org/10.1177/0271121410364250.
- Hayden NK, Hastings RP, Totsika V, Langley E. A population-based study of the behavioral and emotional adjustment of older siblings of children with and without intellectual disability. J Abnorm Child Psychol 2019;47:1409-19. https://doi.org/10.1007/s10802-018-00510-5.
- Schuengel C, van Rest MM, Stanford CE, Hastings RP. Impact of research about the early development of children with intellectual disability: a science mapping analysis. Front Educ 2019;4. https://doi.org/10.3389/feduc.2019.00041.
- Totsika V, Hastings RP, Vagenas D, Emerson E. Parenting and the behaviour problems of young children with an intellectual disability: concurrent and longitudinal relationships in a population-based study. Am J Intellec Dev Disabil 2014;119:422-35. https://doi.org/10.1352/1944-7558-119.5.422.
- Totsika V, Hastings RP, Emerson E, Hatton C. Early years parenting mediates early adversity effects on problem behaviors in intellectual disability. Child Dev 2020;91:e649-e664. https://doi.org/10.1111/cdev.13273.
- Eldevik S, Jahr E, Eikeseth S, Hastings RP, Hughes CJ. Cognitive and adaptive behavior outcomes of behavioral intervention for young children with intellectual disability. Behav Modif 2010;34:16-34. https://doi.org/10.1177/0145445509351961.
- Dykens EM, Fisher MH, Taylor JL, Lambert W, Miodrag N. Reducing distress in mothers of children with autism and other disabilities: a randomized trial. Pediatrics 2014;134:e454-63. https://doi.org/10.1542/peds.2013-3164.
- Singer GH, Ethridge BL, Aldana SI. Primary and secondary effects of parenting and stress management interventions for parents of children with developmental disabilities: a meta-analysis. Ment Retard Dev Disabil Res Rev 2007;13:357-69. https://doi.org/10.1002/mrdd.20175.
- Glidden LM, Floyd FJ, Hastings RP, Mailick MR, Glidden LM, Abbeduto L, et al. APA Handbook of Intellectual and Developmental Disabilities. Washington, DC: American Psychological Association Publications; 2021.
- Hsieh RL, Hsieh WH, Lee WC. Short-term family-centered workshop for children with developmental delays enhances family functioning and satisfaction: a prospective clinical trial. Medicine 2016;95. https://doi.org/10.1097/MD.0000000000004200.
- DaWalt LS, Greenberg JS, Mailick MR. Transitioning together: a multi-family group psychoeducation program for adolescents with ASD and their parents. J Autism Dev Disord 2018;48:251-63. https://doi.org/10.1007/s10803-017-3307-x.
- Lunsky Y, P Hastings R, Weiss JA, M Palucka A, Hutton S, White K. Comparative effects of mindfulness and support and information group interventions for parents of adults with autism spectrum disorder and other developmental disabilities. J Autism Dev Disord 2017;47:1769-79. https://doi.org/10.1007/s10803-017-3099-z.
- Taylor JL, Hodapp RM, Burke MM, Waitz-Kudla SN, Rabideau C. Training parents of youth with autism spectrum disorder to advocate for adult disability services: results from a pilot randomized controlled trial. J Autism Dev Disord 2017;47:846-57. https://doi.org/10.1007/s10803-016-2994-z.
- Picard I, Morin D, De Mondehare L. Psychoeducational program for parents of adolescents with intellectual disabilities. J Policy Pract Intellect Disabil 2014;11:279-92. https://doi.org/10.1111/jppi.12099.
- National Institute for Health and Care Excellence (NICE) . Mental Health Problems in People With Learning Disabilities: Prevention, Assessment, and Management 2016.
- Tellegen CL, Sanders MR. Stepping Stones Triple P – Positive Parenting Program for children with disability: a systematic review and meta-analysis. Res Dev Disabil 2013;34:1556-71. https://doi.org/10.1016/j.ridd.2013.01.022.
- Durand VM, Hieneman M, Clarke S, Wang M, Rinaldi ML. Positive family intervention for severe challenging behavior I: a multisite randomized clinical trial. J Posit Behav Interv 2013;15:133-43. https://doi.org/10.1177/1098300712458324.
- Bovaird T. Beyond engagement and participation: user and community coproduction of public services. Public Adm Rev 2007;67:846-60. https://doi.org/10.1111/j.1540-6210.2007.00773.x.
- Shilling V, Morris C, Thompson-Coon J, Ukoumunne O, Rogers M, Logan S. Peer support for parents of children with chronic disabling conditions: a systematic review of quantitative and qualitative studies. Dev Med Child Neurol 2013;55:602-9. https://doi.org/10.1111/dmcn.12091.
- Association of Directors of Adult Social Services, Local Government Association and NHS England . Supporting People With a Learning Disability and Or Autism Who Display Behaviour That Challenges, Including Those With a Mental Health Condition: Service Model for Commissioners of Health and Social Care Services 2015.
- Scottish Government . National Parenting Strategy: Making a Positive Difference to Children and Young People Through Parenting 2012.
- Gore N, Hastings R, Brady S. Early intervention for children with learning disabilities: making use of what we know. Tizard Learn Disabil Rev 2014;19:2-14. https://doi.org/10.1108/TLDR-08-2013-0037.
- Guralnick MJ. A developmental systems model for early intervention. Infants Young Child 2001;141.
- Coulman E, Gore N, Moody G, Wright M, Segrott J, Gillespie D, et al. Early Positive Approaches to Support (E-PAtS) for families of young children with intellectual disability: a feasibility randomised controlled trial. Front Psychiatry 2021;12.
- Sparrow SS, Cicchetti DV, Saulnier CA. Vineland Adaptive Behavior Scales, Survey Forms Manual. Circle Pines, MN: AGS Publishing; 2016.
- Weiss JA, Lunsky Y. The brief family distress scale: a measure of crisis in caregivers of individuals with autism spectrum disorders. J Child Fam Stud 2011;20:521-8. https://doi.org/10.1007/s10826-010-9419-y.
- Feinberg ME, Brown LD, Kan ML. A multi-domain self-report measure of coparenting. Parent Sci Pract 2012;12:1-21. https://doi.org/10.1080/15295192.2012.638870.
- Pianta RC. Child–Parent Relationship Scale. Charlottesville, VA: University of Virginia; 1995.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10. https://doi.org/10.1186/1471-2288-10-67.
- Johnson J, Atkinson M, Rosenberg R, Schoon I, Joshi H, Smith K, et al. Millennium Cohort Study: Psychological, Developmental, and Health Inventories: User Guide to the Data. London, UK: Centre for Longitudinal Studies, Institute of Education; 2015.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med 1997;4:92-100. https://doi.org/10.1207/s15327558ijbm0401_6.
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2000.
- Varni JW, Seid M, Kurtin PS. PedsQL™ 4.0: reliability and validity of the Pediatric Quality of Life Inventory™ version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800-12. https://doi.org/10.1097/00005650-200108000-00006.
- Smilkstein G. The family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract 1978;6:1231-9.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Furman W, Buhrmester D. Children’s perceptions of the qualities of sibling relationships. Child Dev 1985;56:448-61. https://doi.org/10.2307/1129733.
- Dunst CJ. The family support scale: reliability and validity. J Individ Fam Community Wellness 1984;1:45-52.
- Magaña AB, Goldstein JM, Karno M, Miklowitz DJ, Jenkins J, Falloon IR. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Res 1986;17:203-12. https://doi.org/10.1016/0165-1781(86)90049-1.
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. J Clin Child Psychol 1989;18:167-75. https://doi.org/10.1207/s15374424jccp1802_8.
- MacDonald EE, Hastings RP, Fitzsimons E. Psychological acceptance mediates the impact of the behaviour problems of children with intellectual disability on fathers’ psychological adjustment. J Appl Res Intellect Disabil 2010;23:27-3. https://doi.org/10.1111/j.1468-3148.2009.00546.x.
- Treadwell T, Lavertue N, Kumar VK, Veeraraghavan V. The Group Cohesion Scale-Revised: reliability and validity. Int J Action Methods 2001;54:3-12.
- Beecham J, Knapp MRJ, Thornicroft GJ, Brewin CR, Wing JK. Measuring Mental Health Needs. London: Gaskell; 1992.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- GOV.UK . Advisory Fuel Rates from 1 June 2015 to 29 February 2020 2020. www.gov.uk/government/publications/advisory-fuel-rates/advisory-fuel-rates-1-september-2011-to-29-february-2016 (accessed 15 March 2020).
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- NHS Improvement . 2017/18/Reference/Costs 2018. https://improvement.nhs.uk/resources/reference-costs/ (accessed 2 December 2020).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2019 n.d. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2019/ (accessed 20 February 2020).
- Rutter J, Stocker K. Childcare Costs Survey 2015 2015. www.familyandchildcaretrust.org/sites/default/files/Resource%20Library/Childcare%20cost%20survey%202015%20Final_0.pdf (accessed 15 December 2019).
- National Institute for Health and Care Excellence . British National Formulary 2018. https://bnf.nice.org.uk (accessed 1 August 2018).
- National Institute for Health and Care Excellence . British National Formulary for Children 2018. https://bnfc.nice.org.uk (accessed 1 August 2018).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018 n.d. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2018/ (accessed 20 December 2019).
- UK Parliament . Written Evidence from NHS Direct NHS Trust (ES 31) 2013. https://publications.parliament.uk/pa/cm201314/cmselect/cmhealth/171/171vw25.htm (accessed 2 December 2019).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2013. Canterbury: Personal Social Services Research Unit, University of Kent; 2013.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit; 2016.
- NHS Improvement . 2018/19/National/Cost/Collection/Data 2019. https://improvement.nhs.uk/resources/national-cost-collection/#ncc1819 (accessed 20 February 2020).
- Curtis L, Burns A. Unit Cost of Health and Social Care 2012 2012. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2012/ (accessed 10 December 2019).
- Curtis L, Netten A. Unit Costs of Health and Social Care 2006 2006. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2006/ (accessed 2 February 2020).
- Curtis L. Unit Costs of Health and Social Care 2011 2011. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2011/ (accessed 2 February 2020).
- Curtis L. Unit Costs of Health and Social Care 2013 2013. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2011/ (accessed 15 February 2020).
- Lancsar E, Fiebig DG, Hole AR. Discrete choice experiments: a guide to model specification, estimation and software. PharmacoEconomics 2017;35:697-716. https://doi.org/10.1007/s40273-017-0506-4.
- McFadden D. Computing Willingness to Pay in Random Utility Models. Trade Theory and Econometrics. Essays in Honour of John S Chipman. London: Routledge; 1999.
- Giannotta F, Özdemir M, Stattin H. The implementation integrity of parenting programs: which aspects are most important?. Child Youth Care Forum 2019;48:917-33. https://doi.org/10.1007/s10566-019-09514-8.
- Bessen T, Chen G, Street J, Eliott J, Karnon J, Keefe D, et al. What sort of follow-up services would Australian breast cancer survivors prefer if we could no longer offer long-term specialist-based care? A discrete choice experiment. Br J Cancer 2014;110:859-67. https://doi.org/10.1038/bjc.2013.800.
- Mangham LJ, Hanson K, McPake B. How to do (or not to do) . . . Designing a discrete choice experiment for application in a low-income country. Health Policy Plan 2009;24:151-8. https://doi.org/10.1093/heapol/czn047.
- Ryan M, Kolstad J, Rockers P, Dolea C. How to Conduct a Discrete Choice Experiment for Health Workforce Recruitment and Retention in Remote and Rural Areas: A User Guide with Case Studies. Geneva: World Health Organization and CapacityPlus: World Bank; 2012.
- Tinelli M, Ryan M, Bond C. What, who and when? Incorporating a discrete choice experiment into an economic evaluation. Health Econ Rev 2016;6. https://doi.org/10.1186/s13561-016-0108-4.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2014.
- Franklin M, Thorn J. Self-reported and routinely collected electronic healthcare resource-use data for trial-based economic evaluations: the current state of play in England and considerations for the future. BMC Med Res Methodol 2019;19:1-3. https://doi.org/10.1186/s12874-018-0649-9.
- Husain MJ, Brophy S, Macey S, Pinder LM, Atkinson MD, Cooksey R, et al. HERALD (Health Economics using Routine Anonymised Linked Data). BMC Med Inform Decis Mak 2012;12. https://doi.org/10.1186/1472-6947-12-24.
- Franklin M, Davis S, Horspool M, Kua WS, Julious S. Economic evaluations alongside efficient study designs using large observational datasets: the PLEASANT trial case study. PharmacoEconomics 2017;35:561-73. https://doi.org/10.1007/s40273-016-0484-y.
- Davies JM, Gao W, Sleeman KE, Lindsey K, Murtagh FE, Teno JM, et al. Using routine data to improve palliative and end of life care. BMJ Support Palliat Care 2016;6:257-62. https://doi.org/10.1136/bmjspcare-2015-000994.
- Lugg-Widger F, Angel L, Cannings-John R, Hood K, Hughes K, Moody G, et al. Challenges in accessing routinely collected data from multiple providers in the UK for primary studies: managing the morass. Int J Popul Data Sci 2018;3. https://doi.org/10.23889/ijpds.v3i3.432.
- Lugg-Widger F, Cannings-John R, Angel L, Moody G, Segrott J, Kenkre J, et al. Assessing the impact of specialist home visiting upon maltreatment in England: a feasibility study of data linkage from a public health trial to routine health and social care data. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-018-0294-4.
- Robling M, Bekkers MJ, Bell K, Butler CC, Cannings-John R, Channon S, et al. Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (Building Blocks): a pragmatic randomised controlled trial. Lancet 2016;387:146-55. https://doi.org/10.1016/S0140-6736(15)00392-X.
- Great Britain . National Health Service Act 2006 2006.
- Candlish J, Teare MD, Dimairo M, Flight L, Mandefield L, Walters SJ. Appropriate statistical methods for analysing partially nested randomised controlled trials with continuous outcomes: a simulation study. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-018-0559-x.
- Avery KN, Williamson PR, Gamble C, O’Connell Francischetto E, Metcalfe C, Davidson P, et al. Informing efficient randomised controlled trials: exploration of challenges in developing progression criteria for internal pilot studies. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013537.
Appendix 1 The E-PAtS programme logic model
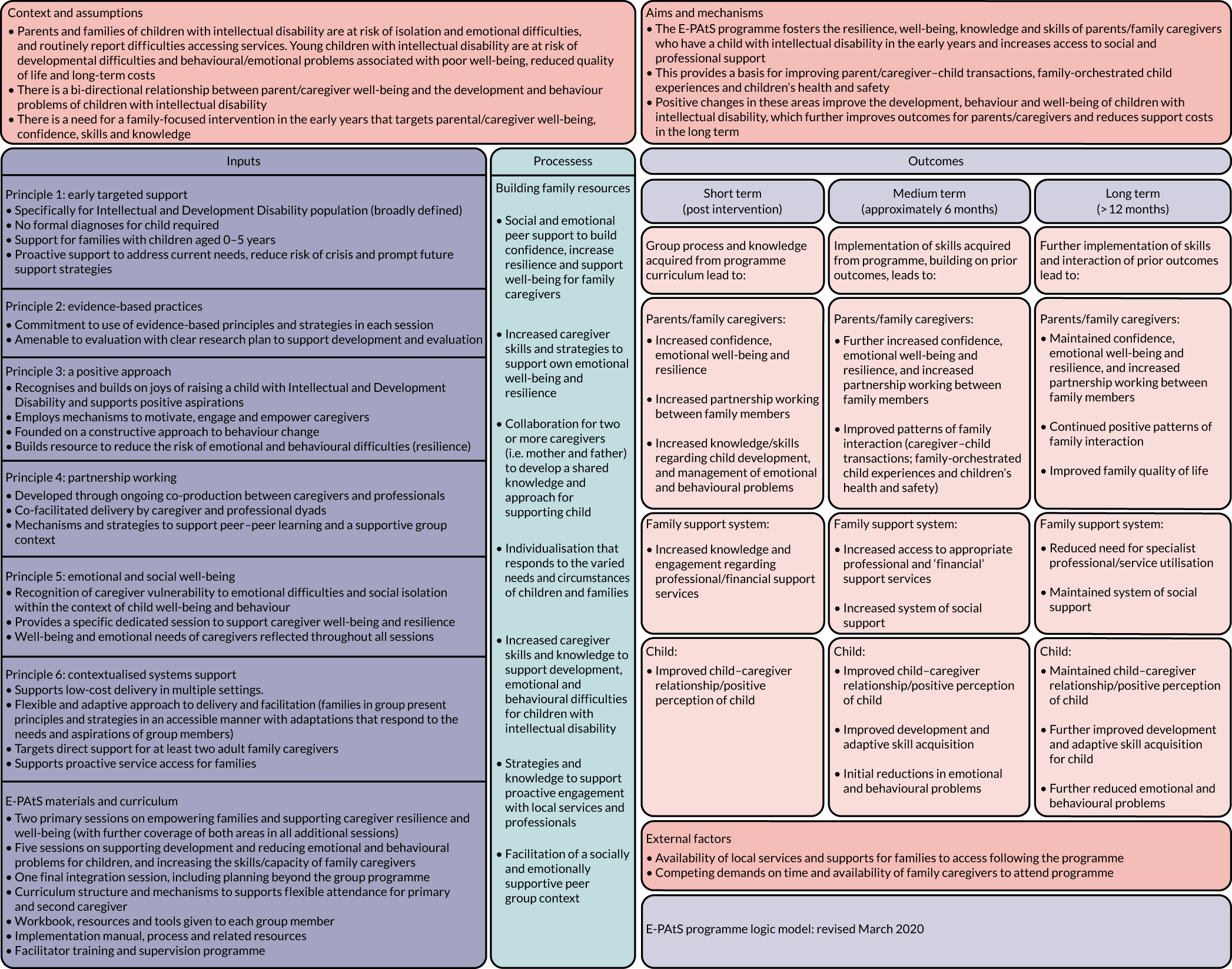
Appendix 2 Participant characteristics by site
| Characteristic | All participants, n (%) | ||
|---|---|---|---|
| Site 1 (N = 52) | Site 2 (N = 25) | Site 3 (N = 18) | |
| Relationship to child | |||
| Biological mother | 32 (62) | 21 (84) | 12 (67) |
| Biological father | 15 (29) | 4 (16) | 3 (17) |
| Adoptive mother | 0 (0) | 0 (0) | 1 (6) |
| Adoptive father | 0 (0) | 0 (0) | 1 (6) |
| Foster mother | 1 (2) | 0 (0) | 1 (6) |
| Grandmother | 2 (4) | 0 (0) | 0 (0) |
| Missing | 2 (4) | 0 (0) | 0 (0) |
| Living arrangements | |||
| Child lives with you full time | 45 (87) | 23 (92) | 18 (100) |
| Child lives with you part time | 4 (8) | 0 (0) | 0 (0) |
| Missing | 3 (6) | 2 (8) | 0 (0) |
| Ethnicity | |||
| Black/African/black British: African | 2 (4) | 5 (20) | 0 (0) |
| Black/African/black British: Caribbean | 1 (2) | 1 (4) | 0 (0) |
| Black: other | 1 (2) | 0 (0) | 0 (0) |
| Mixed: other | 0 (0) | 1 (4) | 0 (0) |
| Ethnic: other | 0 (0) | 1 (4) | 0 (0) |
| White: English/Welsh/Scottish/Northern Irish/British | 39 (75) | 6 (24) | 5 (28) |
| White: Irish | 7 (13) | 0 (0) | 13 (72) |
| White: other | 0 (0) | 6 (24) | 0 (0) |
| Any other ethnic background | 0 (0) | 2 (8) | 0 (0) |
| Prefer not to say | 0 (0) | 1 (4) | 0 (0) |
| Missing | 2 (4) | 2 (8) | 0 (0) |
| Qualifications | |||
| No qualifications | 2 (4) | 1 (4) | 0 (0) |
| Some GCSEs passes or equivalent | 10 (19) | 3 (12) | 2 (11) |
| Five or more GCSEs at A*–C or equivalent | 6 (12) | 2 (8) | 1 (6) |
| Five A/AS Levels or equivalent | 1 (2) | 0 (0) | 1 (6) |
| Higher education but below degree level | 11 (21) | 4 (16) | 6 (33) |
| Degree (e.g. BA, BSC, MA) | 19 (37) | 12 (48) | 8 (44) |
| Do not know | 0 (0) | 1 (4) | 0 (0) |
| Missing | 3 (6) | 2 (8) | 0 (0) |
| Employment | |||
| In a job and currently working for an employer | 25 (8) | 5 (20) | 6 (33) |
| On maternity/paternity/parental leave | 1 (2) | 0 (0) | 0 (0) |
| Self-employed | 3 (6) | 1 (4) | 3 (17) |
| Full-time student | 0 (0) | 0 (0) | 1 (6) |
| Doing voluntary work | 1 (2) | 0 (0) | 0 (0) |
| Looking after home and family | 17 (33) | 10 (40) | 8 (44) |
| Unemployed | 0 (0) | 3 (12) | 0 (0) |
| Do something else | 2 (4) | 4 (16) | 0 (0) |
| Missing | 3 (6) | 2 (8) | 0 (0) |
| Financial situation: total weekly household income | |||
| ≤ £200 | 4 (8) | 3 (12) | 2 (11) |
| Between £201 and £300 | 4 (8) | 4 (16) | 4 (22) |
| Between £301 and £400 | 6 (12) | 6 (24) | 5 (28) |
| Between £401 and £500 | 6 (12) | 4 (16) | 1 (6) |
| Between £501 and £600 | 6 (12) | 2 (8) | 5 (28) |
| Between £601 and £700 | 9 (17) | 2 (8) | 0 (0) |
| Between £701 and £800 | 5 (10) | 0 (0) | 0 (0) |
| Between £801 and £900 | 5 (10) | 0 (0) | 0 (0) |
| Between £901 and £1000 | 0 (0) | 0 (0) | 0 (0) |
| > £1000 | 5 (10) | 2 (8) | 0 (0) |
| Missing | 2 (4) | 2 (8) | 0 (0) |
| Financial situation: how are you managing financially? | |||
| Living comfortably | 8 (15) | 0 (0) | 3 (17) |
| Doing all right | 25 (48) | 8 (32) | 7 (39) |
| Just about getting by | 9 (17) | 10 (40) | 5 (28) |
| Finding it quite difficult | 4 (8) | 3 (12) | 0 (0) |
| Finding it very difficult | 2 (4) | 2 (8) | 1 (6) |
| Missing | 4 (8) | 2 (8) | 2 (11) |
| Financial situation: could you raise £2000 in a week for an emergency | |||
| I could easily raise the money | 11 (21) | 2 (8) | 1 (6) |
| I could, but it would involve some sacrifices | 12 (23) | 4 (16) | 4 (22) |
| I would have to do something drastic | 9 (17) | 4 (16) | 1 (6) |
| I do not think I could raise the money | 17 (33) | 12 (48) | 10 (56) |
| Missing | 3 (6) | 3 (12) | 2 (11) |
| Health | |||
| Very good | 18 (35) | 6 (24) | 12 (67) |
| Good | 17 (33) | 14 (56) | 5 (28) |
| Fair | 12 (23) | 3 (12) | 1 (6) |
| Bad | 0 (0) | 0 (0) | 0 (0) |
| Very bad | 2 (4) | 0 (0) | 0 (0) |
| Missing | 3 (6) | 2 (8) | 0 (0) |
| LTLI | |||
| No | 34 (65) | 18 (72) | 18 (0) |
| Yes | 16 (31) | 5 (20) | 0 (0) |
| Missing | 2 (4) | 2 (8) | 0 (0) |
Appendix 3 Child characteristics by study site
| Characteristic | Reported by main family carer, n (%) | ||
|---|---|---|---|
| Site 1 (N = 38) | Site 2 (N = 22) | Site 3 (N = 14) | |
| Gender of child | |||
| Male | 24 (63) | 16 (73) | 10 (71) |
| Female | 12 (32) | 6 (27) | 4 (29) |
| Missing | 2 (5) | 0 (0) | 0 (0) |
| School/nursery attendance | |||
| Not in school/nursery | 13 (34) | 3 (14) | 8 (57) |
| Mainstream preschool/nursery | 5 (13) | 9 (41) | 0 (0) |
| SRB in mainstream preschool/nursery | 1 (3) | 6 (27) | 0 (0) |
| Mainstream school | 2 (5) | 1 (5) | 1 (7) |
| Special school | 3 (8) | 0 (0) | 0 (0) |
| Special preschool/nursery | 12 (32) | 1 (5) | 4 (29) |
| Missing | 2 (5) | 2 (9) | 1 (7) |
| Visual impairment | |||
| No | 28 (74) | 13 (59) | 11 (79) |
| Yes | 8 (21) | 6 (27) | 3 (21) |
| Missing | 2 (5) | 3 (14) | 0 (0) |
| Hearing impairment | |||
| No | 29 (76) | 16 (73) | 14 (100) |
| Yes | 7 (18) | 3 (14) | 0 (0) |
| Missing | 2 (5) | 3 (14) | 0 (0) |
| Physical health problems | |||
| No | 15 (39) | 16 (73) | 8 (57) |
| Yes | 20 (53) | 3 (14) | 6 (43) |
| Missing | 3 (8) | 3 (14) | 0 (0) |
| Sibling aged 4–16 years | |||
| No | 10 (26) | 9 (41) | 5 (36) |
| Yes | 26 (68) | 13 (59) | 8 (57) |
| Missing | 2 (5) | 0 (0) | 1 (7) |
Appendix 4 Secondary outcomes by trial arm and family carer status
| Measure | Trial arm | |||||
|---|---|---|---|---|---|---|
| Control | Intervention | |||||
| Baseline | 3 months | 12 months | Baseline | 3 months | 12 months | |
| WEMWBS: score range 14–70; higher scores indicate higher levels of mental well-being | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 23 (62) | 18 (49) | 35 (95) | 29 (78) | 20 (54) |
| Useable forms, n (%) of those returned | 35 (100) | 23 (100) | 18 (100) | 35 (100) | 28 (97) | 20 (100) |
| Mean score (SD) | 43.5 (9.5) | 42.0 (10.2) | 43.1 (11.3) | 43.0 (10.6) | 44.4 (9.0) | 45.2 (10.9) |
| Range | 23–62 | 21–60 | 21–65 | 19–66 | 23–59 | 25–62 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 41.8 (6.9) | 45.7 (3.9) | 40.0 (10.4) | 47.2 (10.5) | 51.0 (8.9) | 50.3 (11.0) |
| Range | 30–55 | 41–49 | 26–52 | 36–65 | 40–61 | 37–68 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 28 (60) | 23 (49) | 45 (94) | 35 (73) | 27 (56) |
| Useable forms, n (%) of those returned | 45 (100) | 28 (100) | 23 (100) | 45 (100) | 34 (97) | 27 (100) |
| Mean score (SD) | 43.2 (8.9) | 42.7 (9.4) | 43.4 (11.0) | 43.9 (10.6) | 45.5 (9.2) | 46.5 (10.9) |
| Range | 23–62 | 21–60 | 21–65 | 19–66 | 23–61 | 25–68 |
| HADS anxiety: score range 0–21; higher scores indicate greater anxiety | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (58) | 18 (49) | 37 (100) | 27 (73) | 21 (58) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 18 (100) | 37 (100) | 27 (100) | 21 (100) |
| Mean score (SD) | 10.6 (3.5) | 12.3 (4.7) | 10.6 (4.6) | 10.7 (4.6) | 10.8 (4.9) | 8.2 (4.5) |
| Range | 3–19 | 4–20 | 3–19 | 1–21 | 3–19 | 1–20 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 10.3 (4.5) | 7.6 (3.6) | 7.4 (3.0) | 8.1 (3.0) | 7.2 (4.0) | 7.4 (4.4) |
| Range | 0–18 | 4–13 | 3–11 | 4–12 | 1–11 | 1–14 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 33 (69) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 47 (100) | 33 (100) | 28 (100) |
| Mean score (SD) | 10.6 (3.7) | 11.4 (4.8) | 9.9 (4.4) | 10.1 (4.4) | 10.2 (4.9) | 8.0 (4.4) |
| Range | 0–19 | 4–20 | 3–19 | 1–21 | 1–19 | 1–20 |
| HADS depression: score range 0–21; higher scores indicate higher levels of depression | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 18 (49) | 37 (100) | 27 (73) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 18 (100) | 37 (100) | 27 (100) | 21 (100) |
| Mean score (SD) | 7.7 (3.8) | 8.9 (4.3) | 9.6 (4.2) | 7.6 (4.2) | 7.6 (4.3) | 6.1 (4.1) |
| Range | 1–16 | 3.5–20 | 4–20 | 0–17 | 0–15 | 0–14 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 8.5 (4.4) | 7 (2.9) | 6.4 (3.2) | 5.7 (2.9) | 4.5 (4.1) | 6.0 (5.4) |
| Range | 0–15 | 2–9 | 3–11 | 1–9 | 0–11 | 0–13 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (27) | 23 (49) | 47 (98) | 33 (69) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 47 (100) | 33 (100) | 28 (100) |
| Mean score (SD) | 7.9 (3.9) | 8.6 (4.1) | 8.9 (4.2) | 7.2 (4.0) | 7.1 (4.4) | 6.1 (4.4) |
| Range | 0–16 | 2–20 | 3–20 | 0–17 | 0–15 | 0–14 |
| HADS emotional distress (sum of anxiety and depression subscales): score range 0–42; higher scores indicate greater emotional distress | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (74) | 21 (57) | 18 (49) | 37 (100) | 27 (73) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 18 (100) | 37 (100) | 27 (100) | 21 (100) |
| Mean score (SD) | 18.3 (6.4) | 21.2 (7.6) | 20.2 (8.0) | 18.3 (8.2) | 18.5 (8.7) | 14.3 (8.1) |
| Range | 6–32 | 7.5–32 | 7–34 | 4–38 | 4–32 | 1–32 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 18.8 (8.4) | 14.6 (5.5) | 13.8 (6.1) | 13.8 (5.1) | 11.7 (7.5) | 13.4 (9.0) |
| Range | 0–33 | 6–20 | 6–22 | 7–21 | 1–22 | 1–27 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 33 (69) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 47 (100) | 33 (100) | 28 (100) |
| Mean score (SD) | 18.4 (6.8) | 19.9 (7.7) | 18.8 (8.0) | 17.3 (7.8) | 17.2 (8.8) | 14.1 (8.2) |
| Range | 0–33 | 6–32 | 6–34 | 4–38 | 1–32 | 1–32 |
| VABS child-level variable | ||||||
| Not collected at the 3-month time point | Not collected at the 3-month time point | |||||
| Composite score: standardised score, mean 100 | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 22 (59) | 37 (100) | 20 (54) | ||
| Useable forms, n (%) of those randomised | 35 (100) | 22 (100) | 37 (100) | 20 (100) | ||
| Median score (IQR) | 55 (40–67) | 64.5 (58–69) | 58 (50–66) | 67.5 (58.5–70.5) | ||
| Range | 25–78 | 46–73 | 34–76 | 45–73 | ||
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 9 (90) | 9 (90) | 11 (100) | 7 (64) | ||
| Useable forms, n (%) of those randomised | 9 (100) | 9 (100) | 11 (100) | 7 (100) | ||
| Median score (IQR) | 60 (52–67) | 67 (59–69) | 61 (51–68) | 68 (57–71) | ||
| Range | 47–78 | 57–71 | 36–76 | 53–71 | ||
| Communication: standardised score, mean 100 | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 22 (59) | 37 (100) | 20 (54) | ||
| Useable forms, n (%) of those randomised | 35 (100) | 22 (100) | 37 (100) | 20 (100) | ||
| Median score (IQR) | 44 (26–67) | 63 (52–70) | 55 (34–64) | 61 (52–70.5) | ||
| Range | 20–83 | 39–77 | 20–85 | 40–80 | ||
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 9 (90) | 9 (90) | 11 (100) | 7 (64) | ||
| Useable forms, n (%) of those randomised | 9 (100) | 9 (100) | 11 (100) | 7 (100) | ||
| Median score (IQR) | 47 (40–58) | 64 (61–70) | 55 (42–64) | 61 (57–71) | ||
| Range | 32–83 | 39–73 | 20–75 | 54–76 | ||
| Family APGAR Scale: five items, score range 0–10; higher scores indicate better family function | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 34 (92) | 21 (57) | 18 (49) | 37 (100) | 27 (73) | 21 (57) |
| Useable forms, n (%) of those returned | 34 (100) | 20 (95) | 17 (94) | 37 (100) | 27 (100) | 21 (100) |
| Mean score (SD) | 7.2 (2.4) | 7.4 (2.8) | 6.8 (2.7) | 6.7 (2.9) | 6.9 (3.1) | 6.3 (2.6) |
| Range | 2–10 | 1–10 | 1–10 | 0–10 | 0–10 | 1–10 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 11 (100) | 5 (45) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 11 (100) | 5 (100) | 7 (100) |
| Mean score (SD) | 7.6 (2.5) | 8.0 (2.3) | 5.4 (4.6) | 7.7 (3.1) | 8.0 (2.5) | 6.9 (3.3) |
| Range | 2–10 | 5–10 | 0–10 | 0–10 | 4–10 | 1–10 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 44 (94) | 26 (55) | 23 (49) | 48 (100) | 32 (67) | 28 (58) |
| Useable forms, n (%) of those returned | 44 (100) | 25 (96) | 22 (96) | 48 (100) | 32 (100) | 28 (100) |
| Mean score (SD) | 7.3 (2.4) | 7.5 (2.7) | 6.5 (3.2) | 6.9 (2.9) | 7.1 (3.0) | 6.4 (2.8) |
| Range | 2–10 | 1–10 | 0–10 | 0–10 | 0–10 | 1–10 |
| Family Support Scale: number of informal sources of support available | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 17 (46) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those randomised | 35 (100) | 21 (100) | 17 (100) | 37 (100) | 28 (100) | 21 (100) |
| Median score (IQR) | 9 (8–12) | 10 (9–12) | 11 (9–13) | 9 (7–11) | 7.5 (6–11) | 10 (7–11) |
| Range | 5–13 | 3–13 | 2–13 | 3–13 | 2–13 | 2–12 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those randomised | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Median score (IQR) | 11 (10–13) | 12 (11–13) | 11 (11–12) | 12 (12–12) | 8 (7–13) | 12 (8–13) |
| Range | 6–13 | 11–13 | 10–13 | 9–13 | 7–13 | 7–13 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 22 (47) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those randomised | 45 (100) | 26 (100) | 22 (100) | 47 (100) | 34 (100) | 28 (100) |
| Median score (IQR) | 10 (8–12) | 11 (9–12) | 11 (10–13) | 10 (7–12) | 8 (6–11) | 10 (7.5–11) |
| Range | 5–13 | 3–13 | 2–13 | 3–13 | 2–13 | 2–13 |
| Family Support Scale: number of formal sources of support available | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 17 (46) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those randomised | 35 (100) | 21 (100) | 17 (100) | 37 (100) | 28 (100) | 21 (100) |
| Median score (IQR) | 4 (3–4) | 5 (4–5) | 4 (4–5) | 4 (3–4) | 4 (3.5–5) | 4 (3–4) |
| Range | 1–5 | 3–5 | 3–5 | 1–5 | 2–5 | 2–5 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those randomised | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Median score (IQR) | 5 (4–5) | 5 (4–5) | 4 (4–4) | 4 (4–5) | 4 (3–5) | 5 (4–5) |
| Range | 3–5 | 4–5 | 4–5 | 1–5 | 3–5 | 3–5 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 43 (91) | 26 (55) | 22 (47) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those randomised | 43 (100) | 26 (100) | 22 (100) | 47 (100) | 34 (100) | 28 (100) |
| Median score (IQR) | 4 (3–5) | 4 (4–5) | 4 (4–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Range | 1–5 | 3–5 | 3–5 | 1–5 | 2–5 | 2–5 |
| Mean helpfulness of informal sources of support available: scored 0 (not at all helpful) to 4 (extremely helpful) | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 17 (46) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 17 (100) | 37 (100) | 28 (100) | 21 (100) |
| Mean score (SD) | 1.8 (0.8) | 1.8 (0.7) | 1.6 (0.7) | 2.1 (0.9) | 2.0 (0.8) | 2.0 (1.0) |
| Range | 0.5–3.5 | 0.7–3.0 | 0.5–3.0 | 0.5–4.0 | 0–3.7 | 0.6–3.8 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 1.9 (0.5) | 2.0 (0.6) | 1.5 (0.3) | 1.7 (0.6) | 2.2 (1.1) | 2.2 (1.1) |
| Range | 1.1–2.7 | 1.0–2.7 | 1.1–1.9 | 0.9–2.8 | 0.9–3.8 | 0.8–4.0 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 22 (47) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 22 (100) | 47 (100) | 34 (100) | 28 (100) |
| Mean score (SD) | 1.8 (0.8) | 1.8 (0.7) | 1.6 (0.6) | 2.0 (0.9) | 2.0 (0.8) | 2.0 (1.0) |
| Range | 0.5–3.5 | 0.7–3.0 | 0.5–3.0 | 0.5–4.0 | 0–3.8 | 0.6–4.0 |
| Mean helpfulness of formal sources of support available: scored 0 (not at all helpful) to 4 (extremely helpful) | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 17 (46) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 17 (100) | 37 (100) | 28 (100) | 21 (100) |
| Mean score (SD) | 2.2 (1.0) | 2.2 (0.8) | 1.9 (1.1) | 2.4 (0.9) | 2.4 (0.9) | 2.5 (1.1) |
| Range | 0.6–4.0 | 0.5–3.6 | 0.4–4.0 | 0.8–4.0 | 0.6–4.0 | 0.5–4.0 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (10) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 2.8 (1.1) | 2.7 (0.9) | 2.2 (1.1) | 2.7 (1.2) | 2.8 (1.3) | 2.7 (0.7) |
| Range | 0.7–4.0 | 1.8–4.0 | 0.5–3.5 | 0.2–4.0 | 0.6–4.0 | 2.0–4.0 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 22 (47) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 22 (100) | 47 (100) | 34 (100) | 28 (100) |
| Mean score (SD) | 2.4 (1.0) | 2.3 (0.8) | 2.0 (1.1) | 2.5 (1.0) | 2.5 (0.9) | 2.6 (1.0) |
| Range | 0.6–4.0 | 0.5–4.0 | 0.4–4.0 | 0.2–4.0 | 0.6–4.0 | 0.5–4.0 |
| Positive Gains Scale: seven items, score range 7–35; higher scores indicate higher positive gains | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 18 (49) | 34 (92) | 28 (76) | 20 (54) |
| Useable forms, n (%) of those randomised | 35 (100) | 21 (100) | 18 (100) | 34 (100) | 27 (96) | 20 (100) |
| Median score (IQR) | 13 (9–16) | 14 (11–15) | 12.5 (9–14) | 11.5 (9–16) | 12 (9–15) | 11.5 (8–14.5) |
| Range | 7–24 | 7–19 | 7–19 | 7–23 | 7–35 | 7–20 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those randomised | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Median score (IQR) | 14 (9–15) | 11 (9–12) | 11 (10–13) | 10 (7–14) | 11.5 (10–17) | 9 (9–13) |
| Range | 7–15 | 9–16 | 9–16 | 7–19 | 9–35 | 7–14 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 44 (92) | 34 (71) | 27 (56) |
| Useable forms, n (%) of those randomised | 45 (100) | 26 (100) | 23 (100) | 44 (100) | 33 (97) | 27 (100) |
| Median score (IQR) | 13 (9–15) | 12.5 (10–15) | 12 (9–14) | 11 (8–15) | 12 (9–15) | 11 (8–14) |
| Range | 7–24 | 7–19 | 7–19 | 7–23 | 7–35 | 7–20 |
| CPRS (15 items) conflict: eight items, score range 8–40; higher scores indicate greater conflict | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 18 (49) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 18 (100) | 36 (97) | 28 (100) | 21 (100) |
| Mean score (SD) | 19.6 (6.1) | 21.0 (5.8) | 20.7 (5.8) | 20.0 (6.9) | 20.2 (7.7) | 18.6 (7.1) |
| Range | 11–32 | 10–30 | 11–32 | 8–33 | 8–35 | 8–32 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 11 (100) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (91) | 6 (100) | 7 (100) |
| Mean score (SD) | 16.7 (7.3) | 15.6 (6.1) | 19.0 (8.2) | 16.3 (6.0) | 10.5 (2.6) | 16.4 (8.0) |
| Range | 8–29 | 9–23 | 10–31 | 9–26 | 8–15 | 8–28 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 48 (100) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 46 (96) | 34 (100) | 28 (100) |
| Mean score (SD) | 18.9 (6.4) | 20.0 (6.1) | 20.3 (6.2) | 19.2 (6.8) | 18.5 (8.0) | 18.0 (7.3) |
| Range | 8–32 | 9–30 | 10–32 | 8–33 | 8–35 | 8–32 |
| CPRS (15 items) closeness: seven items, score range 7–35; lower scores indicate a less close relationship | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 18 (49) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those returned | 33 (94) | 19 (90) | 15 (83) | 35 (95) | 27 (96) | 21 (100) |
| Mean score (SD) | 25.2 (5.8) | 25.3 (6.0) | 27.8 (4.1) | 26.6 (4.9) | 28.0 (4.9) | 29.1 (3.8) |
| Range | 13–35 | 11–34 | 19–35 | 17–35 | 19–35 | 22–35 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 11 (100) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 9 (90) | 5 (100) | 4 (80) | 10 (91) | 6 (100) | 7 (100) |
| Mean score (SD) | 28.3 (2.6) | 27.6 (2.8) | 27.0 (1.4) | 27.9 (4.4) | 28.5 (6.9) | 31.2 (3.5) |
| Range | 24–32 | 23–30 | 26–29 | 21–32 | 15–35 | 25–35 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 48 (100) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 42 (93) | 24 (92) | 19 (83) | 45 (94) | 33 (97) | 28 (100) |
| Mean score (SD) | 25.9 (5.4) | 25.8 (5.5) | 27.6 (3.7) | 26.9 (4.7) | 28.1 (5.2) | 29.7 (3.8) |
| Range | 13–35 | 11–34 | 19–35 | 17–35 | 15–35 | 22–35 |
| Child–Parent Activity Index: five items, score range 5–25; higher scores indicate higher frequencies of activities shared with child | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 18 (49) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 18 (100) | 37 (100) | 28 (100) | 21 (100) |
| Mean score (SD) | 20.8 (3.4) | 20.5 (3.2) | 20.9 (2.9) | 20.6 (3.1) | 20.5 (3.7) | 20.2 (3.1) |
| Range | 13–24 | 13–25 | 14–25 | 12–25 | 12–25 | 13–25 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 11 (100) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 11 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 19.9 (3.4) | 19.8 (3.9) | 20.8 (4.1) | 19.7 (3.1) | 21.0 (2.3) | 21.7 (3.2) |
| Range | 14–23 | 16–24 | 14–24 | 14–24 | 18–25 | 16–25 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 48 (100) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 48 (100) | 34 (100) | 28 (100) |
| Mean score (SD) | 20.6 (3.4) | 20.4 (3.3) | 20.9 (3.1) | 20.4 (3.1) | 20.6 (3.4) | 20.6 (3.2) |
| Range | 13–24 | 13–25 | 14–25 | 12–25 | 12–25 | 13–25 |
| EQ-5D-5L: EQ-VAS – score range 0 (worst health) to 100 (best health) | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 23 (62) | 18 (49) | 37 (100) | 29 (78) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 23 (100) | 18 (100) | 37 (100) | 29 (100) | 21 (100) |
| Mean score (SD) | 72.4 (17.6) | 72.3 (17.6) | 68.3 (15.7) | 76.6 (18.0) | 74.9 (13.6) | 73.9 (21.4) |
| Range | 30–95 | 37–95 | 40–100 | 30–100 | 45–100 | 30–100 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 75.0 (12.5) | 82.0 (6.7) | 71.0 (13.9) | 74.0 (21.8) | 71.0 (22.9) | 71.0 (25.1) |
| Range | 50–95 | 75–90 | 50–85 | 40–100 | 40–96 | 30–97 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 28 (60) | 23 (49) | 47 (98) | 35 (73) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 28 (100) | 23 (100) | 47 (100) | 35 (100) | 28 (100) |
| Mean score (SD) | 73.0 (16.5) | 74.0 (16.6) | 68.9 (15.1) | 76.1 (18.7) | 74.2 (15.2) | 73.2 (21.9) |
| Range | 30–95 | 37–95 | 40–100 | 30–100 | 40–100 | 30–100 |
| Index value: score range 0.28 to 1 (perfect health) | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 23 (62) | 18 (49) | 37 (100) | 29 (78) | 21 (57) |
| Useable forms, n (%) of those randomised | 35 (100) | 23 (100) | 18 (100) | 37 (100) | 28 (97) | 20 (95) |
| Median score (IQR) | 0.84 (0.72–0.91) | 0.84 (0.67–1.00) | 0.82 (0.72–0.85) | 0.80 (0.74–0.88) | 0.84 (0.75–0.88) | 0.85 (0.73–1.00) |
| Range | –0.08 to 1.00 | –0.12 to 1.00 | 0.61 to 1.00 | 0.44 to 1.00 | 0.27 to 1.00 | 0.35 to 1.00 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 11 (100) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those randomised | 10 (100) | 5 (100) | 5 (100) | 11 (100) | 6 (100) | 7 (100) |
| Median score (IQR) | 0.83 (0.77–0.88) | 0.77 (0.68–1.00) | 0.74 (0.71–0.80) | 0.84 (0.70–1.00) | 0.88 (0.80–0.88) | 0.77 (0.72–1.00) |
| Range | 0.33–1.00 | 0.35–1.00 | 0.15–1.00 | 0.56–1.00 | 0.71–1.00 | 0.61–1.00 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 28 (60) | 23 (49) | 48 (100) | 35 (73) | 28 (58) |
| Useable forms, n (%) of those randomised | 45 (100) | 28 (100) | 23 (100) | 48 (100) | 34 (97) | 27 (96) |
| Median score (IQR) | 0.84 (0.77–0.88) | 0.80 (0.68–1.00) | 0.80 (0.71–0.85) | 0.84 (0.74–0.88) | 0.84 (0.75–0.88) | 0.85 (0.72–1.00) |
| Range | –0.08 to 1.00 | –0.12 to 1.00 | 0.15 to 1.00 | 0.44 to 1.00 | 0.27 to 1.00 | 0.35 to 1.00 |
| Brief COPE (17 items, three subscales): active avoidance coping – score range 6–24 | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 18 (49) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 18 (100) | 35 (95) | 27 (96) | 21 (100) |
| Mean score (SD) | 13.8 (2.9) | 12.3 (2.4) | 12.7 (2.7) | 13.5 (3.2) | 13.9 (3.3) | 13.1 (3.7) |
| Range | 8–20 | 8–18 | 7–18 | 8–21 | 8–20 | 7–21 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 14.2 (3.7) | 11.0 (2.3) | 10.6 (1.9) | 12.1 (4.5) | 10.7 (2.5) | 11.9 (2.0) |
| Range | 9–20 | 9–15 | 8–13 | 6–19 | 8–15 | 9–14 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 45 (96) | 33 (97) | 28 (100) |
| Mean score (SD) | 13.9 (3.1) | 12.1 (2.4) | 12.3 (2.7) | 13.2 (3.5) | 13.3 (3.4) | 12.8 (3.4) |
| Range | 8–20 | 8–18 | 7–18 | 6–21 | 8–20 | 7–21 |
| Problem-focused coping: score range 5–20 | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 18 (49) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 18 (100) | 36 (97) | 28 (100) | 21 (100) |
| Mean score (SD) | 16.5 (2.6) | 16.6 (2.6) | 17.2 (3.0) | 17.0 (2.7) | 17.5 (2.8) | 17.1 (2.6) |
| Range | 10–20 | 9–20 | 9–20 | 10–20 | 10–20 | 11–20 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 14.4 (2.8) | 13.7 (3.2) | 13.0 (3.3) | 15.0 (2.1) | 16.0 (3.3) | 16.9 (2.1) |
| Range | 10–18 | 10–18 | 9–16 | 10–17 | 11–20 | 14–20 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 46 (98) | 34 (100) | 28 (100) |
| Mean score (SD) | 16.0 (2.7) | 16.0 (2.9) | 16.3 (3.4) | 16.5 (2.6) | 17.2 (2.9) | 17.0 (2.4) |
| Range | 10–20 | 9–20 | 9–20 | 10–20 | 10–20 | 11–20 |
| Positive coping: score range 6–24 | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 21 (57) | 18 (49) | 37 (100) | 28 (76) | 21 (57) |
| Useable forms, n (%) of those returned | 35 (100) | 21 (100) | 18 (100) | 36 (97) | 28 (100) | 21 (100) |
| Mean score (SD) | 18.9 (3.5) | 17.9 (3.7) | 18.3 (3.7) | 18.0 (3.6) | 18.9 (2.7) | 18.8 (2.9) |
| Range | 11–24 | 10–23 | 11–24 | 10–24 | 14–24 | 14–24 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 10 (91) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 10 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 18.5 (3.1) | 19.4 (1.5) | 17.8 (3.3) | 18.0 (2.3) | 18.2 (4.2) | 20.4 (2.6) |
| Range | 13–23 | 17–21 | 14–22 | 13–22 | 11–22 | 17–24 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 26 (55) | 23 (49) | 47 (98) | 34 (71) | 28 (58) |
| Useable forms, n (%) of those returned | 45 (100) | 26 (100) | 23 (100) | 46 (98) | 34 (100) | 28 (100) |
| Mean score (SD) | 18.8 (3.4) | 18.2 (3.4) | 18.2 (3.6) | 18.0 (3.4) | 18.8 (3.0) | 19.2 (2.9) |
| Range | 11–24 | 10–23 | 11–24 | 10–24 | 11–24 | 14–24 |
| Happiness of Relationship Scale: one item scored 1–7; higher scores indicate greater happiness | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 28 (76) | 20 (54) | 16 (43) | 23 (62) | 24 (65) | 19 (51) |
| Useable forms, n (%) of those returned | 28 (100) | 20 (100) | 16 (100) | 23 (100) | 24 (100) | 19 (100) |
| Answered ‘cannot say’, n | 2 | 2 | 1 | 1 | 1 | 2 |
| Median score (IQR) (excluding those who answered ‘cannot say’) | 6 (5–7) | 6 (5–7) | 6 (5–7) | 6 (4–7) | 6 (4–7) | 6 (5–6) |
| Range | 1–7 | 1–7 | 1–7 | 1–7 | 1–7 | 1–7 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 9 (90) | 5 (50) | 5 (50) | 8 (73) | 6 (55) | 6 (55) |
| Useable forms, n (%) of those returned | 9 (100) | 5 (100) | 5 (100) | 8 (100) | 6 (100) | 6 (100) |
| Answered ‘cannot say’, n | 0 | 0 | 0 | 1 | 1 | 0 |
| Median score (IQR) (excluding those who answered ‘cannot say’) | 7 (6–7) | 7 (7–7) | 7 (7–7) | 7 (7–7) | 7 (7–7) | 7 (5–7) |
| Range | 6–7 | 5–7 | 6–7 | 6–7 | 5–7 | 3–7 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 37 (79) | 25 (53) | 21 (45) | 31 (65) | 30 (63) | 25 (52) |
| Useable forms, n (%) of those returned | 37 (100) | 25 (100) | 21 (100) | 31 (100) | 30 (100) | 25 (100) |
| Answered ‘cannot say’, n | 2 | 2 | 1 | 2 | 2 | 2 |
| Median score (IQR) (excluding those who answered ‘cannot say’) | 6 (5–7) | 7 (5–7) | 6.5 (5–7) | 7 (6–7) | 6 (4.5–7) | 6 (5–7) |
| Range | 1–7 | 1–7 | 1–7 | 1–7 | 1–7 | 1–7 |
| Co-Parenting Agreement Scale: four items, score range 0–6; higher scores indicate greater co-parenting agreement | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 28 (76) | 17 (46) | 17 (46) | 23 (62) | 22 (59) | 14 (38) |
| Useable forms, n (%) of those randomised | 28 (100) | 17 (100) | 16 (94) | 23 (100) | 22 (100) | 14 (100) |
| Median score (IQR) | 5.4 (3.8–6.0) | 5.5 (3.8–5.8) | 5.3 (4.0–5.9) | 4.5 (3.5–6.0) | 4.1 (3.5–6.0) | 4.4 (3.3–6.0) |
| Range | 1.0–6.0 | 0.5–6.0 | 0.3–6.0 | 0.5–6.0 | 0.0–6.0 | 2.3–6.0 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 8 (73) | 5 (45) | 4 (36) |
| Useable forms, n (%) of those randomised | 10 (100) | 5 (100) | 5 (100) | 8 (100) | 5 (100) | 4 (100) |
| Median score (IQR) | 5.8 (5.5–5.8) | 5.8 (5.3–6.0) | 5.5 (5.0–5.8) | 5.8 (4.4–6.0) | 4.5 (4.3–6.0) | 6.0 (5.5–6.0) |
| Range | 4.0–6.0 | 4.3–6.0 | 5–5.8 | 1.5–6.0 | 3.5–6.0 | 5.0–6.0 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 38 (81) | 22 (47) | 22 (47) | 31 (65) | 27 (56) | 18 (38) |
| Useable forms, n (%) of those randomised | 38 (100) | 22 (100) | 21 (95) | 31 (100) | 27 (100) | 18 (100) |
| Median score (IQR) | 5.5 (4.3–6.0) | 5.6 (4.3–5.8) | 5.3 (4.8–5.8) | 4.8 (3.5–6.0) | 4.3 (3.5–6.0) | 5.0 (3.3–6.0) |
| Range | 1.0–6.0 | 0.5–6.0 | 0.3–6.0 | 0.5–6.0 | 0–6 | 2.3–6.0 |
| Conflict: one item scored 1–7; higher scores indicate greater exposure to conflict | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 28 (76) | 17 (46) | 18 (49) | 23 (62) | 21 (57) | 15 (41) |
| Useable forms, n (%) of those returned | 28 (100) | 17 (100) | 18 (100) | 23 (100) | 21 (100) | 15 (100) |
| Answered ‘cannot say’, n | 3 | 1 | 2 | 1 | 1 | 2 |
| Median score (IQR) (excluding those who answered ‘cannot say’) | 2 (2–3) | 2 (1–4) | 2 (1.5–3.5) | 2 (1–2) | 2 (1–4) | 2 (1–3) |
| Range | 1–6 | 1–6 | 1–6 | 1–4 | 1–4 | 1–4 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 8 (73) | 5 (45) | 4 (36) |
| Useable forms, n (%) of those returned | 10 (100) | 5 (100) | 5 (100) | 8 (100) | 5 (100) | 4 (100) |
| Answered ‘cannot say’, n | 0 | 0 | 0 | 0 | 0 | 0 |
| Median score (IQR) (excluding those who answered ‘cannot say’) | 1.5 (1–2) | 1 (1–2) | 2 (1–3) | 2 (2–2) | 1 (1–2) | 1.5 (1–2) |
| Range | 1–4 | 1–2 | 1–4 | 1–3 | 1–5 | 1–2 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 38 (81) | 22 (47) | 23 (49) | 31 (65) | 26 (54) | 19 (40) |
| Useable forms, n (%) of those returned | 38 (100) | 22 (100) | 23 (100) | 31 (100) | 26 (100) | 19 (100) |
| Answered ‘cannot say’, n | 3 | 1 | 2 | 1 | 1 | 2 |
| Median score (IQR) (excluding those who answered ‘cannot say’) | 2 (1–3) | 2 (1–4) | 2 (1–3) | 2 (1–2) | 2 (1–4) | 2 (1–3) |
| Range | 1–6 | 1–6 | 1–6 | 1–4 | 1–6 | 1–4 |
| CBCL internalising score | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 20 (54) | 17 (46) | 37 (100) | 28 (76) | 20 (54) |
| Useable forms, n (%) of those returned | 34 (97) | 19 (95) | 14 (82) | 35 (95) | 24 (86) | 18 (90) |
| Mean score (SD) | 20.2 (9.2) | 21.2 (11.2) | 22.4 (12.2) | 20.6 (11.6) | 20.4 (12.8) | 20.4 (13.3) |
| Range | 6–37 | 4–40 | 9–46 | 2–51 | 3–49 | 1–42 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 11 (100) | 6 (55) | 6 (55) |
| Useable forms, n (%) of those returned | 9 (90) | 5 (100) | 5 (100) | 10 (91) | 5 (83) | 6 (100) |
| Mean score (SD) | 15.1 (7.3) | 13.4 (8.6) | 20.2 (11.0) | 16.9 (10.5) | 7.6 (6.2) | 11.3 (13.1) |
| Range | 3–26 | 3–23 | 9–38 | 4–36 | 3–17 | 1–28 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 25 (53) | 22 (47) | 48 (100) | 34 (71) | 26 (54) |
| Useable forms, n (%) of those returned | 43 (96) | 24 (96) | 19 (86) | 45 (94) | 29 (85) | 24 (92) |
| Mean score (SD) | 19.1 (9.0) | 19.5 (11.0) | 21.8 (11.6) | 19.8 (11.3) | 18.2 (12.8) | 18.2 (13.6) |
| Range | 3–37 | 3–40 | 9–46 | 2–51 | 3–49 | 1–42 |
| CBCL externalising score | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 20 (54) | 17 (46) | 37 (100) | 28 (76) | 20 (54) |
| Useable forms, n (%) of those returned | 34 (97) | 19 (95) | 14 (82) | 35 (95) | 24 (86) | 18 (90) |
| Mean score (SD) | 22.0 (9.6) | 24.3 (11.1) | 23.1 (10.7) | 20.6 (11.6) | 19.4 (13.9) | 18.5 (11.9) |
| Range | 6–42 | 2–43 | 5–41 | 4–44 | 0–46 | 1–46 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 11 (100) | 6 (55) | 6 (55) |
| Useable forms, n (%) of those returned | 9 (90) | 5 (100) | 5 (100) | 10 (91) | 5 (83) | 6 (100) |
| Mean score (SD) | 19.4 (10.7) | 16.0 (11.9) | 22.4 (10.4) | 13.3 (9.5) | 9.0 (10.6) | 10.8 (9.5) |
| Range | 3–36 | 2–29 | 4–29 | 2–33 | 1–27 | 1–28 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 25 (53) | 22 (47) | 48 (100) | 34 (71) | 26 (54) |
| Useable forms, n (%) of those returned | 43 (96) | 24 (96) | 19 (86) | 45 (94) | 29 (85) | 24 (92) |
| Mean score (SD) | 21.5 (9.7) | 22.6 (11.5) | 22.9 (10.3) | 19.0 (11.5) | 17.6 (13.8) | 16.6 (11.7) |
| Range | 3–42 | 2–43 | 4–41 | 2–44 | 0–46 | 1–46 |
| CBCL total problem score | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 20 (54) | 17 (46) | 37 (100) | 28 (76) | 20 (54) |
| Useable forms, n (%) of those returned | 34 (97) | 19 (95) | 14 (82) | 35 (95) | 24 (86) | 18 (90) |
| Mean score (SD) | 69.8 (25.4) | 75.8 (32.3) | 75.1 (27.2) | 66.7 (33.1) | 65.3 (38.8) | 62.9 (32.7) |
| Range | 19–120 | 10–129 | 22–120 | 10–142 | 10–140 | 5–115 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 5 (50) | 5 (50) | 11 (100) | 6 (55) | 6 (55) |
| Useable forms, n (%) of those returned | 9 (90) | 5 (100) | 5 (100) | 10 (91) | 5 (83) | 6 (100) |
| Mean score (SD) | 58.9 (30.0) | 51.0 (34.6) | 67.6 (30.6) | 51.3 (28.5) | 30.0 (25.4) | 38.3 (34.1) |
| Range | 13–104 | 7–86 | 16–92 | 13–108 | 9–70 | 3–95 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 25 (53) | 22 (47) | 48 (100) | 34 (71) | 26 (54) |
| Useable forms, n (%) of those returned | 43 (96) | 24 (96) | 19 (86) | 45 (94) | 29 (85) | 24 (92) |
| Mean score (SD) | 67.5 (26.4) | 70.6 (33.6) | 73.2 (27.5) | 63.3 (32.5) | 59.2 (38.9) | 56.8 (34.1) |
| Range | 13–120 | 7–129 | 16–120 | 10–142 | 9–140 | 3–115 |
| Paediatric Quality of Life Inventory: total score, score range 0–100; higher scores indicate better health-related quality of life | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 35 (95) | 20 (54) | 16 (43) | 35 (95) | 27 (73) | 20 (54) |
| Useable forms, n (%) of those returned | 35 (100) | 20 (100) | 16 (100) | 35 (100) | 27 (100) | 20 (100) |
| Mean score (SD) | 54.7 (16.9) | 55.4 (18.8) | 44.4 (22.4) | 60.1 (17.3) | 56.7 (17.8) | 58.9 (14.5) |
| Range | 26–94 | 17–86 | 0–85 | 24–85 | 26–89 | 25–86 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 10 (100) | 4 (40) | 5 (50) | 11 (100) | 6 (55) | 7 (64) |
| Useable forms, n (%) of those returned | 10 (100) | 4 (100) | 5 (100) | 11 (100) | 6 (100) | 7 (100) |
| Mean score (SD) | 56.1 (17.9) | 65.5 (16.8) | 61.9 (7.5) | 66.2 (18.3) | 73.7 (8.3) | 67.7 (23.9) |
| Range | 35–87 | 50–89 | 54–69 | 33–85 | 61–86 | 19–87 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 45 (96) | 24 (51) | 21 (45) | 46 (96) | 33 (69) | 27 (56) |
| Useable forms, n (%) of those returned | 45 (100) | 24 (100) | 21 (100) | 46 (100) | 33 (100) | 27 (100) |
| Mean score (SD) | 55.0 (16.9) | 57.0 (18.6) | 48.5 (21.2) | 61.6 (17.6) | 59.8 (17.7) | 61.2 (17.3) |
| Range | 26–94 | 17–89 | 0–85 | 24–85 | 26–89 | 19–87 |
| Group Cohesion Scale: score range 8–32; higher scores indicate better group cohesion | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 18 (49) | |||||
| Useable forms, n (%) of those returned | 16 (89) | |||||
| Median score (IQR) | 31.0 (27.2–32.0) | |||||
| Range | 8 to 32 | |||||
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 5 (45) | |||||
| Useable forms, n (%) of those returned | 4 (80) | |||||
| Median score (IQR) | 24.5 (23.4–28.0) | |||||
| Range | 23 to 31 | |||||
| All participants | ||||||
| Forms returned, n (%) of those randomised | 23 (48) | |||||
| Useable forms, n (%) of those returned | 20 (87) | |||||
| Median score (IQR) | 29.5 (24.5–32.0) | |||||
| Range | 8 to 32 | |||||
| Strengths and Difficulties Questionnaire (for siblings): 25 items | ||||||
| Number reporting a sibling aged 4–16 years | 25 | 25 | 25 | 22 | 22 | 22 |
| Strengths and Difficulties Questionnaire: Prosocial – five items, score range 0–10 | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 24 (96) | 14 (56) | 11 (44) | 22 (100) | 16 (73) | 13 (59) |
| Useable forms, n (%) of those returned | 24 (100) | 14 (100) | 11 (100) | 22 (100) | 16 (100) | 13 (100) |
| Median score (IQR) | 8.0 (8.0–9.5) | 8.5 (7.0–10.0) | 7.0 (7.0–9.0) | 8.5 (6.0–10.0) | 8.5 (4.5–10.0) | 8.0 (8.0–9.0) |
| Range | 1.3–10.0 | 5.0–10.0 | 1.0–10.0 | 1.0–10.0 | 0.0–10.0 | 5.0–10.0 |
| Second family carer | ||||||
| Number reporting a sibling aged 4–16 years | 8 | 8 | 8 | 8 | 8 | 8 |
| Forms returned, n (%) of those randomised | 8 (100) | 3 (38) | 3 (38) | 8 (100) | 4 (50) | 5 (63) |
| Useable forms, n (%) of those returned | 8 (100) | 3 (100) | 3 (100) | 8 (100) | 4 (100) | 5 (100) |
| Median score (IQR) | 8.4 (5.5–9.5) | 6.0 (5.0–8.0) | 9.0 (6.0–9.0) | 8.5 (6.5–9.0) | 7.5 (5.5–9.0) | 8.0 (6.0–10.0) |
| Range | 2.0–10.0 | 5.0–8.0 | 6.0–9.0 | 1.0–9.0 | 5.0–9.0 | 5.0–10.0 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 32 (97) | 17 (52) | 14 (42) | 30 (100) | 20 (67) | 18 (60) |
| Useable forms, n (%) of those returned | 32 (100) | 17 (100) | 14 (100) | 30 (100) | 20 (100) | 18 (100) |
| Median score (IQR) | 8.0 (7.5–9.5) | 8.0 (7.0–9.0) | 7.5 (7.0–9.0) | 8.5 (6.0–10.0) | 8.5 (5.0–10.0) | 8.0 (6.0–10.0) |
| Range | 1.2–10.0 | 5.0–10.0 | 1.0–10.0 | 1.0–10.0 | 0.0–10.0 | 5.0–10.0 |
| Internalising problems: sum of emotional and peer problems subscale, score range 0–20 | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 24 (96) | 14 (56) | 11 (44) | 22 (100) | 16 (73) | 13 (59) |
| Useable forms, n (%) of those returned | 24 (100) | 14 (100) | 11 (100) | 22 (100) | 16 (100) | 13 (100) |
| Median score (IQR) | 4.5 (3.0–8.5) | 3.5 (3.0–7.0) | 6.0 (4.0–13.0) | 2.0 (1.0–9.0) | 5.5 (3.5–8.5) | 4.0 (3.0–8.0) |
| Range | 0.0–15.0 | 0.0–13.0 | 0.0–15.0 | 0.0–16.0 | 0.0–11.0 | 1.0–17.0 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 8 (100) | 3 (38) | 3 (38) | 8 (100) | 4 (50) | 5 (63) |
| Useable forms, n (%) of those returned | 8 (100) | 3 (100) | 3 (100) | 8 (100) | 4 (100) | 5 (100) |
| Median score (IQR) | 3.5 (0.0–9.0) | 4.0 (0.0–9.0) | 4.0 (2.0–11.0) | 2.5 (1.0–8.5) | 4.0 (1.0–7.0) | 4.0 (3.0–5.0) |
| Range | 0.0–9.0 | 0.0–9.0 | 2.0–11.0 | 0.0–10.0 | 0.0–8.0 | 0.0–6.0 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 32 (97) | 17 (52) | 14 (42) | 30 (100) | 20 (67) | 18 (60) |
| Useable forms, n (%) of those returned | 32 (100) | 17 (100) | 14 (100) | 30 (100) | 20 (100) | 18 (100) |
| Median score (IQR) | 4.5 (2.5–9.0) | 4.0 (3.0–7.0) | 5.5 (4.0–11.0) | 2.0 (1.0–9.0) | 5.5 (2.5–8.0) | 4.0 (3.0–6.0) |
| Range | 0.0–15.0 | 0.0–13.0 | 0.0–15.0 | 0.0–16.0 | 0.0–11.0 | 0.0–17.0 |
| Externalising problems: sum of hyperactivity and conduct, score range 0–20 | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 24 (96) | 14 (56) | 11 (44) | 22 (100) | 16 (73) | 13 (59) |
| Useable forms, n (%) of those returned | 24 (100) | 14 (100) | 11 (100) | 22 (100) | 16 (100) | 13 (100) |
| Median score (IQR) | 7.0 (3.5–9.0) | 6.5 (4.0–9.0) | 9.0 (3.0–11.0) | 4.0 (2.0–7.0) | 6.8 (1.5–10.0) | 4.0 (2.0–5.3) |
| Range | 1.0–12.0 | 2.0–13.0 | 1.0–12.0 | 0.0–15.0 | 0.0–18.3 | 0.0–15.0 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 8 (100) | 3 (38) | 3 (38) | 8 (100) | 4 (50) | 5 (63) |
| Useable forms, n (%) of those returned | 8 (100) | 3 (100) | 3 (100) | 8 (100) | 4 (100) | 5 (100) |
| Median score (IQR) | 8.5 (1.5–10.5) | 5.0 (2.0–9.0) | 7.0 (1.0–11.0) | 5.0 (2.0–6.5) | 8.0 (5.5–10.0) | 6 (4.0–7.0) |
| Range | 1.0–13.3 | 2.0–9.0 | 1.0–11.0 | 1.0–14.0 | 5.0–10.0 | 3.0–13.7 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 32 (97) | 17 (52) | 14 (42) | 30 (100) | 20 (67) | 18 (60) |
| Useable forms, n (%) of those returned | 32 (100) | 17 (100) | 14 (100) | 30 (100) | 20 (100) | 18 (100) |
| Median score (IQR) | 7.0 (3.0–9.0) | 5.0 (4.0–9.0) | 8.0 (3.0–11.0) | 4.5 (2.0–7.0) | 6.8 (3.5–10.0) | 4.5 (3.0–7.0) |
| Range | 1.0–13.3 | 2.0–13.0 | 1.0–12.0 | 0.0–15.0 | 0.0–18.3 | 0.0–15.0 |
| SRQ: warmth, score range 1–5; higher scores indicate higher levels of warmth in relationship | ||||||
| Main family carer | ||||||
| Number reporting a sibling aged 4–16 years | 25 | 25 | 25 | 22 | 22 | 22 |
| Forms returned, n (%) of those randomised | 25 (100) | 14 (56) | 11 (44) | 22 (100) | 15 (68) | 13 (59) |
| Useable forms, n (%) of those returned | 23 (92) | 12 (86) | 8 (73) | 17 (77) | 12 (80) | 11 (85) |
| Mean score (SD) | 3.1 (0.7) | 3.0 (0.5) | 3.0 (0.8) | 3.3 (0.4) | 3.3 (0.9) | 3.5 (0.6) |
| Range | 1.8–4.2 | 2.0–4.0 | 1.5–4.0 | 2.3–4.3 | 2.0–5.0 | 2.5–4.2 |
| Second family carer | ||||||
| Number reporting a sibling aged 4–16 years | 8 | 8 | 8 | 8 | 8 | 8 |
| Forms returned, n (%) of those randomised | 8 (100) | 3 (38) | 3 (38) | 8 (100) | 4 (50) | 5 (63) |
| Useable forms, n (%) of those returned | 7 (88) | 2 (67) | 2 (67) | 7 (88) | 3 (75) | 4 (80) |
| Mean score (SD) | 3.3 (1.2) | 3.8 (0.5) | 3.5 (0.2) | 3.5 (0.6) | 4.0 (0.7) | 3.8 (1.0) |
| Range | 1.0–4.3 | 3.5–4.2 | 3.3–3.7 | 2.7–4.3 | 3.2–4.5 | 2.5–4.8 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 33 (100) | 17 (52) | 14 (42) | 30 (100) | 19 (63) | 18 (60) |
| Useable forms, n (%) of those returned | 30 (91) | 14 (82) | 10 (71) | 24 (80) | 15 (79) | 15 (83) |
| Mean score (SD) | 3.1 (0.8) | 3.1 (0.6) | 3.1 (0.7) | 3.4 (0.5) | 3.4 (0.9) | 3.6 (0.7) |
| Range | 1.0–4.3 | 2.0–4.2 | 1.5–4.0 | 2.3–4.3 | 2.0–5.0 | 2.5–4.8 |
| SRQ: conflict, score range 1–5; higher scores indicate higher levels of conflict in relationship | ||||||
| Main family carer | ||||||
| Forms returned, n (%) of those randomised | 25 (100) | 14 (56) | 11 (44) | 22 (100) | 15 (68) | 13 (59) |
| Useable forms, n (%) of those returned | 23 (92) | 13 (93) | 8 (73) | 20 (91) | 14 (93) | 12 (92) |
| Mean score (SD) | 2.0 (0.8) | 2.3 (0.9) | 2.3 (1.2) | 1.9 (0.8) | 2.2 (0.8) | 2.2 (0.6) |
| Range | 1.0–3.5 | 1.0–4.5 | 1.0–4.0 | 1.0–3.3 | 1.0–3.5 | 1.0–3.0 |
| Second family carer | ||||||
| Forms returned, n (%) of those randomised | 8 (100) | 3 (38) | 3 (38) | 8 (100) | 4 (50) | 5 (63) |
| Useable forms, n (%) of those returned | 7 (88) | 2 (67) | 2 (67) | 8 (100) | 4 (100) | 5 (100) |
| Mean score (SD) | 2.0 (0.8) | 1.8 (1.1) | 2.6 (2.3) | 1.9 (0.6) | 1.9 (0.8) | 1.9 (0.9) |
| Range | 1.0–4.0 | 1.0–2.5 | 1.0–4.3 | 1.0–2.7 | 1.0–3.0 | 1.0–3.0 |
| All participants | ||||||
| Forms returned, n (%) of those randomised | 33 (100) | 17 (52) | 14 (42) | 30 (100) | 19 (63) | 18 (60) |
| Useable forms, n (%) of those returned | 30 (91) | 15 (88) | 10 (71) | 28 (93) | 18 (95) | 17 (94) |
| Mean score (SD) | 2.0 (0.9) | 2.2 (0.9) | 2.4 (1.3) | 1.9 (0.7) | 2.1 (0.8) | 2.1 (0.7) |
| Range | 1.0–4.0 | 1.0–4.5 | 1.0–4.3 | 1.0–3.3 | 1.0–3.5 | 1.0–3.0 |
Appendix 5 Participants’ awareness of and views surrounding routine data collection
| Data | Main family carer, n (%) | |
|---|---|---|
| Control (N = 18) | Intervention (N = 19) | |
| Hospital data | ||
| Were you aware researchers are able to request access to hospital data? | ||
| No | 10 (56) | 13 (68) |
| Yes | 7 (39) | 5 (26) |
| Missing | 1 (4) | 1 (5) |
| Would you be comfortable in agreeing to us accessing your data in a future study? | ||
| Not at all comfortable | 0 (0) | 5 (26) |
| Not very comfortable | 2 (11) | 3 (16) |
| No preference | 7 (38) | 3 (16) |
| Quite comfortable | 5 (28) | 7 (37) |
| Very comfortable | 3 (17) | 1 (5) |
| Missing | 1 (6) | 0 (0) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||
| Not at all comfortable | 0 (0) | 3 (16) |
| Not very comfortable | 1 (6) | 3 (16) |
| No preference | 8 (44) | 3 (16) |
| Quite comfortable | 5 (28) | 8 (42) |
| Very comfortable | 3 (17) | 2 (11) |
| Missing | 1 (6) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your data? | ||
| Definitely less likely to take part | 0 (0) | 3 (16) |
| Slightly less likely to take part | 2 (11) | 3 (16) |
| No difference | 14 (78) | 10 (53) |
| Slightly more likely to take part | 0 (0) | 1 (5) |
| Definitely more likely to take part | 1 (6) | 0 (0) |
| Missing | 1 (6) | 2 (11) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||
| Definitely less likely to take part | 0 (0) | 5 (26) |
| Slightly less likely to take part | 3 (17) | 2 (11) |
| No difference | 13 (72) | 10 (53) |
| Slightly more likely to take part | 1 (6) | 1 (5) |
| Definitely more likely to take part | 1 (6) | 1 (5) |
| School data | ||
| Were you aware researchers are able to request access to school data? | ||
| No | 13 (72) | 14 (74) |
| Yes | 5 (28) | 5 (26) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||
| Not at all comfortable | 0 (0) | 4 (21) |
| Not very comfortable | 1 (6) | 1 (5) |
| No preference | 9 (50) | 5 (26) |
| Quite comfortable | 4 (22) | 7 (37) |
| Very comfortable | 3 (17) | 2 (11) |
| Missing | 1 (6) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||
| Definitely less likely to take part | 0 (0) | 3 (16) |
| Slightly less likely to take part | 2 (11) | 0 (0) |
| No difference | 13 (72) | 13 (68) |
| Slightly more likely to take part | 1 (6) | 1 (5) |
| Definitely more likely to take part | 1 (6) | 1 (5) |
| Missing | 1 (6) | 1 (5) |
| Social care data | ||
| Were you aware researchers are able to request access to social care data? | ||
| No | 13 (72) | 13 (68) |
| Yes | 5 (28) | 6 (32) |
| Missing | 0 (0) | 0 (0) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||
| Not at all comfortable | 0 (0) | 4 (21) |
| Not very comfortable | 1 (6) | 0 (0) |
| No preference | 10 (56) | 7 (37) |
| Quite comfortable | 2 (11) | 6 (32) |
| Very comfortable | 4 (22) | 2 (11) |
| Missing | 1 (6) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||
| Definitely less likely to take part | 0 (0) | 4 (21) |
| Slightly less likely to take part | 2 (11) | 0 (0) |
| No difference | 13 (72) | 13 (68) |
| Slightly more likely to take part | 1 (6) | 1 (5) |
| Definitely more likely to take part | 1 (6) | 1 (5) |
| Missing | 1 (6) | 0 (0) |
Appendix 6 Participants’ awareness of and views surrounding routine data collection by site
| Data | Site 1 | Site 2 | Site 3 | |||
|---|---|---|---|---|---|---|
| Control (N = 13), n (%) | Intervention (N = 15), n (%) | Control (N = 8), n (%) | Intervention (N = 8), n (%) | Control (N = 2), n (%) | Intervention (N = 1), n (%) | |
| Hospital data | ||||||
| Were you aware researchers are able to request access to hospital data? | ||||||
| No | 10 (77) | 11 (73) | 1 (13) | 5 (63) | 2 (100) | 0 (0) |
| Yes | 3 (23) | 4 (27) | 6 (75) | 3 (38) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 0 (0) | 1 (13) | 0 (0) | 0 (0) | 1 (100) |
| Would you be comfortable in agreeing to us accessing your data in a future study? | ||||||
| Not at all comfortable | 0 (0) | 4 (27) | 0 (0) | 2 (25) | 0 (0) | 0 (0) |
| Not very comfortable | 1 (8) | 3 (20) | 1 (13) | 2 (25) | 0 (0) | 0 (0) |
| No preference | 3 (23) | 4 (27) | 4 (50) | 0 (0) | 2 (100) | 0 (0) |
| Quite comfortable | 4 (31) | 3 (20) | 3 (38) | 4 (50) | 0 (0) | 0 (0) |
| Very comfortable | 4 (31) | 1 (7) | 0 (0) | 0 (0) | 0 (0) | 1 (100) |
| Missing | 1 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||||||
| Not at all comfortable | 0 (0) | 3 (20) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Not very comfortable | 0 (0) | 3 (20) | 1 (13) | 2 (25) | 0 (0) | 0 (0) |
| No preference | 4 (31) | 3 (20) | 4 (50) | 0 (0) | 2 (100) | 0 (0) |
| Quite comfortable | 4 (31) | 5 (33) | 3 (38) | 4 (50) | 0 (0) | 0 (0) |
| Very comfortable | 4 (31) | 1 (7) | 0 (0) | 1 (13) | 0 (0) | 1 (100) |
| Missing | 1 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your data? | ||||||
| Definitely less likely to take part | 0 (0) | 3 (20) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Slightly less likely to take part | 0 (0) | 3 (20) | 2 (25) | 2 (25) | 0 (0) | 0 (0) |
| No difference | 11 (85) | 7 (47) | 5 (63) | 4 (50) | 2 (100) | 1 (100) |
| Slightly more likely to take part | 0 (0) | 0 (0) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Definitely more likely to take part | 2 (15) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 2 (13) | 1 (13) | 0 (0) | 0 (0) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||||||
| Definitely less likely to take part | 0 (0) | 3 (20) | 0 (0) | 3 (38) | 0 (0) | 0 (0) |
| Slightly less likely to take part | 0 (0) | 3 (20) | 2 (25) | 1 (13) | 1 (50) | 0 (0) |
| No difference | 11 (85) | 9 (60) | 5 (63) | 2 (25) | 1 (50) | 1 (100) |
| Slightly more likely to take part | 0 (0) | 0 (0) | 1 (13) | 1 (13) | 0 (0) | 0 (0) |
| Definitely more likely to take part | 2 (15) | 0 (0) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| School data | ||||||
| Were you aware researchers are able to request access to school data? | ||||||
| No | 12 (92) | 12 (80) | 3 (38) | 5 (63) | 2 (100) | 0 (0) |
| Yes | 1 (8) | 3 (20) | 5 (63) | 3 (38) | 0 (0) | 1 (100) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||||||
| Not at all comfortable | 0 (0) | 3 (20) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Not very comfortable | 0 (0) | 1 (7) | 1 (13) | 1 (13) | 0 (0) | 0 (0) |
| No preference | 6 (46) | 6 (40) | 5 (63) | 0 (0) | 2 (100) | 1 (100) |
| Quite comfortable | 2 (15) | 3 (20) | 2 (25) | 5 (63) | 0 (0) | 0 (0) |
| Very comfortable | 4 (31) | 2 (13) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Missing | 1 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||||||
| Definitely less likely to take part | 0 (0) | 2 (13) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Slightly less likely to take part | 0 (0) | 1 (7) | 1 (13) | 5 (63) | 1 (50) | 0 (0) |
| No difference | 10 (77) | 11 (73) | 6 (75) | 0 (0) | 1 (50) | 1 (100) |
| Slightly more likely to take part | 0 (0) | 0 (0) | 1 (13) | 1 (13) | 0 (0) | 0 (0) |
| Definitely more likely to take part | 2 (15) | 0 (0) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Missing | 1 (8) | 1 (7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Social care data | ||||||
| Were you aware researchers are able to request access to social care data? | ||||||
| No | 12 (92) | 12 (80) | 2 (25) | 5 (63) | 2 (100) | 0 (0) |
| Yes | 1 (8) | 3 (20) | 6 (75) | 3 (38) | 0 (0) | 1 (100) |
| Would you be comfortable in agreeing to us accessing your child’s data in a future study? | ||||||
| Not at all comfortable | 0 (0) | 2 (13) | 0 (0) | 2 (25) | 0 (0) | 0 (0) |
| Not very comfortable | 0 (0) | 3 (20) | 1 (13) | 0 (0) | 0 (0) | 0 (0) |
| No preference | 7 (54) | 4 (27) | 5 (63) | 2 (25) | 2 (100) | 1 (100) |
| Quite comfortable | 0 (0) | 5 (33) | 2 (25) | 3 (38) | 0 (0) | 0 (0) |
| Very comfortable | 5 (38) | 1 (7) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Missing | 1 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Would it have affected your decision to take part in the E-PAtS programme if we had asked for consent to collect your child’s data? | ||||||
| Definitely less likely to take part | 0 (0) | 2 (13) | 0 (0) | 2 (25) | 0 (0) | 0 (0) |
| Slightly less likely to take part | 0 (0) | 3 (20) | 1 (13) | 0 (0) | 1 (50) | 0 (0) |
| No difference | 10 (77) | 10 (67) | 6 (75) | 4 (50) | 1 (50) | 1 (100) |
| Slightly more likely to take part | 0 (0) | 0 (0) | 1 (13) | 1 (13) | 0 (0) | 0 (0) |
| Definitely more likely to take part | 2 (15) | 0 (0) | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Missing | 1 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
List of abbreviations
- CACE
- complier-average causal effect
- CBF
- Challenging Behaviour Foundation
- CEDAR
- Centre for Educational Development Appraisal and Research
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DCE
- discrete choice experiment
- E-PAtS
- Early Positive Approaches to Support
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FMSS
- Five Minute Speech Sample
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- ID
- identifier
- IQR
- interquartile range
- MHMDS
- Mental Health Minimum Data Set
- NICE
- National Institute for Health and Care Excellence
- NMB
- net monetary benefit
- NPD
- National Pupil Database
- PPI
- patient and public involvement
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SE
- standard error
- SMG
- Study Management Group
- SPIRIT
- Standard Protocol Items: Recommendations for Interventional Trials
- SRQ
- Sibling Relationship Questionnaire
- SSC
- Study Steering Committee
- VABS
- Vineland Adaptive Behaviour Scales
- VAS
- visual analogue scale
- WEMWBS
- Warwick–Edinburgh Mental Wellbeing Scale
