Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as award number 15/129/03. The contractual start date was in March 2017. The draft manuscript began editorial review in October 2022 and was accepted for publication in August 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Burns et al. This work was produced by Burns et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Burns et al.
Chapter 1 Introduction
Parts of this chapter have been reproduced with permission from Cook et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The following text includes minor additions and changes to the original text.
Alcohol harm: a global concern
Reducing alcohol-related harm continues to be a global public health priority, with 5.3% of all global deaths and 5.1% of all disease and injuries being attributable to alcohol. 2 Use of alcohol is widely recognised to harm an individual’s health and social relationships, and increasing evidence highlights the scale of alcohol’s harm to others through second-hand effects. 3–5 It also harms society more generally, as urban areas can become less pleasant and less safe to visit,6 and crime may increase. 7,8 Moreover, the consumption of alcohol contributes significantly to health inequalities. A so-called ‘alcohol harm paradox’ exists where alcohol harm is higher among those living in more deprived areas, even when the amount of alcohol consumed is the same or less as those more advantaged. 9 This is due to patterns of consumption (e.g. heavy episodic binge drinking), lower access to health services, increased alcohol availability with fewer community assets and the accumulative effect of multiple risk factors (e.g. smoking, obesity). 10–12 Overall, alcohol use is a key risk factor for many non-communicable diseases13 (NCD) but currently, the global NCD target to reduce harmful use of alcohol by 10% by 2025 is on a poor trajectory. 14
Interventions to reduce intake and harm from alcohol
Interventions that are effective at reducing alcohol harm can be implemented at an individual level,15 community level16,17 and national level. 18 At the individual level, alcohol identification and brief advice (IBA), otherwise known as alcohol screening and brief interventions (ASBIs), aims to reduce alcohol-related harm through early identification of hazardous or harmful drinking in non-treatment-seeking populations. It has been shown in systematic reviews and meta-analyses to be effective among adults in a variety of settings15,19 with most trials located in primary care settings20 and emergency departments. 21,22 According to the traditional classification system of preventative interventions, ASBIs are a type of secondary prevention intervention designed to lower the prevalence of alcohol use disorders and reduce the potential for future harm by promoting early behaviour change. 23,24 The World Health Organization identifies ASBIs as a recommended ‘best buy’ intervention to reduce alcohol use. 25
However, evidence of implementation of ASBIs as a secondary prevention intervention in non-health community settings is limited. 26 Little is known as to whether alcohol IBA must always be delivered by a professional in order to be effective. While existing research demonstrates that lay health worker roles are an established approach,23 widely used for a range of public health priorities and population groups,27 no previous programmes with a specific focus on alcohol had been published in the literature.
At the community level, accessibility of alcohol is a key determinant of harm, and restricting physical access to alcohol is an additional World Health Organization ‘best buy’ as it is deemed effective, cost-effective and feasible to implement globally. 2,3,25 Internationally, systematic review evidence shows that increased alcohol outlet density and temporal availability are linked to higher levels of crime and poor health. Interventions in and around the alcohol environment that improve the serving practices and standards of licensed premises can lead to small reductions in acute alcohol-related harm. 18
In England, local authorities can address accessibility, serving practices and standards of operation of premises licensed to sell or supply alcohol using the regulatory framework of the Licensing Act 2003. 28 Each local licensing authority must publish a statement of its licensing policy every 5 years, promoting the four statutory objectives of the 2003 Act: the prevention of crime and disorder; public safety; the prevention of public nuisance; and the protection of children from harm. Longitudinal, area-level analysis of UK data sets has shown that, at borough level (i.e. lower-tier local authorities in England), both alcohol-related hospital admissions16 and crime17 reduced faster in areas where more restrictive licensing policies are in place. Using small area-level data [lower-layer super output areas (LSOAs) with a mean population of 1500 persons], alcohol outlet density in Wales has similarly been associated with alcohol-related hospital admissions and crime data. 8 Licensing action could reduce alcohol harm at a community population level through both primary and secondary prevention mechanisms of action since restricting the physical availability of alcohol can benefit the whole population universally, and targeted enforcement action can mitigate the impact of existing harm. 3,24
Powers exist for local people to influence licensing decisions, but such licensing action does not generally happen, and there is a paucity of published evidence on community engagement. 29 Lay people have the ability to influence local alcohol licensing policy and licensing decisions via the local licensing process, and legislation promotes greater community involvement in licensing decisions. Existing studies have identified the need to gain a better understanding of how to support community members to engage, especially those experiencing health inequalities. 29–31 Utilising ‘people power’ has represented a huge untapped resource in existing local regulatory systems; however evidence highlights asymmetries of power as one of the key barriers to community engagement32 and how licensing authorities may prioritise conflict resolution and compromise between licence applicants and members of the public rather than the promotion of existing licensing objectives. 33 Furthermore, where promoting community involvement in licensing decisions is not only ‘encouraged’ but is a legal requirement, concerns exist to ensure it is not tokenistic. Where there has been evidence of successful community-led alcohol controls reducing alcohol harm, further research is needed to develop and test context-specific menus of available powers communities can use, tailored to the specific identities of communities. 34
Asset-based community development
The Communities in Charge of Alcohol (CICA) intervention was designed using an asset-based community development (ABCD) approach, where a health asset is any factor which enhances the ability to create or sustain health and well-being. 35 This is in line with the National Institute for Health and Care Excellence (NICE) guidance on behaviour change, which advocates building on existing community resources and skills. 36 The principles of the approach are to: allow time for communities to realise and acknowledge their individual and collective assets and to rebuild their confidence and networks, enable local people to take the lead and build trust with communities by demonstrating that involvement leads to change. The approach seeks to build community networks, which are health promoting. At the time of the National Institute for Health and Care Research (NIHR) commissioning brief in 2016, ABCD approaches were being promoted widely23 and were attractive in terms of current fiscal challenges and cuts to services, but there was relatively little evidence for their effectiveness. 37
Context to the Communities in Charge of Alcohol evaluation
In 2014, the Greater Manchester Combined Authority (GMCA) agreed a Greater Manchester (GM) Alcohol Strategy 2014–17, which included taking forward a programme of activity to reduce alcohol-related harm while retaining a focus on growth and reform, promoting effective practice within GM and challenging the status quo on key national issues. Within the strategy, there was a particular focus on the role of the community in reducing alcohol harm and the expanded use of licensing and regulatory powers to address alcohol availability. In pursuing these objectives, the GMCA entered into a partnership with the Royal Society for Public Health (RSPH) to develop training for and introduce alcohol health champions (AHCs) in all 10 GM local authority areas in 2017. The principle of community lay health champions has been well established;38–40 the focus on alcohol and the community’s role in licensing is the novel contribution of this study.
This was the first time that GM had attempted to co-ordinate an approach to building health champion capacity across all 10 local authorities. It was underpinned by the GM Health and Social Care Strategic Partnership’s commitment to a ‘Radical Upscale in Prevention’ as one of the four key programmes within the ‘GM Taking Charge’ Strategy. Thus, an important opportunity presented itself, coinciding with the commissioning brief from the NIHR Public Health Research (PHR) Board in 2016 identifying the need for research on the effectiveness of locally delivered interventions to reduce intake and harm caused by alcohol.
Research objectives
The main aim of the research was to evaluate the effectiveness and cost consequences of the community AHC programme, known as CICA.
Primary objective
To determine the effect of the CICA intervention on area-level key health and crime performance indicators.
Outcome evaluation objectives
-
Determine the effect on area-level key health performance indicators: alcohol-related hospital admissions, accident and emergency (A&E) attendances and ambulance call-outs.
-
Determine the effect on key crime indicators (street-level crime data).
-
Determine the effect on key antisocial behaviour (ASB) indicators.
Research questions
-
Does the intervention result in (statistically significant as well as relevant in absolute terms) improvement in health and crime indicators?
Economic evaluation objectives
-
Identify set-up and running costs using a standardised costing exercise (examination of commissioning documents and contracts).
-
Resolve costs by sector (health, ambulance and police) before, during and after CICA setup.
-
Quantify benefits due to reduced hospital admissions, ambulance call-outs, emergency department use, crime and ASB.
Research questions
-
What are the set-up/ongoing costs in terms of in-kind contributions (time of residents, public sector officers, councillors and voluntary organisations)?
-
How much did the set-up phase cost (venue hire, refreshments, training)?
-
How much per year will the process cost to run (advertising, venue hire, external facilitation)?
-
What are the savings in terms of reduced crime, hospital admissions and ambulance call-outs? What are the cost benefits and cost consequences of CICA?
Secondary objectives
To understand the context and factors that enable or hinder the implementation of the intervention, including establishing, operationalising and sustaining the CICA intervention.
Process evaluation objectives
-
Explore policy context and variation in licensing practice, including any impact of devolution in GM.
-
Explore barriers/facilitators at key stages of the intervention (recruitment of AHCs to initial training and cascade training; delivery of initial training and cascade training; using skills beyond the training in AHC activity; retention of AHCs).
-
Explore responses to AHC training, modelling of health behaviours, perceptions of community cohesion and development.
-
Determine the numbers of trainees, brief interventions applied and community awareness events organised/participated in.
-
Examine and quantify the amount and success of community involvement in licensing issues.
-
Determine whether there is a change in composite measures of alcohol availability.
Research questions
-
How was licensing policy operationalised in the local area prior to CICA? Does the context (devolution) impact on licensing?
-
What are the main barriers/critical success factors?
-
How many people were trained, did they engage with the training and did they put it to use?
-
How many brief interventions were applied?
-
Has licensing (and therefore alcohol availability) been influenced by community involvement?
-
Does citizen participation increase as a result of the intervention?
Chapter 2 Methods
Parts of this chapter have been reproduced with permission from Cook et al. 1 and from the CICA trial protocol (available from the NIHR project web page: https://fundingawards.nihr.ac.uk/award/15/129/03) and earlier papers on the process evaluation. 41–44 The CICA trial protocol is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The earlier process evaluation papers are published under a Creative Commons Attribution-Non-Commercial-NoDerivatives (CC BY-NC-ND 4.0), therefore these extracts have been reproduced exactly. See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Study design
Communities in Charge of Alcohol was a complex community-level intervention. Since it was not amenable to conventional randomisation (as recognised in the complex interventions guidance45), it had a quasi-experimental design. 46 This fitted on the ‘continuum of evaluation’,47 which recognised the need for multiple methods/variants in experimental design. 48
Analysis of primary outcomes was made at the area level, comparing CICA areas with control areas. Each local authority defined its own CICA area by selecting pre-existing geographical communities defined by LSOA boundaries. The smallest intervention area encompassed one LSOA, and the largest contained three LSOAs (mid-year population estimates combined: 1600–5500).
With implementation already in the planning phase as part of the GM Alcohol Strategy 2014–17, this evaluation was researcher-influenced but not researcher-controlled. Although researchers had no control over the selection of the areas, the order of roll-out of intervention areas in each local authority was under researcher control. CICA was rolled out as a stepped-wedge randomised trial. It was evaluated using mixed methods to investigate health and crime outcomes, processes and economic effects.
Ethical approval, registrations and study monitoring
Ethical approval was received from the University of Salford Research Ethics Committee on 17/05/17 (reference number: HSR1617–135) and obtained from the University of Bristol (as the host of the outcome evaluation) on 16 May 2019 (reference number: 82762). The trial was registered with the International Standard Randomised Controlled Trial Number registry www.isrctn.com/ISRCTN81942890. The trial protocol was published in April 2018,1 and protocol revisions were published here: www.fundingawards.nihr.ac.uk/award/15/129/03.
A summary of the amendments to the protocol is listed within the evaluation methods. The Analytic Plan for the evaluation (version 3) described in this chapter was uploaded to the Open Science Framework prior to analysis (https://osf.io/9z65w/; dated 8 March 2021).
The outcome evaluation relied on analysis of secondary data from Local Alcohol Profiles for England (LAPE) (Public Health England), Hospital Episode Statistics [National Health Service (NHS) Digital], ambulance call-out data [North West Ambulance Service (NWAS)] and police data obtained initially at the LSOA level. In terms of sensitivity, police data are publicly available at street level. Hospital Episode Statistics are sensitive at LSOA level, although once alcohol-attributable fractions (AAFs) are applied to the data, they are deemed to represent a low risk of disclosure. Nevertheless, appropriate measures were taken to ensure the security of potentially sensitive data sets, including their storage only on secure university file servers. These data were aggregated to compile intervention areas (composed of one to three LSOAs) and their matched controls.
Participants were recruited to take part in the process evaluation and economic evaluation. All participants were provided with full information about the study (see project website) and provided written consent. Participants included volunteer AHCs, key informants and stakeholders in commissioning, service providers and licensing officer roles and members of the public. Alcohol health champions completed consent forms at their first training session prior to filling out the pre-training questionnaire. Potential participants for interviews and focus groups were given a minimum of 1 week to decide whether or not to take part, and written informed consent was obtained prior to the start of the interview or focus group. Data obtained within the process evaluation were anonymised, and each participant was given a unique code, stored separately to the main data file. Consent forms were stored in a separate location to the main data files. Transcripts used pseudonyms in place of real names and are used throughout the reported findings to protect participants’ anonymity. Data were stored on secure university file servers, accessible only to the research team.
To protect the anonymity of participants, since the intervention was at a small area (community) level, the locations of the study areas and the identity of the host local authority are not revealed in this report, and each area is given a (randomly generated) code between 1 and 10.
A protocol was established for local CICA leads to report incidents or adverse events using a standardised form. The process outlined responsibilities for monitoring and reporting from CICA local leads to the Greater Manchester Programme Manager, the research team at the University of Salford, Principal Investigator and Study Steering Committee (SSC). No adverse events or incidents were reported.
The study methods are reported in accordance with the Consolidation Standards of Reporting Trials (CONSORT) statement.
Setting
All GM local authorities within the study setting had higher than England averages for alcohol-related mortality, ranging from 46.7 in Trafford to 71.9 per 100,000 in Manchester. 49 A fifth of all LSOAs in GM were in the highest decile of deprivation nationally (ranging from only 3% in the borough of Trafford to 28% in the City of Manchester). Greater Manchester was heterogeneous in terms of its application of licensing policy; only one local authority was classified as having high licensing policy intensity (two local authorities were medium, five low and two passive in terms of making use of cumulative impact areas and/or refusing licences16).
Intervention description
The description of the intervention is concordant with TIDieR:50 the Template for Intervention Description and Replication and the description below is structured according to the headings of the template.
Brief name
Communities in Charge of Alcohol.
Why (rationale/theory/goal)
Communities in Charge of Alcohol is based on the principles of ABCD. The ABCD mechanism of action in CICA assumes that communities have strengths, motivations and skills to become AHCs who can reduce alcohol harm. This is based on existing health champion models which utilise lay health workers to work in a voluntary capacity to offer brief advice and brief interventions alongside their other daily activities. 23,40 Through CICA, champions are trained to focus on alcohol, receiving additional knowledge and skills to enable them to get involved in local licensing decisions. In ABCD theory, building an infrastructure of alcohol training and support to deliver alcohol harm reduction interventions will positively reinforce the strengths, motivations and skills of the community. See Appendix 1 for logic model.
What (materials)
An AHC role description advertises the CICA programme, and local co-ordinators recruit lay volunteers. Informational material explains the AHC role, what is involved, the requirements for the role and support that is available at all stages of the training and AHC activity (see Appendix 2).
Royal Society for Public Health ‘candidate workbooks’ are used within the training of AHCs (the ‘intervention providers’), which are assessed and externally verified to award successful participants with the Level 2 qualification in ‘Understanding Alcohol Misuse’. Supplies of the alcohol harm assessment tool, Alcohol Use Disorders Identification Test – consumption (AUDIT-C), in scratchcard form (see Figure 1), are issued to AHCs to support them with informal, brief advice conversations. 51
FIGURE 1.
Alcohol use disorders identification test – consumption scratchcard used by AHCs as part of the CICA intervention. Source: Public Health England.

What (procedures)
Using a cascade training model, an accredited and standardised 2-day Train-the-Trainer course is delivered initially by the RSPH and local licensing officers, then cascaded by professionals with the support of the AHC community. In both the Train-the-Trainer and cascade training, delivery is face-to-face in small groups.
In the pre-implementation phase, professionals are designated to be local CICA co-ordinators who prepare for the roll-out of alcohol health training in their area before the first Train-the-Trainer event. They recruit lay volunteers on to AHC courses, support AHCs in developing confidence to put their knowledge and skills into practice and cascade the training to others. The CICA training programme aims to give lay AHCs the confidence and tools to understand and address alcohol use, take action on alcohol licensing and train others to become AHCs (see Table 1).
| Day | Topic/aims |
|---|---|
| Day 1 (full day) | Understanding alcohol misuse |
|
|
| Day 2 (half day) | Licensing action |
|
|
| Day 2 (half day) | Train-the-Trainer |
|
Alcohol health champion activities include: offering informal brief alcohol advice to promote behaviour change among family, friends, colleagues and with the wider community at community events and using the powers that exist in the Licensing Act 2003 that encourages communities to strengthen restrictions in the sale or supply of alcohol. Alcohol health champions are trained to use informal approaches to raise concerns and complaints directly with managers of licensed premises, as well as formal processes to report issues to local licensing authorities, submitting representations or requesting licensing reviews. A community hub approach at a place-based level created an infrastructure of support for AHCs through meetings facilitated by local CICA co-ordinators and attended by local licensing officers.
Who provided
Communities in Charge of Alcohol co-ordinators are professionals working in the intervention case area, employed by the local authority, private or voluntary sector. They are commissioned to provide health and well-being services or alcohol and drug treatment services. Their expertise in health improvement/health promotion or alcohol and drug treatment may or may not include a background in ABCD or working with volunteers. They receive the same training as AHCs, the standardised 2-day Train-the-Trainer course accredited by the RSPH.
Alcohol health champions are lay individuals who share the common place-based characteristic that they live or work within the intervention case area. They attend the accredited and standardised 2-day Train-the-Trainer course with the RSPH (first-generation training) or the two-date cascade training course delivered by the local CICA co-ordinator.
Lay volunteers are recruited from the intervention case areas, include adults aged 18 years and over, and are embedded in the community either through their residency or their work role.
How
Alcohol health champion intervention activities are provided individually or as a group. The AHC activity of providing informal, brief alcohol advice is provided face to face to individuals within the community where AHCs live or work. Alcohol health champions (with support from their co-ordinators) are responsible for deciding exactly how to operationalise the advice-giving. Examples included opportunistic conversations with friends, families, colleagues or community members, as well as more planned activities such as staffing stalls at drop-in community events. Informal licensing action is provided face to face to managers of licensed premises within the community where they live or work. Formal licensing action requires issues to be reported by telephone, on the internet or face to face to a local licensing officer. Formal representations require submission in writing to local authorities on the internet or by post.
Where
Each local authority’s public health team selects a target community to receive CICA, using the following guiding principles as inclusion criteria and making use of a standardised data set available to local authorities:52
-
an area of high alcohol-related harm (defined as high within the local authority rather than in comparison to regional or national average rates)
-
alcohol harm is considered in terms of a combination of indicators
-
alcohol-related crime and ASB
-
alcohol-related hospital admissions
-
weekend evening A&E attendances
-
users of local treatment services
-
hospital recording of location of violent incidents (if available)
-
density of licensed premises in the area or adjoining areas (if available).
A rationale was provided in writing by e-mail from local authority public health commissioning teams, summarising LSOA and middle-layer super output area (MSOA) data used to inform their decisions. The number and type of different alcohol harm indicators chosen varied from 2 to 5.
Of the nine authorities that rolled out CICA, the majority used alcohol hospital admissions as an indicator of high levels of alcohol harm (n = 8), followed by crime (n = 6), A&E attendances (n = 4), indices of multiple deprivation (IMD) (n = 4) and number of licensed premises (n = 4). Three public health teams used numbers in structured community-based alcohol treatment as recorded in the National Drug Treatment Monitoring System (NDTMS),53 previously referred to as Tier 3 interventions. 54 Considering the variation of data underpinning area selection for the CICA intervention, the process evaluation team (SCH) additionally extracted and compared available data on a wider set of area characteristics (all characteristics shown in Table 2). The intervention was planned in all 10 GM local authorities; thus, there were originally 10 sites. These are labelled by randomly generated codes rather than local authority names to protect the confidentiality of the stakeholders and AHC participants.
| Intervention areaa | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 6 | 7 | 8 | 9 | 10 | |
| Size of target area | |||||||||
| No. of LSOAs | 2 | 1 | 1 | 2 | 2 | 3 | 2 | 3 | 2 |
| Mid-year population estimate55 | 2996 | 2139 | 2162 | 3259 | 4244 | 5586 | 3604 | 5220 | 3452 |
| Rationale for choosing area | |||||||||
| Alcohol hospital admissions | ✓b | ✓ | ✓b | ✓ | ✓ | ✓ | ✓ | ✓ | |
| A&E attendances | ✓ | ✓ | ✓ | ✓ | |||||
| Crime | ✓b | ✓c | ✓c | ✓ | ✓ | ✓ | |||
| Domestic violence incidents | ✓ | ||||||||
| No. in community (Tier 3) structured alcohol treatment | ✓ | ✓ | ✓ | ||||||
| Prevalence of higher-risk drinking | ✓b | ||||||||
| % binge drinking adults (MSOA) | ✓b | ✓b | |||||||
| Engagement team presence | ✓ | ||||||||
| No. of licensed premises | ✓ | ✓ | |||||||
| Indices of Deprivation | ✓ | ✓ | ✓ | ✓ | |||||
| Characteristics of area | |||||||||
| Deprivation decile56 | 1, 1 | 1 | 1 | 1, 1 | 1,1 | 1, 2, 2 | 1,1 | 1, 4, 4 | 1, 2 |
| Population: men (%)55 | 48.7 | 56.6 | 46.4 | 45.7 | 47.6 | 48.3 | 50.7 | 49.5 | 53.0 |
| Population: women (%)55 | 51.3 | 43.4 | 53.6 | 54.3 | 52.4 | 51.7 | 49.3 | 50.5 | 47.0 |
| Ethnicity: white57 | 94.0 | 64.0 | 90.0 | 96.3 | 81.0 | 80.0 | 96.0 | 82.0 | 89.0 |
| Social housing (%)58 | 45.0 | 37.1 | 39.6 | 55.8 | 45.0 | 42.0 | 55.0 | 17.6 | 50.0 |
| Home ownership (%)58 | 38.0 | 29.0 | 31.5 | 33.9 | 28.8 | 45.0 | 36.4 | 56.0 | 35.0 |
| Access to health assets and hazards decile59 | 6th, 8th | 10th | 9th | 9th, 9th | 8th | 6th, 7th, 9th | 8th, 9th | 7th, 9th, 10th | 9th |
| No. of licensed premises | 8 | 59 | 0 | 3 | 20 | 17 | 9 | 22 | 20 |
Alcohol health champion activities take place within the geographical boundaries of the community where people live and work. Informal, brief advice conversations take place with family and friends in people’s own homes, at social events or with colleagues in the workplace. Community awareness events take place in local community centres, libraries, health centres or other public spaces. Informal licensing action takes place in licensed premises within the community. Formal licensing action could lead to a Licensing Sub-Committee hearing which would take place at local council offices.
When and how much
In keeping with the ABCD (bottom-up, community-led) approach, AHCs are free to do whatever they are comfortable with; the programme does not dictate where, when or how much activity should take place.
Tailoring
The Level 2 Understanding Alcohol Misuse course is defined as a Level 2 qualification (recognised by Ofqual/Council for the Curriculum, Examinations & Assessment and Qualification Wales) with a standardised syllabus and candidate workbook set by the RSPH. The licensing action half-day training is designed by a local licensing officer to then be adapted according to the regulatory and enforcement processes and procedures within each local authority as per their Statement of Licensing Policy. The Train-the-Trainer course is a 2-day course, whereas the cascade training can be delivered flexibly within the community. Support for AHCs provided by local CICA co-ordinators can be tailored as required.
Outcome evaluation methods
The effectiveness of CICA was measured through the following data and objectives:
-
Determine the effect of the intervention on area-level key health performance indicators: routinely collected alcohol-related hospital admissions (narrow indicator), A&E attendances and ambulance call-outs.
-
Determine the effect of the intervention on key crime indicators (street-level crime data).
-
Determine the effect of the intervention on key ASB indicators.
Key indicators of health and crime were determined based on the literature, discussion between the researchers and with stakeholders from GM and data availability.
Given the nature of the population intervention, which we were not able to randomise to specific areas (i.e. this study was, therefore, a natural experiment evaluation60 rather than a randomised controlled trial), and the relatively small average population effects we would expect from an intervention such as CICA (although for individual events a large impact might be possible), an important component of this evaluation is the application of different evaluation designs as well as different statistical methods (described below) to evaluate the same intervention. Methodological triangulation, following recommendations to improve such natural experiment evaluations for public health,60 strengthens the inferences about effectiveness by triangulating the results from methods and data sets, each with its own unique, inevitable sources of bias. 61
Data set
The intervention was planned to be rolled out across all 10 boroughs in the study at different points in time, in a random order. These areas are referred to as ‘intervention areas’, and each local authority had selected a small area (within their respective district) to target the intervention – these were areas of priority in terms of having high levels of alcohol-related harm and were also areas of significant economic and social deprivation. The random order of roll-out for the 10 areas was generated by the project’s lead statistician (FdV) using statistical software R, independent from the implementation and process evaluation teams.
For the purpose of this evaluation, data were aggregated to the geographical level of the LSOAs, which each have a minimum population of 1000 residents, with the mean population size being 1500. 62 This geographical aggregation level most closely approximates the areas of implementation, which were defined around pre-existing communities (and may therefore not necessarily map directly onto a LSOA). As such, all subsequent statistical analyses were also conducted on data aggregated at the LSOA level and counts or rates of events (see below). The intervention areas varied in size between one and three LSOAs and varied in population size from 1648 to 5586 (mid-year population estimates).
The evaluation covers a 10-year period, with about 7 years pre intervention and a maximum of 3 years after the start of the implementation follow-up until the end of January 2020. For reference, the implementation schedule for CICA is shown in Table 3.
| Area code | Training | Intervention | Follow-up | |
|---|---|---|---|---|
| Start | End | End | ||
| Area 9 | September 2017 | October 2017 | September 2018 | September 2019 |
| Area 10 | September 2017 | October 2017 | September 2018 | September 2019 |
| Area 1 | November 2017 | December 2017 | November 2018 | November 2019 |
| Area 4 | November 2017 | December 2017 | November 2018 | November 2019 |
| Area 8 | January 2018 | February 2018 | January 2019 | January 2020 |
| Area 7 | January 2018 | February 2018 | October 2018 | January 2020 |
| Area 3 | Mar 2018 | April 2018 | September 2018 | January 2020 |
| Area 6 | May 2018 | June 2018 | May 2019 | January 2020 |
| Area 2 | May 2018 | June 2018 | May 2019 | January 2020 |
| Area 5a | January 2020 | |||
For each LSOA, we selected three local control LSOAs and three national control LSOAs for comparison. Further details can be found later in this chapter, in Evaluation and analytic designs.
During the pre-implementation phase of the project, it became clear that the CICA intervention would not be implemented in Area 5 in the time period relevant to the study, and as a result there were only nine areas that progressed to the initial implementation phase (made up of one to three LSOAs each). With the exception of the counterfactual analyses (see below), Area 5 and its matched controls were kept in the data set and served as an additional control set. For the counterfactual analyses, which are conducted at the individual area level prior to combining them to obtain the average effect, Area 5 was not included.
We selected four outcomes for evaluation of alcohol-related community harms, with ambulance call-outs, A&E attendances and numbers of crimes collected separately for weekends and weekdays. In addition, within the crime statistics, we also looked at the incidence of reported ASB separately. This resulted in a total of eight outcomes for evaluation, of which alcohol-related hospital admissions were considered the study’s primary outcome.
-
alcohol-related hospital admissions (narrow measure)
-
A&E attendances weekends
-
A&E attendances weekdays
-
call-outs for ambulance to the area services weekends
-
call-outs for ambulance to the area services weekdays
-
numbers of recorded crimes weekends
-
numbers of recorded crimes weekdays
-
number of recorded ASB incidents.
Alcohol-related hospital admissions were estimated as the AAF of total hospital admissions and were based on the narrow definition of alcohol-attributable. More details on this methodology can be found here. 63,64
A number of further decisions were made prior to analysis of the data. Crimes are more likely to be recorded as being related to alcohol over a weekend, with the Crime Survey of England and Wales also showing that, in 2013–14, victims of violent crime were more likely to report the offender to be under the influence of alcohol at the weekend (70% of crimes are related to alcohol) compared to overall (53%). 65 A similar pattern was observed for ambulance call-outs in the North East of England,66 and we hypothesise that a similar pattern might also be present for A&E attendances. We therefore a priori defined a time period where the likelihood of involvement of alcohol is highest (Friday 3 p.m.–Sunday 3 p.m.) and aggregated these ‘weekend incidents’. Conversely, ‘weekday’ incidents were those occurring from Monday to Friday between 9 a.m. and 5 p.m. each day (note there was a small overlap in timings, but data indicate66 very few incidents occur in this 2-hour timeslot). Because of low numbers, we were not able to also do this for recorded ASB incidents.
Except for the primary outcome of alcohol-related hospital admissions, which necessarily is associated with an indication of the involvement of alcohol, for the other outcomes the involvement of alcohol was also recorded. However, from discussions with experts and initial exploration of this indicator in the GM crime statistics (in preparation of this study), it became clear that the quality of these ‘alcohol-flags’ was questionable and, in any case, missing for a significant proportion of incidents. We therefore included all incidents and did not use the alcohol flags.
In addition to outcome data, we obtained corresponding time series of resident population size, the LSOA-level English IMD56 and the average age of the LSOA residents. We further defined a new variable of the four quarters of each year to account for annual patterns in the outcome, and we defined a ‘time’ variable, which signifies each subsequent time point in the time series. And finally, we defined a 0/1 indicator variable for each time point in each intervention LSOA to indicate whether CICA has started (1) or not yet (0).
For the evaluation of each of the outcomes, we obtained time series data from 2010 through 2020. With the CICA roll-out introduced in 2017–18, this means that analyses are based on 7 full years of pre-intervention time series and up to 3 years of post-roll-out follow-up.
Data sources
Time series data were obtained from several different sources and linked to LSOA and month in one data set for analysis.
Alcohol-related hospital admissions were obtained at LSOA level from the Local Knowledge and Intelligence Service (LKIS) North West of the former Public Health England. For reference, data aggregated at higher levels is available from the LAPE. 49 The time series were aggregated by month and LSOA. LAPE are based on NHS Digital’s Hospital Episode Statistics, and we obtained the sum of AAFs based on the narrow definition from Public Health England. 63,64
Accident and emergency attendances and emergency admissions were obtained from the NHS Digital Hospital Episode Statistics A&E data set following a Data Access Request (DARS) Application (DARS-NIC-268750-B3T4W-v0). Requested data were monthly total numbers of A&E attendances by LSOAs (patients) in the GM area. Two outcomes were created: one for weekends and one for weekdays, as described above.
Data on ambulance call-outs to the LSOA were obtained from the NWAS following a data request to the HRA and Health and Care Research Wales (HCRW) (IRAS ID 261621). Data were all ‘see and treat’ and ‘see and convey’ events for GM aggregated by LSOA and month and for weekend and weekdays (using the same definition of weekends/weekdays as for A&E attendances and emergency admissions above).
Reported street-level crime incidents were obtained through data requested to the GM police authority and included recorded violent, sexual and public order offences (ASB incidents). Data requests were developed with the project collaborator from the GMCA. Reported incident data were aggregated from postal codes to corresponding LSOAs and from individual events to monthly counts. Weekday and weekend time series were generated following the same definition as for A&E attendances and emergency admissions above. Incidents of reported ASB incidents were extracted for separate analyses, as it was hypothesised these might be most likely to change most following the intervention.
Covariate data were obtained from publicly available national statistics data sets by the Office for National Statistics. 67
Prior power calculation
Based on the methodology for stepped-wedge randomised trials outlined by Hussey and Hughes,68 power calculations were performed for the primary outcome ‘alcohol-related hospital admission rates (narrow)’ obtained from the LAPE49 extracted for all 10 GM local authorities. Power analyses were conducted at larger local authority level rather than at the level of the intervention area because the exact areas and comparisons had not yet been determined. The mean standardised alcohol-related hospital admission rate for the year 2014 was 207 (per 100,000 people), with a maximum temporal standard deviation per site of 17.2 (range within sites 5–17) and a coefficient of variation across sites of 4.35. With 10 areas and 12-month follow-up (i.e. when all areas have received the intervention and a minimum of 1-month post-intervention follow-up), and a statistical significance level of 5% and statistical power of 90%, the proposed study would be able to detect a 10% average difference in rates compared to baseline. For an intervention to be effective and cost-effective, a minimal reduction in key indicators of 10% was reasonable. Power calculations for various alternative scenarios were also calculated and are provided in the Analyses Plan (https://osf.io/9z65w/).
Evaluation and analytic designs
As a complex community intervention, it was not possible to use a conventional randomised design (as recognised in the complex interventions guidance45). Communities in Charge of Alcohol was therefore evaluated as a natural experiment. 46 We evaluated the average intervention (treatment) effect (ATE) across all 10 boroughs using four different analytic designs or statistical methods. This form of methodological triangulation was done following recommendations to improve causal inference from natural experiment evaluations. 60 Its aim is to improve causal inference by comparing the results from different ways of obtaining the ATE through use of different study designs, control units and methods, thereby exploring similarities and differences in the different results. The hypothesis being that if different methods provide broadly comparable results in terms of direction of effect and effect size, this would increase our confidence in inferring that an effect might be the result of the intervention. Conversely, if there are differences in effect size, but in particular in direction of effects, this is most likely evidence of artefacts in the data rather than true effects. This way, we reduce the potential for bias from the use of a single study design or analytic method. However, note that analyses are still based on the same data and data generation process (see above), so there remains potential for bias even after triangulation.
Stepped-wedge cluster trial
Design
The stepped-wedge design describes the sequential roll-out of an intervention over time, or in other words, how the intervention is implemented in each of the intervention areas at some time point in the time series. Each intervention LSOA therefore changes from ‘control’ to ‘intervention’ and thus serves as its own control. 69
Analysis
The stepped-wedge design was analysed using hierarchical growth models (similar to previous work16,17) and analysed by multilevel mixed-effects models to account for the repeated measurements in the same areas (i.e. random intercepts), thereby accounting for different levels of the outcome in each area (e.g. alcohol-related hospital admissions in one LSOA will be ‘more similar’ than those in another LSOA, perhaps one with a much lower rate). Theoretically, it is also plausible that the temporal trend in each area differs from that in any other, which can be modelled using random slopes as well. However, exploratory analyses indicated there is insufficient statistical power to incorporate this. The outcome variables were LSOA-level counts and were analysed using mixed-effects negative binomial models (to account for overdispersion70). LSOA resident population sizes were used as offsets in the models. All models were further adjusted for quarter, area-level IMD score, average age in the area and time to account for the secular time trend across the time series. Exploratory analyses indicated that for none of the outcomes, this was a linear increase/decrease, and therefore the time trend was modelled using a basic cubic spline to account for non-linearity. Out of different potential model structures, the final models were determined based on assessment of assumptions regarding distributions of errors and model fit calculated by the Akaike information criterion. All analyses were done in R statistical software using the lme4 package for hierarchical growth modelling.
Local controls
Design
Each intervention area was matched to three other, comparable, control LSOAs. Comparable LSOAs were from the same district (lower tier local authority) but not neighbouring the case area, the latter to avoid bias in the effect estimates because of spillover effects as a result of the intervention. Matching of intervention to control areas was done using propensity score matching based on an a priori selected set of confounding variables (LSOA population density, deprivation, average age and baseline alcohol-related hospital admissions and crime rates) for the year prior to the start of CICA programme (2016). Note that although these are outcome measures, in contrast to propensity score matching, here the propensity scores are only used to identify the most similar control. Matching was done using the ‘nearest neighbours’ algorithm.
Analysis
The final data set contains the time series for 76 LSOAs (19 interventions and 57 matched controls). These have been analysed as controlled Interrupted Time series (cITS)71 using the same hierarchical growth modelling analytic method as used for the stepped-wedge cluster trial, with the difference being that in these analyses, results are not just internally compared but also against trends in the control LSOAs. Unmatched mixed-effects negative binomial models were conducted. All analyses were conducted in R, using the MatchIt package for propensity score matching and lme4 package for statistical analyses.
National controls
Design
The national control analyses are similar to the local control analyses, but each intervention LSOA was matched to a comparable control from the national data set. This was done so that local idiosyncrasies would not bias results and would also completely avoid any issues of spillover. 72 Matching was similarly done using propensity scores based on the 2016 values, although because of the large amount of data (there are 32,844 LSOAs in England56), a prior selection of areas was made based on similarities in the pre-2017 time series of the primary outcome only using ‘dynamic time warping’, which is a statistical methodology that can be used for matching time series. 73 Because of (lack of) data availability, the national control analyses were done only for hospital admissions and A&E admissions.
Analyses
Statistical analyses for the national controls are similar to those of the local controls, as described above. All analyses were conducted in R, using the dtw package for dynamic time-warping and lme4 package for statistical analyses.
Counterfactuals
Design
Alternative to the local control analyses described above, we also approached the evaluation of this design using a synthetic control approach74,75 to estimate counterfactuals of ‘what would have happened had there been no CICA intervention’ for each intervention LSOA separately (henceforth named “counterfactuals”). The difference between the counterfactual and the measured outcomes can then be interpreted as the impact of the intervention. This methodology was previously successfully used in other studies of the impact of local alcohol policies on health and crime. 16,76–78
Analyses
We used Bayesian structural time series to model the pre-intervention time series of the outcome in the intervention area from a weighted combination of the time series in the matched local controls. This model was then used together with the post-intervention time series in the controls to estimate the counterfactual in the intervention areas. The methodology has been described in detail79,80 and in summary. 81 Analyses were done for each intervention LSOA separately, and the LATE was estimated by combining the effects across all areas using meta-analysis. As flagged above, as Area 5 did not end up receiving the intervention, it is excluded from these analyses. All analyses were done in R using the bsts and CausalImpact packages. Meta-analysis was done using the metagen package in R.
Presentation of results
Results are presented as percentage change as a result of the intervention, 95% confidence intervals and p-values. An important assumption for evaluation using cITS is that of parallel trends of the outcome in the intervention and control areas prior to the intervention (with the assumption that this would have continued had there not been an intervention). 71 These are presented – for convenience aggregated for intervention and control LSOAs – graphically in Chapter 3.
Results of Bayesian structural time series are presented as the average percentage change as a result of the intervention across all areas and 95% Bayesian credible intervals (CrIs). We also present the posterior tail area probabilities, calculated as the samples where the 95% CrI excluded the null and which can be interpreted as classical p-values. 79
For triangulation, and ease of comparison, all results of the different methods for each outcome are plotted as forest plots. Because these are not independent study estimates (as normally used in meta-analyses), the summary estimates and confidence intervals are not presented. Forest plots were generated using the meta R package.
Changes to the protocol
Following the withdrawal of an intervention case area in the pre-implementation phase, all references to 10 intervention areas in project documentation were changed to 9 areas. As this protocol change between version 2.0 and 2.1 amended the planned sample size, the statistical power calculations were updated. With only nine intervention areas, but with all other characteristics the same and using the same statistical power calculation methodology, with 90% power, the study was expected to be able to detect 10% differences (or 8% with 80% statistical power). The difference between 9 and 10 intervention areas was approximately 0.1%. The randomisation of areas for roll-out was updated to reflect one intervention area had been removed.
Follow-up of primary outcomes was originally due to end in May 2020. Between version 2.1 and version 3.0 of the protocol, follow-up timescales were reduced from 12 months to 9 months to remove the impact of the national lockdown due to the COVID-19 pandemic, which started in March 2020. This was because the lockdown was likely to have changed the nature and type of alcohol-related harms occurring in year 3 between March 2020 and May 2020.
Process evaluation methods
The design of the process evaluation was informed by Medical Research Council (MRC) guidance for conducting process evaluation of complex public health interventions. 48 The aim was to explore the factors that enabled or hindered the implementation of the intervention. This included establishing, operationalising and sustaining the CICA intervention. The objectives of the process evaluation were as follows:
-
Exploring the policy context and variation in licensing practice, including any impact of devolution in GM.
-
Exploring the barriers/facilitators at key stages of implementing the intervention (recruitment of AHCs to initial training and cascade training, delivery of initial training and cascade training, use of skills beyond the training in AHC activity, retention of AHCs).
-
Exploring the response to AHC training, modelling of health behaviours, perceptions of community cohesion and development.
-
Determining the numbers of trainees, brief interventions applied and community awareness events organised/participated in.
-
Examining and quantifying the amount and success of community involvement in licensing issues.
-
Determining whether there was a change in composite measures of alcohol availability.
The aims and objectives of the process evaluation were achieved using mixed methods to examine the context, acceptability, facilitators and barriers to implementing the intervention (see Appendix 1). Appropriate process analysis techniques were selected for each method.
In the quasi-experimental study, the intervention was not implemented in exactly the same way in each locality. This depended on various local contextual factors, the specific skills, motivations and behaviour of the local AHCs, and the characteristics of the support network provided by the local CICA co-ordinator. The goal of the process evaluation was to capture key contextual factors relating to the recruitment, training and ongoing support of AHCs, in addition to pre-existing decision-making structures. 82
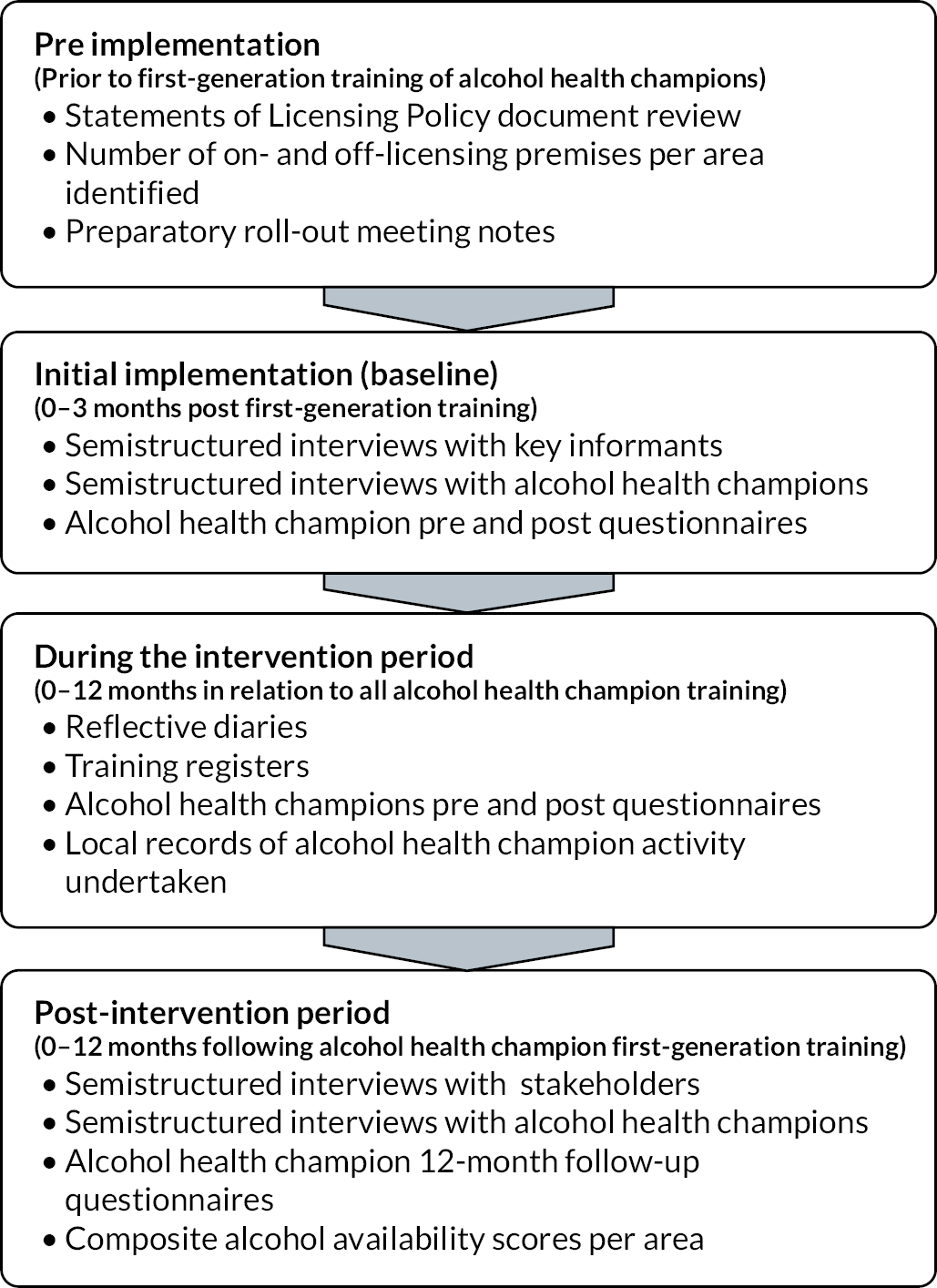
Each phase of the implementation process was explored through relevant and available data capture and methods. Figure 2 provides an overview of the data collection activities pre, during and post the roll-out of the intervention. Data collection required collaboration between stakeholders (AHCs, local co-ordinators and licensing leads) and researchers using mixed methods.
FIGURE 2.
Data collection materials used and processes undertaken across the timeline of the intervention.
Pre-implementation phase
The pre-implementation context was defined as the 2- to 3-month period before the official launch of CICA in each intervention case area. The launch of CICA was marked by the first RSPH Train-the-Trainer event. Data collection in the pre-implementation phase relied on document review and data extraction of secondary data.
Licensing policy context
The document review included a review of the licensing policy context (Statements of Licensing Policy) in each local authority to discover how licensing policy was enacted prior to intervention and the ongoing monitoring of the policy/practice context. A document review was carried out by EJB and SH [patient and public involvement (PPI) representative] on publicly available Statements of Licensing Policy from each of the 10 local authorities (n = 10). These local alcohol licensing policies are legally required to be published by each local Licensing Authority at least once every 5 years, detailing how they will carry out their administrative licensing functions in accordance with the 2003 Act to promote the four licensing objectives: prevention of crime and disorder; public safety; prevention of public nuisance; and the protection of children from harm. 28,83
Document analysis involved skimming (superficial examination), reading (thorough examination) and interpretation using content analysis as an iterative process to organise information into themes, categories and case examples. 84 A directed content analysis approach was taken using predetermined categories85 based on existing research assessing the context of alcohol licensing policy statements in Scotland. 86 These predetermined categories structured the standardised data extraction form used by both members of the research team.
Alcohol availability
Alcohol availability data for CICA intervention areas were obtained from Licensing Authority registers. Each local authority Licensing Unit is responsible for maintaining the register as per Section 8 of the 2003 Act. 28 Information was sought on the number of premises licences granted for both on- and off-licensed sales of alcohol, hours of alcohol sales and size/capacity of premises (where available). Our original protocol stated that we would calculate composite alcohol availability scores from these variables. However, there was no standardised database system shared by Licensing Authorities to maintain Licensing Registers. Therefore, details of hours of alcohol sales and size/capacity limit of premises were not consistently recorded, preventing composite alcohol availability scores from being calculated. Only one consistent data set available was used as the measure of alcohol availability: the number of premises licensed to sell or supply alcohol in each intervention area. Records were exported at a ward level in Microsoft Excel® form. Since ward-level records did not provide the granularity needed for CICA intervention areas, premises licence data were then transferred into Microsoft Access, creating a database file to enable multivalued ‘look up’ fields to obtain alcohol availability data at a LSOA level. Each local licensing authority’s web page was used to identify whether their Licensing Register28,83 was made available to the public to access online.
Preparatory roll-out meetings
Notes from preparatory roll-out meetings were used to explore infrastructure in place in all 10 areas a priori. These audio teleconferencing meetings were held between July 2017 and April 2018, each being held for 2–3 months leading up to each Train-the-Trainer event with key stakeholders from each area, convened by an overall programme manager supporting the co-ordinated implementation of CICA. Meetings were structured around a roll-out checklist created by stakeholders to guide preparation. Meeting notes were shared with the research team as secondary data and evaluated using content analysis by two researchers (EJB and SCH). Units of meaning were defined from items within the meeting checklists as ‘external contextual factors’, that were labelled, grouped into a category (categorisation matrix) and described as a theme. 85 This analysis from a priori qualitative data (2–3 months prior to roll-out) was then revisited as part of a longitudinal design of the process evaluation. At the follow-up phase, relationships were tested between external contextual factors and a key output indicator at the end of the intervention period: total numbers of lay people trained to be AHCs.
Initial implementation phase
The initial implementation context was defined as the baseline position at the start of CICA, captured within the first 3 months from the initial Train-the-Trainer event. Sampling was purposeful. All 22 stakeholders (see Table 4) from 10 local authorities (LA) who had committed to establishing the role of AHCs in their localities were eligible to participate. Two chose not to be interviewed.
| Stakeholder | Background and role in implementing CICA |
|---|---|
| Commissioning leads | Extensive experience of working in local government. Invited to participate in regular meetings prior to implementing the intervention in their area. Some commissioning leads could attend the RSPH Level 2 Understanding Alcohol Misuse training programme for AHCs. |
| Local operational co-ordinators | Employed by their local authority or by a service provider commissioned by their local authority. All operational co-ordinators had experience as practitioners with expertise in working with individuals with moderate/severe addiction difficulties. All were invited to participate in three meetings in advance of the training rolling out in their area. All attended both days of the RSPH training programme in their area, supporting their prospective AHCs. |
| Licensing leads | Licensing leads, employed by their local authorities, had extensive experience in alcohol licensing. Eight of the nine licensing leads attended the RSPH training programme on Day 2 to provide input about the Licensing Act 2003 to prospective AHCs. They were invited to attend the pre-meetings prior to the training rolling out in their area. |
Interviews with 20 of these key informants were held either in person (n = 19) or by telephone (n = 1). All had committed to establishing the role of AHCs in their localities. This included a key stakeholder from the local authority that withdrew from the CICA programme. All were known to the research team through preparatory roll-out meetings. Audio-recorded interviews lasted between 13 and 50 minutes (mean = 26.5 minutes) and were fully transcribed.
Response to alcohol health champion training
Training registers provided numbers of participants trained at all CICA training events as well as details of the role background of attendees (categorised as lay volunteers or paid professionals) to monitor the reach of the training to volunteers from within the target communities. Registers provided a timeline of the total number of CICA training events that took place within the 12-month intervention period, including how many times an intervention area carried out cascade training. Demographic questionnaires were completed by lay volunteers at the beginning of the first training day to record age, gender, ethnicity and highest educational attainment. The abbreviated alcohol screening tool AUDIT-C51 was used as a measure of healthy behaviours, and a free-text question captured reasons for participating in CICA.
Pre- and post-training attitudinal questionnaires surveyed participants’ perceived importance and confidence towards AHC activity on a 5-point Likert scale. Questions asked to what extent they agreed whether it was important to promote healthy lifestyles within their community and get involved in licensing decisions, and their perceived confidence in carrying out different aspects of the role (giving alcohol-related brief advice and/or raising issues about venues selling alcohol). Post-training questionnaires were completed at the end of the last day of training.
Interviews with a convenience sample of newly trained AHCs (n = 5 from n = 3 CICA areas) explored how they responded to the CICA intervention at an early stage to explore ‘sense-making work’ as defined in Normalisation Process Theory as a key component when operationalising a new set of practices. 87 This aimed to understand the intervention and how people begin to start collective action, for example, putting actions into place to enact the intervention. 88 Time since initial training ranged from 3 to 6 months. Data collection comprised a mix of telephone (n = 2) and face-to-face (n = 3) interviews, ranging from 23 to 47 minutes in length. They were audio-recorded, transcribed verbatim and anonymised. Face-to-face interviews took place in private spaces within community settings. A one-off payment to cover travel and time costs was given to interview participants.
Intervention phase
The intervention period commenced in the month subsequent to the initial Train-the-Trainer event and was ongoing for 12 months. Although targets were not imposed or a specified amount of activity expected, local co-ordinators were asked to keep a tally of AHC activity (five out of nine did so). Volunteer champions were invited to complete a reflective diary, which was not used as a tool to check for consistency with local co-ordinators’ tallies but instead to help explore barriers and enablers affecting their role. In other research, diaries have been used as a validation exercise where self-reported data have been assessed for bias;89 in CICA, we did not want the volunteers to feel watched or over-monitored. Reflective diaries were completed by AHCs who consented, and the detail was as much or as little as the AHCs were willing to provide. Diary participants had the choice of using their own online reflective diary, paper diary or a diary kept by their local co-ordinator recording the information on their behalf (a group diary).
Cascade training events were delivered by local CICA co-ordinators with the support of AHCs during the intervention period. Observations of cascade training events (n = 5) were recorded by the research team on a standard form to evaluate fidelity of cascaded training as well as any tailoring of the training.
Follow-up phase
Survey and semistructured interviews with alcohol health champions
The follow-up period within the process evaluation commenced after 12 months. Champions were invited to take part in a survey and interviews and were contacted by both their local co-ordinator as well as the research team. One year post-training, a follow-up questionnaire was sent to AHCs. Questionnaires (n = 11) were completed online (using the Bristol Online Survey Tool). Reasons for loss of champions at the follow-up phase were documented where known, along with factors affecting inactivity. Semistructured interviews were held with AHCs (n = 7) to capture experiences of the CICA intervention activities they took part in. We had originally intended to recruit a purposive sample of those who had or had not remained engaged with the programme. However, because of our earlier experience at 3 months, showing that recruitment for the interview could be problematic, all AHCs were invited to take part. Interviews ranging between 24.37 and 28 minutes (average 40.5 minutes) were audio-recorded and transcribed.
Semistructured interviews with stakeholders
Semistructured one-to-one interviews with local co-ordinators/stakeholders 12 months post implementation of CICA were carried out. Sampling was purposive. Eleven local co-ordinators, representing eight of the nine CICA areas responsible for operationalising CICA, were invited to participate in a telephone or face-to-face interview 12 months post implementation. In terms of role, four were public health practitioners; four were public health commissioners; and three were substance misuse practitioners. Local co-ordinators from all areas except Area 3 and Area 5 participated (the local co-ordinator from Area 3 was no longer in post, and the intervention did not take place in Area 5). Eleven interviews were conducted following written consent: nine face to face and two by telephone. Interviews ranging between 31 and 131 minutes (average 75.90 minutes) were audio-recorded and transcribed. Written consent was gained at the outset of interviews following a period of consideration of a participant information sheet.
Licensing leads
Sampling was purposeful. Licensing leads involved in AHC training from nine LAs were invited by e-mail to participate in a telephone or face-to-face interview 12 months after the first training session for AHCs. Licensing leads from Areas 1, 2, 6, 7, 9 and 10 participated (n = 6). Licensing leads from Areas 3, 4 and 8 did not respond to interview requests. Five telephone interviews were conducted by SCH and one face-to-face interview by EJB. Audio-recorded interviews ranged between 14.6 and 38.3 minutes (average 22.18 minutes).
Licensing records
Licensing records were extracted with local authority Licensing Units where available to validate activity around licensing. This included numbers of new applications for a premises licence (including minor variations), written representations, review applications and any changes to the local authority’s Statement of Licensing Policy.
Focus groups with the community
Community members within two intervention areas were invited to attend a focus group. Local CICA co-ordinators helped advertise the focus groups using adverts/posters in local public spaces and through wider promotion within existing community networks. Focus groups explored: perceptions of alcohol harm within the community, views and opinions about the AHC role and perceptions of community cohesion within the intervention area.
A convenience sample was drawn from two CICA intervention areas (Area 1 and Area 6). Members of the public were reached through adverts in public places (e.g. local library) and via e-mail to existing community networks. Local co-ordinators, familiar with the area, led on recruitment using an electronic PDF advert as well as printed copies of A3 posters and A5 flyers provided by the research team. Participants were unknown to the research team but knew in advance that the focus group was organised by the University of Salford and aimed to give people a chance to ‘have their say about alcohol’ in return for £20 as a token of appreciation.
Three single focus groups90 were facilitated in private rooms within local libraries. A total of 26 participants attended, and written consent was obtained before the start. Two focus groups were held on the same day in June 2019 (Area 1) and one more in February 2020 (Area 6). EJB was supported by CU (administrative support inside the focus group) and SCH (administrative support outside the focus group). EJB explained how the focus group would work, its purpose and ground rules and announced when the audio-recorder would be switched on. A short description was provided of the CICA programme and the role of an AHC. Discussions lasted 38.11–60 minutes (average 48.54 minutes). Audio-recordings were transcribed (field notes not taken). Transcripts were not returned to participants for comment or correction as contact details were not obtained.
Quantitative analysis
Quantitative data from public licensing registers (e.g. on number of licensed premises) were extracted and described. Data from training registers were extracted and summarised. For the pre–post-training questionnaires with AHCs, descriptive statistics were used to summarise AHC demographic characteristics and current level of drinking as categorised by their AUDIT-C score. Related sample sign test statistics were conducted to ascertain changes in attitude following training. Statistical analyses were carried out using IBM SPSS Statistics 26. Training register data and loss at follow-up data were summarised descriptively using Microsoft Excel. A Spearman’s rank correlation test measured the association between the number of pre-implementation external contextual facilitating factors and the number of AHCs trained in the first year. This was followed by Mann–Whitney U-tests comparing the numbers of AHCs trained in areas with and without each individual external contextual factor.
Qualitative analysis
Analysis of documents
Analysis of documents used content analysis, and a summative, deductive approach was taken using the ‘surface structure’ (manifest analysis) – ‘what has been said’ rather than ‘what intended to be said’. Starting with the selection of a unit of analysis, five stages of data analysis were followed: stage one decontextualisation; stage two recontextualisation; stage three categorisation; and stage four compilation. This comprehensive review of the collected data enables information relevant to the research question to be identified. 91
Analysis of interviews and focus groups
Semistructured interviews and focus groups were digitally recorded, fully transcribed verbatim by a transcription service and anonymised. The transcripts were returned as Microsoft Word (Version 2204) documents. A thematic framework method92,93 was used for data analysis. This approach enabled themes to develop both deductively from the research questions and inductively from participants’ testimonies. 94 All data were coded and analysed according to the five stages of framework analysis. Textual data were ‘charted’ in themes relating to key research questions and scrutinised for differences and similarities within themes, keeping in mind the context in which these arise. We used a predominantly inductive approach with both semantic and latent coding.
Familiarisation of the data was done by reading through all the transcripts once while listening to the original audio recordings. Notes were taken based on key recurring ideas that related to the research question. 95,96 An initial thematic framework of possible themes and subthemes was developed based on the interview schedule and emerging concepts from the notes taken. 97 All transcripts were coded according to this framework, a process known as indexing. This was done by inputting all transcripts into NVivo (Version 12 Plus) (QSR International, Warrington, UK) as a singular data set and applying codes to them using the ‘nodes’ feature.
A matrix of the framework was then developed in Microsoft Excel (Version 2206) where each column represents a theme or subtheme, and each row represents a participant. Codes were extracted from NVivo and charted into the framework in the appropriate intersections between the columns (themes) and the rows (participants). As data were charted, the framework was revised as needed, with themes and subthemes merged, split or removed in an iterative process. Summarising notes for each column (themes) and each row (participant) were added to the chart. Charting in this way allowed us to not only synthesise an interpretation of the overall data but also observe and form trends in the data for each participant and compare across participants. Researchers MC, SCH and CU (initial implementation phase) and PAC, CU, ND and EJB (follow-up phase) held review meetings to reflect on thematic development and refine the themes and subthemes. Each theme and subtheme were given a categorical label, and a map was devised to demonstrate the relationships between them. Other steps to maintain the quality of the process included: verbatim transcription, checking transcripts against recordings, being reflexive and exploring data in a nuanced manner. 98,99
Member checking
The findings were presented back to key stakeholders as well as AHCs at a conference, led by the process evaluation team, to share and discuss early CICA project findings. The presentation gained verbal input from attendees, who were invited to comment, in order to check the trustworthiness of findings. 100 The findings resonated with attendees, and no recommendations for amending the themes were suggested. Focus group findings could not be presented back to the public as contact details were not obtained.
Changes to the protocol
In the design stages of CICA, the training aspect of the intervention was intended to be a 3-day course, which had been reflected in version 1.0 of our protocol. Prior to roll-out preparation in each area, the GM Local Leads steering group changed the delivery mode of the training to 2 days. This was following consultation with the RSPH and local areas, who suggested that it would be easier to recruit people for a 2-day programme.
The 3-month interviews with AHCs were not part of our original protocol. This data source was added as an amendment following a discussion about Normalisation Process Theory with our SSC and how a snapshot of AHCs’ attitudes at the outset would contribute to recording their sense-making of the intervention. 87 We recognised that volunteer lay champions were driven by a range of personal motivations to get involved and aimed to explore whether their experience of key training messages (how to deliver brief advice and get involved in licensing activity) may or may not have been coherent with their own values and motivations.
We had initially planned to create a composite score of alcohol availability, making use of data on number of licensed premises, hours of sale and capacity (on-licensed premises only). In theory, this information forms part of licensing applications and should be recorded in the licensing register. However, there was no consistent format, so we were unable to do this. See the discussion chapter for a consideration of its implications.
At 1-year follow-up, we had planned to carry out two focus groups with people who had come into contact with AHCs, given the original premise that by this time each LSOA would have received a significant ‘dose’. However, it became evident that recruiting those who had received brief advice raised a range of issues which had not been anticipated, including ethical issues and potential bias in the sample.
We had also initially hoped to hold interviews with 22 AHCs from a purposive sample of first-generation and second-generation training participants, capturing the experiences of those who engaged in AHC activities and those who did not. However, due to the attrition, we were unable to do this, which led to convenience sampling of all AHCs available. Follow-up questionnaires, intended to be completed by all trained lay AHCs, were completed by only 11 out of 95; these have been omitted from the report since there were too few to analyse.
Economic evaluation methods
The economic evaluation was conducted using a cost–benefit and cost–consequences analysis (CCA) of the CICA programme. A health economics analysis plan (combined with the outcome analysis) was developed and is available here: https://osf.io/9z65w/. The economic evaluation had the following steps:
-
identifying set-up and running costs using a standardised costing exercise (examination of commissioning documents and contracts)
-
resolving costs and benefits by sector: public sector, society and local authority
-
quantifying the value for money of CICA in terms of reduced alcohol-related hospital admissions, A&E use, ambulance call-outs, crime and ASB.
The cost–benefit analysis (CBA) presented in this report was initially developed by the New Economy. The method was developed with the broad participation of different sectors and stakeholders across GM to give a comprehensive figure about the multisectoral impact of interventions. Members of the central government departments contributed to the development of this approach, including HM Treasury; the Department of Work and Pensions; the Department for Business, Innovation and Skills; the Department of Health; the Department for Communities and Local Government; the Department for Education; Ministry of Justice; Home Office; and the Cabinet Office. 101,102 We also present the CCA, disaggregating the analysis according to each outcome. Thus, the stakeholders can see the budget implications of implementing CICA overall and for each of the outcomes included in the analysis. We follow good practice of the New Economy to guide the CBA which also applies to the CCA.
The analysis covered the time frame before and after CICA implementation. That is, we collected information about the outcomes included in the analysis – 1-year pre intervention and the final year of the intervention implementation. Due to the stepped-wedge trial design, the period before and after intervention implementation varied for each area. The economic evaluation included the costs of the intervention, in addition to the fiscal costs and fiscal benefits of the intervention for different agencies in society, such as local authority, NHS and police. Results were presented to show the value for money of CICA from the public sector, society and local authority perspectives.
Identifying set-up and running costs of Communities in Charge of Alcohol
The costs of training, delivery and support elements of the intervention were estimated. The economic evaluation builds on the outcome evaluation by attributing costs to the health performance indicators collected on primary outcomes. UK Treasury-approved methods published by the GMCA underpinned the CBA, and unit costs are based on the GMCA Unit Cost Database. 102
A standard costing exercise used documents and contracts to identify resources and costs required to deliver the CICA intervention in each local authority. Standardised methods allowed comparability of costs. The economic evaluation followed a cost–benefit analysis and CCA which is an approach that is favoured when costs and outcomes fall on a range of budget holders and government agencies, enabling cost–consequence domains to be presented in a disaggregated form. 103,104 This aims to enable decision-makers to assess results using different relevant perspectives.
The key cost categories identified include the set-up cost for the intervention area, comprising staff costs, consumables and overheads (room hire). In terms of consequences, this comprises an analysis of benefits (A&E attendances, alcohol-related hospital admissions, ambulance call-outs, ASB and general crimes).
Costs
We applied a bottom-up micro-costing approach105 to estimate CICA costs incurred during a 1-year time horizon. We mapped and estimated set-up and running costs incurred by four dimensions of the intervention, programme management, first- and second-generation training events and AHCs’ activities.
All costs were entered in the GMCA tool. 102 Costs were categorised into (1) capital costs: one-off investments, for example, design and development of Train-the-Trainer programme; (2) revenue costs: costs which tend to fluctuate in relation to the amount of project activity being undertaken, for example, staff salaries; and (3) in-kind costs: those inputs that are needed in order to make a project a success but which the public purse will not have to pay for, such as a volunteer activity.
We adjusted all costs according to an optimism bias correction recommended by GMCA tool. The correction factors (% increase in costs) adopted a confidence grade which varied according to the data source (e.g. independently audited cost data, formal service delivery contract and others) and age (e.g. current data, between 1 and 2 years old, 2 and 3 years old and 3 and 4 years old).
Capital costs were collected from the GM local authorities through the provision of invoices. Revenue costs were collected through cost diaries filled out monthly by local CICA co-ordinators. Cost diaries included time spent by AHCs undertaking CICA activities (e.g. support meetings, conversations with the local community, attending community events), which were converted into monetary values by using hourly or daily minimum wages to account for the in-kind cost estimates. Table 5 provides detailed information on cost items in British Pounds, source of information and costing approach included in this study.
| Cost domain | Type of cost | Source | Method |
|---|---|---|---|
| Programme management | |||
| Revenue | Time and transportation costs incurred during project meetings:
|
Meeting minutes and local lead diaries | Transportation: unit costs vs. quantity Time cost: (annual incomea/annual number of working hoursb) * total number of meetingsc * average duration of the meetingsd |
| First- and second-generation training | |||
| Capital | Design, development and delivery of training package, accreditation fees | GM local authority invoices | Unit costs vs. quantity |
| Revenue | RSPH qualification and assessment fees, time and miscellaneous (transportation, room hire, catering, printing costs) | GM local authority invoices and local lead diaries | Miscellaneous: unit costs vs. quantity Time cost = the hourly (£17.59) and daily (£140.69) wages self-reported by the participants |
| AHCs | |||
| Revenue | Engagement materials | GM local authority | Unit costs vs. quantity |
| In-kind | Volunteer time in conversations (~11 minutes each) | Local lead diaries | Total number of conversations * 11 minutes. Total time of conversations * hourly minimum wage in UK for 25-year-olds and above in 2018, £7.83 |
Cost–benefit analysis and cost–consequences analysis
The effects of CICA were calculated in terms of alcohol-related hospital admissions, A&E attendances, ambulance call-outs, reported crime and ASB. We assessed the frequency of these outcomes during weekdays and weekends. The economic evaluation provided: (1) fiscal benefits, that is, savings to the public sector due to CICA implementation (e.g. reduction in demand for health service); (2) public value benefits (economic and social benefits), that is, the overall value of CICA to the society; and (3) CICA overall value for money for the local authority. Costs and their source for each CICA outcome are presented in Table 6.
| Outcome | Costsa | Source | ||
|---|---|---|---|---|
| Fiscal | Economic | Social | ||
| Crime: average cost per incident of crime, across all types of crime | £998 | £1133 | £1489 | ‘The Economic and Social Costs of Crime, Second Edition’. |
| ASB further action necessary (cost of dealing with incident) | £510 | N/A | N/A | The Economic and Social Costs of antisocial Behaviour: a review’ (London School of Economics and Political Science, 2003), p. 43. |
| Ambulance call: ambulance services – average cost of call-out, per incident | £238 | N/A | N/A | Reference Cost Collection: National Schedule of Reference Costs – Year 2017–18 – weighted average of currency codes ASS01 and ASS02 (‘AMB’ worksheet). |
| A&E attendance: all scenarios | £166 | N/A | N/A | National Schedule of Reference Costs 2017–18 for NHS trusts and NHS foundation trusts (weighted average of values against HRG code VB01Z–VB11Z). |
| Hospital day cases – average cost per episode | £757 | N/A | N/A | Reference Cost Collection: National Schedule of Reference Costs – Year 2017–18 – weighted average of all day cases HRG data (‘DC’ worksheet). |
The main outcome of the economic evaluation was the net present value (NPV) of CICA, that is the additional value created by implementing the intervention. NPV was calculated considering the fiscal (whether CICA is affordable) and economic (whether the intervention represents the best public value) cases and the local authority. We presented the aggregated CBA results and CCA according to each outcome.
Cost–benefit formulae
| NPV | = | present value of the benefits | − | present value of the costs |
Financial case
| Net present budget impact | = | net present fiscal costs | − | net present cashable fiscal benefits |
| Financial return on investment | = | net present cashable fiscal benefits | / | net present fiscal costs |
| Payback period | = | year in which the cumulative present value of the budgetary savings | > | cumulative present value of the budgetary costs |
Economic case
| Net present public value | = | net present public benefits (Economic and Social) | − | net present public costs |
| Public value for money (benefit-cost ratio) | = | net present public value | − | net present budget impact |
Changes to the protocol
The economic evaluation was carried out as per the protocol.
Chapter 3 Outcome evaluation results
This chapter describes the quantitative evaluation of the effectiveness of the community AHC programme (CICA).
The aims of the CICA Outcome Evaluation were to:
-
determine the effect on area-level alcohol-related hospital admissions, A&E attendances and ambulance call-outs
-
determine the effect on key crime indicators (street-level crime data) and key indicators of ASB.
Data and evaluation of models
An overview of median outcomes pre and post intervention is shown in Table 7. As indicated, any impact from the CICA intervention is likely to be relatively small at most, in particular for ambulance call-outs and reported crimes.
| Outcome | Pre intervention | Post intervention | ||||
|---|---|---|---|---|---|---|
| Median | IQR | Range | Median | IQR | Range | |
| Alcohol-related hospital admissions | 118 | (60–205) | (2–896) | 134 | (67–203) | (2–896) |
| Ambulance weekend | 4 | (2–7) | (0–45) | 5 | (3–8) | (0–45) |
| Ambulance weekday | 4 | (3–7) | (0–57) | 6 | (3–9) | (0–65) |
| A&E weekend | 19 | (15–24) | (4–49) | 21 | (17–27) | (4–60) |
| A&E weekday | 25 | (20–31) | (5–66) | 28 | (23–35) | (5–96) |
| Crime weekend | 2 | (1–3) | (0–45) | 4 | (2–6) | (0–45) |
| Crime weekday | 0 | (0–0) | (0–12) | 2 | (1–4) | (0–41) |
| ASB | 3 | (2–5) | (0–43) | 2 | (1–4) | (0–43) |
Pre-intervention parallel trends in the outcomes are assessed graphically for the local controls in Figures 3 and 4 and for the national controls in Figure 5. While Figures 3 and 4 indicate trends of outcomes in the selected local control LSOAs following those in the CICA intervention LSOAs, for the national controls (see Figure 5), there is some graphical evidence that trends start to converge across the pre-intervention time period. This indicates that inferences about the effect of the CICA intervention from the national comparison analyses should be interpreted with caution.
FIGURE 3.
Comparisons of pre-intervention average trends of: (a) alcohol-related hospital admissions; weekend (b) and weekday (c) ambulance call-outs; and (d) A&E admissions in intervention (CICA) areas (coded 1) and local control areas (coded 0).
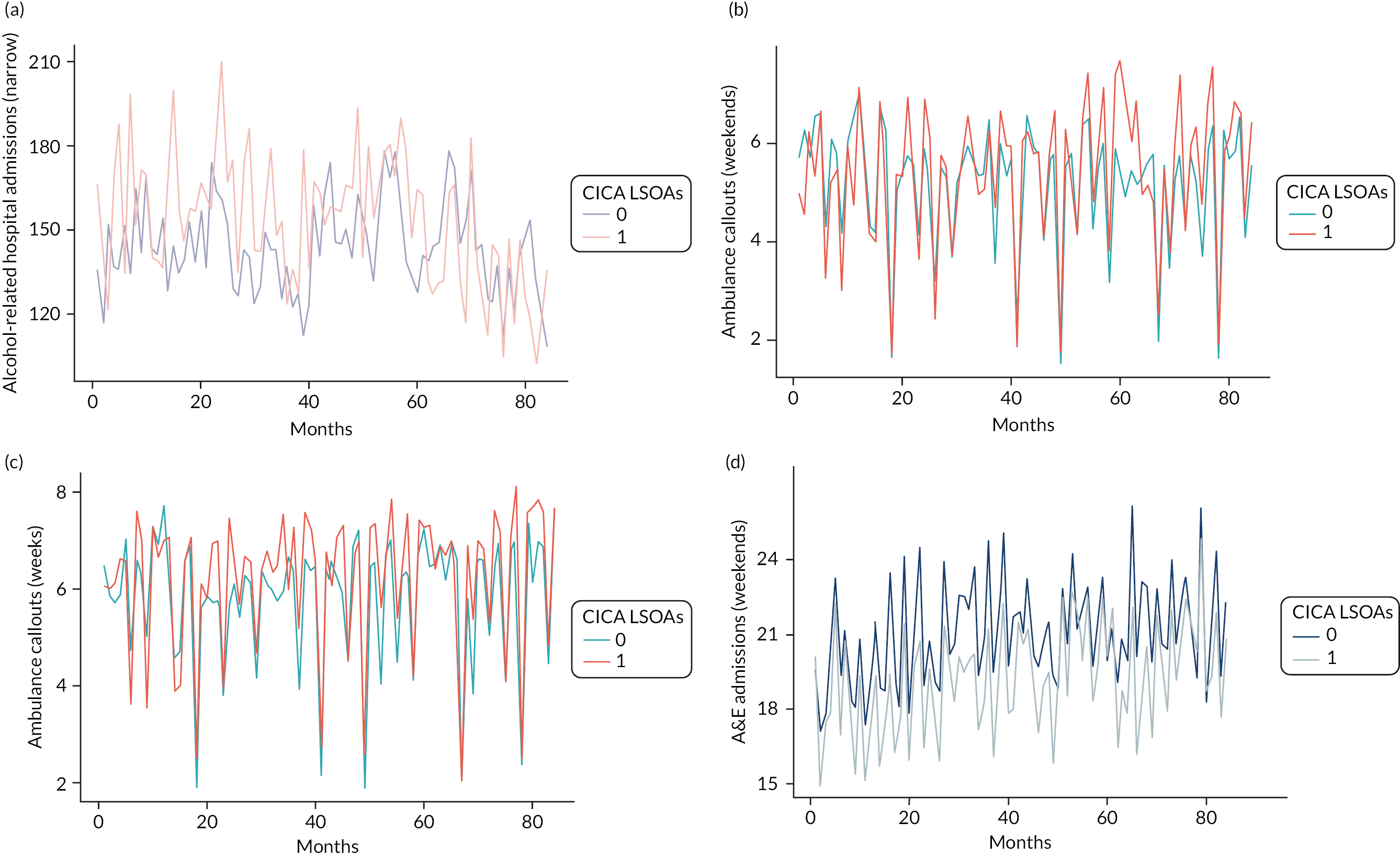
FIGURE 4.
Comparisons of pre-intervention average trends of: (a) alcohol-related A&E admissions; weekend (b) and weekday (c) reported crimes; and (d) reported ASB incidents in intervention (CICA) areas (coded 1) and local control areas (coded 0).
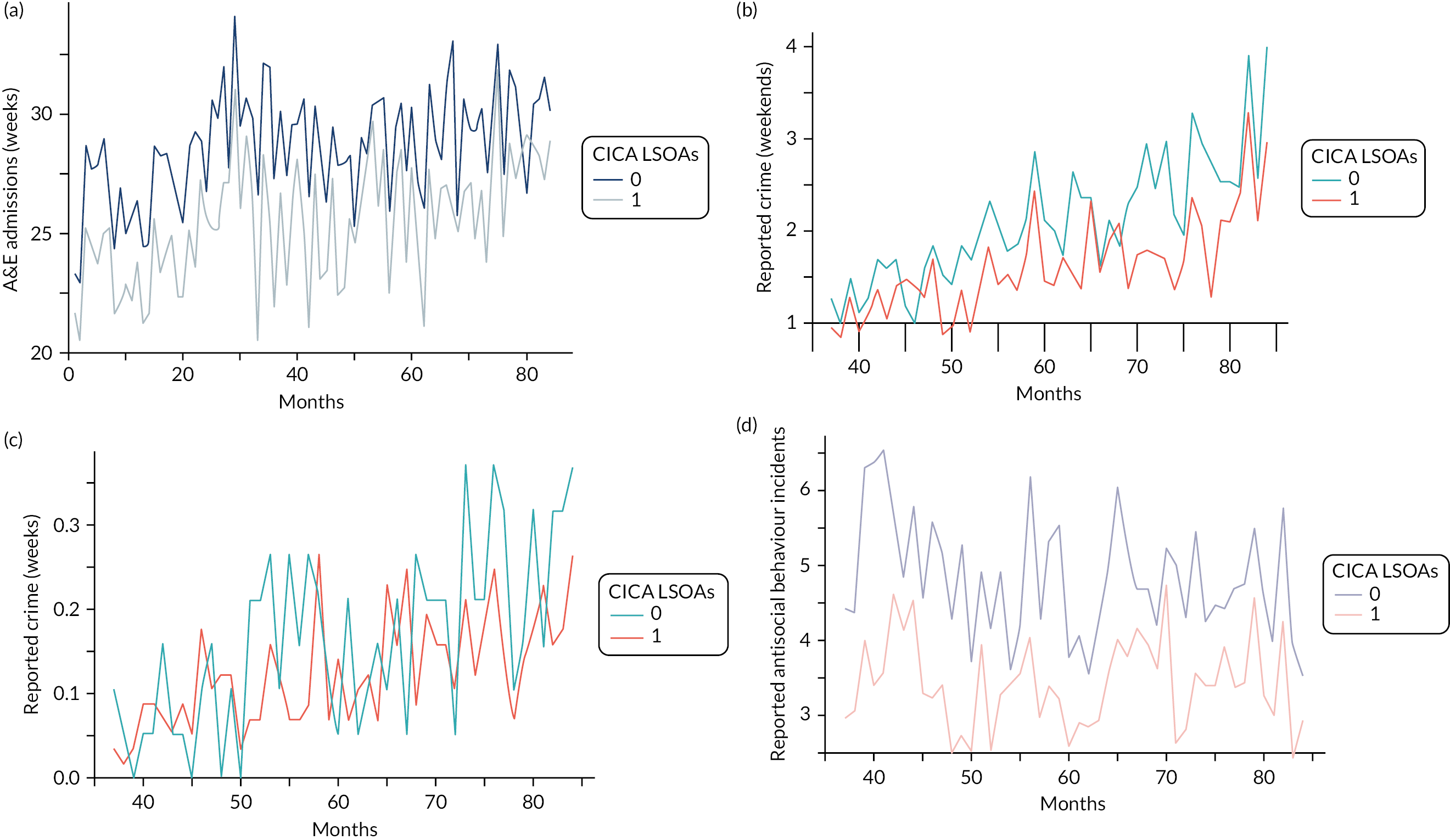
FIGURE 5.
Comparisons of pre-intervention average trends of: (a) alcohol-related admissions and weekend (b) and weekend (c) A&E admissions in intervention (CICA) areas (coded 1) and national control areas (coded 0).
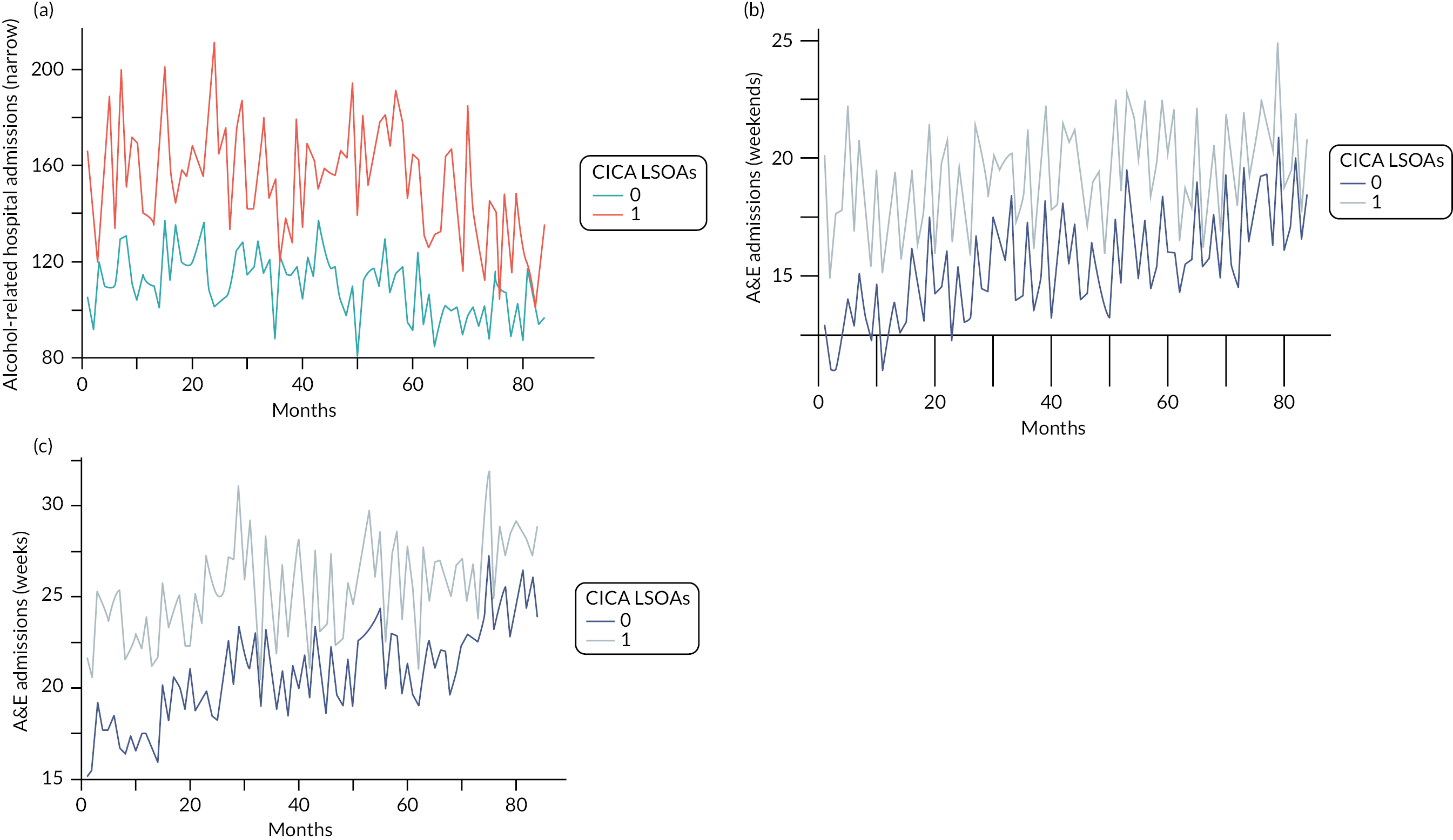
Assessment of performance of the statistical models was done based on evaluation of patterns in the residuals. Broadly speaking, patterns of model residuals confirm that the model assumptions are met, although, for some models, the patterns of residuals could be observed resulting from the low incidence rates of certain events (including zero incidents at some time points). For each of these models, we assessed whether there was evidence of zero inflation (i.e. more counts of zero than expected). There was evidence of this for ambulance call-outs and ASB (assessed using the performance R package), and for these, we reanalysed the data using zero-inflation negative binomial mixed-effects models using the glmmTMB package in R. 106 Results are shown in Appendix 3 and indicate that although point estimates of the ATEs differ, confidence intervals largely overlap, and this alternative modelling would not have impacted on the inferences about effects of the CICA programme. We therefore present the original growth models rather than the zero-inflated model results as part of the main results.
Outcome evaluations
An overview of the results of all statistical analyses is shown in Table 8. A graphical overview of forest plots is shown in Figures 6–9. The primary, stepped-wedge analyses provide weak evidence of an average increase in alcohol-related hospital admissions following the implementation of CICA of about 13%, corresponding to about 20 admissions weekly, although the confidence interval was wide, −1.98 to 31.39, and did not reach statistical significance (p ~ 0.09) (see Table 8). Although this result is comparable to the effect found compared to local controls, this was not confirmed when national controls or counterfactuals were used, which indicated much smaller effect sizes and confidence intervals, including unity: 3.42 (−4.56 to 12.07; p-value 0.41) and 7.14 (−9.76 to 24.04; p-value 0.41), respectively. Nonetheless, all models consistently report an increase in hospital admissions following the introduction of the intervention. This is likely an artefact in the data from some unknown endogenous factor we could not model, as this direction of effect seems highly implausible (at least as a direct result of CICA) (see Figure 6).
| Outcome | Stepped wedge | Local controls | National controls | Counterfactual | ||||
|---|---|---|---|---|---|---|---|---|
| Effect (95% CI) | p-value | Effect (95% CI) | p-value | Effect (95% CI) | p-value | Effect (95% Cr) | p-value | |
| Alcohol-related hospital admissions | 13.43% (−1.98 to 31.39) | 0.09 | 16.36% (7.33 to 26.16) | 0.00 | 3.42% (−4.56 to 12.07) | 0.41 | 7.14% (−9.76 to 24.04) | 0.41 |
| Ambulance weekend | −5.74% (−15.45 to 5.19) | 0.29 | −4.20% (−9.98 to 1.95) | 0.18 | 19.41% (8.14 to 30.68) | 0.00 | ||
| Ambulance weekday | −5.24% (−14.87 to 5.48) | 0.33 | −0.58% (−6.24 to 5.43) | 0.85 | 24.3% (13.40 to 35.23) | 0.00 | ||
| A&E weekend | 6.25% (0.60 to 12.21) | 0.03 | 6.33% (3.28 to 9.47) | 0.00 | 0.28% (−3.10 to 3.77) | 0.87 | 14.36% (7.66 to 21.06) | 0.00 |
| A&E weekday | 1.69% (−3.27 to 6.90) | 0.51 | 6.04% (3.32 to 8.84) | 0.00 | −0.17% (−3.38 to 3.16) | 0.92 | 14.28% (8.01 to 20.55) | 0.00 |
| Crime weekend | 6.34% (−6.01 to 20.32) | 0.33 | 3.36% (−3.95 to 11.23) | 0.38 | 31.10% (7.40 to 54.80) | 0.01 | ||
| Crime weekday | 213.99% (140.08 to 310.62) | 0.00 | 41.74% (22.62 to 63.84) | 0.00 | 1638.09% (−767.77 to 4043.94) | 0.18 | ||
| ASB | −15.61% (−29.79 to 1.43) | 0.07 | 1.64% (−8.44 to 12.82) | 0.76 | −39.30% (−45.03 to −33.57) | 0.00 | ||
FIGURE 6.
Average effect (%) and approximate 95% confidence interval or credible intervals (synthetic controls) of CICA intervention for alcohol-related hospital admissions (narrow definition).
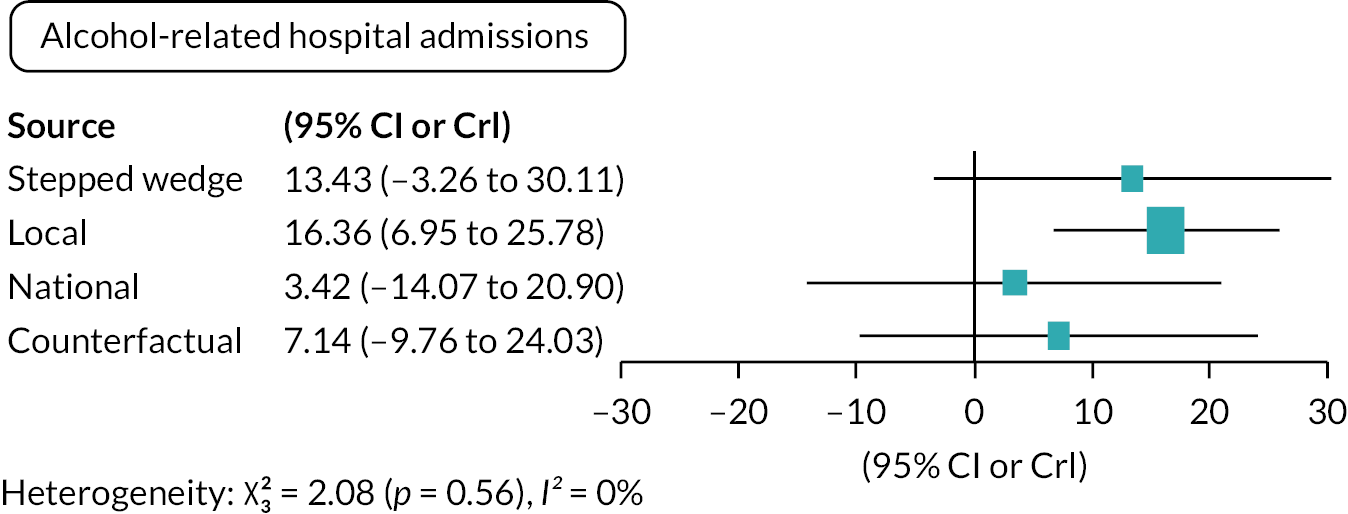
FIGURE 7.
Average effect (%) and approximate 95% confidence interval or credible intervals (synthetic controls) of CICA intervention for: ambulance call-outs during (a) weekdays and (b) weekends.
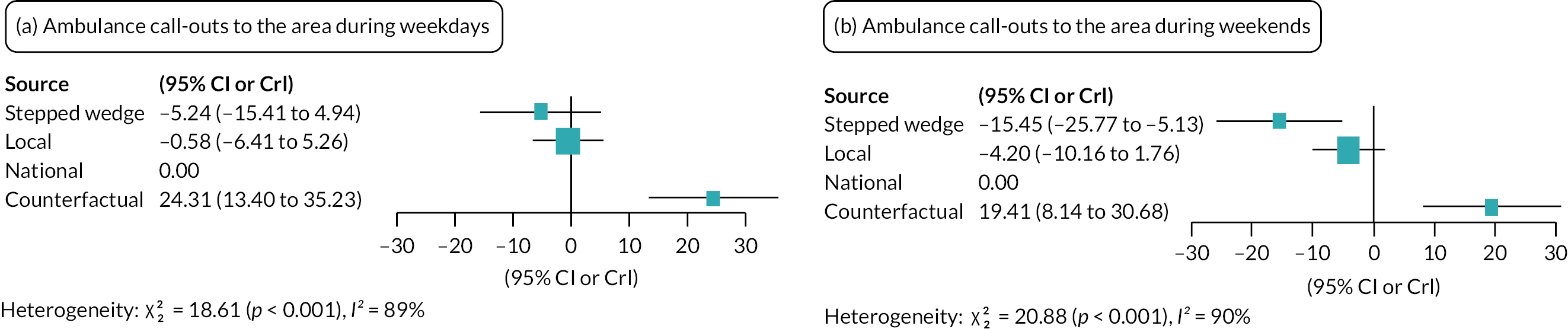
FIGURE 8.
Average effect (%) and approximate 95% confidence interval or credible intervals (synthetic controls) of CICA intervention for A&E attendances during (a) weekends and (b) weekends.
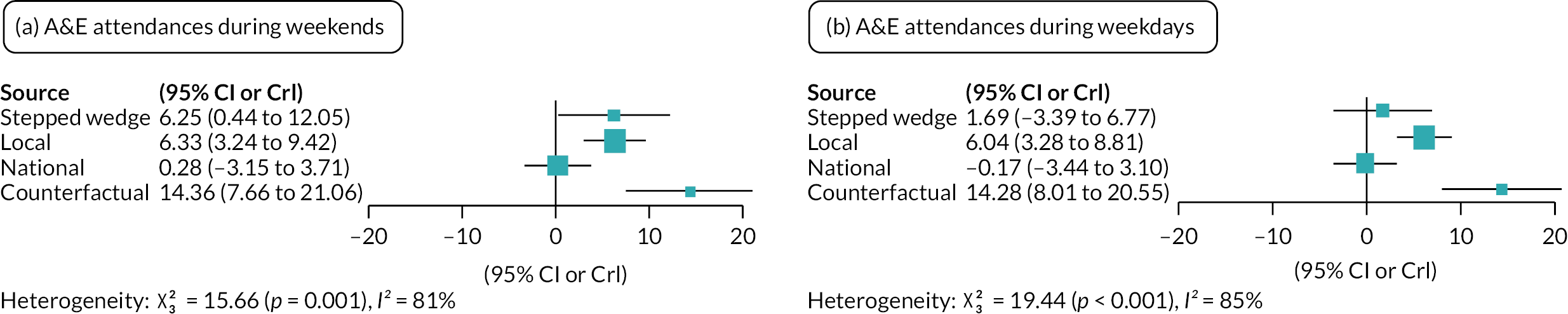
FIGURE 9.
Average effect (%) and approximate 95% confidence interval or credible intervals (synthetic controls) of CICA intervention for reported crimes during (a) weekends and (b) weekdays.
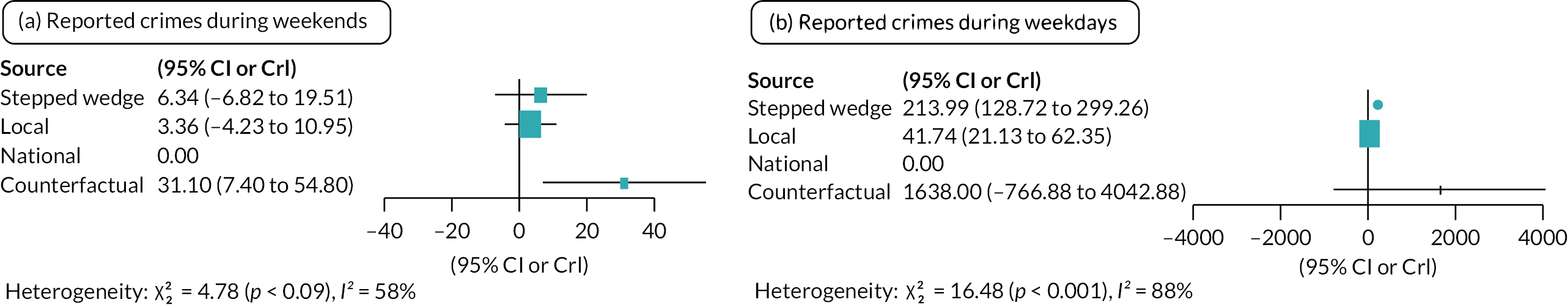
The impact on ambulance call-outs to the areas following the CICA intervention showed an average decrease in call-outs in the weekend as well as for weekdays for both the stepped-wedge and local control analyses, but neither was statistically significant (p > 0.18) (see Table 8 and Figure 7). In contrast, the counterfactual models indicated an increase in call-outs, which was significant and was somewhat larger during weekdays (+24.3%, 13.4–35.2%) compared to weekends (+19.4%, 8.1–30.7%). Regardless, the effect size corresponds to 1–2 call-outs per LSOA per month, indicating that this is unlikely to describe any true effects from the intervention.
Results for A&E attendances similarly show some evidence of an effect of the CICA intervention, but triangulation indicates results are inconsistent (see Table 8 and Figure 8). The number of incidences on average increased following the introduction of CICA, and this is statistically significant for weekends for all methods bar the comparison to national controls (p = 0.87), but not for weekdays for the stepped-wedge analysis (p = 0.51) and national controls (p = 0.92). Effect sizes are small and correspond to < 2 additional admissions per month per LSOA. Given the inconsistency of the results, the small effect size and given that the direction of the effects is against our hypothesis, we infer that these analyses are not indicative of a true effect from the intervention.
There was similarly little evidence of an effect of the CICA intervention on the incidence of reported crimes in weekends (see Table 8 and Figure 9). Even though an average increase following the intervention was observed when compared to the counterfactual of +31.1% (p = 0.01), this was very imprecise (95% CrI 7.4% to 54.8%) and not mimicked by the other analyses which, although the stepped-wedge and local control cITS analyses also suggested an increase in the incidence, were not significant (p = 0.33 and 0.38, respectively). Note that the number of incidents of reported crimes during weekdays was so low, and often none were recorded, that the relative effects of the intervention are meaningless. Whereas the effect for weekend crimes corresponds to approximately two additional reports per LSOA per month on average, and during weekdays, these correspond to less than one.
The stepped-wedge analysis for reported ASB incidence provided weak evidence of an effect in the hypothesised direction and indicated an average reduction of 15.6% (−29.8%, 1.4%) which corresponded to less than one incidence averted per LSOA per month on average (see Table 8 and Figure 10). This was, broadly speaking, confirmed by the counterfactual analyses which indicated an average reduction of 39.3% (95% CrI −45.0% to −33.6%), but not by the comparison to local controls which did not provide any indication of an effect (p = 0.76).
FIGURE 10.
Average effect (%) and approximate 95% confidence interval or credible intervals (synthetic controls) of CICA intervention for reported ASB incidents.
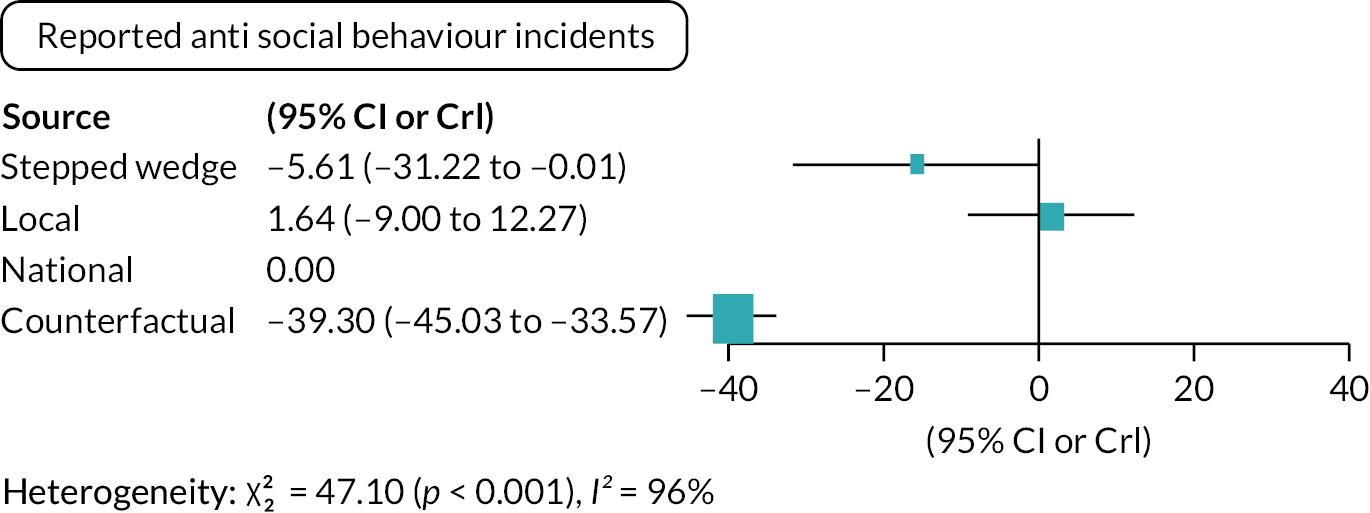
Sensitivity analyses
As outlined in the Analyses Plan, we conducted additional sensitivity analyses for the stepped-wedge design to assess whether there might be a lag between the start of the implementation of the CICA intervention and any measurable effects. We assessed such lagging of effects for 6 and 12 months, and the results are presented in Table 9. Effect estimates vary considerably between the unlagged, 6-month lagged and 12-month lagged results and sometimes differ in direction of change. However, results are imprecise, and confidence intervals largely overlap. For the interpretation of Table 9, it should also be noted that the relative effects presented do not do justice to the absolute effects, which, because of the low incidence, numbers are generally small. Nonetheless, there is no indication of a pattern that would indicate that lagged effects are more likely than the null effects observed in the main analyses.
| Outcome | Stepped wedge | 6 months lag | 12 months lag |
|---|---|---|---|
| Effect (95% CI) | Effect (95% CI) | Effect (95% CI) | |
| Alcohol-related hospital admissions | 13.43% (−1.98 to 31.39) | −10.36% (−23.83 to 5.49) | −5.73% (−21.03 to 12.54) |
| Ambulance weekend | −5.74% (−15.45 to 5.19) | −5.93% (−16.68 to 6.21) | +23.29% (8.40 to 40.24) |
| Ambulance weekday | −5.24% (−14.87 to 5.48) | −8.06% (−18.36 to 3.53) | +19.44% (5.27 to 35.52) |
| A&E weekend | 6.25% (0.60 to 12.21) | 3.71% (−2.37 to 10.18) | +1.81% (−4.56 to 8.60) |
| A&E weekday | 1.69% (−3.27 to 6.90) | +0.98% (−4.45 to 6.72) | +7.57% (−1.59 to 10.73) |
| Crime weekend | 6.34% (−6.01 to 20.32) | −3.37% (−15.23 to 10.15) | −7.23% (−20.16 to 7.78) |
| Crime weekday | 213.99% (140.08 to 310.62) | +54.95% (24.41 to 92.98) | −17.40% (−33.94 to 3.29) |
| ASB | −15.61% (−29.79 to 1.43) | +2.87% (−16.82 to 27.22) | +42.46% (13.76 to 78.39) |
Interpretation
Overall, the analytic results do not indicate that the implementation of the CICA intervention has resulted in measurable effects on any of the health and crime outcomes (see Table 8), and there is similarly little evidence of a lagged period before any such effects are measurable (see Table 9). Although average reductions in incidence following the implementation in the stepped-wedge design were observed for reported ASB (−15.6%) and ambulance call-outs to the area (−5.5% across weekdays and weekends) in agreement with our hypothesised directions of effects, estimates were quite imprecise and mostly non-significant, while they were also not in agreement with the other design and analytic methods. Moreover, even if we would interpret any of these as causally related, for which ASB incidence seems the most likely candidate, average effect sizes are minimal and would have little practical weight.
Chapter 4 Process evaluation results
Parts of this chapter have been reproduced with permission from earlier papers on the process evaluation. 41–44 These are articles published under a Creative Commons Attribution-Non-Commercial-NoDerivatives (CC BY-NC-ND 4.0), and any extracts have been reproduced exactly. See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
The CICA process evaluation explored the context, implementation and response to the CICA intervention at distinct phases, recognising that complex health interventions roll out in identifiable phases or stages. 107,108 As such, the results are organised according to phases: the pre-implementation phase (2–3 months prior to roll-out); the initial implementation phase (within 3–6 months of training); the intervention phase (12-month period of AHC activity from the first month following the initial Train-the-Trainer event) and the follow-up phase (post intervention, at 12 months and beyond).
The initial conception, design and project management of the CICA intervention had commenced in GM prior to the commissioning brief in 2016 and NIHR evaluation award in 2017; therefore it was outside of the scope of the process evaluation. However, time and costs spent on conception, design and project management prior to the pre-implementation phase of CICA were captured within the scope of the economic evaluation (see Chapter 6).
This process evaluation chapter starts with findings from the pre-implementation phase of CICA, during which time all 10 local authorities participated in preparatory roll-out meetings, and document analysis provided insight into each area’s local licensing policy context and infrastructure a priori. While only 9 of the 10 areas progressed to the initial implementation phase, a total of 23 stakeholders participated in baseline interviews, representing all 10 original areas. One hundred and twenty-three people subsequently attended CICA training, and of these ninety-five were volunteers, recruited as intended, living or working in the targeted communities. Training evaluation questionnaire data were collected from 98% of the lay volunteer sample population, representing all nine areas. Cascade training observations took place in five areas. Follow-up interviews were completed with 12 volunteers in 4 areas. After 12 months, seven out of nine areas remained active, with two local authorities withdrawing after 6 and 9 months. Follow-up interviews with 11 stakeholders were carried out in 8 of these areas. To conclude the process evaluation, 26 members of the public from 2 areas attended focus groups.
Pre-implementation phase
Licensing policy context
This document analysis aimed to provide a policy context to each area’s alcohol risk environment, the local authority’s vision for alcohol licensing decisions, and the framework within which volunteers would be working. Statements of Licensing Policy published by each of the 10 local authority areas were examined a priori using 10 items: 7 predetermined categories based on existing research from Scotland86 (marked with *) and three additional items to reflect alcohol licensing practice in England and Wales (item 8) and licensing activity expected of AHCs (items 9–10).
-
presentation and readability*
-
use of evidence*
-
process of consultation*
-
licensed hours for alcohol sales*
-
density/cumulative impact (referred to as ‘overprovision’ in Scotland)*
-
operating conditions, including children’s access*
-
temporary event notices (referred to as ‘occasional licences’ in Scotland)*
-
regard for health (in the absence of 5th licensing objective in England and Wales)
-
community recognition
-
information on how the public can get involved in licensing processes.
Background
None of the Statements of Licensing Policy included in the document review were due for renewal during the CICA intervention period; therefore, the policy context of licensing practice was already established and remained stable throughout each area’s CICA intervention period. Statements of Licensing Policy (referred to as ‘licensing policy’ from here onwards) in England and Wales must be renewed by local licensing authorities every 5 years;83 the anticipated renewal dates in each area ranged from January 2020 to May 2021. All licensing policies were published on the local authority website in either a PDF or Word document that could be downloaded.
Presentation and readability
Length varied between 27 and 92 pages (mean 47 pages). Only two out of nine policies provided details of an author/main point of contact: one signposted the reader to the Licensing Authority office within the local council as a point of contact for ‘any licensing related matter’ (Area 1), and the other provided a named contact for the lead responsible officer (Area 5).
Statements of Licensing Policy are intended to provide clarity for everyone including: ‘..local residents, businesses and licence applicants, who will be able to refer to the statement when making representations or when preparing their application’. 109 A glossary of legalistic language was only provided in four out of nine of the licensing policies. This limited the readability and accessibility of the information. Although a plain language assessment of policy wording is not a requirement within the 2003 Act or Section 182 best practice guidance, none of the policies reviewed had Plain language accreditation or specified that the use of plain language had been considered. 110 The predominant legalistic language used within the policy statements conveyed that they were applicant-focused.
Use of evidence
Guidance to support licensing authorities to fulfil their functions under the 2003 Act emphasises that actions and decisions taken to promote the four licensing objectives should be appropriate, proportionate and evidence-based. 83 Interested parties and Responsible Authorities (RAs) are reciprocally required to provide evidence when making representations. In all policy statements, evidence underpinning policy positions or model conditions was limited, if provided at all. In this excerpt, it is unclear why this recommendation may promote the licensing objectives, what processes and practices are required within the system in order to be effective and how the licensing authority is defining ‘high density’:
It is recommended that radio links or telephone communication systems should be considered for licensed premises in city and town centre leisure areas with a high density of premises selling alcohol.
Area 3
In Area 2, a recommendation was made that applicants and licensed businesses should consider obtaining alcohol IBA training so that members of staff could: ‘recognise when people may have a drinking problem, and how to give them brief advice’, but this did not have an explanatory evidence base.
Three areas highlighted the ‘authority profile’ detailing the number of licensed premises already in operation and the number of Temporary Event Notices issued on average in a year (Areas 1, 4, 9) as underpinning evidence. While two areas cited alcohol-related hospital admission figures as part of a ‘regard for health’, relevant alcohol harm data available to local authorities52 were generally not included. Only one area provided alcohol-related crime, injury and public perception survey data on drunken behaviour in the night-time economy, along with an evidence-based rationale for a framework of opening and closing times for both on- and off-licensed premises:
Taking into account the problems of crime, disorder, nuisance and ASB into the early hours of the morning, we have introduced a framework of opening and closing times for premises …. Off-Licensed Premises 8am–11pm Sun to Sat; On-Licensed Premises 1am Sun to Thurs and 3am Fri and Sat (and BH); Late Night Refreshment 1.30am Sun to Thurs and 3.30am Fri and Sat (and BH) … Applicants should note that there is no guarantee that an application will be granted if the hours of trading fall within this framework. In similar terms, an application will not automatically be rejected because the proposed hours of trading fall outside of the framework. All applications will be considered on their individual merits.
Area 8
In terms of conditions that could be proposed or imposed to prevent crime and disorder and promote public safety. In the following example, the licensing policy explains the expected outcome of adopting a ‘documented glass policy’, naming glasses and bottles as potential weapons:
Operating a documented glass policy for the premises: In the UK, glasses and bottles are the most commonly used weapons in violence occurring in drinking environments. Incidents involving glass tend to result in more severe injuries.
Area 6
While the rationale is provided, suggesting it is an intervention that is evidence-based, references to the source of evidence are not provided.
Process of consultation
The consultation process provides a mechanism for interested parties, such as local residents and community groups, to influence licensing policy principles and licensing practices. The Police Reform and Social Responsibility Bill also removed the ‘vicinity test’ to increase opportunities for members of the public/lay people to get involved in licensing decisions. 111 Across the 10 policy statements, only 1 provided a full list of consultees as an Appendix (Area 4). This is significant in terms of demonstrating transparency in how the process was undertaken and opportunities for meaningful engagement. 86 No detail was given in any of the licensing policies as to what amends were made or rejected as a result of consultation responses.
Licensed hours for alcohol sales
Two areas provided guidance on hours of alcohol sales (Area 8, Area 10). One of these areas, as noted in item 2, provided an evidence-based rationale for their framework. Where no framework was provided, other areas identified particular risk environments that may require stricter conditions: residential areas and takeaways. Two policies did not provide any guidance on hours of alcohol sales and relationships with risk environments; however, in recognition of the 24-hour licensing regime, there was an expectation that the hours of alcohol sales applied for would have to mitigate against any adverse impact on the licensing objectives:
The Authority accepts that as a general principle, the act permits activity which does not undermine the licensing objectives, taking place over 24 hours and 7 days a week. The hours requested… will normally be approved where the applicant can show that the proposal would not, with regard to the licensing objectives, adversely affect the environmental quality, residential amenity and character of any particular area.
Area 1
Density/cumulative impact
Four areas provided some criteria that would be used to assess ‘saturation’ or ‘density’, though not all set out how interested parties, such as local residents or community groups, could make a representation to initiate a cumulative impact assessment and consultation process. At the time of CICA, three areas had at least one special stress policy/cumulative impact policy in effect.
Operating conditions including children’s access
There are three types of conditions that can be attached to a premises licence: proposed (actions and steps the operator voluntarily offers to take to promote the licensing objectives); imposed (actions and steps insisted on within a licensing hearing following relevant representations); and mandatory (a set of conditions that apply to all premises licences, including the Mandatory Conditions Order 2010112 for irresponsible drinks promotions, potable water, age verification and small measures). All licensing policies provided some guidance on example conditions that could be proposed or imposed. However, as identified in item 2, it was not consistently clear if they were evidence-based ‘model conditions’, that is, with a rating of the quality of evidence/strength of recommendations.
Model conditions were themed around the four licensing objectives, with some policies setting out additional conditions to consider for vulnerable groups at higher risk of harm and/or higher-risk alcohol environments: underage drinking; children at risk of sexual exploitation; intoxicated/drunk customers; recreational drug users including the use of new psychoactive drugs; high-volume vertical drinking; alcohol delivery services; hypnotism; and large-scale events. Six out of ten areas explicitly addressed actions and steps that could be proposed or imposed to prevent the illegal sale of alcohol to a person who is drunk (Section 141 of the Licensing Act 2003). No policies detailed how Section 141 would be monitored in terms of compliance and enforcement. 113
Specific conditions recommended to protect children from harm varied, aside from those set out in the Mandatory Conditions Order 2010 in relation to age verification policies. 112 Recognising that the Act promotes free access to children into licensed premises was consistently stated as a principle: ‘It is rarely likely to be necessary that a complete ban on children entering a premises is imposed’ (Area 9). Despite a number of risks identified that may justify increased restrictions or tighter controls (i.e. operating conditions) to protect children from harm, none of the 10 policies recognised the risk of accompanying adults who become drunk or exposure to drunk customers. There were, however, types of alcohol-related selling practices highlighted in three policies to be potential threats to protecting children from harm requiring ‘a more acute need for age restrictions than normal’, namely ‘Happy Hours’ and drinks promotion nights.
Temporary event notices
The ‘light touch’ process to permitting a temporary event for the sale or supply of alcohol does not currently allow interested parties to make representations; only the police and environmental health can object and intervene. 83 Despite this, empowering communities to be aware of the processes available, the number of temporary event notices being permitted and their location, still has significance to the promotion of the licensing objectives, for example, primary schools serving alcohol as part of a temporary event to attract parents. 86 Four of the ten licensing policies explained the process involved to apply for a temporary event notice, with only one providing data on the average number issued each year.
Regard for health
With Directors of Public Health (DPA) appointed as a RA since 2013,114 all licensing policies recognised to some extent the role they can have contributing to licensing decisions. Some emphasised the powers and influence DPA could have promoting the existing four licensing objectives, irrespective of a 5th licensing objective to promote public health:
Local Health Bodies potentially have access to much data that can inform licensing decisions and policy. When such data is presented it will be considered and where links are made to any of the four licensing objectives.
Area 1
Without a 5th Public Health objective within the Licensing Act in England and Wales, two licensing policies stipulated an expectation that operating schedules would set out how they would actively promote health but without evidence-based examples:
[Name of] Council expects applicants for premises licences (and other permissions which allow the sale or supply of alcohol) to include statements in. their operating schedules as to how they will actively promote the protection and improvement of public health. Current holders of premises licences and other permissions which allow the sale or supply of alcohol are also expected to promote the protection and improvement of public health.
Area 9
One policy made more spurious suggestions that conditions could be imposed:
Although the Government did not go as far as introducing a 5th licensing objective of ‘promoting public health’, the introduction of public health as a responsible authority went some way towards starting to reduce alcohol-related health harms through use of licensing legislation. Conditions may be added by way of review of licence if there is a specific public health issue at a premise.
Area 3
Community recognition
Perhaps most pertinent to CICA’s logic model was the extent to which communities were recognised with the local licensing policy statement. This varied, with language used that at times presented as applicant focused rather than balanced with neutrality.
Our officers will always seek to assist applicants in completing applications and considering relevant conditions – particularly with a view to accommodating likely representations from residents and responsible bodies.
Area 7
A potential unintended consequence of language used could deter interested parties from having a voice if they identified as being in the minority:
The Authority acknowledges the advice of DCMS [Department for Digital, Culture, Media and Sport] that the views of local minorities should not be allowed to predominate over the general interests of the community.
Area 1
Promoting liaison and compromise between applicants and local residents was encouraged in 5 of the 10 policies. However, there was no detail or guidance on support available to community members within discussions or mediation meetings.
Information on how the public can get involved in licensing processes
Lastly, since the AHC training would provide lay volunteers with awareness of the processes and procedures available to the public to get involved in licensing decision-making, the document review examined whether the licensing policy itself contained community-centred guidance on how to do it (see Table 10).
| Area | Information aimed at public: submitting representations | Information aimed at public: reporting issues/complaints for compliance and enforcement |
|---|---|---|
| Area 1 | Yes | Yes |
| Area 2 | No | No |
| Area 3 | Partiallya | No |
| Area 4 | No | No |
| Area 6 | Yes | Yes |
| Area 7 | Yes | No |
| Area 8 | Yes | Yes |
| Area 9 | No | No |
| Area 10 | Yes | No |
In contrast to the excerpt highlighted in item 9, which offered support to applicants, none of the policies sought to assist community members in completing representations and considering relevant conditions. Where assistance was signposted, this was to local councillors (Area 1, Area 6, Area 8), and in this context, a local councillor could help if a member of the public has concerns about reprisal.
Preparatory roll-out meetings
All 10 local authorities participated in preparatory roll-out meetings. Analysis of roll-out meeting documentation revealed 12 categories of external contextual factors discussed by stakeholders a priori. These ranged from factors related to identifying a suitable individual or organisation to lead the intervention to the existence of wider political support (see Table 11).
| Keyword themes | Categories of external contextual factors |
|---|---|
| Confirm champions and invite | 1. Healthcare provider in place to co-ordinate the intervention |
| 2. Contract in place with a commissioned service | |
| 3. Staff stability with staff in post at outset | |
| 4. Existing pool of RSPH Level 1 health champions to recruit from | |
| 5. Pool of other volunteers to recruit from | |
| 6. Formality of volunteer arrangements | |
| Confirm RSPH centre status | 7. RSPH training centre status affiliated |
| RSPH qualification | 8. Local CICA co-ordinator registered trainer with RSPH |
| Confirm Public Health/other input | 9. Support from local DPA through the allocation of resources |
| 10. Evident support from elsewhere in the local authority, e.g. elected members | |
| Confirm licensing input | 11. Support from a licensing officer from the local licensing system |
| Licensing information: register of premises | 12. Public licensing register in place |
The number of external contextual factors documented a priori in each intervention area was counted to create an ‘infrastructure score’. From the 12 categories of external contextual factors identified, the maximum possible total baseline ‘CICA infrastructure’ score was 12. Actual scores ranged from 0 (in the area that did not roll out the intervention) to 10 (in three areas), showing the variability in infrastructure in place prior to roll-out (see Table 12).
| CICA area | Infrastructure score |
|---|---|
| Area 1 | 10 |
| Area 2 | 9 |
| Area 3 | 5 |
| Area 4 | 10 |
| Area 5 | 0 |
| Area 6 | 7 |
| Area 7 | 4 |
| Area 8 | 10 |
| Area 9 | 7 |
| Area 10 | 4 |
Initial implementation phase
This comprises analysis of AHC pre- and post-training questionnaires and interviews with AHCs and stakeholders.
In total, 123 participants trained to become AHCs in the nine areas that rolled out CICA: 77% (n = 95) identified as lay people living or working within the community, and 23% attended in their capacity as paid professionals (n = 28). A professional was defined as a person in paid employment with existing specialised knowledge of alcohol, substance misuse and/or public health practice who attended the training as part of their responsibilities for the CICA intervention area. The training clearly reached lay volunteers from within the community, as intended. The number of professionals trained was an indication of the need to build training capacity beyond just one local co-ordinator per area. Of the nine areas, seven completed the full 12-month intervention period, delivering at least one cascade training event.
Training registers
The data collection period for registers was 12 months per area, but due to the staggered roll-out of CICA, register dates spanned a total of 20 months (September 2017 and April 2019). Training register data is differentiated between Train-the-Trainer event attendance (first-generation AHCs) and cascade training attendance (second-generation AHCs). Five Train-the-Trainer events took place, delivered centrally by the RSPH, during which AHCs from each of nine participating areas were trained. Communities in Charge of Alcohol co-ordinators recruited 48 first-generation lay AHCs. A total of 28 professionals were trained to become AHCs at the same time, including local CICA co-ordinators themselves.
At cascade training, 11 events were delivered by the CICA co-ordinators in seven areas. The mean number of months between the initial Train-the-Trainer event and the first cascade training event was 6.9 months, with the shortest gap of only 2 months and the longest 12 months, highlighting wide variation in the number of months it took each area to deliver their first cascade training event and issues experienced gaining momentum. The timeline of cascade training events following the initial Train-the-Trainer event, along with total AHCs trained, is shown in Table 13.
| CICA area | Month number (number of months after initial training) | Total AHCs trained | Total lay people trained | |||
|---|---|---|---|---|---|---|
| Cascade 1 | Cascade 2 | Cascade 3 | Cascade 4 | |||
| Area 1 | Month 6 | – | – | – | 16 | 14 |
| Area 2 | Month 3 | – | – | – | 20 | 17 |
| Area 3 | Did not cascade – withdrew month 6 | 13 | 8 | |||
| Area 4 | Month 12 | – | – | – | 11 | 7 |
| Area 5 | Withdrew before roll-out | 0 | 0 | |||
| Area 6 | Month 10 | – | – | – | 9 | 8 |
| Area 7 | Did not cascade – withdrew month 9 | 7 | 5 | |||
| Area 8 | Month 2 | Month 4 | Month 9 | Month 10 | 22 | 17 |
| Area 9 | Month 7 | Month 10 | – | – | 15 | 13 |
| Area 10 | Month 8 | – | – | – | 10 | 6 |
While seven out of the nine areas held one cascade training event in the first 12 months, only two areas cascaded more than once (a total of 11 cascade events). A further 47 community members were recruited to become second-generation AHCs at cascade events, with a small number of (three) professional participants in attendance. In a sample of five of the seven areas, we carried out a structured observation of the cascade training (n = 5 fidelity forms completed).
Alcohol health champion questionnaire data
Response to alcohol health champion training
In total, 93 out of 95 lay AHCs completed pre- and post-training questionnaires representing nine areas (98% response rate). Nearly three-quarters of lay AHCs (74.2%) were aged between 31 and 60 years old (Table 14). More women were recruited to CICA compared to men (61.3% female), and the majority (69.9%) self-identified as being of white ethnicity. Educational attainment varied, with 9.7% reporting having no qualifications and nearly half (49.5%) having either General Certificate of Secondary Education (GCSE)/National Vocational Qualification (NVQ) Level 2 or A Level/NVQ Level 3 qualifications. In terms of modelling healthy behaviours, almost two-thirds (65.6%) did not drink alcohol at all or were classed as lower-risk drinkers according to AUDIT-C questionnaires. 51 Corroborating this, in pre-training questionnaires, 89.2% of the participants agreed/strongly agreed with the statement that they ‘try to live a healthy lifestyle by not drinking too much’.
| Characteristic | AHC participants | |
|---|---|---|
| n | % | |
| Sex | ||
| Male | 36 | 38.7 |
| Female | 57 | 61.3 |
| Age group | ||
| 18–21 | 2 | 2.2 |
| 22–30 | 12 | 12.9 |
| 31–40 | 16 | 17.2 |
| 41–50 | 29 | 31.2 |
| 51–60 | 24 | 25.8 |
| 61–65 | 3 | 3.2 |
| 65+ | 5 | 5.4 |
| No answer given | 2 | 2.2 |
| Ethnicity | ||
| White | 65 | 69.9 |
| Asian/Asian British | 3 | 3.2 |
| Black/African/Caribbean/Black British | 4 | 4.3 |
| No answer given | 21 | 22.6 |
| Highest qualification gained a | ||
| No formal qualification | 9 | 9.7 |
| NVQ L2, GCSE, O Level or equivalent | 25 | 26.9 |
| NVQ L3, A Level, AS Level or equivalent | 21 | 22.6 |
| NVQ Level 4–5, Certificate of Higher Education or equivalent | 3 | 3.2 |
| NVQ L6, undergraduate degree or equivalent | 17 | 18.3 |
| Other | 2 | 2.2 |
| No answer given | 16 | 17.2 |
| Risk level of alcohol use51 (AUDIT-C) | ||
| 1–4 lower risk drinking | 61 | 65.6 |
| 5–7 increasing risk drinking | 19 | 20.4 |
| 8–10 higher risk drinking | 11 | 11.8 |
| 11–12 possible dependent drinking | 1 | 1.1 |
| Missing data | 1 | 1.1 |
| Participants ‘try to live a healthy lifestyle by not drinking too much’ | ||
| Agree/strongly agree | 83 | 89.2 |
| Neither agree nor disagree | 5 | 5.4 |
| Disagree/strongly disagree | 4 | 4.3 |
| No answer given | 1 | 1.1 |
| Total | 93 | 100.0 |
In a free-text section of the pre-training questionnaire, space was provided for participants to describe their motivations for attending the CICA training. Content analysis was used to categorise units of text into a categorisation matrix and themes (see Figure 11). Three main themes of motivation were identified: lived experience (own harmful drinking or identifying as in recovery); help others (customers, care for my community, for my children); and for own development (personal or professional development, knowledge, skills).
FIGURE 11.
Motivations to attend CICA training.
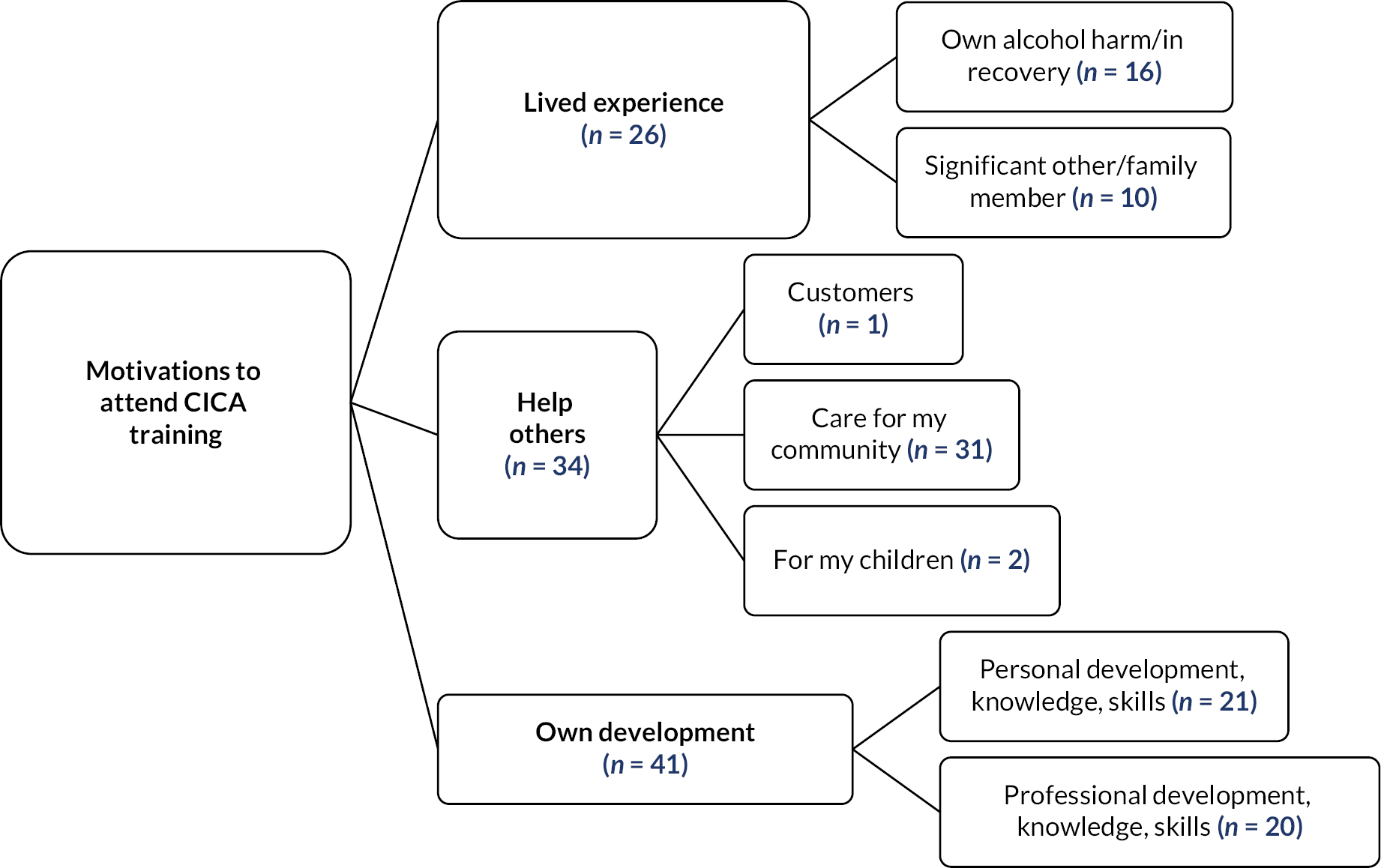
On the final day, at the end of training, post-training questionnaires were completed. These were analysed using the related samples sign test to ascertain any changes in attitude towards AHC role activity post training (Table 15). Nearly all AHCs agreed/strongly agreed that they felt more confident that they could talk about the harms associated with alcohol and give alcohol-related brief advice than they did pre training (91.4% compared with 79.6%) (p < 0.001). The number of AHCs who reported community engagement in local licensing decisions as important increased from 91.4% to 92.5% (p = 0.001). Furthermore, AHCs felt more confident post training that they could raise issues about venues selling alcohol (90.3%, compared with 74.2% pre training) (p < 0.001).
| Positive differences | Negative differences | Number of ties | N | Related samples sign test statistic | p-value | Pre training: agree/strongly agree with statement | Post training: agree/strongly agree with statement |
|---|---|---|---|---|---|---|---|
| Q1 I feel that it is important to promote healthy lifestyles and behaviours within my community | |||||||
| 11 | 7 | 71 | 89 | 11.0 (standardised test statistic 0.7) | 0.480 | 96.8% (n = 90) | 91.4% (n = 85) |
| Q2 I feel confident that I could talk about the harms associated with alcohol and give alcohol-related brief advice to people | |||||||
| 33 | 9 | 46 | 88 | 33.0 (standardised test statistic 3.5) | < 0.001a | 79.6% (n = 74) | 91.4% (n = 85) |
| Q3 I feel that it is important for communities to have a say in alcohol availability in their community and get involved in licensing decisions | |||||||
| 27 | 7 | 55 | 89 | 27.0 (standardised test statistic 3.3) | 0.001a | 91.4% (n = 85) | 92.5% (n = 86) |
| Q4 I feel confident that I could raise issues about venues selling alcohol | |||||||
| 43 | 9 | 37 | 89 | 43.0 (standardised test statistic 4.6) | < 0.001a | 74.2% (n = 69) | 90.3% (n = 84) |
Interviews with stakeholders
Eight themes (see Table 16) report the barriers and facilitators experienced by policy and practitioner stakeholders within the initial implementation phase of CICA. These reflect factors that impacted on the setting up of the AHC role (Themes 1–4) and external factors impacting on the wider implementation of the intervention (Themes 5–8).
| Theme number | Theme description |
|---|---|
| Factors impacting on setting up the AHC role in the community | |
| Theme 1 | Effective recruitment of AHCs |
| Theme 2 | Effective delivery of appropriate training |
| Theme 3 | Getting to grips with the AHC role |
| Theme 4 | Addressing communication challenges |
| Wider external factors impacting on implementation | |
| Theme 5 | Identifying useful assets |
| Theme 6 | Attitudes to community engagement in licensing |
| Theme 7 | Operational challenges |
| Theme 8 | Alignment with strategic, political and policy context |
Factors impacting on setting up the alcohol health champion role
Theme 1: effective recruitment of alcohol health champions
The requirement for volunteers to live or work within the specific geographical areas identified for the intervention (defined by LSOA boundaries) created challenges for recruitment. Many local co-ordinators described recruiting AHCs as ‘being really hard’ or ‘really difficult’. Many appear to have misunderstood the intervention principle1 that the aim of CICA was to build capacity in a specific community as part of a place-based approach. Instead, they referred to the constraints of taking part in the research study:
I think, one, because of the constraints of the areas for the pilot was a bit difficult.
Area H
A second barrier reported related to low levels of existing engagement pre intervention by the provider organisations in the CICA areas. One local co-ordinator described working with a local multiagency team ‘just to go onto the estate every week’ (Area F), while another described having to work through networks of individuals and organisations to access these communities:
speaking to people as much as possible to connect us with people who can connect with people in the communities.
Area G
In some areas, recruitment was facilitated by local co-ordinators investing time and energy by taking potential volunteers ‘for a brew’ (northern English slang for a cup of tea) or by becoming a known face in the community where recruitment would take place. Additionally, social attitudes towards alcohol programmes were reported as a barrier to recruitment:
no-one wants to talk about alcohol, nobody ever wants to talk about alcohol because everybody thinks oh just leave them alone, they’re only having fun, or blah blah blah.
Area D
Implementation was facilitated by enabling local co-ordinators to approach different types of people to become volunteers, including people who had experienced alcohol and substance misuse themselves and who understood the challenges:
some of our participants are recovering alcoholics, they’ve also been kind of, they’ve three or four years some of them had not touched a drop erm, so they know the challenges themselves …
Area A
While accessing potential volunteers through drug and alcohol services or through recovery housing services facilitated recruitment, two local co-ordinators described the challenges they faced working with volunteers drawn from these services. For some, this created additional pressure, anxiety and a sense of being out of their depth in the initial implementation of CICA:
some of them are still battling with their own addiction. They’re also still struggling with loneliness and getting a job and, the many things that happen, you know as a result of them going through a drug and alcohol service. It’s really, I’m finding it really hard. That’s not my, that’s not my job, it’s not my expertise either.
Area F
Two areas developed links with people who wanted to get back into employment:
we worked with the Department of Work and Pensions (DWP) for looking at people who wanted to get employment and who were interested in accessing courses and things like that.
Area G
Some areas recruited members of local public health teams or individuals who had prior experience of working in schools or for organisations such as the police, housing organisations or providers.
Social media, particularly Facebook, appeared to offer potential in facilitating recruitment. However, converting initial interest into actual engagement in training was experienced as far more challenging:
But then social media being social media, when you started chasing people up and going, yeah, that’d be great, if you give me an email address and I’ll get you some information,… it turned out that people seemed to be kind of going, yeah, I’m interested in that but when it actually came to the reality of it they were a little bit less keen.
Area E
Only one local co-ordinator raised early concerns about how to retain AHCs over the long term and embed AHC activity into local plans:
I don’t know, how do you keep them … I don’t know how the other teams are doing it, you know, the other areas are doing it, because if you’re just asking people to just to speak to you once a month, twice a month, it’s not gonna be, it’s gonna die off quite quickly I would say.
Area C
Retention of AHCs was reported as a potential barrier to successful implementation. When volunteers decided ‘it wasn’t for them’, this often resulted in local co-ordinators having to ‘start again’.
Theme 2: the effective delivery of appropriate training
In some areas, the provider was not RSPH accredited, or they did not have access to an accredited RSPH training centre. This was a prerequisite for the training to go ahead, in order for AHCs to receive a formal qualification. Four local co-ordinators reported being unexpectedly required to commit resources to enable accreditation. Where the RSPH accreditation centre was ‘all set up’, commissioners still needed to become familiar with the accreditation processes prior to training roll-out:
so, it’s been, it’s one of those processes, it’s like a getting, getting yourself familiar with it really.
Area E
The training itself was described as ‘intense’, ‘tiring’, ‘a bit of an overload’ and ‘a lot to do in a short space of time’ by stakeholders, but overall, they felt their AHCs responded well and benefitted from being ‘challenged and pushed’. Education and literacy levels were highlighted as potential barriers in three areas:
… there was some people … who, who hadn’t been in education for such a long time and for some of those to feel confident in taking on board the training, I think the training was, there was a lot.
Area A
The concept of cascade training was considered ‘quite daunting’, while some local co-ordinators were concerned that AHCs felt ‘comfortable’ prior to carrying out cascade training and needed ‘plenty of time to get them up to speed’. Another expected the AHCs to cascade the training, including the licensing component, on their own with light touch support:
I’m hoping the first lot of champions that were trained, initially, are going to be able to deliver that training, so I don’t necessarily have to be involved and I can dip in and out if they need me to. But it is about empowering the community, so, once you’ve empowered them, you don’t really want to carry on holding their hand if they don’t need it to be held. But, I’m happy to be there if they need me.
Area E
Other areas felt CICA would be facilitated more effectively if professionals, such as outreach and engagement workers, participated in the initial training to enable them to lead cascade training and support AHCs:
I thought, you know it’s gonna be really relevant to [name] to be on the training. She’s delivered training before so I thought [name] and maybe either [name] or [name] can support each other to deliver it.
Area J
The licensing input was considered a significant factor in developing AHC’s interest in CICA:
the part of it [that] was taking champions and volunteers seriously.
Area D
Those licensing leads interviewed were energised and enthusiastic about the opportunities for AHCs to make a difference from a licensing perspective. They described the AHCs as ‘really positive’, ‘enthusiastic’, ‘keen’ and ‘passionate’, showing significant interest in licensing. This was reflected by one licensing lead feeling:
like a rabbit caught in the headlights because there was a lot of questions.
Area A
Several licensing leads reported how focused the AHCs were in considering how to engage their communities in licensing issues, and one commented on the good, understanding participants showed regarding licensing and the Licensing Act:
Yes, the discussions, they weren’t just sat in silence, they were asking questions of me in my role, they were sharing experiences and how they might engage with their community members, as to rolling the project forward.
Area F
However, one licensing lead identified the training content as too dense, suggesting that more opportunities should be provided to increase relevance to AHCs by focusing discussion on the areas in which they live and making it easier for AHCs to deliver:
but to make it more relevant to the actual champions. Just to maybe relate it to something that they’re aware of. You know, a particular premises, or an experience that they’ve had.
Area E
Consequently, some local co-ordinators were keen to adapt and change the training content for training the future AHCs. This included considering removing some of the licensing elements of the training:
So, I wonder if we could, I don’t know, prune it a bit or change it a bit or just give them what they basically need.
Area E
Theme 3: getting to grips with the AHC role
One local co-ordinator (Area F) identified issues of ‘fit’ for the role and acknowledged that their ‘service user AHCs’ (i.e. those accessing alcohol treatment services) had little previous experience of volunteering. However, this view was not articulated by other local co-ordinators, with one describing their first cohort of AHCs as strong, confident people:
the first cohort of champions were really strong people. There were people from [organisation] and there were a couple of strong individuals from within the community as well, who felt confident.
Area E
Not knowing how or where to start with this new role was highlighted as a challenge for the local co-ordinator:
… the challenge we faced was just understanding to start with where it all fitted in, I think.
Area A
Local co-ordinators described some AHCs as being unclear about their role. Concern was also expressed that role boundaries were not always observed by volunteers from alcohol recovery services when engaging with the local community:
Try and work on things like boundaries, social skills, there’s a hell of a lot to cover because these people think that we are there to help them and sometimes they go back into talking about their experiences and that’s not what the community, you know the alcohol health champion’s role is.
Area F
Despite these challenges, local co-ordinators valued their AHCs and were committed to protecting, developing and encouraging them in their roles:
I want to get ‘em trained up, inducted, get them ID badges. They’ve now got t-shirts, got a full set of kit so I want them getting out there and getting ready for a bit of fun kind of thing.
Area C
Local co-ordinators identified CICA as a stepping stone for AHCs through gaining experience, an accreditation, access to the council’s job pages and confidence:
getting somebody that’s maybe doing nothing at the moment, to get them doing a little bit of voluntary work. They build up their confidence, they apply for a job, maybe working within a school, maybe doing something, you never know and before long, they’ve got a role and you know that, for us, that, that’s the win-win.
Area A
Theme 4: addressing communication challenges
Most local co-ordinators reported finding the right message to ‘sell’ CICA ‘quickly and succinctly’ as a significant barrier:
it was about just having an understanding so we could then sell the product to people, that was the biggest challenge really.
Area A
Local co-ordinators reported time spent discussing CICA with existing LA volunteers or potential volunteers who had indicated interest only to find that they had no connection to the LSOA and therefore did not meet the recruitment ‘criteria’. Local co-ordinators also perceived communication challenges in how volunteers should provide brief advice:
I think if we get too involved with having a conversation, sooner or later there’s either nervous laughter or there’s a sort of ‘oh no, just stop lecturing me, I have a hard job every week, I just want to enjoy myself at the weekend, just leave me alone’.
Area I
However, one local co-ordinator suggested that working with a provider service which offered free personalised support to help improve health and well-being, including conversations around smoking, mental well-being and healthy eating, facilitated brief advice conversations as they took place in the wider context of a person’s well-being:
… with the lifestyle-type service it’s well, we’re not talking about your alcohol today, we’re seeing how you feel about your family you know, or trying to get that motivation, finding the motivation.
Area D
It became evident that different areas had different perceptions regarding what CICA ‘success’ would look like. One local co-ordinator believed the number of licensing reviews initiated in the intervention area would be the main indicator of whether the intervention worked:
specifically from a licensing service point of view if we’re not getting any erm, reviews in from members of the public having been engaged with by an alcohol champion, then from that perspective I think then perhaps from … it’s not been really beneficial on that part, but if we do then erm, obviously it shows that it’s working.
Area A
In contrast, a licensing lead for a different LA felt that initiating reviews was not a key outcome. Rather, the training should lead to more emphasis on community-led mediation, thereby preventing increases in the workload of the local Licensing Committee (Area E).
Wider external factors impacting on implementation (stakeholder analysis)
Theme 5: identifying useful assets
Local co-ordinators described contextual variables, including the availability (or otherwise) of local assets and services (i.e. existing hubs, cafés, networks), as having the potential to affect grassroots mobilisation of volunteers. Free local physical assets were reported as essential, including a central area where people could meet at no cost (community centre, health centre or community café):
[Location] that’s got a community building, and it’s actually originally a pavilion for the bowling greens, but we have access to that at, and no cost to use it for us.
Area B
In areas where multiagency teams (housing, ASB teams, the police, community link workers, employment and welfare services and voluntary sector organisations) worked together, AHCs benefitted by being given practical advice on providing brief advice to community members by these professionals:
The multi-agency team, while they’re litter-picking with the champions say, ‘this is how you do it, this is how you have conversations’ because they don’t have those skills, the champions at the moment to be able to link litter-picking, picking up cans of lager with having a conversation around health or alcohol.
Area F
The presence of established drop-in centres in the locality was seen to facilitate multiagency and place-based working, enabling new networks and relationships. One local co-ordinator described it as a ‘kind of fertile ground’ within which the ABCD model sat well.
However, the range of activities multiagency teams were asked to engage with was reported as making their roles extensive, with concern being highlighted by one local co-ordinator that they were being asked to do too much, and this limited their ability to provide further support to AHCs:
I think money is so tight that multi-agency teams are getting pushed by everybody to add on a bit of this and a bit more, do you know what I mean?
Area F
Some local co-ordinators reported poor formal assets, including a ‘seedy back room’ or no central hub or coherent networks, creating barriers to initial implementation.
Besides the physical (more formal) assets, ‘informal assets’ such as the volunteers themselves, and community activists were considered key facilitators:
it’s [local area] got a number of assets, the [name] centre, which is a former sort of housing office, and obviously [person’s name] is a brilliant community asset so she gets things going in that area.
Area E
Furthermore, if local co-ordinators were known – ‘it’s my patch’ – in the chosen CICA intervention area, this was seen to be facilitative:
I can make use of my contacts and because of my autonomous role out in the community I’m making many more.
Area D
Theme 6: operational challenges
At implementation, some commissioners were unable to commission an appropriate provider organisation to deliver the intervention due to lack of available candidate services. Either relevant ‘service level agreements’ (the contract between the local authority and the service provider) had terminated and new service providers were being commissioned – impacting on roll-out – or there had been no scope to ‘add’ CICA to existing contracts:
we’ve only got the drug and alcohol team who will be helping me to run this and they have recently been decommissioned and a new commissioner, a new provider is starting in April [3 months after initial training].
Area F
Concerns about having the capacity to deliver the essential elements of CICA were frequently emphasised. Area 5 identified a lack of capacity to manage AHC volunteers as curtailing their involvement in CICA:
so even if we could recruit volunteers initially, we certainly couldn’t manage the volunteers, because there’s no post within our organisation as part of the new tender arrangements. So actually, even if you got 10 volunteers, we still couldn’t manage them, we’d have to get someone else to manage them.
Area I
One licensing lead was apprehensive that increasing the knowledge of community members might result in generating more administrative work, leading to Licensing Committee hearings, for which the department would not receive additional funding to manage.
Two stakeholders raised issues about funding for training, specifically in relation to implementing the cascade training, for which no prior funding had been made available:
from promotion, to making leaflets, to delivery and so and forth.
Area G
Similarly, a licensing lead indicated funding constraints would affect implementation despite the view that empowering the community to support preventative approaches was more appropriate than relying on enforcement or requiring the support of drug and alcohol services:
… a further option is to get more areas rolled out, across Greater Manchester. I think that would be absolutely fantastic. But, as I say, we’ll have to see. [LA name] has its own difficulties with funding and I’m pretty sure it wouldn’t automatically happen here, in the scale it possibly needs.
Area F
Despite meetings taking place prior to training roll-out, some local co-ordinators remained confused about CICA until participating in the training (i.e. post recruitment of potential AHCs):
Some of us would come away and actually still email each other and say ‘I don’t really know what we’re doing yet’ and I think for me yeah, I think for me it was only when we did the training I actually started getting a feel of everything.
Area A
Similarly, licensing leads described being unclear about their personal roles and responsibilities, feeling that they ‘came to it cold’ (Area B).
Theme 7: attitudes to community engagement in licensing
Licensing leads acknowledged that at a neighbourhood level there existed a low base of involvement in licensing decision-making, despite expectations from licensing authorities that community members take a proactive investigatory stance to licensing issues. One licensing lead cited the non-reporting of issues which flouted licensing laws, including underage drinking on licensed premises, as evidence:
I am sure that people within the community would have known that that was probably going on but erm, nothing was reported to me in that regard, so we’re starting from zero information from the community.
Area D
A reduction in funding to local authorities was acknowledged as contributing to reduced opportunities for community engagement around licensing:
Things had happened in the past but it kind of all got stopped and lost when there was a lot of, when all the austerity measures were stepping in around 2015.
Area H
For one local co-ordinator, low levels of community engagement were attributed to a ‘fear of reprisals’, as any official representation to the licensing authorities becomes ‘public’:
… and sometimes I have had conversations with members of the public ‘but I don’t want my name going in the public domain’.
Area A
Encouragingly, licensing leads welcomed CICA as an approach that could improve the rate and type of intelligence received by the licensing team:
… best information you can get is from community because they do know what’s going on, on the ground.
Area D
They reflected that building and enhancing new or existing relationships which could support licensing objectives was a positive aim for CICA:
the idea of having local people with knowledge around the licensing system which typically they don’t have as lay people. And then knowing how to effectively engage in the process, yeah, I think there are definitely benefits for that.
Area H
Local co-ordinators and licensing leads commented on the gains that had been made in developing new relationships through the training and the potential for public health improvements through more partnership-based working in the future.
Theme 8: alignment with strategic, political and policy context
Finally, stakeholders reported that implementation as being affected by the extent to which CICA aligned with local alcohol harm strategies and the political and policy contexts of their local areas. Some stakeholders reported variable levels of support from their democratically elected local representative (local councillor), which impacted on perceptions of wider support for a place-based, community-led approach:
I was kind of hoping I’d have a bit more support from the councillor.
Area C
In contrast, some highlighted the significant role of LA DPHs in supporting CICA:
… We’ve got [name of DPH]’s full sort of weight behind not only the alcohol health champions but also the health champion network in general.
Area E
Some local co-ordinators reported issues with commissioning arrangements and others with key role vacancies at the time of implementation (e.g. no full-time commissioning lead), which created barriers in gaining ‘buy-in’:
The problems you’ve got when you’re not commissioned … is, I have to try and get buy-in from that multi-agency team and it’s difficult, one thing I don’t have any influence … it’s different to, to areas where a commissioner is directly commissioning a provider service; and, which a community health promotion like this is embedded into what they do.
Area F
Interviews with lay alcohol health champions
Interviews were carried out with newly trained lay AHCs within the first few months post training. Table 17 details characteristics of interview participants, including the type of service provider leading the co-ordination of CICA in their area. Motivations to take part in CICA ranged from own personal harmful alcohol use (self-identified as ‘in recovery’), family experience of alcohol harm, to a wish to learn more (personal development) and help others in the community.
| Area/participant | Characteristics at time of interview |
|---|---|
| Area 6 | CICA intervention co-ordinated by the drug and alcohol service. One initial training session conducted, and no cascade training rolled out yet between the start of the intervention (September 2017) and the interview (July 2018). CICA training/knowledge/skills beginning to be implemented at wider community support events (e.g. coffee mornings). |
| Peter, Area 6 |
|
| Darren, Area 6 |
|
| Area 8 | CICA intervention co-ordinated by health and well-being services. One initial training session and two cascade training sessions had rolled out since the start of the intervention (September 2017) and the interview (July 2018). CICA training/knowledge/skills started to be implemented at community events (e.g. summer community festival). |
| Amy, Area 8 |
|
| Area 9 | CICA intervention co-ordinated by health and well-being service. One initial training session and two cascade training sessions had rolled out since the start of the intervention (September 2017) and the interview (July 2018). CICA training/knowledge/skills beginning to be implemented at wider health promotion community events. |
| Kathryn, Area 9 |
|
| Grace, Area 9 |
|
Figure 12 shows in a thematic map the overarching themes identified from interviews: (1) perceptions of AHC training; (2) applying knowledge and skills in the AHC role; (3) barriers and facilitators to undertaking the AHC role; and (4) sustaining the AHC role, including thoughts on cascading the training to others.
FIGURE 12.
Thematic map: making sense of the AHC role.
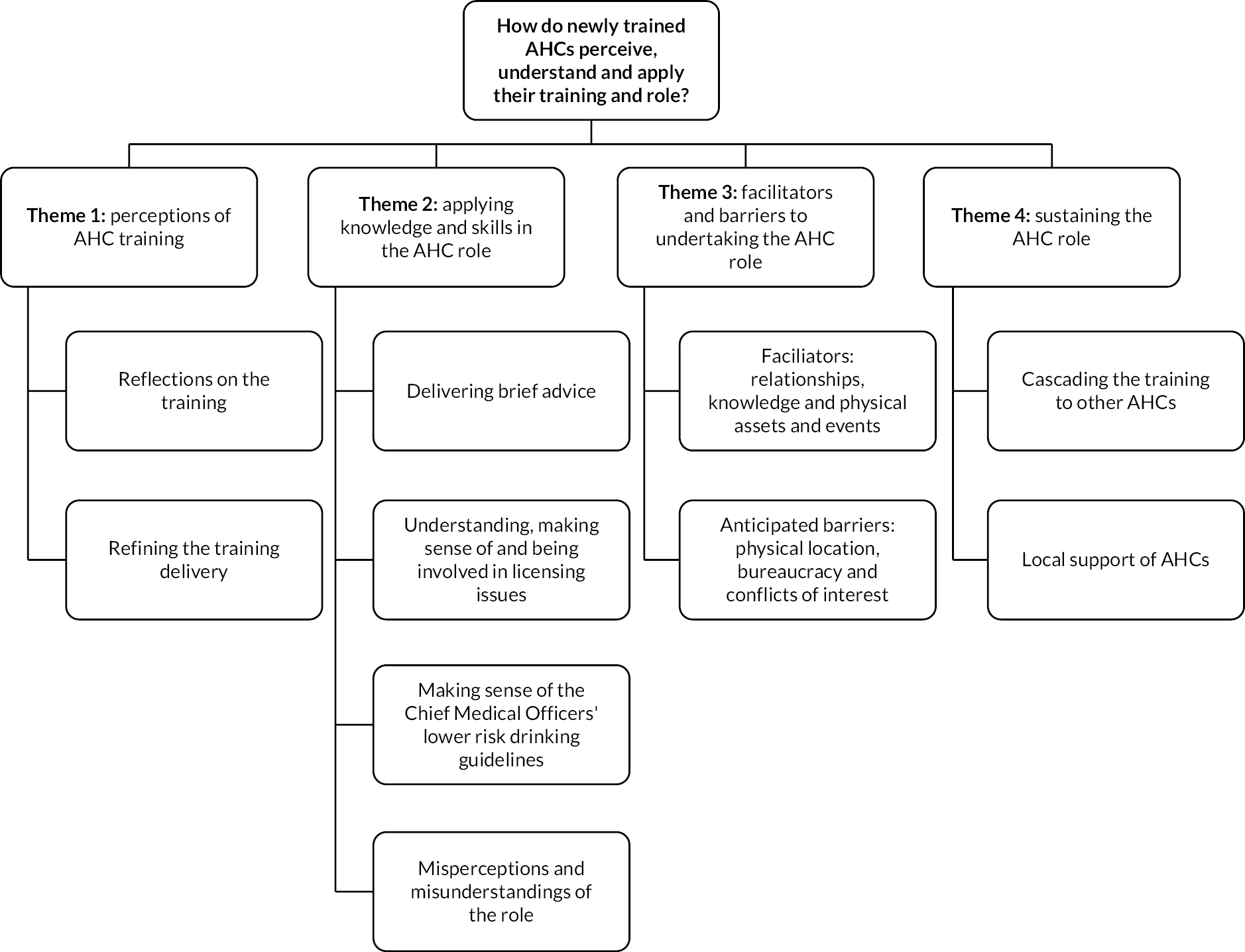
Theme 1: perceptions of alcohol health champion training
Reflections on the training and refining training delivery
Participants expressed pleasure from the training and gaining new knowledge, reporting that they ‘enjoyed it’ and ‘learned quite a lot’ and that it was a positive experience knowing that they ‘can help people’. However, the training content was considered by some AHCs as a lot to fit into a short space of time. Changes in both the language and structure of the training were suggested as something that would be beneficial:
That was difficult for me that day … and [the trainer] was rushed … I would stagger it and I would change some of the language away from what was delivered … I mean it’s not like a job where you’ve got the time to do the induction and ask a colleague and get to know the language.
Peter, Area 6
… I thought it was a bit too much in a short period of time. If we could sort of spread it, then maybe … we had a lot of handouts.
Grace, Area 9
The intensity of the course may not have left enough time for AHCs to explore and evaluate information or to check that all participants had properly understood. There were occasions where misperceptions arose. This included Kathryn, when recounting her experience of an off-licence shop selling alcohol to her intoxicated relative:
… That rule I think should be put on shops as much as pubs so that a law should be made that if they come in in an absolute state [drunk] you should not be allowed to sell them that alcohol … but they can’t if the law isn’t there.
Kathryn, Area 9
However, the Licensing Act 2003 prevents the sale of alcohol to a person who is drunk in both on- and off-licensed premises, which had been explained within the training.
Theme 2: applying knowledge and skills in the alcohol health champion role
Delivering brief advice
Each of the participants spoke about their experiences of giving brief advice about alcohol and signposting to other appropriate services if more specialist support was needed. Alcohol health champions delivered information in various ways, for example, in everyday conversation or as part of wider health and well-being advice. All had used brief advice tools, including an AUDIT-C scratchcard or an ‘alcohol wheel’ (to demonstrate the number of alcohol units and calories in each drink). Some AHCs reflected on the importance of offering non-judgemental advice and approaching the subject gently, giving the conversation a ‘natural flow’ because they did not want to make people ‘feel uncomfortable’. Brief advice on swapping and reducing alcoholic drinks was friendly rather than authoritarian:
… I don’t kind of preach it to them … I would alternate an alcohol drink with a soft drink to try and reduce the amount of units that they’re taking in.
Darren, Area 6
Understanding, making sense of and being involved in licensing issues within the alcohol health champion role
The AHCs demonstrated some positive knowledge of the Licensing Act 2003 following their training. Most were aware of the requirements for responsible retailing regarding drink promotions and checking the age and level of intoxication of individuals purchasing alcohol in accordance with the legislation. Peter, for example, noted that a supermarket in his local community had prominent displays of alcohol at the entrance, which, although not strictly regarded as irresponsible retailing in the Act, was considered by him as drawing attention to the alcohol:
… the first thing you get as you walk through the doors is there’s literally a stand out in the front of the door and the first thing they’ve got on there was alcohol.
Peter, Area 6
However, a different supermarket was reported as showing responsibility by being strict on underage alcohol sales and not selling alcohol to those perceived as intoxicated:
… the girls asked for identification [from underage customer] … the girl who was service on the till refused to serve one gent ‘cos she actually said ‘in my opinion you’ve had enough to drink already’ … it just shows that some stores are taking a stance.
Peter, Area 6
While some AHCs reported a preference for direct action, for instance, by approaching managers of licensed premises, others preferred educating other community members on how to tackle licensing problems. The AHCs highlighted how the training had increased their awareness of the powers available to communities and the need to work collaboratively to address licensing issues:
… if it’s in a residential area, if it’s close to housing, I would say ‘have you spoke to your neighbours?’ … and if you get together as a group and then approach as a group, and I would also say to them don’t feel that you can’t actually get your local council involvedDarren, Area 6
… And it’s knowing that I can talk if somebody came to me complaining or even just an informal discussion with them about their experience with their neighbourhoods then I could encourage them or empower them to go and challenge whatever’s happening.
Grace, Area 9
Making sense of the UK Chief Medical Officers’ lower risk drinking guidelines
Alcohol health champions demonstrated a nuanced understanding of the UK low risk drinking guidance115 (up to 14 units of alcohol per week; 1 unit = 10 ml or 8 g of alcohol). AHCs felt that they are ‘just a recommendation’ and ‘a guide’ and that within those guidelines, people should still be careful. The AHCs showed understanding that people’s responses to alcohol consumption varied, which they shared when giving brief advice, as expressed by Darren:
… it’s a guide ‘cos what you will find, you can have two people of the same body mass, and one person will get drunker quicker than the other person … you just need to be aware that not everybody’s body is the same …
Darren, Area 6
Amy felt that advice needed to be individualised, and even people who were drinking less than the recommended upper limit of the guidelines might still value guidance on reducing alcohol intake:
… I’d still encourage them to cut it down … I’d just go more along the line of well do you think that’s too much? What do you want to be drinking a week? Yeah I think they’re [the guidelines] good just for people to get an idea of where it is that could affect your health massively.
Amy, Area 8
Misperceptions and misunderstandings about the role
The intended role of an AHC was to reduce alcohol-related harm by intervening early through either individual or community action. Informal conversations using the principles of alcohol IBA were aimed primarily at reaching those drinking at hazardous levels to prevent harmful, higher-risk drinking. However, some AHCs viewed CICA as largely directed at those already drinking harmfully, who may possibly be alcohol dependent:
I think [different area] would be better to hit on. In [place] … I’ve seen a lot more alcoholics up there than anything that touches a little bit of this place.
Kathryn, Area 9
The principle of CICA was to have informal conversations where appropriate, with a focus on the quality of the conversations with people who may not otherwise have accessed alcohol advice. There were no pre-set targets for numbers of conversations to be carried out by AHCs. However, some participants were concerned about not having enough conversations with community members about alcohol:
Everyone feels like they’re bring … they’re not getting enough numbers.
Peter, Area 6
This misunderstanding may have meant that AHCs did not consider a conversation as ‘counting’ unless they used tools such as AUDIT-C.
Theme 3: facilitators and barriers to undertaking the alcohol health champion role
Facilitators: relationships, knowledge, physical assets and events
Facilitators to the role were identified as positive relationships between the AHCs enabling them to support one another in their roles, personal attributes and knowledge already possessed by AHCs and key community members and the availability of local physical assets such as libraries and community centres that could be utilised for having conversations. For example, Darren already had an established volunteer role in his local library (a key physical asset), co-ordinating a weekly coffee morning. This gave him the opportunity to network with key, community-based individuals (such as the library manager) and put the CICA training skills into practice, where appropriate, at the coffee mornings with local community members. This started almost immediately after attending the initial training:
… I run an informal coffee morning where there’s basically no boundaries to what we can talk about … and the new manager who’s coming in, she’s all about the library being used as a community hub.
Darren, Area 6
Other existing and established community events were facilitators of the AHC role. Summer carnivals and attendance at health and well-being events, such as wider health promotion events (e.g. incorporating blood pressure tests), enabled AHCs to deliver alcohol advice as part of a larger volunteer team. At these community events, AHCs saw advantages of having a presence alongside drug and alcohol service providers. The informal nature provided a degree of anonymity for those seeking advice without the commitment to seeking out formal alcohol services:
… at the carnival and the stalls … I think it’s so light-hearted … and they are just willing to chat … a couple went to the back of the stall and actually spoke to [local co-ordinator] about serious things that they’re facing … that’s like just off the carnival.
Amy, Area 8
Grace described how AHCs in Area 9 worked alongside other volunteers and healthcare providers as part of wider health promotion events outside the scope of CICA, using the opportunity to offer brief advice about alcohol use:
As an alcohol health champion, I have taken people’s blood pressure and advised them on how they can cut down on their drinking … signposted them to their GPs … yeah, I did that as part of a community.
Grace, Area 9
Life experiences of AHCs were reported as key to the role, and these included being an active member of a community and being a community-minded individual:
Over the years I’ve just blended in with the community and done things … it’s about connecting on a community level.
Peter, Area 6
Barriers: physical location, bureaucracy and conflicts of interest
In this early phase of the intervention, AHCs had not experienced many barriers in offering brief advice, although they were aware of potential barriers. One example was in setting up a drop-in service, which was felt to ‘restrict people’ who were concerned they might be seen attending a particular location, such as a specific café, that they would not normally attend. There were also concerns that members of the wider community might be ‘a bit aggressive’ towards AHCs, although these were hypothetical concerns at this stage of their role.
Negotiating licensing processes was viewed as a potential barrier, ‘full of bureaucracies’. However, when faced with this, Peter felt that it was ‘easier to go in’ to the licensed premises to discuss issues directly than go through the paperwork of putting in an official representation (commenting/complaining in writing to the licensing authority), thus working around the barrier showing a positive example of AHC action. Peter applied his new knowledge of alcohol licensing legislation (Licensing Act 2003) to talk to an initially defensive manager of a pub (public house; licensed to sell/supply alcohol ‘on the premises’), who felt that issues of litter, empty glasses and noise around his premises were ‘not a licensing issue’. To maintain a positive relationship with the local community, Peter reminded the manager of his responsibility to the neighbourhood, and this had the positive outcome of reducing some of the ASB around the premises:
Clear the glasses, tell them if they want a drink go inside but don’t have them sitting out at two and three in the morning chatting away because you’re making money … He said yeah but when I shut the door they’re outside they can do what they want. Well then you need to know, if they’re your clients at the pub, that there’s kids across the road that need sleeping … That’s how it went … ’cos he was being all defensive like, it’s outside the pub, it’s not a licensing thing … and we’re neighbours.
Peter, Area 6
An example of a more definite barrier was identified by Amy, who had a potential conflict of interest regarding taking licensing action due to working part time in a pub. Amy felt ambivalent about raising concerns about a pub setting:
Yeah, I’m not a complainer really. That’s just me … I probably wouldn’t do it for a pub, but I might do it for a shop. ‘Cos I think pubs have to earn a living and I don’t know. I think if you’re going into a pub, you know you want a drink. If you’re going into a shop, I don’t know …
Amy, Area 8
Perhaps more pervading was a potential sociocultural barrier to making complaints within a community: ‘We don’t grass each other up’.
Theme 4: sustaining the alcohol health champion role
Cascading the training to others
At the time of the interviews, four AHCs were looking forward to cascading the training to new AHCs, and one had already been involved in a cascade training session. They suggested ways in which the original training could be developed. There was a feeling that the training needed ‘to be slower’, perhaps held over more days, and the content needed simplifying to ‘change the language’. They felt that they required a refresh of the information and some time to ‘carry out some more research about it’ before they cascaded to others. On the whole, with some of those changes in place, AHCs were confident in and positive about planning the cascade training, not just in their own communities but also beyond the study intervention area:
Well hopefully, like I’ve said to [local co-ordinator], we can then, once we’ve done a bit of training, we can maybe see about extending it to other areas … we can widen the net out.
Darren, Area 6
However, there was a feeling that their role in cascade training in the future should be in assisting rather than leading the training sessions, which they felt less confident about:
I loved it, it was brill … when somebody is on their own … at least you can partner up with them and they don’t feel on their own, having to struggle … I would love to keep helping … but I don’t fancy doing it on my own … If I had to teach one person I could do it. If I had to teach a whole class, no.
Katherine, Area 9
The CICA training programme was accredited by the RSPH, and this was generally seen as positive when recruiting new AHCs because it cemented its importance and identified it as ‘a properly structured piece of training’ that gave the programme a level of approval. Some felt that the RSPH accreditation and qualification were ‘important’ but that there should be some other incentive offered alongside that ‘might be more meaningful’ to new trainees:
… tie it in with something that they need … you can get points and credit towards some education … a bus pass or something … a recognition.
Peter, Area 6
However, the use of accredited training also led to delays because, in some areas, the training centres first needed to be accredited by RSPH. This was frustrating to some AHCs and contributed to difficulties in keeping momentum and retaining new recruits:
We’ve got a number of people interested … in doing the course … it’s this delay of getting the accreditation to do it, it’s the longer it’s going on it might, they might just think ‘oh you mentioned this 2 months ago’ … it’s when you keep putting it off, that’s when you wonder whether or not they’ll just think ‘oh I can’t be bothered now’.
Darren, Area 6
Local support of alcohol health champions
Notwithstanding the types of activities AHCs explored in their role, there was a clear reliance on the local CICA co-ordinator. For some, having a lead professional located within a local health and well-being service appeared to offer a sense of validity:
It’s not as though we’re trying to do it as a community thing without any backing, we’re actually doing it with the backing behind us
Darren, Area 6
For others, the personal attributes of their local co-ordinator made a significant impact on their own sense of self-efficacy and that without the co-ordinator’s encouragement, they would not have stayed involved.
Knowing that the local CICA co-ordinator was available further supported the AHCs’ confidence in the role. This seemed to be particularly helpful in enabling AHCs to manage their role boundaries effectively during brief advice conversations. If the level of information disclosed needed further signposting and support, having quick access to their co-ordinator by e-mail or phone provided reassurance that the AHC was not alone.
Intervention phase
Monitoring of activity
Self-reported data on the provision of brief advice were collected through local co-ordinators and reflective diaries kept by AHCs. Five out of nine CICA co-ordinators kept a tally of AHC activity during the 12-month intervention period as follows:
-
1148 conversations counted
-
251 AUDIT-Cs completed
-
65 community events attended.
The largest tally of conversations was counted and recorded by the co-ordinator in Area 1 (n = 499, 14 lay volunteers), followed by Area 9 (n = 306, 13 lay volunteers), Area 6 (n = 168, 8 lay volunteers) and Area 8 (n = 167, 17 lay volunteers). Community events attended by AHCs mirrored a similar pattern, with Area 1 most active (n = 30), followed by Area 9 (n = 23). The CICA co-ordinator in Area 1 additionally kept a time/cost diary of recorded AHC activity which indicated that AHCs spent on average 11 minutes having an informal, brief advice conversation. Further data from reflective diaries (see Table 18) showed a variety of activities and actions that had taken place (elaborated in textual comments in Appendix 4).
| Area | Number of diary entries | Spoke to someone about alcohol for the first time | Number of community events attended | Licensing issues/activity recorded |
|---|---|---|---|---|
| Online diaries | ||||
| Area 8 | 39 | 35 | 5 | 0 |
| Area 9 | 1 | 4 | 0 | 0 |
| Area 10 | 2 | 9 | 2 | 0 |
| Paper diaries | ||||
| Area 1 | 30 | 117 | 34 | 0 |
| Area 2 | 7 | 14 | 0 | 0 |
| Area 4 | 4 | 97 | 10 | 1 (no detail) |
| Area 9 | 8 | 13 | 5 | 3 |
| Group diaries | ||||
| Area 6 | 8 | 163 | 5 | 3 |
| Area 8 | 12 | 91 | 3 | 0 |
| Area 9 | 1 | 90 | 5 | 1 |
| Totals | 112 | 633 | 69 | 8 |
Four case studies highlight different ways in which AHCs were empowered to take forward other types of licensing action. The first case study demonstrated new community connections made between AHCs and the neighbourhood policing team, whereby they jointly hosted an information stall in the local library to promote reporting of licensing issues directly to the police. The second case study involved brief advice being offered to the owner of a local off-licence who disclosed concerns about their alcohol use. This led to AUDIT-C scratchcards being made available to customers to take away to raise awareness of alcohol units at point-of-sale. In terms of informal licensing action, the third case study involved an AHC noticing antisocial, noisy behaviour outside a local pub. Their knowledge of the Licensing Act 2003 and the licensing objectives gave them confidence to have an informal conversation with the manager, giving the manager the opportunity to improve the operating practices. The final case study demonstrated formal licensing action being taken against an off-licence that had their premises licence suspended. The AHC and local co-ordinator contacted their local licensing officer to report illegal sales, enabling enforcement action to take place. The premises was located outside of the boundary of their CICA area and demonstrated the potential for licensing action as interested parties to reduce harm in the wider neighbourhood.
To monitor the fidelity of cascade training to the Train-the-Trainer model provided by the RSPH and any local tailoring of the training, five observations were recorded by the research team. The five areas observed were: Area 2, Area 6, Area 8, Area 9 and Area 10. Local CICA co-ordinators facilitated the training and were all registered RSPH trainers.
During the cascade training, we observed some tailoring of the original protocol and materials. Firstly, the number of presentation slides was reduced. This was in response to initial feedback highlighting the Train-the-Trainer content had felt too intense. The pacing of the training also differed at cascade events. For example, RSPH workbooks were completed on day one in four areas as per the Train-the-Trainer model, but one area staggered the training delivery and completion of the workbook over 2 days. Overall, the standardised requirements of the RSPH Level 2 ‘Understanding Alcohol Misuse’ qualification workbook directed the cascade training, and this promoted fidelity in delivery.
All observations explained behaviour change using the Transtheoretical Model,116 defining stages of change and Prochaska and DiClemente’s principles of stage-matched interventions. No tailoring was made to introduce more recent behaviour change models such as the COM-B (Capability, Opportunity, Motivation) system. 117 However, some variation was noted in the extent to which cascade training provided more attention to skill development. For example, Area 10 providing a bespoke section on ‘How to start a conversation’ as they had felt such a skill was fundamental to the AHC brief advice role, and Area 8 allocated more time to practise role-playing brief advice conversations in comparison to the Train-the-Trainer event.
The other main area of variation noted was in the delivery of the licensing action training on day 2. The coverage of what counts as evidence and exploring ‘good’ and ‘bad’ examples of representations, as per the original model, was omitted in all five cascade events observed. In the original model, the local licensing officer was invited to cofacilitate the licensing action training section; this occurred in only three out of five areas. In the other two areas, the local co-ordinator delivered the licensing section of the training alone. Since the licensing training was not within the scope of RSPH Level 2 qualification, there was no workbook assessment to prioritise or standardise delivery.
Follow-up phase
Associations between external contextual factors and total alcohol health champions trained
At follow-up, we assessed whether the baseline infrastructure score calculated in the pre-implementation phase was related to the number of alcohol champions trained over the 12-month intervention (see Table 19). At follow-up interview, CICA co-ordinators from 7 out of 10 areas reviewed these initial findings. Six interviews took place during the 12-month follow-up period and one after 9 months when the area withdrew from the project earlier than planned. In six areas, no amendments were made, and in one area, one item was amended following further clarification.
| CICA area | Infrastructure scorea | Total AHCs trained | Total lay people traineda |
|---|---|---|---|
| Area 1 | 10 | 16 | 14 |
| Area 2 | 9 | 20 | 17 |
| Area 3 | 5 | 13 | 8 |
| Area 4 | 10 | 11 | 7 |
| Area 5 | 0 | 0 | 0 |
| Area 6 | 7 | 9 | 8 |
| Area 7 | 4 | 7 | 5 |
| Area 8 | 10 | 22 | 17 |
| Area 9 | 7 | 15 | 13 |
| Area 10 | 4 | 10 | 6 |
The number of lay people trained varied from 0 in Area 5 to 17 in Areas 2 and 8. Although Area 5 had participated in the preparation meetings in the pre-implementation phase, they did not roll out due to the lack of infrastructure in place. A positive correlation (using non-parametric Spearman’s rank correlation coefficient) was found between an area’s total infrastructure score and the total number of lay AHCs trained in the first year (see Table 19, rs = 0.77, p = 0.01).
The numbers of lay AHCs trained in areas with a specific contextual factor were compared to areas without the factor using Mann–Whitney U-tests (see Table 20). From this, four external contextual factors were found to have higher numbers of lay people trained. Those having a healthcare provider in place at the outset to co-ordinate the intervention (p = 0.02); a contract in place with a commissioned service (p = 0.02); a pool of other volunteers to recruit from (p = 0.02); and formal volunteer arrangements (p = 0.03) trained more AHCs.
| External contextual factor content category | Number of areas with characteristic | Mann–Whitney U-test statistic |
Significance |
|---|---|---|---|
| Healthcare providers in place to co-ordinate the intervention | 7 | 21 | 0.02 |
| Contract in place with a commissioned service | 6 | 22.5 | 0.02 |
| Staff stability with staff in post at the outset | 9 | 9 | 0.20 |
| Pool of other volunteers to recruit from | 7 | 21 | 0.02 |
| Existing pool of RSPH Level 1 health champions to recruit from | 0 | – | |
| Formality of volunteer arrangements | 5 | 23 | 0.03 |
| RSPH training centre status affiliated | 5 | 19 | 0.22 |
| Local CICA co-ordinator registered trainer with RSPH | 3 | 17 | 0.18 |
| Support from local DPA through the allocation of resources | 9 | 9 | 0.20 |
| Evident support from elsewhere in the local authority | 3 | 17 | 0.18 |
| Support from a licensing officer from the local alcohol licensing system | 8 | 8.5 | 1.00 |
| Public licensing register in place at the outset | 4 | 13.5 | 0.76 |
Follow-up interviews with stakeholders
Key stakeholders considered factors that influenced the operationalisation and sustainability of CICA, and five themes were initially identified: (1) limited alignment with strategic, political and policy context; (2) navigating intervention assumptions; (3) ability to leverage partnerships; (4) developing new community assets; and (5) practices to facilitate the sustainability of CICA. The strategic context and leveraging partnerships focus on localised issues and will not be explored here. Rather, in these findings, three themes will be explored which are of most interest to a wider audience. Table 21 presents an overview of the themes/subthemes to be discussed.
| Theme | Subthemes |
|---|---|
| 1. Navigating intervention assumptions | 1.1 Widespread community inertia to tackling alcohol harm 1.2 Active role of first-generation AHCs in capacity building 1.3 Retention, not attrition |
| 2. Developing new community assets | 2.1 Capacity, capability and confidence of AHCs and local co-ordinators 2.2 ‘Hand-holding’ AHCs 2.3 Giving brief advice |
| 3. Identifying practices to facilitate the sustainability of CICA | 3.1 Identifying the right ‘place’ and timeline to successfully build community capability 3.2 ‘No Key Performance Indicators – why bother?’ 3.3 Broadening AHCs’ skills and engagement |
Theme 1: navigating intervention assumptions
This theme focuses on the extent to which assumptions underpinning the interventions facilitated the operationalisation of CICA and co-ordinators’ responses to barriers experienced.
Widespread community inertia to tackling alcohol harm
Underpinning CICA was a perception that utilising community advocacy to reduce alcohol harm and the availability of alcohol represented an ‘untapped resource’. 1 However, the extent of community inertia to take action on alcohol harm impacted operationalisation and sustainability. For instance, AHCs and the local co-ordinator in Area 7 found residents reluctant to engage in conversations about alcohol:
I think what we picked up from our regular meetings was, if it’s around healthy eating, you had more engagement and more interest from that community […] soon as you turned it around … well, ‘you know what about alcohol’ or ‘what about cutting down’ or having conversations around promoting safer drinking, it’s just really hard to engage.
Participant 1
In two local authorities, business owners identified alcohol misuse as an issue but paid lip service to supporting community-based action:
She (shop owner) was like, ‘alcohol. I am sick of it’. Going on, ‘Everywhere we go, trying to stop these licences, but there’s nothing we can do about it’, blah blah, blah. We tried […]’Is there anything that we can do? […] ‘come up’ [for the training]. […]. But they just weren’t forthcoming, they just … that was it, the buck stopped.
Participant 3
There was inertia from residents around getting involved in the licensing process, despite frustrations with loud noise from licensed venues. In one area, there was concern expressed about the overall number of licenses issued:
they said ‘there are too many people with licences. […] It’s too easy to get a licence, too many people have licences’, and they wanted … because it was noisy at night and stuff. […] we said, ‘Well, can we come and join your committee and maybe come and have a chat at your committee’, […] but they didn’t actually really want to do anything.
Participant 3
Area 9 utilised the Licensing Public Register during AHC training sessions but described an inertia or lack of interest shown by the AHCs to getting further involved in licensing decision-making:
They were interested at the training but beyond that … and then, if they saw a [blue] sticker (indication of a new licensing or variation to an existing application), that was it! There wasn’t much more of wanting to share that knowledge or do anything about it. And I don’t know whether that’s because of me not pushing it or … I don’t know, I don’t know what the answer is. They’re not really interested, I don’t know.
Participant 11
Active role of first-generation alcohol health champions
The intervention design anticipated that first-generation AHCs would lead on the recruitment for second-generation AHCs; however only two of the areas (Areas 1 and 8) were able to successfully recruit through existing volunteers. In some areas, recruiting through alcohol and drug services for first- or second-generation AHCs impacted on capacity building (see Theme 2) and was limited in terms of leading recruitment activity:
the champions that we chose were … are … have been through the treatment service so you’re dealing with very vulnerable adults complex […] so if I had to do this again […] I think we would really try and get volunteers, which were wider than their Drug and Alcohol service … I think for sustainability.
Participant 1
the second group were mainly still users, as such, they were alcohol-dependent, and that’s why we’ve … probably the wrong group that we recruited on the second phase, really. They weren’t quite ready.
Participant 9
All co-ordinators found people interested in the idea of becoming an AHC, suggesting the underlying premise of CICA was seen to offer value. However, in some areas, neither local co-ordinators nor their AHCs had the capacity to recruit effectively:
I didn’t have the time to do it (publicity to recruit) and I attempted to get the alcohol health champions to do that and get it up and running […] It was probably a bit much for them, and it was certainly too much for me.
Participant 3
As a consequence of first-generation AHCs not recruiting, the need for recurring recruitment driven by the co-ordinator, in hard-to-reach areas was described as ‘hardcore’ (Area 8).
in terms of … the amount of work and effort that goes … to get in volunteers and champions to attend training, it’s quite high.
Participant 1
A further premise underpinning CICA was that first-generation AHCs would roll out cascade training. Co-ordinators from many areas found the AHCs did not have the confidence and skills to be able to deliver cascade training, as originally envisaged:
just to get people to volunteer then we were asking to train them up and ask them to deliver to others … we found … you normally find in these communities that they don’t have the confidence or the skillset to do that.
Participant 1
An assumption that AHCs would be able to deliver the training on their own, having received Train-the-Trainer training, as part of their Level 2 training, was potentially therefore misplaced.
Even in an area which was successful at sustaining CICA beyond 12 months, second-generation champions were experienced very differently to the first cohort, pointing towards challenges underpinning volunteer-based approaches:
I thought they were going to be perfect, to be honest. But you never know, and I just think, again, that’s what the nature, or the risk you’ve got with volunteers, because you can give them as much support as possible, if they’re not ready to engage, then they’re not ready to engage.
Participant 11
Despite these challenges, in one area, a strong group ethos developed between the AHCs, supported by the local experienced volunteer co-ordinator:
And like I say, there’s about four or five of them that, from the first cohort, that have stayed with us. Yeah. Some have gone into paid employment, but they’ve stayed with us, and they’re the ones that basically have kept the momentum going.
Participant 7
Retention not attrition
However, an unexpected consequence of CICA was caused by AHCs moving into paid employment, training or education in all areas, impacting the sustainability of the programme:
when you are training such a small number of people initially, when you have two who are immediately taken out of the picture for other reasons, you’re very much left without enough peer support and, kind of, your momentum really is almost gone almost straightaway.
Participant 8
Interestingly, generally local co-ordinators had no expectation that AHCs would continue to give brief advice or have alcohol-related conversations if they were no longer directly involved with the service they had been working with ‘because they’ve got a life’. This suggests that volunteers’ interest was seen as transitory rather than perceiving community members as engaged ‘assets’ whether or not they remained in contact with their local co-ordinator or service:
And then people started getting jobs, which is absolutely brilliant, but then they lose … obviously they’re not going to carry on having (brief) conversations because they’ve got a life. So, sometimes the success of helping somebody can hinder you. If that makes sense?
Participant 11
In an area that has sustained CICA, the social value that AHCs gain is celebrated as a real success for the programme, despite leading to attrition:
I mean, it is a powerful tool, and that’s why I said that with the CICA Programme, it potentially … for certain individuals it will lead to so many things, given the right support and opportunities. And that’s what we … well, that’s what we’ve been doing, and that’s what we will continue to do.
Participant 9
Theme 2: developing new community assets
This theme focuses on characteristics associated with individuals’ core to the success of CICA, including motivation, skills, confidence, capacity and capability.
Capacity, capability and confidence of alcohol health champions and local co-ordinators
In all areas, CICA was led by local co-ordinators as an additional scope of work, with no additional funding to support implementation in eight of the nine areas. In those areas that were successful in recruiting more than one cohort of AHCs, local co-ordinators detailed the scope of the ‘CICA’ role as ‘difficult’ and included the ongoing recruitment of AHCs, mentoring existing and new AHCs, managing a volunteer team, assessment for the qualification and keeping volunteers engaged:
So yeah, it’s difficult with just a few hours a week, it really is.
Area 9
At 12 months, limited capacity due to lack of funding was identified as a barrier and frustrating:
I don’t think it can be done on the fly. Speaking as somebody who’s been doing it on the fly, you know what I mean? […] it’s been another part of a busy job. […] I’ve been up for it, and it’s been a good experience […] but I think to not have the time and resources to dedicate to it makes it a very frustrating experience.
Participant 5
Continual challenges in recruiting and retaining engagement of AHCs were experienced as demotivating:
I probably at that point was a bit disheartened because I think that was the point where we’d booked for seven people and six cancelled, and I thought, I don’t know what else to do.
Participant 3
Sustainability was also impacted by the capacity, and capability, of local co-ordinators to lead on delivering the cascade training to further cohorts of AHCs. Some local co-ordinators found they struggled to deliver the training and that role would be difficult for ‘a layperson’:
When I delivered the first one, I thought, ‘Wow, it’s going to be very difficult for a layperson who has no experience in brief advice conversations to stand up here for 2 days’. I was struggling.
Participant 11
Despite the challenge for AHCs in delivering cascade training, Area 8 reported proactive engagement from the first-generation AHCs and a successful outcome:
the best part of the training was seeing the first-generation health champions start to deliver the training, and being really nervous and being really unconfident and being really scared and all that kind of stuff, and then just getting up there and going *Boom* and really, really smashing it and I’m thinking ‘wow, you’ve done spectacularly well there’.
Participant 5
While all local co-ordinators found AHCs were unable to lead cascade training events due to limited skills and lack of confidence in some areas, AHCs also lacked confidence to begin brief advice conversations due to the topic:
Other people just felt, well I do drink, people here know that I drink, again, what permission do I have to tell somebody else that they drink too much? And so, I think the topic itself provides a challenge, […]and it can feel hard to have those conversations about how much is too much.
Participant 8
As it became clearer that AHCs lacked the confidence to open brief advice conversations, local co-ordinators used different strategies to strengthen AHCs’ self-efficacy. These included plans to deliver motivational interviewing training (Area 2); buddying the AHC with an experienced support volunteer (Area 9); and developing AHC's broader public health knowledge and understanding and providing additional skills sessions (Area 8).
We […] didn’t feel comfortable that those volunteers, who had passed (the qualification) would be ready to go out and face the community. So myself and [Name of local lead], kind of, went back and had a number of workshops with the first cohort […]. And going through areas again and picking off areas that would be more relevant in terms of having conversations with communities and building up some of that.
Participant 9
Consequently, the AHCs became independent and ‘self-sufficient’ with the capability and confidence to engage with the community:
And now I’ve got good people who go out, even if I’m not here […] they’ll come and pick the green bag up. They’ve got a green bag with everything in; their banner, all the leaflets, the Audit-Cs. And they just pick it up and off they go. So, they might set up in the library here, they might go to the health centre around the corner […] So, they’re very self-sufficient, as long as I keep the bag stocked up, they’ve got a good routine going.
Participant 7
‘Hand holding’ alcohol health champions
Volunteers required far more support on an ongoing basis than was originally envisaged by leads or articulated in terms of the expectations for CICA and became a significant barrier:
It [ongoing support] needed to be far greater than we could reasonably provide.
Participant 8
As local co-ordinators were largely supporting CICA within their existing workloads, the unexpected need to ‘hand hold’ became a barrier which impacted on capacity building and embedding CICA:
, but then when it came to actually going down and doing it [the AHCs going to run a drop in session at a local café], they struggled a bit with that, really. And I don’t feel I had enough time to dedicate to supporting them with that as well.
Participant 5
Some areas set up support sessions ‘every couple of weeks’ (Area 8) for AHCs, where they ‘reiterated what we were trying to do’. In Area 9, the local co-ordinator
sent out a text every Monday morning, ‘This is what we’ve got planned’, […] So, we do ‘What have we done last month?’ A plan for this month and study that, do it and then act upon it.
Participant 11
In one area that has continued to sustain CICA, the effort and demand on the time of the local lead were deemed worthwhile in terms of the results gained:
I think [Name of local co-ordinator] has been there 100 per cent of the time for them, you know, to a point where it was sometimes a bit hand holding and that, kind of, was expensive in terms of his time, because he wasn’t allowed then to do some of his work, because he felt as though he needed to support them. And if you look at the long term of it, it was worth it, because they’re now actually doing things that they don’t need hand holding for.
Participant 9
Here, a managed ‘hand-holding’ approach was used to build AHCs confidence to have brief advice conversations, starting in ‘safer’ spaces such as a health-centre hub:
it was really hand holding to start with, because it had to be … because they were very, very nervous, but now I think they would take on anybody, to be honest.
Participant 9
A different local lead (Area 4) identified that investing the time in ‘hand holding’ to support the development of AHC confidence was integral to building AHC capability and therefore would take ‘time’.
Experiences of giving brief advice
Four out of the eight areas shared examples of AHCs providing brief advice demonstrating successful capacity building. Sustaining interest in delivering brief advice focused on AHCs providing advice to ‘strangers’ rather than family and friends. Evidence was provided of brief advice conversations held in taxis (Area 9), with people met on a canal towpath (Area 6) and with people at carnivals (Areas 1 and 8) for instance:
[Name of AHC] did his very first conversation in the taxi on the way home (from the training day) with the taxi driver. His very first Audit C. And he was buzzing, he was absolutely buzzing about it, which is great.
Participant 11
In Area 9, AHCs learnt how to structure conversations. Evidence was provided of engaging with individuals over a longer timescale – to support a reduction in overall alcohol use – facilitated by goal-setting with the recipient of the brief advice:
and then, we’d have a conversation and we could get somebody to set a goal to reduce their alcohol, […] we’re saying to them, ‘How about you reduce from 14 units to 12 units?’ something like that, […]. If we were setting them a goal […] then we’d call them back in a month and say, ‘How did you get on with that?’ That was one good thing.
Participant 11
Local leads in Areas 1, 4 and 9 warmly recognised the commitment of their AHCs, describing them as being ‘proud’ for ‘everything they’ve done’. Interestingly, local co-ordinators celebrated this success through quantifying brief advice activity and reporting on it:
obviously, we’re delighted that we’ve smashed the 200 hours (CICA volunteer time) in 12 months. To get 200 hours of people’s time, to be out there talking to the community, and be confident and be … and wishing to do that, I think it’s massive. I think it’s massive.
Participant 7
he did the training and he was just at a very high level of his volunteering […] and that was when we went out and did lots of community engagement and we did 300 brief intervention in 15 days.
Participant 4
However, in some areas, volunteers were less comfortable in having brief advice conversations, and the area struggled to effectively operationalise CICA:
The topic made it uncomfortable for some people, and let’s face it, we know health professionals who struggle to have a conversation with people about how much they drink. […].
Participant 8
Theme 3: identifying practices to facilitate the sustainability of Communities in Charge of Alcohol
This theme explores practices that facilitated, or were anticipated that they would facilitate, the sustainment of CICA.
Identifying the right ‘place’ and timeline to successfully build community capability
Most local co-ordinators debated issues around operationalising CICA in the LSOAs chosen. Two local co-ordinators felt that targeting less deprived areas, and with more established patterns of volunteering, may have worked more effectively and enabled the programme to embed:
it has potential I think definitely. The programme lends itself really well to places that are … like very established and run really well […]. Our volunteer groups that have been established a long time that may be … are used to working in this way … I think the model really fits really well with that …
Participant 1
Five local co-ordinators felt the sustainability of CICA was affected by the LSOA-level approach taken to the intervention. Four argued that using a wider geographical footprint within a town or city centre would have supported operationalisation by providing access to different levels of capability within the community to deliver CICA:
I could have imagined taking that community-based model to other places within the borough, and finding we had local residents with the capability, already, to pick up the model and take it somewhere. Yes. I think that the area we focused on – as having a high level of need – it’s much harder to find people who were able to do that.
Participant 8
In relation to taking CICA into other areas within the local authority, one local co-ordinator said:
there’s so much more we can do there, absolutely loads.
Participant 11
One local co-ordinator hypothesised that operationalising CICA in more affluent areas might have more success in creating engagement with the licensing process, due to different ‘tolerance’ levels:
our more affluent areas often make far more complaints and objections around licensed premises than some of our more deprived areas. […]. So, if it’s an area without a huge number of licensed premises and with reasonably high tolerance levels, potentially for some street drinking, or kids having alcohol, or things like that, it [alcohol availability] just might not be an issue for that group of people.
Participant 3
The 12-month timeline for operationalising and evaluating CICA was also seen as problematic. Some local co-ordinators identified 12 months to embed a community-based approach as unrealistic:
It can take years to get stuff established, can’t it? You know what I mean? Especially groups and community groups and stuff. You know, three years, you know? To just … to get it anywhere, into any kind of shape, really.
Participant 5
Consequently, the initial ambition of training 35 AHCs combined with a 12-month time frame skewed activity towards recruitment and training rather than building the capability of the first generation:
It’s almost been like, right we’ve got to get 30 people trained up by next January, and stuff like that. And I think, on reflection, I don’t know how realistic that was, really. And I think that’s again been a bit of a driver for banging training on, when we’ve not really been ready to bang that training on. Rather than thinking, right we’ve got a small group here, let’s grow that.
Participant 5
‘No Key Performance Indicators (KPIs) – why bother?’
Local co-ordinators shared different opinions about targets or goals that hindered or facilitated operationalising CICA. In two areas, recruitment targets were viewed as a barrier. At 12 months, these two areas had struggled to recruit and carry out cascade training, which may explain the negative focus on recruitment targets:
I just think … the way that the CICA is … sort of written around having 30 odd … to have a specific number of cascade … is it 35 or 30? I think … yeah, there was a … an estimate of trying to aim for … building that capacity. I just think … you know maybe that’s just too far … it’s just not achievable really. I think it just has to be whatever works in that area.
Participant 1
For some local co-ordinators, the absence of goals in relation to the number of brief advice conversations expected and the number of AUDIT-Cs required was a barrier, so local-level goals were put in place to encourage and motivate AHCs. In one area, the local co-ordinator found methodically measuring activity so that feedback could be given to both commissioners and the AHCs was motivational, facilitated engagement and ongoing support:
Since we’ve started, we’ve […] seen 571 individuals and spoken to them about alcohol, whether it affects them, their family, a loved one, a neighbour, a work colleague, or somebody in … or just generally by their community. We’ve done 101 mini-Audit-Cs. We’ve given out 652 leaflets at different events. And we’ve done over 200 hours of volunteers completed.
Participant 7
While some AHCs found targets motivating, others were reported as being concerned about being ‘embarrassed’ if they had not had ‘enough’ brief advice conversations which became a barrier and contributed to attrition in one area:
There was always a bit of a concern about a need to do a certain amount of work […] people (the AHCs) perceived, I need to do a certain number of things, otherwise I’m embarrassed to go back and talk to [Name of local co-ordinator], or the other colleagues involved, because I feel like I’ve not done anything.
Participant 8
Some local co-ordinators reported feeling pressured to ensure brief advice conversations were carried out, despite there being no targets. In one area, this was reported as necessary ‘to keep the project afloat’ and to ‘garner a good impression’ with commissioners: Two local co-ordinators identified the CICA work going on in other GM areas as a driver to complete more conversations in some areas:
then, I guess with the local meetings and people going ‘Oh, I’ve done X amount of Audit-Cs, and I’ve done this, and I’ve done that’, and they’re thinking ‘oh shit, right, I need to get some Audit-Cs in, don’t I?’
Participant 5
It can become an issue, perhaps, when a commissioner is telling you, ‘Just get a venue, just use volunteers. So-and-so in town X are doing fine.
Participant 4
Local co-ordinators’ responses to completing a (non-prescribed) number of brief advice interventions begin to demonstrate the complexity of monitoring and evaluating brief advice interventions. The absence of targets at local level left one local co-ordinator to question the use of a ‘blunt instrument’ to determine the success of the CICA intervention:
What do they want from it? Do they want people to drink less? Do they want people to present to A&E less? Do they want less domestic violence? I don’t know, broadly speaking … If you’re going to be using admissions to A&E as a KPI, it’s a very blunt instrument, isn’t it? I don’t necessarily think it proves anything.
Participant 4
Interestingly, none of the local co-ordinators discussed the absence of targets related to licensing activity.
Broadening skills and engagement beyond the alcohol health champion role
Some areas (Areas 1, 8 and 9) found benefit in extending the range of training provided to the AHCs to give them a wider health remit. Using wider conversations about health was seen to facilitate conversations about alcohol consumption:
So, if you’ve got somebody and you’re testing their blood pressure, the next thing you know is you’ve got a card there. So, they can do an Audit-C depending on their age, but they’ve also got the lifestyle risk assessment. […] Then they will talk to people about their smoking and definitely their alcohol, so they’re getting an Audit-C then.
Participant 11
As a result of leading on CICA, some local co-ordinators identified that new volunteers – whether AHCs specifically or broader lifestyle volunteers – would benefit from initial training and the development of underpinning knowledge in public health:
what we are going to do though, from now on, is we are going to do the Level 1 ‘Understanding Public Health’(qualification) […] around obesity, physical activity, healthy eating, all those things, smoking […]. Because public health is the big picture. It affects everybody.
Participant 9
Licensing officer engagement
Licensing officers, delegated as lead officers for the CICA programme for their local area (henceforth referred to as ‘licensing leads’), had been expected to attend and cofacilitate the licensing half-day at both Train-the-Trainer training and cascade training. Table 22 provides an overview of the licensing context by local authority, number of AHCs trained and licensing officer engagement.
| Area characteristics | Intervention areas | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 6 | 7 | 8 | 9 | 10 | |
| Number of licensed premises in intervention area at the start of roll-out | 8 | 59 | 0 | 3 | 20 | 17 | 9 | 22 | 20 |
| Number of first-generation AHCs trained | 10 | 8 | 13 | 7 | 6 | 7 | 9 | 7 | 6 |
| Total number of AHCs trained during intervention period | 16 | 20 | 13 | 11 | 9 | 7 | 22 | 15 | 10 |
| Number of cascade training events held during intervention period | 1 | 1 | 0 | 1 | 1 | 0 | 4 | 2 | 1 |
| First-generation training event attended by licensing lead | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Cascade training event(s) attended by licensing lead | Yes | Yes | N/A | Yes | No | N/A | Yes | Yes | No |
Our logic model (see Appendix 1) anticipated that following alcohol licensing training, community involvement in licensing activities would be measurable using indicators including the number of licences challenged, licence reviews requested, representations made, investigations initiated and issues reported to local licensing authorities. These would act as a proxy for community engagement. Semistructured one-to-one interviews were carried out. Routinely collected data relating to alcohol harm and descriptive statistics of licensing applications were reviewed to understand context.
Five LA licensing units provided data relating to the electoral ward where the target CICA LSOAs were located in 2020 (see Table 23). Wards were chosen as the geography because LSOA-level licensing data were not easily available; typically, there are three or four LSOAs in a ward. Four authorities cited lack of staff capacity for non-provision of data.
| Area characteristics | Intervention areas | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 6 | 7 | 8 | 9 | 10 | |
| Number of LSOAs | 2 | 1 | 1 | 2 | 2 | 3 | 2 | 2 | 2 |
| Availability of a fulla public licensing register | Yes | Yes | No | Yes | No | Yes | No | No | No |
| Licensing data b | |||||||||
| Number of new licensing applications madec | – | – | – | 1d | 2(1) | – | 2(6) | 9(4) | 28(56) |
| Number of full variatione applications made | – | – | – | 0(0) | 3(1) | – | 1(2) | 1(4) | 1(13) |
| Number of minor variationf applications made | – | – | – | 0(0) | 3(4) | – | 1(2) | 0(0) | 0(17) |
| Number of reviews of licences | – | – | – | 0(0) | 0 | – | 0(0) | 0(0) | – |
| Number of licensing representations made on new applications | – | – | – | 0(0) | 1(0) | – | 0(4) | 3(0) | – |
| Number of licensing representations made on full variation applications | – | – | – | 0(0) | 2(3) | – | 0(5) | 0(0) | – |
| Number of licensing representations made on minor variation applications | – | – | – | 0(0) | 0(0) | – | 0(0) | 0(0) | – |
| Number of representations made by AHCs during the intervention period | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Crime rate per 100K pop. in the year preceding CICA roll-out | |||||||||
| Public order offences | 712 | 4810 | 710 | 629 | 1155 | 785 | 467 | 324 | 1164 |
| Sexual offences | 441 | 416 | 376 | 126 | 141 | 109 | 55 | 76 | 58 |
| Violent offences | 1662 | 9251 | 2424 | 881 | 2334 | 1332 | 1483 | 1144 | 1600 |
| Total major offencesg | 2816 | 14,477 | 3510 | 1635 | 3631 | 2226 | 2005 | 1545 | 2822 |
| ASB offences | 2070 | 6846 | 2507 | 1352 | 2405 | 2043 | 1895 | 1316 | 2182 |
| Alcohol harm-related hospital admissions per 100K pop. | |||||||||
| AAFs for hospital admissionsh | 976 | 1335 | 1359 | 572 | 726 | 591 | 1011 | 936 | 970 |
Data on the number of premises licence applications, reviews and representations processed within 12 months prior and 12 months during the CICA intervention were incomplete. Four areas provided data which, to our knowledge, was complete. One further area provided a full set of data but did not clarify which year one licensing application pertained to. Four authorities did not provide data due to COVID-19-related capacity issues. Data were at a larger geography (ward level) but nevertheless showed that activity had been limited, even in the areas with more licensed premises (see Table 22). Alcohol-related hospital admissions varied from 572 to 1359/100,000,121 and rates of major offences ranged from 1545 to 14,477/100,000. Data at such a geographic granularity can be used to support scene setting when making representations at licensing hearings or for more strategic considerations, such as cumulative impact policies. 52
Despite a persistent context of alcohol-related harm, Table 23 suggests that while all areas reported receiving new premises licence applications during the intervention period, only one area (Area 8) recorded receiving any representations to raise concerns. Representations against new applications did increase in Area 8 during the 12-month intervention period, though the licensing lead reported that these were made by LA councillors (elected representatives) rather than community members or public health teams acting as a RA. Four areas recorded applications received for ‘full variations’ to an existing premises licence during the intervention period. A full variation is an application to significantly change a premises licence that could impact on the licensing objectives (e.g. to extend opening hours). However, only two areas (Areas 6 and 8) recorded any representations. Information provided by the Area 6 licensing lead indicated three representations were received objecting to one full variation, with one of these representations made by a resident. It is not known whether this resident was influenced by CICA/AHCs’ work. In Area 10, the number of applications for a full variation increased from 1 to 13 during the intervention period, with no concerns or objections raised.
Licensing policy context at follow-up
Due to the burden on licensing authorities that arose from March 2020 as a result of the COVID-19 pandemic,122 all nine licensing authorities had to delay the full review and renewal of their licensing policy statements. As of September 2022, five were fully reviewed and renewed; two had an interim review while awaiting a full review and consultation; and two were awaiting review (no interim or full review to date). The earliest review and renewal (full review or interim review) were published in December 2020 and the most recent in May 2022.
Before determining the licensing policy, it is a statutory requirement83 of licensing authorities to consult all RAs, including the Director for Public Health. However, it is not a statutory requirement to consult interested parties, such as residents/local community members. In our logic model, training AHCs to engage in the licensing process may have led to involvement in the consultation process if given the opportunity.
Subject to the statutory requirements, it is for each licensing authority to determine the extent of the consultation it should undertake, and whether any particular person or body is representative of the groups described in the 2003 Act. While it is clearly good practice to consult widely, this may not always be necessary or appropriate.
Section 5 of the Licensing Act 2003
It was unknown the extent of the consultations undertaken with ‘interested parties’ in the five areas that had fully reviewed and renewed their licensing policies; details of consultees other than RAs were not provided as identified in the document review at baseline. However, a keyword search for ‘champion’, ‘communities in charge of alcohol’ or CICA yielded one positive result. In their renewed 5-year policy statement, Area 8 recognised the ambition of CICA and the role of AHCs under the section ‘Partnership Working and Enforcement’, stating: ‘Champions learn about alcohol misuse and how to talk to friends and family about alcohol and how to seek support if needed, as well as learning about the licensing process and how they can help if local on and off licensed premises are causing any community concerns’.
Interviews with licensing officers
Three overarching themes were identified regarding barriers and facilitators to operationalising and sustaining CICA specific to community-based activity around licensing activity. Themes, definitions of themes and subthemes are provided in Table 24. Participants have been anonymised. As such, participant numbers do not relate to area numbers identified in Table 22.
| Theme | Theme definition | Subthemes |
|---|---|---|
| 1. Extent of alignment with statutory requirements and political support | The extent of backing from licensing authorities and the formal national, community or system regulations (rules, policies, laws) impacting the intervention |
|
| 2. Ability to operationalise and support local assets | The availability of funding as related to the intervention; and the physical, technical, service and training structures or resources existing in the community or larger system in which the intervention is embedded |
|
| 3. Opportunity for and ability to raise licensing issues | Beliefs, values, customs and practices of the community and licensing processes within which the intervention is embedded in relation to licensing |
|
Theme 1: extent of alignment with statutory requirements and political context
Fit with statutory requirements
The interviews highlighted challenges for communities and RAs in addressing alcohol harm through the existing legal framework if local alcohol harm issues did not directly align with one of the four licensing objectives. Licensing leads highlighted how their practice is guided by statutory requirements which do not include taking a (public) health perspective in England and Wales:
we have a statutory obligation to grant licences to premises or licence holders that have met all the criteria that is set out by the legislation. There are mechanisms that if a premises is not doing what they are supposed to do and promoting the licensing objectives, then those people can be called to task. So, the pathway side of it and the health side of it really for me isn’t our avenue.
Participant 8
Indeed, the impact of alcohol harm at a local level was reported by one licensing lead as something they were largely uninformed about:
I am not involved with the, for instance, the public health people, I don’t see the data on alcohol abuse in certain areas, or anything like that, I wouldn’t be able to comment on the impact locally, but I am sure there is an impact.
Participant 6
While LA public health teams operate as RAs and have the opportunity to comment on licensing applications, Participant 8 indicated that comments were ‘very few and far between’:
Although licensing legislation in Scotland does have public health licensing objective, in England and Wales, it doesn’t. Albeit the public health is what we call a responsible authority and can make comments on licence applications, they are very few and far between.
Participant 8
One licensing lead described how support had been sought by the public health team to understand how they could make effective licensing representations using health data. Advice was provided about relating the objection to the ‘public safety’ licensing objective:
So the sort of thing I discuss with the colleagues from public health is, where you have an area where you’ve got a, sort of, there is public health evidence of high deprivation or wholesale alcohol abuse or something of that nature, if they have that data and those statistics, a relevant representation may be that they will say well, look, … the admissions data for this particular area of [name of LA]- the hospital – these are the number who were treated for alcohol issues or here is this piece of data or that piece of data. And essentially their argument – the last thing that this area needs now is another place selling alcohol or an existing off-licence that is deciding it’s going to open until two o clock in the morning, for example. And their argument would be, well, on the basis of public health and public safety, this shouldn’t be allowed.
Participant 6
Extent of ‘political’ support
None of the licensing leads made any reference to CICA having wider backing from public officials or locally elected council members in their LAs, suggesting alcohol harm was not a political priority at the time. Only one licensing lead highlighted being supported by their line manager regarding their involvement in delivering training to the AHCs:
My Head of Service has been supportive of doing it and allowed me to have the time to go and do the presentations and so on. (Participant 8)
One licensing lead noted that by attending the training of AHCs and gaining greater insight into the ambitions of CICA, their own support for the programme grew:
after I’d been to it my view did change about … because I knew a little bit more about what the aim of it was. So, my view did change, and I thought it was a good idea what was going on.
Participant 3
However, while understanding the ambitions of CICA and the value of developing a community place-based approach, Participant 10 did not view implementing CICA as something for which they had responsibility or ownership. Although not explored or reported explicitly, this may have been a barrier to proactively engaging with AHCs in their area:
I guess I came on board to offer the licensing experience and support, as opposed to … I don’t know, I guess have like ownership or sort of I’m not sure if sort of responsibility, it’s the right word but …You know, if it was my project as it were I wouldn’t have considered it that.
Participant 10
Theme 2: operational concerns and approaches
Funding and capacity to provide ongoing support to alcohol health champions
Despite the national recommendation to encourage greater community involvement in licensing, licensing leads identified how limited funding impacted on their ability, and the ability of wider licensing teams, to engage with the community, including through rolling out CICA:
this is a very commendable project, it’s something that I think that most, if not all of them [licensing managers], want to be involved in, want to try and support, but in practical terms, the levels of support they could give it would be limited, because of the pressures on their licensing teams across the region.
Participant 6
With licensing leads having to absorb their involvement in CICA into their existing workload, two participants identified issues around how ‘capacity’ would impact ongoing ‘commitment and motivation’ and the sustainability of CICA:
I guess it’s getting like a lot of things, it relies on sort of the capacity and I guess commitment and motivation and sort of … I suppose one of the challenges is keeping that up.
Participant 10
Despite legislative guidelines recommending community involvement, Participant 3 indicated that a renegotiation of time related to CICA would be required, suggesting an ongoing challenge of committing capacity to establish, foster and develop community-based relationships:
time is of the essence unfortunately, especially now we’re cut to the quick because I was going to say that to you. If you’re running any more [cascade training courses] I would then have to … we’ve got a new different management structure, I’d have to run it past our management to make sure it was okay that I attended and stuff like that.
Participant 3
Identifying and harnessing useful assets
Given the role AHCs were anticipated to play in licensing activity and the opportunities for licensing leads to cofacilitate AHC training, it was notable across all interviews that discussion about licensing leads engaging with the AHCs themselves over the 12-month intervention period was limited. Interestingly, of the six licensing leads interviewed, two (Areas 6 and 10) reported not being involved in cascade training in their area, despite second-generation training taking place, suggesting that community-based engagement in alcohol licensing activity was not a priority at this time. One licensing lead did reflect on their likelihood to engage further with AHCs. Their perception was that this was more probable if AHCs were proactively bringing issues to the attention of the licensing leads/unit/department; that the lever for engagement was a level of activity and insight at local levels which actively sought out licensing engagement rather than a licensing lead proactively engaging with AHCs around intelligence gathering:
I suppose the key to it is the proactivity and I suppose the areas that there is more engagement, there is maybe a higher degree of proactivity from the person, from the residents, is to ‘look, we have these issues, how can you help us?’ I suppose there is the tendency to think, oh if you don’t hear anything everything’s fine you know and take that approach.
Participant 10
Only one of the licensing leads identified the cohort of trained AHCs as an asset with whom they were working on an ongoing basis to have wider conversations in the community about alcohol harm:
getting feedback from the community in what’s called the [name of LA] ‘Let’s Talk About Alcohol’ campaign and some of the CICA volunteers are involved in coming to those sessions.
Participant 4
This licensing lead identified a need for the LA to harness AHCs’ interest; engage them in relevant alcohol harm reduction activities; and consider ways to retain engagement over the longer term, although it is notable that the activities discussed do not directly relate to licensing decision-making:
perhaps involving them in those projects [the ‘Reducing the Strength’ and ‘Challenge 25’ campaigns] and (…) like keeping them involved, like I said we wouldn’t want them to just attend that training session, hear that information and then be completely detached from, from it. And in terms of scoping that role, like I say it’s just when we do go and, or if public health or whoever it may be, have events on or whatever, they’re involved and brought to them really just so, so they can be part of it and keep their interest, engaged, keep them engaged […]. Because they’re engaged initially at the training session and you wanna keep that engagement ongoing rather than just for that one time, then that’s the key isn’t it?
Participant 4
It was mooted that to gain more impact from AHCs as formal assets, the communities within which they were situated needed to become more aware of the AHCs presence and role:
Making the wider public at large aware of it, so that they know how they could get involved in it and just promoting the fact that there are these volunteers who are in the community, who’ve been trained who have an awareness of how they can get involved and just the promotion of it really.
Participant 4
Involvement in CICA had made some licensing leads reflect on the wider presence of volunteer-led community assets. In one area, where CICA had been less successful at becoming established, the licensing lead reflected on environmental volunteer groups working at a community level but was less aware of sustainable volunteer-based projects focused on ‘social’ outcomes, such as alcohol harm:
we have ‘Friends of Parks’ groups for instance in [name of LA] … I think the approach for the environmental stuff, that’s quite a common thing. Social stuff, I don’t know.
Participant 6
Another licensing lead reflected on the challenges of accessing communities on an ongoing basis due to limited resources. They suggested professionals already working at community level, such as community police officers, could become useful AHCs. This suggests that at 12 months, some licensing leads were still reflecting on how to continue capacity building and develop assets at a local level.
Meaningful training provision
Four licensing leads suggested the licensing element of the training course could be amended to make it more meaningful and appropriate for AHCs as it was ‘a little bit too in-depth’ (Participant 4). Suggestions were made regarding the key licensing elements that needed to be delivered in the training:
Effectively somebody who’s getting involved in a licensing application needs to be aware of the licensing objectives and they need to be aware of the timescale and they need to be aware of the point of contact of where they can make the applications and those are the key elements of it really.
Participant 4
Another licensing lead stated that AHCs only needed to know ‘the basics’:
I think laymen only need to know basics. So, it doesn’t have to be any in depth about this is how licensing works and, you know, maybe about all the law and everything else. They need to know the basics and, you know, people put in application, they put a blue notice up, it’s in the paper. You can then do this at this point.
Participant 3
Licensing leads found that by changing the licensing input at the cascade stage, they felt they gained more ‘buy-in’ from AHCs:
[the training input] being at a higher level wasn’t really suitable or relevant and when it was pitched at the right level, that, that helped with their buy-in.
Participant 4
One licensing lead felt the licensing aspect of the CICA intervention would benefit if AHCs were involved in additional activities to help extend their involvement in licensing beyond the training session:
rather than maybe just having a training session, it’s like right, go away and you know do stuff, or you know … as a variation … you may be, you know, I guess, an ongoing programme.
Participant 10
While licensing leads suggested the licensing content of the course was overly complicated and could be amended to be more appropriate, two officers suggested that getting engaged in licensing issues at a community level was straightforward. One lead stressed that AHCs were ‘told of how simple it can be to get involved’ (Participant 4). A second lead expanded by outlining the approach AHCs and community members should take:
I mean what we do is, every council has to, list the applications – current applications in consultation, on the website. And I guess what we do is we have a link if somebody wants to comment and some guidance notes around submitting the comments and trying to do so effectively. And we include in our policy separate advice on that. So, there’s a section on doing that. And if people are reluctant, how they … I suppose alternative measures for having those concerns raised. So, we do have information that we publicise and have available on how people can engage and do so effectively, and then also equally raise concerns. It’s things like that you can pretty easily do through the website.
Participant 10
Licensing leads therefore felt that processes existed to support community engagement, and this could be achieved ‘pretty easily’. However, licensing leads’ testimonies raised a range of broader factors that may have impacted on the AHCs’ ability to engage in licensing issues within the 12-month period of the CICA intervention.
Theme 3: raising licensing issues
Significant differences existed between the LAs in the number of licensed premises situated within the CICA LSOAs (see Table 22: range: 0–59). Logically, this would suggest some communities had greater opportunity to become involved in the licensing process than others. However, despite this, there were no differences in the perceived level of involvement of AHCs in contesting licensing applications by making representations across LA areas. This was despite the fact that the AHCs had appeared very engaged with the licensing aspect of the training:
I feel like my experience of the volunteers had been that they were all very engaged, certainly with the training and with the scheme. It’s actually from a licensing perspective, getting them to get involved was probably the, the right way of saying that. It’s been … I don’t feel like they’ve been involved as much as we could, as they could have been and as I would have liked, from the start, from the start of the scheme and initiative.
Participant 4
Licensing leads highlighted a range of structural barriers they perceived as impacting community members’ ability to influence licensing decision-making:
Traditional low levels of community involvement
Area 9’s licensing officer stated they received only one community representation during the 12-month intervention period (from a non-CICA area), indicating community engagement in licensing operating from a low base. When discussing community engagement in licensing more generally, a different licensing lead felt public ‘apathy’ was a barrier:
I just feel that there can be a kind of apathy from the public not to get involved in the applications and that it’s just the same in one, from one area to another area. An area where you’ve got particular alcohol problems, density of premises just as much as you would have an area where you’ve not got those issues.
Participant 4
Licensing leads suggested multiple barriers impacted on community members’ willingness to make representations, although these perceptions did not appear to be informed by direct conversations with AHCs. Perceived barriers included the ‘potential for conflict’; lack of anonymity; potential need to attend a Licensing Committee ‘hearing’; and concerns about whether their involvement would have an ‘impact’ on the outcome:
I think they can possibly get deterred from … there’s a range of things. There’s the potential for conflict. The … I suppose they could go to a hearing. There might be some doubts as to how realistic an effect or impact they can have.
Participant 10
Involvement in one particular licensing issue was facilitated by a licensing lead’s personal reassurance to a community member, but there was no suggestion that this involvement was related to one of the CICA areas:
sometimes it comes down to the fear of repercussions, sometimes they feel like they don’t want to get involved because they might have a viewpoint but they don’t want to get involved but I thought it was my job really to reassure them and particularly one of the complainants who changed her mind initially said that she wanted to withhold all her details and obviously so that (pause) only so much weight can be given to that representation if it’s anonymous and everything’s taken out of it if they don’t attend the hearing.
Participant 4
This indicates a potential conflict for community members between wishing to retain their anonymity set against a perception that anonymised community representations limit influence with licensing committees.
Ability to identify alcohol health champion involvement in licensing activity
One of the challenges identified by a number of licensing leads was whether they would be able to know if AHCs were becoming involved in informal licensing activities, for example, informing others about the Licensing Act 2003 or wider education of local community members about licensing. They acknowledged that AHCs could be using their training to inform wider community members of which they would be unaware:
So personally, I couldn’t really say to you, Oh yeah, I know that happened because it was one of the champions. But that doesn’t mean that that hasn’t happened and it’s just word of mouth and it has been one of the champions who said, Well, try that or do this or go to licensing, ask them the question.
Participant 3
I have not had the ‘phone calls in terms of it’s from a CICA project, but if individual X that lives on [Name of street], whatever, has been to the champion and said, all this information is available on the website, I wouldn’t necessarily know.
Participant 8
It was acknowledged that AHCs could utilise other routes for licensing information or support which licensing leads would be unaware of:
it may well be that they don’t necessarily only speak to me on it. They might speak to the licensing advisors (in RAs) which obviously we are dealing with, with numerous conversations every day.
Participant 8
Significantly, one licensing lead indicated ‘a lot of’ licensing applications over a 12-month period were ‘quite minor’ – assumed to mean minor variations – and therefore uncontested (supported by the data in Table 23) which created a challenge regarding ‘objective assessment’ of AHC involvement in increasing community engagement:
It’s difficult to gauge, because often a range of applications we get over a 1-year period, a lot of them will be quite minor and perhaps we won’t get any objections at all, because they won’t be contested by anyone. Others may be more controversial. And it’s hard to gauge whether we would have had more objections or more engagement from the community over any of these, than we would if CICA was in place or not. It’s very difficult to make an objective assessment of that.
Participant 6
One of the challenges identified was that AHC activity would only be recognised if AHCs declared their role or a community member informed licensing that AHCs had played a role, when a representation was made:
I think the only way we could be sure about that, if we have representations made from persons within this groups, and when they made the representation, they actually said well, actually, we are linked with the CICA project and we’ve done a lot of work and we’ve had information from that project and we think, in regard to that, we are going to object and these are the grounds we are going to object. Other than that, they don’t say who they are when they object, it’s difficult to make an objective judgement.
Participant 6
Working with responsible authorities
One lead indicated that the ability of AHCs or community members to address premises licensing issues may be limited unless a co-ordinated multiagency approach was taken to address licensing applications. Notably, the focus here was on licensed premises as settings that create issues relating to crime and disorder:
So perhaps one sort of route could be, with the projects, for those groups that have engaged with the project, when they have one of these issues, perhaps don’t just go straight to the licensing authority, if it’s a concern about crime issues, go and speak to the neighbourhood police officers, and say well, look, we’ve got this application come in, we’re really unhappy about this, because of this, this and this. Would the police be prepared to support us, in terms of putting our objection in?
Participant 6
Furthermore, licensing leads identified that communities are ‘hampered’ if the relevant RA does not object to an application, limiting the power communities have to raise concerns:
One of the issues, when we have a new premises application, a new premises licence application, is sometimes the residents will object and they might say well, we are going to object on the grounds of crime and disorder, that this premises will increase the levels of crime and disorder in the area. And the applicant will say well, hang on a minute, the police haven’t made a relevant representation, the police are quite happy with it and it sort of undermines what the residents are saying, (…) and if police don’t object it sort of hampers the residents, it makes it harder for residents to make their argument. Similarly, if you were saying, well, this premises is very noisy and it keeps residents awake at night and Environmental Health don’t object, then it makes it more difficult to make that argument.
Participant 6
Place-based factors regarding licensing engagement
Licensing leads identified that factors to do with the intervention areas themselves may have impacted on the ability of AHCs to get directly involved in influencing licensing issues within the timescale of the intervention period. For instance, Area 9 has 22 licensed premises. During the interview with the licensing lead, the licensing register was checked regarding applications made during the intervention period. Low levels of activity across the LA overall were reported and confirmed by a later data check (see Table 23). Limited engagement in licensing by AHCs was suggested as a result of limited opportunities to become involved:
I can’t say that I’ve seen any benefit of it [CICA] but I think that is probably because there haven’t been any issues or the type of applications we’ve been having in. I’ve just been having a quick flick (through the register). We have had a couple of applications in [area name] but nothing that would really cause any problems.
Participant 3
A lack of licensing issues that needed pursuing during the time frame of the intervention was also reported by Participant 8:
I am not aware off the top of my head of any real problems within [area name] and any potential reviews that the responsible authorities, be it the police, licensing authority, trading standards, that are calling for review of licences because we’ve got such problems.
Participant 8
This lack of opportunity may in part be due to changes in the overall licensing environment. One licensing lead suggested applications were shifting towards ‘online sales’ and ‘tried-and-tested’ suppliers, such as supermarkets, and that the overall level of engagement in relation to alcohol licensing activity was low:
I’ve not had anything off anybody. We’ve not been inundated with applications, I must admit. And we seem to be changing the face of [area name]. We get applications now more for … like they want to open a business that’s online. So, they want to do the sales online. We get a few of them. We’ve got quite a lot of new developments, haven’t we? So, we’ve got places like, the little shops are now like, the [Names of three large supermarket chains], so they’re more tried-and-tested people.
Participant 3
Similarly, during the interview, the licensing lead in Area 6 (20 licensed premises) did not ‘recall any particular licensing applications’ during the 12-month intervention period.
Opportunities to get involved due to ‘problems with specific premises’ were also perceived by licensing leads as ‘unpredictable’. The likelihood therefore of ‘problem premises’ suddenly appearing in the specific intervention area was perhaps unlikely during the period of the intervention:
equally, if you’re then looking at problems with specific premises, again that’s the only other situation whereby you might need to get involved, and again that’s unpredictable as to whether you know there will be problem premises.
Participant 10
One licensing lead reiterated the focus on intelligence gathering through web-based online forms and digital spaces as a significant ‘place’ for community licensing engagement:
as soon as anybody phones it’s, ‘What’s your email address? I’ll send you the link to this or send you the link to that.
Participant 3
Building community capability
Licensing leads continued to report positive support for the ABCD approach underpinning CICA and the principle of identifying and mobilising individual and community assets:
I thought it was a really good idea (…). And one of the challenges, I guess for members of the public, in licensing is sort of getting to grips, I guess, with the processes and you know I think it can often be a bit daunting. So, the idea of having training and sort of growing experience for them, you know, was a good one.
Participant 10
It was notable, however, that across all interviews, discussion about the AHCs themselves was limited. Only two discussed issues relating to accessing communities to address alcohol harm in the community and a further licensing lead spoke about the sense of social value gained by AHCs. Given the key role AHCs were anticipated to play in delivering the intervention and the role licensing leads were anticipated to have in cofacilitating first- and second-generation AHC training, it is interesting to note the limited conversation related to the volunteers as assets. Only one licensing lead described continuing relationships with their AHCs by the ‘Council’ (LA):
and I see some of the volunteers, now I’ve seen them since at [Provider organisation name] when I’ve gone to meetings and stuff, they’re aware of, of who I am and I’m involved and that yeah, just a friendly face really that can chat about things and how they’re involved because I know that the Council have made use of the CICA volunteers.
Participant 4
Two licensing leads identified a need to understand how CICA could impact on licensing activity at scale. Notably, licensing leads in the nine authorities across GM received no ‘central’ briefing regarding why specific intervention areas had been selected or specific information regarding the intervention theory underpinning the implementation process. A view was shared that a wider network of AHCs operating across a wider footprint may demonstrate an ‘effect’ from the training:
And it’s just I think perhaps it’s because the... like the cohort were from one particular area. Maybe it may take several cohorts from different areas to spread that message around the borough for them to get involved more and that may be how we can see the effect that that training can have.
Participant 4
A different licensing lead questioned whether the way the intervention was set up enabled it to have sufficient ‘reach’ to make a ‘difference’:
The thing I probably wondered about was how does this scale up to an area like [name of LA]. There’s 300,000 residents in [name of LA] and there’s lots of localities probably where we have issues related to deprivation and alcohol with these groups, or there should be. So, I don’t know enough about the programmes to comment on that, but I suppose the question is: does it reach out enough to make a real big difference?
Participant 6
In two different areas, despite neither licensing leads being involved in cascade training, both perceived building community asset capability as positive and empowering the lives of residents:
I think it can only help, in the areas where you have it. Because it’s only going to be a positive thing, because it’s going to help the lives of the residents, living in those areas, and it’s going to empower those people to engage with the licensing authority when the time comes.
Participant 6
It was acknowledged, however, that building community capability ‘needs time’, ‘momentum’ and commitment:
It has potential but it needs time and it needs people who are committed. If you’ve got both those things, then you’ve got the chance of success. But I’d say, particularly sometimes in these communities it’s a struggle, you’ve got to keep at it because people soon lose momentum. You’ve got to not badger people but keep them onboard at regular intervals while something’s in its infancy until it beds in and possibly that’s what didn’t happen here.
Participant 1
One licensing lead acknowledged the opportunity for a consultative role for AHCs in future policy development:
it would be great if there was, I suppose, a real network of these kind of representatives and individuals who I suppose you could engage with, not only in respect of an area, but I suppose in respect of wider licensing issues, and licensing consultations and … I mean, we’ve not done any licensing consultations, but for example you know I would include the CICA rep in any sort of revisions to the policy and things like that.
Participant 10
Interviews with alcohol health champions
After the first 12 months of the intervention, we reviewed the number of lay champions who remained in contact with the local co-ordinator and recorded whether they were active or inactive as an AHC (see Table 25).
| Area (total numbers trained) | In contact Active |
In contact Inactive |
No longer in contact |
|---|---|---|---|
| Area 1 (14) | 8 | 6 | |
| Area 2 (17) | 4 | 3 | 10 |
| Area 3 (8) | 8a | ||
| Area 4 (7) | 3 | 3 | 1 |
| Area 6 (8) | 1 | 3 | 4 |
| Area 7 (5) | 5b | ||
| Area 8 (17) | 4 | 3 | 10 |
| Area 9 (13) | 8 | 2 | 3 |
| Area 10 (6) | 2 | 4 | |
| Totals | 28 | 16 | 51 |
Just over half of the AHCs (54%) who had taken part in training were no longer in contact with the local co-ordinator. Some local co-ordinators were aware of the reasons why these champions had dropped out, such as competing pressures with full-time work or personal life; not feeling able to embed in day-to-day job; feeling isolated when a network of champions did not grow; getting banned from the local community centre; attending training for personal awareness only (did not want to be ‘active’); not understanding why the training was recommended as part of their recovery treatment plan; moving out of the CICA area.
While it was unknown to what extent individuals who lost contact with their local co-ordinator may have continued to use their training in their personal or working lives, we defined ‘active’ as someone who continued to be actively engaged in AHC activities in the AHC community network.
Just under a third of AHCs (29%) remained ‘in contact and active’. Due to the cascade training approach, this number included second-generation champions who may have only recently trained. Of those who were still in contact but ‘inactive’ (n = 16), reasons known to local co-ordinators at 12 months included: securing paid employment; changing volunteer roles (becoming recovery volunteers, domestic abuse campaigning volunteer); returning to study/education; poor health; relapse of harmful/dependent drinking. All active and inactive champions in contact with the local co-ordinator were invited to interview. Due to the reduced target population available, instead of a purposive sampling approach (as per protocol), all those who responded were interviewed.
Seven follow-up interviews were conducted in total, representing four areas: five out of seven AHCs were first-generation AHCs (remained in contact for at least 12 months). Only one participant had also been interviewed within the initial implementation phase. Two overarching themes were identified when examining the champions' experiences after CICA had been running for 12 months. Themes and sub-themes are shown in Table 26. Participants are anonymised.
| Themes | Subthemes |
|---|---|
| 1. Connecting inside and out | 1.1 Growing, progressing, moving forward |
| 1.2 To AUDIT-C or not to AUDIT-C | |
| 1.3 ‘We’re a proper outfit’ | |
| 2. Being in charge of alcohol | 2.1 Power to say no |
| 2.2 Is knowledge power? | |
| 2.3 Branching out |
Theme 1: connecting inside and out
Growing, progressing, moving forward
Looking back on how they had personally developed over the year, champions spoke of how it had boosted their self-esteem and built their confidence to have brief conversations with people about alcohol:
Everyone goes ‘I don’t drink’. ‘Well, if you let me explain …’ and it’s actually given me the confidence to go out and do that, whereas when I first started I was like, ‘Okay it’s fine, it’s fine’ and I was quite shy about it.
First-generation AHC, Participant 1
Additionally, they built confidence being in a large group, recognising how they had changed over the course of the year:
I can sit with twenty people now and do a group, you know, whereas last year I wouldn’t.
First-generation AHC, Participant 2
Some champions spoke about the reason why they joined the training in the first place, to gain more qualifications for their CV and how the experience exceeded their expectations:
when I first come into it, it was kind of yeah, I’ll do this training it’ll be another certificate to add on to my CV and my qualifications to help me grow, progress, moving forward in my own personal development. And I had no pre-conceived expectations, but from doing it, I found it really beneficial, really rewarding.
Second-generation AHC, Participant 3
Some champions spoke about the benefits to their job prospects, not just from the training and experience of AHC activity but also by having a referee in the local co-ordinator, a person they could put down on job applications:
What I’ll say to you, through doing that (CICA), it’s certainly made people that viewed my CV think, well (name of AHC) has been involved in something … that may have helped people think ‘Well he’s worth giving an opportunity to’. The main thing behind that, the (name of local co-ordinator), he’s sort of like helped me with references.
First-generation AHC, Participant 4
To AUDIT-C or not AUDIT-C
The AUDIT-C scratchcard (see Figure 1) was offered to all areas as a resource to support having informal conversations to identify alcohol risk and offer brief advice. Champions interviewed at follow-up spoke extensively about the pros and cons of using the AUDIT-C tool and how it influenced their ability to make connections with people.
We use the AUDIT-C quite a lot to be fair. Most of the time I’ll start off a conversation and then we’ll ask them to fill in the AUDIT-C, and nine times out of ten that works. So I wouldn’t go straight … personally I wouldn’t go straight in with the AUDIT-C, but others find the AUDIT-C as a way to start a conversation, so it’s just personal preference I think.
First-generation AHC, Participant 1
There was a concern that bringing out the AUDIT-C scratchcard could affect the authenticity of the conversation, with concerns that what began as an informal chat could suddenly appear contrived and ‘not what CICA was about’, causing an unintentional disconnect between the AHC and the person:
I found that I didn’t use the AUDIT-C all the time because for me that could be a barrier, because that could for somebody who’s aware that they’re drinking too much, that could be the red flag that ‘oh she’s led me into this’. Do you know what I mean? ‘She’s producing something now, she knew that she was going to produce this’ and if it’s just a conversation you wouldn’t necessarily be that prepared … CICA’s very natural, it’s supposed to be just a conversation, and then all of a sudden, you’re producing this tick list or you know, let’s do this questionnaire kind of thing, and it’s like ooo, maybe that wasn’t as genuine a conversation as I thought it was.
First-generation AHC, Participant 5
Due to the popular use of scratchcards to win a prize, one AHC found that it was an eye-catching and effective conversation starter to help connect with people, but some people were suspicious they were being sold something:
They were fantastic and it’s a … I mean it’s a great icebreaker to start with because you know it’s a scratchcard – oh what’s that? Or they’d say I’m not paying any money. No it’s not that.. just come over. It’s a really nice icebreaker but some people really take notice of them.
First-generation AHC, Participant 6
Not knowing whether using AUDIT-C was making a difference to individuals or the wider community brought up questions for AHCs about how to measure the effects of their activities:
..I could do 30 Audit Cs but that might not even be one of the people that are being antisocial or that have a problem or that present at A&E. So, it’s how do we measure it, is it measurable? At the moment, we don’t think so, and I’m not the only one who says that.
First-generation AHC, Participant 1
Not using AUDIT-C but instead sharing knowledge gained from the CICA training in other ways was found to make a significant difference to a work colleague in an informal, opportunistic conversation:
… one night we had a conversation and just a chat about the training and he was asking me about the training and I said ‘oh it’s great’ you know, and we were just talking, and he kind of, gave a little bit of information about himself, and we were looking at ways that maybe he could reduce that and he said ‘yeah I really need to have a think about it’, and I said ‘well, what do you think you could do first, just to start that?’ and he actually did a month free cos, we worked his units out and he was on something like 70, 80 units a week he was on … so he was quite shocked at that and then he did a month completely alcohol free, and even to this day, you know much later on he’s still aware of it and he does the free month, every time we have the Sobertober … previously he wasn’t and it was kind of accepted and a bit of a joke and a bit of a laugh.
First-generation AHC, Participant 5
‘We’re actually a proper outfit’
Having a clear identity as an AHC was highlighted by a number of participants as being important for role legitimacy, their sense of having the ‘right’ to undertake alcohol health activity, as well as the responsibility:
… people need to know that you’re a proper body. They don’t want to be talking to any Jack Jones out there. It’s not really appropriate, that. You’re dealing with people’s lives here, aren’t you? They’re not just numbers.
First-generation AHC, Participant 4
The support provided to AHCs by the local co-ordinators was extremely valued, but the lack of budget and the quality of engagement/takeaway resources available to them were limited. This reflected negatively on the value of their own role:
Their support is brilliant, I can’t fault them. What I can fault is … they’re wanting us to do something with no budget. We’ve got garbage leaflets that we hand out, that look like they’ve been done on a cigarette box. It’s rubbish, we’ve had no support that way. When we do events, people want something to take away, be it a keyring or whatever, we don’t have any funding whatsoever to do anything like that. That’s my main bug bear, is the funding … I’ve said it from the beginning, I think we need a budget, we need to be able to do something. And we haven’t.. I think we do need to have a face … and then we can show people that we’re actually a proper outfit.
First-generation AHC, Participant 1
Theme 2: being in charge of alcohol
Power to say no
Alcohol health champions interviewed experienced a number of misperceptions about their role and, at times, confrontation. This led to a number of occasions where they said ‘no’:
I had a shop telling me to move when I was talking to someone outside it, and I just said ‘you do not own the street love. And I will stand here and talk to this person’ … I said ‘you do not own this street, that’s your shop and I will not move I am talking’.
Second-generation AHC, Participant 7
Affirming their role boundaries became important in some instances, where they were being asked to fill gaps in statutory service provision for those experiencing serious alcohol harm, such as ‘high impact dependent drinkers’:123
We’ve had a lady from … I can’t remember which housing trust she’s from, but she contacts us regularly to say, ‘This tenant is an alcoholic, that tenant is an alcoholic, can you go and knock on their door and help them?’ ‘No, that’s not what we do’. So, people misinterpreting what we do, but they are contacting us to say this person and that person has a problem.
First-generation AHC, Participant 1
Alcohol health champion activity was not without confrontation, and saying ‘no’ included refusing to cold-calling door to door:
We have had abuse from people that are drunk, and we just leave them to it. We’ve had it in the library, and we’ve had it at an event that we did at [location], but you just brush over it, just leave them to it. They’re only a minute amount of people, so it’s not every time we go somewhere or everything we do … I think if we went out canvassing on the streets or went to people’s doors, like was suggested, the area that it is, I just wouldn’t do that for my own safety, and all the other volunteers feel the same … I don’t think it would work as well.
First-generation AHC, Participant 1
The challenges some volunteers experienced taking part in CICA when still engaged in structured community alcohol treatment led to experiences in one area where instead of explicitly saying ‘no’ to taking part, people voted with their feet and stopped coming:
I felt that stopped people coming to, because, although we were meeting as CICA, these people were still ex-addicts and they were still kind of under a support treatment kind of, not treatment but kind of, it was a support session for them, as well as CICA, and I think, if anything, it would prevent them coming.
First-generation AHC, Participant 5
Is knowledge power?
There were a number of effects and reflections that arose for participants following their licensing training. For one person, the knowledge they gained from the licensing training about the need for ‘evidence’ if reporting licensing issues became a hindrance to taking action:
because I’d not got my mobile phone handy, I couldn’t get the evidence. Because I couldn’t just say ‘Oh, it is such a place’, that’s not good enough, you need the photographic evidence.
First-generation AHC, Participant 4
For some, knowledge of the licensing process was boring or confusing:
No it bored me. I can’t be doing with it. That bit of it just over my head. I’m not good like that.
Second-generation AHC, Participant 7
Despite finding it hard to understand, one champion was interested in being able to have the opportunity to have a refresher:
I’ve not had anything to do with the licensing. To tell you the truth, I didn’t understand it … So, if you ever do that again, I’d like to sit in.
First-generation AHC, Participant 2
Understanding the processes required by licensing authorities to use online public registers, submit representations, and, in some areas, report issues online highlighted the reliance on AHCs having the digital capability to get involved in licensing decisions:
they’re not tech savvy shall we let’s say and that is another like hurdle they have to come to. It is like I can’t do that on computers and stuff and I think if there was another way, you know.
First-generation AHC, Participant 6
There were suggestions to share knowledge gained around licensing by raising awareness with the wider community using a leaflet that AHCs could distribute and use as a conversation tool:
I wouldn’t have even known, at all, I wouldn’t have known we could do that, just as the general public … We can do that, but you can do it as Joe Bloggs as well, and a lot of people don’t know that. Have we used it? No, we’ve never really used it, unfortunately, and I think that’s because the general public, the general Joe Bloggs, as I would have counted myself, we wouldn’t have … Maybe we could put a leaflet together to explain that that might help, so we’ve got something physical to hand out.
First-generation AHC, Participant 1
For some participants, they felt more passionate about the brief advice AHC role activity compared to getting involved in licensing, and it was important to them to have this flexibility to decide how little or much they wanted to use their CICA knowledge and skills:
I suppose there’s been opportunities to, if I wanted to, but I’m more interested in the face-to-face conversations with people within the community. I’m aware of the stuff, and what can be done if issues come up around the licensing and people perceive a shop or a pub kind of becoming a problem, or a nuisance within the area where kids are congregating, at the local shop and shop keepers serving them alcohol when they shouldn’t be. So, I’m aware of that stuff and how to intervene or the people who need to approach to put things in place and be made aware of that stuff, but, as I say, I’m more passionate about the face-to-face stuff with people, within the community, my local, me neighbours, people who live down the street on the estate.
Second-generation AHC, Participant 3
For others, they found the knowledge they gained about alcohol licensing and how to report issues and complaints the most valuable aspect of the CICA training:
Yeah well it helped a lot in many ways, in personal ways. It built me up to be more confident and the teaching around the council reporting way, you know, when you can report to off licences and stuff, that was so valuable. I’m gonna say that is what I got most off the course because I still pass it to people outside … What I would say is if the training, maybe on the audience, it might be delivered a bit slower on the licensing.
First-generation AHC, Participant 6
One participant suggested a missed opportunity within the licensing training to get AHCs signed up to receive notices of applications for their area. They felt that this on-the-spot practical step may have been a simple bridge that local licensing officers could have used to keep in touch with people after the training, keep them informed and remind them how they could put into practice their knowledge:
I’m going to sort that out, I’m going to get the applications for my area coming to my email and I didn’t do it because life’s busy and it doesn’t get done. But had that been set up in the training or given me the opportunity to get that done, then who knows, I’d have opened a few of them and that would have got me learning more … Almost that practical step? Yeah. Just helping that yeah? And it wasn’t hard, but I didn’t do it.
First-generation AHC, Participant 5
Branching out
Alcohol health champions felt that communities needed to have the power to be able to branch out and not be limited to prescribed target areas:
I think it’s daft that we have target areas, to be honest, because our target area is a housing estate. We ain’t going to go up into that housing estate. I went and did a housing association meeting, I ended up doing it on my own because my colleagues, unfortunately, couldn’t do it, and I was waiting for the police to turn up. They were fighting, they were scrapping, it was this one versus that one and it’s like, ‘What on earth?’. And that’s apparently tame for what it normally is. So, I said to (name of local co-ordinator), ‘I’m not going back into one of them’.
First-generation AHC, Participant 1
Branching out within the wider local authority area was seen to have the potential to provide more opportunities for AHC activities, particularly attending community events, as they were considered to be one of the most successful activities they undertook in their role:
… Maybe branch out into the local area, like into [local authority area], because they do a lot of events that we could attend. So for other areas, getting as many events in as possible. Because that’s the easiest way we found of spreading the word.
First-generation AHC, Participant 1
And lastly, allowing time for a community AHC programme to grow and expand was important, not just when branching out within a small community but also wider, recognising the value of small incremental change and ‘planting seeds’:
I see it as yes moving forward and it growing and becoming bigger and getting that message out there to the wider community, not just my local community, to other people … listen I’ve seen this work and benefit people within my community, and other people might not see that straight away, but you see little things and little changes in the way people are thinking, they’re acting and behaviours, and as I say planting them seeds.
Second-generation AHC, Participant 3
Focus groups with communities
Two main overarching themes from the focus group analysis were perceptions of alcohol consumption within society and the felt needs within the community. Themes and subthemes are provided in Table 27. Participants are anonymised within each single session focus group (Focus Group 1, Focus Group 2, Focus Group 3).
| Theme | Subtheme |
|---|---|
| 1. Alcohol consumption ingrained in society |
|
| 2. Felt needs of the community |
|
Theme 1: alcohol consumption ingrained in society
Increasing cultural and social significance
Perceptions that excessive drinking had become normalised in the area were referred to in all three focus groups. This was in the context of alcohol use becoming ‘trendier’ and popularised as an activity:
…people think that there is no such thing as life without booze. You see it on Facebook every day, it’s wine o’clock, everyone’s living for the next drink and that’s not even alcoholics, that’s just, there doesn’t seem to be anything without alcohol.
Focus Group 1, Participant 2
It’s a bit more glorified now isn’t it? And it doesn’t matter I don’t think whatever background you come from, whether you’re from affluent or not affluent, everybody drinks …
Focus Group 2, Participant 1
Now, pubs are quite open to allowing children in, so from an early age that’s what children are seeing. So, they’re considering it normal but it’s not, like you say, a parent going out for a pint, it’s doubles and shots, and they’re watching their parents do this and this is what they’re growing up with. Therefore, they think it’s okay but then they just take it to the next level and then their children think that’s okay.
Focus Group 3, Participant 1
It was suggested that drinking shaped social activities and events, and ‘not drinking’ was seen to be abnormal: ‘They’re sort of insistent, they think you’re being funny by not letting them buy you a proper drink’ (Focus Group 2, Participant 2). In contrast, buying large quantities of alcohol from off-licensed premises was considered to be the norm:
When I’ve been in the supermarket and you see it, particularly a woman with a trolley full of drink, I’m thinking is it all for her? Or is it a party or is it … you can, if you drink a lot now you can get away with it, put two or three bottles of whatever, wine in the … nobody thinks anything of it now.
Focus Group 2, Participant 4
Cycle of community breakdown and alcohol misuse
Unemployment and lower socioeconomic factors were seen to be perpetuating increased use of alcohol, contributing to a sense of community breakdown, intersecting with coexisting health, crime and ASB:
I think we have massive issues here with unemployment, with substance misuse, both drug and alcohol and I wouldn’t say alcohol’s more than drugs … you see it more and more and then obviously there is that increase in issues with mental health and antisocial behaviour, vandalism, poor [name of high street pharmacy] must be shoplifters paradise. And you just see these things and we need help.
Focus Group 2, Participant 1
Levels of ASB, such as littering and noise, were more noticeable in Focus Group 1, along with concerns for violent crime:
These idiots have parties in their back yard that go on all night and when I say all night we’re talking until like five o’clock in the morning, drink, drugs, loud music. Totally no respect for the neighbours or anybody else. If you complain you can receive death threats. And you’re worried about your windows going through.
Focus Group 1, Participant 1
The impact of noise at a hyperlocal level was particularly highlighted, and due to the small proximity, the knock-on effect of feeling vulnerable:
The noise. It’s affected everybody in the street that I live on. In fact I live on a little estate but one party going on all night can affect the whole estate because it’s that small. So it’s really, it is rough, but it leaves you vulnerable.
Focus Group 1, Participant 4
Concerns were expressed about drink spiking, risks of child sexual exploitation and crimes that do not get reported to the police:
… people will either wilfully get them drunk, so they’ll have their drink spiked and they’re taken advantage of and they wake up not knowing what happened and gradually realisation kicks in. Half of them don’t tell anybody, doesn’t get reported to the police, and there are actually groups of people who will target young ladies of the ages of 13 upwards in that situation.
Focus Group 1, Participant 6
As alcohol misuse becomes more visible in the community, participants spoke of how communities break down further: ‘once you’ve destroyed a community it’s difficult to rebuild it’ (Focus Group 1, Participant 1). Having a lost sense of purpose was identified as a factor compounding a cyclical nature to community breakdown:
… people have lost respect for themselves and in having no respect for themselves they’re doing the drinking, they’re doing the drugs to try and find a reason for being. Because a lot of them can’t get jobs, can’t get into work, they’ve lost the sense of being.
Focus Group 1, Participant 4
Increasing accessibility
All three focus group discussions recognised the changing nature of alcohol availability:
You can get alcohol everywhere now … whereas now supermarkets, so it’s much more accessible. So even if you weren’t thinking about it, say if you had an issue with alcohol, you were to go to the supermarket, there’s the alcohol.
Focus Group 2, Participant 5
Accessibility was also defined by its affordability and cheap prices:
You can go to [name of supermarket] now and buy a case of 24 for £11–12, is it? People just stay in now, don’t they? They don’t bother going out.
Focus Group 3, Participant 2
One participant further suggested that areas of deprivation were targeted by the alcohol industry to increase outlet density at the same time as lowering prices:
That’s what the cheap alcohol is all about, and it’s on every corner. It’s difficult to see that in more affluent areas, you wouldn’t go down and see that because it’s just … it’s demographics. They see depravity (sic) appear, so they say, ‘Right, we can approach them and give them what they want at a cheaper price’, and that’s where it gets people.
Focus Group 3, Participant 2
Theme 2: felt needs of the community
Regulation
Some participants perceived larger supermarkets to sell alcohol legally and responsibly but felt more regulation was needed for smaller independent premises:
The supermarkets are brilliant at controlling it, but the smaller shopkeepers, they’re not just selling alcohol at stupid o’clock in the morning, they’re selling drugs over the counter.
Focus Group 1, Participant 3
On-licensed premises, such as pubs, were seen to be more responsible and less profit-driven in comparison to off-licensed premises:
The businesses will still sell to them, therefore contributing to the problem, instead of saying, in a pub, if you were kicking off, they’d go, ‘Right, no more, you’re not having it’. Shops don’t do that; they will willingly sell to anyone because they’re a business and they need to make profit.
Focus Group 3, Participant 1
A small number of participants demonstrated awareness of the licensing procedures required to notify the public when a new premises licence application is submitted:
When you apply to open a … I don’t know, [name of off-licence chain] or whatever, the Council is supposed to put it in writing, that’s why you see it on lamp posts and things … But it’s also, in certain cases, in the paper as well, isn’t it?.
Focus Group 3, Participant 2
However, the meaningfulness of the required approaches to advertising applications to the public was doubted:
Have you looked at the public notices of kind of licences and seen who’s applying for licences? It’s actually has no one ever … you’d think it’s in the Advertiser or whatever …
Focus Group 2, Participant 1
Problems paired with drug use
In Focus Group 1 and Focus Group 2 (Area 1), the felt needs of the community predominantly centred around the prevalence of both alcohol and other drug use and concerns for young people.
Youngsters on parks that are passing things round and the, obviously they’re mixing it with other things, it’s not always just about alcohol. We’ve got a number of dealers that live nearby, there’s parks where you’ve got empty cans. And some people are just throwing them out the cars as they drive by. And I just think, what do you have to do to get these people to just respect the area around them and where people live?
Focus Group 1, Participant 3
Accessibility to other drugs was also seen to be a factor:
I think there’s been a shift … I can remember talking about it when I grew up, access to drugs was far more difficult. I think now you can go anywhere. So I think there’s the kind of alcohol and drugs as a combination and it’s a lifestyle choice.
Focus Group 2, Participant 3
Combining stimulant drugs such as cocaine when going out was perceived to be the norm:
I spoke to a young guy yesterday, he’s 19 years old and he hasn’t been going out and he literally said to me every single person when he goes out is using coke. And I find that quite shocking because it’s so readily available and it’s an expensive drug.
Focus Group 2, Participant 1
Help seeking
Focus Group 3 particularly felt there was a need for an AHC role to act as a bridge, exchanging helpful information about alcohol licensing between authorities and the community:
I definitely think there should be somebody you can go to and say, ‘Look, this is going wrong, is there anything you can do about it?’ Or, ‘Can we change this?’ And somebody needs to be in that role, to go to whoever the hierarchy are and say, ‘Look, we’re getting complaints’, or, ‘You’re being complemented on what you’re doing’, blah blah. And have a say within that community.
Focus Group 3, Participant 2
One proposal was for an AHC to act as a middle person:
It’s just a way of getting the community to actually relate to the Council and vice versa, but using that spokesperson, that middleman or whatever, it would just be easier, wouldn’t it?
Focus Group 3, Participant 5
Having AHCs have a watchful eye over the community was also valued:
… they would be almost like your local community guardian, going around checking if everything is okay within the area, yeah.
Focus Group 3, Participant 6
However, concerns were expressed about potential repercussions for a community member having such an advocacy role:
If you’re stood behind a 13-year-old who’s getting beer, you’re not going to be the one that turns around and says, ‘He’s 13’, because all his mates outside are going to jump you on the way out, or you just don’t know what the consequences are going to be. So, even though it’s a community responsibility, we don’t feel like, as a community, we can be responsible. Which is hard.
Focus Group 3, Participant 1
Perceived negative consequences of an AHC getting involved in licensing were not only associated with young people’s reactions but the wider community:
That would be good in an ideal world, but they would be targeted then, I think, somebody like that. They would get targeted by youths, by people who were drinking and coming out of pubs … If I closed that down, stuff like that, I would be a wanted man.
Focus Group 3, Participant 5
In terms of alcohol brief advice and information seeking, ‘othering’ was evident in the language, stereotyping those who needed help as ‘alcoholics’ or people with addiction now in recovery. Poor responses were described from local services, particularly for people with multiple coexisting issues:
I’ve got friends in recovery who, and friends who aren’t in recovery who need recovery and they’re meeting that same problem. So they go for help with the mental health and they’re just getting shoved away because of drug and alcohol addiction.
Focus Group 1, Participant 2
Another concern was the configuration of community services and stereotyping people who would benefit from structured alcohol treatment:
So for example I’ve got another friend who’s just come into recovery who was a terrible binge drinker, she would cause havoc all the time when she’d had a drink and she did go to [name of service] several years ago and they said because she wasn’t drinking every day, she wasn’t an alcoholic. So that gave her the green light then to go out, be a nuisance, carry on drinking until the point that she’s almost nearly killed herself.
Focus Group 1, Participant 2
Participants valued the informal, brief advice aspect of the AHC role, not just to provide information, signpost, but also to act as a listening ear:
It is that gap that needs to be bridged because there’s so many people who are looking for help but they’ve no idea where to go for it. And how to access it. And so having those alcohol champions visible in places.
Focus Group 1, Participant 2
One participant knew one of the local AHCs as a friend and highlighted some of the positive changes they had seen in them:
… one of my closest friends is actually now an alcohol champion and what it’s done for her and her perspective and being able to make her see and realise was absolutely amazing in 12 months she went from walking with her head down like that and not making eye contact with anybody, to like this and being able to look you straight in the eye and talk to everybody. Because she’s now aware of things that are going on and how to cope with things that she wasn’t aware of before.
Focus Group 1, Participant 4
Chapter 5 Economic evaluation results
The CBA adopted in this study is a valuable tool for understanding the value for money of CICA and investigating whether extra benefits arise from the outweigh costs of its implementation in GM, UK.
Set-up and running costs of Communities in Charge of Alcohol intervention
The total cost to implement CICA, including the optimism bias, was £115,065. Most of the cost was incurred to design and implement the first-generation training activities (£76,050; 66%), followed by the second-generation training (£21,374; 19%), AHCs (£9416; 8%) and project management (£8225; 7%). Analysing each cost element, the training design and delivery and the development of the training package (in the first-generation training component) were the main cost drivers of the intervention (50% of the total costs). The cost to deliver the training was £40,392 or 35% of the total cost. The cost of the design and development of training package was £17,136 or 15% of the total costs. A third cost driver of CICA was time and revenue in all cost components, reaching £37,291 in total, that is 32% of the total cost. The total capital and revenue costs were similar and summed at £58,446 (52%) and £50,806 (44%), respectively (see Table 28). Figure 13 shows all activities included in each cost domain and the types of costs incurred.
| Cost | Type of cost | Total | Optimism bias (%) | Total cost |
|---|---|---|---|---|
| Project management | ||||
| Time | Revenue | 6713 | 10 | 7383 |
| Transportation | Revenue | 765 | 10 | 842 |
| Total 1 | 7478 | 8225 | ||
| First-generation training | ||||
| Design and development of training package | Capital | 16,800 | 2 | 17,136 |
| Training delivery | Capital | 39,600 | 2 | 40,392 |
| Qualification and assessment fees | Revenue | 1200 | 5 | 1260 |
| Travel and venue | Revenue | 3408 | 5 | 3579 |
| Advertising, stationery | Revenue | 220 | 5 | 231 |
| Time | Revenue | 12,811 | 5 | 13,452 |
| Total 2 | 74,039 | 76,050 | ||
| Second-generation training | ||||
| Qualification and assessment fees | Revenue | 1385 | 5 | 1454 |
| Accreditation fee | Capital | 900 | 2 | 918 |
| Room hire | Revenue | 963 | 5 | 1011 |
| Photocopy | Revenue | 264 | 5 | 277 |
| Travel | Revenue | 737 | 5 | 774 |
| Catering | Revenue | 470 | 5 | 484 |
| Time | Revenue | 15,672 | 5 | 16,456 |
| Total 3 | 20,390 | 21,374 | ||
| AHCs activities | ||||
| Engagement materials | Revenue | 3424 | 5 | 3595 |
| Time | In kind | 5292 | 10 | 5821 |
| Total 4 | 8716 | 9416 | ||
| Total | 110,623 | 115,065 | ||
FIGURE 13.
Set-up and running costs of CICA intervention.
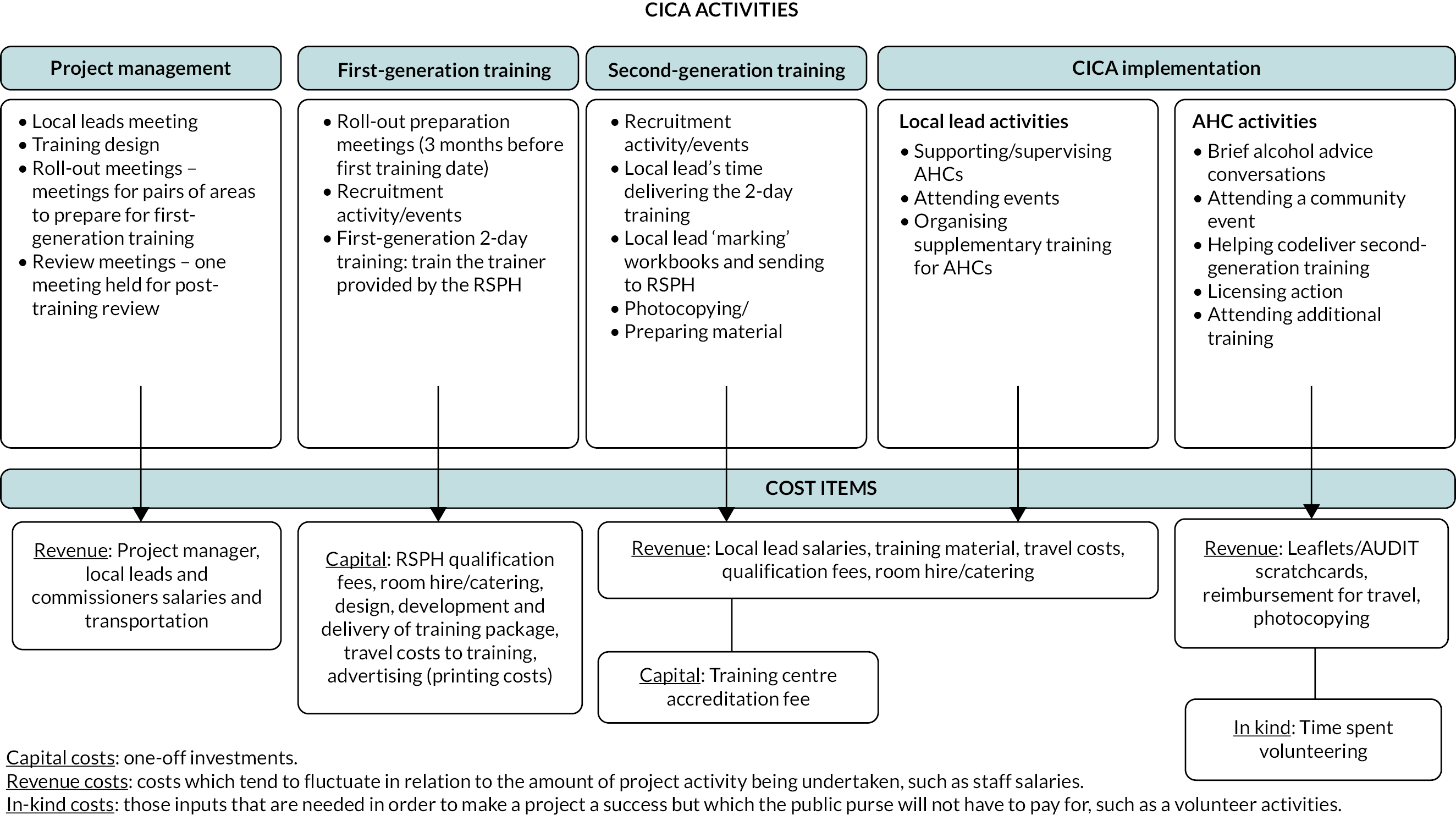
Effectiveness results
In CICA implementation areas, there was an increase of 2% in ambulance calls, whereas, in the control areas, the percentage increased by 11% during the weekends. The weekday figures were similar, with an increment of 2% in CICA areas and 10% in the control areas. The reduction of ASB was identical in CICA and non-CICA regions, 22% and 23%, respectively. We could not find any other significant impact for the rest of the outcomes. Due to the small effect of the intervention on the outcomes included in the analysis, CICA did not present economic or social benefits in GM. CICA had a negative overall financial return on investment (−1.66) and negative public value return on investment (−4.68). There was no fiscal return on investment for the local authority. Table 29 shows the cost–benefit results for the financial and economic cases and local authority.
| Financial case (fiscal CBA) | Financial year (£) | NPV (£) | |||
| 2019–20 | 2043–44 | ||||
| Actual costs | Costs | 115,074.13 | – | ||
| Benefits | −190,740.02 | – | |||
| Discounted costs | Costs | 115,074.13 | – | 115,074.13 | |
| Benefits | −190,740.02 | - | −190,740.02 | ||
| 0 | 0 | 305,814.14 | Net present budget impact | ||
| −1.66 | Overall financial return on investment | ||||
| – | Payback period (years) | ||||
| Economic case (public value CBA) | Financial year | NPV | |||
| 2019–20 | 2043–44 | ||||
| Actual costs | Costs | 115,074.13 | – | ||
| Benefits | −539,079.65 | – | |||
| Discounted costs | Costs | 115,074.13 | – | 115,074.13 | |
| Benefits | −539,079.65 | – | −539,079.65 | ||
| −654,153.77 | Net present public value | ||||
| −2.14 | Public value for money BCR | ||||
| −4.68 | Public value return on investment | ||||
| Local authority | Financial year | Net present value (NPV) | |||
| 2019–20 | 2043–44 | ||||
| Actual costs | Costs | 115,074.13 | – | ||
| Benefits | −232.06 | – | |||
| Discounted costs | Costs | 115,074.13 | – | 115,074.13 | |
| Benefits | −232.06 | – | −232.06 | ||
| 0.00 | Local authority fiscal return on investment | ||||
| – | Payback period (years) | ||||
Chapter 6 Discussion
Overview
Communities in Charge of Alcohol introduced the first alcohol-focused champion role of its kind in 2017 as part of the delivery plan for the GM Alcohol Strategy 2014–17. Developing a dedicated community lay health champion role – an AHC – to reduce alcohol harm at a hyperlocal level across all 10 city region local authorities provided an opportunity to evaluate CICA as a natural experiment. It was critical that an evaluation on this scale and nature occurred, as it presented an important opportunity for evaluating a multicomponent, community-centred public health intervention.
Our research project aimed to evaluate the effectiveness, cost–benefits and cost– consequences of implementing the CICA programme and understand the context and factors that enabled or hindered the intervention. Mixed-methods process evaluation data demonstrated that, among individual AHCs trained, there was significant activity, with local co-ordinators recording hundreds of occasions of brief advice given and qualitative accounts of life-changing conversations. However, we also found that there were significant challenges to setting up and maintaining the intervention: only around a third of the hoped-for number of champions were trained in nine areas, and over two-thirds of those trained were inactive after 12 months. The ambition to empower local people to get involved in licensing decisions to change the alcohol risk environment was not realised.
Given that the ‘dose’ of the intervention was dilute, it was unsurprising that the quantitative outcome analysis, which made use of area-level data, showed no consistent significant effect on rates of health and crime indicators. Consequently, the cost evaluation did not show CICA to be cost-effective.
Discussion of the outcome analysis
The results of the quantitative evaluation of the CICA intervention do not indicate any measurable impact on alcohol-related hospital admissions, A&E admissions or ambulance call-outs to the area, nor on reported crimes or reported ASB incidents specifically as a result of the CICA intervention. Local AHCs as an intervention to engage communities in brief advice and statutory processes to affect alcohol availability in their local area have to date not been implemented elsewhere, so these results cannot be directly compared with results from other evaluations. However, there are a couple of observations that we can make.
Given the type of intervention, which is relatively low key in terms of direct impact, we had hypothesised that likely impacts on hard public health outcomes such as those included in this study (in contrast to softer, more difficult-to-measure outcomes such as impacts on the ‘experience’ of the neighbourhood, feelings of belonging to a community and feelings of safety, for example) were always going to be small at best, particularly with respect to the relatively short time period of up to 3 years from the implementation start date of the programme, in which it would have been difficult to fundamentally change the alcohol environment of a community. Theoretically, once the initial group of local alcohol champions starts engaging with the licensing regime in an area and starts engaging the wider community in this, and if training of additional champions in subsequent rounds were to commence, this could lead to measurable change in the outcomes in this evaluation within several years. However, these findings show that it may be unrealistic to expect this within the confines of the current evaluation.
The data set, both in terms of length of post-intervention period and number of areas included, might just not have been sufficiently large to pick up smaller effects. However, while increasing the sample size may have given us more power to detect smaller effects, such small effects may have been meaningless in terms of making a practical impact.
Where there were statistically significant effects, with the exception of ambulance call-outs and ASB incidence (for most models), these indicated an increase in incidence of these harmful outcomes rather than a decrease following the intervention. Possible explanations are that they are either (1) artefacts in the data where reporting went up significantly nearer the end of the time period in this study, and/or (2) these result from the non-random allocation of the CICA intervention, whereby the intervention was allocated to particular geographical areas where there were concerns over high rates of alcohol harm. If CICA had no effect on these selected outcomes, it is plausible that alcohol-related hospital admissions and crimes increased more in problem areas than in comparable other areas. We attempted it to minimise this bias by matching to comparable control areas, but this might not have been sufficient.
It might have been predicted that, of the two main activities undertaken by AHCs (involvement in licensing and brief advice conversations), the licensing activity would have had greater potential to have a bigger impact on area-level outcomes. Therefore, the finding from the process evaluation, that even after increasing community capacity to influence alcohol availability decision-making at a local level, communities did not engage with statutory processes to affect alcohol availability in their local area is congruent with the null finding in the quantitative analysis. There was initial enthusiasm and confidence expressed post training by AHCs to get involved in alcohol licensing action. However, the licensing context at baseline highlighted that the scope to strengthen restrictions for existing licensed premises at a hyperlocal level varied, with the number of premises licensed to sell or supply alcohol in the target areas ranging from 0 to 59. This variation was consistent with data (where available) on the number of new alcohol licensing applications submitted to the local authority, comparing the 12-month period pre-CICA with the 12-month intervention period during CICA. Alcohol health champions were further limited in putting their training into practice if there were few (or no) new applications to increase the density of licensed premises in the area. Other formal metrics, such as the number of licensing issues positively reported to RAs resulting in a recorded crime or incident of ASB, were unknown.
It was challenging to recruit and retain sufficient volunteers in a specific, small area/community, with the most active areas training 17 champions in the first 12 months. While adjoining LSOAs provided a geographical unit of study for the outcome analysis, this limited the ability to build a groundswell of health assets. Stakeholders, including licensing officers, felt that extending CICA training and CICA activity to a local authority level may provide greater opportunities to mobilise community members in areas where there are higher numbers of licensed premises. As previously noted, in some chosen LSOAs there was little or no opportunity to get involved in alcohol licensing, suggesting the criteria used to select the target areas were not always aligned to the programme’s objectives. However, more than two-thirds of volunteers had become inactive at 12 months, and interviews with local co-ordinators and AHCs indicated that they found licensing processes complex and were reluctant to get involved in licensing action. We also observed, in the documentation review of local alcohol policies, that policies were orientated to support the needs and interests of the applicant, rather than towards persons wishing to raise a concern. This suggests that even with more time and more volunteers, an impact on the health and crime outcomes of this evaluation might not have been conceivable.
Discussion of the process analysis
We assessed the process over four phases: pre-implementation, initial implementation, during the intervention and follow-up. Our aim at the pre-implementation/roll-out phase was to identify the infrastructure at baseline. Existing evaluations have recognised the importance of a supportive infrastructure when implementing new community health champion programmes, but more research is needed to explore what aspects positively influence process indicators such as recruitment, training numbers and retention.
Multicomponent public health interventions such as CICA have interacting individual and community components, influenced by and interacting with contextual factors; they are complex interventions. 124 In terms of degrees of task difficulty, the CICA intervention (as described in ‘intervention description’ in the Methods section) required local co-ordination and project management, continuous volunteer recruitment, support and supervision. The cascade model of AHC training required the organisation of both Train-the-Trainer and delivery of cascade training events. RSPH candidate workbooks required assessment and external verification in order to award volunteers with the Level 2 qualification ‘Understanding Alcohol Misuse’. Licensing officers who may or may not have experience training lay people were expected to codeliver an ‘introduction to alcohol licensing’ at both Train-the-Trainer and cascade training events. The number of organisations involved in the implementation of CICA (RSPH, commissioning teams, service providers and wider stakeholders in the intervention area) led to inherent complexity, as were the fixed procedures required when setting up RSPH-accredited cascade training. While the co-ordination, recruitment, training format, support and supervision of AHCs could be tailored flexibly to the local context in each CICA intervention area, the formal procedures available for members of the public (and therefore AHCs) to influence licensing decisions were fixed within the statutory processes prescribed within the 2003 Act.
In the pre-implementation phase, we identified significant variation between areas in terms of the infrastructure in place to deliver the CICA intervention. For example, some areas struggled to identify a suitable professional to support and co-ordinate at the local level. Ultimately, those areas that had more of the infrastructure were able to train more volunteers. Also in pre-implementation phase, we attempted to measure a baseline composite score of alcohol availability, which was to be based on hours of sale, size of premises (on licensed premises only) and number of premises. Theoretically, this information should have been available to extract from licensing registers. However, in practice, the only variable that could be consistently obtained was the overall number of premises. The lack of structured data and inconsistency in data management systems used means that it is not possible to get an overall picture of alcohol supply in an area, and this hinders the ability to work out which areas have high (or increasing) density and hinders the ability to evaluate outcomes of licensing interventions. However, since AHCs did not tend to take action in the area of licensing, the lack of this process indicator did not affect the conclusions of this study.
Results from the initial implementation phase demonstrated that some AHCs were confident in providing alcohol advice to family members, friends and strangers in their communities. In contrast, a lack of confidence in raising alcohol as a topic is commonly reported as a barrier by health and community-based professionals,26 despite ASBIs continuing to be a WHO ‘best buy’ to reduce hazardous and harmful drinking in primary care. 125 This suggests that lay people with this skill and confidence could be a significant asset for a community, though fidelity as a behaviour change intervention was unknown. In order to perform this role, AHCs required significant support, and universally, local co-ordinators described a high level of personal involvement, which they had not anticipated, to meet the needs of the programme. They noted two-thirds of the AHCs had disengaged at 12 months, and this low engagement may have been attributable to low acceptability of the CICA intervention, both while participating (concurrent acceptability) and afterwards (retrospective acceptability),126 as evidenced further by their lack of participation in any follow-up interviews. The burden of activity for newly trained AHCs included not just putting into practice opportunistic brief advice conversations and getting involved in licensing action, but also helping with wider recruitment and cascade training.
Evaluation at the initial phase of the intervention also revealed that the time taken to establish such an intervention had been underestimated: commissioners and providers seeking to develop assets-based approaches need time to establish confidence and networks within local communities in order to develop a partnership-based approach prior to intervention implementation. Recruitment was challenging, and co-ordinators struggled to ‘sell’ CICA as a product, and despite successfully securing volunteers to attend a 2-day course, individual participants may not have known exactly what they had signed up to. Local co-ordinators celebrated the social value gained by AHCs through gaining new experiences, accreditation and improved confidence. However, these personal successes added to AHC attrition as some subsequently took up employment within 3 months of training, leaving them with insufficient time for the role. Additionally, consistent with previous findings,127 the extent of strategic and political support at a local area level impacted on the success of this phase of implementation. In fact, in one area, despite an original commitment, the intervention was not established.
From a licensing perspective, links between LA licensing teams and AHCs needed to be built from a low level. There were several barriers to AHCs and the community getting involved in the licensing process, including the complexity of training content delivered within a half-day session, its dilution in cascade training as noted in training observations, ‘applicant-centred’ statements of licensing policy and processes, a limited number of licensed premises in the target areas and fear of reprisals. Importantly, licensing leads reported that despite the commitment to promote community involvement in licensing decisions in the 2003 Licensing Act, there were no resources allocated to make it happen. Taking part in CICA highlighted to licensing officers the limited capacity, they had to commit to regular training sessions for the public and to be a source of ongoing support for AHCs. Further concerns were raised around the administrative resources needed if the ambition of CICA was realised, with more reports of issues, complaints and representations to be processed.
A reoccurring theme from the different strands and time points of the process evaluation was a misperception that the CICA brief advice component of the intervention was (or should be) a tertiary intervention, focused on people who had developed a dependence on alcohol. There was a tendency to assume that alcohol harm was something that happened to ‘others’. This came from the co-ordinators in some areas (some of whom recruited from the recovery community, who in turn were motivated to help those like them), the AHCs themselves and also from the community focus groups. This was in contrast to the original theory that brief advice might be most effective in the majority of drinkers as a secondary prevention intervention, that is those who were drinking at increasing or higher risk levels and were not alcohol dependent. Although direct observations to assess intervention fidelity were not possible due to the opportunistic nature of brief conversations, interview findings suggest that this shift may not have necessarily been intervention drift but instead, an innovative adaptation to fit the presenting needs of their community to aid access to community alcohol treatment services. 128
Future iterations of a programme such as CICA would need to take into account this tendency to ‘other’ the issue of alcohol. Indeed, at the outset, we created a ‘dark logic model’ (see Appendix 5),1 which mapped potential unintended consequences. One of these was ‘opportunity harm: missed opportunities to reach at risk groups’. The tendency to focus away from those drinking at just above risky levels was an opportunity harm. These opportunity harms can also lead to direct harms, including potential time delays for at-risk populations. We also identified, a priori,1 that it was feasible that CICA could cause direct harm to those AHCs who were in recovery. While we had some evidence that a few champions were still managing their own alcohol recovery journeys, which caused them personal issues, there was no evidence that these issues were caused directly by participating in CICA.
Discussion of the economic analysis
The economic evaluation followed the quantitative data analysis findings which show no economic and social benefit of CICA on health (alcohol-related hospital admissions, A&E admissions, ambulance call-outs) and non-health outcomes (crimes and ASB).
So far, no economic evaluation has determined the value for money of a complex community-based intervention such as CICA adopting the same outcomes and methodological approach. The cost analysis shows that the main cost driver of CICA was the first-generation training. This is because it includes costs associated with the design and development of the training package (£17,136; 15% of the total costs), which would not be necessary in the case of scale-up of the intervention. In terms of benefits, our results indicate that CICA reduced the likelihood of ambulance calls. However, the intervention areas still presented an increase of 2% in ambulance calls which was smaller than the control areas, where a 10% increase was detected. All other outcomes had similar results in the intervention and control areas.
The current evidence from economic evaluations shows ambiguous results. Some studies have shown a good value for money of community-based interventions in reducing specific health and non-health outcomes; others have shown no significant impact. For example, a well-implemented community action programme targeting on-licensed premises in Stockholm reported a reduction in police-recorded violent crime, and violent crime permeated wider to neighbouring areas. 129 The programme was cost-effective, saving €39 for every €1 invested, and demonstrated a large-scale roll-out, suggesting the intervention is highly feasible. Like CICA, this Stockholm intervention involved community mobilisation to raise awareness of alcohol harm in the community; however Responsible Beverage Service training was delivered to bar servers rather than training to empower community members. Unlike CICA, community mobilisation was supported by strengthened enforcement of alcohol laws, and the violence outcome was analysed through a survey among victims of violence.
A multisectoral economic evaluation130 analysed the value for money of delivering different intensities of a brief intervention by comparing a client information leaflet (CIL), with brief advice, and brief lifestyle counselling. This case study focused on the probation arm of the larger Screening and Intervention Programme for Sensible Drinking (SIPS) in England. The multisectoral economic evaluation was an extension of the ‘impact inventory’ developed by the Second Panel on Cost-Effectiveness in Health and Medicine131 and evaluated the interventions from the perspectives of health and criminal justice sectors. From the criminal justice perspective within the SIPS case study, brief lifestyle counselling reduced crime and costs to the criminal justice system compared to a CIL. In addition, brief lifestyle counselling resulted in a more significant reduction in avoided reconvictions and cost savings compared with a CIL. In the healthcare system sector, brief lifestyle counselling reduced quality-adjusted life-years losses to the victims and the associated healthcare costs. This is a comprehensive economic evaluation as it analysed the cost-effectiveness for two different sectors separately. The CICA economic evaluation also involved different sectors of society (e.g. health, justice, local authority). Still, the cost–benefit analysis and CCA do not provide the results disaggregated by sector. In CICA, AHCs were trained to provide CILs and brief advice, but not brief lifestyle counselling.
In contrast, a review of evidence on the effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol found that community-based interventions, such as mass-media awareness campaigns, are not expensive [implementation cost expressed in international dollars(I$) I$0.20–0.80 per year per person]. 132 However, these interventions do not significantly affect consumption levels or health outcomes. The studies mentioned above have important differences from CICA in terms of their methodological approach to economic evaluation, population and interventions. So, our results are not directly comparable to other studies.
Strengths of the study
The quantitative evaluation of the CICA programme has several strengths. The data set was relatively large and should have been able to detect relatively small impacts on any of the outcomes, if these exist. The researchers had some influence on the time point of when the intervention would be implemented in each of the areas; this was randomised by the researchers and broadly followed which is likely to have minimised bias of areas considered to be most ‘at risk’ being implemented first, for example. A particular strength of this evaluation was the parallel evaluation of the same intervention using four different evaluation designs and three different analytic methods, each with its own strengths and limitations. This methodological triangulation was one of the recommendations to improve natural experiment evaluations. 60 We believe this approach guarded against incorrect inferences that would have likely occurred had we relied on only one of the evaluation designs or analytic methods.
The quantitative outcome evaluation was backed up by a robust process evaluation using mixed methods, which was able to glean significant insight into the barriers and facilitators to establishing an AHC intervention. Findings will also be useful to inform other asset-based community interventions. The process evaluation data were useful to describe the ‘dose’ of the intervention, from which we are able to conclude that the null findings from the outcomes evaluation may not be as a result of the intervention not working but rather that the dose may have been too dilute.
This study adopted a robust economic evaluation approach recommended by the GM local authority. Costs were collected by using a bottom-up approach and corrected by using the optimism bias which gives more accuracy to the cost estimates.
Limitations of the study
This evaluation also had several limitations. Unfortunately, we were not able to obtain all data for all comparisons, and, as a result, comparisons to national controls could not be done for ambulance call-outs and incidence of reported crimes. Although the researchers were able to influence the time when the implementation of the intervention started in each area, they had no influence on the selection of the intervention areas itself. These areas were selected by the respected councils based on considerations of alcohol-related harms to the area, and, as a result, this allocation of the intervention could not be considered as an as-if random process. 60 This is likely to have impacted on the evaluations, and the observation that several of the impact estimates indicated an increase in harms on health and on crime instead of reductions suggest that some bias is likely to have been present despite the successful matching of the local and national control areas to the interventions using propensity scores. Although data sets were large, the number of events recorded per LSOA per month was small for some outcomes. Aggregation over time or over geography could have improved this but would have resulted in analyses that were less specific to the intervention areas and less accurate over time. Although we included both sensitivity analyses and exhaustive methodological triangulation, these were done on a data set on which the information was obtained from the same source (although these differed for each outcome) using the same data generation methodology. If there is some bias resulting from this, it would have been present in all of our analyses, and it is therefore recommended to (also) conduct triangulation of results using different data sets from different sources and using different data generation methods. 61 This evaluation would have benefitted from such additional data, but unfortunately, we were not able to obtain these for this study.
Limitations of the process evaluation included under-recruitment to follow-up interviews with volunteers and focus groups that only representing two areas. Due to the low numbers of alcohol champions remaining engaged in the intervention, the sample size for follow-up was small. Furthermore, we were not able to get the direct views of those champions who had disengaged from the programme. While difficult to do, this could have generated useful information. However, local co-ordinators were well represented in the interviews, and as a result of their regular contact and supervision of champions, they were able to offer good insight into what the champions were experiencing and, for those who dropped out, reasons why they had disengaged.
There were further limitations to monitoring brief advice activity through direct observations because of the risk of Hawthorne effects; therefore, we were unable to assess the competency of AHCs and the fidelity of their conversations to behaviour change techniques. Nor was it possible to talk to any recipients of brief advice in the context of a brief, opportunistic conversation. Diaries were developed in response to this and were used by AHCs across seven areas. Furthermore, the philosophy behind the CICA intervention (asset-based community development) aimed to give champions the skills, confidence and support to utilise them as they saw fit within their community. While some local co-ordinators attempted to count the number of conversations and events each quarter, commissioners did not impose or expect a specified amount of activity from each champion. Since this process activity data were not collected consistently across areas, it was not possible to correlate process activity with the primary outcome data.
Economic evaluation of complex public health interventions may require broader methodological approaches to capture health and non-health costs and benefits and direct and indirect impacts of the interventions. A multisectoral economic evaluation approach would be valuable to determine the value for money of CICA-like interventions from different stakeholders and sectors in the society.
Equality, diversity and inclusion
Participant representation
In terms of protected characteristics,133 we used pre-training questionnaires to capture demographic data. Representation from ethnic minority groups was as follows: 3.2% identified as Asian/Asian British, and 4.3% identified as black/African/Caribbean/Black British. However, no response was provided to the ethnicity monitoring question by 22.6% of participants (n = 21), despite other demographic details being completed within the same form. Maximising participation of ethnic minority communities in research needs to start at the application stage134 and include ethnic minority PPI representation.
A wide age range of participants aged between 18 and 65+ attended (48% aged between 41 and 60). Slightly more women became AHCs compared to men (61%), though representation from transgender communities was unknown. Sexual orientation was not monitored, making the proportion of heterosexual/straight, gay or lesbian, and bisexual participants unknown. We reflected on the gaps in our demographic data collection and the importance of designing research instruments that follow best practices in relation to sexual orientation and trans monitoring. 135
In terms of resources used within the intervention to gain the RSPH Level 2 qualification, participants were required to complete candidate workbooks. It became apparent at the start of the first roll-out training event that participants experienced the learning material as very intense over the 2 days, and writing answers in workbooks was challenging for some who had been out of education or work for some time. The RSPH trainer (at first-generation training events) and local co-ordinators (at cascade training) addressed this by providing reasonable adjustments and support for candidates who expressed concerns about reading and writing, especially at a fast pace. Our pre-training questionnaires indicated that educational qualifications varied, with 9.7% reporting having no qualifications and nearly half (49.5%) having either GCSE/NVQ Level 2 (national qualifications typically taken at age 16) or A Level/NVQ Level 3 qualifications.
Communities in Charge of Alcohol interventions were targeted in communities whose common interest was a shared geographical area where they lived or worked. All areas had high levels of deprivation. While alcohol harm is experienced by all sections of society, research has identified an alcohol-harm paradox whereby people of low socioeconomic status experience greater harm than those of high socioeconomic status, despite drinking the same amount of alcohol or less. 12 Since CICA recruited people directly from communities at a LSOA level, we believe its ABCD design helped ensure that participants, albeit lower than expected numbers, were representative of socioeconomic inclusion groups.
Public involvement in Communities in Charge of Alcohol
Aim of public involvement in the Communities in Charge of Alcohol study
Our strategy for PPI was to actively involve public representatives in all stages of our research, from design to data collection, interpretation and pathways to impact. The GRIPP2 short form has been used here to describe our PPI activities as a tool to improve the quality, transparency and consistency of the international PPI evidence base. 136
The ‘public’ was defined as anyone directly or indirectly affected by alcohol use, its sale or its supply or another person’s drinking. Experts by experience (Alcohol Concern, 2017) included the public, service providers, service users, commissioners and licensing officers/RAs working within or representing the communities chosen as intervention case areas.
Methods used for public involvement
In the design and application stage of CICA, Principal Investigator (PAC) and Co-Investigator (EJB) carried out consultation meetings with public representatives from established community networks. A handout was created with a user-friendly project outline of the logic model. A lay representative, coinvestigator SH, was recruited from one of these community networks to be a co-applicant on the grant application and to represent the study team via membership in the SSC.
The CICA intervention had already been in the design stage at the time of the NIHR grant application. This was outside the influence of the research team. A steering group and ‘local leads’ meetings had been convened by Public Health England, attended by representatives from all 10 GM local authorities. Meetings were co-ordinated by staff from Public Health England who had responsibilities for health and well-being programme management in the North West of England. Face-to-face and teleconference meetings provided a forum for commissioners, service providers and practitioners to exchange ideas about the design of the research and particularly the process evaluation methods of CICA.
During the data collection phases of the study, our public representative (SH) directly participated in aspects of the process evaluation with the process evaluation (University of Salford) team. As a coinvestigator, SH attended monthly investigator meetings between 2017 and 2022 as well as SSC meetings between 2017 and 2021. SH cowrote the PPI sections of the NIHR Progress Reports.
In our pathway to impact plans, we directly recruited and involved AHCs, local co-ordinators and SH to contribute to the co-design of impact activity, the production of creative products and engagement events. A number of methods were used to invite experts with CICA experience to get involved, including storyboard consultation workshops, filming and speaking at engagement events.
Results of public involvement
The positive and negative outcomes of PPI in the study are reported around three key areas of activity: design and application feedback, data collection and pathways to impact.
Design and application feedback
A total of 13 public representatives from 4 different community networks contributed to the design and application stage of the CICA research in March to April 2016.
We met with volunteer health champions (n = 2) from a Level 1 Health Champion network who debated the feasibility of being able to raise alcohol as part of an informal conversation with family, friends and colleagues. This led us to add ‘organising/attending community awareness events’ as an additional secondary outcome measure within the process evaluation.
Forever Manchester, who co-ordinate volunteers involved in ABCD, challenged us on how ABCD theory fitted with our proposal (n = 1). This was because the CICA intervention started with an issue/deficit (alcohol harm) decided by the 10 GM local authorities and not a community’s strengths. This influenced our logic model by clarifying how existing strengths, motivations and skills need to be identified, mapped and recognised, but it also informed our dark logic model, as we hypothesised potential unintended ‘equity harms’.
The LGBT Foundation, which provides advice, support and information to lesbian, gay, bisexual and trans communities, co-ordinates a team of volunteers who patrol city centre areas to support people with issues during a night out. We met the Village Angels’ co-ordinator and one of the volunteers (n = 2), who suggested that people in recovery from alcohol dependence ‘find pride in a sense of recovery and can be highly motivated to volunteer’. Anticipating CICA areas may consider recruiting volunteers to the AHC role from local recovery communities further informed the development of our dark logic model, hypothesising potential unintended ‘opportunity harms’ or ‘direct harms’ that could arise.
Fallowfield Community Guardians are local residents who act on behalf of local residents to influence licensing regulation and enforcement in their area of South Manchester. A consultation meeting was held with six local residents and two local councillors (n = 8). They felt the research was relevant and needed but had a concern that the proposed quantitative outcome measures may not capture what matters to local residents and ‘would not be visible in the data’. They proposed that key performance of indicators of ASB should be measured in addition to reported crime to help address what residents are motivated by to reduce alcohol harm (passive drinking effects), for example, transient noise, litter and deliberate damage (tipping over bins). ASB was subsequently added as an outcome measure.
SH cowrote the plain language summary for our application and created a short video for use within CICA training: sharing her experience getting involved in licensing action and advocacy (reporting issues to local licensing officers) and licensing decisions (making representations against new premises licence applications).
Data collection
Our public representative SH additionally directly participated and was paid for her contribution to aspects of the qualitative research, including training observations as well as a document review of local licensing policies. SH attended Train-the-Trainer CICA events at the beginning of the sequential roll-out in September 2017 and at the end of May 2018. Data extraction was completed with EJB on 10 statements of licensing policy (one per local authority) between April 2019 and July 2019.
Pathways to impact
Three AHCs took part in a storyboarding event in March 2018 with the process evaluation (University of Salford) team along with SH. All were reimbursed for travel expenses, and lunch was provided. The second opportunity for PPI involvement invited AHCs to be part of the filming. Nine AHCs agreed to be filmed for the video, and all were given a voucher as a token of appreciation for their time. The resulting documentary benefitted from being designed by people directly involved in CICA and share their journeys as AHCs, from training to being active in their community, the success of the programme so far and success stories of individuals.
In that same year, November 2018, GM Health and Social Care Partnership launched the ‘Big Alcohol Conversation’ which involved public engagement with 80 local voluntary, community and social enterprise (VCSE) organisations and more than 5000 people. At the engagement launch event with GM’s Mayor Andy Burnham, AHCs spoke on stage about their motivation and experiences as an AHC and the role communities can have to prevent and reduce alcohol-related harm. The AHCs found the experience speaking on stage and having their photo taken with the Mayor of GM personally rewarding and validating to feel part of a high-profile public engagement campaign.
In October 2019, we held an Early Findings CICA Stakeholder Conference, attended by a cross-section of stakeholders, including AHCs. SH also attended the event. The presence of the champions made a positive impact on our project in a number of ways, especially assisting us to sense-check our early process evaluation findings. For example, one AHC told us that they recognised the anticipated mechanisms of action of CICA enacted in his local community at a local meeting he attended. We also heard how participating in the conference had a positive impact on another champion’s self-esteem. She described having never visited/attended a higher education setting before and how the invitation and participation on the day made AHCs feel validated. Two champions also contributed to the making of a new set of short films at the stakeholder event about local area-level impact.
In 2020, as plans to host and attend conferences were disrupted by COVID-19, plans for dissemination activity were adapted. One such activity resulted in the development of a ‘speedy drawing animation’ to promote CICA impact stories. When developing the speedy drawing animation, input was sought again from a sample of AHCs. They received a storyboard containing early ideas, asking for their comments about its accuracy and representativeness. One AHC commented:
The part of engaging advice and encouraging people to take part in AUDIT-C is greatly appreciated because this really helps the advisor to enlighten the person doing the AUDIT-C about where they are at with alcohol consumption and whether they are wanting to make some small changes to make a bigger difference to health and wellbeing.
Our PPI representative shared the positive impact of being actively involved in the CICA project and its research in local licensing activity and how it gave her increased knowledge about health harms from alcohol and extra credibility when participating in licensing objections.
Discussion and conclusions
Overall, PPI involvement had a number of positive effects at different stages of the CICA study. Our public involvement approach was effective in actively engaging public representatives in all stages of our research, from design to data collection, interpretation and pathways to impact. Attrition of volunteers meant that the perspectives of AHCs who contributed to PPI activities were likely to be biased towards those who had been active and invested in CICA.
Reflections/critical perspective of public involvement
A major tenet of community-centred approaches to health and well-being is the use of participatory methods to address and reduce inequalities in power. 40 Members of the public were not actively involved from the outset in the decisions about CICA, so they did not have a say in developing options and deciding together which communities might want to be ‘in charge of alcohol’ in their area. This was outside of researcher control, since the intervention had already been conceived by GM stakeholders and was well into the design process at the outset of this study. Since a CICA ‘community’ was predetermined as a small geographic unit of population, the study assumed people had a ‘shared stake’ in it as a place where they lived or worked, but this was not explored. The geographically imposed boundaries of CICA meant that it was also unknown to what extent communities of interest or identity may have wanted to get involved.
We reflected on differing levels of power sharing within community-centred approaches, opportunities for the public to define their own ‘community’ unit of population in PHR and identifying their own outcomes of interest. With true asset-based approaches, the community works together with the researcher to define the health issues and co-design the intervention. The intervention and the outcomes are not known from the outset. This makes it more difficult to specify the intervention (and therefore the evaluation methods) when applying for research funding. Such applications, which are short on detail on the intervention and the evaluation methods, are less attractive/higher risk for funders if priority is given to ‘robust’ quantitative designs with clearly specified interventions, logic models and evaluation methods.
There is a need to understand the differences between engaging members of the public to take part in a community-based research process compared to patients coming through the door of a clinical setting. Additionally, there is a need to explore the barriers and facilitators to encouraging members of the public from deprived communities to take part.
Chapter 7 Conclusion and future research
To our knowledge, CICA is the first alcohol-focused champion role of its kind to be investigated across multiple intervention sites. It is also the first evaluation of a health champion programme that uses methodological triangulation to strengthen inferences about effectiveness.
There was evidence that lay people trained as AHCs were able to have conversations with members of their communities who were consuming alcohol at higher risk levels, demonstrating a level of skill and confidence that can sometimes be absent in health professionals. AHCs, their co-ordinators and the public valued the role. However, significant infrastructure is needed to support an intervention such as CICA, and time is needed to develop and embed a group of volunteers.
Despite evidence (from the process evaluation) of some planned activity taking place at local level, we were not able to show that CICA was effective, nor was it cost-effective. There are likely to be two main reasons for this. Firstly, the number of champions trained was too small to generate an effect that is measurable at the area-level of analysis. Secondly, the AHCs were less willing (and had less opportunity) to get involved with alcohol licensing decisions. Since licensing policies have an impact at an area level, this theoretically would have been more likely to generate a significant area-level effect. The evidence from this study is that communities continue to struggle to influence statutory processes that affect alcohol availability where they live, and further consideration of how to resource increasing community engagement is necessary. Moreover, despite evidence demonstrating that ASBIs can have a moderate effect on consumption at an individual level, brief interventions may not have a direct effect on the selected primary outcomes at a population level.
Recommendations
The findings of this research have led to several recommendations to support effective implementation of a place-based health promotion utilising community assets:
-
Ensure all stakeholders have a clear understanding of the place-based ‘role’ being implemented, including its scope and purpose.
-
Ensure providers or commissioned services have clear understanding of their own role, anticipated outcomes and the skills and capacity to support inexperienced alcohol/health issue-focused volunteer groups.
-
Prepare the ground at community level, well in advance of a formal implementation period, to build community understanding, support and involvement to aid recruitment at the appropriate time.
-
Develop and resource a multipronged recruitment strategy utilising digital technologies, social media, community influencers, leaflets/posters and word-of-mouth.
-
Be prepared for a longer/sustained period of supporting new champions – especially since the aim is to target areas of high need where existing levels of confidence and literacy might be low.
In terms of AHC activities:
-
Focus the brief advice component of the intervention on the majority of people who use alcohol who are not alcohol dependent/in highest need. There needs to be a conscious effort to reiterate this during set-up, training and ongoing support.
-
Use a systems approach to consider the whole alcohol treatment system as part of the wider infrastructure of support, inclusive of population-based health promotion and prevention.
-
In order to intervene in licensing policy, consider an intervention at a wider scale, providing dedicated community licensing officers with adequate resources and capacity to deliver a training and support programme at a local authority level (average 180,000 population) to mobilise communities in areas where there are higher numbers of licensed premises.
-
Our research suggests that local licensing policy might benefit from a rebalance to become more community-centred, with the support of national policy to address fears of reprisal and setting out standards to increase the inclusivity and accessibility of statutory processes.
In terms of evaluation design:
-
Other natural experiment evaluations should include the kind of triangulation used in this evaluation to guard against overinterpretation of spurious results.
-
Given that the preferred activity of the AHCs was giving brief advice, it is likely that an area-level analysis would not be sensitive enough to measure any effect. Alternative study designs could be sought.
Additional information
Acknowledgements
The authors wish to thank and acknowledge all those who have been key to the implementation of CICA across Greater Manchester including Paul Duffy, Jan Hopkins, the alcohol health champions, local co-ordinators, licensing officers and the Royal Society for Public Health training team. We gratefully acknowledge the advice and support from the study steering group, chaired by Eileen Kaner (Brendan Collins, Andrew Simpkin, Harry Sumnall, Janet Harris, Donald Read and Maria Smolar).
Contributions of authors
Elizabeth J Burns (https://orcid.org/0000-0003-4611-9253) (Lecturer in Mental Health Nursing) prepared the first draft of this report, contributed to the evaluation design, the process evaluation and prepared the results for publication.
Frank de Vocht (https://orcid.org/0000-0003-3631-627X) (Professor in Epidemiology and Public Health) contributed to the evaluation design, generated the random order of sequence in the stepped-wedge design, conducted the outcome evaluation and prepared the results for publication.
Noemia Siqueira (https://orcid.org/0000-0003-0730-8561) (Health Economics Research Associate) conducted the economic evaluation and prepared the results for publication.
Cathy Ure (https://orcid.org/0000-0001-5021-1947) (Lecturer in Public Health) contributed to the process evaluation and prepared the results for publication.
Suzanne Audrey (https://orcid.org/0000-0002-8310-2672) (Senior Research Fellow in Public Health) contributed to the evaluation design, the process evaluation and prepared the results for publication.
Margaret Coffey (https://orcid.org/0000-0001-5837-5532) (Reader in Public Health) contributed to the evaluation design, the process evaluation and prepared the results for publication.
Susan Hare (https://orcid.org/0009-0005-5342-4207) (Fallowfield Community Guardian) contributed to the evaluation design, conducted the licensing policy document review and prepared the results for publication.
Suzy C Hargreaves (https://orcid.org/0000-0003-3240-8230) (Research Assistant) assisted with the process evaluation and prepared the early implementation phase results for publication.
Mira Hidajat (https://orcid.org/0000-0002-7252-9574) (Honorary Senior Research Associate in Epidemiology and Public Health) conducted the analysis of primary outcome measures and prepared the results for publication.
Steve Parrott (https://orcid.org/0000-0002-0165-1150) (Reader in Health Economics) contributed to the health economics evaluation design and prepared the results for publication.
Lauren Scott (https://orcid.org/0000-0003-3129-5123) (Senior Research Associate in Quantitative Research and Evidence Synthesis) contributed to the analysis of primary outcome measures and prepared the results for publication.
Penny A Cook (https://orcid.org/0000-0001-6435-8050) (Professor of Public Health) led the study design and the process evaluation, contributed to the analysis and prepared the results for publication.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/HTMN2101.
Primary conflicts of interest: All authors’ time conducting this research was partially or fully funded by the National Institute for Health and Care Research (NIHR) Public Health Research (PHR) programme. Frank de Vocht reports funding (to his institution) from National Institute for Health and Care Research (NIHR) Public Health Research (PHR) for time on other grants, membership in the NIHR Public Health Research Board and is partly funded by the NIHR Applied Research Collaboration West (ARC West). Frank de Vocht was a member of the PHR Prioritisation group, Efficacy and Mechanism Evaluation (EME) Strategy Advisory Committee, EME Funding Committee and EME Funding Committee Sub-Group Remit and Comp Check. Suzanne Audrey was a member of the National Institute for Health and Care Research (NIHR) Public Health Research (PHR) Funding Board.
Steve Parrott reports funding (to his institution) from Yorkshire Cancer Research and Medical Research Council (MRC) for time on other grants. Penny Cook reports funding (to her institution) from National Institute for Health and Care Research (NIHR) Research for Patient Benefit (RfPB), Medical Research Council (MRC) and Oglesby Charitable Trust for time on other grants. Greater Manchester Health and Social Care Partnership funded the initial Train-the-Trainer costs to set up the intervention, co-ordinated roll-out preparation and facilitated local co-ordinator network meetings. The Royal Society for Public Health delivered the Train-the-Trainer events but played no role in the data collection, data analyses or in the preparation of this report. All other authors declare that they have no competing interests.
Participating investigators
Kate Ardern (former Director of Public Health, Wigan Council) contributed to the intervention and study design and served as a scientific advisor in the drafting of work for publication and dissemination/pathway to impact plan.
Paul Duffy (former Health and Wellbeing Programme Manager, Public Health England North West) provided city region support to local commissioners and local co-ordinators in the design and planning phase of CICA.
Jan Hopkins (Programme Manager, Greater Manchester Health and Social Care Partnership) provided city region support to local commissioners and local co-ordinators in the pre-implementation phases and intervention phases of CICA.
Kiran Kenth (Director of National and Regional Programmes, Royal Society for Public Health) contributed to the design of the intervention and dissemination/pathway to impact plan.
Nadine Mirza (Research Assistant, University of Salford) participated in the analysis of the follow-up phase of the process evaluation.
David Ottiwell (Principal Researcher, Greater Manchester Combined Authority) provided a liaison role between the police and the CICA research team and served as a scientific advisor for the New Economy CBA tool.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review and if appropriate agreements are in place.
Ethics statement
All study procedures were in accordance with the 1964 Helsinki declarations and its later amendments, together with the British Psychological Society’s Ethical Procedures. Ethical approval was received from the University of Salford Research Ethics Committee on 17 May 17 (reference number: HSR1617–135) and obtained from the University of Bristol on 16 May 19 (reference number: 82762).
Information governance statement
NIHR-funded researchers are expected to handle all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Salford is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.salford.ac.uk/privacy.
Department of Health and Social Care disclaimer
This report presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Public Health Research programme or the Department of Health.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Cook PA, Hargreaves SC, Burns EJ, de Vocht F, Parrott S, Coffey M, et al. Communities in charge of alcohol (CICA): a protocol for a stepped-wedge randomised control trial of an alcohol health champions programme. BMC Public Health 2018;18(1):522. https://doi.org/10.1186/s12889-018-5410-0
McGrath M, Reynolds J, Smolar M, Hare S, Ogden M, Popay J, et al. Identifying opportunities for engaging the ‘community’ in local alcohol decision-making: a literature review and synthesis. Int J Drug Policy 2019;74:193–204. https://doi.org/10.1016/j.drugpo.2019.09.020
Ure C, Burns L, Hargreaves SC, Coffey M, Audrey S, Kenth K, et al. Mobilising communities to address alcohol harm: an Alcohol Health Champion approach. Perspect Public Health 2020;140(2):88–90. https://doi.org/10.1177/1757913919899700
Ure C, Burns EJ, Hargreaves SC, Hidajat M, Coffey M, de Vocht F, et al. How can communities influence alcohol licensing at a local level? Licensing officers’ perspectives of the barriers and facilitators to sustaining engagement in a volunteer-led alcohol harm reduction approach. Int J Drug Policy 2021;98:103412. https://doi.org/10.1016/j.drugpo.2021.103412
Ure C, Hargreaves SC, Burns EJ, Coffey M, Audrey S, Ardern K, Cook PA. An asset-based community development approach to reducing alcohol harm: exploring barriers and facilitators to community mobilisation at initial implementation stage. Health Place 2021;68:102504. https://doi.org/10.1016/j.healthplace.2020.102504
Burns EJ, Hargreaves SC, Ure C, Hare S, Coffey M, Hidajat M, et al. ‘A priori’ external contextual factors and relationships with process indicators: a mixed-methods study of the pre-implementation phase of ‘Communities in Charge of Alcohol’. BMC Public Health 2022;22(1):2224. https://doi.org/10.1186/s12889-022-14411-2
Hargreaves SC, Ure C, Burns EJ, Coffey M, Audrey S, Ardern K, Cook PA. A mixed-methods analysis evaluating an alcohol health champion community intervention: how do newly trained champions perceive and understand their training and role? Health Soc Care Commun 2022;30(5):e2737–49. https://doi.org/10.1111/hsc.13717
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
- Cook PA, Hargreaves SC, Burns EJ, de Vocht F, Parrott S, Coffey M, et al. Communities in charge of alcohol (CICA): a protocol for a stepped-wedge randomised control trial of an alcohol health champions programme. BMC Public Health 2018;18. https://doi.org/10.1186/s12889-018-5410-0.
- World Health Organization . Global Status Report on Alcohol and Health 2018. www.who.int/publications/i/item/9789241565639 (accessed May 2023).
- Babor T, Casswell S, Graham K, Huckle T, Livingston M, Rehm J, et al. Alcohol: No Ordinary Commodity: Research and Public Policy. Oxford: Oxford University Press; 2022.
- Laslett A-M, Room R, Waleewong O, Stanesby O, Callinan S. Harm to Others from Drinking: Patterns in Nine Societies. Geneva: World Health Organization; 2019.
- McCarthy R, Mukherjee RAS, Fleming KM, Green J, Clayton-Smith J, Price AD, et al. Prevalence of fetal alcohol spectrum disorder in Greater Manchester, UK: an active case ascertainment study. Alcohol Clin Exp Res 2021;45:2271-81. https://doi.org/10.1111/acer.14705.
- Cook PA, Phillips-Howard PA, Morleo M, Harkins C, Briant L, Bellis MA. The big drink debate: perceptions of the impact of price on alcohol consumption from a large scale cross-sectional convenience survey in north west England. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-664.
- Campbell CA, Hahn RA, Elder R, Brewer R, Chattopadhyay S, Fielding J, et al. Task Force on Community Preventive Services . The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am J Prev Med 2009;37:556-69. https://doi.org/10.1016/j.amepre.2009.09.028.
- Fone D, Dunstan F, White J, Webster C, Rodgers S, Lee S, et al. Change in alcohol outlet density and alcohol-related harm to population health (CHALICE). BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-428.
- Addressing Alcohol Consumption and Socioeconomic Inequalities: How a Health Promotion Approach Can Help. Geneva: World Health Organization; 2021.
- Fone DL, Farewell DM, White J, Lyons RA, Dunstan FD. Socioeconomic patterning of excess alcohol consumption and binge drinking: a cross-sectional study of multilevel associations with neighbourhood deprivation. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-002337.
- Probst C, Kilian C, Sanchez S, Lange S, Rehm J. The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: a systematic review. Lancet Public Health 2020;5:e324-32. https://doi.org/10.1016/S2468-2667(20)30052-9.
- Bellis MA, Hughes K, Nicholls J, Sheron N, Gilmore I, Jones L. The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-2766-x.
- World Health Organization . Global NCD Target: Reduce the Harmful Use of Alcohol 2016. https://apps.who.int/iris/handle/10665/312277 (accessed May 2023).
- Probst C, Manthey J, Neufeld M, Rehm J, Breda J, Rakovac I, et al. Meeting the global NCD target of at least 10% relative reduction in the harmful use of alcohol: is the WHO European region on track?. Int J Environ Res Public Health 2020;17. https://doi.org/10.3390/ijerph17103423.
- O’Donnell A, Anderson P, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, et al. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol 2014;49:66-78. https://doi.org/10.1093/alcalc/agt170.
- de Vocht F, Heron J, Angus C, Brennan A, Mooney J, Lock K, et al. Measurable effects of local alcohol licensing policies on population health in England. J Epidemiol Community Health 2016;70:231-7. https://doi.org/10.1136/jech-2015-206040.
- de Vocht F, Heron J, Campbell R, Egan M, Mooney JD, Angus C, et al. Testing the impact of local alcohol licencing policies on reported crime rates in England. J Epidemiol Community Health 2017;71:137-45. https://doi.org/10.1136/jech-2016-207753.
- Burton R, Henn C, Lavoie D, O’Connor R, Perkins C, Sweeney K, et al. A rapid evidence review of the effectiveness and cost-effectiveness of alcohol control policies: an English perspective. Lancet 2017;389:1558-80. https://doi.org/10.1016/S0140-6736(16)32420-5.
- Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction 2002;97:279-92. https://doi.org/10.1046/j.1360-0443.2002.00018.x.
- Kaner EF, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2018;2. https://doi.org/10.1002/14651858.CD004148.pub4.
- D’Onofrio G, Degutis LC. Preventive care in the emergency department: screening and brief intervention for alcohol problems in the emergency department: a systematic review. Acad Emerg Med 2002;9:627-38.
- Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction 2008;103:368-76; discussion 377. https://doi.org/10.1111/j.1360-0443.2007.02072.x.
- National Institute for Health and Care Excellence . Community Engagement: Improving Health and Wellbeing and Reducing Health Inequalities 2016. www.nice.org.uk/guidance/ng44 (accessed May 2023).
- Offord DR. Selection of levels of prevention. Addict Behav 2000;25:833-42. https://doi.org/10.1016/s0306-4603(00)00132-5.
- World Health Organisation . Tackling NCDs: ‘Best Buys’ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases 2017. https://apps.who.int/iris/handle/10665/259232 (accessed May 2023).
- Derges J, Kidger J, Fox F, Campbell R, Kaner E, Hickman M. Alcohol screening and brief interventions for adults and young people in health and community-based settings: a qualitative systematic literature review. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4476-4.
- Public Health England . Community Champion Approaches: Rapid Scoping Review of Evidence 2021. www.gov.uk/government/publications/community-champion-approaches-rapid-scoping-review-of-evidence (accessed May 2023).
- Licensing Act 2003 n.d. www.legislation.gov.uk/ukpga/2003/17/contents (accessed October 2022).
- McGrath M, Reynolds J, Smolar M, Hare S, Ogden M, Popay J, et al. Identifying opportunities for engaging the ‘community’ in local alcohol decision-making: a literature review and synthesis. Int J Drug Policy 2019;74:193-204. https://doi.org/10.1016/j.drugpo.2019.09.020.
- Kypri K, Maclennan B. Public participation in local alcohol regulation: findings from a survey of New Zealand communities. Drug Alcohol Rev 2014;33:59-63. https://doi.org/10.1111/dar.12094.
- Reynolds J, McGrath M, Halliday E, Ogden M, Hare S, Smolar M, et al. ‘The opportunity to have their say?’ Identifying mechanisms of community engagement in local alcohol decision-making. Int J Drug Policy 2020;85. https://doi.org/10.1016/j.drugpo.2020.102909.
- Fitzgerald N, Winterbottom J, Nicholls J. Democracy and power in alcohol premises licensing: a qualitative interview study of the Scottish public health objective. Drug Alcohol Rev 2018;37:607-15. https://doi.org/10.1111/dar.12819.
- David G, Cooper R, Dixon S, Holmes J. Exploring the implementation of public involvement in local alcohol availability policy: the case of alcohol licensing decision-making in England. Addiction 2022;117:1163-72. https://doi.org/10.1111/add.15699.
- Muhunthan J, Angell B, Hackett ML, Wilson A, Latimer J, Eades A-M, et al. Global systematic review of Indigenous community-led legal interventions to control alcohol. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013932.
- Morgan A, Ziglio E. Revitalising the evidence base for public health: an assets model. IUHPE: Promotion and Education 2007;14:17-22.
- National Institute for Health and Care Excellence (NICE) . Behaviour Change: General Approaches 2007. www.nice.org.uk/guidance/ph6 (accessed May 2023).
- Friedli L. ‘What we’ve tried, hasn’t worked’: the politics of assets based public health1. Critical Public Health 2013;23:131-45. https://doi.org/10.1080/09581596.2012.748882.
- Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, Van Wyk B, et al. Lay health workers in primary and community health care. Cochrane Database Syst Rev 2005. https://doi.org/10.1002/14651858.CD004015.pub2.
- South J, Raine G, White J. Community Health Champions: Evidence Review 2010. https://eprints.leedsbeckett.ac.uk/id/eprint/7368/ (accessed March 2024).
- Public Health England . A Guide to Community-Centred Approaches for Health and Wellbeing: Full Report 2015. www.gov.uk/government/publications/health-and-wellbeing-a-guide-to-community-centred-approaches (accessed May 2023).
- Ure C, Hargreaves S, Burns E, Coffey M, Audrey S, Ardern K, et al. An asset-based community development approach to reducing alcohol harm: exploring barriers and facilitators to community mobilisation at initial implementation stage. Health Place 2021;68. https://doi.org/10.1016/j.healthplace.2020.102504.
- Ure C, Burns EJ, Hargreaves SC, Hidajat M, Coffey M, de Vocht F, et al. How can communities influence alcohol licensing at a local level? Licensing officers’ perspectives of the barriers and facilitators to sustaining engagement in a volunteer-led alcohol harm reduction approach. Int J Drug Policy 2021;98.
- Hargreaves SC, Ure C, Burns EJ, Coffey M, Audrey S, Ardern K, et al. A mixed methods analysis evaluating an alcohol health champion community intervention: how do newly trained champions perceive and understand their training and role?. Health Soc Care Community 2022;30:e2737-49. https://doi.org/10.1111/hsc.13717.
- Burns EJ, Hargreaves SC, Ure C, Hare S, Coffey M, Hidajat M, et al. ‘A priori’ external contextual factors and relationships with process indicators: a mixed methods study of the pre-implementation phase of ‘Communities in Charge of Alcohol’. BMC Public Health 2022;22. https://doi.org/10.1186/s12889-022-14411-2.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: The New Medical Research Council Guidance. BMJ 2008;337:979-83. https://doi.org/10.1136/bmj.a1655.
- Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health.
- Lamont T, Barber N, Pury J, Fulop N, Garfield-Birkbeck S, Lilford R, et al. New approaches to evaluating complex health and care systems. BMJ 2016;352. https://doi.org/10.1136/bmj.i154.
- Moore G, Audrey S, Barker M, Bond L, Bonell C, Cooper C, et al. Process evaluation in complex public health intervention studies: the need for guidance. J Epidemiol Community Health 2014;68:101-2. https://doi.org/10.1136/jech-2013-202869.
- Public Health England . Local Alcohol Profiles for England (March 2016 Update) 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/503879/LAPE_March_2016_official_statistics_commentary.pdf (accessed May 2023).
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Lavoie D. Alcohol identification and brief advice in England: a major plank in alcohol harm reduction policy. Drug Alcohol Rev 2010;29:608-11. https://doi.org/10.1111/j.1465-3362.2010.00224.x.
- Public Health England . Alcohol Licensing: Data for Public Health Teams 2017. www.gov.uk/government/publications/alcohol-licensing-data-for-public-health-teams (accessed May 2023).
- Public Health England . National Drug Treatment Monitoring System (NDTMS): Adult Drug and Alcohol Treatment Business Definitions 2020. www.gov.uk/government/publications/business-definitions-for-adult-drug-and-alcohol-misuse-treatment-providers (accessed May 2023).
- Rush B. Tiered frameworks for planning substance use service delivery systems: origins and key principles. Nord Stud Alcohol Drugs 2010;27:617-36. https://doi.org/10.1177/145507251002700607.
- Office for National Statistics . Mid-2016 Population Estimates for LSOA in England and Wales 2017. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/lowersuperoutputareamidyearpopulationestimates (accessed May 2023).
- Department for Communities and Local Government . English Indices of Deprivation by LSOA 2015. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed May 2023).
- Office for National Statistics . Ethnic Group, NOMIS 2011. www.nomisweb.co.uk/census/2011/ks201ew (accessed May 2023).
- Office for National Statistics . QS403EW – Tenure – People, NOMIS 2011. www.nomisweb.co.uk/census/2011/qs403ew (accessed May 2023).
- Consumer Data Research Centre . Access to Healthy Assets and Hazards Index (AHAH), Consumer Data Research Centre (CDRC) 2019. https://data.cdrc.ac.uk/dataset/access-healthy-assets-hazards-ahah (accessed September 2019).
- de Vocht F, Katikireddi SV, McQuire C, Tilling K, Hickman M, Craig P. Conceptualising natural and quasi experiments in public health. BMC Med Res Methodol 2021;21. https://doi.org/10.1186/s12874-021-01224-x.
- Lawlor DA, Tilling K, Davey Smith G. Triangulation in aetiological epidemiology. Int J Epidemiol 2016;45:1866-86. https://doi.org/10.1093/ije/dyw314.
- Health and Social Care Information Centre . NHS Data Model and Dictionary 2022. www.datadictionary.nhs.uk/nhs_business_definitions/lower_layer_super_output_area.html (accessed May 2023).
- Public Health England . Alcohol-Attributable Fractions for England: An Update 2020. www.gov.uk/government/publications/alcohol-attributable-fractions-for-england-an-update (accessed May 2023).
- Public Health England . Alcohol-Attributable Fractions for England: An Update (Appendix 2: Technical Appendix) 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/890556/Appendix_2_Technical__appendix.pdf (accessed May 2023).
- Office for National Statistics . Violent Crime and Sexual Offences – Alcohol-Related Violence 2015. www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/compendium/focusonviolentcrimeandsexualoffences/2015-02-12/chapter5violentcrimeandsexualoffencesalcoholrelatedviolence#type-of-violence (accessed May 2023).
- Martin N, Newbury-Birch D, Duckett J, Mason H, Shen J, Shevills C, et al. A retrospective analysis of the nature, extent and cost of alcohol-related emergency calls to the ambulance service in an English region. Alcohol Alcohol 2012;47:191-7. https://doi.org/10.1093/alcalc/agr158.
- Office for National Statistics . People, Population and Community 2021. https://www.ons.gov.uk/peoplepopulationandcommunity (accessed May 2023).
- Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemp Clin Trials 2007;28:182-91. https://doi.org/10.1016/j.cct.2006.05.007.
- Brown CA, Lilford RJ. The stepped wedge trial design: a systematic review. BMC Med Res Methodol 2006;6:1-9. https://doi.org/10.1186/1471-2288-6-54.
- Berk R, MacDonald JM. Overdispersion and Poisson regression. J Quant Criminol 2008;24:269-84. https://doi.org/10.1007/s10940-008-9048-4.
- Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 2016;46:348-55. https://doi.org/10.1093/ije/dyw098.
- Brannstrom L, Trolldal B, Menke M. Spatial spillover effects of a community action programme targeting on-licensed premises on violent assaults: evidence from a natural experiment. J Epidemiol Community Health 2016;70:226-30. https://doi.org/10.1136/jech-2015-206124.
- Giorgino T. Computing and visualizing dynamic time warping alignments in R: the dtw package. J Stat Softw 2009;31:1-24. https://doi.org/10.18637/jss.v031.i07.
- Abadie A, Diamond A, Hainmueller J. Synthetic control methods for comparative case studies: estimating the effect of California’s tobacco control program. J Am Stat Assoc 2010;105:493-505. https://doi.org/10.1198/jasa.2009.ap08746.
- Abadie A, Diamond A, Hainmueller J. Synth: an R package for synthetic control methods in comparative case studies. J Stat Softw 2011;42. https://doi.org/10.18637/jss.v042.i13.
- de Vocht F, McQuire C, Brennan A, Egan M, Angus C, Kaner E, et al. Evaluating the causal impact of individual alcohol licensing decisions on local health and crime using natural experiments with synthetic controls. Addiction 2020;115:2021-31. https://doi.org/10.1111/add.15002.
- de Vocht F, Tilling K, Pliakas T, Angus C, Egan M, Brennan A, et al. The intervention effect of local alcohol licensing policies on hospital admission and crime: a natural experiment using a novel Bayesian synthetictime-series method. J Epidemiol Community Health 2017;71:912-8. https://doi.org/10.1136/jech-2017-208931.
- McQuire C, Tilling K, Hickman M, de Vocht F. Forecasting the 2021 local burden of population alcohol-related harms using Bayesian structural time-series. Addiction 2019;114:994-1003. https://doi.org/10.1111/add.14568.
- Brodersen KH, Gallusser F, Koehler J, Remy N, Scott SL. Inferring causal impact using Bayesian structural time-series models. Ann Appl Stat 2015;9:247-74. https://doi.org/10.1214/14-aoas788.
- Scott SL, Varian H. Predicting the present with Bayesian structural time series. Int J Math Model Numer Optim 2014;5:4-23. https://doi.org/10.1504/ijmmno.2014.059942.
- Brodersen KH, Hauser A. An R Package for Causal Inference Using Bayesian Structural Time-Series Models 2017. http://google.github.io/CausalImpact/CausalImpact.html (accessed May 2023).
- Orton L, Halliday E, Collins M, Egan M, Lewis S, Ponsford R, et al. Putting context centre stage: evidence from a systems evaluation of an area based empowerment initiative in England. Crit Public Health 2016;27:477-89. https://doi.org/10.1080/09581596.2016.1250868.
- Home Office . Revised Guidance Issued under Section 182 of the Licensing Act 2003 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/705588/Revised_guidance_issued_under_section_182_of_the_Licensing_Act_2003__April_2018_.pdf (accessed May 2023).
- Bowen GA. Document analysis as a qualitative research method. Qual Res J 2009;9:27-40.
- Hsieh H, Shannon S. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277-88. https://doi.org/10.1177/1049732305276687.
- Alcohol Focus Scotland . Review of Statements of Licensing Policy 2013 to 2016 n.d. www.alcohol-focus-scotland.org.uk/media/85184/Review-of-statements-of-licensing-policy-FINAL.pdf (accessed May 2023).
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- May C. Towards a general theory of implementation. Implement Sci 2013;8.
- Procter S, Mutrie N, Davis A, Audrey S. Views and experiences of behaviour change techniques to encourage walking to work: a qualitative study. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-868.
- Morgan DL. Focus groups. Ann Rev Sociol 1996 n.d.;22:129-52. https://doi.org/10.1146/annurev.soc.22.1.129.
- Bengtsson M. How to plan and perform a qualitative study using content analysis. Nurs Plus Open 2016;2:8-14. https://doi.org/10.1016/j.npls.2016.01.001.
- Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2014.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ (Clin Res Ed) 2000;320:114-6. https://doi.org/10.1136/bmj.320.7227.114.
- Goldsmith L. Using framework analysis in applied qualitative research. Qual Rep 2021;26:2061-76. https://doi.org/10.46743/2160-3715/2021.5011.
- Spencer L, Ritchie J, O’Connor W, . Analysis in Practice. London: SAGE Publications Ltd; 2014.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Braun V, Clarke V. Successful Qualitative Research: A Practical Guide for Beginners. London: SAGE Publications Ltd; 2013.
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 2019;11:589-97. https://doi.org/10.1080/2159676X.2019.1628806.
- O’Brien B, Harris I, Beckman T, Reed D, Cook D. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245-51. https://doi.org/10.1097/ACM.0000000000000388.
- HM Treasury . The Green Book: Central Government Guidance on Appraisal and Evaluation n.d. www.gov.uk/government/publications/the-green-book-appraisal-and-evaluation-in-central-government (accessed March 2024).
- HM Treasury PSTNNE . Supporting Public Service Transformation: Cost Benefit Analysis Guidance for Local Partnerships n.d. www.greatermanchester-ca.gov.uk/what-we-do/research/research-cost-benefit-analysis/ (accessed May 2023).
- Drummond M, Sculpher M, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Brazier J, Ratcliffe J, Salomon J, Tsuchiya A. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford: Oxford University Press; 2017.
- Cunnama L, Sinanovic E, Ramma L, Foster N, Berrie L, Stevens W, et al. Using top-down and bottom-up costing approaches in LMICs: the case for using both to assess the incremental costs of new technologies at scale. Health Econ 2016;25:53-66. https://doi.org/10.1002/hec.3295.
- Brooks ME, Kristensen K, Van Benthem KJ, Magnusson A, Berg CW, Nielsen A, et al. glmmTMB balances speed and flexibility among packages for zero-inflated generalized linear mixed modeling. R J 2017;9:378-400.
- Chamberlain P, Brown CH, Saldana L. The Stages of implementation completion (SIC). Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-116.
- King DK, Shoup JA, Raebel MA, Anderson CB, Wagner NM, Ritzwoller DP, et al. Planning for implementation success using RE-AIM and CFIR frameworks: a qualitative study. Front Public Health 2020;8. https://doi.org/10.3389/fpubh.2020.00059.
- Home Office . Police Reform and Social Responsibility Bill: Change the Requirement for a Licensing Authority to Publish Their Licensing Policy Statement Every Three Years to Every Five Years n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/98128/Licensing-Policy-Statement.pdf (accessed May 2023).
- Morris M. Guest Post: Clarity Is King – The Evidence That Reveals the Desperate Need to Re-Think the Way We Write n.d. https://gds.blog.gov.uk/2014/02/17/guest-post-clarity-is-king-the-evidence-that-reveals-the-desperate-need-to-re-think-the-way-we-write/ (accessed May 2023).
- Home Office . Police Reform and Social Responsibility Bill: Increase the Opportunities for Local Residents or Their Representative Groups to Be Involved in Licensing Decisions by Removing the Vicinity Test for Interested Parties 2011. www.gov.uk/government/publications/licensing-act-2003-removing-the-vicinty-test-for-interested-parties (accessed May 2023).
- Home Office . Guidance on Mandatory Licensing Conditions 2010: For Suppliers of Alcohol and Enforcement Authorities in England and Wales 2014. www.gov.uk/government/publications/guidance-on-mandatory-licensing-conditions (accessed May 2023).
- Quigg Z, Hughes K, Butler N, Ford K, Canning I, Bellis MA. Drink less enjoy more: effects of a multi-component intervention on improving adherence to, and knowledge of, alcohol legislation in a UK nightlife setting. Addiction 2018;113:1420-9. https://doi.org/10.1111/add.14223.
- Public Health England . Alcohol Licensing: A Guide for Public Health Teams n.d. www.gov.uk/guidance/alcohol-licensing-a-guide-for-public-health-teams (accessed May 2023).
- Department of Health . Welsh Government. Department of Health Northern Ireland SG. UK Chief Medical Officers’ Low Risk Drinking Guidelines n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/545937/UK_CMOs__report.pdf (accessed May 2023).
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997;12:38-4. https://doi.org/10.4278/0890-1171-12.1.38.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- OCSI . LSOAs, LEPs and Lookups: A Beginner’s Guide to Statistical Geographies n.d. https://ocsi.uk/2019/03/18/lsoas-leps-and-lookups-a-beginners-guide-to-statistical-geographies/ (accessed May 2023).
- Cheshire West and Chester Council . Statement of Licensing Policy: Licensing Act 2003 n.d. www.cheshirewestandchester.gov.uk/documents/business/licensing/licensing-act/statement-of-licensing-policy/statement-of-licensing-policy-licensing-act-2020.pdf (accessed December 2021).
- Home Office . Minor Variations to Premises Licences or Club Premises Certificates: Guidance for Applicants n.d. www.gov.uk/government/publications/minor-variations-to-premises-licence-application-form (accessed December 2021).
- NHS Digital . Statistics on Alcohol, England 2020 n.d. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-alcohol/2020 (accessed December 2021).
- Fitzgerald N, Manca F, Uny I, Martin JG, O’Donnell R, Ford A, et al. Lockdown and licensed premises: COVID-19 lessons for alcohol policy. Drug Alcohol Rev 2022;41:533-45. https://doi.org/10.1111/dar.13413.
- Alcohol Change UK . The Blue Light Project n.d. https://alcoholchange.org.uk/help-and-support/training/for-practitioners/blue-light-training (accessed May 2023).
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: New Guidance. Medical Research Council; 2008.
- Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, et al. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.e8501.
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2031-8.
- Watson DP, Adams EL, Shue S, Coates H, McGuire A, Chesher J, et al. Defining the external implementation context: an integrative systematic literature review. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3046-5.
- Hall N, Mooney JD, Sattar Z, Ling J. Extending alcohol brief advice into non-clinical community settings: a qualitative study of experiences and perceptions of delivery staff. BMC Health Serv Res 2019;19.
- Mansdotter AM, Rydberg MK, Wallin E, Lindholm LA, Andréasson S. A cost-effectiveness analysis of alcohol prevention targeting licensed premises. Eur J Public Health 2007;17:618-23. https://doi.org/10.1093/eurpub/ckm017.
- Ramponi F, Walker S, Griffin S, Parrott S, Drummond C, Deluca P, et al. Cost-effectiveness analysis of public health interventions with impacts on health and criminal justice: an applied cross-sectoral analysis of an alcohol misuse intervention. Health Econ 2020;30:972-88. https://doi.org/10.1002/hec.4229.
- Walker S, Griffin S, Asaria M, Tsuchiya A, Sculpher M. Striving for a societal perspective: a framework for economic evaluations when costs and effects fall on multiple sectors and decision makers. Appl Health Econ Health Policy 2019;17:577-90. https://doi.org/10.1007/s40258-019-00481-8.
- Anderson P, Chisholm D, Fuhr DC. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet 2009;373:2234-46. https://doi.org/10.1016/S0140-6736(09)60744-3.
- Equality Act 2010 n.d. www.legislation.gov.uk/ukpga/2010/15/contents (accessed October 2022).
- Farooqi A, Jutlla K, Raghavan R, Wilson A, Uddin MS, Akroyd C, et al. Developing a toolkit for increasing the participation of black, Asian and minority ethnic communities in health and social care research. BMC Med Res Methodol 2022;22. https://doi.org/10.1186/s12874-021-01489-2.
- NHS Digital . Sexual Orientation and Why It Is Important to Ask About n.d. https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-sets/mental-health-services-data-set/submit-data/data-quality-of-protected-characteristics-and-other-vulnerable-groups/sexual-orientation (accessed May 2023).
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358. https://doi.org/10.1136/bmj.j3453.
Appendix 1 Logic model
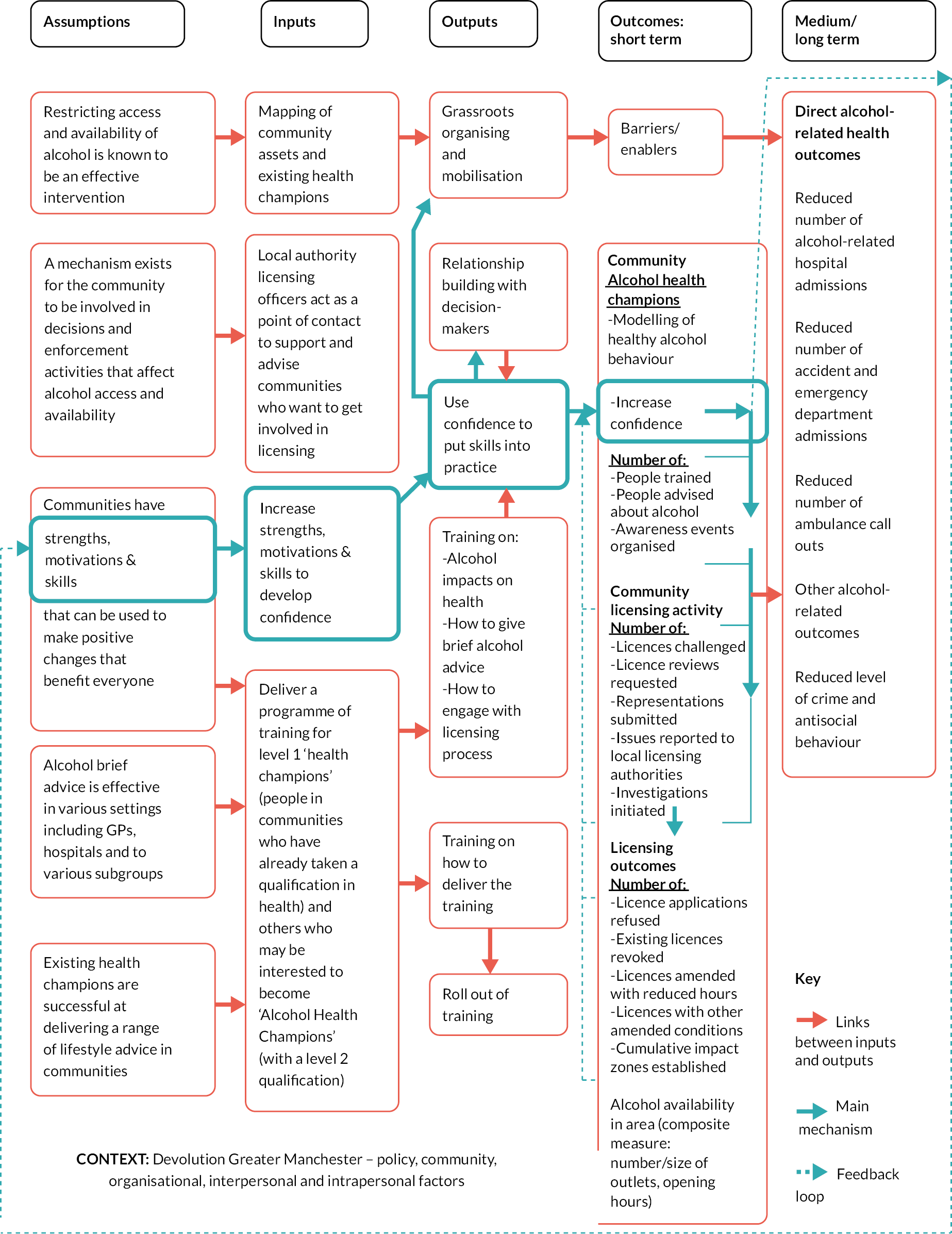
Appendix 2 Alcohol health champion role description
What is an alcohol health champion?
An AHC is someone we will train to:
-
talk about the harms associated with alcohol and give alcohol-related brief advice to people
-
help communities have a say in alcohol availability in their community
-
train others to become AHCs (first AHCs only).
We are looking for people who are enthusiastic about changing their community’s relationship with alcohol. You will get 2 days training to give you the knowledge and skills you need to go out into your local community to improve health and influence how alcohol is sold. You will receive a nationally recognised qualification from the RSPH as part of your training.
What’s involved?
Ways to use your training could include:
-
Having informal conversations about alcohol and health with family, friends and colleagues.
-
Supporting people to reduce drinking through brief advice and/or guiding them towards specialist services. The information you need to do this will be provided in the training.
-
Attending local community social events to speak to people about alcohol and health, for example if you already go to a kids club, a dance lesson or a school event you could speak to other people there about alcohol.
-
With the support of other champions, local NHS services, the local authority or other organisations attend events to promote a healthier relationship with alcohol.
-
Provide local support for communities to get involved with licensing decisions by helping them raise issues with the local authority about venues selling alcohol.
-
Work with other members of the community and professionals to influence alcohol policy in your area and beyond.
What’s not involved?
-
using detailed questionnaires or specialist equipment and techniques to assess people’s health
-
performing medical tests
-
having targets for the number of conversations, referrals or events you attend.
Once we have helped you to develop your skills it will be up to you how (and how often) you use them. You are not expected to do anything you are uncomfortable with. However, as the role is specifically about alcohol you will need to be happy having conversations about alcohol with people who may not be open to that at the start.
Requirements
Alcohol health champions can come from all walks of life. Regardless of where you come from you should want to improve the health and well-being of your community by reducing alcohol-related harm. You should:
-
have enthusiasm for improving the health and well-being of those around you, with a particular interest in supporting people to have a healthier relationship with alcohol
-
be approachable, helpful and interact regularly with members of your community
-
enjoy learning new skills
-
be willing to record the activity you undertake and help us evaluate the success of the project
-
not have any plans to leave the area you live in in the near future
-
be able to understand, read and write English at a reasonable level.
You do NOT need:
-
official qualifications/expert knowledge in health
-
to give up other commitments or work in order to be an AHC – you can make use of the skills you learn however and whenever you see fit.
Support for alcohol health champions
You will receive support at all stages of your training and work as an AHC:
-
Local co-ordinators – these will be your point of contact for the AHC network and will be a link to other people and organisations to support you.
-
Licensing Link – a named link to your local licensing authority who can help you with any queries about licensing.
-
Health Champion Network – there is likely to be an already active group of health champions in your area who can provide a support network. You will be invited to events to meet other champions and participate in further learning.
Source: AHC Plain Language Role Descriptor (2017).
Appendix 3 Zero-inflation negative binomial mixed-effects models
| Outcome | Stepped wedge | Local controls | ||
|---|---|---|---|---|
| Effect (95% CI) | p-value | Effect (95% CI) | p-value | |
| Hospital admissions | No zero incidence reported | |||
| Ambulance weekend | −5.34% (−15.13 to 5.58) | 0.32 | −4.08% (−9.88 to 2.02) | 0.19 |
| Ambulance weekday | −5.11% (−14.70 to 5.56) | 0.33 | −0.33% (−5.99 to 5.68) | 0.91 |
| A&E weekend | No zero incidence reported | |||
| A&E weekday | ||||
| Crime weekend | No evidence of zero inflation | |||
| Crime week | ||||
| ASB | −15.62% (−29.81 to 1.43) | 0.07 | +1.64% (−8.45 to 12.84) | 0.76 |
Appendix 4 Text comments from reflective diaries
Reflective diary comments describing actions taken in the AHC role.
| Action | Comment |
|---|---|
| Spoke to someone about alcohol for the first time | ‘Got a guy to think about cutting down, it’s causing him health concerns. Change brand, no cider, said he would let me know how its going’ (Area 9) |
| ‘I met a colleague for a mtg who was drunk at 9.30 a.m. He openly admits to me about being dependent. We exchange our experiences …. We discussed healthy eating and his pledge to omit drinking on a Monday a weekend detox. We will engage further. Following my training and the completion of an audit-scratch card I have pledged to refrain from alcohol completely’ (Area 4) | |
| Community events attended | ‘The people who approached me and my colleague seemed very motivated and interested in participating in the audit-c. Some very interesting conversations about when people drink, such as wine with a meal. One participant wanted me to show them the way to work out the measure of alcohol volume an unit … Throughout the event some people informed me and my colleague of how they drank more at the weekend but never understood the implications of that model of drinking.. (We) explained how that can be unsafe. However we both ensure that we was (sic) helping and not preaching to them’ (Area 1) |
| ‘Of the four people I spoke to none knew how many units per day/week was recommended. Two men extremely surprised that is now 2–3 units daily for men too. I did an audit-c with two people. One man scored 6.5 points, I informed him this put him at a higher risk of health problems, he agreed to try and cut down the number of glasses of wine each night, or to drink every other night’ (Area 1) | |
| ‘In group got the ladies to do an audit C to show how many units they were actually drinking. Some were surprised and hadn’t realised. Most of the women tend to be binge drinking when they go out’ (Area 2) | |
| Barriers to brief advice activity | ‘Not many people interested today or they saw our “CICA” banner, read it and scurried on saying “I don’t drink” … Again I feel the barrier to overcome is the banner we have, it states “Communities in Charge of Alcohol” and many people looked at this and scurried away saying I’m not an alcoholic’ (Area 1) |
| ‘Someone in the group said to me “you used to drink too much, and you used to post it on Facebook all the times you were having a drink” I was not amused one but about this as I rarely drink more than 3 times a week! How rude to call me out like that in front of a whole group’ (Area 2) | |
| ‘…my confidence knocked over the last couple of weeks from people thinking it’s a joke when I explain what it is I am doing and why, to just being shut down as though my aim is to now lecture them on how much they are drinking’ (Area 8) | |
| Licensing issues/activity recorded | ‘Told a member of the community how to go online and look at licensing – report his local off licence’ (Area 9) |
| ‘A fellow in my flats was interested in licensing and was happy to know you can actually look online who’s applying for licenses to sell alcohol, and ways of appealing licences what I learned from RSPH training’ (Area 9) |
Appendix 5 Dark logic model
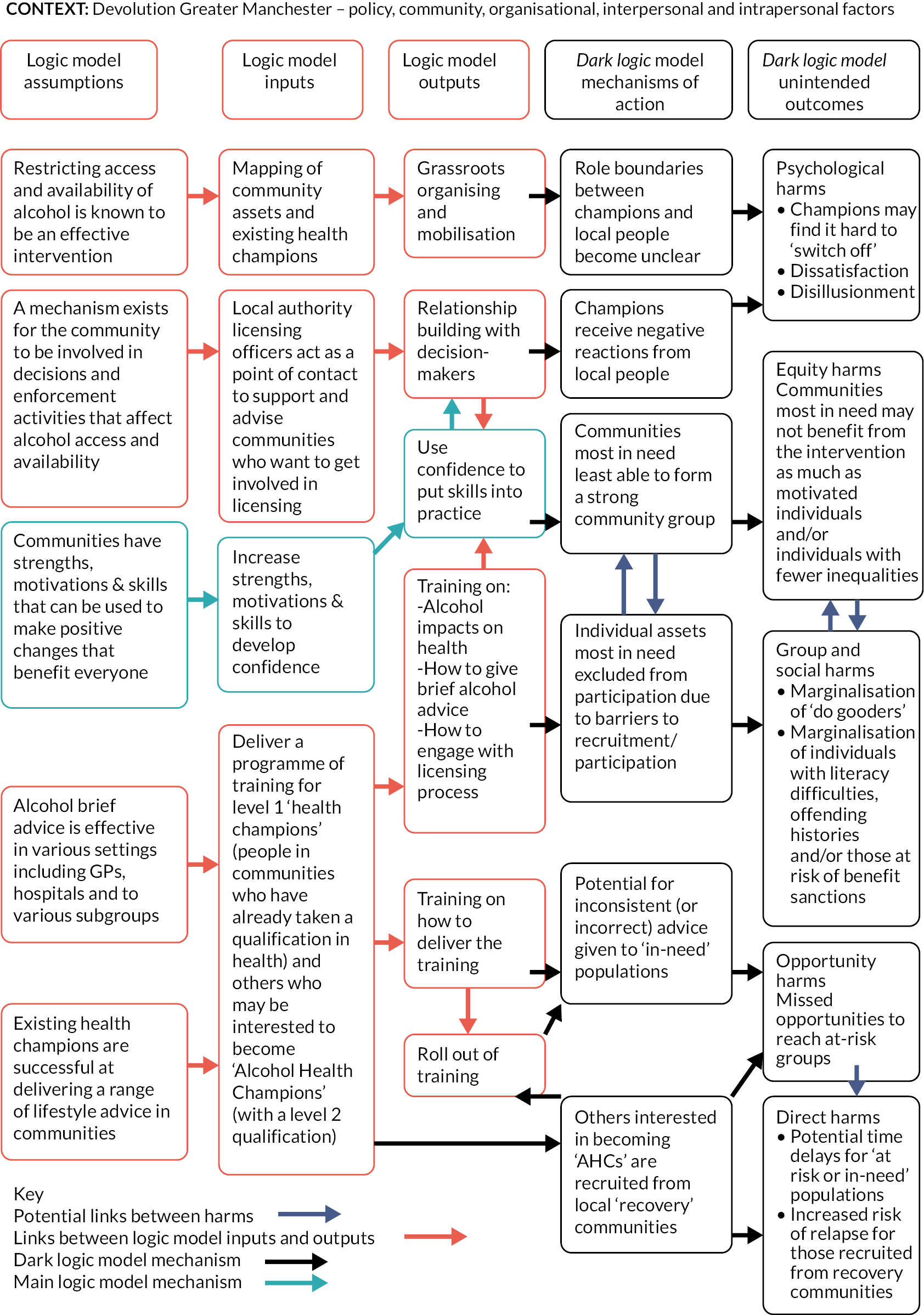
List of abbreviations
- A&E
- accident and emergency
- ABCD
- asset-based community development
- AHC
- alcohol health champion
- ASB
- antisocial behaviour
- ATE
- average intervention (treatment) effect
- CBA
- cost–benefit analysis
- CCA
- cost–consequences analysis
- CICA
- Communities in Charge of Alcohol
- cITS
- controlled Interrupted Time series
- GM
- Greater Manchester
- GMCA
- Greater Manchester Combined Authority
- GMHSCP
- Greater Manchester Health and Social Care Partnership
- IBA
- identification and brief advice
- IQR
- interquartile range
- LAPE
- Local Alcohol Profiles for England
- LSOA
- lower-layer super output area
- MSOA
- middle-layer super output area
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NCD
- non-communicable diseases
- SSC
- Study Steering Committee
