Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as award number 17/44/11. The contractual start date was in December 2018. The draft manuscript began editorial review in January 2023 and was accepted for publication in April 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Holloway et al. This work was produced by Holloway et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Holloway et al.
Chapter 1 Introduction and background
Sections of this chapter have been reproduced from Holloway et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
For individuals in contact with the criminal justice system, the prevalence of at-risk drinking is far higher than in the general population. There is very little evidence of efficacy or effectiveness of alcohol interventions in reducing risky drinking amongst those in the criminal justice system and in particular men on remand in prison. This is compounded by the limited evidence for the optimum timing of delivery, recommended length, content, implementation and economic benefit of an extended alcohol intervention in the prison setting. APPRAISE (A two-arm parallel group individually randomised Prison Pilot study of a male Remand Alcohol Intervention for Self-efficacy Enhancement) will therefore provide vital evidence to inform a future definitive randomised controlled trial (RCT) of an extended alcohol intervention for men on remand in prison. The remainder of this chapter provides the background research and rationale for APPRAISE, presents the study aims and objectives, and concludes by describing the structure of the remaining chapters of this report.
Prevalence of at-risk drinking in the United Kingdom criminal justice system
Hazardous drinking is defined as a repeated pattern of drinking that increases the risk of psychological or physical problems,2 whereas harmful drinking is defined by the presence of these problems. 3 Drinking at hazardous or harmful levels is categorised as risky or at-risk drinking.
The prevalence of at-risk drinking, which includes drinking at levels that harm a person’s health, is far higher amongst those in contact with the criminal justice system (73%). 4–9 In the UK, between 51% and 83% of incarcerated people are classified as risky drinkers. 10 For those on remand in prison, the prevalence is between 62% and 68%. 8 This compares to 35% in the general population. 11 Furthermore, rates of alcohol dependence among those who are incarcerated (43%) are 10 times higher than for the general population. 8
Interventions
Parts of this section have been reproduced from Newbury-Birch et al.,8 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Alcohol brief interventions (ABIs) are a secondary prevention activity, which is aimed at people who are drinking in a pattern that is likely to be harmful to health and/or well-being. They have been frequently shown to be effective in primary health care,12,13 but they are typically delivered by practitioners who are not addiction specialists, to non-treatment, opportunistic populations. 14
ABIs largely consist of two different approaches: simple structured advice, which after screening raises awareness through provision of personalised feedback and advice on steps to reduce drinking behaviour and its adverse consequences; and an extended brief intervention, which generally involves behaviour-change counselling. Extended brief intervention introduces and evokes change by giving the participant the opportunity to explore their alcohol use, as well as their motivations and strategies for change. Both forms share the common aim of helping people to change drinking behaviour to promote health. 14
There is a wide variation in the duration and frequency of ABIs. However, typically they consist of between one and four sessions and are very short in nature (between 5 and 60 minutes). 15 They generally include personalised feedback on alcohol intake in relation to what the recommended limits are and discussion of both health and social risks, and may include setting personal targets which can include psychological and motivational interviewing. 15 One example of this is using the FRAMES (Feedback, Responsibility, Advice, Menus, Empathy, Self-efficacy) approach. 14
Due to the established links between risky drinking and crime and the costs to society, in both health and social care, it is important to find interventions that are effective. It has been shown that interventions that capitalise on the ‘teachable moment’ are conducive to behaviour change, for example where individuals consider their alcohol use within the context of their offending behaviour and its punitive consequences. 16,17
There is robust evidence from systematic reviews and meta-analyses to indicate that short alcohol interventions are effective in reducing alcohol consumption amongst risky drinkers in healthcare settings. 18,19 There is very little evidence of efficacy or effectiveness of alcohol interventions in reducing risky drinking amongst those in the criminal justice system, including the prison system, 20,21 and in particular remand prisoners. However, there has recently been evidence in the UK that alcohol (and drug) interventions can have an effect in reducing recidivism. 22 Furthermore, short alcohol interventions have been shown to reduce recidivism in the probation setting. 7 Nevertheless, there is limited evidence for the optimum timing of delivery, recommended length, content, implementation and economic benefit of an extended alcohol intervention in the prison setting. Likewise, there are weaknesses within the current evidence base with regard to the theoretical underpinnings of such interventions. This risks an intervention with a weak theoretical base and poorly specified ‘active’ ingredients, and which is less likely to deliver the desired outcomes.
Current evidence of alcohol interventions for those in the criminal justice system
A recent systematic review of the efficacy of psychosocial alcohol interventions for incarcerated people found that interventions in the prison setting have the potential to positively impact their relationship with and use of alcohol;21 however, because of small numbers and the use of different outcome measures it was not possible to conduct a meta-analysis or generalise findings. Notably, none of the studies focused on men on remand, as compared with other subgroups within prisons. Remand refers to those who are either unconvicted or convicted and unsentenced, held in custody awaiting trial and/or sentencing.
Rationale for APPRAISE
In 2021, 16% of the prison population in England and Wales, and 19% in Scotland, were remand prisoners. 23,24 This equated to around 12,750 in England and Wales and 1700 in Scotland. Approximately 25% of individuals will not receive a custodial sentence. 25 People spend on average 10 weeks in custody while on remand. 26 During this time, many do not have the opportunity to access mainstream prison health or public health services. 27
It has been shown that there is a complex interplay between individual and contextual factors and risky drinking behaviours and alcohol-related crime. 28 Addressing alcohol harm in prisons, at what can be considered a ‘teachable moment’, where there is an opportunity for people to reflect on their risky drinking and their current position, could potentially reduce the risk of re-offending and costs to society, and help to address health inequalities. 29 While there is an inevitable uncertainty in estimating the costs of alcohol-related crime and disorder, most estimates suggest they represent a considerable economic burden.
A recent Cabinet Office estimate reported that alcohol-related crime in England cost society £21.5 billion. 30 However, this estimate is outdated and there are concerns regarding the assumptions and methodological judgements used in deriving this estimate. 31 Better-quality estimates from four high-income countries placed the total costs of alcohol at 2.6% of gross domestic product (GDP) in 2007, of which 3.5% was made up of law-enforcement costs. 32,33 It has been shown that intervening to reduce alcohol use is cost-effective, generating both long- and short-term savings. Public Health England (PHE) estimated that every £1 invested in effective alcohol treatment brings a social return of £5. Evidence estimates that health savings of £4.3 m and crime savings of £100 m per year can be made as a result of appropriate alcohol interventions. 34 It has also been suggested that providing effective treatment is likely to significantly reduce the costs relating to alcohol as well as increase individual social welfare. 35
In 2017, the Scottish Parliament Health and Sports Committee held an inquiry into prisoner health care to consider how health and social care and medicines in prison are accessed and the effectiveness of health and social care in prison. The Inquiry report set out recommendations for the Scottish government to prepare a strategic plan to address prison social and health care. 36 Furthermore, National Institute for Health and Care Excellence (NICE) Guidelines [NG57]37 for people in prison acknowledge that adequate healthcare provision for prisoners would reduce pressure on community services later.
Theoretical background
The intervention in this study (the APPRAISE study) builds on previous research which has explored the theoretical validity of a self-efficacy-enhancing alcohol intervention,38,39 and was originally tested as part of a pilot cluster RCT in a general hospital setting with evidence of a potential effect. 38 In our recently completed Medical Research Council Public Health Intervention Development (MRC-PHIND) funded PRISM-A (Alcohol Brief Interventions for Male Remand Prisoners) study, we undertook development and refinement of this self-efficacy-enhancing alcohol intervention within the prison setting, working with men on remand to include a synthesis of their views, with reviews of the evidence base and theoretical underpinnings. 40
This current study worked solely with men on remand. We acknowledge that there are also women prisoners who have alcohol-use disorders. There is evidence that women face different issues when imprisoned, and different barriers to services, which are important to note. 41,42
The PRISM-A study with men on remand, carried out in two prisons in the UK, showed a high prevalence of risky drinking [82% scored more than 8 on the Alcohol Use Disorders Test (AUDIT)]. These numbers are comparable to other findings in the prison system in the UK,4–8 but more than three times as high as in primary care settings. 11 In the PRISM-A study, we were able to access, recruit, consent and identify those who were risky drinkers. We also found high levels of willingness of staff and participants to engage with the self-efficacy-enhancing intervention we tested for acceptability, and a willingness to participate in a trial that would involve follow-up at 6 and 12 months. Analysis of 24 in-depth interviews with male remand participants demonstrated strong substantiation that the intervention could help men on remand to develop skills and strategies that would be particularly useful on liberation. We also identified through the interviews a stronger preference amongst the participants for interventions of longer duration and that such interventions should incorporate a post-liberation component.
This is an under-researched area with large gaps in knowledge. A systematic review of alcohol interventions for offenders in the criminal justice setting identified a lack of evidence-based intervention strategies and highlighted the paucity of knowledge in this area, and in particular the lack of UK-based studies and the absence of rigorous studies focusing on men on remand. 8,21
Given the limited evidence on the effectiveness of psychosocial alcohol interventions for men on remand, we aimed to address this gap by carrying out a two-armed individually randomised pilot study to assess the feasibility and acceptability of a self-efficacy-enhancing intervention that had been developed during the PRISM-A study. 40 The results from this study will enable us to undertake a future definitive RCT evaluating its effectiveness and cost-effectiveness.
The study aligns to the MRC framework,43 using mixed methods with two linked phases conducted in two sites in the UK: Scotland and England.
Phase I involves a two-arm, parallel-group, individually randomised pilot study. The pilot evaluation provides data on feasibility and an assessment of the likely impact of the APPRAISE intervention to inform the feasibility of a future definitive multicentre RCT.
Phase II comprises a process evaluation. We have drawn on the MRC framework for process evaluation to guide the planning, design and proposed conduct of the process evaluation. 44 The aim of the process evaluation is threefold: first, to assess how the intervention was implemented, second, to undertake some preliminary exploration of change mechanisms underpinning the intervention and third, to assess the context within which the intervention is delivered.
An additional element was added to the study, as part of the study extension, during and in response to the COVID-19 pandemic. Following approval from National Institute for Health and Care Research (NIHR), we carried out a survey of prisons in Scotland, England and Wales to ascertain what alcohol services are available in male remand prisons and how coronavirus disease discovered in 2019 (COVID-19) has affected these services.
Study aims and objectives
APPRAISE comprised a two-arm, parallel-group, individually randomised, pilot study of a self-efficacy-enhancing psychosocial alcohol intervention for men on remand in prison. It aimed to provide the evidence to support the design of a future definitive multicentre RCT for which new funding would be sought. APPRAISE had the following objectives and questions.
Objective 1: to pilot the study measures and evaluation methods to assess the feasibility of conducting a future definitive multicentre, pragmatic, parallel-group RCT.
-
Is it feasible to conduct a future multicentre RCT of a self-efficacy-enhancing psychosocial alcohol intervention for men on remand?
-
Can we obtain reasonable estimates of the parameters necessary to inform the design and sample size calculation for a future definitive multicentre RCT? This includes standard deviations of potential continuous primary outcomes and estimates of recruitment, retention and follow-up rates.
-
How well do participants complete the questionnaires necessary for a future definitive RCT?
-
Can we collect economic data needed for a future definitive RCT?
-
Can we access recidivism data from the Police National Computer (PNC) databases for trial participants?
-
Can we access health data from routine NHS data sources for trial participants?
Objective 2: to assess intervention fidelity.
-
What proportion of the interventions are delivered as per protocol?
-
Is there any evidence of contamination between the two conditions and/or between those workers delivering the intervention.
-
To what extent was the intervention changing process variables consistent with the underpinning theory?
Objective 3: to qualitatively explore the feasibility and acceptability of a self-efficacy-enhancing psychosocial alcohol intervention and study measures to staff and for men on remand and on liberation.
-
How acceptable are the trial and intervention procedures (including context and any barriers and facilitators) to the following key stakeholders: men on remand in prison and on liberation; prison staff (including healthcare staff); commissioners; policy-makers and third-sector partners?
Objective 4: to assess whether operational progression criteria for conducting a future definitive RCT are met across trial arms and study sites and, if so, develop a protocol for a future definitive trial. Operational progression criteria are based on previous research results. 7
-
Do the two prisons invited to the study agree to take part?
-
Based on knowledge from previous data, do at least 90 eligible participants consent to take part and be randomised across the trial arms?
-
Do at least 70% of participants who consent to the trial receive the intervention?
-
Are at least 60% of those who received the intervention followed up at 12 months across trial arms and study sites?
Objective 5: to carry out a survey to ascertain what alcohol services are available in male remand prisons and how COVID-19 has affected services.
Structure of the report
The report comprises nine chapters, providing details of the background to the study, the rationale for the study, and an account of the research design, methods and findings. Reporting of public patient involvement (PPI) involvement and on equality diversity and inclusion is included. The report concludes by answering whether the study met its aims and objectives, learning from the study, strengths and limitations, while reflecting on the impact of COVID-19 and details of the recommendations for a future definitive trial.
This first chapter has provided the background research and rationale for the study and presented the study aims and objectives. Chapter 2 details the development of the intervention, presents the various elements of the intervention and theoretical underpinnings, and aligns itself to the Template for Intervention Description and Replication (TIDieR) framework. 45 delivery mechanisms as well as the logic model. Intervention training is also described. Chapter 3 reports the pilot trial methods including the management of the study, governance as well as ethics and research clearance. Chapter 4 presents the pilot trial findings, addressing Objectives 1 and 4. Chapter 5 reports the qualitative process evaluation methods. Chapter 6 presents the qualitative process evaluation findings, addressing Objectives 2 and 3. Chapter 7 details the results of the collection and access of economic data and recidivism data for trial participants, addressing Objective 1. Chapter 8 presents the APPRAISE COVID-19 survey methods and results. This was an additional piece of work we agreed with NIHR to carry out during COVID-19 and as part of the study extension period. Chapter 9 presents the discussion, PPI overview, strengths and limitations, recommendations for future RCT and conclusion. The aim of PPI was to provide meaningful engagement with stakeholders who had direct experience of the prison system, ranging from those who have experience of incarceration to those who run third-sector organisations supporting people on release from prison. Our PPI co-applicant was present to contribute in all PMG meetings. The Guidance for Reporting Instrument of Patients and the Public – short form (GRIPP2) form46 identifies the PPI study engagement (see Appendix 1). Finally, recommendations for a future definitive trial are presented. Due to COVID-19, we faced unavoidable modifications to the APPRAISE study. These are reported across chapters at the relevant points. To support completeness of reporting these unavoidable and important modifications to the trial due to COVID-19 (extenuating circumstances), we also completed the CONSERVE checklist9 (see Appendix 2).
Chapter 2 Intervention development
Sections of this chapter have been reproduced from Holloway et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter reports on the origins of the APPRAISE intervention and its theoretical underpinnings, and provides a detailed description of the study intervention itself and the nature of the training for those delivering it. For completeness of the APPRAISE intervention reporting and replicability, the TIDieR checklist is used to support the structure of the chapter (see Appendix 3). 45
Origins and development of the APPRAISE intervention
The APPRAISE intervention is an extended self-efficacy-enhancing alcohol intervention developed for men on remand with self-reported drinking that is harmful or hazardous. The APPRAISE intervention is based on previous ABI research focusing on self-efficacy as an appropriate basis for a single-session ABI intervention to enhance drinking refusal self-efficacy in a general hospital population. 38,39
From this original work, additional intervention modification was undertaken as part of the PRISM-A study on the basis of our learning from interviews with men on remand (n = 24). 40 The aim of these interviews was to explore the acceptability of a self-efficacy-enhancing ABI,40 including listening to feedback regarding the nine elements of the intervention: (1) preliminary discussion, (2) acquiring and providing information, (3) self-monitoring, (4) increasing awareness, (5) situation appraisal and appropriate coping strategies, (6) goal-setting, (7) relapse, (8) self-evaluation/self-reinforcement and (9) culmination. 39,40
The nine intervention elements of the single-session delivery were found to be acceptable to men on remand who were interviewed as part of the PRISM-A study. Feedback regarding frequency and intensity of contact identified a preference for more than one session, with a desire for additional sessions being delivered in the community following liberation. The participants reported that this would provide the opportunity to put the skills gained as a result of the single-session intervention into practice, once liberated, in real-world situations in which alcohol is widely available to them.
This evidence subsequently informed the development and refinement of the single-session ABI to an extended four-session ABI, incorporating a single session to be delivered in the prison setting with the remaining three additional booster sessions to be delivered following liberation.
APPRAISE intervention: theory, elements and logic model
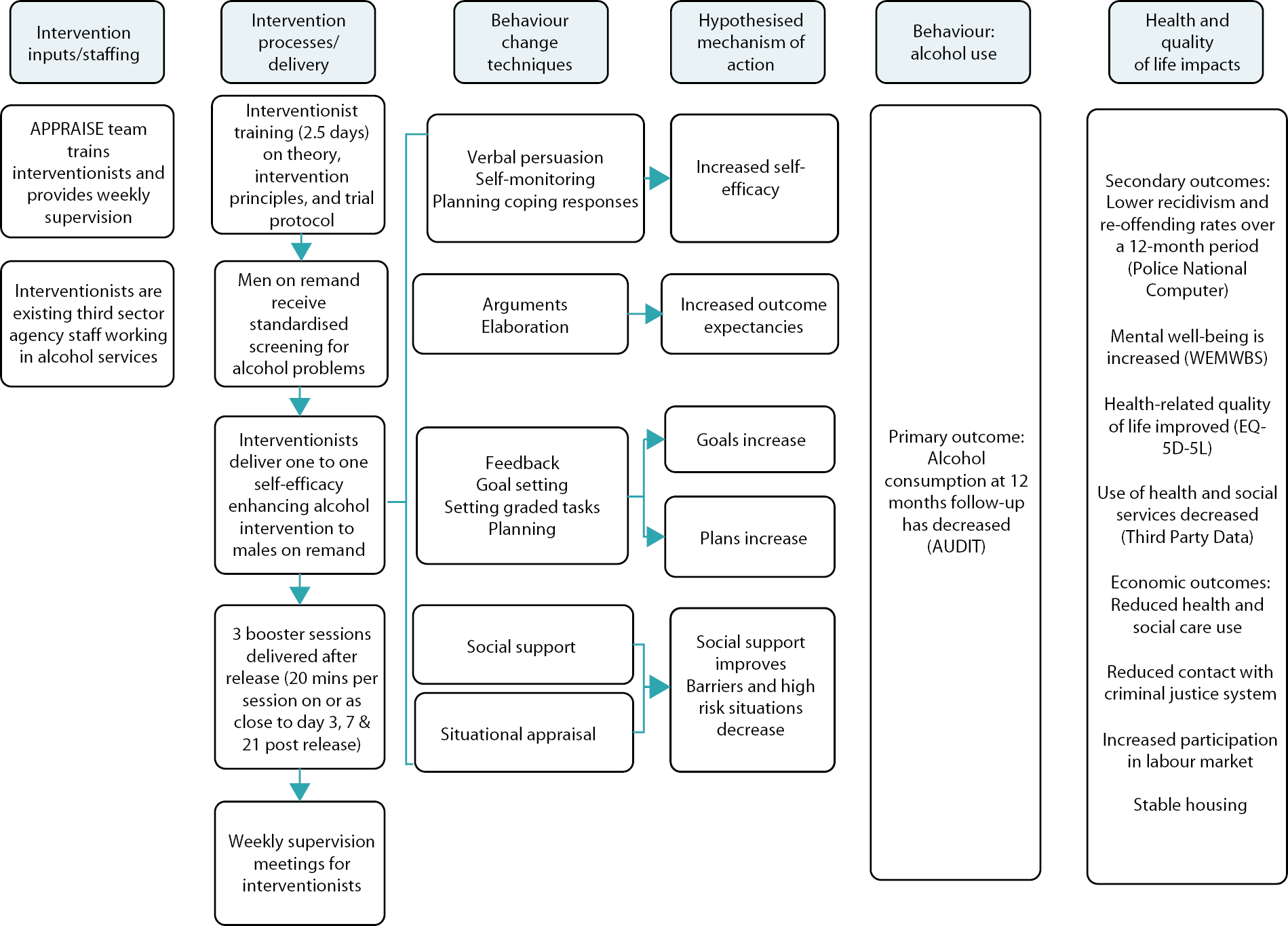
The APPRAISE intervention is based on Social Cognitive Theory and designed to increase self-efficacy and other self-regulatory skills to reduce alcohol consumption. Figure 1 illustrates this process in the APPRAISE logic model. According to the theory, self-efficacy is a central determinant of health behaviour change. 47 Primary sources of self-efficacy that can be targeted through interventions are mastery experience, verbal persuasion, vicarious experience and physiological state. 39,40,47 All these sources of self-efficacy were addressed in the intervention (see Table 1 for all elements of the APPRAISE intervention). Mastery experiences should become more likely due to intervention elements addressing feedback, goal-setting, planning for release, including plans for coping responses, and self-monitoring of the intervention. Verbal persuasion was delivered by the interventionist, as were ways to achieve a calmer physiological state during high-risk situations. The intervention was designed to also increase outcome expectations by delivering arguments and elaborations and seeking social support. The intervention aimed to develop better self-regulation skills, thus enabling individuals to address their alcohol consumption behaviour. Liberation then offered participants the opportunity to implement and act on the targeted behaviours learned in the intervention in their ‘real life’ social context. The aim was for participants to have the ability to develop and build upon these skills and self-belief through success and mastery, with their efforts leading to the adoption and maintenance of reduced alcohol consumption. Reducing alcohol consumption can provide a sense of achievement and success, which should further increase self-efficacy. 39
FIGURE 1.
APPRAISE logic model.
| Opening strategies | |
|---|---|
| Element 1: preliminary discussion | Introduction to APPRAISE study |
| Introduction to APPRAISE | |
| Consent, confidentiality, engagement rules, trust | |
| Element 2: acquiring and providing information | Feedback on AUDIT score |
| Establish perception of impact of alcohol on health and life | |
| Standard units of alcohol | |
| Recommended drinking levels | |
| Alcohol-related health problems | |
| Legal drink/drive limit | |
| Tips on reducing consumption | |
| Where to obtain information/support (prison and liberation) | |
| Element 3: self-monitoring | Diary card – when, where, who, type of drink, why |
| Element 4: increasing awareness | Balance sheet – pros and cons of drinking |
| Physiological sensations identified | |
| Alternative appraisal of somatic sensations identified | |
| Strategies to reduce | |
| Element 5: situation appraisal and appropriate coping strategies | High-risk situations and antecedents of over-drinking identified |
| Alternative coping strategies identified | |
| Coping strategies verbalised by participant | |
| Praise provided | |
| Strategies developed further through co-production | |
| Strategies modelled by interventionist | |
| Participant verbalises strategies and visualises them | |
| Plan for exposure to low-risk situations and avoidance of high-risk situations | |
| General control strategies: reduction in rate of drinking, sipping, drinking low-alcohol drinks and alternating between soft or low-alcohol drinks and higher-alcohol drinks | |
| Element 6: goal-setting | Setting realistic sub-goals (short-term) |
| Facilitating success and increasing motivation | |
| Element 7: relapse | What happens if you relapse |
| What caused the relapse? | |
| How do I understand relapse? | |
| Element 8: self-evaluation and self-reinforcement | Using my alcohol diary as a means of self-evaluation and self-reinforcement |
| Self-congratulations and rewarding my success | |
| What do I attribute my success to? | |
| Element 9: culmination | Reflections and conclusions. Plans and goals reiterated and confirmed |
The six proposed mechanisms of change in the logic model are: self-efficacy, outcome expectations, goals, plans, social support and high-risk situations.
-
Self-efficacy will be measured using: (i) an item on the Readiness to Change Ruler: ‘How confident are you that you could reduce (or stop) drinking when you are released?’ and separately (ii) the Drinking Refusal Self-efficacy Questionnaire.
-
Alcohol expectancy will be measured using the Negative Alcohol Expectancy Questionnaire.
-
Goals will be measured using an item on the Readiness to Change Ruler: ‘How much do you want to reduce (or stop) drinking when you are released?’
-
Plans will be measured using: (i) an item on the Readiness to Change Ruler: ‘How ready are you to reduce (or stop) drinking when you are released?’ and (ii) ‘I have made a detailed plan regarding when, where and how to reduce my drinking’.
-
Social support will be measured using the following items: (i) ‘The people who are important to me support me in reducing my drinking’ and (ii) ‘I have someone I can talk to about reducing my drinking’ in the Readiness to Change Ruler.
-
Barriers and high-risk situations will be measured using the following items: (i) ‘I know in which situations it will be difficult for me to reduce my drinking’ and separately (ii) the question ‘to what extent do you consider this to be a high-risk situation for you?’ in the Drinking Refusal Self-efficacy Questionnaire.
APPRAISE intervention materials
The APPRAISE intervention consisted of three documents:
-
APPRAISE Intervention Tool [V3_20October] (see Appendix 4)
-
Intervention Tool Postcard (Unit card) [V2_25Sept19] (see Appendix 5) and
-
Follow-up Manual [V1_25 Sept19] (see Appendix 6).
These documents together supported the delivery of the behaviour-change methods, linked directly to the determinants/mechanisms of change that focused on the targeted behaviour, in order to achieve the desired outcomes.
-
Document 1: the APPRAISE Intervention Tool was an eight-page, double-sided A5 booklet containing all nine Intervention Elements (Table 1: APPRAISE elements) and was the material used for the first intervention session.
-
Document 2: the Intervention Tool Postcard (Unit card) was postcard-sized and provided brief information about recommended drinking levels and units that was given to individuals to take away with them during Element 2 of the first intervention session.
-
Document 3: the Follow-up Manual was a six-page double-sided A5 booklet for use during all three post-liberation follow-up intervention sessions (Day 3, Day 7 and Day 21). The manual contained Element 1 as a way of re-establishing dialogue following on from the first intervention session, followed by Elements 5–9 of the APPRAISE intervention.
APPRAISE intervention procedures
The APPRAISE intervention was delivered in a safe, non-judgemental environment where engagement rules and trust were affirmed. This was with the aim of enabling and supporting the intervention activities. The APPRAISE Intervention Tool booklet contained ‘Things to remember’ – notes for the interventionist to support the delivery of the intervention elements. This reminded the interventionist of the key areas within each element to be emphasised during intervention delivery. It also provided a mechanism of supporting intervention fidelity in relation to delivery of the intervention changing process variables consistent with the underpinning theory.
While the APPRAISE intervention has specific core elements, the intervention itself was person-centred in that it became individualised during the course of the participant-interventionist conversation and subsequent intervention delivery.
The starting point for this approach was assessing participants’ readiness to change by way of completion of the Readiness to Change Ruler. 48 The scoring then provided information and understanding as to where the participant was in relation to their readiness to change. Similarly high-risk drinking situations were identified during Element 1 to provide further information that would build upon all the elements moving forward. This initial discussion was key to ensuring the interventionist was able to understand, recognise and respond effectively in relation to gauging how participants perceived their drinking and their motivation to change and how they used alcohol in their lives. Discussing answers to both the Readiness to Change Ruler and high-risk situations supported the delivery of an individual realistic starting point for both participant and interventionist. Depending on the results of these elements, each element could then be individualised to participants’ particular needs.
The participants AUDIT score, obtained following screening, was shared with them during Element 2 to feedback and provide information on recommended drinking levels, units and the impact alcohol may have been having on themselves, others and their life on the whole. Giving the Intervention Tool Postcard (Unit card) to the participant provided an easy-to-carry postcard-size information resource which could be studied following intervention sessions and post liberation.
In addition, the booklet had a perforated page that was removed at the end of Element 8 and was given to and kept by the individual receiving the intervention. The page was a takeaway ‘personal planner’ with reinforcement triggers of the key behaviour-change methods and mechanisms.
APPRAISE intervention training
Intervention training was provided at both study sites to members of the Change Grow Live (CGL) team who were supporting the delivery and which included those practitioners who would be delivering the APPRAISE intervention itself.
The aims of the training for interventionists were to:
-
have an awareness and understanding of the APPRAISE intervention
-
understand AUDIT Scores and what they mean
-
have an awareness of the Readiness to Change Ruler and Risky Situation Assessments and why we use them
-
be confident working with the APPRAISE booklet; and
-
be able to deliver the APPRAISE intervention.
The training material ‘(APPRAISE training plan1_VG) (see Appendix 7) for the APPRAISE intervention provides interventionists with:
-
a written brief on the theoretical underpinnings of the intervention
-
paper copies of the three APPRAISE intervention documents
-
paper copy of the APPRAISE elements
-
online narrated review of the three APPRAISE intervention documents
-
intervention delivery video
-
paper copy of the AUDIT instrument; and
-
opportunity to engage in intervention delivery role-play exercises.
On completion of the training, a six-question Likert scale survey (see Appendix 8) as a form of evaluation of the training undertaken was self-completed by interventionists and CGL team members from both study sites (see Intervention implementation).
APPRAISE intervention delivery mode and location
Following completion of baseline assessments and randomisation, those allocated to the intervention arm were invited to attend their first of three intervention sessions. This was delivered face to face by the identified interventionist at each study site. It was delivered in a quiet room either on the residential wing, a landing or in one of the CGL designated rooms and was delivered at both sites by CGL interventionists. Four members of the CGL team from the England study site and two members from the Scotland study site attended the intervention delivery training.
At the beginning of data collection, both study sites had allocated two interventionists. Due to resource capacity and sick leave during the data-collection period, Scotland had one interventionist and England had two interventionists able to deliver the interventions.
We asked the three interventionists for details of their education and previous training experience. This request was made during COVID-19 when we were only able to communicate via e-mail. While there was a willingness to provide the information, due to the incapacity of interventionists to find the time we were unable to obtain that information.
The APPRAISE intervention comprises nine elements (Table 2) to be delivered in four steps: Step 1 comprises a 1 × 40-minute face-to-face session in which the nine elements are covered and delivered by a trained practitioner from CGL in the prison setting. Steps 2, 3 and 4 are 20-minute sessions conducted by phone, on or close to day 3, 7 and 21 post liberation. The post-liberation sessions include elements 1 (preliminary discussion), 5 (situation appraisal), 6 (goal-setting), 7 (relapse), 8 (self-evaluation/self-reinforcement) and 9 (culmination). Table 3 provides details of the intervention sessions, duration, intensity and dose.
| Element | Description |
|---|---|
| Element 1: preliminary discussion | Participants re-introduced to study and APPRAISE, made aware of the purpose of the engagement, emphasising confidentiality, consent and trust. Mirrored aspects of ‘Opening strategies’.48 Readiness to Change Ruler completed and list of high-risk drinking situations identified on a scale of 0–5. |
| Element 2: acquiring and providing information | Focus on participants reported level of alcohol consumption as per screening AUDIT score and their perception of the impact of alcohol on their health and life. Six key pieces of information provided: Standard units of alcohol; Recommended drinking levels; Alcohol-related health problems; Legal drink/drive limit; Tips on reducing consumption; Where to obtain information/support. Intervention Tool Postcard (Unit Card) given to keep. |
| Element 3: self-monitoring | Participant introduced to the idea of keeping a diary post liberation: they are guided through how they would complete the diary with the support of the interventionist. They are informed that the diary will encourage them to reflect and record when, where and with whom, if anyone, they have consumed alcohol, why and what type of drink to enable self-monitoring on liberation, acting as a source of self-evaluation and record of progress.49 |
| Element 4: increasing awareness | Pros and cons of drinking recorded on a balance sheet of drinking. Physiological drinking sensations experienced discussed with strategies to identify and reduce with alternative appraisal of somatic sensations identified, for example alternative stress-relieving strategies, such as relaxation techniques rather than alcoholic drink. |
| Element 5: situation appraisal and appropriate coping strategies | High-risk situations and antecedents of over-drinking identified and alternative coping strategies considered. Situations are identified in order that appropriate coping and response strategies are practised prior to the situation next occurring. Coping strategies verbalised by participant, praise provided and strategies developed further and modelled by interventionist. Participants talk through the strategy and visualise themselves carrying it out (covert modelling). The better ingrained and more automated the response is, the higher one’s self-efficacy and the lower the probability of relapse.50 Avoidance of high-risk situations may be necessary in the first instance (although can be unrealistic) until mastery with low-risk situations is achieved (progressive mastery). Core set of general control strategies also discussed: reduction in rate of drinking, sipping drinks, low-alcohol-content drinks and alternating between soft or low-alcohol and higher-alcohol drinks. |
| Element 6: goal-setting | Realistic sub-goals set, short-term so that unachievable goals initially avoided. Setting proximate goals in relation to self-efficacy development can facilitate success promptly with increase in motivation towards accession to distal goals. This approach likened to a stepladder approach of focusing on the few rungs in front of you. For example, goal may be to reduce quantity of alcohol consumption on certain days of the week. |
| Element 7: relapse | Likelihood of relapse discussed and importance of identifying the events that resulted in the relapse, not attributing relapse to stable causes, such as ability or uncontrollable causes as this can result in lowering of self-efficacy and expectation of future success. Attribution to relapse discussed and focus on appraisal due to unstable causes and not to a personal failure/ability. Majority of relapses occur as a result of emotional distress, social pressure and interpersonal conflicts, therefore appropriate relapse strategies are discussed and practised. |
| Element 8: self-evaluation and self-reinforcement | Reward for success through affective self-reaction, for example, self-congratulations. The alcohol diary is a means of self-evaluation and self-reinforcement, success is attributed to their ability and skill, resulting in feelings of pride. |
| Element 9: culmination | Reflection of preceding discussion, conclusions drawn, praise given on progress and decisions made. Plans and goals reiterated and confirmed. Agreement regarding mobile phone follow-up on liberation. |
| Element | Elements of intervention39 | Enhancing self-efficacy | Delivery mode and location | Number of sessions and location |
|---|---|---|---|---|
| 1 | Preliminary discussion | Verbal persuasion | Face-to-face (P) Mobile phone (L) |
1 (P) 3 (L) |
| 2 | Acquiring and providing information | Verbal persuasion | Face-to-face (P) | 1 (P) |
| 3 | Self-monitoring | Verbal persuasion | Face-to-face (P) | 1 (P) |
| 4 | Increasing awareness | Physiological state | Face-to-face (P) | 1 (P) |
| 5 | Situation appraisal and appropriate coping strategiesa | Vicarious experience | Face-to-face (P) Mobile phone (L) |
1 (P) 3 (L) |
| 6 | Goal-settinga | Verbal persuasion | Face-to-face (P) Mobile phone (L) |
1 (P) 3 (L) |
| 7 | Relapsea | Performance attainment | Face-to-face (P) Mobile phone (L) |
1 (P) 3 (L) |
| 8 | Self-evaluation/self-reinforcementa | Performance attainment | Face-to-face (P) Mobile phone (L) |
1 (P) 3 (L) |
| 9 | Culmination | Performance attainment | Face-to-face (P) Mobile phone (L) |
1 (P) 3 (L) |
APPRAISE post-liberation intervention modifications due to coronavirus disease discovered in 2019
The outbreak of the COVID-19 pandemic had a significant impact on the project. Due to COVID-19 restrictions, access to both study sites for the RAs and research team was halted. It became clear quite quickly that the impact of the pandemic resulted in there being limited or no capacity for the interventionists to follow up on liberation data of those in the intervention group or deliver post-liberation intervention. Prison staff were also unable to provide us with liberation data, as their focus was rightly on the COVID-19 response in prisons. Similarly, RAs were unable to go into the prisons and access liberation data.
Modifications on timing of the post-liberation intervention delivery were made in an attempt to provide flexibility, if there was an opportunity to deliver the post-release interventions. This meant that post-release intervention sessions could still be attempted where possible with the originally intended interval between them maintained to the extent possible (4 days between sessions 2 and 3, and 14 days between sessions 3 and 4).
Chapter 3 Pilot trial methods
Sections of this chapter have been reproduced from Holloway et al.,1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
APPRAISE was a two-arm, parallel-group, individually randomised pilot study of a self-efficacy-enhancing psychosocial alcohol intervention for men on remand in prison. 1 It was intended to provide the evidence to support the design of a future definitive multicentre RCT, for which new funding would be sought.
The study aligned to the MRC framework,43 using mixed methods with two linked phases.
-
Phase I involved a two-arm, parallel-group, individually randomised pilot study. The pilot evaluation provides data to inform the feasibility of a future definitive multicentre RCT.
-
Phase II comprised an embedded process evaluation. The MRC framework for process evaluation guided the planning, design and proposed conduct of the process evaluation. 44
This chapter presents the methods of the Phase I pilot trial with the pilot trial findings presented in Chapter 4, and relates to research Objectives 1 and 4 in our protocol. Objectives 2 and 3 are discussed in later chapters.
The primary research objectives of the Phase I pilot study were:
Objective 1: to pilot the study measures and evaluation methods to assess the feasibility of conducting a future definitive multicentre, pragmatic, parallel-group RCT.
-
Is it feasible to conduct a future multicentre RCT of a self-efficacy-enhancing psychosocial alcohol intervention for men on remand?
-
Can we obtain reasonable estimates of the parameters necessary to inform the design and sample size calculation for a future definitive multicentre RCT? This includes standard deviations of potential continuous primary outcomes and estimates of recruitment, retention and follow-up rates.
-
How well do participants complete the questionnaires necessary for a future definitive RCT?
-
Can we collect economic data needed for a future definitive RCT?
-
Can we access recidivism data from the PNC databases for trial participants?
-
Can we access health data from routine NHS data sources for trial participants?
Objective 4: to assess whether operational progression criteria for conducting a future definitive RCT are met across trial arms and study sites and, if so, develop a protocol for a future definitive trial. Operational progression criteria are based on previous research results. 7
-
Do the two prisons invited to the study agree to take part?
-
Based on knowledge from previous data, do at least 90 eligible participants consent to take part and be randomised across the trial arms?
-
Do at least 70% of participants who consent to the trial receive the intervention?
-
Do at least 60% of those who received the intervention get followed up at 12 months across trial arms and study sites?
Setting and site selection
The study occurred in two study sites hosting men on remand within the prison estate of the Scottish Prison Service (SPS) and His Majesty’s Prison and Probation Service (HMPPS), one in Scotland and one in England respectively.
The complexity of the prison estate cannot be overestimated. Our learning from previous work had highlighted how essential it was to engage with our colleagues within the prison system with regard to the study. Prison governors and associated personnel at both prison sites were involved in discussions regarding the study while we were developing the initial funding application. We had built good operational knowledge as well as relationships with key personnel over the course of securing funding.
The prison governor at each site was the primary gatekeeper and contact for the study team. This proved vital in previous prison research work and again for this study. In the months leading up to data collection commencing, while waiting for ethics approval, we had several meetings with the governors at both study sites and also with appointed research study contacts for day-to-day operations. Visits were made to both prison sites to share details of the study with prison officers, health professionals and CGL over several months. The strong relationships formed were essential to our understanding of the complexities of the prison estates and the day-to-day work carried out there, providing insight into how we could undertake the research study with minimal disruption to the estate operations.
Eligibility criteria
Men detained on remand had to meet the following criteria:
-
Inclusion criteria
-
detained in either the SPS Scottish study site or His Majesty’s Prison Service (HMPS) North East England study site
-
have been in the prison setting for 3 months or less
-
aged 18 years and over
-
informed consent given
-
≥ 8 on the AUDIT screening tool51
-
-
Exclusion criteria
-
previously recruited to the study
-
unable to give informed consent or deemed incompetent/unable to make an informed decision regarding consent
-
identified as a risk to self and/or others by prison staff
-
judged to be under the influence of an illicit substance by prison or research staff
-
currently taking Antabuse
-
on a segregative rule under the prison rules
-
not able to understand the documents, which are in the English language, or agree to the research assistant (RA) working with them to understand them.
-
Prison and/or research staff were responsible for making a subjective judgement as to whether or not a remand person was under the influence of an illicit substance and whether the level of intoxication was likely to have an influence on risk or capacity to understand/consent.
Participant selection and recruitment
The prison staff were key to facilitating the selection and recruitment of study participants at both sites. At the England study site, peer induction workers were also key to this process. The RAs spent time developing good working relationships with prison staff and peer induction workers on the wing. Information regarding males on remand entering the estate was made available to the RA with the selection and recruitment process across both study sites, as outlined in Table 4.
| Scotland | England |
|---|---|
| Men on remand were given PIS by reception staff as part of their admittance. | Men on remand were held on the Induction wing. During the first 3 weeks, men on remand who were eligible were given PIS by the RA where possible. Thereafter, the RA was able to join the daily Induction session and provide the PIS and talk about the research with all new men on remand. |
| Review new arrival list sheet daily. Highlight initial eligibility of potential participants (< 3 months, high risk, Rule 95a). |
Drug and Alcohol Recovery Team (DART) provided list of new arrivals daily. RA reviewed the list. Highlighted initial eligibility of potential participants (< 3 months, high risk). |
| Arrive on wing with list and checked with prison officers any on the list eligible who may be at high risk/excluded/Rule 95. Prison officers would also identify to RA anyone who had expressed an interest to them about participating in the study. RA informed prison officer whom they wished to approach. | Arrive on wing with list and checked with prison officers any on the list eligible who may be at high risk/excluded. Prison officers and Peer Induction would also identify to RA anyone who has expressed an interest to them about participating in the study. RA informed prison officer whom they wished to approach. |
| If approval given, cell number identified and potential participant approached via door hatch. If they agreed to speak with RA, prison officer would open pad door and escort potential participant and RA to the interview room. | If approval given, cell number identified and potential participant approached via door hatch. If they agreed to speak with RA, prison officer would open pad door and escort potential participant and RA to the interview room. |
| Interview room on landing with window. RA would sit on seat nearest the door and potential participant on the other side of the table. RA reaffirmed study information, confirms exclusion and inclusion criteria and consents as appropriate. Following completion prison officer would escort participant back to the cell. If potential participant did not wish to participate, prison officer would escort them back to the cell. | Interview room glass room in middle of wing. RA reaffirmed study information, confirms exclusion and inclusion criteria and consents as appropriate. Following completion prison officer would escort participant back to the cell. If potential participant did not wish to participate, prison officer would escort them back to the cell. |
Consent
The RA at each site reviewed the Participant Information Sheet (PIS) with men on remand who met the eligibility criteria, provided a written and verbal description of the study, answered any questions or queries and then invited them to consider participating. The RA obtained informed consent from those willing to participate. Those who did not wish to participate at this point were thanked for their time and received no further interaction with regard to participating in the study.
We were aware that freedom of consent can easily be undermined for prisoners and those in the criminal justice system, which means these individuals may be more vulnerable to exploitation or abuse by researchers: learning disabilities, illiteracy and language barriers are prevalent within these populations. The prevalence of these characteristics alongside the power differential between researcher and potential participant meant that particular care was needed to ensure that valid, freely given and fully informed consent was achieved. For the purposes of this research, we considered valid consent as underpinned by adequate information being provided to the potential study participants and that they had the capacity to decide for themselves. A capable person would:
-
understand the purpose and nature of the research
-
understand what the research involves, its benefits (or lack of benefits), risks and burdens
-
understand the alternatives to taking part
-
be able to retain the information long enough to make an effective decision
-
be able to make a free choice; and
-
be capable of making this particular decision at the time it needs to be made.
Participants were asked to consent to their data being used for the present study as well as consenting to long-term follow-up (beyond this study) and for appropriate linkage to be conducted.
Stopping rule/discontinuation/withdrawal criteria
Participants were reminded during the trial that they were free to withdraw at any time without having to give a reason and without it affecting their care in the prison setting or on liberation. Where a participant wished to withdraw, we honoured their wish. We also made attempts to ascertain and document the reason for withdrawal, recording this within the case report form (CRF). Participants who requested withdrawal from the study intervention were asked if they would be willing to remain in the study for the purposes of follow-up data collection. Data provided at the point of withdrawal were retained and used in the study analysis, where the patient consented to this.
Potential reasons for participants being withdrawn from the study were: participant withdrawal of consent; RA discretion in the best interest of the participant to withdraw; the RA was informed by Prison, NHS or service staff that it was in the best interests of the participant to withdraw; an adverse event required discontinuation of participation in the trial; or termination of the trial by the sponsor.
Sample size
The aim was to recruit at least 180 participants in total comprising 90 participants per study arm across the two study sites. From prison data obtained from correspondence with SPS and the Ministry of Justice (MoJ), we had estimated that approximately 50% of participants would be liberated while the rest would remain incarcerated, leaving 45 participants per study arm (90 in total) across the two study sites.
The target sample size
-
would enable us to calculate two-sided 95% confidence intervals around proportions recruited, liberated, and dropping out in each study arm with half-widths of < 0.15
-
exceeds the 30 per group recommendation of Lancaster et al.,53 and the 35 participants per group recommendation of Teare et al.,54 for estimating key unknown design parameters, for example standard deviation with sufficient precision when the primary outcome is continuous; and
-
would ensure that within each study arm within each site we were satisfying the minimum 12 per group rule of thumb of Julious for pilot trials. 55
Participant screening
The AUDIT tool51 is considered the ‘gold standard’ alcohol screening instrument and was developed by the World Health Organization (WHO). It is a 10-item screening tool designed to assess alcohol consumption, drinking behaviours and alcohol-related harms. The score is the total sum derived from the 10 questions. Scores range from 0 to 40. A score of 8–15 indicates hazardous/increasing-risk alcohol use, 16–19 indicates harmful/high-risk alcohol use and 20–40 indicates likely dependence. The AUDIT has been used previously in the criminal justice system,7 and was found to be feasible and acceptable with men on remand in the PRISM-A study. 40
After obtaining informed consent, the RAs screened all study participants using the AUDIT. Those with a score of ≥ 8 were considered eligible for the study. Those scoring < 8 on AUDIT were thanked for their time and took no further part in the study. Those with an AUDIT score of ≥ 8 completed the baseline assessment and measures and were then randomised.
Randomisation and blinding
The randomisation process was supported by the Edinburgh Clinical Trials Unit (ECTU). Due to the restriction of the use of electronic equipment and no access to mobile phones by the research team and RAs while in the prison setting, we were unable to use a randomisation system, such as an interactive voice response telephone system or one accessed over the web. Allocation was conducted at the level of the participants, randomised to the active or control intervention using stratified block randomisation by site, via opaque sealed envelopes, based on a predetermined random number allocation carried out by the ECTU. Allocation was conducted by researchers opening the next sequential sealed opaque envelope after consent had been provided and the baseline assessment completed. Therefore, RAs were blind to group allocation at baseline.
The RAs were not involved in the delivery of the active and control interventions but were aware of study allocation of participants as the trial progressed. Allocation concealment was used whereby neither the person delivering the interventions nor the participant was aware of the study allocation until they were irrevocably entered into the trial. Both the trial statistician (RP) and health economists (AS, JB) were blind to group allocation prior to the final analysis and only had details of study participants by study number.
The trial statistician and health economists were only to be unblinded if requested to do so by the Data Monitoring and Ethics Committee Project Steering Group (DMEC), due to safety concerns. This was not necessary during the study and unblinding took place at the final analysis stage.
Self-report primary outcome measure
The proposed primary outcome measure for a future definitive study was total alcohol consumed (in units) in a 28-day period. This can be ascertained using the 28-day timeline followback questionnaire (TLFB-28). 43 Three other variables can be derived from the data: per cent days abstinent, drinks per drinking day (secondary outcome measures) and total number of days where alcoholic drinks are consumed. The TLFB-28 was to be conducted by the RA at time points (TP) 1 and 2.
Self-report secondary outcome measures
Secondary outcomes measures were to be completed at TP0 (baseline), TP1 (6 months) and TP2 (12 months).
Alcohol use frequency, quantity (on a typical occasion) and binge drinking were assessed using the AUDIT. 34 In order to assess the utility of using Average Drinks per Day derived from the AUDIT at 12 months as a primary outcome measure we planned to randomise the order of presentation of TLFB-28 and AUDIT and conduct a levels-of-agreement analysis, using TLFB-28 as a gold standard, to explore whether AUDIT is an acceptable proxy for TLFB-28. The order of presentation of TLFB and AUDIT was to be randomised in advance by a secure remote randomisation service. (See section ‘Follow-up plans post-COVID 19’ for changes to the use of AUDIT and TLFB-28 at TP1 and TP2.)
The following study measures were to be used across the three time points.
Warwick-Edinburgh Mental Well-being Scale
Warwick-Edinburgh Mental Well-being Scale56 comprises 14 items with five response categories, ranging from ‘None of the time’ to ‘All of the time’. The items are all worded positively and cover both feeling and functioning aspects of mental well-being. Items are scored on a range from 1 to 5, providing a total score between 14 and 70.
Drinking Refusal Self-efficacy Questionnaire – revised
This revised version of the DRSEQ57 assesses a person’s belief in his/her ability to resist alcohol. There are 19 items, each scored on a five-point Likert scale. Responses range from 1 (I am very sure I could NOT resist) to 6 (I am very sure I could resist), providing a total score between 19 and 114. A lower score indicates less self-efficacy.
Three subscales can also be calculated: Social Pressure (SP) (score range 5–30), Emotional Relief (ER) (score range 7–42) and Opportunistic (OP) (score range 7–42).
Negative Alcohol Expectancy Questionnaire
The NAEQ58 assesses the extent to which people expect negative consequences to occur if they drink. There are 60 items in the questionnaire. Responses are measured on a five-point Likert scale ranging from 1, which is ‘highly unlikely’, to 5, which is ‘highly likely’, providing a total score between 60 and 300. A lower score indicates more negative expectancies.
The items, themselves, are grouped onto three dimensions (same-day, next-day and continued-drinking expectations). The next-day and continued-drinking dimensions are combined to form the distal expectancy subscale (score range 39–195) and the same-day, the proximal subscale (score range 21–105).
EuroQol-5 Dimensions, five-level version
The EQ-5D-5L59 comprises two parts. The first is a visual analogue scale and the second is a descriptive system. There are five dimensions within the descriptive system: mobility, self-care, usual activities, pain/discomfort, anxiety/depression. Each has five levels: no problems, slight problems, moderate problems, severe problems, and extreme problems. Participants convey their health state by identifying the most appropriate statement in each of the five dimensions. Each dimension score is combined to describe health state. An X is used for the visual analogue score to identify the health of the participant on that particular day.
Readiness to Change Ruler
The Readiness to Change Ruler is used to assess a person’s readiness to change their alcohol use. 10 There are six readiness to change rulers on the assessment form. Each ruler represents a linear scale from 1 to 10, and the participant marks on the ruler their current position in the change process.
The Readiness to Change Ruler was completed immediately prior to and immediately following the initial intervention session. This was carried out by the interventionist as part of the initial intervention delivery.
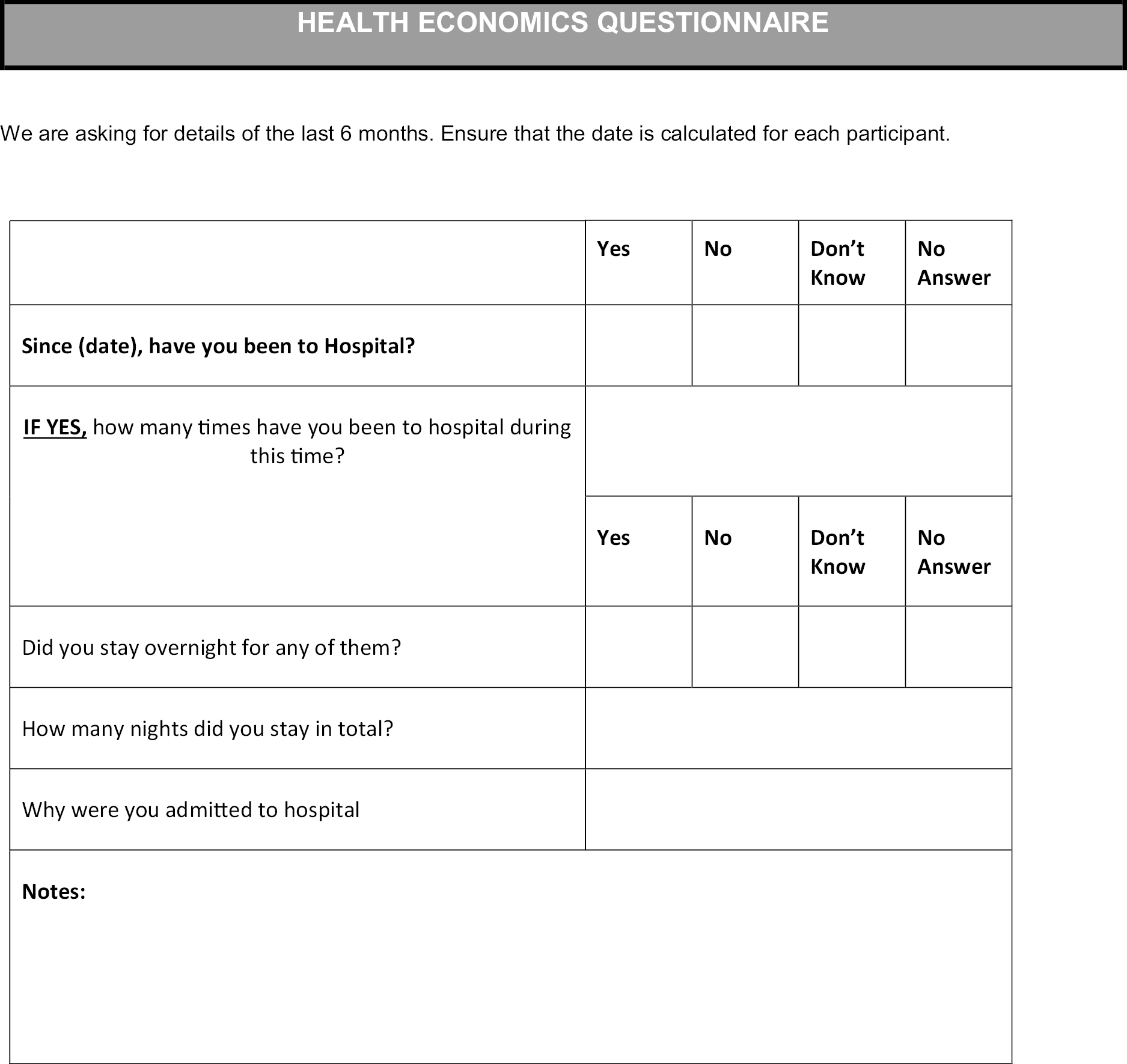
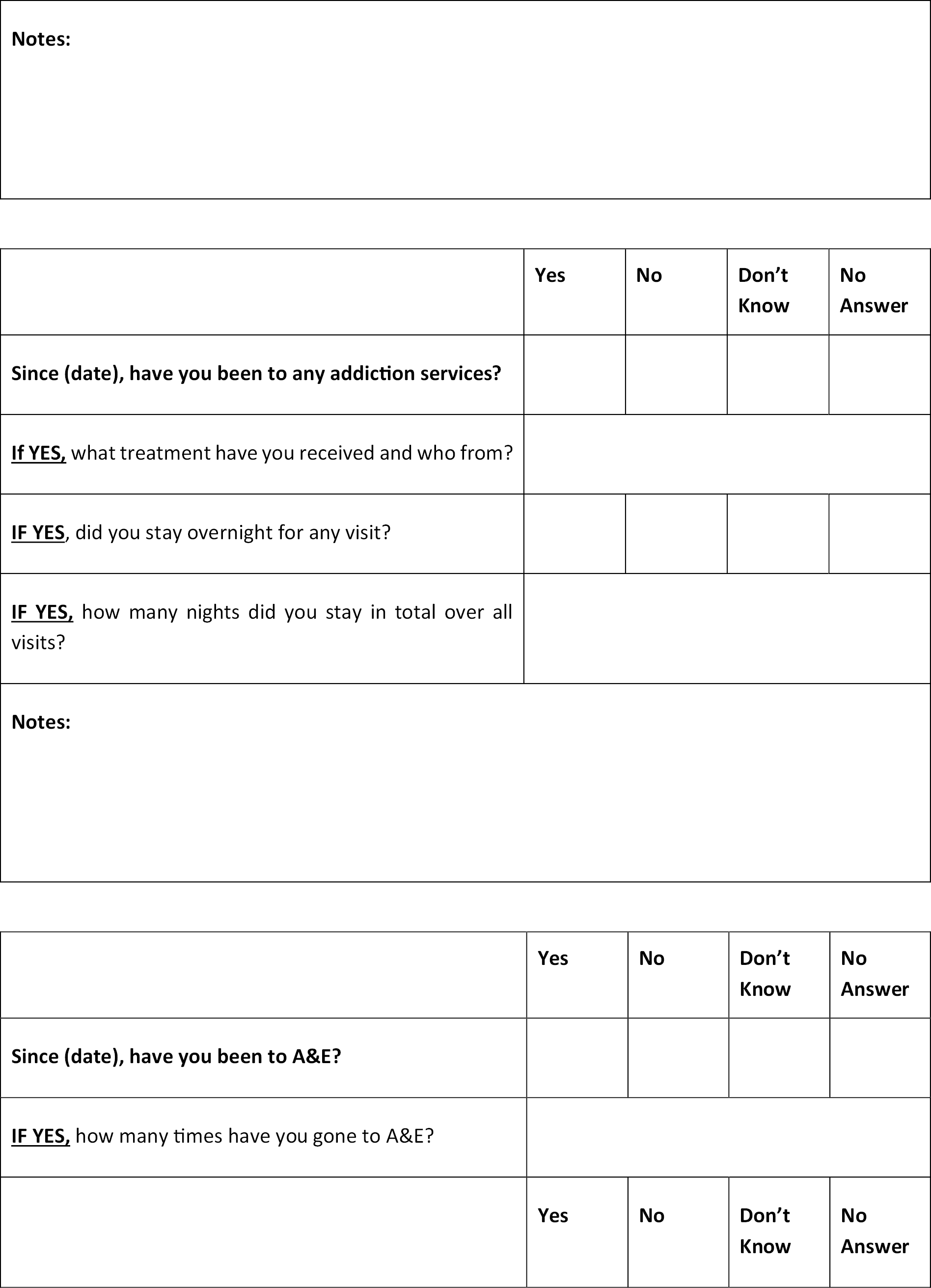
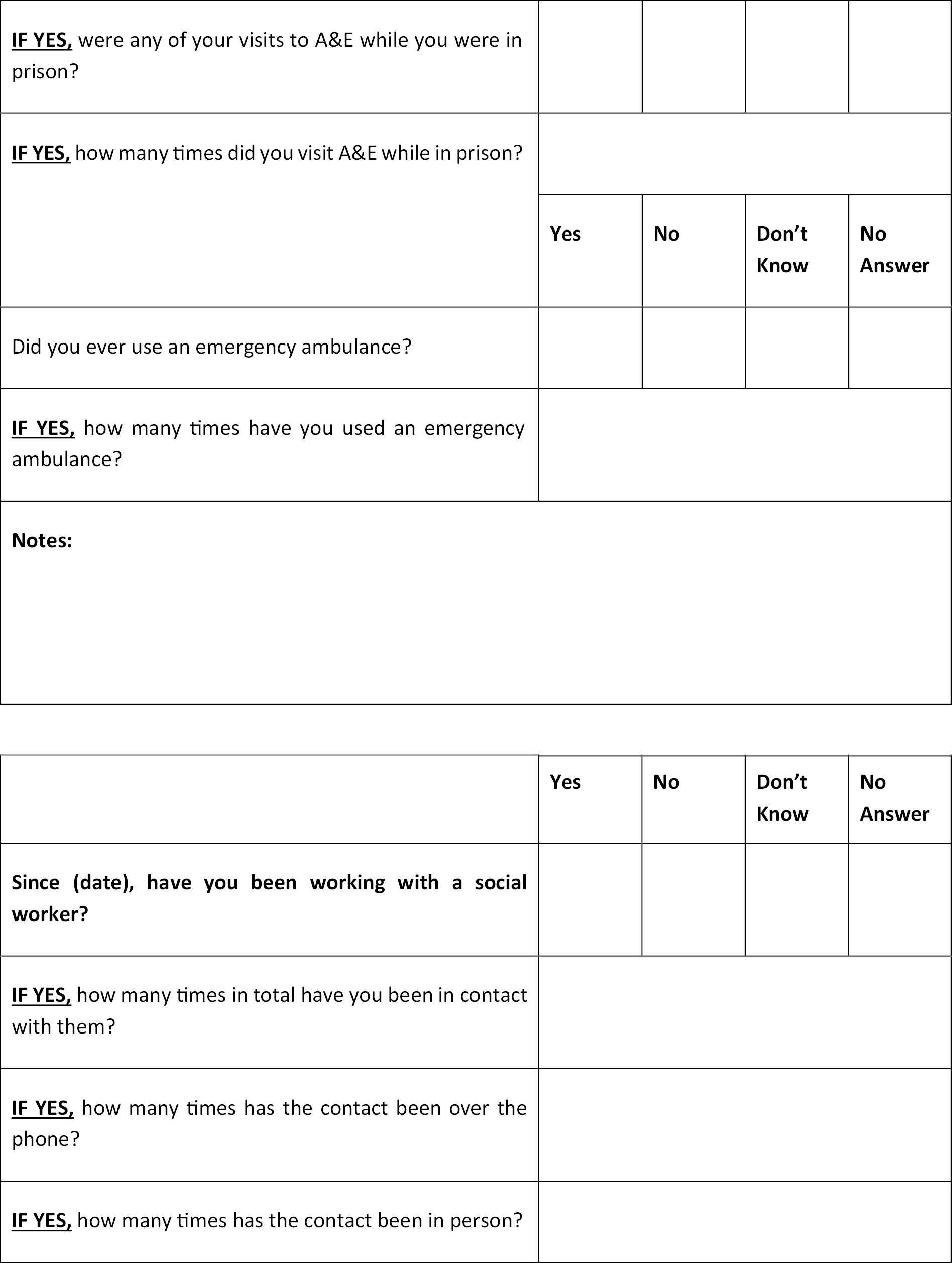
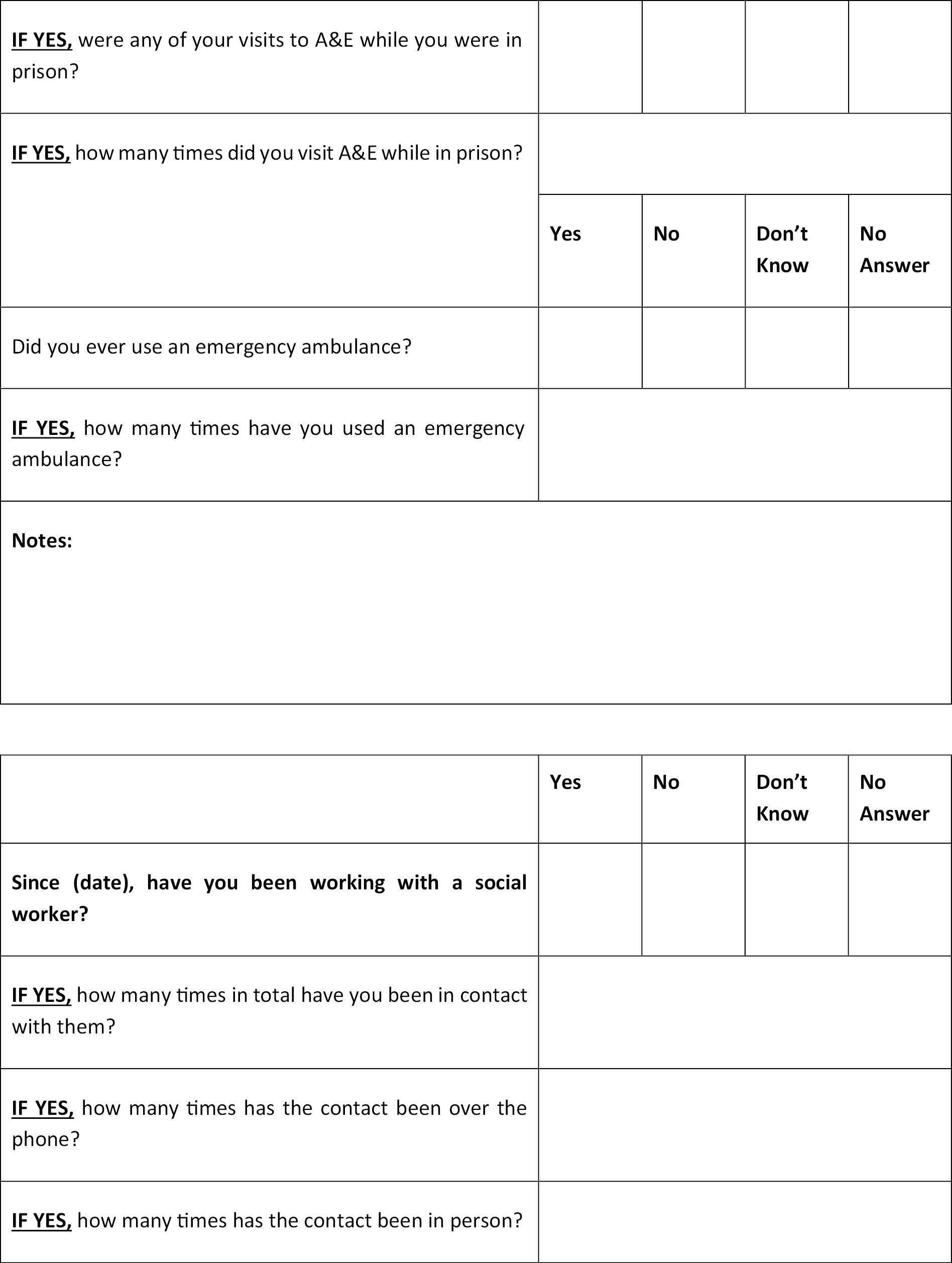
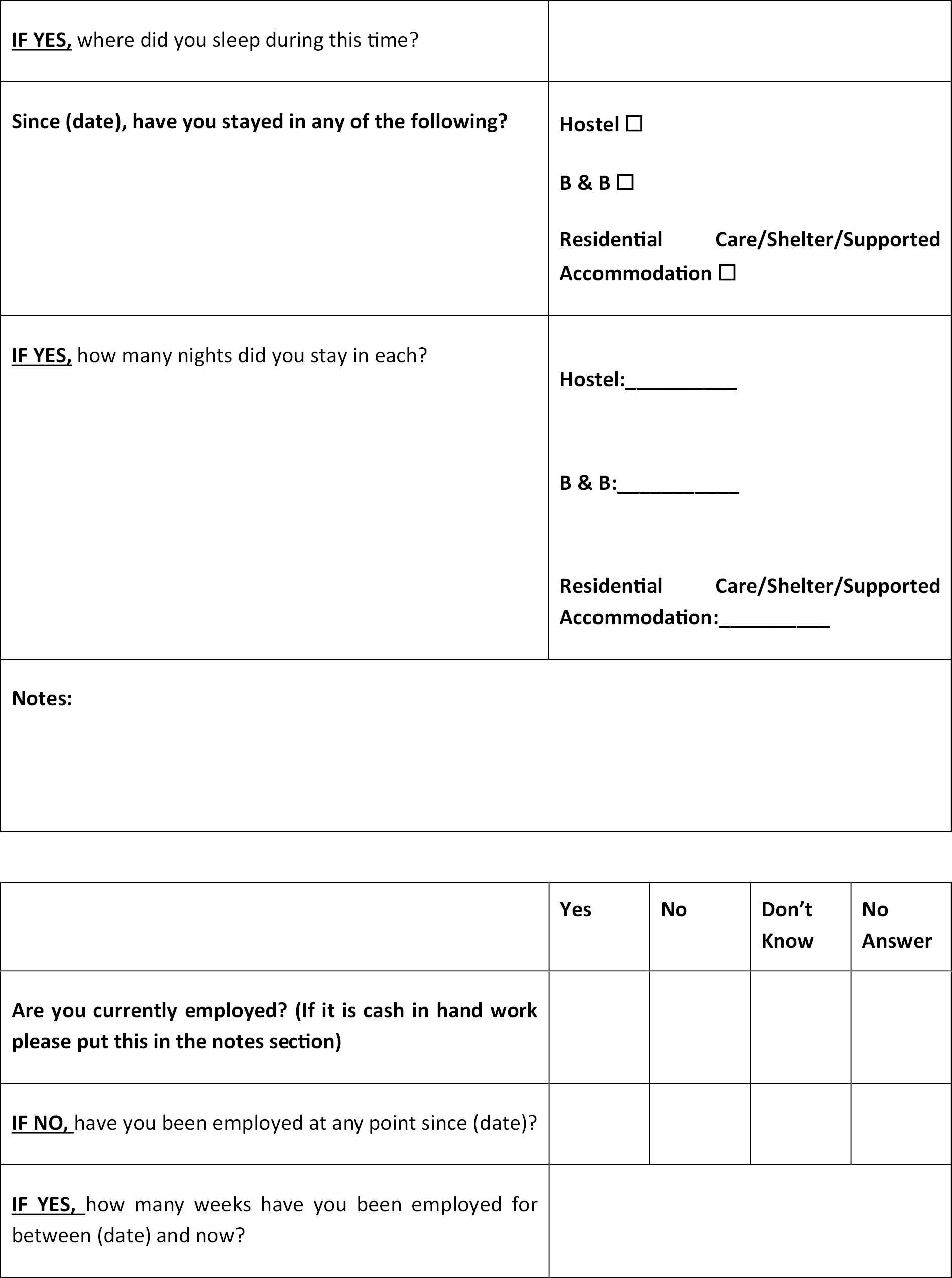
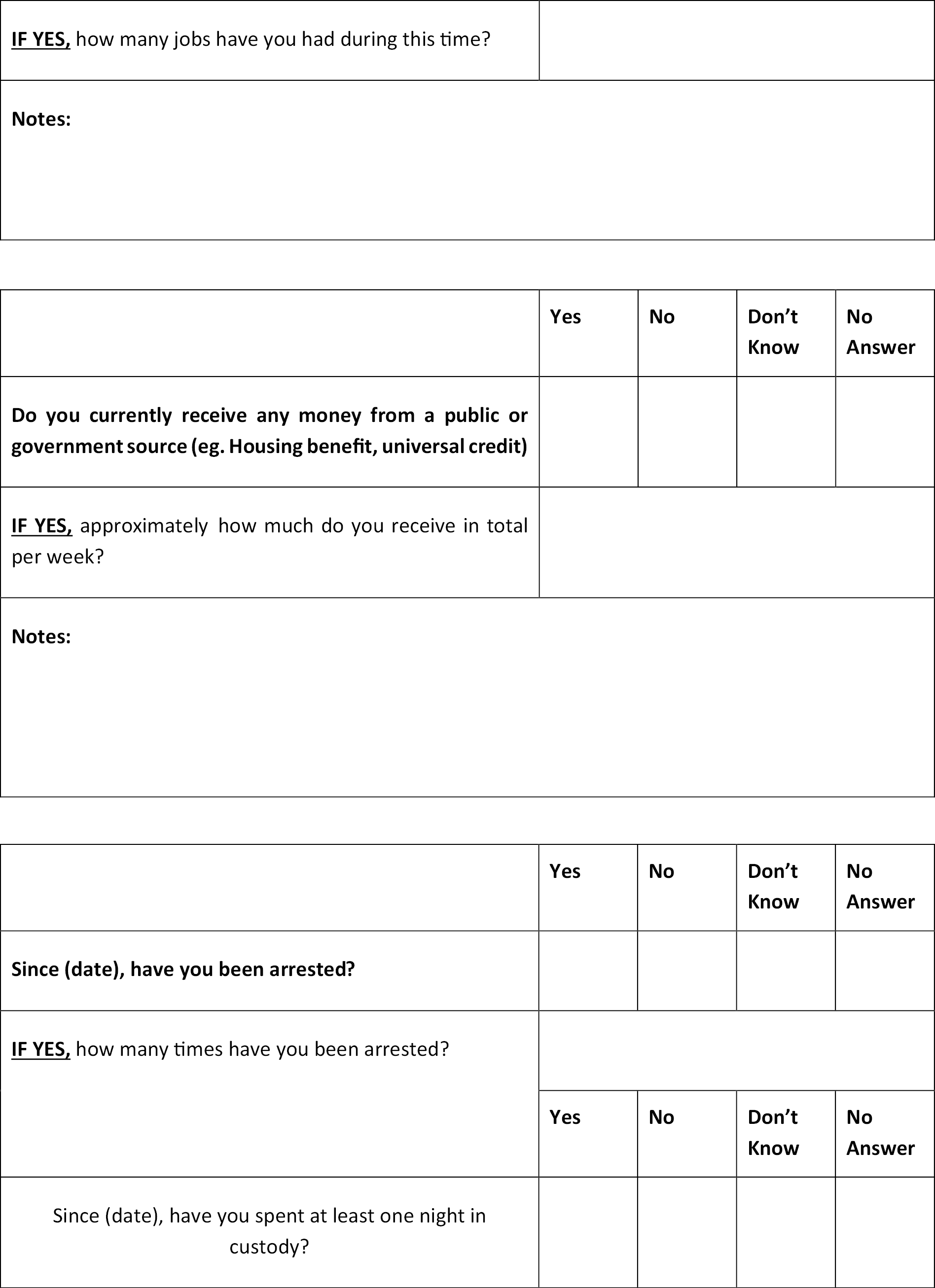
Economic Form 90
We adapted the terminology of the Economic Form 9060 (the Economic Form 90 was originally designed for American context) (see Chapter 7, Methods) to produce a service user questionnaire to determine social costs including in the domains of health and social care use, criminal justice involvement, unemployment, and welfare (see Appendix 9).
Baseline data collection and assessment of outcomes
Baseline data (TP0) collection was conducted prior to randomisation to prevent observer or respondent bias to questions asked or answered at baseline by knowledge of the randomisation group, with follow-up data collected at TP1 (6 months) and TP2 (12 months).
The baseline assessment data were collected via researcher-led completion of hard-copy questionnaires embedded within the Baseline CRF (TP0). Due to restrictions on the use of electronic equipment in the prison estate, we were unable to use electronic devices to record study data on site. The RA was able to answer any questions and offered clarification as needed. The baseline assessment took approximately 35 to 60 minutes. Participants also completed the Participant Locator Form (see Appendix 10). The Locator Form was used to collect information from participants about a range of methods, modes and formats of contacting them at follow-up if they were liberated. Immediately after, participants were randomised, informed of their allocation,61 and thanked for their time.
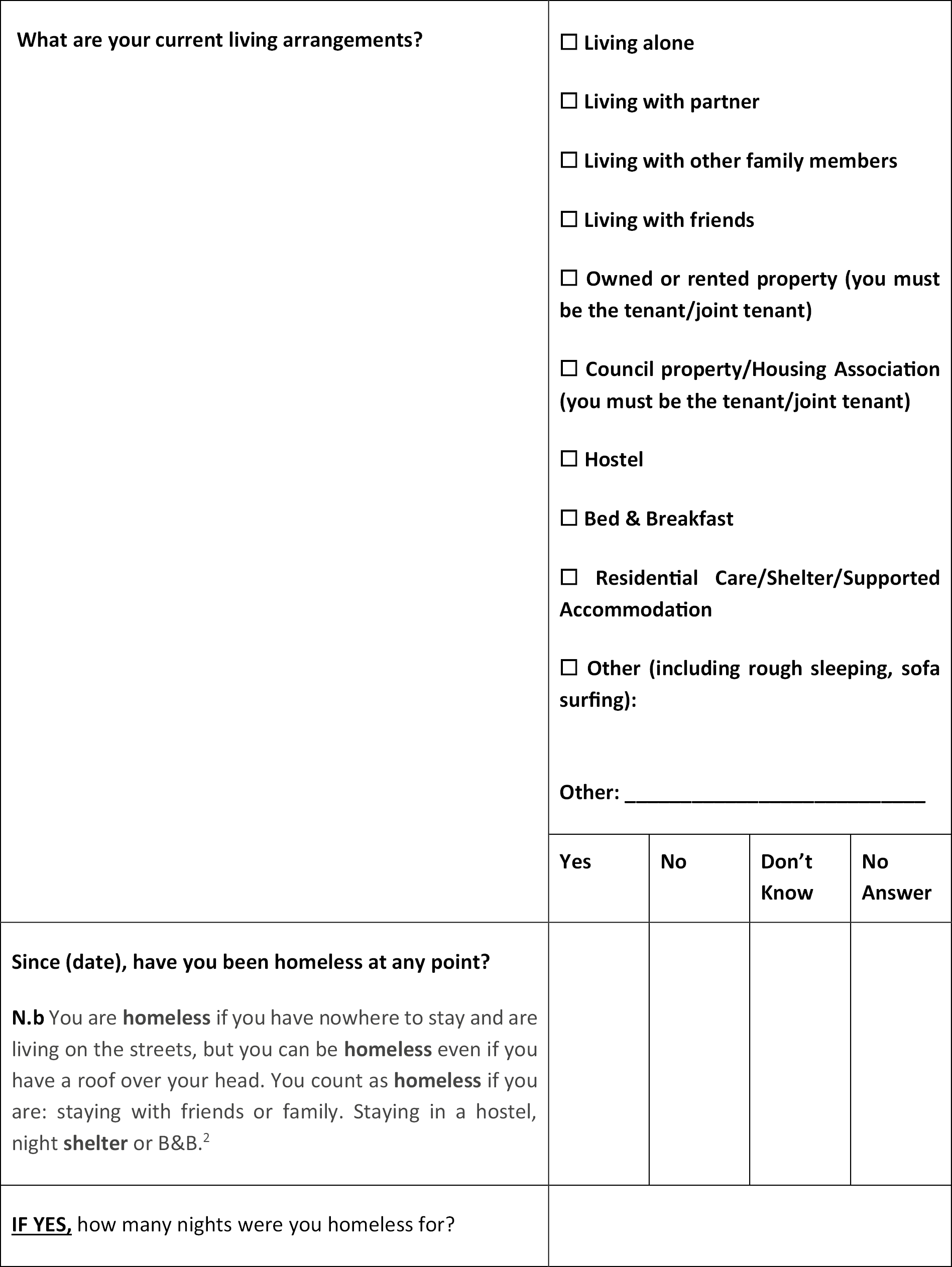
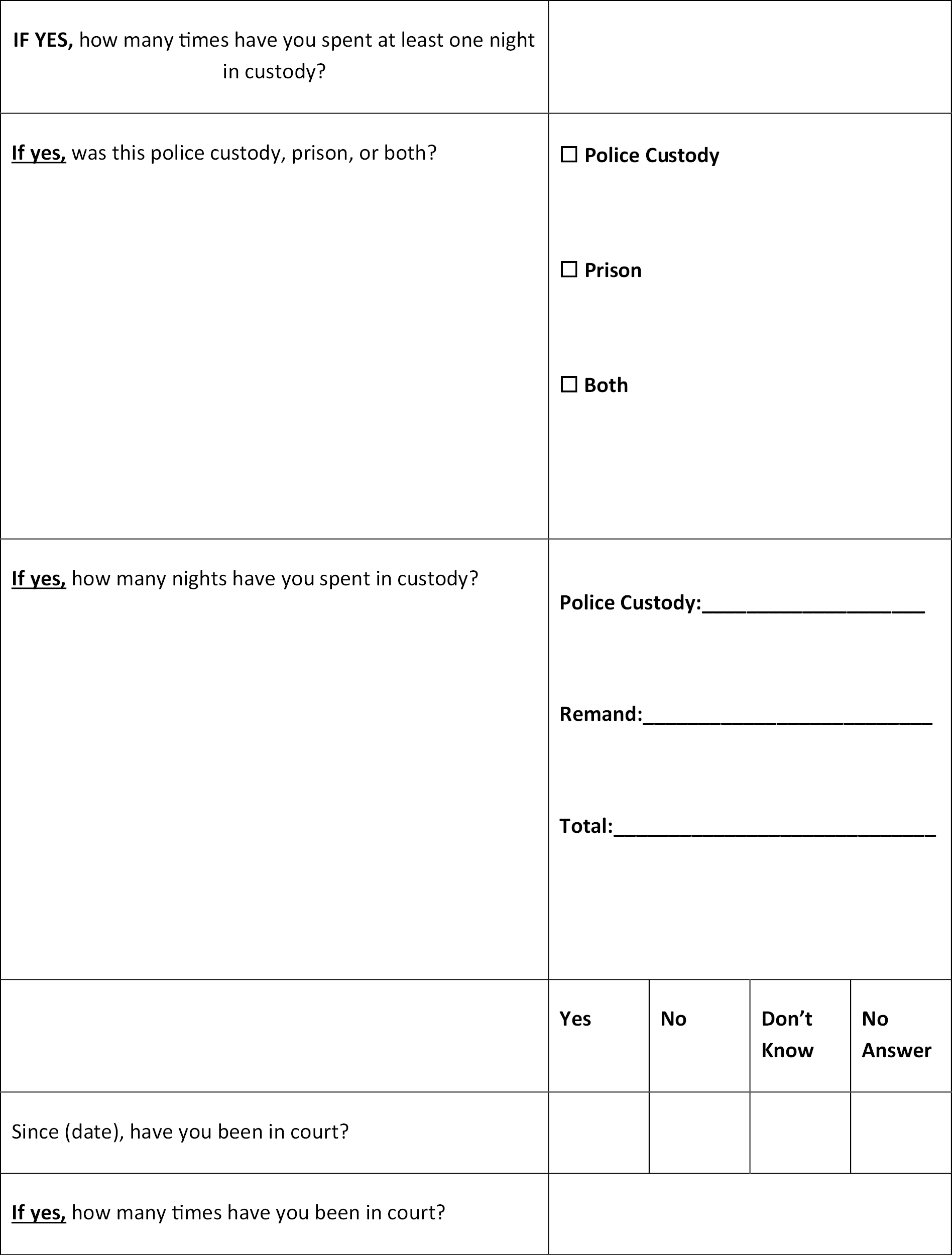
The baseline CRF recorded demographic data on age, known court dates, ethnicity, postcode [Scottish Index of Multiple Deprivation (SIMD)], relationship status, and educational achievement. In addition, baseline data on proposed secondary outcome measures were recorded via the Readiness to Change Ruler,10 the EQ-5D-5L,59 the Warwick-Edinburgh Mental Well-being Scale,56 the Drinking Refusal Self-efficacy Questionnaire – revised,57 the Negative Alcohol Expectancy Questionnaire,58 and a revised version of the Economic Form 90,60 which recorded data relating to hospital and or A/E visits, general practitioner (GP) registration and visits, engagement with Community Psychiatric Nurse, engagement with any addiction services, emergency ambulance use, engagement with social worker, current living arrangements, ever been homeless, employment status, number of arrests and number of court visits.
Control condition (care as usual)
The control condition (care as usual) consisted of similar components at both study sites.
England control condition
All men held on remand are screened by a reception nurse on reception. If a substance misuse need is identified in the screening, they are referred to the Drug and Alcohol Recovery Team (DART) and the team then sees them the following day to complete the triage and comprehensive assessment. Those men who decline the offer of the DART service are then revisited to be given harm-reduction information and a point of contact if they need to self-refer further into their sentence. Posters are displayed around all of the establishment and anyone or any service can refer an individual to DART.
They refer to the relevant community substance misuse treatment service for an individual’s release and ensure the service user understands when and where their appointment is. They also offer additional support through the gate with their Reconnect Navigators, who will support those individuals who are more complex and struggle to engage to their first appointment.
Scotland control condition
For those service users who expressed that they are looking for alcohol support, the support is person-centred and based on the person’s needs. Following assessment, individuals would agree a recovery plan with their worker, the recovery coordinator, and support Scotland Mental Well-Being Scalemay be alcohol awareness, harm reduction, motivational support and relapse prevention. The frequency of this would be dependent on the individuals’ needs and would not be time-limited. People with alcohol issues could be referred to the relevant region’s alcohol service for counselling support if they wanted this. If the individual was returning to the region where the prison was, they would be offered through-care support from a recovery support service. This would include practical support as well as substance misuse support to help them reintegrate back into the community.
Intervention condition
Following completion of baseline assessments and randomisation, those allocated to the intervention arm were invited to attend their first of three intervention sessions. This was delivered face to face by the identified interventionist at each study site. The APPRAISE intervention was delivered at both sites by CGL.
The in-prison and post-liberation elements of the APPRAISE intervention are described in full detail in Chapter 2.
Follow-up data collection
We worked with our PPI co-applicant and former community justice mentor, who mentored men in prison and on liberation, to advise on the strategies to maximise retention and follow-up. These strategies were based on her own experiences of following up her mentees on liberation and were also strategies used by CGL community justice workers. Each study participant provided their preferred method of follow-up by completing the Locator Form at baseline.
Follow-up assessments were to be attempted at 6 months (TP1) and 12 months (TP2) post-randomisation where the participant had been (a) not liberated, (b) liberated and in the community, or (c) liberated and then re-incarcerated. An 8-week window was in place for the follow-up to be completed for both of the time points. If a participant was not contacted at 6 months they were still approached again at 12 months. Follow-up was to be conducted by the RA at each study site. However, due to changes in personnel at both study sites during the study, all follow-ups for both study sites were not conducted by the RA who undertook recruitment and baseline measurements. Feedback from all RAs noted that participants responded to follow-up more positively when it was the RA they knew and remembered from recruitment and baseline. There was a sense of trust that had been built which was less evident when the new RAs were undertaking the follow-ups.
Follow-up plans pre-coronavirus disease discovered in 2019
Participants were initially followed up using one of the following methods, determined by the information they provided at baseline interview as part of the Locator Form completion:
-
by phone call (at varying times and days of the week)
-
via hard copies of the follow-up questionnaire sent by post with an accompanying letter to be completed and returned to the study team via a pre-paid envelope; two reminders were sent; or
-
via hard copy in prison for completion with the RA.
Follow-up plans post-coronavirus disease discovered in 2019
As a result of the impact of COVID-19 on the planned follow-up strategy, modifications were made to the follow-up method, procedures, data collection format, measures, and CRFs. These were discussed by the project management group (PMG) and then at the Trial Steering Committee (TSC). Ethical approval for these amendments was sought and gained.
Additional follow-up approaches were added: text message, WhatsApp, Facebook and an electronic Qualtrics link to the survey sent by phone or e-mail. Follow-ups were to be conducted over the phone by the RA. Where study participants were identified as being incarcerated at follow-up, we would attempt to make appropriate arrangements with the relevant prison to establish if it was possible to visit and undertake the follow-up assessment. Due to the duration of the COVID-19 pandemic, access to the England study site was still not possible and for the Scotland site, although access had started to return, it was restricted and was only possible in a few instances, by which time the study had concluded.
Participants who had given permission to use social media were also sought on Facebook and one attempt to contact them was carried out (we were limited to one attempt as per ethics committee stipulation).
COVID-19 restrictions meant that we were unable to undertake face-to-face interviews. We therefore developed alternative formats of CRFs for participants to complete at 6- and 12-month follow-ups. Our amendment allowed us to send electronic copies via Qualtrics link to participants (if they had consented to us contacting them in this way) and would allow for self-completion using hard copies. We simplified the CRFs to accommodate this and removed the TLFB-28, which required in-person administration. We therefore replaced the AUDIT and TLFB-28 with the extended-item AUDIT-C questionnaire. Previous studies have shown AUDIT-C and the TLFB-28 demonstrating excellent levels of agreement on alcohol consumption. 4 An overall total score of ≥ 5 is deemed as AUDIT-C positive, and indicates increasing or higher-risk drinking. 62
The NAEQ includes three sub-sections. The final sub-section was removed as it was considered as having potential to cause distress when self-completed. This was discussed at length by the PMG and with particular input from our PPI co-applicant. The layout of the Health Econ Form was also simplified to support self-completion.
Statistical methods/analysis plan
The progress of participants through the APPRAISE pilot trial is presented in accordance with CONSORT (Consolidated Standards of Reporting Trials) guidelines40 to allow descriptions of key parameters required for a future RCT: eligibility rates, consent, adherence, retention at follow-up and data completeness of outcome measures.
Overall statistical principles
Analyses were based on a modified intention-to-treat (ITT) population unless otherwise stated. The modified ITT population included all participants who were randomised into the APPRAISE study, if they had provided valid non-missing data for each outcome at the relevant time points. Participants were analysed according to the trial arm they were randomised to, irrespective of the treatment they received, continuing study eligibility, or compliance post randomisation. Participants who discontinued with the intervention, withdrew, or were non-compliant with the protocol were included in the ITT population, provided that valid outcome data were recorded for them.
It was assumed that any missing data were missing-completely-at-random (MCAR). Although a multiple imputation analysis was specified in the protocol paper, this approach is only valid when the proportion of missing data lies between 5% and 40%. 63 Very high amounts of missing data at follow-up meant that no multiple imputation was performed and all missing data were left as missing.
Lancaster et al. 53 recommend that the analysis of a pilot study should be mainly descriptive and focus on confidence intervals. Therefore, the analyses focused on calculating descriptive statistics and two-sided 95% confidence intervals rather than on hypothesis tests or p-values in general. Outliers were identified by viewing boxplots and/or histograms of the outcome variables of interest and were queried at the data-checking stage where an error had been suspected. All analyses included outliers as standard unless otherwise stated.
Primary outcome measure
The primary outcome was to be collected at TP0, TP1 and TP2. The primary outcome for the pilot study was alcohol consumed in the 28 days prior to TP2, assessed using the extended Alcohol Use Disorders Identification Test – Consumption (AUDIT-C). This was calculated using questions 1 and 2 of the AUDIT-C, which address frequency and quantity of alcohol consumed. 64,65 Responses to question 1 were recoded; Never = 0, Monthly or less = 0.25, 2–4 times per month = 0.75, 2–3 times per week 2.5, 4–5 times per week = 4.5, 6 or more times per week = 7. Question 2 was recoded; 1–2 drinks = 1.5, 3–4 = 3.5, 5–6 = 5.5, 7–9 = 8, 10–12 = 11, 12–14 = 13 and more than 14 = 16. The weekly consumption was derived by multiplying the recoded values for question 1 and question 2 together and then multiplying the product by 4 to derive 28-day consumption.
The original AUDIT-C measure is known for right censoring quantity of consumption and as a consequence being less responsive to change in heavy drinkers. Extending the AUDIT-C response categories we aimed to have a trade-off between minimal completion burden and granular data. We initially tested our assumptions about categorisation of consumption in data sets that contained the extended AUDIT-C and TLFB and found minimal benefit of allocating a daily consumption value over 16 units per drinking day, something that has been further confirmed in other studies using the extended AUDIT-C to assess weekly consumption. 66
Secondary outcome measures
The secondary outcome measures are the Readiness to Change Ruler,10 the EQ-5D-5L,59 the Warwick-Edinburgh Mental Well-being Scale,67 the Drinking Refusal Self-efficacy Questionnaire – revised,57 the Negative Alcohol Expectancy Questionnaire,58 and a revised version of the Economic Form 90. 60 Measurements were recorded at baseline (TP0) using a combination of self-completion and researcher-led completion of a hard-copy questionnaire. These measures were to be collected again at 6 months (TP1) and 12 months (TP2) post randomisation where participants were (a) not liberated, (b) liberated and in the community or (c) liberated but back in prison.
Recruitment, adherence and follow-up retention analyses
Trial management data, the Intervention Delivery Logs, and follow-up questionnaires were used to assess recruitment, eligibility, adherence, and retention at follow-up. For recruitment and eligibility, the following trial management data (recorded from the initiation of the trial until full recruitment is reached) were considered by each study site where possible:
-
number entering on remand
-
number given information sheet
-
number approached
-
number consented
-
number randomised and
-
number followed up at each time point.
These numbers were used to calculate appropriate proportions, which are reported for the entire study and by site. Exact 95% confidence intervals were calculated for key overall proportions relating to recruitment, adherence and retention.
Descriptive summaries
Descriptive statistics were calculated for the following variables:
-
baseline characteristics
-
numbers receiving the in-prison and post-liberation intervention
-
duration of the in-prison intervention sessions
-
reasons why the in-prison intervention was not delivered
-
numbers followed-up
-
reasons for being unable to follow-up
-
information on data completeness at baseline and follow-up time points
-
the primary outcome (28-day alcohol consumption)
-
secondary outcomes.
In general, categorical variables were presented as counts and percentages. Discrete and continuous variables were presented using the mean, median, standard deviation (SD), minimum, maximum, and number of responses, split by randomisation group for the entire study and by study site.
A side-by-side boxplot was produced to show the age distribution of participants randomised to each site.
Primary outcome analyses
Means and 95% confidence intervals were calculated for 28-day alcohol consumption in each randomised group and site.
For the primary analysis, the mean difference in alcohol consumption at 12 months post randomisation (TP2) between the two randomisation groups was calculated (with 95% confidence intervals), both overall and stratified by site. Linear regression was used, adjusting for baseline alcohol consumption (TP0).
The mean difference was calculated assuming that any missing outcome data were missing-at-random (MAR) and only patients with AUDIT-C data collected at TP0 and TP2 were included (i.e. we performed a complete-cases analysis).
Secondary outcome analyses
The psychometric measurements were treated as secondary outcomes, and descriptive statistics were calculated based on these, stratified by site and randomised group.
Table 5 contains information on the number and type of measurements for each psychometric tool.
| Tool | Abbreviation | Number and type of measurements |
|---|---|---|
| Alcohol Use Disorders Identification Test for consumption | AUDIT-C | 1 score (0–12) treated as discrete and categorical |
| Readiness to Change Ruler | – | 6 scores (1–10) treated as discrete |
| EQ-5D-5L | – | 5 categorical variables and 1 score (0–100) treated as discrete |
| Warwick-Edinburgh Mental Well-being Scale | WEMWBS | 1 score (14–70) treated as discrete |
| Drinking Refusal Self-efficacy Questionnaire – revised | DRSEQ-R | 1 score (19–114) treated as discrete |
| Negative Alcohol Expectancy Questionnaire | NAEQ | 2 separate scores (21–105; 18–90) treated as discrete |
Information on the derivation of the psychometric outcome measures is provided below, along with details of how missing individual item scores were accounted for in the calculation of total scores.
-
AUDIT-C: the primary outcome is alcohol consumed in the 28 days prior to TP2, assessed using the extended AUDIT-C. This is calculated using questions 1 and 2 of the AUDIT-C, which address frequency and quantity of alcohol consumed. Responses to question 1 were recoded; Never = 0, Monthly or less = 0.25, 2–4 times per month = 0.75, 2–3 times per week = 2.5, 4–5 times per week = 4.5, 6 or more times per week = 7. Question 2 was recoded; 1–2 drinks = 1.5, 3–4 = 3.5, 5–6 = 5.5, 7–9 = 8, 10–12 = 11, 12–14 = 13 and more than 14 = 16. The weekly consumption was derived by multiplying the recoded values for question 1 and question 2 together and then multiplying the product by 4 to derive 28-day consumption. The AUDIT-C was also used to calculate a total score, which was calculated as the sum of the first three questions of the AUDIT questionnaire. The first question was scored as 0 (never), 1 (monthly or less), 2 (2–4 times a month), 3 (2–3 times a week), 4 (4–5 times a week, or 6 or more times a week); the second question scored as 0 (1 to 2), 1 (3 to 4), 2 (5 to 6), 3 (7 to 9), 4 (10 to 12, 12 to 14, or more than 14); and the third question scored as 0 (never), 1 (less than monthly), 2 (monthly), 3 (weekly), 4 (daily or almost daily). If any participants answered ‘Never’ to AUDIT-C Q1 then their overall score was 0. Otherwise, if any of the first three questions were missing then the AUDIT-C was also missing.
-
The Readiness to Change Ruler is used to assess a person’s readiness to change their alcohol use. There are six readiness to change rulers on the assessment form. Each ruler represents a linear scale from 1 to 10, and the participant marks on the ruler their current position in the change process. The score for each question was regarded as the integer value closest to the mark made by the participant on the ruler. No missing-value imputation was performed.
-
EQ-5D-5L consists of five descriptive dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression) and a question on how the respondent would rate their health. Each descriptive dimension has a score of 1–5 with levels: no problems (1), slight problems (2), moderate problems (3), severe problems (4), and unable to or extreme problems (5). The visual analogue score consists of a scale numbered from 0 (‘best health you can imagine’) to 100 (‘worst health you can imagine’). No missing-value imputation was performed.
-
The WEMWBS consists of 14 items with five response categories. Each item was scored on a range from 1 to 5, and a total score was calculated with a possible range of 14 to 70. A higher WEMWBS score indicates a higher level of mental well-being. The total score was treated as missing if 50% or more of the individual items were missing. If fewer than 50% of the items were missing, then each of the missing individual item scores was imputed using the mean of the remaining non-missing questions before calculation of the total score.
-
The DRSEQ-R consists of 19 items with five response categories following a Likert scale. Each item is scored on a range from 1 to 6, providing a total score between 19 and 114. A lower score indicates less self-efficacy to resist alcohol. The total score was treated as missing if 50% or more of the questions were missing. If fewer than 50% of the items are missing, then each of the missing individual item scores was imputed using the mean of the remaining non-missing questions before calculation of the total score.
-
The NAEQ at baseline consists of 60 items with five response categories following a Likert scale. Each item is scored on a range from 1 to 5, with 1 indicating ‘highly unlikely’ and 5 indicating ‘highly likely’. The NAEQ was used to generate two expectancy scores: same day (sum of items 1–21) and next day (sum of items 22–39). 68 Each expectancy score was treated as missing if 50% or more of the questions were missing. If fewer than 50% of the items were missing, then each of the missing individual item scores was imputed using the mean of the remaining non-missing questions before calculation of the expectancy score. A higher score indicates more negative expectancies of drinking alcohol.
Logic model analyses
An exploratory analysis was performed to explore key behavioural markers (mediators) of change and how these may influence the effect of the delivered intervention. The six proposed mechanisms of change were: self-efficacy, outcome expectations, goals, plans, social support and high-risk situations.
In exploratory analysis, Kendall’s tau correlation coefficients were calculated to assess the correlation between each of the mechanisms of change and the primary outcome (AUDIT-C) at 12 months.
Software
Statistical Product and Service Solutions (SPSS) version 27 (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp) was used to produce the side-by-side boxplot of age. RStudio version 1.4.1103 [RStudio Team (2021). RStudio: Integrated Development Environment for R. RStudio, PBC, Boston, MA. www.rstudio.com/] was used to analyse the screening and recruitment data and produce the recruitment graph. All other tables and analyses were produced using statistical analysis system (SAS) software version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics approval
Ethics approval for the study was sought and secured from five different organisations:
-
Integrated Research Application System (IRAS) (East of Scotland Research Ethics Service) REC reference 19/ES/0068, IRAS project ID 261003
-
HMPPS Ministry of Justice, National Research Committee reference 2019240
-
SPS Research Access and Ethics Committee (RAEC) approval letter dated 13 June 2019
-
the University of Scotland School of Health in Social Science Nursing Studies Research Panel approval letter dated 26 September 2019
-
NHS R&D in Scotland (R&D No. 2019/0268).
The University of Edinburgh acted as trial sponsor (CAHSS 18/2/02). A model non-commercial agreement (mNCA) was in place for the England study site but not for the Scotland study site following discussions with Health Research Authority (HRA). The mNCA is strongly recommended as the agreement between sites for clinical trials/investigations; it is not mandatory for a non-commercial study. For the Scotland study site it was not considered the appropriate mechanism for agreement and therefore a site agreement between the Sponsor and the SPS site was drawn up and put in place. The agreement for this took many months of discussion with stakeholders and was a long protracted process causing delays to the start of recruitment at the Scotland study site.
Management of the study
Two groups were in place to support the research management of the study. The PMG was convened and comprised the chief investigator (CI), co-applicants, our PPI member who was also a co-applicant, the Project Manager and researchers from both study sites working on the project. Professor Jeremy Bray chaired the PMG. The frequency of the PMG meetings was determined by the needs of the project. The PMG’s responsibility was to ensure appropriate and timely study implementation. The constitution and composition of the PMG and TSC were in line with NIHR research governance guidelines.
The TSC was appointed to provide independent assessment of the study progress, adherence to the protocol, patient safety and well-being of study participants, consideration of new information of relevance to the progress of the study and support of decision-making on the merits of a future definitive trial. A subcommittee DMEC was also convened following approval from NIHR-PH as this was a pilot feasibility study. It was agreed that because the study was a feasibility study rather that a definitive trial, it was sufficient to have the group as a subcommittee rather than having it sealed off as a separate entity. The terms of reference (ToR) for the TSC with the ToR for the subcommittee added were agreed (see Appendix 11).
Research governance
The study was managed and conducted in accordance with the Medical Research Council’s Guidelines on Good Clinical Practice in Clinical Trials (www.mrc.ac.uk), which included compliance with national and international regulations on the ethical involvement of patients in clinical research (including the Declaration of Helsinki). Before the study commenced, all required approvals were obtained and all conditions of approvals were met. All staff assisting with the study were adequately informed about the protocol and their trial-related duties.
The study was conducted at each site in compliance with the study protocol and all protocol amendments. All forms, reports, and other records were designed to maintain participant confidentiality. All data were held in a secure environment with participants’ information identified by a unique participant identification code. All records were kept in a secure storage area in compliance with the Data Protection Act (2018) and the General Data Protection Regulation (GDPR) 2019 regarding collection, storage, processing and disclosure of personal information. Trial management support was provided by the Clinical Trials Unit we were working with.
Changes to the original study protocol
During the course of the study, a number of amendments were made to the study protocol, the majority as a result of the impact of the COVID-19 pandemic. Several of these changes have been discussed above, but this section provides a comprehensive catalogue of substantial changes. All proposed amendments to the study were discussed by the CI, PMG and TSC. Once agreed, the process involved discussion with the study sponsor, whose responsibility it was to determine if an amendment was substantial or not.
Substantial amendments were submitted to the East of Scotland Research Ethics Service Committee by the CI, on behalf of the sponsor. Once approval was obtained, changes to the study protocol were then implemented. (Table 6 provides details of the substantial protocol changes approved and made.)
| Original aim | Changes to protocol | |
|---|---|---|
| Changes to recruitment | Our original aim was to recruit 180 participants across two prison sites, Scotland (N = 90) and England (N = 90). Recruitment began in England on 2 December 2019 and was completed on 28 February 2020 (N = 90). Recruitment began in Scotland on 15 January 2020 and was halted due to COVID- 19 restrictions on 13 March 2020 (N = 44). |
As a result of COVID-19, recruitment at HMP Scotland was halted on 13 March and a decision to stop any further recruitment was made on 12 June. Total consented: 134. Total included: 132 (90 in England, 42 in Scotland). This change was approved on 16 July 2020. |
| Changes to intervention delivery | Our original aim was to deliver a face-to-face intervention session within the prison to all participants in the intervention condition. It was also our aim to deliver 3 × 20-minute telephone sessions to those who received the first intervention session and were subsequently released from prison. Our aim was to deliver the post-release sessions on or as close as possible to day 3, 7 and 21 post release. | Unfortunately, due to COVID-19 restrictions, outstanding interventions in Scotland (N = 5) were not possible and post-release intervention sessions at both sites were halted. Post-release intervention sessions had to be halted because we were unable to access release data in the prisons. This meant that intervention sessions could not be delivered on or as close as possible to days 3 (session 2), 7 (session 3) and 21 (session 4) post-release. It was agreed that post-release intervention sessions should still be attempted where possible and that the originally intended interval between them should be maintained (4 days between sessions 2 and 3, and 14 days between sessions 3 and 4). |
| Changes to 6- and 12-month follow up timing | Due to the impact of COVID-19, we extended the possible follow-up window from 8 weeks to 12 weeks. This was to allow for both post-release intervention delivery and 6- and 12-month data collection. This change was approved on 21 September 2020. |
|
| Changes to 6- and 12-month follow-up procedures | Due to the impact of COVID-19, face-to-face follow-ups were no longer appropriate. Therefore, an amendment was sought to allow hard copies and electronic copies of the survey to be sent to participants. This change was approved on 21 September 2020. |
|
| Changes to 6- and 12-month CRFs | To allow for the self-completion of questionnaires, a number of changes were required. | |
These changes were approved on 21 September 2020.
|
||
| Changes to interview schedules | To explore the unique impact of COVID-19 on the feasibility of this and any future project, additional questions have been added to our interview guides. The questions will allow us to identify whether changes to service utilisation and delivery have occurred as a result of COVID-19 and establish whether there are likely to be long-term impacts and changes as a result. This will help inform the feasibility of any future trial. This change was approved on 4 September 2020. |
|
| Inclusion of a survey | We have proposed designing and distributing a short survey to all UK prisons with a male remand population to ask what their current ABI delivery process is, how this has been impacted by COVID-19, and whether they would be willing to work with us on a potential future RCT to explore the efficacy of a self-efficacy-enhancing psychosocial alcohol intervention. This information would inform the feasibility of a future RCT. | |
| Changes to proposed end date | We requested a 9-month extension which changed the end date from 31 March to 31 December 2020. This change was approved on 4 September 2020. |
Chapter 4 Pilot trial results
Data regarding the number of participants consented, recruited and randomised to the study are presented. In addition, we present data on baseline characteristics and primary and secondary outcome measures. Information on data completeness across the three time points is provided. Numbers receiving the intervention and numbers followed up are also shown.
Overall study recruitment
Both study sites agreed to take part with the necessary organisation approvals and ethics approvals were secured. Recruitment opened at the England site on 2 December 2019 and closed on 28 February 2020, as the required sample size of 90 participants had been met. The Scotland site opened to recruitment on 15 January 2020 and was halted due to COVID-19 restrictions on 13 March 2020, with 42 individuals recruited to the study. Following discussions with the site governor and the head of research at the Scottish Prison Service, HMP Scotland was closed to any further recruitment on 12 June 2020. Differences in start date between study sites were due to difficulties caused by the model non-commercial agreement (mNCA) requested by the Health Research Authority (see Ethics approval).
Table 7 provides an overview of the screening and recruitment data at the two sites.
| Entering on remand (N = 656) | Given information sheet (N = 705)a | Number approached (N = 182) | Number randomised (N = 132) | |
|---|---|---|---|---|
| England | 497 (75.8) | 384 (54.5) | 134 (73.6) | 90 (68.2) |
| Scotland | 159 (24.2) | 321 (45.5) | 48 (26.4) | 42 (31.8) |
Recruitment methods varied between the two sites as the prison profiles, regimes and access were different. As such, the screening and recruitment data for the two sites are considered in more detail separately.
England study site recruitment
Table 8 summarises the screening and recruitment data for England by week number. Unlike the Scotland site, where all individuals on remand were given an information sheet about the trial, not all of the individuals entering HMP England received an information sheet.
| Week number | Date at start of week | No. (%) entering on remand (N = 497) | No. (%) given info sheet (N = 384) | No. (%) approached (N = 134) | No. (%) randomised (N = 90) |
|---|---|---|---|---|---|
| 1 | 2 December 2019 | 44 (8.9) | 31 (8.1) | 3 (2.2) | 3 (3.3) |
| 2 | 9 December 2019 | 35 (7) | 23 (6) | 3 (2.2) | 1 (1.1) |
| 3 | 16 December 2019 | 28 (5.6) | 19 (4.9) | 10 (7.5) | 2 (2.2) |
| 4 | 6 January 2020 | 47 (9.5) | 43 (11.2) | 19 (14.2) | 6 (6.7) |
| 5 | 13 January 2020 | 45 (9.1) | 38 (9.9) | 15 (11.2) | 9 (10) |
| 6 | 20 January 2020 | 68 (13.7) | 59 (15.4) | 15 (11.2) | 8 (8.9) |
| 7 | 27 January 2020 | 52 (10.5) | 36 (9.4) | 13 (9.7) | 9 (10) |
| 8 | 3 February 2020 | 44 (8.9) | 30 (7.8) | 16 (11.9) | 7 (7.8) |
| 9 | 10 February 2020 | 62 (12.5) | 56 (14.6) | 19 (14.2) | 15 (16.7) |
| 10 | 17 February 2020 | 51 (10.3) | 30 (7.8) | 2 (1.5) | 13 (14.4) |
| 11 | 24 February 2020 | 21 (4.2) | 19 (4.9) | 19 (14.2) | 17 (18.9) |
The number of prisoners on remand at the start of recruitment was not provided by the England site. Reasons why individuals were excluded in England are summarised in Table 9.
| Number (%) of individuals (N = 88) | |
|---|---|
| Self-identified non-drinker | 10 (11.4) |
| Not in pad (cell) | 9 (10.2) |
| Refused | 4 (4.5) |
| Not feeling well | 12 (13.6) |
| Isolation/segregation | 2 (2.3) |
| Risk to others | 6 (6.8) |
| High risk | 8 (9.1) |
| Operational | 5 (5.7) |
| Alcohol-dependant | 11 (12.5) |
| Not able to understand the documents | 10 (11.4) |
| Health care | 10 (11.4) |
| Already participated | 1 (1.1) |
Scotland study site recruitment
Table 10 contains information on the number of individuals entering HMP Scotland on remand by week of recruitment. At the start of recruitment, there were 162 prisoners on remand, and an additional 159 individuals entered the prison on remand during the data-collection period. During recruitment, 195 individuals were excluded, and 86 were not approached due to lack of resources and time.
| Week number | Date at start of week | No. (%) entering on remand (N = 159) | No. (%) randomised (N = 42) |
|---|---|---|---|
| 1 | 13 January 2020 | 7 (4.4) | 4 (9.5) |
| 2 | 20 January 2020 | 23 (14.5) | 6 (14.3) |
| 3 | 27 January 2020 | 16 (10.1) | 5 (11.9) |
| 4 | 3 February 2020 | 22 (13.8) | 4 (9.5) |
| 5 | 10 February 2020 | 13 (8.2) | 2 (4.8) |
| 6 | 17 February 2020 | 17 (10.7) | 5 (11.9) |
| 7 | 24 February 2020 | 15 (9.4) | 5 (11.9) |
| 8 | 2 March 2020 | 25 (15.7) | 5 (11.9) |
| 9 | 9 March 2020 | 21 (13.2) | 6 (14.3) |
Table 11 provides information on the number of screened individuals with 0, 1, 2, 3 or 4 reasons for being excluded from the study.
| Number of reasons | Number (%) of individuals excluded (N = 195) |
|---|---|
| 0 | 9 (4.6) |
| 1 | 165 (84.6) |
| 2 | 19 (9.7) |
| 3 | 1 (0.5) |
| 4 | 1 (0.5) |
Of those who had at least one reason for being excluded at the Scotland site, there was a total of 210 exclusion reasons, and these have been summarised in Table 12. Of note is the largest exclusion reason, which was being on remand for more than 3 months. Being liberated (n = 49) and operational reasons (n = 44) were the second and third most prevalent reasons for exclusion respectively.
| Number (%) of exclusion reasons (N = 210) | |
|---|---|
| More than 3 months on remand | 74 (35.2) |
| Operational reasons (hall) | 44 (21) |
| Transferred | 5 (2.4) |
| Liberated | 49 (23.3) |
| Unable to give informed consent | 1 (0.5) |
| Risk to self | 7 (3.3) |
| Risk to others | 4 (1.9) |
| Segregative rule | 9 (4.3) |
| Not able to understand the documents | 3 (1.4) |
| Sentenced | 5 (2.4) |
| Self-identified non-drinker | 3 (1.4) |
| Awaiting extradition | 3 (1.4) |
| Audit < 8 | 2 (1) |
| Already active participant | 1 (0.5) |
We had not created a standard proforma of consistent categories for exclusion, which resulted in different terminology being used for the exclusion criteria at the two study sites. We also noted that some criteria were much more frequent at one study site compared to the other (there was not much consistency between sites). Following several discussions by the PMG we agreed, for the purposes of the pilot trial and to support our understanding of these differences, that for a future trial we would continue the site-specific reasons and as such the exclusions are reported separately.
Consented and randomised
There were 134 participants who gave informed consent (90 from the England site and 44 from Scotland). A total number of 132 participants were randomised. Two participants from the Scotland site who were consented did not proceed to randomisation. One participant was considered to have lacked capacity and the other scored less than 8 on the AUDIT. Table 13 provides data on the numbers randomised to the intervention and control arms at each study site.
| Site | Both sites | |||||
|---|---|---|---|---|---|---|
| England | Scotland | |||||
| N | % | N | % | N | % | |
| Intervention | 46 | 51 | 22 | 52 | 68 | 52 |
| Control | 44 | 49 | 20 | 48 | 64 | 48 |
| Total | 90 | 100 | 42 | 100 | 132 | 100 |
Randomisation recruitment rates
It was anticipated that recruitment would start on the 1 September 2019 and would last for 4–6 months, with recruitment being quicker in England compared to Scotland. We were predicting this based on our learning from the PRISM-A study. 40 Variations in the speed of recruitment can partially be explained by access opportunities. Due to the different regimes within the prisons, the amount of time on the halls was less in Scotland than in England. The regimes also impacted on the amount of time the researchers were able to be on site. For example, in England the researcher was on site 5 days a week. In Scotland the researcher was on site 3 days a week.
Table 14 contains information on the number of participants randomised by month and by site, with Figure 2 providing a graphical overview of the recruitment rate by site and as a total. The planned rate of recruitment starts from 2 December in Figure 3 to correspond with when the England site was opened to recruitment.
FIGURE 2.
Consolidated Standards of Reporting Trials 2010 flow diagram.
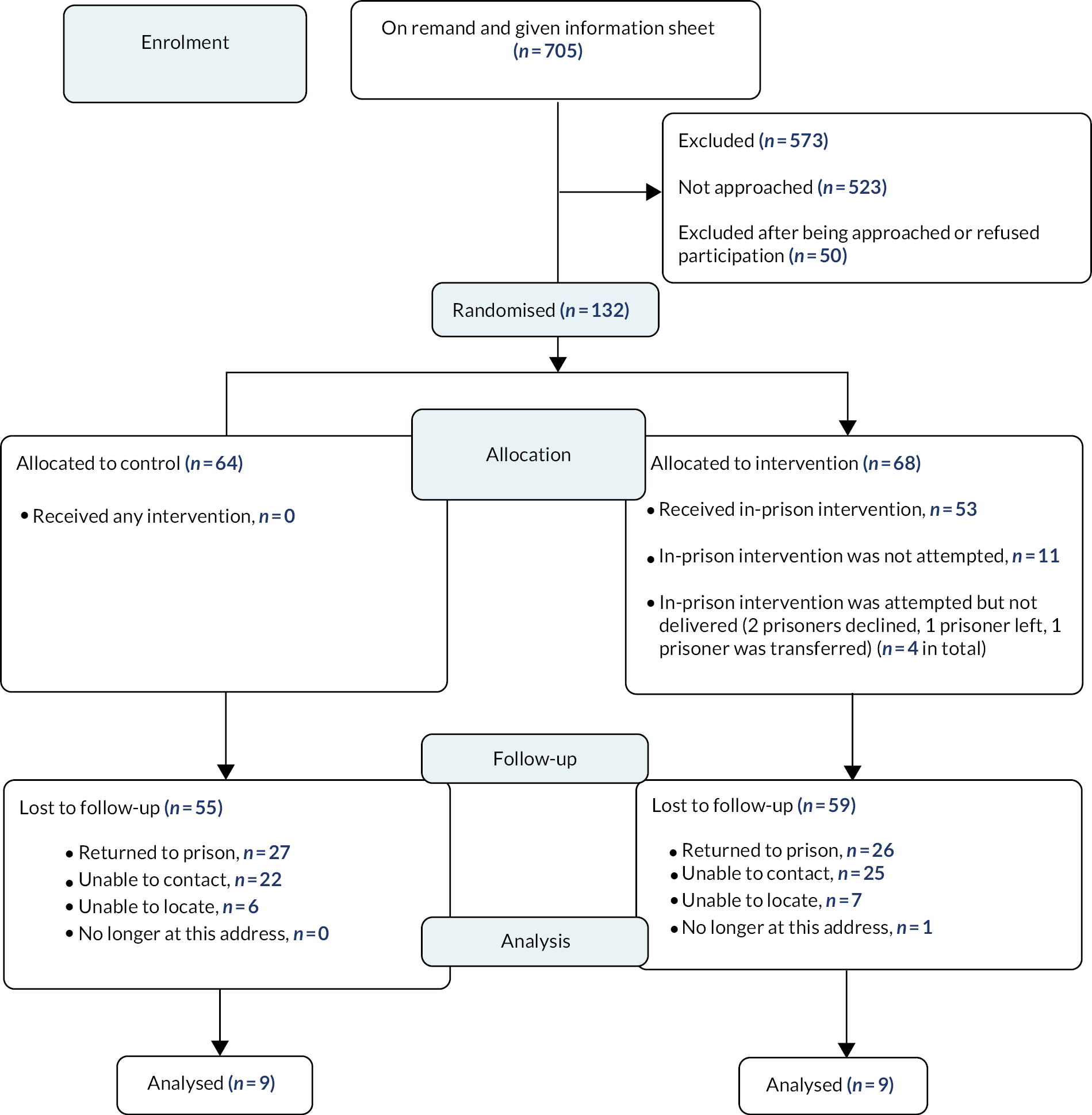
FIGURE 3.
Recruitment graph of planned recruitment and overall recruitment by study site.
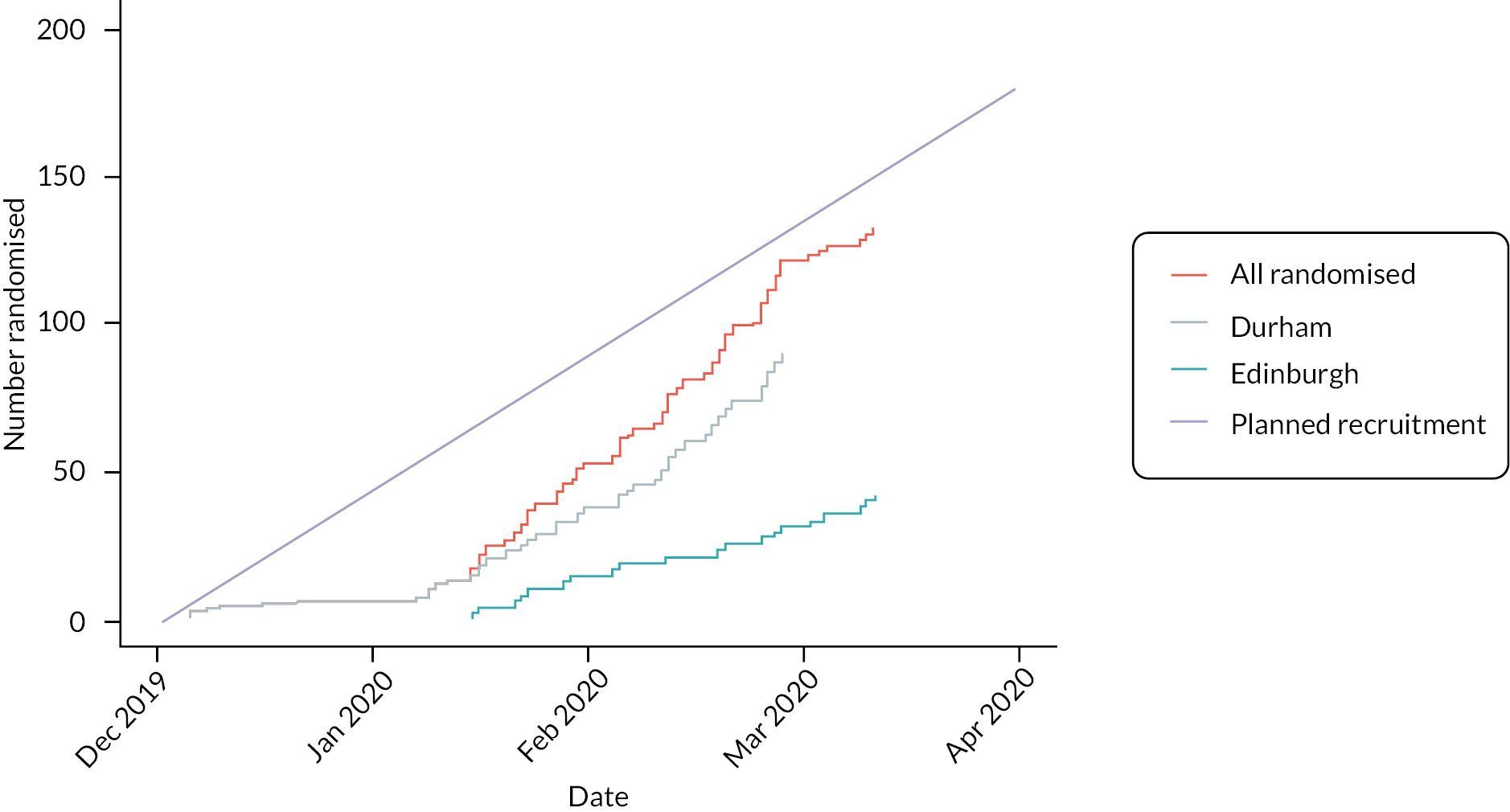
| Month year | England (N = 90) | Scotland (N = 42) | Total (N = 132) |
|---|---|---|---|
| December 2019 | 6 (6.7) | 0 (0) | 6 (4.5) |
| January 2020 | 32 (35.6) | 15 (35.7) | 47 (35.6) |
| February 2020 | 52 (57.8) | 16 (38.1) | 68 (51.5) |
| March 2020 | 0 (0) | 11 (26.2) | 11 (8.3) |
Baseline characteristics
The demographic characteristics of the randomised participants can be found in Tables 15 and 16. The average age of the participants was 34 years (median 31, SD 10), the majority of participants were single [87 (66%)] and considered themselves to be White British or White Scottish. Regarding highest educational achievement, 36% had no formal qualifications, 19% had a recognised trade apprenticeship, 39% had GCSEs or equivalent, 1% had A-levels or equivalent, while 6% were educated to university or college degree level. There was substantial variability in terms of the number of drinks consumed per month at baseline: the SD was 73 (range 5–198 drinks per month). The median number of drinks consumed per month was 80 (mean 94). The mean total score of the AUDIT-C was 9.2 (SD 2.2, range 3 to 12). A total score of < 5 on the AUDIT-C is regarded as low risk, while a score of 5 or more indicates hazardous drinking. Overall, 98% of participants were in the ‘at-risk’ category for drinking based on the AUDIT-C (≥ 5) at baseline, including 23% who recorded the maximum value of 12 on the AUDIT-C (indicating extremely high levels of drinking). Only two participants were considered to be at low risk (2%). These two participants had an AUDIT-C of 9 and were therefore eligible for the study.
| Randomisation allocation | Overall | ||||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||
| N | % | N | % | N | % | ||
| Site | |||||||
| England | Total number of prisoners | 46 | 67.6 | 44 | 68.8 | 90 | 68.2 |
| Ethnicity | |||||||
| White Scottish | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| White British | 45 | 66.2 | 38 | 59.4 | 83 | 62.9 | |
| White Irish | 0 | 0.0 | 2 | 3.1 | 2 | 1.5 | |
| White other | 0 | 0.0 | 1 | 1.6 | 1 | 0.8 | |
| Asian British | 0 | 0.0 | 1 | 1.6 | 1 | 0.8 | |
| Mixed race | 1 | 1.5 | 1 | 1.6 | 2 | 1.5 | |
| Other | 0 | 0.0 | 1 | 1.6 | 1 | 0.8 | |
| Relationship status | |||||||
| Single | 31 | 45.6 | 33 | 51.6 | 64 | 48.5 | |
| In a relationship (same sex or opposite) | 14 | 20.6 | 8 | 12.5 | 22 | 16.7 | |
| Married/civil partnership | 1 | 1.5 | 2 | 3.1 | 3 | 2.3 | |
| Divorced | 0 | 0.0 | 1 | 1.6 | 1 | 0.8 | |
| Highest educational achievement | |||||||
| University degree | 1 | 1.5 | 0 | 0.0 | 1 | 0.8 | |
| College degree | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| A-level/highers/advanced highers | 1 | 1.5 | 0 | 0.0 | 1 | 0.8 | |
| GCSEs/standard grades/National Certificate | 14 | 20.6 | 18 | 28.1 | 32 | 24.2 | |
| Recognised trade apprenticeship | 10 | 14.7 | 8 | 12.5 | 18 | 13.6 | |
| No formal qualifications | 20 | 29.4 | 18 | 28.1 | 38 | 28.8 | |
| Scotland | Total number of prisoners | 22 | 32.4 | 20 | 31.3 | 42 | 31.8 |
| Ethnicity | |||||||
| White Scottish | 17 | 25.0 | 16 | 25.0 | 33 | 25.0 | |
| White British | 2 | 2.9 | 4 | 6.3 | 6 | 4.5 | |
| White Irish | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| White other | 1 | 1.5 | 0 | 0.0 | 1 | 0.8 | |
| Asian British | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| Mixed race | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| Other | 2 | 2.9 | 0 | 0.0 | 2 | 1.5 | |
| Relationship status | |||||||
| Single | 13 | 19.1 | 10 | 15.6 | 23 | 17.4 | |
| In a relationship (same sex or opposite) | 8 | 11.8 | 8 | 12.5 | 16 | 12.1 | |
| Married/civil partnership | 1 | 1.5 | 2 | 3.1 | 3 | 2.3 | |
| Divorced | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| Highest educational achievement | |||||||
| University degree | 2 | 2.9 | 1 | 1.6 | 3 | 2.3 | |
| College degree | 2 | 2.9 | 2 | 3.1 | 4 | 3.0 | |
| A-level/highers/advanced highers | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| GCSEs/standard grades/National Certificate | 10 | 14.7 | 9 | 14.1 | 19 | 14.4 | |
| Recognised trade apprenticeship | 3 | 4.4 | 4 | 6.3 | 7 | 5.3 | |
| No formal qualifications | 5 | 7.4 | 4 | 6.3 | 9 | 6.8 | |
| Both sites | Total number of prisoners | 68 | 100.0 | 64 | 100.0 | 132 | 100.0 |
| Ethnicity | |||||||
| White Scottish | 17 | 25.0 | 16 | 25.0 | 33 | 25.0 | |
| White British | 47 | 69.1 | 42 | 65.6 | 89 | 67.4 | |
| White Irish | 0 | 0.0 | 2 | 3.1 | 2 | 1.5 | |
| White other | 1 | 1.5 | 1 | 1.6 | 2 | 1.5 | |
| Asian British | 0 | 0.0 | 1 | 1.6 | 1 | 0.8 | |
| Mixed race | 1 | 1.5 | 1 | 1.6 | 2 | 1.5 | |
| Other | 2 | 2.9 | 1 | 1.6 | 3 | 2.3 | |
| Relationship status | |||||||
| Single | 44 | 64.7 | 43 | 67.2 | 87 | 65.9 | |
| In a relationship (same sex or opposite) | 22 | 32.4 | 16 | 25.0 | 38 | 28.8 | |
| Married/civil partnership | 2 | 2.9 | 4 | 6.3 | 6 | 4.5 | |
| Divorced | 0 | 0.0 | 1 | 1.6 | 1 | 0.8 | |
| Highest educational achievement | |||||||
| University degree | 3 | 4.4 | 1 | 1.6 | 4 | 3.0 | |
| College degree | 2 | 2.9 | 2 | 3.1 | 4 | 3.0 | |
| A-level/highers/advanced highers | 1 | 1.5 | 0 | 0.0 | 1 | 0.8 | |
| GCSEs/standard grades/National Certificate | 24 | 35.3 | 27 | 42.2 | 51 | 38.6 | |
| Recognised trade apprenticeship | 13 | 19.1 | 12 | 18.8 | 25 | 18.9 | |
| No formal qualifications | 25 | 36.8 | 22 | 34.4 | 47 | 35.6 | |
| N | Mean | SD | Median | Min | Max | |||
|---|---|---|---|---|---|---|---|---|
| Age | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 31.0 | 7.7 | 30.0 | 19.0 | 62.0 | |
| Control | 44 | 34.4 | 12.6 | 30.0 | 19.0 | 86.0 | ||
| Overall | 90 | 32.7 | 10.5 | 30.0 | 19.0 | 86.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 37.3 | 10.1 | 37.5 | 23.0 | 60.0 | ||
| Control | 20 | 34.4 | 9.3 | 33.0 | 22.0 | 55.0 | ||
| Overall | 42 | 35.9 | 9.7 | 34.5 | 22.0 | 60.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 33.1 | 8.9 | 31.0 | 19.0 | 62.0 | ||
| Control | 64 | 34.4 | 11.6 | 31.0 | 19.0 | 86.0 | ||
| Overall | 132 | 33.7 | 10.3 | 31.0 | 19.0 | 86.0 | ||
| Alcohol consumption: number of drinks consumed in previous 28 days according to AUDIT-C | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 75.5 | 66.4 | 33.0 | 8.0 | 198.0 | |
| Control | 44 | 102.1 | 72.3 | 110.0 | 10.5 | 198.0 | ||
| Overall | 90 | 88.5 | 70.2 | 80.0 | 8.0 | 198.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 113.8 | 78.4 | 104.5 | 11.0 | 198.0 | ||
| Control | 20 | 98.0 | 78.4 | 81.0 | 5.5 | 198.0 | ||
| Overall | 42 | 106.3 | 77.9 | 99.0 | 5.5 | 198.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 87.9 | 72.2 | 71.5 | 8.0 | 198.0 | ||
| Control | 64 | 100.8 | 73.6 | 110.0 | 5.5 | 198.0 | ||
| Overall | 132 | 94.2 | 72.9 | 80.0 | 5.5 | 198.0 | ||
| AUDIT-C total score | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 8.7 | 2.1 | 9.0 | 3.0 | 12.0 | |
| Control | 44 | 9.4 | 2.0 | 9.0 | 4.0 | 12.0 | ||
| Overall | 90 | 9.0 | 2.1 | 9.0 | 3.0 | 12.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 9.7 | 2.3 | 9.5 | 5.0 | 12.0 | ||
| Control | 20 | 9.3 | 2.4 | 9.0 | 5.0 | 12.0 | ||
| Overall | 42 | 9.5 | 2.3 | 9.0 | 5.0 | 12.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 9.0 | 2.2 | 9.0 | 3.0 | 12.0 | ||
| Control | 64 | 9.4 | 2.2 | 9.0 | 4.0 | 12.0 | ||
| Overall | 132 | 9.2 | 2.2 | 9.0 | 3.0 | 12.0 | ||
| Readiness to Change Ruler: how much do you really want to stop (or cut down) drinking at the present time? | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 7.2 | 3.5 | 9.0 | 1.0 | 10.0 | |
| Control | 44 | 7.3 | 3.2 | 9.0 | 1.0 | 10.0 | ||
| Overall | 90 | 7.2 | 3.4 | 9.0 | 1.0 | 10.0 | ||
| Scotland | Randomisation allocation | 22 | 7.8 | 2.8 | 9.0 | 1.0 | 10.0 | |
| Intervention | ||||||||
| Control | 20 | 7.6 | 3.0 | 9.5 | 1.0 | 10.0 | ||
| Overall | 42 | 7.7 | 2.9 | 9.0 | 1.0 | 10.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 7.4 | 3.3 | 9.0 | 1.0 | 10.0 | ||
| Control | 64 | 7.4 | 3.1 | 9.0 | 1.0 | 10.0 | ||
| Overall | 132 | 7.4 | 3.2 | 9.0 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: if you decided to stop or cut down drinking right now, how confident do you feel about succeeding with this? | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 7.6 | 2.8 | 9.0 | 1.0 | 10.0 | |
| Control | 44 | 8.2 | 2.1 | 9.5 | 3.0 | 10.0 | ||
| Overall | 90 | 7.9 | 2.5 | 9.0 | 1.0 | 10.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 7.0 | 2.7 | 7.5 | 1.0 | 10.0 | ||
| Control | 20 | 7.3 | 3.0 | 9.0 | 1.0 | 10.0 | ||
| Overall | 42 | 7.1 | 2.8 | 8.0 | 1.0 | 10.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 7.4 | 2.8 | 8.0 | 1.0 | 10.0 | ||
| Control | 64 | 7.9 | 2.4 | 9.0 | 1.0 | 10.0 | ||
| Overall | 132 | 7.6 | 2.6 | 8.5 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: how ready are you to stop (or cut down) drinking right now? | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 8.2 | 2.6 | 10.0 | 1.0 | 10.0 | |
| Control | 44 | 8.3 | 2.6 | 10.0 | 1.0 | 10.0 | ||
| Overall | 90 | 8.2 | 2.6 | 10.0 | 1.0 | 10.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 7.8 | 3.2 | 9.0 | 1.0 | 10.0 | ||
| Control | 20 | 9.0 | 1.9 | 10.0 | 3.0 | 10.0 | ||
| Overall | 42 | 8.4 | 2.7 | 10.0 | 1.0 | 10.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 8.0 | 2.7 | 9.0 | 1.0 | 10.0 | ||
| Control | 64 | 8.5 | 2.4 | 10.0 | 1.0 | 10.0 | ||
| Overall | 132 | 8.3 | 2.6 | 10.0 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: I have someone I can talk to about reducing my drinking | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 7.3 | 3.6 | 10.0 | 1.0 | 10.0 | |
| Control | 44 | 7.9 | 3.0 | 10.0 | 1.0 | 10.0 | ||
| Overall | 90 | 7.6 | 3.3 | 10.0 | 1.0 | 10.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 5.6 | 3.7 | 5.0 | 1.0 | 10.0 | ||
| Control | 20 | 6.5 | 3.9 | 7.5 | 1.0 | 10.0 | ||
| Overall | 42 | 6.0 | 3.8 | 6.5 | 1.0 | 10.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 6.7 | 3.7 | 9.0 | 1.0 | 10.0 | ||
| Control | 64 | 7.5 | 3.3 | 10.0 | 1.0 | 10.0 | ||
| Overall | 132 | 7.1 | 3.5 | 9.5 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: the people who are important to me support me in reducing my drinking | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 7.7 | 3.5 | 10.0 | 1.0 | 10.0 | |
| Control | 44 | 8.5 | 2.6 | 10.0 | 1.0 | 10.0 | ||
| Overall | 90 | 8.1 | 3.1 | 10.0 | 1.0 | 10.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 21 | 6.7 | 3.8 | 8.0 | 1.0 | 10.0 | ||
| Control | 18 | 6.2 | 3.8 | 6.5 | 1.0 | 10.0 | ||
| Overall | 39 | 6.5 | 3.8 | 8.0 | 1.0 | 10.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 67 | 7.4 | 3.6 | 10.0 | 1.0 | 10.0 | ||
| Control | 62 | 7.8 | 3.2 | 10.0 | 1.0 | 10.0 | ||
| Overall | 129 | 7.6 | 3.4 | 10.0 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: I have made a detailed plan regarding when, where and how to reduce my drinking | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 3.2 | 3.2 | 1.0 | 1.0 | 10.0 | |
| Control | 44 | 5.0 | 4.1 | 3.0 | 1.0 | 10.0 | ||
| Overall | 90 | 4.0 | 3.8 | 1.5 | 1.0 | 10.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 3.7 | 3.5 | 1.5 | 1.0 | 10.0 | ||
| Control | 20 | 3.8 | 2.8 | 3.0 | 1.0 | 10.0 | ||
| Overall | 42 | 3.7 | 3.1 | 2.0 | 1.0 | 10.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 3.3 | 3.3 | 1.0 | 1.0 | 10.0 | ||
| Control | 64 | 4.6 | 3.8 | 3.0 | 1.0 | 10.0 | ||
| Overall | 132 | 3.9 | 3.6 | 2.0 | 1.0 | 10.0 | ||
| EQ-5D: mobility | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 1.4 | 0.8 | 1.0 | 1.0 | 4.0 | |
| Control | 44 | 1.1 | 0.5 | 1.0 | 1.0 | 3.0 | ||
| Overall | 90 | 1.3 | 0.7 | 1.0 | 1.0 | 4.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 1.1 | 0.4 | 1.0 | 1.0 | 2.0 | ||
| Control | 20 | 1.8 | 1.0 | 1.0 | 1.0 | 4.0 | ||
| Overall | 42 | 1.4 | 0.8 | 1.0 | 1.0 | 4.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 1.3 | 0.7 | 1.0 | 1.0 | 4.0 | ||
| Control | 64 | 1.3 | 0.7 | 1.0 | 1.0 | 4.0 | ||
| Overall | 132 | 1.3 | 0.7 | 1.0 | 1.0 | 4.0 | ||
| EQ-5D: self-care | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 1.2 | 0.6 | 1.0 | 1.0 | 4.0 | |
| Control | 44 | 1.2 | 0.5 | 1.0 | 1.0 | 3.0 | ||
| Overall | 90 | 1.2 | 0.6 | 1.0 | 1.0 | 4.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 1.4 | 1.0 | 1.0 | 1.0 | 4.0 | ||
| Control | 20 | 1.2 | 0.5 | 1.0 | 1.0 | 3.0 | ||
| Overall | 42 | 1.3 | 0.8 | 1.0 | 1.0 | 4.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 1.2 | 0.8 | 1.0 | 1.0 | 4.0 | ||
| Control | 64 | 1.2 | 0.5 | 1.0 | 1.0 | 3.0 | ||
| Overall | 132 | 1.2 | 0.7 | 1.0 | 1.0 | 4.0 | ||
| EQ-5D: usual activities (e.g. work, study, housework, family or leisure activities) | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 1.4 | 0.7 | 1.0 | 1.0 | 3.0 | |
| Control | 44 | 1.3 | 0.8 | 1.0 | 1.0 | 4.0 | ||
| Overall | 90 | 1.4 | 0.7 | 1.0 | 1.0 | 4.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 2.1 | 1.4 | 1.5 | 1.0 | 5.0 | ||
| Control | 20 | 2.1 | 1.3 | 2.0 | 1.0 | 5.0 | ||
| Overall | 42 | 2.1 | 1.3 | 2.0 | 1.0 | 5.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 1.6 | 1.0 | 1.0 | 1.0 | 5.0 | ||
| Control | 64 | 1.6 | 1.0 | 1.0 | 1.0 | 5.0 | ||
| Overall | 132 | 1.6 | 1.0 | 1.0 | 1.0 | 5.0 | ||
| EQ-5D: pain/discomfort | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 2.3 | 1.3 | 2.0 | 1.0 | 5.0 | |
| Control | 44 | 1.8 | 1.1 | 1.0 | 1.0 | 5.0 | ||
| Overall | 90 | 2.1 | 1.2 | 2.0 | 1.0 | 5.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 1.9 | 1.3 | 1.0 | 1.0 | 5.0 | ||
| Control | 20 | 2.0 | 1.3 | 1.0 | 1.0 | 4.0 | ||
| Overall | 42 | 1.9 | 1.3 | 1.0 | 1.0 | 5.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 2.1 | 1.3 | 2.0 | 1.0 | 5.0 | ||
| Control | 64 | 1.9 | 1.2 | 1.0 | 1.0 | 5.0 | ||
| Overall | 132 | 2.0 | 1.2 | 1.0 | 1.0 | 5.0 | ||
| EQ-5D: anxiety/depression | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 2.9 | 1.2 | 3.0 | 1.0 | 5.0 | |
| Control | 44 | 2.5 | 1.2 | 2.5 | 1.0 | 5.0 | ||
| Overall | 90 | 2.7 | 1.2 | 3.0 | 1.0 | 5.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 3.1 | 1.2 | 3.0 | 1.0 | 5.0 | ||
| Control | 20 | 3.6 | 1.4 | 4.0 | 1.0 | 5.0 | ||
| Overall | 42 | 3.3 | 1.3 | 4.0 | 1.0 | 5.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 3.0 | 1.2 | 3.0 | 1.0 | 5.0 | ||
| Control | 64 | 2.9 | 1.3 | 3.0 | 1.0 | 5.0 | ||
| Overall | 132 | 2.9 | 1.3 | 3.0 | 1.0 | 5.0 | ||
| EQ-5D: visual analogue scale | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 49.7 | 23.0 | 50.0 | 0.0 | 100.0 | |
| Control | 44 | 61.0 | 22.0 | 60.0 | 10.0 | 100.0 | ||
| Overall | 90 | 55.2 | 23.1 | 50.0 | 0.0 | 100.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 22 | 61.4 | 21.1 | 62.5 | 5.0 | 90.0 | ||
| Control | 20 | 61.1 | 21.3 | 62.5 | 20.0 | 100.0 | ||
| Overall | 42 | 61.2 | 20.9 | 62.5 | 5.0 | 100.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 68 | 53.5 | 22.9 | 50.0 | 0.0 | 100.0 | ||
| Control | 64 | 61.0 | 21.6 | 60.0 | 10.0 | 100.0 | ||
| Overall | 132 | 57.1 | 22.5 | 60.0 | 0.0 | 100.0 | ||
| Warwick-Edinburgh Mental Well-being Scale: total score | Site | Randomisation allocation | ||||||
| England | Intervention | 46 | 34.4 | 13.7 | 32.0 | 14.0 | 66.0 | |
| Control | 44 | 40.2 | 10.6 | 39.0 | 19.0 | 63.0 | ||
| Overall | 90 | 37.2 | 12.6 | 36.0 | 14.0 | 66.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 21 | 41.6 | 13.1 | 41.0 | 24.0 | 70.0 | ||
| Control | 20 | 41.3 | 10.4 | 42.5 | 22.0 | 56.0 | ||
| Overall | 41 | 41.4 | 11.7 | 42.0 | 22.0 | 70.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 67 | 36.7 | 13.8 | 35.6 | 14.0 | 70.0 | ||
| Control | 64 | 40.5 | 10.5 | 40.0 | 19.0 | 63.0 | ||
| Overall | 131 | 38.5 | 12.4 | 38.0 | 14.0 | 70.0 | ||
| Drinking Refusal Self-efficacy Questionnaire: total score | Site | Randomisation allocation | ||||||
| England | Intervention | 45 | 72.8 | 24.8 | 73.5 | 22.2 | 114.0 | |
| Control | 44 | 70.8 | 22.2 | 69.6 | 33.8 | 109.8 | ||
| Overall | 89 | 71.8 | 23.4 | 71.0 | 22.2 | 114.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 21 | 58.5 | 20.1 | 55.8 | 27.1 | 99.0 | ||
| Control | 20 | 61.8 | 24.1 | 64.5 | 19.0 | 90.8 | ||
| Overall | 41 | 60.1 | 21.9 | 61.0 | 19.0 | 99.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 66 | 68.2 | 24.2 | 67.6 | 22.2 | 114.0 | ||
| Control | 64 | 68.0 | 23.0 | 68.6 | 19.0 | 109.8 | ||
| Overall | 130 | 68.1 | 23.5 | 68.1 | 19.0 | 114.0 | ||
| Negative Alcohol Expectancy Questionnaire: same-day expectancy score | Site | Randomisation allocation | ||||||
| England | Intervention | 45 | 52.3 | 16.6 | 54.2 | 21.0 | 87.3 | |
| Control | 44 | 55.3 | 18.4 | 54.4 | 23.0 | 105.0 | ||
| Overall | 89 | 53.7 | 17.5 | 54.2 | 21.0 | 105.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 21 | 61.2 | 12.2 | 62.0 | 28.7 | 86.1 | ||
| Control | 19 | 64.8 | 9.7 | 67.2 | 46.2 | 82.0 | ||
| Overall | 40 | 62.9 | 11.1 | 64.6 | 28.7 | 86.1 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 66 | 55.1 | 15.8 | 56.0 | 21.0 | 87.3 | ||
| Control | 63 | 58.1 | 16.8 | 58.0 | 23.0 | 105.0 | ||
| Overall | 129 | 56.6 | 16.3 | 56.0 | 21.0 | 105.0 | ||
| Negative Alcohol Expectancy Questionnaire: next-day expectancy score | Site | Randomisation allocation | ||||||
| England | Intervention | 45 | 41.4 | 16.2 | 39.0 | 18.0 | 71.0 | |
| Control | 44 | 47.9 | 20.1 | 43.9 | 18.0 | 90.0 | ||
| Overall | 89 | 44.6 | 18.5 | 41.3 | 18.0 | 90.0 | ||
| Scotland | Randomisation allocation | |||||||
| Intervention | 21 | 54.8 | 16.9 | 54.0 | 20.0 | 87.0 | ||
| Control | 19 | 60.7 | 12.7 | 62.0 | 38.0 | 88.0 | ||
| Overall | 40 | 57.6 | 15.2 | 58.0 | 20.0 | 88.0 | ||
| Both sites | Randomisation allocation | |||||||
| Intervention | 66 | 45.7 | 17.5 | 45.6 | 18.0 | 87.0 | ||
| Control | 63 | 51.8 | 19.1 | 51.0 | 18.0 | 90.0 | ||
| Overall | 129 | 48.6 | 18.5 | 49.0 | 18.0 | 90.0 | ||
On average, high scores were recorded on the readiness to change ruler at baseline except for the item ‘I have made a detailed plan regarding when, where and how to reduce my drinking’, indicating that most participants had not made a detailed plan regarding when, where and how to reduce their drinking. The EQ-5D item scores suggested that participants had moderate problems with anxiety/depression on average; all other EQ-5D item scores were low on average. The WEMWBS had a mean of 38.5 (SD 12.4), indicating probable clinical depression in most participants.
Figure 4 shows side-by-side boxplots of the ages of participants in each site.
FIGURE 4.
Ages of participants at HMP England and HMP Scotland.
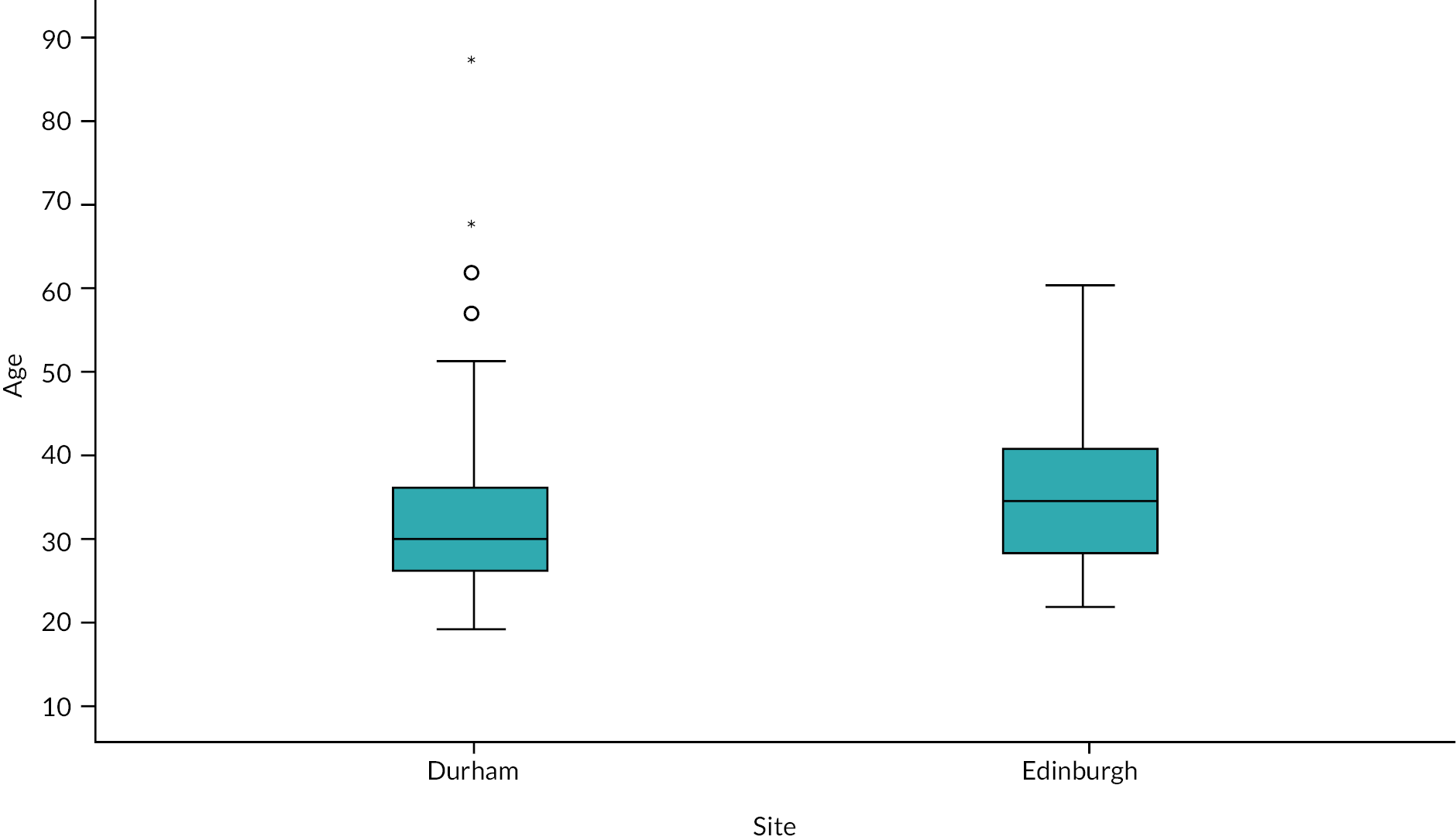
In-prison and post-liberation intervention delivery
Table 17 contains information on whether those randomised to the intervention arm received the in-prison and post-liberation intervention sessions. Out of 68 participants randomised to the intervention condition, 53 received the in-prison intervention session (77.9%, 95% CI 66.2% to 87.1%). This percentage is greater than the 70% threshold specified as one of the criteria necessary for progression to a future larger randomised controlled trial (Objective 4c).
| England (N = 46) | Scotland (N = 22) | Total (N = 68) | |
|---|---|---|---|
| In prison | |||
| Yes | 40 (87) | 13 (59.1) | 53 (77.9) |
| No | 6 (13) | 9 (40.9) | 15 (22.1) |
| First (3 days) post prison | |||
| Yes | 0 (0) | 1 (4.5) | 1 (1.5) |
| No | 40 (87) | 12 (54.5) | 52 (76.5) |
| N/Aa | 6 (13) | 9 (40.9) | 15 (22.1) |
| Second (7 days) post prison | |||
| Yes | 0 (0) | 0 (0) | 0 (0) |
| No | 40 (87) | 13 (59.1) | 53 (77.9) |
| N/Aa | 6 (13) | 9 (40.9) | 15 (22.1) |
| Third (21 days) post prison | |||
| Yes | 1 (2.2) | 0 (0) | 1 (1.5) |
| No | 39 (84.8) | 13 (59.1) | 52 (76.5) |
| N/Aa | 6 (13) | 9 (40.9) | 15 (22.1) |
Reasons for why the in-prison intervention was not delivered are shown in Table 18.
| Site | Both sites | ||
|---|---|---|---|
| England | Scotland | ||
| Session attempted but participant declined | 1 | 1 | 2 |
| Prisoner was sentenced | 0 | 2 | 2 |
| Prisoner was released | 1 | 3 | 4 |
| Prisoner was transferred | 1 | 0 | 1 |
| Session not attempted because the prisoner had a crisis | 0 | 1 | 1 |
| Session not attempted because prisoner had COVID-19 | 0 | 2 | 2 |
| Session not attempted for unknown reason | 3 | 0 | 3 |
| Total | 6 | 9 | 15 |
Only one ‘day-3 post-prison intervention’ session was attempted and was delivered (duration 30 minutes) at the Scotland site. No ‘day-7 post-prison intervention’ sessions were attempted. Only one ‘day-21 post-prison intervention’ session was attempted and was delivered to one participant (duration 30 minutes) at the England site.
The main reasons why participants did not receive the post-prison interventions were (1) they could not be contacted and (2) CGL staff were unable to contact participants due to the impact of the COVID-19 pandemic.
Data for the duration (minutes) of the intervention sessions across both study sites are presented for all but one of the 53 interventions delivered in Table 19. There was a marked difference in the median time taken to deliver the intervention between the two sites: the intervention duration was half an hour in England compared to 1 hour in Scotland. The shortest time for an intervention was only 5 minutes in England, whereas in Scotland it was 30 minutes. The maximum time for delivery was more aligned across sites, being 70 minutes and 80 minutes in England and Scotland, respectively.
| N | Miss | Mean | SD | Median | Min | Max | ||
|---|---|---|---|---|---|---|---|---|
| Duration of session (minutes) | Site | 40 | 0 | 31.8 | 11.2 | 30.0 | 5.0 | 70.0 |
| England | ||||||||
| Scotland | 12 | 1 | 53.8 | 14.9 | 60.0 | 30.0 | 80.0 | |
| Both sites | 52 | 1 | 36.8 | 15.2 | 35.0 | 5.0 | 80.0 | |
Follow-up and withdrawal
There were no formal withdrawals from the study. However, only 3 out of 132 randomised participants recorded any follow-up data at 6 months (2.3%, 95% CI 0.5% to 6.5%), and only 18 out of 132 randomised participants recorded any follow-up data at 12 months (13.6%, 95% CI 8.3% to 20.7%) (Table 20). The low numbers of follow-ups were due to the impact of COVID-19.
| England (N = 90) | Scotland (N = 42) | Total (N = 132) | |
|---|---|---|---|
| 6-month follow-up | |||
| Yes | 0 (0) | 3 (7.1) | 3 (2.3) |
| No | 90 (100) | 39 (92.9) | 129 (97.7) |
| 12-month follow-up | |||
| Yes | 4 (4.4) | 14 (33.3) | 18 (13.6) |
| No | 86 (95.6) | 28 (66.7) | 114 (86.4) |
Tables 21 and 22 show the numbers of follow-ups at 6 and 12 months respectively within each site and randomised allocation group.
| Randomisation allocation | Overall | ||||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||
| N | % | N | % | N | % | ||
| Site | Recording data at TP1 | ||||||
| England | No | 46 | 67.6 | 44 | 68.8 | 90 | 68.2 |
| Yes | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| Total | 46 | 67.6 | 44 | 68.8 | 90 | 68.2 | |
| Scotland | Recording data at TP1 | ||||||
| No | 20 | 29.4 | 19 | 29.7 | 39 | 29.5 | |
| Yes | 2 | 2.9 | 1 | 1.6 | 3 | 2.3 | |
| Total | 22 | 32.4 | 20 | 31.3 | 42 | 31.8 | |
| Both sites | Recording data at TP1 | ||||||
| No | 66 | 97.1 | 63 | 98.4 | 129 | 97.7 | |
| Yes | 2 | 2.9 | 1 | 1.6 | 3 | 2.3 | |
| Total | 68 | 100.0 | 64 | 100.0 | 132 | 100.0 | |
| Randomisation allocation | Overall | ||||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||
| N | % | N | % | N | % | ||
| Site | Recording data at TP2 | ||||||
| England | No | 44 | 64.7 | 42 | 65.6 | 86 | 65.2 |
| Yes | 2 | 2.9 | 2 | 3.1 | 4 | 3.0 | |
| Total | 46 | 67.6 | 44 | 68.8 | 90 | 68.2 | |
| Scotland | Recording data at TP2 | ||||||
| No | 15 | 22.1 | 13 | 20.3 | 28 | 21.2 | |
| Yes | 7 | 10.3 | 7 | 10.9 | 14 | 10.6 | |
| Total | 22 | 32.4 | 20 | 31.3 | 42 | 31.8 | |
| Both sites | Recording data at TP2 | ||||||
| No | 59 | 86.8 | 55 | 85.9 | 114 | 86.4 | |
| Yes | 9 | 13.2 | 9 | 14.1 | 18 | 13.6 | |
| Total | 68 | 100.0 | 64 | 100.0 | 132 | 100.0 | |
Out of the 44 participants receiving the intervention, only 13% were followed up to 12 months. Note that this percentage is much lower than our progression criteria (Objective 4d) specifying that at least 60% of those who received the intervention should be followed up at 12 months across trial arms and study sites. This progression criterion was set prior to the COVID-19 pandemic.
The greatest increase in numbers of those followed up at 12 months was seen at the Scotland site, where we were able to have some access to the prison site and identify where participants were located; however, this was minimal. In England where there was no access to the estate this meant at the time of intervention delivery and follow-ups we did not know who had been liberated and who had not liberated. However, this access remained very limited. Reasons for being unable to follow up at 12 months are shown in Table 23. Out of all 132 randomised participants, 53 (40%) were not liberated or released at 12 months follow-up, 47 (36%) were uncontactable and 14 (11%) could not be located even though they had been released.
| Liberation/release status | Randomisation allocation | Overall | ||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| N | % | N | % | N | % | |||
| Site | Not liberated/released | 24 | 54.5 | 26 | 61.9 | 50 | 58.1 | |
| England | Liberated and in community but unable to contact | 16 | 36.4 | 11 | 26.2 | 27 | 31.4 | |
| Liberated and in community but unable to locate | 4 | 9.1 | 5 | 11.9 | 9 | 10.5 | ||
| Total | 44 | 100 | 42 | 100 | 86 | 100 | ||
| Scotland | Not liberated/released | 2 | 13.3 | 1 | 7.7 | 3 | 10.7 | |
| Liberated and in community but unable to contact | 9 | 60.0 | 11 | 84.6 | 20 | 71.4 | ||
| Liberated and in community but unable to locate | 4 | 26.7 | 1 | 7.7 | 5 | 17.9 | ||
| Total | 15 | 100 | 13 | 100 | 28 | 100 | ||
| Both sites | Not liberated/released | 26 | 44.1 | 27 | 49.1 | 53 | 46.5 | |
| Liberated and in community but unable to contact | 25 | 42.4 | 22 | 40.0 | 47 | 41.2 | ||
| Liberated and in community but unable to locate | 8 | 13.6 | 6 | 10.9 | 14 | 12.3 | ||
| Total | 59 | 100 | 55 | 100 | 114 | 100 | ||
Data completeness
Table 24 contains information on data completeness at baseline and follow-up for all 132 randomised participants. Complete data collection refers to when a participant has recorded data for all relevant questionnaires and outcomes. Incomplete data collection refers to when the participants have recorded data on the primary outcome, but have not recorded data for one or more secondary outcomes.
| Baseline | 6 months | 12 months | |
|---|---|---|---|
| Complete data collection | 127 (96.2) | 1 (0.8) | 11 (8.3) |
| Incomplete data collection | 5 (3.8) | 2 (1.5) | 7 (5.3) |
| No data recorded | 0 | 129 (97.7) | 114 (86.4) |
The information we have collected on data completeness helps us to address Objective 1c (‘How well do participants complete the questionnaires necessary for a future definitive RCT?’). The majority of participants did not complete questionnaires, which was at least partly due to the difficulties in following up participants because of the COVID-19 pandemic and lockdown restrictions. However, considering the small numbers of participants who did complete the questionnaires, nearly half of them (9/21) could not (or would not) complete all the questionnaires or record data in response to every question.
Outcomes
Primary outcome
The intended primary outcome measure for the pilot RCT was the TLFB-28. As outlined in Chapter 3 this was amended to AUDIT-C. Table 25 shows descriptive statistics for estimated alcohol consumption in the previous 28 days at each time point, restricted to those participants with any follow-up information. Please note that alcohol information recorded at baseline may be an underestimate because a different AUDIT questionnaire was used at this time point and the formats of the first few question options were different (e.g. ‘4–5 times a week’ drinking was not distinguished from ‘6 or more times a week’ drinking).
| N | Mean | SD | Median | Min | Max | |||
|---|---|---|---|---|---|---|---|---|
| Both sites | Time point | Randomisation allocation | ||||||
| Baseline | Intervention | 9 | 95.2 | 83.8 | 80.0 | 10.5 | 198.0 | |
| Control | 9 | 107.8 | 70.3 | 110.0 | 11.0 | 198.0 | ||
| Overall | 18 | 101.5 | 75.3 | 104.5 | 10.5 | 198.0 | ||
| 6 months follow-up | Randomisation allocation | |||||||
| Intervention | 2 | 10.8 | 0.4 | 10.8 | 10.5 | 11.0 | ||
| Control | 1 | 11.0 | . | 11.0 | 11.0 | 11.0 | ||
| Overall | 3 | 10.8 | 0.3 | 11.0 | 10.5 | 11.0 | ||
| 12 months follow-up | Randomisation allocation | |||||||
| Intervention | 9 | 106.1 | 159.8 | 16.5 | 0.0 | 448.0 | ||
| Control | 9 | 41.4 | 58.2 | 8.0 | 0.0 | 154.0 | ||
| Overall | 18 | 73.8 | 121.3 | 14.5 | 0.0 | 448.0 | ||
| Site | Time point | Randomisation allocation | ||||||
| England | Baseline | Intervention | 2 | 60.3 | 70.4 | 60.3 | 10.5 | 110.0 |
| Control | 2 | 121.5 | 31.8 | 121.5 | 99.0 | 144.0 | ||
| Overall | 4 | 90.9 | 56.9 | 104.5 | 10.5 | 144.0 | ||
| 12 months follow-up | Randomisation allocation | |||||||
| Intervention | 2 | 13.5 | 4.2 | 13.5 | 10.5 | 16.5 | ||
| Control | 2 | 117.0 | 52.3 | 117.0 | 80.0 | 154.0 | ||
| Overall | 4 | 65.3 | 67.0 | 48.3 | 10.5 | 154.0 | ||
| Scotland | Baseline | Randomisation allocation | ||||||
| Intervention | 7 | 105.2 | 89.6 | 80.0 | 11.0 | 198.0 | ||
| Control | 7 | 103.9 | 79.6 | 110.0 | 11.0 | 198.0 | ||
| Overall | 14 | 104.5 | 81.4 | 95.0 | 11.0 | 198.0 | ||
| 6 months follow-up | Randomisation allocation | |||||||
| Intervention | 2 | 10.8 | 0.4 | 10.8 | 10.5 | 11.0 | ||
| Control | 1 | 11.0 | . | 11.0 | 11.0 | 11.0 | ||
| Overall | 3 | 10.8 | 0.3 | 11.0 | 10.5 | 11.0 | ||
| 12 months follow-up | Randomisation allocation | |||||||
| Intervention | 7 | 132.6 | 174.3 | 24.0 | 0.0 | 448.0 | ||
| Control | 7 | 19.8 | 40.2 | 4.5 | 0.0 | 110.0 | ||
| Overall | 14 | 76.2 | 134.9 | 12.0 | 0.0 | 448.0 | ||
Table 26 shows means and 95% confidence intervals for alcohol consumption (number of drinks consumed in the past 28 days) within each site and randomised group. Note that the amount of missing data is very substantial, so it is difficult to interpret these results.
| Randomisation allocation | Site | Baseline | 6 months | 12 months |
|---|---|---|---|---|
| Intervention | England | 60.3 (0 to 692.4) | – | 13.5 (0 to 51.6) |
| Scotland | 105.2 (22.4 to 188.1) | 10.8 (7.6 to 13.9) | 132.6 (0 to 293.7) | |
| Overall | 95.2 (30.8 to 159.7) | 10.8 (7.6 to 13.9) | 106.1 (0 to 228.9) | |
| Control | England | 121.5 (0 to 407.4) | – | 117.0 (0 to 587.1) |
| Scotland | 103.9 (30.2 to 177.5) | – | 19.8 (0 to 57.0) | |
| Overall | 107.8 (53.7 to 161.8) | – | 41.4 (0 to 86.2) |
For the primary analysis, the mean difference with 95% confidence interval in alcohol consumption at 12 months post randomisation (TP2) between the two randomisation groups was calculated (Table 27), both overall and stratified by site. Linear regression was used, adjusting for baseline alcohol consumption (TP0). Note that the linear regression model for England was based on only four data points and the 95% confidence intervals are extremely wide. Due to the substantial amount of missing data, extreme caution is required when interpreting these results.
| Site | Mean difference intervention – control (95% CI) |
|---|---|
| England | −117.5 (−919.1 to 684.0) |
| Scotland | 112.6 (−42.4 to 267.6) |
| Overall | 67.2 (−57.0 to 191.5) |
Secondary outcomes
Summary statistics of the secondary outcomes are presented in Table 28 for both sites combined. Please see supplementary material for the same tables stratified by site (Tables S1.1 and S1.2 in Report Supplementary Material 1). Although sample sizes are small, the standard deviations reported at 12 months follow-up could be used to inform sample size calculations for future studies in conjunction with the standard deviations reported in the baseline characteristics (see Table 16). This addresses our Objective 1b (‘Can we obtain reasonable estimates of the parameters necessary to inform the design and sample size calculation for a future definitive multicentre RCT?’). This also gives us some insight into Objective 2c (‘To what extent was the intervention changing process variables consistent with the underpinning theory’).
| N | Miss | Mean | SD | Median | Min | Max | |||
|---|---|---|---|---|---|---|---|---|---|
| AUDIT-C total score | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 8.6 | 3.0 | 9.0 | 5.0 | 12.0 | |
| Control | 9 | 0 | 9.9 | 1.8 | 10.0 | 7.0 | 12.0 | ||
| Overall | 18 | 0 | 9.2 | 2.5 | 9.0 | 5.0 | 12.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 4.5 | 2.1 | 4.5 | 3.0 | 6.0 | ||
| Control | 1 | 0 | 6.0 | . | 6.0 | 6.0 | 6.0 | ||
| Overall | 3 | 0 | 5.0 | 1.7 | 6.0 | 3.0 | 6.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 9 | 0 | 6.9 | 4.0 | 6.0 | 0.0 | 12.0 | ||
| Control | 8 | 1 | 4.5 | 4.4 | 4.0 | 0.0 | 10.0 | ||
| Overall | 17 | 1 | 5.8 | 4.2 | 6.0 | 0.0 | 12.0 | ||
| Readiness to Change Ruler: how much do you really want to reduce (or stop) drinking? | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 8.3 | 2.8 | 10.0 | 3.0 | 10.0 | |
| Control | 9 | 0 | 7.6 | 3.6 | 9.0 | 1.0 | 10.0 | ||
| Overall | 18 | 0 | 7.9 | 3.1 | 9.5 | 1.0 | 10.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 4.5 | 6.4 | 4.5 | 0.0 | 9.0 | ||
| Control | 1 | 0 | 10.0 | . | 10.0 | 10.0 | 10.0 | ||
| Overall | 3 | 0 | 6.3 | 5.5 | 9.0 | 0.0 | 10.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 8.1 | 3.1 | 9.5 | 1.0 | 10.0 | ||
| Control | 8 | 1 | 7.0 | 3.9 | 8.5 | 1.0 | 10.0 | ||
| Overall | 16 | 2 | 7.6 | 3.4 | 9.0 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: if you decided to stop or cut down drinking right now, how confident do you feel about succeeding with this? | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 8.4 | 1.5 | 9.0 | 6.0 | 10.0 | |
| Control | 9 | 0 | 8.7 | 1.3 | 9.0 | 6.0 | 10.0 | ||
| Overall | 18 | 0 | 8.6 | 1.4 | 9.0 | 6.0 | 10.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 9.0 | 1.4 | 9.0 | 8.0 | 10.0 | ||
| Control | 1 | 0 | 7.0 | . | 7.0 | 7.0 | 7.0 | ||
| Overall | 3 | 0 | 8.3 | 1.5 | 8.0 | 7.0 | 10.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 6.8 | 3.6 | 8.0 | 1.0 | 10.0 | ||
| Control | 7 | 2 | 7.6 | 1.8 | 7.0 | 6.0 | 10.0 | ||
| Overall | 15 | 3 | 7.1 | 2.9 | 8.0 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: how ready are you to stop (or cut down) drinking right now? | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 9.4 | 1.0 | 10.0 | 7.0 | 10.0 | |
| Control | 9 | 0 | 9.7 | 0.5 | 10.0 | 9.0 | 10.0 | ||
| Overall | 18 | 0 | 9.6 | 0.8 | 10.0 | 7.0 | 10.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 5.0 | 7.1 | 5.0 | 0.0 | 10.0 | ||
| Control | 1 | 0 | 10.0 | . | 10.0 | 10.0 | 10.0 | ||
| Overall | 3 | 0 | 6.7 | 5.8 | 10.0 | 0.0 | 10.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 8.1 | 3.1 | 9.5 | 1.0 | 10.0 | ||
| Control | 7 | 2 | 6.3 | 3.2 | 6.0 | 1.0 | 10.0 | ||
| Overall | 15 | 3 | 7.3 | 3.2 | 8.0 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: I have someone I can talk to about reducing my drinking | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 7.8 | 3.3 | 10.0 | 1.0 | 10.0 | |
| Control | 9 | 0 | 7.1 | 3.8 | 9.0 | 1.0 | 10.0 | ||
| Overall | 18 | 0 | 7.4 | 3.5 | 9.5 | 1.0 | 10.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 7.5 | 3.5 | 7.5 | 5.0 | 10.0 | ||
| Control | 1 | 0 | 0.0 | . | 0.0 | 0.0 | 0.0 | ||
| Overall | 3 | 0 | 5.0 | 5.0 | 5.0 | 0.0 | 10.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 6.8 | 3.7 | 7.5 | 1.0 | 10.0 | ||
| Control | 7 | 2 | 7.0 | 3.2 | 7.0 | 2.0 | 10.0 | ||
| Overall | 15 | 3 | 6.9 | 3.3 | 7.0 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: the people who are important to me support me in reducing my drinking | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 8 | 1 | 8.5 | 1.9 | 9.0 | 5.0 | 10.0 | |
| Control | 9 | 0 | 6.4 | 4.0 | 8.0 | 1.0 | 10.0 | ||
| Overall | 17 | 1 | 7.4 | 3.2 | 8.0 | 1.0 | 10.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 7.5 | 3.5 | 7.5 | 5.0 | 10.0 | ||
| Control | 1 | 0 | 5.0 | . | 5.0 | 5.0 | 5.0 | ||
| Overall | 3 | 0 | 6.7 | 2.9 | 5.0 | 5.0 | 10.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 6.9 | 3.8 | 8.0 | 1.0 | 10.0 | ||
| Control | 7 | 2 | 6.9 | 3.1 | 6.0 | 3.0 | 10.0 | ||
| Overall | 15 | 3 | 6.9 | 3.4 | 8.0 | 1.0 | 10.0 | ||
| Readiness to Change Ruler: I have made a detailed plan regarding when, where and how to reduce my drinking | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 4.7 | 4.2 | 2.0 | 1.0 | 10.0 | |
| Control | 9 | 0 | 3.0 | 2.2 | 3.0 | 1.0 | 7.0 | ||
| Overall | 18 | 0 | 3.8 | 3.4 | 2.5 | 1.0 | 10.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 5.0 | 4.2 | 5.0 | 2.0 | 8.0 | ||
| Control | 1 | 0 | 7.0 | . | 7.0 | 7.0 | 7.0 | ||
| Overall | 3 | 0 | 5.7 | 3.2 | 7.0 | 2.0 | 8.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 6.1 | 3.4 | 6.5 | 1.0 | 10.0 | ||
| Control | 7 | 2 | 5.1 | 2.8 | 5.0 | 1.0 | 10.0 | ||
| Overall | 15 | 3 | 5.7 | 3.0 | 6.0 | 1.0 | 10.0 | ||
| EQ-5D: mobility | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 1.1 | 0.3 | 1.0 | 1.0 | 2.0 | |
| Control | 9 | 0 | 1.6 | 0.9 | 1.0 | 1.0 | 3.0 | ||
| Overall | 18 | 0 | 1.3 | 0.7 | 1.0 | 1.0 | 3.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 2.0 | 1.4 | 2.0 | 1.0 | 3.0 | ||
| Control | 1 | 0 | 1.0 | . | 1.0 | 1.0 | 1.0 | ||
| Overall | 3 | 0 | 1.7 | 1.2 | 1.0 | 1.0 | 3.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 1.5 | 0.8 | 1.0 | 1.0 | 3.0 | ||
| Control | 9 | 0 | 1.2 | 0.4 | 1.0 | 1.0 | 2.0 | ||
| Overall | 17 | 1 | 1.4 | 0.6 | 1.0 | 1.0 | 3.0 | ||
| EQ-5D: self-care | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 1.0 | 0.0 | 1.0 | 1.0 | 1.0 | |
| Control | 9 | 0 | 1.2 | 0.7 | 1.0 | 1.0 | 3.0 | ||
| Overall | 18 | 0 | 1.1 | 0.5 | 1.0 | 1.0 | 3.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 1.0 | 0.0 | 1.0 | 1.0 | 1.0 | ||
| Control | 1 | 0 | 1.0 | . | 1.0 | 1.0 | 1.0 | ||
| Overall | 3 | 0 | 1.0 | 0.0 | 1.0 | 1.0 | 1.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 1.1 | 0.4 | 1.0 | 1.0 | 2.0 | ||
| Control | 9 | 0 | 1.3 | 0.7 | 1.0 | 1.0 | 3.0 | ||
| Overall | 17 | 1 | 1.2 | 0.6 | 1.0 | 1.0 | 3.0 | ||
| EQ-5D: usual activities (e.g. work, study, housework, family or leisure activities) | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 1.9 | 1.4 | 1.0 | 1.0 | 5.0 | |
| Control | 9 | 0 | 1.8 | 1.3 | 1.0 | 1.0 | 5.0 | ||
| Overall | 18 | 0 | 1.8 | 1.3 | 1.0 | 1.0 | 5.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 2.0 | 1.4 | 2.0 | 1.0 | 3.0 | ||
| Control | 1 | 0 | 1.0 | . | 1.0 | 1.0 | 1.0 | ||
| Overall | 3 | 0 | 1.7 | 1.2 | 1.0 | 1.0 | 3.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 1.9 | 1.4 | 1.0 | 1.0 | 4.0 | ||
| Control | 9 | 0 | 1.3 | 0.7 | 1.0 | 1.0 | 3.0 | ||
| Overall | 17 | 1 | 1.6 | 1.1 | 1.0 | 1.0 | 4.0 | ||
| EQ-5D: pain/discomfort | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 2.1 | 1.4 | 1.0 | 1.0 | 4.0 | |
| Control | 9 | 0 | 1.9 | 1.4 | 1.0 | 1.0 | 4.0 | ||
| Overall | 18 | 0 | 2.0 | 1.3 | 1.0 | 1.0 | 4.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 2.5 | 2.1 | 2.5 | 1.0 | 4.0 | ||
| Control | 1 | 0 | 1.0 | . | 1.0 | 1.0 | 1.0 | ||
| Overall | 3 | 0 | 2.0 | 1.7 | 1.0 | 1.0 | 4.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 2.8 | 1.3 | 3.0 | 1.0 | 4.0 | ||
| Control | 9 | 0 | 1.7 | 1.1 | 1.0 | 1.0 | 4.0 | ||
| Overall | 17 | 1 | 2.2 | 1.3 | 2.0 | 1.0 | 4.0 | ||
| EQ-5D: anxiety/depression | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 2.7 | 1.1 | 3.0 | 1.0 | 4.0 | |
| Control | 9 | 0 | 3.1 | 1.8 | 4.0 | 1.0 | 5.0 | ||
| Overall | 18 | 0 | 2.9 | 1.5 | 3.0 | 1.0 | 5.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 1.0 | 0.0 | 1.0 | 1.0 | 1.0 | ||
| Control | 1 | 0 | 2.0 | . | 2.0 | 2.0 | 2.0 | ||
| Overall | 3 | 0 | 1.3 | 0.6 | 1.0 | 1.0 | 2.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 2.9 | 1.7 | 3.0 | 1.0 | 5.0 | ||
| Control | 9 | 0 | 2.8 | 1.3 | 2.0 | 1.0 | 5.0 | ||
| Overall | 17 | 1 | 2.8 | 1.5 | 3.0 | 1.0 | 5.0 | ||
| EQ-5D: visual analogue scale | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 60.0 | 24.7 | 65.0 | 25.0 | 90.0 | |
| Control | 9 | 0 | 71.2 | 15.9 | 70.0 | 50.0 | 90.0 | ||
| Overall | 18 | 0 | 65.6 | 21.0 | 68.0 | 25.0 | 90.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 86.0 | 15.6 | 86.0 | 75.0 | 97.0 | ||
| Control | 1 | 0 | 95.0 | . | 95.0 | 95.0 | 95.0 | ||
| Overall | 3 | 0 | 89.0 | 12.2 | 95.0 | 75.0 | 97.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 9 | 0 | 57.2 | 29.9 | 70.0 | 0.0 | 95.0 | ||
| Control | 9 | 0 | 57.2 | 18.9 | 60.0 | 20.0 | 80.0 | ||
| Overall | 18 | 0 | 57.2 | 24.3 | 60.0 | 0.0 | 95.0 | ||
| Warwick-Edinburgh Mental Well-being Scale: total score | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 46.0 | 12.3 | 42.0 | 28.0 | 70.0 | |
| Control | 9 | 0 | 42.2 | 9.8 | 41.0 | 29.0 | 56.0 | ||
| Overall | 18 | 0 | 44.1 | 10.9 | 42.0 | 28.0 | 70.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 55.0 | 1.4 | 55.0 | 54.0 | 56.0 | ||
| Control | 1 | 0 | 52.8 | . | 52.8 | 52.8 | 52.8 | ||
| Overall | 3 | 0 | 54.3 | 1.6 | 54.0 | 52.8 | 56.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 44.3 | 13.1 | 46.5 | 23.0 | 61.0 | ||
| Control | 9 | 0 | 47.7 | 9.0 | 49.5 | 32.0 | 57.0 | ||
| Overall | 17 | 1 | 46.1 | 10.9 | 49.0 | 23.0 | 61.0 | ||
| Drinking Refusal Self-efficacy Questionnaire: total score | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 73.4 | 19.1 | 79.2 | 39.1 | 96.0 | |
| Control | 9 | 0 | 63.9 | 30.7 | 70.0 | 19.0 | 102.8 | ||
| Overall | 18 | 0 | 68.6 | 25.3 | 76.5 | 19.0 | 102.8 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 2 | 0 | 93.4 | 9.7 | 93.4 | 86.6 | 100.3 | ||
| Control | 1 | 0 | 86.1 | . | 86.1 | 86.1 | 86.1 | ||
| Overall | 3 | 0 | 91.0 | 8.1 | 86.6 | 86.1 | 100.3 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 64.0 | 33.2 | 63.1 | 19.0 | 109.0 | ||
| Control | 8 | 1 | 81.3 | 23.2 | 85.8 | 40.0 | 114.0 | ||
| Overall | 16 | 2 | 72.7 | 29.1 | 82.3 | 19.0 | 114.0 | ||
| Negative Alcohol Expectancy Questionnaire: same-day expectancy score | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 52.7 | 16.6 | 52.5 | 28.7 | 86.1 | |
| Control | 9 | 0 | 57.8 | 14.6 | 63.0 | 35.0 | 75.6 | ||
| Overall | 18 | 0 | 55.2 | 15.4 | 53.3 | 28.7 | 86.1 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 1 | 1 | 29.0 | . | 29.0 | 29.0 | 29.0 | ||
| Control | 0 | 1 | . | . | . | . | . | ||
| Overall | 1 | 2 | 29.0 | . | 29.0 | 29.0 | 29.0 | ||
| TP2 | Randomisation allocation | ||||||||
| intervention | 8 | 1 | 53.9 | 19.7 | 51.0 | 31.0 | 79.3 | ||
| Control | 8 | 1 | 50.3 | 16.0 | 48.7 | 28.0 | 77.0 | ||
| Overall | 16 | 2 | 52.1 | 17.4 | 48.7 | 28.0 | 79.3 | ||
| Negative Alcohol Expectancy Questionnaire: next-day expectancy score | Time point | Randomisation allocation | |||||||
| TP0 | Intervention | 9 | 0 | 47.1 | 18.7 | 47.0 | 20.0 | 82.0 | |
| Control | 9 | 0 | 53.8 | 19.3 | 55.0 | 18.0 | 88.0 | ||
| Overall | 18 | 0 | 50.5 | 18.8 | 49.5 | 18.0 | 88.0 | ||
| TP1 | Randomisation allocation | ||||||||
| Intervention | 1 | 1 | 33.0 | . | 33.0 | 33.0 | 33.0 | ||
| Control | 0 | 1 | . | . | . | . | . | ||
| Overall | 1 | 2 | 33.0 | . | 33.0 | 33.0 | 33.0 | ||
| TP2 | Randomisation allocation | ||||||||
| Intervention | 8 | 1 | 50.1 | 22.6 | 45.5 | 23.0 | 87.2 | ||
| Control | 8 | 1 | 48.4 | 14.5 | 45.0 | 30.0 | 71.0 | ||
| Overall | 16 | 2 | 49.3 | 18.4 | 45.5 | 23.0 | 87.2 | ||
The supplementary material also contains detailed tables of individual questionnaire item scores, overall and split by site (Tables S3.1 to S3.7 in Report Supplementary Material 1).
The secondary outcome results, change from baseline, show the average scores of participants in the intervention and control group at baseline, 6 months and 12 months. Due to missing data and small sample sizes, we are not able to interpret change from baseline to 6 months, nor group differences in change for 6 to 12 months. For change from baseline to 12 months, we can look at patterns of change in the data in mechanisms of change, albeit with caution. Readiness to change does not show increasing or at least maintained values; rather it seems to slightly decrease across items. One exception is the item ‘I have made a detailed plan regarding when, where and how to reduce my drinking’, which increases from baseline to 12 months in both groups (at baseline intervention: M = 4.17, control: 3.0; at 12 months intervention: M = 6.1, control 5.1).
Logic model results
An exploratory analysis was performed to explore key behavioural markers (mediators) of change and how these may influence the effect of the delivered intervention. The six proposed mechanisms of change were: self-efficacy, outcome expectations, goals, plans, social support and high-risk situations.
Summary statistics for the mechanisms of change at each time point and within each randomised group are presented in Report Supplementary Material 1, Tables S2.1 to S2.6.
In exploratory analysis, Kendall’s tau correlation coefficients were calculated to assess the correlation between each of the mechanisms of change and the primary outcome (AUDIT-C) at 12 months. Correlation coefficients and p-values are shown in Table 29, along with valid sample size N that each correlation analysis is based on.
| Mechanism of change | N | Kendall’s tau correlation coefficient | P-value |
|---|---|---|---|
| Self-efficacy: Readiness to Change Ruler: ‘How confident are you that you could reduce (or stop) drinking when you are released?’ | 15 | −0.31 | 0.13 |
| Self-efficacy: Drinking Refusal Self-efficacy Questionnaire Total | 16 | −0.43 | 0.023 |
| Alcohol expectancy: Negative alcohol expectancy questionnaire: Same-day expectancy score | 16 | 0.02 | 0.93 |
| Alcohol expectancy: Negative alcohol expectancy questionnaire: Next-day expectancy score | 16 | 0.11 | 0.55 |
| Goals: Readiness to Change Ruler: ‘How much do you want to reduce (or stop) drinking when you are released?’ | 16 | 0.27 | 0.18 |
| Plans: Readiness to Change Ruler: ‘How ready are you to reduce (or stop) drinking when you are released?’ | 15 | 0.17 | 0.41 |
| Plans: Readiness to Change Ruler: ‘I have made a detailed plan regarding when, where and how to reduce my drinking’ | 15 | −0.19 | 0.34 |
| Social support: ‘The people who are important to me support me in reducing my drinking’ | 15 | −0.26 | 0.22 |
| Social support: ‘I have someone I can talk to about reducing my drinking’ | 15 | −0.22 | 0.28 |
| High-risk situations: How much could I resist drinking when I am out for dinner? | 16 | −0.46 | 0.026 |
| High-risk situations: How much could I resist drinking when someone offers me a drink? | 16 | −0.47 | 0.019 |
| High-risk situations: How much could I resist drinking when my spouse or partner is drinking? | 13 | −0.54 | 0.021 |
| High-risk situations: How much could I resist drinking when my friends are drinking? | 16 | −0.35 | 0.084 |
| High-risk situations: How much could I resist drinking when I am at a pub or club? | 16 | −0.26 | 0.21 |
| High-risk situations: How much could I resist drinking when I am angry? | 16 | −0.34 | 0.088 |
| High-risk situations: How much could I resist drinking when I feel frustrated? | 16 | −0.33 | 0.10 |
| High-risk situations: How much could I resist drinking when I am worried? | 16 | −0.24 | 0.24 |
| High-risk situations: How much could I resist drinking when I feel upset? | 16 | −0.36 | 0.077 |
| High-risk situations: How much could I resist drinking when I feel nervous? | 15 | −0.39 | 0.062 |
| High-risk situations: How much could I resist drinking when I feel sad? | 16 | −0.52 | 0.009 |
| High-risk situations: How much could I resist drinking when I am watching TV? | 15 | −0.47 | 0.031 |
| High-risk situations: How much could I resist drinking when I am at lunch | 16 | −0.48 | 0.019 |
| High-risk situations: How much could I resist drinking when I am on the way home from work? | 15 | −0.53 | 0.012 |
| High-risk situations: How much could I resist drinking when I am listening to music or reading? | 16 | −0.46 | 0.026 |
| High-risk situations: How much could I resist drinking when I am by myself? | 16 | −0.57 | 0.006 |
| High-risk situations: How much could I resist drinking when I have just finished playing sport? | 14 | −0.45 | 0.046 |
| High-risk situations: How much could I resist drinking when I first arrive home? | 16 | −0.57 | 0.006 |
| High-risk situations: How much could I resist drinking when I feel like celebrating? | 16 | −0.13 | 0.52 |
| High-risk situations: Drinking Refusal Self-efficacy Questionnaire Total | 16 | −0.43 | 0.023 |
Mindful of the very small sample sizes and that as such caution should be applied, provisional indications suggest that self-efficacy may be a determinant of alcohol consumption and further exploration of interventions targeting self-efficacy should be considered. We observed moderate correlations between markers of self-efficacy and high-risk situations and alcohol consumption, whereas the correlations between the other mechanisms for change and alcohol consumption were weak.
Serious adverse events
There were no serious adverse events reported during the pilot RCT.
Chapter 5 Process evaluation methods
Sections of this chapter have been reproduced from Holloway et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
In this chapter, we present the methods for Phase II of the study which comprised the process evaluation (addressing Objectives 2 and 3). Elements of the process evaluation, where quantitative data were also collected, were integrated within the pilot trial (Objectives 2a and 2c) with cross-referencing to related results tables for these specific objectives provided. 44
Process evaluation aims and objectives
The new MRC framework for process evaluation guided the planning, design and proposed conduct of the process evaluation. 32 The process evaluation set out to assess intervention fidelity, to consider the extent to which the behaviour change markers were appropriate to the underpinning intervention and to explore the feasibility and acceptability of the APPRAISE intervention and study measures to staff and for men on remand and following liberation. Objectives 2 and 3 set out the key questions that were to be answered.
Objective 2: to assess intervention fidelity
-
What proportion of the interventions are delivered as per protocol?
-
Is there any evidence of contamination between the two conditions and/or between those workers delivering the intervention?
-
To what extent was the intervention changing process variables consistent with the underpinning theory?
Objective 3: to qualitatively explore the feasibility and acceptability of a self-efficacy-enhancing psychosocial alcohol intervention and study measures to staff and for men on remand and on liberation
-
How acceptable are the trial and intervention procedures (including context and any barriers and facilitators) to the following key stakeholders: men on remand in prison and following liberation; prison staff (including healthcare staff); commissioners; policy-makers and third-sector partners?
Process evaluation methods and design
Table 30 summarises the different components of the process evaluation and how they relate to the objectives of the APPRAISE pilot study. It also identifies the main research question for each process evaluation component and the main sources of data that were employed to answer them.
| Process evaluation component | Objective | Main research questions | Data source | Results |
|---|---|---|---|---|
| Implementation (i) Dose: delivered |
2a | What proportion of the interventions were offered and subsequently successfully delivered? | Quantitative data from participant study records, intervention booklets of successful (includes duration) and unsuccessful delivery (includes reasons for latter). | Chapter 4, In-prison and post-liberation intervention delivery, Tables 17–19. |
| Implementation (ii) Dose: quality (fidelity) |
2b | To what extent was the intervention delivered as intended? | Three cases were audio-recorded (with participant consent) of intervention delivery in the 1st APPRAISE session. Data were coded to assess delivery of essential theoretical elements and the use of the Behaviour Change Counselling Index (BECCI)72 to assess intervention fidelity. |
Chapter 6, Intervention implementation results |
| Contamination | 2b | Is there any evidence of contamination between: those who receive the intervention(s) and those who are in the control condition and/or between those workers delivering the intervention? | Qualitative interviews with men on remand from intervention and control arm. Qualitative interviews with intervention workers and non-interventionists at each study site. |
Chapter 6, Contamination results |
| Mechanism of change | 2c | To what extent was the intervention delivery consistent with the underpinning theory? Are the key behavioural markers appropriate for the mechanism of behaviour change? |
Quantitative data from self-reported alcohol self-efficacy and alcohol expectancies. | Chapter 4, Outcomes Table 28; Supplementary Material 1 (Tables S3.1–S3.7) Chapter 4, Logic model results Table 29; Supplementary Material 1 (Tables S2.1–S2.6) |
| 3a | How acceptable is the trial intervention and procedures to men on remand and on liberation? What are the barriers and facilitators? | Qualitative interviews with men on remand in both conditions. | Chapter 6, Remand participants | |
| 3a | How acceptable is the trial intervention and procedures to key stakeholders? What are the barriers and facilitators? | Qualitative interviews with prison staff (including healthcare staff); commissioners; policy-makers and third-sector partners. | Chapter 6, CGL team participants and Stakeholder participants | |
| Context | 3a | What factors will enable the delivery and or impact of the intervention at scale? | Qualitative interviews with stakeholders including prison staff (including healthcare staff); commissioners; policy-makers and third-sector partners. | Chapter 6, Context, Remand participants, CGL team participants and Stakeholder participants |
Both quantitative and qualitative methods were employed to provide the data required to answer the process evaluation questions. The quantitative data providing evidence related to the implementation dose and quality as well as the mechanisms of change associated with the intervention were integrated in the pilot trial. The study participants and wider stakeholder semistructured interviews were conducted separately from the pilot trial. This was due to the impact on access and availability during the COVID-19 pandemic.
In particular, the qualitative interview data analysis sought to provide evidence to verify the feasibility and acceptability of the APPRAISE study intervention to better understand and explain the social processes associated with the intervention through the lens of normalisation process theory (NPT). 69–71
Intervention implementation
To confirm intervention implementation, data collection was planned in two ways: intervention booklets (dose delivered) and audio recordings (dose quality).
Dose delivered
The interventionists were asked to use intervention booklets to record contact attempts, sessions offered, sessions delivered, reasons for unsuccessful delivery, session dates, and duration of sessions to assess whether the intervention was delivered as per protocol (see In-prison and post-liberation intervention delivery, Tables 17–19).
Dose quality (fidelity)
For the intervention condition, we had planned to audio record 20% of sessions delivered at each time point (4 sessions in total × 9 participants = 36) and for the control condition, we had planned to audio record 20% of the care-as-usual interventions (4 sessions in total × 9 participants = 36). However, we were unable to secure approval from the England study site to take in audio recording equipment, which meant that the in-prison intervention and control conditions could not be recorded there. Following discussions with the Scotland study site intervention team, recording control intervention delivery was not deemed feasible or practical.
Interventionists at the Scotland study site were aware that we were recording the intervention delivery sessions for the purposes of undertaking intervention fidelity assessment.
The Audio Recordings and Behaviour Change Counselling Index (BECCI)72 was used to provide insight into the Behaviour Change Counselling Skills of the interventionists from the audio recording of the APPRAISE intervention delivery sessions. To calculate the overall BECCI score, the mean across the item responses is calculated to provide the Practitioner BECCI score. The BECCI mean score will correspond to the points given on the Likert scales on the checklist.
The interventionists at both study sites received training (see Chapter 2, APPRAISE intervention training) and self-completed a six-question Likert scale evaluation (see Appendix 8) on completion of the training.
Contamination
During the qualitative interviews with the participants and interventionists and those delivering care as usual, we explored the possibility of contamination. This was with the purpose of identifying any evidence of contamination between those in the intervention and control arm and/or the intervention and non-intervention (care as usual) workers. We had hoped to note the wing/area in the prison where the participant was located and which other participants in the study they were likely to have most contact with. However, this was not feasible in terms of the practicalities within the running of the estates at each study site and the impact of COVID-19.
Mechanism of change
Quantitative and qualitative data were obtained to explore the mechanisms of change and the extent to which the intervention changing process variables were consistent with the underpinning theory.
The six proposed mechanisms of change in the logic model are: self-efficacy, outcome expectations, goals, plans, social support. These quantitative measures are discussed in APPRAISE intervention: theory, elements and logic model. In the pilot study the causal mechanisms were measured to provide increased understanding of how the delivered intervention influenced change through the quantitative assessment of key behavioural markers (mediators) of change. These were to be assessed at TP0, TP1 and TP2 and an exploratory prognostic analysis undertaken to explore the nature of change within these domains and their relationship to observed outcome.
In addition, we also conducted a qualitative exploration of study participant and stakeholder responses to, and interactions with, the intervention, providing the opportunity to identify acceptability, barriers and facilitators.
Context
We undertook qualitative interviews with study participants and wider stakeholders to contribute to our understanding of the context within which APPRAISE was delivered, to enable the delivery and or impact of the intervention at scale. We also recorded any differences in delivery in and across study sites where local organisational and devolved country contexts may have had implications for future intervention design and delivery.
Eligibility and recruitment to interviews
Those eligible to be interviewed were drawn from those registered in the pilot trial and from a range of stakeholders who had been involved in different aspects of the study or where, if this intervention were to be implemented at scale, they would be involved in some capacity.
Recruitment to all interviews was significantly impacted by the ongoing COVID-19 pandemic. The challenges of being able to locate men on remand hampered our ability to recruit them to take part in the process evaluation interviews. Similarly, the availability and capacity of some stakeholders (commissioners, policy-makers and prison healthcare professionals), as a result of the ongoing COVID-19 pandemic, meant it was not possible to secure interviews. Interviews were conducted at a time convenient to the participant and were conducted by JF and VG.
Sampling
Participants for all the interviews were selected via purposive sampling within three main groups. 73 The proposed number of participants to recruit was 40 interviews in total across the two study sites: men on remand from intervention (n = 8 at each site) [n = 16] and control arm (n = 8 at each site) [n = 16], N = 32; stakeholders (interventionists and those delivering usual care, prison governor, prison officers, commissioners, policy-makers, third-sector partners and prison healthcare professionals) (N = 8). However, due to the impact of COVID-19 we were unable to reach this target.
-
Participant group 1: men on remand who had been enrolled onto the APPRAISE pilot study and had been randomised.
-
Participant group 2: interventionists, who were invited to take part if they had delivered the APPRAISE intervention to study participants.
-
Participant group 3: stakeholders, who were invited to take part if they had been involved in different aspects of the study or where, if this intervention were to be implemented at scale, they would be involved in some capacity.
Informed consent
Each participant was required to provide their informed consent before taking part in an interview. We reinforced to participants that taking part in the interviews was voluntary, even if they had been involved in the main study or had delivered the interventions. It was also imperative to ensure that a participant’s decision to take part was based on a clear understanding of what was involved. All participants, therefore, received a verbal explanation of the study, at the time of the qualitative data collection, even in the case of male remand prisoner participants or APPRAISE interventionists. The verbal explanation included the provision of a PIS and then the interviewer went through all the elements in the PIS. When this had been completed, those in Stakeholder 1 group did not have to provide further written consent at this stage as they had already provided written consent on entering the study, which included taking part in future interviews. For those in Stakeholder 2 and 3 groups, each had to sign a consent form.
All participants were given the opportunity to ask questions or to clarify anything that was not clear, or they did not understand. In addition, all participants were reassured that they did not have to answer any questions that they did not understand or that made them feel uncomfortable and that they could withdraw their consent to taking part, at any time during the interview, and even following data collection.
Data management
During the timeline of the study, the COVID-19 pandemic came into play and therefore many of the interviews had to be conducted virtually using videoconferencing software or via telephone with Dictaphone facility as all interviews were to be transcribed verbatim. In Scotland as COVID-19 restrictions eased in the prison three of the four remand participant interviews were able to take place face to face and were digitally recorded, with the fourth taking place by phone.
Audio files were uploaded securely to a password-protected site by the researchers, from which the approved transcription company was able to access the files. On return, a quality check was conducted to ensure the accuracy of the transcribed files and then all audio recordings were securely destroyed, and the resulting transcripts were stored on password-protected drives at the University of Edinburgh and Teesside University. Upon storage, all interview transcripts were anonymised, with any personal or identifiable participant information being removed, and each transcript was assigned a unique participant number for analysis purposes.
Any pieces of hard-copy data from the Scotland site, such as the completed consent forms with a participant’s name on, were sent by secure courier to the England study team.
Qualitative data analysis
Following the transcription of the interviews, Braun and Clarke’s approach to thematic analysis was used, supporting a structured yet reflexive analytic process. 74 Because of the atheoretical nature of Braun and Clarke’s approach, we chose to use NPT as a lens to support thematic identification. 74
Thematic data analysis is often underpinned by theoretical concepts. In this study, we employed the NPT, an implementation theory, to better understand what the qualitative data could tell us around implementing the APPRAISE intervention for future work.NPT was developed to explore and develop the understanding around the factors affecting whether an intervention can be incorporated into practice, and the context in which the work of the new intervention happens. 69–71 NPT aims to facilitate a better understanding of the challenges arising during the embedding of a new practice by considering the components of four different constructs; Coherence (‘sense-making’), Cognitive Participation (‘relational’ work), Collective Action (‘operational’ work) and Reflexive Monitoring (‘appraisal’ work). 69–71 The theory lends itself well when considering qualitative data around implementing a new intervention in different contexts and in this work was used as a tool to structure the thinking around the different factors arising that would affect the future implementation of the APPRAISE intervention.
The interview data in the APPRAISE study were analysed within each of the three main groups; remand participants, CGL team and wider stakeholders. The first stage consisted of data familiarisation, essentially reading through the transcripts to elicit any initial thoughts and feelings emerging from the data. The next stage involved forming early codes from the data, the process of which is referred to as ‘coding’. A code refers to ‘the most basic segment, or element, of the raw data or information that can be assessed in a meaningful way regarding the phenomenon’. 75 Each transcript was read and coded by JF and was then double coded by GW at data analysis meetings to ensure consistency and refined further or developed further as necessary. The next stages involved the codes being assimilated and emergent data themes were mapped against the four main NPT constructs. Areas of divergence and discrepancy were explored and the data checked for fit.
Chapter 6 Process evaluation results
I think COVID and the impact of COVID, we’ll be dealing with this for a number of years going forward. And I think the longer term effects of COVID, and some of the almost the PTSD from COVID is something that’s going to play out over the next few years
D400S
As described in Chapter 5, quantitative and qualitative methods were employed to provide the data required to answer the process evaluation questions. The results of the implementation dose and quality as well as the mechanisms of change associated with the intervention are presented first. This is then followed by the results from the qualitative interview data, which focused on the feasibility and acceptability of the APPRAISE study intervention as well as any reflections on potential contamination and the context within which the intervention was delivered.
Firstly, it is important to acknowledge that the impact of the COVID-19 pandemic was felt by all participants. The pandemic resulted in prison lockdowns, social distancing and increased social isolation; pandemic measures reduced the prison staff capacity and the space available within the prison.
All participants reported on the impact of the COVID-19 pandemic on mental health. The lockdowns were identified as heightening mental health issues, by facilitating social isolation and reducing available support to the prisoners even further. The stakeholders and the interventionists recalled struggling with the different and ever-changing demands within the prison, while dealing with the unprecedented lack of social contact and restrictions outside of the prison.
Intervention implementation results
To confirm intervention implementation, data collection was planned in two ways: intervention booklets (dose delivered) and audio recordings (dose quality).
Dose delivered results
The full results of the in-prison and post-liberation intervention doses delivered are presented in In-prison and post-liberation intervention delivery, Tables 17–19. To recap, of the 68 participants randomised to the intervention condition, 53 received the in-prison intervention session (77.9%, 95% CI 66.2% to 87.1%). This percentage is greater than the 70% threshold specified as one of the criteria necessary for progression to a future larger randomised controlled trial (Objective 4c). Reasons why the in-prison intervention was not delivered are shown in Table 18. They varied from participant declining, being sentenced, released, transferred, in crises, had COVID-19 and unknown.
Only one ‘day-3 post-prison intervention’ session was attempted and was delivered (duration 30 minutes) at the Scotland site. No ‘day-7 post-prison intervention’ sessions were attempted. Only one ‘day-21 post-prison intervention’ session was attempted and was delivered to one participant (duration 30 minutes) at the England site. The main reasons why participants did not receive the post-prison interventions were (1) they could not be contacted and (2) CGL staff were unable to contact participants due to the impact of the COVID-19 pandemic.
Data for the duration (minutes) of the intervention sessions across both study sites are presented for all but one of the 53 interventions delivered in Table 19. There was a marked difference in the median time taken to deliver the intervention between the two sites: the intervention duration was half an hour in England compared to 1 hour in Scotland. The shortest time for an intervention was only 5 minutes in England whereas in Scotland it was 30 minutes. The maximum time for delivery was more aligned across sites, being 70 minutes and 80 minutes in England and Scotland, respectively.
Dose quality (fidelity) results
Interventionist training evaluation scores
Six practitioners from CGL took part in and participated in the training. Two interventionists and two team leaders at the England site and two interventionists at the Scotland study site (see the section Intervention implementation) completed a five-item ‘agree’ to ‘disagree’ Likert scale evaluation asking the trainees to score the Intervention Training sessions (see Appendix 8). Ratings for the six questions were all 4 and 5, with the exception of three practitioners from England who rated Q5 ‘The videos used during the training were helpful’ a 3. One England practitioner also rated Q3 ‘The training was what I expected’ a 3.
England interventionists and team leaders provided some written evaluation feedback. There was no written evaluation feedback from the Scotland interventionists who completed the training.
-
‘More understanding now’
-
‘Much more info now – trainer knew her stuff and explained really well – video clip delivery not scripted’
-
‘Thank you, nice relaxed training’
-
‘The intervention video – too long and should just be an overview, not full session’.
The Audio Recordings and Behaviour Change Counselling Index scores
During the course of the pilot trial, a total of three intervention sessions were successfully recorded at the Scotland site. Three recordings were reviewed and the BECCI instrument was completed. The mean Practitioner BECCI score for each of the recorded sessions was 4, which indicates the interventionist has been practising BCC to a great extent for all three of the recorded APPRAISE intervention sessions.
Contamination results
During the qualitative interviews with the participants and interventionists and those delivering care as usual, we explored the possibility of contamination. This was with the purpose of identifying any evidence of contamination between those in the intervention and control arm and/or the intervention and non-intervention (care as usual) workers. There was mention of discussion of the study between one of the remand participants and another (see sub-section ‘Coherence: acceptability of the APPRAISE intervention’ in the section ‘Remand participants’ below) but the participant stated that he did not know if the other participant got the intervention or not. No other evidence was obtained of contamination; however, it would be prudent to explore this again in any future work in the absence of a global pandemic, lockdown and restrictions across the prison estate. We had hoped to note the wing/area in the prison where the participant was located and which other participants in the study they were likely to have most contact with. However, this was not feasible in terms of the practicalities within the running of the estates at each study site.
Mechanism of change results
Quantitative and qualitative data were obtained to explore the mechanisms of change. The results of the quantitative data are presented in Chapter 4, Outcomes, Table 28 and Supplementary Material 1, Tables S3.1 to S3.7, and Table 29 and Report Supplementary Material 1, Tables S2.1 to S2.6.
In addition, we also conducted a qualitative exploration of men on remand, and CGL team and stakeholder responses to, and interactions with, the intervention, providing the opportunity to identify mechanisms of change and influencing factors (see section ‘Interview results’ below).
Context
Interviews with the three participant groups contributed to our understanding of the context within which APPRAISE was delivered, to enable the delivery and or impact of the intervention at scale. We also explored any differences in delivery in and across study sites where local organisational and devolved country contexts may haFifteen semive had implications for future intervention design and delivery. The next section provides the interview findings.
Interview results
Fifteen semistructured interviews were conducted with three participant groups from across the two study sites (Scotland and England) and are presented by participant group in Table 31.
| Participant group | Participants | Number of interviews | Participant codes |
|---|---|---|---|
| Participant group 1: remand participants | Male remand prisoner participating in APPRAISE pilot study | 4 | Participant A |
| Participant B | |||
| Participant C | |||
| Participant D | |||
| Participant group 2: CGL team | APPRAISE Interventionists | 6 | E200S |
| E300S | |||
| S100S | |||
| S200S | |||
| S300S | |||
| S600S | |||
| Participant Group 3: wider stakeholders | Prison staff RAs |
5 | E100S |
| E400S | |||
| E500S | |||
| S400S | |||
| S500S |
All remand participants were from the Scotland study site only. For the CGL team and wider stakeholder groups, participants from each of the two study sites were distinguished by their participant code, by using an E for England and an S for Scotland.
Remand participants
A total of four male remand prisoners were interviewed. Due to the COVID-19 regulations, following the completion of the recruitment of participants to the study, England project staff were unable to be granted further face-to-face access to prisoners. Therefore, as previously mentioned, all prison interview participants were from Scotland. The key themes emerging from the remand participants’ reported data aligned to each of the NPT constructs respectively were: Acceptability of the APPRAISE intervention; Utility and Value to ensure ‘buy-in’ in the APPRAISE intervention; Gaining trust and ‘opening up’; and finally Provision of ongoing support to affect change (Table 32). Within each theme there were sub-themes drawn from the data that collectively provided evidence to support our understanding of the experiences of the remand participants interviewed who had received the intervention.
| NPT construct | Theme | Subthemes |
|---|---|---|
| Coherence | Acceptability of the APPRAISE intervention |
|
| Cognitive participation | Utility and Value to ensure APPRAISE intervention ‘buy-in’ |
|
| Collective action | Gaining trust and ‘opening up’ |
|
| Reflexive monitoring | Provision of ongoing support to affect change |
|
Coherence: acceptability of the APPRAISE intervention
When exploring the responses around the initial screening process, using the baseline questionnaire to assess alcohol use, in the main, participants were happy to answer all of the questions in the questionnaire and, in general, the questions appeared to be acceptable to the population group, with only one participant saying they found some questions too personal.
I did feel comfortable about the questions and I understood what they meant, most of them nay bother eh I felt fine answering them
Participant A
Some of them are a bit personal like, but I suppose I felt alright about them, aye
Participant B
The APPRAISE intervention was reported by the remand participants as being useful and having a purpose.
Good because like, like I say, I didn’t ever talk to anybody about, so it’s good to have somebody that you can talk to, and say I’m feeling like this and tempted to like, use drugs or drink
Participant B
It seemed useful, do you know what I mean, to help me out going forward, you know what I mean? Get a better understanding, and not going back to old habits basically
Participant D
In addition, some participants were already able to reflect upon being able to see the benefit of engaging with such an intervention. The data for Participant B also provide evidence of some form of acknowledgement between remand participants about the intervention.
I don’t even know if he got the intervention, but he said he had spoke to yous. And they, it seemed, like he’d already stopped drinking
Participant B
The data suggest that remand participants were cognisant of the APPRAISE intervention and could reflect upon being participants in the study, the purpose of it and how it could be useful.
Cognitive participation: utility and value to ensure APPRAISE intervention ‘buy-in’
When considering the implementation of the APPRAISE intervention on a wider scale, a key contributor to this, which is incorporated within the Cognitive Participation construct of the NPT, is the notion of participants recognising the value of an intervention and hence facilitate their ‘buy-in’. Participants were seen to value the idea that by receiving support to reduce their drinking, it could have a positive impact on other elements of their life, including reducing re-offending and maintaining their relationships. A specific example of this was a participant who talked about being able to see the benefit of the intervention in allowing individuals to reduce their offending rates as a positive consequence of reducing their drinking.
I think it’s important, I believe that most people who have committed offences have been on alcohol or drugs eh? So, I think it is maybe important to hear people like come in prisons and say they can do stuff. And speak about drink, because there’s big problems there, it is. If they didn’t drink, they probably wouldn’t be half the people in prison. If they never had the problems with a drink. Yeah. So, if the good guys get a bit of help, then maybe it would make them not commit their offences and they wouldn’t come back.
Participant A
The notion of possible utility and value of engaging in such an intervention appeared to link to the acceptability to engage and the motivation and willingness to change their current drinking behaviour. Remand participants recognised that they needed help with reducing their alcohol consumption outside of prison, from completing the initial baseline question and intervention session, and hence appeared to welcome receiving support and having a new way of approaching it.
I wanted that support, I wanted that definitely, and into, I wanted that into it as well, you know, how you can change and how you can do better with your life, you know what I mean? It’s just that wee bit knowledge, that what I never had and that goes a long way when you’ve got it and then you’re off doing it, you know what I mean?
Participant C
Within the data, remand participants were seen to talk about not knowing where to go to access or receive the support or help they needed when early in the process of thinking about reducing their alcohol consumption.
If you’ve got that from inside going out, then you’ve got more of a chance I would say of you actually doing it.
Participant C
Therefore, as the first intervention session was delivered within the prison setting, it was seen as beneficial to participants to allow them to consider new habits once liberated.
Collective action: gaining trust and ‘opening up’
The idea of gaining trust and building a rapport during the first intervention session was reported recurrently, and is one which is highly indicative of the Collective Action construct of the NPT. Building and maintaining trust and having staff members who possess the relevant characteristics and qualities to be able to do so was seen to significantly increase the acceptability of the APPRAISE intervention.
some people just cannae, I don’t know they just cannae talk to people, do you know what I mean, for whatever reason, so I, that might be like your only barrier would be like getting through to people and saying, listen were just here to talk about this, if you want to talk but just many people understand why they don’t want to talk to people about things but, but whatever went on in their life basically they’re not willing to share.
Participant B
The issue of being unable or not wanting to talk about or vocalise problems to staff was discussed by the participants. However, one participant talked about feeling more comfortable to talk to a peer and it feeling more acceptable and relatable to engage with someone who had lived experience or who could empathise with an individual’s situation and offer a positive pathway for change.
I mean, not to say you’re intimidating or anything like that. You’re not, but it’s like, men don’t like to talk generally, especially on issues. They kind of close down. But yeah, you need to get some people inside, I guess. You know, so if you get someone here that goes out and reaches out to people in the hall there, that would help I think. It’s easier than them coming to you. If there’s somebody like me going to them, and going like, listen, man, I think that’d be good for you, I’ve done it and I can tell you this, this is what’s helped me, this is what it’s like, you don’t have to be fearful, if you don’t want to, you know what it is, you don’t have to do it. You don’t have to say this. You don’t have to say that. You know but give it a chance.
Participant C
It was clear that being able to open up and to speak to the individual delivering the intervention was important to the prison participants. The same participant talked about the importance of building a rapport with the support worker and gaining a relationship of trust to facilitate the delivery of the intervention.
I’ve got a lot of trust, I’ve got a lot of trust in this lassie. And that’s only because she was helping me, she was helping me with things I didn’t know nothing about, do you know what I mean?
Participant C
The sharing of information with the intervention delivery staff emerged as key. A challenge around the acceptability of the APPRAISE intervention was observed when the prison participants talked about being unable to ‘open up’ and talk to a new interventionist or support worker about their personal experiences or alcohol consumption.
Reflexive monitoring: provision of ongoing support to affect change
When asked about what would improve the intervention session or add to its usefulness or making it worthwhile, participants considered the offer of a continuous and ongoing package of support to be most useful.
Continuous, continuous support, you know what I mean. And letting people know, you’re definitely having the possibility of contacting people, you know, you’re just not being left to your own devices, to your own thoughts.
Participant D
All four participants welcomed the idea of having continuous and ongoing support, that they could access easily and build on the content of the intervention, in times of need for additional support.
The discussion on the post-release intervention sessions identified them as being less acceptable and feasible to remand participants. The remand participants talked about the importance of the post-release intervention support being obtained quickly, before an individual was able to return to their old habits.
I think if that, work, that help was still there right at the gate, waiting for the guy to go out to you’d have many a chance of like benefiting.
Participant C
However, many of the participants reflected upon the challenges of a participant being released from prison and establishing any reduction in their alcohol consumption, regardless of receiving an ABI in prison. They talked about an individual being released from prison and then finding themselves in situations where alcohol was freely accessible again or being in the company of other individuals that they used to drink with or who were drinking around them and falling back into previous risky drinking habits.
I dunno like, some people might work like, aye you might work with people in the jail, and like outside the jail, but it would be a lot harder outside the jail, because obviously other people could come in here with all good intentions of going to interventions, or whatever it may be, but when it gets out there it’s all going to be different, eh?
Participant B
On a more practical point, participants spoke about the difficulties that they would face in contacting an interventionist once they were released and vice versa. One participant talked about lacking a phone, and hence being unable to receive calls to arrange a follow-up session with a support worker or to contact them quickly if he needed any additional support.
You see now, outside everybody expects people to have phones. I was like, I’ve not got a phone, you know what I mean, so, they’d look at me and go, well some of my workers would go, ‘what you’ve not got a phone?’ How, now, wait a minute and they might now think different and go, ‘we need to write you a letter’. You know, and that, a letter can take days to try and get to you, whereas a quick phone call is like there and then isn’t it.
Participant C
Therefore, different methods of keeping in contact with men post-release appeared to be a key area warranting further consideration in future work, to facilitate successful implementation and success of the intervention over time.
Change Grow Live team participants
A total of six members of the CGL team participated in the semistructured interviews. The team members were all responsible for delivering alcohol and substance use interventions, within the prison setting, prior to the study and were all employed by the respective commissioned service provider at the time of the study taking place. This included those who delivered the APPRAISE intervention at both study sites and had received the intervention training. From the CGL team participant data, four key themes emerged: making sense of new ways of intervention practice; engaging in the APPRAISE intervention content; investing in alcohol prevention interventions; and scaling up the APPRAISE intervention (Table 33). Subthemes for each were identified, providing an insight into the context and system within which the intervention was delivered and providing key areas for recommendations if the APPRAISE intervention were to be scaled up and implemented. The CGL team participants reflected upon several factors related to the prison setting and alcohol services that they reported were relevant to the acceptability, feasibility and implementation of the APPRAISE intervention.
| NPT construct | Theme | Sub-themes |
|---|---|---|
| Coherence | Making sense of new ways of intervention practice |
|
| Cognitive participation | Engaging in the APPRAISE intervention content |
|
| Collective action | Investing in alcohol prevention interventions |
|
| Reflexive monitoring | Scaling up the APPRAISE intervention |
|
Coherence: making sense of new ways of intervention practice
In order to deliver the APPRAISE intervention, the CGL team who were to be involved in delivering the intervention and supporting the study were required to undertake APPRAISE training. Even though they were likely to have been delivering/managing/supporting a form of alcohol brief intervention within the prison setting previously, they were asked to complete training. Interview participants were asked about the training they received to determine whether it was fit for purpose and whether it was acceptable and feasible to them. Training is a key part of the NPT’s Coherence construct as it relates to the participants’ understanding of what was expected of them and being able to see the value of a new intervention or practice.
Generally, the training was well received by the interventionists. It was seen to be pitched at an appropriate level for them to understand the components of the APPRAISE ABI and to feel confident with the delivery following the session.
When we came to doing the APPRAISE books we knew exactly, yeah. It went well.
E300S
Even participants who were not feeling enthusiastic about undertaking the training felt that it was a valuable experience and allowed them to gain the skills and knowledge they needed to deliver the intervention.
I was quite keen not to go through it. But I’m glad we did. Because otherwise I wouldn’t have known that tool so well.
S200S
The less acceptable elements of the training appeared to be the role-play components, the amount of paperwork and the overall length of the session. One participant said they did not usually enjoy role-playing in training sessions, but they agreed that it added value to the training, in developing their understanding around the best ways to deliver an intervention to a prisoner.
I’m always apprehensive about role playing. It’s not anybody’s favourite thing to do. But actually, it was, it was quite good.
S200S
The feedback about the length of the training was that the session was too long, and that the content could be covered effectively in a shorter time frame.
I’m thinking maybe even just the one half-day probably would have been enough. Erm, cos yeah, I sort of felt like I had it after the first one, kind of thing.
S100S
In addition, the same participant felt that the amount of materials provided was overwhelming, and that they didn’t have time to look at them post training.
I remember getting a lot of paperwork though, supposed to read through and didn’t. I had every good intention of reading the paperwork. Yes. Just never found the time.
S100S
When talking about the intervention itself and the content, the interventionists were largely positive and indicated that it was well received by both the prisoners and the delivery staff.
everyone we talked to thought it went very well.
E3002
They seemed like the, you know, it was interesting for them, it was a little bit different. Yeah, no, it was, it was good. Yeah, there was a little bit of resistance with some, but not with many, I would say.
S200S
The fact that the ABI was different from the usual treatment and was ‘more structured’ and ‘repetitive’ in content appeared to be a facilitator for wider implementation.
I think there was actually a bit of intrigue around it, just because it was something new and something different. And you tend to find that does sort of pique people’s interest? That actually the idea of this something new, something different. That might be what works for them? Was something worth sort of buying into?
S100S
Being able to see the difference from current ways of working or usual care is part of the Coherence construct of NPT. Being able to identify how the APPRAISE intervention is different and valuing those differences can be a key facilitator of early implementation.
Cognitive participation: engaging in the APPRAISE intervention content
Similarly, to the remand participants, the CGL team participants stressed the importance of staff motivation and encouragement. Building a rapport between the prisoner and the interventionist delivering the intervention meant the prisoner was more likely to share their alcohol consumption habits and engage with the intervention content.
You know, just conversation, building some kind of rapport and relationship.
S200S
That’s the most important thing. Motivation and encouragement that’s the most important thing.
E3002
CGL team participants reported their belief that if the staff were motivated and encouraging when delivering the ABI, the prisoners were more likely to engage and take more from it. This is indicative of the Cognitive Participation construct of the NPT, which considers how key individuals can drive the intervention forward and support the implementation of an intervention. If the APPRAISE interventionists are motivated and can see the value of such an intervention, this could facilitate the implementation further.
The need for staff buy-in is also reflective of the Cognitive Participation construct of NPT, where implementation is supported by the relevant individuals buying into an intervention. The issue of staff capacity and space is encompassed within the Collective Action construct, which relates to the need for those involved in delivery of the intervention to have the motivation, capacity and ability to deliver it.
Collective action: investing in alcohol prevention interventions
From the interviews it was clear that the services and treatment options that were currently available to the men on remand were limited. The interventionists valued an ABI that was targeted at men on remand, as they generally had fewer services available to them, and it provided a window of opportunity to offer support post release.
There are a lot of services in here that are only available for people who have been convicted.
200S
The lack of service and treatment options available to the remand population at the time the interviews were undertaken was accompanied by reports that alcohol consumption was being viewed as less important or the ‘lesser of evils’ within the remand prison setting. One participant labelled alcohol as ‘being continuously left behind’, as the primary focus tended to be on substances that were more likely to cause significant damage in the short term, by overdosing or causing immediate harm.
I think alcohol is left behind a bit. A lot of concentration is on heroin, and methadone. Because the powers that be are so worried about people overdosing, which, obviously we all are.
E300S
CGL team participants reported how it had been eye-opening for the remand prisoners involved in the study to better understand the risks associated with alcohol consumption as opposed to drug use.
On a more practical level and building upon the prison setting as a suitable or feasible location for intervention delivery, a commonly reported issue was the lack of space. All of the participants reported room availability being very limited and often interventionists had struggled to find acceptable rooms to deliver the APPRAISE intervention.
Issues with rooms is kind of permanently a thing. And there, there’s never enough space.
S100S
As the interventionists were delivering the APPRAISE intervention over and above their usual service provision and need for rooms, room availability was even more stretched than usual and available space was very limited.
I couldn’t, because there weren’t enough rooms to facilitate the APPRAISE project, whether it was you in with interviewing somebody or [name removed] over to do the intervention with somebody. And it was just like for goodness sake, but you know. But, again, that’s life. And that’s how it goes. And that is just one of the ties with having such little room in this place.
S100S
more dedicated time, more dedicated space. And at the end of the day, you need, you need that buy in.
S100S
This is reflective of the Collective Action construct of NPT as it highlights the importance of how the host organisation, that is, the prison estate, is able to adequately support the implementation of the new practice; the pressures on suitable room availability could hinder the feasibility of an intervention future roll-out.
Reflexive monitoring: scaling up the APPRAISE intervention
A specific element of the intervention content that the interventionists from the Scotland study site reported they had found was a challenge for men on remand during intervention delivery was in navigating the variable numbering system of different scales. Two CGL team participants talked about the need to standardise the numbering so as to not exclude or frustrate the interventionists during delivery.
But the one thing that confused me and confused a few of the guys that I did the brief intervention with, was the change in the numberings. So, I think one of the, some of them were between one and five, and some of them were between one and 10. And that did throw people off, myself included.
S100S
One participant talked about the difficulties of maintaining implementation fidelity in an ever-changing, dynamic environment, such as the remand prison setting.
different workers have different approaches and different service users have different appointments.
S300S
Similarly, to the remand participants, the CGL team participants found the post-release follow-up sessions to be less acceptable and feasible to conduct in practice. Follow-ups were made challenging by inability to make contact with prisoners post release and this was further hampered by the COVID-19 pandemic, which made it impossible to meet face-to-face. The interventionists reflected upon the different methods of establishing contact with the prisoners. Letters were often seen as helpful, as a tool for prisoners to refer back to, and also sending text messages, prior to making a phone call, to introduce who was calling them.
sending a letter can be quite helpful, because sometimes it’s just that kind of post release panic of trying to get everything sorted out. And then the dust settles, and then they go, ‘Oh, yeah, I was offered that support’.
S100S
I would send that text explaining who I am because I know these guys and they won’t answer numbers they don’t know.
S600S
After being a part of the APPRAISE pilot study, the interventionists appeared to be positive about it being scaled up and extended as a larger study to determine the effectiveness of the intervention and could see the potential of the APPRAISE intervention in the setting.
yeah, I think it’s, a bigger study would be good. Very definitely.
E300S
I quite liked the project. Would be nice to see it done like on a larger scale because I do think it has, it has potential.
S100S
When asked to reflect upon the factors that would enable the delivery and facilitate future scale-up, a key facilitator of the pilot study in the setting was the researcher being able to understand the context and the management of the prison and hence being flexible and accommodating to any unexpected situations that arose.
I would say that the research team was flexible, which was good, and because they appreciated the difficulties and the pressures that we are often under as a team, due to various factors such as staffing, for example.
S300S
Being flexible aided the acceptability of conducting a research study within a prison and the researchers, within the APPRAISE study, were able to build a rapport with staff and support them with any issues as required, which would also be important within a future trial or considering future roll-out.
A commonly talked about barrier to research within the prison was capacity, in addition to the issue of space. Thinking specifically about staff capacity, interventionists talked about already having a high case load of prisoners, prior to working on the APPRAISE study, and therefore they often felt apprehensive about the thought of a research study adding to their burden.
I think concern for anything that we end up doing that’s an addition to somebody’s core duties that they do, there’s always just like, concerns about how that’s fitting in. But then, I think they had a bit more reassurance once it’s like, ‘okay, we’re only going to ask you for this amount of commitment’.
S300S
Therefore, exploring ways to ameliorate these issues would contribute to future feasibility of roll-out. On a positive note, the interventionists were in agreement that the APPRAISE study did not add significantly to their workload in practice. However, it has to be remembered that the majority of the post-liberation intervention delivery did not take place due to COVID-19. And participants did talk about how they thought a larger-scale trial in the future may be more difficult in terms of capacity.
would just be capacity for workers so I guess if it was a larger study, it’s just how?
S300S
Stakeholder participants
The final group of interview participants consisted of stakeholders who were involved with the delivery or the management of the APPRAISE pilot study. This group consisted of five participants ranging from the researcher who was managing one of the study sites and going into the prison to recruit the participants, to prison staff who were involved with the undertaking of the study and recruitment. The four main themes were: understanding the diversity of the prison population for APPRAISE intervention delivery; acceptability and utility of APPRAISE intervention champion; the value of networking; and awareness of the individuality of the prison environment and vulnerability of the remand population. Subthemes emerging from the stakeholder interviews are presented (Table 34).
| NPT construct | Theme | Subthemes |
|---|---|---|
| Coherence | Understanding the diversity of the prison population for APPRAISE intervention delivery |
|
| Cognitive participation | Acceptability and utility of the APPRAISE intervention champion |
|
| Collective action | The value of networking |
|
| Reflexive monitoring | Awareness of the individuality of the prison environment and vulnerability of the remand population |
|
The themes and subthemes emerging from the stakeholder interview data were very similar to those of the interventionist data. Similar findings were reported around the prison’s logistical constraints affecting the APPRAISE intervention feasibility, such as space and staff capacity, the importance of engagement with prisoners and the lack of currently available support for prisoners on remand. Overlapping findings are not discussed further in this section to avoid repetition. The novel themes and subthemes that came out of the stakeholder data were around the intricacies of the prison environment and how it affected the study and intervention delivery, the individual differences across the setting and across the participants, and further barriers and facilitators to delivery of the APPRAISE intervention.
Coherence: understanding the diversity of the prison population for APPRAISE intervention delivery
The need for joined-up care and signposting to different services links to another key finding from the stakeholder data, around understanding the remand prison population. A key facilitator in ensuring that the APPRAISE intervention was acceptable and feasible in practice was the delivery staff being able to understand the population. As the stakeholder group included mainly prison staff, it included people who understood this population well.
we need to understand the cohorts we’re dealing with as well as the remand group, particularly younger drinkers and particularly the kind of thinking around it.
E500S
This included being able to understand that younger drinkers were likely to have different drinking patterns, in comparison to an older population group. Therefore, having an understanding of the diverse population group and how to work with them would be advantageous when considering the future delivery and wider implementation.
A barrier which was reflected upon briefly in the prisoner findings, and directly linked to understanding the population involved, was considering the language used in both the intervention and questionnaire. Several stakeholders who had significant experience working with remand prisoners talked about the need to simplify the language for it to be acceptable for the population. The findings highlighted that the population group often had literacy or comprehension difficulties.
I get that I think some of it is come from, you’re already, you know, evidence based and use trials. You know questionnaires, but you’re working with a different clientele?
E100S
Another stakeholder participant talked about the fact that the language that was acceptable to academics isn’t always acceptable for this population group. This led to the discussion around the need to ‘demystify’ overly complex language.
I think the other things is finally around brief interventions is to demystify an awful lot of language that people use in treatment eh I think academics are the worst for it.
E500S
Cognitive participation: acceptability and utility of the APPRAISE champion
Thinking about some of the findings which might increase the acceptability and utility of the APPRAISE intervention in practice, it was reported by one stakeholder that the use of ‘intervention champions’ could be advantageous. The stakeholder talked about the importance of having an individual, within the prison setting, who clearly saw the purpose of the intervention and who was motivated to engage others to deliver and implement it. The stakeholder participant was able to see the effectiveness of having an intervention champion in other settings, therefore they believed it would be useful to employ this strategy within the remand prison setting.
they become your champions, they do it everywhere else why not do it around this particular intervention, because when they are gone, they trained the next leader.
E500S
This finding is concurrent with the Cognitive Participation construct of the NPT, as it includes the concept that key individuals are responsible for driving an intervention forward. Similarly to the prisoner participants, the stakeholder participants could also see the benefit and relevance of employing people with lived experience of alcohol use or the prison setting, in the intervention delivery process, as it appeared more acceptable to the prisoners.
that’s where lived experiences are really important, peer support, peer mentors, mutual aid groups, recovery networks, visible recovery.
E500S
The discussion around prisoners and their individual needs is linked to another finding that prison staff were often apprehensive about allowing research to be undertaken in the remand setting. One participant talked about how they felt protective of prisoners taking part in research studies and that they had to be able to see the benefit to the prisoner in taking part in the research, before allowing a study to take place.
Some staff are very protective of their prisoners as well and they don’t like to see tours coming in or high school kids coming in, or university guys just coming in, because we don’t want people in our care to be treated like, you know, it’s like a fishbowl.
S400S
This is again reflective of the NPT Cognitive Participation construct, as the stakeholders needed to be able to see the value of the new ABI to the prisoners, before agreeing to take part in the research study.
Collective action: the value of networking
Another perceived facilitator to the APPRAISE intervention delivery was being able to work with other services to create a network and to offer signposting, and stakeholder participants frequently talked about the importance of adopting a ‘joined-up’ approach. One participant talked about promoting a ‘social network’, to support the different treatment services.
If your cat is sick and your car breaks down who do you ring? You don’t ring the same person, so from that perspective that’s why networks are really important, your social networks, so what you need to understand is what social networks and what other services do they buy into, where do they go.
E500S
Working with other services and the sub-theme of trust came across in the findings. This is reflective of the Collective Action construct of NPT, as it includes the concept of participants being able to maintain their trust in each other’s work and expertise throughout the work of an intervention, such as the APPRAISE ABI.
Reflexive monitoring: awareness of the individuality of the prison environment and vulnerability of the remand population
As expected, the remand prison setting was found to be dynamic and largely unpredictable. This meant that there was a constant pressure felt by the prison staff to be able to adapt to the changing environment and situations.
my main interest is in this place is keeping the place safe, keeping it decent, but keeping people alive when they come in, because I manage an awful lot of chaos in a very confined custodial setting.
E400S
They’ve also usually got quite a lot of chaotic things happen in the background.
S400S
Specific challenges that were discussed across the two study sites, and at times which affected the study and recruitment, included prisoners’ illicit drug and alcohol use, physical violence and the prison going into lockdown. Poor mental health was also a commonly reflected-upon issue that added to the unpredictable nature of the population. The reported stigma of being on remand was felt to contribute to this, with one participant reflecting upon the challenges associated with a prisoner adapting to their environment.
Just a week on remand can mean family breakdown, loss of job, loss of status, stigma, self-esteem, down the toilet, you know, so that’s you, you know, you’ve got it branded, is right in the middle of your forehead.
S500S
The trauma experienced by the remand prisoners as reported by one stakeholder participant identified that this also extended to their release, and the APPRAISE study findings indicated that this was a contributing factor to why the follow-ups were difficult in practice (aside from COVID-19), as the prisoners struggled to ‘re-establish their lives’ post release.
And you know that that traumatic, that trauma they’ve just went through, probably might not be the one trauma they have. They’re now leaving custody to try and re-establish their life under a great deal of stress and pressure, and probably are here at least in part due to alcoholism.
S400S
The individual nature of both the prisoners and the prison setting was highlighted. Stakeholder participants commonly reflected that what worked in one prison may not necessarily work in another, due to the individuality of the settings. However, there was a consensus that although there were differences experienced across prisons, there would also be a certain degree of consistency.
obviously quite different in general quite different prisons, but you would expect some consistency.
S400S
The idea of individuality also extended to the prisoners and acknowledging their differences and individual needs. Stakeholders talked about the importance of the services, offered to remand prisoners, not just acting as a tick-box exercise, but being able to adapt and encompass prisoners’ individual differences.
I think, trying to just keep away from a map that’s got tick boxes on it, is better. We need to talk to that individual about their individual needs and how it’s affecting their individual well-being.
S400S
One participant talked about how prisoners were often seen to be excluded and labelled as ‘hard to reach’, due to them not engaging in a particular activity or service. However, this was often more complex than that because prisoners were seen to be likely to be struggling with various issues, or it was found that the service did not meet their needs or was not acceptable to them etc.
services generically are quite often designed where people don’t feel they’re included.
E500S
Therefore, it appeared to be important to consistently appraise the ABI to ensure it is not a ‘one size fits all’ approach and that it meets a range of different prisoners’ needs. This is reflective of the Reflexive Monitoring construct of NPT, which highlights the importance of modifying relational work in the appraisal of a new practice or intervention. Clearly clarifying which components of the ABI can be subject to modifications and which need to exist as ‘core components’ will aid implementation in a future trial.
Summary of findings
Analysis of the 16 interviews highlighted key findings from the qualitative work, in regard to the acceptability and the feasibility of the APPRAISE intervention. The in-prison APPRAISE intervention session appeared to be acceptable and feasible to receive and deliver according to all of the participants we asked. The intervention sessions delivered post liberation appeared to be more challenging in practice and less feasible to complete because of a plethora of different factors, such as being unable to re-establish contact with males upon their release and individuals relapsing to their previous risky alcohol consumption when alcohol was more freely available. Therefore, it would be imperative to explore different ways to make contact with the men post release and to provide more emphasis to strategies of avoiding relapse in future work, if pursuing an intervention which included post-release sessions. Picking up on the value of networking, it may be prudent to explore how the Probation Service could play a role in facilitating making contact with the men post liberation.
The prisoner participants appeared to welcome receiving support for making changes to their alcohol consumption and talked about the utility and value of the intervention in order to ensure buy-in from them. Importantly, they also mentioned the need for the provision of ongoing support and the practicalities of that. Fundamental to the men was the importance of fostering an environment that promoted an individual to feel comfortable and trusting of the interventionist, in order for the men to open up and share their personal experiences and discuss their consumption patterns and potentially other areas of their lives that were relevant to drinking.
The interventionist findings also included the importance of building a rapport with prisoners when undertaking the intervention sessions. In addition, they talked about how the prison setting and culture affected the acceptability and the feasibility of implementing an intervention due to the lack of currently available options to the remand population, the lack of available space in the prison and limited staff capacity. Investing in alcohol prevention interventions were identified as important as other behaviours that impact on health and well-being. The intervention training and content appeared to be largely acceptable and were key to identifying the purpose of the intervention, while understanding the impact of the intervention would facilitate scaling up in the longer term, although it was thought that the time taken and the materials used could be reduced to ensure the feasibility in future roll-out. The delivery significantly benefited from staff buying into the intervention and being motivated and engaged with the content.
The final stakeholder group expressed the need for implementation to fully understand and respond to the diversity across the prison population and the different drinking patterns that may exist. They also believed that the language used could be modified and simplified to be more acceptable for the remand population. In addition, the need to create safe spaces, fostering inclusivity and adaptation to meet the individual needs of the remand population, was identified. An awareness of the vulnerability within the prison environment for those on remand and being cognisant of this in working to implement new interventions within the estate was identified as being required. The relevance of the lived experience and that those with it can have a role to play alongside the wider network of services could shape the implementation of the APPRAISE intervention.
Finally, all participants interviewed appeared to be enthusiastic about facilitating future work in the area and building upon the delivery of the ABI in the APPRAISE study. Researchers were able to introduce the study effectively, develop rapport with the prison staff and maintain flexibility to ensure minimal disruption to the setting, even during the unprecedented COVID-19 pandemic. The fact that participants relayed that the services and treatment options currently available to remand prisoners were extremely limited further highlights the need to broaden the existing services in this area and work towards a future trial of the APPRAISE intervention to determine the APPRAISE intervention effectiveness.
This, therefore, further confirmed the importance of the remand prison setting as a suitable location for delivering the APPRAISE intervention and the importance of the wider network that could support implementation.
Although this did not appear to have a negative impact on delivery, in a future roll-out it may be prudent to condense training sessions and the accompanying materials to ensure that it remains acceptable and feasible to a larger cohort of interventionists.
Chapter 7 Economic study
Were the APPRAISE intervention to demonstrate effectiveness, the next barrier to widespread adoption would be cost efficiency. While stated policy criteria exist in the UK health sector to guide the design of health research,76 the APPRAISE intervention encompasses a wider stakeholder group, including the prison and wider criminal justice system (CJS) stakeholders, and the prisoners themselves. These groups additionally require convincing of value from their own perspective to help alleviate implementation barriers. Hence, a standard health and social care perspective alone may not provide sufficient evidence needed by all parties in their independent decision-making, and a broader taxonomy of outcomes is necessary. Conducting any analysis in a prison setting adds challenges to data collection and analysis, hence the feasibility of collecting data to inform data analysis requires exploring and refining prior to any significant investment in a larger definitive trial. To that end, we present the findings of the APPRAISE economic substudy, including a micro-costing methodology protocol, and a revision of the Economic Form 90 for a UK context,60 and some provisional scoping of routine data sources to support future cost-effectiveness analyses (CEA) in this area. We anticipate this work to be valuable as we believe this to be the first of its kind for an extended ABI in this setting and that the methods we have discussed will likely be relevant and transferable across other ABI settings.
Full details of the wider trial methodology are given elsewhere in this report and in our published study protocol. 1 This chapter focuses exclusively on the economic evaluation pilot study. Specifically, we discuss efforts undertaken to address the study Objectives 1d, 1e and 1f.
-
1d. Can we collect economic data needed for a future definitive RCT?
-
1e. Can we access recidivism data from the PNC databases for trial participants?
-
1f. Can we access health data from routine NHS data sources for trial participants?
To aid UK policy relevance, the base-case costing perspective was based on the NICE recommended NHS and personal social services (PSS) perspective,76 with the addition of criminal justice and prison service costs to future support prison sector buy-in. The economic study focuses on the opportunity cost of intervention implementation from these perspectives. Further planned analyses aimed to widen this to a whole societal perspective with the further inclusion of employment, welfare, and third-sector addiction services, as well as including future cost savings from the NHS and PSS perspectives. For this pilot feasibility study, the base year for all costs was set to the 2020–1 financial year, selected at the latest financial year from which any prisoner provided data on balance internal and external validity. Discounting and inflation adjustments were not necessary as the time horizon for analysis was under 1 year, and all price estimates related directly to the base year. A Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist indicating the location of key economic principles and methods can be found in Appendix 12.
Methods
The economic evaluation pilot study aimed to evaluate the feasibility of collecting economic data to inform design of a potential future RCT of the APPRAISE intervention in a UK prison setting. This had three principal components:
-
development and pilot testing of an activity-based costing (ABC) exercise adapting recommendations from Drummond et al.,77 which aimed to estimate the resources used to deliver the ABI programme, and equivalent usual care, and associated financial cost of these
-
pilot testing of the collection of self-report data on prisoners’ health care, social care, criminal justice, welfare payments, employment, and third-sector addiction-service utilisation at baseline and at 6- and 12-month follow-ups using an adapted Economic Form 9060
-
an examination of the feasibility of accessing recidivism data from the PNC databases, and health data from routine NHS data sources for research purposes within a prisoner population.
Of note are overlaps between potential data items obtainable via components 2 and 3. We sought to compare data quality to both validate our survey data instrument and identify the preferred data-collection approach to provide an informed balance of data quality and participant self-report burden. We initially planned to publish a health economic analysis plan prior to analysis; however, disruptions due to the pandemic necessitated a number of ad hoc adaptations.
The activity-based costing exercise
The proposed ABC exercise was based on the recommendations by Drummond et al.,77 and consisted of four principal steps:
-
Step 1 – a taxonomy of intervention activities was created. A 1-day consultation exercise was held, with both the staff delivering the intervention and the research staff involved in the APPRAISE pilot study, to identify all of the resources that would be required in the implementation of the APPRAISE intervention, at scale, in a future hypothetical roll-out, as opposed to those only required for research purposes. A detailed narrative was constructed, for each study site, which documented the key components of the intervention delivery and the process. The intervention activities were listed in the sequence performed, in relation to each participant, and the resources that were used for each activity.
-
Step 2 – resources used for each activity were measured. The staff delivering the APPRAISE interventions in each study site were asked to note the duration of each intervention activity and the necessary materials and commodities that were required before, during, and after each stage of intervention. Examples of these resources measured included: the time taken to locate participants using their preferred method of contact; the preparation and printing of the intervention materials; and the actual time taken for the delivery of the intervention sessions. Security protocols and procedures prohibited the use of use electronic equipment for recording this information. In order to comply, handwritten research diaries were instead compiled. These were either transcribed verbatim or were scanned and shared retrospectively within the economic research team.
-
Step 3 – identification of unit cost. Where possible, unit costs for each resource use item were identified based on the study invoices and targeted (non-systematic) literature searches or sourced from expert knowledge within the team. Priority was given to the estimates considered to be best fit to a hypothetical future roll out (at scale) where multiple estimates were located.
-
Step 4 – calculation of costs. The resources identified in Step 2 were combined with the unit costs from Step 3 to generate estimations of the costs of each activity.
These calculations are not intended as an accurate estimation of costs of a hypothetical future roll-out, but rather as a demonstration of how these might be calculated in a future trial. Of particular note is that differences in prison procedures would be expected to yield differences in durations and costs of each type of activity, and that a larger study would need to account for this. To this end, separate outputs from Steps 1 and 2 were generated and compared for each site.
Adaptation of the Economic Form 90
The items of the Economic Form 90 were systematically examined in consultation with a UK economist and experts in the prison and addiction-services fields to identify UK equivalents for each entry and anything missing, and remove anything not relevant in a UK context. Questions were additionally rephrased for clarity to a UK reader and PPI input was solicited.
Unit costs for each item were identified by a non-systematic literature search, alongside those from the ABC exercise, with the same preference given to national-level unit costs to maximise relevance to a hypothetical future roll out (at scale).
Examination of Police National Computer and National Health Service data sources
Permission to access PNC and PHS data sets was requested from prison authorities. Upon receipt these were to be examined for data quality and compared to results of the Form 90 survey to cross validate. Results from this comparison would inform the optimal balance of data items to be obtained from each source in a future definitive trial. Consideration was to be given to any missing items, and if these were estimable via other sources, such as literature or modelling.
Results
Disruption due to coronavirus disease discovered in 2019 pandemic
Follow-up data collection for multiple parts of the study became disrupted as researchers were unable to access prison services due to revised safety protocols. This had the following notable impacts on the economic substudy:
-
It was not possible collect the anticipated number of Economic Form 90 surveys, preventing analysis and validation efforts. However, the adaptation process was completed prior to onset of the pandemic, and scoping of potential sources for price weights was possible remotely.
-
Prison staff experienced sharp increases in workloads which they needed to prioritise over research efforts, leading to lower participation rates and possibly different duration of intervention sessions than might be anticipated in a live roll-out.
-
Time spent locating prisoners for post-liberation intervention sessions increased due to additional complexities of doing so remotely that may not reflect future methods.
Activity-based costing exercise
Row headings on Tables 35–37 display the items identified in Stage 1 of the ABC process via day consultation. Tables were then populated in Steps 2–4 detailing all activities, staff costs and the unit cost sources. Separate estimates are provided for the Scotland and England study sites to account for differences in services and local salaries of staff providing services.
Table 35 breaks down staff costs associated with delivering the intervention. The intervention service providers (CGL) at each study site were asked to provide a typical salary cost for the different roles delivering the APPRAISE intervention so that the intervention staff salary cost could be estimated. Values obtained for these, correct at the time of the pilot study undertaking (2020), are included in Table 35. Participant locating time proved more difficult to determine and hence it was more difficult to provide a meaningful estimation of the staff cost associated with it. In the pilot study these tended to be lower-paid staff, such as support workers or administrative staff, attempting to make contact with a participant. The time taken to schedule a follow-up intervention session or to successfully make contact to start the intervention session remotely (by telephone) often varied significantly. Some individuals could be reached quickly (within 10–15 minutes) or it could be ascertained quickly that the listed provided contact methods could no longer be used, for example their phone number was no longer in use or e-mails to their address were bouncing back etc. This was in direct contrast to those who were unable to be reached after frequent attempts, by different methods of contact, or those who would reply once and then would stop replying. Successful completion of follow-up interventions was low, even with large amounts of time spent attempting to make contact. However, it was difficult to establish how much of an effect the COVID-19 pandemic had in this lack of successful contact; thus it needs to be an area to explore further in a future cost analysis, rather than attaching a cost estimate to the participant-contacting time with limited insight.
| APPRAISE activities | England cost | Scotland cost |
|---|---|---|
| Session 1 Approximately 45 minutes with a co-ordinator plus an additional participant-locating cost |
Co-ordinator annual salary cost = £21,630–£21,812 45 minutes |
Co-ordinator annual salary cost = £23,218.59–£26,983.44 45 minutes only |
| Session 2 Approximately 20 minutes with an intervention support worker plus an additional participant-locating cost |
Support worker annual salary cost = £18,213–£19,847 20 minutes |
Support worker annual salary cost = £18,895.07–£19,744.94 20 minutes |
| Session 3 Approximately 20 minutes with an intervention support worker plus an additional participant-locating cost |
Support worker annual salary cost = £18,213–£19,847 20 minutes |
Support worker annual salary cost = £18,895.07–£19,744.94 20 minutes only |
| Session 4 Approximately 20 minutes with an intervention support worker plus an additional participant-locating cost |
Support worker annual salary cost = £18,213–£19,847 20 minutes |
Support worker annual salary cost = £18,895.07–£19,744.94 20 minutes |
Table 36 documents the one-off and the ongoing staff training costs that would be associated with implementing the APPRAISE intervention in practice. Initial APPRAISE interventionist staff training consisted of a one-time in-depth training session lasting approximately 2 hours. This was followed by refresher courses every 6 months typically lasting 20–30 minutes, and weekly 5–10-minute debriefs to allow the intervention staff to catch up with the research staff around their progress and to provide updates and to discuss any concerns or queries. However, disentangling research-only costs from those that would be present in a real-world setting may require separate sampling, and/or may be better handled by attributing varying proportions of activities to each in sensitivity analysis in a next-stage RCT. These staff costs, associated with the intervention delivery training, would vary dependent on the numbers of the different staff roles that were required in each location, and across the two study sites.
| Training | England cost | Scotland cost |
|---|---|---|
| Initial training Generally, 2 hours and dependent on number of staff trained |
Co-ordinator annual salary cost = £21,630–£21,812 Support worker annual salary cost = £18,213–£19,847 |
Co-ordinator annual salary cost = £23,218.59–£26,983.44 Support worker annual salary cost = £18,895.07–£19,744.94 |
| Refresher training Generally, 30 minutes and dependent on number of staff trained |
Co-ordinator annual salary cost = £21,630–£21,812 Support worker annual salary cost = £18,213–£19,847 |
Co-ordinator annual salary cost = £23,218.59–£26,983.44 Support worker annual salary cost = £18,895.07–£19,744.94 |
| Ongoing weekly debrief in prison Generally, 10 minutes and dependent on number of staff |
Co-ordinator annual salary cost = £21,630 - £21,812 Support worker annual salary cost = £18,213 - £19,847 |
Co-ordinator annual salary cost = £23,218.59–£26,983.44 Support worker annual salary cost = £18,895.07–£19,744.94 |
Table 37 presents other resource-utilisation costs required when delivering the APPRAISE intervention. As several of the questionnaires form part of the screening and recruitment process, and prison security processes and procedures prevented all non-paper-based data-collection options, printing costs totalling £6.45 per participant were unavoidable.
| Resource | Resource breakdown | Price per item |
|---|---|---|
| Printing | APPRAISE information booklet | £0.42 |
| Consent form | £0.57 | |
| Participant contact details form | £0.12 | |
| Baseline questionnaire (with AUDIT-C) | £2.43 | |
| APPRAISE alcohol unit postcard | £0.19 | |
| APPRAISE follow-up intervention booklet | £2.60 | |
| Contacting participants | Letters | Printing letter – £0.12 |
| Envelope – £0.11 | ||
| 2nd-class postage – £0.66 | ||
| Telephone calls | £0.25 per minute | |
| Text messages | £0.10 per message | |
| Internet (WhatsApp or social media) | £0.10/MB |
Depending on which session was being undertaken a plethora of different methods may be used to contact participants for follow-up intervention sessions. These included the cost of using a telephone or text messages, sending written letters or using the internet for social media or WhatsApp. In the pilot study, all of the required printing was conducted and costed by the research staff at the University of Edinburgh, which included the follow-up letters. Any further attempts to contact participants or to conduct phone-based follow-up sessions were conducted using a researcher’s phone, but with a new pay-as-you-go sim card. The sim card was free to obtain, but the phone costs have been quoted from the listed provider’s pay-as-you-go costs at the time of the study. Costs of these in future studies or eventual roll-outs may vary, and users of these results may wish to substitute their own local estimates.
Factors, such as rooms in prisons needed to undertake sessions were provided free and so were not included in the pilot ABC exercise. While these are anticipated to have opportunity costs associated with them, costs at a given prison will vary substantially and arguably only incur an opportunity cost if the room was needed for another purpose. Financial values for these are challenging to estimate reliably and may be misleading if they appear overly specific. Nevertheless, their need is noted in a more qualitative sense, with recommendation that future work or roll-outs include these costs and use local estimates for decision purposes where possible.
Adaptation of Economic Form 90
The adapted version of the Economic Form 90 survey developed as part of this study can be found in Appendix 9. While the COVID pandemic prevented data collection, it was still possible to identify candidate sources of price weights for items included in the survey. These are listed in Table 38.
| Item | Unit | Unit cost source | Notes |
|---|---|---|---|
| Healthcare costs | |||
| GP consultations | Per consultation | PSSRU unit costs78 | |
| Practice nurse consultations | Per consultation | PSSRU unit costs | |
| Psychiatrist | Per consultation | PSSRU unit costs | |
| Psychiatric nurse | Per consultation | PSSRU unit costs | |
| Inpatient admissions | Per day | NHS reference costs79/ISD cost book80 | |
| Emergency dept. visits | Per visit | NHS reference costs/ISD cost book | |
| Social care costs | |||
| Social worker in person | Per consultation | PSSRU unit costs | |
| Social worker phone | Per consultation | PSSRU unit costs | |
| Addiction services | |||
| Alcohol services | Per consultation? | PSSRU unit costs | |
| Drug services | Per consultation? | PSSRU unit costs | |
| Third sector | Per consultation? | Recommend local pricing | Costs will depend on organisation in question. Recommend bespoke costing, such as private communications. |
| Criminal justice system costs | |||
| Arrests | Per event | See comments in text below | |
| Custody | Per night | See comments in text below | |
| Prison | Per night | See comments in text below | |
| Hospital security detail | Per night | See comments in text below | |
| Welfare | |||
| Stayed at hostel | Per night | Recommend local pricing | |
| Stayed at B&B | Per night | Recommend local pricing | |
| Residential care/supported accommodation/shelter | Per night | Recommend local pricing | |
| Housing benefit | Total GBP paid | N/A | Recorded in GBP. No price weight required. |
| Universal credit | Total GBP paid | N/A | Recorded in GBP. No price weight required. |
Note that this table provides potential price weight sources as opposed to specific price weights and values for a given base year. This is to provide a guide for future survey users to source weights appropriate to their analysis which may not have been published at time of writing.
While the specific content of each may change in a given year of publication, standard UK price weight sources, such as the Personal Social Services Research Unit (PSSRU) unit costs of health and social care series78 and the NHS reference cost report series79 are likely to be suitable for the majority if not all of the health and social care aspects of the survey. PSSRU additionally has some content for substance misuse including alcohol services, albeit with more limited content.
A small number of items were identified as being likely to require bespoke or local pricing to best reflect the differences in regional availability of services and prices, namely those relating to housing costs and third-sector alcohol services. While a similar argument for local costing could be made for health and social care aspects, housing and third-sector alcohol services are likely to be part of costing perspectives falling out with a national programme or organisation (such as the NHS), but rather on the individual or a programme regional budget.
Price weights for criminal justice aspects may warrant some minor rewording of the survey to better match the granularity of the available sources in the literature. For example, Ramponi et al. break down costs by form of crime (e.g. assault/robbery/criminal damage) rather than as components of system use (e.g. arrest/custody/prison). 81 In the absence of a recurring national publication for such items, researchers may wish to identify price weights prior to survey issue and adapt the questionnaire to suit.
Response rates of Economic Form 90
While the adapted Economic Form 90 was issued at baseline, its follow-up issues were hampered by the pandemic, as shown by Table 39.
| Site | Baseline | 6 months | 12 months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Total | Intervention | Control | Total | Intervention | Control | Total | |
| England | 46 | 44 | 90 | 0 | 0 | 0 | 2 | 2 | 4 |
| Scotland | 22 | 20 | 42 | 2 | 1 | 3 | 7 | 7 | 14 |
| Total | 68 | 64 | 132 | 2 | 1 | 3 | 9 | 9 | 18 |
The baseline data completeness and self-reported responses are shown in Table 40 (health and social care), Table 41 (living arrangements), Table 42 (employment status) and Table 43 (criminal justice service utilisation).
| Item | Intervention | Control | Total | ||||
|---|---|---|---|---|---|---|---|
| Total number of prisoners | 68 | 100.0% | 64 | 100.0% | 132 | 100.0% | |
| Since (date), have you been to hospital? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| No: N, % | 47 | 69.1% | 44 | 68.8% | 91 | 68.9% | |
| Yes: N, % | 21 | 30.9% | 20 | 31.3% | 41 | 31.1% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 21 | 100.0% | 20 | 100.0% | 41 | 100.0% | |
| Visits: mean, SD | 2.4 | 1.70 | 1.7 | 0.90 | 2.1 | 1.40 | |
| If Yes, did you stay overnight? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| No: N, % | 11 | 16.2% | 8 | 12.5% | 19 | 14.4% | |
| Yes: N, % | 10 | 14.7% | 12 | 18.8% | 22 | 16.7% | |
| If Yes, how many nights in total? | Missing/unknown: N, % | 1 | 4.8% | 0 | 0.0% | 1 | 2.4% |
| Answered: N, % | 9 | 42.9% | 12 | 60.0% | 21 | 51.2% | |
| Nights: mean, SD | 10.7 | 9.80 | 4.3 | 7.70 | 7 | 9.00 | |
| Are you registered with a GP? | Missing/unknown: N, % | 1 | 1.5% | 1 | 1.6% | 2 | 1.5% |
| No: N, % | 11 | 16.2% | 9 | 14.1% | 20 | 15.2% | |
| Yes: N, % | 56 | 82.4% | 54 | 84.4% | 110 | 83.3% | |
| If registered, have you visited a GP? | Missing/unknown: N, % | 1 | 1.8% | 0 | 0.0% | 1 | 0.9% |
| No: N, % | 19 | 33.9% | 23 | 42.6% | 42 | 38.2% | |
| Yes: N, % | 36 | 64.3% | 31 | 57.4% | 67 | 60.9% | |
| If Yes, how many times? | Missing/unknown: N, % | 1 | 2.8% | 0 | 0.0% | 1 | –1.5% |
| Answered: N, % | 35 | 97.2% | 31 | 100% | 66 | 98.5% | |
| Visits: mean, SD | 3.1 | 3.00 | 2.9 | 2.60 | 3 | 2.80 | |
| If registered, have you visited a practice nurse? | Missing/unknown: N, % | 1 | 1.8% | 0 | 0.0% | 1 | 0.9% |
| No: N, % | 40 | 71.4% | 45 | 83.3% | 85 | 77.3% | |
| Yes: N, % | 15 | 26.8% | 9 | 16.7% | 24 | 21.8% | |
| If Yes, how many times? | missing/unknown: n, % | 3 | 20.0% | 1 | 11.1% | 4 | 16.7% |
| Answered: N, % | 12 | 80.0% | 8 | 88.9% | 20 | 83.3% | |
| Visits: mean, SD | 2.3 | 1.60 | 2.4 | 1.80 | 2.3 | 1.60 | |
| Missing/unknown: N, % | 1 | 1.5% | 1 | 1.6% | 2 | 1.5% | |
| Since (date), have you been visited by a community psychiatric nurse? | Missing/unknown: N, % | 0 | 0.0% | 1 | 1.6% | 1 | 0.8% |
| No: N, % | 65 | 95.6% | 56 | 87.5% | 121 | 91.7% | |
| Yes: N, % | 3 | 4.4% | 7 | 10.9% | 10 | 7.6% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 3 | 100.0% | 7 | 100.0% | 10 | 100.0% | |
| Visits: mean, SD | 1.7 | 0.60 | 2.4 | 2.20 | 2.2 | 1.90 | |
| Since (date), have you been to any addiction services? | Missing/unknown: N, % | 2 | 2.9% | 1 | 1.6% | 3 | 2.3% |
| No: N, % | 48 | 70.6% | 45 | 70.3% | 93 | 70.5% | |
| Yes: N, % | 18 | 26.5% | 18 | 28.1% | 36 | 27.3% | |
| If Yes, did you stay overnight for any visit? | Missing/unknown: N, % | 2 | 11.1% | 4 | 22.2% | 6 | 16.7% |
| No: N, % | 16 | 88.9% | 14 | 77.8% | 30 | 83.3% | |
| Yes: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | |
| Since (date), have you been to A&E? | Missing/unknown: N, % | 2 | 2.9% | 0 | 0.0% | 2 | 1.5% |
| No: N, % | 31 | 45.6% | 35 | 54.7% | 66 | 50.0% | |
| Yes: N, % | 35 | 51.5% | 29 | 45.3% | 64 | 48.5% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 35 | 100.0% | 29 | 100.0% | 64 | 100.0% | |
| Visits: mean, SD | 1.7 | 1.4 | 1.5 | 0.9 | 1.6 | 1.2 | |
| If Yes, were any of these times when you were in prison? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| No: N, % | 27 | 77.1% | 20 | 69.0% | 47 | 73.4% | |
| Yes: N, % | 8 | 22.9% | 9 | 31.0% | 17 | 26.6% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 8 | 100.0% | 9 | 100.0% | 17 | 100.0% | |
| Visits: mean, SD | 2 | 1.8 | 1.1 | 0.3 | 1.5 | 1.3 | |
| If Yes, did you ever use an emergency ambulance? | Missing/unknown: N, % | 0 | 0.0% | 1 | 3.4% | 1 | 1.6% |
| No: N, % | 16 | 45.7% | 12 | 41.4% | 28 | 43.8% | |
| Yes: N, % | 19 | 54.3% | 16 | 55.2% | 35 | 54.7% | |
| If Yes, how many times? | Missing/unknown: N, % | 1 | 5.3% | 0 | 0.0% | 1 | 2.9% |
| Answered: N, % | 18 | 94.7% | 16 | 100% | 34 | 97.1% | |
| Trips: mean, SD | 1.6 | 1.1 | 1.2 | 0.4 | 1.4 | 0.9 | |
| Since (date), have you been working with a social worker? | Missing/unknown: N, % | 0 | 0.0% | 2 | 3.1% | 2 | 1.5% |
| No: N, % | 51 | 75.0% | 47 | 73.4% | 98 | 74.2% | |
| Yes: N, % | 17 | 25.0% | 15 | 23.4% | 32 | 24.2% | |
| If Yes, how many times have you been in contact? | Missing/unknown: N, % | 2 | 11.8% | 0 | 0.0% | 2 | 6.3% |
| Answered: N, % | 15 | 88.2% | 15 | 100.0% | 30 | 93.8% | |
| Contacts: mean, SD | 14.7 | 12.9 | 10.5 | 8 | 12.6 | 10.8 | |
| If Yes, how many times were by phone? | Missing/unknown: N, % | 4 | 24% | 1 | 7% | 5 | 16% |
| Answered: N, % | 13 | 76% | 14 | 93% | 27 | 84% | |
| Contacts: mean, SD | 3.1 | 4 | 4.8 | 8 | 4 | 6.3 | |
| If Yes, how many times were in person? | Missing/unknown: N, % | 0 | 0% | 0 | 0% | 0 | 0% |
| Answered: N, % | 17 | 100% | 15 | 100% | 32 | 100% | |
| Contacts: mean, SD | 11.9 | 12.7 | 7.4 | 7.1 | 9.8 | 10.5 | |
| If Yes, how many times were while you were in your home? | Missing/unknown: N, % | 4 | 24% | 1 | 7% | 5 | 16% |
| Answered: N, % | 13 | 76% | 14 | 93% | 27 | 84% | |
| Contacts: mean, SD | 10.1 | 15.1 | 0.9 | 1.1 | 5.3 | 11.3 | |
| Since (date), have you tried to access help from any other support services? | Missing/unknown: N, % | 0 | 0.0% | 2 | 3.1% | 2 | 1.5% |
| No: N, % | 52 | 76.5% | 45 | 70.3% | 97 | 73.5% | |
| Yes: N, % | 16 | 23.5% | 17 | 26.6% | 33 | 25.0% | |
| If Yes, how many times? | Missing/unknown: N, % | 3 | 18.8% | 6 | 35.3% | 9 | 27.3% |
| Answered: N, % | 13 | 81.3% | 11 | 64.7% | 24 | 72.7% | |
| Contacts: mean, SD | 4.8 | 5.7 | 9.7 | 8.7 | 7.1 | 7.5 | |
| Item | Intervention | Control | Total | ||||
|---|---|---|---|---|---|---|---|
| What are your current living arrangements? | |||||||
| Living alone | Unchecked | 50 | 73.5% | 44 | 68.8% | 94 | 71.2% |
| Checked | 18 | 26.5% | 20 | 31.3% | 38 | 28.8% | |
| Living with a partner | Unchecked | 55 | 80.9% | 51 | 79.7% | 106 | 80.3% |
| Checked | 13 | 19.1% | 13 | 20.3% | 26 | 19.7% | |
| Living with other family members | Unchecked | 47 | 69.1% | 42 | 65.6% | 89 | 67.4% |
| Checked | 21 | 30.9% | 22 | 34.4% | 43 | 32.6% | |
| Living with friends | Unchecked | 66 | 97.1% | 63 | 98.4% | 129 | 97.7% |
| Checked | 2 | 2.9% | 1 | 1.6% | 3 | 2.3% | |
| Owned or rented property (you must be the tenant/joint tenant) | Unchecked | 64 | 94.1% | 61 | 95.3% | 125 | 94.7% |
| Checked | 4 | 5.9% | 3 | 4.7% | 7 | 5.3% | |
| Council property/housing association (you must be the tenant/joint tenant) | Unchecked | 61 | 89.7% | 58 | 90.6% | 119 | 90.2% |
| Checked | 7 | 10.3% | 6 | 9.4% | 13 | 9.8% | |
| Hostel | Unchecked | 68 | 100.0% | 63 | 98.4% | 131 | 99.2% |
| Checked | 0 | 0.0% | 1 | 1.6% | 1 | 0.8% | |
| Bed and breakfast | Unchecked | 66 | 97.1% | 63 | 98.4% | 129 | 97.7% |
| Checked | 2 | 2.9% | 1 | 1.6% | 3 | 2.3% | |
| Residential care/shelter/supported accommodation | Unchecked | 61 | 89.7% | 64 | 100.0% | 125 | 94.7% |
| Checked | 7 | 10.3% | 0 | 0.0% | 7 | 5.3% | |
| Other (including rough sleeping, sofa surfing) | Unchecked | 59 | 86.8% | 54 | 84.4% | 113 | 85.6% |
| Checked | 9 | 13.2% | 10 | 15.6% | 19 | 14.4% | |
| Since (date), have you been homeless at any point? | Missing/unknown: N, % | 3 | 4.4% | 0 | 0.0% | 3 | 2.3% |
| No: N, % | 44 | 64.7% | 44 | 68.8% | 88 | 66.7% | |
| Yes: N, % | 21 | 30.9% | 20 | 31.3% | 41 | 31.1% | |
| If Yes, how many nights? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 21 | 100.0% | 20 | 100.0% | 41 | 100.0% | |
| Nights: mean, SD | 123.4 | 109 | 97.5 | 77 | 110.8 | 94.5 | |
| Since (date), have you stayed in any of the following? | |||||||
| Hostel | Unchecked | 64 | 94.1% | 62 | 96.9% | 126 | 95.5% |
| Checked | 4 | 5.9% | 2 | 3.1% | 6 | 4.5% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 1 | 50.0% | 1 | 16.7% |
| Answered: N, % | 4 | 100.0% | 1 | 50.0% | 5 | 83.3% | |
| Nights: mean, SD | 28.3 | 14.8 | 3 | -- | 23.2 | 17.1 | |
| Bed and breakfast | Unchecked | 62 | 91.2% | 61 | 95.3% | 123 | 93.2% |
| Checked | 6 | 8.8% | 3 | 4.7% | 9 | 6.8% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 6 | 100.0% | 3 | 100.0% | 9 | 100.0% | |
| Nights: mean, SD | 40 | 70.2 | 58 | 68.6 | 46 | 65.8 | |
| Residential care/shelter/supported accommodation | Unchecked | 59 | 86.8% | 62 | 96.9% | 121 | 91.7% |
| Checked | 9 | 13.2% | 2 | 3.1% | 11 | 8.3% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 1 | 50.0% | 1 | 9.1% |
| Answered: N, % | 9 | 100.0% | 1 | 50.0% | 10 | 90.9% | |
| Nights: mean, SD | 81.3 | 73.1 | 60.0 | -- | 79.2 | 69.2 | |
| Item | Intervention | Control | Total | ||||
|---|---|---|---|---|---|---|---|
| Are you currently employed? | Missing/unknown: N, % | 0 | 0.0% | 1 | 1.6% | 1 | 0.8% |
| No: N, % | 52 | 76.5% | 52 | 81.3% | 104 | 78.8% | |
| Yes: N, % | 16 | 23.5% | 11 | 17.2% | 27 | 20.5% | |
| If No, have you been employed at any point since (date)? | Missing/unknown: N, % | 0 | 0.0% | 1 | 1.9% | 1 | 1.0% |
| No: N, % | 43 | 82.7% | 43 | 82.7% | 86 | 82.7% | |
| Yes: N, % | 9 | 17.3% | 8 | 15.4% | 17 | 16.3% | |
| If Yes, how many jobs have you had during this time? | Missing/unknown: N, % | 3 | 18.8% | 1 | 9.1% | 4 | 14.8% |
| One | 13 | 81.3% | 10 | 90.9% | 23 | 85.2% | |
| If Yes, how many weeks have you been employed between (date) and now? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 16 | 100.0% | 11 | 100.0% | 27 | 100.0% | |
| Weeks: mean, SD | 22.5 | 7.2 | 31.4 | 50.1 | 26.1 | 31.9 | |
| Do you currently receive any money from a public or government source? | Missing/unknown: N, % | 1 | 1.5% | 1 | 1.6% | 2 | 1.5% |
| No: N, % | 17 | 25.0% | 23 | 35.9% | 40 | 30.3% | |
| Yes: N, % | 50 | 73.5% | 40 | 62.5% | 90 | 68.2% | |
| If Yes, approximately how much do you receive in total per week? | Missing/unknown: N, % | 5 | 10.0% | 1 | 2.5% | 6 | 6.7% |
| Answered: N, % | 45 | 90.0% | 39 | 97.5% | 84 | 93.3% | |
| GBP: mean, SD | 114.7 | 93.2 | 117.1 | 75.7 | 115.8 | 85.0 | |
| If No, have you been employed at any point since (date)? | Missing/unknown: N, % | 0 | 0.0% | 1 | 1.9% | 1 | 1.0% |
| No: N, % | 43 | 82.7% | 43 | 82.7% | 86 | 82.7% | |
| Yes: N, % | 9 | 17.3% | 8 | 15.4% | 17 | 16.3% | |
| If Yes, how many jobs have you had during this time? | Missing/unknown: N, % | 3 | 18.8% | 1 | 9.1% | 4 | 14.8% |
| One | 13 | 81.3% | 10 | 90.9% | 23 | 85.2% | |
| If Yes, how many weeks have you been employed between (date) and now? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 16 | 100.0% | 11 | 100.0% | 27 | 100.0% | |
| Weeks: mean, SD | 22.5 | 7.2 | 31.4 | 50.1 | 26.1 | 31.9 | |
| Item | Intervention | Control | Total | ||||
|---|---|---|---|---|---|---|---|
| Since (date), have you been arrested? | Missing/unknown: N, % | 0 | 0 | 0 | 0 | 0 | 0 |
| No: N, % | 0 | 0 | 1 | 1.6% | 1 | 0.8% | |
| Yes: N, % | 68 | 1 | 63 | 98.4% | 131 | 99.2% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 68 | 100% | 63 | 100.0% | 131 | 100.0% | |
| Times: mean, SD | 2.4 | 3.6 | 2.7 | 2.4 | 2.5 | 2.1 | |
| Since (date), have you spent at least one night in custody? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| No: N, % | 1 | 1.5% | 0 | 0.0% | 1 | 0.8% | |
| Yes: N, % | 67 | 98.5% | 64 | 100.0% | 131 | 99.2% | |
| If Yes, was this police custody, prison, or both? | Missing/unknown: N, % | 1 | 1.5% | 0 | 0.0% | 1 | 0.8% |
| Police custody: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | |
| Prison: N, % | 2 | 2.9% | 2 | 3.1% | 4 | 3.0% | |
| Both: N, % | 65 | 95.6% | 62 | 96.9% | 127 | 96.2% | |
| If Yes, how many nights spent on remand? | Missing/unknown: N, % | 1 | 1.5% | 1 | 1.6% | 2 | 1.5% |
| Answered: N, % | 66 | 98.5% | 63 | 98.4% | 129 | 98.5% | |
| Nights: mean, SD | 15.3 | 24.2 | 24 | 42 | 19.5 | 34.2 | |
| If Yes, how many nights spent in police custody? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Answered: N, % | 67 | 100.0% | 64 | 100.0% | 131 | 100.0% | |
| Nights: mean, SD | 18.6 | 24.2 | 27 | 42.2 | 22.7 | 34.4 | |
| Since (date), have you been in court? | Missing/unknown: N, % | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| No: N, % | 1 | 1.5% | 0 | 0.0% | 1 | 0.8% | |
| Yes: N, % | 67 | 98.5% | 64 | 100.0% | 131 | 99.2% | |
| If Yes, how many times? | Missing/unknown: N, % | 0 | 0.0% | 1 | 1.6% | 1 | 0.8% |
| Answered: N, % | 67 | 100.0% | 63 | 98.4% | 130 | 99.2% | |
| Times: mean, SD | 2.3 | 2.2 | 2.6 | 2.6 | 2.5 | 2.4 | |
Completeness of the survey at baseline was generally very good, with only three questions having over five missing entries.
Feasibility of accessing Police National Computer and National Health Service service use data
Although it is possible that COVID-19 played a role in our inability to obtain these data, we do not think that the pandemic was solely responsible. Two key issues are at play: prisoner confidentiality and data systems. We found that gaining approval to obtain the PNC or NHS identifiers was difficult to impossible due to a combination of prison and data-protection concerns. Although these concerns may fade as more evidence of the benefits of the APPRAISE intervention mounts, we conclude that it is very likely that these concerns will still exist for a definitive trial, and possibly be even more salient for some stakeholders in that context. Exacerbating the confidentiality issues were data-system issues that prevented data access on a large scale. Although this issue depends on the jurisdiction, in each of our two jurisdictions (Scotland and England) at least one of the data sources required case-by-case data extraction at some step of the process. We could not extract either PNC or NHS data on a large scale in either England or Scotland, making the use of such data prohibitively costly for a definitive RCT.
Discussion
We aimed to assess the feasibility of collecting economic data to inform the design of a potential future RCT of APPRAISE in a UK prison setting. We did not seek to provide a definitive measurement of cost, but rather inform methods by which they could be measured in a future trial. This has been achieved with mixed results. While many of the issues faced were a result of the COVID-19 pandemic, it is important to separate ambiguity of findings due to extenuating circumstances from findings of issues in data collection. Data obtained despite such circumstances are still likely to be viable without them, if not more so, and we were able to document the stages of an ABC exercise and provide discussion around how to assess the costs associated with implementing the APPRAISE intervention. We believe this to be one of the first pieces of work in this area and the methods that we have presented can be applied more broadly to determine the costs associated with implementing a similar intervention in practice.
While not the aim of the study, we have also provided early estimates of some of the costs associated with the implementation of the APPRAISE intervention, in two different prison systems. There were important differences between the two different sites, primarily around the differing roles and numbers of members of prison and intervention staff involved, the location of delivery and availability of rooms and the level of access to prisoner data at the time of data collection. Such differences are inevitable given the heterogeneity of prison regimes in general in terms of local service provision, facilities, staff and the management of each prison site. Nevertheless, the ABC process itself as described could be reapplied to new contexts, and elements of the activities observed, such as necessary paperwork and durations of phone sessions would reasonably be expected to be common to other settings.
There were challenges in separating research-specific costs from those which might reasonably be expected in a practice. For example, in the England site the researcher recruiting the participants to the study was unable to access the prison database to identify further potential participants and their current location. This meant that the process of identification was more cumbersome at times and it may have taken longer to locate eligible participants, which would likely increase the staff cost associated with the intervention. Assuming that, in a real-world setting, intervention staff or prison staff would have access to such databases and would not need to spend the extra time locating individuals for their APPRAISE intervention, the time taken may not accurately reflect that needed in a live roll-out. In relation to this, prison staff costs were intentionally excluded in the staff costs listed in Table 35 because, while they were involved and helped with the process of locating participants within the research trial setting, it is currently unclear what role they would play in practice. Such details will need to reflect the final design of an intervention or will need to be explored in future work, though we have no reason to believe the ABC approach could not be used to do so.
The COVID-19 pandemic is also likely to have influenced the follow-up and the retention of study participants. This issue is common to the study as a whole rather than to economic assessment in particular, and is discussed in broader terms in other chapters of this report. Specific to the economic evaluation pilot, substantial time was spent by intervention staff trying to locate participants for their follow-up interventions and often being unable to access the information they required or finding that participant court dates had been moved or postponed due to COVID-19. More time spent locating participants for the post-liberation intervention sessions has direct implications on the cost of the APPRAISE intervention, as it obviously increases the staff costs associated with the intervention. Disentangling the direct impact of the COVID-19 pandemic on locating participants remotely from the normal challenges of this population was not possible in this pilot study. Follow-up in the CJS is often very complicated and it is frequently challenging to retain participants within a study due to a number of logistical reasons, mostly being unable to re-establish contact with them. 82 Consequently, this is something to consider when planning for a future RCT with the APPRAISE intervention and ensuring that the lower-paid staff, such as administrative or support workers, could be responsible for locating participants to reduce overall costs, if deemed necessary.
The timing of the first COVID lockdowns in 2020 had a significant effect on the participant recruitment and the study’s data collection after both prison sites went into an immediate lockdown. Hence limited data could be collected for the remaining duration of the pilot, post April 2020. As a result, it also became difficult to work with prison staff due to their sharply increased workloads and new unforeseen pressures. The majority of any further interactions were conducted virtually (via telephone or e-mail), rather than the face-to-face meetings and follow-ups as planned. This is extremely likely to have had an effect on the information we were able to collect around the cost estimates. For some specific items, such as the cost of space in the prison, we were unable to obtain meaningful estimates. Context is critical for this factor, as costs of this are expected to vary substantially between prisons. It may be sufficient to note the duration for which a private room is required, and allow users of this information to apply their own local estimates where necessary.
We were able to adapt the Economic Form 90 to a UK context and provide a list of candidate price weight sources for future use. We were also able to issue the survey to 132 prisoners at baseline with very high completeness, though follow-up time points were heavily disrupted by the pandemic. Of note, the baseline survey was researcher-administrated. It is not possible to know how well the survey would have been completed in follow-up time points without the confounding of the pandemic; however, the completeness at baseline at least implies the form was well accepted and understood. Completeness included questions relating to criminal justice activity, suggesting that any adaptation of the questionnaire to allow for more bespoke or specific price weights to be applied is likely to be viable following a similar format.
Disruptions to data collection prohibited our ability to validate the survey against routine data sources. The matter may be rendered a moot point as PNC and NHS data proved too difficult to obtain at large scale for this population, thus suggesting they should not be included as part of a definitive RCT. Some element of prisoner self-report was always anticipated to be unavoidable; however, the loss of routine data as a potential alternative source places increased importance on validation of the revised Economic Form 90. While the original Economic Form 90 has been validated for a US alcohol treatment population,60 larger-scale future trials would be advised to build in a pilot stage to validate and potentially refine our adapted UK version prior to full-scale administration.
Chapter 8 Prison survey
In this chapter, we present the methods undertaken and the results obtained from conducting a survey to further understand the alcohol services provided in male remand prisons across England, Wales and Scotland and how the COVID-19 pandemic has affected them. A short online survey was distributed to all prison governors of male remand prisons in England, Wales and Scotland. The survey questions were largely closed questions with simple ‘yes’ or ‘no’ responses, but some open-ended questions were included to obtain a more in-depth understanding in specific areas. Out of the 55 prison governors invited to take part in the survey by e-mail, 17 completed the survey.
Background
During 2020 and the subsequent years that followed; the COVID-19 pandemic was seen to have a monumental impact across the world. 83 It affected every aspect of society from the increased demands on the healthcare system, the negative effects on employment and businesses and the adverse effects on mental health, with individuals being left isolated from friends and family. 83,84 The prison population was not spared from the impact of the pandemic, and both positive and negative implications associated with the prisoner and prison staff mental health outcomes have been reported. 85,86 Prisons across the world immediately went into lockdown. 87 This left prisoners being unable to maintain contact with their family and friends and they often found themselves isolated and confined to their cells for extended periods of time, in order to minimise the risk of a COVID-19 outbreak within the prison. 85,88 Although in one study this was argued to have led to a reduction in the cases of self-harm being reported,86 it was also said to contribute to the deepening of the pains of imprisonment in another. 89
As expected there has been an outpouring of research projects focusing on the different impacts of the pandemic, across different populations. There have been examples of research focusing on the impact of COVID-19 within the prison setting. 85–89 However, to date there has been no research which has specifically focused on the impact to the alcohol treatment services, which were routinely available to prisoners pre pandemic. Although the APPRAISE feasibility study commenced in 2019, the data collection and the follow-ups spanned across the pandemic years of 2020 and 2021. The restrictions imposed caused a significant impact on the research study. The study’s recruitment process was significantly affected by the prisons going into lockdown, with Scotland’s recruitment having to be halted before reaching the desired target sample. In addition, the follow-ups were hampered by being unable to be undertaken face to face and often it proved difficult to confirm the location of prisoners, with court dates and release dates being postponed as a result of the pandemic.
As the world started opening up again and restrictions began to ease, it felt salient to conduct a survey, within the APPRAISE study, that explored the impact of the COVID-19 pandemic on prisons and the availability of the alcohol treatment services. The purpose of the survey was to give more context to the delays experienced in the APPRAISE study, but also to establish the wider implications of the lockdown on services for alcohol within the prison. As the APPRAISE study focused on male remand prisoners, the survey sought to include all prisons within England, Wales and Scotland that held male remand prisoners. The alcohol treatment services that worked within the prison and were the intervention workers used to deliver the APPRAISE intervention (CGL) were largely unable to complete the data collection due to the pandemic. This impacted hugely on the data collected and hence the findings of the study. Therefore, we anticipated by undertaking this survey it would help us to understand what the prisons did in relation to alcohol services throughout the pandemic, and to fill in the gaps in our data that the research team were not able to complete.
Aims and objectives
The aim of conducting the survey, as a component of the APPRAISE study, was to further understand the alcohol services that are currently provided in male remand prisons across England, Wales and Scotland and how the COVID-19 pandemic has affected their delivery.
The specific objectives to achieve the above aim were:
-
to establish what alcohol services are currently provided within male remand prisons
-
to explore the prison governors’ understanding of alcohol brief interventions
-
to understand how the COVID-19 pandemic has impacted the services available in male remand prisons
-
to identify whether the impact of the COVID-19 pandemic upon services could be avoided in the future.
Methods
Survey design
The survey was developed to ask questions related to the delivery of alcohol brief interventions and other alcohol treatment services, within the prison setting, in order to ascertain what services the prison currently provided. Questions were largely closed, with ‘yes’ or ‘no’ responses, but did include some open-ended questions to obtain a more in-depth understanding in specific areas. The latter part of the survey asked participants whether services were affected by the COVID-19 pandemic and, if so, what could be done to ameliorate this in the future. The survey also provided participants with the opportunity to say whether there was anything that was not asked that they wished to express around the impact of the pandemic. The survey finished by asking whether any participants would be willing to engage with the research team in the context of a future study in remand prisons. It was made clear that this response was in no way binding, but simply a way of gauging an initial expression of interest for planned future work.
The survey was distributed online using the JISC tool (www.onlinesurveys.ac.uk/), which was used to both develop and distribute the survey. By using an online platform it ensured that the survey was accessible across a wide geographical reach and that participants did not need to return hard copies, avoiding a pitfall for completion. In addition, by using the online platform it also allowed the survey data to be transferred to SPSS for analysis, which avoided security being compromised by surveys being returned and entered by hand. JISC also allowed the scheduling of e-mail reminders to be sent to prospective participants reminding them about completing the survey.
Setting
The primary setting of the APPRAISE study was two specific remand prison sites in England, Wales and Scotland. However, to get a broader range of responses across different remand prisons the survey component was extended to invite all prison governors, across England, Wales and Scotland, working within prisons with men on remand to take part in the survey.
Sampling and recruitment
As the contact details for prison governors are freely available online, online searches were conducted to obtain the e-mail addresses of all of the governors, across the UK. E-mails were then sent to each prison governor which included a link to the online survey, alongside an information leaflet. The information leaflet was used to explain the purpose of the survey and what the participants’ responses would be used for.
Consent
The survey asked all participants to provide their informed consent, before completion, via a consent form built into the start of the survey. It stated that participation was voluntary and that participants did not have to answer any questions that made them feel uncomfortable. It also reassured participants that all personal details, such as names and places, would be removed, in order to ensure they were not identifiable from their responses. In addition, participants were informed that they could withdraw their consent at any point during the survey and could even withdraw their responses following its completion. It was stated that participants could withdraw their responses, for up to 2 weeks, following the completion of the survey, by contacting the lead researcher and hence the respective contact details were supplied.
Data analysis
Analysis of the survey data took place once all surveys were anonymised. SPSS was employed to analyse the survey data obtained. As the survey primarily consisted of yes or no responses the data analysis mainly consisted of percentage calculations. For the more open-ended questions, simple thematic analysis was undertaken to ascertain qualitative statements, which could be used to draw conclusions and answer the survey’s objectives.
Data management
All contact with prospective participants was undertaken electronically, along with the creation of all necessary research materials. Any data collected was stored in accordance with GDPR 2016/679. The exported data were stored in a shared folder on a secure network drive which was only accessible by the research team. All identifiable information was removed from the survey results, in order to protect the identity of participants. A password-protected database was stored in a secure network folder at Teesside University, which contained the prison names and the survey IDs, in order to assist the removal of a participant’s responses, if they requested to remove themselves from the study. This file was securely deleted once the survey had concluded and the survey withdrawal period had closed. Teesside University acted as the data processor and data owner. Data and research materials were also stored in a Microsoft Teams group which was only accessible to members of the research team and was used to upload, store and circulate all relevant study files and documents securely.
Ethics
Although the APPRAISE study obtained ethical clearance from the University of Edinburgh, a separate ethics application was submitted to Teesside University ethics within the school of Social Sciences, Humanities and Law, for this survey component – 7 October 2021 (2021-6427). Ethical clearance was also obtained from HMPPS on 21 December 2021 (HMPPS 2019-2240) via an amendment to the original approval of the overall APPRAISE study. Participants were notified that their survey responses would be confidential, and only if they disclosed something which indicated a risk to them or someone else would it potentially be necessary to breach confidentiality. In this case the procedure involved the project supervisor being informed, and if deemed appropriate the project supervisor would take further action based on the safeguarding protocol. However, confidentiality did not need to be broken across any of the included participants.
Results
Obtained sample
Out of the 59 prisons in the UK, successful e-mail invitations were sent to 55 governors inviting them to take part in the survey by e-mail; 17 completed the survey. Difficulties were encountered during this part of the research process due to the apparent turnover in staff undertaking the prison governor role. Many e-mail invitations were returned as not being able to be delivered and more investigating had to be carried out.
Governors were asked to disclose the capacity of their prison and, from those who answered, the smallest prison held 577, and the largest 1600.
Findings
The findings of the survey are presented below in relation to the objectives discussed above. The response rate of 17 out of 55 completing the survey needs to be borne in mind when considering the study findings. It may be that those prisons that were more engaged in alcohol services responded and as such self-selected.
Current alcohol services within male remand prisons
The survey showed a wealth of knowledge on the different services offered within prisons with men on remand. The survey gathered information on both the service providers and the services offered. These services included:
-
Alcoholics Anonymous (AA) sessions: 58.8% (n = 10).
-
NHS services: 35.3% (n = 6).
-
Psychotherapy/Counselling/11 support: 29.4% (n = 5).
-
In-cell work packs: 23.5% (n = 4).
-
Smart recovery: 17.6% (n = 3).
-
Support services via community partners: 11.8% (n = 2).
-
Group work: 11.8% (n = 2).
-
Detox services: 11.8% (n = 2).
-
Substance misuse services: 5.8% (n = 1).
-
CJSW Addictions team: 5.8% (n = 1).
The above services are provided by a broad range of providers. These included: NHS services, AA sessions, Change Grow Live, DART (drug and recovery team), Inclusion team, criminal justice social worker (CJSW) Addictions team, Chaplaincy support, Scotland and Midlothian Offender Recovery Service (EMORS), Dfodol, trained prison staff, SPS, Forward Trust, Drugs Action, Turning Point and third-sector services. The most frequently mentioned provider was NHS services (n = 10, 41.2%).
Governors’ understanding of alcohol brief interventions
All governors were asked about their knowledge of alcohol brief interventions. When initially asked, 82.4% (n = 14) stated that they did know what the intervention was.
The survey then asked all governors if to the best of their knowledge their prison delivered alcohol brief interventions. Ten (58.8%) said that they thought their prison did deliver the intervention. Within the survey they were then given some information on what the intervention entails and asked again if they knew if they were delivering them. This time, more governors declared that they think they are delivering the intervention (n = 11, 64.7%). This shows that the knowledge of the intervention helped with making a decision about whether alcohol brief interventions are being delivered.
One of the questions at the end of the survey asked those who wished to, to leave an e-mail address if they were interested in taking part in any future trial around alcohol brief interventions. For this question, 64.7% (n = 11) did express this interest, showing an interest in developing their alcohol provisions further.
The impact of the coronavirus disease discovered in 2019 pandemic upon services available in male remand prisons
The pandemic undoubtedly affected the alcohol services within the prisons with men on remand in England, Scotland and Wales and that were included in the overall APPRAISE study (HMP England and HMP Scotland). The survey also established this, with 15 of the 17 prisons (88.2%) answering yes to ‘did the pandemic impact alcohol services within your prison?’.
The impact on services was answered in an open question, with governors giving detailed responses to the question of how services were impacted. A summary of some of the service impact is as follows:
-
group sessions being suspended
-
face-to-face sessions being suspended
-
services suspended – being unable to attend the prison
-
staffing issues
-
interventions being reduced
-
a lack of resources.
The majority of governors mentioned the services that entailed group sessions being affected (n = 8, 47.1%). This and all of the barriers were due to not being able to see the men face to face and the social distancing measures in place. The conditions imposed on the prison by government to stop the spread of the COVID-19 virus and keep the men and staff safe meant staff and organisations other than prison officers and healthcare staff were unable to enter the prison. There were some prison governors who mentioned an attempt at using telephone support but due to staffing pressures this was unsuccessful too. Staff numbers were limited due to isolation rules or being vulnerable or (potentially) contagious.
This has shown that although there are some services being carried out with in-cell packs, most alcohol services rely on face-to-face intervention work, mostly in groups, and carried out by outside organisations.
Interestingly, we asked the prison governors about ‘other services’ delivered in the prison and whether or not these were impacted by the pandemic. In this instance, 100% (n = 17) answered ‘yes’. The reasons for impact were all the same as those mentioned above in relation to the disruption to alcohol services. While the majority of services mentioned were related to drugs and smoking, there were also other services disrupted, such as health care, therapeutic services, gambling support, education, religious services, the gym and, importantly, the overall regime of the prison.
Best practice to avoid any future disruption to services
When asked whether the disruptions due to the pandemic would have a long-term effect on the prison, there was a divide between responses, with 41.2% (n = 7) stating they felt it would, and 58.5% (n = 10) stating no, they would not. Those that felt the affect would be felt for a long time had different reasons for this. However, most responses discussed that this was from the fact that there was a long gap in services, and the impact of that having a long-term effect, for example, not having treatment and falling more unwell. One governor discussed the DART team not having access to the prisoners, which ultimately led to fewer services now being delivered, and these have not yet been fully increased back to pre-pandemic levels. All of those who responded stated they were unable to say when they thought this long-term affect would end, but one governor predicted ‘years to come’.
Every governor who answered the survey had an opinion on how best to avoid a future disruption. First, we gave options as to what they thought would lead to less disruption should a pandemic arise in the future. The most favoured appeared to be something tangible for the prisoners to work on in their cells:
-
online sessions: 76.5% (n = 13)
-
workbook/paper sessions: 82.4% (n = 14)
-
staff continuing interventions but wearing full personal protective equipment (PPE): 70.6% (n = 12).
PPE featured heavily in some of the open-ended questions and was considered a barrier to overcoming further disruption if not dealt with more quickly in a future pandemic.
Other suggestions given by those who returned the survey included comments about better provisions for in-cell phones, or in some circumstances the praising of purple visits which allowed video calls. This highlighted some good that came from the learning of the COVID-19 pandemic and new innovations. Aside from comments regarding a better, more appropriate use of technology should this ever happen again, one governor commented on the services being seen as ‘essential’ and therefore not something that is withdrawn in the same way it was in 2020.
Chapter 9 Discussion and conclusions
Sections of this chapter have been reproduced from Holloway et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
For individuals in contact with the criminal justice system, the prevalence of at-risk drinking is far higher than in the general population. There is very little evidence of efficacy or effectiveness of alcohol interventions in reducing risky drinking amongst those in the criminal justice system and in particular men on remand in prison. This is compounded by the limited evidence for the optimum timing of delivery, recommended length, content, implementation and economic benefit of an extended alcohol intervention in the prison setting. APPRAISE aimed to provide vital evidence to inform a future definitive RCT of an extended alcohol intervention for men on remand in prison.
APPRAISE specifically aimed to undertake a two-arm, parallel-group, individually randomised pilot study of a self-efficacy-enhancing psychosocial alcohol intervention for men on remand in prison.
Results relating to objectives are detailed in the individual chapters and summarised below.
Objective 1
To pilot the study measures and evaluation methods to assess the feasibility of conducting a future definitive multicentre, pragmatic, parallel-group RCT.
-
1a. Is it feasible to conduct a future multicentre RCT of a self-efficacy-enhancing psychosocial alcohol intervention for men on remand?
We cannot say that it is feasible to conduct a future definitive trial as we were unable to follow up participants – of course COVID-19 played a part in the low response rates but, at this present stage, with the results we have we are not yet in a position to move this work forward to a definitive study.
-
1b. Can we obtain reasonable estimates of the parameters necessary to inform the design and sample size calculation for a future definitive multicentre RCT? This includes standard deviations of potential continuous primary outcomes and estimates of recruitment, retention and follow-up rates.
Yes, but only partially. We can obtain reasonable estimates of standard deviations of outcomes based on the baseline data collected. However, the amount of valid data collected at follow-up was too little to be able to provide us with reliable estimates of parameters for outcomes at follow-up.
The pre-pandemic recruitment data give us reasonable estimates of recruitment rates in a future trial. However, the retention and follow-up rates we observed in the APPRAISE trial were likely to have been heavily influenced by the COVID-19 pandemic and associated lockdown measures, and therefore these are not reliable indicators of what they might be in a future trial.
-
1c. How well do participants complete the questionnaires necessary for a future definitive RCT?
At baseline there was a very small amount of missing data for a few questionnaires/outcomes, for example, ‘Readiness to Change Ruler: The people who are important to me support me in reducing my drinking’, and for the ‘Drinking Refusal Self-Efficacy Questionnaire’ and for the ‘Negative Alcohol Expectancy Questionnaire’. The amount missing was very similar between sites at baseline. At follow-up, the amount of missing data was very substantial in both sites. We were able to do slightly better at the Scotland site because ‘we were able to have some access to the prison site and identify where participants were located’. In addition, the same researcher conducted the majority of the follow-ups in Scotland at 12 months as conducted the recruitment and baseline measures, which may have had an effect on participants’ willingness to respond. However, numbers are small so we must be cautious with this assertion. In terms of data completeness of the questionnaires at each site, this was similar between the sites (Report Supplementary Material 1 S1.1 and S1.2). It is, however, really difficult to read too much into the differences because the numbers completing data at each site were so small. Similarly, the different questionnaires had similar amounts of missing data at follow-up (see Table 28) and we cannot really say too much about differences of ±1 or ±2. In summary, we did not find any notable differences across the different sites/instruments. However, it could be that self-completion was a factor; at baseline the questionnaire was not self-completed, but RA-delivered. In addition, we also observed and reflected on the suitability of certain questions, particularly if the questionnaire was to be self-completed (which was reflected in later amendments) and this would warrant further consideration in future research for this population.
-
1d. Can we collect economic data needed for a future definitive RCT?
We were able to design and implement an ABC study that provided detailed estimates of the implementation costs of the APPRIASE intervention. That we could do this despite COVID-19 complications suggests that our methodology will be appropriate for a definitive RCT. We nonetheless note that additional attention needs to be devoted to some aspects of our ABC study. In particular, more attention should be devoted to assessing the prison space needed to deliver the intervention and more attention should be given to separating research costs from true intervention costs when it comes to scheduling follow-up intervention visits. We were also able to modify the Economic Form 90 for use with a UK prison population and found no evidence that it was difficult for study subjects to complete. However, were unable to validate the data-collection instrument and recommend that such validation be part of a definitive trial.
-
1e. Can we access recidivism data from the PNC databases for trial participants?
-
1f. Can we access health data from routine NHS data sources for trial participants?
Although it is possible that COVID-19 played a role in our inability to obtain these data, we do not think that it was solely responsible. Two key issues are at play: prisoner confidentiality and data systems. We found that gaining approval to obtain the PNC or NHS identifiers was difficult to impossible due to a combination of prison and ethics board concerns. Although these concerns may fade as more evidence of the benefits of the APPRAISE intervention mounts, we conclude that it is very likely that these concerns will still exist for a definitive trial, and possibly be even more salient for some stakeholders in that context. Exacerbating the confidentiality issues were data-system issues that prevented data access on a large scale. Although this issue depends on the jurisdiction, in each of our two jurisdictions at least one of the data sources required case-by-case data extraction at some step of step of the process. We could not extract either PNC or NHS data on a large scale in either England or Scotland, making the use of such data prohibitively costly for a definitive RCT.
Objective 2
To assess intervention fidelity
-
2a. What proportion of the interventions are delivered as per protocol?
We recorded three of the in-prison interventions. They all scored highly and had maximum scores on the BECCI Scale.
-
2b. Is there any evidence of contamination between the two conditions and/or between those workers delivering the intervention?
We did not find any evidence of contamination between workers delivering the intervention. At the Scotland study site, the intervention was only delivered by one interventionist. In England two interventionists were delivering the intervention. There was mention of discussion of the study between one of the remand participants and another (see sub-section ‘Coherence: acceptability of the APPRAISE intervention’ in Remand participants) but the participant stated that he didn’t know if the other participant got the intervention or not. No other evidence was obtained of contamination; however, it would be prudent to explore this again in any future work in the absence of a global pandemic, lockdown and restrictions across the prison estate.
-
2c. To what extent was the intervention changing process variables consistent with the underpinning theory?
Table 28 shows the results for changes in process variables (secondary outcomes). The available data do not allow answering the question if the change in process variables from baseline to 6 and 12 months was greater in the intervention group than in the control group in central process variables (goals, self-efficacy, outcome expectations, according to social cognitive theory), as we were able to obtain only limited data for change in mediators (especially at 6 months) and only a small number of participants were released, which precludes interpretation of change in mediators after release from prison. We found small and inconsistent changes in process variables with considerable variation. Therefore, we cannot answer this research question.
Objective 3
To qualitatively explore the feasibility and acceptability of a self-efficacy-enhancing psychosocial alcohol intervention and study measures to staff and for men on remand and on liberation.
-
3a. How acceptable are the trial and intervention procedures (including context and any barriers and facilitators) to the following key stakeholders: men on remand in prison and on liberation; prison staff (including healthcare staff); commissioners; policy-makers and third-sector partners?
The qualitative process evaluation showed that the trial and intervention procedures were acceptable to staff and men on remand. We found that it was important for an individual to feel comfortable and trusting of an interventionist before sharing their personal experiences and consumption. Staff did report that the prison setting and resources could affect the work due to the lack of available space and the limited staff capacity. However, in general participants believed that delivering the APPRAISE intervention did not significantly increase their workload. The intervention training and content appeared to be largely acceptable, although the length and content could have been condensed. The APPRAISE intervention delivery benefited from buying into the intervention and being motivated and engaged with the content.
Similar findings were found around the prison’s logistical issues affecting the APPRAISE intervention delivery feasibility, such as space and staff capacity, the importance of engagement with prisoners and the lack of currently available support for prisoners on remand from the stakeholder interviews. Additional themes and subthemes that emerged were around the intricacies of the prison environment and how it affected the study and intervention delivery, the individual differences across the setting and across the participants and also further barriers and facilitators to delivery of the ABI.
A key finding, observed in all three participant groups, was that the in-prison APPRAISE sessions were deemed to be more acceptable and feasible than the post-liberation intervention sessions. This was observed due to a plethora of different factors, such as being unable to re-establish contact with males upon their release and individuals relapsing to previous risky alcohol consumption when alcohol becomes more freely available.
Objective 4
To assess whether operational progression criteria for conducting a future definitive RCT are met across trial arms and study sites and, if so, to develop a protocol for a future definitive trial. Operational progression criteria are based on previous research results. 6
A large proportion of this study was carried out during the COVID-19 pandemic and as such we cannot demonstrate the full extent to how this affected the study. However, we did not meet the criteria for developing a protocol for a future definitive study.
-
4a. Do the two prisons invited to the study agree to take part?
Yes. Both Scotland and England prisons agreed to take part in the study and stayed involved until COVID-19 restrictions closed access to the project down.
-
4b. Based on knowledge from previous data, do at least 90 eligible participants consent to take part and be randomised across the trial arms?
No. Although in the England site, where recruitment began earlier than the Scotland site, we recruited 90 participants, the COVID-19 pandemic and associated lockdown restrictions meant that we were not able to enter the prison and therefore could not achieve the target of 90 participants in the Scotland site (n = 42). However, in a future study without lockdown restrictions we are confident that the required number of participants can be recruited.
-
4c. Do at least 70% of participants who consent to the trial receive the intervention?
Yes, partially. Of the 68 consented and randomised to the trial 53/68 (78% of participants) received the in-prison intervention, although much lower numbers received the post-prison component of the intervention. Only one participant received the day-3 post-liberation intervention, none received the day-7 post-liberation intervention, and one person received the 21-day post-liberation intervention, at least in part because of the COVID-19 context. A post-prison-liberation component of the intervention may not be viable in a future trial.
-
4d. Are at least 60% of those who received the intervention followed up at 12 months across trial arms and study sites?
No. Only 13% (18/132) of those who received the intervention were followed up at 12 months. Although the COVID-19 pandemic was undoubtedly a factor in the low percentage followed up, we observed high percentages of participants who were not released at 12 months; this was worsened by COVID-19 because of the number of those on remand awaiting trial due to suspended and closed courts; or of those who were released, many could not be contacted or could not be located. We consider this to be the greatest barrier in designing a future trial that will achieve satisfactory follow-up rates.
Objective 5
To ascertain what alcohol services are available in male remand prisons and how COVID-19 has affected services.
From 59 prisons in Scotland and England, successful e-mails were sent to 55 prison governors. Seventeen (31%) were completed. A limitation of the study was the barriers to freely accessing governor e-mails. While this was handled by a gatekeeper who worked for SPS for the Scottish prisons, no such facilitation took place in England, and while most e-mails were freely available, many were not. Two-thirds of the sample were interested in hearing more about ABIs.
-
5a. What alcohol services are currently provided within male remand prisons?
There are a wide range of services from a wide variety of providers. The most common were AA sessions (59%), NHS services (35%) and psychotherapy, counselling or 1--1 support (29%).
-
5b. To explore the prison governors’ understanding of brief interventions.
Two-thirds of the governors understood what ABIs are and that they were being delivered.
-
5c. To understand how the COVID-19 pandemic has impacted the services available in male remand prisons.
We found that the COVID-19 pandemic had a devastating affect across all prisons in relation to the services they provide. It was also useful to establish what the prison governors deemed important learning from the pandemic, in this instance mostly around PPE and a better use of technology.
-
5d. To identify whether the impact of the COVID-19 pandemic upon services could be avoided in the future.
There were major impacts in relation to services during COVID-19 which included all sessions being suspended and there being staffing issues and a lack of resources.
Patient and public involvement
Patient and public involvement (PPI) has informed and influenced the development of the study through various stages. PPI representatives involved in the research design include: those with experience of being in prison and the criminal justice system, a social enterprise group, prison employees and NHS staff. At the time of the study conception and development, our PPI co-applicant, Sharon Mercado (SM), was a community justice mentor (CJM) at the Wise Group. As part of our PPI work, she brought together service user representatives and held a participatory workshop with men who had experience of being in prison on remand. The aim of the workshop was to discuss and provide suggestions and feedback regarding development of the study design. Their views informed and influenced the study design: need for pictorial information for study material to address literacy/readability; strategies to maximise follow-up by obtaining contact details of family/significant others, homeless shelters and community justice support workers. SM was a member of the PRISM-A study Advisory Board and has continued to work with us as a co-applicant on the APPRAISE study, where she informed the research design and follow-up strategy using experience of her own follow-up work as a CJM with prisoners on liberation. SM continued to provide input throughout the duration of the study as a member of the PMG and in the recommendations for a future definitive trial. Wider PPI was present through TSC membership where we also had wider representation.
The PPI was an extremely positive experience for the team and the study benefited hugely from all their input. This was particularly the case when we were reviewing the impact of COVID on follow-up and considering the mitigations we could take moving to self-completion questionnaires, change of primary outcome measure and adaptations to some of the secondary outcome measures. The input from SM was key. The impact of COVID and the subsequent restrictions on face-to-face meetings did have a negative effect on PPI engagement. The face-to-face meetings were key for the relationships we had been building and meeting face-to-face with PPI colleagues was always a positive experience for everyone.
Reflections and lessons learned from patient and public involvement involvement
Our reflections and learning of our PPI engagement in the APPRAISE study was that we should in future look to strengthen the PPI presence within any future studies. It would have been useful to have created a PPI-led space for the PPI members for them to have the opportunity to meet away from the PMG and TSC. On reflection the TSC and PMG meetings could be quite technical at times, with language used that PPI colleagues felt they were less familiar with. As SM was the sole PPI member of the PMG, in future it would be useful to have a minimum of two members to have a more balanced group. If we created a separate PPI space where PPI members could meet outside of formal meetings to set the agenda, it could be used as a safe space for them to discuss and provide regular feedback to the TSC and PGM. It may be possible to also run workshops linked to the study but also to have informal activity too. With SM we would generally meet ahead of the PMG and have refreshments together; this worked well and has informed the idea of a separate PPI space for PPI colleagues.
SM has provided her own insightful reflections on the research study in relation to what went well and what could have been done differently to improve the PPI representation and involvement. These reflections and recommendations, in her own words, are presented here.
Engaging with offenders is not easy. It takes time and patience and recognising that sometimes, despite the willingness to engage, it doesn’t always happen the way you anticipated.
Holding a focus group needs careful planning especially as you need to make sure that those attending will feel safe, and anything said is confidential. Offenders’ lives, especially those that are involved with substance misuse/alcohol, are chaotic. Therefore, making sure those attending are not going to meet anyone else that they have issues with (enemies, debts etc.) requires input. Despite all the support to attend (incentives were included, food vouchers, travel expenses), the focus group was not attended by all those invited. However, even with a small number, input was good. Those still on remand were also on an individual basis asked for input regarding the information leaflets, and what works best in terms of follow-up appointments after liberation.
To summarise, the whole experience was challenging. Regardless of the research, working with offenders/ex-offenders can be difficult, especially with those who due to their alcoholism can have chaotic lives. This makes it hard to continue engagement with follow-up appointments. There are things that can be done which may assist in getting increased involvement.
-
Building up more trust and spending more time with the offender can help. Rather than just a few engagements, have a few more or enlist support from other agencies working with the offender just to build up the momentum and remind the offender of the research project. This could prevent the offender from disengaging.
-
Better offender tracking after liberation. Some people may have a mentor or a support worker: find out (hopefully before liberation) who is currently working and keep up communication with them, they may be able to inform you of a person’s whereabouts.
-
Offering incentives may help. Whilst offering financial incentives (£20 per community engagement), it can help. It is recommended that any financial rewards are given in food/shop vouchers or pre-payment energy support.
-
Invite those who are now in recovery and have recent relevant experience to come and talk to the research team at the start of the project. It can be a good opportunity to find out more about the lives of those affected by alcohol and why engagement or non-engagement happens.
Equality, diversity and inclusion
Equality, diversity and inclusion (EDI) was a core value of the purpose of our research by the very nature of the setting of the research, the focus on alcohol-related harm and the population we were focusing on. Conducting the study required EDI to be at the forefront of our work from inception with our awareness of the lack of evidence, to meeting ethical approval requirements and working within the criminal justice system. An overview of our experience and reflections are provided in relation to participants, the evidence base, the study design, the research team and PPI representation.
Population characteristics and optimising participation
We are aware that undertaking research within the prison setting is challenging and not commonplace and for trials research it is even less common. The challenge is increased even further when there is a focus on the remand population. The study was developed and conceptualised by drawing on the collective experiences of the research team, our previous research and work with those incarcerated and from the published literature. From this we had a unique understanding of our population and who should be in the study. In our previous research we had undertaken interviews with men in prison who were on remand and asked them specifically how we could optimise participation in a future trial. We had also undertaken interviews with prison service colleagues providing care in the prison setting. Their reflections and insights directly informed the study design and how we approached the research as described in Chapter 3 to be as inclusive as possible. We also purposely undertook the study in two different prison estates to explore how the impact of the variations in category of the prison population and the estate regimes impacted participation. This was a factor from our previous work we had become aware of and remains a key factor for researchers to consider in any future studies along with the use of digital technology from the use of digital recorders to use of mobile phones.
Gaps in the evidence base
To the best of our knowledge we are not aware of any other trials for men on remand focusing on the delivery of a self-efficacy-enhancing extended alcohol brief intervention, at least in the UK, hence the need to undertake the pilot trial. The key gap that remains for this particular population is how best to design a study that provides an optimum follow-up process. We have provided recommendations in Chapter 9 for future studies.
Encouraging under-represented groups
Our PPI engagement with service users during the conception and design phase of the study supported the development of the study material through use of images and the material layout. This was specifically with the aim of optimising accessibility and inclusion.
Research team inclusivity and development opportunities
Our research team comprised a range of under-represented stakeholder groups and individuals largely seen in our TSC membership. The research team also had a good gender balance with a larger percentage of women and early-career research representation evident as co-authors. The ethos and values of the team ensured development-supported opportunities were available to take on key elements of the study, for example, process evaluation interviews and data analyses and COVID survey. Similarly, we provided development opportunities for those coming from a non-research background, for example, our co-applicant service user (SM) and our researcher who collected the baseline data at the England study site.
Patient and public involvement representation
Our PPI representation is outlined in the section Patient and public involvement. The study participants were representative of those from our previous work with this population. The impact of COVID has been described elsewhere in the report. Our additional COVID impact survey provided some further data on how this population were affected in relation to the delivery of alcohol services during the pandemic.
Strengths and limitations
Strengths of the study
-
The APPRAISE study, to the best of our knowledge, is the first pilot trial of an alcohol-focused self-efficacy-enhancing intervention for men on remand.
-
The study provides significant insight into the feasibility and acceptability of pilot trials for this particular population.
-
The ethical approval process for the prison setting across devolved countries provided useful insights into how to navigate the submission and approvals process across a range of ethics committees.
-
The study provided good evidence of the feasibility of recruitment, training interventionists and subsequent in-prison delivery of the APPRAISE intervention to 73% of men on remand, randomised to the intervention, within a highly complex prison setting.
-
The economic findings provide valuable insights, as we believe this to be the first of its kind for this type of intervention in this setting and that the methods discussed will likely be relevant and transferable across other settings.
-
Useful insight regarding the access to PNC and NHS service use data was obtained.
-
The process evaluation provided useful insights into the perspectives of the remand participants, intervention delivery team and wider stakeholders on the acceptability and feasibility of implementation of the intervention.
Limitations of the study
-
Protracted multiple ethical approvals across devolved countries and processes meant a significant delay in recruitment commencing, particularly for the Scotland site.
-
We were unable to deliver the post-liberation elements of the intervention.
-
The onset of the COVID-19 pandemic resulted in prison restrictions and no access to the prison site, meaning we were unable to identify if participants had been released or not at 6 months, with no access still at the England site at 12 months and very limited access at the Scotland site at 12 months.
-
Although the COVID-19 pandemic was undoubtedly a factor in the low percentage followed up, only 13% (18/132) of those who received the intervention were followed up at 12 months.
-
Changes to the study protocol to include self-completion of follow-up data may have made it difficult for participants to complete the survey and resulted in larger proportions of missing data as opposed to RA survey completion at baseline, where missing data were minimal.
-
We did not include probation services in the trial, which on reflection would have strengthened our post-liberation follow-up process.
Recommendations regarding a definitive randomised trial
From the study progression criteria for a full RCT, we have identified the following recommendations:
-
Buy-in for a research trial of this nature in prison requires significant pre-study trust and relationship development, buy-in from the prison estate, governor, prison officers, peer mentors and embedded third-sector services.
-
Recruitment and randomisation of men on remand to a future APPRAISE RCT are possible, with trust in the research team an important factor.
-
Training team members of existing alcohol services to deliver APPRAISE as per protocol is possible.
-
Delivery of the in-prison APPRAISE intervention is possible and would require appropriate space, time and team member capacity.
-
Economic evaluation is possible.
-
Post-liberation intervention delivery would only be possible if there was a robust follow-up process identified and in place.
-
Six-month and 12-month follow-up would only be possible if there was a robust follow-up process identified and in place. What that might look like needs to be carefully considered, explored and understood in an already complex liberation and rehabilitation statutory and non-statutory agency landscape. This may be achieved through the use of in-depth individual case studies or a realist data-capture approach to cover this period.
-
Further exploration of the inclusion of and collaboration with the probation service in the service delivery and implementation of the APPRAISE intervention may offer higher success rates of post-liberation intervention delivery and a more robust follow-up process.
-
Further exploration of the feasibility of utilising routinely collected data to evaluate outcomes post prison release is also warranted, for example, presentation at community alcohol services, presentation to GPs, and/or liver function test readings on routinely collected blood-test investigations.
-
Future research funding amongst prisoner populations must be made available to address the feasibility issues identified in this pilot trial so that a best-practice framework can be developed and utilised by research teams seeking to conduct much-needed research amongst this under-served group.
Conclusion
Addressing alcohol harm in prisons, at what can be considered a ‘teachable moment’, where there is an opportunity for reflection on their risky drinking and their current position, could potentially reduce the risk of re-offending and costs to society, while helping address health inequalities. For those on remand in prison, the prevalence of at-risk drinking is between 62% and 68%. 7
Many men on remand do not have the opportunity to access mainstream prison health or public health services. An intervention such as APPRAISE offers an opportunity to provide an extended behavioural-based alcohol intervention to men on remand. The APPRAISE study has identified that despite the complexities of ethical approval and the time taken to build relationships and trust, it is possible to undertake key elements of a future RCT, but not all, namely follow-up. Further focused research needs to be undertaken to explore, identify and develop a robust process and system to optimise follow-up post liberation. A recent pilot trial in prisons has shown promise in this area, having identified satisfactory follow-up at 6 months, but not at 12 months. 90
The evidence base to meet the needs of men on remand in relation to risky drinking remains weak. However, there are opportunities to build on the work of APPRAISE to ensure that those in the prison setting have equal access to interventions that have the potential to positively impact their relationship with and use of alcohol.
Additional information
Acknowledgements
There are so many people we would wish to thank and who have made this study possible. Firstly, we would like to thank the men who made this study possible, working with us in the prison setting, giving their time with the hope of making positive change happen not only for them but for others. We are forever grateful. Also, we thank all those working within the prison service and in particular the governors at both study sites, who supported us from an idea to a reality and paved the way, along with their teams, to enable the study to take place and provide an opportunity for the men within their care. We would also like to thank the teams of CGL in Scotland and England who took the time to learn about the APPRAISE study. They collaborated with us in the hope that we could provide alcohol support to men on remand in prison and on liberation. They were committed and so wonderful to work with. Together they met with us on numerous occasions, discussing how the study could be conducted, with their willingness, support and advice making this such a positive experience. Finally, thanks to Sharon Mercado, who has worked with us and has become our most valued and trusted team member, always there to give us insights into how we could improve the study design and the documentation and adapting the study when the pandemic struck. Thank you for being you.
The authors would like to thank the funders for their support throughout and offer a particular thank you to Hannah Sainsbury, Research Manager (Monitoring), NIHR Evaluation, Trials and Studies Coordinating Centre (NETSCC), for her continued support. We would like to also thank the sponsor, the University of Edinburgh, Charlotte Smith, Research Governance Manager, the University of Edinburgh College of Arts, Humanities and Social Sciences, and the Research Support Office.
Finally but importantly, we would like to thank the Trial Steering Committee members (Professor Frank Sullivan (Chair), Professor Olivia Wu, Dr Fergus Daly, Hon Professor Alex McMahon, Dr Justina Murray, Ms Joanne O’Connor, Ms Jessica Davidson, Dr James Carnie, Mr Frank Reilly, Ms Tracey Stewart, Professor Anne Whittaker, Ms Alison Douglas, Mr Pete White and Mr Nigel Johnson) for their support and advice throughout.
Acknowledgement of participating investigator
Mr Kieran Lynch contributed as a scientific advisor, critically reviewed the study proposal and contributed to the conception and design of the study. Acknowledgement does not imply endorsement of the study’s data and conclusions. Written permission to be acknowledged was obtained from the participating investigator.
Contributions of authors
Aisha Holloway (https://orcid.org/0000-0003-3070-3703) Professor of Nursing Studies, University of Edinburgh, Chief Investigator, made a substantial contribution to the conception and design of the study, protocol development, contribution to the analysis and interpretation of data, oversaw all aspects of the study, substantial contribution to the drafting of the final report, drafting and revising it critically for important intellectual content and provided approval of the version to be submitted to NIHR.
Gillian Waller (https://orcid.org/0000-0003-1873-3766) RF, Research Fellow, University of Teesside, made a substantial contribution to the conception and design of the health economics project and subsequent literature reviews, and to the analysis and interpretation of data for the work of the APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Jennifer Ferguson (https://orcid.org/0000-0002-1719-269X) RF, Senior Lecturer in Criminology, University of Teesside, made a substantial contribution to the conception and design of the health economics project and subsequent literature reviews, and to the acquisition, analysis and interpretation of data for the work of the APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Victoria Guthrie (https://orcid.org/0000-0002-3920-2342) SRF, Improvement Lead, Community Justice Scotland, made a contribution to the conception, design and methods of the APPRAISE project, protocol development, intervention training, contribution to the acquisition of data, contributed to drafting the work and provided approval of the version to be submitted to NIHR.
Jamie Brian Smith (https://orcid.org/0000-0003-0097-6102) RA, Research Associate, Charité University, made a substantial contribution to the conception and design of the APPRAISE project, protocol development, intervention training, contribution to the acquisition of data, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Joanne Boyd (https://orcid.org/0009-0004-8503-1005) RA, Trainer, County Durham Drug and Alcohol Recovery Service, made a substantial contribution to the conception and design of the APPRAISE project, protocol development, intervention training, contribution to the acquisition of data, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Sharon Mercado, PPI. Contributed substantially to the study from conception to design, contributed to the development of study material for participants, advised on recruitment, data collection and follow-up on liberation within prison services, contributing to the drafting of the final report for important intellectual content and approved the final version for publication.
Jessica Rees (https://orcid.org/0000-0002-1495-2470) Statistician, University of Edinburgh, made a substantial contribution to the analysis and interpretation of data for the work of the APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Richard Anthony Parker (https://orcid.org/0000-0002-2658-5022) Senior Statistician, University of Edinburgh, made a substantial contribution to the conception, design, analysis and interpretation of data for the work of the APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Andrew Stoddart (https://orcid.org/0000-0002-1958-3897) Senior Health Economist, University of Edinburgh, made a substantial contribution to the conception and design of the health economics aspect of the APPRAISE project and to the analysis and interpretation of data, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Jeremy W Bray (https://orcid.org/0000-0001-7712-160X) Professor of Economics, UNC Grennsboro, made a substantial contribution to the conception and design of the health economics aspect of the APPRAISE project and to the analysis and interpretation of data, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Simon Coulton (https://orcid.org/0000-0002-7704-3274) Professor of Health Services Research, University of Kent, made a substantial contribution to the conception, design and methods of the study, protocol development, contribution to the analysis and interpretation of data, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Kate Hunt (https://orcid.org/0000-0002-5873-3632) Professor in Behavioural Sciences and Health, University of Stirling, made a substantial contribution to the conception and design of the APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Gertraud Stadler (https://orcid.org/0000-0002-1935-8200) Professor for gender-sensitive prevention research, Charité University, made a substantial contribution to the conception and design of the logic model and health behaviour change design of the project, to the analysis and interpretation of data for the work of the APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Arun Sondhi (https://orcid.org/0000-0002-4748-5522) Researcher, Open University, made a contribution to the conception and design of the PNC and health data aspect of APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Pam Smith (https://orcid.org/0000-0001-7660-0289) Emeritus Professor, University of Edinburgh, made a contribution to the conception and design of the APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Rosie Stenhouse (https://orcid.org/0000-0002-1253-2544) Senior Lecturer, University of Edinburgh, made a contribution to the conception and design of the APPRAISE project, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
Philip Conaglen (https://orcid.org/0000-0002-8605-7045) Public Health Consultant, NHS Lothian, made a contribution to the conception and design of the APPRAISE project, contributed to the drafting of the work and provided approval of the version to be submitted to NIHR.
Aziz Sheikh (https://orcid.org/0000-0001-7022-3056) Professor of Primary Care Research, University of Edinburgh, made a contribution to the conception and design of the APPRAISE project, contributed to the work and provided approval of the version to be submitted to NIHR.
Dorothy Newbury-Birch (https://orcid.org/0000-0003-0065-8649) Professor of Alcohol and Public Health, Teesside University, made a substantial contribution to the conception and design of the study, protocol development, contribution to the analysis and interpretation of data, oversaw all aspects of the study, contributed to the drafting of the final report for important intellectual content and provided approval of the version to be submitted to NIHR.
All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/KNWT4781.
Primary conflicts of interest: Aisha Holloway reports grants from the RCN Foundation, The Burdett Trust for Nursing; consulting fees from WHO, and non-executive director roles from the Law Society Scotland, and the Florence Nightingale Foundation.
Richard Anthony Parker reports support from NHS Lothian and NIHR; participation on HSDR Board.
Andrew Stoddart reports grants from the NIHR and MRC.
Simon Coulton reports grants from the NIHR and Youth Endowment Fund; consulting fees from Youth Endowment Fund and NIHR Journals Library; participation on NIHR PHR/RGfAR and HTA Boards.
Kate Hunt reports grants from NIHR; participation on NIHR PHR Boards and COVID-19 Review.
Arun Sondhi reports grants from NHS England, College of Policing and Norfolk Police Crime Commissioner.
Dorothy Newbury-Birch reports grants from Durham City Council, NIHR, South Tees HDRC, Middlesbrough County Council; co-president of INEBRIA to September 2024.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All requests for data should be sent to the corresponding author. Access to available anonymised data may be granted following review.
Ethics statement
Ethics approval was sought and secured from (1) IRAS (East of Scotland Research Ethics Service) REC reference 19/ES/0068, IRAS project ID 261003; (2) HMPPS Ministry of Justice, National Research Committee reference 2019-240; (3) SPS Research Access and Ethics Committee (RAEC) approval letter dated 13 June 2019; (4) the University of Edinburgh School of Health in Social Science Nursing Studies Research Panel approval letter dated 26 September 2019; (5) NHS R&D in Scotland (R&D No. 2019/0268). The University of Edinburgh acted as trial sponsor (CAHSS 18/2/02).
Information governance statement
The University of Edinburgh is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Edinburgh is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.ed.ac.uk/data-protection/contact. The University of Edinburgh is the Data Processor.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Public Health Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Holloway A, Watson H, Starr G. How do we enhance problem drinkers’ self efficacy?: a nurse administered intervention. J Subst Use 2006;11:375–86.
Holloway A, Watson H, Arthur A, McFadyen A, Starr G, McIntosh J. An evaluation of drinking refusal self-efficacy and minimal interventions for potential problem drinkers in a general hospital setting. Addiction 2007;102:1762–70.
Holloway A, Landale S, Ferguson J, Newbury-Birch D, Parker R, Smith P, Sheikh A. Alcohol Brief Interventions (ABIs) for male remand prisoners: protocol for development of a complex intervention and feasibility study (PRISM-A). BMJ Open 2017;4:e014561. https://doi.org/10.1136/bmjopen-2016-014561
Holloway A, Guthrie V, Waller G, Smith J, Boyd J, Mercado S, et al. A two-arm parallel-group individually randomised prison pilot study of a male remand alcohol intervention for self-efficacy enhancement: the APPRAISE study protocol. BMJ Open 2021;11:e040636.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
- Holloway A, Guthrie V, Waller G, Smith J, Boyd J, Mercado S, et al. A two-arm parallel-group individually randomised prison pilot study of a male remand alcohol intervention for self-efficacy enhancement: the APPRAISE study protocol. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-040636.
- Saunders J, Lee N. Hazardous alcohol use: its delineation as a subthreshold disorder, and approaches to its diagnosis and management. Compr Psychiatry 2000;41:95-103.
- World Health Organisation . The Role of General Practice Settings in the Prevention and Management of the Harm Done by Alcohol 1992.
- Coulton S, Newbury-Birch D, Cassidy P, Dale V, Deluca P, Gilvarry E, et al. Screening for alcohol use in criminal justice settings: an exploratory study. Alcohol Alcohol 2012;47:423-7.
- Brown N, Newbury-Birch D, McGovern R, Phinn E, Kaner E. Alcohol screening and brief intervention in a policing context: a mixed methods feasibility study. Drug Alcohol Rev 2010;29:647-54.
- Newbury-Birch D, Harrison B, Brown N, Kaner E. Sloshed and sentenced: a prevalence study of alcohol use disorders amongst offenders in the North East of England. Int J Prison Health 2009;5:201-11.
- Newbury-Birch D, Coulton S, Bland M, Cassidy P, Dale V, Deluca P, et al. Alcohol screening and brief interventions for offenders in the probation setting (SIPS Trial): a pragmatic multicentre cluster randomised controlled trial. Alcohol Alcohol 2014;49:540-8.
- Newbury-Birch D, McGovern R, Birch J, O’Neill G, Kaner H, Sondhi A, et al. A rapid systematic review of what we know about alcohol use disorders and brief interventions in the criminal justice system. Int J Prison Health 2016;12:57-70.
- Orkin AM, Gill PJ, Ghersi D, Campbell L, Sugarman J, Emsley R, et al. CONSERVE Group . Guidelines for reporting trial protocols and completed trials modified due to the COVID-19 pandemic and other extenuating circumstances: the CONSERVE 2021 statement. JAMA 2021;326:257-65. https://doi.org/10.1001/jama.2021.9941.
- Heather N, Smailes D, Cassidy P. Development of a readiness ruler for use with alcohol brief interventions. Drug Alcohol Depend 2008;98:235-40.
- Funk M, Wutzke S, Kaner E, Anderson P, Pas L, McCormick R, et al. World Health Organization Brief Intervention Study Group . A multi country controlled trial of strategies to promote dissemination and implementation of brief alcohol intervention in primary health care: findings of a WHO collaborative study. J Stud Alcohol 2005;66:379-88.
- Fitton L, Bates A, Hayes A, Fazel S. Psychiatric disorders, substance use, and executive functioning in older probationers. Crim Behav Ment Health 2018;28:447-59. https://doi.org/10.1002/cbm.2094.
- Kaner EFS, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2018;2. https://doi.org/10.1002/14651858.CD004148.pub4.
- Miller W, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York: Guildford Press; 1991.
- Haighton CA, Newbury-Birch D, Kaner EFS. Screening and Interventions in Medical Settings Including Brief Feedback-focused Interventions. Interventions for Addiction 2013;3:287-98. https://doi.org/10.1016/B978-0-12-398338-1.00030-0.
- Babor TF, Grant M. From clinical research to secondary prevention: international collaboration in the development of the alcohol use disorders identification test (AUDIT). Alcohol Health Res World 1989;13:371-4.
- Haighton C, Newbury-Birch D, Durlik C, Sallis A, Chadbourn T, Porter L, et al. Optimising Making Every Contact Count (MECC) interventions: a strategic behavioural analysis. Health Psychol 2021;40:960-73. https://doi.org/10.1037/hea0001100.
- Kaner EFS, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007;2.
- O’Donnell A, Kaner E, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, et al. The impact of brief interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol 2014;49:66-78.
- Heather N. Spreading alcohol brief interventions from health care to non-health care settings: is it justified?. Drugs: Educ Prev Policy 2016;23:359-64.
- Newbury-Birch D, Ferguson J, Landale S, Giles EL, McGeechan GJ, Gill C, et al. A systematic review of the efficacy of alcohol interventions for incarcerated people. Alcohol Alcohol 2018;53:412-25. https://doi.org/10.1093/alcalc/agy032.
- Ministry of Justice, Public Health England . The Impact of Community-Based Drug and Alcohol Treatment on Re-Offending 2017.
- Ministry of Justice . Prison Population Projections 2021 to 2026, England and Wales 2021.
- Sturge G. UK Prison Population Statistics. London: House of Commons Library; 2023.
- Ministry of Justice . Table Q4.4 Criminal Justice Statistics Quarterly: December 2015 2016.
- Prison Reform Trust . Prison: The Facts – Bromley Briefings 2016.
- Prison Reform Trust . Alcohol and Re-Offending – Who Cares? 2004.
- Graham L, Parkes T, McAuley A, Doi L. Alcohol Problems in the Criminal Justice System: An Opportunity for Intervention. Denmark: World Health Organization, Regional Office for Europe; 2012.
- Revolving Doors Agency . BALANCING ACT. Addressing Health Inequalities Among People in Contact With the Criminal Justice System: A Briefing for Directors of Public Health 2013.
- Public Health England . Guidance Alcohol and Drug Prevention, Treatment and Recovery: Why Invest? 2018. https://www.gov.uk/government/publications/alcohol-and-drug-prevention-treatment-and-recovery-why-invest/alcohol-and-drug-prevention-treatment-and-recovery-why-invest (accessed 9 August 2022).
- Bhattacharya A. Which cost of alcohol? What should we compare it against?. Addiction 2017;112:559-65.
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009;373:2223-33.
- Public Health England . The Public Health Burden of Alcohol and the Effectiveness and Cost-Effectiveness of Alcohol Control Policies: An Evidence Review 2018.
- Public Health England . Alcohol & Drugs Prevention, Treatment &Amp; Recovery: Why Invest? 2013.
- Raistrick D, Heather N, Godfrey C. Review of the Effectiveness of Treatment for Alcohol Problems. London: National Treatment Agency for Substance Misuse, Department of Health; 2006.
- Health and Sport Committee . Healthcare in Prisons. SP Paper 135, 5th Report (Session 5) 2017.
- National Institute for Health and Clinical Excellence . NG57 Physical Health of People in Prison - HSC (SQSD) 2017.
- Holloway A, Watson H, Arthur A, A McFayden, Starr G, McIntosh J. An evaluation of drinking refusal self-efficacy and minimal interventions for potential problem drinkers in a general hospital setting. Addiction 2007;102:1762-70.
- Holloway A, Watson H, Starr G. How do we enhance problem drinkers’ self efficacy?: a nurse administered intervention. J Subst Use 2006;11:375-86.
- Holloway A, Landale S, Ferguson J, Newbury-Birch D, Parker R, Smith P, et al. Brief interventions for male remand prisoners: protocol for a complex intervention framework development and feasibility study (PRISM-A). BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014561.
- Tuchman E. Women and addiction: the importance of gender issues in substance abuse research. J Addict Dis 2010;29:127-38.
- Crewe B, Hulley S, Wright S. The gendered pains of life imprisonment. Brit J Criminol 2017;57:azw088-78.
- Medical Research Council . A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health 2000.
- Moore G, Audrey S, Barker M, Bond L, Bonnell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358. https://doi.org/10.1136/bmj.j3453.
- Bandura A. Health promotion from the perspective of the social cognitive theory. Psychol Health 1998;13:623-49.
- Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. Br J Addict 1992;87:743-54. https://doi.org/10.1111/j.1360-0443.1992.tb02720.x.
- Hartz C, Plant M, Watts M. Alcohol and Health: A Handbook for Nurses, Midwives and Health Visitors. London: Medical Council on Alcoholism; 1990.
- Kok G, Den Boer D, DeVries H, Gerards F, Hospers HJ, Mudde AN. Self-efficacy: Thought Control of Action. Washington, DC: Hemisphere; 1992.
- Saunders J, Aasland O, Babor T, de F, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption – II. Addiction 1993;88:791-804.
- The Prisons and Young Offenders Institutions (Scotland) Rules 2011 No. 331 Part 10 2011.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. https://doi.org/10.1111/j. 2002.384.doc.x.
- Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-264.
- Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 2005;4:287-91.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Young R, Knight RG. The Drinking Expectancy Questionnaire: a revised measure of alcohol-related beliefs. J Psychopathol Behav Assess 1989;11:99-112.
- McMahon J, Jones BT. The negative alcohol expectancy questionnaire. J Assoc Nurses Substance Abuse 1993;12.
- EuroQol G. EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Bray JW, Zarkin GA, Miller WR, Mitra D, Kivlahan DR, Martin DJ, et al. Measuring economic outcomes of alcohol treatment using the Economic Form 90. J Stud Alcohol Drugs 2007;68:248-55. https://doi.org/10.15288/jsad.2007.68.248.
- Kypri K, Wilson A, Attia J, Sheeran P, McCambridge J. Effects of study design and allocation on self-reported alcohol consumption: randomized trial. Trials 2015;16.
- Babor TF, Higgins Biddle J, Saunders J, Monteiro M. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. Geneva: World Health Organization. Department of Mental Health and Substance Dependence; 2001.
- Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials – a practical guide with flowcharts. BMC Med Res Methodol 2017;17. https://doi.org/10.1186/s12874-017-0442-1.
- Coulton S, Bland M, Crosby H, Dale V, Drummond C, Godfrey C, et al. Effectiveness and cost-effectiveness of opportunistic screening and stepped-care interventions for older alcohol users in primary care. Alcohol Alcohol 2017;52:655-64. https://doi.org/10.1093/alcalc/agx065.
- Deluca P, Coulton S, Alam MF, Boniface S, Donoghue K, Gilvarry E, et al. Screening and brief interventions for adolescent alcohol use disorders presenting through emergency departments: a research programme including two RCTs. Programme Grants Appl Res 2020;8:1-144. https://doi.org/10.3310/pgfar08020.
- Dutey-Magni P, Brown J, Holmes J, Sinclair J. Concurrent validity of an estimator of weekly alcohol consumption (EWAC) based on the extended AUDIT. Addiction 2022;117:580-9. https://doi.org/10.1111/add.15662.
- Tennant A, Badley EM. Investigating non-response bias in a survey of disablement in the community: implications for survey methodology. J Epidemiol Community Health 1991;45:247-50.
- Jones BT, McMahon J. Negative alcohol expectancy predicts post-treatment abstinence survivorship: the whether, when and why of relapse to a first drink. Addiction 1994;89:1653-65. https://doi.org/10.1111/j.1360-0443.1994.tb03766.x.
- May C, Mair FS, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009;4.
- May CR, Albers B, Bracher M, Finch TL, Gilbert A, Girling M, et al. Translational framework for implementation evaluation and research: a normalisation process theory coding manual for qualitative research and instrument development. Implement Sci 2022;17. https://doi.org/10.1186/s13012-022-01191-x.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8:1-11.
- Lane C, Huws-Thomas M, Hood K, Rollnick S, Edwards K, Robling M. Measuring adaptations of motivational interviewing: the development and validation of the behavior change counseling index (BECCI). Patient Educ Couns 2005;56:166-73. https://doi.org/10.1016/j.pec.2004.01.003.
- Etikan I, Musa SA, Alkassim RS. Comparison of convenience sampling and purposive sampling. Am J Theor Appl Stat 2016;5:1-4.
- Clarke V, Braun V. Encyclopedia of Critical Psychology. New York: Springer; 2014.
- Elliott V. Thinking about the coding process in qualitative data analysis. Qual Rep 2018;23:2850-61.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Curtis L, Burns A. Unit Costs of Health & Social Care 2020. Canterbury: PSSRU, University of Kent; 2020.
- Department of Health . Reference Costs 2019–20 2019.
- ISD Scotland . ISD Cost Book n.d. www.isdscotland.org/Health-Topics/Finance/Costs/Detailed-Tables/ (accessed 9 August 2022).
- Ramponi F, Walker S, Griffin S, Parrott S, Drummond C, Deluca P, et al. Cost-effectiveness analysis of public health interventions with impacts on health and criminal justice: an applied cross-sectoral analysis of an alcohol misuse intervention. Health Econ 2021;30:972-88. https://doi.org/10.1002/hec.4229.
- Addison M, McGovern R, Angus C, Becker F, Brennan A, Brown H, et al. Alcohol screening and brief intervention in police custody suites: pilot cluster randomised controlled trial (AcCePT). Alcohol Alcohol 2018;53:548-59. https://doi.org/10.1093/alcalc/agy039.
- Chakraborty I, Maity P. COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci Total Environ 2020;728.
- Kumar S. Unaccounted for water and the performance of water utilities: an empirical analysis from India. Water Policy 2010;12:707-21.
- Johnson L, Gutridge K, Parkes J, Roy A, Plugge E. Scoping review of mental health in prisons through the COVID-19 pandemic. BMJ Open 2021;11.
- Hewson T, Green R, Shepherd A, Hard J, Shaw J. The effects of COVID-19 on self-harm in UK prisons. BJPsych Bulletin 2021;45:131-3.
- Suhomlinova O, Ayres TC, Tonkin MJ, O’Reilly M, Wertans E, O’Shea SC. Locked up while locked down: prisoners’ experiences of the COVID-19 pandemic. Br J Criminol 2021;62:279-98.
- Minson S. The Impact of COVID-19 Prison Lockdowns on Children With a Parent in Prison. Centre for Criminology, University of Oxford; 2021.
- Maycock M. ‘COVID-19 has caused a dramatic change to prison life’. Analysing the impacts of the COVID-19 pandemic on the pains of imprisonment in the Scottish Prison Estate. Br J Criminol 2022;62:218-33.
- Byng R, Lennox C, Kirkpatrick T, Quinn C, Anderson R, Brand SL, et al. Development and evaluation of a collaborative care intervention for male prison leavers with mental health problems: the Engager research programme. Programme Grants Appl Res 2022;10:1-46. https://doi.org/10.3310/MMWC3761.
- Linsley P, Roll C. Health Promotion for Nursing Students. London: SAGE Publications Ltd; 2023.
Appendix 1 GRIPP2 short form
| Section and topic | Item | Reported on page no. |
|---|---|---|
| 1: Aim | Report the aim of PPI in the study | Structure of the report. p. 5 |
| 2: Methods | Provide a clear description of the methods used for PPI in the study | Patient and public involvement. p. 109–10 |
| 3: Study results | Outcomes – report the results of PPI in the study, including both positive and negative outcomes | Patient and public involvement. p. 109–10 |
| 4: Discussion and conclusions | Outcomes – comment on the extent to which PPI influenced the study overall. Describe positive and negative effects | Patient and public involvement. p. 109–10 |
| 5: Reflections/critical perspective | Comment critically on the study, reflecting on the things that went well and those that did not, so others can learn from this experience | Patient and public involvement. p. 109–10 |
Appendix 2 CONSERVE-CONSORT
Use CONSERVE-CONSORT for completed trial reports and CONSERVE-SPIRIT for trial protocols.
| CONSERVE-CONSORT Extension: [DATE] | |||||
|---|---|---|---|---|---|
| Item | Item title | Description | Page no. | ||
| CONSORT number and item | No change | Impacta | Mitigating strategyb | Page no. | |
| I. | Extenuating circumstances | Describe the circumstances and how they constitute extenuating circumstances. | Overall study recruitment. p. 31 | ||
| II. | Important modifications | a. Describe how the modifications are important modifications. | Changes to the original study protocol. p. 28 | ||
| b. Describe the impacts and mitigating strategies, including their rationale and implications for the trial. | Changes to the original study protocol, Table 6. pp. 28–29 | ||||
| c. Provide a modification timeline. | Changes to the original study protocol. p. 28 | ||||
| III. | Responsible parties | State who planned, reviewed and approved the modifications. | Changes to the original study protocol. p. 28 CI, PMG, TSC, study sponsor |
||
| IV. | Interim data | If modifications were informed by trial data, describe how the interim data were used, including whether they were examined by study group, and whether the individuals reviewing the data were blinded to the treatment allocation. | N/A | ||
| For each row, if important modifications occurred check ‘direct impact’ and/or ‘mitigating strategy’ and describe the changes in the trial manuscript or supplement. Check ‘no change’ for items that are unaffected in the extenuating circumstance. | |||||
| 1 | Title and abstract | No change | |||
| 2 | Introduction | No change | |||
| 3 | Methods: trial design | No change | |||
| 4 | Methods: participants | No change | |||
| 5 | Methods: interventions | No change | |||
| 6 | Methods: outcomes | Yes | Change of primary outcome measure | Follow-up data collection pp. 44–6 | |
| 7 | Methods: sample size | Yes | None | Changes to the original study protocol. p. 51 | |
| 8–10 | Methods: randomisation | No change | |||
| 11 | Methods: blinding | No change | |||
| 12 | Methods: statistical methods | Yes | Focus was on descriptive analyses and baseline characteristics given the low numbers providing follow-up data | Statistical methods/analysis plan. p. 46 | |
| 13 | Results: participant flow | No change | |||
| 14 | Results: recruitment | No change | |||
| 15 | Results: baseline data | No change | |||
| 16 | Results: numbers analysed | Yes | Reduced sample size at follow-up and so focus was on descriptive analyses and baseline characteristics | Statistical methods/analysis plan. p. 46 | |
| 17 | Results: outcomes and estimation | Yes | Change of primary outcome measure | Follow up data collection | |
| 18 | Results: ancillary analyses | Yes | Could not do originally planned exploratory analyses comparing agreement and full logic model analyses | Statistical methods/analysis plan. p. 49 | |
| 19 | Results: harms | No change | |||
| 20 | Discussion: limitations | Yes | None | Equality, diversity and inclusion. pp. 154–5 | |
| 21 | Discussion: generalisability | Yes | None | Strengths and limitations. p. 155 | |
| 23 | Other information: registration | No change | |||
| 24 | Other information: protocol | Yes | Protocol was updated to reflect changes | Changes to the original study protocol, Table 6 | |
| 25 | Other information: funding | Yes | Study extension secured and additional survey conducted focusing on impact of alcohol services for men on remand during COVID-19 | Survey Chapter 8 | |
Appendix 3 Template for Intervention Description and Replication Checklist
The TIDieR (Template for Intervention Description and Replication) Checklist:
Information to include when describing an intervention and the location of the information
| Item numbera | Item | Where locatedb | |
|---|---|---|---|
| Primary paper (page or appendix number) | Otherc (details) | ||
| BRIEF NAME | |||
| 1. | Provide the name or a phrase that describes the intervention. | Origins and development of the APPRAISE intervention, p. 7 | |
| WHY | |||
| 2. | Describe any rationale, theory, or goal of the elements essential to the intervention. | APPRAISE intervention: theory, elements and logic model, pp. 7–10 | |
| WHAT | |||
| 3. | Materials: describe any physical or informational materials used in the intervention, including those provided to participants or used in intervention delivery or in training of intervention providers. Provide information on where the materials can be accessed (e.g. online appendix, URL). | APPRAISE intervention materials, p. 10 | |
| 4. | Procedures: describe each of the procedures, activities, and/or processes used in the intervention, including any enabling or support activities. | APPRAISE intervention procedures, pp. 10–11 | |
| WHO PROVIDED | |||
| 5. | For each category of intervention provider (e.g. psychologist, nursing assistant), describe their expertise, background and any specific training given. | APPRAISE intervention training, p. 11 | |
| HOW | |||
| 6. | Describe the modes of delivery (e.g. face-to-face or by some other mechanism, such as internet or telephone) of the intervention and whether it was provided individually or in a group. | APPRAISE Intervention delivery mode and location; APPRAISE post-liberation intervention modifications due to COVID-19, pp. 11–14 | |
| WHERE | |||
| 7. | Describe the type(s) of location(s) where the intervention occurred, including any necessary infrastructure or relevant features. | APPRAISE Intervention delivery mode and location; APPRAISE post-liberation intervention modifications due to COVID-19, pp. 11–14 | |
| WHEN and HOW MUCH | |||
| 8. | Describe the number of times the intervention was delivered and over what period of time including the number of sessions, their schedule, and their duration, intensity or dose. | APPRAISE Intervention delivery mode and location; APPRAISE post-liberation intervention modifications due to COVID-19, pp. 11–14 Table 3 |
|
| TAILORING | |||
| 9. | If the intervention was planned to be personalised, titrated or adapted, then describe what, why, when and how. | APPRAISE intervention procedures, pp. 10–11 APPRAISE post-liberation intervention modifications due to COVID-19, pp. 13–14 |
|
| MODIFICATIONS | |||
| 10. d | If the intervention was modified during the course of the study, describe the changes (what, why, when, and how). | APPRAISE post liberation intervention modifications due to COVID-19, pp. 13–14, Randomisation and blinding, p. 19 |
|
| HOW WELL | |||
| 11. | Planned: if intervention adherence or fidelity was assessed, describe how and by whom, and if any strategies were used to maintain or improve fidelity, describe them. | Process evaluation aims and objectives – context, pp. 97–100 Table 30 |
|
| 12. d | Actual: if intervention adherence or fidelity was assessed, describe the extent to which the intervention was delivered as planned. | Chapter 6, pp. 67–82 | |
Appendix 4 APPRAISE intervention tool (V3_20October)

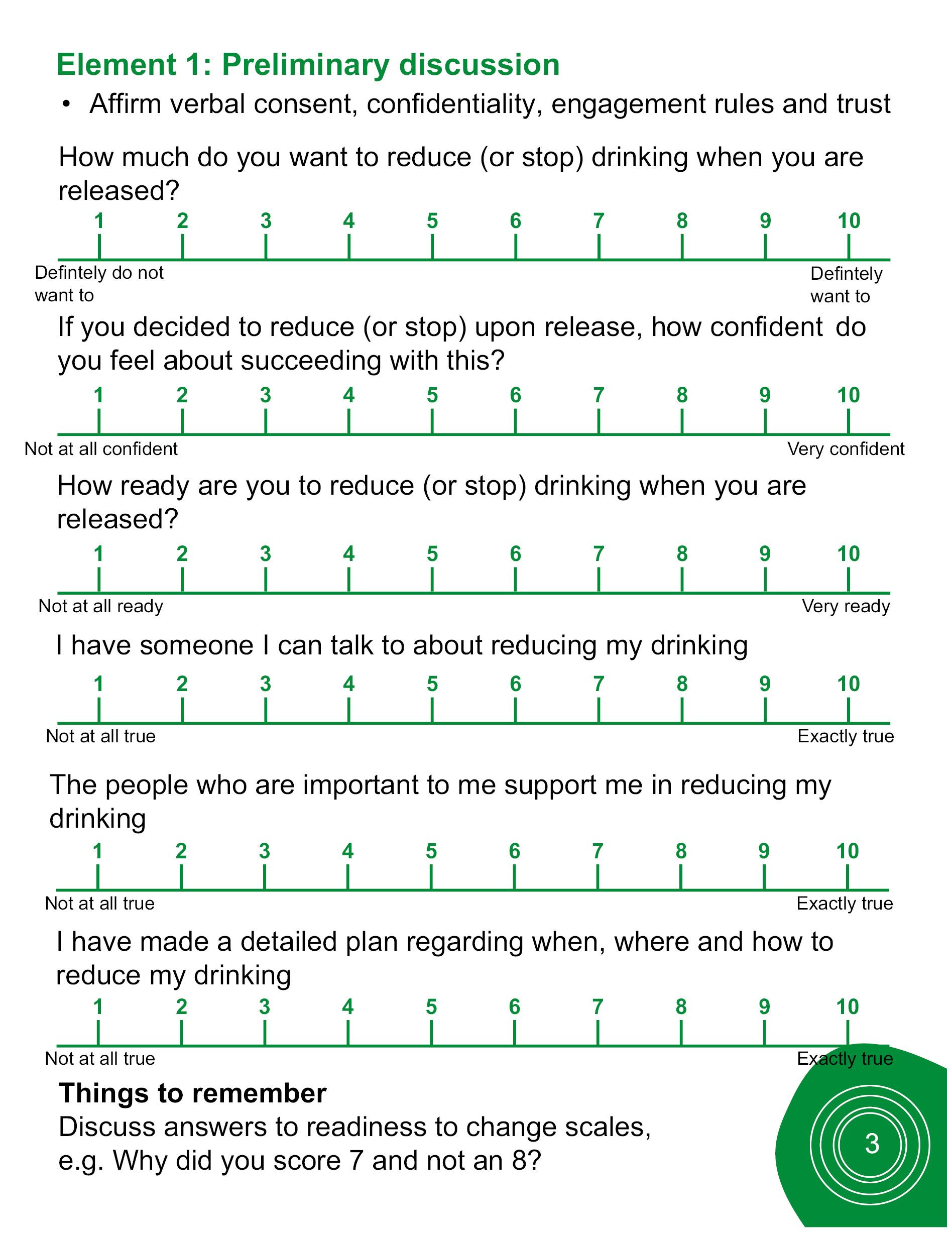
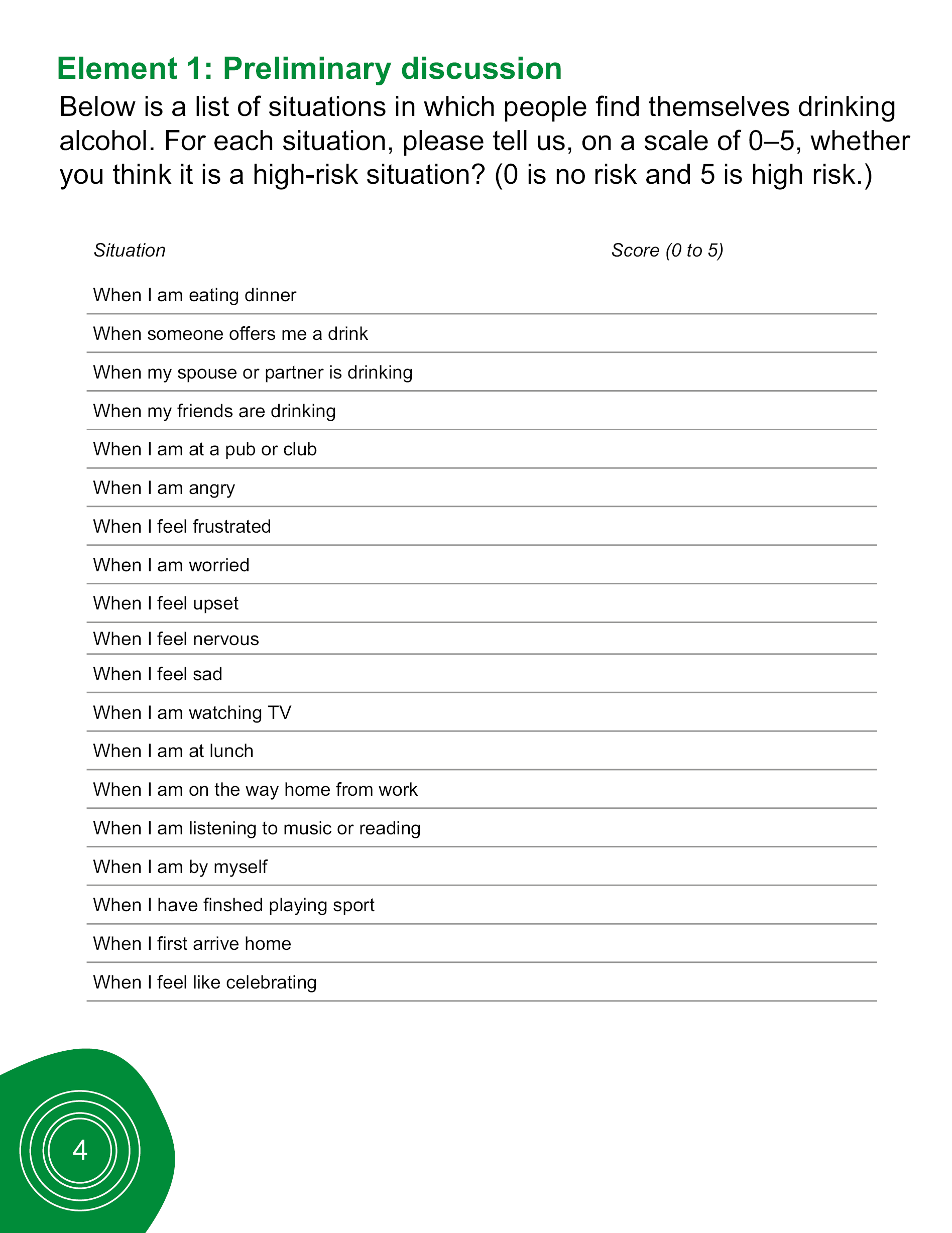

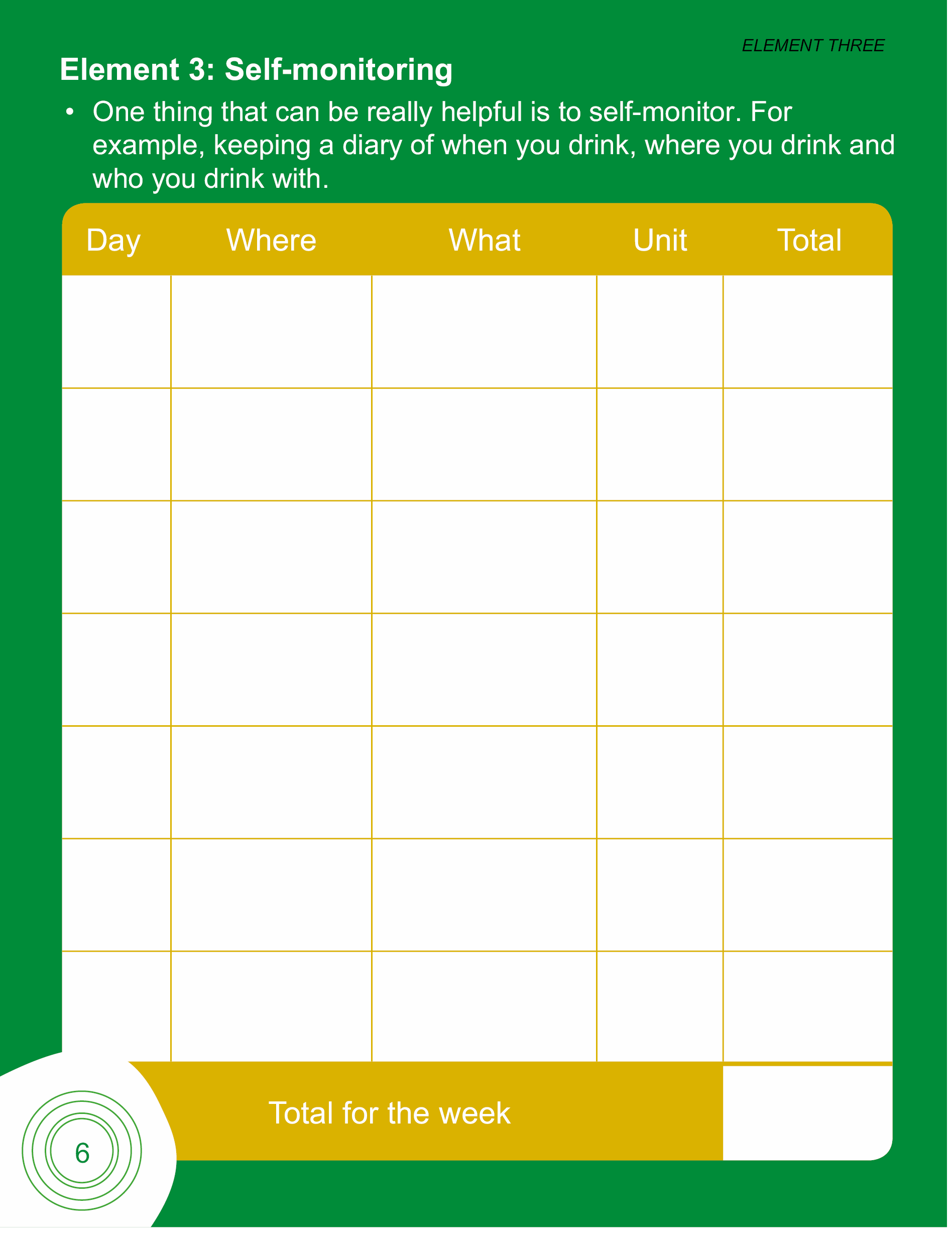
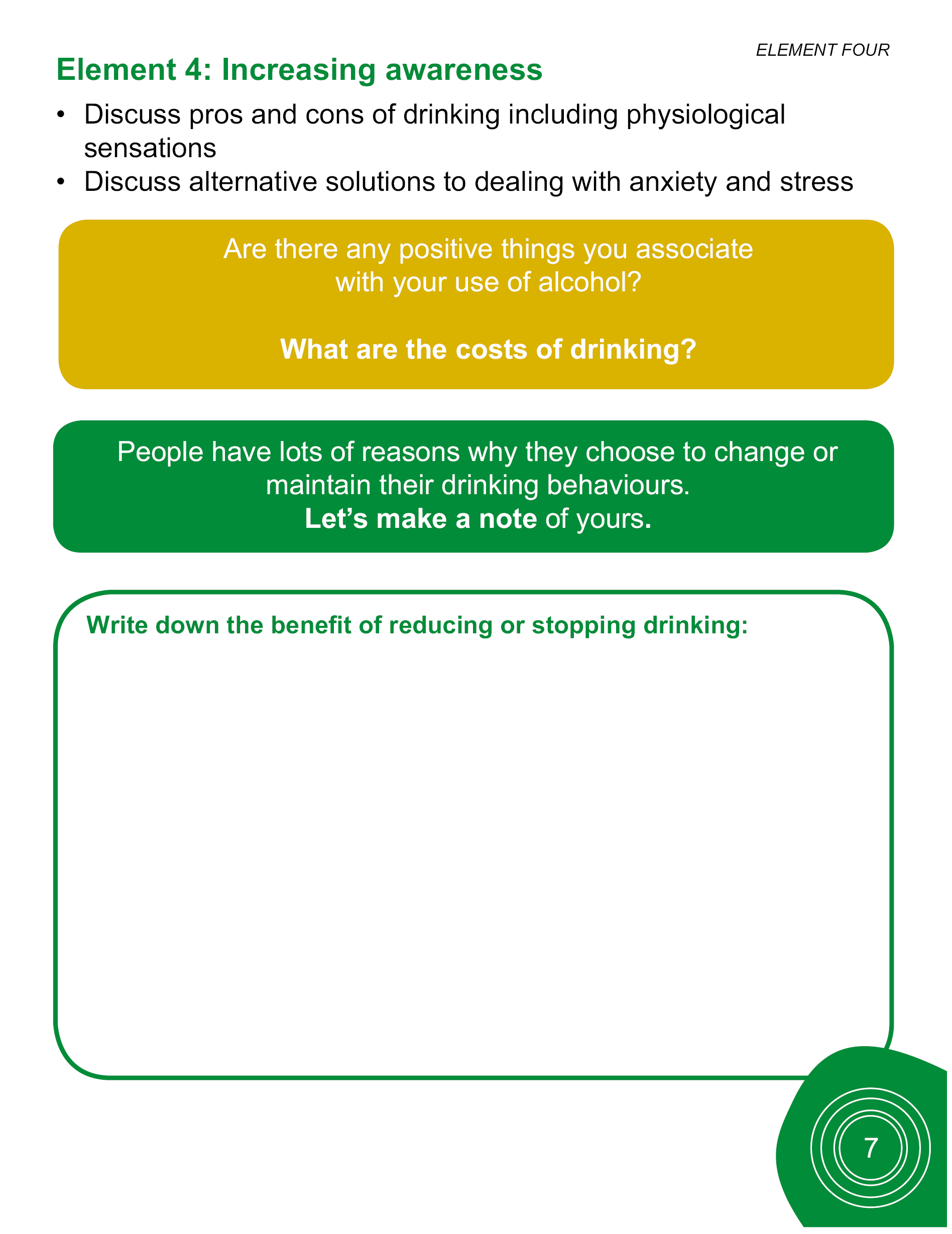
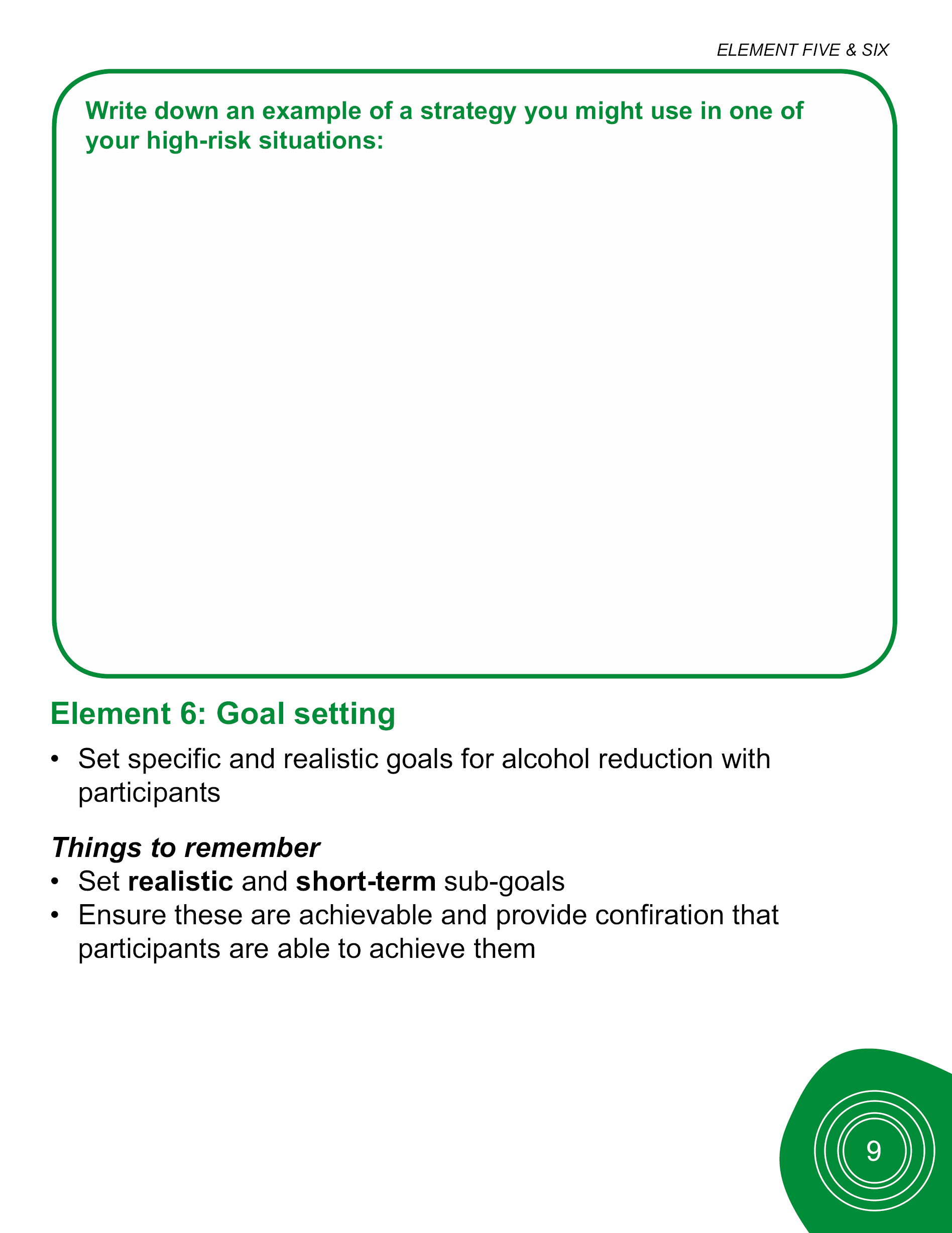
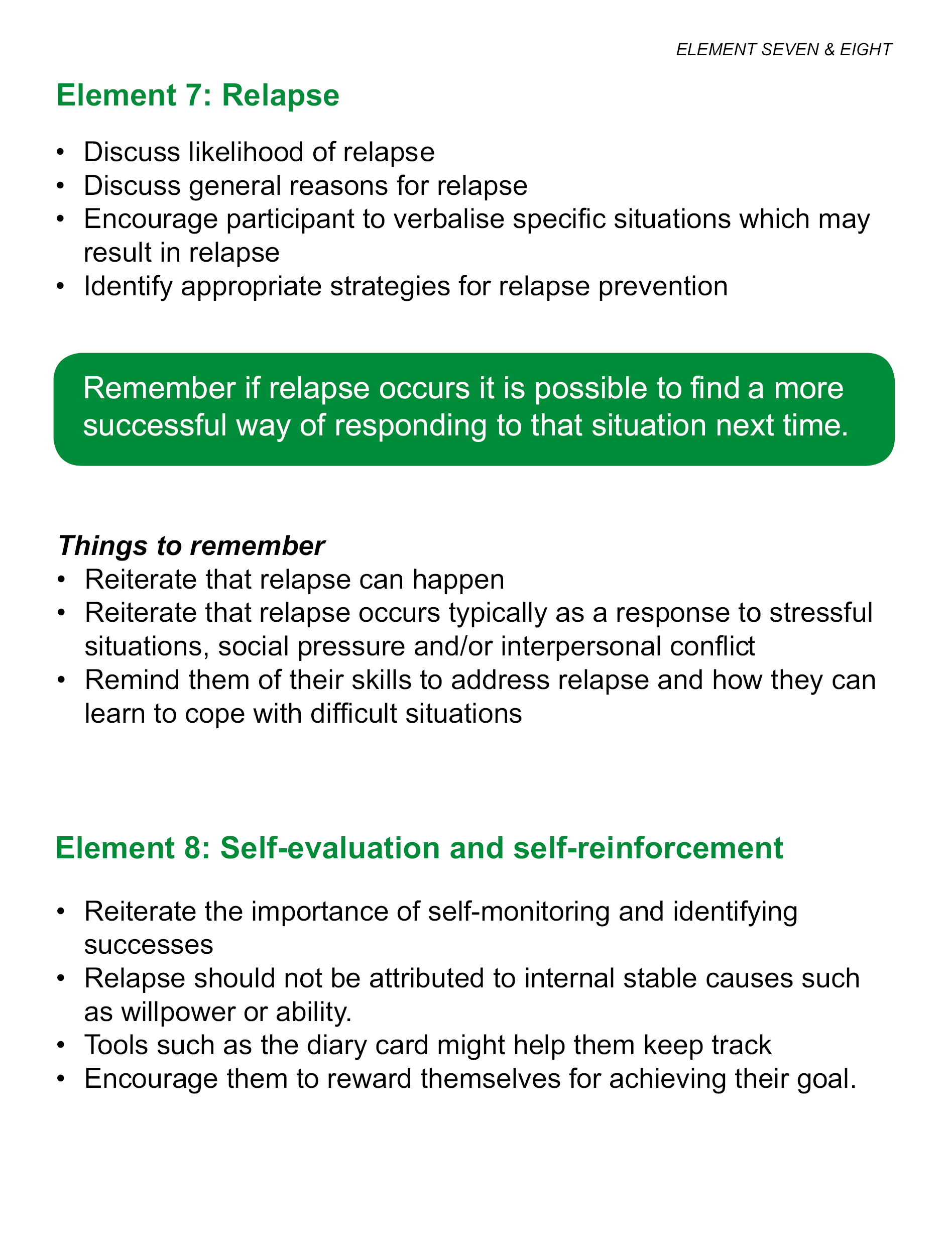
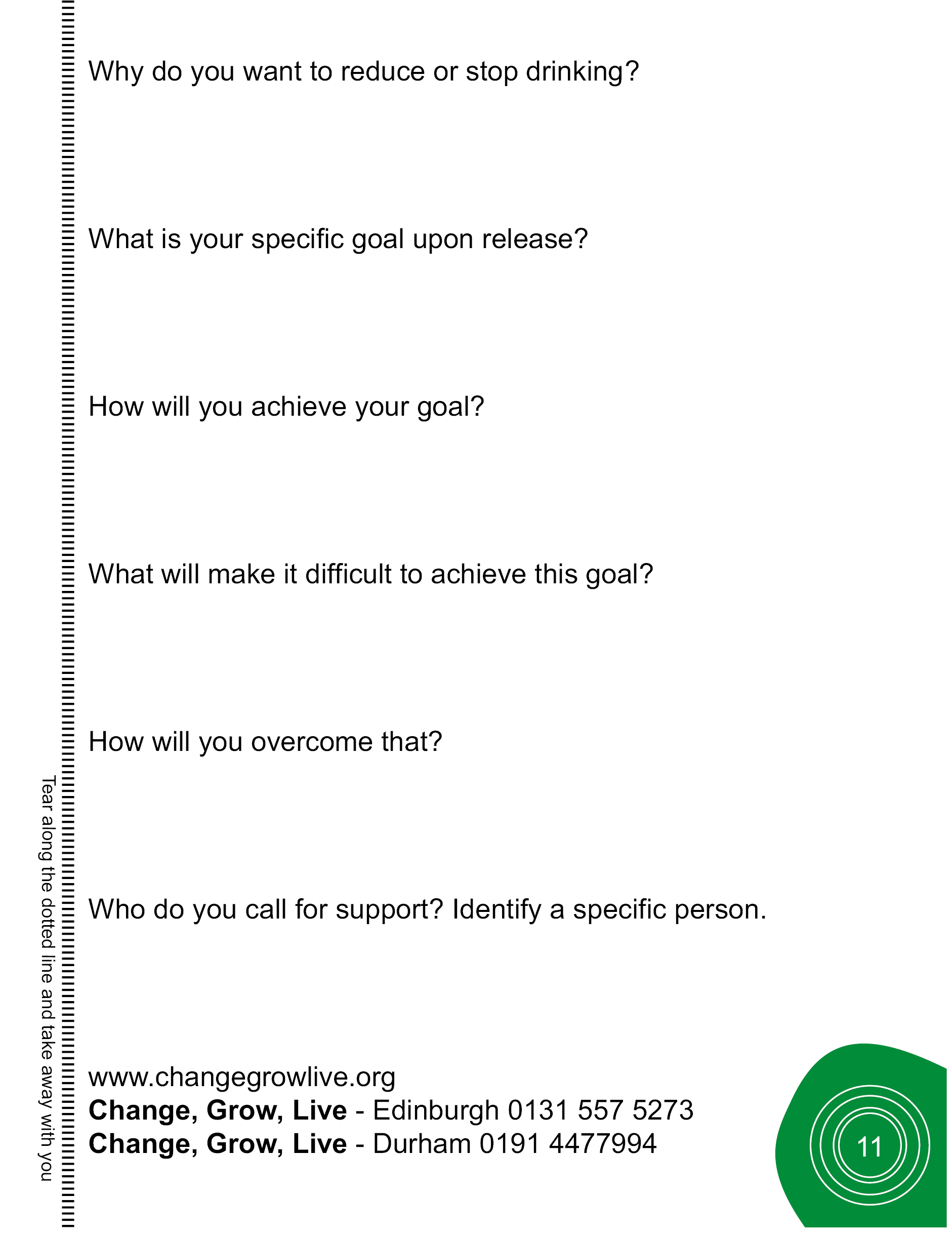
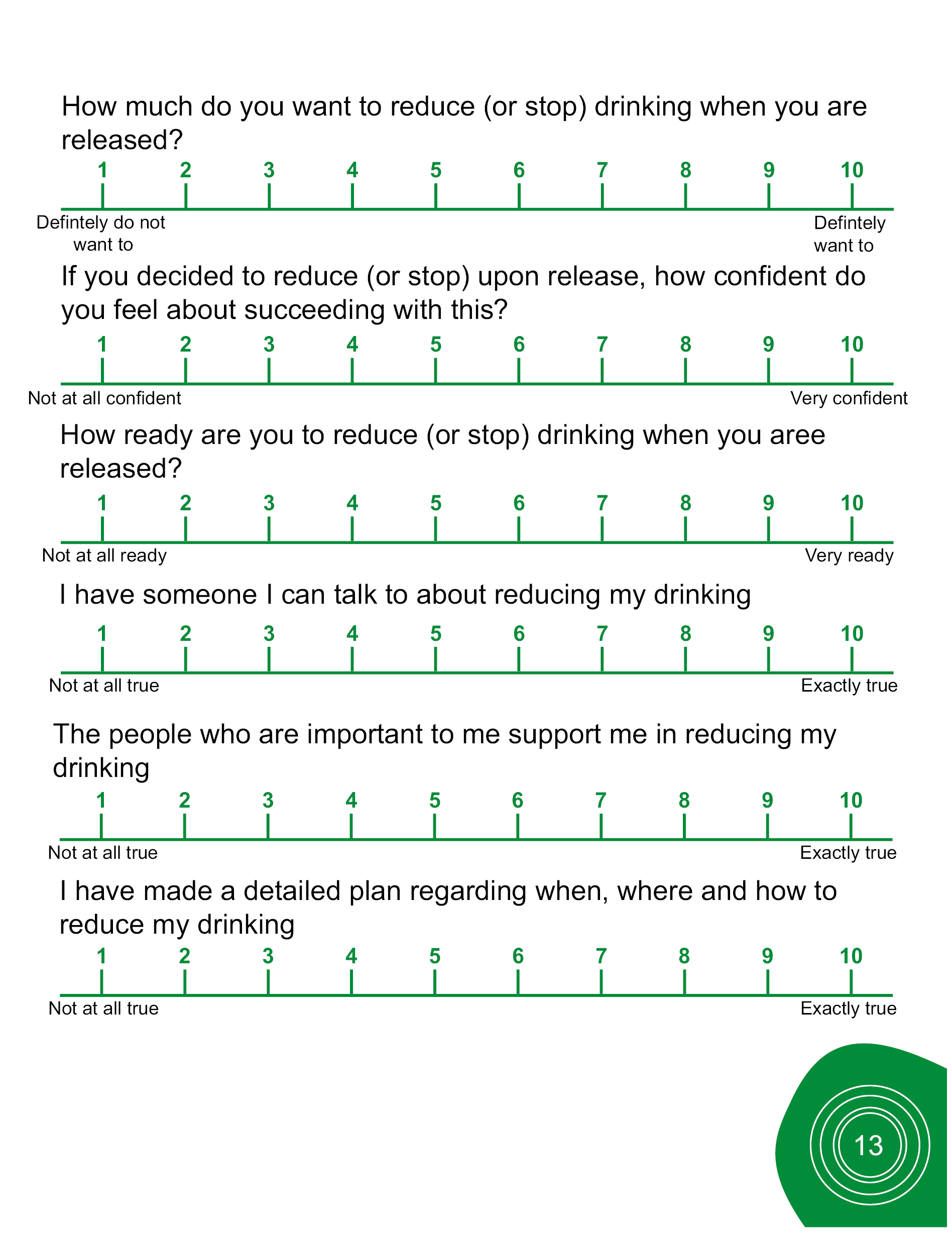
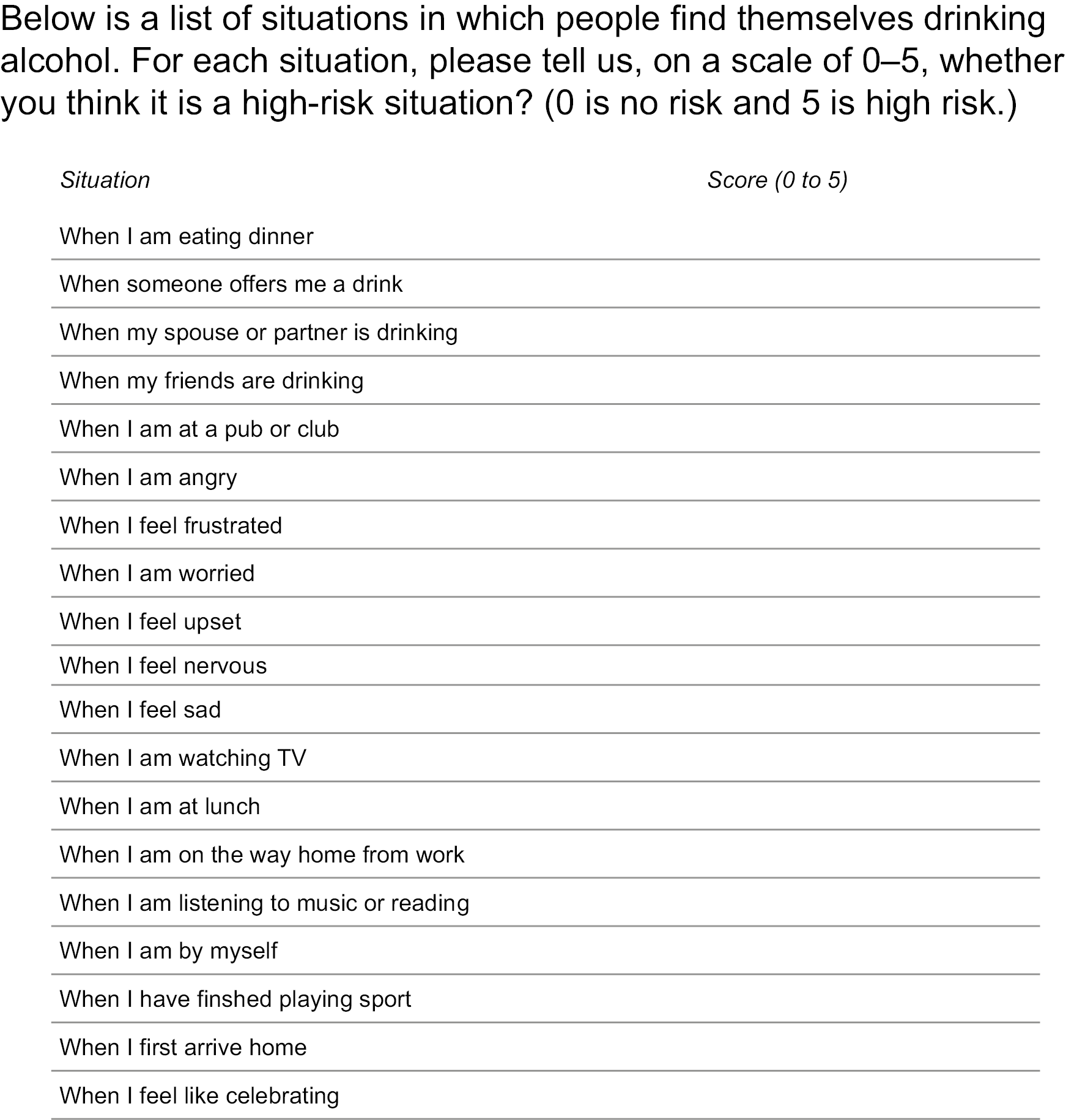

Appendix 5 Intervention tool postcard (Unit card) (V2_25Sept19)
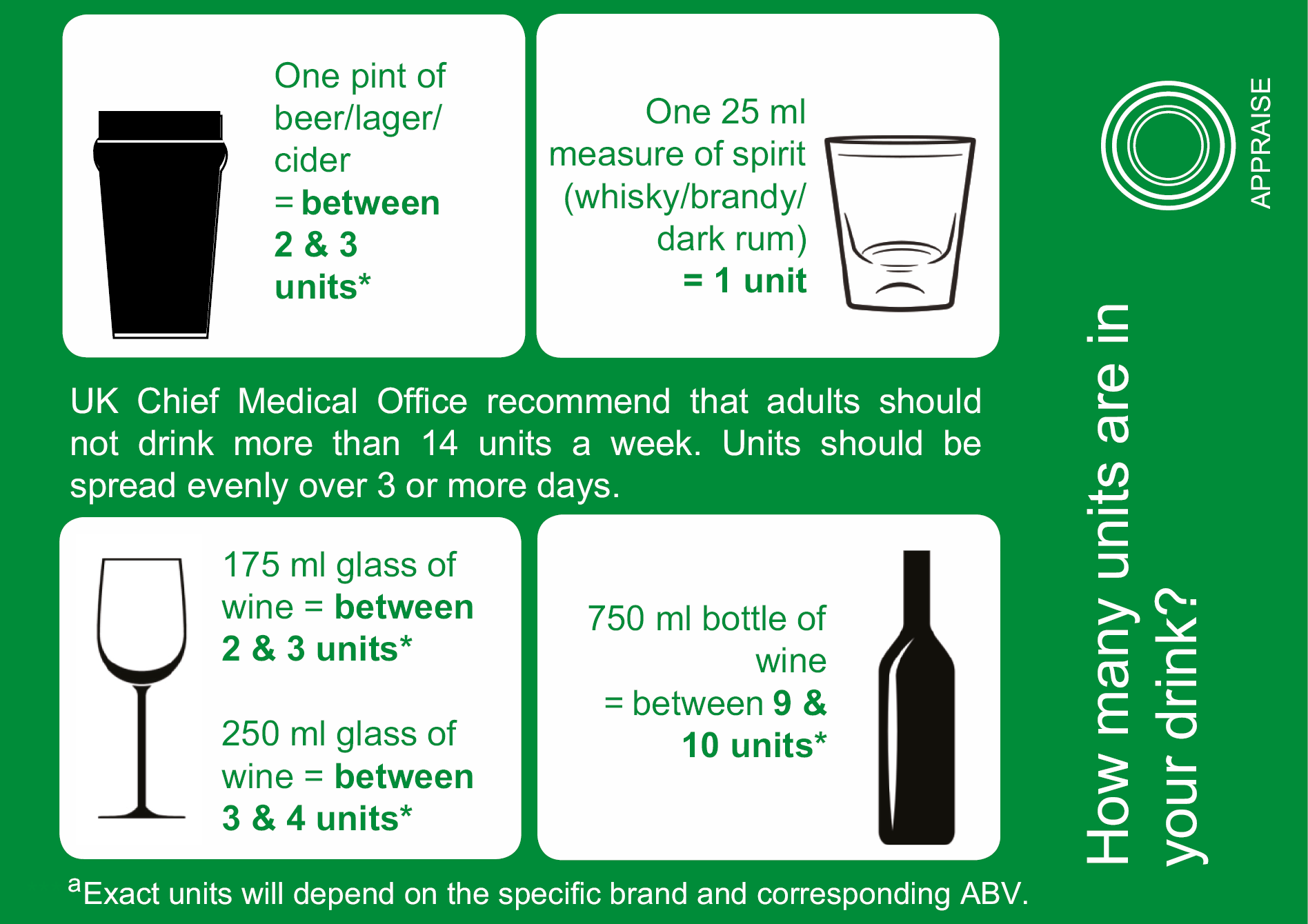

Appendix 6 Follow-up manual (V1_25 Sept19)


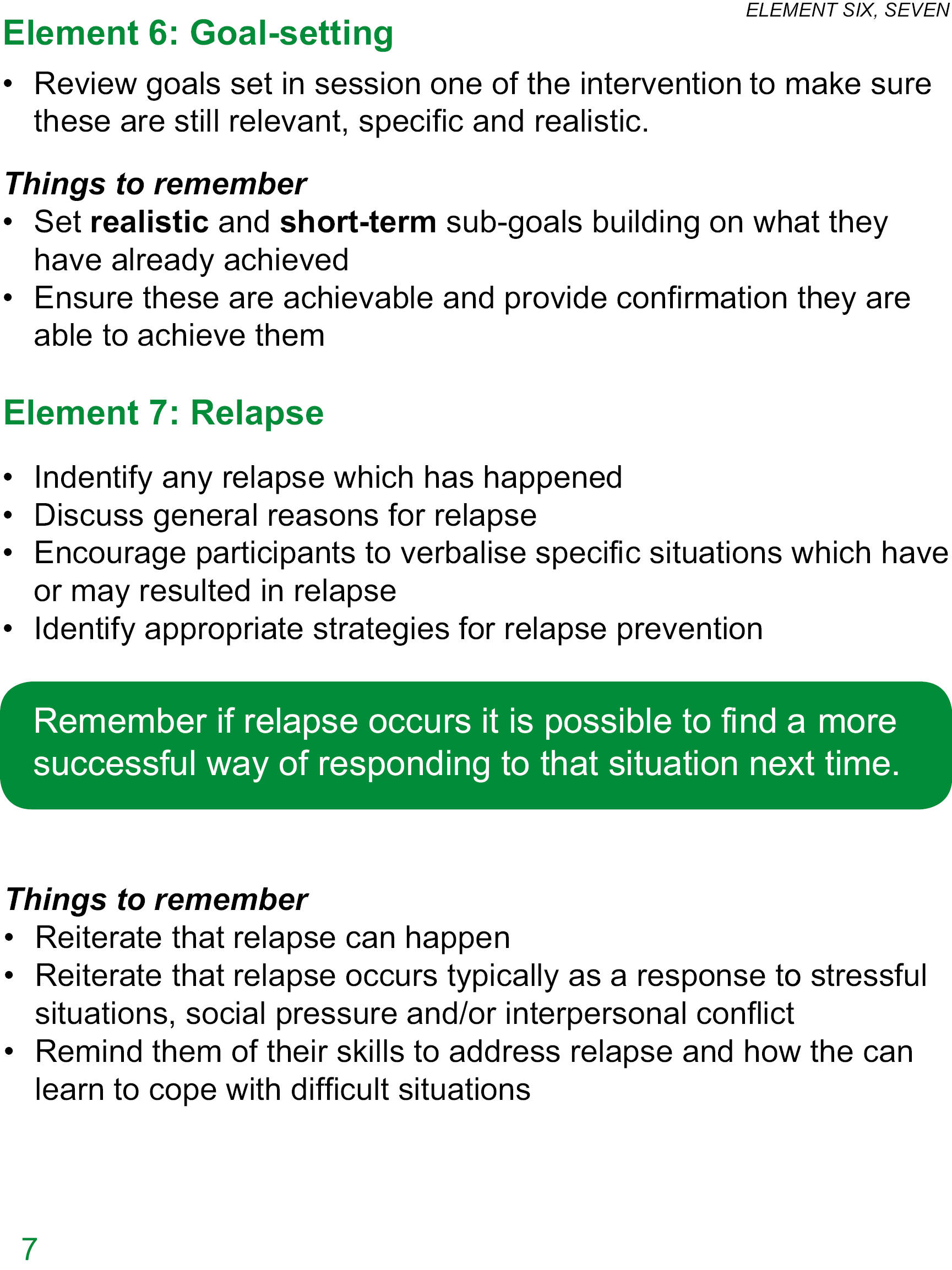

Appendix 7 APPRAISE training part 1
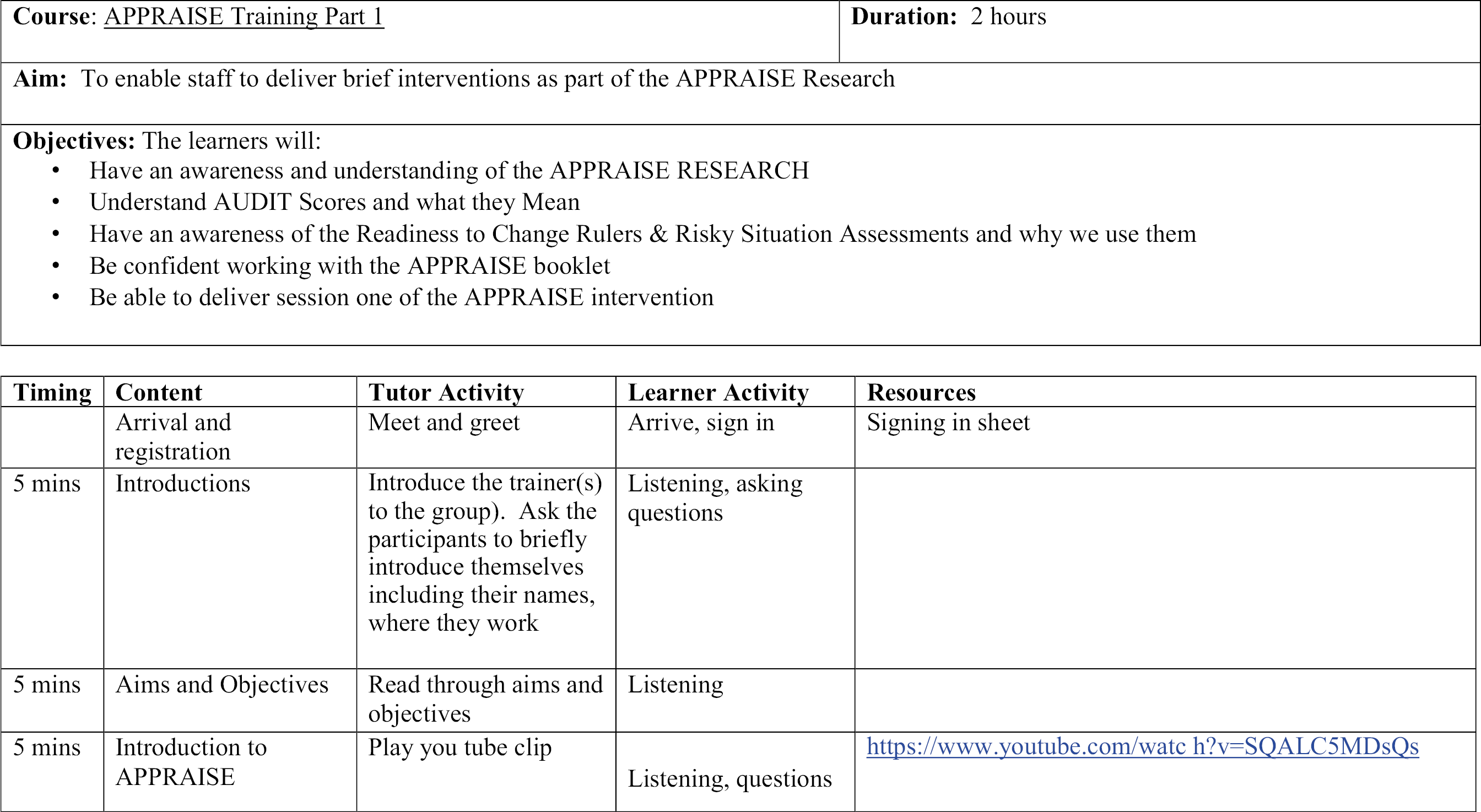
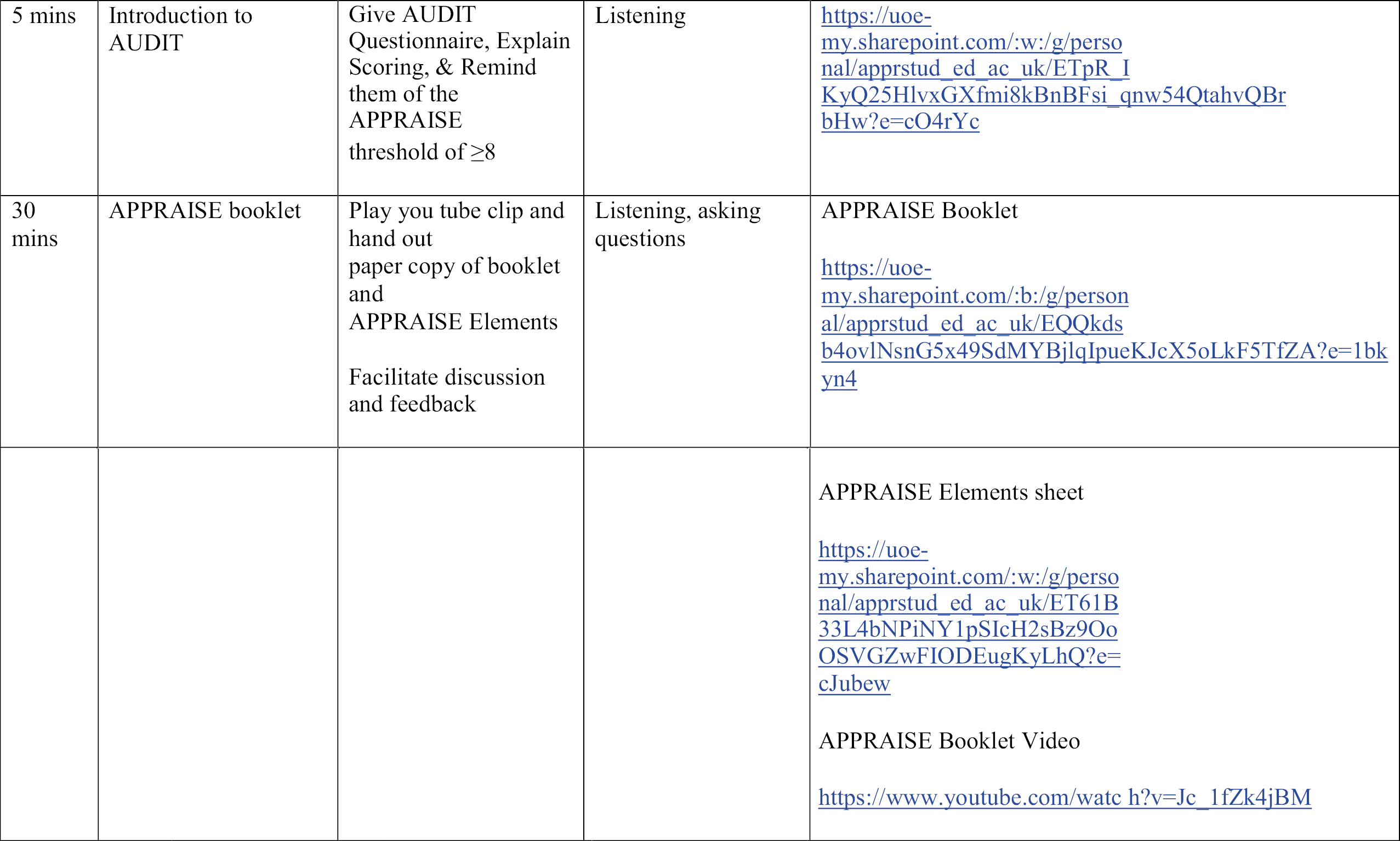
Appendix 8 Six-question Likert scale survey
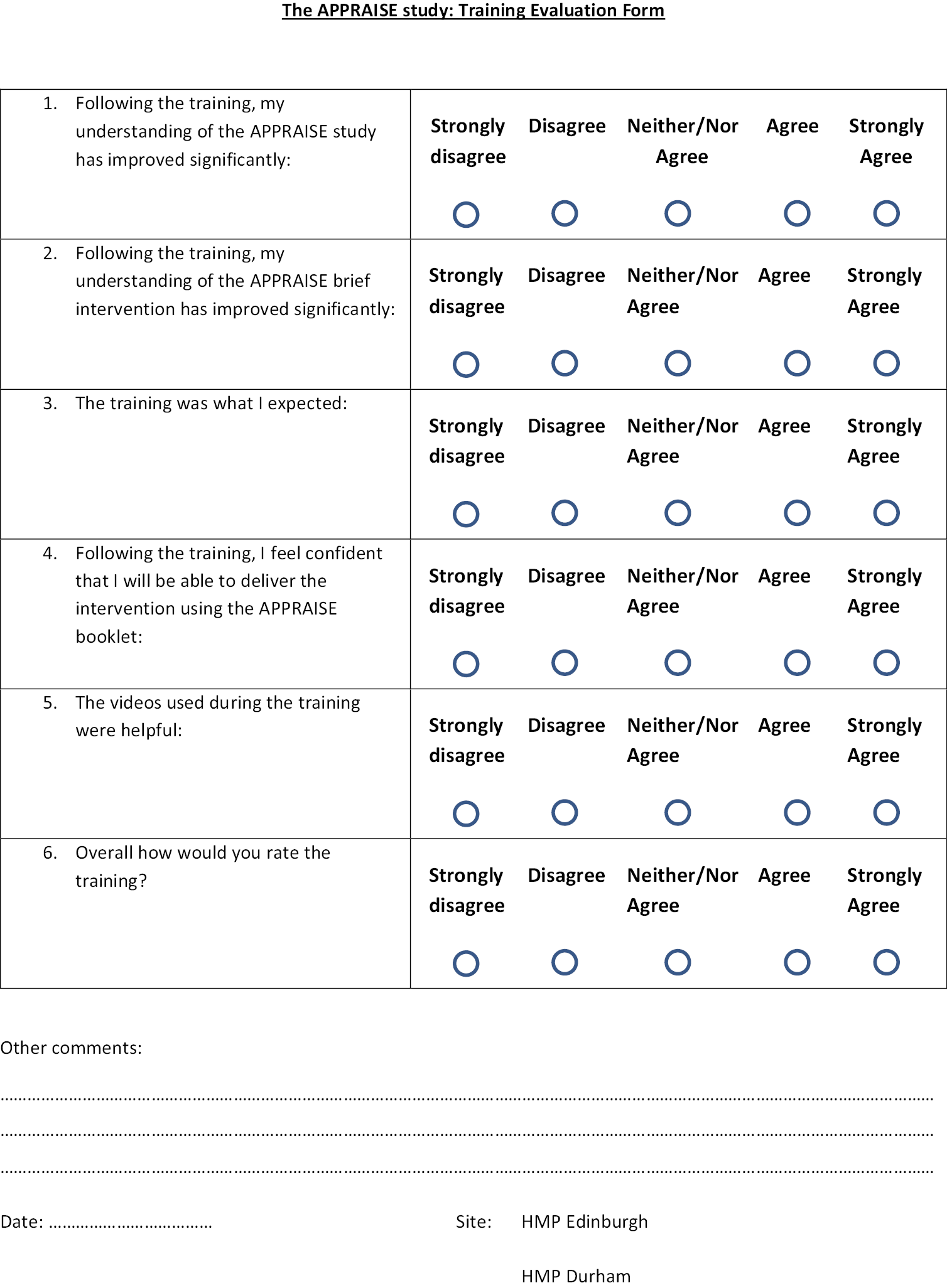
Appendix 10 Participant Locator Form
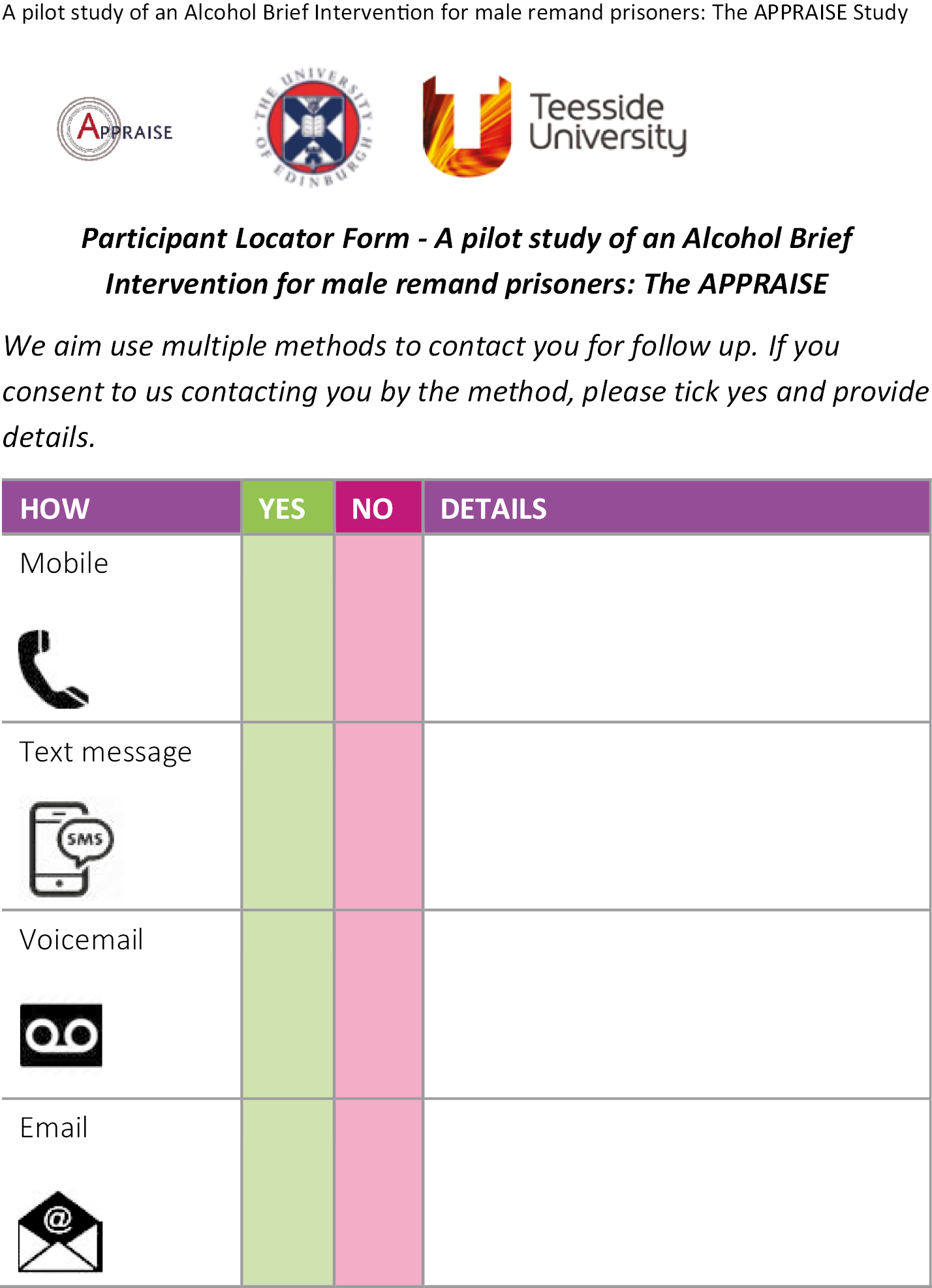
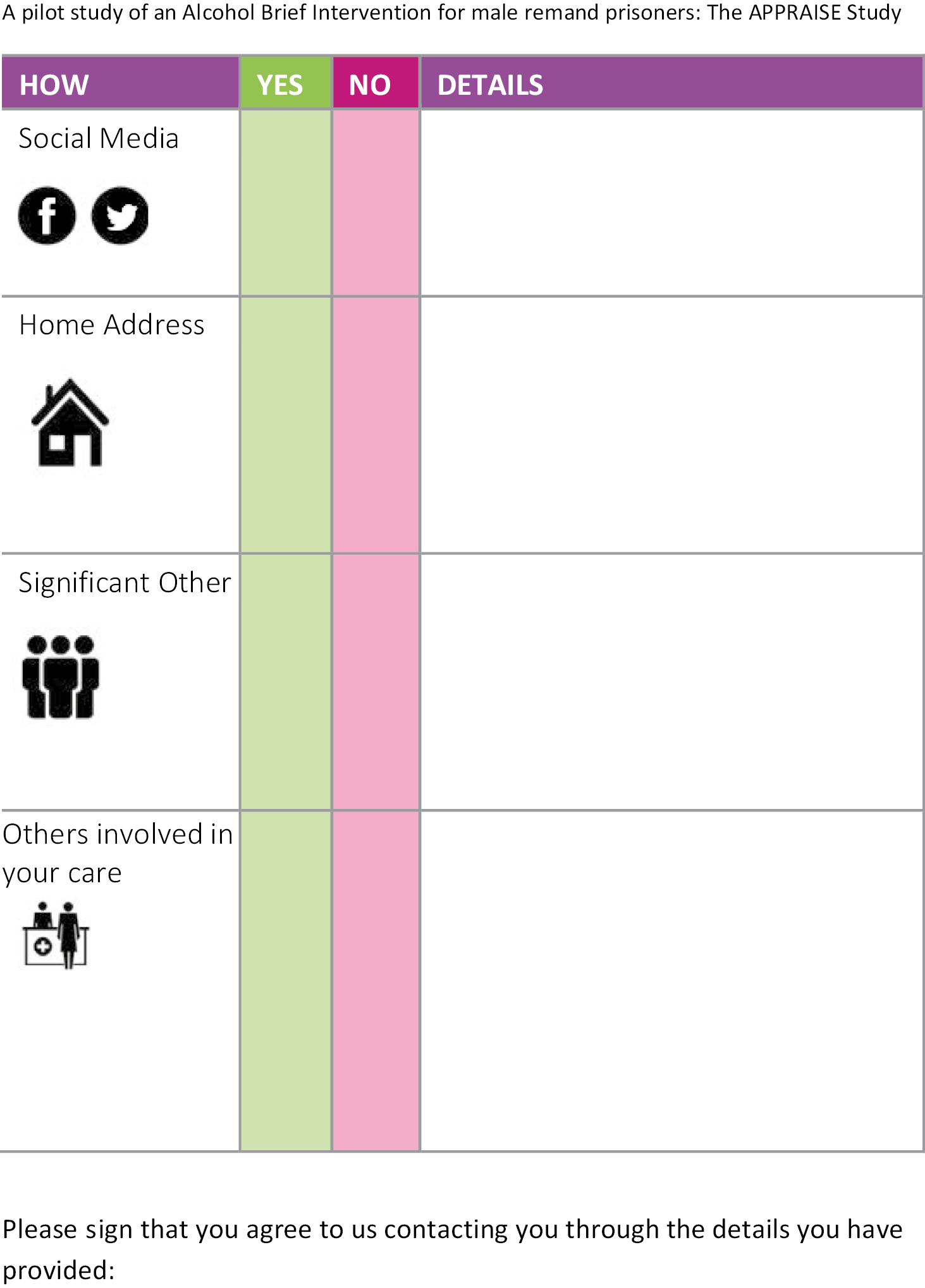
Appendix 11 Trial Steering Committee and Subcommittee terms of reference

A two-arm parallel-group individually randomised Prison Pilot study of a male Remand Alcohol Intervention for Self-efficacy Enhancement: the APPRAISE study
Terms of reference for the Trial Steering Committee (TSC)
These ToR will guide the scientific, administrative and operational direction of the APPRAISE Study.
Chief investigator (CI): Professor Aisha Holloway, School of Health and Social Science, the University of Edinburgh
Aims and objectives
The TSC has the primary aims of monitoring implementation of the APPRAISE feasibility trial, providing an independent assessment of the data analysis and determining if a future trial is merited.
The TSC has the following objectives:
-
Provide overall supervision of the trial on behalf of the trial sponsor and funder and ensure it is conducted to rigorous standards.
-
Comment on the progress of the trial and adherence to protocol.
-
Consider new information of relevance to the research question.
-
Provide advice, through the chair, to the chief investigator and trial funder on all appropriate aspects of the trial.
-
Provide evidence to support any requests for extensions.
In addition to the TSC, the chair plus three members of the TSC (who specialise in health economics, statistics, and qualitative methodology and analysis) will form a subcommittee responsible for data monitoring and ethics.
The subcommittee has the following objectives:
-
To monitor the data and make recommendation to the TSC on whether there are any ethical or safety reasons why the trial should not continue.
-
To ensure that the safety, rights and well-being of the trial participants remain paramount.
-
The subcommittee will consider the need for any interim analysis.
-
The subcommittee is the only body who, if necessary, will have access to the unblinded data.
Meeting
The TSC will meet bi-annually. Members are able to join the meeting by teleconferencing. A meeting will be considered quorate when at least seven members are in attendance. Aisha Holloway and Victoria Guthrie will be responsible for calling, organising and minuting the meeting.
The subcommittee will meet prior to the TSC meeting. Members are able to join the meeting by teleconferencing. There is no quorate to this meeting. Jamie Smith will be the administrator of this group and responsible for minuting the meeting.
Duration: the group will function for the entire duration of the APPRAISE study.
Membership
Current membership is as follows:
| Name | Position |
|---|---|
| Professor Frank Sullivan (Chair) | Professor of Primary Care Medicine, Director of Research |
| Professor Olivia Wu | Professor of Health Technology Assessment (Health Economics and Health Technology Assessment), Director of the HEHTA Research Unit |
| Dr Fergus Daly | Statistician at Frontier Science |
| Hon Professor Alex McMahon | Chair of the National Prisoner Health Care Network, Executive Director, Nursing, Midwifery, and Allied Health Professionals, Executive Lead, REAS and Prison Healthcare, NHS Lothian |
| Dr Justina Murray | CEO Scottish Families Affected by Drugs and Alcohol |
| Ms Joanne O’Connor | Director at Junction 42 |
| Ms Jessica Davidson | Senior Clinical Forensic Charge Nurse |
| Dr James Carnie | Director of Research and Evaluation at the Scottish Prison Service |
| Mr Frank Reilly | Director at the Scottish Recovery Network |
| Ms Tracey Stewart | Community Alcohol-Related Damage Service (CARDS) Volunteer Co-ordinator at Rowan Alba |
| Dr Anne Whittaker | Associate Professor and Clinical Academic |
| Ms Alison Douglas | Chief Executive at Alcohol Focus Scotland |
| Mr Pete White | Chief Executive at Positive Prison? Positive Future |
| Mr Nigel Johnson |
Appendix 12 Consolidated Health Economic Evaluation Reporting Standards 2022 checklist
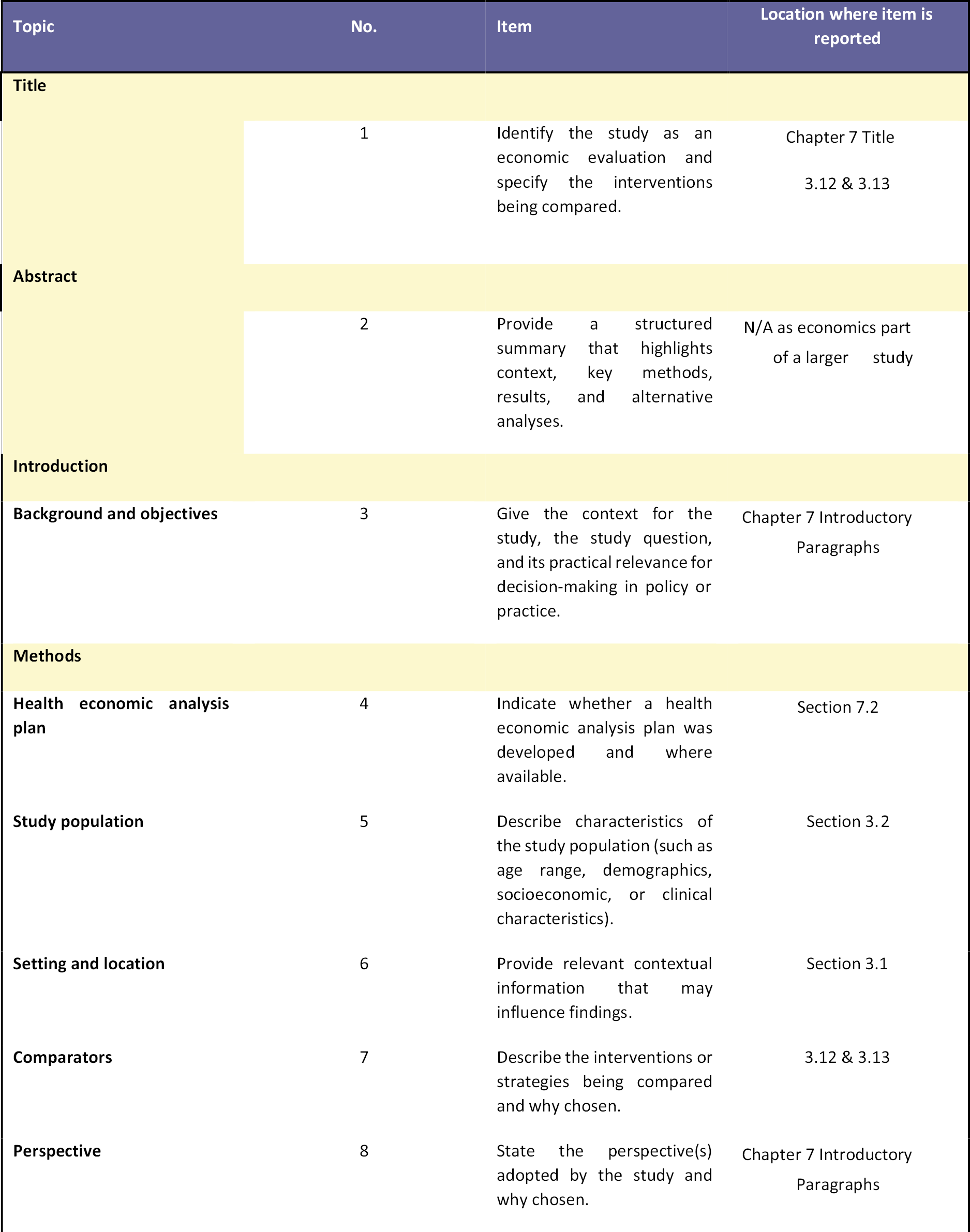
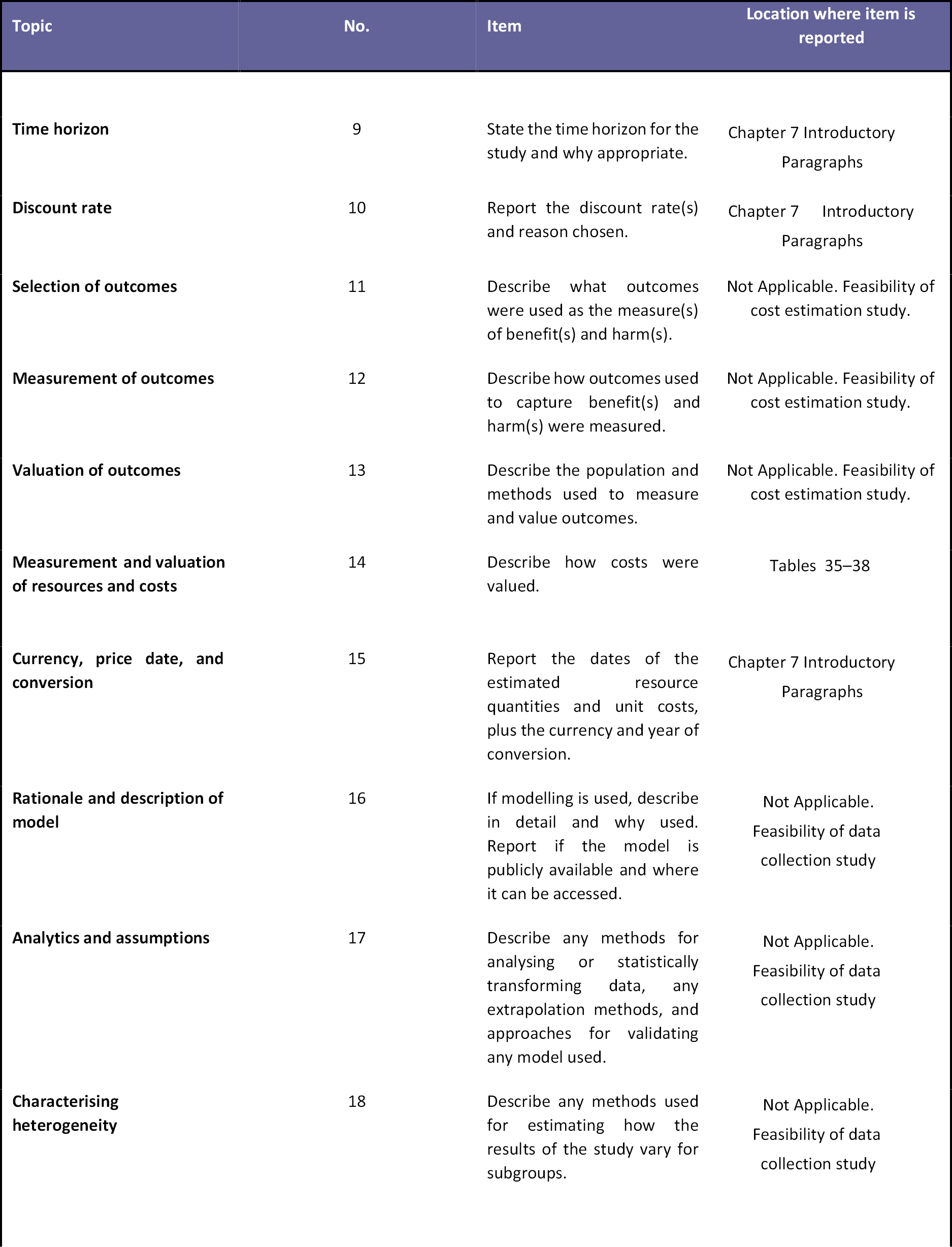
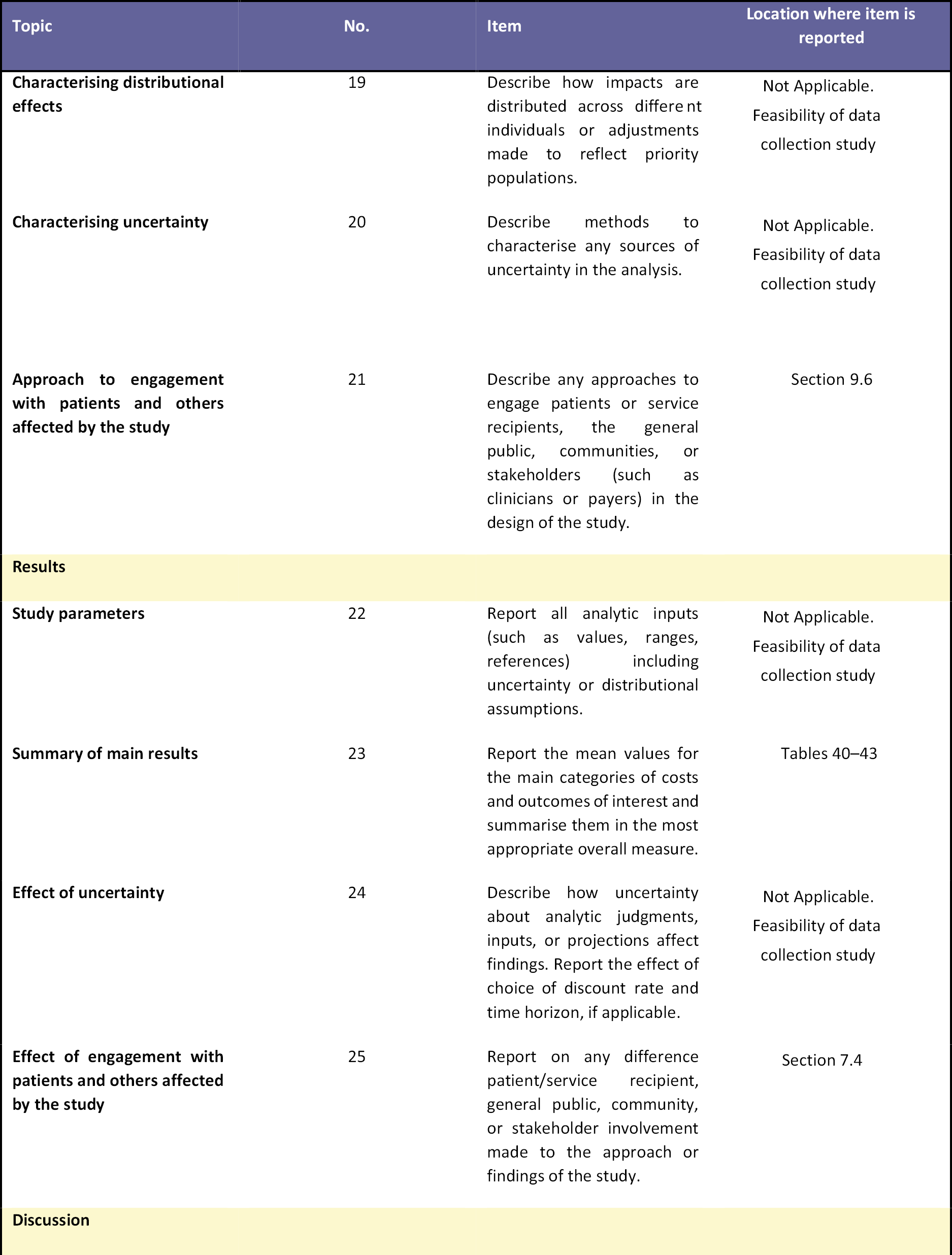
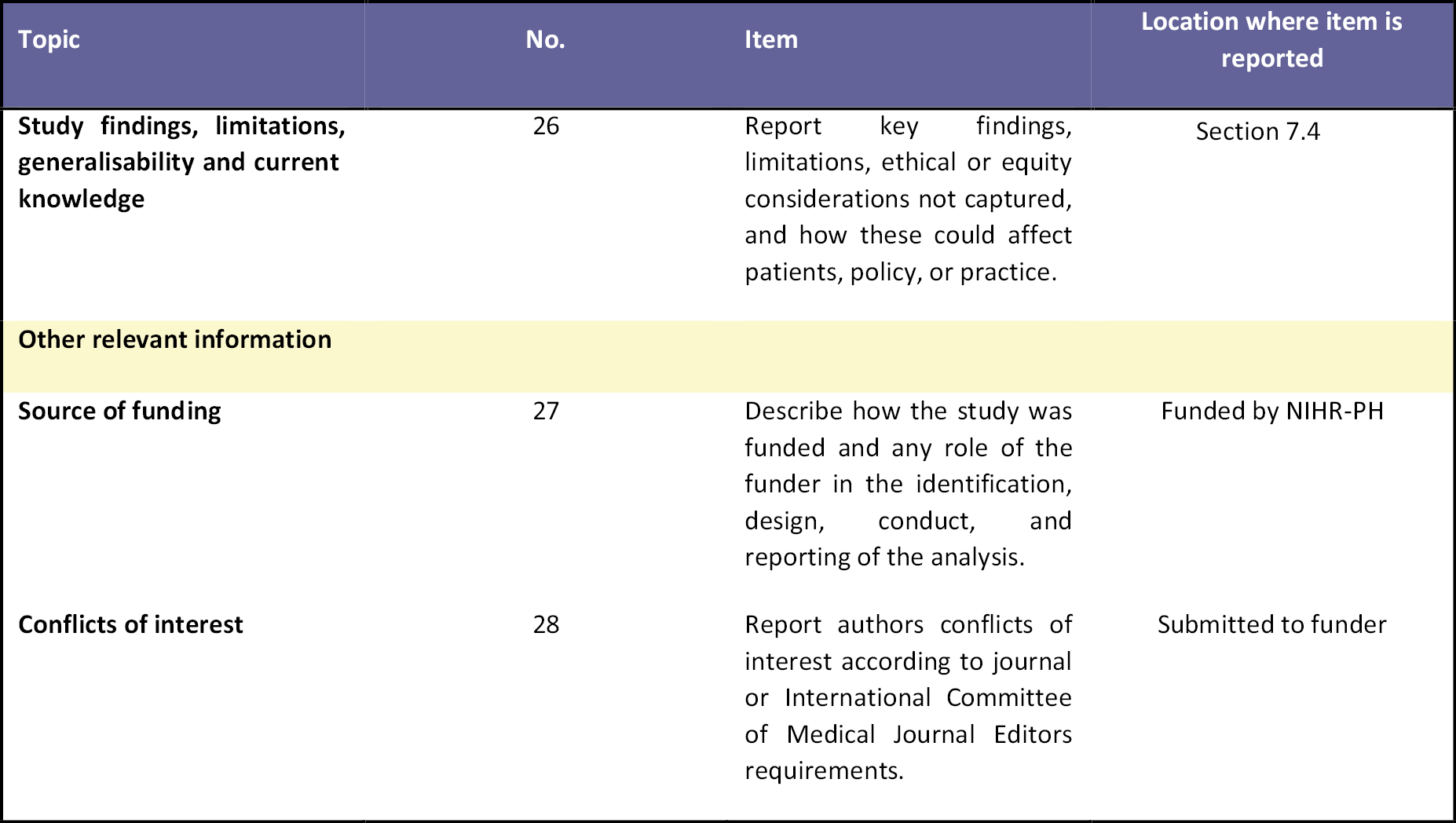
List of abbreviations
- AA
- Alcoholics Anonymous sessions
- ABC
- activity-based costing
- ABI
- alcohol brief intervention
- APPRAISE
- A two-arm parallel group individually randomised Prison Pilot study of a male Remand Alcohol Intervention for Self-efficacy Enhancement
- AUDIT
- Alcohol Use Disorders Identification Test
- AUDIT-C
- Alcohol Use Disorders Identification Test – Consumption
- BECCI
- Behaviour Change Counselling Index
- CEA
- cost-effectiveness analysis
- CGL
- Change Grow Live
- CHEERS
- Consolidated Health Economic Evaluation Reporting Standards
- CI
- chief investigator
- CJM
- community justice mentor
- CJS
- criminal justice system
- CJSW
- criminal justice social worker
- CONSORT
- Consolidated Standards of Reporting Trials
- COVID-19
- coronavirus disease discovered in 2019
- CRF
- case report form
- DART
- Drug and Alcohol Recovery Team
- DMEC
- Data, Monitoring and Ethics Committee
- DRSEQ-R
- Drinking Refusal Self-efficacy Questionnaire – revised
- ECTU
- Edinburgh Clinical Trials Unit
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FRAMES
- Feedback, Responsibility, Advice, Menu, Empathy, Self-efficacy
- GDP
- gross domestic product
- GDPR
- General Data Protection Regulation
- GP
- general practitioner
- HMPPS
- His Majesty’s Prison and Probation Service
- HMPS
- His Majesty’s Prison Service
- HRA
- Health Research Authority
- IRAS
- Integrated Research Application System
- ITT
- intention-to-treat
- MAR
- missing-at-random
- MCAR
- missing-completely-at-random
- mNCA
- model non-commercial agreement
- MoJ
- Ministry of Justice
- MRC
- Medical Research Council
- MRC-PHIND
- Medical Research Council Public Health Intervention Development
- NAEQ
- Negative Alcohol Expectancy Questionnaire
- NHS
- National Health Service
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NPT
- normalisation process theory
- PHE
- Public Health England
- PIS
- Participant Information Sheet
- PMG
- project management group
- PNC
- Police National Computer
- PPE
- personal protective equipment
- PPI
- patient and public involvement
- PRISM-A
- Alcohol Brief Interventions for Male Remand Prisoners
- PSS
- personal social services
- RA
- research assistant
- RAEC
- Research and Access Ethics Committee
- RCT
- randomised controlled trial
- SAS
- statistical analysis system
- SD
- standard deviation
- SIMD
- Scottish Index of Multiple Deprivation
- SPS
- Scottish Prison Service
- SPSS
- statistical package for social science
- TIDieR
- Template for Intervention Description and Replication
- TLFB-28
- timeline followback-28
- ToR
- terms of reference
- TP
- time point
- TSC
- Trial Steering Committee
- UK
- United Kingdom
- WEMWBS
- Warwick-Edinburgh Mental Well-being Scale
- WHO
- World Health Organization
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/KNWT4781).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.