Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3005/05. The contractual start date was in December 2010. The final report began editorial review in December 2012 and was accepted for publication in June 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Catherine Law is Director of the NIHR Public Health Research Programme, Editor-in-Chief of the Public Health Research journal and a former member of the NIHR Journals Library Board. Helen Roberts is a member of the NIHR Journals Library Editorial Group.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Law et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
Levels of childhood overweight and obesity have been rising steadily over the past decade. In 2010, 31% of 2- to 15-year-old boys and 29% of girls were overweight or obese; figures for obesity alone were 17% and 15% respectively. 1 Comparable figures in 1995 showed that 24% of boys and 26% of girls were overweight or obese, with 11% and 12% respectively classed as obese. 1 Although the rise in prevalence appears to be levelling off,2 rates of childhood overweight remain high.
Childhood overweight arises because of an imbalance between energy intake and expenditure. This is linked to increased sedentary behaviour (particularly related to screen-based entertainment), low physical activity and patterns of diet such as consuming high-fat and high-sugar foods and drinks. 3 These behaviours are potentially modifiable, but the causes of childhood overweight also need to be considered at a societal level as the features of ‘obesogenic’ environments which promote obesity often operate at levels largely beyond families’ control. 4,5
Compared with their peers with healthy weight, overweight children have a higher risk of a range of adverse health and other outcomes. These include fatty liver disease, childhood-onset type 2 diabetes mellitus, adverse cardiovascular risk profiles, impaired psychological health, low self-esteem and being a perpetrator and/or victim of bullying. 5,6 Both the prevalence and adverse consequences of childhood overweight and obesity are underestimated by parents. 7 This may reflect general desensitisation to seeing excess body fatness, such that overweight among children is seen as normal, fatalism (‘nothing can be done about it’), optimism (‘they’ll grow out of it’) or denial of a stigmatising problem. 8 Childhood obesity is a risk factor for adult obesity, and so is associated with an increased risk of premature mortality and morbidity from a range of adult conditions. 5,6 In addition to its substantial health impact, obesity is projected to have significant future cost implications for the NHS. Using a microsimulation model, it has been estimated that the NHS costs of managing obesity and its consequences in England will reach £9.7B by 2050,3 around 10% of NHS expenditure at 2007 levels. The societal costs of obesity, including those from lost productivity and premature death, are projected to be £49.9B in 2050. 3,9
Despite the scale of childhood overweight, and a large research endeavour, relatively few effective interventions for the prevention or treatment of childhood overweight have been described. Authoritative syntheses of evidence, both international10,11 and applied to UK settings,5,9,12 for treatment of childhood overweight and obesity have noted that there is insufficient evidence to recommend one programme over another, although principles of effective interventions have been established. In addition to the changes needed to the obesogenic environment,13 these principles include addressing diet and physical activity, behaviour change, involvement of the family and a positive emphasis on managing a healthy lifestyle for the whole family.
Evaluation of a scaled-up weight management intervention
In this study we examine a weight management intervention, Mind, Exercise, Nutrition, Do it! (MEND) 7–13 (www.mendcentral.org). It is one of a suite of interventions offered by MEND Central, a limited company delivering weight management interventions from early childhood to adulthood. MEND 7–13 is a multicomponent family-based intervention which aims to support families of overweight and obese children to adopt and sustain healthy lifestyles. Children are eligible for the programme if they are aged 7–13 years and are overweight or obese (referred to as overweight throughout this document, unless otherwise specified), defined as exceeding the 91st centile of the UK 1990 growth charts. 14 The programme was shown to be effective in reducing body mass index (BMI) and improving self-esteem after 6 months and 1 year in a randomised controlled trial (RCT). 15
The MEND 7–13 intervention meets the guidelines for weight management interventions outlined above. 9 It combines principles of nutritional and sports science with those from psychology, learning and social cognitive theories and the study of therapeutic processes. It seeks to address three components necessary for individual-level behavioural change – education, skills training and motivational enhancement16 – while recognising the need to engage multiple, interacting systems of influence within the family context. 17 It was developed on the basis of literature and expert guidance9 and to be delivered in community settings. Because of the importance of family involvement for behaviour change, the programme requires a parent or carer to attend all sessions.
The intervention was ‘scaled up’ rapidly across England from 2007. Scaling up has been defined as:
. . . a policy that builds on one or more interventions with known effectiveness and combines them into a programme delivery strategy designed to reach high, sustained, and equitable coverage, at adequate levels of quality, in all who need the interventions[.]
p. 154118
There is a lack of information about what happens when public health interventions deemed to be effective under research conditions are scaled up for delivery under service conditions. 19 This arises partly because outcome data are often not collected and/or collated during service delivery. We drew on data collected by MEND 7–13 delivery partners (individuals and organisations who co-ordinate and run local MEND programmes) and collated and held by MEND Central. Data were available for > 20,000 children referred to MEND 7–13, to examine characteristics of this scaled-up weight management programme.
Using quantitative and qualitative methods, we aimed to assess whether and how MEND contributes to tackling childhood overweight under service conditions, how it works in different contexts, for whom and why. We addressed these aims through the following specific research questions (which are addressed in Chapters 2–6).
-
What are the characteristics of children who take part in MEND, a family-based intervention for childhood overweight and obesity, when implemented at scale and under service conditions?
-
How do the outcomes associated with participation in MEND vary with the characteristics of children [sex, socioeconomic circumstances (SEC) and ethnicity], MEND centres (type of facility, funding source and programme group size) and areas where children live (in relation to area-level deprivation and the obesogenic environment)?
-
What is the cost of providing MEND, per participant, to the NHS and personal social services (PSS), how does this vary and how is it related to variation in outcome?
-
What is the salience and acceptability of MEND to those who commission it, those who participate in full, those who participate but drop out and those who might benefit but do not take up the intervention?
-
What types of costs, if any, are borne by families (and by which members) when participating in MEND, and in sustaining a healthy lifestyle afterwards?
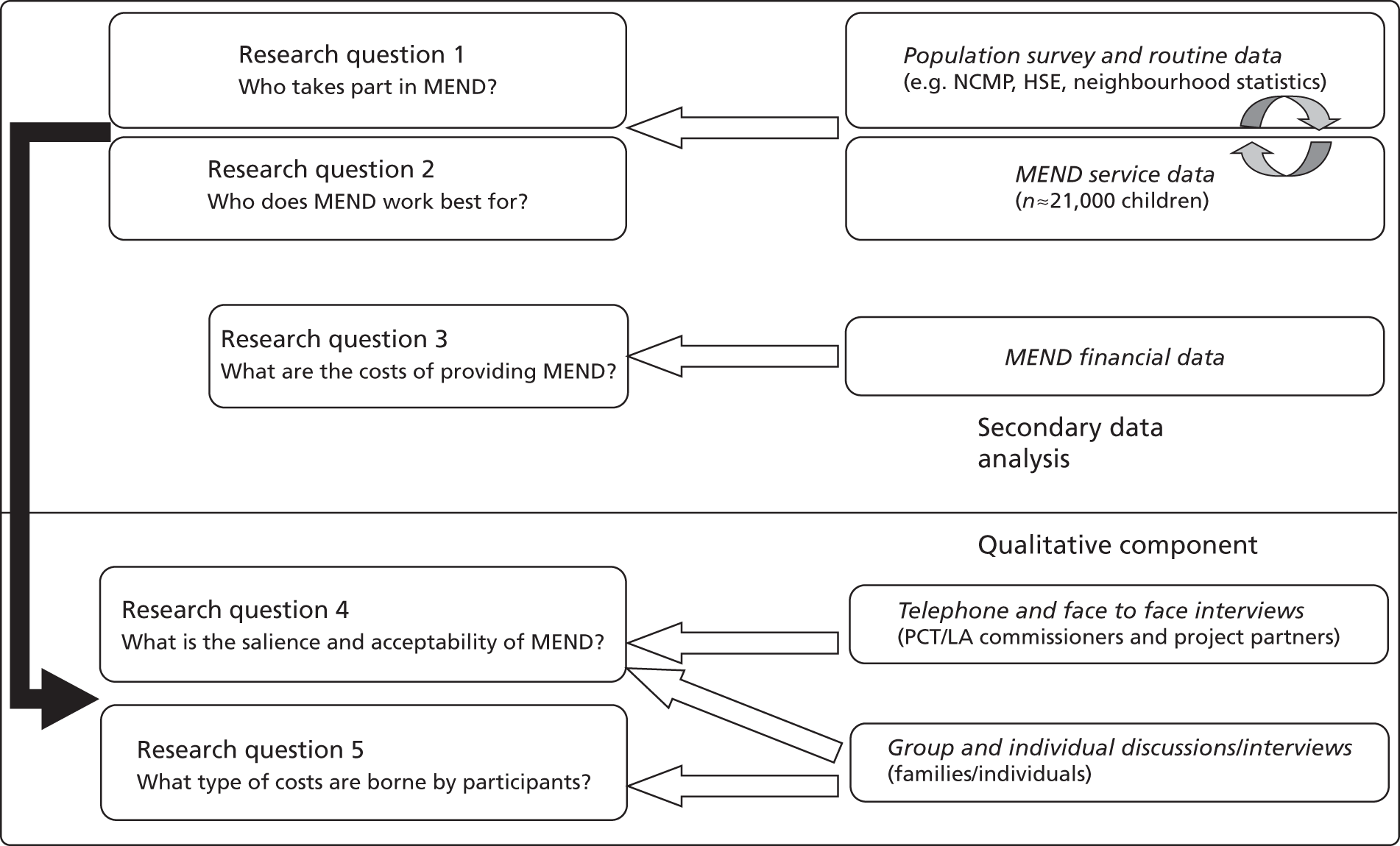
These questions, their rationale and the methods used to address them are summarised in Figure 1 and described briefly here. Further detail is given in Chapters 2–6.
FIGURE 1.
Schematic of study design. HSE, Health Survey for England; LA, local authority; NCMP, National Child Measurement Programme; PCT, primary care trust.
Research question 1: Who takes part in MEND?
Children living in disadvantaged SEC are more likely to be overweight than their more advantaged peers. 20 In addition, the proportion of children who are overweight varies by ethnic group. 21 Research also suggests that some families (those in more advantaged SEC, for example) may be more likely to access or benefit from services which support behaviour change. 22
Given the socioeconomic and ethnic inequalities in childhood overweight and potential inequities in the use of services (including weight management services), we examined the question of who takes part in the MEND 7–13 programme. To do this, we used service data from MEND 7–13 and information from routine data sources about the characteristics of children who would be eligible to take part in the programme. MEND 7–13 participants were described by their age, sex, ethnicity, SEC and characteristics of their residential neighbourhood. The MEND 7–13 participants’ sociodemographic profiles were then compared with those of respondents to three nationally representative surveys [the Health Survey for England (HSE), the Millennium Cohort Study (MCS) and the National Child Measurement Programme (NCMP)]. This analysis is described in full in Chapter 2.
Research question 2: Who does MEND work best for?
Interventions might work less well for some groups than others, and so create or exacerbate inequalities through differential effectiveness. 23 Research suggests that some groups (again, those with more favourable SEC) may be more receptive to interventions aimed at promoting healthy patterns of diet and physical activity. 24 MEND 7–13 (like some other weight management interventions) was evaluated in a relatively small (n = 116) RCT15 which (in common with similar intervention studies) was not designed to investigate whether effects varied by sex, ethnicity or SEC. Therefore, questions remain about whether outcomes associated with participation in MEND 7–13, weight management programmes more generally, and indeed public health programmes in general, vary with these characteristics. 23 We examined how changes in outcomes associated with participation in MEND 7–13 varied by the sociodemographic characteristics of participants and the places where they lived.
Interventions need to be understood as part of a complex system, rather than one-off events which can be understood in isolation. 25 The substantial variations in the contexts where the MEND 7–13 service was delivered, combined with the large size of the data set, allowed us to estimate how changes in outcomes varied by characteristics of programmes and contexts. We estimated whether outcomes associated with MEND 7–13 were moderated by obesogenic characteristics of the environment (such as the density of fast food outlets or access to green space in the local neighbourhood). We also estimated whether differences in programmes accounted for differences in outcomes.
Randomised controlled trials are often conducted with highly selected populations in academic settings,10 meaning that conclusions about effectiveness cannot necessarily be generalised for all groups in the population. 26 In the case of MEND 7–13, the RCT was delivered only to children who were obese, although both overweight and obese children are eligible for the MEND 7–13 service following its implementation into practice. Additionally, as discussed above, once scaled up, the service was delivered across a wide range of contexts. There was therefore significant potential for outcomes under service conditions to vary from those observed in the RCT.
Although the RCT of MEND followed children up for 12 months, such long-term follow-up of participants in large-scale service interventions is unusual and would be costly. Our analyses could only assess changes associated with participation in the MEND 7–13 programme from the first to the penultimate sessions (the time of the last measurement), a period of 10 weeks. We compared unpublished RCT data over a comparable period of follow-up with these service data.
These analyses are described in full in Chapters 3 and 4.
Research question 3: What are the economic costs of MEND?
Evaluations of this type are developed in part to inform decision-making by those considering whether or not to commission weight management interventions like MEND 7–13. The economic costs of interventions are clearly an important component of such decisions. We aimed to analyse cost data for MEND 7–13 to estimate the overall cost of delivery and to characterise the types of costs which were involved in running the programme, over and above the costs of the programme itself.
Although our initial intention (as illustrated in Figure 1, research question 3) was to conduct a de novo analysis of MEND financial data, in the course of reviewing the literature we identified work which had recently estimated these costs for MEND 7–13 on a national and local level. These sources were reviewed and used for our analysis rather than repeating work already undertaken. This analysis is described in full in Chapter 4.
Research questions 4 and 5: What is the salience and acceptability of MEND to those who commission and use it, and what types of costs are borne by participants?
Proponents of the evidence and effectiveness agendas27 have long understood the importance of collaborating with citizen, policy, funding and practitioner users if research is to influence practice. 28 Literature on the difficulties of implementation, the tension between programme fidelity and responsiveness to local needs and the importance of context29–31 informed our approach to research questions 4 and 5.
Our qualitative research was designed to address the salience and acceptability of the intervention to users, non-users and providers. Hawe et al. 32 point to the context-level factors which may affect intervention uptake, success, and sustainability and which include primary care agencies and local adaptation of an intervention. In the course of our study, the NHS was undergoing fundamental reorganisation as a result of proposals subsequently set out in the Health and Social Care Act 2012. Commissioners and service delivery partners, never professionals with time on their hands, were experiencing considerable churn in the system, and we were concerned to capture insights from these provider groups as early as possible in the study. They were selected from a database provided by MEND Central. The interviews were designed to explore the ways in which commissioning and recommissioning decisions were made, what worked well or less well, and the tension between programme fidelity and responsiveness to local context (see Appendix 14 for topic guide). Our findings from these interviews are set out in Chapter 5.
Families were selected from the same MEND database as that used in the quantitative analysis, up to 4 years after they had participated in a MEND 7–13 programme. Interviews began with open questions about family make up and memories about MEND, followed by discussions of barriers and levers to participation, costs and benefits within the family, and life after MEND (see Appendix 14 for topic guide). Our findings from these interviews are set out in Chapter 6.
Roles of the research team
The study was designed and planned by the investigators and project partners. Quantitative analyses were undertaken by Jamie Fagg, supported by team members with expertise in public health epidemiology, policy and health inequalities in childhood (Catherine Law), geographies of health and community evaluation (Steve Cummins) and statistical expertise in child growth, multilevel modelling and the handling of missing data (Tim Cole and Harvey Goldstein). The analysis of the costs of MEND 7–13 was co-ordinated by Steve Morris, a health economist.
Qualitative work was co-ordinated by Helen Roberts. Families and commissioners were purposively selected for recruitment using criteria set out in our grant application. The methods of operationalising these criteria were developed by Jamie Fagg in discussion with the qualitative research team. Families and commissioners were selected by Jamie Fagg, and Hannah Lewis contacted and recruited respondents to the study. Interviews were conducted and analysed by a team of four experienced qualitative researchers (Helen Roberts, Katherine Tyler, Patricia Lucas and Lisa Arai). Additional work on the analysis and report of the commissioner study was conducted by Sally Stapely.
The team members met regularly in the context of the project management group and within subgroups to take part in the planning, management and reporting of the project.
Data from MEND 7–13 were transferred to the Institute of Child Health research team by employees of MEND Central (Paul Sacher, Paul Chadwick and Duncan Radley). They also provided advice on some aspects of the design and development of the project and the technical details of the intervention but did not participate in the analysis of the data (see Management of competing interests). Analyses of the NCMP were commissioned from the National Obesity Observatory (NOO).
The project overall was managed by Catherine Law. Jamie Fagg co-ordinated and managed the project on a day-to-day basis, with support from Hannah Lewis and Chloe Parkin.
Public involvement
The protocol for the project was discussed with the National Children’s Bureau’s (NCB’s) young person’s Public health, Education, Awareness, Research (PEAR) group in 2009. The group’s suggestions (see Appendix 3) informed the successful grant application and the planning of the project. Findings from the study were presented to the comparable NCB Research Advisor’s Group in July 2012 for their feedback (see Appendix 3), which is reflected in the discussion of our results (see Chapter 7).
Ethical considerations
We applied for three sets of ethical approval reflecting the three distinct components of our study. The first two applications were to UCL Ethics Committee for the quantitative secondary data analysis and the qualitative study of families. The committee granted approval for the quantitative study in October 2010 (ref. 2677/002) and for the qualitative study in February 2011 (ref. 2842/001).
As the third element of the study involved a qualitative study of commissioners, many of whom were based in the NHS, we sought NHS Research Ethics (NRES) permission. The NRES committee that reviewed our application deemed this component of the study to be a service evaluation not requiring NRES permission (East London Research Ethics committee ref. 11/H0703/3). As a service evaluation it was also exempt from the need to seek ethics permission from UCL Ethics Committee. We conducted this component of the project with reference to the framework for research ethics produced by the Economic and Social Research Council (ESRC). 33
Management of competing interests
MEND describes itself as a social enterprise – an ethical business which aims to benefit society in general. In the UK, MEND has two operating arms: MEND Central, a limited company, and MEND Places, a not-for-profit company originally set up to provide a route for donations to subsidise places for families on the MEND programme. To date, all those commissioning MEND 7–13 placed funding through MEND Central. As discussed above, three members of the project management group (Sacher, Chadwick and Radley) were employees of MEND Central Ltd. Sacher and Chadwick are also shareholders. They therefore had an interest in MEND Central’s success.
The MEND programme was aimed at 7- to 13-year-olds, based on research undertaken at the Institute of Child Health. Under a contractual relationship, the Institute of Child Health received a proportion of the revenues generated from this programme. These sums were less than £10,000 per annum between 2007 and 2010. The Institute used these funds to support nutrition research and none of the research team had access to these funds, nor works in the department where the funds were held.
Given that results from the project might support, threaten or have no effect on MEND Central’s success, our grant application and subsequent protocol set out governance measures to ensure that these competing interests, and the interests of project stakeholders, were managed appropriately. The project was run according to these measures, with minor variations approved by the National Institute for Health Research (NIHR). Details of governance procedures were agreed with the project advisory group (PAG) (see Appendix 1 for PAG terms of reference). The policy on competing interests was also agreed with this group; see Appendix 2 for full details.
Chapter 2 Who takes part in the MEND 7–13 programme?
What are the characteristics of children who take part in MEND, a family-based intervention for childhood overweight and obesity, when implemented at scale and under service conditions?
Background
We were interested in how far the sociodemographic characteristics of children who were referred to and participated in MEND 7–13 reflected those of the population who were eligible for the intervention. As emphasised by Glasgow et al. ,34 assessment of the reach of interventions is, alongside effectiveness, an important step when considering the population-level impact on health. In particular, research should assess two aspects of reach. First, to what extent are participants in interventions representative of the target population? Second, how far do interventions reach their target population in terms of the percentage who are referred, take up the intervention and complete the intervention? We draw on MEND 7–13 service data and routine data sources to address these issues in this chapter.
Data
MEND 7–13 service-level data
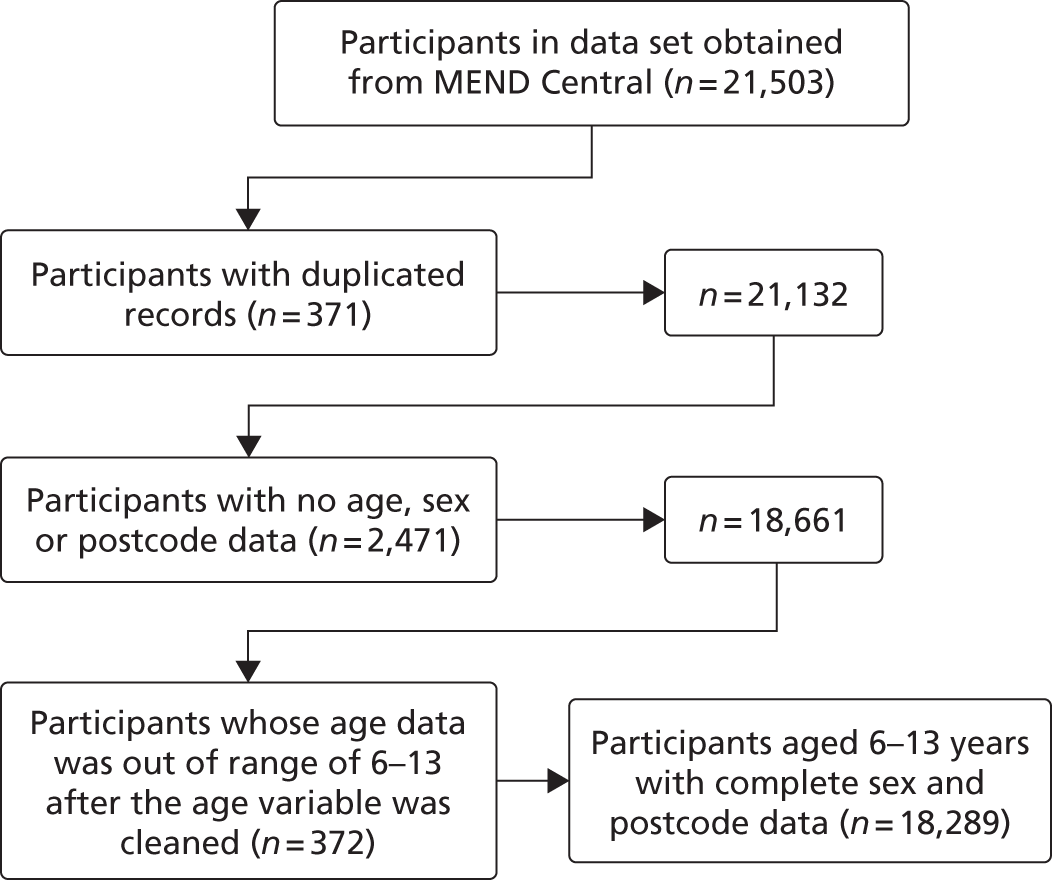
Service-level data about the MEND 7–13 programme were collected by local MEND programme managers and collated by MEND Central between January 2007 and December 2010. All analyses of service data (n = 21,503) were also restricted to those with no duplicate observations in the data set and those with completely observed information for age, sex and postcode (Figure 2).
FIGURE 2.
Derivation of analysis sample, excluding participants with duplicate records, partially observed data on age, sex or postcode and those outside the age range 6–13 years.
Outcome variables: adiposity, psychosocial health and lifestyle
All outcome variables (Table 1) were measured at baseline (the first session of the programme) and follow-up (the penultimate session). The primary outcome used in the study was change in body mass index (BMI), calculated from height and weight [(weight/height)2] measured by MEND 7–13 staff. We also investigated change in age- and sex-standardised BMI (zBMI), self-esteem measured by a modified version of the Rosenberg self-esteem scale35 (participant reported), participant psychological distress measured by the Strengths and Difficulties Questionnaire (SDQ, parent-reported version),36 and questions devised by MEND Central about participants’ levels of physical activity and the healthiness of their diets (both parent reported). Analyses of these outcomes are reported in detail in Chapters 3 (changes in BMI and zBMI) and 4 (changes in psychosocial and lifestyle outcomes).
| Variable | Measured at baseline (B) or follow-up (F) | Data management of MEND Central data by the ICH team | Variable (coding) |
|---|---|---|---|
| Birthdate | B | No additional data management at ICH | Date (day/month/year) |
| Measurement date | B and F | No additional data management at ICH | Date (day/month/year) |
| Age | B and F | Derived from birth and measurement dates | Continuous (accurate to day) |
| Sex | B | No additional data management at ICH | Girls (0)/boys (1) |
| Height | B and F | Outliers removed at ICH | Continuous (nearest 0.1 cm) |
| Weight | B and F | Outliers removed at ICH | Continuous (nearest 0.1 kg) |
| BMI | B and F | BMI calculated at ICH from height and weight | Continuous (kg/m2) |
| Change in BMI | F – B | Baseline subtracted from follow-up | Continuous (kg/m2) |
| zBMI | B and F | zBMI calculated at ICH from UK 1990 data, age, sex, height and weight | Continuous (standardised units) |
| Change in zBMI | F – B | Baseline subtracted from follow-up | Continuous (standardised units) |
| Self-esteem (on Rosenberg self-esteem scale) | B and F | Scale calculated at ICH using published instructions | Continuous (range 0–30) |
| Change in self-esteem | F – B | Baseline subtracted from follow-up | Continuous |
| SDQ | B and F | Scale calculated at ICH using published instructions | Continuous (range 0–42) |
| Categorical baseline SDQ score | B | Derived at ICH using published instructions | Categorical (normal = 0–13 symptoms, borderline = 14–16 symptoms, abnormal = 17–37 symptoms) |
| Change in SDQ score | F – B | Baseline subtracted from follow-up | Continuous |
| PA | B and F | Items (walking and cycling) selected and collated at ICH | Continuous (hours in last week spent walking or cycling) |
| Change in PA | F – B | Baseline subtracted from follow-up | Continuous |
| Diet | B and F | Scale collated by ICH staff using MEND coding matrix (provided in Appendix 12) | |
| Change in diet | F – B | Baseline subtracted from follow-up | Continuous |
| Ethnicity | B | Collated at ICH from multiple classifications provided by MEND Centrala | White (0), Asian (1), black (2), other (3) |
| Family structure | B | No additional data management at ICHa | Couple (0), single parent (1) |
| Housing tenure | B | Derived at ICH from rental status and owner-occupation variables provided by MEND Centrala | Owned (0), social rented (1), private rented (2) |
| Employment status of primary earner | B | No additional data management at ICHa | Yes (0), no (1) |
| Residential postcode of MEND 7–13 participants | B | Incomplete postcodes coded as missing; those with clear errors were cleaned with algorithms developed at ICH (e.g. WCI = WC1) | Standard postcode format |
| Attendance at MEND sessions | Each session | Did not differentiate between missing data and non-attendance. Cleaned using assumptions developed at ICH in consultation with MEND Central | Categorical: non-completers < 25% of sessions attended (0), partial completers 25–75% of sessions attended (1), completers > 75% of sessions attended (3) |
| Programme-level variables | |||
| Group size | B | Derived using participant and programme identifiers | Continuous (range from 1–20) and categorical: 1–5 (1), 6–9 (2), 10+ (3) |
| Number of programmes to date for programme manager | B | Derived using measurement date, programme and programme manager identifier | Continuous (ranging from 1–32) |
| Rounding of height measures | B | Derived using height, participant and programme identifiers | Binary (0 if < 20% of programme participants equal to 0 or 0.5 cm, 1 if > 20% rounded) |
| Rounding of weight measures | B | Derived using height, participant and programme identifiers | Binary (0 if < 20% of programme participants equal to 0 or 0.5 kg, 1 if > 20% rounded) |
Demographic and socioeconomic variables
Age at the first and penultimate sessions was used in the derivation of zBMI at baseline and follow-up. Otherwise, age at baseline was used as a covariate in the study. Sex and ethnicity (white, Asian, black or other, as reported by parents) were also used.
Socioeconomic circumstances were reported by parents. These included family structure, housing tenure and parental employment (whether the ‘primary earner’ in the household was employed or not at baseline). Employment status was not differentiated by subcategories, such as ‘self-employed’ or ‘retired’. It was only collected in 2009 and 2010 and so we used multiple imputation methods to impute values for 2007 and 2008.
Attendance
In theory, attendance was logged by MEND 7–13 local staff at each session. Where a value of 0 had been entered on the service database it was difficult to know whether this was because managers had not collected attendance data or because the child did not attend the session. To separate those who did not attend from cases where information had not been recorded, we derived a variable indicating valid entries for those observations where the programme manager had entered a value of 1 for at least one other child for every session in the programme (some sessions were completely blank; this was taken to indicate lack of data entry rather than lack of attendance). Out of 13,998 children who started the programme (and had age, sex, postcode, measurement year and BMI data recorded in the first session), 7862 (58%) had valid attendance data. Otherwise, attendance data were either missing or judged to be invalid and coded as missing. The number of MEND sessions per programme changed from 18 to 20 in 2008, because the two measurement sessions were not recorded as sessions prior to 2008. This means that the total number of recorded sessions differed, but that the times of measurement and the period from the first observation of outcomes to the last was the same. Attendance was measured as a percentage (not a count) of sessions attended.
There is little consensus on what constitutes completion and attrition in paediatric weight management interventions. 37 Reflecting this uncertainty, we drew three groups based on the percentage of sessions that they attended, which we called non-completers (< 25% of sessions attended), partial completers (25–75% attended) and completers (> 75% of sessions attended).
Programme-level variables
Variables which were constant within programmes but varied between them (hereafter called ‘programme-level’ variables) included participant group size, the number of programmes delivered by each programme manager to date, and rounding of height and weight data. Group size was derived by calculating the number of children in each MEND programme at baseline (Table 2 shows group size distribution within the data set). The number of programmes delivered by each programme manager was derived using the measurement date of the first session of each programme combined with the identification number of each programme manager. This variable was used as a proxy for the amount of experience a team had for running a programme. However, it is important to note that a programme manager did not necessarily have the same role at each venue at which MEND 7–13 programmes were delivered. Specifically, some programme managers do run programmes themselves but others may manage delivery teams who run programmes; programme managers may run teams across single or multiple venues; and having the same programme manager over time does not mean that delivery teams remain constant (Duncan Radley, MEND Central, 2012, personal communication).
| Programme group size (number of children at baseline) | Number of programmes | Total % | Cumulative % |
|---|---|---|---|
| 1 | 43 | 2.22 | 2.22 |
| 2 | 55 | 2.84 | 5.05 |
| 3 | 97 | 5.00 | 10.05 |
| 4 | 207 | 10.67 | 20.72 |
| 5 | 223 | 11.49 | 32.22 |
| 6 | 230 | 11.86 | 44.07 |
| 7 | 233 | 12.01 | 56.08 |
| 8 | 227 | 11.70 | 67.78 |
| 9 | 173 | 8.92 | 76.70 |
| 10 | 152 | 7.84 | 84.54 |
| 11 | 110 | 5.67 | 90.21 |
| 12 | 81 | 4.18 | 94.38 |
| 13 | 47 | 2.42 | 96.80 |
| 14 | 36 | 1.86 | 98.66 |
| 15 | 15 | 0.77 | 99.43 |
| 16 | 7 | 0.36 | 99.79 |
| 17 | 1 | 0.05 | 99.85 |
| 18 | 1 | 0.05 | 99.90 |
| 19 | 2 | 0.10 | 100.00 |
| Total | 1940 | 100 |
As a proxy for data quality we estimated the degree of rounding of height and weight measurements by programme staff. MEND Central recommend that height is measured to the nearest 0.1 cm, using a stadiometer accurate to 0.1 cm, and weight to the nearest 0.1 kg, using electronic scales accurate to 0.1 kg, following standardised procedures. They also provide training to all delivery staff in taking these measurements. To estimate whether there was rounding at the programme level, we calculated the percentage of baseline measures at 0 or 0.5 kg (for weight) or 0 or 0.5 cm (for height). We then calculated which programmes had > 20% of measures rounded to these intervals, indicating that there was possible rounding.
Comparator data – representing the ‘MEND-eligible’ population
The ‘MEND-eligible’ population comprised those children who were living in England during the period when MEND was scaled up (2007–10), who were overweight and within the observed age range for participants on the programme. We estimated the size and sociodemographic composition of the MEND-eligible population using three ’comparator’ data sets: the HSE, the MCS and the NCMP. From these data sets we derived subsets representative of children in the MEND-eligible population.
Health Survey for England 2007–10
The HSE is an annual, nationally representative cross-sectional survey of English children and adults. 2 In 2007–10 the survey was boosted with additional samples of 0- to 15-year-olds. We pooled information from the years 2007–10 for overweight children aged 6–13 years (n = 2799). It included information on sex, ethnicity, housing tenure, employment status of household reference person and family structure. Where subcategories for these variables were available (i.e. retirement in employment status) these were merged so that the variables could be compared with the MEND 7–13 data (see Table 27 in Appendix 5 for full details of coding in comparators and MEND). The survey design (a cluster randomised sampling strategy, booster sampling, inverse probability weights, pooling of 2007–10 data sets and restriction to a subpopulation defined by an age range of 6–13 years and overweight) was accounted for using survey commands in the statistical package Stata 11.2 (StataCorp LP, College Station, TX, USA). This meant that prevalence and percentages calculated from the data were representative of overweight children aged 6–13 years and resident in England between 2007 and 2010.
Millennium Cohort Study wave four
The MCS is following the lives of 18,819 children born in the UK in 2000–2. We used information taken from children living in England in wave four of the study (n = 8728) when they were aged 6–8 years inclusive. This was restricted to those who were overweight (n = 1533). 38 MCS respondents were categorised by sex, ethnicity, housing tenure, employment status of the household reference person and family structure (see Table 27 in Appendix 5). As with the HSE, the survey design [a cluster randomised sampling strategy, booster sampling of socioeconomically deprived areas and those with high percentages of black and minority ethnic (BME) groups, inverse probability weights, attrition over time, and the use of a subpopulation who were overweight and resident in England] was accounted for using survey commands in the statistical package Stata. This meant that prevalence and percentages calculated from the data were representative of overweight children aged 6–8 years, born in England in 2000–1 and eligible for MEND 7–13 between 2006 and 2009.
National Child Measurement Programme 2007–10
The NCMP records height and weight measurements of children in Reception (typically aged 4–5 years) and Year 6 (aged 10–11 years) school classes. 39 We commissioned analysis of data from the NOO on 10- to 11-year-old children who were overweight in 2007–8, 2008–9 and 2009–10 (n = 379,756). Specifically, we obtained percentages of overweight children by sex and ethnic group. The NCMP does not collect SEC information other than at the neighbourhood level, where urban/rural status and deciles of the Income Deprivation Affecting Children Index (IDACI) 2007 relative to England as a whole are available (see Routine small area-level data). Data from the NCMP were nationally representative. In the years between 2007 and 2009 participation rates were judged to potentially impact on calculations of prevalence or percentages, and therefore figures were adjusted. There was no adjustment in 2009–10 as analysis suggested that selective participation would not introduce appreciable bias to estimates. 40
Subsets of MEND data set used in this chapter
For the analyses in this chapter, the MEND service-level data were divided into three subsets of participants (MEND-HSE, MEND-MCS and MEND-NCMP), each drawn to be comparable with their respective comparator by age and time period. Thus, 18,289 children (all children with observed data for age, sex and postcode) were referred to and contacted MEND (discussed as ‘referrals’ throughout) and were comparable in terms of age (6–13 years) and time period (2007–10) with the HSE data. Of these, 13,998 had BMI measured at the first session and are discussed as ‘starters’, while 8311 starters completed > 75% of sessions and are referred to throughout as ‘completers’. This is the MEND-HSE subsample.
The MEND-MCS subset is made up of 4391 children referred to MEND Central when they were aged 6–8 years inclusive. This subsample was not restricted to the MCS data collection period (mainly in 2008) as this would have severely reduced the numbers, and hence the power for comparison. Of the 4391 referrals, 3360 were starters and 2010 were completers. Although MEND 7–13 was aimed at 7- to 13-year-olds, in practice 317 children (1.6%) who participated were aged 6 years, and we included these participants in our analyses to increase the statistical power to compare MEND participants with MCS respondents.
The MEND-NCMP subsample included 6004 children referred to MEND who would have been in Year 6 in 2007–8, 2008–9 or 2009–10, and who were therefore comparable with the pooled NCMP data. Of these, 4615 were starters and 2711 were completers.
Routine small area-level data
All the individual data sets (MEND, HSE, MCS and NCMP) contained the residential postcodes of respondents. These data were not routinely available for these data sets but were linked to the MEND 7–13 data set by the Institute of Child Health team, to the HSE by the National Centre for Social Research (NatCen), to the MCS by the Centre for Longitudinal Studies (based at the Institute of Education, University of London) and to the NCMP by the NOO. This was then used to describe which of 34,378 lower super output areas (LSOAs) across England the respondents and their families lived in. LSOAs are statistically designed to have a minimum of 1000 residents but average 1500 residents. Using the LSOA identifiers we linked in the IDACI 2007 deciles41 and an indicator of urban/rural status to the MEND and comparator data sets. For analyses reported in Chapters 3 and 4 we also linked in measures of the food and built environment (described below) to the MEND data sets. We decided not to use composite indicators of multiple deprivation such as the Index of Multiple Deprivation 200741 as we wished to assess which specific components were independently associated with our outcomes.
The IDACI 2007 measures the percentage of income-deprived households with children aged 0–15 years in the LSOA. Households are defined as income-deprived if they are in receipt of means-tested benefits such as Jobseeker‘s Allowance or child tax credits. 41 The majority of underlying data sources were collected in 2005, although some are based on 2001 census data. Therefore, this index slightly predates the MEND and comparator data sets. However, it is unlikely that the decile ranking of LSOAs would vary in the 2-year period between measurement of most of the IDACI data and the measurement of the individual data sets. Deciles of the index were calculated relative to the deprivation ranking of all English LSOAs. Thus, MEND participants and survey respondents living in a LSOA classified as decile 10 live in an area which is among the 10% most deprived areas in England (as opposed to within the data set) for children.
In addition to IDACI 2007, we used an index developed for the Department for Environment, Food and Rural Affairs. 42 The index divides England into grid squares, classifying those with more than 10,000 people as ‘urban’. Rural categories are assigned using geospatial statistics to categorise communities as ‘town’ and ‘fringe’ (described throughout this report as ‘suburban’), or as ‘villages’, ‘isolated hamlets’ or ‘dispersed communities’ (described here as ‘rural’). This index was available at the LSOA level and was linked into our data sets.
We also described the environmental characteristics of participants’ residential LSOAs, which might constrain physical activity or be associated with unhealthy or healthy diets, and so moderate the effect of MEND 7–13. We examined physical land use characteristics, specifically the percentage of green space and the percentage of roads in each LSOA. Land use data were linked from the Generalised Land Use Database constructed in 2005. 43 These land use components were inversely correlated (i.e. as the percentage of green space increases, the percentage of roads in an area decreases) and therefore would violate assumptions of collinearity in regression models. Therefore, we combined them into a single ‘built environment’ variable using factor analysis, with a low value indicating a LSOA with a high percentage of green space and low road density. The Local Index of Child Well-being44 includes a relevant measure of access to sports facilities as well as the percentage of green space as two of five underlying environmental measures. However, we decided not to use this composite indicator as we wished to assess which specific components were independently associated with our outcomes.
To examine the characteristics of the local food environment in the MEND data we linked in information from the national Ordnance Survey Points of Interest data set,45 which lists the postcode locations of all food retail outlets in England on an annual basis. Following previous work examining the relationship between food availability and overweight and obesity in 9- to 10-year-old children,46 supermarkets and fruit and vegetable stores were classified as ‘healthy’ and takeout/fast-food outlets and convenience stores as ‘unhealthy’. Population data downloaded at the LSOA level from the mid-year population estimates for England47 were used in conjunction with the Points of Interest data to derive two density measures of the number of healthy and unhealthy food outlets per 1000 population in the LSOA in 2007.
Methods
Percentage of MEND-eligible population referred to, starting and completing MEND 7–13
We estimate the percentages of the MEND-eligible population who were referred to, started and completed MEND 7–13 as the number of children referred to, starting and completing the programme divided by the size of the MEND-eligible population. We also calculated the percentage of the MEND-eligible population who started or completed the programme who were obese (as opposed to overweight or obese) when they started the programme.
The MEND-eligible population (the denominator) was estimated three times, using the HSE, MCS and NCMP. The HSE allowed us to estimate the prevalence of children aged 6–13 years who were overweight or obese between 2007 and 2010. We applied this prevalence to the Office for National Statistics (ONS) mid-year population estimates of 6- to 13-year-olds between the same years48 to estimate the MEND-eligible population aged 6–13 years.
Sweep four of the MCS was collected in 2007 and 2008, providing information about children who were born in England between August 2000 and September 2001. These children were aged 6–8 years when they were surveyed. We used the estimates of the MCS population size (537,000 children born between August 2000 and September 2001) as reported by Plewis et al. 49 As with the HSE, we applied the sweep four prevalences of overweight and obesity, which were adjusted for sampling design including attrition.
The NCMP measures the BMI of children in Year 6, predominantly aged 10–11 years. This population cannot be readily represented using ONS population estimates of 10- or 11-year-olds as the school year spans the period of interest for mid-year estimates. Instead, we used the observed population counts from the NCMP as our denominator.
Missingness and multiple imputation
Data were missing for sociodemographic and outcome variables to varying degrees (Table 3). This was attributable to systematic reasons for some variables; for example, parental employment status was only collected in 2009–10, and self-esteem was measured by the Harter personality profile instead of the Rosenberg self-esteem scale until mid-2008.
| Variable | Missing data (n) | Percentage |
|---|---|---|
| Ethnicity | 4595 | 32.8 |
| Family structure | 5028 | 35.9 |
| Housing tenure | 4949 | 35.4 |
| Employment status of primary earner | 8804 | 62.9 |
| Percentage of sessions attended | 5811 | 41.5 |
| BMI (follow-up) | 4435 | 31.7 |
| Self-esteem (baseline) | 5902 | 42.2 |
| Self-esteem (follow-up) | 8895 | 63.5 |
| SDQ score (baseline) | 1000 | 7.1 |
| SDQ score (follow-up) | 5760 | 41.1 |
| PA (baseline) | 8218 | 58.7 |
| PA (follow-up) | 11,821 | 84.4 |
| Diet (baseline) | 1389 | 9.9 |
| Diet (follow-up) | 5899 | 42.1 |
This number of missing data were considered to have the potential to introduce systematic bias to observed associations, and to reduce both the statistical power of models to detect associations and the precision of estimates. Therefore, we decided to impute missing values using multiple imputation. This is a general approach to producing valid inferences when analysing partially observed epidemiological data. 50 Multiple imputation assumes that data are missing at random (MAR), and that differences between the missing values and the observed values can be explained by differences in the observed data. Therefore, a multiple imputation approach will not, in theory, account for missing data arising from factors not included in the multiple imputation model [where data are missing not at random (MNAR)] or those where the participants with missing data do not differ from those with complete data [where data are missing completely at random (MCAR)]. However, it is important to note that whereas multiple imputation explicitly makes this assumption, other techniques, such as discarding cases with only partially observed data (complete case analysis), implicitly make similar assumptions (MCAR in the case of complete case analysis51). Furthermore, although it may be difficult to verify why data are missing (i.e. how far the MAR assumption is correct) in any given analysis, studies which simulate different missing data patterns have demonstrated that multiple imputation tends to be more robust to departures from these assumptions than available alternatives such as the complete case approach. 52
Multiple imputation for our data set was complicated by two characteristics of the missing data. Firstly, because data were multilevel, participants were not randomly distributed in the population but grouped through attendance at programmes. This meant that the reasons for the data to be missing might vary between participants but also between programmes (when, for example, staff did not input any responses for a particular programme). To take account of this we estimated multiple imputation models using the REALCOM-IMPUTE software (REALCOM, Centre for Multilevel Modelling, University of Bristol, Bristol, UK). 53 This software imputed missing data while taking account of the multilevel nature of the missingness. The second complicating feature was that we had 15 variables which were only partially observed (i.e. had missing data) and these were a mixture of categorical and continuous variables. The imputation of the missing values needed to be conducted in a single model to ensure that the relationships between the variables were estimated as precisely as possible. Again, the REALCOM software allowed these joint models to be fitted, while taking account of the multilevel structure described above.
In summary, we assumed that the reasons for missing data could be explained by the variables included in the multiple imputation model (i.e. all outcomes, sociodemographic, attendance, neighbourhood and programme-level factors, height and weight rounding, and random variation between programmes).
Differences between sociodemographic characteristics of MEND 7–13 participants and the MEND-eligible population
Percentages for the MEND subsamples and comparators were calculated, taking into account survey design where necessary (see Comparator data – representing the ‘MEND-eligible’ population). Differences in percentages were calculated for each MEND subsample (MEND-HSE, MEND-MCS and MEND-NCMP) by subtracting from them the corresponding comparator percentage (HSE, MCS or NCMP). The statistical significance of the differences at the 5% level was then tested using tests of the equality of percentages for two independent samples.
Calculation of differences in percentages for the imputed variables was a three-stage process. First, 10 data sets were imputed from the master data set by the multiple imputation model described above (stage 1). Following this, 10 tests of the equality of percentages were conducted, producing 10 sets of differences (and their variances) in percentages (stage 2). Finally, these parameters were combined into final estimates using Rubin’s rules,54 which take into account the variation introduced by the imputation procedure (stage 3).
These calculations were repeated for all the imputed socioeconomic variables (i.e. ethnicity, family structure, housing tenure and employment status). The process was repeated for the MEND-MCS and MEND-NCMP data sets, which were also imputed and compared with the percentages in the MCS and the NCMP.
Sensitivity analyses were conducted with the MEND-HSE data set to examine whether the sociodemographic composition of MEND participants varied by year. We repeated comparisons of the MEND-HSE data and the MEND-eligible population for starters and completers using complete case data, imputed data for overweight children excluding obese children, and imputed data for obese children.
Differences in neighbourhood income deprivation gradient between MEND 7–13 participants and comparators
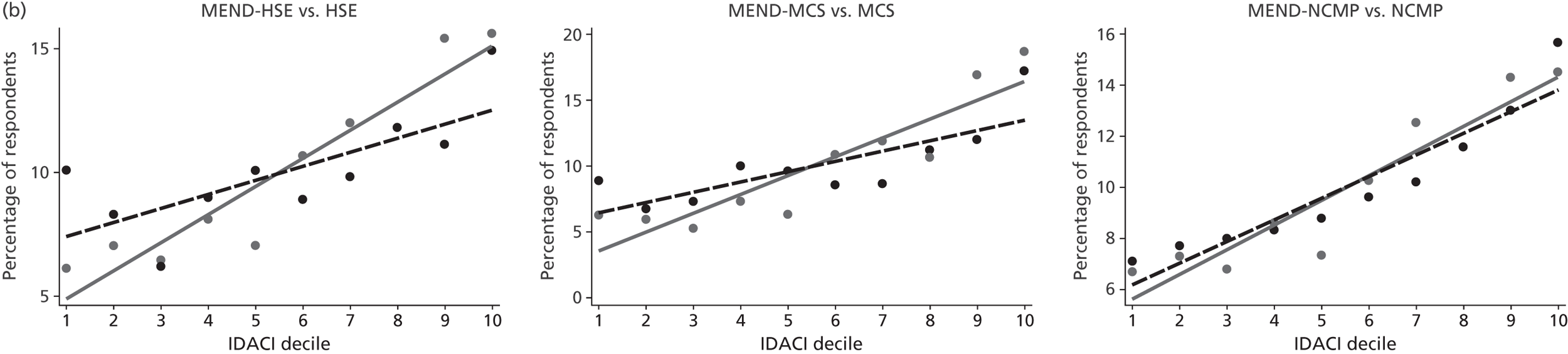
We tested for differences in the social gradients of participants in the MEND programme by examining IDACI 2007 deciles graphically. The statistical differences in slopes were tested using regression models where the outcome was the percentage of participants by deprivation in each MEND subsample (MEND-HSE, MEND-MCS and MEND-NCMP) and comparators (HSE, MCS and NCMP) (for further details see Appendix 7). This analysis was repeated, where data existed, for those referred to MEND 7–13, those who attended < 75% of sessions (low to medium attendance) and those who attended > 75% of sessions (high attendance).
Determinants of completion of MEND 7–13
A multilevel poisson regression model was used to estimate the relative risk ratios of children completing the programme. A multilevel model was needed because participants were nested within programmes and so were not statistically independent from each other (a violation of the assumptions of single-level regression models). Relative risks ratios were calculated with 95% confidence intervals (CIs). We examined unadjusted and adjusted associations between completion and BMI at baseline (BMI at the first session), SDQ score at baseline, age, sex, ethnicity, family structure, housing tenure, employment status of the primary earner, IDACI 2007 decile, built environment, urban/rural status, group size and the number of previous programmes per programme manager.
We fitted the final multilevel model in MLwiN Version 2.25 (MLwiN, Centre for Multilevel Modelling, University of Bristol, Bristol, UK),55 fitting a model for each of the 10 imputed data sets in turn before combining the coefficients and standard errors using Rubin’s rules54 as implemented by the Stata 11.2 multiple imputation commands.
The model was estimated using multiply-imputed data for 13,998 participants. As with the calculation of differences in percentages described above, the relative risk ratios and standard errors derived from analysis of all ten data sets were calculated using Rubin’s rules as implemented by the Stata 11.2 missing data (mi est) commands.
Age was grand-mean centred, subtracting the mean across the whole sample from each observation. This means that relative risk ratios from the model could be interpreted as ‘for each year of age greater than the average the risk of completion increases/decreases by . . .’
We categorised all continuous covariates apart from age as this facilitated interpretation. We categorised the SDQ as normal (0–13 symptoms reported), borderline (14–17 symptoms reported) and abnormal (≥ 17 symptoms reported), following the wording and guidance of the score’s developers. 36
Findings
What percentage of the MEND-eligible population are referred to, start and complete MEND 7–13?
Estimates of the size of the MEND-eligible population were calculated using prevalence and population estimates data presented in Table 4. The prevalences of overweight and obesity were smallest in the youngest children (in the MCS) and highest in the NCMP data (for Year 6 children).
| Percentage of 6- to 13-year-olds in 2007–10 (HSE) (95% CI) | Percentage of 6- to 8-year-olds in 2008 (MCS) (95% CI) | Percentage of 10- to 11-year-olds in 2007–10 (NCMP) (95% CI) | |
|---|---|---|---|
| Overweight | 23.3 (22.4 to 24.1) | 17.7 (16.8 to 18.7) | 25.4 (25.4 to 25.5) |
| Obese | 10.7 (10.1 to 11.4) | 8.0 (7.3 to 8.8) | 11.7 (11.7 to 11.8) |
Table 5 shows the population estimates by the age range of the comparator surveys. Across the entire age range of the MEND 7–13 programme (6- to 13-year-olds), 4.4 million children would have been eligible for the programme and just under half (2.0 million) of those eligible would have been obese.
| MEND-eligible population size | Number of 6- to 13-year-olds in 2007–10 (HSE) | Number of 6- to 8-year-olds in 2008 (MCS) | Number of 10- to 11-year-olds in 2007–10 (NCMP) |
|---|---|---|---|
| All children | 18,804,500a | 567,000b | N/Ac |
| MEND-eligible: overweight | 4,372,080 | 100,566 | 379,756 |
| MEND-eligible: obese | 2,020,648 | 45,466 | 175,375 |
Of the 21,132 children who self-referred or were referred to MEND, 18,289 had complete age, sex and postcode data. These children constituted 0.42% of the MEND-eligible population (Table 6). A total of 13,998 started a MEND programme, constituting 0.32% of the MEND-eligible population; the 8311 who completed the programme constituted 0.19%. The percentages of those who were referred, started and completed were higher for 6- to 8-year-olds. The percentages who were referred, started and completed were estimated to be higher for 10- to 11-year-olds (Year 6 children), reflecting the high percentage of MEND 7–13 children in that age range (mean age of MEND children at baseline was 10.7 years). Percentages reduced from referral through starters and completers in the same way for the age ranges 6–13, 6–8 and 10–11 years.
| MEND 7–13 (n) | Percentage of MEND-eligible populationa | |||||
|---|---|---|---|---|---|---|
| Number of 6- to 13-year-olds in 2007–10 (HSE) | Number of 6- to 8-year-olds in 2008 (MCS) | Number of 10- to 11-year-oldsb in 2007–10 (NCMP) | Percentage of 6- to 13-year-olds in 2007–10 (HSE) | Percentage of 6- to 8-year-olds in 2008 (MCS) | Percentage of 10- to 11-year-oldsb in 2007–10 (NCMP) | |
| Overweight | ||||||
| Referrals | 18,289 | 983 | 6004 | 0.42 | 0.97 | 1.58 |
| Starters | 13,998 | 919 | 4615 | 0.32 | 0.91 | 1.22 |
| Completersc | 8311 | 571 | 2711 | 0.19 | 0.57 | 0.71 |
| Obesed | ||||||
| Starters | 11,796 | 825 | 3795 | 0.58 | 1.81 | 2.17 |
| Completersc | 7024 | 508 | 2236 | 0.35 | 1.12 | 1.27 |
The percentages of obese children referred to the programme could not be calculated because anthropometry was not measured until participants started the programme. The percentages of obese children who started and completed MEND 7–13 were higher than when overweight (including obese) children were considered (see Table 6). Starters aged 6–13 years who were obese accounted for 0.58% and completers accounted for 0.35% of the MEND-eligible population who were obese.
Differences between the sociodemographic characteristics of MEND 7–13 participants and those of the MEND-eligible population
We investigated how MEND referrals, starters and completers compared with the MEND-eligible population. Characteristics of all data sets compared in the analyses are available for reference (see Tables 28 and 29). Differences between the MEND referrals and children in the MEND-eligible population are reported only in the text (only sex- and area-level data were available for referrals) and, for starters and completers, sociodemographic differences and the p-values of these differences are reported in Table 7. A negative value for the difference in the proportions indicates that proportionally fewer children of that group were in the MEND participant subsample than might be expected given the proportion of children in that group in the comparator data set (and, by extension, in the MEND-eligible population). Figure 3 presents graphs showing the distribution of MEND subsets and comparator data sets by deciles of deprivation. The results are discussed below.
| Variables | Section A: starters (attended at least one session) | Section B: completers (attended > 75% of sessions) | ||||
|---|---|---|---|---|---|---|
| MEND 7–13 vs. comparator | MEND 7–13 vs. comparator | |||||
| HSE difference in percentages (p) | MCS difference in percentages (p) | NCMP difference in percentages (p) | HSE difference in percentages (p) | MCS difference in percentages (p) | NCMP difference in percentages (p) | |
| Adiposity | ||||||
| Overweight excl. obese | –38.1 (< 0.001) | –40.0 (< 0.001) | –36.0 (< 0.001) | –38.0 (< 0.001) | –39.8 (< 0.001) | –36.3 (< 0.001) |
| Obese | +38.1 (< 0.001) | +40.0 (< 0.001) | +36.0 (< 0.001) | +38.0 (0.000) | +39.8 (< 0.001) | +36.3 (< 0.001) |
| Sex | ||||||
| Boy | –7.1 (< 0.001) | –11.2 (< 0.001) | –8.0 (< 0.001) | –9.6 (< 0.001) | –14.4 (< 0.001) | –10.3 (< 0.001) |
| Ethnicity | ||||||
| White | –2.3 (0.014) | –5.9 (< 0.001) | +2.3 (0.004) | –1.1 (ns) | –4.0 (0.007) | +3.6 (0.001) |
| Asian | +3.0 (< 0.001) | +7.3 (< 0.001) | +4.8 (< 0.001) | +2.4 (0.003) | +5.9 (< 0.001) | +4.1 (< 0.001) |
| Black | +0.2 (ns) | +0.3 (ns) | –4.6 (< 0.001) | –0.2 (ns) | –0.7 (ns) | –5.1 (< 0.001) |
| Other | –0.9 (0.025) | –1.7 (0.022) | –2.6 (< 0.001) | –1.1 (0.016) | –1.2 (0.100) | –2.8 (< 0.001) |
| Family structure | ||||||
| Lone parent | +4.0 (0.020) | +6.1 (0.002) | – | +1.0 (ns) | +3.3 (ns) | – |
| Housing tenure | ||||||
| Owned | –10.1 (< 0.001) | –12.6 (< 0.001) | – | –5.3 (< 0.001) | –6.7 (0.001) | – |
| Social | +6.7 (< 0.001) | +5.1 (0.007) | – | +2.7 (0.009) | +1.1 (ns) | – |
| Private | +3.4 (< 0.001) | +7.5 (< 0.001) | – | +2.6 (0.001) | +5.7 (< 0.001) | – |
| Employment status of primary earner | ||||||
| Unemployed | +5.5 (< 0.001) | +7.9 (< 0.001) | – | +2.2 (0.039) | +4.4 (0.012) | – |
| Urban/rural | ||||||
| Urban | +6.9 (< 0.001) | +5.4 (< 0.001) | +4.4 (< 0.001) | +6.0 (< 0.001) | +4.4 (< 0.001) | +3.1 (< 0.001) |
| Suburban | –2.5 (< 0.001) | –1.4 (ns) | –1.2 (0.003) | –1.9 (0.001) | –1.2 (ns) | –0.5 (ns) |
| Rural | –4.5 (< 0.001) | –4.0 (< 0.001) | –3.3 (< 0.001) | –4.1 (< 0.001) | –3.2 (< 0.001) | –2.8 (0.000) |
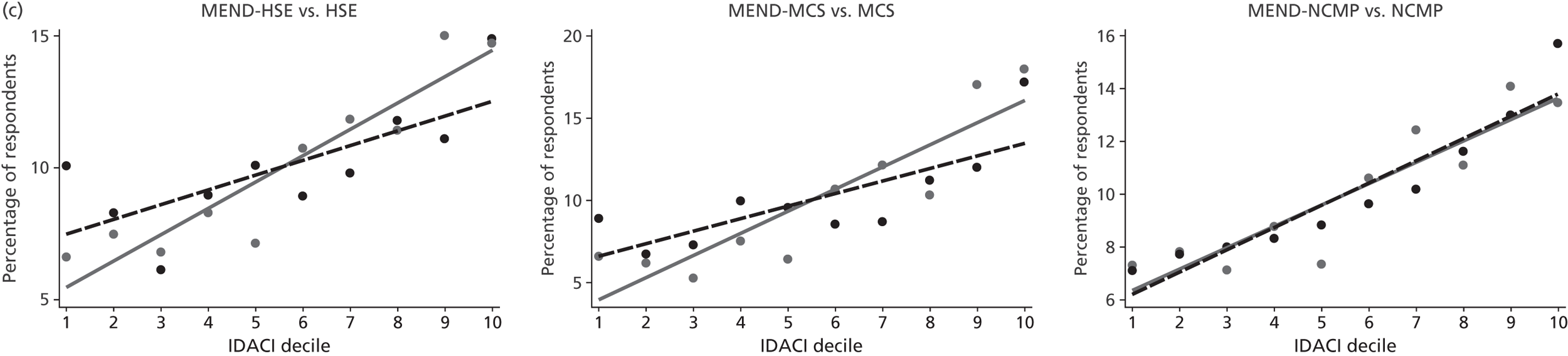
FIGURE 3.
Percentages of MEND participants and comparator respondents by decile of IDACI 2007, where decile 10 is the most deprived. The dashed black line is the socioeconomic gradient, estimated by linear regression of the MEND-eligible population (represented by HSE, MCS and NCMP). The solid grey line is the socioeconomic gradient of the MEND participants (MEND-HSE, MEND-MCS and MEND-NCMP respectively). Black and grey spots are comparator- and MEND-observed proportions respectively. (a) Social gradient by IDACI decile of MEND referrals vs. comparators; (b) social gradient by IDACI decile of MEND starters vs. comparators; and (c) social gradient by IDACI decile of MEND completers (> 75% of sessions attended) vs. comparators.
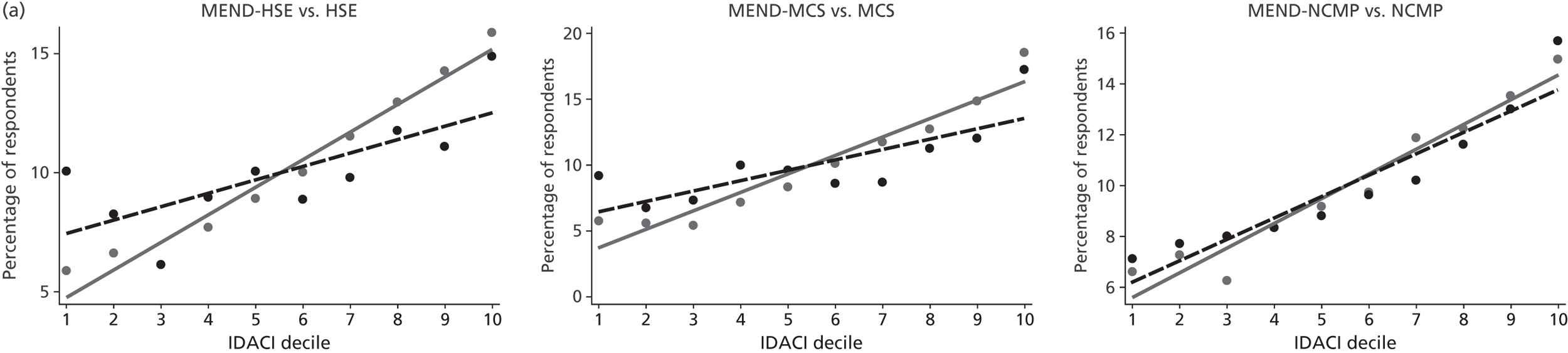
Who was referred to MEND?
Results for all three comparisons (MEND-HSE referrals vs. HSE, MEND-MCS referrals vs. MCS and MEND-NCMP referrals vs. NCMP) were broadly consistent. Fewer boys [−6.3% (p < 0.001) in HSE vs. MEND-HSE, −10.7% (p < 0.001) in MCS vs. MEND-MCS and −7.0% (p < 0.001) in NCMP vs. MEND-NCMP] were referred to MEND relative to the MEND-eligible population. Conversely, more girls were referred than might be expected.
More urban children [+7.1% (p < 0.001) in HSE vs. MEND-HSE, +5.0% (p < 0.001) in MCS vs. MEND-MCS and +4.4% (p < 0.001) in NCMP vs. MEND-NCMP] were referred to MEND relative to the MEND-eligible population. Conversely, children living in suburban and rural locations were less likely to be referred to MEND.
There was a steeper social gradient by IDACI 2007 decile in those referred to MEND 7–13 than in the MEND-eligible population (see Figure 3a). Broadly speaking, this means that proportionally more children were referred to MEND 7–13 from the most deprived areas than might be expected given the proportions of MEND-eligible children in those areas. These differences in gradients were statistically significant for those aged 6–13 years (HSE data) and 6–8 years (MCS data) but not for the Year 6 children (NCMP data). See the regression models in Appendix 7 (Table 33) for model coefficients.
Who started on MEND?
MEND starters were more likely to be obese than those in the MEND-eligible population. Specifically, 84% (95% CI 83.7 to 84.9%) of children aged 6–13 years who started MEND in MEND-HSE exceeded the 98th centile of the UK 1990 growth charts,14 whereas the comparable figure from the HSE was 46%.
Sociodemographically, in line with the analysis of those who were referred to MEND, there were lower proportions of boys in each of the MEND starter subsets than in the MEND-eligible population (see section A of Table 7). There were proportionally more MEND starters from Asian groups than in the MEND-eligible population (but not from black groups, where differences were non-significant), and proportionally fewer from white and other ethnic groups.
Proportionally more MEND starters than children in the MEND-eligible population lived with a lone parent (see section A of Table 7). The pattern was similar for housing tenure, where higher proportions of MEND starters lived in social or private rented housing; and also for parental employment, with higher proportions of MEND starters living in households where the primary earner was unemployed.
The results show that compared with the MEND-eligible population, MEND starters were more likely to live in urban neighbourhoods and less likely to live in rural and suburban neighbourhoods (although the suburban difference was non-significant for the MCS vs. MEND-MCS comparison).
As with referrals, there was a steeper social gradient by small-area deprivation among those who started MEND than in the MEND-eligible population (see Figure 3b). Proportionally more children from the most deprived areas started MEND than might be expected given the proportions of MEND-eligible children in those areas. These differences in gradients were statistically significant for those aged 6–13 years (HSE data) and 6–8 years (MCS data) but not for the Year 6 children (NCMP data). See the regression models in Appendix 7 (Table 33) for model coefficients.
Who completed MEND?
The sociodemographic distribution of the children who completed the MEND programme was, when compared with the MEND-eligible population, similar to that of MEND referrals and starters in terms of direction (see sections A and B in Table 7 and Who was referred to MEND?). That is, there were proportionally more girls and Asian children in the completers sample than in the MEND-eligible population, and proportionally fewer white children (although the HSE vs. MEND-HSE comparison was non-significant). There were proportionally fewer MEND completers than MEND-eligible children living in owner-occupied and proportionally more living in private rented housing. However, although proportionally more MEND completers lived with lone parents, with a parent who was unemployed or in rented accommodation, these differences were not statistically significant. As with the referrals and starters comparisons, MEND 7–13 completers were more likely to live in urban areas.
There were differences in the results between completers and starters in terms of the size and statistical significance of the results. The difference between the MEND-eligible population and MEND subsamples was greater for boys and girls when the completers findings were compared with the starters. The size of the differences was also smaller for the SEC in completers compared with starters.
Proportionally more MEND completers came from the most deprived areas than might be expected given the proportions of MEND-eligible children in those areas (see Figure 3c). These differences in gradients were statistically significant for those aged 6–13 years (HSE data) and 6–8 years (MCS data) but not for the Year 6 children (NCMP data). See the regression models in Appendix 7 (Table 33) for model coefficients.
Sensitivity analyses
The analyses described above were conducted for all MEND 7–13 referrals, starters and completers who were overweight. However, the majority of MEND participants were obese. To test whether the distribution of MEND 7–13 was steeper by IDACI 2007 decile because of the differential adiposity of the MEND 7–13 and comparator samples, we repeated analyses for obese children only (see Appendix 6, Table 30) and overweight children excluding those who were obese (see Appendix 6, Table 31). Results were very similar.
Some variables in the service data were only partially observed, so that the complete case data set was significantly smaller than the number of participants in MEND. Basing the analysis on this would have reduced the power to detect genuine variations in the outcome, and could have introduced bias. We addressed this limitation using multilevel multiple imputation, which relies on the assumption that the data were MAR. By making comparisons based on imputed data we were able to maximise power and minimise bias. While the MAR assumption could not be directly tested, we ran sensitivity analyses of the final multivariable models with complete case data (as recommended for this type of analysis50). Results were similar between the complete case and the multiple imputation models (see Appendix 6, Table 32), implying that bias introduced by missingness due to MAR was minimal. However, the multiple imputation findings are presented because the variation in the sample is more accurately estimated by these models. Sensitivity analyses suggested that the sociodemographic characteristics of the MEND starters and completers did not vary systematically by year of participation (data not reported).
Determinants of completion of MEND 7–13
The relative risk of completion (recorded as attending > 75% of sessions) varied by sociodemographic, neighbourhood and programme-level characteristics (Table 8). The second column of Table 8 presents the results from models of the unadjusted relative risks of completion. Covariates which were significantly associated with the relative risk of completing from these univariable models were carried forward to a multivariable model (presented in the final column). The unadjusted results show that SDQ score at baseline, sex, family structure, housing tenure, employment status of the primary earner, IDACI 2007 decile, programme group size and the number of previous programmes per programme manager were associated with the relative risk of completing. Conversely, BMI at baseline, age, ethnicity and urban/rural status were not. These variables were not carried forward to the multivariable model.
| Parameters | Single variable models uRR (95% CI) |
Multivariable model aRR (95% CI) |
|---|---|---|
| Intercept | – | 0.85 (0.76 to 0.95)** |
| BMI at baseline (ref. 91st–95th centile) | ||
| 95–98th centile | 1.02 (0.91 to 1.14) | – |
| > 98th centile | 1.00 (0.92 to 1.10) | – |
| SDQ score at baseline (ref. ‘normal’) | ||
| ‘Borderline’ | 0.95 (0.89 to 1.02) | 0.97 (0.90 to 1.04) |
| ‘Abnormal’ | 0.88 (0.83 to 0.93)*** | 0.91 (0.86 to 0.97)** |
| Age (years) | 0.99 (0.97 to 1.00) | |
| Sex (ref. girls) | ||
| Boys | 0.90 (0.86 to 0.95)*** | 0.91 (0.87 to 0.96\)*** |
| Ethnicity (ref. white) | ||
| Asian | 0.94 (0.87 to 1.00) | – |
| Black | 0.91 (0.82 to 1.00) | – |
| Other | 0.94 (0.83 to 1.08) | – |
| Family structure (ref. couples) | ||
| Lone parents | 0.87 (0.82 to 0.92)*** | 0.93 (0.88 to 0.98)* |
| Housing tenure (ref. owner-occupied) | ||
| Social rented | 0.80 (0.75 to 0.85)*** | 0.88 (0.82 to 0.95)*** |
| Private rented | 0.86 (0.80 to 0.92)*** | 0.90 (0.84 to 0.97)** |
| Employment status of primary earner (ref. employed) | ||
| Unemployed | 0.84 (0.79 to 0.89)*** | 0.93 (0.87 to 0.98)* |
| IDACI 2007 deciles [ref. decile 1 (least deprived)] | ||
| 2 | 1.00 (0.88 to 1.14) | 1.01 (0.89 to 1.15) |
| 3 | 0.97 (0.86 to 1.09) | 0.99 (0.88 to 1.12) |
| 4 | 0.95 (0.84 to 1.08) | 0.98 (0.87 to 1.11) |
| 5 | 0.92 (0.82 to 1.04) | 0.96 (0.84 to 1.08) |
| 6 | 0.87 (0.78 to 0.97)* | 0.92 (0.82 to 1.03) |
| 7 | 0.86 (0.77 to 0.97)* | 0.93 (0.82 to 1.04) |
| 8 | 0.84 (0.75 to 0.95)** | 0.93 (0.82 to 1.05) |
| 9 | 0.81 (0.73 to 0.91)*** | 0.91 (0.80 to 1.02) |
| 10 (most deprived) | 0.74 (0.66 to 0.83)*** | 0.85 (0.76 to 0.96)** |
| Urban/rural status (ref. urban) | ||
| Suburban | 1.09 (1.00 to 1.20) | – |
| Rural | 1.10 (0.98 to 1.22) | – |
| Programme group size (ref. one to five participants) | ||
| Six to nine participants | 0.93 (0.86 to 1.01) | 0.93 (0.86 to 1.01) |
| ≥ 10 participants | 0.83 (0.76 to 0.90)*** | 0.84 (0.77 to 0.91)*** |
| Number of programmes per manager (ref. < 10) | ||
| ≥ 10 | 0.91 (0.85 to 0.98)* | 0.93 (0.86 to 0.99)* |
The multivariable model showed that, on average, children with higher than expected symptoms of psychological distress (‘abnormal’) at baseline were less likely to complete than those with ‘normal’ symptoms (see adjusted relative risk ratios in Table 8). Boys were less likely to complete the programme than girls.
All four markers of SEC were independently associated with completion (see the final column of Table 8). Children living with a lone parent were less likely to complete compared with those living with two parents. Children living in social or private rented housing were less likely to complete than those living in owner-occupied housing. Children living in households where the primary earner was unemployed were less likely to complete than those in households where the primary earner was employed. Finally, children living in the most deprived neighbourhoods were less likely to complete the programme.
Families who started MEND 7–13 programmes in groups with > 10 people were less likely to complete than those who started in groups of one to five children. However, there was no statistical difference in completion between those in groups of six to nine children and those in groups of one to five children. Children attending programmes where managers had run ≥ 10 previous programmes were less likely to complete than those where managers had run < 10 programmes.
As noted previously (see MEND 7–13 service-level data), there is no agreed definition of a completer. 56 We tested relationships between completion and covariates using a lower threshold of attendance at 60% of sessions to define completion (see Appendix 8 for results). The direction and statistical significance of relationships were similar.
Discussion
Percentage of the MEND-eligible population referred to, starting and completing MEND 7–13
Our analysis shows that only a small percentage of the MEND-eligible population were referred to, started and completed MEND 7–13 programmes. As MEND 7–13 has been reported as the largest intervention of its type in England in a recent mapping study of such schemes,57 this serves to illustrate the challenge for scaling up family-based lifestyle interventions to the population level.
Those who started and completed the programme were more likely to be obese compared with the MEND-eligible population, indicative perhaps that children and families principally self-refer or are referred when levels of adiposity are perceived by families or professionals as already particularly high. The percentage of MEND-eligible children referred to the scheme was slightly higher for 10- to 11-year-olds, which might reflect the role of the NCMP as a health promotion intervention which raises awareness of childhood overweight.
Differences between sociodemographic characteristics of MEND 7–13 participants and those of the MEND-eligible population
Our results showed that in comparison with the MEND-eligible population, proportionally more children who started or completed MEND lived in less favourable SEC (indicated by employment status of the primary earner, family structure and housing tenure). Relative to the MEND-eligible population, proportionally more of those who started or completed a MEND 7–13 programme were girls, Asian and urban-dwelling, and proportionally fewer were of white or other ethnicities. Finally, relative to the MEND-eligible population, proportionally more MEND 7–13 starters and completers were obese, rather than overweight but not obese.
We also found that there were socioeconomic gradients in referral to, starting or completing MEND 7–13 at the neighbourhood level. In the MEND-HSE and MEND-MCS comparisons, the proportions of MEND 7–13 participants were higher for those living in the most deprived areas relative to the MEND-eligible population. In the MEND-NCMP comparison, proportions of MEND 7–13 participants by deprivation were similar to the proportions in the MEND-eligible population. In none of the comparisons was provision of MEND 7–13 in the most deprived neighbourhoods less than expected. This is an interesting finding as it suggests that referral to MEND 7–13 was equitable, in the sense that children from more deprived communities were more likely to be referred or to self-refer to the scheme than those living in more advantaged circumstances.
Finally, MEND children were more likely to live in urban areas and less likely to live in suburban and rural areas than children in the MEND-eligible population. This applied to those who were referred to MEND and also to starters and completers.
Many of the differences between the MEND-eligible population and the MEND referrals, starters and completers were statistically significant but not large in magnitude. Therefore, we conclude that the provision and/or uptake of MEND 7–13 did not appear to compromise and, if anything, promoted participation of those from more disadvantaged circumstances and from ethnic minority groups. This suggests that participation in MEND 7–13, when it was implemented at scale across England, had the potential to make a contribution to tackling health inequalities.
The reasons for the differences between the MEND-eligible population and MEND referrals, starters and completers might be owing to factors related to the differential supply of the service (programmes may be more likely to be commissioned in deprived localities) and/or the differential uptake of the service (families in more disadvantaged SEC may be more likely to take up the programme). We were not able to examine these factors.
Determinants of completion of MEND 7–13
Completers differed from starters. Completers were less likely to be psychologically distressed at baseline than starters. This is consistent with the findings of previous work. 58 Specifically, girls were more likely to complete than boys. This finding was inconsistent with the results of previous research,59 which found no sex difference in dropout rates (dropout rather than completion was measured in previous work). Completion of MEND 7–13 was not associated with ethnicity in unadjusted models. This was in contrast to previous research suggesting that children from BME groups were more likely to drop out of paediatric weight management programmes. 58,59 The difference in findings might reflect the fact that the previous studies were based in different countries (the Netherlands59 and the USA58) with different ethnic, cultural and other contexts.
Family structure, housing tenure, parental employment and neighbourhood deprivation were all independently associated with completion of the programme. All associations were in the same direction, with more disadvantaged families less likely to complete. The same associations were not observed in the study by de Niet et al. ,59 where levels of parental education, maternal employment status and family structure were not associated with dropout between 0 and 3 months. These differences might be explained because the intervention had a lower level of parental involvement (parents only attended three sessions) than that of MEND 7–13.
Programme group size and the number of programmes delivered by the programme manager were both associated with rates of completion. We have not identified other studies which tested whether these types of variables were associated with attrition or completion. However, further analysis of these types of process factors at the programme level, and their relationship with completion of child weight management programmes delivered under service conditions, would be valuable.
The model therefore gives some insight into the predictors of completion of weight management programmes conducted in the English context. It is notable that although there were associations between sex and SEC and the likelihood of completion, these relative risks of completion did not alter the direction of MEND versus MEND-eligible differences for starters and completers, although differences were reduced in magnitude and sometimes attenuated to non-significance (see Who completed MEND?).
Strengths and weaknesses of the study
Data availability prevented us from making identical comparisons of the MEND subsample with each routine data set. For example, family structure was not established in exactly the same way in any of the three data sets (MEND 7–13, HSE and MCS). However, results were consistent across two comparisons (MEND 7–13 with MCS and MEND 7–13 with HSE) which gave us confidence that results were not overly sensitive to differences in variables or measurement. Moreover, we drew on three family socioeconomic variables from two studies (the MCS and HSE). The results from all three variables in both data sets were consistent. We also linked neighbourhood deprivation data into all three samples. Although this is measured at the area level, and so is less appropriate for making inferences at the individual level, it was also consistent with the results from the family SEC data in the sense that participation in MEND 7–13 was proportionate for each decile of neighbourhood deprivation. Taken together, the proportion of MEND 7–13 participants who were living in socioeconomically deprived circumstances was similar or slightly higher than expected given the proportion of children in these circumstances in the MEND-eligible population.
The analysis of attendance may be biased owing to the ways in which the service managers reported attendance. Specifically, we could not differentiate between a missing response (where the data were not entered) and a child who was reported by the programme manager as not attending. For this reason, the number of completers reported in the MEND subsets may have been less than the actual number. In addition, this may have introduced systematic bias into the results if those who were missing as opposed to non-attendees differed in terms of the socioeconomic variables of interest. We attempted to mitigate this last possibility by multiply imputing the attendance and SEC variables, to minimise bias due to differences between participants with complete data and those with partially observed data.
The MEND 7–13 programme was predominantly delivered to obese rather than overweight children. Within a population which is generally overweight (including obese), socioeconomic gradients may be steeper for those who are obese. However, sensitivity analyses suggested that the differences in adiposity between the MEND participants and those in the MEND-eligible population did not explain the findings.
Wider context
Most current work on scaled-up interventions refers to those delivered in low- to middle-income countries, and studies which have evaluated scale-up of public health interventions in higher-income countries are relatively rare. 60 It is unusual to have comprehensive, population-level information about public health interventions and the degree to which they reach populations at particular risk. 61 This study therefore adds to this literature by estimating how far a weight management intervention, when scaled up, was available to overweight and obese children in the population.
To summarise, the provision and/or uptake of MEND 7–13 did not appear to compromise and, if anything, promoted participation of those from more disadvantaged circumstances and from ethnic minority groups. This suggests that participation in MEND 7–13, when it was implemented at scale across England, had the potential to make a contribution to tackling health inequalities. However, this potential was mitigated to some extent because, having started a programme, completion was relatively less likely for those participants living in less favourable SEC and for boys.
Headline findings from Chapter 2
Using an estimate of how many children aged 6–13 years were overweight in England, just under 0.5% were referred to a MEND programme between 2007 and 2010, while 0.2% completed the programme.
Comparing the characteristics of children in MEND programmes with those of all children who were overweight in England suggests that children from more disadvantaged SEC and those from Asian or ‘other’ ethnic groups were more likely to be referred to, start and complete MEND 7–13.
Specifically, the programme is used slightly more by:
-
girls compared with boys
-
children from Asian groups (and slightly less by white and ‘other’ groups, while similar proportions are from black groups)
-
those who live in socioeconomically deprived circumstances, compared with those who are less deprived
-
children living in urban areas compared with suburban or rural areas.
Participants were less likely to complete MEND 7–13 if they:
-
were reported as psychologically distressed at baseline
-
were boys compared with girls
-
lived in more socioeconomically deprived circumstances
-
attended a MEND 7–13 programme with > 10 participants at baseline
-
attended a MEND 7–13 programme where the manager had managed > 10 programmes previously.
Chapter 3 Characteristics associated with changes in BMI and zBMI
How do outcomes associated with participation in MEND vary with the characteristics of children (sex, SEC and ethnicity), MEND centres (type of facility, funding source and programme group size) and areas where children live (in relation to area-level deprivation and the obesogenic environment)?
Background
To our knowledge, no studies have examined variations in outcomes from a childhood weight management intervention delivered under service conditions at the population level. In the two chapters which follow, we address this research gap. This chapter addresses the question for outcomes of change in body fatness measured by change in absolute BMI and zBMI.
As part of this analysis, we also aimed to benchmark changes in BMI estimated from service data on MEND 7–13 programmes delivered in the community against those observed in the RCT15 of the programme.
Data
This analysis draws upon the MEND service data described previously (see Chapter 2, MEND 7–13 service-level data). Chapter-specific outcomes and covariates are described below.
Outcomes
The primary outcome was change in BMI after participation in MEND. BMI was calculated at baseline and follow-up [using (weight/height)2]. BMI measures weight after taking account of an individual’s height, and where it exceeds the 91st centile of the UK 1990 growth charts14 it can be used as a measure of overweight, a proxy for having excess fat. A reduction in BMI can therefore be interpreted as a reduction in excess fat. Where this is an average value across a group such as the MEND 7–13 participants, it will likely reflect that the group predominantly reduced levels of excess fat (one of the aims of the intervention), but that a minority either maintained or even increased their levels. Change in BMI was calculated by subtracting baseline BMI from follow-up BMI, so that 0 on the measure indicates no change, a positive value indicates an increase in BMI and a negative value indicates a reduction in BMI. We took an average reduction in BMI to be evidence of the programme assisting families in child weight management at a population level.
To compare the changes with those commonly reported in reviews10 of childhood obesity interventions, we also measured change in BMI after standardising baseline and follow-up BMI for age and sex. This was done using the UK 1990 BMI growth reference,14 created using Cole’s lambda-mu-sigma (LMS) method,62 which standardises BMI for age and sex. Standardised BMI is termed zBMI. As with BMI, change in zBMI was calculated by subtracting baseline zBMI from follow-up zBMI. Also as with BMI, a fall in zBMI implies a reduction in excess fat, whereas a rise indicates increased excess fat.
In our analysis, the two outcome measures, change in BMI and change in zBMI, lead to broadly similar conclusions. Change in BMI is more comprehensible than change in zBMI, and this is why it is the main focus of the report.
Covariates
Participant-level variables included BMI at baseline, sex, age and ethnicity; characteristics of families included housing tenure, parental unemployment, lone parent or couple status; and characteristics of LSOAs included IDACI 2007 deciles, a measure of built environment, food outlet density and urban/rural status. Programme-level variables included group size, number of previous programmes per programme manager and rounding of height and weight measurements. These variables were described in Chapter 2 (see MEND 7–13 service-level data).
In this section we also examine whether participant-reported global self-esteem is associated with change in BMI. We measure global self-esteem using an adapted form of the widely validated Rosenberg self-esteem scale. 35 The scale measures global self-esteem by asking MEND participants to state to what extent they agree with 10 statements about themselves (listed in Box 1). The Rosenberg scale was originally designed for use with adolescents35 and few studies have used it with children within the age range targeted by MEND 7–13. However, the response format was judged by staff at MEND Central to be too confusing for younger children, and so was modified to more fully reflect the cognitive abilities of younger children. In addition, some of the original constructs measured in the scale used American terminology, and these statements were modified by MEND Central to be more accessible to children in the UK (for example, including ‘happy’ in brackets as an alternative to ‘satisfied’ in statement 1 – all 10 MEND-modified statements are listed in Box 1 for reference). Responses to each statement were on a four-point symmetric agree–disagree scale where the coding is given in brackets: ‘a lot like me (0)’, ‘a bit like me (1)’, ‘not like me (2)’ or ‘not at all like me (3)’. Where statements were negative (i.e. statements 2, 5, 6, 8 and 9 in Box 1), these were reverse coded to be positive. The score was then calculated by summing the statements together so that a high value was indicative of high self-esteem.
-
I am satisfied (happy) with myself.
-
At times/I feel I am no good at all.
-
I feel there are a number of good things about me.
-
I do things as well as most other children my age.
-
I do not have much to be proud of.
-
I feel useless at times.
-
I feel that I am as good as everyone else.
-
I wish I liked myself more.
-
I tend to feel that I am a failure.
-
I have a positive (good) view of myself.
Missingness
Chapter 2 (see Missingness and multiple imputation) described how we used multiple imputation to address issues of missingness in variables required for the analysis. We used the same approach in the analysis reported in this chapter. We imputed values on covariates where BMI (and therefore zBMI) at baseline and follow-up, age, sex, neighbourhood and programme variables were completely observed (n = 9563).
In addition to exploring sources of variation in change in BMI and variation in change in self-esteem, we wanted to examine how baseline self-esteem related to change in BMI. For this specific model, we estimated models where baseline self-esteem and change in BMI were both completely observed (n = 4962).
Randomised controlled trial data and the randomised controlled trial-comparable subset of the MEND data
We pooled the service data and data from the intervention arm in the MEND RCT. 15 The RCT was not part of the current study. The RCT data (previously unpublished in trial reports) relate to changes in BMI over the course of the programme. This period (10-week follow-up) is the same as that for the service data. The RCT was restricted to 8- to 12-year-old participants who were obese (exceeded the 98th centile of the UK 1990 growth charts14), whereas MEND 7–13 services in the community are available to those who are overweight and aged 7–13 years. To ensure a valid comparison, the pooled sample was restricted to participants in the RCT intervention arm (n = 47) and those in the service data who were obese and of the same age as RCT participants (n = 8054), for whom data were recorded at baseline and follow-up.
Methods
Regression to the mean
Data obtained before and after interventions are subject to measurement error, biological variation, intrasubject variability and other influences unrelated to the intervention. As a result, the correlations between serial measurements taken from individuals over time are less than perfect, and this leads to regression to the mean. 63 Regression to the mean is a statistical phenomenon such that, on average, the change in BMI over time is greater in subjects whose BMI at baseline is more extreme; thus, there is an inverse association between BMI at baseline and BMI change even in the absence of any intervention effect. 64 Regression to the mean confounds the interpretation of BMI change associated with an intervention. To address this, estimation of intervention effects needs to include adjustment of the outcome (change in BMI and zBMI in this chapter and change in secondary outcomes presented in Chapter 4) for the baseline value. We undertook this adjustment in all analysis models. The adjustment cannot adjust perfectly for confounding by regression to the mean as it accounts for two separate effects simultaneously: conventional regression to the mean, and unmeasured confounding by variables which are associated with BMI at baseline and change in BMI but are not measured by other covariates in the model.
Multilevel analysis of change in body mass index
In this chapter we used multilevel linear regression models to examine the outcomes of change in BMI and change in zBMI, as these outcomes were continuous. Multilevel regression models make the assumption that residuals at the participant and programme levels are normally distributed. We checked this assumption by graphing the residuals from the unadjusted models and found that residuals at both levels met these assumptions. We calculated the Bayesian information criterion (BIC) for models to assess whether the addition of parameters such as random intercepts and slopes, polynomials and interactions improved the fit of the model parsimoniously. The BIC is a measure of a model’s overall fit, penalised for its parametric complexity. The BIC decreases if parameters added to the model improve the fit over and above the increase in parametric complexity. Following recommendations for the use of Bayesian criteria for model selection, we considered a decrease in BIC of 1–2 as only weak evidence of improved fit while decreases ≥ 3 were considered positive to strong. 65
Our preliminary analysis involved a five-stage series of multilevel models. Complete case data (n = 2150) were used to evaluate whether complex parameters (random intercepts and slopes, polynomials and interaction terms) were required in the multivariate model. Complete case data were used as the BIC cannot be computed for multiply-imputed data.
We hypothesised that relationships between variables might vary with age, sex, ethnic group and whether the children lived with lone parents or parents in a couple. We tested these a priori interactions for change in BMI and change in zBMI (see the description of the stages of the analysis, below, for further details).
A series of models were fitted to estimate associations with change in BMI. To ensure that associations were not ruled out because of a lack of power, we used data that were completely observed for each pairwise comparison (i.e. for the age models, data were completely observed for change in BMI, baseline BMI and age).
The first five stages, using complete case data sets, are summarised below.
-
Compare single-level and multilevel models to test whether a multilevel model is necessary (complete case data to compute change in BIC).
-
Assess whether the relationship between BMI at baseline and change in BMI was linear or polynomial to determine how to adjust for baseline BMI in subsequent models (complete case data to compute change in BIC).
-
Estimate ‘baseline-adjusted’ associations between covariates and change in BMI. These multilevel models were adjusted for BMI at baseline. Models were based on fully observed data for change in BMI, BMI at baseline and each covariate in turn to maximise power.
-
Assess whether a random slope for each coefficient improves the fit compared with stage 3. The random slopes allow the coefficients to vary between programmes (complete case data to compute change in BIC).
-
Assess whether prespecified interaction terms improve the fit of models over and above those including just the main effects specified in the interaction (i.e. the BIC of a model including an age-by-sex interaction was compared with the BIC of a model including age and sex but no interaction).
The sixth, seventh and eighth stages of the analysis used multiply-imputed data. As with the multilevel modelling described in Chapter 2 (see Methods, Determinants of completion of MEND 7–13), we fitted models in MLwiN 2.25 and combined analyses across all 10 data sets using Rubin’s rules54 as implemented by the Stata 11.2 multiple imputation commands. These stages are described below.
-
6. Fit multivariable model including all significant covariates, and interactions or random slopes which improved fit with imputed data.
-
7. Repeat multivariable model of change in BMI, replacing outcome with change in zBMI and replacing BMI at baseline with zBMI at baseline.
-
8. We also explored whether self-esteem at baseline was associated with change in BMI, using the Rosenberg self-esteem scale data collected in 2009/10.
We report the intercept of the model, which describes change in BMI for a given ‘reference group’. We characterised this reference group as girls, and for other categorical variables (e.g. ethnicity or family structure) we chose the largest category as the reference category (e.g. white, parents living as a couple, etc.). For continuous variables (e.g. age), the reference category was the average value (e.g. 10.7 years).
Comparisons with randomised controlled trial results
The RCT and service data were also compared using a multilevel regression model. Again, the outcome was change in BMI. For this analysis, the principal covariate of interest was a binary variable indicating whether participants were included in the RCT or the service data. Two multivariable models were estimated, the first estimating differences in change in BMI between the RCT and service data after adjusting for any differences in baseline BMI, age and sex. The second also included ethnicity and housing tenure in addition to the first model, in order to adjust for differences in samples by ethnic group and SEC.
Findings
Description of MEND participants
On average, BMI declined by 0.7 kg/m2 among MEND participants, which equated to a reduction of 0.2 units of zBMI. The sample was approximately normally distributed in terms of BMI change (Figure 4). The histogram shows that although BMI was maintained or reduced for the majority of participants (n = 7661, 80.1%), it also increased for some participants (n = 1902, 19.9%). A larger majority maintained or decreased their zBMI (n = 8441, 88.3%) with a corresponding smaller minority increasing their zBMI (n = 1122, 11.7%).
FIGURE 4.
Histogram of change in BMI (n = 9563).
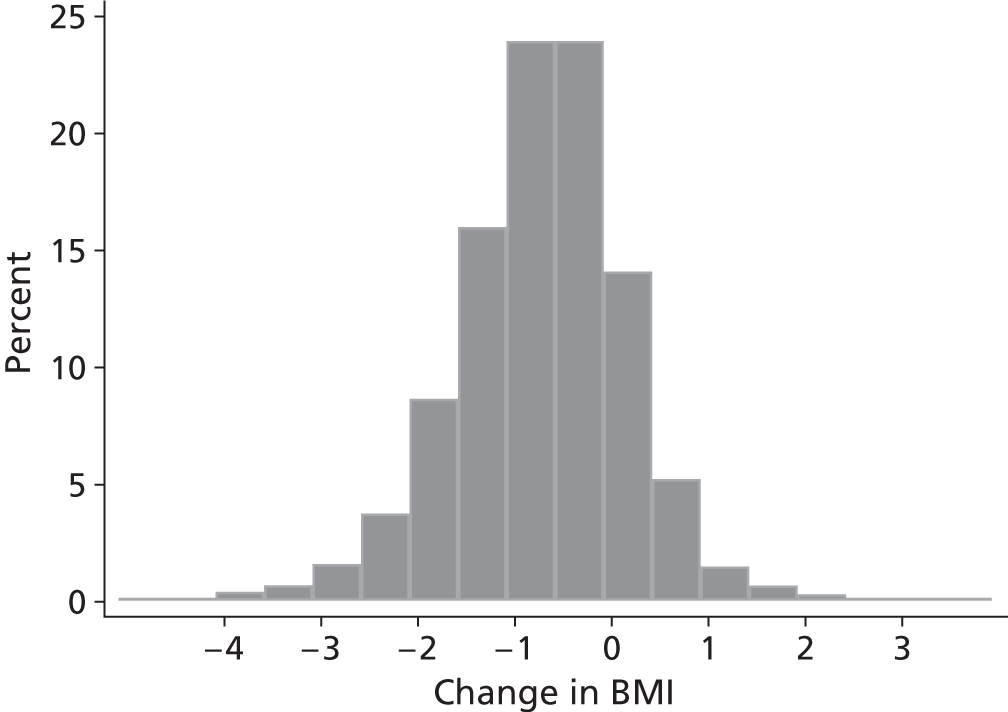
Of 8368 children who were obese at baseline, 8.8% were overweight at follow-up and 0.07% (n = 6) were normal weight. Of 1195 children who were overweight at baseline, 0.4% (n = 38) were obese at follow-up, while 2.8% (n = 264) were normal weight. Demographically, MEND participants were normally distributed by age, centred on a mean of approximately 10 years (Table 9). A disproportionate number of MEND 7–13 participants were girls and from white ethnic groups. Socioeconomically, most MEND participants lived with a parent/carer who considered themselves to be in a couple, reported that they owned their residence and were employed. Higher proportions lived in neighbourhoods which were income deprived relative to England as a whole, and which were urban and built up.
| Imputed data set (n = 9563) |
Complete case data set (n = 2150) |
|
|---|---|---|
| Mean (95% CI) | ||
| BMI change (kg/m2) | –0.7 (–0.7 to –0.7) | –0.7 (–0.7 to –0.7) |
| BMI at baseline (kg/m2) | 26.8 (26.7 to 26.9) | 26.5 (26.3 to 26.7) |
| BMI at follow-up (kg/m2) | 26.1 (26.0 to 26.2) | 25.8 (25.6 to 25.9) |
| zBMI change | –0.2 (–0.2 to –0.2) | –0.2 (–0.2 to –0.2) |
| zBMI at baseline | 2.7 (2.7 to 2.7) | 2.6 (2.6 to 2.6) |
| zBMI at follow-up | 2.5 (2.5 to 2.5) | 2.4 (2.4 to 2.5) |
| Age (years) | 10.4 (10.3 to 10.4) | 10.5 (10.4 to 10.5) |
| IDACI 2007 decile | 0.3 (0.3 to 0.3) | 0.2 (0.2 to 0.4) |
| Built environment score | 0.2 (0.2 to 0.2) | 0.1 (0.1 to 0.2) |
| Number of previous programmes per programme manager | 5.8 (5.6 to 5.9) | 8.0 (7.7 to 8.3) |
| Group size (number of participants) | 8.6 (8.5 to 8.6) | 8.7 (8.6 to 8.9) |
| Percentage | ||
| Sex | ||
| Girls | 55.3 | 56.2 |
| Boys | 44.7 | 43.8 |
| Ethnicity | ||
| White | 76.5 | 76.5 |
| Asian | 13.4 | 10.6 |
| Black | 6.2 | 8.0 |
| Other | 3.9 | 4.9 |
| Family structure | ||
| Couples | 67.1 | 67.2 |
| Lone parents | 33.0 | 32.8 |
| Housing tenure | ||
| Owner occupied | 56.9 | 61.4 |
| Social rented | 28.6 | 25.3 |
| Private rented | 14.5 | 13.3 |
| Employment status | ||
| Employed | 76.4 | 77.7 |
| Unemployed | 23.6 | 22.3 |
| Urban/rural | ||
| Urban | 88.5 | 88.4 |
| Towns | 6.9 | 6.3 |
| Villages | 4.6 | 5.4 |
| Sessions attended | ||
| Non-completers | 2.0 | 0.6 |
| Partial completers | 25.0 | 15.6 |
| Completers | 73.0 | 83.8 |
| Height rounding | ||
| Not rounded | 3.7 | 10.6 |
| Rounded | 96.3 | 89.4 |
| Weight rounding | ||
| Not rounded | 41.3 | 49.3 |
| Rounded | 58.7 | 50.74 |
Using the definitions of ‘completion’ chosen for this study (non-completers attended < 25%, partial completers attended 25–75% and completers attended > 75% of sessions), only a very small minority of the sample were non-completers. This is not surprising because to be part of the change in BMI sample (or any other change outcome sample), the children needed fully observed BMI data at baseline and follow-up. A quarter of the sample partially completed the programme whereas the majority completed the programme.
In terms of data quality, most programmes rounded height measurements to 0.5 or 1 cm. A smaller majority rounded weight measurements.
Examination of the overlap in CIs suggests that there are few differences between the imputed and complete case samples in regard to age, sex, ethnicity, housing tenure, residential neighbourhood deprivation, built environment or urban/rural status and programme group size. The imputed proportions were lower for completers and conversely higher for partial completers.
Modelling to inform multilevel models of change in body mass index
The first stage of the analysis compared an unadjusted single-level model of change in BMI with an unadjusted multilevel model of change in BMI. Estimating the between-programme intercept improved the fit of the model (single-level model BIC = 7434, multilevel model BIC = 7354, change in BIC = –79.9). Between-programme variation in change in BMI explained 16% of the overall variation.
The second stage of the analysis tested whether change in BMI was associated with BMI at baseline on a linear or quadratic scale. The multilevel model showed a significant quadratic effect of BMI at baseline. However, the BICs were similar (linear model BIC = 7304, quadratic model BIC = 7303). 65 Thus, subsequent models in the analysis adjusted for BMI at baseline as a linear term only. On average, children with higher BMI at baseline declined slightly more in BMI than those with lower BMI at baseline. Figure 5 illustrates this relationship.
FIGURE 5.
Relationship between BMI at baseline and change in BMI (n = 9563).
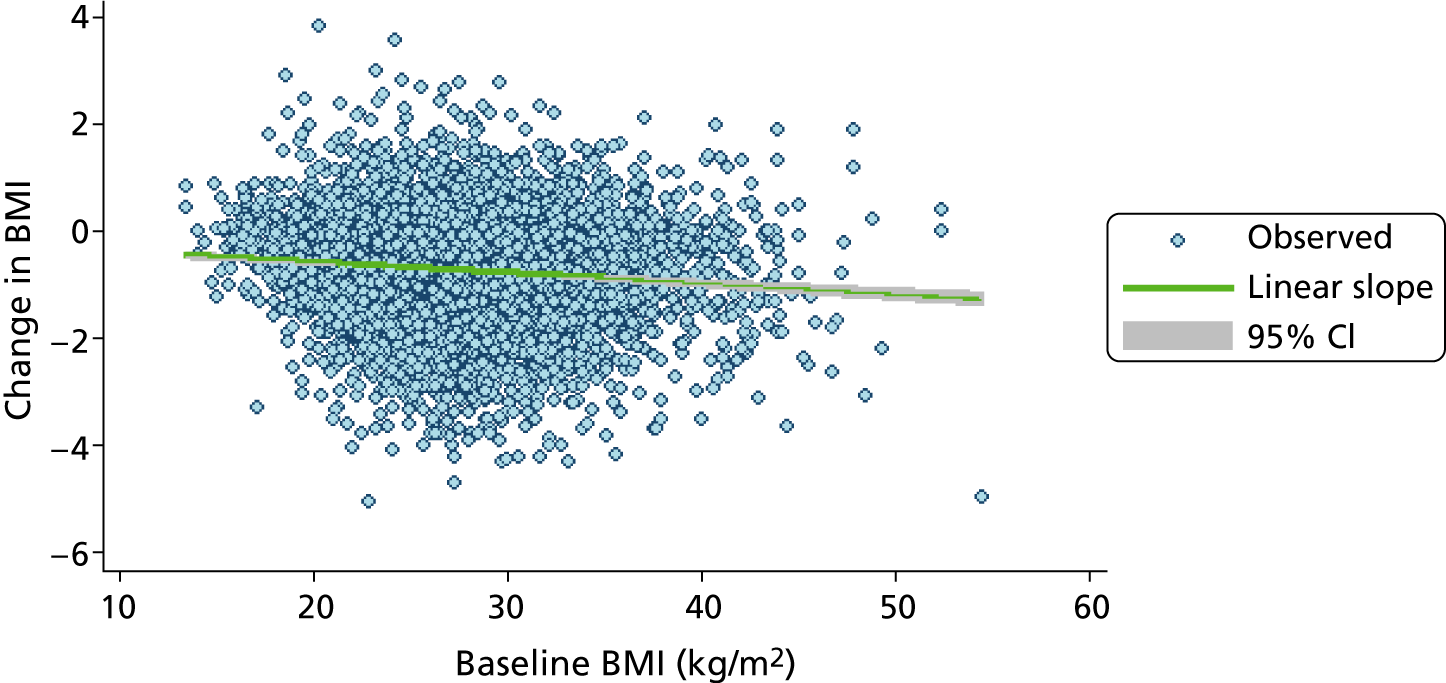
The third stage of the analysis used baseline-adjusted models to explore which variables to use in the final multivariate model. After adjustment for BMI at baseline, most variables were significantly associated with change in BMI (Table 10). Food environment variables for both healthy and unhealthy environments were non-significant and were omitted from later models, as were variables measuring rounding of height and weight.
| Variables | Change in BMI adjusted for baseline BMI, B (SE) | Change in zBMI adjusted for baseline zBMI, B (SE) |
|---|---|---|
| Age (years) | 0.013 (0.0054)* | 0.014 (0.00098)*** |
| Sex (ref. girls) | ||
| Boys | –0.072 (0.017)*** | –0.0050 (0.0034) |
| Ethnicity (ref. white) | ||
| Asian | 0.30 (0.036)*** | 0.054 (0.0072)*** |
| Black | 0.21 (0.039)*** | 0.033 (0.0079)*** |
| Other | 0.14 (0.046)** | 0.025 (0.0092)** |
| Family structure (ref. parents in a couple) | ||
| Lone parents | 0.048 (0.023)* | 0.013 (0.0045)** |
| Housing tenure (ref. owner occupied) | ||
| Social rented | 0.086 (0.025)*** | 0.020 (0.0049)*** |
| Private rented | 0.035 (0.031) | 0.0047 (0.0063) |
| Parental employment (ref. employed) | ||
| Unemployed | 0.16 (0.033)*** | 0.031 (0.0068)*** |
| IDACI 2007 decile (higher score denotes ‘more deprived’) | 0.32 (0.051)*** | 0.062 (0.010)*** |
| Built environment score (higher score denotes ‘more built up’) | 0.050 (0.010)*** | 0.0087 (0.0021)*** |
| Urban/rural status (ref. urban) | ||
| Towns | –0.098 (0.036)** | –0.019 (0.0072)** |
| Villages | –0.085 (0.042)* | –0.013 (0.0084) |
| Healthy food outlets (ref. none) | ||
| One to two healthy outlets | 0.0083 (0.022) | 0.0036 (0.0043) |
| Three or more healthy outlets | 0.0048 (0.063) | –0.0039 (0.013) |
| Unhealthy food outlets (ref. none) | ||
| One to two unhealthy outlets | –0.020 (0.020) | –0.0027 (0.0040) |
| Three to four unhealthy outlets | –0.017 (0.028) | 0.0025 (0.0055) |
| Five or more unhealthy outlets | 0.039 (0.033) | 0.0064 (0.0066) |
| Number of previous programmes per programme manager | 0.0042 (0.0021)* | 0.00062 (0.00041) |
| Group size (number of participants) | 0.014 (0.0039)*** | 0.0027 (0.00078)*** |
| Attendance (ref. completer, attended > 75% of sessions) | ||
| Non-completer (attended < 25% of sessions) | 0.50 (0.12)*** | 0.083 (0.024)*** |
| Partial completer (attended 25–75% of sessions) | 0.27 (0.031)*** | 0.049 (0.0062)*** |
| Height rounding | ||
| Rounded | –0.10 (0.065) | –0.021 (0.013) |
| Weight rounding | ||
| Rounded | –0.044 (0.024) | –0.0079 (0.0048) |
Results were broadly similar for change in zBMI and change in BMI. However, sex and number of previous programmes per programme manager were not associated with the change in zBMI and so were not carried forward to the multivariable model.
A fourth set of models investigated whether the relationships between each covariate and the change in BMI varied randomly between programmes (Table 11). Adding a random slope increased BIC in every case so no random slopes were included. Similarly, the a priori-specified two-way interaction terms all increased BIC, so they too were omitted from the multivariable model.
| Variation between programmes by covariates | Change in BIC |
|---|---|
| Age random slope | 14 |
| RI varies with sex | 0 |
| RI varies with ethnicity | 29 |
| RI varies with family structure | 12 |
| RI varies with housing tenure | 34 |
| RI varies with parental unemployment | 0 |
| IDACI 2007 random slope | 15 |
| Built environment random slope | 15 |
| RI varies with urban/rural status | 33 |
| RI varies with number of healthy food outlets | 7 |
| RI varies with number of unhealthy food outlets | 43 |
| Number of previous programmes per programme manager random slope | 15 |
| Group size random slope | 15 |
| RI varies with attendance | 50 |
| RI varies with height rounding | 0 |
| RI varies with weight rounding | 8 |
| A priori interaction terms | |
| Age*baseline BMI | 2 |
| Sex*baseline BMI | 7 |
| Ethnicity*baseline BMI | 23 |
| Age*sex | 44 |
| Lone parent*built environment | 8 |
Multivariable models of change in BMI and zBMI
The multivariable models of change in BMI, based on the imputed and complete case data sets, appear in Table 12. Model 1 was based on 10 imputed data sets (n = 9563) where the missing covariates (including BMI at baseline) and missing change in BMI were imputed. The intercept shows that the average change in BMI associated with the intervention was −0.76 kg/m2 for those children belonging to the reference group. The characteristics of the reference group in interpreting this finding are therefore important. The group comprised white girls, of average BMI for MEND participants at baseline, living in favourable SEC (having parents who are in a couple, owner occupiers and employed) and who had completed at least 75% of the MEND programme. This group lived in urban neighbourhoods with average levels of deprivation and built environment and attended MEND programmes with around nine attendees at baseline where the programme manager had run around six previous programmes.
| Parameters | Model 1: change in BMI (imputed, n = 9563), B (SE) | Model 2: change in BMI (complete case, n = 2150), B (SE) |
|---|---|---|
| Fixed part | ||
| Intercept | –0.76 (0.021)*** | –0.80 (0.036)*** |
| BMI at baseline | –0.022 (0.0020)*** | –0.030 (0.0042)*** |
| Age (years) | 0.018 (0.0054)*** | 0.020 (0.011) |
| Sex (ref. girls) | ||
| Boys | –0.085 (0.017)*** | –0.060 (0.035) |
| Ethnicity (ref. white) | ||
| Asian | 0.15 (0.037)*** | 0.20 (0.065)** |
| Black | 0.15 (0.040)*** | 0.10 (0.072) |
| Other | 0.088 (0.046) | 0.11 (0.083) |
| Family structure (ref. parents in a couple) | ||
| Lone parents | 0.011 (0.020) | –0.0086 (0.041) |
| Housing tenure (ref. owner occupied) | ||
| Social rented | 0.020 (0.024) | 0.0040 (0.049) |
| Private rented | 0.0085 (0.033) | –0.063 (0.057) |
| Parental employment (ref. employed) | ||
| Unemployed | 0.060 (0.026)* | 0.16 (0.049)** |
| IDACI 2007 decile (higher score denotes ‘more deprived’) | 0.15 (0.061)* | 0.055 (0.12) |
| Built environment score (higher score denotes ‘more built up’) | 0.012 (0.013) | 0.023 (0.026) |
| Urban/rural status (ref. urban) | ||
| Towns | –0.033 (0.040) | –0.14 (0.082) |
| Villages | –0.0071 (0.047) | –0.00082 (0.089) |
| Number of previous programmes per programme manager | 0.0033 (0.0020) | 0.0067 (0.0030)* |
| Group size (number of participants) | 0.0087 (0.0039)* | 0.013 (0.0072) |
| Attendance (ref. completer, attended > 75% of sessions) | ||
| Non-completer (attended < 25% of sessions) | 0.21 (0.074)** | –0.022 (0.24) |
| Partial completer (attended 25–75% of sessions) | 0.13 (0.027)*** | 0.23 (0.049)*** |
| Random part | ||
| Between programmes | 0.11 (0.0080)*** | 0.096 (0.015)*** |
| Between participants | 0.63 (0.010)*** | 0.58 (0.020)*** |
Body mass index fell more in children with higher baseline BMI. Demographically, BMI fell more in younger rather than older children, boys rather than girls and white rather than Asian or black ethnic groups. Socioeconomically, BMI fell more in children whose parents were employed, those living in areas with low proportions of income-deprived families (i.e. low IDACI 2007 scores) and those who attended groups that were larger at baseline. BMI fell less in partial completers and non-completers compared with completers.
Model 2 used complete data (n = 2150) (see the final column of Table 12). The results for models 1 and 2 were similar in direction, though coefficients in the latter model were non-significant for age, sex, black groups, IDACI 2007 decile, group size and non-completers, reflecting the smaller sample size. One coefficient, the number of previous programmes per programme manager, was only significant in model 2.
Results for change in zBMI (Table 13) were broadly similar to the results for change in BMI, except that the baseline BMI/zBMI coefficient was negative for BMI and positive for zBMI, and both were highly significant.
| Parameters | Model 1: change in zBMI (imputed, n = 9563), B (SE) |
Model 2: change in zBMI (complete case, n = 2150), B (SE) |
|---|---|---|
| Fixed part | ||
| Intercept | –0.18 (0.0038)*** | –0.18 (0.0069)*** |
| zBMI at baseline | 0.029 (0.0024)*** | 0.021 (0.0049)*** |
| Age (years) | 0.015 (0.00099)*** | 0.012 (0.0020)*** |
| Ethnicity (ref. white) | ||
| Asian | 0.029 (0.0074)*** | 0.043 (0.014)** |
| Black | 0.022 (0.0079)** | 0.014 (0.015) |
| Other | 0.017 (0.0090) | 0.019 (0.017) |
| Family structure (ref. parents in a couple) | ||
| Lone parents | 0.0033 (0.0040) | –0.00058 (0.0086) |
| Housing tenure (ref. owner occupied) | ||
| Social rented | 0.0081 (0.0047) | 0.0060 (0.010) |
| Private rented | 0.0031 (0.0067) | –0.010 (0.012) |
| Parental employment (ref. employed) | ||
| Unemployed | 0.0099 (0.0050)* | 0.024 (0.010)* |
| IDACI 2007 decile (higher score denotes ‘more deprived’) | 0.034 (0.012)** | 0.013 (0.026) |
| Built environment score (higher score denotes ‘more built up’) | 0.0017 (0.0026) | 0.0032 (0.0055) |
| Urban/rural status (ref. urban) | ||
| Towns | –0.0082 (0.0078) | –0.014 (0.017) |
| Villages | –0.000071 (0.0092) | –0.00033 (0.019) |
| Group size (number of participants) | 0.0018 (0.00077)* | 0.0029 (0.0015) |
| Attendance (ref. completer, attended > 75% of sessions) | ||
| Non-completer (attended < 25% of sessions) | 0.034 (0.015)* | –0.013 (0.049) |
| Partial completer (attended 25–75% of sessions) | 0.023 (0.0051)*** | 0.042 (0.010)*** |
| Random part | ||
| Between programmes | 0.0045 (0.00032)*** | 0.0044 (0.00069)*** |
| Between participants | 0.024 (0.00039)*** | 0.025 (0.00087)*** |
Magnitude of changes in BMI and zBMI
In order to interpret how the results from the multivariable models related to changes in BMI and zBMI we calculated the amount of change which would be expected for key subgroups after adjustment for covariates. We selected subgroups on the basis that they were significantly different from the intercept in the model, and using extreme but meaningful categories (for example, 7 and 13 years were chosen as the extremes of the intended age range for MEND 7–13).
The findings (Table 14) show that all subgroups reduced in BMI and zBMI on average. The top 10% of the sample in terms of BMI showed the greatest BMI reduction overall (0.90 kg/m2). Non-completers reduced the least but still reduced their BMI by 0.55 kg/m2 and their zBMI by 0.15 kg/m2. Other groups reduced in BMI by 0.61 kg/m2 (Asian children), 0.70 kg/m2 (children with unemployed parents) and 0.73 kg/m2 (children living in the most deprived neighbourhoods). The range of the reduction in BMI for group sizes ranging from two to 18 participants was −0.68 kg/m2 to −0.82 kg/m2.
| Subgroups | Change in BMI | Change in zBMI |
|---|---|---|
| Reference group (intercept from models) | –0.76 | –0.18 |
| Baseline BMI | ||
| 10th centile of MEND participant BMI (BMI = 21.59, zBMI = –0.911) | –0.64 | –0.21 |
| 90th centile of MEND participant BMI (BMI = 33.2, zBMI = 0.867) | –0.90 | –0.16 |
| Age (years) | ||
| 7 years | –0.81 | –0.23 |
| 13 years | –0.71 | –0.14 |
| Sex | ||
| Girls | –0.76 | N/A |
| Ethnicity | ||
| Asian | –0.61 | –0.16 |
| Black | –0.67 | –0.16 |
| Parental employment status | ||
| Unemployed | –0.70 | –0.17 |
| IDACI 2007 decile | ||
| Threshold for least deprived 10% of LSOAs in England (IDACI 2007 score = 0.04) | –0.79 | –0.19 |
| Threshold for most deprived 10% of LSOAs in England (IDACI 2007 score = 0.48) | –0.73 | –0.17 |
| Completion | ||
| Non-completers (attended < 25% of sessions) | –0.55 | –0.15 |
| Group size (eight to nine participants on average, ranging from one to 19) | ||
| 2 participants | –0.82 | –0.19 |
| 18 participants | –0.68 | –0.16 |
Self-esteem at baseline and change in body mass index
Table 15 explores the relationship between change in BMI and self-esteem, using the imputed self-esteem data set (n = 4962) (models 1 and 2). Model 1 omits baseline self-esteem while model 2 includes it. Model 2 shows that self-esteem at baseline is weakly associated with change in BMI; for each extra unit of self-esteem (measured on a 0–30 scale), BMI falls by 0.0048 kg/m2 less. This means that, after adjustment for covariates, participants whose level of self-esteem at baseline was average (16.78) reduced in BMI by −0.79 kg/m2. For those whose self-esteem was one standard deviation (6.89) above the mean at baseline, BMI reduced less (by −0.76 kg/m2), and for those whose self-esteem was one standard deviation below, BMI reduced more (by −0.83 kg/m2). Model 3 in Table 15 shows that in the complete case model baseline self-esteem was not significantly related to change in BMI.
| Parameters | Model 1: no self-esteem (imputed), B (SE) | Model 2: self-esteem (imputed), B (SE) | Model 3: complete case, B (SE) |
|---|---|---|---|
| Fixed part | |||
| Intercept | –0.79 (0.027)*** | –0.79 (0.027)*** | –0.79 (0.040)*** |
| BMI at baseline | –0.024 (0.0028)*** | –0.023 (0.0029)*** | –0.030 (0.0047)*** |
| Baseline self-esteem | – | 0.0048 (0.0018)** | 0.0026 (0.0028) |
| Age (years) | 0.020 (0.0073)** | 0.022 (0.0073)** | 0.022 (0.012) |
| Sex (ref. girls) | |||
| Boys | –0.091 (0.024)*** | –0.095 (0.024)*** | –0.076 (0.038)* |
| Ethnicity (ref. white) | |||
| Asian | 0.21 (0.047)*** | 0.20 (0.048)*** | 0.19 (0.070)** |
| Black | 0.13 (0.051)* | 0.12 (0.052)* | 0.096 (0.077) |
| Other | 0.074 (0.058) | 0.071 (0.058) | 0.13 (0.092) |
| Family structure (ref. parents in a couple) | |||
| Lone parents | 0.024 (0.028) | 0.026 (0.028) | –0.025 (0.044) |
| Housing tenure (ref. owner occupied) | |||
| Social rented | 0.019 (0.032) | 0.021 (0.032) | 0.0028 (0.054) |
| Private rented | 0.0090 (0.040) | 0.011 (0.040) | –0.057 (0.062) |
| Parental employment status (ref. employed) | |||
| Unemployed | 0.084 (0.034)* | 0.087 (0.034)* | 0.16 (0.053)** |
| IDACI 2007 decile | 0.16 (0.080) | 0.15 (0.080) | 0.069 (0.13) |
| Urban/rural status (ref. urban) | |||
| Towns | –0.064 (0.048) | –0.064 (0.048) | –0.18 (0.080)* |
| Villages | –0.042 (0.058) | –0.043 (0.058) | –0.033 (0.091) |
| Number of previous programmes per programme manager | 0.0028 (0.0024) | 0.0028 (0.0024) | 0.0063 (0.0033) |
| Group size (number of participants) | 0.0051 (0.0050) | 0.0050 (0.0050) | 0.011 (0.0078) |
| Attendance (ref. completer, attended > 75% of sessions) | |||
| Non-completer (attended < 25% of sessions) | 0.17 (0.10) | 0.17 (0.10) | –0.27 (0.30) |
| Partial completer (attended 25–75% of sessions) | 0.14 (0.032)*** | 0.14 (0.031)*** | 0.21 (0.055)*** |
| Random part | |||
| Between programmes | 0.10 (0.011)*** | 0.10 (0.011)*** | 0.11 (0.018)*** |
| Between participants | 0.61 (0.014)*** | 0.61 (0.014)*** | 0.57 (0.022)*** |
Results were broadly similar to those shown in Table 12 (change in BMI in a larger sample size of 9563, with no baseline self-esteem included). However, whereas associations between change in BMI and IDACI 2007 decile, non-completers versus completers and group size were non-significant in Table 15, they were significant in Table 12.
Sensitivity analyses of modelling of change in body mass index
We considered it essential to adjust for BMI at baseline before selecting the other covariates. However, we anticipate that, for comparison with previous work, some readers may be interested in the univariable relationships between change in BMI and the covariates without adjustment for BMI at baseline. Associations from multilevel models with the imputed data but without adjustment for BMI at baseline are presented in Appendix 8 (see Table 34).
Comparison of change in body mass index observed in service and randomised controlled trial settings
The mean change in BMI in service-level data for 8- to 12-year-old obese children was −0.71 kg/m2 after adjustment for BMI at baseline, age and sex (Table 16). The coefficient for the RCT shows that the BMI of those in the RCT reduced by 0.17 kg/m2 more, but this difference was not statistically significant. After adjustment for ethnicity and housing tenure the change in BMI in service-level data was −0.79 kg/m2, and for those in the RCT it reduced by 0.25 kg/m2 more. Again, this difference was not statistically significant.
| Parameters | Adjusted for demographic factors, B (SE) | Adjusted for ethnicity, demographic and SEC factors, B (SE) |
|---|---|---|
| Fixed part | ||
| Intercept | –0.71 (0.017)*** | –0.79 (0.025)*** |
| RCT (ref. service level) | –0.17 (0.13) | –0.25 (0.13) |
| BMI at baseline | –0.010 (0.0033)** | –0.012 (0.0039)** |
| Age | 0.016 (0.011) | 0.020 (0.014) |
| Sex (ref. girls) | ||
| Boys | –0.082 (0.024)*** | –0.055 (0.029) |
| Ethnicity (ref. white) | ||
| Asian | – | 0.29 (0.049)*** |
| Black | – | 0.26 (0.049)*** |
| Other | – | 0.13 (0.058)* |
| Housing tenure (ref. owner occupied) | ||
| Social rented | – | 0.10 (0.032)** |
| Private rented | – | 0.052 (0.042) |
Discussion
Changes in body mass index associated with MEND 7–13 delivered under service conditions
Our principal objective in this chapter was to investigate how outcomes associated with MEND 7–13 varied according to participant, family, neighbourhood and programme factors. However, before the results relating to this objective are discussed, we discuss whether or not MEND 7–13, when delivered under service conditions at the population level, was associated with any reduction in BMI.
Our findings show that MEND 7–13, as delivered across the country in the service setting, was associated with a mean reduction in BMI of 0.76 kg/m2. Previous work suggests that there are unlikely to be large increases in height over a 10-week follow-up period,66 which means that a reduction in BMI associated with MEND suggests that the programme may be associated with weight maintenance or weight loss. An outcome of weight maintenance/loss is in line with current national guidance on paediatric weight management interventions from the National Institute for Health and Care Excellence (NICE). 9
Beyond knowing that average BMI is reduced in the programme, it may also be instructive to consider how much of a reduction in BMI might be important from a clinical perspective. However, there is little consensus as to what constitutes a clinically significant effect. Meta-analyses reported by Cochrane reviewers10 of four lifestyle treatments for childhood overweight and obesity suggest that treatment interventions for children aged < 12 years lead to changes in zBMI of −0.06 at 6-month follow-up. This reduction in zBMI was described by the authors as both ‘statistically significant and clinically relevant’ (p. 16). Therefore, the magnitude of the reduction of 0.18 in zBMI observed in the MEND 7–13 service might also be considered ‘clinically relevant’ but it is important to note that the findings reported here relate to a shorter follow-up (10 weeks) than the Cochrane review findings (6-month follow-up). As a targeted intervention, the magnitude of the reductions in BMI and zBMI noted here might be important for the health of overweight and obese children at the population level. However, as with the debate on whether the findings are clinically relevant, there are few sources available which suggest by how much BMI might need to reduce following a scaled-up intervention for it to be important at the population level. Changes observed in the service data were not significantly different from the change in BMI observed in the intervention arm of the MEND RCT (Sacher et al. 15). This suggests that BMI fell by a similar amount under research and service conditions during the programme (and that changes were of a similar order of magnitude), although these results should be treated cautiously owing to the small sample size of the RCT intervention arm. As we discuss above, it would be interesting to consider whether this difference was important from a clinical or population health perspective. However, in the absence of a clear consensus view on the size of a clinically relevant difference between groups, or what constitutes an important reduction at the population level, we cannot comment further.
In the MEND RCT, the reduction in BMI seen by the end of the intervention was maintained at 12 months. 15 We did not have service data at a comparable follow-up to assess whether changes were maintained after MEND 7–13 was delivered in service settings (discussed in more depth below; see Strengths and limitations of the study).
We note that our findings do not reflect an assessment of the effectiveness of MEND 7–13, or a comparative analysis of MEND 7–13 versus alternative weight management or health promotion schemes.
Variations in outcomes associated with MEND 7–13
The extent of the reduction in BMI varies with BMI at baseline, demographic group, family SEC and neighbourhood deprivation, group size and levels of attendance at the programme. Similar variations were also observed for models using change in zBMI as an outcome and where complete data were used. Our findings suggest that reductions in excess fat associated with this weight management intervention were smaller for those living in less favourable SEC and in black and Asian groups. However, statistically significant variation between groups does not necessarily equate to variation which is clinically relevant. As discussed above, a reduction in zBMI of 0.06 can be considered a ‘clinically relevant’ threshold. Even the groups which experienced statistically significantly smaller reductions in average BMI (for example, older children, girls or Asian children) still reduced their zBMI by more than 0.06 on average (see Table 14).
Higher baseline zBMI was associated with a smaller reduction in zBMI, whereas higher baseline BMI was associated with a larger reduction in BMI. We investigated the underlying reasons for this, finding that these different patterns might be expected given the ways that age and sex standardisation impact differentially on the variability of baseline BMI/zBMI and on the relationships between age, sex and change in BMI/zBMI. These patterns are discussed in more detail in Appendix 10.
We have found no studies which have systematically tested how the impact of weight management interventions varies according to demographic factors. Review articles have suggested that this is a key area for future research. A recent review of reviews23 examining the differential effectiveness of interventions by SEC found no studies which examined this question for change in BMI or change in zBMI (although diet and physical activity interventions were found; see Chapter 4, Change in lifestyle behaviours associated with MEND 7–13).
Our study investigated whether or not self-esteem at baseline was associated with change in BMI after adjustment for BMI at baseline and other covariates. We found that higher levels of self-esteem were associated with slightly smaller reductions in BMI; conversely, children with lower self-esteem reduced in BMI more. This may be because children who have lower self-esteem before the programme have more potential to benefit from MEND than children whose self-esteem is already high. Although several intervention studies have examined self-esteem as a secondary outcome in weight management intervention studies (see Griffiths et al. 67 for a recent review), we have found none which examined self-esteem as a moderator of weight management interventions.
Baseline-adjusted models showed that change in BMI associated with MEND was not associated with variations in local food environments. Thus, participants living in areas with a high density of fast food and other unhealthy food outlets did not reduce in BMI less than those living in areas with a lower density. Conversely, participants living in areas with high proportions of healthy outlets did not reduce in BMI more than those living in areas with less healthy outlets. This suggests that any changes associated with the programme were, in the short term, apparently resistant to differential exposure to food environments that either promote or constrain a healthy diet. This is perhaps not surprising in the UK context; despite the popular characterisation of ‘food deserts’ (areas where healthy food is less readily available), the evidence that variations in the availability of healthy food in the local environment are associated with levels of overweight is relatively weak. 68,69
Change in BMI was not independently associated with characteristics of the built environment or with urban/rural status. Although participants living in more built-up areas did reduce less in BMI, and those in rural and suburban areas reduced more, when these variables were included in a model which also adjusted for neighbourhood deprivation (IDACI 2007 decile) and family socioeconomic status, these relationships were attenuated to non-significance. This suggests that the unadjusted differences may have been due to differences between urban and rural areas in terms of families’ SEC.
Change in BMI was associated with levels of attendance at the programme; completers showed greater reductions in BMI than partial completers and non-completers. This supports the assertion that the variations in the outcome are attributable to participation in the intervention. This is important because our study did not have access to measurements for controls who did not receive the intervention. This means that we cannot make causal assertions about whether or not changes in BMI observed among MEND participants were attributable to the intervention itself (as opposed to another temporal change).
Strengths and limitations of the study
This analysis was based on a service-level data set collected under service (or ‘real world’) conditions across all regions of England. The data set was large enough to have substantial statistical power to identify associations between change in BMI and factors at the individual, family, neighbourhood and programme levels when modelled in a multivariable regression. The availability of such data to examine how interventions operate is a major strength as it allows us to quantify changes associated with such programmes delivered under a wide range of circumstances across the country.
We have noted challenges associated with using the MEND service data in terms of missingness and our methods of mitigating these issues using multiple imputation (see Chapter 2, Strengths and weaknesses of the study). The same discussion also applies to these analyses of change in BMI and change in zBMI.
The statistical power to relate sociodemographic and programme factors to change in BMI was a strength of the study. However, as with most secondary data sets, there were other variables which we would have liked to examine which were not measured at the family level, such as parental BMI and parental lifestyle factors which may have moderated the programme’s relationship with participants’ BMI. In addition, there was substantial unexplained random variation between programmes accounting for approximately 16% of the variation in change in BMI. This may well be explained by features which were unmeasured in the service data, such as variations in facilitator qualifications and experience, or features of the venues where sessions were delivered. Again, it would have been useful to explore how these factors related to changes in outcome, and service organisations might consider how to routinely collect such information.
MEND Central recommends anthropometry equipment and trains delivery partners in measurement. However, programmes did not record what equipment was used and so we could not check how far programmes adopted this guidance. In addition, when we analysed the height data, many measurements appeared to have been rounded. As this study was based on service data, the staff delivering programmes were also responsible for the data collection. Therefore, it is possible that observer bias may have influenced the measurement of results. This is not uncommon in routine data collection and it has been demonstrated to impact on estimates of prevalence. 70 Our analysis considered height and weight rounding at the programme level, and these were not found to be associated with change in BMI in baseline-adjusted models; however, it is possible that observer bias may remain.
The analysis allowed us to estimate variations in change in BMI as the primary outcome. In the absence of controls we cannot attribute changes in BMI to the programme itself, as children may have been participating in other interventions elsewhere. However, it is unlikely that secular changes would account for changes in such a short time period. In addition, although there were issues with data quality in terms of height and weight rounding, it is unlikely that these could systematically have biased the results. That said, as with all studies, and especially those utilising data not collected under research conditions, there may have been other, unmeasured sources of error which may have introduced bias and we cannot assess how this may have impacted on our findings.
Most interventions measured under research conditions report change at periods of follow-up, typically 6 or 12 months. In this study, data were not available beyond the end of the programme. This limitation is probably common if using service-level data. Although the estimates derived here cannot be used to comment on the sustainability of the intervention effect over a longer time period, the intervention’s effectiveness was assessed under research conditions at 6 months and 1 year in a RCT. 15 The change in BMI and zBMI at the end of the programme was similar in both the RCT and our analysis.
Headline findings from Chapter 3
Participation in MEND 7–13 was associated with ‘clinically relevant’ average reductions in BMI overall, and in all socioeconomic and ethnic groups.
Although all groups reduced in BMI by a ‘clinically relevant’ amount, reductions were greater for:
-
children who had higher BMI at the start of the programme
-
boys
-
younger children
-
white children
-
children living in a family where the primary earner was employed
-
children living in less deprived neighbourhoods where a social gradient in change in BMI was observed independently of family SEC
-
children who attended a smaller MEND 7–13 programme
-
children who completed the programme, compared with those who were partial or non-completers.
This suggests that, although referral to, participation in and completion of MEND 7–13 may enhance equity (see Chapter 2), the outcomes associated with the programme may have the potential to widen inequalities.
There were differences between MEND programmes in terms of children’s average reduction in BMI. However, characteristics of the food and built environment did not independently moderate changes in BMI associated with the programme. BMI reductions under service and RCT conditions were of similar magnitude.
Chapter 4 Characteristics associated with changes in secondary outcomes and MEND costs
How do outcomes associated with participation in MEND 7–13 vary with the characteristics of the children (sex, ethnicity and family SEC), MEND programmes (data quality, programme group size, percentage of programme sessions attended) and areas where children live (area-level deprivation and the obesogenic environment)?
What are the costs of providing MEND? What are the factors likely to affect the cost of providing MEND? What is the relationship between the variation in the cost of providing MEND and the outcomes of participants?
Background
Interventions such as MEND 7–13 aim primarily to help children and families address weight management and so support the loss of excess fat. However, they also aim to impact on other outcomes associated with childhood overweight, such as low self-esteem, high psychological distress, low levels of physical activity and poor diet. In this chapter, we examine how variation in these outcomes is associated with individual-, neighbourhood- and programme-level factors.
Two recent studies71,72 have undertaken detailed analyses of the cost of providing MEND 7–13, and we summarise these here. We also examine variation in the costs of providing MEND 7–13 under service conditions, which other studies have not done. In addition, we investigate the extent to which the factors influencing the costs of providing MEND 7–13 affect outcomes. Note that our analysis does not aim to calculate the incremental cost of MEND 7–13 (in terms of the cost of providing MEND 7–13 minus cost savings from reduction in future obesity-related costs), nor the incremental cost-effectiveness of MEND 7–13 versus a comparator (see Appendix 11 for details of calculations of these for MEND 7–13 by other authors).
Data
In this section we draw on the MEND 7–13 service data relating to overweight children who attended MEND 7–13 between 2007 and 2010 (described in full in Chapter 2, MEND 7–13 service-level data).
Secondary outcomes
The four secondary outcomes were change in self-esteem, change in SDQ score, change in physical activity and change in diet. These are defined as follows.
Change in self-esteem was assessed using the Rosenberg scale35 (described in Chapter 3, Covariates; a higher score indicates higher self-esteem). Change in self-esteem ranges theoretically from −30 to 30, and was derived by subtracting baseline self-esteem from self-esteem at follow-up.
Change in psychological distress was assessed using change in SDQ score. A positive value on change in SDQ score means that the participant’s level of psychological distress increased. The SDQ score ranges theoretically from −50 to 50, and was derived by subtracting baseline SDQ score from SDQ score at follow-up.
Change in physical activity was measured by the difference in the number of hours spent walking or cycling in the previous week, as reported by parents in the first and last sessions of the intervention. We excluded values at baseline or follow-up which exceeded 20 hours of exercise (affecting between 1.2 and 3.4% of participants) as unrealistic. Change in physical activity could therefore range theoretically from −20 to 20 hours, and was derived by subtracting physical activity at baseline from physical activity at follow-up.
The diet score was developed for use in the MEND 7–13 programme. The score measures ‘MEND-friendliness’, a construct to assess a combination of diet and food behaviours considered to reflect a healthy balanced diet. The score is derived from parent reports on 14 items that assess:
-
the types of foods the child eats
-
how much the child eats
-
how the food is prepared and eaten
-
the adult’s perspective on the child’s food.
Responses are scored 0 (‘MEND unfriendly’), 1 (‘MEND neutral’) or 2 (‘MEND friendly’), and summed over the items to create a score out of 28. A higher score indicates that the child’s diet and food behaviour is ‘MEND friendly’. The coding matrix (provided by MEND Central) is reproduced in Appendix 12.
Covariates
The set of covariates at the participant, neighbourhood and programme levels used in models of change in secondary outcomes was the same as that used for change in BMI (see Chapter 3, Covariates). The only difference was that instead of adjusting for BMI at baseline we adjusted for each secondary outcome at baseline (for example, we adjusted for self-esteem at baseline for the model of change in self-esteem).
Missingness
As with the analyses of change in BMI, data were missing for ethnicity, family structure, housing tenure, employment status and session attendance. Data were handled using multilevel multiple imputation models (see Chapter 3, Missingness).
Methods
Multilevel models of secondary outcomes
The analytic sequence for changes in self-esteem, SDQ score, physical activity and diet was the same as that used for change in BMI (see Chapter 3, Multilevel analysis of change in body mass index).
Bivariate multilevel model
We also examined a bivariate multivariable model of change in self-esteem and change in BMI. This allowed us to model changes in self-esteem and BMI simultaneously (using the imputed data for change in self-esteem and change in BMI described in Chapter 2, Missingness and multiple imputation). This type of model directly estimates the covariance between changes in self-esteem and BMI (although inferences about the direction of causality cannot be made). It also shows whether characteristics associated with change in BMI were associated with change in self-esteem in the same way.
Cost of providing MEND 7–13
To identify the cost of providing MEND 7–13 we originally planned to undertake a de novo analysis of selected currently and previously funded MEND 7–13 programmes. However, we identified two recently conducted studies that evaluated the cost of providing MEND 7–13 and reported results in sufficient detail for our analysis. 71,72 These studies were undertaken separately and yielded similar results so we felt that further independent analysis was unnecessary. Based on these studies we present figures for the cost of providing a MEND 7–13 programme. We also calculated the mean cost of providing MEND 7–13 per participant, using published figures and our own calculations based on the number of children who started each MEND 7–13 programme. We focus on the number of starters because it is relatively straightforward to define, and because this is likely to be the basis on which local programme running costs (e.g. staffing and venue hire) are calculated. Costs were calculated from the perspective of the NHS and PSS and reported in UK£2010/11.
To identify the factors likely to affect the cost of providing MEND 7–13 we undertook interviews with staff at MEND Central, and examined the main drivers of the cost of providing MEND 7–13 from the two studies described above. Group size was identified by MEND staff as a factor likely to affect the cost of providing MEND 7–13. Data on group size were taken from the same sources used in Chapter 3.
To identify the relationship between variation in the cost of providing MEND 7–13 and the outcomes of participants we used the analysis for research question 2 (see Chapter 3) to identify, where possible, whether or not the factors likely to affect the cost of providing MEND 7–13 affected the outcomes of participating in MEND 7–13.
Findings
Description of MEND 7–13 participants
The complete case and imputed data sets for change in self-esteem and change in SDQ score are described in Table 17. Those for change in diet and change in physical activity are shown in Table 18. Changes in the secondary outcomes showed that self-esteem increased by 3.2 units, SDQ score (i.e. psychological distress) decreased by 2.9, parent-reported walking and cycling increased by 0.8 hours a week and the MEND-friendliness of children’s diets increased by 6.1 units.
| Change in self-esteem | Change in SDQ score | |||
|---|---|---|---|---|
| Imputed (n = 5078) | Complete case (n = 1852) | Imputed (n = 8127) | Complete case (n = 1918) | |
| Mean (95% CI) | ||||
| Self-esteem/SDQ score change | 3.2 (3.0 to 3.3) | 3.1 (2.7 to 3.3) | –2.9 (–3.1 to –2.8) | –2.8 (–3.0 to –2.5) |
| Self-esteem/SDQ score at baseline | 16.8 (16.6 to 17.0) | 17.0 (16.6 to 17.3) | 13.1 (13.0 to 13.3) | 12.9 (12.5 to 13.2) |
| Self-esteem/SDQ score at follow-up | 20.0 (19.8 to 20.2) | 20.0 (19.7 to 20.3) | 10.2 (10.1 to 10.4) | 10.1 (9.8 to 10.4) |
| Age (years) | 10.4 (10.3 to 10.4) | 10.5 (10.4 to 10.6) | 10.4 (10.3 to 10.4) | 10.5 (10.4 to 10.6) |
| IDACI 2007 decile | 0.3 (0.3 to 0.3) | 0.3 (0.2 to 0.3) | 0.3 (0.3 to 0.3) | 0.2 (0.2 to 0.3) |
| Built environment score | 0.2 (0.2 to 0.2) | 0.2 (0.1 to 0.2) | 0.2 (0.2 to 0.2) | 0.1 (0.1 to 0.2) |
| Number of previous programmes per programme manager | 6.9 (6.7 to 7.1) | 7.9 (7.6 to 8.3) | 5.9 (5.7 to 6.0) | 8.1 (7.8 to 8.5) |
| Group size (number of participants) | 8.6 (8.5 to 8.7) | 8.8 (8.6 to 8.9) | 8.6 (8.6 to 8.7) | 8.8 (8.7 to 8.9) |
| Percentages | ||||
| Sex | ||||
| Girls | 55.5 | 56.8 | 55.4 | 56.0 |
| Boys | 44.5 | 43.3 | 44.6 | 44.0 |
| Ethnicity | ||||
| White | 76.6 | 76.2 | 77.1 | 77.0 |
| Asian | 12.0 | 10.4 | 12.6 | 9.9 |
| Black | 6.9 | 8.5 | 6.5 | 8.3 |
| Other | 4.5 | 4.9 | 3.9 | 4.9 |
| Family structure | ||||
| Couple | 65.8 | 67.2 | 66.8 | 66.9 |
| Lone parent | 34.3 | 32.8 | 33.2 | 33.1 |
| Housing tenure | ||||
| Owner occupied | 57.1 | 61.5 | 57.2 | 61.4 |
| Social rented | 28.4 | 25.3 | 28.3 | 25.4 |
| Private rented | 14.6 | 13.2 | 14.5 | 13.2 |
| Employment status of primary earner | ||||
| Employed | 76.0 | 77.5 | 76.3 | 77.3 |
| Unemployed | 24.0 | 22.5 | 23.7 | 22.7 |
| Urban/rural | ||||
| Urban | 87.9 | 88.4 | 88.5 | 88.2 |
| Towns | 7.4 | 6.7 | 7.0 | 6.7 |
| Villages | 4.7 | 4.9 | 4.6 | 5.2 |
| Sessions attended | ||||
| Non-completers | 2.0 | 0.4 | 1.9 | 0.4 |
| Partial completers | 24.2 | 14.8 | 23.8 | 15.2 |
| Completers | 73.8 | 84.8 | 74.3 | 84.4 |
| Height rounding | ||||
| Not rounded | 5.6 | 10.0 | 3.6 | 10.2 |
| Rounded | 94.4 | 90.0 | 96.4 | 89.8 |
| Weight rounding | ||||
| Not rounded | 44.5 | 50.1 | 41.7 | 50.5 |
| Rounded | 55.5 | 50.0 | 58.4 | 49.5 |
| Change in PA | Change in diet | |||
|---|---|---|---|---|
| Imputed (n = 2024) | Complete case (n = 610) | Imputed (n = 7859) | Complete case (n = 1848) | |
| Mean (95% CI) | ||||
| PA/diet change | 0.8 (0.7 to 0.9) | 0.7 (0.5 to 0.9) | 6.1 (6.0 to 6.2) | 5.5 (5.3 to 5.7) |
| PA/diet at baseline | 2.5 (2.4 to 2.6) | 2.7 (2.6 to 2.9) | 16.5 (16.4 to 16.6) | 16.5 (16.3 to 16.7) |
| PA/diet at follow-up | 3.3 (3.2 to 3.4) | 3.5 (3.3 to 3.7) | 22.6 (22.5 to 22.7) | 22.0 (21.8 to 22.2) |
| Age (years) | 10.4 (10.3 to 10.5) | 10.5 (10.4 to 10.7) | 10.4 (10.3 to 10.4) | 10.4 (10.4 to 10.5) |
| IDACI 2007 decile | 0.2 (0.2 to 0.3) | 0.2 (0.2 to 0.2) | 0.3 (0.3 to 0.3) | 0.3 (0.2 to 0.3) |
| Built environment score | 0.1 (0.1 to 0.2) | 0.1 (0.0 to 0.2) | 0.2 (0.2 to 0.2) | 0.1 (0.1 to 0.2) |
| Number of previous programmes per programme manager | 6.0 (5.7 to 6.2) | 6.6 (6.1 to 7.0) | 5.9 (5.7 to 6.0) | 8.1 (7.7 to 8.4) |
| Group size (number of participants) | 8.8 (8.6 to 8.9) | 9.0 (8.7 to 9.2) | 8.6 (8.6 to 8.7) | 8.8 (8.6 to 8.9) |
| Percentages | ||||
| Sex | ||||
| Girls | 54.8 | 58.2 | 55.2 | 55.6 |
| Boys | 45.2 | 41.8 | 44.8 | 44.4 |
| Ethnicity | ||||
| White | 79.8 | 80.2 | 76.7 | 76.0 |
| Asian | 11.8 | 10.3 | 12.7 | 10.2 |
| Black | 5.2 | 6.4 | 6.6 | 8.8 |
| Other | 3.3 | 3.1 | 4.0 | 5.0 |
| Family structure | ||||
| Couple | 65.3 | 69.7 | 66.9 | 67.2 |
| Lone parent | 34.7 | 30.3 | 33.1 | 32.8 |
| Housing tenure | ||||
| Owner occupied | 60.0 | 67.1 | 57.2 | 61.0 |
| Social rented | 26.0 | 23.0 | 28.5 | 26.1 |
| Private rented | 14.0 | 10.0 | 14.3 | 12.9 |
| Employment status of primary earner | ||||
| Employed | 78.0 | 80.5 | 76.5 | 77.3 |
| Unemployed | 22.0 | 19.5 | 23.5 | 22.7 |
| Urban/rural | ||||
| Urban | 87.0 | 88.7 | 88.5 | 87.9 |
| Towns | 8.3 | 5.9 | 7.0 | 6.7 |
| Villages | 4.6 | 5.4 | 4.6 | 5.3 |
| Sessions attended | ||||
| Non-completers | 2.0 | 0.5 | 1.9 | 0.3 |
| Partial completers | 26.7 | 14.9 | 24.0 | 15.2 |
| Completers | 71.3 | 84.6 | 74.1 | 84.5 |
| Height rounding | ||||
| Not rounded | 2.7 | 7.7 | 3.7 | 10.1 |
| Rounded | 97.3 | 92.3 | 96.3 | 89.9 |
| Weight rounding | ||||
| Not rounded | 40.6 | 46.1 | 41.4 | 50.4 |
| Rounded | 59.4 | 53.9 | 58.6 | 49.6 |
As with the data on change in BMI (see Table 9), the imputed and complete case data were very similar in terms of the estimated proportions in the data. The sociodemographic distribution of MEND 7–13 participants in the change in BMI data set was described previously (see Chapter 3, Description of MEND participants and Table 9). The sociodemographic composition of the participants in the secondary outcome data sets (see Tables 17 and 18) was similar to that of the data set looking at change in BMI.
Modelling to inform multilevel models of change in secondary outcomes
The fit of all models was improved by multilevel modelling (changes in BIC in comparisons of single and multilevel models were −18 for self-esteem, −6 for SDQ score, −5 for physical activity and −21 for diet). The percentages of variation explained by between-programme variation differed by outcome as follows: 8.2% for change in self-esteem; 6.2% for change in SDQ score; 7.6% for change in physical activity; and 11.0% for change in diet. These were lower than the 16.0% observed for change in BMI (see Chapter 3).
The set of variables included in the final model was identified independently for each outcome by fitting a series of preliminary multilevel models, one for each covariate after adjustment for the outcome at baseline. As with the analysis of change in BMI, the covariates significant at the 5% level were carried forward. The density of healthy or unhealthy food outlets and changes in self-esteem and SDQ score were not tested as they were not considered applicable.
Self-esteem at baseline, ethnicity, parental employment status, IDACI 2007 decile, the number of programmes run by the programme leader up to that point, and attendance were all carried forward to the change in self-esteem model. The remaining covariates were not associated with change in self-esteem (Table 19, model 1).
| Variables | Model 1: change in self-esteem (n = 1852), B (SE) | Model 2: change in SDQ score (n = 1918), B (SE) | Model 3: change in PA (n = 610), B (SE) | Model 4: change in diet (n = 1848), B (SE) |
|---|---|---|---|---|
| Age | –0.074 (0.046) | –0.043 (0.028) | 0.041 (0.028) | –0.034 (0.021) |
| Sex (ref. girls) | ||||
| Boys | 0.079 (0.16) | 0.56 (0.099)*** | 0.14 (0.096) | –0.25 (0.074)*** |
| Ethnicity (ref. white) | ||||
| Asian | –1.32 (0.30)*** | 0.51 (0.20)* | –0.13 (0.20) | –1.03 (0.15)*** |
| Black | 0.0018 (0.34) | –0.32 (0.21) | –0.14 (0.23) | –0.60 (0.16)*** |
| Other | –0.53 (0.39) | –0.18 (0.26) | –0.051 (0.28) | –0.35 (0.19) |
| Family structure (ref. couple) | ||||
| Lone parent | –0.32 (0.20) | 0.16 (0.13) | –0.094 (0.12) | –0.085 (0.094) |
| Housing tenure (ref. owner occupied) | ||||
| Social rented | –0.24 (0.21) | 0.25 (0.13) | 0.50 (0.14)*** | 0.097 (0.10) |
| Private rented | 0.53 (0.27) | –0.26 (0.17) | 0.14 (0.18) | 0.20 (0.13) |
| Parental employment (ref. employed) | ||||
| Unemployed | –0.51 (0.23)* | 0.19 (0.18) | 0.36 (0.17)* | –0.11 (0.14) |
| IDACI 2007 decile (high score denotes ‘more deprived’) | –1.36 (0.45)** | 1.15 (0.27)*** | 0.74 (0.28)** | –0.30 (0.22) |
| Built environment score (high score denotes ‘more built up’) | –0.046 (0.091) | 0.11 (0.056)* | 0.0098 (0.056) | –0.14 (0.044)** |
| Urban/rural status (ref. urban) | ||||
| Towns | 0.37 (0.32) | –0.15 (0.20) | 0.087 (0.18) | 0.35 (0.15)* |
| Villages | –0.021 (0.38) | –0.41 (0.24) | –0.026 (0.23) | 0.40 (0.18)* |
| Healthy food outlets (ref. none) | ||||
| One to two | – | – | 0.21 (0.12) | 0.15 (0.092) |
| Three or more | – | – | –0.49 (0.32) | 0.090 (0.27) |
| Unhealthy food outlets (ref. none) | ||||
| One to two | – | – | 0.025 (0.11) | –0.12 (0.085) |
| Three to four | – | – | 0.030 (0.15) | 0.10 (0.12) |
| Five or more | – | – | 0.079 (0.18) | –0.047 (0.14) |
| Number of previous programmes per programme manager | –0.031 (0.014)* | 0.027 (0.0094)** | –0.0085 (0.011) | –0.040 (0.0082)*** |
| Group size | –0.012 (0.029) | 0.032 (0.018) | –0.024 (0.019) | –0.052 (0.016)*** |
| Attendance (ref. completer, > 75% of sessions attended) | ||||
| Non-completer (< 25% of sessions attended) | –0.25 (1.24) | 1.32 (0.73) | –0.55 (0.76) | –0.56 (0.58) |
| Partial completer (25–75% of sessions attended) | –0.71 (0.29)* | 0.49 (0.18)** | –0.21 (0.19) | –0.83 (0.14)*** |
| Height rounding | ||||
| Rounded | 0.36 (0.40) | –0.88 (0.30)** | 0.072 (0.36) | 1.02 (0.26)*** |
| Weight rounding | ||||
| Rounded | 0.31 (0.18) | –0.023 (0.11) | –0.0071 (0.12) | 0.22 (0.098)* |
Baseline SDQ score, sex, ethnicity, IDACI 2007 decile, measure of built environment, the number of programmes run by the programme leader up to that point, attendance and the amount of height rounding at the programme level were all carried forward to the change in SDQ score model. Other covariates were not associated with change in SDQ score (see Table 19, model 2).
Baseline hours of physical activity, housing tenure, parental employment status and IDACI 2007 decile were carried forward to the change in physical activity model. Other covariates were not associated with change in physical activity (see Table 19, model 3).
Baseline diet score, sex, ethnicity, measure of built environment, urban/rural status, the number of programmes run by the programme leader up to that point, group size, attendance, height and weight rounding were carried forward to the change in diet model. Other covariates were not associated with change in diet (see Table 19, model 4).
The next stage of the analysis tested random slopes for each outcome. None of the modelled random slopes improved the fit of the change in self-esteem model so none were included (Table 20). In contrast, the between-programme intercept in change in SDQ score varied by employment status (change in BIC = –16). For this reason, this random effect was included in the multivariable model of change in SDQ score. No other random slopes improved the fit of the model (see Table 20). Inclusion of random slopes for the change in physical activity and change in diet models did not improve fit so the final models for these outcomes excluded these parameters (see Table 20).
| Random slope | Model 1: change in self-esteem (n = 1852) (change in BIC) | Model 2: change in SDQ score (n = 1918) (change in BIC) | Model 3: change in PA (n = 610) (change in BIC) | Model 4: change in diet (n = 1848) (change in BIC) |
|---|---|---|---|---|
| Age random slope | 12 | 7 | 4 | DNC |
| RI varies by sex | DNC | 11 | DNC | 13 |
| RI varies by ethnicity | 31 | 6 | DNC | 48 |
| RI varies by family structure | 11 | DNC | 24 | 9 |
| RI varies by housing tenure | 7 | 8 | 4 | 8 |
| RI varies by parental unemployment | 4 | –16 | –1 | 3 |
| IDACI 2007 random slope | 14 | 5 | DNC | 9 |
| n previous programmes per programme manager random slope | 13 | DNC | DNC | DNC |
| Group size random slope | 17 | DNC | DNC | 14 |
| RI varies by attendance | 58 | 38 | 30 | 6 |
The a priori two-way interactions described in Chapter 3 (see Multilevel analysis of change in body mass index) were tested for each secondary outcome, but none were included in any of the multivariable models (Table 21).
| Hypothesis | Model 1: change in self-esteem (n = 1852) (change in BIC) | Model 2: change in SDQ score (n=1918) (change in BIC) | Model 3: change in PA (n = 610) (change in BIC) | Model 4: change in diet (n = 1848) (change in BIC) |
|---|---|---|---|---|
| Age*baseline BMI | 7 | 7 | 0 | 6 |
| Sex*baseline BMI | 7 | 7 | 5 | 8 |
| Ethnicity*baseline BMI | 22 | 10 | 19 | 18 |
| Age*sex | 8 | 8 | 3 | 8 |
Multivariable models of changes in secondary outcomes
As each outcome is measured on a different scale, each set of results is presented with the range, mean and standard deviation of the score at baseline to aid interpretation. Increases in self-esteem and physical activity and improved diet can all be interpreted as ‘beneficial’ changes, whereas an increase in SDQ score represents an increase in psychological distress and would therefore be interpreted as an ‘adverse’ change.
Change in self-esteem
Self-esteem increased on average by just under half a standard deviation (change = 3.53 units, scale range = 0–30, mean at baseline = 16.8, standard deviation = 7.0). Self-esteem increased less for children whose baseline self-esteem was above average, and for Asian children compared with white children (but not for children from black or other ethnic groups, who were no different to white children) Table 22.
| Parameters | Model 1: change in self-esteem (n = 5078), B (SE) | Model 2: change in SDQ score (n = 8127), B (SE) | Model 3: change in PA (n = 2024), B (SE) | Model 4: change in diet (n = 7859), B (SE) |
|---|---|---|---|---|
| Fixed part | ||||
| Intercept | 3.53 (0.13)*** | –2.65 (0.31)*** | 0.55 (0.36) | 6.05 (0.31)*** |
| Baseline | –0.41 (0.012)*** | –0.34 (0.0073)*** | –0.53 (0.021)*** | –0.62 (0.0084)*** |
| Sex (ref. girls) | ||||
| Boys | – | 0.54 (0.099)*** | – | –0.21 (0.074)** |
| Ethnicity (ref. white) | ||||
| Asian | –0.72 (0.28)** | 0.053 (0.20) | – | –0.61 (0.16)*** |
| Black | 0.16 (0.34) | –0.50 (0.22)* | – | –0.55 (0.17)*** |
| Other | –0.42 (0.39) | –0.26 (0.26) | – | –0.31 (0.19) |
| Housing tenure (ref. owner occupied) | ||||
| Social rented | – | – | 0.34 (0.15)* | – |
| Private rented | – | – | 0.095 (0.18) | – |
| Parental employment (ref. employed) | ||||
| Unemployed | –0.30 (0.26) | 0.091 (0.16) | 0.16 (0.19) | – |
| IDACI 2007 decile | –0.85 (0.49) | 1.04 (0.31)*** | 0.32 (0.31) | – |
| Built environment score | 0.041 (0.062) | – | –0.0041 (0.054) | |
| Urban/rural status (ref. urban) | ||||
| Towns | – | – | 0.23 (0.17) | |
| Villages | – | – | 0.25 (0.20) | |
| Group size | 0.0073 (0.029) | – | – | –0.029 (0.016) |
| Previous programmes per programme manager | – | 0.022 (0.0094)* | – | –0.033 (0.0082)*** |
| Attendance | ||||
| Non-completer | –0.45 (0.64) | 1.05 (0.49)* | – | –0.86 (0.38)* |
| Partial completer | –0.50 (0.32) | 0.43 (0.14)** | – | –0.46 (0.14)*** |
| Height rounding (ref. < 20%) | ||||
| Rounded | – | –0.84 (0.30)** | –0.0092 (0.36) | 0.83 (0.26)** |
| Weight rounding (ref. < 20%) | ||||
| Rounded | – | – | – | 0.22 (0.097)* |
| Random part | ||||
| Between programmes | 1.79 (0.37)*** | 0.87 (0.21)*** | 0.49 (0.10)*** | 1.49 (0.13)*** |
| Between programmes (covariance) | – | –0.14 (0.38) | – | – |
| Between programmes (unemployed) | – | 2.60 (0.93)** | – | – |
| Between participants | 30.8 (0.68)*** | 18.0 (0.34)*** | 4.28 (0.15)*** | 9.47 (0.17)*** |
Relationship between change in self-esteem and change in body mass index
Change in self-esteem and change in BMI negatively covary at the programme and individual levels (see between-programme and between-participant covariance terms in Table 23). This means that when BMI falls, self-esteem rises. However, the direction of causality cannot be inferred.
| Parameters | Change in BMI, B (SE) | Change in self-esteem, B (SE) |
|---|---|---|
| Fixed part | ||
| Intercept | –0.79 (0.027)*** | 3.40 (0.17)*** |
| BMI at baseline | –0.023 (0.0029)*** | –0.11 (0.019)*** |
| Self-esteem at baseline | 0.0048 (0.0018)** | –0.42 (0.012)*** |
| Age | 0.022 (0.0073)** | 0.023 (0.050) |
| Sex (ref. girls) | ||
| Boys | –0.095 (0.024)*** | 0.10 (0.16) |
| Ethnicity (ref. white) | ||
| Asian | 0.20 (0.048)*** | –0.83 (0.29)** |
| Black | 0.12 (0.052)* | 0.36 (0.34) |
| Other | 0.071 (0.058) | –0.48 (0.39) |
| Family structure (ref. couple) | ||
| Lone parent | 0.026 (0.028) | –0.28 (0.21) |
| Housing tenure (ref. owner occupied) | ||
| Social rented | 0.021 (0.032) | 0.25 (0.25) |
| Private rented | 0.011 (0.040) | 0.67 (0.28)* |
| Parental employment | ||
| Unemployed (ref. employed) | 0.087 (0.034)* | –0.30 (0.27) |
| IDACI 2007 decile | 0.15 (0.080) | –0.85 (0.54) |
| Urban/rural status (ref. urban) | ||
| Towns | –0.064 (0.048) | 0.17 (0.32) |
| Villages | –0.042 (0.058) | –0.25 (0.39) |
| Group size | 0.0050 (0.0050) | 0.0088 (0.029) |
| Previous programmes per programme manager | 0.0028 (0.0024) | –0.032 (0.014)* |
| Attendance (ref. completer, > 75% of sessions attended) | ||
| Non-completer (< 25% of sessions attended) | 0.17 (0.10) | –0.56 (0.71) |
| Partial completer (25–75% of sessions attended) | 0.14 (0.031)*** | –0.55 (0.24)* |
| Random part: programme | ||
| Between-programme variance (BMI change) | 0.10 (0.011)*** | |
| Between-programme covariance (BMI change, self-esteem change) | –0.10 (0.045)* | |
| Between-programme variance (self-esteem change) | 1.56 (0.36)*** | |
| Random part: participants | ||
| Between-participant variance (BMI change) | 0.61 (0.014)*** | |
| Between-participant covariance (BMI change, self-esteem change) | –0.50 (0.068)*** | |
| Between-participant variance (self-esteem change) | 29.9 (0.67)*** | |
The bivariate multivariable model (Table 23) extends the model of change in BMI moderated by self-esteem (see Table 15, model 1) by modelling change in self-esteem and change in BMI simultaneously. The associations from the bivariate multilevel model of change in self-esteem and change in BMI did not differ substantively from the univariate models of change in BMI and change in self-esteem.
The bivariate multivariable model shows that BMI and self-esteem at baseline are independently associated with change in BMI (higher BMI at baseline is associated with a larger fall in BMI; higher self-esteem is associated with a smaller fall in BMI). Higher baseline BMI and higher baseline self-esteem were both associated with a smaller increase in self-esteem (Table 22).
Change in Strengths and Difficulties Questionnaire
Strengths and Difficulties Questionnaire fell on average by just over one-third of a standard deviation (change = –2.65 units, scale range = 0–37, mean at baseline = 12.9, standard deviation at baseline = 7.1). This change is indicative of a reduction in psychological distress. SDQ score fell less for children with lower SDQ score at baseline; boys compared with girls; white children compared with black children; children living in more income-deprived neighbourhoods; children in programmes where the programme manager had delivered more programmes; non-completers and partial completers compared with completers; and those participating in programmes where height data were not rounded (see Table 22, model 2). Although there were no fixed effects by employment status, the between-programme variation in change in SDQ score was larger for participants whose parents were unemployed than for those whose parents were in employment.
Change in physical activity
Physical activity (hours of walking and cycling in the previous week, as reported by parents at baseline and follow-up) increased on average by just under one-quarter of a standard deviation (change = 0.55 hours, scale range = 0–14, mean at baseline = 2.5, standard deviation = 2.3). Physical activity increased less for those whose baseline physical activity was higher; it increased more for those who lived in socially rented accommodation.
Change in diet
The MEND-friendliness of participants’ diets increased on average by more than one standard deviation (change = 6.05 units, scale range = 1–28, mean at baseline = 16.5, standard deviation = 4.4). MEND-friendliness increased less for those who had a more MEND-friendly diet at baseline; boys; Asian and black children compared with white children; those attending programmes where programme managers had managed more programmes; non-completers and partial completers compared with completers; and those in programmes where height and weight data were not rounded.
Cost of providing MEND 7–13
As noted, cost data were derived from two recent evaluations of the MEND 7–13 programme. 71,72
Techakehaki and Hutton71 calculated the costs of providing MEND 7–13 to all eligible children across England from an NHS and PSS perspective in UK£2010/11. Their analysis was based on activity data collected from the MEND 7–13 programme based on four cost components: programme set up; participant recruitment; programme activities; and evaluation and monitoring. For each of these items, fixed costs such as office rental and variable costs such as staffing, equipment and materials were included. Costs were not itemised by cost component. They were calculated by contract size and weighted by the number of children attending programmes with different contract sizes. Mean costs per participant were calculated by dividing the total programme costs by the number of children in the programme (it is not stated if these are numbers starting or completing the programmes, or some other measure of participation). Using this approach, Techakehaki and Hutton71 calculated that the mean cost of the programme per participant was £416.
Steeds72 calculated the total costs of MEND 7–13 programmes in South Gloucestershire, England between May 2008 and November 2009. The analysis was based on a detailed study of the costs of providing seven MEND 7–13 programmes within the region. Costs were disaggregated into local programme costs, comprising start-up costs and running costs, and costs incurred from MEND 7–13 Central to organise and run local programmes. Total costs were reported for seven programmes, and the base year for costs was assumed to be 2008/9. The costs are summarised in Table 24; they have been converted into mean costs per programme and inflated to UK£2010/11 values using the NHS Hospital and Community Health Services Pay and Prices Index. 73 The cost per participant, based on a reported 10 children per programme (figures for a subset of four programmes suggested that 46 children started these programmes and 36 completed them), was £399.
| Cost component | Cost (£) | % of totala |
|---|---|---|
| Local programme costs | ||
| Start-up costs | ||
| Posters and flyers | 59 | 1 |
| Programme co-ordinator | 1181 | 30 |
| Measurement equipment | 59 | 1 |
| Subtotal | 1299 | 33 |
| Running costs | ||
| Theory leader | 827 | 21 |
| Exercise leader | 413 | 10 |
| Venue hire | 827 | 21 |
| Printing | 52 | 1 |
| Swimming hire | 103 | 3 |
| Administration | 52 | 1 |
| Subtotal | 2274 | 57 |
| MEND Central costs | ||
| Training course | 148 | 4 |
| Sports equipment | 44 | 1 |
| Programme resources | 15 | 0 |
| Hand-outs | 103 | 3 |
| MEND kit bags | 103 | 3 |
| Subtotal | 413 | 10 |
| Total | 3986 | 100 |
Based on these figures, the cost per programme is around £4000, and the mean cost of providing MEND 7–13 per participant is £399–416.
Factors likely to affect the cost of providing MEND 7–13
Broadly, the factors affecting the mean cost of providing MEND 7–13 per participant are those that affect local programme costs and MEND Central costs (as these are the two components of the cost per MEND 7–13 programme, the numerator in the calculation of the cost per participant), and the number of participants in each programme, i.e. the programme group size (the denominator in the calculation of the cost per participant).
More specifically in terms of local programme costs, as shown in Table 24, the main cost components are staff costs (programme co-ordinator, theory leader and exercise leader), accounting for around 60% of the cost per programme, and venue hire, accounting for around 20%. Assuming these figures are largely representative of all MEND 7–13 programmes, they are the main factors likely to affect local programme costs. Staff costs will vary depending on the specialism, qualifications and level of experience of staff. For example, as shown by Curtis73 (see table 17.2), the salary of qualified allied health professionals (AHPs) at Agenda for Change Pay Band 7 is more than twice that of unqualified AHPs at Pay Band 3 (mean annual basic salary per full-time equivalent £37,600 vs. £17,500). In terms of both staff costs and venue hire, local programme costs will be lower when these can be provided by in-kind support at zero or negligible financial or opportunity cost; for example, via the free use of unoccupied rooms.
MEND Central costs are likely to depend on the size of the contract between MEND Central and those commissioning MEND 7–13 programmes locally. For example, commissioners drawing up larger contracts with MEND Central are likely to be able to negotiate lower costs per participant.
Steeds72 reported a programme group size of 10 children per programme. Using the data analysed in Multivariable models of changes in secondary outcomes and Chapter 3, Multivariable models of change in BMI and zBMI, we calculated the programme group sizes at the first session of 1940 MEND 7–13 programmes (see Table 2). The mean, median, mode, interdecile range and overall range were 8.6, 8, 7, 5–13 and 1–19 respectively. If we applied the mean value in these data to the costs per programme calculated by Steeds,72 then the mean cost of providing MEND 7–13 per starting participant would increase to around £463. If we applied the programme group size values based on the limits of the interdecile range, then the costs would vary between £307 and £797.
The costs presented above are based on mean programme sizes, using data on the mean number of children starting MEND programmes. Programme size could instead be based on the mean number of children completing programmes, and, assuming the completion rate of programmes is less than 100%, this would increase the cost of providing MEND per participant. Using our definition of completers as those attending > 75% of sessions, the completion rate based on imputed data for participants who started the programme was 59.9%. If we applied this to the mean 8.6 children who started each MEND programme, then 5.2 children completed each programme on average and the cost per completer was £773. If we applied the completion rate to the limits of the interdecile range for starters, then the costs would vary between £511 and £1329.
Relationship between the variation in the cost of providing MEND 7–13 and the outcomes of participants
As noted, the factors likely to affect costs are staff costs (which will vary depending on the specialism, qualifications and level of experience of staff), venue hire costs, contract size and programme group size. What evidence is there that these factors affect the outcomes of participating in MEND 7–13? Using the analysis we undertook to address changes in outcomes (see Multivariable models of changes in secondary outcomes and Chapter 3, Multivariable models of change in BMI and zBMI), we were unable to obtain data on the specialism, qualifications or level of experience of local staff and so could not assess the impact of these factors on outcomes. In terms of venue hire costs, we did not know if the venue was provided at zero or negligible cost. We were also unable to obtain other possible proxies such as the type of facility where the programme was delivered. We could not find out the size of the contract between MEND Central and those commissioning the programmes; however, we did include funding source [whether primary care trust (PCT), Big Lottery Fund (BLF) or another organisation], and this was found to have a non-significant impact on outcomes, except in one instance (Table 25).
| Variables | Change in BMI (n = 2150), B (SE) | Change in zBMI (n = 2150), B (SE) | Change in self-esteem (n = 1852), B (SE) | Change in SDQ score (n = 1918), B (SE) | Change in PA (n = 610), B (SE) | Change in diet (n = 1848), B (SE) |
|---|---|---|---|---|---|---|
| Funding source (ref. PCTs and local government) | ||||||
| BLF | 0.050 (0.027) | 0.0097 (0.0054) | 0.085 (0.27) | 0.13 (0.12) | 0.032 (0.14) | 0.011 (0.11) |
| Other organisations | –0.083 (0.061) | –0.014 (0.012) | 0.39 (0.59) | –0.015 (0.26) | 0.37 (0.27) | 0.78 (0.23)*** |
Programme group size slightly moderated change in BMI but no other outcomes (see Multivariable models of changes in secondary outcomes and Chapter 3, Multivariable models of change in BMI and zBMI).
Programme group size was found to have a statistically significant impact on outcomes (see Multivariable models of changes in secondary outcomes and Chapter 3, Multivariable models of change in BMI and zBMI), with larger group size being associated with smaller BMI reductions. Hence, larger programme group size is associated with lower costs per participant, but worse outcomes.
Therefore, there is limited evidence that the factors affecting the cost of providing MEND 7–13 are related to the outcomes of participating in MEND 7–13. We found evidence of an effect for programme group size but not for other factors, as we did not have sufficient data for the analyses of specialism, qualifications and level of experience of staff, venue hire and contract size.
Discussion
Changes in psychological health associated with MEND 7–13
On average, MEND 7–13 was associated with improvements in self-reported global self-esteem and reductions in parent-reported psychological distress (change in SDQ score). Conservatively, this can be interpreted as showing that MEND 7–13 does not adversely impact on children’s psychological health (i.e. it does no harm). More liberally, it suggests that participation in weight management interventions such as MEND may have at least short-term benefits for psychological health when delivered under real-world conditions. This is consistent with evidence from childhood weight management programmes delivered under research conditions. 67,74
Variations in psychological outcomes associated with MEND 7–13
Higher baseline self-esteem and Asian compared with white ethnicity were associated with lower levels of improvement in self-esteem. Otherwise, change in self-esteem did not vary by sociodemographic, neighbourhood or programme characteristics.
Benefits associated with the programme, in terms of reduced parent-reported participant psychological distress (change in SDQ score), also varied by participant characteristics. Psychological distress reduced less in children with lower baseline psychological distress (consistent with regression to the mean); boys compared with girls; white compared with black ethnic groups; children living in more deprived neighbourhoods; those who attended programmes where the manager had delivered a higher number of previous programmes; those who completed < 75% of sessions compared with ‘completers’; and those who attended programmes where height rounding was common. Although change in psychological distress was not associated with family structure, housing tenure or parental employment status, between-programme variation was higher for participants with unemployed parents.
Thus, change in psychological distress was associated with more covariates than change in self-esteem. Self-esteem and psychological distress are conceptually and operationally distinct, and therefore liable to vary in different ways with the same covariates. Furthermore, SDQ is reported by parents whereas self-esteem is reported by participants. SDQ scores may partially reflect children’s and parents’ distress, and might therefore be affected by factors which influence both children’s and parents’ mental health. The same is not true for self-esteem, which is self-reported. Therefore, it might be expected (as was found here) that the parent-reported measure (psychological distress) would be associated with a wider range of factors than the participant-reported measure (self-esteem).
Covariation in changes in self-esteem and change in body mass index
The bivariate model of changes in self-esteem and BMI allowed us to show that self-esteem at baseline and BMI at baseline were both independently associated with changes in self-esteem and BMI. This is important when considering the longstanding debate about the direction of the relationship between changes in self-esteem and BMI, as it shows that all possibilities are supported by the data. This is perhaps consistent with a model whereby self-esteem and BMI genuinely covary, rather than one causing variations in the other. To our knowledge, no other studies have investigated BMI and mental health outcomes in a bivariate model to assess this possibility.
Change in lifestyle behaviours associated with MEND 7–13
Parent reports suggested that their children’s physical activity (walking and cycling) increased after participation in MEND 7–13. Higher levels of physical activity at the start of the intervention were associated with smaller increases over the course of the intervention. No individual-, family-, neighbourhood- or programme-level covariates were associated with change in physical activity, apart from housing tenure; families living in social rented accommodation increased their physical activity more than owner occupiers. This suggests that the intervention is associated in a similar way for most participants and their families across the service, once baseline physical activity is taken into account.
The finding that SEC did not moderate physical activity outcomes (apart from slightly larger increases in physical activity among children living in social rented accommodation) is broadly consistent with a recent review which draws together the limited evidence base to suggest that physical activity interventions are equally effective for low and high socioeconomic groups. 23 However, as physical activity did not vary with any other covariates, the lack of a statistically significant difference associated with SEC should be interpreted with caution because of the known errors in reported physical activity. 75
The results show that the MEND-friendliness of participants’ reported diets increased over the course of the MEND 7–13 programme. Those with more MEND-friendly diets at baseline reported a smaller increase, as did boys compared with girls, Asian and black children when compared with white children (there was no significant difference between other ethnic groups and white children), children in programmes where the number of previous programmes per manager was higher, non-completers and partial completers compared with those completing the programme, and those in programmes where height and weight measures were often rounded.
Cost of providing MEND
In summary, we met the aims of our analysis as follows:
-
The cost of providing MEND is around £4000 per programme. The mean cost per starting participant is £463 and the mean cost per completer is £773.
-
The cost per participant varies according to:
-
local programme costs, which are affected by, among other things, the number and type of staff employed, administration costs and venue hire
-
the costs incurred from MEND Central, which are affected by the size of the contract between the purchaser/deliverer and MEND
-
the number of participants on each programme.
-
-
There is limited evidence that the factors affecting the cost of providing MEND are related to the variation in outcomes. We found evidence that larger programme group size is associated with lower costs per participant but smaller BMI reductions per participant. In other cases there is no evidence because we do not have sufficient data to undertake appropriate analyses (e.g. with regards to the specialism, qualifications and level of experience of staff, venue hire and contract size).
Strengths and limitations
All the secondary outcomes were reported by participants in the intervention or their parents. As such, all are subject to sources of bias which can affect the internal validity of measures. These might include social desirability bias; for example, respondents might be less likely to report feelings of low self-esteem or psychological distress because of stigma surrounding these issues. Positive outcomes might be inflated because the questionnaires were distributed by the same people who managed the intervention.
The psychological measures used in the study have been validated against several different populations. However, the majority of the research literature uses multicomponent measures of self-esteem67 (as opposed to the adapted Rosenberg measure used here) and no studies were found which had used the SDQ in this context.
A recent Cochrane review of childhood obesity interventions10 suggests that there are considerable challenges in measuring lifestyle behaviours such as physical activity and diet, and recommends that research uses measures that have been validated to ensure that the data reliably measure the behaviours of interest. Our analyses of dietary patterns and physical activity were based on scales which have not been validated in previous research studies. Accordingly, the findings from these scales should be treated with caution and the results cannot be compared directly with those of other studies.
Headline findings from Chapter 4
Psychosocial and lifestyle outcomes associated with MEND
Psychosocial (self-reported self-esteem and parent-reported psychological distress) and lifestyle (parent-reported physical activity and diet) outcomes improved overall. These varied by group:
-
Improvements in self-esteem were smaller where baseline self-esteem was higher and for Asian compared with white children, but otherwise did not vary.
-
Reduction in psychological distress was smaller for children who were less distressed at baseline; boys; black compared with white children; those living in more deprived neighbourhoods; children attending programmes delivered by managers who had delivered larger numbers of previous programmes; those who did not complete the programme; and those who attended programmes where height data were rounded.
-
Increases in physical activity were smaller for those who were more physically active at baseline and those living in owner-occupied compared with social rented accommodation, but otherwise did not vary sociodemographically or by completion status.
-
Dietary improvements were smaller for those who had healthier diets at baseline; boys; Asian and black children compared with white children; those attending programmes delivered by managers who had delivered larger numbers of previous programmes; children who did not complete the programme; and children who attended programmes where height or weight data were rounded.
Costs of providing MEND
The cost of providing MEND is around £4000 per programme. The mean cost per starting participant is £463 and the mean cost per completer is £773. The cost per participant varies according to:
-
local programme costs, which are affected by, among other things, the number and type of staff employed, administration costs and venue hire
-
the costs incurred from MEND Central, which are affected by the size of the contract between the purchaser/deliverer and MEND
-
the number of participants on each programme.
There is limited evidence that the factors affecting the cost of providing MEND are related to the variation in outcomes.
Chapter 5 The salience and acceptability of MEND to commissioners and delivery partners
What is the salience and acceptability of MEND to those who commission it?
Background
Real-world evaluations of public health interventions such as MEND have the potential to inform commissioning and recommissioning decisions. 76
The context of our work with commissioners was a time of change in the NHS leading up to the publication of the 2010 White Paper Healthy Lives, Healthy People: Our Strategy for Public Health in England. 77 At the time of our interviews, there was uncertainty surrounding the place of public health in the new structures, and the wider environment was one of fiscal restraint. Commissioners deal with the purchase of services. MEND is free for families, but it is not cost free. At the time of the study, the programme received multiple sources of financial support including funding from PCTs and the BLF. At the start of our study, BLF funding for MEND stood at 66% (see MEND data described in Chapter 2).
Our sampling strategy drew on both commissioners in the traditional NHS sense of those purchasing services, and those commissioned to deliver a service. Our decision to take this broad view had a contextual driver. Between the submission of our grant and the study being carried out, the NHS landscape was changing, with an increasing emphasis on choice and competition. We took the view that interviewing those commissioned to deliver services as well as those purchasing them was likely to be helpful in terms of informing future provision. This was endorsed in our initial interviews with our project partners, who were commissioners in PCTs and emphasised the importance of those delivering services and developing partnerships.
The complete list of contract holders provided as a sampling frame by MEND Central included both commissioners and delivery partners. MEND described delivery partners as including public or private leisure centres, charities such as the Young Men’s Christian Association (YMCA), or housing associations, employing staff trained by MEND to co-ordinate and run local MEND programmes and receiving grant funding via MEND to deliver them. Staff included leisure centre managers, fitness instructors and community activity managers knowledgeable about the practical and logistical aspects of running MEND. Commissioners were described as purchasers with a duty to commission local health and well-being services for the population, typically with a public health background (but not necessarily with a specialist interest in obesity services). At the time of the study, commissioners worked largely in public health teams in a PCT or local authority. Their focus was on meeting national and local targets and developing the local health-care strategy and local area agreements that determine health priorities. Commissioners purchased services directly from MEND and had separate contracts with delivery partners.
Our work with commissioners was designed to investigate:
-
commissioning decisions
-
the tension between programme fidelity and responsiveness to local context, circumstances and service users.
Methods
Recruitment
From a full list of 151 contract holders, shortlists were developed to meet inclusion criteria for a maximum variation sample. There was a geographical spread of interviews, with commissioners and delivery partners located in London, the south-west and the north-east of England.
We selected commissioners according to the sociodemographics of the local population (index of multiple deprivation and area ethnic composition), the type of organisation (PCT or not) and contracting details (number of programmes contracted and current contracting status). The sampling approach is fully described in Appendix 13.
Although there were few refusals, a considerable number of commissioners could not be contacted during this period of rapid change in the NHS.
Twenty commissioners and nine delivery partners were recruited into the study. Some delivery partners had been delivering MEND for some time, whereas other commissioners were new in post.
The recruitment of interviewees is described in Figure 6.
FIGURE 6.
Recruitment process for commissioner interviews. Please note that 54 individuals were contacted but the final sample increased to 66 because of onward referral. ICH, Institute of Child Health.
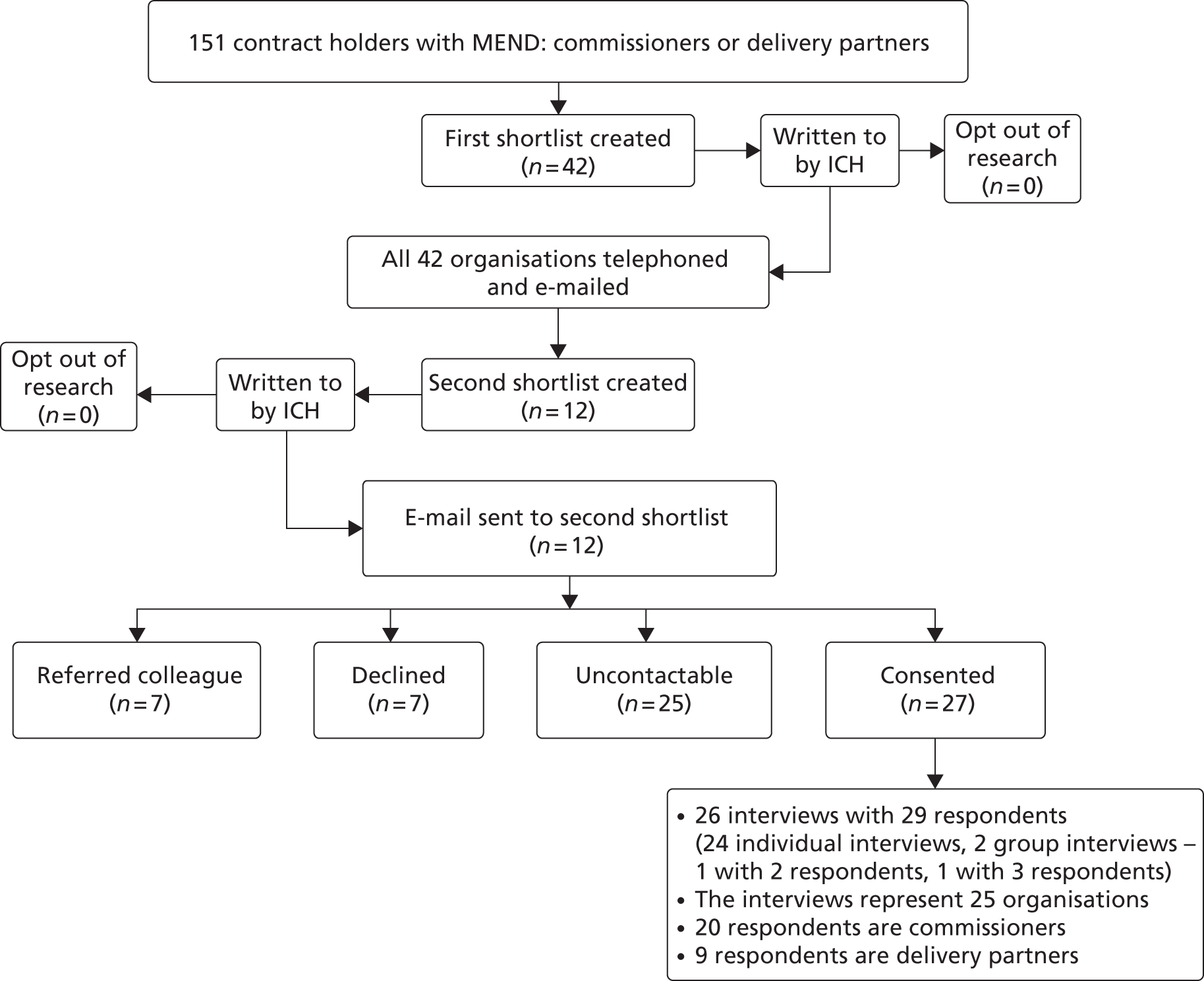
Interviews
Our proposal described recruiting up to 30 commissioners in the expectation that we were unlikely to generate significant new data after that point. In the event, 29 interviewees took part in 26 interviews (see Figure 6) in 2011. They included those who had commissioned MEND and those who had managed it or contributed to the programme delivery. Interviewees included health and well-being development officers, strategic leads for obesity, medically qualified public health consultants and MEND operations managers or co-ordinators. For some commissioners, MEND had been commissioned or was running by the time they had taken up post. Not all had observed the delivery of the MEND programme first hand but those who had not had access to reports from colleagues.
Interviews with commissioners were largely conducted by telephone, with five face-to-face meetings. Consent forms and information sheets were sent in advance and the interview started only once written/e-mailed consent had been received. Some interviewees asked to see the topic guide before being interviewed and this was provided, with the caveat that this was a guide and not a questionnaire. All interviewees agreed to the interview being audio recorded. Interviewees took a highly professional approach. Despite our interviewing them at a time of considerable professional uncertainty for many, we found them generous with their time, thoughtful in expressing their views and experience, and well prepared. Some had gathered data or papers in advance or offered to send them subsequently. Some expressed concerns related to confidentiality, particularly where they had criticisms of the scheme. Although the information sheets emphasised that the research was independent of MEND, several respondents were aware of the relationship between MEND and UCL Institute of Child Health (see Chapter 1, Management of competing interests). The interview material reported here has all identifiers removed.
The topic guide (see Appendix 14) for the interviews was developed on the basis of our proposal to the NIHR and was adapted following initial interviews with commissioners on our advisory group. The wording was further adapted according to whether we were interviewing delivery-partner contract holders or commissioners. Interviews typically lasted around 45 minutes. Encrypted data were sent to a secure drop box facility and then uploaded using a secure file transfer system for transcription. Verbatim transcriptions were returned to the qualitative research team after removal of identifying features such as names.
For ease, the term ‘commissioner’ will be used to refer to both delivery partners and commissioners, unless otherwise stated. Individuals are identified using unique interview numbers (e.g. C6).
Analysis
Before commencing analysis, the qualitative researchers held a team workshop, also attended by JF and our colleague Hannah Lewis (who had dealt with recruitment), to discuss the strengths and weaknesses of various approaches to analysing our three data sets (family, individual and commissioners). The constant comparative approach, which compares new emerging concepts from the data, guided our thinking and we decided that a framework analysis, enabling us to draw on this, was the best way to analyse data from both the commissioners and the families.
The interviews were analysed using framework analysis, drawing on work by Ritchie et al. 78 This involves familiarisation with the data and drawing up a thematic framework on the basis of research questions and interview data. Summaries of data are indexed, mapped and tabulated by case and theme within this framework to allow analysis and interpretation and reconsideration of themes.
Findings
Our findings are grouped under three broad themes which emerged from the data. First, the context for commissioning decisions is described, including the changing organisational context and cost and funding issues. Next, commissioners’ perceptions of the acceptability of MEND to families in their localities are reported, including their understanding of staffing needs for their populations. Finally, we report the views of commissioners about the delivery of MEND to their local populations in the light of local diversity.
The context for commissioning MEND
A changing public health
At the time of the interviews the changing NHS and evolving public health agenda dominated interviewees’ accounts, with concern expressed about the ways in which changes would affect working practices, working conditions and commissioning public health services: ‘it’s just all up in the air’ (C31).
Some interviewees’ working roles had recently changed, such that they had taken up new posts during a process of restructuring. Future responsibility for programmes such as MEND was not always apparent:
Because things have changed so much from where we started in terms of our own internal structure, in terms of the NHS. The provider-commissioning split . . . if you were in commissioning, then you weren’t supposed to be doing . . . direct service provision which is basically what MEND is. So, you know, that at the moment we don’t actually have anybody in provider services who would be responsible for this.
C5
At the time of our interviews, the roles of clinical commissioning groups (CCGs) and local authorities in public health commissioning were unclear. Where the future involvement of local authorities in public health was discussed by commissioners, there was speculation that local authorities might not be interested in taking up services which focused on a single issue:
I think it’s a question of yes, who could fund what, and how might you package it in a way that [a] local authority would feel comfortable . . . For instance, the local authority is more used to doing what you’d call universal services than targeted services . . . Obesity might just be one problem amongst a whole series of other issues that the family is confronting.
C2
Costs and funding concerns
The issue of future funding raised concerns from NHS commissioners about what local authorities might value. In the world of commissioners, decisions are predicated on whether or not a programme ‘fits’ within the terms of a budget, and whether or not it is affordable. Some commissioners discussed whether or not childhood obesity was a local priority. If it was, they had funds to allocate, in one case paying a neighbouring area for a service they did not have the resources to provide themselves. But even in areas with higher than average childhood obesity, there may be (and usually were) other pressing public health problems. Most of the MEND programmes whose commissioners or delivery partners we interviewed had been supported by Big Lottery funding which, at the time of concluding the study, was no longer available. Those interviewees who wanted to recommission MEND were uncertain as to how future budgets would be organised and what funds would be accessible:
[F]rom a national top-down level, they’ve got issues because of the GP consortia. We don’t know what they’ll look like, or where money is going to be housed. A lot of people locally are having conversations with me to say, ‘we’ve got to keep MEND going’, but there is no money there, and at the end of the day, we can’t run MEND without a budget.
C39
These concerns were compounded by the perceived high cost of MEND. Particularly in the context of uncertain funding, the cost of the MEND programmes was seen as prohibitive:
[I]t does cost a lot of money, and I’m not sure what we get for that money.
C54
[I]t’s an expensive programme because along with the delivery costs, it has proved to be very expensive per family.
C10
A distinction was made between absolute costs and value for money. Interviewees reported figures of £30,000 a year for the licence to run the programme, £87,000 to run seven programmes, £215,000 to run it for 3 years and £400–900 per family, depending on how many families attended a programme. Some felt that the costs could be justified in relation to savings over the long term, but the case might be difficult to make: ‘Even with the quality, I’m not quite so sure it merits the cost. Even the training handbook was expensive; we thought it was at the time’ (C28).
Staffing costs were reported as the highest outgoing and, as most costs were fixed, retention of families could be a problem for commissioners. One explained: ‘If not enough people join in, we wouldn’t run that programme, but if people drop out, it wouldn’t change what we pay to MEND or the exercise coaches or the nutritionist. They’re there anyway’ (C7).
One interviewee expressed unease regarding the profit to be had from both the context producing unhealthy weight gain in children, and its treatment.
[T]he people making the profit, you know the children being made obese because we have large industries who are promoting all the things that are making our children obese, you know, fast food, cheap non-nutritional food, including electronic items that keep children in their own homes rather than running around and playing and all of those factors. So if the causes of obesity are profit-related, the treatment becomes profit-related as well[.]
C2
Others described less tangible costs relating to responding to MEND Central, for example, pressure to provide rapid information without necessarily receiving reciprocal feedback.
MEND expects a lot from the commissioners . . . they want all the reports done straight after the programme.
C10
A similar view was expressed by interviewees C3 and C4, experienced commissioners with substantial experience of the programme and of childhood obesity, who were interviewed together.
A bit that was missing was feedback from national [MEND], in terms of, we’re running our programmes locally, but it’s very difficult to know how we’re doing compared to other boroughs or nationally . . .
There were conferences and network events and things but it felt quite like we were being mined for information and not as much coming back in terms of well, how is it working nationally, how are we doing compared to others[.]
C3 and C4 (pair interview)
One commissioner (C65) who was otherwise positive about MEND commented that putting in the hard work needed to recruit families was a problem. Commissioners expected to put in extra resources to get started, but were frustrated if, once on the road, the scheme was not able to deliver as a free-standing intervention without additional support.
Commissioning and recommissioning decisions
Most interviewees had not been involved at the beginning of the decision to commission MEND in their areas, but had come in during the process or after programmes were up and running. They did, however, have responsibility for future commissioning decisions, and some had commissioned MEND elsewhere in the past.
Interviewees suggested that one pragmatic reason for commissioning MEND was its readiness and availability, especially, some indicated, in terms of facilitating delivery on local public sector agreements (LPSAs):
It was useful in that . . . the LPSA target had to be delivered in terms of DALYs [disability-adjusted life years] and we were able to use the MEND programme in quite a structured way to deliver on the DALYs[.]
C3
I think we chose it because it was easy, and it was off the shelf[.]
C10
I think with all the resources that they provide . . . MEND was kind of . . . already planned, already set up ready, it was easier for us to take on MEND than looking to set up a child weight management project ourselves because we just didn’t have time . . .
C65
Some interviewees, however, baulked at what they saw as aggressive marketing:
[T]he reason we were all a bit anti-MEND was partly . . . because of the very aggressive marketing approach they’ve taken . . . [when] MEND had literally just started . . . they had a cohort of 12 children, and [there was] a photograph of the Minister taken with them . . . And we were so impressed by the fact that they had actually hooked the Minister when they had absolutely no substance to what they . . . But then, over time, bless ‘em, the evidence has shown it does have an effect[.]
C111
The importance of the evidence underpinning MEND was highlighted as key to the decision-making to commission MEND in the first place: ‘The main reason that we commissioned it was because of the RCT, I think it came out that year, and . . . that’s why we’re delivering MEND’ (C35).
Some interviewees also suggested that, as an evidence-informed programme, MEND had the support of local PCTs. In considering recommissioning MEND, there was a range of views as to the success of the programmes and whether or not MEND had been or would be recommissioned. Some interviewees questioned the effectiveness of the programmes they had run, commenting on recruitment difficulties and relatively small changes in outcomes. Some suggested that because of poor retention and missing data, it was difficult to evaluate the impact of the programmes.
For others, results were very positive:
We’ve got a very good evaluation report so everything was meticulously recorded and the results are really excellent. That’s why we’re very pleased with the outcome of the programme and it’s been very highly thought of both here and elsewhere[.]
C48
However, the long-term impact of MEND was less clear:
[I]t really comes down to three very important questions which are the key questions for . . . well, all commissioners and providers of obesity services at the moment which is what outcome, over what period of time, for what unit cost so that’s what we’re trying to have a discussion with DH [the Department of Health] and MEND[.]
C64
Certainly, in considering recommissioning MEND, interviewees would have liked more data on maintenance of outcomes and longer-term follow-up of families. Although MEND was considered intensive, it was sometimes regarded as too short a programme to enable long-term behaviour change: ‘For me, 10 weeks, 10 weeks is not enough. It’s not sufficient to make any long-lasting changes, and therefore I don’t think it’s a sensible thing to do without that longer-term back up’ (C5).
Some interviewees reported commissioning alternatives to MEND, or sometimes services in parallel with MEND which were viewed as cheaper, equivalent or better: ‘MEND is not rocket science . . .’ and ‘MEND haven’t got the kind of copyright on what they’re doing anymore, and there are about three or four different products on the market’ (C15).
Interviewees suggested longer-term programmes for continued engagement with families, and in some areas follow-up programmes such as family exercise clubs had been implemented. As a result of difficulties in recruiting and retaining both staff and families, one area had implemented its own 20-week rolling programme, so that new families could continually join.
This was seen by commissioners as providing the flexibility to devise content to suit their own localities, and supported the view expressed by some interviewees that investing in high-quality staff with good skills could bring worthwhile returns.
One commissioner felt that:
The fundraising so far has worked quite well. In terms of commissioning I think now, nothing to do with MEND or [name] but to do with local commissioning and local development, we’re now in a position where . . . our major weakness was we didn’t have the information, adequate information, on which to judge whether things were working so there was quite a leap of faith in commissioning if you like for a while.
C9
This commissioner was drawing on several models of service for the local population and wanted to use the best available evidence in making commissioning decisions:
The Department of Health guidance has been useful, but even that doesn’t guarantee the outcomes . . . So that’s the weaknesses from a commissioner point of view, knowing what is the best model to deliver the outcomes. I think I’m commissioning the best available knowledge at the moment, but I don’t know whether it’s going to be effective in the longer term. I mean, we have done a cost-effectiveness review of our local service, children’s weight management, on last year’s data which won’t be as good as this year’s data and it did come out very positive. I . . . got someone else to do it who was a public health trainee and it came out very positively . . . when you measured in terms of QALYs [quality-adjusted life-years] for weight management, but, you know, that’s just a piece of information. So as a commissioner I don’t feel I have quite strong enough certainty of the evidence.
C9
Thus, although MEND had originally been welcomed as a readily usable, evidence-based programme, there was a desire for further evidence on outcomes in the longer term. MEND was no longer seen as unique in having an evidence base, so commissioners were considering developing their own weight management programmes to suit their own localities or commissioning what they saw as comparable but cheaper programmes.
Engaging with families for children
MEND’s family-based approach was largely endorsed by interviewees. They valued the active involvement of parents and carers, but acknowledged that this brought challenges for recruitment and retention. They also emphasised the need for skilled staff who could engage with families, including families who might have multiple health or social needs.
Referral, recruitment and participation
There was a range of referral routes into MEND, including GP referrals, referrals via the school nurse and self-referrals, leading one interviewee to comment that ‘it’s all a bit chaotic’ (C15).
A delivery partner described one of their strategies:
What I do is I always e-mail all the GPs for every programme we start, and they might not refer directly, but they’ll give the information to the person in the surgery and then they’ll self-refer. A lot of people self-refer.
C7
Some commissioner interviewees suggested more focused recruitment, such as identifying children who were pre-diabetic and conducting motivational interviews to assess readiness for change. The NCMP was seen as helping to identify ‘hot spots for obesity’ and target recruitment. Staff were not able to access NCMP data to recruit specific families, but in some places information about MEND went out with the letters to parents: ‘they get information on what they can do, including weight management, not only weight management . . . from MEND’ (C9).
Recruitment was often reported as poor. Some interviewees suggested that there was a stigma to attending a weight management programme which might be viewed as a ‘Fat Club’: ‘with any programme there are always going to be stigmas to certain things in life; and programmes especially that you run, especially if you’re talking about the less active and those who are obese’ (C38).
Others referred to difficulties in engaging hard-to-reach groups:
[I]t is very hard sometimes to engage parents, mainly because there are a lot of low-income families. You’ve got [name] estate, which is one of the top four per cent of council estates in the country for deprivation. There are low-income families, single-parent families, and there are a lot of kids in care[.]
C39
In some cases, previous attendees on MEND programmes had helped to engage such families, and recruitment had improved. However, it was suggested that the multiple problems of, for instance, asylum seekers and refugees meant that they were unlikely to want to engage with a programme such as MEND:
[O]bviously they came with a bundle of additional problems . . . language, mental health issues, they’d been abused, they’d come to a new country and tried to settle in, so we had those to contend with as well. I think the children at the schools, they were able to adapt . . . but to engage the parents when their primary thought was to stay in England, the UK – it’s less around budgeting and balancing your food, it’s more about feeding your kids and getting your kids clothed and staying in the country[.]
C28
Poor retention was reported as resulting in the cancellation of MEND programmes. Although two interviewees reported maintaining 80% and 90% of programme attendees until the end of the sessions, attrition was generally perceived as high, sometimes with half or more of the families dropping out. What was considered to be reasonable retention varied. For some interviewees, completion by half of the recruited families was considered adequate. But for others this was not satisfactory: ‘so we roughly have maximum fifty per cent retention, which is absolutely appalling’ (C10). Other interpretations of completion related to regular attendance: ‘Back then, when we were looking at MEND . . . if they missed half, but they still came every other week, we’d still count that as a completer’ (C47).
In summary, how and whether or not families are engaged with MEND was described as variable. There was a diversity of referral routes, recruitment could be difficult and hard-to-reach groups might not engage with the MEND programmes. Definitions of completion were inconsistent, although interviewees generally regarded retention as poor.
Family engagement and commitment
Interviewees generally valued the family-based approach to MEND, whereby changing the family was placed at the heart of changing the child’s behaviour and relationship with food: ‘I think that’s key to the 10 weeks because if you don’t change the parents, then nothing changes at home anyway’ (C14).
Such changes referred to issues such as family motivation in weight management and understanding family food culture, given that parents normally manage much of the access to food at home (influenced by their children who, in turn, were influenced by advertisements and peers – sometimes referred to as ‘pester power’). In addition, interviewees suggested that families got a lot out of engaging with other parents and carers: ‘they like the fact that they’re in a forum where they can speak to other parents who are like-minded or are going through similar circumstances and I think it’s nice to be part of that’ (C54).
Development of links with other services was seen as crucial to engagement with families: ‘we’ve developed partnerships through . . . MEND, linking with, like we said, the sports centres, schools, GPs, dieticians. We’ve got a real raft of people who back the programme’ (C31).
The biggest barrier to active engagement with MEND was felt to be the time commitment, particularly during the school week:
We do understand that it’s evidence based, tried, tested and proven that this set format works but then you’re up against [it] if you can’t get the parents to commit to it. I mean it is a heck of a commitment; twice a week for 2 hours for 10 weeks[.]
C31
Interviewees described parents having to take children to different activities, and several reported that parents had to bring other children with them to MEND sessions. One commissioner reported that the imam of the local mosque was approached to discuss the importance of MEND because programmes conflicted with children’s attendance at mosque. Another concern was that parents from disadvantaged families might not be able to reconcile paid and unpaid work and child care demands with those of attending MEND: ‘But it is also being sensitive to how much else they’ve got going on, and if you’re working with deprived families who’ve got parents working two jobs each and three or four children to manage, it’s difficult’ (C4).
Interviewees described consulting families on the best time to run programmes during the week, with consideration given to running MEND sessions at the weekend. One reported allowing families back on to programmes to work on what they had missed: ‘But that’s not recommended practice really is it for what we do? But we’re working with real people with real lives here . . . sometimes what’s dreamt up in academia doesn’t . . . fit with working, with real people in the community’ (C31).
In addition to the time commitment, practical issues such as access to, and choice of, venues were considered. Public transport was described as problematic, particularly in rural areas.
One aspect of family engagement relates to the wider environment for health, which may take on increased salience given the move of responsibility for local health improvement to local authorities. MEND Central suggests that family-based treatment programmes are based on helping the family cope with an obesogenic environment, and potentially creating a micro-environment/family culture that can help protect against the worst excesses of this. Given this, we asked commissioners whether or not they were aware of the programme going beyond a protective micro-environment to ‘prime’ either commissioners or families to act on the wider environment. Although the commissioners we spoke to were very aware of the wider determinants, when asked whether or not they were aware of participation in MEND impacting on preconditions for obesity, only one gave an example:
I’m not aware of anything actually chang[ing] or getting done. But I do know that a lot of parents have been quite, sort of shocked, when they speak to the nutritionist and . . . get from their children, what they really eat in school. And I know several of them have said, well, I’m going to take this up with the head teacher . . . And some of them have actually questioned how little physical exercise there is on at school, erm, but whether or not anything has actually changed from that, I don’t know.
C7
Staff capability and addressing complex needs within the family
A key consideration for interviewees was who was actually delivering the programmes. The importance of a skilled delivery team was highlighted, an issue sometimes affected by a high turnover of skilled staff:
Unfortunately this is going to sound more negative on the whole programme to be honest, but because of how the programme’s run, a lot of instructors did not always stay around for that long so we were continuingly training new instructors, and looking for more people to do the programmes[.]
C52
Staff needed good interpersonal and teaching skills to keep families motivated and to explain the content of the programme in a way that they could understand:
[I]t’s the personalities of the deliverers . . . great rapport with a difficult-to-reach target group . . . So it’s about the personalities of the people involved plus the knowledge and the skills, their experience, it’s the whole package . . . from my point of view[.]
C31
[I]t’s important to have the knowledge but also to be able to put that over to whatever client group you’ve got in front of you . . . rather than using jargon[.]
C30
Good recruitment and retention of staff and appropriate staff training beyond obesity issues were highlighted, with one interviewee insisting that all MEND delivery staff were trained up to level 2 in safeguarding:
[W]hen you’re dealing with families who have multiple difficulties in their life . . . those difficulties . . . appear in the room. And that is quite a strain on the people who are trying to run those programmes, who may not necessarily be trained to deal with those kinds of issues[.]
C40
[. . .] they have got a weight issue but actually they’ve also got maybe ADHD [attention deficit hyperactivity disorder] or they’ve got severe learning difficulties or they are a particularly troubled family, maybe they’re under social services or there’s a team around the child. We are starting to find that we’re getting more of those children which MEND I don’t think is appropriate for, that people just don’t know where else to send them[.]
C54
A number of interviewees did not feel that MEND was appropriate for children with complex needs, with interviewees reporting that they referred children with attention deficit hyperactivity disorder or Down syndrome to other programmes.
So if they have any comorbidities, complex needs, under social services, we’re worried about them . . . if there’s anything we’re concerned about, they stay under the specialist service . . . It’s far more tailored . . . It was developed locally, NHS side, and . . . our sessional workers are excellent, but we’d still be worried about some children going to a MEND programme who . . . especially if they’re children in need, or they’re on the Child Protection Register, things like that . . . I just feel as though if they’re at a MEND programme we can’t really get a sessional worker to come and feed back. Although they can report back to us, I think it’s better if there’s a health professional for the teams[.]
C66
Interviewees made the point that staff–client interaction was critical: ‘it’s too simplistic from MEND’s point of view. “Here’s the solution in a box. All you have to do is work through our manual, and you’ll deliver a good programme” ’ (C5).
It was suggested in a commissioner interview that MEND is costed on the basis that almost anyone can do it following basic training, but several commissioners only trusted high quality staff that were more expensive. They wanted to invest in their staff:
So to deliver it, it’s relatively straightforward because there’s a book to work from, and MEND themselves I believe, if someone goes on the training, you don’t have to be a qualified nutritionist to deliver but, but we always use a qualified nutritionist because – well the training lasts 2 days, but the questions that come up, you wouldn’t be able to [answer] them unless you had quite a good grounding in nutrition. We decided we would always use a qualified nutritionist rather than someone who had just been on the MEND training. So I don’t know if that’s a down side of it, but that’s what we’ve decided.
C7
Delivering MEND for local populations
The sociodemographic and ethnic diversity of families was considered important, along with the content and delivery of MEND programmes and local adaptations in enabling better engagement with families on the programme.
Sociodemographic and ethnic diversity
Interviewees were well aware of the link between obesity and deprivation and the association between obesity and some minority ethnic groups. The sociodemographic profiles within the areas where MEND had been implemented varied, with both urban and rural areas including affluent and poor neighbourhoods. Interviewees described ‘pockets of deprivation’ in their localities, including parts of London, where individuals and communities in a small area may be at opposite ends of the socioeconomic spectrum.
Interviewees were familiar with local data on childhood obesity, with one commissioner, for instance, reporting that around 25% of Year 6 (10- to 11-year-old) children in their locality were obese. NCMP data were used to support recruitment efforts for MEND which targeted districts where child obesity levels were known to be high. In terms of ethnic diversity, there were high numbers of BME populations in some districts where MEND was provided, with one interviewee reporting a particularly high percentage including asylum seekers and refugees:
[W]hen we’ve done more analysis, as you know, it’s similar elsewhere, with a strong association with deprivation and strong association with ethnicity, particularly our west African communities and some of our mixed communities . . . When we plotted out a trajectory of how we would like to try and tackle this issue, it wasn’t necessarily about bringing down the rates, it was about levelling off and halting the rise of obesity[.]
C3
However, in another area it was not the BME population that caused concern: ‘So our problem population is white British, not BME, which is unhelpful because all the national stuff on health and equality is about BME groups’ (C15).
Obesogenic aspects of the localities were discussed, including the high numbers of fast food outlets, lack of access to outdoor play and poor public transport, particularly in rural areas. Other factors discussed were low employment and high levels of depression, alcohol abuse and domestic violence. Understanding the profile of the local populations where MEND is being implemented was seen as key to recruitment and addressing inequalities, with some acknowledging that need could not necessarily be ‘read off’ from demographic data.
Content and delivery of MEND
Commissioner and service delivery-partner interviewees were largely positive about the content of MEND materials in terms of the topics covered, though some disliked the terms ‘MEND friendly’ and ‘MEND unfriendly’, which they considered confusing or counter to the premise of eating certain foods in moderation. There was also a suggestion that MEND materials were insufficiently ethnically sensitive. For example, it was pointed out that many families from Asian backgrounds used local markets rather than going to the supermarket, and that ‘label reading’ advice provided in MEND materials did not translate to unpackaged foods.
There was a suggestion from some commissioners that MEND was ‘too academic’ or ‘too middle class’, which was seen as a problem for parents who had disengaged from education:
It’s like school, it’s like a test[.]
C35
Some of them felt it was a bit patronising, and almost a bit school-y, a bit like we were delivering lessons. We took that learning and we tried to really mould our programme to do the opposite.
C47
There was felt to be a lot of homework and form-filling and, in general, MEND programmes were described as demanding good literacy skills and fluency in English. Some interviewees reported no concerns in relation to literacy or English-language skills, but others suggested that these are important in that some parents on their MEND programmes could not read or had dyslexia:
[I]t’s an education for the adults, isn’t it? . . . It depends what area you’re working in . . . I’m working in a disadvantaged area, literacy skills and numeracy skills are at a lower scale so it’s difficult to judge, without having done this in a more affluent area[.]
C28
Where parents were not fluent in English, there was a demand for interpreters on the MEND programmes and translation of materials, or for MEND delivery staff fluent in community language(s). Although MEND materials were praised, a few interviewees concluded that MEND was not sufficiently inclusive for some BME populations or for children with special educational needs. It was suggested that MEND materials might need to be more visual. One MEND scheme had specifically designed one-to-one sessions on weight management for children with complex needs, and another commissioner used a different provider for this.
Tailoring ‘the solution in the box’
A number of interviews discussed what was viewed by some as inflexible delivery of the MEND programme, resulting from the perception that it is ‘a solution in a box’. Changes to MEND to suit the local context had been implemented by some delivery teams, although there was a tension between local adaptations and programme fidelity:
[M]y initial feeling . . . coming from a research background, was that that’s a really bad idea because we’re not working from an evidence base. But having now been . . . on the coalface for 3 years, I feel slightly more inclined to understand . . . why people do that . . . [They] . . . know their own population . . . their delivery team. They want to give people the chance to use those skills and make sure what they’re delivering is useful in their own locality[.]
C5
Another interviewee reported that MEND actively encouraged staff to adapt the delivery of sessions to meet the local context:
But to be honest, MEND always said use what is the best fit for you locally. You know, nationally, top down, with all the programmes we deliver, if they just said deliver it one way you would never get anything achieved or done[.]
C39
Adaptations were referred to in terms of meeting the needs of the local population, and tended to be small-scale. Modifications which had been implemented included timing sessions around school holidays, ‘breaking down’ MEND materials for groups in which literacy levels had been low, and adapting sessions to the group, depending on the group interaction and participants’ understanding. Translation and visual adaptation of materials were described:
[. . .] it was because we have a culturally diverse community in [place], so what we do is tailor our programmes to meet that diversity. A lot of the items that are produced may not necessarily be in English because you’ve got to deal with that kind of dimension so we use a number of approaches to tackle the diversity issues. So we use different languages. It just depends on who you’re seeing really . . . we try and do things to make them visual. So that is how we try and tailor things[.]
C48
Similarly, in one locality where most families used local markets for shopping, participants were encouraged to discuss their own diets in sessions; in one MEND programme, the list of foods was expanded to include more ‘Asian’ foods. There was also a suggestion that the exercise component of MEND was not as structured as the other components, so some exercise activities were altered (e.g. using dance mats), with the children asked what activities they wanted to do the following week.
Suggestions for future local adaptations included reducing the time commitment to the programme, which was considered substantial; for example, requiring families to attend key sessions only but with other optional sessions available. Other suggestions included having more practical activities such as cookery sessions, ensuring translation of materials into community languages and providing follow-up or ‘graduate’ services and internet-based programmes. The perceived high cost and a lack of fit to local context had led some interviewees’ teams to develop their own programmes:
I think in rural areas it struggles because it’s about getting people to a set location at a set time for 2 hours, whereas what we’ve done with some of the other services that we’ve designed ourselves now is more about 1 hour, getting people to local locations to them that works, and being able to have that 2- or 4-week break between sessions which allows them to make changes.
C52
Discussion
The changing NHS, the evolving public health agenda and a climate of austerity dominated interviewees’ accounts, with anxiety expressed as to how changes would affect working practices, working conditions, and the commissioning and future provision of public health services. In the light of this, there may be a response bias, with those with whom we were able to make contact and who responded positively more than usually knowledgeable and interested in the evidence base (such as it is), and with something they wanted to say about MEND.
Original decisions to commission MEND were influenced by the well-publicised trial, lottery funding and a sense that, although expensive, the programme would offer value for money as an intervention to reduce child overweight and obesity. With hindsight and with the ending of Big Lottery funding, the cost was seen as a problem, and increasingly so within an uncertain public health environment. For some, cheaper alternative programmes used or developed locally were described as an attractive option.
Commissioners identified a need for greater planning and resourcing of engagement with families before and after the programme, and delivery teams with the skills and expertise to engage with a range and complexity of needs as well as confidence in delivering the programme itself. Implementing MEND flexibly in the highly diverse socioeconomic and ethnic profiles of local populations was recognised as difficult, and underlined the need for good contemporaneous data and longer-term follow-up in order to make sound commissioning decisions.
Engaging with families was seen as critical, but recruitment and retention were viewed as generally poor, partly as a result of the demanding time commitment to the programme. Whereas the logic of involving parents was very much liked by commissioners, only one addressed the issue of children who might want to attend, but whose parents could or would not. It was felt that MEND should be implemented in a way that takes account of varying literacy and English-language skills, reflecting the highly diverse socioeconomic and ethnic profiles of the local population. MEND as it stands was viewed as unlikely to be appropriate for everyone, and children with special educational needs were particularly mentioned. However, as one interviewee pointed out, need cannot be ‘read off’ from deprivation, education and ethnicity.
Engagement is partly dependent on a skilled delivery team, who in some cases face the challenge of complex needs in the family. From that point of view, programmes such as MEND were seen by some as an opportunity for capacity-building locally. Another positive feature of MEND from the commissioners’ point of view was that it draws together behavioural, educational and physical elements of change. Although the RCT and the links to an evidence base made commissioning decisions easier to justify to PCTs, there was some uncertainty about how decision-making would play in the new public health environment of local government, where complexity is well understood and single-issue solutions are viewed with some scepticism. In summary, there were tensions, with those whom we interviewed liking MEND for being ‘evidence-based’ and ‘off the shelf’ or ’a solution in a box’, while acknowledging that it is ‘only as good as the staff’ and requires significant backstage organisation.
Headline findings from Chapter 5
Findings from our discussions with commissioners and service delivery partners suggest that the salience and acceptability of the scheme were positively influenced by:
-
the perception of MEND as evidence based and ready for easy implementation – ‘a solution in a box’
-
MEND’s emphasis on involving families.
Concerns which might influence future commissioning included:
-
uncertainty surrounding changes to the NHS and the organisation of services
-
the end of Big Lottery funding and, given that this was no longer available, what was seen by some as the relatively high cost of MEND both financially and in terms of data requests from MEND Central
-
the evidence gap on longer-term outcomes
-
variable participation and completion rates for MEND, which influenced perceptions of value for money
-
concerns in relation to planning and resourcing skill sets for delivery to diverse populations and children and families with complex health and social needs.
Chapter 6 The salience, acceptability and costs of MEND to individuals and families
What is the salience and acceptability of MEND to those who participate in full, those who participate but drop out and those who might benefit but do not take up the intervention?
What types of costs, if any, are borne by families (and by which members) when participating in MEND, and in sustaining a healthy lifestyle afterwards?
Background
The work with commissioners highlighted the way in which a RCT showing a positive effect was influential in terms of commissioner decision-making. Given that, in addition to high quality research evidence, the ways in which those on the receiving end feel about an intervention is crucial for implementation, we explored this with both parents and children. Although the context in which we conducted interviews with individuals and families may not have been as volatile as that faced by commissioners, our interviews took place in a climate of rising unemployment, increased public awareness of childhood obesity and anxiety about the economy.
This section reports findings from face-to-face family-based group and individual interviews with MEND participants. We explored with them the salience and acceptability of MEND and the types of costs, if any, borne by families when participating in MEND, and in trying to sustain a healthy lifestyle afterwards.
Methods
Interviews
Data were gathered through individual and family-based group interviews. A topic guide was developed by the qualitative team, informed by the literature, discussions with the wider project management group, the advisory group and the commissioner interviews. Transcripts from the first family interviews were reviewed by the research team and the topic guide was refined. The guide was a tool, not a rule, and was used to map rather than constrain our discussions. In order to make sense of MEND from the participants’ perspectives, we needed to elicit their narratives. Interviews began with open questions about family make up and memories of MEND, after which families were encouraged to take the lead with prompts towards the following broad topics:
-
the opportunities and trade-offs presented by participation in a MEND programme
-
costs and benefits within the family
-
access to schemes
-
positive and/or negative experiences of participation.
Researchers were alert to whom within the group had opportunities to speak, and managed conversations in order that everyone could contribute.
Sampling strategy and recruitment
As it is a requirement of the MEND programme that the child be accompanied by a parent or carer, our sample was based on family units. We aimed to recruit 30 families: 10 high attenders, 10 less frequent attenders and 10 who had not taken part despite eligibility and initial interest. We recruited families in three regions of England: the London area, the north-east and the south-west.
MEND records, which are designed to include contact details for both MEND participants and people who did not take part after an initial referral or contact, were used to purposively select a sample of families. We anticipated that 50% of those approached might choose to take part. Using anonymised data on attendance and demographics from 657 families, a sample of 68 families was derived with the intention of achieving variation by ethnicity (50% white/50% BME), housing tenure (50% owner occupied/50% council or private rental), family structure (50% with two parents/50% single parent), number of MEND sessions attended (as above) and local deprivation (highest and lowest 30% in the English Index of Multiple Deprivation). Full details of the sampling strategy are supplied in Appendix 15.
MEND Central wrote to these 68 families with information about the study, inviting them to opt out by contacting the research team if they did not wish to take part. If no response was received after 21 days, a research associate telephoned families in order to complete recruitment. Families who could not be contacted on the first call were telephoned up to three times and voice messages were left. Where phone numbers were invalid, or no message could be left, a second letter was sent asking families to phone or text the research team if they wished to take part.
This was supplemented by three additional methods of recruiting low and non-attenders. Firstly, we tried ‘snowballing’ from the families interviewed, and one additional family was recruited through this method. Secondly, we advertised in sports centres where MEND was or had been offered (see Appendix 16). Thirdly, we placed advertisements on a parenting website in each of the three research areas (see Appendix 16). We know that these website advertisements were read (though not necessarily by MEND families); in one location, for instance, the advert was viewed 53,737 times and clicked on 26 times. Neither method of advertising yielded additional participants.
The primary contact, usually the parent, was asked to take part in a group interview comprising the index child, the parent who attended MEND sessions, and, if they wished, up to two other family members or friends whom they considered important to their child’s weight management (parents, carers, siblings or others who might influence the impact of MEND on the family’s day-to-day living).
We had intended to follow up the family interview with up to 30 individual interviews with a participant from the initial interview, to generate accounts which might have been unvoiced in a group interview. We planned to recruit those who might be willing to engage in greater detail about their experiences of MEND, possibly offering an alternative narrative to that characterising the group interview. We planned to prioritise voices which were more muted in the interviews, anticipating that this might occur with children. In fact, by the end of the majority of family interviews, it was clear that the interviewees had exhausted all they had to say. Just eight individual interviews took place, two of which were with family members who had missed the group interviews. The individual interviews were unstructured, reflecting on discussions which had taken place in the group interviews and, where necessary, using prompts from the family topic guide.
Most families chose to be interviewed in their homes. Two preferred to be interviewed by telephone, one was interviewed in a quiet space in a library, one in their family shop and one at a relative’s home. Each person who took part in interviews was given a £10 gift voucher to thank them for their time. The length of interviews was determined by the preferences of the families. Each lasted at least 45 minutes and most were longer. After 1 hour, interviewers offered regular time checks and opportunities to end, but participants often appeared to enjoy the discussion and were happy to continue. The interviews with families and individuals were conducted between October 2011 and July 2012.
Ethics, informed consent and data protection
The work was approved by the UCL Ethics Committee (2842/001). Amendments were submitted to allow further advertising for participants in the under-represented categories. Age-appropriate participant information and consent forms were used, including versions for children with learning disabilities. Families were provided with information several weeks prior to participation, and the research was explained in person before interviews began. All parents and children were asked for written consent, except for one very young child who gave verbal consent. Translation/interpretation was offered to families for whom English was an additional language. Researchers ensured that all members of the family (including children) were given the opportunity to opt out of the research, and some children did choose to leave interviews before they ended. Researcher safety for interviewers was addressed by ensuring that another member of the research team had details of interview locations and mobile telephone contact details.
Interviews were recorded and encrypted sound files were sent to a secure drop box facility and then for transcription. Verbatim transcriptions, with identifying features removed, were returned to the qualitative team. Hard copies of consent forms were securely archived.
Analysis
As with the commissioner interviews, data were analysed using framework analysis. 78 The qualitative researchers collaborated to develop the initial framework for data management. All contributed to tabulating data within this, including both individual and family group data. One team member drew up a list of higher-order themes and interpretations, extended after discussion with the whole team. We took into account issues raised by the NCB’s young people’s PEAR group (see Chapter 1, Public involvement), consulted prior to the research proposal being submitted, including the accessibility of MEND, how it fitted into parents’ busy lives, the potential for positive peer groups and the potential for attending MEND to be stigmatising.
As an aim of individual interviews had been to hear from those with ‘alternative perspectives’, a further analysis was carried out to explore tensions between participants’ accounts within group interviews, or between group and one-to-one interviews within the same family. A framework approach was used where participants’ accounts were at odds, or where participants challenged or contradicted one another, and a typology was developed to describe these.
Findings
Recruited sample
Of 68 families contacted, 10 declined to take part (15%), 18 did not respond to calls or voicemails (26%), 14 had invalid phone numbers and did not respond to letters (21%) and 26 (38%) agreed to be interviewed. Of these, 22 went on to be interviewed and 4 declined on further contact. One further family was recruited through snowballing. Appendix 15 provides further details on recruitment.
We interviewed 23 families comprising 64 individuals, including 22 mothers (one a foster mother), six fathers, two grandmothers, two aunts, 12 male and 12 female child MEND participants, five brothers of child participants, eight sisters of child participants and one family friend. Our sample included adult participants who worked in health or social care, including two who had at some time been responsible for commissioning decisions about MEND.
Although our final sample captures variation across most of the dimensions of interest (Table 26), there was a larger proportion of owner occupiers and MEND completers than planned. Most had attended earlier programmes (most families were referred in 2008). This afforded an opportunity to explore participants’ reflections on change over time. In order to ensure anonymity, individuals are identified using a unique family number and a brief descriptor (e.g. ‘father, F4’).
| Characteristic | Number of families interviewed (%) |
|---|---|
| Region | |
| South-west | 9 (39) |
| South-east | 7 (30) |
| North-east | 7 (30) |
| Year of first session | |
| 2008 | 10 (43) |
| 2009 | 5 (22) |
| 2010 | 7 (30) |
| 2011 | 1 (4) |
| Housing tenure | |
| Owner occupier | 16 (70) |
| Social housing | 3 (13) |
| Privately rented | 4 (17) |
| Family structure | |
| Lone parent | 11 (including one foster parent) (48) |
| Couple | 12 (52) |
| Ethnicity | |
| Bangladeshi/Bangladeshi British | 2 (9) |
| Pakistani/Pakistani British | 4 (17) |
| Other Asian | 1 (4) |
| Black African | 1 (4) |
| Black British – Caribbean | 1 (4) |
| White British | 13 (57) |
| Mixeda | 0 (0) |
| MEND completion status | |
| Unknownb | 10 (43) |
| Moderate attendance (actual range 44–72% of sessions attended) | 6 (26) |
| High attendance (actual range 85–100% of sessions attended) | 7 (30) |
Some families initially found it difficult to remember details of MEND, but talking jogged their memories and most participants had clear views on what they had found useful, enjoyable and difficult about MEND, both at the time and looking back. We were aware that these interviews were sometimes difficult for families; unhappiness with weight was expressed by adults and children, and family members disagreed, contradicting each other’s memories and interpretations of events. Occasionally, children expressed unhappiness that their parents had not made changes that they wanted; some parents felt that their children were resistant to change.
Where mothers and fathers were both present in interviews, mothers had the most to say but fathers too made important contributions. In four cases, men (one grandfather and three fathers) had chosen not to take part in interviews, but were in fact present. Two of the fathers who were ‘listening in’ in this way asked to join the conversation and were consented.
Our findings fall into four main sections mapping on to our research questions about the salience, acceptability and costs of the programme to families, and the perceived costs of maintaining a healthy lifestyle afterwards. The first section explores reports of why families attended and who made the decision to do so. The second explores experiences of attendance, including positive experiences, barriers to attending and perceived costs associated with attending. Finally, we consider long-term change as understood by families, beginning by setting out perceptions of long-term change, and perceptions about costs and constraints associated with trying to maintain behaviours promoted by MEND after the programme had finished.
Referral to MEND and decision to attend
Most families self-referred, having seen leaflets or heard about MEND from friends or family who knew that parents were concerned about diet or weight. Four families were referred through some part of the health service (e.g. a nutritionist) and in one case a community worker recruited a group of local families to MEND and arranged shared transport for them. Schools were an important source of information, including leaflets received with NCMP letters. The impetus for contacting/attending was not always clear in discussions, but reasons offered fell into four areas: experience of bullying, transition to secondary school, concerns about diet or weight, and concerns about other health problems.
The most common reason given was that children had experienced bullying, and parents and children felt that losing weight might reduce this: ‘I used to get bullied a lot about it. I just decided to drop the weight and stuff’ (boy, F18).
This chimes with children’s focus on the social impact of overweight observed in other studies,79,80 and in our study this was often associated with the transition to secondary school. This seemed to be an important moment, because of fear or experience of bullying at the ‘teenage school’ (F61) and because it was a time of transition for the children. There was a sense that they could either capitalise on changes for the better, or slip back into familiar habits.
A small number of parents were worried about their child having a poor diet and felt that MEND might be useful in correcting this. Many families (parents and children) said that they were worried about excess weight, although parents seldom explicitly used the term: ‘I heard about it from my friend [name] because her lad was like [son’s name], you know, a big lad’ (mother, F61).
Several parents referred to their own weight. One father (F4) said of himself, ‘I’m not the smallest person in Britain’. Overweight was sometimes identified as a family problem: ‘we knew there was an issue in our family and we didn’t want our children to end up like our parents or us either’ (mother, F70).
Some parents described weight gain, and attending MEND in the context of another problem for the child such as learning disabilities, cystic fibrosis or endocrine problems:
[I]t’s kind of a genetic hormone imbalance, he can be prone to weight gain so he was starting to put on weight at a certain stage and I just happened to see a leaflet advertising the MEND programme and I thought, ‘Oh, that’s something . . .’ I couldn’t afford to go and hire a private dietician or anything, so it was something I was able to go to[.]
Father, F57
Despite some shifts in the domestic division of labour nationally and internationally,81 it remains largely mothers who protect and promote the health of children. In our study, responsibility for undertaking MEND lay largely with women. In almost all families, the mother was behind the decision to attend. Most often it was she who heard about the scheme, decided the child should attend and persuaded him or her to sign up:
I think it was basically both of us. Mum said to me, ‘Oh, there’s this going on, would you like to maybe try it for a week or so, see how it goes, don’t like it, don’t have to go, if we do, stay there.’
Girl, F26
In some cases this was not negotiated: ‘you just told us one day we’re going’ (boy, F50).
Only in one case – that of a father parenting alone – was a mother not the route by which the family entered MEND. Where children lived with both of their parents (n = 11), the mother accompanied the child to MEND in all but one family. This was often described as being because mothers worked part-time or had more flexible working arrangements than their partners. Only five fathers reported ever attending any MEND sessions; two regularly accompanied their sons and three went to some sessions when asked or when their partner could not attend. Other family members also helped out; grandmothers, aunts and older sisters attended when parents could not. It was very common for siblings to attend alongside the child participating in MEND, usually because there was no other child care available. In two families more than one child in the family was referred to MEND.
In the interviews, non-attending adults told us that it simply was not possible for them to attend because of their work, but they felt they played a role in supporting changes at home and that they did what they could: ‘You had me running around the bloody field. What do you mean I didn’t get involved?’ (father, F27).
Two families felt that the wrong decision had been made about which adult should attend MEND. In family 67, the mother attended with her daughter, but felt in retrospect that as her partner did most of the food shopping, changes in diet would have been more successful if he had attended instead. In family 4, the father and his son attended, but the mother felt excluded from MEND and believed that the lack of change in their diet was because she did not know what she was supposed to do: ‘Because that’s the problem with not going, I was relying on two boys to bring the information back’ (mother, F4). Her partner agreed that lack of communication had impeded family change following MEND, but her son felt that they had left the information for her, and it was her responsibility to read it.
Family experiences of attending MEND
Having fun and feeling supported
Many families reported positive experiences. The supermarket tour, sharing recipes and food, and swimming sessions were highlights. Children’s main memories of MEND were often the games they played in the activity sessions. The children had enjoyed trying new activities in the company of children of similar build. Cousins who had attended together (F55) were quick to claim confidence in new areas:
I was good at the rowing machine.
Daughter, F55
I was good at the running machine.
Niece, F55
The youngest MEND participant that we interviewed told us his main memory was that it had been ‘funny’ learning: ‘how to [do] back flips and front flips. Running backwards and falling over backwards’ (boy, F70).
Both adults and children enjoyed some of the practical lessons and valued the concrete steps they could take. Although some thought these elements a bit of an ‘idiot’s guide’ (mother, F67) most found something of value. For example, teaching children to read labels for themselves and distributing cups for portion control were described as useful, clear and practical components of the programme: ‘They were very basic . . . not basic, that’s not the word I need, very strong in telling you exactly what you should or shouldn’t eat and the amounts’ (grandmother, F57).
Children liked being recognised as important decision-makers about their eating, as others82 have described.
She enjoyed the family side of it when we all sat together, and then you were paired off with a group of people, chatting . . . I think she felt, ‘Oh, I’m an adult here because I’m getting treated like an adult, not like a child.’
Mother, F26 (individual interview)
Exposure to new foods was often a success. Families described trying foods that they would never otherwise have bought or cooked, and these changes were often things that families felt had ‘stuck’.
All of the families found the groups friendly and welcoming (though few made friendships which lasted beyond the course) and many valued the social acceptance received in the groups, describing talking about shared problems and knowing that ‘you’re not the only one’ (and that some others are worse off), which made it easier to exercise.
The positive support from the social group was key to MEND. Where the social group was not successful, for instance, in terms of the age mix, children found it difficult:
[S]ome of the other people were about three/four years older and they were really tall so I had to look up to see them.
Girl, F67
I felt quite grown up really because I was the oldest and sometimes it was a good thing but sometimes it was a bad thing because I thought, ‘Well I know all this already, so what’s the point?’
Girl, F25
I felt a bit embarrassed when we went walking through to the pool and all you saw was someone under 10, under 10, under 10, then me, then another under 10, under 10 . . . I vividly remember this conversation, ‘It will be all kids,’ and [mother] went, ‘No, I bet there is someone your age.’ There was not one person my age, no one close to being my age.
Boy, F56
Responding to the suggestion from commissioners that MEND was too middle class, we asked families about the social mix of the groups. Families perceived MEND differently; there was a suggestion among some that MEND was more geared towards the needs of less well-off families: ‘we’re not . . . I work, my husband works, so we’ve got two incomes coming in. So we’re mostly probably not the target family [for MEND] in terms of our position in an income scale’ (mother, F25).
One mother (F50) told us the other parents were ‘not educated, not someone you could have that level of communication with’ and she felt they had more in common with the families she worked with in her professional role. This was not a common view, and mostly parents enjoyed the mix of families they met:
. . . I quite enjoyed the sessions. There’s different people that you’re interacting with . . . as a family we didn’t used to do a lot of socialising . . . So actually getting out and about and meeting these sorts of people it was different[.]
Father, F4
The final important source of support for families was their wider social and family network, although this could have a positive or negative impact. For some, the extended family facilitated attendance at MEND because they provided child care or transport, or attended when parents could not. However, some also spoke about a lack of support, including grandparents ‘treating’ their grandchildren with unhealthy food:
Their grandmother gives them treats . . . They are spoilt when they are there[.]
Mother, F53
She used to give us sweets every day[.]
Boy, F51
Many festivals and celebrations include special meals, and families spoke about these being difficult times to keep to a healthy diet. Friends were important, because their approval mattered. Children were wary about whether or not they would ever discuss weight or MEND with their friends, because they would not want to offend them by implying they were overweight. This sensitivity created difficulties around lunchtime at school; healthy meals were often not acceptable to their friends and children would therefore reject them. One boy (F26) described how he used to make vegetable soup to take to school but: ‘I never ate it because of the smell. I thought the smell was repulsive. I used to do that to my friends, just open it on the bus and they used to go, “Oh, what is that smell?” ’
Some participants, whose family roots were in low- and middle-income countries, described a less obesogenic lifestyle and environment: ‘my great granddad . . . the day before he died he was still working on the fields’ (father, F51).
Barriers to attendance
Although most of the families in our sample had maintained high attendance, they spoke about the challenge of fitting MEND into their lives. All of the families discussed difficulties with attending the sessions, and several commented on the high dropout rates among other families. They often attributed not taking part or dropping out early among other families to parental commitments; another mother ‘was quite busy with the nurs[ing]’ (girl, F26), while others were seen as lacking commitment and ‘were just a bit lazy’ (mother, F61).
Combining attending MEND with all the other demands on family time was often very difficult for parents and children. Working hours often determined which adult could attend. Several parents in our sample worked shifts, often into the evening and changing on rotation. Children also had to fit MEND around other activities such as sports, after-school clubs, school work and time in the mosque. The needs of all the children in the family had to be considered, not just the child who was attending MEND. As one mother (F67) put it: ‘My neighbour says, “you’re in and out of that house like a fiddler’s elbow”. I drop one off, come back, go and get the other one. Tuesdays is my worst nightmare, worst nightmare’.
One boy saw this as not worth the effort:
I just thought the whole thing was a bit of waste of time because like half an hour to get there and half to get back, so that’s an hour already, and we were there for like an hour and a half, so that’s like two and a half hours out of the day. With that I could be playing football or something[.]
Boy, F50
The timing of sessions caused difficulties, particularly for younger children. Where sessions were organised for early evening, families were rushing to get there after school and work, and children were tired and hungry:
We were swimming at four and then doing MEND at half four and he was eating a packed lunch almost surreptitiously in the corner because he was starving[.]
Mother, F70
[T]hey’re coming from the school right into the mosque, half an hour, coming out from the mosque and stayed in the MEND, that is very tiring and draining for them . . . sometimes we took things [food] with us[.]
Mother, F45
However, if sessions were held later they were felt to finish too late. Both parents and children mentioned that they disliked coming out of the sessions when it was already dark. One mother (F13) told us: ‘by the time you get back, it’s nine o’clock, it’s way past their bedtime, they go to bed at eight o’clock’.
Families acknowledged that it would not have been possible to find a time that suited everyone, but that problems with timing made attending the sessions hard.
For a few, the venues selected for MEND presented barriers. For some the venue was several miles away (one family travelled 16 miles). Although most families drove to MEND, this could cause difficulties when the family car was needed elsewhere and/or driving through rush hour traffic was involved.
A few thought the venues themselves were unsuitable because they were uncomfortable in some way (cold or damp) or did not suit the needs of the programme itself:
The place that they were I think it was the café, but we had to move all the tables and chairs so that was a bit of a . . . they could have done with like a proper sports hall, you know, long length because they were a bit limited in terms of space.
Mother, F61
Some of the educational elements were disliked. One child described MEND as being more like prison than school because it did not involve going anywhere. Families did not like repetition of information, nor did they like waiting around when facilitators were getting organised or spending time maintaining discipline in the group.
[. . .] we just kind of did the same thing I think so we just got bored[.]
Boy, F50
I think some of the sessions were a bit boring . . . just going through all the wholemeal stuff and what goes into it and what makes it healthier. But she just dragged it on a bit too much[.]
Mother/aunt, F55
One family (F28) pointed out that the materials were not appropriate for those who could not read or write and that they all got ‘fed up’ with all the paperwork. Most families had thrown away their MEND folder or relegated it to a dusty corner, although some retrieved it to show to interviewers.
The qualities of the facilitator were important to families. Often parents were keen to stress that facilitators were nice people; they were described as ‘marvellous’ (grandmother, F57) and ‘fabulous’ (mother, F21) and the children told us they ‘made it fun’ (boy, F51). However, this did not necessarily mean that the people we interviewed thought that they were doing a good job. Several parents felt they did not have the necessary professional skills or knowledge to carry the programme:
They were dead enthusiastic. I personally didn’t think they knew as much maybe as what they should have known[.]
Older sister, F28
[I]t’s the credibility of being confident in what you’re trying to do and I’m not so sure the person had actually gone through the package in any great depth . . . It felt like she was just reading off a . . . She was a lovely lady[.]
Mother, F27
Some felt that leaders lacked skills, particularly in managing a group of children, and behaviour could be out of hand or unsafe. There was also a concern that facilitators did not always have the life experience to help. They were seldom parents themselves and were sometimes described as being ‘thin’ or, in one case, ‘looking anorexic’ (mother, F67). Experiences of poor facilitation undermined families’ confidence in the programme.
Perceived costs of MEND participation
Parents most often told us that their participation was constrained by the time cost, rather than the financial cost. One mother of three children, one with special needs, whose husband often works away from home, said: ‘I just felt like I’d invested a lot of time, forget about the money, but a lot of time and effort’ (F67).
The main message from parents was that they would find a way to pay for the things their children need: ‘I don’t mind paying for something if he likes doing it. I mean, my parents will help out, you know, because they know he likes doing it, they don’t mind’ (mother, F61).
The same mother also told us that money had been ‘tight’ lately, and that ‘there isn’t a lot of money to spend on healthiest food: I mean I’m a single mum, you know, I can’t go out and buy all this decent low fat food, all the yogurt’. She and others discussed the fact that low-cost ranges and low-cost supermarkets do not include the healthier alternatives they had been encouraged to buy, such as lean mince or turkey breasts. As for the more exotic foods they had tried with MEND: ‘at the end it was all healthy stuff, but it was more expensive’ (girl, F26).
Others said that some food costs had gone down because they ate less meat, or there was less waste because they were making things with fruit and vegetables, but also that it need not be expensive to eat healthily: ‘Nowadays they’re [fruit] a pound a bowl . . . And they’re everywhere. So there’s no excuse saying it’s expensive’ (mother, F13).
Any change in costs to families was related to prior buying habits. A study of food prices has suggested that although a change from low-cost food purchased at budget supermarkets does carry a cost, families may be able to keep costs to a minimum if they have the time and resources to seek out the keenest prices. 83
Many of the barriers to attending MEND described by parents would probably have resulted in financial costs, but were not identified as such by families. Time off work, child care and, in particular, driving to the venue were likely to have carried costs. Several families said it was easy to attend because the venue was just a short drive away, but did not identify this as costly because they already owned and ran a car: ‘The only cost would be travelling there, but you drive anyway‘ (foster mother, F28).
Similarly, several parents arranged shifts or child care differently in order to attend MEND, and this was not perceived as a new cost, but part of the ordinary running of family arrangements.
Alongside time, the greatest perceived burden on families was the emotional demand. Parents spoke about this, and of people crying in sessions. They were aware that the children sometimes found the sessions emotionally demanding. An exchange with one father (F57) describes his observations:
. . . I think the children are crying out for help, but they don’t know what’s going wrong and why they are the way they are. And it’s kind of the parents’ fault really and it just makes them aware of that. I think some of them feel quite upset and bad about it.
So do people get upset in some of the classes?
Yeah, a couple of the kids did when they kind of get up to introduce themselves and why they’ve come to the MEND programme.
This could be perceived as intrusive and inappropriate:
And then it was almost like they were trying to look for some psychological reason . . . and I should imagine everyone has a psychological reason, but it was almost like they were looking for something deep and meaningful. I thought to myself, ‘I haven’t come here to be psychoanalysed’ which is what I felt that the leaders were trying to do.
Mother, F67
Although on the one hand children described enjoying the opportunity to exercise with others with weight problems, there was an emotional cost to attending a weight intervention programme.
The top, I didn’t like the top . . . I got out of the car, launched it on, and then launched a coat over it. It was just really embarrassing . . .
Why didn’t you want people to see you?
Just if they laughed or something, called me names.
Did people know what MEND was about?
I didn’t tell anyone. I just said I had to go to the leisure centre after school.
Costs associated with maintaining a healthy lifestyle
This section describes the costs and constraints reported by families in maintaining the healthy behaviours instigated following their involvement with MEND. As well as questions about financial costs, our questions on salience reported in this chapter include discussing weight change post MEND. This frequently led on to discussing broader post-MEND behaviours and family life. Like the commissioners who would have liked more data on longer-term outcomes, families too felt that what happened longer term was important. Despite the fact that many children and parents reported that the children’s weight had dropped or at least stabilised in the short term, long-term improvement was rarely reported. Parents also talked about the costs, both financial and emotional, of ‘MEND-friendly’ behaviours, and parents and sometimes children expressed disappointment with themselves, and sometimes with others, when they had been unable to maintain changes: ‘He was maintaining his weight. You were actually growing into the same weight, weren’t you, because he hasn’t actually put more weight on, he’s actually grown into the weight he’s got‘ (mother, F68).
Children and parents in families where children did lose or maintain their weight often described concerted, co-ordinated family behaviour changes made to achieve this. Most families who took part in the study were able to identify changes they had been able to make during MEND, such as avoiding takeaway food, not keeping crisps, sweets or fizzy drinks in the home, switching to healthier options (semi-skimmed milk, whole grains, more fish and less meat), avoiding fatty foods (cooking less fatty food, eating more vegetables and salads, cooking more food from scratch and, conversely, buying fewer prepared meals), using smaller plates and controlling portion sizes. Children described starting organised activities (tag rugby, wrestling, Guides) or walking to school; several families had invested in exercise machines, in one case explicitly because this was felt to be safer than going outside (son, F14).
Where long-term change in weight status had been achieved (not always attributed to MEND), there was consensus that this could be triggered by an important life transition for the child, such as moving to senior school, and/or by being supported from the outside, for example by teachers’ interest, or by new opportunities for play, such as getting older and having more independence.
I think it was just a combination of everything. We changed how he ate. And then he started walking to school and back, and now he’s got the dog.
Mother, F18
Just getting out and about with friends doing stuff instead of being confined to the house.
Father, F67
I think most things happened after the MEND programme. They put in your head what you need to do, and it’s up to you to follow it through. And being on the MEND programme twice a week was enough to concentrate on while we were on the programme. So the rest . . . we kind of got the knowledge, and then took it away and did something with it.
Mother, F18
I think it was kind of like a turning point for me . . . when I finished that, like I changed so much. I’m so much more careful with the things I eat now, what exercise I do. I try and walk to and from school now. I basically changed the way I feel about eating and exercising and stuff . . . If it was just one person, say me, it wouldn’t have been as easy as I wouldn’t have had the support of my family[.]
Girl, F27
But participants also talked about the difficulty of maintaining change and felt discouraged if their efforts did not bring about weight loss.
It changed my knowledge. I’m not saying I stuck to a lot of what they said[.]
Foster mother, F28
She’s taller, but compared to other big girls, she does have a weight issue . . . We are telling her, she’s still got the hula hoop since the MEND programme[.]
Mother, F45
Thus, as well as the costs of participating in MEND, families described a range of costs associated with trying to maintain healthy behaviours and what made it difficult to do so.
Social/emotional costs
For children, choosing the healthy option often meant being the odd one out:
[M]e and my brother had to make our own way to school and so I used to walk and he used to get the bus . . .
Girl, F50
I do find that most of my friends they have the unhealthy food in their house and they’re allowed to eat it[.]
Boy, F26
This, and frustration with the slow impact of behaviour change, could be painful: ‘But [swimming] just didn’t help at all, even when I wasn’t having snacks afterwards, it just didn’t help . . . I didn’t lose weight. I was just staying the same, even putting [it] on‘ (girl, F26).
For some parents it was very difficult not to allow children to have what they wanted: ‘It breaks my heart sometimes when I say no to them [about sweets]‘ (mother, F53).
One mother spoke about the damage she felt had been done to her relationship with her daughter by spending her teenage years fighting about food. Her daughter (F25) admitted that: ‘When I’m in a really bad mood I blame my mum‘. She both acknowledged that her diet was her choice and responsibility, and blamed her mother for giving her bad habits and allowing her to make unhealthy choices. Both mother and daughter felt they were to blame and were unhappy about their weight.
In many discussions there was an implied or explicit moral judgement about children being overweight.
All the kids, you see them with handfuls of sweets and it’s to put them over until the mothers are ready to do their tea[.]
Mother, F28
I think if people can’t pay a bit of bus fare to get a free swimming session for the children then what can you do? The government can’t afford to subsidise every little bit.
Foster mother, F28
Tensions and contradictions were evident in some family discussions with participants wanting to ‘do the right thing‘ in relation to weight and weight management. Aside from differing memories of programme logistics, such as timing and frequency, most differences arose out of participants asserting or defending their moral character, or challenging someone else’s, in relation to their behaviour or weight. For example, one child (F14) contested his mother’s claim that they visited the sports centre to check for activities at the beginning of the previous month, saying, ‘it was more than six months ago’. Several children disputed that they had regained weight lost on MEND: ‘I didn’t put anything on’ (child, F49).
Some participants’ narratives indicated how this moral framework could reinforce or intensify positive or negative experiences of MEND and feelings of success or failure, so that they fell into virtuous or vicious circles of engagement (or not) with the programme or with healthy living subsequently:
. . . this doesn’t mean to be rude to other people, but I think having said that, when she turned up, she was one of the smaller ones there and I think it made her realise that, you know, things weren’t as bad as she saw it. I think she just thought she was huge . . .
Mother, F27
Achieving co-ordinated family effort
Nudges towards unhealthy consumption are everywhere. 84 One woman, whose family came from Bangladesh originally, described how their assumptions about a safe and healthy environment for children in the UK had to be unlearned in favour of constant watchfulness: ‘the grannies, they don’t really give attention to that sort of thing, losing weight or keeping your health . . . because they think the children of this society will be all right . . .’ (aunt, F49).
Checking up on eating and exercise, on the other hand, requires vigilance both within and beyond the family; for example, in family 26 the mother described going to great lengths to make arrangements with the mother of her daughter’s friend to ensure their girls’ shopping trips did not end in a fast food restaurant. It was clear from interviews that for families where tensions ran high and parents juggled complex, fluid roles with little support (e.g. shift work or living apart), achieving these levels of co-operation could be a challenge. Parents in several families discussed how moving between households meant that there was less control over a healthy diet – with a risk of not being able to control what a child ate at the father’s house or of the child being given two meals. One mother (F67), who initially described herself as ‘lazy’ for not keeping up with MEND recommendations, later said ‘there’s only so much I can do’. For some families, the degree of planning and organisation needed to achieve MEND exercises had been beyond their resources:
So what was the hardest challenge you were asked to do?
I don’t think there really was one because . . .
You didn’t do them.
Some of . . .
Some of them he did.
Yeah, some of them I did, but for the rest somebody didn’t set them.
You were supposed to self-set, [son].
Yeah, but self-set with parent’s assistance.
I think that’s the thing in one respect, it was one of those things I started, thought it was a good plan, but I’m not sure I necessarily had the backing of both of them to do it. Both of them ended up doing it, but I didn’t necessarily have the backing of both of them to do it.
And then you . . .
Like things like challenges didn’t get set. At the end of the day, [son] would have been sort of 10, 9 or 10, and you can’t expect him to set his own challenges on his own without your assistance. And if he hasn’t got your assistance and your backing then it was going to fail to start with and [son] had no hope.
Maintaining change required willingness not just from the child but across members of the family, to sustain the personal costs of giving up favoured foods or activities and taking on new, possibly less liked, foods or activities. Independence on the part of the child was often named as one of the things that made changes easier to maintain, either because children were able to do more alone or because they took responsibility themselves for changes: ‘You’ve got to want to lose weight yourself before anything will work’ (girl, F50).
However, conflicts of priorities across the generations were often clear:
She [mother] still has white bread, don’t you . . . Which means then [daughter] technically gets white bread because that’s what mam likes[.]
Daughter, F28
I think it would have been nice to carry on the sports . . . But now mum can’t take us swimming and then as well all the family could have gone and it could have been like a family club to go to the swimming baths . . . You (Mother) wouldn’t have liked that idea but I would.
F67
One mother (F14) did not want her son to play outside ‘because of the chest infection that he’s had’, because ‘there’s a neighbour upstairs and she does a lot of shouting’, and because in the winter ‘you need to eat to keep warm’; she felt that he was active because ‘kids make their own entertainment . . . all this technology stuff with the phones and . . . stuff like that’.
Some parents told researchers that they had reduced food intake and switched to healthier options, but when they described their children’s diet it seemed extra meals or calorific snacks were creeping back in (e.g. offering snacks such as pizza or sandwiches to replace biscuits or crisps).
Environmental constraints and controls on children’s choices
For many families there were actual or perceived environmental constraints on the choices that children might want to make. Although all participants might agree that children should be able to make those choices, neighbourhoods were not necessarily safe, nor exercise activities accessible for children:
I don’t really feel too safe going out on my own just doing stuff especially on a bike because I have a BMX but I don’t want it to get robbed, because it almost got robbed last year or 2 years ago . . .
Son, F14
The child in one family used a wheelchair and could only walk with support for short distances. This family lived in a built-up area with major roads nearby and few pedestrian crossings or pavements, so there was no real opportunity for her to walk outside of her home.
Families described cuts in local services that removed healthy activities (such as school swimming lessons) or weight-loss programmes as contributing to increased weight among children. One mother (F2) spoke about the fact that advertising may be misleading, questioning why advertisers are allowed to state that something is healthy when it is not. This mother told us that parents were often blamed and the real causes of weight problems ignored; she gave as an example professionals blaming poor feeding for her daughter’s slow growth during infancy, which was later explained by a diagnosis of cystic fibrosis.
Sustaining non-‘normal’ behaviours in busy, changing family life
Participants spoke of MEND as a one-off event which takes place at a particular point in a family’s life and is easy to leave behind: ‘Like a new jumper you wear it for quite a long time and then afterwards it just goes old and sometimes you just go, No I don’t want that, I’ll go back on to the usual ones’ (daughter, F45).
They also talked about a desire to move on, to return to ‘normal’. Many reported keeping to MEND changes as much as possible, but reverting to unhealthy options (particularly takeaways) at busy or ‘special’ times, such as when they are on holiday from school or ‘if people are coming over’ (mother, F56).
[If] you’re running around like a loony trying to run a house, keep a job down, send the kids everywhere, pick them up, doing all that, then you think ‘I’m starving’ and you just grab something.
Mother, F26
The changing circumstances of family life contributed to this. When a mother signs up for MEND she makes a commitment to attend, but families are not static. Circumstances change over time and this can make avoiding falling ‘back on to the usual’ even more of a challenge. Families in our sample had experienced divorces, deaths, births, and moving jobs and homes over the period since they had first contacted MEND. These changed the context within which MEND was operating and sometimes made it more difficult for families to take on the changes MEND recommended. For example, family 51 moved to a new area and the daughter (who was overweight) had to use a school bus which left immediately after classes. She and her father spoke about her disappointment that she could not join after-school clubs.
More than one Bangladeshi or Pakistani family described moving to healthier foods as switching to ‘non-Asian’ foods, as they perceived Asian foods as unhealthy: ‘change it to make it healthier, and not just having Asian food all the time, like samosas, which is all fried stuff. We very rarely fry now. We grill’ (mother/aunt, F55).
Feeling that ‘Asian’ food is unhealthy and to be avoided implies a change that rejects cultural norms and identity. This risks creating conflict, also described by Rawlins et al. ,85 between healthy eating and traditional practices, and one mother (F53) told us that her own mother flatly contradicted the view that using lots of cooking oil was unhealthy.
Maintaining change without support from MEND
Because there’s no reinforcement afterwards it kind of went off[.]
Aunt, F57
Although participants had found it very difficult to find time to attend MEND, they described needing support and re-engagement with changes in the context of a ‘safe’ and stable group, such as the MEND group. They felt that the ongoing support offered by MEND was inappropriate. The few families who had attended MEND follow-up activities had been disappointed that none of the families they knew were there. These were activities offered to all families who had completed MEND, and those who went felt uncomfortable because ‘they were all strangers’ (girl, F26). Few had logged on to the MEND website and, in any case, providing a screen-based format was seen as contradicting MEND advice: ‘There we are exercising twice a week and they say, “go and sit at a computer”. I just couldn’t get my head round that at the time’ (mother, F67).
Although some children had started organised activities after MEND, others disliked the fact that these tend to be ‘mixed’ (mother, F68) rather than solely for children with weight problems.
The story of one family (F26) illustrates something of what might have been helpful from follow-up activities after MEND. The family was interviewed together, and the girl who had attended MEND was very forthcoming. Her mother therefore held back to let her talk, and a follow-up one-to-one interview was held with the mother. During this second interview, the mother told the interviewer that her daughter was not usually very chatty with strangers and the family had been surprised how much she wanted to talk about MEND. Following MEND her daughter had wanted to go shopping with her and was keen to cook for herself, but over time she had lost interest. However, the interview had revitalised her, and she was using the MEND folder and cooking again. This mother felt she might have underestimated the importance to her daughter of being able to talk about diet and weight, both topics that her daughter found difficult.
Discussion
These findings highlight how issues underpinning the salience and acceptability (or not) of the programme varied for different family members at different times during families’ experiences of MEND. Mothers mostly described initiating attendance on the basis of concerns about their child’s overweight and bullying. Though children also described sharing these concerns, many had an equal worry about what MEND would involve and the risk of stigma from participation.
On attending, most families, both parents and children, described finding the programme fun and the facilitators supportive. Children reported enjoying the opportunity to play games and activities in a ‘safe’ atmosphere with other children with concerns about weight. Families liked the fact that facilitators engaged with both parents and children, and enjoyed hands-on demonstrations that supported healthier eating, innovative ways to learn about the fat and sugar content of foods, sharing recipes and trying new foods. Nonetheless, children often found the information sessions boring and the age range of the group too great. Mothers also expressed concerns about the quality of delivery, and facilitators’ knowledge (both professional and experiential) and skills in working with children.
Both parents and children found it hard to fit the MEND programme into family life. Sessions clashed with after-school activities and parents’ work and could mean late bedtimes, and some travelled a considerable distance to venues. Family life is full of compromises; there is no good time for families to be part of a programme like MEND. Therefore, decisions regarding what gets prioritised are very important in understanding whether programmes can be acceptable. Priorities are generally set by mothers and are determined by logistics and necessities, but also by more intangible dimensions. Mothers wanted to make time for MEND because they felt it was important, particularly when children were being bullied, felt socially isolated and were unhappy about their bodies and themselves. This means that families can and did make time to attend MEND, but they found it harder to maintain changes when these external pressures were removed; that is, when children felt better about themselves and when there was no class to go to.
Families identified a significant cost of MEND attendance in terms of ‘time and effort’ (mother, F67). Few emphasised financial costs, or even recognised these, in terms of travel expense or time off work. It was the emotional cost of sessions, and of attempts at healthy living after MEND, that was demonstrated in families’ narratives. Just as many children and mothers reported struggling to fit attendance at the programme into daily life, some also described feelings of failure, guilt and blame around their perceived inability to maintain MEND-friendly behaviours in a MEND-unfriendly world. This meant that success in MEND was related to the distance to travel to achieve MEND friendliness. Whereas some86 suggest that weight loss in children is likely to take place in families ready to make changes, we argue that living in circumstances which facilitate change was more important for the families to whom we spoke. For family 18, for instance, involvement with MEND coincided with acquiring a dog and having greater access to exercise, and families 26 and 57 identified MEND as arriving at a moment when there was both motivation and opportunity for change. In contrast, for those whose current habits (including nudges from the wider environment) are far from the MEND ideal, the experience of failure undermines attempts to maintain ‘good behaviour’. They focus on the small lessons and tricks that they can achieve, but do not feel able to tackle the totality of change needed. Their desire for ongoing support from MEND supports this interpretation. MEND could be understood as supporting families’ learning about how to survive in an obesogenic world, not least by offering them a place in which to learn and exercise with others facing similar difficulties.
A systematic review of parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children concurs with many concerns expressed by parents in this study about family interactions and child weight. 87 Like the present study, this notes the negative impact of feeling blamed for child overweight.
Families in this review felt fatalistic about overweight, believing that for their children it was inevitable or an intractable result of child behaviours. 87 Parents seek to normalise weight and interpret it as largely indicative of health. 88 Children, in contrast, are more concerned with the social impact of overweight. 79,80 The interchange between family members is less often studied, and conflicts between parents and children, exposed in interviews, suggest that acknowledging and resolving these conflicts within treatment programmes may be helpful. Such conflicts in motivation resulting in ambivalence towards weight loss programmes elsewhere86 would suggest this is the case. This research also confirms the observation made elsewhere86 that relationships between facilitators and children are important, but beyond that, we would suggest that the credibility of the trainer (both professional and experiential) matters to families. Parents were keen to offer balanced views, so that any criticism of MEND in interviews tended to be followed by a comment about something they valued, preceded by the phrase ‘to be fair’. This was most pronounced in discussions about facilitators, who were frequently described as ‘good people’ if poor facilitators. Parents may have wanted to model ‘fairness’ for children present, particularly in front of an outsider (the interviewer). Also problematic were discussions of feelings of guilt and of parents experiencing a sense of failure if their child had not reached a healthy weight. These tensions might account for some of the conflicting accounts we heard.
In summary, all families found some value in MEND and individual elements of the programme were appreciated and valued. However, in terms of creating a ‘micro-environment’ to protect against the wider obesogenic environment, few families felt that MEND had made a big difference to weight or lifestyle, while the stresses on family time and, for some, feelings of failing to rise to the challenges of MEND were considerable. MEND’s perceived lack of impact may reflect families’ feelings about the distance to travel in terms of changes required. Where MEND was understood as requiring relatively small changes, it could be perceived as making little additional impact (for example, changing cooking oil or having semi-skimmed milk). Others, however, felt there was a large gap between their existing behaviours, their circumstances, the wider environment and MEND recommendations which, with MEND alone, they did not feel they had the capacity to bridge.
Study limitations
An important limitation of the study was our failure to recruit people referred to the scheme but who did not attend. This was due to limitations in the selection procedure applied to the contact data set. Although it is not uncommon for those who do not engage with a service to be under-represented in data sets,89 our experience in recruiting such samples in the past had been less problematic, and in particular we had found that people who decline or drop out of programmes are not reluctant to say why.
Some features of research governance may have made it more difficult for us to recruit to this study. Our recruitment process was lengthy. At the request of the ethics committee, the letter of invitation to take part in this study was followed by a 21-day ‘cooling off’ period before researchers could make contact. Families were not reluctant to opt out once telephoned, but none did so during the 21 days, suggesting that the time lag may not have been helpful to participants or researchers. After the delayed contact, many had no recollection of having received a letter, or said they had thrown it away or had read it but forgotten what it had said. For those who agreed to an interview, there was often a further delay in order to find a time when family members could meet the researcher. This long process was evidently unattractive to people for whom the intervention was a distant memory, lower on their agendas as participants than on ours as researchers. We believe that for low-risk studies such as this one, direct contact from researchers and a shorter opt-out period is likely to reduce barriers without compromising participants’ opportunities to opt out.
Finally, we may not have provided sufficient incentive for families to consider taking part. In recent work with an advisory group of parents for another study, parents suggested three changes to information materials that are needed to make them attractive. Firstly, written information should be as parsimonious as possible, as too much written detail is off-putting; such detail is better described in person by the researcher once initial interest has been shown. Secondly, it would be appropriate to emphasise the ‘thank you’ payment offered for those taking part in research. Thirdly (and this is perhaps the most difficult to achieve), the parents wanted reassurance that their contribution would make a difference to policy or practice. The careful wording and long information sheets that have evolved from more complete research governance may put families off taking part, and researchers may want to consider in what circumstances written information may not be the most appropriate strategy.
The sample of families recruited here does not claim to be representative. Rather, it offers a range of views and experiences which help to understand service delivery and service acceptability. However, ‘refusers’ are missing voices, and as those we interviewed are ‘compliers’ both in terms of MEND attendance and allowing us to interview them, it is likely that our work presents a less rounded picture than would have been the case had we been able to learn from low or non-attenders. Young people who may have wanted to attend but could not as there was no family member to accompany them, or parents unable to persuade their overweight child to attend, are unrepresented in this study.
In addition to the lack of low and non-attenders, we recruited fewer individuals than planned, but believe that this did not have a significant impact on findings. Families sufficiently motivated to attend MEND together, and to then agree to a research interview as a group, may be so familiar with the give and take of family discourse that the silenced and the overtalkative were uncommon. Siblings did not seem to be constrained in their teasing or squabbles because an interviewer was present and observing family exchanges allowed researchers to better understand the dynamics of the household. 90 The additional analyses we undertook identified convergence or divergence of narratives, and demonstrated occasions when children were able to use the interview to challenge their parents.
Headline findings from Chapter 6
Family findings which relate to the salience and acceptability of MEND
There were no interviews in which no one in the family felt they had benefitted, but few felt that they had managed long-term change.
Referral to MEND
-
Referral was mainly by self-referral and was mainly the mother’s decision (with variable support from the child). The basis for attendance tended to be underlying health problems, bullying, the transition to secondary school or a last resort (‘we’d tried everything else’).
Positive experiences
-
Many children valued the social acceptance; talking about shared problems, finding that they were ‘not the only one’ (and that some are worse off than them), and being with others with a similar body shape and range of sporting ability made exercising easier.
-
Useful tips for parents: the value of using measuring cups and learning to read labels, and not keeping stocks of sweets or fizzy drinks in the house.
-
Children learned to cook, helped to make the family shop ‘MEND friendly’, became more independent (‘I don’t need to nag any more’), spent more time ‘out and about’ and set targets for themselves.
-
Particular experiences: swimming, taking a supermarket tour and sharing recipes.
-
Facilitators (particularly exercise instructors) were well liked personally.
Things families find hard
-
Timings for parents: competing with their work commitments; there is no ‘good’ time for families.
-
Timings for children: hunger, tiredness, other after-school commitments and sessions finishing in the dark in winter time.
-
Locations of sessions, especially where there was no, or poor, public transport; some venues were unsuitable.
-
The age mix of sessions meant that being the oldest or youngest was hard.
-
Engaging with the behaviours that MEND recommends.
-
Family dynamics and MEND: decisions about who did or did not go to sessions, other families being supportive or otherwise, family change and the emotional demands of addressing childhood obesity.
What types of costs are borne by families when participating in MEND, and in sustaining a healthy lifestyle afterwards?
-
Costs are mostly associated with a move to higher-quality food.
-
‘Treats‘: ‘bad’ food was still thought of as a treat.
-
‘We find a way’: parents prioritise spending on things to benefit their children.
-
Time costs have to be negotiated with work and child-care arrangements (a hidden financial cost).
-
Transport costs: probably underestimated by parents (e.g. ‘It was only a 10-minute drive away’).
-
Social/emotional cost of making/maintaining behaviour changes generally unsupported by the wider environment.
Chapter 7 Discussion
In this final chapter we discuss some of the overarching and intersecting issues which emerged from our analyses, and which are best commented on from the perspective of the whole study rather than in relation to the individual research questions. We have separated these into issues relating to our methods and to our findings.
Methods
The evaluation exploited a relatively unusual opportunity to use service data from a scaled-up intervention. Service data are valuable for this type of analysis, in comparison with data collected under research conditions, because they allow researchers to quantify how the intervention outcomes vary when delivered in the real world. They also offer considerably more statistical power than could be achieved from primary research data collection. However, it is useful to discuss the challenges of working with such data.
A problem which is not unique to service data, but which constituted a significant challenge, was the extent of missing data on variables central to the analysis. We mitigated the potential for this to bias our findings and reduce the precision of estimates by using multilevel multiple imputation models. However, multiple imputation assumes that patterns underlying missing data are associated with variables measured in the models. We undertook sensitivity analyses throughout the quantitative analysis, repeating models with complete case data, to examine how results differed from those estimated on multiple imputation data. 50
Challenges of using routine data for research
Data collected through service provision are normally intended for monitoring or other service delivery purposes, rather than in anticipation of research. For example, the MEND 7–13 data did not distinguish whether attendance data were missing owing to reporting error or actual non-attendance. This meant that there was a degree of uncertainty about the construct validity of attendance variables. Although we retrospectively addressed these biases to some extent using data cleaning and multiple imputation, these types of issues are, like missingness, best addressed at the data collection stage.
Where possible, we have conducted analyses to test the sensitivity of our findings to analytic decisions. For example, in Chapter 2 we estimated differential completion, where completers were defined as those attending > 75% of sessions. However, there is a lack of consensus in the literature about what constitutes completion, and therefore we also estimated the model with completers defined at a 60% threshold. Results were similar, giving us confidence that the findings were not threshold dependent.
Design issues
Our analysis explored internal variations in a specific subgroup of the population: children who were overweight or obese. In study design this is, in essence, a large case series. We did not have a comparator group who had not gone through the intervention, and therefore we cannot make causal inferences about whether or not the programme achieved changes in outcomes beyond what might be expected over a similar period for children who were overweight but did not receive this intervention. This means that we cannot make assertions about whether or not the intervention was effective or differentially effective. We were, however, able to explore whether or not the outcomes associated with the intervention varied for subgroups of children participating in MEND under service conditions.
Perspectives from quantitative and qualitative work
The mixed-methods approach used here allowed us to reflect on the MEND intervention from three distinct angles: the quantifiable outcomes, the perceptions of families and the perceptions of commissioners. The commissioner/service delivery and family studies were designed to derive expert views from those receiving, commissioning or delivering the intervention within the context of a sampling strategy designed to achieve maximum variation. The quantitative work aimed to summarise the average change in weight management and psychosocial outcomes associated with participation in the MEND 7–13 programme.
Our quantitative analysis was based on short-term prospective data, whereas the qualitative analysis was based on retrospective recall of the programme over a longer time period. Both had distinct advantages and disadvantages. The quantitative analysis showed that, on average, there were short-term benefits in terms of weight management and psychosocial well-being, but our data could not be used to comment on longer-term changes. In contrast, the qualitative work suggested that although families perceived short-term benefits (there were none who felt that nothing had been gained from the programme), these were felt to be relatively modest and difficult to sustain in the longer term in an obesogenic environment. Whereas, in the short term, the commissioners commented favourably on the evidence-informed ‘solution in a box’, concern was expressed about the longer-term cost implications once Big Lottery funding was no longer available.
Gaining information from families who did not engage with MEND
People referred to a programme or intervention who do not take it up, or who withdraw, are of particular interest to researchers and those charged with commissioning services. This is especially important when the per capita cost of the programme, relative to the population health gain, is at least partly conditional on achieved recruitment and retention rates.
Families who were referred to MEND 7–13 but who did not attend, or attended few sessions, were under-represented in the qualitative component of the study and had less data available in the quantitative component. As discussed in Chapter 2 (see Findings, Determinants of completion of MEND 7–13), those in less well-off circumstances who started the programme were less likely to complete than those who were better off. However, when we compared starters (including completers) and completers with the MEND-eligible population, the differences suggested that participation in MEND 7–13 was socioeconomically and ethnically equitable even after differential completion was taken into account.
We did not have sufficient information to identify those referred to the programme accurately, and this led to a lack of information in the qualitative study relating to the perceived acceptability of the MEND 7–13 prior to attendance, and reasons for dropping out of the programme early. This was important because some of the commissioners interviewed expressed concerns about retention rates in the programmes. It is a limitation of our study that as a result of data problems at the sampling stage described above, our findings do not include the perspectives of those who were referred to the programme but did not attend, or dropped out early on. Participants in the qualitative component were eloquent in telling us what had made attending and engaging hard. We can only surmise that these or other difficulties were even less surmountable for the non-attendees or those who dropped out early.
Tackling inequalities in childhood overweight
An ecological model of health91 suggests that overweight and obesity are determined by multiple layers of influence. This model has been influential in the development of research into the policy response to complex issues such as childhood overweight, which are unequally distributed across society. It plays an important role in the understanding of health over the life course and geographical variations. MEND 7–13 and similar interventions do not claim to address overweight and obesity by acting on the wider determinants of health emphasised in the social model of health. Instead, they address more proximal causes such as health-related behaviours at the individual and family levels.
This study has considered how wider determinants interact with family-based interventions in service settings. Despite increasing interest in the translation of research findings into practice,92 this appears to represent a novel contribution to the literature on childhood weight management interventions. In this light, we reflect on the ways in which a family-based intervention might relate to social inequalities in health, and how it operates in context.
Intervention-generated inequalities
MEND 7–13 has been scaled up to include many families across the country, so it is important to consider what our findings mean in terms of the potential impact of the scaled-up programme on population-level inequalities in health. The evidence base for interventions delivered in a community setting is relatively small and equivocal,23,93 with a lack of information on how outcomes associated with family-based weight management interventions for children vary by ethnicity and SEC. This is an important gap given the variation in overweight and obesity for these groups. Inequity might arise at several points in the delivery of a programme, from differential access to differential outcomes. These pathways are discussed below with respect to the findings from our project before general conclusions for population-level health inequalities are drawn out.
Socioeconomic and ethnic inequalities in access
The Marmot review of health inequalities uses the concept of ‘proportionate universalism’ to recommend that interventions are applied right across the social gradient in health, but with a scale and intensity proportionate to the level of disadvantage. 22 As a programme for childhood overweight and obesity, MEND 7–13 is targeted at an ‘at-risk’ group: overweight children and their families. However, beyond this it is not targeted at particular sociodemographic groups, unlike other interventions such as Sure Start Children’s Centres. 94 Inequalities in referral to, starting and completing the programme might arise through unequal provision of services (supply-side factors) or unequal uptake (demand-side factors).
We found that there were proportionally more girls participating in MEND 7–13 than there were in the MEND-eligible population (see Chapter 2), but otherwise MEND 7–13 participants were sociodemographically similar to those in the MEND-eligible population. Overall, our quantitative findings suggested that referral to, starting and completing MEND were ethnically and socioeconomically equitable.
In interviews with commissioners of MEND 7–13, disadvantage and the ethnic composition of the local population were frequently cited as the rationale behind commissioning weight management programmes (see Chapter 5, Delivering MEND for local populations).
Differences in outcomes by ethnic and socioeconomic group
The current evidence for differential effects by SEC in multicomponent interventions is equivocal. 23 We found that family and neighbourhood deprivation moderated associations between participation in MEND 7–13 and change in BMI. This is consistent with the views of some commissioners who suggested that the content of the intervention was too ‘middle class’ – ‘it’s like school’ (C35) (see Chapter 5, Delivering MEND for local populations) – or insufficiently attuned to families with complex needs. This was not a view necessarily shared by all participants in family interviews; some of the more middle-class interviewees felt that MEND was geared towards the needs of less well-off families (see Chapter 6, Family experiences of attending MEND).
Although reductions in BMI were ‘clinically relevant’ in all groups, we found evidence that the programme outcomes varied between broad ethnic groups after taking into account SEC (see Chapters 3 and 4). This was consistent with interviews with commissioners who identified variations in food cultures – with some populations more likely to shop in street markets than in supermarkets – as one of the issues undermining successful delivery. They also discussed difficulties with staffing the programme for those who spoke little English. Families themselves recognised the role of ethnic variations in food culture [for example, some Asian families identified Asian food, and Asian celebratory meals, as typically unhealthy (see Chapter 6, Family experiences of attending MEND)]. However, these variations in outcomes may relate to wider cultural factors, including the ethnicity of facilitators of the programme and competing educational and religious after-school commitments for children (referred to in family interviews). These observations align with a growing recognition that public health interventions need to be culturally sensitive and benefit from working closely with service users, including different ethnic groups. 85
Implications for population health and inequalities
More than 20,000 children and families living in England were referred, or self-referred, to MEND 7–13 between 2007 and 2010. However, it is important to remember that those 20,000 families who made a phone call to MEND represented around 0.4% of the population of overweight children who would have been eligible to attend MEND 7–13 at that time. This means that they may be a relatively select subgroup of families, motivated sufficiently to act on concerns about their child’s weight and to contact an organisation like MEND Central. We do not know to what degree this level of motivation might be present in the overall population of overweight and obese children and their families. Thus, one interpretation of our quantitative findings is that, on average, MEND 7–13 was associated with reductions in BMI and improved psychological outcomes for families and children with particular levels of motivation (see Chapters 3 and 4). Our qualitative work suggests that families were more likely to identify circumstances which facilitate change, rather than levels of motivation, as a driver. For one family, for instance, involvement with MEND coincided with acquiring a dog and having greater access to exercise. Others identified MEND as arriving at a moment when there was both motivation and opportunity for change. This is a difference in perspective rather than a rebuttal of the ‘motivation’ argument, but one which highlights the complexity to which we refer below (see Interventions in the real world, a reflection on complexity).
The data allowed us to investigate how the intervention might be associated with differential outcomes by SEC and ethnicity. These variations were calculated over a large sample size for each subgroup. This means that there was an increased risk of the study identifying relationships which were statistically significant but of no clinical importance. We found that in absolute terms, MEND 7–13 was associated with ‘clinically relevant’ BMI change on average for all ethnic and socioeconomic groups. However, as discussed above, in relative terms white children and those living in more favourable SEC did do better than children from BME groups and those living in less favourable SEC.
MEND 7–13 as an intervention in context
Implications of findings for translational research in public health
In order to generalise from a study of this kind, findings must be understood as part of a framework linking intervention development, public health decision-making and population health. One such framework was put forward by Ogilvie et al. 93 and is reproduced in Figure 7. We consider where our study contributes to this framework. Findings from evidence syntheses directly and indirectly influence policy responses and commissioning decisions (‘Public realm’ box in Figure 7; see Chapter 5, Findings). The ability of organisations to scale up delivery of an intervention in practice will determine how available the intervention is, and how far it is taken up by all groups in the population (‘Professional practice’ box in Figure 7; see Chapter 2, Findings). The salience and acceptability (‘Professional practice’ box; see Chapter 6, Findings) of the programme may partially determine how far the programme is taken up and subsequently engaged with by families (and by which types of families). The intervention may then determine changes in individual and family behaviours which may translate to small changes in population health behaviours (‘Health-related behaviour’ box in Figure 7; see Chapter 4, Findings) and population-level health (‘Heath and well-being’ box in Figure 7; see Chapters 3 and 4).
FIGURE 7.
Translational framework for public health research (adapted from Ogilvie et al. , 200993).
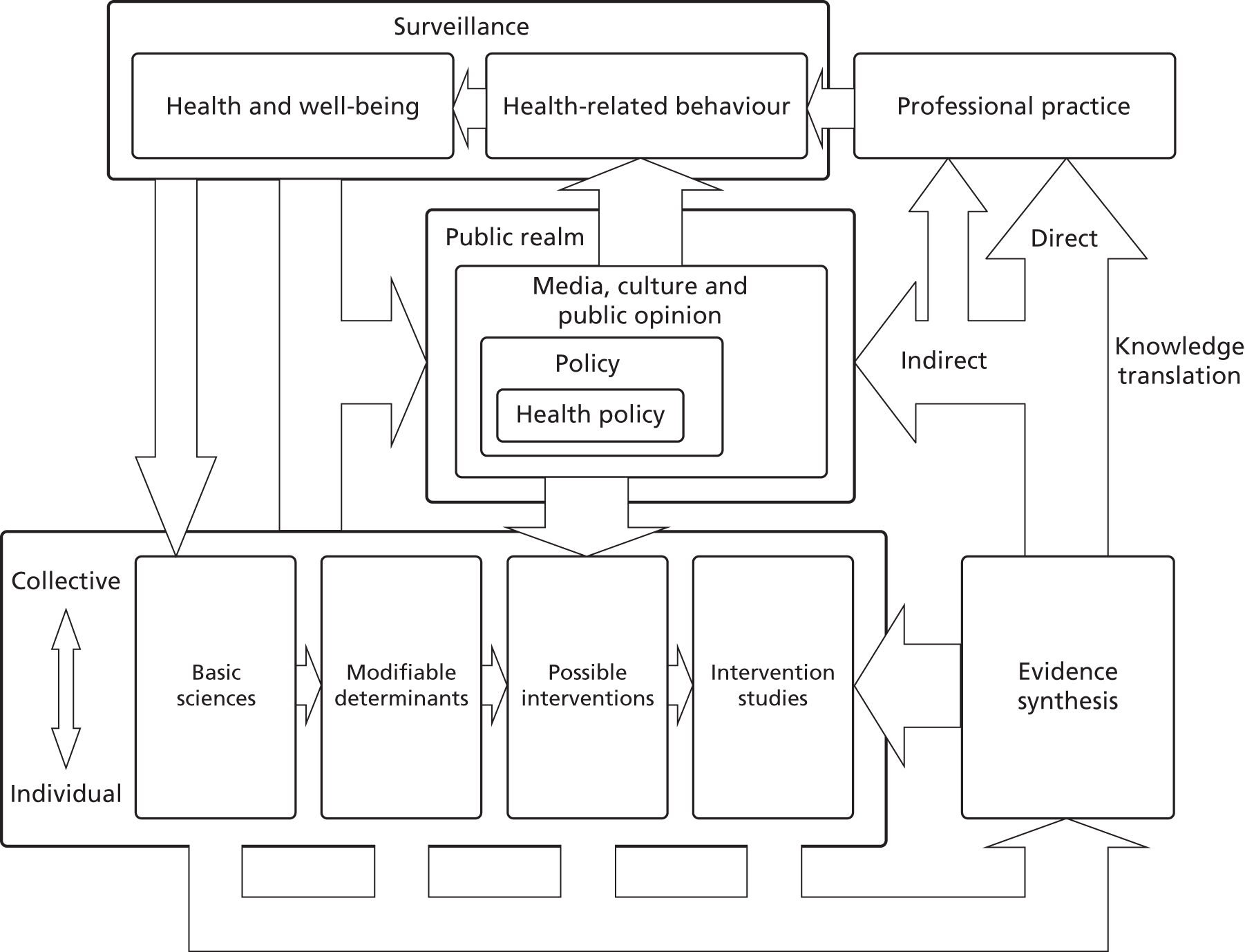
Currently, and to our knowledge, no studies have assessed how family-based childhood weight management interventions operate in the real world, although a study to examine the scale up of an adult weight intervention has been outlined. 95 Our study evaluated one family-based intervention and it is difficult for us to say that our findings are generalisable to other weight management interventions for children, or to other community-level interventions. However, the model of study we have undertaken might be useful in evaluating other interventions shown to be effective in RCTs when rolled out at scale. Research designed to explore the real-world impact of other interventions should continue to be developed.
The sensitivity of MEND 7–13 to the obesogenic environment
Obesogenic environments are generally discussed with reference to their role in the development of overweight and obesity at the population level96,97 and, following from that, as environmental determinants to be modified by area-based intervention. 98 Obesogenic environments have not, to our knowledge, been empirically tested with respect to their interaction with family-based weight management interventions, partially because individual-level intervention studies are rarely statistically powered to test whether or not outcomes are moderated by factors such as the availability of healthy food and the nature of the built environment. In this study we had a large enough sample to examine whether families’ food and/or built environments might lead to variations in the outcomes associated with participating in MEND 7–13; in particular, whether or not children and families living in environments which were more obesogenic may have been less likely to benefit from participation. Families interviewed were receptive to healthy food messages but some reported not always being able to afford these foods, or that they were not available in low-cost supermarkets (see Chapter 6, Perceived costs of MEND participation). Other families found that healthier food was not more expensive. When investigated using service-level data, we found no differences in outcomes for those living in areas which were very dense in terms of fast food and other unhealthy outlets compared with areas with high proportions of healthy outlets. This suggests that any changes associated with the programme are, in the short term, apparently resistant to differential exposure to food environments which either promote or constrain a healthy diet. This is perhaps not surprising in the UK context; despite the popular characterisation of ‘food deserts’ (areas where healthy food is less readily available), the evidence that variations in the availability of healthy food in the local environment are associated with levels of overweight is relatively weak. 68,69 Although the quantitative analysis did take into account the local retail environment in terms of fast food shops and access to healthy food, it is important to note that qualitative work highlighted that exposure to highly calorific foods may go beyond this environment, and that festivals and celebrations may also have a role. In addition, food environments measured in the quantitative analyses, using broad exposures such as fast food restaurant density, may not be precise enough to estimate relationships with short-term change in outcomes. Finally, although the quantitative analysis took into account broad sociodemographic characteristics of families, it could not examine detailed characteristics of families’ lives suggested by the qualitative work, such as school meals or the influence of grandparents, which might help the family to keep unhealthy foods out of children’s diets.
In addition to energy intake, energy expenditure is a central component of overweight and obesity, and evidence suggests that interventions may be able to influence this by increasing physical activity. However, the degree of physical activity that children (in particular) can pursue is subject to the constraints and affordances of local built environments, such as the availability of green space, and family resources including the time of parents and other carers. In this study we found unadjusted associations between the built environment and change in BMI. These were attenuated to non-significance in multivariable models (see Chapter 3, Modelling to inform multilevel models of change in BMI and Multivariable models of change in BMI and zBMI) but the unadjusted associations were consistent with reports by participants in qualitative family interviews that when they tried to change their physical activity behaviours they felt constrained by their local environment.
In the qualitative work, participants valued the opportunities afforded by the programme to exercise in a non-competitive environment with others of similar build. The lack of such opportunities following the programme was considered by some to be a problem.
MEND as an event in the life course
The children who are referred to and participate in MEND 7–13 are, by definition, overweight or obese. The natural history of this group is one associated with adiposity in early life which is likely to track into adolescence and adulthood. Moreover, children who are overweight at this point may well live in families where parents struggle to maintain healthy lifestyles. In the context of this natural history, MEND 7–13 and other short-term interventions tend to be one-off events, of relatively short duration in the life course. Many families struggled to remember the programme in detail until prompted in family interviews (see Chapter 6, Recruited sample).
That said, most families did report having gained something positive from the experience of participation in MEND, with some also reporting changing aspects of their lifestyles (see Chapter 6, Family experiences of attending MEND). However, several things made it difficult to sustain changes associated with the intervention in the longer term. These sometimes related to the constraints imposed by the wider environment (as discussed in the section above), or could be due to the changeability of family life or simply the ‘pull’ of normal ways of living, not accompanied by the time, financial and emotional costs associated with participation in the programme. Although MEND Central runs a website giving MEND graduates a forum to stay in touch, feedback from family interviews suggests that this was perceived as somewhat ironic, and of course counter to advice to be less sedentary (see Chapter 6, Perceived costs of MEND participation). Families’ concerns about sustainability were also shared to some extent by commissioners, who felt that MEND 7–13 was supportive while it was running but needed to continue to support families in the longer term.
Our quantitative findings showed that younger children reduced in BMI more than older children. This suggests that interventions such as MEND 7–13 might be more effective when families have more control over children’s lifestyles. On the other hand, qualitative data suggested that, in some cases, parental and family influence actually limited children’s engagement with physical activity or new foods. Selective uptake, whereby more proactive parents, whose children may benefit more from weight management interventions, take part in programmes such as MEND at an earlier point in their child’s growth, might also account for these differences.
Interventions in the real world, a reflection on complexity
Tony Delamothe, writing in the BMJ on complexity theory,99 refers to the work of Shiell et al. ,100 saying:
. . . evaluating complex interventions is a doddle beside the challenges of evaluating the effects of interventions on complex systems. In complex systems ‘everything is interconnected, changes in one part of the system feed through to other parts of the system and feedback on themselves.’ [Quote from Shiell et al.] Attributing causality is difficult.
Family-based weight management schemes are only one way that overweight and obese children can be encouraged to adopt healthier lifestyles. For this reason, we have situated our findings in the light of the social model of health and with reference to health inequalities, obesogenic environments, life course theory and frameworks of translational research.
Recommendations for further research on weight management programmes for children
Further research should aim to address the following questions:
-
How sustainable are positive changes associated with weight management interventions when they are delivered under service conditions, and is there potential for less positive changes to be reduced?
-
What is the cost-effectiveness of weight management interventions from a societal perspective, and, in order to determine this:
-
what reduction in BMI following weight management interventions is ‘clinically relevant’;
-
what reduction in BMI following weight management interventions is important for population health;
-
what is the long-term impact of child weight management programmes on weight and disease risk; and
-
what is the health-related quality of life of children (and their families) in different weight/obesity categories (to enable QALYs to be calculated)?
-
-
How can information on children and families who attend, and who do not attend interventions be collected over longer periods of follow-up?
-
What features of programme implementation influence programme effectiveness?
-
To what extent can findings from weight management programmes be translated to community-based health promotion interventions?
Acknowledgements
Contributions of authors
Catherine Law (Professor of Public Health and Epidemiology, UCL Institute of Child Health) led the study, contributed to all parts of the quantitative components and co-authored the final report.
Tim Cole (Professor of Medical Statistics, UCL Institute of Child Health) advised on the statistical analysis and interpretation of the growth data and contributed to the final report.
Steven Cummins (Professor of Population Health, London School of Hygiene and Tropical Medicine) supervised collation and interpretation of environmental data and contributed to the final report.
James Fagg (Research Associate, UCL Institute of Child Health) contributed to day-to-day project management and all parts of the quantitative components. He carried out the statistical analyses and contributed to the qualitative components. He co-authored Chapters 1–4 and 7 of the report and contributed to the remainder.
Stephen Morris (Professor of Health Economics, UCL Department of Applied Health Research) led the economics components, co-authored Chapter 4 and contributed to the final report.
Helen Roberts (Professor of Child Health Research, UCL Institute of Child Health) led the qualitative work, contributed to all parts of the qualitative components, co-authored Chapters 5 and 6, and contributed to the final report.
Other members of the project management group and their contributions
Dr Lisa Arai (Senior Lecturer, School of Health & Social Care, University of Teesside) contributed to the qualitative components and co-authored Chapters 5 and 6.
Dr Patricia Lucas (Senior Lecturer, School of Policy Studies, University of Bristol) contributed to the qualitative components, co-authored Chapters 5 and 6 and contributed to the final report.
Dr Katherine Curtis-Tyler (Senior Lecturer, School of Health Sciences, City University, London) contributed to the qualitative components, co-authored Chapters 5 and 6 and contributed to the final report.
Dr Sally Stapely (Senior Lecturer, School of Health & Social Care, University of Teesside) worked on the analysis of the commissioner interviews and co-authored Chapter 5.
Professor Harvey Goldstein (Professor of Social Statistics, UCL Institute of Child Health) advised on statistical analysis of missingness, and provided technical support for multiple imputation using REALCOM and multilevel modelling.
MEND Central colleagues (Mr Paul Sacher, Dr Paul Chadwick and Dr Duncan Radley) contributed by collating MEND 7–13 data, organising the transfer of quantitative data to the UCL Institute of Child Health, advising on the intervention delivery and the technical details of the data set, and commenting on the final report.
Other acknowledgements
The authors wish to thank the following:
Children, families, commissioners and delivery partners who agreed to be interviewed for the study.
The Centre for Policy Research team at UCL Institute of Child Health: Hannah Lewis for assistance with the recruitment of families and commissioners, organisation of the transcription of qualitative interviews, assistance in coding of secondary outcomes and contributing to the presentation and drafting of the report; Chloe Parkin for support in collating the ethics applications and proofreading early drafts of the final report; Steve Hope for proofreading the final report; and Anna Pearce for assistance with the analysis of the MCS.
Members of the independent PAG, who were as follows: Professor Mitch Blair (Chair), Mrs Fiona El Achkar, Dr Ann Marie Connolly, Mrs Reeta Mahey, Professor Mary Rudolf, Dr Helen Walters and Dr Wendy Wills.
Colleagues at NatCen for linking in neighbourhood and BMI z-score data to the HSE and providing syntax for deriving variables, to describe lone- and couple-parent families and to adjust for the design of the survey.
Colleagues at the Centre for Longitudinal Studies (Institute of Education, University of London) for linking in neighbourhood data to the fourth sweep of the MCS.
Colleagues at the NOO for assisting with the analysis of the NCMP.
Young people from the NCB PEAR group and the NCB Research Advisors group for their assistance with the design and interpretation of the project in workshops facilitated by NCB colleagues.
Colleagues at MEND Central for assisting with the logistics of family and commissioner recruitment (e.g. sending letters to families).
The research was conducted at the UCL Institute of Child Health, Centre for Paediatric Epidemiology and Biostatistics (CPEB). The CPEB was supported in part by the Medical Research Council (MRC) in its capacity as the MRC Centre of Epidemiology for Child Health. Research at the UCL Institute of Child Health and Great Ormond Street Hospital for Children receives a proportion of funding from the Department of Health’s NIHR Biomedical Research Centres funding scheme.
Publications
Fagg J, Cole TJ, Cummins S, Goldstein H, Morris S, Radley D, et al. After the RCT – who comes to a family-based intervention for childhood overweight or obesity when it is implemented at scale in the community? JECH 2014; in press.
Fagg J, Chadwick P, Cole TJ, Cummins S, Goldstein H, Lewis H, et al. From trial to population: a study of a family-based community intervention for childhood overweight implemented at scale. Int J Obes 2014; 29 July 2014 Advance Online Publication.
Lucas P, Curtis-Tyler K, Arai L, Stapley S, Fagg J, Roberts H. What works in practice: user and provider perspectives on the acceptability, affordability, implementation, and impact of a family-based intervention for child overweight and obesity delivered at scale. BMC Public Health 2014;14:614.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Craig R, Mindell J. Health Survey for England – 2010: Respiratory Health. Report of the 2010 Health Survey for England. Leeds: NHS Information Centre; 2011.
- Aresu M, Bécares L, Brage S, Chaudhury M, Doyle-Francis M, Esliger D, et al. Health Survey for England 2008: Volume 1. Physical Activity and Fitness. Leeds: NHS Information Centre; 2009.
- McPherson K, Marsh T, Brown M. Foresight. Tackling Obesities: Future Choices – Modelling Future Trends in Obesity and the Impact on Health. London: Department for Innovation, Universities and Skills; 2007.
- Reilly JJ. Tackling the obesity epidemic: new approaches. Arch Dis Child 2006;91:724-6. http://dx.doi.org/10.1136/adc.2006.098855.
- Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J. Foresight. Tackling Obesities: Future Choices – Project Report. London: Government Office for Science; 2007.
- Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, et al. Health consequences of obesity. Arch Dis Child 2003;88:748-52. http://dx.doi.org/10.1136/adc.88.9.748.
- Parry LL, Netuveli G, Parry J, Saxena S. A systematic review of parental perception of overweight status in children. J Ambulat Care Manag 2008;31:253-68. http://dx.doi.org/10.1097/01.JAC.0000324671.29272.04.
- Baur LA. Childhood obesity: practically invisible. Int J Obes Relat Metab Disord 2005;29:351-2. http://dx.doi.org/10.1038/sj.ijo.0802931.
- Obesity: Guidance on the Prevention, Identification and Management of Overweight and Obesity in Adults and Children. London: NICE; 2006.
- Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev 2009;1.
- Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics 2010;125:e396-418. http://dx.doi.org/10.1542/peds.2009-1955.
- Management of Obesity in Children and Young People. Edinburgh: SIGN; 2003.
- Egger G, Swinburn B. An ecological approach to the obesity pandemic. BMJ 1997;315:477-80. http://dx.doi.org/10.1136/bmj.315.7106.477.
- Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995;73:25-9. http://dx.doi.org/10.1136/adc.73.1.25.
- Sacher PM, Kolotourou M, Chadwick PM, Cole TJ, Lawson MS, Lucas A, et al. Randomized controlled trial of the MEND program: a family-based community intervention for childhood obesity. Obesity 2010;18:S62-8. http://dx.doi.org/10.1038/oby.2009.433.
- Fisher JD, Fisher WA, DiClemente R, Crosby R, Kegler M. Emerging Theories in Health Promotion Practice and Research. San Francisco, CA: Jossey Bass Publishers; 2002.
- Christensen P. The health-promoting family: a conceptual framework for future research. Soc Sci Med 2004;59:377-87. http://dx.doi.org/10.1016/j.socscimed.2003.10.021.
- Victora CG, Hanson K, Bryce J, Vaughan JP. Achieving universal coverage with health interventions. Lancet 2004;364:1541-8. http://dx.doi.org/10.1016/S0140-6736(04)17279-6.
- Edwards N. Scaling-up Health Innovations and Interventions in Public Health: A Brief Review of the Current State-of-the-Science n.d.
- Shrewsbury V, Wardle J. Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990–2005. Obesity 2008;16:275-84.
- Becker E, Boreham R, Chaudhury M, Craig R, Deverill C, Doyle M, et al. Health Survey for England 2004: Volume 1. The Health of Minority Ethnic Groups. Leeds: NHS Information Centre; 2006.
- Marmot M, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, et al. Fair Society, Healthy Lives. The Marmot Review. London: The Marmot Review; 2010.
- Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Comm Health 2013;67:190-3. http://dx.doi.org/10.1136/jech-2012-201257.
- Research Report: Public Attitudes to Public Health Policy. London: The King’s Fund; 2004.
- Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Comm Psychol 2009;43:267-76. http://dx.doi.org/10.1007/s10464-009-9229-9.
- Cartwright N. A philosopher’s view of the long road from RCTs to effectiveness. Lancet 2011;377:1400-1. http://dx.doi.org/10.1016/S0140-6736(11)60563-1.
- Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. BMJ 1998;317:465-8.
- Chalmers I. What do I want from health research and researchers when I am a patient?. BMJ 1995;310:1315-18. http://dx.doi.org/10.1136/bmj.310.6990.1315.
- Glass N. What works for children – the political issues. Child Soc 2001;15:14-20. http://dx.doi.org/10.1111/j.1099-0860.2001.tb00198.x.
- Glass N. Sure Start: where did it come from and where is it going?. J Child Serv 2006;1:51-7.
- Hoddinott P, Britten J, Pill R. Why do interventions work in some places and not others: a breastfeeding support group trial. Soc Sci Med 2010;70:769-78. http://dx.doi.org/10.1016/j.socscimed.2009.10.067.
- Hawe P, Shiell A, Riley T, Gold L. Methods for exploring implementation variation and local context within a cluster randomised community intervention trial. J Epidemiol Comm Health 2004;58:788-93. http://dx.doi.org/10.1136/jech.2003.014415.
- ESRC Framework for Research Ethics (FRE) 2010. Swindon: ESRC; 2010.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM Framework. Am J Public Health 1999;89:1322-7. http://dx.doi.org/10.2105/AJPH.89.9.1322.
- Rosenberg M. Society and the Adolescent Self-image. Princeton, NJ: Princeton University Press; 1965.
- Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Skelton JA, Beech BM. Attrition in paediatric weight management: a review of the literature and new directions. Obes Rev 2011;12:e273-81. http://dx.doi.org/10.1111/j.1467-789X.2010.00803.x.
- Hansen K, Jones E, Joshi H, Budge D. Millennium Cohort Study Fourth Survey: a User’s Guide to Initial Findings. London: Centre for Longitudinal Studies, Institute of Education, University of London; 2010.
- Ridler C, Townsend N, Dinsdale H, Mulhall C, Rutter H. National Child Measurement Programme: Detailed Analysis of the 2007/08 National Dataset. London: National Obesity Observatory; 2009.
- National Child Measurement Programme: England, 2009/10 School Year. Leeds: Health and Social Care Information Centre; 2010.
- Noble M, McLennan D, Wilkinson K, Whitworth A, Dibben C, Barnes H. English Indices of Deprivation 2007. London: Communities and Local Government; 2008.
- Bibby P, Shepherd J. Developing a New Classification of Urban and Rural Areas for Policy Purposes – the Methodology. London: DEFRA; 2004.
- Generalised Land Use Database Statistics for England 2005. London: Department for Communities and Local Government; 2007.
- Local Index of Child Well-Being 2009. London: Department for Communities and Local Government; 2009.
- Points of Interest 2007–09. Southampton: Ordnance Survey; 2011.
- Harrison F, Jones AP, van Sluijs EM, Cassidy A, Bentham G, Griffin SJ. Environmental correlates of adiposity in 9–10 year old children: considering home and school neighbourhoods and routes to school. Soc Sci Med 2011;72:1411-19.
- Lower Super Output Area Population Estimates – Mid-2007. Newport: ONS; 2010.
- Population Estimates for England and Wales – Mid-2002 to Mid-2010 Revised (National). Newport: ONS; 2012.
- Plewis I. Millennium Cohort Study First Survey: Technical Report on Sampling. London: Centre for Longitudinal Studies, Institute of Education, University of London; 2004.
- Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b2393.
- Schafer JL. Multiple imputation: a primer. Stat Method Med Res 1999;8:3-15. http://dx.doi.org/10.1191/096228099671525676.
- King G, Honaker J, Joseph A, Scheve K. Analyzing incomplete political science data: an alternative algorithm for multiple imputation. Am Pol Sci Rev 2001;95:49-6.
- Carpenter JR, Goldstein H, Kenwood MG. REALCOM-IMPUTE software for multilevel multiple imputation with mixed response types. J Stat Software 2011;45:1-14.
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley and Sons; 1987.
- Rasbash J, Steele F, Browne W, Goldstein H. A User’s Guide to MlWin: Version 2.10. Bristol: Centre for Multilevel Modelling, University of Bristol; 2009.
- Managing Overweight and Obesity Among Children and Young People. London: NICE; 2013.
- Aicken C, Roberts H, Arai L. Mapping service activity: the example of childhood obesity schemes in England. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-310.
- Zeller M, Kirk S, Claytor R, Khoury P, Grieme J, Santangelo M, et al. Predictors of attrition from a pediatric weight management program. J Pediatr 2004;144:466-70. http://dx.doi.org/10.1016/j.jpeds.2003.12.031.
- de Niet J, Timman R, Jongejan M, Passchier J, van den Akker E. Predictors of participant dropout at various stages of a pediatric lifestyle program. Pediatrics 2011;127:e164-70. http://dx.doi.org/10.1542/peds.2010-0272.
- Mangham LJ, Hanson K. Scaling up in international health: what are the key issues?. Health Policy Plan 2010;25:85-96. http://dx.doi.org/10.1093/heapol/czp066.
- Katikireddi SV, Higgins M, Bond L, Bonell C, Macintyre S. How evidence based is English public health policy?. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d7310.
- Cole TJ, Green PJ. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 1992;11:1305-19. http://dx.doi.org/10.1002/sim.4780111005.
- Galton F. Regression towards mediocrity in hereditary stature. J Anthropolog Institute GB Ireland 1886;15:246-63. http://dx.doi.org/10.2307/2841583.
- Allison DB, Loebel AD, Lombardo I, Romano SJ, Siu CO. Understanding the relationship between baseline BMI and subsequent weight change in antipsychotic trials: effect modification or regression to the mean?. Psychiatr Res 2009;170:172-6. http://dx.doi.org/10.1016/j.psychres.2008.10.007.
- Raftery AE. Bayesian model selection in social research. Sociol Method 1995;25:111-63. http://dx.doi.org/10.2307/271063.
- Cole TJ. A chart to link child centiles of body mass index, weight and height. Eur J Clin Nutr 2002;56:1194-9. http://dx.doi.org/10.1038/sj.ejcn.1601473.
- Griffiths LJ, Parsons TJ, Hill AJ. Self-esteem and quality of life in obese children and adolescents: a systematic review. Int J Pediatr Obes 2010;5:282-304. http://dx.doi.org/10.3109/17477160903473697.
- Cummins S, Macintyre S. Food environments and obesity – neighbourhood or nation?. Int J Epidemiol 2006;35:100-4. http://dx.doi.org/10.1093/ije/dyi276.
- Macdonald L, Ellaway A, Ball K. Is proximity to a food retail store associated with diet and BMI in Glasgow, Scotland?. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-464.
- Townsend N, Rutter H, Foster C. Variations in data collection can influence outcome measures of BMI measuring programmes. Int J Pediatr Obes 2011;6:491-8. http://dx.doi.org/10.3109/17477166.2011.605897.
- Techakehaki W, Hutton J. Economic Evaluation of the National Child Weight Management Programme: MEND. York: York Health Economics Consortium; 2010.
- Steeds J. MEND Programme Evaluation May 2008–November 2009. Bristol: Community Sport and Active Lifestyles, South Gloucestershire Council; 2010.
- Curtis L. Unit Costs of Health and Social Care 2011. Kent: Personal Social Services Research Unit, University of Kent; 2012.
- Lowry KW, Sallinen BJ, Janicke DM. The effects of weight management programs on self-esteem in pediatric overweight populations. J Pediatr Psychol 2007;32:1179-95. http://dx.doi.org/10.1093/jpepsy/jsm048.
- Taber DR, Stevens J, Murray DM, Elder JP, Webber LS, Jobe JB, et al. The effect of a physical activity intervention on bias in self-reported activity. Ann Epidemiol 2009;19:316-22. http://dx.doi.org/10.1016/j.annepidem.2009.01.001.
- Ells LJ, Cavill N. Treating Childhood Obesity Through Lifestyle Change Interventions. A Briefing Paper for Commissioners. Oxford: National Obesity Observatory; 2009.
- Healthy Lives, Healthy People: Our Strategy for Public Health in England. London: The Stationery Office; 2010.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice: a Guide for Social Science Students and Researchers. London: Sage; 2003.
- Rees R, Oliver K, Woodman J, Thomas J. The views of young children in the UK about obesity, body size, shape and weight: a systematic review. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-188.
- Murtagh J, Dixey R, Rudolf M. A qualitative investigation into the levers and barriers to weight loss in children: opinions of obese children. Arch Dis Child 2006;91:920-3. http://dx.doi.org/10.1136/adc.2005.085712.
- Crompton R. Employment and the Family: the Reconfiguration of Work and Family Life in Contemporary Societies. Cambridge: Cambridge University Press; 2006.
- Curtis P, James A, Ellis K. Children’s snacking, children’s food: food moralities and family life. Child Geog 2010;8:291-302. http://dx.doi.org/10.1080/14733285.2010.494870.
- Banks J, Williams J, Cumberlidge T, Cimonetti T, Sharp DJ, Shield JP. Is healthy eating for obese children necessarily more costly for families?. Br J Gen Pract 2012;62:1-5. http://dx.doi.org/10.3399/bjgp12X616300.
- Hastings G. Why corporate power is a public health priority. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e5124.
- Rawlins E, Baker G, Maynard M, Harding S. Perceptions of healthy eating and physical activity in an ethnically diverse sample of young children and their parents: the DEAL prevention of obesity study. J Hum Nutr Diet 2012;26:132-44. http://dx.doi.org/10.1111/j.1365-277X.2012.01280.x.
- Twiddy M, Wilson I, Bryant M, Rudolf M. Lessons learned from a family-focused weight management intervention for obese and overweight children. Public Health Nutr 2012;15:1310-17. http://dx.doi.org/10.1017/S1368980011003211.
- Pocock M, Trivedi D, Wills W, Bunn F, Magnusson J. Parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children: a systematic review of qualitative studies. Obes Rev 2010;11:338-53. http://dx.doi.org/10.1111/j.1467-789X.2009.00648.x.
- Lucas P, Arai L, Baird J, Kleijnen J, Law C, Roberts H. A systematic review of lay views about infant size and growth. Arch Dis Child 2007;92:120-7. http://dx.doi.org/10.1136/adc.2005.087288.
- Robson C. Real World Research: a Resource for Social Scientists and Practitioner-Researchers. Oxford: Blackwell Publishing; 2002.
- Punch S. ‘I felt they were ganging up on me’: interviewing siblings at home. Child Geog 2007;5:219-34.
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA and London: Harvard University Press; 1979.
- Khoury MJ, Gwinn M, Ioannidis JPA. The emergence of translational epidemiology: from scientific discovery to population health impact. Am J Epidemiol 2010;172:517-24. http://dx.doi.org/10.1093/aje/kwq211.
- Ogilvie D, Craig P, Griffin S, Macintyre S, Wareham N. A translational framework for public health research. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-116.
- Melhuish E, Belsky J, Leyland AH, Barnes J. Effects of fully-established Sure Start Local Programmes on 3-year-old children and their families living in England: a quasi-experimental observational study. Lancet 2008;372:1641-7. http://dx.doi.org/10.1016/S0140-6736(08)61687-6.
- O’Hara BJ, Bauman AE, Eakin EG, King L, Haas M, Allman-Farinelli M, et al. Evaluation framework for translational research: case study of Australia’s Get Healthy Information and Coaching Service®. Health Promot Pract 2012;14:380-9. http://dx.doi.org/10.1177/1524839912456024.
- Swinburn BA, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prevent Med 1999;29:563-70. http://dx.doi.org/10.1006/pmed.1999.0585.
- Obesity: Working with Local Communities. London: NICE; 2012.
- Kremers SPJ, de Bruijn G-J, Droomers M, van Lenthe F, Brug J. Moderators of environmental intervention effects on diet and activity in youth. Am J Prevent Med 2007;32:163-72. http://dx.doi.org/10.1016/j.amepre.2006.10.006.
- Delamothe T. Complexity theory. BMJ 2008;336. http://dx.doi.org/10.1136/bmj.39602.443785.47.
- Shiell A, Hawe P, Gold L. Complex interventions or complex systems? Implications for health economic evaluation. BMJ 2008;336:1281-3. http://dx.doi.org/10.1136/bmj.39569.510521.AD.
- Hollingworth W, Hawkins J, Lawlor DA, Brown M, Marsh T, Kipping RR. Economic evaluation of lifestyle interventions to treat overweight or obesity in children. Int J Obes 2012;36:559-66. http://dx.doi.org/10.1038/ijo.2011.272.
Appendix 1 Terms of reference of the project advisory group
Introduction
This document outlines the terms of reference for the PAG for the population-level evaluation of the MEND programme.
Membership of the project advisory group
The group will be composed of (including the chair): two commissioners, two academics, two service users (parents) and Catherine Law, the principal investigator on the project.
All grant applicants, project partners and members of the project management group will receive the advisory group meeting papers, and be invited to attend as observers.
Remit
-
To advise on the conduct and progress of the Population-Level Evaluation of MEND (PLEM) project.
-
To agree and monitor processes for addressing potential conflicts of interest that may arise.
-
To consider the final report and advise on its implementation.
This remit will be reviewed and confirmed by the PAG as necessary.
Details of project advisory group meetings
Frequency: The PAG will be convened on May 23rd 2011. Two further meetings will be held, one before August 2012, and a second before December 2012.
Location: Meetings will be held at the UCL Institute of Child Health.
Appendix 2 Policy agreed by the project advisory group for the management of competing interests
In the draft version of this policy presented to the PAG, we referred throughout to ‘conflicts of interest’, a term which is widely used. The PAG recommended that it may be more appropriate to use the term ‘competing interests’. We have revised the wording of the policy accordingly, apart from where conflicts of interests are used in direct quotes – in these cases we consider the terms to be synonymous.
Introduction
This paper sets out the nature of competing interests in academic research generally and in relation to the PLEM project. It then sets out proposals for managing these interests.
Actions
-
The members of the PAG were invited to note any competing interests that they have.
-
The PAG was asked to comment on and approve the current and proposed arrangements for managing competing interests.
What are competing interests?
Competing interests (or conflicts of interest) have been defined by the US National Academies as ‘any financial or other interest which conflicts with the service of the individual because it (1) could significantly impair the individual’s objectivity or (2) could create an unfair competitive advantage for any person or organization’ [National Academies. Policy on Committee Composition and Balance and Conflicts of Interest for Committees Used in the Development of Papers. 2003. Available online (accessed on April 11th 2011) www.nationalacademies.org/coi/bi-coi_form-0.pdf]. Quite frequently in health research, complete avoidance of competing interests is not possible if the research is to go ahead. Furthermore, ‘there is no moral or ethical failing in having a conflict of interest; the problem occurs when conflicts are not disclosed appropriately and when conflicts are allowed to bias research teaching or practice’ [Friedman PJ. The troublesome semantics of conflict of interest. Ethics Behavior 1992;2(4):245–51].
Who might have competing interests in the Population-Level Evaluation of MEND project?
Financial competing interests
Three members of the project management group (Sacher, Chadwick and Radley) are employees of MEND Central Ltd. Sacher and Chadwick are also shareholders. They therefore have an interest in MEND Central’s success. Results from the project might support, threaten or have no effect on MEND Central’s success.
The MEND programme was aimed at 7- to 13-year-olds, based on research undertaken at UCL Institute of Child Health. Under a contractual relationship, UCL Institute of Child Health receives a small proportion of the revenues generated from this programme. These sums have been less than £10,000 p.a. for the last 3 years. UCL Institute of Child Health uses these funds to support nutrition research and none of the project management group has access to these funds, nor works in the department where they are held.
Other competing interests
Researchers in the project management group may predict particular results which may influence discussion and interpretation, or may have known intellectual positions on which their reputations may rest. In addition, some results may be easier to publish than others. These competing interests are common in health research, though are not often articulated.
Processes to manage competing interests
To date
Discussions to manage competing interests took place prior to submission of the grant application in April 2010 and again after reviewers’ comments on that proposal had been received (May 2010). A number of measures were proposed to manage competing interests in the grant application and these are the basis of the proposals in this paper. In addition, in response to reviewers’ comments, Sacher and Chadwick shifted from being project co-applicants to project partners. This move was accepted by the funding body in June 2010. Sacher and Chadwick remain on the project management group as project partners. In addition, a third member of MEND Central’s staff, Duncan Radley (MEND Central Research Manager) has also joined the project management group to directly support the involvement of MEND Central in the project.
To assess whether further action was required, CL discussed the issues with the following:
-
Dr Peter Davison, Director of the Health Technology Assessment programme, NIHR National Evaluations, Trials and Studies Coordinating Centre.
-
Dr Vic Larcher, Consultant Paediatrician and Ethicist, Great Ormond Street Hospital NHS Trust.
-
Professor Sir Michael Rawlins, Chairman of National Institute for Health and Clinical Excellence (Helen Roberts also attended this meeting).
Two common themes were transparency and proportionality (i.e. taking steps in proportion to the magnitude of the competing interest and the risk of this affecting the research and being open about both what competing interests might exist and what these steps are).
Going forward
In our grant application we proposed a range of measures to address competing interests. Having received approval of these measures from the PAG, we now intend to follow these measures. The text below has minor adaptations of language but not meaning from that submitted in our grant application (for example, we originally referred to PAG as a Study Steering Group in our application).
We propose a Programme Advisory Group (PAG), to be chaired by an independent academic or commissioner. We propose that the composition of members (including the chair) will be two commissioners, two academics, two service users (parents) and the principal investigator of this application. Co-investigators and project partners will be invited to be observers. The PAG will oversee the conduct of the study and will be asked particularly to ensure that processes to address potential competing interests are adhered to. These include:
Project partners from MEND will not take part in data analysis (quantitative or qualitative), though they will be involved in planning the analysis and in discussions relating to interpretation.
The results of the data analysis (and if they request it, the primary data) will be presented to the PAG prior to report or paper writing being commenced.
The reports of the results will be scrutinised by the PAG and checked against the presentation of the results made earlier.
We have further developed the protocol to mitigate risks related to competing interests.
Qualitative component
Risks of selection bias have been mitigated by separating the tasks carried out by researchers in sample selection from the tasks of MEND Central, who supply information only. Selection of both commissioners and families who participated in MEND is made by Institute of Child Health researchers on the project management group according to pre-specified criteria which aim to achieve maximum variation in the samples. MEND supply contact information on the selected sample. Follow-up of commissioners and families approached is also made by researchers from the project management group.
Input to the topic guides for commissioners and families: the topics to be covered were set out in our application and ethics approval documents. Inevitably, in qualitative research which asks open questions, respondents may themselves raise issues not in the topic guide. All members of the project management group, including those employed by MEND, have had an opportunity to comment on the application. Final decisions on questions asked, and the ways they are asked will rest with the qualitative researchers. While we do not foresee difficulties, any which arise will be reported to the advisory group chair.
Quantitative component
Data have been transferred from MEND Central to the Institute of Child Health. We will note MEND Central’s data preparation protocols but will carry out all data preparation (checking for outliers, assessing missing data, etc.) within the Institute of Child Health research team.
Catherine Law and Helen Roberts
16th June 2011
Appendix 3 Engagement with the National Children’s Bureau
Public health, Education, Awareness, Research group session, 27 July 2009.
Introduction
Public health, Education, Awareness, Research was a group of young people which aimed to increase young people’s involvement with public health research. It was facilitated by the NCB with funding from the Wellcome Trust (2007–10). At its annual residential meeting in 2009, Catherine Law (CL) worked with the group as part of the development of the grant proposal which the NIHR subsequently funded. CL first described the MEND intervention and her proposed research questions. In small groups, PEAR members then discussed scenarios on hypothetical potential participants of MEND. The introductory PowerPoint and the scenarios are given below.
Children in the PEAR group were then ask to consider the following scenarios.
Responses to individual scenarios
Ola
-
Her family are not encouraging healthy lifestyles. She needs to reduce the amount of time she spends doing sedentary activity.
-
School dinners may be a healthier option for her (depending on what she has in her lunchbox).
-
She might go to MEND, but her parents might not want to as they are overweight themselves and they might not have enough time.
Alize
-
Rather a sad person and may be comfort eating.
-
Probably does little exercise because of social isolation.
-
Might not go to MEND because of language and transport issues. On the other hand this might be a good way to make friends.
Jon
-
Lazy and following the family pattern.
-
May not know about healthy lifestyles. Also, his mother is very busy.
-
Might not go to MEND as he is lazy and his mother might be too busy to go with him. Can he go by himself?
Naufil
-
Eats well and is privileged but doesn’t use what is on offer enough.
-
Needs a confidence boost – this would help him increase his physical activity at school.
-
Also needs to think about active transport.
-
Probably would go to MEND because he might like the peer support and it might increase his confidence.
General themes
-
Accessibility and fitting into parents’ (busy) lifestyles.
-
Many group members felt parents would be unwilling to go to MEND because of the time commitment. This was more commonly expressed than children and young people being unwilling.
-
Attending MEND may be seen as a stigma and a stimulus for bullying.
-
There was lots about the social aspects of MEND and the positive peer group support it might provide.
National Children’s Bureau Young Research Advisors session, 14 July 2012
Introduction
This section reports on the NCB Young Research Advisors consultation session about the PLEM project on 14 July 2012. The aim of the session was to find out how young people interpreted the PLEM results, and to establish whether their interpretations provided additional insights to be considered by the researchers.
The session was introduced by presenting a short overview of MEND 7–13 as a weight management intervention for children and their families and an overview of the methodologies used in the population-level evaluation.
The young people were split into three groups and then each group was presented with a page of findings from the qualitative and quantitative work (see Findings sheets), and a worksheet with relevant questions (see Feedback about the information sheets). Some questions were specific to each group to allow the children and young people to actively engage with the work, while two questions were given to all the groups and related to what they thought the findings might mean for MEND and whether they were useful. Each group then had 10 minutes to report back their findings and discussion to the rest of the advisors and then there was a short discussion before the session ended.
Individual group responses
Group 1 thought that:
-
Families will have to devote time to MEND, and change their schedules so that it does not clash with other priorities. Families might need to arrange extra support in order to attend MEND, such as child care.
-
If one family member is unemployed, he or she will have more time to look after the children. Unemployed parents might not be able to afford healthy foods.
-
Religion might be a bigger priority than attending MEND.
-
Some ethnic groups might eat more fatty foods and therefore do worse on MEND than other ethnic groups.
MEND could improve its intervention by:
-
surveying parents of 7- to 13-year-olds about the timings of MEND sessions
-
changing session times and frequency as required (sessions should not necessarily have set times)
-
providing or signposting exercise classes and other support after MEND finishes
-
promoting MEND within schools; however, this should be done discreetly so that children are not embarrassed if they want to go to MEND
-
focusing sessions on cheaper, healthy food/budgeting/lifestyle for unemployed parents
-
highlighting healthier options of cultural foods
-
making the parents aware of the benefits of MEND
-
having supportive parents.
These findings are useful because:
-
they can now give support and extra help to the children who need it
-
child obesity is a big problem
-
statistics allow the intervention to have more impact.
Group 2 thought that:
-
Losing weight makes you feel more confident about your appearance/body, and feeling like you are doing something about your weight may improve your self-esteem.
-
Meeting other people ‘like me’ will make you feel like you are not alone in being overweight.
-
Older children are more conscious of their weight. When you are younger you don’t understand why people look at you, but as you get older you are exposed to different people’s opinions which may influence what you think.
-
When you start secondary school you meet new people.
-
When you are younger it is easier to change and to make it a long-term change.
-
Overall – you will be more successful if you want to make the changes.
MEND might work because:
-
the ‘commitment’, having to physically go to something, is better than doing it alone
-
it is a sustainable way for children to manage their weight because it is a lifestyle change
-
it presents scientific evidence, which means children are more likely to attend
-
support and advice is given, which means children are more likely to want to go
-
children are given help to go through it, rather than simply being told what they need to do
-
it brings back people’s confidence and provides mental support
-
it is sociable; other people also attend.
These findings are useful because:
-
It is important to get the children’s views; there is a need to find out what users think in order to make MEND better, as this will lead to an increase in the number of users.
-
There is currently no evaluation, and therefore no way of knowing whether or not it is effective.
Group 3 thought that:
-
It is important that both parents and children attend MEND as this provides support and motivation, and parents will remember things from the sessions. Parents are also in charge of shopping and so should attend MEND sessions.
-
However, perhaps it is not essential that parents attend the sessions with their children, as children should take responsibility for themselves.
-
The number of fast food outlets in a child’s neighbourhood did not have any effect on the reduction in BMI because fast food might be too expensive and children might not like it.
Children who attended more sessions might do better because:
-
they get to do more exercise
-
they are more motivated
-
they set more aims and goals
-
they have diet plans.
MEND could improve its intervention by:
-
offering incentives (e.g. gym passes, free t-shirts and pens, grocery vouchers)
-
doing more advertising, e.g. within schools
-
providing more statistics as evidence of how well it works
-
linking with Change4Life
-
educating people about what is contained in food
-
promoting the ‘traffic light’ system (of food labelling) because it is good
-
providing alternative exercise to sport, as some people do not like sports
-
promoting sports
-
giving advice on supplements.
Summary of young research advisors’ thoughts
-
Family: the role of the child’s family is important as it will affect attendance at MEND and the success of MEND; however, as children get older they should rely less on their families and take more responsibility for their own weight.
-
Self-esteem: MEND may improve self-esteem, not just because of improved appearance but because of the process of taking control over one‘s weight and having the social support of other overweight children.
-
Age: as children get older they are more aware of how people view them and are more exposed to people’s opinions. The younger children are, the easier it is to make changes.
-
The young people thought that weight management interventions could be optimised by:
-
providing flexible access
-
providing post-intervention support
-
being accessed discreetly within schools
-
being practical and conscious of food costs
-
being tailored to different cultures
-
offering incentives for attendance and weight loss
-
linking with public health campaigns or big businesses
-
using statistics in their promotion
-
providing a range of physical activities
-
educating people on what is contained in food.
-
-
The young people felt that this research is valuable because:
-
obesity is a serious and large problem
-
the results can be used to improve weight management interventions
-
children’s views were taken into account in the qualitative component
-
there is currently no other population-level evaluation of a weight-loss intervention.
-
Appendix 4 Notes relating to child and researcher safety for ethics
Family study
We conducted all interviews with families using a child protection protocol. This protocol covered situations where researchers were provided with, or become aware of, information which raised concerns about the safety or welfare of someone who is under 18 years old. Young people’s safety is of paramount importance. If the researcher identified a potential child protection or other safety concern, the protocol outlined the steps which the researcher would take.
Researcher as well as participant safety is important, and we put in place control measures to mitigate risks. The location and time of interviews was logged centrally and researchers liaised with the central team after the interview to ensure that they remained safe.
Appendix 5 Coding of MEND, Health Survey for England and Millennium Cohort Study socioeconomic circumstances and black and minority ethnic variables
| Analysis variables | Variables in original MEND data | HSE subcategories | MCS subcategories |
|---|---|---|---|
| Ethnicity | |||
| White | Any other white background; white; white British; white Irish | 2007: white 2008–10: white British; white Irish; any other white background |
White British; white Irish; any other white background |
| Asian | Any other Asian background; Asian or Asian British – Bangladeshi; Asian or Asian British – Indian; Asian or Asian British – Pakistani; Chinese | 2007: Asian or Asian British 2008–10: Asian or Asian British – Indian; Asian or Asian British – Pakistani; Asian or Asian British – Bangladeshi; any other Asian/Asian British background; Chinese |
Asian/Asian British – Indian; Asian/Asian British – Pakistani; Asian/Asian British – Bangladeshi; Chinese; any other Asian background |
| Black | Any other black background; black or black British – African; black or black British – Caribbean | 2007: black or black British 2008–10: black or black British – Caribbean; black or black British – African; any other black/black British background |
Black/black British – Caribbean; black/black British – African; any other black background |
| Other | Any other ethnic group; any other mixed background; mixed – white and Asian; mixed – white and black; African; mixed – white and black Caribbean | 2007: mixed, Chinese or other ethnicity 2008–10: mixed – white and black Caribbean; mixed – white and black African; mixed – white and Asian; any other mixed background |
Mixed – white and black Caribbean; mixed – white and black African; mixed – white and Asian; any other mixed background; any other background |
| Employment status | |||
| Employed | Primary earner (implicitly defined by respondent) is ‘employed’ | In paid employment or self-employed (or temporarily away) | Couples are employed if either or both partners are in work/on leave; lone parents are employed if they are in work/on leave |
| Not employed | Primary earner (implicitly defined by respondent) is ‘unemployed’ (’Undisclosed’ defined as missing) |
On a government scheme for employment training; doing unpaid work for a business that you own, or that a relative owns; waiting to take up paid work already obtained; looking for paid work or a government training scheme; intending to look for work but prevented by temporary sickness; permanently unable to work because of long-term sickness or retired from paid work; looking after home or family; doing something else (specify) | Couples are unemployed if both partners are not in work; lone parents are unemployed if they are not in work |
| Housing tenure | |||
| Owner occupied | Owner occupied; owner occupied: owned with mortgage or loan; living rent-free; owner occupied: owned outright; owner occupied: shared ownership | Own it outright; buying it with the help of a mortgage or loan; pay part rent and part mortgage (shared ownership) | Own outright; own – mortgage/loan; part rent/part mortgage (shared equity) |
| Social rented | Local authority/council; housing association; housing co-operative; charitable trust or registered social landlord; social rented – other social rented; social rented – rented from council | Rent from the local authority/council/new town development; a housing association or co-operative or charitable trust; employer (organisation) of a household member | Rent from local authority; rent from housing association |
| Private rented | Employer of a household member; private landlord or letting agency; other; relative or friend of a household member | Rent from another organisation; a relative/friend (made prior to living at this property) of a household member; employer (individual) of a household member; letting agency or another individual private landlord; live here rent-free | Rent privately |
| Family structure | |||
| Lone parent | Parent/carer self-defines as not ‘in a couple’ | Mother or father single; separated; divorced; widowed | One parent/carer |
| Couple | Parent/carer defines themselves as ‘in a couple’ | Mother or father either married or cohabiting with partner | Two parents/carers |
Appendix 6 Further details of analyses in Chapter 2
The following tables describe the comparator and MEND data sets used to calculate differences in percentages. Individual and family characteristics are described in Tables 28 and 29.
| Variables | Section A: comparators | Section B: referrals | Section C: startersa | Section D: completersa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HSE (%) | MCS (%) | NCMP (%) | MEND-HSE (%) | MEND-MCS (%) | MEND-NCMP (%) | MEND-HSE (%) | MEND-MCS (%) | MEND-NCMP (%) | MEND-HSE (%) | MEND-MCS (%) | MEND-NCMP (%) | |
| Overweight (excluding obese) | 53.8 | 54.8 | 53.8 | n/a | n/a | n/a | 15.7 | 14.6 | 17.8 | 15.8 | 14.9 | 17.8 |
| Obese | 46.2 | 45.2 | 46.2 | n/a | n/a | n/a | 84.3 | 85.4 | 82.2 | 84.2 | 85.1 | 82.5 |
| n | 2799 | 1533 | 379,756 | n/a | n/a | n/a | 13,998 | 3360 | 4615 | 8311 | 2010 | 2711 |
| Sex | ||||||||||||
| Boy | 53.0 | 54.9 | 55.0 | 46.7 | 44.1 | 48.0 | 45.9 | 43.8 | 47.0 | 43.5 | 41.2 | 44.7 |
| n | 2799 | 1708 | 379,756 | 18,289 | 4391 | 6004 | 13,998 | 3360 | 4615 | 8419 | 2060 | 2713 |
| Ethnicity | ||||||||||||
| White | 79.6 | 78.2 | 76.2 | n/a | n/a | n/a | 76.7 | 72.6 | 78.1 | 77.9 | 73.6 | 78.8 |
| Asian | 10.0 | 9.3 | 7.2 | n/a | n/a | n/a | 13.6 | 16.3 | 12.4 | 12.9 | 15.7 | 12.1 |
| Black | 5.7 | 7.0 | 10.5 | n/a | n/a | n/a | 5.9 | 6.7 | 5.9 | 5.5 | 6.3 | 5.8 |
| Other | 4.7 | 5.5 | 6.2 | n/a | n/a | n/a | 3.8 | 4.4 | 3.6 | 3.7 | 4.4 | 3.4 |
| n | 2798 | 1688 | 289,491 | n/a | n/a | n/a | 13,998 | 3360 | 4615 | 8419 | 2060 | 2713 |
| Family structure | ||||||||||||
| Lone parent | 30.5 | 27.1 | n/a | n/a | n/a | n/a | 34.5 | 34.4 | 34.3 | 31.3 | 30.8 | 30.9 |
| Couple | 69.5 | 72.9 | n/a | n/a | n/a | n/a | 65.5 | 65.6 | 65.7 | 68.7 | 69.2 | 69.1 |
| n | 804 | 1708 | n/a | n/a | n/a | n/a | 13,998 | 3360 | 4615 | 8419 | 2060 | 2713 |
| Housing tenure | ||||||||||||
| Owned | 63.5 | 59.8 | n/a | n/a | n/a | n/a | 53.7 | 49.0 | 55.3 | 58.6 | 54.5 | 59.5 |
| Social | 25.2 | 29.9 | n/a | n/a | n/a | n/a | 31.3 | 33.5 | 30.0 | 27.7 | 29.5 | 26.8 |
| Private | 11.3 | 10.3 | n/a | n/a | n/a | n/a | 15.0 | 17.4 | 14.7 | 13.8 | 16.1 | 13.7 |
| n | 2793 | 1639 | n/a | n/a | n/a | n/a | 13,998 | 3360 | 4615 | 8419 | 2060 | 2713 |
| Employment status of the primary earner | ||||||||||||
| Employed | 79.4 | 79.4 | n/a | n/a | n/a | n/a | 74.0 | 71.5 | 74.7 | 77.1 | 75.5 | 78.2 |
| Unemployed | 20.6 | 20.6 | n/a | n/a | n/a | n/a | 26.0 | 28.5 | 25.3 | 22.9 | 24.5 | 21.8 |
| n | 2753 | 1577 | n/a | n/a | n/a | n/a | 13,998 | 3360 | 4615 | 8419 | 2060 | 2713 |
| Variables | Section A: comparators | Section B: referrals | Section C: starters | Section D: completers | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HSE (%) | MCS (%) | NCMP (%) | MEND-HSE (%) | MEND-MCS (%) | MEND-NCMP (%) | MEND-HSE (%) | MEND-MCS (%) | MEND-NCMP (%) | MEND-HSE (%) | MEND-MCS (%) | MEND-NCMP (%) | |
| Urban/rural | ||||||||||||
| Urban | 82.1 | 84.3 | 84.2 | 89.2 | 89.6 | 88.6 | 89.0 | 6.1 | 88.6 | 88.4 | 88.8 | 88.1 |
| Suburban | 8.9 | 7.7 | 8.2 | 6.4 | 6.1 | 7.0 | 6.5 | 5.8 | 7.0 | 6.8 | 6.7 | 7.2 |
| Rural | 9.0 | 7.9 | 7.7 | 4.4 | 4.3 | 4.4 | 4.5 | 5.2 | 4.4 | 4.8 | 4.6 | 4.7 |
| n | 2799 | 1698 | 370,890 | 18,289 | 4391 | 6004 | 13,998 | 3360 | 4615 | 8419 | 2060 | 2713 |
| IDACI 2007 decile | ||||||||||||
| 1 (least deprived) | 10.1 | 8.9 | 7.1 | 5.9 | 5.7 | 6.6 | 6.0 | 6.1 | 6.6 | 6.8 | 7.0 | 7.5 |
| 2 | 8.3 | 6.7 | 7.7 | 6.6 | 5.6 | 7.2 | 6.9 | 5.8 | 7.2 | 7.9 | 6.5 | 8.2 |
| 3 | 6.1 | 7.3 | 8.0 | 6.1 | 5.4 | 6.3 | 6.3 | 5.2 | 6.7 | 6.9 | 5.3 | 7.1 |
| 4 | 9.0 | 9.9 | 8.3 | 7.7 | 7.2 | 8.4 | 7.9 | 7.1 | 8.5 | 8.6 | 7.6 | 9.1 |
| 5 | 10.0 | 9.6 | 8.8 | 8.9 | 8.3 | 9.2 | 6.9 | 6.3 | 7.2 | 7.3 | 6.5 | 7.8 |
| 6 | 8.9 | 8.6 | 9.6 | 10.0 | 10.0 | 9.7 | 10.5 | 10.7 | 10.1 | 10.3 | 10.6 | 9.8 |
| 7 | 9.8 | 8.7 | 10.2 | 11.5 | 11.7 | 11.9 | 11.8 | 11.6 | 12.3 | 11.8 | 12.2 | 12.2 |
| 8 | 11.8 | 11.2 | 11.6 | 13.0 | 12.7 | 12.2 | 13.2 | 12.4 | 12.9 | 12.9 | 11.7 | 12.8 |
| 9 | 11.1 | 12.0 | 13.0 | 14.3 | 14.9 | 13.5 | 15.2 | 16.5 | 14.1 | 14.2 | 16.0 | 13.3 |
| 10 (most deprived) | 14.9 | 17.2 | 15.7 | 15.9 | 18.5 | 15.0 | 15.3 | 18.4 | 14.3 | 13.1 | 16.6 | 12.1 |
| n | 2799 | 1694 | 370,853 | 18,289 | 4391 | 6004 | 13,998 | 3360 | 4615 | 8419 | 2060 | 2713 |
| Variables | Section A: starters (attended at least one session) | Section B: completers (attended > 75% of sessions) | ||||
|---|---|---|---|---|---|---|
| MEND 7–13 vs. comparator | MEND 7–13 vs. comparator | |||||
| HSE, difference (p) | MCS, difference (p) | NCMP, difference (p) | HSE, difference (p) | MCS, difference (p) | NCMP, difference (p) | |
| Sex | ||||||
| Boy | –5.11 (< 0.001) | –9.88 (< 0.001) | –5.20 (< 0.001) | –7.25 (< 0.001) | –13.95 (< 0.001) | –7.12 (< 0.001) |
| Ethnicity | ||||||
| White | –1.72 (0.072) | –4.95 (0.004) | +2.56 (0.003) | –0.39 (0.715) | –4.95 (0.037) | +4.77 (< 0.001) |
| Asian | +2.19 (0.005) | +6.62 (< 0.001) | +4.13 (< 0.001) | +0.93 (0.289) | +6.40 (0.001) | +2.86 (0.002) |
| Black | +0.44 (0.384) | +0.24 (0.804) | –4.23 (< 0.001) | +0.40 (0.481) | +0.68 (0.610) | –5.00 (< 0.001) |
| Other | –0.91 (0.027) | –1.91 (0.014) | –2.56 (< 0.001) | –0.93 (0.052) | –2.13 (0.059) | –2.72 (< 0.001) |
| Family structure | ||||||
| Lone parent | +4.55 (0.009) | +6.63 (< 0.001) | – | 0.48 (0.788) | +2.16 (0.398) | – |
| Housing tenure | ||||||
| Owned | –10.89 (< 0.001) | –12.98 (< 0.001) | – | –3.49 (0.007) | –3.24 (0.251) | – |
| Social | +7.28 (< 0.001) | +5.23 (0.008) | – | +1.52 (0.186) | –1.44 (0.581) | – |
| Private | +3.61 (< 0.001) | +7.75 (< 0.001) | – | +1.97 (0.019) | +4.67 (0.010) | – |
| Employment status of the primary earner | ||||||
| Unemployed | +5.52 (< 0.001) | +7.47 (< 0.001) | – | +1.09 (0.390) | +3.38 (0.270) | – |
| Urban/rural | ||||||
| Urban | +6.84 (< 0.001) | +5.12 (< 0.001) | +4.39 (< 0.001) | +5.39 (< 0.001) | +3.21 (0.082) | +2.93 (0.002) |
| Suburban | –2.45 (< 0.001) | –1.35 (0.157) | –1.32 (0.003) | –1.58 (0.015) | –0.88 (0.517) | –0.82 (0.256) |
| Rural | –4.39 (< 0.001) | –3.77 (< 0.001) | –3.17 (< 0.001) | –3.81 (< 0.001) | –2.33 (0.086) | –2.20 (0.002) |
| Variables | Section A: starters (attended at least one session) | Section B: completers (attended > 75% of sessions) | ||||
|---|---|---|---|---|---|---|
| MEND 7–13 vs. comparator | MEND 7–13 vs. comparator | |||||
| HSE, difference (p) | MCS, difference (p) | NCMP, difference (p) | HSE, difference (p) | MCS, difference (p) | NCMP, difference (p) | |
| Sex | ||||||
| Boy | –17.53 (< 0.001) | –18.74 (< 0.001) | –21.22 (< 0.001) | –19.47 (< 0.001) | –24.31 (< 0.001) | –23.90 (< 0.001) |
| Ethnicity | ||||||
| White | –5.59 (< 0.001) | –11.28 (0.001) | +1.00 (0.545) | –6.88 (< 0.001) | –10.31 (0.034) | +0.89 (0.738) |
| Asian | +7.39 (< 0.001) | +11.24 (< 0.001) | +7.92 (< 0.001) | +7.68 (< 0.001) | +8.66 (0.016) | +8.02 (< 0.001) |
| Black | –0.93 (0.144) | +0.58 (0.752) | –6.23 (< 0.001) | –0.59 (0.514) | +2.40 (0.401) | –7.16 (< 0.001) |
| Other | –0.87 (0.135) | –0.54 (0.736) | –2.79 (0.001) | –0.21 (0.801) | –0.75 (0.766) | –1.85 (0.184) |
| Family structure | ||||||
| Lone parent | +1.24 (0.534) | +2.98 (0.474) | – | –0.02 (0.992) | +3.87 (0.482) | – |
| Housing tenure | ||||||
| Owned | –6.17 (< 0.001) | –10.34 (0.018) | – | –4.47 (0.034) | –12.67 (0.045) | – |
| Social | +3.59 (0.016) | +4.21 (0.255) | – | +0.34 (0.859) | +0.73 (0.894) | – |
| Private | +2.58 (0.016) | +6.13 (0.017) | – | +4.14 (0.004) | +11.94 (0.003) | – |
| Employment status of the primary earner | ||||||
| Unemployed | +5.14 (0.001) | +10.53 (0.002) | – | +3.92 (0.056) | +13.48 (0.012) | – |
| Urban/rural | ||||||
| Urban | +7.50 (< 0.001) | +7.20 (0.004) | +4.34 (0.001) | +7.96 (< 0.001) | +6.27 (0.118) | +4.43 (0.036) |
| Suburban | –2.54 (0.001) | –1.94 (0.300) | –0.64 (0.505) | –3.24 (0.003) | –0.69 (0.817) | –0.84 (0.596) |
| Rural | –4.96 (< 0.001) | –5.26 (0.005) | –3.80 (< 0.001) | –4.72 (< 0.001) | –5.59 (0.059) | –3.69 (0.017) |
| Variables | Section A: starters (attended at least one session) | Section B: completers (attended > 75% of sessions) | ||||
|---|---|---|---|---|---|---|
| MEND 7–13 vs. comparator | MEND 7–13 vs. comparator | |||||
| HSE, difference (p) | MCS, difference (p) | NCMP, difference (p) | HSE, difference (p) | MCS, difference (p) | NCMP, difference (p) | |
| Ethnicity | ||||||
| White | –4.97 (0.000) | –9.23 (0.000) | –0.03 (0.971) | –3.33 (0.001) | –8.24 (0.000) | 2.41 (0.044) |
| Asian | 0.89 (0.182) | 5.80 (0.000) | 2.62 (0.000) | 0.23 (0.762) | 6.13 (0.000) | 2.19 (0.003) |
| Black | 3.12 (0.000) | 3.49 (0.001) | –1.79 (0.001) | 2.46 (0.000) | 3.08 (0.030) | –3.48 (0.000) |
| Other | 0.96 (0.049) | –0.06 (0.946) | –0.90 (0.036) | 0.64 (0.242) | –0.97 (0.415) | –1.23 (0.070) |
| Family structure | ||||||
| Lone parent | 4.38 (0.012) | 6.43 (0.000) | – | 0.22 (0.902) | 2.14 (0.376) | – |
| Housing tenure | ||||||
| Owned | –10.87 (0.000) | –13.23 (0.000) | – | –3.55 (0.004) | –4.24 (0.109) | – |
| Social | 7.47 (0.000) | 5.73 (0.002) | – | 1.56 (0.155) | –1.25 (0.610) | – |
| Private | 3.40 (0.000) | 7.50 (0.000) | – | 1.99 (0.016) | 5.49 (0.001) | – |
| Employment status of the primary earner | ||||||
| Unemployed | 6.09 (0.000) | 8.84 (0.000) | – | 0.80 (0.495) | 5.93 (0.032) | – |
Appendix 7 Regression models estimating differences in Income Deprivation Affecting Children Index slopes for MEND participants and the MEND-eligible population
| Variables | HSE vs. MEND-HSE, B (SE) | MCS vs. MEND-MCS, B (SE) | NCMP vs. MEND-NCMP, B (SE) |
|---|---|---|---|
| Section A: referrals | |||
| Intercept of gradient (comparator) | 7.476 (0.838)*** | 5.762 (1.152)*** | 5.367 (0.598)*** |
| MEND intercept of gradient | –3.902 (1.186)** | –4.418 (1.630)* | –1.082 (0.846) |
| Comparator gradient | 0.459 (0.135)** | 0.771 (0.186)*** | 0.842 (0.096)*** |
| MEND vs. comparator gradient | 0.709 (0.191)** | 0.803 (0.263)** | 0.197 (0.136) |
| n | 20 | 20 | 20 |
| Section B: starters | |||
| Intercept of gradient (comparator) | 7.476 (0.812)*** | 5.762 (1.133)*** | 5.367 (0.568)*** |
| MEND intercept of gradient | –3.291 (1.149)* | –3.950 (1.603)* | –0.693 (0.804) |
| Comparator gradient | 0.459 (0.131)** | 0.771 (0.183)*** | 0.842 (0.092)*** |
| MEND vs. comparator gradient | 0.598 (0.185)** | 0.718 (0.258)* | 0.126 (0.130) |
| Section C: completers | |||
| Intercept of gradient (comparator) | 7.476 (0.812)*** | 5.762 (1.137)*** | 5.367 (0.558)*** |
| MEND intercept of gradient | –3.559 (1.148)** | –4.163 (1.608)* | –0.701 (0.789) |
| Comparator gradient | 0.459 (0.131)** | 0.771 (0.183)*** | 0.842 (0.090)*** |
| MEND vs. comparator gradient | 0.647 (0.185)** | 0.757 (0.259)** | 0.127 (0.127) |
| n | 20 | 20 | 20 |
Appendix 8 Differential completion for completion defined at 60% of sessions attended instead of 75%
| Parameter | 60% of sessions attended, OR (95% CI) |
|---|---|
| Intercept | 0.96 (0.87 to 1.07) |
| SDQ at baseline (ref. normal) | |
| Borderline | 0.96 (0.91 to 1.02) |
| Abnormal | 0.93 (0.89 to 0.98)** |
| Sex (ref. girls) | |
| Boys | 0.94 (0.89 to 0.98)** |
| Family structure (ref. couple) | |
| Lone parent | 0.95 (0.90 to 1.00)* |
| Housing tenure (ref. owner occupied) | |
| Social rented | 0.92 (0.87 to 0.98)** |
| Private rented | 0.94 (0.88 to 1.00)* |
| Employment status of the primary earner (ref. employed) | |
| Unemployed | 0.94 (0.89 to 0.99)* |
| IDACI 2007 deciles (ref. decile 1, least deprived) | |
| 2 | 0.98 (0.88 to 1.10) |
| 3 | 1.00 (0.90 to 1.11) |
| 4 | 0.97 (0.88 to 1.08) |
| 5 | 0.96 (0.86 to 1.07) |
| 6 | 0.94 (0.85 to 1.04) |
| 7 | 0.95 (0.86 to 1.05) |
| 8 | 0.93 (0.84 to 1.03) |
| 9 | 0.92 (0.83 to 1.02) |
| 10 (most deprived) | 0.90 (0.82 to 1.00) |
| Group size (ref. one to five participants) | |
| Six to nine | 0.94 (0.88 to 1.02) |
| ≥ 10 | 0.88 (0.82 to 0.95)*** |
| Number of previous programmes per programme manager (ref. < 10) | |
| ≥ 10 | 0.92 (0.87 to 0.98)** |
Appendix 9 Unadjusted associations between covariates and change in body mass index
| Variable | Unadjusted multilevel models, B (SE) |
|---|---|
| Age | –0.0081 (0.0050) |
| Sex (ref. girls) | |
| Boys | –0.072 (0.017)*** |
| Ethnicity (ref. white) | |
| Asian | 0.33 (0.036)*** |
| Black | 0.20 (0.039)*** |
| Other | 0.15 (0.046)*** |
| Family structure (ref. couple) | |
| Lone parent | 0.038 (0.023) |
| Housing tenure (ref. owner occupied) | |
| Social rented | 0.071 (0.025)** |
| Private rented | 0.030 (0.032) |
| Parental employment (ref. employed) | |
| Unemployed | 0.16 (0.033)*** |
| IDACI 2007 decile | 0.31 (0.051)*** |
| Built environment score | 0.050 (0.010)*** |
| Urban/rural status (ref. urban) | |
| Towns | –0.10 (0.036)** |
| Villages | –0.092 (0.043)* |
| Number of healthy food outlets (ref. none) | |
| One to two | 0.010 (0.022) |
| Three or more | 0.015 (0.064) |
| Number of unhealthy food outlets (ref. none) | |
| One to two | –0.021 (0.020) |
| Three to four | –0.019 (0.028) |
| Five or more | 0.035 (0.033) |
| Number of previous programmes per programme manager | 0.0052 (0.0021)* |
| Group size | 0.014 (0.0039)*** |
| Attendance (ref. completer) | |
| Non-completer | 0.47 (0.12)*** |
| Partial completer | 0.26 (0.032)*** |
| Height rounding (ref. not rounded) | |
| Rounded | –0.11 (0.065) |
| Weight rounding (ref. not rounded) | |
| Rounded | –0.045 (0.024) |
Appendix 10 Relationship between baseline BMI and zBMI with changes in BMI and zBMI: the role of age and sex
The relationship between BMI change and BMI at baseline applies across the range of ages and for boys and girls, which together increase the variability of BMI at baseline, but much less so BMI change. Conversely, zBMI is already adjusted for age and sex, and hence the variability in baseline zBMI is much smaller. There is a positive correlation between zBMI at baseline and zBMI change, whereby higher zBMI at baseline is associated with a smaller reduction in zBMI change. This same correlation is masked with BMI, where the age–sex variability, which is broadly uncorrelated with BMI change, introduces noise and weakens the correlation between baseline and change, in the classic form of regression to the mean.
The relationship between BMI and age is non-linear, and it may differ in shape between the sexes. Thus, BMI change adjusted for BMI at baseline, age and sex introduces complex age–sex-related patterns to the residuals, whereas zBMI is adjusted for age and sex using separate non-linear curves. For this reason, the age and sex coefficients for BMI change and zBMI change are very likely to differ in form, and one should prefer the zBMI model to the BMI model. However, in other respects the two models are very similar, particularly in terms of the significance or non-significance of other covariates.
Appendix 11 Cost-effectiveness details from previous research
Techakehaki and Hutton71 investigated the cost-effectiveness of making MEND available to all eligible children in England versus not doing so. Using a 17-year time horizon they calculated that the cost of providing MEND 7–13 would be £551.2M and the reduction in future obesity-related medical costs would be £216M. The incremental cost was therefore £335.15M. Accounting for these savings reduced the incremental costs by 40%.
Techakehaki and Hutton71 calculated that the incremental cost per QALY gained of making MEND available to all eligible obese children in England, versus not doing so, was £1671. Hollingworth et al. 101 estimated the lifetime cost-effectiveness of lifestyle interventions to treat overweight and obese children. Their analysis was based on published estimates of the costs and benefits of lifestyle interventions evaluated in 10 RCTs, including a RCT of MEND. 15 Their central estimate of the incremental cost per life-year gained was £13,589. Uninflated figures from this report were also used in the cost-effectiveness analysis undertaken by Hollingworth et al. 101
Appendix 12 Matrix for coding of the MEND diet questionnaire
| Questionnaire item | Response scoring | ||||
|---|---|---|---|---|---|
| 1. How often does your child eat breakfast? | Rarely = 0 | Few times a month = 0 | Few times a week = 0 | Most days of the week = 2 | Every day = 2 |
| 2. How many cups of fluids (water or other drinks) does your child have per day? | Less than 2 = 0 | 2–4 = 0 | 4–6 = 0 | 6–8 = 2 | More than 8 = 2 |
| 3. My child drinks fizzy sugary drinks | Rarely = 2 | Once a week = 2 | A few times a week = 0 | Once a day = 0 | A few times a day= 0 |
| 4. How many portions of fruits and vegetables does your child eat per day? | None = 0 | Less than 2 = 0 | 2–4 = 0 | 4–5 = 2 | More than 5 = 2 |
| 5. My child eats white bread | Rarely = 0 | Once a week = 1 | A few times a week = 0 | Once a day = 0 | A few times a day = 0 |
| 6. My child eats wholewheat or wholegrain bread | Rarely = 0 | Once a week = 0 | A few times a week = 2 | Once a day = 2 | A few times a day = 2 |
| 7. My child eats crisps | Rarely = 2 | Once a week = 2 | A few times a week = 1 | Once a day = 0 | A few times a day = 0 |
| 8. My child eats sweets or chocolates | Rarely = 2 | Once a week = 2 | A few times a week = 1 | Once a day = 0 | A few times a day = 0 |
| 9. My child eats takeaways, e.g. burgers, Chinese, Indian, kebabs, pizza, etc. | Rarely = 2 | Once a week = 2 | A few times a week = 0 | Once a day = 0 | A few times a day = 0 |
| 10. Can you understand the nutrition labels on foods and drinks? | Rarely = 0 | Occasionally = 0 | Sometimes = 1 | Often = 2 | Always = 2 |
| 11. How often do you cook from fresh at home? | Rarely = 0 | Occasionally = 0 | Sometimes = 1 | Often = 2 | Always = 2 |
| 12. My family eats meals together at the table | Rarely = 0 | Occasionally = 0 | Sometimes = 1 | Often = 2 | Always = 2 |
| 13. What type of milk does your child have at home? | Fat-free (or skim) = 2 | Low-fat (1%) or plain soy, rice = 2 | 2% milk = 0 | Whole milk or flavoured ‘milk-style’ drinks (milkshakes, soy or rice) = 0 | My child does not drink milk |
| 14. I am happy with the variety (types) of foods my child eats | Not at all = 0 | Somewhat = 1 | Very = 2 | ||
Appendix 13 MEND commissioner sampling strategy
Introduction
The aim of this strategy was to develop a sample to maximise variation across five dimensions of interest and to ensure representation of some commissioners with high numbers of MEND contracts.
The variables and strategy used are described, as is the sample drawn from the data (see Table 37).
Description of methodology and sample
MEND provided a list of 151 commissioners and delivery partners (both terms defined below) with summary information on their organisational background and contracting history. We used a maximum variation purposive sample to select respondents along the five dimensions of interest in the study (area deprivation, area ethnic demographics, number of MEND contracts, whether or not the organisation was a PCT and whether or not it was a current contract holder). We also planned to try to recruit one of nine commissioners who contracted large numbers of programmes (> 40 programmes).
MEND defines delivery partners and commissioners in the following way.
A delivery organisation is typically a leisure centre (public or private), charity (e.g. YMCA) or sometimes a housing association that is employing staff who are trained by MEND to co-ordinate and run local MEND programmes. They have most commonly received grant funding via MEND to deliver programmes though some of them have sourced their own budgets. Their motives to deliver MEND are generally around wanting to provide health and wellbeing services for the local community and generate income for their facilities. The staff we work with in these roles are often leisure centre managers, fitness instructors, community activity managers. They are knowledgeable about running MEND, in particular the practical/logistical aspects and have a good understanding of the local population and the participant demographics. Generally they are less focussed on data and outcomes which are primary concerns for commissioners.
The commissioner is a purchaser only and has a formal duty to commission local health and wellbeing services to suit their population. They typically have a public health background (not necessarily in obesity) and reside within public health teams in a PCT or (more recently) local authority. They are focussed on meeting national and local targets and develop local healthcare strategy and local area agreements that determine health priorities. Following NHS reforms in 08/09 (to separate commissioning from service delivery), commissioners are not involved at all in service provision – they select, monitor and manage their chosen service providers. They purchase services directly from MEND and have separate contracts with their delivery partner. Our relationship with them is focussed on maximising the local impact of their programmes, providing data to evidence impact etc. For MEND, they are particularly focussed on participation levels, retention, participant demographics, outcomes and cost.
MEND Central, 2011, personal communication
Our original proposal described a sampling of ‘commissioners’. Our research aims were to understand the ‘salience and acceptability of MEND for those who commission it’ and to undertake an ‘exploration of the tension between programme fidelity and responsiveness to local context, circumstance and service users. Examples will be sought of modifications made to programmes and the perceived consequences of these.’ We felt that the full list of contract holders would be valuable to use as a sampling frame, as all of these organisations have a perspective on these dimensions of our study. To ensure that we had sufficient numbers of both, we aimed to sample equal proportions of PCT and non-PCT organisations.
Stage 1: maximum variation purposive sample
We were interested in five dimensions of variation. This was analogous to drawing a sample with six binary dimensions, leaving 25 (32) possible profiles of participants. These profiles were identified in the data using Stata version 11. Two commissioners were selected from each profile. Where there were multiple participants per profile, the commissioners within that profile were ranked by multiple deprivation score and selected according to the highest (for those in the most deprived profiles) or lowest (for the least deprived profiles) deprivation scores.
We aimed to recruit 30 commissioners and anticipated that 50% might opt out of the study when we contacted them. We oversampled to allow for this attrition. The first pass over the data left a sample too small for our criterion of at least 60 respondents; a second pass using the same method produced an overall sample of 68 participants.
Detailed breakdown of dimensions of variation
1. Organisation type
Almost half of the MEND commissioners were based in PCTs. The others were mainly based in local authorities, leisure providers and educational establishments (see Table 37). We therefore grouped commissioners as ‘PCT’ or ‘not PCT’.
2. Number of programmes contracted
Almost all commissioners contracted MEND on a relatively small-scale basis of between one and 40 programmes each. In fact, a majority commissioned only one to seven programmes. We classified commissioners as ‘low’ (one to seven programmes) or ‘medium’ (eight to 40 programmes) on this basis.
3. Current contracting status
Commissioners whose last programme had a start date of 2011 or 2012 were considered ‘current’ commissioners (interviews were conducted in 2011), whereas those whose last programme was due to end in 2010 or before were classified as ‘past’ commissioners.
4. Area-level multiple deprivation
The Index of Multiple Deprivation 2007 was linked to the organisation postcode of each commissioner and delivery partner at the PCT level. PCTs were classified as ‘high deprivation’ if they were in the highest tertile of deprivation relative to all PCTs in England. They were classified as ‘low deprivation’ if they were in the lowest tertile.
5. Area-level ethnic composition
Black and minority ethnic status was operationalised as anyone in the PCT who was not classified as white British. Thus, BME groups included mixed ethnicities, black and Asian ethnicities, white Irish and white ‘other’. This categorisation masks important heterogeneity within and between BME groups. However, where commissioners work in PCTs with high proportions of these groups, it is likely that this will inform their commissioning decisions.
Primary care trusts were classified as ‘high BME’ or ‘low BME’ depending on whether or not the proportion of the population which was of BME status exceeded the English median of 12%.
Stage 2: critical-case sampling
A small number of organisations (n = 13) commissioned between 41 and 119 programmes. The project team believed that these organisations might have a different perspective on commissioning, and these were included in the sampling strategy.
Sample drawn from the sampling frame
Using the sampling strategies described above a long list of 76 commissioners was drawn from the overall list of 151. This sample is described in Table 37 by the five dimensions of variation outlined as part of the strategy: deprivation, ethnicity, PCT status, current contracting status and number of programmes contracted. The table shows that at this stage, i.e. prior to recruitment, the sample was broadly balanced (i.e. 50/50) along the five dimensions of variation.
| Variable | Sample (N = 76), n (%) | Overall (N = 151), n (%) |
|---|---|---|
| Deprivation tertiles | ||
| 1 (least deprived 33% in England) | 42 (55.3) | 62 (41.1) |
| 2 (around median 33% in England) | 5 (6.6) | 47 (31.1) |
| 3 (most deprived 33% in England) | 29 (38.2) | 42 (27.8) |
| Percentage of BME groups in PCT population | ||
| ≤ median 10% | 35 (46.1) | 76 (50.3) |
| > 10% | 41 (53.9) | 75 (49.7) |
| PCT status | ||
| Non-PCT (local authority, leisure organisation, other) | 40 (52.6) | 88 (58.3) |
| PCT | 36 (47.4) | 63 (41.7) |
| Commissioning status | ||
| Current (last programme in 2011–12) | 34 (44.7) | 63 (43.8) |
| Past (last programme in 2007–10) | 42 (55.3) | 81 (56.3) |
| Number of contracted programmes per commissioner | ||
| Low (one to seven) | 26 (34.2) | 62 (41.1) |
| Medium (eight to 39) | 37 (48.7) | 76 (50.3) |
| High (40+) | 13 (17.1) | 13 (8.6) |
| Total number of commissioners | 76 (100.0) | 151 (100.0) |
From sample to recruitment
We aimed to achieve a final sample size of approximately 30 commissioners. To ensure that we did not over-recruit, we initially drew a subsample of 46 commissioners from the longlist of 76. We returned this list to MEND and 42 sets of contact details could be found on their database.
We contacted all 42 commissioners by letter and they were given the opportunity to opt out of the research by contacting us. None opted out and all were contacted by telephone and e-mail. Each commissioner was telephoned or e-mailed (where a telephone number was not available) at least three times. As a result, 21 consented to be interviewed.
We sampled a further 12 commissioners in order to achieve the nine further interviews. All 12 commissioners in the second round of recruitment were given the opportunity to opt out by contacting us. None did so. As in the first round, each commissioner was telephoned or e-mailed (where a telephone number was not available) at least three times. As a result, an additional six commissioners consented to be interviewed (Figure 8).
FIGURE 8.
Algorithm of commissioner recruitment. Owing to snowballing figures this will not add up to 54 (the original number of commissioners contacted). ICH, Institute of Child Health.
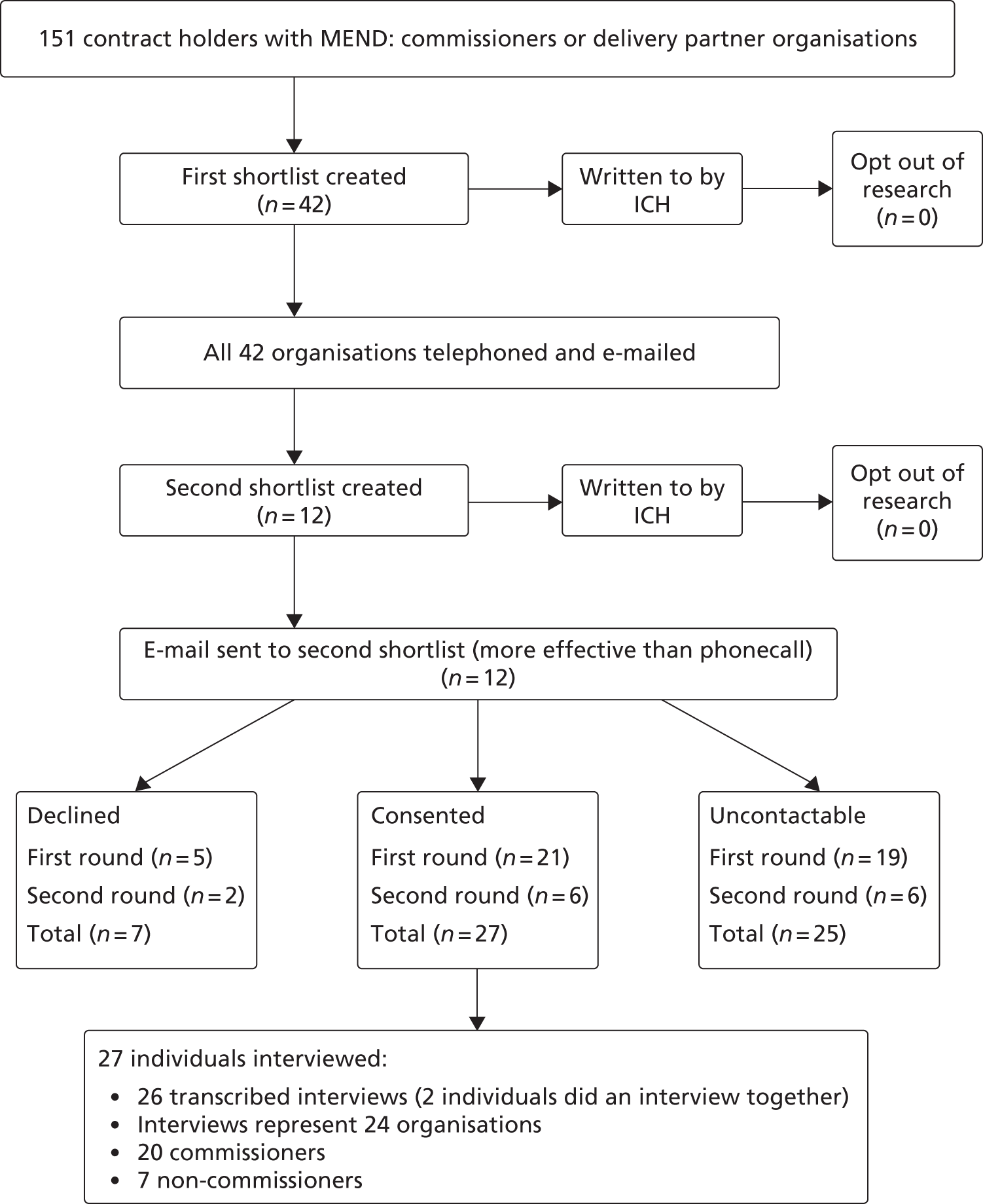
Appendix 14 Topic guides for commissioners/delivery partners and families
Appendix 15 MEND family sampling strategy
The aim of this strategy was to develop a sample to maximise variation across five dimensions of interest (multiple deprivation at the small area level, family structure, parent-reported participant ethnicity, housing tenure and MEND completion status). In addition, we decided that families living in very rural areas should be purposively selected as they are under-represented in the full sample. We aimed to recruit 30 families, anticipating that this would be sufficient to reach data saturation. We assumed that at least 50% of those contacted might choose not to take part in the study, and that our sampling strategy should therefore include contact with at least 60 families.
Basis for sample selection
Information on 22,060 participants who had been referred to the MEND programme was used as a sampling frame to draw our qualitative sample. We first used convenience sampling to select participants in the geographic areas in which we were working, followed by a maximum variation purposive sample to select respondents along the five dimensions of interest in the study. This was supplemented with selection of rural respondents as critical cases if they were not picked up using the maximum variation sampling frame. Finally, we used snowballing and advertising to contact families not reached through these methods.
Stage 1: convenience sampling of a regional subsample
A subsample (n = 1492) was drawn of participants in areas reachable by researchers based in the south-east (n = 376), south-west (n = 426) and north-east (n = 690) of England. The local authorities making up each region are listed below:
-
south-east: Hackney, Newham, Tower Hamlets
-
south-west: Bath and North East Somerset, Birmingham, Bristol, Gloucester, North Somerset, Reading, Somerset, South Gloucestershire, Swindon, Wiltshire
-
north-east: Blyth Valley, Castle Morpeth, Chester-le-Street, Darlington, Derwentside, Durham, Easington, Gateshead, Hartlepool, Middlesbrough, Newcastle upon Tyne, North Tyneside, North Yorkshire, Redcar and Cleveland, South Tyneside, Stockton-On-Tees, Sunderland, Teesdale, Tynedale, Wansbeck.
Stage 2: maximum variation purposive sample
The five variables used to systematically draw out a maximum variation sample are described below. Across the five dimensions of interest there were 64 possible profiles of participants (i.e. 64 unique combinations across five dimensions with eight categories in total). Of these possible profiles, only 48 were present in the subsample identified in stage 1 (identified in the data using Stata version 11). Where only one participant met the profile, they were selected. Where there were multiple participants per profile, the participants were ranked by multiple deprivation score and selected according to the highest (for those in the most deprived deciles) or lowest (for the least deprived deciles) deprivation scores. Sixty-eight participant families were identified using this method, and recruitment followed methods described in the main report (see Chapter 6, Sampling strategy and recruitment).
Family structure, ethnicity and housing tenure
MEND programme managers collate questionnaires from parents which report family structure, participant ethnicity and housing tenure information. There were considerable numbers of missing data on all the MEND programme-reported information (42% of families did not report family structure status, 41% did not report housing tenure and 38% did not report ethnicity). Although participants with missing data may be distinct from those with complete data in interesting ways, we took a decision to exclude families with missing data. Missingness on one or more variables would have prevented us from selecting families across all dimensions of variation, and as one of our aims in the study was to look at inequalities, we felt that this was the better of the choices open to us. The sample size of our data set with complete data on all variables was 825.
The question on family structure relates to single-parent families in comparison with couples. Family structure was sampled so as to try to pick up 50% of single parents and 50% of couples across the whole sample. This was disproportionate to the overall MEND data set, where single parents made up only 36% (see Table 26).
Housing tenure was sampled to pick up 50% of owner-occupied tenures and 50% of council and private rental tenures, a situation which broadly reflects the overall composition of the MEND participants.
Our sample was drawn to comprise 50% from black and Asian groups and 50% from white groups. This decision was made because young people (aged 0–15 years) from these groups are strongly represented in the south-east (Asian and black) and south-west (Asian) sample areas (Table 38). Overall, MEND participants in our subsample were predominantly white (69%), but Asian (21%) and black (5%) groups made up significant minorities, whereas other groups (including mixed-ethnicity families) were only minimally represented (see Table 38).
| Ethnic group | South-west (%) | North-east (%) | South-east (%) |
|---|---|---|---|
| White | 83.4 | 95.0 | 47.7 |
| Mixed | 4.4 | 1.7 | 8.2 |
| Black | 2.6 | 0.4 | 20.5 |
| Asian | 8.6 | 2.2 | 20.9 |
| Other | 1.1 | 0.4 | 2.6 |
Multiple deprivation
Multiple deprivation at the LSOA level (mean population size across England approximately 1500 residents) was described using the English Index of Multiple Deprivation 2007. 41 We linked this to our subsample using residential postcode. This variable was complete for all 825 participants. To maximise variation in multiple deprivation, we sampled those who lived in areas which were in the 30% of most deprived areas in England (top tertile) and the 30% least deprived areas (bottom tertile).
Completion status
The project team aimed to identify four categories of completion status. The first group (‘referrals’) includes participants who were referred to MEND, registered with the company but did not subsequently attend the programme (had no BMI data measured). This group made up almost one-third (28.5%) of MEND’s records. Three other groups were identified based on the percentage of sessions that they attended, corresponding loosely to non-completers (< 25%), partial completers (25–75%) and completers (> 75%). Overall, 33.6% of MEND participants completed the programme (i.e. attended more than 75% of sessions), 16.8% partially completed the programme and 21.2% only attended 25% of the sessions. MEND records were used to purposively select to approximately reflect this balance in our sample, so that our sample of 68 included proportionate numbers of those whose MEND records suggested they had not confirmed, or had attended < 25%, 25–75% or > 75% of all sessions.
Stage 3: critical-case sampling of urban/rural status
We specified a priori that we would seek to examine urban/rural status as a dimension. Accordingly, we linked an urban/rural classification scheme developed by Bibby et al. ,42 which classified the residential LSOA of each respondent as urban (> 10,000 people in the locality), suburban (urban fringe and towns) or rural (villages and isolated hamlets). Examination of urban/rural status in our subsample showed that there were only 10 respondents who lived in villages or isolated hamlets. This was not sufficient to cross-tabulate with the other variables. Therefore, we chose to use a critical-case strategy to identify two rural participants, one from the north-east and one from the south-west, if the sampling matrix did not pick up any rural participants. In the event, this was not necessary because the sampling matrix picked up two rural participants meeting our criteria.
Stage 4: additional recruitment strategies
We monitored sample recruitment against our desired sample characteristics, and identified those under-recruited from the sample described here. This sample was therefore supplemented with families recruited through snowballing from interviewees and advertising in leisure centres and on the internet. This method is described in the main report (see Chapter 6, Sampling strategy and recruitment).
Achieved sample
Of the 68 families contacted, 21 (30.8%) took part in interviews. Recruitment figures are shown in Figure 9.
FIGURE 9.
Recruitment to the family study. IMD, Index of Multiple Deprivation.
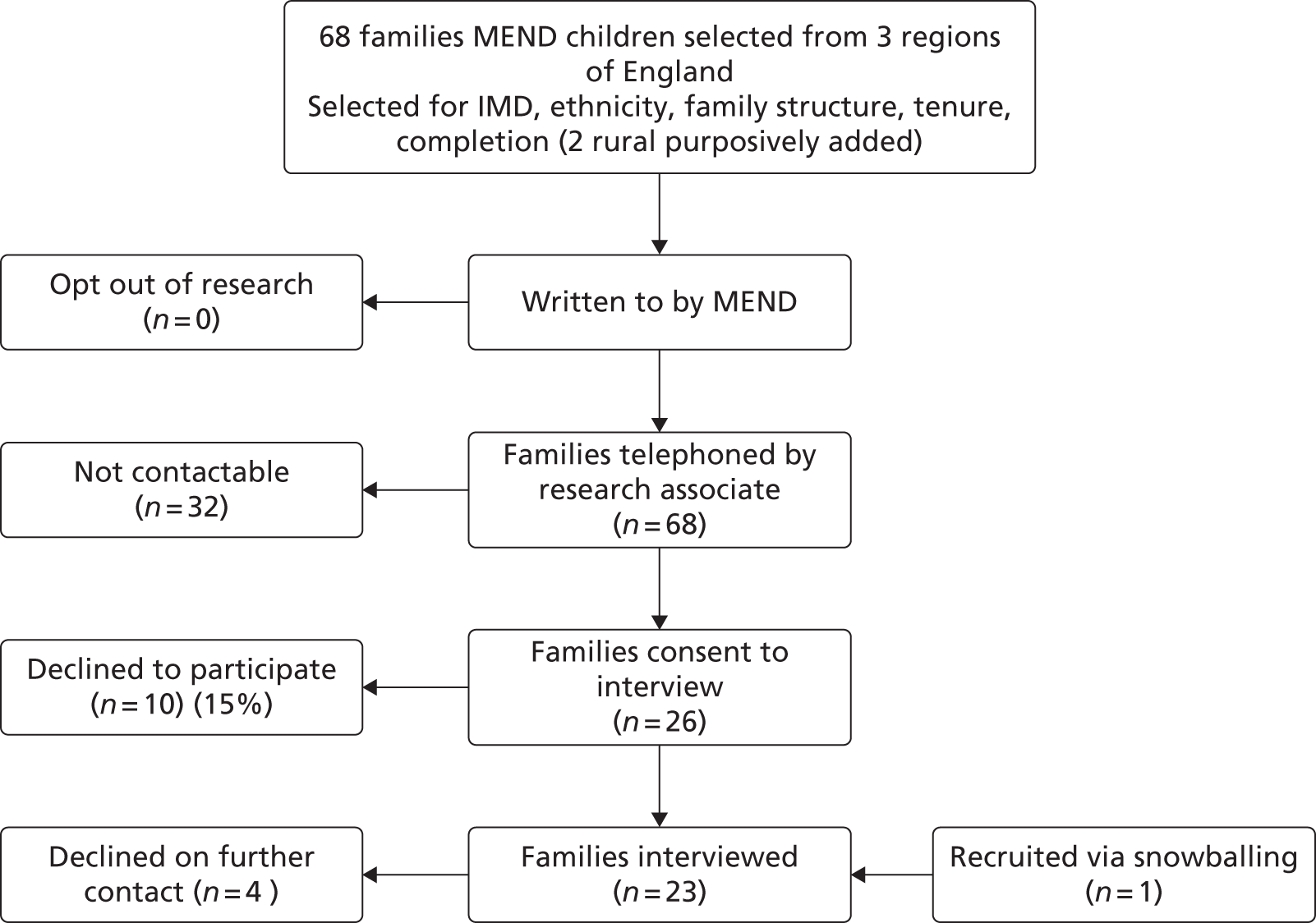
Reflections on the sampling strategy
The final recruited sample is reported in Table 26 of the main report. The sampling strategy was successful in achieving variation across all factors except MEND completion status. Few family records in the MEND Central database were complete for all variables.
Between 2007 and 2010, the MEND Central database did not distinguish between missing values and non-attendance when attendance data were entered by programme managers (this has now been changed).
The qualitative sample had to be drawn while cleaning measures were being developed, and therefore the sample drawn is based on the data and knowledge of the data set prior to cleaning. This had little impact for most dimensions (because we only sampled families for whom data were recorded on ethnicity, housing tenure, etc.) but it did affect our ability to assess the extent to which we had accurately sampled families by completion status.
Missingness of data on MEND attendance also had a substantial impact on the sample drawn in terms of non-completers and referrals. As qualitative work proceeded, we found that families often disputed the MEND attendance data we had used to sample them as low, medium, high or non-attenders. Indeed, families consistently reported higher attendance than MEND recorded – and those with low recorded attendance could often give detailed accounts of individual sessions. In line with this, the one family recorded as referred but not confirmed on a MEND programme had clearly attended (and had the tee shirt to prove it). Accordingly, we checked our achieved sample against cleaned attendance records, and found that the attendance records of a high proportion of our recruited sample (9/22; 40%) would have been judged to be invalid if we had been able to draw our sample after the wider data cleaning (see Chapter 2, MEND 7–13 service-level data). In fact, all those whom we recruited on the basis of low or no attendance (n = 6) were judged to have invalid attendance records.
We believe that because of the particular nature of missing attendance data, it was not possible to use MEND Central records to accurately identify families according to completion status, at least for referrals and non-completers. Only 67% of records had attendance records judged valid (555 of 825 participants in the subsample). Thus, although the MEND database was, in principle, a useful sampling frame, with hindsight this method was not able to identify unconfirmed and low-attendance families. Stage 4 describes the steps taken to try to recruit additional families with low attendance.
Appendix 16 Parent advertisements
FIGURE 10.
Poster displayed in leisure centres.
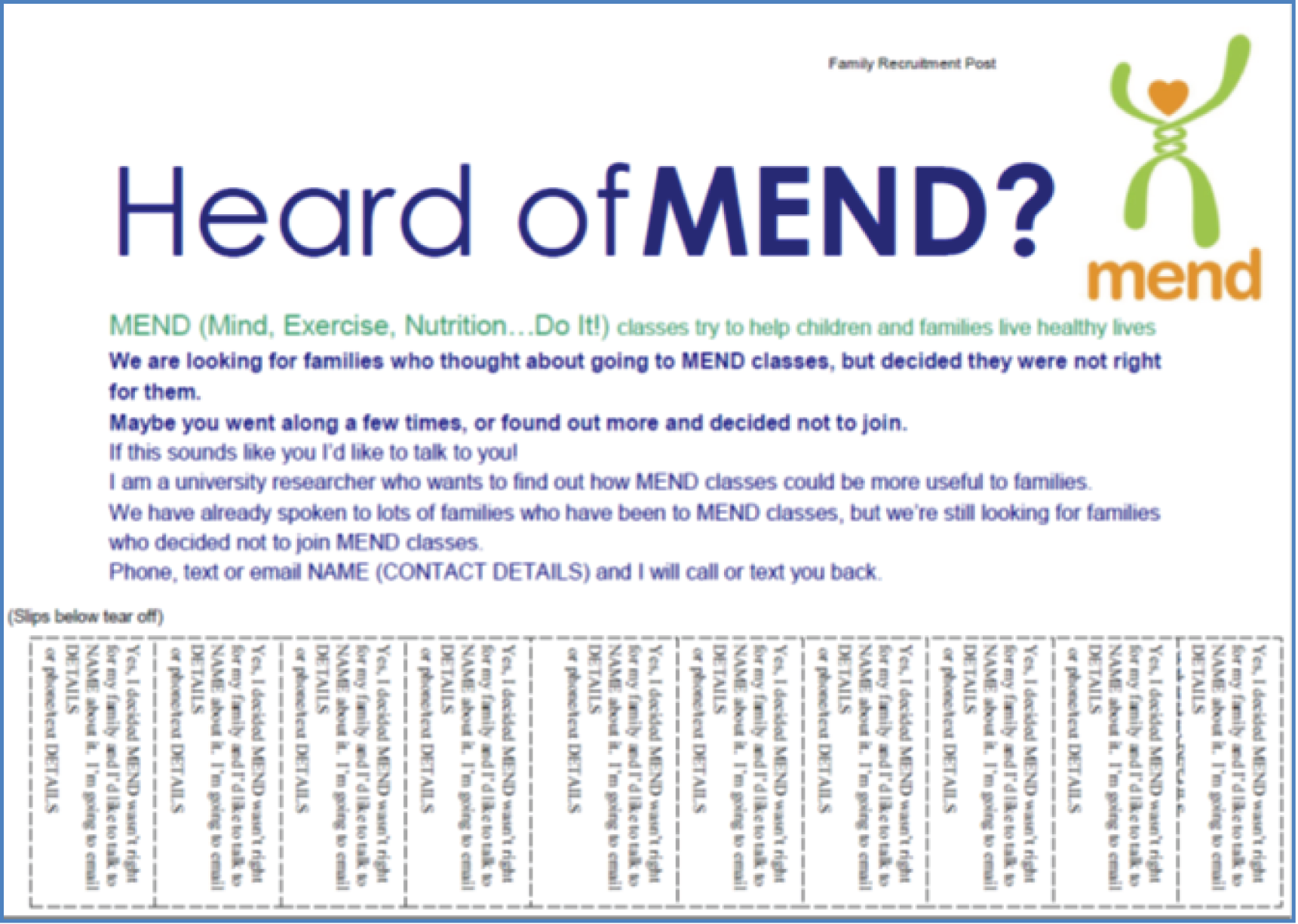
FIGURE 11.
Clickable internet advertisement for a parent forum.
Automated response to e-mail:
Subject: Thanks for getting in touch! I don’t work for MEND – I am a researcher who is trying to find out more about what families think about the MEND scheme.
MEND (Mind, Exercise, Nutrition, Do it!) classes try to help children and families live healthy lives. We are looking for families who thought about going to MEND classes, or started but decided they were not right for them. Maybe you went along a few times, or found out more and decided not to join. If this sounds like you I’d like to talk to you!
Glossary
- MEND 7–13
- Mind, Exercise, Nutrition, Do it! (MEND) weight management intervention for children who are overweight and aged 7–13 years.
- MEND Central
- Organisation which sells MEND interventions to commissioners and delivery partners.
- MEND-eligible population
- Children living in England between January 2007 and December 2010 (when MEND data were collected) who are of the same age as MEND children and are overweight.
- Overweight
- A child, or group of children, whose body mass index exceeds the 91st centile of the UK 1990 growth charts. In this report, this term always includes those children who are obese (exceed the 98th centile of the UK 1990 growth charts) unless otherwise stated.
- zBMI
- Body mass index standardised by age and sex using UK 1990 growth charts.
List of abbreviations
- BIC
- Bayesian information criterion
- BLF
- Big Lottery Fund
- BME
- black and minority ethnic
- BMI
- body mass index
- CI
- confidence interval
- HSE
- Health Survey for England
- IDACI
- Income Deprivation Affecting Children Index
- LSOA
- lower super output area
- MAR
- missing at random
- MCAR
- missing completely at random
- MCS
- Millennium Cohort Study
- MEND
- Mind, Exercise, Nutrition, Do it!
- NatCen
- National Centre for Social Research
- NCB
- National Children’s Bureau
- NCMP
- National Child Measurement Programme
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NOO
- National Obesity Observatory
- NRES
- NHS Research Ethics
- ONS
- Office for National Statistics
- PAG
- project advisory group
- PCT
- primary care trust
- PEAR
- Public health, Education, Awareness, Research
- PLEM
- Population-Level Evaluation of MEND
- PSS
- personal social services
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SDQ
- Strengths and Difficulties Questionnaire
- SEC
- socioeconomic circumstances
- UCL
- University College London
- YMCA
- Young Men’s Christian Association