Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3010/14. The contractual start date was in July 2011. The final report began editorial review in July 2013 and was accepted for publication in April 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Bambra et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
There is growing evidence of the impact of overweight and obesity on short- and long-term functioning, health and well-being. 1 Internationally, childhood obesity rates continue to rise in some countries (e.g. Mexico, India, China, Canada), although there is emerging evidence of a slowing of this increase or a plateauing in some age groups. However, in most European countries, the USA and Australia,2,3 socioeconomic inequalities in obesity and risk factors for obesity are widening. 1,4–7 Obesity is causally linked to chronic diseases such as diabetes, coronary heart disease, stroke, hypertension, osteoarthritis and certain forms of cancer. 8 It is predicted that, as the UK population grows and ages, the burden of diseases associated with obesity will cost the NHS £10B per year by 20504 and will result in escalating numbers of early deaths as well as long-term incapacity and associated reductions in quality of life. 8 Childhood obesity is a particular concern and it is widely accepted that there is a link between childhood obesity and morbidity and mortality in later life. 9,10 Tackling obesity is therefore rightly highlighted as one of the major contemporary public health policy challenges and vital in terms of addressing health inequalities. 4,8 The seminal Foresight review of obesity also highlighted the importance of taking a whole-systems approach to tackling the ‘obesity epidemic’,4 whereby interventions target the broader societal determinants of obesity. 5 This is because the aetiology of obesity is complex; it is the outcome of important structural drivers in the food system (such as upsizing to increase sales, use of extracted fat, replacement of fat by sugar, marketing directed at children through the education system and social media) and in the contemporary organisation of society (e.g. ‘labour-saving’ devices, cities designed for cars, long working hours, lack of green space).
Inequalities in obesity
Childhood obesity is associated with social and economic deprivation in developed countries worldwide, with higher prevalence in the lowest-income quintile. 11–14 In the UK, cross-sectional data from a recent Health Survey for England15 have shown strong associations between adult and childhood obesity and a number of socioeconomic status (SES) indicators (Index of Multiple Deprivation, Income Deprivation Affecting Children Index, eligibility for free school meals, household income and household occupation-based social class). In some areas, childhood obesity rates in the most deprived quintile were almost double those in the least deprived quintile. 15,16 Longitudinal data from a UK cohort found that SES differences in childhood obesity began to emerge at 4 years of age and continued to widen as age increased. 17 Data from longitudinal analyses suggest that social disadvantage accumulated throughout the life course impacts on widening inequalities in obesity into adulthood. 11
There are also socioeconomic inequalities in the distribution of obesity risk factors. Obesity has multiple but inter-related aetiological dimensions such as diet and physical activity as well as biological or genetic components. In adults, evidence suggests that a socioeconomic gradient exists in physical activity levels, with low-income groups participating in exercise to a lesser extent. In children, however, studies are inconsistent regarding the distribution of physical activity levels across the socioeconomic strata, with some studies suggesting that there is no relationship between SES and participation in physical activity. Similarly, in terms of diet, studies have found that those in the higher socioeconomic groups have more healthy diets than those in the lower socioeconomic groups. Giskes et al. 18 conducted a systematic review of socioeconomic inequalities in dietary intakes associated with weight gain and overweight or obesity among European adults. Their synthesis of 47 empirical studies found a consistent association between low fruit and vegetable consumption and deprivation.
Policy context
Addressing inequalities in obesity therefore has a very high profile on the public health agenda in the UK and internationally. However, there is a lack of accessible policy-ready evidence on what works in terms of interventions to reduce inequalities in obesity. Existing systematic reviews examine only the effects of interventions that reduce overall levels of obesity, as opposed to the effects on inequalities in obesity. There is therefore no information to help policy-makers and commissioners of services assess what types of interventions are most effective at reducing inequalities in obesity. This evidence gap has been noted in the recent report of the Priority Public Health Conditions Task Group 8 of the Department of Health-commissioned Strategic Review of Health Inequalities in England Post 2010 (Marmot review)19,20 in that an overt call was made for evidence syntheses on what types of interventions work to reduce inequalities in obesity prevalence, how and in what circumstances. The Evidence for Policy and Practice Information and Co-ordinating Centre report into childhood obesity also called for future systematic reviews to examine the effectiveness of interventions in reducing inequalities and improving the obesity levels of disadvantaged groups. 21 Similarly, at the international level, Robertson et al. 6 identified the need for ‘evidence of the reach and penetration of interventions in lower income groups’ as a priority area for research (p. 10). Internationally, importance is also attached to ‘the development and testing of social determinants of health indicators and intervention impact evaluation’ by the World Health Organization (WHO) Commission on the Social Determinants of Health (p. 20). 22 It is critical for policy-making in this area then that evidence on the effectiveness of different types of interventions at tackling inequalities is systematically identified, appraised and synthesised.
Further, there is increasing recognition among policy-makers that to effectively tackle complex health problems such as obesity and to reduce health inequalities requires integrated policy action across different intervention levels (individual, community, society) as well as across the life course (childhood and adulthood). 4,11 The organisation and implementation of such interventions is also important. 23 Against this backdrop we conducted two systematic reviews to address this deficit in the knowledge base by reviewing primary studies of the effectiveness of interventions to reduce SES inequalities in obesity in a whole-systems way. The reviews therefore examine public health interventions at the individual, community and societal levels. 24 They also examine the organisation, implementation and delivery of such interventions.
Intervention framework
To support the conduct of the reviews we developed a novel framework for how inequalities in obesity might be tackled (Table 1). This shows that interventions are characterised by their level of action and their approach to tackling inequalities. Following Whitehead,25 there are four levels of interventions to tackle inequalities: strengthening individuals (person-based strategies to improve the health of disadvantaged individuals), strengthening communities (improving the health of disadvantaged communities and local areas by building social cohesion and mutual support), improving living and school environments (reducing exposure to health-damaging material and psychosocial environments across the whole population) and promoting healthy macro policy (improving the macroeconomic, cultural and environmental contexts that influence the standard of living achieved by the whole population). According to Graham and Kelly,26 these interventions are underpinned by one of three different approaches to health inequality: disadvantage (improving the absolute position of the most disadvantaged individuals and groups), gap (reducing the relative gap between the best- and worst-off groups) or gradient (reducing the entire social gradient). Interventions are thus either targeted (such as individual-level interventions that are underpinned by health as disadvantage) or universal (such as living and school condition interventions that potentially influence the entire social gradient in health). In the systematic reviews, the interventions that we identify for inclusion must not only fulfil these criteria but also present appropriate analyses, that is, the SES of the targeted group or, for universal studies, outcomes by different SES groupings. Included studies will be grouped according to this framework (with acknowledgement that some interventions, such as Sure Start, might be cross-cutting; see Whitehead25). Examples of interventions at each level and for each approach are shown in Table 1.
| Approach to tackling health inequality | Level of intervention | ||||
|---|---|---|---|---|---|
| Individual | Community | Societal | |||
| Strengthening Individuals | Strengthening communities | Improving living and school/work conditions | Promoting healthy macro policies | ||
| Disadvantage | Targeted | Health education, health promotion and social marketing; diet and exercise advice and counselling; weight-management advice and monitoring; conditional cash transfers; lifestyle counselling; exercise on prescription | Community health and fitness centres; health trainers; school-based exercise programmes; group or community-based exercise programmes; group, community or school-based diet, lifestyle or weight-management advice and counselling; healthy eating campaigns in schools; group or community organised education or support; localised point of sale social marketing; neighbourhood-based physical activity programmes | ||
| Gap | |||||
| Gradient | Universal | Access to physical fitness facilities (e.g. gym subsidies); availability of healthy food; green spaces, walk-ability and the built environment; traffic light labelling | Restrictions on advertising high-fat and high-sugar foods; food prices and agricultural subsidies (e.g. changing the Common Agricultural Policy); fiscal measures to regulate supply and demand (e.g. taxing high-fat and high-sugar foods) | ||
Chapter 2 Part 1: how effective are public health interventions at reducing socioeconomic inequalities in obesity among children?
Review methods
The review was carried out following established criteria for the good conduct and reporting of systematic reviews. 27,28 The full review protocol was published in BMC Systematic Reviews29 and is registered with the PROSPERO International Prospective Register of Systematic Reviews (registration no. CRD42011001740). A study steering group comprising key stakeholders from the UK policy and research communities, international representatives, a statistician and a health economist guided the research.
Interventions
The review examined interventions at the individual, community and societal level that might reduce inequalities in obesity among children aged 0–18 years (including prenatal), in any setting, in any country. The review utilised the intervention framework (see Table 1) to group studies into different types, with acknowledgement that some interventions might be multilevel. We defined individual-level interventions as those that included individualised/one-to-one health promotion, education, advice, counselling or subsidy and which were conducted in a health-care or research setting or in participants’ homes; community-level interventions as group-based health promotion-, education-, advice-, counselling- or subsidy-only interventions, or interventions conducted in a community setting (e.g. a school, community centre, sports centre, shop); societal (environmental)-level interventions as those that included a change in environment or access to an environment; and societal (macro)-level interventions as macrolevel policies such as taxation, advertising restrictions or subsidies. Interventions were also classified in terms of whether they took a gradient approach (‘universal’ interventions) or a disadvantaged approach (‘targeted’ interventions). This distinction is described further in Outcomes. The review considered public health strategies that might reduce existing inequalities in the prevalence of obesity (i.e. effective targeted interventions or universal interventions that work more effectively in low-SES groups) as well as those interventions that might prevent the development of inequalities in obesity (i.e. universal interventions that work along the SES gradient). For the purpose of this review, treatment interventions were defined as those that allowed participants to take part in the study only if they have a body mass index (BMI) (or some other proxy for body fat) at or above a certain threshold. Preventative interventions were defined as those that allowed participants with any BMI to take part in the study, even if the study was targeted at groups who have a higher than average BMI (and potentially all of the participants in the study were overweight or obese). Treatment interventions that involve drugs or surgery, and laboratory-based studies, were excluded from the review.
Study design
A rigorous and inclusive international literature search was conducted for all intervention studies that aimed to reduce childhood obesity that were either targeted at disadvantaged individuals, communities or society or aimed at reducing childhood obesity universally but analysed and presented the effects of the intervention by SES. We included randomised and non-randomised controlled trials (RCTs). We also included prospective and retrospective cohort studies (before-and-after studies), with or without control groups, and prospective repeat cross-sectional studies with or without control groups. Studies with a duration of at least 12 weeks (combination of intervention and follow-up) were included, an inclusion criterion used in previous Cochrane reviews of obesity interventions. 30,31
Search strategy
The following nine electronic databases were searched (host sites given in parentheses): MEDLINE (Ovid), EMBASE (Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (NHS Evidence Health Information Resources), PsycINFO (NHS Evidence Health Information Resources), Social Science Citation Index (Web of Science), Applied Social Sciences Index and Abstracts (ASSIA) [Cambridge Scientific Abstracts (CSA)], International Bibliography of the Social Sciences (IBSS) (EBSCOhost), Sociological Abstracts (CSA) and the NHS Economic Evaluation Database [NHS Centre for Reviews and Dissemination (CRD)].
A trained information scientist (HJM) developed and implemented the electronic searches. All databases were searched from their start date (e.g. MEDLINE starts in 1946) to 10 October 2011. All searches are detailed in Appendix 1. We did not exclude papers on the basis of language, country or publication date.
The electronic database searches were supplemented with website and grey literature searches. The websites searched were the National Obesity Observatory, the Association for the Study of Obesity, the National Obesity Forum, the Department of Health, the International Association for the Study of Obesity and the WHO and the grey literature repositories searched were the Obesity Learning Centre and NHS Evidence. We hand searched the bibliographies of all included studies and requested relevant information on unpublished and in-progress research from key experts in the field. In addition, we hand searched the last 2 years of the most common five journals revealed by the electronic searches (International Journal of Obesity, Preventative Medicine, Medicine and Science in Sport and Exercise, American Journal of Clinical Nutrition and Journal of the American Dietetic Association).
Outcomes
In terms of outcomes, we included studies only if they included a primary outcome that is a proxy for body fat (weight and height, BMI, waist measurement/waist to hip proportion, percentage fat content, skinfold thickness, ponderal index in relation to childhood obesity). Data on related secondary outcomes (such as physical activity levels, dietary intake, blood results such as cholesterol and glucose levels) were also extracted from those included studies that had a primary outcome. We included both measured and self-reported outcomes.
Universal intervention studies were included only if they examined differential effects with regard to SES (education, income, occupation, social class, deprivation, poverty). We only included targeted intervention studies that had been targeted specifically at disadvantaged groups (e.g. children of the unemployed, lone parents, low income groups) or were conducted in deprived areas (e.g. schools in deprived areas). Data on the organisation, implementation and delivery of interventions were extracted by adapting and refining the Egan et al. 23 methodological tool for the assessment of the implementation of complex public health interventions in systematic reviews (Box 1). Although most of the existing constructs in the Egan et al. tool (originally designed for workplace interventions) were relevant to our review, we made the following refinements: the themes ‘manager support’ and ‘employer support’ were removed and the themes ‘delivery fidelity’, ‘sustainability of the intervention’ and ‘stakeholder support’ were added.
A – Motivation – why was the intervention implemented (e.g. to reduce obesity)?
B – Theoretical underpinning (e.g. social cognitive theory, nudge).
C – Implementation context (social, economic, political, managerial).
D – Experience of intervention team (planners and implementers).
E – Consultation and/or collaboration processes (planning and delivery stages) (e.g. consultation with parents/community, participatory research methods used).
F – Delivery fidelity – was the intervention delivered as intended?
G – Sustainability of the intervention – strength of the institution implementing the intervention; integration of activities into existing programmes/services/curriculum, etc.; training/capacity-building component; community involvement/participation.
H – Stakeholder support.
I – Resources described (e.g. time, money, staff and equipment)?
J – Differential effects and population characteristics described (e.g. ethnicity, gender, age)?
Adapted from Egan et al. 23
Data extraction and quality appraisal
The initial screening of titles and abstracts was conducted by one reviewer (FCH), with a random 10% of the sample checked by a second reviewer (HJM). Agreement between the reviewers was fair (kappa = 0.66) and discrepancies between reviewers mainly resulted from the main reviewer (FCH) being more inclusive. The screening of the full papers was conducted by one reviewer (FCH), with a random 10% of the sample checked by a second reviewer (HJM). Agreement between the reviewers was also fair at this stage (kappa = 0.72). Data extraction was conducted by one reviewer (FCH – individual and community; CLB – societal; CDS – multilevel) using established data extraction forms27,32–37 (see Appendix 2) and was independently checked by a second reviewer (HJM, FCH or JMC). The methodological quality of the included studies was appraised independently by two reviewers (FCH, HJM, CLB or CDS) using the Cochrane Public Health Review Group-recommended Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Quantitative Studies38 (see Appendix 3). Any discrepancies were resolved through discussion between the authors and, if consensus was not reached, through discussion with the project lead (CLB). We used the quality appraisal criteria for descriptive purposes only and to highlight variations between the studies.
Analysis and synthesis
Because of the heterogeneity of the studies it was possible to use meta-analysis only for a minority of the included studies (some of the community-level and environment-level experimental studies only). Effect estimates from suitable experimental studies were pooled in meta-analysis by use of the R statistics package ‘metafor’ (The R Foundation for Statistical Computing, Vienna, Austria). Random-effects models were used to summarise the estimates if the test for heterogeneity was significant (defined conservatively as p < 0.20) or if the I2 statistic was moderate or high (> 50%). Publication bias was explored through the use of Egger’s test.
Sensitivity analysis was performed for the meta-analysed studies by investigating whether the heterogeneity between studies can be explained by study type (preventative or targeted) or effect type (diet plus physical activity, diet only or physical activity only). The two variables were included in the meta-analysis model and subgroup analysis was performed for a variable with a significant difference between the outcomes. The extent of the sensitivity analyses depended on the available data.
When meta-analysis was not possible, narrative synthesis was conducted. In keeping with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines39 and our protocol,29 the narrative synthesis examines the effects of (1) individual-, (2) community- and (3) societal-level (macro and environmental) public health interventions on socioeconomic inequalities in obesity, using the multidimensional framework outlined in Table 1. We focus on differential effectiveness by SES. Interventions are also grouped when possible according to the age group targeted: prenatal, early years and primary and secondary school age interventions (as well as generic all-age interventions). There were insufficient data to enable the conduct of any demographic subgroup analysis by age, gender or ethnicity. However, the age range of children is noted using the following categorisation from a previous Cochrane review:31 prenatal, preschool age (0–5 years), primary school age (6–12 years) and secondary school age (13–18 years).
Changes from the original protocol
Two changes were made from the original protocol (which is available to view at www.nets.nihr.ac.uk/__data/assets/pdf_file/0017/55223/PRO-09-3010-14.pdf; accessed 18 July 2014):
-
A considerably higher number of articles were identified from the database searches than had been anticipated (n = 56,967). This resulted in a very high number of full papers that required review (n = 1418) and a much larger than expected number of studies meeting the final review inclusion criteria (n = 76). On the basis of practicality and to complete the review in a reasonable time frame we did not contact all authors of studies (n = 1418) on the general population effects of interventions to reduce obesity for any unpublished data that they might have that related to SES inequalities.
-
In our original protocol we stated that we would use the Cochrane system of domain-based quality appraisal for randomised studies and a different tool (such as the Newcastle–Ottawa scale) for the quality appraisal of non-experimental studies. However, the Cochrane Public Health Review Group now recommends the EPHPP Quality Assessment Tool for Quantitative Studies for quality appraisal and we used this instead as it covers both experimental and non-experimental studies, making it easier for interpretation by readers.
Studies included in the review
A total of 76 unique studies (from 85 papers40–124) were included in the review. There were 1140–43,46–54 unique studies of individual-level interventions (nine40–43,46–52 treatment, one54 prevention and one53 treatment and prevention); 5244,45,55–106 studies of community-level interventions (2044,45,59,60,84,87,88,90–92,96–106 treatment, 3255–58,61–83,85,86,89,93–95 prevention); 10107–121 environmental-level societal studies (nine107–112,114–121 prevention and one113 treatment and prevention); and three122–124 multilevel studies (all prevention). There were no studies of the policy-type societal-level interventions. The process of inclusion and exclusion of studies is detailed in Figure 1. Details of included studies by intervention level are provided in Appendix 5. Full summaries of each study are provided in Appendix 6.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for child studies.

The included studies were of varying study designs, with 4248,50,53,54,57–59,62,63,67–69,71,73–81,83,84,86,87,89,90,93–97,98,102,103,106–119,124 experimental (largely cluster trials) and 3440–47,49,51,52,55,56,60,61,64–66,70,72,82,85,88,91,92,96,97,99–101,104,105,120–123 observational studies. The majority of studies came from the USA and Europe, including two from the UK46,91,92 (Figure 2). There were no included studies on prenatal interventions, 19 on preschool-aged children, 61 on primary school children and 21 on secondary age children (a number of studies included children from more than one age group). Studies largely used BMI (n = 68) or the prevalence of obesity (n = 17) as the main outcome. Very few studies examined differential intervention effects by SES (n = 25), with the vast majority of included studies being of the targeted variety (n = 51), for example studies of interventions targeted at low-income children or schools in deprived areas. There were few high-quality studies (n = 15), with the majority being of only low (n = 30) or moderate (n = 31) quality. Descriptions of how interventions were implemented were also very mixed.
FIGURE 2.
The geographical distribution of the included child studies.

Studies excluded from the review
Figure 1 details the process of inclusion and exclusion of studies from the review. The reasons for the exclusion of papers at the full paper stage (n = 1339) are available from the authors on request. The most common reason for exclusion was lack of data by SES.
Results of the review
Individual-level interventions
Overview
Eleven individual-level studies were identified that met the review inclusion criteria. 40–43,46–54 Because of heterogeneity in terms of study design and main outcomes, as well as the generally poor quality of data reporting in the studies (e.g. studies seldom reported means and standard deviations), it was not possible to conduct meta-analysis for this subset of interventions. The 11 studies are therefore synthesised narratively in terms of whether they followed a universal (n = 740,41,46,48–53) or a targeted (n = 442,43,47,54) approach. The results are also summarised in Table 37 (universal-approach studies) and Table 38 (targeted-approach studies) (see Appendix 5), with effect size data presented (when possible) in Tables 2–5 and implementation information provided in Tables 39 and 40 (see Appendix 5).
The majority of the studies (n = 840–43,46–50) were of weight-management diet and physical activity treatment programmes for childhood obesity conducted in medical/health-care or university settings. In addition, one study investigated a home-based obesity treatment programme51,52 and two studies, one treatment53 and one prevention,54 investigated interventions delivered primarily in participants’ homes. Four47,48,53,54 studies were conducted in the USA, two40,49,50 in Australia and one each in the UK,46 Germany,51,52 Belgium,41 New Zealand43 and Spain. 42 One study was published in a Spanish-language journal42 and one study was published in both German- and English-language journals. 117–119 The remaining studies were published in English-language journals.
The numbers of participants in the studies varied considerably, between n = 16 and n = 445, and the median follow-up time was 12 months (range 3–48 months). The studies were conducted among children aged from 0 to 18 years, with five42,43,46,48,53 including those of preschool age (from 0 to 5 years), 1040–43,46–54 including primary school-aged children (aged 6–12 years) and six40,41,43,46,47,49,54 including secondary school-aged children (aged 13–18 years). There were four48,50,53,54 experimental studies and seven40–43,46,47,49,51,52 observational studies. Seven40,42,47–50,53,54 of the studies were of moderate quality and the remaining studies were of low quality (using the EPHPP tool; see Appendix 3). All of the studies used measured primary outcomes. All of the studies reported some elements of how the intervention was implemented (see Appendix 5, Tables 39 and 40), particularly in terms of motivation, context and resources.
Universal interventions
Three48,50,53 experimental studies and four40,41,46,49,51,52 observational studies took a universal approach and measured outcomes between SES groups (see Appendix 5, Table 37). One experimental study evaluated a home-based intervention intended to reduce the sedentary behaviours (television viewing and computer use) of children (aged 4–7 years) who were either at risk of becoming overweight or obese or already overweight or obese. 53 The active control group received general information on parenting tips, activities and recipes. The study found more favourable intervention effects in terms of a reduced BMI for participants from a low-SES background than for those from a high-SES background. This study was of moderate quality although it had a relatively small final sample size (n = 67). Another moderate-quality experimental study of a health-care setting-based obesity treatment programme (compared with usual care) for preschool children (aged 2–6 years)48 found more favourable results in those of low-SES than in those of high-SES in terms of reduction in BMI (Table 2). The final experimental study (no-intervention control) of a health-care setting-based obesity treatment programme (moderate quality)50 found no relationship between SES and intervention effects on BMI, waist circumference or prevalence of obesity in children aged 5–10 years (see Table 2).
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Nutrition and physical activity interventions | ||||||||
| Taveras et al. 201148 | ||||||||
| BMI (kg/m2) | 160 | 0.27 | 1.39 | 153 | 0.26 | 1.11 | 0.01 (–0.21 to 0.23) | Higher-income group |
| BMI (kg/m2) | 88 | 0.4 | 1.59 | 38 | 1.42 | 1.79 | –0.62 (–1.01 to –0.23) | Lower-income group |
| BMI (kg/m2) | 147 | 0.18 | 1.33 | 127 | 0.27 | 1.13 | –0.07 (–0.31 to 0.17) | Higher-education group |
| BMI (kg/m2) | 106 | 0.49 | 0.16 | 65 | 0.91 | 1.61 | –0.42 (–0.73 to –0.11) | Lower-education group |
| Wake et al. 200950 | ||||||||
| BMI (kg/m2) | 127 | 0.6 | 2.45 | 115 | 0.7 | 2.16 | –0.04 (–0.29 to 0.21) | SES did not modify the effect of the intervention on BMI |
Four observational studies also followed a universal approach40,41,46,49,51,52 (Table 3). These observational studies found more beneficial effects in low-SES groups than in high-SES groups. Two studies (both of low quality) investigating the effects of obesity treatment programmes that targeted both diet and physical activity behaviours in children aged 2–18 years46 and 7–17 years41 found no association between SES indicators and outcomes, although the study by Sabin et al. 46 found a hospital obesity service to be effective in reducing BMI overall. One moderate-quality study found that a treatment programme targeting diet behaviours was more effective in high-SES children aged 10–17 years. 40,49 One low-quality study investigating a home-based diet and physical activity counselling intervention for overweight and obese children (mean age 6.5 years) found that the intervention was less effective in children of low SES than in those of high SES. 51,52 This study had a long duration (4 years); however, it had a very small final sample size (n = 16) and subgroup analysis should be treated with caution.
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Nutrition-only interventions | ||||||||
| Baxter et al. 201140 | ||||||||
| BMI z-score | 88 | –0.12 | 0.41 | NA | NA | NA | –0.29 (–0.58 to 0) | Higher social advantage associated with weight loss |
| Nutrition and physical activity interventions | ||||||||
| Langnäse et al. 200451 | ||||||||
| BMI (kg/m2) | 11 | –0.6 | 7.4 | 10 | 7.5 | 11.5 | –0.82 (–1.7 to 0.06) | High SES |
| BMI (kg/m2) | 15 | 5.2 | 8.3 | 16 | 2.2 | 6 | 0.41 (–0.3 to 1.12) | Low SES |
| BMI z-score | 11 | –0.3 | 0.5 | 10 | 0.1 | 0.7 | –0.63 (–1.51 to 0.25) | High SES |
| BMI z-score | 15 | –0.02 | 0.4 | 16 | –0.1 | 0.4 | 0.19 (–0.52 to 0.9) | Low SES |
| Waist-to-height ratio | 11 | –4.7 | 2.8 | 10 | –2.3 | 8.5 | –0.37 (–1.23 to 0.49) | High SES |
| Waist-to-height ratio | 15 | –0.6 | 10.8 | 16 | –3.5 | 12.6 | 0.24 (–0.47 to 0.95) | Low SES |
| % fat mass | 11 | –3.2 | 26.9 | 10 | 16.2 | 38.2 | –0.57 (–1.45 to 0.31) | High SES |
| % fat mass | 15 | –1.1 | 19.3 | 16 | 17 | 30.9 | –0.68 (–1.41 to 0.05) | Low SES |
| Fat mass (kg) | 11 | 6.6 | 47.2 | 10 | 37.4 | 69.2 | –0.51 (–1.37 to 0.35) | High SES |
| Fat mass (kg) | 15 | 21.2 | 27.6 | 16 | 32.4 | 53.3 | –0.25 (–0.96 to 0.46) | Low SES |
| FFM (kg) | 11 | 13.5 | 11.3 | 10 | 12.8 | 4.8 | 0.08 (–0.78 to 0.94) | High SES |
| FFM (kg) | 15 | 17.2 | 11.7 | 16 | 10.5 | 9.4 | 0.61 (–0.12 to 1.34) | Low SES |
| Braet 200641 | ||||||||
| Adjusted BMI (%) | 110 | –28.94 | 29.38 | NA | NA | NA | –0.99 (–1.26 to –0.72) | SES not a predictor of weight loss |
| Sabin et al. 200746 | ||||||||
| BMI z-score | 58 | –0.3 | 5.79 | NA | NA | NA | –0.05 (–0.42 to 0.32) | No correlation between Townsend score and fall in BMI z-score |
Targeted interventions
One experimental54 and three observational42,43,47 studies examined targeted individual-level interventions. The one experimental study (no-intervention control) was of moderate quality. 54 It found that a home-based mentor-based health promotion and obesity prevention intervention for children aged 11–16 years reduced the prevalence of obesity and reduced percentage body fat and increased the fat-free mass of the overweight and obese participants (Table 4). Of the three observational studies that followed a targeted approach, two investigated the effects of obesity treatment programmes based in a health-care setting, one in children aged 10–14 years47 and the other in those aged 2–13 years. 42 These moderate-quality studies both found improvements in at least one obesity-related outcome: a reduction in BMI47 and a reduction in the prevalence of obesity but not in BMI42 (Table 5). The other study investigated the effects of a more general nurse-led healthy lifestyle clinic that followed a holistic approach to health needs defined by each patient (not necessarily obesity). 43 This low-quality study found no intervention effect on BMI in patients aged 0–18 years.
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Nutrition and physical activity interventions | |||||||
| Black et al. 201054 | |||||||
| BMI z-score | 89 | 0.01 | 1.19 | 90 | 0.06 | 1.12 | –0.04 (–0.33 to 0.25) |
| % body fat | 89 | –2.2 | 10.58 | 90 | 1.15 | 11.59 | –0.3 (–0.59 to –0.01) |
| Fat mass (kg) | 89 | 0.26 | 11.31 | 90 | 2.71 | 9.1 | –0.24 (–0.53 to 0.05) |
| FFM (kg) | 89 | 5.68 | 9.95 | 90 | 4.77 | 9.82 | 0.09 (–0.2 to 0.38) |
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Nutrition and physical activity interventions | |||||||
| Fernandez De Velasco Galan et al. 200842 | |||||||
| BMI (kg/m2) | 69 | –1.94 | 3.26 | NA | NA | NA | –0.6 (–0.93 to –0.27) |
| Smith et al. 201047 | |||||||
| BMI (kg/m2) | 23 | –0.52 | 5.75 | NA | NA | NA | –0.09 (–0.68 to 0.5) |
Community-level interventions
Overview
Fifty-two community studies44,45,55–106 (from 54 papers) were identified that met the review inclusion criteria. Because of heterogeneity in terms of study design and main outcomes, as well as the generally poor quality of data reporting in the studies (e.g. studies seldom reported means and standard deviations), it was possible to conduct meta-analysis for only a small subset of interventions in this category (n = 13 targeted interventions). The fifty-two studies are therefore synthesised narratively in terms of whether they followed a universal (n = 1644,45,57,64,74–77,86,88,96–98,100–102,104,105) or a targeted (n = 3654,56,58–63,65–73,78–85,87,89–95,99,103,106) approach. The results are also summarised in Table 41 (universal-approach studies) and Table 42 (targeted-approach studies) (see Appendix 5). Effect size data (when possible) are displayed in Tables 6–9. The meta-analysis of the 13 suitable studies is reported separately at the end of this section with the raw data in Table 10. The implementation information for each study is contained in Tables 43 and 44 (see Appendix 5).
The majority of the studies (n = 3055–75,77–86) investigated interventions that were conducted in school (including preschool/kindergarten and after-school) settings. The setting of one of these studies was not clearly reported;60 however, the intervention was based around school semesters and therefore it is assumed that it was a school-based intervention. Seven studies investigated interventions conducted in community centres or community venues such as sports centres76,87–93 and two studies took place in Head Start centres (preschool centres similar to the UK’s Sure Start centres). 94,95 One study took place in both community centres and homes. 106 Ten studies investigated group-based childhood obesity treatment programmes. Seven of these were conducted in medical/health-care or university settings. 44,45,96–102 In the other three studies the settings were not clearly reported but each investigated group-based weight-management programmes and read as if they were held in medical or university settings. 103–105
The majority of the studies (n = 3255–58,61–83,85,86,89,93–95) were public health interventions that aimed to promote a healthy weight, either by preventing overweight and obesity in those of a healthy weight or reducing weight in those already overweight or obese until they reached a healthy weight. These interventions were targeted at populations of children regardless of their weight status, whereas the remaining 20 studies44,45,59,60,84,87,88,90–92,96–106 were treatment interventions for overweight and obese children. Sixteen44,45,57,64,74–77,86,88,96–98,100–102,104,105 followed a universal approach and either included subgroup analysis of different SES groups or explored associations between SES and intervention outcomes. The remaining 36 studies55,56,58–63,65–73,78–85,87,89–95,99,101,103,106 were targeted at low-SES or disadvantaged groups or areas.
The majority of the studies were from the USA (n = 31);55–62,70–71,76,80–85,90,93–97,99,101–106 in addition, four were conducted in Germany,44,45,72,100 three in Chile65–67 and two in each of Australia,69,78 Brazil,79,87 France64,86 and Denmark72,88 (the study reported by Nemer et al. 72 was conducted in both Germany and Denmark). Of the remaining studies there was one each from Israel,73 the Netherlands,63 Peru,89 Sweden,68 New Zealand,77 Finland98 and the UK. 91,92 Five studies were published in foreign-language journals,45,65,66,74,87 although two of the studies also had results published in English-language journals. 44,75
Most of the studies (n = 4244,45,55–59,61–63,65–67,70,72,74–88,90–93,96–103,105,106) were conducted among primary school-age children (aged 6–12 years), 10 studies61,64–66,73,77,82,87,89,94,95 were conducted among preschool groups (aged 0–5 years) and 1444,45,59,60,68,69,71,72,91,92,96,99–101 were conducted among secondary school-age children (aged 13–18 years) (14 studies spanned multiple age groups). Thirteen57,63,67,76,79,83,86,87,89,90,93,94,98 of the studies were of high quality, 1844,45,64–66,69,71,78,81,82,84,88,96,100–102 were of moderate quality and 2155,56,58–62,70,72–75,77,80,85,95,97,99,104–106 were of low quality (using the EPHPP tool; see Appendix 3). All of the studies included measured primary outcomes and all reported some elements of how the intervention was implemented (see Appendix 5, Tables 43 and 44), particularly in terms of motivation and context.
Universal interventions
Seven57,74–77,86,98,102 experimental studies followed the universal approach, with five57,74,75,77,98,102 evaluating diet and physical activity interventions and the other two76,86 evaluating physical activity-focused interventions.
Five studies,57,76,86,98,102 four of high quality57,76,86,98 and one of moderate quality,102 found no differences in intervention effects by SES. One school-based cardiovascular disease risk factor reduction intervention comprising nutrition and physical activity education and physical activity sessions was effective at reducing skinfold thickness in children aged 8–10 years (compared with usual care);57 one intervention aimed at increasing physical activity through education, extra physical education classes and activity events reduced the rate of increase in BMI in children aged 11–12 years for up to 3 years but this was not maintained at 4 years (compared with usual care);86 one intervention aimed at reducing sedentary behaviour (television viewing and video game use) in children aged 8–9 years reduced a number of obesity-related outcomes (BMI, triceps skinfold thickness, waist circumference and waist-to-hip ratio) (compared with usual care);76 and two smaller (n < 150) studies investigated health-care setting-based obesity treatment programmes in children aged 7–9 years (compared with usual care)98 and 8–12 years (compared with a low-intensity intervention) (Table 6). 102
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Physical activity-only interventions | ||||||||
| Robinson 199976 | ||||||||
| BMI (kg/m2) | 92 | 0.29 | 3.72 | 100 | 0.71 | 3.77 | –0.11 (–0.38 to 0.16) | No differences in results when adjusted for parental education |
| Triceps skinfold thickness (mm) | 92 | 0.92 | 6.01 | 100 | 2.49 | 5.35 | –0.28 (–0.57 to 0.01) | |
| Waist (cm) | 92 | 3.09 | 9.44 | 100 | 4.92 | 8.91 | –0.2 (–0.47 to 0.07) | |
| Hip (cm) | 92 | 3.75 | 8.43 | 100 | 4.09 | 8.56 | –0.04 (–0.31 to 0.23) | |
| Waist-to-height ratio | 92 | 0 | 0.06 | 100 | 0.02 | 0.05 | –0.36 (–0.65 to –0.07) | |
| Nutrition and physical activity interventions | ||||||||
| Kalavainen et al. 200798 | ||||||||
| Weight loss for height (%) | 35 | –6.8 | 6.2 | 35 | –1.8 | 6.2 | –0.8 (–1.29 to –0.31) | No association between social class and change in outcomes |
| BMI (kg/m2) | 35 | –0.8 | 1 | 35 | 0 | 1.1 | –0.75 (–1.24 to –0.26) | |
| BMI z-score | 35 | –0.3 | 0.3 | 35 | –0.2 | 0.3 | –0.33 (–0.8 to 0.14) | |
One study of low quality did, however, find that a school-based obesity prevention intervention was effective at reducing the prevalence of overweight in high-SES children but not in low-SES children (mean age 6.3 years) (compared with no intervention),74,75 and another study of low quality found that another school-based obesity prevention intervention showed a trend (although not significant) towards more favourable intervention effects in higher-SES schools in terms of body fat increases over 2 years in younger children (5 years old at baseline) but not in older children (10 years old at baseline) (compared with no intervention). 77 Both of these studies had large sample sizes (n = 135277 and n = 176474,75) and long follow-up durations (277 and 474,75 years).
Nine44,45,64,88,96,97,100,101,104,105 observational studies also followed a universal approach. One of these studies followed both universal and targeted approaches as the study population was predominantly those of low SES but within this the results were also broken down by an indicator of SES (receiving Medicaid or not). 101 One study of moderate quality that included the evaluation of two levels of intervention found that a basic obesity information provision intervention was effective at reducing BMI of low-SES preschool children (aged 3–4 years) but not of children of higher SES. 64 This study also found that a reinforced intervention of obesity information provision along with a diet and physical activity education programme was effective at reducing BMI of children in both SES groups.
Seven studies44,45,88,96,97,100,101,105 of group- or community-based obesity treatment programmes (five of moderate quality44,45,88,96,100,101 and two of low quality97,105) found that the programmes led to reductions in BMI or percentage overweight and that the intervention effects were the same across different SES groups (Table 7). Each of these studies was conducted in children aged 7–12 years and/or adolescents aged 13–18 years. Jelalian et al. 104 also found that BMI or weight reductions were not associated with SES in a group-based weight control programme in children aged 13–18 years (low-quality study; overall results not reported). However, one low-quality study of a group-based weight loss intervention in a sample aged 8–12 years reduced the per cent overweight overall but larger reductions were observed in higher-SES children. 97
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Nutrition and physical activity interventions | ||||||||
| Heinberg et al. 201096 | ||||||||
| BMI (kg/m2) | 104 | –0.7 | 8.19 | NA | NA | NA | –0.09 (–0.36 to 0.18) | No difference in SES between those who lost weight and those who did not |
| Pott et al. 201045 | ||||||||
| BMI z-score | 116 | –0.3 | 0.33 | NA | NA | NA | –0.91 (–1.18 to –0.64) | No difference in parent education between those who lost weight and those who did not |
Targeted interventions
Twenty-three58,59,62,63,67–69,71,73,78–80,81,83,84,87–90,93–95,103,106 experimental studies followed a targeted approach (Table 8). Eleven58,59,63,67,73,81,83,89,93,94,103 examined interventions that targeted both diet and physical activity behaviours; 1068,69,71,78,80,84,88,90,95,106 investigated interventions that targeted physical activity and sedentary behaviours only; and two62,79 investigated interventions targeting diet behaviours only. Thirteen55,56,60,61,65,66,70,72,82,85,91,92,99,101 observational studies followed a targeted approach, with 1155,56,60,65,66,70,72,82,85,99,101 investigating interventions targeting diet and physical activity behaviours and two investigating interventions that targeted physical activity behaviour (Table 9).
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Nutrition-only interventions | |||||||
| Sichieri et al. 200979 | |||||||
| BMI (kg/m2) | 434 | 0.32 | 1.49 | 493 | 0.22 | 0.31 | 0.1 (–0.04 to 0.24) |
| Physical activity-only interventions | |||||||
| Alves et al. 200887 | |||||||
| BMI (kg/m2) | 39 | –0.3 | 3.17 | 39 | 0.3 | 2.91 | –0.2 (–0.65 to 0.25) |
| Lubans et al. 201169 | |||||||
| BMI (kg/m2) | 50 | –0.7 | 1.08 | 50 | 0 | 1.19 | –0.62 (–1.01 to –0.23) |
| BMI z-score | 50 | –0.3 | 0.36 | 50 | –0.1 | 0.36 | –0.55 (–0.94 to –0.16) |
| Body fat (%) | 50 | –6.7 | 3.97 | 50 | –4.9 | 3.96 | –0.45 (–0.84 to –0.06) |
| Myers 200871 | |||||||
| BMI (kg/m2) | 44 | 0.02 | 1.47 | 59 | 0.21 | 0.84 | –0.17 (–0.56 to 0.22) |
| Robinson et al. 200390 | |||||||
| Waist (cm) | 28 | 0.62 | 14.21 | 33 | 1.08 | 13.26 | –0.03 (–0.54 to 0.48) |
| BMI (kg/m2) | 134 | 1.28 | 0.9 | 127 | 1.24 | 1.01 | 0.04 (–0.2 to 0.28) |
| BMI z-score | 134 | 0.26 | 0.19 | 127 | 0.24 | 0.19 | 0.11 (–0.13 to 0.35) |
| Waist (cm) | 134 | 4.15 | 2.21 | 127 | 4.25 | 2.54 | –0.04 (–0.28 to 0.2) |
| Triceps skinfold thickness (mm) | 134 | 1.49 | 3.01 | 127 | 1.93 | 2.74 | –0.15 (–0.39 to 0.09) |
| Weintraub et al. 200884 | |||||||
| BMI (kg/m2) | 9 | 0.22 | 5.2 | 12 | 0.36 | 4.64 | –0.03 (–0.89 to 0.83) |
| BMI z-score | 9 | –0.09 | 0.47 | 12 | 0 | 0.31 | –0.22 (–1.08 to 0.64) |
| Nutrition and physical activity interventions | |||||||
| Bellows 200794 | |||||||
| BMI (kg/m2) | 96 | 0.19 | 1.91 | 105 | –0.08 | 1.69 | 0.15 (–0.12 to 0.42) |
| BMI z-score | 96 | 0.13 | 1 | 105 | –0.01 | 0.99 | 0.14 (–0.13 to 0.41) |
| Figueroa-Colon et al. 199659 | |||||||
| BMI (kg/m2) | 12 | –3.8 | 3.2 | 7 | 0.2 | 0.9 | –1.45 (–2.49 to –0.41) |
| % ideal body weight | 12 | –24.3 | 20 | 7 | –0.3 | 5.9 | –1.39 (–2.43 to –0.35) |
| Hamad et al. 201189 | |||||||
| BMI z-score | 279 | 0.05 | 1.35 | 319 | –0.18 | 1.35 | 0.17 (0.01 to 0.33) |
| Janicke et al. 2011103 | |||||||
| BMI z-score | 22 | 0.012 | 0.23 | 11 | 0.03 | 0.16 | –0.09 (–0.82 to 0.64) |
| Jansen et al. 201163a | |||||||
| BMI (kg/m2) | 657 | 0.42 | 2.88 | 729 | 0.5 | 2.93 | –0.03 (–0.13 to 0.07) |
| Waist (cm) | 657 | 1.02 | 8.27 | 729 | 2.13 | 8.38 | –0.13 (–0.23 to –0.03) |
| Jansen et al. 201163b | |||||||
| BMI (kg/m2) | 583 | 0.76 | 4.11 | 653 | 0.71 | 3.96 | 0.01 (–0.11 to 0.13) |
| Waist (cm) | 583 | 2.78 | 11.08 | 653 | 3.43 | 11.14 | –0.06 (–0.18 to 0.06) |
| Kain et al. 200467c | |||||||
| BMI (kg/m2) | 1146 | 0 | 3.6 | 491 | 0.3 | 3.2 | –0.09 (–0.19 to 0.01) |
| BMI z-score | 1146 | –0.12 | 0.95 | 491 | –0.02 | 0.87 | –0.11 (–0.21 to –0.01) |
| Triceps skinfold thickness (mm) | 1146 | –0.5 | 6.2 | 491 | –0.8 | 5.75 | 0.05 (–0.05 to 0.15) |
| Waist (cm) | 1146 | –0.9 | 10.27 | 491 | 0.9 | 9.1 | –0.18 (–0.28 to –0.08) |
| Kain et al. 200467d | |||||||
| BMI (kg/m2) | 995 | 0.3 | 3.85 | 454 | 0.2 | 3.8 | 0.03 (–0.09 to 0.15) |
| BMI z-score | 995 | –0.04 | 0.9 | 454 | –0.07 | 0.91 | 0.03 (–0.09 to 0.15) |
| Triceps skinfold thickness (mm) | 995 | 0.5 | 6.2 | 454 | 0.9 | 6.5 | –0.06 (–0.18 to 0.06) |
| Waist (cm) | 995 | 0.8 | 9.9 | 454 | 1.1 | 9.6 | –0.03 (–0.15 to 0.09) |
| Nemet et al. 201173 | |||||||
| BMI (kg/m2) | 376 | –0.25 | 0.04 | 349 | –0.18 | 0.04 | –1.75 (–1.93 to –1.57) |
| BMI (%) | 376 | –6.4 | 0.8 | 349 | –5.9 | 0.8 | –0.62 (–0.78 to –0.46) |
| Walter et al. 198583 | |||||||
| Ponderosity index | 805 | 0.1 | 1.95 | 310 | 0.1 | 1.86 | 0 (–0.14 to 0.14) |
| Triceps skinfold thickness (mm) | 805 | 1.1 | 6.25 | 310 | 1.2 | 5.6 | –0.02 (–0.16 to 0.12) |
| Willet 199693 | |||||||
| BMI (kg/m2) | 18 | 2.6 | 5.16 | 22 | 2.6 | 7.27 | 0 (–0.63 to 0.63) |
| % overweight | 18 | 11.9 | 22.91 | 22 | 12.4 | 41.01 | –0.01 (–0.64 to 0.62) |
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Physical activity-only interventions | |||||||
| Rudolf et al. 2006,91 200492 | |||||||
| BMI z-score | 48 | –0.07 | 0.16 | NA | NA | NA | –0.44 (–0.85 to –0.03) |
| Nutrition and physical activity interventions | |||||||
| Annesi 201055a | |||||||
| BMI (kg/m2) | 139 | –0.05 | 0.5 | NA | NA | NA | –0.1 (–0.34 to 0.14) |
| Annesi 201055b | |||||||
| BMI (kg/m2) | 61 | –0.48 | 0.74 | NA | NA | NA | –0.65 (–1.02 to –0.28) |
| Annesi et al. 200756c | |||||||
| BMI (kg/m2) | 62 | –1.24 | 4.65 | NA | NA | NA | –0.27 (–0.62 to 0.08) |
| Body composition | 62 | –1.44 | 7.27 | NA | NA | NA | –0.2 (–0.55 to 0.15) |
| Annesi et al. 200756d | |||||||
| BMI (kg/m2) | 51 | –0.84 | 11.53 | NA | NA | NA | –0.07 (–0.46 to 0.32) |
| Body composition | 51 | –0.9 | 5.03 | NA | NA | NA | –0.18 (–0.57 to 0.21) |
| Annesi et al. 200756e | |||||||
| BMI (kg/m2) | 66 | –1.09 | 3.7 | NA | NA | NA | –0.29 (–0.62 to 0.04) |
| Body composition | 66 | –2.67 | 6.7 | NA | NA | NA | –0.4 (–0.75 to –0.05) |
| Annesi et al. 200756f | |||||||
| BMI (kg/m2) | 62 | –1.06 | 6.98 | NA | NA | NA | –0.15 (–0.5 to 0.2) |
| Body composition | 62 | –1.07 | 4.82 | NA | NA | NA | –0.22 (–0.57 to 0.13) |
| Kain et al. 200965g | |||||||
| BMI z-score | 98 | –0.06 | 0.86 | NA | NA | NA | –0.07 (–0.34 to 0.2) |
| Waist (cm) | 98 | 1.3 | 5.2 | NA | NA | NA | 0.25 (–0.02 to 0.52) |
| Kain et al. 200965h | |||||||
| BMI z-score | 213 | –0.04 | 0.9 | NA | NA | NA | –0.04 (–0.24 to 0.16) |
| Waist (cm) | 213 | 1.5 | 8.2 | NA | NA | NA | 0.18 (–0.02 to 0.38) |
| Kain et al. 200965i | |||||||
| BMI z-score | 211 | 0.03 | 0.98 | NA | NA | NA | 0.03 (–0.17 to 0.23) |
| Waist (cm) | 211 | 0.6 | 9.4 | NA | NA | NA | 0.06 (–0.14 to 0.26) |
| Kain et al. 201066 | |||||||
| BMI z-score | 714 | –0.11 | 1.05 | NA | NA | NA | –0.1 (–0.2 to 0) |
| Moore et al. 200970 | |||||||
| Weight percentile | 126 | 1.6 | 23.76 | NA | NA | NA | 0.07 (–0.18 to 0.32) |
| BMI percentile | 126 | 0.3 | 25.95 | NA | NA | NA | 0.01 (–0.24 to 0.26) |
| Topp et al. 200982 | |||||||
| BMI (kg/m2) | 49 | 0.2 | 6.5 | NA | NA | NA | 0.03 (–0.36 to 0.42) |
| BMI percentile | 49 | –0.2 | 26.15 | NA | NA | NA | –0.01 (–0.4 to 0.38) |
| % body fat | 49 | –0.2 | 15.75 | NA | NA | NA | –0.01 (–0.4 to 0.38) |
| Fat weight (lb) | 49 | 1.4 | 30.17 | NA | NA | NA | 0.05 (–0.34 to 0.44) |
| Lean weight (lb) | 49 | 2.3 | 15.7 | NA | NA | NA | 0.15 (–0.24 to 0.54) |
| Weight-to-height ratio | 49 | –0.01 | 0.06 | NA | NA | NA | –0.17 (–0.56 to 0.22) |
Diet and physical activity
Eleven58,59,63,67,73,81,83,89,93,94,103 of the experimental studies investigated interventions that targeted both diet and physical activity behaviours: nine58,63,67,73,81,83,89,93,94 obesity prevention programmes (eight school- or after-school-based interventions and one targeted at parents receiving microcredit loans) and two59,103 weight loss treatment programmes (one school-based and one group-based intervention).
Four58,59,63,67 of the 11 studies (two of high quality and two of low quality; all using no-intervention control groups) found that the intervention investigated led to decreases in obesity-related outcomes among those aged 6–12 years: BMI58,59 (boys only67), percentage overweight (6–9 years only),63 percentage above ideal body weight,59 triceps skinfold thickness (boys only)67 and waist circumference67 (boys aged 6–9 years only63). The prevalence of overweight was also reduced in the low-quality study of preschool children by Nemet et al. 73 (with a no-intervention control group). The remaining six81,83,89,93,94,103 studies of children in similar age groups found no intervention effects; four of these were rated as being of high quality83,89,93,94 and two were rated as being of moderate quality. 81,103 Two studies used an active control group (receiving interventions unrelated to nutrition or physical activity),81,93 one study compared a nutrition-only intervention with the same intervention with a physical activity component added94 and the remaining studies used no-intervention or usual-care control groups.
There were also eleven observational studies of diet and physical activity-targeted interventions, six of which recorded reductions in BMI55,56,60,66,72,101 along with reductions in body composition,56 body fat,101 triceps skinfold thickness,60 waist circumference60 and obesity prevalence;66 however, four of these studies were of low quality55,56,60,72 and two of moderate quality. 66,101 The remaining five studies (three of low quality70,85,99 and two of moderate quality65,82) found no changes in any obesity-related outcome from baseline to follow-up. 65,70,82,85,99
Physical activity and sedentary behaviours
Ten68,69,71,78,80,84,87,90,95,106 of the targeted experimental studies investigated interventions that targeted physical activity and sedentary behaviours only. Six68,69,71,78,80,95 of these studies investigated obesity prevention interventions (all school or preschool based) and four84,87,90,106 investigated obesity treatment programmes (two based in community centres and homes, one school based and one conducted in a disadvantaged Brazilian community).
Five of the studies (including two treatment studies) found at least one beneficial intervention effect on obesity or related outcomes (BMI,69,78,84,87 weight,80 skinfold thickness,80 prevalence of obesity69 and prevalence of overweight69). One of these studies was of high quality,87 three were of moderate quality69,78,84 and one was of low quality. 80 Four of the studies78,80,84,87 were conducted in children aged from 6 to 12 years (one also included 5-year-olds87) and the other69 was conducted in adolescents. One of the studies used a wait list control group,69 another used an active control group (health education programme)84 and the remaining studies used a no-intervention/usual-care control group.
The remaining five studies68,71,90,95,106 (including two treatment studies) found no intervention effects. Of these studies, one was rated as being of high quality,90 two were of moderate68,71 and two were of low quality. 95,106 One of the studies was conducted with preschool children,95 two with children from the age group 6–12 years90,106 and two with adolescents. 68,71 Two studies used an active control group (general health intervention)90,106 and three studies used no-intervention/usual-care control groups. 68,71,95
Two observational studies examined physical activity-only interventions. One low-quality study found a reduction in BMI91,92 and one other low-quality study found no changes in outcomes. 61
Diet only
Two of the targeted experimental studies (with no-intervention control groups) investigated interventions targeting diet behaviours only. 62,79 Both studies, one of high quality79 and one of low quality,62 were school-based prevention studies and found no intervention effects on BMI in children from the age group 6–12 years.
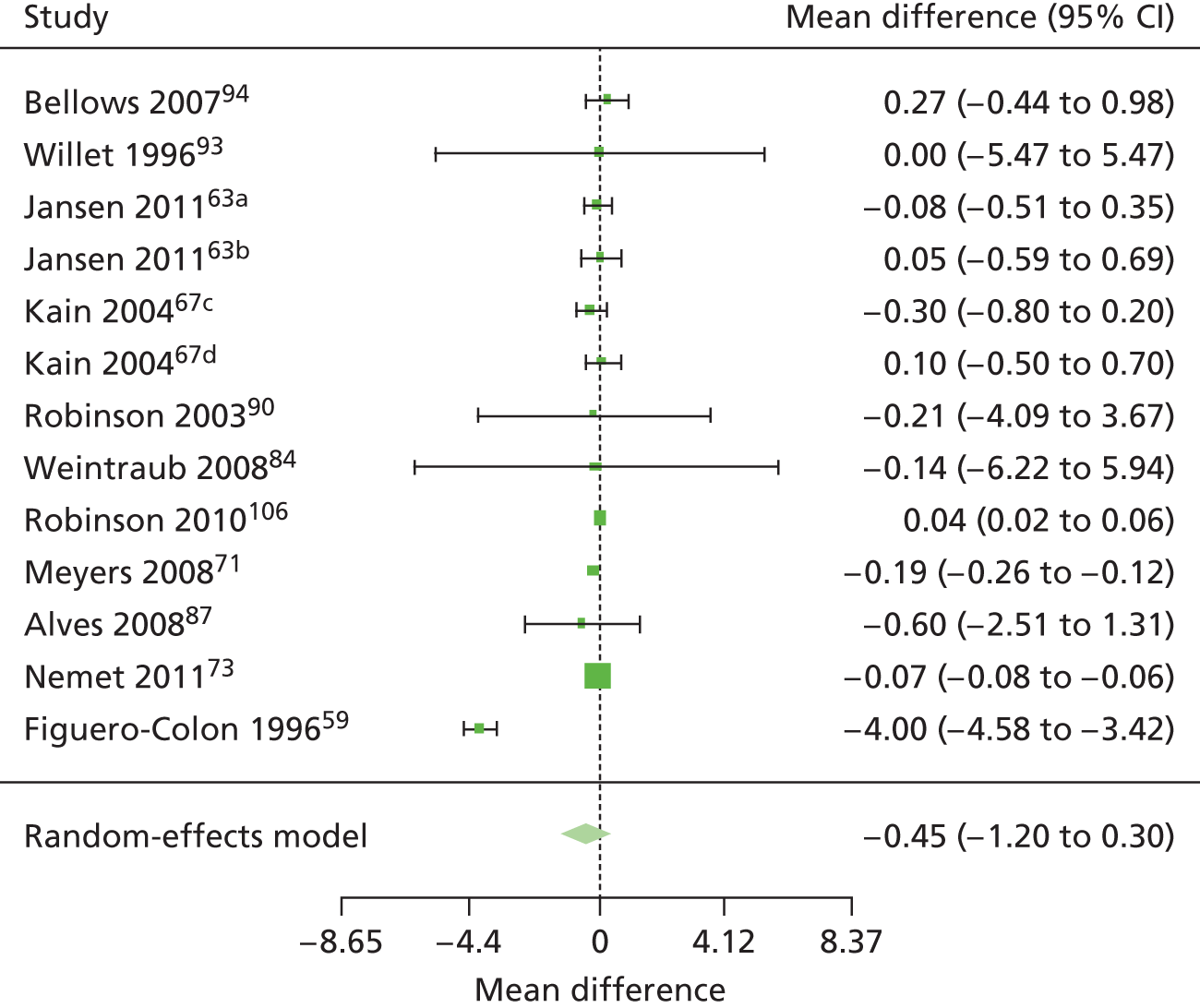
Meta-analysis of community-level interventions
Effect estimates were pooled for the 11 experimental studies of physical activity/diet interventions for which there were sufficient data in terms of sample size and mean and standard deviation values for both the control group and the intervention group, both before and after the intervention (Table 10). 59,63,67,71,73,84,87,90,93,94,106 Two studies reported effects seperately by group: boys and girls67 and 6–9 years and 10–12 years;63 therefore, two sets of data are included in the analysis for each of these studies. The common outcome was BMI change. A random-effects model (in R statistics package ‘metafor’) was used to incoporate heterogeneity between studies, which may have been a result of differences in the interventions as well as in the samples (e.g. age). The level of heterogeneity means that the results of the meta-analysis should be treated with caution. Using Egger’s test (z = 0.0242, p = 0.9807), there is no indication of publication bias. Mean differences and 95% confidence intervals (CIs) are presented for the pooled BMI data.
| Study | Intervention | Control | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| Bellows 200794 | 96 | 0.19 | 2.69 | 105 | –0.08 | 2.39 |
| Willet 199693 | 18 | 2.6 | 7.3 | 22 | 2.6 | 10.29 |
| Jansen et al. 201163a | 657 | 0.42 | 4.07 | 729 | 0.5 | 4.15 |
| Jansen et al. 201163b | 583 | 0.76 | 5.81 | 653 | 0.71 | 5.6 |
| Kain et al. 200467c | 1146 | 0 | 5.09 | 491 | 0.3 | 4.52 |
| Kain et al. 200467d | 995 | 0.3 | 5.44 | 454 | 0.2 | 5.37 |
| Robinson et al. 200390 | 28 | 0.5 | 7.69 | 33 | 0.71 | 7.71 |
| Weintraub et al. 200884 | 9 | 0.22 | 7.36 | 12 | 0.36 | 6.57 |
| Robinson et al. 2010106 | 134 | 1.28 | 0.07 | 127 | 1.24 | 0.08 |
| Myers 200871 | 44 | 0.02 | 0.22 | 59 | 0.21 | 0.1 |
| Alves et al. 200887 | 39 | –0.3 | 4.48 | 39 | 0.3 | 4.12 |
| Nemet et al. 201173 | 376 | –0.25 | 0.04 | 349 | –0.18 | 0.04 |
| Figueroa-Colon et al. 199659 | 12 | –3.8 | 0.92 | 7 | 0.2 | 0.34 |
Figure 3 shows the resulting forest plot. Only one of the 11 studies59 shows a positive effect for the intervention. The summary meta-analysis suggests that overall the interventions did not significantly reduce BMI among children (random-effects model pooled mean difference estimate of –0.45, 95% CI –1.20 to –0.30). There was evidence of subtantial heterogeneity between studies (I2 = 71.74%, p = 0.0047). A sensitivity analysis, which adjusted for moderators (prevention compared with treatment, physical activity intervention compared with physical activity and diet intervention, and study quality), was conducted and this also found that there was no significant intervention effect [described further in Analysis of the robustness of the results (sensitivity analyses)].
FIGURE 3.
Random-effects meta-analysis of BMI change: child community-level intervention studies. a, 6–9 years; b, 10–12 years; c, boys; d, girls.
Societal-level interventions: environment
Overview
No studies of ‘healthy macro policies’ such as restrictions on advertising high-fat foods or agricultural subsidies were located that met the systematic review inclusion criteria (see Figure 1). However, in terms of improving living and working conditions, 10107–121 ‘societal-level’ studies were located that examined multicomponent school environment and education interventions intended to prevent increases in childhood obesity or overweight (summarised in Table 45). All of the studies evaluated interventions in disadvantaged areas (targeted approach). Eight studies examined the combined impact of nutritional education or physical activity alongside changing elements of the school food environment, particularly in terms of introducing nutritional standards for food sold in schools or introducing water fountains. 107–119 One study examined the effects of a school breakfast programme120 and one examined increased access to healthy meals and physical activity. 121
Most studies were conducted in the USA (n = 7107–111,113–116,121), with one each from Germany,117–119 Chile112 and Mexico. 120 There were no UK studies. Two studies112,120 were published in Spanish-language journals and one study117 was published in German, along with two English articles. 118,119 The other seven107–111,114,115 studies were all published in English-language journals. The studies were conducted among children aged from 3 to 17 years, with two studies conducted with children aged 0–5 years,114,121 six conducted with children aged 6–12 years107–111,115–119 and one conducted with children aged 13–18 years. 112 The age of the participants was not reported in the study by Perman et al. 113 but this study included schoolchildren. There were seven107–111,113–119 experimental studies and three112,120,121 observational studies. Seven107–109,112,114,116–119,121 of the studies were of high or moderate quality (using the EPHPP tool; see Appendix 3), with all including independently measured primary outcomes. Most of the studies reported some elements of how the intervention was implemented (see Appendix 5, Table 46), particularly in terms of motivation and delivery fidelity.
Because of heterogeneity in terms of study design and main outcomes, as well as the generally poor quality of data reporting in the studies (e.g. studies seldom reported means and standard deviations), it was possible to conduct meta-analysis for only a small subset of interventions in this category (n = 4 targeted interventions). The 10 studies are, therefore, synthesised narratively. The results are also summarised in Table 45 (see Appendix 5). Effect size data (when possible) are reported in Tables 11 and 12. The meta-analysis of the four107–110 suitable studies is reported separately at the end of this section, with the raw data used provided in Tables 13 and 14.
Targeted interventions
The seven107–111,113–119 experimental studies (five107–109,114,116–119 of moderate quality and two110,111,113,115 of low quality; all using no-intervention control groups) all examined targeted interventions among deprived populations, mostly of children from the 6–12 years age group, with one study carried out with preschool children. The interventions were of promising – albeit only limited and inconsistent – effectiveness as, although most did not reduce the prevalence of overweight and obesity or necessarily prevent new incidence of overweight and obesity (confirmed by the meta-analysis; see Meta-analysis of environmental-level interventions), they did tend to slow down the rate of incidence or weight or BMI gain among poorer children and thus decrease the size of the growth in the SES gap in prevalence (Table 11). In other words, they slowed the epidemic increase in risk of overweight or obesity among the low-income children under study.
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Nutrition-only interventions | |||||||
| Foster et al. 2010108 | |||||||
| BMI z-score | 2307 | –0.05 | 1.05 | 2296 | –0.01 | 1.08 | –0.04 (–0.1 to 0.02) |
| Waist (cm) | 2307 | 4.6 | 14.95 | 2296 | 5.3 | 14.8 | –0.05 (–0.11 to 0.01) |
| Perman et al. 2008113 | |||||||
| BMI (kg/m2) | 166 | –3.57 | 29.55 | 184 | –1.39 | 25.68 | –0.08 (–0.3 to 0.14) |
| Muckelbauer et al. 2011117 | |||||||
| BMI z-score | 1641 | 0.005 | 0.289 | 1309 | 0.007 | 0.295 | –0.01 (–0.09 to 0.07) |
Two observational studies112,120 (one120 of low quality and one112 of moderate quality) found no significant intervention effects, one in children from the 6–12 years age group and one in adolescents, whereas another, better-quality study121 found a decrease in obesity prevalence but not overweight in preschool children (Table 12).
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Nutrition-only interventions | |||||||
| Ramirez-Lopez et al. 2005120 | |||||||
| BMI (kg/m2) | 254 | 17.1 | 0.1 | 106 | –0.1 | 0.2 | 125.19 (116.04 to 134.34) |
| Body fat (%) | 254 | 29.2 | 0.1 | 106 | –0.5 | 0.2 | 216.17 (200.37 to 231.97) |
| No. overweight and obese (%) | 254 | 17.4 | 10.8 | 106 | –1 | 8.06 | 1.83 (1.58 to 2.08) |
| No. obese (%) | 254 | 17.4 | 10.8 | 106 | –3 | 9.99 | 1.93 (1.66 to 2.2) |
Meta-analysis of environmental-level interventions
Effect estimates were pooled for four of the five experimental studies of nutritional interventions for which there were useable data107–110 in relation to two common outcomes: differences in prevalence of overweight and obesity (four studies107–110) and differences in prevalence of obesity (three studies108–110). Random-effects models were used in all cases to incorporate heterogeneity between studies. The heterogeneity between studies may have been a result of differences in the interventions as well as in the samples (e.g. age). Odds ratios (ORs) and 95% CIs are presented for the pooled prevalence data.
Prevalence of overweight and obesity
The four studies107–111 show a range of effectiveness, with the summary meta-analysis suggesting that overall the nutritional interventions did not significantly reduce the prevalence of overweight and obesity among children aged 4–11 years (random-effects model pooled OR estimate of 0.85, 95% CI 0.71 to 1.02) (Figure 4). There was evidence of subtantial heterogeneity between studies (I2 = 71.74%, p = 0.0047) and this meta-analysis result should be treated with caution. Using Egger’s test (z = –0.6706, p = 0.5025), there is no indication of publication bias. Raw data for the studies included in the meta-analysis are presented in Table 13.
FIGURE 4.
Random-effects meta-analysis of the prevalence of overweight and obesity: societal-level intervention studies.
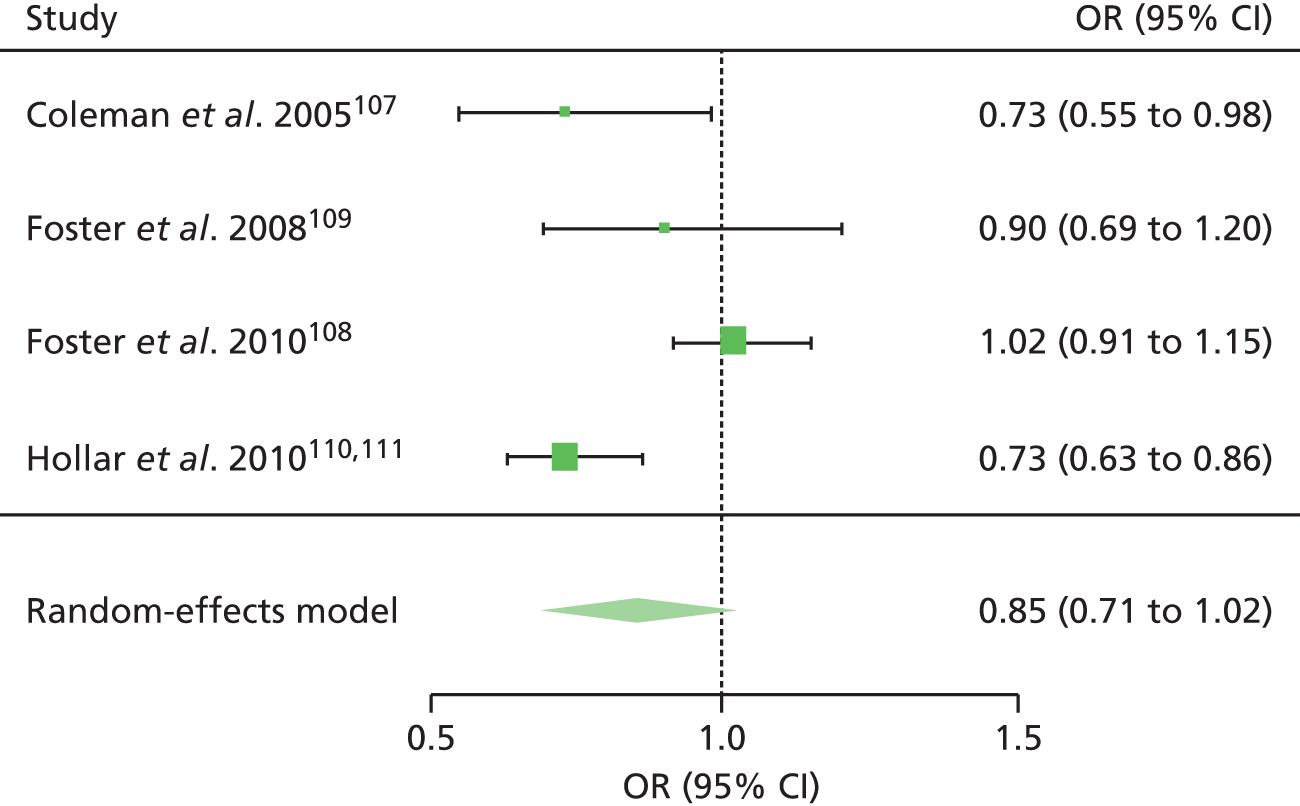
| Study | Treatment | Overweight, n | Not overweight, n | OR (95% CI) |
|---|---|---|---|---|
| Coleman et al. 2005107 | Intervention | 147 | 253 | |
| Control | 152 | 192 | 0.73 (0.55 to 0.98) | |
| Foster et al. 2008109 | Intervention | 204 | 275 | |
| Control | 164 | 201 | 0.90 (0.69 to 1.20) | |
| Foster et al. 2010108 | Intervention | 1057 | 1250 | |
| Control | 1038 | 1258 | 1.02 (0.91 to 1.15) | |
| Hollar et al. 2010110,111 | Intervention | 1207 | 1825 | |
| Control | 350 | 387 | 0.73 (0.63 to 0.86) |
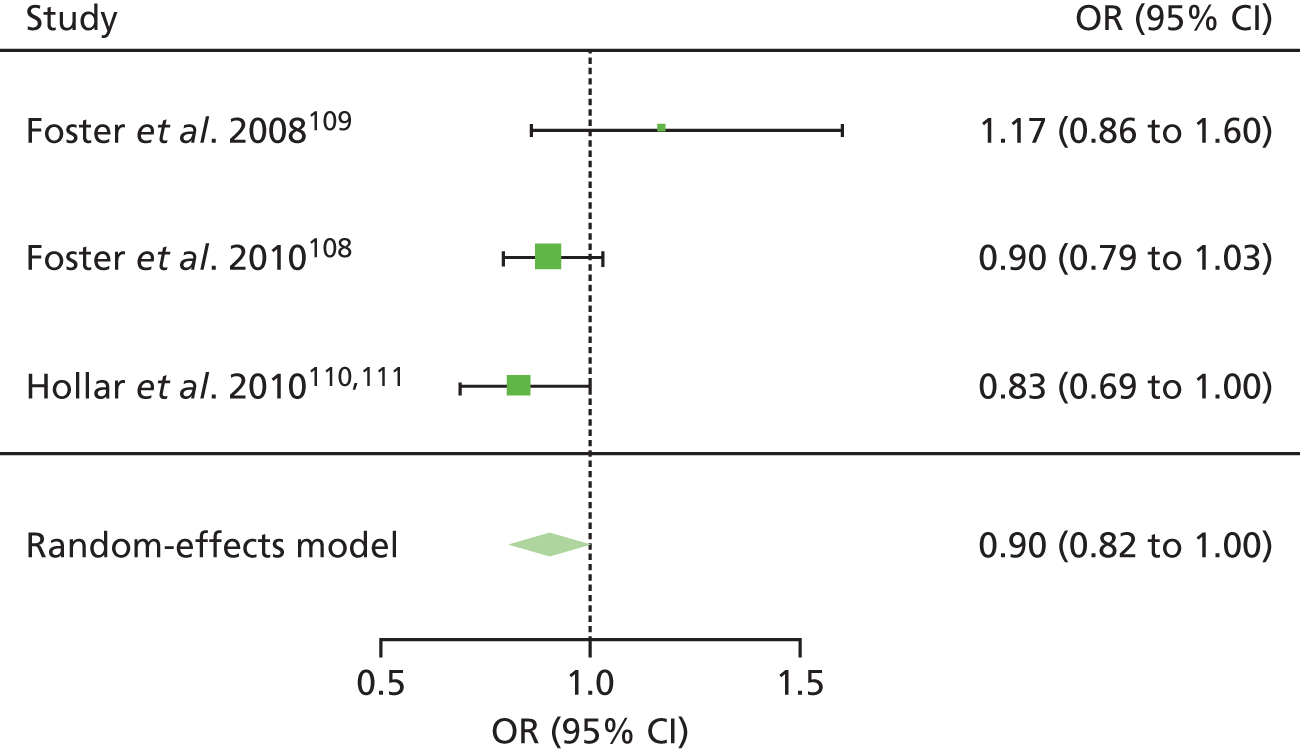
Prevalence of obesity
Three studies108–110 all found that nutritional interventions did not significantly reduce the prevalence of obesity among children aged 4–11 years and this is reinforced by the summary meta-analysis (random-effects model pooled OR estimate of 0.92, 95% CI 0.79 to 1.06) (Figure 5). There was no evidence of heterogeneity between studies (I2 = 0%, Q = 3.46, p = 0.1765). Using Egger’s test (z = 1.1820, p = 0.2372), there was no indication of publication bias. Raw data for the studies included in the meta-analysis are presented in Table 14.
FIGURE 5.
Random-effects meta-analysis of the prevalence of obesity: societal-level intervention studies.
Societal-level interventions: healthy macro policies
No studies identified.
Multilevel interventions: individual, community and societal (environmental)
Overview
Three studies,122–124 although described as community level, contained elements that spanned each of the levels of interventions described in our framework (see Table 1) – individual, community and societal (environmental). Each of these studies investigated obesity prevention interventions that primarily took place in school settings but also involved the wider community through partnership (capacity-building) approaches. Two of the studies were conducted in the USA122,123 and one was conducted in Australia. 124 All of the studies were published in English-language journals. Because of heterogeneity in intervention types, meta-analysis was not conducted and the studies are therefore synthesised narratively in terms of whether they followed a universal (n = 2122,124) or a targeted (n = 1123) approach. The results are also summarised in Tables 47 and 48 (see Appendix 5). The effect size data of the studies (when possible) are reported in Tables 15 and 16. The implementation information is contained in Tables 49 and 50 (see Appendix 5).
Universal approach
Two of the studies, one experimental124 and one observational,122 followed a universal approach and explored differential effects by SES. The high-quality experimental study by Sanigorski et al. 124 found favourable effects (significantly lower increases) for waist circumference and BMI z-score in the intervention group compared with the no-intervention control group although BMI changes were no different (Table 15). There was no association between SES and intervention effects in the intervention schools; however, lower SES was associated with a greater gain in body fat and waist circumference in the control schools. The low-quality observational study by Chomitz et al. 122 also found non-stratified decreases in BMI z-score and prevalence of obesity (Table 16).
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Nutrition and physical activity interventions | ||||||||
| Sanigorski et al. 2008124 | ||||||||
| BMI (kg/m2) | 833 | 16.7 | 3.47 | 974 | 1.3 | 3.26 | 4.57 (4.39 to 4.75) | Lower SES associated with a greater increase in outcomes in the control group but not in the intervention group |
| BMI z-score | 833 | –0.39 | 0.93 | 974 | –0.02 | 0.88 | –0.41 (–0.51 to –0.31) | |
| Waist (cm) | 833 | 61.8 | 10.28 | 974 | 4.2 | 9.93 | 5.71 (5.49 to 5.93) | |
| Waist-to-height ratio | 833 | 0.43 | 0.05 | 974 | –0.01 | 0.05 | 7.97 (7.7 to 8.24) | |
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Nutrition and physical activity interventions | ||||||||
| Chomitz et al. 2010122 | ||||||||
| BMI z-score | 1053 | –0.53 | 1.01 | –0.52 (–0.6 to –0.44) | High SES | |||
| BMI z-score | 803 | –0.29 | 1.06 | –0.27 (–0.37 to –0.17) | Low SES | |||
Targeted approach
One low-quality observational study by Hoelscher et al. 123 targeted a low-income school population. It observed larger decreases in the number of children who were overweight but not obese in the schools receiving an obesity prevention intervention with community involvement than in the schools receiving the obesity prevention intervention with no community involvement.
Synthesis of the ‘best-available’ international evidence
This review used very broad study inclusion criteria and conducted a very wide search to capture the entire evidence base on the effects of interventions to reduce inequalities in obesity among children. This has resulted in the inclusion of a total of 76 unique studies on the effects of individual (n = 11), community (n = 52), societal (n = 10) and individual, community and societal (n = 3) interventions. This is a very large evidence base and much larger than anticipated. To make sense of it for policy and practice, this section focuses on synthesising only the ‘best-available’ evidence for each intervention type (n = 23). For the individual-level interventions (n = 4), the ‘best-available’ international evidence is provided by moderate-quality experimental studies; for the community-level interventions (n = 13) and the individual-, community- and societal-level interventions (n = 1), the ‘best-available’ international evidence is provided by high-quality experimental studies; and for the societal (environmental)-level interventions (n = 5), the ‘best-available’ evidence is provided by moderate-quality experimental studies. The findings of the ‘best-available’ evidence studies are summarised in Table 17. Overall, this shows very clearly that the various interventions either reduced inequalities in obesity (i.e. they reduced the prevalence of obesity-related outcomes among low-SES groups or they closed the SES gap) or had no effect, with no studies reporting a negative impact (i.e. increasing the gap in obesity-related outcomes). In the following sections the results of these international studies are synthesised in more detail by intervention type.
| Study | Impact on inequalities in obesity |
|---|---|
| Individual-level interventions (experimental, moderate quality, n = 4) | |
| Taveras et al. 201148 | + |
| Epstein et al. 200853 | + |
| Black et al. 201054 | + |
| Wake et al. 200950 | 0 |
| Community-level interventions (experimental, high quality, n = 13) | |
| Kain et al. 200467 | + (in boys) |
| Jansen et al. 201163 | + |
| Alves et al. 200887 | + |
| Sichieri et al. 200979 | + (in girls) |
| Simon et al. 200886 | 0 |
| Bingham 200257 | 0 |
| Kalavainen et al. 200798 | 0 |
| Robinson 199976 | 0 |
| Bellows 200794 | 0 |
| Walter et al. 198583 | 0 |
| Willet 199693 | 0 |
| Hamad et al. 201189 | 0 |
| Robinson et al. 200390 | 0 |
| Societal-level interventions (experimental, moderate quality, n = 5) | |
| Foster et al. 2008109 | + |
| Foster et al. 2010108 | + |
| Heath and Coleman 2003,116 Coleman et al. 2005107 | + |
| Muckelbauer et al. 2009,118,119 2011117 | + |
| Williams et al. 2004114 | 0 |
| Individual/community/societal-level interventions (experimental, high quality, n = 1) | |
| Sanigorski et al. 2008124 | + |
Individual-level interventions
Four high-quality experimental studies examined individual interventions, three universal48,50,53 and one targeted. 54 Two of the studies examined tailored weight loss programmes delivered through primary care for children of all SES. 48,50 One study investigated a screen time-reduction intervention that aimed to reduce television and computer use in overweight children of all SES. 53 The final study examined a mentor-based health promotion programme for black adolescents of low SES. 54 One study48 included children of preschool age (0–5 years), two studies50,53 included children of primary school age (6–12 years) and one54 study included children of secondary school age (13–18 years). Three of the studies were conducted in the USA48,53,54 and one50 in Australia. The studies of tailored weight loss programmes found either more beneficial effects in the lower-SES groups or no differential effect by SES after 1 year. The screen time-reduction intervention found beneficial effects in low-SES children but not in high-SES children, both in the short term and long term. The mentor-based health promotion intervention maintained (did not decrease or increase) obesity-related outcomes in all low-SES children and had beneficial effects for those who were overweight and obese in the long term.
Tailored weight loss programmes (n = 2)
One RCT50 and one cluster RCT48 followed a universal approach and examined primary care-delivered tailored weight loss programmes (face-to-face counselling on healthy diet and physical activity behaviours) in boys and girls of all SES in the USA48 and Australia. 50 The cluster RCT48 of 445 children aged 2–6 years found that a 1-year intervention led to no changes in BMI overall. However, BMI increased to a lesser extent in the intervention group than in the control group among children with a household income of ≤ $50,000 (intervention group change 0.4 kg/m2; control group change 1.42 kg/m2; adjusted difference –0.93 kg/m2; p = 0.01). There was no intervention effect in the subgroup of children with a household income > $50,000. The RCT50 of 245 children aged 5–10 years found that, following a 12-week intervention, there were no significant differences between the intervention group and the control group in BMI, waist circumference or number overweight or obese at 6 or 12 months, and SES did not modify the intervention effect.
Screen time-reduction intervention
A RCT following a universal approach53 investigated the effects of a screen time-reduction intervention aimed at reducing television viewing and computer use in 67 children aged 4–7 years in the USA. Overall, there were greater reductions in BMI z-score over 24 months in the intervention group than in the control group (p < 0.05 for group × time interaction). In the low-SES group there was a statistically significant between-group difference for change in BMI z-score from baseline to 6 months (mean difference between groups –0.17; p = 0.002), 12 months (–0.20; p = 0.02), 18 months (–0.17; p = 0.04) and 24 months (–0.26; p = 0.05). There were no statistically significant between-group differences in the high-SES group.
Mentor-based health promotion intervention
A RCT54 investigated the effects of an 11-week mentor-based health promotion intervention (healthy eating and physical activity education and counselling) in 179 black adolescents aged 11–16 years from low-income communities. After 2 years there was no difference between the intervention group and the control group with regard to change in BMI z-score from baseline; however, the percentage of overweight and obese participants was decreased in the intervention group compared with the control group. Overall, there were no between-group differences in change in percentage body fat, fat mass or fat-free mass but the intervention was effective at reducing percentage fat (β = –1.54; p = 0.003) and fat mass (β = –1.31; p = 0.025) and increasing fat-free mass (β = 1.41; p = 0.021) in participants who were overweight or obese.
Community-level interventions
In total, 13 high-quality experimental studies examined community-level interventions: four universal57,76,86,98 and nine63,67,79,83,87,89,90,93–95 targeted. Eight of the studies examined the effects on obesity-related outcomes of school-based health promotion interventions (three among children of all SES57,76,86 and five among children of low-SES63,67,79,83,94), three evaluated group-based weight loss programmes87,90,98 (one among children of all SES98 and two among low-SES children87,90) and two89,93 evaluated group-based weight gain prevention educational interventions in low-SES children (one targeted parents only89). Half of the studies (n = 657,76,83,90,93,94) were conducted in the USA with four conducted in South American countries (two from Brazil79,87 and one each from Chile67 and Peru89) and three conducted in Europe (the Netherlands,63 Finland98 and France86). The majority of the studies (n = 1057,63,67,76,79,83,86,87,90,93,98) included children of primary school age (6–12 years); three89,94,95 studies included children of preschool age (0–5 years). None of the studies included adolescents (13–18 years). All of the studies included boys and girls (usually an approximately 50/50 mix) with the exception of two studies90,93 that included girls only.
The evidence from school-based health promotion interventions suggests that nutrition and physical activity education combined with exercise sessions may be effective in school-aged children (6–12 years) after reasonably long follow-up times (≥ 6 months) both when targeted at low-SES populations and when delivered universally to children of all SES (and there were no differential effects by SES), but may not be effective in preschool-aged children in the short term. Education-only interventions (diet and/or physical activity) are not so consistently effective in low-SES school-aged children. Screen time-reduction interventions may also be effective in school-aged children (6–12 years) after 6 months, with no differential effects by SES.
The evidence from group-based weight loss programmes suggests that family-based educational and behavioural weight loss programmes may be beneficial in terms of short-term weight loss and long-term weight maintenance and work equally across the social class gradient in school-aged children (aged 6–12 years); and exercise-based weight loss programmes may result in short-term weight loss among low-SES school-aged children.
The evidence from group-based weight gain prevention educational interventions suggests that these interventions do not lead to beneficial effects after a relatively long follow-up period (1 year) in low-SES preschool and primary school-aged children.
School-based health promotion interventions (n = 8)
Eight high-quality experimental studies examined school-based health promotion interventions. Five studies investigated nutrition and physical activity education combined with exercise sessions;57,63,67,86,94 two studies examined education-only interventions (diet and/or physical activity);79,83 and one study examined a screen time-reduction intervention. 76
Five studies examined nutrition and physical activity education combined with exercise sessions. 57,63,67,86,94 Overall, the results suggest that these types of interventions are effective in school-aged children (6–12 years) when targeted at low-SES populations and when delivered to children of all SES (no differential effects by SES) after reasonably long follow-up times (≥ 6 months) but may not be effective in preschool children in the short term.
A cluster RCT57 that followed a universal approach investigated the effects of a cardiovascular disease risk factor reduction intervention delivered over 8 weeks to 985 schoolchildren aged 8–10 years in the USA. There was a significant reduction in the sum of skinfolds from baseline to 1 year in the intervention group compared with the control group (log of sum of skinfolds mean change: intervention group –0.060, control group –0.032; p = 0.0422). There was no relationship between intervention effects and SES of the children. A non-randomised cluster controlled trial67 of a 6-month nutrition and physical activity education intervention in low-SES schools in Chile (n = 3084 children aged 11 years on average) found positive effects for boys (e.g. the BMI z-score decreased significantly in the intervention schools whereas in the control schools there was very little change: –0.12 vs. –0.02; p < 0.001) but not for girls. A cluster RCT63 examined the effects of an 8-month diet and physical intervention (Lekker Fit!) in low-income, multiethnic, inner-city schools in the Netherlands (n = 2416 children aged 6–12 years). The intervention consisted of exercise sessions and nutrition, physical activity and healthy lifestyle education. In the younger children (6–9 years) there was no intervention effect for BMI; however, increase in waist circumference was significantly lower in the intervention group than in the control group (difference between groups –1.29 cm; 95% CI –2.16 cm to –0.42 cm). The prevalence of overweight in the intervention group also increased to a lesser extent than in the control group.
A randomised cluster trial86 that followed a universal approach examined the effects on the prevention of overweight of a 4-year, school-based, multicomponent education and exercise intervention to increase physical activity in 732 children aged 11–12 years in France. At 4 years’ follow-up, although there were no differential effects by SES, there was also no significant difference in overall BMI. A cluster RCT94 investigated the effects of an 18-week intervention, Food Friends Get Movin’ with Mighty Moves™, in 201 low-income, minority preschool children in the USA. The intervention comprised physical activity sessions and nutrition education sessions, and cartoon characters (Food Friends®) were used to introduce and support new skills and topics. There were no significant effects on BMI after 18 weeks.
Two cluster RCTs examined education-only interventions (health promotion around diet and/or physical activity) that were targeted at children aged 9–11 years from low-SES schools in the USA83 and Brazil. 79 One cluster RCT79 of an 8-month intervention to reduce sugar-sweetened beverage intake in schools in Brazil (n = 927 children aged 10–11 years) encouraged water consumption through competitions, promotions and the provision of water bottles. There were no significant differences between groups for all children; however, for girls – but not boys – who were overweight at baseline there was a significant reduction in BMI in the intervention group (regression coefficient –0.01; p = 0.009). However, the US cluster RCT83 showed no intervention effect of an education-only intervention after 1 year.
A cluster RCT76 investigated a screen time-reduction intervention and showed beneficial effects in children aged 8 and 9 years after 6 months that were not associated with child SES. The intervention included a teacher-delivered classroom course that was intended to increase pupils’ self-regulation of television and video game use; it included a 10-day ‘TV turn-off challenge’, educational materials disseminated to parents and installation of domestic television usage monitors. Post intervention, children in the intervention group had statistically significant relative reductions in BMI (adjusted difference –0.45 kg/m2, 95% CI –0.73 kg/m2 to –0.17 kg/m2; p = 0.002) as well as triceps skinfold thickness (adjusted difference –1.47 mm, 95% CI –2.41 mm to –0.54 mm; p = 0.002), waist circumference (adjusted difference –2.30 cm, 95% CI –3.27 cm to –1.33 cm; p < 0.001) and waist-to-hip ratio (adjusted difference –0.02, 95% CI –0.03 to –0.01; p < 0.001). The results did not differ by SES.
Group-based weight loss programmes (n = 3)
Three high-quality experimental studies examined group-based weight loss programmes. One study examined a family-based education and behavioural weight loss programme98 and two studies examined exercise-based weight loss programmes,87,90 one of which also incorporated a screen time-reduction intervention. 90
A RCT98 investigated the effects of a 6-month family-based education and behavioural therapy programme compared with a standard treatment programme in 69 obese children aged 7–9 years in Finland. Children and their parents in the intervention group each attended 15 health behaviour sessions. Intervention children lost more weight for their height than those receiving the routine treatment after 6 months (intervention group mean 6.8% reduction, control group mean 1.8% reduction; p = 0.001) and 12 months (intervention group mean 3.4% reduction, control group mean 1.8% increase; p = 0.008). There was a greater decrease in BMI in intervention children than in control children (intervention group change –0.8, control group change 0.0; p = 0.003). There was no association between SES and outcomes.
The two studies investigating exercise-based weight loss programmes found promising short-term (< 6 months) results among primary school-aged children from the USA90 and Brazil. 87 A randomised controlled pilot study90 investigated the effects of a 12-week culturally appropriate exercise session and screen time-reduction intervention [Stanford Girls health Enrichment Multisite Studies (GEMS)] among 61 low-income African American girls aged 8–10 years in the USA. From baseline to post intervention there were no significant differences between groups for changes in BMI and waist circumference; however, a trend towards better outcomes in the intervention group was noted. A RCT87 investigated the effects of a similar 6-month exercise session intervention in 68 overweight children aged 5–10 years from a disadvantaged area in Brazil. After 6 months weight gain was less in the intervention group than in the control group [difference in change (intervention group – control group) –1.37 kg; p < 0.001] and there was a significant decrease in BMI in the intervention group compared with the control group [difference in change (intervention group – control group) –0.53 kg/m2; p = 0.049].
Group-based weight gain prevention educational interventions (n = 2)
Two high-quality experimental studies investigated the effects of group-based weight gain prevention educational interventions and found that the interventions did not lead to beneficial effects after a relatively long follow-up period (1 year) in preschool89 and primary school-aged93 children. A non-randomised controlled study93 investigated the effects of a mother and daughter 12-week culturally specific group-based weight gain prevention educational intervention among 40 low-SES, African American girls aged 7–12 years in the USA (mean age 10.0 years). The intervention consisted of weekly 1-hour sessions that included education on healthy eating, obesity risks, physical activity and behaviour change, and practical exercise and cooking sessions. No intervention effects were observed for obesity outcomes after 1 year of follow-up. A RCT89 investigated the effects, on children aged < 5 years, of a health education intervention delivered to 1501 microcredit clients in Peru (microcredit involves the provision of small loans to families who are too poor to borrow from traditional lending institutions). The health education intervention was delivered by trained loan officers over 8 months and covered basic child health provision and discussion of clients’ own experiences and problem-solving. There were no differences between the control group and the intervention group from baseline to 1 year of follow-up in the change in percentage of children who were overweight and in mean BMI z-scores.
Societal-level interventions
The ‘best-available’ evidence for environmental interventions comes from five moderate-quality experimental studies that were all conducted in low-SES schools (targeted approach). 107–109,114,116–119 All of the studies examined multifaceted school-based obesity prevention interventions. Four of the studies were from the USA107–109,114,116 and one was from Germany. 117–119 Four of the studies included children of primary school age (6–12 years)107–109,116–119 and one included preschool children (0–5 years). 114 The evidence from these relatively long-term (> 8 months) studies suggests that multifaceted school-based obesity prevention interventions are effective at reducing or preventing increases in obesity-related outcomes in low-SES primary school-aged children (6–12 years) but may not be effective among low-SES preschool children. No studies investigated macrolevel interventions.
A randomised cluster trial109 examined the effects of a 2-year School Nutrition Policy Initiative (a multifaceted educational and environmental intervention to increase nutritional knowledge and the availability of healthy food) in 844 children aged 11 years in a deprived area of the USA. Sodas, crisps and other high-calorie snacks were no longer sold in vending machines or cafeterias. At the 2-year follow-up, the incidence of overweight was 33% less in the intervention group (OR 0.67, 95% CI 0.47 to 0.96) and the prevalence of overweight was 35% less (adjusted OR 0.65, 95% CI 0.54 to 0.79). The reduction in prevalence was particularly effective for black pupils (adjusted OR 0.59, 95% CI 0.38 to 0.92).
Another randomised cluster trial108 examined the effects of a similar multifaceted educational and environmental intervention in 4603 children aged 11 years from low-SES schools in the USA. The 30-month study found non-significant differences in the prevalence of overweight and obesity in both the intervention group and the control group. However, the mean BMI z-score (p = 0.04) and waist-to-hip ratio were significantly lower in the intervention group (p = 0.04). There were significantly more cases of remission in the intervention group, with overweight or obese pupils at baseline having a 21% lower chance of being obese at follow-up than control group pupils (OR 0.79, 95% CI 0.63 to 0.98).
A non-randomised cluster trial by Williams et al. 114 examined the effects of an 8-month Healthy Start intervention to improve cardiovascular health in 676 low-SES preschool children. At post-intervention follow-up there were non-significant differences between the intervention group and the control group in the prevalence of obesity or overweight or in BMI z-scores.
A non-randomised cluster trial107,116 examined the effects of the 2-year preventative CATCH (Child and Adolescent Trial for Cardiovascular Health) initiative on 744 children aged 8 years from low-SES schools. At the 2-year follow-up, the percentage of children who were overweight and obese increased significantly for both girls and boys in the intervention group and the control group; however, the rate of increase was significantly lower in intervention schools (girls: intervention group increased by 2%, control group increased by 13%; boys: intervention group increased by 1%, control group increased by 9%; p < 0.05).
One randomised cluster trial117–119 examined the effects of a 10-month school-based educational and environmental intervention to increase water consumption in 2950 children aged 8 years from a deprived area in Germany. The intervention entailed the installation of water fountains in schools alongside education. At 10 months’ follow-up, the prevalence of overweight (BMI) was unchanged in the intervention group but increased in the control group. The risk of becoming overweight was significantly reduced in the intervention group compared with the control group (OR 0.69, 95% CI 0.48 to 0.98; p = 0.04).
Individual-, community- and societal-level interventions
The ‘best-available’ evidence for the multilevel individual, community and societal (environmental) interventions comes from one high-quality experimental study124 that examined the effects of a 3-year community capacity-building intervention (Be Active Eat Well) among 1807 children aged 4–12 years in Australia. The intervention was designed by a number of key organisations to build the community’s capacity to create its own solutions to promoting healthy eating, physical activity and a healthy weight and was delivered universally in all intervention schools. After 3 years, children in the intervention schools showed significantly lower increases in waist circumference (–3.14 cm) and BMI z-score (–0.11) than children in the control schools. There was no association between SES measures and intervention effects in the intervention schools; however, lower SES was associated with a greater gain in body fat and waist circumference in the control schools. Therefore, the intervention halted the widening of inequalities in obesity that would normally occur naturally over time.
Synthesis of UK evidence
To further aid the translation of our results into UK policy and practice, this section focuses on synthesising only the UK evidence for each intervention type. There were just two studies conducted in the UK, both observational in design and of weak methodological quality. One was an individual-level study that followed a universal approach46 and the other was a community-level study that followed a targeted approach. 91,92 The findings of these UK studies are summarised in Table 18 and described in the following sections.
| Study | Study type, quality | Impact on inequalities in obesity |
|---|---|---|
| Individual-level intervention | ||
| Sabin et al. 200746 | Observational, low quality | 0 |
| Community-level intervention | ||
| Rudolf et al. 2004,92 200691 | Observational, low quality | + |
Individual-level intervention
An uncontrolled prospective cohort (uncontrolled before-and-after) study conducted by Sabin et al. 46 investigated the effects of a primary care educational and behavioural weight loss programme among 61 children aged 2–18 years (approximately 50% girls). The study followed a universal approach in that the service was open to children of all SES and the study explored whether or not SES influenced a child’s level of success. After at least 1 year, 28% of participants achieved the target reduction in BMI [BMI standard deviation score (SDS) reduction of at least 0.5 or obtained normal BMI centiles for age]. There was no significant correlation between SES and BMI SDS reduction nor were there any differences in SES between achievers and non-achievers.
Community-level intervention
An uncontrolled prospective pilot cohort study91,92 explored the effects of a community-based counselling weight loss programme (WATCH IT) among 48 children aged 8–16 years (approximately 50% girls) living in deprived areas in the UK. There was no significant change in BMI SDS at 3 months; however, the BMI SDS was significantly reduced at 6 months’ follow-up (change –0.07; p < 0.01) (the intervention was particularly effective in girls and those aged ≥ 13 years).
Implementation
Using the implementation tool (see Box 1) we recorded information about how the interventions were implemented, organised and delivered. In this section we synthesise the main themes from across the 76 studies. More detailed analyses of implementation data are presented by intervention type and study in Tables 39 and 40 (individual-level interventions), Tables 43 and 44 (community-level interventions), Table 46 (societal-level interventions) and Tables 49 and 50 (multilevel interventions) (see Appendix 5).
Motivation
The majority of the studies clearly described the motivation behind the intervention investigated. The main motivation was to reduce or prevent obesity and/or overweight, or a combination of the two. In some cases this was in a particular population (e.g. low-SES, African American). In some studies the general motivation was the improvement of health and in some studies the focus was on the prevention of disease risk factors, including excessive weight/body fat. Only three studies did not clearly report a motivation behind the intervention. 62,80,110,111,115
Theory
Twenty-nine studies47,48,50,54–56,62,63,68–70,76,78,81,82,86,88,90–92,94,95,98,106,112,117–119,121,122,124 reported a theoretical underpinning of the intervention (or evaluation of the intervention). A number of studies reported using multiple theories, frameworks and/or approaches. The most commonly reported theory informing the interventions was social cognitive theory (reported by 11 studies), followed by social learning theory (three studies), self-efficacy theory (three studies), the theory of planned behaviour (two studies) and community-based participatory approaches (two studies). Other theories or frameworks reported included the chronic care model, the behavioural epidemiology framework, behavioural- and solution-oriented therapy, the social marketing framework, the transtheoretical model of behaviour change, self-care deficit nursing theory, behavioural choice theory, the bottom-up approach to health promotion and concept of empowerment (collective/community control over the design and implementation of interventions) and child quality theory.
Context
Twenty studies55–57,59,60,62,65,66,69,70,78–80,82,84,87,88,110,111,115,120 did not report the context in which the intervention was developed/delivered. For the remaining studies the most commonly reported context was social, usually led by the research team or a health-care or community group. Four studies reported a political context to their study: the intervention investigated by Hawthorne et al. 61 was developed in response to the Child Nutrition and Women, Infants and Children Reauthorisation Act in the USA; the intervention investigated by Hamad et al. 89 was guided by the WHO Integrated Management of Childhood Illness strategy; Ibarra and Alarcón113 evaluated an intervention developed as part of a university social responsibility agenda and inspired by the WHO Healthy Schools Initiative; and Frisvold and Lumeng121 studied the effects of changes to childcare settings that were influenced by national policies: the ‘War on Poverty’ in 1965 and welfare reform in the mid-1990s.
Experience
Fifty-eight of the studies40,42,43,46–52,54–59,62–68,71–75,77–85,87–94,96,98,100,101,103–119,122,124 reported some information regarding the experience of either those who developed the intervention or those who delivered it. In all of these cases interventions were delivered by those with appropriate experience or by those who were trained by others with appropriate experience. In some studies interventions were developed and delivered by multidisciplinary teams. In a number of cases, however, some details of experience were lacking, for example the experience of those delivering the intervention may have been reported but details of who developed the intervention were not given or were unclear, and vice versa.
Consultation/collaboration
Only 20 studies54,62,68,70,72,73,77,81,84,90,94,95,106,107,109,112,113,116,122–124 reported that some degree of consultation/collaboration took place and, within these studies, the level of detail provided varied as well as the level of consultation and/or collaboration. For example, in the study by Perman et al. ,113 a coalition between academic and community partners (including health departments, food retailers and banks) was formed and planning meetings were held with the teachers involved in the intervention, whereas in the study by Moore et al. 70 focus groups with children and teachers informed just a small part of the intervention. The majority of consultations appeared to take place during the planning stages; however, some studies did report extensive consultation at all stages of the research. 122,124
Delivery fidelity
Thirty-five studies40,47–50,55,56,61,62,65–67,71,73,76–78,81–83,86,87,89,90,91,92,95,97,103,106–112,115–119,123 reported details about whether the intervention was delivered as intended or about methods that were put in place to ensure delivery fidelity. This information included data on session attendance, completion rates of intervention components, observation of sessions, quality control audits, staff and researcher records/logs and additional evaluation such as interviews and focus groups with participants and intervention staff members. Methods used to ensure delivery fidelity included standardised training, the use of standardised manuals, practice ‘role-play’ sessions with feedback and regular meetings with trainers/supervisors/more experienced members of the intervention team, and observations of sessions.
Sustainability
Information regarding intervention sustainability was reported for 26 studies. 43,48,50,57,61,63,66,67,69,71–75,86,89,91,92,94,96,101,107,110–113,115–119,121,122 In a number of studies, interventions were integrated into existing health services and school curriculums and were delivered by existing or non-specialised staff. Some studies reported the continuation and expansion of interventions beyond the study. 63,72,107,116,122 However, problems affecting sustainability were reported in some studies66,89,101,121 and reliance on highly motivated staff, volunteers and/or in-kind contributions was reported in others. 61,86,91,92,113 One study relied on the intervention being unsustainable as intervention schools were later assigned as control schools. 74,75,125
Stakeholder support
Twenty studies50,59,61,62,67,70,72,73,81–84,86,89,98,107,112,113,116,123,124 provided information on stakeholder support. Stakeholders included general practitioners (GPs), community groups/individuals, health departments, volunteer groups/individuals, schools, teachers, parents, participants and funders. Stakeholder involvement and feedback were used to indicate stakeholder support but in most cases stakeholder support was implied by the authors without formal evaluation.
Resources
Information on resources was well documented, being reported by 57 studies;40,42,44,46–58,60–64,67–73,77–80,82–84,86–93,96–98,100–104,107,108,113,116–119,121,124 however, the information provided was mostly related to time, staff and equipment rather than the actual costs of the interventions or parts of the interventions, which were reported by just 11 studies. 50,72,77,80,90,93,107,108,113,116–119,121
Differential effects
Subgroup differential effects were also explored by the majority of the studies (n = 4740–42,44,46,48,50–57,61,63–67,73,76–79,86,88,90–92,94,96–98,100,103,106,107,109–112,114–116,121–124). As well as the 23 studies40,41,44,46,48–53,57,64,76,77,88,96–98,100,101,104,105,122,124 reporting differential effects by an indicator of SES (universal approach studies), other differential effects were explored for age, gender, ethnicity, weight status, geographical location (e.g. rural vs. urban), session attendance, parental marital status and parent variables (e.g. BMI, ethnicity).
Analysis of the robustness of the results (sensitivity analyses)
Sensitivity analysis was conducted for both of the meta-analyses. For the meta-analysis of the 13 community-level studies,57,63,67,76,79,83,86,87,89,90,93–95,98 the sensitivity analysis adjusted for three types of moderator: (1) prevention compared with treatment, (2) physical activity compared with physical activity and diet interventions and (3) study quality. The environment meta-analysis adjusted for quality only (because of the small number of studies). These analyses are described in detail in the following sections.
Sensitivity analysis for the meta-analysis of community-level studies
The heterogeneity between the studies, as shown earlier, may be attributable to study-specific characteristics such as type of study [prevention (P) compared with treatment (T)], quality of the study (high, moderate or low) and intervention type (physical activity only or diet only or physical activity and diet). In the meta-analysis model we accounted for these mediators and the results are presented in Table 19. There is a statistically significant difference between the different types of study (P and T). Additionally, there is a significant difference between intervention types, with physical activity-only studies reporting a higher intervention effect than physical activity and diet studies. There is also a significant effect of quality score. The Q-statistic measure for heterogeneity between the studies is no longer significant (4.2188, p = 0.8369).
| Variable | Estimate | SE | p-value | 95% CI |
|---|---|---|---|---|
| Intercept | –4.1935 | 0.2971 | < 0.0001 | (–4.7757 to –3.6112) |
| Study type (ref. = P) | ||||
| T | –3.8941 | 0.2947 | < 0.0001 | (–4.4717 to –3.3164) |
| Diet (ref. = diet and PA) | ||||
| PA only | 4.0040 | 0.2949 | < 0.0001 | (3.4260 to 4.5820) |
| Quality score (ref. = moderate) | ||||
| High | 4.1397 | 0.3218 | < 0.0001 | (3.5089 to 4.7705) |
| Low | 4.1235 | 0.2971 | < 0.0001 | (3.5412 to 4.7057) |
Given that the original heterogeneity between the studies is explained by the moderators (study type, intervention type and quality score), it would be desirable to perform the meta-analysis on a homogeneous set of studies. Table 20 shows the distribution of studies by study type, intervention type and quality score. Among all of the possible combinations, only the combination of preventative study, diet and physical activity intervention and high quality includes more than three homogeneous studies.
| Study type | Effect type | Quality score | ||
|---|---|---|---|---|
| High | Moderate | Low | ||
| P | Diet and PA | 6 | 0 | 1 |
| PA only | 0 | 1 | 0 | |
| T | Diet and PA | 0 | 0 | 1 |
| PA only | 2 | 1 | 1 | |
Figure 6 shows the forest plot for the preventative studies that have a quality score of high and include a diet and physical activity intervention. The individual-level studies do not show significant intervention effects and consequently the overall pooled effect is also insignificant. The Q-statistic (2.1074, I2 = 0%, p = 0.8341) measure of heterogeneity is not significant, which implies that these studies are homogeneous. The result is still that there is no significant intervention effect (pooled effect size –0.04, 95% CI –0.29 to 0.20).
FIGURE 6.
Random-effects meta-analysis of BMI change for the high-quality, preventative studies of diet and physical activity interventions. a, 6–9 years; b, 10–12 years; c, boys; d, girls.

Sensitivity analysis for the meta-analysis of societal (environmental) studies
For both outcomes – the prevalence of overweight and obesity and the prevalence of obesity – the low-quality study by Hollar et al. 110,111 was excluded and the random-effects meta-analysis was re-run. The results were as follows. For the prevalence of obesity and overweight the pooled effect size based on the three better-quality studies107–109 was an OR of 0.91 (95% CI 0.75 to 1.1). There was also less heterogeneity (I2 = 55.54%, Q = 4.52, p = 0.1040) between the remaining studies. 107–109 For the two better-quality studies of the prevalence of obesity,108,109 the pooled estimate of the OR was 0.99 (95% CI 0.77 to 1.26). As with the full meta-analysis, these sensitivity analyses suggest that, overall, the nutritional interventions did not significantly reduce the prevalence of overweight and obesity or obesity only among children.
Discussion
Summary of results
Individual-level interventions
In total, we located 11 studies of individual-level interventions. 40–43,46–54 The ‘best-available’ international evidence comes from four48,50,53,54 moderate- or high-quality experimental studies and suggests that tailored weight loss programmes work equally well across the SES gradient and can even have more beneficial effects in the lower-SES groups; screen time-reduction interventions can have beneficial effects in low-SES children but not high-SES children, both in the short term and the long term; and mentor-based health promotion interventions can have beneficial long-term effects among disadvantaged children who are most at risk (overweight and obese). This evidence suggests that interventions of this type may help reduce SES inequalities in obesity. There were no studies that assessed the cost-effectiveness of interventions.
The UK evidence comes from one46 low-quality observational study of a primary care educational and behavioural weight loss programme that found positive results across the SES gradient.
Community-level interventions
In total, we located 5244,45,55–106 studies of community-level interventions. The ‘best-available’ international evidence comes from 1357,63,67,76,79,83,86,87,89,90,93,94,98 high-quality experimental studies which suggest that school-based nutrition and physical activity education combined with exercise sessions can be effective in low-SES school-aged children and when delivered universally to children of all SES groups after reasonably long follow-up times (≥ 6 months), but may not be effective in preschool children in the short term. School-based education-only interventions are not as consistently effective in low-SES children, and school-based screen time-reduction interventions can be equally effective across the SES gradient after 6 months. Family-based educational and behavioural group weight loss programmes can be beneficial in terms of short-term weight loss and long-term weight maintenance and work equally across the social class gradient. Group-based exercise-only weight loss programmes may result in short-term weight loss among low-SES school-aged children. Group-based weight gain prevention educational interventions have no effect in low-SES preschool and school-aged children. There were no studies that assessed the cost-effectiveness of interventions.
The UK evidence comes from one91,92 low-quality observational study of a community-based counselling weight loss programme, which found no effect initially but BMI reductions in low-SES children in the longer term (6 months).
Societal-level interventions
In total, we located 10107–121 studies of societal (environmental)-level interventions but no studies of societal (macro)-level interventions. The ‘best-available’ international evidence for the environmental interventions comes from five107–109,114,116–119 moderate-quality experimental studies and suggests that multifaceted school-based obesity prevention interventions are effective at reducing or preventing increases in obesity-related outcomes in low-SES children aged 6–12 years but may not be effective among low-SES preschool children.
There were no UK studies of societal-level interventions.
Individual-, community- and societal-level interventions
In total, we located three122–124 studies of multilevel interventions that spanned each of the individual, community and societal levels described in our framework. The ‘best-available’ international evidence comes from one124 high-quality experimental study, which found that a community capacity-building intervention halted the widening of inequalities in obesity that was observed in the control community.
There were no UK studies of multilevel interventions.
Table 21 illustrates where the included child studies fit within our framework described in Table 1.
| Approach to tackling health inequality | Level of intervention | |||
|---|---|---|---|---|
| Individual | Community | Societal | ||
| Strengthening individuals | Strengthening communities | Improving living and school conditions | Promoting healthy macro policies | |
| Disadvantage (targeted) | All studies (n = 4) Best evidence (n = 1) Mentor-based health promotion for children from low-income communities UK evidence (n = 0) |
All studies (n = 36) Best evidence (n = 9) School-based nutrition and physical activity education with/without exercise sessions; group-based weight loss programmes; group-based weight gain prevention educational interventions UK evidence (n = 1) Community-based counselling weight loss programme (WATCH IT) |
All studies (n = 10) Best evidence (n = 5) Multifaceted educational and environmental interventions UK evidence (n = 0) |
(n = 0) |
| Gradient (universal) | All studies (n = 7) Best evidence (n = 3) Tailored weight loss programmes; screen time-reduction intervention UK evidence (n = 1) Primary care educational and behavioural weight loss programme |
All studies (n = 16) Best evidence (n = 4) School-based nutrition and physical activity with exercise sessions; school-based screen time-reduction intervention; group-based weight loss programmes UK evidence (n = 0) |
(n = 0) | (n = 0) |
What works to reduce inequalities in obesity, for whom and where?
The ‘best-available’ international evidence for the effectiveness of individual-level interventions (n = 4)48,50,53,54 in reducing inequalities in obesity among children suggests that tailored weight loss programmes may have more beneficial effects on obesity-related outcomes in lower-SES groups than in higher-SES groups in the longer term (1 year); that a mentor-based health promotion intervention also seemed effective in preventing an increase in obesity-related outcomes in SES children (but not reducing them) and that this particularly benefited those who were overweight and obese (1 year); and that, most notably, a screen time-reduction intervention (aimed at reducing television viewing and computer use in 67 children aged 4–7 years in the USA) found beneficial effects for up to 2 years in low-SES children but not high-SES children.
Similarly, the ‘best-available’ international evidence for the effectiveness of community-level interventions (n = 13)57,63,67,76,79,83,86,87,89,90,93,94,98 included evidence of some effective interventions in the short and long term among school-aged children (aged 6–12) but not among adolescents (no studies) or preschool children (not effective in the short or long term). There was evidence of longer-term effectiveness (> 6 months) in reducing obesity-related outcomes among school-aged children (6–12 years) of (1) school-based nutritional and physical activity education and exercise sessions and (2) school-delivered screen time-reduction interventions, with no differential effects by SES. There was evidence of short-term effectiveness (up to 6 months) in reducing obesity-related outcomes among school-aged children (6–12 years) of targeted (1) family-based educational and behavioural weight loss programmes and (2) exercise-based weight loss programmes.
We found only five107–109,114,116–119 moderate-quality experimental studies of the effects of more upstream environmental interventions and no studies of the effects of macro-level policy interventions on obesity-related outcomes among children. All of the studies examined multifaceted school-based obesity prevention interventions. The evidence suggests that multifaceted school-based obesity prevention interventions (educational and environmental interventions typically including nutritional education and/or physical activity and an environmental modification component such as increasing the availability of healthy food) are effective in the medium to longer term (> 8 months) at reducing or preventing increases in obesity-related outcomes in low-SES school-aged children (6–12 years) but may not be effective among low-SES preschool children. Similarly, a multilevel community capacity-building intervention was effective in preventing a widening of inequalities in obesity over the long term (up to 3 years) among schoolchildren aged 4–12 years.
There were just two46,91,92 studies conducted in the UK, both observational in design, with small sample sizes (< 75) and of low methodological quality. There was no evidence of effectiveness in terms of reducing inequalities in obesity-related outcomes of an individual-level primary care educational and behavioural weight loss programme for children aged 2–18 years. However, a community-based counselling weight loss programme targeted at children aged 8–16 years in a deprived area found reductions in BMI after 6 months and the intervention was particularly effective in girls and those aged ≥ 13 years.
It is important to reflect on ‘for whom’ and ‘where’ the interventions were – or more usually were not – effective. The ‘best-available’ international evidence was typically for interventions conducted in the USA or South America. However, caution should be applied in trying to extrapolate the effectiveness of the various individual-, community- and societal-level interventions beyond these countries. This is especially the case as the UK evidence base was extremely small (n = 2) and so provides little insight into how such interventions could work in the UK. However, the ‘best-available’ international evidence does suggest that interventions are universally much more effective among school-aged children (aged 6–12 years) than among preschool children. There were no studies of adolescents. This is such a consistent finding that it may also be applicable to the UK context and suggests that it is at the primary-school level that we need to intervene. Interventions appeared to be equally effective for boys and girls, although some studies did not distinguish their results by gender. Most of the studies were of interventions targeted at low-SES children/areas and often of ‘treatment’ interventions for those already overweight/obese. In terms of ‘where’ interventions appeared to be effective, the ‘best-available’ evidence was dominated by school-delivered interventions, which suggested that targeted school-based interventions appear, in general, to be effective. This supports the ‘whole school approach’ to tackling childhood obesity. The findings of effectiveness are therefore very much limited to the effectiveness of school-based interventions for low-income, primary school-aged children (6–12 years), particularly in the USA.
In terms of barriers to and facilitators of interventions, although most of the studies provided data for motivation, context and experience of the intervention team and resources, the type and level of information provided varied substantially for each of the domains, making comparisons between the studies difficult. There were no apparent differences between interventions that were successful in reducing inequalities in obesity and those that were not. For example, in terms of study motivation, it may be hypothesised that studies that focused primarily on reducing obesity would be more successful at reducing inequalities in obesity than those that aimed to improve health in general; however, both successful and unsuccessful studies reported both motivations. There appeared to be no differences in the experience of the intervention team between successful and unsuccessful interventions (e.g. trained or professional facilitators were reported for both). Additionally, the reporting of resources (incentives, supportive materials, contact time and training of facilitators) did not appear to be related to outcomes.
Implications for research
The evidence suggests that the direction of research and evaluation in this field would benefit from looking into how to implement effectively to scale interventions to manage childhood obesity, sustain the impacts over time and ensure equitable outcomes. We recommend larger, longer-term studies, powered to detect the small changes that are likely to be found and including an assessment of equity impacts, to enable translation of research findings into effective public health approaches for managing childhood obesity.
The nature of the evidence base has a number of implications for public health researchers. Most notably, although we found a very large international evidence base, the evidence found was largely observational and of moderate to low quality. It is worth noting that, for the same type of intervention, observational studies are more likely to show positive effects than experimental studies. It is reasonable to suggest, therefore, that the most useful information on the way in which obesity (preventative or treatment) interventions impact on health inequalities comes from moderate- to high-quality experimental studies of universal interventions. These were particularly lacking in the UK evidence base and in methodological terms the UK evidence did not compare well with studies from the USA. There were also very few studies of societal-level interventions, which might be expected to have more of an impact on the gradient in obesity. 29 We did search for reports of observational studies of societal interventions that we are aware of, and which might have met our inclusion criteria, for example EPODE (Ensemble Prévenons l’Obésité Des Enfants; see www.epode-international-network.com/; accessed 16 September 2014), Sure Start (see www.gov.uk/find-sure-start-childrens-centre; accessed 16 September 2014) and Healthy Towns (www.theguardian.com/society/2008/nov/10/obesity-healthy-towns1; accessed 16 September 2014); however, we were not able to find any relevant evidence.
The majority of interventions that we included in this review took a targeted approach to tackling obesity and were concerned with weight loss (‘treating’ existing obesity) rather than preventing weight gain (‘preventing’ obesity). These ‘treatment’ interventions are more likely to show positive effects than prevention interventions. 31 The targeted approach also has limitations because even when interventions are effective among low-income groups they are only able to reduce the health inequalities gap; they have little effect on the wider social gradient. Most studies were school based and aimed at primary school-aged children. We also found no studies that assessed the cost-effectiveness of interventions and meta-analysis could be conducted only on a minority of studies given their heterogeneity.
Our results suggest a need for more experimental studies of the effectiveness and cost-effectiveness of interventions to reduce inequalities in childhood obesity, particularly in (1) adolescents, (2) in the UK and (3) in terms of macro-level interventions that potentially address the entire gradient. There has been a real missed opportunity to evaluate the effects of such ‘real-world’ interventions, and future interventions (such as Fulfilling Lives: A Better Start, a Big Lottery-funded programme in Newcastle) could benefit from including such analysis.
Implications for public health
Our review has found a large international evidence base but only limited effectiveness of interventions with the potential to reduce SES inequalities in obesity. The body of evidence in this review provides some support for the hypothesis that obesity management interventions in children can be effective and that they do not increase health inequalities. Interventions need to be developed that can be embedded into ongoing practice and operating systems, rather than implementing interventions that are resource intensive and cannot be maintained long term. This review also highlights that, although we may now have a good understanding of the range of interventions that are feasible for use in reducing the risk of childhood obesity, we lack the knowledge of which specific intervention components are most effective to ensure that the equity gradient is reduced. Being able to answer this question is of critical importance to decision-makers.
The review provides evidence of significant positive outcomes for the more disadvantaged. There was no evidence of a widening of health inequalities as a result of obesity management interventions. In addition, the relatively large number of studies of interventions targeting disadvantaged population groups provides useful information about the implementation strategies needed for obesity prevention efforts targeting these high-risk groups. We advocate for an assessment of outcomes by measures of equity, such as those indicated by PROGRESS (Place of residence, Race/ethnicity, Occupation, Gender, Religion, Education, Socioeconomic status and Social capital), if a general population is targeted.
In relation to which interventions could now be implemented by the UK public health community, the findings of this review are mainly limited to non-UK evidence and we cannot assume that such interventions will be effective outside their country context. It is also difficult to distinguish which specific components of intervention programmes are necessary to achieve beneficial impacts on obesity in children across all SES groups. However, our review has found tentative evidence of some interventions with the potential to reduce SES inequalities in obesity. Most notably, school-delivered educational and combined educational and environmental interventions that are targeted at low-SES primary school-aged children appear to have some effectiveness in the long term in reducing obesity-related outcomes among such children. The evidence suggests that interventions of this type may therefore be worth commissioning in the UK by clinical commissioning groups or local authorities who wish to target services at low-income primary school children or children in deprived areas. However, these interventions could benefit from being piloted first and thoroughly evaluated using an experimental design.
Strengths and limitations
This review was very extensive as an extremely thorough search was conducted of the international literature, using very broad intervention inclusion and exclusion criteria, which has ensured that the entire relevant experimental and observational evidence base has been captured. However, we located few evaluations of societal-level interventions and this was probably because we did not include non-experimental study designs. The quality of the review is also high as double screening was applied and both data extraction and quality appraisal were independently checked. We also examined the implementation of the interventions and paid attention to the context within which interventions were carried out. However, the review is still subject to some methodological limitations as, for example, the quality assessment tool, although described as a tool for public health interventions, seemed to favour those that followed a more clinical model. We particularly found the blinding question unhelpful as it mostly resulted in moderate scores. The implementation tool was practical but enabled only a brief summary of implementation factors to be provided. The theoretical framework adapted from the health inequalities literature meant that most interventions were categorised as community-level interventions and we encountered difficulties in determining in which section of the framework particular interventions should sit. One final limitation that may be of particular relevance to the non-UK evidence base is our exclusion of studies that examined ethnic inequalities, which may have reduced the number of US studies identified, in which ethnicity is often used as a proxy for SES.
Chapter 3 Part 2: how effective are interventions at reducing socioeconomic inequalities in obesity among adults?
Review methods
The review will follow the same procedure as carried out for the systematic review of the effectiveness of public health interventions at reducing socioeconomic inequalities in obesity among children (see Chapter 2). The full review protocol was published in Systematic Reviews126 and is registered with the PROSPERO International Prospective Register of Systematic Reviews (registration no. CRD42013003612).
Interventions
The review examined public health interventions at the individual, community and societal level that might reduce inequalities in obesity among adults aged ≥ 18 years in any setting, in any country. The review utilised the intervention framework (see Table 1) to group studies into different types, with acknowledgement that some interventions might be multilevel. We defined individual-level interventions as those that included individualised/one-to-one health promotion, education, advice, counselling or subsidy and which were conducted in a health-care or research setting or in participants’ homes; community-level interventions as group-based health promotion, education, advice, counselling or subsidy interventions, or interventions conducted in a community setting (e.g. a workplace, community centre, sports centre, shop); societal (environmental)-level interventions as those that included a change in environment or access to an environment; and societal (macro)-level interventions as macrolevel policies such as taxation, advertising restrictions or subsidies. Interventions were also classified in terms of whether they took a gradient approach (‘universal’ interventions) or a targeted approach (‘targeted’ interventions). This distinction is described further in Outcomes. The review considered public health strategies that might reduce existing inequalities in the prevalence of obesity (‘treatment’ interventions) as well as those interventions that might prevent the development of inequalities in obesity (‘prevention’ interventions). Clinical interventions such as those using drugs or surgery and laboratory-based studies were excluded from the review.
Study designs
A rigorous and inclusive international literature search was conducted for all randomised and non-RCTs, prospective and retrospective cohort studies (with/without control groups) and prospective repeat cross-sectional studies (with/without control groups) of the effectiveness of public health interventions at reducing inequalities in obesity among adults. Studies with a duration of at least 12 weeks (combination of intervention and follow-up) were included, an inclusion criterion used in previous Cochrane reviews of interventions. 30,31
Search strategy
The following nine electronic databases were searched (host sites given in parentheses): MEDLINE (Ovid), EMBASE (Ovid), CINAHL (EBSCOhost), PsycINFO (EBSCOhost), Social Science Citation Index (Web of Science), ASSIA (CSA), IBSS (EBSCOhost), Sociological Abstracts (CSA) and the NHS Economic Evaluation Database (NHS CRD).
A trained information scientist (HJM) developed and implemented the electronic searches. All databases were searched from their start date (e.g. MEDLINE starts in 1946) to the 11 October 2012. All searches are detailed in Appendix 1. We did not exclude papers on the basis of language, country or publication date.
The electronic database searches were supplemented with website and grey literature searches. The websites searched were the National Obesity Observatory, the Association for the Study of Obesity, the National Obesity Forum, the Department of Health, the International Association for the Study of Obesity and the WHO, and the grey literature repositories searched were the Obesity Learning Centre and NHS Evidence. We hand searched the bibliographies of all included studies and requested relevant information on unpublished and in-progress research from key experts in the field. In addition, we hand searched the last 2 years of the most common five journals revealed by the electronic searches (International Journal of Obesity, Preventative Medicine, Medicine and Science in Sport and Exercise, American Journal of Clinical Nutrition and Journal of the American Dietetic Association).
Outcomes
In terms of outcomes, we included studies only if they included a primary outcome that is a proxy for body fat (weight and height, BMI, waist measurement/waist-to-hip proportion, percentage fat content, skinfold thickness, ponderal index in relation to childhood obesity). Data on related secondary outcomes (such as physical activity levels, dietary intake, blood results such as cholesterol and glucose levels) were also extracted from those included studies that had a primary outcome. We included both measured and self-reported outcomes.
Studies were included only if they examined differential effects with regard to SES (education, income, occupation, social class, deprivation, poverty) or the intervention had been targeted specifically at disadvantaged groups or were conducted in deprived areas. The former are referred to as ‘universal’ interventions and the latter as ‘targeted’ (see Chapter 2, Interventions). Data on the organisation, implementation and delivery of interventions were extracted by adapting and refining the methodological tool for the assessment of the implementation of complex public health interventions in systematic reviews of Egan et al. 23 (see Box 1). Although most of the existing constructs in the Egan et al. tool (originally designed for workplace interventions) were relevant to our review, we made the following refinements: the themes ‘manager support’ and ‘employer support’ were removed and the themes ‘delivery fidelity’, ‘sustainability of the intervention’ and ‘stakeholder support’ were added.
Data extraction and quality appraisal
The initial screening of titles and abstracts was conducted by one reviewer (FCH) with a random 10% of the sample checked by a second reviewer (HJM or JMC). Agreement between the reviewers was fair (kappa = 0.68). The screening of the full papers was conducted by one reviewer (FCH) with a random 10% of the sample checked by a second reviewer (JMC). Agreement between the reviewers at this stage was good (kappa = 0.93). Data extraction and methodological quality appraisal of the included studies was conducted by one reviewer (FCH or JMC) using established data extraction forms23,27,32–35,37 and was checked by a second reviewer (FCH or JMC). Any discrepancies were resolved through discussion between the authors and, if consensus was not reached, through discussion with the project lead (CLB). The methodological quality of the included studies was also appraised using the Cochrane Public Health Review Group-recommended EPHPP Quality Assessment Tool for Quantitative Studies,38 which includes, among other things, an examination of the sampling strategy, response and follow-up rates, intervention integrity and statistical analyses and an assessment of adjustment for confounders. The quality appraisal criteria were used for descriptive purposes and to highlight variations between studies.
Analysis and synthesis
Because of the heterogeneity of the included studies, it was possible to use meta-analysis only for a minority of the studies (some of the individual-level and community-level studies only). Effect estimates from suitable experimental studies were pooled in meta-analysis by use of the R statistics package ‘metafor’ for the community interventions. Random-effects models were used to summarise the estimates if the test for heterogeneity was significant (defined conservatively as p < 0.20) or if the I2 statistic was moderate or high (> 50%). Publication bias was explored through the use of Egger’s test.
When meta-analysis was not possible, narrative synthesis was conducted. In keeping with PRISMA guidelines39 and our protocol,126 the narrative synthesis examines the effects of (1) individual-, (2) community- and (3) societal-level (macro and environmental) public health interventions on socioeconomic inequalities in obesity, using the multidimensional framework outlined in Table 1. We focus on differential effectiveness by SES. There were insufficient data to enable the conduct of any demographic subgroup analyses by age, gender or ethnicity.
Changes from the original protocol
Two changes were made from the original protocol (which is available to view at www.nets.nihr.ac.uk/__data/assets/pdf_file/0017/55223/PRO-09–3010–14.pdf):
-
A considerably higher number of articles were identified from the database searches than had been anticipated (n = 70,730). This resulted in a very high number of full papers that required review (n = 3142) and a much higher than expected number of studies meeting the final review inclusion criteria (n = 103). On the basis of practicality and to complete the review in a reasonable time frame, we did not contact all authors of studies (n = 3142) on the general population effects of interventions to reduce obesity for any unpublished data that they might have that related to SES inequalities.
-
In our original protocol we stated that we would use the Cochrane system of domain-based quality appraisal for randomised studies and a different tool (such as the Newcastle–Ottawa scale) for the quality appraisal of non-experimental studies. However, the Cochrane Public Health Review Group now recommends the EPHPP Quality Assessment Tool for Quantitative Studies for quality appraisal and we used this instead as it covers both experimental and non-experimental studies, making it easier for interpretation by readers.
Studies included in the review
In total, 103 separate studies (reported in 103 papers43,65,66,103,127–231) were included in the review. There were 33 studies43,127–150,152,154–158 of individual-level interventions (12 treatment,132,133,135,136,138,141,142,147–150,155 21 prevention43,127–131,134,137,139,140,143–146,152,154,156–158); 60 studies65,66,103,153,159–176,178–214,225,230,231 of community-level interventions (32 treatment,153,159,160,164,165,168–170,173,175,176,178,179,182–184,186–189,191–193,195,196,200,201,203,207,208,212,230 27 prevention,65,66,103,161–163,167,171,172,174,180,181,185,190,194,197–199,202,204–206,209–211,213,214,231 one treatment and prevention166); eight215–222 societal (environmental)-level studies (eight prevention); and two223,224 societal (macro)-level studies (two prevention). The process of inclusion and exclusion of studies is detailed in Figure 7. Included studies are summarised by intervention type in Appendix 5. Full summaries of each study are provided in Appendix 7.
FIGURE 7.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for adult studies.
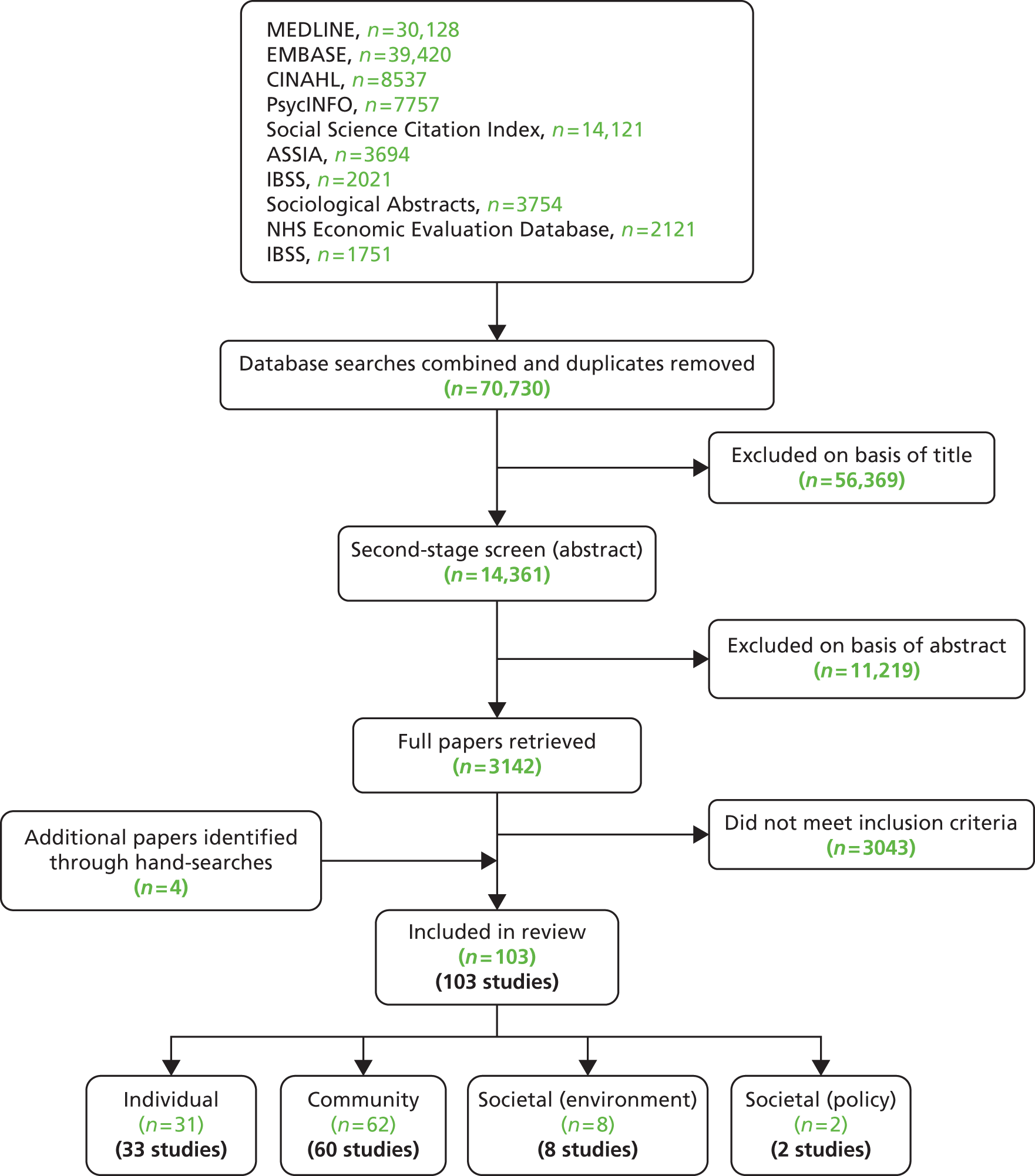
The included studies were of varying study designs, with 4165,66,103,128–130,132–136,138,139,148–150,152,166–171,174,176,179,180,182–184,186–189,197–200,209–212,219,225,230 experimental and 6243,127,131,140–147,153–165,172,173,175,178,181,185,190–196,200–208,213–218,220–224,231 observational studies. The majority of the studies came from the USA (n = 62127,129–134,136,138,145,150,154,155,164–172,174–176,178,179,181–186,190,191,193,195,196,198–200,202,203,205,206,210,213,214,219–224,230,231) and Europe (n = 30128,135,140,141,143,144,146,147,153,156,159–161,189,192,197,208,215–218), including 12 from the UK135,141,143,147,153,189,192,208,218 (Figure 8). Studies largely had body weight or BMI as the main outcome. Most of the included studies were targeted at low-SES adults (n = 6743,65,66,103,128,132,134–137,140,141,143–148–150,152–160,164–171,174,176,178–185,197–199,200–217,223–225,230,231) although there was a reasonable number of studies that examined differential intervention effects by SES (n = 36127,129–131,138–146,161–163,172,173,175,186–196,218,219,221,222). There were some high-quality studies (n = 23128–131,133,135,136,140,150,157,167,176,183,186,189,197–200,210,211,225,230) but the majority were only of low (n = 4743,65,66,127,138,139,141–144,146–149,152,153,155,156,159,161–166,169–173,178,180,188,193,195,196,201,204–206,208,213,214,218,223,224) or moderate (n = 33103,132,134,137,145,154,158,160,168,174,175,179,182,184,185,187,190–192,194,200,202,203,207,209,212,215–222,231) quality. Descriptions of how interventions were implemented were also very mixed.
FIGURE 8.
The geographical distribution of the included adult studies.
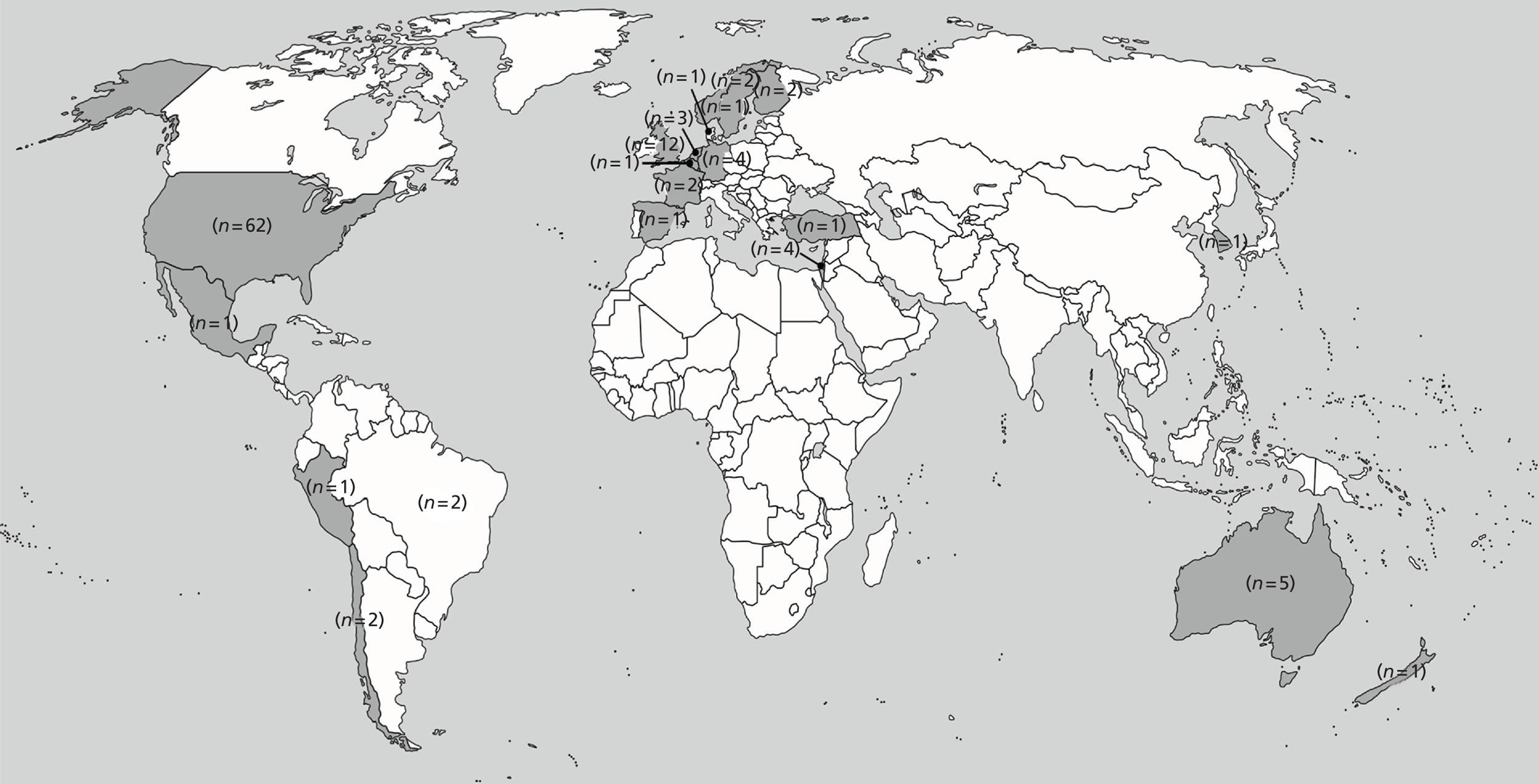
Studies excluded from the review
Figure 7 details the process of inclusion and exclusion of studies from the review. The reasons for the exclusion of papers at the full paper stage (n = 3043) are available from the authors on request. The most common reason for exclusion was lack of data by SES.
Results of the review
Individual-level interventions
Overview
Thirty-three43,127–150,152,154–158 individual-level studies were identified that met the review inclusion criteria. Because of heterogeneity in terms of study design and main outcomes, it was possible to conduct meta-analysis for only a small subset of studies in this category (n = 4133,135,136,152 for weight change and n = 4132,135,149,152 for BMI change, all targeted interventions). The 33 studies are therefore synthesised narratively in terms of whether they followed a universal (n = 13127,129–131,138–146) or a targeted (n = 2043,128,132,134–137,140,141,143–148-150,152,154–158) approach. The results are also summarised in Table 51 (universal-approach studies) and Table 52 (targeted-approach studies) (see Appendix 5). Effect size data (when possible) are presented in Tables 22–25 and the meta-analysis is reported separately at the end of this section, with the raw data included reported in Tables 26 and 27. Implementation information for each study is provided in Tables 53 and 54 (see Appendix 5).
Most of the studies (n = 2143,127–131,134,137,139,140,143–146,152,154,156–158) were prevention-type studies (they included participants regardless of their weight status). The other 12 studies132,133,135,136,138,141,142,147–150,155 were treatment studies in participants who were already overweight or obese. The greatest number of studies were conducted in health-care settings or study/university settings (n = 1943,131,133,134,136–138,141,143,144,147,150,152,155,157,158), with five129,130,135,148,149 studies conducted in participants’ homes (or in the home environment, e.g. shopping vouchers for fruit and vegetables), two128,142 delivered remotely by telephone or through the internet and seven127,132,139,140,145,146 being mass media or population-wide campaigns or prevention activities. Thirteen127,129–134,136,138,145,150,154,155 of the studies were conducted in the USA, with two127 of those also being conducted in Sweden. In addition, seven135,141,143,147,152 studies were conducted in the UK, three each in Australia,139,142,148,149 Israel137,157,158 and the Netherlands140,156 and one each in Finland,144 Germany,146 Spain128 and New Zealand. 43 One study was published in a foreign-language journal. 128 Seven129–136 studies targeted women only, with two133,136 targeting only African American women, two131,134 targeting pregnant women and one135 targeting mothers who were 6–18 weeks post partum. One137 study targeted men only and one128 recruited participants from industrial workplaces, resulting in a predominantly male sample.
The numbers of participants in the studies varied considerably, between n = 9 and n = 14,078 (median sample size 687), and the median follow-up time was 12 months (range 3–72 months). Eight of the studies were of high methodological quality (using the EPHPP tool; see Appendix 3), six were of moderate quality and the remaining studies were of low quality. All of the studies reported some elements of how the intervention was implemented (see Appendix 5, Tables 53 and 54), with 21 studies scoring ≥ 6.
Universal interventions
Three129,130,138,139 experimental and 10127,131,140–146 observational studies followed a universal approach (all diet and physical activity studies). One study145 was of moderate quality and three129–131,140 were of high quality, with the remaining studies of low quality. All of the experimental studies found no differential effects by SES. One found that a financial incentive weight loss programme (compared with a non-financial incentive weight loss programme) led to weight loss (low quality);138 one observed no intervention or differential effects of a weight prevention programme (no contact control; high quality);129,130 and one found that, although in the final (low-quality) study weight increased after a nurse-delivered counselling cardiovascular disease risk prevention intervention (usual-care control), there were no differential effects by occupation139 (Table 22).
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Nutrition and physical activity interventions | ||||||||
| Volpp et al. 2008138a | ||||||||
| Weight (lb) | 19 | –14 | 10.2 | 19 | –3.9 | 9.1 | –1.02 (–1.69 to –0.35) | No differential effects by income |
| Volpp et al. 2008138b | ||||||||
| Weight (lb) | 19 | –13.1 | 12.6 | 19 | –3.9 | 9.1 | –0.82 (–1.49 to –0.15) | No differential effects by income |
| Edye et al. 1989139 | ||||||||
| Weight (kg) | 861 | –1 | 4.11 | 1076 | –1.25 | 3.94 | 0.06 (–0.04 to 0.16) | No differential effects by occupation |
One high-quality observational study found that an intervention to prevent excess gestational weight gain had more beneficial effects among low-income women than among high-income women131 (Table 23). A high-quality study observed beneficial intervention effects (BMI and waist circumference) after a population-wide/mass media cardiovascular disease prevention programme in both moderate to high and low-SES groups. 140 Three studies (all low quality) observed beneficial effects of weight-management programmes141,142 and a health trainer-led prevention programme,143 with no differential effects by SES. One low-quality study found beneficial effects of a national diabetes prevention programme in terms of weight, BMI and waist circumference reductions, which were similar across all SES groups144 (see Table 23). Two further studies of a mass media campaign (moderate quality)145 and a population-wide cardiovascular disease prevention programme (low quality)146 also found no differential effects by SES; however, no beneficial changes were observed in either study. One population-based health promotion intervention was evaluated using two different study designs (therefore this counted as two studies; both low quality) in two different countries (Sweden and the USA). 127 The evaluation using a controlled prospective cohort design found no differential effects by education but also no decreases in BMI in both countries, whereas the evaluation using serial cross-sectional surveys observed adverse effects (increases in BMI) both overall and in those with a low level of education in Sweden, but no intervention or differential effects in the USA or when data from the two countries were pooled.
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Nutrition and physical activity interventions | ||||||||
| Olson et al. 2004131 | ||||||||
| Gestational weight gain (kg) | 158 | 0.59 | 4.75 | 359 | 1.31 | 5.6 | –0.13 (–0.33 to 0.07) | Significant intervention effect for weight gain in low-income women only |
| Rautio et al. 2011144a | ||||||||
| Weight (kg) | 376 | –1.38 | 5.06 | NA | NA | NA | –0.27 (–0.41 to –0.13) | Low level of education |
| Weight (kg) | 549 | –1.63 | 5.99 | NA | NA | NA | –0.27 (–0.39 to –0.15) | Intermediate level of education |
| Weight (kg) | 79 | –0.88 | 4.16 | NA | NA | NA | –0.21 (–0.52 to 0.1) | High level of education |
| BMI (kg/m2) | 375 | –0.44 | 1.62 | NA | NA | NA | –0.27 (–0.41 to –0.13) | Low level of education |
| BMI (kg/m2) | 546 | –0.56 | 1.69 | NA | NA | NA | –0.33 (–0.45 to –0.21) | Intermediate level of education |
| BMI (kg/m2) | 79 | –0.29 | 1.35 | NA | NA | NA | –0.21 (–0.52 to 0.1) | High level of education |
| Waist circumference (cm) | 358 | –1.58 | 5.34 | NA | NA | NA | –0.3 (–0.46 to –0.14) | Low level of education |
| Waist circumference (cm) | 531 | –1.75 | 5.2 | NA | NA | NA | –0.34 (–0.46 to –0.22) | Intermediate level of education |
| Waist circumference (cm) | 79 | –0.14 | 4.55 | NA | NA | NA | –0.03 (–0.34 to 0.28) | High level of education |
| Rautio et al. 2011144b | ||||||||
| Weight (kg) | 643 | –1.48 | 5.92 | NA | NA | NA | –0.25 (–0.37 to –0.13) | Low level of education |
| Weight (kg) | 1137 | –1.38 | 5.31 | NA | NA | NA | –0.26 (–0.34 to –0.18) | Intermediate level of education |
| Weight (kg) | 193 | –0.78 | 3.96 | NA | NA | NA | –0.2 (–0.4 to 0) | High level of education |
| BMI (kg/m2) | 643 | –0.57 | 2.18 | NA | NA | NA | –0.26 (–0.38 to –0.14) | Low level of education |
| BMI (kg/m2) | 1135 | –0.52 | 1.96 | NA | NA | NA | –0.27 (–0.35 to –0.19) | Intermediate level of education |
| BMI (kg/m2) | 191 | –0.34 | 1.47 | NA | NA | NA | –0.23 (–0.43 to –0.03) | High level of education |
| Waist circumference (cm) | 618 | –1.5 | 5.47 | NA | NA | NA | –0.27 (–0.39 to –0.15) | Low level of education |
| Waist circumference (cm) | 1089 | –1.33 | 5.9 | NA | NA | NA | –0.23 (–0.31 to –0.15) | Intermediate level of education |
| Waist circumference (cm) | 183 | –1.47 | 4.98 | NA | NA | NA | –0.3 (–0.52 to –0.08) | High level of education |
Targeted interventions
Nine128,132–136,148–150,152 experimental and eleven43,137,140,141,143,147,154–158 observational studies followed a targeted approach (interventions targeted at low-SES adults or low-SES areas) (Tables 24 and 25 respectively). Four experimental studies (two of strong quality,133,135 one of moderate quality132 and one of weak quality148,149) observed beneficial intervention effects on obesity-related outcomes. Three of these studies were weight-management treatment programmes with diet and physical activity components133,135,136,147 (two usual-care controls133,136,147 and one lower-intensity intervention control135) and one was a physical activity and nutrition programme for sedentary older adults (no-intervention control). 148,149 A high-quality pilot study (using an enhanced standard care control) found no beneficial effects of a diabetes prevention programme for overweight adults, although there was a trend towards a reduction in body weight. 150 One high-quality study found a beneficial intervention effect of a telephone-based counselling intervention (participants were recruited from a manufacturing company but the intervention was home based) in terms of weight loss and BMI. 128 Two studies (both of moderate quality) found no beneficial effects of an intervention to prevent excessive gestational weight gain (standard care control)134,151 or a diet-only culturally appropriate fruit and vegetable promotion programme (with an active control; fruit and vegetable gift card only vs. gift card plus health education). 132 One moderate-quality study even observed an adverse effect on waist circumference of a lifestyle helper intervention using behavioural counselling (vs. a lifestyle helper intervention without behavioural counselling), although there was no effect on BMI. 152
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Nutrition and physical activity interventions | |||||||
| Sierra et al. 2010128 | |||||||
| BMI (kg/m2) | 3085 | –0.05 | 2.267052 | 1707 | 0.16 | 2.32 | –0.09 (–0.15 to –0.03) |
| Weight | 3085 | –0.09 | 0.283382 | 1707 | 0.13 | 5.27 | –0.07 (–0.13 to –0.01) |
| Waist circumference (cm) | 3085 | –0.7 | 10.72 | 1707 | –0.14 | 10.12 | –0.05 (–0.11 to 0.01) |
| Weerts and Amoran 2011132 | |||||||
| Weight (lb) | 4 | –6.05 | 3.93 | 5 | 3.68 | 4.06 | –2.16 (–3.81 to –0.51) |
| Craigie et al. 2011135 | |||||||
| Body fat (%) | 22 | –1.5 | 0.8 | 14 | –0.5 | 1.4 | –0.91 (–1.62 to –0.2) |
| Burke et al. 2011,148 2012149 | |||||||
| Waist-to-hip ratio | 176 | –0.02 | 0.085147 | 199 | –0.01 | 0.09 | –0.11 (–0.31 to 0.09) |
| Hillier et al. 2012152 | |||||||
| Waist circumference (cm) | 31 | –0.3 | 17.75 | 24 | –0.7 | 12.70 | 0.03 (–0.5 to 0.56) |
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Nutrition and physical activity interventions | |||||||
| Jackson et al. 2007147 | |||||||
| BMI (kg/m2) | 28 | –3.97 | 5.58 | NA | NA | NA | –0.71 (–1.26 to –0.16) |
| Weight (kg) | 29 | –10.48 | 18.41 | NA | NA | NA | –0.57 (–1.1 to –0.04) |
| Gardner et al. 2012143 | |||||||
| BMI (kg/m2) | 3759 | –1.77 | 2.45 | NA | NA | NA | –0.72 (–0.76 to –0.68) |
| Verheijden et al. 2012156 | |||||||
| BMI (kg/m2) | 816 | 0.2 | 4.65 | NA | NA | NA | 0.04 (–0.06 to 0.14) |
| Abramson et al. 1979137 | |||||||
| Weight (kg) | 211 | –0.1 | 11.45 | 709 | 0.3 | 10.65 | –0.04 (–0.2 to 0.12) |
| Abramson et al. 1981157a | |||||||
| Weight (kg) | 216 | –0.1 | 11.55 | 733 | 0.3 | 11.18 | –0.04 (–0.2 to 0.12) |
| Abramson et al. 1981157b | |||||||
| Weight (kg) | 308 | –0.9 | 12.05 | 779 | –0.1 | 11.80 | –0.07 (–0.21 to 0.07) |
| Johnson and Meadows 2010154c | |||||||
| Weight (lb) | 13 | –10 | 57.52 | NA | NA | NA | –0.17 (–0.93 to 0.59) |
| Johnson and Meadows 2010154d | |||||||
| Weight (lb) | 13 | 4 | 62.74 | NA | NA | NA | 0.06 (–0.7 to 0.82) |
Of the observational studies, three140,143,147 diet and physical activity interventions (two of weak quality143,147 and one of high quality140) led to favourable intervention effects in terms of weight loss and BMI: one weight-management treatment programme,147 one health trainer-led prevention programme143 and one population-wide/mass media cardiovascular disease prevention programme. 140 One physical activity-only intervention investigating a dog-walking programme also improved obesity-related outcomes (moderate-quality study). 154 A clinic-based nurse health promotion (diet and physical activity) intervention for overweight participants saw beneficial effects in those who were classified as full adherers, but this effect was lost when all participants were included in the analysis (low-quality study). 155 Marshall et al. 43 did not find any beneficial effects in terms of BMI or waist circumference in those attending a nurse-led healthy lifestyle clinic (low-quality study) and Verheijden et al. 156 saw no changes in BMI following a mass media campaign except for a small decrease in non-Dutch people following a second campaign (low-quality study).
Three studies,137,157,158 using different populations, evaluated the Community syndrome of Hypertension, Atherosclerosis and Diabetes (CHAD) programme in Israel. The preliminary study (moderate quality) in a sample of men found no beneficial effects in terms of body weight or prevalence of overweight. 137 The evaluation of the first 5 years of the programme observed reductions in the prevalence of overweight overall and BMI in women (high-quality study);157 however, these beneficial effects were not observed in the evaluation of the second 5 years of the programme, although it is worth noting that a different study design was used (moderate-quality study). 158
Meta-analysis of targeted individual-level interventions
Effect estimates were pooled for the five132,133,135,136,149,152 experimental studies of targeted physical activity/diet interventions for which there were sufficient data in terms of sample size, means and standard deviations for both the control group and the intervention group, both at baseline and at follow-up. Common outcomes identified for meta-analysis were weight change (n = 4133,135,136,152) and BMI change (n = 4132,135,149,152).
Random-effects models were used in all cases as the test for heterogeneity was significant (p < 0.20) and/or the I2 statistic was moderate or high (> 50%). This heterogeneity may have been a result of differences in the interventions as well as in the samples (e.g. age). This level of heterogeneity means that the results of the meta-analysis should be treated with caution.
Individual-level interventions: weight change
Results for effects of interventions on weight were pooled for the experimental studies with usable data (n = 4133,135,136,152) and, using Egger’s test (–0.3452, p = 0.7300), there was no indication of publication bias. In Figure 9 the random-effects model shows a signficant pooled effect in favour of the intervention (mean difference –1.52, 95% CI –2.53 to –0.52). There was no evidence of heterogeneity (I2 = 38.85%, p = 0.2565) between the studies. Table 26 shows the raw data included in the meta-analysis.
FIGURE 9.
Random-effects meta-analysis of weight change: adult individual-level studies.
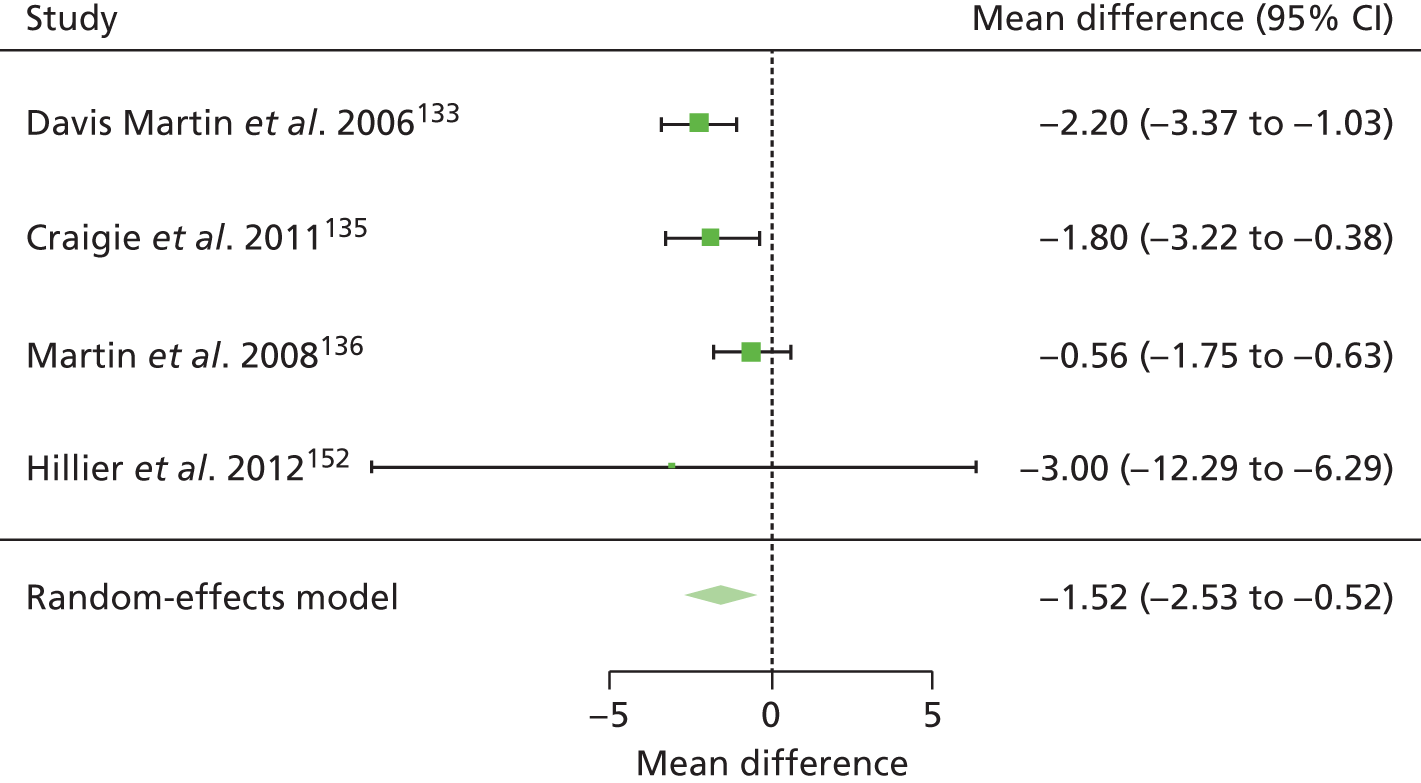
Individual-level interventions: body mass index change
Results for BMI were pooled for the experimental studies with usable data (n = 4132,135,149,152). Using Egger’s test (0.2071, p = 0.8360) there was no indication of publication bias. In Figure 10 the random-effects model shows a significant, albeit small, pooled effect in favour of the intervention (mean difference –0.85, 95% CI –1.72 to 0.02). There was evidence of substantial heterogeneity (I2 = 65.87%, p=0.0583) between the studies. Table 27 shows the raw data included in the meta-analysis.
FIGURE 10.
Random-effects meta-analysis of BMI change: adult individual-level studies.

Community-level interventions
Overview
Sixty community studies (from 62 papers)65,66,103,153,159–176,178–200,202–214,225,230,231 were identified that met the review inclusion criteria. Because of heterogeneity in terms of study design and main outcomes, it was possible to conduct meta-analysis only for a small subset of interventions in this category (n = 1365,103,168,179,182,183,198,211,212,230 for weight, n = 965,66,179,182,198,209,212,230 for BMI change and n = 365,66,179 for waist circumference change; all targeted interventions). The 60 studies are therefore synthesised narratively in terms of whether they followed a universal approach (n = 16161–163,172,173,175,186–196) or a targeted approach (n = 4465,66,103,153,159,160,164–171,174,176,178–185,197–200,202–214,225,230,231). The results are also summarised in Table 55 (universal-approach studies) and Table 56 (targeted-approach studies) (see Appendix 5). Effect size data (when possible) are presented in Tables 28–30. The meta-analysis of the 25 outcomes is reported separately at the end of this section along with the raw data in Tables 31–33. Implementation information for each study is provided in Tables 57 and 58 (see Appendix 5).
Twenty-seven65,66,103,161–163,167,171,172,174,180,181,185,198,190,194,197,199,201,202,205,206,209–211,213,214,231 of the studies were aimed at the prevention of obesity and 32153,159,160,164,165,168–170,173,175,176,178,179,182–184,186–189,191–193,195,196,200,201,203,204,207,208,212,225,230 were aimed at the treatment of obesity (these studies included participants who were overweight and/or obese only). One study166 used both prevention and treatment strategies. Twenty-five164,166–169,176,178,181–184,190,196,198,203,204,207,209,210,212–214,225,231 studies were conducted in community settings (e.g. community centres, churches and schools), 1765,66,159,162,163,170–174,187,191,193,194,199,200,205,206 were workplace interventions, seven153,180,185,192,195,211,230 were conducted in health-care settings, two165,188,202,208 were conducted in both health-care and community settings, two160,161 investigated health insurance training courses, one179 was conducted in a university, one189 investigated a diet club and one201 a weight loss training camp. The four103,175,186,197 remaining studies investigated group-based interventions but their settings were unclear.
The majority of the studies were conducted in the USA (n = 42164–172,174–176,178,179,181–186,190,191,193,195,196,198–200,202,203,205,206,210,213,214,230,231), one of which202 was conducted at the USA/Mexico border. Four studies153,189,192,208 were conducted in the UK. Three studies159–161 were carried out in Germany and two each in Australia,194,211 Brazil162,163,212 and Chile. 65,66 There was one study from each of the following countries: Denmark,173 Israel,188 Korea,197 Mexico201 and Turkey. 204 Five of the studies were published in foreign-language journals: three in German,159–161 one in Spanish (Chile)65 and one in Portuguese (Brazil). 162,163
In the majority of studies, more women participated than men. Twenty-three164–169,174,176,178–180,182–184,188,197,199,200,203,212–214,225,230 studies were exclusively targeted at women, with six targeting mothers in particular. 164–169 Six studies were conducted in manufacturing companies;159,170–174 with the exception of the study by Grandjean et al. ,174 which targeted blue-collar female employees, the participants in these studies were predominantly men. Two studies targeted men only. 153,175 Six studies explicitly targeted African Americans (five176,179,180,200,230 of which also included only women), two studies recruited Mexican American women only,182–184 one study recruited Filipinos only (predominantly women)185 and one study recruited Latino women only. 167
The study populations varied considerably, with between 19 and 10,368 individuals included (median sample size 99) and a median follow-up time of 6.5 months (range 3–48 months). Thirteen of the studies were of high methodological quality,167,171,176,183,186,189,197–200,210,211,225,230 21 were of moderate quality103,160,168,174,175,179,182,184,185,187,190–192,200,202–204,207,209,212 and the remaining 26 were of low quality65,66,153,159,161–166,169,170,172,173,178,180,188,193,195,196,201,205,206,208,213,214 (using the EPHPP tool; see Appendix 3). All of the studies reported some elements of how the intervention was implemented (see Appendix 5, Tables 57 and 58), with 43 studies scoring ≥ 6.
Universal studies
Four experimental studies (two diet and physical activity studies,186,187 one diet-only study189 and one physical activity-only study188) followed the universal approach (Table 28). In one of the diet and physical activity studies (high quality), no relationship was found between the intervention effect of a weight loss programme based on behavioural education and social support (vs. a behavioural weight loss programme without social support) and the education status of participants, although the intervention was ineffective overall for weight maintenance. 186 In the other diet and physical activity study (moderate quality), a workplace telephone- and internet-based weight loss intervention was effective at reducing body weight and waist circumference compared with an information provision-only control group and the intervention effect was not affected by the participants’ level of education. 187 A low-quality study investigating the effectiveness of adding an exercise session component to a weight loss programme found that both the intervention group and the active control group (weight loss programme without an exercise component) lost weight to the same extent and that there were no differences in weight loss between employed and unemployed women in the intervention group (although employed women did lose more weight than unemployed women in the control group). 188 In the diet-only experimental study two types of diet (low-carbohydrate vs. low-fat diet) were compared in a diet club in the UK for the treatment of overweight (high-quality study). 189 The low-carbohydrate diet appeared to be more beneficial in the short term (3 months), especially in those of low SES, but this effect was lost after 1 year. Neither diet was effective overall in either social group after 1 year.
| Outcome | Intervention | Control | Effect size (95% CI) | SES analysis | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | |||
| Physical activity-only interventions | ||||||||
| Neumark-Sztainer et al. 1995188 | ||||||||
| Weight (kg) | 13 | –4.6 | 2.8 | 11 | –3.9 | 5 | –0.17 (–0.97 to 0.63) | No difference in weight loss between employed and non-employed in the intervention group (employed lost more weight than unemployed in the control group) |
| Nutrition and physical activity interventions | ||||||||
| Wing and Jeffrey 1999186a | ||||||||
| Weight (kg) | 36 | –6.1 | 4.7 | 29 | –5.3 | 6.8 | –0.14 (–0.63 to 0.35) | Employment did not affect overall weight loss |
| Wing and Jeffrey 1999186b | ||||||||
| Weight (kg) | 38 | –8.7 | 6.3 | 33 | –8.8 | 6.6 | 0.02 (–0.45 to 0.49) | Employment did not affect overall weight loss |
| van Wier et al. 2009187c | ||||||||
| Weight (kg) | 332 | –2.7 | 14.15 | 321 | –1 | 13.30 | –0.12 (–0.28 to 0.04) | Education level had no effect on intervention effects |
| Waist circumference (cm) | 236 | –4 | 10.15 | 231 | –2 | 9.90 | –0.2 (–0.38 to –0.02) | |
| van Wier et al. 2009187d | ||||||||
| Weight (kg) | 329 | –2.1 | 14.15 | 321 | –1 | 13.30 | –0.08 (–0.24 to 0.08) | Education level had no effect on intervention effects |
| Waist circumference (cm) | 235 | –3.3 | 10.25 | 231 | –2 | 9.90 | –0.13 (–0.31 to 0.05) | |
Twelve observational studies (10 nutrition and physical activity studies,161,172,173,175,190–193,195,196 one diet-only study162,163 and one physical activity-only study194) followed the universal approach. Four moderate-quality studies175,190–192 and three low-quality studies161,173,193 found that the interventions investigated [four weight-management programmes, two health promotion (prevention) interventions and one workplace weight loss competition] led to reductions in BMI or weight overall and that SES indicators were not associated with these intervention effects. Another low-quality study investigating a workplace-based telephone coaching health promotion (prevention) intervention observed reductions in body weight that did not differ across income groups;172 there was even a tendency for more weight loss in those who were less educated (although this was not statistically significant). The moderate-quality physical activity study (a pedometer-based workplace health promotion intervention) observed reductions in waist circumference overall and no differential intervention effects by level of education. 194 A low-quality study found no differences in education level between those who were successful in a group-based weight loss programme and those who were unsuccessful,195 and another low-quality study found no association between employment status and weight gain during the maintenance period following a commercial weight loss programme. 196 Although these studies do not show any strong evidence of reducing SES inequalities in obesity, they do show promising results for the prevention of such inequalities. However, one low-quality study showed that the Workers’ Food Program in Brazil had adverse effects (weight gain, increase in overweight rates) in workers of low SES but not in those of high SES,162,163 suggesting that this intervention may contribute to the development of SES inequalities in obesity.
Targeted interventions
Twenty-four65,66,103,166–171,174,176,179,180,182–184,197–200,209–212,225,230 experimental studies followed the targeted approach (Table 29). Sixteen65,66,103,166–171,179,182,184,197–200,230 of these studies examined interventions with diet and physical activity components, five176,183,209–211,225 examined interventions with a diet component only and three174,180,212 were physical activity-only interventions. Twenty153,159,164,165,178,181,185,200–208,213,214,231 observational studies followed the targeted approach (Table 30). Sixteen153,159,164,178,185,200–208 of these studies targeted both diet and physical activity, one160 contained a diet component only and three181,213,214,231 were physical activity-only interventions.
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Nutrition-only interventions | |||||||
| Howard-Pitney et al. 1997210 | |||||||
| BMI (kg/m2) | 183 | 0 | 0.2 | 168 | 0 | 0.2 | 0 (–0.22 to 0.22) |
| Physical activity-only interventions | |||||||
| Grandjean et al. 1996174 | |||||||
| Weight (kg) | 20 | –2 | 13.11 | 17 | 0.7 | 11.38 | –0.22 (–0.87 to 0.43) |
| Nutrition and physical activity interventions | |||||||
| Krummel et al. 2010166 | |||||||
| Weight (lb) | 28 | 2.9 | 11.8 | 36 | 2.9 | 10.7 | 0 (–0.49 to 0.49) |
| BMI (kg/m2) | 28 | 0.54 | 1.9 | 36 | 0.54 | 1.8 | 0 (–0.49 to 0.49) |
| Waist circumference (inches) | 28 | –0.8 | 2 | 36 | –0.44 | 2 | –0.18 (–0.67 to 0.31) |
| Nichols 1995179 | |||||||
| BMI (kg/m2) | 20 | –0.95 | 1.05 | 17 | 0.32 | 1.03 | –1.19 (–1.9 to –0.48) |
| Outcome | Intervention | Control | Effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean Δ | SD | n | Mean Δ | SD | ||
| Physical activity-only interventions | |||||||
| Clark et al. 2003213a | |||||||
| Weight (lb) | 36 | 3.55 | 8.94 | NA | NA | NA | 0.4 (–0.07 to 0.87) |
| BMI (kg/m2) | 36 | 0.25 | 1.56 | NA | NA | NA | 0.16 (–0.31 to 0.63) |
| Waist circumference (mm) | 34 | 2.56 | 4.65 | NA | NA | NA | 0.55 (0.06 to 1.04) |
| Clark et al. 2003213b | |||||||
| Weight (lb) | 17 | 1.31 | 9.54 | NA | NA | NA | 0.14 (–0.53 to 0.81) |
| BMI (kg/m2) | 17 | –0.34 | 1.63 | NA | NA | NA | –0.21 (–0.88 to 0.46) |
| Waist circumference (mm) | 17 | 2.18 | 5.01 | NA | NA | NA | 0.44 (–0.25 to 1.13) |
| Clark et al. 2003213c | |||||||
| Weight (lb) | 18 | –4.26 | 8.48 | NA | NA | NA | –0.5 (–1.17 to 0.17) |
| BMI (kg/m2) | 18 | –1.12 | 1.67 | NA | NA | NA | –0.67 (–1.34 to 0) |
| Waist circumference (mm) | 18 | –0.94 | 4.89 | NA | NA | NA | –0.19 (–0.84 to 0.46) |
| Carlin 2009214 | |||||||
| Weight (lb) | 59 | –2.54 | 9.41 | NA | NA | NA | –0.27 (–0.62 to 0.08) |
| BMI (kg/m2) | 59 | –0.59 | 14.91 | NA | NA | NA | –0.04 (–0.39 to 0.31) |
| Zoellner et al. 2007181 | |||||||
| BMI (kg/m2) | 66 | –0.3 | 9.4 | NA | NA | NA | –0.03 (–0.36 to 0.3) |
| Waist circumference (cm) | 66 | –1.4 | 7.36 | NA | NA | NA | –0.19 (–0.52 to 0.14) |
| Nutrition and physical activity interventions | |||||||
| Clarke et al. 2007164 | |||||||
| Weight (lb) | 93 | –0.3 | 83.15 | NA | NA | NA | 0 (–0.29 to 0.29) |
| Gill 1998203 | |||||||
| Weight (lb) | 105 | 2.6 | 36.21 | NA | NA | NA | 0.07 (–0.2 to 0.34) |
| Rickel 2008200d | |||||||
| Weight (kg) | 43 | –6.83 | 0.76 | NA | NA | NA | –8.99 (–10.4 to –7.58) |
| BMI (kg/m2) | 43 | –2.6 | 0.29 | NA | NA | NA | –8.97 (–10.38 to –7.56) |
| Rickel 2008200e | |||||||
| Weight (kg) | 181 | –10.1 | 0.37 | NA | NA | NA | –27.3 (–29.3 to –25.3) |
| BMI (kg/m2) | 181 | –4.08 | 0.14 | NA | NA | NA | –29.14 (–31.28 to –27) |
| Perez-Lizaur et al. 2011204f | |||||||
| Weight (kg) | 278 | 1.42 | 15.76 | NA | NA | NA | 0.09 (–0.07 to 0.25) |
| BMI (kg/m2) | 278 | 3.57 | 9.09 | NA | NA | NA | 0.39 (0.21 to 0.57) |
| Waist circumference (cm) | 242 | –2 | 17.60 | NA | NA | NA | –0.11 (–0.29 to 0.07) |
| Perez-Lizaur et al. 2011204g | |||||||
| Weight (kg) | 173 | –1.95 | 14.72 | NA | NA | NA | –0.13 (–0.35 to 0.09) |
| BMI (kg/m2) | 173 | –0.78 | 5.29 | NA | NA | NA | –0.15 (–0.37 to 0.07) |
| Waist circumference (cm) | 158 | –4.68 | 8.88 | NA | NA | NA | –0.53 (–0.75 to –0.31) |
| Balcazar et al. 2009202 | |||||||
| Weight (lb) | 85 | –3 | 40 | NA | NA | NA | –0.08 (–0.37 to 0.21) |
| BMI (kg/m2) | 85 | –1 | 7.52 | NA | NA | NA | –0.13 (–0.42 to 0.16) |
| Christiansen et al. 2007201 | |||||||
| Weight (kg) | 99 | –7 | 34.01 | NA | NA | NA | –0.21 (–0.48 to 0.06) |
| Gray et al. 2009153 | |||||||
| Weight (kg) | 80 | –4.98 | 34.59 | NA | NA | NA | –0.14 (–0.45 to 0.17) |
| BMI (kg/m2) | 80 | –1.29 | 16.11 | NA | NA | NA | –0.08 (–0.39 to 0.23) |
| Waist circumference (cm) | 80 | –7.53 | 48.05 | NA | NA | NA | –0.16 (–0.47 to 0.15) |
| Hajek et al. 2010208 | |||||||
| Weight (kg) | 39 | –4.5 | 34.41 | NA | NA | NA | –0.13 (–0.58 to 0.32) |
| Pescatello et al. 2001205h | |||||||
| BMI (kg/m2) | 139 | 0.3 | 3.00 | 59 | 0.7 | 2.35 | –0.14 (–0.45 to 0.17) |
| Waist circumference (cm) | 139 | 1.7 | 9.62 | 59 | 3.2 | 8.62 | –0.16 (–0.47 to 0.15) |
| Pescatello et al. 2001205i | |||||||
| BMI (kg/m2) | 278 | 0.5 | 4.25 | NA | NA | NA | 0.12 (–0.04 to 0.28) |
| Waist circumference (cm) | 278 | 2.5 | 11.91 | NA | NA | NA | 0.21 (0.03 to 0.39) |
Diet and physical activity
Sixteen65,66,103,166–171,179,182,184,197–200,230 of the targeted experimental studies investigated interventions that contained both diet and physical activity components. Eight65,66,103,167,171,197–199 of the studies were prevention studies, seven168–170,179,182,184,200,230 were treatment studies and one166 contained both prevention and treatment elements. Results were almost equally divided with seven65,170,171,179,182,184,197,198 of the studies (two of low quality,65,170 two of moderate quality179,182,184 and three of high quality170,197,198) reporting positive intervention effects [two workplace health promotion interventions with no-treatment controls,65,171 two culturally sensitive weight loss programmes179,198 (one information-only control179), a workplace weight loss programme,170 a group-based health training obesity prevention programme using a wait-list control197 and a culturally tailored diabetes prevention programme with a usual-care control182,184] and eight66,103,166–169,177,199 of the studies (three of low quality,66,166,199 two of moderate quality103,168 and three of high quality167,177,179) reporting no intervention effects [three workplace-based health promotion interventions66,166,199 (one wait-list control and two with no-intervention controls), two group-based weight-management programmes167,168 (one with self-guided controls and one with a wait-list control), two culturally tailored weight-management programmes169,177 (one health education-only control and one usual-care control) and a family-based weight-management programme vs. an individual standard care control intervention that targeted overweight children but also involved parents103]. One high-quality study reported no effects in low-SES African American women but positive effects in low-SES Caucasian women following a culturally tailored weight-management intervention compared with an education-only control group. 200
Sixteen153,159,164,178,185,200–208 of the targeted observational studies contained both diet and physical activity components. Most of these studies investigated weight loss treatment programmes (n = 10153,164,200–203,207,208), with one being a residential weight loss camp. 201 The remainder of the studies (n = 6185,202,204–206) were prevention studies targeted at participants of any weight status. Again, the results appear to be divided, with seven studies159,185,202–206 (three of low quality159,205,206 and four of moderate quality185,202–204) finding no intervention effects (a workplace weight-management programme, a culturally appropriate weight-management programme, two workplace cardiovascular disease prevention programmes and three community group-based health promotion programmes delivered by community workers) and nine153,159,164,165,178,200,201,207,208 studies (seven of low quality153,160,164,165,178,201,208 and two of moderate quality200,207) finding positive intervention effects in terms of obesity-related outcomes (eight group-based weight-management programmes and a weight loss camp). One low-quality study205 also observed some adverse effects (increases in BMI and waist circumference) after a cardiovascular health awareness programme. 205
Diet only
Five176,183,209–211,225 of the targeted experimental studies contained a diet-based intervention only (two treatment176,183 and three prevention209–211 studies). Four176,209–211 of the studies (one of moderate quality209 and three of high quality176,210,211) investigated group-based health promotion programmes (two210,211 comparing modified programmes with usual programmes and one209 with an information provision-only control) and a peer-led176 weight-management programme (vs. a low-intensity control) and found no intervention effects on obesity-related outcomes. One high-quality study observed clinically (but not statistically) significant weight losses following a group-based weight-management programme (vs. standard care) for low-SES Mexican American women. 183
There was just one targeted observational study with a diet but no physical activity component. 160 This moderate-quality study found favourable effects after a health insurance programme for overweight adults.
Physical activity only
Three174,180,212 of the targeted experimental studies focused on physical activity behaviours only (one treatment212 and two prevention174,180 studies; one of low quality180 and two of moderate quality174,212). All of the interventions were for women only; they included an exercise session treatment intervention for overweight and obese women (with a no-intervention control),212 a community walking programme (with a minimal-treatment control)180 and a workplace exercise programme (with a no-intervention control). 174 All of these studies found positive intervention effects for at least one obesity-related outcome. Three181,213,214 of the observational targeted studies also focused on physical activity behaviours only (all prevention studies; two of low quality213,214 and one of moderate quality181); they investigated the effects of a community walking programme,181 an exercise intervention for older women213 and access to a community gym. 214 Again, all of these studies found beneficial intervention effects for at least one obesity-related outcome.
Meta-analysis of targeted community-level interventions
Effect estimates were pooled for the targeted experimental studies for which there were sufficient data in terms of sample size, means and standard deviations for both the control group and the intervention group, both at baseline and at follow-up. Meta-analysis was conducted for a small subset of intervention outcomes (n = 1365,102,168,179,182,183,198,211,212,230 for weight, n = 965,66,179,182,198,209,212,230 for BMI and n = 365,66,179 for waist circumference).
Random-effects models were used in all cases as the test for heterogeneity was significant (p < 0.20) and/or the I2 statistic was moderate or high (> 50%). This heterogeneity may have been a result of differences in the interventions as well as in the samples (e.g. age). This level of heterogeneity means that the results of the meta-analysis should be treated with caution.
Community-level interventions: weight change
Results were pooled for all of the experimental community-level studies with usable data (n = 1365,103,168,179,182,183,198,211,212,230 outcomes). Using Egger’s test (–0.4645, p = 0.6423) there is no indication of publication bias. In Figure 11 the random-effects model shows no significant pooled effect in favour of the intervention (mean difference –0.73, 95% CI –1.56 to 0.11). There was no evidence for significant heterogeneity (I2 = 20.40%, p = 0.5420) between the studies. The raw data included in the meta-analysis are shown in Table 31.
FIGURE 11.
Random-effects meta-analysis of weight change: adult community-level studies. a, individual intervention group vs. control group; b, family intervention group vs. control group; c, white/Anglo women; d, African American women; e, Hispanic women.
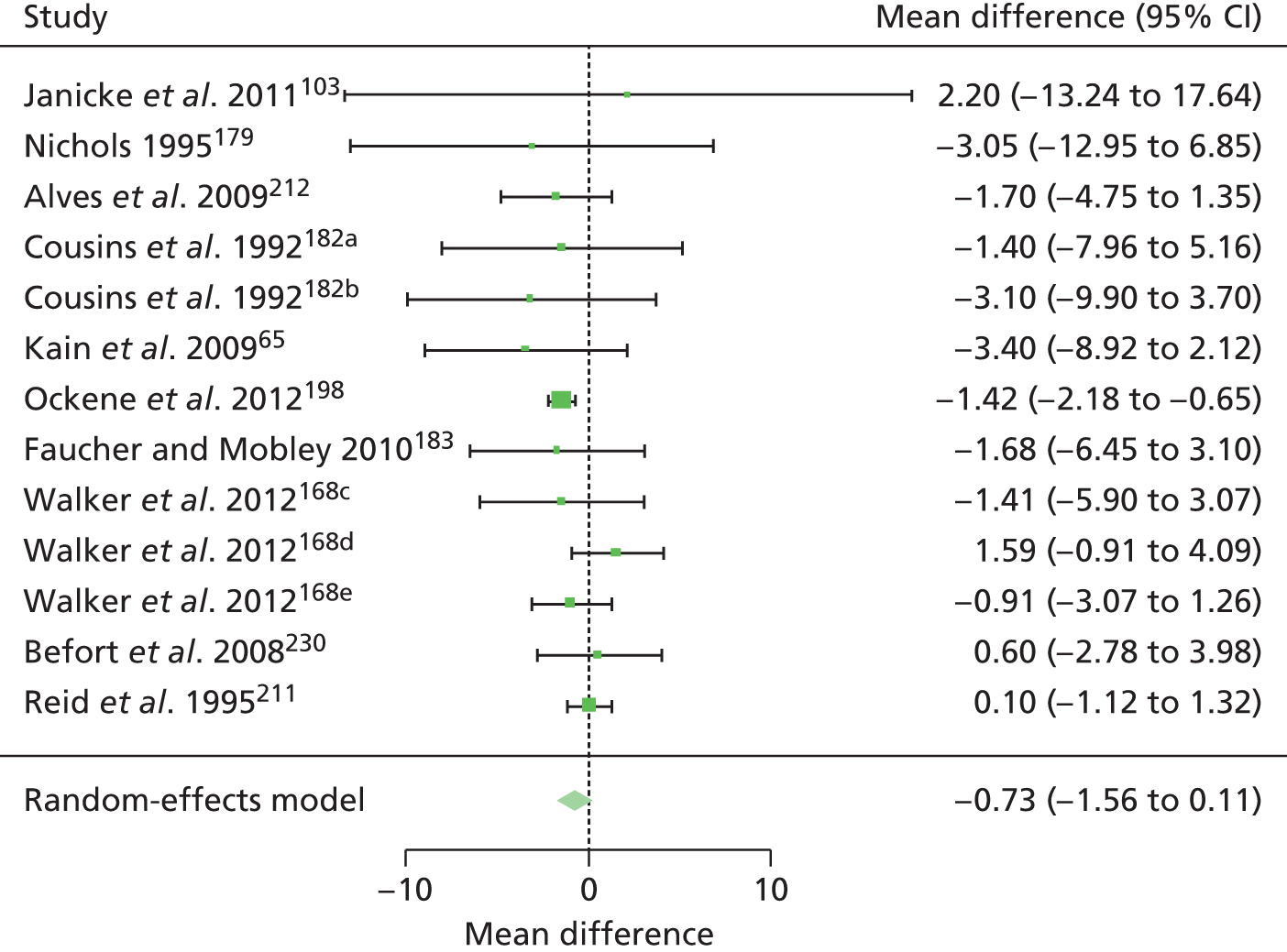
| Study | Intervention | Control | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| Janicke et al. 2011103 | 22 | 1.6 | 26.01 | 11 | –0.6 | 18.56 |
| Nichols 1995179 | 20 | –2.39 | 16.03 | 17 | 0.66 | 14.67 |
| Alves et al. 2009212 | 78 | –1.3 | 8 | 78 | 0.4 | 11.15 |
| Cousins et al. 1992182a | 32 | –2.1 | 14.05 | 27 | –0.7 | 11.66 |
| Cousins et al. 1992182b | 27 | –3.8 | 13.72 | 27 | –0.7 | 11.66 |
| Kain et al. 200965 | 38 | –1.5 | 9.08 | 19 | 1.9 | 10.45 |
| Ockene et al. 2012198 | 147 | –1.13 | 2.78 | 142 | 0.28 | 3.79 |
| Faucher and Mobley 2010183 | 7 | –2.94 | 3.4 | 5 | –1.27 | 4.62 |
| Walker et al. 2012168c | 8 | –2.59 | 6.21 | 8 | –1.17 | 1.81 |
| Walker et al. 2012168d | 9 | 1.5 | 2.85 | 11 | –0.09 | 2.81 |
| Walker et al. 2012168e | 5 | –1 | 1.85 | 9 | –0.09 | 2.18 |
| Befort et al. 2008230 | 14 | –2.6 | 4.2 | 19 | –3.2 | 5.7 |
| Reid et al. 1995211 | 76 | –0.4 | 4.44 | 73 | –0.5 | 3.05 |
Community-level interventions: body mass index change
Results were pooled for all of the experimental community-level studies with usable data (n = 965,66,179,182,198,209,212,230 outcomes). Using Egger’s test (–0.7140, p = 0.4752) there is no indication of publication bias. In Figure 12 the random-effects model shows a significant pooled effect in favour of the intervention (mean difference –0.31, 95% CI –0.57 to –0.06). There was no evidence of substantial heterogeneity (I2 = 21.73%, p = 0.7227) between the studies. The raw data included in the meta-analysis are shown in Table 32.
FIGURE 12.
Random-effects meta-analysis of BMI change: adult community-level studies. a, Individual group vs. control; b, family group vs. control.

| Study | Intervention | Control | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| Nichols 1995179 | 20 | –0.95 | 8.4 | 17 | 0.32 | 9.12 |
| Befort et al. 2008230 | 14 | –1 | 1.5 | 19 | –1.1 | 2 |
| Cullen et al. 2009209 | 318 | –0.3 | 0.42 | 240 | –0.1 | 0.56 |
| Alves et al. 2009212 | 78 | –0.6 | 4.67 | 78 | 0.1 | 4.87 |
| Ockene et al. 2012198 | 147 | –0.4 | 0.92 | 142 | 0.11 | 1.64 |
| Cousins et al. 1992182a | 32 | –0.8 | 7.28 | 27 | –0.3 | 7.29 |
| Cousins et al. 1992182b | 27 | –1.6 | 7.1 | 27 | –0.3 | 7.29 |
| Kain et al. 200965 | 38 | –0.4 | 5.8 | 19 | 1 | 5.51 |
| Kain et al. 201066 | 28 | –0.3 | 5.23 | 19 | –0.4 | 5.51 |
Community-level interventions: waist circumference change
Results were pooled for all of the experimental community-level studies with usable data (n = 365,66,179). Using Egger’s test (0.3589, p = 0.7197) there is no indication of publication bias. In Figure 13, the random-effects model shows a significant pooled effect in favour of the intervention (mean difference –4.26, 955 CI –4.83 to –3.69). Table 33 shows the raw data included in the meta-analysis.
FIGURE 13.
Random-effects meta-analysis of waist circumference change: adult community-level studies. a, Individual group vs. control; b, family group vs. control.

Societal-level interventions: environment
Overview
Eight215–222 environmental studies were identified that met the review inclusion criteria. All studies were aimed at prevention and combined some environmental-level changes with individual- and community-level interventions. Three studies conducted community-wide environmental interventions,215–217,222 one study incorporated both a community-wide and a workplace intervention218 and four studies conducted workplace interventions. 219–221 The results are summarised in Table 59 (universal-approach studies) and Table 60 (targeted-approach studies) (see Appendix 5), with implementation information provided in Tables 61 and 62 (see Appendix 5).
Most studies were conducted in the USA (n = 5219–222), with two215–217 from Norway and one218 from the UK. All of the studies were published in English and one was also published in Norwegian. 217 One of the studies was an experimental study219 and seven were observational studies. 215–218,222 Six of the studies were of moderate quality215–217,219,222 (using the EPHPP tool; see Appendix 3), with all using independently measured primary outcomes. Half of the studies215–219,221 reported most elements of how the intervention was implemented (see Appendix 5, Tables 61 and 62; high scores between 6 and 9), particularly in terms of motivation and delivery fidelity, but the other half218,220,222 reported only a few elements of implementation (scoring between 4 and 5). Two of the studies scored low on the quality appraisal because of the study design, having no control and using self-reported health measures. Because of heterogeneity in terms of study design and main outcomes, we could not conduct a meta-analysis of the eight environmental studies.
Universal interventions
The experimental study by Lemon et al. 219 (moderate quality; no-intervention control), which examined a universal intervention among a working-age population (aged 18–69 years) that combined environmental components (modification to stairways and canteens through the use of signs and improved street lighting and gritting) with other non-environmental components (including a social marketing campaign, farmers’ markets, walking groups, educational displays, newsletters and a website), showed adverse BMI intervention effects for lower-SES individuals. This study found that weight gain was most likely to be prevented in the groups with a higher income and a higher educational level, thus revealing that such environmental modifications may not be effective in narrowing socioeconomic inequalities in obesity but may increase them, although it is unclear whether this was solely the effect of the environmental modifications or a combination of these modifications and other aspects of the intervention (e.g. educational material).
Six observational studies followed the universal approach. Scoggins et al. 221 examined the effects of environmental modifications in the workplace (such as decorating stairways and replacement of unhealthy food in vending machines with healthy food) using two study designs: a 1-year controlled cohort study (moderate quality) and a 5-year uncontrolled cohort study (low quality). In both studies favourable weight loss effects for lower-SES adults were observed. This therefore suggests that such environmental modifications in the workplace may have favourable effects for lower-SES individuals. The observational study (moderate quality) by VanWormer et al. ,220 which also examined the effects of aesthetic stairwell enhancements and access to healthy food/beverages as well as other non-environmental interventions (such as the use of pedometers and website step-tracking to encourage physical activity, improved scale access for self-weighing, worksite advisory groups and site-wide publicity on nutrition and physical activity), found no difference in BMI change across SES groups. Therefore, these studies show contradictory results for the effect of environmental modifications in the workplace and community wide on lower-SES groups.
A controlled cohort study215–217 in those aged 30–67 years explored the intervention effects of environmental modifications (improved street lighting, pavement gritting and labelling of walking trails to increase the accessibility of areas for physical activity) and non-environmental modifications (including specifically designed leaflets, individual counselling, biannual fitness tests, organised walking groups and indoor group activity sessions) and found that the net proportion who increased their body mass was significantly lower in the intervention district than in the control district. This was found across all educational groups; however, it was more pronounced in low-SES men, thus showing potential favourable intervention effects on lower-SES groups as well as improvements across the social gradient.
One repeat cross-sectional study (moderate quality) conducted by Carleton et al. 222 explored the intervention effects of community-wide, environmental components (grocery store food labelling and healthy hearts menus) combined with non-environmental components (exercise courses and nutrition programmes at the public library) and found that BMI was lower in the intervention district than in the control district (similar to the results of the Jenum et al. study215–217). The other repeat cross-sectional study (low quality) by Tudor-Smith et al. ,218 which examined multiple interventions (both community wide and in the workplace) consisting of both environmental modifications (food labelling in a major grocery retailer, a restaurant and canteen scheme to increase the availability of healthy food choices, and smoke-free areas) and non-environmental modifications (smoking cessation television series), had significant biases that prevented the detection of intervention effects and differences between SES groups. These biases included possible contamination in the reference area because of other health promotion activities taking place there and the fact that the sample size for the reference area was too small to give it enough statistical power for the detection of likely net intervention effects.
Targeted interventions
One of the observational studies reported in the universal interventions section also followed a targeted approach as it was delivered in two low-SES districts. 215,216 The study explored the intervention effects of environmental modifications (improved street lighting, pavement gritting, and labelling of walking trails to increase accessibility of areas for physical activity) and non-environmental modifications (including specifically designed leaflets, individual counselling, biannual fitness tests, organised walking groups, and indoor group activity sessions) and found that the net proportion who increased their body mass was significantly lower in the intervention district than in the control district. Therefore, this intervention appeared to be effective in a low-SES population.
Societal-level interventions: macro
Two studies were identified that met the review inclusion criteria. 223,224 Both studies were aimed at prevention and were targeted at low-SES individuals/families. One study was based in the home223 whereas the other was a population-wide study. 224 The results are summarised in Table 63 (targeted-approach studies), with implementation information provided in Table 64 (see Appendix 5).
Both of the studies were observational studies and were conducted in the USA and published in English. They were both rated as being of low quality (using the EPHPP tool; see Appendix 3) because of not including a control group, the use of self-reported health measures and not reporting withdrawals/follow-ups when applicable. Because of the non-experimental study designs, we could not conduct a meta-analysis of these two studies.
Targeted interventions
The two studies investigated the effects on obesity-related outcomes of the US Food Stamp Program (now called the Supplemental Nutrition Assistance Program), which is aimed at low-income families. The study by Kaushal224 was a natural experiment that took advantage of a change in the federal law that denied a subgroup of the population access to the programme. The results from this study suggest that the Food Stamp Program had no effect on BMI. The second study investigated the effects of the Food Stamp Program in women using longitudinal data from the Panel Study of Income Dynamics. 223 The results were presented by food security status. There was no change in body weight in those who were persistently food secure, or those who changed food security status, but increases in body weight were associated with Food Stamp Program participation in those who were persistently food insecure (the most deprived group). These results suggest that the Food Stamp Program may be associated with increases in weight in low-income, food-insecure women that could potentially increase SES inequalities in obesity. However, the authors concluded that participation in the Food Stamp Program does not necessarily cause weight gain.
Synthesis of the ‘best-available’ international evidence
This review used very broad study inclusion criteria and conducted a very wide search to capture the entire evidence base on the effects of interventions to reduce inequalities in obesity among adults. This resulted in the inclusion of 103 unique studies on the effects of individual (n = 33127–150,152,155–158), community (n = 6065,66,103,153,159–176,178–200,202–214,225,230,231) and societal (n = 10215–224) interventions. This is a very large evidence base and much larger than anticipated. To make sense of it for policy and practice, this section focuses on synthesising only the ‘best-available’ evidence for each intervention type (n = 20). For the individual-level (n = 5129,130,133,135,136,150) and community-level (n = 12167,171,176,183,186,189,197–200,211,225,230) interventions, the ‘best-available’ international evidence is provided by high-quality experimental studies (randomised and non-RCTs, randomised and non-randomised cluster trials); for the societal (environmental)-level interventions (n = 1219), the ‘best-available’ international evidence is provided by moderate-quality experimental studies; and for the societal (macro)-level interventions (n = 2223,224), the ‘best-available’ international evidence is of low quality and observational in design (retrospective cohort and repeat cross-sectional studies). The findings of the ‘best-available’ evidence studies are summarised in Table 34. Overall, this shows very clearly that the various interventions either reduced inequalities in obesity (i.e. they reduced the prevalence of obesity-related outcomes among low-SES groups or they closed the SES gap) or had no effect, with only one study reporting a negative impact (i.e. it increased the gap in obesity-related outcomes). In the sections below the results of these international studies are synthesised in more detail by intervention type.
| Study | Impact on inequalities in obesity |
|---|---|
| Individual-level interventions (experimental, high quality; n = 5) | |
| Cragie et al. 2011135 | + |
| Davis Martin et al. 2006133 | + |
| Whittemore et al. 2009150 | + |
| Jeffery and French 1997,129 1999130 | 0 |
| Martin et al. 2008136 | 0 |
| Community level-interventions (experimental, high quality; n = 12) | |
| Erfurt et al. 1991171 | + |
| Ockene et al. 2012198 | + |
| Kisioglu et al. 2004197 | + |
| Faucher 2008,225 Faucher and Mobley 2010183 | 0 |
| Rickel 2008200 | 0 |
| Auslander et al. 2000176 | 0 |
| Baron et al. 1986189 | 0 |
| Befort et al. 2008230 | 0 |
| Campbell et al. 2002199 | 0 |
| Olvera et al. 2010167 | 0 |
| Reid et al. 1995211 | 0 |
| Wing et al. 1999186 | 0 |
| Societal (environmental)-level interventions (experimental, high quality; n = 1) | |
| Lemon et al. 2010219 | – |
| Societal (macro)-level interventions (observational, low quality; n = 2) | |
| Kaushal 2007224 | 0 |
| Jones and Frongillo 2006223 | 0 |
Individual-level interventions
Five high-quality experimental studies examined individual interventions: four targeted133,135,136,150 and one universal. 129,130 Four of the five studies were from the USA129,130,133,136,150 and all of the studies included all women or majority women participant groups. The four targeted studies examined tailored weight loss programmes delivered via primary care for low-income groups. 133,135,136,150 They found that these programmes can have positive short-term effects (up to 9 months) but that these are not sustained longer term (after 12 months). The universal study found that an educational intervention had no effect on preventing weight gain. 129,130
Tailored weight loss programmes (n = 4)
Two RCTs,133,136 a randomised controlled pilot study135 and a cluster randomised controlled pilot study150 examined primary care-delivered tailored weight loss programmes (monthly face-to-face lifestyle counselling on a healthy diet and physical activity behaviours) targeted at low-income populations.
One RCT of 106 low-income African American women found that, after 6 months, the intervention group demonstrated a significant weight loss [–2.0 kg, standard deviation (SD) 3.2 kg] compared with the control group (+0.2 kg, SD 2.9 kg; p = 0.03). 133 Another study, a small (n = 36) randomised controlled pilot study of overweight post-partum women living in areas of moderate to high deprivation in the UK, found that, after 12 weeks, body weight loss was significantly greater in the intervention group than in the comparison group (–1.6 kg vs. 0.2 kg; p = 0.018), with significant improvements in BMI (–0.7 kg/m2 vs. 0.1 kg/m2; p = 0.009) and percentage body fat (–1.5% vs. –0.5%; p = 0.029) too. 135 However, there were no significant differences in waist circumference or physical activity. A cluster randomised controlled pilot study investigated the effects of a tailored weight loss programme in 51 low-income adults (majority women) considered to be at high risk of diabetes in four areas of the USA. 150 After 6 months, 25% of the intervention group achieved a clinically significant weight loss compared with only 11% of the control group. However, physical activity and nutritional changes were similar among the control and intervention groups. Intention-to-treat analysis from another RCT showed that, after 9 months, weight loss among 86 low-income African American women was significantly higher in the intervention group than in the control group (–1.52 ± 3.72 kg vs. 0.61 ± 3.37 kg; F = 12.32; p < 0.01) although this was not sustained at 12 months (F = 3.80; p = 0.10). 136
Weight gain prevention educational intervention (n = 1)
The high-quality RCT that took a universal approach investigated the effects of a weight gain prevention educational intervention (consisting of a monthly newsletter with healthy behaviour messages) among low- and high-income women in the USA. 129,130 After 1 year the intervention improved weight among high-income women only, but after 3 years there were no significant intervention effects on weight for either the high-income group or the low-income group.
Community-level interventions
Twelve167,171,176,183,186,189,197–200,211,225,230 high-quality experimental studies examined community-level interventions: 11167,171,176,183,186,197–200,211,225,230 targeted and one189 universal. Seven of the studies176,186,197,198,200,211,230 examined the effects on weight outcomes among low-income adults of community-based group health education and counselling interventions; two171,199 evaluated workplace-delivered group health education and counselling interventions; and two167,183,225 examined family-based group education or physical activity interventions. The one universal study189 evaluated the differential effects of a diet club on weight loss by social class. The vast majority of the studies were from the USA (one each from the UK,189 Australia211 and Turkey197) and all except three studies171,198,211 had only women participants or a female majority. Some of the studies had very small sample sizes as they were pilot studies and many had active controls (usually standard care using individual-level interventions).
The seven targeted studies176,186,197,198,209,211,230 of community-based group health education and counselling found that behavioural weight loss programmes among low-income men and women can have short-term (4 months) but not long-term (7 months) positive effects on weight loss; that group lifestyle counselling interventions had limited effects, with one study211 reporting short-term positive effects on weight loss and two167,171 reporting no effects; and that group-based health education interventions were of limited effectiveness as two studies176,230 found no effects after 3 months and one197 found some positive effects on weight loss among low-income women at 6 months. The universal study189 found that a community diet club had short-term positive effects (3 months) on weight loss, particularly among low-SES participants, but that there was no significant longer-term effect (1 year). Two studies171,199 examined workplace-delivered group interventions and obtained divergent results: one study found positive long-term effects (3 years) of an extensive and complex health promotion, counselling and physical activity intervention on weight loss and weight maintenance among blue-collar men, whereas a study of blue-collar women employees found no long-term effect (5 years) on BMI of a lay health advisor programme. One study210 examined interventions that were delivered in school settings. One167 examined a physical activity intervention for low-income mothers and daughters, whereas the other200 examined a culturally tailored education programme. Neither found an intervention effect.
Community-based group interventions (n = 9)
Nine high-quality experimental studies examined community-based group health education and counselling interventions. Two177,186 studies examined behavioural weight loss programmes; three198,200,211 studies examined group lifestyle counselling interventions; three176,183,197,225 studies evaluated community-based group health education interventions; and the universal study189 examined a community-based diet club.
Two studies examined behavioural weight loss programmes among low-income men and women in the USA. 177,186 Together their findings suggest that such interventions have short-term (4 months) but not long-term (7 months) positive effects on weight loss. A RCT compared the effects on weight loss of a professionally delivered behavioural therapy active control condition (e.g. problem-solving, assertion, stimulus control) and a behavioural therapy and social support intervention among 136 low-income men and women in the USA. 186 The intervention showed short-term weight loss (up to 4 months) but this was not sustained at 7 and 10 months’ follow-up. A small randomised controlled pilot study177 investigated the effects of a culturally adapted weekly behavioural weight loss group programme with motivational interviewing compared with a behavioural weight loss group programme plus health education (active control) in 33 lower-income African American women. There were significant positive effects after 4 months on weight loss, calorie intake, percentage of calories from fat, and fruit and vegetable servings per day in both groups.
Three studies examined group lifestyle counselling interventions compared with an active control condition. 198,200,211 One198 found a short-term effect on weight loss among low-income Latino women whereas the other two200,211 found no intervention effect. A RCT evaluated a community-based, culturally tailored group lifestyle counselling intervention among 288 low-income (majority female) Latinos in the USA. 198 The intervention group lost significantly more weight after 12 months than the control group (intervention effect –2.5 lb; p = 0.04), with a significant decrease in BMI (–0.46 kg/m2; p = 0.04). A RCT in a low-income urban area of Australia examined the intervention effects on 149 participants of a one-off group lifestyle counselling session (lasting 2 hours) on the reduction of cardiovascular risk factors among those at high risk (majority male participants). 211 The control group received a pamphlet about reducing cardiovascular risk factors. After 6 months there were no significant weight changes either between or within groups. A RCT conducted by Rickel investigated a 12-month extended-care group counselling intervention (face-to-face group sessions vs. individual sessions delivered by telephone) compared with an education-only control condition following a weight loss intervention in 224 obese women living in low-SES areas of the USA. 200 The interventions had no effect overall on weight regain compared with the control group.
Three studies evaluated community-based group health education interventions. 176,183,197,225 The two US studies176,183,225 found no effects after 3 months whereas the Turkish study197 found some positive effects on weight loss after 6 months. A small randomised controlled pilot study compared the effects of a community centre-delivered, culturally adapted group nutritional education intervention with individual counselling (active control) on weight loss among 19 low-income Mexican American women in the USA. 183,225 There were no significant differences in weight loss in the intervention group compared with the control group after 5 months (2.9 kg vs. 1.3 kg; p = 0.47). A RCT investigated the effects of a 3-month peer educator-led group-based dietary skills development intervention among 239 obese low-income African American women in the USA. 176 The control group received a self-help workbook and a half-day workshop. There were no significant differences between the intervention group and the control group in BMI or weight. A RCT examined the effects of a group-based health education intervention among 400 women from a low-income area of Turkey. 197 The intervention group reported significant changes in lifestyle behaviours, leading to reductions in BMI (p = 0.014) and an increase in those with an ideal BMI (86 vs. 60; p = 0.009) after 6 months.
A small RCT carried out in the UK took a universal approach. 189 It compared the effects by social class status of weekly community diet clubs that used two different weight-reducing diets: a low-carbohydrate diet compared with a low-fat/high-fibre diet. Moderate weight losses were observed among 119 participants (majority women) in both diet groups after 3 months but there was no significant difference between the groups at the 1-year follow-up. Both diets worked equally well among the higher-SES participants (social class I or II), with the low-carbohydrate diet particularly effective at 3 months among the lower-SES participants (social classes III–V) (weight loss 5.0 kg vs. 3.0 kg; 95% CI of difference 0.3 kg to 3.9 kg).
Workplace-delivered group interventions (n = 2)
Two studies examined workplace-delivered group interventions, with divergent results. 171,199 A cluster RCT171 investigated the effects of four well-being interventions (active control condition – health screening only; intervention A – health screening and health education; intervention B – health screening, health education and follow-up counselling; intervention C – health screening, health education, follow-up counselling and organised workplace activities) among 690 overweight (majority male) blue-collar workers across four manufacturing worksites in the USA. At 3 years’ follow-up there was a significant intervention effect as, although the control group gained weight, intervention groups A and B experienced no weight change and intervention group C lost weight (p < 0.001). A RCT conducted by Campbell et al. 199 examined a 5-year workplace health promotion programme among 859 low-skilled women workers in the USA. The intervention consisted of two strategies: (1) individualised computer-tailored health messages and (2) a lay health advisors programme. There were no significant changes in BMI in either of the study groups.
Family-based group education interventions (n = 2)
Two US studies examined family interventions that were delivered in school settings. 167,210 Neither found an intervention effect. A RCT investigated the effects of a 12-week intensive school-based physical activity intervention compared with a less-intensive physical activity control condition among 92 daughter and mother dyads in a low-income Latino community in the USA. 167 There were no significant differences in maternal BMI at the end of the 12-week intervention. A second RCT tested the effectiveness of a professionally delivered, tailored group education intervention to prevent heart disease in 242 adults in the USA with low incomes and low literacy levels (the Stanford Nutrition Action Program; SNAP). 210 It consisted of a 6-week, tailored, classroom-based intervention followed by a 12-week maintenance intervention. It was compared with non-tailored general nutritional group interventions. There were no significant changes in BMI in the SNAP group compared with the control group.
Societal-level interventions
The ‘best-available’ evidence for the environmental interventions comes from one moderate-quality experimental study that took a universal approach and examined an intervention that modified the work environment. 219 It suggested that a multifaceted workplace weight prevention intervention could actually increase SES inequalities in obesity-related outcomes. The ‘best-available’ evidence for the macro-level interventions comes from two low-quality observational studies that took a targeted approach and examined the effects of the US Food Stamp Program, a welfare programme for people with a low income or with no income. 223,224 Together, the studies found little evidence of a relationship between participation and weight change. All three studies were from the USA and two219,223 included mainly women participants.
Societal: environmental-level interventions (n = 1)
The cluster RCT of 648 (majority female) participants in the USA investigated the effects of a multifaceted workplace weight prevention intervention on hospital employees. 219 The intervention included a social marketing campaign, interpersonal support groups and environmental strategies to promote physical activity and healthy eating. This included stairway signs, cafeteria signs, farmers’ markets, walking groups, challenges, workshops, educational displays, newsletters, a project website, a project information centre and print materials. The study suggested that, after 24 months of participation, the intervention reduced the average BMI. However, there were differential effects, with participants educated to a higher level more likely to prevent weight gain and participants with a lower level of education least likely to prevent weight gain.
Societal: macro-level interventions (n = 2)
A retrospective cohort study of 5503 US women found that a US$2000 increase in food stamps had no significant effect on weight change unless women were persistently food insecure (the very poorest), in which case a US$2000 increase in food stamps was associated with a significant increase in weight (β = 7.78; p < 0.05). 223 A retrospective repeat cross-sectional study of low-income men and women also found no significant effects on obesity of the US Food Stamp Program. 224
Synthesis of UK evidence
The majority of the international studies were from the USA. To further aid the translation of our results into UK policy and practice, this section focuses only on synthesising the UK evidence for each intervention type. In total, seven135,141,143,147,152 individual-level, four153,189,192,208 community-level and one218 societal (environmental)-level intervention studies were conducted in the UK. Just three135,152,189 of the studies were experimental studies (RCTs and cluster RCTs), two135,189 of high quality and one152 of low quality. The remaining studies were observational in design (uncontrolled prospective cohort studies). The findings of these UK studies are summarised in Table 35 and described in the following sections.
| Study | Study type, quality | Impact on inequalities in obesity |
|---|---|---|
| Individual-level interventions (n = 7) | ||
| Craigie et al. 2011135 | Experimental, high quality | + |
| Morrison et al. 2011141 | Observational, low quality | + |
| Gardner et al. 2012143 | Observational, low quality | + |
| Jackson et al. 2007147 | Observational, low quality | + |
| Morrison et al. 2011141 | Observational, low quality | 0 |
| Hillier et al. 2012152 | Experimental, low quality | 0 |
| Gardner et al. 2012143 | Observational, low quality | – |
| Community-level interventions (n = 4) | ||
| Gray et al. 2009153 | Observational, low quality | + |
| Hajek et al. 2010208 | Observational, low quality | + |
| Baron et al. 1986189 | Experimental, high quality | 0 |
| Lloyd and Khan 2011192 | Observational, moderate quality | 0 |
| Societal (environmental)-level interventions (n = 1) | ||
| Tudor-Smith et al. 1998218 | Observational, low quality | 0 |
Individual-level interventions (n = 7)
There were seven135,141,143,147,152 UK studies of individual-level interventions: two135,152 with an experimental design (a randomised controlled pilot study and a cluster RCT) and five141,143,147 with an observational design (uncontrolled prospective cohort studies, uncontrolled retrospective cohort studies and an uncontrolled before-and-after exploratory study) (two of the observational studies used both a targeted and a universal approach and therefore each of these were treated as two studies for the purpose of this review). Four135,141 of the studies investigated tailored weight loss interventions delivered in primary care and three143,147,152 investigated obesity prevention interventions delivered by health advisors (professionals and volunteers).
Tailored weight loss interventions
Four studies135,141,147 (one experimental high-quality study135 and three low-quality observational studies141,147) investigated tailored weight loss interventions delivered in primary care. The results from these studies suggest that tailored weight loss programmes delivered in primary care can have positive short- and long-term effects on obesity-related outcomes in low-SES groups and are equally effective across the SES gradient. A small (n = 36) randomised controlled pilot study of a primary care-delivered tailored weight loss programme targeted at overweight post-partum women living in areas of moderate to high deprivation in the UK found that, after 12 weeks, body weight loss was significantly greater in the intervention group than in the comparison group (–1.6 kg vs. 0.2 kg; p = 0.018), with significant improvements in BMI (–0.7 kg/m2 vs. 0.1 kg/m2; p = 0.009) and percentage body fat (–1.5% vs. –0.5%; p = 0.029) too. 135 However, there were no significant differences in waist circumference or physical activity. A small (n = 29) uncontrolled before-and-after exploratory study investigated the effects of a 52-week specialised health visitor-led therapeutic weight loss programme delivered at a primary care health-care centre located in a moderately deprived area in the UK. 147 Body weight and BMI were significantly reduced from baseline at 13 weeks (body weight –5.34 kg; BMI –2.01 kg/m2), 27 weeks (body weight –8.09 kg; BMI –3.04 kg/m2) and 52 weeks (body weight –10.48 kg; BMI –3.97 kg/m2; p = 0.000 for all). A larger (n = 809) uncontrolled prospective cohort study investigated the short-term effects of a 16-week behavioural weight loss programme among primarily low-SES patients in the UK (Scotland). 141 This study was both targeted and universal (two studies). At post-intervention follow-up, 36% of the participants had achieved a clinically successful weight loss of ≥ 5 kg and there were no differences in the prevalence of success across the SES gradient.
Health advisor-delivered obesity prevention interventions
Three studies143,152 (one low-quality experimental study152 and two low-quality observational studies143) examined obesity prevention interventions that were delivered by health advisors. The results from these studies suggest that a volunteer health advisor counselling intervention is ineffective in low-SES groups and that a health trainer programme, although effective in all SES groups, may be more effective among the least deprived. A small (n = 63) cluster RCT assessed the effectiveness of a 1-year volunteer health advisor counselling intervention in deprived areas of the UK. 152 There were no significant changes in BMI or weight change after 1 year but there was a significant increase in waist circumference (mean change 3.6 cm, 90% CI 0.8 cm to 6.3 cm) compared with the control group. A large (n = 3759) retrospective uncontrolled cohort study evaluated the NHS Health Trainer Service (HTS) targeted at disadvantaged patients in the UK (England and Wales). 143 The study also followed a universal approach as it explored differential effects by SES (and it was therefore treated as two studies for this review). Health trainers support clients to achieve healthy eating and physical activity goals. The mean duration of HTS attendance was 6.14 months. At the post-intervention follow-up, BMI was reduced by 1.77 points (95% CI –1.69 points to –1.85 points; p < 0.001), from 34.03 kg/m2 to 32.26 kg/m2. Overweight/obesity prevalence decreased from 94.7% to 91.0% and the proportion of obese clients decreased from 72.3% to 60.1%. Clients from the least deprived 80% of the population achieved a greater BMI change than the most deprived clients (0.28 BMI points; p = 0.001).
Community-level interventions (n = 4)
There were four153,189,192,208 UK studies of community-level interventions, one high-quality experimental study,189 one moderate-quality observational study192 and two low-quality observational studies. 153,208 All of the studies examined group-based weight loss programmes (diet clubs, commercial and behavioural programmes) and the results suggest that these programmes have positive effects in the short term in low-SES groups or equally across the SES gradient. However, a small amount of evidence suggests that these positive effects are not maintained in the long term.
A small RCT of a community-level intervention took a universal approach. 189 It compared the effects by social class status of weekly community diet clubs in the UK that used two different weight-reducing diets: a low-carbohydrate diet compared with a low-fat/high-fibre diet. Moderate weight losses were observed among 119 participants (majority women) in both diet groups after 3 months but there was no significant difference at the 1-year follow-up. Both diets worked equally well among the higher-SES participants (social class I or II), with the low-carbohydrate diet particularly effective at 3 months among the lower-SES participants (social classes III–V) (weight loss 5.0 kg vs. 3.0 kg; 95% CI of difference 0.3 kg to 3.9 kg). A large (n = 2456) uncontrolled prospective cohort study, also following a universal approach, investigated the short-term effects of a 12-week commercial weight loss programme. 192 The programme was used as part of a health service obesity treatment model (Healthy Choices) in the UK, with overweight and obese patients referred to the programme. Overall, participants lost on average 4.7 kg after 12 weeks, with completers losing 6.1 kg and dropouts losing 2.2 kg. In total, 44% of all participants achieved > 5% weight loss and were classified as being successful. Importantly, there was no statistical difference in successful weight loss outcomes between deprivation quintiles.
A small (n = 80) uncontrolled prospective cohort study investigated the short-term effects of a health service-led 12-week group-based behavioural weight loss programme targeted at men living in deprived areas of Scotland. 153 On average, participants lost 4.98 kg and 44% achieved the weight loss target of 5–10%. Similarly, a small (n = 39) uncontrolled before-and-after pilot study investigated the effects of a 6-week group-based behavioural weight loss programme incorporating a ‘buddy system’ conducted in localities of high deprivation in the UK. 208 The average weight loss at 3 months was 4.5 kg (4.7% of baseline body weight; p < 0.001).
Societal-level interventions (n = 1)
There was one UK study of a societal (environmental)-level intervention, with a weak observational study design. 218 The repeat cross-sectional study used two independent cross-sectional surveys in Wales (intervention) and north-east England (control) to assess the efficacy of the Heartbeat Wales cardiovascular disease prevention programme. Obesity-relevant interventions included food labelling and nutrition education with a major grocery retailer, a restaurant and canteen scheme to increase the availability of healthy food choices and a widespread worksite health promotion programme. There were no intervention effects on the prevalence of overweight and there were no differential effects by SES.
Implementation
Note: For the purposes of our analysis of intervention implementation, we used data from 94 studies43,65,66,103,127–231 (studies containing multiple study designs are reported as one study).
Using the implementation tool (see Box 1), we recorded information about how the interventions were implemented, organised and delivered. In this section we synthesise the main themes from across the 94 studies included in the adult review. More detailed analyses of implementation data are presented by intervention type and for each study in Tables 53 and 54 (individual-level interventions), Tables 57 and 58 (community-level interventions), Tables 61 and 62 [societal (environmental)-level interventions] and Table 64 [societal (macro)-level interventions] (see Appendix 5).
Motivation
All of the studies clearly described the motivation behind the intervention investigated. The main motivation was to reduce or prevent obesity and/or overweight or a combination of the two. In some cases this was in a particular population (e.g. low-SES men/women/families/communities or an African American population). Some studies gave as a general motivation the improvement of health and some were focused on the prevention of disease risk factors that included excessive weight/body fat. A minority of studies focused on diabetes prevention, the reduction of hypertension, lowering cholesterol levels, improving physical activity or reducing food insecurity.
Theory
Almost half of the studies (n = 45133–135,141–143,145–147,150,152,155,164,165,167–170,172,173,176,179–181,183,185,187,190,196,198–204,206,210,215–217,219,222,230) reported a theoretical underpinning of the intervention (or evaluation of the intervention). A number of studies reported multiple theories, frameworks and/or approaches. The most commonly reported theory informing the interventions was social cognitive theory, followed by the transtheoretical model of behaviour change, social learning theory, self-efficacy theory and the theory of planned behaviour. Other theories or frameworks reported included community capacity, community organisation theory, the cultural humility framework, the interaction model of client health behaviour, the health action process approach, the theory of diffusion of innovations, Jayne Felgen’s I2E2 model,232 social problem-solving theory, the stages of change model, the self-management of care model, the precede–proceed model, health behaviour change theory, the ecological model of change, social support models, positive deviance methods, cognitive restructuring, behavioural science theories, behavioural compliance management, behaviour therapy, communication theory, patient-centred counselling, motivational interviewing, economic theory, the social marketing framework, the bottom-up approach to health promotion and the concept of empowerment (collective/community control over the design and implementation of interventions) and participatory approaches.
Context
Only one study193 did not report the context in which the intervention was developed/delivered. For all of the other studies the most commonly reported context was social, usually led by health-care professionals, the research team or a community group. Five studies162,163,218,223,224 reported a political context to their studies: the intervention investigated by Veloso and Santana163 and Veloso et al. ,162 the Programa de Alimentação do Trabalhador (PAT), brought into law in 1976, was part of the National Program of Feeding and Nutrition implemented in response to 67% of the population being calorific deficient (in the 1940s, revised in the 1970s); the intervention investigated by Tudor-Smith et al. 218 was guided by the Welsh Office and the Health Education Council; and Jones and Frongillo223 and Kaushal224 evaluated the effects of a national food stamp programme aimed at reducing food insecurity and meeting the nutritional needs of low-income families. One study, that by Hwang et al. ,173 had an economic focus, examining the effects of financial incentives for behaviour change.
Experience
Sixty-five of the studies43,65,66,103,128–133,135–137,139,141–147,150,152,153,155,157,158,160,164,166–173,176,178,179,182–184,192,193,195,196,198,200–204,206,207,209–212,214–217,230 reported some information regarding the experience of either those who developed the intervention or those who delivered it. It appears that in all of these cases the interventions were delivered by those with appropriate experience or by those who were trained by others with appropriate experience. Many of the interventions were developed and delivered by multidisciplinary teams. However, there were some studies that were lacking in detail. For example, some studies were quite broad in their reporting (i.e. health-care professionals or researchers) but did not specify who delivered the intervention or the number of years of experience of those delivering the intervention and/or the number of years of training received by those delivering the intervention.
Consultation/collaboration
Only 27 studies127,132,136,146,147,150,152,160,166,168,169,171,176,178,179,181,183,185,193,197–199,202,204,207,214–217,231 reported that some degree of consultation/collaboration took place and, within these studies, the level of detail provided varied as well as the level of consultation and/or collaboration. For example, Hillier et al. 152 collaborated with local community and voluntary organisations to invite their members to act as community champions. Although the recruitment rate of community champions was lower than desired, this study sought to include local community members in the development and delivery of the intervention. Another study by Nichols179 consulted a small sample of African American women to test the feasibility and acceptability of a culturally tailored health improvement intervention.
Delivery fidelity
Forty-three studies66,103,128,132–136,150,155,161,164,166–170,175,176,178,180,181,187–192,194,195,198,200,204,207,209,210,213,214,219,221,224,231 reported details about whether the intervention was delivered as intended or about methods that were put in place to ensure delivery fidelity. This information included data on session attendance, compliance to the intervention, quality control procedures, process evaluations and supervision of the intervention (by the project lead), mainly through site visits. Three studies103,166,177 used a similar technique for ensuring delivery fidelity. They each recorded the respective interventions using audio tapes to ensure that they were being delivered appropriately. One study, by Davis Martin et al. ,133 used an automated computer-based intervention programme, which ensured a standardised method of intervention delivery.
Sustainability
Information regarding intervention sustainability was reported for 45 studies. 43,65,66,127,131–134,136,137,141,143,146,147,150,153,154,156,158,160–163,166,167,171,178,183,192,193,196–198,202,207,209,214–217,220–224 In a number of studies, interventions were integrated into existing national programmes, health services, workplaces, commercial programmes and community services. Some studies reported the continuation and expansion of interventions beyond the study. 143,215,216 However, problems affecting sustainability were reported in some studies. For example, Scoggins et al. 221 discussed the willingness of employees as a significant resource and how it was important to incentivise employees to participate in the programme. Cost-effectiveness was also reported in some studies, for example VanWormer et al. 220 examined the cost-effectiveness of self-weighing and self-management strategies and Kisioglu et al. 197 discussed the cost-effectiveness of health education and leaflets. Equally, some studies reported on the potential barriers to sustainability, for example the high cost of gift cards132 or the overall intervention costs. 156
Stakeholder support
Twenty-nine studies65,127,129,130,132,135,147,152,153,164,176,178,183,185,188,190,194,195,198,200,201,207–209,211,215–219 provided information on stakeholder support. Stakeholders included health departments, local health authorities, communities, participants, universities, the National Heart, Lung, and Blood Institute and local political and lay leaders. At times, stakeholder involvement and feedback were used to indicate stakeholder support, but in many cases stakeholder support was implied by the authors without formal evaluation.
Resources
Information on resources was well documented by the majority of studies. However, the information provided was mostly related to time, staff and equipment rather than the actual costs of the intervention or parts of the intervention, which were reported by only six studies. 138,156,171,180,198,223
Differential effects
Subgroup differential effects were also explored by some of the studies (n = 42103,127,131,138–145,156–158,160–163,168,172,173,175,186,188,189–196,200,201,204,206,215–222,224). As well as the 30 studies127,131,138–140,142–145,161–163,172,173,175,186,188,189–196,215–222,224 reporting differential effects by an indicator of SES, other differential effects were explored for age, gender, ethnicity, type of work shift, income, weight loss attempts, number of scales at home, geographical location (e.g. rural vs. urban), marital status, social support, language, depression and baseline outcome variables (e.g. BMI or weight).
Analysis of the robustness of the results (sensitivity analyses)
Sensitivity analysis was conducted for weight and BMI changes from the adult community-level studies. The studies were grouped by the combination of study type and effect type and meta-analysis was repeated for combinations with more than two studies. There was an insufficient number of studies to analyse the sensitivity of adult individual-level studies.
Figure 14 shows the forest plot from the meta-analysis of weight change in the adult community-level targeted studies with the intervention type diet plus physical activity. All of the individual studies show non-significant intervention effects, except for Ockene et al. ,198 and consequently the overall pooled effect is also non-significant (pooled effect size –0.81 kg, 95% CI –1.85 kg to 0.22 kg). There is no indication of heterogeneity between the studies (I2 = 16.25%, p = 0.6532).
FIGURE 14.
Random-effects meta-analysis of weight change: adult community-level studies. a, Individual intervention group vs. control group; b, family intervention group vs. control group; c, white/Anglo women; d, African American women; e, Hispanic women.

Figure 15 shows the forest plot from the meta-analysis of BMI change in the adult community-level targeted studies with the intervention type diet plus physical activity. All of the individual studies show non-significant intervention effects, except for Ockene et al. 198 However, the overall pooled effect is significant (pooled effect size –0.48 kg/m2, 95% CI –0.78 kg/m2 to –0.18 kg/m2), which may be attributed to the strong intervention effect in the study by Ockene et al. 198 There was no indication of heterogeneity between the studies (I2 = 0%, p = 0.8795), as previously observed in the meta-analysis results of BMI change.
FIGURE 15.
Random-effects meta-analysis of BMI change: adult community-level studies. a, Individual intervention group vs. control group; b, family intervention group vs. control group.
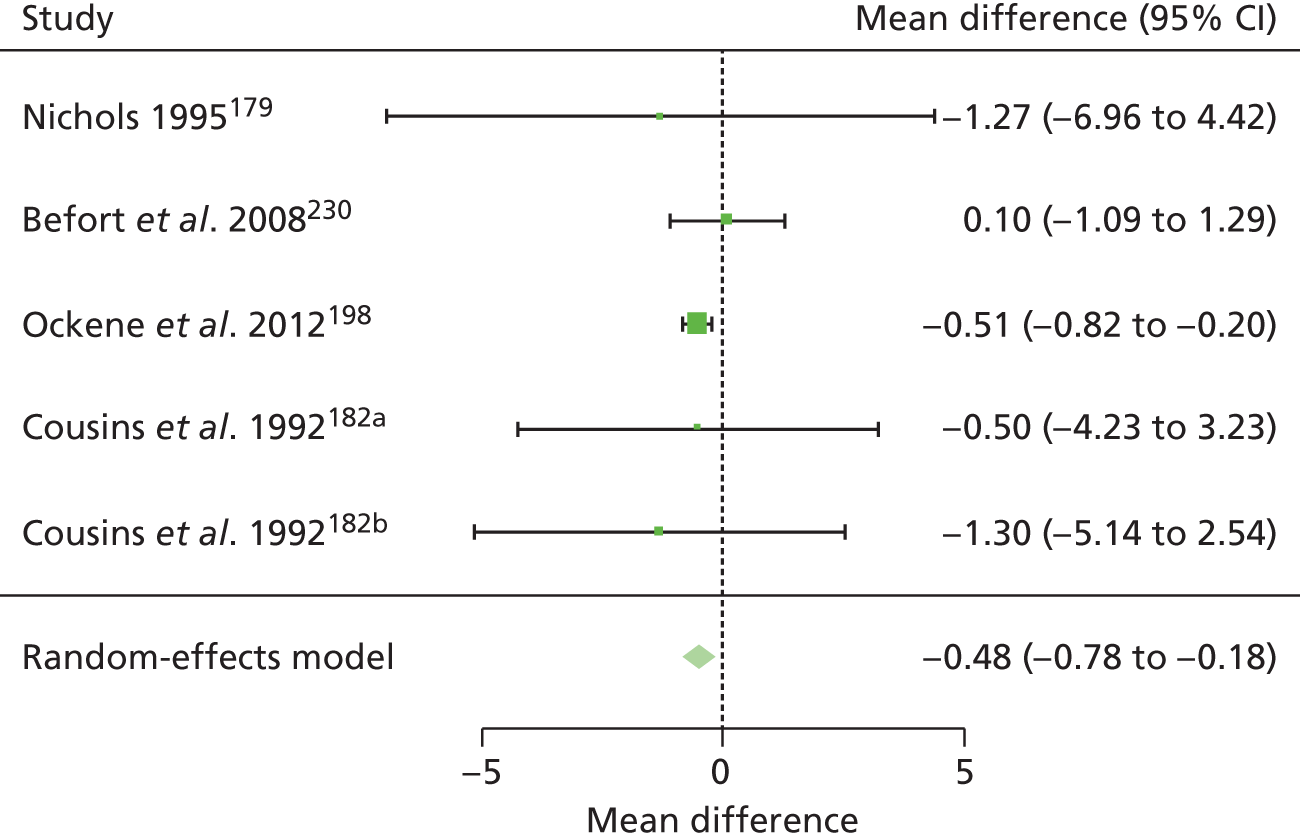
Discussion
Summary of results
Individual-level interventions
In total, we located 33 studies43,127–150,152,154–158 of individual-level interventions. The ‘best-available’ international evidence from five129,130,133,135,136,150 high-quality experimental studies suggests that primary care-delivered tailored weight loss programmes targeted at low-income groups can have positive short-term effects on weight outcomes (up to 9 months) but that these are not sustained in the longer term (after 12 months). Health education interventions have little long-term impact on weight outcomes in high- or low-income groups. These individual-level interventions therefore seem to provide only short-term reductions in obesity-related outcomes among low-SES groups. The impacts on SES inequalities in obesity are therefore likely to be very small and short-lived. No studies assessed the cost-effectiveness of the interventions.
The UK evidence comes from seven135,141,143,147,152 studies (two135,152 experimental and five141,143,147 observational) and suggests that tailored weight loss programmes delivered in primary care can have positive short- and long-term effects on obesity-related outcomes in low-SES groups and are equally effective across the SES gradient.
Community-level interventions
In total, we located 60 studies65,66,103,153,159–176,178–200,202–214,225,230,231 of community-level interventions. The ‘best-available’ international evidence from 12167,171,176,183,186,189,197–200,211,225,230 high-quality experimental studies suggests that community-based behavioural weight loss interventions and community diet clubs have short-term (3 months) but no longer-term positive effects on weight loss. Group-based lifestyle counselling interventions have limited effects, as do group-based health education interventions. Workplace studies suggest that longer-term positive effects on obesity-related outcomes require more complex, multifaceted interventions. School-based physical activity and education interventions for adults have little effect. No studies assessed the cost-effectiveness of the interventions.
The UK evidence comes from four153,189,192,208 studies (one experimental189 and three observational153,192,208) and suggests that group-based weight loss programmes (diet clubs, commercial and behavioural programmes) have positive effects in the short term in low-SES groups or equally across the SES gradient. However, these positive effects are not maintained in the long term.
Societal-level interventions
In total, we located eight215–222 studies of societal (environmental)-level interventions and two223,224 studies of societal (macro)-level interventions. The ‘best-available’ international evidence for the environmental interventions comes from one moderate-quality experimental study219 and two low-quality observational studies. 223,224 The experimental study took a universal approach and examined an intervention that modified the work environment. It suggested that a multifaceted workplace weight prevention intervention could actually increase SES inequalities in obesity-related outcomes. The two low-quality observational studies took a targeted approach and examined the effects of the US Food Stamp Program. Together, the studies found little evidence of a relationship between participation and weight change. No studies assessed the cost-effectiveness of the interventions.
The UK evidence base consists of one low-quality observational study218 of a multifaceted cardiovascular disease prevention programme (that included food labelling, the increased availability of healthy food choices and a worksite health promotion programme). There were no intervention effects on the prevalence of overweight and there were no differential effects by SES.
Table 36 illustrates where the included adult studies fit within our framework described in Table 1.
| Approach to tackling health inequality | Level of intervention | |||
|---|---|---|---|---|
| Individual | Community | Societal | ||
| Strengthening individuals | Strengthening communities | Improving living and school conditions | Promoting healthy macro policies | |
| Disadvantage (targeted) | All studies (n = 20) Best evidence (n = 4) Tailored weight loss programmes UK evidence (n = 5) Primary care tailored weight loss programmes; volunteer health advisor counselling intervention; NHS HTS |
All studies (n = 44) Best evidence (n = 11) Community-based group health education and counselling; workplace-delivered group health education and counselling; family-based group education or physical activity UK evidence (n = 2) Group-based behavioural weight loss programme |
All studies (n = 1) Best evidence (n = 0) UK evidence (n = 0) |
All studies (n = 2) Best evidence (n = 2) Supplemental Nutrition Assistance Program (formally known as the Food Stamp Program) for low-income families in the USA UK evidence (n = 0) |
| Gradient (universal) | All studies (n = 13) Best evidence (n = 1) Weight gain prevention educational intervention UK evidence (n = 2) Primary care tailored weight loss programme; NHS HTS |
All studies (n = 16) Best evidence (n = 1) Diet club UK evidence (n = 2) Diet club; commercial weight loss programme (part of the NHS primary care pathway) |
All studies (n = 7) Best evidence (n = 1) Multifaceted workplace weight prevention intervention UK evidence (n = 1) Cardiovascular disease prevention programme Heartbeat Wales |
(n = 0) |
What works in reducing inequalities in obesity, for whom and where?
The ‘best-available’ international evidence on the effectiveness of individual-level interventions to reduce inequalities in obesity among adults suggests that tailored weight loss programmes targeted at low-income groups have positive effects on weight outcomes but that these are sustained only in the short term (up to 9 months). Similarly, the ‘best-available’ international evidence on the effectiveness of community-level interventions also found that, of the various intervention types reviewed, community-based weight loss interventions, including behavioural weight loss interventions and community diet clubs, had consistent effects on obesity-related outcomes. However, again, these positive effects were only short term in nature (3 months), with no longer-term positive effects detected in the included studies. This is in keeping with previous research into the general effectiveness of obesity reduction interventions, which has found only short-term benefits of interventions, with weight regain in the longer term. 226,227 The community-level workplace studies suggested that longer-term positive effects on obesity-related outcomes require more complex, multifaceted interventions. This is in keeping with the Foresight obesity review,4 which highlighted the complex multifactorial nature of inequalities in obesity and therefore the need for sophisticated and longer-term interventions to reduce them. However, in our review, the evidence that we found on more upstream ‘multifactorial’ interventions – the societal ones – suggests that such interventions were not actually effective in reducing inequalities in obesity. The evidence base here was very small, though, (n = 10215–224) and covered a wide range of interventions.
The findings of the UK studies, although not as methodologically strong (of the 12 studies135,141,143,147,152,153,189,192,208,219 only three135,152,189 were experimental), were nonetheless broadly in keeping with those of the ‘best-available’ international studies. The UK evidence base includes examples of individual-level tailored weight loss programmes that are effective in the short term (3–6 months) in reducing obesity-related outcomes among low-income groups (e.g. Craigie et al. ’s135 study of a post-partum weight loss programme and Jackson et al. ’s147 small study of a health visitor-led weight-management intervention) or which are equally effective across the social gradient (e.g. Morrison et al. ’s141 study of the NHS Glasgow and Clyde Weight Management Service). However, such findings were not universal (e.g. Hillier et al. ’s152 study of a volunteer health advisor counselling intervention in Middlesbrough found no evidence of effectiveness and the study of NHS health trainers in England and Wales by Gardner et al. 143 found that, although the intervention was effective in all SES groups, it was more effective among the least deprived). At the community level, UK studies found that diet clubs were effective among all SES groups in the short term but not in the longer term (e.g. Baron et al. ,189 Lloyd and Khan192). Similarly, there was some UK evidence that community-based, targeted, behavioural weight loss interventions were also effective in reducing obesity-related outcomes among the most deprived (e.g. Gray et al. ,153 Hajek et al. 208). At the societal level, the UK evidence base was very small (n = 1218) and showed no evidence of effectiveness.
It is important to reflect on ‘for whom’ and ‘where’ the interventions were – or more usually were not – effective. The ‘best-available’ international evidence was typically of interventions in the USA, perhaps reflecting their more sophisticated approach to experimental design. However, as the UK evidence base is in keeping with the international findings, it seems plausible to cautiously extrapolate the short-term effectiveness of individual-level tailored weight loss programmes, community-level behavioural weight loss interventions and community diet clubs beyond the USA. However, both the ‘best-available’ international evidence base and the UK evidence base are populated by studies with exclusively or majority female participant groups. This is in keeping with general obesity studies, in which only 10–30% of participants in weight loss programmes are men. 228 In the case of the international evidence, often the interventions were targeted at African American or Latin American women. The findings of effectiveness are, therefore, very much limited to effectiveness among low-income women in the USA and the UK. In terms of ‘where’ interventions were effective, then, the ‘best-available’ evidence suggests that primary care-delivered interventions and those based in community settings (including workplaces) were the more effective. The value of primary care-based interventions is also reflected in the UK evidence.
In terms of barriers to and facilitators of interventions, although most of the studies provided data for motivation, context, experience of the intervention team and resources, the type and level of information varied substantially for each of the domains, making comparisons between the studies difficult. There were no apparent differences between interventions that were successful in reducing inequalities in obesity and those that were not. For example, in terms of study motivation it may be hypothesised that studies that primarily focused on reducing obesity would be more successful at reducing inequalities in obesity than those that aimed to improve health in general; however, both successful and unsuccessful studies reported both motivations. There appeared to be no differences in the experience of the intervention team between successful and unsuccessful interventions (e.g. trained or professional facilitators were reported for both) and interventions reporting a level of resources (incentives, supportive materials, contact time and training of facilitators) did not appear to be related to outcomes.
Implications for research
The nature of the evidence base has a number of implications for public health researchers. Most notably, although we found a very large international evidence base, the evidence found was largely observational and of moderate to low quality. This was particularly the case for the UK evidence base, which was surprisingly small (n = 12135,141,143,147,152,153,189,192,208,219) and in methodological terms did not compare well with the US evidence base. There were also very few studies of societal-level interventions (n = 10215–224), which might be expected to have more of an impact on the gradient in obesity. 126 This was particularly the case in terms of the macro policy-level interventions as the few studies that were found (n = 2223,224), did not necessarily have obesity as their main outcome or indeed motivation behind the intervention (e.g. the US Food Stamp Program was not motivated by a desire to reduce obesity). Similarly, the vast majority of interventions that were evaluated took a targeted approach to reducing SES inequalities in obesity, with only a minority of studies examining the effects of interventions across the SES gradient. The targeted approach has limitations as, even when interventions are effective among low-income groups, they are only able to reduce the health inequalities gap and have little effect on the wider social gradient. The included studies, especially the UK studies and the better-quality international studies, were almost exclusively of women. The findings of effectiveness are therefore limited to women, given that weight loss is embedded in sociocultural contexts, including those relating to gender. 229 We also found no studies that assessed the cost-effectiveness of the interventions and meta-analysis could be conducted only on a minority of studies given their heterogeneity.
Our results suggest a need for more experimental studies of the effectiveness and cost-effectiveness of interventions to reduce inequalities in obesity among both men and women, particularly in the UK and especially in terms of macro-level interventions that potentially address the entire gradient.
Implications for public health
Our review has found a large international evidence base but only limited effectiveness of interventions with the potential to reduce SES inequalities in obesity. Most notably, primary care-delivered tailored weight loss programmes targeted at individuals from low-income groups and community-based weight loss interventions appeared to have effectiveness – at least in the short term – among low-income women, internationally and in the UK. The evidence suggests that these interventions may therefore be worth commissioning by clinical commissioning groups or local authorities who wish to target services at low-income women or at women in deprived areas. However, to be effective in the longer term, such interventions could benefit from being of a longer duration and supplemented with subsequent weight maintenance interventions. The evidence also suggests that some adaptation may be required for the interventions to be effective among men.
Strengths and limitations
This review was very extensive as an extremely thorough search was conducted of the international literature, with very broad inclusion and exclusion criteria, which has ensured that the entire relevant experimental and observational evidence base was captured. However, we located few evaluations of societal-level interventions and this was probably because we did not include non-experimental study designs. The quality of the review is also high as double screening was applied and both data extraction and quality appraisal were independently checked. We also examined the implementation of interventions and paid attention to the context within which interventions were undertaken. However, the review is still subject to some methodological limitations, for example the quality assessment tool, although described as a tool for public health interventions, seemed to favour those that followed a more clinical model. We particularly found the blinding question unhelpful as it mostly resulted in moderate scores. The implementation tool was practical but enabled only a brief summary of implementation factors to be produced. A more qualitative approach to assessing implementation may indeed be better, as Egan et al. 23 themselves conclude. The theoretical framework adapted from the health inequalities literature meant that most studies were categorised as community-level interventions and we encountered difficulties in determining in which section of the framework particular interventions should sit. One final limitation that may be of particular relevance to the non-UK evidence base is our exclusion of studies that examined ethnic inequalities, which may have reduced the amount of US literature, in which ethnicity is often used as a proxy for SES. This means that there may be additional studies of value in the international literature that have not been included in this UK-funded review.
Chapter 4 Conclusions of the child and adult reviews
Our reviews found a large international evidence base, with the better-quality studies suggesting that individual-, community-, societal- and multilevel interventions that aim to prevent, reduce or manage obesity do not increase inequalities; that some universal interventions reduced the gradient in obesity; and that many targeted interventions are effective in decreasing obesity among lower-SES groups.
Implications for public health
Our review has found a large international evidence base but only limited effectiveness of interventions with the potential to reduce SES inequalities in obesity. The body of evidence in this review provides some support for the hypothesis that obesity management interventions in children and adults can be effective and that they do not increase health inequalities. Interventions that can be embedded into ongoing practice and operating systems need to be developed, rather than implementing interventions that are resource intensive and cannot be maintained long term. These reviews also highlight that, although we may now have a good sense of the range of interventions that are feasible for use in reducing the risk of obesity, we lack the knowledge of which specific intervention components are most effective in ensuring that the equity gradient is reduced. Being able to answer this question is of critical importance to decision-makers.
The reviews provide evidence of significant positive outcomes for the more disadvantaged. There was no evidence of a widening of health inequalities as a result of obesity management interventions. In addition, the relatively large number of studies of interventions targeting disadvantaged population groups provides useful information about the implementation strategies needed for obesity prevention efforts targeting these high-risk groups. We advocate for an assessment of outcomes by measures of equity, such as those indicated by PROGRESS, if a general population is targeted.
In relation to which interventions could be implemented by the UK public health community, the findings of this review are very limited to non-UK evidence and we cannot assume that such interventions will be effective outside their country context. It is also difficult to distinguish which specific components of intervention programmes are necessary to achieve the beneficial impacts on obesity in adults and children across all SES groups (our implementation tool found very little evidence of consistent factors behind successful interventions, for example in terms of empowerment/participation). However, our review has found tentative evidence of some interventions with the potential to reduce SES inequalities in obesity in children:
-
School-based and environmental interventions targeted at low-SES children appear to have evidence of effectiveness – and over the longer term – in reducing obesity-related outcomes among low-income primary school-aged children. For example, the School Nutrition Policy Initiative (a 2-year multifaceted educational and environmental intervention in low-income schools in the USA) increased nutritional knowledge and the availability of healthy food and reduced the prevalence of overweight by 35%. 109
-
Multilevel interventions that use community empowerment mechanisms, for example, may also be effective in reducing the widening of inequalities in obesity among children. For example, the Australian Be Active Eat Well community capacity-building intervention was designed by a number of key organisations to build the community’s capacity to create its own solutions to promoting healthy eating, physical activity and healthy weight and was delivered universally in all intervention schools. After 3 years, children in the intervention schools showed significantly lower increases in waist circumference and BMI.
The evidence reviewed here suggests that interventions of this type may therefore be worth commissioning in the UK by clinical commissioning groups or local authorities who wish to target services at low-income primary school children or children in deprived areas. However, these interventions may need to be piloted first and thoroughly evaluated using an experimental design.
Similarly, among adults, there is evidence that the following interventions targeted at individuals from low-income groups have some effectiveness – at least in the short term – in reducing SES inequalities in obesity, at least among low-income women, internationally and in the UK:
-
Primary care-delivered tailored weight loss programmes – there is evidence from UK and US studies132,134,135,149 that monthly face-to-face lifestyle counselling on a healthy diet and physical activity behaviours, targeted at low-income women, can be effective in reducing body weight. For example, a UK study of a 12-week intervention found significant reductions in BMI, body weight and percentage body fat among overweight post-partum women living in areas of moderate to high deprivation. 134
-
Community-based weight loss interventions (diet clubs, commercial and behavioural programmes) have positive effects in the short term in low-SES groups or equally across the SES gradient. 152,176,185,207 For example, a behavioural therapy (e.g. problem-solving, assertion, stimulus control) and social support (peer delivered in groups) intervention was effective at reducing weight among low-income men and women in the USA. 185
These interventions may therefore be worth commissioning by clinical commissioning groups or local authorities who wish to target services at low-income women or at women in deprived areas. However, to be effective in the longer term, such interventions will need to be of a longer duration and supplemented with subsequent weight maintenance interventions. They may also need to be adapted to be effective among men.
Research recommendations
This review suggests that research and evaluation in this field would benefit from focusing on how to implement interventions effectively to scale, sustain the impacts over time and ensure equitable outcomes of interventions to manage childhood obesity. We recommend larger, longer-term studies, powered to detect the small changes that are likely to be found, with assessments of equity impacts, to enable translation of research findings into effective public health approaches for managing childhood obesity.
The nature of the evidence base has a number of implications for public health researchers. Most notably, although we found a very large international evidence base, the quality of the evidence found was largely observational and of moderate to low quality. This was particularly the case with the UK evidence base, which was surprisingly small and in methodological terms did not compare well with the US evidence base. It is worth noting that, for the same type of intervention, observational studies are more likely to show positive effects than experimental studies. It is reasonable to suggest, therefore, that the most useful information on the way in which obesity (prevention or treatment) interventions impact on health inequalities is from moderate- to high-quality experimental studies of universal interventions. The large evidence base found resulted from the very inclusive nature of our search strategy and future research into the effects of interventions on health inequalities may wish to reflect on this – how far systematic reviewers search (in terms of databases and the study designs of included studies) is a difficult issue as there is a concern about missing potentially relevant studies, but there also needs to be a trade-off in terms of time, money and the quality of the studies found.
There were also very few studies of societal-level interventions, which might be expected to have more of an impact on the gradient in obesity. 29 This was particularly the case in terms of macro policy-level interventions, as the few studies that were found did not necessarily have obesity as their main outcome or indeed motivation behind the intervention (e.g. the US Food Stamp Program was not motivated by a desire to reduce obesity). Similarly, the vast majority of interventions that were evaluated took a targeted approach to reducing SES inequalities in obesity, with only a minority of studies examining the effects of interventions across the SES gradient. The latter probably reflects a tendency among researchers, practitioners and funders to focus at this level when evaluating interventions as the evaluation of complex interventions is difficult and often gives equivocal results. Few studies were found that evaluated more upstream interventions; this is not evidence of a lack of effectiveness, rather a lack of evaluation evidence for this type of intervention. It is also the case that effectiveness was seldom sustainable over time. We did search for reports of observational studies of societal interventions that we are aware of, and which might have met our inclusion criteria, for example EPODE, Sure Start and Healthy Towns; however, we were unable to find any relevant evidence.
The majority of interventions that were included in the reviews took a targeted approach to tackling obesity and were concerned with weight loss interventions (‘treating’ existing obesity) rather than interventions that aim to prevent weight gain (‘preventing’ obesity). These ‘treatment’ interventions are more likely to show positive effects than ‘prevention’ interventions. 31 The targeted approach also has limitations as even when interventions are effective among low-income groups they are only able to reduce the health inequalities gap and have little effect on the wider social gradient. Most of the child studies were school-based and aimed at primary school-aged children. The adult studies, especially the UK studies and the better-quality international studies, almost exclusively included women. The findings of effectiveness are therefore limited to women, given that weight loss is embedded in sociocultural contexts, including those relating to gender. 228 We also found no studies that assessed the cost-effectiveness of interventions and meta-analysis could be conducted only on a minority of studies, given their heterogeneity.
Our results suggest a need for more evaluations of the effects of interventions on SES inequalities in child and adult obesity, particularly in terms of the following:
-
priority 1 – country context: the UK
-
priority 2 – population groups: adolescents and adult men
-
priority 3 – intervention types: macro-level interventions that potentially address the entire gradient (such as taxes on high-fat foods or a television advertising ban on fast foods) and multilevel interventions that, for example, use community empowerment mechanisms to reduce inequalities in obesity
-
priority 4 – study designs: experimental studies of effectiveness and cost-effectiveness.
There has been a real missed opportunity to evaluate the effects of such ‘real-world’ interventions, and future interventions (such as Fulfilling Lives: a Better Start – see www.children-ne.org.uk/fulfilling-lives-better-start; accessed 16 September 2014) should include such analysis. There is therefore a need to review the possibility of conducting secondary analysis of existing intervention data sets (e.g. Healthy Towns, Change4Life – see www.nhs.uk/Change4Life/Pages/what-is-change-for-life.aspx; accessed 6 October 2014) to assess whether or not it is possible to retrospectively explore the effects of these UK interventions (that aim to manage obesity) on SES inequalities. We would also encourage all funders of such initiatives in the future to build a robust evaluation into such national programmes, or work alongside others who might conduct an evaluation (e.g. funded through the NIHR Public Health Research programme). Research in this area is increasing rapidly in line with the increasing prevalence of obesity in developed countries and so regular updating of this review will be required.
Acknowledgements
We would like to thank the members of our project steering group for their time and advice throughout the review: Goof Buijs (Netherlands Institute for Health Promotion and Disease Prevention, Woerden, the Netherlands), Richard Cookson (University of York, UK), Liam Hughes (Local Government Improvement and Development, London, UK), Mike Kelly (University of Cambridge, UK), Louise Potvin (University of Montreal, Canada) and Martin White (Newcastle University, UK). We would also like to thank Jayne Kenworthy of the Wolfson Research Institute for Health and Wellbeing, Durham, UK, for her administrative support.
This project was funded by the National Institute for Health Research Public Health Research programme (project number 09/3010/14).
Contributions of authors
Clare L Bambra (Professor, Public Health Policy) was responsible for overall co-ordination and project management. She provided methodological and conceptual input, analysis and synthesis input and, together with Frances C Hillier, led the drafting of the report and the preparation of the results for publication.
Frances C Hillier (Research Associate, Public Health Nutrition) was responsible for data collection, analysis and synthesis and, together with Clare L Bambra, led the drafting of the report and the preparation of the results for publication.
Joanne-Marie Cairns (Research Associate, Public Health Policy) contributed to data collection and analysis and the drafting of the report.
Adetayo Kasim (Statistician, Biomedicine) conducted the meta-analysis and contributed to the drafting of the report.
Helen J Moore (Lecturer, Public Health Nutrition) designed and conducted the searches and contributed to the data collection and the drafting of the report.
Carolyn D Summerbell (Professor, Public Health Nutrition) provided analysis and synthesis input and contributed to the drafting of the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
Publications
Cairns JM, Bambra CL, Hillier-Brown FC, Moore HJ, Summerbell CD. Weighing up the evidence: a systematic review of the effectiveness of workplace interventions to tackle socio-economic inequalities in obesity [published online ahead of print 14 October 2014]. J Public Health 2014. doi: 10.1093/pubmed/fdu077
Hillier-Brown FC, Bambra CL, Cairns JM, Kasim A, Moore HJ, Summerbell CD. A systematic review of the effectiveness of individual, community and societal level interventions at reducing socioeconomic inequalities in obesity amongst adults [published online ahead of print 12 May 2014]. Int J Obes (Lond) 2014. doi:10.1038/ijo.2014.75.
Hillier-Brown FC, Bambra CL, Cairns JM, Kasim A, Moore HJ, Summerbell CD. A systematic review of the effectiveness of individual, community and societal level interventions at reducing socioeconomic inequalities in obesity amongst children. BMC Public Health 2014;14:834.
References
- Obesity: Preventing and Managing a Global Epidemic: Report of a WHO Consultation of Obesity. WHO technical report series 894. Geneva: World Health Organization; 2000.
- Rokholm B, Baker JL, Sørensen TIA. The levelling off of the obesity epidemic since the year 1999 – a review of evidence and perspectives. Obes Rev 2010;11:835-46. http://dx.doi.org/10.1111/j.1467-789X.2010.00810.x.
- Olds T, Maher C, Zumin S, Péneau S, Lioret S, Castetbon K, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes 2011;6:342-60. http://dx.doi.org/10.3109/17477166.2011.605895.
- Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J, et al. Tackling Obesities: Future Choices – Project Report. London: Government Office for Science; 2007.
- Friel S, Chopra M, Satcher D. Unequal weight: equity oriented policy responses to the global obesity epidemic. BMJ 2007;335:1241-3. http://dx.doi.org/10.1136/bmj.39377.622882.47.
- Robertson A, Lobstein T, Knai C. Obesity and Socio-Economic Groups in Europe: Evidence Review and Implications for Action. Report to the European Commission 2007. http://ec.europa.eu/health/ph_determinants/life_style/nutrition/documents/ev20081028_rep_en.pdf (accessed 16 September 2014).
- Organisation for Economic Co-operation and Development . Obesity and the Economics of Prevention: Fit Not Fat 2010. www.oecd-ilibrary.org/social-issues-migration-health/obesity-and-the-economics-of-prevention_9789264084865-en (accessed 16 September 2014).
- Healthy Weight, Healthy Lives: A Cross-Government Strategy for England. London: The Stationery Office; 2008.
- Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, et al. Health consequences of obesity. Arch Dis Child 2003;88:748-52. http://dx.doi.org/10.1136/adc.88.9.748.
- White M, Adamson A, Chadwick T, Dezateux C, Griffiths L, Howel D, et al. The Changing Social Patterning of Obesity: an Analysis to Inform Practice and Policy Development. Final Report to the Policy Research Programme. London: Department of Health; 2007.
- Law C, Power C, Graham H, Merrick D. Obesity and health inequalities. Obes Rev 2007;8:19-22. http://dx.doi.org/10.1111/j.1467-789X.2007.00312.x.
- Shrewsbury V, Wardle J. Socioeconomic Status and adiposity in childhood: a systematic review of cross-sectional studies 1990–2005. Obesity 2008;16:275-84. http://dx.doi.org/10.1038/oby.2007.35.
- El-Sayed A, Scarborough P, Galea S. Socioeconomic inequalities in childhood obesity in the United Kingdom: a systematic review of the literature. Obes Facts 2012;5:671-92. http://dx.doi.org/10.1159/000343611.
- El-Sayed A, Scarborough P, Galea S. Unevenly distributed: a systematic review of the health literature about socioeconomic inequalities in adult obesity in the United Kingdom. BMC Public Health 2012;12. http://dx.doi.org/10.1186/1471-2458-12-18.
- Health Survey for England – 2011: Volume 1 – Health, Social Care and Lifestyles. London: NatCen Social Research; 2012.
- National Child Measurement Programme: England, 2011/12 School Year. London: Department of Health; 2012.
- Howe LD, Tilling K, Galobardes B, Smith GD, Ness AR, Lawlor DA. Socioeconomic disparities in trajectories of adiposity across childhood. Int J Pediatr Obes 2011;6. http://dx.doi.org/10.3109/17477166.2010.500387.
- Giskes K, Avendano M, Brug J, Kunst AE. A systematic review of studies on socioeconomic inequalities in dietary intakes associated with weight gain and overweight/obesity conducted among European adults. Obes Rev 2010;11:413-29. http://dx.doi.org/10.1111/j.1467-789X.2009.00658.x.
- Bambra C, Joyce KE, Maryon-Davies A. Priority Health Conditions – Task Group 8 Report to the Strategic Review of Health Inequalities in England Post-2010 (Marmot Review). London: University College London; 2009.
- Bambra C, Joyce K, Bellis M, Greatley A, Greengross S, Hughes S, et al. Reducing health inequalities in priority public health conditions: using rapid review to develop proposals for evidence-based policy. J Public Health (Oxf) 2010;32:496-505. http://dx.doi.org/10.1093/pubmed/fdq028.
- Woodman J, Lorenc T, Harden A, Oakley A. Social and Environmental Interventions to Reduce Childhood Obesity: a Systematic Map of Reviews. London: EPPI-Centre; 2008.
- Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008.
- Egan M, Bambra C, Petticrew M, Whitehead M. Reviewing evidence on complex social interventions: appraising implementation in systematic reviews of the health effects of organisational-level workplace interventions. J Epidemiol Community Health 2009;63:4-11. http://dx.doi.org/10.1136/jech.2007.071233.
- Chow CK, Lock K, Teo K, Subramanian S, McKee M, Yusuf S. Environmental and societal influences acting on cardiovascular risk factors and disease at a population level: a review. Int J Epidemiol 2009;38:1580-94. http://dx.doi.org/10.1093/ije/dyn258.
- Whitehead M. A typology of actions to tackle social inequalities in health. J Epidemiol Community Health 2007;61:473-8. http://dx.doi.org/10.1136/jech.2005.037242.
- Graham H, Kelly M. Health Inequalities: Concepts, Frameworks and Policy. London: Health Development Agency; 2004.
- Undertaking Systematic Reviews of Research on Effectiveness. CRD’s Guidance for Carrying Out or Commissioning Reviews. York: Centre for Reviews and Dissemination, University of York; 2001.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) 2011.
- Bambra C, Hillier F, Moore H, Summerbell C. Tackling inequalities in obesity: a protocol for a systematic review of the effectiveness of public health interventions at reducing socioeconomic inequalities in obesity amongst children. Syst Rev 2012;1. http://dx.doi.org/10.1186/2046-4053-1-16.
- Shaw K, Gennat H, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev 2006;4.
- Waters E, de Silva-Sanigorski A, Hall B, Brown T, Campbell K, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12. http://dx.doi.org/10.1002/14651858.CD001871.pub3.
- Bambra C, Egan M, Thomas S, Petticrew M, Whitehead M. The psychosocial and health effects of workplace reorganisation. 2. A systematic review of task restructuring interventions. J Epidemiol Community Health 2007;61:1028-37. http://dx.doi.org/10.1136/jech.2006.054999.
- Bambra C, Whitehead M, Sowden A, Akers J, Petticrew M. ’A hard day’s night?’ The effects of Compressed Working Week interventions on the health and work-life balance of shift workers: a systematic review. J Epidemiol Community Health 2008;62:764-77. http://dx.doi.org/10.1136/jech.2007.067249.
- Bambra CL, Whitehead MM, Sowden AJ, Akers J, Petticrew MP. Shifting schedules: the health effects of reorganizing shift work. Am J Prev Med 2008;34:427-34. http://dx.doi.org/10.1016/j.amepre.2007.12.023.
- Deeks J, Dinnes J, D’Amico R, Sowden A, Sakarovitch C, Song F, et al. Evaluating non-randomised intervention studies. Health Technol Assess 2003;7. http://dx.doi.org/10.3310/hta7270.
- Egan M, Bambra C, Thomas S, Petticrew M, Whitehead M, Thomson H. The psychosocial and health effects of workplace reorganisation. 1. a systematic review of interventions that aim to increase employee participation or control. J Epidemiol Community Health 2007;61:945-54. http://dx.doi.org/10.1136/jech.2006.054965.
- Joyce K, Pabayo R, Critchley J, Bambra C. Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst Rev 2010;2. http://dx.doi.org/10.1002/14651858.CD008009.pub2.
- Effective Public Health Practice Project . Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies 2009. www.ephpp.ca/tools.html (accessed 1 September 2011).
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b2700.
- Baxter KA, Ware RS, Batch JA, Truby H. Predicting success: factors associated with weight change in obese youth undertaking a weight management program. Obes Res Clin Pract 2013;7:e147-54. http://dx.doi.org/10.1016/j.orcp.2011.09.004.
- Braet C. Patient characteristics as predictors of weight loss after an obesity treatment for children. Obesity 2006;14:148-55. http://dx.doi.org/10.1038/oby.2006.18.
- Fernandez De Velasco Galan JJ, Pascual De La Pisa B, Benitez Cambra MR. Control of childhood obesity in primary care. Acta Pediatr Esp 2008;66:13-9.
- Marshall B, Floyd S, Forrest R. Clinical outcomes and patients’ perceptions of nurse-led healthy lifestyle clinics. J Prim Health Care 2011;3:48-52.
- Pott W, Albayrak O, Hebebrand J, Pauli-Pott U. Treating childhood obesity: family background variables and the child’s success in a weight-control intervention. Int J Eat Disord 2009;42:284-9. http://dx.doi.org/10.1002/eat.20655.
- Pott W, Frohlich G, Albayrak O, Hebebrand J, Pauli-Pott U. Conditions for success in a lifestyle intervention weight-reduction programme for overweight or obese children and adolescents. Z Kinder Jugendpsychiatr Psychother 2010;38:351-60. http://dx.doi.org/10.1024/1422-4917/a000059.
- Sabin MA, Ford A, Hunt L, Jamal R, Crowne EC, Shield JPH. What factors are associated with a successful outcome in a weight management programme for obese children?. J Eval Clin Pract 2007;13:364-8. http://dx.doi.org/10.1111/j.1365-2753.2006.00706.x.
- Smith AE, Annesi JJ, Walsh AM, Lennon V, Bell RA. Association of changes in self-efficacy, voluntary physical activity, and risk factors for type 2 diabetes in a behavioral treatment for obese preadolescents: a pilot study. J Pediatr Nurs 2010;25:393-9. http://dx.doi.org/10.1016/j.pedn.2009.09.003.
- Taveras EM, Gortmaker SL, Hohman KH, Horan CM, Kleinman KP, Mitchell K, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch Pediatr Adolesc Med 2011;165:714-22. http://dx.doi.org/10.1001/archpediatrics.2011.44.
- Truby H, Baxter K, Ware R, Batch J. Successful weight loss for adolescents: what can diet offer?. Obes Res Clin Pract 2011;5. http://dx.doi.org/10.1016/j.orcp.2011.08.072.
- Wake M, Baur LA, Gerner B, Gibbons K, Gold L, Gunn J, et al. Outcomes and costs of primary care surveillance and intervention for overweight or obese children: the LEAP 2 randomised controlled trial. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3308.
- Langnäse K, Asbeck I, Mast M, Müller MJ. The influence of socio-economic status on the long-term effect of family-based obesity treatment intervention in prepubertal overweight children. Health Educ 2004;104:336-43. http://dx.doi.org/10.1108/09654280410564105.
- Pust S, Langnäse K, Asbeck I, Geisler C, Danielzik S, Müller MJ. Influence of socio-economic state on the outcome of a family-based intervention for overweight children as part of the Kiel Obesity Prevention Study (KOPS). Int J Obes Relat Metab Disord 2004;28.
- Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med 2008;162:239-45. http://dx.doi.org/10.1001/archpediatrics.2007.45.
- Black MM, Hager ER, Le K, Anliker J, Arteaga SS, Diclemente C, et al. Challenge! Health promotion/obesity prevention mentorship model among urban, black adolescents. Pediatrics 2010;126:280-8. http://dx.doi.org/10.1542/peds.2009-1832.
- Annesi JJ. Initial body mass index and free-time physical activity moderate effects of the Youth Fit for Life treatment in African-American pre-adolescents. Percept Mot Skills 2010;110:789-800. http://dx.doi.org/10.2466/pms.110.3.789-800.
- Annesi JJ, Faigenbaum AD, Westcott WL, Smith AE, Unruh JL, Hamilton FG. Effects of the Youth Fit For Life protocol on physiological, mood, self-appraisal, and voluntary physical actitivity changes in African American preadolescents: contrasting alter-school care and physical education formats. Int J Clin Health Psychol 2007;7:641-59.
- Bingham M. Mediators and Moderators of the Effects of a Children’s Heart Health Intervention 2002.
- de Heer H. Project l.e.a.N.: An After-School Health and Exercise Program for Elementary School Children in El Paso, Texas 2009.
- Figueroa-Colon R, Franklin FA, Lee JY, von Almen TK, Suskind RM. Feasibility of a clinic-based hypocaloric dietary intervention implemented in a school setting for obese children. Obes Res 1996;4:419-29. http://dx.doi.org/10.1002/j.1550-8528.1996.tb00250.x.
- Fletcher A, Cooper JR, Helms P, Northington L, Winters K. Stemming the tide of childhood obesity in an underserved urban African American population: a pilot study. ABNF J 2009;20:44-8.
- Hawthorne A, Shaibi G, Gance-Cleveland B, McFall S. Grand Canyon Trekkers: school-based lunchtime walking program. J Sch Nurs 2011;27:43-50. http://dx.doi.org/10.1177/1059840510391669.
- Hoffman JA, Thompson DR, Franko DL, Power TJ, Leff SS, Stallings VA. Decaying behavioral effects in a randomized, multi-year fruit and vegetable intake intervention. Prev Med 2011;52:370-5. http://dx.doi.org/10.1016/j.ypmed.2011.02.013.
- Jansen W, Borsboom G, Meima A, Zwanenburg EJV, MacKenbach JP, Raat H, et al. Effectiveness of a primary school-based intervention to reduce overweight. Int J Pediatr Obes 2011;6:e70-7. http://dx.doi.org/10.3109/17477166.2011.575151.
- Jouret B, Ahluwalia N, Dupuy M, Cristini C, Negre-Pages L, Grandjean H, et al. Prevention of overweight in preschool children: results of kindergarten-based interventions. Int J Obes (Lond) 2009;33:1075-83. http://dx.doi.org/10.1038/ijo.2009.166.
- Kain J, Concha F, Salazar G, Leyton B, Del Pilar Rodriguez M, Ceballos X, et al. Obesity prevention in preschool and schoolchildren attending public schools from a district of Santiago, Chile: pilot project 2006. Arch Latinoam Nutr 2009;59:139-46.
- Kain J, Leyton B, Concha F, Salazar G, Lobos L, Vio F. Effect of counselling school teachers on healthy lifestyle on the impact of a program to reduce childhood obesity. Rev Med Chile 2010;138:181-7.
- Kain J, Uauy R, Albala, Vio F, Cerda R, Leyton B. School-based obesity prevention in Chilean primary school children: methodology and evaluation of a controlled study. Int J Obes Relat Metab Disord 2004;28:483-93. http://dx.doi.org/10.1038/sj.ijo.0802611.
- Lindgren EC, Baigi A, Apitzsch E, Bergh H. Impact of a six-month empowerment-based exercise intervention programme in non-physically active adolescent Swedish girls. Health Educ J 2011;70:9-20. http://dx.doi.org/10.1177/0017896910379366.
- Lubans DR, Morgan PJ, Aguiar EJ, Callister R. Randomized controlled trial of the Physical Activity Leaders (PALs) program for adolescent boys from disadvantaged secondary schools. Prev Med 2011;52:239-46. http://dx.doi.org/10.1016/j.ypmed.2011.01.009.
- Moore JB, Pawloski LR, Goldberg P, Kyeung MO, Stoehr A, Baghi H. Childhood obesity study: a pilot study of the effect of the nutrition education program Color My Pyramid. J Sch Nurs 2009;25:230-9. http://dx.doi.org/10.1177/1059840509333325.
- Myers DA. The Effect of a Virtual Skill and Fitness Trainer in Physical Education Classes on Student Heart Rates, Body Mass Index, Fitness Level, and Student Perceptions 2008.
- Nemer L, Schweizer C, von Hoff K, Fernandes Guerreiro AI. Improving Children’s Health and the Environment: Examples from the WHO European Region. Copenhagen: WHO Regional Office for Europe; 2009.
- Nemet D, Geva D, Eliakim A. Health promotion intervention in low socioeconomic kindergarten children. J Pediatr 2011;158:796-801. http://dx.doi.org/10.1016/j.jpeds.2010.10.040.
- Plachta-Danielzik S, Landsberg B, Lange D, Langnäse K, Müller MJ. 15 years of the Kiel Obesity Prevention Study (KOPS). Results and its importance for obesity prevention in children and adolescents. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2011;54:304-12. http://dx.doi.org/10.1007/s00103-010-1229-2.
- Plachta-Danielzik S, Pust S, Asbeck I, Czerwinski-Mast M, Langnäse K, Fischer C, et al. Four-year follow-up of school-based intervention on overweight children: the KOPS study. Obesity 2007;15:3159-69. http://dx.doi.org/10.1038/oby.2007.376.
- Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA 1999;282:1561-7. http://dx.doi.org/10.1001/jama.282.16.1561.
- Rush E, Reed P, McLennan S, Coppinger T, Simmons D, Graham D. A school-based obesity control programme: Project Energize. Two-year outcomes. Br J Nutr 2012;107:581-7. http://dx.doi.org/10.1017/S0007114511003151.
- Salmon J, Ball K, Hume C, Booth M, Crawford D. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: switch-play. Int J Obes (Lond) 2008;32:601-12. http://dx.doi.org/10.1038/sj.ijo.0803805.
- Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr 2009;12:197-202. http://dx.doi.org/10.1017/S1368980008002644.
- Stephens MB, Wentz SW. Supplemental fitness activities and fitness in urban elementary school classrooms. Fam Med 1998;30:220-3.
- Story M, Sherwood NE, Himes JH, Davis M, Jacobs DR, Cartwright Y, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethn Dis 2003;13:S54-64.
- Topp R, Jacks DE, Wedig RT, Newman JL, Tobe L, Hollingsworth A. Reducing risk factors for childhood obesity: the Tommie Smith Youth Athletic Initiative. West J Nurs Res 2009;31:715-30. http://dx.doi.org/10.1177/0193945909336356.
- Walter HJ, Hofman A, Connelly PA, Barrett LT, Kost KL. Primary prevention of chronic disease in childhood: changes in risk factors after one year of intervention. Am J Epidemiol 1985;122:772-81.
- Weintraub DL, Tirumalai EC, Haydel KF, Fujimoto M, Fulton JE, Robinson TN. Team sports for overweight children: the Stanford Sports to Prevent Obesity Randomized Trial (SPORT). Arch Pediatr Adolesc Med 2008;162:232-7. http://dx.doi.org/10.1001/archpediatrics.2007.43.
- Williams AD, Warrington V. Get Fit Kids: a feasibility study of a pedometer-based walking program. Bariatr Nurs Surg Patient Care 2011;6:139-43. http://dx.doi.org/10.1089/bar.2011.9957.
- Simon C, Schweitzer B, Oujaa M, Wagner A, Arveiler D, Triby E, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obes (Lond) 2008;32:1489-98. http://dx.doi.org/10.1038/ijo.2008.99.
- Alves JGB, Gale CR, Souza E, Batty GD. Effect of physical exercise on bodyweight in overweight children: a randomized controlled trial in a Brazilian slum. Cad Saude Publica 2008;24:S353-9. http://dx.doi.org/10.1590/S0102-311X2008001400020.
- Grønbaek HN, Madsen SA, Michaelsen KF. Family involvement in the treatment of childhood obesity: the Copenhagen approach. Eur J Pediatr 2009;168:1437-47. http://dx.doi.org/10.1007/s00431-009-0944-x.
- Hamad R, Fernald LCH, Karlan DS. Health education for microcredit clients in Peru: a randomized controlled trial. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-51.
- Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis 2003;13:S65-77.
- Rudolf M, Christie D, McElhone S, Sahota P, Dixey R, Walker J, et al. WATCH IT: a community based programme for obese children and adolescents. Arch Dis Child 2006;91:736-9. http://dx.doi.org/10.1136/adc.2005.089896.
- Rudolf M, Sahota P, Walker J. A community-based approach for the treatment of childhood obesity: a pilot study. Int J Obes Relat Metab Disord 2004;28.
- Willet SL. Health Risk Reduction Among African-American Females: A One Year Follow-Up 1996.
- Bellows LL. Development and Evaluation of Food Friends Get Movin’ With Mighty Moves(TM), a Physical Activity Program to Prevent Obesity in Low-Income Preschoolers 2007.
- Winter SM, Sass DA. Healthy & ready to learn: examining the efficacy of an early approach to obesity prevention and school readiness. J Res Child Educ 2011;25:304-25. http://dx.doi.org/10.1080/02568543.2011.580211.
- Heinberg LJ, Kutchman EM, Berger NA, Lawhun SA, Cuttler L, Seabrook RC, et al. Parent involvement is associated with early success in obesity treatment. Clin Pediatr 2010;49:457-65. http://dx.doi.org/10.1177/0009922809337531.
- Kalarchian MA, Levine MD, Arslanian SA, Ewing LJ, Houck PR, Cheng Y, et al. Family-based treatment of severe pediatric obesity: randomized, controlled trial. Pediatrics 2009;124:1060-8. http://dx.doi.org/10.1542/peds.2008-3727.
- Kalavainen MP, Korppi MO, Nuutinen OM. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. Int J Obes (Lond) 2007;31:1500-8. http://dx.doi.org/10.1038/sj.ijo.0803628.
- Ranstrom BB. Taking Steps Together: A Family Centered, Lifestyle Education and Behavioral Modification Program for Overweight and Obese Children and Their Families 2009.
- Reinehr T, Brylak K, Alexy U, Kersting M, Andler W. Predictors to success in outpatient training in obese children and adolescents. Int J Obes Relat Metab Disord 2003;27:1087-92. http://dx.doi.org/10.1038/sj.ijo.0802368.
- Woolford SJ, Sallinen BJ, Clark SJ, Freed GL. Results from a clinical multidisciplinary weight management program. Clin Pediatr 2011;50:187-91. http://dx.doi.org/10.1177/0009922810384845.
- Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med 2004;158:342-7. http://dx.doi.org/10.1001/archpedi.158.4.342.
- Janicke DM, Gray WN, Mathews AE, Simon SL, Lim CS, Dumont-Driscoll M, et al. A pilot study examining a group-based behavioral family intervention for obese children enrolled in Medicaid: differential outcomes by race. Child Health Care 2011;40:212-31. http://dx.doi.org/10.1080/02739615.2011.590394.
- Jelalian E, Hart CN, Mehlenbeck RS, Lloyd-Richardson EE, Kaplan JD, Flynn-O’Brien KT, et al. Predictors of attrition and weight loss in an adolescent weight control program. Obesity 2008;16:1318-23. http://dx.doi.org/10.1038/oby.2008.51.
- Mockus DS. Weight Loss Success Among Overweight Children: What Predicts Short-Term Outcome? 2011.
- Robinson TN, Matheson DM, Kraemer HC, Wilson DM, Obarzanek E, Thompson NS, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med 2010;164:995-1004. http://dx.doi.org/10.1001/archpediatrics.2010.197.
- Coleman KJ, Tiller CL, Sanchez J, Heath EM, Sy O, Milliken G, et al. Prevention of the epidemic increase in child risk of overweight in low-income schools: the El Paso coordinated approach to child health. Arch Pediatr Adolesc Med 2005;159:217-24. http://dx.doi.org/10.1001/archpedi.159.3.217.
- Foster GD, Linder B, Baranowski T, Cooper DM, Goldberg L, Harrell JS, et al. A School-based intervention for diabetes risk reduction. N Engl J Med 2010;363:443-53. http://dx.doi.org/10.1056/NEJMoa1001933.
- Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics 2008;121:e794-802. http://dx.doi.org/10.1542/peds.2007-1365.
- Hollar D, Lombardo M, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS, et al. Effective multi-level, multi-sector, school-based obesity prevention programming improves weight, blood pressure, and academic performance, especially among low-income, minority children. J Health Care Poor Underserved 2010;21:93-108. http://dx.doi.org/10.1353/hpu.0.0304.
- Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS. Effect of a two-year obesity prevention intervention on percentile changes in body mass index and academic performance in low-income elementary school children. Am J Public Health 2010;100:646-53. http://dx.doi.org/10.2105/AJPH.2009.165746.
- Ibarra PJ, Alarcón RM. Malnutrition by excess among school-age children. Rev Chil Pediatr 2010;1:506-14. http://dx.doi.org/10.4067/S0370-41062010000600004.
- Perman JA, Young TL, Stines E, Hamon J, Turner LM, Rowe MG. A community-driven obesity prevention and intervention in an elementary school. J Ky Med Assoc 2008;106:104-8.
- Williams CL, Strobino BA, Bollella M, Brotanek J. Cardiovascular risk reduction in preschool children: the ‘Healthy Start’ project. J Am Coll Nutr 2004;23:117-23. http://dx.doi.org/10.1080/07315724.2004.10719351.
- Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS. Healthier options for public schoolchildren program improves weight and blood pressure in 6- to 13-year-olds. J Am Diet Assoc 2010;110:261-7. http://dx.doi.org/10.1016/j.jada.2009.10.029.
- Heath EM, Coleman KJ. Adoption and Institutionalization of the Child and Adolescent Trial for Cardiovascular Health (CATCH) in El Paso, Texas. Health Promot Pract 2003;4:157-64. http://dx.doi.org/10.1177/1524839902250770.
- Muckelbauer R, Libuda L, Clausen K, Kersting M. Approaches for the prevention of overweight through modified beverage consumption in the elementary school setting: the ‘trinkfit’ study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2011;54:339-48. http://dx.doi.org/10.1007/s00103-010-1224-7.
- Muckelbauer R, Libuda L, Clausen K, Reinehr T, Kersting M. A simple dietary intervention in the school setting decreased incidence of overweight in children. Obes Facts 2009;2:282-5. http://dx.doi.org/10.1159/000229783.
- Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics 2009;123. http://dx.doi.org/10.1542/peds.2008-2186.
- Ramirez-Lopez E, Grijalva-Haro MI, Valencia ME, Ponce JA, Artalejo E. Effect of a School Breakfast Program on the prevalence of obesity and cardiovascular risk factors in children. Salud Publica Mex 2005;47:126-33.
- Frisvold DE, Lumeng JC. Expanding exposure: can increasing the daily duration of head start reduce childhood obesity?. J Hum Resour 2011;46:373-402. http://dx.doi.org/10.1353/jhr.2011.0026.
- Chomitz VR, McGowan RJ, Wendel JM, Williams SA, Cabral HJ, King SE, et al. Healthy Living Cambridge Kids: a community-based participatory effort to promote healthy weight and fitness. Obesity 2010;18:S45-53. http://dx.doi.org/10.1038/oby.2009.431.
- Hoelscher DM, Springer AE, Ranjit N, Perry CL, Evans AE, Stigler M, et al. Reductions in child obesity among disadvantaged school children with community involvement: the Travis County CATCH trial. Obesity 2010;18:S36-44. http://dx.doi.org/10.1038/oby.2009.430.
- Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes (Lond) 2008;32:1060-7. http://dx.doi.org/10.1038/ijo.2008.79.
- Danielzik S, Pust S, Müller MJ. School-based interventions to prevent overweight and obesity in prepubertal children: process and 4-years outcome evaluation of the Kiel Obesity Prevention Study (KOPS). Acta Paediatr Suppl 2007;96:19-25. http://dx.doi.org/10.1111/j.1651-2227.2007.00165.x.
- Bambra C, Hillier F, Moore H, Cairns-Nagi J, Summerbell C. Tackling inequalities in obesity: a protocol for a systematic review of the effectiveness of public health interventions at reducing socioeconomic inequalities in obesity among adults. Syst Rev 2013;10. http://dx.doi.org/10.1186/2046-4053-2-27.
- Weinehall L, Lewis C, Nafziger AN, Jenkins PL, Erb TA, Pearson TA, et al. Different outcomes for different interventions with different focus! A cross-country comparison of community interventions in rural Swedish and US populations. Scand J Public Health 2001;29:46-58.
- Sierra MC, Bonacho EC, Garcia AG, Moraga MR, Gutierrez JCS, Barrientos AC, et al. Effectiveness of a preventive intervention strategy based on structured telephone interviews in a working population with a moderate to high cardiovascular risk. Aten Primaria 2010;42:498-505. http://dx.doi.org/10.1016/j.aprim.2010.05.003.
- Jeffery RW, French SA. Preventing weight gain in adults: design, methods and one year results from the Pound of Prevention study. Int J Obes 1997;21:457-64. http://dx.doi.org/10.1038/sj.ijo.0800431.
- Jeffery RW, French SA. Preventing weight gain in adults: the pound of prevention study. Am J Public Health 1999;89:747-51. http://dx.doi.org/10.2105/AJPH.89.5.747.
- Olson CM, Strawderman MS, Reed RG. Efficacy of an intervention to prevent excessive gestational weight gain. Am J Obstet Gynecol 2004;191:530-6. http://dx.doi.org/10.1016/j.ajog.2004.01.027.
- Weerts SE, Amoran A. Pass the fruits and vegetables! A community–university–industry partnership promotes weight loss in African American women. Health Promot Pract 2011;12:252-60. http://dx.doi.org/10.1177/1524839908330810.
- Davis Martin P, Rhode PC, Dutton GR, Redmann SM, Ryan DH, Brantley PJ. A primary care weight management intervention for low-income African-American women. Obesity 2006;14:1412-20. http://dx.doi.org/10.1038/oby.2006.160.
- Jackson RA, Stotland NE, Caughey AB, Gerbert B. Improving diet and exercise in pregnancy with Video Doctor counseling: a randomized trial. Patient Educ Couns 2011;83:203-9. http://dx.doi.org/10.1016/j.pec.2010.05.019.
- Craigie AM, Macleod M, Barton KL, Treweek S, Anderson AS. WeighWell team . Supporting postpartum weight loss in women living in deprived communities: design implications for a randomised control trial. Eur J Clin Nutr 2011;65:952-8. http://dx.doi.org/10.1038/ejcn.2011.56.
- Martin PD, Dutton GR, Rhode PC, Horswell RL, Ryan DH, Brantley PJ. Weight loss maintenance following a primary care intervention for low-income minority women. Obesity 2008;16:2462-7. http://dx.doi.org/10.1038/oby.2008.399.
- Abramson JH, Hopp C, Gofin J, Gofin R, Makler A, Habib J, et al. A community program for the control of cardiovascular risk factors: a preliminary evaluation of the effectiveness of the CHAD program in Jerusalem. J Community Health 1979;5:3-21. http://dx.doi.org/10.1007/BF01321566.
- Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA 2008;300:2631-7. http://dx.doi.org/10.1001/jama.2008.804.
- Edye B, Mandryk J, Frommer M, Healey S, Ferguson D. Evaluation of a worksite programme for the modification of cardiovascular risk factors. Med J Aust 1989;150.
- Schuit AJ, Wendel-Vos GCW, Verschuren WMM, Ronckers ET, Ament A, Van Assema P, et al. Effect of 5-year community intervention Hartslag Limburg on cardiovascular risk factors. Am J Prev Med 2006;30:237-42. http://dx.doi.org/10.1016/j.amepre.2005.10.020.
- Morrison DS, Boyle S, Morrison C, Allardice G, Greenlaw N, Forde L. Evaluation of the first phase of a specialist weight management programme in the UK National Health Service: prospective cohort study. Public Health Nutr 2012;15:28-3. http://dx.doi.org/10.1017/S1368980011001625.
- Neve M, Morgan PJ, Collins CE. Weight change in a commercial web-based weight loss program and its association with website use: cohort study. J Med Internet Res 2011;13. http://dx.doi.org/10.2196/jmir.1756.
- Gardner B, Cane J, Rumsey N, Michie S. Behaviour change among overweight and socially disadvantaged adults: a longitudinal study of the NHS Health Trainer Service. Psychol Health 2012;27:1178-93. http://dx.doi.org/10.1080/08870446.2011.652112.
- Rautio N, Jokelainen J, Oksa H, Saaristo T, Peltonen M, Niskanen L, et al. Socioeconomic position and effectiveness of lifestyle intervention in prevention of type 2 diabetes: one-year follow-up of the FIN-D2D project. Scand J Public Health 2011;39:561-70. http://dx.doi.org/10.1177/1403494811408482.
- Fortmann SP, Williams PT, Hulley SB, Maccoby N, Farquhar JW. Does dietary health education reach only the privileged? The Stanford Three Community Study. Circulation 1982;66:77-82. http://dx.doi.org/10.1161/01.CIR.66.1.77.
- Helmert U, Shea S, Greiser E, Maschewsky Schneider U. Effects of 3.5 years of community intervention on social class gradients for cardiovascular disease risk factors in the German Cardiovascular Prevention Study. Ann Epidemiol 1993;3:S36-43.
- Jackson C, Coe A, Cheater FM, Wroe S. Specialist health visitor-led weight management intervention in primary care: exploratory evaluation. J Adv Nurs 2007;58:23-34. http://dx.doi.org/10.1111/j.1365-2648.2007.04226.x.
- Burke L, Jancey J, Howat P, Lee A, Kerr D, Shilton T, et al. Preliminary physical activity findings from a home-based Physical Activity and Nutrition Program for Seniors (PANS). J Sci Med Sport 2011;14. http://dx.doi.org/10.1016/j.jsams.2011.11.163.
- Burke L, Lee AH, Pasalich M, Jancey J, Kerr D, Howat P. Effects of a physical activity and nutrition program for seniors on body mass index and waist-to-hip ratio: a randomised controlled trial. Prev Med 2012;54:397-401. http://dx.doi.org/10.1016/j.ypmed.2012.03.015.
- Whittemore R, Melkus G, Wagner J. Translating the diabetes prevention program to primary care: a pilot study. Nurs Res 2009;58:2-12. http://dx.doi.org/10.1097/NNR.0b013e31818fcef3.
- Abramson JH, Gofin J, Hopp C, Schein MH, Naveh P. The CHAD program for the control of cardiovascular risk factors in a Jerusalem community: a 24-year retrospect. Isr J Med Sci 1994;30:108-19.
- Hillier FC, Batterham AM, Nixon CA, Crayton AM, Pedley CL, Summerbell CD. A community-based health promotion intervention using brief negotiation techniques and a pledge on dietary intake, physical activity levels and weight outcomes: lessons learnt from an exploratory trial. Public Health Nutr 2012;15:1446-55. http://dx.doi.org/10.1017/S1368980011002862.
- Gray CM, Anderson AS, Clarke AM, Dalziel A, Hunt K, Leishman J, et al. Addressing male obesity: an evaluation of a group-based weight management intervention for Scottish men. J Mens Health 2009;6:70-81. http://dx.doi.org/10.1016/j.jomh.2008.11.002.
- Johnson RA, Meadows RL. Dog-walking: motivation for adherence to a walking program. Clin Nurs Res 2010;19:387-402. http://dx.doi.org/10.1177/1054773810373122.
- Buchholz SW, Wilbur J, Miskovich L, Gerard P. An office-based health promotion intervention for overweight and obese uninsured adults: a feasibility study. J Cardiovasc Nurs 2012;27:68-75. http://dx.doi.org/10.1097/JCN.0b013e3182112829.
- Verheijden MW, van Dommelen P, van Empelen P, Crone MR, Werkman AM, van Kesteren NMC. Changes in self-reported energy balance behaviours and body mass index during a mass media campaign. Fam Pract 2012;29:i75-81. http://dx.doi.org/10.1093/fampra/cmr133.
- Abramson JH, Gofin R, Hopp C, Gofin J, Donchin M, Habib J. Evaluation of a community program for the control of cardiovascular risk factors: the CHAD program in Jerusalem. Isr J Med Sci 1981;17:201-12.
- Gofin J, Gofin R, Abramson JH, Ban R. Ten-year evaluation of hypertension, overweight, cholesterol, and smoking control: the CHAD program in Jerusalem. Community Syndrome of Hypertension, Atherosclerosis and Diabetes. Prev Med 1986;15:304-12. http://dx.doi.org/10.1016/0091-7435(86)90049-6.
- Hugk D, Winkelvoss E. Ambulatory weight reduction program and possible effects on lipid and purine metabolism. Z Gesamte Inn Med 1985;40:126-9.
- Zuber J, Gromus B, Potreck-Rose F, Koch U. Differentielle Indikation zur ambulanten Gruppentherapie der Adipositas – am Beispiel der ‘Interdisziplinären Therapie der Adipositas’. Psychother Psychosom Med Psychol 1992;42:110-19.
- Kliche T, Schreiner-Kürten K, Wanek V, Koch U. Health promotion effectiveness: testing the German statutory health insurance agencies evaluation system in health promotion, and preliminary findings from 212 health training courses. Gesundheitswesen 2011;73:258-63. http://dx.doi.org/10.1055/s-0030-1249040.
- Veloso IS, Santana VS, Oliveira NF. The Brazilian Workers’ Food Program and its impact on weight gain and overweight. Rev Saude Publica 2007;41:769-76. http://dx.doi.org/10.1590/S0034-89102007000500011.
- Veloso IS, Santana VS. Impact of the worker food program in Brazil. Rev Panam Salud Publica 2002;11:24-31.
- Clarke KK, Freeland-Graves J, Klohe-Lehman DM, Milani TJ, Nuss HJ, Laffrey S. Promotion of physical activity in low-income mothers using pedometers. J Am Diet Assoc 2007;107:962-7. http://dx.doi.org/10.1016/j.jada.2007.03.010.
- Jordan KC, Freeland-Graves JH, Klohe-Lehman DM, Cai G, Voruganti VS, Proffitt JM, et al. A nutrition and physical activity intervention promotes weight loss and enhances diet attitudes in low-income mothers of young children. Nutr Res 2008;28:13-20. http://dx.doi.org/10.1016/j.nutres.2007.11.005.
- Krummel D, Semmens E, MacBride AM, Fisher B. Lessons learned from the mothers’ overweight management study in 4 West Virginia WIC offices. J Nutr Educ Behav 2010;42:S52-8. http://dx.doi.org/10.1016/j.jneb.2010.02.012.
- Olvera N, Bush JA, Sharma SV, Knox BB, Scherer RL, Butte NF. BOUNCE: a community-based mother-daughter healthy lifestyle intervention for low-income Latino families. Obesity 2010;18:S102-4. http://dx.doi.org/10.1038/oby.2009.439.
- Walker LO, Im EO, Vaughan MW. Communication technologies and maternal interest in health-promotion information about postpartum weight and parenting practices. J Obstet Gynecol Neonat Nurs 2012;41:201-15. http://dx.doi.org/10.1111/j.1552-6909.2011.01333.x.
- Chang MW, Nitzke S, Brown R. Design and outcomes of a Mothers in Motion behavioral intervention pilot study. J Nutr Educ Behav 2010;42:S11-21. http://dx.doi.org/10.1016/j.jneb.2010.01.010.
- Dennison KF, Galante D, Dennison D, Golaszewski T. A one year post-program assessment of a computer-assisted instruction (CAI) weight management program for industrial employees: lessons learned. J Health Educ 1996;27:38-42. http://dx.doi.org/10.1080/10556699.1996.10603162.
- Erfurt JC, Foote A, Heirich MA. Worksite wellness programs: incremental comparison of screening and referral alone, health education, follow-up counseling, and plant organization. Am J Health Promot 1991;5:438-48. http://dx.doi.org/10.4278/0890-1171-5.6.438.
- Rohrer JE, Naessens JM, Liesinger J, Tulledge-Scheitel S, Vanhouten H. A telephonic coaching program has more impact when body mass index is over 35. Obes Res Clin Pract 2010;4:e65-72. http://dx.doi.org/10.1016/j.orcp.2009.09.002.
- Hwang G, Yoon C, Jung H, Kim Y. Evaluation of an incentive-based obesity management program in workplace. Int J Occup Saf Ergon 2011;17:147-54.
- Grandjean PW, Oden GL, Crouse SF, Brown JA, Green JS. Lipid and lipoprotein changes in women following 6 months of exercise training in a worksite fitness program. J Sports Med Phys Fitness 1996;36:54-9.
- Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist RA, Kurth CL, Johnson SL. Correlates of weight loss and its maintenance over two years of follow-up among middle-aged men. Prev Med 1984;13:155-68. http://dx.doi.org/10.1016/0091-7435(84)90048-3.
- Auslander W, Haire-Joshu D, Houston C, Williams JH, Krebill H. The short-term impact of a health promotion program for low-income African American women. Res Soc Work Pract 2000;10:78-97.
- Befort CA, Donnelly JE, Sullivan DK, Ellerbeck EF, Perri MG. Group versus individual phone-based obesity treatment for rural women. Eat Behav 2010;11:11-7. http://dx.doi.org/10.1016/j.eatbeh.2009.08.002.
- Lasco RA, Curry RH, Dickson VJ, Powers J, Menes S, Merritt RK. Participation rates, weight loss, and blood pressure changes among obese women in a nutrition-exercise program. Public Health Rep 1989;104:640-6.
- Nichols GJ. Testing a Culturally Consistent Behavioral Outcomes Strategy for Cardiovascular Disease Risk Reduction and Prevention in Low Income African American Women 1995.
- Wilbur J, McDevitt JH, Wang E, Dancy BL, Miller AM, Briller J, et al. Outcomes of a home-based walking program for African-American women. Am J Health Promot 2008;22:307-17. http://dx.doi.org/10.4278/ajhp.22.5.307.
- Zoellner J, Connell CL, Santell R, Fungwe T, Strickland E, Avis-Williams A, et al. Fit for life steps: results of a community walking intervention in the rural Mississippi delta. Prog Community Health Partnersh 2007;1:49-60. http://dx.doi.org/10.1353/cpr.0.0009.
- Cousins JH, Rubovits DS, Dunn JK, Reeves RS, Ramirez AG, Foreyt JP. Family versus individually oriented intervention for weight loss in Mexican American women. Public Health Rep 1992;107:549-55.
- Faucher MA, Mobley J. A community intervention on portion control aimed at weight loss in low-income Mexican American women. J Midwifery Womens Health 2010;55:60-4. http://dx.doi.org/10.1016/j.jmwh.2009.03.014.
- Foreyt JP, Ramirez AG, Cousins JH. Cuidando El Corazon – a weight-reduction intervention for Mexican Americans. Am J Clin Nutr 1991;53:1639-41S.
- Fernandes R, Braun KL, Spinner JR, Sturdevant C, Ancheta SJ, Yoshimura SR, et al. Healthy Heart, Healthy Family: a NHLBI/HRSA collaborative employing community health workers to improve heart health. J Health Care Poor Underserved 2012;23:988-9. http://dx.doi.org/10.1353/hpu.2012.0097.
- Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol 1999;67:132-8. http://dx.doi.org/10.1037/0022-006X.67.1.132.
- van Wier MF, Dekkers JC, Hendriksen IJM, Smid T, van Mechelen W. Phone and e-mail counselling are effective for weight management in an overweight working population: a randomized controlled trial. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-6.
- Neumark-Sztainer D, Kaufmann NA, Berry EM. Physical activity within a community-based weight control program: program evaluation and predictors of success. Public Health Rev 1995;23:237-51.
- Baron JA, Schori A, Crow B, Carter R, Mann JI. A randomized controlled trial of low carbohydrate and low fat/high fiber diets for weight loss. Am J Public Health 1986;76:1293-6. http://dx.doi.org/10.2105/AJPH.76.11.1293.
- Merrill RM, Aldana SG, Greenlaw RL, Salberg A, Englert H. Chronic disease risk reduction with a community-based lifestyle change programme. Health Educ J 2008;67:219-30. http://dx.doi.org/10.1177/0017896908094639.
- Jeffery RW, Forster JL, Snell MK. Promoting weight control at the worksite: a pilot program of self-motivation using payroll-based incentives. Prev Med 1985;14:187-94. http://dx.doi.org/10.1016/0091-7435(85)90034-9.
- Lloyd A, Khan R. Evaluation of Healthy Choices: a commercial weight loss programme commissioned by the NHS. Perspect Public Health 2011;131:177-83. http://dx.doi.org/10.1177/1757913911408258.
- Stunkard AJ, Cohen RY, Felix MR. Weight loss competitions at the worksite: how they work and how well. Prev Med 1989;18:460-74. http://dx.doi.org/10.1016/0091-7435(89)90006-6.
- Freak-Poli RL, Wolfe R, Walls H, Backholer K, Peeters A. Participant characteristics associated with greater reductions in waist circumference during a four-month, pedometer-based, workplace health program. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-824.
- Mattfeldt-Beman MK, Corrigan SA, Stevens VJ, Sugars CP, Dalcin AT, Givi MJ, et al. Participants’ evaluation of a weight-loss program. J Am Diet Assoc 1999;99:66-71. http://dx.doi.org/10.1016/S0002-8223(99)00018-8.
- Lowe M, Miller-Kovach K, Phelan S. Weight-loss maintenance in overweight individuals one to five years following successful completion of a commercial weight loss program. Int J Obes Relat Metab Disord 2001;25:325-31. http://dx.doi.org/10.1038/sj.ijo.0801521.
- Kisioglu AN, Aslan B, Ozturk M, Aykut M, Ilhan I. Improving control of high blood pressure among middle-aged Turkish women of low socio-economic status through public health training. Croat Med J 2004;45:477-82.
- Ockene IS, Tellez TL, Rosal MC, Reed GW, Mordes J, Merriam PA, et al. Outcomes of a Latino community-based intervention for the prevention of diabetes: the Lawrence Latino Diabetes Prevention Project. Am J Public Health 2012;102:336-42. http://dx.doi.org/10.2105/AJPH.2011.300357.
- Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, et al. Effects of a tailored health promotion program for female blue-collar workers: Health Works for Women. Prev Med 2002;34:313-23. http://dx.doi.org/10.1006/pmed.2001.0988.
- Rickel KA. Response of African-American and Caucasian Women in a Rural Setting to a Lifestyle Intervention for Obesity 2008.
- Christiansen T, Bruun JM, Madsen EL, Richelsen B. Weight loss maintenance in severely obese adults after an intensive lifestyle intervention: 2- to 4-year follow-up. Obesity 2007;15:413-20. http://dx.doi.org/10.1038/oby.2007.530.
- Balcazar H, Alvarado M, Cantu F, Pedregon V, Fulwood R. A promotora de salud model for addressing cardiovascular disease risk factors in the US-Mexico border region. Prev Chronic Dis 2009;6.
- Gill DS. Testing a Biopsychosocial Model of Health Behavior: A Community Intervention for Reducing Obesity in Mexican-American Women 1998.
- Perez-Lizaur AB, Fernandez AC, Balcazar H. Cardiovascular health promotion in a Mexican population. FASEB J 2011;25.
- Pescatello LS, Murphy D, Vollono J, Lynch E, Bernene J, Costanzo D. The cardiovascular health impact of an incentive worksite health promotion program. Am J Health Promot 2001;16:16-20. http://dx.doi.org/10.4278/0890-1171-16.1.16.
- Williams A, Wold J. Nurses, cholesterol, and small work sites: innovative community intervention comparisons. Fam Community Health 2000;23:59-75. http://dx.doi.org/10.1097/00003727-200010000-00007.
- Goldfinger JZ, Arniella G, Wylie-Rosett J, Horowitz CR. Project HEAL: peer education leads to weight loss in Harlem. J Health Care Poor Underserved 2008;19:180-92. http://dx.doi.org/10.1353/hpu.2008.0016.
- Hajek P, Humphrey K, McRobbie H. Using group support to complement a task-based weight management programme in multi-ethnic localities of high deprivation. Patient Educ Couns 2010;80:135-7. http://dx.doi.org/10.1016/j.pec.2009.10.017.
- Cullen KW, Lara Smalling A, Thompson D, Watson KB, Reed D, Konzelmann K. Creating healthful home food environments: results of a study with participants in the expanded food and nutrition education program. J Nutr Educ Behav 2009;41:380-8. http://dx.doi.org/10.1016/j.jneb.2008.12.007.
- Howard-Pitney B, Winkleby MA, Albright CL, Bruce B, Fortmann SP. The Stanford Nutrition Action Program: a dietary fat intervention for low-literacy adults. Am J Public Health 1997;87:1971-6. http://dx.doi.org/10.2105/AJPH.87.12.1971.
- Reid C, McNeil JJ, Williams F, Powles J. Cardiovascular risk reduction: a randomized trial of two health promotion strategies for lowering risk in a community with low socioeconomic status. J Cardiovasc Risk 1995;2:155-63. http://dx.doi.org/10.1097/00043798-199504000-00012.
- Alves JG, Gale CR, Mutrie N, Correia JB, Batty GD. A 6-month exercise intervention among inactive and overweight favela-residing women in Brazil: the Caranguejo Exercise Trial. Am J Public Health 2009;99:76-80. http://dx.doi.org/10.2105/AJPH.2007.124495.
- Clark DO, Stump TE, Damush TM. Outcomes of an exercise program for older women recruited through primary care. J Aging Health 2003;15:567-85. http://dx.doi.org/10.1177/0898264303253772.
- Carlin CA. The Impact of Voluntary Participation in a Community Fitness Center on the Health and Well-Being of African American Women over 40 Years of Age 2009.
- Jenum AK, Anderssen SA, Birkeland KI, Holme I, Graff-Iversen S, Lorentzen C, et al. Promoting physical activity in a low-income multiethnic district: effects of a community intervention study to reduce risk factors for type 2 diabetes and cardiovascular disease: a community intervention reducing inactivity. Diabetes Care 2006;29:1605-12. http://dx.doi.org/10.2337/dc05-1587.
- Jenum AK, Lorentzen CA, Ommundsen Y. Targeting physical activity in a low socioeconomic status population: observations from the Norwegian ‘Romsås in Motion’ study. Br J Sports Med 2009;43:64-9. http://dx.doi.org/10.1136/bjsm.2008.053637.
- Jenum AK, Lorentzen C, Graff-Iversen S, Anderssen S, Ødegaard AK, Holme I, et al. Can area-based public health strategies reduce the social gradient in health? The ‘Romsås in Motion’ study – background, main results and lessons learnt. Norsk Epidemiol 2007;17:49-57.
- Tudor-Smith C, Nutbeam D, Moore L, Catford J. Effects of the Heartbeat Wales programme over five years on behavioural risks for cardiovascular disease: quasi-experimental comparison of results from Wales and a matched reference area. BMJ 1998;316:818-22. http://dx.doi.org/10.1136/bmj.316.7134.818.
- Lemon SC, Zapka J, Li W, Estabrook B, Rosal M, Magner R, et al. Step ahead: a worksite obesity prevention trial among hospital employees. Am J Prev Med 2010;38:27-38. http://dx.doi.org/10.1016/j.amepre.2009.08.028.
- VanWormer JJ, Linde JA, Harnack LJ, Stovitz SD, Jeffery RW. Self-weighing frequency is associated with weight gain prevention over 2 years among working adults. Int J Behav Med 2012;19:351-8. http://dx.doi.org/10.1007/s12529-011-9178-1.
- Scoggins JF, Sakumoto KN, Schaefer KS, Bascom B, Robbins DJ, Whalen CL. Short-term and long-term weight management results of a large employer-sponsored wellness program. J Occup Environ Med 2011;53:1215-20. http://dx.doi.org/10.1097/JOM.0b013e3182338676.
- Carleton RA, Lasater TM, Assaf AR, Feldman HA, McKinlay S. The Pawtucket Heart Health Program: community changes in cardiovascular risk factors and projected disease risk. Am J Public Health 1995;85:777-85. http://dx.doi.org/10.2105/AJPH.85.6.777.
- Jones SJ, Frongillo EA. The modifying effects of food stamp program participation on the relation between food insecurity and weight change in women. J Nutr 2006;136:1091-4.
- Kaushal N. Do food stamps cause obesity? Evidence from immigrant experience. J Health Econ 2007;26:968-91. http://dx.doi.org/10.1016/j.jhealeco.2007.01.006.
- Faucher MA. Promotoras de salud and portion control: a community intervention aimed at weight loss in low-income Mexican-American women. J Midwifery Womens Health 2008;53. http://dx.doi.org/10.1016/j.jmwh.2008.05.015.
- Curioni CC, Lourenco PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes Relat Metab Disord 2005;29:1168-74. http://dx.doi.org/10.1038/sj.ijo.0803015.
- Wu T, Gao X, Chen M, Van Dam RM. Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: a meta-analysis. Obes Rev 2009;10:313-23. http://dx.doi.org/10.1111/j.1467-789X.2008.00547.x.
- Wilkins D, White A, Pettifer M. Hazardous Waist: Tackling Male Weight Problems. Abingdon: Radcliffe Publishing; 2007.
- Wolfe B, Smith J. Different strokes for different folks: why overweight men do not seek weight loss treatment. J Eat Disord 2002;10:115-24. http://dx.doi.org/10.1080/10640260290081687.
- Befort CA, Nollen N, Ellerbeck EF, Sullivan DK, Thomas JL, Ahluwalia JS. Motivational interviewing fails to improve outcomes of a behavioral weight loss program for obese African American women: a pilot randomized trial. J Behav Med 2008;31:367-77. http://dx.doi.org/10.1007/s10865-008-9161-8.
- Zoellner J, Connell C, Powers A, Avis-Williams A, Yadrick K, Bogle M. Does a six-month pedometer intervention improve physical activity and health among vulnerable African Americans? A feasibility study. J Phys Act Health 2010;7:224-31.
- Koloroutis M, Felgen JA, Wright D, Pearson C, Manthey M. Relationship-Based Care. A Model for Transforming Practice. Minneapolis, MN: Creative Health Care Management; 2004.
- Hollingshead A. Four Factor Index of Social Status. New Haven, CT: Yale University; 1975.
- Census . Census: Standard Area Statistics n.d. http://casweb.mimas.ac.uk/ (accessed 1 October 2014).
- Canadian Association for Health, Physical Education, Recreation and Dance . Canadian Active Living Challenge n.d. www.cahperd.ca//node/414/ (accessed 29 September 2014).
- Welk GJ, Blair SN, Welk GJ, Meredith MD. FITNESSGRAM Reference Guide. Dallas, TX: Cooper Institute; 2001.
- Joyner B. Reliability of criterion-referenced standards of the FITNESSGRAM PACER. Georgia Assoc Health Phys Ed Recreation Dance J 1997;31:14-5.
- McKenzie TL, Sallis JF, Nader PR. SOFIT: System for Observing Fitness Instruction Time. J Teach Phys Ed 1991;11:195-209.
- Brigance A. Brigance Diagnostic Inventory of Early Development-II (IED-II). North Billerica, MA: Curriculum Associates; 2004.
- Hoelscher DM, Kelder SH, Pérez A, Day RS, Benoit JS, Frankowski RF, et al. Changes in the regional prevalence of child obesity in 4th, 8th, and 11th grade students in Texas from 2000–2002 to 2004–2005. Obesity (Silver Spring) 2010;18:1360-8. http://dx.doi.org/10.1038/oby.2009.305.
- Hoelscher DM, Day RS, Lee ES, Frankowski RF, Kelder SH, Ward JL, et al. Measuring the prevalence of overweight in Texas schoolchildren. Am J Public Health 2004;94:1002-8. http://dx.doi.org/10.2105/AJPH.94.6.1002.
- Maccoby N, Farquhar JW, Wood PD, Alexander J. Reducing the risk of cardiovascular disease: effects of a community-based campaign on knowledge and behavior. J Community Health 1977;3:100-14. http://dx.doi.org/10.1007/BF01674232.
- Nutrition During Pregnancy. Washington, DC: National Academy Press; 1990.
- Rollnick S, Butler CC, Kinnersley P, Gregory J, Mash B. Motivational interviewing. BMJ 2010;340:1242-5. http://dx.doi.org/10.1136/bmj.c1900.
- Scottish Intercollegiate Guidelines Network . Management of Obesity 2010. www.sign.ac.uk/pdf/sign115.pdf (accessed June 2013).
- Resnicow K, McCarty F, Blissett D, Wang T, Heitzler C, Lee RE. Validity of a modified CHAMPS physical activity questionnaire among African-Americans. Med Sci Sports Exerc 2003;35:1537-45. http://dx.doi.org/10.1249/01.MSS.0000084419.64044.2B.
- Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol 1986;124:453-69.
- National Institute for Health and Care Excellence . Obesity: The Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children 2006. http://guidance.nice.org.uk/CG43/guidance (accessed 17 September 2014).
- Obesity in Scotland: Integrating Prevention with Weight Management. Edinburgh: SIGN; 1996.
Appendix 1 Search strategies
MEDLINE (host: Ovid)
URL: http://library.dur.ac.uk/record=b2044620a&searchscope=1
Database searched from inception to 10 October 2011 (child review) and from inception 11 October 2012 (adult review).
Dates of searches: 10 October 2011 (child review); 11 October 2012 (adult review).
| 1 | “Body Weights and Measures”/ |
| 2 | (BMI or Body Mass Index).ti,ab. or Body Weight/ or obesity.ti,ab. or obese.ti,ab. or overweight.ti,ab. or weight gain.ti,ab. or weight loss.ti,ab. or exp OBESITY/ or Body fat.ti,ab. or Fat mass.ti,ab. or Weight control$.ti,ab. or Weight maintain$.ti,ab. or Adipos$.ti,ab. or Adipose tissue.ti,ab. or Skinfold thickness.ti,ab. or Waist circumference.ti,ab. or Waist hip ratio.ti,ab. or WHR.ti,ab. |
| 3 | 1 or 2 |
| 4 | Health Promotion/ or health promotion.ti,ab. or health behaviour.ti,ab. or health behavior.ti,ab. or (policy and (social or school or food or public or urban or environmental or fiscal)).ti,ab. or urban planning.ti,ab. or city planning.ti,ab. or built environment.ti,ab. or social environment.ti,ab. or physical environment.ti,ab. or cultural environment.ti,ab. or urban environment.ti,ab. or school environment.ti,ab. or neighbourhood.ti,ab. or community.ti,ab. or societal.ti,ab. or social interventions.ti,ab. or community interventions.ti,ab. or obesogenic environment.ti,ab. or individual level.ti,ab. or lifestyle.ti,ab. or individual.ti,ab. or tax$.ti,ab. or subsid$.ti,ab. or price$.ti,ab. or health education.ti,ab. or social marketing.ti,ab. or (diet and (advice or counselling)).ti,ab. or (exercise and (advice or counselling)).ti,ab. or weight management.ti,ab. or cash transfer$.ti,ab. or lifestyle counselling.ti,ab. or behavioural counselling.ti,ab. or behavioral counselling.ti,ab. or exercise on prescription.ti,ab. or exercise.ti,ab. or health trainer$.ti,ab. or school.ti,ab. or workplace.ti,ab. or campaign$.ti,ab. or (access adj1 facilities).ti,ab. or green space.ti,ab. or walk?ability.ti,ab. or food label$.ti,ab. or food advert$.ti,ab. |
| 5 | (evaluat$ or effective$ or Intervention or RCT or experiment$ or randomi?ed controlled trial$ or clinical randomi?ed controlled trial$ or cluster randomi?ed controlled trial$ or double blind randomi?ed controlled trial$ or randomi?ed consent design or single blind randomi?ed controlled trial$ or randomi?ed or placebo or random$ or trial or quasi?experiment$ or pre$test or post$test or trial or time series or evaluat$ or intervention$ or “before and after” or intervention$ or community trial or non?randomi?ed or repeat$ or repeat$ measures).ti,ab. or (exp Clinical Trial/ or exp Randomized Controlled Trial/ or exp Randomization/ or exp Double-Blind Method/ or exp Single-Blind Method/ or exp Cross-Over Studies/) or clinical trial.ti,ab. or latin square.ti,ab. or random$.ti,ab. or exp Evaluation/ or clinical trial.ti,ab. or clinical trial.pt. or (before adj1 after adj1 (stud$ or trial$ or design$)).ti,ab. or random$.ti,ab. or (quasi?experimental or pseudo?experimental).ti,ab. or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed).ti,ab. or ((population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) adj3 (intervention$ or prevention or policy or policies or program$ or project$)).ti,ab. |
| 6 | 3 and 4 and 5 |
| 7 | limit 6 to humans |
EMBASE (host: Ovid)
URL: http://library.dur.ac.uk/record=b2044208a&searchscope=1
Database searched from inception to 10 October 2011 (child review) and from inception 11 October 2012 (adult review).
Dates of searches: 10 October 2011 (child review); 11 October 2012 (adult review).
| 1 | “Body Weights and Measures”/ |
| 2 | (BMI or Body Mass Index).ti,ab. or Body Weight/ or obesity.ti,ab. or obese.ti,ab. or overweight.ti,ab. or weight gain.ti,ab. or weight loss.ti,ab. or exp OBESITY/ or Body fat.ti,ab. or Fat mass.ti,ab. or Weight control$.ti,ab. or Weight maintain$.ti,ab. or Adipos$.ti,ab. or Adipose tissue.ti,ab. or Skinfold thickness.ti,ab. or Waist circumference.ti,ab. or Waist hip ratio.ti,ab. or WHR.ti,ab. |
| 3 | 1 or 2 |
| 4 | Health Promotion/ or health promotion.ti,ab. or health behaviour.ti,ab. or health behavior.ti,ab. or (policy and (social or school or food or public or urban or environmental or fiscal)).ti,ab. or urban planning.ti,ab. or city planning.ti,ab. or built environment.ti,ab. or social environment.ti,ab. or physical environment.ti,ab. or cultural environment.ti,ab. or urban environment.ti,ab. or school environment.ti,ab. or neighbourhood.ti,ab. or community.ti,ab. or societal.ti,ab. or social interventions.ti,ab. or community interventions.ti,ab. or obesogenic environment.ti,ab. or individual level.ti,ab. or lifestyle.ti,ab. or individual.ti,ab. or tax$.ti,ab. or subsid$.ti,ab. or price$.ti,ab. or health education.ti,ab. or social marketing.ti,ab. or (diet and (advice or counselling)).ti,ab. or (exercise and (advice or counselling)).ti,ab. or weight management.ti,ab. or cash transfer$.ti,ab. or lifestyle counselling.ti,ab. or behavioural counselling.ti,ab. or behavioral counselling.ti,ab. or exercise on prescription.ti,ab. or exercise.ti,ab. or health trainer$.ti,ab. or school.ti,ab. or workplace.ti,ab. or campaign$.ti,ab. or (access adj1 facilities).ti,ab. or green space.ti,ab. or walk?ability.ti,ab. or food label$.ti,ab. or food advert$.ti,ab. |
| 5 | (evaluat$ or effective$ or Intervention or RCT or experiment$ or randomi?ed controlled trial$ or clinical randomi?ed controlled trial$ or cluster randomi?ed controlled trial$ or double blind randomi?ed controlled trial$ or randomi?ed consent design or single blind randomi?ed controlled trial$ or randomi?ed or placebo or random$ or trial or quasi?experiment$ or pre$test or post$test or trial or time series or evaluat$ or intervention$ or “before and after” or intervention$ or community trial or non?randomi?ed or repeat$ or repeat$ measures).ti,ab. or (exp Clinical Trial/ or exp Randomized Controlled Trial/ or exp Randomization/ or exp Double-Blind Method/ or exp Single-Blind Method/ or exp Cross-Over Studies/) or clinical trial.ti,ab. or latin square.ti,ab. or random$.ti,ab. or exp Evaluation/ or clinical trial.ti,ab. or clinical trial.pt. or (before adj1 after adj1 (stud$ or trial$ or design$)).ti,ab. or random$.ti,ab. or (quasi?experimental or pseudo?experimental).ti,ab. or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed).ti,ab. or ((population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) adj3 (intervention$ or prevention or policy or policies or program$ or project$)).ti,ab. |
| 6 | 3 and 4 and 5 |
| 7 | limit 6 to humans |
| 8 | limit 7 to last year |
International Bibliography of the Social Sciences (host: EBSCOhost)
URL: http://library.dur.ac.uk/record=b2044596a&searchscope=1
Database searched from inception to 10 October 2011 (child review) and from inception 11 October 2012 (adult review).
Dates of searches: 10 October 2011 (child review); 11 October 2012 (adult review).
| S5 | all((BMI OR Body Mass Index) OR (obesity) OR (obese) OR (overweight) OR (weight gain) OR (weight loss) OR (Body fat) OR (Fat mass) OR (Weight control*) OR (Weight maintain*) OR (Adipos*) OR (Adipose tissue) OR (Skinfold thickness) OR (Waist circumference) OR (Waist hip ratio) OR (WHR)) AND all((health promotion) OR (health behaviour) OR (health behavior) OR (policy AND (social OR school OR food OR public OR urban OR environmental OR fiscal)) OR (urban planning) OR (city planning) OR (built environment) OR (social environment) OR (physical environment) OR (cultural environment) OR (urban environment) OR (school environment) OR (neighbourhood) OR (community) OR (societal) OR (social interventions) OR (community interventions) OR (obesogenic environment) OR (individual level) OR (lifestyle) OR (individual) OR (tax*) OR (subsid*) OR (price*) OR (health education) OR (social marketing) OR (diet AND (advice OR counselling)) OR (exercise AND (advice OR counselling)) OR (weight management) OR (cash transfer*) OR (lifestyle counselling) OR (behavioural counselling) OR (behavioral counselling) OR (exercise on prescription) OR (exercise) OR (health trainer*) OR (school) OR (workplace) OR (campaign*) OR (access NEAR/1 facilities) OR (green space) OR (walk*ability) OR (food label*) OR (food advert*)) AND ((evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*))Limits applied Databases: Narrowed by: Entered date: 10/ 2011 - 10/ 2012 |
| S4 | all((BMI OR Body Mass Index) OR (obesity) OR (obese) OR (overweight) OR (weight gain) OR (weight loss) OR (Body fat) OR (Fat mass) OR (Weight control*) OR (Weight maintain*) OR (Adipos*) OR (Adipose tissue) OR (Skinfold thickness) OR (Waist circumference) OR (Waist hip ratio) OR (WHR)) AND all((health promotion) OR (health behaviour) OR (health behavior) OR (policy AND (social OR school OR food OR public OR urban OR environmental OR fiscal)) OR (urban planning) OR (city planning) OR (built environment) OR (social environment) OR (physical environment) OR (cultural environment) OR (urban environment) OR (school environment) OR (neighbourhood) OR (community) OR (societal) OR (social interventions) OR (community interventions) OR (obesogenic environment) OR (individual level) OR (lifestyle) OR (individual) OR (tax*) OR (subsid*) OR (price*) OR (health education) OR (social marketing) OR (diet AND (advice OR counselling)) OR (exercise AND (advice OR counselling)) OR (weight management) OR (cash transfer*) OR (lifestyle counselling) OR (behavioural counselling) OR (behavioral counselling) OR (exercise on prescription) OR (exercise) OR (health trainer*) OR (school) OR (workplace) OR (campaign*) OR (access NEAR/1 facilities) OR (green space) OR (walk*ability) OR (food label*) OR (food advert*)) AND ((evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*))Databases: |
| S3 | (evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*)Databases: |
| S2 | all((health promotion) or (health behaviour) or (health behavior) or (policy and (social or school or food or public or urban or environmental or fiscal)) or (urban planning) or (city planning) or (built environment) or (social environment) or (physical environment) or (cultural environment) or (urban environment) or (school environment) or (neighbourhood) or (community) or (societal) or (social interventions) or (community interventions) or (obesogenic environment) or (individual level) or (lifestyle) or (individual) or (tax*) or (subsid*) or (price*) or (health education) or (social marketing) or (diet and (advice or counselling)) or (exercise and (advice or counselling)) or (weight management) or (cash transfer*) or (lifestyle counselling) or (behavioural counselling) or (behavioral counselling) or (exercise on prescription) or (exercise) or (health trainer*) or (school) or (workplace) or (campaign*) or (access NEAR/1 facilities) or (green space) or (walk*ability) or (food label*) or (food advert*))Databases: |
| S1 | all((BMI or Body Mass Index) or (obesity) or (obese) or (overweight) or (weight gain) or (weight loss) or (Body fat) or (Fat mass) or (Weight control*) or (Weight maintain*) or (Adipos*) or (Adipose tissue) or (Skinfold thickness) or (Waist circumference) or (Waist hip ratio) or (WHR)) |
Applied Social Sciences Index and Abstracts (ASSIA) (host: CSA)
URL: http://library.dur.ac.uk/record=b2603336a&searchscope=1
Database searched from inception to 10 October 2011 (child review) and from inception 11 October 2012 (adult review).
Dates of searches: 10 October 2011 (child review); 11 October 2012 (adult review).
| S5 | ((BMI or Body Mass Index) or (obesity) or (obese) or (overweight) or (weight gain) or (weight loss) or (Body fat) or (Fat mass) or (Weight control*) or (Weight maintain*) or (Adipos*) or (Adipose tissue) or (Skinfold thickness) or (Waist circumference) or (Waist hip ratio) or (WHR)) AND ((health promotion) or (health behaviour) or (health behavior) or (policy and (social or school or food or public or urban or environmental or fiscal)) or (urban planning) or (city planning) or (built environment) or (social environment) or (physical environment) or (cultural environment) or (urban environment) or (school environment) or (neighbourhood) or (community) or (societal) or (social interventions) or (community interventions) or (obesogenic environment) or (individual level) or (lifestyle) or (individual) or (tax*) or (subsid*) or (price*) or (health education) or (social marketing) or (diet and (advice or counselling)) or (exercise and (advice or counselling)) or (weight management) or (cash transfer*) or (lifestyle counselling) or (behavioural counselling) or (behavioral counselling) or (exercise on prescription) or (exercise) or (health trainer*) or (school) or (workplace) or (campaign*) or (access NEAR/1 facilities) or (green space) or (walk*ability) or (food label*) or (food advert*)) AND ((evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*))Limits appliedDatabases: Narrowed by: Entered date: 10/ 2011 - 10/ 2012 |
| S4 | ((BMI or Body Mass Index) or (obesity) or (obese) or (overweight) or (weight gain) or (weight loss) or (Body fat) or (Fat mass) or (Weight control*) or (Weight maintain*) or (Adipos*) or (Adipose tissue) or (Skinfold thickness) or (Waist circumference) or (Waist hip ratio) or (WHR)) AND ((health promotion) or (health behaviour) or (health behavior) or (policy and (social or school or food or public or urban or environmental or fiscal)) or (urban planning) or (city planning) or (built environment) or (social environment) or (physical environment) or (cultural environment) or (urban environment) or (school environment) or (neighbourhood) or (community) or (societal) or (social interventions) or (community interventions) or (obesogenic environment) or (individual level) or (lifestyle) or (individual) or (tax*) or (subsid*) or (price*) or (health education) or (social marketing) or (diet and (advice or counselling)) or (exercise and (advice or counselling)) or (weight management) or (cash transfer*) or (lifestyle counselling) or (behavioural counselling) or (behavioral counselling) or (exercise on prescription) or (exercise) or (health trainer*) or (school) or (workplace) or (campaign*) or (access NEAR/1 facilities) or (green space) or (walk*ability) or (food label*) or (food advert*)) AND ((evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*))Databases: |
| S3 | (evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*)Databases: |
| S2 | (health promotion) or (health behaviour) or (health behavior) or (policy and (social or school or food or public or urban or environmental or fiscal)) or (urban planning) or (city planning) or (built environment) or (social environment) or (physical environment) or (cultural environment) or (urban environment) or (school environment) or (neighbourhood) or (community) or (societal) or (social interventions) or (community interventions) or (obesogenic environment) or (individual level) or (lifestyle) or (individual) or (tax*) or (subsid*) or (price*) or (health education) or (social marketing) or (diet and (advice or counselling)) or (exercise and (advice or counselling)) or (weight management) or (cash transfer*) or (lifestyle counselling) or (behavioural counselling) or (behavioral counselling) or (exercise on prescription) or (exercise) or (health trainer*) or (school) or (workplace) or (campaign*) or (access NEAR/1 facilities) or (green space) or (walk*ability) or (food label*) or (food advert*)Databases: |
| S1 | (BMI or Body Mass Index) or (obesity) or (obese) or (overweight) or (weight gain) or (weight loss) or (Body fat) or (Fat mass) or (Weight control*) or (Weight maintain*) or (Adipos*) or (Adipose tissue) or (Skinfold thickness) or (Waist circumference) or (Waist hip ratio) or (WHR)Databases: |
Sociological Abstracts (host: CSA)
URL: http://library.dur.ac.uk/record=b2603341a&searchscope=1
Database searched from inception to 10 October 2011 (child review) and from inception 11 October 2012 (adult review).
Dates of searches: 10 October 2011 (child review); 11 October 2012 (adult review).
| S5 | ((BMI or Body Mass Index) or (obesity) or (obese) or (overweight) or (weight gain) or (weight loss) or (Body fat) or (Fat mass) or (Weight control*) or (Weight maintain*) or (Adipos*) or (Adipose tissue) or (Skinfold thickness) or (Waist circumference) or (Waist hip ratio) or (WHR)) AND ((health promotion) or (health behaviour) or (health behavior) or (policy and (social or school or food or public or urban or environmental or fiscal)) or (urban planning) or (city planning) or (built environment) or (social environment) or (physical environment) or (cultural environment) or (urban environment) or (school environment) or (neighbourhood) or (community) or (societal) or (social interventions) or (community interventions) or (obesogenic environment) or (individual level) or (lifestyle) or (individual) or (tax*) or (subsid*) or (price*) or (health education) or (social marketing) or (diet and (advice or counselling)) or (exercise and (advice or counselling)) or (weight management) or (cash transfer*) or (lifestyle counselling) or (behavioural counselling) or (behavioral counselling) or (exercise on prescription) or (exercise) or (health trainer*) or (school) or (workplace) or (campaign*) or (access NEAR/1 facilities) or (green space) or (walk*ability) or (food label*) or (food advert*)) AND ((evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*))Limits applied Databases: Narrowed by: Entered date: 10/ 2011 - 10/ 2012 |
| S4 | ((BMI or Body Mass Index) or (obesity) or (obese) or (overweight) or (weight gain) or (weight loss) or (Body fat) or (Fat mass) or (Weight control*) or (Weight maintain*) or (Adipos*) or (Adipose tissue) or (Skinfold thickness) or (Waist circumference) or (Waist hip ratio) or (WHR)) AND ((health promotion) or (health behaviour) or (health behavior) or (policy and (social or school or food or public or urban or environmental or fiscal)) or (urban planning) or (city planning) or (built environment) or (social environment) or (physical environment) or (cultural environment) or (urban environment) or (school environment) or (neighbourhood) or (community) or (societal) or (social interventions) or (community interventions) or (obesogenic environment) or (individual level) or (lifestyle) or (individual) or (tax*) or (subsid*) or (price*) or (health education) or (social marketing) or (diet and (advice or counselling)) or (exercise and (advice or counselling)) or (weight management) or (cash transfer*) or (lifestyle counselling) or (behavioural counselling) or (behavioral counselling) or (exercise on prescription) or (exercise) or (health trainer*) or (school) or (workplace) or (campaign*) or (access NEAR/1 facilities) or (green space) or (walk*ability) or (food label*) or (food advert*)) AND ((evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*))Databases: |
| S3 | (evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or (clinical trial or latin square or random* or clinical trial) or (before NEAR/1 after NEAR/1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or (population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) or (intervention* or prevention or policy or policies or program* or project*)Databases: |
| S2 | (health promotion) or (health behaviour) or (health behavior) or (policy and (social or school or food or public or urban or environmental or fiscal)) or (urban planning) or (city planning) or (built environment) or (social environment) or (physical environment) or (cultural environment) or (urban environment) or (school environment) or (neighbourhood) or (community) or (societal) or (social interventions) or (community interventions) or (obesogenic environment) or (individual level) or (lifestyle) or (individual) or (tax*) or (subsid*) or (price*) or (health education) or (social marketing) or (diet and (advice or counselling)) or (exercise and (advice or counselling)) or (weight management) or (cash transfer*) or (lifestyle counselling) or (behavioural counselling) or (behavioral counselling) or (exercise on prescription) or (exercise) or (health trainer*) or (school) or (workplace) or (campaign*) or (access NEAR/1 facilities) or (green space) or (walk*ability) or (food label*) or (food advert*)Databases: |
| S1 | (BMI or Body Mass Index) or (obesity) or (obese) or (overweight) or (weight gain) or (weight loss) or (Body fat) or (Fat mass) or (Weight control*) or (Weight maintain*) or (Adipos*) or (Adipose tissue) or (Skinfold thickness) or (Waist circumference) or (Waist hip ratio) or (WHR)Databases: |
NHS Economic Evaluation Database (host: NHS CRD)
URL: www.cochrane.org/editorial-and-publishing-policy-resource/nhs-economic-evaluation-database
Database searched from inception to 10 October 2011 (child review) and from inception 11 October 2012 (adult review).
Dates of searches: 10 October 2011 (child review); 11 October 2012 (adult review).
| 1 | descriptor Body Weights and Measures explode all trees in Economic Evaluations |
| 2 | MeSH descriptor Obesity explode all trees in Economic Evaluations |
| 3 | BMI or Body Mass Index or Body Weight or obesity or obese or overweight or weight gain or weight loss or Body fat or Fat mass or Weight control* or Weight maintain* or Adipos* or Adipose tissue or Skinfold thickness or Waist circumference. or Waist hip ratio or WHR in Economic Evaluations |
| 4 | (#1 OR #2 OR #3) |
| 5 | MeSH descriptor Health Promotion explode all trees in Economic Evaluations |
| 6 | health promotion or health behaviour or health behavior or (policy and (social or school or food or public or urban or environmental or fiscal)) or urban planning or city planning or built environment or social environment or physical environment or cultural environment or urban environment or school environment or neighbourhood or community or societal or social interventions or community interventions or obesogenic environment or individual level or lifestyle or individual or tax* or subsid* or price* or health education or social marketing or (diet and (advice or counselling)) or (exercise and (advice or counselling)) or weight management or cash transfer* or lifestyle counselling or behavioural counselling or behavioral counselling or exercise on prescription or exercise or health trainer* or school or workplace or campaign* or (access adj1 facilities) or green space or walk?ability or food label* or food advert* in Economic Evaluations |
| 7 | (#5 OR #6) |
| 8 | (evaluat* or effective* or Intervention or RCT or experiment* or randomi?ed controlled trial* or clinical randomi?ed controlled trial* or cluster randomi?ed controlled trial* or double blind randomi?ed controlled trial* or randomi?ed consent design or single blind randomi?ed controlled trial* or randomi?ed or placebo or random* or trial or quasi?experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non?randomi?ed or repeat* or repeat* measures) or clinical trial or latin square or random* or exp Evaluation/ or clinical trial or clinical trial.pt. or (before adj1 after adj1 (stud* or trial* or design*)) or random* or (quasi?experimental or pseudo?experimental) or (nonrandomi?ed or non?randomi?ed or pseudo?randomi?sed or quasi?randomi?ed) or ((population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) adj3 (intervention* or prevention or policy or policies or program* or project*)) in Economic Evaluations |
| 9 | (#4 AND #7 AND #8) from 2011 to 2012 |
| 10 | (#4 and #7 and #8) from 2011 to 2012 in Economic Evaluations |
Social Science Citation Index (host: Web of Science)
URL: http://apps.webofknowledge.com/UA_GeneralSearch_input.do?product=UA&search_mode=GeneralSearch&SID=Z1j5YrUOJ8scTdhR1Nv&preferencesSaved
Database searched from inception to 10 October 2011 (child review) and from inception 11 October 2012 (adult review).
Dates of searches: 10 October 2011 (child review); 11 October 2012 (adult review).
| 1 | TS=(Body Weights and Measures) |
| 2 | TS=(BMI or Body Mass Index) or TS=(obesity) or TS=(obese) or TS=(overweight) or TS=(weight gain) or TS=(weight loss) or TS=(Body fat) or TS=(Fat mass) or TS=(Weight control*) or TS=(Weight maintain*) or TS=(Adipos*) or TS=(Adipose tissue) or TS=(Skinfold thickness) or TS=(Waist circumference) or TS=(Waist hip ratio) or TS=(WHR) |
| 3 | #1 or #2 |
| 4 | TS=Health Promotion |
| 5 | TS=(health promotion) or TS=(health behaviour) or TS=(health behavior) or TS=(policy and (social or school or food or public or urban or environmental or fiscal)) or TS=(urban planning) or TS=(city planning) or TS=(built environment) or TS=(social environment) or TS=(physical environment) or TS=(cultural environment) or TS=(urban environment) or TS=(school environment) or TS=(neighbourhood) or TS=(community) or TS=(societal or social interventions) or TS=(community interventions) or TS=(obesogenic environment) or TS=(individual level) or TS=(lifestyle) or TS=(individual) or TS=(tax*) or TS=(subsid*) or TS=(price*) or TS=(health education) or TS=(social marketing) or TS=(diet and (advice or counselling)) or TS=(exercise and (advice or counselling)) or TS=(weight management) or TS=(cash transfer*) or TS=(lifestyle counselling) or TS=(behavioural counselling) or TS=(behavioral counselling) or TS=(exercise on prescription) or TS=(exercise) or TS=(health trainer*) or TS=(school) or TS=(workplace) or TS=(campaign*) or TS=(access N1 facilities) or TS=(green space) or TS=(walk$ability) or TS=(food label*) or TS=(food advert*) |
| 6 | #4 or #5 |
| 7 | TS=(Clinical Trials) OR TS=(Randomized Controlled Trials) or TS=(Double-Blind Studies) or TS=(Single-Blind Studies) or TS=(Crossover Design) |
| 8 | TS=(evaluat* or effective* or Intervention or RCT or experiment* or randomi$ed controlled trial* or clinical randomi$ed controlled trial* or cluster randomi$ed controlled trial* or double blind randomi$ed controlled trial* or randomi$ed consent design or single blind randomi$ed controlled trial* or randomi$ed or placebo or random* or trial or quasi$experiment* or pre*test or post*test or trial or time series or evaluat* or intervention* or “before and after” or intervention* or community trial or non$randomi$ed or repeat* or repeat* measures) or TS=(clinical trial) or TS=(latin square) or TS=(random*) or TS=(clinical trial) or TS=(before N1 after N1 (stud* or trial* or design*)) or TS=(random*) or TS=(quasi$experimental or pseudo$experimental) or TS=(nonrandomi$ed or non$randomi$ed or pseudo$randomi$sed or quasi$randomi$ed) or TS=((population level or population based or population orientated or population oriented or community level or community based or community orientated or community oriented) N3 (intervention* or prevention or policy or policies or program* or project*)) |
| 9 | #7 or #8 |
| 10 | #3 and #6 and #9 |
Appendix 2 Data extraction form
| Part 1: Bibliographic details | |||||
|---|---|---|---|---|---|
| Study ID | |||||
| Author (first) | |||||
| Journal | |||||
| Year | |||||
| Volume | |||||
| Pages | |||||
| Language | |||||
| Type (e.g. full paper, conference proceeding, unpublished report) | |||||
| Corresponding author and contact details | |||||
| In/out reviewer initials | Data extraction reviewer initials | ||||
| Date in/outed | Date data extracted | ||||
| Part 2: Eligibility (in/out) | |||||
| For this review do you think that this study should be (please circle): | |||||
| Include (child review) | Include (adult review) | Contact author – child (for SES data) | Contact author – adult (for SES data) | Exclude | Unsure |
| Does this study fall into any of the following categories? Societal Workplace Low to mid income | |||||
| Comments: | |||||
| 1 | Does the study investigate a public health intervention aimed at preventing or treating obesity NOT specifically targeted at participants with critical illness or severe comorbidities? (Y/N/unclear) | ||||
| 2 | Is the study a randomised or non-randomised controlled trial, a prospective or retrospective cohort study (with/without control groups) or a prospective repeat cross-sectional study (with/without control groups)? (Y/N/unclear) | ||||
| 3 | Does the study include an outcome that is a proxy for body fatness (weight and height; body mass index; waist measurement/waist-to-hip proportion; percentage fat content; skinfold thickness; ponderal index in relation to childhood obesity)? (Y/N/unclear) | ||||
| 4 | Does the study examine differential effects with regard to socioeconomic status (education, income, occupation, social class, deprivation, poverty) OR Is the intervention targeted specifically at disadvantaged groups (e.g. described as disadvantaged, low-SES, low income) or deprived areas? (Y/N/unclear) | ||||
| 5a | Does the study report outcomes in children aged between 0 and 18 years? (Y/N/unclear) | ||||
| 5b | Does the study report outcomes in adults aged ≥ 18 years? (Y/N/unclear) | ||||
| 6 | Does the study involve both ‘before and after’ measures? (Y/N/unclear) | ||||
| 7 | Is the duration of the study (combination of intervention and follow-up) ≥ 12 weeks? (Y/N/unclear) | ||||
| Part 3: Type of intervention | |||||
| 3a | Type of obesity intervention and intervention details | ||||
| 3b | Level of intervention (individual, community, societal – working/living conditions or macro policy) | ||||
| 3c | Approach to targeting inequality (disadvantaged group only/gap between top and bottom groups/gradient – all socioeconomic groups) | ||||
| Part 4: Study population | |||||
| 4a | Setting | ||||
| 4b | Population targeted | ||||
| 4c | Sex (baseline sample) | ||||
| 4d | Age (baseline sample) | ||||
| 4e | Country in which study was conducted | ||||
| 4f | Date study was conducted | ||||
| Part 5: Study design and methods | |||||
| 5a | Study design | ||||
| 5b | Method of sampling (simple random, stratified, cluster, etc.) | ||||
| 5c | Total population (number who could take part, e.g. total school population) | ||||
| 5d | Baseline sample size and rate | ||||
| 5e | Time between baseline and follow-ups | ||||
| 5f | Follow-up response rate | ||||
| 5g | Final sample size | ||||
| 5h | Is confounding from attrition/non-response explored? Are adjustments made? | ||||
| 5i | Is information about other potential confounders obtained (e.g. concurrent interventions, not all intervention group exposed)? | ||||
| 5j | Other concerns about bias | ||||
| Part 6: Control group selection (if applicable) | |||||
| 6a | Method of selecting control group (randomised or matched, etc.) | ||||
| 6b | Is demographic confounding between intervention and control groups explored? Any adjustments made? | ||||
| 6c | Contamination between intervention and control group? | ||||
| Part 7: Outcome measures | |||||
| 7a | Obesity measure (state if independently measured, i.e. by health professional, researcher, or self-reported) | ||||
| 7b | SES measure | ||||
| 7c | Physical activity | ||||
| 7d | Diet intake | ||||
| 7e | Biochemical outcomes (e.g. cholesterol, glucose) | ||||
| Part 8: Results | |||||
| 8a | Obesity outcomes (differential effects by SES group if applicable) | ||||
| 8b | Physical activity | ||||
| 8c | Diet intake | ||||
| 8d | Biochemical outcomes | ||||
| 8e | Study authors’ key conclusions | ||||
| 8f | Do you agree with the authors’ conclusions? | ||||
| Part 9: Implementation | |||||
| 9a | Motivation (Why was the intervention implemented? Most likely to reduce obesity – state whether treatment or prevention) | ||||
| 9b | Theoretical underpinning (e.g. social cognitive theory, nudge, theory of planned behaviour) | ||||
| 9c | Implementation context (social, economic, political, managerial) | ||||
| 9d | Experience of intervention team (planners and implementers) | ||||
| 9e | Consultation and/or collaboration processes (planning and delivery stages) (e.g. consultations with parents/community, participatory research methods used) | ||||
| 9f | Delivery fidelity – was the intervention delivered as intended? If applicable, extent to which the programme has been modified over time, and extent to which the programme may be considered a new or different programme as a result of modification | ||||
| 9g | Sustainability – strength of the institution implementing the intervention; integration of activities into existing programmes/services/curriculum/etc.; training/capacity building component; community involvement/participation | ||||
| 9h | Stakeholder support | ||||
| 9i | Resources (time, money, staff and equipment) | ||||
| 9j | Differential effects and population characteristics (e.g. ethnicity, gender, age) | ||||
| Part 10: Miscellaneous | |||||
| 10a | Funding source | ||||
| 10b | Secondary publications | ||||
| 10c | Correspondence required (request for clarification of methods or results) | ||||
| 10d | Comments/summary | ||||
Appendix 3 Example completed quality appraisal form

| Study | Craigie 2011 |
| Reviewer initials | FH |
| Date | 19/03/13 |
Quality assessment tool for quantitative studies
Component ratings
A) Selection bias
Q1 Are the individuals selected to participate in the study likely to be representative of the target population?
-
Very likely
-
Somewhat likely
-
Not likely
-
Can’t tell
Q2 What percentage of selected individuals agreed to participate?
-
80–100% agreement
-
60–79% agreement
-
< 60% agreement
-
Not applicable
-
Can’t tell
| Rate this section | Strong | Moderate | Weak |
|---|---|---|---|
| See dictionary | 1 | 2 | 3 |
B) Study design
Indicate the study design
-
Randomised controlled trial
-
Controlled clinical trial
-
Cohort analytical (two-group pre + post)
-
Case–control
-
Cohort [one-group pre + post (before and after)]
-
Interrupted time series
-
Other specify ____________________________
-
Can’t tell
Was the study described as randomised? If no, go to component C.
No Yes
If yes, was the method of randomisation described? (See dictionary)
No Yes
If yes, was the method appropriate? (See dictionary)
No Yes
| Rate this section | Strong | Moderate | Weak |
|---|---|---|---|
| See dictionary | 1 | 2 | 3 |
C) Confounders
Q1 Were there important differences between groups prior to the intervention?
-
Yes
-
No
-
Can’t tell
The following are examples of confounders:
-
Race
-
Sex
-
Marital status/family
-
Age
-
SES (income or class)
-
Education
-
Health status
-
Pre-intervention score on outcome measure
Q2 If yes, indicate the percentage of relevant confounders that were controlled [either in the design (e.g. stratification, matching) or analysis]?
-
80–100% (most)
-
60–79% (some)
-
< 60% (few or none)
-
Can’t tell
| Rate this section | Strong | Moderate | Weak |
|---|---|---|---|
| See dictionary | 1 | 2 | 3 |
D) Blinding
Q1 Was (were) the outcome assessor(s) aware of the intervention or exposure status of participants?
-
Yes
-
No
-
Can’t tell
Q2 Were the study participants aware of the research question?
-
Yes
-
No
-
Can’t tell
| Rate this section | Strong | Moderate | Weak |
|---|---|---|---|
| See dictionary | 1 | 2 | 3 |
E) Data collection methods
Q1 Were data collection tools shown to be valid?
-
Yes
-
No
-
Can’t tell
Q2 Were data collection tools shown to be reliable?
-
Yes
-
No
-
Can’t tell
| Rate this section | Strong | Moderate | Weak |
|---|---|---|---|
| See dictionary | 1 | 2 | 3 |
F) Withdrawals and dropouts
Q1 Were withdrawals and dropouts reported in terms of numbers and/or reasons per group?
-
Yes
-
No
-
Can’t tell
-
Not applicable (i.e. one-time surveys or interviews)
Q2 Indicate the percentage of participants completing the study (If the percentage differs by group, record the lowest)
-
80–100%
-
60–79%
-
< 60%
-
Can’t tell
-
Not applicable (i.e. retrospective case–control)
| Rate this section | Strong | Moderate | Weak | |
|---|---|---|---|---|
| See dictionary | 1 | 2 | 3 | Not applicable |
G) Intervention integrity
Q1 What percentage of participants received the allocated intervention or exposure of interest?
-
80–100%
-
60–79%
-
< 60%
-
Can’t tell
Q2 Was the consistency of the intervention measured?
-
Yes
-
No
-
Can’t tell
Q3 Is it likely that subjects received an unintended intervention (contamination or co-intervention) that may influence the results?
-
Yes
-
No
-
Can’t tell
H) Analyses
Q1 Indicate the unit of allocation (circle one)
Community organisation/institution practice/office individual
Q2 Indicate the unit of analysis (circle one)
Community organisation/institution practice/office individual
Q3 Are the statistical methods appropriate for the study design?
-
Yes
-
No
-
Can’t tell
Q4 Is the analysis performed by intervention allocation status (i.e. intention to treat) rather than the actual intervention received?
-
Yes
-
No
-
Can’t tell
Global rating
Component ratings
Please transcribe the information from the grey boxes on pages 1–4 onto this page. See dictionary on how to rate this section.
| A) Selection bias | Strong | Moderate | Weak | |
| 1 | 2 | 3 | ||
| B) Study design | Strong | Moderate | Weak | |
| 1 | 2 | 3 | ||
| C) Confounders | Strong | Moderate | Weak | |
| 1 | 2 | 3 | ||
| D) Blinding | Strong | Moderate | Weak | |
| 1 | 2 | 3 | ||
| E) Data collection method | Strong | Moderate | Weak | |
| 1 | 2 | 3 | ||
| F) Withdrawals and dropouts | Strong | Moderate | Weak | |
| 1 | 2 | 3 | Not applicable |
Global rating for this paper (circle one):
-
Strong (no weak ratings)
-
Moderate (one weak rating)
-
Weak (two or more weak ratings)
With both reviewers discussing the ratings:
Is there a discrepancy between the two reviewers with respect to the component (A–F) ratings?
No Yes
If yes, indicate the reason for the discrepancy
-
Oversight
-
Differences in interpretation of criteria
-
Differences in interpretation of study
Final decision of both reviewers (circle one): 1 Strong 2 Moderate 3 Weak
Appendix 4 List of included studies
Child individual-level interventions [11 studies (13 papers)]
Baxter KA, Ware RS, Batch JA, Truby H. Predicting success: factors associated with weight change in obese youth undertaking a weight management program. Obes Res Clin Pract 2013;7:e147–54.
Black MM, Hager ER, Le K, Anliker J, Arteaga SS, Diclemente C, et al. Challenge! Health promotion/obesity prevention mentorship model among urban, black adolescents. Pediatrics 2010;126:280–8.
Braet C. Patient characteristics as predictors of weight loss after an obesity treatment for children. Obesity 2006;14:148–55.
Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med 2008;162:239–45.
Fernandez De Velasco Galan JJ, Pascual De La Pisa B, Benitez Cambra MR. Control of childhood obesity in primary care. [Control de la obesidad infantil en atencion primaria.] Acta Pediatr Esp 2008;66:13–19.
Langnäse K, Asbeck I, Mast M, Müller MJ. The influence of socio-economic status on the long-term effect of family-based obesity treatment intervention in prepubertal overweight children. Health Educ 2004;104:336–43.
Marshall B, Floyd S, Forrest R. Clinical outcomes and patients’ perceptions of nurse-led healthy lifestyle clinics. J Prim Health Care 2011;3:48–52.
Pust S, Langnäse K, Asbeck I, Geisler C, Danielzik S, Müller MJ. Influence of socio-economic state on the outcome of a family-based intervention for overweight children as part of the Kiel Obesity Prevention Study (KOPS). Int J Obes Relat Metab Disord 2004;28(Suppl. 1):S201.
Sabin MA, Ford A, Hunt L, Jamal R, Crowne EC, Shield JPH. What factors are associated with a successful outcome in a weight management programme for obese children? J Eval Clin Pract 2007;13:364–8.
Smith AE, Annesi JJ, Walsh AM, Lennon V, Bell RA. Association of changes in self-efficacy, voluntary physical activity, and risk factors for type 2 diabetes in a behavioral treatment for obese preadolescents: a pilot study. J Pediatr Nurs 2010;25:393–9.
Taveras EM, Gortmaker SL, Hohman KH, Horan CM, Kleinman KP, Mitchell K, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch Pediatr Adolesc Med 2011;165:714–22.
Truby H, Baxter K, Ware R, Batch J. Successful weight loss for adolescents: what can diet offer? Obes Res Clin Pract 2011;5:S10.
Wake M, Baur LA, Gerner B, Gibbons K, Gold L, Gunn J, et al. Outcomes and costs of primary care surveillance and intervention for overweight or obese children: the LEAP 2 randomised controlled trial. BMJ 2009;339:b3308.
Child community-level interventions [52 studies (54 papers)]
Alves JGB, Gale CR, Souza E, Batty GD. Effect of physical exercise on bodyweight in overweight children: a randomized controlled trial in a Brazilian slum. [Efeito do exercicio fisico sobre peso corporal em criancas com excesso de peso: Ensaio clinico comunitario randomizado em uma favela no Brasil.] Cad Saude Publica 2008;24(Suppl. 2):S353–9.
Annesi JJ. Initial body mass index and free-time physical activity moderate effects of the Youth Fit for Life treatment in African-American pre-adolescents. Percept Mot Skills 2010;110:789–800.
Annesi JJ, Faigenbaum AD, Westcott WL, Smith AE, Unruh JL, Hamilton FG. Effects of the Youth Fit For Life protocol on physiological, mood, self-appraisal, and voluntary physical actitivity changes in African American preadolescents: contrasting alter-school care and physical education formats. Int J Clin Health Psychol 2007;7:641–59.
Bellows LL. Development and Evaluation of Food Friends Get Movin’ with Mighty Moves(TM), a Physical Activity Program to Prevent Obesity in Low-Income Preschoolers. PhD thesis. Fort Collins, CO: Colorado State University; 2007.
Bingham M. Mediators and Moderators of the Effects of a Children’s Heart Health Intervention. PhD thesis. Chapel Hill, NC: University of North Carolina at Chapel Hill; 2002.
de Heer H. Project l.e.a.n.: an After-School Health and Exercise Program for Elementary School Children in El Paso, Texas. PhD thesis. El Paso, TX: University of Texas; 2009.
Figueroa-Colon R, Franklin FA, Lee JY, von Almen TK, Suskind RM. Feasibility of a clinic-based hypocaloric dietary intervention implemented in a school setting for obese children. Obes Res 1996;4:419–29.
Fletcher A, Cooper JR, Helms P, Northington L, Winters K. Stemming the tide of childhood obesity in an underserved urban African American population: a pilot study. ABNF J 2009;20:44–8.
Gronbaek HN, Madsen SA, Michaelsen KF. Family involvement in the treatment of childhood obesity: the Copenhagen approach. Eur J Pediatr 2009;168:1437–47.
Hamad R, Fernald LCH, Karlan DS. Health education for microcredit clients in Peru: a randomized controlled trial. BMC Public Health 2011;11:51.
Hawthorne A, Shaibi G, Gance-Cleveland B, McFall S. Grand Canyon Trekkers: school-based lunchtime walking program. J Sch Nurs 2011;27:43–50.
Heinberg LJ, Kutchman EM, Berger NA, Lawhun SA, Cuttler L, Seabrook RC, et al. Parent involvement is associated with early success in obesity treatment. Clin Pediatr 2010;49:457–65.
Hoffman JA, Thompson DR, Franko DL, Power TJ, Leff SS, Stallings VA. Decaying behavioral effects in a randomized, multi-year fruit and vegetable intake intervention. Prev Med 2011;52:370–5.
Janicke DM, Gray WN, Mathews AE, Simon SL, Lim CS, Dumont-Driscoll M, et al. A pilot study examining a group-based behavioral family intervention for obese children enrolled in Medicaid: differential outcomes by race. Child Health Care 2011;40:212–31.
Jansen W, Borsboom G, Meima A, Zwanenburg EJV, MacKenbach JP, Raat H, et al. Effectiveness of a primary school-based intervention to reduce overweight. Int J Pediatr Obes 2011;6:e70–7.
Jelalian E, Hart CN, Mehlenbeck RS, Lloyd-Richardson EE, Kaplan JD, Flynn-O’Brien KT, et al. Predictors of attrition and weight loss in an adolescent weight control program. Obesity 2008;16:1318–23.
Jouret B, Ahluwalia N, Dupuy M, Cristini C, Negre-Pages L, Grandjean H, et al. Prevention of overweight in preschool children: results of kindergarten-based interventions. Int J Obes (Lond) 2009;33:1075–83.
Kain J, Uauy R, Albala, Vio F, Cerda R, Leyton B. School-based obesity prevention in Chilean primary school children: methodology and evaluation of a controlled study. Int J Obes Relat Metab Disord 2004;28:483–93.
Kain J, Concha F, Salazar G, Leyton B, Del Pilar Rodriguez M, Ceballos X, et al. Obesity prevention in preschool and schoolchildren attending public schools from a district of Santiago, Chile: pilot project 2006. [Prevencion de obesidad en preescolares y escolares de escuelas Municipales de una Comuna de Santiago de Chile: Proyecto piloto 2006.] Arch Latinoam Nutr 2009;59:139–46.
Kain J, Leyton B, Concha F, Salazar G, Lobos L, Vio F. Effect of counselling school teachers on healthy lifestyle on the impact of a program to reduce childhood obesity. [Estrategia de prevencion de obesidad en escolares: efecto de un programa aplicado a sus profesores (2007–2008).] Rev Med Chile 2010;138:181–7.
Kalarchian MA, Levine MD, Arslanian SA, Ewing LJ, Houck PR, Cheng Y, et al. Family-based treatment of severe pediatric obesity: randomized, controlled trial. Pediatrics 2009;124:1060–8.
Kalavainen MP, Korppi MO, Nuutinen OM. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. Int J Obes (Lond) 2007;31:1500–8.
Lindgren EC, Baigi A, Apitzsch E, Bergh H. Impact of a six-month empowerment-based exercise intervention programme in non-physically active adolescent Swedish girls. Health Educ J 2011;70:9–20.
Lubans DR, Morgan PJ, Aguiar EJ, Callister R. Randomized controlled trial of the Physical Activity Leaders (PALs) program for adolescent boys from disadvantaged secondary schools. Prev Med 2011;52:239–46.
Mockus DS. Weight Loss Success among Overweight Children: What Predicts Short-Term Outcome? PhD thesis. San Diego, CA: University of California; 2011.
Moore JB, Pawloski LR, Goldberg P, Kyeung MO, Stoehr A, Baghi H. Childhood obesity study: a pilot study of the effect of the nutrition education program Color My Pyramid. J Sch Nurs 2009;25:230–9.
Myers DA. The Effect of a Virtual Skill and Fitness Trainer in Physical Education Classes on Student Heart Rates, Body Mass Index, Fitness Level, and Student Perceptions. PhD thesis. Richmond, VA: Virginia Commonwealth University; 2008.
Nemer L, Schweizer C, von Hoff K, Fernandes Guerreiro AI. Improving Children’s Health and the Environment: Examples from the WHO European Region. Copenhagen: WHO Regional Office for Europe; 2009.
Nemet D, Geva D, Eliakim A. Health promotion intervention in low socioeconomic kindergarten children. J Pediatr 2011;158:796–801.
Plachta-Danielzik S, Pust S, Asbeck I, Czerwinski-Mast M, Langnäse K, Fischer C, et al. Four-year follow-up of school-based intervention on overweight children: the KOPS study. Obesity 2007;15:3159–69.
Plachta-Danielzik S, Landsberg B, Lange D, Langnäse K, Müller. [15 years of the Kiel Obesity Prevention Study (KOPS). Results and its importance for obesity prevention in children and adolescents.] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2011;54:304–12.
Pott W, Albayrak O, Hebebrand J, Pauli-Pott U. Treating childhood obesity: family background variables and the child’s success in a weight-control intervention. Int J Eat Disord 2009;42:284–9.
Pott W, Frohlich G, Albayrak O, Hebebrand J, Pauli-Pott U. Conditions for success in a lifestyle intervention weight-reduction programme for overweight or obese children and adolescents. Z Kinder Jugendpsychiatr Psychother 2010;38:351–60.
Ranstrom BB. Taking Steps Together: a Family Centered, Lifestyle Education and Behavioral Modification Program for Overweight and Obese Children and their Families. PhD thesis. Fargo, ND: North Dakota State University; 2009.
Reinehr T, Brylak K, Alexy U, Kersting M, Andler W. Predictors to success in outpatient training in obese children and adolescents. Int J Obes Relat Metab Disord 2003;27:1087–92.
Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA 1999;282:1561–7.
Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis 2003;13(Suppl. 1):S65–77.
Robinson TN, Matheson DM, Kraemer HC, Wilson DM, Obarzanek E, Thompson NS, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med 2010;164:995–1004.
Rudolf M, Sahota P, Walker J. A community-based approach for the treatment of childhood obesity: a pilot study. Int J Obes Relat Metab Disord 2004;28(Suppl. 1):S202.
Rudolf M, Christie D, McElhone S, Sahota P, Dixey R, Walker J, et al. WATCH IT: a community based programme for obese children and adolescents. Arch Dis Child 2006;91:736–9.
Rush E, Reed P, McLennan S, Coppinger T, Simmons D, Graham D. A school-based obesity control programme: Project Energize. Two-year outcomes. Br J Nutr 2012;107:581–7.
Salmon J, Ball K, Hume C, Booth M, Crawford D. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: switch-play. Int J Obes (Lond) 2008;32:601–12.
Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr 2009;12:197–202.
Simon C, Schweitzer B, Oujaa M, Wagner A, Arveiler D, Triby E, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obes (Lond) 2008;32:1489–98.
Stephens MB, Wentz SW. Supplemental fitness activities and fitness in urban elementary school classrooms. Fam Med 1998;30:220–3.
Story M, Sherwood NE, Himes JH, Davis M, Jacobs DR Jr, Cartwright Y, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethn Dis 2003;13(Suppl. 1):S54–64.
Topp R, Jacks DE, Wedig RT, Newman JL, Tobe L, Hollingsworth A. Reducing risk factors for childhood obesity: the Tommie Smith Youth Athletic Initiative. West J Nurs Res 2009;31:715–30.
Walter HJ, Hofman A, Connelly PA, Barrett LT, Kost KL. Primary prevention of chronic disease in childhood: changes in risk factors after one year of intervention. Am J Epidemiol 1985;122:772–81.
Weintraub DL, Tirumalai EC, Haydel KF, Fujimoto M, Fulton JE, Robinson TN. Team sports for overweight children: the Stanford Sports to Prevent Obesity Randomized Trial (SPORT). Arch Pediatr Adolesc Med 2008;162:232–7.
Willet SL. Health Risk Reduction among African-American Females: A One Year Follow-Up. PhD thesis. Evanston, IL: Northwestern University; 1996.
Williams AD, Warrington V. Get Fit Kids: a feasibility study of a pedometer-based walking program. Bariatr Nurs Surg Patient Care 2011;6:139–43.
Winter SM, Sass DA. Healthy & ready to learn: examining the efficacy of an early approach to obesity prevention and school readiness. J Res Child Educ 2011;25:304–25.
Woolford SJ, Sallinen BJ, Clark SJ, Freed GL. Results from a clinical multidisciplinary weight management program. Clin Pediatr 2011;50:187–91.
Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med 2004;158:342–7.
Child societal (environmental)-level interventions [10 studies (15 papers)]
Coleman KJ, Tiller CL, Sanchez J, Heath EM, Sy O, Milliken G, et al. Prevention of the epidemic increase in child risk of overweight in low-income schools: the El Paso coordinated approach to child health. Arch Pediatr Adolesc Med 2005;159:217–24.
Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics 2008;121:e794–802.
Foster GD, Linder B, Baranowski T, Cooper DM, Goldberg L, Harrell JS, et al. A school-based intervention for diabetes risk reduction. N Engl J Med 2010;363:443–53.
Frisvold DE, Lumeng JC. Expanding exposure: can increasing the daily duration of head start reduce childhood obesity? J Hum Resour 2011;46:373–402.
Heath EM, Coleman KJ. Adoption and Institutionalization of the Child and Adolescent Trial for Cardiovascular Health (CATCH) in El Paso, Texas. Health Promot Pract 2003;4:157–64.
Hollar D, Lombardo M, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS, et al. Effective multi-level, multi-sector, school-based obesity prevention programming improves weight, blood pressure, and academic performance, especially among low-income, minority children. J Health Care Poor Underserved 2010;21(Suppl.):93–108.
Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS. Effect of a two-year obesity prevention intervention on percentile changes in body mass index and academic performance in low-income elementary school children. Am J Public Health 2010;100:646–53.
Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS. Healthier options for public schoolchildren program improves weight and blood pressure in 6- to 13-year-olds. J Am Diet Assoc 2010;110:261–7.
Ibarra PJ, Alarcon RM. Malnutrition by excess among school-age children. [Mal nutricion por exceso en escolares.] Rev Chil Pediatr 2010;1:506–14.
Muckelbauer R, Libuda L, Clausen K, Reinehr T, Kersting M. A simple dietary intervention in the school setting decreased incidence of overweight in children. Obes Facts 2009;2:282–5.
Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics 2009;123:e661–7.
Muckelbauer R, Libuda L, Clausen K, Kersting M. Approaches for the prevention of overweight through modified beverage consumption in the elementary school setting: the ‘trinkfit’ study. [Ansatze der ubergewichtspravention durch verbessertes trinkverhalten im setting grundschule: Die ‘trinkfit‘-studie.] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2011;54:339–48.
Perman JA, Young TL, Stines E, Hamon J, Turner LM, Rowe MG. A community-driven obesity prevention and intervention in an elementary school. J Ky Med Assoc 2008;106:104–8.
Ramirez-Lopez E, Grijalva-Haro MI, Valencia ME, Ponce JA, Artalejo E. Effect of a School Breakfast Program on the prevalence of obesity and cardiovascular risk factors in children. [Impacto de un Programa de Desayunos Escolares en la prevalencia de obesidad y factores de riesgo cardiovascular en ninos sonorenses.] Salud Publica Mex 2005;47:126–33.
Williams CL, Strobino BA, Bollella M, Brotanek J. Cardiovascular risk reduction in preschool children: the ‘Healthy Start’ project. J Am Coll Nutr 2004;23:117–23.
Child multilevel interventions [three studies (three papers)]
Chomitz VR, McGowan RJ, Wendel JM, Williams SA, Cabral HJ, King SE, et al. Healthy Living Cambridge Kids: a community-based participatory effort to promote healthy weight and fitness. Obesity 2010;18(Suppl. 1):S45–53.
Hoelscher DM, Springer AE, Ranjit N, Perry CL, Evans AE, Stigler M, et al. Reductions in child obesity among disadvantaged school children with community involvement: the Travis County CATCH Trial. Obesity 2010;18(Suppl. 1):S36–44.
Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes (Lond) 2008;32:1060–7.
Adult individual-level interventions [33 studies (31 papers)]
Abramson JH, Hopp C, Gofin J, Gofin R, Makler A, Habib J, et al. A community program for the control of cardiovascular risk factors: a preliminary evaluation of the effectiveness of the CHAD program in Jerusalem. J Community Health 1979;5:3–21.
Abramson JH, Gofin R, Hopp C, Gofin J, Donchin M, Habib J. Evaluation of a community program for the control of cardiovascular risk factors: the CHAD program in Jerusalem. Isr J Med Sci 1981;17:201–12.
Buchholz SW, Wilbur J, Miskovich L, Gerard P. An office-based health promotion intervention for overweight and obese uninsured adults: a feasibility study. J Cardiovasc Nurs 2012;27:68–75.
Burke L, Jancey J, Howat P, Lee A, Kerr D, Shilton T, et al. Preliminary physical activity findings from a home-based Physical Activity and Nutrition Program for Seniors (PANS). J Sci Med Sport 2011;14:e79.
Burke L, Lee AH, Pasalich M, Jancey J, Kerr D, Howat P. Effects of a physical activity and nutrition program for seniors on body mass index and waist-to-hip ratio: a randomised controlled trial. Prev Med 2012;54:397–401.
Craigie AM, Macleod M, Barton KL, Treweek S, Anderson AS, on behalf of the WeighWell team. Supporting postpartum weight loss in women living in deprived communities: design implications for a randomised control trial. Eur J Clin Nutr 2011;65:952–8.
Davis Martin P, Rhode PC, Dutton GR, Redmann SM, Ryan DH, Brantley PJ. A primary care weight management intervention for low-income African-American women. Obesity 2006;14:1412–20.
Edye B, Mandryk J, Frommer M, Healey S, Ferguson D. Evaluation of a worksite programme for the modification of cardiovascular risk factors. Med J Aust 1989;150:574, 576–8, 581.
Fortmann SP, Williams PT, Hulley SB, Maccoby N, Farquhar JW. Does dietary health education reach only the privileged? The Stanford Three Community Study. Circulation 1982;66:77–82.
Gardner B, Cane J, Rumsey N, Michie S. Behaviour change among overweight and socially disadvantaged adults: a longitudinal study of the NHS Health Trainer Service. Psychol Health 2012;27:1178–93.
Gofin J, Gofin R, Abramson JH, Ban R. Ten-year evaluation of hypertension, overweight, cholesterol, and smoking control: the CHAD program in Jerusalem. Community Syndrome of Hypertension, Atherosclerosis and Diabetes. Prev Med 1986;15:304–12.
Helmert U, Shea S, Greiser E, Maschewsky Schneider U. Effects of 3.5 years of community intervention on social class gradients for cardiovascular disease risk factors in the German Cardiovascular Prevention Study. Ann Epidemiol 1993;3(Suppl.):S36–43.
Hillier FC, Batterham AM, Nixon CA, Crayton AM, Pedley CL, Summerbell CD. A community-based health promotion intervention using brief negotiation techniques and a pledge on dietary intake, physical activity levels and weight outcomes: lessons learnt from an exploratory trial. Public Health Nutr 2012;15:1446–55.
Jackson C, Coe A, Cheater FM, Wroe S. Specialist health visitor-led weight management intervention in primary care: exploratory evaluation. J Adv Nurs 2007;58:23–34.
Jackson RA, Stotland NE, Caughey AB, Gerbert B. Improving diet and exercise in pregnancy with Video Doctor counseling: a randomized trial. Patient Educ Couns 2011;83:203–9.
Jeffery RW, French SA. Preventing weight gain in adults: design, methods and one year results from the Pound of Prevention study. Int J Obes 1997;21:457–64.
Jeffery RW, French SA. Preventing weight gain in adults: the pound of prevention study. Am J Public Health 1999;89:747–51.
Johnson RA, Meadows RL. Dog-walking: motivation for adherence to a walking program. Clin Nurs Res 2010;19:387–402.
Marshall B, Floyd S, Forrest R. Clinical outcomes and patients’ perceptions of nurse-led healthy lifestyle clinics. J Prim Health Care 2011;3:48–52.
Martin PD, Dutton GR, Rhode PC, Horswell RL, Ryan DH, Brantley PJ. Weight loss maintenance following a primary care intervention for low-income minority women. Obesity 2008;16:2462–7.
Morrison DS, Boyle S, Morrison C, Allardice G, Greenlaw N, Forde L. Evaluation of the first phase of a specialist weight management programme in the UK National Health Service: prospective cohort study. Public Health Nutr 2012;15:28–38.
Neve M, Morgan PJ, Collins CE. Weight change in a commercial web-based weight loss program and its association with website use: cohort study. J Med Internet Res 2011;13:e83.
Olson CM, Strawderman MS, Reed RG. Efficacy of an intervention to prevent excessive gestational weight gain. Am J Obstet Gynecol 2004;191:530–6.
Rautio N, Jokelainen J, Oksa H, Saaristo T, Peltonen M, Niskanen L, et al. Socioeconomic position and effectiveness of lifestyle intervention in prevention of type 2 diabetes: one-year follow-up of the FIN-D2D project. Scand J Public Health 2011;39:561–70.
Schuit AJ, Wendel-Vos GCW, Verschuren WMM, Ronckers ET, Ament A, Van Assema P, et al. Effect of 5-year community intervention Hartslag Limburg on cardiovascular risk factors. Am J Prev Med 2006;30:237–42.
Sierra MC, Bonacho EC, Garcia AG, Moraga MR, Gutierrez JCS, Barrientos AC, et al. Effectiveness of a preventive intervention strategy based on structured telephone interviews in a working population with a moderate to high cardiovascular risk. Aten Primaria 2010;42:498–505.
Verheijden MW, van Dommelen P, van Empelen P, Crone MR, Werkman AM, van Kesteren NMC. Changes in self-reported energy balance behaviours and body mass index during a mass media campaign. Fam Pract 2012;29(Suppl. 1):i75–81.
Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA 2008;300:2631–7.
Weerts SE, Amoran A. Pass the fruits and vegetables! A community–university–industry partnership promotes weight loss in African American women. Health Promot Pract 2011;12:252–60.
Weinehall L, Lewis C, Nafziger AN, Jenkins PL, Erb TA, Pearson TA, et al. Different outcomes for different interventions with different focus! A cross-country comparison of community interventions in rural Swedish and US populations. Scand J Public Health 2001;29:46–58.
Whittemore R, Melkus G, Wagner J. Translating the diabetes prevention program to primary care: a pilot study. Nurs Res 2009;58:2–12.
Adult community-level interventions [60 studies (62 papers)]
Alves JG, Gale CR, Mutrie N, Correia JB, Batty GD. A 6-month exercise intervention among inactive and overweight favela-residing women in Brazil: the Caranguejo Exercise Trial. Am J Public Health 2009;99:76–80.
Auslander W, Haire-Joshu D, Houston C, Williams JH, Krebill H. The short-term impact of a health promotion program for low-income African American women. Res Soc Work Pract 2000;10:78–97.
Balcazar H, Alvarado M, Cantu F, Pedregon V, Fulwood R. A promotora de salud model for addressing cardiovascular disease risk factors in the US-Mexico border region. Prev Chronic Dis 2009;6:A02.
Baron JA, Schori A, Crow B, Carter R, Mann JI. A randomized controlled trial of low carbohydrate and low fat/high fiber diets for weight loss. Am J Public Health 1986;76:1293–6.
Befort CA, Donnelly JE, Sullivan DK, Ellerbeck EF, Perri MG. Group versus individual phone-based obesity treatment for rural women. Eat Behav 2010;11:11–17.
Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, et al. Effects of a tailored health promotion program for female blue-collar workers: Health Works for Women. Prev Med 2002;34:313–23.
Carlin CA. The Impact of Voluntary Participation in a Community Fitness Center on the Health and Well-being of African American Women over 40 Years of Age. PhD thesis. Philadelphia, PA: University of the Sciences in Philadelphia; 2009.
Chang MW, Nitzke S, Brown R. Design and outcomes of a Mothers in Motion behavioral intervention pilot study. J Nutr Educ Behav 2010;42:S11–21.
Christiansen T, Bruun JM, Madsen EL, Richelsen B. Weight loss maintenance in severely obese adults after an intensive lifestyle intervention: 2- to 4-year follow-up. Obesity 2007;15:413–20.
Clark DO, Stump TE, Damush TM. Outcomes of an exercise program for older women recruited through primary care. J Aging Health 2003;15:567–85.
Clarke KK, Freeland-Graves J, Klohe-Lehman DM, Milani TJ, Nuss HJ, Laffrey S. Promotion of physical activity in low-income mothers using pedometers. J Am Diet Assoc 2007;107:962–7.
Cousins JH, Rubovits DS, Dunn JK, Reeves RS, Ramirez AG, Foreyt JP. Family versus individually oriented intervention for weight loss in Mexican American women. Public Health Rep 1992;107:549–55.
Cullen KW, Lara Smalling A, Thompson D, Watson KB, Reed D, Konzelmann K. Creating healthful home food environments: results of a study with participants in the expanded food and nutrition education program. J Nutr Educ Behav 2009;41:380–8.
Dennison KF, Galante D, Dennison D, Golaszewski T. A one year post-program assessment of a computer-assisted instruction (CAI) weight management program for industrial employees: lessons learned. J Health Educ 1996;27:38–42.
Erfurt JC, Foote A, Heirich MA. Worksite wellness programs: incremental comparison of screening and referral alone, health education, follow-up counseling, and plant organization. Am J Health Promot 1991;5:438–48.
Faucher MA. Promotoras de salud and portion control: a community intervention aimed at weight loss in low-income Mexican-American women. J Midwifery Womens Health 2008;53:482.
Faucher MA, Mobley J. A community intervention on portion control aimed at weight loss in low-income Mexican American women. J Midwifery Womens Health 2010;55:60–4.
Fernandes R, Braun KL, Spinner JR, Sturdevant C, Ancheta SJ, Yoshimura SR, et al. Healthy Heart, Healthy Family: a NHLBI/HRSA collaborative employing community health workers to improve heart health. J Health Care Poor Underserved 2012;23:988–9.
Foreyt JP, Ramirez AG, Cousins JH. Cuidando El Corazon – a weight-reduction intervention for Mexican Americans. Am J Clin Nutr 1991;53(Suppl.):1639–41S.
Freak-Poli RL, Wolfe R, Walls H, Backholer K, Peeters A. Participant characteristics associated with greater reductions in waist circumference during a four-month, pedometer-based, workplace health program. BMC Public Health 2011;11:824.
Gill DS. Testing a Biopsychosocial Model of Health Behavior: A Community Intervention for Reducing Obesity in Mexican-American Women. Ann Arbor, Ml: ProQuest Information & Learning; 1998.
Goldfinger JZ, Arniella G, Wylie-Rosett J, Horowitz CR. Project HEAL: peer education leads to weight loss in Harlem. J Health Care Poor Underserved 2008;19:180–92.
Grandjean PW, Oden GL, Crouse SF, Brown JA, Green JS. Lipid and lipoprotein changes in women following 6 months of exercise training in a worksite fitness program. J Sports Med Phys Fitness 1996;36:54–9.
Gray CM, Anderson AS, Clarke AM, Dalziel A, Hunt K, Leishman J, et al. Addressing male obesity: an evaluation of a group-based weight management intervention for Scottish men. J Mens Health 2009;6:70–81.
Hajek P, Humphrey K, McRobbie H. Using group support to complement a task-based weight management programme in multi-ethnic localities of high deprivation. Patient Educ Couns 2010;80:135–7.
Howard-Pitney B, Winkleby MA, Albright CL, Bruce B, Fortmann SP. The Stanford Nutrition Action Program: a dietary fat intervention for low-literacy adults. Am J Public Health 1997;87:1971–6.
Hugk D, Winkelvoss E. Ambulatory weight reduction program and possible effects on lipid and purine metabolism. Z Gesamte Inn Med 1985;40:126–9.
Hwang G, Yoon C, Jung H, Kim Y. Evaluation of an incentive-based obesity management program in workplace. Int J Occup Saf Ergon 2011;17:147–54.
Janicke DM, Gray WN, Mathews AE, Simon SL, Lim CS, Dumont-Driscoll M, et al. A pilot study examining a group-based behavioral family intervention for obese children enrolled in Medicaid: differential outcomes by race. Child Health Care 2011;40:212–31.
Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist RA, Kurth CL, Johnson SL. Correlates of weight loss and its maintenance over two years of follow-up among middle-aged men. Prev Med 1984;13:155–68.
Jeffery RW, Forster JL, Snell MK. Promoting weight control at the worksite: a pilot program of self-motivation using payroll-based incentives. Prev Med 1985;14:187–94.
Jordan KC, Freeland-Graves JH, Klohe-Lehman DM, Cai G, Voruganti VS, Proffitt JM, et al. A nutrition and physical activity intervention promotes weight loss and enhances diet attitudes in low-income mothers of young children. Nutr Res 2008;28:13–20.
Kain J, Concha F, Salazar G, Leyton B, Del Pilar Rodriguez M, Ceballos X, et al. Obesity prevention in preschool and schoolchildren attending public schools from a district of Santiago, Chile: pilot project 2006. [Prevencion de obesidad en preescolares y escolares de escuelas Municipales de una Comuna de Santiago de Chile: Proyecto piloto 2006.] Arch Latinoam Nutr 2009;59:139–46.
Kain J, Leyton B, Concha F, Salazar G, Lobos L, Vio F. Effect of counselling school teachers on healthy lifestyle on the impact of a program to reduce childhood obesity. [Estrategia de prevencion de obesidad en escolares: efecto de un programa aplicado a sus profesores (2007–2008).] Rev Med Chile 2010;138:181–7.
Kisioglu AN, Aslan B, Ozturk M, Aykut M, Ilhan I. Improving control of high blood pressure among middle-aged Turkish women of low socio-economic status through public health training. Croat Med J 2004;45:477–82.
Kliche T, Schreiner-Kürten K, Wanek V, Koch U. Health promotion effectiveness: testing the German statutory health insurance agencies evaluation system in health promotion, and preliminary findings from 212 health training courses. [Gesundheitswirkungen von Pravention: Erprobung des Evaluationssystems der Krankenkassen im Individualansatz und erste Befunde aus 212 Gesundheitskursen.] Gesundheitswesen 2011;73:258–63.
Krummel D, Semmens E, MacBride AM, Fisher B. Lessons learned from the mothers’ overweight management study in 4 West Virginia WIC offices. J Nutr Educ Behav 2010;42(Suppl.):S52–8.
Lasco RA, Curry RH, Dickson VJ, Powers J, Menes S, Merritt RK. Participation rates, weight loss, and blood pressure changes among obese women in a nutrition-exercise program. Public Health Rep 1989;104:640–6.
Lloyd A, Khan R. Evaluation of Healthy Choices: a commercial weight loss programme commissioned by the NHS. Perspect Public Health 2011;131:177–83.
Lowe M, Miller-Kovach K, Phelan S. Weight-loss maintenance in overweight individuals one to five years following successful completion of a commercial weight loss program. Int J Obes Relat Metab Disord 2001;25:325–31.
Mattfeldt-Beman MK, Corrigan SA, Stevens VJ, Sugars CP, Dalcin AT, Givi MJ, et al. Participants’ evaluation of a weight-loss program. J Am Diet Assoc 1999;99:66–71.
Merrill RM, Aldana SG, Greenlaw RL, Salberg A, Englert H. Chronic disease risk reduction with a community-based lifestyle change programme. Health Educ J. 2008;67:219–30.
Neumark-Sztainer D, Kaufmann NA, Berry EM. Physical activity within a community-based weight control program: program evaluation and predictors of success. Public Health Rev 1995;23:237–51.
Nichols GJ. Testing a Culturally Consistent Behavioral Outcomes Strategy for Cardiovascular Disease Risk Reduction and Prevention in Low Income African American Women. PhD thesis. College Park, MD: University of Maryland; 1995.
Ockene IS, Tellez TL, Rosal MC, Reed GW, Mordes J, Merriam PA, et al. Outcomes of a Latino community-based intervention for the prevention of diabetes: the Lawrence Latino Diabetes Prevention Project. Am J Public Health 2012;102:336–42.
Olvera N, Bush JA, Sharma SV, Knox BB, Scherer RL, Butte NF. BOUNCE: a community-based mother-daughter healthy lifestyle intervention for low-income Latino families. Obesity 2010;18(Suppl. 1):S102–4.
Perez-Lizaur AB, Fernandez AC, Balcazar H. Cardiovascular health promotion in a Mexican population. FASEB J 2011;25:974.3.
Pescatello LS, Murphy D, Vollono J, Lynch E, Bernene J, Costanzo D. The cardiovascular health impact of an incentive worksite health promotion program. Am J Health Promot 2001;16:16–20.
Reid C, McNeil JJ, Williams F, Powles J. Cardiovascular risk reduction: a randomized trial of two health promotion strategies for lowering risk in a community with low socioeconomic status. J Cardiovasc Risk 1995;2:155–63.
Rickel KA. Response of African-American and Caucasian Women in a Rural Setting to a Lifestyle Intervention for Obesity. PhD thesis. Gainesville, FL: University of Florida; 2008.
Rohrer JE, Naessens JM, Liesinger J, Tulledge-Scheitel S, Vanhouten H. A telephonic coaching program has more impact when body mass index is over 35. Obes Res Clin Pract 2010;4:e65–72.
Stunkard AJ, Cohen RY, Felix MR. Weight loss competitions at the worksite: how they work and how well. Prev Med 1989;18:460–74.
van Wier MF, Dekkers JC, Hendriksen IJM, Smid T, van Mechelen W. Phone and e-mail counselling are effective for weight management in an overweight working population: a randomized controlled trial. BMC Public Health 2009;9:6.
Veloso IS, Santana VS. Impact of the worker food program in Brazil. [Impacto nutricional do programa de alimentacao do trabalhador no Brasil.] Rev Panam Salud Publica 2002;11:24–31.
Veloso IS, Santana VS, Oliveira NF. The Brazilian Workers’ Food Program and its impact on weight gain and overweight. Rev Saude Publica 2007;41:769–76.
Walker LO, Im EO, Vaughan MW. Communication technologies and maternal interest in health-promotion information about postpartum weight and parenting practices. J Obstet Gynecol Neonat Nurs 2012;41:201–15.
Wilbur J, McDevitt JH, Wang E, Dancy BL, Miller AM, Briller J, et al. Outcomes of a home-based walking program for African-American women. Am J Health Promot 2008;22:307–17.
Williams A, Wold J. Nurses, cholesterol, and small work sites: innovative community intervention comparisons. Fam Community Health 2000;23:59–75.
Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol 1999;67:132–8.
Zoellner J, Connell C, Powers A, Avis-Williams A, Yadrick K, Bogle M. Does a six-month pedometer intervention improve physical activity and health among vulnerable African Americans? A feasibility study. J Phys Act Health 2010;7:224–31.
Zoellner J, Connell CL, Santell R, Fungwe T, Strickland E, Avis-Williams A, et al. Fit for life steps: results of a community walking intervention in the rural Mississippi delta. Prog Community Health Partnersh 2007;1:49–60.
Zuber J, Gromus B, Potreck-Rose F, Koch U. Differentielle Indikation zur ambulanten Gruppentherapie der Adipositas – am Beispiel der ‘Interdisziplinären Therapie der Adipositas’. Psychother Psychosom Med Psychol 1992;42:110–19.
Adult societal (environmental)-level interventions [eight studies (eight studies)]
Carleton RA, Lasater TM, Assaf AR, Feldman HA, McKinlay S. The Pawtucket Heart Health Program: community changes in cardiovascular risk factors and projected disease risk. Am J Public Health 1995;85:777–85.
Jenum AK, Anderssen SA, Birkeland KI, Holme I, Graff-Iversen S, Lorentzen C, et al. Promoting physical activity in a low-income multiethnic district: effects of a community intervention study to reduce risk factors for type 2 diabetes and cardiovascular disease: a community intervention reducing inactivity. Diabetes Care 2006;29:1605–12.
Jenum AK, Lorentzen C, Graff-Iversen S, Anderssen S, Ødegaard AK, Holme I, et al. Can area-based public health strategies reduce the social gradient in health? The ‘Romsas in Motion’ study – background, main results and lessons learnt. [Kan lokalbaserte strategier bidra til a redusere sosiale helseforskjeller? MoRo-prosjektet – Bakgrunn, hovedresultater og erfaringer.] Norsk Epidemiol 2007;17:49–57.
Jenum AK, Lorentzen CA, Ommundsen Y. Targeting physical activity in a low socioeconomic status population: observations from the Norwegian ‘Romsas in Motion’ study. Br J Sports Med 2009;43:64–9.
Lemon SC, Zapka J, Li W, Estabrook B, Rosal M, Magner R, et al. Step ahead: a worksite obesity prevention trial among hospital employees. Am J Prev Med 2010;38:27–38.
Scoggins JF, Sakumoto KN, Schaefer KS, Bascom B, Robbins DJ, Whalen CL. Short-term and long-term weight management results of a large employer-sponsored wellness program. J Occup Environ Med 2011;53:1215–20.
Tudor-Smith C, Nutbeam D, Moore L, Catford J. Effects of the Heartbeat Wales programme over five years on behavioural risks for cardiovascular disease: quasi-experimental comparison of results from Wales and a matched reference area. BMJ 1998;316:818–22.
VanWormer JJ, Linde JA, Harnack LJ, Stovitz SD, Jeffery RW. Self-weighing frequency is associated with weight gain prevention over 2 years among working adults. Int J Behav Med 2012;19:351–8.
Adult societal (macro)-level interventions [two studies(two papers)]
Jones SJ, Frongillo EA. The modifying effects of food stamp program participation on the relation between food insecurity and weight change in women. J Nutr 2006;136:1091–4.
Kaushal N. Do food stamps cause obesity? Evidence from immigrant experience. J Health Econ 2007;26:968–91.
Appendix 5 Additional tables
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 3) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions (n = 1) | ||||||
| Epstein et al. 200853 | RCT 24 months’ follow-up Final sample: 67 Quality: Moderate |
Participants’ homes, USA Age: 4–7 years BMI: ≥ 75th percentile At risk of overweight or overweight/obese |
Treatment/prevention: Intervention to reduce television viewing and computer use – duration of use regulated, monetary incentives for reduced use and newsletters containing information and advice Implementation: 4 |
Gradient intervention effect compared between low-SES group and high-SES group | BMI z-score (low SES) | ↓ |
| BMI z-score (high SES) | ↔ | |||||
| Nutrition and physical activity interventions (n = 2) | ||||||
| Taveras et al. 201148 | Cluster RCT [10 clusters, two arms; five clusters (matched) per arm] 1 year of follow-up Final sample: 445 Quality: Moderate |
10 primary care paediatric centres, USA Age: 2–6 years 48% girls Obese and high risk of obesity |
Treatment: Weight-management programme (High Five for Kids) – diet and physical activity education and counselling and behavioural–cognitive therapy Implementation: 8 |
Gradient: Results analysed by household income | BMI | |
| High income | ↔ | |||||
| Low income | ↓ | |||||
| Wake et al. 200950 | RCT 12 months’ follow-up Final sample: 245 Quality: Moderate |
45 family medical practices, Australia Age: 5–10 years 61% girls Overweight or mildly obese |
Treatment: Primary care obesity management programme (LEAP2) – screening for overweight/obesity followed by GP-administered counselling (diet and physical activity) Implementation: 9 |
Gradient: Investigation of SES as a moderator of intervention effect | BMI | ↔ |
| Waist circumference | ↔ | |||||
| No. overweight/obese | ↔ | |||||
| Physical activity | ↔ | |||||
| Diet | ↔ | |||||
| SES did not modify any intervention effect | ||||||
| Observational studies (n = 4) | ||||||
| Nutrition-only interventions (n = 1) | ||||||
| Baxter et al. 2013,40 Truby et al. 201149 | Prospective cohort (uncontrolled before/after) study 12 weeks’ follow-up Final sample: 88 Quality: Moderate |
Paediatric hospital, Australia Age: 10–17 years 69% girls Obese |
Treatment: Weight reduction programme – weight reduction diet (Eat Smart study) Implementation: 6 |
Gradient: Relationship between SES and BMI change | BMI z-score | ↓ |
| Higher social advantage associated with weight loss | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 3) | ||||||
| Braet 200641 | Prospective cohort (uncontrolled before/after) study 2 years’ follow-up Final sample: 110 Quality: Weak |
1 inpatient clinic, Belgium Age: 7–17 years 66% girls Obese |
Treatment: 10-month inpatient treatment programme for childhood obesity – nutrition education with daily physical activity, and cognitive–behavioural therapy Implementation: 3 |
Gradient: Explored SES as a predictor of weight loss | SES did not predict weight loss | |
| Langnäse et al. 2004,51 Pust et al. 200452 | Prospective (controlled) cohort study 4 years’ follow-up Final sample: 16 Quality: Weak |
Homes, Germany Age: 6.5 years Percentage male/female not reported Overweight/obese |
Treatment: Home-based counselling including diet and physical activity education Implementation: 5 |
Gradient: Outcomes of low SES vs. high SES | BMI SDS | ↔ |
| Fat mass | ↓ | |||||
| Fat-free mass | ↑ | |||||
| Waist-to-hip ratio | ↔ | |||||
| Physical activity | ↔ | |||||
| Television viewing | ↔ | |||||
| Fruit and vegetable intake | ↔ | |||||
| Low-fat milk intake | ↑ | |||||
| Snacks | ↔ | |||||
| Intervention was less effective in those of low SES than in those of high SES | ||||||
| Sabin et al. 200746 | Prospective cohort (uncontrolled before-and-after) study ≥ 1 year of follow-up Final sample: 62 Quality: Weak |
Hospital outpatient clinic, UK Age: 2–18 years 54% girls Obese |
Treatment: Hospital multidisciplinary obesity service – consultations with paediatrician, dietitian and health and exercise specialist and weekly exercise sessions Implementation: 5 |
Gradient: Investigation of any relationship between SES and intervention outcomes | BMI z-score | ↓ |
| SES had no effect on intervention outcomes | ||||||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 1) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 1) | ||||||
| Black et al. 201054 | RCT 24 months’ follow-up Final sample: 179 Quality: Moderate |
Homes and community sites, USA Age: 11–16 years 49% girls |
Prevention: Mentor-based health promotion and obesity prevention programme (Challenge!) – session with mentors including food preparation, exercise, goal-setting, progress discussions and provision of information and recipes; rap music video promoting healthy eating and physical activity Implementation: 7 |
Disadvantage: Low-income communities | No. overweight/obese | ↓ |
| BMI z-score | ↔ | |||||
| Normal weight | ||||||
| % body fat | ↔ | |||||
| Fat mass | ↔ | |||||
| Fat-free mass | ↔ | |||||
| Obese/overweight | ||||||
| % body fat | ↓ | |||||
| Fat mass | ↓ | |||||
| Fat-free mass | ↑ | |||||
| Physical activity | ↔ | |||||
| Energy intake | ↔ | |||||
| Fat intake | ↔ | |||||
| Saturated fat intake | ↔ | |||||
| Calcium intake | ↔ | |||||
| Fruit intake | ↔ | |||||
| Vegetable intake | ↔ | |||||
| Snack/dessert intake | ↓ | |||||
| Milk intake | ↔ | |||||
| Non-diet soda intake | ↔ | |||||
| Fried food intake | ↔ | |||||
| Observational studies (n = 3) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 3) | ||||||
| Fernandez De Velasco Galan et al. 200842 | Prospective cohort (uncontrolled before-and-after) study 2 years’ follow-up Final sample: 69 Quality: Moderate |
Health centre, Spain Age: 2–13 years Percentage male/female not reported Overweight and obese |
Treatment: Education programme promoting correct eating habits and physical activity in overweight and obese children Implementation: 5 |
Disadvantage: Population from areas of medium to low and low SES; areas in need of social transformation | BMI | ↔ |
| No. obese | ↓ | |||||
| Marshall et al. 201143 | Prospective cohort (uncontrolled before-and-after) study ≥ 3 months’ follow-up Final sample: 162 Quality: Weak |
17 health-care practices, New Zealand Age: 0–18 years |
Treatment: Nurse-led healthy lifestyle clinic – including diabetes, diet/nutrition and cardiovascular clinic. Holistic approach to health needs defined by patient Implementation: 4 |
Disadvantage: Children living in high-deprivation areas | BMI | ↔ |
| Smith et al. 201047 | Prospective cohort (uncontrolled before-and-after) study 12 weeks’ follow-up Final sample: 23 Quality: Moderate |
Physicians’ offices, USA Age: 10–14 years Obese |
Treatment: Obesity treatment programme – physical activity sessions, nutrition consultations, food demonstrations and behavioural skills training Implementation: 6 |
Disadvantage: Area where substantial number of minority and low-income families reside; 95% of participants covered by Medicaid | BMI | ↓ |
| Physical activity | ↑ | |||||
| Total cholesterol | ↓ | |||||
| LDL cholesterol | ↔ | |||||
| HDL cholesterol | ↔ | |||||
| Glucose/insulin ratio | ↔ | |||||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 3) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions (n = 1) | |||
| Epstein et al. 200853 | A: Motivation | Reduction of obesity-related sedentary behaviours in children at risk of obesity | 4 |
| C: Context | Social – researcher led | ||
| I: Resources | Television allowance devices, monthly newsletters, financial incentives (up to US$2 per week for intervention group; US$2 per week for control group) | ||
| J: Differential effects | SES | ||
| Nutrition and physical activity interventions (n = 2) | |||
| Taveras et al. 201148 | A: Motivation | Reduction of BMI in obese and risk of obese children | 8 |
| B: Theory | Chronic care model | ||
| C: Context | Social – health care led | ||
| D: Experience | Programme implemented by nurse practitioners, physicians and medical assistants | ||
| F: Delivery fidelity | 56% of participants completed two of six intervention activities | ||
| G: Sustainability | Intervention components were designed to be sustainable in a real-world primary care setting. Existing staff were trained to deliver the intervention | ||
| I: Resources | Negotiated that insurance companies pay for up to four visits in the first year. Participants received payments at each data collection time point | ||
| J: Differential effects | Gender and household income | ||
| Wake et al. 200950 | A: Motivation | Reduce BMI gain in overweight or mildly obese children | 9 |
| B: Theory | Designed using an intervention mapping technique within a behavioural epidemiology framework | ||
| C: Context | Social – researcher and health care led | ||
| D: Experience | Research team: Paediatrician, academics, researchers, head of nutrition and food services and GPs | ||
| F: Delivery fidelity | GPs completed simulated patient consultations, which were observed and marked. Further training given to those with low scores. In total, 37% attended all four intervention sessions, 22% attended three, 21% attended two, 12% attended one and 9% attended none | ||
| G: Sustainability | Integrated into existing primary care services but not effective and therefore not sustainable | ||
| H: Stakeholder support | Appears well supported by GPs who participated | ||
| I: Resources | Cost to health sector for BMI surveillance, GP recruitment and training was A$152,000. Cost for consultations was A$1317 per intervention child and A$81 per control child | ||
| J: Differential effects | No differential effects by SES or session attendance | ||
| Observational studies (n = 4) | |||
| Nutrition-only interventions (n = 1) | |||
| Baxter et al. 201340 (Truby et al. 201149) | A: Motivation | Treatment of obesity in children | 6 |
| C: Context | Social – researcher led | ||
| D: Experience | Delivered by paediatric dietitians with training in behaviour modification | ||
| F: Delivery fidelity | Standardised manual used | ||
| I: Resources | Eight dietary sessions and six telephone calls | ||
| J: Differential effects | SES and weight status | ||
| Physical activity only interventions – none | |||
| Nutrition and physical activity interventions (n = 4) | |||
| Braet 200641 | A: Motivation | Treatment of obesity in children previously unsuccessful in an outpatient programme | 3 |
| C: Context: | Social – researcher led | ||
| J: Differential effects | Age and baseline weight | ||
| Langnäse et al. 2004,51 Pust et al. 200452 | A: Motivation | Treatment of overweight and obesity | 5 |
| C: Context | Social – researcher led | ||
| D: Experience | Study team included nutritional scientists | ||
| I: Resources | Five 45- to 90-minute sessions during 5–10 weeks | ||
| J: Differential effects | SES | ||
| Sabin et al. 200746 | A: Motivation | Stabilising weight in younger children (< 7 years) and reducing weight in older children | 5 |
| C: Context | Social – health care led | ||
| D: Experience | Paediatrician, paediatric dietitian and exercise specialist | ||
| I: Resources | Three monthly appointments: Paediatrician consultation (30 minutes first session, 25 minutes each follow-up session), dietitian (15–30 minutes) and exercise specialist. Free weekly 2-hour exercise session | ||
| J: Differential effects | Age and gender (none by SES) | ||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 1) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 1) | |||
| Black et al. 201054 | A: Motivation | Health promotion and prevention of obesity | 7 |
| C: Context | Social – researcher led | ||
| B: Theory | Social cognitive theory | ||
| D: Experience | Mentors were trained college students | ||
| E: Consultation | Intervention developed with the assistance of an advisory board of black adolescents | ||
| I: Resources | 12 sessions with mentor; 40 hours of mentor training and weekly supervision | ||
| J: Differential effects | Weight status | ||
| Observational studies (n = 3) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 3) | |||
| Fernandez De Velasco Galanet al. 200842 | A: Motivation | Promotion of correct eating and physical activity in overweight and obese children | 5 |
| C: Context | Social – researcher led | ||
| D: Experience | Intervention delivered by paediatricians | ||
| I: Resources | Initial 15-minute consultation and follow-up after 1 month with paediatrician (follow-up consultations thereafter for 2 years every time child visited health centre, even if reason not related to weight) | ||
| J: Differential effect | Gender explored but no differential effect | ||
| Marshall et al. 201143 | A: Motivation | Improve general health in deprived populations | 4 |
| C: Context | Social – health service led | ||
| D: Experience | Registered nurses | ||
| G: Sustainability | Integrated into existing service – clinics grew locally from work happening within the general practice | ||
| Smith et al. 201047 | A: Motivation | Reduction of BMI in obese preadolescents for the prevention of type 2 diabetes | 6 |
| B: Theory | Social cognitive theory and self-efficacy theory | ||
| C: Context | Social – researcher led | ||
| D: Experience | Intervention delivered by a registered dietitian and credentialed exercise specialist | ||
| F: Delivery fidelity | Periodic assessment of adherence to protocol by implementers | ||
| I: Resources | Two 45-minute physical activity sessions per week for 12 weeks, four 45-minute nutrition consultations and two 60-minute food demonstration sessions | ||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 7) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions (n = 2) | ||||||
| Robinson 199976 | Cluster randomised trial (two clusters, two arms; one cluster per arm) 6 months’ follow-up Final sample: 192 Quality: Strong |
Two schools, USA Age: 8–9 years 45% girls |
Prevention: Education course to reduce television and video game use including a 10-day television turn off; home television usage monitor; parental education materials Implementation: 5 |
Gradient: No differences in results by parental education | BMI | ↓ |
| Triceps skinfold thickness | ↓ | |||||
| Waist circumference | ↓ | |||||
| Waist-to-hip ratio | ↓ | |||||
| Hip circumference | ↔ | |||||
| Television/video games | ↓ | |||||
| Sedentary behaviour | ↔ | |||||
| Physical activity | ↔ | |||||
| Cardiovascular activity | ↔ | |||||
| Television meals | ↓ | |||||
| Television snacks | ↔ | |||||
| High-fat food | ↔ | |||||
| Simon et al. 200886 | Cluster randomised trial (eight clusters, two arms; four clusters per arm) 48 months’ follow-up Final sample: 732 Quality: Strong |
Eight schools, eastern France Age: 11–12 years 50% girls |
Prevention: Physical activity education and increase in number of physical activity classes, ‘cycling to school’ days and sports events Implementation: 8 |
Gradient: No differences in results by parental occupation | BMI | ↓ |
| Overweight | ↓ | |||||
| % body fat | ↔ | |||||
| Fat mass index | ↓ | |||||
| Fat-free mass index | ↔ | |||||
| Physical activity | ↑ | |||||
| Television/video use | ↓ | |||||
| Active commuting | ↔ | |||||
| Nutrition and physical activity interventions (n = 5) | ||||||
| Bingham et al. 200257 | Cluster RCT (12 clusters, two arms; number per arm not clearly stated) 1 year of follow-up Final sample: 985 Quality: Strong |
12 schools, USA Age: 8–10 years 51% girls |
Prevention: Cardiovascular disease risk factor reduction intervention – education (including nutrition and physical activity) and physical activity sessions Implementation: 5 |
Gradient: Investigated relationship between SES and outcomes | Skinfold thickness | ↓ |
| Cardiovascular fitness | ↔ | |||||
| SES was not found to be a moderator of the intervention effect on obesity or fitness outcomes | ||||||
| Kalavainen et al. 200798 | RCT 12 months’ follow-up Final sample: 69 Quality: Strong |
Health-care centre, Finland Age: 7–9 years 60% girls Obese |
Treatment: Family-based group treatment programme – diet and physical activity education and behavioural therapy Implementation: 7 |
Gradient: Association between social class and outcomes explored | Weight loss for height | ↓ |
| BMI | ↔ | |||||
| BMI SDS | ↓ | |||||
| No association between social class and change of weight for height, BMI or BMI z-score | ||||||
| Plachta-Danielzik et al. 2007,75 201174 | Quasi-RCT 8 years’ follow-up Final sample: 1192 Quality: Weak |
? schools, Germany Age: 6.3 years 50% girls |
Prevention: Intervention included healthy eating and physical activity education Implementation: 4 |
Gradient: Results reported by low, middle and high SES | 4-year follow-up | |
| Body weight | ↔ | |||||
| Body fat | ↔ | |||||
| BMI | ↔ | |||||
| BMI SDS | ↑ | |||||
| 8-year follow-up: | ||||||
| BMI SDS | ↔ | |||||
| 4-year incidence of overweight (high SES only) | ↓ | |||||
| 8-year BMI SDS (high SES only) | ↓ | |||||
| Rush et al. 201277 | Cluster RCT (124 clusters, two arms; 62 per arm) 2 years’ follow-up Final sample: 1352 Quality: Weak |
124 schools, New Zealand Age: 5 or 10 years 51% girls |
Prevention: School-based exercise sessions, nutrition education and healthy eating initiatives; parent education sessions; and community events Implementation: 7 |
Gradient: Explored school SES as a confounder of intervention effects | 5- to 7-year-olds | |
| BMI SDS | ↔ | |||||
| % body fat SDS | ↓ | |||||
| 10–12 year olds | ||||||
| BMI SDS | ↔ | |||||
| % body fat SDS | ↔ | |||||
| Favourable (but non-significant) intervention effects on body fat in higher- SES schools in 5- to 7-year-olds | ||||||
| Wrotniak et al. 2004102 | Three RCT (results combined) 24 months’ follow-up Final sample: 142 Quality: Moderate |
University-based weight control programme, USA Age: 8–12 years 59% girls Overweight and obese |
Treatment: Family-based weight-management control programmes – diet and physical activity education, physical activity sessions and goal-setting Implementation: 3 |
Gradient: Investigation of SES as a predictor of intervention effect | No relationship between SES and child BMI z-score change | |
| Observational studies (n = 9) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 9) | ||||||
| Grønbæk et al. 200988 | Prospective cohort (uncontrolled before-and-after) study 6 months’ follow-up Final sample: 81 Quality: Moderate |
Community centre, Denmark Age: 10–12 years Obese |
Treatment: Obesity treatment programme – nutrition education, physical activity sessions, psychological sessions and monitoring of behaviours and weight Implementation: 5 |
Gradient: Investigated SES predictors of BMI change | BMI z-score | ↓ |
| No significant relationships between indicators of SES and BMI change | ||||||
| Heinberg et al. 201096 | Prospective cohort (uncontrolled before-and-after) study 12 weeks’ follow-up Final sample: 104 Quality: Moderate |
Hospital outpatient clinic, USA Age: 7–18 years Overweight |
Treatment: Paediatric obesity treatment programme (Healthy Kids, Healthy Weight) – improving diet, increasing physical activity and increasing behaviour change skills Implementation: 6 |
Gradient: Investigated whether or not there were any SES differences between those who were successful and those who were unsuccessful | BMI | ↓ |
| No differences in SES between those who lost weight and those who did not | ||||||
| Jelalian et al. 2008104 | Prospective cohort (uncontrolled before-and-after) study 4 months’ follow-up Final sample: 62 Quality: Weak |
Setting not reported, USA Age: 13–18 years Overweight and obese |
Treatment: Cognitive–behavioural weight control programme combined with either peer-based adventure therapy or aerobic exercise Implementation: 5 |
Gradient: Investigated relationship between SES and outcomes | SES was not associated with change in BMI or ≥ 5% weight loss | |
| Jouret et al. 200964 | Cluster controlled cohort study 2 years’ follow-up Final sample: 1663 Quality: Moderate |
119 kindergartens, France Age: 3–4 years 51% girls |
Prevention: Basic strategy (information provision) vs. reinforced strategy (information and education programme) Implementation: 5 |
Gradient: Kindergartens in underprivileged area vs. kindergartens not in underprivileged area | Underprivileged | |
| BMI z-score (basic) | ↓ | |||||
| BMI z-score (reinforced) | ↓ | |||||
| Non-underprivileged | ||||||
| BMI z-score (basic) | ↔ | |||||
| BMI z-score (reinforced) | ↓ | |||||
| Kalarchian et al. 200997 | Prospective cohort (uncontrolled before-and-after) study – using data relevant to this review 6 months’ follow-up Final sample: 87 Quality: Weak |
University medical centre, USA Age: 8–12 years Obese |
Treatment: Family-based intervention – calorie-restricted diet; behavioural therapy for increasing physical activity, reducing sedentary behaviours and reducing unhealthy eating habits Implementation: 5 |
Gradient: Investigated relationship between SES and intervention outcomes | Per cent overweight | ↓ |
| Higher income associated with larger reductions in per cent overweight | ||||||
| Mockus 2011105 | Prospective cohort (uncontrolled before-and-after) study 20 weeks’ follow-up Final sample: 150 Quality: Weak |
Setting not reported, USA Age: 7–12 years Overweight and obese |
Treatment: Family-based weight loss programme – Traffic Light Diet, individualised physical activity plans and behaviour modification training Implementation: 5 |
Gradient: Investigated relationship between SES and intervention outcomes | Per cent overweight | ↓ |
| No relationship between SES and change in per cent overweight | ||||||
| Pott et al. 2009,44 201045 | Prospective cohort (uncontrolled before-and-after) study 12 months’ follow-up Final sample: 116 Quality: Moderate |
Paediatric practices, Germany Age: 7.5–15.5 years Obese |
Treatment: Family-based weight reduction programme (Fit Kids) – behavioural therapy and diet and physical activity education Implementation: 4 |
Gradient: Investigated whether or not there were any SES differences between those who were successful and those who were unsuccessful | BMI z-score | ↓ |
| No SES differences between those who lost weight and those who did not | ||||||
| Reinehr et al. 2003100 | Prospective cohort (uncontrolled before-and-after) study 1 year of follow-up Final sample: 55 Quality: Moderate |
Outpatient health clinic, Germany Age: 7–15 years Mixed Obese |
Treatment: Outpatient obesity management programme (Obeldicks) – behaviour therapy, nutrition education, exercise therapy, psychological therapy and parent courses Implementation: 5 |
Gradient: Compared SES indicators of those who were successful and those who were unsuccessful | BMI z-score | ↓ |
| No differences in SES indicators between those who were successful and those who were unsuccessful, except those who were more unsuccessful lived in single-parent families | ||||||
| Woolford et al. 2011101 | Retrospective cohort 24 weeks’ follow-up Final sample: 48 Quality: Moderate |
University, USA Age: 12–18 years Obese |
Treatment: Multidisciplinary weight-management programme (MPOWER) – nutrition and physical activity education, behavioural therapy (motivational interviewing) and exercise sessions Implementation: 6 |
Gradient: Investigated relationship between insurance status and outcomes | BMI | ↓ |
| % body fat | ↓ | |||||
| No association between insurance and outcomes | ||||||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 23) | ||||||
| Nutrition-only interventions (n = 2) | ||||||
| Hoffman et al. 201162 | Cluster RCT (four clusters, two arms; two clusters per arm) 3.5 years’ follow-up Final sample: 166 Quality: Weak |
Four schools, USA Age: 6.2 years 49% girls |
Prevention: Educational intervention to promote fruit and vegetable consumption Implementation: 6 |
Disadvantage: Low-SES school (91% of pupils received free or reduced-price lunch) | BMI z-score | ↔ |
| Fruit and vegetable intake | ↑ | |||||
| Sichieri et al. 200979 | Cluster RCT (47 clusters, two arms; 23 clusters in intervention arm, 24 in control arm) 8 months’ follow-up Final sample: 927 Quality: Strong |
22 schools (47 classes), Brazil Age: 10–11 years 53% girls |
Prevention: Educational intervention to reduce consumption of sugar-sweetened beverages and encourage water consumption Implementation: 4 |
Disadvantage: Children from low-SES families | BMI | ↔ |
| Carbonated beverages | ↓ | |||||
| Fruit juices | ↔ | |||||
| Physical activity-only interventions (n = 10) | ||||||
| Alves et al. 200887 | RCT 6 months’ follow-up Final sample: 68 Quality: Strong |
Community, Brazil Age: 5–10 years 49% girls Overweight |
Treatment: Physical activity sessions three times per week Implementation: 4 |
Disadvantage: Children from a disadvantaged area | BMI | ↓ |
| Lindgren et al. 201168 | Cluster RCT (wait list control) (eight clusters, two arms; four clusters per arm) 6 months’ follow-up Final sample: 62 Quality: Moderate |
Eight schools, Sweden Age: 13–19 years 100% girls |
Prevention: Empowerment-based exercise programme with some education Implementation: 6 |
Disadvantage: Recruitment from schools representative of low-SES areas | BMI | ↔ |
| Cardiovascular fitness | ↔ | |||||
| Lubans et al. 201169 | Cluster RCT (wait list control) (four clusters, two arms; two clusters per arm) 6 months’ follow-up Final sample: 82 Quality: Moderate |
Four schools, Australia Age: 14.3 years 100% boys |
Prevention: Physical Activity Leaders programme: sports sessions, interactive seminars, lunchtime activities (peer-student led), handbooks, leadership sessions, monitoring and Physical Activity Leader accreditation Implementation: 4 |
Disadvantage: Low-SES schools | BMI | ↓ |
| BMI z-score | ↓ | |||||
| Prevalence of overweight | ↓ | |||||
| Prevalence of obesity | ↓ | |||||
| Body fat | ↔ | |||||
| Waist circumference | ↔ | |||||
| Physical activity | ↔ | |||||
| Muscular fitness | ↔ | |||||
| Sugar-containing drinks | ↓ | |||||
| Fruit intake | ↔ | |||||
| Vegetable intake | ↔ | |||||
| Water intake | ↔ | |||||
| Myers 200871 | Cluster non-RCT (two clusters, two arms; one cluster per arm) 15 weeks’ follow-up Final sample: 103 Quality: Moderate |
Two schools, USA Age: 13–14 years 45% girls |
Prevention: Virtual skills and fitness trainer Implementation: 6 |
Disadvantage: Schools located in lower-SES areas | BMI | ↔ |
| Cardiovascular fitness | ↔ | |||||
| Robinson et al. 200390 | RCT (pilot) 12 weeks’ follow-up Final sample: 60 Quality: Strong |
Community centres and homes, USA Age: 8–10 years 100% girls At risk of obesity |
Treatment: Dance classes and television viewing reduction intervention (GEMS) targeting African American girls at risk of obesity Implementation: 8 |
Disadvantage: Recruited from low-income neighbourhoods | BMI | ↔ |
| Waist circumference | ↔ | |||||
| MVPA | ↔ | |||||
| Television/video game use | ↔ | |||||
| Household television use | ↓ | |||||
| Energy intake | ↔ | |||||
| % fat intake | ↔ | |||||
| Robinson et al. 2010106 | RCT 2 years’ follow-up Final sample: 225 Quality: Weak |
Community centres and homes, USA Age: 8–10 years 100% girls At risk of obesity |
Treatment: Dance classes and television viewing reduction intervention (GEMS) targeting African American girls at risk of obesity Implementation: 8 |
Disadvantage: Recruited from low-income neighbourhoods | BMI z-score | ↔ |
| Waist circumference | ↔ | |||||
| Triceps skinfold thickness | ↔ | |||||
| Physical activity | ↔ | |||||
| Energy intake | ↔ | |||||
| % energy from fat | ↔ | |||||
| BP | ↔ | |||||
| Total cholesterol | ↓ | |||||
| HDL cholesterol | ↔ | |||||
| LDL cholesterol | ↓ | |||||
| Triglycerides | ↔ | |||||
| Glucose | ↔ | |||||
| Insulin | ↔ | |||||
| Salmon et al. 200878 | Group RCT (17 clusters, two arms; number per arm not reported) 12 months’ follow-up Final sample: 268 Quality: Moderate |
Three schools (17 classes), Australia Age: 10–11 years 51% girls |
Prevention: Physical activity education, self-monitoring, contract setting and practical skills training Implementation: 5 |
Disadvantage: Schools located in low-SES areas | BMI | ↓ |
| Physical activity | ↑ | |||||
| Television viewing | ↑ | |||||
| Electronic game use | ↔ | |||||
| Stephens and Wentz 199880 | Cluster RCT (two clusters, two arms; one cluster per arm) 15 weeks’ follow-up Final sample: 89 Quality: Weak |
Two schools, USA Age: 8–10 years 50% girls |
Prevention: Supplemental fitness programme in addition to usual physical education lessons Implementation: 2 |
Disadvantage: Schools attended predominantly by children from black and low-income families | Weight | ↓ |
| Skinfold thickness | ↓ | |||||
| Cardiovascular fitness | ? | |||||
| Flexibility | ↑ | |||||
| Systolic BP | ↔ | |||||
| Diastolic BP | ↔ | |||||
| Weintraub et al. 200884 | RCT 6 months’ follow-up Final sample: 21 Quality: Moderate |
After-school club, USA Age: 9.9 years % male/female not reported Overweight |
Treatment: After-school team sports (football) programme Implementation: 5 |
Disadvantage: Racial/ethnic minority children from low-income families | BMI | ↔ |
| BMI z-score | ↓ | |||||
| Total physical activity | ↔ | |||||
| Moderate physical activity | ↔ | |||||
| Vigorous physical activity | ↔ | |||||
| Screen time | ↔ | |||||
| Winter and Sass 201195 | Cluster RCT (four clusters, two arms; two clusters per arm) 24 weeks’ follow-up Final sample: 405 Quality: Weak |
Four Head Start centres, USA Age: 3–5 years 48% girls |
Prevention: Home- and school-based multilevel obesity prevention and school readiness programme (Healthy & Ready to Learn) Implementation: 4 |
Disadvantage: Low-income, predominantly Latino population | BMI | ↔ |
| Physical activity | ↔ | |||||
| Gross motor skills | ↑ | |||||
| Nutrition and physical activity interventions (n = 11) | ||||||
| Bellows 200794 | Cluster RCT (eight clusters, two arms; number per arm not reported) 18 weeks’ follow-up Final sample: 201 Quality: Strong |
Eight Head Start centres, USA Age: 3–5 years 46% girls |
Prevention: Food Friends Get Movin’ with Mighty Moves (TM) intervention – physical activity sessions and nutrition education Implementation: 7 |
Disadvantage: Low-income, ethnic minority preschoolers | BMI z-score | ↔ |
| Physical activity | ↔ | |||||
| Cardiovascular fitness | ↑ | |||||
| Flexibility | ↑ | |||||
| Gross motor skills | ↑ | |||||
| de Heer 200958 | Nested RCT (one intervention class and one control class per school) 4 months’ follow-up Final sample: 931 Quality: Weak |
Seven schools (14 classes) (after-school) USA Age: 8–11 years 48% girls |
Prevention: After-school health and exercise programme – an exercise component based on the CATCH physical activity programme and a health education component Implementation: 4 |
Disadvantage: Participants were predominantly from a socioeconomically disadvantaged Hispanic population | BMI | ↓ |
| Aerobic fitness | ↔ | |||||
| Sedentary behaviour | ↓ | |||||
| Diet | ↔ | |||||
| Figueroa-Colon et al. 199659 | Cluster RCT (two clusters, two arms; one cluster per arm) 6 months’ follow-up Final sample: 15 Quality: Weak |
Two schools, USA Age: 8–13 years 42% girls Super obese |
Treatment: Weight loss intervention – high-protein, low-calorie diet (10 weeks) followed by a hypocaloric diet; exercise sessions; and behaviour modification Implementation: 3 |
Disadvantage: Schools serving low- to middle-SES families | % ideal body weight | ↓ |
| BMI | ↓ | |||||
| Systolic BP | ↔ | |||||
| Diastolic BP | ↔ | |||||
| Total cholesterol | ↔ | |||||
| HDL cholesterol | ↓ | |||||
| LDL cholesterol | ↔ | |||||
| Triglycerides | ↔ | |||||
| Hamad et al. 201189 | RCT 1 year of follow-up Final sample: 454 Quality: Strong |
Microcredit institution, Peru Age: < 5 years |
Prevention: Microcredit loan with the addition of health education sessions vs. microcredit loan only (active control) Implementation: 7 |
Disadvantage: Children of families receiving microcredit | BMI | ↔ |
| % overweight | ↔ | |||||
| Janicke et al. 2011103 | RCT 9 months’ follow-up Final sample: 33 Quality: Moderate |
Setting unclear, USA Age: 6–12 years 47% girls Overweight or obese |
Treatment: Family-based weight-management programme – diet, physical activity and behaviour management education; diet and physical activity monitoring; group support and problem-solving Implementation: 6 |
Disadvantage: Participants enrolled in the Medicaid programme | BMI z-score | ↔ |
| Jansen et al. 201163 | Cluster RCT (20 clusters, two arms; 10 clusters per arm) 8 months’ follow-up Final sample: 2416 Quality: Strong |
20 schools, the Netherlands Age: 6–12 years 51% girls |
Prevention: Nutrition, active living and healthy lifestyle education, three physical education lessons per week and voluntary additional after-school sport and play activities Implementation: 7 |
Disadvantage: Low-income, inner-city, multiethnic schools | Younger children | |
| BMI | ↔ | |||||
| Waist circumference | ↓ | |||||
| % overweight | ↓ | |||||
| Cardiovascular fitness | ↑ | |||||
| Older children | ||||||
| BMI | ↔ | |||||
| Waist circumference | ↔ | |||||
| % overweight | ↔ | |||||
| Cardiovascular fitness | ↔ | |||||
| Kain et al. 200467 | Non-randomised cluster controlled trial (five clusters, two arms: three clusters in intervention arm, two in control arm) 6 months’ follow-up Final sample: 3086 Quality: Strong |
Five schools, Chile Age: 10.6 years 47% girls |
Prevention: Nutrition education (children and parents), extra time in physical education lessons, encouragement of physical activity during daily recess, healthy snacks in vending machines (voluntary), incentives for healthy eating and sports equipment for schools Implementation: 7 |
Disadvantage: Low-SES schools (35% of children received the School Lunch Program) | Boys’ BMI z-score | ↓ |
| Boys’ triceps skinfold thickness | ↓ | |||||
| Boys’ waist circumference | ↓ | |||||
| Girls’ BMI z-score | ↔ | |||||
| Girls’ triceps skinfold thickness | ↔ | |||||
| Girls’ waist circumference | ↔ | |||||
| Cardiovascular fitness | ↑ | |||||
| Flexibility | ↑ | |||||
| Nemet et al. 201173 | Cluster RCT (30 clusters, two arms; 15 clusters per arm) 1 school year of follow-up Final sample: 725 Quality: Weak |
30 kindergartens, Israel Age: 5.2 years 45% girls |
Prevention: Nutrition lectures, games and story reading, nutrition and physical activity songs, nutritional information for parents, exercise training and Healthy Day Festivals Implementation: 9 |
Disadvantage: Kindergartens for low-SES communities | BMI | ↔ |
| BMI percentile | ↔ | |||||
| No. overweight | ↓ | |||||
| No. obese | ↔ | |||||
| Cardiovascular fitness | ↑ | |||||
| Story et al. 200381 | Randomised controlled pilot study 12 weeks’ follow-up Final sample: 53 Quality: Moderate |
After-school, three schools, USA Age: 8–10 years 100% girls |
Prevention: After-school obesity prevention programme for African American girls (Minnesota GEMS) Implementation: 7 |
Disadvantage: African American girls from low-income families | BMI | ↔ |
| Waist circumference | ↔ | |||||
| Physical activity | ↔ | |||||
| Dietary intake | ↔ | |||||
| Walter et al. 198583 | Cluster RCT (22 clusters, two arms; 14 clusters in intervention arm, eight in control arm) 1 year of follow-up Final sample: 1115 Quality: Strong |
22 schools, USA Age: 9 years 49% girls |
Prevention: Know Your Body curriculum focusing on nutrition, physical fitness and smoking prevention Implementation: 6 |
Disadvantage: Children from low-income families | Ponderosity index | ↔ |
| Triceps skinfold thickness | ↔ | |||||
| Cardiovascular fitness | ↔ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Total cholesterol | ↓ | |||||
| HDL cholesterol | ↔ | |||||
| Willet 199693 | Non-RCT 1 year of follow-up Final sample: 40 Quality: Strong |
Community, USA Age: 7–12 years 100% girls |
Prevention: Mother and daughter culturally specific obesity prevention programme (based on the Know Your Body health education curriculum) Implementation: 3 |
Disadvantage: Low-SES African American girls | BMI | ↔ |
| % overweight | ↔ | |||||
| % fat intake | ↔ | |||||
| % saturated fat intake | ↔ | |||||
| Cholesterol intake | ↔ | |||||
| BP | ↔ | |||||
| Observational studies (n = 13) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions (n = 2) | ||||||
| Hawthorne et al. 201161 | Prospective cohort (uncontrolled before-and-after) study 16 weeks’ follow-up (post intervention) Final sample: 1074 (83%) Quality: Weak |
10 schools, USA Age: 5–12 years 51% girls |
Prevention: Structured lunchtime walking programme Implementation: 8 |
Disadvantage: Conducted in low-SES schools | BMI percentile | ↔ |
| Waist circumference | ↔ | |||||
| Cardiovascular fitness | ↑ | |||||
| Rudolf et al. 2004,92 200691 | Prospective cohort (uncontrolled before-and-after) study (pilot phase) 6 months’ follow-up Final sample: 48 Quality: Weak |
Sports and community centres, UK Age: 8–16 years 52% girls Obese |
Treatment: Community-based obesity treatment programme (WATCH IT) – individual counselling and support for increasing physical activity; group activity sessions; and group parenting sessions Implementation: 8 |
Disadvantage: Deprived neighbourhoods | BMI SDS | ↓ |
| Nutrition and physical activity interventions (n = 11) | ||||||
| Annesi 201055 | Prospective cohort (uncontrolled before-and-after) study 12 weeks’ follow-up Final sample: 200 Quality: Weak |
After-school care, USA Age: 7–12 years 51% girls |
Prevention: Youth Fit for Life programme – physical activity sessions; self-management and self-regulation skills; small amount of nutrition and general health education Implementation: 6 |
Disadvantage: African American children of lower-middle and lower SES | BMI | ↓ |
| Physical activity | ↑ | |||||
| Annesi et al. 200756 | Prospective cohort (uncontrolled before-and-after) study 12 weeks’ follow-up Final sample: 241 Quality: Weak |
10 YMCA after-school care sites and one school, USA Age: 10.1 years 53% girls |
Prevention: Youth Fit for Life programme (after-school programme vs. physical education class) – physical activity sessions; self-management and self-regulation skills; small amount of nutrition and general health education Implementation: 6 |
Disadvantage: African American children of lower-middle and lower SES | BMI | ↓ |
| Body composition | ↓ | |||||
| Strength | ↑ | |||||
| Flexibility | ↑ | |||||
| Endurance | ↑ | |||||
| Physical activity | ↑ | |||||
| Fletcher et al. 200960 | Pilot prospective cohort (uncontrolled before-and-after) study 10 months’ follow-up Final sample: 12 Quality: Weak |
Setting unclear, USA Age: 13–17 years 92% girls Overweight and obese |
Treatment: Two weight reduction interventions – Kids for Healthy Eating and Exercising (KHEE) club. Early intervention for overweight adolescents; intensive intervention for obese adolescents Implementation: 2 |
Disadvantage: Adolescents from families eligible for Medicaid | BMI | ↓ |
| Waist circumference | ↓ | |||||
| Triceps skinfolds | ↓ | |||||
| Kain et al. 200965 | Prospective pilot cohort (uncontrolled before-and-after) study 5 months’ follow-up Final sample: 522 Quality: Moderate |
Seven schools, Chile Age: 4–10 years % male/female not reported |
Prevention: National validated nutrition education programme, physical activity education, teachers trained to improve physical education lessons and sports equipment provided Implementation: 4 |
Disadvantage: Schools in areas of medium to low SES in which 35% of children were classed as vulnerable (received free school meals) | BMI z-score | ↔ |
| Waist circumference | ↔ | |||||
| No. overweight | ↔ | |||||
| No. obese | ↔ | |||||
| Fitness (pre-kindergarten to year 2) | ↑ | |||||
| Fitness (year 3 to year 4) | ↓ | |||||
| Kain et al. 201066 | Prospective cohort (uncontrolled before-and-after) study 2 years’ follow-up Final sample: 741 Quality: Moderate |
Seven schools, Chile Age: 4–9 years % male/female not reported |
Prevention: National validated nutrition education programme, physical activity education, teachers trained to improve physical education lessons and sports equipment provided Implementation: 5 |
Disadvantage: Schools in areas of medium to low SES in which 35% of children were classed as vulnerable (received free school meals) | BMI z-score | ↓ |
| No. obese | ↓ | |||||
| Moore et al. 200970 | Prospective cohort (uncontrolled before-and-after) study 3 months’ follow-up Final sample: 126 Quality: Weak |
Two schools, USA Age: 9–11 years 63% girls |
Prevention: Color My Pyramid intervention – nutrition education with small amount of physical activity education Implementation: 5 |
Disadvantage: Half of school pupils in the school breakfast programme – indicator of low SES | BMI percentile | ↔ |
| Physical activity | ↑ | |||||
| Diet behaviour | ↑ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↔ | |||||
| Nemer et al. 200972 | Prospective cohort (uncontrolled before-and-after) study 3 years’ follow-up Final sample: 500 Quality: Weak |
Schools, Denmark and Germany Age: 10–14 years |
Prevention: Cooking courses, physical activity classes and food shopping trips Implementation: 7 |
Disadvantage: Schools in socially underprivileged districts | BMI | ↓ |
| Ranstrom 200999 | Prospective cohort (uncontrolled before-and-after) study 10–15 weeks’ follow-up Final sample: 20 Quality: Weak |
Paediatric clinic, USA Age: 7–17 years Overweight and obese |
Treatment: Family-based weight loss programme (Taking Steps Together) – nutrition and physical activity education, exercise classes, behaviour modification techniques and telephone check-ins Implementation: 5 |
Disadvantage: Low-income families | BMI percentage | ↔ |
| Physical activity | ↑ | |||||
| Computer/television use | ↔ | |||||
| Fruit intake | ↔ | |||||
| Vegetable intake | ↔ | |||||
| Milk type | ↓ | |||||
| Sugared drink intake | ↓ | |||||
| Water intake | ↔ | |||||
| Topp et al. 200982 | Prospective cohort (uncontrolled before-and-after) study 14 weeks’ follow-up (post intervention) Final sample: 79 Quality: Moderate |
School, USA Age: 5–10 years 51% girls |
Prevention: Physical activity sessions with nutrition education Implementation: 6 |
Disadvantage: Children from low-income families | BMI percentile | ↔ |
| % body fat | ↔ | |||||
| Fat weight | ↔ | |||||
| Lean weight | ↑ | |||||
| Waist-to-hip ratio | ↔ | |||||
| Cardiovascular fitness | ↑ | |||||
| Bread and grain intake | ↔ | |||||
| Green vegetable intake | ↑ | |||||
| Yellow vegetable intake | ↔ | |||||
| Fruit intake | ↔ | |||||
| Fruit juice intake | ↓ | |||||
| Milk intake | ↔ | |||||
| Added sugar intake | ↔ | |||||
| Sweetened beverages | ↔ | |||||
| Fat intake | ↔ | |||||
| Williams and Warrington 201185 | Prospective cohort study (non-completers used as comparison group) 12 weeks’ follow-up Final sample: 231 Quality: Weak |
Six schools, USA Age: 8–11 years 58% girls |
Prevention: Pedometer-based walking programme with nutrition education (Get Fit Kids) Implementation: 3 |
Disadvantage: Low-SES schools (80% of pupils received free/reduced-price meals) | BMI | ↔ |
| BMI percentile | ↔ | |||||
| Physical activity | ↑ | |||||
| Woolford et al. 2011101 | Retrospective cohort study 24 weeks’ follow-up Final sample: 48 Quality: Moderate |
University, USA Age: 12–18 years Obese |
Treatment: Multidisciplinary weight-management programme (MPOWER) – nutrition and physical activity education, behavioural therapy (motivational interviewing) and exercise sessions Implementation: 6 |
Disadvantage: Majority of participants from low-income families | BMI | ↓ |
| % body fat | ↓ | |||||
| No association between insurance and outcomes | ||||||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 7) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions (n = 2) | |||
| Robinson 199976 | A: Motivation | Prevent the onset of obesity | 5 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social – researcher led | ||
| F: Delivery fidelity | Not all pupils conformed to the switch off (67%) or kept within the weekly viewing target (55%); content and delivery of lessons not independently checked | ||
| J: Differential effects | Intervention group more likely to have parents with a college education than the control group (45% vs. 21%; p < 0.01) | ||
| Simon et al. 200886 | A: Motivation | Increase physical activity by changing attitudes, promoting the social support of parents and teachers and making the environment more supportive of physical activities | 8 |
| B: Theory | Theory led | ||
| C: Context | Researcher led | ||
| F: Delivery fidelity | > 90% of pupils attended the educational classes; mean participation time in optional physical exercise activities of at least 30 minutes per week increased from 25% in year 1 to 65% in year 4 | ||
| G: Sustainability | Involvement of community leaders expected to enhance it | ||
| H: Stakeholder support | Community leaders, club organisers, community agencies | ||
| I: Resources | Co-ordination of partners and supervision of activities main costs | ||
| J: Differential effects | Age, parental occupation, gender | ||
| Nutrition and physical activity interventions (n = 5) | |||
| Bingham 200257 | A: Motivation | Cardiovascular disease risk factor reduction | 5 |
| D: Experience | Delivered by teachers using American Heart Association school-site kits | ||
| G: Sustainability | The intervention was easily implemented using existing physical education programmes and lesson plans by teachers not trained as physical education specialists | ||
| I: Resources | Three 20-minute physical activity sessions per week and two education sessions per week for 8 weeks | ||
| J: Differential effects | Rural vs. urban and ethnicity | ||
| Kalavainen et al. 200798 | A: Motivation | Treatment of obesity | 7 |
| B: Theory | Behavioural- and solution-oriented therapy | ||
| C: Context | Social – researcher led | ||
| D: Experience | Delivered by experienced dietitians, schools nurses and advanced nutrition students | ||
| H: Stakeholder support | Sessions were well attended by parents and positive parent evaluations of the sessions were received | ||
| I: Resources | 15 sessions (90 minutes) for both parent and child | ||
| J: Differential effects | Gender and baseline weight | ||
| Plachta-Danielzik et al. 2007,75 201174 | A: Motivation | Reduce prevalence of childhood obesity | 4 |
| C: Context | Social | ||
| D: Experience | Medics and dietitian developed the intervention | ||
| G: Sustainability | Intervention was unsustainable as intervention schools were allocated as control schools 1 year later | ||
| Rush et al. 201277 | A: Motivation | Improve child health | 7 |
| C: Context | Social – led by district health board | ||
| D: Experience | Teachers or graduates in the fields of exercise and nutrition or physical exercise | ||
| E: Consultation | Consultation with schools to develop individualised action plans | ||
| F: Delivery fidelity | Shorter duration of intervention in lower-SES schools | ||
| I: Resources | 11 Team Energize staff responsible for six to eight schools each; calculated cost < NZ$40 per child per year | ||
| J: Differential effects | Ethnicity, age and SES | ||
| Wrotniak et al. 2004102 | A: Motivation | Reduction of obesity outcomes in overweight and obese children | 3 |
| C: Context | Social – researcher led | ||
| I: Resources | 16 weekly meetings followed by two biweekly (two of the trials) and two monthly meetings; meetings included 15–30 minutes with the therapist and a 30-minute group session; parents paid a deposit that was returned after minimal session attendance and the 6- and 12-month follow-ups; families were paid at the final follow-up data collection time point | ||
| Observational studies (n = 9) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 9) | |||
| Grønbæk et al. 200988 | A: Motivation | Reduction of BMI in obese children | 5 |
| B: Theory | Social learning theory | ||
| D: Experience | Trained sports coaches, certified clinical nutritionist and authorised psychologist | ||
| I: Resources | 118 hours in total for all sessions | ||
| J: Differential effects | Ethnicity | ||
| Heinberg et al. 201096 | A: Motivation | Reduction of weight/BMI in overweight children | 6 |
| C: Context | Social – health-care service led | ||
| D: Experience | Dietitian, exercise physiologist and behaviouralist | ||
| G: Sustainability | Developed by and integrated within a health-care setting | ||
| I: Resources | Weekly 2-hour sessions for 12 weeks | ||
| J: Differential effects | Gender, age and ethnicity | ||
| Jelalian et al. 2008104 | A: Motivation | Weight reduction in overweight and obese adolescents | 5 |
| C: Context | Social – researcher led | ||
| D: Experience | Programme delivered by doctoral-level psychologists with experience in adolescent weight management and an exercise physiologist or physical therapist | ||
| I: Resources | Five 30-minute cognitive–behavioural therapy sessions per week plus weekly peer-based adventure therapy or traditional exercise sessions for 16 weeks | ||
| J: Differential effects | Gender, ethnicity | ||
| Jouret et al. 200964 | A: Motivation | Prevention of overweight in preschool children | 5 |
| C: Context | Social – health-care and academic collaboration | ||
| D: Experience | Study physician and family physicians, dietitian and teachers | ||
| I: Resources | Study physician and family physicians, dietitian and teachers; training sessions for teachers; flyers and letters to parents; posters; five 20-minute classroom sessions per year; audio cassettes and story books; and information packs for parents | ||
| J: Differential effects | School area | ||
| Kalarchian et al. 200997 | A: Motivation | Treatment of severe obesity | 5 |
| C: Context | Social – researcher led | ||
| F: Delivery fidelity | Session attendance was recorded (50% attendance) | ||
| I: Resources | 20 × 60-minute group meetings | ||
| J: Differential effects | Family income, attendance, baseline per cent overweight and change in parental BMI | ||
| Mockus 2011105 | A: Motivation | Predict weight loss success in overweight children | 5 |
| C: Context | Social – researcher led | ||
| D: Experience | Programme delivered by graduate students in psychology and doctoral researchers | ||
| I: Resources | Weekly sessions: child-only group session followed by 20-minute family session | ||
| J: Differential effects | Baseline per cent overweight | ||
| Pott et al. 200944 | A: Motivation | Reduction of BMI in obese children | 4 |
| C: Context | Social – health service led | ||
| I: Resources | Biweekly behavioural therapy and dietary training sessions and weekly exercise sessions for 3 months; weekly exercise sessions and monthly parent meetings for 9 months | ||
| J: Differential effects | Age | ||
| Reinehr et al. 2003100 | A: Motivation | Reduce BMI in obese children | 5 |
| C: Context | Social – health-care service led | ||
| D: Experience | Programme team included paediatricians, dietitians, psychologists and exercise physiologists | ||
| I: Resources | Intensive phase = six parental, six behaviour therapy, six nutrition and three to six exercise therapy sessions; establishing phase = individual psychological therapy and three to six exercise therapy sessions; and accompanying phase = three to six exercise therapy sessions and individual care when required | ||
| J: Differential effects | Age, sex, BMI, SES, single-parent family | ||
| Woolford et al. 2011101 | A: Motivation | Treatment of obesity in adolescents | 6 |
| C: Context | Social – researcher led | ||
| D: Experience | Developed and implemented at the University of Michigan, Ann Arbor, MI, USA; delivered by a paediatrician, psychologist, dietitian, social worker and exercise physiologist | ||
| G: Sustainability | Programme was housed at an academic centre that had the advantage of personnel and infrastructure to maintain the programme; however, unlikely to be located in area that all patients can access easily and patients may have to travel long distances, adding a burden for families most at need | ||
| I: Resources | Group and individual biweekly sessions and weekly exercise session for 24 weeks | ||
| J: Differential effects | Explored but not found for age, sex, race or insurance | ||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 23) | |||
| Nutrition-only interventions (n = 2) | |||
| Hoffman et al. 201162 | B: Theory | Social learning theory | 6 |
| D: Experience | Intervention was implemented by school staff | ||
| E: Consultation | Meetings held with teachers | ||
| F: Delivery fidelity | Unannounced observations; staff completed logs and student interviews; fidelity data indicated that intervention components designed to be implemented daily were implemented on the majority of school days; the classroom DVD was implemented as intended in years 1 and 2 but rarely in year 3 | ||
| H: Stakeholder support | Teachers and principals supported the intervention | ||
| I: Resources | Daily loudspeaker announcements, instructional DVD, activity books and stickers. Programme implemented entirely by school staff | ||
| Sichieri et al. 200979 | A: Motivation | Prevention of excess weight gain | 4 |
| D: Experience | Classroom sessions were delivered by trained research assistants | ||
| I: Resources | 10 classroom sessions (1 hour), promotional banners, water bottles, fliers and magnets for parents | ||
| J: Differential effects | Gender and baseline weight status | ||
| Physical activity-only interventions (n = 10) | |||
| Alves et al. 200887 | A: Motivation | Increase physical activity in overweight children to reduce BMI | 4 |
| D: Experience | Implemented by physical education students supervised by a professor of education | ||
| F: Delivery fidelity | Some intervention participants did not attend all of the sessions | ||
| I: Resources | Three weekly 50-minute sessions for 6 months | ||
| Lindgren et al. 201168 | A: Motivation | Increase physical activity in low-SES non-active adolescent girls | 6 |
| B: Theory | Health promotion using a bottom-up approach and the concept of empowerment | ||
| C: Context | Social – led by the Sport Federation | ||
| D: Experience | Intervention implemented by the Sport Federation; trained exercise leaders and sports coaches delivered the intervention | ||
| E: Consultation | Participatory planning approach was used at the programme design stage and participants’ interests and concerns were central to the process | ||
| I: Resources | Two co-ordinators, four exercise leaders (two also co-ordinators) and sports coaches; two 1-hour sessions offered for 26 weeks | ||
| Lubans et al. 201169 | A: Motivation | Obesity prevention in low-SES low-active adolescent boys | 4 |
| B: Theory | Social cognitive theory | ||
| G: Sustainability | Students were trained to deliver parts of the intervention to reduce the burden on teachers and improve sustainability; the intervention was provided at no cost to the school or students | ||
| I: Resources | Intervention delivered by teachers and trained students; 10 × 90-minute enhanced sport sessions, three 30-minute interactive sessions, eight 30-minute lunchtime physical activity sessions, six 30-minute physical activity leadership sessions; equipment = handbooks and pedometers | ||
| Myers 200871 | A: Motivation | Increase moderate- to vigorous-intensity physical activity and physical fitness and prevent obesity | 6 |
| C: Context | Managerial – intervention assignment determined by school division | ||
| D: Experience | Intervention supervised by teachers who received training pre intervention | ||
| F: Delivery fidelity | Virtual trainer used for only 32% of the time | ||
| G: Sustainability | Intervention is potentially sustainable as incorporated into existing physical education lessons | ||
| I: Resources | Computerised video unit and projector required; teacher training | ||
| Robinson et al. 200390 | A: Motivation | Prevent obesity in low-SES African American girls | 8 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social – researcher led | ||
| D: Experience | Trained college students/recent college graduates from dance troupes/organisations; intervention specialist (television reduction) | ||
| E: Consultation | Community members were extensively involved in designing the study | ||
| F: Delivery fidelity | Participation data reported | ||
| I: Resources | Dance classes 5 days per week for 3 months; each session included 45–60 minutes of dance plus 30 minutes of theory/talks, healthy snack and homework time; five lessons of television reduction intervention; payment for completing data collection: US$25 at baseline, US$75 at follow-up | ||
| J: Differential effects | Baseline BMI (trend towards greater intervention effect) | ||
| Robinson et al. 2010106 | A: Motivation | Prevent obesity in low-SES African American girls | 8 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social – researcher led | ||
| D: Experience | Trained college students/recent college graduates from dance troupes/organisations; intervention specialist (television reduction) | ||
| E: Consultation | Community members were extensively involved in designing the study | ||
| F: Delivery fidelity | Lower than projected intervention dose for dance classes because of venue change and transport difficulties | ||
| I: Resources | Dance classes 5 days per week, 12 months per year (excluding school holidays); each session included 1 hour of homework and 45–60 minutes of dance; dance performance and awards every 8 weeks; a total of 24 lessons of a television reduction intervention over 2 years | ||
| J: Differential effects | Marital status of parent/guardian | ||
| Salmon et al. 200878 | A: Motivation | Prevent excess weight gain, reduce time spent on screen behaviours and promote participation and enjoyment of physical activity | 6 |
| B: Theory | Social cognitive theory and behavioural choice theory | ||
| D: Experience | Intervention delivered by qualified physical education teachers | ||
| F: Delivery fidelity | 88% attendance at behavioural modification group and fundamental skills group lessons; 57–62% completion of homework; 92% completion of classroom tasks; 70% participation rate in intervention contracts | ||
| I: Resources | 19 (40- to 50-minute) lessons for both behavioural modifications and fundamental skills conditions; intervention specialist teacher (physical education teacher) | ||
| J: Differential effects | Gender | ||
| Stephens and Wentz 199880 | D: Experience | Delivered by trained medical students | 2 |
| I: Resources | 2-day orientation session for students; three 35-minute sessions per week for 15 weeks; no additional equipment or financial commitment was required | ||
| Weintraub et al. 200884 | A: Motivation | BMI reduction in overweight, low-income, minority children | 5 |
| D: Experience | Intervention delivered by trained undergraduate and medical students | ||
| E: Consultation | Intervention implemented in collaboration with school district personnel; feasibility study and clinics with community-informed development | ||
| H: Stakeholder support | Child and parent support for programme was high; an additional session was added in month 5 at the request of children and parents | ||
| I: Resources | 135-minute session three to four times per week; shin pads, uniforms, water bottles, certificates and medals | ||
| Winter and Sass 201195 | A: Motivation | Prevention of obesity in low-income, minority children | 4 |
| B: Theory | Social cognitive theory | ||
| E: Consultation | Promotores (trained Latino neighbourhood leaders) assisted in training and provided an important cultural interface between parents and researchers | ||
| F: Delivery fidelity | Multiple strategies used to enhance and assess treatment fidelity, including intervention manual, intermittent integrity checks by researchers (monitoring visits and interviews) and an evaluation questionnaire for teachers and parents to identify successes or barriers to implementation | ||
| Nutrition and physical activity interventions (n = 11) | |||
| Bellows 200794 | A: Motivation | Prevent obesity | 7 |
| B: Theory | Social learning theory and social marketing framework | ||
| D: Experience | Intervention delivered by teachers | ||
| E: Consultation | Formative research (focus groups and interviews) with parents and teachers | ||
| G: Sustainability | Classroom teachers were used to facilitate programme activities, allowing for future sustainability of the programme and the potential for increased expansion | ||
| I: Resources | Four 15- to 20-minute physical activity sessions per week for 18 weeks; one 15- to 20-minute nutritional education session per week for 12 weeks; materials = teacher activity binder, musical CD, rubber mats, flashcards, puppets, basic physical education equipment (bean bags, balls, etc.), parent materials, story books, games and placemats | ||
| J: Differential effects | Age and weight status | ||
| de Heer 200958 | A: Motivation | Increase physical activity and prevent obesity | 4 |
| C: Context | Social – researcher led | ||
| D: Experience | Exercise component delivered by student teachers; health education component taught by community health workers | ||
| I: Resources | Teachers were paid a small stipend | ||
| Figueroa-Colon et al. 199659 | A: Motivation | Weight reduction in super-obese children | 3 |
| D: Experience | Implemented by a paediatrician, psychologist and nutritionist in collaboration with a physical education instructor and school nurse | ||
| H: Stakeholder support | Efforts of committed staff, school officials, peers and family involvement was essential for the success of the intervention | ||
| Hamad et al. 201189 | A: Motivation | Improve the general health of disadvantaged children | 7 |
| C: Context | Political – response to the WHO Integrated Management of Childhood Illness strategy | ||
| D: Experience | Delivered by microcredit loan officers who received a small amount of training | ||
| F: Delivery fidelity | Results from additional evaluation suggests that some loan officers demonstrated more knowledge and a greater ability to engage with clients than others | ||
| G: Sustainability | Intervention implemented within an existing service; however, loan officers expressed frustration at being requested to educate clients on topics with which they were not very familiar and without financial compensation for the extra time spent | ||
| F: Stakeholder support | Loan officers expressed frustration | ||
| I: Resources | Monthly 30-minute session for 8 months | ||
| Janicke et al. 2011103 | A: Motivation | Reduction of obesity, especially in low-SES populations | 6 |
| C: Context | Social – researcher led | ||
| D: Experience | Intervention delivered by master’s-level graduate students and postdoctoral fellow in clinical psychology; all received 8 hours of training and had previous experience in behavioural approaches to weight management | ||
| F: Delivery fidelity | Lead researcher reviewed audio tapes of group treatment sessions to assist with supervision of interventionists and help ensure treatment fidelity | ||
| I: Resources | 12 weekly 90-minute sessions; 8 hours of interventionist training | ||
| J: Differential effects | Change in parental BMI and ethnicity | ||
| Jansen et al. 201163 | A: Motivation | Weight reduction and prevention of obesity in low-SES children | 7 |
| B: Theory | Theory of planned behaviour and ecological model | ||
| C: Context | Social – researcher led | ||
| D: Experience | Delivery by professional physical education teacher, regular classroom teacher and local sports clubs | ||
| G: Sustainability | All but one school continued the intervention after the study period; the intervention was implemented in another 60 schools in Rotterdam and the classroom curriculum was implemented in approximately 700 schools in the Netherlands | ||
| I: Resources | Three physical education sessions per week, two after-school physical activity sessions and three classroom lessons plus an introduction lesson; staff: professional physical education teacher, regular classroom teacher and local sports club class | ||
| J: Differential effects | Age | ||
| Kain et al. 200467 | A: Motivation | Reduction and prevention of obesity in low-SES children | 7 |
| C: Context | Social – researcher led in response to government’s Health Promotion Program | ||
| D: Experience | Trained nutritionists and physical education teachers implemented the intervention | ||
| F: Delivery fidelity | Degree of implementation of the nutrition education programme varied by school (school B 100%; school C 85%; school A 80%); provision of extra physical activity and active recess was successfully implemented; implementation varied by school: the lower the enrolment rate, the better the degree of adherence; additional physical education classes were well liked by children and 80% of teachers thought that they should be a permanent part of the school curricula | ||
| G: Sustainability | The provision of extra physical activity time was incorporated into the schools’ curricula | ||
| H: Stakeholder support | Teacher support varied by school; parental involvement was difficult to achieve | ||
| I: Resources | Extra 90 minutes of physical education per week; two meetings with parents; and basic sports equipment provided (duration and number of classroom nutrition education sessions not reported) | ||
| J: Differential effects | Gender; weight status at baseline | ||
| Nemet et al. 201173 | A: Motivation | Prevention of obesity | 9 |
| C: Context | Social – led by a multidisciplinary team | ||
| D: Experience | Intervention was developed by health professionals (paediatricians, dietitians and an exercise physiologist) along with youth exercise coaches and preschool staff | ||
| E: Consultation | Preschool staff were involved in the intervention development | ||
| F: Delivery fidelity | Adherence to the programme was followed on a weekly basis by the study co-ordinator and by the professional youth coach | ||
| G: Sustainability | The programme was incorporated into the existing preschool core curriculum and delivered mainly by preschool staff; therefore, the programme did not require the major investment of time or financial expenses | ||
| H: Stakeholder support | The programme was supported by the schools | ||
| I: Resources | Six 45-minute physical activity sessions per week (one session per week delivered by professional youth coach); remainder of the physical activity sessions and nutritional education delivered by preschool teachers | ||
| J: Differential effects | Effects by gender and weight status explored but no differences found | ||
| Story et al. 200381 | A: Motivation | Prevention of obesity in African American girls | 7 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social – researcher led | ||
| D: Experience | Delivered by trained African American GEMS staff | ||
| E: Consultation | Extensive formative research with girls, parents, community leaders and youth workers helped develop the intervention | ||
| F: Delivery fidelity | Intervention staff completed checklists after every session (attendance, completion of activity, level of participation); each session was observed by project staff; family event attendance was recorded; parents completed evaluation forms | ||
| H: Stakeholder support | Parent satisfaction was high and all would recommend to other parents | ||
| Walter et al. 198583 | A: Motivation | Prevention of chronic disease risk factors (including obesity) | 6 |
| C: Context | Social – researcher led | ||
| D: Experience | Intervention delivered by teachers trained by researchers | ||
| F: Delivery fidelity | Adherence to teaching protocols was ascertained through a system of teacher monitoring, which included documentation of attendance at training workshops and number of lessons taught and classroom visits by research staff | ||
| H: Stakeholder support | The intervention programme was feasible and acceptable to school personnel, students and parents | ||
| I: Resources | 2 hours of teaching per week by regular teacher; teachers trained in three half-day workshops; monthly meetings between teachers and trainers; and equipment including teacher guides, student workbooks and worksheets, health passports, videotapes, posters and calendars | ||
| Willet 199693 | A: Motivation | Prevention of obesity in low-income African American girls | 3 |
| D: Experience | Delivered by advanced doctoral students in clinical psychology and registered dietitians | ||
| I: Resources | 1-hour sessions per week for 12 weeks; US$5 gift certificate per mother/daughter pair each week; US$35 per mother/daughter pair for each data collection event | ||
| Observational studies (n = 13) | |||
| Nutrition only interventions – none | |||
| Physical activity only interventions (n = 2) | |||
| Hawthorne et al. 201161 | A: Motivation | Increase opportunities for physical activity during the school day | 7 |
| C: Context | Social and political – programme implemented by a non-profit health community department in response to the Child Nutrition and Women, Infants and Children Reauthorization Act; helped school meet legislative requirement | ||
| F: Delivery fidelity | Cheating was reported in some schools | ||
| G: Sustainability | Sustainability is dictated by school administration and requires commitment from community partners | ||
| H: Stakeholder support | There was a lack of parental volunteers; school nurse encouragement provided momentum for the programme | ||
| I: Resources | Staff/volunteers to supervise walking; 0.25-mile walking trail; incentive and mileage card; sessions on 3 days a week for 16 weeks | ||
| J: Differential effects | Differential effects were explored but none found | ||
| Rudolf et al. 2004,92 200691 | A: Motivation | Treatment of obesity in disadvantaged children | 8 |
| B: Theory | Underpinned by motivational and solution-focused approaches | ||
| C: Context | Social – community driven | ||
| D: Experience | Delivered by health trainers and sports coaches trained, supported and supervised by a team leader, dietitian, psychologist and paediatrician | ||
| F: Delivery fidelity | Implementers received training and ongoing support and supervision | ||
| G: Sustainability | Good will, untold time and energy needed to ensure programme was incorporated into management structures across agencies (NHS and leisure services) | ||
| I: Resources | Weekly individual sessions, weekly exercise sessions and parent sessions; four part-time health trainers employed; clinic space, sports facilities and coaches supplied at no cost | ||
| J: Differential effects | Age and gender | ||
| Nutrition and physical activity interventions (n = 11) | |||
| Annesi 201055 | A: Motivation | Prevention of obesity in normal weight and treatment in overweight/obese | 6 |
| B: Theory | Self-efficacy theory | ||
| D: Experience | Implementers were trained YMCA staff | ||
| F: Delivery fidelity | Quality assurance was completed every 2 weeks by outside evaluators to ensure treatment fidelity | ||
| I: Resources | Three 45-minute sessions per week for 12 weeks; workbooks provided; displays and posters | ||
| J: Differential effects | Baseline weight and physical activity status | ||
| Annesi et al. 200756 | A: Motivation | Increase physical activity in preadolescent African Americans to reduce and prevent overweight/obesity | 6 |
| B: Theory | Social cognitive theory and self-efficacy theory | ||
| D: Experience | Delivered by trained instructors, either after-school counsellors formally untrained in exercise methods or physical education specialists | ||
| F: Delivery fidelity | YMCA wellness instructors performed quality control audits | ||
| I: Resources | Two or three 45-minute sessions per week; instructors trained for 4–5 hours | ||
| J: Differential effects | Gender | ||
| Fletcher et al. 200960 | A: Motivation | Treatment of overweight and obesity in underserved adolescents | 2 |
| I: Resources | Kids for Healthy Eating and Exercising (KHEE) club meetings once a week (overweight participants); KHEE club activities every day (obese); chaperoned field trips for all participants and parents | ||
| Kain et al. 200965 | A: Motivation | Prevention of obesity | 4 |
| D: Experience | Nutrition education programme developed by the Instituto de Nutrición y Tecnologia de Alimentos (Institute of Nutrition and Food Technology); intervention delivered by trained teachers; research team included biochemist, master in public health, nutritionist, physician and statistician | ||
| F: Delivery fidelity | Nutrition education programme only partially implemented (training later than intended): 60% implementation for preschoolers, 50% for years 1–4 | ||
| J: Differential effects | Age | ||
| Kain et al. 201066 | A: Motivation | Prevention of obesity | 5 |
| D: Experience | Nutrition education programme developed by the Instituto de Nutrición y Tecnologia de Alimentos (Institute of Nutrition and Food Technology); intervention delivered by trained teachers; research team included biochemist, master in public health, professor of education, nutritionist, physician and statistician | ||
| F: Delivery fidelity | Some activities were supervised by project nutritionist | ||
| G: Sustainability | Intervention was incorporated into the existing curriculum; limited time for teacher training; low teacher motivation | ||
| J: Differential effects | Gender | ||
| Moore et al. 200970 | A: Motivation | Prevention of obesity | 5 |
| B: Theory | Self-care deficit nursing theory | ||
| E: Consultation | Focus groups with children and teachers informed development of a small part of the intervention: the educational computer game | ||
| H: Stakeholder support | The short course for teachers appeared to increase teacher ‘buy-in’ to the project | ||
| I: Resources | Teacher and school administer training delivered by researchers; six classes taught by researchers | ||
| Nemer et al. 200972 | A: Motivation | Ensure adequate physical activity in children | 7 |
| C: Context | Social – led by health professional, Ministry of Health, Ministry of Education, Municipality Health Office, teachers and community sports associations | ||
| D: Experience | Nutritionists, sports therapists and psychologists developed each training module | ||
| E: Consultation | Teachers part of the project team | ||
| G: Sustainability | Integrated into the regular school day and elements will be implemented in the school curriculum on a permanent basis; the programme has been expanded to other schools | ||
| H: Stakeholder support | Project supported by a number of stakeholders and partners | ||
| I: Resources | > US$100,000; paid staff: 10 for planning, 45 for implementation and 14 for evaluation | ||
| Topp et al. 200982 | A: Motivation | Prevention of obesity | 6 |
| B: Theory | Transtheoretical model of behaviour change | ||
| D: Experience | Intervention delivered by local track coaches, research staff, health department employees, local high-school students, nurses, nursing students and a registered dietitian; research staff administering the intervention had limited experience at the beginning of the intervention in conducting physical activity interventions with children, particularly in underserved areas | ||
| F: Delivery fidelity | Parents were not as involved with the intervention as was envisaged | ||
| H: Stakeholder support | Support was provided by a health department, school, university, fruit company and community group; lower support from parents than envisaged | ||
| I: Resources | Three 90-minute after-school sessions for 14 weeks; local track coaches, research staff, health department employees, high-school students, nurses, nursing students and a registered dietitian; equipment included water bottles, t-shirts and notepads | ||
| Williams and Warrington 201185 | A: Motivation | Increase physical activity and prevent obesity | 3 |
| C: Context | Social – researcher led | ||
| D: Experience | Programme overseen by a board-certified family medicine physician and managed by a master’s-qualified registered nurse | ||
| Woolford et al. 2011101 | A: Motivation | Treatment of obesity in adolescents | 6 |
| C: Context | Social – researcher led | ||
| D: Experience | Developed and implemented at the University of Michigan, Ann Arbor, MI, USA. Delivered by a paediatrician, psychologist, dietitian, social worker and exercise physiologist | ||
| G: Sustainability | Programme was housed at an academic centre that had the advantage of personnel and infrastructure to maintain the programme; however, unlikely to be located where all patients can access easily and patients may have to travel long distances, adding burden for families most at need | ||
| I: Resources | Group and individual biweekly sessions and weekly exercise session for 24 weeks | ||
| J: Differential effects | Explored but not found for age, sex, race or insurance | ||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 7) | ||||||
| Nutrition-only interventions (n = 7) | ||||||
| Coleman et al. 2005,107 Heath and Coleman 2003116 | Non-randomised cluster trial (eight clusters, two arms; four clusters per arm) 24 months’ follow-up Final sample: 744 (intention to treat) Quality: Moderate |
Eight schools, USA Age: 8 years 47% girls |
Prevention: Reduction in fat content of school food plus nutrition education and physical activity Implementation: 9 |
Disadvantage: Conducted in low-income areas | Overweight and obese | ↓ |
| Obese | ↔ | |||||
| Weight | ↔ | |||||
| Waist-to-hip ratio | ↔ | |||||
| BMI | ↔ | |||||
| Fitness | ↔ | |||||
| Foster et al. 2008109 | Randomised cluster trial (10 clusters, two arms; number per arm not reported) 24 months’ follow-up Final sample: 844 Quality: Moderate |
10 schools, USA Age: 11 years 54% girls |
Prevention: Nutrition education, social marketing, parent outreach and nutritional standards for school food Implementation: 6 |
Disadvantage: Schools had > 50% subsidised or free school meals | Overweight | ↓ |
| Obesity | ↔ | |||||
| BMI | ↔ | |||||
| Sedentary activity | ↓ | |||||
| Physical activity | ↔ | |||||
| Energy consumed | ↔ | |||||
| Fat consumption | ↔ | |||||
| Fruit and vegetables | ↔ | |||||
| Foster et al. 2010108 | Randomised cluster trial (42 clusters, two arms; 21 clusters per arm) 30 months’ follow-up Final sample: 4603 Quality: Moderate |
42 schools, USA Age: 11 years 53% girls |
Prevention: Nutritional standards for school food plus education, social marketing and physical activity Implementation: 5 |
Disadvantage: Pupils entitled to subsidised or free school meals | Overweight and obese | ↔ |
| Obese | ↔ | |||||
| Waist-to-hip ratio | ↓ | |||||
| BMI | ↓ | |||||
| Glucose | ↔ | |||||
| Insulin | ↓ | |||||
| Hollar et al. 2010110,111,115 | Non-randomised cluster trial (five clusters, two arms; four clusters in intervention arm, one in control arm) 18 months’ follow-up Final sample: 1197 Quality: Weak |
Five schools, USA Age: 8 years 51% girls |
Prevention: Nutrition content of school-provided meals and snacks plus healthy lifestyle education, increased physical activity and school fruit and vegetable garden Implementation: 4 |
Disadvantage: Pupils entitled to subsidised or free school meals | Overweight | ↔ |
| Obesity | ↔ | |||||
| BMI | ↓ | |||||
| Weight | ↓ | |||||
| Muckelbauer et al. 2009,118,119 2011117 | Randomised cluster trial (32 clusters, two arms; 17 clusters in intervention arm, 15 in control arm) 10 months’ follow-up Final sample: 2950 Quality: Moderate |
32 schools, Germany Age: 8 years 50% girls |
Prevention: School water fountains alongside lessons on the importance of water consumption, provision of water bottles, target setting for consumption Implementation: 7 |
Disadvantage: Conducted in disadvantaged areas | Overweight | ↓ |
| BMI | ↔ | |||||
| Water intake | ↑ | |||||
| Juice intake | ↔ | |||||
| Soft drink intake | ↔ | |||||
| Perman et al. 2008113 | Non-randomised cluster controlled trial (two clusters, two arms; one cluster per arm) 9 months’ follow-up Final sample: 350 Quality: Weak |
Two schools, USA School children Boys and girls |
Prevention and treatment: Healthy breakfast and lunch plus School Health Advisory Council whole-school universal nutrition education and in-class physical activity; targeted group (overweight children): education sessions for parents, motivation and good choices group sessions, after-school fun activities, mentors and behavioural support and incentives Implementation: 7 |
Disadvantage: Children from low-income families (57% annual household income < US$10,000; 93% of children on free or reduced-price lunch) | BMI percentile (whole school) | ↓ |
| BMI percentile (overweight children) | ↔ | |||||
| Williams et al. 2004114 | Non-randomised cluster trial (9 clusters, 3 arms; 3 clusters per arm) 8 month follow-up Final sample: 676 Quality: Moderate |
9 preschools, USA 4 years 49% girls |
Prevention: Food service changes plus parental outreach and nutritional education; food service changes plus parental out reach Implementation: 4 |
Disadvantage: Families with incomes below the national poverty level | Overweight Obesity BMI Serum cholesterol Total cholesterol |
↔ ↔ ↔ ↓ ↓ |
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions – none | ||||||
| Observational studies (n = 3) | ||||||
| Nutrition-only interventions (n = 3) | ||||||
| Frisvold and Lumeng 2011121 | Retrospective cohort (controlled before-and-after) study 6 months’ follow-up Final sample: 1532 Quality: Strong |
Preschools, USA Age: 3–5 years 49% girls |
Prevention: Head Start childcare and associated nutritious food and physical activity Implementation: 6 |
Disadvantage: Children below the poverty line | Obesity | ↓ |
| Overweight | ↔ | |||||
| BMI | ↔ | |||||
| Ibarra and Alarcón 2010112 | Prospective cohort (uncontrolled before-and-after) study 24 months’ follow-up Final sample: 472 Quality: Moderate |
One school, Chile Age: 14–17 years 56% girls |
Prevention: Healthy eating lessons and activities added to the school curriculum alongside changing the school kiosk into a healthy eating kiosk Implementation: 9 |
Disadvantage: Conducted in a disadvantaged area | Obesity | ↔ |
| Obesity risk | ↔ | |||||
| Calorie intake | ↔ | |||||
| Ramirez-Lopez et al. 2005120 | Prospective cohort (controlled before-and-after) study 9 months’ follow-up Final sample: 360 Quality: Weak |
17 municipalities, Mexico Age: 6–10 years |
Prevention: School breakfast programme Implementation: 0 |
Disadvantage: Targeted at low-income children | Overweight | ↔ |
| Obesity | ↔ | |||||
| BMI | ↔ | |||||
| % fat | ↔ | |||||
| Total cholesterol | ↔ | |||||
| Serum triglycerides | ↔ | |||||
| Fasting glucose | ↔ | |||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions – none | ||||||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 7) | |||
| Nutrition-only interventions (n = 7) | |||
| Coleman et al. 2005,107 Heath and Coleman 2003116 | A: Motivation | Improve cardiovascular health | 9 |
| C: Context | Social – initiated by a community organisation | ||
| D: Experience | Task force comprised individuals with expertise in nutrition and exercise from school districts, higher education, hospitals and clinics, state organisations and non-profit groups | ||
| E: Consultation | Task force consulted but no mention of parents | ||
| F: Delivery fidelity | Implemented differently from the national programme. Food content was assessed: intervention schools met per cent fat content target in year 2 only, but fat content was consistently lower than in controls schools for all years. Sodium target was not met. Physical activity goal was met in intervention and control schools | ||
| G: Sustainability | Further funding was awarded and training for cafeteria workers so that they are more engaged | ||
| H: Stakeholder support | Support was high from all stakeholders (funders, planning committees, teachers, school administrators, food service staff) | ||
| I: Resources | US$8500 per school over 4 years | ||
| J: Differential effects | Gender | ||
| Foster et al. 2008109 | A: Motivation | Reduce overweight and obesity, particularly in low-SES children | 6 |
| C: Context | Social – initiated by a community organisation | ||
| D: Experience | Planned by the community organisation (Food Trust) with support from the municipality. Teachers and support staff were trained by the research team | ||
| E: Consultation | Task force adapted national nutrition guidance for use in the schools. The community organisation and the school food service were involved | ||
| F: Delivery fidelity | Teachers participated in an average of 10.4 hours of training and provided 48 hours of nutritional education | ||
| J: Differential effects | Ethnicity, age, gender | ||
| Foster et al. 2010108 | A: Motivation | Reduce prevalence of obesity and overweight | 5 |
| C: Context | Social: researcher led | ||
| D: Experience | Study investigators were experienced in conducting research in schools | ||
| F: Delivery fidelity | Structured observations suggested that intervention components were implemented as planned 90% of the time | ||
| I: Resources | Staff and equipment as well as study incentive costs for schools of US$9000–12,000 each, plus US$120 per pupil | ||
| Hollar et al. 2010110,111,115 | D: Experience | Dietitian involved in school food changes; professional gardeners assisted with school gardens | 4 |
| F: Delivery fidelity | Physical activity intervention was intended to be the use of pedometers but this was changed to 15 minutes of desk-side activity per day after the pedometers broke in year 2 | ||
| G: Sustainability | School gardeners used to sustain the gardens | ||
| J: Differential effects | SES, ethnicity, gender | ||
| Muckelbauer et al. 2009,118,119 2011117 | A: Motivation | Prevention of overweight in children in deprived areas through increased water consumption | 7 |
| B: Theory | Theory of planned behaviour | ||
| C: Context | Social: researcher led | ||
| D: Experience | Researchers with expertise in health and pedagogy | ||
| F: Delivery fidelity | 94% of teachers implemented one out of four lessons, 85% implemented two out of four lessons and 16% implemented all lessons; motivation targets were used at least once by 68% of teachers and regularly by 24% of teachers, and in 71% of classes the regular use of the water bottles was organised | ||
| G: Sustainability | 49% of teachers reported that water bottle use did not disturb teaching and the study authors commented on long-term compliance | ||
| I: Resources | Teacher time, water fountains at €2500 each and water bottles at €13 per child per year | ||
| Perman et al. 2008113 | A: Motivation | Reduce obesity and slow weight gain in those already overweight/obese | 7 |
| C: Context | Social – community driven; community–academic partnership | ||
| D: Experience | Physicians, residents, nurses, medical students, nursing students, public health students, extension agents and elementary teachers and staff volunteered in the programme | ||
| E: Consultation | Coalition of academic and community partners [including University of Kentucky Colleges of Agriculture, Education, Nursing and Public Health; Lexington-Fayette County Health Department; YMCA of Central Kentucky; Community Trist bank; and God’s Pantry (food retailer)]; planning meetings held with teachers to ensure genuine investment in the programme and provide important insights | ||
| G: Sustainability | Reliance on volunteers and partner/stakeholder in-kind contributions | ||
| H: Stakeholder support | Support was high from volunteer groups and individuals; parental participation was low | ||
| I: Resources | Cost of the programme in actual cash outlay was approximately US$16,000 but this does not include in-kind contributions from community partners of professional time, supplies and memberships | ||
| Williams et al. 2004114 | A: Motivation | Cardiovascular health improvement | 4 |
| C: Context | Part of the Head Start programme | ||
| D: Experience | Administered by registered dietitians with teachers trained in use of the curriculum | ||
| J: Differential effects | Ethnicity and gender examined | ||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions – none | |||
| Observational studies (n = 3) | |||
| Nutrition-only interventions (n = 3) | |||
| Frisvold and Lumeng 2011121 | A: Motivation | Reduce poverty (including improving health of disadvantaged groups) | 6 |
| B: Theory | Child quality theory | ||
| C: Context | Political – began with War on Poverty in 1965; full-day structure introduced as a result of welfare reform in the mid-1990s | ||
| G: Sustainability | Public sector budget cuts reduced the availability of the intervention | ||
| I: Resources | State-funded initiative with US$1.6M given to the provider of the evaluated intervention for 1 year | ||
| J: Differential effects | Age, gender | ||
| Ibarra and Alarcón 2010112 | A: Motivation | Prevention of obesity | 9 |
| B: Theory | Early intervention for long-term health behaviour change | ||
| C: Context | Researcher led as part of a university social responsibility agenda and inspired by the WHO Healthy Schools initiative | ||
| D: Experience | The researchers increased the awareness of obesity and nutrition among the teachers who would deliver the intervention | ||
| E: Consultation | Meetings with pupils, parents, teachers and school directors were carried out to gain support for the intervention in the planning stages. Economic concerns about changing the food sold by the kiosk were expressed and this led to a compromise in the type/extent of healthy food sold | ||
| F: Delivery fidelity | Focus groups showed that teachers’ knowledge of healthy eating increased and questionnaires showed increased nutritional knowledge among pupils | ||
| G: Sustainability | Education was integrated into the curriculum on a long-term basis but there were no comments about the long-term sustainability of the kiosk | ||
| H: Stakeholder support | Kiosk owner issues noted | ||
| J: Differential effects | Age and gender were examined | ||
| Ramirez-Lopez et al. 2005120 | No implementation information reported | 0 | |
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions – none | |||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 1) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 1) | ||||||
| Sanigorski et al. 2008124 | Quasi-experimental including cluster RCT 3 years’ follow-up Final sample: 1807 Quality: Strong |
Community (environmental and policy), Australia Age: 4–12 years ≈50% girls |
Prevention: Community capacity-building programme. Intervention targeted a variety of diet, physical activity and sedentary behaviours Implementation: 8 |
Gradient: SES | Body weight | ↓ |
| Waist circumference | ↓ | |||||
| BMI | ↔ | |||||
| BMI z-score | ↓ | |||||
| No association between intervention effect and SES; SES was associated with weight gain in the control group | ||||||
| Observational studies (n = 1) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 1) | ||||||
| Chomitz et al. 2010122 | Prospective cohort study without controls 3 years’ follow-up Final sample: 1858 Quality: Weak |
Community (environmental and policy), USA Age: 5–11 years 48.5% girls |
Prevention: Community-based intervention targeting a variety of diet, physical activity and sedentary behaviours Implementation: 7 |
Gradient: Income | BMI z-score | ↓ |
| Obese | ↓ | |||||
| Overweight | ↔ | |||||
| Ideal weight | ↑ | |||||
| Similar intervention effects in low- and high-income participants | ↓ | |||||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Observational studies (n = 1) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 1) | ||||||
| Hoelscher et al. 2010123 | Serial cross-sectional intervention study 1 year of follow-up Final sample: 1107 Quality: Weak |
Elementary schools, USA Age: 9–10 years 53% girls |
Prevention: School-based intervention using a ‘whole-school approach’ vs. the same but with an additional educational course to promote community partnership working. Targeted a variety of diet, physical activity and sedentary behaviours Implementation: 7 |
Disadvantage | Percentage of students > 85th percentile | ↓ |
| Percentage of students > 95th percentile | ↔ | |||||
| Vigorous physical activity | ↔ | |||||
| Physical activity participation | ↔ | |||||
| Television viewing | ↓ | |||||
| Video game use | ↔ | |||||
| Computer use | ↓ | |||||
| Breakfast | ↑ | |||||
| Milk | ↔ | |||||
| Fruit and vegetables | ↑ | |||||
| Sugar-sweetened drinks | ↔ | |||||
| Unhealthy Food Index | ↓ | |||||
| Healthy Food Index | ↔ | |||||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 1) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 1) | |||
| Sanigorski et al. 2008124 | A: Motivation | Reduce the prevalence of childhood obesity | 8 |
| B: Theory | Socioecological model and community-based participatory approach | ||
| C: Context | Social | ||
| D: Experience | Mixed. Development of the intervention was extensive and involved users and other stakeholders (capacity-building approach) | ||
| E: Consultation | Consultation extensive at all stages of the research process. Capacity-building approach used | ||
| H: Stakeholder support | Very good | ||
| I: Resources | Approximately 6789 total person-hours required to deliver the intervention | ||
| J: Differential effects | SES explored – no effects found | ||
| Observational studies (n = 1) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 1) | |||
| Chomitz et al. 2010122 | A: Motivation | Reduce the prevalence of childhood obesity | 7 |
| B: Theory | Socioecological model and community-based participatory approach | ||
| C: Context | Social | ||
| D: Experience | Development of the intervention was extensive and involved users and other stakeholders | ||
| E: Consultation | Extensive at all stages of the research process | ||
| G: Sustainability | Elements of the intervention continued beyond 3 years and local policy and practice changed | ||
| J: Differential effects | Explored but none found | ||
| Study | Domain | Details | Score |
|---|---|---|---|
| Observational studies (n = 1) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 1) | |||
| Hoelscher et al. 2010123 | A: Motivation | Reduce the prevalence of childhood obesity | 7 |
| B: Theory | Socioecological models and social cognitive theory | ||
| C: Context | Social | ||
| E: Consultation | Programme components developed by working in a community participatory manner with district leaders and teachers, and a community action team was formed to develop partnerships between the school and the community | ||
| F: Delivery fidelity | BasicPlus + community schools performed better on nearly all classroom process measures and the school-level co-ordination and leadership process measures | ||
| H: Stakeholder support | High levels of support | ||
| J: Differential effects | Gender and ethnicity | ||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 3) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 3) | ||||||
| Edye et al. 1989139 | RCT 3 years’ follow up Final sample: 1937 Quality: Weak |
Study centre, Australia Age: male 35.8–36.7 years; female 29.1–29.7 years % male/female not reported |
Prevention: Physician-delivered medical interview and counselling session; diet advice for weight and cholesterol reduction and energy intake control and exercise; nurse-delivered counselling sessions Implementation: 5 |
Gradient: Explored differential effects by occupation | Weight | ↑ |
| Proportion not fit | ↓ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↔ | |||||
| Cholesterol | ↑ | |||||
| No differential effects by occupation | ||||||
| Jeffery and French 1997,129 1999130 | RCT 3 years’ follow-up Final sample: 809 Quality: Strong |
Homes, USA Age: 20–45 years 100% female (used for gradient analysis) |
Prevention: Pound of Prevention study – diet and physical activity education (via monthly e-mails) with or without a lottery incentive; additional voluntary activities (e.g. group sessions and dance classes) Implementation: 6 |
Gradient: High income vs. low income (women only) | Body weight | ↔ |
| No interaction between intervention and participant type (low-income or high-income women) | ||||||
| Volpp et al. 2008138 | RCT (three groups) 16 weeks’ follow-up Final sample: 52 Quality: Weak |
Health-care setting, USA Age: 30–70 years 5.3% female BMI: 30–40 kg/m2 |
Treatment: Weight loss programme without financial incentives vs. weight loss programme with deposit contract vs. weight loss programme with lottery Implementation: 4 |
Gradient: Exploratory subgroup analysis of weight loss patterns by income | Weight | ↓ |
| No differential effects by income | ||||||
| Observational studies (n = 10) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 10) | ||||||
| Fortmann et al. 1982145 | Prospective cohort (uncontrolled before-and-after) study 3 years’ follow-up Final sample: 687 Quality: Moderate |
Mass media campaign, USA Age: 35–59 years Male and female |
Prevention: Stanford Three Community Study – dietary and physical activity health education delivered in various media: television and radio programmes and public service announcements, newspaper columns, billboards and other communications Implementation: 6 |
Gradient: Outcomes reported for each SES group | Weight | ↔ |
| Dietary cholesterol | ↔ | |||||
| Dietary saturated fat | ↔ | |||||
| Plasma cholesterol | ↔ | |||||
| No significant differences across SES groups for these outcome measures | ||||||
| Gardner et al. 2012143 | Uncontrolled before-and-after study 6 months’ follow-up (mean) Final sample: 3759 Quality: Weak |
Health-care setting, UK (England and Wales) Age: > 18 years 79% female |
Prevention: NHS HTS – health trainers (lay community members) trained in behaviour change techniques to provide individualised support to clients to achieve health behaviour goals Implementation: 7 |
Gradient: BMI change among each deprivation quintile explored | BMI | ↓ |
| Those from the least deprived 80% of the population achieved a greater BMI change than the most deprived | ||||||
| Helmert et al. 1993146 | Repeat cross-sectional study 3.5 years’ follow-up Final sample: 14,078 Quality: Weak |
Community, Germany Age: 25–69 years 52% female |
Prevention: German Cardiovascular Prevention (GCP) study – multicentre, community-based initiative promoting public information, training of professionals and lay individuals, and support of self-help activities Implementation: 5 |
Gradient: Explored intervention effect on social class gradients for cardiovascular disease risk factors | Obesity prevalence | ↔ |
| Hypertension prevalence | ↔ | |||||
| No intervention effects on SES gradient | ||||||
| Hypercholesterolaemia, men | ↔ | |||||
| Hypercholesterolaemia, women | ↑ | |||||
| In women, the intervention blunted the rise in SES gradient | ||||||
| Morrison et al. 2012141 | Prospective cohort (uncontrolled before-and-after) study 16 weeks’ follow-up Final sample: 809 Quality: Weak |
Health-care setting, UK (Scotland) Age: men 47.5 years; women 44.6 years 74% female BMI: ≥ 30 kg/m2 |
Treatment: NHS Glasgow and Clyde Weight Management Service – 600-kcal deficit diet and activity changes advised, supported with cognitive–behavioural approaches Implementation: 7 |
Gradient: Compared rate of success in each SES group | 36% achieved ≥ 5kg of weight loss (clinically successful) No differences in prevalence of success across SES gradient |
|
| Neve et al. 2011142 | Retrospective uncontrolled cohort study 15 months’ follow-up Final sample: 614 Quality: Weak |
Web based, Australia Age: 18–75 years 88% female BMI: ≥ 22 kg/m2 |
Treatment: Commercial web-based weight loss programme (the Biggest Loser Club Australia); used weight-management strategies based on elements of social cognitive theory Implementation: 6 |
Gradient: Compared SES in successful and unsuccessful participants | Body weight | ↓ |
| 37% achieved ≥ 5% weight loss | ||||||
| No differences in SES status between those who were successful and those who were not successful | ||||||
| Olson et al. 2004131 | Prospective cohort analytical study (with a historical control) 1 year of follow-up Final sample: 517 Quality: Strong |
Hospital/primary care clinic, USA 100% female (pregnant) Age: 20–40 years |
Prevention: The intervention had two major components: a clinical component, including guidance about and monitoring of gestational weight gain by health-care providers using new tools in the obstetric chart, and a by-mail patient education programme Implementation: 6 |
Gradient: Reported effects by income (low/high) | Weight gain Weight retention Significant intervention effect for weight gain in low-income women (smaller % weight gain in intervention group than in control group and significantly smaller proportion of intervention group women retained ≥ 2.27 kg at 1 year post-partum) |
↔ ↔ |
| Rautio et al. 2011144 | Prospective cohort study 1 year of follow-up Final sample: 2977 Quality: Weak |
Health-care centres, Finland Age: 20–64 years 67% female Increased risk of diabetes |
Prevention: FIN-D2D project – health check-up with nurse including short counselling session on lifestyle changes (including diet and physical activity; individual or group sessions for lifestyle change support) Implementation: 5 |
Gradient: Reported effects in different education and occupation groups | Body weight | ↓ |
| BMI | ↓ | |||||
| Waist circumference | ↓ | |||||
| BP | ↓ | |||||
| Total cholesterol | ↓ | |||||
| LDL cholesterol | ↓ | |||||
| HDL cholesterol | ↑ | |||||
| Triglycerides | ↓ | |||||
| Intervention effect the same across SES groups except BP not decreased to the same extent in low-educated women as in higher-educated women | ||||||
| Schuit et al. 2006140 | Cohort analytical (two groups pre and post test) study One intervention area and one reference area (control) 5 years’ follow-up Final sample: 3114 Quality: Strong |
Community, the Netherlands Age: 31–70 years ≈50% female |
Prevention: 790 interventions were implemented (1993–2003); 500 were major interventions (193 diet, 361 physical activity and nine anti-smoking). Examples include computer-tailored nutrition education, nutrition education tours in supermarkets, public–private collaboration with the retail sector, television programmes, food labelling, smoke-free areas, walking and bicycling campaigns, stop-smoking campaign, commercials on local television and radio, newspaper articles and pamphlet distribution Implementation: 3 |
Gradient | BMI | ↓ |
| Waist circumference | ↓ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Glucose | ↓(F) | |||||
| Cholesterol | ↔ | |||||
| This intervention significantly benefited both moderate to high and low SES groups (BMI and waist circumference) | ||||||
| Weinehall et al. 2001127 | Prospective cohort study with comparison 5 year follow-up Final sample: 690 Quality: Weak |
Community, Sweden and USA Age: 45.2 years (Sweden); 47.2 years (USA) 51.6% female (Sweden); 52.8% female (USA) |
Prevention: Population-based health promotion and individually oriented disease prevention activities: health messages (including healthy eating and physical activity) promoted throughout communities; screening of cardiovascular risk factors and appropriate medical counselling/information provision/follow-up medical care Implementation: 7 |
Gradient: Subgroup analysis of intervention effects by education | Sweden, USA and pooled | |
| BMI | ↔ | |||||
| No difference by education | ||||||
| Weinehall et al. 2001127 | Serial cross-sectional study with comparison 5 years’ follow-up Final sample: ≈2500 Quality: Weak |
Community, Sweden and USA Age: 45.2 years (Sweden); 47.2 years (USA) 51.6% female (Sweden); 52.8% female (USA) |
Prevention: Population-based health promotion and individually oriented disease prevention activities: health messages (including healthy eating and physical activity) promoted throughout communities; screening of cardiovascular risk factors and appropriate medical counselling/information provision/follow-up medical care Implementation: 7 |
Gradient: Subgroup analysis of intervention effects by education | Sweden | |
| BMI | ↑ | |||||
| Overall and with low level of education | ||||||
| USA and pooled | ||||||
| BMI | ↔ | |||||
| No difference by education | ||||||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 9) | ||||||
| Nutrition-only interventions (n = 1) | ||||||
| Weerts and Amoran 2011132 | Randomised control pilot study 3 months’ follow-up Final sample: 9 Quality: Moderate |
Healthy Start centres, USA Age: 18–44 years 100% female BMI: ≥ 25 kg/m2 |
Treatment: Fruit and vegetable promotion – culturally appropriate health education plus gift card for fruit and vegetables only vs. health education plus gift card for all groceries (active control) Implementation: 8 |
Disadvantage: Low-income women | Body weight | ↓ |
| BMI | ↓ | |||||
| All fruit and vegetables | ↔ | |||||
| Raw, fresh fruit and vegetables | ↓ | |||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 8) | ||||||
| Burke et al. 2011,148 2012149 | RCT 6 months’ follow-up Final sample: 375 Quality: Weak |
Participants’ homes, Australia Age: 60–70 years 48% female Sedentary |
Treatment: Physical Activity and Nutrition for Seniors (PANS) – information on dietary guidelines, recommended physical activity levels and goal-setting; exercise chart, calendar and bimonthly newsletters; pedometer and resistance band (for exercises suggested) provided; e-mail and telephone support and non-compulsory group meetings Implementation: 2 |
Disadvantage: Residents of low- to medium-SES areas | BMI | ↔ |
| Waist-to-hip ratio | ↓ | |||||
| Craigie et al. 2011135 | Randomised controlled pilot study 12 weeks’ follow-up Final sample: 36 Quality: Strong |
Participants’ homes, UK Mean age: 30 years 100% female BMI: > 25 kg/m2, 6–18 months post-partum |
Treatment: Post-partum weight loss programme (WeighWell) – face-to-face consultations and telephone support from trained lifestyle counsellor; motivational interviewing techniques, calorie-reduced diet and physical activity goals Implementation: 7 |
Disadvantage: Women living in areas of moderate to high deprivation | Body weight | ↓ |
| BMI | ↓ | |||||
| % body fat | ↓ | |||||
| Waist circumference | ↔ | |||||
| Physical activity | ↔ | |||||
| Davis Martin et al. 2006133 | RCT 6 months’ follow-up Final sample: 106 Quality: Strong |
Two medical centres, USA Age: 18–62 years 100% female Overweight and obese |
Treatment: Tailored and culturally appropriate weight-management programme – physician delivered; individual recommendations and strategies provided by health psychologist, registered dietitian and exercise physiologist Implementation: 7 |
Disadvantage: Low-income, African American women | Body weight | ↓ |
| Hillier et al. 2012152 | Cluster RCT (12 clusters, two arms; six clusters per arm) 12 months’ follow-up Final sample: 63 Quality: Weak |
Health centre and homes in 12 public health localities, UK 63–86% female Mean age: 42–49 years |
Prevention: Community challenge health promotion intervention; pledge to improve elements of dietary intake and physical activity; lifestyle helper delivered sessions; reflective listening; understanding client’s motivation and readiness to change Implementation: 6 |
Disadvantage: Low SES | Diet | ↔ |
| BMI | ↔ | |||||
| Waist circumference | ↑ | |||||
| Physical activity | ↔ | |||||
| Jackson et al. 2011134 | RCT > 14 weeks’ follow-up Final sample: 287 Quality: Moderate |
Three public hospitals, two academic practices, one community hospital, USA Age: ≥ 18 years 100% female < 26 weeks of gestation |
Prevention: Computerised, multimedia, interactive Video Doctor – conducts in-depth behavioural risk assessments, delivers tailored counselling messages (diet and physical activity) and produces printed output for both the patient and the clinician Implementation: 6 |
Disadvantage: Majority of participants were Medicaid recipients | Excessive gestational weight gain | ↔ |
| Martin et al. 2008136 | RCT 18 months’ follow-up Final sample: 86 (intention to treat) Quality: Strong |
Primary care setting, USA 100% female Age: 18–65 years Overweight or obese (BMI > 25 kg/m2) |
Treatment: Tailored weight loss intervention delivered by primary care physician; monthly counselling sessions; topics included weight loss, decreasing dietary fat, increasing physical activity, barriers to weight loss and healthy alternatives when eating out and shopping Implementation: 7 |
Disadvantage: Low-income minority women | Weight loss | ↔ |
| Sierra et al. 2010128 | Non-RCT 1 year of follow-up Final sample: 4792 Quality: Strong |
Telephone based, Spain Age: Majority > 45 years 5% female Increased risk of cardiovascular disease |
Prevention: Routine health screen plus telephone intervention vs. health screen only – feedback from health screen, appropriate lifestyle advice, monitoring of behaviour Implementation: 5 |
Disadvantage: Majority of sample were manual workers | Body weight | ↓ |
| BMI | ↓ | |||||
| Waist circumference | ↔ | |||||
| Glucose | ↔ | |||||
| Triglycerides | ↔ | |||||
| Total cholesterol | ↓ | |||||
| LDL cholesterol | ↓ | |||||
| HDL cholesterol | ↔ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Whittemore et al. 2009150 | Cluster randomised controlled pilot study (four clusters, two arms; two clusters per arm) 6 months’ follow-up Final sample: 51 Quality: Strong |
Four health-care practices, USA 92% female Mean age: ≈46 years BMI: ≥ 25 kg/m2 |
Treatment: Diabetes prevention programme for overweight and obese adults – separate individual sessions with nurse and nutritionist; culturally relevant education on nutrition and exercise; behavioural support in identifying goals and problem-solving barriers to change; motivational interviewing Implementation: 8 |
Disadvantage: Participants had moderately low incomes | Body weight | ↓(trend) |
| BMI | ↔ | |||||
| Waist circumference | ↔ | |||||
| Diet | ↔ | |||||
| Physical activity | ↑(trend) | |||||
| Homeostasis model assessment | ↔ | |||||
| Glucose | ↔ | |||||
| Insulin | ↔ | |||||
| LDL cholesterol | ↔ | |||||
| HDL cholesterol | ↑(trend) | |||||
| Observational studies (n = 11) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions (n = 1) | ||||||
| Johnson and Meadows 2010154 | Uncontrolled before-and-after study 26–50 weeks’ follow-up Final sample: 26 Quality: Moderate |
Two Housing Association subsidised inner-city high-rise resident buildings, USA Age: ≥ 40 years 54% female |
Prevention: Dog-walking programme – participants walked dogs (certified by College of Veterinary Medicine) with handlers. Started with 10 minutes three times a week and advanced to 20 minutes three times a week and then 20 minutes five times a week Implementation: 5 |
Disadvantage: Residents of subsidised housing | Site 1 (50-week duration): | |
| Body weight | ↓ | |||||
| BMI | ↓ | |||||
| Site 2 (26-week duration): | ||||||
| Body weight | ↔ | |||||
| BMI | ↔ | |||||
| Nutrition and physical activity interventions (n = 10) | ||||||
| Abramson et al. 1979137 | Controlled prospective cohort study 54 months’ follow-up Final sample: 920 Quality: Moderate |
Family health-care practices, Israel Age: ≥ 35 years 100% male |
Prevention: CHAD programme. Primary aim was to reduce BP. Face-to-face counselling (and small-group component) with family physicians and nurses Implementation: 5 |
Disadvantage: Residents of housing projects | Body weight | ↔ |
| Prevalence of overweight | ↔ | |||||
| Physical activity | ↔ | |||||
| Diet | ↑ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Cholesterol | ↔ | |||||
| Abramson et al. 1981157 | Controlled prospective cohort study 5 years’ follow-up Final sample: 2038 Quality: Strong |
Family health-care practices, Israel Age: ≥ 35 years 53% female |
Prevention: CHAD programme. Primary aim was to reduce BP. Face-to-face counselling (and small-group component) with family physicians and nurses Implementation: 6 |
Disadvantage: Residents of housing projects | Body weight | ↓(F) |
| Prevalence overweight | ↓ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Cholesterol | ↔ | |||||
| Buchholz et al. 2012155 | Prospective cohort (uncontrolled before-and-after) pilot study 6 months’ follow-up Final sample: 122 Quality: Weak |
Two free health-care clinics, USA 89% female Mean age: 47 years BMI: ≥ 25 kg/m2 |
Treatment: Clinic-based nurse-delivered health promotion intervention – 30-minute one-to-one session each month for 6 months; nutrition and physical activity education; feedback on current behaviours; goal-setting and monitoring; self-monitoring; US$5 food voucher at each session Implementation: 6 |
Disadvantage: Medically uninsured adults registered to free health-care clinics | BMI (all participants) | ↔ |
| BMI (full adherers, n = 23) | ↓ | |||||
| Gardner et al. 2012143 | Uncontrolled before-and-after study 6 months’ follow-up (mean) Final sample: 3759 Quality: Weak |
Health-care setting, UK (England and Wales) Age: > 18 years 79% female |
Prevention: NHS HTS – health trainers (lay community members) trained in behaviour change techniques to provide individualised support to clients to achieve health behaviour goals Implementation: 7 |
Disadvantage: Socially disadvantaged population | BMI | ↓ |
| Gofin et al. 1986158 | Uncontrolled prospective cohort study 5 years’ follow-up Final sample: 441 Quality: Moderate |
Family health-care practices, Israel Age: ≥ 25 years % male/female not reported |
Prevention: CHAD programme. Primary aim was to reduce BP. Face-to-face counselling (and small-group component) with family physicians and nurses Implementation: 6 |
Disadvantage: Residents of housing projects | Body weight | ↔ |
| Prevalence of overweight | ↔ | |||||
| BP | ↓ | |||||
| Prevalence of hypertension | ↓ | |||||
| Jackson et al. 2007147 | Prospective cohort (uncontrolled before-and-after) exploratory study 52 weeks’ follow-up Final sample: 29 Quality: Weak |
Health-care centre, UK 70% female Mean age: 56 years BMI: ≥ 30 kg/m2 |
Treatment: Specialist health visitor-led weight-management intervention – biweekly sessions; diet and physical activity education; supportive infrastructure; goal-setting and problem-solving; evidence of progress; focuses on building a therapeutic relationship Implementation: 8 |
Disadvantage: Health centre in a moderately deprived location | Body weight | ↓ |
| BMI | ↓ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Glucose | ↔ | |||||
| Cholesterol | ↔ | |||||
| Cakes, desserts, snacks | ↔ | |||||
| Fruit and vegetables | ↔ | |||||
| Marshall et al. 201143 | Uncontrolled before-and-after study ≥ 3 months’ follow-up Final sample: 2681 Quality: Weak |
17 health-care providers, New Zealand Age: 19–95 years Gender not reported |
Prevention: Nurse-led healthy lifestyle clinic – targeting diabetes, smoking cessation, diet/nutrition, women’s health, cardiovascular and asthma/respiratory clinics. Holistic approach to health needs defined by the patient Implementation: 5 |
Disadvantage: Patients living in high-deprivation areas | BMI | ↔ |
| Waist circumference | ↔ | |||||
| Systolic BP | ↔ | |||||
| Cardiovascular disease risk | ↔ | |||||
| HbA1c | ↔ | |||||
| Morrison et al. 2012141 | Prospective cohort (uncontrolled before-and-after) study 16 weeks’ follow-up Final sample: 809 Quality: Weak |
Health-care setting, UK (Scotland) Age: men 47.5 years; women 44.6 years 74% female BMI ≥ 30 kg/m2 |
Treatment: NHS Glasgow and Clyde Weight Management Service – 600-kcal deficit diet and activity changes advised, supported with cognitive–behavioural approaches Implementation: 7 |
Disadvantage: Majority of participants from the least deprived SES group | 36% achieved ≥ 5 kg of weight loss (clinically successful) No differences in prevalence of success across SES gradient |
|
| Schuit et al. 2006140 | Controlled prospective cohort study 5 years’ follow-up Final sample: 3114 Quality: Strong |
Hartslag Limburg, the Netherlands Age: 31–70 years ≈50% female |
Prevention: 790 interventions were implemented (1993–2003); 500 were major interventions (193 diet, 361 physical activity and nine anti-smoking). Examples include computer-tailored nutrition education, nutrition education tours in supermarkets, public–private collaboration with the retail sector, television programmes, food labelling, smoke-free areas, walking and bicycling campaigns, stop-smoking campaign, commercials on local television and radio, newspaper articles and pamphlet distribution Implementation: 3 |
Disadvantage: Almost 50% in low-income areas | BMI | ↓ |
| Waist circumference | ↓ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Glucose | ↓(F) | |||||
| Cholesterol | ↔ | |||||
| Verheijden et al. 2012156 | Cohort study 18 months’ follow-up Final sample: 816 Quality: Weak |
The Netherlands Campaign 1: general population; campaign 2: low-SES men Mean age: 45 years 55% female |
Prevention: Mass media campaign by the Netherlands Nutrition Centre. Focus on weight control by promotion of energy balance behaviour and physical activity Implementation: 5 |
Disadvantage: Low-SES men (campaign 2 only) | Campaign 1 | |
| BMI | ↔ | |||||
| Physical activity | ↔ | |||||
| Food choices | ↔ | |||||
| Campaign 2 | ||||||
| BMI (non-Dutch only) | ↓ | |||||
| Physical activity | ↔ | |||||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 3) | |||
| Nutrition only interventions – none | |||
| Physical activity only interventions – none | |||
| Nutrition and physical activity interventions (n = 3) | |||
| Edye et al. 1989139 | A: Motivation | Prevention: Reduce cardiovascular disease risk factors | 5 |
| C: Context | Social – health care led | ||
| D: Experience | Physician and nurse | ||
| I: Resources | Physician and nurse; sphygmomanometer | ||
| J: Differential effects | SES, gender | ||
| Jeffery and French 1997,129 1999130 | A: Motivation | Weight gain prevention | 6 |
| C: Context | Social | ||
| D: Experience | Four local health departments. Health department personnel actively involved in developing intervention materials and delivering face-to-face components of the intervention | ||
| G: Sustainability | Newsletters cost-effective | ||
| H: Stakeholder support | Four local health departments | ||
| I: Resources | Health department nutritionists | ||
| Volpp et al. 2008138 | A: Motivation | Reduce obesity | 4 |
| C: Context | Social – researcher led | ||
| I: Resources | The average amount of money earned was US$378.49 in the deposit contract condition (paid in by participants) and US$272.80 in the lottery condition. All participants were given US$20 at each monthly weigh-in | ||
| J: Differential effects | Age, income, initial BMI and ethnicity explored | ||
| Observational studies (n = 10) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 10) | |||
| Fortmann et al. 1982145 | A: Motivation | Reduce risk of cardiovascular disease | 6 |
| B: Theory | Family–community model | ||
| C: Context | Social | ||
| D: Experience | Biomedical experts and social scientists | ||
| I: Resources | Mass media campaign: television and radio programmes and public service announcements, newspaper columns, billboards and other communications. Pamphlets and cookbooks were also distributed by direct mail | ||
| J: Differential effects | SES, gender, language spoken | ||
| Gardner et al. 2012143 | A: Motivation | Improve health in disadvantaged populations | 7 |
| B: Theory | Control theory, health action process approach and social cognitive theory | ||
| C: Context | Social – health service led | ||
| D: Experience | Team of health psychologists designed and developed the intervention and provided long-term support. Health trainers were lay community members with appropriate training | ||
| G: Sustainability | Incorporated into existing services (and continues to be) | ||
| I: Resources | Majority of health trainers operate in a paid role (58%) but a considerable proportion are voluntary | ||
| J: Differential effects | SES, ethnicity, duration of the NHS HTS, health trainer–client ethnicity match, baseline scores of outcome variables (including BMI) | ||
| Helmert et al. 1993146 | A: Motivation | Prevention of cardiovascular disease | 5 |
| B: Theory | Social learning theory, theory of diffusion of innovations | ||
| C: Context | Social | ||
| D: Experience | Health professionals and medical associations | ||
| E: Consultation | Collaboration with health professionals and medical associations; health committees created | ||
| G: Sustainability | One aim of the study was that communities would continue the intervention after the study had finished | ||
| Morrison et al. 2012141 | A: Motivation | Reduce prevalence of obesity | 7 |
| B: Theory | Cognitive–behavioural approaches | ||
| C: Context | Social – health service led | ||
| D: Experience | Dietitians, psychologists and physiotherapists | ||
| G: Sustainability | Integrated into existing health service | ||
| I: Resources | Nine fortnightly sessions delivered by dietitian with referral to psychologist if/when required. Group rather than individual sessions – more likely to be cost-effective | ||
| J: Differential effects | Age, gender, baseline BMI and SES explored | ||
| Neve et al. 2011142 | A: Motivation | Reduce overweight and obesity | 6 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social – commercial company led | ||
| D: Experience | Programme developed by commercial company SP Health Co. One of the authors was a consultant dietitian to the company | ||
| I: Resources | Programme subscription cost A$16.50–79.95 per month (dependent on number of months subscribed to) (approx. £11–55) | ||
| J: Differential effects | Explored age, gender, baseline BMI, ethnicity, SES, remoteness, days since enrolment, days of membership, other weight loss strategy use and intervention satisfaction | ||
| Olson et al. 2004131 | A: Motivation | Prevention of excessive gestational weight gain | 6 |
| C: Context | Social – health care led | ||
| D: Experience | Health-care professionals (does not specify who) | ||
| G: Sustainability | May not be sustainable as based in primary care setting and there will be limited time available for counselling within this context of care; however, the more general patient education was carried out using newsletters | ||
| I: Resources | Health-care professionals, newsletters | ||
| J: Differential effects | SES | ||
| Rautio et al. 2011144 | A: Motivation | Prevention of type 2 diabetes | 5 |
| C: Context | Social – health care led | ||
| D: Experience | Nurses | ||
| I: Resources | Nurses, health screen, individual and group sessions | ||
| J: Differential effects | SES, gender | ||
| Schuit et al. 2006140 | A: Motivation | Cardiovascular disease prevention | 3 |
| C: Context | Social | ||
| J: Differential effects | Gender and high/low SES | ||
| Weinehall et al. 2001127 (two study designs) | A: Motivation | Prevention of cardiovascular disease | 7 |
| C: Context | Social – community and health department driven | ||
| E: Consultation | Intervention components were planned and implemented in close association with people affected by the programmes. In Sweden there was collaboration with local associations, sports clubs, the media and food retailers. In the USA there was collaboration with the Healthy Heart Program Advisory Committee (comprising community leaders), community task forces and local health committees, together with community agencies and organisations, health providers, unique local media, churches and schools | ||
| G: Sustainability | Large amount of community involvement and participation. The Swedish programme was incorporated into existing services; the US programme relied on volunteers from the community | ||
| H: Stakeholder support | Stakeholder support appeared high | ||
| I: Resources | Low-budget interventions. The Swedish programme required almost no additional financial support; however, the US programme relied on health department funding and volunteers | ||
| J: Differential effects | Gender and education | ||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 9) | |||
| Nutrition only interventions (n = 1) | |||
| Weerts and Amoran 2011132 | A: Motivation | Alleviate food insecurity and promote weight loss among low-income African American women | 8 |
| C: Context | Social – community–university–industry partnership | ||
| D: Experience | Health educator of same ethnic and cultural background | ||
| E: Consultation | Partnership included community group, which allowed reach to priority individuals | ||
| F: Delivery fidelity | Shopping receipts were returned to ensure that gift cards were used correctly | ||
| G: Sustainability | Partnership appeared to work well. Industry partner provided in-kind funding for gift cards – would this be sustainable in a larger intervention? | ||
| H: Stakeholder support | Partnership appeared to work well – no problems reported | ||
| I: Resources | Health educator provided by community group (four 15-minute sessions with each participant); industry partner provided in-kind funding for gift cards (four US$40 gift cards for each participant) | ||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 8) | |||
| Burke et al. 2011,148 2012149 | A: Motivation | Prevention of obesity in older adults | 2 |
| C: Context | Social – researcher led | ||
| Craigie et al. 2011135 | A: Motivation | Reduce weight gained during pregnancy in post-partum women | 7 |
| B: Theory | Motivational interviewing | ||
| C: Context | Social – researcher led | ||
| D: Experience | Trained lifestyle counsellor (no further details) | ||
| F: Delivery fidelity | Intervention was successfully delivered face-to-face and by telephone call to 100% of the intervention participants | ||
| H: Stakeholder support | All participants reported their experience positively overall; all intervention recipients described the intervention as useful; one-to-one format of the intervention was particularly well received (rather than group sessions) | ||
| I: Resources | Trained lifestyle counsellor; three face-to-face consultations (home visits); minimum of three telephone calls; weight loss booklet | ||
| Davis Martin et al. 2006133 | A: Motivation | Reduce overweight and obesity | 7 |
| B: Theory | Social cognitive theory, transtheoretical model | ||
| C: Context | Social | ||
| D: Experience | Multidisciplinary research team consisting of a physician, health psychologist, registered dietitian and exercise physiologist | ||
| F: Delivery fidelity | Site visits in months 1 and 3 at which the principal investigator of the study randomly selected five intervention participants and tracked all aspects of the their office visit, including directly observing the physician-administered treatment in the examination room | ||
| G: Sustainability | The intervention was incorporated into the physicians’ normal schedule and required minimal time on the part of both the physician and the patient | ||
| I: Resources | Six monthly 15-minute consultations with the physician. Individualised materials and recommendations prepared by the remaining intervention team: health psychologist, registered dietitian and exercise physiologist | ||
| Hillier et al. 2012152 | A: Motivation | Prevention of obesity | 6 |
| B: Theory | Theory of planned behaviour and social cognitive theory | ||
| C: Context | Social | ||
| D: Experience | Researchers were International Society for the Advancement of Kinanthropometry-accredited level 1 anthropometrists trained in waist circumference measurement; lifestyle helpers were trained in recruitment and motivational interviewing/brief negotiation techniques (intervention group only) | ||
| E: Consultation | Community champions and public health authorities | ||
| H: Stakeholder support | Local health authorities | ||
| Jackson et al. 2011134 | A: Motivation | Prevention of excessive gestational weight gain through improvement of diet and physical activity behaviours | 6 |
| B: Theory | Motivational interviewing | ||
| C: Context | Social | ||
| F: Delivery fidelity | Automated computer-based programme ensures a standardised method of intervention delivery | ||
| G: Sustainability | Incorporated into routine prenatal care | ||
| I: Resources | Video Doctor component took 10–15 minutes to complete. Participants received US$30 and US$40 for completing the baseline and follow-up data collection sessions respectively | ||
| Martin et al. 2008136 | A: Motivation | Weight loss (treatment) | 7 |
| C: Context | Social – health care led | ||
| D: Experience | Physicians received training to undertake the intervention | ||
| E: Consultation | Consultation with physicians about delivery of the intervention | ||
| F: Delivery fidelity | Project co-ordinator was on site for each physician visit to ensure the intervention protocol was adhered to | ||
| G: Sustainability | Integrated into primary care setting (too brief an intervention – needs to be longer and more frequent) | ||
| I: Resources | Handouts, culturally specific recipe menus and books and US$35 reimbursement (for time, transportation and childcare) | ||
| Sierra et al. 2010128 | A: Motivation | Reduce cardiovascular disease risk factors | 5 |
| C: Context | Social | ||
| D: Experience | Trained health staff in call centres (teams of doctors and nurses) | ||
| F: Delivery fidelity | Compliance to recommendations – 85% of those completing the intervention followed recommendations, 73% knew the risk factors and 33% knew their own risk level; 52% had given their letter to their GP | ||
| I: Resources | Routine health screen; three telephone calls; trained health staff in call centres (doctors and nurses) | ||
| Whittemore et al. 2009150 | A: Motivation | Prevention of type 2 diabetes | 8 |
| B: Theory | Behavioural science theories | ||
| C: Context | Social | ||
| D: Experience | Nurses and nutritionists | ||
| E: Consultation | Pre-intervention participatory phase to modify intervention protocol for easy implementation by nurses | ||
| F: Delivery fidelity | Attendance for in-person sessions was high at 96%. Completion of telephone calls for the lifestyle programme was problematic, with only a 37% success rate. Implementation of the lifestyle programme took 9.3 months compared with the outlined protocol of 6.5–7 months; this was because of nurse practitioner illnesses, rescheduling of participant appointments and end of year holidays. Implementation of the standard care nurse practitioner protocol was 80%, implementation of the standard care nutrition protocol was 92% and nurse practitioner implementation of the lifestyle protocol was 76%. All nurse practitioners reported that motivational interviewing was the most challenging aspect of the protocol to implement. Protocol implementation increased over time. Time constraints resulted in difficulty implementing the protocol as nurse practitioners were encouraged to complete sessions in 20 minutes to maintain their office schedule | ||
| G: Sustainability | Integrated into existing health-care services | ||
| I: Resources | 20- to 30-minute individual session with nurse; 45-minute individual session with nutritionist | ||
| Observational studies (n = 11) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions (n = 1) | |||
| Johnson and Meadows 2010154 | A: Motivation | Increase physical activity in disadvantaged populations | 5 |
| C: Context | Social – researcher led | ||
| F: Delivery fidelity | Adherence rates were 72% in site 1 and 52% in site 2 | ||
| G: Sustainability | Programme appeared to be feasible for implementation in other settings, although careful planning, implementing and testing is required. Pet Assisted Love and Support (PALS) was an existing programme | ||
| I: Resources | Trained handlers required; cost and equipment for care and transportation of the dogs; suitable footwear was purchased for each participant. Logistically complex intervention | ||
| Nutrition and physical activity interventions (n = 10) | |||
| Abramson et al. 1979137 | A: Motivation | Control of cardiovascular disease risk factors | 5 |
| C: Context | Social | ||
| D: Experience | Family physicians and nurses | ||
| G: Sustainability | Integrated into existing services | ||
| I: Resources | Costs of care are covered by medical insurance and in some cases by social welfare arrangements | ||
| Abramson et al. 1981157 | A: Motivation | Control of cardiovascular disease risk factors | 6 |
| C: Context | Social | ||
| D: Experience | Family physicians and nurses | ||
| G: Sustainability | Integrated into existing services | ||
| I: Resources | Costs of care are covered by medical insurance and in some cases by social welfare arrangements | ||
| J: Differential effects | Sex | ||
| Buchholz et al. 2012155 | A: Motivation | Reduce obesity in medically uninsured adults | 6 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social – health care led | ||
| D: Experience | Registered nurses, nurse practitioner researcher | ||
| F: Delivery fidelity | Selected visits were observed to assess for fidelity; attendance of session reported (only 19% attended all sessions) | ||
| I: Resources | Six monthly 30-minute sessions; pedometers and food diaries; US$5 food vouchers per session; reminder telephone calls and telephone calls and letters to reschedule missed appointments; registered nurse | ||
| Gardner et al. 2012143 | A: Motivation | To improve health in disadvantaged populations | 7 |
| B: Theory | Control theory, health action process approach and social cognitive theory | ||
| C: Context | Social – health service led | ||
| D: Experience | Team of health psychologists designed and developed the intervention and provided long-term support. Health trainers were lay community members with appropriate training | ||
| G: Sustainability | Incorporated into existing services (and continues to be) | ||
| I: Resources | Majority of health trainers operate in a paid role (58%) but a considerable proportion are voluntary | ||
| J: Differential effects | SES, ethnicity, duration of the NHS HTS, health trainer–client ethnicity match, baseline scores of outcome variables (including BMI) | ||
| Gofin et al. 1986158 | A: Motivation | Control of cardiovascular disease risk factors | 6 |
| C: Context | Social | ||
| D: Experience | Family physicians and nurses | ||
| G: Sustainability | Integrated into existing services | ||
| I: Resources | Costs of care are covered by medical insurance and in some cases by social welfare arrangements | ||
| J: Differential effects | Sex | ||
| Jackson et al. 2007147 | A: Motivation | Reduce obesity | 8 |
| B: Theory | Jayne Felgen’s I2E2 model232 | ||
| C: Context | Social – health care led | ||
| D: Experience | Specialist health visitor | ||
| E: Consultation | Partnership approach – focuses on building a therapeutic relationship between the health visitor and the participant rather than weight loss per se | ||
| G: Sustainability | Integrated into existing health service | ||
| H: Stakeholder support | Overall, participants found the intervention acceptable both in terms of content and in terms of delivery | ||
| I: Resources | 1-hour initial session followed by biweekly 20-minute consultations; health visitor | ||
| Marshall et al. 201143 | A: Motivation | Improve health (general) | 5 |
| C: Context | Social – health service led | ||
| D: Experience | Registered nurses | ||
| G: Sustainability | Integrated into existing service – clinics grew locally from the work happening within the general practice | ||
| I: Resources | Registered nurses; clinic time not reported | ||
| Morrison et al. 2012141 | A: Motivation | Reduce the prevalence of obesity | 7 |
| B: Theory | Cognitive–behavioural approaches | ||
| C: Context | Social – health service led | ||
| D: Experience | Dietitians, psychologists and physiotherapists | ||
| G: Sustainability | Integrated into existing health service | ||
| I: Resources | Nine fortnightly sessions delivered by dietitian with referral to psychologist if/when required. Group rather than individual sessions – more likely to be cost-effective | ||
| J: Differential effects | Age, gender, baseline BMI and SES explored | ||
| Schuit et al. 2006140 | A: Motivation | Cardiovascular disease prevention | 3 |
| C: Context | Social | ||
| J: Differential effects | Gender and high/low SES | ||
| Verheijden et al. 2012156 | A: Motivation | Focus on weight control by promotion of energy balance behaviour and physical activity | 5 |
| C: Context | Social | ||
| G: Sustainability | No – too expensive | ||
| I: Resources | ≈€850,000 | ||
| J: Differential effects | Favourable short-term effects on food choice attention among low-SES participants and long-term effects on BMI in non-Dutch participants (for those who reported exposure to mass media campaigns), although effects are small | ||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (total n = 4) | ||||||
| Nutrition-only interventions (n = 1) | ||||||
| Baron et al. 1986189 | RCT 1 year of follow-up Final sample: 119 Quality: Strong |
Diet clubs, UK Age: 16–70 years 85% female Overweight |
Treatment: Diet clubs with weekly group meetings that followed either a low-carbohydrate diet or a low-fat/high-fibre diet (both ≈1000–1200 kcal per day) Implementation: 5 |
Gradient: Explored diet effects by social class | Body weight | ↔ |
| Low-carbohydrate diet more effective than low-fat/high-fibre diet in lower-SES group at 3 months but this effect not observed at 1 year | ||||||
| Physical activity-only interventions (n = 1) | ||||||
| Neumark-Sztainer et al. 1995188 | RCT 7 months’ follow-up Final sample: 24 Quality: Weak |
Health centre, Israel Age: 25–50 years 100% female Obese |
Treatment: The addition of an exercise component to a weight loss programme (run as part of the CHAD programme); 1 hour per week exercise training and home exercise guidance Implementation: 7 |
Gradient: Explored occupation status as predictor of intervention success | Weight loss | ↓ |
| No difference in weight loss between employed and non-employed in intervention group (but employed lost more weight than unemployed in active control) | ||||||
| Nutrition and physical activity interventions (n = 2) | ||||||
| Wing and Jeffery 1999186 | RCT 10 months’ follow-up Final sample: 136 Quality: Strong |
Setting unclear, USA Age: 22–55 year olds ≈50% female |
Treatment: 4-month treatment with/without social support; 16 weekly group meetings led by a behaviour therapist, a nutritionist or both; individual weigh-in; review of self-monitoring records; lecture or discussion period; problem-solving, assertion, stimulus control, developing social support, dealing with high-risk situations, cognitions and strategies for long-term maintenance Implementation: 5 |
Gradient: Reported effects by employment status | Weight (participants recruited with friends – social support but only significant months 0–4) | ↓ |
| Employment did not affect overall weight loss | ||||||
| van Wier et al. 2009187 | RCT (three arms: telephone, internet and control) 6 months’ follow-up Final sample: 982 (intention to treat) Quality: Moderate |
Work settings (MN, USA) Overweight employees with BMI ≥ 25 kg/m2 Mean age: 43 years 65.1–69.5% female |
Treatment: Three-arm RCT. Two arms received a 6-month lifestyle intervention with behaviour counselling by either telephone (telephone group) or e-mail (internet group). The third arm received usual care in the form of lifestyle brochures (control group); 10 biweekly counselling sessions by telephone and e-mail Implementation: 6 |
Gradient: Subgroup analysis by education | Telephone group | |
| Body weight | ↓ | |||||
| Waist circumference | ↓ | |||||
| Physical activity | ↓ | |||||
| Fat intake | ↓ | |||||
| Fruit intake | ↔ | |||||
| Vegetable intake | ↔ | |||||
| Internet group | ||||||
| Body weight | ↓ | |||||
| Waist circumference | ↓ | |||||
| Physical activity | ↔ | |||||
| Fat intake | ↔ | |||||
| Fruit intake | ↔ | |||||
| Vegetable intake | ↔ | |||||
| Education had no effect on the intervention | ||||||
| Observational studies (n = 12) | ||||||
| Nutrition-only interventions (n = 1) | ||||||
| Veloso and Santana 2002,163 Veloso et al. 2007162 | Retrospective cohort group with non-randomised comparison group > 1 year of follow-up Final sample: 10,368 Quality: Weak |
Workplaces, Brazil Working age 22% female |
Prevention: Workers’ Food Program (PAT) – coupons or food provided in workplace; recommends main meals of 1400 calories and minor meals of 300 calories, and 6% protein Implementation: 5 |
Gradient: Explored intervention effects compared with comparison group in SES subgroups | Body weight | ↑ |
| Prevalence of overweight | ↑ | |||||
| Food programme increased weight and the prevalence of overweight in low-SES workers but not high-SES workers | ||||||
| Physical activity-only interventions (n = 1) | ||||||
| Freak-Poli et al. 2011194 | Prospective cohort study 4 months’ follow-up Final sample: 604 Quality: Moderate |
Ten workplaces, Australia Mean age ≈40 years 57% female |
Prevention: Pedometer-based workplace health intervention – target of at least 10,000 steps per day for 125 days; weekly encouragement e-mails; website for logging daily steps, accessing additional health information, communication among participants and comparing team progress Implementation: 6 |
Gradient: Explored educational differences | Waist circumference | ↓ |
| Between baseline and the 4-month follow-up, participants who had completed tertiary education at baseline had a 2.1 cm larger reduction in waist circumference than participants who had not completed tertiary education at baseline | ||||||
| Nutrition and physical activity-only interventions (n = 10) | ||||||
| Hwang et al. 2011173 | Prospective cohort study 3 months’ follow-up Final sample: 62 Quality: Weak |
Electronics company in Korea High BMI workers (> 27 kg/m2) Mean (SD) age: 33.6 (7.4) years 88.4% male |
Treatment: 3-month incentive-based obesity management programme (Turn Fat into Gold) – each participant awarded one gold medal for each kilogram of body fat lost; counselling by factory nurses, self-help group, free gym facilities, trainers and health information; health information by e-mail Implementation: 6 |
Gradient: Explored occupation (office vs. factory workers) | BMI | ↓ |
| Body weight | ↓ | |||||
| Body fat | ↓ | |||||
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Cholesterol | ↓ | |||||
| Exercise | ↑ | |||||
| Night eating | ↔ | |||||
| Dining together | ↔ | |||||
| Drinking | ↔ | |||||
| Similar significant effects for both office and factory workers except that diastolic BP and exercise changed significantly only in factory workers | ||||||
| Jeffery et al. 1984175 | Uncontrolled before-and-after study 2 years’ follow-up Final sample: 81 Quality: Moderate |
Setting unclear, USA Mean age: 53 years 100% male Obese |
Treatment: 15-week behavioural programme – weekly group meetings, financial contracts for weight reduction, diet and exercise instruction and behavioural skills training Implementation: 5 |
Gradient: Explored occupation and education as predictors of weight loss | Body weight | ↓ |
| Education and occupation were not predictors of weight loss | ||||||
| Jeffery et al. 1985191 | Uncontrolled before-and-after study 6 months’ follow-up Final sample: 34 Quality: Moderate |
Workplace, USA 86% female Mean age: 42 years |
Treatment: Payroll-based incentive plan – US$5 minimum deduction from bimonthly pay check, repaid to participant if met weight loss goals; weigh-ins; group education sessions – diet, physical activity and modification of social and environmental factors; weight loss manual; monitoring of diet intake Implementation: 5 |
Gradient: Results reported for different occupation categories | Body weight | ↓ |
| No differences in weight lost or percentage reaching goal between occupation categories: faculty, professional/technical, secretary/clerical | ||||||
| Kliche et al. 2011161 | Uncontrolled before-and-after study 3 months’ follow-up Final sample: 718 Quality: Weak |
Health insurance courses, Germany Age: 19–68 years 80% female |
Prevention: Health promotion training courses run by three major German health insurers: one that focused on increasing physical activity, one that focused on nutrition and one that focused on stress Implementation: 6 |
Gradient: Education explored as a confounder | BMI | ↓ |
| Physical activity | ↑ | |||||
| Diet behaviour | ↑ | |||||
| Education had no effect on the overall intervention effects | ||||||
| Lloyd and Khan 2011192 | Prospective cohort (uncontrolled before-and-after) study 12 weeks’ follow-up Final sample: 2456 Quality: Moderate |
Health-care settings, UK Age: 18–91 years 87% female BMI: ≥ 28 kg/m2 |
Treatment: Commercial weight loss programme commissioned by health service (Weight Watchers or Slimming World) –12 weekly group-based sessions; practical advice and guidance for weight loss Implementation: 7 |
Gradient: SES of successful vs. unsuccessful participants | Body weight | ↓ |
| No differences in number successful (> 5% weight loss) and number unsuccessful between deprivation quintiles | ||||||
| Lowe et al. 2001196 | Retrospective (uncontrolled) cohort study 1–5 years’ follow-up Final sample: 1002 Quality: Weak |
Community venues, USA Age: Majority 35–54 years 96% female Overweight |
Treatment (maintenance phase): Commercial weight loss programme (Weight Watchers) – weekly group meetings; food, physical activity and behaviour modification plans; educational materials; role model, peer leader; social support; weigh-ins; goal-setting Implementation: 7 |
Gradient: Relationship between employment status and weight gain explored | Employment status did not predict weight gain | |
| Mattfeldt-Beman et al. 1999195 | Uncontrolled before-and-after study 18 months’ follow-up Final sample: 281 Quality: Weak |
Clinical centres, USA Age: 30–54 years 27% female Mild obesity |
Treatment: Weight loss programme delivered by multidisciplinary team; 14 weekly 90-minute group sessions, contact at least once a month up to 18 months. Focused on self-management of energy intake, exercise and individually set behaviour goals Implementation: 7 |
Gradient: Education status of those successful and those unsuccessful | There were no significant differences in education status between those who were successful, those who relapsed and those who were unsuccessful | |
| Merrill et al. 2008190 | Uncontrolled before-and-after study 18 months’ follow-up Final sample: 211 Quality: Moderate |
Community settings, USA Age: ≥ 18 years 70% female |
Prevention: Coronary Health Improvement Project (CHIP) – 4-week health education course including topics on diet, physical activity and cardiovascular disease and risk factors; preset dietary and exercise goals were encouraged Implementation: 7 |
Gradient: Explored relationship between family income, education and employment status and weight loss | BMI | ↓ |
| Systolic BP | ↔ | |||||
| Diastolic BP | ↔ | |||||
| Total cholesterol | ↔ | |||||
| LDL cholesterol | ↓ | |||||
| HDL cholesterol | ↑ | |||||
| Triglycerides | ↔ | |||||
| Glucose | ↔ | |||||
| Only change in glucose associated with SES – more favourable effects for those not employed | ||||||
| Rohrer et al. 2010172 | Retrospective cohort study 6 months’ follow-up Final sample: 936 Quality: Weak |
Workplace, USA Age: 18+ years Adult employees 64.1% male |
Prevention: Telephone coaching programme. Coaches called participants up to seven times. Coaching was based on collaborative goal-setting and included self-management health education Implementation: 6 |
Gradient: Explored education and income in subgroup analysis | Body weight change | ↓ |
| Weight loss did not differ significantly by income. There was a tendency for more weight loss in less educated groups but this was not statistically significant | ||||||
| Stunkard et al. 1989193 | Prospective cohort (uncontrolled before-and-after) study 12 weeks’ follow-up Final sample: 1146 Quality: Weak |
Fifteen workplaces, USA Age: 38 years 52% female Overweight |
Treatment: Workplace weight loss competitions – weekly weigh-ins; weight loss advice; team-mate support; public awareness of progress; cash incentive for winning team Implementation: 6 |
Gradient: Blue-collar vs. white-collar employees | Body weight No association between work type and weight loss, and similar percentages of blue-collar and white-collar employees meeting goals in subsample |
↓ |
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 24) | ||||||
| Nutrition-only interventions (n = 5) | ||||||
| Auslander et al. 2000176 | RCT 3 months’ follow-up Final sample: 239 Quality: Strong |
Community, USA Age: 25–55 years 100% female Obese |
Treatment: Eat Well Live Well (EWLW) health promotion intervention – peer education focusing on nutrition skills tailored to individuals’ stage of change; social support from group sessions Implementation: 9 |
Disadvantage: Low-income African American women | BMI | ↔ |
| Body weight | ↔ | |||||
| Fat intake | ↓ | |||||
| Cullen et al. 2009209 | RCT 4 months’ follow-up Final sample: 558 Quality: Moderate |
Expanded Food and Nutrition Education Program (EFNEP) classes, USA Mean age: 35 years 97% female |
Prevention: Modified Texas EFNEP vs. usual EFNEP. Six education sessions with the addition of videos to promote guided discussion and problem-solving; weekly goal-setting and goal review; new handouts Implementation: 8 |
Disadvantage: Low-income families | BMI | ↔ |
| Dietary intake | ||||||
| Energy | ↔ | |||||
| Fat | ↔ | |||||
| Saturated fat | ↔ | |||||
| Fibre | ↔ | |||||
| Fruit and 100% juice | ↔ | |||||
| Vegetables | ↔ | |||||
| Whole milk | ↔ | |||||
| 2% fat milk | ↔ | |||||
| Low-fat/fat-free milk | ↔ | |||||
| Sweetened beverages | ↔ | |||||
| Water | ↔ | |||||
| Faucher 2008,225 Faucher and Mobley 2010183 | RCT 5 months’ follow-up Final sample: 19 Quality: Strong |
Community centre, USA Mean age: 35 years 100% female BMI ≥ 25 kg/m2, obese |
Treatment: Weight loss pilot study – nutritional intervention aimed at portion control; culturally sensitive and foods prepared in a culturally/economically specific way for low-income Mexican American families Implementation: 8 |
Disadvantage: Low SES by income | Weight loss | ↓(CS) |
| Howard-Pitney et al. 1997210 | RCT 19 weeks’ follow-up Final sample: 242 Quality: Strong |
Community setting, USA Mean age: 31 years 85% female |
Prevention: SNAP – 20-month classroom-based intervention; nutrition education (appropriate for low-literacy, low-income and Hispanic population); topics included the major sources of dietary fat including meat, dairy foods, desserts, snacks and solid and liquid fats, the food guide pyramid, food label reading and low-fat eating when away from home; 12-week maintenance period with six contacts Implementation: 7 |
Disadvantage: Low SES | BMI | ↔ |
| Dietary fat | ↓ | |||||
| Saturated fat | ↓ | |||||
| Blood cholesterol | ↔ | |||||
| Reid et al. 1995211 | RCT 6 months’ follow-up Final sample: 149 Quality: Strong |
Community health centre, Australia Mean age: 41 years ≈40% female |
Prevention: Group counselling sessions lasted 1.5–2 hours and were conducted in small groups by a trained community health nurse; covered smoking cessation, dietary modification and non-pharmacological lowering of BP; emphasis on reduction of saturated fat intake; practical advice on cooking and shopping; session attendance with partners encouraged Implementation: 6 |
Disadvantage: Low-SES area | Weight | ↔ |
| Physical activity | ↑ | |||||
| Systolic BP | ↔ | |||||
| Diastolic BP | ↔ | |||||
| Dietary intake (alcohol) | ↔ | |||||
| Physical activity-only interventions (n = 3) | ||||||
| Alves et al. 2009212 | RCT 6 months’ follow-up Final sample: 146 Quality: Moderate |
Grounds of local church, Brazil Age: 20–60 years 100% female BMI: ≥ 25 kg/m2 |
Treatment: Three 50-minute exercise sessions each week for 6 months incorporating aerobic moderate-intensity physical activity and supervised by physical education instructor Implementation: 4 |
Disadvantage: Residents of a disadvantaged area | BMI | ↓ |
| Body weight | ↓ | |||||
| Grandjean et al. 1996174 | RCT 24 weeks’ follow-up Final sample: 37 Quality: Moderate |
Workplace, USA 100% female Sedentary |
Prevention: Workplace exercise programme – walking, jogging, cycling or a combination at least 3 days per week for 24 weeks (individualised exercise prescription) carried out at workplace fitness facility Implementation: 3 |
Disadvantage: Blue-collar employees | Weight | ↓ |
| % body fat | ↓ | |||||
| Aerobic fitness | ↑ | |||||
| Total cholesterol | ↔ | |||||
| HDL cholesterol | ↔ | |||||
| LDL cholesterol | ↔ | |||||
| Triglycerides | ↔ | |||||
| Wilbur et al. 2008180 | Cluster RCT (no. of clusters not described) 48 weeks’ follow-up Final sample: 143 Quality: Weak |
Community health centres, USA Age: 40–65 years 100% female |
Prevention: Walking programme: 24-week intensive adoption phase, 24-week maintenance phase; tailored walking prescription, health information, problem-solving and goal-setting; workshops/group sessions and follow-up telephone contact Implementation: 5 |
Disadvantage: Moderate- to low-income African American women | BMI | ↔ |
| Waist circumference | ↓ | |||||
| Physical activity | ↔ | |||||
| Aerobic fitness | ↑ | |||||
| Nutrition and physical activity interventions (n = 16) | ||||||
| Befort et al. 2008230 | Randomised controlled pilot study 16 weeks’ follow-up Final sample: 33 Quality: Strong |
Community health centre, USA Age: ≥ 18 years 100% female Obese (BMI 30–50 kg/m2) |
Treatment: Culturally appropriate behavioural weight loss programme (BWLP) plus motivational interviewing vs. BWLP plus health education. BWLP included calorie-reduced diet, self-monitoring and food and physical activity guidance Implementation: 6 |
Disadvantage: Lower-income African American women | Body weight | ↔ |
| BMI | ↔ | |||||
| Energy intake | ↔ | |||||
| Fat intake | ↔ | |||||
| Fruit and vegetable intake | ↔ | |||||
| Physical activity | ↔ | |||||
| Campbell et al. 2002199 | Cluster RCT (nine clusters, two arms; four clusters in intervention group, five in delayed intervention group) 18 months’ follow-up Final sample: 538 Quality: Strong |
Nine worksites, USA No mean age provided 100% women |
Prevention: Health Works for Women – two strategies: (1) individualised computer-tailored health messages combined with health behaviour change theory, communication theory, social marketing and new technology; (2) a natural helpers programme at the workplace (lay health advisor) designed to affect behavioural and social change through the ‘natural’ social networks of individuals Implementation: 5 |
Disadvantage: Low-SES workplaces | BMI | |
| Fruit/vegetable intake | ↑ | |||||
| Fat intake (after 6 months only) | ↓ | |||||
| Strengthening and flexibility exercise | ↑ | |||||
| Chang et al. 2010169 | RCT 8 months’ follow-up Final sample: 38 Quality: Weak |
Special Supplemental Nutrition Program for Women, Infants, and Children sites, USA 18–34 years 100% female (mothers) |
Treatment: 10-week, theory-based, culturally sensitive intervention messages were delivered via a series of five chapters on a DVD and complemented by five peer support group teleconferences Implementation: 7 |
Disadvantage: Low SES | Body weight | ↔ |
| Cousins et al. 1992,182 Foreyt et al. 1991184 | RCT 1 year of follow-up Final sample: 86 Quality: Moderate |
Community, USA Age: 18–45 years 100% female 20–100% above ideal body weight |
Treatment: Culturally sensitive family-based weight loss programme: Cuidando el Corazon – 24 weekly classes and 6 monthly classes taught by bilingual registered dietitians; low-fat eating plan, nutrition information, recipes, exercise plan and behaviour modification strategies Implementation: 4 |
Disadvantage: Low-income and education Mexican American women | Body weight | ↓ |
| BMI | ↓ | |||||
| Dennison et al. 1996170 | Controlled (quasi-experimental) trial 1 year of follow-up Final sample: 30 Quality: Weak |
Two workplaces, USA Age: 47 years 10% female 20–35% over ideal weight |
Treatment: Weigh to Go programme – nutrition information; computerised food intake and activity analysis and feedback; personal guidelines; incentives for weight loss (t-shirts, lunch bags, books) Implementation: 6 |
Disadvantage: Blue-collar workers | Weight loss | ↓(CS) |
| Energy intake | ↔ | |||||
| Polyunsaturated fatty acid intake | ↓ | |||||
| Monounsaturated fatty acid intake | ↓ | |||||
| Saturated fatty acid intake | ↓ | |||||
| Protein intake | ↔ | |||||
| Fibre intake | ↔ | |||||
| Carbohydrate intake | ↔ | |||||
| Sodium intake | ↔ | |||||
| Erfurt et al. 1991171 | Cluster RCT (four clusters, four arms; one cluster per arm) 3 years’ follow-up Final sample: 1883 (effect size results based on 809 – overweight group only) Quality: Strong |
Four workplaces, USA Age: 39–43 years Predominantly male |
Prevention: Workplace Wellbeing interventions – four levels: screening only (control) vs. screening + health education (A) vs. screening + health education + follow-up counselling (B) vs. screening + health education + follow-up counselling + organised activities (C) Implementation: 6 |
Disadvantage: Manufacturing worksites (predominantly blue-collar employees) | Body weight: | |
| All overweight employees (n = 690) | ||||||
| Intervention A | ↔ | |||||
| Intervention B | ↔ | |||||
| Intervention C | ↓ | |||||
| Participants in the weight loss interventions (n = 238) | ||||||
| Intervention A | ↔ | |||||
| Intervention B | ↓ | |||||
| Intervention C | ↓ | |||||
| Janicke et al. 2011103 | RCT 9 months’ follow-up Final sample: 33 Quality: Moderate |
Setting unclear, USA Age: 40.1 years Parents/caregivers of overweight or obese children |
Prevention: Family-based weight-management programme targeting children – diet, physical activity and behaviour management education; diet and physical activity monitoring; group support and problem-solving Implementation: 6 |
Disadvantage: Participants enrolled in Medicaid programme | Body weight | ↔ |
| Kain et al. 200965 | Non-randomised controlled pilot study 5 months’ follow-up Final sample: 57 Quality: Weak |
Workplaces (schools), Chile Teachers Age/sex not reported |
Prevention: Teacher intervention: three 15-minute counselling sessions on healthy eating and physical activity, plus goal-setting with nutritionist Implementation: 6 |
Disadvantage: Medium- to low-SES area | BMI | ↓ |
| Waist circumference | ↓ | |||||
| Total and HDL cholesterol | ↔ | |||||
| Triglycerides | ↔ | |||||
| Kain et al. 201066 | Non-RCT 2 years’ follow-up Final sample: 47 Quality: Weak |
Workplaces (schools), Chile Teachers Age/sex not reported |
Prevention: Teacher intervention: three 15-minute counselling sessions on healthy eating and physical activity, plus goal-setting with nutritionist Implementation: 6 |
Disadvantage: Medium- to low-SES area | BMI | ↔ |
| Waist circumference | ↔ | |||||
| Physical activity | ↑ | |||||
| Glucose | ↓ | |||||
| Total cholesterol | ↔ | |||||
| LDL cholesterol | ↔ | |||||
| HDL cholesterol | ↑ | |||||
| Triglycerides | ↔ | |||||
| Kisioglu et al. 2004197 | RCT 6 months’ follow-up Final sample: 400 Quality: Strong |
Setting unclear, Turkey 34.1 years 100% women |
Prevention: Health training support, nutrition educational material; encouragement to participate in the ongoing education programme. One to three intervention programmes were conducted per day over 25 days Implementation: 6 |
Disadvantage: Low SES | BMI Nutrition Physical activity BP |
↓ ↑ ↑ ↔ |
| Krummel et al. 2010166 | Randomised controlled pilot trial 1 year of follow-up Final sample: 64 Quality: Weak |
Women, Infants, and Children offices and churches, USA Age: > 18 years 100% female |
Treatment/prevention: Mothers’ Overweight Management Study (MOMS) – counselling session with dietitian; goals for eating, physical activity and other aspects of weight management; monthly newsletters; 10 facilitated discussion group sessions; monthly personalised feedback on self-monitoring records for nutrition and physical activity behaviours Implementation: 8 |
Disadvantage: Low-SES mothers (participants of Special Supplemental Nutrition Program for Women, Infants, and Children) | Body weight | ↔ |
| BMI | ↔ | |||||
| Waist circumference | ↔ | |||||
| Energy intake | ↔ | |||||
| Fat intake | ↔ | |||||
| Fibre intake | ↔ | |||||
| Physical activity | ↔ | |||||
| Nichols 1995179 | RCT 12 weeks’ follow-up Final sample: 37 Quality: Moderate |
University, USA Age: 24–72 years 100% female BMI ≥ 25 kg/m2 or 20% above ideal body weight |
Treatment: Weight loss programme delivered by trained facilitator with similar cultural preference; 12 weekly sessions including diet, physical activity and health education; behavioural strategies; monetary incentives; and group support Implementation: 6 |
Disadvantage: Low-income African American women | BMI | ↓ |
| Body weight | ↓ | |||||
| Waist circumference | ↓ | |||||
| Hip circumference | ↓ | |||||
| Waist-to-hip ratio | ↔ | |||||
| Saturated fat | ↓ | |||||
| Total fat | ↓ | |||||
| Moderate physical activity | ↑ | |||||
| Hard physical activity | ↑ | |||||
| Very hard physical activity | ↔ | |||||
| BP | ↔ | |||||
| Cholesterol | ↓ | |||||
| Fasting blood glucose | ↔ | |||||
| Ockene et al. 2012198 | RCT 1 year of follow-up Final sample: 288 Quality: Strong |
Lawrence, MA, USA Most study activities held in the Lawrence Senior Centre Mean age: 51.37–52.37 years 72.22–76.67% female |
Prevention: Lawrence Latino Diabetes Prevention Program (LLDPP) – lifestyle intervention for weight loss and diabetes risk reduction. Community-based, literacy-sensitive and culturally tailored intervention. Included three individual and 13 group counselling sessions (between 0.5 and 1.5 hours) over a 12-month period Implementation: 9 |
Disadvantage: Low-SES area | Weight | ↓ |
| BMI | ↓ | |||||
| Physical activity | ↔ | |||||
| Dietary intake (fat) | ↓ | |||||
| HbA1c | ↓ | |||||
| Olvera et al. 2010167 | RCT 12 weeks’ follow-up Final sample: 35 Quality: Strong |
Community locations, USA Mean age: ≈35 years 100% female (mothers) |
Prevention: Healthy lifestyle intervention (Behavior Opportunities Uniting Nutrition, Counseling, and Exercise; BOUNCE) – 12-week intervention: three 45-minute structured group aerobic or sports sessions or free-play recreational activities per week; two 45-minute nutrition sessions per week; one 45-minute behavioural counselling session per week Implementation: 7 |
Disadvantage: Low-income women | BMI | ↔ |
| Physical activity | ↔ | |||||
| Rickel 2008200 | RCT 12 months’ follow-up Final sample: 224 Quality: Strong |
Cooperative Extension Service offices, USA Age: 50–75 years 100% female BMI ≥ 30 kg/m2 |
Treatment: Extended care after a culturally tailored lifestyle intervention – contact twice per month, face-to-face vs. telephone vs. education only (newsletters) control Implementation: 8 |
Disadvantage: Counties with low levels of educational attainment and low household incomes (African American and Caucasian) | Body weight Caucasians | ↓ |
| Body weight African Americans | ↔ | |||||
| Both intervention conditions vs. control (no differences in weight change between intervention groups) | ||||||
| Walker et al. 2012168 | RCT 13 weeks’ follow-up Finale sample: 50 Quality: Moderate |
Community settings: Family or school-based clinics, USA Age: 24.6 years 100% women Overweight, post-partum women |
Treatment: 13-week school-based clinics – topics included improved eating patterns, portion sizes (MyPyramid), choices when eating out and shopping, cooking methods, increasing fruit and vegetable intake, identifying and managing mindless eating, personal barriers to and benefits of weight loss, and increasing physical activity Implementation: 8 |
Disadvantage: Low SES | Weight | ↔ |
| Health Behaviour Inventory (including physical and activity and nutrition) | ↔ | |||||
| Observational studies (n = 20) | ||||||
| Nutrition-only interventions (n = 1) | ||||||
| Zuber et al. 1992160 | Uncontrolled before-and-after study 1 year of follow-up Final sample: 372 Quality: Moderate |
Health insurance programme, Germany Age: 15–76 years 86% female 20% over ideal weight |
Treatment: Health insurance programme – 24 group sessions over 6 months, follow-up of four after-care sessions within a year; goal-setting, group support, nutrition, medicine and dietetic education/advice and monitoring; psychological concepts Implementation: 7 |
Disadvantage: Majority of participants of low to medium or low SES | Body weight | ↓ |
| Prevalence of overweight | ↓ | |||||
| Physical activity-only interventions (n = 3) | ||||||
| Carlin 2009214 | Uncontrolled prospective cohort study 6 months’ follow-up Final sample: 66 Quality: Weak |
Community fitness centres, USA Age: ≥ 40 years 100% female |
Prevention: Community fitness centre attendance – access to convenient, safe and pleasant fitness centres with fully-equipped gyms and personal trainers; US$20 per member per month participation fee; individual fitness assessments and personalised exercise plan based on participants’ personal goals and fitness level Implementation: 8 |
Disadvantage: Communities that are disadvantaged, underinsured or uninsured | Body weight | ↓ |
| Clark et al. 2003213 | Cohort study 1 year of follow-up Final sample: 73 Quality: Weak |
Community settings (church and community centre), USA Age: > 50 years 100% women |
Prevention: Exercise classes – 20 minutes chair-based or standing leg and arm movements and up to 30 minutes of indoor walking. Participants were encouraged to attend at least three exercise classes per week Implementation: 5 |
Disadvantage: Low SES | Weight | ↓ |
| BMI | ↓ | |||||
| Hip circumference | ↓ | |||||
| Abdominal circumference | ↔ | |||||
| Thigh circumference | ↔ | |||||
| Arm circumference | ↔ | |||||
| Waist circumference | ↓ | |||||
| Triceps skinfold thickness | ↓ | |||||
| Abdomen skinfold thickness | ↔ | |||||
| Suprailiac skinfold thickness | ↔ | |||||
| Body fat | ↔ | |||||
| Physical activity | ↑ | |||||
| Zoellner et al. 2007,181 2010231 | Prospective cohort study 6 months’ follow-up Final sample: 66 Quality: Moderate |
Community setting, USA Mean age: 44 years 98% females |
Prevention: ‘Fit for life’ steps intervention – pedometer based; encouraged to exercise 10,000 steps per day but instructed to set realistic and personalised weekly goals; walking teams led by coaches; monthly educational sessions Implementation: 6 |
Disadvantage: Low-SES area | BMI | ↔ |
| Waist circumference | ↓ | |||||
| Body fat | ↔ | |||||
| Steps per day | ↔ | |||||
| Activity classification | ↔ | |||||
| BP | ↓ | |||||
| Fasting total cholesterol | ↔ | |||||
| HDL cholesterol | ↑ | |||||
| LDL cholesterol | ↔ | |||||
| Triglyceride | ↔ | |||||
| Glucose | ↔ | |||||
| Nutrition and physical activity interventions (n = 16) | ||||||
| Balcazar et al. 2009202 | Prospective cohort study 12 months’ follow-up Final sample: 85 Quality: Moderate |
Community based in health-care settings (US–Mexico border) Age/sex not clearly reported |
Prevention: Salud para su Corazón – Educational programme with eight lessons (group delivery). Educational sessions were delivered several times per week, once per week or every other week for a total intervention period of 2–3 months Implementation: 8 |
Disadvantage: Low SES | BMI | ↔ |
| Waist circumference | ? | |||||
| Weight | ? | |||||
| LDL cholesterol | ↓ | |||||
| HDL cholesterol | ↔ | |||||
| HbA1c | ↔ | |||||
| Systolic BP | ↔ | |||||
| Diastolic BP | ↔ | |||||
| Triglycerides | ↓ | |||||
| Christiansen et al. 2007201 | Retrospective cohort follow-up study 4 years’ follow-up Final sample: 99 Quality: Weak |
Weight loss camp, Denmark Age: 32.9 years 72.3% female Severely obese |
Treatment: Weight loss camp with a focus on physical activity. Intervention included a diet and exercise programme (group-based exercise). Intervention lasted 21 weeks (mean) Implementation: 7 |
Disadvantage: Low SES by income | Weight loss | ↓ |
| Weight maintenance | Yes | |||||
| Clarke et al. 2007164 | Uncontrolled before-and-after study 24 weeks’ follow-up Final sample: 93 Quality: Weak |
Community centres and clinics, USA Age: 18–45 years 100% female (mothers) BMI ≥ 25 kg/m2 |
Treatment: Eight weekly lessons; 30 minutes of physical activity; group discussion; recommendations for physical activity, healthful eating and behaviour modification; goal-setting; and physical activity monitoring Implementation: 7 |
Disadvantage: Low-income mothers | Body weight | ↓ |
| Fernandes et al. 2012185 | Prospective cohort study 12 months’ follow-up Final sample: 92 Quality: Moderate |
Health centre, USA Age: 68.5 years 83.8% female |
Prevention: ‘Healthy heart, healthy family’ curriculum intervention – 2-hour weekly sessions for 11 weeks delivered by community health workers; encouragement to undertake exercise, physical activity and community gardening; after 11 weeks, monthly activities promoting heart-healthy behaviours around themes such as Heart Day, Family Day and Mother’s Day Implementation: 6 |
Disadvantage: Low SES (low-income Filipinos) | BMI | ↔ |
| Waist circumference | ↔ | |||||
| Physical activity | ↑ | |||||
| Healthier dietary intake | ↑ | |||||
| Cholesterol | ↓ | |||||
| LDL cholesterol | ↓ | |||||
| High cholesterol | ↑ | |||||
| Blood glucose | ↓ | |||||
| BP (significant after 6 months but not 12 months) | ↔ | |||||
| Gill 1998203 | Uncontrolled before-and-after study (with a controlled element) 12 months’ follow-up Final sample: 105 Quality: Moderate |
Community venues, USA Age: 17–65 years 100% female BMI 25–40 kg/m2 |
Treatment: Unidos En Salud – weekly 90-minute classes co-led by a bilingual registered dietitian and a behavioural specialist (6 months), followed by weekly support groups run by peer leaders (6 months); included nutrition education, behaviour modification, physical activity and fostering of social support Implementation: 5 |
Disadvantage: Women from a low-income town | Body weight | ↔ |
| Physical activity | ↔ | |||||
| Dietary fat avoidance | ↓ | |||||
| Goldfinger et al. 2008207 | Uncontrolled before-and-after pilot study 1 year of follow-up Final sample: 21 Quality: Moderate |
Community, USA Age: 68 years 81% female BMI ≥ 25 kg/m2 |
Treatment: Project HEAL: Healthy Eating, Active Lifestyles – peer-led weight-management programme; weekly action plans, group feedback and support; key diet and physical activity messages Implementation: 8 |
Disadvantage: Low-income community | Body weight | ↓ |
| Fat intake | ↔ | |||||
| Dietary cholesterol | ↔ | |||||
| Fruit and vegetable intake | ↑ | |||||
| Fast food intake | ↔ | |||||
| Physical activity | ↔ | |||||
| Sedentary time | ↓ | |||||
| BMI | ↓ | |||||
| Gray et al. 2009153 | Prospective cohort (uncontrolled before-and-after) study 12 weeks’ follow-up Final sample: 80 Quality: Weak |
Health-care clinic, UK Age: 24–75 years 100% male Obese |
Treatment: Camelon weight-management group programme – weekly group sessions; Scottish Intercollegiate Guidelines Network and National Institute for Health and Care Excellence guidelines; behavioural modification techniques; promoting physical activity and healthful diet (not energy restriction) Implementation: 6 |
Disadvantage: One of the 20% most deprived communities in Scotland | Body weight | ↓ |
| BMI | ↓ | |||||
| Waist circumference | ↓ | |||||
| Hajek et al. 2010208 | Prospective cohort (uncontrolled before-and-after) study 3 months’ follow-up Final sample: 39 Quality: Weak |
Community centres and hospital, UK 90% female Mean age: 44 years |
Treatment: Weight Action Programme (WAP) – six weekly treatment sessions and two 1-hour follow-up visits; combines standard cognitive–behavioural interventions with structured individually tailored tasks and a group-oriented social support (‘buddy’) system Implementation: 4 |
Disadvantage: Localities of high deprivation | Body weight | ↓ |
| Hugk and Winkelvoss 1985159 | Uncontrolled before-and-after study 1 year of follow-up Final sample: 50 Quality: Weak |
Workplace, Germany Age: 22–67 years 5% female Obese |
Treatment: Outpatient weight reduction programme; individual doctor interviews discussing current behaviours, diet, lifestyle; nutrition and physical activity education; calorie-reduced diet Implementation: 3 |
Disadvantage: Industrial workers | Body weight | ↔ |
| Total cholesterol | ↔ | |||||
| Triglycerides (moulders only) | ↑ | |||||
| Jordan et al. 2008165 | Prospective cohort (uncontrolled before-and-after) study 24 weeks’ follow-up Final sample: 93 Quality: Weak |
Clinics and community centres, USA Age: ≥ 18 years 100% female (mothers) BMI ≥ 25 kg/m2 |
Treatment: Nutrition and physical activity intervention – incorporating recommendations for healthful eating, behaviour modification and physical activity; education; monitoring; counselling; practical skills; behaviour therapy; calorie-prescribed diets; exercise sessions Implementation: 4 |
Disadvantage: Low-income mothers | BMI | ↓ |
| Body fat | ↓ | |||||
| Waist circumference | ↓ | |||||
| Lasco et al. 1989178 | Prospective cohort study 3 months’ follow-up Final sample: 70 Quality: Weak |
Community settings (health clinic, YMCA and a school), USA Age: 18–59 years 100% female Obese |
Treatment: 10-week exercise and nutrition intervention (Community Health Assessment and Promotion Project; CHAPP) – nutrition education; food sampling; healthy cooking demonstrations and recipe sharing; water aerobics, low-impact aerobic dance and walking Implementation: 8 |
Disadvantage: Low SES by income | Weight | ↓ |
| Systolic BP | ↓ | |||||
| Diastolic BP | ↓ | |||||
| Perez-Lizaur et al. 2011204 | Prospective cohort study 3 months’ follow-up Final sample: 452 (+ 22 promotores) Quality: Moderate |
Community and domestic (home) settings, Mexico Age: ≤ 60 years, 56.3% women Age: > 60 years, 43.7% women |
Prevention: Salud para su Corazón – cardiovascular health promotion and disease prevention education programme; 22 health promoters (promotores de salud) delivered the curriculum; 2-hour sessions per week and nine lessons in total in the curriculum; 12-week intervention Implementation: 8 |
Disadvantage: Low SES | Promotores | |
| Physical activity | ↑ | |||||
| Dietary (all) | ↓ | |||||
| Age ≤ 60 years | ||||||
| BMI | ↔ | |||||
| Weight | ↔ | |||||
| Waist circumference | ↔ | |||||
| Physical activity | ↑ | |||||
| Salt and sodium, cholesterol and fat intake | ↓ | |||||
| BP | ↔ | |||||
| Glucose | ↔ | |||||
| Age > 60 years | ||||||
| BMI | ↔ | |||||
| Weight | ↔ | |||||
| Waist circumference | ↔ | |||||
| Physical activity | ↑ | |||||
| Salt and sodium intake | ↓ | |||||
| BP | ↑ | |||||
| Glucose | ↑ | |||||
| Pescatello et al. 2001205 | Prospective controlled cohort study 4 years’ follow-up Final sample: 198 Quality: Weak |
Workplace, USA Mean age: 41 years 87% female |
Prevention: Cardiovascular Health Awareness Program (CHAP) – Annual cardiovascular screens and results counselling (individualised feedback and methods to adopt or maintain healthy lifestyle behaviours); encouragement to participate in formal group education and behavioural support programmes held at the workplace and off site Implementation: 3 |
Disadvantage: Benefit-eligible employees | BMI | ↔ |
| Waist circumference | ↔ | |||||
| Waist-to-hip ratio | ↔ | |||||
| Total cholesterol | ↔ | |||||
| Total/HDL cholesterol ratio | ↔ | |||||
| HDL cholesterol | ↔ | |||||
| LDL cholesterol | ↔ | |||||
| Triglycerides | ↔ | |||||
| Glucose | ↔ | |||||
| BP | ↔ | |||||
| Pescatello et al. 2001205 | Prospective uncontrolled cohort study 4 years’ follow-up Final sample: 278 Quality: Weak |
Workplace, USA Mean age: 41 years 87% female |
Prevention: Cardiovascular Health Awareness Program (CHAP) – annual cardiovascular screens and results counselling (individualised feedback and methods to adopt or maintain healthy lifestyle behaviours); encouragement to participate in formal group education and behavioural support programmes held at the workplace and off site Implementation: 3 |
Disadvantage: Benefit-eligible employees | BMI | ↑ |
| Waist circumference | ↑ | |||||
| Waist-to-hip ratio | ↔ | |||||
| Total cholesterol | ↔ | |||||
| Total/HDL cholesterol ratio | ↓ | |||||
| HDL cholesterol | ↔ | |||||
| LDL cholesterol | ↓ | |||||
| Triglycerides | ↑ | |||||
| Glucose | ↓ | |||||
| BP | ↔ | |||||
| Rickel 2008200 | Uncontrolled before-and-after study 6 months’ follow-up Final sample: 224 Quality: Moderate |
Cooperative Extension Service offices, USA Age: 50–75 years 100% female BMI ≥ 30 kg/m2 |
Treatment: Culturally tailored lifestyle intervention for weight loss – 24 weekly 90-minute group sessions led by interventionists; goal-setting; progress feedback; skills related to cognitive–behavioural self-management, healthful eating behaviours and physical activity practice Implementation: 8 |
Disadvantage: Counties with low levels of educational attainment and low household incomes (African American and Caucasian) | Body weight | ↓ |
| Fitness | ↑ | |||||
| MVPA | ↑ | |||||
| Energy intake | ↓ | |||||
| Saturated fat intake | ↓ | |||||
| BP | ↓ | |||||
| LDL cholesterol | ↓ | |||||
| Triglycerides (Caucasians only) | ↓ | |||||
| C-reactive protein | ↓ | |||||
| HbA1c | ↓ | |||||
| Williams and Wold 2000206 | Prospective cohort (uncontrolled before-and-after) study 1 year of follow-up Final sample: 71 Quality: Weak |
Two workplaces, USA Working age |
Prevention: Mobile nursing cardiovascular risk factor identification programme – screening; individualised education-based interview focused on dietary and physical activity behaviour change; follow-up report and letter Implementation: 6 |
Disadvantage: Workplaces in areas of low-income residents | BMI | ↔ |
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 4) | |||
| Nutrition-only interventions (n = 1) | |||
| Baron et al. 1986189 | A: Motivation | Reduce obesity | 5 |
| C: Context | Social – researcher led | ||
| F: Delivery fidelity | Co-operation of the participants was excellent. The two groups reported contrasting dietary changes. At 3 months those in the low-carbohydrate group decreased their fibre intake and those in the low-fat group increased their fibre intake; consumption of bread and potatoes decreased markedly among the low-carbohydrate group; and consumption of cheese, milk and meat decreased among the low-fat group. After 1 year there were smaller differences between the groups although the difference in dietary fibre intake between the groups remained substantial | ||
| I: Resources | Weekly group meetings; group leaders | ||
| J: Differential effects | SES, age, gender, baseline BMI | ||
| Physical activity-only interventions (n = 1) | |||
| Neumark-Sztainer et al. 1995188 | A: Motivation | Reduce obesity | 7 |
| C: Context | Social – health service led | ||
| D: Experience | Nutritionist, physician and physical education instructor | ||
| F: Delivery fidelity | On average participants completed one-third of the recommended programme. Reported levels of physical activity were higher among the exercise group than among the non-exercise group | ||
| H: Stakeholder support | Programme satisfaction was high | ||
| I: Resources | Weekly group meetings for 3 months; 1-hour exercise session per week; participants paid US$20 for the entire course; nutritionist, physician and physical education instructor | ||
| J: Differential effects | SES, baseline BMI | ||
| Nutrition and physical activity interventions (n = 2) | |||
| Wing and Jeffery 1999186 | A: Motivation | Treatment | 5 |
| C: Context | Social – health care led | ||
| D: Experience | Behaviourist and nutritionist | ||
| I: Resources | Behaviour therapist and nutritionist; meal plans, grocery lists and diaries; balance beam scale and stadiometer | ||
| J: Differential effects | No significant differential effects (gender, employment, social support) | ||
| van Weir et al. 2009187 | A: Motivation | Obesity reduction – weight management (treatment) | 6 |
| B: Theory | Behaviour therapy | ||
| C: Context | Social | ||
| D: Experience | Two dietitians, two movement scientists, and two researchers | ||
| F: Delivery fidelity | 80% of telephone group and 74% of internet group had at least one counselling session | ||
| I: Resources | Pedometers; staff: two dietitians, two movement scientists and two researchers | ||
| Observational studies (n = 12) | |||
| Nutrition only interventions (n = 1) | |||
| Veloso and Santana 2002,163 Veloso et al. 2007162 | A: Motivation | Ensure adequate nourishment for low-income workers | 5 |
| C: Context | Political – part of the National Program of Feeding and Nutrition implemented in response to 67% of the population being calorific deficient (in the 1940s, revised in the 1970s); Workers’ Food Program (PAT) brought into law in 1976 | ||
| G: Sustainability | Existing national programme | ||
| I: Resources | Food coupons or food provided in the workplace | ||
| J: Differential effects | SES, baseline weight status | ||
| Physical activity-only interventions (n = 1) | |||
| Freak-Poli et al. 2011194 | A: Motivation | Chronic disease prevention | 6 |
| C: Context | Social | ||
| F: Delivery fidelity | Lack of assessment and evaluation | ||
| H: Stakeholder support | Global Corporate Challenge | ||
| I: Resources | Pedometers | ||
| J: Differential effects | Education | ||
| Nutrition and physical activity interventions (n = 10) | |||
| Hwang et al. 2011173 | A: Motivation | Treatment | 6 |
| B: Theory | Economic theory | ||
| C: Context | Social and economic | ||
| D: Experience | Nurse | ||
| I: Resources | Gold medal incentives | ||
| J: Differential effects | Office vs. factory workers (SES) | ||
| Jeffery et al. 1984175 | A: Motivation | Reduce obesity in men | 5 |
| C: Context | Social – researcher led | ||
| F: Delivery fidelity | 85% attendance at sessions | ||
| I: Resources | 15-week programme | ||
| J: Differential effects | SES, age, sex | ||
| Jeffery et al. 1985191 | A: Motivation | Improve health in the workplace | 5 |
| C: Context | Social – researcher led | ||
| F: Delivery fidelity | 12% attended fewer than half the weigh-ins | ||
| I: Resources | 6-month programme; bimonthly weigh-ins and group education sessions; weight loss manual and food record; payroll-based incentives (US$5 minimum deduction from bimonthly pay check, repaid to participants when they met weight loss goals) | ||
| J: Differential effects | SES, age, weight status at baseline | ||
| Kliche et al. 2011161 | A: Motivation | Improve health | 6 |
| C: Context | Social | ||
| F: Delivery fidelity | Participants were referred to courses appropriate to their needs – nobody received inappropriate care | ||
| G: Sustainability | Integrated into existing health insurance company practice | ||
| I: Resources | Approximately nine sessions (approximately 10–13 hours) | ||
| J: Differential effects | Age, gender, education | ||
| Lloyd and Khan 2011192 | A: Motivation | Reduce obesity | 7 |
| C: Context | Social – health service led | ||
| D: Experience | Commercial weight loss programme group leaders | ||
| F: Delivery fidelity | Attendance data collected (64% attended ≥ 10 sessions) | ||
| G: Sustainability | Referral to existing commercial weight loss programmes | ||
| I: Resources | Vouchers for 12 weekly sessions of existing commercial weight loss programme | ||
| J: Differential effects | Age, sex, SES, baseline BMI | ||
| Lowe et al. 2001196 | A: Motivation | Reduce obesity | 7 |
| B: Theory | Cognitive restructuring | ||
| C: Context | Social | ||
| D: Experience | Successful programme graduates | ||
| G: Sustainability | Well-established commercial weight-management programme | ||
| I: Resources | Weekly group meetings; written educational materials | ||
| J: Differential effects | Age, employment, sex and marital status | ||
| Mattfeldt-Beman et al. 1999195 | A: Motivation | Prevention of hypertension | 7 |
| C: Context | Social | ||
| D: Experience | Registered dietitians, exercise physiologists and psychologists | ||
| F: Delivery fidelity | Central training and quality control procedures were used to ensure that study guidelines were followed at each of the centres | ||
| H: Stakeholder support | Many of the intervention components were rated as useful by the majority of the participants | ||
| I: Resources | 14 weekly 90-minute group sessions followed by contact at least once a month up to 18 months (included group meetings, brief weigh-ins or individual counselling sessions); registered dietitians, exercise physiologists and psychologists | ||
| J: Differential effects | Explored age, education, race, marital status and gender | ||
| Merrill et al. 2008190 | A: Motivation | Reduce cardiovascular risk factors | 7 |
| B: Theory | Learning theory | ||
| C: Context | Social – researcher led | ||
| F: Delivery fidelity | Mean participation at each session was 89% | ||
| H: Stakeholder support | Formal evaluation revealed that 98% of participants enjoyed the classes | ||
| I: Resources | 4-week programme, four 2-hour classes per week | ||
| J: Differential effects | Explored age, gender, race, marital status, annual family income, education and employment status | ||
| Rohrer et al. 2010172 | A: Motivation | Obesity prevention through weight loss programme | 6 |
| B: Theory | Stages of change model and self-management of care model | ||
| C: Context | Social | ||
| D: Experience | Coaches were not licensed professional counsellors but were trained before the study | ||
| I: Resources | Coaches | ||
| J: Differential effects | Gender, age, race and income explored | ||
| Stunkard et al. 1989193 | A: Motivation | Reduce cardiovascular risk | 6 |
| D: Experience | Intervention planned, co-ordinated and administered by workplace Heart Health Committee with minimal assistance from County Health Improvement Program staff. No professionally trained staff took part in weigh-ins | ||
| E: Consultation | Intervention planned, co-ordinated and administered by workplace Heart Health Committee with minimal assistance from County Health Improvement Program staff | ||
| G: Sustainability | Intervention run by workplace with little assistance from professionals; weigh-ins carried out at lunchtimes (15 minutes of staff time donated by workplaces, 15 minutes donated by staff) | ||
| I: Resources | Cost-effectiveness: US$0.92 per 1% of body weight lost; interventions run by workplace with little assistance from professionals; 16-page manual per participant; posters; incentive (US$5 paid by each participant and US$5 by management); weekly weigh-ins (lunchtimes plus 15 minutes of staff time donated by workplaces, 15 minutes donated by staff) | ||
| J: Differential effects | Occupation type, sex, age | ||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 24) | |||
| Nutrition-only interventions (n = 5) | |||
| Auslander et al. 2000176 | A: Motivation | Reduce risk of non-insulin-dependent diabetes among low-income African American women | 9 |
| B: Theory | Stages of change theory and community organisation theory | ||
| C: Context | Social – collaborative partnership of health professionals and peer educators of a social service agency | ||
| D: Experience | Dietitians, social workers, health educators and trained peer educators | ||
| E: Consultation | Community organisation theory: peer educators assisted in the development and implementation of the programme; a community sponsor/lead agency was selected; neighbourhood ownership and decision-making were facilitated through steering committees of volunteers from the neighbourhood; community values were integrated into the programme; and community empowerment strategies were employed | ||
| F: Delivery fidelity | Process evaluation: sessions were randomly selected for audio-taping and evaluation by two independent raters to determine the degree of content delivered and by a registered dietitian to determine the accuracy of the content; 89–91% of the content was delivered and the accuracy was 89% | ||
| G: Sustainability | Integrated into the community – capacity-building approach | ||
| H: Stakeholder support | Appeared to be well supported | ||
| I: Resources | Six group sessions and six individual sessions over 3 months; dietitians, social workers, health educators and trained peer educators; peer educator training: three half-day sessions per week over 4 months | ||
| Cullen et al. 2009209 | A: Motivation | Prevention of obesity | 8 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social | ||
| D: Experience | Trained paraprofessional teachers | ||
| F: Delivery fidelity | 46 intervention sessions in 29 classes were observed. Fidelity to the class session structure was high (> 80%), except for problem-solving in the final discussion (76%) | ||
| G: Sustainability | Existing programme (running since 1968) | ||
| H: Stakeholder support | Participants reported that a number of the intervention components were useful and staff comments were also very positive | ||
| I: Resources | Six weekly sessions; six 5-minute videos; class binder with handouts and recipes; trained teachers; US$20 for each participant at each data collection session | ||
| Faucher and Mobley 2010183 | A: Motivation | Treatment (weight loss) | 8 |
| B: Theory | Cultural humility framework | ||
| C: Context | Social | ||
| D: Experience | Certified midwife, promotores de salud (lay health advisors), a primary researcher and research assistant | ||
| E: Consultation | Collaboration with promotores de salud | ||
| G: Sustainability | Promotora model – integration into health-care system (through nurse-midwives) | ||
| H: Stakeholder support | University Research Committee and the Dean’s Grant, Baylor University, and the Louise Herrington School of Nursing, Baylor University, TX, USA | ||
| I: Resources | Incentives: fridge magnets, measuring cups, make-up, jewellery, fragrances, shower gels; materials: portion control aids (tennis balls, posters, etc.); staff: listed above | ||
| Howard-Pitney et al. 1997210 | A: Motivation | Prevention of heart disease | 7 |
| B: Theory | Social learning theory | ||
| C: Context | Social | ||
| D: Experience | Professional health educators | ||
| F: Delivery fidelity | Class attendance was high (both intervention and control groups) | ||
| H: Stakeholder support | National Heart, Lung, and Blood Institute (National Institutes for Health) | ||
| I: Resources | Staff | ||
| Reid et al. 1995211 | A: Motivation | Reduction of cardiovascular disease risk factors | 6 |
| C: Context | Social – health care led | ||
| D: Experience | Trained community health nurse | ||
| G: Sustainability | Simple and inexpensive programme that could easily be duplicated in other community health centres | ||
| H: Stakeholder support | Two community health-care centres | ||
| J: Differential effects | No statistically significant differences reported between those with a high level of education and those with a low level of education | ||
| Physical activity-only interventions (n = 3) | |||
| Alves et al. 2009212 | A: Motivation | Reduce obesity in a disadvantaged population | 4 |
| C: Context | Social – researcher led | ||
| D: Experience | Trained physical education instructor | ||
| I: Resources | Three 50-minute exercise sessions each week for 6 months; trained physical education instructor | ||
| Grandjean et al. 1996174 | A: Motivation | Reduce cardiovascular disease risk factors in female employees | 3 |
| C: Context | Social – researcher led | ||
| I: Resources | Workplace fitness facility | ||
| Wilbur et al. 2008180 | A: Motivation | Increase physical activity in African American women | 5 |
| B: Theory | Interaction model of client health behaviour, social cognitive theory and transtheoretical model | ||
| C: Context | Social – researcher led | ||
| F: Delivery fidelity | Walking adherence recorded | ||
| I: Resources | Individualised orientation session, four weekly targeted workshops, weekly telephone calls for 3 weeks, biweekly for 14 weeks and monthly during maintenance phase; African American group facilitator; heart rate monitors, walking logbooks, waist packs, magnets and discount coupons to buy walking shoes; US$50 per participant per data collection point | ||
| Nutrition and physical activity interventions (n = 16) | |||
| Befort et al. 2008230 | A: Motivation | Reduce obesity in African American women | 6 |
| B: Theory | Motivational interviewing | ||
| C: Context | Social – researcher led | ||
| D: Experience | Master’s-level counsellor or dietitian trained by a doctoral-level clinical psychologist | ||
| F: Delivery fidelity | Counselling sessions were audio-taped and 25% of tapes were randomly selected and reviewed during weekly supervision. A standardised checklist was used to rate the extent to which counsellors captured the overall spirit of motivational interviewing and adhered to motivational interviewing strategies | ||
| I: Resources | 90-minute weekly sessions for 16 weeks plus four additional motivational interviewing sessions (two in person, two by telephone); trained counsellor | ||
| Campbell et al. 2002199 | A: Motivation | Improve nutrition and physical activity (prevention) | 5 |
| B: Theory | Ecological model of change, health behaviour change theory and communication theory, social cognitive theory, stages of change transtheoretical framework and social support models | ||
| C: Context | Social | ||
| E: Consultation | Lay health advisor part of the community under study; focus groups undertaken to develop appropriate tailoring variables, message content, language and literacy level for the tailored messages | ||
| F: Delivery fidelity | Partial intervention for delayed intervention group | ||
| Chang et al. 2010169 | A: Motivation | Treatment (weight loss) | 7 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social – community | ||
| D: Experience | Women, Infants, and Children educators (received 1 day of training) | ||
| E: Consultation | Community partnership, community advisory group and peer advisory group | ||
| F: Delivery fidelity | Compliance with intervention was examined (quite low compliance) | ||
| I: Resources | Monetary incentives | ||
| Cousins et al. 1992,182 Foreyt et al. 1991184 | A: Motivation | Cardiovascular risk reduction in obese Mexican American women | 4 |
| C: Context | Social – researcher led | ||
| D: Experience | Bilingual registered dietitians | ||
| I: Resources | 24 weekly classes and six monthly classes; bilingual manual; bilingual registered dietitians | ||
| Dennison et al. 1996170 | A: Motivation | Reduce overweight in employees | 6 |
| B: Theory | Activated health education model | ||
| C: Context | Social – researcher led | ||
| D: Experience | Certified health educator, registered dietitian and exercise technician | ||
| F: Delivery fidelity | Men felt uncomfortable discussing personal weight-management problems with women present; contracting aspect was not well responded to (involving family/friends as contracting partners) | ||
| I: Resources | Computers | ||
| Erfurt et al. 1991171 | A: Motivation | Reduce cardiovascular disease risk factors | 6 |
| C: Context | Social | ||
| D: Experience | Included medical staff – programme was provided by an external hospital-based health promotion team | ||
| E: Consultation | Wellness committee that included worksite management, labour and medical department representatives helped plan, co-ordinate and carry out activities | ||
| G: Sustainability | Programme activities were implemented into the workplace but were carried out during break times and before/after work | ||
| I: Resources | Part-time wellness counsellors located at the workplace (independent of personnel department); cost of full group programmes ranged from US$50 to US$100 per participant (workplace paid for two-thirds and employee for one-third) | ||
| Janicke et al. 2011103 | A: Motivation | Reduction of child obesity, especially in low-SES populations | 6 |
| C: Context | Social – researcher led | ||
| D: Experience | Intervention delivered by master’s-level graduate students and postdoctoral fellow in clinical psychology. All received 8 hours of training and had previous experience in behavioural approaches to weight management | ||
| F: Delivery fidelity | Lead researcher reviewed audio tapes of group treatment sessions to assist with supervision of interventionists and help ensure treatment fidelity | ||
| I: Resources | 12 weekly 90-minute sessions; 8 hours of interventionist training | ||
| J: Differential effects | Change in child BMI, ethnicity | ||
| Kain et al. 200965 | A: Motivation | Prevent obesity | 6 |
| C: Context | Social | ||
| D: Experience | Education programme and materials developed by the Instituto de Nutrición y Tecnología de los Alimentos; trained nutritionist, classroom teachers and physical education teachers; research team included biochemist, master in public health, nutritionist, physician and statistician | ||
| G: Sustainability | Counselling with teachers was limited – lack of time, fit in with children’s breaks; time limitations of teachers – need to bring in external professionals | ||
| H: Stakeholder support | Successfully included teachers in the intervention; teachers very satisfied with the intervention – interest in their health and support of health professional | ||
| I: Resources | Teacher training – three group sessions of 90 minutes | ||
| Kain et al. 201066 | A: Motivation | Prevent obesity | 6 |
| C: Context | Social | ||
| D: Experience | Trained nutritionists, teachers and physical education teachers; research team included biochemist, master in public health, professor of education, nutritionist, physician and statistician | ||
| F: Delivery fidelity | Nutritionist supervised some activities | ||
| G: Sustainability | Few possibilities for training time; low teacher motivation | ||
| I: Resources | Staff: research team included biochemist, master in public health, professor of education, nutritionist, physician and statistician | ||
| Kisioglu et al. 2004197 | A: Motivation | Prevention of hypertension and obesity (through health education) | 6 |
| C: Context | Social – health care led | ||
| D: Experience | Health-care professionals | ||
| E: Consultation | Muhtars (socially active leaders) emphasised the importance of women visiting the health centre | ||
| G: Sustainability | Intervention is cost-effective (health education and leaflets) | ||
| I: Resources | Health experts, leaflets | ||
| Krummel et al. 2010166 | A: Motivation | Reduce post-partum weight gain/obesity in low-SES women | 8 |
| C: Context | Social – researcher led | ||
| D: Experience | Nutritionists, exercise physiologists, psychologist and health educator | ||
| E: Consultation | Focus groups to inform intervention development and intervention material testing with Women, Infants, and Children participants not eligible for the study | ||
| F: Delivery fidelity | Facilitators were taped for two practice groups and feedback was given; attendance of sessions was low (57% of participants did not attend any sessions) and therefore exposure to the intervention was low | ||
| G: Sustainability | Incorporated into existing Women, Infants, and Children service but attendance was low | ||
| H: Stakeholder support | Facilitators and those who attended sessions were positive about their experiences but attendance was low | ||
| I: Resources | One counselling session with a Mothers’ Overweight Management Study (MOMS) dietitian; 10 group discussion sessions; monthly newsletters; nutritionists, exercise physiologists, psychologist and health educator | ||
| Nichols 1995179 | A: Motivation | Improve health of low-income African American women | 6 |
| B: Theory | Precede–proceed model, social and behavioural compliance management | ||
| C: Context | Social – researcher led | ||
| D: Experience | Pharmacist trained in social and behavioural compliance management, physician, nutritionist, clinical psychologist and exercise physiologist | ||
| E: Consultation | Preliminary study conducted in a small group of African American women to test the feasibility and acceptability of concepts and processes of the intervention | ||
| I: Resources | 12 weekly sessions; trained facilitator; US$50 given before and after the intervention (incentive) and US$10 given each week (for travel and attendance); prizes awarded each week | ||
| Ockene et al. 2012198 | A: Motivation | Diabetes prevention [Lawrence Latino Diabetes Prevention Program (LLDPP)] | 9 |
| B: Theory | Social cognitive theory and patient-centred counselling | ||
| C: Context | Social – health care led | ||
| D: Experience | Post high-school education and some with undergraduate degree in nutrition | ||
| E. Consultation | Focus groups conducted with Latino community | ||
| F: Delivery fidelity | Extensive training in the delivery of the intervention protocol, including the nutritional and exercise aspects of the intervention, the theoretical background, and training in motivational counselling and group management skills. Training included role plays and mock intervention sessions led by a behavioural psychologist and a senior registered dietitian. Booster training sessions conducted semi-annually | ||
| G: Sustainability | Collaborative project with community organisation support | ||
| H: Stakeholder support | Collaboration between the Greater Lawrence Family Health Center, the Lawrence Senior Centre, the YWCA of Greater Lawrence and investigators from the Worcester and Lowell campuses of the University of Massachusetts | ||
| I: Resources | US$661 per participant for the LLDPP intervention (less than standard care in the control group, which is US$1399 per participant) | ||
| Olvera et al. 2010167 | A: Motivation | Obesity prevention through the promotion of physical activity | 7 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social | ||
| D: Experience | Child psychologist and licensed counsellor, registered dietitian/nutrition educators, trained Cooper Institute (Dallas, TX) fitness specialists and two additional instructors | ||
| F: Delivery fidelity | Process evaluation completed: lessons were monitored and evaluated by instructor assistants; quite high attendance rates reported | ||
| G: Sustainability | Intervention was designed to be cost-effective by utilising existing resources within the community | ||
| I: Resources | Materials: educational materials, sports equipment; staff: child psychologist and licensed counsellor, registered dietitian/nutrition educators, trained Cooper Institute fitness specialists and two additional instructors | ||
| Rickel 2008200 | A: Motivation | Reduce obesity – particularly in African Americans | 8 |
| B: Theory | Social problem-solving theory | ||
| C: Context | Social – researcher led | ||
| D: Experience | Bachelor’s- and master’s-level interventionists | ||
| F: Delivery fidelity | Attendance rates recorded; interventionists followed a structured protocol | ||
| H: Stakeholder support | Participants reported satisfaction with the programme | ||
| I: Resources | Treatment phase: 24 weekly 90-minute group sessions; extended care: in-person or telephone contact twice per month; bachelor’s- and master’s-level interventionists | ||
| J: Differential effects | Ethnicity | ||
| Walker et al. 2012168 | A: Motivation | Promote weight loss in overweight post-partum women (treatment) | 8 |
| B: Theory | Social cognitive theory, positive deviance methods and cognitive–behavioural strategies | ||
| C: Context | Social – health care led | ||
| D: Experience | Registered dietitian | ||
| E: Consultation | Local knowledge derived from focus groups and community advisors | ||
| F: Delivery fidelity | Distance to and timings of meetings acted as barriers to participating and weight loss | ||
| I: Resources | Pedometer; stationery – for guidelines; electronic scales; stadiometer | ||
| J: Differential effects | Weight losses, although not statistically significant, were achieved by white/Anglo and Hispanic women | ||
| Observational studies (n = 20) | |||
| Nutrition-only interventions (n = 1) | |||
| Zuber et al. 1992160 | A: Motivation | Reduce obesity | 7 |
| C: Context | Social | ||
| D: Experience | Clinical psychologist, diet assistant and doctor | ||
| E: Consultation | 3-year evaluation previously conducted that included piloting materials | ||
| G: Sustainability | Aim during aftercare was to convert the professionally led groups to self-help groups | ||
| I: Resources | 24 × 2-hour sessions over 6 months, follow-up with four therapist-led aftercare sessions within a year; clinical psychologist (all sessions), diet assistant (12–16 sessions) and doctor (eight sessions) | ||
| J: Differential effects | Baseline weight status | ||
| Physical activity-only interventions (n = 3) | |||
| Carlin 2009214 | A: Motivation | Prevent unnecessary disease and disability by enhancing access to preventative health services, co-ordinating efforts for more efficient delivery of care and supporting community members to take control of their own health | 8 |
| B: Theory | Transtheoretical model of health behaviour change | ||
| C: Context | Social – health care led | ||
| D: Experience | Personal trainers | ||
| E: Consultation | Steering committee of local community organisations, health-care providers, universities and governmental organisations | ||
| F: Delivery fidelity | Exercise frequency: median 5.8 visits per month (Healthy People 2010 target five visits per week). One-third of participants achieved a moderate level of exercise frequency (8–12 exercise visits per month). Participants remained active for a median of 16.5 months and one-third were active for > 2 years | ||
| G: Sustainability | An existing service with community partnership collaboration | ||
| I: Resources | Fitness centres with fully-equipped gyms and personal trainers; US$20 per member per month participation fee (no contract required) | ||
| Clark et al. 2003213 | A: Motivation | Improve physical activity (prevention) | 5 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social | ||
| D: Experience | Research assistant | ||
| F: Delivery fidelity | Adherence levels examined (moderate, little and no) | ||
| Zoellner et al. 2007,181 2010231 | A: Motivation | Obesity prevention through the promotion of physical activity | 6 |
| B: Theory | Transtheoretical model and social support model | ||
| C: Context | Social – health care led | ||
| E: Consultation | Guided by community input (via a workshop) | ||
| F: Delivery fidelity | Quality control measures were implemented by ensuring that one Agricultural Research Service member and three university members were present during all data collection procedures | ||
| I: Resources | Pedometers | ||
| Nutrition and physical activity interventions (n = 16) | |||
| Balcazar et al. 2009202 | A: Motivation | Cardiovascular health promotion | 8 |
| B: Theory | Community capacity | ||
| C: Context | Social – health-care setting | ||
| D: Experience | Community members (promotores), medical providers, medical support staff, certified diabetes educators, administrators and board of directors – integrated training system was put in place | ||
| E: Consultation | With community members (promotores); collaboration among staff from the National Heart, Lung, and Blood Institute (NHLBI; National Institutes for Health) and Health Resources and Services Administration’s (HRSA) Bureau of Primary Health Care and researchers from the University of Texas School of Public Health (to provide consultation, mentorship and guidance to community health centre staff, promotores and other personnel involved in the intervention) | ||
| G: Sustainability | Community-based participatory research was a strength (based on community capacity-building principles); activities were integrated into existing medical providers (health centres); well-developed curriculum | ||
| H: Stakeholder support | NHLBI, HRSA, University of Texas School of Public Health | ||
| I: Resources | Curriculum manuals and staff as above | ||
| Christiansen et al. 2007201 | A: Motivation | Treatment (weight loss and maintenance) | 7 |
| B: Theory | Cognitive theory | ||
| C: Context | Social – commercial weight loss camp | ||
| D: Experience | A multidisciplinary group that included dietitians, physical therapists and a psychologist | ||
| H: Stakeholder support | Danish National Board of Health, the Aarhus County for Public Health and the Society of Physiotherapists in Denmark | ||
| I: Resources | Staff listed above; commercial weight loss camp – had to pay to attend unless on income support but does not state how much | ||
| J: Differential effects | Gender | ||
| Clarke et al. 2007164 | A: Motivation | Increase physical activity of overweight and obese low-income mothers | 7 |
| B: Theory | Self-efficacy theory | ||
| C: Context | Social – researcher led | ||
| D: Experience | Professor of nutrition, assistant professor of nursing and nutrition graduate students | ||
| F: Delivery fidelity | Attendance rate averaged 74% | ||
| H: Stakeholder support | Majority of participants evaluated the programme positively | ||
| I: Resources | Eight weekly lessons (including 30 minutes of physical activity); instructor | ||
| Fernandes et al. 2012185 | A: Motivation | Obesity prevention | 6 |
| B: Theory | Transtheoretical model of behaviour change | ||
| C: Context | Social – health care led | ||
| E: Consultation | Community health workers | ||
| H: Stakeholder support | National Heart, Lung, and Blood Institute (National Institutes for Health) | ||
| I: Resources | Pedometers, water bottles, healthy snacks | ||
| Gill 1998203 | A: Motivation | Reduction of obesity in Mexican American women | 5 |
| B: Theory | Biopsychosocial model of health behaviour | ||
| C: Context | Social – researcher led | ||
| D: Experience | Bilingual registered dietitian, master’s-level behavioural specialist and trained peer leaders | ||
| I: Resources | Treatment: 6 months of weekly 90-minute classes; maintenance: 6 months of weekly support groups; 4 hours of peer leader training; bilingual registered dietitian, master’s-level behavioural specialist and trained peer leaders | ||
| Goldfinger et al. 2008207 | A: Motivation | Reduction of obesity in non-white, low-income communities | 8 |
| C: Context | Social – diabetes coalition led | ||
| D: Experience | Community and academic partners; trained peer leaders | ||
| E: Consultation | East Harlem Diabetes Center of Excellence community–academic coalition – operates on the principles of community-based participatory research, an egalitarian collaboration among community, clinical and public health leaders | ||
| F: Delivery fidelity | Participants attended an average of six of the eight sessions (75%) | ||
| G: Sustainability | Community-based participatory research; project sought to weave itself into the fabric of the vibrant Harlem community | ||
| H: Stakeholder support | Appeared to be well supported by all partners | ||
| I: Resources | Trained peer leader; eight sessions over 10 weeks | ||
| Gray et al. 2009153 | A: Motivation | Reduce obesity in low-SES men | 6 |
| C: Context | Social – health care led | ||
| D: Experience | Community nurses and dietitians | ||
| G: Sustainability | Integrated into existing health services | ||
| H: Stakeholder support | Positive feedback from participants and spouses/partners | ||
| I: Resources | 20-minute pre-programme assessment; 12-week programme (weekly 60-minute evening sessions); post-programme meetings (four per year); community nurses and dietitians | ||
| Hajek et al. 2010208 | A: Motivation | Reduce obesity | 4 |
| C: Context | Social | ||
| H: Stakeholder support | Programme received high ratings from participants | ||
| I: Resources | Six weekly treatment sessions and two 1-hour follow-up visits | ||
| Hugk and Winkelvoss159 | A: Motivation | Reduce obesity in workers | 3 |
| C: Context | Social | ||
| I: Resources | Workplace health centre; doctor | ||
| Jordan et al. 2008165 | A: Motivation | Reduce obesity in low-SES women | 4 |
| B: Theory | Social cognitive theory | ||
| C: Context | Social – researcher led | ||
| I: Resources | 8-week programme, 2-hour sessions (frequency not reported) | ||
| Lasco et al. 1989178 | A: Motivation | Treatment (obesity reduction) | 8 |
| C: Context | Social | ||
| D: Experience | Public health educators | ||
| E: Consultation | Community collaboration – the impetus for the intervention came from the community | ||
| F: Delivery fidelity | High participation rates (70% attended ≥ 10 sessions) | ||
| G: Sustainability | Community involvement was key to the success of this intervention | ||
| H: Stakeholder support | Department of Community Health, Emory University, Atlanta, GA, and the Centers for Disease Control | ||
| I: Resources | Diaries, food samples, cookbook, resources for exercise classes, rewards (certificates, towels, shirts, sweatshirts, sweat bands, make-up, trampoline, bicycle and Walkman) | ||
| Perez-Lizaur et al. 2011204 | A: Motivation | Cardiovascular health promotion and disease prevention | 8 |
| B: Theory | Social marketing, social action, social learning, social efficacy and planned behaviour | ||
| C: Context | Social | ||
| D: Experience | 5 days of training provided (promotores) | ||
| E: Consultation | Community members (promotores) and collaboration with research team at the University of Texas | ||
| F: Delivery fidelity | Sessions were supervised by a team of researchers who visited different sites at least once every 2 weeks | ||
| I: Resources | Materials included a manual and educational resources (i.e. flip charts, fotonovela) | ||
| J: Differential effects | Age (</> 60 years) | ||
| Pescatello et al., 2001205 (two study designs) | A: Motivation | Reduce coronary artery disease in the workforce | 3 |
| C: Context | Social | ||
| I: Resources | Annual health screening and individualised feedback; US$100–150 incentive; group-based education and support programmes | ||
| Rickel 2008200 | A: Motivation | Reduce obesity – particularly in African Americans | 8 |
| B: Theory | Social problem-solving theory | ||
| C: Context | Social – researcher led | ||
| D: Experience | Bachelor’s- and master’s-level interventionists | ||
| F: Delivery fidelity | Attendance rates recorded; interventionists followed a structured protocol | ||
| H: Stakeholder support | Participants reported satisfaction with the programme | ||
| I: Resources | Treatment phase: 24 weekly 90-minute group sessions; extended care: in-person or telephone contact twice per month; bachelor’s- and master’s-level interventionists | ||
| J: Differential effects | Ethnicity | ||
| Williams and Wold 2000206 | A: Motivation | Reduce cholesterol levels in worksite employees | 6 |
| B: Theory | Transtheoretical model | ||
| C: Context | Social | ||
| D: Experience | Nurses, research staff and students | ||
| I: Resources | Screening programme; individual education-based interview; follow-up letter and report; nurses | ||
| J: Differential effects | Geographical location (urban vs. rural) | ||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies (n = 1) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 1) | ||||||
| Lemon et al. 2010219 | Cluster RCT – pair matched [six clusters, two arms; three clusters (matched) per arm] 24 months’ follow-up intervention group and 12 months’ follow-up control group Final sample: 648 (intention to treat) Quality: Moderate |
Six hospital worksites, USA Age: 18–65 years ∼80% female |
Prevention: Four-strategy intervention including a social marketing campaign, environmental strategies promoting physical activity, environmental strategies promoting healthy eating and strategies promoting interpersonal support. Types of intervention strategies included stairway signs, cafeteria signs, farmers’ markets, walking groups, challenges, workshops, educational displays, newsletters, project website, project information centre and print materials Implementation: 7 |
Gradient: Explored education | BMI | ↔ |
| The group most likely to prevent weight gain was that with a higher educational status | ||||||
| Observational studies (n = 6) | ||||||
| Nutrition-only interventions (n = 2) | ||||||
| Carleton et al. 1995222 | Repeat cross-sectional study with comparison community 8.5 years’ follow-up Final sample: 2075 Quality: Moderate |
Community wide, USA Age: 18–64 years > 50% women (between 54% and 60%) |
Prevention: Multiple community-wide interventions including grocery store shelf labelling of low-fat foods, installation of a multiple-station exercise course, nutrition programmes at the public library and restaurant menu healthy heart highlights Implementation: 4 |
Gradient: Explored by education | BMI | ↓ |
| Total cholesterol | ↔ | |||||
| Systolic BP | ↔ | |||||
| Diastolic BP | ↔ | |||||
| BMI decrease most pronounced in those with a lower level of education | ||||||
| Tudor-Smith et al. 1998218 | Repeat cross-sectional study 5 years’ follow-up Final sample: 17,579 Quality: Weak |
Wales and north-east England, UK Age: 18–64 years Gender not reported |
Prevention: Heartbeat Wales health promotion programme that sought to prevent cardiovascular disease. Interventions included smoking cessation television series with BBC Wales and HTV, food labelling and nutrition education with a major grocery retailer, a restaurant and canteen scheme to increase the availability of healthy food choices and smoke-free areas and a worksite health promotion programme with the Confederation of British Industry (CBI) Wales Implementation: 4 |
Gradient: Manual workers vs. non-manual workers (head of household) | Overweight prevalence | ↔ |
| Exercise | ↔ | |||||
| Unhealthy dietary choices | ↔ | |||||
| Healthy dietary choices | ↔ | |||||
| No significant differences between manual and non-manual workers | ||||||
| Physical activity only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 4) | ||||||
| Jenum et al. 2006,215 2007217 and 2009216 | Prospective controlled cohort study 3 years’ follow-up Final sample: 1776 Quality: Moderate |
Two districts, Norway Age: 30–67 years 54–57% female |
Prevention: Romsås in Motion – culturally sensitive physical activity classes organised for immigrants attending Norwegian language classes. Environmental changes also made during this intervention, including the labelling of walking trails within the district, improving street lighting and gritting of pavements and trails in the winter to increase accessibility to areas for physical activity and thereby reinforce self-efficacy and perceived behavioural control Implementation: 9 |
Gradient: Results reported by educational group | Body mass | ↓(M) |
| BMI | ↓(M) | |||||
| Resting heart rate | ↓(M) | |||||
| Systolic BP | ↓ | |||||
| Total/HDL cholesterol | ↓(M) | |||||
| Triglycerides | ↓ | |||||
| Body mass results were similar across all educational groups | ||||||
| Scoggins et al. 2011221 | Controlled cohort study 1 year of follow-up Final sample: 19,559 Quality: Moderate |
Worksite, USA Age: 18–69 years 49.9% female |
Prevention: Healthy Incentives weight-management intervention sponsored by employer – environmental modifications (e.g. decorating stairwells and prompting stair use, healthy options in vending machines, room converted to free gym, garden for employees to grow healthy food) plus individual action plans encouraging healthy activities, weight management, exercise, nutrition, stress management and smoking cessation; monthly electronic newsletter, website and poster campaigns Implementation: 6 |
Gradient: Explored intervention effects by level of education | BMI | |
| All participants | ↓ | |||||
| College graduates | ↓ | |||||
| Some college education | ↓ | |||||
| High-school education only | ↓ | |||||
| High-school education-only group had the biggest reduction in BMI | ||||||
| Scoggins et al. 2011221 | Cohort study 5 years’ follow-up Final sample: 10,432 Quality: Weak |
Worksite, USA Age: 18–69 years 49.9% female |
Prevention: Healthy Incentives weight-management intervention sponsored by employer – environmental modifications (e.g. decorating stairwells and prompting stair use, healthy options in vending machines, room converted to free gym, garden for employees to grow healthy food) plus individual action plans encouraging healthy activities, weight management, exercise, nutrition, stress management and smoking cessation; monthly electronic newsletter, website and poster campaigns Implementation: 6 |
Gradient: Explored intervention effects by level of education | BMI | |
| All participants | ↓ | |||||
| College graduates | ↔ | |||||
| Some college education | ↓ | |||||
| High-school education only | ↓ | |||||
| VanWormer et al. 2012220 | Prospective cohort study (had control groups but merged into one group for analysis) 24 months’ follow-up Final sample: 1222 Quality: Moderate |
Six worksites in St Paul, MN, USA Mean age: 44.2 years 61% female |
Prevention: HealthWorks intervention – healthy foods/beverages made affordable, access modifications to healthy foods, aesthetic stairwell enhancements, free access to pedometers and website step-tracking tools, improved scale access for self-weighing (including balance beam scales placed at various locations within the workplace such as restrooms), worksite advisory groups and site-wide publicity of nutrition and physical activity Implementation: 5 |
Gradient: Explored education | Body weight (more frequent self-weighers and obese at baseline) | ↓ |
| No differential effects by level of education | ||||||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies – none | ||||||
| Observational studies (n = 1) | ||||||
| Nutrition-only interventions – none | ||||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions (n = 1) | ||||||
| Jenum et al. 2006,215 2007217 and 2009216 | Prospective controlled cohort study 3 years’ follow-up Final sample: 1776 Quality: Moderate |
Two districts, Norway Age: 30–67 years 54–57% female |
Prevention: Romsås in Motion – culturally sensitive physical activity classes organised for immigrants attending Norwegian language classes. Environmental changes also made during this intervention, including the labelling of walking trails within the district, improving street lighting and gritting of pavements and trails in the winter to increase accessibility to areas for physical activity and thereby reinforce self-efficacy and perceived behavioural control Implementation: 9 |
Disadvantage: Low SES (income) and gradient | Body mass | ↓(M) |
| BMI | ↓(M) | |||||
| Resting heart rate | ↓(M) | |||||
| Systolic BP | ↓ | |||||
| Total/HDL cholesterol | ↓(M) | |||||
| Triglycerides | ↓ | |||||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies (n = 1) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 1) | |||
| Lemon et al. 2010219 | A: Motivation | Weight gain prevention and promotion of physical activity | 7 |
| B: Theory | Ecological frameworks, self-efficacy, social networks and social cognitive theory | ||
| C: Context | Social (workplace) | ||
| F: Delivery fidelity | Intervention participation rates (quite low, from 4.8% to 12.9% for weekly or more regular participation in the intervention) | ||
| H: Stakeholder | National Heart, Lung, and Blood Institute (National Institutes for Health) | ||
| I: Resources | Materials: weekly newsletter, recipe books, print materials, signs, resistance bands, US$20 gift cards | ||
| J: Differential effects | Education, income, age, ethnicity and work patterns | ||
| Observational studies (n = 6) | |||
| Nutrition-only interventions (n = 2) | |||
| Carleton et al. 1995222 | A: Motivation | Cardiovascular disease prevention | 4 |
| B: Theory | Social learning theory | ||
| C: Context | Social | ||
| J: Differential effects | Age, gender and education | ||
| Tudor-Smith et al. 1998218 | A: Motivation | Cardiovascular disease prevention | 4 |
| C: Context | Social and political | ||
| H: Stakeholder | The Welsh Office and the Health Education Council (Wales) | ||
| J: Differential effects | Gender, age and manual vs. non-manual | ||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 4) | |||
| Jenum et al. 2006,215 2007217 and 2009216 | A: Motivation | Increase physical activity and reduce cardiovascular disease risk factors | 9 |
| B: Theory | Social cognitive learning theory, ecological models, empowerment and participatory approaches | ||
| C: Context | Social | ||
| D: Experience | Health and welfare workers; local political and lay leaders | ||
| E: Consultation | Local political and lay leaders and health and welfare workers were involved in the planning and implementation stages | ||
| G: Sustainability | The physical activity groups still meet (> 5 years after the project period) | ||
| H: Stakeholder | Local political and lay leaders as well as funding sources (Norwegian Institute of Public Health, the Directorate for Health and Social Affairs, the Norwegian Research Council, the Norwegian Foundation for Health and Rehabilitation and the Romsås District Administration) | ||
| I: Resources | Leaflets, fitness tests, counselling sessions, improving street lighting, labelling of walking trails and gritting of pavements (no costs mentioned) | ||
| J: Differential effects | Age (< 50 and > 50 years) and gender | ||
| Scoggins et al. 2011221 (two study designs) | A: Motivation | Weight management | 6 |
| C: Context | Social (workplace) | ||
| G: Sustainability | Employers must be willing to commit significant resources and incentivise employees to join the programme | ||
| F: Delivery fidelity | High participation rates (> 90%) | ||
| I: Resources | Monetary incentives, marketing resources | ||
| J: Differential effects | BMI, sex, age, race/ethnicity, education | ||
| VanWormer et al. 2012220 | A: Motivation | Weight gain prevention | 5 |
| C: Context | Social | ||
| G: Sustainability | Self-weighing is a low-cost and straightforward self-management strategy | ||
| I: Resources | Pedometers, stairwell enhancement modifications, publicity | ||
| J: Differential effects | Age, sex, race, education, marital status, depression, number of weight loss attempts, perceived pounds needed to gain before attempting weight loss, number of scales in the home and BMI | ||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies – none | |||
| Observational studies (n = 1) | |||
| Nutrition-only interventions – none | |||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions (n = 1) | |||
| Jenum et al. 2006,215 2007217 and 2009216 | A: Motivation | Increase physical activity and reduce cardiovascular disease risk factors | 9 |
| B: Theory | Social cognitive learning theory, ecological models, empowerment and participatory approaches | ||
| C: Context | Social | ||
| D: Experience | Health and welfare workers; local political and lay leaders | ||
| E: Consultation | Local political and lay leaders and health and welfare workers were involved in the planning and implementation stages | ||
| G: Sustainability | The physical activity groups still meet (> 5 years after the project period) | ||
| H: Stakeholder | Local political and lay leaders as well as funding sources (Norwegian Institute of Public Health, the Directorate for Health and Social Affairs, the Norwegian Research Council, the Norwegian Foundation for Health and Rehabilitation and the Romsås District Administration) | ||
| I: Resources | Leaflets, fitness tests, counselling sessions, improving street lighting, labelling of walking trails and gritting of pavements (no costs mentioned) | ||
| J: Differential effects | Age (< 50 and > 50 years) and gender | ||
| Study | Design and quality appraisala | Setting and participants | Interventionb and implementationc | Inequalityd | Summary resultse,f | |
|---|---|---|---|---|---|---|
| Experimental studies – none | ||||||
| Observational studies (n = 2) | ||||||
| Nutrition-only interventions (n = 2) | ||||||
| Jones and Frongillo 2006223 | Retrospective uncontrolled cohort study 2 years’ follow-up Final sample: 5503 Quality: Weak |
Homes, USA Age: 18–74 years 100% female |
Prevention: Food Stamp Program – financial assistance for purchasing food for low- and no-income people living in the USA Implementation: 4 |
Disadvantage: Low-income families Gradient: Results reported by food poverty status |
Body weight | |
| Persistently food secure | ↔ | |||||
| Became food secure | ↔ | |||||
| Became food insecure | ↔ | |||||
| Persistently food insecure | ↑ | |||||
| Kaushal 2007224 | Serial cross-sectional study (natural study) 8 years’ follow-up Final sample: 68,318 Quality: Weak |
Population wide, USA Age: 21–54 years 26% female |
Prevention: Food Stamp Program – investigation of the 1996 federal law change denying immigrants access to the programme Implementation: 5 |
Disadvantage: Low education (proxy for low income) | BMI | |
| Women | ↔ | |||||
| Unmarried mothers | ↔ | |||||
| Men | ↔ | |||||
| Physical activity-only interventions – none | ||||||
| Nutrition and physical activity interventions – none | ||||||
| Study | Domain | Details | Score |
|---|---|---|---|
| Experimental studies – none | |||
| Observational studies (n = 2) | |||
| Nutrition-only interventions (n = 2) | |||
| Jones and Frongillo 2006223 | A: Motivation | Reduce food insecurity | 4 |
| C: Context | Political | ||
| G: Sustainability | Existing programme | ||
| I: Resources | Full participation: US$2000 worth of food stamps | ||
| Kaushal 2007224 | A: Motivation | Reduce food insecurity and meet nutritional needs of low-income families | 5 |
| C: Context | Political | ||
| F: Delivery fidelity | Participation rates | ||
| G: Sustainability | National programme | ||
| J: Differential effects | Gender | ||
| Physical activity-only interventions – none | |||
| Nutrition and physical activity interventions – none | |||
Appendix 6 Detailed summaries of the included child studies
Individual-level interventions
Universal approach: experimental studies (n = 3)
Taveras et al.48
Method: Cluster RCT.
Participants: A total of 10 primary care paediatric offices in Massachusetts, USA, were divided into five pairs matched on practice size and racial/ethnic composition. One office from each pair was randomly assigned to the intervention condition and the other was assigned to the usual-care control condition. There was a baseline response of 15% and a final sample size of 445 children (94% follow-up response rate).
Intervention: This study investigated a health-care weight-management programme, High Five for Kids, aimed at children aged 2–6 years who were obese or at risk of obesity (overweight with at least one overweight parent). The 1-year intensive intervention consisted of consultations and telephone calls with a paediatric nurse trained in motivational interviewing. Behaviours targeted included reducing television viewing and sugar-sweetened beverage consumption. Primary and acute care services were reorganised to support the programme.
Outcomes: This study presents results after the intensive intervention and there are plans to follow participants for a further year during a less intensive maintenance period. Height and weight were measured by medical assistants (blinding status not reported). The primary outcome was BMI. In all participants there was no significant intervention effect on BMI observed. However, in those with a household income of ≤ US$50,000, BMI increased to a lesser extent in the intervention group than in control children (intervention group change 0.4 kg/m2; control group change 1.42 kg/m2; adjusted difference –0.93 kg/m2; p = 0.01). There was no intervention effect in the subgroup of children with a household income > US$50,000. However, lower-income children had a higher BMI at baseline, which may also explain the larger effect, and so results will need to be explored further.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Wake et al.50
Method: RCT
Participants: GPs were recruited from 45 family medical practices in Melbourne, Australia, and trained to deliver the intervention. Children attending the practices were all invited to take part in the BMI screening survey and those identified as overweight and obese were invited to participate in the weight-management trial. There was a baseline response of 27% and a final sample of 245 children (95% follow-up response rate).
Intervention: This study investigated the effects of a primary care weight-management programme in overweight and mildly obese children aged 5–10 years (mean age 7.5 years, 61% girls). Trial participants were randomised into the intervention or the control condition after stratification by GP and overweight compared with obese status. The programme followed a universal approach and included children from all SES levels and explored whether or not SES was a moderator of any of the intervention effects. The intervention group received four GP-administered counselling consultations over 12 weeks, in which physical activity and nutrition behaviour topics were discussed and healthy lifestyle goals were set.
Outcomes: Height, weight and waist circumference were measured by researchers blinded to each child’s group status. Physical activity was assessed using accelerometry and also from parent-reported activity diaries. Nutrition scores were derived from parent-reported food diaries. There were no significant differences between the intervention group and the control group at 6 or 12 months for BMI, waist circumference, number overweight or obese or physical activity (moderate- to vigorous-intensity physical activity, total counts or high vs. low activity) (unadjusted or adjusted difference). Slightly higher nutrition scores were observed in the intervention group than in the control group at 6 and 12 months but these results lost significance after adjustment for age, baseline values, baseline raw BMI and SES. Post hoc analysis found no evidence at the 5% level in adjusted models that SES modified the effect of the intervention on BMI, physical activity or nutrition.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Epstein et al.53
Method: RCT
Participants: Families were recruited to the study through newspaper advertisements, flyers and direct mailings. Families agreeing to participate were randomised into the intervention group or the control group after stratification by child gender. There was a baseline response rate of 38% and a final sample size of 67 families (follow-up response rate of 96%).
Intervention: The intervention aimed to reduce the amount of television viewing and computer use in children at risk of becoming overweight and obese (BMI ≥ 75th percentile; mean age 6.0 years, 47% girls). The intervention followed a universal approach whereby intervention effects were compared between children of low SES and children of high SES (groups were divided at the mean SES of the study sample; SES measured using the Four Factor Index of Social Status233). The intervention consisted of fitting a television allowance monitor to all televisions and computer monitors in the homes of participants, which monitored and regulated television and computer use. Monetary incentives were provided to children who used less than their allocated time for television and computer use, along with parental and project team praise. Monthly newsletters providing information and advice supported the intervention.
Outcomes: Height and weight were measured using standard procedures (blinding status not reported). In the low-SES group there was a statistically significant between-group difference for change in BMI z-score from baseline to 6 months (mean difference between groups –0.17; p = 0.002), 12 months (–0.20; p = 0.02), 18 months (–0.17; p = 0.04) and 24 months (–0.26; p = 0.05). There were no statistically significant between-group differences in the high-SES group.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Universal approach: observational studies (n = 4)
Langnäse et al.,51 Pust et al.52
Method: Non-randomised controlled cohort study
Participants: There was a baseline response rate of approximately 40% and a sample size of 52 children after 1 year and 16 children in the intervention group after 4 years (follow-up response rates of 96% and 57% after 1 and 4 years respectively). This study was part of the larger Kiel Obesity Prevention Study (KOPS), which also included a universal obesity prevention intervention. Children were referred to the study by school physicians, local paediatricians and the health office. Participation in the intervention was voluntary and those who did not wish to participate were invited to act as a control group and given monetary incentives for data collection. A reference group of normal-weight children was also recruited from participants of the KOPS prevention intervention.
Intervention: This study investigated the effects of a family-based obesity treatment intervention in children living in Kiel, Germany (BMI ≥ 90th percentile, mean age 6.6 years). The intervention consisted of five counselling sessions delivered in the homes of participants by a trained nutritionist over a period of 5–10 weeks. The counselling sessions covered diet, physical activity and sedentary behaviour topics and treatment was individualised to families’ personal preferences and current behaviours.
Outcomes: Height, weight, waist and hip circumferences and skinfolds (triceps, biceps, subscapular and suprailiac) were measured using standard techniques (blinding status of the assessor not reported) and BMI SDS, waist-to-hip ratio and body composition were determined. Physical activity, sedentary behaviour (television viewing) and diet intake (fruit and vegetables, cold cuts, low-fat milk products, cheese and snacks) data were collected using validated questionnaires completed by parents. After 1 year, a decrease in fat mass and an increase in fat-free mass were observed in the intervention group compared with the control group (fat mass change: intervention group –2.8%, control group 17.0%, p < 0.05; fat-free mass change: intervention group 15.6 kg, control group 11.1 kg, p < 0.05) but there were no differences between groups for change in BMI SDS or waist-to-hip ratio. Subgroup analysis showed that, in the intervention group, compared with high-SES children, low-SES children had greater increases in weight and BMI (weight: low SES 18.7 kg, high SES 13.4 kg, p < 0.05; BMI: low SES 5.2 kg/m2, high SES – 0.6kg/m2, p < 0.05) and a smaller decrease in BMI SDS (low SES –0.02, high SES –0.3, p < 0.05). There were no SES effects on changes in any outcome variables in the control and normal-weight reference group. After 4 years there was a decrease in mean fat mass in the intervention group (–3.5%, p < 0.05) and an increase in mean fat mass in the control group (3.0%, p < 0.05). In the intervention group, fat mass decreased by 8.3% in high-SES children but increased by 1.5% in low-SES children. Secondary outcomes were reported at the 1-year follow-up only. 51 The intervention was more effective at increasing low-fat milk product intake in children of high SES than in low SES children [high SES: index change 1.0 (SD 1.8) to 2.0 (SD 1.8), p < 0.05; low SES: index change 1.0 (SD 1.8) to 2.0 (1.0), p ≥ 0.05]. There were no significant SES effects on intervention outcomes for any other dietary or physical activity/sedentary behaviour variables. This study followed a universal approach and conducted subgroup analysis by SES (high vs. low; based on parental education).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Sabin et al.46
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Obese children were referred to the obesity service where they received 3-monthly consultations with a paediatrician, dietitian and health and exercise specialist, who provided healthy lifestyle, diet and physical activity education and advice, problem-solving and goal-setting. Families were also invited to attend free weekly exercise sessions. There was a baseline response of 92% and a final sample size of 61 children (those with at least 1 year of follow-up data or discharged from the programme because of successfully meeting BMI reduction targets; 49% follow-up response rate).
Intervention: This study investigated the effects of a hospital-based obesity service aimed at obese children [mean (range) age 11.7 (2.2–17.8) years, 54% girls]. The study followed a universal approach in that the service was open to children of all SES and the study explored whether or not SES influenced a child’s level of success.
Outcomes: Height and weight were measured (blinding not reported but appears unlikely) and BMI scores were calculated using UK reference data. The Townsend material deprivation score234 was used as the measure of a child’s SES. After at least 1 year, 28% of participants achieved the target reduction (BMI SDS reduction of at least 0.5 or obtained normal BMI centiles for age). There was no significant correlation between SES and BMI SDS reduction or any differences in SES between achievers and non-achievers.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Braet41
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Children were referred to the programme by medical doctors. The study included a random selection of 150 patients who had entered the programme between September 1996 and September 1999 and who were followed up for 2 years. There was a 73% follow-up response rate (final sample size 110 children).
Intervention: This study investigated the effectiveness of a 10-month inpatient treatment programme for obese children who had previously been unsuccessful after receiving an outpatient treatment programme (BMI > 90th percentile, mean age 12.7 years, 66% girls). The study followed a universal approach and explored SES (among other variables) as a predictor of weight loss. Patients lived in the treatment centre for 10 months and had all meals provided and participated in organised exercise sessions (10 hours per week). The programme did not use a calorie-restricted diet approach but focused on a healthy lifestyle and taught children to make healthy food choices. Cognitive–behavioural techniques were used as tools for behaviour change.
Outcomes: The primary outcome was BMI, and SES was determined using the Hollingshead Four Factor Index of Social Status. 233 At the 2-year follow-up there was a total mean weight loss of 27% from baseline (significance not reported) and 77% of patients had reduced their BMI by 10%. BMI reduction was not predicted by a patient’s SES.
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Baxter et al.,40 Truby et al.49
Our database searches identified an abstract from Truby et al. 49 reporting on results of the Eat Smart study. In turn, we identified a full paper by the research team40 that described the study and results in more detail but for a lower number of participants. Although this paper was published after our database searches were run, we have included it for the write-up along with the more up-to-date findings reported in the accompanying abstract. 49
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Participants (BMI > 90th percentile; mean age 13.2 years, 69% girls) were referred to the programme by health professionals. The data reported in the full paper40 were for a final sample size of 88 children (follow-up response rate of 86%); the abstract49 included an additional 37 children (final sample size 125; follow-up response rate not reported).
Intervention: The Eat Smart study investigated the effects of a 12-week weight-management programme consisting of weight control diets for obese children.
Outcomes: The study followed a universal approach and explored the relationship between SES and weight change. Height and weight were measured (blinding status of assessors not reported) at baseline and post intervention and SES was assessed using the Socio-Economic Index for Areas (SEIFA). Overall, there was a mean reduction in BMI z-score of 6.3% in both samples after 12 weeks. Higher social advantage was associated with a decrease in BMI z-score (effect size of SEIFA ≥ 70th percentile –0.055; p = 0.02) in the smaller sample and this effect remained with the addition of the extra 37 participants (data not presented but narrative report in abstract).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Targeted approach: experimental studies (n = 1)
Black et al.54
Method: RCT.
Participants: Adolescents were recruited from schools and an existing cohort study and were randomised into the intervention or the control condition after stratification by growth history, BMI z-score, gender and age. The baseline response rate was not reported. The follow-up response rate was 76% and the final sample included 179 adolescents.
Intervention: This was a mentor-based health promotion and obesity prevention programme targeted at black adolescents (mean age 13.3 years, 49% girls) from low-income communities and delivered in participants’ homes and at community venues (e.g. parks and convenience stores). Intervention participants received 12 sessions aimed at encouraging physical activity and healthy eating and delivered by a trained college student mentor. The sessions included goal-setting and planning using motivational interviewing techniques and progress discussions, as well as physical activities and practical food preparation and tasting. Parent participation was also encouraged and recipes and information were provided for the family.
Outcomes: Measurements were taken at baseline, post intervention (after 11 weeks) and at 24 months. Height and weight were measured by blinded researchers and body composition was assessed using dual-energy radiograph absorptiometry. Physical activity counts and play-equivalent physical activity were determined using accelerometry, and dietary intake was self-reported using a food frequency questionnaire. There was no difference between the intervention group and the control group in change in BMI z-score from baseline to post intervention or 24 months; however, the percentage of overweight and obese participants decreased in the intervention group from baseline to 24 months compared with the control group. Overall, there was no between-group difference in change in percentage body fat, fat mass or fat-free mass at either follow-up time point; however, when the analysis was stratified by weight category, the intervention was effective at reducing the percentage of fat (β = –1.54; p = 0.003) and fat mass (β = –1.31; p = 0.025) and increasing fat-free mass (β = 1.41; p = 0.021) from baseline to 24 months in participants who were overweight or obese. Overall, there were no intervention effects on physical activity counts or time spent in play-equivalent physical activity; however, the intervention was effective at increasing play-equivalent physical activity from baseline to post intervention in those who were overweight or obese (β = 29.22; p = 0.009) but this effect was lost at 24 months. There were no significant differences between intervention and control participants in changes in the majority of the diet behaviours assessed (energy, total fat, saturated fat, calcium, fruit, vegetables, milk, non-diet soda and fried food intake) but a significant reduction in snacks/dessert consumption was observed post intervention (β = –2.21; p=0.001) and at 24 months (β = –0.69; p = 0.026). A decrease in fruit intake was also observed post intervention in the intervention group compared with the control group (β = –0.41; p = 0.021) but no difference was observed at 24 months.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Targeted approach: observational studies (n = 3)
Marshall et al.43
Method: Observational prospective cohort study.
Participants: Patients were referred to the clinic and treated holistically for health needs defined by the patient. Nurses referred patients on to other professionals if required. Data collected at the clinics included height, weight and systolic blood pressure. Data analysed in this study were measurements recorded at each patient’s first and last visit to the clinic (duration varied from 3 months to several years). Data were analysed for 100 children (aged 0–12 years) and 62 adolescents (aged 13–18 years).
Intervention: This study investigated a nurse-led healthy lifestyle clinic that targeted diabetes, smoking cessation, diet/nutrition, women’s health, cardiovascular and asthma/respiratory conditions in patients from high-deprivation communities.
Outcomes: There were no significant changes in BMI or systolic blood pressure in adolescents or in BMI in children between the first and the last visits to the clinic.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Smith et al.47
Method: Prospective cohort (uncontrolled before-and-after) pilot study.
Participants: A total of 23 children were recruited to the study and there was a 100% follow-up response rate. Participants were referred to the programme by physicians and nurses and approximately 60% of those referred agreed to participate.
Intervention: This study investigated a 12-week behavioural treatment programme for obese preadolescents (BMI ≥ 95th percentile, mean age 11.7 years, % male/female not reported) on type 2 diabetes risk factors. The intervention was conducted in a physician’s office located in an area populated by a substantial number of minority and low-income families. The intervention consisted of two weekly physical activity sessions with an exercise specialist and four nutrition consultations and two food demonstration sessions with a registered dietitian and incorporated family support, goal-setting and cognitive–behavioural skills.
Outcomes: Measurements were taken at the beginning and end of the programme (blinding status of assessors not reported). Height and weight were measured using standard procedures; the number of days when ≥ 60 minutes of voluntary physical activity (not including mandatory physical education classes) was carried out in a typical week was self-reported using a single-item questionnaire; and blood was taken to determine total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol and the glucose/insulin ratio. From baseline to post intervention there was a significant reduction in BMI (from 33.1 kg/m2 to 32.6 kg/m2) and this change was associated with treatment (associated BMI change –0.52 kg/m2) rather than maturation (associated BMI change 0.27 kg/m2; p = 0.04). There was a significant increase in days per week when ≥ 60 minutes of voluntary physical activity was carried out (mean difference 1.25 days; p = 0.001) and there was a significant reduction in total cholesterol (mean difference 15.4 mg/dl; p = 0.02). There was no change in LDL or HDL cholesterol or in the glucose/insulin ratio.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Fernandez et al.42
Method: Prospective cohort study.
Participants: Overweight and obese children aged 2–13 years were identified through a blanket BMI screening programme of all paediatric patients of the health centre and were invited to participate in the intervention. Of the 74 children identified as obese or overweight, only five did not participate (recruitment response rate of 93%), and all 69 children who did participate were followed for 2 years (100% follow-up response rate).
Intervention: This study investigated a health promotion intervention targeted at overweight and obese children, delivered in a health centre serving areas in need of social transformation (medium to low and low SES) in Seville, Spain. The intervention consisted of an initial 15-minute consultation with a paediatrician for each child and his or her family at which healthy eating and physical activity education was provided verbally and backed up by written materials. A second consultation was then carried out after 1 month at the latest to check on the child’s progress and discuss any difficulties encountered in establishing healthy behaviours. This was then repeated every time the child visited the paediatrician during the 2 years of the study, even if the reason for the visit was not related to overweight or obesity. At each visit height and weight were measured by the paediatrician.
Outcomes: Over 2 years there was a reduction in, or stabilisation of, BMI in 44% of the children. The mean BMI reduction was 1.94 kg/m2 (95% CI 1.17 kg/m2 to 2.70 kg/m2); however, this was not significant (p = 0.27). In terms of weight categories, 44% of the children who were classified as overweight at baseline had moved into the normal weight category at 2 years (p < 0.001) and 52% of those who were obese at baseline were classified as overweight at 2 years (p < 0.001).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Community-level interventions
Universal approach: experimental studies (n = 7)
Bingham 200257
Method: Cluster RCT.
Participants: A total of 12 elementary schools in North Carolina, USA, were randomly assigned to the intervention group or the control group after stratification by geographical region (six schools in each group). The baseline response rate was not reported. There was a 74% follow-up response rate resulting in a final sample size of 985 children.
Intervention: This study investigated a cardiovascular disease risk factor reduction intervention in schoolchildren (mean age 8.9 years, 51 girls). The intervention was delivered over 8 weeks and included physical activity sessions (three 20-minute sessions per week) and education sessions (delivered twice a week) based on the American Heart Association school-site kits and covering topics such as healthy heart, nutrition, smoking and physical activity. Data were collected at baseline, post intervention and at 1 year of follow-up.
Outcomes: The obesity outcome measured was the sum of skinfolds taken by trained researchers (blinding status not reported; errors of measurement were accounted for in the analysis). Height and weight measurements were also taken but were not used in the analysis relevant to this review. Cardiovascular fitness was determined using peak oxygen uptake (VO2max. ) measurements. There was a significant reduction in the sum of skinfolds from baseline to follow-up in the intervention group compared with the control group (log of sum of skinfolds mean change: intervention group –0.060, control group –0.032; p = 0.0422) but no intervention effect on VO2max. SES did not function alone or in interaction with the intervention as a moderator explaining intervention effects on the sum of skinfolds or VO2max. This study followed a universal approach in that children of all SES were included in the study and the relationship between SES and intervention effects was explored in post-hoc analysis.
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Plachta-Danielzik et al.74,75
Method: Quasi-RCT.
Participants: The recruitment rate was 41% and the final sample included 1764 children (35% follow-up response rate) after 4 years and 1192 children (24% follow-up response rate) after 8 years.
Intervention: This study investigated an intervention to promote healthy eating and physical activity and a healthy weight, which was delivered universally to six cohorts of children in the first grade (mean age 6.3 years, 50% girls) in the intervention schools. The aim of KOPS was to reduce the prevalence of overweight and obesity in schoolchildren attending schools in Kiel, Germany. The method of allocation of schools to the intervention was unclear, but schools were re-randomised each year so that all schools had the opportunity to be an intervention school. The risk of contamination between groups was high and baseline differences in SES between groups existed.
Outcomes: The primary outcomes were change in BMI, BMI SDS and triceps skinfold thickness. Trained staff conducted the anthropometric measurements using established guidelines (blinding status not reported). Physical activity and dietary intake data (along with other information) were collected using a survey. There were no differences in change in the primary outcomes after 4 and 8 years between the children in the control group and those in the intervention group. The cumulative 4-year incidence of overweight was lower only in intervention children from families of a high SES. After 8 years a significant decrease in BMI SDS was observed in high-SES intervention children compared with high-SES control children. No intervention effects were observed in low- or middle-SES children.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Rush et al.77
Method: Cluster RCT.
Participants: Two age groups were followed over 2 years: children who were 5 years old and children who were 10 years old at baseline. At baseline, 3034 children were recruited (response rate of 47%; 51% girls) and there was a final sample size of 1352 children (692 intervention group; 45% follow-up rate).
Intervention: This study investigated a school-based intervention, Project Energize, that was conducted in 124 schools in New Zealand. Project Energize aimed to improve the health of children through exercise sessions, nutrition education and healthy eating initiatives, parent education sessions and community events. The schools were stratified by rurality and SES and randomly assigned to the intervention or the control condition (62 schools in each group). Each school was assigned a Project Energize team member who supported regular teachers to deliver classes and assisted schools to develop individualised action plans and goals.
Outcomes: Height, weight, body fat (using bioelectrical impedance) and blood pressure measurements were taken by registered public health nurses (blinding status not reported) at regular intervals throughout the intervention. After 2 years, no differences in BMI between the intervention group and the control group were observed in either age group. However, in those who were aged 5 years at baseline, there was a smaller increase in percentage body fat in the intervention group than in the control group (intervention group change 0.65%, control group change 0.79%, intervention group – control group –0.14%, 95% CI –0.26% to –0.01%). In addition, although there were no significant differential intervention effects, there was a trend towards more favourable effects on body fat in higher-SES schools in the sample of children aged 5 years at baseline. There was no difference between groups in blood pressure changes in this sample but in the sample of those aged 10 years at baseline there was a decrease in systolic blood pressure SDS in the intervention group and an increase in the control group (intervention group change –0.18, control group change 0.05, intervention group – control group –0.23, 95% CI –0.43 to –0.02) and the intervention was marginally (but not significantly) more effective at reducing systolic blood pressure in higher-SES schools than in lower-SES schools.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Wrotniak et al.102
Method: Three RCTs (results combined).
Participants: Participants were recruited to the studies through physician referrals, posters and newspaper and television adverts. Between the trials there was a 29% recruitment rate and a final sample size of 142 after 24 months (65% follow-up response rate).
Interventions: This study investigated the relationship between SES and BMI z-score change in family-based behavioural obesity treatment programmes. Each trial investigated the effects of obesity treatment programmes conducted at the University of Buffalo, NY, USA. The programmes all contained similar components: an educational programme based on the Traffic Light Diet; a physical activity programme; education on changing the home environment; and behavioural strategies (goal-setting/contract-making).
Outcomes: Height and weight were measured by research staff (blinding status not reported) for the majority of the participants and were self-reported for 3% of the participants (data were adjusted for underestimation). The primary outcome was change in BMI z-score after 6 months and 24 months. This study found that SES did not predict child BMI z-score change at either 6 or 24 months, which suggests that the obesity treatment programmes did not lead to SES inequalities in obesity outcomes.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Kalavainen et al.98
Method: RCT.
Participants: There was a baseline response rate of approximately 10% and a final sample size of 69 children (follow-up response rate of 99%). The study was conducted in a health-care centre in Finland and was advertised through newspaper articles and by school nurses.
Intervention: The study investigated a 6-month family-based treatment programme for obesity compared with routine treatment in obese children aged 7–9 years (weight for height 120–200%; mean age 8.1 years; 60% girls). The study followed a universal approach and explored the association between social status and changes in obesity outcomes. Children who volunteered to participate were randomised to either the intervention or the standard treatment condition after stratification for weight for height. Children and their parents in the intervention group each attended 15 sessions of 90 minutes promoting healthy eating, increasing physical activity and decreasing sedentary behaviours using education and behavioural therapy. Parents were targeted as the main agents of change and were responsible for inducing necessary changes at home. Children in the standard treatment group attended two 30-minute appointments with a school nurse and received information booklets for their family.
Outcomes: Height and weight were measured by non-blinded researchers and school nurses and weight-for-height scores were determined using Finnish national growth charts. Social class was determined based on parental education. Intervention children lost more weight for height than those receiving the routine treatment post intervention (intervention group mean 6.8% reduction, control group mean 1.8% reduction; p = 0.001) and at 12 months’ follow-up (intervention group mean 3.4% reduction, control group mean 1.8% increase; p = 0.008). At post intervention there was a greater decrease in BMI in intervention children than in routine treatment control children (intervention group –0.8 kg/m2, control group 0.0 kg/m2; p = 0.003) and also in BMI SDS (intervention group –0.3, control group 0.2; p = 0.022). At 12 months’ follow-up there was a smaller increase in BMI in the intervention group than in the routine treatment group (intervention group 0.1 kg/m2, control group 0.8 kg/m2; p = 0.016). However, in terms of BMI SDS, only a trend of a greater decrease in the intervention group was observed. There was no association between social class and change of weight for height, BMI or BMI SDS at any time point.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Robinson76
Method: Randomised cluster trial.
Participants: The intervention was delivered to all pupils (aged 8–9 years at baseline; 45% girls) in one primary school in California, USA, with another sociodemographically matched school in the same area acting as a control. Randomisation was at the school level with a 90% intervention group baseline response (85% control group) and a final sample size of 192, with 92 in the intervention group (a follow-up response rate of 97%).
Intervention: This study investigated a school-based educational intervention to reduce television and video game usage. The intervention consisted of an 18-hour teacher-delivered classroom course that was intended to increase pupils’ self-regulation of television and video game use. The intervention also included a 10-day television turn-off challenge, educational materials disseminated to parents and the installation of domestic television usage monitors. The intervention lasted for 6 months.
Outcomes: The primary outcomes were BMI, triceps skinfold thickness, waist circumference and hip circumference and waist-to-hip ratio. Blinded trained staff conducted the adiposity measurements using established guidelines. Physical activity (self-report by children/parents: hours per week of television/video games, other sedentary behaviour, physical activity and cardiovascular fitness through school-delivered shuttle tests) and diet intake (self-report by children/parents: meals and snacks in front of the television, daily servings of high-fat foods) were also recorded. Baseline obesity measures were the same in each group (p > 0.01) but intervention group pupils were more likely to have parents with a college education than control group pupils (45% vs. 21%; p < 0.01).
At 6 months’ follow-up, as would be expected for children in this age group, all measures increased. However, compared with the control group, children in the intervention group had statistically significant relative reductions in BMI (intervention group change 18.67 kg/m2 to 18.81 kg/m2, control group change 18.1 kg/m2 to 18.81 kg/m2; adjusted difference –0.45 kg/m2, 95% CI –0.73 kg/m2 to –0.17 kg/m2; p = 0.002), triceps skinfold thickness (intervention group change 14.55 mm to 15.47 mm, control group change 13.97 mm to 16.46 mm; adjusted difference –1.47 mm, 95% CI –2.41 mm to –0.54 mm; p = 0.002), waist circumference (intervention group change 60.48 cm to 63.57 cm, control group change 59.51 cm to 64.73 cm; adjusted difference –2.30 cm, 95% CI –3.27 cm to –1.33 cm; p < 0.001) and waist-to-hip ratio (intervention group change 0.83 to 0.83, control group change 0.82 to 0.84; adjusted difference –0.02, 95% CI –0.03 to –0.01; p < 0.001). There were also significant relative decreases in the intervention group for television viewing (intervention group change 15.35 hours to 8.8 hours per week, control group change 15.46 hours to 14.46 hours per week; adjusted difference –5.53 hours, 95% CI –8.64 hours to –2.42 hours; p < 0.001), video game use (intervention group change 2.57 hours to 1.32 hours per week, control group change 3.85 hours to 4.24 hours per week; adjusted difference –2.54 hours, 95% CI –4.48 hours to –0.60 hours; p = 0.01) and meals in front of the television (intervention group change 2.38 to 1.70, control group change 1.84 to 1.99; adjusted difference –0.54, 95% CI –0.98 to –0.12; p = 0.01). There were non-significant differences between the intervention group and the control group at follow-up for hip circumference, physical activity, other sedentary behaviour, cardiovascular fitness, high fat intake and television snacking.
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Strong |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Simon et al.86
Method: Randomised cluster trial.
Participants: The baseline response was 91% and the final sample size was 732, with 374 in the intervention group (a follow-up response rate of 77%). The intervention was targeted at secondary school pupils (aged 11–12 years at baseline; 50% girls) in eastern France. Randomisation was at the school level with four matched pairs (by geographical location, city size and location or not in a low-SES neighbourhood) of schools randomly selected from 77 schools in the region. The intervention status of schools in the pairs was also randomised. The study took a gradient approach to inequality, examining the effects of the intervention by parental occupational class.
Intervention: This study investigated a school-based educational and environmental intervention to increase physical activity. The multicomponent intervention involved physical activity and sedentary behaviour education (15 classes over 4 years), new opportunities for voluntary non-competitive physical activity at lunchtime and break time and after school and ‘cycling to school’ days and sports events. The intervention was in addition to the standard French school curriculum, which requires three 50-minute exercise classes per week (control condition). The intervention lasted for 4 years.
Outcomes: The primary outcome was change in BMI and age- and gender-adjusted BMI (French reference values). Data were also collected on the incidence of overweight, body fat, fat mass index, fat-free mass index, self-reported physical activity, television and video use and active commuting to school. Biochemical outcomes were also monitored (plasma glucose, total and HDL cholesterol, triacylglycerols and insulin). Data were collected by qualified professionals and validated questionnaires were used for the self-reported elements. There were no differences by age, sex or outcomes at baseline. However, there were some significant differences in terms of SES, with the intervention group having fewer lower occupational class pupils than the control group (low, middle and high occupational status: intervention group 14%, 64% and 22%; control group 19%, 66% and 15% respectively; p < 0.01).
At 4 years’ follow-up, although there was a non-significant difference at the 5% level in overall BMI between the intervention group and the control group, the intervention group did show a lower increase in BMI at follow-up than the control group in years 2 and 3 (relative mean difference between the intervention group and the control group: year 2 –0.26 kg/m2, 95% CI –0.43 kg/m2 to –0.08 kg/m2; year 3 –0.29 kg/m2, 95% CI –0.51 kg/m2 to –0.07 kg/m2), but this did not persist into year 4 (–0.25 kg/m2, 95% CI –0.51 kg/m2 to 0.01 kg/m2). The accumulated incidence of overweight was lower in the intervention group than in the control group at 4 years (p < 0.01): 4.2% new cases of overweight in the intervention group compared with 9.8% in the control group (OR 0.41, 95% CI 0.22 to 0.75). There was also a strong intervention interaction with baseline weight (p < 0.01). Baseline non-overweight pupils in the intervention group saw significant decreases in BMI, adjusted BMI and the fat mass index compared with baseline non-overweight pupils in the control group. For example, relative to the non-overweight pupils in the control group, BMI in the intervention group decreased from 2 years’ follow-up onwards (year 1 –0.04 kg/m2, 95% CI –0.16 kg/m2 to 0.08 kg/m2; year 2 –0.18 kg/m2, 95% CI –0.36 kg/m2 to –0.01 kg/m2; year 3 –0.34 kg/m2, 95% CI –0.55 kg/m2 to –0.13 kg/m2; year 4 –0.33 kg/m2, 95% CI –0.57 kg/m2 to 0.08 kg/m2). There was a non-significant effect relative to the control group for body fat or the fat-free mass index for the non-overweight pupils at baseline. Self-reported physical activity at 4 years’ follow-up was significantly higher in the intervention group (79% at least one additional activity) than in the control group (47% at least one additional activity) (OR 2.34, 95% CI 1.66 to 3.31). Television/video use was reduced in the intervention group (difference of –16 minutes per day, 95% CI –29 minutes to –2 minutes) compared with the control group. There was a significant difference between the groups in HDL cholesterol at 4 years’ follow-up (3.43 mg/100ml, 95% CI 1.73 mg/100ml to 5.13 mg/100ml) but non-significant differences for the other biochemical markers and for active commuting.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Universal approach: observational studies (n = 9)
Jouret et al.64
Method: Prospective cohort study with retrospective comparison group.
Participants: A random sample of 156 kindergartens from a total of 344 were invited to take part in the intervention. Of these, 79 kindergartens agreed to participate. The baseline response rate was 48% and there was a final sample of 1253 children in the intervention groups (70% follow-up response rate) after 2 years. Comparison data from 40 kindergartens, matched to the intervention kindergartens for demographic characteristics, for 410 children were retrospectively retrieved from school records. The total baseline sample consisted of children aged 3–4 years (51% girls).
Intervention: This study investigated two intensities of an obesity prevention intervention. The basic intervention (BI) consisted of providing obesity-related information to parents and teachers and screening for overweight at baseline. Those identified as overweight were referred to a family practitioner for follow-up care. The reinforced intervention (RI) followed the basic strategy with the addition of an educational programme that focused on healthy nutrition habits, physical activity and reducing television viewing. The intervention followed a universal approach in that a sample of kindergartens of all SES were targeted and then results from kindergartens located in disadvantaged areas were compared with those from kindergartens in non-disadvantaged areas.
Outcomes: Height and weight were measured by the study physician (therefore not blinded) and children were classified as being at risk of overweight using French reference curves for BMI. There were no differences between either intervention group and the comparison group in anthropometric outcomes at baseline. In kindergartens located in underprivileged areas the prevalence of overweight in the two intervention groups was significantly lower than in the comparison group at the end of the study, but there were no differences between the intervention groups (BI 12.2%, RI 17.0%, control group 36.8%; BI vs. control group p < 0.001, RI vs. control group p = 0.00, BI vs. RI p = 0.317). Change in BMI z-score was also lower in the intervention groups than in the comparison group but there were no differences between the intervention groups (BI change 0.35, RI change 0.50, control group change 1.35; BI vs. control group p < 0.0001, RI vs. control group p < 0.0001, BI vs. RI p = 0.388). In non-underprivileged areas, no differences were seen either at baseline or at the end of the study between groups for prevalence of overweight. Change in BMI z-score was lower in the RI group than in the BI group and the comparison group (BI change 0.39, RI change 0.22, control group change 0.41; BI vs. control group, p = 0.548; RI vs. control group, p = 0.011; BI vs. RI, p = 0.006).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Grønbæk et al.88
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Obese children (weight > 40% above the median Danish weight for height) were referred to the programme by school nurses, family practitioners and school teachers (mean age 10.9 years; 56% girls). There was a 75% baseline response rate and a final sample size (after 6 months) of 81 children (81% follow-up response rate).
Intervention: This study investigated a community-based obesity treatment programme. The programme consisted of a 6-month intensive phase followed by a 1-year maintenance phase (total duration 18 months); however, the association between SES and BMI change was investigated using data collected after the 6-month intensive phase only and therefore, for the purpose of this review, only the intensive phase of this study will be reported. The intervention consisted of individual and group nutrition education sessions, cooking sessions, a guided shopping trip and physical activity sessions and guidance.
Outcomes: Height and weight were measured by project staff members. Based on intention-to-treat analysis, 68% of the children experienced a reduction in BMI SDS during the 6-month intensive phase. The only significant predictor of BMI SDS change was ethnicity. Weight loss was lower in children of immigrants of non-European origin than in those of Danish or European origin. Weight loss also tended (close to significance) to be lower if the father had limited education and if the family owned, rather than rented, their residence. It is worth noting that significantly more children with unemployed mothers and mothers with limited school attendance dropped out of the study.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Reinehr et al.100
Method: Prospective cohort study.
Participants: A total of 75 children (aged 7–15 years) took part in the programme, of whom 27 (36%) were still in the overweight category after treatment (20 of these dropped out of the programme but were still included in the analysis).
Intervention: The study investigated an outpatient clinic weight-management programme for obese children. The programme consisted of three phases: a 3-month intensive phase of parental sessions, behaviour therapy, nutrition education and exercise therapy; a 6-month establishing phase of individual psychological therapy and exercise therapy; and 3 months spent accompanying the families back to everyday life including individual care if needed and exercise therapy.
Outcomes: Height and weight were measured by programme staff and therefore were unlikely to be blinded. There were no differences between children who reduced their weight and those who were unsuccessful in the type of school of the child, the mother’s education and the father’s education. However, those living in single-parent families were more likely to be unsuccessful (10% successful, 30% unsuccessful; p = 0.03), although multiple regression analysis showed that single-parent family was not an independent factor associated with BMI z-score reduction.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Heinberg et al.96
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: The baseline response rate was 88% and the final sample included 104 children (71% follow-up response rate).
Intervention: This study investigated a hospital-based paediatric obesity treatment programme (Healthy Kids, Healthy Weight) in overweight children (mean age 11.4 years; 64% girls). The study followed a universal approach in that children of all SES participated in the programme and the study explored whether or not there were any SES differences between those who successfully lost weight and those who did not. The programme consisted of a 12-week multifamily behavioural-based intervention aimed at increasing physical activity, decreasing sedentary activity, improving diet and increasing behaviour change skills (e.g. goal-setting, monitoring diet and activity behaviours).
Outcomes: Height and weight were measured by trained but non-blinded research staff at each weekly meeting. Overall, 76% of participants reduced their BMI from pre to post intervention and a significant decline in BMI was shown [t(1,102) = 41.0; p < 0.001]. In addition, 28% of participants lost ≥ 2 kg, a clinically significant weight loss. There were no differences in SES between those who lost weight and those who did not, including those who lost ≥ 2kg and those who did not.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Pott et al.44,45
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Obese children were referred to the programme (mean age 11.5 years; 54% girls). The baseline response rate was not reported. There was an 85% follow-up response rate resulting in a final sample of 116 children. Results from this study were initially reported by Pott et al. in 200944 for a sample of 95 children and then extended results, which included results from additional participants (n = 116), were reported in 2010. 45 The results from these articles were extremely similar and therefore, for this review, we will report the most up-to-date results. 45
Intervention: This study investigated a family-based weight reduction programme conducted in local paediatric practices in Siegen, Germany. The study followed a universal approach whereby children of all SES were recruited and differences between those who responded to the programme (> 5% reduction in BMI SDS) and those who did not were explored. The programme consisted of a 3-month intervention phase in which participants attended biweekly behavioural therapy sessions, a biweekly dietary training course and weekly physical exercise sessions. This was followed by a 9-month maintenance phase consisting of the weekly exercise sessions plus monthly group or individual parent sessions.
Outcomes: Height and weight were measured by programme staff (therefore not blinded) at baseline and each week during the programme. After 12 months there was a mean (SD) reduction in BMI SDS of 0.3 (0.33). BMI SDS was reduced in 85% of the children and 68% reduced their BMI SDS by > 5% (classified as responders). There was no difference in parent education (or employment status44) between responders and non-responders.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Kalarchian et al.97
Method: Prospective cohort (uncontrolled before-and-after) study [the full study was a RCT; however, using the data relevant to this review, this study is treated as a prospective cohort (uncontrolled before-and-after) study].
Participants: The baseline response rate was 30% and the final sample size was 87 children in the intervention group (follow-up response rate of 90%).
Intervention: This study investigated a family-based obesity treatment programme for severely obese children (BMI ≥ 97th percentile; mean age 10.2 years; 57% girls) conducted at a university medical centre in Pittsburgh, PA, USA, compared with usual care. The intervention consisted of a calorie-restricted diet (Stoplight Eating Plan) and behavioural strategies were taught to increase physical activity, reduce sedentary behaviours and reduce unhealthy eating habits.
Outcomes: Height and weight were measured by independent but non-blinded assessors and per cent overweight was calculated as the per cent over the median BMI for age and gender. The subgroup analysis found that 6-month decreases in child per cent overweight in the intervention group were associated with higher income (β = –5.57 ± 0.04; p < 0.001).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Mockus105
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: There was a low baseline response rate of 18% and a final sample size of 150 children (follow-up response rate of 74%). Participants were recruited through media outlets, postings and referrals from paediatricians’ offices.
Intervention: This study investigated a 20-week family-based weight loss programme in overweight children (20–100% overweight; mean age 9.9 years; 70% girls) in San Diego, CA, USA. Participants followed the Traffic Light Diet, aimed at reducing calorie intake and improving food choice, and an individualised physical activity plan. They also received behaviour modification training in which several techniques were taught including self-monitoring, positive reinforcement, stimulus control and modelling.
Outcomes: Height and weight were measure at baseline and post intervention (blinding status of assessors not reported) and per cent overweight was calculated as a ratio of the child’s BMI to the 50th percentile BMI for children according to sex and age. The Hollingshead Four Factor Index233 was used to calculate participant SES. Overall, the intervention led to a significant decrease in per cent overweight of 11% (p < 0.001). There was no correlation between SES and change in per cent overweight (r = –0.049; p = 0.553).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Jelalian et al.104
Method: Prospective cohort (uncontrolled before-and-after) study [the full study design was a RCT; however, results from the control group were not considered in this analysis and the results from each intervention group were combined; therefore, for the purpose of this review the study is treated as a prospective cohort (uncontrolled before-and-after) study].
Participants: The baseline response rate was 19% and the final sample size was 62 (a follow-up response rate of 82%). Participants were recruited through newspaper advertisements.
Intervention: This study investigated a weight control programme for overweight and obese adolescents. The participants (mean age 14.5 years; 71% girls) were assigned to a cognitive weight control programme that included a calorie-restricted diet, physical activity prescription, behavioural techniques (e.g. self-monitoring, motivation, goal-setting and relapse prevention) and parent nutrition and physical activity education, along with either peer-based adventure therapy (Outward Bound activities) or traditional cardiovascular physical activity sessions.
Outcomes: Height and weight were measured at baseline and post intervention (4 months) but the blinding status of the assessors was not reported. Regression analysis revealed that SES was not associated with change in BMI or weight loss of ≥ 5% from baseline to post intervention.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Woolford et al.101
Method: Retrospective cohort study.
Participants: The baseline response rate was not reported. There was a follow-up response rate of 72%, resulting in a final sample size of 48 adolescents. Although there were no exclusion criteria based on SES, the majority of participants were from low-income families and, in addition, the authors retrospectively explored the relationship between participants’ insurance status and obesity-related outcomes.
Intervention: This study investigated a clinical multidisciplinary weight-management programme (MPOWER) at the University of Michigan, Ann Arbor, MI, USA, and was targeted at obese adolescents (BMI ≥ 95th percentile; mean age 14.5 years; 71% girls) who were referred to the programme by their primary care physician. The programme followed a targeted and a universal approach. The 24-week intervention consisted of individual and group (including parents) sessions delivered by a multidisciplinary team consisting of a paediatrician, a psychologist, a dietitian, a social worker and an exercise physiologist. The sessions included nutrition and physical activity education, exercise sessions and behavioural techniques such as goal-setting and problem-setting (using motivational interviewing).
Outcomes: Height and weight were measured and body fat was assessed using bioelectrical impedance at the first and last visit (blinding status of assessor not reported). From baseline to post intervention there was a mean reduction in BMI of 2.3 units and a mean reduction in per cent body fat of 5.1%. Changes in BMI and body fat were not associated with participants’ insurance status.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Targeted approach: experimental studies (n = 23)
Nemet et al.73
Method: Cluster RCT.
Participants: Thirty kindergartens located in low-SES communities (criteria set by the Israeli Central Bureau of Statistics) in the Sharon area, Israel, were randomly assigned to either the intervention or the control condition (15 in each group). The recruitment rate was not reported. The final sample included 725 children, with 376 in the intervention group (follow-up response rate of 91%).
Intervention: This study investigated a nutrition and physical activity intervention in kindergartens located in low-SES communities. The intervention was delivered during 1 school year. Intervention children received nutrition education delivered by their preschool teachers and participated in daily exercise sessions. Teachers were also provided with a CD of songs about nutrition and exercise, written by a famous Israeli children’s songwriter. Parents and children were invited to two Healthy Day Festivals that included lectures and games based on the major themes of the intervention.
Outcomes: Anthropometric measurements (the primary outcome was BMI percentile) were taken by experienced technicians who were blinded to the children’s group assignment, and fitness was assessed using a 10-m shuttle run at the beginning and end of the programme. There were no differences in the change of BMI percentile from baseline to post intervention between the intervention group and the control group, with significant decreases in BMI percentile in both. However, the number of overweight children in the intervention group decreased by 32% compared with an 18% reduction in the control group (p < 0.05). The intervention also led to a greater improvement in cardiovascular fitness compared with the control group (intervention group increase by approximately 17 laps vs. control group decrease by approximately two laps) and this increase occurred in both boys and girls and in overweight and obese children.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Bellows94
Method: Cluster RCT.
Participants: Eight Head Start centres in Colorado, USA, were enrolled in the study, with four being randomly assigned to the intervention and four to act as controls after being matched for geographical location (urban vs. rural). At baseline, 274 children were recruited (response rate not reported; age 51.4 months; 56% girls) and there was a final sample size of 201 (73.3% follow-up response rate).
Intervention: This study investigated a diet and physical activity intervention, Food Friends Get Movin’ with Mighty Moves, in low-income, minority preschool children. The intervention consisted of physical activity sessions four times a week for 18 weeks and one nutrition education session each week for 12 weeks. Cartoon characters (Food Friends) were used to introduce and support new skills and topics.
Outcomes: Data were collected at baseline and post intervention. Anthropometric measurements were taken by trained researchers (blinding status not reported); fitness was assessed using sit and reach, sit-up and shuttle run tests; gross motor skills were assessed using the Peabody Developmental Motor Scales test; and physical activity was measured using pedometers. There were no significant differences in BMI and BMI z-score between the intervention group and the control group at baseline. After controlling for classroom, ethnicity, gender and age, there were no significant differences between the groups at follow-up. The intervention group showed a significant increase in the number of laps completed in the 3-minute shuttle run from baseline to post intervention (change 1.61; p = 0.01), whereas there was no change in the control group. After controlling for covariants, a significant difference by treatment was found for the sit and reach test (intervention group 29.0 inches, control group 28.7 inches; difference between groups p = 0.03). Gross motor skills improved in the intervention group (change in gross motor quotient 5.73; p < 0.0005) but not in the control group. No treatment effect was found for physical activity levels from baseline to post intervention.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Kain et al.67
Method: Non-randomised cluster controlled trial.
Participants: Five schools were selected from three different cities in Chile: in two cities a control and an intervention school were assigned by the county education authority based on perceived overweight prevalence and willingness of the schools to participate; in the remaining city only one school met the inclusion criteria and was assigned to the intervention. All of the schools were classified as being of low SES using the criterion of 35% of children receiving the School Lunch Program. Recruitment rates were not reported. The baseline sample (n = 3577) had a mean age of 11 years and 47% were girls. The final sample size was 3086, with 2141 pupils in the intervention group (a follow-up response rate of 86%).
Intervention: This study investigated a nutrition and physical activity intervention in low-SES schools. The intervention was implemented during the school year for 6 months and consisted of classroom-based nutrition education for the pupils and nutrition education for parents during two meetings; special activities and competitions to support the nutrition education (e.g. stickers awarded for eating healthy snacks to win a physical activity-related prize); physical activity education and encouragement based on the Canadian Active Living Challenge;235 provision of an extra 90 minutes of physical activity per week; encouragement of physical activity during one recess period per day; and the provision to schools of basic sports equipment. Communication with vending machine providers also took place to encourage the provision of healthier snacks.
Outcomes: Baseline measurements were taken at the beginning of the school year and follow-up measures at the end of the school year. Anthropometric primary outcomes were BMI, BMI z-score, triceps skinfold thickness and waist circumference. Trained researchers, with good inter- and intraobserver reliability for triceps skinfold thickness and waist circumference, conducted the anthropometric measurements but blinding was not reported. Cardiovascular fitness (20-m shuttle run) and lower back flexibility were also measured. Consistent with the non-random assignment of the schools, at baseline the proportion of obese children, BMI z-score, BMI percentile and waist circumference were higher and physical fitness indices were worse (lower values) in the experimental schools than in the control schools. The effect of the intervention over time was evaluated based on changes in outcome values between baseline and follow-up.
The outcome data were analysed by gender. In boys, the average BMI remained unchanged in the intervention group over time (19.5 kg/m2 at baseline and follow-up), whereas it increased in the control group (change 18.9 kg/m2 to 19.2 kg/m2), as would be expected for this age. There was a significant interaction by group assignment and time, after adjusting for baseline BMI values (p < 0.001). The BMI z-score declined significantly in the intervention schools (from 0.63 to 0.51) whereas it remained unchanged in the control schools (0.48 and 0.46 at baseline and follow-up respectively). The group × time interaction was significant (p < 0.001). Triceps skinfold thickness decreased non-significantly over time in both groups (intervention group mean change 12.8 mm to 12.3 mm, control group mean change 12.3 mm to 11.5 mm, group × time interaction p = 0.14), but waist circumference declined in the intervention group and increased in the control group (intervention group mean change 67.4 cm to 66.5cm, control group mean change 64.6 cm to 65.5 cm, group × time interaction p < 0.0001). In girls, none of the anthropometric outcomes were significantly affected by the intervention. Cardiovascular fitness and flexibility improved in the intervention schools and declined or remained the same in the control schools for both boys (20-m shuttle run: intervention group mean change 3.7 to 5 stages, control group mean change 3.96 to 3.96 stages, group × time interaction p < 0.001; flexibility: intervention group mean change 21.3 cm to 23.6 cm, control group mean change 23.4 cm to 22.0 cm, group × interaction p < 0.001) and girls (20-m shuttle run: intervention group mean change 2.6 to 3.3 stages, control group mean change 2.9 to 2.6 stages, group × time interaction p < 0.0001; flexibility: intervention group mean change 22.9 cm to 25.7 cm, control group mean change 24.0 cm to 23.0 cm, group × interaction p < 0.0001). The intervention had no effect on the pattern of sales of health foods by the kiosks.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Jansen et al.63
Method: Cluster RCT.
Participants: Schools were located in low-income, inner-city neighbourhoods. Twenty schools were paired according to size, proportion of migrants and neighbourhood. One school from each pair was randomly assigned to the intervention group and the other school in the pair was assigned to the control group. There was a 95% baseline response rate and a final sample of 2416 children (follow-up response rate of 92%).
Intervention: This study investigated a school-based diet and physical activity intervention (Lekker Fit!) to reduce weight in low-income, multiethnic, inner-city schools (pupils aged 6–12 years; 51% girls). The intervention consisted of the implementation of three physical education sessions per week, additional sport and play activities outside school hours (attendance was voluntary) and education on healthy nutrition, active living and a healthy lifestyle.
Outcomes: Baseline measurements were taken at the beginning of the school year and follow-up measures at the end of the school year by non-blinded research staff. The primary outcomes were BMI, waist circumference and prevalence of overweight. At baseline, intervention children aged 10–12 years had a higher BMI and waist circumference and lower cardiovascular fitness than control children of the same age; however, baseline values were controlled for during the data analysis. In the younger children (6–9 years) there was no intervention effect for BMI; however, the increase in waist circumference was significantly smaller in the intervention group than in the control group (intervention group change 59.1 cm to 60.1cm, control group change 58.7 cm to 60.8 cm; difference between groups –1.29 cm, 95% CI –2.16 cm to –0.42 cm). The prevalence of overweight in the intervention group also increased to a lesser extent than in the control group (intervention group increase 1.3%, control group increase 4.3%; OR 0.53, 95% CI 0.36 to 0.78). No intervention effects were found for BMI, waist circumference or prevalence of overweight in the older children. Cardiovascular fitness improved in the intervention group compared with the control group in the younger age group (intervention group change 4.33 to 5.61 laps, control group change 5.59 to 6.09 laps; difference between groups 0.57 laps, 95% CI 0.13 laps to 1.01 laps). No intervention effect was found in older children for cardiovascular fitness.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Walter et al.83
Method: Cluster RCT.
Participants: All 22 elementary schools in a single school district took part, of which 14 schools were randomly assigned as intervention schools and eight were randomly assigned as control schools. The baseline response rate was 69% and the final sample size was 1115 children (follow-up response rate of 71%).
Intervention: This study investigated the Know Your Body curriculum, which aimed to reduce cardiovascular risk factors by educating children in low-income schools on nutrition, physical fitness and cigarette smoking prevention (pupils aged 9 years; 49% girls).
Outcomes: Measurements were taken by trained professional personnel but it was not stated whether or not they were blinded. Outcomes were the ponderosity index, triceps skinfold thickness, post-exercise heart rate recovery, blood pressure and plasma cholesterol (total and HDL). There were no significant differences between the control group and the intervention group in mean change from baseline to follow-up (observed or adjusted) of the ponderosity index, triceps skinfold thickness, heart rate recovery or HDL cholesterol. Systolic blood pressure increased by a lesser extent in the intervention group than in the control group (intervention group change 104.9 mmHg to 106.6 mmHg, control group change 104.0 mmHg to 108.1 mmHg; adjusted mean difference –1.9 mmHg; p = 0.000) and diastolic blood pressure decreased by a greater extent in the intervention group than in the control group (intervention group change 73.6 mmHg to 70.5 mmHg, control group change 74.1 mmHg to 72.5 mmHg; adjusted mean difference –1.8 mmHg; p = 0.000). Total cholesterol decreased in the intervention group and increased in the control group (intervention group change 173.3 mg/100 ml to 172.7 mg/100 ml, control group change 170.1 mg/100 ml to 171.7 mg/100 ml; adjusted mean difference –3.1 mg/100 ml; p = 0.032).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Willet93
Method: Non-randomised controlled study.
Participants: This study investigated a mother and daughter culturally specific obesity prevention programme aimed at low-SES, African American girls living in a community in Chicago, IL, USA (mean age 10.0 years).
Intervention: The intervention was implemented over 12 weeks and consisted of weekly 1-hour sessions led by advanced doctoral clinical psychology students and registered dietitians. The sessions included education on healthy eating, obesity risks, physical activity and behaviour change, and practical exercise and cooking sessions.
Outcomes: Measurements were taken at baseline, post intervention and at 1 year by blinded personnel. Height, weight and blood pressure were measured using standard procedures and dietary intake was assessed using a food frequency questionnaire. There were no significant multivariate group × time intervention effects for any of the outcomes: BMI, per cent overweight (using the 50th percentile weight for height), percentage of fat calorie intake, percentage of saturated fat calorie intake, cholesterol intake and blood pressure.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
de Heer58
Method: Nested RCT.
Participants: The baseline response rate was approximately 50% and the final sample size was 931, of which 323 were in the intervention group (follow-up response rate not reported).
Intervention: This study investigated an after-school health and exercise programme in predominantly socioeconomically disadvantaged Hispanic children aged 8–11 years (mean age 9.6 years; 48% girls) from seven elementary schools in Texas, USA. Two classes in each school were randomly invited to take part in the intervention, which consisted of an exercise component based on the CATCH physical activity programme,116 in which students were encouraged to achieve at least 30 minutes of daily physical activity and were provided with opportunities to participate in a variety of enjoyable physical activities, and a health education component that covered topics such as ‘eating fruit and vegetables’, ‘reading food labels’ and ‘what is diabetes?’.
Outcomes: Height and weight were measured by researchers blinded to the participants’ group allocation. Aerobic fitness was assessed using the PACER bleep test236 and sedentary behaviour and diet intakes were self-reported using a questionnaire. In all students BMI was reduced from baseline to post intervention but this decrease was larger in the intervention group than in the control group (intervention group –0.200 kg/m2, control group –0.116 kg/m2), although the significance of the between-group difference was not reported. Aerobic capacity increased in both groups (intervention group 21.26 laps to 25.09 laps, p = 0.000; control group 21.95 to 24.28 laps, p = 0.000) but the between-group differences for these changes were not reported. Television viewing during the week decreased in the intervention group (from 3.39 hours to 3.07 hours; p < 0.01), as did video game use during the week (from 2.78 hours to 2.55 hours; p < 0.05), and there were no changes observed in the control group. There were no changes from baseline to post intervention in weekend television viewing or video game use for either group. Both groups increased fruit intake (intervention group change 2.35 to 2.55, p < 0.05; control group change 2.31 to 2.44, p < 0.05) but also sweet intake (intervention group change 1.56 to 1.71, p < 0.05; control group change 1.63 to 1.73, p < 0.05) and there were no changes in intake of fruit juice or French fries in either group. Again, between-group differences were not reported for the sedentary behaviour or diet intake outcomes.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Strong |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Story et al.81
Method: Randomised controlled pilot study.
Participants: Participants (mean age 9.3 years) from low-income families were recruited through three schools that served as sites for delivery of the after-school intervention and were randomised to either the intervention or the control condition. In total, 54 girls were recruited to the study (baseline response rate not reported) and 26 were assigned to the intervention. Only one control participant did not complete the follow-up (follow-up response rate of 98%).
Intervention: This study investigated a culturally appropriate after-school obesity prevention programme for African American girls (Minnesota GEMS). The after-school intervention was delivered by trained African American project staff and included culturally appropriate, fun, interactive activities incorporating nutrition and physical activity education, healthy snack preparation and exercise. Water bottles, t-shirts, pedometers, jump ropes and bracelets were provided to intervention participants. Family involvement was also encouraged through weekly family packs, family nights, telephone calls to parents and organised neighbourhood walks.
Outcomes: Measurements were taken (blinding status of assessors not reported) at baseline and after completion of the 12-week intervention. Height, weight and waist circumference were measured; physical activity was assessed using an accelerometer and the GEMS Activity Questionnaire; and dietary intake data were collected using 24-hour recalls. As was expected in a pilot study of short duration and including a small sample size, there was no significant difference between the intervention group and the control group in change in BMI, waist circumference, objectively measured physical activity, self-reported physical activity or any of the dietary variables (fruit and vegetable, sweetened beverage, water, energy and fat intake). However, trends were observed for improvements in a number of the variables and the programme was found to be feasible and acceptable.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Weak |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Figueroa-Colon et al.59
Method: Cluster RCT.
Participants: Participants were recruited from two schools that served families of low to middle SES. Each school was randomised to either the intervention group or the control group and a screening programme was implemented to identify those who were super obese. The baseline response rate was 30% and the final sample included 15 children (follow-up response rate of 79%).
Intervention: This study investigated a weight loss programme aimed at children who were super obese (> 140% ideal body weight; mean age 10.6 years; 42% girls). The intervention was delivered by a paediatrician, a psychologist and a nutritionist in collaboration with the school’s physical education instructor and nurse and consisted of dietary restriction (high-protein, low-calorie diet for 10 weeks followed by a hypocaloric diet for 16 weeks), nutrition education, exercise sessions, behaviour modification and peer and familial support.
Outcomes: Data were collected at baseline, 10 weeks and 6 months. Height, weight, blood pressure and biochemical assessments were taken by programme staff, who were therefore not blinded to the children’s group status. From baseline to 6 months there were significant decreases in the intervention group for percentage of ideal body weight (–24.3%; p < 0.002) and BMI (–3.8 kg/m2; p < 0.002). There were no changes in percentage of ideal body weight or BMI in the control group. There were no changes in blood pressure in either group and the only change in biochemical variables was a decrease in HDL cholesterol in both groups (intervention group change 48 mg/dl to 44 mg/dl; p < 0.004; control group change 51 mg/dl to 44 mg/dl; p < 0.05).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Hamad et al.89
Method: RCT.
Participants: Existing clients of a microcredit, government-run, not-for-profit institution in Peru were randomised into the intervention group or the control group (loan only with no health education). The baseline response rate was 88% and the final sample size was 1501 (a follow-up response rate of 80%).
Intervention: This study investigated the effect of a health education intervention delivered to microcredit clients (microcredit involves the provision of small loans to families too poor to borrow from traditional lending institutions) on their children aged < 5 years. The health education intervention was delivered by trained loan officers. Monthly 30-minute sessions were delivered over 8 months consisting of basic child health provision, discussion of clients’ own experiences and problem-solving and information about interactions with health-care providers to empower caregivers during clinic visits.
Outcomes: Although the prevention of obesity was not a concern in this study, the height and weight of the clients’ children were measured (blinding status of the assessor not reported) at baseline and at the 1-year follow-up and changes in obesity-related measures were reported. There were no differences in the change in the percentage of children who were overweight and the change in mean BMI z-score from baseline to follow-up between the control group and the intervention group.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Janicke et al.103
Method: RCT.
Participants: The baseline response rate was 55% and the final sample included 33 child–parent dyads (83% follow-up response rate). Families were recruited through primary care clinics, schools, newspaper articles and community presentations in four cohorts and were randomised to the intervention or the active control in child–parent dyads. Assignment to the groups was unbalanced to ensure that sufficient dyads were allocated to the treatment group for optimal group functioning.
Interventions: This study investigated a group-based family behavioural weight-management intervention compared with individual standard treatment in families receiving Medicaid with an overweight or obese child aged 6–12 years (mean age 9.1 years; 47% girls). Those in the intervention group were asked to attend 12 weekly 90-minute group sessions covering nutrition, physical activity and behaviour management topics and monitored their behaviours using food logs and pedometers. The sessions also offered group support and problem-solving. The standard care programme consisted of three 60-minute sessions over 12 weeks in which individual families met with a treatment team member and received nutrition and physical activity education, advice on problem-solving and a progress review.
Outcomes: Height and weight measurements were taken by a trained research team member (blinding status not reported) and BMI z-scores were calculated using Centers for Disease Control data. No significant treatment effect on BMI z-scores was observed post treatment or at 9 months.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Moderate |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Salmon et al.78
Method: Group RCT.
Participants: This study included children (aged 10–11 years; 51% girls) from three schools located in low-SES areas of Melbourne, Australia. The baseline response rate was 77% and the final sample included 268 children (follow-up response rate of 88%).
Intervention: This study investigated a physical activity intervention aimed at preventing excess weight gain, reducing time spent in screen behaviours and improving fundamental movement skills among children. Children were randomised by school class into one of four conditions: a behavioural modification group (BM), a fundamental skills group (FMS), a combined BM/FMS group and a control group who received the usual curriculum.
Outcomes: Anthropometric measurements were taken by trained, non-blinded staff members; physical activity data were collected using accelerometry; and screen behaviours were self-reported. The intervention lasted approximately 9 months and data were collected at baseline, post intervention and at 6 and 12 months post intervention. Outcomes included age- and sex-adjusted BMI, moderate- and vigorous-intensity physical activity and time spent watching television, using the computer and playing electronic games. There was a significant intervention effect on BMI post intervention in the combined BM/FMS group compared with the control group (adjusted difference in mean change –1.88 kg/m2; p < 0.01) and these effects were maintained at the 12-month follow-up (adjusted difference in mean change –1.53 kg/m2; p < 0.05). Those who were in the combined BM/FMS group were also > 60% less likely to be overweight or obese at all follow-up time points than those in the control group. No intervention effects on BMI were observed in the BM and FMS groups. There was a significant increase in vigorous-intensity physical activity in the BM group compared with the control group from baseline to post intervention (adjusted difference in mean change 2.8 minutes; p < 0.05) and from baseline to 12 months post intervention (adjusted difference in mean change 2.8 minutes; p < 0.05), and there were significant increases in both vigorous- and moderate-intensity physical activity in the FMS group compared with the control group from baseline to post intervention (adjusted difference in mean change: vigorous-intensity physical activity 7.8 minutes, p < 0.01; moderate-intensity physical activity 10.4 minutes, p < 0.01) and these changes were maintained at 12 months post intervention (adjusted difference in mean change: vigorous-intensity physical activity 7.7 minutes, p < 0.01; moderate-intensity physical activity 9.5 minutes, p < 0.05). There were no significant changes in physical activity levels in the combined BM/FMS group.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Stephens and Wentz80
Method: Cluster RCT.
Participants: Few data were provided on recruitment and follow-up response rates. The final sample size was 89 children (8–10 years; 50% girls).
Intervention: This study investigated a fitness programme that supplemented existing physical education and was delivered in schools attended predominantly by children from black and low-income families. One school was randomised into the intervention group and one school was randomised into the control group. The programme consisted of three activity sessions per week with a small amount of nutrition, exercise or disease prevention education at the end of each session.
Outcomes: Measurements were taken by researchers (blinding status not reported) at baseline and post intervention (15 weeks). Outcomes included weight, skinfold thickness (sum of triceps and calf), heart rate response to submaximal exercise (step test), resting heart rate, flexibility and blood pressure (systolic and diastolic). Weight increased from baseline to post intervention in both groups but to a lesser extent in the intervention school (intervention group change 25.4 kg to 25.8 kg, control group change 26.1 kg to 27.0 kg; p < 0.001) and there was a significant decrease in skinfold thickness in the intervention group compared with the control group (intervention group change 25 ml to 23 ml, control group change 26 ml to 28.5 ml; p < 0.01). Maximal and recovery heart rate values reduced significantly in the intervention group compared with the control group (maximal: intervention group change 140 beats per minute to 125 beats per minute, control group change 144 beats per minute to 146 beats per minute, p < 0.05; recovery: intervention group change 108 beats per minute to 88 beats per minute, control group change 112 beats per minute to 123 beats per minute, p < 0.05). Systolic and diastolic blood pressure increased in both groups with no significant differences between the groups.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Lubans et al.69
Method: Cluster RCT with a wait-list control.
Participants: Four low-SES schools (out of six invited) from the Hunter Region, NSW, Australia, consented to take part in the study. The schools were then randomised into the intervention or the wait-list control condition after baseline measurements had been taken. In total, 100 low-active boys were recruited at baseline (mean age 14.3 years) and there was an 82% follow-up response rate at 6 months, resulting in a final sample of 82 boys, with 30 in the intervention group.
Intervention: This study investigated a peer leader-based Physical Activity Leaders programme in low-active adolescent boys in disadvantaged schools.
Outcomes: Height, weight and waist circumference were measured by trained, non-blinded research staff; body fat composition was determined using bioelectrical impedance; physical activity levels were assessed using pedometers; and diet intakes were self-reported using a dietary food frequency questionnaire. There were significant reductions in BMI and BMI z-score in the intervention group compared with the control group from baseline to follow-up (mean between-group difference: BMI –0.8 kg/m2, p < 0.001; BMI z-score –0.2, p < 0.001), which resulted in a significant reduction in the number of boys classified as overweight or obese (χ2 = 4.68, p = 0.03). There was also a significant intervention effect for body fat composition (mean between-group difference –1.8%, p = 0.04). No between-group differences were observed for waist circumference, muscular fitness or physical activity (steps per day). There was a significant reduction in the number of boys drinking ≥ 250 ml of sugar-containing drinks per day in the intervention group compared with the control group (intervention group change 42% to 32%, control group change 48% to 56%; p < 0.05) but no differences between groups for fruit, vegetable or water intake.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Weak |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Lindgren et al.68
Method: Cluster RCT with a wait-list control.
Participants: Eight schools that were representative of low-SES areas in south-west Sweden were randomly allocated to the intervention and control conditions (four in each group). There was a 61% baseline response rate and a final sample size of 62 girls, with 27 in the intervention group (56% follow-up response rate).
Intervention: This study investigated a 6-month empowerment-based exercise programme in non-physically active adolescent girls (mean age 15.4 years) from low-SES schools.
Outcomes: Height and weight were measured by researchers (blinding status not reported) and physical fitness was determined using a submaximal work test. Between-group analysis at baseline and after the intervention revealed no significant change in BMI or physical fitness after the intervention.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Moderate |
Myers 200871
Method: Cluster non-RCT.
Participants: In total, 103 children were included (a recruitment response rate of 86%) and there were no dropouts over the 15 weeks. The intervention consisted of physical education lessons led by the virtual trainer for 12 of the 15 weeks.
Intervention: This study investigated a virtual skills and fitness trainer intervention compared with traditional physical education lessons in schools located in lower-SES areas in Virginia, USA (pupils aged 13–14 years; 45% girls). The virtual trainer intervention was implemented in one predetermined school identified by the district’s school division. A school with a similar demographic and student population was then chosen as the control school. The trainer led classes through fitness routines and motivational tips were promoted by celebrities, games, popular music and cartoons.
Outcomes: Height and weight were measured by physical education teachers who were therefore not blinded to the intervention condition. Cardiovascular fitness level was determined using the 20-minute PACER fitness test. 237 No significant differences were observed in change in BMI or fitness level pre to post intervention between the intervention group and the control group. However, the virtual trainer was used for only 32% of the potential time and it was argued that there was an insufficient difference in physical education lessons between the schools.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Robinson et al.90
Method: Randomised controlled pilot study.
Participants: Participants were recruited through community centres, after-school programmes, community youth leaders, schools, community events, churches and fliers advertising the study. In total, 61 girls were recruited to the study (baseline response rate not reported) and only one girl dropped out before the end of the study (98% follow-up response rate).
Intervention: This study investigated a culturally appropriate dance and television viewing reduction intervention that was targeted at low-income African American girls at risk of obesity (BMI ≥ 50th percentile for age and at least one overweight parent/guardian; mean age 9.5 years) living in low-SES areas of California, USA. After baseline measurements had been taken, the girls were randomised into the intervention group or the active control group. The control group received an information-based health education programme to promote a healthy diet and activity patterns. The intervention (Stanford GEMS) consisted of an after-school dance programme (GEMS Jewels dance classes) and a home-based television viewing reduction intervention (START; Sisters Taking Action to Reduce Television) as well as newsletters sent to parents. All instructors, home visitors and data collectors were female African Americans who were culturally matched providers and role models.
Outcomes: Anthropometric measurements (height, weight and waist circumference) were taken by trained and blinded researchers; physical activity behaviours were assessed using accelerometry and the GEMS Activity Questionnaire; and diet intake was assessed using 24-hour recalls. From baseline to post intervention there were no significant differences between groups for changes in BMI and waist circumference; however, a trend towards better outcomes in the intervention group was noted. There were increases in objectively measured and self-reported physical activity in the intervention group compared with the control group but these were not significant. Total house television use was significantly reduced in the intervention group compared with the control group [difference between groups for change (0–4 scale) –0.56; p = 0.007]. There was a small, non-significant difference in energy intake, favouring the control group, and a small, non-significant difference in per cent energy derived from fat, favouring the intervention group.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Robinson et al.106
Method: Full RCT.
Participants: Low-SES African American girls and their families were recruited from schools, community centres, churches and community events. There was a baseline response rate of 48% from 543 families who expressed an interest in the study and were prescreened (baseline sample mean age 9.4 years). The final sample size was 225, with 134 families in the intervention group (follow-up response rate of 86%).
Intervention: This study investigated a culturally appropriate dance and television viewing reduction intervention that was targeted at low-income African American girls at risk of obesity (BMI ≥ 50th percentile for age and at least one overweight parent/guardian) living in low-SES areas of California, USA. After completing the baseline measurements families were stratified by the girls’ baseline BMI and randomly assigned to the intervention or an active control (health education intervention) condition.
Outcomes: Data were collected every 6 months for 2 years. Anthropometric measurements were taken by trained, blinded researchers, demonstrating good test–retest reliability (0.99) for waist circumference and skinfold measurements. Physical activity was measured using accelerometry (counts per minute and moderate- to vigorous-intensity activity) and sedentary behaviours were self-reported (television and videotape viewing and video game and computer use). Diet outcomes (energy intake and percentage of energy from fat) were assessed using 24-hour recall. Fasting serum insulin, glucose and lipid levels were measured. The intervention effect was assessed based on mean changes of outcome variables per year. There were no significant intervention effects compared with the active control for BMI, BMI z-score, waist circumference or triceps skinfold. However, exploratory subgroup analysis revealed that parent/guardian marital status was a significant moderator of treatment effect and that girls in the intervention group who had unmarried parents/guardians had a slower gain in BMI than those in the active control group. There were no significant differences between groups for changes in physical activity, sedentary behaviours or dietary outcomes. Fasting total and LDL cholesterol decreased significantly more among girls in the treatment group than among girls in the control group (p < 0.001 in both cases), but there were no intervention effects for any of the other biochemical outcomes measured.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Winter and Sass95
Method: Cluster RCT.
Participants: Recruitment and follow-up response rates were not reported. A total of 405 children were sampled from the centres and multiple imputation techniques were used to treat any missing data.
Interventions: This study investigated a preschool and home-based intervention aimed at preventing obesity and increasing school readiness in preschool, low-income, minority children (mean age 50 months; 48% girls). Four Head Start centres, matched on the basis of geographical location, size and demographics of clients, located in a high-poverty, low-income neighbourhood in south Texas, USA, were randomly assigned to the intervention or the control group (two in each group). The Healthy and Ready to Learn intervention included child activities that were carried out at school and at home with teachers and parents, respectively, designed to improve children’s language and literacy skills while encouraging good health habits. Parents received training that focused on the demonstration and practice of activities to help ensure parents’ success in implementing the activities with their children. Teachers received training to increase the awareness of risks associated with overweight and encouraged behaviours and practices to promote healthy lifestyles in children. Parents and teachers also received explicit lesson plans and step-by-step instructions for the activities, along with equipment and materials.
Outcomes: Height and weight were measured using standard techniques. Observation techniques were used to assess physical activity levels during guided physical activity sessions in a subsample of the children238 and to assess gross motor skills. 239 There was no time × treatment effect observed for BMI or physical activity levels determined using SOFIT238 (System for Observing Fitness Instruction Time); however, the intervention did lead to improved gross motor skills (time × treatment effect for non-locomotor skills = 1.15, p = 0.007; locomotor skills = 1.02, p = 0.05).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Weintraub et al.84
Method: RCT.
Participants: Children were recruited to the programme through primary care physicians’ offices and clinics, schools and community centres. In total, 21 children were recruited to the study (recruitment rate not reported) and there were no dropouts over the 6 months.
Intervention: This study investigated an after-school team sports programme aimed at overweight racial/ethnic minority children from low-SES neighbourhoods (BMI ≥ 85th percentile; mean age 9.9 years). After baseline measurements had been conducted, the children were randomised into either the intervention group or an active control group, who received a traditional nutrition and health education programme. The sports team intervention consisted of a football (soccer) programme delivered by trained undergraduate and medical students. Sessions were run on 3 or 4 days per week and included 75 minutes of activity. Shin guards, uniforms and water bottles were provided to each player and at the end of the programme certificates and medals were awarded.
Outcomes: Data were collected by trained, non-blinded researchers at baseline, 3 months and 6 months. Height and weight were measured and physical activity was assessed using accelerometry. Screen-time data (television viewing and computer and videogame use) were collected using self-report questionnaires. Significant reductions in BMI z-score in the intervention group compared with the control group were observed at both 3 months (adjusted intervention group – control group difference –0.07; p = 0.04) and 6 months (adjusted intervention group – control group difference –0.08; p = 0.04). Physical activity levels were increased in the intervention group compared with the control group at 3 months (total activity adjusted intervention group – control group difference 105.7 minutes, p = 0.04; moderate physical activity adjusted intervention group – control group difference 10.6 minutes, p = 0.03; vigorous physical activity adjusted intervention group – control group difference 4.4 minutes, p = 0.02), but there were no significant differences at 6 months. There were no differences between the groups for changes in screen behaviour at either follow-up point.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Alves et al.87
Method: RCT.
Participants: Children who were registered with a family health programme were invited to take part in the study. In total, 78 children were recruited at baseline and 39 were randomly assigned to the intervention group and 39 to the control group. There was an 87% follow-up response rate resulting in a final sample of 68 children, with 30 in the intervention group.
Intervention: This study investigated a physical activity intervention in overweight children (BMI ≥ 85th percentile; mean age 7.91 years; 49% girls) from a slum in Recife, Pernambuco State, Brazil. The 6-month intervention consisted of three weekly 50-minute physical activity sessions delivered by physical education students who were supervised by a professor of education. The sessions were carried out in addition to the children’s normal physical education lessons and included activities of moderate to vigorous intensity.
Outcomes: Height and weight were measured at baseline and post intervention (blinding status of assessors not reported). After 6 months both groups had increased their weight significantly but weight gain was less in the intervention group [difference in change (intervention group – control group) –1.37 kg; p < 0.001]. There was a significant decrease in BMI in the intervention group compared with controls [difference in change (intervention group – control group) –0.53 kg/m2; p = 0.049].
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Hoffman et al.62
Method: Cluster RCT.
Participants: Four urban public schools were randomised into either the intervention group or the control group (two in each group). There was a recruitment response rate of 50% and a final sample of 166 children, with 85 in the intervention group (follow-up response rate of 56%).
Interventions: This study investigated an intervention encouraging the consumption of fruit and vegetables in young children from low-SES schools (mean age 6.2 years; 49% girls). The intervention was delivered from the beginning of 2006 to June 2008 and data were collected pre intervention and during the intervention in years 1, 2 and 3, with follow-up data collection in spring 2009. The intervention incorporated classroom education using an instructional DVD, school-wide daily loudspeaker announcements, take-home activity books and stickers awarded for fruit and vegetable intake.
Outcomes: Anthropometric measurements were taken by a non-blinded researcher and fruit and vegetable consumption was determined through observation of lunchtime intakes and weighed plate waste by blinded researchers (moderate to almost perfect agreement between researchers). BMI z-scores did not differ between intervention pupils and control pupils at any of the follow-up time points. Intervention children consumed more fruit at lunchtime than control children in years 1 and 2 of the intervention (year 1 difference 22 g, 95% CI 14 g to 30 g, p < 0.0001; year 2 difference 15 g, 95% CI 6 g to 23 g, p < 0005). There were no differences between the groups in year 3 or at follow-up (3.5 years). Lunchtime vegetable consumption was higher in the intervention group than in the control group in years 1, 2 and 3 (year 1 difference 7 g, 95% CI 3 g to 10 g, p < 0.005; year 2 difference 3 g, 95% CI –0.5 g to 6.5 g, p < 0.05; year 3 difference 3 g, 95% CI –0.2 g to 6.7 g, p < 0.05) but there were no differences between the groups at follow-up.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Sichieri et al.79
Method: Cluster RCT.
Participants: Twenty-two schools in Rio de Janeiro, Brazil, were randomised to either the intervention or the control condition after stratification by BMI. There was a baseline response rate of 97% and a final sample size of 927 children (follow-up response rate 82%).
Interventions: This study investigated a school-based education intervention aimed at reducing sugar-sweetened beverage intake in schools attended mainly by low-SES students (mean age 10.9 years; 53% girls). The intervention consisted of classroom activities that included quizzes and games and song and drawing competitions. Banners promoted water consumption and water bottles were provided for children and teachers.
Outcomes: Measurements were taken at the beginning and end of the school year. Height and weight were measured by research staff (blinding status not reported) and beverage intake was assessed using an interviewer-administered 24-hour recall and short food frequency questionnaire. From baseline to the end of the study, BMI increased in both groups, with no significant differences between the groups. Among students who were overweight at baseline there was a significant reduction of BMI in the intervention group compared with the control group in girls (regression coefficient –0.01; p = 0.009) but not in boys. There was an approximately four times greater reduction in carbonated beverage intake in the intervention group compared with the control group (mean change: intervention group –69.0 ml/day, control group –13.0 ml/day; p = 0.03).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Targeted approach: observational studies (n = 13)
Topp et al.82
Method: Prospective cohort study.
Participants: The intervention was conducted in one school in Kentucky, USA, where pupils were from low-income families, and was targeted at children aged 5–10 years (mean age 8 years; 51% girls). The baseline recruitment response rate was not reported. There was a 78% follow-up response rate resulting in a final sample size of 49 children.
Intervention: This study investigated the Tommie Smith Youth Athletic Initiative, a physical activity intervention with some nutrition education, targeted at a school attended by children from low-income families. The 14-week initiative consisted of three after-school sport and fun activity sessions per week. Nutrition education was delivered for half of one of the sessions per week. Incentives such as water bottles, t-shirts and notepads were awarded for completion of weekly homework.
Outcomes: Measurements were taken pre and post intervention (blinding not reported) and primary outcomes were BMI percentile, body composition, waist-to-hip ratio, cardiovascular fitness indicators and diet intake. The intervention had no effect on BMI percentile, percentage body fat, fat weight or waist-to-hip ratio but lean weight increased on average by 2.3 lb per child (p < 0.00). Improvements were observed in the cardiovascular fitness indicators of maximum heart rate (change –6.3; p < 0.00), cardiovascular fitness score using a 3-minute step test (change 6.6; p < 0.00) and 1- and 2-minute heart rate recovery (1-minute change –8.7, p < 0.04; 2-minute change –5.2, p < 0.05). There was a significant increase in green vegetable intake (change 0.45–0.66; p < 0.2) and a decrease in fruit juice intake (change 1.23–0.72; p < 0.02) from baseline to follow-up. A number of eating behaviours were unchanged and did not meet recommended levels.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Annesi et al.,56 Annesi55
Methods: Two prospective cohort studies.
Participants: In the earlier study by Annesi et al. 56 there was a final sample size of 241 children (mean age 10.1 years; 53% girls; recruitment and follow-up rates not reported). In the later study by Annesi55 the final sample size was 200 children (mean age 9.8 years; 51% girls; recruitment and follow-up rates not reported).
Intervention: This study investigated the Youth Fit for Life programme, an after-school obesity prevention and treatment programme in African American children of lower-middle and lower SES. The programme consisted of three 45-minute sessions per week for 12 weeks. The sessions included cardiovascular activities, resistance exercises, a review of self-management and self-regulatory skills and general health and nutrition education. In the earlier study56 the programme also included a version that was delivered during physical education lessons. The content of the physical education sessions was similar to the content of the sessions delivered in the after-school programme but instead of three sessions only two sessions were delivered per week.
Outcomes: In the earlier study56 height, weight and skinfolds (triceps and calf) were measured (blinding status of assessors not reported) and BMI and body composition were determined at baseline and post intervention. Indicators of fitness were also assessed [strength (number of push-ups completed in 1 minute), flexibility (shoulder stretch) and endurance (distance run/walked in 6 minutes)] and voluntary physical activity was self-reported using a validated single-item questionnaire. The results were reported separately for boys and girls. BMI and body composition improved in both boys and girls receiving either the after-school intervention or the physical education intervention. In boys there were no differences in the changes between treatment conditions; however, in girls, body composition (% fat) improved to a greater extent in the after-school group (after-school group –2.52%, physical education lessons group –1.07%; p = 0.004). In boys, improvements in strength and flexibility but not endurance were observed for both groups. Strength and endurance improved to a greater extent in the after-school group than in the physical education lessons group [change in strength (number of push-ups completed in 1 minute on a 3-second cadence): after-school group 3.52, physical education lessons group 1.18, p = 0.011; change in endurance (distance covered during a 6-minute run/walk): after-school group 193.55 m, physical education lessons group 41.52 m, p < 0.001]. In girls, there were improvements in strength in both groups (after-school group change 7.87 to 10.60, p < 0.001, physical education lessons group change 9.55 to 11.18, p < 0.001) but only those in the after-school group improved their flexibility and endurance [change in flexibility (distance from fingers touching behind the back) 2.05 cm to 0.08 cm, p = 0.003; change in endurance 603 m to 755 m, p = 0.026]. The increase in days of voluntary moderate- to vigorous-intensity physical activity per week was significant for both groups (boys and girls combined) (after-school group change 2.2 to 2.91 days, p < 0.001; physical education lessons group change 2.38 to 3.13 days, p = 0.005). There was no difference in the change between groups.
The main aim of the later study55 was to investigate differential effects of the Youth Fit for Life after-school intervention by weight status and physical activity level. This study included normal-weight, overweight and obese participants. Height and weight were measured at baseline and post intervention (blinding status of assessor not reported). Voluntary physical activity was measured using the validated single-item questionnaire in a subsample of children (n = 47). BMI was reduced in both normal-weight and overweight/obese children, in contrast to the increases that were expected, although the statistical significance of these changes and differences was not reported. Reductions in BMI were significantly greater in those who were overweight/obese than in normal-weight children (mean change: overweight/obese –0.48 kg/m2, normal weight –0.05 kg/m2; p < 0.001). Reductions in BMI in the obese group were not significantly different from those in the overweight group. Increases in voluntary physical activity were significantly greater in children who were insufficiently active than in those who were already sufficiently active (mean change in days/week of voluntary physical activity: insufficiently active 2.39, sufficiently active 0.28; p < 0.001).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate/weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Moore et al.70
Method: Prospective cohort study.
Participants: There was a reported 35% response rate and a final sample size of 126 children (aged 9–11 years; 63% girls); however, recruitment and retention numbers were not clearly reported and therefore the follow-up response rate is unknown.
Intervention: This study investigated the Color My Pyramid intervention in two low-SES schools in Washington DC, USA. The intervention consisted of nutrition and physical activity education, including an educational computer game, taught in six sessions over 3 months. The intervention in each school differed slightly but the results were combined when investigating intervention effects on obesity outcomes, nutrition behaviour, physical activity and blood pressure.
Outcomes: Anthropometric and blood pressure measurements were carried out by non-blinded researchers and physical activity and nutrition self-care practices were self-reported. There was no significant change in weight for age or BMI percentile from baseline to follow-up and there were no significant changes in the proportion of children in each weight status category. There were significant increases in physical activity (change 31 to 60 minutes per day; p < 0.001) and in the nutrition self-care practice score (change 155 to 162; p = 0.05) and a significant decrease in systolic blood pressure (change 114 mmHg to 108 mmHg; p < 0.001) but no change in diastolic blood pressure.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Kain et al.65
Method: Pilot prospective cohort study.
Participants: Children aged 4–10 years (pre-kindergarten to year 4) were randomly selected from school lists from seven schools in Santiago, Chile. The number of children recruited at baseline (n = 586) exceeded the number required by the study to reach statistical power (n = 400). There was an 89% follow-up response rate, resulting in a final sample of 522 children.
Intervention: This study investigated a school-based obesity prevention programme conducted in schools of medium to low SES (35% of children received free school meals). The intervention was conducted for 5 months and consisted of a nationally validated nutrition education programme and improved physical education lessons delivered by trained teachers. In addition to the child intervention, a subsample of teachers also received a health improvement intervention consisting of individual counselling sessions with a trained nutritionist at which they could discuss healthy eating and physical activity and set goals to improve behaviours. However, the child results presented in this study include all of the children who took part, regardless of whether or not their teacher had received the teacher intervention.
Outcomes: Height, weight and waist circumference were measured by a trained nutritionist (blinding status not reported) before and after the intervention period. Cardiovascular fitness was also assessed at these time points using a 6-minute walking test administered by trained physical education teachers. There was no change in BMI z-score, waist circumference, prevalence of obesity or prevalence of overweight from baseline to post intervention, although trends in the desired direction were noted for BMI z-score and prevalence of obesity in younger children. Indicators of cardiovascular fitness improved in younger children (pre-kindergarten to year 2) but worsened in older children (years 3 and 4).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Kain et al.66
Method: Prospective cohort study.
Participants: All children attending the seven middle- to low-SES schools in Santiago, Chile, took part in the intervention as it was incorporated into the existing curriculum. A total of 741 children completed the baseline and follow-up data collection measurements (78% follow-up response rate). In this study, results for all children are presented along with a subgroup analysis of children whose teachers received the intervention (n = 412) and children whose teachers did not receive the intervention (n = 237) (92 children could not be included in this analysis as their teacher either did not complete the intervention or did not provide enough data).
Intervention: This study investigated a nutrition education programme based on the pilot study65 and teachers were again trained to improve physical education lessons; however, in this study physical education teachers delivered the training to other teachers. As in the pilot study, a subsample of teachers (teachers from four of the schools) also received individualised counselling sessions with a trained nutritionist. The teachers’ eating and physical activity behaviours were also assessed at these sessions and the results were used to guide the discussions and goal-setting.
Outcomes: Height, weight and waist circumference were measured by trained nutritionists (blinding status not reported) at baseline and after the 2-year intervention. In the overall sample, reductions from baseline to follow-up were observed for BMI z-score (change 1.03 to 0.92; p < 0.0001) and prevalence of obesity (change 20.1% to 18.3%; p < 0.05). However, when these results were explored by gender, a decrease in the prevalence of obesity was observed for girls (change 18.8% to 15.4%; p < 0.05) but not for boys (change 21.5% to 21.0%; not significant). In the subgroup analysis a decrease in the prevalence of obesity was observed in children whose teacher did not receive the teacher intervention (change 20.7% to 16.5%; p < 0.05), although when exploring the results by gender there was only a decrease in girls (change 20.6% to 14.7%; p < 0.05). There was no change in the prevalence of obesity in all children whose teacher received the teacher intervention; however, a reduction was observed in girls (change 18.1% to 15.7%; p < 0.05). For BMI z-score, for those whose teacher received the intervention, no changes were observed for all children or for boys and girls separately. In children whose teacher did not receive the intervention, there was no change in BMI z-score overall, but a significant reduction did occur in boys (change 1.03 to 0.81; p = 0.0037).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Williams and Warrington85
Method: Prospective cohort study.
Participants: A convenience sampling method was used in which children who did not complete the programme acted as a comparison group for those who did. There was a baseline response rate of 83% and a final sample size of 231 (follow-up response rate of 55%), of whom 56 (24%) completed the programme.
Intervention: This study investigated a 12-week pedometer walking programme conducted in six low-SES schools (pupils aged 8–11 years; 58% girls). The intervention consisted of physical activity monitoring using pedometers provided to the children. Teachers received suggestions about how to engage children and how to include step counting into the curriculum. The children also received nutrition education in the form of written material and hands-on experience.
Outcomes: Height and weight were measured by a project team member at the beginning and end of the intervention period (blinding status not reported) and pedometer-determined step counts were self-recorded by participants. There were no significant differences between completers and non-completers at baseline or at post intervention for BMI or BMI percentile. In the completers only, step counts increased from baseline to post intervention (change 6567 to 10,804 steps; p = 0.001).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Nemer et al.72
Method: Case study from the WHO-Europe report of examples of health initiatives throughout Europe.
Participants: Baseline recruitment and follow-up response rates were not reported; 500 children (aged 10–14 years) took part in the intervention.
Intervention: This study investigated a school-based intervention designed to ensure adequate levels of physical activity in children attending low-SES schools in Germany and Denmark.
Outcomes: Details of the evaluation were limited. After 3 years it was reported that BMI was reduced (data not reported).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Woolford et al.101
Method: Retrospective analysis.
Participants: The baseline response rate was not reported. There was a follow-up response rate of 72%, resulting in a final sample size of 48 adolescents. The programme was conducted at the University of Michigan, MI, USA, and was targeted at obese adolescents (BMI ≥ 95th percentile; mean age 14.5 years; 71% girls) who were referred to the programme by their primary care physician. The programme followed a targeted and a universal approach. Although there were no exclusion criteria based on SES, the majority of participants were from low-income families and, in addition, the authors retrospectively explored the relationship between the participants’ insurance status (Medicaid recipient or not) and obesity-related outcomes.
Intervention: This study investigated a clinical multidisciplinary weight-management programme (MPOWER). The 24-week intervention consisted of individual and group (including parents) sessions delivered by a multidisciplinary team consisting of a paediatrician, a psychologist, a dietitian, a social worker and an exercise physiologist. The sessions included nutrition and physical activity education, exercise sessions and behavioural techniques such as goal-setting and problem-solving (using motivational interviewing).
Outcomes: Height and weight were measured and body fat was assessed using bioelectrical impedance at the first and last visit (blinding status of assessor not reported). From baseline to post intervention there was a mean reduction in BMI of –2.3 units and a mean reduction in per cent body fat of –5.1%. Changes in BMI and body fat were not associated with participants’ insurance status.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Ranstrom99
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Participants were referred to the programme by primary health-care providers. Recruitment and retention rates were not clearly reported. There was a final sample size of 20 children and their families.
Intervention: This study investigated a family-based overweight and obesity treatment programme conducted in a paediatric clinic in North Dakota, USA, targeted at children from low-income families (mean age 9.9 years; 75% girls). Families were asked to attend at least 10–12 sessions over a 3- to 4-month period. The sessions included nutrition and physical activity education and practical exercises and activities. Participants were also asked to set weekly nutrition and exercise goals and progress was monitored using a sticker chart. Telephone check-in calls were also used to keep in touch with families who could not attend all of the sessions.
Outcomes: Measurements were taken at baseline and post intervention. Height and weight were measured (blinding status of the assessor was not reported) and daily physical activity level, computer/television use per day and dietary intakes were self-reported. The majority of the participants maintained their BMI percentage from baseline to post intervention (group mean changes not reported). There was an increase in hours of physical activity per day (mean change 0.92 hours; p = 0.011) but no change in computer/television use. There was a significant reduction in sugared drink consumption per day (mean change –0.5 servings; p = 0.013) and a significant change in milk type (mean change –0.36; p = 0.012), but there were no changes in fruit, vegetable or water intake.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Hawthorne et al.61
Method: Prospective cohort study.
Participants: Grand Canyon Trekkers was implemented in 10 low-SES schools in north-east Phoenix, AZ, USA (pupils aged 5–12 years; 51% girls). There was a baseline response rate of 22% and a final sample size of 1074 children (83% follow-up response rate).
Intervention: This study investigated a structured lunchtime walking programme, Grand Canyon Trekkers, in low-income, primarily Hispanic schoolchildren. Children completed a 0.25-mile walking trail 3 days a week for 16 weeks. Mileage cards were provided for monitoring progress and incentives were awarded at predetermined mileage intervals. Teachers also received incentives for modelling positive physical behaviour.
Outcomes: Anthropometric measurements were taken by nursing students (blinding unlikely) and cardiovascular fitness was assessed using a 20-m shuttle run at baseline and post intervention. No significant changes in BMI percentile or waist circumference were observed from baseline to post intervention. Cardiovascular fitness increased by 37% from baseline to post intervention in the entire sample (all ages and weight status and both genders).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Moderate |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Rudolf et al.91,92
Method: Prospective pilot cohort (uncontrolled before-and-after) study.
Participants: Participants (mean age 12.2 years; 52% girls) were recruited through health professional referral or self-referral. The recruitment response rate was not reported. The final sample included 48 children (follow-up response rate of 51%).
Interventions: This study investigated an obesity treatment programme (WATCH IT) conducted in community settings and aimed at obese children living in deprived areas in Leeds, UK. The WATCH IT programme was delivered by trained health trainers and sports coaches and consisted of frequent individual sessions at which participants received motivational counselling, encouragement and support; weekly 1-hour group activity sessions; and group parenting sessions.
Outcomes: Height and weight measurements were collected at baseline, 3 months and 6 months by non-blinded project staff. There was no significant change in BMI SDS at 3 months; however, BMI SDS was significantly reduced at 6 months’ follow-up (–0.07; p < 0.01). Subgroup analysis revealed significant reductions in BMI SDS in girls (–0.07; p = 0.02) and those aged ≥ 13 years (–0.13; p < 0.01) from baseline to 6 months.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Moderate |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Fletcher et al.60
Method: Pilot prospective cohort study.
Participants: The setting of this intervention was unclear. It took place in the USA and children were identified from regularly scheduled Medicaid screenings at the UNACARE Health Centre. The intervention was targeted at children aged 3–17 years (92% girls). The baseline recruitment rate was not reported but 12 children participated in the study. It seems that there was a 100% follow-up response rate resulting in a final sample size of 12 children; however, this was not clear.
Intervention: This study was a pilot study investigating the Kids for Healthy Eating and Exercise (KHEE) club, which was a weight control programme specifically designed for African American children lasting for 10 months.
Outcomes: Measurements included weight loss, waist girth, triceps skinfold thickness, dietary intake and physical activity. The intervention resulted in > 10% weight loss and a > 4-inch waist girth decrease for all participants as well as a significant decrease in triceps skinfold thickness (p < 0.005). Improvements were also observed for physical activity and dietary intake with 75% reporting continued exercise on three or more days per week and 80% increasing their daily intake of fruit and vegetables (to five per day).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Societal (environmental)-level interventions
Universal approach: experimental studies
None.
Universal approach: observational studies
None.
Targeted approach: experimental studies (n = 7)
Foster et al.109
Method: Randomised cluster trial.
Participants: The intervention was targeted at five schools (pupils aged 11 years at baseline; 54% girls) in deprived areas of Philadelphia, PA, USA, with five matched schools acting as control schools. Deprivation was defined as a school at which > 50% of pupils received free school meals. Schools were randomly sampled from 27 eligible in the state and allocation was also randomised at the school level, stratified by school size and food provision. There was a 70% baseline response and a final sample size of 844, with 479 in the intervention group (a follow-up response rate of 63%).
Intervention: This study investigated the School Nutrition Policy Initiative, a school-based educational and environmental intervention to increase nutritional knowledge and the availability of healthy food. The multifaceted School Nutrition Policy Initiative (delivered by a community organisation and funded by national government) included staff training (10 hours per year for teachers on nutritional education and parent outreach; nutrition teaching materials provided), nutrition education (50 hours per pupil per year), social marketing (promotional competitions to promote healthy eating, healthy food branding logos and promotional slogans), parent outreach (home and school meetings, encouragement of healthy eating and physical activity) and environmental changes (all foods sold on school premises were changed to meet national nutritional standards, which meant that sodas, crisps and other high-calorie snacks were no longer sold in vending machines or cafeterias; calorie content labelling). The intervention lasted for 2 years.
Outcomes: The primary outcome was the independently measured incidence of obesity and overweight (% of those of normal weight/underweight at baseline who became overweight or obese) and secondary outcomes were age- and sex-adjusted BMI z-score, the prevalence of obesity or overweight and remission (% no longer overweight/obese). Self-reported sedentary activity, physical activity, total energy consumed (kJ), fat consumption (g) and fruit and vegetable servings were also assessed using a validated questionnaire. Baseline measures were the same in each group (p > 0.05), with an obesity prevalence of 26.7% and an overweight prevalence of 16.7% in the intervention group. At 2 years’ follow-up, the incidence of overweight was 33% less in the intervention group (intervention group 7.46% vs. control group 14.9%; adjusted OR 0.67, 95% CI 0.47 to 0.96) and the prevalence of overweight was 35% less (intervention group 16.28% baseline to 14.61% follow-up vs. control group 15.89% baseline to 20% follow-up; adjusted OR 0.65, 95% CI 0.54 to 0.79). The reduction in prevalence was particularly effective for black pupils (adjusted OR 0.59, 95% CI 0.38 to 0.92). Sedentary behaviour was 4% lower in the intervention group than in the control group (adjusted OR 0.96, 95% CI 0.94 to 0.99). However, there were non-significant differences in the incidence or prevalence of obesity, remission, changes in BMI and the other self-reported outcomes.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Weak |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Foster et al.108
Method: Randomised cluster trial.
Participants: The intervention was targeted at 21 low-income schools (pupils aged 11 years at baseline; 53% girls) in seven different states in the USA, with 21 matched schools acting as control schools. A low-income school was defined as one at which > 50% of pupils received free school meals (average 77%). Schools volunteered to participate but allocation was randomised at the school level. There was a 57% baseline response rate and a final sample size of 4603, with 2307 in the intervention (a follow-up response rate of 72%).
Intervention: This study investigated an integrated educational, physical activity and food environment intervention. The integrated intervention included healthy lifestyle education, changes to the quantity and quality of foods sold on school premises (vending machines or cafeterias) and increased time spent engaged in physical activity. These changes were reinforced by social marketing. The intervention lasted for 30 months.
Outcomes: The primary outcome was the independently measured prevalence of obesity and overweight, with BMI, waist-to-hip ratio, remission (% no longer overweight/obese) and glucose and insulin levels as secondary outcomes. Baseline measures were the same in each group (p > 0.05), with an obesity prevalence of 30.1% and an overweight prevalence of 20.2% in the intervention group. At follow-up there were reductions in the prevalence of overweight and obesity in both the intervention group and the control group, with non-significant differences between the groups. However, the mean BMI score (p = 0.04) and waist-to-hip ratio (p = 0.04) were significantly lower in the intervention group. There were significantly more cases of remission in the intervention group, with overweight or obese pupils at baseline having a 21% lower chance of being obese at follow-up than control group pupils (OR 0.79, 95% CI 0.63 to 0.98). There were non-significant differences in glucose levels but insulin levels were lower in the intervention group (p = 0.04).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Williams et al.114
Method: Non-randomised cluster trial.
Participants: The interventions were delivered in six Head Start preschools (average age 4 years at baseline; 49% girls) in New York City, NY, USA, with three similar schools acting as control schools. Head Start schools serve low-income communities (below the poverty line). The study sampling and intervention allocation at the school level was not described. There was a 95% baseline response rate and a final sample size of 676, with 233 and 181 in the two intervention groups (86% response rate).
Interventions: This study investigated two Healthy Start interventions to improve cardiovascular health (cholesterol was the primary outcome). The two interventions were (1) food service changes, parental outreach and nutritional education and (2) food service changes and parental outreach. The food service changes reduced the fat content of school-served foods and the parental component involved ‘take-home’ educational materials on preschool learning and three to four school-based meetings per year on health themes. The education supplement was teacher delivered and focused on healthy eating. The intervention lasted for 8 months.
Outcomes: The primary outcome was change in total and serum cholesterol with changes in the prevalence of obesity and overweight, as well as BMI z-score. At follow-up, there were non-significant differences between the intervention group and the control group in the prevalence of obesity or overweight or BMI z-score, although serum and total cholesterol both decreased in both of the intervention groups (p < 0.01).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Heath and Coleman,116 Coleman et al.107
Method: Non-randomised cluster trial.
Participants: The intervention was targeted at four schools (pupils aged 8 years at baseline; 47% girls) in deprived areas of Texas, USA, with four geographically matched schools acting as control schools. Low income was defined in terms of US Department of Education Title 1 school status, in which the majority of pupils are from families below or around the poverty line. Intervention and control schools were randomly sampled from those eligible in the area. There was a 94% baseline response rate and a final sample size of 744, with 400 in the intervention group (a follow-up response rate of 83%).
Intervention: This study investigated the CATCH initiative, a school-based educational and environmental intervention to increase nutritional knowledge and physical activity and provide healthier school food. The multifaceted CATCH programme (delivered by a community organisation and funded by national government) included nutrition education, increased levels of physical activity (the amount of moderate- to vigorous-intensity physical activity was to increase to > 40% of class time, subsidies were provided for new sports equipment) and environmental changes (school meals to have < 30% of total calories, sodium content to between 600 mg and 1000 mg and saturated fat to be < 10% of total calories). The intervention lasted for 2 years.
Outcomes: The primary outcome was the independently measured prevalence of obesity (% of those above the 95th percentile for BMI) and overweight (% of those above the 85th percentile for BMI), with BMI, waist-to-hip ratio and weight also measured. Physical fitness was also assessed using a fitness test. There were differences at baseline between the intervention group and the control group for girls but not for boys in terms of percentage overweight and obese (26% control group, 30% intervention group; p < 0.01) but no adjustments were made in the analysis. At 2 years’ follow-up, the percentage of those who were overweight and obese increased significantly for both girls and boys in the intervention group and the control group; however, the rate of increase was significantly lower in intervention schools: intervention group girls increased by 2% from 30% to 32% and control group girls increased by 13% from 26% to 39%; intervention group boys increased by 1% from 40% to 41% and control group boys increased by 9% from 40% to 49% (p < 0.05). The prevalence of obesity did not increase for girls although there were increases for boys in both the intervention group (5%) and the control group (8%) (difference not significant). There were non-significant intervention effects on weight, waist-to-hip ratio and BMI, and the passing rate for the fitness test decreased in all children but to a lesser extent in boys but not girls in the intervention schools (mean change boys: control group –29%, 95% CI –35% to –23%, intervention group –13%, 95% CI –18% to –8%; mean change girls: control group –19%, 95% CI –25% to –13%, intervention group –16%, 95% CI –22% to –10%).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Hollar et al.110,111,115
Method: Non-randomised cluster trial.
Participants: The intervention was delivered in four schools (average pupil age 8 years at baseline; 51% girls) in Florida, USA, with one school acting as a control school. The intervention was delivered to all pupils but the analysis focused on the results for those with a low income, defined in terms of entitlement to free (family income < 130% of the federal poverty line guidelines) or reduced-price (family income 130–185% of the poverty line guidelines) school meals. The study used convenience sampling and intervention allocation at the school level was also non-random. There was an 82% baseline response and a final sample size of 1197, with 196 in the intervention group (no follow-up response rate reported).
Intervention: This study investigated the Healthier Options for Public Schoolchildren (HOPS) programme. The intervention combined healthy lifestyle education and a physical activity component (15 minutes per day) with improvements to the nutritional content of school-provided meals and snacks (increased fibre and lower fat) and a school fruit and vegetable garden. The intervention lasted for 18 months.
Outcomes: The outcomes were changes in the prevalence of obesity and overweight, as well as BMI and weight z-scores. Baseline measures were the same in each group (p > 0.05), with an obesity prevalence of 17.6% and an overweight prevalence of 7.3% in the intervention group. At follow-up, there were non-significant differences between the intervention group and the control group in the prevalence of obesity or overweight. However, BMI (intervention group 0.71, control group 1.05; p < 0.05) and weight (intervention group 0.65, control group 0.95; p < 0.05) z-scores showed larger decreases in the intervention group than in the control group and there were larger decreases in BMI percentile in the intervention group (intervention group –1.73, control group –0.47; p < 0.007).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Perman et al.113
Methods: Non-randomised cluster controlled study.
Participants: The intervention school was selected because it exhibited risk factors for childhood obesity – low-income families, minority population (67% African American, 13% Hispanic) – and was located in a neighbourhood where outdoor opportunities for physical activity were limited. A non-intervention school was selected as a comparison school (matching or the investigation of differences between the schools was not reported). Baseline response rates were not reported. There was a final sample size of 350 children for the school-wide intervention (follow-up response rate not reported) and 27 children in the targeted intervention group (68% follow-up response rate), who were matched to a comparison group by BMI, age and gender (n not reported).
Interventions: This study investigated a community-driven universal school-based diet and physical activity intervention and a targeted intervention for overweight children in a school attended by children from low-income families. The universal, school-wide intervention consisted of nutrition education, in-class physical activity, healthy breakfasts and lunches and a School Health Advisory Council. The targeted intervention included the addition of education sessions for parents (including cooking sessions), motivation and good choices group sessions, after-school fun activities, mentors and behavioural support and incentives such as healthy snacks, t-shirts, 1-year membership to the Young Men‘s Christian Association (YMCA) and scholarship savings bonds.
Outcomes: The primary outcome was BMI percentile, calculated using measured height and weight (blinding not reported) and an appropriate BMI-for-age growth chart. For the school-wide population there was no significant difference in BMI percentile between the intervention school and the control school at baseline but post intervention the BMI percentile of the intervention children was significantly lower than that of the control children (intervention group 68.6, control group 75.5; p = 0.027). There was no significant difference in BMI percentile between the targeted intervention group and the targeted control group at baseline or post intervention.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Targeted approach: observational studies (n = 3)
Ramirez-Lopez et al.120
Method: Prospective cohort (controlled before-and-after) study.
Participants: The study data were taken from 17 municipalities in Sonora State, Mexico (pupils aged 6–10 years at baseline; boys and girls). The final sample included 360 children (intervention group 254, control group 106), with a follow-up response rate of 59%.
Intervention: This study investigated a Mexican national school breakfast programme. The breakfast programme had been run in Mexico since 1929 and was available to pupils from low-income families. The programme provided 25–27% of daily nutritional needs. The follow-up period was 9 months.
Outcomes: The main outcomes were BMI, prevalence of overweight and obesity (independently measured using weight and height and with reference to national distributions) and percentage of body fat, with biochemical indicators (total cholesterol, serum triglycerides, fasting glucose) as secondary outcomes. There were no significant differences in any of the outcomes over time in the intervention group or between the intervention group and the control group at follow-up.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Ibarra and Alarcón112
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: The intervention was targeted at one secondary school (pupils aged 14–17 years at baseline; 56% girls) in a deprived small town in Chile. Deprivation was defined as high levels of unemployment and poverty. The sample frame was all pupils in years 1–3 of the secondary school and there was a 90% baseline response rate and a final sample size of 472 (follow-up response rate of 100%).
Intervention: This study investigated a school-based educational and environmental intervention that included nutritional education alongside a healthy eating kiosk. Pupil education involved standard teacher-led classroom sessions on healthy eating and obesity and the inclusion of nutritional education in physical education classes, as well as a school play and an art mural to promote healthy eating. Parents were also invited to nutritional information dissemination events (including the play) and were provided with information about nutrition and obesity within the school. The school kiosk was transformed into a healthy eating kiosk, as defined by the Chilean Ministry of Health. The intervention period was 24 months.
Outcomes: The primary outcome was obesity and risk of obesity (measured using weight and height and with reference to national distributions), with calorie intake relative to need as a secondary outcome. Researchers conducted the adiposity measurements whereas calorie consumption data were self-reported. The study reported that the risk of obesity decreased from 28% to 25% at 24 months’ follow-up, the prevalence of obesity increased from 10% to 12% and the prevalence of risk of obesity reduced from 18% to 13%. Average daily calorie intake decreased from 115% of calories needed to 102%. Differences by sex were noted, with higher reductions in the risk of obesity and calorie intake among boys than among girls. No statistical analysis was presented by the study authors, but 95% CI calculations by the systematic review team found that none of the reported changes were statistically significant at the 5% level.
Quality appraisal
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Frisvold and Lumeng121
Method: Retrospective cohort (controlled before-and-after) study.
Participants: This study was based in Michigan, USA (children aged 3–5 years at baseline; 49% girls). Low income was defined as around or below the federal poverty level. The sample frame was all children enrolled in one Head Start provider in Michigan and there was a final sample size of 1532, with 327 in the intervention group (a follow-up response rate of 87%).
Interventions: This study investigated Head Start childcare classes with associated increased access to nutritional meals and physical activity. The study compared the effects of full-day Head Start childcare with the effects of half-day childcare. The Head Start programme has been run nationally since 1965, providing childcare for low-income children on a half-day basis. This was expanded in 2000 to also provide full-day childcare as part of a wider welfare reform initiative to enhance maternal employment. The Head Start programme provides nutritionally balanced meals (with full-day attendance providing 50–66% of daily nutritional needs) as well as physical activity and playgrounds.
Outcomes: Routinely collected administrative data were pooled for five annual Head Start cohorts, with outcomes measured at baseline and 6 months later by the Head Start employees. Data were compared for the half-day and full-day cohorts. The outcomes examined were BMI and the prevalence of obesity and overweight (national distributions). At baseline, 17% of full-day (intervention group) and 17% of half-day (intervention group) children were obese; at follow-up this had decreased to 12% and 16%, respectively, with a statistically significant (p = 0.04) additional decrease among the full-day intervention group of almost four percentage points. Decreases in the prevalence of overweight were non-significant, as were changes in BMI.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Moderate |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Muckelbauer et al.117–119
Method: Randomised cluster trial.
Participants: The intervention was targeted at 17 primary schools (pupils aged 8 years at baseline; 50% girls) in deprived urban areas of Dortmund, Germany, with 15 primary schools in deprived urban areas of Essen, Germany, acting as control schools. Area deprivation was defined as > 15% unemployment, > 5% welfare receipt and > 5% non-German residents. Randomisation was at the city level, with schools randomly sampled within the two cities. There was an 87% intervention group baseline response rate (80% control group) and a final sample size of 2950, with 1641 in the intervention group (a follow-up response rate of 95%).
Intervention: This study investigated a school-based educational and environmental intervention to increase water consumption. The intervention entailed the installation of water fountains in the schools alongside four 45-minute (total 180 minutes) teacher-delivered lessons on the importance of water consumption, the provision of water bottles for pupils and encouragement to fill them each day (including target-setting for consumption from month 3 and new bottles in month 5). The intervention lasted for 10 months.
Outcomes: The primary outcome was BMI, with BMI SDS and beverage consumption (water, soft drinks, fruit juice) as secondary outcomes. Health-care professionals conducted the adiposity measurements (German reference values) whereas beverage consumption data were self-reported and collected by the school teachers. Baseline measures were the same in each group (p > 0.05) except for fruit juice consumption, which was slightly higher in the intervention group (p = 0.032). At 10 months’ follow-up, the prevalence of overweight (BMI) was 23.5% (baseline 23.4%) in the intervention group and 27.8% (baseline 25.9%) in the control group. The risk of becoming overweight (adjusted for the prevalence of overweight at baseline and clustering according to school) was significantly reduced in the intervention group compared with the control group (OR 0.69, 95% CI 0.48 to 0.98; p = 0.04). The incidence rate of overweight (number of newly diagnosed overweight children at follow-up in relation to the number of non-overweight children) was significantly lower in the intervention group (3.8%) than in the control group (6.0%) (p = 0.018). In contrast, the remission rate of overweight and obesity (number of participants no longer overweight/obese at follow-up divided by all overweight/obese participants at baseline) among the subgroup of overweight children did not differ significantly between the groups. In terms of beverage consumption there was a significant increase in water consumption in the intervention group compared with the control group (adjusted difference 1.1 glasses per day, 95% CI 0.7 to 1.4 glasses per day; p < 0.001). There were non-significant differences between the intervention group and the control group at follow-up in BMI SDS, juice consumption and soft drink consumption (p > 0.40).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Individual-, community- and societal-level interventions
Universal approach: experimental studies (n = 1)
Sanigorski et al.124
Method: Quasi-experimental study.
Participants: Children aged 5–12 years were eligible to participate in the evaluation (mean age of those participating was just over 8 years), and about half of those participating were female (54% in the intervention group, 50% in the control group). Of the eligible 1726 participants in the intervention group at baseline, 1001 agreed to take part in the evaluation (58%) and 84% of these were assessed at follow-up. Of the eligible 2687 participants in the control group at baseline, 1183 agreed to take part in the evaluation (44%) and 83% of these were assessed at follow-up. The area of Australia in which this study was conducted, the Barwon South Western region of Victoria, is a socioeconomically disadvantaged area compared with state-wide averages.
Interventions: This study investigated a 3-year community capacity-building intervention (Be Active Eat Well) to reduce the prevalence of overweight and obesity in children aged 4–12 years attending preschools or primary schools in Colac, a town in the Barwon South Western region of Victoria, Australia. Be Active Eat Well is a multifaceted community capacity-building intervention that was designed to build the community’s capacity to create its own solutions to promoting healthy eating, physical activity and healthy weight in children aged 4–12 years and their families. It was designed, planned and implemented by a number of key organisations in Colac, working in partnership, and was delivered in preschools and primary schools.
Outcomes: Measurements were collected by trained researchers from children who agreed to participate in the evaluation of the intervention in all four preschools and all six primary schools in Colac at baseline and at 3 years’ follow-up. The same measurements were taken in the control schools, which were also in the Barwon South Western region of Victoria, but at least > 30 km away from Colac, using the probability proportional to size method.
The primary outcomes were change in BMI, BMI z-score and waist circumference at 3 years. Trained staff conducted the anthropometric measurements using established guidelines (blinding status not reported). Physical activity and dietary intake data (along with other information) were collected from some children using a 16-question survey. Children in the intervention schools showed significantly lower increases in waist circumference (–3.14 cm) and BMI z-score (–0.11) than children in the control schools. SES was assessed using four different indices: mother’s education, father’s education, household income and an area-level indicator of SES called the Socioeconomic Index for Areas. The adjusted regression coefficients between the changes in anthropometric measures and the four indices of SES were not statistically significant in the intervention group, that is, the intervention did not increase health inequalities. However, the same analyses in the control group resulted in significant negative regression coefficients between all four indices of SES and change in anthropometric outcomes (except for household income and change in waist circumference), that is, lower-SES was associated with a greater gain in body fat and waist circumference.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Universal approach: observational studies (n = 1)
Chomitz et al.122
Method: Uncontrolled study.
Participants: Baseline measurements were collected from all children in kindergarten to fifth grade in 13 schools (mean age 7.7 years; 48% girls) as part of a state-wide routine surveillance service, and end-point/outcome data were taken from the same group of children 3 years later. Of the eligible 3561 participants at baseline, 1858 (52%) were assessed at 3 years.
Interventions: This study investigated a 3-year community-based intervention (Healthy Living Cambridge Kids) to reduce the prevalence of overweight and obesity in children aged 5–11 years attending schools in Cambridge, MA, USA. The intervention was developed using the socioecological model and community-based participatory research principles. Healthy Living Cambridge Kids is a multicomponent intervention targeting the community, schools, families and individuals. The intervention included city policies and community awareness campaigns, physical education enhancements, food service reforms, farm-to-school-to-home programmes and family outreach and ‘BMI and fitness reports’. These reports were a form of individualised feedback sent to all children and their families on an annual basis.
Outcomes: The primary outcomes were change in BMI z-score, and change in the percentage of children in the four weight status categories at 3 years. Trained staff conducted the height and weight measurements using established guidelines (blinding status not reported). For the whole sample, the BMI z-score decreased significantly by a mean of 0.04 over 3 years. The percentage of children in the obese category decreased significantly from 20.2% to 18.0% over 3 years, and the changes in the overweight, ideal weight and underweight categories were from 16.8% to 17.4% (not significant), 61.0% to 63.4% (significant) and 2.1% to 1.2% (significant) respectively. When these data were analysed by income status or race, the results were particularly informative. Similar decreases in the percentage of children in the obese category (about 2%) were seen in the high- and low-income groups, even though the baseline levels of obesity were 28% in the low-income group and 14% in the high-income group. Of importance (as it was a concern highlighted by some stakeholders during the development of the intervention), there was no significant increase in underweight in any group during the 3-year intervention period, and in most of the groups the percentage of underweight children decreased significantly.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Weak |
| C) Confounders | Weak |
| D) Blinding | Weak |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Targeted approach: experimental studies
None.
Targeted approach: observational studies (n = 1)
Hoelscher et al.123
Method: Serial cross-sectional intervention study.
Participants: Baseline measurements were taken from all children in one school year (fourth grade, aged 9–10 years; 53% girls) and end-point/outcome data were taken from a different group of children in the same schools (fourth graders) 1 year later. Although 97 schools were included in the study, only 30 (15 in each group) were included for analysis in this paper. Fifty-nine of the 97 schools were classified as low-income schools and 15 of these low-income schools were selected to receive the CATCH BPC intervention [a universal school-based intervention (CATCH BP) plus the additional promotion of community partnerships] ‘based on input from school district leaders regarding perceptions of the school principal, PE teachers, and school faculty support’ (p. S38),123 although the details of what criteria were used for selection are not clear. The remaining 44 low-income schools were compared with these 15 CATCH BPC schools in terms of ethnic profile and SES and the best-matched 15 schools were selected to receive the CATCH BP intervention. It is unclear from the data provided what the baseline or end-point response rate was but it is stated that approximately 1100 students participated at both time points.
Interventions: This study investigated a universal school-based intervention (CATCH BP) compared with CATCH BP plus the additional promotion of community partnerships (CATCH BPC) to reduce the prevalence of overweight and obesity in children aged 9–10 years attending low-income schools in Texas, USA. The interventions were developed using a ‘whole-school approach’ and incorporated elements of socioecological models and social cognitive theory. The schools receiving the CATCH BP intervention were provided with an evidence-based co-ordinated school health programme, training, materials and facilitator support visits. The CATCH BPC schools received the additional promotion of community partnerships, with the aim of integrating community members and organisations into schools, local decision-making and action, and workshops.
Outcomes: The primary outcome was prevalence of overweight and obesity (> 85th percentile) and the prevalence of obesity (> 95th percentile). Trained staff conducted the height and weight measurements using established guidelines, but it is unclear if they were blinded to which schools were receiving which intervention. Physical activity and dietary intake data were collected using a modified version of the School Physical Activity and Nutrition (SPAN) questionnaire. 240,241 At baseline, the prevalence [mean standard error (SE)] of overweight and obesity, and obesity, in fourth graders appeared lower in the CATCH BP group than in the CATCH BPC group [42.0% (0.02%) vs. 47.4% (0.02%) and 23.9% (0.02%) vs. 27.5% (0.02%) respectively]. A smaller difference between groups may have been expected if the method of allocation of schools to intervention type had been randomisation. At 1 year, the prevalence rates [mean (SD)] for children in the same schools who were now fourth graders were more similar between the CATCH BP group and the CATCH BPC group [40.7% (0.02%) vs. 39.1% (0.02%) and 22.0% (0.02%) vs. 23.9% (0.02%) respectively]. However, compared with the CATCH BP group, the prevalence of overweight and obesity in children attending schools that received the CATCH BPC intervention had decreased more at 1 year [difference in change between groups –7.0% (0.05%)]. The difference in change between groups for the prevalence of obesity was not significant. There were also significant relative changes in favour of the CATCH BPC group for some of the diet and sedentary behaviours assessed (% who had breakfast, intake of fruit and vegetables, unhealthy food index, % who watched > 2 hours of television per day and % who spent > 2 hours per day on a computer). No differences were found for any of the physical activity/sport/vigorous physical activity behaviours or, of particular interest, the number of sugar-sweetened beverages consumed per day.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Weak |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Not applicable |
| Global rating | Weak |
Appendix 7 Detailed summaries of the included adult studies
Individual-level interventions
Universal approach: experimental studies (n = 3)
Volpp et al.138
Method: RCT.
Participants: A total of 958 veterans were invited by mail to take part in the study, of whom 57 were recruited using inclusion criteria of age between 30 and 70 years and BMI of between 30 kg/m2 and 40 kg/m2 (baseline recruitment rate 5.9%; 5.3% female). After 16 weeks, 52 participants remained in the study (follow-up response rate 91%).
Interventions: This study investigated two weight loss programmes with financial incentives compared with a weight loss programme without financial incentives (active control). The two financial incentive interventions were a lottery-based intervention in which participants played a lottery and received earnings if they achieved or lost more than their target weight, and a deposit contract condition in which participants invested their own money, which they lost if they did not achieve their weight goal. After an initial consultation with a dietitian, covering diet and exercise strategies, participants were weighed each month by non-blinded study staff. Participants in both financial incentive groups weighed themselves and received feedback (including financial or potential financial earnings) by text message each day.
Outcomes: After 16 weeks, mean weight loss was greater in each of the incentive groups (lottery group: 13.1 lb, p = 0.02, 95% CI of the difference in means 1.95 lb to 16.40 lb; deposit contract group: 14.0 lb, p = 0.006, 95% CI of the difference in means 3.69 lb to 16.43 lb; control: 3.9 lb, 95% CI of the difference in means 0.20 lb to 13.2 lb). Although only 10.5% (95% CI 1.3% to 33.1%) of control participants attained the 16-lb weight loss goal, about half of the incentive participants did (lottery group: 52.6%, 95% CI 28.9% to 75.6%; deposit contract group: 47.4%, 95% CI 24.5% to 71.1%; p = 0.01). The odds of achieving the 16-lb weight loss goal were significantly greater in both the deposit contract group (OR 7.7, 95% CI 1.4 to 42.7) and the lottery group (OR 9.4, 95% CI 1.7 to 52.7) compared with the control group.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Weak |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Edye et al.139
Method: RCT.
Participants: The total number of eligible participants was difficult to determine because of mobility but it is estimated that the participation rate was between 35% and 45%. A total of 2489 participants were eligible from the 4607 who volunteered to participate. Participants were randomised into the intervention group or the reference group (using random numbers allocation). In total, 1937 participants (77.8%) were included in the 3-year follow-up. The mean age of male participants was between 35.8 and 36.7 years and the mean age of female participants was between 29.1 and 29.7 years. The ratio of men to women in the study was not reported.
Interventions: This study investigated individual counselling in the worksite in Sydney, Australia, in adults with mildly elevated levels of cardiovascular risk factors. The intervention group received a 40-minute medical interview followed by a 15- to 20-minute counselling session with a physician. Advice was given on diet, aimed at weight and cholesterol reduction. Pamphlets were also given that were produced by the New South Wales Department of Health. Additionally, three 20-minute counselling sessions were provided by a nurse (at monthly intervals). The reference (control) group received an explanation of risk factors from a physician but no further intervention.
Outcomes: The outcome measures were independently measured weight (by a nurse; blinding not reported), proportion not fit (based on heart rate after exercise), systolic and diastolic blood pressure and cholesterol. After 3 years, in the intervention group there was an increase in mean weight (baseline 71.7 kg ± 0.28 kg, follow-up 72.8 kg ± 0.29 kg; p < 0.01) and cholesterol (baseline 5.5 mmol/l ± 0.02 mmol/l, follow-up 5.8 mmol/l ± 0.02 mmol/l; p <0.01) and a reduction in systolic blood pressure (baseline 124.5 mmHg ± 0.31 mmHg, follow-up 122.2 mmHg ± 0.30 mmHg; p < 0.01) but no statistically significant effects on diastolic blood pressure. The proportion who were not fit also decreased (baseline 59.6% ± 1.1%, follow-up 47.9% ± 1.1%; p < 0.01). However, the Bonferroni-corrected results showed that none of the results were statistically significant when the 56 comparisons were made (eight occupations compared with the risk factor measurements listed above). Therefore, this RCT indicates that a programme of individual counselling by occupational health personnel at the worksite, which was directed towards the amelioration of risk factors for coronary heart disease, did not achieve major long-term improvements, although the intervention appeared to have some small effect on systolic blood pressure in men who were aged ≥ 40 years or in men who were employed in the administrative category. In terms of narrowing inequalities in obesity, this study does not suggest that individual counselling sessions would have a significant effect on any occupational group.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Jeffery and French129,130
Method: RCT.
Participants: A total of 1226 participants aged 20–45 years were recruited at baseline (228 men, 594 high-income women and 404 low-income women; 81% female overall). After 3 years there was a 72% follow-up response rate, resulting in a final sample of 809 adults. Participants were recruited through a variety of methods including telephone solicitation, newspaper advertising and mailings to a large workplace. To ensure that a representative low-SES sample was recruited, recruitment efforts were also targeted at low-SES areas and face-to-face recruitment of women participating in the Special Supplemental Nutrition Program for Woman, Infants, and Children was carried out.
Interventions: This study investigated a weight gain prevention intervention, Pound of Prevention. Participants were randomly assigned to one of three groups: a non-contact control group, an education-only intervention and an education plus lottery incentive intervention. The education intervention consisted of messages promoting regular weighing, eating more fruit and vegetables, reducing the consumption of high-fat foods and increasing exercise levels, delivered primarily through a monthly newsletter. Every 6 months participants were also offered the opportunity to attend additional intervention activities such as weight control classes run by nutritionists, physical activity educational seminars, dance classes and home-based walking competitions, as well as being offered gym membership. In addition, the education plus lottery incentive group had the chance to win $100 each month.
Outcomes: The primary outcome was weight change, which was measured using standard techniques (blinding status of the assessor was not reported) at baseline and after 1 and 3 years’ follow-up. At 1 year there were no significant between-group differences (education intervention vs. education plus lottery vs. control) in terms of weight change for either high- or low-income women; however, a trend was observed that indicated a potential adverse effect of the intervention, with low-income intervention women (both intervention groups combined) gaining more weight than low-income control women. In high-income women there was a trend towards a desirable intervention effect. At 3 years, again there were no significant intervention effects and there were no significant interactions between treatment and participant type (men or low-income women or high-income women).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Universal approach: observational studies (n = 10)
Weinehall et al.127 (two study designs)
Methods: Quasi-experimental study incorporating a longitudinal cohort study and a serial cross-sectional study.
Participants: A total of 690 participants completed the longitudinal study and approximately 2500 participants took part in each cross-sectional survey (baseline recruitment and follow-up response rates not reported).
Interventions: This study investigated two low-budget population-wide cardiovascular disease prevention interventions, one conducted in Sweden and the other conducted in the USA. Both interventions involved population-based health promotion (health messages, including healthy eating and physical activity, promoted throughout communities) and individually oriented disease prevention activities (screening of cardiovascular risk factors and appropriate medical counselling/information provision/follow-up medical care), although each intervention was developed independently and was designed to fit the local social and political conditions in each country. The Swedish intervention focused most strongly on the improvement of nutrition, whereas in the USA prevention and cessation of smoking was the primary concern.
Outcomes: Data were collected at two time points for both studies: at baseline and 5 years. Height, weight, cholesterol and blood pressure measurements were taken by study staff following standard procedures (blinding status not reported). After 5 years, in Sweden there were no differences in BMI changes between the intervention group and the reference population in the cohort study overall (change: intervention group 25.3 kg/m2 to 25.8 kg/m2, control group 25.0 kg/m2 to 25.5 kg/m2; p = 0.880) or in either education group. However, in the cross-sectional study, BMI significantly increased in the intervention group (change: intervention group 25.3 kg/m2 to 26.0 kg/m2, control group 25.3 kg/m2 to 25.4 kg/m2; p = 0.31) as well as in the lower education group (change: intervention group 25.7 kg/m2 to 26.9 kg/m2, control group 26.4 kg/m2 to 26.3 kg/m2; p = 0.007). In the USA, no significant differences between the intervention group and the reference group for changes in BMI were observed in either the cohort study or the cross-sectional study (increases were observed in both groups). When data from both countries were pooled there were no significant differences in BMI change between the intervention group and the reference group for either the longitudinal comparison or the cross-sectional comparison. In Sweden, significant decreases in cholesterol in the intervention group compared with the reference population were observed in both the cohort study (change: intervention group 6.65 mmol/l to 6.16 mmol/l, control group 6.31 mmol/l to 6.39 mmol/l; p = 0.003) and the cross-sectional study (change: intervention group 6.82 mmol/l to 6.02 mmol/l, control group 6.36 mmol/l to 6.21 mmol/l; p = 0.000). In the cohort study, this effect was observed in the lower education group (change: intervention group 7.27 mmol/l to 6.46 mmol/l, control group 6.60 mmol/l to 6.67 mmol/l; p = 0.010) but not in the higher education group (change: intervention group 6.08 mmol/l to 5.96 mmol/l, control group 6.11 mmol/l to 6.20 mmol/l; p = 0.363). Significant decreases were observed in both educational groups in the cross-sectional study. With regard to systolic blood pressure, no differences between groups were observed overall in the cohort study, but a reduction was observed in the higher education group (change: intervention group 123.9 mmHg to 121.7 mmHg, control group 124.0 mmHg to 127.7 mmHg; p = 0.011). In the cross-sectional study, systolic blood pressure was decreased overall (change: intervention group 129.1 mmHg to 125.1 mmHg, control group 128.4 mmHg to 128.0 mmHg; p = 0.003) and in the higher education group (change: intervention group 123.5 mmHg to 119.9 mmHg, control group 123.1 mmHg to 123.3 mmHg; p = 0.014) but not in the lower education group. For diastolic blood pressure, in the cohort study a reduction was observed overall in the intervention group compared with the control group (change: intervention group 84.1 mmHg to 83.4 mmHg, control group 80.4 mmHg to 84.2 mmHg; p = 0.001) and this effect was observed in the higher education group (change: intervention group 82.0 mmHg to 81.5 mmHg, control group 79.1 mmHg to 83.6 mmHg; p = 0.007) but not in the lower education group. No significant differences between groups were observed in the cross-sectional comparison. In the USA, no differences between groups were observed overall in either the cohort study or the cross-sectional study for changes in cholesterol and diastolic and systolic blood pressure. However, in the cohort study, systolic blood pressure increased in the low-education intervention group and decreased in the low-education reference group (change: intervention group 78.3 mmHg to 79.7 mmHg, control group 79.3 mmHg to 77.6 mmHg; p = 0.033). When data from the two countries were pooled, cohort comparisons found decreases in systolic blood pressure in the higher-education group (p = 0.013) but no other intervention effects. Cross-sectional comparisons found a significant decrease in cholesterol levels in the higher-education group only (p = 0.021) and no other intervention effects.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Neve et al.142
Method: Retrospective uncontrolled cohort study.
Participants: All participants of a commercial web-based weight loss programme (n = 11,341) were invited to take part in the study; 5625 agreed to take part and 614 completed the survey (5.4% response rate; mean age 38.3 years; 88% female).
Intervention: This study investigated a commercial web-based weight loss programme (the Biggest Loser Club Australia) in adults aged 18–75 years with a BMI ≥ 22 kg/m2. Participants of the programme paid a subscription charge and could choose to take part in the programme for 1, 3, 4 or 12 months. The study included a mix of participants with different subscription durations. The intervention was developed and run by a commercial company and used weight-management strategies based on elements of social cognitive theory.
Outcomes: The programme was evaluated using a follow-up survey conducted 15 months post enrolment and results were compared with baseline records. Weight and height measurements were self-reported by participants at both baseline and follow-up. Success was classified as weight loss of ≥ 5%. After 15 months, the median (interquartile range) weight change was –2.0 kg (–8.0 to –1.8 kg) and 37% of the sample was classified as successful. There were no differences in SES status between those who were successful and those who were non-successful.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Morrison et al.141
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Of the 3170 patients who were referred to the Glasgow and Clyde Weight Management Service, 2156 patients opted to participate (68% baseline response rate; 74% female; approximate average age mid-forties) and 809 patients completed the programme (38% follow-up response rate). The majority of the patients who were referred to the service were from the most deprived SES groups.
Intervention: This study investigated a UK NHS weight-management programme, the Glasgow and Clyde Weight Management Service. The programme was delivered by dietitians with support from psychologists. Physiotherapists were also part of the programme team. The 16-week programme consisted of nine fortnightly sessions. A 600-kcal (2510-kJ) deficit diet and activity changes were advised and these changes were supported with cognitive–behavioural approaches such as goal-setting, self-monitoring, cognitive restructuring and relapse prevention.
Outcomes: Objective height and weight measurements were taken pre and post intervention, although methods and assessors were not clearly reported. Success was defined as achieving a weight loss of ≥ 5 kg. Of those patients who completed the programme, 35.5% lost at least 5 kg. Among the completers there were no differences along the SES gradient in the prevalence of success. Additional analyses revealed that patients from the least deprived group were least likely to complete the programme; however, this would be expected as the majority of the sample was from this group, but this finding does have implications for the development of SES inequalities in obesity. These results highlight the need to improve recruitment strategies in low-SES populations.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Gardner et al.143
Method: Uncontrolled before-and-after study (using data from routine health service records).
Participants: During the study period health trainers were encouraged but not compelled to record data in the national database; therefore, of 24,986 eligible clients, only 3759 (15% response rate; 79% female; highest proportion in the 36–45 years age group) had suitable data recorded and were used in the analysis.
Intervention: This study investigated the NHS HTS in the UK (England and Wales). The HTS is a nationwide public health initiative based on individualised support for disadvantaged people. The service was designed and developed by a team of psychologists, who also provided long-term support during implementation. Health trainers are lay community members who typically come from the same background as the target group and are trained in evidence-based behaviour change techniques. Health trainers support clients to achieve health behaviour goals and, for the purpose of this study, clients who set primary goals relating to healthy eating and physical activity (rather than alcohol or smoking) were included in the analysis. The number of sessions between the health trainer and client varied according to client need or engagement, but the mean duration of HTS attendance was 6.14 months.
Outcomes: Data were collected at the first contact session and at the final assessment, when all of the sessions needed had been completed. The height and weight data recorded were a mixture of objectively measured and self-reported data; however, it was not recorded which of these measures was used in each instance. Overall, BMI was reduced by 1.77 points (95% CI –1.69 kg/m2 to –1.85 kg/m2; p < 0.001), from 34.03 kg/m2 to 32.26 kg/m2. Overweight/obesity prevalence decreased from 94.7% to 91.0%, and the proportion of obese clients decreased from 72.3% to 60.1%. Clients from the least deprived 80% of the population achieved a greater BMI change than the most deprived clients (0.28 BMI points; p = 0.001). However, multiple linear regression analysis found that deprivation did not predict BMI change. Clients with physical activity goals reported a 171% increase in the number of intensive physical activity sessions per week, from 0.63 to 1.71 (d = 0.46), and the proportion of clients engaging in five or more intensive sessions weekly increased from 3.9% to 11.6%. The number of moderate physical activity sessions per week increased by 56%, from 3.06 to 4.77 (d = 0.42), and the proportion undertaking five or more moderate sessions weekly increased from 24.4% to 45.5%. Physical activity and fruit and vegetable or fried snack consumption changes were not associated with deprivation. Clients with healthy eating goals reported a 70% increase in fruit and vegetable intake, from 3.08 to 5.23 daily portions (d = 0.97). The proportion of clients consuming five or more portions of fruit and vegetables increased from 24.8% to 60.5%. Mean fried snack consumption decreased by 60%, from 1.99 to 0.79 servings per day (d = 0.85). Deprivation was not associated with physical activity or fruit and vegetable or fried snack consumption changes.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Fortmann et al.145
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: A final sample of 687 adults provided data for the baseline and 3-year surveys. It was difficult to calculate the exact follow-up response rate from the information provided; however, a related paper on the Stanford Three Community Study reported a follow-up response rate of 72% after 2 years. 242
Intervention: This study investigated the effects of a community-wide mass media campaign aimed at preventing cardiovascular disease (the Stanford Three Community Study) on risk factors across different SES groups. Dietary and physical activity health education was delivered via television and radio programmes, public service announcements, newspaper columns, billboards and other communications in two towns in northern California, USA. To evaluate the campaign, sample surveys were conducted with a random sample of adults aged 35–59 years from the towns’ populations. This study used data from the two intervention towns only; the data used were collected in the first survey conducted at baseline and the fourth survey conducted 3 years later. During the surveys, participants completed a medical examination (blinding status of the medical professionals not reported) that included measures of weight, plasma cholesterol and dietary intake (using a validated questionnaire delivered by trained interviewers).
Outcomes: After 3 years there were no significant differences across SES groups for changes in weight, dietary cholesterol, dietary saturated fat and plasma cholesterol (adjusting for sex, age and language group). There was a trend of improved dietary cholesterol and dietary saturated fat intake in lower-SES groups (change in cholesterol: least deprived –20.6 mg/day, most deprived –37.6 mg/day, p = 0.36; change in saturated fat: least deprived –19.7 g/day, most deprived change –34.8 g/day, p = 0.30).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Helmert et al.146
Method: Serial cross-sectional study.
Participants: The initiative was delivered in six regions of the Federal Republic of Germany, and a reference sample of individuals was obtained from 200 sample points within the remaining Federal Republic of Germany. Surveys were conducted with adults aged 25–69 years, at baseline and 3.5 years into the initiative, in both the intervention and the reference regions (baseline n = 16,338; follow-up n = 14,078; response rates 66–74%).
Intervention: This study investigated the multicentre community-wide German Cardiovascular Prevention (GCP) initiative. The programme aimed to promote public information, train professionals and lay individuals and support self-help activities. Education was provided on topics including elevated blood pressure, healthy nutrition, improved physical activity and promotion of non-smoking. Health committees were formed to provide community-wide co-ordination in the production and distribution of health goods and services. The programme involved public persons, groups and organisations in the community and the appropriate use of mass media. Special efforts were made to involve physicians and medical associations.
Outcomes: At each survey, height, weight, blood pressure and cholesterol measurements were taken by trained medical staff (blinding status not reported) to determine the prevalence of obesity, uncontrolled hypertension and hypercholesterolaemia. There was no significant change between the baseline survey and the follow-up survey in the prevalence of obesity and the intervention effect was not significant in men or women (regression coefficient b = 1.5, p ≥ 0.1 for both). There was no significant effect of the intervention on the social class gradient of the prevalence of obesity in either sex (men: b = 0.4, p ≥ 0.1; women: b = –1.7, p ≥ 0.1); therefore, a higher prevalence remained in those of a low SES but the difference between high and low SES did not increase. In terms of the prevalence of uncontrolled hypertension, there was no significant intervention effect in men, nor was there an intervention effect on the SES gradient in men. In women, there was no significant effect of the intervention. At baseline there was a significant association between uncontrolled hypertension and SES (higher prevalence among those of a lower SES) and this increased at the second survey. However, there was a significant effect of the intervention in blunting this increase in the social gradient for uncontrolled hypertension in women (b = –1.6, p = 0.008). For the prevalence of hypercholesterolaemia, there was no intervention effect in men and in women an increase occurred in the intervention areas compared with the reference areas. However, there were no significant associations with SES in either sex.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Weak |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Not applicable |
| Global rating | Weak |
Rautio et al.144
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Participants were recruited through opportunistic screening at primary health-care settings, public places and events and through the internet. In total, 8584 adults (67% female; mean age approximately 52 years) were recruited at baseline. The final sample size was 2977 at 1 year of follow-up (follow-up response rate of 34%).
Intervention: This study investigated a type 2 diabetes prevention intervention (FIN-D2D) in a cohort of men and women in Finland. The FIN-D2D programme consisted of health checks conducted by local nurses at which participants received a short counselling session on lifestyle changes. Participants were then directed to individual visits or group sessions to receive support for lifestyle changes and diet, physical activity, weight-management, lifestyle and diabetes education.
Outcomes: Outcomes included changes in weight, BMI and waist circumference (measured by non-blinded nurses) after 1 year, along with changes in blood pressure and blood lipids. Results were reported by education category (low, intermediate and high) and occupation category (manual, non-manual, not employed and retired). From baseline to 1 year, decreases were observed in weight, BMI and waist circumference in all education and occupation categories and there were no differential effects between these groups. The blood lipid and blood pressure outcomes also changed in the favourable direction with the exception of blood pressure in women, in whom greater decreases were observed in the intermediate- and high-education groups compared with the low-education group.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Olson et al.131
Method: Cohort analytical study.
Participants: The total eligible population was not reported. In total, 560 participants were assessed at baseline and 517 (92.3%) completed the 1 year post-partum follow-up. The majority of women (93–94%) were aged between 20 and 40 years.
Intervention: This study investigated clinical counselling and patient education for pregnant women in New York, NY, USA. The study included an intervention cohort group and a historical control group. The intervention was based in a hospital/primary care clinic and consisted of two major components: a clinical component, including guidance about and monitoring of gestational weight gain by health-care providers using new tools in the obstetric chart, and a by-mail patient education programme.
Outcomes: The outcome measure was weight (independently measured by health-care professionals – blinding unlikely). Both weight gain during pregnancy and weight retention post-partum were measured. Overall, gestational weight gain did not differ significantly between the control group and the intervention group (14.80 ± 4.68 kg vs. 14.10 ± 4.5 kg; p = 0.09), nor did the proportion of women gaining more than the recommended amount of weight during pregnancy (45% vs. 41%; p = 0.30 – not significant). However, for low-income women there was a significant difference between the control group and the intervention group in the proportion exceeding the recommended weight gain. Among the low-income women, 52% of the control group gained more than the recommended amount of weight compared with 33% of the intervention group (p < 0.01). When the intervention effect was further examined within low-income women by early pregnancy BMI group, the impact of the intervention was seen in both overweight women and women of normal BMI. A total of 72% of the overweight women in the control group gained more than the recommended amount of weight compared with 44% in the intervention group (p = 0.04). Among women of normal BMI, 45% of the women in the control group gained more than the recommended amount of weight compared with 29% in the intervention group (p = 0.05). No effect of the intervention was detected in high-income women. Weight retention was also examined at 1 year post partum and the adjusted analysis showed that it did not differ significantly between the control group and the intervention group (1.31 ± 50 kg vs. 0.59 ± 4.75 kg; p = 0.14). However, the unadjusted analysis showed that there was a significant difference between the control group and the intervention group in the two subgroups of women (low- and high-income women). A significantly smaller proportion of intervention group women retained ≥ 2.27 kg at 1 year post partum in the low-income and overweight BMI subgroups (25% vs. 55%; p = 0.04); in the high-income and normal BMI subgroup the difference between the proportions approached statistical significance (24% vs. 36%; p = 0.07).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Schuit et al.140
Methods: Cohort analytical study.
Participants: Of the 4059 potentially eligible participants in the intervention area, 3000 were recruited (the authors aimed to recruit 3000 in the intervention group, with an estimated response rate of 65%). In the reference group (control), out of a total of 1115 eligible participants, 895 participated in the study. The attrition rate was low, with 81% of the intervention group and 85% of the reference group completing the 5-year follow-up.
Interventions: This study investigated a cardiovascular disease prevention programme in Hartslag Limburg, the Netherlands, in men and women aged from 31 to 70 years. The aim of the study was to encourage participants to become more active, reduce their fat intake and stop smoking. Between 1999 and 2003, 790 interventions were implemented, of which 500 were major interventions (193 diet, 361 physical activity and nine anti-smoking interventions). Examples of intervention activities include computer-tailored nutrition education, nutrition education tours in supermarkets, public–private collaboration with the retail sector, television programmes, food labelling, smoke-free areas, the creation of walking and bicycling campaigns, a stop-smoking campaign, commercials on local television and radio, newspaper articles and pamphlet distribution.
Outcomes: The outcome measures in the study were BMI, waist circumference, blood pressure, non-fasting glucose level and total cholesterol. Because of some missing values on SES (n = 13), BMI (n = 5), waist circumference (n = 8), blood pressure (n = 21), cholesterol (n = 278) and glucose (n = 205), analyses were performed on between 2834 and 3114 men and women. Change in BMI and waist circumference was significantly different between the intervention group and the reference group at the 5-year follow-up. The adjusted difference in mean change in BMI was –0.38 kg/m2 for men and –0.25 kg/m2 for women and the adjusted difference in mean change in waist circumference was –2.9 cm for men and –2.1 cm for women. For moderate- to high- and low-SES subgroups, the adjusted difference in mean change in BMI was –0.34 kg/m2 and –0.27 kg/m2, respectively, and the adjusted difference in mean change in waist circumference was –2.4 cm and –2.6 cm respectively. These differences were statistically significant. Change in blood pressure was significantly different between the intervention group and the reference group at the 5-year follow-up. The adjusted difference in mean change in blood pressure was –7.8 mmHg for men and –5.5 mmHg for women (systolic) and –5.1 mmHg for men and –4.4 mmHg for women (diastolic). In women only, the mean changes in non-fasting glucose level and total cholesterol were also significantly different between the intervention group and the reference group (–0.23 mmol/l and 0.11 mmol/l respectively). There were no significant changes in HDL cholesterol (men and women) or glucose (men). For moderate- to high- and low-SES subgroups, the adjusted difference in mean change in blood pressure was –7.2 mmHg and –6.1 mmHg (systolic) and –4.6 mmHg and –4.9 mmHg (diastolic), respectively, and the adjusted difference in mean change in non-fasting glucose level was –0.23 mmol/l and 0.18 mmol/l respectively. These results were statistically significant and so this intervention benefited both moderate- to high- and low-SES groups (blood pressure and glucose level). There were no significant changes in cholesterol levels between moderate- to high- and low-SES groups.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Targeted approach: experimental studies (n = 9)
Davis Martin et al.133
Method: RCT.
Participants: Of 205 eligible women, 144 completed the baseline assessment [baseline recruitment rate 70%; mean age 42.97 years (standard care), 40.69 years (intervention)] and there was a final sample size of 106 (74% follow-up response rate).
Intervention: This study investigated a tailored, culturally appropriate weight-management programme delivered in a primary care setting and designed for low-income African American women. The intervention was delivered by physicians during six monthly 15-minute consultations. The individualised tailored materials, recommendations and strategies were developed by a health psychologist, registered dietitian and exercise physiologist using data on current behaviours and preferences of each participant at the baseline assessment visit. Eight physicians from two medical centres were randomised to provide either the tailored intervention (and receive the appropriate training) or usual care (control) so that there were two intervention and two control physicians at each medical centre. Participants were recruited from among clinic attendees and their group allocation was determined by the assignment of their physician.
Outcomes: Height and weight measurements were taken at baseline and post intervention using standard techniques (blinding status of assessors was not reported). The intervention group demonstrated a significant weight loss [mean (SD) –2.0 (3.2) kg; differed significantly from 0 (t4 = 3.8, p = 0.02)] whereas the control group gained weight [mean (SD) +0.2 (2.9) kg; p = 0.03]. A greater percentage of intervention participants than standard care participants lost weight by month 6 (79% vs. 47%; p = 0.03). Intervention participants achieved an average 1.78% loss in body weight and standard care participants showed an average 0.19% gain in body weight, although this difference was non-significant (p = 0.05). Among the 48 intervention participants, six (12.5%) achieved ≥ 5% weight loss compared with three (5.2%) of the standard care participants.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Jackson et al.134
Method: RCT.
Participants: Of 625 women assessed for eligibility, 412 completed a behavioural assessment (66% baseline recruitment rate). Eighty-two of these women were assigned to another study and nine women withdrew or became ineligible for the study, leaving a baseline sample of 321 (158 intervention group, 163 usual-care group). There was an 89% follow-up response rate, with 287 women (134 intervention, 153 control) completing the study.
Intervention: This study investigated the effect of a computerised, multimedia, interactive Video Doctor brief intervention compared with usual care on excessive gestational weight gain in low-income pregnant women. The intervention was incorporated into routine prenatal care and took 10–15 minutes to complete. The Video Doctor uses strategies based on motivational interviewing and simulates an ideal conversation with a health-care provider. It conducts in-depth behavioural risk assessments, delivers tailored counselling messages (targeting diet and physical activity) and produces printed output for both the patient and the clinician. Participants (< 26 weeks’ gestation) were recruited through clinic advertisements, self-referral, clinical staff or clinician referral and by direct recruitment by research assistants in waiting rooms. At baseline, all participants completed a computerised baseline assessment, after which the computer randomly assigned them to either the intervention or the control condition. Those assigned to the intervention continued with the Video Doctor intervention before their routine prenatal care appointment. Those assigned to the control condition did not interact with the Video Doctor and proceeded to their usual-care medical appointment. Participants from both groups were invited back for a follow-up assessment (at which intervention participants also received a Video Doctor refresher) after at least 4 weeks.
Outcomes: Gestational weight gain was calculated as delivery weight (taken from medical records) minus pre-pregnancy weight (self-reported during the baseline assessment). Weight gain above Institute of Medicine (IOM) guidelines243 was considered excessive. The proportion of women gaining weight above IOM guidelines did not differ between the groups. Approximately one-third of participants in both groups gained weight within the recommended guidelines, 53% gained more than the recommended amount of weight and 14% gained less than the recommended amount of weight [relative risk (RR) for excessive weight gain 1.06, 95% CI 0.83 to 1.36]. Mean weight gain also did not differ between the groups in those with a term delivery (intervention 33.4 lb, control 33.6 lb; p = 0.95). There was no difference between groups in weight gain from enrolment to delivery (mean 20.7 lb; p = 0.91) nor in pounds gained per week of gestation (mean 0.86 lb per week; p = 0.79). Of note, 13% had already gained more than the IOM-recommended amount before entering the study.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Moderate |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Craigie et al.135
Method: Randomised controlled pilot study.
Participants: Participants were recruited through community groups, general practices (that had at least 30% of their patients classified as living within the most deprived 15% of the Scottish Index of Multiple Deprivation areas), support workers, newspaper advertising and posters in community settings. Participants were randomly assigned to either the intervention or the control condition. Fifty-two women completed the baseline assessment and were randomised (29 intervention group, 23 control group; mean age 30 years). There was a final sample size of 36 (22 intervention group, 14 control group; follow-up response rate 69%).
Intervention: This study investigated a weight loss programme for overweight post partum women living in areas of moderate to high deprivation (UK). The 12-week intervention consisted of three face-to-face (one per month) consultations with a trained lifestyle counsellor, with support between the consultations over the telephone (minimum of three calls), also with the lifestyle counsellor. The lifestyle counsellor used motivational interviewing techniques244 and provided a personalised dietary prescription of estimated energy requirements minus 500 kcal along with verbal and written guidance on food groups, frequency of consumption and portion size. Personalised physical activity goals were also set towards achieving 150 minutes of moderate- to vigorous-intensity activity per week. Participants were provided with 4-week walking plans, a pedometer and a weight logbook for self-monitoring, along with a weight loss booklet. The control group also received the weight loss booklet but had no further contact over the 12 weeks (a post-study consultation with a lifestyle counsellor was provided to those in the control group).
Outcomes: Height, weight, skinfold and waist circumference measurements were taken by a research assistant blinded to group allocation. An objective measure of physical activity (minutes of moderate- to vigorous-intensity physical activity per day) was also recorded using a physical activity monitor (SenseWear™; Bodymedia Inc., Pittsburgh, PA, USA). Body weight loss was achieved by 73% of the intervention group compared with 36% of the comparison group. Weight loss of clinical significance (reduction of 5% body weight245) was achieved by 9% of the intervention group compared with 0% of the comparison group. Although the study was not powered to show change between the intervention group and the control group, there was a significantly greater change in the intervention group than in the control group for body weight (intervention –1.6 kg vs. control 0.2 kg; p = 0.018), BMI (intervention –0.7 kg/m2 vs. control 0.1 kg/m2; p = 0.009) and percentage body fat (intervention –1.5%, control –0.5%; p = 0.029). There were no between-group differences for change in waist circumference or objectively measured physical activity.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Burke et al.148,149
Method: RCT.
Participants: Of 913 eligible participants, 478 were recruited at baseline (52% baseline recruitment rate; mean age 66 years; 48% female) and there was a final sample size of 375 (79% follow-up response rate; 176 intervention group, 199 control group).
Intervention: This study investigated the Physical Activity and Nutrition for Seniors (PANS) intervention for sedentary older adults. The home-based intervention was conducted for 6 months and consisted of the provision of a specially designed booklet containing information on dietary guidelines, recommended physical activity levels and goal-setting. This was supplemented with additional written materials including an exercise chart, a calendar and bimonthly newsletters. A pedometer (for physical activity monitoring) and a resistance band (for strength exercises suggested in the booklet) were also provided. E-mail and telephone support from a group guide was given, and there was also the option to attend non-compulsory group meetings. The control group received no materials or contact other than when providing data. Participants living in low to medium SES neighbourhoods were recruited from the Australian Federal Electoral Roll and were randomly assigned to either the intervention or the control condition.
Outcomes: Self-reported measures of height, weight and waist and hip circumference were given at baseline and post intervention. After 6 months, no significant changes in BMI were observed for either group. There was a significant decrease in waist-to-hip ratio from baseline to post intervention in the intervention group (baseline 0.94, follow-up 0.92; p = 0.001) but not in the control group (baseline 0.93, follow-up 0.92; p = 0.58). However, between-group differences in changes in BMI and waist-to-hip ratio were not reported. Generalised estimating equation model analysis found that, after controlling for demographic and other confounders, the intervention group demonstrated a significant reduction in waist-to-hip ratio relative to the control group [coefficient –1.16 (SE 0.55); p = 0.03]. No change in BMI was apparent for both groups through the group × time interaction term. Additional analyses found similar results; however, the effect of the group × time interaction term became marginal for waist-to-hip ratio [coefficient –1.01 (SE 0.55); p = 0.06].
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Martin et al.136
Method: RCT.
Participants: The total number of eligible participants was not reported but the study included 137 women aged 18–69 years. Only women who were classified as either overweight or obese were included (BMI > 25 kg/m2). Also, women had to have an annual income of < $16,000 to participate in the intervention.
Intervention: This study investigated a tailored weight loss intervention in a primary care setting. The intervention lasted for 6 months and consisted of six counselling meetings (lasting ≈15 minutes each). Topics of the monthly meetings included introductory information on weight loss (month 1), ways to decrease dietary fat (month 2), ways to increase physical activity (month 3), dealing with barriers to weight loss (month 4) and healthy alternatives when eating out and shopping (month 5). Also, there was one maintenance session (month 6) that addressed motivational levels. The outcome measure was weight change (kg).
Outcomes: Intention-to-treat analysis showed that, after 9 months, the intervention group was more successful at maintaining a lower weight from baseline than the standard care group. Weight change from baseline of the intervention group was –1.52 ± 3.72 kg and this differed significantly from the weight change of the standard care group (0.61± 3.37 kg; F = 12.32; p < 0.01). A total of 13% of the intervention participants maintained at least 5% weight loss from their baseline weight at month 9 compared with 7% of the standard care group, but this was not statistically significant (p = 0.39). At 12 months after baseline, the weight change of the intervention group (–1.38 ± 3.69 kg) was no longer significantly greater than the weight change of the standard care group (–0.16 ± 3.63 kg; F = 3.80; p = 0.10). Somewhat surprisingly, the standard care group demonstrated a decrease in weight between 9 and 12 months’ follow-up. The proportion of participants who maintained at least 5% weight loss was almost identical at 12 months (10% intervention group, 11% standard care group; p = 0.81). At 18 months’ follow-up the weight change of the intervention group (–0.49 ± 3.33 kg) was not significantly greater than the weight change of the standard care group (0.07 ± 3.75 kg; F = 0.85; p = 0.39). At month 18, only 7% of the intervention group participants maintained 5% weight loss whereas 12% of the standard care participants achieved 5% weight loss, but this difference was not significant (p = 0.40). The results of the completers-only analysis were consistent with these results. At month 9, participants in the intervention group lost significantly more weight (–2.21 kg) than those in the standard care group (0.68 kg; p < 0.01). However, at months 12 (1.97 vs. 0.19 kg; p = 0.07) and 18 (–0.88 vs. 0.09; p = 0.28) there were no significant differences in weight loss between the intervention group and the standard care group. Interestingly, women who completed the 9- and 18-month follow-up assessments had lower educational levels than participants lost to attrition.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Hillier et al.152
Method: Cluster RCT.
Participants: A total of 128 participants agreed to take part in the study and were measured at baseline (total eligible population not reported). In the intervention group 86% of the participants were women whereas in the control group 63% were women. The mean age of participants ranged from 41.6 to 49.1 years. There were two follow-ups at 6 and 12 months. A final sample of 63 (49% follow-up response rate) completed the 12-month follow-up.
Intervention: This study investigated a health promotion intervention in deprived areas of Middlesbrough, UK. The intervention consisted of a community challenge (pledge) to improve dietary intake and physical activity habits over a 1-year period. Student lifestyle helpers delivered the one-to-one intervention. Intervention sessions covered techniques such as reflective listening, understanding client’s motivation and readiness to change.
Outcomes: The primary outcomes were percentage of food energy from fat, number of portions of fruit and vegetables consumed and minutes of moderate- to vigorous-intensity physical activity undertaken. Secondary outcomes were BMI and weight and waist circumference, which were measured independently by the researcher (blinding status not reported). The results showed that there were no significant changes in BMI or weight but there were significant changes in waist circumference (mean change 3.6 cm, 90% CI 0.8 cm to 6.3 cm) compared with the control group, which was unexpected. There were no significant changes in physical activity or dietary intake.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Whittemore et al.150
Method: Cluster randomised controlled pilot study.
Participants: Four nurse practitioner primary care practice sites were randomly assigned to either the intervention or the standard care control group. Within these sites, nurses invited a convenience sample of adults at high risk of type 2 diabetes to participate in the study. Of the 88 eligible adults who were invited, 58 agreed to participate in the study (66% recruitment rate; 92% female; mean age approximately 46 years; moderately low income). There was an 88% follow-up response rate after 6 months, resulting in a final sample of 51 (24 in the intervention group).
Intervention: This study investigated a type 2 diabetes prevention programme for adults considered at high risk of diabetes (age ≥ 65 years and BMI ≥ 25 kg/m2 or age < 64 years and BMI ≥ 25 kg/m2 and another risk factor for diabetes) delivered by nurses in health-care practices. The study compared a lifestyle change programme against enhanced standard care (active control). In both conditions, participants received written information about diabetes prevention and attended a 20- to 30-minute individual session with a nurse on the importance of a healthy lifestyle for the prevention of type 2 diabetes along with a 45-minute individual session with a study nutritionist. Participants were encouraged to follow a healthy diet (limit calories, fat and processed foods), lose 5–7% of their initial weight through diet and exercise and increase their exercise level gradually with a goal of at least 30 minutes of exercise (e.g. walking) on 5 days per week. In addition, during the sessions, nurses in the lifestyle change programme provided culturally relevant education on nutrition, exercise and type 2 diabetes prevention; behavioural support in identifying lifestyle change goals and problem-solving barriers to change; and motivational interviewing when participants were unable to achieve lifestyle goals.
Outcomes: Height, weight and waist circumference were measured by trained research assistants blinded to the experimental condition. Blood samples were also collected for glucose tolerance, insulin resistance and blood lipid measurements and data on physical activity and diet behaviours were collected using a validated self-report questionnaire. At 6 months, weight losses were observed in both groups. However, participants in the intervention group demonstrated a trend towards a greater per cent weight loss (p = 0.08) than participants in the control group, and 25% of intervention participants achieved a weight loss goal of 5% compared with 11% of standard care participants. Participants in both groups also improved nutrition behaviour and increased exercise behaviour, with intervention participants demonstrating a trend towards a greater improvement in exercise (p = 0.08). The percentage of participants meeting the exercise goal of 150 minutes per week increased in the intervention group (from 29% to 46%) and was relatively stable in the control group (from 39% to 40%). Intervention participants also demonstrated a trend towards higher cholesterol HDL levels (p = 0.21) than control participants but there were no significant differences or trends with respect to other clinical variables.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Weerts and Amoran132
Method: Randomised controlled pilot study.
Participants: Participants were recruited from among existing participants of the Magnolia project, a federal Health Start initiative in the USA addressing racial disparities in maternal and child health and whose priority population was low-income women. The first 21 participants who consented to the project were randomised into either the intervention group or the control group.
Intervention: This study investigated a fruit and vegetable promotion intervention in overweight low-income African American women (aged 18–44 years). The study was developed and implemented by a community–university–industry partnership. All participants received four 15-minute brief counselling sessions (at baseline and at 1, 2 and 3 months) with a health educator (an African American women employed by the community group who knew participants well) covering behavioural techniques and nutritional education. Each participant also received a colourful handout that matched the advice given during the session. Finally, each participant received a US$40 grocery gift card (provided in kind by the industry partner, a large supermarket chain with stores located in the neighbourhood) at each of the counselling sessions. The difference between the groups was that intervention participants were instructed to use the gift card to purchase fresh fruit and vegetables only whereas the control group could spend the gift card on any type of groceries.
Outcomes: There were significant differences between the groups at each time point for changes in weight (baseline to 1 month: intervention –2.85 lb, control 3.68 lb, p = 0.002; baseline to 2 months: intervention –1.90 lb, control 3.68 lb, p = 0.022; baseline to 3 months: intervention –6.05 lb, control 3.68 lb, p = 0.008) and BMI (baseline to 1 month: intervention –0.5 kg/m2, control 0.8 kg/m2, p = 0.005; baseline to 2 months: intervention –0.38 kg/m2, control 1.12 kg/m2, p = 0.018; baseline to 3 months: intervention –1.10 kg/m2, control 0.68 kg/m2, p = 0.008). The mean increase in intake of raw, freshly prepared fruit and vegetables only was significantly greater in the intervention group than in the control group from baseline to month 3 (intervention 1.29 cups, control 0.15 cups, p = 0.042), but there were no significant differences at any other time point or for all fruit and vegetables.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Moderate |
Sierra et al.128
Method: Non-RCT.
Participants: Following the initial health screen, 5035 increased-risk participants agreed to take part in the study (baseline recruitment rate of 69%), of whom 3085 were contacted by the health team. Of the participants who the team were unable to contact, 1707 took part in the follow-up health check, resulting in a final sample of 4792 (6% female; 71% aged ≥ 45 years; follow-up response rate 95%).
Intervention: This study investigated a structured telephone intervention in addition to a routine health screening programme in manual workers at increased risk of cardiovascular disease in Spain. Participants were recruited through a routine workplace health screen that included anthropometric and blood pressure measurements and measurement of glucose, triglycerides and cholesterol levels. The participants were given feedback from the results of their health screen and appropriate advice for healthy lifestyle changes based on recommendations of the European Council for Cardiovascular Disease Prevention. Participants were also given letters to pass on to their own doctor containing the results of their health screen. Those deemed at increased risk of cardiovascular disease, as determined using the SCORE criteria, were also contacted by telephone at 1, 4 and 8 months after the health screen by a trained health staff member (doctor or nurse) located in a Spanish accident and health insurance company call centre. During the calls participants were reminded of their results of the health screen and their awareness of risk and compliance to the recommendations given were assessed. The participants at increased risk who the health team failed to contact but who completed the follow-up health screen were used as the control group.
Outcomes: After 1 year there were significant reductions in weight and BMI in the intervention group compared with the comparison group (whose weight and BMI increased) (weight: intervention –0.9 kg, control 0.13 kg, p = 0.017; BMI: intervention –0.05 kg/m2, control 0.16 kg/m2, p < 0.001). There were no significant differences between the groups for changes in waist circumference, triglycerides, HDL cholesterol and glucose. Total and LDL cholesterol reduced to a greater extent in the intervention group than in the comparison group (total cholesterol: intervention –20.20 mg/dl, control –15.66 mg/dl, p < 0.0001; LDL cholesterol: intervention –21.00 mg/dl, control 17.69 mg/dl, p = 0.001), as did diastolic and systolic blood pressure (diastolic blood pressure: intervention –3.82 mmHg, control –2.39 mmHg, p = 0.0001; systolic blood pressure: intervention –6.73 mmHg, control –4.05 mmHg, p = 0.0001).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Moderate |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Targeted approach: observational studies (n = 9)
Abramson et al.,137,157 Gofin et al.158
Method: Three observational studies.
Participants: A preliminary controlled before-and-after study137 investigated the effects of the CHAD programme in a population of men aged ≥ 35 years at the beginning of the programme. From a total population of 1615 men, 1269 took part in the baseline survey (baseline recruitment rate 79%). A total of 920 completed the follow-up survey after approximately 54 months (73% follow-up response rate). A controlled prospective cohort (before-and-after) study157 investigated the first 5-year effects of the CHAD programme in men and women, also aged ≥ 35 years at baseline. A total of 2679 were recruited at baseline for the study (87% recruitment rate), of whom 76% completed data collection at 5 years, resulting in a final sample size of 2038 (524 in the intervention group; 53% female). The final study was an uncontrolled prospective cohort study158 that evaluated the effects of the second 5 years of the CHAD programme. This study included a younger sample than the previous study (men and women aged ≥ 25 years at the beginning of the programme). Of the 652 men and women who completed the baseline survey, 441 provided weight data after 5 years (68% follow-up response rate).
Intervention: This study investigated the CHAD programme, which was implemented in four housing projects in one neighbourhood in Israel. The CHAD programme was an integral part of a family practice operated by the neighbourhood community health centre. Care was based on standardised examination methods, uniform treatment guidelines and defined surveillance regimes for those at specified levels of risk. An individualised programme was developed for each person that included recommendations for screening and other examinations, drug treatment, counselling and ongoing surveillance. The main mode of care was face-to-face counselling carried out by family physicians and nurses and, in addition, small discussion groups were conducted with physicians and nurses, aimed at invoking group pressure and support for behaviour change. Individuals were encouraged to reduce their intake of calories and saturated fats, to stop smoking and to increase their levels of physical activity. An adjacent neighbourhood not exposed to the organised intervention was used as a comparison group in two of the studies. 137,157
Outcomes: In the preliminary study137 body weight, blood pressure and cholesterol measurements were taken at each time point by examiners blinded to the study conditions using standard procedures. No differences between the intervention group and the control group were observed for changes in body weight (intervention –0.1 kg, control +0.3 kg; p = 0.09) or cholesterol (intervention –6.0 mg/100 ml, control –3.6 mg/100 ml; p = 0.38) from baseline to follow-up. There were also no differences in changes in the prevalence of overweight or self-reported physical activity between the groups. However, the intervention group did experience greater decreases than the control group in systolic and diastolic blood pressure, which were the primary outcomes of this study (systolic blood pressure: intervention –4.4 mmHg, control –1.1 mmHg, p = 0.012; diastolic blood pressure: intervention –4.5 mmHg, control –2.6 mmHg, p = 0.043). In addition, the total proportion who stated that they had kept to a diet for reasons connected with weight, cholesterol, heart disease and/or blood pressure was greater in the intervention group than in the control group (intervention 37%, control 23.3%, p = 0.0002, summary OR 9 : 1).
In the controlled prospective cohort (before-and-after) study,157 body weight, blood pressure and cholesterol measurements were taken at each time point using standard procedures by examiners blinded to the study conditions. Overall, weight decreased to a significantly greater extent in CHAD participants than in control participants [net reduction (CHAD – control) 0.6 kg, p < 0.01], although subgroup analysis revealed that this effect was found only among women. Prevalence of overweight in the CHAD participants reduced by 13% over 5 years, which was significantly different from the control participants [net reduction (CHAD – control) 4.0%, p < 0.025], although in this case the effect was observed only in men.
In the final study158 weight was measured by a non-blinded physician or nurse. After 5 years there was no significant change in the CHAD group in mean body weight (data not reported) or the prevalence of overweight (5-year change: men 30% to 32%; women 42% to 43%).
Quality assessment (Abramson et al.137)
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Quality assessment (Abramson et al.157)
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Moderate |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Quality assessment (Gofin et al.158)
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Marshall et al.43
Method: Observational, prospective cohort study.
Participants: Data were analysed for 2681 adults (aged 19–95 years; 45% between 40 and 59 years).
Intervention: This study investigated a nurse-led healthy lifestyle clinic that targeted diabetes, smoking cessation, diet/nutrition, women’s health and cardiovascular and asthma/respiratory conditions in patients from communities with high levels of deprivation. Patients were referred to the clinic and treated holistically for the health needs defined by the patient. Nurses referred patients on to other professionals if required. Data collected at the clinics included height, weight, waist circumference, systolic blood pressure, glycosylated haemoglobin level and cardiovascular disease risk. Data analysed in this study were measurements recorded at each patient’s first and last visit to the clinic (duration varied from 3 months to several years).
Outcomes: There were no significant changes in weight, BMI, waist circumference, systolic blood pressure, glycosylated haemoglobin level or cardiovascular disease risk between the first and the last visits to the clinic.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Buchholz et al.155
Method: Prospective cohort (uncontrolled before-and-after) pilot study.
Participants: In total, 123 adults were recruited at baseline (89% female; mean age 47 years); however, only 23 attended all six sessions.
Intervention: This study investigated a lifestyle health promotion intervention delivered by nurses in two free health clinics for overweight and obese uninsured adults in the USA. The intervention consisted of six monthly 30-minute one-to-one sessions with a registered nurse who provided nutrition and physical activity education and feedback on current behaviours and worked with participants to set appropriate goals and monitor progress at subsequent visits. Participants were also provided with a food diary and a pedometer so that they could monitor behaviours between visits. A US$5 food voucher was also given to participants at each session.
Outcomes: Height and weight were measured at baseline and post intervention at 6 months (blinding status of assessor not reported). Overall, there was no significant difference in change in BMI from baseline to 6 months. However, for those who attended all sessions (n = 23) there was a significant decrease in BMI (from 37.27 kg/m2 to 36.67 kg/m2; p = 0.27).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Jackson et al.147
Method: Prospective cohort (uncontrolled before-and-after) exploratory study.
Participants: Participants were recruited through referrals by health professionals and attended an initial 1-hour session with the health visitor followed by biweekly consultations for 52 weeks. Eighty-nine participants were recruited at baseline (39% recruitment rate; 70% female; mean age 56 years); however, just 29 completed the intervention up to 52 weeks (33% follow-up response rate).
Interventions: This study investigated a specialised health visitor-led weight-management programme delivered at a primary care health-care centre located in a moderately deprived area in the UK. The intervention was based on Jayne Felgen’s I2E2 model,232 which focuses on building a therapeutic relationship with the participant rather than weight loss per se. This approach is based on four key elements of change: inspiration (shared goal-setting, reflection, problem-solving, positive affirmation and reinforcement), infrastructure (accessible local services), education (healthy eating and physical activity) and evidence (of current behaviours and progress). Height, weight and blood pressure were measured at baseline and 13, 27 and 52 weeks. Blood samples were also taken to determine fasting blood glucose and cholesterol levels. Diet behaviour data were collected using a self-report questionnaire.
Outcomes: Body weight and BMI were significantly reduced from baseline at all three follow-up time points (body weight: week 13 –5.34 kg, week 27 –8.09 kg, week 52 –10.48 kg; p = 0.000 for all) and significant time effects were observed for the 29 participants who completed all 52 weeks. Significant decreases in systolic and diastolic blood pressure were also observed at all follow-up time points, and there was a significant increase in fruit and vegetable consumption at all follow-up time points. Significant reductions in intake of cakes, desserts and snacks were observed initially (from baseline to week 13) but these were not maintained at the longer follow-ups.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Verheijden et al.156
Method: Cohort study.
Participants: Out of a total eligible population of 1200, 1030 (86%) took part in the study. In total, 55% of the participants were women and the mean age was 45 years. Outcome measurements were taken at the following time periods: November 2007, March 2008, November 2008 and March 2009. The follow-up response rate in March 2009 was 79% (n = 816).
Intervention: This study investigated a programme promoting physical activity and energy balance behaviour. The programme consisted of a mass media campaign by the Netherlands Nutrition Centre.
Outcomes: Self-reported height and weight measures were used to calculate the primary outcome, BMI. Level of physical activity and food choices were also examined. The results showed that there were significant long-term effects on BMI in the Dutch group only. BMI was less likely to increase among people with a non-Dutch ethnicity who had been exposed to the second campaign wave (targeted low SES) (BMI –0.6 kg/m2; p = 0.001). There were no statistically significant effects for physical activity. On average, low-SES respondents with exposure to the second campaign wave reported having increased their attention to their food choices compared with other respondents (p = 0.02), with an average change of 0.60 points (on a 5-point scale).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Johnson and Meadows154
Method: Uncontrolled before-and-after study.
Participants: Thirty residents initially signed up to the intervention (baseline recruitment rate not reported) and 26 completed the programme (mean age 55 years; 54% female; 13 at each site; 87% follow-up response rate).
Interventions: This study investigated a graduated dog walking programme for residents of subsidised housing. The study took part at two separate inner-city high-rise buildings where residents aged ≥ 40 years were invited to take part. Walking dogs, brought to the sites by their owners or study staff, were from the College of Veterinary Medicine’s Pet Assisted Love and Support (PALS) animal-assisted activity programme (dogs were screened for health and behaviour). Participants walked dogs along with their handler using a two-leash system along pre-measured routes in the neighbourhoods surrounding their building. Participants began with walks of 10 minutes three times per week and then advanced to 20 minutes three times per week and 20 minutes five times per week. The intervention lasted 50 weeks at one of the sites (site 1) and 26 weeks at the other site (site 2). Height and weight measurements were taken by study staff (therefore not blinded to the study condition).
Outcomes: At site 1 significant reductions in weight and BMI were observed after 50 weeks (mean weight change –14.4 lb, p = 0.013; mean BMI change –1.90 kg/m2, p = 0.021). However, at site 2, no changes were observed after the 26-week intervention (mean weight change –5 lb, p = 0.29; mean BMI change 0.77 kg/m2, p = 0.91).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Morrison et al.141
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Of the 3170 patients who were referred to the service, 2156 patients opted to participate (68% baseline response rate; 74% female; approximate average age mid-forties) and 809 patients completed the programme (38% follow-up response rate).
Intervention: This study investigated a UK NHS weight-management programme, the Glasgow and Clyde Weight Management Service. The programme was delivered by dietitians with support from psychologists. Physiotherapists were also part of the programme team. The 16-week programme consisted of nine fortnightly sessions. A 600-kcal (2510-kJ) deficit diet and activity changes were advised and these changes were supported with cognitive–behavioural approaches such as goal-setting, self-monitoring, cognitive restructuring and relapse prevention. The majority of the patients who were referred to the service were from the most deprived SES groups. Objective height and weight measurements were taken pre and post intervention (methods and assessors not clearly reported). Success was defined as achieving a weight loss of ≥ 5 kg.
Outcomes: Of those patients who completed the programme, 35.5% lost at least 5 kg. Among the completers there were no differences along the SES gradient in prevalence of success. Additional analyses revealed that patients from the least deprived group were least likely to complete the programme; however, this would be expected as the majority of the sample was from this group, but this finding does have implications for the development of SES inequalities in obesity. These results highlight the need to improve recruitment strategies in low-SES populations.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Gardner et al.143
Method: Uncontrolled before-and-after study using data from routine health service records.
Participants: During the study period health trainers were encouraged but not compelled to record data in the national database; therefore, of 24,986 eligible clients, only 3759 (15% response rate; 79% female; highest proportion in the 36–45 years age group) had suitable data recorded and were used in the analysis.
Intervention: This study investigated the NHS HTS in the UK (England and Wales). The HTS is a nationwide public health initiative based on individualised support for disadvantaged people. The service was designed and developed by a team of psychologists, who also provided long-term support during the intervention implementation. Health trainers are lay community members who typically come from the same background as the target group and who are trained in evidence-based behaviour change techniques. Health trainers support clients to achieve health behaviour goals and, for the purpose of this study, clients who set primary goals relating to healthy eating and physical activity (rather than alcohol or smoking) were included in the analysis. The number of sessions between the health trainer and client varied according to client need or engagement but the mean duration of HTS attendance was 6.14 months.
Outcomes: Data were collected at the first contact session and at the final assessment, when all of the sessions needed had been completed. The height and weight data recorded were a mixture of objectively measured and self-reported data; however it was not recorded which of these measures was used in each instance. Overall, BMI was reduced by 1.77 points (95% CI –1.69 kg/m2 to –1.85 kg/m2; p < 0.001), from 34.03 kg/m2 to 32.26 kg/m2. Overweight/obesity prevalence decreased from 94.7% to 91.0% and the proportion of obese clients decreased from 72.3% to 60.1%. Clients from the least deprived 80% of the population achieved a greater BMI change than the most deprived clients (0.28 points; p = 0.001). However, multiple linear regression analysis found that deprivation did not predict BMI change. Clients with physical activity goals reported a 171% increase in the number of intensive physical activity sessions per week, from 0.63 to 1.71 (d = 0.46), and the proportion of clients engaging in five or more intensive sessions weekly increased from 3.9% to 11.6%. The number of moderate physical activity sessions per week increased by 56%, from 3.06 to 4.77 (d = 0.42), and the proportion undertaking five or more moderate sessions weekly increased from 24.4% to 45.5%. Clients with healthy eating goals reported a 70% increase in fruit and vegetable intake, from 3.08 to 5.23 daily portions (d = 0.97). The proportion of clients consuming five or more portions of fruit and vegetables increased from 24.8% to 60.5%. Mean fried snack consumption decreased by 60%, from 1.99 to 0.79 servings per day (d = 0.85). Deprivation was not associated with changes in physical activity or fruit and vegetable or fried snack consumption.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Schuit et al.140
Method: Cohort analytical study.
Participants: Of the 4059 potentially eligible participants in the intervention area, 3000 were recruited (the authors aimed to recruit 3000 in the intervention group, with an estimated response rate of 65%). In the reference group (control), out of a total of 1115 eligible participants, 895 participated in the study. The attrition rate was low, with 81% of the intervention group and 85% of the reference group completing the 5-year follow-up.
Intervention: This study investigated a cardiovascular disease prevention programme in Hartslag Limburg, the Netherlands, in men and women aged from 31 to 70 years. The aim of the study was to encourage participants to become more active, reduce their fat intake and stop smoking. Between 1999 and 2003, 790 interventions were implemented, of which 500 were major interventions (193 diet, 361 physical activity and nine anti-smoking interventions). Examples of intervention activities include computer-tailored nutrition education, nutrition education tours in supermarkets, public–private collaboration with the retail sector, television programmes, food labelling, smoke-free areas, the creation of walking and bicycling campaigns, a stop-smoking campaign, commercials on local television and radio, newspaper articles and pamphlet distribution.
Outcomes: The outcome measures in the study were BMI, waist circumference, blood pressure, non-fasting glucose level and total cholesterol. Because of some missing values on SES (n = 13), BMI (n = 5), waist circumference (n = 8), blood pressure (n = 21), cholesterol (n = 278) and glucose (n = 205), analyses were performed on between 2834 and 3114 men and women. At the 5-year follow-up change in BMI and waist circumference was significantly different between the intervention group and the reference group. The adjusted difference in mean change in BMI was –0.38 kg/m2 for men and –0.25 kg/m2 for women and the adjusted difference in mean change in waist circumference was –2.9 cm for men and –2.1 cm for women. For moderate- to high- and low-SES subgroups, the adjusted difference in mean change in BMI was –0.34 kg/m2 and –0.27 kg/m2, respectively, and the adjusted difference in mean change in waist circumference was –2.4 cm and –2.6 cm respectively. These differences were statistically significant. Change in blood pressure was significantly different between the intervention group and the reference group at the 5-year follow-up. The adjusted difference in mean change in blood pressure was –7.8 mmHg for men and –5.5 mmHg for women (systolic) and –5.1 mmHg for men and –4.4 mmHg for women (diastolic). In women only, the mean changes in non-fasting glucose level and total cholesterol were also significantly different between the intervention group and the reference group (–0.23 mmol/l and 0.11 mmol/l respectively). There were no significant changes in HDL cholesterol (men and women) or glucose (men). For moderate- to high- and low-SES subgroups, the adjusted difference in mean change in blood pressure was –7.2 mmHg and –6.1 mmHg (systolic) and –4.6 mmHg and –4.9 mmHg (diastolic), respectively, and the adjusted difference in mean change in non-fasting glucose level was –0.23 mmol/l and 0.18 mmol/l respectively. These results were statistically significant and so this intervention benefited both moderate- to high- and low-SES groups (blood pressure and glucose level). There were no significant changes in cholesterol levels between moderate- to high- and low-SES groups.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Community-level interventions
Universal approach: experimental studies (n = 4)
Wing and Jeffery186
Method: RCT.
Participants: The study participants were aged from 22 to 55 years (mean age 42.5 years). The total eligible population is not reported. In total, 166 participants agreed to participate in the study and were randomised into one of four treatment conditions: (1) recruited alone and standard behavioural treatment; (2) recruited alone and standard behavioural treatment plus social support; (3) recruited with friends and standard behavioural treatment; (4) recruited with friends and standard behavioural treatment plus social support. The male-to-female ratio was 18 : 20 in group 1, 26 : 22 in group 2,18 : 22 in group 3 and 20 : 20 in group 4.
Intervention: This study investigated a 4-month behavioural lessons and social support intervention to support weight loss and maintenance in Pennsylvania and Minneapolis, USA. Behavioural lessons focused on such topics as problem-solving, assertion, stimulus control, developing social support, dealing with high-risk situations, cognitions and strategies for long-term maintenance. The intervention involved weekly group meetings for 16 weeks. Meetings were led by a behavioural therapist, a nutritionist or both and included an individual weigh-in, a review of self-monitoring records and a lecture or discussion period. Follow-up measurements were taken at 7 and 10 months. In total, 136 of the participants (82%) completed the 10-month follow-up.
Outcomes: The outcome measures were BMI and weight. Participants recruited with friends had an overall weight loss of 8.7 kg whereas those recruited alone had an overall weight loss of 5.8 kg. The significant difference in overall weight loss occurred during months 0–4 and after this initial difference there were no significant differences among the four treatment conditions for overall weight loss. There were no significant differences in weight loss maintenance between the four groups. The effects of the recruitment approach and social support on maintaining weight loss were significant (p < 0.05). Employment did not affect overall weight loss.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
van Wier et al.187
Method: Three-armed RCT.
Participants: Out of a total eligible workplace population of 2615, 1336 (53%) were assessed at baseline and 64% of these (n = 886) completed the 6-month follow-up. The mean age of participants was 43 years for all three arms. Between 65.1% and 69.5% of the participants were female.
Intervention: The study examined a weight-management intervention in overweight adults in various workplace settings in Minnesota, USA. There were two intervention arms (telephone and internet groups) and one control arm (standard group). The two intervention arms received a 6-month lifestyle intervention with behaviour counselling (10 biweekly sessions) by either telephone or e-mail. The control arm received usual care in the form of lifestyle brochures.
Outcomes: The primary outcome measure was body weight (measured by trained research personnel; blinding not reported). The secondary outcome measures were waist circumference, physical activity and dietary intake. There were significant weight losses in all three groups. In the main analysis (all subjects regardless of intervention adherence), there was a significant weight loss of 1.5 kg (95% CI –2.2 kg to –0.8 kg) in the telephone group compared with the control group. For the internet group the corresponding figure was 0.6 kg (95% CI –1.3 kg to –0.01 kg). The difference between the telephone group and the internet group was not statistically significant. In the secondary analysis (complete cases only), there was a significant weight loss of 1.6 kg (95% CI –2.2 kg to –1.0 kg) in the telephone group and 1.1 kg (95% CI –1.7 kg to –0.5 kg) in the internet group compared with the control group. Compared with the control group, waist circumference decreased significantly by 1.9 cm (95% CI –2.7 cm to –1.0 cm) in the telephone group and 1.2 cm (95% CI –1.7 cm to –0.5 cm) in the internet group. No significant differences were found between the two intervention groups. The comparison between the telephone group and the control group showed statistically significant changes for physical activity (increase) and fat intake (decrease). Education was treated as a possible confounder and was therefore controlled for in these analyses.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Baron et al.189
Method: RCT.
Participants: At baseline, 135 overweight participants (mean age 40 years; 85% female) were randomised to either the low-carbohydrate or the low-fat diet club. After 1 year the final sample size was 119 participants (88% follow-up response rate).
Intervention: This study investigated diet clubs using two different weight-reducing diets: a low-carbohydrate diet compared with a low-fat/high-fibre diet. Each diet club held weekly meetings for 3 months run by a group leader and both diets provided approximately 1000–1200 kcal per day. Participants planned their own menus with the assistance of group leaders and study investigators and were given diet instruction sheets.
Outcomes: Height and weight measurements were taken (assumed by non-blinded diet club staff) at baseline, post intervention (3 months) and at 1 year. Moderate weight losses were observed in both diet groups after 3 months but most of this had been regained at 1 year. Participants on the low-carbohydrate diet lost more weight on average than those on the low-fat/high-carbohydrate diet at 3 months (5.0 kg vs. 3.7 kg; 95% CI of difference 0.0 kg to 2.5 kg) but there was no significant difference in weight lost between the groups at the 1-year follow-up (2.3 kg vs. 1.6 kg; 95% CI of difference –1.2 kg to 2.6 kg). Both diets worked equally well among the more upper class participants (social class I or II) but among those of a lower social class (III–V) the low-carbohydrate diet was particularly effective at 3 months (weight loss: low-carbohydrate diet 5.0 kg, low-fat diet 3.0 kg; 95% CI of difference 0.3 kg to 3.9 kg), although at 1 year there was no significant difference between groups for this social group (weight loss: low-carbohydrate diet 2.6 kg, low-fat diet 0.5 kg; 95% CI of difference –0.7 kg to 4.8 kg).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Neumark-Sztainer et al.188
Method: RCT.
Participants: The final sample size was 24 (57% follow-up response rate).
Intervention: This study investigated an additional exercise component in a weight loss programme (a subprogramme of the CHAD programme). Obese women from the CHAD programme were invited to participate in the weight loss programme. Forty-two women aged 25–50 years were recruited at baseline (recruitment rate not reported) and were randomly assigned to either the weight loss programme with the additional exercise component (intervention group) or the weight loss programme without the exercise component (active control group). All participants attended group sessions run by a nutritionist or a physician where they received nutrition guidance and education and learnt behavioural modification skills. The intervention group also received 1 hour of physical activity instruction from a physical education instructor and a home exercise programme (six 25-minute exercise sessions per week).
Outcomes: Weight was measured by the programme nutritionist at baseline, post intervention (month 3), 2 months post intervention (month 5) and 5 months post intervention (month 8). Both groups lost weight after the initial intervention (intervention group –3.8 kg, control group –3.6 kg) and continued to lose weight 2 months post intervention (intervention group –4.7 kg, control group –4.3 kg). There were no significant differences in weight loss between the groups at either time point. At 5 months post intervention weight loss appeared to be maintained in the intervention group (weight change from baseline –3.9 kg) and increased in the control group (weight change from baseline –4.6kg); however, by this stage the sample sizes were very small and the results should be treated with caution. In the intervention group there were no significant differences in weight loss between women who were employed and women who were not employed; however, in the control group women who were employed lost more weight than women who were unemployed.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Universal approach: observational studies (n = 12)
Freak-Poli et al.194
Method: Prospective cohort study.
Participants: A total of 762 eligible participants were recruited from 10 workplaces but only 671 completed the waist circumference baseline measurement; 539 participants (80%) completed the 4-month follow-up. In total, 57% were female and the mean age for a low-risk waist circumference was 38 ± 10 years and for a high-risk waist circumference was 43 ± 10 years.
Intervention: This study investigated a 4-month work-based physical activity health programme intervention in workplaces in Melbourne, Australia. The programme involved wearing a visible step-count pedometer with a target of at least 10,000 steps per day for 125 days. Weekly encouragement e-mails were sent and a website was used for logging daily steps, accessing additional health information, communication among participants and comparing team progress.
Outcomes: The outcome measure was waist circumference (independently measured by trained staff; blinding not reported). The results showed that participants who were not meeting waist circumference guidelines at baseline responded positively to the programme and had a 2.9-cm larger reduction in waist circumference than participants who were meeting waist circumference guidelines. For every extra centimetre of waist circumference at baseline, a 0.12-cm loss in waist circumference was observed at 4 months. Similarly, participants with a high baseline risk of type 2 diabetes had a 2.2-cm larger reduction in waist circumference than participants with a low baseline risk of type 2 diabetes [statistically significant (p < 0.001) and a clinically significant reduction for high-risk individuals]. There was also a noticeable difference according to education group: between baseline and the 4-month follow-up, participants who had completed tertiary education at baseline had a 2.1-cm larger reduction in waist circumference than participants who had not completed tertiary education at baseline.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Moderate |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Merrill et al.190
Method: Uncontrolled before-and-after study.
Participants: A volunteer sample was recruited by targeted advertising through Centres of Excellence, Coronary Health Improvement Project alumni groups, corporate client sites and the Swedish American Health System. In total, 348 participants were recruited at baseline (baseline recruitment rate not reported; 70% female) and there was a final sample size of 211 participants (61% follow-up response rate; follow-up 18 months).
Intervention: The Coronary Health Improvement Project investigated a 4-week health education course aimed at reducing cardiovascular risk factors. The intervention was aimed at all adults aged ≥ 18 years, and associations with intervention effects and SES indicators were explored. The health education course covered topics including atherosclerosis, coronary risk factors, obesity, dietary fibre, smoking, diabetes, hypertension, hypercholesterolaemia, dietary fat and cholesterol, exercise, osteoporosis, cancer, lifestyle and health, the optimal diet, behavioural change and self-worth. Participants were encouraged to follow pre-set dietary (a more plant-based diet, which emphasised unrefined food and was low in fat and high in fibre) and exercise (walking or some other form of exercise for at least 30 minutes a day) goals.
Outcomes: Participants were given a pedometer so that they could keep a log of the miles walked each day. Height and weight measurements were taken by trained programme staff (blinding status unclear) at baseline and at 6, 12 and 18 months. Fasting blood samples and blood pressure measurements were also taken. After 18 months, mean BMI was significantly reduced (–0.9 kg/m2, 95% CI –1.2 kg/m2 to –0.6 kg/m2), with 66% of the participants decreasing their BMI. After adjusting for baseline quartile groupings, the effects of annual family income, education and employment status on BMI were not significant. There were no significant changes for systolic blood pressure, diastolic blood pressure, total cholesterol, triglycerides or glucose; however, LDL cholesterol was significantly decreased (–4.5 mg/dl, 95% CI –8.5 mg/dl to –0.5 mg/dl) and HDL cholesterol was significantly increased (+4.4 mg/dl, 95% CI 3.4 mg/dl to 5.4 mg/dl) after 18 months. After adjusting for baseline quartile groupings, the effects of annual family income, education and employment status on systolic blood pressure, diastolic blood pressure, total cholesterol, LDL and HDL cholesterol and triglycerides were not significant. However, for glucose, after adjusting for baseline quartile groupings, those not employed were significantly more likely to lower their glucose level (OR 2.2, 95% CI 1.1 to 4.6).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Mattfeldt-Beman et al.195
Method: Uncontrolled before-and-after study.
Participants: In total, 308 participants were recruited to the intervention and the final sample size after 18 months was 281 (91% follow-up response rate; mean age 43 years; 27% female).
Intervention: This study investigated a 14-week weight loss programme. The intervention was targeted at adults aged 30–54 years with mild obesity (115–160% of ideal body weight) and blood pressure at the high end of the normal range. The weight loss programme was delivered by a multidisciplinary team and focused on self-management of energy intake, exercise and individually set behaviour goals. The aim of the intervention was gradual weight loss at a rate of 1–2 lb per week (minimum weight reduction of 10 lb), to be maintained for the 18-month duration of the study. During the 14-week intervention, weekly 90-minute group sessions were delivered. During the maintenance phase to 18 months’ follow-up (from baseline), participants received contact at least once a month through group meetings, brief weigh-ins or individual counselling sessions.
Outcomes: Weight measurements were taken at baseline and 18 months by independent assessors who were blinded to the intervention. After 18 months, 42% of the participants were classified as successful (defined as a loss of ≥ 10 lb and not regaining > 50% of weight lost). There were no significant differences in education status between those who were successful and those who were not successful.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Kliche et al.161
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Participants were referred to a health promotion training course through doctor referral or through media advertising. At baseline, 1671 signed up to the courses (80% female; mean age 49 years; 71% baseline recruitment rate); 718 completed the 3-month follow-up (43% follow-up response rate).
Intervention: This study investigated health promotion training courses run by major health insurers in Germany. There were three types of course available: one that focused on increasing physical activity, one that focused on nutrition and one that focused on stress. Each course consisted of modules that focused on specific health goals. The courses consisted of, on average, nine group-based sessions.
Outcomes: Self-reported height, weight, physical activity and diet behaviour data were collected at baseline, post intervention and at 3 months follow-up. Overall, there was a small but significant decrease in BMI from baseline to post intervention to 3 months (27.24 kg/m2, 27.00 kg/m2 and 26.9 kg/m2 respectively; p = 0.000). Physical activity and healthful dietary behaviour increased from baseline to post intervention and, although they then decreased slightly at 3 months, levels were still higher than at baseline (physical activity scores: 3.66, 3.98 and 3.75 respectively, p = 0.000; diet scores: 3.85, 4.22 and 4.07 respectively, p = 0.000). When explored as a confounder, the participants’ level of education had no effect on the intervention effect, suggesting that the intervention had the same effect across SES groups. However, most of the participants had a lower level of education.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Stunkard et al.193
Method: Prospective cohort study.
Participants: In total, 1177 employees from the 15 workplaces volunteered to participate (mean age 38 years; 57% female) and attrition was low (97% follow-up response rate), resulting in a final sample size of 1146. A subsample of employees from one workplace that contained similar numbers of white- and blue-collar workers (final n = 195) was also used to conduct additional analysis to explore any differential effects by work type.
Intervention: This study investigated a workplace weight loss competition. The competitions took place in 15 workplaces (mostly manufacturing but also banks and a community college) and were implemented primarily by committees of workplace employees (with a small amount of assistance from professionals). Teams of employees volunteered to participate and competitions were conducted between and within workplaces. The 12-week intervention consisted of weekly weigh-ins at which teams and team-mates could interact with each other and weight loss advice was provided. After 12 weeks, the team who lost the most weight received a cash prize (each participant paid US$5, matched by workplace management, at the beginning of the competition). Weight loss progress was publicised using posters and weigh-ins were conducted in public spaces at lunchtimes.
Outcomes: The outcome used was change in weight from baseline to post intervention. Including data from all workplaces, weight losses were large in those who were initially > 10% overweight (6.3 kg for men and 4.4 kg for women). In those who were mildly overweight, men lost 3.4 kg and women lost 2.9 kg. Type of worksite (blue collar vs. white collar) showed no association with weight loss in regression analysis, suggesting that competitions were equally effective in achieving weight loss in both types of worksite. In the subsample of employees, the intervention seemed to work equally as well in both groups: 50% of blue-collar workers reached their weight loss goal compared with 44% of white-collar workers. It is worth noting, however, that blue-collar workers were less likely to enter the competitions (overall and subsample data).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Lloyd and Khan192
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: A total of 2456 patients (87% female; mean age 51 years) were given vouchers to attend 12 weekly group sessions run by either Slimming World or Weight Watchers at which they received practical advice and guidance for weight loss. Height and weight were measured at baseline and after 12 weeks (blinding status of assessor not reported) and success was defined as a weight loss of > 5%. Follow-up measurements were taken for all participants, even those defined as dropouts (attended < 10 sessions); therefore, in terms of the study there was a 100% follow-up response rate.
Intervention: This study investigated a health service obesity treatment model (Healthy Choices) in the UK in which overweight and obese patients were referred to a commercial weight loss programme for 12 weeks.
Outcomes: Overall, on average, participants lost 4.7 kg after 12 weeks, with completers losing 6.1 kg and dropouts 2.2 kg. In total, 44% of all participants achieved a > 5% weight loss and were classified as being successful. Importantly, there was no statistical difference in successful weight loss outcome between deprivation quintiles.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Lowe et al.196
Method: Retrospective (uncontrolled) cohort study.
Participants: Participants for the study were identified through a database of lifetime members of Weight Watchers and telephone interviews were conducted with a random subsample of 1002 adults (recruitment rate not reported; 96% female; majority in the 35–54 years age range).
Intervention: This study investigated weight regain in participants who had previously participated in a commercial weight loss programme (Weight Watchers) and had reached their weight goal 1–5 years previously. The Weight Watchers programme consists of weekly group session led by successful programme graduates (peer role models), who offer social support. Participants receive food (moderately energy deficient), physical activity (30 minutes on most days) and behaviour modification plans, along with written educational materials. Weight loss goals are determined by each individual member and weigh-ins are conducted at each session so that progress can be monitored.
Outcomes: Weight data were self-reported by participants although these were corrected using data from a subsample who had their weight measured. On average, participants had regained 5.8 kg (56% of initial weight loss), although, as would be expected, weight regain was greatest in those who had reached their weight loss goal the longest time ago (5 years vs. 1 year; F = 23.1; p < 0.001). Over half of the sample (57%) maintained ≥ 5% weight loss and 80% remained below the weight that they were before beginning the programme. However, less than one-third (28%) of the participants had remained within 5 lb of their goal weight. Simultaneous regression analysis revealed no relationship between employment status and weight regain.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Not applicable |
| Global rating | Weak |
Veloso and Santana,163 Veloso et al.162
Method: Retrospective cohort study with a non-intervention comparison group.
Participants: The study included data from workers who had completed at least two surveys. In the 2002 publication,163 preliminary analysis and results were presented (n = 8454), whereas in the 2007 publication162 a more inclusive and comprehensive analysis was undertaken (n = 10,368); we will focus on these later results for the purpose of this review.
Intervention: This study investigated a national Workers’ Food Program (PAT) that was implemented in Brazil in the 1970s with the aim of ensuring adequate nourishment for low-income workers. Workplaces registered to PAT provided food or coupons to their workers to ensure that they received a main meal of at least 1400 calories, minor meals of at least 300 calories and a diet of 6% protein. Data were taken from routine annual workplace health monitoring surveys carried out between 1995 and 2000 from workplaces registered to PAT, workplaces using another food programme (not PAT) and workplaces that did not use any programme.
Outcomes: The 2007 study162 found that, overall, weight and incidence of overweight increased per year to a greater extent in workplaces implementing a food programme (PAT or another) than in workplaces with no programme (RR/OR of weight gain: PAT 1.71, 95% CI 1.45 to 2.00, other food programme 2.00, 95% CI 1.70 to 2.35; RR/OR of being overweight: PAT 1.91, 95% CI 1.26 to 2.91, other food programme 2.13, 95% CI 1.41 to 3.23; no programme = reference). When exploring the effects of the food programmes in different SES groups (determined by occupation), the 2007 study162 found that these adverse effects occurred in low-SES workers (and medium-SES workers for incidence of overweight) but not in high-SES workers. The 2002 study163 found similar patterns for incidence of weight gain but not overweight (for which adjusted analyses revealed no intervention effects or differences by SES groups). The authors concluded that the adverse effects of the Workers’ Food Program and other food programmes may be a result of the programmes reflecting the needs of the Brazilian population when they were first implemented but not being appropriate for the current population’s needs.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Moderate |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Hwang et al.173
Method: Prospective cohort study.
Participants: The approximate total workforce was 6000 but the total eligible population who could participate in the study was not reported. Employees had to have a BMI of > 27 kg/m2. In total, 88.4% of the participants were men and the mean age was 33.6 ± 7.4 years.
Intervention: This study investigated a work-based obesity management programme called the Midas Project in an electronics company in Pyungtaik, Korea. The programme lasted for 3 months. It was incentive based and the catchphrase was ‘Turn fat into gold’, with each participant being awarded one gold medal for each kilogram of body fat lost during the programme. Major elements of the programme included counselling by factory nurses, self-help groups, free gym facilities, trainers and health information seminars/bulletins. Small group meetings took place with the company nurse for an hour every week to discuss any problems. Participants also received health information by e-mail on a weekly basis.
Outcomes: The primary objective outcome measures included changes in BMI, body weight, body fat, systolic and diastolic blood pressure and cholesterol. Other self-reported measures included exercise, night eating, dining together, drinking, smoking and sleeping. The results showed that, of the independently measured objective health measures, BMI, body weight, body fat and systolic and diastolic blood pressure significantly decreased (–1 kg/m2, –3.7 kg, –2.1 kg, –5.4 mmHg and –4.7 mmHg respectively, all p < 0.05); cholesterol increased by 8 mg/dl but this was not statistically significant. Subgroup analyses between office and factory workers also showed very similar results, with significant decreases in all but cholesterol for factory workers and all but diastolic blood pressure and cholesterol for office workers. Therefore, the intervention had favourable effects in both office and factory workers for all obesity outcomes. Self-reported lifestyle measures did not show any significant changes except for exercise, for which there was a statistically significant increase for factory workers.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Rohrer et al.172
Method: Retrospective cohort study.
Participants: A total of 936 participants out of 10,489 eligible participants (9%) took part in a telephone coaching weight-management programme (64.1% male, mean age 48.7 years). In total, 100% of the participants completed the 6-month follow up.
Interventions: This study investigated a telephone coaching programme in a large manufacturing company in the USA. The coaching was based on collaborative goal-setting and included self-management health education. Goal categories included understanding principles of weight management, incorporating more physical activity into the daily routine, increasing exercise, following food pyramid guidelines and following recommended portion sizes.
Outcomes: The primary outcome measure was body weight change (based on self-reported measures of weight). The results showed that, overall, the mean change in weight was –1.8 kg (–4.0 lb), with a range from a gain of 18 kg to a loss of 48 kg. Weight loss was statistically and clinically significant (p < 0.001). Individuals with a higher BMI (> 35 kg/m2) lost more weight (p = 0.001). Weight loss did not differ significantly between genders, age groups, different racial groups or different income levels. There was a tendency for more weight loss in less educated groups but this was not statistically significant.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Targeted approach: experimental studies (n = 24)
Janicke et al.103
Method: RCT.
Participants: There was a baseline response rate of 55% and a final sample size of 33 child–parent dyads (83% follow-up response rate). Families were recruited through primary care clinics, schools, newspaper articles and community presentations in four cohorts and were randomised to the intervention and active control groups in child–parent dyads. Assignment to the groups was unbalanced to ensure that sufficient dyads were allocated to the treatment group for optimal group functioning.
Intervention: This study investigated a group-based family behavioural weight-management intervention compared with individual standard treatment in families receiving Medicaid with overweight or obese children aged 6–12 years. Although the primary focus of the intervention was to reduce obesity-related outcomes in the children, weight changes of the parents/caregivers were also monitored. The intervention group was asked to attend 12 weekly 90-minute group sessions covering nutrition, physical activity and behaviour management topics, and monitored their behaviours using food logs and pedometers. The sessions also offered group support and problem-solving. The standard care programme consisted of three 60-minute sessions over 12 weeks at which individual families met with a treatment team member and received nutrition and physical activity education, problem-solving and a progress review.
Outcomes: Height and weight measurements were taken by a trained research team member (blinding status not reported) and BMI z-scores were calculated. No significant treatment effect on parent/caregiver weight was observed post treatment or at 9 months.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Moderate |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Nichols179
Method: RCT.
Participants: Community health workers and university secretaries were invited to take part in the study through personal contact and referrals from friends. Participants were randomised into the intervention group or a control group in which they were instructed to self-manage their weight loss (this group were offered the intervention after the 12-week study). In total, 41 women were recruited at baseline (approximately 56% recruitment rate; mean age 51 years). Three control participants dropped out and there were missing data for another control participant, resulting in a final sample size of 37 (90% follow-up response rate).
Intervention: This study investigated a 12-week weight loss intervention for overweight low-income African American women. Weekly group sessions were delivered by a trained African American facilitator with similar cultural preferences. The sessions included health education on obesity and cardiovascular disease risk factors; skills development in dietary monitoring and tracking through keeping a food and exercise diary; techniques for healthy caloric food choices; meal planning; demonstrations for healthy lifestyle options; recommendations for healthy outcomes in setting (realistic) goals for risk factor reduction and prevention; and facilitated group discussions of psychosocial indices of depression, self-concept and general well-being. A combination of change strategies was used in the intervention, including self-monitoring, stimulus control, rewards, stress management, problem-solving, cognitive–behavioural and relapse prevention approaches. Behavioural strategies used were individualised to each participant depending on what was suitable for him or her. Participants were given individualised food plans based on US Department of Agriculture guidelines for a healthful diet (specific energy intake was not prescribed) and were encouraged to perform at least 15–30 minutes of physical activity five to several times per week. Participants and facilitators served as a formal structured support group (rather than informal unstructured support, i.e. from family and friends) and a buddy system was used in which participants made 10- to 15-minute calls to each other once a week to check up on progress, offer encouragement and prevent relapses. Finally, a weekly prize was awarded to the participant who lost the most weight and small monetary incentives were given to those who had accomplished their goal for the week.
Outcomes: Height, weight, waist, hip, body composition and blood pressure (intervention group only) measurements were taken by a trained clinical evaluator blinded to experimental condition. Blood samples were also taken to determine cholesterol and fasting glucose levels. Physical activity and dietary intake data were collected using self-report questionnaires. BMI decreased in the intervention group from baseline to post intervention and increased in the control group (intervention group –0.95 kg/m2, control group 0.32 kg/m2; between-group difference –1.27 kg/m2; p < 0.001), as did body weight (intervention group –2.39 kg, control group 0.66 kg; between-group difference –3.05 kg; p < 0.001), body fat (intervention group –7.5 lb, control group 7.98 lb; between-group difference –15.54 lb; p < 0.05), per cent body fat (intervention group –2.38%, control group 3.59%; between-group difference –5.97%; p < 0.001) and waist and hip circumferences (waist: intervention group –1.33 inches, control group 0.35 inches, between-group difference –1.68 inches, p < 0.001; hip: intervention group –1.50 inches, control group 0.04 inches, between-group difference –1.54 inches, p < 0.001). However, there were no significant between-group differences for changes in waist-to-hip girth. Lean body mass increased in the intervention group and decreased in the control group (intervention group 1.72 lb, control group –4.93 lb; between-group difference 6.65 lb; p < 0.01), as did the lean-to-fat ratio (intervention group 0.16, control group –0.24; between-group difference 0.40; p < 0.001).
In terms of physical activity levels, the intervention group increased levels of weekday moderate activity whereas the control group decreased levels (intervention group 244 kcal/week, control group –178 kcal/week; between-group difference 421.57 kcal/week; p < 0.001). There were no significant changes in weekend moderate activity from baseline to post intervention in either group and no between-group differences. Weekday hard activity increased to a greater extent in the intervention group than in the control group (intervention group 393 kcal/week, control group 30 kcal/week; between-group difference 363 kcal/week; p < 0.03), as did weekend hard activity (intervention group 504 kcal/week, control group –30 kcal/week; between-group difference 534 kcal/week; p < 0.001). There were no significant between-group differences in changes in weekday or weekend very hard activity levels. With regard to dietary intake, there were significantly greater reductions in saturated fat intake (intervention group –3.49% energy, control group –0.51% energy; between-group difference –2.98% energy; p < 0.005) and total dietary fat (intervention group –10.84% energy, control group –1.79% energy; between-group difference –9.05% energy; p < 0.001) in the intervention group than in the control group. There was no significant change in cholesterol levels in the intervention group; however, there was an increase in the control group resulting in a significant between-group difference (intervention group –3.30 mg/dl, control group 13.40 mg/dl; between-group difference 16.7 mg/dl; p < 0.04). There were no significant between-group differences in change from baseline to post intervention for fasting glucose levels and there was no significant change in blood pressure from baseline to follow-up in the intervention group.
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Befort et al. 2008230
Method: Small randomised controlled pilot study.
Participants: Participants were recruited from a community health centre that served predominantly lower-income African Americans using flyers and a staffed table in the health clinic lobby and by word of mouth. In total, 44 women were recruited at baseline and randomised into either the intervention group (n = 21) or a comparison condition (n = 23) (mean age 44 years). After the 16-week intervention the final sample size was 33 (14 in the intervention group; 75% follow-up response rate).
Intervention: This study investigated a 16-week behavioural weight loss programme plus motivational interviewing compared with a behavioural weight loss programme plus health education in lower-income African American women. The behavioural weight loss programme was delivered in 90-minute weekly sessions by a doctoral-level psychologist and a master’s-level counsellor or dietitian. All participants received an individual calorie and fat intake goal and were instructed to self-monitor food intake and physical activity. Cultural adaptations included the following: (1) social support was emphasised with dedicated sharing time and by addressing ways to build support among existing networks; (2) barriers related to transportation, neighbourhood safety, literacy and other stressors were discussed and childcare during meetings was provided when feasible; (3) guidance about food and physical activity were made relevant to cultural practices, for example by discussing alternatives to preferred high-fat meats and highlighting existing physical activity programmes in the community; (4) preferences for larger body sizes were recognised and the health benefits of 5–10% weight loss were highlighted; (5) African American community leaders who had succeeded at weight loss were invited as peer mentors; (6) participants developed group names for themselves (e.g. ‘Jazzy Women Taking It Off’ and ‘Dedicated Divas’) to increase programme ownership; and (7) sessions were less didactic and more interactive in nature. Participants in the intervention group received four motivational interviewing sessions (two in person and two by telephone) in addition to the behavioural weight loss programme sessions. The first session focused on building motivation and commitment for attending the programme and changing behaviours by discussing relevant past experiences and clarifying connections between core values and motivation to lose weight. The remaining three sessions focused on relevant target behaviours (e.g. problem foods, barriers to being physically active) that were identified. Consistent with the behavioural weight loss programme, the majority of each session was spent eliciting change talk by exploring participants’ motivations and confidence for changing the target behaviour, linking the behaviour to core values and/or discussing the pros and cons of change. Sessions ended with a global summary and, if appropriate, development of a behavioural action plan based on participants’ self-identified goals. Participants in the comparison group received four health education sessions (two in person and two by telephone) in addition to the behavioural weight loss programme. These sessions intentionally avoided topics that were directly relevant to weight loss and participants chose four topics from six options: breast, colon or cervical cancer screening, smoking cessation, helping others quit smoking and improving sleep.
Outcomes: Height and weight were measured at baseline and post intervention (blinding status of assessor not reported) and dietary intake and physical activity data were collected using self-reported recall methods. From baseline to post intervention, both groups lost a significant amount of weight (intervention group –2.6 kg, control group –3.2 kg; p-value not reported) and achieved a significant decrease in daily food intake (intervention group –434 kcal, control group –486 kcal) and per cent kcal from fat (intervention group –3.4%, control group –5.5%) and a significant increase in fruit and vegetable servings per day (intervention group 1.2, control group 2.0). There were no significant changes in physical activity levels for either group. There were no significant differences between the groups for diet, physical activity or weight outcomes (p = 0.13–0.95) and the between-group effect sizes were trivial to small (Cohen’s d = –0.04 to –0.27).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Cousins et al.,182 Foreyt et al.184
Method: RCT.
Participants: Mexican American women were recruited to the study through media promotion and personal contacts in the local community, primarily through churches and health agencies. At baseline, 168 participants were recruited and randomised to one of the three conditions after stratification by weight. After 12 months, 86 participants remained in the study (51% follow-up response rate; mean age 33.4 years), with 27 in the family-based group.
Intervention: This study investigated a culturally sensitive family-based weight loss programme compared with an individual-based programme and a manual-only intervention in the Cuidando el Corazon study of Mexican American women. All of the study groups received a bilingual manual consisting of a low-fat eating plan, nutrition information, recipes (for fat-modified traditional Mexican American foods), an exercise plan and behaviour modification strategies. Information was also included on maintaining weight loss, emphasising problem-solving, and preventing relapses. The individual- and family-based groups also attended 24 weekly classes and six monthly classes taught by bilingual registered dietitians. The individual group sessions provided individualised instruction in nutrition, feedback on subjects’ food records and instruction in the use of behaviour modification techniques for weight loss. Classes also included group exercise, food tastings, cooking demonstrations and videotaped instructions on preparing low-fat foods. The family-based intervention sessions contained similar information to the individual classes; however, the classes were designed for families (participants and their husbands and children) and encouraged all family members to adopt more healthful eating and exercise habits. This group also received a modified version of the Cuidando el Corazon manual that included information on partner support and parenting skills to encourage family changes in eating and exercise behaviours.
Outcomes: Height and weight were measured using standard techniques at baseline and 3, 6 and 12 months (blinding status of assessor not reported). Multivariate analysis of variance with repeated measures yielded a significant group × time interaction for BMI (Wilk’s lambda = 0.7817, p < 0.003), indicating an intervention effect over time. There were significant group × time interactions for the comparison (manual-only) group and individual group (Wilk’s lambda = 0.7797, p < 0.003) and the comparison group and family-based group (Wilk’s lambda = 0.7329, p < 0.001) comparisons. The individual group compared with family-based group comparison did not yield a significant group × time interaction (Wilk’s lambda = 0.9668, p < 0.599).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Moderate |
Rickel200
Method: RCT.
Participants: Participants had been recruited for the weight loss intervention through direct mailings, media articles, radio announcements and community presentations. As the main purpose of the study was to compare effects in different ethnic groups (African American vs. Caucasian), both culturally sensitive approaches and direct solicitation to community groups were used to attract a demographically representative sample. The study reported no dropouts during the extended care phase and there was a final sample of 224 women (43 African American, 181 Caucasian; mean age 58–60 years).
Intervention: This study investigated two types of extended care following a weight loss intervention. The two extended care interventions, one including face-to-face group sessions and one delivered by telephone, were provided for 12 months and were compared against an education-only control condition in which information was sent in a newsletter. Participants completing the weight loss intervention were randomised into one of the three conditions. All participants received contact twice each month (face-to-face group sessions at a County Cooperative Extension Service office, by telephone or by newsletter). The intervention conditions included goal-setting and problem-solving and provided support and reinforcement for continued efforts in weight management.
Outcomes: The study consisted of two components that were considered as two separate studies for the purpose of this review. The experimental component of the study investigated the effects of two extended care programmes (described in more detail in the observational studies section) on obese women living in low-SES counties in the USA. The outcome measure for this study was weight, which was measured during a medical examination conducted by a mobile clinical assessment team led by a licensed registered nurse (blinding status not reported) before and after the extended care phase. There were no significant differences in weight regain between the two intervention conditions for either African Americans or Caucasians. African American participants in the face-to-face group sessions condition regained 3.02 ± 4.38 kg whereas those assigned to telephone-based individual counselling regained 1.03 ± 6.07 kg (between-group difference p = 0.35). However, the difference between the groups could be considered clinically significant. Caucasian participants in the face-to-face group sessions condition regained 0.76 ± 6.19 kg and those in the telephone-based individual counselling condition regained 1.39 ± 6.12 kg (between-group difference p = 0.55; no clinical significance). For African Americans there was no difference in weight regain between those assigned to an extended care programme and those assigned to the control condition (extended care 1.67 ± 1.03 kg, control 1.34 ± 1.56 kg; p = 0.85). However, Caucasians assigned to an extended care programme regained significantly less weight than those assigned to the control condition (extended care 1.03 ± 0.58 kg, control 4.23 ± 0.83 kg; p = 0.002).
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Krummel et al.166
Method: Randomised controlled pilot trial.
Participants: Participants were recruited using passive methods (Women, Infants, and Children bulletin board, newspaper/cable/radio advertisements, flyers at local businesses, church bulletins, mailings) and active recruitment by physicians, Women, Infants, and Children staff (breastfeeding counsellors, nutritionists) and Mothers’ Overweight Management Study (MOMS) staff (education classes, clinic days in waiting rooms). At baseline, 151 women (36% recruitment rate; mean age 27 years) were recruited and randomised into either the intervention group (peer guided; n = 78) or comparison group (self-guided; n = 73). After 1 year, 64 women remained in the study (28 intervention group, 36 comparison group; follow-up response rate 42%).
Intervention: The MOMS study investigated a weight-management programme for post partum low-SES mothers including group discussion sessions compared with a self-management approach. All participants attended one counselling session with a MOMS dietitian at which they received a lifestyle plan containing goals for eating, physical activity and other aspects of weight management, and personal feedback; monthly newsletters; and incentives (MOMS tote bag, t-shirt, Teflon pan, make-up, veggie toys and a raffle for gift cards). Those in the self-management group were left to manage their own weight whereas the peer-guided group was enrolled in 10 facilitated discussion group sessions and received monthly personalised feedback on self-monitoring records for nutrition and physical activity behaviours. Both groups were followed for 1 year.
Outcomes: At baseline and follow-up, height, weight and waist circumference were measured (blinding status of assessor reported). Dietary intake data were collected using a 7-day food record and physical activity data (steps per day) were collected using pedometers. After 1 year there were no statistically significant differences between the groups in any of the outcome variables (weight, BMI, waist circumference, energy intake, fat intake, fibre intake, steps per day). Process evaluation revealed that attendance at the intervention group sessions was very low (57% of the participants did not attend any of the sessions); therefore, intervention exposure was low, which may explain the lack of intervention effect observed.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Erfurt et al.171
Method: Cluster randomised controlled/quasi-experimental trial.
Participants: Initially, between 75% and 88% of the worksite employees at four manufacturing workplaces took part in the first health screen. Of these employees, a random sample of 2300 was selected to take part in the second follow-up health screen, of whom 1883 completed (82% follow-up response rate), 690 of whom were classed as overweight. Participants were predominantly male blue-collar workers and were aged between 39 and 43 years.
Interventions: This study investigated workplace well-being interventions in four manufacturing workplaces. The four worksites were randomised into the active control condition (health screening only), intervention A (health screening and health education), intervention B (health screening, health education and follow-up counselling) and intervention C (health screening, health education, follow-up counselling and organised activities). Health screening included measurement of blood pressure, weight and history of cigarette smoking. In the control site, no additional interventions were implemented by the study team; however, the workplace was free to take part in wellness studies independent of the study. The health education component comprised media promotion following health screening and health improvement classes (twice a year). A part-time health educator was also assigned to work with a health committee (with representatives from the workplaces’ management, labour and medical departments). For the follow-up counselling component (for those with one or more cardiovascular disease risk factors: high blood pressure, ≥ 20% overweight and/or smoker in intervention B, and any employee who had been screened in intervention C), participants were contacted approximately once every 6 months by a wellness counsellor (located at the worksite) and received counselling about their current risk status and explored how they might change their risks. The participants also received mailings and telephone calls to their home and memos and telephone calls to their work station. Participants could also choose from a menu of approaches: guided self-help, one-to-one formal consultation, mini-group interventions or full-group classes. Finally, the worksite-organised activities included informal health networks and peer support groups such as buddy systems, specific interest health promotion groups such as walking clubs and site-wide health promotion such as weight loss contests. Employees completed the health screen again after 3 years when follow-up weight measurements were taken (blinding status of assessor not reported).
Outcomes: Comparing those who were overweight at baseline and who were rescreened after 3 years (n = 690), the control group gained 3.1 lb (change from baseline p < 0.01), the intervention A and B groups maintained their weight and the intervention C group lost 4.7 lb (change from baseline p < 0.001). In those who actively took part in weight loss interventions offered (n = 238), those in the control group and the intervention A group maintained their weight (no significant changes from baseline), those in the intervention B group lost on average 5 lb (change from baseline p < 0.001) and those in the intervention group C group lost on average 6.4 lb (change from baseline p < 0.01).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Dennison et al.170
Method: Quasi-experimental study.
Participants: In total, 93 workers were recruited at baseline (majority blue-collar production workers; recruitment rate not reported) and the final sample size was 30 after 1 year (90% men, average age approximately 47 years; follow-up response rate 32%).
Intervention: This study investigated a computer-assisted instruction weight-management programme for overweight employees of an automobile manufacturing company (two worksites). Employees volunteered to take part in the study and were eligible if they were 20–35% over their ideal weight. In one worksite, participants were randomly assigned to either a computer-assisted programme consisting of nutrition information and assessment of diet and physical activity behaviours in which the participant interacted with the computer software (intervention group A) or the same intervention but in which a project staff member completed the computer software program (intervention group B). A group of employees from the second worksite acted as a non-randomised control group and received no intervention.
Outcomes: The interventions were conducted for 8 weeks and follow-up data were collected after 1 year. Data collected were weight (blinding status of assessor not reported) and dietary intake using 3-day self-reported food records. There were no statistically significant changes in weight for any of the groups or between groups; however, the final sample was very small and unlikely to be large enough to detect statistically significant effects. The intervention group who interacted with the computer program did achieve a clinically significant average weight loss of 20.3 lb (intervention group B lost 2.3 lb and the control group gained 2 lb). After combining the data for the two intervention groups, significant differences in change in polyunsaturated, monounsaturated and saturated fat intake were observed between the intervention group and the control group (polyunsaturated: intervention group –8.74 g, control group 5.47 g, p = 0.01; monounsaturated: intervention group –13.28 g, control group 7.65 g, p = 0.003; saturated: intervention group –10.90 g, control group 3.51 g, p = 0.027). There were no significant between-group differences for change in total calories, protein, fibre, carbohydrate or sodium.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Ockene et al.198
Method: RCT.
Participants: Out of 440 eligible subjects, 312 (70.9%) agreed to participate in the study (162 intervention group, 150 control group). In total, 72.2% of the intervention group were female and 76.7% of the control group were female. The mean age for both groups was similar (51.4 years in the intervention group, 52.4 years in the control group). In total, 288 (94%) of the participants underwent the 1-year follow-up.
Intervention: This study investigated a community-based, literacy-sensitive and culturally tailored intervention in Lawrence, MA, USA. This lifestyle intervention, called the Lawrence Latino Diabetes Prevention Program (LLDPP), aimed to promote weight loss and diabetes risk reduction in low-income Latinos. Most study activities were held in the Lawrence Senior Centre. This was a collaborative study between the Greater Lawrence Family Health Center, the Lawrence Senior Centre, the Young Women’s Christian Association (YWCA) of Greater Lawrence and investigators from the Worcester and Lowell campuses of the University of Massachusetts. The RCT had one intervention and one control group. The intervention group received three individual and 13 group counselling sessions (between 0.5 and 1.5 hours) over a 12-month period. The intervention was based on principles of social cognitive theory and patient-centred counselling.
Outcomes: The primary outcome measures were weight loss (measured) and glycated haemoglobin (HbA1c). BMI was calculated from weight and height measurements. Physical activity, dietary intake, glucose, insulin and blood pressure were also examined. The results showed that intervention group participants lost significantly more weight than control group participants (intervention effect –2.5 lb; p = 0.04). This was associated with a significant reduction in HbA1c (intervention effect –0.10%; p = 0.09). The intervention also led to a significant decrease in BMI (–0.46 kg/m2; p = 0.04).The intervention group also showed a significantly greater reduction in the percentage of dietary calories from fat (intervention effect –2.02%; p = 0.04) and there was a trend for a greater reduction in the percentage of calories from saturated fat (intervention effect –0.65% vs. –0.43%; p = 0.08). In addition, there was an increase in dietary fibre intake (intervention effect 3.13 g/day vs. 1.98 g/day; p = 0.07). Insulin resistance improved significantly in the intervention group compared with the control group (median homeostasis model assessment – insulin resistance: intervention group –0.36, control group –0.06). There were no statistical changes in physical activity.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Campbell et al.199
Method: RCT.
Participants: The total eligible population was not reported. Nine out of 19 (47%) eligible worksites participated, with a total of 859 participants at baseline. In total, 538 participants (62.6%) completed the baseline, 6-month and 18-month measurements.
Intervention: This study investigated a 5-year workplace health promotion programme called Health Works for Women in North Carolina, USA. The intervention consisted of two strategies: (1) individualised computer-tailored health messages combined with health behaviour change theory, communication theory, social marketing and new technology and (2) a natural helpers (lay health advisors) programme at the workplace designed to affect behavioural and social change through the ‘natural’ social networks of individuals in a given community. In the intervention group 55% were aged 18–39 years, 27% were aged 40–49 years and 17% were aged 50+ years. In the delayed intervention group 50% were aged 18–19 years, 30% were aged 40–49 years and 20% were aged 50+ years. There were two follow-ups at 6 and 18 months following the intervention.
Outcomes: The primary outcome measure was BMI (based on independent measures of height and weight; blinding not reported). Dietary intake and physical activity were also measured (questionnaire data). The results showed that there were no significant changes in BMI in either of the study groups. At 6 months, the intervention group showed a higher level of combined strengthening and flexibility exercise (p < 0.05) than the delayed intervention group. At 18 months, this was still statistically significant (p < 0.01). After 18 months’ follow-up, in the intervention group there was a statistically significant increase in intake of fruit and vegetables (0.7 servings/day, p < 0.05) compared with no change in the delayed intervention group (it was not statistically significant after 6 months; the increase became significant only after 18 months). After 6 months’ follow-up, there was a statistically significant decrease in dietary fat score of approximately 3 g in the intervention group compared with no change in the delayed intervention group (p < 0.05), although this was not statistically significant at 18 months.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Walker et al.168
Method: RCT.
Participants: Out of 172 eligible women, 71 (41.3%) agreed to participate in the study. There were two follow-ups, at 7 and 13 weeks. In total, 50 women (70%) completed the measurements at 13 weeks. The mean (SD) age of participants was 24.6 (4.8) years.
Intervention: This study investigated the promotion of weight loss in low-income, overweight, post partum white/Anglo, African American and Hispanic women in the USA. Intervention groups met weekly for 2 hours over 13 weeks. Meetings took place in either family-based or school-based clinics. Topics covered in the weekly meetings included improved eating patterns, including portion sizes with reference to MyPyramid, choices when eating out, grocery shopping and modifying cooking methods for self and family, increasing fruit and vegetable intake and identifying and managing mindless eating; personal barriers to and benefits of weight loss; and strategies to increase the intensity and duration of daily physical activity. A registered dietitian gave women personalised written guidelines that recommended a low-calorie diet (1500–1600 kcal for non-breastfeeding women or 2200–2400 kcal for breastfeeding women). Culturally relevant materials for ethnic-specific adaptations were provided. Women were also given pedometers to encourage physical activity.
Outcomes: The outcome measures were weight (independently measured; blinding not reported), physical activity and dietary intake (both measured using the Self-Care Inventory). The results showed that there was no statistically significant weight loss in any of the ethnic groups (white/Anglo: intervention group –5.7 ± 13.7 lb, control group –2.6 ± 4.0 lb, p = 0.553; African-American: intervention group 3.3 ± 6.3 lb, control group –0.2 ± 6.2 lb, p = 0.224; Hispanic: intervention group –2.2 ± 4.1 lb, control group –0.2 ± 4.8 lb, p = 0.448).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Kisioglu et al.197
Method: RCT.
Participants: Out of 1017 eligible women aged 20–50 years in the Yenice region of Turkey, 430 were randomised into either the intervention group (n = 214) or the control group (n = 216). The authors aimed for a recruitment rate of 20% (because of a 20% prevalence of hypertension in Turkey), which they obtained for each group. However, 30 women dropped out before baseline measurements were taken for the following reasons: moved away, did not attend the centre or aged > 50 years. Therefore, 400 women out of the 1017 who were eligible (40.3%) were included at baseline. There was no attrition; 100% (400 women) completed the study up to 6 months’ follow-up.
Intervention: This study investigated a health training course that was developed to better control high blood pressure in middle-aged (20–50 years) women in Turkey. The intervention aimed to prevent hypertension and obesity. The intervention included health education in group settings and information leaflets that explained the unhealthy impacts of addictive behaviours (alcohol, smoking, etc.) and poor nutrition (consumption of fatty and oily foodstuffs, etc.).
Outcomes: The outcome measures were BMI, nutrition, physical activity and blood pressure. The results showed that this public health intervention programme for hypertension control and prevention caused significant changes in the lifestyles of participating women (BMI, nutrition and exercise). A significant difference in BMI distribution was found between the intervention group and the control group after the intervention (p = 0.014). Similarly, the number of women with a normal BMI in the intervention group was significantly higher than the number of women with a normal BMI in the control group (86 vs. 60 respectively) after the intervention (p = 0.009). Additionally, the number of women with a normal BMI increased significantly after the intervention (p = 0.001). The women in the intervention group reduced the use of salt, oils and fats in their cooking, especially margarine and butter. Also, after the intervention most women from the intervention group preferred boiling and baking to frying, with a 31.9% decrease in frying and a 15.74% increase in boiling; the difference was significant compared with the control group. The level of exercise also increased significantly in the intervention group compared with the control group (p = 0.001). The reduction in blood pressure after the intervention was insignificant (p = 0.310).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Strong |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Strong |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Strong |
Kain et al.65
Method: Non-randomised controlled pilot study.
Participants: It is unclear how many eligible teachers there were in the schools that could have participated in this study and the baseline number of participants is not reported. There was a 5-month follow-up with a final sample size of 57 teachers. The mean age/sex of the teachers were not reported.
Intervention: This study was a pilot study of an obesity prevention intervention in schools in the Santiago district of Chile. The teacher intervention included three 15-minute counselling sessions on healthy eating and physical activity plus goal-setting with a nutritionist.
Outcomes: The outcome measures were weight, BMI and waist circumference (all independently measured by the nutritionist; blinding not reported). In addition, total and HDL cholesterol and triglycerides were measured. The results show that there were decreases in weight (–1.5 kg), BMI (–0.4 kg/m2) and waist circumference (–2 cm) in the intervention group and increases in these outcome measures in the control group (weight +1.9 kg, BMI +1 kg/m2, waist circumference +2.2 cm). However, only the increases in the control group were statistically significant. There were no significant differences in the biochemical measures (cholesterol or triglycerides).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Kain et al.66
Method: Non-RCT.
Participants: The total number of eligible teachers who could participate in this full study was not reported. At baseline, 47 teachers (28 in the intervention group and 19 in the control group) were included but it was not reported how many of the teachers completed the 2-year follow-up. Sex and age were not reported for the teachers in the study.
Intervention: This study investigated an obesity prevention intervention (as described in Kain et al. 65) with a 2-year follow-up in schools in the Santiago district of Chile.
Outcomes: The outcome measures were the same as in Kain et al. 65 as well as physical activity and dietary intake. There were no differences between groups or over time for BMI or waist circumference. In total, 67% of the teachers increased their levels of physical activity, 61% increased fruit intake, 68% increased vegetable intake and 85% decreased bread intake (significant decrease). Two biochemical measures changed significantly: HDL cholesterol increased and glucose decreased.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Olvera et al.167
Method: RCT.
Participants: In total, 46 daughter–mother dyads were recruited (n = 92) from two elementary schools, grades 3–6. Recruitment was conducted primarily through flyers mailed to Latino family homes.
Intervention: This study investigated a healthy lifestyle programme, BOUNCE (Behavior Opportunities Uniting Nutrition, Counseling, and Exercise), that sought to promote physical activity in daughters. The 12-week intervention consisted of three 45-minute structured group aerobic or sports sessions or free-play recreational activities per week; two 45-minute nutrition sessions per week and one 45-minute behavioural counselling session per week. The control group received one 45-minute session per week, which included written educational materials (covering various nutritional and counselling topics) and light-intensity aerobics or sports.
Outcomes: The primary outcome measure was physical activity. Secondary outcomes were dietary intake and BMI. There were no significant differences in physical activity levels of mothers between the intervention group and the control group (p = 0.40). Dietary intake results were reported only for daughters. In terms of BMI, there was no significant difference between the intervention group and the control group mothers at the end of the 12-week intervention.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Chang et al.169
Method: RCT.
Participants: The baseline sample size was 129. There were two follow-ups at 2 and 8 months. At 8 months’ follow-up, 38 participants (29.5%) completed the study. The mean age of the intervention group was 25.53 years and the mean age of the control group was 25.12 years.
Intervention: This study investigated a culturally sensitive intervention in Special Supplemental Nutrition Program for Women, Infants, and Children sites in southern Michigan, USA. The intervention was aimed at 18- to 34-year-old overweight and obese women. It comprised theory-based, culturally sensitive intervention messages delivered using a series of five chapters on a DVD over 10 weeks, complemented by five peer support group teleconferences. Intervention participants viewed the DVD, which featured peers from the target audience, at home and participated in peer support group teleconferences at convenient locations led by Women, Infants, and Children educators.
Outcomes: The outcome measures were body weight (independently measured; staff were blinded – single blinded, no mention of participant blinding), self-reported physical activity and dietary intake, and glucose levels. After 8 months the adjusted analysis showed an intervention effect size of –0.03 kg (95% CI –0.73 kg to 0.67 kg) and –0.28 mg/dl (95% CI –0.98 mg/dl to –0.42 mg/dl) for body weight and blood glucose respectively. However, these were not statistically significant although changes in body weight and blood glucose showed apparent trends consistent with the study’s hypotheses. There were also no significant intervention effects for the secondary outcomes (physical activity or dietary intake).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Cullen et al.209
Method: Cluster RCT.
Participants: A total of 100 existing Texas Expanded Food and Nutrition Education Program (EFNEP) classes were randomised, by city, to either the new intervention or the standard active control condition. Clients from each of these classes were then invited to participate in the study and provide written consent. Of the 100 classes, 54 were assigned to the new intervention condition and 46 to the control condition. Of the total 1252 clients, 1006 were recruited to the study (80% baseline recruitment rate; 97% female, mean age 35 years). After 4 months’ follow-up the final sample size was 558 clients (318 in the intervention group; 56% follow-up response rate).
Intervention: This study investigated a modified version of the Texas EFNEP compared with the standard Texas EFNEP. The EFNEP has been providing food and nutrition education to low-income families since 1968 throughout 50 states and six territories in the USA. The standard Texas EFNEP class comprises six sessions covering the following topics: (1) nutrition basics and portion size, (2) breakfast and snacks, (3) fruits and vegetables, (4) dairy and meat, (5) breads and grains and (6) smart shopping. The sessions also include discussion and food preparation. The new intervention (named Building Healthy Families: Step by Step) included the following additional components: six 5-minute videos dealing with home food and eating issues to promote guided discussion and problem-solving; weekly goal-setting and goal review; and new handouts that supported class session materials.
Outcomes: At baseline and follow-up height and weight were measured by trained staff members; however, it was impossible to blind them to the intervention condition. Dietary intake data were collected using 24-hour dietary food records completed by the client at the data collection sessions. After 4 months’ follow-up there were no changes in BMI from baseline in either group and no significant between-group differences. With regard to dietary intake, there were significant desirable changes at follow-up for total energy intake and consumption of regular vegetables, 2% milk, whole milk, fibre and sweetened beverages for both groups. However, there were no significant between-group differences in changes in dietary intakes.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Moderate |
Auslander et al.176
Method: RCT.
Participants: A total of 301 women were recruited to the study and there was a 79% follow-up response rate, resulting in a final sample of 239 women after 3 months.
Intervention: This study investigated a 3-month health promotion intervention that focused on dietary skills for obese low-income African American women. African American women aged 25–55 years and with a > 20% ideal body weight were recruited to the study through a social service agency that served as the programme’s sponsor and through advertisements in neighbourhood newspapers that are targeted to African American audiences and were randomised to either the intervention or the control condition. The intervention was founded on stages of change theory and community organisation theory and consisted of six group sessions and six individual sessions with a peer educator who had no previous background in nutrition or education but who had been trained by a team of dietitians, social workers and health educators. The group sessions focused on nutrition skills and aimed to foster social support among the participants, and the individual sessions encouraged participants to apply skills learnt in the group sessions and were tailored to the participants’ stage of change. The control group received a self-help workbook that reflected the content of the group sessions and were offered a half-day workshop on healthy, low-fat eating.
Outcomes: Height and weight were measured at baseline and post intervention (blinding status of assessor not reported) and dietary fat intake was assessed using a validated food frequency questionnaire. Results of the analysis of covariance revealed no significant differences between the intervention group and the control group for post-test means (adjusted for pre-test means) of BMI or weight. However, there was a significant between-group difference for fat intake (% energy from fat: intervention group 33.3%, control group 36.2%; p = 0.03).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Weak |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Reid et al.211
Method: Randomised parallel-group trial.
Participants: Out of 225 eligible subjects, 164 (72.9%) agreed to participate in the study and were randomised into one of two groups: counselling (n = 85) or pamphlet (n = 79). On average, 62% of the participants were men and the mean age was 40.8 years. There were two follow-ups at 3 and 6 months. There was a 91% follow-up response rate with 149 participants completing the 6-month follow-up.
Intervention: This study investigated a single-group counselling session (lasting 1.5–2 hours) on the reduction of cardiovascular disease risk factors in adults aged 18–65 years with a moderate to high risk score (> 65) in the northern suburbs of Melbourne, Australia. The trial was based in community health centres or worksites and was led by a community health nurse. The content of the session was directed towards three major risk factors, covering smoking cessation, dietary modification and non-pharmacological lowering of blood pressure. The major emphasis of the sessions was on a reduction in saturated fat intake. Low-fat cooking information and information on the identification of low-fat foods in supermarkets was provided. Participants were encouraged to attend the session with their partners. The parallel group (control) received a specifically designed pamphlet containing information about reducing the impact of cardiovascular disease risk factors. The pamphlet was written in a simple way with cartoons.
Outcomes: The outcome measures were body weight, physical activity levels, dietary intake, blood pressure and cholesterol levels. Body weight was measured independently. The results show that there were no statistically significant body weight changes either between or within groups. After 6 months’ follow-up, the increase in regular physical activity from baseline was 50% for the counselling group and 16% for the pamphlet-only group. After 6 months’ follow-up, 33% of the participants in the counselling group indicated that they had modified their diet and had a lower fat intake compared with 19.2% in the pamphlet-only group. The proportion of participants in the counselling group who indicated that they added salt to food fell from 22% at baseline to 7% after 3 and 6 months (p < 0.05). In the pamphlet-only group there were no statistically significant reductions in salt intake. The counselling group showed a reduced fat intake, which explained 7% of the variance in cholesterol level (p = 0.0016). Systolic blood pressure fell by 4.8 mmHg in the counselling group and 4.4 mmHg in the pamphlet-only group at 3 months’ follow-up and by 5.5 mmHg and 5.3 mmHg, respectively, at 6 months’ follow-up. These differences were not statistically significant between groups; however, within the pamphlet group the difference was statistically significant (p = 0.013). Diastolic blood pressure fell by 3.9 mmHg in the counselling group and 3.1 mmHg in the pamphlet-only group at 3 months’ follow-up and by 4.2 mmHg and 3.8 mmHg, respectively, at 6 months’ follow-up. Again, these differences were not statistically significant between groups but were statistically significant within groups (p = 0.046 counselling group, p = 0.022 pamphlet-only group). In both groups, a 5% reduction in total plasma cholesterol level was seen after 3 months, with no further reduction after 6 months. The difference between groups was not statistically significant but within the pamphlet-only group the difference was statistically significant (p = 0.02).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Weak |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Howard-Pitney et al.210
Method: RCT.
Participants: In total, 351 participants took part in the study, of whom 69% completed all three data collections at baseline, 7 weeks (1 week after the 6-week intervention) and 19 weeks (1 week after the subsequent 12-week intervention). In total, 85% of the participants were women and the mean age was 31 years. Classes were the unit of allocation and analysis.
Intervention: This study investigated SNAP in San Jose, CA, USA. SNAP was developed to prevent heart disease in adults on a low income and with low literacy levels. SNAP is a classroom-based intervention that lasted 20 months (1993–4). It was composed of two parts: a 6-week, classroom-based intervention followed by a 12-week maintenance intervention. The curriculum was developed to match the structure of the general nutrition classes (control), which typically included six 90-minute sessions. The curriculum was taught by one of two professional nutrition health educators. The total eligible population is not reported.
Outcomes: The outcome measures were BMI, nutritional knowledge and dietary intake. There were no statistically significant changes in BMI but the SNAP classes led to significantly greater improvements than general nutrition classes in nutrition knowledge [t(II) = 4.93, p < 0.0004], nutrition attitudes towards eating a low-fat diet [t(II) = 2.87, p < 0.02] and self-efficacy for achieving a low-fat diet [t(II) = 2.28, p < 0.04]. Food Frequency Questionnaire data showed significant changes in the percentage of calories from total fat [t(II) = –3.04, p < 0.01] and saturated fat [t(II) = –2.76, p < 0.01]. Participants in both the SNAP and the general nutrition classes consumed fewer total and saturated fat calories at the first follow-up than at baseline; however, those in the SNAP classes did not reduce their consumption significantly more than those in the general nutrition classes.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Faucher and Mobley183
Method: Small RCT pilot study.
Participants: The total eligible population was not reported. In total, 24 low-income Mexican American women were recruited. At 5 months’ follow-up, 19 women completed the study (11 intervention and 8 control women; 79.2%). The mean age of participants was 34.9 years.
Intervention: This study investigated a community-based weight loss intervention in low-income Mexican American women in the USA. As part of the intervention, nutritional education aimed at portion control was compared with standard care counselling on weight loss. The intervention consisted of four 2-hour classes. The curriculum included meal sampling, recipe sharing and use of portion control aids such as tennis balls, a deck of cards, the palm of the hand, the thumb tip, a super-sized poster, measuring aids and portion control plates. All classes were culturally sensitive and foods prepared were culturally/economically specific to low-income Mexican American families.
Outcomes: The outcome measure was weight loss (independently measured but does not state who took the measurements). The results showed that women in the intervention group lost more weight than women in the standard care group, although this difference was not statistically significant. Mean (SD) weight loss in the intervention group was 6.57 (7.5) lb (2.9 kg) whereas mean weight loss in the standard care group was 2.8 (10.3) lb (1.3 kg) (p = 0.47). Although this weight loss was not statistically significant, it is potentially clinically significant.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Strong |
Alves et al.212
Method: RCT.
Participants: A total of 156 women were recruited at baseline (mean age approximately 38 years). Only 10 participants dropped out of the study (94% follow-up response rate) resulting in a final sample of 146 women.
Intervention: This study investigated a group-based exercise intervention targeting overweight women living in a Brazilian slum. The intervention lasted for 6 months and consisted of three 50-minute exercise sessions each week supervised by a trained physical education instructor. Each exercise session was aerobic in nature, consisting of a 5-minute warm-up followed by 40 minutes of moderate-intensity exercise (such as walking and rhythmical continuous movements in time to fast-tempo music) and a 5-minute cool down. Participants were recruited from Caranguejo, a favela (slum) in the north-eastern city of Recife and were randomised either to the intervention condition or to the no-intervention control condition.
Outcomes: Height and weight measurements were taken in both groups at baseline and after 6 months (blinding status of assessor not reported). Case-by-case analyses were conducted and, as weight and height differences between the groups at baseline were present, adjusted analyses were also conducted. The mean difference in weight and BMI between the intervention group and the control group was –1.69 kg (95% CI –2.36 kg to –1.03 kg) and –0.63 kg/m2 (95% CI –0.97 kg/m2 to –0.30 kg/m2) respectively (p < 0.001 for both weight and BMI). After adjustment for baseline differences in height and weight, these results changed little: mean difference in weight and BMI between the treatment group and the control group was –1.66 kg (95% CI –2.34 kg to –0.98 kg) and –0.62 kg/m2 (95% CI –0.9 kg/m2 to –0.28 kg/m2) respectively (p < 0.001 for both weight and BMI). Using case-by-case analysis and after adjustment for baseline differences in height and weight, women in the treatment group showed a significant decrease in both body weight (mean difference –1.81 kg, 95% CI –2.54 kg to –1.08 kg) and BMI (mean difference –0.68 kg/m2, 95% CI –1.04 kg/m2 to –0.31 kg/m2) at the 6-month follow-up (p < 0.001 for both weight and BMI).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Wilbur et al.180
Method: Cluster RCT.
Participants: Two communities, each served by a community health centre, were randomly assigned to either the intervention condition or the control (minimal intervention) condition and women were recruited from each community via print materials distributed throughout the communities, publicity at health fairs and community gatherings, and social networking by study participants. Therefore, participants were allocated to either the intervention condition or the control condition depending on the community in which they lived. There was a recruitment rate of 55% resulting in a baseline sample of 281 (156 intervention group; mean age 49 years). After 48 weeks the final sample size was 143 (84 intervention group; 51% follow-up response rate).
Intervention: This study investigated an enhanced-treatment walking programme for sedentary moderate- to low-SES African American women aged 40–65 years, compared with a minimal-treatment walking programme. Both programmes included an orientation session at which participants received a tailored walking prescription and health information and were taught about problem-solving and goal-setting. Each participant’s target was to walk three times per week within the target heart rate for 20–30 minutes. All participants received heart monitors, walking logbooks, waist packs, magnets and discount coupons to buy walking shoes. In addition to this, the intensive treatment group attended four weekly workshops/group sessions run by a peer group facilitator (same ethnicity and with ties to the community). These sessions covered topics such as the benefits of walking, overcoming personal and environmental barriers to walking and anticipating and handling relapses. Each session also included a 10-minute video featuring six African American role models discussing the workshop topic. The workshops were followed by tailored staff telephone calls weekly for 3 weeks, biweekly for 14 weeks and monthly during a 24-week maintenance phase.
Outcomes: Although weight loss was not a focus of the intervention, height, weight and waist circumference measurements were taken by staff who were not part of the intervention team (although it was not reported if they were blinded to the participants’ experimental condition). Physical activity levels were self-reported using the Centers for Disease Control Behavioural Risk Factor Surveillance System survey and aerobic fitness was assessed using an incremental treadmill exercise test. Using data from completers only, there were no significant changes in BMI from baseline to 24 weeks and 48 weeks in either group. There was no significant change in waist circumference in the control group, but there was a significant reduction in the intervention group between baseline and 24 and 48 weeks [baseline: 37.9 inches, 24 weeks: 37.5 inches (p = 0.044), 48 weeks: 37.3 (p = 0.001)]. There were increases in the number of participants meeting physical activity recommendations in both groups from baseline to 24 weeks and 48 weeks. There was a significant increase in aerobic fitness (time spent on treadmill) from baseline to 24 and 48 weeks in the intervention group [baseline: 11.5 minutes, 24 weeks: 11.9 minutes (p = 0.011), 48 weeks: 11.9 (p = 0.024)] but not in the control group. There was no significant group × time interaction for any of the outcomes.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Grandjean et al.174
Method: Small RCT.
Participants: In total, 37 women volunteered to participate in the study and were randomised to either the exercise programme or a no-intervention control condition.
Intervention: This study investigated a 24-week workplace exercise programme in female blue-collar employees. Participants of the exercise programme received an individualised exercise prescription that involved walking, jogging, cycling or a combination of any of these on at least 3 days per week for 24 weeks. Exercise was carried out at a workplace fitness facility (encouraged) but could also be carried out outside if it was more convenient.
Outcomes: Before and after the intervention period, height, weight and body fat (seven skinfold sites) measurements were taken (blinding status of assessor not reported), along with blood samples to determine cholesterol (total, HDL cholesterol, very LDL cholesterol and LDL cholesterol) and triglyceride levels. A treadmill test was used to determine VO2max. as a measure of aerobic fitness. After 24 weeks, the intervention group lost an average of 2 kg whereas the control group maintained body weight (between-group difference p < 0.025). Both groups significantly reduced their percentage body fat (change: intervention group 27.6 ± 6.5 to 23.5 ± 5.4, p < 0.05; control group 28.7 ± 7.5 to 26.6 ± 5.8, p < 0.05). The difference in change in percentage body fat between the groups approached but did not reach significance (p < 0.056). The intervention group also increased VO2max. (change: 1.88 ± 0.39 l/minute to 2.16 ± 0.33 l/minute, p < 0.05) whereas there was no change in the control group (between-group difference p < 0.0006). There were no between-group differences in changes in cholesterol or triglyceride levels from baseline to post intervention.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Moderate |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Moderate |
Targeted approach: observational studies (n = 20)
Carlin214
Method: Uncontrolled prospective cohort study.
Participants: This study included data from 66 African American women aged at least 40 years (mean age 60.5 years) who had used a community fitness centre for 6 months. Although weight was not used as an inclusion criterion, the sample was on average obese, with a mean BMI of 33.6 kg/m2 at baseline. The number of eligible women who had signed up to the centre initially was not reported; however, the average attrition rate for all members was 49.7%, defined as those who drop out of the exercise programme within the first 2 months of membership.
Intervention: This study investigated weight changes in African American women from low-SES communities who had attended a community fitness centre for 6 months. Users of the fitness centre were recruited through local advertising, community awareness efforts and word of mouth and through the local hospital’s rehabilitation clinic (where continued exercise after physical therapy was encouraged). Attendance, and frequency, were entirely voluntary and exercise was self-directed and self-paced. However, those who did attend had access to a convenient, safe and pleasant community fitness centre with a fully-equipped gym and personal trainer; an individual fitness assessment followed by creation of a personalised exercise plan including aerobic and strength training, based on a participant’s personal goals and fitness level; and reassessments every 3 months. There was a $20 per member per month participation fee although no contract was required.
Outcomes: Weight was measured at each assessment session by health centre staff, who were therefore not blinded to the study condition. After 6 months the median per cent weight loss was 1% (1 lb weight loss) and 7% of participants (n = 5) achieved a medically significant weight loss of at 5% of their initial body weight. Attendance rate data were also collected and, although participants did not meet the recommended levels of five exercise sessions per week, they did achieve a moderate level of exercise frequency (8–12 exercise visits per month).
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Goldfinger et al.207
Method: Uncontrolled before-and-after pilot study.
Participants: Participants were recruited through flyers circulated at a local black church. In total, 31 participants signed up to the study at baseline and 21 provided data at the 1-year follow-up (68% follow-up response rate).
Intervention: This study investigated a peer-led weight-management programme in a sample of low-income African Americans (mean age 68 years, 81% female). The intervention consisted of eight sessions delivered over 10 weeks by a trained peer leader. During the sessions weekly action plans were developed and group feedback and support were given. The intervention concentrated on the following key messages: (1) portion control; (2) filling half the plate with fruit and vegetables of multiple colours at each meal; (3) drinking calorie-free beverages; (4) cutting fat; (5) making daily life more active; and (6) eating healthy food on a budget and at fast-food venues.
Outcomes: Body weight was measured by trained research assistants (blinded to baseline weight) and diet and physical activity data were collected using self-report tools at baseline, 10, 22 and 33 weeks and 1 year. Initially, post intervention at 10 weeks, participants had lost a mean of 4.4 lb or 2.2% of their baseline body weight (p < 0.001). Additional follow-up data at 22 weeks, 32 weeks and 1 year showed continued weight loss. At 1 year, participants had lost a mean of nearly 10 lb or 5% of their initial body weight (range +1.5% to −17.7%; p = 0.001). At 10 weeks, participants had significantly decreased their daily total fat intake from 87.7 g to 80.1 g (p = 0.046), their daily saturated fat intake from 23.4 g to 20.6 g (p = 0.046) and their daily cholesterol intake from 261.9 mg to 237.0 mg (p = 0.046). These changes were maintained at 22 weeks but not at 1 year. Although daily servings of fruit and vegetables did not increase significantly initially post intervention, significant increases were observed at 22 weeks and 1 year (from 3.7 to 4.4 servings per day from baseline to 1 year; p = 0.039). There were no changes in fast-food intake at any of the time points. The number of days per week that participants engaged in > 30 minutes of moderate exercise did not increase significantly at any of the follow-up time points. However, the amount of sedentary time, defined as hours per day that participants spent watching television, videos or DVDs, decreased by > 1 hour per day at 10 weeks (p = 0.034) and by nearly 3 hours at 1 year (p < 0.001).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Clarke et al.164
Method: Uncontrolled before-and-after study.
Participants: Participants were recruited via fliers posted at Special Supplemental Nutrition Program for Women, Infants, and Children clinics, public health clinics and community centres. At baseline, 93 mothers were recruited for the intervention (53% aged between 26 and 39 years) although it is unclear how many completed data collection at 24 weeks.
Intervention: This study investigated an 8-week group-based weight loss programme for overweight and obese low-income mothers, with follow-up at 24 weeks. The intervention consisted of eight weekly lessons that included class discussions and 30 minutes of exercise. The participants shared ideas for establishing exercise goals, reducing barriers and identifying sources of social support. The instructor led physical activities that mothers could continue on a daily basis, such as walking, resistance training and video exercise tapes. Mothers were instructed to exercise at least 5 days a week for 45 minutes per session at a moderate intensity, equivalent to a brisk walk. Pedometers were provided for the monitoring of physical activity. The diet component of the programme consisted of menu planning with ethnic foods, cooking demonstrations and information on recipe modifications, portion control, food budgeting and the energy content of fast foods. Behaviour topics that were presented included social support, self-monitoring, role modelling by successful dieters and stress management.
Outcomes: Self-reported height and weight were confirmed by direct measurements but the blinding status of the assessors was not reported. After 24 weeks, the total weight loss from baseline was –6.9 lb (range –41 lb to 10.2 lb; p < 0.05).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Gill203
Method: Uncontrolled before-and-after study with a controlled component.
Participants: At baseline, 268 women (134 intervention group, 134 wait-list control group; mean age 41 years) were recruited to the study. After the treatment phase, 232 participants completed data collection (116 in each group; follow-up response rate of 87%). Of the 134 intervention participants entering the study, 105 remained after completion of the maintenance phase (follow-up response rate of 78%).
Intervention: This study investigated a weight loss programme, Unidos En Salud, aimed at overweight and obese Mexican American women from a low-income town in Texas, USA. The programme consisted of two phases: a 6-month treatment phase followed by a 6-month maintenance phase. A wait-list control group, recruited at the same time as the intervention group but who waited 6 months before entering the treatment phase, was used as a comparison group to the intervention group after the treatment phase. During the treatment phase, weekly 90-minute classes were co-delivered by a bilingual registered dietitian and a master’s-level behavioural specialist (both members of the participants’ community) and included nutrition education, behaviour modification, physical activity and fostering of social support. During the maintenance phase, weekly support groups were run by peer leaders (who had been selected from among the participants and who received 4 hours’ training), with one class per month led by the professionals. The intervention was based on the Cuidando El Corazon programme, which is also included in this review;182,184 however, this modified programme used more experimental learning techniques and less written materials and education components.
Outcomes: All data collection measurements were taken by trained staff members familiar to the participants (therefore it was assumed that they were not blinded to the experimental condition). Weight was measured using standard techniques; physical activity data were collected using the 7-day Physical Activity Recall (PAR) questionnaire; and dietary fat avoidance was measured using a 0- to 7-point scale based on the Saturated Fat/Cholesterol Avoidance Scale. Both self-reported methods had been evaluated in populations that were comparable to the study participants. After the first 6 months (treatment phase), no significant changes in weight were observed in either the intervention group or the control group (intervention group –1.8 (SD 7.3) lb, p = not significant; control group –1.0 (SD 8.08) lb, p = not significant) (between-group differences not reported). However, significant increases in physical activity and fat avoidance were observed in the intervention group but not in the control group [change in physical activity (hours/day): intervention group 0.28 (SD 0.75), p < 0.005; control group –0.21 (SD –0.80), p = not significant; change in fat avoidance: intervention group 0.38 (SD 0.44), p < 0.005; control group 0.14 (SD 0.40), p = not significant]. Using data from the intervention group only, there were no changes in any of the outcomes during the second 6 months (maintenance phase). Overall, from baseline to post maintenance, there were no significant changes in weight or physical activity (increases in physical activity during the treatment phase were not maintained) but there was a significant increase in fat avoidance [change 0.34 (SD 0.41), p < 0.005]. Therefore, although fat avoidance did not increase further over the maintenance phase, the improvements made during treatment were maintained after 6 months.
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Rickel200
Method: Uncontrolled before-and-after study.
Participants: Obese women aged 50–75 years were recruited through culturally sensitive direct mailings, media articles, radio announcements and community presentations. A total of 286 African American and Caucasian women were recruited at baseline (approximately 90% recruitment rate) and a final sample size of 224 women completed the intervention (78% follow-up response rate).
Intervention: This study investigated a culturally tailored weight loss programme for obese low-SES African American or Caucasian women. The 6-month intervention consisted of 24 weekly 90-minute group sessions led by an interventionist (bachelor’s and/or master’s level). During sessions, participants (1) reported on, and received feedback about, their previous week’s progress in reaching eating and physical activity goals; (2) learned skills related to cognitive–behavioural self-management, healthful eating behaviours and physical activity practice; and (3) identified specific behavioural goals for the coming week, receiving encouragement from fellow group participants. Certain procedures of this initial lifestyle treatment were culturally tailored to suit the special needs and issues of rural women, for example the provision of a recipe booklet providing recipes and cooking tips for preparing traditional African American and Southern dishes with lower-fat, lower-calorie, and lower-sodium ingredients. Some of the sessions included cooking demonstrations and food tastings.
Outcomes: Weight and blood pressure were measured and blood samples were taken to determine LDL cholesterol, triglyceride, C-reactive protein and HbA1c levels at baseline and post intervention by a mobile clinical assessment team led by a licensed registered nurse (blinding status not reported). Fitness levels were determined using a 6-minute walk test and data on physical activity were collected using the CHAMPS Physical Activity Questionnaire. 246 Energy and saturated fat intakes were determined from data collected using the Block 95 Food Questionnaire. 247 Weight was significantly reduced in both ethnicity groups from baseline to post intervention [mean (SE) change in weight: African American –6.83 (0.76) kg, p < 0.05; Caucasian –10.10 (0.37) kg, p < 0.05]. Reductions were also observed in systolic blood pressure, diastolic blood pressure, LDL cholesterol, HbA1c and C-reactive protein in both African American and Caucasian women; however, a reduction in triglycerides was observed only in Caucasian women. Fitness and physical activity levels were improved in all participants, and all participants decreased energy and fat intakes.
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Hugk and Winkelvoss159
Method: Prospective cohort study.
Participants: The final sample size included 50 workers who were overweight at baseline (approximately 5% female, age 22–67 years; recruitment and follow-up response rates not reported) and who had the job roles of smelter, moulder and fettler.
Intervention: This study investigated a workplace weight reduction programme conducted in an industrial manufacturing company in Germany. Although a comparison group was included in the study, follow-up data for this group were not reported and therefore we will treat this study as an uncontrolled before-and-after study. The programme consisted of an individual doctor interview conducted in the workplace health centre. During the interview current lifestyle and diet behaviours of participants were discussed and appropriate diet and physical activity advice and education was provided. A reduced-calorie diet was also recommended. The aim of the study was for participants to lose 5 kg on average after 1 year.
Outcomes: Baseline and 1-year data included weight and total cholesterol and triglyceride levels. After 1 year the participants did not lose any weight on average and therefore the programme aim was not met. There were no significant changes in total cholesterol or triglyceride levels, except for an increase in triglycerides in those who were moulders.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Fernandes et al.185
Method: Prospective cohort (one-group pre/post) study.
Participants: The intervention was delivered to 99 participants (mean age 68.5 years, 83.8% females) at Kokua Kalihi Valley (a federally qualified health centre in Hawaii). There was a low attrition rate, with 92 out of 99 participants completing the intervention at 12 months’ follow-up.
Intervention: This study investigated a community health worker-delivered curriculum intervention designed to prevent cardiovascular disease in low-income Filipino Americans. The curriculum consisted of 11 weekly group sessions on a healthy heart and healthy family educational topics. The intervention was culturally and linguistically tailored.
Outcomes: The primary outcomes were BMI, waist circumference, biochemical outcomes (including blood pressure, fasting blood glucose, fasting lipid profile and glycosylated haemoglobin), food consumption and physical activity. At 12 months’ follow-up there were no statistically significant changes in BMI and waist circumference. Mean total cholesterol decreased from 186.25 mg/dl at baseline to 170.88 mg/dl at 12 months (p = 0.001); mean LDL cholesterol decreased from 114.43 mg/dl to 103.40 mg/dl (p = 0.013); and mean fasting blood glucose decreased from 117.95 mg/dl to 109.07 mg/dl (p = 0.003). However, HDL cholesterol was 3.3 mg/dl lower (worse) at 12 months (p = 0.003). Blood pressure reductions were seen at 6 months [systolic blood pressure decreased from 122.60 mmHg to 116.61 mmHg at 6 months (p = 0.001); diastolic blood pressure decreased from 74.24 mmHg to 71.35 mmHg at 6 months (p = 0.03)] but were not sustained at 12 months.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Perez-Lizaur et al.204
Method: Pre- and post-test cohort study.
Participants: Out of approximately 700 eligible people, 452 (68%) plus 22 health promoters (promotores) agreed to participate in the study. In total, 43.7–56.3% of the participants were women, with 86.9% of the promotores also women. The mean age of the promotores was 46.13 ± 13.5 years, the mean age of adults ≤ 60 years was 44.6 ± 11.7 years and the mean age of adults > 60 years was 70.4 ± 7.8 years. There was a 3-month follow-up with no attrition reported.
Intervention: This was a pilot feasibility study that examined a curriculum-based cardiovascular health promotion programme. Promotores delivered the 12-week intervention (2-hourly sessions per week with a total of nine lessons) in the Alvaro Obregon district of Mexico city.
Outcomes: The outcome measures were prevalence of obesity, BMI (independently measured by personnel from the Nutrition Clinic of the Universidad Iberoamericana Department of Health), blood pressure, fasting glucose and self-reported physical activity and dietary intake. The results show that the prevalence of obesity decreased from 48.9% to 43.4% but there were no significant changes in BMI for any participants or in biochemical measures (blood pressure and glucose) for adults aged ≤ 60 years. Adults aged > 60 years had significantly higher (p < 0.05) mean (SD) glycaemia values during pre measures than adults aged ≤ 60 years [129.91 (73.91) vs. 104.87 (37.40) respectively], and compared with post measures within the same age group [129.91 (73.91) vs. 116.66 (52.14) respectively]. Mean (SD) systolic blood pressure during post measures among adults aged > 60 years was significantly higher (p < 0.05) than among adults aged ≤ 60 years [140.99 (21.05) vs. 120.24 (17.03) respectively], and compared with pre measures within the same age group [140.99 (21.05) vs. 125.98 (23.19) respectively]. There were significant changes in the percentage of positive responses about exercising for 10 minutes three times per week (significantly higher, p < 0.05) during post test compared with pre test among adults in this age group (19.8% vs. 52.5% and 30.6% vs. 65.0%) for adults ≤ 60 years. For adults aged > 60 years there were also significant changes in the percentage of positive responses about exercising for 10 minutes three times per week, getting off the bus and walking, walking more and exercising for three times per week (significantly higher, p < 0.05) during post test compared with pre test (31.9% vs. 56.0%; 38.2% vs. 59.8%; 56.9% vs. 82.5%; and 39.8% vs. 76.1%, p < 0.001, respectively). Lastly, ‘taking action’ to modify lifestyle behaviours significantly increased, from 31.5% to 63%. Promotores showed significant improvements in all areas of the heart-healthy habits. Adults aged ≤ 60 years had statistically significant changes in four out of five dietary categories (salt and sodium intake, reduced cholesterol and fat intake, maintained or reduced healthy weight and increased physical activity). Adults aged > 60 years had a statistically significant change only in salt and sodium intake (p < 0.001).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Balcazar et al.202
Method: Pre- and post-test cohort study.
Participants: The total eligible population who could have participated in the study is not reported. At baseline there were 256 participants. There were three follow-ups at 3, 6 and 12 months and the final sample size at 12 months was 85 (33% follow-up response rate). The sex and age of participants were not reported.
Intervention: This study investigated a cardiovascular health promotion programme called Salud para su Corazón conducted in four health-care settings in high-risk low-income Hispanic communities in the US–Mexico border region. The intervention consisted of an educational programme comprising eight lessons (group delivery). Educational sessions were delivered several times per week, once per week or every other week for a total intervention period of 2–3 months.
Outcomes: The outcome measures were weight, waist circumference, BMI, physical activity, self-reported dietary intake, cholesterol, triglycerides, HbA1c and systolic and diastolic blood pressure. Mean BMI did not statistically significantly change after 6 or 12 months. There were significant changes in waist circumference after 6 months: waist size decreased from 37.4 inches at baseline to 36.1 inches at 6 months after the intervention. Weight decreased but the decrease was not statistically significant. Physical activity results were reported only for 3 and 6 months. The proportion of participants who reported engaging in physical activity after 3 months of follow-up showed a significant increase from baseline and this change was maintained after 6 months of follow-up (data not shown). The authors also report that significant improvements in heart-healthy behaviours were observed (data not shown). Participants increased the frequency of reporting their consumption of healthy amounts of salt and sodium, cholesterol and fat, and engaging in behaviours related to healthy eating for adequate weight. There were statistically significant decreases from baseline to 6 months after the intervention for three clinical outcomes: diastolic blood pressure, LDL cholesterol level and HbA1c. Only LDL cholesterol and triglyceride levels showed significant decreases from baseline to 12 months after the intervention.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Lasco et al.178
Method: Cohort study.
Participants: Out of 190 eligible women, 72 (37.9%) participated in the study. In total, 70 participants (97.2%) completed the 3-month follow-up.
Intervention: This study investigated the Community Health Assessment and Promotion Project (CHAPP) in Atlanta, GA, USA. This was a 10-week exercise and nutrition intervention targeted at low-income obese black women aged between 18 and 59 years. The nutrition component initially consisted of a 1-hour lecture but this was changed to short presentations followed by food sampling sessions at the suggestion of the participants. Sessions usually lasted for 30 minutes and consisted of demonstrations of healthy cooking techniques and recipe sharing. The exercise component consisted of water aerobics, low-impact aerobic dance and walking.
Outcomes: Outcome measures included weight (independently measured but does not state who took measurements or whether or not assessors were blinded) and blood pressure (diastolic and systolic). The results showed that 55% of the participants weighed less 3 months after the intervention (average weight loss 2.8 lb). The most weight gained was 17 lb and the most weight lost was 59 lb. After 3 months, diastolic blood pressure was lower among 47% of the participants (average decrease for all participants 2.8 points). For systolic blood pressure, 56% showed a decrease (average decrease for all participants 5.8 points).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Christiansen et al.201
Method: Retrospective cohort follow-up study.
Participants: Out of 354 eligible individuals, 249 (70.3%) participated. There were two follow-ups (2 and 4 years) and the final sample size was 249 at the 4-year follow-up. In total, 72.3% of participants were women and the mean age was 39.2 years.
Intervention: This study investigated a weight loss camp for low-income, severely obese participants in Denmark. The intervention consisted of a combination of diet and exercise over 21 weeks. The lifestyle modification programme consisted of a conventional low-calorie diet, structured physical activity and cognitive therapy. The programme was supervised by a multidisciplinary group that included dietitians, physical therapists and a psychologist. Participants had a prescribed diet (2190 kcal/day) based on Nordic Nutrition Recommendations, with a dietary composition of 55–60% carbohydrates, 15% protein and < 30% fat. Participants were weighed on a weekly basis. There was also an education programme whereby participants were instructed to calculate their food intake, to estimate an appropriate portion size and to use different behavioural strategies in their home environment to maintain achieved weight loss. Physical activity was also core to the intervention. For at least 120 minutes per day, all participants took part in structured physical activities supervised by a physical therapist. The exercise programme consisted of group-based activities such as swimming, aerobic exercise, strength training, walking and ergometer bicycling with an estimated intensity of 50–60% VO2max.
Outcomes: Outcomes measures were weight loss and maintenance. Weight loss was both self-reported and independently measured (does not state whether or not blinding took place). The results reveal that weight regain for all subjects at follow-up after 2–4 years (mean 42.9 months) was 13.2 ± 19 kg, resulting in weight loss maintenance of 5.3% of initial body weight. No difference in relative weight loss maintenance was observed between genders or among three cohorts (2–4 years’ follow-up). Successful weight loss maintenance, defined as maintaining weight loss of ≥ 10%, was obtained in 28.9% of all subjects and was similar among the three separate cohorts (p = 0.9). In addition, no gender difference was observed (men 30% vs. women 28%; p = 0.86). Subjects with successful weight loss maintenance of ≥ 10% reported significantly higher levels of daily physical activity than subjects with weight loss maintenance of < 10%.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Not applicable |
| Global rating | Moderate |
Jordan et al.165
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: In total, 114 women were recruited from Women, Infants, and Children clinics, community centres and churches (44% recruitment rate). After 24 weeks the final sample size was 93 (82% follow-up response rate).
Intervention: This study investigated a nutrition and physical activity intervention for overweight and obese low-income mothers in the USA. The intervention was delivered over 8 weeks and sessions incorporated recommendations for healthful eating, behaviour modification and physical activity; education; monitoring; counselling; practical skills; behaviour therapy; calorie prescribed diets; and exercise.
Outcomes: The primary outcomes were weight, waist circumference and percentage body fat (using bioelectrical impedance) (blinding status of assessors not reported). At 24 weeks, significant decreases from baseline in body weight (−2.7 kg; p < 0.001), percentage body fat (−0.8%; p < 0.01) and waist circumference (−12.1 cm; p < 0.001) were observed.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Gray et al.153
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: Obese men (aged 24–75 years) were recruited to the programme through their GPs. There was a recruitment rate of 14%, with 110 men recruited at baseline, and 80 men completed the programme (follow-up response rate 73%).
Intervention: This study investigated a health service-led group-based weight-management intervention for men living in deprived areas of Scotland, UK (the Camelon weight-management group programme). The 12-week intervention consisted of weekly group sessions that were based on National Institute for Health and Care Excellence (NICE)248 and Scottish Intercollegiate Guidelines Network249 guidelines and promoted physical activity and a healthful diet (no energy restriction) and covered behavioural modification techniques.
Outcomes: Height, weight and waist circumference were measured by programme staff at baseline and after 12 weeks. On average, participants lost 4.98 kg and 44% achieved the NICE and Scottish Intercollegiate Guidelines Network weight loss target of 5–10%.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Weak |
Pescatello et al.205 (two study designs)
Method: Uncontrolled prospective cohort (before-and-after) study and controlled prospective cohort design (using a self-selected comparison group).
Participants: At baseline, 621 employees were recruited to the programme (recruitment rate of 34%; 87% female, mean age 41 years).
Intervention: This study investigated a workplace-based Cardiovascular Health Awareness Program (CHAP) in benefit-eligible employees from a hospital in the USA. Two study designs, using slightly different samples, were used to evaluate the programme; therefore, for the purpose of this review, each study design is counted as a separate study. The CHAP intervention consisted of annual cardiovascular screens followed by a counselling session at which individualised feedback based on the results of the screening was given. Participants were encouraged to participate in formal group education and behavioural support programmes that were held at the workplace and off site. Employees were given a US$100 incentive to participate in the programme.
Outcomes: Outcomes included changes in BMI, waist circumference and waist-to-hip ratio (measurements taken by assessors blinded to CHAP participation status), blood lipids and glucose and blood pressure.
First, an uncontrolled prospective cohort (before-and-after) study design was used to evaluate the overall effects of CHAP in all participants. For this study there was a final sample size of 278 participants after 4 years (45% follow-up response rate). After 4 years, increases in BMI [adjusted change from baseline 0.5 kg/m2, standard error of the mean (SEM) 0.2 kg/m2; p < 0.034] and waist circumference (adjusted change from baseline 2.5 cm, SEM 0.7 cm; p = 0.001) were observed, along with increases in triglycerides (adjusted change from baseline 16.0 mg/dl, SEM 6.1 mg/dl; p = 0.009). However, favourable decreases in the total cholesterol/HDL cholesterol ratio (adjusted change from baseline –0.11, SEM 0.06; p = 0.007), LDL cholesterol (adjusted change from baseline –6.7 mg/dl, SEM 1.2 mg/dl; p = 0.009) and fasting blood glucose (adjusted change from baseline –1.7 mg/dl, SEM 1.2 mg/dl; p = 0.018) were also observed.
Second, a controlled prospective cohort design (using a self-selected comparison group) was used to investigate effects in participants who participated in the additional CHAP activities (formal group education and behavioural support programmes; intervention group) and those who did not (control group). This study had a final sample size of 198 (139 in the additional activities intervention group; follow-up response rate of 32%) after 4 years. There were no statistically significant differences between the groups for changes in any of the outcomes although, surprisingly, the control group showed greater improvements for most of the outcomes, with the exception of BMI and waist circumference, which appeared to increase to a lesser extent in the intervention group participants.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong/moderate |
| C) Confounders | Moderate |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Williams and Wold206
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: A total of 77 employees were recruited from two small workplaces and followed for 1 year.
Intervention: This study investigated a workplace mobile nursing cardiovascular disease risk factor identification programme aimed at reducing cholesterol levels and conducted in an area of low-income and low-education residents considered ‘working poor’ (low income but ineligible for benefits) in the USA. The intervention consisted of screening for risk factors followed by an individualised education-based interview focusing on dietary and physical activity behaviour change and based on the individual’s transtheoretical change stage. A follow-up report based on measured values for height, weight, blood pressure and cholesterol and a letter that reinforced the interview discussion were then mailed to participants.
Outcomes: There were no statistically significant changes in BMI from baseline to 1 year in either rural or urban participants.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Strong |
| Global rating | Weak |
Hajek et al.208
Method: Uncontrolled before-and-after pilot study.
Participants: A total of 162 participants (90% female, mean age 44 years) were recruited through advertisements and weight data were collected from 39 at 3 months (24% follow-up rate).
Intervention: This study investigated a health behaviour modification weight-management programme conducted in localities of high deprivation in the UK. The programme consisted of six weekly group-based treatment sessions that incorporated structured individually tailored tasks and a group-oriented social support system (‘buddy’ system) as well as two 1-hour follow-up visits.
Outcomes: The average weight loss at 3 months was 4.5 kg (4.7% of baseline body weight; p < 0.001).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Zuber et al.160
Method: Prospective cohort (uncontrolled before-and-after) study.
Participants: A total of 372 participants completed the 1-year programme (mean age 41 years, 86% female; approximate follow-up response rate 80%).
Intervention: This study investigated a weight loss programme provided by a health insurance company in Germany for low- to medium- and low-SES adults. The programme consisted of 24 sessions conducted over 6 months by a clinical psychologist, diet assistant and doctor. These sessions provided nutrition, medicine and dietetic education and advice and addressed psychological concepts such as motivation, hopes and fears. Four therapist-led after-care sessions were then delivered over a further 6 months and were gradually transformed to self-help groups. Participants were self-referred or referred by a doctor to the programme and were eligible if they were at least 20% over their ideal weight as calculated using Broca’s index.
Outcomes: After 6 months, participants had lost 11 kg on average and the prevalence of overweight had reduced by 18%. After 1 year there was an average weight loss of 9 kg. Weight loss was greatest in participants who were the most overweight (> 70% over their ideal weight) but the authors concluded that the weight loss was clinically insufficient and that more therapy may be required for this group.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Clark et al.213
Method: Cohort study.
Participants: The total number of eligible participants was 412, of whom 123 were recruited (29.9% of total population). The mean age of participants was 63.7 years. A random sample of women was recruited through primary care referral and the researchers. There was a 1-year follow up with a 58.5% follow-up response rate (n = 72).
Intervention: This study investigated a community-based exercise intervention for predominantly low-income women aged > 50 years. Exercise classes were held once a day (Monday–Friday) and consisted of 20 minutes of chair-based or standing leg and arm movements and up to 30 minutes of indoor walking. The classes were held in either a church or a community centre. Participants were encouraged to attend at least three exercise classes per week.
Outcomes: The outcome measures included physical activity intensity, self-reported exercise self-esteem, weight, body fat, BMI, hip and waist circumference and skinfold thickness (obesity measurements were independently measured). The results show that there were differences in change over time between the no-adherence group and the moderate-adherence group for weight, BMI, hip and waist circumference and triceps skinfold. In all cases the no-adherence group worsened whereas the moderate-adherence group improved. In terms of weight, the no-adherence group gained 3.6 lb whereas the moderate-adherence group lost 4.3 lb. This net difference of 8 lb represents approximately a 4% weight difference between the groups after 1 year. Self-reported physical activity minutes per week increased in the moderate-adherence groups but did not change significantly in the no- and little-adherence groups. The difference between groups was statistically significant (p = 0.004).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Zoellner et al.181,231
Method: Prospective cohort study.
Participants: Of the eligible population (n = 88), 83 (94%) agreed to participate in the study. In total, 97% of the participants were female and the mean (SD) age was 46.1 (12.8) years. At 6 months’ follow-up, 80% (n = 66) completed the study.
Intervention: This study investigated a 6-month community walking intervention that targeted African Americans. The Fit for Life steps intervention programme was developed and implemented by the Hollandale Nutrition Intervention Research Initiative. Participants were given pedometers and were asked to keep a pedometer diary to encourage them to undertake physical activity. The intervention included individualised weekly goals. Participants were encouraged to exercise for 10,000 steps per day but were instructed to set realistic and personalised weekly goals. Walking teams were led by coaches and there were monthly educational sessions.
Outcomes: The outcome measures were BMI, body weight, body composition and waist circumference, which were objectively measured. There was no significant difference in BMI. Participants exhibited a significant improvement in waist circumference (–1.4 inches; p < 0.001). There was a trend for the reported average number of minutes spent walking to increase from baseline to 3 months (+31.76 minutes/day) and then to decline from 3 months to 6 months (–10.7 minutes/day), although this was not statistically significant. Additionally, there were significant improvements in systolic blood pressure (–4.3 mmHg; p < 0.001) and HDL cholesterol (+7.9 mg/dl; p < 0.001) from baseline to 6 months. However, there were no significant differences in diastolic blood pressure, blood glucose, total cholesterol, LDL cholesterol and triglycerides.
Quality appraisal
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Societal (environmental)-level interventions
Universal approach: experimental studies (n = 1)
Lemon et al.219
Method: Cluster RCT.
Participants: Out of 1593 eligible employees, 806 (51%) participated in the study (386 intervention group and 420 control group). A total of 648 participants (80%) completed the 24-month follow-up. Only 18- to 65-year-olds were included in the study. In total, 78.3% in the intervention group and 84.2% in the control group were women.
Intervention: This study investigated a four-strategy weight prevention intervention for hospital employees based in six worksites in Massachusetts, USA. The four strategies consisted of a social marketing campaign, environmental strategies promoting physical activity, environmental strategies promoting healthy eating and strategies promoting interpersonal support. Types of intervention strategies include stairway signs, cafeteria signs, farmers’ markets, walking groups, challenges, workshops, educational displays, newsletters, a project website, a project information centre and print materials. The intervention was designed to promote organisational and social norms related to healthy eating and physical activity in the worksite. Gift cards (US$20) were given to participants who completed each follow-up (12 and 24 months) as incentives for completion.
Outcomes: The primary outcome measure was change in BMI (calculated based on objective measures by trained staff). A secondary outcome measure was a dichotomous indicator of weight gain prevention from baseline to the 24-month follow-up. The results show that there was no significant intervention impact on change in BMI. Average adjusted BMI in the intervention and control conditions was 28.4 kg/m2 and 29.0 kg/m2 at baseline, 28.7 kg/m2 and 29.1 kg/m2 at 12 months and 28.9 kg/m2 and 29.4 kg/m2 at 24 months respectively. Analysis examining the association between extent of intervention participation and change in BMI suggested a positive relationship (greater participation resulted in reduced BMI). Differential effects on weight gain prevention were found. The group most likely to prevent weight gain was characterised by a higher proportion of employees who were non-Hispanic white, aged > 50 years, of higher educational and income levels and obese and who worked the first shift and had no patient care responsibilities. The group least likely to prevent weight gain included a higher proportion of employees who were non-white, middle-aged (41–50 years) and of lower educational and income levels and who worked the second or third shift. This therefore highlights the unequal positive benefits of this workplace intervention in terms of SES.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Weak |
| B) Study design | Strong |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Universal approach: observational studies (n = 6)
Scoggins et al.221 (two study designs)
Method: A 1-year controlled cohort study and a 5-year uncontrolled cohort study.
Participants: Out of 23,226 potentially eligible participants, 19,559 were recruited. The age of participants ranged between 18 and 69 years and 49.9% were women.
Intervention: This study investigated Healthy Incentives, a worksite wellness programme in Seattle, USA, that comprised individual action plans as well as environmental modifications to the workplace. Examples of individual action plans included maintaining an exercise journal and joining Weight Watchers at Work. Environmental modifications in the workplace involved opening up and decorating the stairwell to encourage taking the stairs (prompts were also used) and replacing unhealthy options with healthy items in vending machines. The objective of this programme was to compare changes in BMI in participants in the Healthy Incentives programme with changes in a national sample of people insured through their employers (Medical Expenditure Panel Survey, used as a control).
Outcomes: The outcome measure was change in BMI (based on self-reported health and not an objective measure and so potentially some bias). The results show that during the first year intervention participants lost weight on average (–0.80%, p < 0.01) whereas control respondents gained weight on average (0.31%, p < 0.01). As a result, intervention participants lost 1.10% (p < 0.01) of their body weight relative to the control respondents. The 5-year intervention cohort also lost weight on average (–0.47%, p < 0.01), but not as much as first-year participants (–0.80% minus –0.47% = –0.33%, p < 0.01). Differential effects for the following confounders were also examined: BMI, sex, age, race/ethnicity and education. The difference in BMI growth rates between 1-year and control participants becomes more negative with BMI category (normal: –0.59%, p < 0.01; overweight: –1.24%, p < 0.01; obese: –1.74%, p < 0.01). The BMI growth rate for 5-year participants is larger than the growth rate for 1-year participants except for obese participants (–1.17%, p < 0.01). First-year female participants lost weight relative to the control respondents faster than male participants (–1.28% vs. –0.92%, p = 0.15 not significant). Five-year female participants lost weight faster than male participants (–0.79% vs. –0.15%, p < 0.01). First-year participants aged < 30 years lost weight relative to control respondents much more slowly than older participants (18–29 years: −0.35%, p = 0.41; 30–39 years: −1.27%, p < 0.01; 40–49 years: −1.06%, p < 0.01; 50–59 years: −1.11%, p < 0.01; 60–69 years: −1.33%, p < 0.01). The BMI growth rate for 5-year participants decreased with age and was greater than the growth rate for first-year participants for every age group except for participants aged ≥ 60 years (−1.92%, p < 0.01). First-year African American participants lost weight relative to the control respondents faster than any other racial group (−2.08%, p < 0.01) followed in descending order by Hispanics (−1.66%, p < 0.01), whites (−1.13%, p < 0.01) and Asian Americans (−0.33%, p = 0.44). The BMI growth rate for 5-year participants by racial group followed the same pattern, with African Americans losing the most weight and Asian Americans losing the least. Finally, and importantly, first-year participants who graduated from college lost weight at a slower rate relative to the control respondents than participants with less formal education (college graduate: –0.88%, p < 0.01; some college education: –1.41%, p < 0.01; high-school education only: –1.45%, p < 0.01).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
VanWormer et al.220
Method: Controlled cohort study.
Participants: The total eligible worksite population was not reported. A sample of 1747 employees was recruited to this study and 1407 (81%) completed the 24-month follow-up. In total, 1222 of these 1407 met the eligibility criteria for analysis; 61% were women and the mean age was 44.2 ± 10.3 years.
Intervention: This study investigated the HealthWorks environmental intervention, which included six organisations in the Minneapolis–St Paul, MN, USA, metropolitan area, focused on making changes to the work environment designed to promote and support physical activity, reducing calorific consumption, and self-weighing. Despite initially being an experimental study, the study design changed to an observational study as both the intervention group and the control group results were combined as the authors state that the two groups were statistically indistinguishable. As part of the intervention, healthy foods/beverages were made affordable, access modifications to healthy foods and aesthetic stairwell enhancements were made, there was free access to pedometers and website step-tracking tools and improved scale access for self-weighing (including balance beam scales placed at various locations within the workplace such as restrooms), worksite advisory groups were set up and there was site-wide publicity of nutrition and physical activity. Three worksites were randomised into the intervention group and three were randomised into the control (no treatment) group.
Outcomes: The outcome measure was body weight change, which was measured independently by trained staff using calibrated digital scales. Covariates considered were age, sex, race/ethnicity, education, marital status, self-weighing frequency, smoking, diabetes, high blood pressure, depression, number of weight loss attempts, perceived pounds needed to gain before attempting weight loss, number of scales in the home and BMI. The initial crude model indicated that both daily and weekly self-weighing at the 24-month follow-up were significantly associated with weight change. Specifically, participants who reported self-weighing daily and participants who reported self-weighing weekly had lost 1.8 kg and 0.9 kg, respectively, more than participants who reported self-weighing monthly. Further modelling revealed a significant interaction between follow-up self-weighing frequency and baseline BMI (–1.497; p < 0.001). A final multivariate regression model revealed that the direction of the interaction was such that the greatest weight loss was observed for participants who were obese at baseline and reported self-weighing daily at 24 months’ follow-up [mean (SD) –4.4 (0.8) kg]. In contrast, the largest weight gain was observed for participants with a healthy BMI at baseline and who reported self-weighing monthly at 24 months’ follow-up [mean (SD) 2.1 (0.4) kg]. The authors also examined differential effects for age, race, education, marital status, study condition, baseline self-weighing, smoking, diabetes, high blood pressure, depression, weight loss attempts, required weight gain for action and number of scales in the home and found no statistically significant differences in weight change.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Strong |
| Global rating | Moderate |
Jenum et al.215–217
Method: Controlled prospective cohort study.
Participants: Out of 6149 eligible subjects, 2950 (48%) took part in the study. After 3 years’ follow-up, 1776 (60%) completed the study. The age of participants ranged from 30 to 67 years and the mean age was 49 ± 10 years in the intervention group and 48.9 ± 9 years in the control group. In total, 57% of the intervention group were women and 54% of the control group were women.
Intervention: This study investigated the Romsås in Motion intervention programme in Oslo, Norway, which included strategies to increase awareness of, improve knowledge of and change attitudes towards physical activity, implemented through the use of specifically designed leaflets, reminders of the health benefits of using stairs compared with lifts, local meetings, stands and mass media communication activities. To increase self-efficacy and perceived behavioural control for physical activity, participants were provided with individual counselling during biannual fitness tests, and walking groups and group sessions for indoor activity were organised for participants during the whole intervention period. These group activities were expected to enhance perceived social support for physical activity through the involvement of family and friends. Environmental changes were also made during the intervention including the labelling of walking trails within the district, improving street lighting and gritting of pavements and trails in winter to increase accessibility for physical activity and thereby reinforce self-efficacy and perceived behavioural control. This study followed a targeted approach as it was conducted in two low-SES districts, but within this the study investigated differential effects by education level. Therefore, the study also followed a universal approach and is regarded as two studies for the purposes of this review.
Outcomes: The outcome measures include objectively measured body mass in light clothes using an electronic device (DS 102; Arctic Heading, Tønsberg, Norway), BMI, self-reported physical activity, resting heart rate, systolic blood pressure and cholesterol, HDL cholesterol, triglyceride and glucose levels. Blinding was not described in the study. The results showed that, in the intervention district, body mass was reduced in 23.7% and increased in 37.9% of the participants, compared with 15.6% and 44.5%, respectively, in the control district. The net proportion who increased their body mass was significantly lower in the intervention district than in the control district (p < 0.01); this was found overall (14.2%; p < 0.001) and across educational groups (increase in weight was independent of educational level). Mean body mass increased less in the intervention district than in the control district, but a significant interaction for district/sex and district/age was found, with district differences most marked in men and participants aged < 50 years. In men, a net reduction of 1.2 kg (95% CI 0.6 kg to 1.9 kg) was found, whereas there was no net reduction in women (0.3 kg, 95% CI –0.4 kg to 0.9 kg). Women had the poorest results for body mass. After 3 years’ follow-up, BMI was significantly lower in men (–0.42 kg/m2, 95% CI –0.63 kg/m2 to –0.21 kg/m2; p < 0.001). There was no statistically significant difference in BMI in women. Men increased their self-reported heavy physical activity more than women, and mean resting heart rate was also reduced among men. Women aged < 50 years had the poorest results for physical activity. The reported physical activity outcomes were slightly reduced but remained significant after adjustments for differences between districts at baseline with respect to education, work participation, disability pension, BMI and prevalence of diabetes (heavy physical activity: β unadjusted/adjusted: 0.178, p = 0.001/0.157, p = 0.007; stages of change: β unadjusted/adjusted: 0.22, p < 0.001/0.152, p = 0.014). Favourable changes were found for both sexes in systolic blood pressure and serum triglyceride levels and for men in resting heart rate, serum total cholesterol/HDL cholesterol ratio and glucose level. The significant estimates for net changes in body weight (men: β unadjusted/adjusted: –1.2, p < 0.001/–1.1, p = 0.005), systolic blood pressure (both sexes), resting heart rate and mean levels of lipids (men) remained fairly stable after similar adjustments.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Carleton et al.222
Method: Repeat cross-sectional study.
Participants: Random-sample, cross-sectional surveys were conducted with 18- to 64-year-olds (mean age 39 years) between 1984 and 1991. Participants were tracked through a computer-based process evaluation system. Out of 5241 participants (first- and second-wave surveys), 2925 were re-examined approximately 8.5 years later. In total, > 50% were women (between 54% and 60%).
Intervention: This study investigated the Pawtucket Heart Health Program in Rhode Island, USA. A control New England city was selected as a comparator. The objective of this study was to investigate whether or not community-wide education changed cardiovascular disease risk factors and disease risk in Pawtucket compared with a comparison community in New England. The multiple community-wide interventions included grocery store shelf labelling of low-fat foods, installation of a multiple-station exercise course, nutrition programmes at the public library and restaurant menu healthy heart highlights.
Outcomes: The outcome measures included BMI (objectively measured by staff), total cholesterol level, systolic and diastolic blood pressure and smoking. The results showed that Pawtucket participants maintained a relatively stable BMI throughout whereas the comparison city (control) participants’ BMI values increased steadily, resulting in a significant difference between the two cities. The city difference for BMI (0.62 kg/m2) between the baseline minus the post-intervention survey values was also significant. The BMI city differential occurred predominantly in men, in those aged < 35 years and in those with a lower level of education. No statistically significant between-city differences were seen in blood cholesterol levels and systolic and diastolic blood pressure. Although the mean cholesterol level fell from baseline values of 204.2 mg/dl (SEM 5.28 mmol/l) and 205.5 mg/dl (SEM 5.31 mmol/l) to 199.1 mg/dl (SEM 5.14 mmol/l) and 200.8 mg/dl (SEM 5.19 mmol/l) in Pawtucket and the comparison city, respectively, there were no significant city differences across the duration of the study. Also, there was no statistically significant between-city differences in smoking.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Weak |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Not applicable |
| Global rating | Moderate |
Tudor-Smith et al.218
Method: Repeat cross-sectional study.
Participants: The study used two independent cross-sectional surveys (1985 and 1990) in both Wales (intervention) and north-east England (control), UK, to assess the efficacy of a cardiovascular disease prevention programme. The surveys were randomly stratified and the lowest response rates in Wales were 67% and 61% for the self-completion surveys in 1985 and 1990 respectively. In north-east England the lowest response rates were 64% and 61% respectively. Mean age and sex were not reported but the age of participants ranged from 18 to 64 years.
Intervention: This study investigated the Heartbeat Wales cardiovascular disease prevention programme. This health promotion programme consisted of the following interventions: smoking cessation television series with BBC Wales and HTV, food labelling and nutrition education with a major grocery retailer, a restaurant and canteen scheme to increase the availability of healthy food choices and smoke-free areas and a worksite health promotion programme with the Confederation of British Industry (CBI) Wales.
Outcomes: The outcome measures included dietary choices in food consumption (including healthy and unhealthy food choices), smoking attitudes, exercise and prevalence of overweight (BMI > 24 kg/m2 for women or > 25 kg/m2 for men, based on self-reported measures in the surveys). Community-level and subgroup analyses showed that there were no intervention effects between manual and non-manual SES groups for any of the outcome measures above. The overweight intervention effect ratio was 1.07 (95% CI 0.89 to 1.28) and 1.02 (95% CI 0.87 to 1.19) for manual and non-manual occupation groups respectively. There were no significant differences in any of the outcome measures according to SES.
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Weak |
| C) Confounders | Moderate |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Not applicable |
| Global rating | Weak |
Targeted approach: experimental studies
None.
Targeted approach: observational studies (n = 1)
Jenum et al.215–217
Method: Controlled prospective cohort study.
Participants: Out of 6149 eligible subjects, 2950 (48%) took part in the study. After 3 years’ follow-up, 1776 (60%) completed the study. The age of participants ranged from 30 to 67 years and the mean age was 49 ± 10 years in the intervention group and 48.9 ± 9 years in the control group. In total, 57% of the intervention group were women and 54% of the control group were women.
Intervention: This study investigated the Romsås in Motion intervention programme in Oslo, Norway. It followed a targeted approach as it was conducted in two low-SES districts, but within this the study investigated differential effects by education level. Therefore, the study also followed a universal approach and is regarded as two studies for the purpose of this review. The intervention programme included strategies to increase awareness of, improve knowledge of and change attitudes towards physical activity, implemented through the use of specifically designed leaflets, reminders of the health benefits of using stairs compared with lifts, local meetings, stands and mass media communication activities. To increase self-efficacy and perceived behavioural control for physical activity, participants were provided with individual counselling during biannual fitness tests, and walking groups and group sessions for indoor activity were organised for participants during the whole intervention period. These group activities were expected to enhance perceived social support for physical activity through the involvement of family and friends. Environmental changes were also made during the intervention including the labelling of walking trails within the district, improving street lighting and gritting of pavements and trails in winter to increase accessibility for physical activity and thereby reinforce self-efficacy and perceived behavioural control
Outcomes: The outcome measures include objectively measured body mass in light clothes using an electronic device (DS 102; Arctic Heading, Tønsberg, Norway), BMI, self-reported physical activity, resting heart rate, systolic blood pressure and cholesterol, HDL cholesterol, triglyceride and glucose levels. Blinding was not described in the study. The results showed that, in the intervention district, body mass was reduced in 23.7% and increased in 37.9% of the participants, compared with 15.6% and 44.5%, respectively, in the control district. The net proportion who increased their body mass was significantly lower in the intervention district than in the control district (p < 0.01); this was found overall (14.2%; p < 0.001) and across educational groups (increase in weight was independent of educational level). Mean body mass increased less in the intervention district than in the control district, but a significant interaction for district/sex and district/age was found, with district differences most marked in men and participants aged < 50 years. In men, a net reduction of 1.2 kg (95% CI 0.6 kg to 1.9 kg) was found, whereas there was no net reduction in women (0.3 kg, 95% CI –0.4 kg to 0.9 kg). Women had the poorest results for body mass. After 3 years’ follow-up, BMI was significantly lower in men (–0.42 kg/m2, 95% CI –0.63 kg/m2 to –0.21 kg/m2; p < 0.001). There was no statistically significant difference in BMI in women. Men increased their self-reported heavy physical activity more than women, and mean resting heart rate was also reduced among men. Women aged < 50 years had the poorest results for physical activity. The reported physical activity outcomes were slightly reduced but remained significant after adjustments for differences between districts at baseline with respect to education, work participation, disability pension, BMI and prevalence of diabetes (heavy physical activity: β unadjusted/adjusted: 0.178, p = 0.001/0.157, p = 0.007; stages of change: β unadjusted/adjusted: 0.22, p < 0.001/0.152, p = 0.014). Favourable changes were found for both sexes in systolic blood pressure and serum triglyceride levels and for men in resting heart rate, serum total cholesterol/HDL cholesterol ratio and glucose level. The significant estimates for net changes in body weight (men: β unadjusted/adjusted: –1.2, p < 0.001/–1.1, p = 0.005), systolic blood pressure (both sexes), resting heart rate and mean levels of lipids (men) remained fairly stable after similar adjustments.
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Strong |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Strong |
| F) Withdrawals and dropouts | Moderate |
| Global rating | Moderate |
Societal (macro)-level interventions
Universal approach: experimental studies
None.
Universal approach: observational studies
None.
Targeted approach: experimental studies
None.
Targeted approach: observational studies (n = 2)
Jones and Frongillo223
Method: Retrospective cohort study.
Participants: Data from 5503 women were used in the analysis.
Intervention: This study investigated a Food Stamp Program implemented in the USA in women using longitudinal data from the Panel Study of Income Dynamics. The Food Stamp Program provides financial assistance for purchasing food to low- and no-income people. The Panel Study of Income Dynamics included data on Food Stamp Program participation and the self-reported weight of participants.
Outcomes: Results from analysis controlling for changes in covariates and time-invariant covariates revealed that a US$2000 increase in food stamp participation had no effect on weight change among women who were persistently food secure. Among women who changed food insecurity status, a US$2000 increase in food stamp benefits was associated with a small and insignificant difference in weight change (became food secure: β = 2.98, p = not significant; became food insecure: β = 1.50, p = not significant). In women who remained food insecure, a US$2000 increase in food stamps was associated with a significantly significant increase in weight change (β = 7.78, p < 0.05).
Quality assessment
| Item | Authors’ judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Moderate |
| C) Confounders | Weak |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Weak |
| Global rating | Weak |
Kaushal224
Method: Natural study.
Participants: Using data from two serial cross-sectional surveys the analysis was based on 68,318 observations.
Intervention: This study investigated the effects of a US Food Stamp Program on obesity. The 1996 Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) changed immigrant eligibility for the Food Stamp Program, resulting in denied access to the programme. The study used national (self-reported) BMI data taken before and after 1996 and compared immigrants with a low level of education (who became ineligible for the programme after 1996) with US-born participants with a low level of education (who remained eligible).
Outcomes: From pre to post PRWORA the average BMI of foreign-born low-educated women increased by 0.72 BMI units, whereas the average BMI of US-born low-educated women increased by 1.11 BMI units (difference between groups −0.34 units), although the difference was not statistically significant (p ≤ 0.1). When looking at low-educated unmarried mothers only, an increase in BMI after PRWORA was also observed and the increase was relatively lower (0.63 BMI units) for foreign-born unmarried mothers than for US-born unmarried mothers (1.17 units; difference between groups −0.47 units), although this difference was not statistically significant (p ≤ 0.1). The rise in BMI among low-educated foreign-born men (0.8 BMI units) was slightly less than the increase experienced by low-educated US-born men (0.95 BMI units; difference between groups –0.12), but again the between-group difference was insignificant (p > 0.1).
Quality assessment
| Item | Author’s judgement |
|---|---|
| A) Selection bias | Moderate |
| B) Study design | Weak |
| C) Confounders | Strong |
| D) Blinding | Moderate |
| E) Data collection methods | Weak |
| F) Withdrawals and dropouts | Not applicable |
| Global rating | Weak |
Glossary
- Experimental studies
- Randomised and non-randomised controlled trials and cluster trials.
- Ideal weight
- < 85th percentile (within the bottom 85% of the population weight distribution).
- Obese
- ≥ 95th percentile (within the top 5% of the population weight distribution).
- Observational studies
- Prospective and retrospective cohort studies (before-and-after studies), with or without control groups, and prospective repeat cross-sectional studies with or without control groups.
- Overweight
- ≥ 85th percentile (within the top 15% of the population weight distribution).
List of abbreviations
- ASSIA
- Applied Social Sciences Index and Abstracts
- BI
- basic intervention
- BM
- behavioural modification
- BMI
- body mass index
- CATCH
- Child and Adolescent Trial for Cardiovascular Health
- CHAD
- Community syndrome of Hypertension, Atherosclerosis and Diabetes
- CHAP
- Cardiovascular Health Awareness Program
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CRD
- Centre for Reviews and Dissemination
- CSA
- Cambridge Scientific Abstracts
- EFNEP
- Expanded Food and Nutrition Education Program
- EPHPP
- Effective Public Health Practice Project
- EPODE
- Ensemble, Prévenons L’Obésité Des Enfants
- FMS
- fundamental skills
- GEMS
- Girls health Enrichment Multisite Studies
- GP
- general practitioner
- HbA1c
- glycated haemoglobin
- HDL
- high-density lipoprotein
- HTS
- Health Trainer Service
- IBSS
- International Bibliography of the Social Sciences
- IOM
- Institute of Medicine
- KOPS
- Kiel Obesity Prevention Study
- LDL
- low-density lipoprotein
- MOMS
- Mothers’ Overweight Management Study
- NICE
- National Institute for Health and Care Excellence
- OR
- odds ratio
- PAT
- Programa de Alimentação do Trabalhador
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROGRESS
- Place of residence, Race/ethnicity, Occupation, Gender, Religion, Education, Socioeconomic status and Social capital
- PRWORA
- Personal Responsibility and Work Opportunity Reconciliation Act
- RCT
- randomised controlled trial
- RI
- reinforced intervention
- RR
- relative risk
- SD
- standard deviation
- SDS
- standard deviation score
- SE
- standard error
- SEM
- standard error of the mean
- SES
- socioeconomic status
- SNAP
- Stanford Nutrition Action Program
- VO2max.
- peak oxygen uptake
- WHO
- World Health Organization