Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3010/06. The contractual start date was in June 2011. The final report began editorial review in January 2014 and was accepted for publication in June 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Professor Peter Donnan has received research grants in the past from GlaxoSmithKline, Pfizer, Otsuka and Amgen Inc. He is also a member of the New Drugs Committee of the Scottish Medicines Consortium. Dr Adrian Brady has received research grants from Merck, Servier, AstraZeneca and Bayer, has provided consultancy to Merck USA and Bayer Germany, and been awarded lecture fees and/or honoraria from Merck, Servier, AstraZeneca, Boehringer Ingelheim, Pfizer and Bayer. Eleanor Grieve has received unrestricted research funds from Cambridge Weight Plan.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research, or similar, and contains language which may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Wyke et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
The problem of obesity and male obesity
Rising levels of obesity are a major challenge to public health. There are expected to be 11 million more obese adults in the UK by 2030, accruing up to 668,000 additional cases of diabetes mellitus, 461,000 cases of heart disease and stroke, 130,000 cases of cancer, and up to 6.3 million lost quality-adjusted life-years (QALYs), with associated medical costs set to increase by £1.9–2.0B per year by 2030. 1
In Scotland, more men (69%) than women (60%) are overweight or obese,2 and the UK prevalence of male obesity is among the highest in Europe1 and forecast to increase at a faster rate than female obesity in the next 40 years. It is likely that the link between obesity and socioeconomic deprivation, already evident in women, will soon appear in men. 2 Compared with women, men may be more vulnerable to adverse health consequences of obesity. At all ages, men are diagnosed with type 2 diabetes mellitus at lower body mass index (BMI) than women3 and adult men are more insulin resistant than women, a finding that is associated with difference in fat distribution. 4
Men, existing weight loss programmes and the potential of sporting organisations
Although 5–10% weight loss can produce significant health benefits,5 men are under-represented in trials of weight loss interventions (only 27% of participants are men),6 in referrals to commercial weight management programmes (between 11%7 and 13%8 of men) and in NHS weight management services (23% of men). 9 As a recent systematic review of approaches to the management of obesity in men concludes: ‘That men are under-represented suggests that methods to engage men in services, and the services themselves, are currently not optimal’. 10
Men’s reluctance to enrol in weight management programmes in part reflects a failure to recognise gender differences in societal processes that contribute to becoming overweight or obese. For example, greater body size is often associated with masculinity,11 leading some men to be concerned about being too thin and less likely to diet than women. 12–14 Indeed, men often view dieting as ‘feminine’15 and are more likely to use exercise to control their weight. 13 In addition, men tend to have poorer nutrition knowledge than women, to be resistant to healthy eating campaigns16 and to be less aware of links between diet and ill health. 13,17 Alcohol may pose an additional problem for weight management for men;18,19 Scottish men drink around twice as much as Scottish women. 20 However, evidence suggests that when gender issues are used to inform programme design, men will engage with appropriately gender-sensitised weight management interventions and lose weight. 10,21
Another reason men may not enrol on weight loss programmes is the setting in which they are delivered. There is a common perception that commercial slimming groups are mainly for women. 22 However, recently the potential of professional sporting organisations to reduce health inequalities by providing access to hard-to-reach populations, including men, has been recognised. 23,24 Although some research has demonstrated the potential of professional sports clubs, particularly football clubs,24–26 to engage men in lifestyle changes, there have been no published controlled studies. 10,26
The Football Fans in Training (FFIT) intervention uses the traditionally male environment of football clubs,27 existing loyalty to football teams and the opportunity to participate in men-only groups to maximise men’s engagement with an evidence-based, gender-sensitised weight management programme. 28 FFIT is delivered under the auspices of the Scottish Premier League (SPL) Trust [which became the Scottish Professional Football League (SPFL) Trust in June 2013]. 29 During the 2011–12 season, nearly 2 million fans passed through SPL club turnstiles. 30
The FFIT is delivered in 12 weekly sessions at club stadia by community coaches trained in diet, nutrition, physical activity and behaviour change techniques (BCTs) to a standard delivery protocol. This intensive weight loss phase is followed by a 9-month minimal contact weight maintenance phase including periodic post programme e-mail prompts and one face-to-face reunion session at the club. The programme’s development is described in Gray et al. 28 and its components are detailed in Chapter 2, Interventions.
Rationale for current study
Project team members have collaborated with the SPL Trust (now the SPFL Trust) to design, implement and evaluate FFIT since June 2009. This partnership has complemented the Trust’s remit to increase Scottish professional football clubs’ community engagement and this is wholly supported by premier league clubs. 29 We developed the evidence-based programme,28 conducted an initial evaluation of the delivery of the pedometer-based walking programme to ensure that it was appropriate for men31 and conducted a feasibility study funded by the Chief Scientist Office (CSO) (CZG/2/504). 32 The feasibility study was conducted in one small and one large club in 2010/11 and demonstrated that men could be recruited to a randomised trial in this context, FFIT was successful in recruiting the target group (mean BMI 34.5 kg/m2 ± 5.0 kg/m2), retention through the trial was good (> 80% at 12 weeks and 6 months; > 75% at 12 months) and men would be likely to engage with the programme (76% attended at least 80% of available programme delivery sessions, and qualitative data examined their enthusiasm for the programme and the context). 31,32 We also found that the programme was likely to be successful; by 12 weeks, the intervention group had lost significantly more weight than the comparison group (4.6% vs. –0.6%; p < 0.001) and many maintained this to 12 months (intervention group baseline 12 month weight loss: 3.5%; p < 0.001). 32
These results supported the decision to conduct the full randomised controlled trial (RCT) reported here.
Note: previous publication of some of the results
Some of the methods and results presented in this report have been previously reported. The design, methods and main results of the RCT were published in The Lancet. 33 The ‘draw’ of the football club setting to attract men to weight management who were at high risk of ill health and who would not otherwise have attended a weight management programme was published in BMC Public Health. 34
Chapter 2 Methods
Setting
A total of 13 professional football clubs in Scotland, including the 12 football clubs constituting the SPL in the 2011–12 football season, and the club relegated to Division 1 at the end of the 2010–11 football season participated in the study.
Overview of study design
We undertook a two-arm, pragmatic, RCT to evaluate delivery of the FFIT programme in 13 Scottish professional football clubs in 2011–12. Men were randomised to intervention or comparator in a 1 : 1 ratio, stratified by club.
Randomisation of individuals within clubs (rather than randomisation of clubs) was chosen for two reasons. First, individual randomisation is more efficient unless contamination is a major risk35 and, second, the SPL Trust was required to deliver the programme in all clubs at the same time.
Assessment of the primary outcome (mean difference in weight loss between groups at 12 months) was blinded.
A summary of the protocol is available at www.thelancet.com/protocol-reviews/11PRT8506. 36
Recruitment strategies and contact with men
At the time of the trial, funding from the Scottish Government and The Football Pools had been secured for three deliveries of the FFIT programme (August to December 2011, February to April 2012 and August to December 2012) in 13 clubs, and the funders required the SPL Trust to provide two deliveries of FFIT in the 2011–12 season. We needed to recruit sufficient men to fill all available places in the three deliveries because the trial design compares men randomly allocated to the FFIT programme in September 2011 with those randomly allocated to a waiting list comparison group starting the FFIT programme 12 months later and we needed to ensure that comparison group participants could not ‘leak’ into vacancies on the non-trial delivery programme. This meant that our recruitment target was inflated from 720 to 1080 (see Sample size for the calculation).
Formal recruitment commenced on 2 June 2011 and continued until the week before the baseline measurements in each club, which took place between 11 August 2011 and 20 September 2011. Participants randomly allocated to the delivery in August to December 2011 formed the intervention group and those randomly allocated to the August to December 2012 delivery formed the waiting list comparison group and undertook the programme after the 12-month trial outcomes had been completed. Those allocated to the February to April 2012 delivery did not participate in the trial.
Our multifaceted recruitment strategy was informed by the feasibility study, which suggested that club-based strategies were likely to be most effective and that men may need multiple prompts before signing up. 32 Box 1 lists the various strategies we adopted to recruit the numbers needed over a very limited time period. Club-based recruitment included advertisements on SPL, club and fans websites, in-stadia advertising (poster/flyers with endorsement from club personalities), active involvement of local supporters’ organisations, advertisements in the club and Scottish Football Association e-newsletters. We also employed fieldworkers to approach potentially eligible men on match days to ask if they would like to register an interest in FFIT. Between 16 July and 17 September 2011, our recruitment staff attended 25 pre-season ‘friendlies’, early-season home games and club open days.
Posters/flyers with endorsement from club personalities; end of season home match advertising (except at Hibernian); active involvement of local supporters’ organisations (Kilmarnock, Motherwell, Hibernian, Hamilton and Aberdeen).
Online publicity including SPL website, club websites, fan websites, some club e-newsletters.
Publicity in media NewspapersLocal papers: Evening Telegraph, 3 May 2011; The Courier, 6 May 2011; Evening Times, 31 May 2011; Paisley Daily Express, 18 May 2011; and The Inverness Courier, 9 September 2011.
National papers: The Sunday Times, 17 April 2011; Daily Record, 13 June 2011; Sunday Post, 10 July 2011; Metro, 11 July 2011; and Daily Record, 11 July 2011.
TV and radio coverageBBC Radio Scotland: John Beattie show, lunchtime, 2 May 2011; Call Kay, morning, 17 June 2011; ‘On the Ball’, 18 June 2011; FFIT documentary, 18 June 2011 and 9 July 2011; STV: The Hour, teatime 17 May 2011.
Workplace advertisingLocal councils: Perth and Kinross, Glasgow City, North, South and East Ayrshire, North Lanarkshire and Highland.
Other employers: Glasgow Benefits Office, Wiseman’s dairies, HBOS, Clydesdale Bank, Scottish Qualifications Authority, Her Majesty’s Inspectorate of Education, Thomas Cook, Mahle (Kilmarnock), Aviva, BP, Longannet Power Station, Dell Scotland, HP Scotland, Microsoft Scotland, Oracle, Scottish Business in the Community, Scottish Enterprise, all companies at City Park in Glasgow, Morris and Spottiswood and Adecco (Scotland).
OtherFFIT Facebook® (Facebook, Inc., Menlo Park, CA, USA) page, FFIT website (www.spl-ffit.co.uk), FFIT participant online diary February to June.
BBC, British Broadcasting Corporation; BP, British Petroleum; HBOS, Halifax Bank of Scotland; HP, Hewlett Packard; STV, Scottish Television.
We made a concerted effort to achieve media coverage. We were successful in attracting articles in local and national newspapers (see Box 1), a video blog filmed by a British Broadcasting Corporation (BBC) Scotland sports presenter who took part in one of the pilot deliveries of FFIT, a 1-hour-long documentary on BBC Radio Scotland and interviews with members of the research team and participants in the pilot FFIT programme on Radio Scotland and Scottish Television. As part of our recruitment drive, we ran a five-a-side tournament for ‘graduates’ of the pilot FFIT programme on 18 June 2011 at St Mirren’s home stadium, which formed an excellent focus for some of this publicity. We invited the BBC to contribute a team (made up of sports presenters and three former Scottish international football players) to participate and this event was the focus of live coverage on BBC Radio Scotland’s ‘On the Ball’ football programme. It is possible that articles and events attracted other media coverage that we were not aware of during the recruitment period.
Other strategies included e-mails to staff through local employers (see Box 1) and word of mouth. Men who took part in the pilot FFIT programme told their family, friends and work colleagues about the programme and some also put up leaflets in their workplaces. An incentive (a £50 football club shop voucher) was offered to the FFIT graduate who generated the highest enrolment rate of eligible men in the FFIT study.
All publicity invited men to contact the research team by short message service (SMS) text, e-mail or telephone to register their interest in the study by providing their contact details and self-reported weight, height, trouser waist size and date of birth. They were also asked where they heard about the study. Men who gave their name to recruitment staff on match days were subsequently telephoned by the research team to confirm their interest in the study and to collect full contact and self-report information. All men whose self-reported BMI (calculated from self-reported weight and height) and age suggested they were eligible for the study were invited to participating club stadia for formal eligibility assessment.
Participants
Men were eligible if they:
-
were aged 35–65 years in 2011/12
-
had an objectively measured BMI of at least 28 kg/m2
-
completed the Physical Activity Readiness Questionnaire (PAR-Q)37
-
consented to randomisation and
-
consented to weight, height and waist measurements (this was a requirement for taking part in the FFIT programme imposed by Scottish Government, irrespective of the trial).
The age limits reflect recognition that overweight and obese men in their mid-to-late thirties may experience an attitudinal shift towards their health and weight,38 and focusing on men in the middle years can maximise the potential effectiveness of lifestyle interventions. 39 The older age limit reflects opinions that for those over the age of 65 years, physical activity programmes may be more effective when targeted specifically.
The decision to include only men with a BMI of at least 28 kg/m2 was made for three reasons. First, we had previously reported the power for men of being told that they were ‘obese’ as a motivator for them to want to lose weight40 and that those labelled ‘overweight’ were more likely to challenge the validity of BMI categories. 41 We thought that ‘approaching obese’ would be similarly motivational. Second, men with a BMI of at least 28 kg/m2 would also be more likely to benefit from weight loss. Third, in our feasibility study we had found that men liked being with others with similar weight loss goals. 28
The PAR-Q is a self-screening tool to help identify those who should seek medical advice prior undertaking exercise. If any of the men had answered ‘yes’ to any of the seven questions, fieldwork staff were instructed to recommend that men consulted their general practitioner (GP) prior to commencing the FFIT programme. Although answering ‘no’ to all questions was not an inclusion criterion for FFIT, with participants’ permission, copies of the PAR-Q forms were given to the community coaches so that they could check whether or not men had any pre-existing medical conditions and help the men exercise appropriately.
Because of the SPL Trust’s whole-hearted commitment to collaborating in a rigorous evaluation of FFIT, it was not possible for eligible men to access the FFIT programme unless they agreed to be randomly allocated to any one of the three programmes starting in September 2011, February 2012 or September 2012.
The SPL Trust also required participants to consent to weight, height and waist measurements, but men were free to opt out of additional measures/procedures relating to the trial’s secondary and process outcomes. Men were excluded if they had participated in FFIT previously.
If men’s blood pressure, as measured at baseline, contraindicated vigorous exercise (systolic ≥ 160 mmHg and/or diastolic ≥ 100 mmHg), they were initially able to take part in the classroom sessions only and the incremental, pedometer-based walking programme; they were advised that they would be able to take part in more intense in-stadia training once they had provided coaches with evidence of a reduction in their blood pressure.
Interventions
All men measured at baseline were informed of their weight and BMI, given a British Heart Foundation booklet, So You Want to Lose Weight?, which offered detailed advice on weight management,42 were advised to see their GP if baseline readings for blood pressure exceeded pre-specified levels, and met the coaches, who talked broadly about the FFIT programme and gave information of the timing of the programme at their club.
The FFIT programme was developed and optimised during our feasibility study and the content of the programme is described in detail elsewhere. 28 The programme adheres strictly to national guidance for weight management programmes. 5,43 The behavioural aspects of the programme were not based on any single theory of behaviour because, as Michie et al. 44 suggest, single theories contain so many overlapping constructs that there is no good basis for deciding which would be appropriate. Here we briefly describe the way in which the programme was gender sensitised, its dietary and physical activity components, the evidence-based BCTs45 used, the format through which it was developed and the training delivered to coaches.
Gender sensitivity
The FFIT was designed to work with, rather than against, prevailing conceptions of masculinity28,31,34 and gender sensitised in relation to the context, content and style of delivery. 31 The traditionally male environment of football clubs and men-only groups led by club community coaches provided a masculinised context for the delivery of key messages.
The programme content was developed to be attractive to men. It provided information on weight loss presented simply (‘science but not rocket science’), included a separate session on alcohol reinforced by demonstration of the size of units and discussion of alcohol’s potential role in weight management, and provided men with a physical representation of the amount of weight lost to date at week 7 for them to hold. In addition, materials ‘branded’ with club insignia were provided; for example, T-shirts in their club colours and with the FFIT logo were provided for men to wear when attending the programme and the programme notes were branded with club-specific insignia.
Finally, the style of delivery of the programme was participative, with coaches facilitating interactive learning through discussion of key points and encouraging camaraderie, ‘team bonding’ and ‘banter’ to facilitate discussion of sensitive subjects.
Dietary components
The dietary component of FFIT was designed to deliver a 600-kcal daily deficit (from estimated daily energy requirements)5,46 through the gradual adoption of more nutrient-dense foods and reduction of portion size, particularly of energy-dense foods, as well as the reduction of snacks, sugary and alcoholic drinks. Classroom activities were aimed at encouraging participants to make dietary changes that suited their individual circumstances and eating preferences, to weigh themselves each week and to keep a personal record of their weekly weight loss. Men were encouraged to make changes to their diet informed by the recommended balance of food groups indicated in the ‘Eatwell Plate’47,48 and make small, gradual and achievable changes to their normal diet. Key messages for dietary habits indicated in Cancer Research UK’s ‘ten top tips’49 were highlighted as the men moved towards a programme to maintain weight loss in the longer term.
Physical activity components
The FFIT had two physical activity components: an incremental pedometer-based walking programme shown to increase physical activity50,51 and pitch-side physical activity sessions led by club community coaching staff.
The men set individual daily brisk walking goals and recorded their progress each week in step count diaries provided in programme notes and reported back to the group during the weekly classroom sessions. Our feasibility work had shown that the walking programme was highly acceptable to men; participants described the pedometers as a very useful technology for motivation, self-monitoring and goal setting. In addition, the men reported finding they (re)gained fitness quickly through walking, which in turn enabled them to participate in other forms of physical activity that they also enjoyed (such as playing football). 31 As the programme progressed, they were encouraged to supplement walking with more vigorous activity (e.g. gym membership).
The pitch-side physical activity sessions taught men how to increase fitness through structured activities. Training was tailored to individual fitness levels and ability and included aerobic (e.g. walking, stair climbing, jogging), muscle strengthening (e.g. weight/circuit training) and flexibility (e.g. warm-up/cool-down activities) exercises. 52 Participants were taught to use the rating of perceived exertion (RPE) scale to ensure their activity was appropriate for their own fitness level and was performed at moderate intensity. The men were encouraged to consider how they could continue these activities in community settings using community resources, to continue to meet to train together post programme and to avoid compensatory behaviours (e.g. increased snacking or television viewing) that can undermine weight loss following physical activity. 53,54
Behaviour change techniques
Using the BCTs Taxonomy v1,45 37 specific BCTs are used in FFIT. 28 However, the programme draws most heavily on self-monitoring, implementation intentions, goal setting and review, and feedback on behaviour, all of which are associated with control theory55 and have been shown to be effective in physical activity and healthy eating interventions. 56–58 The programme also encourages social support, which has been shown to be effective in weight loss interventions57 and relapse prevention strategies. Further key techniques used in FFIT draw on other theoretical accounts of behaviour change (e.g. social cognitive theory and self-regulation)59 and include information on consequences, identification of barriers to change, verbal persuasion about capability, instruction in performing new behaviours, graded tasks to encourage increases in self-efficacy and social comparison.
Format of the programme
The FFIT was delivered free of charge by community coaching staff, employed by individual clubs and trained to standard protocols, to groups of up to 30 overweight/obese men (participant to coach ratio of 15 : 1) over 12 weekly sessions at the club’s home stadium. Each 90-minute session combined advice on healthy diet with physical activity. The balance of classroom and physical activity sessions changed over the 12 weeks; later weeks focused more on physical activity as men became fitter and the classroom element was shorter and focused on revision. 28 A club-branded information booklet (including tables to record self-monitored weight loss and step counts) was given to each participant.
Based on evidence from previous group-based physical activity programmes,60,61 we encouraged coaches to create a welcoming, supportive climate from the outset to encourage group cohesion. This included sharing some of their own experiences and allowing plenty of time for group interactions. Delivery notes reminded them which key tasks to deliver each week (summarised in Table 1). Nevertheless, the programme was cumulative in that each week built on what had been learnt in previous weeks and there was repeated practice of BCTs such as goal setting, self-monitoring and action planning with interactive problem-solving. Coaches were available at the end of each session if any man wanted to discuss issues individually.
| Session | Number of key tasks per session |
|---|---|
| Session 1. Getting started | |
| KT1. Introduce men to aim of programme ‘how to eat better, be more active and stay that way in the long term’ | 5 |
| KT2. Getting to know one another and sharing ideas and experiences | |
| KT3. Influences on choosing what to eat and control over food and eating | |
| KT4. Energy balance (intake vs. output) | |
| KT5. Food diary homework | |
| Session 2. What are we eating? | |
| KT6. Explanation of food groups and eating a healthy diet using Eatwell Plate (less fatty and sugary foods, more fruit and vegetables, whole-wheat bread and pasta and brown rice) | 3 |
| KT7. Food diaries compared with healthy eating recommendations and smaller portions | |
| KT8. SMART goal setting introduced | |
| Session 3. Making changes | |
| KT9. Review of SMART goals | 6 |
| KT10. Avoiding compensation | |
| KT11. Example of individualised healthy eating plans | |
| KT12. Health benefits associated with 5–10% long-term weight loss | |
| KT13. Personal weight loss targets | |
| KT14. Importance of support from others | |
| Session 4. Thinking about physical activity | |
| KT15. Review of SMART goals | 4 |
| KT16. Health benefits of physical activity | |
| KT17. Overcoming barriers to physical activity | |
| KT18. Local amenities for physical activity | |
| Session 5. Thinking about drinking | |
| KT19. SMART goal setting | 5 |
| KT20. Alcohol and weight gain | |
| KT21. Alcohol units | |
| KT22. Planning your drinking | |
| KT23. Cutting down on sugary drinks (fizzy and tea/coffee) | |
| Session 6. Halfway down | |
| KT24. Stages of change | 3 |
| KT25. Introduction to setbacks and strategies for dealing with them | |
| KT26. Measurements taken to review progress | |
| Session 7. How are we doing? | |
| KT27. Physical representation of individual weight loss to date (e.g. sandbag) | 3 |
| KT28. SMART goals and weight loss reviewed | |
| KT29. Reflection on how things are going so far | |
| Session 8. What to look out for | |
| KT30. Understanding food labels and choosing healthier foods | 2 |
| KT31. Importance of regular meals and breakfast | |
| Session 9. Practical stuff | |
| KT32. Making favourite meals healthier | 3 |
| KT33. Eating out sensibly | |
| KT34. Damage limitation for takeaways | |
| Session 10. Myths and moods | |
| KT35. Common ideas about healthy living | 3 |
| KT36. Triggers for setbacks and how to avoid them | |
| KT37. SMART goals reviewed | |
| Session 11. Making progress? | |
| KT38. Food diaries revisited | 3 |
| KT39. The energy balance and eating plans revisited | |
| KT40. Locus of control revisited | |
| Session 12. Looking forward | |
| KT41. Review of progress and next steps | 2 |
| KT42. Final measurements taken and recorded | |
| Total number of key tasks in the 12-week programme | 42 |
The 12-week active phase was followed by a ‘light-touch’, weight maintenance phase with six post-programme e-mail prompts over 9 months and a group reunion at the club 6 months after the end of the weekly sessions. E-mail prompts were designed to be easy to deliver and did not require coaches to interact with participants; however, this meant that they were largely passive and consisted of periodic reminders to enact some of the behavioural skills learnt on the programme. Table 2 provides some more detail of their content.
| Content | BCT reminded to use | |
|---|---|---|
| 1 | Football Fans in Training: how’s it going? | |
| Restatement that coach enjoyed working with them and hopes they are keeping the weight they lost off and keeping up lifestyle changes | Self-monitoring of behaviour and outcome of behaviour; goal setting for behaviour and goal setting for outcome; problem-solving | |
| Reminder to weigh themselves weekly or daily; to continue to monitor daily activity; to plan for set-backs and to remember to use SMART goals if going off-track | ||
| 2 | Football Fans in Training: still going well? | |
| Reminder to check current step count and consider whether or not it was as high as at the end of the programme | Discrepancy between current behaviour and goal; action planning; social support/encouragement | |
| Suggested ways to increase if not as high | ||
| Recommend getting in touch with others who had done FFIT via Facebook® (Facebook, Inc., Menlo Park, CA, USA) site to help get active again | ||
| 3 | Football Fans in Training: still on target? | |
| Reminder to check 5–10% weight loss target from baseline and current weight. Reminder of health benefits of losing weight | Goal setting for behaviour and outcome; discrepancy between current behaviour and goal; health consequences | |
| Reminder to set some SMART goals for eating well if off-track and suggested ways to make small dietary changes | ||
| Reminder that they will be meeting up again for 9-month reunion in club and will see other guys to discuss how will be doing | ||
| 4 | Football Fans in Training: looking forward | |
| Restatement that coach enjoyed seeing some people at 9-month reunion and reminder to keep in touch with other guys for support | Social support/encouragement; goal setting for behaviour and outcome | |
| Reminder to check their progress, set some goals if not achieving them and check their confidence to achieve goals | ||
| 5 | Football Fans in Training: reflecting on progress | |
| Reminder to check whether eating and exercise routines are still healthy and make SMART goals if no longer on track, reminder that has been successful in past and that has skills to be so again. Suggestion that other men have used use if-then plans to plan for difficult situations | Focus on past success; verbal persuasion to boost self-efficacy; goal setting for behaviour and outcome; problem-solving | |
| 6 | Football Fans in Training: FFIT for life? | |
| Consider how many ‘top tips for weight loss’ still use. Reminder to use SMART goals to achieve them if not using. Information about some people has found FFIT to be life changing. Good luck for future | Goal setting for behaviour and outcome | |
The 9-month reunion meeting was designed to allow men to share experiences of successes and difficulties in maintaining weight loss post FFIT, set new specific, measurable, achievable, realistic, time-limited (SMART) goals and take part in a group physical activity session.
Coach training
Coaches received group-based training over 2 days and detailed delivery notes. Within these notes, separate sections for each week of the programme described the ‘key tasks’ for the session (see Table 1), the equipment and preparation required, a suggested order of activities and the detailed content for that session. The coaches’ delivery notes incorporated and cross-referenced to the participant notes.
The length of the training was limited by the availability of the coaches. It was delivered face to face in a central location (although some coaches still had to travel for up to 4 hours to attend) and took place over a period of 2 days, timed to fit in the training around a full programme of other activities.
The aim of the training was to foster full competence in delivering the programme and a sense of ownership of the delivery of the programme in their own club while adhering to the delivery of key tasks. Training was designed to build on coaches existing strengths, to teach them how to deliver each element of the programme and how to use their existing skills to create a positive, welcoming climate. Training was interactive to allow coaches to discuss their experience of delivering each component and exchange practical tips. It highlighted key elements of the programme (the use of pedometers, the Eatwell Plate, the alcohol session, the ‘key tasks’ for each week) and emphasised the importance of applying BCTs, in particular self-monitoring, goal setting and action planning and relapse prevention; personalisation of each element of the programme to suit individual men’s abilities and circumstances; and encouraging mutually supportive interaction between participants.
The delivery of the programme, but not its core components, had to be flexible to allow coaches to adapt the programme to suit their club’s facilities, their own skills set, the limitations and abilities of the specific men enrolled on their programme and external factors such as the weather, the rearrangement of club match fixtures or the timing of the recommended ‘guest appearance’ of a club celebrity (recommended for week 6) to suit the club celebrity’s diary. Coaches were also encouraged to respond to group interactions and queries while ensuring that the key tasks in each session were covered.
In relation to physical activity, coaches were encouraged to use their own experience and the facilities available within their club to devise interesting and varied physical activity sessions. The training included a practical session in which coaches shared and demonstrated ideas about how to adapt flexibility, cardiac fitness and strength exercises for overweight, potentially very unfit men. Coaches were instructed that they should reinforce the use of the RPE scale in every session,62 to ensure that men were exercising at a moderate intensity level.
The coach and participant notes have been made available for others’ use. These can be requested from the FFIT research website, which can be accessed at www.ffit.org.uk. 63
Aim and objectives
The aim of this study was to determine whether or not FFIT, a gender-sensitised, weight loss, physical activity and healthy living programme delivered in SPL football clubs, can help men aged 35–65 years with a BMI of at least 28 kg/m2 achieve a reduction in body weight that is at least 5% more than any reduction seen in the comparison group 12 months after the start of their participation in FFIT.
Three further objectives related to the investigation of secondary, health economic and process outcomes:
Secondary outcomes to investigate whether or not involvement with FFIT:
-
reduces body weight by at least 5% at 12 weeks
-
reduces waist circumference and percentage body fat at 12 weeks and 12 months
-
increases physical activity and reduces sedentary behaviour at 12 weeks and 12 months
-
improves eating habits at 12 weeks and 12 months
-
reduces alcohol consumption at 12 weeks and 12 months
-
reduces blood pressure at 12 weeks and 12 months
-
increases positive affect and self-esteem, and improves quality of life (QoL) at 12 weeks and 12 months.
We also examined the difference in area under the trend line of weight loss from baseline to 12 months as a measure of the effect of the intervention across all time periods.
Cost-effectiveness to investigate whether or not FFIT has the potential to provide a cost-effective use of resources.
Process outcomes to investigate:
-
programme reach
-
participants’ reasons for continuing with or opting out of FFIT
-
the extent to which coaches deliver FFIT as designed
-
participants’ views of FFIT: including satisfaction, acceptability and any unexpected outcomes
-
coaches’ experiences of delivering FFIT: including satisfaction, acceptability and any unexpected outcomes
-
participants’ experiences of maintaining weight loss and lifestyle changes in the longer term.
Under Procedures below, we report on the measures and processes of data collection for primary and secondary trial outcomes. Chapter 3 reports the results of the trial, Chapter 4 reports the economic analyses, including methods and results, and Chapter 5 reports process outcomes.
Outcome assessment
Outcome measures are set with reference to National Obesity Observatory guidance for the evaluation of weight management interventions. 64
Primary outcome
The primary outcome was mean difference in weight loss between groups at 12 months, expressed as absolute weight and as a percentage.
Secondary outcomes
-
Weight loss at 12 weeks.
-
Reduction in waist circumference and body fat at 12 weeks and 12 months.
-
Physical activity: changes in self-reported frequency and duration of walking, moderate activity, vigorous activity and sedentary behaviour over the last 7 days at 12 weeks and 12 months as measured by the International Physical Activity Questionnaire (IPAQ) Short Form. 65
-
Eating habits: changes in self-reported intake of key contributors to weight gain (e.g. fast foods, chocolate bars, chips, pies, sugary drinks), expressed as estimated intake of fatty foods, sugary foods and fruit and vegetables at 12 weeks and 12 months.
-
Changes in self-reported alcohol consumption over the last 7 days at 12 weeks and 12 months measured using an alcohol diary over a week66 and expressed as units of alcohol per week.
-
Reduction in resting blood pressure at 12 weeks and 12 months.
-
Psychological outcomes: (1) changes in positive and negative affect as measured by the Positive and Negative Affect Schedule (PANAS),67 (2) changes in self-esteem as measured by the Rosenberg Self-Esteem (RSE) scale68 and (3) changes in health-related quality of life (HRQoL) as measured by the Short Form questionnaire-12 items (SF-12),69 all at 12 weeks and 12 months.
-
Difference in area under the trend line of weight loss from baseline to 12 months.
Procedures
Timing of measurements
Outcomes were measured at baseline, 12 weeks and 12 months according to the measurement schedule shown in Table 3. Demographic characteristics were measured at baseline. Copies of the questionnaires are available on request.
| Time | Demographic characteristics | Height | Weight | Waist | BMI | Blood pressure | Modified DINE questionnaire | IPAQ | Self-reported alcohol | PANAS | RSE scale | SF-12 and resource use |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| 12 weeks | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| 12 months | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
The fieldwork team
Data were collected by teams of fieldworkers, educated at least to degree level. Each team in each measurement session had a designated team leader and a fieldwork nurse responsible for blood pressure measurement. Staff were trained to standard measurement protocols by experienced research and survey staff in the Medical Research Council (MRC)/CSO Social and Public Health Sciences Unit. Training took place over 2 days and emphasised strict adherence to protocol to minimise detection bias. Field staff wore T-shirts branded with FFIT research logos at all measurement sessions. Figure 1 illustrates the measurement team spirit that was encouraged.
FIGURE 1.
Fieldwork team arriving at a 12-month in-stadia measurement session.

Baseline data
All men who had registered an interest in FFIT prior to the baseline measures in their club (and whose self-reported BMI and date of birth suggested they were eligible to take part) were sent a letter of invitation to attend an appointment at an in-stadia measurement session at their club. They were asked to confirm or rearrange their appointment date and time by e-mail or telephone. Eligibility criteria were confirmed through objective measurement of height and weight.
Outcome measurement
The 12-week measures
The intervention group 12-week measurements were taken around the time of the final FFIT programme session. We telephoned participants to make appointments and sent written reminders in advance by e-mail or letter according to the individual’s preference. Men who did not attend the stadia for these measurements were telephoned to arrange individual measurements at home.
Men who had dropped out of the FFIT programme were invited to the measurement sessions by telephone and, if that was difficult for them, they were offered a home visit for measurement. Any men who had dropped out of the programme, and men in the comparison group, were offered travel expenses and a £20 club shop gift voucher in appreciation of their time. FFIT intervention group participants were not offered a club gift voucher because their 12-week measurements followed on immediately after the programme completed, but they were offered travel expenses if the made a special journey to take attend the 12-week measurements.
To avoid risk of contamination, 12-week in-stadia measurements for the comparison group were held on a different evening from the intervention group measurement sessions.
The 12-month measures
The 12-month measurement sessions for both groups were held at club stadia. To maximise retention at 12 months, the men were (1) sent an advanced reminder that follow-up measurements were imminent, using a personalised letter sent 4–5 weeks ahead of the measurement dates at their club; (2) telephoned within a fortnight of the reminder letter to arrange a personal appointment time; (3) sent an e-mail (or letter) around a week before their appointment and a SMS text reminder the day before; (4) offered a home visit if attending the stadium was difficult; and (5) offered a £40 club voucher to thank them for their time.
Measurement protocols: objectively measured outcomes
Weight (kg) was recorded using electronic scales (Tanita HD 352™, Middlesex, UK) with participants wearing light clothing, no shoes and with empty pockets. Height (cm) was measured without shoes using a portable stadiometer (Seca Leicester™, Chino, CA, USA). Waist circumference was measured twice (three times, if the first two measurements differed by 5 mm or more) and the mean of all recorded measurements calculated. Resting blood pressure was measured using a digital blood pressure monitor (Omron HEM-705CP™, Buckinghamshire, UK) by a fieldwork nurse. All equipment was calibrated prior to fieldwork.
Measurement protocols: outcomes based on self-report
Participants completed self-administered questionnaires. Fieldworkers assisted any participant who appeared to have literacy problems and, whenever possible, checked questionnaires before the participant left the measurement session to minimise missing data.
Measurement of adverse events
An adverse event was defined as any injury or newly diagnosed health condition (e.g. high blood pressure, diabetes mellitus) that occurred while a man was registered on the FFIT programme, whether or not it was related to his participation in FFIT. A serious adverse event was defined as an adverse event that included at least one of the following: an event requiring hospitalisation or prolonged medical attention, an event that is immediately life-threatening (such as a cardiac arrest), a fatal event. Any serious adverse events were reported immediately to the chairperson or the Trial Steering Committee. A report of all adverse events was provided at every meeting of the Data Monitoring and Ethics Committee.
At the baseline and 12-week measurements, men were given a pre-paid postcard and details about how to report any adverse events. In addition, coaches (and the researchers who conducted the observations of the programmes) were also asked to report any adverse events that came to their attention. At the 12-month measurements, all participants were asked whether or not they had experienced any adverse events since their last contact with the research team.
All adverse events were categorised by a member of the research team according to their severity and whether or not they were related to participation in FFIT. When possible, serious adverse events and any adverse events for which relatedness to participation in FFIT was not clear were followed up by a telephone call to the participant. Adverse events that occurred before the baseline measurement period or after the August to December 2012 delivery of FFIT had started were not recorded.
Preparation of self-reported variables for analysis
Physical activity
Following standard procedures described in the IPAQ scoring protocol,70 we calculated and reported sedentary time, and metabolic equivalent (MET) minutes per week from self-reported walking, vigorous and moderate exercise and a measure of total MET minutes.
Diet
We used the adapted Dietary Instrument for Nutrition Education (DINE) questionnaire to collect data on self-reported frequency of intake of different food types and the dietary question referred to the last 7 days. The full DINE questionnaire can take a considerable time to complete and can be difficult for some participants. Recent evidence on dietary factors influencing weight gain highlights items not included in the tool (e.g. sugary drinks); therefore, we adapted the DINE questionnaire to reduce participant burden and capture information on additional relevant markers. From these data, we calculated a fatty food score, a fruit and vegetable score and a sugary food score.
Description of items included in the adopted Dietary Instrument for Nutrition Education questionnaire
Participants reported how many times (over the last 7 days) they had consumed a serving of cheese, beef burgers or sausages, beef, pork or lamb, fried food, chips, bacon or processed meat, pies, quiches or pastries, crisps and fast food. We also asked about the amount of milk used in a day (for drinking or in cereal, tea or coffee) and what kind of milk is usually used (full cream, semi-skimmed or skimmed). They also reported how many times a day they had consumed fruit and vegetables, chocolate or sweets, and biscuits and sugary drinks (fizzy drinks, diluting juice or fruit juice).
Scoring food frequencies
Food frequency categories differed for different food types and we converted the DINE questionnaire food frequency categories as described in Table 4.
| Food type | Scoring of frequencies |
|---|---|
| Cheese, beef burgers or sausages, beef, pork or lamb, chips and fried food | 0 times = 1 |
| 1–2 times = 2 | |
| 3–5 times = 6 | |
| ≥ 6 times = 9 | |
| Pies, quiches and pastries | 0 times = 1 |
| 1–2 times = 2 | |
| 3–5 times = 5 | |
| ≥ 6 times = 8 | |
| Bacon or processed meat and crisps | No times = 1 |
| 1–2 times = 2 | |
| 3–5 times = 5 | |
| ≥ 6 times = 6 | |
| Milk amount | Less than one-quarter of a pint = 1 |
| About one-quarter of a pint = 2 | |
| About half a pint = 3 | |
| ≥ 1 pint = 4 | |
| Sugary drinks | Less than once = 1 |
| 1–2 times = 2 | |
| 3–5 times = 3 | |
| ≥ 6 times = 4 | |
| Biscuits, chocolate and sweets | Less than once = 1 |
| 1–2 times = 2 | |
| 3–5 times = 4 | |
| ≥ 6 times = 6 | |
| Fruit and vegetables | Less than once = 0.5 |
| 1–2 times = 1.5 | |
| 3–5 times = 4 | |
| ≥ 6 times = 6 |
Alcohol intake
Following Emslie et al. ,66 we converted responses to the 7-day recall diary for alcohol to standard units equivalent to 8 g of pure alcohol (half a pint of ordinary beer, lager or cider, one small glass of wine and one measure of spirits each contain 1 unit of alcohol). We calculated total number of units reported in the last week.
Psychological outcomes
Scores for both the RSE scale and the short form of the PANAS were normalised so that values could be calculated for participants who had missed one or two items contributing to each scale. The PANAS-normalised scale scores range from 1 to 5, with higher scores indicating higher negative affect and higher positive affect. Similarly, higher scores on the RSE scale (normalised range 0–3) indicate better self-esteem.
Scores on QoL using the SF-12 were summarised scores for mental and physical health following standard algorithms. 69
Changes to outcomes after trial commencement
The protocol stated that the secondary outcomes of weight loss at 12 weeks and reduction in waist circumference and body fat at 12 weeks and 12 months would be reported as percentages. To be consistent with best statistical practice71 these were reported as absolute differences. All changes made, together with their rationale, are summarised in Table 5.
| Original outcome as expressed in the protocol | Changed outcome | Rationale for change |
|---|---|---|
| Percentage weight loss at 12 weeks | Weight loss at 12 weeks | To be consistent with best statistical practice, which recommends reporting absolute differences |
| Percentage reduction in waist circumference and body fat at 12 weeks and 12 months | Reduction in waist circumference and body fat at 12 weeks and 12 months | |
| Eating habits: changes in self-reported intake of key contributors to weight gain (e.g. fast foods, chocolate bars, chips, pies, sugary drinks) at 12 weeks and 12 months using questions adapted from the DINE questionnaire | Eating habits: we calculated dietary intake scores for fatty food, sugary food and fruit and vegetables | There were 17 separate variables included in our adapted DINE questionnaire; to reduce reporting burden we summarised these into three scores indicative of healthy changes that men could have made to their diets |
| Changes in self-reported alcohol consumption over the last 7 days at 12 weeks and 12 months measured using an alcohol diary over a week and expressed as units of alcohol per week, and changes in football-associated alcohol consumption | Changes in self-reported alcohol consumption over the last 7 days at 12 weeks and 12 months, measured using an alcohol diary over a week and expressed as units of alcohol per week | On reflection we realised that the questions we had developed to assess football-related alcohol intake lacked external validity and we focused our analysis only on total alcohol consumption |
Sample size
The study was powered to detect a 5% mean difference in percentage weight loss between the intervention and comparison groups at 12 months, with standard deviation (SD) of 19.9%, 80% power and a two-sided significance level. A total of 250 men were required in each trial arm and based on our feasibility study,32 the sample size was inflated to 360 men in each arm to allow for 30% attrition.
Randomisation
Following baseline measurement the randomisation sequence was generated by the Tayside Clinical Trials Unit (TCTU) statistician using SAS (v 9.2; SAS Institute Inc., Cary, NC, USA), blocked (block size between two and nine depending on how many participants were recruited at a club) and stratified by club. The allocation sequence was sent in a password-protected file to a database manager (not part of the research team) who assigned individuals to each group. All those allocated to the intervention group were telephoned within 3 weeks of baseline measurements at each club to notify them of their allocation and the date, time and place of the first FFIT session. This was confirmed in writing. Those allocated to the waiting list comparison group were informed of their allocation by letter and given information about when they should expect to hear from the research team over the following 12 months. They were reassured that they had a guaranteed place on the FFIT programme in their club commencing August/September 2012.
Blinding
To blind the measurement of the primary outcome at the 12-month measurement, session weight was the first measure taken and was taken by fieldworkers employed only for 12-month measures (and who, therefore, had not met the men before), who were trained to minimise interaction with men until weight had been recorded and was in a screened-off area to prevent interaction with others. Blinding for other measures was not possible.
Statistical methods
All analyses were conducted as intention to treat on randomised participants, with all available data in mixed models as recommended by White et al. 72 All outcome variables were continuous. If the distribution was not normal, we carried out a logarithmic transformation to achieve normality and results comparing intervention with comparators were subsequently expressed as the ratio of geometric means (RGM) with corresponding 95% confidence interval (CI). We used multiple linear regression for all analyses and baseline measure, group allocation and club (to allow for stratification by club) were included as fixed effects in adjusted models.
To assess whether or not the intervention effect on the primary outcome and four selected secondary outcomes differed between subgroups of the study population we conducted pre-specified subgroup analyses by adding allocation group by subgroup factor interaction terms to the models. 73 The four selected secondary outcomes were total MET minutes/week, fatty food score, sugary food score and positive affect. Potential moderating variables were age, marital status, Scottish Index of Multiple Deprivation (SIMD) from postcode of residence, location of measurement (stadium vs. home), orientation to masculine norms, affiliation to football, whether or not attended a formal weight management programme in the last 3 months, smoking, housing tenure, education, ethnicity, employment status, joint pain, injuries and limiting long-standing illness (LSI).
Changes are presented as mean (95% CI) unless otherwise specified.
We conducted sensitivity analyses for the primary outcome (1) multiple imputation for missing data assuming data missing at random,72 (2) added club as a random variable to account for possible clustering74 and (3) repeated measures analysis using results from both 12 weeks and 12 months.
All analyses were conducted using SAS (v 9.3; SAS Institute Inc., Cary, NC, USA) by the TCTU statistician who was blinded to group allocation.
Changes to protocol
There were no changes to protocol except those concerned with the way that outcomes were expressed. See Table 5.
Public involvement
Extensive public engagement was built into the development of the FFIT intervention and the evaluation design. This principally involved ongoing engagement during the programme development phase with key stakeholders (the SPL Trust, the football clubs and the programme delivery funders) and consultation with men who took part in the first pilot deliveries of FFIT at 11 clubs in the 2010–11 football season. Input from the coaches, the SPL Trust and the target group of men thus all fed directly into the final shaping of the intervention and the research design.
Representatives of the SPL Trust were actively involved throughout the development of the delivery protocol for the pilot FFIT programme. Following these initial meetings, we also met with community managers from the football clubs who would be involved in the pilot programme prior to the finalisation of the pilot delivery protocol. These meetings allowed the community managers to input into the programme design and to discuss the importance of undertaking a programme that was evidence based and generalisable, and of gathering gold standard evidence of its effectiveness by conducting an evaluation using a randomised design. We also met with the coaches who were delivering the autumn 2010 pilot programme at a training workshop in October 2010 to ask for feedback on the initial sessions. At the end of the autumn 2010 delivery, we held in-depth interviews with coaches at the two clubs which took part in our pilot trial to obtain their views about the programme and research design and received written feedback from coaches at the other clubs. 28 In addition, CMG visited all clubs during spring 2011 to observe delivery sessions of the second pilot programme and to speak informally to the coaches and in April 2011 we fed back the emerging the pilot findings at a plenary meeting organised by the SPL Trust at the National Football Stadium, Hampden Park. All comments were carefully considered in the development of the final version of the FFIT programme that was delivered in the intervention arm of the trial as reported by Gray et al. 28
The views and experiences of the men who participated in the pilot deliveries also fed into the development of the intervention. All men taking part in the autumn 2010 pilot deliveries were asked to complete a programme evaluation form, which asked for their suggestions for changes. Men at the two clubs involved in the feasibility study also took part in focus groups following the autumn 2010 and spring 2011 pilot deliveries where they gave their views on the content of the programme and on the planned research procedures for the RCT. 28,32 In addition, when a reviewer of the grant application for this trial suggested that the evidence on men and health raised questions about whether or not men would engage with the pedometer-based walking programme, we undertook a series of semistructured telephone interviews (n = 27) with men from a number of clubs who had taken part in the autumn 2010 pilot deliveries, to ask them about their experience of this aspect of the programme. These interviews strongly reinforced our first hand experiences that men saw the pedometer-based walking programme as an appropriate way to begin to regain some fitness and (re-)engage with physical activity;31 furthermore, it demonstrated that this was a part of the programme that was highly valued by our target group (men aged 35–65 years with a BMI ≥ 28 kg/m2).
Participants in the pilot deliveries of FFIT in 2010/11 were also engaged in outreach work on FFIT prior to and during our intense period of recruitment to this trial. Many participated in various public engagement activities including the five-a-side football tournament held in June 2011 at St Mirren Football Club for ex-participants and a video diary made by a BBC journalist, Paul Bradley, who took part in the spring 2011 pilot FFIT programme, which illustrated week by week (each week being filmed at a different club) the atmosphere that the programme sought to foster in order to engage men. Throughout the summer of 2011 (July and August), participants from the pilot deliveries took part in TV, radio and newspaper interviews about their experiences of FFIT (including a 1-hour-long BBC Radio Scotland documentary about the programme that was first broadcast on 18 June 2011). They also played an active role in recruitment by telling their friends and family about the programme, advertising it in their workplaces and local community venues (e.g. libraries) and supporting fieldworkers during match day visits to home fixtures. In February 2012, a half-hour TV documentary on FFIT, which involved interviews with several participants from the autumn 2011 deliveries of FFIT (the intervention group in the trial), was screened on BBC 2 Scotland. Finally, in September 2013, representatives from each of the groups of men who undertook the intervention in autumn 2011 readily agreed to come to a bespoke event at Hampden Park to talk about their experiences of FFIT for future dissemination purposes, including the FFIT research website (www.ffit.org.uk). 63
Chapter 3 Results: the randomised controlled trial
Participant flow
Figure 2 shows participant flow through the trial. Of the 1231 men registering an interest during the recruitment period, 483 were excluded from the trial (101 decided against participation, 76 had a BMI < 28 kg/m2, 306 were allocated to the non-trial delivery of FFIT). Three hundred and seventy-four were randomly allocated to the intervention group and 374 to the comparison group. One comparison group participant subsequently withdrew and requested we destroy his data.
FIGURE 2.
Flow of participants through the FFIT RCT. a, After randomisation, one participant requested to have all of his data destroyed. Reprinted with permission from Elsevier (The Lancet, 2014, 383, 1211–21). 33

Recruitment
As described below (see Baseline data), formal recruitment commenced on 2 June 2011 (although preparations for recruitment had begun in anticipation of receiving the grant award) and continued until the week before the baseline measurements in each club, between 11 August 2011 and 20 September 2011. Figure 3 shows that recruitment started slowly, probably because in Scotland the 2010/11 season had closed and the 2011/12 season had yet to begin. As the clubs and media coverage geared up for the start of the season, and we were able to recruit men at games, recruitment speeded up so that we exceeded our target of 1110 men.
FIGURE 3.
Recruitment to the FFIT study from May to September 2011.

Baseline data
Table 6 shows baseline characteristics of participants (n = 747), including total self-reported MET-minutes per week. FFIT attracted men from across the socioeconomic spectrum, but few from ethnic minority groups.
| Variable | FFIT (n = 374) | Comparison group (n = 373) | Total (n = 747) |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Age (years) | 47.0 (8.07) | 47.2 (7.89) | 47.1 (8.0) |
| Ethnicity | |||
| White – British/Scottish/Irish/other | 367 (98.1) | 368 (98.7) | 735 (98.3) |
| Other | 5 (1.4) | 2 (0.5) | 7 (1.0) |
| Missing | 2 (0.5) | 3 (0.8) | 5 (0.7) |
| SIMD (% living in quintiles) | |||
| 1 (most deprived) | 65 (17.4) | 66 (17.6) | 131 (17.5) |
| 2 | 69 (18.4) | 62 (16.6) | 131 (17.5) |
| 3 | 62 (16.6) | 60 (16.0) | 122 (16.3) |
| 4 | 82 (21.9) | 84 (22.5) | 166 (22.2) |
| 5 | 89 (23.8) | 99 (26.5) | 188 (25.1) |
| Missing | 7 (1.9) | 3 (0.8) | 10 (1.3) |
| Employment status | |||
| Paid work | 322 (86.1) | 304 (81.5) | 626 (83.8) |
| Education or training | 3 (0.8) | 5 (1.4) | 8 (1.1) |
| Unemployed | 9 (2.4) | 18 (4.8) | 27 (3.6) |
| Not working due to long-term sickness or disability | 8 (2.1) | 8 (2.1) | 16 (2.1) |
| Retired | 14 (3.7) | 18 (4.8) | 32 (4.3) |
| Other | 17 (4.6) | 19 (5.0) | 36 (4.8) |
| Missing | 1 (0.3) | 1 (0.3) | 2 (0.3) |
| Education | |||
| No qualifications | 37 (9.9) | 34 (9.1) | 71 (9.5) |
| Standard Grades/Highers | 115 (30.8) | 126 (33.7) | 241 (32.3) |
| Vocational or HNC/HND | 133 (35.6) | 107 (28.7) | 240 (32.1) |
| University education | 75 (20.1) | 81 (21.7) | 156 (20.9) |
| Other | 14 (3.7) | 25 (6.7) | 39 (5.2) |
| Housing tenure | |||
| Owner-occupied | 280 (74.8) | 283 (75.8) | 563 (75.3) |
| Other | 94 (25.2) | 90 (24.2) | 184 (24.7) |
| Marital status | |||
| Married | 249 (66.6) | 269 (72.1) | 518 (69.3) |
| Living with partner | 55 (14.7) | 40 (10.7) | 95 (12.7) |
| Other | 70 | 64 | 134 |
| Objectively measured outcomes | |||
| Weight (kg) | 110.3 (17.9) | 108.7 (16.6) | 109.5 (17.3) |
| Waist circumference (cm) | 118.7 (12.3) | 118.0 (11.1) | 118.4 (11.7) |
| BMI (kg/m2) | 35.5 (5.1) | 35.1 (4.8) | 35.3 (4.9) |
| Body fat (% total weight) | 31.8% (5.7) | 31.5% (5.2) | 31.7% (5.5) |
| Missing | 7 | 3 | 10 |
| Blood pressure (mm/Hg) | |||
| Systolic blood pressure | 139.4 (17.6) | 141.2 (14.9) | 140.3 (16.3) |
| Diastolic blood pressure | 88.2 (10.3) | 89.5 (10.1) | 88.8 (10.2) |
| Missing | 0 | 2 | 2 |
| Participants with BMI < 30 kg/m2 | 35 (9.4) | 40 (10.7) | 75 (10.0) |
| Self-reported outcomes | |||
| Total MET-minutes/week | 1188 (396–2559) | 1173 (396–2559) | 1188 (396–2559) |
| Missing | 3 | 2 | 5 |
| DINE-based measures | |||
| Fatty food score (range 10–58) | 23.3 (7.1) | 23.4 (7.1) | 23.3 (7.1) |
| Fruit and vegetable score (range 1–6) | 2.3 (1.7) | 2.3 (1.7) | 2.3 (1.7) |
| Sugary food score (range 3-16) | 6.0 (2.7) | 6.2 (2.9) | 6.1 (2.8) |
| Total alcohol consumption (units per week) | 16.5 (17.4) | 17.0 (17.4) | 16.7 (17.4) |
| Self-esteem (normalised RSE score, range 0–3) | 1.1 (0.5) | 1.1 (0.5) | 1.1 (0.5) |
| Positive affect (normalised PANAS score, range 1–5) | 3.2 (0.7) | 3.2 (0.7) | 3.2 (0.7) |
| Missing | 1 | 0 | 1 |
| Negative affect (normalised PANAS score, range 1–5) | 1.7 (0.6) | 1.7 (0.6) | 1.7 (0.6) |
| HRQoL (SF-12) | |||
| Mental aspects | 48.9 (10.1) | 48.3 (9.2) | 48.6 (9.7) |
| Missing | 1 | 0 | 1 |
| Physical aspects | 47.0 (7.9) | 47.7 (7.5) | 47.4 (7.7) |
| Missing | 1 | 0 | 1 |
Table 7 shows baseline levels of self-reported physical activity in relation to whether activity was vigorous, moderate or walking (reported in MET-minutes/week) or time spent sitting on a week day in the last 7 days.
| Variable | FFIT (n = 374) | Comparison group (n = 373) | Total (n = 747) |
|---|---|---|---|
| Vigorous MET-minutes/week | 0 (0–720) | 0 (0–720) | 0 (0–720) |
| Missing | 4 | 3 | 7 |
| Moderate MET-minutes/week | 0 (0–360) | 0 (0–360) | 0 (0–360) |
| Missing | 3 | 2 | 5 |
| Walking MET-minutes/week | 462 (132–1188) | 396 (99–1039) | 445 (99–1188) |
| Missing | 4 | 2 | 6 |
| Time spent sitting on a week day in last 7 days | 480 (300–600) | 420 (300–600) | 450 (300–600) |
| Missing | 75 | 72 | 147 |
Numbers analysed
After randomisation, one participant allocated to the comparison group withdrew and requested that all of his data be destroyed. This left 374 participants in the intervention group and 373 in the comparison group. Retention was high, although it varied between intervention and comparison groups (see Figure 2). At 12 weeks, measurements were obtained for 91% of participants: 330 out of 374 (88%) in the intervention group and 347 out of 373 (93%) in the comparison group. At 12 months, measurements were obtained for 92% of participants: 333 out of 373 (89%) in the intervention group and 355 out of 373 (95%) in the comparison group. All analyses were conducted as intention to treat on randomised participants with all available data.
Outcomes
Primary outcome: weight at 12 months
At 12 months, mean weight loss among men in the intervention group was 5.56 kg (95% CI 4.70 kg to 6.43 kg) and 0.58 kg (95% CI 0.04 kg to 1.12 kg) in the comparison group (Table 8).
| Variable | FFIT (n = 374) | Comparison group (n = 373) | ||
|---|---|---|---|---|
| n | Mean (95% CI) | n | Mean (95% CI) | |
| Change in weight from baseline (kg) | 333 | –5.56 (–6.43 to –4.70) | 355 | –0.58 (–1.12 to –0.04) |
| % change in weight from baseline | 333 | –4.96 (–5.71 to –4.20) | 355 | –0.52 (–1.00 to –0.03) |
The mean difference in weight loss between groups, adjusted for baseline weight and club, was 4.94 kg (95% CI 3.95 kg to 5.94 kg) and the mean difference in percentage weight loss at 12 months, similarly adjusted, was 4.36% (Table 9).
| Variable | Difference between groups | p-value |
|---|---|---|
| Change in weight from baseline (unadjusted) (kg) | –4.11 (–6.75 to –1.47) | 0.0023 |
| Change in weight from baseline (adjusted for baseline weight and club) (kg) | –4.94 (–5.94 to –3.95) | < 0.0001 |
| % change in weight from baseline (unadjusted) | –4.36 (–5.09 to –3.64) | < 0.0001 |
| % change in weight from baseline (adjusted for baseline weight and club) | –4.36 (–5.08 to –3.64) | < 0.0001 |
Sensitivity analyses on primary outcome: change in weight at 12 months
The sensitivity analyses gave similar results to the main analysis (Table 10). Using multiple imputation, assuming data were missing at random, to account for missing data the mean difference in weight loss between groups adjusted for baseline weight and club was 4.93 kg (95% CI 3.92 kg to 5.94 kg). Adding club as a random effect to account for possible clustering, the mean difference in weight loss between groups adjusted for baseline weight was 4.94 kg (95% CI 3.83 kg to 6.04 kg). Using repeated measures to make use of weight loss data from both 12 weeks and 12 months found that the mean difference in weight loss between groups at 12 months, adjusted for baseline weight and club, was 5.28 kg (95% CI 4.62 kg to 5.94 kg) (see Table 10).
| Model | Difference between groups | p-value |
|---|---|---|
| Multiple imputation model (adjusted for weight at baseline and club) | –4.93 (–5.94 to –3.92) | < 0.0001 |
| Club as a random effect (adjusted for baseline weight) | –4.94 (–6.04 to –3.83) | < 0.0001 |
| Repeated measures model (adjusted for weight at baseline and club) | –5.28 (–5.94 to –4.62) | < 0.0001 |
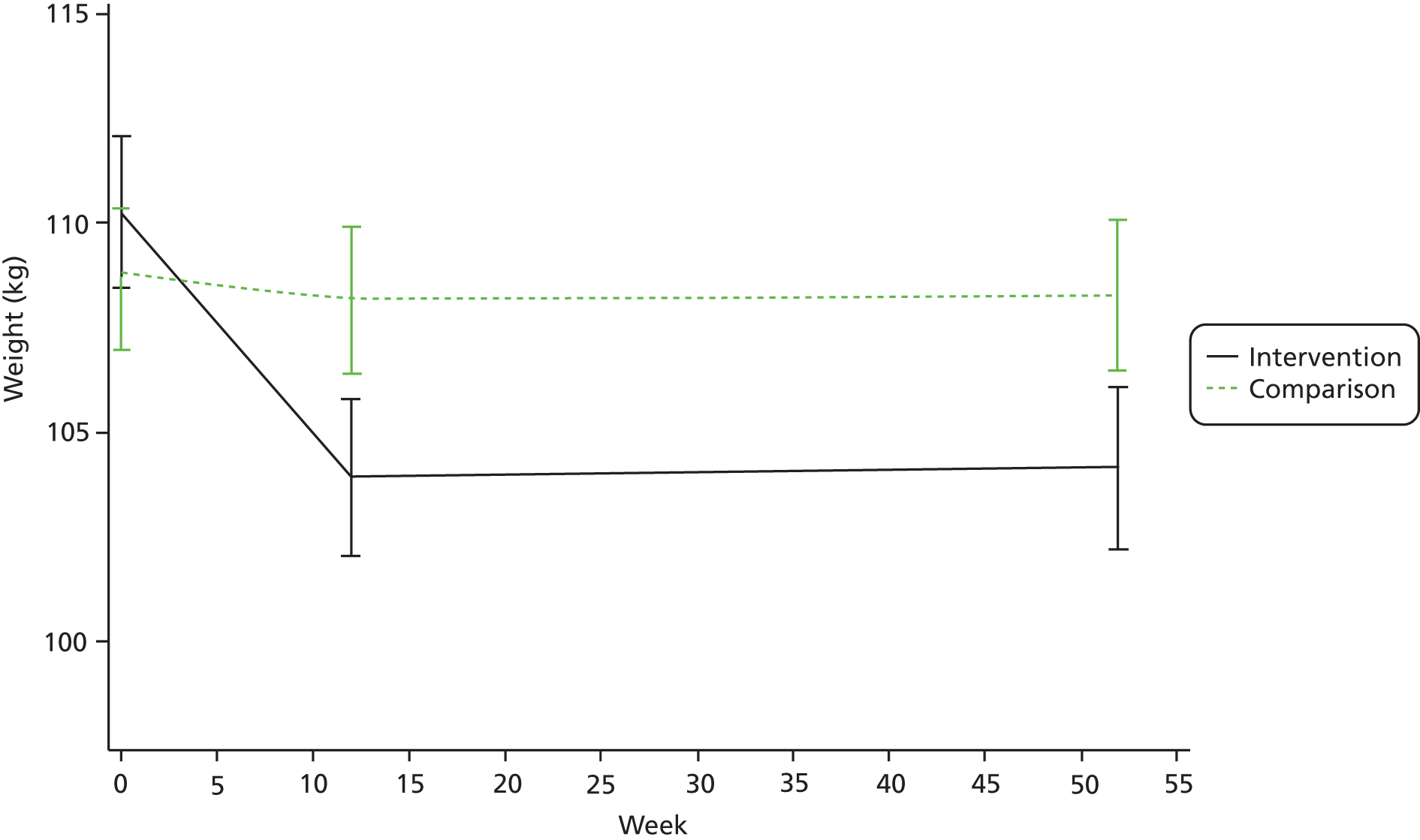
As shown in Figure 4, participants lost most weight over the period that coincided with the 12 weekly sessions delivered in the clubs.
FIGURE 4.
Mean weight (kg, 95% CI) in participants allocated to the FFIT weight loss programme or waiting list comparison group 12 weeks and 12 months after baseline measurement. Note that the y-axis (weight) does not start at zero. Reprinted with permission from Elsevier (The Lancet, 2014, 383, 1211–21). 33
Subgroup analyses on primary outcome
In order to investigate potential differential effects on the primary outcome by subgroup, we investigated associations between pre-specified subgroups (see Chapter 2, Statistical methods) and weight loss at 12 months. Table 11 shows which variables were significantly associated with weight loss in univariate analyses.
| Variable | ANOVA F-value | p-value |
|---|---|---|
| Age (years) | 26.02 | < 0.0001 |
| Number of long-standing illnesses | 9.88 | 0.002 |
| Fatty food score | 10.06 | 0.002 |
| Conformity to masculine norms | 5.81 | 0.016 |
| Employment status | 2.08 | 0.024 |
| Fruit and vegetable score | 4.63 | 0.032 |
| Joint pain | 4.82 | 0.029 |
| Housing tenure | 2.20 | 0.053 |
| SIMD (quintile) | 2.08 | 0.080 |
| Affiliation to football | 0.98 | 0.47 |
| Any attempts to lose weight in last 3 months | 0.26 | 0.61 |
| Ethnicity | 0.69 | 0.63 |
| Ever smoked | 0.24 | 0.79 |
| Highest educational status | 0.86 | 0.53 |
| Number of injuries | 1.78 | 0.18 |
| Marital status | 0.75 | 0.61 |
| SIMD (decile) | 1.32 | 0.22 |
| Sugary food score | 0.49 | 0.48 |
| Trained at club they supported | 0.21 | 0.64 |
Table 12 demonstrates that in multiple regression analyses including only those variables which had shown significant association with weight loss in univariate analysis together with weight at baseline and treatment group, the only significant associations were weight at baseline and treatment group. That is, the pre-specified subgroup analyses found no significant additional predictors of primary outcome and the intervention effect did not vary significantly by age, marital status, deprivation of area participants’ residence, location of measurement (stadium vs. home), orientation to masculine norms, affiliation to football, whether or not attended a formal weight management programme in last 3 months, smoking, housing tenure, education, ethnicity, employment status, joint pain, injuries and number of long-standing illnesses.
| Variable | Estimate (95% CI) | p-value |
|---|---|---|
| Treatment group (FFIT vs. comparison) | 0.94 (0.92 to –0.97) | < 0.0001 |
| Weight at baseline | –4.94 (–3.95 to –5.94) | < 0.0001 |
| Club | 0.637 | |
| Age (years) | 0.051 | |
| Fatty food score | 0.999 | |
| Fruit and vegetable score | 0.652 | |
| Number of long-standing illnesses | 0.182 | |
| Joint pain | 0.713 | |
| Conformity to masculine norms | 0.600 | |
| Employment status | 0.428 | |
| SIMD (quintile) | 0.311 |
Secondary outcomes
More men in the intervention group (39.04%, 130/333) than the comparison group (11.27%, 40/355) achieved at least 5% weight loss at 12 months (RR 3.47, 95% CI 2.51 to 4.78) and more had a BMI below 30 kg/m2 (Table 13).
| Variable | FFIT (N = 374) | Comparison group (N = 373) | Relative risk (95% CI) | |||
|---|---|---|---|---|---|---|
| n | n (%) | n | n (%) | |||
| Percentage who achieve at least 5% weight loss | 12 weeks | 329 | 154 (46.81) | 347 | 24 (6.92) | 6.77 (4.52 to 10.13) |
| 12 months | 333 | 130 (39.04) | 355 | 40 (11.27) | 3.47 (2.51 to 4.78) | |
| Percentage with a BMI < 30 kg/m2 | 12 weeks | 329 | 85 (25.84) | 347 | 44 (12.68) | 2.04 (1.46 to 2.84) |
| 12 months | 333 | 85 (25.53) | 355 | 48 (13.52) | 1.89 (1.37 to 2.60) | |
Table 14 shows changes in other secondary outcomes at 12 weeks and 12 months, before and after adjusting for baseline measure and clubs. These analyses show similarly positive results.
| Variable | FFIT (n = 374) | Comparison group (n = 373) | Mixed models, difference between groups, mean (95% CI) | Mixed models, difference between groups, mean (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| N | Mean (95% CI) or median (interquartile range) | N | Mean (95% CI) or median (interquartile range) | Unadjusted | p-value | Adjusteda | p-value | |
| Objectively measure outcomes | ||||||||
| Change in weight (kg) | ||||||||
| 12 weeks | 329 | −5.80 (−6.33 to −5.27) | 347 | −0.42 (−0.76 to −0.09) | −3.93 (−6.47 to −1.38) | 0.0026 | −5.18 (−6.00 to −4.35) | < 0.0001 |
| 12 months | 329 | −5.23 (−5.69 to −4.78) | 347 | −0.37 (−0.67 to −0.07) | −4.72 (−5.45 to −3.99) | < 0.0001 | −4.71 (−5.44 to −3.98) | < 0.0001 |
| Change in waist circumference (cm) | ||||||||
| 12 weeks | 329 | −6.70 (−7.28 to −6.13) | 345 | −1.00 (−1.43 to −0.56) | −4.88 (−6.72 to −3.04) | < 0.0001 | −5.57 (−6.41 to −4.72) | < 0.0001 |
| 12 months | 318 | −7.34 (−8.18 to −6.49) | 353 | −2.04 (−2.63 to −1.46) | −4.47 (−6.31 to −2.63) | < 0.0001 | −5.12 (−5.97 to −4.27) | < 0.0001 |
| Change in BMI (kg/m2) | ||||||||
| 12 weeks | 329 | −1.87 (−2.04 to −1.70) | 347 | −0.14 (−0.25 to −0.03) | −1.36 (−2.09 to −0.63) | 0.0003 | −1.66 (−1.93 to −1.40) | < 0.0001 |
| 12 months | 333 | −1.79 (−2.07 to −1.51) | 355 | −0.20 (−0.38 to −0.02) | −1.27 (−2.00 to −0.54) | 0.0007 | −1.56 (−1.82 to −1.29) | < 0.0001 |
| Change in % body fat | ||||||||
| 12 weeks | 276 | −2.70 (−3.21 to −2.23) | 260 | −0.30 (−0.62 to 0.09) | −1.77 (−2.70 to −0.84) | 0.0002 | −2.16 (−2.81 to −1.51) | < 0.0001 |
| 12 months | 271 | −2.20 (−2.88 to −1.60) | 312 | 0.00 (−0.40 to 0.43) | −1.92 (−2.83 to −1.00) | < 0.0001 | −2.15 (−2.78 to −1.52) | < 0.0001 |
| Change in systolic blood pressure (mmHg) | ||||||||
| 12 weeks | 295 | −7.50 (−9.14 to −5.89) | 280 | −3.50 (−4.97 to −2.00) | −5.41 (−7.70 to −3.12) | < 0.0001 | −4.51 (−6.36 to −2.67) | < 0.0001 |
| 12 months | 318 | −7.90 (−9.54 to −6.25) | 351 | −6.60 (−7.98 to −5.31) | −3.58 (−5.76 to −1.39) | 0.0025 | −2.27 (−4.01 to −0.54) | 0.0171 |
| Change in diastolic blood pressure (mmHg) | ||||||||
| 12 weeks | 295 | −3.70 (−4.77 to −2.70) | 280 | −1.50 (−2.53 to −0.54) | −3.10 (−4.56 to −1.64) | < 0.0001 | −2.51 (−3.71 to −1.32) | < 0.0001 |
| 12 months | 318 | −4.60 (−5.63 to −3.60) | 351 | −3.80 (−4.74 to −2.96) | −2.16 (−3.55 to −0.76) | 0.0014 | −1.36 (−2.48 to −0.24) | 0.0102 |
| Self-reported physical activity | ||||||||
| Changes in total MET–minute/week (walking, vigorous and moderate exercise) | ||||||||
| 12 weeks | 325 | 1485 (IQR 339–3435) | 341 | 0 (IQR −840–747) | 2.43 (IQR 1.92–3.07) | < 0.0001 | 2.38 (IQR 1.90–2 .98) | < 0.0001 |
| 12 months | 310 | 1219 (IQR 54–3111) | 347 | 375 (IQR −414–1800) | 1.51 (IQR 1.12–2.04) | 0.0.007 | 1.49 (IQR 1.11–1.99) | 0.008 |
| Self-reported eating and alcohol intake | ||||||||
| Change in DINE-based measures | ||||||||
| Fatty food score | ||||||||
| 12 weeks | 330 | −5.60 (−6.39 to −4.86) | 345 | −1.40 (−2.03, −0.77) | −4.45 (−5.35 to −3.55) | < 0.0001 | −4.39 (−5.16 to −3.61) | < 0.0001 |
| 12 months | 318 | −4.50 (−5.32 to −3.74) | 353 | −1.70 (−2.32 to −1.13) | −2.72 (−3.62 to −1.82) | < 0.0001 | −2.74 (−3.52 to −1.96) | < 0.0001 |
| Fruit and vegetable score | ||||||||
| 12 weeks | 330 | 1.60 (1.39 to 1.81) | 347 | 0.20 (0.03 to 0.41) | 1.26 (1.03 to 1.57) | < 0.0001 | 1.32 (1.07 to 1.57) | < 0.0001 |
| 12 months | 333 | 0.80 (0.60 to 1.07) | 355 | 0.30 (0.11 to 0.49) | 0.53 (0.26 to 0.80) | 0.0001 | 0.54 (0.29 to 0.79) | < 0.0001 |
| Sugary food score | ||||||||
| 12 weeks | 330 | −2.10 (−2.43 to −1.84) | 345 | −0.70 (−0.95 to −0.39) | −1.57 (−1.91 to −1.22) | < 0.0001 | −1.52 (−1.83 to 1.21) | < 0.0001 |
| 12 months | 318 | −1.30 (−1.62 to −0.97) | 353 | −0.50 (−0.81 to −0.25) | −0.93 (−1.28 to −0.59) | < 0.0001 | −0.87 (−1.18 to −0.56) | < 0.0001 |
| Change in alcohol consumed (units per week) | ||||||||
| 12 weeks | 329 | −6.20 (−7.58 to −4.79) | 345 | −2.10 (−3.43 to −0.68) | −5.14 (−7.43 to −2.86) | < 0.0001 | −4.47 (−6.09 to −2.86) | < 0.0001 |
| 12 months | 318 | −4.20 (−5.55 to −2.87) | 353 | −2.20 (−3.39 to −0.96) | −3.40 (−5.69 to −1.11) | 0.0037 | −2.59 (−4.21 to −0.97) | 0.0017 |
| Self-reported psychological health and QoL outcomes | ||||||||
| Change in self-esteem (Rosenberg score) | ||||||||
| 12 weeks | 330 | 0.30 (0.24 to 0.32) | 344 | 0.10 (0.05 to 0.12) | 0.17 (0.10 to 0.25) | < 0.0001 | 0.19 (0.14 to −0.24) | < 0.0001 |
| 12 months | 317 | 0.30 (0.22 to 0.30) | 350 | 0.10 (0.10 to 0.17) | 0.11 (0.03 to 0.18) | 0.0052 | 0.12 (0.07 to 0.17) | < 0.0001 |
| Change in positive affect (PANAS score) | ||||||||
| 12 weeks | 328 | 0.50 (0.45 to 0.59) | 344 | 0.10 (0.01 to 0.14) | 0.45 (0.34 to 0.55) | < 0.0001 | 0.44 (0.36 to 0.53) | < 0.0001 |
| 12 months | 317 | 0.30 (0.27 to 0.41) | 350 | 0.10 (0.01 to 0.14) | 0.29 (0.18 to 0.39) | < 0.0001 | 0.28 (0.19 to 0.36) | < 0.0001 |
| Change in negative affect (PANAS score) | ||||||||
| 12 weeks | 329 | −0.20 (−0.21 to −0.11) | 344 | −0.10 (−0.11 to −0.01) | −0.08 (−0.16 to 0.00) | 0.0591 | −0.09 (−0.15 to −0.03) | 0.0039 |
| 12 months | 317 | −0.20 (−0.24 to −0.13) | 350 | −0.10 (−0.14 to −0.05) | −0.07 −(0.15 to −0.01) | 0.0998 | −0.08 (−0.15 to −0.02) | 0.0079 |
| Change in mental HRQoL (SF-12 score) | ||||||||
| 12 weeks | 328 | 3.20 (2.33 to 4.12) | 345 | 1.50 (0.66 to 2.39) | 2.56 (1.12 to 4.00) | 0.0005 | 2.01 (0.89 to 3.12) | 0.0004 |
| 12 months | 316 | 1.90 (0.93 to 2.83) | 351 | 1.60 (0.82 to 2.42) | 0.97 (0.47 to 2.42) | 0.1861 | 0.50 (−0.62 to 1.62) | 0.3822 |
| Change in physical HRQoL (SF-12 score) | ||||||||
| 12 weeks | 328 | 3.30 (2.53 to 4.00) | 345 | 0.40 (−0.33 to 1.12) | 2.00 (0.77 to 3.24) | 0.0015 | 2.60 (1.60 to 3.60) | < 0.0001 |
| 12 months | 316 | 2.30 (1.48 to 3.21) | 351 | 0.20 (−0.62 to 0.93) | 1.30 (0.06 to 2.54) | 0.0400 | 1.89 (0.89 to 2.90) | 0.0002 |
In relation to objectively measured secondary outcomes, adjusting for baseline measure and club, the mean difference in reduction at 12 months in waist circumference was 5.12 cm (95% CI 4.27 to 5.97 cm) and in BMI was 1.56 kg/m2 (95% CI 1.29 to 1.82 kg/m2). Differences in changes in all other objectively measured secondary outcomes, including weight loss at 12 weeks, % body fat at 12 weeks and 12 months, and systolic and diastolic blood pressure at 12 weeks and 12 months were also all in favour of the intervention and highly statistically significant (p < 0.0001, except for systolic BP at 12 months where p = 0.017) (see Table 14). There was clear attenuation of effect between the end of 12-week programme and 12-month measurements.
In relation to eating and drinking alcohol, Table 14 demonstrates that reductions in the fatty food and sugary food scores were greater for participants in the FFIT programme than in the comparison group at 12 weeks, and these differences remained highly significant at 12 months (p < 0.0001) although, again, there was considerable attenuation of the effects between 12 weeks and 12 months. Similarly, positive changes in reported eating patterns were seen for the fruit and vegetable score; the differences in the increase seen in fruit and vegetable consumption were highly significant (p < 0.0001) at 12 weeks and 12 months, in favour of the intervention (see Table 14). They also reported drinking less units of alcohol per week; the mean difference in units of alcohol reported being drunk between groups, adjusted for baseline units and club, was 4.47 (95% CI –6.09 to –2.86) at 12 weeks and 2.59 (95% CI –4.21 to –0.97) at 12 months (see Table 14).
In relation to changes in self-reported QoL and mental health, Table 14 illustrates that FFIT also resulted in greater improvements in self-esteem and positive affect at 12 weeks and 12 months in the intervention than the comparison groups, and greater reductions in negative affect at 12 weeks and 12 months. Similarly, there were greater improvements in scores on physical aspects of QoL as measured by the SF-12 at 12 weeks and 12 months, but the greater improvements in mental HRQoL in the intervention group at 12 weeks were no longer significantly different from the comparison group at 12 months (see Table 14). As with all other outcomes, there was attenuation of the differences between the two groups between 12 weeks and 12 months.
In relation to self-reported physical activity, as the changes in MET-minutes were highly positively skewed, the standard linear-mixed models were not valid and so linear modelling on natural log-transformed was implemented for total MET-minutes/week. Table 14 illustrates that the increase in total MET-minutes per week was greater in the intervention group than the comparison group with an adjusted RGM at 12 months of 1.49 (IQR 1.11–1.99) for total MET-minutes, in other words roughly 50% higher in the intervention.
To further investigate changes in self-reported physical activity in addition to log-transformations, we applied a repeated measures analysis using data from 12 weeks and 12 months in relation to total activity but also whether activity was vigorous, moderate or walking (reported in MET-minutes/week) and time spent sitting on a week day in the last 7 days.
Table 15 illustrates that the repeated measures analysis gave very similar results to the standard analysis in relation to increase in total MET-minutes per week. The results also indicated that when total activity is subdivided into the constituent elements, the improvement in physical activity was greatest for vigorous (RGM 4.63, 95% CI 2.64 to 8.12), followed by moderate (RGM 2.10, 95% CI 1.22 to 3.62) and then walking (RGM 1.31, 95% CI 0.91 to 1.89) (see Table 15). It is also clear that there was considerable attenuation in the effects between 12 weeks and 12 months, although there were still highly significant differences between the groups at 12 months for vigorous and moderate physical activity at 12 months, though not in walking.
| Variable | FFIT (n = 374) | Comparison group (n = 373) | Mixed models (repeated measures): difference between groups (FFIT comparison) mean (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Median (interquartile range) | n | Median (interquartile range) | Unadjusted ratio RGM (95% CI) | Adjusteda ratio RGM (95% CI) | ||||
| Changes in total MET minutes/week (walking, vigorous and moderate physical activity) | 12 weeks | 325 | 1485 (339–3435) | 341 | 0 (–840–747) | 3.94 (2.84 to 5.47) | < 0.0001 | 3.79 (2.77 to 5.20) | < 0.0001 |
| 12 months | 310 | 1219 (54–3111) | 347 | 375 (–414–1800) | 1.53 (1.10 to 2.12) | 0.011 | 1.49 (1.09 to 2.05) | 0.013 | |
| Changes in vigorous MET minutes/week | 12 weeks | 324 | 360 (0–1640) | 340 | 0 (0–240) | 10.64 (5.92 to 19.12) | < 0.0001 | 9.21 (5.26 to 16.10) | < 0.0001 |
| 12 months | 309 | 440 (0–1680) | 346 | 0 (0–720) | 5.23 (2.90 to 9.44) | < 0.0001 | 4.63 (2.64 to 8.12) | < 0.0001 | |
| Changes in moderate MET minutes/week | 12 weeks | 325 | 160 (0–840) | 339 | 0 (–120–240) | 9.29 (5.34 to 16.14) | < 0.0001 | 9.48 (5.53 to 16.26) | < 0.0001 |
| 12 months | 310 | 0.0 (0–720) | 346 | 0.0 (0–360) | 2.03 (1.16 to 3.53) | 0.013 | 2.10 (1.22 to 3.62) | 0.007 | |
| Changes in walking MET minutes/week | 12 weeks | 324 | 528 (0–1353) | 340 | 0 (–280.5–396) | 3.20 (1.22 to 5.37) | < 0.0001 | 3.39 (2.35 to 4.88) | < 0.0001 |
| 12 months | 311 | 222.8 (–99–956.3) | 348 | 99 (–198–693) | 1.41 (0.96 to 2.07) | 0.080 | 1.31 (0.91 to 1.89) | 0.151 | |
| Changes in time spent sitting on a week day in last 7 days (minutes) | 12 weeks | 236 | –60 (–180–0) | 248 | –30 (–120–60) | 0.86 (0.79 to 0.94) | 0.001 | 0.85 (0.78 to 0.93) | 0.0005 |
| 12 months | 235 | –60 (–180–0) | 260 | –15 (–120–60) | 1.00 (0.92 to 1.09) | 0.99 | 0.96 (0.88 to 1.04) | 0.314 | |
There was some evidence of a reduction in time spent sitting in the intervention group, especially at 12 weeks (RGM 0.85, 95% CI 0.78 to 0.93) but these effects were modest; at 12 weeks self-reported sitting time was 15% lower in the intervention group relative to the comparison group (p = 0.0005). However, at 12 months there was no statistically significant difference in sitting time (see Table 15 between groups).
Adverse events
Eight serious adverse events were reported: five in the intervention and three in the comparison group. Two appeared to be, or were reported as, related to participation in FFIT: one participant ruptured an Achilles tendon while playing football and the other was told by his doctor that intermittent abdominal pains from gall stones could have been aggravated or caused by weight or dietary changes.
A total of 211 adverse events were reported: 107 events reported by 96 men in the intervention and 104 events in the comparison group reported by 92 men. Ten appeared to be, or were reported as, related to participation in FFIT: five occurred at FFIT sessions, three elsewhere (two when running; one playing football) and it was unclear where the other two occurred. Seven of the men reported leg injuries (often ligament damage), one a dislocated shoulder, one leg and shoulder injuries and one a head collision (with another participant at a FFIT session). Another 11 adverse events could have been related to participation in FFIT, but the research team were unable to contact the men to confirm this. Of these, five occurred playing football and two when running; it was not clear where the remainder had happened. Six involved leg injuries and the others were reported as neck, leg, groin, hand and collar bone injuries.
Chapter 4 Economic evaluation: methods and results
Introduction
The aim of the economic evaluation was to determine the cost-effectiveness of the FFIT programme compared with no active intervention. No intervention was used as the comparator as, in the absence of the FFIT intervention, this was the most likely alternative for this population. Throughout the analyses, the waiting list comparison group was used as the source of data for the ‘no active intervention’ group. The evaluation was undertaken from the NHS and Personal Social Service perspective favoured by the National Institute for Health and Care Excellence (NICE).
An initial, short-term analysis estimates the cost-effectiveness of FFIT compared with no active intervention over the period of the trial. This analysis requires the assumption that there are no differences in costs or effects between the intervention and comparison groups beyond the 12-month trial follow-up period. A second, longer-term analysis employs a model to estimate additional costs and benefits over the participants’ lifetime in order to provide an estimate of the lifetime cost-effectiveness of FFIT compared with no active intervention. Further details of each analysis are provided in the sections below.
Within-trial analysis
Introduction
The aim of the within-trial analysis was to estimate the immediate impacts (in terms of costs and effects) associated with the FFIT intervention in order to establish the cost-effectiveness of the intervention compared with no active intervention. The within-trial analysis compared the FFIT intervention group with the waiting list comparison group in terms of (1) costs incurred over the 12-month period, (2) number of men achieving and maintaining a 5% weight reduction over 12 months and (3) QALYs gained over the 12-month period.
Methods
Resource use and costs
The cost calculation included the resources required to manage and run the programme (Table 16), as well as self-reported health-care resource use and GP-prescribed medications.
| Item | Unit cost (£) | Units | Total cost of intervention (£) |
|---|---|---|---|
| SPL/club costs | |||
| Club running costs | 3544.00 | Per club | 46,072.00 |
| SPL Trust management cost | 10,000.00 | Per season | 5000.00 |
| Equipment costs (per unit) | |||
| Scales | 131.00 | Per club | 1703.00 |
| Height measure | 30.50 | Per club | 396.50 |
| Waist measures | 8.80 | Per club | 114.40 |
| Blood pressure monitor | 65.00 | Per club | 845.00 |
| Food plate and plastic food display | 144.00 | Per club | 1872.00 |
| Material costs (per unit) | |||
| Pedometer | 6.60 | Per participant + spare | 2917.20 |
| Participant guide | 7.00 | Per participant | 2639.00 |
| Coaches guide | 3.50 | Per coach | 182.00 |
| Roll out costs | 61,741.10 | ||
The principal part of the intervention cost is the £3544 cost of running the intervention in each club. This covers all the clubs costs involved in providing the intervention, including club-level management, staff time and venue hire and club-based recruitment activities. In addition, the SPL Trust management cost of £5000 per season covers the cost of training the coaches, the SPL-level management and co-ordination of the intervention across the clubs and marketing and additional recruitment. In addition to these costs, there are a number of resources required to provide the intervention. These include equipment to measure the height, weight, blood pressure and waist circumference of the participants, plus a display plate (Eatwell Plate)47 to illustrate the appropriate proportion of food stuffs to each from the five main food groups and portion sizes, and materials to deliver the intervention (including a pedometer and booklet for each participant and booklets for coaches). Each club was assumed to receive one complete set of equipment per year (with the exception of the waist measures of which each club was assumed to be provided with four sets per year), with the assumption that each club provided the intervention twice in each year. The materials were assumed to be provided per participant/coach, with the addition of a few spares. All resources required to deliver the intervention were costed according to the price paid to purchase them at the start of the trial (September 2011). Overall, the cost of providing the intervention in all SPL clubs was estimated to be £61,741, equivalent to £165 per FFIT participant.
In addition to the intervention costs, data were collected at each time point (baseline, 12 weeks and 12 months) from each participant relating to the number and type of any NHS resources used in the preceding 12-week period. This included visits to the GP, practice nurse or physiotherapist and any attendances at accident and emergency. Unit costs for each of these visits were taken from Personal Social Services Research Unit (PSSRU) 2011/12 (Table 17). 75
| Type of health professional visit | Unit cost (£) | Notes |
|---|---|---|
| GP visit | 43.00 | Per patient contact in surgery (assumed 11.7 minutes). Includes direct care staff costs |
| Practice nurse visit | 13.25 | Per patient contact in surgery (assumed 15 minutes) |
| Physiotherapist | 16.50 | Per patient contact in community (assumed 30 minutes) |
| A&E | 41.00 | Walk-in service, not admitted |
Data were also collected at each time point relating to any inpatient stays and outpatient appointments in the preceding 12-week period. Unit costs were taken from Information and Statistics Division Scotland tariffs for 2012 and, when necessary, NHS reference costs for 2011/12. 76–78
Finally, self-reported data were collected at each time point regarding GP prescriptions of antidepressants, painkillers, asthma, pain gels/creams, anti-inflammatories and sleeping tablets in the preceding 12 weeks. These medications were identified as the most likely to be affected by the intervention and were pre-specified on the advice of our clinical advisor; diabetes mellitus medication was not included in this list it was not expected to be affected by the intervention over the within-trial period. Other prescribed medications were also excluded from the analysis. In addition, because the analysis used an NHS and Personal Social Service perspective, we excluded over-the-counter medications. Medications were costed using unit costs for a typical prescription from the British National Formulary76 (Table 18).
| Kind of medication | Unit cost (£) | Drug costed |
|---|---|---|
| Asthma | 2.19 | Beconase |
| Antidepressants | 0.96 | Citalopram: 20 mg, 28-tablet pack |
| Painkillers | 4.70 | Cocodamol: 8 mg, 100-tablet pack |
| Anti-inflammatories | 3.23 | Diclofenac: 25 mg, 28-tablet pack |
| Sleeping tablets | 0.86 | Diazepam: 5 mg, 28-tablet pack |
| Gels/creams | 3.89 | Ibuprofen: maximum strength 10% w/w, 50-g pack |
In the economic evaluation, as in the main analyses, we did not take account of missing resource use data. For NHS resource use, the proportion of missing responses across all time points ranged from 1.3% to 2.3% across the different categories. The proportion of missing responses for medications was less than 2% across the different categories.
We used 12 weeks as the time frame over which participants were asked to recall their resource use, as longer periods have potentially been found to be subject to greater recall bias. 79
Table 19 shows that at baseline comparison group participants had higher inpatient costs.
| Type of cost | Intervention (£) | Comparison (£) |
|---|---|---|
| GP | 48,074.00 | 52,732.33 |
| Nurse | 5913.92 | 6545.50 |
| A&E | 3020.33 | 5507.67 |
| Physiotherapy | 1930.50 | 2860.00 |
| Concomitant medications | 3941.99 | 3757.61 |
| Inpatient | 24,277.98 | 54,171.00 |
| Outpatient | 35,213.23 | 33,495.89 |
| Total baseline costs | 22,371.95 | 159,069.99 |
Outcome measurement
The initial outcome measure for the within-trial analysis is the number of men achieving and maintaining the 5% weight reduction over 12 months, as measured at the 12-month follow-up.
In addition, self-report SF-12 data were collected at baseline, 12 weeks and 12 months. These values were converted into utility weights using the Short Form questionnaire-6 Dimensions algorithm. 75,80,81 Table 20 details the mean utility score associated with FFIT and no active intervention at each time point (baseline, 12 weeks and 12 months) with and without adjustment for missing data.
| Analysis | Baseline utilities | 12-week utilities | 12-month utilities |
|---|---|---|---|
| Intervention | |||
| With missing data | 0.78 | 0.83 | 0.80 |
| Adjusted for missing values | 0.78 | 0.82 | 0.80 |
| No active intervention | |||
| With missing data | 0.77 | 0.79 | 0.79 |
| Adjusted for missing values | 0.77 | 0.79 | 0.78 |
The area under the curve method was used to determine the overall utility for each participant over the trial period. 82 This provides a utility weighting, similar to a QALY, but measured over a 12-month period. Change from baseline has been used to account for differences in the average baseline values between the intervention and comparison groups, to give an estimate of the utility change over the year for each participant.
Analysis
The within-trial effectiveness is presented both in terms of the number of men achieving and maintaining a 5% weight reduction over 12 months, and QALYs gained over 12 months. The individual-level data on achieving and maintaining a 5% weight reduction are summed to provide the number attaining this outcome in each group, while the individual-level QALY data are averaged within each group (intervention, comparison). Differences in the average utility change between the intervention and comparison groups give an estimate of the QALYs gained from the intervention, assuming no differences beyond the 12-month follow-up period. Effect results are presented as mean values with CIs.
The cost associated with each individual is determined as the sum of the per participant intervention cost (for the FFIT intervention group), plus the cost of NHS resource use, plus any medication cost. The individual costs are averaged within each group to give an estimate of the average cost associated with the FFIT intervention and the comparison groups. The incremental cost associated with the FFIT intervention is the difference between the average cost of the FFIT intervention group and the average cost of the comparison group. Cost results are presented as mean values with CIs.
The incremental cost-effectiveness associated with the FFIT intervention is then presented in terms of incremental cost per additional individual achieving and maintaining the 5% weight reduction over 12 months and the incremental cost per QALY gained. Discounting of costs and outcomes is not required owing to the 12-month time frame of the within-trial analysis.
The uncertainty surrounding the estimates of incremental costs, incremental effects and cost-effectiveness was investigated through the use of bootstrapping with 10,000 iterations. The uncertainty surrounding the cost-effectiveness results are presented on the cost-effectiveness plane and summarised on a cost-effectiveness acceptability curve.
Results
The total costs associated with the FFIT intervention group were estimated to be £254,579 (£680 per participant), compared with total costs for the ‘no active intervention group’ of £177,025 (£475 per participant), giving an incremental cost of £77,554 (£205 per participant) (Table 21).
| Analysis | Cost per person (£) | Utility change over 12 months | Total costs (£) | Breakdown of costs | |||
|---|---|---|---|---|---|---|---|
| Primary care (£) | Secondary care (£) | Medication (£) | FFIT costs (£) | ||||
| FFIT | 680 | 0.029 | 254,579 | 72,281 | 116,156 | 4892 | 61,250 |
| No active intervention (comparison) | 475 | 0.014 | 177,025 | 73,634 | 95,874 | 7517 | 0 |
| Incremental | 205 | 0.015 | 77,554 | –1353 | 20,282 | –2625 | 61,250 |
At the 12-month follow-up, 130 men in the FFIT intervention group and 40 men in the comparison group had achieved and maintained a 5% weight reduction. The incremental cost of FFIT was estimated as £862 per additional man achieving and maintaining a 5% weight reduction at 12 months.
The results illustrate that FFIT is more expensive than no active intervention, with an additional cost of £205 per individual (95% CI £27 to £386). This is driven mostly by the additional cost of the intervention. The results also indicate that FFIT is more effective in terms of QALYs, with a gain in QALYs of 0.015 (95% CI 0.003 to 0.027) (see Table 21). As a result, the FFIT intervention is associated with an incremental cost-effectiveness of £13,847 per QALY gained.
Figure 5 shows the uncertainty surrounding the estimates of the costs and effects on the incremental cost-effectiveness plane. The figure shows that there is no uncertainty surrounding the existence of a cost difference – FFIT is more expensive than no active intervention (i.e. all the incremental costs are positive), although there is some uncertainty about the extent of the cost difference. In addition, the figure shows that there is some uncertainty about whether or not FFIT is more effective than no active intervention (i.e. a few of the incremental QALYs are negative) and there is considerable uncertainty about the extent of the effect difference.
FIGURE 5.
Incremental cost-effectiveness plane for FFIT intervention compared with no active intervention (within-trial analysis).

The cost-effectiveness acceptability curve (Figure 6) illustrates the probability that the FFIT intervention is cost-effective for any given value of the cost-effectiveness threshold. For a cost-effectiveness threshold of £20,000/QALY, the probability that FFIT is cost-effective, compared with no active intervention, is 0.72. This probability rises to 0.89 for a cost-effectiveness threshold of £30,000/QALY.
FIGURE 6.
Cost-effectiveness acceptability curve for FFIT intervention (within-trial analysis). Reprinted with permission from Elsevier (The Lancet, 2014, 383, 1211–21). 33

Lifetime analysis
Introduction
The within-trial cost-effectiveness analysis assumes that there are no differences in QALYs between the intervention and comparison groups beyond the 12-month trial follow-up period. The aim of the lifetime analysis was to estimate the longer-term implications (in terms of cost or effect) of the FFIT intervention in order to establish the long-term cost-effectiveness of the intervention compared with no active intervention. The analysis involved linking the short-term impacts identified within the trial period to longer-term impacts through the use of a model. As such, the initial step involved a review of published models undertaken in this area. Following this review a model structure was selected and this is presented below followed by the results of the lifetime analysis.
Review of existing models
We reviewed a variety of models in the area of weight management and physical activity. These models were generally one of two types:
-
Risk factor models: these link risk scores to impacts on health outcomes and are driven by changes in the risk factors that compose the risk score. These models have been presented both in terms of population-level changes and as individual-level models.
-
Behaviour change models: these link health/risk behaviours (e.g. smoking, physical activity) with health outcomes and are driven by changes in these health behaviours. These behaviour change models are typically individual-level models projecting the impact of individual behaviour change on individual health outcomes.
Bending et al. 83 adapted and developed a model to estimate cost-effectiveness for interventions that promote physical activity for a NICE report on physical activity interventions in the workplace. 83 This risk factor model employed the Framingham risk profiles84 and Lindström et al. 85 risk equations to estimate the probabilities of developing coronary heart disease (CHD), stroke and type 2 diabetes mellitus within a 10-year period based on age, gender, cholesterol, blood pressure, BMI, smoking and diabetes mellitus status. These probabilities were combined with published evidence of effectiveness to estimate the number of cases of disease that would be averted by a proportion of the sedentary population taking up certain levels of physical activity. Estimates, from the literature, of the utility and cost impact of these diseases were applied to generate lifetime health and cost estimates. 83
Brennan et al. 86 used a behavioural model to establish the likely cost-effectiveness of various walking and cycling interventions for a NICE report. 86 The model estimated the statistical relationships between levels of walking and cycling and overall physical activity using data from the Health Survey for England. This allowed direct evidence of intervention effects on walking and cycling to be converted into overall changes in physical activity levels. These changes in physical activity were then transformed into changes in life expectancy using the relationship observed between physical activity and relative risk of mortality from a long-term prospective study. 87 Finally, the model employed national life tables and evidence on average HRQoL to estimate discounted QALYs, costs of the interventions if rolled out across the country and lifetime cost per QALY gained. 86
The Prevent model, developed by Gunning-Schepers,88 converts changes in behaviour into changes in exposure to risk factors. Various studies have been published89–91 using this model to estimate the effect of behaviour changes such as smoking, alcohol consumption and physical activity on incidence of disease and mortality. Recently, Dallat et al. 91 used the Prevent model to assess the cost-effectiveness of an urban regeneration project by modelling the impact of the intervention on ischaemic heart disease, type 2 diabetes mellitus, stroke, colon and breast cancer to the year 2050.
Haby et al. 92 assessed the impacts of behaviour changes in diet, physical activity or both, brought about by preventative childhood obesity interventions, on energy imbalance. A model then determined the impact of these energy deficits on changes in weight. Published data were used to translate mean changes in weight to mean changes in BMI, assuming no change in height. 92 Potential impact fractions were used to assess the impact of the changes in BMI on the prevalence of risk factors for heart disease, stroke, type 2 diabetes mellitus, osteoarthritis and obesity-related cancers. This, in turn, was used to estimate the impact on mortality, morbidity and changes in lifetime disability-adjusted life-years saved. 92
The Foresight Programme developed a two-part modelling process to predict future levels of obesity in England. 93 The first part utilised a cross-sectional analysis of data from the Health Survey for England and implemented a non-linear regression analysis to derive BMI projections for the English population in 2050. The second part generated a longitudinal analysis using microsimulation to simulate successful obesity interventions and consequent changes in obesity-related diseases and NHS expenditure. 93 Foresight modelling estimates for 2050 indicate that 60% of adult men, 50% of adult women and 25% of children could be obese. 93 Costs attributable to overweight and obesity are estimated at £10B to the NHS in 2050, with wider costs to society estimated to reach £49.9B. 93 Two further studies1,94 have employed the Foresight model to evaluate interventions in childhood obesity and to project future trends in obesity prevalence, diseases and costs. However, the Foresight model is not published in a peer-reviewed journal and was not available to us.
Methods
Following the review of the existing models and in consultation with project collaborators the decision was taken to employ a risk factor model, developed by colleagues at the University of Glasgow, Glasgow, UK, with funding from Scotland’s CSO (two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014), to project the longer-term impacts of FFIT.
The cardiovascular disease (CVD) model for Scotland (also known as the ‘HELP’ model; two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014) was chosen because it is an established model employing a risk score developed for the Scottish population, supplemented with Scottish data on costs and health outcomes, to examine long-term health outcomes. The model uses ASSIGN risk factors published in Tunstall-Pedoe et al. 95 to predict both CVD events and death from all non-CVD causes, including, for example cancers and respiratory diseases. The model utilises data from the Scottish Heart Health Extended Cohort (SHHEC),96 which measured the ASSIGN risk factors, linked through Scottish Morbidity Records (SMRs) and General Register Office for Scotland, to identify all hospital events and death records. As such, the model provides a prediction of life expectancy, long-term costs and outcomes for individuals based on their risk score. For more details on ASSIGN please see http://assign-score.com. 96
HELP model
The objective in developing HELP was to build a model capable of undertaking economic evaluation to inform Scotland’s approach to primary prevention (two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014). Predictions of life expectancy from the model closely match those published in national life tables (two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014). The structure of the state transition model is shown in Figure 7. Using the nine ASSIGN97 risk factors as parameter inputs, the HELP model predicts life-years gained, QALYs and lifetime costs.
FIGURE 7.
Structure of the state transition model. The numbers in brackets refer to Equations 1–7. CBVD, cerebrovascular disease.
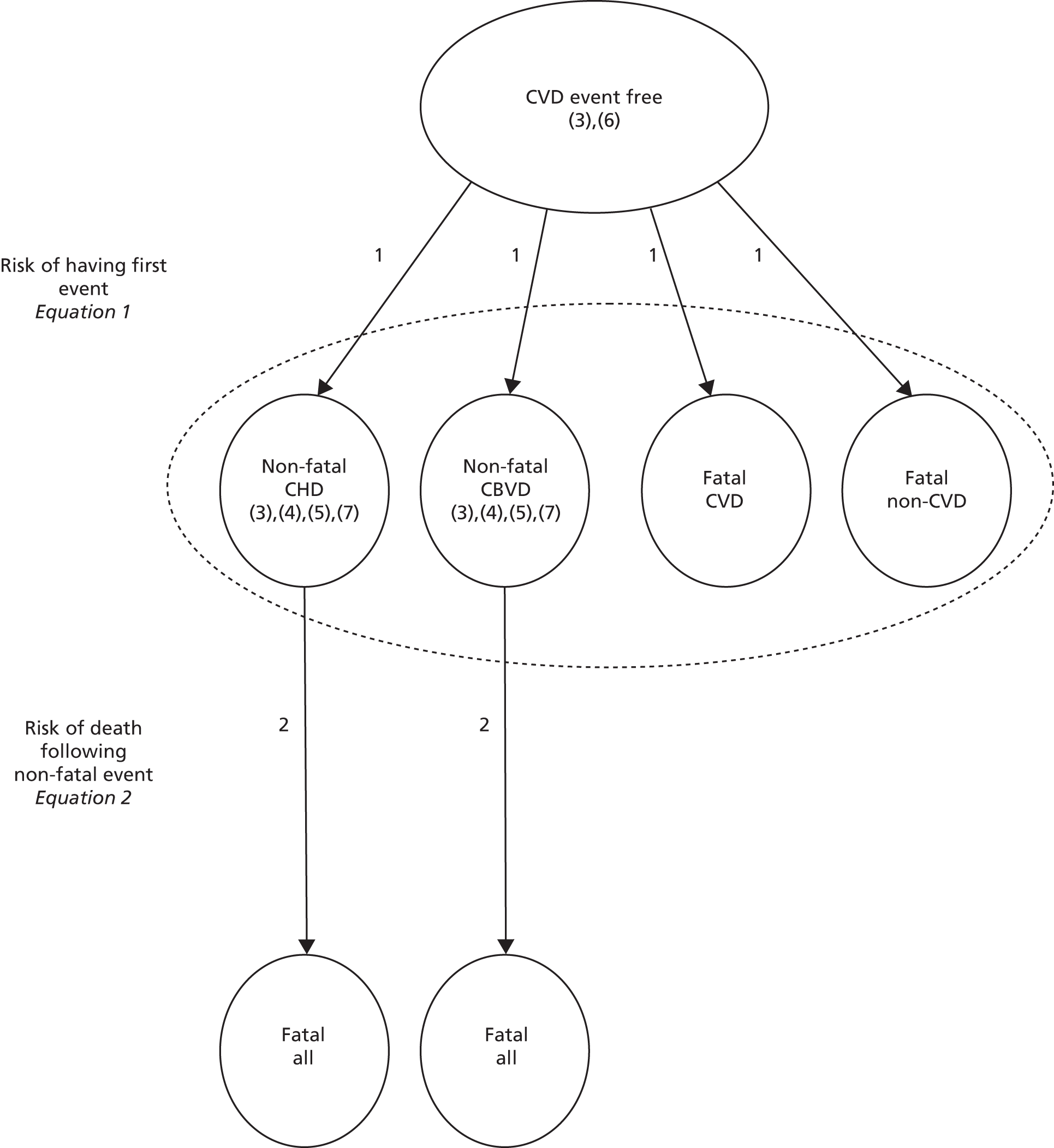
The numbers in brackets in Figure 7 refer to the following equations:
Life expectancy
Individuals are assumed to be free from CVD at the point that they enter the model. Each individual is allocated a risk score based on their ASSIGN97 risk variables. These variables include age, gender, family history of CHD and stroke, postcode (linked to SIMD), diabetes mellitus, systolic blood pressure, number of cigarettes smoked per day, total and HDL cholesterol. It is this individual risk score that determines the risk of experiencing an initial event [non-fatal CHD, non-fatal cerebrovascular disease (CBVD), fatal CVD and fatal non-CVD] (see Equation 1). Individuals subsequently transit into one of four ‘competing’ events, non-fatal CHD hospitalisation, non-fatal CBVD hospitalisation, death from CVD and death from non-CVD causes. Survival analysis was used to model the cause-specific hazards of these competing first events. As not all SHHEC participants had experienced a first event by the end of follow-up, a parametric approach was used to extrapolate and provide estimates of the total remaining life expectancy. The predicted cumulative incidence of events was calculated from the cause-specific hazards and the probability of surviving from any of the competing events at a given time. Those individuals for whom the initial event is non-fatal will experience a fatal event at some point in the future, the risk of which is a determined by a combination of their age at initial event, family history and SIMD (see Equation 2; two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014). Each individual’s life expectancy is determined as the sum of the time to the initial event plus the time to the fatal event (for those whose initial event is not fatal).
Quality-of-life adjustment
Quality-of-life adjustment is made in three ways as an individual transits through the model to account for background morbidity (see Equation 3), impact of experiencing a first non-fatal CVD event (see Equation 4) and impact of experiencing subsequent non-fatal CVD events (see Equations 4 and 5). These are then combined to generate overall quality-adjusted life expectancy (two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014).
For background morbidity, Scottish Health Survey (SHeS) 200398 cross-sectional survey data were used to generate a preference-based weighted HRQoL score for each age group (Table 22). 75 These scores were used to weight survival probabilities in all arms of the model (two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014).
| Age (years) | Utility |
|---|---|
| 25–34 | 0.8310 |
| 35–44 | 0.8200 |
| 45–54 | 0.8060 |
| 55–64 | 0.8010 |
| 65–74 | 0.7880 |
| > 74 | 0.7740 |
These utility scores were then adjusted to account for the experience of non-fatal events using utility decrements (Table 23) also estimated using data from SHeS 2003 (two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014).
| Event | Utility decrement |
|---|---|
| Angina | 0.0891 |
| Myocardial infarction | 0.0403 |
| Irregular heartbeat | 0.0499 |
| Stroke | 0.0938 |
| Intermittent claudication | 0.0199 |
| Other cardiac | 0.0336 |
Lifetime health service costs
Individuals accumulate health service costs as they transit through the model. These costs are a mixture of age-related costs (associated with increasing comorbidities) and costs associated with the experience of specific events. The linked SHHEC and SMRs data set provides information on all hospital episodes (two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014). These episodes were costed using method 1 in Geue et al. 99 to generate annual age-related health-care costs. Costs accumulate in the period prior to the initial event (see Equation 6) and following a non-fatal CVD event (see Equation 7).
More details on the HELP model are available on request.
Employing the HELP model for the longer-term analysis of Football Fans in Training
Within the longer-term analysis, the HELP model is used simply as a means to extrapolate the trial results. The model utilises individual sampling that enables us to generate estimates of long-term cost and outcomes for each individual within the trial population with which to supplement the trial data. This allows us to estimate the longer-term costs and outcomes associated with the FFIT intervention compared with no active intervention. As such, the model is populated with the 12-month data concerning the individual participants’ risk factors. These data are used to generate a post-intervention risk score from which the model generates a post-intervention estimate of life expectancy, a post-intervention estimate of QALYs as well as an estimate of cumulative lifetime hospital costs for each participant. The impact of the FFIT intervention is based on the differences between these estimates for the participants who received the FFIT intervention and those who were part of the waiting list comparison group.
It was necessary to make a number of assumptions and adjustments in order to use the HELP model within the longer-term FFIT analysis. All but three of the nine ASSIGN97 risk factors were collected for participants at baseline, 12 weeks and 12 months. The remaining three risk factors (family history of CHD/stroke, total cholesterol and HDL cholesterol) were not available for the participants. In order to generate an ASSIGN score these risk factors were imputed for each participant using information from other Scottish sources.
Family history of CHD/stroke is defined as an immediate family member (mother, father or sibling) being diagnosed with heart disease or stroke before the age of 60 years. 100 A participant may also be classed as having a family history if two or more of their aunts, uncles or cousins suffered CHD/stroke before age 60 years, despite not having a mother, father or sibling affected. The Midspan Family study101 is a cardiorespiratory investigation of two generations of a population based in the west of Scotland. The original Renfrew/Paisley study102 contained a cohort of 4064 married couples from 1972–6. In 1996, their offspring were traced and 2338 attended the cardiorespiratory examination and completed the survey questionnaire. From this data set we were able to find a proportion estimate of family history to apply to our study population (Professor Michaela Benzeval, University of Essex, 2013, personal communication). The proportion was based on men with at least one parent who experienced or died of CHD/stroke in our population of interest: men with a BMI ≥ 28 kg/m2, aged 35–65 years. This proportion (121/313) was then applied randomly to our study population, resulting in 38% of both intervention and comparison groups having a family history CHD/stroke.
Using this approach to estimate family history has limitations. Generalisability is questionable as the Midspan population is specific to the offspring of a west of Scotland general population, whereas our sample is from all over Scotland. In addition, the definition of family history varied slightly from the ASSIGN risk score definition as information from the Midspan Family Study was only available on parents. Finally, the proportion with a family history is likely to be an underestimate, as it was based on self-reported data rather than hospital admissions data. However, as family history is not influenced by the intervention, these limitations should not impact the incremental analysis.
Data on total and HDL cholesterol for men aged 35–65 years with a BMI ≥ 28 kg/m2 were available from the west of Scotland Twenty-07 study. 103 From these data, multivariate regression equations were estimated through discussion with clinical colleagues to relate total and HDL cholesterol to age, BMI, SIMD, education, diabetes mellitus and smoking status (Tables 24 and 25). The approach to estimate total and HDL cholesterol for each participant in this way was discussed and agreed with clinical colleagues, who suggested that activity, weight loss and diabetes mellitus would all effect HDL cholesterol more than total cholesterol. Note that we are not attempting to estimate the impact of behaviour change on cholesterol change, an approach which was deemed inappropriate by our clinical colleagues.
| Variable | Regression coefficient | 95% CI |
|---|---|---|
| Age (1-year increase) | –0.0068598 | –0.192659 to 0.0055462 |
| BMI (unit increase) | –0.0450094 | –0.0781239 to –0.0118948 |
| SIMD (unit increase) | –0.0066748 | –0.013775 to 0.0004254 |
| Intermediate vs. higher education | 0.0676622 | –0.2250695 to 0.3603939 |
| Basic vs. higher education | 0.2754775 | –0.0712515 to 0.6222065 |
| Diabetes mellitus vs. none | –0.883468 | –1.431325 to –0.3356115 |
| Ex-smoker vs. non-smoker | –0.1088097 | –0.3963641 to 0.1787446 |
| Current smoker vs. non-smoker | 0.2003869 | –0.1046881 to 0.0505462 |
| Constant term | 7.601214 | 6.345408 to 8.857019 |
| Variable | Regression coefficient | 95% CI |
|---|---|---|
| Age (1-year increase) | –0.0035155 | –0.0088002 to 0.0017692 |
| BMI (unit increase) | 0.0020153 | –0.0031141 to 0.0030424 |
| SIMD (unit increase) | –0.0000358 | –0.0031141 to 0.0030424 |
| Intermediate vs. higher education | –0.0872548 | –0.2098335 to 0.0353239 |
| Basic vs. higher education | –0.083006 | –0.2273535 to 0.0613415 |
| Diabetes mellitus vs. none | –0.01753 | –0.2294473 to 0.1943874 |
| Ex-smoker vs. non-smoker | 0.1154253 | –0.0057461 to 0.2365966 |
| Current smoker vs. non-smoker | 0.1083991 | –0.0237426 to 9.2405409 |
| Constant term | 1.577714 | 1.053263 to 2.1022164 |
The equation for total cholesterol was based on a sample of 337 men, while the equation for HDL cholesterol was based on a sample of 317 men. Note that those with higher BMI were more likely to be on statins, lowering their cholesterol and, thus, explaining the negative coefficient in the results in Tables 24 and 25.
Analysis
The long-term effectiveness is presented in terms of both life-years gained and QALYs. These estimates are generated for each individual as the sum of the individual’s within-trial outcome (in terms of life-years or QALYs) and the individual’s estimate of life expectancy generated from the HELP model (in terms of life-years or QALYs).
The long-term cost associated with each individual is determined by the sum of the individual’s within-trial cost and the individual’s estimate from the HELP model.
The longer-term estimates of life expectancy, QALYs and costs were all discounted at a rate of 3.5% following guidance from the UK NICE. 104
The cost and effects of the FFIT intervention are calculated by averaging the costs and effects of the individual participants who received the FFIT intervention; the same process is undertaken for members of the waiting list comparison group to determine the costs and effects associated with no active intervention. The incremental cost associated with the FFIT intervention is the difference between the average cost of the FFIT intervention group and the average cost of the comparison group. The incremental effects associated with the FFIT intervention are taken as the difference in the average effects (in terms of life-years or QALYs) between the FFIT intervention group and the comparison group. The incremental cost-effectiveness associated with the FFIT intervention is then presented in terms of incremental cost per life-year gained and incremental cost per QALY gained.
Probabilistic analysis
In order to estimate the uncertainty in the model estimates, we undertook a probabilistic sensitivity analysis allowing for uncertainty in the estimation of all of the parameters within the model. Running this analysis required simulating 1000 draws from the probability distributions for each of the parameters and using each of these 1000 draws to estimate the life expectancy, QALYs and lifetime costs for each of the participants, generating an estimate of the average costs, life-years and QALYs for each group for each draw.
The resulting uncertainty in the incremental costs and effects associated with the intervention is plotted on the incremental cost-effectiveness plane. The cost-effectiveness acceptability curve presents the uncertainty surrounding the cost-effectiveness of the FFIT intervention compared with no active intervention.
Finally, the uncertainty surrounding the decision to implement the FFIT intervention was formally assessed, in terms of the associated costs and consequences, within a value of information (VOI) analysis. The expected value of perfect information (EVPI) provides a monetary valuation of the impact of the uncertainty surrounding the decision between FFIT and no active intervention every time that a decision is made. This per-decision amount is scaled up according to the frequency of the decision in order to provide a population-level value of the uncertainty. This valuation provides an estimate of the maximum return achievable, for the population, from reducing uncertainty through further research and can be used to determine whether or not it is potentially worthwhile undertaking further research around the effectiveness or cost-effectiveness of FFIT compared with no active intervention.
Within the VOI analysis of the FFIT intervention, the eligible population was specified as Scottish men aged 35–65 years identified over the next 3 years with a BMI ≥ 30 kg/m2; that is a population of 365,000 men.
Scenario analysis
Uncertainty about the long-term sustainability of behavioural change (structural uncertainty) is examined through a scenario analysis that limits the time frame for the risk reduction impact of the intervention. This was achieved by changing the hazard ratios utilised within the model 5 years after the intervention.
Results
Table 26 presents the results of the probabilistic analysis in terms of the average lifetime costs and QALYs per participant in each group.
| Costs variable | Cost (£) | Life-years | QALYs |
|---|---|---|---|
| FFIT | 19,452 | 66.94 | 65.59 |
| No active intervention | 18,378 | 66.51 | 65.21 |
| Incremental | 1074 | 0.43 | 0.38 |
The results illustrate that FFIT is more expensive than no active intervention, with an average additional cost of £1074 per individual (95% CI £780 to £1298). The results also indicate that the FFIT intervention is also marginally more effective with an average increase of 0.43 life-years (95% CI 0.32 to 0.56 life-years) and 0.38 QALYs (95% CI 0.25 to 0.55 QALYs). As a result, the FFIT intervention is associated with an incremental cost-effectiveness of £2810 per QALY gained (£2535 per life-year gained).
Figure 8 shows the uncertainty surrounding the estimates of the lifetime incremental costs and effects. The figure shows that there is no uncertainty surrounding the existence of a cost difference – FFIT is more expensive than no active intervention (i.e. all the incremental costs are positive), although there is some uncertainty about the extent of the cost difference. In addition, the figure shows that there is no uncertainty surrounding the existence of a difference in effect (i.e. all the incremental QALYs are positive), although there is uncertainty about the extent of the effect difference.
FIGURE 8.
Incremental cost-effectiveness plane (lifetime analysis).

Figure 9 presents the cost-effectiveness acceptability curve for the lifetime analysis. This demonstrates that when the decision-maker is willing to pay £20,000 or £30,000 per QALY, there is no uncertainty that FFIT is cost-effective compared with a no active intervention alternative, with a probability of 1. In fact, this is the case for any value of the cost-effectiveness threshold beyond £5000 per QALY, as such if the decision-maker is willing to pay more than this value there is no uncertainty that FFIT is cost-effective.
FIGURE 9.
Cost-effectiveness acceptability curve for FFIT intervention (lifetime analysis).
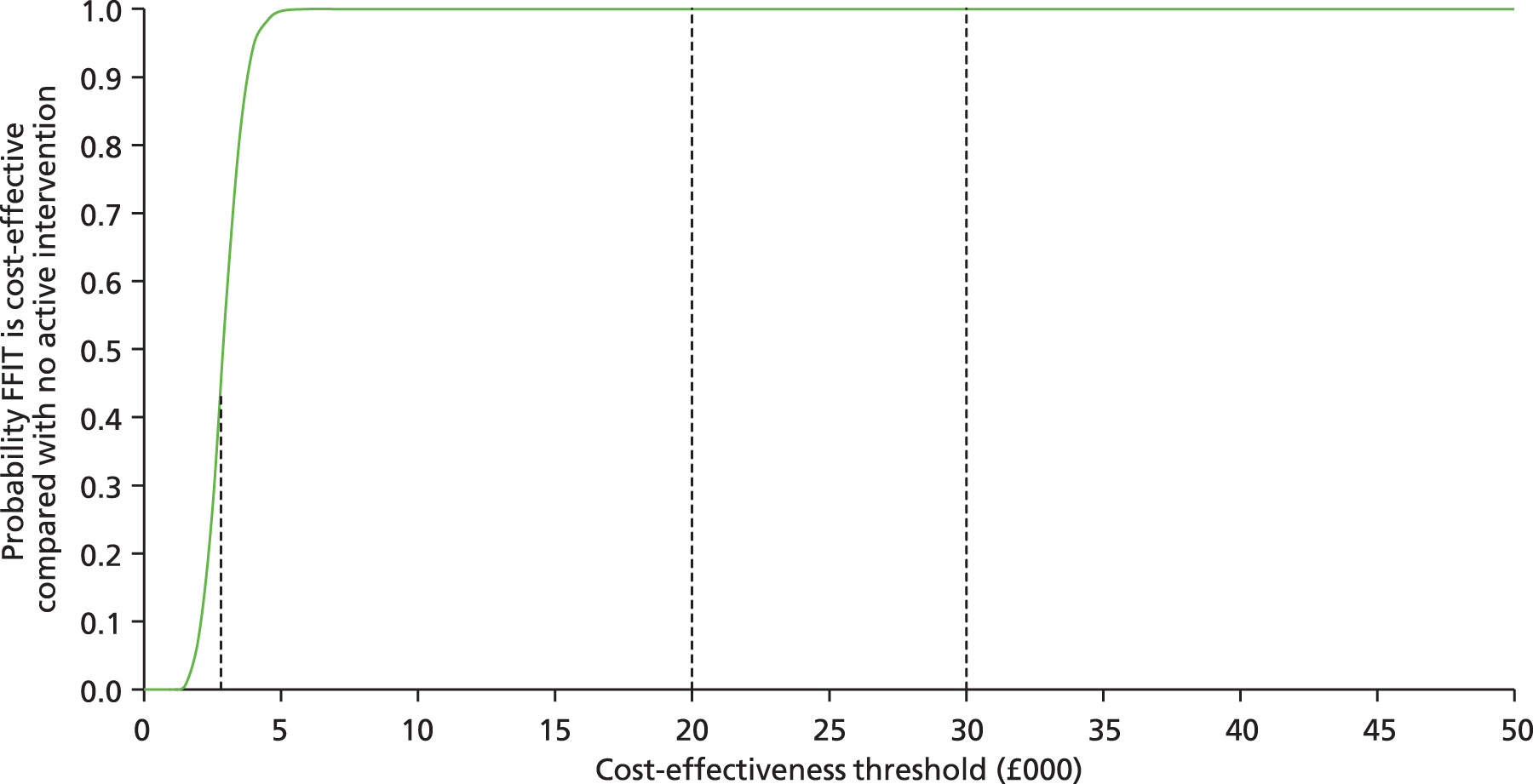
Figure 10 presents the EVPI associated with the decision between FFIT and no active intervention for each instance of the decision (individual eligible man). This illustrates that for any value of the cost-effectiveness threshold above £5000 per QALY (i.e. when the decision-maker is willing to pay > £5000 per QALY) there is little value associated with further research and data collection.
FIGURE 10.
The EVPI for each eligible man aged 35–65 years.

Figure 11 presents the EVPI associated with the decision to implement FFIT (compared with no active intervention) for a Scottish population of men aged 35–65 years identified with a BMI ≥ 30 kg/m2 over the next 3 years. Again, the figure shows that there is very little value associated with further research and data collection if the decision-maker is willing to pay > £5000 per QALY. For cost-effectiveness thresholds below this level, there is considerable value in undertaking further research: up to £25M for a willingness to pay of £3000 per QALY. This reflects the increasing level of certainty concerning the cost-effectiveness of the FFIT intervention as cost-effectiveness thresholds rise from £2810 per QALY (the level at which FFIT becomes cost-effective) to £5000 per QALY (for which there is no uncertainty). For the range of thresholds generally employed within the UK (£20,000–30,000 per QALY) there is no uncertainty about implementing FFIT and, consequently, no potential value in undertaking further research.
FIGURE 11.
The EVPI for a population of men aged 35–65 years with a BMI ≥ 30 kg/m2.
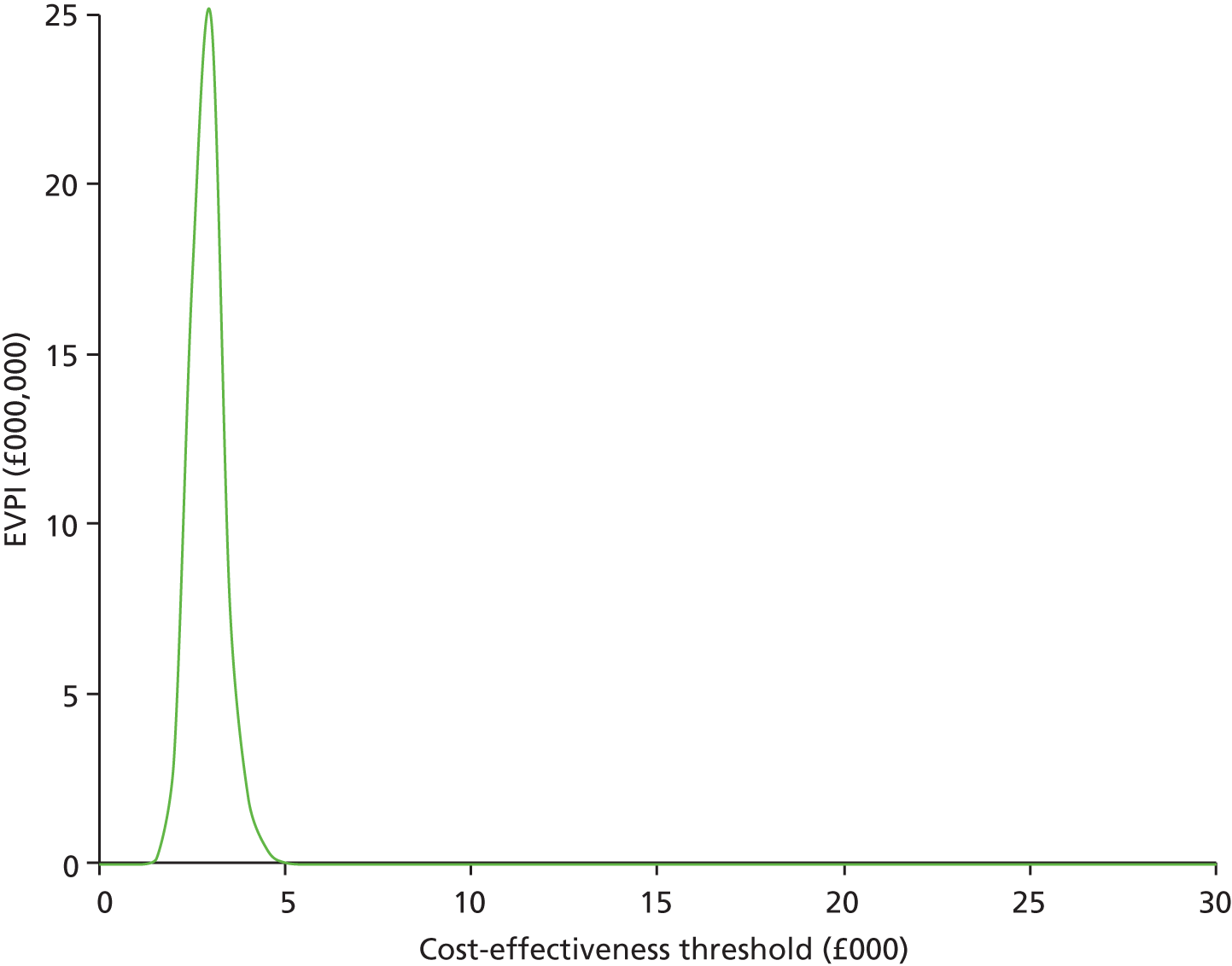
The results of a scenario analyses (Table 27) is limiting the beneficial behaviour change impact of the intervention to 5 years indicates that FFIT remains more expensive than no active intervention, although the average additional cost is reduced to £289.00 per individual (95% CI £0.12 to £503.00). The results also indicate that the FFIT intervention remains marginally more effective, with an average increase of 0.21 life-years (95% CI 0.12 to 0.31 life-years) and 0.25 QALYs (95% CI 0.12 to 0.38 QALYs). The overall result is to improve the cost-effectiveness of the FFIT intervention; incremental cost-effectiveness ratio (ICER) £1174 per QALY gained (£1384 per life-year gained). This counterintuitive result is because restricting the behaviour change has a greater impact on the life-years and QALYs associated with FFIT intervention than the no active intervention group (reducing the incremental outcomes associated with FFIT). In addition, the reduction in life-years and QALYs has a greater impact on the lifetime costs associated with the FFIT intervention than the no active intervention (reducing the incremental costs associated with FFIT). These two effects, when combined in a ratio, lead to a fall in the additional cost per QALY associated with FFIT.
| Cost variable | Cost (£) | Life-years | QALYs |
|---|---|---|---|
| FFIT | 17,924 | 65.68 | 64.36 |
| No active intervention | 17,635 | 65.47 | 64.12 |
| Incremental | 289 | 0.21 | 0.24 |
If altering the behaviour change assumption were assumed to only impact outcomes with costs (and incremental costs) remaining at their original levels, the impact would be to increase the ICER associated with FFIT to £4475 per QALY compared with no active intervention.
Chapter 5 Process evaluation: methods and results
Introduction
The process evaluation investigated six process outcomes:
-
process outcome 1: programme reach
-
process outcome 2: participants’ reasons for continuing with or opting out of FFIT
-
process outcome 3: the extent to which coaches deliver FFIT as designed (fidelity)
-
process outcome 4: participants’ views of FFIT including satisfaction, acceptability and any unexpected outcomes (participants’ experiences of taking part)
-
process outcome 5: coaches’ experiences of delivering FFIT including satisfaction, acceptability and any unexpected outcomes (coaches’ experiences of taking part)
-
process outcome 6: participants’ experiences of maintaining weight loss and lifestyle changes in the longer term.
In this chapter we describe the methods of data collection (data sources) and analysis used to address each process outcome. We then present results in relation to each outcome in turn and, finally, present our conclusions from the process evaluation.
Methods
Data sources and data collection
We used mixed methods and nine data sources to address the process outcomes. Figure 12 shows which sources of data (1–9) were used to address each process outcome (1–6).
FIGURE 12.
Sources of data used to address process outcomes.

Data source 1: self-reports on online registration form and registration telephone calls
On registration, men were asked to provide their name, contact details, date of birth, the club they wished to attend and their self-reported trouser waist size, height and weight. When the research team telephoned men who had registered an initial interest in FFIT (either online or when approached at football games), 98% (1206/1231) were asked how they had heard about FFIT and a single response was recorded.
Data source 2: baseline questionnaire
The methods of data collection for the baseline questionnaire and measurements are reported in Chapter 2, Procedures and baseline characteristics of trial participants are reported in Chapter 3, Baseline data. In this chapter, we use age and objectively measured BMI and waist circumference to compare FFIT trial participants with men in the general population. Categories of waist circumference (‘low’ < 94 cm; ‘high’ ≥ 94 cm and < 102 cm; ‘very high’ ≥ 102 cm) and BMI (‘overweight’ BMI 28–29.99 kg/m2; ‘mild obesity’ BMI 30–34.99 kg/m2; ‘moderate obesity’ BMI 35–39.99 kg/m2 and ‘extreme obesity’ BMI > 40 kg/m2) were used to assess risk of future ill health following Scottish Intercollegiate Guidelines Network (SIGN) guidelines. 43 Comparison figures for similarly aged men in the Scottish population were obtained from the SHeS 2011. 2
Data source 3: telephone interviews with men who opted out of Football Fans in Training
At 12 weeks, participants were contacted by the research team to arrange post-intervention measurements. At this point, 46 participants (12% of the original intervention group) informed the research team that they had left the intervention while it was still being delivered. During this telephone call, a brief structured exit survey was undertaken by telephone with any men who had opted out of FFIT (see Appendix 1). This asked about their reasons for joining, why they stopped attending, whether or not their attendance had changed them in any way and any suggestions for improvements to the programme (and whether or not this would have encouraged them to stay on the programme). It also invited them to make any additional comments not covered by these questions.
Data source 4: club coaches’ weekly attendance sheets
Club coaches were asked to keep a record of attendance at each of the 12 weekly sessions. Coaches for 12 of the 13 clubs (covering 356 of the 374 men allocated to the intervention arm) were able to provide these; one club (Club09) suffered a computer failure that resulted in the loss of their attendance record.
Data source 5: observations of programme deliveries
Three researchers were trained to conduct observations of the intervention delivery. Across the 13 clubs, 26 sessions were observed (observations were distributed so that each of the 12 sessions was observed at least twice and every club was observed twice). Table 28 details which sessions were observed in each of the clubs.
| Club | First session observed | Second session observed |
|---|---|---|
| Club01 | 4 | 11 and 12a |
| Club02 | 2 | 6 |
| Club03 | 5 | 10 |
| Club04 | 4 | 12 |
| Club05 | 6 | 9 |
| Club06 | 1 | 10 |
| Club07 | 3 | 12 |
| Club08 | 2 | 8 |
| Club09 | 3 | 11 |
| Club10 | 3 | 8 |
| Club11 | 2 | 7 |
| Club12 | 1 | 9 |
| Club13 | 5 | 7 |
Researchers were introduced to the men by the coach at the beginning of each session. The researcher explained their role as observer, gave the men an opportunity to ask questions and asked for their consent to observe, take notes, audio-record the classroom session and video-record the physical activity session. They reassured participants that the researcher would leave the session if anyone did not wish to give their consent. Men in all sessions consented to be observed.
As soon as possible after observing the session, researchers wrote detailed notes using a proforma that focused on the extent to which coaches delivered key tasks for the session as specified in the programme delivery guide and identification of particularly good practice and/or any problems/issues with the delivery (see Appendix 2). Researchers listened to the audio-recording of the classroom session and watched the video of the physical activity session and supplemented their proforma notes with any relevant observations which had not already been captured. The key tasks for each session were designed to deliver core educational messages (see Table 1). In total, there were 42 key tasks to be delivered in 12 classroom sessions, as shown in Table 1. Observers rated whether or not key tasks had been ‘delivered’ or ‘not delivered’ and recorded reasons for their rating.
Data source 6: programme evaluation questionnaire
We asked men in the intervention group to complete a questionnaire to evaluate their experiences of the FFIT programme (the exit questionnaire is available from the authors on request). This was administered at 12-month measurement sessions after completion of all other measures. It was completed by 316 out of 333 men (95%) who attended the 12-month measurement sessions and 316 out of 374 men (84%) who were randomised to the intervention group. The questionnaire asked how useful they found key aspects of the programme including physical activity, diet, goal setting, weight loss, group interactions and support.
Data sources 7 and 8: participant focus group discussions
We conducted two sets of focus group discussions (FGDs), the first soon after the delivery of the intervention programme was completed (data source 7: 12-week FGDs) and the second after the 12-month follow-up measurements had been completed at each club (data source 8: 12-month FGDs). At each time point, one FGD was conducted at each of the 13 clubs.
For the 12-week FGDs, men who had consented to additional research-related contact and who had attended the programme for at least 6 weeks were approached to ask if they would be willing to take part in a group discussion on their views of the programme. Of 295 men contacted, 133 (45%) indicated interest in taking part. Up to six men per club were invited to take part in a 60-minute focus group. If men were not available or did not wish to attend at the chosen time, additional men were contacted from the list (if numbers permitted) until five or six men per club had confirmed they could take part. The 12-week FGDs covered how they had heard about FFIT and their reasons for taking part; perceptions of any impacts the programme had; which, if any, aspects of the programme had enabled them to make changes; any negative experiences; and any suggestions for changes that could be made to improve the programme (see Appendix 3). In total, 63 men participated in the 12-week FGDs across the 13 clubs (Table 29).
| Club | 12-week FGDs | 12-month FGDs |
|---|---|---|
| Club01 | 2 | 4 |
| Club02 | 5 | 6 |
| Club03 | 6 | 6 |
| Club04 | 4 | 6 |
| Club05 | 6 | 5 |
| Club06 | 5 | 5 |
| Club07 | 5 | 5 |
| Club08 | 5 | 4 |
| Club09 | 4 | 6 |
| Club10 | 6 | 4 |
| Club11 | 4 | 5 |
| Club12 | 5 | 6 |
| Club13 | 6 | 6 |
| Total | 63 | 68 |
We wanted to ensure that the 12-month FGDs (which were conducted following final 12-month measurements) included a mix of men who had been variously successful in achieving and maintaining weight loss to 12 months. We e-mailed 280 men who had consented to additional research-related contact and 143 (51%) indicated that they were willing to take part. Again, up to six men per club were invited and if they were not available or did not wish to attend at the chosen time, additional men were contacted from the list (if numbers permitted) until five or six men per club had confirmed they could take part. In total, 68 men participated in the 12-month FGDs across the 13 clubs (see Table 29). The topic guide focused on what had helped and hindered men’s attempts to maintain weight loss, increased physical activity and a healthier diet (see Appendix 3).
With participants’ consent we audio- and video-recorded all FGDs. They were transcribed verbatim and checked for accuracy. As part of the consent procedure, men were assured that they could withdraw from the discussion at any time, they could choose not to answer any questions and their participation/lack of participation would not affect future participation in FFIT-related or other activities at their club. Participants were given a £20 club shop voucher to thank them for participation and offered reimbursement for any travel expenses incurred.
Data source 9: coach interviews
We conducted semistructured interviews with coaches who had delivered the programme at each club as soon as possible after the 2011 delivery was completed. At one club, all three coaches involved were interviewed together, at eight clubs two coaches were interviewed together, at one club both coaches were interviewed individually and at the remaining three clubs the main coach was interviewed individually.
As part of the consent procedure, coaches were assured that they could terminate the interview at any time or choose not to answer any question and that their participation/lack of participation would not affect future participation in FFIT.
The topic guide included questions about coaches’ experiences of delivering the programme, elements they thought were effective/less effective, aspects that were difficult to deliver and any changes they would like to suggest for future versions of the FFIT programme. Interviews were conducted at the clubs, lasted up to 1 hour, were audio-recorded, transcribed verbatim and checked for accuracy.
Analysis
Qualitative data from focus group discussions, coach interviews and observational data
We used a structured, thematic, approach to analyse transcripts from FGDs, coach interviews and qualitative data from observations. 105–107 First, transcripts were repeatedly read and coded to broad themes reflecting the research questions covered in the process evaluation. For the 12-week focus group data, these broad themes were reasons for participating in FFIT, reasons for continuing with FFIT and satisfaction with/acceptability of FFIT. For the 12-month FGDs, themes relating to participant experiences of maintaining weight loss and lifestyle change were identified. For coach interview data, broad themes were experiences of delivering FFIT, satisfaction and acceptability of FFIT and any adaptations made during the delivery of FFIT.
Second, all data coded to these ‘broad themes’ were read independently by two researchers who noted all subthemes that were present, including both anticipated subthemes that related to the main research questions and any unanticipated themes or topics. 106 This mixed approach ensured that the full range of participants’ views was captured. 107 Third, the two researchers compared the themes they had identified and collectively agreed a coding framework based on these.
Fourth, each broad theme was recoded by one researcher to the agreed coding framework to ensure that all material of relevance to these analytical categories was captured. Finally, the same researcher produced an extended descriptive summary of each analytical category using data extracts to illustrate each point. This summary was read by the second researcher to double-check that all views were covered and then used to write this report.
In conducting our analysis we were particularly mindful of the capabilities, opportunities, motivation and behaviour (COM-B) model of behaviour change108 and the ROMEO logic model by Robertson et al. 10 The COM-B model argues that for behaviour change people need the right combination of capabilities, opportunities and motivation. The opportunity and motivation aspects of the COM-B model were especially useful for explaining data relating to reasons for participation. The ROMEO logic model describes the important influence of wider environments and culture and of family, friends and workplace interactions on individuals’ ‘weight loss journeys’; this was particularly useful in interpreting extrapersonal factors that drew men to the programme, why they engaged with FFIT and influenced the weight loss trajectories men followed after the programme finished. In conducting the analysis of men’s experiences of maintenance, we also drew on self-determination theory (SDT), which argues that maintenance of weight loss-related behaviours is associated with the satisfaction of three universal psychological needs: autonomy (volition), relatedness and competence. 109 Thus, men may be more likely to succeed in maintaining their weight loss, increased physical activity and healthier diet if they have developed internalised self-regulation and have integrated their new behaviours with other aspects of their personal identity; feel optimally challenged to perform the new behaviours; and feel meaningfully connected to others.
Quantitative data from the baseline questionnaire, the programme evaluation questionnaire and exit survey
Categories of waist circumference (‘low’, < 94 cm; ‘high’, ≥ 94 cm and < 102 cm; ‘very high’, ≥ 102 cm) and BMI (‘overweight’, 28–29.99 kg/m2; ‘mild obesity’, 30–34.99 kg/m2; ‘moderate obesity’, 35–39.99 kg/m2; and ‘extreme obesity’, > 40 kg/m2) were used to assess risk of future ill health. Descriptive statistics were used to examine men’s satisfaction with the programme, as reported in the programme questionnaire at 12 months, and men’s reasons for dropping out of the programme, as recorded in the exit survey.
Results
Process outcome 1: programme reach
In this section we report the start of men’s ‘weight loss journeys’10 by considering who the FFIT programme managed to reach and how these men were engaged.
Reach
In order to attract sufficient numbers to the FFIT trial within a very constrained recruitment period, we needed multiple recruitment strategies (see Chapter 2, Recruitment strategies and contact with men and/or Chapter 3, Recruitment). Potential participants could therefore have been exposed to information on the upcoming FFIT programmes from multiple sources (e.g. leafleting at football matches, workplace fliers/e-mails, word of mouth) and we are unable to provide a clear denominator for any estimation of reach. Here then, we consider ‘reach’ in relation to the kinds of men who chose to participate in FFIT.
The baseline demographic characteristics of trial participants (see Table 6) demonstrate that FFIT was successful in reaching men from across the socioeconomic spectrum. However, in comparison with the general population, fewer participants were not in paid work (17.2% in FFIT compared with 22.4% of men aged 35–64 years in the Scottish population)110 and fewer were from non-white ethnic backgrounds (98.3% of FFIT participants described themselves as ‘white’ compared with 96.2% in the total Scottish population). 111
The FFIT succeeded in attracting men who were at high risk of ill health on the basis of their BMI, waist circumference and blood pressure. 34 As reported in Chapter 3, mean BMI was 35.3 kg/m2 (SD 4.9 kg/m2). Over 90% of participants had a BMI ≥ 30 kg/m2; 44% were classed as mildly obese, 31% as moderately obese and 17% as extremely obese. Mean weight was 109.5 kg (SD 17.3 kg) and mean waist circumference was 118.4 cm (SD 11.7 cm); all but two men had a high (4%) or very high waist circumference (96%). Mean systolic and diastolic blood pressure readings were 140 mmHg and 89 mmHg, respectively. Table 30 compares FFIT RCT participants with male SHeS respondents of similar ages2 according to health risk category. 34 On the basis of their BMI and waist circumference, FFIT trial participants were at much higher risk of future ill health (type 2 diabetes mellitus, hypertension and CVD); around 10 times more men were classed as being at ‘extremely high’ risk (21%, 16% and 12% of FFIT participants aged 35–44 years, 45–54 years and 55–65 years, respectively, as compared with 2%, 2% and 1% of Scottish men of the same age). A further 223 out of 311 men (72%) aged 35–44 years, 212 out of 290 men (73%) aged 45–54 years and 116 out of 146 men (80%) aged 55–65 years were at ‘very high’ risk, compared with 25%, 25% and 32% of Scottish men, respectively.
| Waist circumference and BMI classification | Health risk category according to SIGN guidelines43 | All FFIT | Age categories (years) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| FFIT 35–44 | SHeS 35–44 | FFIT 45–54 | SHeS 45–54 | FFIT 55–65 | SheS 55–64 | ||||||
| n | n | % | % | n | % | % | n | % | % | ||
| Overweight | |||||||||||
| Low waist circumference | No increased risk | 2 | 1 | 0.3 | 19.4 | 1 | 0.3 | 14.6 | 0 | 0.0 | 9.3 |
| High waist circumference | Increased | 18 | 4 | 1.3 | 17.7 | 10 | 3.4 | 19.7 | 4 | 2.7 | 21.3 |
| Very high waist circumference | High | 37 | 13 | 4.2 | 6.2 | 17 | 5.9 | 8.2 | 7 | 4.8 | 16.4 |
| All | 57 | 18 | 5.8 | 43.2 | 28 | 9.6 | 42.5 | 11 | 7.5 | 47.0 | |
| Obesity I | |||||||||||
| Low waist circumference | Increased | 0 | 0 | 1.9 | 0.4 | 0 | 0.0 | 1.2 | 0 | 0.0 | – |
| High waist circumference | High | 11 | 6 | 0.0 | 2.8 | 3 | 1.0 | 5.8 | 2 | 1.4 | 0.9 |
| Very high waist circumference | Very high | 318 | 114 | 36.7 | 22.4 | 131 | 45.2 | 18.3 | 73 | 50.0 | 25.5 |
| All | 329 | 120 | 38.6 | 25.7 | 134 | 46.2 | 25.3 | 75 | 51.4 | 26.5 | |
| Obesity II | |||||||||||
| Low waist circumference | Very high | 0 | 0 | 0.0 | – | 0 | 0.0 | – | 0 | 0.0 | – |
| High waist circumference | Very high | 1 | 0 | 0.0 | – | 1 | 0.3 | – | 0 | 0.0 | – |
| Very high waist circumference | Very high | 232 | 109 | 35.1 | 2.8 | 80 | 27.6 | 6.3 | 43 | 29.5 | 6.9 |
| All | 233 | 109 | 35.1 | 2.8 | 81 | 27.9 | 6.3 | 43 | 29.5 | 6.9 | |
| Obesity III | |||||||||||
| Low waist circumference | Extremely high | 0 | 0 | 0.0 | – | 0 | 0.0 | – | 0 | 0.0 | – |
| High waist circumference | Extremely high | 0 | 0 | 0.0 | – | 0 | 0.0 | – | 0 | 0.0 | – |
| Very high waist circumference | Extremely high | 128 | 64 | 20.6 | 1.7 | 47 | 16.2 | 2.0 | 17 | 11.6 | 1.1 |
| All | 128 | 64 | 20.6 | 1.7 | 47 | 16.2 | 2.0 | 17 | 11.6 | 1.1 | |
| Total | 747 | 311 | – | – | 290 | – | – | 146 | – | – | |
Furthermore, despite being sufficiently concerned about their weight to register for the FFIT programme, only 3.6% had attended a commercial weight management programme and only 1.7% a primary care-based programme in the 3 months prior to undertaking FFIT. 34
Routes to recruitment
Men expressing an interest in FFIT reported hearing about the programme from a range of different sources. The most widely reported sources of information about the programme were match-day recruitment (reported by 327 men, 27% of the 1206 who were asked to identify what led them to join the programme). At least 13% (154/1206) of potential participants also reported hearing about the programme through club websites, articles or news pieces in the media (newspaper, radio and TV) and through word of mouth. Several other sources were mentioned by a small minority of men (< 10% of participants) including work-based advertisement (6%, 77/1206), posters at the clubs (5%, 55/1206), other club associations (4%, 45/1206), fans’ websites (3%, 40/1206) and GPs (1%, 9/1206).
Accounts from participants in the 12-week FGDs confirm findings from our feasibility study. 32 The most common account was of having heard or read about the programme from multiple sources. For example:
I’d actually, I had heard, coming to one of the home games, there was, like, folk out sort of talking to people periodically. We just happened to be walking past somebody when I heard – that was probably the first I heard of it, and then I’d picked it up in the work through someone in the work, who was actually sort of involved wi’ [with] the measuring side of it. So she’d kind of highlighted the fact that, you know, did I know fans [who would be interested]? I don’t know if it was a subtle hint!
Participant 1, Club12, 12-week FGD
This extract also points to the importance for some men of interactions with others in their decision-making about whether or not to engage with the programme. Other examples suggest some men were strongly encouraged to sign up by family members and some needed prompts from multiple sources before a final decision to sign up. Collectively, the data suggest that it is important to use multiple media outlets when advertising for recruitment and that each source can reinforce another and that making it as easy as possible for men to make the decision to participate is important.
Process outcome 2: reasons for participating/opting out
Reasons for participation: personal motivations and the ‘draw’ of the football club
During the 12-week FGDs, participants were asked about their motivations for signing up for the FFIT programme. They offered multiple and overlapping explanations. This included a range of personal or family ‘push’ factors, such as wanting to regain a more youthful, better functioning or less compromised body. For example:
Well, I used to play football, [. . .] and when I had to chuck it, I kept playing fives [five-a-side], but I was kidding mysel’ on, and you’re no’ doing the same training but you continue to eat the same way you always did, and you continue to drink on the Saturday wi’ [with] your mates, the same way you did. And year on year, it [weight] just crept up to the point where I think I hit about sixteen stone, and I thought I need to dae [do] something aboot [about] it. And I did try to do something aboot [about] it, and it worked for a wee while, and then lapsed again, and then this came up through the work [advert about FFIT] and I thought, ‘I’m going to [Club12 ground],’ so my motivation was to lose the weight and get back fit again . . .
Participant 3, Club12, 12-week FGD
The opportunity to stave off or fight back health problems was frequently raised. One participant explained how when he was approached by a member of the recruitment team at a home game he connected his weight to his musculoskeletal health:
He said they were looking for fat bastards, and I’d had trouble wi’ [with] my knees because of the additional weight I’d been putting on. I knew I had to do something, so it just sort of fitted in.
Participant 5, Club13, 12-week FGD
Similarly, another participant noted that concerns about his high blood pressure prompted him to think about joining FFIT to lose weight.
I just wanted to lose weight. I mean, I’ve been on blood pressure tablets for, I dunno [don’t know] – three or four years. That’s something I’ve never particularly taken seriously, but you should take it seriously, obviously. It’s not a good thing. My doctor’s often said to me, ‘Lose that weight, you never know, you might come off that medication!’ Well, there’s a goal in itself, I suppose.
Participant 2, Club08, 12-week FGD
Another very commonly mentioned ‘push’ factor was a desire to ‘be there’ for family. This referred both to the present, what they wanted to be able to do now with or for family members, and to the future, through an expressed desire to survive long enough to support their families over coming decades and to see their children grow up. As one man put it, when describing why he took part in FFIT:
And plus the fact I’ve got a nine-year-old daughter, and she was beginning, it was beginning to tell when, if she was even swimming, I was swimming with her and I couldnae [couldn’t] keep up with her. She’s only nine, and that was the real, you know, sort of slap in the face, if you like, for me to say to myself, ‘well, I’ve really got to do something,’ because she’s getting fitter and fitter. She’s only nine, but what happens when she’s twelve and I can hardly run a hundred yards withoot [without], you know, breathing really heavy?
Participant 6, Club10, 12-week FGD
These push factors correspond to what the ROMEO model10 describes as history and personal motivations for weight loss.
At the same time, they were powerful ‘pull’ factors that drew the men to the programme. The most important of these were the programme’s delivery within the football club; being with people like them (men who were perceived to be like-minded and like-bodied); and the group format with opportunities to interact with other men. The football club setting was very important for most of the focus group participants and was frequently discussed as a very important ‘pull’ factor.
I think the big pull was you’re actually going to [Club12] to do it. So you’re going to a club where you’re spending a lot of time, anyway, coming to watch games and following the team. And, a bit like saying, well, like-minded [Club12] fans, and that’s really, I think that was the big pull in for me.
Participant 1, Club12, 12-week FGD
Equally important in many discussions was knowing that the programme would be for people like them: men who liked football and were of similar ages, sizes and levels of fitness. The following exchange is a good example:
I think the thing, also, about what we went through, as well, was, I mean, the common denominator is football. We all like football, you know? And that gets us all going.
Of course it does.
That was it.
The good thing, to me, is I didnae [didn’t] like going to a gym. I would prefer to go to a class, or have somebody telling you what to dae [do] and what not to dae [do]. It was kinda like, I don’t want to go to a gym and see all the younger ones, the fitter ones – and you got a kinda, you look roon [around] and you think they’re looking at ye [yourself]. ‘He’s that fat he cannae [can’t] even dae [do] that.’ And that was the kinda thing I liked. You come here, everybody was in the same boat – everybody was between a certain age and overweight, coz that’s how I got into it.
Club10, 12-week FGD
Linked to the importance of being in a group of like-minded (and like-bodied) men was the feeling that pursuing weight loss in a group setting would make the task easier:
Yeah, that was part of it as well, and as you says aboot being at [Club09 stadium] – that was another draw, being at your local club, being about the place. I just agree with what everybody’s saying – coz you’re doing it in a group, it’s so much easier. You’re encouraging each other and you’re happy to see other people getting on and losing weight – no’ just the losing weight.
Participant 3, Club09, 12-week FGD
These ‘pull’ factors correspond to what the ROMEO model10 describes as engagement. Men saw the programme as being in the right setting and circumstances to support them in losing weight and commonly articulated that the FFIT programme was an ‘ideal’ opportunity to translate an emerging or conscious desire to lose weight into action:
I’ve struggled with my weight since, maybe, early twenties and I’ve tried various diets, various things, and you seem to get to a stage where you’re successful, then you fall back out the way again. So, when I seen this advertised in the paper . . . the main thing that drew us to it was because it’s [Club07]. You’re going to be involved at [Club07], whether it just be at the ground, stadium . . . That was what really attracted me to it.
Participant 1, Club07, 12-week FGD
There were many similar examples of men discussing the synergy between their (developing or long-standing) motivation to lose weight or get fit (‘push’ factors) and the opportunity to take part in a programme in their club (‘pull factors’) and the ways in which this encouraged their initial engagement.
Figure 13 illustrates how the combination of ‘push’ and ‘pull’ factors, together with the increasing awareness of the opportunity to enrol for FFIT provided by the multifaceted recruitment strategy, were sufficient to encourage men to register their interest in the programme. Thus, in line with the COM-B model, the focus group data repeatedly provided accounts of men who wanted, and were motivated, to lose weight for whatever reason and for whom the FFIT programme was an appealing opportunity to engage.
FIGURE 13.
Factors attracting men to take part in FFIT: the power of the ‘draw’ of the football club for themselves and other like-minded/like-bodied men. Reprinted with permission from Hunt K, Gray C, Maclean A, Smillie S, Bunn C, Wyke S. Do weight management programmes delivered at professional football clubs attract and engage high risk men? A mixed-methods study. BMC Public Health 2014;14:50. 34
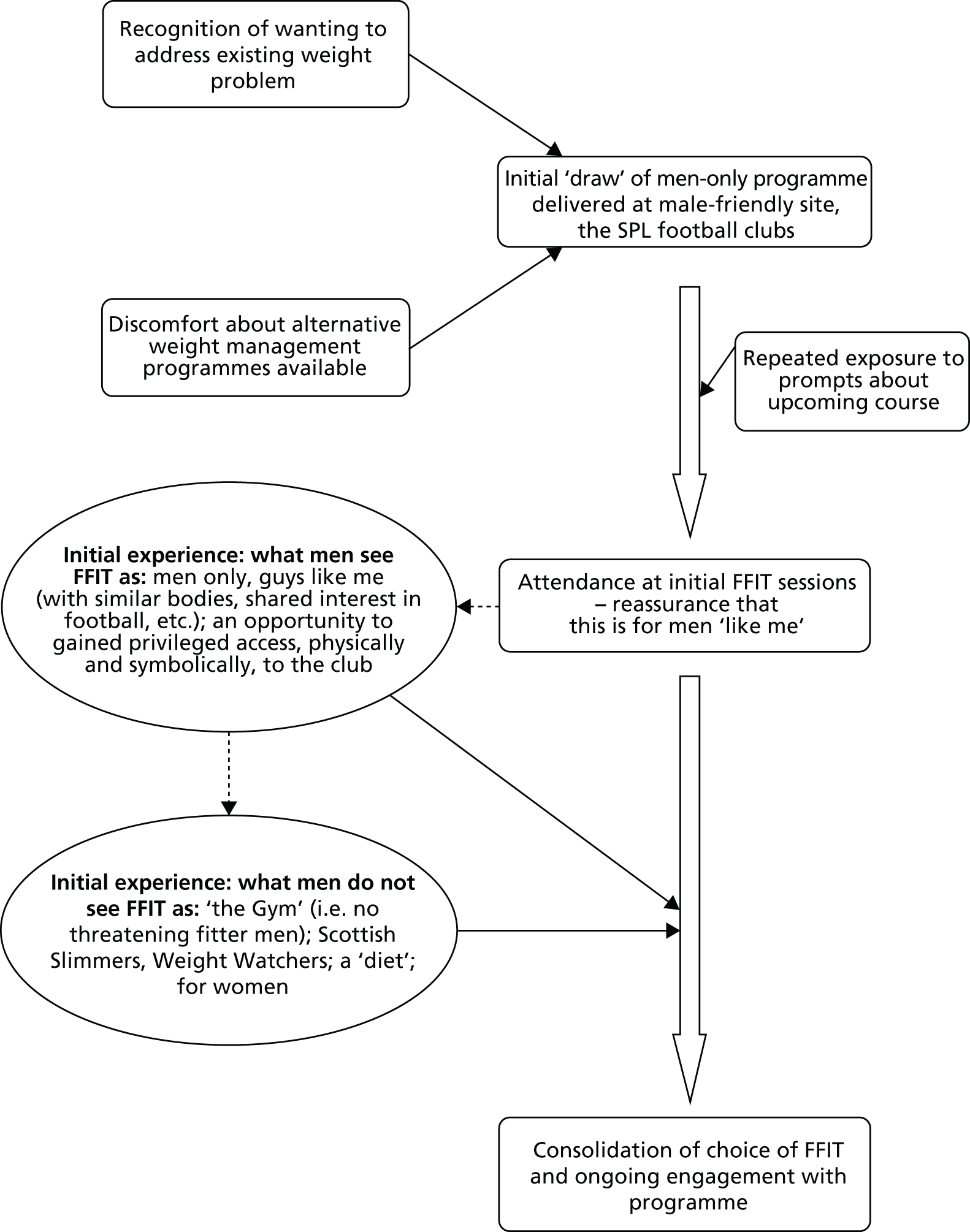
The powerful combination of ‘push’ and ‘pull’ factors is illustrated in some men’s accounts of overcoming deep-seated barriers to taking part in a weight management programme. For example, one man described how his experience of attending baseline measurement in his club’s grounds and discussion with the club coach afterwards had helped him to overcome long-held anxieties about tackling his weight problems:
I remember the first time . . . when you got weighed and all that sort of stuff [. . .] and I genuinely, I just didnae [don’t] want to be here. I felt very nervous aboot [about] the whole thing, . . . It was very embarrassing. It’s not now, but at the time, it was. At the time, I was like, ‘Oh, this is terrible,’ and aye, measuring my waist, and I came in here . . . That was the first time I met [Club07 Coach 1], and I genuinely thought, ‘After I get out [of] here, I’m just going in the car, ignore the phone calls, ignore the e-mails, I’m not daen [doing] that. That’s ridiculous.’ And I sat in here with [Coach 1], and he was telling us, ‘Right, you know, of course we train here, at [Club07’s stadium].’ And I thought, ‘That’s good. I wouldn’t mind training here at [Club07’s stadium] . . .’ And after that, he said, ‘Aye, ken [you know] what we’ll do, we’ll get you some training gear . . . you’ll be running aboot [about] in the training gear.’ And honestly, I couldnae [couldn’t] get the grin off my face. I was like a bairn [child]. I thought, ‘I want to be training at [Club07’s stadium],’ with the, you know, aye, with the kit.
Participant 4, Club07, 12-week FGD
Others expressed their worries about weight management in different ways, such as a fear of being so overweight, unwell or unfit that they might be rejected when they applied for FFIT.
Men’s very early experience of the programme reinforced their view that FFIT was the right programme for them and increased early engagement (see Figure 13). Men articulated this in relation to gaining privileged access to club facilities (e.g. home/away changing rooms, the tunnel, pitch side), as noted in the two examples below:
I’m a fan, and I think that helped a lot . . . the fact that I was coming to [Club05 stadium] and going into the changing room and stuff like that . . . I mean, it was just nice. And you felt kinda part of it . . .
The fact, walking about the stadium, up and doon [down] the stairs.
Club05, 12-week FGD
Just the enjoyment of coming along and being involved in the club . . . even walking round [Club04 stadium], to me, was an exciting part of the Monday night . . . walking up and down the terraces. You might only be restricted to one area when you come to a game, but, you know, the fact that you’ve got carte blanche, you can go wherever you like, other than the pitch.
Participant 1, Club04, 12-week FGD
Thus, FFIT was able to harness men’s initial desire to ‘do something’ about their weight, fitness and health with the deep symbolic and cultural attachments to the football clubs that many participants held. Many had supported their club since they were boys and the chance to take part in a weight management programme which gave them enhanced physical and symbolic access to that club, its coaches and like-minded fans was sufficiently powerful to overcome any reservations they may have felt about signing up for the programme (see Figure 13).
As discussed later, this powerful attachment to the club was also important in retaining men’s engagement with FFIT once they had started on the programme (see Process outcome 2: reasons for participating/opting out).
Attendance and opting out of Football Fans in Training
Across the 12 clubs for which we have data, attendance was high. Participants attended a mean of 8.7 (SD 3.7) sessions during the 12-week programme; 78.9% of men (281/356) attended at least six sessions; and 61.8% attended at least 10 sessions (Table 31).
| Number of FFIT sessions attended | Number of participants | Row % (base n = 356) | Cumulative % |
|---|---|---|---|
| 12 | 74 | 20.8 | 20.8 |
| 11 | 87 | 24.4 | 45.2 |
| 10 | 59 | 16.6 | 61.8 |
| 9 | 29 | 8.1 | 69.9 |
| 8 | 15 | 4.2 | 74.1 |
| 7 | 10 | 2.8 | 76.9 |
| 6 | 7 | 2.0 | 78.9 |
| 5 | 13 | 3.7 | |
| 4 | 6 | 1.7 | |
| 3 | 11 | 3.1 | |
| 2 | 18 | 5.1 | |
| 1 | 11 | 3.1 | |
| 0 | 16 | 4.5 | |
| Total | 356 | 100 |
However, although attendance at the main 12-week programme was high, attendance at the 9-month ‘reunion’ was quite poor; 72% (261/365) did not attend. This may have been because the sessions coincided with the Euro 2012 football championship or because they were held in the ‘closed’ season when we know men often switch off from football. However, it may also indicate less interest in the programme 6 months after the main sessions had been completed.
Some men did drop out of the programme. Examination of participant attendance week by week over the 12-week programme (Figure 14) demonstrated that there was an initial drop-in attendance between sessions 1 and 5, after which attendance remained relatively stable until the final two sessions, when a further small drop-off was observed.
FIGURE 14.
Number of participants attending FFIT by delivery session (of 356 for whom we have attendance data).
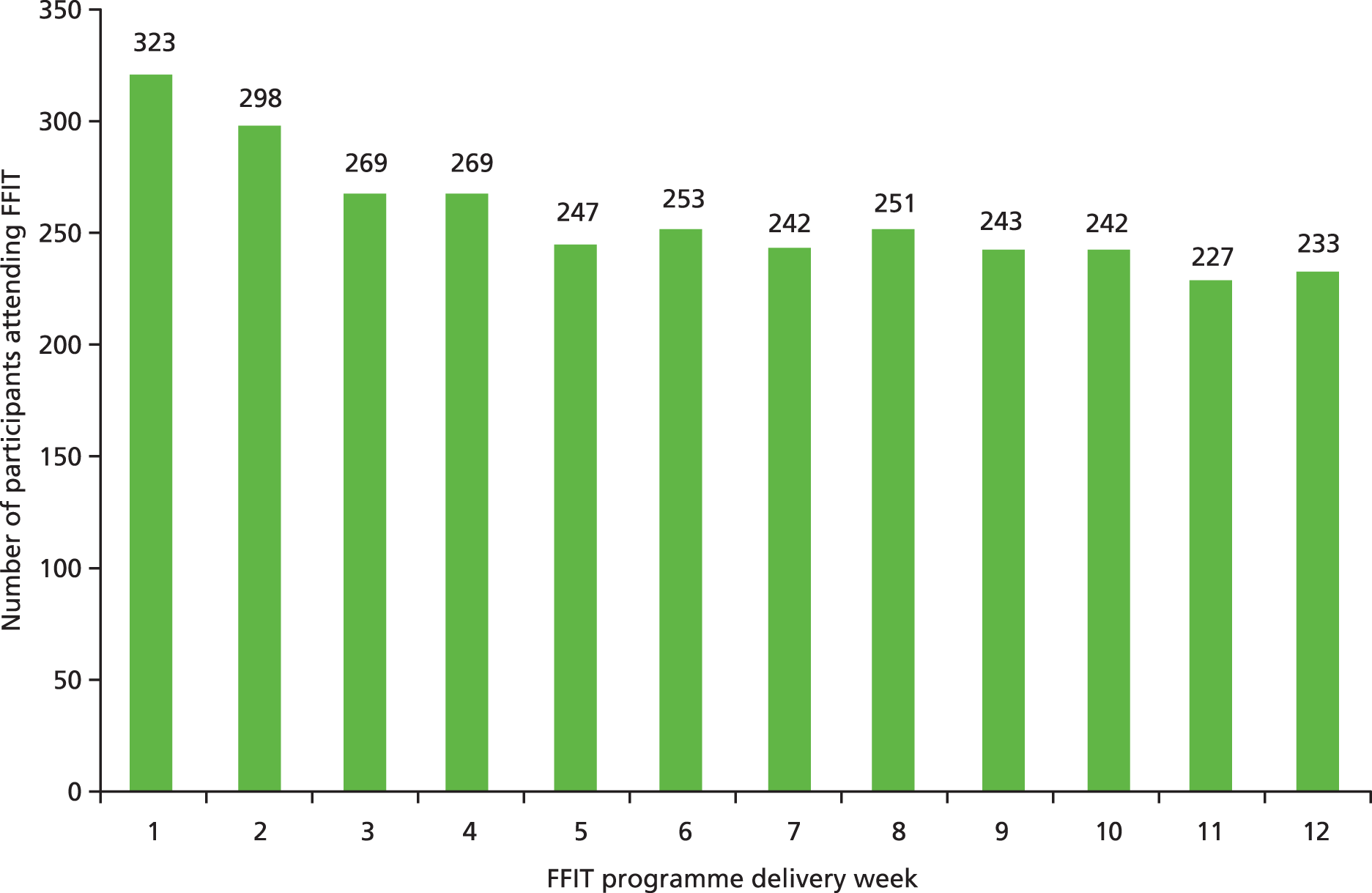
Table 32 shows the results from exit telephone interviews with the 46 ‘drop-outs’ whom we were able to contact. The most common reason cited for dropping out was changes to work patterns that meant they could no longer attend (19/46, 41% of ‘drop-outs’). Much less common were course-related issues, although seven men (15% of ‘drop-outs’) reported not being able to continue because of injury. Only one man said that he left FFIT because he did not like the classroom sessions and only two cited dislike of the physical activity sessions as their reason for dropping out. Of the 16 ‘other reasons’ cited, four men said that the course did not meet their expectations and one felt he was not making sufficient progress. Not only were programme-related reasons for leaving the course uncommon, but some men stressed in the exit survey that they felt that FFIT had had a positive effect on their lives or health: 20% (9/46) reported that they had lost weight; 43% (20/46) said they had improved their eating habits and 24% said they were doing more exercise (11/46).
| Reason | Number of times cited (% of all 46 responders to exit survey) |
|---|---|
| Changes to work commitments | 19 (41) |
| Injury | 7 (15) |
| Health reasons | 5 (11) |
| Changes to family commitments | 3 (7) |
| Could not devote the time needed | 3 (7) |
| Did not like exercise sessions | 2 (4) |
| Did not like classroom sessions | 1 (2) |
| Other | 16 (35) |
Process outcome 3: the extent to which coaches deliver Football Fans in Training as designed (fidelity)
To address objective process outcome 3 we draw on data from the observations, the coach interviews after the initial 12 weekly sessions at the club and the weekly attendance sheets to consider whether or not the coaches delivered the programme as intended, the extent to which the coaches were judged to have delivered the key tasks in observed sessions and any problems or challenges with delivery identified in coach interviews and the researchers’ observation field notes.
In the 12 clubs for which we have attendance records, all but two delivered 12 sessions over a 12-week delivery period as intended: one club (Club01) had to combine sessions 11 and 12 because of operational problems and another (Club04) had to cancel session 11 because of snow.
As we described under Data source 5: observations of programme deliveries, we observed two sessions in each club (26 in all) and each session of the 12-week programme was observed in at least two clubs. Therefore, we were able to calculate the number (%) of key tasks that could be delivered in each observed session and the number (%) of key tasks that observers judged to have been delivered as intended (Table 33).
| Delivery week | Number of key tasks in delivery session | Number of sessions observed | Total key tasks that should have been delivered in the sessions observed | Number (%) key tasks judged to have been delivered as intended |
|---|---|---|---|---|
| 1 | 5 | 2 | 10 | 9 (90) |
| 2 | 3 | 3 | 9 | 8 (89) |
| 3 | 6 | 3 | 18 | 11 (61) |
| 4 | 4 | 2 | 8 | 8 (100) |
| 5 | 5 | 2 | 10 | 10 (100) |
| 6 | 3 | 2 | 6 | 6 (100) |
| 7 | 3 | 2 | 6 | 6 (100) |
| 8 | 2 | 1a | 2 | 2 (100) |
| 9 | 3 | 2 | 6 | 6 (100) |
| 10 | 3 | 2 | 6 | 5 (83) |
| 11 | 3 | 2 | 6 | 6 (100) |
| 12 | 2 | 3 | 6 | 4 (67) |
| Total | 42 | 26 | 93 | 81 (87) |
Of 93 key tasks that should have been delivered in observed sessions, the observers judged that 81 (87%) tasks were delivered. Table 33 shows that in weeks 3 and 12, fewer key tasks were judged complete by observers. Session 3 contained the most key tasks (n = 6), meaning that it was extremely challenging to deliver in a single week. Coaches were trained to ensure that delivery was highly interactive and to exercise flexibility in terms of the content and timings of each session to allow full discussion of the key points. The coaches were encouraged to reflect after each session, noting any key tasks they had not managed to deliver and to ensure these were delivered in future sessions. In session 12, two clubs did not record the final measurements because these had already been done by the research fieldwork team.
All coaches interviewed reported that the programme was enjoyable and easy to deliver. However, when pressed they identified some challenges, including the enthusiasm of the men during discussion of some of the key points. For example:
I think the notes are very comprehensive. If you’ve read through them beforehand and you’ve got them in front of you, it’s quite an easy programme to follow, and most of the talking points, if not all of them, that you’re asked to invite the men to talk about are very relevant, and they work really well in getting them discussing the issues and topics that are required. And it’s, again, just looking at being flexible – so it might say ten minutes in the book, but it might take twenty minutes if you get a good discussion going about it. And just fitting the rest of the programme around that, whether you curtail something else in the programme. But everything in it is relevant. And it’s just individual preference of how much time you want to spend on each thing.
Coach 1
Spend on each thing, yeah.
So some things you want to spend a bit longer, sometimes, not quite, or just the time, more.
Club06, 12-week coach interview, coach 1
Although the coaches welcomed the interactive nature of the sessions, there was evidence that on occasion this did cause some problems. For example:
I tend to find you just get caught up in questions from the guys which is, obviously they’re needing that information so you try and give them that but you then become side-tracked. So you might very well miss stuff and I kinda feel that I did miss things like just simple things like explaining, I don’t know, I can’t remember off the top of my head right now but eh like wholemeal bread instead of white bread and things like that. Brown rice instead of white rice.
Club11, 12-week coach interview, coach 2
The observation notes provided some detail about ways in which coaches modified programme delivery when time was short. For example, on occasion very little time was allowed for a warm-down period after the physical activity session. Similarly, in later sessions the coaches did not always remind the men about their step count targets. Sometimes, when small-sided football games were used as part of a physical activity session, observers noted that these made it difficult for individuals to regulate their level of exertion: participants tended to push themselves further than they should have done. This emphasises the importance of including the RPE to help structure appropriate physical activity, particularly for those who are less fit.
Taken together, these data suggest that the frequency and coverage of the key tasks of the FFIT intervention were delivered largely as intended in the sessions observed. Coaches delivered almost all of the key tasks and largely succeeded in incorporating flexibility with regard to the recommended timings to allow the men to discuss relevant issues, while ensuring all of the important messages were delivered. Nevertheless, a weakness of our approach is that we were unable to observe all FFIT sessions in each club and we recognise that the observation and coach interview data may not capture any issues or departures from the delivery protocol that arose at other times. For example, during the 12-month FGDs, it emerged that operational problems had led to a delay in men receiving their pedometers in one club:
Aye, and one of the things that helped me a lot was the pedometer. Because once we got it, and we were a while getting it, because it was about just how little you actually moved about and then you were making a bid tae try and get a bit better for the next week . . .
That’s right, yeah.
And next week. So . . .
It was week 6 that we actually got that.
Aye, that was it and you’re supposed to get it in week two.
Club12, 12-month FGD
Process outcome 4: participants’ views of Football Fans in Training, including satisfaction, acceptability and any unexpected outcomes (participants’ experiences)
We now consider men’s satisfaction with the programme, the extent to which different elements proved acceptable to them and any suggestions they made for potential improvements. This section focuses on the intervention stage of participants’ weight loss journeys, in relation to the interactions between participants and with coaches during the programme, the content of the programme, the context in which it was delivered and the relationships that emerged with and between these factors. 10
Satisfaction and acceptability
Overall, both men expressed very high levels of satisfaction with the programme and found its content highly acceptable, as succinctly illustrated in one interchange at the end of a FGD when participants were asked for their final reflections on the programme as a whole:
I would just have said it was one of the best 12 weeks.
Aye, it was brilliant.
That’s one of the best things I’ve ever done in my life.
To me, it’s life changing. It was life changing, you know? Hopefully, you know, that you know, it will keep it up. I know I’m determined, I will keep it up.
Club02, 12-week FGD
Such spontaneous and enthusiastic praise was common, as one participant said:
I honestly can’t praise it enough. I thought it was great.
Club03, 12-week FGD, participant 6
A number of factors, which are considered in turn below, are particularly salient in explaining these high levels of satisfaction: (1) the football club setting, (2) the delivery of the programme by club coaches, (3) men’s enjoyment of interactions in the group and of being with men like themselves, (4) the content of the course and, (5) their experience of bodily changes over the 12-week programme.
The football club: branding and setting
We describe above how participants cited the location of the programme in the stadium and its close association with the football club as powerful ‘draws’ to the programme in the first place (see Reasons for participation: personal motivations and the ‘draw’ of the football club). These factors appeared to be equally important in men’s continued engagement with the programme and were elements that men consistently said they liked about FFIT. For example:
One of the things that I found, and it’s such a simple thing, [. . .] the booklet you got, first of all, from the club, with all the information on it – and I’m sure it’s identical in all the other clubs had it – but the fact that they did the [Club03] crest on it, then, you kind of felt as if, yeah, you were part of a bigger thing, doing it. I know it seems like a really small, stupid thing, but that really did kinda hook me.
You actually thought, at the end of the day, once you leave your group, you had your [Club03] jersey. You were actually doing it for [Club03], as well, not just yourself.
Aye, that’s right.
Club03, 12-week FGD
This exchange highlights the importance participants placed on symbolic representations of FFIT’s proximity to the club – the crests on the booklets and the team shirts – that were harnessed in the intervention (see Chapter 2, Gender sensitivity). Another group conceptualised the connection engendered with club in terms of being part of the ‘fans’ team’:
There’s an ownership wi’ [with] the club, or I suppose ‘ownership’ is probably not the right word, but you definitely feel a connection to the club that you maybe didn’t have before. Even just the T-shirts we all got.
Aye.
Aye, it’s like an identity. It’s almost as if it’s you become, I know this sounds crazy, but I had this in my head that it’s all like, you know, I’m part of the team, the fans’ team, you know? And it’s nothing to do with that, but there is a kind of psychological part of that, as well – but I think that was one of the things that kept me going, as well.
Club12, 12-week FGD
Thus, participation in the programme seemed to engage a new, enhanced, relationship to the club, symbolised through tangible markers or symbols. This enhanced closeness was also apparent in the way the men spoke of their enjoyment of being in the club grounds. For example:
I think the other good thing was it’s actually held here, in [Club08 stadium]. I remember, I think it was week 1 or week 2 and it was [FFIT participant] said, ‘You know, it’s unbelievable! We’re here and we’re in the stadium and, you know, we can go out to the park and things like that!’ And that was encouraging a lot more than anything else.
Yeah.
A couple of people said, in our group that, ‘Why did you not have it at [Club08 training ground]?’ And they says, ‘Well, we thought yous would all want to come here [stadium], rather than go to [training ground].’ He says, ‘Well, we could have went up to [training ground] one or two weeks of the course, like.’ And then most people said, ‘No, this is what we come for, to see this place [Club08 stadium].’
Club08, 12-week FGD
Other men expressed pleasure at getting access to parts of the stadium they would otherwise not see, such as the changing rooms or warm-up facilities. Thus, the physical setting of the stadium provided a direct, ongoing motivation for continuing with the programme. This shows that the physical, not just the cultural, connection to their clubs was important for galvanising participant attendance, that the setting was as important as the branding.
Taken together, the data on the importance of the football club as both setting and brand suggest that another angle of analysis could usefully be added to the micro level of the ROMEO model by Robertson et al. :10 the importance of objects. This resonates with Latour’s suggestion that inanimate objects play an active role in the social, acting as mediators of social relationships that are far more durable than transient interactions. 112 The fact that men cited the club-crested T-shirts and books that they received and the stadia in which the intervention took place as significant reasons for continuation and satisfaction suggests that this analytical approach holds value and should be carefully considered in the development and delivery of interventions; other health interventions might increase engagement if they are able to integrate objects that are symbolically valued by participants.
The delivery of the programme by club coaches
When talking about their experiences of FFIT, participants often spontaneously attributed their high level of commitment to FFIT to the positive interactions they had had with the coaches that led the sessions. For example,
And I think the two people that were running it were, you know, could have a laugh and, you know, there was wee jibes and jokes, so it was . . .
Yeah, it wasnae [wasn’t] somebody just up there rattling change in their pocket and talking at you.
Aye.
Club01, 12-week FGD
The importance of the genuine interest in the men that the coaches had shown was felt to set the tone for a sociable, enjoyable and motivational environment for participants; they had succeeded in promoting a very positive motivational climate in which the group could operate. Another aspect of the sessions that participants valued highly was the positive group interactions between participants on the programme and this too was something that was attributed to the coaches’ style of facilitation:
And I think the club coach was a big part of that, bonding everybody together and I think we’re lucky we got such a – he’s a good guy. He knows what, he’s very good at what he, at doing it and presenting it. So everybody felt quite comfortable as soon as he started on you.
Participant 5, Club07, 12-week FGD
Thus, coaches played a central role in the formation of the group and the fostering of group cultures. This was seen to be down to the engaging, knowledgeable and sociable approach they adopted while delivering the intervention, which really encouraged the building of relationships and to a genuine interest that they had in the participants.
Enjoyment of group interactions
Men’s active enjoyment of group interactions and the relationships they developed with each other while on the programme was also an important contributor to the very high levels of reported satisfaction with FFIT. There were three features to this: team spirit, the sociability of the group and a sense of solidarity deriving from being with men very much like themselves.
All groups made reference to the team spirit engendered among those that participated in FFIT. For example:
I think self-encouragement is, we’re there, because we’re part of a group, we were all encouraging each other. It’s not, you were no longer an individual. You were part of a team, and [. . .] I think it helped, and even although you had the book to start with, you could have flicked through the whole book yourself and worked it out yourself – I think you wanted the encouragement, as well, by going on to the next stage and having a wee bit of explanation. You can learn a lot from books, but the practical side, you learn a heck of a lot more from the practical side than you do from just the written word.
Participant 1, Club08, 12-week FGD
For this participant, the importance of working with others in maintaining commitment to and attendance at the programme was vital. As another participant put it:
There was a team spirit and you didnae [didn’t] want to let the team down, you know?
Participant 1, Club03, 12-week FGD
This was also reflected in responses to the programme evaluation questionnaire; 277/316 (88%) of respondents reported that it was ‘quite’ or ‘very’ useful to hear how other men were getting on during the course of the 12 weekly session highlighting the vicarious learning that is a feature of group-based interventions. 113,114
Related to team spirit was discussion of the sociable atmosphere in which the programme was delivered. The men joked, teased and supported one another and laughed together about incidents they related to each other, as illustrated by the next extract:
And the craic.
And the craic was great.
The biggest thing, I think, in life, is laughing because, you know, aw [all] the chemicals go off and you know . . .
[. . . discussion about a particular night].
But things like that was just, and like, wee bits of banter when we’re in the gym, or playing fitba [football] or that – you’d have a wee craic with somebody. And the laughter, when I played football – no’ at a great level, like – but I used to prefer the training bit to the actually going oot [out] and somebody trying to kick lumps out of you. And that was the environment we were working in. It was almost, coz we had training every week, you know?
And it was completely non-threatening.
Yeah.
Club02, 12-week FGD
Thus, within the football club setting, coaches and participants between them created a supportive, cohesive, non-threatening environment in which humour was experienced. This appeared to give meaning to the experience of taking part in FFIT that was said to be an important reason for continuing with the programme. For many, this was likened to other forms of sociality that they enjoyed in their day-to-day lives:
It was [like] going to the pub for the banter withoot [without] the drink.
Aye.
[Laughing.]
You know? That’s what it was.
Right enough, it just aboot [about] was.
Club13, 12-week FGD
The comparison of the atmosphere within the sessions to the geniality, comfort and sense of belonging that men might experience with their friends in the pub, points not just to men’s enjoyment of the sociality of the programme, but also to the ability of the programme to support group cohesion and demonstrates that its design successfully tapped into cultural frames that appeal to men.
Alongside enjoyment of the sociality and team spirit, participants often commented on the importance of the programme being aimed at people like themselves, in relation to age, love of football, love of their club and being aimed specifically at men only. For example:
I think it was quite good because your peers were people of possibly similar age, or within a reasonable age bracket of yourself. You were no gonna [going to], aye, you werenae [weren’t] gonna have your twenty-year-old who could, maybe is slightly overweight, who’ll find it easy to lose where, when you’re a wee bit older, it’s a lot harder.
Participant 1, Club08, 12-week FGD
The fact that the intervention was aimed at older men was often reported to be extremely important. Another perspective on commonality, a shared interest in the club, was frequently brought up:
The good thing was, straight from the start, we all had something in common with each other. Rather than being sixteen strangers, we’d all something in common, and that was the club and a love for it.
Two things in common. We were fat and we supported [Club03].
Sorry, we were cuddly and supported [Club03], and that was the big factor. So no matter, you met up the first few weeks, you didn’t know each other’s names, we immediately were able to converse with each other easily.
Club03, 12-week FGD
Thus, the combination of a shared passion and a shared problem allowed for the rapid consolidation of a group that they wanted to remain a part of and to high levels of cohesion. Others commented on another commonality, the fact that the programme was targeted at men, and contrasted FFIT to commercially available weight management programmes:
I think we were quite happy it was just men, to be honest. We spoke about going to Weight Watchers or that . . . but we were saying that, a lot of things are set up and it is mainly female – so it was good to see something that was just for male.
For guys.
[. . .]
That’s right. I think the majority felt that Weight Watchers was not for us. That was very much a women’s thing.
That’s a ladies’ thing.
Club08, 12-week FGD
Another group expressed these commonalities (and a humour typical of the groups) between participants very succinctly:
We’re all similar, old, fat gits.
Yeah, exactly.
You know? And that was it.
You could count five points we all have in common, right? One – age. One – weight, yeah? [Club03] supporters, yeah? I’ve ran oot [out] of ideas on that.
All want to lose weight, all want to get fit.
Uh huh.
Male.
Hair falling out.
Yeah.
No, mine’s fell out.
Every single one of us [over talking] has sort of, OK, I’ll say three, four, five things in common, and that’s the pulling thing for the whole lot.
Club03, 12-week FGD
The humour, facilitated through group interactions and the tone set early on by the coaches, not only contributed to men’s enjoyment of FFIT, but was seen as an important factor in enhancing participants’ engagement with the course content:
You know, outside what we did [i.e. activities to lose weight before FFIT], we’re doing it because we feel we have to do it, whereas, what we did here [on FFIT programme], we wanted to do it. It was a pleasure, it was enjoyable, and it was great meeting the guys.
No, they were. I think they were, there’s eh, you get a bit of a laugh with it, as well. It wasnae [wasn’t] all, you know – it was a kind of learning, a wee bit of fun and exercise with a bit of fun, as well. So, although there was a serious side to it, there was also the, there was a wee bit of [pause] I mean, [pause] at some points, it was laugh a minute.
Club12, 12-week FGD
For participants, behavioural changes encouraged by FFIT were transformed from an obligation – ‘we feel we have to do it’, to a desire – ‘ we wanted to do it’. Yet, this enjoyment enhanced, rather than detracted from, the ‘serious side’ of the programme: humour and fun were seen to facilitate learning and exercise, not impede them. It suggests that the high levels of group identity, which formed over the course of the programme, actually helped men to be even more committed to the changes they were making to their lifestyles. We turn now to men’s views of the course content.
The course content
The men (and coaches, see Process outcome 6: participants’ experiences of maintaining weight loss and lifestyle changes in the longer term) discussed how much they enjoyed and appreciated the actual content of the programme, in terms of classroom activities, physical activity sessions and ‘homework’ and skills they learnt on how to make behavioural changes. The content was seen as one of the reasons the programme ‘was so good’. Men commented on the style of delivery of the programme, which was non-didactic and based on adult learning techniques and on the value of graduated learning and the practicality of the skills learnt. They also valued the walking programme, the pedometers as tools for self-monitoring their progress with the walking programme, the self-monitoring of weight more generally and, to a lesser extent, the SMART goal setting. We discuss each of these in turn.
Men appeared to value the way in which the programme materials, supported by the style of delivery of these materials, encouraged them to build autonomy and take personal responsibility for their own behaviours. For example:
They’re giving us the tools – aye, but they’re not telling us what to do. They’re saying, ‘You can do this. This would be beneficial to you.’ They gave us that booklet and all the other tools and let us take them away.
It’s up to you.
And we’ve done what we’ve done with the basic information – and that’s what’s changed us all. It’s, you know what I mean? Yes, the course has helped, and all the work that they’ve done and everything else. They’ve given us the tools and the opportunity, and we’ve taken it away, and everybody’s nurtured it in a different way.
Club10, 12-week FGD
For participant 5 (Club10), then, the information was delivered in an empowering way as ‘tools’ to be used, not orders to be followed. The tools could be adapted and used in ways relevant and meaningful in the context of their own lives.
The modular, graduated, nature of the programme was also discussed in relation to building knowledge and skills over time. When one group was asked what it was about the programme that helped them make the positive changes they had just been discussing, a participant said:
I think coz it was in bite-sized chunks, you know? It was just like a week, every week was something different, so you could get stuck into it for a week, type thing. It wasnae [wasn’t] like overloading, trying to maybe do different things, coz that would probably switch me off, trying to change diet portion control, going shopping, trying to, you know, look at the labels, etc. It was bite-sized chunks with an education. It was like going through modules, for want of a better word, which was quite good for me.
Participant 5, Club08, 12-week FGD
By breaking down the programme’s educational content into ‘bite-sized chunks’, which were ‘like going through modules’, participant 5 (Club08) felt that the course facilitated positive change, a view endorsed by the coaches (see Process outcome 6: participants’ experiences of maintaining weight loss and lifestyle changes in the longer term). He appreciated being able to focus on one new aspect of lifestyle change at a time.
Responses to the programme evaluation questionnaire also suggested that the course’s educational content was important. The vast majority judged that the information about diet (302/316, 96%), food portion sizes (300/316, 95%), regular eating (291/316, 92%), daily calories and personal eating plans (296/316, 94%) was either ‘quite’ or ‘very’ useful. These judgements were supported by comments in the focus groups. The information on portion sizes and nutrition was particularly memorable for participants, as the following illustrates:
I got most of . . . the thing out the course I liked was the fact that I didnae [didn’t] know much aboot [about] food labels and nutrition and what to eat and portion sizes – so the whole start of the course, rather than the exercise – the whole nutrition and aw [all] that, getting aw that in was good, because then I could sit doon [down] and say, ‘Well, haud [hold] on. Looking at these Weight Watchers boxes and that, they arenae [aren’t] good for you because there’s still a lot of fat in them through cheese and aw [all] that,’ which I never knew about. And then it’s going home and educating my family to say, ‘Well, we need to, instead of having this, we need to have that because, even though it does say it’s good for you, it’s no’.’ So it was good to go back and educate my family, plus, then, empty oot [out] the cupboards and start again, and mair [more] fruit, and if I didn’t like certain fruit, put it in a smoothie, and then you could have it, rather than just say, ‘I cannae [can’t] eat that coz I don’t like it.’ Bung it in a smoothie. You can have it then, because you’re drinking it all in the one. So it was an education in food.
Participant 2, Club12, 12-week FGD
Thus, the information relating to portion sizes, nutritional values and food choice was a highly valued part of FFIT for many participants. They learnt to renegotiate their understanding of what an appropriate portion was for different foodstuffs and the course provided them with skills to scrutinise the content of the foods and to think about ways to include more nutritious foodstuffs into their daily diet.
More generally, participants commented on how useful they found the basic information and the very practical tips they discussed in the sessions, as illustrated in the following exchange:
It’s good stuff, aye. It’s good.
It is really basic stuff. Nobody ever really has told me that before.
It’s good quality information, wasn’t it? It was good quality information.
Aye. People think it’s going to be rocket science when you tell them what it is. You point to your pedometer, and then you say, ‘By the way, you watch your portion controls and, you know, naan breads, this. . .’. Remember the naan bread?
Aye. ‘Stop eating half the stuff that comes with curry!’. It’s, like you say, no’ rocket science at all.
Aye, and folk get surprised when you tell them.
Club02, 12-week FGD
Many participants expressed enthusiasm about the new information and understandings they had gained about diet and physical activity. They appreciated the way in which the programme was set out to explain the importance of balancing calorific input and output while also providing skills to make easy, practical, changes to achieve this. One participant suggested that this ‘scientific’ or ‘technical’ focus was one of the reasons the programme was so appealing to many men:
And the other, the part of the programme that helped, I think, again, for guys, there was a technical aspect to it, as well, you know? There was a scientific, technical background, and I think guys, especially, will react to stuff like that, when it’s put factual[ly] – it’s not airy-fairy and there it is.
Participant 2, Club01, 12-week FGD
This resonates with culturally prevalent perceptions of gender roles and interests, which tend to cast men as practical, device loving and scientific. While these norms have and should be questioned, it is noteworthy that men perceived the FFIT intervention to be sufficiently ‘scientific’ and ‘technical’, but yet accessible and credible, expressed by some men through references to ‘science’ but not ‘rocket science’.
We have previously demonstrated that men who took part in the pilot deliveries of FFIT responded extremely well to the walking programme as a first step towards regaining increased physical fitness and were enthusiastic about being able to monitor their progress with the pedometers provided. 31 In the FGDs presented here, men also repeatedly reinforced the views expressed by men on the earlier deliveries of FFIT and discussed how the walking programme supported them to build up their physical activity, typically from low levels of fitness, in a slow and graduated manner they felt suited them well. For example:
I think the pace of the course was good . . . if they put us in the gym the first week, most of us wouldn’t have came back in week two. I’d have been out.
Participant 4, Club13, 12-week FG
Walking is all I could have coped with, when I started out you know.
Yeah.
There’s no way I could have done anything else. I couldn’t have gone into a gym.
Yeah.
I certainly couldn’t have gone out running, jogging or anything.
Participant 6, Club05, 12-week FGD
The suggestion that the walking programme was a well-received component of FFIT was supported by responses to the programme evaluation questionnaire: 298 out of 316 (94%) of participants rated advice on walking either ‘quite’ or ‘very’ useful. In the FGDs, the pedometer was again seen as a key tool for monitoring and, thus, supporting achievement of their physical activity goals. It was seen as ‘the best thing’:
I think for me, personally, I started to think about what I’m putting in my mouth, now, and I started to think about an increase in exercise. The pedometer, for me, was brilliant because it made me go out and, I work in an office job, now – when I was a kid, I was very healthy, very active, played a lot of football, was super fit – but going into an office, you get out of the way of it. I was doing zilch exercise, and it [pedometer] gave you that incentive to go for a fifteen minute walk on my lunch break, and I started doing that, just to get my steps up – but it was for me. It made me change a lifestyle thing, change a habit into a good habit and then start doing more exercise.
Participant 3, Club13, 12-week FG
Thus, the pedometers provided participants with a tangible way of engaging with and adjusting their levels of physical activity. These data are again supported by the results from the programme evaluation questionnaire, which showed that 91% (288/316) found the pedometer either ‘very’ or ‘quite’ useful. The pedometer thus appeared to provide men with a concrete externalisation of their levels of activity that rendered an otherwise abstract and unmeasured aspect of their life visible and easy to manipulate.
One of the key BCTs known to be effective in weight management is goal setting and this is a key component of FFIT, in relation to both eating and physical activity. In response to direct questioning on how useful SMART goals were, some men discussed the difficulties they first had with setting SMART goals as well as how they used them effectively, at least in early parts of the course:
The first one [goal-setting exercise], when you first got to it, you didnae [didn’t] really ken [know] – then he sort of told you to change your goals to sort of exercise and try something different.
It was difficult. I mean, we had the first set of goals – and I can’t even remember what my first one was. Lose three pounds in one week or something. Don’t eat chocolate, I think, or something. And then, as the weeks went by, it was difficult to set yourself different goals – coz it was really the same thing you were doing every week, you know? The goals were the same goals, sort of thing.
Aye, you changed yoursel’ [yourself] right from the start, didn’t you? Coz everybody sort of said, well, I think it was after the portion size, I sort of looked at myself and thought, ‘Right, well, I’m really going to have to drastically change the way I’m going,’ you know what I mean? So from there it was like, well, what are my goals? Well, I’ll put another fifteen hundred steps on. Right, no problem. I’ll eat more veg. Well, I have been doing that. I’ll cut out another thing and I’ll cut out another – you know what I mean?
Club10, 12-week FGD
Although the SMART goals proved to be ‘difficult’, as participant 1 (Club10) notes, participant 5 was able to recount the processes that this technique led him through, demonstrating the impact it had on his thinking, from the initial realisation that he needed to change his lifestyle through to the tangible and incremental actions he identified to help him achieve this change.
However, success in identifying and implementing SMART goals was not uniform and not all men found them useful:
To be honest wi’ [with] you, I didnae [didn’t] buy into that part of it at all, because I knew what, I knew, myself, what I was wanting to achieve, and I didn’t – you know, I wrote them down, then thought, ‘Right, ok, we’ll try and do so many of these extra steps this week,’ you know? But eventually, I did, I ended up just chucking it, because I thought to myself, ‘If I keep to the step thing,’ you know, the increasing the steps, ‘and if I keep to the eating bit, I should be ok’, you know? I mean, for some, maybe some people found it helpful – I don’t know.
Participant 1, Club01, 12-week FGD
Thus, although the principle of goal setting is clearly important in the early stages of the programme, only some participants reported making use of SMART goal setting as the programme progressed, at least for eating goals. As Dombrowski et al. 58 suggest, different techniques may be more useful in the initiation rather than the maintenance phases of weight management.
Despite these mixed views of SMART goals, most participants found understanding their weight loss target to be useful, as reinforced by data from the programme evaluation questionnaire [in which 280 out of 316 (89%) participants reported it was ‘quite’ or ‘very’ useful to know their 5–10% weight loss target].
Experiencing successes
The experience of success, of progress, both individually and as a ‘team’, was reported to be highly motivating for participants. As one commented, when asked why the men kept coming back to the FFIT sessions:
It’s the success. Success, because it breeds success, doesn’t it, you know? If you’re doing well and you get off to a good start, you want to improve and to go on and lose weight, and then you’re, the sort of team thing comes in, where you’re part of a team and you want to go forward as part of the team, and to make sure that we all do the same things and we’re trying to encourage each other, as well.
Participant 3, Club08, 12-week FGD
Thus, the programme was seen to work, not just theoretically, but through, embodied, experiences:
I think also it works, or it certainly worked for the majority of people who went on it. I mean, I’ve done diets, etc. and not lost a jot, and the fact that, you know, you’re going on the scales every week and I was losing weight was incentive. I think, probably, halfway through, if I hadn’t been losing weight, I probably would have dropped out – but the fact that I was losing it, it was working, and it’s continued to do so very easily, you know? Obviously reducing your calorie intake slightly – I mean, I haven’t changed my life, eating-wise, hugely. Me breakfast, I certainly have, but other than that, I haven’t changed it. It’s actually the walking, and the walking has made the huge difference to me [. . .].
And what kept you coming back, week after week?
The fact it was working.
Aye.
Yeah.
Club05, 12-week FGD
For many, then, the achievements they realised each week led them to continue to attend the programme and fuelled their high levels of satisfaction with the programme overall. Many expressed a sense of personal achievement, particularly when they had tangible evidence (such as looser clothes) or external verification (such as others commenting on how they looked) of their successes:
I think one of the nicest things, when you lose your weight, if you’ve been successful, to put on a pair of trousers you’ve no’ had on for three or four years, and you know, just that nice feeling to think, ‘Oh my goodness me’ you know? Your notches on your belt and all the different signs that you track.
[. . .]
I think you get, I mean, when people, when somebody notices you get a wee bit, you feel a wee bit pleased, you know? If somebody hasn’t seen you for a wee while and they say to you, ‘Have you lost weight?’ And you think, ‘Well,’ you know, you know you have, coz you’ve got the letter telling you – I think you do get a wee bit, aye, you feel quite pleased and quite, and a wee bit proud, you know? Coz it’s not, nobody can do it for you. It’s all very much been your own efforts. I mean, it is a very personal achievement, and you do feel, you get a wee bit, aye, you feel quite proud and quite pleased when people are noticing. [. . .] And I think when people are telling you you’re looking better, it’s a circular thing, you know? Just self-perpetuates, that’s really what I’d say.
Club08, 12-week FGD
Further discussion of the importance of tangible markers of success emerged when participants and coaches commented on the use of physical representations of weight loss in session 7 of the programme:
Yeah, I couldnae [couldn’t] believe it, when you were handed the [sand]bag and [coach 2] said, ‘Feel that weight!’ Because we didn’t know [at first] what it was all about. ‘That’s what you’ve lost in the last . . .’ what was it, 6 weeks, about week 6 or something, wasn’t it?
I’d lost eight bags of it [physical representation of actual weight loss], yeah, which was quite incredible, yeah.
Yeah, could not believe it!
That was the thing, when you seen the bags lying, you thought one was for every person that was there, but they gave you four. You’re saying, ‘No, no, that’s not for me!’
The other thing that amazed me was that lump of rubber which represented the fat.
Club08, 12-week FGD
Thus, the sandbags and other physical objects (e.g. replica lumps of fat in week 11), which were used to render weight loss visible and tangible, were another successful component of the programme. Men’s recollections of seeing and handling these objects convey some of the excitement they felt at the time – ‘I couldnae believe it’ (participant1, Club08,12-week FGD) and ‘it was amazing’ (participant 3 Club08_12-week FGD).
When we explicitly asked about unexpected outcomes, the only ones mentioned, usually partly in jest, were the need to buy new clothes:
Do you know the only thing, it’s costing me a fortune!
On clothes.
In clothes.
Club10, 12-week FGD
In summary, men recounted a strong experience of enjoyment while taking part in the programme and expressed very high levels of satisfaction with, and acceptability of, the programme. Several factors were repeatedly raised in discussions about what motivated them to keep coming along to the programme: the positive atmosphere fostered by coaches, the physical environment of the football club setting, feeling a part of and closer to the club (symbolised by the T-shirts and other branded physical objects), the enjoyment of the group interactions and feeling part of a ‘team’ indicating high levels of group cohesion and the satisfaction of learning tips and techniques for behaviour change for themselves and for others. Together these built to deliver tangible experiences of success in reaching their weight and physical activity goals, which kept the vast majority of men engaged throughout the 12-week programme.
Process outcome 5: coaches’ experiences of delivering the Football Fans in Training intervention
In many ways the coaches’ experiences of delivering FFIT mirrored the positive aspects of the programme that had been valued by men. They had observed, and enjoyed, the excitement and engagement that men felt in coming to the club each week. They also noted the largely positive interactions between the men that allowed them to learn from each other’s experiences as well as from the formal course materials. And they also felt that the structure of the programme worked well:
I think it all kind of linked well with each other, like in terms of the weeks. Obviously we started off in terms of obviously the diet and then adding, having a little bit of physical activity and then obviously increasing the physical activity as you went along obviously helped with that. And then I think obviously having the weeks where you then obviously have the alcohol and things like that. Just giving them that sort of weeks where they do have sort of different things. So, it’s not always just about the food, not always just about the physical activity. So, there are sort of weeks that sort of break up that sort of stuff, but then there are things that do. So, I do feel it kind of all linked in well together.
Club13, 12-week coach interview, coach 2
Like the participants, the coaches also recognised the usefulness of the pedometers in helping men get into routines of increasing physical activity and of self-monitoring. When the coaches in Club10 were asked what they thought about the use of pedometers within the programme, they said:
Massive.
Aye cause it [pedometer] keeps them going, eh? Cause, they keep going, like they get into that sorta addictive sort of mode ae [of] checking every, like every day going ‘Right, I still need to go and dae [do] another thousand’. So they go out and they’ll like, they’ll drag their dog out who’s already been for aboot [about] five walks that day and they take him roon [round] the block just to get like those extra steps up. So they’re constantly monitoring themself on this pedometer.
Club10, 12-week coach interview
Another aspect of the programme that the coaches felt was very powerful was men’s reactions to seeing each other receive the tangible feedback on their actual weight loss halfway through the programme:
I think, going back to the difference that the, the sessions that made the difference, I don’t know what week it was, but it was when they got to see, I think it was the halfway point, when we gave them bags of sands to show them what they’d lost.
Week 6.
. . . and you could see it, they were like ‘Whoa!’.
[Week] six or seven, yeah.
. . . that’s, and I mean the guys were taking the bags of sand home with them to show their wives.
To show their missus.
How much they’d lost because you could say to them well you’ve lost four kilograms or whatever and they’d be like ‘Oh all right’ but when you actually give them it, they’re like ‘Whoa!’. One guy, [FFIT participant], he had these bags in his hand, loads of bags eh? And it almost weighed the same as his kid. I think his kid was like three years old or something eh? And he was like ‘I can’t believe it!’.
Club10 12-week coach interview
Thus, here we see how the halfway session could be one of ‘the sessions that made the difference’ because it allowed men to make real life comparisons between the weight they had lost and an object they could hold, equating this to something meaningful in their lives, such the weight of a small child.
However, there were three areas that coaches felt could sometimes present difficulties. The first was the pressure of time. This was spoken about in relation to the actual delivery of the session and related to a tension they sometimes felt between allowing men to have a discussion that appeared important for a particular issue and needing to leave enough time to deliver all the key tasks for that week of the programme. A further time-related issue emerged from the coach interviews and this was a concern that other demands and pressures of their job as community coaches within the club could place on the time needed to attend fully to the paperwork that accompanied FFIT deliveries:
I think, wae [with] the overall programme, is that most of the guys [coaches at other clubs] that are responsible for delivering this . . . are football development officers, so they’ve already got a real hectic programme in place, anyway. So they’re out doing development squads and loads of other stuff, and they’ve got lots of other stuff that they’re involved in, lots of different programmes. We’re the same, here at [Club08] – we’ve got education programme and social programmes, but we’ve all got small staff, in that predominantly, it’s one person or two people if you’re really, really lucky. So if something comes through that requires a lot of admin, the guys are like ‘Oopf!’, you know? [. . .] So I think, when there’s a lot ae [of] admin there, the guys are like ‘Phew, I’m gonna have to give more time to doing this.’
Club08, 12-week coach interview, coach 1
Despite considerable enthusiasm for the programme and what it can deliver for men and for society, coaches could feel under considerable time pressure while trying to get through this addition to their workload with few club resources. These pressures could influence the fidelity of intervention delivery if adequate support is not provided.
The second area that the coaches sometimes found difficulties with was overcoming differential engagement with SMART goal setting. They described this as something that suited some men but not others:
SMART goals tends to be something that’s kinda come from business, I think, and it’s a bit touchy-feely, airy-fairy. I think the guys come in with the same SMART Goal every week, and it’s trying to kinda progress them there on from it. It’ll work for some. Some people think differently. Some people like to list things and categorise things and how they work it out in their head and how I’m going to get from A to B. Some just do it a different way. So it’ll fit for some people. It won’t fit for all of them, though. Yeah.
Club01, 12-week coach interview, coach 1
Given that coaches and men (see The course content) noted such a range of reactions to SMART goals, it might be suggested that future interventions consider deploying a range of approaches to goal setting. This could help increase engagement by ensuring that approaches that have negative associations (e.g. SMART goals and work/business), can be replaced where necessary with an approach that is more acceptable.
The final aspect of the programme coaches sometimes found challenging, related to a medical responsibility they often felt towards participants. Although participants were screened for their readiness to take part in physical activity (see Chapter 2, Physical activity components) and strict blood pressure cut-offs were put in place for those at the highest risk of an over exertion-induced health event (see Chapter 2, Participants), coaches were aware that these precautionary measures were by no means fail-safe.
Mm hmm, and I suppose there’s things like guys who maybe have high blood pressure and that sort of thing, that has to be . . .
Things you maybe don’t – obviously, we don’t deal with that in a football centre, or one of the coaches wouldn’t have to deal with this. You’re working with a wider range of age as well.
That’s certainly an issue. That is certainly an issue from our perspective, the fact that we do first aid courses for sports injury or emergency first aid. The client group that we have, Football Fans in Training, are completely different and probably, I think, the benefit of having someone with more medical background and medical knowledge would be, I think it would be important. I think it would be important because we’re dealing with guys, here, who, as I say, at the start of each course, someone at one of the clubs will die during this course – not because of the course, but just because of the condition that that type, that person is in. Now, fingers crossed, that’s never happened so far, on site or on course, but who’s to say it wouldn’t happen? And that added responsibility for a coach, I think’s extremely demanding.
Club05, 12-week coach interview
Thus, some coaches expressed concern about the amount of responsibility they felt they carried in relation to men’s health risks. Accounts such as these suggest that the FFIT programme could include more detailed first aid, medical emergency and medical risk training for coaches, with a particular focus on the kinds of issues that men eligible for FFIT are more at risk of experiencing. They also point to the importance of coaches adhering to the guidance to make sure men work at a level of exertion that is appropriate to their own level of fitness. Alternatively, coaches could be relieved of some of the sense of responsibility by a waiver signed by men themselves that they are happy to bear any responsibility.
From the interview data presented here, we are able to conclude that the programme was highly acceptable to the coaches who delivered the FFIT programme. They reported enjoying the delivery experience, finding the course well structured and resourced, and felt comfortable dealing with the questions asked by participants. Coaches also judged the pedometers, self-monitoring and tangible weight loss feedback (in the form of sandbags or a lump of fat) to be central to the success of the programme and stressed that the group context in which these BCTs were practised strengthened their efficacy. Alongside these positive judgements, coaches pointed to the challenge of fitting FFIT into their busy coaching schedules, the need for a more diversified approach to goal setting and the benefit they feel they would receive from more detailed training in how to respond to exercise-related medical emergencies in the overweight and obese men that FFIT targets.
Process outcome 6: participants’ experiences of maintaining weight loss and lifestyle changes in the longer term
We now consider men’s experiences of maintaining the weight loss, physical activity and dietary changes they had made during the initial 12 weekly sessions at their club once these had finished. During the 9 months following the active phase of FFIT (i.e. until 12 months after they had started the programme), participants received ‘light-touch’ weight loss maintenance support incorporating six passive e-mail prompts (see Chapter 2, Format of the programme) and a poorly attended reunion 9 months after they started [see Process outcome 3: the extent to which coaches deliver FFIT as designed (fidelity)]. The results below draw on the 12-month FGDs to describe men’s experiences of trying to maintain weight loss post programme, and include perspectives from men who had been successful and less successful in maintaining weight loss. We describe factors that facilitated and hindered attempts at maintaining weight loss in turn. As described under Qualitative data from focus group discussions, coach interviews and observational data, our analysis was guided by SDT,109 which describes processes essential for behavioural persistence and psychological well-being, including feelings of autonomy through the internalisation of motivations, increasing feelings of relatedness and of competence in performing behaviours.
Factors that facilitated weight loss maintenance
During the FFIT programme, the coaches had provided clear, easy-to-follow advice about how to lose weight by adopting healthier eating habits. The men were shown practical examples of how to reduce portion sizes and how to make better food choices (by swapping energy-dense foods for nutrition-dense foods) and learned about the benefits of regular mealtimes. This learning was reinforced through group discussion about adapting this information for their personal situations and the use of goal setting and action planning. At 12 months, members of the FGDs who had successfully maintained weight loss described following the lessons learnt on eating in ways that best suited their own lifestyle:
We stick to the Eatwell Plate, we’ve got that up in the kitchen which is good, it’s a good reminder, you know, when you’re doing the shopping we check out all the, you know, the various fat content, sugar, salt, things like that.
Participant 5, Club02, 12-month FGD
Instead of eating at 11, 12 o’clock at night when I come home from work (having a big plate of food), stopping suppertime, 5, 6 o’clock, no matter what I’m doing, and having a meal. I’ve managed to do that. I’ve had breakfast in the morning, dinner and I have a supper at night. And it’s just maintaining that, and then that stops all form of binge eating, grabbing what you can sorta stuff, you know? It’s just certainly giving you a structure for eating like that.
Participant 1, Club06, 12-month FGD
My eating habits have totally changed and that’s since I’ve started the programme to now, and I don’t think I’ll ever go back to where I was. I mean, even things like, it’s just a small thing, but I got a tub of Mackie’s ice-cream, you know, the two litre, and before, I was sitting with that and eat it, maybe not eat it all obviously, but you know, I’d eat part of it. And now what I’ve learnt is, because what [coach 1] was saying . . . I put it into a bowl, I put the ice cream away, so that I’m only eating that specific amount, rather than eating a whole lot.
Participant 6, Club07, 12-month FGD
These extracts illustrate how being able to make autonomous choices about how to change their eating habits had helped the men sustain the improvements in the longer term.
Another way that FFIT had tried to support weight loss maintenance was by promoting the ongoing use of self-monitoring, which has been shown to be associated with weight loss maintenance. 58 Towards the end of the active phase, the men were encouraged to continue to weigh themselves regularly and to use their pedometers to monitor and record their physical activity levels as part of their weight loss maintenance strategy. Many (but not all) men had found this advice helpful:
I find that the pedometer, even now it’s my conscience. If I can look back 7 days and say, ‘Phew, I’m only averaging about 7000. I usually should be doing eight or nine’, it’ll make me go for a longer walk some time later in the week.
Participant 2, Club10, 12-month FGD
[Weighing myself] it’s my motivation. It’s the fact ‘Shit I’ve put on four pounds here in a fortnight!’ So it motivates me to do a bit more, eat a bit better so that’s my own self-monitoring motivator and that’s what I’ve always stuck to myself. ‘Cause if I didn’t do it then I just would not bother my shirt, you know.
Participant 3, Club09, 12-month FGD
Once again, the FGDs provided evidence of how men had made their own choices over how to apply advice around ongoing self-monitoring: some continued to use their pedometer, others to weigh themselves regularly, while one man described using internalised somatic and psychological cues to regulate his eating and physical activity. For some participants, maintaining weight loss remained effortful and while there was little evidence that men had continued to use SMART goal setting and review, some had found the action planning they had learned to use during FFIT was helpful in maintaining behavioural change:
I think the thing for me is actually the planning of stuff because you tend to need to plan a bit more about your activity. You know about how, if you want tae walk you’re gonna have to plan about ‘When am I gonna walk?’ An’ also I quite often end up staying at hotels or whatever for work, an’ you have to know, ‘What am I gonna eat? Where am I gonna eat?’ So you have to do a bit more planning about how you do that. [. . .] You have to sort of try an’ work something out there so you don’t end up goin’ to [a bakery] or whatever.
You have to plan your [food] shop as well.
Yeah (nodding).
Club05, 12-month FGD
A clear message that was emphasised during FFIT was the importance of men feeling comfortable with the changes they made to their eating habits and not feeling they had to totally deprive themselves of foods they really enjoyed. Many of the men who had been successful in maintaining their weight loss had adopted a flexible approach (e.g. allowing themselves to eat unhealthy foods on occasion). Men who had tried to follow a more rigid eating regimen during the active phase had found this more difficult to sustain afterwards:
My diet changed a wee bit because I wasn’t sorta eating healthily or as much as I was when I was involved in the twelve-week programme. I don’t know if that was me, just, I don’t know, it’s, just found it quite difficult to stick to the eating plan because, you know, you had, for that twelve-week period, I done so well losing so much weight and I don’t know if I found it, did I find it boring or some of the things that? I know I’ve gotta try and eat five bits of fruit every single day, and I just found or, you know, your veg as well, sometime I just couldn’t do it.
Participant 1, Club08, 12-month FGD
Finally, following the active phase of FFIT, the coaches sent participants e-mail prompts every 6–8 weeks that were designed to support the maintenance of weight loss, physical activity and healthy eating and the men were invited back to attend the 9-month reunion meeting at their club. There was some confusion in the FGDs over the 9-month meeting. Some men appeared unclear whether they had attended it or not and, as we saw under Attendance and opting out of Football Fans in Training, very few had attended the sessions. The utility of the e-mail prompts was also the subject of some debate:
The prompts have been good from [Club02 coach] and some of his prompts about getting through yourselves as well, just to say, ‘Look, you know, how are you doing?’ and that type of thing. You felt, still feel part of it even though [. . .] no I found them, you know, they’re very good, you know, ‘cause it gets you thinking again, you know, right okay, you know. And there’s this, you know, we’re doing this and we’re doing that. That type of thing.
Participant 5, Club02, 12-month FGD
I just got the impression these were e-mails that had been sent by the people at [Club01] so they can fulfil the criteria required to get to do this Football Fans in Training. ‘We did what we had to do, we had to send out an e-mail periodically.’ It didn’t seem that it was anything really in it. It was just a case of, ‘Right we’ve now met every criteria we’ve to complete the thing.’ That’s all I felt it was. I didn’t get anything from that, to be honest wi’ [with] you.
Participant 1, Club01, 12-month FGD
It therefore appears that few of the men had found the ‘light-touch’ components of the weight maintenance phase of FFIT particularly useful. They preferred to select the tools and BCTs that were most salient to them and which best suited their lifestyles as they tried to maintain their weight loss, physical activity and healthy eating.
Self-determination theory also argues that people who feel intrinsically motivated (e.g. who do something because they find it interesting or beneficial) are more likely to sustain a behaviour than those who are extrinsically motivated109 (e.g. who do something because someone else has told them to, such as eating smaller portions because the FFIT coach has suggested you do it). The contributions within the FGDs of men who had successfully maintained weight loss were certainly congruent with SDT as we show below.
Deci and Ryan109 describe three stages in the internalisation of regulation. The first stage is ‘introjection’, when a person manages to regulate his or her own behaviours, but this is driven by external values. The result is that positive (e.g. pride in personal achievement) and negative emotions and external factors become important sources of motivation. There was evidence of this in the FGDs:
I think the information you got has increased the guilt conscience more. There’s a bit o’ [of] that in there to be honest. There’s a bit o’[of] that that said ‘Jeez, I suppose I better do something!’ Not the driving factor, but certainly in there.
Participant 1, Club09, 12-month FGD
Something that was never mentioned when we did all this course was we were talking, we don’t buy crisps now, we don’t buy chocolate things. I reckon I probably spend ten quid a week less ‘cos I’m not buying the rubbish that I was eating before in the evening.
Participant 2, Club02, 12-month FGD
Although introjected regulation of behaviour is more likely to persist than external regulation, it remains relatively unstable. Recognition that a healthier lifestyle can save money may be an example of introjected behaviour, but it also shows some elements of the second stage of internalisation, ‘identification’, when people recognise and accept the value of a behaviour for them. Deci and Ryan109 argue that as identification is associated with greater regulatory stability, it should be more effective than introjection in supporting behavioural persistence. Many of the FGD participants described their appreciation of how much better their positive lifestyle had made feel in themselves:
I would start to eat more greens, more – what I call wet food, you know. The vegetables, you know, the stuff that’s carrying more water and towards the end of it, it clears out my system, it allows you to breathe, you feel fitter [. . .] you feel healthier, you feel more able to function.
Participant 3, Club01, 12-month FGD
We all know once you’ve done the exercise how you get a buzz out of it – endocrines is it or . . .?
Participant 2, Club10, 12-month FGD
Endorphins?
Endorphins, aye. But, you start to – I wouldnae [wouldn’t] say you start to be a junkie on them, but your day does feel different if you’ve done that, and I now have that discipline.
Participant 2, Club10, 12-month FGD
The third stage of the internalisation process, ‘integration’, occurs when people fully assimilate their new behaviours with other aspects of their personal values and identity. The result is complete self-regulation, which is the most stable form of regulation and is most likely to support long-term maintenance of weight loss-related behaviours. A few of the men who had been successful in maintaining their weight loss appeared to have achieved a new, coherent sense of self:
I used to, when I was out in the car look at people runnin’ out in the street thinkin’, ‘God, they’re really keen, they’re [pause] look at that idiot!’ But that’s now me [points thumb at self]. So it’s . . . I dunno, it’s just a perception, I couldn’t have done it before. An’ even things like runnin’ across the road to the shop when it’s rainin’ an’ runnin’ back to the office. I’m not outta [out of] breath when I come back in an’. . . you realise that and you remind yourself how much better you’ve become because of it.
Participant 3, Club03, 12-month FGD
However, a FGD among men who had experienced mixed success in weight loss at 12 months suggested they had been less successful in internalising their new behaviours:
I don’t feel that, I don’t feel I’ve changed at all but I feel that, you know, that my habits have changed and, you know, eating habits.
As I was saying, I’m wi’ [with] you on that, it’s like I think I’m the same person, but I know a lot of my habits have changed. I mean, is changing your habits changing the person? I don’t really think so.
Club07, 12-month FGD
Taking part in FFIT therefore helped some men internalise extrinsic motivation and develop different degrees of self-regulation of their new weight loss-related behaviours. Many appeared to have moved beyond ‘introjection’ to ‘identification’ and a few appeared to have developed the highly stable ‘integrated’ self-regulation that SDT suggests is most likely to be associated with long-term maintenance of behaviour change.
Self-determination theory suggests that for fully integrated motivation (regulation), two other universal needs are necessary – feelings of relatedness and of competence. Again, there is evidence of increasing experiences of each of these as facilitators of maintenance of weight loss.
We have seen how much men enjoyed interacting with one another in the 12-week programme (see Enjoyment of group interactions). In some clubs, men had continued to meet up to exercise together regularly after the 12 weekly active phase of FFIT had ended suggesting very high levels of group cohesion and social identification. Some of these ongoing groups were organised by the FFIT coaches and a couple were held at the clubs; others were organised by the men themselves and took place at local community venues. FGD participants appreciated these opportunities to keep meeting up, irrespective of how well they were doing in maintaining their weight loss:
I was still struggling, but the coach organising the Monday night thing was a Godsend to me ‘cause I coulda [could have] easily have just slipped into bad habits again.
Participant 4, Club13, 12-month FGD
Aye, it’s really like . . . I mean, the physical activities, I wouldn’t say almost are a by-product of it, but, you know, we go round there and everybody’s sorta common goals or aims; and, like I say, we’ve got common setbacks a lot of us, you know, and things like that. And you, and like you say, it’s like a support group, as such, ‘cause we’re all in there, everybody’s there for the same reason sorta thing, so it’s a good sorta almost like a, what’s the word I’m looking for? . . . Safety valve almost, you know?
Participant 5, Club07, 12-month FGD
Some men were not able to make these meetings; others had taken part in FFIT at a club where ongoing groups had not been set up. They described experiencing a real sense of loss when the active phase of FFIT had ended:
I would like tae have seen it [the active phase] just a wee bit longer . . . Even if it had went doon [down] from every week to know, maybe once a month or something like that? I think it would still have gave everybody the wee incentive to go along, share their experiences an’ things like that. Pass on like the good habits, the bad habits – the good an’ bad times an’ things like that . . .
Participant 1, Club05, 12-month FGD
For other men, leading a healthier, more active lifestyle had helped them to become more involved in family life. For them, this was a really positive benefit that helped them maintain the changes they had made:
I must admit my kids have kept me goin’ an’ a lot of the—an’ they’re now startin’ to drag their mother out as well when they’re wantin’ to go oot [out] for runs on their bikes an’ things, an’ that’s made a big difference [touches nose] to keepin’ you goin’ when you get . . . If you’re havin’ a – you want tae [to] have . . . or feel like being lazy or tired, I’ve got one [child] at five an’ one at ten an’ they just want to be goin’ all the time. So it does give you a good feelin’ when they’ll come tae [to] me if they want to go an’ do somethin’ that involves either runnin’ aboot [about] or cyclin’ aboot [about] an’ the mum gets left, so . . .
Participant 6, Club03, 12-month FGD
For many men, feeling meaningfully connected to other people, both their peers from the programme and family members, was a valued outcome from taking part in FFIT and this continued to be an important factor for many in the period after the active phase. However, as the extracts demonstrate, satisfaction of relatedness was not necessarily associated with autonomy and increased well-being and, for some men, it was particularly important when things were not going well.
People are more likely to engage in healthy lifestyle behaviours when they have the necessary skills to perform them, and find them interesting and optimally challenging. 108 FFIT provided the men with a range of skills and knowledge about how to lose weight by improving their eating habits and becoming more active and the coaches were trained to further support the development of a feeling of competence through providing positive feedback about the men’s efforts and achievements. Men who had done well in maintaining their weight loss spoke with confidence about applying what that had learnt from participation in FFIT:
I feel I’m more knowledgeable about things as well. I mean obviously those were the main things, but I mean for instance food advertising and what they put on the labelling is a disgrace. It wouldn’t be allowed in other fields, and yet you know they can get away with it. They’re misleading, it’s pretty bad actually, it’s pretty bad and I’m aware of that now . . . it’s changed the way I look at things.
Participant 2, Club13, 12-month FGD
So, I mean, I went out and bought a slow cooker and started cooking things like that, just using fresh vegetables putting things like that in it, meat joi— getting proper big meat joints and actually cooking them off and doing things like that.
Participant 3, Club11, 12-month FGD
Practice theory describes how ‘novices’ learn experientially and assimilate new behaviours into their routinised practice to become ‘full practitioners’. 115,116 The FGD participants’ narratives revealed a trajectory of increasing competence, confidence and habit formation.
I think now right the exercise . . . is a part of your way of life . . . used to be your work, sleep, up again, work, sleep . . . Now you make time, either once a day or at least a couple of times a week, to go and do that wee bit [of] exercise. Now it’s, it just pushes you right on.
Participant 2, Club10, 12-month FGD
As their feeling of competence and expertise increased, men described how they and others viewed themselves differently. Some changed from ‘novice learner’ to fully practising ‘carriers of practice’ who took pleasure in sharing their new knowledge with their family and friends:
Everything about my life – and my children – even my children, you know what I mean . . . We’ll walk to the shops, you know what I mean? Or they’ll take their bikes. Any chance they’ve got to come out wi’ [with] me they’ll do it, so they’ve started tae [to] get more exercise, they’ve started to watch what they’re eating, they’ll not have chocolate cereal in the morning, they’ll have normal cereal or they’ll have porridge or that so . . . It’s not just my aspect on life, it’s theirs as well that’s sorta benefited from twelve weeks.
Participant 1, Club10, 12-month FGD
The racquetball has been a revelation . . . Absolutely love it [participant 1 agrees]. And, you know, I’ve got to the point where I’m trying to sort of get of some of my workmates involved in playing as well now and I’m back down south next week and I phoned up my brother-in-law and said ‘Do you fancy a game of racquetball?’, sort of thing, so he’s gonna give it a go.
Practice theory 4, Club08, 12-month FGD
The preceding sections have shown that men made autonomous choices over which tools and techniques they continued to use to maintain their weight loss and positive lifestyle changes after the active phase of FFIT. Many succeeded in developing some degree of internalised self-regulation and those who were successful in maintaining their weight loss and lifestyle changes spoke with confidence about applying their new knowledge both in their own lives and to influence other people. However, although continuing to meet up with other men they perceived as being ‘like them’ was important for many FGD participants, this was not always associated with weight loss maintenance nor the development of self-regulation; men who found it difficult to maintain their weight loss and lifestyle changes also valued the continuing camaraderie and social support from their peers. Many of the men reported facing a number of challenges in maintaining the changes they had made after the active phase of FFIT ended. The next section examines these problems.
Factors that hindered weight loss maintenance
As we have seen in Chapter 3, although there was a large difference in outcomes between the intervention and control group, less than half of the intervention group maintained at least a 5% weight loss at 12 months. Participants in the 12-month focus groups described a range of difficulties and issues they had encountered in trying to maintain their weight loss and positive lifestyle changes in the longer term, including specific events and more generalised barriers.
Most men reported some degree of success in maintaining increased physical activity levels after the end of the 12 weekly sessions. However, the most commonly reported barrier to remaining physically active was injury, which often occurred as a result of men’s increased activity levels:
Couple of times wi’ [with] me, I reckon I picked up [. . .] injury after injury at five-a-sides, and it was really frustrating ‘cos I really enjoy it . . . I can hardly do anything for . . . I mean, I can hardly get oot [out] o’ bed. So that’s the thing that kinda puts me, sort of puts me back a bit. But that’s . . . I maybe go back down tae [to] just doing walking and cycling and just doing stuff that’s no’ gonna have much impact in terms of your muscles and your bones so, and I could probably get by with that.
Practice theory 4, Club12, 12-month FGD
A number of men reported that changes at work had played a major role on their ability to maintain their physical activity levels after the active phase of FFIT. Sometimes these changes had a positive effect (e.g. starting new job and standing up all day), but more often the impact was negative:
I’m less active now ‘cos I’ve moved offices. I used to park my car in near the [Local Bridge] and walk to my office. But, my office moved to the other side of the city centre, and it’s now half an hour walk instead of fifteen minute walk. But I can’t really afford an hour of my day walking to and from my car, and plus trying to get home and everything. So, I now get the underground, so that’s less walking.
Practice theory 1, Club01, 12-month FGD
Three reported how health problems had limited the amount of physical activity they were able to do, as illustrated here:
Sadly after the course finished, I put on a couple of pounds over Christmas and New Year, which I wasn’t too concerned about – got back on track in January – and I suffered much more serious haemorrhaging in my right eye, which I was very, very disappointed with because I’d got my blood sugar down and I’d lost a couple of stone in weight, and that really put me on the back foot. For six months I couldn’t exercise, or I probably could have if I’d gone to a gym, but I had been doing all my work outside, walking and running in the streets. I couldn’t drive at night, so that restricted me as well.
Practice theory 3, Club12, 12-month FGD
Taken together, these extracts suggest that adopting a flexible approach (finding different activities to suit different circumstances) is important for overcoming specific barriers to remaining physically active in the long term.
Most of the men had also experienced challenges to maintaining healthy eating presented by holidays and other special occasions (e.g. Christmas, weddings). A common response (as had been emphasised in the course material) was to view these events as temporary lapses that could be overcome by using the techniques and strategies they had learnt on FFIT:
Everything noo [now] is great. I was on holiday for the last fortnight there, I was in Florida, and I did put two or three pound on. But I came back on Monday there, and this is now Friday, and I’ve lost a pound again. Just because eating salads and stuff and goin’ tae [to] the gym again.
Practice theory 2, Club12, 12-month FGD
However, occasionally, major events in men’s personal lives had totally undermined their efforts to maintain change:
My brother passed away, which is one o’ the difficult things. My dad became unwell, and so that was, that, a lot o’ [of] that’s kinda impinged in, you know . . . when my brother died, basically he died in his early fifties, so it’s young. But it was his heart that caused problems, so you think that well that kinda would inspire you. But to a certain extent that was probably one of the worst times where, you know, things were going wrong, and it was just, you know, feeling bad and eating.
Practice theory 5, Club09, 12-month FGD
In addition to the challenges posed by specific events, the men reported a number of other, more generalised, problems they had encountered in trying to maintain their weight loss and positive lifestyle changes. These included not being able to find enough time to be physically active:
But I think this last year for me has been kinda busy, and the bits that you don’t need tae [to] do get kinda left behind. So it will, so I think when you’re that busy, sometimes when you get in at night and you think, ‘Right, I need tae go for a walk’, and you’re thinking, ‘Do you know, just no’ got the energy’.
Well, it’s winter time isn’t it . . .
And it’s just, there’s no’ enough time in the day. Then tae just, you know, sit back and gather your thoughts and things.
Club09, 12-month FGD
Despite discussion of strategies to overcome the negative influence Scotland’s weather could have on people’s motivation to be physically active during the active phase of FFIT, a number of participants still reported they struggled to keep active when the weather was bad:
Weather’s the worst one, absolutely by a mile, because you would go, I would be, I’d be out playing golf and I’d gone for a walk. See when I’m on holiday, guaranteed, absolutely guaranteed, when I’m on holiday, other when I was on a cruise to be fair, but normally after dinner her [wife] and I’ll go, and we can walk for Britain – literally hours on end, walk. And it’s great, pleasure walking at night, cool breeze, all that – lovely. Come hame [home] that’s . . . it’s pissing from the heavens, an’ I think, ‘Nah, we’ll no’ bother’ [participant 2 nods], just sit in.
Practice theory 1, Club09, 12-month FGD
For some men, the cost of healthy food and access to exercise facilities were significant obstacles to maintaining a healthy lifestyle:
Well, I find it’s price of the stuff, prices you oot [out] o’ [of] the market. See, I’m the oldest here. Now I’m a pensioner now, so it’s difficult when you, when you’re on the State Pension, especially when you’re trying to pay for electricity, gas and stuff like that. And I’ve got my, gotta keep my car running.
P6, Club08, 12-month FGD
I find it’s quite disappointing that sort of like [local public leisure facilities] are probably one of the most expensive ones in, you know, sort of, in Scotland. If you look at the prices of, you know, municipal leisure centres and all that around the rest of the country, [local public leisure facility]’s really quite poor in terms of what they charge.
P4, Club08, 12-month FGD
Finally, while other people were an important source of support for many men, their influence was not always positive or helpful:
My brother split up wi’ [with] his missus, come doon [down], ‘Would you like a glass o’ water?’ ‘No! I’ve just spilt up wi’ [with] my missus!’ ‘Right, have a beer then.’ (Laughter.) I don’t want a beer, you know? So there is a sorta wee daft things that go on. I can’t believe his missus has left – that’s really inconsiderate of her! Now I’ve got tae [to] drink one beer . . . (laughter). ‘Have you any crisps?’ Oh, he’s only wantin’ crisps as well! (laughter). I’m on a diet here!
Participant 1, Club05, 12-month FGD
In summary, although many of the men who took part in the 12-month FGDs appeared to be doing well in maintaining their weight loss and lifestyle changes, most had faced some challenges in the period since the active phase of FFIT ended. These included specific events such as injuries, changes at work, holidays, ill health and bereavement, and more generalised issues such as time and financial pressures, the weather and negative social influences. However, some of the men also reported how they had overcome these challenges through taking a flexible approach to being active and using the relapse prevention strategies (regular self-monitoring and recording of weight and/or physical activity, SMART goal setting) they had learnt on FFIT.
Chapter 6 Discussion
Introduction
Rising levels of obesity, particularly in men, and men’s lower participation in existing weight management programmes6 mean that there is a clear need for innovation in the design and delivery of programmes to attract overweight/obese men. 117,118 Professional sports clubs, and specifically professional football clubs in the UK, are increasingly seen as settings that can attract men to health promoting activities. 24,25 Pringle et al. 24 suggest that ‘the product [i.e. football/EPL (English Premier League)] . . . the place (club stadia and facilities), people (players and management) and processes (including communication, marketing and the product delivery infrastructure)’ all contribute to their appeal. 24 Our developmental28 and pilot work on FFIT31,32 and the process evaluation for this trial34 attest to the power and cultural currency of this ‘draw’ for many men.
However, if the ‘draw’ of the football club is to be used to maximum public health benefit (and for maximum benefit for individual men), it is important that programmes delivered in these popular locations are based on best evidence about what works and reach those men most likely to benefit.
Our team have collaborated with the SPL Trust (now SPFL Trust) to design, implement and evaluate the FFIT programme. We have reported the development of the evidence-based programme28 and on the conduct of a feasibility study. 32 In this report we build on existing peer-reviewed papers33,34 to present the full findings of a RCT, health economic and process evaluation of the FFIT Programme.
Interpretation
This trial has shown that a 12-session, gender-sensitised, weight management and healthy living programme with subsequent light-touch weight loss support (including six e-mail prompts and a reunion session at 9 months) can help men achieve significant changes in objectively measured weight, waist circumference, body fat, BMI, blood pressure and self-reported physical activity, dietary intake, alcohol consumption and measures of psychological and physical well-being 12 months after baseline measurement. Mean weight loss in the intervention group fell only 0.04% short of 5% weight loss and is likely to be of clinical benefit. The only predictors of weight loss at 12 months were participation in the programme and baseline weight (with relationship with age of borderline significance); all other potential mediators and moderators that were pre-specified in our protocol were unrelated to weight loss.
Although the difference in weight loss in favour of the intervention group was highly statistically significant, as in other weight management research119 we found small improvements in the comparison group in terms of mean weight loss, and 11% of these men (compared with 39% in the intervention group) had also lost at least 5% of their baseline body weight. We suggest a number of potentially interacting explanations. First, it could be argued that all of the men who attended the baseline measures recognised that they wished to lose weight and were motivated, to some extent at least, to lose weight. Second, the experience of undergoing the baseline measurements prior to randomisation (including measures of mental and physical well-being and self-esteem, etc.) may have had the effect of heightening their awareness of the need to lose weight as all men were shown where their current objectively measured height and weight placed them on the ‘BMI Wheel’ and were told that the evidence suggested benefits to weight loss among those who were classified as obese. Any men with blood pressure readings over pre-specified thresholds were also advised to consult their GP for advice. These measurements were successfully repeated in a high percentage (93%) of the comparison group 12 weeks later and this may have provided a second prompt or ‘wake-up call’ about their weight and overall health. Third, following the baseline measurements, all men were given an advice booklet (British Heart Foundation’s So You Want to Lose Weight?42) and had the chance to speak briefly to the coach about the impending FFIT programmes. Together, these factors may have been sufficient to help a minority of men in the ‘waiting list’ comparison group to lose weight independently, or to motivate them to find alternative resources to do so (although we know that a very small proportion had used existing NHS or commercial weight management programmes in the 3 months prior to any of the measurement sessions). Fourth, it is possible that some men allocated to the comparison group may have known men in the intervention group, or men who participated in the pilot deliveries of FFIT, and gleaned some details about the approach taken to weight loss in FFIT. Finally, our recruitment activities within clubs may also have changed men’s views about the acceptability of weight loss in men in general, or among their football-supporting peers in particular. Taken together, these factors suggest that the difference in weight loss between the groups is a conservative estimate of what FFIT can deliver. It also raises the possibility that there may be some men who can be motivated to achieve weight loss independently if primed or motivated in the right settings and manner.
A recent systematic review reported only 11 other RCTs investigating interventions to reduce male obesity,10 of which only three were of interventions combining dietary and physical activity advice with support for behavioural change (the approach shown to be most effective). 10 Only two of these three trials, both internet-based programmes with some one-to-one support, reported outcomes for both intervention and comparison groups to 12 months. 118,120 The weight loss reported in FFIT was substantially greater than the mean differences in weight loss of 2.20 kg (95% CI 1.25 kg to 5.65 kg)118 and 0.60 kg (95% CI 0.14 kg to 1.52 kg)120 reported at 12 months in these trials. FFIT is a more intense, although relatively inexpensive, group-based programme and is gender sensitised not only in content (as others also are118,120,121), but also context (the football club) and style of delivery (participative, peer-supported learning). This gave the men opportunities for direct group interactions in a valued environment, which were seen clearly to enhance the cohesion of the group and formation of a group identity, and the chance to build networks of social support during, and in some cases after, the programme. These differences may explain why weight loss was greater in FFIT than in earlier trials.
The weight loss that the FFIT intervention group achieved at 12 weeks was comparable to that reported in a UK study of primary care referral to a 12-week commercial weight management programme. 7 Stubbs et al. 7 report greater weight loss and percentage weight loss in men [weight loss at around 12 weeks: mean (SD) 5.8 kg (4.9 kg) in men and 3.8 kg (3.5 kg) in women; per cent weight loss at around 12 weeks –4.9% (4.0%) in men and –3.9% (3.5%) in women]. However, only 11% of the 34,271 participants were men and outcome data were available only up to the last session attended (with outcome measures collected as part of routine data collection within the referral programme) so there are no comparable data at 12 months.
The increase in self-reported physical activity suggests that men in the intervention group had taken the physical activity message ‘on board’ and changed their habits to include vigorous activity (such as attending the gym or playing five-a-side football) as well as more moderate activities including walking. Greatest differences in self-reported physical activity were seen at 12 weeks, but many were maintained to 12 months. The difference in total activity reported between the two groups at 12 months (844 MET minutes/week) equates to approximately 3–4 hours of walking, although the greatest difference between the groups was in MET minutes/week spent in vigorous activity. Qualitative data from the process evaluation supported our earlier findings about the popularity and utility of the pedometer-based walking programme as a means of helping men regain some fitness. 31 These data taken together suggest that the combination of regaining fitness through a walking programme, combined with the experience of undertaking physical ‘training’ activities guided by the coach each week, may have enhanced men’s confidence and motivation to take up new forms of physical activity or restart more vigorous activities that they had enjoyed earlier in their lives.
The intervention appears to have had an immediate effect on reducing self-reported sitting time at 12 weeks. However, this difference was not maintained to 12 months. This suggests that, if the reduction of sedentary time is an important primary or secondary outcome of this type of intervention, this element of the programme needs further development to give greater emphasis and support to reducing sedentary time.
The reduced frequency of reported consumption of fatty foods, sugary foods (including drinks) and alcohol suggests that weight loss was in part due to decreased caloric intake. It is not possible to assess whether or not the total decrease amounted to the 600 kcal deficit recommended. However, the reduction in all food categories, and in reported portion sizes, indicate that a range of strategies were utilised, including reduced frequency of intake of main meal items, snacks and drinks. The range of high-fat foods included in the modified DINE questionnaire matched those targeted in the intervention (cheese, processed meats, fried foods and whole milk). Reduction in the consumption of these foods indicates a reduction in saturated fats as well as total calories, which is desirable for reduced cardiovascular risk, and it seems likely from qualitative data about reductions in portion size that changes in quantities eaten will also have contributed to lower energy intake.
The reported increase in fruit and vegetable consumption indicates that men took on board the strong messages that this was an area of consumption that they should strive to increase, at the expense of foods from less healthy food groups. Hence, the data suggest that the overall balance of the men’s diet changed and the overall diet quality improved. Consumption of a greater proportion of plant-based items is associated with reduction of cancer and cardiovascular risk (especially combined with weight loss). 122 The increased consumption score for fruits and vegetables of 1.6 indicates an increase of one to two portions per day. Even modest increases in fruits and vegetables (e.g. increases by one portion per day) are associated with a significant reduction in CVD risk. In addition, increasing fruit and vegetable consumption by as little as an extra apple a day could cut the risk of dying early from any cause by 20% (irrespective of age, blood pressure or smoking status). 123 Current intakes of fruit and vegetables in Scottish men are estimated at three portions per day and trend data show no increase in intake in men in the general population despite significant public health efforts. 2
The short-term within-trial cost-effectiveness analysis demonstrated that the FFIT intervention was inexpensive to deliver, with an additional cost of just £205 per participant. This analysis also indicated that FFIT is more effective than no active intervention, both in terms of numbers of men achieving and maintaining a 5% weight loss at 12 months (130 compared with 40) and in terms of QALYs (with a utility change of 0.029 over 12 months compared with a change of 0.014). As such, the within-trial analysis demonstrated that the FFIT intervention was cost-effective, with an additional cost per man achieving and maintaining the 5% weight loss at 12 months of £862 and an incremental cost of £13,847 per QALY gained.
A within-trial analysis assumes that there are no differences in costs and QALYs between the groups beyond the trial follow-up period. Our second analysis employed an established Cardiovascular Disease Model for Scotland (two unpublished articles by Lewsey JD, Lawson KD, Ford I, Fox K, Ritchie LD, Tunstall-Pedoe H, et al. , University of Glasgow, 2014) in order to investigate the additional costs and benefits which accrue over the participants’ lifetimes so that we could provide an estimate of the lifetime cost-effectiveness of FFIT compared with no active intervention.
The model we used projects life expectancy, utility-adjusted life expectancy and lifetime costs based on the risk factors of individual participants’ as measured at 12 months. The lifetime analysis demonstrates that FFIT remains more expensive than no active intervention, with an average additional cost of £1074 per individual (95% CI £780 to £1298). Nevertheless, the results also suggest that FFIT remains more cost-effective, with an average increase of 0.43 life-years (95% CI –0.32 to 0.56 life-years) and 0.38 QALYs (95% CI –0.25 to 0.55 QALYs). As a result, the FFIT intervention is associated with an incremental cost-effectiveness of £2810 per QALY gained (£2535 per life-year gained). A scenario analysis, limiting the longer-term impact of the FFIT intervention to 5 years, demonstrated that FFIT remains more expensive and more effective, with a cost-effectiveness estimated between £1174 to £4475 per QALY gained (compared with no active intervention) depending on the assumptions made about the impact on longer-term costs.
All of these estimates are well below the threshold range of £20,000 to £30,000 per QALY used by NICE and comparable to the cost-effectiveness of community-based physical activity interventions (US$14,000–69,000 per QALY) found in a review by Roux et al. 124 in 2008 and the estimates of cost-effectiveness of behavioural interventions (US$235–30,419 per QALY) found in the review by Griffiths et al. 125 in 2012.
The data from the process evaluation on what attracted men to the FFIT programme demonstrated the complex interplay between ‘push’ and ‘pull’ factors to the programme, but also the over-riding power of the football club to help men overcome cultural barriers to group-based weight management. Push factors included concerns about their future health and wanting to ‘being there’ for their families, in the present and the future, able to actively fulfil roles they valued as fathers, sons, husbands and so on. This suggests that strong and positive masculine ideals of men as ‘providers’, which have been shown to motivate South Asian men to seek prompt health care for coronary symptoms,126 can also be relevant as motivations for weight loss. Pull factors included the football club setting, the potential to get an ‘insider’ view of the club and the opportunity to be with other people like them.
Our findings are consistent with the COM-B model of behaviour change by Michie et al. ,108 which suggests that both motivation and opportunity are necessary for behaviour change (as well as capability which we discuss below). The multiple invitations from different sources to take part in the programme made it relatively easy for men who had already considered weight loss to take part.
They are also consistent with the ROMEO model by Robertson et al. ,10 which emphasises the importance of extrapersonal factors that drew men to the programme; we found that FFIT was able to harness an initial desire to ‘do something’ about their weight, fitness and health through the deep symbolic and cultural attachments to the football clubs that many, though not all, participants held.
The process evaluation clearly demonstrated high levels of satisfaction with and acceptability of the FFIT programme, based on a combination of factors. Coaches were encouraged in both face-to-face pre-delivery training and in training manuals to value the participants, to share experiences and to create a positive environment. Participant reports suggest that this was very successful and that the supportive, participative, atmosphere fostered by coaches in which laughter and enjoyment was fostered alongside the ‘serious’ business of behaviour change was important in the success of the programme. These findings are congruent with the creation of the positive motivational climate known to be important for behaviour change in sport and exercise science. 127
Equally important in participant discussions was the physical environment of the football club setting which enhanced participants’ sense of being a part of and closer to the club (symbolised by the club T-shirts and other branded programme materials they were given). Participants also discussed their real enjoyment of group interactions during the course and feelings of being part of a ‘team’ and the satisfaction of learning ‘tips’ and techniques for behaviour change for themselves and for others. Together, these factors suggest that at least part of the reason that group interventions work is through the promotion of high levels of group cohesion, the creation of a ‘social identity’ as a group or team and the opportunities for vicarious learning. All of these factors have previously been proposed as mechanisms through which group-based therapies and group-based motivational interviewing could operate. 113,114 Together the factors men reported enjoying built to deliver tangible experiences of success in reaching their weight and physical activity goals which kept the vast majority of men engaged throughout the 12-week programme.
Coaches also enjoyed delivering the programme and thought the course was well structured. They felt comfortable dealing with the questions asked by participants. They also delivered the programme largely as intended. However, they highlighted the ongoing challenge of fitting FFIT into their busy coaching schedules, often in resource-poor environments, suggesting that a clear business model and support from public health organisations may be needed for long-term implementation of the programme in these settings.
Findings from FGDs at 12 months suggest that those men who were successful in maintaining longer-term changes had used the lessons they had learnt flexibly in the context of their own lives, using self-monitoring of both weight and step counts and adapting what they ate according to their personal circumstances. They also suggest, consistent with SDT,109 that self-regulation of behaviours had become integrated for some; what had once been new behaviours had become everyday and almost unremarkable so that they represented a new sense of identity, as the kind of person who eats well and is physically active. These qualitative findings support other research that suggest that physical activity programmes based on SDT may be effective in supporting behaviour change in the long-term. 128
Nevertheless, some men had found it extremely difficult to maintain the changes they had made during the 12-week programme, reporting a combination of stressful life events, social commitments as well as the high cost of some activities as barriers. This suggest that further developments to the programme may be needed to enhance the maintenance of longer-term changes in some men.
Strengths and limitations
The FFIT programme has a number of strengths and some limitations. One of the major strengths of the programme, relevant to the generalisability of the programme, was that it was conceived in partnership between the SPL Trust and Scottish universities. This partnership was possible because the support for public health the programme offered was congruent with SPL and clubs commitment to community engagement, discussed in Chapter 1, Rationale for current study.
In addition, it was specifically designed with few exclusion criteria so as to increase generalisability. It attracted men from across the socioeconomic spectrum, reflecting the reach of football across social groups. 129 We report elsewhere that FFIT succeeded in attracting men at high risk of future disease, among whom only 3.6% had attended a commercial weight management programme and only 1.7% a primary care-based programme in the 3 months prior to undertaking FFIT. 34 Thus, FFIT succeeded in reaching high-risk men who were not attracted to other weight management programmes. However, unlike health-related initiatives within the English Premier League,26 FFIT attracted few men from ethnic minority groups. In part, this reflects the lesser degree of ethnic diversity in many parts of Scotland, but this is something that should be further addressed in other research and development projects.
The programme was evidence based and the qualitative process evaluation suggests it succeeded in creating a positive motivational climate which fostered behaviour change through providing information and teaching the use of BCTs in a group-based context that participants could enjoy while dealing with serious and potentially sensitive issues. However, there is some evidence from the process evaluation that SMART goal setting did not suit everyone. There is increasing evidence that although goal setting is an effective technique to initiate behaviour change it may be less important in the maintenance of those changes. 58
Coach training was interactive, built on coaches’ existing experience and skills, and took place over 2 days. It was supported with written coaching materials that included prompts for coaches on which tasks were essential to deliver in each week. Coaches reported finding FFIT easy to deliver and they were able to deliver the programme’s content largely as intended. We also found that any variation in the delivery of FFIT between coaches in clubs was not sufficient to effect the main outcomes; club was not significantly associated with outcomes in any of the analyses undertaken. Nevertheless, in line with best practice,130 it might have been even better to have trained coaches for longer with some observed practice and feedback and to have provided some ‘top-up’ training in the middle of the programme deliveries. Neither of these options was feasible because of resource constraints and coach workload; we had limited resource to train them and coaches had no more time in which to attend training.
Although the between-group differences clearly demonstrate FFIT’s effectiveness, around 60% of participants, who we know were motivated enough to join the programme in the first place, did not achieve 5% weight loss at 12 months. This suggests that there are many improvements that could be made and we return to this when we consider further research.
Finally, the data from process evaluation suggest that the ‘light-touch’ maintenance programme of passive e-mail prompts and the relatively poorly attended 9-month reunion session in each club is unlikely to have contributed to the overall programme’s effectiveness.
The evaluation also had key strengths and weaknesses. It was pragmatic and we were able to blind measurement of the primary outcome through careful fieldwork procedures. Although the objective measurement of physical activity would have been desirable, it was logistically impossible given the number of men involved in the trial and the fact that the SPL Trust required the intervention to be delivered in all clubs at the same time.
We exceeded our recruitment and retention targets and participating men fully reflected the socioeconomic mix of football supporters in general. Nevertheless, we are aware that those attracted to the programme were already at least partly motivated to make changes to the lifestyles given the right opportunity. FFIT is an innovative and successful programme, but it may not attract those who have not already, even at some subconscious level, considered weight loss. In addition, FFIT is unlikely to attract those who are actively disinterested in football or other sports and other approaches will be necessary. FFIT is thus only one part of, but not the whole, solution to the public health problem of rising levels of obesity in men. Nonetheless, it provides evidence of men’s enthusiasm for making positive changes in their life and health when presented with the tools and the opportunity packaged in ways that are congruent with dominant cultural constructions of masculinity.
Our approach to assessing fidelity was pragmatic in the context of the resources available to us and limited coach time for research. Best practice in the measurement of fidelity would have included assessment of coach competencies and an assessment of the fidelity of delivery in each week. 130,131 Constraints on coach and researcher time and resources, already discussed, meant that these data were impractical to collect.
The cost-effectiveness analyses have a number of strengths and limitations. The HELP model underlying the lifetime analysis is based on the ASSIGN score, which is the preferred screening tool for CVD risk in Scotland. 96 HELP uses risk factors that were measured during the trial within a patient-level simulation to predict the long-term health consequences in terms of survival, comorbidities, QoL and costs for each individual. These estimates are combined with those from the within-trial analysis in what Griffiths et al. 125 describe as a mixed-methods approach and which is accepted as best practice for economic evaluation.
The main strengths of the HELP model relate to the data sources, modelling methods used, and the fact that validation and calibration of the model is more advanced than is usually undertaken for other models of this type. It uses data from the Scottish population in the estimation of the risk, projections of life expectancy, comorbidity and as the source of cost and utility inputs. The SHHEC survey96 linked to all national hospital discharge and death records allows individuals to be followed up for a long time (median survival time to first event was almost 21 years). These linked data allow a competing risk analysis to be undertaken to estimate the association between risk factors and CVD and non-CVD outcomes using a single cohort of individuals. Estimates between risk variables and events were made continuously when possible. This enhances the discriminatory ability of the model so that no averaging across groups is required (common in cohort state transition models). HELP also has the ability to assess cost-effectiveness over the lifetime of individuals. This is in contrast to many other models which project potential impacts over shorter periods (e.g. the NICE Programme Development Group projected potential impacts of changes in legislation, for example salt reduction, over a period of only 10 years). 132 HELP model predictions accurately reproduced observed events in a randomised trial (West of Scotland Coronary Prevention Study) and life expectancy predictions have been calibrated to contemporary Scottish life tables. In addition, the analysis involves a probabilistic sensitivity analysis to estimate the uncertainty as recommended by Griffiths et al. 125
However, there are limitations associated with the HELP model used for the longer-term extrapolation. It does not take into account other risk factors and outcome measurement used in the FFIT trial and not all of the risk factors required by for the ASSIGN score were measured within the trial population. Cholesterol and family history had to be imputed from external sources. This limits the ability of the ASSIGN score to produce an accurate prediction of risk for each individual. Although family history is an important element in the ASSIGN score, it is not affected by the intervention and, as such, will not impact the incremental analysis. Weight loss is, in contrast, not a risk factor in the model but it is the main outcome of the trial reported here. Despite not being a risk factor within the ASSIGN risk score, the impact of weight loss is included in the long-term model, and thus projections of future events, indirectly through its influence on the other risk factors that are used within the model presented here.
In addition, the HELP model predicts hospitalisations so less serious events that could be treated in a primary care setting are not explicitly modelled. The result is that the projection of lifetime costs in the model is limited to hospital costs; primary care costs are not included. These costs may be considerable especially following a non-fatal event (e.g. stroke). Nevertheless, although this impacts on the estimate of the individual’s total cost, it should not impact on the incremental cost unless there is a large disparity in the number of events between the intervention and waiting list comparison groups.
The within-trial analysis also has a number of limitations. The costing of medications is limited to GP prescriptions of antidepressants, painkillers, asthma, pain gels/creams, anti-inflammatories and sleeping tablets. Other prescribed medications and over-the-counter medications are excluded from the analysis. The exclusion of over-the-counter medications, and nearly all the medications included here are available over the counter, is a limitation of utilising the NHS perspective preferred by NICE as opposed to taking a wider societal perspective. These exclusions will affect the estimate of the total cost for each individual but will only affect the incremental cost if the use of other prescribed or over-the-counter medications differs markedly between the intervention and waiting list comparison groups over time.
Finally, we acknowledge that NICE prefers the use of European Quality of Life-5 Dimensions (EQ-5D) questionnaire, rather than the SF-12 to generate health utilities. At the time that the trial was planned there was uncertainty about whether or not the EQ-5D would be responsive to change in such a ‘healthy’ population. As a result, a decision was made to use the SF-12 as it served to provide both physical and mental summary component scores as well as health utility scores for the economic analysis.
Further research
We have shown the FFIT programme to be effective in supporting men to achieve weight loss 12 months after starting the programme. For lasting public health benefit it is necessary for this weight loss to be retained over the long-term. Follow-up of the cohort and further data linkage to NHS resource use data sets would enable investigation of whether or not the programme was able to support weight loss in the very long term.
Although the programme was effective at a group level, just over 60% of participants were not successful in achieving or maintaining 5% weigh loss from baseline and the programme can clearly be improved. This suggests that further research is necessary to optimise the programme and we agree with other commentators that further research is necessary to improve maintenance to weight loss into the long term. 58,133 The processes involved in maintaining weight loss may be quite different to those involved in initiating weight loss.
In future programme development we will place even greater emphasis on BCTs known to be effective in maintenance of behaviours (especially self-monitoring of both behaviour and outcome)58 and on approaches that provide even greater support for the development of intrinsic motivations128 so that it is possible for the practical and emotional barriers to weight loss maintenance reported by participants to be overcome.
Our qualitative analyses suggest that group interaction between the participants and the coaches, and between participants themselves, created high levels of group cohesion and a social identity which themselves supported change. However, many men who did not succeed in maintaining weigh loss also reported the importance of the group support. It would be useful to understand exactly how, in the context of a warm, positive, atmosphere promoted by coaches, peer group interaction operates and to harness this learning for further group programme development. In addition, although the FFIT programme was clearly successful, we are not sure what is the optimal length for a programme; we would certainly advocate experimentation with different approaches to a ‘light-touch’ ongoing programme.
Our finding that men in the comparison group also lost weight and that by 12 months 11% of them had lost up to 5% of their baseline body weight is not unusual. Comparison group participants in the recently published BeWEL trial to evaluate the impact of a diet and physical activity intervention on weight change in people at increased risk of colorectal cancer and other obesity-related comorbidities also lost 0.78 kg (95% CI 0.19 kg to 1.38 kg) compared with weight loss of 3.50 kg (95% CI 2.70 kg to 4.30 kg) in the comparison group. 119 Taken together, these findings suggest that much more research is necessary to understand the minimum requirements for weight loss support.
We are confident that our results have excellent generalisability to other football-based settings. Indeed, we believe that the results have relevance for lifestyle improvement programmes delivered through other types of sports club. We see no reason why FFIT, or something very like it, could not achieve similar results if adapted for delivery through, for example, rugby or cricket clubs. We also think that the model could be adapted to attract some women or families to weight management of physical activity programmes and would like to see the model extended to lower league or non-professional sports club settings. Nevertheless, the organisational barriers and resource constraints are considerable and it would be useful to investigate how resourcing and other organisational barriers can be overcome to implement the FFIT model effectively on a wide scale.
Chapter 7 Conclusions
Rising levels of obesity and lower participation in existing weight management programmes among men demand high-quality evaluation of innovative programmes in community settings to extend the evidence base for cost-effective strategies to support weight loss in men.
The evidence presented in this report demonstrates that the football setting proved highly effective in attracting and engaging overweight and obese men from a wide range of social backgrounds and that the programme engaged them in health behavioural changes in ways that were congruent with keys aspects of their identities. The degree of men’s engagement with the programme challenges a predominant view of ‘masculinity’ as somehow intrinsically linked to negative behaviours in relation to health;134 our results suggest that there is greater potential for engaging men in positive health behaviours, through linking more healthful behaviours to prevalent constructions of masculinity.
The report has also clearly demonstrated that FFIT, an evidence-based programme, gender sensitised in context, content and style of delivery, was effective in helping a significant proportion of men to achieve clinically important weight loss sustained to 12 months. A cost-effectiveness analysis suggested that the approach was cost-effective with QoL gains well below the threshold range of £20,000 to £30,000 per QALY used by NICE. The evidence we present suggests that public health commissioners and other organisations committed to public health improvement should consider whether or not the FFIT programme could be delivered in their jurisdiction.
Acknowledgements
We are grateful to the FFIT participants who took part in the research. We have been very heartened by the feedback that we have received from men about their participation in FFIT. We also warmly thank the club coaches in the football clubs (Aberdeen Football Club, Celtic Football Club, Dundee United Football Club, Dunfermline Athletic Football Club, Hamilton Academical Football Club, Heart of Midlothian Football Club, Hibernian Football Club, Inverness Caledonian Thistle Football Club, Kilmarnock Football Club, Motherwell Football Club, Rangers Football Club, St Johnstone Football Club and St Mirren Football Club) who delivered the FFIT programme.
Our wholehearted thanks also go to members of the survey office at MRC/CSO Social and Public Health Sciences Unit, Glasgow University, Glasgow, UK, and to the fieldwork team leaders and fieldworkers for their dedicated and careful work on the project. Particular thanks go to Alice Maclean, Alan Pollock, Mark Robinson, Susan Smillie, David Walker and Karen Wood. We also are also grateful to the UK Clinical Research Network registered TCTU for support in data entry and data management.
We are extremely grateful to current and former colleagues at the SPL Trust, now the SFPL Trust (Billy Singh, Mark Dunlop, Stuart MacPhee), for their support in developing, delivering and evaluating FFIT. We are pleased that our strong collaboration in this endeavour was recognised in our joint nomination and selection as a finalist in the Scottish Council for Voluntary Organisations’ Partnership Award for 2012 and that the SPL gained other awards in recognition of their excellent work in delivering FFIT (Winner of the Physical Activity and Health Alliance, Community Wide Programmes Award, 2012; Herald Society Award for SPL Trust for FFIT for Health provider of year 2011; European Professional Football League, Best Practice Award in Social Responsibility category, 2011). We are also grateful to Jim Leishman and Adrian Brady, who as cogrant holders on the project collaborated in the training of the coaches.
We would also like to thank the Scottish Executive Health Department CSO for funding the feasibility pilot that preceded this RCT (CZG/2/504) and to the MRC who funded Kate Hunt and additional developmental research through the MRC/CSO Social and Public Health Sciences Unit (SPHSU) Gender and Health programme (5TK50/25605200-68094).
Many people contributed to the development of FFIT. We would particularly like to acknowledge current and former colleagues at the SPL Trust (Euan Miller, Billy Singh, Mark Dunlop, Stuart MacPhee) and Jim Leishman and colleagues at the Camelon Men’s Health Clinic.
Contributions of authors
Sally Wyke (Deputy Director, Institute of Health and Wellbeing, health social sciences), in close collaboration particularly with Kate Hunt and Cindy Gray and others as specified below, wrote the original grant application, developed the intervention, designed the trial, measurement schedules and qualitative topic guides, contributed to the design and delivery of the training of the community coaches and interpreted the findings. She was coprincipal investigator with Kate Hunt of the project reported here, and coprincipal investigator on the earlier feasibility pilot study with Kate Hunt and Cindy Gray. She and Kate Hunt jointly drafted this report (with input from other authors as specified below).
Kate Hunt (Associate Director, health social sciences), in close collaboration particularly with Sally Wyke and Cindy Gray and others as specified below, wrote the original grant application, developed the intervention, designed the trial, measurement schedules and qualitative topic guides, contributed to the design and delivery of the training of the community coaches, and interpreted the findings. She was coprincipal investigator with Sally Wyke of the project reported here and coprincipal investigator on the earlier feasibility pilot study with Sally Wyke and Cindy Gray. She oversaw the fieldwork training and conduct with Cindy Gray and contributed expertise in gender and health in the gender-sensitisation of the programme. She and Sally Wyke jointly drafted this report (with input from other authors as specified below).
Cindy M Gray (Lord Kelvin Adam Smith Fellow, health psychology), in close collaboration particularly with Sally Wyke and Kate Hunt and others as specified below, wrote the original grant application, developed the intervention, designed the trial, measurement schedules and qualitative topic guides and interpreted the findings. She co-ordinated recruitment to the trial, developed the training materials and manuals for participants and coaches, oversaw the training of the coaches, liaised with the clubs at all stages of the development and delivery of the intervention and the fieldwork and oversaw the fieldwork training and conduct with Kate Hunt. She drafted part of the process evaluation chapter (see Chapter 5) and provided detailed critical comments on the full report. Cindy was a grant holder on project and the project manager until December 2012.
Elisabeth Fenwick (Professor of Health Economics) was a grant holder and contributed to the original grant application. She designed and oversaw the economic evaluation and wrote the economic evaluation sections of the report.
Christopher Bunn (research fellow, sociology) was the project manager from January to December 2013. He led analysis, drafted most of the process evaluation chapter (see Chapter 5) and provided detailed critical comments on the full report.
Peter T Donnan (Professor of Statistics) was a grant holder on this project and contributed to the design of the trial and the original grant application. He oversaw and interpreted the statistical analysis and provided critical comments on chapters reporting the trial methods and results.
Petra Rauchhaus (research fellow, statistics) undertook the statistical analyses and oversaw the quantitative data management at the University of Dundee, Dundee, UK. She provided comments on chapters reporting the trial methods and results (see Chapters 2 and 3).
Nanette Mutrie (Professor, Sports Psychology) contributed to the design of the intervention (in particular providing expertise on physical activity) and the trial, the original grant application, the design and delivery of the training of the community coaches, provided critical additions and comments on the trial results, particularly in relation to physical activity, and made critical comments on the report. She was a grant holder on this project and on the earlier feasibility pilot study.
Annie S Anderson (Professor of Public Health Nutrition) contributed to the design of the intervention (in particular providing expertise on diet and dietary behaviour change) and the trial, the original grant application, provided critical comments on the trial results, particularly in relation to diet, and made critical comments and additions to the Report. She was a grant holder on this project and on the earlier feasibility pilot study.
Nicole Boyer (research assistant, health economics) undertook the economic analysis with Eleanor Grieve and Elisabeth Fenwick and provided critical comments on the economic evaluation chapter (see Chapter 4).
Adrian Brady (Associate Professor, University of Glasgow and Consultant Cardiologist, Glasgow Royal Infirmary) was a grant holder on the project. He provided clinical oversight of the programme and contributed to the analyses of adverse events. He commented on the health economics chapter and provided critical feedback throughout the project.
Eleanor Grieve (research fellow, health economics) undertook the economic analysis with Nicole Boyer and Elisabeth Fenwick and provided critical comments on the economic evaluation chapter (see Chapter 4).
Alan White (Professor of Men’s Health) was a grant holder on the project. He provided comments on the grant application and the final report.
Catherine Ferrell (survey manager) wrote the fieldwork protocols, designed the databases and contributed to the Standard Operating Procedures. She developed training protocols and oversaw quality assurance of fieldwork and measurements. She gave critical comment on the plain English summary.
Elaine Hindle (survey support officer) developed questionnaires, oversaw database management and delivery of fieldwork timetables. She gave critical comment on the plain English summary.
Shaun Treweek (Professor of Health Services Research) contributed to the design of the intervention and the trial, the original grant application, provided critical comments on the trial results and the cost-effectiveness analysis and gave detailed critical comments on the report. He was a grant holder on this project and on the earlier feasibility pilot study.
Publications
Hunt K, Wyke S, Gray CM, Anderson AS, Brady A, Bunn C, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet 2014;383:1211–21.
Hunt K, Gray C, Maclean A, Smillie S, Bunn C, Wyke S. Do weight management programmes delivered at professional football clubs attract and engage high risk men? A mixed-methods study. BMC Public Health 2014;14:50.
Wyke S, Hunt K, Gray C. 11 PRT/8506: Football Fans in Training (FFIT): a pragmatic randomised controlled trial of a gender-sensitised weight loss and healthy living programme delivered to men aged 35–65 years by Scottish Premier League football clubs (ISRCTN32677491). Lancet 2012. URL: www.thelancet.com/protocol-reviews/11PRT8506 (accessed 29 July 2014).
Other publications related to FFIT, from research funded by CSO and MRC/CSO Social and Public Health Sciences Unit are:
Gray C, Hunt K, Mutrie N, Anderson A, Leishman J, Dalgarno L, et al. Football Fans in Training: the development and optimisation of an intervention delivered through professional sports clubs to help men lose weight, become more active and adopt healthier eating habits. BMC Public Health 2013;13:232.
Hunt K, McCann C, Gray C, Mutrie N, Wyke S. ‘You have got to walk before you run’. Positive evaluations of a walking programme as part of a gender sensitised weight management programme delivered to men through professional football clubs. Health Psychol 2013;32:57–65.
Gray C, Hunt K, Mutrie N, Anderson A, Treweek S, Wyke S. Weight management for overweight and obese men delivered through professional football clubs: a pilot randomized trial. Int J Behav Nutr Phys Act 2013;10:121.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378:815-25. http://dx.doi.org/10.1016/S0140-6736(11)60814-3.
- Bradshaw P, Bromley C, Corbett J, Day J, Doig M, Dowling S, et al. The Scottish Health Survey. Volume 1: Adults. Edinburgh: The Scottish Government; 2012.
- Logue J, Walker JJ, Colhoun HM, Leese GP, Lindsay RS, McKnight JA, et al. Do men develop type 2 diabetes at lower body mass indices than women?. Diabetologia 2011;54:3003-6. http://dx.doi.org/10.1007/s00125-011-2313-3.
- Sattar N. Gender aspects in type 2 diabetes mellitus and cardiometabolic risk. Best Pract Res Clin Endocrinol Metab 2013;27:501-7. http://dx.doi.org/10.1016/j.beem.2013.05.006.
- Obesity: The Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. London: NICE; 2006.
- Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomised controlled trials of lifestyle weight loss interventions. Obesity 2012;20:1234-9. http://dx.doi.org/10.1038/oby.2011.140.
- Stubbs RJ, Pallister C, Whybrow S, Avery A, Lavin J. Weight outcomes audit for 34,271 adults referred to a primary care/commercial weight management partnership scheme. Obes Facts 2011;4:113-20. http://dx.doi.org/10.1159/000327249.
- Jebb SA, Ahern AL, Olson AD, Aston LM, Holzapfel C, Stoll J, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet 2011;378:1485-92. http://dx.doi.org/10.1016/S0140-6736(11)61344-5.
- Ross HM, Laws R, Reckless J, Lean M. Counterweight Project Team . Evaluation of the Counterweight Programme for obesity management in primary care: a starting point for continuous improvement. Br J Gen Pract 2008;58:548-54. http://dx.doi.org/10.3399/bjgp08X319710.
- Robertson C, Archibald D, Avenell A, Douglas F, Hoddinott P, van Teijlingen E, et al. Systematic reviews and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol Assess 2014;18. http://dx.doi.org/10.3310/hta18350.
- Stibbe A. Health and the social construction of masculinity in Men’s Health magazine. Men Masc 2004;7:31-5. http://dx.doi.org/10.1177/1097184X03257441.
- Pliner P, Chaiken S, Flett GL. Gender differences in concern with body weight and physical appearance over the life span. Pers Soc Psychol Bull 1990;16:263-73. http://dx.doi.org/10.1177/0146167290162007.
- Kiefer I, Rathmanner T, Kunze M. Eating and dieting differences in men and women. J Mens Health Gender 2005;2:194-201. http://dx.doi.org/10.1016/j.jmhg.2005.04.010.
- McPherson KE, Turnbull JD. Body image satisfaction in Scottish men and its implications for promoting healthy behaviours. Int J Mens Health 2005;4:3-12. http://dx.doi.org/10.3149/jmh.0401.3.
- Gough B. ‘Real men don’t diet’: an analysis of contemporary newspaper representations of men, food and health. Soc Sci Med 2007;64:326-37. http://dx.doi.org/10.1016/j.socscimed.2006.09.011.
- Gough B, Conner MT. Barriers to healthy eating amongst men: a qualitative analysis. Soc Sci Med 2006;62:387-95. http://dx.doi.org/10.1016/j.socscimed.2005.05.032.
- Fraser GE, Welch A, Luben R, Bingham SA, Day NE. The effect of age, sex, and education on food consumption of a middle-aged English cohort: EPIC in East Anglia. Prev Med 2000;30:26-34. http://dx.doi.org/10.1006/pmed.1999.0598.
- Health Survey for England. Leeds: NHS Information Centre; 2010.
- Duvigneaud N, Wijndaele K, Matton L, Deriemaeker P, Philippaerts R, Lefevre J, et al. Socio-economic and lifestyle factors associated with overweight in Flemish adult men and women. BMC Public Health 2007;7. http://dx.doi.org/10.1186/1471-2458-7-23.
- Scottish Health Survey 2010. Edinburgh: Scottish Government; 2010.
- Young MD, Morgan PJ, Plotnikoff RC, Callister R, Collins CE. Effectiveness of male-only weight loss and weight loss maintenance interventions: a systematic review with meta-analysis. Obes Rev 2012;13:393-408. http://dx.doi.org/10.1111/j.1467-789X.2011.00967.x.
- Bye C, Avery A, Lavin J. Tackling obesity in men – preliminary evaluation of men-only groups within a commercial slimming organization. J Hum Nutr Diet 2005;18:391-4. http://dx.doi.org/10.1111/j.1365-277X.2005.00642.x.
- Drygas W, Ruszkowska J, Philpott M, Bjorkstrom O, Parker M, Ireland R, et al. Good practices and health policy analysis in European sports stadia: results from the ‘Healthy Stadia’™ project. Health Prom Int 2013;28:157-65. http://dx.doi.org/10.1093/heapro/dar088.
- Pringle A, Zwolinsky S, Smith A, Robertson S, McKenna J, White A. The pre-adoption demographic and health profiles of men participating in a programme of men’s health delivered in English Premier League football clubs. Public Health 2011;125:411-16. http://dx.doi.org/10.1016/j.puhe.2011.04.013.
- Brady AJB, Perry C, Murdoch DL, McKay G. Sustained benefits of a health project for middle-aged football supporters, at Glasgow Celtic and Glasgow Rangers Football Clubs. Eur Heart J 2010;31:2966-8.
- Pringle A, Zwolinsky S, McKenna J, Daly-Smith A, Robertson S, White A. Effect of a national programme of men’s health delivered in English Premier League football clubs. Public Health 2013;127:18-26. http://dx.doi.org/10.1016/j.puhe.2012.10.012.
- Ireland R, Watkins F. Football fans and food: a case study of a football club in the English Premier League. Public Health Nutr 2010;13:682-7. http://dx.doi.org/10.1017/S1368980009991765.
- Gray C, Hunt K, Mutrie N, Anderson A, Leishman J, Dalgarno L, et al. Football Fans in Training: the development and optimization of an intervention delivered through professional sports clubs to help men lose weight, become more active and adopt healthier eating habits. BMC Public Health 2013;13. http://dx.doi.org/10.1186/1471-2458-13-232.
- ESPN FC n.d. http://spfl.co.uk/spfl-trust/ (accessed 14 October 2013).
- Scottish Premier League . Scottish Premier League Stats: Team Attendance – 2011–12 2012. http://espnfc.com/stats/attendance/_/league/sco.1/year/2011/scottish-premiership?cc=5739 (accessed 13 December 2013).
- Hunt K, McCann C, Gray CM, Mutrie N, Wyke S. ‘You’ve got to walk before you run’: positive evaluations of a walking program as part of a gender-sensitised, weight-management program delivered to men through professional football clubs. Health Psychol 2013;32:57-65. http://dx.doi.org/10.1037/a0029537.
- Gray C, Hunt K, Mutrie N, Anderson A, Treweek S, Wyke S. Weight management for overweight and obese men delivered through professional football clubs: a pilot randomized trial. Int J Behav Nutr Phys Act 2013;10. http://dx.doi.org/10.1186/1479-5868-10-121.
- Hunt K, Wyke S, Gray CM, Anderson AS, Brady A, Bunn C, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet 2014;383:1211-21. http://dx.doi.org/10.1016/S0140-6736(13)62420-4.
- Hunt K, Gray C, Maclean A, Smillie S, Bunn C, Wyke S. Do weight management programmes delivered at professional football clubs attract and engage high risk men? A mixed-methods study. BMC Public Health 2014;14. http://dx.doi.org/10.1186/1471-2458-14-50.
- Torgerson DJ. Contamination in trials: is cluster randomisation the answer?. BMJ 2001;322:355-7. http://dx.doi.org/10.1136/bmj.322.7282.355.
- Wyke S, Hunt K, Gray C. 11 PRT 8506: Football Fans in Training (FFIT): A Pragmatic Randomised Controlled Trial of a Gender-Sensitised Weight Loss and Healthy Living Programme Delivered to Men Aged 35–65 Years by Scottish Premier League Football Clubs (ISRCTN32677491) 2012. www.thelancet.com/protocol-reviews/11PRT8506 (accessed 29 July 2014).
- Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Can J Sport Sci 1992;17:338-45.
- Calasanti T, Pietila I, Ojala H, King N. Men, bodily control, and health behaviors: the importance of age. Health Psychol 2013;32:15-23. http://dx.doi.org/10.1037/a0029300.
- Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J, et al. Foresight TACKLING Obesities: Future Choices – Project Report. London: Department of Innovation Universities and Skills; 2007.
- Gray CM, Anderson AS, Clarke AM, Dalziel A, Hunt K, Leishman J, et al. Addressing male obesity: an evaluation of a group-based weight management intervention for Scottish men. J Mens Health 2009;6:70-81. http://dx.doi.org/10.1016/j.jomh.2008.11.002.
- Gray C, Hunt K, Lorimer K, Anderson A, Benzeval M, Wyke S. Words matter: a qualitative investigation of which weight status terms are acceptable and motivate weight loss when used by health professionals. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-513.
- So You Want to Lose Weight?. London: British Heart Foundation; 2009.
- Management of Obesity: A National Clinical Guideline. Edinburgh: SIGN; 2010.
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26-33. http://dx.doi.org/10.1136/qshc.2004.011155.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: building an International Consensus for the Reporting of Behavior Change Interventions. Ann Behav Med 2013;46:81-95. http://dx.doi.org/10.1007/s12160-013-9486-6.
- Management of Obesity: A National Clinical Guideline. Edinburgh: SIGN; 2012.
- Public Health England, Welsh Government, the Scottish Government and the Food Standards Agency in Northern Ireland . Your Guide to the Eatwell Plate: Helping You Eat a Healthier Diet n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/237282/Eatwell_plate_booklet.pdf (accessed 29 July 2014).
- Public Health England, The Welsh Government, The Scottish Government, The Food Standards Agency in Northern Ireland . The Eatwell Plate n.d. www.nhs.uk/livewell/goodfood/documents/eatwellplate.pdf (accessed 25 May 2014).
- Cancer Research UK . Ten Top Tips – Weight Loss Tips Based on Scientific Evidence n.d. http://info.cancerresearchuk.org/healthyliving/obesityandweight/tentoptips/ (accessed 25 May 2014).
- Baker G, Gray SR, Wright A, Fitzsimons C, Nimmo M, Lowry R, et al. The effect of a pedometer-based community walking intervention ‘Walking for Wellbeing in the West’ on physical activity levels and health outcomes: a 12-week randomised controlled trial. Int J Behav Nutr Phys Act 2008;5. http://dx.doi.org/10.1186/1479-5868-5-44.
- Fitzsimons C, Baker G, Gray S, Nimmo M, Mutrie N. the Scottish Physical Activity Research Collaboration (SPARColl) . Does physical activity counselling enhance the effects of a pedometer-based intervention over the long-term: 12-month findings from the Walking for Wellbeing in the west study. BMC Public Health 2012;12. http://dx.doi.org/10.1186/1471-2458-12-206.
- O’Donovan G, Blazevich AJ, Boreham C, Cooper AR, Crank H, Ekelund U, et al. The ABC of physical activity for health: a consensus statement from the British Association of Sport and Exercise sciences. J Sports Sci n.d.;28:573-91. http://dx.doi.org/10.1080/02640411003671212.
- King NA, Caudwell P, Hopkins M, Byrne NM, Colley R, Hills AP, et al. Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss. Obesity 2007;15:1373-83. http://dx.doi.org/10.1038/oby.2007.164.
- Manthou E, Gill JMR, Wright A, Malkova D. Behavioral compensatory adjustments to exercise training in overweight women. Med Sci Sports Exerc 2010;42:1221-8. http://dx.doi.org/10.1249/MSS.0b013e3181c524b7.
- Carver CS, Scheier MF. Control-theory – a useful conceptual-framework for personality-social, clinical, and health psychology. Psychol Bull 1982;92:111-35. http://dx.doi.org/10.1037/0033-2909.92.1.111.
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. http://dx.doi.org/10.1037/a0016136.
- Greaves C, Sheppard K, Abraham C, Hardeman W, Roden M, Evans P, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-119.
- Dombrowski SU, Sniehotta FF, Avenell A, Johnston M, MacLennan G, Araújo-Soares V. Identifying active ingredients in complex behavioural interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: a systematic review. Health Psychol Rev 2012;6:7-32. http://dx.doi.org/10.1080/17437199.2010.513298.
- Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Dec Process 1991;50:248-87. http://dx.doi.org/10.1016/0749-5978(91)90022-L.
- Mutrie N, Campbell AM, Whyte F, McConnachie A, Emslie C, Lee L, et al. Benefits of supervised group exercise programme for women being treated for early stage breast cancer: pragmatic randomised controlled trial. BMJ 2007;334. http://dx.doi.org/10.1136/bmj.39094.648553.AE.
- Mutrie N, Campbell A, Barry S, Hefferon K, McConnachie A, Ritchie D, et al. Five-year follow-up of participants in a randomised controlled trial showing benefits from exercise for breast cancer survivors during adjuvant treatment. Are there lasting effects?. J Cancer Surviv 2012;6:420-30. http://dx.doi.org/10.1007/s11764-012-0233-y.
- Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med 1970;2:92-8.
- The FFIT Research Group . Football Fans in Training Research Website 2013. www.ffit.org.uk (accessed 31 July 2014).
- Standard Evaluation Framework for Weight Management Interventions. National Health Service; 2009.
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381-95. http://dx.doi.org/10.1249/01.MSS.0000078924.61453.FB.
- Emslie C, Lewars H, Batty GD, Hunt K. Are there gender differences in levels of heavy, binge and problem drinking? Evidence from three generations in the west of Scotland. Public Health 2009;123:12-4. http://dx.doi.org/10.1016/j.puhe.2008.06.001.
- Thompson ER. Development and validation of an internationally reliable short-form of the positive and negative affect schedule (PANAS). JCCP 2007;38:227-42.
- Rosenberg M. Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press; 1965.
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. J Clin Epidemiol 1998;51:1171-8. http://dx.doi.org/10.1016/S0895-4356(98)00109-7.
- International Physical Activity Questionnaire . IPAQ Scoring Protocol n.d. https://sites.google.com/site/theipaq/scoring-protocol (accessed 14 October 2013).
- Vickers A. The use of percentage change from baseline as an outcome in a controlled trial is statistically inefficient: a simulation study. BMC Med Res Methodol 2001;1. http://dx.doi.org/10.1186/1471-2288-1-6.
- White IR, Carpenter J, Horton NJ. Including all individuals is not enough: lessons for intention-to-treat analysis. Clin Trials 2012;9:396-407. http://dx.doi.org/10.1177/1740774512450098.
- Pocock SJ, Assmann SE, Enos LE, Kasten LE. Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Stat Med 2002;21:2917-30. http://dx.doi.org/10.1002/sim.1296.
- Lee KJ, Thompson SG. The use of random effects models to allow for clustering in individually randomized trials. Clin Trials 2005;2:163-73. http://dx.doi.org/10.1191/1740774505cn082oa.
- Brazier JE, Roberts J. The Estimation of a Preference-Based Measure of Health From the SF-12. Med Care 2004;42:851-9. http://dx.doi.org/10.1097/01.mlr.0000135827.18610.0d.
- British National Formulary n.d. www.bnf.org/bnf/index.htm (accessed 16 August 2013).
- Personal Social Services Research Unit . Unit Cost of Health and Social Care 2011 n.d. www.pssru.ac.uk/project-pages/unit-costs/2011/index.php (accessed 16 August 2013).
- Information Services Division Scotland n.d. www.isdscotland.org/ (accessed 16 August 2013).
- Bhandari A, Wagner T. Self-Reported Utilisation of Health Care Services: improving Measurement and Accuracy. Med Care Res Rev 2006;63:217-35. http://dx.doi.org/10.1177/1077558705285298.
- McCabe C, Brazier J, Gilks P, Tsuchiya A, Roberts J, O’Hagan A, et al. Using rank data to estimate health state utility models. J Health Econ 2006;25:418-31. http://dx.doi.org/10.1016/j.jhealeco.2005.07.008.
- Kharroubi SA, Brazier JE, Roberts J, O’Hagan A. Modelling SF-6D health state preference data using a nonparametric Bayesian method. J Health Econ 2007;26:597-612. http://dx.doi.org/10.1016/j.jhealeco.2006.09.002.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. http://dx.doi.org/10.1002/hec.944.
- Bending M, Beale S, Hutton J. NICE: An Economic Analysis of Workplace Interventions that Promote Physical Activity. York: York Health Economics Consortium; 2008.
- Anderson KM, Odell PM, Wilson PWF, Kannel WB. Cardiovascular disease risk profiles. Am Heart J 1991;121:293-8. http://dx.doi.org/10.1016/0002-8703(91)90861-B.
- Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care 2003;26:725-31. http://dx.doi.org/10.2337/diacare.26.3.725.
- Brennan A, Blake L, Hill-McManus D, Payne N, Woods HB, Blank L. NICE Public Health Programme: Walking and Cycling: Local Measures to Promote Walking and Cycling as Forms of Travel or Recreation: Health Economics and Modelling Report. Sheffield: School of Health and Related Research (ScHARR): University of Sheffield; 2012.
- Andersen L, Schnohr P, Schroll M, Hein H. All-cause mortality associated with physical activity during leisure time, work, sports, and cycling to work. Arch Intern Med 2000;160:1621-8. http://dx.doi.org/10.1001/archinte.160.11.1621.
- Gunning-Schepers L. The health benefits of prevention: a simulation approach. Health Policy 1989;12:1-255.
- Bronnum-Hansen H. How good is the prevent model for estimating the health benefits of prevention?. J Epidemiol Comm Health 1999;53:300-5. http://dx.doi.org/10.1136/jech.53.5.300.
- Soerjomataram I, de Vries E, Engholm G, Paludan-Muller G, Bronnum-Hansen H, Storm HH, et al. Impact of a smoking and alcohol intervention program on lung and breast cancer incidence in Denmark: an example of dynamic modeling with Prevent. Eur J Cancer 2010;46:2617-24. http://dx.doi.org/10.1016/j.ejca.2010.07.051.
- Dallat MAT, Soerjomataram I, Hunter RF, Tully MA, Cairns KJ, Kee F. Urban greenways have the potential to increase physical activity levels cost-effectively. Eur J Public Health 2014;24:190-5. http://dx.doi.org/10.1093/eurpub/ckt035.
- Haby MM, Vos T, Carter R, Moodie M, Markwick A, Magnus A, et al. A new approach to assessing the health benefit from obesity interventions in children and adolescents: the assessing cost-effectiveness in obesity project. Int J Obes 2006;30:1463-75. http://dx.doi.org/10.1038/sj.ijo.0803469.
- Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J, et al. Foresight Tackling Obesities: Future Choices – Project Report 2nd edn. London: Department of Innovation Universities and Skills; 2007.
- Hollingworth W, Hawkins J, Lawlor DA, Brown M, Marsh T, Kipping RR. Economic evaluation of lifestyle interventions to treat overweight or obesity in children. Int J Obes 2012;36:559-66. http://dx.doi.org/10.1038/ijo.2011.272.
- Tunstall-Pedoe H, Woodward M, Tavendale R, A’Brook R, McCluskey MK. Comparison of the prediction by 27 different factors of coronary heart disease and death in men and women of the Scottish Heart Health Study: cohort study. BMJ 1997;315:722-9. http://dx.doi.org/10.1136/bmj.315.7110.722.
- NHS Scotland . Scottish Heart Health Extended Cohort (SHHEC) 2014. http://assign-score.com/about/shhec/ (accessed 15 May 2014).
- Woodward M, Brindle P, Tunstall-Pedoe H. SIGN group on risk estimation . Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC). Heart 2007;93:172-6. http://dx.doi.org/10.1136/hrt.2006.108167.
- Scottish Executive . The Scottish Health Survey 2003 2005. www.scotland.gov.uk/Publications/2005/11/25145024/50251 (accessed 29 July 2014).
- Geue C, Lewsey J, Lorgelly P, Govan L, Hart C, Briggs A. Spoilt for choice: implications of using alternative methods of costing hospital episode statistics. Health Econ 2012;21:1201-16. http://dx.doi.org/10.1002/hec.1785.
- Tunstall-Pedoe H, Woodward M. Appendices from Heart Paper Published Online November 2006 Print February 2007 Modified to Include Rheumatoid Arthritis October 2013 Onwards 2006. http://assign-score.com/downloads/HeartAppxUpdate2013.pdf (accessed 6 June 2014).
- Hart C, McConnachie A, Upton M, Watt G. Risk factors in the Midspan family study by social class in childhood and adulthood. Int J Epidemiol 2008;37:604-14. http://dx.doi.org/10.1093/ije/dyn052.
- Hawthorne VM, Watt GCM, Hart CL, Hole DJ, Smith GD, Gillis CR. Cardiorespiratory disease in men and women in urban Scotland – base-line characteristics of the Renfrew–Paisley (Midspan) study population. Scott Med J 1995;40:102-7.
- Benzeval M, Der G, Ellaway A, Hunt K, Sweeting H, West P, et al. Cohort profile: west of Scotland Twenty-07 study: health in the community. Int J Epidemiol 2009;38:1215-23. http://dx.doi.org/10.1093/ije/dyn213.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ 2006;40:405-14. http://dx.doi.org/10.1111/j.1365-2929.2006.02467.x.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Corbin J, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol 1990;13:3-21. http://dx.doi.org/10.1007/BF00988593.
- Michie S, van Stralen M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-42.
- Deci E, Ryan R. The ‘what’ and ‘why’ of goal pursuits: human needs and the self-determination of behavior. Psychol Inq 2000;11:227-68. http://dx.doi.org/10.1207/S15327965PLI1104_01.
- National Statistics for Scotland . Local Area Labour Markets in Scotland – Statistics from the Annual Population Survey 2012 2013. www.scotland.gov.uk/Publications/2013/05/6728/downloads (accessed 14 August 2013).
- Scottish Government . Summary: Ethnic Group Demographics n.d. www.scotland.gov.uk/Topics/People/Equality/Equalities/DataGrid/Ethnicity/EthPopMig (accessed 14 August 2013).
- Latour B. Reassembling the Social: An Introduction to Actor-Network-Theory. Oxford: Oxford University Press; 2005.
- Yalom ID. The Theory and Practice of Group Psychotherapy. New York, NY: Basic Books; 1985.
- Wagner CC, Ingersoll KS. Motivational Interviewing in Groups. New York, NY: The Guildford Press; 2013.
- Shove E, Pantzar M, Watson M. The Dynamics of Social Practice: Everyday Life and How it Changes. London: Sage; 2012.
- Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991.
- Morgan PJ, Collins CE, Plotnikoff RC, Cook AT, Berthon B, Mitchell S, et al. Efficacy of a workplace-based weight loss program for overweight male shift workers: the Workplace POWER (Preventing Obesity Without Eating like a Rabbit) randomized controlled trial. Prev Med 2011;52:317-25. http://dx.doi.org/10.1016/j.ypmed.2011.01.031.
- Morgan PJ, Lubans D, Collins CE, Warren J, Callister R. 12-month outcomes and process evaluation of the SHED-IT RCT: an internet-based weight loss program targeting men. Obesity 2011;19:142-51. http://dx.doi.org/10.1038/oby.2010.119.
- Anderson AS, Craigie AM, Caswell S, Treweek S, Stead M, Macleod M, et al. The impact of a bodyweight and physical activity intervention (BeWEL) initiated through a national colorectal cancer screening programme: randomised controlled trial. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g1823.
- Patrick K, Calfas K, Norman G, Rosenberg D, Zabinski M, Sallis J, et al. Outcomes of a 12-month web-based intervention for overweight and obese men. Ann Behav Med 2011;42:391-40. http://dx.doi.org/10.1007/s12160-011-9296-7.
- Morgan PJ, Warren JM, Lubans DR, Collins CE, Callister R. Engaging men in weight loss: experiences of men who participated in the male only SHED-IT pilot study. Obes Res Clin Pract 2011;5:e239-48. http://dx.doi.org/10.1016/j.orcp.2011.03.002.
- Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Washington, DC: World Cancer Research Fund/American Institute of Cancer Research; 2007.
- Khaw K-T, Bingham S, Welch A, Luben R, Wareham N, Oakes S, et al. Relation between plasma ascorbic acid and mortality in men and women in EPIC-Norfolk prospective study: a prospective population study. Lancet 2001;357:657-63. http://dx.doi.org/10.1016/S0140-6736(00)04128-3.
- Roux L, Pratt M, Tengs TO, Yore MM, Yanagawa TL, Van Den Bos J, et al. Cost effectiveness of community-based physical activity interventions. Am J Prev Med 2008;35:578-88. http://dx.doi.org/10.1016/j.amepre.2008.06.040.
- Griffiths UK, Anigbogu B, Nanchahal K. Economic evaluations of adult weight management interventions: a systematic literature review focusing on methods used for determining health impacts. Appl Health Econ Health Policy 2012;10:145-62. http://dx.doi.org/10.2165/11599250-000000000-00000.
- O’Brien R, Hunt K, Hart G. ‘It’s caveman stuff, but that is to a certain extent how guys still operate’: men’s accounts of masculinity and help seeking. Soc Sci Med 2005;61:503-16. http://dx.doi.org/10.1016/j.socscimed.2004.12.008.
- Roberts GC, Treasure DC. Advances in Motivation in Sport and Exercise. Champaign, IL: Human Kinetics; 2012.
- Teixeira P, Carraca E, Markland D, Silva M, Ryan R. Exercise, physical activity, and self-determination theory: a systematic review. International. J Behav Nutr Phys Act 2012;9. http://dx.doi.org/10.1186/1479-5868-9-78.
- Barclays Premier League . Research and Insight, Season 2011–2012 2012. http://fansurvey.premierleague.com/ (accessed 16 August 2013).
- Bellg A, Borrelli B, Resnick B, Hecht J, Minicucci D, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004;23:443-51. http://dx.doi.org/10.1037/0278-6133.23.5.443.
- Breckon JD, Johnston LH, Hutchison A. Physical activity counseling content and competency: a systematic review. J Phys Act Health 2008;5:398-417.
- Prevention of Cardiovascular Disease. NICE Public Health Guidance 25. London: NICE; 2010.
- Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g2646.
- Courtenay W. Constructions of masculinity and their influence on men’s well-being: a theory of gender and health. Soc Sci Med n.d.;50:1385-401. http://dx.doi.org/10.1016/S0277-9536(99)00390-1.
Appendix 1 Exit questionnaire
Appendix 2 Example programme observation proforma
Appendix 3 Participant focus group and coach interview topic guides
Football Fans in Training 12-week focus group topic guide
Introduction
-
Aims of group – first, I want to find out what you thought of the FFIT programme, how being involved with it has changed your life, and any changes you would like to see made to it.
-
I am simply here as a sort of chairperson to make sure that everyone gets a chance to speak. What you have to say is important to me and the other researchers so please don’t be afraid of speaking your mind.
-
I will audio- and video-tape the discussion, and the recordings will kept for 10 years after the project finishes, but everything you say will be in strictest confidence.
-
Questions and consent forms.
-
Start by getting the men to introduce themselves and say what was their most memorable football game (for voice identification).
Discussion
-
Why did you join the FFIT Programme?
-
What did you want to achieve when you came along?
-
What are the main differences being on the programme has made to you? Positive and negative (Prompts: weight-loss, following better eating habits, taking more exercise, drinking less, having more energy, feeling better, injury)?
-
What was it about the programme that helped you make these changes? Why?
-
Was there anything about the programme that was not so helpful? Why?
-
What did you think about using club coaches to deliver the programme? What did you feel about external staff being brought into help?
-
Did you know that we had selection criteria for joining? What did you think about that? (Prompt age range/BMI/waist) How did these affect group dynamics?
-
Was there anything else you would have liked to have been included in the programme? (Prompt: continuing support) How would this have changed the programme, do you think?
-
Was there anything you don’t think should have been included in the programme?
-
Why did you keep coming to the programme?
-
Did your being on the programme have any effect on your family? If so, how and why?
-
Would you like to see the club offering any other kinds of programmes to supporters?
Summary
At end of discussion, summarise what has been said and ask men if there is anything else they would like to add.
Football Fans in Training 12-month focus group
Introduction
-
Aims of group – I want to find out how you have been getting on with your weight management and exercise in the 12 months since you joined the FFIT programme at [Club Name]. We particularly want to know what information or ‘tricks’ that you learned from FFIT have been useful in helping you maintain the changes over the last 9 months or so. I would also like you to be honest about the difficulties and problems you have faced too.
-
I am simply here as a sort of chairperson to make sure that everyone gets a chance to speak. What you have to say is important to me and the other researchers so please don’t be afraid of speaking your mind.
-
I will audio- and video-tape the discussion, and the recordings will kept for 10 years after the project finishes, but everything you say will be in strictest confidence.
-
Questions and consent forms.
-
Start by getting the men to introduce themselves and say what was their most memorable football game (for voice identification).
General
-
Looking back at taking part in the FFIT programme and the time since, would you say that it has affected any aspect of your day-to-day life or your health?
Eating
-
Thinking about your eating habits, what were the main changes you managed to make, if any, while on the FFIT programme at [Club Name].
-
Which of those changes have you managed to maintain over the nine months since the programme ended?
-
What difficulties have you faced in trying to maintain the changes to your eating habits?
-
What have you found helpful in maintaining the changes to your eating habits?
Physical activity
-
Thinking about physical activity now, what were the main changes you managed to make, if any, while on the FFIT programme at [Club Name].
-
Which of those changes have you managed to maintain over the nine months since the programme ended?
-
What difficulties have you faced in trying to maintain the changes to your physical activity level?
-
What have you found helpful in maintaining the changes to your physical activity level?
Anything else?
-
Are there any other changes you have made to your lifestyle as a result of being on the FFIT programme? If yes, how have you found maintaining these since the programme ended?
Overall impact
-
Finally, 12 months on, what would you say are the main impacts being on the FFIT programme has made on your life/or the lives of those around you?
Summary
At end of discussion, summarise what has been said and ask men if there is anything else they would like to add.
Football Fans in Training face-to-face interview with coaches
-
Can you tell me about your programme? (Prompts: no. of men, date and time and why these were chosen.)
-
How do you feel it went?
-
How did you find it to deliver? Any specific problems?
-
How did you find the training sessions (helpful/not helpful)? What could have been done differently?
-
How did you find the support you were given to deliver the programme (Prompts: from the SPL, from the programme trainers?)
-
What did you think was good about the programme?
-
What did you think was not so good about the programme?
-
Which parts of the programme did you think were effective in helping the men to lose weight? Why?
-
Which elements did you think were effective in helping the men to increase physical activity? Why?
-
Were there any elements that you thought weren’t useful for helping the men to lose weight? Why?
-
Were there any elements that you thought weren’t useful for helping the men to increase physical activity? Why?
-
Did you find anything particularly helpful in allowing you to deliver the programme? If so, what?
-
Was there anything that made delivery of the programme more difficult? (Prompt age range; different physical activity abilities.)
-
How did you feel about dealing with questions the men asked?
-
Are there any changes you would like to see made to any aspect of the programme? (Prompt: more information; targeting different men) Why?
-
Would you like to see the club offering any other kinds of programmes to supporters?
Summary
At end of interview, summarise what has been said and ask the trainers if there is anything else they would like to add.
List of abbreviations
- BBC
- British Broadcasting Corporation
- BCT
- behaviour change technique
- BMI
- body mass index
- CBVD
- cerebrovascular disease
- CHD
- coronary heart disease
- CI
- confidence interval
- COM-B
- capabilities, opportunities, motivation and behaviour
- CSO
- Chief Scientist Office
- CVD
- cardiovascular disease
- DINE
- Dietary Instrument for Nutrition Education questionnaire
- EQ-5D
- European Quality of Life-5 Dimensions questionnaire
- EVPI
- expected value of perfect information
- FFIT
- Football Fans in Training
- FGD
- focus group discussion
- GP
- general practitioner
- HDL
- high-density lipoprotein
- HRQoL
- health-related quality of life
- ICER
- incremental cost-effectiveness ratio
- IPAQ
- International Physical Activity Questionnaire
- LSI
- limiting long-standing illness
- MET
- metabolic equivalent
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- PANAS
- Positive and Negative Affect Schedule
- PAR-Q
- Physical Activity Readiness Questionnaire
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- RGM
- ratio of geometric means
- RPE
- rating of perceived exertion
- RSE
- Rosenberg Self-Esteem scale
- SD
- standard deviation
- SDT
- self-determination theory
- SF-12
- Short Form questionnaire-12 items
- SHeS
- Scottish Health Survey
- SHHEC
- Scottish Heart Health Extended Cohort
- SIGN
- Scottish Intercollegiate Guidelines Network
- SIMD
- Scottish Index of Multiple Deprivation
- SMART
- specific, measurable, achievable, realistic, time-limited
- SMR
- Scottish Morbidity Record
- SMS
- short message service
- SPFL
- Scottish Professional Football League
- SPL
- Scottish Premier League
- TCTU
- Tayside Clinical Trials Unit
- VOI
- value of information