Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 11/3001/16. The contractual start date was in September 2012. The final report began editorial review in August 2014 and was accepted for publication in December 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Barber et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Physical activity and the preschool years
The preschool years are considered a critical period for establishing healthy lifestyle behaviours such as physical activity. 1 The benefits of engaging in regular physical activity in the preschool years are numerous, with one of the most significant being the promotion of healthy weight and prevention of obesity during childhood. 2–5 The prevalence of overweight and obesity in preschool children has doubled in recent decades,6 and in the mid-2000s over one-third of preschool children in the UK and USA were overweight or obese. 7 Despite the widespread belief that the prevalence of childhood obesity is still escalating, contemporary high-quality studies suggest a slowing in the rate of rise in some developed countries, including the UK. 8,9 Although this appears promising, levels still remain high and are heterogeneous within countries. 8 For example, in England childhood obesity is higher in urban areas, in children from deprived backgrounds and in certain ethnic minority groups including black and Asian populations. 10 South Asian school-aged children are reported to have substantially lower levels of physical activity than white Europeans. 11 These particularly low levels may contribute to the increased risks of obesity, coronary heart disease (CHD) and diabetes seen in South Asian adults living in the UK. 12 The cause of obesity has not been fully identified but it is probable that reduced physical activity and increased sedentary behaviour are important contributing factors. 3,4 Lower time spent in moderate to vigorous physical activity (MVPA) during the early years has been shown to be associated with higher fat mass (+0.75 kg for girls and +0.61 kg for boys in the lowest compared with the highest quartiles). 2 Additionally, reduced MVPA at age 5 years increases fat mass at age 8 and 11 years: for every 10 minutes per day of MVPA at age 5 years, fat mass has been reported to decrease by 0.2 kg at age 8 and 11 years. 2 Furthermore, levels of MVPA have been inversely associated with measures of central adiposity in children aged 3–8 years. 5
Observational and experimental studies have shown that regular physical activity has other important health and social implications for preschool children. Physical activity is valuable for developing motor skills, enhancing bone and muscle development and developing social competence. 13,14 Furthermore, regular physical activity in this age group may also have beneficial effects on cardiovascular disease (CVD) risk factors such as blood pressure and blood lipids. 14–16 Finally, levels of physical activity track through early childhood17 and into adulthood;18,19 therefore, establishing habitual physical activity early in life may be key to remaining active throughout the lifespan.
Current levels of habitual physical activity in preschool children in the UK, and internationally, are unclear. Methodological differences in the objective measurement of physical activity have resulted in a wide variation of levels reported. Daily physical activity levels have been reported to be as low as 90 minutes20 and as high as 569 minutes21 in the UK. Levels of 127 minutes per day have been reported in Belgium, Australia and the USA22–24 and levels of 402 minutes per day have been reported in Portugal and the USA. 23,25 This large variation in reported physical activity behaviour, even within countries, is likely to be because of the application of different intensity cut-points to accelerometry data (i.e. cut-point non-equivalence26) between different research groups, rather than actual behavioural differences within and between countries. Despite the lack of clarity regarding the extent to which preschoolers engage in physical activity, it has been clearly identified that health-enhancing physical activity declines markedly during childhood,27 with this decline potentially beginning in the early years. 28 Therefore, the promotion of physical activity in the preschool years is critical to slow the rate of this age-related decline.
UK physical activity policy for preschool children
The importance of engaging preschool children in daily physical activity was brought to the forefront in July 2011 with the publication of the UK’s first physical activity guidelines for the under 5s in the Chief Medical Officer’s (CMO) report Start Active, Stay Active. 29 The report recommends 180 minutes of physical activity (light, moderate and vigorous intensity) each day and states that the volume of physical activity is more important than the intensity. Physical activity should be spread throughout the day and should include active play (activities that involve movements of all the major muscle groups) and the development of locomotor, stability and object-control skills.
These guidelines are a significant step towards recognising the importance of physical activity promotion for preschool children; however, guidelines themselves do not change behaviour. The determinants of physical activity in young children are unclear. One systematic review that studied correlates of preschoolers’ physical activity found that boys were more active than girls and that a parent’s level of physical activity and a child’s time spent outdoors had a positive association with physical activity. 30 Members of our team (SEB and DDB) are currently updating this systematic review. The preliminary findings confirm the results from the previous review with regard to sex and time spent outdoors. Additionally, the individual preschool that the child attends has been associated with physical activity level, suggesting policy and environmental impacts on preschool activity levels. This finding is further supported by a systematic review of physical activity in school-aged children, which suggests that environments allowing easy access to physical activity are important. 31 The CMO report states that a ‘concerted and committed action to create environments and conditions that make it easier for people to be more active’ is needed (p. 8). 29 The guidelines also highlight the need for activities to promote movement in the early years and the need to recognise that local communities can have a strong influence on behaviour. The report suggests that investment should be made in community-level programmes in settings such as school playgrounds. We have developed and pilot tested such an intervention, Preschoolers in the Playground (PiP), in the city of Bradford, an area of ethnic diversity and social deprivation in West Yorkshire, UK.
Components of successful interventions
The literature identifies several features likely to lead to successful physical activity interventions and these have informed the development of the PiP intervention.
Theoretical underpinning
The utility of basing health promotion interventions on sound theoretical frameworks is well expounded. 32 A systematic review33 conducted by members of our team (CDS, HJM) reported that the predominant behaviour change theory used in successful childhood obesity prevention interventions is Bandura’s social cognitive theory. 34,35 This theory describes behaviour change as an interaction between personal, environmental and behavioural factors. Personal and environmental factors provide the framework for understanding behaviour. The personal concepts include skills, self-efficacy, self-control and outcome expectancies whereas the environmental concepts include availability (e.g. provision of space for physical activity) and opportunity for social support (e.g. a group setting). The review also reported that providing information on behaviour–health links appeared to be an important component in childhood obesity prevention and physical activity interventions.
An outdoor setting
Enhancing environmental and cultural practices that support children to be more active throughout the day are thought to be promising strategies to prevent childhood obesity, particularly if the children perceive the activities as being fun. 36 Time spent outdoors has been shown to correlate with physical activity levels in preschool children30 and outdoor play is associated with a lower risk of overweight. 37 School and preschool playgrounds provided a potential opportunity to intervene to increase physical activity levels. Indeed, in school-aged children, outdoor playground interventions have been shown to increase daily physical activity. 38,39 Furthermore, some studies have reported that factors related to increased MVPA in playground interventions include greater provision of equipment38,39 and greater play space per child. 40 However, a recent systematic review concluded that further research is needed to elucidate which intervention strategies and playground characteristics are most effective. 41 Interventions in preschool playgrounds supervised by preschool teachers have had mixed success. Adding portable play equipment in a US preschool playground increased physical activity levels in 3- to 5-year-olds. 42 In contrast, in Belgium, no change in physical activity levels of 4- and 5-year-olds was reported after providing playground markings or play equipment or both in the preschool playground. 43 The authors concluded that creating an activity-friendly environment may not be sufficient to promote physical activity in preschoolers and regular infusions of different equipment with more guidance and encouragement from adults to play in an active way are required. Currently, there is no evidence regarding preschool playground interventions in the UK.
Seasonality and weather conditions can present barriers to participation in outdoor play for children. 44,45 Emerging literature is beginning to focus on the importance of season in physical activity promotion and weight management. Two recent studies in the UK21 and Denmark46 have examined seasonal variations in preschool children’s physical activity levels. In both studies, overall, children were significantly less active during the winter months than in the spring, summer and autumn. The Danish study also examined differences in activity patterns across seasons according to body mass index (BMI) status. Children in the highest tertile of BMI had a flatter activity profile throughout the year than children in the lowest tertile. Those in the lowest tertile showed a curved pattern, with activity peaking between June and August at around 200 counts per minute (measured via accelerometry) greater than their higher BMI counterparts. Although not statistically significant, these different activity patterns between normal and overweight people have also been observed in adult populations. 47 Thus, the establishment of annual patterns of physical activity, with levels peaking in the summer months, may begin during the preschool years and possibly track into childhood, contributing towards the prevention of childhood obesity. This emerging research highlights the need to consider seasonality when designing and evaluating the effectiveness of interventions. The PiP intervention was conducted in three waves that were staggered across the year to examine the impact of season on the feasibility and acceptability of the intervention.
Parental involvement
Parental engagement should be a key part of any intervention in the preschool years48 and the suggestion that adult encouragement is required to increase active play is supported by findings from a systematic review of preschool obesity prevention interventions. 49 The 12 interventions reported in this systematic review were conducted in a variety of settings (preschool/childcare, home, group, primary care and mixed settings) and included a physical activity component. Home-based interventions appeared to be the most successful at increasing physical activity despite the small sample sizes of studies and poor adherence to the interventions. This is perhaps because of parental involvement in the interventions, which has been suggested to be vital for facilitating behaviour change during the early years. 33 Mothers in particular are considered to play a major role in establishing a child’s healthy lifestyle behaviours50 and this, in part, may be indirectly through modelling of behaviours. 51
Since the PiP pilot trial started in September 2012 more physical activity interventions for preschoolers have reported a parent or family component. A recent German preschool physical activity intervention with strong and active parental involvement found statistically significant increases in physical activity, reductions in sedentary time and improved perceived general health and quality of life 1 year post intervention. 52 Using a participatory approach, parents were supported to develop and implement their own physical activity-promoting activities for their children in a preschool centre. This study is a good example of capitalising on a setting where preschool children and their parents congregate and involving parents in activities to promote and model physical activity. Another study from the UK demonstrated a statistically significant increase in preschoolers’ physical activity levels immediately after receiving a 10-week active play programme that targeted the whole family. 53 Families were invited to attend five sessions of active play and parent education. Although these recent studies are promising, the changes in physical activity have not been clinically meaningful and thus further research and intervention development is required for this age group.
A further intervention in Belgium (ToyBox) used a preschool-based curriculum plus passive family involvement (giving newsletters, tip cards and posters) approach. 54 This intervention demonstrated effectiveness for boys or children from high-socioeconomic status (SES) preschools only and not girls or children from low-SES preschools. Given that boys and children of a higher SES level have higher levels of physical activity,10,30 this intervention actually generated further health inequalities. These studies with a parental component indicate that active parental involvement rather than just passive parent education may be required to elicit improvements in preschoolers’ physical activity levels and prevent further health inequalities. The development of preschool physical activity interventions that focus on increasing physical activity levels in groups with particularly low levels, including girls, low-SES children and ethnic minority groups, requires particular attention.
Health inequalities and interventions
As demonstrated by the ToyBox study in Belgium,54 interventions aimed at improving public health outcomes can inadvertently exacerbate health disparities when they are differentially effective for those from different socioeconomic positions or ethnic populations. This can occur during a number of stages of intervention implementation including provision of, or access to, the intervention, uptake of the intervention and compliance to the intervention. For example, in the ToyBox study, the lower-SES families may not have read the newsletters provided or implemented changes from the ‘tips’ given, whereas the higher-SES families may have done so, thus widening the inequalities.
There is some guidance regarding the types of public health interventions likely to reduce inequalities. A rapid overview of systematic reviews55 concluded that ‘downstream’ interventions that seek to directly alter the adverse health behaviour are more likely to increase inequalities whereas ‘upstream’ interventions that focus on the wider circumstances that produce the behaviour are more likely to have a positive equality impact. Interventions that are targeted at the most disadvantaged groups may also reduce health disparities. A recent Canadian study demonstrated that a ‘whole school-based’ physical activity promotion intervention targeted at low-SES schools reduced inequalities in physical activity. 56 Furthermore, members of our group (HJM, CDS) have recently conducted a systematic review of the effectiveness of interventions aimed at reducing inequalities in childhood obesity-related outcomes (including physical activity). 57 The review concluded that school-based interventions targeted at low-SES children may have some beneficial effects in reducing inequalities, although the evidence is not conclusive. It recommends that participants should be engaged in the development of interventions to prevent intervention-generated inequalities. Shared decision-making in interventions may be more beneficial to disadvantaged groups than to those with higher literacy or SES. 58
Successful early interventions that are effective and reduce health inequalities have a high potential return in terms of health, social and economic benefits for children throughout their lives. Early childhood problems often translate into lifelong inequalities in health and well-being, and the preschool period is seen as a key period for intervention. The Marmot review of health inequalities59 concluded that ‘giving every child the best start in life’ was its ‘highest priority recommendation’.
Development and description of the Preschoolers in the Playground intervention
The PiP intervention was developed in 2011 following the publication of the UK CMO’s guidance for physical activity in the under 5s,29 consideration of potentially effective intervention components, strategies to reduce health inequalities and focus groups with mothers of preschool children.
The predominant behaviour change theory used in successful childhood obesity prevention interventions32 is Bandura’s social cognitive theory34,35 and, therefore, social cognitive theory was used to direct the intervention development and appropriate behaviour change techniques utilised. The intervention was based in an outdoor environment, the primary school playground, and had strong parental involvement, with parents actively playing with their child during the intervention sessions. The intervention was an ‘upstream’ community-level intervention that focused on changing the traditional use of the local primary school playground and school play equipment, allowing groups of parents and their preschool children to use the facilities to play actively outdoors in a safe environment. It was also ‘downstream’, with direct engagement from preschoolers and their parents. The intervention was targeted at the two most deprived quintiles of the Index of Multiple Deprivation (IMD) in Bradford and at both white and South Asian families to tackle health inequalities in physical activity levels (see Appendix 1). The intervention was developed in conjunction with parents through focus groups that explored typical physical activity in preschoolers and the barriers to and facilitators of physical activity. 60 Six focus groups with a total of 17 white and Pakistani mothers and caregivers (English and Urdu speaking) were conducted at children’s centres in the poorest IMD areas in Bradford. Mothers reported that their children were innately active and enjoyed playing outside. Lack of time was a major barrier to physical activity. Mothers minimised the amount of ‘journeys’ that they made and were put off organised activity sessions, finding it inconvenient to leave the house with young children. Other barriers to outdoor physical activity included ‘feeling that their neighbourhood was an unsafe place to play outdoors’ and ‘needing help from another adult to take the children to the park’. Additionally, the season, the weather and having to take public transport to parks were also identified as barriers. Key facilitators for physical activity were having someone to help during activities and having activities available locally. There was little variation in the reported barriers and facilitators between ethnicities.
Site of delivery of the intervention and timing of the sessions
Local primary school playgrounds were chosen as the site for delivering the PiP intervention. It was anticipated that using the school setting for the intervention would overcome some of the barriers to participation in physical activity for preschool children reported by parents in the focus groups. For example, the intervention would be available locally and would fit into family routines and the playground is an enclosed space that can be supervised easily. Furthermore, the intervention would be accessible to hard-to-reach families, who often do not attend other community-based children’s activities such as those held at children’s centres. Primary school playgrounds (or children’s centre playgrounds when located on the primary school site) were made available to parents and preschool children at times when parents were likely to be attending school (e.g. dropping off or picking up older children from school or young children from nursery). These times were chosen to capitalise on times of the day that parents are already out of the house and minimised the number of journeys to activities that parents had to make (identified as a barrier in focus groups). Six PiP sessions per week for 30 weeks (three school terms) were available to families. This number of sessions was chosen to meet the need for flexibility, which was highlighted at the focus groups. Families were encouraged to attend at least three of these sessions each week. Each PiP session lasted for 30 minutes. There were two phases of the intervention, the initiation phase (10 weeks: one school term), which was supervised and facilitated by a member of school staff, and the maintenance phase, which was unsupervised (20 weeks: two school terms).
Intervention facilitators
Following consultations with two staff members from two schools, parental involvement workers or nursery teachers were suggested as appropriate facilitators to deliver the intervention. It was thought that by training existing staff the intervention would be more sustainable. The initiation phase (10 weeks) was facilitated by parental involvement workers and/or nursery teachers employed by schools/children’s centres. These facilitators undertook a 2-hour training session using the PiP manual and were accompanied during the first session by the lead researcher (SEB) who developed the PiP intervention. Subsequent telephone support from the lead researcher was offered to facilitators during the intervention period as and when they requested it.
The Preschoolers in the Playground manual
The PiP manual was developed as a resource for the facilitators. It included a background section explaining how the intervention had been developed, an explanation of the facilitators’ role and what was expected of them, an equipment list detailing the play equipment that would be required to deliver the intervention (all play equipment was standard school physical education equipment), information about the importance of physical activity in the early years, guidelines for physical activity in preschoolers and information about giving effective praise, encouragement and positive reinforcement. The manual also described the session timings and structure of the sessions. A guide on how to deliver the first session was also provided for support. The manual included a description of the ‘statue game’ used in sessions to gather the group together, a description of 20 structured play games called PiP-PoPs, five handouts to be photocopied for parents and instructions on facilitating 10 discussions (one per week) with parents about physical activity-related topics (more detail is given in Content of the Preschoolers in the Playground intervention and Appendix 2). At the back of the manual was a paperwork section that included a register of attendance and adverse event reporting forms. The manual was reviewed by five early years workers and minor revisions were made before the start of the intervention (e.g. changing the order of the contents in the manual). The manual was also modified during the delivery of the intervention following feedback from the facilitators delivering the intervention (e.g. language was clarified).
Structure of the Preschoolers in the Playground sessions
Each PiP session lasted for 30 minutes and included two 5-minute structured play activities (PiP-PoPs), 15 minutes of free play (during this time handouts were given out and guided discussions conducted) and 5 minutes for an active tidy-up. Play activities were designed to be of light physical activity (LPA) and MVPA. There is some evidence to suggest that as little as an extra 10 minutes per day of MVPA significantly reduces fat mass. 2 Furthermore, 56 minutes per day of MVPA in boys and 42 minutes in girls aged 5–8 years has been reported to improve metabolic status assessed from a composite score of various CVD risk factors. 61 Given the sporadic nature of physical activity in very young children, and that between 25% and 70% of total physical activity (TPA) in preschoolers has been classified as MVPA,23,62,63 it was estimated that during a 30-minute session the children would spend at least 10 minutes in MVPA and that this could contribute towards the amount of MVPA required for health benefits. Furthermore, it was thought that a 30-minute session would be more acceptable to both schools and families.
During the maintenance phase (20 weeks) playgrounds remained available to parents and their preschool children six times a week for 30 minutes at specific times to coincide with the ‘school run’, as allocated by the schools/children’s centres. For the purposes of the pilot trial, the PiP facilitator took a register of attendees at the beginning of the sessions but did not give formal supervision.
Content of the Preschoolers in the Playground intervention
The following sections provide a detailed description of the content of the PiP intervention. Table 1 summarises the content, evidence for the content and associated behaviour change techniques for both the initiation and the maintenance phases of the intervention.
| Content | Initiation (I) or maintenance (M) phase | Evidence to support content | Behaviour change technique |
|---|---|---|---|
| Provision of playground area at a time that coincides with families’ daily routine (dropping off at/picking up from school/nursery) | I, M | Social cognitive theory (environmental factors);34,35 focus group reports: activity sessions need to fit into other daily routines60 | Environmental changes |
| Provision of outdoor play equipment during sessions | I, M | Social cognitive theory (environmental factors)34,35 | Environmental changes |
| Facilitator to give telephone support and encourage families to attend the sessions | I, M | Social cognitive theory (behavioural factors)34,35 | Social processes of support/encouragement |
| Group sessions | I, M | Recommendation for preschool obesity interventions32 | Social processes of support/encouragement |
| Supervision at the session from the facilitator | I | Focus group reports: parents need extra support to feel confident and safe playing with their children outside60 | Social processes of support/encouragement |
| Facilitator to encourage children to be physically active and give rewards (praise and ‘well done’ stickers) | I | Social cognitive theory (behavioural factors);34,35 recommendation for preschool obesity interventions48 | Social processes of support/encouragement |
| Facilitator to support parents to give positive reinforcement to their child’s physical activity | I | Social cognitive theory (behavioural factors);34,35 parent involvement is important for children’s behaviour change49,52,53 | Modelling, social processes of support/encouragement, increasing skills, rehearsal of skills |
| Facilitator to encourage outdoor play between parent and child outside of the intervention | I | CMO report29 | Social processes of support/encouragement |
| Facilitator to provide information (verbally) and leaflets and facilitate parent discussions on the link between physical activity and health and provide guidelines for physical activity and sedentary behaviour in under 5s | I | Social cognitive theory (personal factors);34,35 recommendation for preschool obesity interventions32 | Provide information regarding behaviour, provide information on consequences, social processes of support/encouragement |
| Ideas for active games provided and these games and activities are fun for children | I (facilitator), M (instruction cards) | Social cognitive theory (personal factors);34,35 CMO report;13 recommendation for preschool obesity interventions48 | Increasing skills, skill rehearsal, modelling, graded tasks |
| Facilitator to teach two 5-minute structured parent and child games to develop children’s observational learning, locomotor, stability and object-control skills | I | Social cognitive theory (personal factors);34,35 CMO report29 | Increasing skills, skill rehearsal, modelling, graded tasks |
| Facilitator to modify play activities to suit the different needs of children in the group | I | CMO report29 | Graded tasks |
| Children have 20 minutes of free play | I | CMO report29 | Environmental changes |
| Facilitator to ensure regular infusions of different play equipment during free play | I | Recommendation for preschool playground interventions43 | Environmental changes |
| Play equipment given out once a week to support families to play at home | I (three schools only) | Social cognitive theory (environmental factors and behavioural factors);34,35 CMO report29 | Rewards/incentives, skill rehearsal |
Structured play activities
There were 20 different PiP-PoPs (structured play activities) and facilitators were asked to teach each PiP-PoP at least once during the 10-week period. The PiP-PoP activities were designed to promote active play (activities that involve movements of all of the major muscle groups) and the development of locomotor, stability and object-control skills (as recommended by the Start Active, Stay Active report29). Ideas on how to modify each PiP-PoP to make it easier or harder depending on each child’s ability were also given.
Free play
At the beginning of the free-play segment of sessions, facilitators were instructed to bring out two or three pieces of equipment and then bring out additional equipment later on in the segment to ensure a flow of different equipment. Facilitators were instructed to allow all of the children to decide what they would like to play with and then to support the parents to do this, encouraging all of the children to explore and use their imagination.
Guided discussions and handouts
The facilitators were asked to guide discussions with parents on physical activity-related topics each week during the initiation phase. For some of the discussions there were accompanying handouts for parents to take home. The discussion topics were:
-
what to wear for outdoor play (supplemented by a handout)
-
giving praise and encouragement (supplemented by a handout)
-
why physically active play is important (including physical activity guidelines for preschoolers; supplemented by a handout)
-
help your child move and play every day (supplemented by a British Heart Foundation leaflet)
-
active parents have active kids (supplemented by a handout)
-
outdoor spaces near me (supplemented by a handout)
-
playing as a family
-
couch potatoes
-
games I used to play
-
continuing to be active.
Active tidy-up
At the end of each initiation session families were encouraged to tidy up the playground in a playful and active way. For example, facilitators may have asked the group to collect all the balls up and jump back to put them in the carrier. It was anticipated that, by including an active tidy-up, when families began the maintenance phase with no facilitator this would continue and the school playground would be left tidy at the end of each PiP session.
Changes to the intervention
Before the PiP intervention commenced, a change was made to the duration of the intervention, from 36 weeks (12 weeks in the initiation phase and 24 weeks in the maintenance phase) to 30 weeks (10 weeks in the initiation phase and 20 weeks in the maintenance phase); blocks of 10 weeks were better suited to school term times. During the PiP intervention, changes were made to the content of the intervention. These included the addition of weekly, take-home play equipment during the initiation phase, with £15 spent per child. This action implemented the behaviour change techniques of providing rewards for participation and skill rehearsal. The take-home play equipment included items that would allow parents and children to recreate at home the PiP-PoPs that they had learned in the sessions. The kit included:
-
PiP kit bag
-
PiP-PoP game cards
-
hoop
-
skipping rope
-
beanbag
-
ball
-
bat
-
collector bag
-
chalk
-
water pot and brush.
A further change was the addition of telephone support provided by facilitators to parents who, for unknown reasons, had not attended three consecutive sessions (one week of the intervention). A change to the delivery of the intervention was also made: schools were given the option to reduce the number of sessions offered to four per week after the first 3 weeks of the intervention if two sessions were poorly attended.
Chapter 2 Methods
Study design
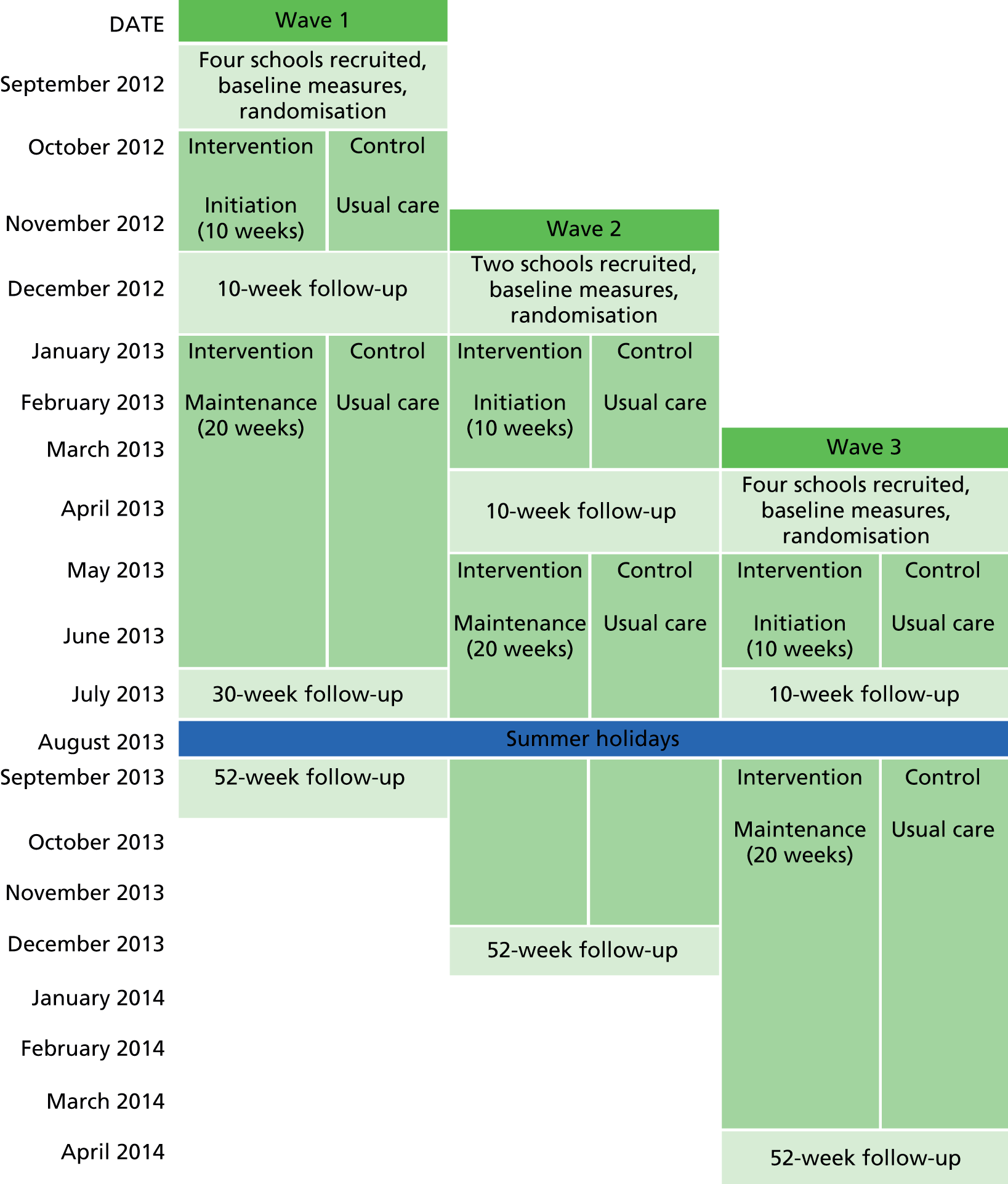
The design of this pilot study was based on guidance from the UK Medical Research Council for developing and evaluating complex interventions. 64 Figure 1 shows the trial design: a two-armed pilot cluster randomised controlled trial (RCT) with economic and qualitative evaluations. The two arms were the PiP intervention and usual practice (control). Recruitment, randomisation and the intervention or control period took place in three waves. Wave 1 commenced in the autumn 2012 school term, wave 2 commenced in the spring 2013 school term and wave 3 commenced in the summer 2013 school term. This staggered approach allowed the examination of seasonal variations in the feasibility of the intervention as well as mimicking one approach that could be taken in a full cluster RCT. The intervention consisted of a 10-week initiation phase (one school term) followed by a 20-week maintenance phase (two school terms). Further details of the intervention are provided in Chapter 1 (see Development and description of the Preschoolers in the Playground intervention). Follow-up was at 10 weeks (mid-intervention), 30 weeks (at the end of the intervention) and 52 weeks. For waves 2 and 3, the follow-ups at 30 weeks (immediately after the intervention) and 52 weeks (1 year after baseline assessment) fell at the same time because of the school holidays occurring during the middle of the intervention period (see Figure 1); this meant that 30-week data were collected from wave 1 children only. It was not possible for schools, participants and facilitators to be blind to allocation because of the nature of the intervention. It was planned that researchers would be blind to allocation; however, many of the parents informed staff of their child’s trial status. It was also planned that the statistician and health economist would be blind to allocation; however, because of sickness of the blinded statistician an unblinded statistician conducted the analysis. The health economist was blinded. Ethics approval for the study was secured from the National Research Ethics Service (NRES) Committee Yorkshire and the Humber – Bradford (reference 12/YH/0334) and complied with the Declaration of Helsinki. 65
FIGURE 1.
Study design: a pilot cluster RCT conducted in three waves.
Setting
The high levels of deprivation in Bradford and the multiethnic nature of Bradford’s population made it an ideal setting in which to trial this preschool physical activity intervention. Bradford is the sixth largest metropolitan borough in England with a population of approximately 500,000 and includes some of the most deprived areas in the UK. 66 The National Child Measurement Programme for 2010–11 reported that 22% of Bradford’s children in reception classes (similar to the national average) and 35% in year 6 (higher than the national average) were overweight or obese. 67 In addition, overall there are very low levels of participation in school sport in the city. 67 Half of all babies born in Bradford are of South Asian origin68 and 60% of these are born into the poorest 20% of the population of England and Wales, based on the IMD. 66
Sample size
It was anticipated that at least 150 children from 10 schools with 15 children at each school would be recruited. This would give five schools with a total of 75 children in the PiP intervention arm and five schools with a total of 75 children in the control arm.
Recruitment of schools and participants
School recruitment
The study was initially publicised to primary schools through advertising and presentations at education conferences and events hosted for Bradford primary school staff. Letters were also sent to eligible schools (those located in the two poorest quintiles of the IMD for Bradford) (see Appendix 1). Schools were asked to contact the researchers if they were interested in taking part in the study. Interested schools were then contacted and visited to discuss the study further. Schools that were located in different areas of the city of Bradford (Bradford South, Bradford West, Bradford East and Shipley) were selected to take part. Each study site completed a study site agreement, which was signed by the head teacher and chair of governors. To express thanks for participating in the pilot trial, all schools received a donation of £200 towards play equipment. Because the children were of preschool age and were not attending the primary schools, those affiliated to the schools in the control arm did not have access to the play equipment during the trial period.
Participant recruitment
Families from participating schools, and families who used children’s services affiliated with the schools (e.g. nearby children’s centres or nurseries), were approached to take part in the trial. Recruitment was carried out through letters home with school-going children and through face-to-face conversations with community research assistants in school playgrounds and children’s centres or nurseries. A participant information sheet (see Appendix 3) was given to participants before they attended a baseline measurement appointment. Written informed consent was obtained before any data were collected at the baseline measurement session. To account for the linguistic diversity among the study population, research staff recruiting families and conducting measurements and questionnaires were bilingual and undertook these tasks in either English or Urdu. 68 Urdu is the language spoken and understood by Pakistanis; it is also spoken and understood in many parts of Bangladesh. For Bangladeshi participants who did not fully understand Urdu, the consent form was audio recorded in Sylheti and participants were asked to sign a paper copy of the consent form (translations and transliterations were prepared in collaboration with Born in Bradford staff, according to standard Born in Bradford procedures68). All families received a £10 voucher for a children’s shop (Mothercare or the Early Learning Centre) as a thank-you for attending each study measurement session (baseline and 10, 30 and 52 weeks’ follow-up) and for participating in a qualitative interview.
Inclusion and exclusion criteria
Children were included if they were aged between 18 months and 4 years and were available to complete three school terms of the intervention before going into the reception class (first year of school). For wave 1, children were eligible if they were born between 1 September 2008 and 5 March 2011. For wave 2, children were eligible if they were born between 1 September 2009 and 7 July 2011. For wave 3, children were eligible if they were born between 1 September 2009 and 6 November 2011. Children were excluded if a parent or legal guardian was unable to provide informed consent.
Randomisation
Randomisation was conducted by the York Trials Unit Randomisation Service using a secure computer system after baseline data were collected. Schools were allocated on a 1 : 1 basis to the intervention arm or the control arm. The first four schools (wave 1) were randomised using block randomisation with a block size of four. The remaining schools (two in wave 2 and four in wave 3) were allocated using minimisation. Minimisation is a largely non-random method of treatment allocation in trials and is particularly useful when there are a small number of units to be randomised and balance is desired across a number of variables. Treatment allocations are determined by which would lead to a better balance between groups in the variables of interest.
In Bradford ethnic groups tend to cluster in localities and thus the predominant ethnicity of pupils attending the schools was used as a minimisation factor with two levels (< 50% South Asian pupils and > 50% white pupils). When schools were recruited into the study, an assumption was made that the ethnicity of participants recruited at each school would reflect the ethnic groups of pupils attending each school. IMD was not used as a minimisation factor because all of the schools were in the two poorest quintiles of the IMD for Bradford. Furthermore, Bradford is particularly skewed towards a high IMD and, thus, this was not felt necessary.
Aims and objectives
The aim of the study was to undertake a pilot cluster RCT of an outdoor playground-based physical activity intervention (PiP) to assess the feasibility of a full-scale cluster RCT of the PiP intervention. The specific objectives were to determine:
-
the feasibility and acceptability of the recruitment strategy for schools and families and whether or not there was a difference in recruitment rate between ethnic groups
-
follow-up and attrition rates during the trial and whether or not there was a difference between trial arms and ethnic groups
-
the acceptability of the trial procedures
-
the feasibility of collecting the outcome measures and whether or not there was a difference between trial arms and ethnic groups
-
the influence of financial incentives on trial participation
-
attendance to, and acceptability of, the intervention, whether or not there was a difference between ethnic groups and whether or not attendance varied by season
-
the fidelity of programme implementation
-
the capability and capacity of schools to deliver and incorporate the intervention within existing services
-
the effect of participation in the intervention on health outcomes and whether or not there were any differences between ethnic groups
-
estimates of effect size, typical cluster sizes and intraclass correlation coefficients (ICCs) to enable an accurate sample size calculation for a full trial
-
preliminary assessment of the potential cost-effectiveness of PiP and an estimate of the value of further research
-
whether or not links can be established between short-term outcomes and long-term quality of life, potentially including across sectors
-
whether or not it is appropriate to apply for further funding for a full-scale RCT.
Data collection and analysis
To answer each of the study’s objectives a multimethods approach was used to collect and analyse the data. The following three sections describe how the quantitative data, the health economics data and the qualitative data were collected. Methodology for each study objective describes how the data were analysed to answer each of the objectives. Throughout the report participants are grouped according to ethnicity. The predominant ethnicity of pupils attending the school is used to describe cluster-level ethnicity. At the participant level a child’s ethnicity (as reported by his or her parent) is used, except when data specifically relate to the parent [i.e. for the European Quality of Life-5 Dimensions (EQ-5D), Comprehensive Quality of Life Scale – Adult (ComQol-A5) and General Self-Efficacy Scale questionnaires]. White refers to participants who were white European (white British, white Irish, white Polish) and South Asian refers to participants who were of Pakistani, Bangladeshi or Indian heritage; the other group included participants who were of African, Burmese and dual heritage (white and Asian and Chinese and Indian).
Quantitative data
Trial recruitment, attrition and follow-up
Community research assistants logged all trial contacts with participants and the outcomes of these contacts on a central database system. Data relating to trial recruitment, attrition and follow-up were captured.
Health outcomes
Each parent and his or her participating child were invited to attend a measurement session in a private room at their school to collect health outcome data at baseline and at 10, 30 (for wave 1 participants only) and 52 weeks’ follow-up. When families were unable to attend the appointment at the school, a community research assistant visited their home to conduct the measurement session. Community research assistants used standardised paper and electronic forms to record data from participants. The measurement sessions were child friendly with toys and play equipment available to entertain the children and put them at ease.
Child’s physical activity
At the measurement session a triaxial Actigraph GT3X+ accelerometer (15-second epochs; Actigraph Pensacola, FL, USA) was placed on the child on a belt around his or her waist (anterior to the iliac crest). Parents were asked to place the accelerometer on their child in this position during waking hours for the subsequent 7 days including at least 1 weekend day. 69 Parents were provided with a diary to record the times that the accelerometer was put on and taken off their child. Further details about the processing and analysis of accelerometry data are provided in Objective 4: feasibility of collecting the outcome measures and whether or not there was a difference between trial arms and ethnic groups and Objective 9: the effect of participation in the intervention on health outcomes and whether or not there were any differences between ethnic groups, Physical activity.
Child’s height and weight and waist and upper arm circumferences
Body mass was measured in standard clothing conditions (lightweight clothing) using regularly calibrated Seca electronic scales (Medical Scales and Measuring Systems, Birmingham, UK). Height was measured using a Leicester Height Measure (Harlow Healthcare, Harlow, UK). Waist circumference was measured at the midpoint between the lowest rib and the iliac crest. Upper arm circumference was measured at the mid-point between the acromion process of the scapula and the olecranon process. Further details about the analysis of these data are presented in Objective 9: the effect of participation in the intervention on health outcomes and whether or not there were any differences between ethnic groups, Anthropometry.
Parent well-being and self-efficacy
Parents completed the ComQol-A570,71 to assess their well-being; they also completed the General Self-Efficacy Scale. 72 Details regarding how these data were analysed are provided in Objective 4: feasibility of collecting the outcome measures and whether or not there was a difference between trial arms and ethnic groups.
Intervention attendance, fidelity and environment
Intervention attendance
The PiP facilitators completed a standardised register for each PiP session (both initiation and maintenance phases) to record attendance. This included recording who attended the PiP session with the child. Withdrawals from the intervention (i.e. parents who gave notification that they no longer wanted to attend the intervention) were also recorded by either the PiP facilitator or the study co-ordinator. Facilitators were provided with adverse event reporting forms and were instructed to contact the study co-ordinator immediately if an adverse event occurred.
Intervention fidelity
Fidelity was assessed in line with guidance from the National Institutes for Health (NIH) Behavior Change Consortium. 73 To assess adherence to the intervention protocol an observer attended two sessions in the initiation phase at each intervention school; intervention delivery was scored on a scale from 1 to 4 (with 1 relating to poor adherence and 4 relating to complete adherence) in relation to five key intervention factors:
-
delivery as per manual, which consists of four subcomponents
-
supervision
-
support given to parents
-
encouragement of children
-
infusion of play equipment.
Some sessions were observed by two individuals, with each scoring independently. When this was the case, the average score for each component was used.
Playground and local environment
To assess whether or not the school and local environment impacted on the intervention, the study co-ordinator visited each school before it was allocated to either the intervention arm or the control arm and completed a standardised form detailing the playground and the local environment.
Health economics data
Child and parent health-related quality of life
At each of the measurement sessions parents completed the EQ-5D instrument74 to report on their own health-related quality of life (HRQoL); they also completed the Pediatric Quality of Life Inventory (PedsQL)75 regarding their child’s HRQoL. The PedsQL items were slightly different for infants (aged 13–24 months) and toddlers (aged 2–4 years). Further details regarding the analysis of the two instruments are provided in Objective 11: preliminary assessment of the potential cost-effectiveness of Preschoolers in the Playground and an estimate of the value of further research, Health-related quality of life outcomes.
Injuries and health service use
Parents were asked to recall their child’s use of hospital services [overnight stay, day hospital attendance, outpatient visit, accident and emergency (A&E) department attendance, day-case surgery] and contact with health professionals within the last 3 months. This was recorded on a standardised form (see Appendix 5). Further details about the analysis of these data are given in Objective 11: preliminary assessment of the potential cost-effectiveness of Preschoolers in the Playground and an estimate of the value of further research, Resource use and unit costs.
Qualitative data
Interviews were carried out with parents in both the intervention arm and the control arm and with PiP facilitators and head teachers in the intervention arm. The methods used to carry out the interviews are described here. How the data collected were used to meet each study objective is described in Methodology for each study objective.
All of the interviews used a semistructured topic guide (see Appendix 6) to ensure consistency. The questions were as open-ended as possible to enable participants to raise issues that were important to them. The wording and order of the topics covered also varied between interviews to ensure that each interview was informal and open-ended to suit individual participants. 76 Interviews were audio recorded digitally with the exception of the wave 1 interviews with parents (see the following section).
Parent interviews
The aim was to interview approximately 16–20 parents/carers (up to 15 parents/carers from the intervention arm and up to five from the control arm) at the 10-week follow-up time point. A maximum variation sampling strategy77 was employed to achieve diversity on three key characteristics for which views about the PiP study might be expected to differ. First, the wider PiP study was interested in understanding potential differences in feasibility between South Asian and white families; we therefore sought to include a mix of South Asian and white parents/carers in this qualitative component. Second, of parents/carers allocated to the intervention arm, we aimed to interview parents who had continued to attend the PiP intervention as well as those who had never attended or who had dropped out. Third, we intended to interview a mix of mothers, fathers, grandparents and carers. We found that it was only parents who were attending measurement and PiP sessions with their children and, thus, for the remainder of this report we refer only to parents.
Parents were asked to consent to take part in an interview when they were recruited to the PiP trial. From those who consented, the study co-ordinator purposively selected parents to be interviewed on the basis of their ethnicity, (non-) attendance at the PiP intervention (intervention arm only) and parental role. Parents were then recruited in one of two ways: either a community research assistant asked parents if they would be willing to be interviewed when booking the 10-week measurement session or the study co-ordinator telephoned the parents and requested them to take part in an interview. By this time both of these individuals were known to the parents and could vouch for the trustworthiness of the interviewer, hence facilitating recruitment. 78 Parents received a £10 gift voucher for Mothercare or the Early Learning Centre on completion of the interview.
Parents were interviewed after completing their 10-week measurement session. Interviews lasted between 6 and 19 minutes and were conducted in English. The wave 1 interviews were undertaken over the telephone in the week following the 10-week measurement session. This was because of very bad weather (snow) and the school Christmas holidays commencing immediately after the end of the 10-week initiation phase of the intervention. Because of a technical fault with the digital recorder these interviews were not recorded; instead, the interviewer took detailed notes whilst conducting the interview. The wave 2 and wave 3 interviews were conducted face to face immediately after the measurement session had been completed (either in the parent’s home or at the school).
Facilitator and head teacher interviews
In each of the five intervention schools we intended to interview the PiP facilitators with responsibility for delivering the intervention at the 10-week follow-up time point and the head teachers at the 52-week follow-up time point. The study co-ordinator contacted each PiP facilitator and head teacher by telephone/e-mail to arrange their participation in this qualitative component. This included providing a participant information sheet (see Appendix 7) and the consent form (see Appendix 8) and subsequently arranging a date/time for the interview.
The PiP facilitators were interviewed face to face in school. The exception was one PiP facilitator in a wave 1 school who was interviewed over the telephone (as with the wave 1 parents this was because of bad weather and the Christmas break). PiP facilitator interviews lasted between 13 and 31 minutes. Head teachers were interviewed on the telephone and these interviews lasted between 12 and 16 minutes.
Thematic analysis of the interviews
The audio recordings were transcribed verbatim with anonymisation of all personal data. The detailed notes taken for the wave 1 parent interviews were used as data. These interview data were then analysed using thematic analysis, which is a method of ‘identifying, analysing and reporting patterns (themes) within the data’ (p. 79). 79 This a useful approach for producing qualitative analyses suited to informing policy and programme development. 79 The six phases of thematic analysis were as follows.
-
Familiarisation. The researcher became immersed in the raw data by ‘repeated reading’ of the transcripts and listed key ideas for coding.
-
Generating initial codes. Initial codes and a coding framework were developed, informed predominantly by the objectives of this qualitative component (a deductive approach), although novel views expressed by participants were also captured (an inductive approach). 4 The interview data were then coded to this framework using the ATLAS.ti data management software package (version 6.2; ATLAS.ti Scientific Software Development, Corvallis, OR, USA). Data from the three participant groups (parents, PiP facilitators and head teachers) were coded to the same framework with additional codes created for each particular group when necessary.
-
Searching for themes. The codes were then organised into potential themes and subthemes. At this point similarities and differences in views ‘within’ and ‘across’ the three participant groups were explored.
-
Reviewing themes. The coded data within each potential theme were reviewed and the themes modified to ensure that they formed a coherent pattern. Each theme was then reviewed to see if it ‘worked’ in relation to the entire data set.
-
Defining and naming themes. A short paragraph was produced for each theme and subthemes to define the ‘essence’ of the theme/subthemes and names were allocated.
-
Producing the report. The thematic analysis was written up.
Methodology for each study objective
Objective 1: feasibility and acceptability of the recruitment strategy for schools and families and whether or not there was a difference in the recruitment rate between ethnic groups
The numbers (and percentages) of schools approached, recruited and randomly assigned were summarised, as were the number of children who were approached, the number screened, the number of parents who consented to further contact and the number taking part. The reasons for parents declining to be contacted further about the study were tabulated. The flow of schools and children through the study was presented in a Consolidated Standards of Reporting Trials (CONSORT) flow diagram. Consent status was also summarised by parents’ ethnicity. Characteristics of the schools (location, presence of children’s centre on site, number of pupils on roll, percentage free school meals (FSMs), percentage white, percentage South Asian and percentage with English as an additional language) were summarised alongside allocated trial arm. The characteristics of participating children and parents were summarised by trial arm both overall and as analysed. As analysed were those individuals who were included in the primary analysis who had baseline and week 52 MVPA data that both met the wear time criterion (see Objective 4: feasibility of collecting the outcome measures and whether or not the was a difference between trial arms and ethnic groups).
The characteristics of the parents, PiP facilitators and head teachers who were interviewed for the qualitative component were tabulated. Parent and head teacher reasons for taking part in the study were explored, as were parents’ views on recruitment and the information that they were given about the study.
Objective 2: follow-up and attrition rates during the trial (in particular, whether or not there was a difference between trial arms and ethnic groups)
A CONSORT diagram was produced to display the follow-up and attrition rates during the trial.
The numbers (and proportions) of children providing accelerometer data, questionnaire data (including anthropometry data) and both were summarised over time for the whole trial, by trial arm and by ethnicity. The numbers of children withdrawing from the trial were summarised alongside the reasons for withdrawal and ethnicity. The numbers of communications required for follow-up visits were also summarised.
Objective 3: acceptability of the trial procedures
Qualitative analysis of the interviews explored parents’ understanding of the trial procedure, including randomisation. The acceptability of randomisation, the accelerometer and the measurement sessions was also examined.
Objective 4: feasibility of collecting the outcome measures and whether or not there was a difference between trial arms and ethnic groups
Physical activity data were downloaded from accelerometers and reduced using Actilife software version 5 (Actigraph Pensacola, FL, USA). Non-wear time was defined as consecutive zero counts of ≥ 10 minutes. 80 Parent-completed wear-time logs were checked for periods when the monitor was not worn and matched against Actigraph data. To determine the minimum wear time (i.e. daily wear hours and number of wear days) required to achieve a reliable estimate of habitual physical activity, that is, an ICC value of ≥ 0.8, the Spearman–Brown prophecy formula was applied to participants’ baseline accelerometer data. 81 This resulted in a wear-time criterion of at least 6 hours of wear time on any 3 days for data to be included in the analysis (see Appendix 9 for a table of these results). The number and proportion of data meeting the wear-time criterion were assessed overall, by trial arm, by ethnicity and over time.
Completion rates for anthropometric measurements (height, weight, BMI and waist and upper arm circumferences) and for questionnaires [children: infant (13–24 months) and toddler (2–4 years) PedsQL; parents: EQ-5D, ComQol-A5 and General Self-Efficacy Scale] were assessed. These summaries were presented overall, by trial arm, by ethnicity and over time.
Objective 5: influence of financial incentives on trial participation
Parent and head teacher views on the influence of financial incentives on trial participants were explored through qualitative analysis.
Objective 6: attendance to, and acceptability of, the intervention, whether or not there was a difference between ethnic groups and whether or not attendance varied by season
The number of schools and number of children providing attendance data to the PiP intervention sessions were summarised by initiation and maintenance phase and overall. For those children attending at least one session, the average number of sessions attended was summarised [mean, standard deviation (SD), median, minimum and maximum values]. The data were provided overall, by school (and wave/season) and by ethnicity.
Quantitative data were used to examine parents’ and PiP facilitators’ views on the acceptability of the PiP intervention, parents’, PiP facilitators’ and head teachers’ views on reasons why participants did not attend and parents’ and facilitators’ acceptability of the maintenance sessions. These data are presented alongside the qualitative data.
Objective 7: fidelity of programme implementation
Summary statistics were produced for the fidelity scores relating to each of the five key intervention factors: delivery as per manual, supervision, support given to parents, encouragement of children and infusion of play equipment. The delivery as per manual factor has four components; summary statistics were presented for each component separately and for the combined total score.
Objective 8: capability and capacity of schools to deliver and incorporate the intervention within existing services
Summary statistics were presented for the playground and local environment factors by trial arm and overall. Head teacher views on capability and capacity and benefits to the schools and suggestions for improving the PiP intervention were all explored through analysis of the qualitative interviews. PiP facilitators’ experiences of delivering the intervention, the training that they received and their views on the PiP manual were also examined and are summarised.
Objective 9: The effect of participation in the intervention on health outcomes and whether or not there were any differences between ethnic groups
Health outcome data were processed as detailed in the following sections.
Physical activity
After the application of the wear-time criterion (see Objective 4: feasibility of collecting the outcome measures and whether or not there was a difference between trial arms and ethnic groups), vaild accelerometer data were analysed and time spent in different physical activity intensity levels was calculated from the vertical axis activity counts using the thresholds shown in Table 2. These cut-points, which were derived by Pate et al. 82 for children aged 3–5 years, were selected as they have been cross-validated under free-living conditions and have been found to have better agreement with directly observed physical activity than other published Actigraph intensity cut-points in children aged 16–35 months. 83 The percentages of children meeting the physical activity guideline of 180 minutes per day (TPA) were also calculated.
| Physical activity level | Counts per 15-second epoch | Equivalent counts per minute |
|---|---|---|
| TPA | ≥ 38 | ≥ 149 |
| Light | 38–419 | 149–1679 |
| Moderate to vigorous | ≥ 420 | ≥ 1680 |
| Sedentary | ≤ 37 | ≤ 148 |
Anthropometry
Body mass and height were measured and used to calculate BMI. These were then converted to age- and sex-adjusted z-values relative to the World Health Organization (WHO) 2006 growth standard84 using the least mean squares method. The percentage of overweight children in each arm, defined as having a BMI z-value of > +1.04 (= 85th centile), was recorded. Waist and upper arm circumference were also measured.
Parent well-being and self-efficacy
Parent well-being was measured using the ComQol-A5. The questionnaire asked both subjective and objective questions relating to seven domains (material well-being, health, productivity, intimacy, safety, place in community and emotional well-being). A mistake was made when administering the questionnaire and one page relating to the subjective domains was not included. Thus, only the objective data were analysed. The objective score on each domain was the aggregate of the three objective questions on each domain. The General Self-Efficacy Scale consisted of 10 items, each with four levels. The final composite score was obtained by summing the response levels on all dimensions (lower values indicating better self-efficacy).
Health outcome analysis
Appropriate summary statistics were calculated in Stata version 12 (StataCorp LP, College Station, TX, USA) following the intention-to-treat principle for each of physical activity, anthropometry, parent well-being and self-efficacy. Data were summarised for each time point overall, by trial arm and by ethnicity. A graph of the changes in MVPA over time by group and ethnicity was presented. When statistical testing was undertaken, statistical significance was assessed at the 5% level and 95% confidence intervals (CIs) were calculated where appropriate.
Objective 10: estimates of effect size, typical cluster sizes and intraclass correlation coefficients to enable an accurate sample size calculation for a full trial
The main aim of this study was to establish practicality, feasibility, recruitment rates and the sample size to inform a full-scale trial and, although it is unlikely that the small sample size would result in effectiveness being established, the primary outcome for a full trial, daily MVPA, was analysed to mimic practice in a full-scale trial. Results from this analysis must be treated as preliminary and interpreted with caution. 85,86 As the number of clusters is low, cluster summary statistics were utilised rather than multilevel modelling. 87,88 The analysis was carried out using school as the unit of analysis and the mean MVPA per day for the individuals in the school as the outcome variable. A weighted linear regression model was used to compare the PiP intervention arm and the control arm weighted by the number of participants followed up in each cluster and adjusted for the baseline average MVPA per day for each cluster. A sample size calculation was undertaken using the relevant information from the pilot study.
Objective 11: preliminary assessment of the potential cost-effectiveness of Preschoolers in the Playground and an estimate of the value of further research
Preliminary assessment of the potential cost-effectiveness
To make a preliminary assessment of the likely cost-effectiveness of the PiP intervention compared with usual practice in the context of the pilot trial, a cost-effectiveness analysis was conducted. When subgroup analysis was carried out, the whole group was analysed first and then the same analysis was repeated for both white and South Asian groups separately. The perspective was the NHS and Personal Social Services and 2012–13 costs were used. Costs and outcomes [as measured by quality-adjusted life-years (QALYs) and the PedsQL questionnaire] are not discounted as the time horizon was 1 year only, that is, the period that the study covered.
The outcome used to capture parents’ HRQoL was QALYs. QALYs are the product of the health state of each individual and the time spent in that state. The health state of each parent was evaluated using the EQ-5D instrument. The EQ-5D is a validated generic health-related preference-based measure consisting of five items that cover mobility, self-care, usual activities, pain and anxiety and depression, each with three levels of severity. This generates 245 possible health states, including ‘death’ and ‘unconsciousness’. The EQ-5D scores collected at baseline and 10 and 52 weeks were transformed into HRQoL weights using the UK general population tariff, which assigns societal values to each health state. 89,90 Subsequently, QALYs accumulated over the 52 weeks of the trial period were derived for each individual applying the area under the curve (AUC) method. 91 In this approach, the HRQoL weights are multiplied by the respective length of time to produce the QALYs using the following equation:
where Q denotes the weight derived from the EQ-5D score at the time point t.
The HRQoL of children was assessed using the PedsQL questionnaire, which consists of four multidimensional scales, that is, physical functioning, emotional functioning, social functioning and school functioning, with a total of 23 items. Each item is assigned a value from 0 to 100 and a summary score is produced by summing all of the items over the number of items answered across all of the scales. Three summary scores can be estimated: total scale score (23 items), physical health summary score (eight items) and psychosocial health summary score (15 items). A higher score indicates a better health state. 92 For the purpose of this study the total scale score was used.
Parents recalled their child’s use of NHS services. All unit costs of the resources used were taken from the NHS reference cost database93 and the Personal Social Services Research Unit (PSSRU),94,95 adjusted to 2012–13 prices when necessary (Table 3).
| Description | Mean cost (£) | Unit | Source |
|---|---|---|---|
| Hospital services | |||
| Overnight stay (short) | 735.59 | Per person per day | Weighted average of the costs of a non-elective inpatient (short stay) and an elective inpatient stay across paediatric services93 |
| Overnight stay (long) | 933.35 | Per person per day | Weighted average of the costs of a non-elective inpatient (long stay) and an elective inpatient stay across paediatric services93 |
| Day hospital attendancea | 799.61 | Per attendance | Weighted average of the cost of day cases93 |
| Outpatient appointment | 184 | Per attendance | Weighted average of the cost of outpatient attendances across paediatric services93 |
| A&E | 115 | Per attendance | A&E services93 |
| Day-case surgery | 1099 | Per attendance | Weighted average of the cost of paediatric surgery across all paediatric surgery services93 |
| Dentist | 38.15 | Per hour | Review Body on Doctors’ and Dentists’ Remuneration 201496 |
| Dermatologist | 140 | Per attendance | Paediatric dermatology93 |
| ENT | 95 | Per attendance | Paediatric ENT93 |
| Consultant for learning disabilities | 101 | Per hour | Consultant: psychiatric, PSSRU 201395 |
| Non-hospital services | |||
| General practitioner | 45 | Per patient contact lasting 11.7 minutes | PSSRU 201395 |
| General practitioner home visit | 114 | Per 23.4-minute consultation including travel | PSSRU 201395 |
| Practice nurse | 13.43 | Per 15.5-minute consultation | PSSRU 201395 |
| Practice nurse home visit | 21.53 | Per visit | PSSRU 201094b |
| Occupational therapist home visit | 47.36 | Per visit | PSSRU 201094b |
| Speech and language therapist | 45.21 | Per hour of client contact | PSSRU 201094b |
| Speech and language therapist home visit | 47.36 | Per visit | PSSRU 201094b |
| Physiotherapist | 45.21 | Per hour | PSSRU 201094b |
| Clinical/child psychologist | 134 | Per hour | PSSRU 201395 |
| Children’s social worker | 218 | Per hour | PSSRU 201395 |
| Health visitor | 59 | Per hour of patient-related work | Cost per hour of patient-related work, PSSRU 201395 |
| Special help teacher | 47.36 | Per visit | Speech and language therapist home visit, PSSRU 201094b |
| Family support worker | 49 | Per hour of client-related work | PSSRU 201395 |
| NHS Direct | 25.53 | Per call | |
Costing for overnight hospital stays was differentiated between participants who spent only 1 night in hospital and those who stayed for > 1 night, based on the distinction reported in the NHS reference costs database. 93 Those who were admitted for only 1 night were assigned a ‘short overnight stay’ cost, which was calculated as a weighted average of the cost of an elective inpatient stay and the cost of a short non-elective inpatient stay across paediatric services. Those who remained in hospital for > 1 night were attached a ‘long overnight stay’ cost, that is, a weighted average of the cost of an elective inpatient stay and the cost of a long non-elective inpatient stay across paediatric services (see Table 3). The cost per day of an inpatient stay was also varied substantially in the sensitivity analysis (see Chapter 3).
In addition, a detailed costing of the PiP intervention was performed (Table 4). The cost of the intervention consisted of two components: the salary of the PiP facilitator (based on the salary of a parental involvement worker) and the cost of training. A pro-rata annual salary of £18,144, increased by 25% to account for on-costs, was assumed for PiP facilitators, which resulted in a £14.69 hourly wage assuming that they worked for 30 hours per week over a period of 39 weeks and 10 days. 97 In total, 11 PiP facilitators were recruited in the trial, of whom five delivered six 30-minute PiP sessions per week for a period of 10 weeks. In future, the training of PiP facilitators would most likely be performed by experienced sports development officers and, therefore, would be costed using a £30,000 annual salary (37.5 hours per week for 42.7 working weeks per year),98 assuming £10,000 additional on-costs to account for national insurance and pension charges. The training involved a one-off session of 2.5 hours provided to each school. Furthermore, a total of three additional support visits to intervention schools were needed and telephone support was provided throughout the trial period. Forty 5-minute calls were included in the cost of training, that is, two calls per school in the initiation phase and two calls per school in the maintenance phase (Table 5). Alternative assumptions about the cost of the intervention were employed in the sensitivity analysis.
| Description | Mean cost (£) | Source |
|---|---|---|
| PiP facilitator | 14.69a | Prospects Online97 |
| PiP facilitator training | 24.98a | Prospects98 |
| Description | n | Use |
|---|---|---|
| PiP facilitator training | 5 | 2.5 hours |
| Telephone support to PiP facilitator | 40a | 5 minutes |
| Support visit to intervention school | 3 | 40 minutes |
| PiP facilitator | 5 | 60 × 30-minute PiP sessions |
Missing data arose when participants did not fully complete the follow-up questionnaires or missed one or more follow-up interviews. In the base-case analysis, missing data were imputed by multiple imputation (MI) using predictive mean matching. Complete-case analysis (excluding participants with missing data) was carried out as a sensitivity analysis.
The MI model included all variables related to costs, EQ-5D scores and PedsQL scores at the three data collection points. The total costs incurred by each individual at baseline, 10 weeks and 52 weeks were inserted in the model after being aggregated on two levels: total primary care costs and total secondary care costs.
The questionnaire at 52 weeks’ follow-up collected data on resource use during the previous 3 months (i.e. 13 weeks) to reduce the risk of recall bias and hence no resource use data were collected between weeks 11 and 39. Therefore, in all analyses and for all participants, costs were imputed during this period based on mean weekly health-care expenditure for that participant during the other two follow-up periods, that is, during weeks 0–10 and 40–52 (excluding the cost of intervention). These imputations were incorporated into the system of MI to reflect uncertainty.
Parents were asked whether or not their child had used any other health services in addition to those stated in the questionnaire. Parents who did not answer this question but who had provided data for the other resource items in the questionnaire were assumed to have made zero use of additional health services. For participants who had missing data for all resource items included in the questionnaire, the use of additional resources was treated as missing as well.
Cost-effectiveness analysis
A seemingly unrelated regression (SUR) model was used to estimate the mean difference in costs and mean difference in QALYs per participant over 52 weeks for the PiP intervention relative to usual practice. The SUR model consisted of two regression equations. In the first equation, the number of QALYs was the dependent variable and intervention group and baseline EQ-5D score were the covariates. The baseline EQ-5D index was included in this equation to adjust the estimation of QALYs for differences in baseline HRQoL across individuals. In the second equation, the total cost over the entire trial period was the dependent variable and intervention was the covariate. This model was preferred over ordinary least squares regression as it accounts for the potential correlation of the error terms across the equations. 99 The outcomes of the regression analysis were used to calculate the incremental cost-effectiveness ratio (ICER). The ICER formally compares the incremental costs and effects associated with intervention(s). Conventionally, NHS treatments in England are considered to be cost-effective by the National Institute for Health and Care Excellence if the ICER is < £20,000 per QALY gained. 99 For interventions that are associated with an ICER between £20,000 and £30,000 per QALY gained, there needs to be evidence that the intervention is innovative and/or that HRQoL is not captured adequately and/or that there is considerable uncertainty around the ICER. As the ICER goes above £30,000 per QALY gained, this evidence needs to be stronger. 99 Assuming that the health benefits followed a normal distribution, a cost-effectiveness acceptability curve was also produced to graphically represent the probability that the PiP intervention is cost-effective for a range of threshold values of a QALY.
Objective 12: whether or not links can be established between short-term outcomes and long-term quality of life, potentially including across sectors
A computerised search of online electronic databases was carried out to identify studies that examined the relationship between physical activity or obesity indices (such as BMI and waist and upper arm circumference) and health outcomes in later stages of life. As the focus of this review was the link with longer-term outcomes, emphasis was put on identifying literature related to health outcomes in adults, but studies with reported associations in children or adolescents were not excluded. Two searches were conducted in a range of databases, including MEDLINE and the Education Resources Information Center (ERIC): (1) Pre-schoolers AND Physical Activity AND (Long Term Outcomes OR Cohort/Longitudinal Studies) and (2) Pre-schoolers AND (Physical Activity OR Obesity) AND (Risk Factors OR Predictors OR CVD OR Diabetes OR Cancer) AND Adults. The results were then sifted for potentially relevant studies by the information specialist who conducted the searches. Relevant studies were identified and scanned and information was extracted regarding study characteristics (year, study design, country, population), type of outcome measured (physical activity, adiposity/obesity) and associated health conditions.
Changes to the protocol
A summary of changes to the intervention and trial is presented in Table 6. At the outset of the study we intended to recruit eight schools and 120 participants. However, early results showed lower than expected attendance to the intervention in the winter months and therefore a decision was made to recruit two additional schools and approximately 30 more participants to better test the feasibility of the intervention starting in the summer term. This new target of 10 schools and 150 participants was presented in our published protocol in Trials. 100 In an oversight in the Trials-published protocol, the objective to examine the differences in recruitment, follow-up, attrition and the effect of the intervention between white and South Asian participants was not included. This was included in the original proposal and subsequent updated protocols submitted to the Public Health Research programme board.
| Original protocol | Amended protocol |
|---|---|
| Intervention | |
| Duration 36 weeks | Duration 30 weeks |
| Addition of take-home play equipment, one piece each week | |
| Additional support given to parents to attend via a telephone call from the facilitator | |
| Six sessions provided per week | Schools could reduce the number of sessions provided to four if two sessions were poorly attended |
| Trial | |
| Recruitment target of eight schools and 120 children | Recruitment target of 10 schools and 150 children |
Chapter 3 Results
For each of the study’s objectives the relevant quantitative, qualitative and health economic results are reported. Objective 13, whether or not it is appropriate to apply for further funding for a full-scale RCT, is addressed in the discussion section.
Objective 1: feasibility and acceptability of the recruitment strategy for schools and families and whether or not there was a difference in the recruitment rate between ethnic groups
Recruitment of schools
In total, 27 schools were approached to take part in the study, 13 with predominantly South Asian pupils and 14 with predominantly white pupils. Of these, 15 (56%) expressed an interest in taking part (11 with predominantly South Asian pupils and four with predominantly white pupils). Nine did not respond to the invitation to take part and three declined. The reasons for declining were no space in the playground during school time (n = 1) and changes in school management (n = 2). Ten schools were recruited to the study (six with predominantly South Asian pupils and four with predominantly white pupils); this equates to 37% of those who were approached to take part. Table 7 shows the characteristics of the recruited schools. The smallest school had one class per year group and the largest had three classes per year group. All schools had a high proportion of children receiving FSMs. The schools with a high proportion of South Asian pupils also had very high numbers of children who spoke English as an additional language.
| School | Trial arm | Wave | Location | Children’s centre on site | Number of classes per year group | Eligible for FSMs any time during the last 6 years (all pupils), % | Reception class pupils South Asian,a % | Reception class pupils white,a % | English not first language (all pupils), % |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Intervention | 1 | Bradford South | No | 2 | > 50 | 33 | 65 | 10–20 |
| 2 | Intervention | 1 | Bradford West | No | 3 | 30–50 | 96 | 1 | 90–100 |
| 3 | Intervention | 2 | Bradford East | Yes | 1 | > 50 | 57 | 37 | 40–50 |
| 4 | Intervention | 3 | Bradford West | No | 2 | > 50 | Predominantly white | 20–30 | |
| 5 | Intervention | 3 | Bradford East | No | 2 | 30–50 | 80 | 12 | 70–80 |
| 6 | Control | 1 | Bradford East | No | 2 | 30–50 | 97 | 2 | 90–100 |
| 7 | Control | 1 | Bradford East | No | 2 | 30–50 | 90 | 5 | 80–90 |
| 8 | Control | 2 | Bradford North | No | 2 | > 50 | 23 | 73 | 10–20 |
| 9 | Control | 3 | Bradford East | No | 3 | 30–50 | 83 | 1 | 70–80 |
| 10 | Control | 3 | Bradford West | Yes | 2 | > 50 | Predominantly white | 30–40 |
Recruitment of participants
In total, 341 children were screened for inclusion in the study and the parents of 305 (89%) of these children agreed to be contacted further about the study. The reasons for parents declining to be contacted further about the study are summarised in Table 8. The main reason for declining was that parents were too busy.
| Reason | n (%) |
|---|---|
| Too busy | 15 (41.7) |
| Not interested | 6 (16.7) |
| No reason given | 4 (11.1) |
| School too far away from home | 4 (11.1) |
| Relative unwell | 2 (5.6) |
| Child attending nursery | 1 (2.8) |
| Critical asthma/epilepsy | 1 (2.8) |
| Other | 3 (8.3) |
| Total | 36 (100) |
The CONSORT diagram in Figure 2 illustrates the flow of participants through the study. Of the 305 parents who agreed to be contacted about the study, 164 (54%) consented to take part in the study. The ethnicity of the recruited parents by consent status is summarised in Table 9.
FIGURE 2.
Cluster CONSORT flow diagram.
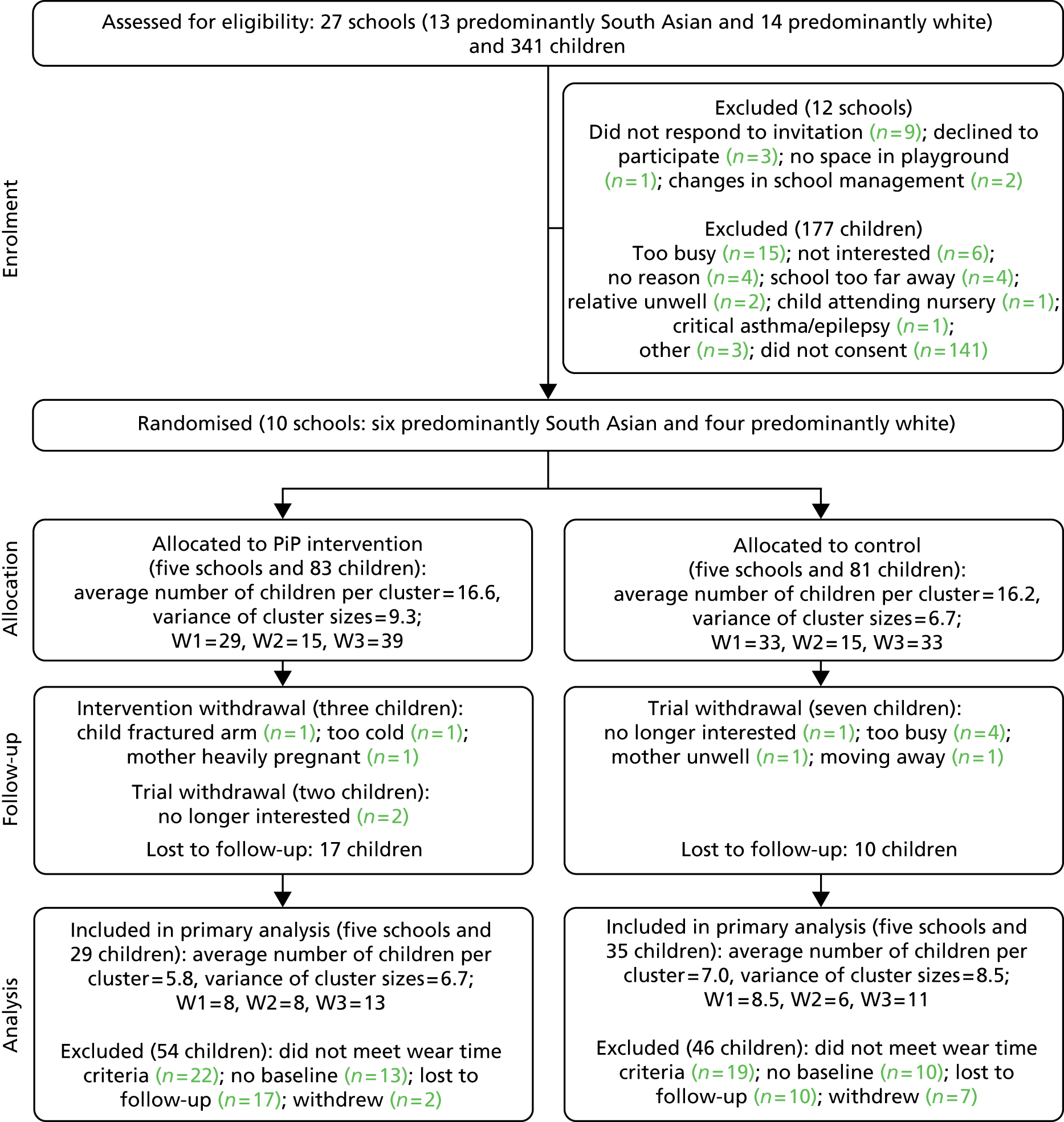
| Ethnicity | Consent, n (%) | Total, N (%) | |
|---|---|---|---|
| Yes | No | ||
| White | 62 (66.0) | 32 (34.0) | 94 (30.8) |
| South Asian | 77 (52.4) | 70 (47.6) | 147 (48.2) |
| Other | 3 (17.6) | 14 (82.4) | 17 (5.6) |
| Missing | 22 (46.8) | 25 (53.2) | 47 (15.4) |
Table 9 shows that, of those who agreed to be contacted further about the study, a higher proportion of the white parents (66%) than the South Asian (52%) or other (18%) parents then consented to take part. In total, 47 (15%) parents did not state their ethnicity and 22 (47%) of these consented to take part in the study.
Randomisation and participant characteristics
Five schools and 83 children were randomised to receive the PiP intervention and five schools and 81 children were randomised to the control arm. The characteristics of the participating children and parents are shown in Table 10. The mean age of the children in the study was 2.8 (SD 0.7) years and the mean age of parents attending the baseline measurement session was 30.6 (SD 5.6) years. There was an equal proportion of female and male children (53% and 48%, respectively) in the study and there were more South Asian (57%) than white (37%) or other (6%) children. A similar pattern of ethnicity was seen for the parents at baseline (South Asian 54%, white 44% and other 2%).
| Characteristic | As randomised | As analysed | ||||
|---|---|---|---|---|---|---|
| Intervention (n = 83) | Control (n = 81) | Total (n = 164) | Intervention (n = 29) | Control (n = 35) | Total (n = 64) | |
| Age (years), mean (SD) | ||||||
| Child | 2.7 (0.7) | 2.9 (0.7) | 2.8 (0.7) | 2.8 (0.7) | 2.8 (0.8) | 2.8 (0.8) |
| Parent | 29.4 (5.3) | 31.7 (5.6) | 30.6 (5.6) | 30.9 (5.9) | 33.2 (5.4) | 32.2 (5.7) |
| Gender, n (%) | ||||||
| Child | ||||||
| Female | 43 (52.4) | 42 (52.5) | 85 (52.5) | 14 (50.0) | 17 (50.0) | 31 (50.0) |
| Male | 39 (47.6) | 38 (47.5) | 77 (47.5) | 14 (50.0) | 17 (50.0) | 31 (50.0) |
| Parent | ||||||
| Mother | 80 (96.4) | 77 (95.1) | 157 (95.7) | 28 (96.6) | 32 (91.4) | 60 (93.8) |
| Father | 3 (3.6) | 4 (4.9) | 7 (4.3) | 1 (3.5) | 3 (8.6) | 4 (6.3) |
| Ethnicity, n (%) | ||||||
| Child | ||||||
| White | 35 (42.7) | 25 (30.9) | 60 (36.8) | 9 (31.3) | 9 (25.7) | 18 (28.1) |
| South Asian | 43 (52.4) | 50 (61.7) | 93 (57.1) | 19 (65.5) | 25 (71.4) | 44 (68.8) |
| Other | 4 (4.9) | 6 (7.4) | 10 (6.1) | 1 (3.5) | 1 (2.9) | 2 (3.1) |
| Parent | ||||||
| White | 34 (44.2) | 28 (43.1) | 62 (43.7) | 9 (33.3) | 9 (33.3) | 18 (33.3) |
| South Asian | 41 (53.3) | 36 (55.4) | 77 (54.2) | 17 (63.0) | 18 (66.7) | 35 (64.8) |
| Other | 2 (2.6) | 1 (1.5) | 3 (2.1) | 1 (3.7) | 0 (0.0) | 1 (1.9) |
Randomisation achieved balance across age, gender and parental ethnicity and attrition did not impact on the balance achieved at baseline, as seen in the ‘as-analysed’ sample (those included in the primary analysis). There was a slight imbalance in children’s ethnicity, with a higher percentage of white children in the intervention group. Table 11 summarises gender by ethnicity of the children in the study. In total, 45% of the white children were female, 57% of the South Asian children were female and 60% of the other children were female.
| Gender | White, n (%) | South Asian, n (%) | Other, n (%) | Total, N (%) |
|---|---|---|---|---|
| Female | 27 (45.0) | 52 (57.1) | 6 (60.0) | 85 (52.8) |
| Male | 33 (55.0) | 39 (42.9) | 4 (40.0) | 76 (47.2) |
| Total | 60 (100.0) | 91 (100.0) | 10 (100.0) | 161 (100.0) |
Recruitment and characteristics of those who participated in the qualitative component of the study
Parents
Fifteen parents were interviewed (Table 12). Five were from the control arm and 10 were from the intervention arm; five were in wave 1, seven were in wave 2 and only two were in wave 3. Interviews were booked with more wave 3 parents, including those from the control arm; however, these parents did not attend. Most of the interview participants were mothers. One interview included both a mother and a father. Across interview participants there was a mix of ethnicity and levels of attendance at the PiP sessions. The lack of diversity in parental role reflected the profile of parents attending the PiP measurement sessions and intervention.
| Participant ID | Trial arm | Wave | Parental role | Ethnicity | Self-reported attendance to PiP sessions |
|---|---|---|---|---|---|
| P01 | Control | 1 | Father | White | NA |
| P02 | Control | 1 | Mother | Pakistani | NA |
| P03 | Intervention | 1 | Mother | White | No sessions |
| P04 | Intervention | 1 | Mother | White | Four sessions |
| P05 | Intervention | 1 | Mother | White | A few sessions |
| P06 | Control | 2 | Mother | Pakistani | NA |
| P07 | Control | 2 | Mother | White | NA |
| P08 | Control | 2 | Mother | White | NA |
| P09 | Intervention | 2 | Mother | White | No sessions |
| P10a | Intervention | 2 | Mother | White | One session |
| P10b | Father | White | |||
| P11 | Intervention | 2 | Mother | White | No sessions |
| P12 | Intervention | 2 | Mother | White | No sessions |
| P13 | Intervention | 3 | Mother | Pakistani | Most sessions |
| P14 | Intervention | 3 | Mother | Pakistani | Most sessions |
Preschoolers in the Playground facilitators
Seven PiP facilitators from the five intervention schools were interviewed (Table 13). Two interviews included two PiP facilitators.
| Participant ID | Wave | School |
|---|---|---|
| F01 | 1 | 1 – white |
| F02a | 1 | 2 – South Asian |
| F02b | ||
| F03a | 2 | 3 – South Asian |
| F03b | ||
| F04 | 3 | 4 – South Asian |
| F05 | 3 | 5 – white |
Head teachers
Two head teachers from two of the five intervention schools were interviewed (Table 14). All five head teachers were approached to be interviewed; one declined saying that the PiP facilitator was better placed to comment on the study and two did not respond to the invitation.
| Participant ID | Wave | School |
|---|---|---|
| H01 | 1 | 2 – South Asian |
| H02 | 3 | 5 – white |
Head teachers’ reasons for taking part in the study (Box 1)
In discussing the reasons for agreeing to their school taking part in the PiP study, both head teachers identified perceived benefits for the children and the parents: linking health with education, engaging the parents in ‘meaningful activities’ with their children and promoting learning in children. Although both of the schools were either currently, or had previously been, involved with other Born in Bradford initiatives and were supportive of the Born in Bradford programme (see www.borninbradford.nhs.uk; accessed 6 March 2015), this was not the reason for participating in the PiP study. Similarly, although the £200 that the schools had received to spend on play equipment had been used to buy equipment for use after the end of the study, this was also not the reason why they had chosen to take part.
I think Born in Bradford is, is a fantastic initiative really and we’re hoping to get lots of information from, from that, and, and in, inform what we do in school, and it’s a great opportunity to work more closely with health, which I think has been an issue over a long period of time, and, and this one, when it’s about pre-schoolers and outside activities, you know, is, is, is right up our street really.
Right. Would you have taken part if it hadn’t been in, linked to Born in Bradford?
Possibly, because I think there’s, you know, we all know that health and education need to be more closely linked together and, as I say, anything that’s working in, in a mutual way is beneficial.
H01
I can’t really remember [why took part], but it was just, it was just something really, you know, useful; it was to encourage some playful play and just be involved, you know, with your children’s learning; and we just felt, knowing the area that we were in, it was anything to try and engage our parents in work with their children . . . See I’d more or less just started as head; and we’re in a very deprived area of Bradford, and we did have a lot of issues, you know, getting our parents to engage with their children in some meaningful activities, you know, and they, they were coming into school with extremely low language skills, and it was just anything to try and encourage the parents to, I suppose, play in a productive way with their children.
H02
Financial incentive
Well maybe it’s not about just what we’re gonna get, it’s what we can do for the children. So it depends, I mean I don’t know what other heads’ll think, but I mean I, I don’t want a great, you know, I don’t want a lot of monetary value, it might be that we get a few extra skipping ropes, or if it was, say, an extra half a dozen, I don’t know, tennis racquets or just small, just even small bits of equipment like that that you could then use on the playground afterwards, you know, not wobble boards and things that are a bit dangerous. It could be some, you know, just say half a dozen space hoppers or, you know, just something that is usable again.
H02
Parents’ reasons for taking part in the study (Box 2)
Parents offered a variety of reasons why they had agreed to participate in the PiP study. These were most commonly related to the perceived benefits of the study rather than what study participation entailed. The majority of parents explained that they viewed the PiP study as being ‘good’ for their child, which was why they had agreed to take part. When asked to elaborate on this, most talked about wanting to be involved in something that might directly benefit their child, other children or their child’s school. For some this was simply about the study’s focus on children, whereas for others it was related to the focus on physical activity. Two parents discussed how they saw the PiP study as an opportunity to introduce their child to the school environment before they started nursery in the next academic year. For many the PiP study appeared to be trusted to deliver these perceived benefits because it was part of the wider Born in Bradford programme. Several parents explained that they were already taking part in the Born in Bradford programme and so they were familiar with this type of research and/or they wanted to ‘give something back’.
Owt to do with kids . . . we might as well, we don’t want to lose out.
P10a
My daughter has eczema so we want to take part if can make a difference to her or other children with problems.
P05
Focus on physical activity
Well obviously you want your kids to be active, don’t you.
P11
I wanted her to play in the playground for half an hour ‘cause she’s very inactive. She doesn’t play at home much.
P14
Opportunity to introduce child to the school environment
I just wanted [name of child] to come into school and start participating in school . . . she’ll get to know the children and play, share, learn colours.
P14
To benefit the school
Like if, if it was just some randomer out on the street, I would, I wouldn’t bother, you know I’d just walk straight past ‘em but because they were at school, and it involves the school and stuff like that, then it’s, I’m willing to do it . . . if it’s obviously to help the school.
P14
Link to the Born in Bradford programme
I have been in BIB for years. I wanted to help as BIB helped me [identified a health problem before her baby was born].
P14
Because when [name of daughter] were born it were, she was part of that Born in Bradford thing . . . Yeah, ‘cause I did like loads of surveys when I were carrying ‘er in maternity, like little office bit. I did a few surveys there . . . Yeah, yeah, yeah. Cause she’s part of that Teddy Bear Picnic as well, aren’t yah?
P14
Requirements of the study
I didn’t see any harm in it, it just seemed like quite a simple straightforward thing . . . everyone else was ignoring him [the community research assistant].
P14
Relevance of trial arm allocation
Cause for her I wanted her to be active and join the playground. Measuring [being in the control arm], you know I’m not gonna get nothing out of that, you’re just gonna measure her, you were just get information for your research but not for her.
P14
Only one parent commented that the requirements of the PiP study had influenced her decision to participate. She was already involved with the Born in Bradford programme and perceived the PiP study to be relatively straightforward. She also explained that she had felt sorry for the community research assistant standing in the snow with a clipboard. Parents were not directly asked if being in the intervention or the control arm would affect their decision to take part and only one parent stated that they would not have taken part if put in the control arm because she had particularly wanted her daughter to attend the playground sessions.
Parents’ views on recruitment and study information (Box 3)
All but one parent described being approached by the community research assistant in the school playground or at the nursery or children’s centre to take part in the PiP study. The one exception was a mother who had learnt about the study from her sister-in-law and sought out the community research assistant to volunteer to take part. Parents were generally positive about being approached in this way and this appeared to be associated with the friendly manner of the community research assistants and the assumption that the school/nursery/children’s centre had endorsed the PiP study. Several parents explained that they had received a subsequent follow-up telephone call from a PiP researcher to make an appointment for the first measurement session. One parent had telephoned the Born in Bradford office herself as she was so keen to take part.
Friendly, yeah she were lovely, yeah. She spoke to me first and explained it all and then asked me if I wanted to do it.
P07
Study endorsed by school
I don’t usually like being approached by people in town. This was OK as was in the school playground so you are more trusting.
P01
Contacted the Born in Bradford office to take part
But what I did, I’m one of the odd ones [laughs] when I got the letter then half-term came in between and then I rang the actual office, the Born in Bradford, and I spoke to one of the colleagues there and then she told me that someone, some people will be already there and I will send you the information through post. I received the permission through post through the half-term.
P13
Community research assistant translated written study information
Yeah, because I am, sorry, but I’m tell her, I said my reading problem, I’m not properly read, but I said you some explain and I understand what she said.
P06
Well informed about the study
I’m a weird one, I probably read it about five times . . . it, it was straight to the point everything that’s gonna get involved and what you’re, what you’re, what you’re participating for, why your children are participating. Yeah, I do remember all of it . . . it’s perfect.
P13
I was told a few times about it [laughs] . . . Yeah, it kind of got a bit, not too much, but you know ‘cause they were phoning me and sending me letters and I was, was having to meet ‘em at the school, so I think I was very well informed [laughs].
P11
Positive feedback on the written study information
I was given lots of good information.
P01
There were nothing I didn’t like. Liking it tells you step by step what you’re gonna do and what will, what it’ll involve.
P07
Over half of the parents interviewed had no particular recollection of the written study information (participant information sheet; see Appendix 3) that they had received and were unable to comment on it other than saying that they thought it had been ‘OK’. Two parents for whom English was not their first language said that they had only seen the participant information sheet in English and had been unable to read it but that the community research assistant had explained the study to them verbally, which had helped with their understanding. Other parents commented that the study information was clear both from the conversation with the community research assistant and in the written information that they were given to take home. Two parents commented that they had felt very informed about the study, each for different reasons. One had read the leaflet five times and the other explained that the PiP team had telephoned/met with her on many occasions to discuss the study (this parent’s son did not attend any of the PiP sessions and so she had received telephone calls to encourage attendance). Despite parents expressing confidence that they understood the PiP study, with further probing it was clear that many had limited understanding about the processes of the study (see Parents’ understanding of the study procedures).
Finally, parents in waves 2 and 3 were shown the participant information and consent forms during the interview. They still had little to say about this written information although commonly described liking that the study was explained step-by-step, using a question and answer format and bullet points. Only one parent made a suggestion for improving these resources, which was to include more colour and pictures to make them look more appealing.
Objective 2: follow-up and attrition rates during the trial and whether or not there was a difference between trial arms and ethnic groups
The CONSORT diagram (see Figure 2) displays the follow-up and attrition rates for the pilot trial. At 10 and 52 weeks 82.3% and 83.5% of participants, respectively, provided data (accelerometry and/or questionnaire data, including anthropometric data).
Table 15 summarises attendance at the measurement sessions. At baseline 88% of participants provided any accelerometer data, at 10 weeks 76% provided any data and at 52 weeks 78% provided any data. These figures include all children who provided data irrespective of whether or not they met the wear-time criterion (any 3 days with at least 6 hours of wear). There was little difference between trial arms in the percentages providing accelerometer data across time. However, slightly higher responses were seen among South Asian children than among white children. Responses for questionnaire data were slightly higher than the percentages providing accelerometer data, with 100% of baseline, 81% of 10-week and 81% of 52-week data being provided. Again, little difference was seen between trial arms and a slightly higher percentage of South Asian children than white children attended measurement sessions. The numbers and percentages of children providing both any accelerometer data and questionnaire data demonstrated a similar pattern to those described above, with 88% providing both sets of data at baseline, 74% providing both sets of data at 10 weeks and 77% providing both sets of data at 52 weeks.
| Group variable | Baseline, n (%) | 10 weeks, n (%) | 52 weeks, n (%) |
|---|---|---|---|
| Providing any accelerometer data | |||
| Overall | 145 (88.4) | 124 (75.6) | 128 (78.0) |
| Randomised group | |||
| Intervention | 73 (88.0) | 65 (78.3) | 64 (77.1) |
| Control | 72 (88.9) | 59 (72.8) | 64 (79.0) |
| Ethnicity | |||
| White | 50 (83.3) | 47 (78.3) | 43 (71.7) |
| South Asian | 84 (90.3) | 71 (76.3) | 80 (86.0) |
| Other | 10 (100.0) | 5 (50.0) | 4 (40.0) |
| Not stated | 1 (100.0) | 1 (100.0) | 1 (100.0) |
| Questionnaire data | |||
| Overall | 164 (100.0) | 133 (81.1) | 132 (80.5) |
| Randomised group | |||
| Intervention | 83 (100.0) | 66 (79.5) | 68 (81.9) |
| Control | 81 (100.0) | 67 (82.7) | 64 (79.0) |
| Ethnicity | |||
| White British | 60 (100.0) | 48 (80.0) | 43 (71.7) |
| South Asian | 93 (100.0) | 79 (85.0) | 81 (87.1) |
| Other | 10 (100.0) | 5 (50.0) | 7 (70.0) |
| Not stated | 1 (100.0) | 1 (100.0) | 1 (100.0) |
| Both sets of data | |||
| Overall | 145 (88.4) | 122 (74.4) | 126 (76.8) |
| Randomised arm | |||
| Intervention | 73 (88.0) | 64 (77.1) | 64 (77.1) |
| Control | 72 (88.9) | 58 (71.6) | 62 (76.5) |
| Ethnicity | |||
| White | 50 (83.3) | 46 (76.7) | 42 (70.0) |
| South Asian | 84 (90.3) | 70 (75.3) | 79 (85.0) |
| Other | 10 (100.0) | 5 (50.0) | 4 (40.0) |
| Not stated | 1 (100.0) | 1 (100.0) | 1 (100.0) |
Table 16 shows the number of communications made for all participants who attended the 10- and 52-week follow-up visits.
| Number of communications | Number of participants at 10 weeks | Number of participants at 52 weeks |
|---|---|---|
| 1 | 100 | 72 |
| 2 | 20 | 20 |
| 3 | 8 | 18 |
| 4 | 2 | 4 |
| 5+ | 3 | 18 |
It took between one and nine communications (telephone calls, text messages, face-to-face conversations in the school playground with parents) for the children to attend the 52-week follow-up visit. The average number of communications was 2.2 and the median was 1. The average number of calls to those who were lost to follow-up was 4.75. In total, 44 parents changed their contact telephone number over the duration of the trial and 24 changed their address.
A total of nine children withdrew from the trial (five white, three South Asian and one other; two from the intervention group and seven from the control group). The reasons for withdrawal are summarised in Table 17. The most frequent reasons for withdrawal from the trial were being too busy and no longer interested in taking part.
| Reason for withdrawal from trial | Trial arm | Ethnicity |
|---|---|---|
| No longer interested | Intervention | White |
| No longer interested | Intervention | White |
| No longer interested | Control | South Asian |
| Too busy | Control | South Asian |
| Too busy | Control | Other |
| Too busy | Control | White |
| Too busy | Control | White |
| Mother unwell | Control | South Asian |
| Moving away from area | Control | White |
Objective 3: acceptability of the trial procedures
Parents’ understanding of the study procedures (Box 4)
During the interviews it was clear that, although most parents claimed to understand the design and processes of the PiP study, in reality many were quite confused, particularly about the concept of randomisation and its implication for their participation. One parent explained that she had not really understood what the study entailed when she turned up for the first measurement session. Several parents did not understand the interview question, ‘What did you think about being randomised to the two groups in the study?’ Others understood randomisation to mean ‘picked by chance’ (P13); however, they did not appear to recognise its relevance to the PiP study. Examples of confusion included thinking that randomisation was about the PiP sessions being offered in the morning or afternoon, uncertainty about which trial arm the child’s school was allocated to despite having discussed attendance at the PiP sessions and thinking that the schools with the most children were chosen for the PiP intervention. Only one parent (in the control arm) commented that randomisation seemed unfair.
To be honest, when I went [to the first measurement session] I wasn’t really sure what I were going for [laughs].
P09
Confusion about randomisation
Well obviously I didn’t know why they were just picking one [school], so they, they never explained why.
P11
Yeah, she said is morning and some is afternoon, she’s go for afternoon class, so and she said that in the two sessions.
P06
Do you know which group you’re, you were put in?
No. I don’t know really. I don’t know.
P12
I thought the most school that had the most parents, that’s why they got chosen [for the PiP intervention].
P13
Randomisation is unfair
At [name of school], they haven’t been picked for exercise bit . . . which I thought were a bit unfair. I think they should all, if you’re part of this, then I think you should, should all do it.
P07
Preschoolers in the Playground facilitator view
No, I don’t think they [parents] understand that they’re part of a big programme that’s happening and a big research thing. I’m not sure that they understood that fully to be honest.
F02a
The PiP facilitators had mixed views about how well they thought the parents at their school had understood the study. Indeed, one facilitator believed that the low attendance at the PiP sessions was because of a lack of understanding.
Using the accelerometer (Box 5)
Most parents said that using the accelerometer belt was easy and this judgement seemed to be based primarily on how they perceived it was for the child to wear the belt. Parents generally described their child as ‘being fine’ with wearing the belt. Some explained how their child had really liked wearing it. Examples included a boy who thought that he was a ‘Power Ranger’ when wearing it and did not want to take it off at night or return it to the community research assistant at the end of the week. Another boy thought that it was his ‘Sportacus’ belt and liked the flashing light on it and a girl was described as feeling ‘important’ when wearing the belt. There were also examples of children being less keen to wear the belt, particularly when tired or unwell. The comfort or discomfort of the belt also made a difference, with one parent describing how she distracted her daughter when putting the belt on as it kept swivelling around, and tightening it to stop this was uncomfortable for the little girl. Indeed, several parents mentioned that the belt either moved or pinched the child when tight. Another practical issue mentioned by one father was that a small part of the accelerometer kept coming off (and could be swallowed by the child). One parent suggested that the accelerometer could look more child friendly, perhaps by being a different colour.
Yeah, she han’t bothered. It han’t phased her, yeah.
P07
Yeah, he loves the belt, he loves the belt, he thinks he’s a Power Ranger with the belt, so . . . Oh it’s the, it’s easy when you put it on in the morning, but when you take it off in the night it’s, it’s hard because he says, oh I have to leave it on, I’m gonna have a, oh it’s harder taking it off at night, but when he’s gone to sleep I just pull it off, so he doesn’t know it’s off, because you have to take it off at night don’t you? . . . and then obviously then you have to, have to have a fight, but when I had to give it, after 7 days, oh my God, I remember, oh he was like, oh I have, I said, I said ‘OK, I promise you I’ll, I’ll promise you’ll get another belt for you’. I had to say that to him, and then we ended up getting a Power Ranger suit because then he forgot about the belt [laughs].
P13
He was absolutely like put it on and he’s like exercising [laughs] running down to the school to show ‘em all that he’s got this belt on, ‘cause he just thought it was like a Sportacus belt, so he was just, he was happy with it . . . He’s very specific. He wanted it at the front and I had to keep, I’d, I’d turn it round and I’d lift his top up and he’d have it back there again, ‘cause they said it had to be on his side. But if they’ve still got readings off it, then it’s, it’s not a problem is it? . . . He was usually wanting it there so he could see the green bit flickering. Obviously he couldn’t see it on his side.
P11
She loves it, she loves wearing belt. I think it makes her think she’s important, so [laughs]. Don’t, don’t yah? Surprises me though ‘cause she, ‘cause she keeps it on and she knows not to move it, which is not normal for her [laughs].
P10a
Practical issues
She has times where, if she’s tired or anything, she’ll say ‘I don’t want it on’ and I have to sort of try and do it when she’s not looking [laughs]. Well it works sometimes, it depends if I can distract her and then sort of have her looking at me and something like that. But no, she does pretty well with it. Yeah, we do OK . . . And I tell you what I do find difficult is keeping it on the right-hand side, on the hip bone where it’s supposed to be.
Does it swivel round?
It does, yeah, and I, I had it sort of tight enough but if I’d have tightened it more she’d have been uncomfortable.
P09
I do think they could do with making something a bit better for a child of her age, ‘cause she, she’s fine with it, but quite often you’ve got to move it back into place, ‘cause if she’s moving about and stuff, it’s moving. So it does need summat a bit more so it’ll stay in that spot . . . Like a, like a harness sort of one where it’ll keep in, keep there would be fine. The other problem is it, it’s got small parts on it, as well, that come off. That’s why I take, I take ‘em off when she’s got it on, because the little cap comes off, which she put in her mouth, and also the strap comes off that holds the cap in place, so they’re not secure. So children under age of . . . It’s a choking hazard, in’t it, so? I think, I think it’s a cap for the USB socket on the top, because they must download the data, but it’s not secure.
P10b
Support from the community research assistant
Again staff excellent we had a girl from [name of town] who gave us the belt the first time. Really impressed staff phoned up to see how we’re getting on with it. Second time we missed the appointment [at the children’s centre] so she came to the house, went through the same information as the first time. I said they didn’t need to but they said they wanted to be sure which is great.
P05
Parents were asked to ensure that their child wore the belt for 7 days over a week and to complete a diary of when the belt was worn. A few mentioned that they had sometimes forgotten to put the belt on their child and in some cases the child had reminded them. As with handling the belt, completing the diary appeared to be ‘fine’ for parents. Once again, the community research assistants were commended on their instructions and support for parents.
Measurement sessions (Box 6)
There were mixed views about the location of the measurement sessions, with a few parents not minding where they took place, some liking the sessions being at school and others preferring the sessions to be at home. When a preference was expressed this seemed to be related to convenience, for example tied in with the school drop-off or coming to the house when a parent was unable to attend the sessions in the school. The happiness of the child and the comfort of the surroundings were also mentioned. All of the parents from one school in wave 2 commented that the room was very small or that they had been moved from room to room during the second (10-week) measurement session.
As long as [name of son]’s happy to do it wherever, I am.
P11
[School is preference] because I drop my children off to school anyway.
P14
I’m not bothered either way [where the measurement sessions are held]. The only thing I would say is that the, at the school we were in a very small room, it it were like were just, it were a bit like a cupboard, to be honest . . . So in a way it were more comfortable here [at home].
P09
Length of the sessions
They [the measurement sessions] were very straightforward and simple, yeah no problem. It took 20 minutes.
P01
I think she were having problems with her lap top, if I remember rightly. But I think we were in there about an hour; but it might have been co’ it were first session, so there might have been different, more questions in on it.
P10a
Child’s engagement with the session
No he doesn’t [mind being measured], you can tell he doesn’t.
P13
He’s happy to do it . . . last time . . . as soon as she was like come and measure yourself he was away. He was, he was having fun. It was all about him, so he was having fun.
P11
The girl was very good with [name of son], gave him paper and crayons when I answered questions.
P01
I liked it [the measurement session] [name of daughter] didn’t, she were a bit wary, so . . . she wouldn’t just, she wouldn’t stay still, she kept on wanting to come out.
P12
Questions about parents
Well the thing about the mental health, obviously no one’s going to admit to that anyway [laughs]. But yeah, that, that question seemed a bit weird to me, where you’re asking the parents what mental health state they’re in. Oh I can’t, I think I’m a bit insane [laughs].
What were you expecting, what would you expect the questions to be about?
Well about the kids. I wouldn’t expect it to be like the safety questions and stuff. How safe do you feel, and stuff like that, you wouldn’t expect . . . I remember talking to a girl from the school and she was horrified that they’d asked her, you know, about her mental health, and I was just like, well, you know, they’re just questions, you know. It, I, I’m not fussed like that.
P11
It goes a bit too much, but yeah, it were all right [laughs]. Yeah. Quite easy but it just goes on a bit too much. They’re sort of quite repetitive, some of the questions are quite repetitive.
P07
I find them a bit odd how they’re, they’re very personal towards me and not so much about [name of daughter]. I don’t, I, it’s meant to be about her so why are the questions at me? So no, I don’t mind answering it, it’s just a bit odd [laughs].
P10a
I do dislike the fact that obviously they’re asking really personal questions like income, etc. etc. But I, was that like related to the whole research, that depends, I don’t know . . . Yeah, I do find, I do personally think that they are personal questions, and like income and, etc. and so forth, I’m not, I’m not, I’m, I’m not embarrassed or anything anyhow I’m happy to give the information out, but some people might find it really like, oh I don’t want to give that information out.
P13
Yeah, some is easy but some is hard for me because I’m no understand . . . that’s why is Urdu for easily for me.
P06
I’d rather fill them [the questions] in myself because a lot of the questions are personal. Obviously like the first questions that were asked, like the, the simple ones, they’re, they’re . . . that’s fine. But in the personal questions like you just don’t want them to like, like shout it out.
Interviewer: And would you prefer to do them on like a laptop or paper and pen?
Laptop or paper or pen . . . No, I don’t mind.
P07
Parents were generally accepting about the length of time that the measurement sessions took, despite describing some of the sessions as taking up to an hour. Reasons offered for these longer sessions included the volume of paperwork to complete, poor organisation (being moved from room to room during the session) and the tablet not working. They also tended to report that their children were fine or even enjoyed being measured and several commended the approach of the community research assistants who were observed as engaging well with the children, making the session fun and having a friendly approach. Two parents described slightly different experiences: one explained that his son had been grumpy at the second session but attributed that to him being ill; another discussed that her daughter had been a bit wary. Nevertheless, both of these children completed all of the measurements.
The one component of the measurement sessions that many parents were less positive about was the set of questions about themselves (rather than about their child). There were several issues mentioned: confusion as to the purpose of these questions (rather than focusing on the child’s physical activity); the perception that they were very long and repetitive; and their personal nature, particularly the mental health questions but also the questions on income (these questions are from the ComQol-A5). One mother for whom English was her second language said that she would have preferred the questions to be translated for her. A couple of parents spoke about a preference to complete the questions on paper or using a tablet rather than being asked them verbally; this again was related to the personal nature of the questions.
Objective 4: feasibility of collecting the outcome measures and whether or not there was a difference between trial arms and ethnic groups
Feasibility of accelerometry
The number and proportion of data meeting the wear-time criterion (any 3 days with at least 6 hours of wear) overall, by trial arm and by ethnicity are presented in Table 18.
| Group variable | Baseline, n (%) | 10 weeks, n (%) | 52 weeks, n (%) |
|---|---|---|---|
| Overall | 113 (68.9) | 87 (53.0) | 87 (53.0) |
| Randomised arm | |||
| Intervention | 55 (66.3) | 44 (53.0) | 42 (50.6) |
| Control | 58 (71.6) | 43 (53.1) | 45 (55.6) |
| Ethnicity | |||
| White | 22 (36.7) | 28 (46.7) | 28 (46.7) |
| South Asian | 44 (47.3) | 55 (59.1) | 56 (60.2) |
| Other | 3 (30.0) | 3 (30.0) | 3 (30.0) |
| Not stated | 1 (100.0) | 1 (100.0) | 0 (0.0) |
Overall, 68.9% of baseline data, 53.0% of 10-week data and 53.0% of 52-week data met the wear-time criterion. There was little difference across trial arms but a higher percentage of South Asian children met the wear-time criterion than white children. Only 64 children (39%), 29 from the intervention arm and 35 from the control arm, provided accelerometer data that met the wear-time criterion at both baseline and 52 weeks.
Feasibility of other health outcomes
The feasibility of the anthropometric measurements, the ComQol-A5 and the General Self-Efficacy Scale in terms of completion rates at each time point is presented in Table 19.
| Characteristic | Height, n (%) | Weight, n (%) | Upper arm circumference, n (%) | Abdominal circumference, n (%) | ComQol-A5, n (%) | General Self-Efficacy Scale, n (%) |
|---|---|---|---|---|---|---|
| Baseline | ||||||
| Overall | 145 (88.4) | 151 (92.1) | 121 (73.8) | 126 (76.8) | 147 (89.6) | 163 (99.4) |
| By arm | ||||||
| Intervention | 72 (86.8) | 74 (89.2) | 55 (66.3) | 60 (72.3) | 75 (90.4) | 83 (100.0) |
| Control | 73 (90.1) | 77 (95.1) | 66 (81.5) | 66 (81.5) | 72 (88.9) | 80 (98.8) |
| By ethnicity | ||||||
| White | 49 (81.7) | 51 (85.0) | 46 (76.7) | 45 (75.0) | 53 (88.3) | 59 (98.3) |
| South Asian | 86 (92.5) | 89 (95.7) | 64 (68.8) | 70 (75.3) | 85 (91.4) | 93 (100.0) |
| Other | 10 (100.0) | 10 (100.0) | 10 (100.0) | 10 (100.0) | 8 (80.0) | 100 (100.0) |
| 10 weeks | ||||||
| Overall | 110 (67.1) | 116 (70.7) | 86 (52.4) | 88 (53.7) | 115 (70.1) | 130 (79.3) |
| By arm | ||||||
| Intervention | 53 (63.9) | 58 (69.9) | 45 (54.2) | 47 (56.6) | 62 (74.7) | 64 (77.1) |
| Control | 57 (70.4) | 58 (71.6) | 41 (50.6) | 41 (50.6) | 53 (65.4) | 66 (81.5) |
| By ethnicity | ||||||
| White | 40 (66.7) | 42 (70.0) | 35 (58.3) | 36 (60.0) | 42 (70.0) | 48 (80.0) |
| South Asian | 65 (69.9) | 69 (74.2) | 46 (49.5) | 47 (50.5) | 68 (73.1) | 76 (81.7) |
| Other | 4 (40.0) | 4 (40.0) | 4 (40.0) | 4 (40.0) | 4 (40.0) | 5 (50.0) |
| 52 weeks | ||||||
| Overall | 115 (70.1) | 118 (72.0) | 97 (59.2) | 103 (62.8) | 125 (76.2) | 131 (79.9) |
| By arm | ||||||
| Intervention | 58 (69.9) | 60 (72.3) | 50 (60.2) | 53 (63.9) | 65 (78.3) | 68 (81.9) |
| Control | 57 (70.4) | 58 (71.6) | 47 (58.0) | 50 (61.7) | 60 (74.1) | 63 (77.8) |
| By ethnicity | ||||||
| White | 36 (60.0) | 39 (65.0) | 34 (56.7) | 36 (60.0) | 41 (68.3) | 43 (71.7) |
| South Asian | 72 (77.4) | 72 (77.4) | 57 (61.3) | 61 (65.6) | 77 (82.8) | 81 (87.1) |
| Other | 6 (60.0) | 6 (60.0) | 6 (60.0) | 6 (60.0) | 6 (60.0) | 6 (60.0) |
| Both baseline and 52 weeks | ||||||
| Overall | 101 (61.6) | 107 (65.2) | 68 (56.2) | 74 (58.7) | 113 (68.9) | 130 (79.3) |
| By arm | ||||||
| Intervention | 50 (60.2) | 53 (63.9) | 33 (60.0) | 36 (60.0) | 60 (72.3) | 68 (81.9) |
| Control | 51 (63.0) | 54 (66.7) | 35 (53.0) | 38 (57.6) | 53 (65.4) | 62 (76.5) |
| By ethnicity | ||||||
| White | 28 (46.7) | 31 (51.7) | 25 (54.4) | 25 (55.6) | 36 (60.0) | 42 (70.0) |
| South Asian | 67 (72.0) | 69 (74.2) | 37 (57.8) | 43 (61.4) | 71 (83.5) | 81 (87.1) |
| Other | 6 (60.0) | 6 (60.0) | 6 (60.0) | 6 (60.0) | 5 (50.0) | 6 (60.0) |
From Table 19 we can see that the quality of life and self-efficacy questionnaires had the highest response rates at baseline, week 52 and both baseline and week 52. The ComQol-A5 had 69% of data available at both baseline and week 52 and the General Self-Efficacy Scale had 79% of data available at both baseline and week 52. The anthropometry data response rates for those with baseline and week 52 data ranged from 56% for upper arm circumference to 65% for body mass, with height (62%), BMI z-value (57%) and waist circumference (59%) falling between these two figures. Higher response rates were seen among South Asian children than among white children for all measures apart for upper arm circumference.
Feasibility of conducting an economic analysis
The overall completion rates for both the EQ-5D and the PedsQL were at least 70% at each time point, whereas those for resource items did not fall below 80% (Table 20).
| Outcome | Baseline, n (%) | Week 10, n (%) | Week 52, n (%) |
|---|---|---|---|
| EQ-5D | |||
| Control arm | 56 (69) | 50 (62) | 64 (79) |
| Intervention arm | 70 (84) | 64 (77) | 61 (73) |
| Total | 126 (77) | 114 (70) | 125 (76) |
| PedsQL | |||
| Control arm | 81 (100) | 67 (83) | 60 (74) |
| Intervention arm | 83 (100) | 62 (75) | 63 (76) |
| Total | 164 (100) | 129 (79) | 123 (75) |
| Resource items | |||
| Control arm | 80 (99) | 67 (83) | 64 (79) |
| Intervention arm | 82 (99) | 64 (77) | 68 (82) |
| Total | 162 (99) | 131 (80) | 132 (81) |
Objective 5: influence of financial incentives on trial participation (Box 7)
If we were running the study again and there wasn’t any vouchers?
No, I wouldn’t [take part].
P06
How important are the gift vouchers in terms of encouraging you to take part?
Well for her [the daughter], yeah, very important, ‘cause it goes to her, so . . .
It’s like a reward for ‘em, in’t it, so . . .
P10a and P10b
A nice gesture
To begin with vouchers were important but then we forgot and so they were a nice surprise. To be honest we’d have done the study anyway.
P01
I think I would have took part anyway but I mean they’re just a bonus, so. I mean, like I said, I can go and get him a game or something, so but I always, I always seem to get roped into stuff like answering questions and people and . . . [laughs].
P11
Value and cash/gift voucher
Yeah, I think that’s fine for her because, well she’s a 3-year-old, £10 is a lot of money for a, for a 3-year-old.
P10a
Cash is better. I have not used the vouchers. Some people might want more than £10 if they are not working. I am not working any more so more would be better.
P04
I prefer the gift vouchers, because cash obviously you’re just gonna use it on yourself, but with Mothercare vouchers you are . . . tend to use it on the child that’s taking part in it. Basically it’s for her, she’s the one that, she’s the one that’s doing the hard work, I’m just bringing her to them.
And how, what do you think about the amount of the gift voucher? Is it £10 each time?
£10 yeah, yeah, good.
Views on having a voucher for Mothercare or the Early Learning Centre
And would you prefer cash instead of vouchers or . . .?
I’m not fussed. Yeah. I, I think if it was used, if it was used as cash on some people, that it wouldn’t get spent on the kids. You know, ‘cause obviously it’s Mothercare vouchers, you’ve got no choice but to spend it on your kids. Cause there, I know there are a few people out there that would use it on themselves [laughs].
And do you think, what, what do you think about the amount?
I think it’s really good, yeah. Although Mothercare is quite expensive [laughs]. Last time we went we managed to get him a, a packet of underpants. That was all we came out with [laughs]. He didn’t actually have enough for any of the toys in there, so. So this time he’s . . .
So this’ll be better with £20?
Yeah, ‘cause, like I said, them, them games for that thing, they’re like £20 each, so when you said it was £20, like going to get him a new game then [laughs].
Yeah. Not pants.
Yeah [laughs]. He’s got enough underpants now [laughs].
P11
To be, to be honest, I’d probably say it’d be better cash rather than the gift vouchers ‘cause Mothercare is expensive . . . whereas if you’ve got the cash, you could go to somewhere like B and M’s [a discount home store] and you could get a lot more for the money than what you would at, £10 at Mothercare you can’t get a lot, but if you put that to B and M’s you’d probably get summat like four or five toys, so . . .
Plus you can’t use the vouchers online neither.
P10a and P10b
I mean I’m quite happy with Mothercare and Early Learning, ‘cause that, I do go there. But no, to me it’s fine as it is.
P09
No, that’s fine [vouchers for Mothercare/Early Learning Centre], me and my sister both participated in it, in it, so she’s got, she’ll end up having 30 and I’ll have, we’re plan, planning to buy something really big for the garden, yeah.
P13
Well I don’t, you know, monetary values are, are always good for the child, you know, for the, for the parents round here. I mean [sighs] we do a lot with Asda vouchers, that, that seems to be the, the payment of choice round here, people say, well they just spend it on booze or fags; but actually they don’t always, you know, they do spend it on quite nice things for the children. Even, even if they buy an extra, I suppose, ready-made lasagne, at least it’s a tea, isn’t it?
H02x
Timing
But it, was there an incentive for the parents, for the parents? If the parents attended for a certain percentage of the 12 weeks, they were entitled to a photo shoot, that initiative attracted five parents. But I think that was done at the beginning of the project rather than at the end of the project [laughs]. It would be better to do [laughs] if you’re going to run any sort of a sweetener, it’s better to run it at the end, with our parents.
H01
I think it’s nice that they’ve got something at the end, but I think a bit, what they could have done was waited, and perhaps, you know, different equipment each week and then done a little goody bag at the end with the different things in, giving them it then rather than more, more at the start, because some of our parents are quite canny, once they’ve got their freebie they don’t bother so much [laughs].
H02
There were no differences in parents’ views on incentives by ethnicity or level of attendance at the PiP intervention. When the parental involvement workers and head teachers offered an opinion these are included.
Parents were given a £10 gift voucher for Mothercare or the Early Learning Centre on completion of each measurement session and also for taking part in an interview. Two of the parents said that they would not have taken part in the study without the incentives (although this slightly contradicted what parents had said earlier about their reasons for taking part: no one indicated that incentives were the reason why they had participated). Another two parents commented that the vouchers were important as they could be used to buy something for the child. The rest of the parents seemed to view the vouchers as a nice gesture but certainly not the reason for participating (see Parents reasons for taking part in the study).
There were also mixed views on the value and type of voucher. Most parents thought that the value of £10 was about right and, when they offered an explanation, they stated that this was because the work that they had been asked to do was fairly minimal or that £10 was quite a lot for a small child. Others did not think that the value of the incentive mattered. Two parents suggested that a higher value of incentive would be better, one because she was not currently working. The importance of spending the money on the child emerged again here. It did not seem to matter whether the incentive was in the form of cash or a voucher as long as it was spent on the child; some acknowledged that the voucher format ensured that this happened. The key issue that emerged about incentives was the inappropriateness of giving a voucher for Mothercare or the Early Leaning Centre as these were perceived by about two-thirds of parents to be expensive shops where the £10 voucher had relatively little value. The other one-third of parents liked these shops (and their focus on the child) and either were saving the vouchers to buy something substantial or had already shopped there. One of the head teachers mentioned that her school typically uses Asda vouchers with parents and her perception was that parents do spend the money on something for the child and that this could be a hot dinner, which would be acceptable.
Both head teachers questioned the value of providing an incentive at the start of the PiP intervention and suggested that it would have been better to keep it until the end to motivate parents to continue to attend.
Objective 6: attendance to, and acceptability of, the intervention, whether or not there was a difference between ethnic groups and whether or not attendance varied by season
Attendance to the intervention
Attendance data for the PiP intervention sessions were available for 83 children from the five intervention schools and are summarised in Tables 21 and 22 by initiation and maintenance phase.
| Summary | School 1 (wave 1) | School 2 (wave 1) | School 3 (wave 2) | School 4 (wave 3) | School 5 (wave 3) | Overall |
|---|---|---|---|---|---|---|
| Initiation | ||||||
| Timing | Autumn 2012 | Autumn 2012 | Winter 2012/spring 2013 | Summer 2013 | Summer 2013 | |
| Number of children | 13 | 16 | 15 | 18 | 21 | 83 |
| Attended any session, n (%) | 6 (46.2) | 10 (62.5) | 6 (40.0) | 15 (83.3) | 17 (81.0) | 54 (65.1) |
| Number of sessions attended | ||||||
| Mean (SD) | 1.8 (1.0) | 2.3 (1.4) | 10.7 (10.6) | 10.8 (10.7) | 13.6 (9.8) | 9.1 (9.6) |
| Median (min.–max.) | 1.5 (1–3) | 2 (1–5) | 10 (1–21) | 5 (1–28) | 17 (1–29) | 3 (1–29) |
| Maintenance | ||||||
| Timing | Winter 2012/spring and summer 2013 | Winter 2012/spring and summer 2013 | Summer and autumn 2013 | Autumn and winter 2012/spring 2013–14 | Autumn and winter 2012/spring 2013–14 | |
| Number of children | 13 | 16 | 15 | 18 | 21 | 83 |
| Attended any session, n (%) | 0 (0.0) | 0 (0.0) | 3 (20.0) | 4 (22.2) | 6 (28.6) | 13 (15.7) |
| Number of sessions attended | ||||||
| Mean (SD) | 0.0 (0.0) | 0.0 (0.0) | 8.3 (1.2) | 3.0 (2.3) | 5.0 (3.7) | 5.2 (3.4) |
| Median (min.–max.) | 0 (0–0) | 0 (0–0) | 9 (7–9) | 3 (1–5) | 4.5 (1–11) | 4.5 (1–11) |
| Overall | ||||||
| Number of children | 13 | 16 | 15 | 18 | 21 | 83 |
| Attended any session, n (%) | 6 (46.2) | 10 (62.5) | 6 (40.0) | 15 (83.3) | 17 (81.0) | 54 (65.1) |
| Number of sessions attended | ||||||
| Mean (SD) | 1.8 (1.0) | 2.3 (1.4) | 14.8 (15.2) | 11.6 (12.1) | 15.4 (11.6) | 10.3 (11.5) |
| Median (min.–max.) | 1.5 (1–3) | 2 (1–5) | 14.5 (1–30) | 5 (1–33) | 5 (1–33) | 3.0 (1–35) |
| Number of sessions attended | Week, n (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total, n | |
| Initiation phase | |||||||||||
| 0 | 19 (35.2) | 28 (51.9) | 20 (37.0) | 34 (63.0) | 30 (55.6) | 31 (57.4) | 36 (66.7) | 31 (57.4) | 37 (68.5) | 39 (72.2) | 54 |
| 1 | 23 (42.6) | 7 (13.0) | 15 (27.8) | 3 (5.6) | 8 (14.8) | 6 (11.1) | 8 (14.8) | 6 (11.1) | 8 (14.8) | 9 (16.7) | 54 |
| 2 | 5 (9.3) | 7 (13.0) | 5 (9.3) | 7 (13.0) | 2 (3.7) | 6 (11.1) | 3 (5.6) | 6 (11.1) | 2 (3.7) | 6 (11.1) | 54 |
| 3 | 6 (11.1) | 10 (18.5) | 10 (18.5) | 6 (11.1) | 10 (18.5) | 8 (14.8) | 7 (13.0) | 9 (16.7) | 7 (13.0) | 0 (0.0) | 54 |
| 4 | 1 (1.9) | 1 (1.9) | 4 (7.4) | 4 (7.4) | 4 (7.4) | 3 (5.6) | 0 (0.0) | 2 (3.7) | 0 (0.0) | 0 (0.0) | 54 |
| 5 | 0 (0.0) | 1 (1.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 54 |
| 6 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 54 |
| Maintenance phase | |||||||||||
| 0 | 7 (53.8) | 6 (46.2) | 9 (69.2) | 8 (61.5) | 10 (76.9) | 9 (69.2) | 2 (15.4) | 7 (53.8) | 8 (61.5) | 10 (76.9) | 13 |
| 1 | 1 (7.7) | 7 (53.8) | 4 (30.8) | 5 (38.5) | 3 (23.1) | 3 (23.1) | 6 (46.2) | 6 (46.2) | 5 (38.5) | 3 (23.1) | 13 |
| 2 | 4 (30.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (7.7) | 4 (30.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 13 |
| 3 | 1 (7.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (7.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 13 |
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 13 |
| 5 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 13 |
| 6 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 13 |
Across the intervention schools 54 of the 83 children (65%) attended one or more sessions during the initiation phase and 13 of the 83 children (16%) attended one or more sessions during the maintenance phase. Among those children who attended at least one session during the initiation phase, the average number of sessions attended was 9.1 (SD 9.6 sessions), with a median of three sessions attended (minimum–maximum 1–29 sessions), and among those children who attended at least one session during the maintenance phase, the average number of sessions attended was 5.2 (SD 3.4 sessions), with a median of 4.5 sessions attended (minimum–maximum 1–11 sessions). Attendance was much higher during the summer term initiation phase than during the autumn or winter/spring initiation phase. Attendance was also much higher in the initiation phase than in the maintenance phase. It was recommended that children attend 30 sessions in the initiation phase and 60 sessions in the maintenance phase (n = 90 overall). None of the schools provided the second term of the maintenance phase and, thus, the maximum number of sessions that families could have attended was 60.
The recommended number of sessions per week was three; in weeks 1–9, between six and 10 children (11.1–18.5%) attended three sessions. In week 10, no children attended the recommended number of sessions. Just under half of the participants (n = 23, 42.6%) attended one session in the first week; between three and 15 pupils (5.6–27.8%) attended one session per week in the remaining 9 weeks. The proportion of participants attending no sessions a week rose from 35.2% in the first week to 72.2% in week 10 and, with the exception of week 3, was between 51.9% and 68.5% in the interim weeks. Attendance data for the maintenance phase were available for three of the five intervention schools. In total, 13 children attended at least one maintenance session. No participants attended more than the recommended three sessions per week and only in weeks 1 and 7 did any children attend the recommended number of sessions (in both cases one child attended the three sessions). Mostly, participants did not attend any sessions per week (between 46.2% and 76.9%); the exceptions were weeks 2, 7 and 8 when around half attended one session (n = 6, 46.2%). Table 23 presents the attendance data by ethnicity for those children who attended at least one session.
| Summary | White | South Asian | Other |
|---|---|---|---|
| Initiation | |||
| n (%) | 19 (54.3) | 30 (69.8) | 4 (100.0) |
| Mean (SD) | 10.7 (12.1) | 11.3 (11.8) | 2.5 (2.4) |
| Median (min.–max.) | 3 (1–33) | 4.5 (1–35) | 1.5 (1–6) |
| Maintenance | |||
| n (%) | 3 (20.0) | 4 (22.2) | 6 (28.6) |
| Mean (SD) | 28.7 (1.2) | 28.3 (6.6) | 26.0 (8.0) |
| Median (min.–max.) | 28 (28–30) | 30.5 (19–33) | 26.5 (12–35) |
| Overall | |||
| n (%) | 19 (54.3) | 30 (69.8) | 4 (100.0) |
| Mean (SD) | 10.7 (12.1) | 11.3 (11.8) | 2.5 (2.4) |
| Median (min.–max.) | 3 (1–33) | 4.5 (1–35) | 1.5 (1–6) |
Attendance at the PiP intervention sessions was higher among South Asian children than among white children. Among those children who attended at least one session, the average number of sessions attended for white children was 10.7 (SD 12.1 sessions), with a median of three sessions attended (minimum–maximum 1–33 sessions), and for South Asian children was 11.3 (SD 11.8 sessions), with a median of 4.5 sessions attended (minimum–maximum 1–35 sessions).
Three children withdrew from the intervention (one white and two South Asian). The reasons given for withdrawal were (1) that it was too cold, (2) that the child was injured and (3) that the mother was heavily pregnant. Throughout the duration of the intervention there were no adverse events reported.
Acceptability of the intervention (Box 8)
Only five parents who were interviewed in the intervention arm had actually attended any PiP sessions; two of these had attended most sessions (and provide the most detail about the sessions), two had attended a few/four sessions and one father had attended only once, explaining that he was not impressed with the delivery of the session. The views presented here are, therefore, based on a very small number of parents.
Children enjoyed them . . . they do exercise at nursery but, but this was with different staff so good. They used balls and skipping ropes.
P04
We have enjoyed ourselves. It’s like every week it was something different. Something different every day and my [name of child] loves playing with balls and the cricket bat.
P13
Observed benefits to the children
When she started she was very clingy, you know she wouldn’t do anything, she wouldn’t move around, she just wanted to hold me and look, she was interested in what the other children were doing, she wasn’t doing it herself, but over the weeks, so I’ve noticed the change in her. So you know she’s picking the beanbag up, she loves the beanbag.
P14
She loves the balancing game, that’s her favourite game, even when we have free play for 5 minutes, that’s the game she will go, she will pick up her, the rope up for herself, lay it on the floor, get a bucket and put the beanbag on her head.
P14
And first time we really, really come to the session he only knew the colour blue, he always wanted to play with the blue, but now we’ve learnt red so now we play with red colour [laughs].
P13
Yeah, he’s brilliant with other children, he says to them ‘You bat and I will ball then we swap over OK?’ He shares a lot now, which is good, which is good to see. He’s made more friends I guess that’s the best thing.
P13
They’re lovely, the beanbags they get. So I feel like, we’ve been collecting them so the games that we play here we go and play at home as well, so with the hoops and the beanbags, and my other children love them as well.
P14
Because I’m dragging the equipment up before me, they do a little bit of free play before we begin even. They’ve normally started kicking the ball, they just do, they don’t in the beginning the first few weeks they’ve probably hung around and waiting for me to start, now as soon as there’s a ball or a hoop, they’re off basically.
F05
Then I’ll say to ‘em let’s tidy up now, it’s time to finish, and then they just get, they get that expression on their faces like, do we have to go now, that kind of face, and I’m thinking oh did you really enjoy that? [Laughs]
F03b
Benefits to the parents
Yeah, they’re [PiP sessions] very, very good. The activities they play, it’s like I didn’t know that you can play such games with a beanbag, with a hoop, with balancing you know, these are games I will not play with her. So coming to these sessions, I’ve picked up games . . . Talking to the other parents and, you know, it’s really nice.
P14
They [the leaflets] were good as well, first one we got was even if it’s raining, things you can wear, your wellies and things like that. Second one was like, I can’t remember now.
P14
Shame that only myself and one other parent there.
P05
We left the PiP-PoPs out, the ones that we’d already done, so that the children could, and the mums could do it again if they wanted to, during their free, free play session.
And did they?
Yes, they did.
F02a
When we model it from the first session it’s getting to, used to it, and then eventually they [the parents] would know what to do. The more we did we had more fun, I think because we were getting more confident at delivering it and the parents were getting more confident with us as well, yeah and the kids.
F02b
And of course the child is getting important transition work as well. A lot of the children I have start nursery in September, so they’ve been able to, we’re right near nursery so [name of nursery teacher]’s been coming out and meeting them . . . so it’s been really valuable, we couldn’t have picked a better time to do it really [summer term].
F02b
They had, they were able to have a ball, oh beanbags they went home with, skipping rope, paint, brush and pot, hula hoop, scarf, ball and a bat . . . they’ve all said that they play with the stuff at home.
F03a
Why only attended one session
She [the parental involvement worker] didn’t seem to know what she were doing, to be honest, the lass who took it. So I think it were the first time she’d ever done it, so it were a bit, stood around outside basically, for half an hour, so didn’t really do much.
P10b
Four of the five parents were very positive about the PiP sessions. They saw them as fun for the children and commented on the variety of games and equipment that the children had enjoyed playing with during free play and in the PiP-PoPs. The two parents who had frequently attended the sessions identified how their children had developed over the 10 weeks, not only in initiating playing active games but also in developing confidence, learning colours, sharing toys with other children and making friends with children who would also be starting nursery in the following September. The wave 3 parents reported that they had received a piece of play equipment at each PiP session that they attended, which they then used at home.
The PiP facilitators also spoke about how they thought the children had enjoyed the sessions, offering examples of how children started playing with equipment whilst the facilitator was setting it up for the session and how they looked sad when the session ended.
Parents also spoke about the benefits to themselves of attending the sessions, namely making new friends, enjoying doing something with their child, being more active themselves and learning how to undertake active play with their child at home. One mother had enjoyed translating for the other parents. Parents did not talk particularly about the leaflets that they had received at the PiP sessions, with only one mother mentioning them (she could only remember the leaflet about what to wear in wet weather). Finally, the parent from wave 1 who had attended a few PiP sessions in the winter months observed that the sessions would have been better if more parents and children had attended.
The PiP facilitators also offered some suggestions of how parents had benefited from coming to the PiP sessions. They talked mainly about how they had seen parents develop in confidence in playing with their children, illustrated by them using the PiP-PoPs during the free-play sessions. One facilitator described how she had undertaken lots of modelling with parents at the start of the 10 weeks but gradually over time she had been able to do less as the parents knew what to do themselves. Two PiP facilitators also mentioned that these were parents and children who did not know each other before attending and so it was nice that they had met new people. Facilitating the transition to nursery was also mentioned in this regard. Finally, the wave 2 and wave 3 PiP facilitators spoke about the play equipment that the parents received for attending the sessions that they could then use at home, a further perceived benefit of participation.
Reasons for not attending the intervention (Boxes 9 and 10)
Of the parents from the intervention arm who were interviewed, four had not attended any PiP sessions, two had attended ‘a few’ sessions, two had attended regularly and two (parents of the same child) attended one session. Parents were asked directly why they had not attended the PiP sessions and why they thought other parents may not have attended. The PiP facilitators were also asked for their views on the reasons for low attendance to the sessions.
One time I had an appointment.
P04
Didn’t go to any as my daughter was in hospital for several weeks at a time.
P03
Bug that has gone through all three kids, me and husband so a good few weeks we were affected by that.
P05
I will not be going this time as I don’t work at the school any more and don’t want to go there.
P04
I missed some because one of my twins has asthma and can’t be out in the cold.
P04
Yeah they all call sick, I mean they’re [the children] always picking up things.
F02a
Timing and location of the sessions
My daughter is in nursery until 11.45 and then she needs to nap when she gets home, so hard to get to afternoon session. This term I will ask nursery if I can take her out 20 minutes in the morning to do the exercise, should be ok as it’s at the same place.
P05
To be honest what puts me off is the first session is 8.50 to, I think it’s 9.20. Yeah what put me off, the timings. Because mine don’t go to [name of school where PIP sessions run] I wouldn’t be able to get there while just sort of 9 and that would be the session I would prefer to do . . . the afternoon’s not that good because a lot of times she would go to sleep as well.
P09
Yeah ours [PIP sessions] are in the mornings because I prefer it like that, ‘cause I come and drop my eldest then I take, bring [name of child] with me in the mornings and we join the sessions.
P13
But apparently the thing is [name of child’s] Mum said that the afternoon sessions don’t work out good for her because I think he’s be, he’s asleep or something like that.
F03b
So there are kind of reasons, you know, for, for other parents not being able to attend because of work commitments.
F01
Thursday afternoon seems to be the worst one for some reason, that’s, I think I’ve had two Thursday sessions where nobody’s attended.
F05
Because mainly we thought of that time because on a Thursday, Thursday afternoon, we got [name of other activity] from 1 ‘til 3, so initially we have 12.30 ‘til 1 [for PIP] thinking on a Thursday, any that did come hopefully may stay for the whole session for, or at least part of the session for the [name of other activity], but that didn’t really work. So [F03a] said to try it half 11 so that, people coming out of nursery could come in, or people coming to nursery could come half an hour before.
And has that worked better?
No it’s just the same [laughs].
F03b
Yeah she comes Thursday twice . . . because she works the rest of the days, so she gets her three in by doing that, yeah.
F03a
I think the timings are very, have really helped with my numbers. I think if they’d have been later on then we wouldn’t have as, as many as we have had.
F05
Nursery have been good ‘cause one little boy on the study, he is in morning nursery but nursery let him come out for the first half an hour to do PiP with his Mum.
F04
The weather
I think it’s the weather, because I, I keep thinking they’ve started this at, at a ridiculous time. Mind you it is March and I suppose you might not expect this [laughs]. But when it first started I think it were January and it were freezing, and it was snowing, and I’m thinking well people aren’t gonna turn up, it’s just so cold, to be stood outside for half an hour in the freezing cold. Maybe sort of end of March/April time might have been a bit better time to start it. And, I, I think you’d probably find a lot of people think that.
P09
I am not bothered by the weather. We go out in all sorts and I like to get out of the house.
P03
Some parents said it was too cold to stand around. It’s OK for me as I have two to chase round all the time, inside would be better.
P04
It’s just the bad weather and children being ill, nothing you can change. Giving vouchers for parents to come might work but it isn’t why parents haven’t been.
P05
I think there was a couple of the, the sessions where it involved the parents actually sitting on the floor, and I think again that was something they wouldn’t really want to do when it was so cold and possibly wet, do you know what I mean?
F01
I think it’s ‘cause of the weather. We had two parents that came out of them that didn’t come back again, but that day they came it was absolutely freezing.
F03a
Yesterday afternoon I had nobody turn up and it was absolutely, I mean it could have been ‘cause it was absolutely scorching.
F05
The attendance was a problem ‘cause of the time of the year. The weather played a huge, a major factor in the parent, getting the parents to attend. Any adverse weather and attendance fell there. If a similar project was to be run again it would be better in the summer.
H01
Did not know about the sessions
Do you know, I weren’t even told about that, I didn’t get a letter, nobody phoned me. I could have took him but no one told me.
P11
But most parents have kept the excuse, oh we didn’t know [about the PiP sessions]. But we’ve got their mobile numbers, so we text ‘em on a Friday night, and then on a Monday, on a Monday the text goes out again to remind ‘em that they’ve got a PiP session, so they can’t say they didn’t know.
F03a
If I’ve had a bad week for attendance first thing Monday morning after the first PiP session, if I’ve time I will sit down and ring non-attenders and ask for reasons. I mean I have had, I think its three that haven’t answered phone calls or replied to messages and haven’t been to one session, so they’ve just vanished basically.
F05
More flyers going out, posters up, people to talk to them before it actually started, I think that would help a lot. Yeah, have maybe a meeting before the thing starts, and have bilingual staff there to explain to them exactly what it is. Maybe show things to them, you know, like the PiP-PoP cards or something, you know, some visual stuff. You said about a DVD before. Maybe something like that for the parents, to say, look, this is what we’re gonna be doing, something for them to see.
F02a
But you know, all in all, you know going through everything that they were expected to do [for the PiP study] and the time that they were expected to give up, it wasn’t a big surprise actually. I think it was when there was a mention of home visits, as soon as that, that became, you know, something, that was a requirement of the, the research. We had quite a few parents that, that seemed to back off.
F01
They were kind of in an area where there might be other people that could see, you know, I, I’m just thinking of other ways. You know, maybe if it was inside . . . in a big, maybe a big hall or something, where I know it wouldn’t be other people walking around outside, that could be something that might have appealed to the slightly more.
F01
You see that, that could be some of the problem that we’ve had getting the parents here, because at the beginning it was different people running the session, and they didn’t know the parents as well and, you know, visa versa.
F02b
General reluctance to take part in school-based activities
It’s the not understanding things and being a bit wary.
F02a
Because when we put events on or we invite them to things, we do provide things like refreshments . . . for no charge . . . we sometimes put raffles in and encourage them to come, because they’ll get a free raffle ticket and we do get a handful of parents then . . . So it’s kind of swings and roundabouts.
F01
I do think some of them have been, do you know, when they first got the voucher for the belt, I think once they got that, a few, not all of them, a few of ‘em have just decided, well I won’t bother now, I’ve got me voucher.
F05
Do your parents typically get involved in, in initiatives that you run at the school?
It’s not the split between the Bangladeshis and Pakistan, Pakistanis, it’s the, the diverse range of, of parents and what they actually do with their children. So we’ve got parents that are absolutely fantastic, you’d say had sort of middle-class values for their children, high aspirations, lots of work done at home, really strong family units, really through to the really deprived end of the scale where parents spend very little time with their children, very little time together some of the families. I mean they, they sort of work in shifts, some of the dads work in restaurants and don’t get home till 3 o’clock in the morning and then take the children to school and then they go to bed, and then they don’t see the children again, you know. So it’s the deprivation factor rather than where the children are from, which is, is the real barrier. So it’s those, those are the children, those are the parents that we need to work with, those that . . .
H01
Parents offered a variety of reasons for not attending the PiP sessions. Some of these were related to family issues rather than to the PiP sessions, for example competing priorities or the child and/or other family members being ill. One mother also described stopping attending as she no longer worked at the school and did not want to go there. This parent’s child had asthma, which also deterred her from attending as the child was unable to be out in the cold. The PiP facilitators also acknowledged that lots of children were unwell in the winter months.
The timing and location of the PiP sessions were also discussed by several parents, particularly in the context of their children’s routines. Some parents talked about the afternoon sessions clashing with the time that their child would be having a nap whereas for other parents the sessions clashed with child-minder days or nursery; one mother said that she would ask if her daughter could leave nursery 20 minutes early to attend PiP sessions. Another parent (who had been recruited to the study through a children’s centre) had children attending a different school and so could not get to the sessions in time. The PiP facilitators also alluded to difficulties with the timing of the sessions for some of the parents, particularly mentioning children’s nap times and competing commitments of full-time employment and English lessons (for South Asian parents). They were able to identify the sessions that were less popular and in one school they had changed the timing of the afternoon sessions so that they did not clash with a particular activity running at the nursery: however, this did not improve attendance.
For the parents who attended regularly the timings and location worked as anticipated, linking with school drop-off and pick-up times. One of the facilitators described how one mum had ‘made it work’ by attending two sessions on one day each week to fit all three sessions in around her employment. One of the PiP facilitators in a wave 3 school, where attendance at the PiP sessions was better, commented that the timing of the sessions worked well. Another described how the nursery had been flexible in letting a boy come out of nursery to attend the PiP session.
The bad weather was discussed by all seven intervention arm parents in waves 1 and 2 and was offered as a reason why ‘other parents and children’ may not have attended. Interestingly, although none of these parents had attended regularly and four had not attended any sessions, they did not see the weather as the reason why ‘they’ themselves had not attended. The PiP facilitators also talked about the negative influence of the weather, suggesting that it was to be expected that parents did not return when they had been sat on the cold, wet ground outside in ‘freezing’ weather. A facilitator in wave 3 described the opposite problem of parents not bringing their children because it was too hot. A head teacher from a wave 1 school also alluded to the cold weather as a reason why parents in his school had not attended.
Finally, two parents said that they did not know about the PiP sessions and would have gone if they had known (the PiP facilitator at this school said that she had telephoned these parents on several occasions to encourage them to attend). In fact, it was clear from the interviews with all of the PiP facilitators that they had regularly texted or telephoned parents to try to encourage them to attend and they did not accept that parents were unaware of the PiP sessions.
The PiP facilitators offered some additional reasons why they thought that the parents had not attended the PiP sessions (which parents themselves did not mention). Some were related to the study, namely a lack of promotion of the study at the schools, the ‘burden’ of the measurement sessions and that these sessions might involve home visits, the embarrassment of being watched doing the PiP sessions in the playground and the challenge of bringing two children to the sessions. In one school there had been a staff change and the facilitator who took over the running of the sessions suggested that, because of wider timetabling issues, the original facilitator did not know the parents very well, which did not help with attendance. Another facilitator also commented on the importance of knowing the parents and that the ones who attended were the ones that she knew and the ones who had not come she did not know.
Finally, the other reasons related more to a general nervousness of parents and reluctance to take part in school activities. One facilitator described how the school relies on incentives (e.g. refreshments) to encourage parents to come to events. Related to this was the suggestion by two PiP facilitators that parents had attended only to receive the gift vouchers and that once they realised that these were only for the measurement sessions they had stopped coming. Both of the head teachers who were interviewed spoke about the children who would most benefit from attending being the ones whose families are the most difficult to engage in school activities.
Acceptability of the maintenance sessions (Box 11)
Following 10 weeks of PiP sessions led by a PiP facilitator, the next term’s sessions were to be led by parents, without supervision. PiP facilitators were asked in their interviews whether or not they thought that parents would continue to attend once they were no longer leading the sessions. Two PiP facilitators were not confident that the sessions would work without them being there because they believed that someone needed to take the lead. Another two facilitators were more positive because they thought that there were some parents who were regular attenders who were very capable of running the sessions, but they were less sure that parents with less confidence would continue to attend.
And you know it’s on and you know it’s there, because they can see me out on the playground, ‘cause most of them know me anyway from other things, and I think they just feel like there’s someone there to guide them really.
F04
I think we’ll definitely get the ones, the couple that were always coming, but I don’t know about the others, we’ll have to really give it a big push, see, try and get them to come, won’t we?
F02a
The parents that I have that come to most sessions, they would be really good at organising that, I know they would, they’d be, I’ve already started talking to them about it, ‘cause they are still gonna come for some of the sessions they just can’t guarantee all three with the boys being in nursery in the morning. So I think they’ll be absolutely fine with that, but the parents that I would be left with, I think, I think they’d be OK after a little bit, a while, they’re not as confident as the ones that I would have liked.
F05
I think it would because we know how to play these games now. Sometimes [facilitator] she’s like, oh once or twice she didn’t attend it, but some other teacher attended, so we were actually telling that teacher, oh this is what we have to do.
P14
The likelihood of the PiP sessions running in the maintenance phase was also explored with parents interviewed in wave 3. Both parents, who had attended regularly, thought that the maintenance sessions could work because as a group of parents they now knew what to do. These were the same parents who the facilitator had identified as being capable of leading the sessions.
Objective 7: fidelity of programme implementation
Adherence to the intervention protocol was assessed at each of the five intervention schools. In total, 10 observations were undertaken but only eight of these are included in the summaries as on two occasions there were two individuals making independent observations on the same session. For these repeated observations the average scores on each component were calculated. A summary of the fidelity scores across the five key intervention factors is provided in Table 24.
| Fidelity component assessed | Mean (SD) | Median (min.–max.) |
|---|---|---|
| Delivery as per manual | ||
| Welcome and 5 minutes of structured play | 3.69 (0.46) | 4 (3–4) |
| Encourage families to seek other physical activities on non-intervention days | 2.13 (1.09) | 1.75 (1–4) |
| Information on guidelines for physical activity for under 5s given | 2.00 (1.41) | 1 (1–4) |
| 5 minutes of structured play and goodbye | 3.44 (1.05) | 4 (1–4) |
| Total score | 11.25 (3.30) | 10.25 (7–15) |
| Supervision | 3.56 (0.73) | 4 (2–4) |
| Support given to parents | 3.31 (0.96) | 4 (2–4) |
| Encouragement of children | 3.81 (0.37) | 4 (3–4) |
| Infusion of play equipment | 3.56 (0.50) | 3.75 (3–4) |
| Total fidelity score | 29.13 (5.74) | 29.50 (21–35) |
As shown in Table 24, there was good adherence for most of the key intervention factors assessed. Two factors that had poorer adherence were encouraging families to seek other physical activities on non-intervention days and providing information on guidelines for physical activity for under 5’s. The mean total fidelity score was 29.13 (SD 5.74) out of a total possible score of 36, highlighting overall good adherence to the intervention protocol.
Objective 8: capability and capacity of schools to deliver and incorporate the intervention within existing services
Playground and local environment
Table 25 displays the summary statistics of the playgrounds and local environments of the schools by trial arm and overall.
| Characteristics | Intervention (n = 5) | Control (n = 5) | Overall (n = 10) |
|---|---|---|---|
| Playground surface, n (%) | |||
| Concrete | 3 (60.0) | 4 (80.0) | 7 (70.0) |
| Concrete and rubber | 2 (40.0) | 1 (20.0) | 3 (30.0) |
| Fixed equipment available | 3 (60.0) | 3 (60.0) | 6 (60.0) |
| Grassed area available | 4 (80.0) | 2 (40.0) | 6 (60.0) |
| Playground markings | 4 (80.0) | 5 (100.0) | 9 (90.0) |
| Covered area | 3 (60.0) | 2 (40.0) | 5 (50.0) |
| Location on school site, n (%) | |||
| Nursery | 3 (60.0) | 3 (60.0) | 6 (60.0) |
| Primary | 2 (40.0) | 2 (40.0) | 4 (40.0) |
| Proximity to busy road (metres) | |||
| Mean (SD) | 375 (362.7) | 116 (118.4) | 245.5 (288.7) |
| Median (min.–max.) | 325 (0–975) | 100 (0–300) | 187.5 (0–975) |
| Proximity to local park with fixed play equipment (metres) | |||
| Mean (SD) | 346 (350.7) | 402 (327.5) | 374 (321.3) |
| Median (min.–max.) | 275 (75–950) | 500 (50–850) | 287.5 (50–950) |
In total, 70% of schools had a concrete playground surface, 60% had fixed play equipment and 60% had a grassed area available. Playground markings were present in 90% of schools, 50% had a covered area in the playground and 60% were located in the nursery. The average proximity to a busy road was 246 (SD 289) metres, with a median proximity of 188 (minimum–maximum 0–975) metres. The average proximity to a local park with fixed play equipment was 374 (SD 321) metres, with a median proximity of 288 (minimum–maximum 50–950) metres. There were large differences between trial arms in the average proximity to a busy road and the average proximity to a local park with fixed play equipment, with the intervention schools being further away from busy roads and in closer proximity to a local park with fixed play equipment. However, the number of schools in the comparison is low.
Head teacher views on the capability and capacity of schools to deliver the intervention (Box 12)
When asked about the capability and capacity of the school to deliver the PiP intervention the wave 3 school head teacher explained that it had taken a little time to organise the timing of the sessions and that a building project that was happening at the time had reduced the space available. Both head teachers described how they had incorporated the work into their staff’s existing workloads. One head teacher was clear that he viewed this as a cost to the school because it took that person away from their normal work; furthermore, this member of staff was more senior than a nursery nurse. The other head teacher described how the school was well staffed with a good budget so this was less of a concern. For different reasons neither head teacher saw delivering the intervention to be sustainable in the long term. The first head teacher stated that the Born in Bradford programme would need to provide staff to continue to deliver the PiP sessions. The second head teacher explained that parents at her school do not ‘stick with’ any initiatives for very long and so the PiP sessions would need to recruit new families continually to run long term.
There was a little bit just getting the times, you know, the time slots organised, but once we got over that that worked OK. We were in the middle of a building project at the same time, so that was a bit difficult for space, you know, for, for where the children could, you know, use the, the usable space; that was a little bit of a worry. But, you know, we got over it.
H02
Staff roles and costs
Well, I mean it, it was a 12-week project so it wasn’t particularly a, a long period of time. We provided a couple of members of staff to keep the project running, a nursery nurse and our [Special Educational Needs] SEN teacher. The two members of staff spent half, about an hour a week for 12 weeks, so, I mean it had got a cost to the school in, in what we were actually doing, quite a high cost really. It did take ‘em away from their normal job, so yeah. I mean obviously the SEN person, they’re a senior member of staff so I mean they’re, they’re more expensive than a nursery nurse. On the whole, the project did impact on children and staffing at [name of school].
H01
Well we already had a PIW [parental involvement worker], we already had our PIW, so we just, it was just part of her role. So we just, we just modelled it round, because, you know, we, we do that often, we look at, you know, what, what our staff do, and if there’s anything that we think’s worthwhile them doing, we can easily move their, their role around, ‘cause we are quite, we’re quite well-staffed here and we’ve got quite a good budget. So, you know, you, you look at it and you think well 6/8/10 weeks for an hour a week, yeah, it’s the cost of an hour a week, but, you know, we’ll just do it and hopefully it’ll have some impact.
H02
Sustainability
Born in Bradford would need to provide more staff in the future should the project run again.
Rather than rely on you providing the staff?
Yeah, all the time, yeah. So it’s, it’s more of a partnership thing.
H01
Certainly, I don’t think anything for us long term is, is viable, because the parents, a bit like the children, have a bit of a short attention span . . . because once, once they’ve been doing something for a little while, they’ll not stick at it. But if it was a 6-week course, you know, a start, a finish and a goody bag at the end, or a whatever at the end, you know, and a cup of coffee and a biscuit before they finish, that sort a thing, a short burst of activity, and then maybe a few weeks or half a term off and then start again, I think that’s better for our parents . . . and then, you know, maybe get some new people joining in as well.
H02
Benefits to the school (Box 13)
The head teachers identified some benefits of the PiP intervention for their staff as well as for the families. In terms of the staff, one head teacher commented that they now recognised the importance of encouraging parents to play outside with their children and were going to build this more into the nursery programme in the next year using the PiP manual, which was identified as being easy to use (see Preschoolers in the Playground facilitators views’ on previous experience, training, the Preschoolers in the Playground manual and follow-up support). The other head teacher described how the parents who took part were engaged in playing with their children. She also mentioned better attendance at nursery and more ‘engaged’ parents this year, which she said might have been related to those children attending the intervention.
The project made the nursery staff more aware of the work that needs to be done with parents playing outside. Parents do not seem to realise the importance of play. Nursery will be looking into encouraging parents to play next year. The facts received from Born in Bradford have been very easy to follow and these will be able to be used in the future to encourage nursery parents.
H01
Impact on families
Certainly the parents that were engaged, you know, they were, they were active with children, and they were doing, you know, you know, things that they would never have done, ideas for sort of ball games and play activities and just other people are modelling good language. So it’s all very subjective really, but what, what I can say is the children that have come into our nursery this year, whether it’s just because more parents are working, but their attendance is better. So I, I can’t say it was the project, ‘cause I don’t know exactly who was all on the project now, but certainly the, the parents are coming to us, you know, they, they’ve been more involved with their children’s learning this year.
H02
Suggestions for improving the intervention (Box 14)
The head teachers were asked for their thoughts on how the PiP intervention could be improved in the future. In responding to this both spoke about the importance of thinking about the types of families attending the schools. The first head teacher proposed more ‘joined-up thinking’ between health and education so that initiatives such as the PiP intervention are part of a more strategic, longer-term approach focusing on children from the most disadvantaged families. The second head teacher spoke about the importance of getting the ‘right person’ in to recruit to the study and conduct the measurement sessions, someone who the parents could relate to. She commented that the PiP staff were quite young and perhaps looked a bit ‘academic’.
Well I think it’s, the, the answer is for health and education to work really closely together. I would do absolutely anything to help you. But it’s about working with health visitors, children on the child protection register, children at risk and all those, that are known to health and education, but we don’t share enough information about those parents and what we’re going to do with them. So I think it needs to be far more focused. We’re, we’re probably not as strategic as we could be . . . a more focused strategic approach on the families that were in, in the poorest group that we thought we could have a real impact on, you know, I think it’d be an interesting study. But 12 weeks wouldn’t be, wouldn’t do it really.
H01
Ensuring that the staff are ‘right’
I, I think we’ve just got to be a bit careful who comes and runs them [the PiP measurement sessions], because if you’ve got both; I mean I can’t quite remember, but some of them were quite young, I think, that came to, to run the initial study, and that can be maybe the personnel both, you know, if they’re maybe young, youngsters out of uni, it’s a bit, oh gosh, look at them, who do they think they are, sorta thing. It’s just the location of us; we’re very white, white estate, predominantly free school, well 66% of our children free school meals, high area of unemployment, low self-worth, low self-esteem, you know . . . and I think you’ve just got to be careful personnel that you put into there. You’ve got to have sort of, you know, people with a little bit of life experience, say ‘Come on, have a go’ you know, rather than it look too aca, if it looks academic, you know, if it looks a bit academic, a bit high brow, a bit university based, it will turn some of our parents off. If it’s quite low key, you know, a little bit of information and this is what we’re doing, that works better for us.
H02
Preschoolers in the Playground facilitators’ experiences of delivering the PiP sessions (Boxes 15 and 16)
All of the PiP facilitators said that they had enjoyed running the PiP sessions, with those in the wave 1 and 2 schools suggesting that it would have been better had more parents attended as this would have created a different atmosphere.
The PiP facilitators were asked to describe how they had delivered the PiP sessions, reflecting on how they had used the suggested format (in the training manual) of warm-up, PiP-PoP, free play, PiP-PoP. What emerged clearly was that they had been flexible in their delivery, using their experience of working with children as well as getting to know the children to adapt the activities. Half of the PiP facilitators explained that they would decide when to initiate the free play and PiP-PoPs according to how engaged (or not) the children and their parents were. Specifically, they did not break up free play ‘for the sake of it’ if it was going well, and conversely the PiP-PoPs were used as a way of re-engaging the families when they appeared bored during free play.
A number of factors informed which PiP-PoPs the PiP facilitators chose to use. Most important was what would work for the children in terms of the number of children in the session, their ages (associated physical development and concentration span) and their mood, as well as what would promote learning. All of the PiP facilitators could name the PiP-PoPs that the children in their sessions most enjoyed and they commented that they used these the most often and adapted them when they did not work. The popular PiP-PoPs were the statue game, the spaceships and planets game, Mr Crocodile, chalks and water painting, balancing along the skipping rope, the hula hoop and throwing balls. Finally, two of the PiP facilitators explained that they had started off using the PiP-PoPs that they felt most comfortable with and which others talked about, taking into account how the parents were responding to the activities.
It’s been interesting and it’s been enjoyable.
F04
I really enjoyed doing it, but I just really wish that there’d been more parents come, ‘cause it would’ve been a, a completely different atmosphere.
F02a
Flexible approach to the whole session
I’ve just been flexible with it. As long as they get a PiP-PoP, they have a play, we have a little bit of a chat, encourage the parents, in my eyes that is covering everything that the manual’s asked me to do.
F04
So, you know, we, so it, sometimes, as the time went on, and you got to know your children you also got to know their likes and what they liked doing.
F03a
I didn’t always do the PiP-PoP straight away, I’ll do it halfway through because when they’re coming in . . . rather than me stopping them from exploring and finding what we’ve put out, I just want them to go and just have a play.
F03a
If they do start, if I feel that they’re starting to get a bit bored and fed up and that the parents are getting bored, I pull ‘em all together again.
F04
Adapting the PiP-PoPs to the children
I do start off with a PiP if I have more than two children; if I have less than two I tend to do a smaller PiP, do you know like the jumping lines and things, and buzzy bees, we just adapt it to fit the lesser numbers. With the bigger numbers the ball rolling is really popular especially when we all join together and make a big circle.
F04
Some will play it [the PiP-PoP] for a long time. Some will play it for a short time. I’ve tried to like free, flow freely, because there’s a difference between your 2-year-olds and your 3-year-olds. Some of the 2-year-olds, it’s quite hard to do some of the organised games with them because they just want to run around.
F04
I think it’s looking at the children’s stages and ages, and then thinking which’d be suitable for, you know the children that are coming and then you know at which PiP-PoP is suitable for them and which of them you’ll know that they’ll be able to do. Cause there’s certain ones in there that I don’t think some of them children might be able to do, but there’s no harm in trying them to see if they do work.
F03b
I tried the river hopping one and the, the, the children were just stood there watching me and the parents doing it [laughs] which is good, we were modelling it [laughs] but yeah . . .
Was it too advanced for them?
Yeah, yeah, so, because I, I tried the, the rope, well I’d obviously put it too far away, at first, so it were kind of, made it, but I don’t think the concept of jumping over the river was, it, they just didn’t get that one.
F03a
Depending on the children’s moods as well, Monday morning can be very hard, you can have lots of grumpy toddlers [laughs] and they’re not the easiest of age range to get together to do an activity. So sometimes some do it [the PiP-PoP] and some play alongside with their parents.
F05
And the hopscotch, I’ve just recently introduced that, they haven’t, it’s the, it’s not, I keep putting it out ‘cause I do think that, I find that a good one because it introduces numbers and things and, and jumping and things like that.
F04
Favourite PiP-PoPs
The statues . . . we always did that first . . . we returned to ones [PiP-PoPs] that I knew they’d really enjoyed, so did that again . . . I think they like the chalks and the, the painting . . . ‘cause we got a nice big board for them to do that on and I think they enjoyed that. They enjoyed the sort of balancing along the skipping rope as well . . . And the balls, they loved the balls, passing balls . . . the buggies and the dolls, and they liked that yeah.
F02a
They really like the spaceships and planets game . . . They do, they like quite a lot. Surprising they like Mr Crocodile on the wall.
F04
But you see I, you see some of the PiP-PoPs I keep for the play, like the water painting, they love the water painting and the, the hula hoop, they, they find that, and the throwing the ball as well.
F03a
PiP-PoPs that facilitators feel confident to deliver
The first, the first, the first couple of weeks I chose the easy ones and that were fab, like the I-Spy which I thought, although that was easy.
F03a
Adapting the PiP-PoPs to the parents
I’ve tried to be flexible how I’ve run the sessions depending on how the parents are responding.
F05
The PiP facilitators talked about using a wide range of equipment during the PiP sessions. Some of this was required equipment highlighted in the PiP manual, for example hoops, balls, beanbags and skipping ropes. Other pieces, including a ‘windy box’, a climbing frame, a trampoline and a sand pit, the PiP facilitators introduced themselves. As with the structure of the PiP sessions, it was clear that the PiP facilitators thought carefully about which equipment they used, introducing additional equipment when the children were no longer engaging with the equipment already set out for the session, and using the same equipment that the children were being given to take home and use so that the parents and children had some ideas of how to play at home.
As part of the PiP sessions the PiP facilitators were expected to guide discussions each week and to give out a handout. These handouts focused on matters such as giving praise and encouragement and why active play is important (see Chapter 1, Guided discussions and handouts). For many of the PiP facilitators it was evident that the handouts did not feature heavily in the sessions. Indeed, one facilitator said that she did not remember seeing the leaflets and another stated that it was hard to get a discussion about the handouts going within the sessions. Others described how they had thought about which handouts to distribute, deliberately staggering the distribution of the handouts to not overload parents with too much information and ensuring that parents received the handout about what to wear in different weathers when the weather was particularly hot.
The PiP facilitators described varied parental responses to the handouts, with some parents asking questions and others ‘pulling a face’ and putting the handout in their bag. Two PiP facilitators said that some of their parents were not very confident about physical activity and that the handouts did contain new information for those parents. Another facilitator thought that it was her ‘more capable’ parents who engaged more with the handouts. The ‘Active parents have active kids’ and the ‘What to wear for outdoor play’ handouts were those most frequently mentioned as being liked by parents.
I got the windy box out once, ‘cause it was really windy. ‘Cause it’s got all stuff that blows in the wind, you know, like windmills, bells that you can hang up, and they really like that box ‘cause they can be running around with it. If you run it’ll turn.
F03a
There was obviously the hoops, there was balls, beanbags, skipping ropes. There were things already in place in the outdoor area, there was one of the rickety bridges. I can’t remember the technical term for those [laughs] but things they can climb on and the balancing beams and the stepping stones, you know, so the things already fixed within the area.
F01
Introducing additional equipment
Depends if they were going back to their mum or not, and just, just looking, you know and not taking notice of anything that was out there, or if I’d start, say if the balls were out if they were not kicking the ball, or if I was kicking the ball and they were just ignoring it, then sort of, right, it’s time to go get something else out [laughs] just to get their interest again really.
F03a
Handouts
I don’t remember seeing the leaflets, but it could have been [name of other facilitator] that, that did that, I’m not sure.
F01
No, because generally we don’t, I give them to take home. I explain a little bit what it’s about, but I’ll leave it for them to read at home really, and there’s not been a lot of feedback. But I have, for the first few weeks did ask them, did you get last week’s, have you got this one, just talking about making, at the beginning we started to talk about make sure you’re dressed appropriately and things, which is the week 1 leaflet. But it’s just very hard to do all those things in a session.
F04
The hand-outs, we, we didn’t actually give all of the handouts out. We gave some of them out and talked to the parents about them. I’ve still got some spare ones there so I could always hand them on afterwards as well. But yes, they were, they were really good, they were really informative, nice and simple. Yeah, I quite liked those . . . Yeah, well we handed out a couple, two or three I think, and we, I didn’t do it every session ‘cause I thought it would be too, too much information all at once, it was kind of like every week or every other week, because obviously we didn’t have a lot coming either [laughs]. So it was basically when they were there grab one, talk about the handout and, you know, and then take it home. But yeah, I think they were very good, the handouts, I liked them, yeah.
F02a
And is there a sort of timetable for giving out the leaflets or is it up to you?
No, not in the manual, it’s entirely up to me, they’re not in any order, yeah.
So how have you decided?
I’ve gone with the weather actually because the, the first leaflet I gave out was dressing for appropriate weather, eating well, so depending on, like this week with the weather as well, with it being hot, I’ve got the what to wear as well, I’ve got that one back out again and, do you know, ‘cause we, we have had a few that didn’t come at first but then they’ve started coming in the last week. So it’s just knowing, do you know, keeping on top of who I’ve given what and then remembering and touching base with the ones that haven’t had that leaflet.
F05
Yeah. They were fine. Yeah, they, they asked a few questions about some of them, the clothing one and things like, and things to eat, and stuff like that. Yes, yeah, they were quite interested. So I think they were really good.
F02a
Some, some of them find ‘em really informative, but, I mean I have some really experienced parents as well who, who just, do you know, have a look, pull a face and put it in their bag, but [laughs].
F05
Do you know it, it makes for a good discussion, we can talk about it, and I mean especially the, the adults ball of exercise, you know, with the house, the housework being a big chunk of that exercise, that always gets some good conversation going, yeah.
F05
So some of our mums are not very confident with things, and so they did, which is really good, they do ask, don’t they, they do ask us?
F02a
And do you think that it’s new information for these parents, new ideas?
For some parents, whereas some parents may be all, doing it all the time but not realising that they’re doing it, and it’s making a big difference. Like some basic stuff as praise, they don’t know that they’re constantly doing that with their child, sometimes giving that praise, but whereas having that leaflet they’re just thinking I do that naturally, it’s just, it’s just there.
F03b
Preschoolers in the Playground facilitators views’ on previous experience, training, the Preschoolers in the Playground manual and follow-up support (Box 17)
The PiP facilitators were asked what types of skills and experience someone would need to run the PiP sessions. All of them talked about the importance of having previous experience of working with children and their parents. It meant that they were confident in leading the sessions, could ‘think on their feet’ and could adapt the sessions when needed, as well as having a good rapport with children and parents. One facilitator said that it was important to enjoy working with children. Several also explained that it had helped that they already knew many of the families coming to the PiP sessions through working at the nursery and running baby yoga. The PiP facilitators did not think that they had needed to have previous experience of physical activity because that was provided in the training and manual. Indeed, without exception the PiP facilitators described the training session and the manual as helpful in providing them with useful information, ideas and confidence to deliver the PiP sessions in a flexible way. A few acknowledged that the brief training, which really ‘just involved working through the manual’, was sufficient because they were already experienced in working with children. They also valued the offer of follow-on support from the PiP research team, although no PiP facilitators mentioned accessing this.
At least knowledge or experience of working with parents and children, being able to think from the top of your head as well, being able to, ‘cause it’s OK doing a PiP-PoP but if its, if something not’s going right that you’re able to think quite quickly how to, to move it on . . . but also enjoying playing games yourself really [laughs]. I facilitate baby yoga here and I do a lot of work in the nursery. So I do know quite a few of the parents and I, I am quite confident on speaking to them and getting them to do things, so I felt, yeah I felt quite confident in doing it all and I’ve really enjoyed it.
F03b
You need to be good with children and work with children obviously, you need to be able to think on your feet and to be able to change things and adapt things.
F04
We’ve got rapport with the parents, ‘cause we’ve both been here a long time and we know the families quite well, so it’s nice that we’ve got that bond with them . . . I think that helped immensely. I mean if I, if we didn’t have the confidence, and then parents didn’t have the confidence in us, I, I phew, I don’t think it would’ve worked at all.
F02a
‘Cause it’s all in the manual, and the PiP-PoPs, it tells you all what to do so you don’t really need to have that much experience in the physical side of it.
F02b
Training and manual
Yeah, she went through it all, she, she had the book with her, or this book should I say, and went through everything quite detailed. Yeah, it were really, yeah, yeah, because at my first session, although I’d, I’d taken the book home and [laughs] gone through everything, but yeah, I felt quite confident the first, first couple of sessions of doing it because of what she’d, she’d gone through, yeah.
Is there anything else that we could have included in the training you think that would help to run the sessions?
Hmm, for me personally, no, it was OK, but then I’d got that little bit, I had that experience.
F03a
And how useful have you found the manual and the training?
Really useful, it’s really easy to read as well, it’s really informal and like, and all the time it’s saying, do you know, it’s not, nothing’s set in, in stone.
F05
The manual was really helpful as well, yeah, there was a lot of new ideas, a lot of information, it was, it was really simple and, and very easy to understand.
F02a
Follow-on support
Yeah. Well I felt that I could contact somebody if I needed to, about things, ‘cause the, all the information was in there again, in the manual, who to ring, the numbers and everything else, yeah. So yeah, I found that quite . . .
Was there anything that you, you did contact us about?
I don’t think so.
F02a
Objective 9: the effect of participation in the intervention on health outcomes and whether or not there were any differences between ethnic groups
Physical activity
The baseline physical activity measures are summarised in Table 26.
| Characteristic | As randomised, mean (SD) | As analysed, mean (SD) | ||
|---|---|---|---|---|
| Intervention (n = 55) | Control (n = 58) | Intervention (n = 29) | Control (n = 35) | |
| Minutes spent in MVPA per day | 64.2 (26.3) | 62.0 (22.9) | 65.6 (26.7) | 61.9 (23.7) |
| Minutes spent in LPA per day | 212.8 (44.1) | 212.6 (40.2) | 224.1 (41.6) | 219.2 (36.8) |
| Minutes spent sedentary per day | 317.7 (89.1) | 287.4 (64.8) | 342.8 (89.3) | 296.8 (61.5) |
| Minutes of TPA per day | 277.0 (60.2) | 274.6 (56.0) | 289.7 (57.2) | 281.1 (53.1) |
| Percentage of children spending ≥ 180 minutes per day in physical activity, n/N (%) | 53/55 (96.4) | 55/58 (94.8) | 29/29 (100.0) | 33/35 (94.3) |
The average time spent in MVPA per day was 63.1 (SD 24.5) minutes, in light activity was 212.7 (SD 41.9) minutes and sedentary was 302.2 (SD 78.7) minutes. The average total time spent in physical activity per day was 275.8 (SD 57.8) minutes and 96% of children achieved a total of 180 minutes or more of physical activity per day. Randomisation achieved balance across most measures. There were slight imbalances in the minutes spent in MVPA, in light activity and sedentary per day in the as-analysed comparisons, with the intervention group having slightly higher values for MVPA and light activity and being more sedentary than the control group.
Table 27 shows the physical activity data for participants at 10 and 52 weeks.
| Characteristic | Intervention, mean (SD) | Control, mean (SD) | Total, mean (SD) |
|---|---|---|---|
| 10 weeks, n | 44 | 43 | 87 |
| 52 weeks, n | 42 | 45 | 87 |
| Minutes spent in MVPA per day | |||
| 10 weeks | 61.77 (25.21) | 62.12 (22.88) | 61.94 (23.95) |
| 52 weeks | 72.62 (30.35) | 74.30 (25.46) | 73.49 (27.78) |
| Minutes spent in light activity per day | |||
| 10 weeks | 212.85 (39.44) | 200.43 (45.09) | 206.72 (42.54) |
| 52 weeks | 220.89 (37.44) | 219.14 (43.14) | 219.98 (40.26) |
| Minutes spent sedentary per day | |||
| 10 weeks | 317.96 (102.58) | 303.72 (68.99) | 310.92 (87.39) |
| 52 weeks | 335.67 (102.43) | 302.52 (65.59) | 318.52 (86.49) |
| Minutes of TPA per day | |||
| 10 weeks | 274.62 (49.26) | 262.55 (61.14) | 268.66 (55.46) |
| 52 weeks | 293.51 (52.04) | 293.44 (59.32) | 293.47 (55.60) |
| Percentage of children spending ≥ 180 minutes per day in physical activity, n/N (%) | |||
| 10 weeks | 44/44 (100.0) | 41/43 (95.3) | 85/87 (97.7) |
| 52 weeks | 41/42 (97.6) | 44/45 (97.8) | 85/87 (97.7) |
The mean number of minutes spent in MVPA per day was lower in the intervention group than in the control group at both 10 weeks [61.8 (SD 25.2) minutes vs. 62.1 (SD 22.9) minutes] and 52 weeks [72.6 (SD 30.4) minutes vs. 74.3 (SD 25.5) minutes]. The mean number of minutes spent in light activity per day was higher in the intervention group than in the control group at both 10 weeks [212.9 (SD 39.4) minutes vs. 200.4 (SD 45.1) minutes] and 52 weeks [220.9 (SD 37.4) minutes vs. 219.1 (SD 43.1) minutes]. The mean number of minutes spent sedentary per day was higher in the intervention group than in the control group at both 10 weeks [318.0 (SD 102.6) minutes vs. 303.7 (SD 69.0) minutes] and 52 weeks [335.7 (SD 102.4) minutes vs. 302.5 (SD 65.6) minutes]. Hence the intervention group appeared to be undertaking less MVPA and more light activity and to be more sedentary than the control group. The total number of minutes spent in physical activity per day was higher in the intervention group than in the control group at 10 weeks [274.6 (SD 49.3) minutes vs. 262.6 (SD 61.1) minutes] but the two groups were similar at 52 weeks [293.5 (SD 52.0) minutes vs. 293.4 (SD 59.3) minutes]. A similar pattern was seen for the percentage of children undertaking 180 minutes of physical activity a day at 10 weeks (n = 44, 100% vs. n = 41, 95.3%) and at 52 weeks (n = 41, 97.6% vs. n = 44, 97.8%).
Trial arm and ethnic group differences
Figure 3 and Table 28 summarise the accelerometer data by ethnicity. Different results are seen by ethnic group. For white children, the number of minutes spent in MVPA per day was lower in the intervention group than in the control group at both 10 and 52 weeks; however, for South Asian children it was slightly higher in the intervention group than in the control group at 10 weeks and very similar between the two groups at 52 weeks. Although these differences by ethnicity are demonstrated in the raw means, these results must be interpreted with caution, as there appears to be an imbalance in MVPA scores at baseline between the intervention group and the control group for white children for those included in the analysis (i.e. baseline and 52-week data) and these summaries are based on data for 18 white children (nine intervention and nine control children; see Figure 3). For white children, the number of minutes spent in light activity per day was lower in the intervention group than in the control group at both 10 and 52 weeks; however, for South Asian children the number of minutes spent in light activity per day was higher in the intervention group than in the control group at both 10 and 52 weeks. No differences in the number of minutes spent sedentary per day were apparent between ethnic groups. For white children, the number of minutes of TPA per day was lower in the intervention group than in the control group at 10 and 52 weeks; however, the reverse was seen for South Asian children, with more minutes of TPA per day in the intervention group than in the control group at both 10 and 52 weeks. All white and South Asian children were undertaking at least 180 minutes of physical activity a day at 10 weeks but at 52 weeks different patterns were seen by ethnic group. For white children the control group had a higher number of children undertaking at least 180 minutes of TPA per day; however, for South Asian children the intervention group had a higher number meeting the criterion.
FIGURE 3.
Mean minutes of MVPA per day at baseline and week 52 by group and ethnicity (white and South Asian). The top graphs include all children at each time point who provided enough accelerometry data. The bottom graphs include just the children who provided enough accelerometry data at both baseline and 52 weeks’ follow-up.
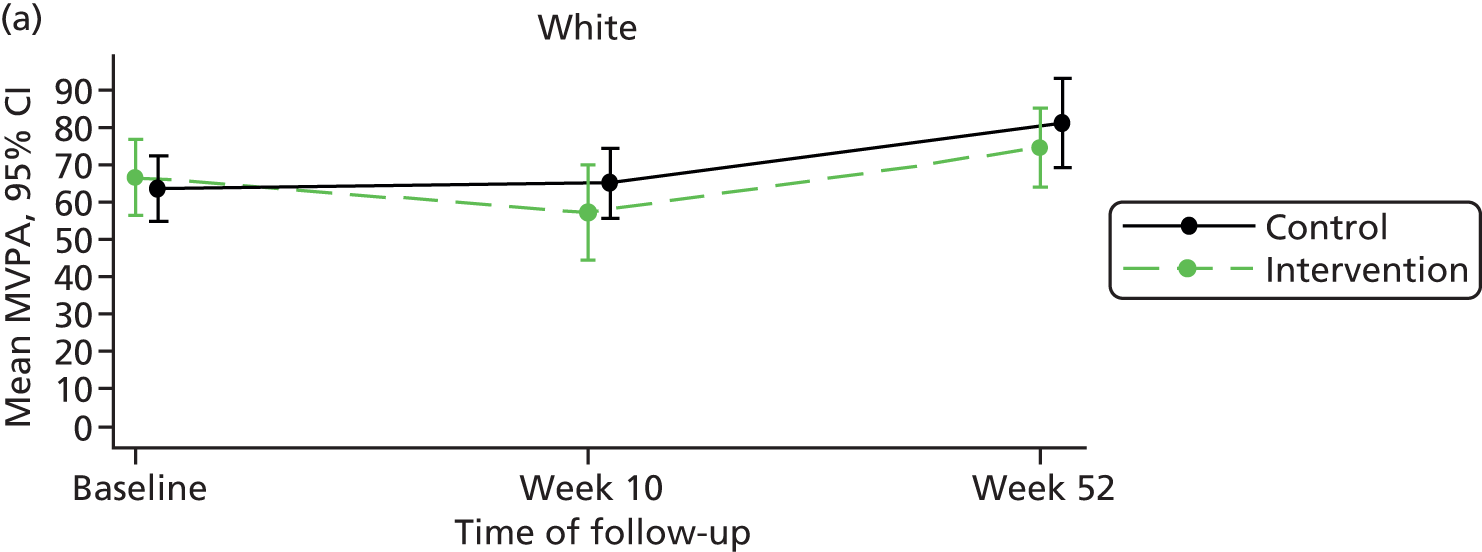
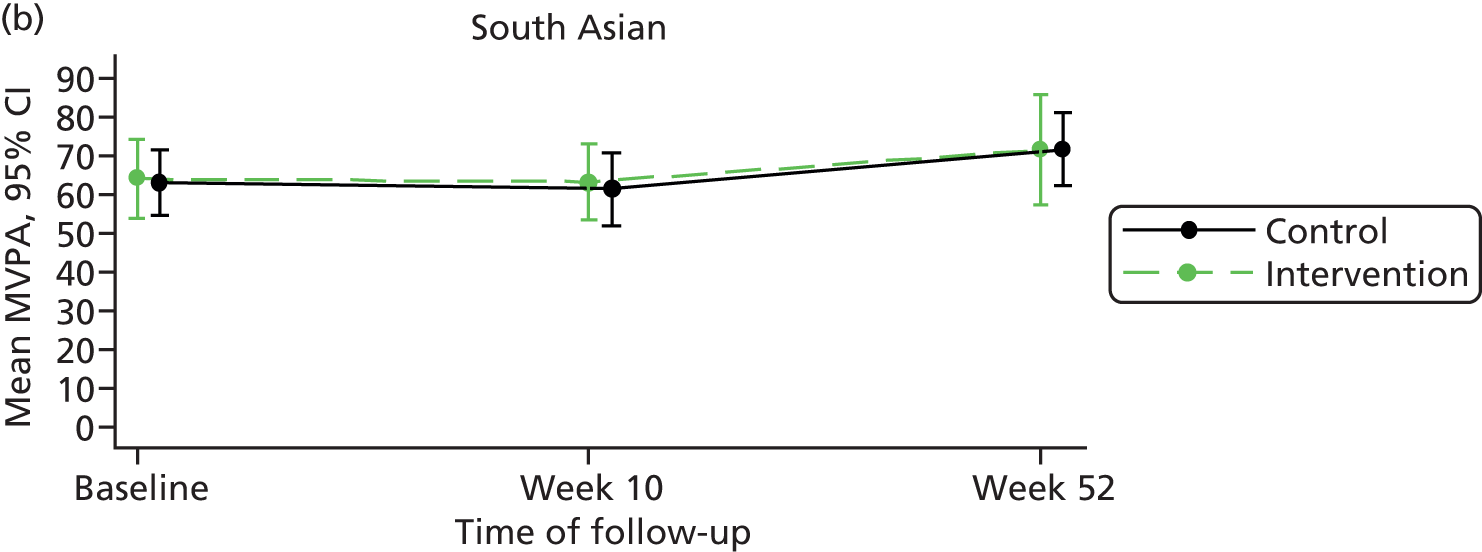
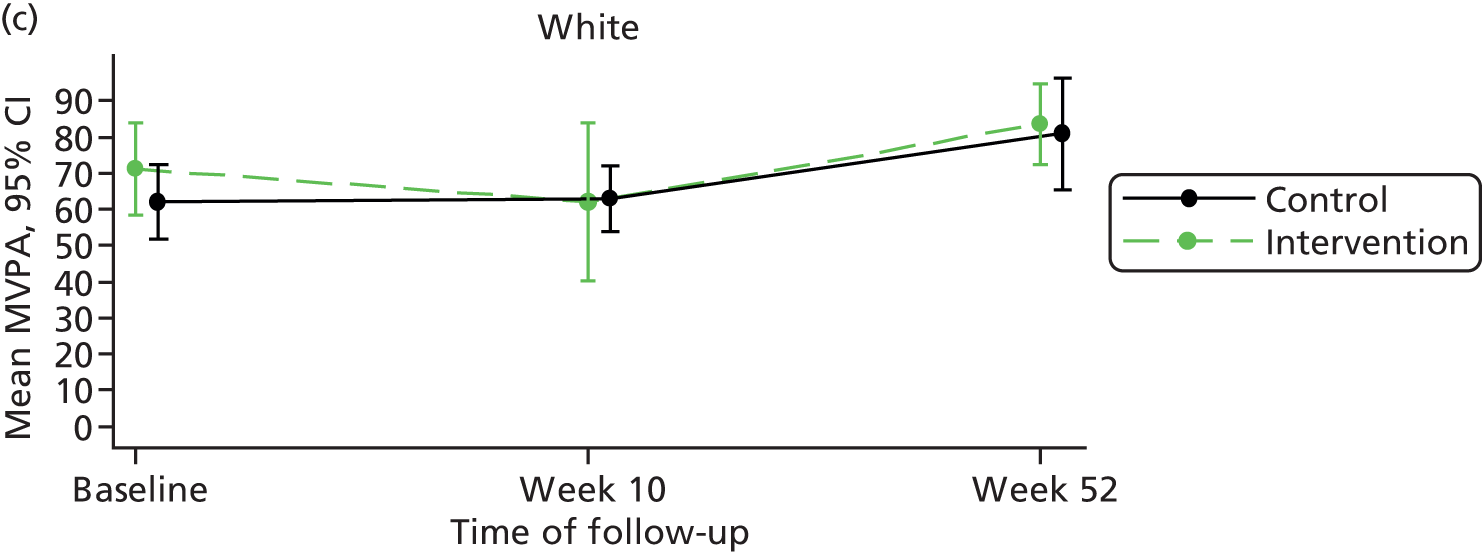

| Characteristic | 10 weeks, mean (SD) | 52 weeks, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Intervention | Control | Total | Intervention | Control | Total | |
| White, n | 14 | 14 | 28 | 16 | 12 | 28 |
| South Asian, n | 28 | 27 | 55 | 24 | 32 | 56 |
| Minutes spent in MVPA per day | ||||||
| White | 57.2 (24.6) | 65.0 (18.0) | 61.1 (21.5) | 74.6 (21.3) | 81.1 (21.3) | 77.4 (21.1) |
| South Asian | 63.2 (26.2) | 61.3 (25.3) | 62.3 (25.5) | 71.5 (35.3) | 71.6 (27.1) | 71.6 (30.6) |
| Minutes spent in light activity per day | ||||||
| White | 211.5 (43.8) | 212.5 (43.4) | 212.0 (42.8) | 219.7 (47.8) | 229.6 (37.8) | 224.0 (43.3) |
| South Asian | 213.2 (39.3) | 193.1 (45.1) | 203.3 (43.0) | 223.3 (28.9) | 214.0 (44.9) | 218.0 (38.8) |
| Minutes spent sedentary per day | ||||||
| White | 337.7 (111.7) | 313.4 (85.3) | 325.5 (98.3) | 334.2 (130.4) | 294.5 (78.5) | 317.2 (111.2) |
| South Asian | 308.9 (102.1) | 302.1 (50.5) | 305.5 (80.3) | 333.4 (86.5) | 304.2 (61.9) | 316.7 (74.2) |
| Minutes of TPA per day | ||||||
| White | 268.8 (54.2) | 277.5 (57.8) | 273.1 (55.1) | 294.3 (58.0) | 310.7 (51.2) | 301.3 (54.8) |
| South Asian | 276.4 (49.1) | 254.4 (62.0) | 265.6 (56.4) | 294.8 (46.2) | 285.6 (61.8) | 289.5 (55.4) |
| Percentage of children spending ≥ 180 minutes per day in physical activity, n/N (%) | ||||||
| White | 14/14 (100.0) | 14/14 (100.0) | 28/28 (100.0) | 15/16 (93.8) | 12/12 (100.0) | 27/28 (96.4) |
| South Asian | 28/28 (100.0) | 25/27 (92.6) | 53/55 (96.4) | 24/24 (100.0) | 31/32 (96.9) | 55/56 (98.2) |
Anthropometry
Table 29 summarises the baseline anthropometry data and Table 30 shows the 10- and 52-week follow-up data.
| Characteristic | As randomised, mean (SD) | As analysed, mean (SD) | ||
|---|---|---|---|---|
| Intervention (n = 83) | Control (n = 81) | Intervention (n = 29) | Control (n = 35) | |
| Height (cm) | 92.4 (7.3) | 93.1 (6.9) | 93.5 (8.2) | 92.8 (7.8) |
| Body mass (kg) | 14.1 (2.5) | 14.3 (2.3) | 14.4 (2.6) | 14.3 (2.6) |
| Abdominal circumference (cm) | 50.0 (3.8) | 50.2 (3.9) | 49.6 (3.4) | 50.6 (4.3) |
| Arm circumference (cm) | 16.9 (1.8) | 17.3 (3.9) | 17.0 (1.8) | 18.3 (5.9) |
| BMI z-value | 0.6 (1.1) | 0.8 (1.1) | 0.5 (1.1) | 1.0 (1.1) |
| Overweight (BMI z-value ≥ 1.04) | 24 (33.8) | 29 (39.7) | 8 (30.8) | 12 (40.0) |
The average height of children in the study was 92.8 (SD 7.1) cm, with an average body mass of 14.2 (SD 2.4) kg, abdominal circumference of 50.0 (SD 3.8) cm and arm circumference of 17.1 (SD 3.1) cm. The average BMI z-value was 0.7 (SD 1.1) and the number of children with a BMI z-value of ≥ 1.04 was 53 (32.3%). Randomisation achieved balance across most anthropometry measures and attrition did not impact on the balance achieved at baseline in the as-analysed sample across most measures. There was a slight imbalance in BMI z-value in the as-analysed comparison, with the intervention group having a slightly lower BMI z-value (and subsequently a lower percentage of overweight children) than the control group.
| Characteristic | Intervention | Control | Total | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Body mass (kg) | ||||||
| 10 weeks | 58 | 14.6 (2.6) | 58 | 14.6 (2.3) | 116 | 14.6 (2.4) |
| 52 weeks | 60 | 16.1 (2.8) | 58 | 16.4 (2.8) | 118 | 16.2 (2.8) |
| Height (cm) | ||||||
| 10 weeks | 53 | 95.0 (6.8) | 57 | 95.1 (6.4) | 110 | 95.1 (6.6) |
| 52 weeks | 58 | 100.2 (7.2) | 57 | 100.8 (6.7) | 115 | 100.5 (6.9) |
| BMI z-value | ||||||
| 10 weeks | 71 | 0.5 (1.2) | 73 | 0.7 (1.2) | 144 | 0.6 (1.2) |
| 52 weeks | 54 | 0.2 (1.2) | 53 | 0.3 (1.2) | 107 | 0.3 (1.2) |
| Waist circumference (cm) | ||||||
| 10 weeks | 47 | 49.6 (3.7) | 41 | 50.4 (4.8) | 88 | 49.9 (4.2) |
| 52 weeks | 53 | 51.1 (4.1) | 50 | 52.2 (4.8) | 103 | 51.6 (4.5) |
| Upper arm circumference (cm) | ||||||
| 10 weeks | 45 | 17.0 (1.4) | 41 | 17.8 (5.5) | 86 | 17.4 (3.9) |
| 52 weeks | 50 | 17.5 (2.1) | 47 | 17.6 (1.5) | 97 | 17.5 (1.8) |
Table 30 shows that there was little difference in average body mass and height between the intervention group and the control group at 10 and 52 weeks. The average BMI z-value at 10 and 52 weeks was slightly lower in the intervention group than in the control group. At 10 weeks the average BMI z-value in the intervention group was 0.5 (SD 1.2) and in the control group was 0.7 (SD 1.2) and at 52 weeks the average BMI z-value in the intervention group was 0.2 (SD 1.2) and in the control group was 0.3 (SD 1.2). The average waist and upper arm circumference at 10 and 52 weeks were slightly lower in the intervention group than in the control group. At 10 weeks the average waist circumference in the intervention group was 49.6 (SD 3.7) cm and in the control group was 50.4 (SD 4.8) cm and at 52 weeks the average waist circumference in the intervention group was 51.1 (SD 4.1) cm and in the control group was 52.2 (SD 4.8) cm. Similarly, at 10 weeks upper arm circumference in the intervention group was 17.0 (SD 1.4) cm and in the control group was 17.8 (SD 5.5) cm and at 52 weeks upper arm circumference in the intervention group was 17.5 (SD 2.1) cm and in the control group was 17.6 (SD 1.5) cm.
Quality of life and general self-efficacy
Table 31 shows parents’ well-being and general self-efficacy at baseline.
| Characteristic | As randomised, mean (SD) | As analysed | ||
|---|---|---|---|---|
| Intervention (n = 83) | Control (n = 81) | Intervention (n = 29) | Control (n = 35) | |
| ComQol-A5 total objective scorea | 73.2 (8.0) | 75.2 (7.1) | 74.7 (7.6) | 76.3 (6.9) |
| General Self-Efficacy Scale scoreb | 30.3 (5.7) | 29.2 (5.4) | 30.6 (4.6) | 30.0 (5.3) |
The average total objective quality-of-life score was 74.2 (SD 7.6) and the average general self-efficacy score was 29.7 (SD 5.6). Randomisation achieved balance across both measures and attrition did not impact on the balance achieved at baseline in the as-analysed sample across both measures.
Table 32 shows the individual domains of well-being at 10 and 52 weeks’ follow-up.
| Objective | Intervention | Control | Total | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Material well-being | ||||||
| 10 weeks | 63 | 9.4 (1.8) | 56 | 9.3 (2.1) | 119 | 9.4 (1.9) |
| 52 weeks | 65 | 9.3 (1.8) | 62 | 9.4 (2.0) | 127 | 9.3 (1.9) |
| Health | ||||||
| 10 weeks | 64 | 13.6 (1.8) | 62 | 13.8 (1.5) | 126 | 13.7 (1.6) |
| 52 weeks | 66 | 13.4 (1.6) | 62 | 13.9 (1.4) | 128 | 13.7 (1.5) |
| Productivity | ||||||
| 10 weeks | 64 | 9.3 (1.8) | 65 | 9.6 (2.0) | 129 | 9.4 (1.9) |
| 52 weeks | 67 | 9.0 (2.1) | 64 | 9.2 (1.8) | 131 | 9.1 (2.0) |
| Intimacy | ||||||
| 10 weeks | 64 | 11.3 (3.1) | 65 | 12.2 (2.3) | 129 | 11.8 (2.8) |
| 52 weeks | 67 | 11.4 (2.7) | 64 | 12.3 (2.2) | 131 | 11.8 (2.5) |
| Safety | ||||||
| 10 weeks | 64 | 12.3 (1.7) | 66 | 12.2 (1.7) | 130 | 12.0 (2.5) |
| 52 weeks | 67 | 12.3 (1.8) | 64 | 12.2 (1.8) | 131 | 12.3 (1.8) |
| Place in community | ||||||
| 10 weeks | 64 | 8.0 (2.1) | 66 | 7.9 (1.9) | 130 | 8.0 (2.0) |
| 52 weeks | 67 | 7.9 (1.8) | 64 | 8.2 (1.5) | 131 | 8.1 (1.7) |
| Emotional well-being | ||||||
| 10 weeks | 63 | 9.2 (2.4) | 66 | 9.3 (2.1) | 129 | 9.3 (2.2) |
| 52 weeks | 66 | 9.4 (2.2) | 64 | 9.6 (2.1) | 130 | 9.5 (2.1) |
| Total score | ||||||
| 10 weeks | 62 | 72.7 (9.2) | 53 | 74.0 (6.7) | 115 | 73.3 (8.1) |
| 52 weeks | 65 | 72.4 (7.5) | 60 | 74.5 (7.1) | 125 | 73.4 (7.4) |
At 10 weeks the mean overall total score for objective well-being was lower in the intervention group than in the control group [intervention 72.7 (SD 9.2); control 74.0 (SD 6.7)] and a similar pattern was present at 52 weeks [intervention 72.4 (SD 7.5); control 74.5 (SD 7.1)]. However, there was little change in scores between the two time points.
Trial arm and ethnic group differences
Tables 33 and 34 summarise the total scores for objective quality of life and general self-efficacy, respectively, by trial arm and ethnicity.
| Total score | Intervention | Control | Total | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| 10 weeks | ||||||
| White | 27 | 69.8 (11.0) | 15 | 77.3 (6.7) | 42 | 72.5 (10.2) |
| South Asian | 32 | 75.2 (6.3) | 36 | 72.7 (6.2) | 68 | 73.9 (6.3) |
| 52 weeks | ||||||
| White | 24 | 71.1 (9.0) | 17 | 77.1 (7.7) | 41 | 73.6 (8.9) |
| South Asian | 36 | 73.5 (6.6) | 41 | 73.7 (6.2) | 77 | 73.6 (6.3) |
For white parents, the average ComQol-A5 score was lower in the intervention group than in the control group at both 10 and 52 weeks; however, for South Asian parents the average score was higher in the intervention group than in the control group at 10 weeks and was similar between the two groups at 52 weeks.
| Total score | Intervention | Control | Total | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| 10 weeks (overall) | 64 | 31.1 (6.4) | 66 | 30.9 (5.0) | 130 | 31.0 (5.7) |
| White | 28 | 29.1 (7.3) | 20 | 31.0 (4.7) | 48 | 29.9 (6.3) |
| South Asian | 33 | 32.7 (4.4) | 43 | 30.8 (5.1) | 76 | 31.6 (4.9) |
| 52 weeks (overall) | 68 | 31.8 (5.5) | 63 | 31.9 (4.3) | 131 | 31.9 (5.0) |
| White | 26 | 32.5 (5.3) | 17 | 31.4 (4.6) | 43 | 32.0 (5.0) |
| South Asian | 37 | 31.6 (5.4) | 44 | 32.2 (4.0) | 81 | 31.9 (4.7) |
The average self-efficacy score at 10 weeks was 31.1 (SD 6.4) in the intervention arm and 30.9 (SD 5.0) in the control arm and at 52 weeks was 31.8 (SD 5.5) in the intervention group and 31.9 (SD 4.3) in the control group. Again, different patterns were seen for average scores between white and South Asian parents. For white parents the scores were lower in the intervention arm than in the control arm at 10 weeks and were higher in the intervention arm than in the control group at 52 weeks; however, the reverse was seen for the South Asian parents.
The average total objective quality-of-life score was 74.2 (SD 7.6) and the average general self-efficacy score was 29.7 (SD 5.6). Randomisation achieved balance across both measures and attrition did not impact on the balance achieved at baseline in the as-analysed sample across both measures.
Objective 10: estimates of effect size, typical cluster sizes and intraclass correlation coefficients to enable an accurate sample size calculation for a full randomised controlled trial
Analysis of the primary outcome (mean daily moderate to vigorous physical activity at 52 weeks)
The analysis for the primary outcome measure included 64 children (39%) who had both baseline and 52-week outcome data. At baseline the average time spent in MVPA per day was 63.1 (SD 24.5) minutes. The number of minutes spent in MVPA per day was lower in the intervention arm than in the control group at 10 weeks [61.8 (SD 25.2) vs. 62.1 (SD 22.9) minutes].
At 52 weeks the number of minutes spent in MVPA per day was very similar across trial arms (mean difference 0.39, 95% CI –16.26 to 17.04 minutes), although the results are not statistically significant (p = 0.96). The ICC for the primary analysis was estimated to be zero. On inspection of the data it appeared that there was a plausible but outlying child who had a low baseline MVPA level but the highest MVPA level at 52 weeks and so we undertook a sensitivity analysis to explore the impact on the results of excluding this individual from the analysis. In the sensitivity analysis the average number of minutes spent in MVPA was higher in the control group than in the intervention group (mean difference –3.19, 95% CI –18.06 to 11.68), although the results are not statistically significant (p = 0.63). The ICC for the primary analysis excluding the outlying child was estimated to be 0.02.
Sample size calculation
A full RCT would require a sample size of 600 children at 38 schools (16 children per school). This is based on a previous study by Specker et al. 101 and data from the pilot trial. The study by Specker et al. 101 found higher average daily accelerometer counts in gross than in fine motor groups at follow-up [mean (SD) 27.7 (8.8) vs. 31.0 (8.4), p = 0.03]; this translates into an approximate effect size of 0.38. To detect an effect size of 0.3, assuming 80% power, we require 352 participants (176 per group). Using an ICC of 0.02 and an average cluster size of 15 from our pilot data we estimate that there will be a design effect of approximately 1.28 [using 1 + (n – 1) * ICC]. On this basis, to detect 0.3 of a standardised difference between the groups would require enrolling 31 schools and 452 children. However, from our pilot data the pre-/post-test correlation between MVPA at baseline and MVPA at 52 weeks was 0.6. Taking this into account suggests that 20 schools and 300 children would be sufficient. Allowing for a potential loss to follow-up of 50% for the primary outcome (based on experience from the pilot trial), the final sample size needed is 600 children and thus 38 schools (16 children per school).
Objective 11: preliminary assessment of the potential cost-effectiveness of the Preschoolers in the Playground intervention and an estimate of the value of further research
Costs of health care
At baseline and at each follow-up, parents were asked to recall their child’s health and social care service use during the past 3 months. Table 35 demonstrates the mean cost of each type of health-care service at each time point. The accrued costs for each resource used have been calculated based on the number of observations that have available data for any cost item and hence n varies by group and time point.
| Item | Baseline (£), mean (SD) | Weeks 0–10 (£), mean (SD) | Weeks 11–39a (£), mean (SD) | Weeks 40–52 (£), mean (SD) | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention (n = 83) | Control (n = 81) | Intervention (n = 64) | Control (n = 67) | Intervention (n = 58) | Control (n = 62) | Intervention (n = 68) | Control (n = 64) | |
| Hospital services | ||||||||
| Overnight stay | 67.47 (431.99) | 0 (0) | 628.22 (3637.36) | 8.45 (69.13) | 906.02 (4811.13) | 11.51 (90.61) | 32.45 (152.18) | 0 (0) |
| Day hospital attendance | 105.97 (714.88) | 69.10 (259.03) | 57.66 (262.08) | 137.71 (335.53) | 201.91 (888.18) | 236.42 (495.58) | 82.31 (439.91) | 49.98 (195.08) |
| Outpatient appointment | 17.73 (93.62) | 61.33 (156.67) | 35.38 (187.03) | 29.58 (76.09) | 93.23 (353.48) | 92.68 (271.32) | 35.18 (111.30) | 40.25 (155.40) |
| A&E | 8.31 (34.93) | 9.94 (32.51) | 12.44 (31) | 13.20 (35.30) | 22.88 (53.73) | 32.02 (74.79) | 8.46 (30.24) | 10.78 (33.79) |
| Day case surgery | 26.48 (241.26) | 0 (0) | 13.21 (105.67) | 0 (0) | 18.38 (139.96) | 0 (0) | 0 (0) | 0 (0) |
| Dentist | 0 (0) | 0 (0) | 0.92 (5.15) | 0 (0) | 1.28 (6.81) | 0 (0) | 0.56 (4.63) | 0 (0) |
| Dermatologist | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3.04 (23.18) | 0 (0) | 2.06 (16.98) | 0 (0) |
| ENT | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2.07 (15.73) | 0 (0) | 1.40 (11.52) | 0 (0) |
| Consultant for learning disabilities | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2.20 (16.72) | 4.11 (32.35) | 1.49 (12.25) | 3.16 (25.25) |
| Non-hospital services | ||||||||
| General practitioner | 37.41 (44.90) | 48.33 (83.52) | 26.50 (33.07) | 23.08b (32.32) | 90.38 (109.87) | 84.93 (91.50) | 43.01 (64.32) | 45 (53.79) |
| General practitioner home visit | 2.75 (17.59) | 1.41 (12.67) | 0 (0) | 2.62 (21.43) | 0 (0) | 3.57 (28.08) | 0 (0) | 0 (0) |
| Practice nurse | 1.13 (6.36) | 1.49 (6.01) | 0.32 (1.81) | 0.46 (2.80) | 3.66 (14.36) | 2.82 (10.73) | 2.57 (10.44) | 1.68 (6.10) |
| Practice nurse home visit | 1.58 (14.27)c | 0 (0)d | 0.78 (6.21) | 0 (0) | 1.08 (8.23) | 0 (0) | 0 (0) | 0 (0) |
| Occupational therapist home visit | 1.73 (15.69)c | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Speech and language therapist | 9.26 (60.23) | 2.79 (10.95) | 7.06 (52.28) | 2.60 (9.21) | 16.71 (81.95) | 21.01 (92.54) | 4.65 (33.27) | 13.42 (70.08) |
| Speech and language therapist home visit | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Physiotherapist | 0.54 (4.96) | 2.79 (16.53) | 7.61 (60.86) | 1.04 (5.96) | 11.57 (88.09) | 4.17 (27.77) | 0.66 (5.48) | 2.12 (16.95) |
| Clinical/child psychologist | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 5.83 (44.37) | 0 (0) | 3.94 (32.50) | 0 (0) |
| Children’s social worker | 0 (0) | 0 (0) | 5.24 (29.41) | 0 (0) | 7.29 (38.92) | 0 (0) | 0 (0) | 0 (0) |
| Health visitor | 0 (0) | 0 (0) | 1.42 (7.96) | 0.68 (5.54) | 3.26 (14.18) | 0.92 (7.27) | 1.74 (10.04) | 0 (0) |
| Special help teacher | 0 (0) | 0 (0) | 0 (0) | 48.94 (400.57) | 0 (0) | 66.68 (525.03) | 0 (0) | 0 (0) |
| Family support worker | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2.13 (11.37) | 0 (0) | 1.44 (8.34) | 0 (0) |
| NHS Direct | 0 (0) | 0.32 (2.84) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Total cost (excluding the PiP intervention costs) | 283.75 (1005.01) | 199.40 (345.60) | 796.76 (4081.88) | 272.05 (684.46) | 1392.9 (6038.49) | 568.63 (1080.08) | 221.92 (580.41) | 166.38 (285.69) |
| Total costs from week 0 to week 52 (excluding the PiP intervention costs) | – | – | 2529.52 (10,827.63) | 1019.61 (1949.22) | ||||
Figure 4 summarises the mean cost per participant by randomised arm for participants for whom complete cost data were available at both week 10 and week 52 (n = 58 for the intervention group and n = 61 for the control group). Costs were extrapolated from week 11 to week 39 based on mean resource use in the other two follow-up periods as no data were collected in the trial for this period. Participants in the intervention arm tended to generate higher costs over the whole trial period but there was not a statistically significant difference in total cost per participant between trial arms (p = 0.23).
FIGURE 4.
Total resource use costs over weeks 0–10, weeks 11–39 and weeks 40–52. Intervention costs have been excluded.
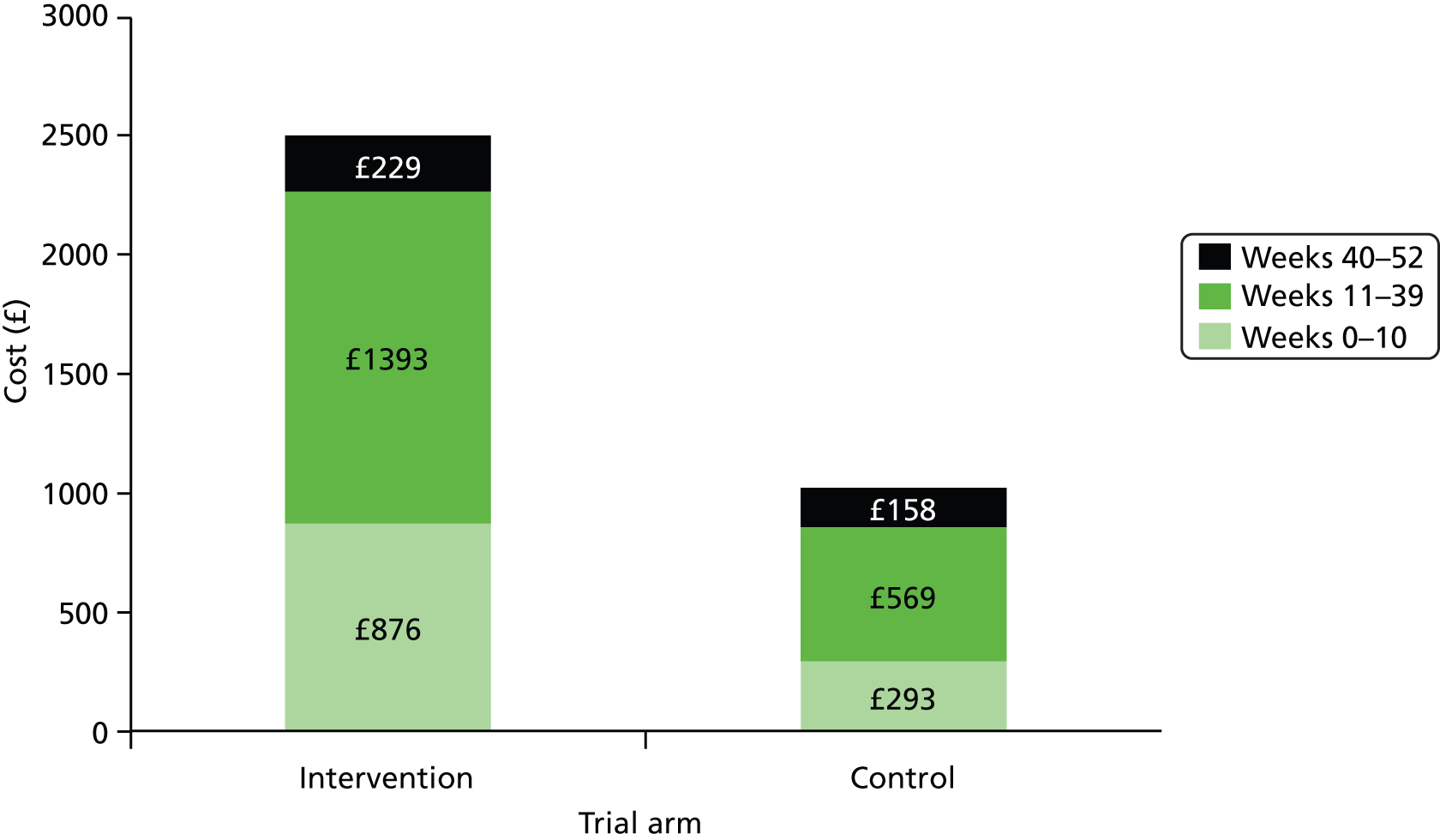
Health-related quality of life
European Quality of Life-5 Dimensions questionnaire
Parents’ HRQoL at each data collection point was measured using the EQ-5D questionnaire. Table 36 shows the proportion of participants in each health state of the EQ-5D for whom HRQoL data were available (126 parents at baseline, 124 parents at 10 weeks and 125 parents at 52 weeks).
| Item | Level of severity | % of participants in health state | |||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||
| Baseline (n = 70) | 10 weeks (n = 64) | 52 weeks (n = 61) | Baseline (n = 56) | 10 weeks (n = 60) | 52 weeks (n = 64) | ||
| Mobility | 1 | 98.57 | 93.75 | 95.08 | 96.43 | 88.24 | 92.19 |
| 2 | 1.43 | 6.25 | 4.92 | 3.57 | 11.76 | 7.81 | |
| 3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Self-care | 1 | 100.00 | 100.00 | 95.08 | 98.21 | 96.0 | 96.88 |
| 2 | 0.0 | 0.0 | 4.92 | 1.79 | 4.0 | 1.56 | |
| 3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.56 | |
| Usual activities | 1 | 92.86 | 90.63 | 93.44 | 96.43 | 90.20 | 92.19 |
| 2 | 7.14 | 9.38 | 6.56 | 3.57 | 9.80 | 7.81 | |
| 3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Pain/discomfort | 1 | 82.86 | 78.13 | 90.16 | 78.57 | 76.47 | 70.31 |
| 2 | 11.43 | 14.06 | 3.28 | 17.86 | 11.76 | 23.44 | |
| 3 | 5.71 | 7.81 | 6.56 | 3.57 | 11.76 | 6.25 | |
| Anxiety/depression | 1 | 87.14 | 85.94 | 93.44 | 85.71 | 74.51 | 76.56 |
| 2 | 10.00 | 14.06 | 6.56 | 14.29 | 25.49 | 20.31 | |
| 3 | 2.86 | 0.0 | 0.0 | 0.0 | 0.0 | 3.13 | |
Figure 5 shows the mean EQ-5D index at baseline, 10 weeks and 52 weeks by randomised arm (without MI). The estimates of the means were derived from the observations with available EQ-5D data at each time point (Table 37). HRQoL tended to decrease in both groups at 10 weeks followed by a slight increase at 52 weeks. Despite the similar pattern, overall the PiP intervention appeared to improve parents’ HRQoL marginally, leading to an overall increase in score of 0.023, whereas in the control group the EQ-5D index of parents decreased by 0.063. A different pattern was observed in the complete-case analysis, that is, when only participants with complete cost, EQ-5D and PedsQL data were taken into account in the calculation of the mean EQ-5D scores (Table 38). In this case parents’ HRQoL showed a steady improvement from baseline to week 52 in the intervention group compared with a steady decline in the control group.
FIGURE 5.
Mean EQ-5D index of HRQoL at baseline and follow-up by trial arm. The scores at each time point have been derived from all participants with available data at that time point.
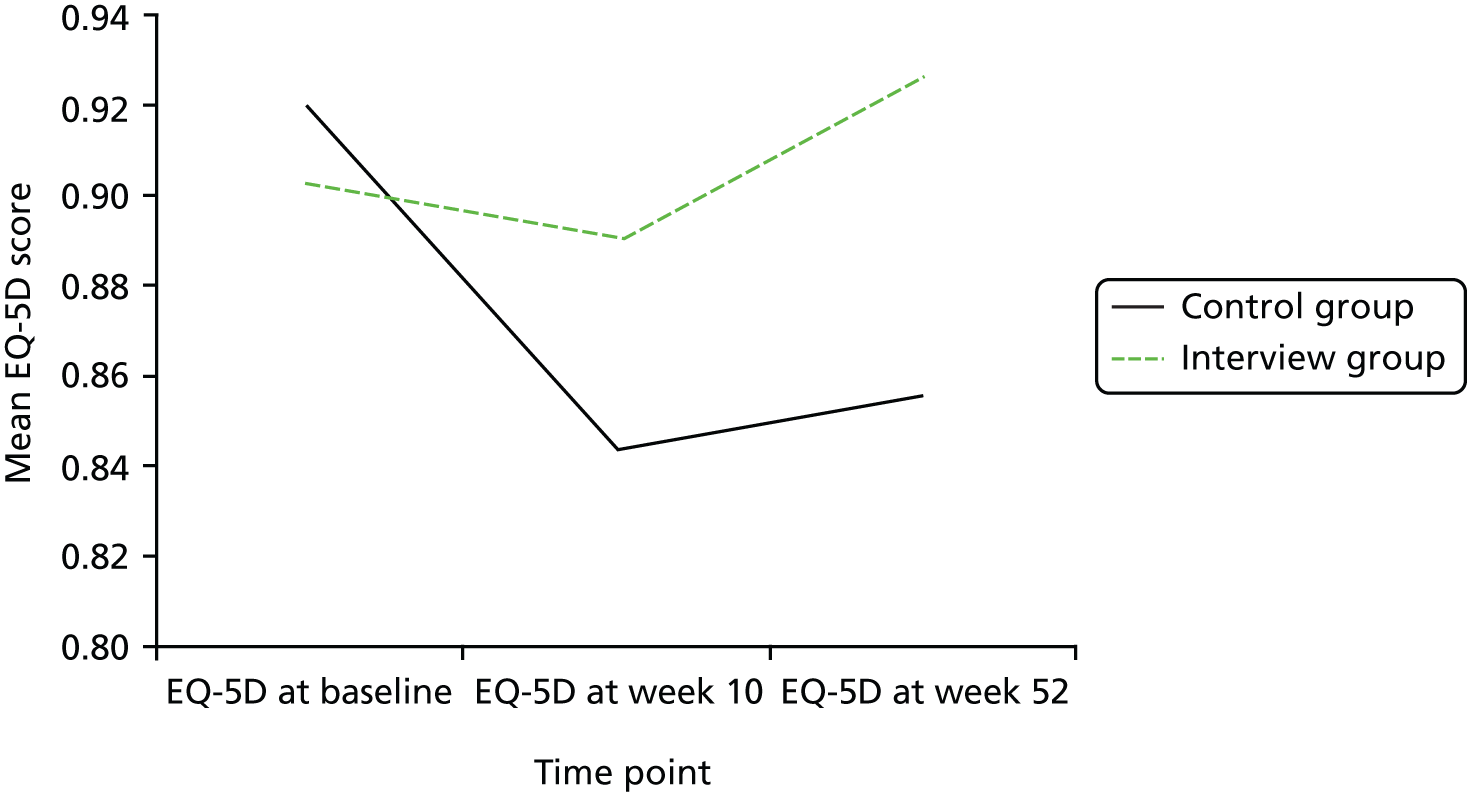
| Time point | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 70 | 0.90 (0.22) | 56 | 0.92 (0.18) |
| 10 weeks | 64 | 0.89 (0.23) | 50 | 0.85 (0.28) |
| 52 weeks | 61 | 0.93 (0.23) | 64 | 0.86 (0.25) |
| Difference in means from baseline to 52 weeks | 0.02 | –0.06 | ||
| Time point | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 38 | 0.92 (0.18) | 34 | 0.94 (0.12) |
| 10 weeks | 38 | 0.92 (0.19) | 34 | 0.84 (0.28) |
| 52 weeks | 38 | 0.97 (0.16) | 34 | 0.83 (0.27) |
| Difference in means from baseline to 52 weeks | 0.05 | –0.2 | ||
Pediatric Quality of Life Inventory
Parents were asked to complete the PedsQL questionnaire at baseline, 10 weeks and 52 weeks to measure the HRQoL of the infants and toddlers. In both groups children’s quality of life showed a deterioration from baseline to 10 weeks, which was followed by an improvement at 52 weeks (Figure 6). Infants and toddlers in the control arm had a higher mean score at 52 weeks than those in the intervention arm. However, as Table 39 shows, that score was lower than the baseline score and reflected a decrease in HRQoL of 0.2 units from baseline to 52 weeks, whereas children in the intervention arm demonstrated an overall improvement in HRQoL of 1.5 units over the same period.
FIGURE 6.
Mean PedsQL index of HRQoL at baseline and follow-up by trial arm. The scores at each time point have been derived from all participants with available data at that point.

| Time point | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 83 | 89.22 (7.37) | 81 | 91.76 (6.31) |
| 10 weeks | 62 | 87.96 (9.02) | 67 | 87.28 (10.68) |
| 52 weeks | 63 | 90.72 (7.62) | 60 | 91.56 (7.06) |
| Difference in means from baseline to 52 weeks | 1.50 | –0.20 | ||
Imputation of missing data
Of the 164 participants in the trial, 89 provided EQ-5D and PedsQL data at both 10 weeks and 52 weeks; 28 had missing data at 10 weeks only, 22 had missing data at 52 weeks only and 25 had missing data at both time points. MI was used to impute missing data (costs, EQ-5D scores and PedsQL scores) following the predictive mean matching approach. The imputation produced five imputed data sets, based on which the means of the outcomes were estimated.
The mean estimates of the EQ-5D index and the PedsQL index derived from the entire trial population were similar to those of the available case analysis, showing a decrease in HRQoL in both groups at 10 weeks and subsequent improvement at 52 weeks (Tables 40 and 41, respectively). Overall, however, the health gains over the entire trial period were higher for the intervention group than for the control group (change in mean score from baseline to 52 weeks for the intervention group vs. the control group: 0.0343 vs. –0.0568 for EQ-5D and 1.97 vs. 0.18 for PedsQL).
| Time point | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 83 | 0.90 (0.03) | 81 | 0.92 (0.02) |
| 10 weeks | 83 | 0.89 (0.03) | 81 | 0.84 (0.04) |
| 52 weeks | 83 | 0.93 (0.03) | 81 | 0.86 (0.03) |
| Difference in means from baseline to 52 weeks | 0.03 | –0.06 | ||
| Time point | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 83 | 89.22 (0.81) | 81 | 91.76 (0.70) |
| 10 weeks | 83 | 88.37 (1.17) | 81 | 87.53 (1.21) |
| 52 weeks | 83 | 91.19 (0.86) | 81 | 91.94 (0.95) |
| Difference in means from baseline to 52 weeks | 1.97 | 0.18 | ||
Cost-effectiveness analysis
Total population
Table 42 shows the mean incremental QALYs and mean incremental costs compared with usual practice. MI was performed to deal with missing data and a SUR model was used to estimate the mean total costs and QALYs from the imputed data sets. After adjusting for baseline differences in EQ-5D score, the PiP intervention appeared to improve parents’ HRQoL by 0.058 QALYs at an increased cost of £1137 per participant compared with the control arm. Estimates of both incremental costs and effects are associated with considerable uncertainty with all CIs crossing zero.
| Mean incremental QALYs (compared with control) | 95% CI | Mean incremental cost (compared with control) (£) | 95% CI (£) | ICER (£ per QALY) | |
|---|---|---|---|---|---|
| MI, n = 164a | |||||
| PiP intervention | 0.06 | –0.01 to 0.13 | 1136.62 | –940.08 to 3213.33 | 19,588 |
| Complete cases, n = 72b | |||||
| PiP intervention | 0.11 | 0.05 to 0.18 | 2686.24 | –1748.32 to 7120.79 | 23,895 |
Overall, in the MI analysis the PiP intervention appeared to be borderline cost-effective with an ICER of £19,588 per QALY gained. However, this estimate is surrounded by a considerable amount of uncertainty. The probability that the PiP intervention is cost-effective is 0.507 at a cost-per-QALY threshold of £20,000, 0.656 at a threshold of £30,000 and 0.807 at a threshold of £50,000. Figure 7 illustrates the uncertainty associated with the estimate of the ICER, that is, the probability of the PiP intervention being cost-effective at various thresholds.
FIGURE 7.
Cost-effectiveness acceptability curve controlling for baseline utility: MI analysis.

Cluster analysis
A cluster analysis by school was also performed. For this the outcomes and the uncertainty were adjusted for 10 clusters, as many as the schools recruited in the trial. As Table 43 shows, the resulting CIs were tighter for costs but somewhat wider for QALYs than those of the base case. The ICER remained unaffected.
| Mean incremental QALYs (compared with control) | 95% CI | Mean incremental cost (compared with control) (£) | 95% CI (£) | ICER (£ per QALY) | |
|---|---|---|---|---|---|
| MI, n = 164a | |||||
| PiP intervention | 0.06 | –0.05 to 0.17 | 1136.62 | –903.50 to 3176.75 | 19,587 |
Subgroup analysis
A subgroup analysis was undertaken to explore differences in the effect of the PiP intervention on costs and QALYs across participants of different ethnicity. White intervention group participants appear to accrue on average £1737 more than their peers in the control group for only marginal health gains (0.0063 QALYs), yielding a prohibitive ICER of £275,203 per QALY. Hence the PiP intervention cannot be deemed cost-effective for white populations. In contrast, the intervention is likely to be cost-effective for the South Asian subpopulation, as the mean incremental cost per participant is £539 and the mean incremental QALYs are 0.0577, yielding an ICER of £9346 per QALY. The ICER for the subgroup that consists of people of other origins appears to be prohibitively high. Notably, all outcomes are uncertain, as all CIs include zero (Table 44).
| Mean incremental QALYs (compared with control) | 95% CI | Mean incremental cost (compared with control) (£) | 95% CI (£) | ICER (£ per QALY) | |
|---|---|---|---|---|---|
| MI, n = 164a | |||||
| White (n = 61) | |||||
| PiP intervention | 0.01 | –0.09 to 0.10 | 1736.79 | –2984.64 to 6458.22 | 275,203 |
| South Asianb (n = 93) | |||||
| PiP intervention | 0.06 | –0.03 to 0.15 | 539.25 | –1258.25 to 2336.75 | 9346 |
| Other (n = 10) | |||||
| PiP intervention | 0.13 | –0.16 to 0.41 | 2201.67 | –11,045.08 to 15,448.42 | 17,620 |
Sensitivity analysis
A complete-case analysis was conducted as a sensitivity analysis. Complete cases (n = 72) consisted of participants who had no missing data for any cost, EQ-5D or PedsQL item at baseline, 10 weeks or 52 weeks. This analysis resulted in slightly higher incremental costs and QALYs for the PiP intervention (see Table 42) than with MI, which produced an ICER of £23,895 per QALY gained. The results of the complete-case analysis were not statistically significant in terms of incremental costs, with wide CIs that crossed zero.
Figure 8 captures the uncertainty associated with the estimates.
FIGURE 8.
Cost-effectiveness acceptability curve controlling for baseline utility: complete-case analysis.

Cluster analysis
As in the base case, adjusting for clusters in the complete-case analysis affected the results only slightly. The resulting CIs were wider for the health gains and tighter for the incremental costs but the outcomes and hence the ICER remained nearly unchanged (Table 45). The ICC estimate was near zero, suggesting that values within the same clusters (i.e. schools) did not tend to be similar (ICC: 0.161 for QALYs, 0.021 for total costs, 0.104 for PedsQL).
| Mean incremental QALYs (compared with control arm) | 95% CI | Mean incremental cost (compared with control arm) (£) | 95% CI (£) | ICER (£ per QALY) | |
|---|---|---|---|---|---|
| Complete cases, n = 72a | |||||
| PiP intervention | 0.11 | –0.00 to 0.23 | 2686.24 | –1658.35 to 7030.83 | 23,890 |
Subgroup analysis
The subgroup analysis in the complete case showed similar results to those of the subgroup analysis in the base case (MI). The intervention in the white group was dominated as it led to a lower quality of life and higher costs than in the control group, whereas it was likely to be cost-effective in the South Asian group (ICER £10,329 per QALY). Importantly, the health gains in this subpopulation were statistically significant in this analysis (Table 46).
| Mean incremental QALYs (compared with control arm) | 95% CI | Mean incremental cost (compared with control arm) (£) | 95% CI (£) | ICER (£ per QALY) | |
|---|---|---|---|---|---|
| Complete cases, n = 72a | |||||
| White (n = 28) | |||||
| PiP intervention | –0.02 | –0.09 to 0.05 | 4350.54 | –5545.21 to 14,246.29 | Dominated |
| South Asian (n = 41) | |||||
| PiP intervention | 0.17 | 0.08 to 0.26 | 1745.20 | –2006.50 to 5496.90 | 10,329 |
| Other (n = 3) | |||||
| PiP intervention | –0.05 | –1.18 to 1.08 | 342.09 | –4225.96 to 4910.14 | Dominated |
One-way sensitivity analysis
A one-way sensitivity analysis was performed to explore the sensitivity of the base-case and complete-case analysis results to variation in the cost of the intervention, that is, the cost of the parental involvement workers and their trainers. Each of these two cost items was varied by ±20%. The results showed that the impact of varying the intervention cost was minor (Table 47). In addition, the cost per inpatient day was varied as hotel costs may be more appropriate in some instances. This reduced the cost per day to £424.36 and generated a considerably lower ICER than in the base case, that is, £8824 per QALY (£12,290 per QALY in the complete-case analysis). This scenario represents a ‘best case’, as it assumes that only hotel costs occur during the entire hospital inpatient stay and does not consider the higher costs that are usually observed in the initial period of a hospitalisation. Therefore, this reflects a lower extreme than in the base case, which assumes that the high cost per day of a hospital stay occurring in the initial period is maintained for the entire stay, and hence leads to a conservative estimate of the ICER.
| ICER (£ per QALY), base case | ICER (£ per QALY), costs –20% | ICER (£ per QALY), costs +20% | |
|---|---|---|---|
| MI | |||
| Cost of PiP facilitator | 19,588 | 19,497 | 19,680 |
| Cost of PiP trainer | 19,588 | 19,570 | 19,607 |
| Complete case | |||
| Cost of PiP facilitator | 23,895 | 23,848 | 23,942 |
| Cost of PiP trainer | 23,895 | 23,885 | 23,904 |
Objective 12: whether or not links can be established between short-term outcomes and long-term quality of life, potentially including across sectors
Nine studies102–110 examined associations between childhood adiposity/obesity and health conditions in adult life and six studies102,103,111–114 reported links between obesity or physical activity and associated health conditions in childhood or adolescence. One study14 reported evidence of an association between physical activity and obesity in childhood.
Short-term links
Obesity as the exposure measure
Obesity was the exposure measure in three102,103,114 of the seven studies14,102,103,111–114 that examined short-term associations between physical activity or obesity and health status. A non-intervention prospective cohort study in the UK studied the relationship between insulin resistance and current weight in 5-year-old children. 114 The results suggested that insulin resistance was positively correlated with current weight (at 5 years) in both sexes, but more strongly so in girls than in boys. As children grew older a counterintuitive relationship was observed: a negative association between fat mass (BMI, skinfold thickness and percentage fat) and insulin resistance. In particular, all indices of body fatness were reported to rise progressively and significantly between 5 and 7 years, whereas insulin levels and HOMA-IR (an index of insulin resistance) fell substantially. Lee103 studied the consequences of obesity in childhood for a wide range of health conditions. The findings were based on a literature review and a regional cohort study in Singapore. Positive associations were reported between childhood obesity and obstructive sleep apnoea (prevalent in 33–94% of obese children), hypertension (20–30% of the sample), glucose intolerance (17.4% of the sample), dyslipidaemia, non-alcoholic fatty liver disease (26.4% of the sample), type 2 diabetes mellitus (4.5% of the sample), menstrual abnormalities, gallstones and metabolic syndrome (24.4% of the sample). These findings should be treated with caution as the paper was confounded by serious limitations: the evidence was not derived from a systematic review and the search strategy and inclusion criteria for the articles identified were not described. Moreover, the patient population relevant to the literature search and countries of the studies included were not reported. Finally, the relevance of the outcomes to a UK population is dubious as the paper was largely focused on a regional cohort study and it is reported that obese Asian children may be more prone to worse health measures than white European children. 103 A Canadian report on childhood obesity102 reported a positive link between obesity and acute respiratory infection. A potential relationship with hypertension was also suggested. The studied population was slightly older than the children in the PiP study and therefore the generalisability of the results to the PiP sample should be considered carefully. Moreover, the findings related to measurements conducted > 20 years ago.
Physical activity as the exposure measure
Of the four studies14,111–113 in which physical activity was the exposure measure, one examined associations with educational attainment,111 one with CVD risk score112 and one with memory and attention. 113 The fourth study, a systematic literature review conducted by Timmons et al. ,14 examined the relationship between higher levels of physical activity and adiposity. Dills et al. 111 used data from the Early Childhood Longitudinal Survey Kindergarten Class of 1998–1999 to evaluate how recess and physical education impact on students’ learning for kindergarteners through to fifth graders. The results showed that time spent in recess and physical education was unlikely to affect student test scores. For example, an additional 49 minutes per week of physical education in kindergarten improved reading test score gains by a statistically insignificant 0.05 SDs. Jimenez-Pavon et al. 112 collected cross-sectional data from a longitudinal study to explore the relevance of physical activity for combating CVD risk in children aged 2–9 years. The study involved eight European countries (Italy, Estonia, Cyprus, Belgium, Sweden, Germany, Hungary and Spain). In boys aged < 6 years, the odds ratio (OR) for CVD risk was statistically significantly elevated in the least active quintile of TPA (OR 2.58, 95% CI 1.07 to 6.18) compared with the most active quintile as well as in the second least active quintile of vigorous physical activity (OR 2.91, 95% CI 1.25 to 6.82). Finally, a cross-sectional longitudinal study113 conducted in Switzerland examined the relationship between aerobic fitness and motor skills and memory and attention in preschoolers (mean age 5.2 years). This study found that, in young children, higher baseline aerobic fitness and motor skills were related to a better spatial working memory and/or attention at baseline and to some extent also to their future improvements over the following 9 months.
The systematic literature review by Timmons et al. 14 examined the relationship between higher levels of physical activity and adiposity. In this study, low-quality evidence pertaining to infants (aged from 1 month to 1 year) and low- to high-quality evidence in preschoolers (aged 3.1–4.9 years) suggest that increased or higher levels of physical activity are positively associated with improved measures of adiposity. In particular, increased levels of physical activity were found to be associated with lower skinfold thickness in infants whereas, in preschoolers, three115–117 of the seven relevant papers identified reported that higher levels of physical activity were associated with improved measures of adiposity in childhood. The review concluded that investing in physical activity during the early years has health benefits later in life, particularly with respect to adiposity. No quantitative analyses of the collected evidence were performed because of the dearth of information identified; the evidence was synthesised and presented only in narrative fashion. However, this study was well reported in terms of the search methods and inclusion criteria for the identified studies as well as quality assessment results for each study that met the inclusion criteria. Moreover, the populations included were mostly from the USA and Western European countries and their age ranges were similar to the age range of the participants in the PiP RCT.
Long-term links
Childhood obesity has been reported to pertain to a number of health conditions in adult life. Extrapolating the findings of the systematic review by Timmons et al. 14 it could be hypothesised that increased physical activity in children may positively affect their long-term HRQoL by reducing obesity levels and, in turn, the risk of future health disorders. The exploration of such links between health outcomes in children and their potential consequences in adult life was the main focus of the literature review.
Of the body of evidence included in the review, in all nine studies102–110 that explored the links between short-term outcomes and long-term outcomes obesity was the exposure measure and eight102,103,105–108,110,118 out of the nine studies reported evidence of an association with cardiometabolic morbidity in adulthood. Additional health conditions explored included asthma105,108 and various types of cancer. 105,108,109
Coronary heart disease and atherosclerosis
Six papers102–105,107,108 examined the association between childhood obesity and vascular diseases later in life, in particular CHD and atherosclerosis. Three103,105,108 of the four papers that studied a potential link with adult CHD reported a positive association whereas one104 found no significant association. The systematic reviews of Park et al. 105 and Reilly and Kelly,108 which involved populations mostly from Western European countries and the USA, found consistent evidence that overweight and obese children and adolescents had a statistically significant risk of CHD as adults. Both reviews were well reported, with search strategies and inclusion criteria described in detail and a quality assessment performed for each source of evidence. In addition, Reilly and Kelly108 included only recent studies in their review (2002–10). Because of the diverse nature of the outcomes, study designs and effect measures included in the selected studies, data in both reviews were synthesised and presented in a narrative fashion. Similar evidence of a positive association was reported by Lee. 103 The fourth study, by Lloyd et al. ,104 identified one study,119 which found no significantly increased risk of CHD incidence in adults who were classified as overweight or obese as children.
The study by Lloyd et al. 104 also reported the existence of mixed evidence with regard to the association of childhood obesity with atherosclerosis in adulthood. More specifically, it presented three studies120–122 with evidence of a positive association between childhood BMI and carotid intima–media thickness, an indicator of atherosclerosis, and two studies123,124 with non-significant results. A significantly positive correlation was also identified in the longitudinal study of Raitakari et al. 107 of 3596 children and adolescents aged 3–18 years in Finland, whereas a retrospective study of the Canadian Task Force on the Periodic Health Examination102 of 902 men found no link.
Hypertension
Three104,105,108 of the studies looked at the impact of childhood BMI on adult hypertension. Reilly and Kelly108 found three papers125–127 that reported a significant increase in adult hypertension with overweight and obesity during childhood and adolescence (population age range 7–15 years). Park et al. ’s105 systematic review identified five studies126–130 which suggested that an increased BMI or overweight in children aged 1–19 years was associated with an increased risk of hypertension in adulthood (age 18–45 years). ORs for obesity in childhood ranged from 1.35 at 7 years to 3.75 at 16–19 years. The evidence provided by the third study104 was less consistent as four studies126,131–133 showed a significant positive association, two studies127,134 showed a non-significant positive correlation and two studies135,136 showed no statistically significant associations. The age of the population across the three studies104,105,108 varied from 1 to 19 years.
Cholesterol and triglycerides
Three studies102,106,118 provided evidence related to childhood BMI and adult levels of cholesterol and triglycerides. A British birth cohort study was conducted by Pinto Pereira and Power106 to examine the links between life-course BMI, birthweight and lipid levels in mid-adulthood. The cohort consisted of 3927 men and 3897 women born in 1958. Weight and height were recorded at birth and at 7, 11, 16, 23, 33 and 45 years. This study found a negative association between childhood BMI and longer-term cholesterol levels. In particular, in terms of per unit (kg/m2) BMI at 45 years, total cholesterol was more elevated in women in the lowest BMI tertile at 7 years than in women in the highest BMI tertile. Moreover, obesity or overweight in childhood but not thereafter was unrelated to lipid levels compared with the never obese. Of the other two studies, the Canadian Task Force102 reported no association between childhood BMI and adult levels of cholesterol and triglycerides and Lloyd et al. 118 found no conclusive evidence (two studies131,137 reported a significant positive correlation between childhood BMI and adult levels of cholesterol and triglycerides, one study136 reported a non-significant negative correlation and one study133 reported no statistically significant associations). A similar pattern of association between childhood BMI and triglyceride levels later in life was found by Lloyd et al. (two studies131,133 found a significant positive correlation with childhood BMI, one study136 found a non-significant negative correlation and one study138 found no statistically significant associations).
Insulin and diabetes
Three103,105,108 of the four studies102,103,105,108 that looked at childhood obesity and the associated risk of diabetes in adult life found a positive correlation. Nine128,139–146 of the 10 relevant studies identified by Park et al. 105 showed that, for type 2 diabetes, ORs for a 1-unit increase in BMI SD score ranged from 1.22 at school entry to 2.04 at age 16 years, whereas one study147 found no association between overweight at ages 13–18 years and diabetes at age 73 years. Reilly and Kelly108 reported evidence that showed a significant increase in diabetes risk with overweight and obesity at age 5 years (adjusted OR 2.6, 95% CI 1.3 to 5.2). Non-conclusive evidence was also reported for the link with adult insulin levels. 118
Cancer
Three studies105,108,109 reported associations with different types of cancers in adulthood but the evidence was conclusive in only one of them. Robinson et al. 109 conducted a systematic review of the association between prostate cancer and body size in childhood and young adulthood and found null or weak associations between them. The measures used included BMI and early-adult waist circumference. The review, including the search methods and inclusion criteria used, was well reported. Moreover, a meta-analysis was performed and the statistical methods used in the evidence synthesis were described in detail. A potential bias in these results could stem from the fact that BMI was self-reported in the majority of studies. In addition, the population studied was quite diverse (USA 43%, Western Europe 33%, Australia and China 24%) and therefore the generalisability of these results to the UK population should be considered with caution.
Stroke
Three studies104,105,108 reported results related to the risk of stroke in adulthood for obese children. Park et al. 105 did not find consistent evidence and the majority of the evidence sources referred to adolescents. One study148 reported in the review found that each unit increase in BMI at age 2 years and 7 years was associated with a reduced risk of all stroke [hazard ratio (HR) 2 years: 0.84, 95% CI 0.77 to 0.92; 7 years: 0.85, 95% CI 0.76 to 0.94) whereas another119 found no evidence of an association between risk of stroke and overweight status at primary school entry. Lloyd et al. ’s104 systematic review found no significantly increased risk of stroke in adults who were classified as overweight or obese as children whereas Reilly and Kelly108 found statistically significant evidence of an increased risk of stroke for the top 2.5% of the BMI distribution at age 4–6 years compared with all others (HR 2.41, 95% CI 1.00 to 5.86).
Obesity
A study published in 1994102 found that infants and children who are obese are at somewhat increased risk of becoming obese adults. However, the correlations were reported to be low and the probability that an individual obese infant will be an obese adult was also reported to be low. A more recent study107 reported that being obese in adolescence (between 12 and 18 years) carries about a fourfold increased risk of being obese in adulthood 21 years later (at 33–39 years). However, the outcomes principally concerned adolescents and not young children.
Mortality
Adult mortality associated with childhood BMI was considered in four papers. 102,105,108,118 Park et al. 105 found five studies149–153 which showed that an increased BMI in childhood/adolescence was associated with an increased risk of mortality and Reilly and Kelly108 reported that childhood/adolescent obesity was significantly associated with premature mortality (HR ranging from 1.4 to 2.9). Lloyd et al. ’s104 systematic review found similar evidence of a positive correlation. The fourth paper102 reported that ‘severe obesity in childhood has been linked to higher age-adjusted death rates among adults, but there is no association between moderate childhood obesity and higher death rates unless other risk factors are present’ (p. 875).
Other health conditions
Additional long-term health outcomes identified in the literature review included asthma, renal disease, polycystic ovary syndrome and mortality from type 2 diabetes. This evidence either showed no significant associations with childhood obesity or physical activity (renal disease102 and mortality118) or concerned adolescents (polycystic ovary syndrome and asthma108). An Australian study153 presented in the literature review of Park et al. 105 showed that being overweight at age 7 years was associated with adult-onset asthma in women (OR 3.1), whereas a British cohort study154 from the same review showed no association between being overweight at age 10 years and having asthma at age 26 years.
Patient and public involvement in the Preschoolers in the Playground pilot trial
We had strong engagement with the public during the PiP pilot trial, including with both parents and school staff. The Born in Bradford cohort study has a dedicated parent governors group that meets every 2 months. During the course of the trial we consulted with this group of parents (of white and South Asian ethnicity) on two occasions. Members of the group made useful comments about the trial and the intervention and thought that the trial procedures (including the accelerometers) and the intervention were acceptable. They also suggested changes to clarify the participant information sheets. The group recommended that the intervention was more visible in the school playground and as a result of this we produced outdoor banners with the PiP logo and session times for each participating school.
We hosted a meeting at a primary school in Bradford and invited both staff and parents along. At the meeting we asked them to comment on some of the trial procedures and aspects of the intervention. To engage with schools, the teachers recommended showing evidence that the trial has a community element or that participation in the study enhances a school’s Office for Standards in Education, Children’s Services and Skills (Ofsted) report. Parents were asked what might help them to attend the PiP sessions; the group felt that the play kit was a good motivational tool. Members of the group also suggested that, outside of the PiP sessions, an indoor venue where parents could meet and socialise might improve attendance. Parents who have older children at the school may have children in private nursery and it was suggested that private nurseries should be visited for PiP recruitment as well as those attached to schools.
Teachers and other school staff could not commit enough time to sit on the trial steering group and so we used a variety of other engagement channels to seek their opinions and guidance:
-
We hosted one meeting of a teacher panel, which included a head teacher, two early years workers and an educational psychologist, all from schools not involved in the PiP study.
-
We attended the Bradford Primary Improvement Partnership meeting. This meeting is for the head teachers of all of the primary schools in the district (n = 155).
-
The Born in Bradford programme ran the September 2014 session of Bradford’s quarterly Public Forum for Education, which is for workers from across the education sector and any members of the public. There were > 100 participants at this event.
-
The Born in Bradford programme also hosted two conferences presenting research relating to health and education, specifically for staff working in the education sector. The PiP study was presented at both conferences and delegates were asked for their opinions of the study. In general, the study and the intervention were well received. Staff concerns were around how to engage parents, given previous experiences of poor commitment to events hosted at school, but they also reported that the intervention was appealing as it offered a new and different way to engage with families.
At these meetings and conferences many of the schools that were not eligible to take part in the pilot trial expressed an interest in taking part in the future.
A further public engagement event was carried out with families. Each year the Born in Bradford programme holds an event for families in the city. In 2013 this was a Teddy Bear’s picnic. At the Teddy Bear’s picnic we set up PiP-PoP active games for the children to play and consulted with children and parents. The games were found to be enjoyable for children to participate in. In October 2014, the Born in Bradford programme hosted ‘BiB-Fest’, a family festival with the purpose of disseminating research findings. A video of children and parents participating in the PiP intervention was shown to explain to families about the intervention and research. A researcher spoke to families whilst they were watching and families reported that the intervention was appealing to them.
Chapter 4 Discussion
The PiP intervention was designed following the 2011 CMO’s report Start Active, Stay Active,29 which gave specific physical activity guidelines for children aged 0–5 years. At the time of development there were few interventions specifically for preschool children and none with long-term follow-up. A meta-analysis of physical activity interventions for preschoolers (mean age 4.1 years) published between 2004 and 2011155 reported a small to moderate short-term effect on TPA (Hedges g = 0.44, SD 0.86) and a moderate short-term effect on MVPA (Hedges g = 0.51, SD 0.88). Two more recent interventions have reported small increases in physical activity levels or reductions in sedentary behaviour that have been sustained over a longer term. 52,54 In a parent and child participatory intervention hosted in German preschools, at 6 months’ follow-up children in the intervention group were 11 minutes less sedentary (p < 0.05) and 4% more physically active (p > 0.05) each day than control children. 52 In an intervention delivered in Belgian preschools, time spent in MVPA was on average 7.2 minutes greater in the intervention group at 12 months’ follow-up (p < 0.05) than in control children. 54 These results are promising; however, they may not be clinically meaningful given that the changes reported were small (< 10 minutes difference in MVPA). Furthermore, the intervention in Belgium reported a positive effect of the intervention only in boys and high SES children. 54 The development of preschool physical activity interventions that focus on increasing physical activity levels in groups with particularly low levels, including girls, low SES children and ethnic minority groups, requires further attention.
Research has indicated that there are components of interventions that may increase the success of a physical activity intervention. These include theoretical underpinning using social cognitive theory,33,34,35 using an outdoor setting37–40 and parental involvement in the intervention. 49–54 The PiP intervention was designed to incorporate these components and had input from target group parents. It takes an upstream and a downstream targeted approach, focusing on deprived communities and ethnic minority groups with the anticipation of reducing health inequalities. In the pilot trial of the intervention we aimed to evaluate the feasibility of conducting a full-scale trial and the acceptability of the intervention in a deprived and multiethnic population (predominantly white and South Asian). The study had 13 objectives, which were met using a multimethods approach (quantitative, qualitative and health economic analyses). A discussion of each objective is provided in the following sections, including a summary of the key findings, a comparison with other studies (when appropriate), interpretation and suggestions for future research.
Objective 1: feasibility and acceptability of the recruitment strategy for schools and families and whether or not there was a difference in the recruitment rate between ethnic groups
The PiP pilot trial demonstrated that the recruitment strategy for schools was feasible, with 37% of schools approached agreeing to take part. In physical activity interventions based in preschool centres, recruitment rates of centres have varied widely, from 28%54 to 100%. 156 A recent study of a UK primary school-based physical activity intervention for children aged 8–11 years reported a school recruitment rate of 41%. 157 As our PiP intervention was hosted in the primary school setting, this is perhaps the best study to draw comparisons with, and our recruitment rate was similar to the rate in this study. We did, however, find a marked difference in engagement between schools with predominantly South Asian pupils and schools with predominantly white pupils. Of the schools approached, 85% of those with predominantly South Asian pupils expressed an interest in taking part, whereas only 29% of those with predominantly white pupils expressed an interest in taking part.
All of the schools approached to take part in the study were located within some of the most deprived areas of the country; this is reflected in the number of children at the schools eligible for FSMs. The average percentage of children eligible for FSMs at these schools was 48%, which is 2.7 times higher than the national average of 18%. These schools serving deprived communities have many competing priorities aside from education, and the differences in engagement with the study may reflect these priorities.
The head teachers of two of the schools that received the intervention reported that the most deprived families were the hardest for the school to reach, that the PiP study offered a new way to engage with families and that this was one of the main reasons why they had decided to take part in the study. They remarked that, through the PiP intervention, parents and preschool children could become familiar with the school environment. Additionally, they highlighted that the PiP intervention provided a way for parents to engage in meaningful activities with their children and that this can benefit language skills and learning. One of the head teachers also acknowledged the importance of the link between health and education. These insights can inform future health research within an education setting. They show that it is important for health researchers to consider the priorities of education professionals and to describe the potential benefits that health research may have for education when engaging with schools to take part in studies.
In the PiP pilot trial 48% of parents eligible for the study agreed to take part. This is slightly better than recruitment rates reported in similar studies evaluating preschool physical activity interventions. The Belgium ToyBox intervention54 reported a recruitment rate for children of 39% and two physical activity interventions in Liverpool reported recruitment rates of 36%156 and 42%53 for a preschool-based intervention and a family-focused group-based intervention respectively.
Interestingly, and in contrast to the results for school recruitment, there was a slightly higher consent rate for white parents (n = 62, 66.0%) than for South Asian parents (n = 77, 52.4%) among those who agreed to be contacted about the study. The reasons for this are unclear but it is unlikely to be the result of a language barrier as the community research assistants recruiting at predominantly South Asian schools were bilingual; indeed, in the qualitative interviews one South Asian mother with limited English commented that she appreciated the community research assistant translating the study information for her.
Parents emphasised the importance of trusting the community research assistants when they were initially approached about taking part in the study. The trust came from knowing that the school was working in partnership with the researchers and endorsing the research. Parents said that they participated in the study because the focus was on their child, that they thought that it was a good way to introduce their child to the school environment and learning and that they wanted to help the school. Only one parent said that she wanted her child to play and be more active. Again, this highlights the mainly educational motivations for taking part and suggests that these should be clearly stated in the potential benefits section of the participant information sheet. When asked about the participant information sheet, parents reported that it was acceptable but could be made more appealing by adding pictures and colours. To improve recruitment one head teacher from a predominantly white school suggested making the study more familiar to parents from areas of high deprivation. She remarked that the study looked a bit academic (the community research assistants and information given) and that this might have discouraged parents with low self-esteem who live in an area of high unemployment from taking part.
Objective 2: follow-up and attrition rates during the trial and whether or not there was a difference between trial arms and ethnic groups
Overall, there were good levels of follow-up, with 82.3% and 83.5% of participants providing data (accelerometry, questionnaire or anthropometry) at 10 and 52 weeks respectively. Indeed, retention to the PiP study was better than in other similar trials, which have reported retention at follow-up to be between 68% and 75%. 49 There was no difference in follow-up rates between trial arms at any time point and rates were higher in the South Asian children than in the white children. Thus, although, as discussed above, consent rates were higher in the white families, they were less likely to remain engaged in the study. In the interview with the head teacher from the predominantly white school, she mentioned that this is also the school’s experience of their parents: that they do not ‘stick at it’ (see Box 12).
Only nine participants (5%) withdrew from the trial, with more withdrawing from the control arm (n = 7) than the intervention arm (n = 2). This suggests that taking part in the intervention and undergoing the measurements was not overly burdensome for the participants randomised to the intervention arm of the trial. To ensure good follow-up rates, especially in a hard-to-reach, deprived population, there is a time and resource implication. Almost one-quarter of participants required three or more communications for them to attend the 52-week measurement session and > 10% required five or more communications. It is important that these participants are not excluded from research and that sufficient resources and strategies are built into research study plans to ensure their inclusion. We found that 44 parents changed their contact telephone number over the duration of the trial and 24 changed their address. Therefore, in future research it is suggested that participants are asked to provide as many contact details as possible, such as an e-mail address, Facebook details and the contact details of a significant other.
Objective 3: acceptability of the trial procedures
Parents reported that the information that they received about the study and the trial procedures was, in general, acceptable. However, there was a lack of understanding about the concept of randomisation and the PiP facilitators did not think that parents had a good understanding about what the study entailed. One way to improve understanding of the trial could be to produce a short video to supplement the information in the participant information sheet, including a visual representation of what randomisation is as well as a parent, child and community research assistant completing a measurement session, with a voice-over in a relevant language for participants.
There were mixed opinions about the best location for measurement sessions and parents liked the flexible approach of providing school-based sessions with the option of a home visit. Parents reflected that providing toys and activities for the children during measurement sessions made them enjoyable for the children and they greatly valued the flexibility and helpfulness of the community research assistants. Parents reported feeling uncomfortable about answering questions relating to their own mental health and income from the ComQol-A5 and did not find this long and repetitive questionnaire acceptable.
Parents remarked that using the accelerometer was easy; this seemed to be based on how they perceived it was for their child to wear the monitor. Some parents commented that the belt used to secure the monitor in position around the waist did not stay in the same position and they had to readjust it throughout the day. One parent said that the monitors could be more visually appealing to the children and another mentioned that they sometimes forgot to put the monitor on their child. Despite the mainly favourable reports on using the accelerometer, the feasibility data show that few children wore the accelerometer for the requested time period (7 days) and many did not provide enough data (≥ 6 hours on any 3 days) to be included in the analysis. A discussion on how to improve compliance to the accelerometry protocol is provided in the following section.
Objective 4: feasibility of collecting the outcome measures and whether or not there was a difference between trial arms and ethnic groups
In the PiP pilot trial accelerometers were used to measure physical activity because of their ability to capture physical activity at a high frequency over an extended period and their established reliability and validity. 158,159 However, there are methodological issues to consider when working with accelerometers. The quality and number of data generated is dependent on compliance to wearing protocols, and therefore sufficient data being available to provide a reliable estimate of habitual activity. The minimum wearing criterion reported in the preschool literature ranges from ≥ 1 hours on each of ≥ 3 days to a minimum of 8 hours per day for 7 days. 160 There is also variation in published cut-point thresholds used to reduce accelerometer count data into intensity minutes, with five sets of different preschool cut-points commonly used. 69 Intensity thresholds should be selected if the original sample and calibration activities are reflective of the participant population and there is cross-validation evidence to support their use. Therefore, because of the lack of consensus on wear time criteria and intensity cut-points we derived our own sample-specific criterion using the Spearman–Brown prophecy formula (see Appendix 9), which resulted in a minimum wear-time criterion of 6 hours on at least 3 days. We chose to use the cut-points of Pate et al. 82 as they had been cross-validated under free-living conditions. 83
At baseline, 69% of children in the pilot trial met the wear-time criterion. This is comparable to adherence rates seen in other studies assessing physical activity using a similar wear-time criterion to ours, which report around 70% adherence to accelerometer protocols. 52,159 In the pilot trial we asked participants to wear the accelerometer at baseline and at all follow-up time points. Although parents reported that the accelerometer was acceptable, the number of participants meeting the wear-time criterion was low, with only 39% of participants providing enough data at both baseline and 52 weeks’ follow-up to be included in the analysis.
It is difficult to draw comparisons with other studies because of the lack of methodological consensus for measuring physical activity in children as young as those in this study (mean age 2.8 years). Indeed, very few studies have assessed physical activity in children aged < 3 years. Similar RCTs of physical activity interventions with slightly older preschool children that have used accelerometry as the primary outcome (mean age approximately 5 years) report compliance at both baseline and follow-up ranging from 42% to 70%. 52–54,156 These studies tended to use nursery staff to administer the accelerometers and check that children were wearing them.
Since the conclusion of the PiP pilot trial we have conducted a study to test strategies to improve accelerometry wear time. In total, 67 preschool children were recruited from four primary schools in the two highest IMD categories in Bradford. Three of these schools had been involved in the pilot trial and one school had not. Two schools had predominantly white pupils and two predominantly South Asian pupils, thus the study population was similar to that in the pilot trial. Children were excluded from taking part if they had previously been participants in the PiP pilot trial. Parents were asked to secure the Actigraph accelerometer around their child’s waist for ideally 6 and at least 3 days and for 7 hours on each day. They were also asked to complete a diary of wear time. In addition:
-
Nursery staff were made aware of which children should be wearing accelerometers and offered support to parents and children.
-
Parents received a daily reminder by telephone or text message to put the accelerometer on their child.
-
Accelerometers were checked to see whether or not valid wear-time criteria had been met when they were collected from families.
-
The monitor was left for longer with the family if wear-time criteria had not been met.
-
A desirable incentive (a goodie bag of toys) was offered rather than a voucher.
-
All monitors were checked before each measurement time point to ensure that those that were malfunctioning were not distributed.
The newly employed strategies increased the number of children with valid accelerometry data at both baseline and 10 weeks’ follow-up, from 39% in the pilot trial to 60% in the improvement study. These new strategies would be used in a full-scale trial of the PiP intervention.
In addition to collecting accelerometry data to measure physical activity, it may also be useful to assess physical activity using a questionnaire as a secondary outcome in future research. Although questionnaire data, especially parent reported, are not as valid as objective data such as accelerometry data, in the pilot trial we found very good completion rates for questionnaires. In total, 79% of parents completed the General Self-Efficacy Scale at both baseline and 52 weeks’ follow-up. Even the ComQol-A5, which parents reported to be unacceptable, had reasonable completion rates (69% of participants provided data at both baseline and 52 weeks’ follow-up). These data illustrate that questionnaires are feasible measurement tools for this population. Members of our group have been developing a physical activity questionnaire for use with UK preschool children; preliminary results have shown the questionnaire to have acceptable levels of validity and reliability.
In terms of the secondary outcomes for the study, completion of height and weight measurements decreased over time, with 88% of children completing both measurements at baseline and only 65% completing both measurements at 52 weeks. This resulted in 57% of children having BMI data available for both time points and being included in the analysis. This may be a result of research fatigue on the behalf of participants. To reduce the likelihood of this occurring, subsequent research may consider measuring height and weight at baseline and 52 weeks’ follow-up only, to assess the long-term effects of the intervention on indices of obesity.
A similar pattern was also observed for waist and upper arm circumference, with only 45% and 41% of children, respectively, providing data at both baseline and 52 weeks’ follow-up; the lower rates of completion obtained may be because these measures were taken towards the end of the measurement session, which was relatively long (approximately 1 hour) for young children with short attention spans.
The completion rates for the outcomes related to the economic evaluation of the PiP intervention (EQ-5D, PedsQL and health service use) were sufficient (77% and 76% for the EQ-5D and 100% and 75% for the PedsQL at baseline and 52 weeks respectively). The data provided were useable, rendering a preliminary cost-effectiveness analysis feasible. A new version of the EQ-5D has recently been developed (EQ-5D-5L) that has five levels instead of three levels for each health dimension. 161 This version may be more reliable and sensitive for use within public health settings whilst remaining feasible and thus is recommended for use in future trials that are similar to the PiP trial.
For all of the health outcomes there was little difference in completion rates between trial arms. Completion rates were higher for South Asian children than for white children across all measures and at all time points with the exception of upper arm circumference.
Objective 5: influence of financial incentives on trial participation
Parents were given a £10 gift voucher for Mothercare/Early Learning Centre on completion of each measurement session and for taking part in an interview. Some parents thought that the vouchers were important and encouraged them to take part and others thought that they were a nice gesture. However, parents did also report feeling uncomfortable about answering the questions relating to income and money in the ComQol-A5 and may have been reluctant to disclose how important monetary support is to them. One head teacher who was interviewed reflected that monetary value was important to the families attending her school and that the incentive was good for the children living in deprived areas. She commented that Asda vouchers were used by the school and she perceived that these were usually used for goods relating to the children. A recent review of strategies to increase retention in trials162 concluded that monetary incentives and offers of monetary incentives improved postal and electronic responses to questionnaires. However, there was a lack of research and no conclusions were drawn on the impact of incentives on attendance at trial measurement sessions.
In the PiP pilot trial the consensus from parents was that it was important that the incentive is spent on the child and a voucher ensured that this would happen. Most parents felt that the vouchers were of the right value but that the type of voucher was inappropriate, with two-thirds of parents commenting that they were for expensive shops where they had relatively little value. For future research it is important to consider the type of incentive that is appropriate and useful to the participant population.
Objective 6: attendance to, and acceptability of, the intervention, whether or not there was a difference between ethnic groups and whether or not attendance varied by season
Attendance to the initiation phase
Overall, only 65% of children attended one or more sessions during the initiation phase. The number of children attending at least one session was lowest during the winter initiation phase (wave 2) at 40% but was double this during the summer initiation phase (wave 3) at > 80%. In the autumn initiation phase (wave 1) those who ever attended came to very few sessions, whereas in the winter and summer initiation phases those who ever attended had a mean attendance of 10 sessions, equating to one session per week, with some children attending between two and three sessions per week.
Participants in the PiP intervention group were encouraged to attend three 30-minute sessions per week (equating to 90 minutes of exposure to the intervention per week). This is greater than in other similar preschool physical activity interventions: the Belgium ToyBox intervention54 and two physical activity interventions (one based in preschools156 and the other a family-focused group-based intervention57) all requested that the intervention be delivered in one 1-hour session per week. These studies reported small to moderate effects of the intervention on MVPA (up to 7.2 additional minutes of physical activity per day). Given this emerging evidence, we propose encouraging families to attend at least two and ideally three PiP sessions per week, which equates to an exposure of between 60 and 90 minutes per week. Unfortunately, these and other studies of group-based parent and child lifestyle interventions have not reported their attendance rates and therefore our data cannot be compared.
The interviews with parents showed that one clear reason for poor attendance during the initiation phase in waves 1 and 2 was the poor weather, with all seven parents interviewed mentioning this. Indeed, during the autumn of 2012 there were several extended periods of heavy rainfall and between January and April 2013 there were several weeks of significant snowfall and very low temperatures. Additionally, the PiP facilitators acknowledged that many children were unwell during the winter months and commented that running the intervention during the summer months or in an indoor environment would be better. The possibility of accommodating PiP sessions in an indoor setting within the school as an alternative during the winter months was explored in conversations with the schools (outside of the qualitative interviews); however, it was not feasible in the majority of schools because of restricted indoor space.
Another reason given for poor attendance was the sessions not fitting in with the children’s daily routines. However, the parents who regularly attended stated that the timings and location worked well for them. The timings of the sessions were agreed on by the schools following randomisation and therefore one way to overcome this would be to work with the schools to set the session times before recruiting families. Parents could then be made aware of the session timings before committing to the intervention. This mirrors what already occurs in practice for preschool-organised, group activity sessions and this would also be the case if the intervention was rolled out at scale.
The PiP facilitators suggested that attendance could have been improved by the school promoting the intervention more and by reducing the burden of the measurement sessions (which they thought discouraged parents from participating in the entire study including the PiP sessions). They reflected that it was important that the facilitators were familiar to the parents. This stresses the importance of using existing school staff to deliver the PiP sessions rather than bringing in new ‘specialist’ staff. One method often used by schools to increase familiarity is for outreach workers to visit families at home (this is sometimes part of the role of a parental involvement worker); however, this is resource intensive. Instead, a welcome ‘fun day’ session, with refreshments for parents, could be used as a way for the PiP facilitators to meet new parents before the start of the intervention. In addition, for those parents whose children use the school nursery, the facilitators could introduce themselves during drop-off/pick-up times.
Acceptability of the initiation phase
Parents and facilitators commented that the PiP sessions were varied and fun and that the children had very much enjoyed taking part. One facilitator reflected that the sessions became more enjoyable over time as everyone’s confidence improved and the children settled into the routine of the sessions. Only one parent had a negative experience of the one session he attended, reporting that it was the first session and that the facilitator did not know what she was doing.
Parents, PiP facilitators and head teachers all commented that the intervention was beneficial to children, parents and the school. Children and parents had learned new active games to play together and children had developed their confidence, learning colours, sharing and making friends. Parents reported that they had benefited from taking part; they had enjoyed doing something with their child, being more active themselves and making new friends. Both the structured PiP-PoP games and the free-play sections of the intervention were well accepted and enjoyed by children, parents and facilitators. Different children and different groups had their favourite PiP-PoP activities, which they enjoyed re-enacting during free play. Facilitators also commented on how they bought out different equipment during free play to sustain the active play.
The PiP facilitators and head teachers reflected on how parents had grown in confidence in playing with their children over the duration of the initiation phase, learning new activities and engaging with their children in a way that they had not done before, modelling good language and meeting other parents whose children would be attending the same nursery. Another benefit of the intervention reported by a facilitator at one of the wave 3 schools was that it was a good way to support transition into nursery, with parents and children becoming familiar with the staff in the nursery where many would be starting in the next academic year. The head teacher of the other wave 3 school commented that there had been better attendance at nursery following the initiation phase of the PiP study and that parents had been more involved in their child’s learning. The other head teacher interviewed commented that taking part in the PiP intervention had made the nursery staff more aware of the importance of parents and children playing outside together and planned to build this into the school’s nursery programme using the PiP manual the following year.
The PiP facilitators commented that the PiP manual and the training for the PiP intervention were easy to understand and helpful in providing them with useful information, ideas and confidence to deliver the intervention in a flexible way. They did not feel that they required any previous experience in delivering physical activity sessions but did emphasise the importance of previous experience of working with both children and parents.
There was a mixed response to the guided discussions and handouts in the intervention. One facilitator could not remember seeing the leaflets and another found it hard to guide the discussion within the short time of the sessions. This facilitator commented that she gave out the leaflets but received little feedback. Two other facilitators described the leaflets and discussions as useful but did not want to overload the parents with information. One way to improve on this could be to provide the information in a different format, such as a short film of a group of parents discussing each topic, which parents could view online and then discuss with facilitators at the PiP sessions.
Changes made to the initiation phase of the intervention and their acceptability
During waves 2 and 3 of the intervention a new behaviour change technique was introduced: families received a new piece of play equipment each week when they attended at least one session (see Chapter 1, Changes to the intervention, for a list of equipment). The wave 3 parents reported using the equipment at home and the PiP facilitator confirmed that parents had told her that they had been using the equipment at home.
A further change in wave 3 was the addition of telephone support from facilitators to parents who had, for unknown reasons, not attended three consecutive sessions (one week of the intervention). PiP facilitators reported telephoning and texting those who had not attended sessions but often they received no reply and these families did not attend. This was also the difficulty we experienced when contacting some of the parents for measurement sessions and may reflect the frequency with which some parents change their telephone numbers.
A change to the delivery of the intervention was also made: schools were given the option to reduce the number of sessions offered to four per week after the first 3 weeks of the intervention if there were two sessions that were poorly attended. This change was made before wave 3 of the intervention, in which attendance was much better, and neither of the wave 3 schools implemented this change.
Maintenance phase attendance and acceptability
During the maintenance phase only 16% of children attended any sessions. Attendance was low across all waves, ranging from 0% attendance in wave 1 to 29% of children attending any session in wave 3 (school 5). Of those children who attended at least one session, the average number of sessions attended was 5.2 (SD 3.4 sessions), with a median of 4.5 sessions (minimum–maximum 1–11 sessions). Before the maintenance phase facilitators were asked whether or not they thought that parents would attend. Two thought that the maintenance phase would not work because parents would need someone to lead them and two were more confident because they felt that parents who were regular attendees were capable of running the sessions. Subsequent conversations with facilitators during the maintenance phase about poor attendance revealed that changes in family routines and circumstances, particularly children starting nursery or preschool or changing nursery days or times but also mothers returning to work, advancing pregnancies, poor weather, lack of visibility of the intervention without a facilitator and school building work, hampered attendance during the maintenance phase. The head teacher at one school indicated that, with the maintenance phase, the intervention was too long and that parents attending the school do not engage in long-term programmes. A recent meta-analysis of the effectiveness of physical activity interventions for preschoolers highlighted the importance of having professionals lead intervention sessions. 155 This study found that interventions led by teachers had a larger effect on MVPA levels than interventions led by parents. One previous study maintained a preschool physical activity intervention over 3 years using newsletters and a radio programme to give parents information about physical activity. 163 This strategy could be used in the PiP intervention to sustain behaviour change. Families would receive a newsletter/video link during the summer holidays (after the 10-week initiation phase) including reminders about physical activity guidelines, PiP games, physical activities that they can do as a family and what is available to them locally. This newsletter/video would be repeated each school term for the subsequent year (autumn, spring and summer terms) and would include details of local physical activities available to families. These behaviour change techniques of ‘prompts and cues’ and ‘information regarding the behaviour’ fit within social cognitive theory, targeting behavioural and personal factors.
Ethnic group differences
Attendance at the PiP intervention sessions was higher among South Asian children than among white children. Among those children who attended at least one session, the average number of sessions attended for white children was 10.7 (SD 12.1 sessions), with a median of three sessions attended (minimum–maximum 1–33 sessions), and for South Asian children was 11.3 (SD 11.8 sessions), with a median of 4.5 sessions attended (minimum–maximum 1–35 sessions). The qualitative analysis found no clear differences between ethnic groups regarding the acceptability of the intervention. This pattern of disengagement has been seen throughout the trial, with fewer white participants attending measurement sessions and providing outcome data. These findings may be the result of social differences, specifically social capital. In the PiP pilot trial we found that the ethnic minority South Asian families were more willing to engage in health research and health behaviours and this may be because they have better social networks, are more involved in the community, are less isolated and are more familiar with group activities than poor white parents. Being part of a minority ethnic group and sharing culture and social support networks may be protective for health, even in economically deprived contexts. This is illustrated by research in the USA on the ‘Latina paradox’. 164 Latina women had comparable birth outcomes with white women of better SES and McGlade et al. 164 argue that this was because systems of family, friends, community members and lay health workers provide support.
Objective 7: fidelity of programme implementation
Assessing the fidelity of health interventions is important for interpreting results and the likely success of the intervention if rolled out. The mean total fidelity score of the PiP intervention was 29.1 (SD 5.7) out of a total possible score of 36 (81% adherence), highlighting good adherence overall to the intervention protocol. Few preschool physical activity trials report on the fidelity of the intervention, One teacher-led preschool structured play physical activity intervention from the USA165 reported an average of 70% adherence across different domains included in the analysis (duration of sessions and delivery according to instructions). The two areas with poorer adherence in the PiP intervention were ‘providing information on guidelines for physical activities for the under 5’s’ and ‘encouraging families to seek other physical activities’. These two areas should have been covered in the guided discussion and handouts section of the PiP sessions, which were received with mixed feelings (refer to Acceptability of the initiation phase). Including an information video for parents as suggested in Acceptability of the initiation phase may be one way to meet this intervention objective. Furthermore, these films could also provide parents with information about other local physical activity opportunities, for example toddler and parent dance groups at children’s centres or soccer groups.
Objective 8: capacity of schools to deliver and incorporate the intervention within existing services
The two head teachers who were interviewed had different views on the capacity of their school to deliver the intervention. Both had incorporated the delivery of the intervention into the workloads of existing staff. In one school, the PiP facilitators were nursery staff and the head teacher felt that the intervention took the staff members away from their normal work. The intervention would therefore not be sustainable without additional funding for a facilitator. In the other school, the head teacher described how the school was well staffed, with a good budget. In this school the PiP facilitator was a parental involvement worker whose role it is to work with and support families. This seemed to be a more appropriate member of staff to facilitate the intervention as it was more easily incorporated into their workload. At this school the head teacher commented that she did not think that the intervention would be sustainable as parents at her school do not engage in long-term interventions. She suggested that an intervention of a shorter duration, from 6 weeks to one term, would be more acceptable and sustainable. As mentioned in Maintenance phase attendance and acceptability, this recommendation would be included in a revised version of the intervention. Gordon et al. ’s155 recent meta-analysis of physical activity interventions for preschool children emphasised the importance of the delivery site and showed that effective interventions were delivered in a learning environment (usually a preschool setting), whereas home-based interventions were associated with a small negative effect on indices of physical activity. This highlights the importance of using school/preschool sites for health promotion and strengthens the point that one of the head teachers made when interviewed, that there is a need for more ‘joined-up thinking’ between health and education so that initiatives such as the PiP intervention are part of a more strategic, longer-term approach.
Objective 9: the effect of participation in the intervention on health outcomes and whether or not there were differences between ethnic groups
Summary statistics were presented for health outcomes overall, by trial arm and by ethnicity. The mean number of minutes spent in MVPA per day was lower in the intervention group than in the control group at both 10 weeks [61.8 (SD 25.2) vs. 62.1 (SD 22.9) minutes] and 52 weeks [72.6 (SD 30.4) vs. 74.3 (SD 25.5) minutes]. The mean number of minutes spent in light activity per day was higher in the intervention group than in the control group at both 10 weeks [212.9 (SD 39.4) vs. 200.4 (SD 45.1) minutes] and 52 weeks [220.9 (SD 37.4) vs. 219.1 (SD 43.1) minutes]. The mean number of minutes spent sedentary per day was higher in the intervention group than in the control group at both 10 weeks [318.0 (SD 102.6) vs. 303.7 (SD 69.0)] and 52 weeks [335.7 (SD 102.4) vs. 302.5 (SD 65.6)].
Differences were observed in summary statistics by ethnicity. South Asian children showed very small improvements in time spent in MVPA following the intervention whereas white children did not. The trends identified from the descriptive summaries should be interpreted with caution as the number of children with available data in each ethnic group is small and there is also the possibility of attrition bias.
Objective 10: estimates of effect size, typical cluster sizes and intraclass correlation coefficients to enable an accurate sample size calculation for a full randomised controlled trial
Estimates of effect size, typical cluster sizes and ICCs were presented for all children with available data and a sensitivity analysis excluding an outlier. The sample size for a full trial was calculated to be 600 children and 38 schools (16 children per school).
Objective 11: preliminary assessment of the potential cost-effectiveness of the Preschoolers in the Playground intervention and an estimate of the value of further research
The economic evaluation compared the costs and QALYs of the PiP intervention with those of usual practice (the control arm). In the base case, which involved MI of missing data, the intervention appeared to have a positive impact on parents’ quality of life and was also more costly than usual practice (i.e. no intervention). These results, however, were not statistically significant. The incremental cost per QALY of the intervention compared with usual practice was £19,588 and therefore at current threshold values of a QALY it can be inferred that the PiP intervention is borderline cost-effective, although there is significant uncertainty surrounding this estimate. The primary analysis also found that the HRQoL of toddlers and infants was higher in the control group at week 52 but the overall change from baseline PedsQL score was larger in the intervention group, suggesting higher health gains in the latter, although not statistically significant.
A number of additional analyses were conducted. These concurred with the base-case results and the conclusion that the intervention is borderline cost-effective appears to be robust to a range of different assumptions. These results should, however, be treated with caution. The differences in costs and QALYs were not statistically significant; the causal mechanism whereby the intervention would improve parents’ HRQoL without impacting on children’s QoL is not immediately obvious. These results and mechanisms could be evaluated further in a large-scale trial. An exploratory subgroup analysis was also undertaken, which demonstrated that the PiP intervention is likely to be cost-effective in the South Asian participants (ICER of £9346 per QALY in the base case and £10,329 per QALY in the complete-case analysis) but not in the white participants. However, this difference may be a result of the higher attendance rates for the South Asian participants than for the white participants.
The benefits of the PiP intervention are likely to be seen over the longer term as established by the literature review. The current analysis, which is solely based on the period of the trial, is therefore unlikely to capture all of the costs and benefits associated with the intervention. It would be expected that extending the time horizon over the longer term would strengthen the cost-effectiveness argument in favour of the intervention.
Objective 12: whether or not links can be established between short-term outcomes and long-term quality of life, potentially including across sectors
An extensive body of evidence was identified by the literature review that explored associations between short-term and long-term health outcomes. The papers focused on childhood obesity as the exposure measure. The directions of the associations across the disease areas varied widely between studies but the links between childhood obesity and risk of CHD, atherosclerosis and hypertension in adulthood appeared to be consistent, with the majority of studies showing positive correlations. Overall, the evidence from the literature review corroborated other evidence that exists which associates overweight/obesity indices in childhood with health status later in life. As the study from Timmons et al. 14 suggests, physical activity interventions could be applied in children to improve obesity indices and hence potentially reduce the occurrence of adverse health conditions in adult life.
Objective 13: whether or not it is appropriate to apply for further funding for a full-scale randomised controlled trial
There were two criteria for success of the pilot trial. These were:
-
no more than 40 schools approached to recruit 10 schools to the study and at least 15 preschool children recruited at each school
-
at least 70% retention at 10 weeks (this figure is based on results from previous physical activity interventions in this age group, which have reported retention rates at 6 months of 70–75%49).
The pilot trial was successful in meeting the two criteria for progression. In total, 27 schools were approached to take part in the study and 10 were recruited (six predominantly South Asian schools and four predominantly white schools); this equates to 37% of those who were approached to take part. In total, 164 children were recruited to the study, an average of 16 children per school. The retention rate was 82.3% at 10 weeks and 83.5% at 52 weeks. This exceeds the retention rates reported in a review of preschool obesity prevention interventions by Hesketh and Campbell,49 which found retention to trials to be between 70% and 75%.
Although the progression criteria were met, the lower than expected attendance to the intervention should be considered when judging whether or not it is appropriate to apply for further funding for a full-scale trial. Emerging evidence from successful interventions suggests that a 60-minute dose of physical activity each week has small to moderate effects on MVPA levels (up to 7.2 additional minutes of physical activity per day). Therefore, families attending the modified PiP intervention would be encouraged to attend at least two and ideally three PiP sessions per week, equating to an exposure of between 60 and 90 minutes per week. The qualitative data from the pilot trial and the PPI consultations have informed several strategies (see Proposed changes to the intervention) to increase attendance, from an average of one session per week in the pilot trial to at least two sessions per week for the full trial.
Strengths and limitations of the Preschoolers in the Playground pilot trial
The PiP pilot trial used a multimethod approach (quantitative, qualitative and health economic analyses), which few other evaluations of preschool physical activity interventions have done, and thus a thorough evaluation of the trial procedures, the intervention and the likely value of conducting a full trial has been conducted. In the PiP pilot trial we were able to engage with hard-to-reach poor white families and ethnic minority groups, who are often under-represented in research. We achieved good recruitment and retention rates but found that to sustain engagement there is a higher resource need. Resources are required to track and make contact with the participants in the trial and to support them to attend intervention sessions and complete the study outcome measures. In the PiP study we asked parents to put an accelerometer on their child for 7 days. When families are living chaotic lives with financial pressures, putting an accelerometer on their child is not a priority. A relatively low number of participants was included in the analysis of data because few had accelerometry data at baseline and 52 weeks’ follow-up. This is a limitation of the pilot trial and we have conducted further research and implemented new strategies to improve adherence to the accelerometry protocol.
The PiP intervention was well developed, was based on a theoretical framework and was informed by the existing literature and by parents with preschool children. The three-wave design of the study allowed us to make changes and improve the intervention in an iterative manner throughout the study and we were able to examine the impact of delivering the intervention during different seasons. We had poorer than expected attendance rates to the intervention. In the initiation phase this was primarily because of families not attending during the cold and wet autumn and winter months and in the maintenance phase this was possibly because of the lack of a facilitator. Because of this we propose modifying the intervention so that it is delivered during the summer months only and always by a facilitator (see Proposed changes to the intervention). Indeed, teacher-led interventions have previously been found to be more effective than parent-led interventions for preschool children. 154 Consequently, the data relating to the effect of the intervention on health outcomes in this report do not reflect the likely effect of the proposed modified intervention. We have identified several strategies that could be used to maximise attendance to the modified summer term-only intervention, described in Proposed changes to the intervention, and we propose to review other group-based preschool play programmes to identify other possible strategies that we could employ to increase attendance.
Lessons learned
The findings from the PiP pilot trial can help to modify the PiP intervention, inform a full-scale trial of the PiP intervention and also provide advice for researchers planning to conduct public health interventions with schools and deprived and ethnically diverse populations. The following sections provide a description of the proposed modifications to the PiP intervention and a list of recommendations for a full trial and for other researchers.
Proposed changes to the intervention
To improve the intervention the following changes are proposed:
Modifications aimed at increasing attendance
-
The intervention would be delivered during the summer term. Emerging evidence suggests that establishing high levels of physical activity in the summer months promotes healthy weight in preschool children, regardless of lower activity levels during the winter. 46 It is, therefore, suggested that a summer term-only intervention would still have benefits for health.
-
The intervention would be delivered for 10 weeks only (the initiation phase). One head teacher commented that families may be more inclined to engage in a shorter, one term-only intervention led by a facilitator. This was also suggested by teaching staff who were independent of the PiP pilot trial during a PPI group meeting.
-
Families would be encouraged to attend at least two and ideally three intervention sessions per week (60–90 minutes of intervention exposure).
-
Each family would receive a text reminder about session days and times each week with information about the free take-home play equipment for that week.
-
The timings of the sessions would be agreed on by the schools and set before recruiting families. Parents would be made aware of the session timings before committing to the intervention.
-
Facilitators would become familiar with families before the start of the intervention by hosting a welcome ‘fun day’ session with refreshments for parents and would also introduce themselves to parents whose children use the school nursery before the start of the intervention.
-
Engagement with schools would occur earlier so that all staff members were aware of the intervention and could support the families taking part to attend. More visible promotional materials would be put up in schools, children’s centres and local groups to remind families and early years workers that the intervention is ongoing.
-
As an incentive to attend, refreshments and some social time for parents would be provided at the end of the sessions.
Other modifications to the intervention
-
The information given to parents in the guided discussions and leaflets would be produced in an online video format, showing parents having the discussions, to increase the likelihood that the information is received and to reduce the time needed to cover these topics in the sessions. Facilitators would support parents to watch the videos and would answer any questions.
-
To sustain the behaviour change from the initiation phase of the intervention, families would be provided with information about other local active playgroups or activities, for example toddler and parent dance groups at children’s centres or soccer groups. Families would be asked if they would like to join these groups and contact details could be passed to organisers. This behaviour change technique of ‘prompts and cues’ fits within social cognitive theory, targeting behavioural factors.
-
A further sustainability strategy would be to recontact families with a newsletter/video link during the summer holidays after the 10-week initiation phase and include reminders about PiP games and physical activities that they can do as a family and reminders about what is available to them locally. This newsletter/video would be repeated each school term for the subsequent year (autumn, spring and summer terms), including details of relevant and local activities available to families. These behaviour change techniques of ‘prompts and cues’ and ‘information regarding the behaviour’ fit within social cognitive theory, targeting behavioural and personal factors.
List of recommendations for a full trial and for other researchers
-
Few trials of preschool physical activity interventions conduct qualitative interviews, assess fidelity, report attendance or conduct a health economic evaluation. Including these in research studies is a recommendation for other researchers when designing evaluations of interventions in the future.
-
Build in sufficient time and resources to research plans to ensure successful follow-up of, and extra support for, hard-to-reach participants.
-
With very young children consider the impact of multiple measures over time on research fatigue and minimise measurements when it is possible to do so.
-
The ComQol-A5 questionnaire was not acceptable to parents because of the sensitive questions about mental health and income. It would not be used in a full trial of the PiP intervention.
-
Ensure that study materials are appealing to participants by using colours and pictures and that they can be easily understood. Consider supplementing the participant information sheet with an online video to describe the study procedures visually, including randomisation.
-
Ask participants to provide as many different contact details as possible.
-
Incentives for research appear to be important in deprived communities; the type of incentive that is appropriate and useful to the participant population must be considered.
-
To recruit schools into health research, consider the priorities of education professionals and describe the potential benefits that fit with these priorities, for example parents and children becoming familiar with the school.
-
Consider the motivation for families to take part in the study (in the PiP trial this was mainly social and learning) and describe these potential benefits in the study information. Be aware that these may not match up with the intended primary outcome of the study (in the PiP trial increasing physical activity).
-
Ensure that participants can identify with the research staff who are conducting recruitment, for example the researchers can translate study materials into relevant languages for participants and are not ‘too academic’.
Chapter 5 Conclusion
The aim of this study was to undertake a pilot cluster RCT of the PiP intervention to assess the feasibility of a full-scale cluster RCT using a multimethods approach. We found our recruitment strategy to be successful, reported a good retention rate to the trial, found the trial procedures to be acceptable and found that incentives were important for participation in the trial. We have identified and tested strategies, which improved adherence to the accelerometer protocol. The successful strategies would be implemented in a full trial. The intervention was found to be acceptable to both schools and families and was perceived as beneficial. Schools were able to incorporate the intervention into the roles of staff members and the parental involvement worker was said to be best placed to deliver the intervention. The fidelity of the delivery of the intervention was good. We have proposed some modifications to the intervention to improve attendance and thus effectiveness and sustainability. The research and intervention were more acceptable to the South Asian families approached, who were more willing than the white families approached to engage in both the PiP trial and the intervention.
A preliminary assessment of the potential cost-effectiveness of the PiP intervention was conducted. The intervention was found to be borderline cost-effective and a literature review established that links could be made between short-term outcomes and long-term quality of life. We have shown that it is feasible to conduct a full-scale RCT of the PiP intervention and have calculated a sample size of 600 participants from 38 schools for the full trial.
Acknowledgements
Thank you to all of the helpful school and children’s centre staff we worked with on the study and a big thank you to all of the parents and children who participated. We acknowledge the hard work of the community research assistants who conducted recruitment and collected the data for the study. Over the course of the trial the community research assistants were Sameera Ali, Zille Rabab, Asma Hussain, Gulnaz Akhtar, Julia Blackburn, Yazmin Razaq and Rizwana Lawrence. We also acknowledge Hannah Buckley for her help with the analysis plan and Christina Giannopoulou for her work preparing the health economics section of the report. Finally, we acknowledge the study steering group committee for their expert advice during the course of the study. This group consisted of Professor Greet Cardon (Ghent University), Professor Judy Hutchings (Bangor University) and Andrew Scully (Bradford University).
Contributions of authors
All authors were members of the internal steering group for the trial, read drafts and provided revisions on the content of the report and have given final approval for submission. In addition, their individual contributions are as follows:
Sally E Barber (Principal Research Fellow) was the PiP trial manager and first author.
Shaheen Akhtar (Programme Co-ordinator) was the PiP study co-ordinator and was responsible for data management.
Cath Jackson (Senior Research Fellow) was responsible for qualitative data collection and the analysis, preparation and presentation of the qualitative results.
Daniel D Bingham (PhD student) was responsible for the management of accelerometry data collection and wrote Appendix 9 regarding the accelerometry wear-time decisions.
Catherine Hewitt (Senior Statistician) was responsible for the statistical analysis and the preparation and presentation of the quantitative results.
Ash Routen (Postdoctoral Research Associate) was responsible for analysis of the accelerometry data and contributed to writing the physical activity results and discussion.
Gerry Richardson (Senior Health Economist) was responsible for analysis of the health economic data and the preparation and presentation of the health economic results.
Hannah Ainsworth (Research Fellow) provided trial support from the York Trials Unit and contributed to writing the design and methodology sections.
Helen J Moore (Postdoctoral Research Associate) provided expertise in children’s physical activity interventions and contributed to the analysis and presentation of the physical activity data.
Carolyn D Summerbell (Professor of Human Nutrition) provided expertise in childhood obesity and contributed to the review of the literature and writing of the introduction and discussion.
Kate E Pickett (Professor of Epidemiology) provided expertise in health inequalities, contributed to writing the introduction and contributed to the discussion.
Claire O’Malley (PhD student) contributed to the analysis and presentation of the physical activity data.
Shirley Brierley (Public Health Consultant) provided a link to practice and made revisions to the discussion section.
John Wright (Professor of Epidemiology and Child Health) was the Principal Investigator, reviewed the whole manuscript and had overall responsibility for the study.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Reilly JJ. Physical activity, sedentary behaviour and energy balance in the preschool child: opportunities for early obesity prevention. Proc Nutr Soc 2008;67:317-25. http://dx.doi.org/10.1017/S0029665108008604.
- Janz KF, Kwon S, Letuchy EM, Eichenberger Gilmore JM, Burns TL, Torner JC, et al. Sustained effect of early physical activity on body fat mass in older children. Am J Prev Med 2009;37:35-40. http://dx.doi.org/10.1016/j.amepre.2009.03.012.
- Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med 2000;154:220-6. http://dx.doi.org/10.1001/archpedi.154.3.220.
- Department of Health . At Least Five a Week: Evidence on the Impact of Physical Activity and Its Relationship to Health n.d. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/ (accessed 31 July 2014).
- Martinez-Gomez D, Eisenmann JC, Tucker J, Heelan KA, Welk GJ. Associations between moderate-to-vigorous physical activity and central body fat in 3–8-year-old children. Int J Pediatr Obes 2011;6:e611-14. http://dx.doi.org/10.3109/17477166.2010.533775.
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295:1549-55. http://dx.doi.org/10.1001/jama.295.13.1549.
- Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J 2006;1:11-25. http://dx.doi.org/10.1080/17477160600586747.
- Olds T, Maher C, Zumin S, Péneau S, Lioret S, Castetbon K, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes 2011;6:342-60. http://dx.doi.org/10.3109/17477166.2011.605895.
- Schmidt Morgen C, Rokholm B, Sjöberg Brixval C, Schou Andersen C, Geisler Andersen L, Rasmussen M, et al. Trends in prevalence of overweight and obesity in Danish infants, children and adolescents – are we still on a plateau?. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0069860.
- NHS Information Centre for Health and Social Care . National Child Measurement Programme 2010 2011 n.d. https://catalogue.ic.nhs.uk/publications/public-health/obesity/nati-chil-meas-prog-eng-2010–2011/natichil-meas-prog-eng-2010–2011-rep1.pdf (accessed 31 July 2014).
- Fischbacher CM. How physically active are south Asians in the United Kingdom? A literature review. J Public Health 2004;26:250-8. http://dx.doi.org/10.1093/pubmed/fdh158.
- Owen CG. Ethnic and gender differences in physical activity levels among 9–10-year-old children of white European, south Asian and African-Caribbean origin: the Child Heart Health Study in England (CHASE study). Int J Epidemiol 2009;38:1082-93. http://dx.doi.org/10.1093/ije/dyp176.
- Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med 1999;153:409-18. http://dx.doi.org/10.1001/archpedi.153.4.409.
- Timmons BW, LeBlanc AG, Carson V, Connor Gorber S, Dillman C, Janssen I, et al. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl Physiol Nutr Metab 2012;37:773-92. http://dx.doi.org/10.1139/h2012-070.
- Shea S, Basch CE, Gutin B, Stein AD, Contento IR, Irigoyen M, et al. The rate of increase in blood pressure in children 5 years of age is related to changes in aerobic fitness and body mass index. Pediatrics 1994;94:465-70.
- Sääkslahti A, Numminen P, Varstala V, Helenius H, Tammi A, Viikari J, et al. Physical activity as a preventive measure for coronary heart disease risk factors in early childhood. Scand J Med Sci Sports 2004;14:143-9. http://dx.doi.org/10.1111/j.1600-0838.2004.00347.x.
- Jones RA, Hinkley T, Okely AD, Salmon J. Tracking physical activity and sedentary behaviour in childhood: a systematic review. Am J Prev Med 2013;44:651-8. http://dx.doi.org/10.1016/j.amepre.2013.03.001.
- Shankaran S, Bann C, Das A, Lester B, Bada H, Bauer CR, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Risk for obesity in adolescence starts in early childhood. J Perinatol 2011;31:711-16. http://dx.doi.org/10.1038/jp.2011.14.
- Herman KM, Craig CL, Gauvin L, Katzmarzyk PT. Tracking of obesity and physical activity from childhood to adulthood: the Physical Activity Longitudinal Study. Int J Pediatr Obes 2009;4:281-8. http://dx.doi.org/10.3109/17477160802596171.
- O’Dwyer MV, Foweather L, Stratton G, Ridgers ND. Physical activity in nonoverweight and overweight UK pre-school children: preliminary findings and methods of the Active Play Project. Sci Sports 2011;26:345-9. http://dx.doi.org/10.1016/j.scispo.2011.01.006.
- Hesketh KR, McMinn, AM, Ekelund U, Sharp S, Collings PJ, Harvey NC, et al. Objectively measured physical activity in four-year-old British children: a cross-sectional analysis of activity patterns segmented across the day. Int J Behav Nutr Phys Act 2014;11. http://dx.doi.org/10.1186/1479-5868-11-1.
- Hinkley T, Salmon J, Okely AD, Crawford D, Hesketh K. Preschoolers’ physical activity, screen time and compliance with recommendations. Med Sci Sports Exerc 2012;44:458-65. http://dx.doi.org/10.1249/MSS.0b013e318233763b.
- Beets MW, Bornstein BS, Dowda M, Pate RR. Compliance with national guidelines for physical activity in US pre-schoolers: measurement and interpretation. Pediatrics 2011;127:658-64. http://dx.doi.org/10.1542/peds.2010-2021.
- Cardon GM, De Bourdeaudhuij IM. Are preschool children active enough? Objectively measured physical activity levels. Res Q Exerc Sport 2008;79:326-32. http://dx.doi.org/10.1080/02701367.2008.10599496.
- Vale S, Silva P, Santos R, Soares-Miranda L, Mota J. Compliance with physical activity guidelines in preschool children. J Sports Sci 2010;28:603-8. http://dx.doi.org/10.1080/02640411003702694.
- Bornstein DB, Beets MW, Byun W, Welk G, Bottai M, Dowda M, et al. Equating accelerometer estimates of moderate-to-vigorous physical activity: in search of the Rosetta stone. J Sci Med Sport 2011;14:404-10. http://dx.doi.org/10.1016/j.jsams.2011.03.013.
- Nader PR, Bradley RH, Houts RM, McRitchie SL, O’Brien M. Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA 2008;300:295-30. http://dx.doi.org/10.1001/jama.300.3.295.
- Taylor RW, Murdoch L, Carter P, Gerrard DF, Williams SM, Taylor BJ. Longitudinal study of physical activity and inactivity in preschoolers: the FLAME study. Med Sci Sports Exerc 2009;41:96-102. http://dx.doi.org/10.1249/MSS.0b013e3181849d81.
- Department of Health . Start Active, Stay Active 2011. www.gov.uk/government/uploads/system/uploads/attachment_data/file/216370/dh_128210.pdf (accessed 31 July 2014).
- Hinkley T, Crawford D, Salmon J, Okely AD, Hesketh K. Preschool children and physical activity: a review of correlates. Am J Prev Med 2008;34:435-41. http://dx.doi.org/10.1016/j.amepre.2008.02.001.
- Lakshman R, Paes V, Hesketh H, O’Malley C, Moore H, Ong K, et al. Protocol for systematic reviews of determinants/correlates of obesity related dietary and physical activity behaviours in young children (preschool 0 to 6 years): evidence mapping and syntheses. Syst Rev 2013;2. http://dx.doi.org/10.1186/2046-4053-2-28.
- Nutbeam D. The challenges to provide evidence in health promotion. Health Promot Int 1999;14:99-101. http://dx.doi.org/10.1093/heapro/14.2.99.
- Nixon CA, Moore HJ, Douthwaite W, Gibson EL, Vogele C, Kreichauf S, et al. behalf of the ToyBox study group . Identifying effective behavioural models and behaviour change strategies underpinning successful pre-school and school-based obesity prevention interventions aimed at four to six year olds: a systematic review. Obes Rev 2012;13:106-17. http://dx.doi.org/10.1111/j.1467-789X.2011.00962.x.
- Bandura A. Social Learning Theory. New York, NY: General Learning Press; 1977.
- Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: Freeman; 1997.
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12. http://dx.doi.org/10.1002/14651858.CD001871.pub3.
- Velduis L, Vogel I, Renders CM, Rossem L, Oenema A, HiraSing RA, et al. Behavioural risk factors for overweight in early childhood: the ‘Be active, eat right’ study. Int J Behav Nutr Phys Act 2012;9. http://dx.doi.org/10.1186/1479-5868-9-74.
- Ridgers ND, Fairclough SJ, Stratton G. Variables associated with children’s physical activity levels during recess: the a-CLASS project. Int J Behav Nutr Phys Act 2010;7. http://dx.doi.org/10.1186/1479-5868-7-74.
- Taylor RW, Farmer VL, Cameron SL, Meredith-Jones K, Williams SM, Mann JI. School playgrounds and physical activity policies as predictors of school and home time activity. Int J Behav Nutr Phys Act 2011;8. http://dx.doi.org/10.1186/1479-5868-8-38.
- Cooper AR, Page AS, Wheeler BW, Hillsdon M, Griew P, Jago R. Patterns of GPS measured time outdoors after school and objective physical activity in English children: the PEACH project. Int J Behav Nutr Phys Act 2010;7. http://dx.doi.org/10.1186/1479-5868-7-31.
- Broekhuizen K, Scholten AM, de Vries SI. The value of (pre)school playgrounds for children’s physical activity level: a systematic review. Int J Behav Nutr Phys Act 2014;11. http://dx.doi.org/10.1186/1479-5868-11-59.
- Hannon JC, Brown BB. Increasing preschoolers’ physical activity intensities: an activity-friendly preschool playground intervention. Prev Med 2008;46:532-6. http://dx.doi.org/10.1016/j.ypmed.2008.01.006.
- Cardon G, Labarque V, Smits D, De Bourdeaudhuij I. Promoting physical activity at the pre-school playground: the effects of providing markings and play equipment. Prev Med 2009;48:335-40. http://dx.doi.org/10.1016/j.ypmed.2009.02.013.
- Brockman R, Jago R, Fox KR. Children’s active play: self-reported motivators, barriers and facilitators. BMC Public Health 2011;10. http://dx.doi.org/10.1186/1471-2458-11-461.
- Irwin JD, He M, Bouck LM, Tucker P, Pollett GL. Preschoolers’ physical activity behaviours: parents’ perspectives. Can J Public Health 2005;96:299-303.
- Brasholt M, Chawes B, Kreiner-Møller E, Vahlkvist S, Sinding M, Bisgaard H. Objective assessment of levels and patterns of physical activity in preschool children. Pediatr Res 2013;74:333-8. http://dx.doi.org/10.1038/pr.2013.99.
- Clemes SA, Hamilton SL, Griffiths PL. Summer to winter variability in the step counts of normal weight and overweight adults living in the UK. J Phys Act Health 2011;8:36-44.
- Summerbell CD, Moore HJ, Vögele C, Kreichauf S, Wildgruber A, Manios Y, et al. behalf of the ToyBox study group . Evidence-based recommendations for the development of obesity prevention programs targeted at preschool children. Obes Rev 2012;13:129-32. http://dx.doi.org/10.1111/j.1467-789X.2011.00940.x.
- Hesketh KD, Campbell KJ. Interventions to prevent obesity in 0–5 year olds: an updated systematic review of the literature. Obesity 2010;18:S27-35. http://dx.doi.org/10.1038/oby.2009.429.
- Pollard TM, Rousham EK, Colls R. Intergenerational and familial approaches to obesity and related conditions. Ann Hum Biol 2011;38:385-9. http://dx.doi.org/10.3109/03014460.2011.591658.
- Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr 2005;24:83-92. http://dx.doi.org/10.1080/07315724.2005.10719448.
- De Bock F, Genser B, Raat H, Fischer JE, Renz-Polster H. A participatory physical activity intervention in preschools: a cluster randomized controlled trial. Am J Prev Med 2013;45:64-7. http://dx.doi.org/10.1016/j.amepre.2013.01.032.
- O’Dwyer MV, Fairclough SJ, Knowles Z, Stratton G. Effect of a family focused active play intervention on sedentary time and physical activity in preschool children. Int J Behav Nutr Phys Act 2012;1. http://dx.doi.org/10.1186/1479-5868-9-117.
- De Craemer M, De Decker E, Verloigne M, De Bourdeaudhuij I, Manios Y, Cardon G. ToyBox study group . The effect of a kindergarten-based, family-involved intervention on objectively measured physical activity in Belgian preschool boys and girls of high and low SES: the ToyBox-study. Int J Behav Nutr Phys Act 2014;11. http://dx.doi.org/10.1186/1479-5868-11-38.
- Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health 2013;67:190-3. http://dx.doi.org/10.1136/jech-2012-201257.
- Vander Ploeg KA, Maximova K, McGavock J, Davis W, Veugelers P. Do school-based physical activity interventions increase or reduce inequalities in health?. Soc Sci Med 2014;112:80-7. http://dx.doi.org/10.1016/j.socscimed.2014.04.032.
- Hillier-Brown FC, Bambra CL, Cairns-Nagi JM, Kasim A, Moore HJ, Summerbell CD. A systematic review of the effectiveness of individual, community and societal level interventions at reducing socioeconomic inequalities in obesity-related outcomes amongst children. BMC Public Health 2014;14. http://dx.doi.org/10.1186/1471-2458-14-834.
- Durand MA, Carpenter L, Dolan H, Bravo P, Mann M, Bunn F, et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLOS One 2014;9. http://dx.doi.org/10.1371/journal.pone.0094670.
- Marmot M . Fair Society, Healthy Lives: A Strategic Review of Health Inequalities in England Post-2010 2010. www.marmotreview.org/AssetLibrary/pdfs/Reports/FairSocietyHealthyLives.pdf (accessed 31 July 2014).
- Costa S, Clemes S, Barber S, Griffiths P, Cameron N. Barriers and Facilitators for the Regular Practice of Physical Activity in White and Pakistani Toddlers n.d.
- Metcalf BS, Voss LD, Hosking J, Jeffery AN, Wilkin TJ. Physical activity at the government-recommended level and obesity-related health outcomes: a longitudinal study (Early Bird 37). Arch Dis Child 2008;93:772-7. http://dx.doi.org/10.1136/adc.2007.135012.
- Vale S, Santos R, Soares-Miranda LM, Moreira CM, Ruiz JR, Mota JA. Objectively measured physical activity and body mass index in preschool children. Int J Pediatr 2010;2010. http://dx.doi.org/10.1155/2010/479439.
- Vale S, Trost S, Ruiz JJ, Moreira P, Mota J. Physical activity guidelines and preschooler’s obesity status. Int J Obes (Lond) 2013;37:1352-5. http://dx.doi.org/10.1038/ijo.2013.109.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- World Medical Association . WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects n.d. www.wma.net/en/30publications/10policies/b3/ (accessed 5 February 2015).
- Department of Communities and Local Government . The English Indices of Deprivation 2010 n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/6871/1871208.pdf (accessed 31 July 2014).
- Department of Health . Health Profile 2011: Bradford n.d. www.apho.org.uk/default.aspx?QN = HP_METADATA&AreaID = 50328 (accessed 31 July 2014).
- Born in Bradford Collaborative Group . Born in Bradford, a cohort study of babies born in Bradford and their parents: protocol for recruitment phase. BMC Public Health 2008;8. http://dx.doi.org/10.1186/1471-2458-8-327.
- Cain KL, Sallis JF, Conway TL, Van Dyck D, Calhoon L. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health 2013;10:437-50.
- Cummins RA. The Comprehensive Quality of Life Scale: Development and Evaluation. Presented at the Health Outcomes and Quality of Life Measurement Conference, Canberra, 14–15 August 1995. Health Outcomes Bulletin 1995;7:7-14.
- Cummins RA, McCabe MP, Romeo Y, Gullone E. Validity Studies the Comprehensive Quality of Life Scale (Comqol): instrument development and psychometric evaluation on college staff and students. Educ Psychol Meas 1994;54. http://dx.doi.org/10.1177/0013164494054002011.
- Schwarzer R, Jerusalem M, Weinman J, Wright S, Johnston M. Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs. Windsor: NFER-NELSON; 1995.
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Treatment Fidelity Workgroup of the NIH Behavior Change Consortium . Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004;23:443-51. http://dx.doi.org/10.1037/0278-6133.23.5.443.
- Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 2012;7:1717-27. http://dx.doi.org/10.1007/s11136-012-0322-4.
- Varni JW, Limbers CA, Neighbors K, Schulz K, Lieu JEC, Heffer RW, et al. The PedsQL™ infant scales: feasibility, internal consistency, reliability and validity in healthy and ill infants. Qual Life Res 2011;20:45-5. http://dx.doi.org/10.1007/s11136-010-9730-5.
- Mack N, Woodsong C, MacQueen K, Guest G, Namey E. Qualitative Research Methods a Data Collector’s Field Guide. Research Triangle Park, NC: Family Health International; 2009.
- Patton MQ. Qualitative Evaluation and Research Methods. Newbury Park, CA: Sage; 1990.
- Emmel N, Hughes K, Greenhalgh J, Sales Al. Accessing socially excluded people – trust and the gatekeeper in the researcher–participants relationship. Sociol Res Online 2012;12.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Loprinzi PD, Trost SG. Parental influences on physical activity behaviour in preschool children. Prev Med 2010;50:129-33. http://dx.doi.org/10.1016/j.ypmed.2009.11.010.
- Stanley JC, Thorndike RL. Educational Measurement. Washington, DC: American Council of Education; 1971.
- Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity 2006;14:2000-6. http://dx.doi.org/10.1038/oby.2006.234.
- Trost SG, Fees BS, Haar SJ, Murray AD, Crowe LK. Identification and validity of accelerometer cut-points for toddlers. Obesity 2012;20:2317-19. http://dx.doi.org/10.1038/oby.2011.364.
- WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. Geneva: WHO; 2006.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. http://dx.doi.org/10.1111/j. 2002.384.doc.x.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10. http://dx.doi.org/10.1186/1471-2288-10-67.
- Bland JM, Kerry SM. Trials randomised in clusters. BMJ 1997;315. http://dx.doi.org/10.1136/bmj.315.7108.600.
- Kerry SM, Bland JM. Analysis of a trial randomised in clusters. BMJ 1998;316. http://dx.doi.org/10.1136/bmj.316.7124.54.
- Kind P, Spilker B. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia, PA: Lippincott-Raven; 1996.
- Dolan PCG, Kind P, Williams A. A Social Tariff for EuroQol: Results from a UK General Population Survey. York: University of York, Centre for Health Economics; 1995.
- Matthews JN, Altman DG, Campbell MJ, Royston P. Analysis of serial measurements in medical research. BMJ 1990;300:230-5. http://dx.doi.org/10.1136/bmj.300.6719.230.
- Varni JW. The PedsQL™ 4.0 Measurement Model for the Paediatric Quality of Life Inventory™ Version 4.0: Administration Guidelines 2004. www.pedsql.org/pedsqladmin.html (accessed 8 July 2014).
- Department of Health . NHS Reference Costs 2012 to 2013 2013. www.gov.uk/government/publications/nhs-reference-costs-2012-to-2013 (accessed 21 May 2014).
- Curtis L. Unit Costs of Health and Social Care 2010. Canterbury: PSSRU, University of Kent; 2010.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: PSSRU, University of Kent; 2013.
- Curran P. Review Body on Doctors’ and Dentists’ Remuneration n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/288697/Doctors___Dentists_42nd_report.pdf (accessed 8 March 2015).
- Prospects Online . Parental Involvement Worker n.d. www.prospectsonline.co.uk/detail.aspx?id = 2171 (accessed 31 July 2013).
- Prospects . Sports Development Officer: Job Description n.d. www.prospects.ac.uk/sports_development_officer_job_description.htm (accessed 31 July 2013).
- Willan AR, Jeffrey AHB, Hoch S. Regression methods for covariate adjustment and subgroup analysis for non-censored cost-effectiveness data. Health Econ 2004;13:461-75. http://dx.doi.org/10.1002/hec.843.
- Barber SE, Jackson C, Akhtar S, Bingham DD, Ainsworth H, Hewitt C, et al. ‘Pre-schoolers in the playground’ an outdoor physical activity intervention for children aged 18 months to 4 years old: study protocol for a pilot cluster randomised controlled trial. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-326.
- Specker B, Binkey T. Randomized trial of physical activity and calcium supplementation on bone mineral content in 3-to-5 year old children. J Bone Miner Res 2003;18:885-92. http://dx.doi.org/10.1359/jbmr.2003.18.5.885.
- Canadian Task Force on the Periodic Health Examination . Periodic health examination, 1994 update: 1. Obesity in childhood. CMAJ 1994;150:871-9.
- Lee YS. Consequences of childhood obesity. Ann Acad Med Singapore 2009;38:75-81.
- Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and adult cardiovascular disease risk: a systematic review. Int J Obes (Lond) n.d.;34:18-2. http://dx.doi.org/10.1038/ijo.2009.61.
- Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev 2012;13:985-1000. http://dx.doi.org/10.1111/j.1467-789X.2012.01015.x.
- Pinto Pereira SM, Power C. Life course body mass index, birthweight and lipid levels in mid-adulthood: a nationwide birth cohort study. Eur Heart J 2013;34:1215-24. http://dx.doi.org/10.1093/eurheartj/ehs333.
- Raitakari OT, Juonala M, Viikari JS. Obesity in childhood and vascular changes in adulthood: insights into the Cardiovascular Risk in Young Finns Study. Int J Obes (Lond) 2005;29:S101-4. http://dx.doi.org/10.1038/sj.ijo.0803085.
- Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 2011;35:891-8. http://dx.doi.org/10.1038/ijo.2010.222.
- Robinson WR, Poole C, Godle PA. Systematic review of prostate cancer’s association with body size in childhood and young adulthood. Cancer Causes Control 2008;19:793-80. http://dx.doi.org/10.1007/s10552-008-9142-9.
- Silverwood RJ, Pierce M, Hardy R, Thomas C, Ferro C, Savage C, et al. Early-life overweight trajectory and CKD in the 1946 British birth cohort study. Am J Kidney Dis 2013;62:276-84. http://dx.doi.org/10.1053/j.ajkd.2013.03.032.
- Dills AKM, Hillary N, Rotthoff KW. Recess, physical education and elementary school student outcomes. Econ Educ Rev 2011;30:889-900. http://dx.doi.org/10.1016/j.econedurev.2011.04.011.
- Jimenez-Pavon D, Konstabel K, Bergman P, Ahrens W, Pohlabeln H, Hadjigeorgiou C, et al. Physical activity and clustered cardiovascular disease risk factors in young children: a cross-sectional study (the IDEFICS study). BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-172.
- Niederer I, Kriemler S, Gut J, Hartmann T, Schindler C, Barral J, et al. Relationship of aerobic fitness and motor skills with memory and attention in preschoolers (Ballabeina): a cross-sectional and longitudinal study. BMC Pediatr 2011;11. http://dx.doi.org/10.1186/1471-2431-11-34.
- Wilkin TJ, Voss LD, Metcalf BS, Mallam K, Jeffery AN, Alba S, et al. Metabolic risk in early childhood: the EarlyBird Study. Int J Obes Relat Metab Disord 2004;28:S64-9. http://dx.doi.org/10.1038/sj.ijo.0802807.
- Moore LL, Nguyen US, Rothman KJ, Cupples LA, Ellison RC. Preschool physical activity level and change in body fatness in young children. The Framingham Children’s Study. Am J Epidemiol 1995;142:982-8.
- Moore LL, Gao D, Bradlee ML, Cupples LA, Sundarajan-Ramamurti A, Proctor MH. Does early physical activity predict body fat change throughout childhood?. Prev Med 2003;37:10-7. http://dx.doi.org/10.1016/S0091-7435(03)00048-3.
- Klesges RC, Klesges LM, Eck LH, Shelton ML. A longitudinal analysis of accelerated weight gain in pre-school children. Pediatrics 1995;95:126-30.
- Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Int J Obes (Lond) 2012;36:1-11. http://dx.doi.org/10.1038/ijo.2011.186.
- Lawlor DA, Leon DA. Association of body mass index and obesity measured in early childhood with risk of coronary heart disease and stroke in middle age: findings from the Aberdeen children of the 1950s prospective cohort study. Circulation 2005;111:1891-6. http://dx.doi.org/10.1161/01.CIR.0000161798.45728.4D.
- Freedman DS, Patel DA, Srinivasan SR, Chen W, Tang R, Bond MG, et al. The contribution of childhood obesity to adult carotid intima-media thickness: the Bogalusa Heart Study. Int J Obes (Lond) 2008;32:749-56. http://dx.doi.org/10.1038/sj.ijo.0803798.
- Oren A, Vos LE, Uiterwaal CS, Gorissen WH, Grobbee DE, Bots ML. Change in body mass index from adolescence to young adulthood and increased carotid intima-media thickness at 28 years of age: the Atherosclerosis Risk in Young Adults study. Int J Obes Relat Metab Disord 2003;27:1383-90. http://dx.doi.org/10.1038/sj.ijo.0802404.
- Raitakari OT, Juonala M, Viikari JS. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood. The Cardiovascular Risk in Young Finns Study. JAMA 2003;290:2277-83. http://dx.doi.org/10.1001/jama.290.17.2277.
- Freedman DS, Dietz WH, Tang R, Mensah GA, Bond MG, Urbina EM, et al. The relation of obesity throughout life to carotid intima-media thickness in adulthood: the Bogalusa Heart Study. Int J Obes Relat Metab Disord 2004;28:159-66. http://dx.doi.org/10.1038/sj.ijo.0802515.
- Juonala M, Raitakari M, Viikari JSA, Raitakari OT. Obesity in youth is not an independent predictor of carotid IMT in adulthood. The Cardiovascular Risk in Young Finns Study. Atherosclerosis 2006;185:388-93. http://dx.doi.org/10.1016/j.atherosclerosis.2005.06.016.
- Ford CA, Nonnemaker JM, Wirth KE. The influence of adolescent body mass index, physical activity, and tobacco use on blood pressure and cholesterol in young adulthood. J Adolesc Health 2008;43:576-83. http://dx.doi.org/10.1016/j.jadohealth.2008.06.010.
- Li L, Law C, Power C. Body mass index throughout the life-course and blood pressure in mid-adult life: a birth cohort study. J Hypertens 2007;25:1215-23. http://dx.doi.org/10.1097/HJH.0b013e3280f3c01a.
- Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obes Res 2005;13:163-9. http://dx.doi.org/10.1038/oby.2005.21.
- Barker DJ, Eriksson JG, Forsén T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol 2002;31:1235-9. http://dx.doi.org/10.1093/ije/31.6.1235.
- Barker DJ, Forsén T, Eriksson JG, Osmond C. Growth and living conditions in childhood and hypertension in adult life: a longitudinal study. J Hypertens 2002;20:1951-6. http://dx.doi.org/10.1097/00004872-200210000-00013.
- Israeli E, Korzets Z, Tekes-Manova D, Tirosh A, Schochat T, Bernheim J, et al. Blood-pressure categories in adolescence predict development of hypertension in accordance with the European guidelines. Am J Hypertens 2007;20:705-9. http://dx.doi.org/10.1016/j.amjhyper.2007.01.020.
- Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics 2001;108:712-18. http://dx.doi.org/10.1542/peds.108.3.712.
- Lauer RM, Clarke WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics 1989;84:633-41.
- Sinaiko AR, Donahue RP, Jacobs DR. Circulation 1999;99:1471-6. http://dx.doi.org/10.1161/01.CIR.99.11.1471.
- Hardy R, Wadsworth ME, Langenberg C, Kuh D. Birthweight, childhood growth, and blood pressure at 43 years in a British birth cohort. Int J Epidemiol 2004;33:121-9. http://dx.doi.org/10.1093/ije/dyh027.
- Burke V, Beilin LJ, Dunbar D, Kevan M. Associations between blood pressure and overweight defined by new standards for body mass index in childhood. Prev Med 2004;38:558-64. http://dx.doi.org/10.1016/j.ypmed.2003.09.023.
- Wright CM, Parker L, Lamont D, Craft AW. Implications of childhood obesity for adult health: findings from thousand families cohort study. BMJ 2001;323:1280-4. http://dx.doi.org/10.1136/bmj.323.7324.1280.
- Lauer RM, Lee J, Clarke WR. Factors affecting the relationship between childhood and adult cholesterol levels: the Muscatine study. Pediatrics 1988;82:309-18.
- Salonen MK, Kajantie E, Osmond C, Forsén T, Ylihärsilä H, Paile-Hyvärinen M, et al. Role of childhood growth on the risk of metabolic syndrome in obese men and women. Diabetes Metab 2009;35:94-100. http://dx.doi.org/10.1016/j.diabet.2008.08.008.
- Al Mamun A, Cramb SM, O’Callaghan MJ, Williams GM, Najman JM. Childhood overweight status predicts diabetes at age 21 years: a follow-up study. Obesity (Silver Spring) 2009;17:1255-61. http://dx.doi.org/10.1038/oby.2008.660.
- Eriksson JG, Forsén T, Tuomilehto J, Osmond C, Barker DJ. Early growth and coronary heart disease in later life: longitudinal study. BMJ 2001;322:949-53. http://dx.doi.org/10.1136/bmj.322.7292.949.
- Hypponen E, Power C, Smith GD. Prenatal growth, BMI, and risk of type 2 diabetes by early midlife. Diabetes Care 2003;26:2512-17. http://dx.doi.org/10.2337/diacare.26.9.2512.
- Lawlor DA, Martin RM, Gunnell D, Galobardes B, Ebrahim S, Sandhu J, et al. Association of body mass index measured in childhood, adolescence, and young adulthood with risk of ischemic heart disease and stroke: findings from 3 historical cohort studies. Am J Clin Nutr 2006;83:767-73.
- Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation 2010;122:1604-11. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.940809.
- Morrison JA, Glueck CJ, Horn PS, Wang P. Childhood predictors of adult type 2 diabetes at 9- and 26-year follow-ups. Arch Pediatr Adolesc Med 2010;164:53-60. http://dx.doi.org/10.1001/archpediatrics.2009.228.
- Nguyen QM, Srinivasan SR, Xu JH, Chen W, Berenson GS. Changes in risk variables of metabolic syndrome since childhood in pre-diabetic and type 2 diabetic subjects: the Bogalusa Heart Study. Diabetes Care 2008;31:2044-9. http://dx.doi.org/10.2337/dc08-0898.
- Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 2011;364:1315-25. http://dx.doi.org/10.1056/NEJMoa1006992.
- Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med 1992;327:1350-5. http://dx.doi.org/10.1056/NEJM199211053271904.
- Osmond C, Kajantie E, Forsén TJ, Eriksson JG, Barker DJ. Infant growth and stroke in adult life: the Helsinki birth cohort study. Stroke 2007;38:264-70. http://dx.doi.org/10.1161/01.STR.0000254471.72186.03.
- Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Davey Smith G. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr 1998;67:1111-18.
- Bjorge T, Engeland A, Tverdal A, Smith GD. Body mass index in adolescence in relation to cause-specific mortality: a follow-up of 230,000 Norwegian adolescents. Am J Epidemiol 2008;168:30-7. http://dx.doi.org/10.1093/aje/kwn096.
- Engeland A, Bjørge T, Søgaard AJ, Tverdal A. Body mass index in adolescence in relation to total mortality: 32-year follow-up of 227,000 Norwegian boys and girls. Am J Epidemiol 2003;157:517-23. http://dx.doi.org/10.1093/aje/kwf219.
- Neovius M, Sundstrom J, Rasmussen F. Combined effects of overweight and smoking in late adolescence on subsequent mortality: nationwide cohort study. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b496.
- Nieto FJ, Szklo M, Comstock GW. Childhood weight and growth rate as predictors of adult mortality. Am J Epidemiol 1992;136:201-13.
- Burgess JA, Walters EH, Byrnes GB, Giles GG, Jenkins MA, Abramson MJ. Childhood adiposity predicts adult-onset current asthma in females: a 25-yr prospective study. Eur Respir J 2007;29:668-75. http://dx.doi.org/10.1183/09031936.00080906.
- Gordon ES, Tucker P, Burke SM, Carron AV. Effectiveness of physical activity interventions for preschoolers: a meta-analysis. Res Q Exerc Sport 2013;84:287-94. http://dx.doi.org/10.1080/02701367.2013.813894.
- O’Dwyer MV, Fairclough SJ, Ridgers ND, Knowles ZR, Foweather L, Stratton G. Effect of a school-based active play intervention on sedentary time and physical activity in preschool children. Health Educ Res 2013;28:931-42. http://dx.doi.org/10.1093/her/cyt097.
- Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g3256.
- Esliger DW, Tremblay MS. Technical reliability assessment of three accelerometer models in a mechanical setup. Med Sci Sports Exerc 2006;38:2173-81. http://dx.doi.org/10.1249/01.mss.0000239394.55461.08.
- Van Cauwenberghe E, Gubbels J, De Bourdeaudhuji I, Cardon G. Feasibility and validity of accelerometer measurments to assess physical activity in toddlers. Int J Behav Nutr Phys Act 2011;8. http://dx.doi.org/10.1186/1479-5868-8-67.
- Hinkley T, O’Connell E, Crawford D, Hesketh K, Salmon J. Assessing volume of accelerometry data for reliability in preschool children. Med Sci Sports Exerc 2012;44:2436-41. http://dx.doi.org/10.1249/MSS.0b013e3182661478.
- Oemar M, Janssen B. EQ-5D-5L User Guide. Basic Information on How to Use the EQ-5D-5L Instrument n.d. www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/UserGuide_EQ-5D-5L_v2.0_October_2013.pdf (accessed 2 February 2015).
- Brueton VC, Tierney JF, Stenning S, Meredith S, Harding S, Nazareth I, et al. Strategies to improve retention in randomised controlled trials: a Cochrane systematic review and meta-analysis. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2013-003821.
- Sääkslahti A, Nummienen P, Salo P, Tuominen J, Helenius H, Valimski I. Effects of a three-year intervention on children’s physical activity physical activity from age 4 to 7. Pediatr Exerc Sci 2004;16:167-80.
- McGlade MS, Saha S, Dahlstrom ME. The Latina paradox: an opportunity for restructuring prenatal care delivery. Am J Public Health 2004;94:2062-5. http://dx.doi.org/10.2105/AJPH.94.12.2062.
- Alhassan S, Whitt-Glover MC. Intervention fidelity in a teacher-led program to promote physical activity in preschool-age children. Prev Med 2014;69:S34-6. http://dx.doi.org/10.1016/j.ypmed.2014.07.024.
Appendix 1 Bradford Schools by Level of Deprivation (2010)
| Establishment number | School | Locality | IMD value | IMD rank | IDACI value | IDACI rank | FSM value | FSM rank |
|---|---|---|---|---|---|---|---|---|
| Nursery | ||||||||
| 3801008 | Abbey Green Nursery School and Children’s Centre | BW2 | 62.9 | 1/7 | 0.53 | 1/7 | 1.7 | 4/7 |
| 3801012 | Canterbury Nursery School and Centre for Children and Families | BE3 | 53.8 | 3/7 | 0.52 | 2/7 | 2.2 | 3/7 |
| 3801001 | Hirst Wood Nursery School | SH1 | 21.8 | 7/7 | 0.18 | 7/7 | 0.0 | 6/7 |
| 3801002 | Lilycroft Nursery School | BW2 | 52.0 | 4/7 | 0.49 | 4/7 | 3.1 | 2/7 |
| 3801009 | Midland Road Nursery School and Children Centre | BW2 | 59.1 | 2/7 | 0.52 | 3/7 | 6.5 | 1/7 |
| 3801010 | St Edmund’s Nursery and Children’s Centre | BW1 | 44.3 | 5/7 | 0.42 | 5/7 | 1.6 | 5/7 |
| 3801000 | Strong Close Nursery School and Children’s Centre | KE1 | 33.3 | 6/7 | 0.30 | 6/7 | 0.0 | 6/7 |
| Nursery averages | 46.7 | 0.42 | 2.2 | |||||
| Primary | ||||||||
| 3802173 | Addingham Primary School | KE2 | 7.1 | 150/155 | 0.06 | 151/155 | 5.8 | 139/155 |
| 3802146 | Aire View Infant School | KE2 | 15.0 | 133/155 | 0.12 | 130/155 | 9.5 | 121/155 |
| 3803000 | All Saints’ CE Primary School (Bradford) | BE3 | 54.0 | 21/155 | 0.48 | 29/155 | 26.5 | 40/155 |
| 3803026 | All Saints’ CE Primary School (Ilkley) | KE2 | 4.7 | 154/155 | 0.04 | 154/155 | 0.9 | 154/155 |
| 3802001 | Allerton Primary School | BW1 | 35.7 | 78/155 | 0.32 | 77/155 | 22.9 | 62/155 |
| 3802150 | Ashlands Primary School | KE2 | 7.6 | 148/155 | 0.07 | 148/155 | 7.5 | 133/155 |
| 3802184 | Atlas Community Primary School | BW2 | 63.8 | 5/155 | 0.54 | 14/155 | 31.3 | 27/155 |
| 3803360 | Baildon CE Primary School | SH1 | 13.2 | 142/155 | 0.11 | 137/155 | 17.8 | 86/155 |
| 3802102 | Bankfoot Primary School | BE3 | 44.2 | 57/155 | 0.39 | 59/155 | 16.3 | 92/155 |
| 3802020 | Barkerend Primary School | BE2 | 65.9 | 2/155 | 0.61 | 3/155 | 25.6 | 45/155 |
| 3802166 | Ben Rhydding Primary School | KE2 | 5.5 | 153/155 | 0.06 | 152/155 | 5.6 | 140/155 |
| 3802062 | Blakehill Primary School | BE1 | 22.0 | 115/155 | 0.14 | 123/155 | 7.4 | 134/155 |
| 3802075 | Bowling Park Primary School | BE3 | 50.7 | 31/155 | 0.44 | 41/155 | 23.8 | 56/155 |
| 3802107 | Brackenhill Primary School | BS2 | 36.3 | 75/155 | 0.37 | 64/155 | 17.4 | 88/155 |
| 3802009 | Bradford Moor Community Primary School | BE2 | 57.7 | 16/155 | 0.54 | 13/155 | 24.6 | 49/155 |
| 3803031 | Burley and Woodhead CE Primary School | KE2 | 4.4 | 155/155 | 0.04 | 155/155 | 1.9 | 153/155 |
| 3802203 | Burley Oaks Primary School | KE2 | 7.3 | 149/155 | 0.07 | 149/155 | 3.3 | 151/155 |
| 3802036 | Byron Primary School | BE2 | 59.9 | 11/155 | 0.58 | 8/155 | 20.5 | 73/155 |
| 3802087 | Carrwood Primary School | BS3 | 61.4 | 10/155 | 0.60 | 5/155 | 52.0 | 4/155 |
| 3802094 | Cavendish Primary School | BE1 | 40.0 | 68/155 | 0.32 | 76/155 | 32.3 | 23/155 |
| 3803024 | Clayton CE Primary School | BW1 | 22.8 | 114/155 | 0.15 | 121/155 | 12.3 | 109/155 |
| 3802015 | Clayton Village Primary School | BW1 | 28.6 | 89/155 | 0.22 | 97/155 | 23.6 | 58/155 |
| 3802186 | Copthorne Primary School | BW3 | 42.2 | 64/155 | 0.44 | 43/155 | 19.7 | 80/155 |
| 3802110 | Cottingley Village Primary School | SH2 | 21.9 | 117/155 | 0.20 | 107/155 | 13.3 | 105/155 |
| 3802111 | Crossflatts Primary School | SH2 | 14.3 | 134/155 | 0.11 | 132/155 | 7.2 | 136/155 |
| 3802024 | Crossley Hall Primary School | BW3 | 37.3 | 71/155 | 0.36 | 68/155 | 23.7 | 57/155 |
| 3802112 | Cullingworth Village Primary School | SH2 | 15.0 | 132/155 | 0.12 | 131/155 | 13.4 | 104/155 |
| 3802167 | Denholme Primary School | SH2 | 20.2 | 120/155 | 0.18 | 116/155 | 16.2 | 93/155 |
| 3803028 | East Morton CE Primary School | SH2 | 10.5 | 146/155 | 0.09 | 142/155 | 4.7 | 143/155 |
| 3802147 | Eastburn Junior and Infant School | KE2 | 13.2 | 141/155 | 0.11 | 136/155 | 4.0 | 147/155 |
| 3802120 | Eastwood Primary School | KE1 | 52.4 | 27/155 | 0.47 | 34/155 | 24.0 | 55/155 |
| 3802113 | Eldwick Primary School | SH2 | 8.9 | 147/155 | 0.09 | 144/155 | 3.9 | 149/155 |
| 3802103 | Fagley Primary School | BE1 | 54.0 | 22/155 | 0.49 | 23/155 | 39.0 | 10/155 |
| 3802084 | Farfield Primary School | BS1 | 43.3 | 60/155 | 0.36 | 67/155 | 44.7 | 7/155 |
| 3802183 | Farnham Primary School | BW3 | 47.4 | 39/155 | 0.45 | 39/155 | 20.0 | 76/155 |
| 3802065 | Fearnville Primary School | BS3 | 53.9 | 23/155 | 0.49 | 22/155 | 38.0 | 12/155 |
| 3802177 | Feversham Primary School | BE2 | 63.7 | 6/155 | 0.60 | 4/155 | 17.5 | 87/155 |
| 3805201 | Foxhill Primary School | BS2 | 16.4 | 128/155 | 0.11 | 138/155 | 6.9 | 137/155 |
| 3802027 | Frizinghall Primary School | BW2 | 36.3 | 74/155 | 0.38 | 63/155 | 19.8 | 78/155 |
| 3802182 | Girlington Primary School | BW1 | 48.8 | 37/155 | 0.48 | 27/155 | 20.7 | 72/155 |
| 3802157 | Glenaire Primary School | SH1 | 30.8 | 88/155 | 0.25 | 88/155 | 26.1 | 42/155 |
| 3802034 | Green Lane Primary School | BW2 | 64.6 | 3/155 | 0.57 | 9/155 | 29.2 | 32/155 |
| 3802033 | Greengates Primary School | BE1 | 40.6 | 67/155 | 0.31 | 78/155 | 22.0 | 67/155 |
| 3802093 | Grove House Primary School | BE1 | 25.6 | 104/155 | 0.22 | 98/155 | 10.7 | 114/155 |
| 3802114 | Harden Primary School | SH2 | 11.1 | 145/155 | 0.08 | 145/155 | 4.2 | 146/155 |
| 3802121 | Haworth Primary School | KE3 | 18.4 | 124/155 | 0.14 | 124/155 | 9.7 | 119/155 |
| 3802038 | Heaton Primary School | BW2 | 35.6 | 79/155 | 0.39 | 58/155 | 30.8 | 30/155 |
| 3803308 | Heaton St Barnabas’ CE Primary School | BW2 | 33.4 | 84/155 | 0.34 | 74/155 | 19.6 | 81/155 |
| 3802142 | High Crags Primary School | SH1 | 45.7 | 48/155 | 0.35 | 70/155 | 30.7 | 31/155 |
| 3805203 | Hill Top CE Primary School | BS1 | 28.0 | 94/155 | 0.23 | 93/155 | 12.0 | 110/155 |
| 3805204 | Hollingwood Primary School | BS2 | 24.6 | 108/155 | 0.21 | 103/155 | 16.6 | 91/155 |
| 3802196 | Holybrook Primary School | BE1 | 57.2 | 18/155 | 0.49 | 21/155 | 46.6 | 6/155 |
| 3802123 | Holycroft Primary School | KE1 | 49.8 | 34/155 | 0.49 | 25/155 | 31.0 | 29/155 |
| 3803379 | Home Farm Primary School | BS2 | 32.0 | 86/155 | 0.26 | 86/155 | 26.0 | 43/155 |
| 3802029 | Horton Grange Primary School | BW3 | 46.9 | 42/155 | 0.45 | 37/155 | 22.5 | 65/155 |
| 3802180 | Horton Park Primary School | BE3 | 66.2 | 1/155 | 0.66 | 1/155 | 53.3 | 3/155 |
| 3802169 | Hothfield Junior School | KE2 | 14.2 | 135/155 | 0.11 | 135/155 | 8.2 | 127/155 |
| 3802168 | Hoyle Court Primary School | SH1 | 14.0 | 138/155 | 0.10 | 140/155 | 10.2 | 117/155 |
| 3803304 | Idle CE Primary School | BE1 | 17.3 | 126/155 | 0.11 | 133/155 | 7.7 | 131/155 |
| 3802124 | Ingrow Primary School | KE3 | 36.5 | 73/155 | 0.29 | 83/155 | 37.3 | 14/155 |
| 3802195 | Iqra Community Primary School | BW2 | 57.3 | 17/155 | 0.50 | 18/155 | 37.3 | 15/155 |
| 3805207 | Keelham Primary School | BW1 | 18.7 | 123/155 | 0.13 | 125/155 | 3.3 | 150/155 |
| 3803363 | Keighley St Andrew’s CE Primary School | KE1 | 52.2 | 28/155 | 0.48 | 30/155 | 20.1 | 75/155 |
| 3805200 | Killinghall Primary School | BE2 | 52.6 | 26/155 | 0.49 | 24/155 | 24.5 | 51/155 |
| 3802198 | Knowleswood Primary School | BS3 | 62.9 | 9/155 | 0.58 | 7/155 | 42.5 | 8/155 |
| 3802041 | Lapage Primary School and Nursery | BE2 | 59.1 | 12/155 | 0.56 | 10/155 | 29.2 | 33/155 |
| 3802126 | Laycock Primary School | KE1 | 42.6 | 62/155 | 0.42 | 47/155 | 36.8 | 17/155 |
| 3802127 | Lees Primary School | KE3 | 14.1 | 136/155 | 0.08 | 147/155 | 8.2 | 125/155 |
| 3802090 | Ley Top Primary School | BW1 | 46.0 | 45/155 | 0.40 | 55/155 | 31.6 | 25/155 |
| 3802043 | Lidget Green Primary School | BW3 | 45.0 | 50/155 | 0.45 | 40/155 | 31.4 | 26/155 |
| 3802044 | Lilycroft Primary School | BW2 | 50.4 | 32/155 | 0.48 | 28/155 | 24.2 | 53/155 |
| 3802002 | Lister Primary School | BW2 | 48.9 | 36/155 | 0.47 | 33/155 | 24.0 | 54/155 |
| 3802128 | Long Lee Primary School | KE3 | 24.5 | 110/155 | 0.20 | 104/155 | 13.4 | 103/155 |
| 3802145 | Low Ash Primary School | SH1 | 28.6 | 90/155 | 0.20 | 105/155 | 12.9 | 107/155 |
| 3803023 | Low Moor CE Primary School | BS1 | 26.0 | 103/155 | 0.20 | 110/155 | 15.0 | 96/155 |
| 3802199 | Lower Fields Primary School | BS3 | 45.9 | 46/155 | 0.41 | 50/155 | 34.9 | 19/155 |
| 3802179 | Margaret McMillan Primary School | BW2 | 45.4 | 49/155 | 0.45 | 38/155 | 20.8 | 70/155 |
| 3802048 | Marshfield Primary School | BE3 | 44.9 | 52/155 | 0.41 | 48/155 | 19.8 | 79/155 |
| 3802192 | Menston Primary School | KE2 | 6.1 | 151/155 | 0.06 | 150/155 | 4.3 | 145/155 |
| 3802154 | Merlin Top Primary School | KE1 | 44.9 | 51/155 | 0.44 | 42/155 | 53.6 | 2/155 |
| 3802185 | Miriam Lord Community Primary School | BW2 | 58.4 | 14/155 | 0.51 | 17/155 | 19.9 | 77/155 |
| 3805206 | Myrtle Park Primary School | SH2 | 16.4 | 129/155 | 0.13 | 126/155 | 18.5 | 85/155 |
| 3802170 | Nessfield Primary School | KE3 | 27.2 | 99/155 | 0.22 | 101/155 | 14.3 | 99/155 |
| 3802054 | Newby Primary School | BE3 | 55.6 | 19/155 | 0.47 | 32/155 | 25.0 | 48/155 |
| 3802197 | Newhall Park Primary School | BS3 | 40.7 | 66/155 | 0.36 | 66/155 | 22.5 | 64/155 |
| 3805205 | Oakworth Primary School | KE3 | 13.5 | 140/155 | 0.08 | 146/155 | 5.4 | 141/155 |
| 3802130 | Oldfield Primary School | KE3 | 19.5 | 122/155 | 0.14 | 122/155 | 7.3 | 135/155 |
| 3803353 | Our Lady and St Brendan’s Catholic Primary School | BE1 | 42.4 | 63/155 | 0.35 | 73/155 | 28.7 | 34/155 |
| 3803372 | Our Lady of Victories Catholic Primary School | KE1 | 44.7 | 53/155 | 0.41 | 49/155 | 20.8 | 71/155 |
| 3803375 | Oxenhope CE Primary School | KE3 | 12.4 | 144/155 | 0.09 | 143/155 | 6.3 | 138/155 |
| 3802064 | Parkland Primary School | BE1 | 44.7 | 54/155 | 0.35 | 71/155 | 40.5 | 9/155 |
| 3802132 | Parkwood Primary School | KE1 | 44.0 | 58/155 | 0.40 | 57/155 | 36.9 | 16/155 |
| 3803377 | Peel Park Primary School | BE2 | 47.1 | 40/155 | 0.43 | 45/155 | 26.8 | 39/155 |
| 3802101 | Poplars Farm Primary School | BE1 | 23.9 | 111/155 | 0.20 | 111/155 | 10.6 | 115/155 |
| 3802115 | Priestthorpe Primary School | SH2 | 17.1 | 127/155 | 0.18 | 115/155 | 14.2 | 100/155 |
| 3802086 | Princeville Primary School | BW3 | 47.0 | 41/155 | 0.50 | 19/155 | 22.2 | 66/155 |
| 3802052 | Reevy Hill Primary School | BS1 | 48.3 | 38/155 | 0.41 | 52/155 | 34.5 | 20/155 |
| 3803365 | Riddlesden St Mary’s CE Primary | KE1 | 34.3 | 82/155 | 0.31 | 79/155 | 18.6 | 84/155 |
| 3805202 | Russell Hall Primary School | BS2 | 20.4 | 119/155 | 0.16 | 119/155 | 19.1 | 82/155 |
| 3802097 | Ryecroft Primary School | BS3 | 64.4 | 4/155 | 0.62 | 2/155 | 53.9 | 1/155 |
| 3802140 | Saltaire Primary School | SH2 | 20.8 | 118/155 | 0.18 | 117/155 | 11.2 | 112/155 |
| 3802174 | Sandal Primary School and Nursery | SH1 | 12.4 | 143/155 | 0.10 | 139/155 | 8.8 | 124/155 |
| 3802055 | Sandy Lane Primary School | SH2 | 25.1 | 106/155 | 0.25 | 87/155 | 15.5 | 95/155 |
| 3802178 | Shibden Head Primary School | BS2 | 16.0 | 130/155 | 0.11 | 134/155 | 7.6 | 132/155 |
| 3803366 | Shipley CE Primary School | SH1 | 28.2 | 93/155 | 0.29 | 82/155 | 17.0 | 90/155 |
| 3802077 | Shirley Manor Primary School | BS1 | 39.2 | 69/155 | 0.37 | 65/155 | 38.5 | 11/155 |
| 3802095 | Southmere Primary School | BS2 | 41.5 | 65/155 | 0.41 | 53/155 | 31.7 | 24/155 |
| 3802194 | Springwood Community Primary School | BW2 | 63.3 | 7/155 | 0.56 | 11/155 | 27.6 | 37/155 |
| 3803369 | St Anne’s Catholic Primary School | KE1 | 36.2 | 76/155 | 0.33 | 75/155 | 11.9 | 111/155 |
| 3803333 | St Anthony’s Catholic Primary School (Clayton) | BW1 | 26.4 | 102/155 | 0.20 | 108/155 | 8.9 | 123/155 |
| 3803373 | St Anthony’s Catholic Primary School (Shipley) | SH1 | 26.9 | 101/155 | 0.23 | 94/155 | 22.7 | 63/155 |
| 3803334 | St Clare’s Catholic Primary School | BE1 | 44.6 | 55/155 | 0.40 | 56/155 | 34.0 | 21/155 |
| 3803335 | St Columba’s Catholic Primary School | BS3 | 50.8 | 30/155 | 0.45 | 36/155 | 27.6 | 38/155 |
| 3803354 | St Cuthbert and the First Martyrs’ Catholic Primary | BW1 | 36.2 | 77/155 | 0.35 | 72/155 | 7.9 | 130/155 |
| 3803351 | St Francis’ Catholic Primary School | BE1 | 24.8 | 107/155 | 0.19 | 113/155 | 9.0 | 122/155 |
| 3803016 | St James’ Church Primary School | BW1 | 44.5 | 56/155 | 0.38 | 62/155 | 50.8 | 5/155 |
| 3803352 | St John The Evangelist Catholic Primary School | BS2 | 27.8 | 96/155 | 0.22 | 102/155 | 9.7 | 120/155 |
| 3805208 | St John’s CE Primary School | BS3 | 46.3 | 43/155 | 0.41 | 51/155 | 20.9 | 69/155 |
| 3803367 | St Joseph’s Catholic Primary School (Bingley) | SH2 | 13.6 | 139/155 | 0.13 | 127/155 | 8.2 | 126/155 |
| 3803338 | St Joseph’s Catholic Primary School (Bradford) | BE3 | 54.4 | 20/155 | 0.47 | 31/155 | 24.4 | 52/155 |
| 3803370 | St Joseph’s Catholic Primary School (Keighley) | KE3 | 33.6 | 83/155 | 0.28 | 84/155 | 16.0 | 94/155 |
| 3803021 | St Luke’s CE Primary School | BE1 | 34.6 | 81/155 | 0.28 | 85/155 | 26.2 | 41/155 |
| 3803347 | St Mary’s and St Peter’s Catholic Primary School | BE2 | 63.2 | 8/155 | 0.58 | 6/155 | 24.6 | 50/155 |
| 3803355 | St Matthew’s Catholic Primary School | BW1 | 45.7 | 47/155 | 0.39 | 60/155 | 25.4 | 47/155 |
| 3803013 | St Matthew’s CE Primary School | BE3 | 43.4 | 59/155 | 0.39 | 61/155 | 28.1 | 35/155 |
| 3803310 | St Oswald’s CE Primary School | BW3 | 52.1 | 29/155 | 0.51 | 16/155 | 36.1 | 18/155 |
| 3803301 | St Paul’s CE Primary School | BS1 | 25.6 | 105/155 | 0.20 | 106/155 | 7.9 | 129/155 |
| 3803034 | St Philip’s CE Primary School | BW1 | 49.7 | 35/155 | 0.50 | 20/155 | 12.9 | 108/155 |
| 3803313 | St Stephen’s CE Primary School | BE3 | 53.5 | 25/155 | 0.46 | 35/155 | 15.0 | 97/155 |
| 3803371 | St Walburga’s Catholic Primary School | SH1 | 23.1 | 113/155 | 0.19 | 114/155 | 4.9 | 142/155 |
| 3803349 | St William’s Catholic Primary School | BW1 | 42.9 | 61/155 | 0.40 | 54/155 | 14.2 | 100/155 |
| 3803350 | St Winefride’s Catholic Primary School | BS1 | 28.4 | 91/155 | 0.22 | 100/155 | 10.2 | 116/155 |
| 3802134 | Stanbury Village School | KE3 | 15.1 | 131/155 | 0.10 | 141/155 | 0.9 | 155/155 |
| 3802148 | Steeton Primary School | KE2 | 27.0 | 100/155 | 0.24 | 90/155 | 10.1 | 118/155 |
| 3802081 | Stocks Lane Primary School | BS2 | 20.1 | 121/155 | 0.15 | 120/155 | 2.8 | 152/155 |
| 3802057 | Swain House Primary School | BE1 | 31.0 | 87/155 | 0.24 | 92/155 | 25.8 | 44/155 |
| 3802058 | Thackley Primary School | BE1 | 17.5 | 125/155 | 0.12 | 129/155 | 4.3 | 144/155 |
| 3803368 | The Sacred Heart Catholic Primary School | KE2 | 6.0 | 152/155 | 0.06 | 153/155 | 3.9 | 148/155 |
| 3802060 | Thornbury Primary School | BE2 | 58.0 | 15/155 | 0.52 | 15/155 | 31.2 | 28/155 |
| 3802061 | Thornton Primary School | BW1 | 24.5 | 109/155 | 0.20 | 109/155 | 14.7 | 98/155 |
| 3802200 | Thorpe Primary School | BE1 | 33.1 | 85/155 | 0.24 | 91/155 | 23.4 | 60/155 |
| 3803362 | Trinity All Saints CE Primary School | SH2 | 23.7 | 112/155 | 0.22 | 95/155 | 21.1 | 68/155 |
| 3802135 | Victoria Primary School | KE1 | 46.1 | 44/155 | 0.43 | 46/155 | 13.5 | 102/155 |
| 3802071 | Wellington Primary School | BE1 | 27.6 | 97/155 | 0.19 | 112/155 | 10.9 | 113/155 |
| 3802193 | Westbourne Primary School | BW2 | 58.9 | 13/155 | 0.54 | 12/155 | 23.4 | 59/155 |
| 3803378 | Westminster CE Primary School | BE2 | 50.2 | 33/155 | 0.43 | 44/155 | 25.5 | 46/155 |
| 3802073 | Whetley Primary School | BW1 | 53.9 | 24/155 | 0.48 | 26/155 | 17.2 | 89/155 |
| 3802074 | Wibsey Primary School | BS1 | 28.4 | 92/155 | 0.22 | 99/155 | 20.3 | 74/155 |
| 3802117 | Wilsden Primary School | SH2 | 14.1 | 137/155 | 0.12 | 128/155 | 7.9 | 128/155 |
| 3803030 | Windhill CE Primary School | SH1 | 36.6 | 72/155 | 0.30 | 81/155 | 28.0 | 36/155 |
| 3803035 | Woodlands CE Primary School | BS1 | 21.9 | 116/155 | 0.16 | 118/155 | 13.1 | 106/155 |
| 3802078 | Woodside Primary School and Children’s Centre | BS1 | 34.9 | 80/155 | 0.35 | 69/155 | 37.5 | 13/155 |
| 3802202 | Worth Valley Primary School | KE3 | 38.0 | 70/155 | 0.30 | 80/155 | 32.8 | 22/155 |
| 3802100 | Worthinghead Primary School | BS1 | 27.9 | 95/155 | 0.22 | 96/155 | 23.0 | 61/155 |
| 3803036 | Wycliffe CE Primary School | SH1 | 27.4 | 98/155 | 0.25 | 89/155 | 18.8 | 83/155 |
| Primary averages | 35.1 | 0.31 | 20.3 | |||||
| Secondary/academy | ||||||||
| 3804077 | Aire Valley School | BW2 | 44.7 | 12/28 | 0.43 | 11/28 | 34.3 | 5/28 |
| 3806907 | Appleton Academy | BS1 | 35.8 | 14/28 | 0.30 | 16/28 | 26.4 | 14/28 |
| 3804064 | Beckfoot School | SH2 | 24.4 | 24/28 | 0.22 | 24/28 | 13.0 | 21/28 |
| 3804022 | Belle Vue Boys’ School | BW2 | 49.8 | 6/28 | 0.47 | 5/28 | 32.1 | 11/28 |
| 3804041 | Belle Vue Girls’ School | BW2 | 47.1 | 10/28 | 0.45 | 7/28 | 27.4 | 13/28 |
| 3805400 | Bingley Grammar School | SH2 | 17.1 | 27/28 | 0.15 | 27/28 | 8.3 | 27/28 |
| 3806906 | Bradford Academy | BS3 | 48.3 | 7/28 | 0.43 | 12/28 | 31.9 | 12/28 |
| 3804001 | Buttershaw Business and Enterprise College | BS1 | 36.6 | 13/28 | 0.31 | 13/28 | 33.3 | 7/28 |
| 3804100 | Carlton Bolling College | BE2 | 57.7 | 2/28 | 0.53 | 2/28 | 34.9 | 4/28 |
| 3804111 | Challenge College | BW2 | 58.3 | 1/28 | 0.52 | 3/28 | 35.1 | 3/28 |
| 3806908 | Dixons Allerton Academy | BW1 | 46.6 | 11/28 | 0.44 | 9/28 | 32.2 | 10/28 |
| 3806905 | Dixons City Academy | BE3 | 35.3 | 15/28 | 0.31 | 14/28 | 10.8 | 24/28 |
| 3804613 | Feversham College | BE2 | 51.1 | 4/28 | 0.48 | 4/28 | 33.7 | 6/28 |
| 3804101 | Grange Technology College | BW3 | 47.5 | 9/28 | 0.45 | 8/28 | 32.8 | 8/28 |
| 3805401 | Hanson Academy | BE1 | 30.1 | 20/28 | 0.24 | 23/28 | 13.2 | 20/28 |
| 3804502 | Ilkley Grammar School | KE2 | 6.3 | 28/28 | 0.06 | 28/28 | 2.4 | 28/28 |
| 3804616 | Immanuel College | BE1 | 31.0 | 19/28 | 0.24 | 21/28 | 19.4 | 16/28 |
| 3805404 | Laisterdyke Business and Enterprise College | BE2 | 57.5 | 3/28 | 0.53 | 1/28 | 43.3 | 1/28 |
| 3805402 | Oakbank School | KE3 | 29.6 | 21/28 | 0.25 | 19/28 | 19.0 | 17/28 |
| 3804112 | Parkside School | SH2 | 19.4 | 26/28 | 0.15 | 26/28 | 9.2 | 26/28 |
| 3804069 | Queensbury School | BS2 | 23.8 | 25/28 | 0.19 | 25/28 | 15.8 | 19/28 |
| 3804600 | St Bede’s Catholic Grammar School | BW2 | 34.7 | 17/28 | 0.30 | 15/28 | 11.9 | 22/28 |
| 3804611 | St Joseph’s Catholic College | BW2 | 34.9 | 16/28 | 0.30 | 17/28 | 11.8 | 23/28 |
| 3804610 | The Holy Family Catholic School | KE1 | 31.1 | 18/28 | 0.27 | 18/28 | 9.2 | 25/28 |
| 3805403 | Thornton Grammar School | BW1 | 29.1 | 22/28 | 0.24 | 22/28 | 20.1 | 15/28 |
| 3804074 | Titus Salt School | SH1 | 28.6 | 23/28 | 0.24 | 20/28 | 17.5 | 18/28 |
| 3804036 | Tong High School | BS3 | 50.5 | 5/28 | 0.46 | 6/28 | 37.3 | 2/28 |
| 3806909 | University Academy Keighley | KE1 | 47.5 | 8/28 | 0.43 | 10/28 | 32.5 | 9/28 |
| Secondary/academy averages | 37.7 | 0.34 | 23.2 | |||||
| Special | ||||||||
| 3807032 | Beechcliffe Special School | KE1 | 24.6 | 7/7 | 0.20 | 7/7 | 25.0 | 5/7 |
| 3807031 | Chellow Heights Special School | BW2 | 39.2 | 4/7 | 0.35 | 4/7 | 15.0 | 7/7 |
| 3807035 | Delius Special School | BE2 | 49.1 | 1/7 | 0.45 | 1/7 | 38.5 | 4/7 |
| 3807034 | Hazelbeck Special School | SH2 | 40.4 | 3/7 | 0.36 | 3/7 | 43.9 | 1/7 |
| 3807036 | High Park School | BS1 | 36.9 | 5/7 | 0.33 | 5/7 | 40.8 | 3/7 |
| 3807030 | Phoenix Special School | KE1 | 30.1 | 6/7 | 0.27 | 6/7 | 22.0 | 6/7 |
| 3807033 | Southfield School | BW3 | 42.7 | 2/7 | 0.37 | 2/7 | 43.1 | 2/7 |
| Special averages | 37.6 | 0.33 | 32.6 | |||||
Appendix 2 Intervention materials
Appendix 3 Participant information sheet
Appendix 4 Consent form: parents
Appendix 5 Health service use reporting form
Appendix 6 Qualitative interview semistructured topic guides
Interview topic guide for parents/carers
Introductions
-
Talk through participant information sheet for the interview.
-
Provide opportunity for questions about the interview.
-
Reconfirm the parent’s/carer’s consent to take part and for the interview to be recorded (if not take notes).
Experience of taking part in the PiP pilot trial
Recruitment and randomisation
1. Can you tell me how did you first hear about the PiP study?
Prompts:
-
Letter sent home from school.
-
Spoke to community research administrator in playground.
-
Approached at child’s nursery.
2. What was your initial reaction to receiving the invitation to take part in the PiP study?
Prompts:
-
What were your reasons for deciding to take part?
-
Would it make a difference if the study was linked to someone famous, e.g. Bradford City FC?
3. What did you think about the way that you were recruited to the PiP study?
Prompts:
-
Send a reply slip back.
-
Phoned by the community research administrator.
-
What did you like/dislike about this process? How could we improve this?
4. What do/did you like/dislike about the written information about the study (look through invitation letter, information sheet, consent form and reply slip with parent)?
Prompts:
-
English or Urdu version.
-
How could we improve these?
5. What did you think about being randomised to one of the two groups in the study?
Prompts:
-
What do you understand randomisation to mean?
-
How did you feel about being in the intervention/control group? Why was that?
Data collection (including accelerometry) and measurement time points
6. So far we have asked you and your child to attend two measurement sessions. How have you found these?
Prompts:
-
How many times did you manage to come along?
-
If you missed any, what would have helped you to attend? (time/place)
-
What did you like/dislike about these sessions?
-
How might we improve these measurement sessions for parents and children?
7. What did you think about the questionnaire that we asked you to fill in?
Prompt:
-
How might we make it easier for parents to fill in these questionnaires, i.e. complete at the appointment/complete at home/send back/complete over the phone.
8. How did you find recording your child’s levels of physical activity over 6 days using a diary and the accelerometer that we gave you?
Prompts:
-
What went well?
-
What went less well?
-
How can we make this easier for parents?
Incentives
9. Can I ask how important were the gift vouchers in encouraging you to take part in the PiP study? Will they encourage you to finish the study (two more school terms)?
Prompt:
-
Why is that?
10. Would you prefer vouchers or cash? How much do you think is the right amount?
Experience of taking part in the playground intervention
(Intervention group only; control group parents go to Q15)
11. What did you think of the PiP playground sessions?
Prompts:
-
What did you like about them?
-
What did you dislike?
-
What did your child do in the sessions?
-
How can we improve the sessions?
-
Did you know the other parents and children there?
12. Approximately how many sessions a week did your child attend?
Prompts:
-
Who came with the child to the sessions?
-
Did you go to the morning or afternoon sessions (a mix of both) – why was that?
-
If you did not manage to attend why was that?
-
Was three times a week the right number of times – prefer more or less?
13. How might we encourage more parents and children to come along to the sessions?
Prompt:
-
Were you aware that you would be given some play equipment to take home? Did that make a difference?
14. Do you think your child has benefited from coming to the PiP playground sessions?
-
Confidence.
-
Fitter.
-
Better at playing outside.
-
Sleep better.
-
Better behaved.
14. Do you think you have benefited from coming to the PiP playground sessions?
-
Confident in playing outside with child.
-
Fitter.
Interview topic guide for PiP facilitators
Introductions
-
Talk through the reasons for the interview.
-
Provide opportunity for questions about the interview.
-
Confirm the parental involvement worker’s consent to take part and for the interview to be recorded (if not take notes).
Experience of leading the PiP playground sessions
1. What has been your experience of leading the PiP playground session?
Prompts:
-
How have you found doing it?
-
What has gone well? What has gone less well?
2. Can you tell me what a typical 30-minute PiP playground session looked like?
Prompts:
-
Roughly how many children and parents were there?
-
(Why do you think so few parents and children attended?)
-
How did you go about organising the sessions? What types of activities did you include?
-
What worked well/less well?
3. How about the 5-minute structured parent and child play sessions, what did they include?
Prompts:
-
How did they go?
-
How did you modify the activities for different children?
-
What worked well/less well?
4. What type of equipment was available for the sessions?
Prompts:
-
Did the parents and children use it?
-
What other equipment would you suggest we make available?
5. How did you go about working with the parents to encourage their children and to find other opportunities for activity for their children?
Prompts:
-
How did that go?
-
What worked well/less well?
6. How did you use the PiP leaflets with parents?
Prompts:
-
How did that go?
-
Which leaflets worked well/less well?
7. How did you find the training and the PiP manual?
Prompts:
-
How useful were they in helping you run the PiP sessions?
-
How did you use the manual?
-
How can we improve them?
-
Was there enough support for you? (why/why not?)
8. How do you think we could improve the PiP playground sessions?
9. Finally, is there anything else you want to tell us about the PiP study?
End interview
Thank the participant and let them know that they will receive a summary of the findings of the PiP study at the end of the project.
Interview topic guide for head teachers (telephone interview)
Introductions
Talk through the participant information sheet for the interview, provide an opportunity for questions about the interview and reconfirm the head teacher’s consent to take part.
1. Experience of the playground intervention.
Can you tell me what has been your experience of hosting the PiP playground sessions in your school?
Prompt:
-
From the perspective of the school, how has it gone? What has gone well/less well?
2. Have the sessions impacted on the school day? How?
Prompt:
-
What changes (if any) would you recommend we made?
3. In the first term the playground sessions were led by a parent involvement worker but after that the sessions were not formally supervised. Did that make any difference to the school?
Prompt:
-
How? Which did you prefer? Why is that?
4. Do you have any advice for us about encouraging other schools to take part?
Prompts:
-
What are your thoughts on the benefits to schools of hosting the PiP playground sessions?
-
What about the disadvantages?
-
What types of incentives (e.g. vouchers, cash) do you think are appropriate for schools? What level (£) of incentives do you think are appropriate?
5. Finally, is there anything else you want to tell us about the PiP playground sessions or the wider research study?
End interview
Thank the participant and let them know that they will receive a summary of the findings of the PiP study in due course.
Appendix 7 Qualitative study participant information sheet: facilitators and head teachers
Participant information sheet for facilitators
Participant information sheet for head teachers
Appendix 8 Consent form: facilitators and head teachers
Consent form for facilitators
Consent form for head teachers
Appendix 9 Spearman–Brown prophecy methods and tables
The aim of this document is to describe the process and calculations that have been applied to determine the minimum accelerometer wear time (daily wear hours and number of wear days) for participants of the PiP pilot trial. This document is directly addressing the following statement within the PiP protocol:
Data presented in this document were used by members of the internal steering group to decide what wear-time criterion will be applied to the accelerometer-derived data.
Methods
The PiP baseline data were cleaned and processed using Actigraph (v6) software according to the protocol described in Chapter 2, Objective 4: Feasibility of collecting the outcome measures and whether or not there was a difference between trial arms and ethnic groups and Objective 9: The effect of participation in the intervention on health outcomes and whether or not there were any differences between ethnic groups.
Data for participants who wore the accelerometer for a minimum of 3 days and with a daily wear time of 3 hours, 4 hours, 5 hours, 6 hours, 7 hours, 8 hours and 9 hours were separately scored using the Actilife software and were then exported to Microsoft Excel (2010; Microsoft Corporation, Redmond, WA, USA) for further data cleaning (comparison with wear-time logs). Using data from a minimum of 3 days with a minimum of 3 hours of wear time, paired t-tests or Wilcoxon matched-pairs tests between weekday and weekend day wear time, physical activity [TPA, moderate physical activity (MPA), LPA, vigorous physical activity (VPA)] and sedentary time were conducted to establish whether or not inclusion of a weekend day is required within the reliability analyses. Comparison tests were also conducted for the percentage of time being spent in TPA and MVPA (%TPA and %MVPA); this was so the confounding factor of wear time is controlled for.
To establish wear-time reliability specific written coding for Stata version 12 was used to randomly choose 3 days of data out of the different hourly increments for each participant. Single-day ICCs (two-way mixed models and absolute agreement) were then calculated using IBM SPSS Statistics version 21 (IBM Corporation, Armonk, NY, USA) for %TPA, %LPA, %MVPA and %sedentary time. The Spearman–Brown prophecy formula (see below) was then applied to determine the number of days required at each of the estimated single-day ICC values to meet reliabilities of 0.7 and 0.8. To establish a minimum wear time all results calculated by the Spearman–Brown prophecy formula were rounded up; therefore, both 2.1 and 2.7 were rounded up to 3 (days). If the weekend compared with weekday analysis concluded that there were any differences between weekdays and weekends then the process was repeated but with 2 weekdays and 1 weekday chosen at random.
Spearman–Brown prophecy:
For example:
Results
Table 48 describes the physical activity data from participants (n = 125) who have at least 3 days of data with a minimum 3 hours of wear time.
| Activity | Mean | SD | Min. | Max. |
|---|---|---|---|---|
| Sedentary time | 201.6 | 49.0 | 91.1 | 331.9 |
| LPA | 191.9 | 46.0 | 102.0 | 329.7 |
| MPA | 45.2 | 16.1 | 12.9 | 95.5 |
| VPA | 12.8 | 7.7 | 0.0 | 46.7 |
| MVPA | 58.0 | 22.5 | 14.3 | 120.2 |
| TPA | 249.9 | 60.5 | 116.3 | 402.5 |
| Wear time | 452.4 | 89.8 | 242.8 | 633.3 |
| %LPA | 42.1 | 4.3 | 31.2 | 54.5 |
| %MVPA | 13.0 | 4.6 | 3.4 | 23.8 |
| %TPA | 55.1 | 7.0 | 37.9 | 73.2 |
Table 49 presents the results of the comparison tests between weekdays and weekends. There was no significant difference between the amount of wear time during weekdays and the amount of wear time during weekend days, although the p-value was not too far from being significant (p = 0.09). The only significant differences between weekdays and weekends were found for TPA and LPA; however, when controlling for wear time, TPA (%TPA) was not significantly different, although LPA (%LPA) was.
| Test | Mean | SD | t | p-value |
|---|---|---|---|---|
| Paired t-test | ||||
| Wear time weekday | 458.6516 | 91.28941 | 1.71 | 0.09 |
| Wear time weekend | 476.574 | 115.68922 | ||
| Sedentary time weekday | 204.9949 | 49.36484 | 0.83 | 0.41 |
| Sedentary time weekend | 209.4053 | 65.17377 | ||
| LPA weekday | 194.9531 | 47.64251 | 1.99 | 0.05 |
| LPA weekend | 204.5801 | 54.37704 | ||
| TPA weekday | 253.6568 | 59.49854 | 2.08 | 0.04 |
| TPA weekend | 267.1687 | 76.7268 | ||
| %LPA weekday | 42.1564 | 4.24874 | 2.22 | 0.03 |
| %LPA weekend | 43.0 | 5.1 | ||
| %MVPA weekday | 13.0587 | 4.70116 | 0.02 | 0.98 |
| %MVPA weekend | 13.0495 | 5.58735 | ||
| %TPA weekday | 55.2151 | 6.62817 | 1.55 | 0.12 |
| %TPA weekend | 56.0938 | 8.67456 | ||
| Mean | SD | z | p-value | |
| Wilcoxon test | ||||
| MPA weekday | 45.8901 | 15.32617 | 1.02 | 0.31 |
| MPA weekend | 48.2828 | 22.28786 | ||
| VPA weekday | 12.8136 | 7.95915 | 0.86 | 0.39 |
| VPA weekend | 14.3058 | 10.77923 | ||
| MVPA weekday | 58.7037 | 21.57791 | 1.17 | 0.24 |
| MVPA weekend | 62.3434 | 31.6582 | ||
From these findings and also considering that the sample number was reduced from 125 to 103 to include those participants with both weekday and weekend days, it is logical not to have a wear-time criterion that must include weekend days.
Table 50 outlines the single-day ICCs and the estimated number of days calculated by the Spearman–Brown prophecy formula required to reach reliabilities of 0.7 and 0.8. For %TPA, %MVPA and %sedentary time, a wear time of 6 or 7 hours requires 3 days of wear to reach a reliability of 0.8. For %LPA, 4 days is required for reliability; however, %LPA is not the main outcome variable of the study. Results for 4 and 5 hours of wear time required different numbers of wear days to reach reliability for different variables. Additionally, choosing a wear time of 7 hours or longer drastically decreased the sample size. Looking at the results but also referring to the sample sizes stated within the table, 6 hours on any 3 days as the minimum wear time would be the best compromise.
| Number of hours from any 3 random days | Number of participants | Outcome (%) | Single-day ICC | 95% CI | p-value | 0.8 reliability days | 0.7 reliability days |
|---|---|---|---|---|---|---|---|
| 9 hours | 36 | %TPA | 0.45 | 0.25 to 0.64 | < 0.01 | 4.89 | 2.85 |
| %LPA | 0.61 | 0.43 to 0.76 | < 0.01 | 2.56 | 1.49 | ||
| %MVPA | 0.56 | 0.38 to 0.73 | < 0.01 | 3.14 | 1.83 | ||
| %sedentary time | 0.45 | 0.25 to 0.64 | < 0.01 | 4.89 | 2.85 | ||
| 8 hours | 66 | %TPA | 0.60 | 0.47 to 0.72 | < 0.01 | 2.67 | 1.56 |
| %LPA | 0.55 | 0.42 to 0.68 | < 0.01 | 3.27 | 1.91 | ||
| %MVPA | 0.63 | 0.50 to 0.74 | < 0.01 | 2.35 | 1.37 | ||
| %sedentary time | 0.60 | 0.47 to 0.72 | < 0.01 | 2.67 | 1.56 | ||
| 7 hours | 83 | %TPA | 0.60 | 0.47 to 0.72 | < 0.01 | 2.67 | 1.56 |
| %LPA | 0.54 | 0.40 to 0.65 | < 0.01 | 3.41 | 1.99 | ||
| %MVPA | 0.62 | 0.49 to 0.74 | < 0.01 | 2.45 | 1.43 | ||
| %sedentary time | 0.6 | 0.47 to 0.72 | < 0.01 | 2.67 | 1.56 | ||
| 6 hours | 101 | %TPA | 0.58 | 0.45 to 0.66 | < 0.01 | 2.90 | 1.69 |
| %LPA | 0.51 | 0.40 to 0.62 | < 0.01 | 3.84 | 2.24 | ||
| %MVPA | 0.59 | 0.45 to 0.66 | < 0.01 | 2.78 | 1.62 | ||
| %sedentary time | 0.58 | 0.45 to 0.66 | < 0.01 | 2.90 | 1.69 | ||
| 5 hours | 112 | %TPA | 0.59 | 0.49 to 0.68 | < 0.01 | 2.78 | 1.62 |
| %LPA | 0.55 | 0.42 to 0.68 | < 0.01 | 3.27 | 1.91 | ||
| %MVPA | 0.54 | 0.40 to 0.65 | < 0.01 | 3.41 | 1.99 | ||
| %sedentary time | 0.59 | 0.49 to 0.68 | < 0.01 | 2.78 | 1.62 | ||
| 4 hours | 125 | %TPA | 0.57 | 0.47 to 0.66 | < 0.01 | 3.02 | 1.76 |
| %LPA | 0.44 | 0.33 to 0.55 | < 0.01 | 5.09 | 2.97 | ||
| %MVPA | 0.54 | 0.44 to 0.63 | < 0.01 | 3.41 | 1.99 | ||
| %sedentary time | 0.57 | 0.33 to 0.55 | < 0.01 | 3.02 | 1.76 | ||
| 3 hours | 125 | %TPA | 0.58 | 0.12 to 0.79 | < 0.01 | 2.90 | 1.69 |
| %LPA | 0.46 | 0.25 to 0.62 | < 0.01 | 4.70 | 2.74 | ||
| %MVPA | 0.56 | 0.32 to 0.71 | < 0.01 | 3.14 | 1.83 | ||
| %sedentary time | 0.58 | 0.12 to 0.79 | < 0.01 | 2.90 | 1.69 |
List of abbreviations
- A&E
- accident and emergency
- BMI
- body mass index
- CHD
- coronary heart disease
- CI
- confidence interval
- CMO
- Chief Medical Officer
- ComQol-A5
- Comprehensive Quality of Life Scale – Adult
- CONSORT
- Consolidated Standards of Reporting Trials
- CVD
- cardiovascular disease
- EQ-5D
- European Quality of Life-5 Dimensions
- FSM
- free school meal
- HR
- hazard ratio
- HRQoL
- health-related quality of life
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- IMD
- Index of Multiple Deprivation
- LPA
- light physical activity
- MI
- multiple imputation
- MPA
- moderate physical activity
- MVPA
- moderate to vigorous physical activity
- OR
- odds ratio
- PedsQL
- Pediatric Quality of Life Inventory
- PiP
- Preschoolers in the Playground
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SES
- socioeconomic status
- SUR
- seemingly unrelated regression
- TPA
- total physical activity
- VPA
- vigorous physical activity