Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 10/3007/06. The contractual start date was in April 2013. The final report began editorial review in December 2014 and was accepted for publication in April 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
We confirm that there are no conflicting or competing interests in respect of DeltaNet International Ltd as the Anderson Peak Performance (APP) gateway and the companies responsible for website and logo design.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Stansfeld et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background and rationale
Background
There is empirical evidence, including several meta-analyses, showing that the psychosocial work environment impacts on employee well-being and mental health and risk of sickness absence. 1–4 Job strain, in terms of high demands and low decision latitude, low social support at work from managers and colleagues, effort–reward imbalance, organisational injustice and job insecurity have been related to an increased risk of common mental disorders, depressive disorders and sickness absence. Mental ill health at work has enormous costs to the economy: in 2007 the Sainsbury Centre for Mental Health estimated that the total cost to UK employers of absenteeism, presenteeism and staff turnover was £25.9B. 5 The Organisation for Economic Co-operation and Development (OECD) estimates that mental ill health costs the UK economy £70B every year, of which 53% relates to loss of employment and productivity. 6 In the UK, 40% of overall sickness absence is a result of mental health problems, amounting to 70 million working days lost to psychiatric sickness absence per year. 5 There is consensus that employee health is a public health priority and the responsibility of employers and employees as well as health services. 7,8
Stress management interventions
Stress management interventions in the workplace target either the individual or the organisation9–11 and may act at primary, secondary or tertiary preventative levels. Most interventions to manage stress and mental illness at work have targeted the individual, usually at a secondary or a tertiary prevention level, using a clinical intervention such as cognitive–behavioural therapy or treatment of depressive illness with medication. 4,12 A meta-analysis of individually targeted health promotion13 has shown that it is not especially effective. However, the logic of the research findings linking the psychosocial environment to mental health suggests that primary preventative interventions are needed that can be delivered through the workplace. 14
Organisational interventions
So far, evaluations of organisational interventions for workplace stressors are limited, although there have been some process evaluations using qualitative methods and case studies to identify manager competencies needed for dealing with workplace stress and to examine how management standards are used in large organisations. 15–17 Three reviews of interventions within organisations11,18,19 showed mixed evidence of benefit in terms of health outcomes; van der Klink et al. ’s19 meta-analysis of 48 studies of occupational stress interventions showed that the majority of interventions were delivered to individuals rather than targeting the organisation and often involve cognitive–behavioural techniques. 20
Organisational approaches to improving mental health
Examining organisational-level interventions, Egan et al. 21 reviewed action research studies testing Karasek’s22 job strain model of the health effects of the combination of high job demands and low decision latitude or control over work. An elaborated version of this model includes the ameliorative effects of work social support on the health effects of job strain. Eight studies in this review reported benefits of the intervention for job control and participation; seven reported significant overall health improvements including for mental health questionnaire scores; and four studies reported decreased job demands post intervention accompanied by improved health outcomes in each instance. Improved support was also associated with improved health in the majority of studies in which it was measured. In those studies in which control, demand or support were recorded as unchanged or worsened, health outcomes often remained unchanged. 21 Furthermore, Bambra et al. 23 reviewed studies of workplace reorganisation involving increasing skill discretion, teamworking and decision latitude in diverse occupational groups. Nineteen of these studies included a control group but none was a randomised study. Again, the results were mixed; however, the teamworking interventions did improve the work environment by increasing support.
Organisational approaches to reducing sickness absence
Michie and Williams24 reviewed six studies and found that training and organisational approaches to increase participation and decision-making and increased work support and communication led to reduced sickness absence. The difference between ‘healthy’ and ‘unhealthy’ workplaces in terms of the psychosocial as opposed to the physical environment was attributed to the quality of leadership and the competence and awareness of management throughout the organisation. 24
Methodological problems in organisational interventions
Systematic and meta-analytic reviews conclude that there is a notable scarcity of randomised controlled trials (RCTs) of organisational-level interventions. This partly reflects the difficulty in organising RCTs;25 the insufficient length of follow-up;19,26 and difficulties finding similar clusters for randomisation. 27 Nevertheless, these difficulties are not insurmountable, as exemplified by the WellWorks project, which included a RCT on cancer prevention strategies in 24 organisations in Massachusetts. 28 In summary, there have been insufficient methodologically robust RCTs to test whether or not organisational-level psychosocial interventions are effective in improving the well-being of employees and reducing sickness absence. In general, there is little knowledge of what works at an organisational level to improve employee well-being. A RCT of a participatory intervention involving action planning with nurses and sharing good practice and obstacles was associated with changes in work characteristics but not mental health29 and a participatory risk management intervention in an Australian public sector organisation was associated with significant improvements in job design, training and morale and a reduction in organisational sickness absence duration. 30 There are undoubtedly difficulties in carrying out RCTs in organisations in which there are many complex influences on the behaviour and well-being of employees and managers. However, although it may not be possible to adjust for all confounding factors, previous research has indicated that it is possible to execute RCTs in organisational settings. 24
This study aimed to build on the existing research to pilot an organisational-level management intervention to test the acceptability of a trial, the feasibility of recruitment, the components of the intervention, adherence and the likely effectiveness of the intervention before submitting it to rigorous RCT methodology.
Management standards
In this study we used an organisational-level intervention based on the Health and Safety Executive (HSE) management standards for work-related stress. 31,32 These psychosocial interventions were the first national approach that sought to reduce the incidence of work-related stress at source by applying a risk assessment process to triggers of work-related stress. An integral part of that process was the development of the management standards indicator tool. 31 This consists of 35 questions designed to assess adherence to the six management standards (change, control, demands support, relationships and role). The indicator tool provides a way for an organisation to identify potential hotspots where sources of stress exist and each of the six stressor areas is accompanied by a description of the desirable states to be achieved (the management standards), which are seen to reflect high levels of health, well-being and organisational performance. The basis of the management standards approach is to test or compare the states to be achieved with the actual conditions that currently exist within an organisation. This helps employers identify the underlying causes of workplace stress and think about how they might be prevented through practical improvements using organisational-level interventions. 33 We sought to test the benefits of using the management standards as a tool that can promote health in the workplace when used to improve management understanding and develop more effective competencies, rather than only as a method of assessing risk and compliance with standards. As the management standards are concerned with the prevention of work-related stress, it is apparent that the application of the six standard areas in the promotion of mental health is useful in the design of packages to improve well-being and reduce stress and sickness absence. Donaldson-Feilder et al. 34 found that previous competency frameworks for management did not cover all the six areas of the management standards.
Manager competencies
The HSE and the Chartered Institute of Personnel and Development have worked together in a collaborative research programme with input from employers and employees to develop a set of competencies and behaviours perceived as being the most relevant and appropriate for helping managers to be better at managing work-related stress. The Management Competency Framework35 has four overarching competencies with an additional twelve subcompetencies. Each competency has associated behaviours, both positive and negative, which allow organisations to identify areas of management strengths and development needs around the skills necessary for tackling work-related stress. There has been significant interest and uptake of the Management Competency Framework by the human resources (HR) community, enabling new action plans for managers with regards to their current and future training needs. 36,37
An adapted version of the management standards for managers in small- and medium-sized enterprises (SMEs) has been evaluated by Gaskell et al. ,38 who concluded that it offered ‘time-poor’ SME managers a quick and easy method for identifying problems and the mechanisms for dealing with them. This study focused on improving manager competencies to deal with stress at work within the framework of the HSE management standards.
Rationale for the pilot study
An efficient and potentially cost-effective way of improving the psychosocial work environment is training managers to provide more effective supportive management for employees; this support should make employees feel valued and help managers recognise stressful and unfair conditions in the workplace. When applied to managers at all levels, such interventions can be transmitted through work relationships to change the organisational culture. We decided to focus the intervention on line managers for employees, as these managers would have the most effect on employees and might be under most pressure from both above and below. We planned to test the acceptability, feasibility, risks and likely effectiveness of a primary preventative intervention that provides knowledge and skills about management standards and their implementation in terms of managing stress at work and promoting well-being. This is a pilot study and we did not expect to obtain definitive results on the effectiveness of the intervention as we were not powered to do so. Rather, we wished to assess the likely magnitude of the effect of the intervention as a guide for the future trial.
The intervention was delivered in the form of a guided e-learning education program provided as part of a continuing professional development (CPD) process. The advantage of targeting our intervention at managers who are line managers for a number of employees is that this is potentially a cost-effective way of influencing employees’ well-being. The study randomised the intervention to ‘clusters’ consisting of groups of managers and those employees whom they supervise. It has an advantage over approaching employees directly as managers have more power to change working conditions and these changes will apply to a number of employees in specific work groups. A cluster design allowed us to select managers and the employees working with them in service configurations in which they were carrying out the same types of tasks with similar groups of participants. Potentially, the cluster design also allowed us to recruit groups of managers who work in close proximity on similar tasks and who could share experiences in the facilitated meetings. We attempted to match up employees with their managers involved in the study.
The e-learning intervention allows managers to access the intervention at the most convenient time for them and to be supportive and perhaps facilitate change in working conditions. It can also be returned to again and again and was delivered in weekly or fortnightly instalments to make it more manageable to engage with within a busy working life. The hosting system for the e-learning package also enabled take-up (access, duration and frequency) to be measured so that the influence of intensity of package use could be assessed. The package is interactive (inviting reflection, requiring participants to make decisions during case studies, integrating real-life practical activities) and therefore is likely to engage the interest of the managers involved. The e-learning package could be applied to the whole cluster simultaneously. Thus, middle managers, who are particularly vulnerable to stress, benefit from the intervention directly through their own e-learning.
Several commercial organisations have developed e-learning programs based on management standards but there is no clear evidence of the effectiveness of such programs. In this pilot study we tested the likely effectiveness of an established e-learning program. We chose to use the Anderson Peak Performance (APP) e-learning package Managing Employee Pressure at Work [see www.andersonpeakperformance.co.uk (accessed 25 May 2015)], which is based on HSE management standards and addresses many of the aspects of workplace stress identified in observational research. It has been used in a number of public and private organisations by its originator Rosemary Anderson but its effectiveness has not been formally tested. A comparison of face-to-face stress intervention workshops led by an instructor with an e-learning format suggests that both formats can lead to significant reductions in reported stress, although attrition is significantly higher in the e-learning format. 39 Although there are a number of e-learning tools on stress at work, very few focus on what managers can do to reduce stress among their employees, which is a key feature of the APP e-learning package.
Objectives
The overall aim of the main randomised trial was to evaluate whether or not an e-learning health promotion intervention using management standards applied by managers improved employees’ well-being and reduced sickness absence in clusters selected from an organisation compared with similar clusters in the same organisation where it was not applied.
In this pilot study we tested within separate clusters of the same organisation:
-
the acceptability of the trial
-
the feasibility of recruitment
-
the components of the intervention
-
adherence
-
the likely effectiveness of the intervention.
With regard to adherence, in the protocol we stated that ‘The acceptability of the intervention to managers will be assessed by managers’ engagement with the intervention and their attitudes to the intervention using qualitative methods’. Adherence was not explicitly defined.
As the aim of a pilot study is to prepare for and improve on the design for a full RCT, we formulated a set of progression criteria to assess the likely success of such a future trial and identify measures for improvement. We hoped to see the following results for progression to the main trial to occur:
-
An increase in well-being scores of at least 3% among those employees whose managers completed the intervention compared with employees from the control cluster whose managers did not complete the intervention.
-
Recruitment of 80% of the eligible sample and 80% follow-up of the recruited sample of employees (up to 20% withdrawal from the study), with at least 60% of managers invited actively engaging with the intervention.
-
The acceptability of the intervention and the trial would be judged by the responses of managers to the intervention and the responses of employees to the trial, using data from the qualitative study.
-
The feasibility of the outcome measures and their collection would be assessed by the response rate to the online and paper questionnaires for employees, at least 60% coverage of recruited employees and the ease of availability of sickness absence data.
The decision to progress would also take into account whether or not simple procedures had been identified that are likely to improve rates of recruitment, retention and adherence, taking all measures together rather than in isolation. The overall costs and benefits of the pilot study intervention were also assessed to judge whether or not these would support a full trial.
In the protocol (version 3) our criteria for progression were as described in the following section.
Study progression
Progression to the main study will be assessed in terms of fulfilment of the pilot study objectives: sufficient trial recruitment; acceptability of, use of and adherence to the e-learning program by managers; acceptability of the trial to employees and managers; and the feasibility of the outcome measures and their collection. We estimate that progression to the main study would occur if there is an increase in well-being scores of at least 3% among those employees whose managers completed the intervention compared with those employees from the control cluster whose managers did not complete the intervention. We would aim for 80% recruitment and a 80% follow-up rate, with at least 60% of managers actively engaging with the intervention. The decision to progress will also take into account whether or not simple procedures have been identified that are likely to improve rates and taking all measures together rather than in isolation. We will also assess the overall costs and benefits of the pilot to judge whether or not these would support a full trial.
Patient and public involvement
Public involvement in the research was carried out through the steering group, which included a union member and a member of a mental health charity. Both contributed to fine-tuning the design of the study and to the management of the research. In particular, they were helpful in making suggestions about the content of the employee questionnaire and about ways to engage research staff and managers.
In addition, we held meetings with trust managers a month before the start of the study. As there were no ‘patients’ involved in this study and the relevant ‘public’ involved in this study were employees, we felt that managers and employees were the relevant groups to discuss the study with. This was very helpful in engaging the target audience and the discussion with the managers helped to refine the study methodology. Feedback was used to identify the best channels to communicate with managers during the intervention, for instance managers tended to favour telephone and face-to-face contact with the facilitator rather than web-based interaction. We also received helpful pointers about possible concerns regarding the understanding of cluster selection and randomisation and the confidentiality of the employee questionnaires, which helped us in the set-up of communications with the targeted participants.
Chapter 2 Methods
Introduction to the mixed-methods approach
The pilot study was designed as a ‘mixed-methods’ study, incorporating a qualitative component alongside a RCT. The benefits of a mixed-methods design are increasingly acknowledged40–42 in terms of helping to illuminate the processes of a trial, the acceptability of a trial and intervention and possible reasons why an intervention does or does not work and to draw out the learning from a study.
Trial methods
Trial design
This trial was designed as the precursor of a cluster, single-blind RCT of a site-level intervention. It was conducted at a single organisation with four clusters of employees and the managers who supervise them. Each of the clusters was equivalent to one service unit within the recruited organisation, either for a specific geographical location or for a separate organisational unit. Each cluster was expected to consist of about 10–15 managers responsible for 5–20 employees each. It was expected that 100 employees per cluster would give consent. The clusters were randomly assigned to either the intervention group or the control group at a ratio of 3 : 1. In total, we expected to recruit 30–40 managers from three clusters randomised to the intervention and about 400 employees from all four clusters.
Participants
We recruited a single organisation to participate in the pilot study that was receptive to using a CPD approach to adopting management standards. Inclusion criteria included the organisation’s ability to provide usable data on sickness absence and to allow internet access at work for its staff.
The four clusters were identified and selected in collaboration with stakeholders at the organisation. Although no strict selection criteria were defined in the protocol, we sought to include clusters of comparable size, with similar organisational and hierarchical structures and areas of activity and with relative separation in terms of either geographical location or organisational structure, to minimise contagion effects between intervention and control group clusters.
Within the selected four clusters we aimed to invite all employees and their immediate line managers to participate in the study. Potential participants were identified with the help of the organisation’s own research team, who acted as local study champions, and with the use of the organisation’s electronic staff records. Participants were classified as either employees or managers for the purpose of the study. We excluded staff for whom the intervention was unlikely to have an effect because they would not remain in the organisation for the duration of the study: the long-term sick, those with a notified pregnancy and staff on fixed-term contracts due to expire during the course of the trial.
During recruitment, these exclusion criteria were amended to explicitly exclude managers as well as employees on long-term absences and to exclude managers and employees with other types of contracts known to expire or terminate during the course of the trial (e.g. because of retirement). This amendment was a clarification of the eligibility criteria that became necessary during the recruitment process and did not alter the pool from which the participants were recruited. Long-term sickness absence, often the result of severe illness or very entrenched work problems or both, was unlikely to be influenced by a short-term intervention such as that applied in the study and thus employees with long-term sickness absence were excluded.
Potential participants were invited to take part by the local research team and given a participant information sheet and asked to sign an informed consent form for participation in the study. There were two different information sheets, one customised for employees and one for managers. Participants who gave written informed consent to take part in the study were allocated a three-digit unique participant identification number for pseudo-anonymisation. Participants who were invited to take part in the qualitative research interviews or focus group were asked to give a short separate informed consent for the recording and use of the interview data.
Procedure for the follow-up of employees
Employees recruited to the study were invited to complete a work, health and well-being questionnaire at baseline (i.e. before the start of the study intervention) and at follow-up (after the end of the intervention). Questionnaires were completed online by employees but paper copies were offered to those who were unwilling or unable to complete online questionnaires.
After registration, employees received an automated e-mail with the questionnaire log-in instructions. In case of non-response, the reminder procedure was as follows:
-
two automated e-mail reminders were sent out to participants who had not completed the questionnaire, 7 days apart
-
one personalised e-mail reminder was sent by the trial manager if no response was received
-
local research staff then attempted telephone contact with the participants who had not responded
-
paper questionnaires were then offered to those employees who had not responded by this point.
Intervention
Name of the intervention
The intervention involved a guided application of the APP e-learning program Managing Employee Pressure at Work for managers. A summary of the intervention timeline is given in Figure 1.
FIGURE 1.
Intervention timeline.

Aims of the intervention
The e-learning package Managing Employee Pressure at Work is an already established e-learning health promotion program for managers with a focus on the six management standards domains: change, control, demands, relationship, role and support. This psychosocial program aims to help managers identify sources of stress, understand the link with mental and physical illness and improve managers’ capacity for helping employees proactively improve their well-being and deal with stressful working conditions. The intended focus is on improving social support for employees, improving communication, improving organisational justice, providing more information about job change and making sure that employees’ work is valued. The intervention also involved guidance in the form of face-to-face sessions and support from a study facilitator.
The e-learning program was designed to help managers understand:
-
the concept of pressure at work, the link with mental and physical ill health, the need to take this seriously and the personal and team/organisational benefits for doing so
-
how to work proactively with their teams to identify collective problems and find solutions
-
how to spot if an employee has a problem and work with the individual to find suitable acceptable solutions
-
how to support individual employees who are experiencing problems
-
their legal duty of care
-
how to avoid personal injury claims and how to carry out a HSE-compatible risk assessment if required
-
how their own management style may add to or reduce pressure on their employees.
The intended mechanism of the intervention was as follows. Through participation in the e-learning program, the completion of e-learning activities and consultation with the facilitator, managers change their behaviour towards employees and the workplace conditions. The change in managers’ behaviour results in improved well-being and reduced stress among employees. Increased well-being is also related to employees subsequently being less likely to take sickness absence.
Incentivisation
Staff were incentivised to use the intervention through management ‘buy-in’, publicity and receiving a certificate of completion as part of CPD. The project was presented to senior managers and managers targeted for study participation at two local meetings a month before the start of recruitment, with the endorsement of executives within the organisation. Executives verbally agreed to allow allocated time for managers to complete the e-learning. Senior managers also received access to the same e-learning program as the targeted managers. We presented the program in a way that attempted to incentivise middle managers to participate, showing that this could improve their working life.
Content of the intervention and procedures
The intervention consisted of two face-to-face educational sessions with a facilitator, the modular e-learning program and ongoing e-mail or telephone support from the facilitator. The e-learning program consisted of a series of linked topics with case examples, additional activities that could be completed outside the e-learning environment and an assessment activity in the form of a quiz. The HSE management standard domains are dealt with across several of the e-learning program modules and are not distinct to any one module.
In module 1 pressure and demands are identified and discussed. In module 3 the Health and Safety at Work Act 197443 is explained as well as the need to carry out risk assessments for stress at work. Reference is made to the health and safety guidance on work-related stress44 and the indicator tool. 31 In module 4 each of the six risk factors is introduced and dealt with in terms of manager competencies. Modules 5 and 6 each take the HSE five-step approach [educate to understand the causes of stress, identify the problems, determine ways to improve, record (devise an action plan), take action and review]. In module 5 proactive solutions are suggested including increasing control and social support. The structure of the modules is described in Table 1.
| Title and content | Additional activities for managers to apply to their current work situation | Duration of e-learning module alone (without activities) |
|---|---|---|
| Introduction and benchmarking quiz This module explains how the program is structured. It introduces each module and how to navigate the program. It shows how to access extra information and activities. It also looks at the obstacles to successfully tackling stress at work and explains the benefits of taking part. The introductory quiz is introduced as being for research purposes only |
None | 10 + 10 minutes |
| Module 1: Why tackle employee pressure at work? Health issues The physiological, psychological and behavioural symptoms of stress, how they can affect an employee’s health and well-being and how to spot them; how to more effectively motivate employees |
Activity on motivation | 30 minutes |
| Module 2: Why tackle employee pressure at work? Economic issues The economic reasons why organisations need to address pressure at work |
None | 10 minutes |
| Module 3: Why tackle employee pressure at work? Legal issues The legal reasons why organisations need to address pressure at work and the legislation most commonly associated with this |
None | 10 minutes |
| Module 4: What can a manager do? A management competency topic What managers can do to reduce pressure for employees, the causes of pressure at work and how general management skills and behaviour can reduce pressure at work |
Management styles and behaviours including suggestions for working with teams and colleagues | 20 minutes; additional time to work with teams and colleagues |
| Module 5: Being proactive – helping your team How to identify problems common to a team, how to work with the team to make improvements and how to make an action plan for these improvements |
Developing an action plan | 10 minutes |
| Module 6: Being proactive – helping individuals Why it is important to be aware of an individual’s concerns at work, how to identify problems that employees might be experiencing and how to work with individuals to find solutions to problems at work and stressful situations that require managers to take action |
Interactive case study | 30 minutes; additional time to work with the team and produce an action plan (will vary) |
| Final quiz and confirmation of successful completion 15 randomised questions to check participants’ understanding |
None | 10 minutes |
For the purposes of defining the content and the amount of engagement that managers would show with the e-learning program, modules 1–6 were defined as the ‘main’ learning modules of the program.
The content of the e-learning program Managing Employee Pressure at Work is proprietary to APP and not publicly accessible. The content of the e-learning program was reviewed by the research team before the start of the intervention. The e-learning program was adopted for use in the study without any changes, with the exception of the quiz. The standard e-learning program contains a quiz only at the end of the program, consisting of 10 questions randomised from a bank of 40 questions. To make the assessment more demanding and to allow for an assessment of managers’ knowledge gained from the intervention, the questionnaire was extended to 15 questions from a bank of 75 questions, with additional questions based around the HSE management standards, and duplicated, so that participants would also complete an introductory quiz against which to benchmark their scores on the final quiz.
Duration and schedule of the intervention
The intervention was presented over a 3-month period. The same intervention, including the same e-learning package, was used for all managers in those clusters randomised to the intervention. Having provided written informed consent, the recruited managers were sent a welcome e-mail and invited to take part in an induction session.
The intervention started with the face-to-face induction session conducted by the study facilitator. Three separate induction sessions were held, one for each of the three clusters of managers randomised to the intervention, in separate geographical locations within the participating organisation, at a date convenient for the participating managers. The induction sessions lasted between 90 and 120 minutes. The principal aim of the induction session was to engage the managers in the program by motivating them to take part in the training, by initiating an exchange among their peers on the topic of stress and stress management and by introducing them to the content and technical aspects of the e-learning program. A detailed programme of these sessions is given in Appendix 3. Managers unable to attend the induction session were sent an introductory handout by the trial manager and were contacted by telephone by the study facilitator to brief them on the program, offer support and answer any questions. Attendance at facilitated sessions was documented by circulating an attendance register.
The e-learning program was then applied in weekly to fortnightly instalments:
-
weeks 1 and 2: completion of the introduction and benchmarking quiz after attendance at the induction meeting
-
week 3: completion of modules 1–3
-
week 4: catch-up week, time to carry out motivational activity contained in module 1
-
week 5: completion of module 4
-
week 6: catch-up week, time to carry out activity on management competency contained in module 4
-
week 7: completion of module 5
-
week 8: catch-up week, time to carry out group activity contained in module 5
-
week 9: follow-up face-to-face meeting with the facilitator
-
week 10: completion of module 6 and final quiz
-
week 11: catch-up week.
Participants were provided with a suggested timeline to follow when working through the program (see Appendix 3). During weeks 1 and 2, only the introductory module and the benchmarking quiz were accessible online, to prevent participants from accessing the main content modules before completing the initial benchmarking quiz. From week 3 onwards, all of the remaining modules were made available online and participants were essentially free to complete the program at their own pace, that is they could also complete the remaining modules in one session if they wished. It was, however, stressed that the activities should take place in adherence to the timeline so that they would be able to receive support and have the opportunity to discuss their experiences with the facilitator and at the follow-up meeting.
A second face-to-face session took place with the facilitator after the scheduled completion of module 5. Again, three sessions were held, one for each of the clusters randomised to the intervention. The aim of this follow-up session was to provide an opportunity for managers to discuss their learning, give feedback on the program and discuss their experience with the activities contained within the modules.
After completion of the e-learning program, participants were provided with a certificate of completion. A generic, electronic e-learning certificate automatically became available at the end of the final online quiz module if participants answered at least 10 out of 15 questions correctly. The quiz could be retaken an unlimited number of times. At the end of the study we provided a tailored, Guided E-learning for Managers (GEM) study-specific certificate in paper format to all participants who had completed all of the main e-learning modules, based on the final full uptake data report.
The e-learning program remained accessible to all participating managers until the end of the follow-up period (i.e. for an additional 3 months during which follow-up sickness absence data were collected and while employees completed the follow-up questionnaire), allowing managers to revisit any topics should they wish.
Completion of the e-learning program itself was expected to take around 2.5 hours without any interruptions. Including the completion of the embedded activities, it was expected to take around 4 hours, although more time could be spent on the activities if desired. Finally, adding attendance at the face-to-face sessions with the facilitator, the entire guided e-learning intervention would be expected to take between 7 and 8 hours.
Delivery of the intervention
The guidance for the intervention was provided by a study facilitator recruited especially for this project, a consultant and trainer in organisational health with experience in stress management and the provision of corporate training. The facilitator received 2 days of training from the developer of the e-learning program, a chartered psychologist with 18 years’ experience of working with organisations. The content of this training is summarised in Appendix 3.
The face-to-face induction and follow-up sessions were held on site, at facilities provided by the participating organisation. They were led by the facilitator and attended by the participating managers as well as the qualitative researcher. Care was taken to create an environment in which managers could discuss issues around work and stress freely and confidentiality.
The e-learning program was hosted by DeltaNet International Ltd (Loughborough, UK), who provided unique log-in usernames and temporary passwords for each participating manager. The trial manager sent an e-mail to each individual manager containing a link to the online log-in page for the program, together with log-in information. Managers were required to change their password at their first log-in. They were then free to access the program as many times as desired, from any location and web browser that supported the Adobe Flash plug-in and had JavaScript enabled. The program included a reminder function for any participants who might have forgotten their password and the trial manager was available by telephone and e-mail in case of any technical issues. Each learner’s personal e-learning program home page offered an overview and short description of the different modules and displayed the status of completion for each module, to allow participants to track their progress. Each individual module opened in a pop-up window.
Tailoring of the intervention
The e-learning program and the two face-to-face sessions form the core of the intervention. Additionally, guidance and support from the facilitator was adapted to the participants based on their needs, whether they were able to attend the face-to-face sessions and whether they could be reached for a follow-up telephone conversation. The facilitator would offer support to managers by telephone and/or e-mail to discuss any issues that came up and would attempt to contact managers who had fallen behind on their e-learning schedule. All participants received fortnightly e-mail prompts from the trial manager to complete modules when they became due; non-responders received additional weekly e-mail reminders to complete any overdue modules.
Lastly, we planned that the intervention should be embedded within the participating organisation’s existing policies on stress management. Participating managers therefore received information on existing internal sources of support for dealing with employee stress in the form of a handout entitled Health and Well-being Support Available to Managers, including contact details for various internal support services such as occupational health and staff support and psychological well-being services.
Assessment of adherence
Use of the program was monitored to measure uptake of the intervention by managers. The system logged the number of times each participating manager accessed each module, the duration of access per module and the score on each attempt at both quiz modules. The system automatically logged out users after 30 minutes of inactivity. Weekly uptake reports provided by the e-learning host detailed the number of modules that were completed, not started or incomplete. A final report provided at the end of the intervention additionally detailed the number of times and the length of time that managers spent accessing each module and the scores for each attempt at the baseline and follow-up quiz. The system recorded and reported only the overall scores for the quiz modules for each participant; individual answers to the quiz were not stored, neither was any information entered by participants in any activities integrated within the main learning modules (e.g. text boxes inviting reflection).
Control group treatment
Managers in the cluster allocated to the control group were not recruited to the study and were not given any form of control intervention. They were informed by the local research team of their cluster allocation and asked not to reveal their allocation to their teams. Managers in the control group were offered access to the e-learning program at the end of the study after all follow-up data collection was complete; one control cluster manager took up this offer. This control group access to the e-learning program was not monitored or evaluated in terms of uptake, as this was not within the scope of the study.
Outcomes
The primary outcomes of this pilot study related to acceptability, feasibility and participation.
Adherence to the e-learning intervention
Manager adherence was defined in the protocol as the number of times that managers logged on to the e-learning program. Additionally, it emerged during the intervention that the protocol had not specified a minimum level of engagement to qualify as adherent for the purposes of measuring differing effects between employees whose managers did engage with the intervention and employees whose managers did not engage with the intervention. The number of times that a manager logged on to the program emerged as a poor measure of adherence or engagement, as non-adherent managers could log on without spending a meaningful amount of time with the program, whereas an actively engaged manager could log on once and complete the entire e-learning program in one sitting. Completing the modules contained within the program was a much more meaningful measure. Active engagement with or adherence to the intervention by managers was therefore operationally defined during data collection and before analysis and required managers to have completed at least 50% of the six main learning modules of the e-learning program.
Acceptability of the intervention to managers
The acceptability of the intervention to managers was assessed by managers’ engagement with the intervention and their attitude to the intervention, assessed in individual interviews with managers and in the focus group.
Acceptability of the trial to managers and employees
We assessed the acceptability of the trial to managers and employees using individual interviews with managers and employees and a focus group with managers post intervention.
Feasibility of the trial
The feasibility of the trial was measured for employees and managers by participation and retention rates in the study and the ease of availability of sickness absence data at the cluster level and economic data at the individual level.
Participation of managers
For managers, participation was assessed as the percentage of managers who gave written informed consent to take part in the study, the percentage of participating managers who attended the induction session and the number of times that managers logged on to the program (see Adherence to the e-learning intervention).
Participation of employees
For employees, participation was measured by the giving of consent to take part in the study (presented as the percentage of employees who were approached) and response rates to the baseline and follow-up questionnaires (presented as the percentage of those consenting). Additionally, demographic details in terms of age band, sex and salary band were collected for employees who dropped out of the study between baseline and follow-up and these were compared with the demographic details for the overall trust workforce.
The following are the outcome measures of the main randomised trial, which we also piloted in this study; all employee outcomes were assessed at baseline (i.e. for a period of 3 months before the start of the intervention) and at follow-up (i.e. for a period of 3 months, starting 1 month after completion of the intervention).
Managers’ knowledge gained from the program
This was assessed by comparing scores achieved by managers in the e-learning quiz at the beginning and at the end of the intervention. The quiz was based on a bank of 75 multiple choice questions, out of which 15 questions were randomly selected for each quiz selection. Scores were presented as percentages.
Employee well-being
Pre–post changes in levels of well-being were assessed using the Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS),45 a brief 14-item scale assessing aspects of positive mental health, including both hedonic and eudaimonic perspectives. The score ranges from 14 to 70 with 70 representing perfect well-being. The WEMWBS score is presented as the mean [standard deviation (SD)] and the difference between baseline and follow-up comparing the intervention and control groups after adjusting for baseline. This is presented as an effect size with [95% confidence interval (CI)].
In this pilot study we estimated the SD of change in well-being over 3 months and the intracluster correlation coefficient (ICC) between the four clusters.
Sickness absence
Periods of sickness absence were requested for all employees who gave consent to the study, in an anonymised format, using the existing reporting system of the organisation recruited. Although it is not possible to link these individuals to their GEM study identification number, the number of individuals whose records were not found and hence who cannot be assumed not to be absent was reported back to the trial team.
The sickness absence data collected included the employee age group, sex, income band and dates of sickness absence. The sickness absence data were categorised as ‘short term’ (< 7 days), ‘medium term’ (7–21 days) or ‘long term’ (> 21 days). Sickness absence was calculated as the number of days absent between 1 May 2013 and 31 July 2013 for baseline and between 1 January 2014 and 31 March 2014 for follow-up. If an employee was sick over the weekend, the weekend days were included even though they may not have been working days lost. This was because employees worked for an NHS trust and many worked at weekends. Separate periods of sickness were added together to calculate the total number of days absent. Long-term sickness absence was defined as > 21 consecutive days within the data collection period. Employees with long-term absence were excluded from the overall analysis of sickness absence. Thus, some employees might have had the beginning or end of a long absence within the data collection period but not be coded as having a long-term absence.
Although we did not expect to see changes in sickness absence in this study, the pilot study allowed us to test the process of data collection.
Self-reported sickness absence
In addition to the sickness absence reported from the organisational reporting systems, we also asked employees in the employee questionnaire to report the number of days taken off sick, including weekends, over the previous 3 months. We did not ask about individual periods of sickness absence and so omitted anyone who had been sick for > 21 days in total from the self-reported sickness absence analysis.
Psychological distress
Psychological distress was measured using the 12-item General Health Questionnaire (GHQ-12). 46 The GHQ-12 score is reported as a mean and percentage above 3, the threshold used to identify mental health problems.
Because of error, the wrong item responses were reproduced for question 12 (happiness) on the baseline questionnaire, with ‘not at all’/‘no more than usual’/‘rather more than usual’/‘much more than usual’ presented to the employees instead of ‘more so than usual’/‘about the same as usual’/‘less so than usual’/‘much less than usual’. For the main analysis the first 11 items were used and multiplied by 12/11 for both baseline and follow-up time points. Thus, the same method was used at both time points. Appendix 2 compares the GHQ-12 scoring based on 11 items with that based on 12 items and that based on 11 items with the 12th item classified as ‘missing’.
Psychosocial work characteristics
Psychosocial work characteristics were measured using the standardised assessment tools within the employee questionnaire based on the job strain model (control and demands),22 work social support47 and effort–reward imbalance48 using abbreviated versions for epidemiological studies. 49 Questionnaire items relating to these outcomes are reproduced in Appendix 1.
Job strain is defined as the combination of high psychological demands and low decision latitude. The GEM questionnaire has been designed to capture information on the following work characteristic dimensions: work demands, skill discretion, decision authority and social support. Decision latitude is derived as the sum of decision authority and skill discretion. Job strain is the decision latitude score subtracted from the work demand score. All items have been presented on a scale from 0 to 100, with 100 representing high support for support-related scales and high demand for demand-related scales. Job strain is measured on a scale from –100 to 100, with 100 representing highly demanding roles with low levels of autonomy and –100 representing highly autonomous jobs with low demand.
A modified version of the effort–reward ratio was computed for each employee according to the formula e/(r × c), where e is the sum score of the effort scale, r is the sum score of the reward scale (with reversed polarity, which means that low scores indicate high distress resulting from a lack of recognition) and c defines a correction factor for different numbers of items in the nominator and denominator. Effort uses the same items as work demand and reward uses the same items as supervisor relationship but both are scaled from 1 to 100 to avoid dividing by zero. The correction factor was set to 1 as both effort and reward are measured on the same scale from 1 to 100. As a result, a value close to zero indicates a favourable condition (relatively low effort, relatively high reward), whereas values > 1 indicate an effort–reward imbalance.
We also assessed additional work characteristics such as work conflict, change at work, supervisor relationships (five items from the Chartered Institute of Personnel and Development Employee Outlook surveys scored on a 5-point Likert scale from ‘strongly agree’ to ‘strongly disagree’), supervisor support (two items), job insecurity, clarity of information (with two items on sufficient and consistent information from supervisors) and stressfulness. All items except stressfulness are presented on a scale from 0 to 100, with job stressfulness presented on a scale from 0 to 10. For all scales mean scores are presented.
Additionally, we also assessed employee health behaviours (smoking and alcohol consumption) and social support outside work. Problems with drinking alcohol were assessed using the four-item CAGE (Cut down, Annoyed, Guilty, Eye-opener) instrument. 50 Participants who responded positively to two or more items were classified as having an alcohol problem. Perceived social support was assessed using four items (‘people who make me feel happy’/‘people who make me feel loved’/‘people who can be relied on’/‘people who give support’) out of the seven items used in the Health Survey for England. 51 Those responding positively to all items were classified as having perceived social support.
Safety considerations
The pilot study allowed us to study any risks of the intervention. Given the nature of the intervention and the absence of any routine clinical assessments or reporting procedures as part of this study, there was no systematic documentation of adverse events or adverse effects.
Potentially, we thought that managers could misinterpret the program and adopt maladaptive management strategies. However, the intervention was laid out in such a way that it was easy to comprehend, was organisationally supported and was sanctioned as being part of the HR and professional development strategies. Potentially, some managers could have become distressed by recognising that their previous management practices had not been ideal or that new techniques may be more time-consuming, requiring them to relinquish some control or be involved in more teamwork. We organised an e-mail or telephone-based discussion option for managers to discuss with the study facilitator any issues that arose with the program. The facilitator was asked to report any harms identified to the study team. Negative experiences by managers during the guided e-learning intervention, and by employees as a consequence of their manager’s participation, could be documented qualitatively in a sample of in-depth interviews.
The questionnaires for well-being (WEMWBS) and psychological distress (GHQ-12) are too non-specific to identify clinically significant distress reliably within individual distress. In case psychological distress was reported directly to the research team, protocol guidelines were in place to guide participants to relevant sources of support. Any such direct reports would be reported anonymously for the purposes of the safety evaluation of the study.
Sample size
The study was designed to recruit 120 employees from four clusters, expecting that 100 employees per cluster would consent. The response rate was estimated to within 3.8 percentage points, for example 76.1% to 83.9%. Measurements of intervention acceptability could be estimated from those managers who consented to the intervention, expected to be 40 individuals. If the take-up was 80% the 95% CI would be 64% to 91%. We envisaged recruiting 30–40 managers, each responsible for 5–20 employees. The pilot study was designed to provide evidence for the basic assumptions in our sample size calculations, to strengthen our calculations for the main study. From earlier literature on well-being measures52 the ICC was expected to have a value of about 0.07. Eldridge and Kerry53 showed that ICC estimates from small studies are dependent on the number of individuals and therefore four clusters provide a reasonable estimate. In this pilot study we estimated the likely effect size with its 95% CIs.
Randomisation
Three clusters, rather than individual participants, were randomly allocated to the intervention group and one cluster was randomised to the control group. This was to fit the aims of the trial, which were to test the recruitment process and obtain information about the implementation of the intervention. All managers within a specific intervention cluster were provided with the same intervention. One simple randomisation step was undertaken by an independent statistician. Randomisation of clusters was scheduled to take place after employees had been recruited and before recruitment of the corresponding managers, as only managers in clusters randomised to the intervention would be actively involved in the study.
Blinding
Employees were blinded to whether or not their managers had been randomised to the intervention or the control group. Managers in both groups were asked not to reveal their allocation to their teams.
As managers in the three intervention clusters only were recruited into the study, and as allocation to the intervention or the control group was self-evident, participating managers could not be blinded to their allocation. Likewise, the study facilitator and qualitative researcher were aware of the allocations.
As this was a cluster randomised study and no medical intervention was applied that would require emergency treatment, unblinding procedures were not applicable. Participants were informed of their allocation at the end of the study.
Members of the research team were kept blinded with regard to identification of the intervention and control group clusters and were unblinded only on a need-to-know basis. Members of the local team responsible for the recruitment of employees were not told of the allocation until the end of recruitment. Researchers performing analyses on the quantitative and economic data were blinded to the allocation until the main analyses had been performed.
On recruitment, each participant was allocated with a three-digit unique study identification number. These numbers were predefined and allocated in groups to one of the four clusters. This allowed for participants to be allocated to the correct clusters without identifying the cluster.
Statistical methods
The analyses were carried out using Stata version 12 (StataCorp LP, College Station, TX, USA). Pilot study analyses were descriptive and no formal statistical analyses were conducted to determine the effectiveness of the intervention,54 although CIs are presented. Participation rates are presented for each cluster and overall and 95% CIs for rates have been presented without adjustment for clustering. Effectiveness comparing the intervention and control clusters was estimated using a random-effects model with restricted maximum likelihood estimation. As the random-effects model assumes a large sample for the number of clusters, the CIs were calculated using the standard error from the model and the t-distribution with 2 degrees of freedom instead of the normal distribution. Post-hoc analyses were carried out to assess changes in well-being scores for employees of managers who did or did not engage with the intervention, as well as for employees of managers who changed position during the course of the study. This analysis used a random-effects model but did not adjust for the small number of clusters as the comparison was within rather than between clusters.
The same method was used to assess sickness absence but only employees who did not have an episode of sickness absence > 21 days were included.
Qualitative methods
Interviews with key informants
An aim of the qualitative study was to describe the policy and organisational context within which the overall study took place and the thinking behind the study and intervention. To address this, the qualitative study began by identifying ‘key informants’ for in-depth interview. We interviewed members of the study team and scientific steering committee, senior managers at the NHS trust and those involved with the development and implementation of the guided e-learning intervention. We followed up suggestions from these informants of additional key informants (e.g. other researchers in the field of work stress and well-being). We undertook 14 in-depth key informant interviews, using the topic guide in Appendix 4 as a basis for discussion. We were particularly interested in exploring what key informants identified as critical topics and questions for the study to ask managers and employees. We also asked informants to identify relevant literature, both published and ‘grey literature’. Most interviews were conducted face to face; when this was difficult to arrange (three cases) the interview took place by telephone. Ten of the 14 interviews were audio recorded and transcribed; in the others the qualitative researcher took extensive notes.
Interviews with managers
A key aim of the qualitative study was to explore managers’ views about the study and their experience of the guided e-learning intervention and of managing stress in the workplace. We adopted a narrative approach to interviewing,55 meaning that interview questions encouraged respondents to recount stories of specific (anonymised) cases and incidents, as a way of eliciting a rich and reflective account of the complexities of managing stress at work. A narrative methodology focuses on concrete and situated practice, rather than on abstract perspectives, as is typical of other interview methods. We asked managers to talk through a specific case in which an employee who they line managed had experienced stress and how they had managed that particular case. We took a similar narrative approach to asking questions about the managers’ experience of studying the guided e-learning intervention. The interview schedule is reproduced in Appendix 4.
We adopted a purposive approach to sampling managers for interview to ensure a heterogeneous sample, including men and women from across the intervention and control group clusters. In total, 21 managers (out of the 41 in the intervention clusters who had consented to participate in the GEM study) were approached for interview and of these 11 agreed (the remaining 10 did not respond to the e-mail invitation or a reminder), giving a response rate of 52% among managers in the intervention groups. Eight managers from the control cluster were invited to interview and two agreed (five did not respond to the e-mail and one replied that she no longer held a managerial position). Thus, we undertook a total of 13 in-depth interviews with managers (10 women and three men, which reflects the female–male ratio among the managers participating in the trial).
In total, 10 of the 11 managers interviewed from the intervention groups were defined by the trial as ‘adherent’ (i.e. had completed three or more of the main e-learning modules of the intervention). A limitation of the qualitative sample was therefore that it included only one manager from the ‘non-adherent’ group of managers. Furthermore, as consent had not been gained for this purpose, we were unable to approach managers in the trust who did not participate in the GEM study, although their views would have been of interest.
Manager interviews took place between March and May 2014 (≥ 2 months after they had participated in the guided e-learning intervention) and lasted between 17 and 38 minutes. All interviews were audio recorded, transcribed and anonymised.
Interviews with employees
An aim of the qualitative study was to build a picture of how employees conceptualised and experienced stress and well-being at work and their perceptions of their managers’ role in managing stress. The aim was that these qualitative data would help with interpreting the quantitative findings of the trial.
As with managers, we adopted a purposive approach to sampling employees for interview. To avoid possible influence on employees’ questionnaire responses, we approached employees for interview after they had completed their follow-up questionnaire. In total, 36 employees from across the four clusters in the study were invited for interview (from the sample of 163 employees who had completed their follow-up questionnaire by this time). Ten employees responded (a low response rate of 28%) but we were unable to fix interviews with two of these employees and subsequently undertook a total of eight employee interviews (six women and two men, again reflecting the male–female ratio in the trial employee sample). The sample consisted of two employees from each of the four clusters.
Interviews took place in March and April 2014. As with the manager interviews, we drew on a narrative methodology to elicit employee stories of specific instances of stress at work. Interviews lasted between 10 and 27 minutes. The interview schedule is reproduced in Appendix 4.
Additional data from employees
The baseline and follow-up questionnaires for employees included a free-text box in which employees were invited to make additional comments at the end of the questionnaire. In total, 59 employees out of the 350 who completed the baseline questionnaire provided additional comments and 56 out of the 291 who completed the follow-up questionnaire gave additional comments.
The original study proposal included a suggestion to conduct focus groups with employees. However, given the relatively low response rate to our request for individual interviews with employees, and the rich data that we collected from those who did agree to interview, a decision was taken to not collect focus group data. In total, 12 employees attended the study dissemination meetings (see following section) and contributed to the group discussions at these events.
Observation of study meetings for managers
Meetings between managers involved in the study provided an opportunity to collect observational data. The qualitative researchers and/or study facilitator took field notes, written up in full after the meetings. We observed 10 meetings:
-
A preliminary meeting at the trust in April 2013 to launch the study in the trust and introduce the study and intervention to managers, attended by approximately 20 managers.
-
Three facilitator-led induction meetings for managers in October 2013 to introduce the intervention (see Appendix 3 for details). A total of 26 managers attended these meetings. The meetings constituted the first of two face-to-face ‘educational sessions’ with a facilitator and as such were part of the ‘guided’ component of the guided e-learning intervention.
-
Three ‘follow-up’ facilitator-led meetings in December 2013. These meetings formed the second of the face-to-face educational sessions with the facilitator.
-
A ‘feedback’ meeting for managers in April 2014. This meeting was convened specifically as a qualitative focus group discussion and was audio recorded and transcribed. All interviewed managers from the intervention groups were invited, of whom six (out of 11) accepted and three (one from each of the intervention clusters) attended on the day. The qualitative researcher gave a short presentation of the preliminary interview findings and managers were then invited to comment on the validity of the research interpretations and to reflect as a group on their participation in the study. The trial manager and qualitative researcher facilitated the group discussion.
-
Two study dissemination meetings were held in September 2014 to disseminate the overall study findings to trust staff. Three managers and three employees attended one meeting and one manager and nine employees attended the other. In addition, the meetings were attended by trust staff who had helped manage the research and by the e-learning program developer.
Observation of steering committee and study team meetings
The qualitative researchers acted as participant observers at the two steering committee meetings held during the course of the study and the monthly study team meetings. Research notes, minutes of meetings and associated documentation were considered data sources for qualitative analysis. We were particularly interested in documenting and exploring how the relationship between the quantitative and the qualitative components of the study unfolded in practice and how the qualitative data were perceived as adding value to the trial (or not). Our findings on this aspect of the study will be reported in a separate paper.
Qualitative analysis
Data analysis took place concurrently with data collection, enabling progressive focusing on emerging themes. Two qualitative researchers were engaged in close readings of the transcripts of interviews and meetings, observational field notes and associated documentation. We individually and collectively identified themes emerging from the data, both within subsets of the data (i.e. themes emerging from key informant interviews, from manager interviews and from employee interviews) and across the data set. We discussed our preliminary findings with members of the study team, individually and at team meetings, and with the steering committee and drew on these discussions to interrogate our data further and develop our in-depth analysis.
In keeping with the narrative approach to interviewing, we drew on a narrative approach to analysis of the interview data. This meant that we paid particular attention to the story as a whole that respondents told rather than simply focusing on segments of text. The aim was that this approach would generate a rich picture of the subjective and situated experiences of workplace stress and the guided e-learning intervention.
Dissemination of the results
As part of this pilot study it was planned to disseminate our findings specifically among the study participants, as promised to them, to receive additional feedback. We designed a printed newsletter that was supplied to all participants and conducted two local feedback meetings for study participants at which we presented and discussed our findings. We have also presented the results at the following conferences: a Public Health England-sponsored conference on Work, Health and Wellbeing in Manchester (10 November 2014); the UK National Work-Stress Network annual conference in Birmingham (22–23 November 2014); and the European Association of Work and Organisational Psychology Conference held in Oslo, Norway (20–23 May 2015). Some parts of the GEM study were also presented at an ISER seminar at the University of Essex on 19 January 2015. Our website has been updated and will refer to published GEM study results in the future [see www.gemstudy.net (accessed 3 June 2015)]. Three papers are also in preparation: a mixed-methods paper reporting the results of the pilot study led by Stephen Stansfeld, which has been submitted for publication; a review paper of e-learning approaches in work stress management led by Tarani Chandola, targeted at an occupational medicine audience; and a mixed-methods paper with a qualitative focus co-led by Jill Russell and Lee Berney, aimed at a social science audience.
Chapter 3 Trial results
Participant flow
Inclusion of clusters
We recruited the clusters and participants from a mental health NHS trust in the north of England (participating organisation). The flow of clusters and participants is represented in Figure 2.
FIGURE 2.
Participant flow diagram.
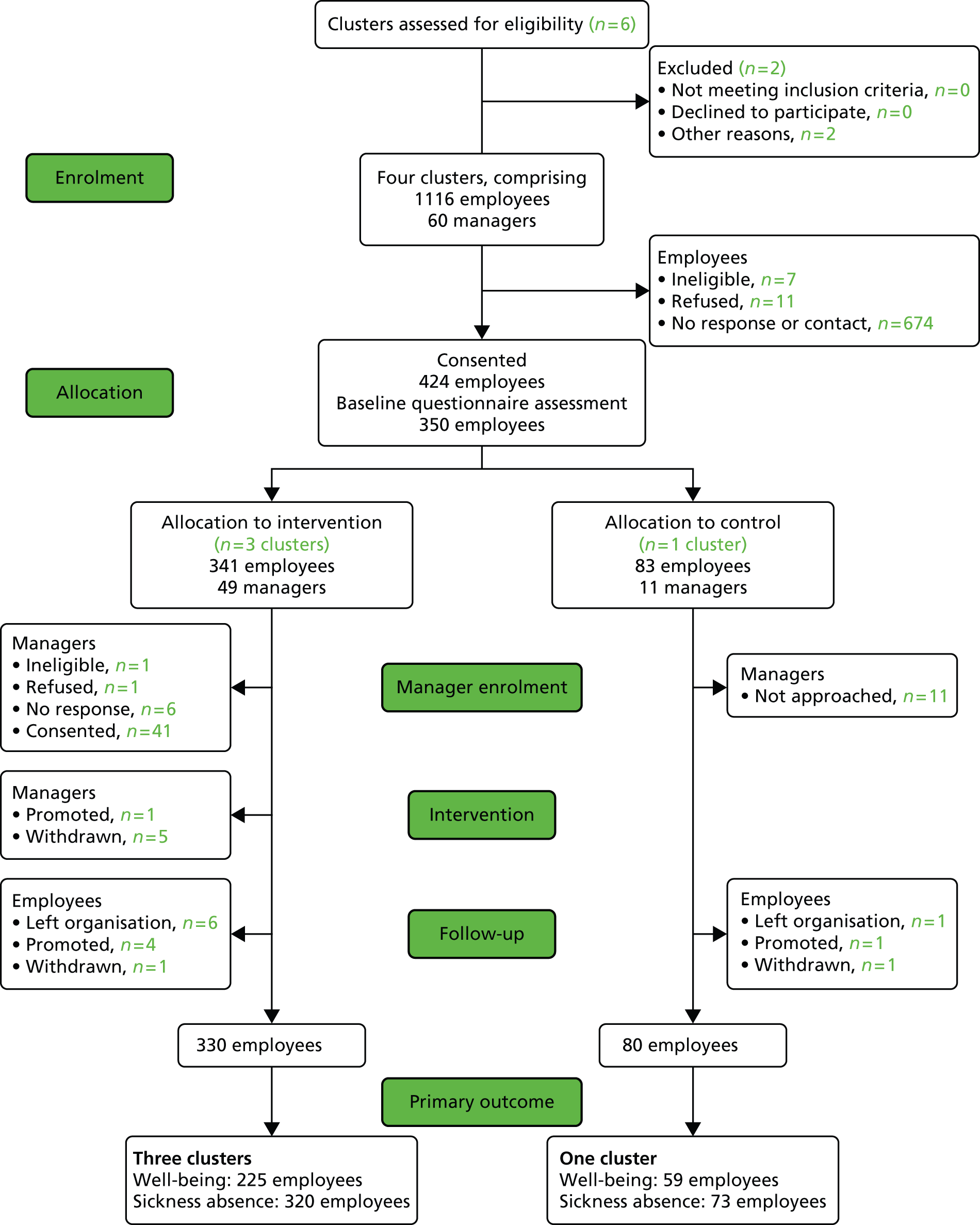
Six clusters from within this organisation were considered for inclusion in the trial. In one cluster the workforce composition and organisational structure was considered too different for comparison with other clusters. Another cluster had insufficient availability of employment data. These two clusters are marked as not included for ‘other reasons’ in Figure 2.
The four selected clusters that took part in the study consisted of three adult mental health services working in separate geographical areas of the participating trust and the teams caring for adults with learning disabilities within the same trust. There were between 199 and 330 employees reported to be working in each cluster who were targeted for participation in the study (Table 2). It should be noted that the total number of targeted employees (n = 1116) is based on estimates given at the local sites on enquiry by the recruiting staff and is higher than the number of staff expected based on figures indicated by local stakeholders when we selected the organisation (n = 650). These employees were managed by between 11 and 19 managers per cluster (Table 3 and see Figure 2).
| Details of employees | Cluster 1 | Cluster 2 | Cluster 3 | All intervention clusters | Cluster 4 | Total |
|---|---|---|---|---|---|---|
| No. of employees invited (no. of employees approached personally by recruiting staff) | 323 (142) | 264 (174) | 330 (204) | 917 (520) | 199 (129) | 1116 (649) |
| Ineligible | 0 | 1 | 5 | 6 | 1 | 7 |
| Refused | 2 | 7 | 1 | 10 | 1 | 11 |
| Consented (% of those approached) | 100 (70) | 126 (72) | 115 (56) | 341 (66) | 83 (64) | 424 (65) |
| Baseline questionnaire (% of those consented) | 89 (89) | 101 (80) | 93 (81) | 283 (83) | 67 (81) | 350 (83) |
| Paper based | 21 (19 + 2a) | 14 (13 + 1a) | 28 (27 + 1a) | 63 (59 + 4a) | 10 | 73 (69 + 4a) |
| Online | 68 | 87 | 65 | 220 | 57 | 277 |
| Follow-up questionnaire (% of those consented) | 77 (77) | 86 (68) | 68 (59) | 231 (68) | 60 (72) | 291 (69) |
| Paper based | 20 | 27 | 22 | 69 | 10 | 79 |
| Online | 57 | 59 | 46 | 162 | 50 | 212 |
| Primary outcome analysis (% of those consented) | 74 (74) | 85 (67) | 66 (57) | 225 (66) | 59 (71) | 284 (67) |
| Sickness absence data (% of those consented) | 93 (93) | 120 (95) | 107 (93) | 320 (94) | 73 (88) | 393 (93) |
| Details of managers | Cluster 1 | Cluster 2 | Cluster 3a | All intervention clusters |
|---|---|---|---|---|
| Managers invited | 19 | 17 | 13 | 49 |
| Ineligible | 1 | 0 | 0 | 1 |
| Refused | 1 | 0 | 0 | 1 |
| Consented (% of those invited) | 12 (63) | 17 (100) | 12 (92) | 41 (84) |
| Consented but no employees in the study | 0 | 2 | 0 | 2 |
| Adherence to the intervention | ||||
| Completed fewer than three modules | 6 | 9 | 5 | 20 |
| Completed three or more modules | 6 | 8 | 7 | 21 |
| Primary outcome analysis: no. of employees whose managers | ||||
| Did not consent | 16 | 0 | 3 | 19 |
| Completed fewer than three modules | 20 | 38 | 28 | 86 |
| Completed three or more modules | 38 | 47 | 35 | 120 |
| Primary analysis: managers changing role during study | ||||
| No. of managers | 2 | 5 | 2 | 9 |
| No. of employees of these managers | 12 | 28 | 12 | 52 |
Inclusion of participants
Employees were recruited by the local research team (clinical study officers and research facilitators), who visited the various teams across the four clusters and attended local team meetings to introduce the study. Many of the teams were visited several times during recruitment to meet the targets. Teams were spread over a large geographical area, many employees were working off site and the meetings were never attended by all staff at any given visit, so not all employees could be contacted personally. The local research team reported contacting 649 employees (58%) during these visits. In total, 424 employees gave written informed consent to take part and baseline questionnaires were completed for 350 (83%). Of these questionnaires, 277 were completed online, 69 were completed on paper only and four were started online and completed on paper. At follow-up, 291 of the employees who had previously completed the questionnaire at baseline completed the follow-up questionnaire and 284 of these also completed the WEMWBS, the primary end point. Thus, 67% (95% CI 62% to 71%) of employees consenting provided primary outcome data at follow-up.
Baseline and follow-up sickness absence data were available for 393 employees (93%, 95% CI 90% to 95%). Data for 368 employees were available from the participating trust HR database and data for an additional 25 employees were available from three local council HR departments, as these were social services employees working within the trust. Reasons for non-availability of sickness absence data were participant withdrawal (as a result of consent withdrawal, leaving the organisation or promotion); staff on service-level agreement contracts, student contracts or other specific contracts with no centralised sickness absence records or records being kept elsewhere; no response from one local council; and administrative failure (records could not be located).
Of the 424 employees who gave consent to take part in the study, 14 were withdrawn from the study: seven left the organisation, five were promoted to manager level and thus were no longer included in employee data collection and two actively withdrew consent to participate during the follow-up data collection phase (one indicated that the questionnaire did not meet expectations and the other did not give a reason).
Of the 41 managers who gave consent to take part in the study, six withdrew during the intervention. One was promoted and no longer managed the employees included in the study (this manager was then replaced in the study by her successor) and five withdrew their consent for a variety of reasons (personal reasons n = 1, time constraints n = 3, no reason given n = 1). One of the managers who withdrew did so after engaging in the intervention sufficiently to qualify as adherent (completing three e-learning modules) and is therefore included in some of the analyses.
The different trust services recruited as clusters in this study went through different degrees of organisational change during the course of the study. Although no systematic, quantitative data were collected to document changes in roles, it emerged during data collection and in interactions with managers that nine managers changed position during the study (see Table 3): one was promoted before the start of the intervention and no longer managed staff on the study (this manager was thus not included in the primary analysis of employee outcomes); four had been newly appointed to their position at the start of the intervention (they had previously been recruited as employees to the study and then were promoted); four changed position and went on to manage different teams of employees within the same cluster; and one took on a different function (not otherwise specified) in the last month of the follow-up data collection period.
Recruitment and follow-up
After receipt of all necessary ethics permissions, the participating site was activated for recruitment on 1 June 2013 and recruitment of participants was initiated. The first participant gave written informed consent on 6 June 2013.
Baseline questionnaire data collection took place in parallel with employee recruitment. After registration employees were sent a link to complete an online questionnaire or were offered a paper questionnaire in case of non-response. The first questionnaire was completed on 28 June 2013. Baseline sickness absence data from the organisational HR systems were collected for the period from 1 May to 31 July 2013.
It was planned that recruitment and baseline data collection should proceed in the following phases:
-
June/July 2013 – recruitment of employees and completion of baseline questionnaires
-
end of July 2013 – randomisation of clusters
-
August 2013 – recruitment of managers from the three clusters randomised to the intervention arm.
By the end of July 2013, just over half of the targeted 400 employees had been recruited; however, randomisation of clusters and recruitment of managers could not be delayed for administrative reasons, as the intervention had to be scheduled within a specific time and deployed to all participating clusters at the same time. Recruitment of employees and completion of baseline questionnaires therefore continued after randomisation and the start of manager recruitment, but care was taken to keep employees and dedicated recruitment personnel blinded to the treatment allocation of the four clusters.
Randomisation of the clusters took place on 23 July 2013. Cluster 4 (the learning disabilities service) was randomly assigned to the control and clusters 1–3 (three regional adult mental health services) were assigned to the intervention. The first managers were recruited to the study on 26 July 2013 (date of informed consent).
The 424th and last employee was recruited to the study on 1 October 2013. The last baseline questionnaire was completed on 8 October 2013 and received on 9 October 2013. The 41st and last manager was recruited to the study on 17 October 2013. This late recruit was a newly appointed manager who replaced a previously recruited manager who had been promoted and was no longer managing employees in the study. Recruitment therefore ended on 17 October 2013.
The intervention began on 9 October 2013 with the first of three separate induction meetings for managers. The intervention officially ended on 20 December 2013 with the end of the scheduled e-learning timeline, although the e-learning program remained available for the managers in the intervention group until April 2014. Although according to the protocol the intervention should have lasted for 2–3 months, in practice the e-learning package was applied over 10 weeks after attending the initial face-to-face meeting and it remained available for participating managers to access for the entire follow-up period.
The follow-up data collection phase started on 1 January 2014. Sickness absence data from the organisational HR systems were collected for the period from 1 January to 31 March 2014. Paper follow-up questionnaires were sent to 73 employees who initially responded to the paper version of the baseline questionnaire on 13 January 2014; it was expected that this would improve the response rate as it was likely that employees would prefer to complete a paper questionnaire at follow-up if they had opted for this at baseline. E-mails requesting employees to complete the online questionnaire were sent on 29 January 2014 to the remaining 274 employees. Three employees were not sent a follow-up questionnaire as they had been promoted to manager status since their baseline questionnaire response and were therefore withdrawn from the study as employees. The last follow-up employee questionnaire was received on 10 April 2014. The end-of-study date was 28 April 2014, which was the date of the last in-depth interview conducted for the qualitative research.
Numbers analysed
Employees analysed
In total, 1116 employees worked in the four clusters of whom 649 attended recruitment meetings. Of these, 424 (i.e. 65%, 95% CI 62% to 69%) consented to take part, 341 in the three intervention group clusters and 83 in the control group cluster (see Table 2). Of those consenting to take part, 350 or 83% (95% CI 79% to 86%) completed a baseline questionnaire and 291 or 69% (95% CI 64% to 72%) also completed a follow-up questionnaire. The proportion consenting of those approached was lower in cluster 3. The proportion completing the baseline questionnaire was similar across all clusters at > 80%. The proportion completing the follow-up questionnaire was lower in cluster 3 than in the other clusters.
Complete well-being outcome data based on the WEMWBS for both baseline and follow-up were available from 284 employees overall (225 in the intervention group, 59 in the control group). Baseline and follow-up HR-reported sickness absence data were available for 393 employees overall (320 in the intervention group, 73 in the control group). For the sickness absence outcome, 93% (95% CI 90% to 95%) of employees’ data were thus available for analysis.
Managers analysed
In total, 60 managers were responsible for the employees across all four clusters included in the study. The three clusters randomised to the intervention arm included 49 managers, who were invited to take part in the study. The remaining 11 managers in the control group cluster were not invited to take part in the study; they were informed of their allocation by the local research team and offered access to the e-learning program after the end of follow-up data collection.
Of the 49 managers invited to take part in the study, 41 gave written informed consent (between 12 and 17 managers per cluster). Of the remaining eight managers, one was ineligible, one refused consent and the remaining six did not respond to the invitation during the recruitment period.
Although we aimed to recruit managers to match employees, not all employees in the intervention group had a manager allocated who also participated in the study. Overall, 19 employees included in the primary analyses did not have a manager who participated in the study; most of these (n = 16) were from cluster 1, where the largest number of potentially eligible managers did not give consent, with the remaining three from cluster 3.
Conversely, every manager recruited to the study was managing at least one employee in the study at inclusion. However, two of these managers in cluster 2 were classified as not having an employee allocated during the study for the purposes of the primary outcome analysis: one manager was promoted and was no longer managing employees on the study and one manager was jointly managing a number of employees with another manager but did not adhere to the e-learning program and thus, for the purposes of distinguishing between outcomes of employees with adherent and non-adherent managers, this manager could not be included in the analysis.
Table 3 also shows the numbers of managers who adhered to the intervention and the numbers of employees managed by these managers who also have well-being data available for both baseline and follow-up; a total of 120 employees in the three intervention clusters were included in the analysis of the primary outcome for the subgroup of managers who achieved adherence in the intervention.
Baseline data
The demographic characteristics of employees were broadly similar between the intervention group (three clusters) and the control group (Table 4). There was a greater proportion of women (85%) in the control group than in the intervention group (74%). There also tended to be more employees aged > 50 years in the intervention group (40%) than in the control group (31%). Similar proportions were married or cohabiting, had children or had responsibility for supporting a family member. A greater proportion in the intervention group (58%) than in the control group (45%) felt that their job interfered with their family life. More employees in the control group (25%) than in the intervention group (15%) were at band 7 or higher; however, similar proportions of employees were in charge of others.
| Characteristic | Control (n = 67), n (%) | Intervention (n = 283), n (%) | Total (n = 350), overall % (range of % or means within each cluster) |
|---|---|---|---|
| Female | 57 (85) | 209 (74) | 76 (60 to 85) |
| Age (years) | |||
| > 50 | 21 (31) | 112 (40) | 38 (31 to 47) |
| < 30 | 6 (9) | 21 (7) | – |
| 30–39 | 9 (13) | 52 (18) | – |
| 40–49 | 31 (46) | 98 (35) | – |
| 50–59 | 21 (31) | 102 (36) | – |
| > 60 | 0 (0) | 10 (4) | – |
| Married or cohabitinga | 49 (73) | 210 (74) | 74 (68 to 79) |
| Children | 32 (48) | 117 (41) | 43 (37 to 48) |
| Supporting a family memberb | 14 (21) | 60 (21) | 21 (16 to 28) |
| Reported that family life interferes with workb | 17 (26) | 80 (28) | 28 (26 to 30) |
| Reported that job interferes with family lifec,d | 30 (45) | 160 (58) | 54 (45 to 68) |
| Working part timeb | 17 (26) | 78 (28) | 27 (24 to 32) |
| No. of hours worked per week, mean (SD)e | 35.3 (8.7) | 36.6 (6.8) | 36.4 (35.3 to 36.9) |
| Employee band 7 or higherf,g | 17 (25) | 42 (15) | 17 (8 to 25) |
| In charge of othersh | 12 (18) | 48 (17) | 17 (16 to 18) |
Health at baseline was similar in employees from both the intervention clusters and the control cluster (Table 5) but the number of days of absence reported was higher in the control group than in the intervention group. It was notable that both clusters had a large proportion of employees who scored > 3 on the GHQ-12 (39% in the control group and 35% in the intervention group).
| Characteristic | Control (n = 67), n (%) | Intervention (n = 283), n (%) | Total (n = 350), overall % (range of % or means within each cluster) |
|---|---|---|---|
| Poor healtha | 11 (16) | 44 (16) | 16 (10 to 21) |
| Disability or limited activities | 10 (15) | 39 (14) | 14 (11 to 17) |
| Smokerb | 11 (16) | 60 (21) | 20 (16 to 30) |
| Problems with drinkingc | 8 (12) | 32 (12) | 11 (7 to 15) |
| Self-reported sickness absence in the past 3 monthsd,e | 14 (22) | 74 (26) | 25 (21 to 31) |
| No. of days of absence reported, mean (range)f | 2.7 (0 to 90) | 1.9 (0 to 70) | 2.0 (1.1 to 2.7) |
| WEMWBS score, mean (SD) | 50.4 (8.0) | 51.0 (8.3) | 50.8 (49.5 to 51.7) |
| GHQ-12 score, mean (SD)g,h | 3.0 (3.3) | 2.8 (3.4) | 2.8 (2.5 to 3.0) |
| GHQ-12 score of > 3h | 26 (39) | 98 (35) | 35 (31 to 41) |
| Perceived social support: some lacki | 13 (19) | 61 (22) | 21 (18 to 25) |
Table 6 shows the comparability of the intervention and control groups when those who did not complete a follow-up questionnaire were excluded.
| Characteristic/outcome | Control (n = 60), n (%) | Intervention (n = 231), n (%) |
|---|---|---|
| Female | 51 (85) | 172 (74) |
| Age > 50 years | 20 (33) | 93 (40) |
| Working part time | 15 (25) | 67 (29) |
| Employee band 7 or higher | 16 (27) | 38 (17) |
| Poor health | 11 (18) | 36 (16) |
| Disability or limited activities | 10 (17) | 34 (15) |
| Smoker | 8 (13) | 44 (19) |
| Problems with drinking | 8 (13) | 28 (12) |
| Self-reported sickness absence in the past 3 months | 14 (25) | 59 (26) |
| WEMWBS score at baseline, mean (SD) | 50.5 (7.9) | 50.8 (8.4) |
| GHQ-12 score at baseline, mean (SD) | 3.2 (3.4) | 2.8 (3.5) |
| GHQ-12 score of > 3 | 24 (40) | 82 (36) |
Baseline population demographics were comparable to trust-wide demographics. In total, 79% of trust staff are female and this was reflected in the GEM study participant population (76%). Similarly, 38% of GEM study employees were part-time workers, comparable to a trust-wide proportion of 40%, and 27% of the GEM study population was aged > 50 years compared with 35% of trust employees.
Outcomes and estimation
Trial feasibility
In summary, we were able to consent and recruit adequate numbers of employees to fulfil our sample size predictions at the start of the study. With 424 employees recruited, we slightly exceeded the target of 400 employees, although this corresponds to only 38% of employees reported to be working in the targeted clusters. In total, 84% of managers in the intervention group clusters consented to take part in the trial and we achieved a good matching of managers and their corresponding employees. However, the poor adherence of managers overall to the intervention casts doubt on the feasibility of a future trial as currently organised, unless effective measures can be identified to increase manager engagement (see Participation of managers and adherence to the e-learning program).
Economic data on the cost of the intervention and the cost of sickness absence were readily available (see Chapter 5). Data on health service use were present in the baseline and follow-up questionnaires and there was a high level of completeness of the health service data (see Table 22), although participants did not provide full data on medication use. As our sample of employees was largely a healthy population, it may not be profitable to pursue health cost data in a full trial using a similar population.
Central HR-reported sickness absence data were available for > 90% of employees, but it did require additional effort to access sickness absence data from the local authorities for employees in social services. This involved obtaining data from four local councils, only three of which were able to fulfil our requests.
With regard to retention in the study, very few employees actively withdrew consent (n = 2); an additional 12 employees were lost because of promotion or because they left the organisation. Additionally, there was some loss in terms of responses to the questionnaire, although 83% of employees who had given consent responded to the baseline questionnaire and 69% responded to the follow-up questionnaire. The characteristics of employees who completed the follow-up questionnaires and the characteristics of those who did not are provided in Table 7.
| Characteristic/outcome | Completed (n = 291), n (%) | Not completed (n = 59), n (%) | p-value |
|---|---|---|---|
| Female | 223 (77) | 43 (73) | 0.54 |
| Age > 50 years | 113 (39) | 20 (34) | 0.48 |
| Working part time | 82 (28) | 13 (22) | 0.35 |
| Employee band 7 or higher | 56 (19) | 4 (7) | 0.025 |
| Poor health | 47 (16) | 8 (14) | 0.62 |
| Disability or limited activities | 44 (15) | 5 (8) | 0.18 |
| Smoker | 52 (18) | 19 (32) | 0.014 |
| Problems with drinking | 36 (13) | 4 (7) | 0.25 |
| Self-reported sickness absence in the past 3 months | 73 (26) | 14 (25) | 0.89 |
| Well-being score at baseline, mean (SD) | 50.8 (8.3) | 50.8 (7.1) | 0.96 |
| GHQ-12 score at baseline, mean (SD) | 2.9 (3.5) | 2.4 (3.0) | 0.29 |
| GHQ-12 score of > 3 | 106 (37) | 18 (31) | 0.33 |
There was very little difference in the baseline characteristics of employees between those who completed the follow-up questionnaire and those who did not complete the follow-up questionnaire, but completers were statistically significantly more likely to be in job band 7 or above (19% vs. 7%; p < 0.025) and statistically significantly less likely to smoke (18% vs. 32%; p < 0.014).
The retention of managers was more difficult. Five managers out of 41 recruited withdrew consent during the intervention, most because of time constraints, and one manager was lost as a result of being promoted. In addition, a significant number of managers did not adhere sufficiently to the e-learning program (see following section).
Participation of managers and adherence to the e-learning program
Of the 49 managers working in the intervention group clusters, 41 (84%) gave consent to take part in the trial.
Twenty-six managers (63.4%) attended the introductory meeting for the e-learning program and 18 managers (43.9%) attended the follow-up meeting after module 5 (Table 8).
| Intervention component | Managers consented (n = 41) | |
|---|---|---|
| n (%) | Mean (SD) | |
| Attended the introduction meeting | 26 (63.4) | |
| Completed the initial quiz; time (minutes) spent logged on | 31 | 21.0 (40.7) |
| Completed the introductory module; time (minutes) spent logged on | 26a | 8.7 (11.0) |
| Completed module 1; time (minutes) spent logged on | 24b | 23.2 (24.1) |
| Completed module 2; time (minutes) spent logged on | 22 | 7.3 (6.0) |
| Completed module 3; time (minutes) spent logged on | 21 | 11.9 (9.8) |
| Completed module 4; time (minutes) spent logged on | 19b | 20.1 (13.9) |
| Completed module 5; time (minutes) spent logged on | 19 | 14.9 (19.4) |
| Completed module 6; time (minutes) spent logged on | 17 | 27.4 (23.7) |
| Completed the final quiz | 15 | |
| Attended the meeting after module 5 | 18 (43.9) | |
| Quiz score (possible range 0 to 100) at introductionc | 20 | 61 (13) |
| Quiz score at introduction among managers who completed at least three modules | 14 | 60 (14) |
| Quiz score at the end of the program among managers who completed at least three modules | 15 | 74 (12) |
| Time (minutes) spent logged on to the program among those who completed at least three modules | 21 | 124 (62) |
| No. of times logged on: all intervention managersd | 41 | 5.6 (6.1) |
| No. of times logged on: managers who completed at least three modules | 21 | 10.5 (4.6) |
Managers who completed at least three modules of the intervention spent a mean of 124 minutes logged on to the e-learning program. However, managers who completed at least three modules spent only a mean of 13 minutes (range 5 to 34 minutes) on the initial quiz compared with 38 minutes (range 5 to 240 minutes) spent by those who did not complete at least three modules.
Of 41 managers, only 21 (51%) achieved the minimum requirement of having completed three of the main e-learning modules to qualify as ‘adherent’. We did not include participation in the activities recommended within the e-learning program as part of the definition of adherence. Table 8 details how many managers completed each module. Modules were completed in sequence by all participating managers, that is, no modules were skipped. The number of managers completing each module therefore gives a representation of the stages at which managers stopped logging into the program. It is notable that the highest number of managers dropped out before the introductory module.
Managers who fell behind on completing the e-learning program received e-mail reminders from the trial manager, which was followed up by telephone by the facilitator, who kept a record of contacts with managers. Lack of time was quoted as the principal reason for non-completion, which corresponds to findings from qualitative research. No manager quoted problems with the program content itself and none of the managers made use of the option to contact the facilitator by telephone or e-mail to discuss topics or issues arising from the program. Two managers quoted technical issues, which were quickly resolved.
The relatively low adherence of managers also meant that only 120 out of 225 intervention group employees who provided complete WEMWBS data for analysis had a manager who adhered to the intervention (see Table 10).
Managers’ knowledge gained from the program
Managers who completed at least three modules of the intervention had a mean quiz score of 60 at baseline, increasing to 74 at the end of the intervention, and spent a mean of 124 minutes logged on to the e-learning program (see Table 8). No individual manager had a reduced quiz score at follow-up compared with baseline. As only 15 managers completed the final quiz, there is limited quantitative information in these results, although there is a trend towards a knowledge gain. A baseline score of 60 increasing to 74 at the end of the intervention would validate the finding from the qualitative research that managers already had a high level of knowledge about stress management, as well as the finding that managers did find the program informative and that some aspects of the program were new to them (see Chapter 4).
As the format of the quiz was multiple choice it was also difficult to produce questions that really tested participant knowledge. It was sometimes possible to guess answers, even though an effort was made to make the questions as challenging as possible and questions were randomly selected for each participant so that they answered different questions in the initial and follow-up quizzes.
Well-being
There was a decline in well-being score as measured by the WEMWBS between baseline and follow-up in both the intervention clusters and the control cluster (Table 9). The mean score declined from 50.4 to 49.0 in the control cluster and from 51.0 to 49.9 in the intervention clusters. The overall intervention effect after adjusting for clustering and baseline values was very small, with a difference of 0.5 points between the intervention group and the control group in favour of the intervention (95% CI –3.2 to 4.2).
| Outcome | Group | n | Baseline, mean (SD) | Follow-up, mean (SD) | Difference between baseline and follow-up (95% CI) | Intervention effect adjusted for baseline and clustering (95% CI)a |
|---|---|---|---|---|---|---|
| Well-being score | Control | 59 | 50.4 (8.0) | 49.0 (8.5) | –1.4 (–2.8 to 0.0) | |
| Intervention | 225 | 51.0 (8.3) | 49.9 (8.3) | –1.1 (–1.9 to 0.2) | 0.5 (–3.2 to 3.7) (slightly favours intervention) | |
| Days off sick from HR datab | Control | 66 | 0.9 (2.0) | 1.0 (1.7) | 0.1 (–0.4 to 0.6) | |
| Intervention | 294 | 1.2 (3.2) | 1.6 (3.7) | 0.4 (–0.1 to 0.9) | 0.6 (–1.4 to 2.6) (slightly favours control) | |
| Days off sick self-reportb | Control | 51 | 1.2 (3.5) | 1.3 (3.8) | 0.1 (–0.8 to 0.9) | |
| Intervention | 198 | 1.0 (3.0) | 1.3 (3.4) | 0.3 (–0.3 to 0.9) | 0.1 (–2.2 to 2.4) |
In post-hoc analyses employees whose managers did not engage with the intervention, either through not consenting or through not completing at least three modules, had a worse mean WEMWBS score at baseline than those whose managers did engage with the intervention (49.8 vs. 52.0; difference 2.3, 95% CI 0.1 to 4.4) (Table 10). The fall in WEMWBS score was significantly less among employees whose managers adhered to the intervention than among those whose managers did not (–0.7 vs. –1.6; adjusted difference 1.6, 95% CI 0.1 to 3.2). Employees whose manager changed role during the study had a higher baseline mean WEMWBS score than employees whose manager did not change role (53.5% vs. 50.2%; difference –3.2, 95% CI –5.8 to –0.7). At follow-up, employees had a similar mean well-being score (49.9%) regardless of whether or not their manager changed role. The adjusted difference was –2.3 (95% CI –4.2 to –0.5), suggesting that employees whose manager changed role during the study had a larger fall in well-being than those whose managers did not change role.
| Outcome | Manager status | n | Baseline, mean (SD) | Follow-up, mean (SD) | Difference between baseline and follow-up (95% CI) | Adherence effect adjusted for baseline and clustering (95% CI) |
|---|---|---|---|---|---|---|
| Well-being score, mean (SD) | Manager adherent | 120 | 52.0 (8.6) | 51.4 (8.8) | –0.7 (–1.8 to 0.5) | |
| Manager not adherent | 105 | 49.8 (7.9) | 48.2 (7.5) | –1.6 (–2.8 to –0.3) | 1.6 (0.1 to 3.2) | |
| Well-being score, mean (SD) | Manager not changing role | 173 | 50.2 (8.5) | 49.9 (8.6) | –0.3 (–1.3 to 0.5) | |
| Manager changing role | 52 | 53.5 (7.3) | 49.9 (7.4) | –3.6 (–5.5 to –1.7) | –2.3 (–4.2 to –0.5) | |
| Days off sick self-report, mean (SD)a | Manager adherent | 107 | 0.7 (2.5) | 1.1 (3.1) | 0.4 (–0.4 to 1.1) | |
| Manager not adherent | 91 | 1.6 (3.8) | 1.4 (3.5) | 0.2 (–0.9 to 1.3) | –0.5 (–1.5 to 0.4) |
Self-reported sickness absence excluding long-term sickness absence
The mean number of self-reported days off sick was 1.2 in the control group at baseline and 1.0 in the intervention group. At follow-up, the mean number of self-reported days off sick was 1.3 in both groups (see Table 9). No evidence of any intervention effect was seen.
The mean number of self-reported days off sick at baseline was 0.7 among employees whose managers were adherent to the program and 1.6 among employees whose managers were not adherent to the program (see Table 10). The mean number of self-reported days off sick increased among employees whose managers were adherent but decreased among employees whose manager was not adherent, although the differences were very small.
Human resources-reported sickness absence excluding long-term sickness absence
An intervention effect of 0.6 (95% CI –1.4 to 2.6) in favour of the control group was observed for HR-reported sickness absence excluding long-term sickness absence. In total, 27% of employees from the control group and 30% from the intervention group were registered as taking sickness absence at baseline from the central HR database (Table 11). This increased to 37% and 35%, respectively, at follow-up (Table 12).
| Variable | Control (n = 73) n (%) | Intervention (n = 320), n (%) | Total (n = 393), overall % or mean (range of % or means within each cluster) |
|---|---|---|---|
| Employees recording absence | 20 (27) | 97 (30) | 30 (27 to 38) |
| Days of absence for all lengths of sickness absence, mean (SD) | 2.3 (7.4) | 2.4 (8.5) | 2.4 (2.2 to 2.5) |
| Employees with short-term absence only | 15 (21) | 70 (22) | 22 (20 to 25) |
| Employees with absence of 7–21 days | 3 (4) | 19 (6) | 6 (4 to 11) |
| Employees with absence of > 21 days | 2 (3) | 8 (3) | 3 (2 to 3) |
| Absence for psychological reasona | 2 (3) | 16 (5) | 5 (3 to 7) |
| No. of days absent for those taking any sick leave, mean (SD) | |||
| All (n = 20/97b) | 8.3 (12.6) | 7.9 (14.0) | |
| Among female employees (n = 15/79b) | 9.7 (14.3) | 7.0 (11.2) | |
| Among employees aged > 50 years (n = 4/32b) | 13.0 (20.0) | 9.6 (15.1) | |
| Among those in a high salary band (n = 12/50b) | 10.5 (15.9) | 8.7 (14.8) | |
| Variable | Control (n = 73), n (%) | Intervention (n = 320), n (%) | Total (n = 393), overall % or mean (range of % or means within each cluster) |
|---|---|---|---|
| Employees recording absence | 27 (37) | 114 (35) | 36 (28 to 44) |
| Days of absence for all lengths of sickness absence, mean (SD) | 4.6 (15.6) | 4.4 (13.4) | 4.4 (1.6 to 7.2) |
| Employees with short-term absence only | 20 (27) | 74 (23) | 24 (14 to 31) |
| Employees with absence of 7–21 days | 2 (3) | 22 (7) | 6 (3 to 8) |
| Employees with absence of > 21 days | 5 (7) | 18 (6) | 6 (1 to 9) |
| Absence for psychological reasona | 4 (5) | 19 (6) | 6 (5 to 8) |
| No. of days absent for those taking any sick leave, mean (SD) | |||
| All (n = 27/114b) | 12.1 (24.0) | 12.6 (20.1) | |
| Among female employees (n = 22/87b) | 14.0 (26.3) | 12.5 (20.4) | |
| Among employees aged > 50 years (n = 9/43b) | 2.4 (2.2) | 13.9 (19.5) | |
| Among those in a high salary band (n = 16/61b) | 7.9 (21.2) | 10.1 (17.3) | |
Psychological distress
Mean GHQ-12 score declined slightly in the control group between baseline and follow-up whereas it increased slightly in the intervention group between baseline and follow-up, although these differences were not statistically significant (Table 13). There was a small reduction in mean GHQ-12 score between baseline and follow-up among employees whose managers were adherent whereas there was a small increase in mean GHQ-12 score between baseline and follow-up among employees of managers who were not adherent (Table 14).
| Outcome | Group | n | Baseline, mean (SD) | Follow-up, mean (SD) | Difference between baseline and follow-up (95% CI) | Intervention effect adjusted for baseline and clustering (95% CI) |
|---|---|---|---|---|---|---|
| GHQ-12 score, mean (SD) | Control | 59 | 3.2 (3.4) | 2.9 (3.7) | –0.3 (–1.1 to 0.4) | 0.2 (–2.0 to 2.5) |
| Intervention | 216 | 2.8 (3.5) | 2.9 (3.5) | 0.0 (–0.4 to 0.5) | ||
| Supervisor relationships, mean (SD) | Control | 59 | 74 (21) | 75 (19) | 0.9 (–5.6 to 7.4) | –3.3 (–14.1 to 7.5) |
| Intervention | 224 | 72 (20) | 71 (21) | –1.5 (–3.8 to 0.9) | ||
| Supervisor support, mean (SD) | Control | 59 | 87 (23) | 86 (21) | –0.8 (–8.7 to 7.0) | –3.2 (–19.2 to 12.9) |
| Intervention | 228 | 80 (23) | 80 (24) | –0.1 (–3.1 to 2.8) |
| Outcome | Manager status | n | Baseline, mean (SD) | Follow-up, mean (SD) | Difference between baseline and follow-up (95% CI) | Adherence effect adjusted for baseline and clustering (95% CI) |
|---|---|---|---|---|---|---|
| GHQ-12 score, mean (SD) | Manager adherent | 118 | 2.6 (3.2) | 2.4 (3.2) | –0.2 (–0.8 to 0.4) | |
| Manager not adherent | 98 | 3.1 (3.6) | 3.4 (3.8) | 0.3 (–0.3 to 1.0) | –0.7 (–1.5 to –0.0) | |
| Supervisor relationships, mean (SD) | Manager adherent | 119 | 77 (19) | 75 (20) | –1.6 (–4.7 to 1.6) | |
| Manager not adherent | 105 | 67 (19) | 66 (21) | –1.3 (–4.8 to 2.1) | 3.1 (–1.3 to 7.4) | |
| Supervisor support, mean (SD) | Manager adherent | 122 | 84 (19) | 84 (20) | –0.2 (–3.9 to 3.4) | |
| Manager not adherent | 106 | 75 (25) | 75 (26) | 0.0 (–4.8 to 4.8) | 4.4 (–0.9 to 9.7) |
Psychosocial work characteristics
Supervisory relationships tended to decline slightly in the intervention group compared with the control group across the study. There was also a non-statistically significant decline in supervisor support in the intervention group employees compared with the control group employees (see Table 13). Supervisor support improved among employees whose managers were adherent to the program, taking into account the adjusted difference, compared with employees whose managers were not adherent to the program between baseline and follow-up, although these results were not statistically significant (see Table 14).
Job strain is measured on a scale from –100 to 100, where 100 represents a highly demanding role with low levels of autonomy (high job strain) and –100 represents a highly autonomous job with low demand (low job strain). The actual range is approximately –80 to 80, which corresponds to the findings from the Whitehall II study. 56 Psychosocial work characteristics, including supervisor relationships and information, job insecurity, work social support and job strain, were very similar between the groups at baseline (Table 15). Similarly, there were very few differences in psychosocial characteristics between the groups at follow-up, although no formal tests of statistical significance were carried out (Table 16).
| Characteristic | Control (n = 67), mean (SD) | Intervention (n = 283), mean (SD) | Total (n = 350), overall mean (range of means within each cluster) |
|---|---|---|---|
| Supervisor relationships and information (range 0 to 100, where 100 is very good) | |||
| Supervisor relationshipsa | 76 (20) | 72 (20) | 73 (70 to 76) |
| Sufficient information from managementb | 79 (25) | 76 (24) | 76 (74 to 79) |
| Clear information from managementb | 76 (26) | 73 (26) | 73 (72 to 76) |
| Job insecurity (range 0 to 100, where 100 is very insecure)b | 49 (22) | 41 (20) | 43 (39 to 49) |
| Social support (range 0 to 100, where 100 is very supportive) | |||
| Social supportb | 90 (14) | 84 (17) | 85 (83 to 90) |
| Colleague supportb | 93 (12) | 87 (17) | 88 (87 to 93) |
| Supervisor supportb | 88 (22) | 81 (23) | 82 (78 to 88) |
| Job strain | |||
| Work demand score (range 0 to 100, where 100 is very demanding)c | 64 (18) | 67 (18) | 66 (63 to 69) |
| Decision authority (range 0 to 100, where 100 is highly autonomous)b | 75 (18) | 66 (18) | 68 (63 to 75) |
| Skill discretion (range 0 to 100, where 100 is highly autonomous)d | 82 (16) | 75 (20) | 76 (73 to 82) |
| Decision latitude (range 0 to 100, where 100 is highly autonomous)b | 78 (14) | 71 (16) | 72 (68 to 78) |
| Job strain (work demand–decision latitude) (range –100 to 100, where positive means high job strain and negative means low job strain)e | –14 (25) | –4 (26) | –6 (–14 to –1) |
| Effort–reward ratio (> 1 indicates greater effort–reward imbalance)e,f | 1.07 (1.34) | 1.37 (4.64) | 1.31 (1.01 to 2.07) |
| Work conflict (range 0 to 100, where 100 represents a lot of conflict)b | 33 (19) | 39 (20) | 38 (33 to 40) |
| Change at work (range 0 to 100, where 100 is always consulted about change)b | 56 (28) | 51 (27) | 52 (47 to 56) |
| Job stress (range 1 to 10, where 10 is very stressful)c | 6.0 (2.0) | 6.4 (2.2) | 6.3 (6.0 to 6.5) |
| Characteristic | Control (n = 60), mean (SD) | Intervention (n = 231), mean (SD) | Total (n = 291), overall mean (range of means within each cluster) |
|---|---|---|---|
| Supervisor relationships and information (range 0 to 100, where 100 is very good) | |||
| Supervisor relationshipsa | 75 (19) | 71 (20) | 72 (67 to 75) |
| Sufficient information from managementb | 77 (24) | 73 (24) | 74 (71 to 77) |
| Clear information from managementb | 76 (25) | 72 (26) | 72 (70 to 76) |
| Job insecurity (range 0 to 100, where 100 is very insecure)b | 41 (21) | 40 (20) | 40 (35 to 46) |
| Social support (range 0 to 100, where 100 is very supportive) | |||
| Social supportb | 90 (15) | 83 (17) | 84 (80 to 90) |
| Colleague supportb | 94 (12) | 86 (18) | 88 (84 to 94) |
| Supervisor supportb | 86 (21) | 80 (24) | 81 (76 to 86) |
| Job strain | |||
| Work demand score (range 0 to 100, where 100 is very demanding)c | 63 (17) | 70 (17) | 68 (63 to 72) |
| Decision authority (range 0 to 100, where 100 is highly autonomous)d | 73 (18) | 65 (18) | 67 (63 to 73) |
| Skill discretion (range 0 to 100, where 100 is highly autonomous)e | 78 (16) | 72 (20) | 73 (70 to 78) |
| Decision latitude (range 0 to 100, where 100 is highly autonomous)d | 75 (14) | 68 (17) | 70 (67 to 75) |
| Job strain (work demand–decision latitude) (range –100 to 100, where positive means high job strain and negative means low job strain)f | –12 (23) | 1 (26) | –1 (–12 to 6) |
| Effort–reward ratio (> 1 indicates greater effort–reward imbalance)g | 1.01 (0.98) | 1.21 (4.64) | 1.16 (1.01 to 1.26) |
| Work conflict (range 0 to 100, where 100 represents a lot of conflict)b | 36 (20) | 42 (21) | 40 (36 to 45) |
| Change at work (range 0 to 100, where 100 is always consulted about change)b | 54 (25) | 48 (25) | 49 (41 to 54) |
| Job stress (range 1 to 10, where 10 is very stressful)h | 5.9 (2.2) | 6.4 (2.1) | 6.3 (5.9 to 6.5) |
Intracluster correlation coefficients
Intracluster correlation coefficients were lower than the 0.07 estimated in advance but the CIs were very wide and in some cases uninformative (Table 17). A reasonable ICC for self-reported measures of well-being would be 0.012 but for HR sickness absence it should be higher, at around 0.03.
| Outcome | ICC (95% CI) |
|---|---|
| WEMWBS score | 0.00 (not estimable) |
| GHQ-12 score | 0.012 (0.0001 to 0.46) |
| Self-reported sickness absence | 0.008 (0.00003 to 0.69) |
| Supervisor relationships | 0.00 (not estimable) |
| Supervisor support | 0.008 (0.00003 to 0.66) |
| HR sickness absence | 0.0003 (0.000 to 1) |
Ancillary analyses
We carried out further analyses to assess whether or not the psychosocial work characteristics in the employees of those managers who were fully engaged in the program differed from the psychosocial work characteristics of those employees whose managers were not fully engaged in the program (Table 18). There was a reduction in job strain across the study in employees of adherent managers compared with non-adherent managers. There was little effect on work stress and effort–reward imbalance. Job insecurity diminished fairly substantially among employees of adherent managers compared with employees of non-adherent managers.
| Outcome | Manager status | n | Baseline, mean (SD) | Follow-up, mean (SD) | Difference between baseline and follow-up (95% CI) | Adherence effect adjusted for baseline and clustering (95% CI) |
|---|---|---|---|---|---|---|
| Job strain | Manager not adherent | 100 | 2.1 (25.5) | 7.2 (24.7) | –5.2 (–9.1 to –1.2) | |
| Manager adherent | 121 | –7.7 (27.7) | –3.9 (26.8) | –3.8 (–7.7 to 0.0) | –4.6 (–9.6 to 0.4) | |
| Difference at baselinea | 277, 8.9 (95% CI 2.7 to 15.0) | |||||
| n | Baseline, n (%) | Follow-up, n (%) | Odds ratio for adherence effect, adjusted for baseline and clustering (95% CI) | |||
| Work stress | Manager not adherent | 105 | 77 (73.3) | 76 (72.4) | ||
| Manager adherent | 121 | 79 (65.3) | 79 (65.3) | 0.8 (0.4 to 1.7). | ||
| Difference at baselineb | 278, χ2 p-value = 0.401 | |||||
| Insecurity | Manager not adherent | 104 | 10 (9.6) | 7 (6.7) | ||
| Manager adherent | 123 | 8 (6.5) | 11 (8.9) | 2.9 (0.7 to 12.2) | ||
| Difference at baselineb | 280, χ2 p-value = 0.272 | |||||
| Effort–reward imbalance | Manager not adherent | 105 | 48 (45.7) | 55 (52.4) | ||
| Manager adherent | 122 | 40 (32.8) | 44 (36.1) | 0.6 (0.3 to 1.1) | ||
| Difference at baselineb | 280, χ2 p-value = 0.183 | |||||
Finally, we wished to examine whether or not the intervention had differing effects within certain subgroups. In particular, we wished, as discussed in the original application, to compare well-being and self-reported sickness absence in employees from lower job bands with well-being and self-reported sickness absence in employees from higher job bands. In addition, we compared well-being and self-reported sickness absence in the following groups: men and women, those aged < 50 years and those aged ≥ 50 years, those working full time and those working part time and those who had worked for the NHS for ≤ 2 years and those who worked for the NHS for > 2 years. The differences were relatively small and there was little evidence of greater effects in any particular subgroup (Table 19).
| Outcome | Control | Intervention | ||||||
|---|---|---|---|---|---|---|---|---|
| n | Baseline, mean (SD) | Follow-up, mean (SD) | Difference (95% CI) | n | Baseline, mean (SD) | Follow-up, mean (SD) | Difference (95% CI) | |
| WEMWBS score | ||||||||
| Male | 8 | 49.1 (6.7) | 50.1 (8.0) | 1.0 (–2.5 to 4.4) | 57 | 51.6 (8.0) | 50.2 (9.6) | –1.4 (–3.2 to 0.3) |
| Female | 51 | 50.6 (8.2) | 48.9 (8.6) | –1.8 (–3.4 to –0.3) | 168 | 50.8 (8.5) | 49.8 (7.9) | –1.0 (–2.0 to –0.1) |
| Aged < 50 years | 39 | 51.0 (7.1) | 49.0 (8.7) | –2.0 (–3.9 to –0.2) | 135 | 50.7 (8.6) | 49.3 (8.7) | –1.4 (–2.6 to –0.3) |
| Aged ≥ 50 years | 20 | 49.3 (9.5) | 49.1 (8.2) | –0.2 (–2.2 to 1.7) | 90 | 51.4 (7.9) | 50.9 (7.7) | –0.6 (–1.8 to 0.5) |
| Job band < 6 | 25 | 49.4 (8.5) | 47.4 (9.8) | –2.0 (–4.7 to 0.6) | 107 | 51.4 (8.1) | 50.3 (8.3) | –1.1 (–2.4 to 0.1) |
| Job band ≥ 6 | 34 | 51.2 (7.6) | 50.2 (7.2) | –1.0 (–2.6 to 0.5) | 117 | 50.6 (8.6) | 49.6 (8.4) | –1.0 (–2.2 to 0.1) |
| Full-time employees | 43 | 49.2 (8.0) | 47.8 (8.7) | –1.4 (–3.2 to 0.3) | 157 | 50.4 (8.3) | 49.2 (8.2) | –1.2 (–2.3 to –0.2) |
| Part-time employees | 15 | 53.8 (7.2) | 52.1 (7.0) | –1.7 (–4.1 to 0.6) | 66 | 52.6 (8.4) | 51.7 (8.3) | –0.8 (–2.2 to 0.5) |
| Worked ≤ 2 years in the NHS | 7 | 51.9 (7.0) | 48.1 (14.2) | –3.7 (–10.1 to 2.6) | 26 | 49.7 (6.8) | 50.7 (6.7) | 1.0 (–1.2 to 3.1) |
| Worked > 2 years in the NHS | 51 | 50.2 (8.2) | 49.0 (7.6) | –1.2 (–2.6 to 0.1) | 195 | 51.1 (8.6) | 49.9 (8.6) | –1.3 (–2.3 to –0.4) |
| Days off sick from self-reporta | ||||||||
| Male | 8 | 1.3 (2.3) | 0.5 (1.4) | –0.8 (–2.1 to 0.4) | 50 | 0.5 (1.5) | 1.0 (3.4) | 0.5 (–0.6 to 1.5) |
| Female | 43 | 1.2 (4.1) | 1.4 (3.7) | 0.2 (–0.8 to 1.1) | 148 | 1.2 (3.4) | 1.5 (3.4) | 0.2 (–0.6 to 0.9) |
| Aged < 50 years | 34 | 0.5 (1.5) | 0.9 (2.1) | 0.4 (–0.4 to 1.1) | 123 | 1.0 (2.8) | 1.4 (3.7) | 0.4 (–0.5 to 1.2) |
| Aged ≥ 50 years | 17 | 2.6 (6.2) | 2.0 (5.3) | –0.6 (–2.7 to 1.4) | 75 | 1.1 (3.4) | 1.3 (3.0) | 0.1 (–1.0 to 1.1) |
| Job band < 6 | 22 | 2.4 (5.5) | 1.7 (4.7) | –0.6 (–2.3 to 1.0) | 97 | 1.1 (3.2) | 1.4 (3.0) | 0.3 (–0.6 to 1.1) |
| Job band ≥ 6 | 29 | 0.4 (1.4) | 1.0 (2.1) | 0.6 (–0.3 to 1.4) | 100 | 1.0 (2.9) | 1.3 (3.8) | 0.3 (–0.7 to 1.2) |
| Full-time employees | 36 | 1.3 (3.8) | 1.7 (4.0) | 0.4 (–0.4 to 1.1) | 138 | 1.1 (3.2) | 1.2 (3.2) | 0.2 (–0.6 to 0.9) |
| Part-time employees | 14 | 1.3 (4.3) | 0.4 (0.9) | –0.9 (–3.3 to 1.4) | 58 | 1.0 (2.7) | 1.5 (3.8) | 0.5 (–0.8 to 1.7) |
| Worked ≤ 2 years in the NHS | 6 | 0.0 (0.0) | 0.2 (0.4) | 0.2 (–0.2 to 0.5) | 23 | 0.7 (1.7) | 0.7 (2.2) | 0 (–1.0 to 0.9) |
| Worked > 2 years in the NHS | 44 | 1.4 (4.1) | 1.5 (3.7) | 0.0 (–1.0 to 0.9) | 171 | 1.1 (3.2) | 1.4 (3.6) | 0.3 (–0.5 to 1.0) |
Harms
No harms or adverse effects to employees or managers were reported during the study, neither to the facilitator, the qualitative researcher or another member of the research team. There were no reported adverse effects of either the trial or the intervention.
Chapter 4 Qualitative results
This chapter presents the findings from the qualitative study. In presenting these findings we draw on data from interviews with key informants (quotes referenced as KI), managers (quotes referenced as M) and employees (quotes referenced as E), observations of meetings, a group discussion with managers and open-ended responses from employee questionnaires. Throughout the chapter we present storied accounts from managers and employees of specific cases of stress to illuminate the ways in which respondents spoke about their own experiences of workplace stress.
The context within which the study took place
The study took place at a time of considerable change and uncertainty within and beyond the NHS. Respondents cited pressures on NHS funding, restrictions on housing and other state benefits and the impact of the Francis inquiry57 into failings in NHS care as all affecting overall staff morale and well-being and having, in the words of one respondent, ‘knock-on effects for the stress levels of people’ (KI10).
At the local level, a major organisational change took place in the trust leading up to the period of study, which was thought to have significantly impacted on workforce stress levels (see Reorganisation, job insecurity and poor communication about change). Indeed, there was a perception among many that stress levels were higher than they had ever previously been.
At the time of the study, the trust had been engaged in a number of ‘healthy workplace’ initiatives in addition to the guided e-learning intervention. For example, several managers mentioned their involvement in ‘resilience training’, although most managers reported that before the guided e-learning intervention they had not received any specific training in managing employee stress. Nevertheless, by virtue of their employment in a NHS mental health trust respondents were likely to have significant awareness of and sensitivity to issues of stress and mental health well-being, and some mentioned that they were undertaking further study in the field of mental health. At the same time, working in a mental health trust providing services for mentally vulnerable patients was identified as having its own particular stresses and strains.
The trust has a stress prevention and management policy that references the HSE management standards for work-related stress. 32 The policy outlines the trust’s commitment to ‘identify, assess and subsequently eliminate, or reduce, work related stressors’. In our interviews with managers and employees, no reference was made to this policy.
Experiences of stress at work
Overall, the different groups of respondents (managers, employees and key informants) identified similar influences on workplace stress. Key sources of workplace stress were organisational change, job insecurity and poor communication, an increased volume of work and lack of resources to deal with it and organisational culture. These aspects of workplace stress reflect those identified by the HSE management standards32 on which the guided e-learning intervention is based. Respondents also identified some additional sources of stress: the physical environment, the nature of mental health work and the pressures of family life events and ill health. These influences on stress at work are less discernible in the e-learning materials.
In talking about workplace stress, respondents conveyed the ‘double-edged’ nature of pressure and stress: how what might be perceived as stress by one person might be experienced as pressure under which they thrive by another. Respondents thus emphasised the very individual nature of stress and how in terms of tackling stress at work the ‘one size fits all approaches won’t work’.
I actually love my job. I really enjoy it. I probably work better under pressure. I really enjoy problem solving. And I enjoy kind of working in different ways and new ways, and I’m always interested in different ways of working, and what’s going on, and how things are working.
M8
Some people deal with it [stress] in a better way. And I’ve always considered myself to be of that ilk, but knowing and seeing what I’ve gone through I’ve realised that it is a fine line that we all tread. And I think none of us quite knows which event or what sequence of events will take us to, you know, that breaking point in which, you know, for our own safety and our own sanity we’ve probably got to sort of step back. And I do think that some people are able to take these sorts of things on board a little bit better and deal with them, but it’s not easy at times.
E5
Reorganisation, job insecurity and poor communication about change
A major reorganisation within the trust during the period of the study was identified as a key source of stress for both managers and employees, with staff redeployed to different departments or reassigned to a different job role but not necessarily a new job band. Mention was made of ‘90 days to possible redundancy’ letters having been sent out in 2012, before the start of the study. Respondents spoke of the stress of uncertainty and job insecurity, of feelings of being out of control and decisions being taken elsewhere:
I don’t think in general any of us are working in a healthy environment. Because the constant changes that are happening, constant redesigns that are going on, everybody’s unsettled.
M5
And I think my concern about it is that most of the problems and stress-inducing aspects of work that we feel are beyond our control, completely beyond our control, and I don’t think that helps at all because things are foisted on us really. I think there’s an awful, to me, a yawning gulf between those who make the decisions and impose these things and the rest of us. I feel personally that voices aren’t heard . . . but it was very comforting to know everybody else felt the same.
M3, feedback meeting
As indicated in the previous quote, there was a view that poor communication ‘from the top’ had exacerbated the stress of reorganisational change:
. . . the process and the communication that people had going through that process was absolutely abysmal and it only added to the sense of worsening morale and not really knowing where the service was going. Lots of concerns about individual practitioners but also the team and how that would function, but more importantly how that was going to have a knock on effect to service users.
M9
In Box 1, one manager tells the story of the impact of reorganisation on his team and on one employee in particular.
One [member of staff] who is very, let me just try and think of the wording for it, very committed, very conscientious, always increasingly finding it difficult because he couldn’t give his clients what they needed so that weighed heavy on him, couldn’t get his documentation up to date because that’s a demand from management that your documentation is up to date and trying to fulfil all those roles is really difficult. So we had supervision and it’s particularly since the change of this new redesign and what I tried to do with him is spend time out of the office so that he wasn’t part of things going on in the office so that he could quietly get on with some of his documentation in a quiet environment, tried to hold back any allocations for a bit until he felt more on top of his work . . . . So I did listen and I did what I could but he could accept I was limited because the expectation on the team from higher management. I actually declared the service unsafe because the other stress on the team was that two [members of staff] went off on long-term sick and I realised I’d got to allocate all those cases because we haven’t got any [staff] that have light [caseloads] any more and so that put extra strain and at that point I declared the service unsafe.
. . . we keep on being told that there’s no money for extra staff. We ended up with a member of staff [from another team] coming over into our team and that was only because I fought for it because I said, ‘Look staff can’t continue under these levels’. But that person ended up resigning and he was brilliant, no job to go to, so I suppose using that as an example he was very positive about my input, he wasn’t positive about the higher management and . . . how they’ve managed this redesign and the pressure they’ve put on staff and he was very vocal about that on leaving. But I felt my hands were tied, I’d done as much as I could because I tried to support him through it . . . that came out on his exit interview and everything and when he resigned saying the job was untenable.
M1
Volume of work and lack of resources
Respondents identified a marked increase in the volume of work in recent years, but at the same time they felt that they had fewer resources to deal with the increase:
When a CPN [community psychiatric nurse] goes off sick or somebody in the community goes off sick, we’re generally not allowed to cover that with bank staff, so the team has to soak up the pressure. So in the last 12 months, we have had three staff off on long-term sick. So if you think they have an average caseload of 25 each, that’s 75 more patients that the rest of the team has got to look after.
M8
We can have say 13 referrals come in one morning and you’ve got five staff and they could be all urgent and they all need assessing and so that’s the stress for the workers and the stress for me is sort of managing that I suppose, trying to help them find solutions to manage their work.
M10
Managers spoke about how their jobs had changed in recent years, with more and more administrative demands on their time and also how more HR functions had been devolved from HR to managerial level, turning line managers into ‘part-time HR managers’:
It just seems there’s more and more and more things that have to be met . . . . The demands of having to meet the paperwork and the timelines and the guidance and the policy expectations, you’re constantly getting these performance data spreadsheets saying well, this is missing, this information needs to be updated and it’s just, you’re catching yourself coming back really. Being able to prioritise work, you’ve only got so many hours in a day to be able to do the bits you need to get done.
M9
The increased demands of documentation were identified as affecting all staff – employees as well as managers.
Overall, the feedback from managers at the facilitator-led induction meetings was summarised by the facilitator as consisting of concerns about ‘high demands, low control’.
Organisational culture and attitudes
Several respondents spoke of the negative effects of organisational culture, with one making the suggestion of a ‘blame culture’:
I think a lot of the stress isn’t so much about the service users. The stress is about the organisation’s attitude to the staff, if something doesn’t quite work out right, so you know obviously if we see 2500 people a year, a high proportion of them are people who’ve harmed themselves, so proportionally we will have more people killing themselves that come through our service than anywhere else but the trust response to that is extremely negative and there is a blame culture.
M3
Key informants from outside the trust identified broad trends in the workplace impacting on stress, with organisations becoming more and more ‘data-driven, rather than people-driven’ (KI1), performance management seen as a tool to identify employees as weak and failing, rather than as needing to be helped and supported, and ‘macho attitudes’ – ‘if you can’t take the heat, get out of the kitchen’ (KI5).
Discussion at the facilitator-led induction and follow-up meetings for managers conveyed considerable negativity about organisational culture and attitudes. The facilitator noted among managers a ‘concern that the number of investigations, disciplinaries and capability processes have increased . . . not feeling appreciated for what they’ve done/achieved – the focus is only on recognising what hasn’t been done/achieved’.
The physical environment
A common problem identified by employees and managers was the physical working environment. Common concerns were a lack of space, hot, overcrowded and noisy offices and ‘hot-desking’:
I think the stresses for the staff are rooms. Rooms are a big, big stress . . . . the availability to have rooms to work out of. This building isn’t adequate for the amount of therapists we’ve got. We’ve got people working out in satellite clinics but we also have to have, obviously, a core of staff here. They’re just juggling rooms on an hourly basis.
M6
It seems to be in vogue . . . but the actual experience of working in a hot desk room is causing lots more stress than it’s ever solved. The staff have been coming to me saying the rates of sickness are increasing, they’re unable to hear themselves think sometimes so their own stress levels in getting through things are [rising].
M9
It’s very hot, it’s very noisy, your desks, you’re literally in a row next to each other so you haven’t got any private real space, you’ve got a locker which you keep everything in basically. Being an OT [occupational therapist] I do lots of different assessments, I have quite a few OT different things and I’ve got nowhere to put them, so they’re all shoved in a drawer and I have all my clients that I’m working on in little folders, then I have to get the whole drawer out to try and find that one folder that might be at the bottom, put them back in and then think ‘Oh, I’ve got to do that’ get them all out. And it’s really had a major impact, the closeness, you can’t hear on the phone, you can’t concentrate.
E7
The nature of mental health work
It was clear from respondents that the nature of the work that they were undertaking could be inherently stressful:
The stresses had built up from an incident when I was on the night shift, when a colleague of mine was badly injured. So there were issues around that, which led to other issues with management, and I suppose I wasn’t reacting very well to the stresses, and you know, it just sort of built up and built up. So I’d a few discussions with my ward manager at the time, who was supportive, very supportive and . . . but I decided that I was okay, I can struggle on through. And I think it was the straw that broke the back. And . . . in my case it was a patient who just decided to target me for a day that finally just broke me.
E5
At the same time, respondents identified the positives of working with this client group:
The positives [of the job] for me are absolutely the clients. I am very passionate about recovery and so the people that I work with, the fact that I can work with them for up to 2 years so I really get to know them inside out. So building up therapeutic relationships there is extremely satisfying.
E8
Family pressures and personal health
One of the striking findings to emerge from manager and employee narratives of employee stress was how their accounts invariably started with a description of the employee as a family carer, as having an elderly mother or a sick relative, or as coping with a bereavement, or having grandchildren who needed looking after whilst the parents were going through a messy divorce, or having various other ‘private personal stresses’. As one respondent commented: ‘It’s not really work stress so much as it’s personal stress. But of course it does have an impact on one’s work life’ (KI13) Several of the stories of stress at work that we present here convey the complex, intertwined nature of personal and workplace stresses (Boxes 2 and 3):
[I was] very, very stressed. I kind of . . . it gets to that point when you think, I just can’t do it. And it might sometimes be personal stress and work stress and everything all happening at the same time, which it usually does doesn’t it? It’s never just one thing or another.
E8
I was just separated from my husband, literally the month I started [the job], then I had loads of health problems with my mum and she passed away shortly afterwards. Loads going on in my life at the time and I just didn’t . . . well, I wasn’t good to be honest . . . . and there was particular trouble on the ward with a client and some of the family involved and it all went wrong on there big time. A lot of people were redeployed, some moved for other reasons and it just ended up a big massive enquiry. I was off long term for 6 months during that time. I never thought . . . to be honest I never thought I’d come back to work, I didn’t, it was that bad you know. . . . me personally I’ve got loads of respect for [managers] that were supporting me then.
E3
I’d had a lot of personal pressure as well as work and, so basically I felt like I had 24/7 constant stuff to deal with and then my caseload at that time, because it can fluctuate, you know, was particularly difficult with quite a few patients that needed a lot of things doing and I just, I knew that I was stressed because I was just moving things, and that’s a sign for me. I know that if I’m moving things and I’m feeling it up here, I’m not effective. So I went to, it was one of the managers I went to, and I was just quite tearful and said, ‘I really at the moment am struggling’. So we looked, he went through my caseload and we prioritised, he helped me prioritise because I was quite bad, and he said to me, ‘If you need to come in a bit later, you do that’, I mean obviously I kept tabs with him, telling him what I was doing, ‘and if you need any support with any of your cases’ he practically helped me with something. It just went like that, he took the pressure off and just because I was at that point where I was like, normally I can sort stuff out, I just couldn’t. And for about a month he monitored me, and that saved me being off. Just saying to me, ‘look, if things get too much go sit in the car, you know, read a book for 10 minutes to get your mind out of all this’ because it was, you know, if you want me to go through the list with you, it just helped with getting through that period of time.
E7
Views on ‘competencies’ required for managing stress at work
Interviews with managers and employees illuminated the ‘competencies’ that respondents thought were required to manage stress at work. Respondents spoke of the need for managers to have an ‘open door’, be accessible, approachable, supportive, compassionate, a good listener and understanding, look for solutions to problems, give staff confidence that they could confide in their manager and have a culture of honesty and openness:
I think knowing that there’s a manager’s support in all that is worth a fortune, really, for someone. They know people are seeing their manager being aware of the stresses that they’re under and being able to express as much in the way of listening and understanding and helping within the system in as many ways as they can to support that person. I think that’s what employees really need, they just don’t want to be left with all this to try and cope because then they’ll implode, sort of break down and next thing they go off with stress.
M3, feedback meeting
I like to feel that they are open and honest. They will share things where they can share things. They are always there if you’ve got a query, a question, a problem and I think if approached in the right way will always be on board with trying to solve that, rather than taking a sort of an authoritative approach that, you know . . . if there’s maybe some aspect of work that maybe it hasn’t happened as well as it should do the approach would be a fairly informal ‘Let’s talk about this, let’s find a way forward’, using supervision, using appraisal and the like rather than . . . I know in some areas it would automatically become almost disciplinary or a capability issue, yeah. So it’s like trying to find a way forward rather than punishing you for it.
E4
In Box 3 several of these attributes are identified, as an employee describes how her manager supported her through a stressful period.
Emotional intelligence and sensitivity
You can have a commitment or a strategic goal around mental health but actually what really matters to people is when they come in on a day-to-day basis what’s their relationship like with their line manager? And if line managers don’t possess that emotional intelligence in terms of being able to spot signs and symptoms, motivate, lead, inspire, when there is an issue of course and an individual is not able to relate to their line manager and they go off sick for any reason, it’s incredibly difficult to get them back into the workplace . . . it is all about middle managers and it’s about their behaviour and about their emotional intelligence and about how they go about conducting themselves on a day-to-day basis.
KI5
The various competencies for managing stress at work identified by managers and employees can perhaps best be encapsulated in the concept of emotional sensitivity. Emotional sensitivity requires a connection both with one’s own emotions and with the emotions of others and has been identified as being critical to workplace health. 58 Yet surprisingly, the HSE management standards and the e-learning program pay little overt attention to this concept. In Box 4 a manager illustrates this ‘competency’, describing how he draws on compassion and his own ‘personal beliefs and personal values’.
It’s more of a personal nature for this member of staff. She’s going through a very difficult break up of a marriage, got young children too . . . it’s all blown up and all . . . really struggling, really having difficulties with it. I’m going out to see her on a fairly regular basis – I’ve been out to see her today, actually. Going out, giving all the support I can refer her to occupational health, refer her to staff support. It’s a really difficult one because I’m sitting there saying, ‘Yes, yes. I hear that you’re not ready to come back. Yes, I hear what you’re saying to me’, but on the other side of that is the fact that there’s a service need. She had a caseload of patients that we’ve had to share out with other people now, not everybody wants to go to another therapist. Therapy’s quite individualised and quite thought-provoking, and you’re sharing your soul to the devil, so to speak, aren’t you? That’s how it feels. So that’s difficult because it’s that balance of I hear what you’re saying, you’re in a really horrible place, I can’t imagine anything worse for you, but on the other side of that, I’ve got to get you back into work somehow . . . I think I’ve had to draw on compassion. I think I’ve had to draw on knowing the policy, knowing what I can and cannot allow her to do. The return to work policy, the phased return, all of that, I’ve had to look on that. I think I’ve had to draw my own personal beliefs and my own personal values, really, and be able to stand up and say, ‘I hear what you’re asking as a trust. I hear what you’re saying as a trust’ but I’m the person that’s in there, I’m the person that’s dealing with this individual, you know, I’ll bring her in to fail and that’s how I feel at the moment. I think she’s too fragile, too vulnerable to come back in at this precise moment but I’m also aware that if I take that to a more senior manager they may say I hear what you’re saying but she needs to get back in.
M6
‘Juggling’ priorities
Although the guided e-learning intervention was focused on reducing stress and increasing well-being in employees, it quickly became apparent that managerial stress was also a key issue (Box 5). At the same time as talking about managing stress in their employees, managers easily slipped into talking about their own stress.
A recent example that landed on my desk, I was asked to investigate a serious untoward incident with a deadline of 3 weeks and, well, the last 10 days of that I’m on holiday and there were lots of reasons why it probably wasn’t appropriate and my diary was already full apart from, I think, two afternoons. So I said all that, in response, and basically the person involved said ‘oh, how can we support you in this? Would you give me all your diary commitments?’ So I then gave permission for my e-calendar to this person, who wasn’t my immediate manager, it was someone else more senior and then she came back and she said ‘oh, let me know if you would like any support in cancelling any meetings’ but basically the thing is, do it. And files this thick arrived in the post the next morning, I’ve got another load that thick since. I was hoping to take my last day’s leave of this financial year’s leave last Wednesday and I had to cancel that because no way could I possibly fit it in. I’ve got client commitments as well and obviously they are sacrosanct, I’ve left the client commitments, but apart from today, and I thought really I should be cancelling this but it was basically hard luck, you’ll do it even though I have reasonably, as far as I’m concerned, argued or responded to say I really am not the right person to be doing this at this time. And it’s just that attitude: you’ll do it.
M3, feedback meeting
A central aspect of managing stress as a manager was the ability to ‘juggle’ – to juggle between organisational demands and employee needs (Box 6). Managers saw themselves as pushed in both directions, as ‘the damp-proof course in the organisation, nothing permeates in either direction’:
I’ve got a member of staff who is still with me, who, last year was for some time, has been the main carer for her father, and who’s become increasingly frail. Last year he was diagnosed with cancer, and was only given a couple of months to live. He subsequently lasted several more months than that. But, obviously, this caused her additional stress because it wasn’t only her work she had to juggle. She had to sort out carers to go in when she was in work, and also when she wasn’t in work . . . . So she had a lot of stress around that . . . . She also had a sister with learning disabilities who, although didn’t live with them, was sort of there in the background, and I think a lot of it was she was thinking how was she going to support her if anything happened to the father. So there were lots of stresses around that.
I think [managing stress] for her it was very much about thinking outside the box [manager describes how she introduced flexible working hours for this employee]. What is it that I could do as a manager to support her as much as I could, to prevent her going off sick, because she would’ve gone off sick . . . And we were able to prevent that. And I suppose a lot of it for me was being able to empathise with her; having gone through bereavement of a close family member myself. You can think what would’ve been good for me at that time.
M2
I suppose you wear two hats as such because one, you want to look after the individuals and the employee, you want to do the kind of best for them, you want to make sure that they are being supported in every possible way, kind of physically, mentally. You want to ensure the other hat is a . . . the organisation is still working and that the team itself is still working, that the people are picking up his patients. So you’ve got a foot in both camps because you’re trying to be the manager and look after the welfare of everyone including all the staff, all your patients. And then you kind of, on an individual basis, you’re trying to look after that person’s mental health you’re trying to be there for them, you’re trying to give as much empathy as possible. You are always trying to kind of . . . it’s like kind of juggling two balls and all of a sudden you drop a ball.
M8
If you’re getting stuff fed down to you without really understanding where you’re coming from, my priority that day isn’t to update a spreadsheet that they need to put through to their contracting discussions, my priority is actually getting a staff member out to see that person who’s just tried to hang themselves or something. So the pragmatic things I have to get done on a daily basis to maintain a service or to reduce the risks to individuals but then there’s the pressure from people from a corporate point of view in terms of running an organisation and all the governance that goes with that and sometimes the two just don’t tally up.
M9
The ‘difficult place’ that managers found themselves in was something acknowledged by employees:
I think the manager role is a key role and I’m aware of the annual staff questionnaires that are done and I think for this trust one of the positive things that’s come out has been a lot of people have felt the first level line manager as being supportive. Where it’s fallen down has been with sort of more senior managers who maybe don’t have that relationship or whose own pressures are very different ones, increasingly financial ones aren’t they? So I see a split, a disjoint if you like between what’s happening for . . . what the senior managers are doing, what middle managers are doing, I think sort of middle managers are probably getting the worst of both worlds. There is pressure from them on the top to perform, to hit targets, to achieve financial outcomes and then from the lower levels with all the everyday aspects of running a service and everything that goes with it. So I think they are in a very difficult place.
E4
Managers also described how they had to juggle different aspects of their role, as both a manager and a practitioner:
I think getting the balance between managing my own workload and my own priorities, supporting the staff, and everything that involves with sort of the performance management and that sort of thing. And also doing clinical work as well, . . . it’s almost like having lots of balls up in the air and juggling with them.
M5
Some managers felt that they had ended up as managers by default rather than by design – ‘I was a good nurse but now all of a sudden I’ve been told “you’re good at nursing, do management” ’ (M8).
Another source of stress identified by managers was the feeling that the stress they were supposed to be managing for their employees was often out of their control, perhaps because it was something that senior managers had imposed, or because it was to do with an aspect of organisational life or policy over which they had little influence. Although many employees acknowledged and accepted this situation, for others it was a source of frustration: ‘Well if you do raise issues she’ll just say, “well there is nothing I can do about it, we’re all in the same boat” ’, said one employee (E6).
Experiences of the guided e-learning intervention
In this section we report on the views of the 13 managers in our interview sample. We were unable to elicit the views of those managers who did not participate in the study. All of the intervention managers in our sample were defined as ‘adherent’ (i.e. had completed three or more e-learning modules). Thus, our sample consisted of a motivated group, keen to engage with the educational opportunity offered by the e-learning program. One respondent described her motivation in the following way:
Firstly, as a manager, I wanted to feel more confident and competent at dealing with my workforce and learning how to do it differently, or even just reflecting on the way that I do things, so that, you know, I’m consolidating my knowledge and experience. So that was my first sort of motivation. The second motivation was to help the staff, because I knew that the staff were also going to be getting involved in terms of giving feedback about how I manage.
M5
Feedback at the manager meetings that we observed indicated that some groups of managers had been nominated to participate in the study. At the preliminary trust meeting about the study the head of HR reported that ‘about half the managers attending have volunteered and the others have been chosen to participate’. At the ‘feedback’ meeting (April 2014) one manager commented:
When I found out I was taking part in the study, it was in a ward managers’ meeting, it was like we’re the ward managers so there was no choice, just we’re doing it, which is fine for me because I thought oh I see, but I was really pleasantly surprised.
M1
Overall, managers reported many positive aspects of the study and the e-learning program. They were overwhelmingly positive about their interactions and communication with the study team and the program was considered easy to access and straightforward to use, ‘looked professional’ and was visually appealing:
It’s easy to use, it’s user friendly, it’s simple, it looked nice, there were useful tools that were in there. It was a tool I’d go back to if I could, stuff that was in there that you could draw upon at later dates. I think that would be useful.
M9
Managers generally found the material within the program applicable and relevant. A few managers commented that the e-learning program had introduced them to new concepts, such as underemployment as a cause of stress and ‘presenteeism’. Respondents were positive about the ‘layered’ approach to information in the program, which meant that they could engage with the material in more or less depth as they found helpful:
I think it gave just the right amount of information, I don’t think it blew you away with shedloads of unnecessary information and it came up with cases and it came up with, you know, the legal framework around discrimination say, so I thought that was quite good and then you clicked on things that you could elaborate on and get more information and there was other stuff that I managed to get which I thought was quite handy for my dissertation in fact. You know, when it’s the further information bits you could click on or the resources as well. So that was quite good.
M3
A tool for reflection and validating practice
For most managers the key value of the e-learning program was not the new knowledge that they acquired from it but the way in which it ‘backed up’ existing knowledge and encouraged reflection on managerial practice. In this sense, managers felt that it validated their own practice and thus helped build confidence:
It made me kind of more aware of the kind of processes and made me more aware of some of the things I was actually doing, probably was doing subconsciously, but it kind of backed me up.
M8
I suppose it wasn’t any news to me about things that people suffer when they’re under stress but then I don’t think it does any harm to do it as a reminder.
M1
I don’t think there was much in there that I don’t already apply to everyday practice. I guess it’s about reaffirming that that is what we should be doing with specific people. It’s having that toolkit almost isn’t it of things?
M2
I quite enjoyed the course because I didn’t really see things that were totally shocking to me or, ‘Oh! You should be doing that’. It reinforced that my way of doing it is all right, it’s acceptable . . . . So I found that course sort of validated some of the stuff that I already do and sort of sends a message to me that carry on doing it that way.
M4
It is a good package in that it invited reflection, and it certainly invited you to draw on past experiences yourself, which is a bit . . . I think I particularly took that bit away. Because there was one exercise, I thought, ‘Oh, this is really good’. It was where there was a question about thinking about managers you’ve had in the past and can you think of someone who you would have rated as a good manager? And what are the qualities of that person? And that was quite useful really, it really helped me to reflect, and then also the same thing for a bad manager . . . and what it was that that person was doing that was poor in terms of stress levels and that sort of thing. Now, I thought that was particularly good.
M7
A few managers, particularly those who had a background in psychology, found the information in the e-learning program too basic and would have liked more in-depth and advanced sections. Arguably, this finding is unsurprising among a group of experienced managers (respondents had been in post for between 3 and 25 years) working in the field of mental health.
I probably found [it] a little bit repetitive, or a little bit basic, probably because of my own level of knowledge that’s all. And obviously, quite a lot of it’s based on psychology, isn’t it? From that point of view, it’s granny and sucking eggs, I think.
M7
I think the content could have been a bit harder, but I suppose . . . looking back at it, I suppose it depends what or how long you have been a manager.
M8
I can’t really key into anything that I’ve picked up from the [e-learning modules] that I wasn’t already aware of or trying to use.
M9
The problem of time
Although senior managers had emphasised at the beginning of the study that the e-learning program could be studied in work time, one of the biggest problems that managers expressed about the e-learning intervention was finding the time to engage with it. Managers working in outreach settings spoke of ‘snatching time here and there’ (on a laptop in their car between clients or at lunch). Managers working on wards or in open plan offices spoke of being frequently interrupted. Some managers who did have their own private office spoke of ‘blitzing it’ – coming in to their office early, or staying late after work, and working through it in one 3-hour block, putting a notice on the door that they were not to be disturbed for a few hours. For one, time had clearly been a factor in not managing to complete the modules. At the facilitator-led follow-up meeting it emerged that ‘completing’ modules did not necessarily mean that managers had undertaken the suggested activities, with several mentioning lack of time as the reason for this:
It was finding the time in the day just to sit down and be able to do it sat at my desk without some other priority or somebody knocking at my door with another question. That was really it, it was not time-consuming or anything necessarily it was just literally finding enough time . . . I found it was useful, it was something I would want . . . I didn’t get far enough through to really be able to say actually, this could have been done differently or . . .
M9
My own initial thought was, ‘Where am I going to find the time?’ I want to do it, happy to do it. I think it’s good for me, on a personal level as well as a work level. But where was I going to find the time . . . I don’t think I gave it the time it deserved . . . I was interrupted all the time.
M6
I was interrupted. I tried to do it between . . . whenever times I wasn’t either doing supervision or going to meetings. And I think it ended up I tried a number of times, but I got interrupted so often that in the end I kind of just shut me door, locked me door, pretended I wasn’t in and blitzed, did a good 3 hours of it.
M8
The problem of senior management support
A clear recommendation from those involved in the development of the guided e-learning intervention and others involved in researching the management of workplace stress17,37 is the need for explicit commitment (‘buy-in’) of senior management. Indeed, those involved in developing the HSE management standards for work-related stress32 argue that, for an initiative to be successful, it needs to be ‘top led and bottom fed’:
One part of the process is we recommend setting up a tripartite steering group: senior management, local management and union reps to work together so that ultimately there is engagement. We came up with this wonderful phrase many years ago: it’s top-led, bottom-fed. And that’s it in a nutshell – without that, it doesn’t work. We found that through our bitter experience. If it’s all coming up from the bottom, it doesn’t work because you haven’t got the buy-in at the top to make the changes necessary. Conversely, if it’s all being fed down and the bottom aren’t engaged, they don’t participate and they don’t change their behaviours.
KI2
Senior management ‘buy-in’ included encouraging managers to participate in the intervention, perhaps ensuring that there was protected time for managers to engage with the intervention, engaging with the findings of the research and having a commitment to addressing the implications of study findings. Although the GEM study team put in a considerable amount of time and resources to try and ensure that senior management were on board in this way, and initially they seemed to be, by the end of the study it was felt that the initial support shown had not been sustained. The facilitator noted that at facilitator-led follow-up meetings for managers:
. . . there was an overwhelming feeling that there was a lack of senior management commitment to the program and the organisation had not supported them to do the e-learning as had been promised.
The facilitator (who had experience of similar initiatives in other organisations) reflected that:
. . . this is quite the norm in health and well-being programmes. They are often introduced to tick the boxes and are not followed through as recommended in good practice. Even when senior managers mean well programmes do not get the support that is initially agreed as other priorities take over.
There was also a disappointing turnout at the final dissemination meeting at the trust, with only two senior managers in attendance. We found it difficult to schedule interviews with senior managers at the trust and some interviews were brief and rushed. One senior manager reflected that arguably more could have been done to encourage greater engagement in the study:
We need to do more on selling it. So that lead-in stuff, although we did those briefings, and I was part of the briefings . . . with hindsight I think I’d do more. I think there’s a bit about how we then sell the management interest bit, ‘cos I think probably where we have not helped you . . . I think is there’s not been enough sort of day-to-day senior management attention to it and encouragement of it.
KI10
Some managers expressed cynicism about the trust’s motives for taking part in the study and concern that the trust could be seen as shifting responsibility for its duty of care to employees on to managers. Some voiced concerns about whether the trust would ignore or act on their comments or on the wider findings of the study:
I think the one thing I’d like to say is . . . I’d love to feel that senior management and the trust board and everyone do really look at this and see what comes out of it because I feel it will, like most other things, fall on deaf ears. But it would be really nice to feel that they do engage with the whole process and they do listen to some of the things their managers are saying . . . It would be nice to think the trust would embrace it as part of the core training for managers because I think managers, until fairly recently at least, in their training they were really just looking at policies and procedures, there was nothing really to do with the human resources, the people they were expected to manage. And all these human issues that do come up. Now anything like this should be trying to restore some or at least achieve some balance because really it’s the people in an organisation that is the main resource isn’t it?’
M3, feedback meeting
At the facilitator-led meetings for managers, in addition to expressions of cynicism, additional reassurances were sought that no individual’s views would be identifiable from the data, arguably reflecting a certain degree of anxiety and mistrust of senior management.
Views on e-learning
A central feature of the intervention was its primary mode of educational delivery: e-learning. Originally, the stress management course developed by APP consisted of a 2-day, face-to-face event. APP reported that, as a solution to organisations increasingly asking for more material to be included in less time, they developed e-learning modules, with the intention of delivering them alongside facilitated face-to-face meetings as part of a ‘blended learning’ package.
In the case of the GEM study, the face-to-face element consisted of two facilitator-led meetings that took place in October and December 2013. The first ‘induction’ meeting was held before the managers started the e-learning intervention and the second ‘follow-up’ meeting took place after the managers had completed a number of the modules. Further details of these meetings can be found in Chapter 3 and Appendix 3.
In general, managers were ambivalent about e-learning as a mode of educational delivery. On the one hand they identified certain advantages: the flexibility of when, where and at what pace to study and the ability to return to material:
And that flexibility, and it’s the direct stuff. I think the trouble with face to face, you might be having an off day or something like that, and you’ve trudged along to something and you’ve not really derived as much as you could out of it. And there isn’t really any time to go back, you can’t rewind and go through it again, can you? So I think the medium was very good, the presentation was good, it was nicely, clearly done.
M7
At the same time, e-learning was thought to be not as ‘engaging’ or as ‘real’ an experience as face-to-face learning. One key informant (KI1) suggested that e-learning can easily become a ‘a “click-click-click-click” exercise’ and this view was evident in some managers’ reservations about e-learning. Furthermore, the advantage of flexibility was sometimes seen as a disadvantage:
I do like the e-learning but if you go on a training session, face to face, then you’re taken away from the environment, aren’t you? You’re taken out and you’ve got that time – that dedicated time – to learn. Whereas doing it e-learning it’s easy to just get distracted.
M10
The ambivalent views expressed by managers towards e-learning echoed those of the GEM developer:
My view is that e-learning’s got the advantage you can go back as many times as you want; you can learn the stuff and you can do it in your own time, and it’s cheaper and it’s quicker. But it’s not as good in my view as face to face because people need to talk, they need to learn and support each other.
KI13
Most managers favoured a ‘blended’ approach, with more emphasis on face-to-face learning than had been the case with the guided e-learning intervention:
I think a lot of the content of it, I think if we’re looking at people trying to develop and learn, should be done face to face and then perhaps followed up by the e-learning package, almost to sort of consolidate your knowledge rather than learn it. Because it’s very different, isn’t it, learning how to recognise signs in people than it is to actually see it and you know I don’t know how you’d do it face to face, but I think people would get a lot more out of it when they’re learning how to do the job, face to face.
M5
To me it would have been nice to do the initial meeting, go away and do two modules and then get together and kind of have a brief discussion.
M8
In this sense, some managers saw e-learning not so much as a replacement for face-to-face learning but as a supplement to it. Those managers who attended the study induction and follow-up meetings with the facilitator were positive about the benefits of meeting face to face in a group. The meetings provided a forum in which managers could engage in discussion with other managers. Some managers reported working in isolation from others at a similar grade and it was reassuring for them to hear that their colleagues were experiencing similar pressures and confronting similar issues at the trust. They had also found it useful to hear others’ views of the e-learning program:
And it was quite good to hear the other people in the room were having similar things, similar issues, similar thoughts, similar concerns. And it was good to express those concerns, I suppose, in a safe environment with no people higher up from myself looking down on you and judging you. So from that perspective, it was quite . . . it felt like a safe environment, just to discuss openly some of the issues that as managers we were concerned about and had raised.
M8
A key informant reflected on the beneficial effect of this shared learning experience:
So what the intervention is facilitating is networking, which could have good effects on the managers’ well-being which in turn leads to well-being effects for the employee [but] in a sense, disentangling that from the actual e-learning intervention would be quite hard to do.
KI6
Reflections on the guided e-learning intervention as an approach to improving employee well-being
The qualitative study elicited a range of reflections about the extent to which the guided e-learning intervention might be expected to ‘work’ as an approach to improving employee well-being.
Embedding the intervention into organisational culture and processes
First, there was the widespread view that interventions such as this one need to be embedded into wider organisational processes and an overall culture of staff development. This view was most clearly expressed by a key informant who had undertaken research in the field:
The package shouldn’t be a ‘one-shot’ deal. There should be follow-up conversations with the managers of the managers, building this into a development process. Any kind of management development needs to be integrated into other initiatives so that it’s not seen as a bolt-on or standalone. It needs to be seen as integrated and woven into a broader process of managing well-being and of developing managers, and that it’s built into all the other HR processes, so performance management and development actually include the review of ‘How did you get on on that course?’ ‘What did you learn?’ ‘Are you integrating it?’ ‘What’s the next step?’ ‘How are you implementing things?’
KI14
A senior manager in the trust echoed this viewpoint. She spoke of the need for a ‘coaching culture’ within which managers could develop their management skills:
Anything we do needs to be linked together with a coaching culture that comes with it and where it becomes the norm that you actually refer to the online module, where it becomes a norm that you actually ask for help and support with a coaching element . . . . And any other training with the managers that’s happening all needs to come together so that as a manager, whether I’m newly appointed, whether I’m halfway through, whether I’m coming to the end, whatever, I can look at that part and think, right okay, which one of those do I need to either refresh myself with, or do I need to have a look at that?
K12
These reflections relate to the views reported above about the need for more ‘buy-in’ from senior management, suggesting that a limitation of the intervention was that too often it was seen as a ‘one-shot’ deal, a standalone initiative rather than fully integrated into organisational processes and practice.
Offering the intervention to a wider group of staff
A number of respondents reflected on the decision to target the intervention at ‘band 7′ middle managers. Some suggested widening its availability to more senior managers ‘right up to chief executive level’ and to more junior staff who may be about to have some managerial or supervisory responsibilities. There was also a viewpoint that perhaps those who could most benefit from the intervention were those who did not take up the offer of it.
The tension between ‘blinding’ trial participants and the e-learning program’s interactive learning activities
The GEM study design involved ‘blinding’, that is managers who received the intervention were instructed not to tell their employees that they were participating in the trial. The rationale behind this was to reduce the bias that could be induced in employees’ responses to questions on well-being and their work environment at follow-up if they knew that their managers were taking part in the intervention. Interviews with employees indicated that blinding had mostly worked and that employees were unaware of their manager’s involvement (or not) in the study, although one employee reported that her manager had explained that she was being ‘trained up to manage stress with people better’ and the questionnaire was ‘part of her evaluation’ (E8). In one or two cases managers revealed that they had told their employees that they were participating in the study and in other cases, although the managers had not explicitly informed their employees that they were taking part, they indicated that some members of their teams had suspected that they were involved with the study:
The few in the team that signed up to do it knew that I’m doing something because obviously I had to give them the paperwork to sign up to do the course with me. I’ve never reminded them again that I’m doing it. Some know what it’s about. One of the lads actually said to me the other day, ‘Do you know why I keep getting e-mails off this flaming GEM place? What do they want?’ And I laughed and he went, ‘Ah . . . it’s about you, isn’t it?’ And I went, ‘Yeah’ and he went, ‘Oh, I’ll do it. I’ll do it’. He thought it was some staff survey that he wasn’t going to participate in.
M6
Alongside the trial requirements for blinding, the e-learning materials included activities to prompt managers to discuss aspects of their learning with their employees and to ask for feedback on their management style. One activity asked managers to conduct a ‘stress survey’ with their employees to identify and discuss problems and to work together to find solutions. Specifically, the activity encouraged managers to discuss the results of the survey and the causes of stress in the workplace at a team meeting. None of our respondents commented on this potential tension between the demands of the trial and suggested learning strategies, although in the facilitator-led meetings one manager mentioned that, when she had asked an employee how she felt about something, the employee asked if the manager was asking because she was in the study! The facilitator reflected that, in her view:
. . . it is impossible to carry out the research without employees knowing some managers are taking part, and if they behave differently it is possible that their motivation will be perceived as due to the study rather than concern.
How a short educational intervention might change attitudes and behaviour
The theory of change underpinning the GEM study was that the guided e-learning intervention would lead to changes in managers’ knowledge, attitudes and behaviour, which would impact on the well-being of their employees. In our qualitative interviews we tried to capture examples of managers ‘putting the intervention into practice’, in other words, examples of how they had applied their learning from the intervention to support employees’ well-being. However, we found that in practice when managers spoke about instances of managing employee stress they drew broadly on ‘experiential knowledge’ rather than isolating any specific learning that they could attribute to the guided e-learning intervention.
Some scepticism was expressed about the extent to which a guided e-learning intervention might be expected to impact on entrenched attitudes and beliefs:
There are some old style managers who think stress is a weakness, all that rubbish, that type of thing. And I don’t know, I don’t think your module is going to address that, they’ve already probably seen what you’re talking about, I think that’s people’s beliefs and attitude and that needs to be addressed in a different way.
M4
A viewpoint that emerged during the study from key informants and members of the study team was that arguably the short timescale of the GEM study militated against the likelihood of observable effects of the intervention:
. . . the big question is whether the e-learning package would induce long-lasting changes in the managers, behaviour change. We’re talking about behavioural change and the vast literature on behavioural change says it’s a slow process.
KI6
Managers similarly expressed some concerns about the timescales of the study. At a preliminary meeting to introduce the study to managers, one commented: ‘The period between the intervention and the second data collection is very short. How are we expected to implement things?’ (field notes from observation of preliminary meeting to launch study, April 2013).
Chapter 5 Health economics evaluation
Methods
Microcosting of the Guided E-learning for Managers intervention
A microcosting of the e-learning education program for managers included a bottom-up construction of the costs associated with setting up and delivering the program. The intervention consisted of three parts: an initial introductory session with managers followed by self-learning and a review meeting. The course running costs included the facilitator’s wages and travel expenses, the managers’ salaries and travel expenses, administration costs (administrator’s and meeting organisers’ salaries), the software licence fee and telephone/internet costs. Organisation overheads were not included. The cost of the intervention also included the cost of training the facilitator, who attended a 2-day course conducted by the developer of the e-learning program. Facilitator training costs included the trainer’s wages, the facilitator’s wages and facilitator travel and subsistence costs. The costs of the training facilities (venue and computers) were not included as these were provided by the trust. Microcosting also excluded costs associated with piloting the intervention (e.g. study-related consultations, qualitative research, study-specific modifications of the e-learning program).
Cost of the intervention per participant
The estimated cost of the intervention per participant (manager and employee) was based on two numbers: the number of managers randomised to the intervention group (n = 49) and the lowest number of managers who participated in any one of the three parts of the intervention (n = 18). For the purposes of analysis it was assumed that each manager supervised seven employees (341 consented employees divided by 49 managers). The average cost per participant (manager and employee) was estimated with and without facilitator training.
Sickness absence
Data on sickness absence of employees over the 3-month period were collected at baseline and follow-up. Self-reported sickness absence data were extracted from employees’ questionnaires whereas HR-reported sickness absence data were provided by the trust/social services along with the pay scales of employees. Both self-reported and HR-reported sickness absences were costed using the friction cost method. 59
Use of health-care services by participants
Data on the use of health-care services by employees over the past month were extracted from self-completed questionnaires at baseline and follow-up. These included the number of contacts with a GP, a nurse and other specialists as well as outpatient attendances, inpatient stays and accident and emergency (A&E) admissions. Questions were also asked about the number of medicines taken by employees over the past month. Individual-level resource use data were combined with unit costs to calculate the total cost of health service use for each participant. The use of health-care services was costed using the Unit Costs of Health and Social Care 2012. 60 Unit costs that were not available from this source were obtained from NHS Reference Costs 2012–13. 61 Tests and investigations were costed using the NHS Reference Costs 2012–13, direct access diagnostic and pathology services. 61 The average unit costs (all NHS trusts) were used given that there was insufficient information about the types of outpatient and inpatient appointments. The unit costs used for costing health-care services use are shown in Appendix 5.
Health-related quality of life
Health-related quality of life was measured at baseline and follow-up using the European Quality of Life-5 Dimensions three-level version (EQ-5D-3L). The EQ-5D-3L measure is recommended by the National Institute for Health and Care Excellence62 and aims to measure the extent of problems across the domains of mobility, self-care, usual activities, pain/discomfort and anxiety/depression, using three levels (no problems, moderate problems and severe problems).
Data analysis
Data analysis was conducted using Microsoft Excel 2012 (Microsoft Corporation, Redmond, WA, USA) and Stata version 12.1 on an intention-to-treat basis using a non-imputed data set. Two estimates of sickness absence were considered: one based on self-reported data and the other on HR-reported sickness absence. HR-reported data contained sickness absence data outside the 3-month period, which were removed from the analysis. HR-reported sickness absence was costed using the Agenda for Change pay scale 2013/14 (provided by the participating NHS trust) and the social services pay scale 2013 (provided by three local authorities). Self-reported sickness absence was costed using the pay scale indicated by the employees in the follow-up questionnaire. A mid-range salary was assumed for estimating the cost of employment.
Two estimates of intervention costs were used in the economic analysis: one based on the number of managers randomised to the intervention group (n = 49) and the other based on the lowest number of managers who participated in any one of the three parts of the intervention (n = 18).
Data on the use of health-care services over 1 month were extracted from the employee questionnaires. Unit costs were assigned to each service category and multiplied by the number of contacts.
The EQ-5D-3L domain scores were converted to preference-based scores. EQ-5D-3L scores at baseline and follow-up were then aggregated to estimate the total quality-adjusted life-years (QALYs) for each participant using the area under the curve method (trapezoid).
Results
Microcosting of the Guided E-learning for Managers intervention
The intervention was delivered in the form of an e-learning education program for managers provided as part of a CPD process. The intervention was conducted by a freelance facilitator who was trained by the developer of the e-learning program. The study randomised the intervention to three clusters – groups of managers and those employees who they supervised. The e-learning package was applied to the whole cluster simultaneously. The intervention consisted of an initial introductory session with managers followed by self-learning and a review meeting. The facilitator also provided support to managers by e-mail and telephone.
Costs included in the costing of the intervention were:
-
the trainer’s wages
-
the facilitator’s wages
-
the managers’ salaries
-
the meeting organisers’ salaries
-
the administrator’s salary
-
the facilitator’s travel costs including overnight accommodation and subsistence
-
the software licence fee
-
telephone costs.
Costs excluded from intervention cost were:
-
costs associated with piloting the intervention (e.g. study-related consultations, qualitative research, adaptation of the e-learning software)
-
costs of the venue and computers (provided by the trust).
In total, 49 managers were randomised to the intervention group. One manager was ineligible, one refused and six did not reply to the invitation to take part. Nevertheless, given that employees supervised by these managers participated in the study, they were included in the analysis. Therefore, our analyses are based on 49 managers. In total, 26 managers attended the introductory meeting and 18 managers attended the review meeting. E-learning was initiated by 31 managers. One manager withdrew half-way through the e-learning program and therefore was not included in the costing. Five managers did not engage with the intervention at any stage.
It was assumed that managers were released from work to attend the introductory session and the review session (0.5 days each session), as well as to undertake e-learning (4 hours as suggested by the program developer). The average travel cost to attend the training sessions was assumed to be £10 per day.
The trainer’s and facilitator’s wages and other intervention-related expenses were based on invoices. Managers’ salaries were based on the NHS Agenda for Change pay scale 2013/14. Most managers were at band 7. As obtaining managers’ pay scales was not feasible, a mid-range salary was assumed. The meeting organisers’ salaries were estimated at band 6 (mid-range). The administrator’s salary was calculated using the Queen Mary University of London pay scale 2013 grade 5 (mid-range). To all salaries were added 24% on-costs (including pension and employer’s National Insurance contribution). 60 The itemised intervention costs and their sources are listed in Table 20.
| Expenditure type | Cost (£) | Description | Reference |
|---|---|---|---|
| E-learning course | |||
| Salaries/wages | |||
| Facilitator | 3500.00 | Six face-to-face sessions plus e-mail and telephone support | Invoice |
| Managers (group course) | 3718.54 | 2 × half-days (26 managers first meeting, 18 managers second meeting) | NHS Agenda for Change pay scale 2013/14, band 7 mid-range |
| Managers (self-learning) | 2704.39 | 4 hours, 30 managers (six withdrawn, five did not engage) | NHS Agenda for Change pay scale 2013/14, band 7 mid-range |
| Meeting organisers (trust) | 188.73 | 10 hours | NHS Agenda for Change pay scale 2013/14, band 6 mid-range |
| Administrator (university) | 733.99 | 30 hours | Queen Mary University of London pay scale 2013, grade 5 mid-range |
| Subtotal (salaries/wages) | 10,845.65 | ||
| Facilitator’s travel costs (including overnight accommodation and subsistence) | 1088.40 | Three courses, 6 days | Invoice |
| Managers’ travel costs | 440.00 | 2 days (26 managers first meeting, 18 managers second meeting) | Assumption £10 per day |
| Software licence | 5000.00 | 50 users | Licence fee |
| Administration (e-mails, telephone calls) | 30.00 | SIM card, top-up | Invoice |
| Subtotal (course) | 17,404.05 | ||
| Facilitator training | |||
| Salaries/wages | |||
| Trainer | 1500.00 | 3 days (2 days of facilitator training + 1 day of support to facilitator during the intervention) | Invoice |
| Facilitator | 2000.00 | 2 days of training and 2 days of familiarisation with the intervention and preparation of the manager training sessions | Invoice |
| Subtotal (salaries/wages) | 3500.00 | ||
| Facilitator’s travel costs (including subsistence) | 58.60 | 2 days | Invoice |
| Subtotal (training) | 3558.60 | ||
| Total cost of intervention | 20,962.65 | ||
The total cost of the intervention was £20,963, of which £17,404 was the cost of running the course and £3559 was the cost of training the facilitator.
More than two-thirds of the total running costs were wages/salaries (£14,346), which included payments to the facilitator and program developer and managers’ salaries (who were released from work to undertake the training). The second highest category of costs was the software licence fee (£5000).
Cost of the intervention per participant
The cost of the intervention was estimated both per manager and per employee, reflecting the fact that the intervention was delivered to managers and sickness absence data were collected for employees. Given that the intervention consisted of several parts with different numbers of managers involved, our estimations of cost per participant were based on two figures: the number of managers randomised to the intervention group (49 managers supervising 349 employees) and the lowest number of managers who attended any one of the three parts of the intervention (18 managers supervising 125 employees). Costs are shown with and without the costs of facilitator training to reflect the fact that, having been trained, the facilitator can deliver courses to a larger number of managers. The costs of the intervention per participant are shown in Table 21. Depending on the assumptions made, the cost of the intervention per manager varied from £494 to £1062, which translates into a cost per employee of £71–153.
| Costing scenario | No. of participants | Cost per participant (£) |
|---|---|---|
| Cost per manager | ||
| Including facilitator training | 49 | 566.92 |
| Excluding facilitator training | 49 | 494.30 |
| Including facilitator training | 18 | 1062.49 |
| Excluding facilitator training | 18 | 864.79 |
| Cost per employee | ||
| Including facilitator training | 341 | 81.46 |
| Excluding facilitator training | 341 | 71.03 |
| Including facilitator training | 125 | 152.67 |
| Excluding facilitator training | 125 | 124.27 |
Description of the health economics data set
Health economics data were derived from two sources: a self-completed questionnaire and HR-reported sickness absence data. Health economics questionnaires were completed by 347 employees at baseline (intervention n = 280, control n = 67) and 291 employees at follow-up (intervention n = 231, control n = 60). HR data were requested for 417 employees (intervention n = 336, control n = 81). The completeness of the health economics data set is shown in Table 22. Completeness varied from 61% to 94%, with higher proportions of missing data at follow-up. The largest proportion of missing data related to medication use as employees preferred not to answer the question about their medication use.
| Data set | Baseline | Follow-up | ||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (n = 341) | Control (n = 83) | Intervention (n = 341) | Control (n = 83) | |||||
| n | % | n | % | n | % | n | % | |
| HR-reported sickness absence | 320 | 94 | 73 | 88 | 320 | 94 | 73 | 88 |
| Self-reported sickness absence | 269 | 79 | 62 | 75 | 222 | 65 | 55 | 66 |
| Health-care services use | 226 | 66 | 67 | 81 | 228 | 67 | 59 | 71 |
| Medication use | 252 | 74 | 61 | 73 | 208 | 61 | 55 | 66 |
| EQ-5D-3L | 275 | 81 | 67 | 81 | 228 | 67 | 59 | 71 |
| EQ-5D-VAS | 272 | 80 | 67 | 81 | 229 | 67 | 59 | 71 |
Sickness absence
Human resources- and self-reported sickness absence and associated costs are shown in Tables 23 and 24 respectively. The tables show the average number of sickness days per employee in the intervention and control groups at baseline and follow-up. There were no significant differences in sickness absence between the intervention and control groups at either baseline or follow-up, although the average number of sickness days was higher at follow-up in both groups. The cost of HR-reported sickness absence was marginally higher in the intervention group than in the control group; however, this difference in cost was not statistically significant. Self-reported sickness absence was lower than HR-reported sickness absence. There may be several reasons for this discrepancy: (1) an unwillingness of employees to provide data on sickness absence; (2) problems with recall of the number of sickness days; and (3) employees being on sick leave at the time of completion. We therefore used HR-reported sickness absence data in the cost-offset analysis.
| Sickness absence | Intervention (n = 320) | Control (n = 73) | Difference in means | SE | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Days off work | ||||||
| Baseline | 2.41 | 8.53 | 2.26 | 7.44 | 0.15 | 1.08 |
| Follow-up | 4.44 | 13.36 | 4.47 | 15.56 | –0.03 | 1.79 |
| Cost (£) | ||||||
| Baseline | 339 | 1694 | 282 | 1038 | 57 | 207 |
| Follow-up | 512 | 1505 | 471 | 1745 | 41 | 201 |
| Sickness absence | Intervention | Control | Difference in means | SE | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Days off work | ||||||
| Baseline (intervention n = 269, control n = 62) | 1.86 | 7.06 | 2.68 | 11.86 | –0.82 | 1.15 |
| Follow-up (intervention n = 222, control n = 55) | 3.38 | 11.41 | 4.05 | 14.24 | –0.67 | 1.81 |
| Cost (£) | ||||||
| Baseline (intervention n = 268, control n = 62) | 241 | 1118 | 375 | 1956 | –134 | 185 |
| Follow-up (intervention n = 219, control n = 55) | 330 | 1385 | 412 | 1190 | –82 | 203 |
Cost of health-care services
The use of health-care resources by employees was analysed at baseline and follow-up. Table 25 shows the average monthly number of contacts with primary and secondary health-care services and the use of medication by employees over 1 month. On average, there were 1–1.5 contacts with health-care services per month in this population group. There were no significant differences in the use of health-care resources by participants between the intervention group and the control group. Approximately half of the employees in the intervention and control groups did not take any medication. The average number of medicines used by employees was slightly lower in the intervention group than in the control group both at baseline and follow-up, although these differences were not significant. Given that employees did not provide sufficient information on the formulation and dosage of medicines, we were unable to estimate the cost of medication. It should be mentioned that the average medication use was low in this population group, reflecting the fact that this group was taken from the general working population.
| Service/medication use | Baseline | Follow-up | ||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (n = 277) | Control (n = 67) | Intervention (n = 228) | Control (n = 59) | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Service | ||||||||
| GP | 0.65 | 1.55 | 0.63 | 0.93 | 0.56 | 1.20 | 0.64 | 1.57 |
| Nurse | 0.21 | 1.01 | 0.18 | 0.39 | 0.14 | 0.53 | 0.05 | 0.22 |
| Other specialist | 0.54 | 1.54 | 0.52 | 3.09 | 0.49 | 2.52 | 0.24 | 0.90 |
| Inpatienta | 0.03 | 0.26 | 0 | 0 | 0.07 | 0.41 | 0.05 | 0.22 |
| Day casea | 0.03 | 0.18 | 0.02 | 0.12 | 0.04 | 0.21 | 0 | 0 |
| A&Ea | 0.04 | 0.20 | 0 | 0 | 0.03 | 0.17 | 0.02 | 0.13 |
| Intervention (n = 252) | Control (n = 61) | Intervention (n = 208) | Control (n = 55) | |||||
| n | % | n | % | n | % | n | % | |
| Medicines | ||||||||
| No medicines | 147 | 58 | 33 | 54 | 115 | 55 | 26 | 47 |
| One medicine | 39 | 15 | 11 | 18 | 49 | 24 | 16 | 29 |
| Two medicines | 28 | 11 | 5 | 8 | 25 | 12 | 7 | 13 |
| Three medicines | 19 | 8 | 8 | 13 | 9 | 4 | 3 | 5 |
| More than three medicines | 19 | 8 | 4 | 7 | 10 | 5 | 3 | 5 |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Average number of medicines per person | 0.98 | 1.50 | 1.08 | 1.55 | 0.84 | 1.26 | 0.93 | 1.15 |
Resource use data were combined with unit costs to calculate the costs of health-care services over 1 month. The costs of health-care services used by participants are summarised in Table 26. The largest proportion of costs was associated with outpatient consultations; this was followed by GP consultations. The average total cost of health-care services was higher at follow-up than at baseline in both the intervention group and the control group. However, these differences were not statistically significant.
| Service | Baseline (£) | Follow-up (£) | ||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (n = 277) | Control (n = 67) | Intervention (n = 228) | Control (n = 59) | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| GP | 27 | 63 | 26 | 38 | 23 | 49 | 26 | 64 |
| Nurse | 5 | 22 | 4 | 8 | 3 | 11 | 1 | 5 |
| Other specialist | 47 | 153 | 42 | 273 | 41 | 182 | 56 | 275 |
| Inpatienta | 15 | 158 | 0 | 0 | 40 | 248 | 31 | 134 |
| Day casea | 18 | 124 | 10 | 85 | 24 | 144 | 0 | 0 |
| A&Ea | 5 | 23 | 0 | 0 | 4 | 20 | 2 | 15 |
| Total cost | 122 | 328 | 84 | 293 | 139 | 496 | 117 | 394 |
Health-related quality of life
The health-related quality of life of employees was compared using both the EQ-5D-3L descriptive system and the visual analogue scale (VAS) (Table 27). The average EQ-5D-3L score derived from the descriptive system ranged between 0.85 and 0.89, which is comparable with the UK national norms for the EQ-5D. 63 There was a slightly higher health-related quality of life in the intervention group than in the control group when measured using the EQ-5D descriptive system. In contrast, the VAS showed slightly higher values in the control group than in the intervention group. None of these differences was statistically significant.
| EQ-5D score | Intervention | Control | Difference in means | SE | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| EQ-5D-3L | ||||||
| Baseline (intervention n = 275, control n = 67) | 0.8873 | 0.1373 | 0.8700 | 0.1953 | 0.0172 | 0.0205 |
| Follow-up (intervention n = 229, control n = 59) | 0.8778 | 0.1761 | 0.8519 | 0.2132 | 0.0259 | 0.0269 |
| Total QALYs (intervention n = 228, control n = 59) | 0.2205 | 0.0335 | 0.2156 | 0.0477 | 0.0049 | 0.0054 |
| EQ-5D-VAS | ||||||
| Baseline (intervention n = 272, control n = 67) | 80.53 | 15.40 | 80.69 | 14.95 | –0.16 | 2.09 |
| Follow-up (intervention n = 228, control n = 59) | 77.73 | 17.95 | 78.08 | 16.87 | –0.35 | 2.59 |
Complete EQ-5D-3L data (baseline and follow-up) were obtained for 229 participants in the intervention group and 59 participants in the control group, which enabled the calculation of QALYs. The mean total QALYs were marginally higher in the intervention group than the control group, although there was a high degree of uncertainty around these estimates.
The EQ-5D-3L health profiles were constructed for five domains (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) (Table 28). There was a small decrease in the proportion of employees who experienced moderate anxiety/depression following the introduction of the intervention.
| EQ-5D domains | Baseline | Follow-up | ||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (n = 275) | Control (n = 67) | Intervention (n = 229) | Control (n = 59) | |||||
| n | % | n | % | n | % | n | % | |
| Mobility | ||||||||
| I have no problems in walking about | 257 | 93 | 61 | 91 | 216a | 95 | 53 | 90 |
| I have some problems in walking about | 18 | 7 | 6 | 9 | 12a | 5 | 6 | 10 |
| I am confined to bed | 0 | 0 | 0 | 0 | 0a | 0 | 0 | 0 |
| Self-care | ||||||||
| I have no problems with self-care | 275 | 100 | 67 | 100 | 226a | 99 | 59 | 100 |
| I have some problems washing or dressing myself | 0 | 0 | 0 | 0 | 2a | 1 | 0 | 0 |
| I am unable to wash or dress myself | 0 | 0 | 0 | 0 | 0a | 0 | 0 | 0 |
| Usual activities (e.g. work, study, housework, family or leisure activities) | ||||||||
| I have no problems with performing my usual activities | 245 | 89 | 59 | 88 | 206 | 90 | 50 | 85 |
| I have some problems with performing my usual activities | 29 | 11 | 8 | 12 | 22 | 10 | 9 | 15 |
| I am unable to perform my usual activities | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Pain/discomfort | ||||||||
| I have no pain or discomfort | 187 | 68 | 45 | 67 | 158 | 69 | 40 | 68 |
| I have moderate pain or discomfort | 86 | 31 | 20 | 30 | 68 | 30 | 17 | 29 |
| I have extreme pain or discomfort | 2 | 1 | 2 | 3 | 3 | 1 | 2 | 3 |
| Anxiety/depression | ||||||||
| I am not anxious or depressed | 196 | 71 | 50 | 75 | 168a | 74 | 43 | 73 |
| I am moderately anxious or depressed | 79 | 29 | 15 | 22 | 58a | 25 | 13 | 22 |
| I am extremely anxious or depressed | 0 | 0 | 2 | 3 | 2a | 1 | 3 | 5 |
Cost-offset analysis
Cost–benefit analysis included two estimates of average intervention costs (£81 and £153) per employee (reflecting variation in the numbers of managers involved in the different parts of the intervention) and the average HR-reported sickness absence over 3 months at follow-up. The results of the cost-offset analysis are summarised in Table 29. The estimated net cost was more negative in the intervention group than in the control group for both intervention costs (£81 and £153). Analyses indicated that the intervention did not have a positive impact on the net cost.
| Costs and benefits | Intervention (£), mean (SD) | Control (£), mean (SD) | Difference (£), mean (SE) |
|---|---|---|---|
| Costs | |||
| Intervention £81 | 81 | 0 | 81 |
| Intervention £153 | 153 | 0 | 153 |
| Benefits | |||
| HR-reported sickness absence | –512 (1505) | –471 (1745) | –41 (–201) |
| Net benefit | |||
| Net cost (intervention £81) | –593 | –471 | –122 |
| Net cost (intervention £153) | –665 | –471 | –194 |
Chapter 6 Discussion
Introduction
In this chapter we explore the implications of our results, interpret the findings and suggest future research directions. Specifically, we revisit each of the study objectives (to test the acceptability of the trial and intervention, the feasibility of recruitment and participation, the components of the intervention, adherence to the intervention and the likely effectiveness of the intervention) and identify what we have learned from the pilot study. We also review what we have learnt from the health economics evaluation, identify and reflect on the limitations of the study and present recommendations for taking the research forward.
What did we learn about the acceptability of the trial and intervention?
The study set out to assess the acceptability of the trial and the intervention by eliciting the views of managers and employees. As stated in Chapter 2, a limitation of the qualitative sample was that it included only one manager from the ‘non-adherent’ group of managers. Furthermore, as consent had not been gained for this purpose, we were unable to approach managers in the trust who did not participate in the study, although their views would have been of interest. We found that the trial and intervention were acceptable to those employees and managers who participated: no respondent identified any aspect of the research that they found unacceptable and many respondents made positive comments about the conduct of the trial and the intervention itself, as described in Chapter 4. Arguably, a further indicator of the acceptability of the trial to employees was the high retention rates achieved in the questionnaire survey (see following section).
We suggest that the construct of acceptability, although widely used in trials, has in fact limited meaning and value in that it artificially reduces complex phenomena to a unidimensional ‘yes’/‘no’ variable. In keeping with the study protocol and objectives we have reverted to using the term ‘acceptability’ to convey that none of our respondents found the intervention ‘unacceptable’; however, our narrative methodology enabled us to paint a much richer and more nuanced picture of respondents’ experiences of the intervention.
What did we learn about the feasibility of recruitment to the trial and participation in it and the feasibility of data collection?
Our study supported the feasibility of recruitment to the trial. We met recruitment targets for both employees and managers, although achieving this proved to be a resource-intensive process, as we expected. Recruitment was greatly aided by being able to use the onsite trust research team to approach participants. Many employee teams required several visits during the recruitment phase of the study for recruitment targets to be reached. Making contact with employees was not straightforward – teams were spread over a large geographical area, reflecting the dispersal of trust services, many employees worked off site and recruitment meetings were attended only by some staff. This may have resulted in reduced levels of recruitment.
Recruitment of employees took longer than expected and this meant that to keep within the time frame of the study not all employees could be recruited before the clusters needed to be randomised; however, we mitigated this by keeping staff who recruited employees blinded to the allocation.
We found no evidence of recruitment bias among employees in terms of gender and part-time working; however, compared with all trust employees, the study population was slightly younger. In terms of employee participation in the trial, there was a fall-off in the participation of employees between consent and baseline questionnaire completion, but a high retention rate between the initial questionnaire and follow-up. This was achieved by sending frequent e-mail reminders to employees to complete the online questionnaire and giving employees the option to complete a paper version of the questionnaire, which some chose to do.
There was good initial recruitment of managers: 41 out of 49 managers who were approached agreed to take part in the study. It appears that some groups of managers were nominated by senior managers to take part in the trial.
In terms of manager participation in the trial, a sizeable number dropped out at the very beginning of the study (between recruitment and the beginning of the e-learning intervention) and disappointingly only half of the managers completed three or more modules of the e-learning intervention (see What did we learn about adherence to the intervention?). Attendance at the facilitator-led induction meeting was good (with almost two-thirds of managers participating) but attendance dropped to just over 40% for the follow-up meeting. Only three managers attended the qualitative focus group, again a lower than expected level of participation.
We found some evidence that the managers who were more engaged with the study in the sense of completing more of the e-learning program were managing employees who had higher employee well-being scores both at baseline and at follow-up. One interpretation of this finding is that the group of managers who were more ‘effective’ at managing stress in their employees were more likely to participate in the study. It could also be the case that in some settings stress levels were very high, employee well-being levels were low and the managers were too stressed to complete the intervention. This latter group is a group who we would like to have engaged as they might have particularly benefited from the intervention. It is notable that levels of psychological distress were high among employees from both the intervention group and the control group compared with the rate in the general population.
Our findings on recruitment and participation need to be interpreted within the wider context described in Chapter 4: considerable organisational change and uncertainty within the trust, resulting in particular pressures on staff time and resources. Arguably this context made staff less responsive to additional demands on their time, such as the invitation to participate in the study. Furthermore, we found evidence of low levels of trust between staff and senior management and cynicism about the trust’s motivation for participating in the study. Participants also asked for reassurance that the research was unconnected to any internal trust monitoring and that the findings would be anonymised. These could perhaps have been factors affecting staff willingness to be involved in the study.
As noted elsewhere in this report, a mental health trust was a very particular organisation within which to undertake a study of stress and well-being. It could be argued that those working in the field of mental health would be more likely to be interested in our study, which would have helped with recruitment and participation; conversely, it could be argued that familiarity with mental health issues may mean that staff were less interested in joining the study, as they may feel that they know about most of the issues around work stress already.
We found that it was feasible to collect sickness absence data using the trust HR systems and that it was also feasible to obtain sickness absence data from social services when employees were employed by social services rather than the trust. We also found that it was feasible to collect data to carry out economic analyses using questionnaire results from employees, although as the employees largely consisted of a healthy population it may not be profitable to examine health service use as an outcome in a further study of a similar population.
Apart from members of our steering group, patient and public involvement involved discussion with managers and employees before the study and also two meetings to feed back our results to employees and managers after the study. Our study had no ‘patients’; instead, our participants to whom the results might be generalised were employees and managers working for the same organisation. In workplace studies the relevant portion of the general public to whom the study results are relevant are employees; hence, engagement with the wider general public would be less meaningful.
What did we learn about the components of the intervention?
We considered the components of the intervention in terms of the different modes of delivery of the educational intervention (e-learning, face-to-face meetings and telephone and e-mail support from a facilitator) and the content of the educational intervention.
We found that the managers who we interviewed were ambivalent about e-learning as a mode of educational delivery (and, as reported in Chapter 4, these managers had all completed three or more modules and so arguably were likely to be more positive about e-learning than those who engaged less). Managers identified both benefits and limitations of e-learning; most favoured a ‘blended’ approach, with more emphasis on face-to-face learning than had been the case with the guided e-learning intervention. There was a strong sense that managers liked hearing from each other at the face-to-face meetings, both about their experiences of the intervention and more widely about the problems of managing stress at work, and found this shared learning experience supportive. Managers made no use of the telephone and e-mail support offered by the facilitator, perhaps suggesting that this is an unnecessary component of the intervention.
In terms of the content of the intervention, we found that managers emphasised how they found the modules reaffirming of existing knowledge rather than necessarily providing them with significant amounts of new knowledge (arguably an unsurprising finding among a study population with considerable experience in the field of mental health). The program was considered no less useful for this. Indeed, managers welcomed the opportunity that the material provided to reflect on practice.
Given our finding that some managers dropped out of the study shortly after taking the initial quiz, it is possible that this aspect of the program was off-putting to some participants, especially as some of the managers who did not progress seemed to spend longer online on the initial modules than managers who went on to complete more modules.
An important finding was the contrast between the focus of the e-learning materials, that is on the competencies that managers require to manage stress at work as defined by the HSE management standards,32 and the sorts of competencies that managers and employees identified when recounting specific instances of stress and managerial support. In their accounts managers and employees emphasised what we have referred to as ‘emotional sensitivity’ (being compassionate, listening, ‘being human’, etc.),58 an aspect of competency not explicitly addressed in the e-learning program, although it was implicitly covered in some aspects of the program, such as in module 6 (Being proactive – helping individuals).
Furthermore, in talking about stress at work, employees and managers highlighted factors that they felt were beyond line managerial control (family pressures and personal health, the physical environment, the specific pressures of working in a mental health trust), conveying a rather different picture of employee stress from that presented in the e-learning modules.
What did we learn about adherence to the intervention?
Managers were deemed to have ‘adhered’ to the intervention if they completed at least three (i.e. half) of the six main e-learning modules. Given that only half (51%) of the managers achieved this, adherence was considered to be relatively low, although, as stated earlier, most of the ‘non-adherers’ stopped after the quiz and before the introductory module. Unfortunately (but perhaps unsurprisingly), those managers in the ‘non-adherent’ group did not take up the invitation to be interviewed and so we have little information from this group as to why they did not continue with the modules (except from the facilitator’s reports stating that in follow-up telephone calls to non-adherent managers no one gave negative feedback on the intervention itself).
What we know very clearly from those who we interviewed and from meetings that we observed is that time was a critical issue for all managers and thus is likely to have been a significant factor in non-adherence. From our monitoring of login times we found that ‘non-adherent’ managers spent more than twice as long logged in to the initial quiz as adherent managers, suggesting that they either found it more time-consuming to complete or were distracted by other duties while still logged on to the module. It seems that managers found it difficult to set aside time for the e-learning intervention in the way that they might for attending a meeting. This highlights the need for dedicated, protected time, which needs to be not only verbally agreed by senior management but also followed up and ascertained by any future study teams.
Our qualitative findings highlighted how in the group of managers defined by the trial as ‘adherent’ many spoke of not having had time to complete the suggested activities that formed part of the learning materials. This finding raises a question about the validity of the definition of ‘adherence’ adopted by the trial, in the sense of measuring meaningful engagement with the educational materials. Furthermore, there was the problem of the tension between the blinding requirements of the trial (meaning that managers were instructed not to tell their employees that they were studying the GEM program) and the learning activities themselves, which encouraged managers to engage in dialogue with their employees and seek feedback from them. There was thus conflict between the demands of the trial and the educational intervention and this perhaps militated against managers engaging as fully and successfully as possible with the educational intervention.
Our finding that there were higher levels of well-being in employees of ‘adherent’ managers both before and after the intervention implies that these managers were already having an impact on their employees’ well-being irrespective of the intervention. In this sense adherence could be considered as a marker for positive qualities in a manager.
What did we learn about the likely effectiveness of the intervention?
There was only a very small effect of the intervention on employee well-being and little effect on sickness absence. It is important to acknowledge that this was a pilot study and we did not therefore expect to test the effectiveness of the intervention definitively and the study was not powered to do so. The lack of a positive effect of the intervention on well-being and sickness absence must be interpreted in this context.
However, our study provided a wealth of learning about the possible factors influencing the likely effectiveness of the intervention and we identified the following potential explanations for our findings:
-
Seasonal effects. Data collection for the baseline questionnaire took place from June to September and for the follow-up questionnaire from January to April. There are well-known seasonal fluctuations in national sickness absence rates,64 with a peak in late winter, which could have affected our results.
-
Random variability. The CIs around the magnitude of the effect of the intervention were wide, given the relatively small numbers involved in the study, and thus our results do not provide a definitive test of the effectiveness of the intervention. Nevertheless, the size of the observed intervention effect was much less than the 3% change expected before the study.
-
Selection effects at baseline. Employees who were on sick leave at baseline were excluded from the study, perhaps leading to lower levels of sickness absence at baseline in the recruited sample than could be expected in the trust as a whole. By follow-up the recruited sample might be expected to have higher levels of sickness absence as part of the normal course of illness in an employed sample, more representative of the trust as a whole. Thus, one possible reason for the increase in levels of sickness absence at follow-up may be because employees who were off sick at baseline were not included in the study.
-
Sensitivity of the well-being measure. The WEMWBS has proved to be a useful measure of well-being and to sensitive to change in other studies. 65 However, it could be criticised as not being sufficiently work directed as it measures overall subjective well-being influenced by non-work-related factors as well as work-related factors. Nevertheless, if there had been a significant change in well-being at work as a result of the intervention it might reasonably be expected to have altered the WEMWBS score.
-
Time interval between the intervention and the follow-up employee well-being measurement. The constraints of the time frame of the pilot study meant that the interval between the end of the intervention and the employee follow-up questionnaire was relatively short – between 1 and 3 months. A benefit of this short interval was that it perhaps helped to reduce attrition and minimise the impact of organisational change (see the following point). However, it also meant that there was little time for any behavioural change among managers to take effect in terms of employee well-being.
-
Confounding effects of organisational change. The reorganisation that took place in the trust meant that one-quarter of managers in our sample changed roles during the study. This may have diluted the effect of any potential behaviour change encouraged by the intervention. Our finding that employee well-being was significantly lower in employees managed by this group of managers lends some support to our hypothesis of a relationship between manager practice and employee well-being.
-
The characteristics of this group of managers. The managers in this study all had considerable experience of mental health issues by virtue of working in a mental health trust and interviews with managers and employees indicated that many managers were ‘already doing’ what was suggested in the e-learning program. As such, it may be that this group already had relatively high levels of competency in supporting employees’ mental health and thus were less likely to be responsive to the educational intervention than a group with little experience of mental health issues.
-
The educational intervention. Educational theory suggests that for an intervention to be effective it needs to encourage ‘deep’ and ‘active’ learning. 66 Our findings that the guided e-learning intervention promoted reflection on practice (through the e-learning modules and face-to-face meetings) are suggestive of an effective learning approach. However, other findings (that managers felt that e-learning could easily become an overly mechanistic ‘click-click’ exercise and that they had insufficient time to engage with the learning activities and were in any case restricted by the requirements of the trial in engaging fully in the activities) indicated shortcomings in the educational experience, which may have limited the effectiveness of the intervention.
-
The study’s logic model. The theory of change underpinning this study was that a 7- to 8-hour guided e-learning educational intervention about management competencies as defined by the HSE would lead to changes in managers’ knowledge, attitudes and behaviour, which would impact on the well-being of their employees within 1–3 months of the managers undertaking the intervention. Our study, along with the work of others,37 has highlighted the complex nature of managing stress at work. In practice, managers and employees described the importance of ‘experiential’ knowledge and ‘emotional sensitivity’ (what some call ‘practical wisdom’) in managing stress; a non-linear relationship between changes in knowledge, attitudes and behaviour; how managers, in effect middle managers, were also employees experiencing their own stresses (particularly in relationships with senior managers); and how employee well-being was affected by many factors beyond the workplace. Given this complex picture, it was perhaps overoptimistic to expect to see clear evidence of an effect of the intervention in this pilot study.
What did we learn from the economic evaluation?
The pilot study provided estimates of intervention costs, sickness absence costs, health-care service costs and QALYs to inform the full-scale study. In terms of the feasibility of data collection for the economic evaluation, we were able to collect adequate data on intervention costs and the costs of sickness absence.
An important outcome of this pilot study was the estimation of the costs of the Guided E-learning for Managers intervention. The cost of the intervention per employee varied from £71 to £153 depending on the number of managers involved in different stages of the intervention and on whether or not we included facilitator training costs. For the purpose of the health economics analysis we included 2 days of facilitator training in our estimations. It should be mentioned that, once trained, the facilitator is able to deliver courses to a larger number of managers. Therefore, the cost of the intervention per employee is likely to be lower in the future. Given that the cost of the intervention is highly dependent on the number of employees supervised by each manager (seven employees on average in our case), we would expect the intervention to be less costly in settings with higher numbers of employees per manager.
A new organisation using the program would as a matter of course be given training and guidance on factors such as obtaining senior management commitment, the promotion of the program in the organisation and the motivation of employees with regard to using the program. This would be included in the cost of the program.
In this study we did not aim to compare costs and outcomes between the intervention group and the control group as adjusting the data for clustering effects would be problematic because of the small number of clusters. However, we provided non-adjusted estimates of costs and QALYs to inform future research. Our preliminary analyses suggest that:
-
Given that this intervention is targeted towards the general population, which is relatively healthy, we are not likely to see significant shifts in QALYs or large changes in the use of health-care resources in the intervention group.
-
The outcome of the economic evaluation largely depends on the cost of the intervention and productivity losses resulting from sickness absence. Therefore, in the full-scale study, preference should be given to other methods of health economics evaluation, such as cost–consequences analysis, rather than cost-effectiveness analysis.
In terms of the economic evaluation, the costs were high partly because of the small sample size. Not all of the costs that were specific to this study could necessarily be separated and thus the costs of future studies using this methodology are likely to be lower. Also, we costed for 2 days of training for the facilitator in this study but once the facilitator is trained he or she would not need further training to facilitate the program in a new organisation. Moreover, in a new study the organisation might want to provide the facilitator from in-house resources to save on costs.
Although the health economics analysis was based on a comparison between the intervention group and the control group, this pilot study was not powered to detect significant differences between the two groups.
In general, we concluded that the costs of e-learning would be reduced in a larger sample. Health economics data collection was shown to be feasible but will require a full trial for a definitive and detailed cost–benefit analysis. A recent review showed mixed results of the cost-effectiveness and financial return of worksite mental health interventions. 67
Limitations of the study
-
For reasons of confidentiality we were unable to link sickness absence to questionnaire data. This would have allowed us to explore differences in rates of sickness absence in subgroups defined by sociodemographic variables such as job band or between full-time and part-time employees. We were therefore unable to explore whether or not the intervention might have had a greater or lesser impact on sickness absence for certain subgroups. The anonymised sickness absence reports that we obtained from HR included basic employee demographics and the status of their manager’s engagement in the study, but these aspects could not be systematically analysed because this information was available only for employees who had a sickness absence in the two data collection periods and not for the employees who had no sickness absence in either period.
-
Other than the e-learning quiz as a measure of knowledge gained from the intervention, the study did not include any quantitative measure of the impact of the intervention on the managers themselves, including any change in manager behaviour, although it is possible that the intervention had some impact on manager well-being and this could have been a proximate outcome of the study. It would have been helpful to have had some quantitative measure of whether or not managers’ behaviours had changed as an intermediate outcome on the pathway to influencing employee well-being.
-
Information on the number of employees approached was difficult to obtain. No information was available on how many non-consenting employees each manager was managing. Information on managers who changed position during the study was not collected in a systematic manner, but we estimated this information through direct contact with managers and through the local research team, although it was unavailable for managers in the control group.
-
Because of a misprint there was an error in the answer codes for one of the 12 questions of the GHQ-12, and psychological distress scores therefore need to be interpreted with some care in this study. However, the sensitivity analyses showed that different methods of correction used to derive a full GHQ-12 score all yielded comparable results (see Appendix 2) and we would therefore maintain that this did not influence the analyses of whether or not the intervention had an impact on psychological distress.
-
Adherence was defined in terms of adherence to the e-learning part of the intervention and did not include participation in the activities recommended in the e-learning program. Moreover, although the intervention was acceptable to managers who took part, we do not know what the managers who dropped out or who did not consent thought about the intervention.
-
It was unfortunate that randomisation resulted in the learning difficulties service being allocated to the control group and the three acute mental health services being allocated to the intervention group. There were differences in the types of employees and the mode of organisation of services between the learning difficulties service and the acute mental health services, which might have contributed to unmeasured confounding factors in the analysis.
-
For reasons of confidentiality we were not able to obtain data on full-time equivalents (FTEs) for part-time employees. Therefore, for the purposes of the health economics analysis we assumed 0.5 FTE for part-time workers. For full-time employees who were on two different pay grades we assumed 0.5 FTE for each grade.
-
It is very difficult to fully adjust for all potential confounding factors in workplace studies. Managers’ behaviours can be influenced by their own senior managers’ behaviours, which we did not take account of in this study. Lack of consistent senior manager engagement with the project, in the context of major organisational change taking place at different times in different parts of the organisation, limited the controlled execution of the study.
Recommendations for taking the research forward
Modify the educational intervention
The pilot study indicated that it would be useful to modify the educational intervention in a full trial. Although the intervention was formally seen as ‘blended learning’ and was labelled a ‘guided e-learning intervention’, in practice more emphasis was given to the e-learning aspects of the intervention. Given the positive feedback from managers about the face-to-face components, and what we know from educational research about the value of peer support in encouraging effective learning,68 a further study should consider developing this aspect of the intervention. For example, we could have up to two additional face-to-face sessions with managers to discuss the manager competency indicator tool results and to share experiences of putting the suggestions from the guided e-learning intervention into management practice.
We should also consider further ways of developing the interactive nature of the educational intervention. One way to do this would be to involve managers more in the development of the intervention. Thus, there should be more involvement of managers in the redesign of the training with a parallel process evaluation to check the acceptability and usability of the intervention. Furthermore, educational research has identified four dimensions of interaction that can improve learning: interaction between learners, interaction between learner and teacher, interaction between learner and educational content and interaction between learner and the context in which he or she is applying the learning. In a further study we should look closely at the opportunities in the educational intervention to develop these dimensions of interactive learning. For example, we would include activities in the modules that encourage managers to discuss with each other both their self-assessments on the manager competency indicator tool and their teamworking initiatives. We would further develop the learning activities within the e-learning program and incorporate them into the face-to-face sessions. Given the significance of interactive learning, we would modify our definition of adherence to include completion of the intervention’s learning activities and involvement in the face-to-face element of the intervention.
One suggestion that emerged from colleagues working in this field was to include the manager competency indicator tool within the intervention to complement the e-learning program and provide a method for managers to examine their own strengths and weaknesses as a manager. This would include discussion of the results of the indicator tool with fellow managers and, potentially, feedback from their employees. Feedback from employees has been identified in previous studies as having a powerful effect on managers’ behaviours. Although incorporating feedback from employees into the intervention would have the benefit of improving interactions between managers and employees, and would potentially change managers’ behaviours towards employees, it is also possible that it could bias employees’ questionnaire responses. One way that this could be overcome would be to request feedback from only two or three employees, who would then be excluded from the follow-up analyses, although we could still collect their follow-up questionnaires to test for bias. In practice, if there were only a few employees working for each individual manager it might be logistically difficult to obtain these data.
We should also consider modifying the content of the educational intervention to take on board our findings about the broad nature of ‘manager competency’. The picture of managing stress at work conveyed by this study suggests that the intervention should include material on, for example, how managers might develop their emotional sensitivity, ways of ‘juggling’ the competing demands on both managers and employees and more explicit recognition of the factors affecting stress that managers feel that they have little or no control over (but which they may still be able to help employees cope with). Further courses offering a range of different modules tailored to managers’ needs could be examined as an alternative way forward.
We should reassess the purpose and value of the quiz at the beginning and end of the e-learning intervention and consider whether or not this might have put some managers off continuing with their learning.
Improve manager engagement
In a further study we would want to improve manager adherence. By ‘improved adherence’ we mean aspiring to both encourage all recruited managers to take part in the study, including those who are reluctant to take part, and encourage managers to complete all modules of the intervention and attend the face-to-face element. An alternative reading of this would be to focus on the enthusiastic managers who are keen to take part as there is a suggestion that these adherent managers are more likely to have a positive effect on the well-being of their employees, as well-being fell less across the study among employees whose managers were adherent. On the other hand, the non-adherent managers may be more likely than the adherent managers to need their skills updating using the intervention.
We suggest that we could achieve improved manager engagement by:
-
Spending longer with senior managers and possibly undertaking senior manager training to help them understand the importance of this work and hence offer greater support. This means obtaining support at the chief executive officer and executive board level. This could be carried out through presentations to the board. It would also need an ‘informal’ agreement with the organisation about what would be expected from both the research team and the organisation. Regular meetings with senior representatives of the organisation would be essential, including the exchange of information about study progress. At the same time employee confidentiality must be scrupulously maintained. When possible there needs to be union involvement in parallel with management ‘buy-in’. Although we had union involvement in this study it was on a fairly informal basis.
-
Encouraging senior managers to provide messages to the managers stressing the reasons for and the importance of changing their behaviour and hence participating in the e-learning.
-
Better engaging the immediate line managers of participating managers and obtaining their commitment to allocate time to the intervention and embed the intervention in their ongoing line management practices as an accepted part of CPD. Much CPD in NHS settings is now mandatory and, although making this intervention mandatory has implications in terms of motivation to take part and ethical issues in terms of a trial, it is not unreasonable to expect that management training should be expected of those employees who have management responsibilities.
-
Checking with senior managers that this legitimisation of the intervention as part of everyday management practice and allowing time for it has happened and following it up with both senior managers and participating managers. We suggest that greater involvement of senior managers could help to embed the intervention in the local work culture, increase acceptance of its use by managers and permit managers to spend more time on the intervention.
-
Incorporating an established self-assessment tool for manager skills, such as the manager competency indicator tool,34 into the intervention. This tool could help managers identify their own areas of strengths and weaknesses in terms of managing employees and in peer discussion gain further insight and help each other change behaviours in a positive direction.
In a further study we would want to ensure that those managers who did not engage or who engaged suboptimally were included in qualitative interviews to explore more fully the factors influencing engagement levels.
Collect additional data from managers
The pilot study has highlighted that to some extent the distinction between ‘employee’ and ‘manager’ is an artificial one. Managers are also employees experiencing considerable stress and a further study should give this issue further consideration. For example, the study could collect data on how the intervention affects managers’ well-being by measuring their well-being score as a more proximate outcome before and after the intervention. We could also explore collecting indicators of manager behaviour change.
We would also want to measure organisational change (specifically the extent of change in managerial positions and roles) and estimate its effect on managers’ engagement with the intervention.
Embedding the intervention into organisational processes
A clear recommendation to emerge from the qualitative findings and other research in this area33 is the need for interventions such as this to not be ‘standalone’ but to be embedded into organisational culture and processes. This could be achieved, for example, by using other staff development opportunities to reflect on the opportunities for and barriers to learning being put into practice, by linking the intervention with initiatives such as management coaching and mentoring and perhaps by opening up the intervention to a wider range of staff (different levels of managers and perhaps employees about to become managers) in an organisation. However, these sorts of recommendations are likely to be in conflict with the requirements of scientific testing in a controlled trial (blinding, reducing the influence of confounding variables, lack of contamination and so on). These requirements could be overcome at least in part by enrolling control group managers into the study and providing them with a control intervention (such as a basic briefing on stress management), which would allow intervention group managers to apply the intervention activities fully with their employees without necessarily lifting the blind.
Improving recruitment processes
Given that recruitment took longer and was more resource intensive than expected, we should allow additional time and resources in a full study. We could also develop strategies and materials to market the study to participants, for example additional leaflets emphasising ‘what is in it for them’, using a unified, recognisable image for the study, and being even more present during the launch and recruitment process. Recruiting an organisation that has less geographical spread than the pilot study organisation would undoubtedly aid this, although the geographical spread in this study may have helped with maintaining blinding.
Modifying the study timetable
The study timetable should take account of known seasonal effects on sickness absence, as noted earlier. The findings of the pilot study indicate that we should extend the time interval between the intervention and the follow-up questionnaire to allow more time for any changes in employee well-being to take effect.
General recommendations for intervention research in the workplace
It is important to understand as much about an organisation as possible and how it functions before a study is started. There is a need for extensive preparatory work with the organisation selected before any quantitative data collection begins. Effort should be made to ensure senior management’s support for the intervention and to include strategies to sustain that commitment. Ideally, the intervention should be developed with employers and managers or at least be tailored to them. It is essential to carry out a mixed-methods study so that the context and the impact of the intervention can be understood.
Generalisability
It is not known whether the difficulties encountered with manager recruitment were specific to this organisation or not. We have learned that e-learning is welcomed by some managers but not others. The mixed-methods approach involving questionnaire surveys of employees and interviews with managers and employees has been successful here and could be generalised to other types of organisations, such as the private sector, with different types of management structure, to test what types of intervention might be feasible and might be likely to yield productive results in terms of well-being and sickness absence.
Conclusion
We carried out a pilot study of a guided e-learning intervention for managers designed to improve employee well-being and reduce levels of sickness absence in a mental health trust. We recruited sufficient numbers of employees and managers. Managers who participated in the intervention found the guided e-learning intervention and the trial acceptable. We piloted methods for collecting sickness absence data and data for economic evaluation and found that this was feasible. There was only a very small effect of the intervention on employee well-being and little effect on sickness absence but the study was not powered to examine this definitively. The fall in well-being score across the study was much less among the employees of managers who adhered to the study. The study would have benefited from ensuring greater commitment from senior managers to the study and also greater engagement from managers and employees. We have identified several ways in which the study could be improved and have made suggestions for further research.
We conclude from the results of our pilot study that we should carry out further research to develop the blended e-learning intervention and refine the study design and methodology to improve adherence to the intervention. We conclude that it is feasible to carry out an economic evaluation of the intervention. The mixed-methods approach that we adopted in the pilot study was very valuable in illuminating the acceptability of the intervention and the reasons for adherence and non-adherence and for understanding the influence of the study context. We recommend that the future study should also take a mixed-methods approach.
Acknowledgements
This project was funded by the National Institute for Health Research Public Health Research programme (project number 10/3007/06).
Contributors to the project
The team would like to thank the following people:
-
Rosemary Anderson for the provision of the e-learning program, for advice and support during the planning of the research, including the intervention timeline and the quiz module extension, for the training of the facilitator and for the practical advice on the conduct of the guided e-learning intervention.
-
Gill Weston for conducting the induction and follow-up workshop sessions with participating managers, contributing to the planning of the e-learning conduct and reminder systems and following up participants by telephone and e-mail.
-
Darren Hockley and colleagues at DeltaNet International Ltd for hosting and providing access to the APP e-learning program, managing access and providing manager uptake data reports.
-
Pat Mottram and colleagues from the research team at Cheshire and Wirral Partnership NHS Foundation Trust for their support with regard to recruitment and data collection.
-
Senior members from Cheshire and Wirral Partnership NHS Foundation Trust for their support of the intervention and the research project.
-
Staff from Cheshire and Wirral Partnership NHS Foundation Trust, Cheshire West and Chester Council, Cheshire East Council and Wirral Council for their help in procuring anonymised sickness absence data.
-
Mike Waring, Sandy Smith, Tom Power and Arouna Woukeu at the Pragmatic Clinical Trials Unit (Queen Mary University of London) for the set-up and maintenance of the trial database and advice on data security matters; Charlotte Clark at the Centre for Psychiatry (Queen Mary University of London) for her contribution to study planning and design; and Richard Hooper at the Pragmatic Clinical Trials Unit (Queen Mary University of London) and Mel Smuk at the Centre for Psychiatry (Queen Mary University of London) for additional statistical support.
-
Amy Hoon, Anitha Manivannan and Zuhur Balayah at the Pragmatic Clinical Trials Unit (Queen Mary University of London) for support and advice on matters of quality assurance and Nancy Schumann and Natasha Stevens at the Pragmatic Clinical Trials Unit (Queen Mary University of London) for project management and administrative support.
-
Amanda Fahy at the Centre for Psychiatry (Queen Mary University of London) for data management support.
-
Joanna Gilbert (YourBrandedArt) for the design of the logo and newsletter for participants and Gary Schwartz (PodPros) for the design and maintenance of the study website.
-
Mansel Aylward (Public Health Wales), Dame Carol Black (Nuffield Trust), Keith Whitfield and Andy Smith (Cardiff University), Andrew Oswald (Warwick University), Colin Mackay (Health and Safety Executive), Geoff Smith (National Association of Schoolmasters Union of Women Teachers) and Peter White (Queen Mary University of London) for their advice as members of the scientific steering committee.
-
James Shearer (King’s College London) for reviewing the health economics evaluation.
-
Emma Donaldson-Feilder (Affinity Health at Work) for her advice regarding use of the line manager competency indicator tool and 360-degree feedback.
-
All of the participating employees, managers and key informants for giving up their time to contribute to this research project.
Other acknowledgements
The WEMWBS was funded by the Scottish Executive National Programme for Improving Mental Health and Well-Being, commissioned by NHS Health Scotland and developed by the University of Warwick and the University of Edinburgh and is jointly owned by NHS Health Scotland, the University of Warwick and the University of Edinburgh.
The EQ-5D™ questionnaire is a trademark and copyright of the EuroQol Group.
Contribution of authors
Stephen A Stansfeld (Professor in Psychiatry, Queen Mary University of London) was the chief investigator. He contributed to the study design, study management, the oversight of study conduct and the initial writing and final editing of the report.
Lee Berney (Qualitative Researcher, Queen Mary University of London) conducted the interviews and focus group meeting with study participants and contributed to data collection and the writing of the report.
Kamaldeep Bhui (Professor in Psychiatry, Queen Mary University of London) contributed to the study design, the original project submission and reviewing the report.
Tarani Chandola (Professor in Medical Sociology, University of Manchester) contributed to the study design and management, the review of existing research on e-learning interventions and writing of the report.
Céire Costelloe (Statistician, Queen Mary University of London) contributed to the statistical analysis and writing of the report.
Natalia Hounsome (Health Economist, Queen Mary University of London) planned and performed the health economics analysis and contributed to writing of the report.
Sally Kerry (Reader in Medical Statistics, Queen Mary University of London) contributed to the study design and led on the statistical analysis and writing of the report
Doris Lanz (Trial Manager, Queen Mary University of London) contributed to study co-ordination, data collection and day-to-day project management and the writing of the report.
Jill Russell (Senior Lecturer in Health Policy and Evaluation, Queen Mary University of London) contributed to the study design, oversaw and reviewed the qualitative research and contributed to the writing of the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Stansfeld S, Candy B. Psychosocial work environment and mental health – a meta-analytic review. Scand J Work Environ Health 2006;32:443-62. http://dx.doi.org/10.5271/sjweh.1050.
- Head J, Kivimaki M, Martikainen P, Vahtera J, Ferrie JE, Marmot MG. Influence of change in psychosocial work characteristics on sickness absence: the Whitehall II study. J Epidemiol Community Health 2006;60:55-61. http://dx.doi.org/10.1136/jech.2005.038752.
- Netterstrom B, Conrad N, Bech P, Fink P, Olsen O, Rugulies R, et al. The relation between work-related psychosocial factors and the development of depression. Epidemiol Rev 2008;30:118-32. http://dx.doi.org/10.1093/epirev/mxn004.
- Bhui KS, Dinos S, Stansfeld SA, White PD. A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health 2012;2012. http://dx.doi.org/10.1155/2012/515874.
- Mental Health at Work: Developing the Business Case. London: Sainsbury Centre for Mental Health; 2007.
- Mental Health and Work: United Kingdom. Paris: OECD Publishing; 2014.
- Black C. Working for a Healthier Tomorrow. London: The Stationery Office; 2008.
- Boorman S. NHS Health and Wellbeing Review. Leeds: COI for the Department of Health; 2009.
- Cahill J. Psychosocial aspects of interventions in occupational safety and health. Am J Ind Med 1996;29:308-13. http://dx.doi.org/10.1002/(SICI)1097-0274(199604)29:4<308::AID-AJIM6>3.0.CO;2-K.
- Cooper CL, Dewe PJ, O’Driscoll MP. Organizational Interventions. Organizational Stress: a Review and Critique of Theory, Research, and Applications. Thousand Oaks, CA: Sage Publications; 2001.
- Marine A, Ruotsalainen J, Serra C, Verbeek J. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev 2006;4. http://dx.doi.org/10.1002/14651858.cd002892.pub2.
- Briner RB. Improving stress assessment: toward an evidence-based approach to organizational stress interventions. J Psychosom Res 1997;43:61-7. http://dx.doi.org/10.1016/S0022-3999(97)00010-X.
- Kuoppala J, Lamminpaa A, Husman P. Work health promotion, job well-being, and sickness absences – a systematic review and meta-analysis. J Occup Environ Med 2008;50:1216-27. http://dx.doi.org/10.1097/JOM.0b013e31818dbf92.
- LaMontagne AD, Martin A, Page KM, Reavley NJ, Noblet AJ, Milner AJ, et al. Workplace mental health: developing an integrated intervention approach. BMC Psychiatry 2014;14. http://dx.doi.org/10.1186/1471-244X-14-131.
- Blache J, Borza A, De Angelis K, Frankus E, Gabbianelli G, Korunka C, et al. BOIT, Burnout Intervention Training for Managers and Team Leaders: A Practice Report. Vienna: die Berater; 2011.
- Donaldson-Feilder E, Lewis R, Yarker J. Preventing Stress: Promoting Positive Manager Behaviour. CIPD Insight Report. London: CIPD Publications; 2009.
- Mackay C, Palferman D, Bauer GF, Jenny GJ. Salutogenic Organizations and Change. Dordrecht: Springer; 2013.
- Richardson KM, Rothstein HR. Effects of occupational stress management intervention programs: a meta-analysis. J Occup Health Psychol 2008;13:69-93. http://dx.doi.org/10.1037/1076-8998.13.1.69.
- van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. The benefits of interventions for work-related stress. Am J Public Health 2001;91:270-6. http://dx.doi.org/10.2105/AJPH.91.2.270.
- Tan L, Wang MJ, Modini M, Joyce S, Mykletun A, Christensen H, et al. Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Med 2014;12. http://dx.doi.org/10.1186/1741-7015-12-74.
- Egan M, Bambra C, Thomas S, Petticrew M, Whitehead M, Thomson H. The psychosocial and health effects of workplace reorganisation. 1. A systematic review of organisational-level interventions that aim to increase employee control. J Epidemiol Community Health 2007;61:945-54. http://dx.doi.org/10.1136/jech.2006.054965.
- Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Admin Sci Q 1979;24:285-309. http://dx.doi.org/10.2307/2392498.
- Bambra C, Egan M, Thomas S, Petticrew M, Whitehead M. The psychosocial and health effects of workplace reorganisation. 2. A systematic review of task restructuring interventions. J Epidemiol Community Health 2007;61:1028-37. http://dx.doi.org/10.1136/jech.2006.054999.
- Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med 2003;60:3-9. http://dx.doi.org/10.1136/oem.60.1.3.
- Gardell B, Gustavsen B. Work environment research and social change: current developments in Scandinavia. J Organ Behav 1980;1:3-17.
- Martin A, Sanderson K, Cocker F. Meta-analysis of the effects of health promotion intervention in the workplace on depression and anxiety symptoms. Scand J Work Environ Health 2009;35:7-18. http://dx.doi.org/10.5271/sjweh.1295.
- Kompier M. Job Design and Well-Being. The Handbook of Work and Health Psychology. Chichester: Wiley; 2003.
- Sorensen G, Stoddard A, Ockene JK, Hunt MK, Youngstrom R. Worker participation in an integrated health promotion/health protection program: results from the WellWorks project. Health Educ Q 1996;23:191-203. http://dx.doi.org/10.1177/109019819602300205.
- Uchiyama A, Odagiri Y, Ohya Y, Takamiya T, Inoue S, Shimomitsu T. Effect on mental health of a participatory intervention to improve psychosocial work environment: a cluster randomized controlled trial among nurses. J Occup Health 2013;55:173-83. http://dx.doi.org/10.1539/joh.12-0228-OA.
- Dollard MF, Gordon JA. Evaluation of participatory risk management work stress intervention. Int J Stress Manag 2014;21:27-42. http://dx.doi.org/10.1037/a0035795.
- Cousins R, Mackay CJ, Clarke SD, Kelly C, Kelly PJ, McCaig RH. ‘Management standards’ and work-related stress in the UK: practical development. Work Stress 2004;18:113-36. http://dx.doi.org/10.1080/02678370410001734322.
- MacKay CJ, Cousins R, Kelly PJ, Lee S, McCaig RH. ‘Management standards’ and work-related stress in the UK: policy background and science. Work Stress 2004;18:91-112. http://dx.doi.org/10.1080/02678370410001727474.
- Mackay CJ, Palferman D, Saul H, Webster S, Packham C, Biron C, et al. Improving Organizational Interventions for Stress and Well-Being. London: Routledge; 2012.
- Donaldson-Feilder E, Yarker J, Lewis R. Line management competence: the key to preventing and reducing stress at work. Strategic HR Rev 2008;7:11-6. http://dx.doi.org/10.1108/14754390810853110.
- Yarker J, Donaldson-Feilder E, Lewis R, Flaxman P. Management Competencies for Preventing and Reducing Stress at Work. Identifying and Developing the Management Behaviours Necessary to Implement the HSE Management Standards. London: Health and Safety Executive; 2007.
- Lewis R, Yarker J, Donaldson-Feilder E, Flaxman P, Munir F. Using a competency-based approach to identify the management behaviours required to manage workplace stress in nursing: a critical incident study. Int J Nurs Stud 2010;47:307-13. http://dx.doi.org/10.1016/j.ijnurstu.2009.07.004.
- Donaldson-Feilder E, Yarker J, Lewis R. Preventing Stress in Organisations. How to Develop Positive Managers. Hoboken, NJ: Wiley-Blackwell; 2011.
- Gaskell L, Hickling N, Stephens P. The Suitability of HSE’s Risk Assessment Process and Management Standards for Use in SMEs. Norwich: Her Majesty’s Stationery Office; 2007.
- Eisen KP, Allen GJ, Bollash M, Pescatello LS. Stress management in the workplace: a comparison of a computer-based and an in-person stress-management intervention. Comput Hum Behav 2008;24:486-96. http://dx.doi.org/10.1016/j.chb.2007.02.003.
- Lewin S, Glenton C, Oxman AD. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: methodological study. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3496.
- O’Cathain A, Murphy E, Nicholl J. Why, and how, mixed methods research is undertaken in health services research in England: a mixed methods study. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-85.
- O’Cathain A, Thomas KJ, Drabble SJ, Rudolph A, Goode J, Hewison J. Maximising the value of combining qualitative research and randomised controlled trials in health research: the QUAlitative Research in Trials (QUART) study – a mixed methods study. Health Technol Assess 2014;18. http://dx.doi.org/10.3310/hta18380.
- Health and Safety at Work Act 1974. London: The Stationery Office; 1974.
- Managing the Causes of Work-Related Stress: A Step-by-Step Approach using the Management Standards. Sudbury: HSE Books; 2007.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. http://dx.doi.org/10.1186/1477-7525-5-63.
- Goldberg DP, Williams P. A User’s Guide to the GHQ. Windsor: NFER Nelson; 1988.
- Karasek R. Low social control and physiological deregulation – the stress–disequilibrium theory, towards a new demand–control model. Scand J Work Environ Health 2008;6:S117-35.
- Siegrist J. Chronic psychosocial stress at work and risk of depression: evidence from prospective studies. Eur Arch Psychiatry Clin Neurosci 2008;258:S115-19. http://dx.doi.org/10.1007/s00406-008-5024-0.
- Stansfeld SA, Clark C, Caldwell T, Rodgers B, Power C. Psychosocial work characteristics and anxiety and depressive disorders in midlife: the effects of prior psychological distress. Occup Environ Med 2008;65:634-42. http://dx.doi.org/10.1136/oem.2007.036640.
- Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry 1974;131:1121-3.
- Craig R, Mindell J. Volume 3: Social Capital and Health. London: Information Centre; 2007.
- Ijzelenberg W. Prevention of Work-Related Musculoskeletal Complaints 2006.
- Eldridge S, Kerry S. A Practical Guide to Cluster Randomised Trials in Health Services Research. London: John Wiley; 2012.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. http://dx.doi.org/10.1111/j. 2002.384.doc.x.
- Muller J, Crabtree BF, Miller WF. Doing Qualitative Research. London: Sage Publications; 1999.
- Stansfeld SA, Shipley MJ, Head J, Fuhrer R. Repeated job strain and the risk of depression: longitudinal analyses from the Whitehall II study. Am J Public Health 2012;102:2360-6. http://dx.doi.org/10.2105/AJPH.2011.300589.
- Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Fineman S. Understanding Emotion at Work. London: Sage Publications; 2003.
- van den Hout WB . The value of productivity: human-capital versus friction-cost method. Ann Rheum Dis 2010;69. http://dx.doi.org/10.1136/ard.2009.117150.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: Personal Social Services Research Unit, University of Kent; 2012.
- NHS Reference Costs 2012–2013. London: Department of Health; 2013.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. Discussion paper 172. York: Centre for Health Economics, University of York; 1999.
- Nuffield Trust and the Health Foundation . NHS Staff Sickness Absence 2014. www.qualitywatch.org.uk/indicator/nhs-staff-sickness-absence (accessed 8 December 2014).
- Maheswaran H, Weich S, Powell J, Stewart-Brown S. Evaluating the responsiveness of the Warwick Edinburgh Mental Well-Being Scale (WEMWBS): group and individual level analysis. Health Qual Life Outcomes 2012;10. http://dx.doi.org/10.1186/1477-7525-10-156.
- Brookfield S. Understanding and Facilitating Adult Learning. Buckingham: Open University Press; 1986.
- Hamberg-van Reenen HH, Proper KI, van den Berg M. Worksite mental health interventions: a systematic review of economic evaluations. Occup Environ Med 2012;69:837-45. http://dx.doi.org/10.1136/oemed-2012-100668.
- Foley G. Understanding Adult Education and Training. Sydney: Allen & Unwin; 2000.
Appendix 1 Employee questionnaire excerpts
Appendix 2 General Health Questionnaire 12 items correction: sensitivity analysis
A sensitivity analysis was conducted to compare different methods of calculating the GHQ-12 score at baseline and follow-up, which was coded incorrectly in the baseline questionnaire.
Three different methods were used to calculate the GHQ-12 score at baseline and follow-up from the study questionnaires. These methods were used to rectify a printing error on the baseline questionnaire. In the baseline questionnaire the wrong item responses were reproduced for question 12 (happiness), with ‘not at all’/‘no more than usual’/‘rather more than usual’/‘much more than usual’ presented to employees instead of ‘more so than usual’/‘about the same as usual’/‘less so than usual’/‘much less than usual’. For the main analysis the first 11 items were used and multiplied by 12/11 for both the baseline and the follow-up time points; thus, the same method was used at both times.
In the sensitivity analysis we conducted the same analysis using different derived values for the GHQ-12 score. The methods compared were as follows:
-
method 1 – the GHQ-12 score was derived using the first 11 items of the GHQ-12 scoring system scaled up by dividing by 11 and multiplying by 12
-
method 2 – the GHQ-12 score was derived using the 12 items of the GHQ-12 scoring system with the scoring of the 12th item reversed
-
method 3 – the GHQ-12 score was derived using the first 11 items of the GHQ-12 scoring system with the 12th item deemed to be ‘missing’.
As indicated in Table 30, all three methods produced similar results and using one method rather than another did not result in any changes to the conclusions regarding the effect of the GEM intervention on GHQ-12 score.
| Method | Group | n | GHQ-12 score | Difference between baseline and follow-up (95% CI) | Intervention effect adjusted for baseline and clustering (95% CI) | |
|---|---|---|---|---|---|---|
| Baseline, mean (SD) | Follow-up, mean (SD) | |||||
| 1 | Control | 59 | 3.2 (3.4) | 2.9 (3.7) | –0.3 (–1.1 to 0.4) | |
| Intervention | 216 | 2.8 (3.5) | 2.9 (3.5) | 0.0 (–0.4 to 0.5) | 0.2 (–2.2 to 2.6) | |
| 2 | Control | 59 | 3 (3.2) | 2.7 (3.6) | –0.3 (–1.1 to 0.4) | |
| Intervention | 216 | 2.7 (3.6) | 2.7 (3.4) | 0.0 (–0.4 to 0.5) | 0.2 (–2.0 to 2.5) | |
| 3 | Control | 59 | 2.9 (3.1) | 2.6 (3.4) | –0.3 (–1.1 to 0.4) | |
| Intervention | 216 | 2.6 (3.2) | 2.6 (3.2) | 0.0 (–0.4 to 0.4) | 0.2 (–2.0 to 2.4) | |
Appendix 3 Detailed description of the intervention
Content of the facilitator training
Overall aims
The overall aim of the facilitator training was to:
-
make sure that the facilitator was familiar with the operation and content of the e-learning package and understood all of the information and activities in the program
-
discuss the content and delivery of the management induction session and the subsequent support session, to take place half-way through the study programme.
It was decided to break the training into two 1-day sessions, 1 month apart. The facilitator was given access to the program 1 month before training commenced so that she could start to become familiar with the contents and operation.
The training was conducted by the author of the e-learning program.
Day 1: familiarisation with the program
The aims of this day were to:
-
familiarise the facilitator with the operation of the program
-
familiarise the facilitator with the content of the program
-
point out and discuss the major learning points of the program
-
discuss the areas that managers may find more challenging and determine how to deal with possible questions
-
introduce the facilitator to the question bank used in the benchmarking questionnaire and ensure that she is satisfied with the answers
-
answer any questions that the facilitator may have about the program
-
outline the content of the induction session.
Introductory module
This module first explains why the organisation is providing the program and provides information to facilitate manager buy-in. It then describes the obstacles to tackling stress in this manner and how these can be overcome. It was decided to demonstrate this module as part of the manager induction session to allow the facilitator to familiarise managers with the look and content of the program and to explain how it works. This was to be carried out using a CD and screenshots.
Along with the discussion of the introductory module, the programme for the induction session was also outlined and discussed. The facilitator then arranged this into a 2-hour format and PowerPoint® presentation (Microsoft Corporation, Redmond, WA, USA), which was discussed at the second facilitator training day (see later for the final programme for the face-to-face sessions).
The author and facilitator then worked through each of the remaining program modules. The facilitator made notes about any salient points to be aware of and jotted down any further points that needed to be included in the induction session. These are outlined in the following sections.
General points to note:
-
A main point was to make sure that the managers read all of the content, including the ‘additional information’ options. It was recognised that there may be a desire to skip this additional information and so it was decided that the facilitator would explain that some of the information in the ‘additional information’ sections may well be in the quiz.
-
It was also deemed necessary for the managers to carry out all of the activities and it would be emphasised that only by doing all of these activities would the managers obtain the maximum benefit from the program. The content of the program is outlined in the following sections under the module headings, with particular points for the facilitator to be aware of listed at the end of each section.
-
Managers should be told that they can contact the facilitator for support at any time during the day and be given her contact details. They should also be told at the outset to schedule the support session after completion of module 4.
-
Managers should also be encouraged to form their own support/discussion groups.
Module 1: why tackle pressure at work? Health issues
In this module the manager will learn about the physiological symptoms of stress and how these can lead to more serious physical illness, about the psychological symptoms of stress and how these can lead to mental ill health and about the behavioural symptoms of stress both at home and at work and how lack of pressure can also have an effect on an employee’s health and well-being. The manager will also learn how to more effectively motivate his or her employees.
Points to note:
-
Learning about signs and symptoms of pressure should be straightforward but managers may still be unsure of the difference between stress and pressure.
-
Managers may have questions to ask about motivating employees. If they try some of the techniques described they may want to discuss their attempts with the facilitator. The facilitator needs to be familiar with the suggestions.
Module 2: why tackle pressure at work? Economic issues
In this module the manager will learn about the economic reasons why organisations need to address pressure at work.
Points to note:
-
Managers may have problems calculating absence rates and Bradford scores.
-
Managers may not see the point of these calculations.
-
Managers may have differing opinions on presenteeism.
-
Managers may have different opinions on why people take time off work and wish to discuss these.
Module 3: why tackle pressure at work? Legal issues
In this module the manager will learn about the legal reasons why organisations need to address pressure at work and the legislation most commonly associated with this.
Points to note:
-
This topic is quite a text-heavy module and may prove difficult for some managers.
-
As the topic refers to managers’ legal duties they may be keen to check that they have understood the salient points correctly.
-
They may find it difficult to understand if they have skipped reading the Walker case in detail, thinking that it is just an example. In actual fact it is used to illustrate salient points.
Module 4: what can a manager do?
In this module the manager will learn what he or she can do to reduce pressure for his or her employees, the causes of pressure at work and how general management skills and behaviour can reduce pressure at work.
Points to note:
-
This is quite a large module and may require the most facilitator support.
-
Managers are asked to assess their own management behaviour and try out new ideas. They may like support and reassurance while doing this.
-
If they ask colleagues for feedback they may want to discuss this.
-
More time is allowed in the research timeline for this and a support session is being held for managers to discuss.
Module 5: being proactive – helping your team
In this module the manager will learn how to identify problems common to his or her team, how to work with his or her team to make improvements and how to make an action plan for these improvements.
Points to note:
-
This is quite a short module but managers may have questions about running sessions with their teams and making action plans. They should be encouraged to print off and complete an action plan for their team.
Module 6: being proactive – helping individuals
In this module the manager will learn why it is important to be aware of an individual’s concerns at work, how to identify problems that employees might be experiencing, how to work with individuals to find solutions to problems at work and about stressful situations that require them to take action.
Points to note:
-
There is a lot of information in this module and so it would be easy to overlook some of it.
-
The facilitator should not miss the sections on managing talking to employees over the telephone.
-
The facilitator should be familiar with how the five points for helping individuals link to the legal issues. There may be questions on this.
-
Managers may want to discuss some of the suggestions for when they should talk to their employees. The facilitator needs to be aware of the HR policies about this as they should not contradict these.
-
A controversial issue is whether or not a manager should contact an employee when he or she is absent. Again, the facilitator needs to be aware of the HR policies about this as they should not contradict these.
Quiz module
Finally, the author and facilitator worked through all 75 questions of the pre- and post-study assessment quiz to ensure that the facilitator understood and was happy with the answers should a manager query any of his or her own responses.
Day 2: determining the content and delivery of the manager induction and follow-up sessions
This took place in the week before the induction session was due.
Aims:
-
to discuss the content of the management induction session and review and revise the program and PowerPoint presentation
-
to determine the time scale
-
to discuss the content of the follow-up session.
It was decided that a particular effort should be made to get all managers on board by emphasising our thanks for their co-operation and making sure that they understood the benefits that they could gain from the project. As all programmes are more effective with support from the top, a message was to be included from the HR director stating that he took the programme seriously and would support anyone following it as instructed. It was also deemed necessary to reassure the managers that they were not being assessed and that confidentiality would be maintained throughout.
Finally, the importance of adhering to the timeline and completing all of the activities was to be stressed.
Once the intervention was under way, the itinerary was reviewed to check that it was still acceptable. As nobody had actually contacted the facilitator to ask questions or give feedback, it was decided to proceed as agreed, although the facilitator was given permission to adapt the material accordingly based on her experience and points raised by the participants.
Content of the face-to-face manager sessions
Induction session: before the start of the e-learning program
Introduction
-
Thank you for taking part.
-
Housekeeping arrangements.
-
Ask delegates to very briefly introduce themselves.
-
Aims and objectives for the session.
-
Commitment from their organisation.
-
Message from the head of HR.
The research study
-
Why we are doing the research – brief background information.
-
What the research entails – managers’ role.
-
Information from the research team – basic information on how a randomised trial works and how it is being carried out within the organisation.
-
Role of the qualitative researcher.
Confidentiality and reassurance
-
Reassurance on confidentiality throughout the study.
-
Cluster RCT, with data held securely.
-
Emphasise the need for confidentiality between participants. Do not reveal what group you are in. Managers should not share information with others who are not part of the research.
-
Reassurance – we want it to be a positive and beneficial exercise.
-
Managers are not being examined/tested – results of the employee questionnaires will be amalgamated so scores are not linked to any individual manager.
-
The employees do not know who is following the program and so managers will not be assessed by their employees.
-
Discussions with the facilitator are confidential.
-
Reassurance: it is the program that is being tested, not the managers.
-
Right to withdraw.
Group exercise
-
What is your experience of work-related stress?
-
How may this course help you/your team?
Benefits
What is in it for the managers?
-
contribute to improving working life
-
develop your management competencies
-
improving manager health and well-being
-
happier, healthier, more engaged employees – less time spent by the manager trying to sort out issues
-
duty of care
-
CPD – certificate of successful completion.
Getting to know the program: how to use it
-
Login details.
-
Quiz pre and post – explain the reason for these; reassure: it is not about being tested with the pre-course quiz.
-
Post-course quiz – a score of ≥ 67% will allow them to be presented with a certificate of successful completion.
-
Demonstrate the program structure and how the program works.
-
Explain that the program consists of an introductory module and six learning modules.
-
Emphasise that they must study all of the additional information and activities, even if they seem simple.
-
Some activities can be printed off to make implementation easier.
-
Emphasise the need to complete the activities in modules 1, 4 and 5 and to be prepared to talk about their work at the second facilitator meeting.
-
Emphasise the need to implement the advice in module 6 (working with individuals) on an ongoing basis.
Group exercise
-
Obstacles and enablers to tackling pressure at work.
-
Use introduction to reiterate.
The research process: timeline
-
Explain the process and timeline including the catch-up time available if busy or on holiday. Time for activities and informal meetings.
-
Explain that they are welcome to study the program all at once if they wish as long as they carry out the activities as suggested by the timeline.
Support
-
Explain the availability of support:
-
from the facilitator
-
from the organisation – managers receive a handout specific to their organisation detailing the internal support available to them
-
from the trial manager – for technical queries.
-
-
Managers can meet informally if they wish – can do this in the spare weeks between the study modules. Emphasise that they are not to share information with anyone not in a study group.
-
Facilitator to inquire whether they want to ask questions by e-mail and whether they want to share their questions and responses.
Follow-up session
-
Reason for a facilitated discussion session and follow-up
-
What would managers like to discuss?
Follow-up session programme: after completion of module 5
Introduction
-
Housekeeping.
-
Welcome back.
-
Thanks for coming back.
-
Setting the agenda for the session including their suggestions and qualitative researcher suggestions.
-
Flip chart exercise, asking the participants what met their expectations from the e-learning program and what differed from their expectations of the e-learning program.
Icebreaker video
-
To build positive affect, helping participants to learn, relax and interact more.
-
Video addresses preconceptions of what stress management is about, e.g. massage – although lovely does not address the problems.
-
Introduce self and answer the question, ‘Were your expectations of the program different from what you have been experiencing so far?’
-
Complete two flip charts – what was the same, what is different.
Feedback
-
Progress and status update.
-
Thoughts on the program.
-
How have you got on?
-
Would you have found it helpful to have a get together sooner, e.g. after the module 1 motivation exercise?
Studying activity 1: motivation (module 1)
-
What was easier and what was more difficult?
-
Have you encountered any difficulties/obstacles?
-
Anything you would have liked to help you?
-
Suggestions on what worked and what didn’t work.
-
Success stories.
Studying activity 2: management competencies (module 4)
-
What was easier and what was more difficult?
-
Have you encountered any difficulties/obstacles?
-
Suggestions on what worked and what didn’t work.
-
Anything you would have liked to help you?
-
Success stories.
-
Discuss management competencies and how they can improve.
Studying activity 3: helping your team (module 5)
-
What was easier and what was more difficult?
-
Have you encountered any difficulties/obstacles?
-
Suggestions on what worked and what didn’t work.
-
Anything you would have liked to help you?
-
Success stories.
What’s coming up next
-
Introduction to the final module ‘Helping individuals’.
-
Hand out adapted timeline (final module was put back by 1 week).
-
Any concerns?
-
Is there anything that might help you?
-
Refer to policies and procedures.
Working together
-
Importance of peer support – sounding out a colleague can build confidence, issues of confidentiality in sharing information.
-
How have you been working together?
-
If so how have you found it?
-
If not, would you find it helpful?
-
Would you have liked another meeting?
Wrap up
-
Opportunity to share more ideas and tips or raise more concerns.
-
Certificate and dissemination.
-
Answer further questions.
Appendix 4 Qualitative study: interview topic guides
Key informant topic guide
-
Respondent’s background and relevance to project.
-
Perceptions of workplace stress: key issues, causes, factors fostering and hindering efforts to reduce workplace stress and absenteeism, current systems/procedures in place (the perceived advantages, benefits and/or deficiencies of current approaches).
-
E-learning interventions: experience of/attitude towards current practice. How e-learning fits in with/builds on existing strategies.
-
Possible influences on (a) the delivery of the intervention and (b) the effects of the intervention.
-
Suggestions of relevant individuals, organisations and literature to follow up.
Manager topic guide
Part A: context
Tell me about your job, your role and the place/department in which you work.
Prompts
-
Role as a manager.
-
What are the key workplace stresses that you face in your daily work? [Leave open for respondent to talk about his or her own stresses (home or work) or stresses that he or she manages in his or her employees, but prompt to talk about both.]
-
Positive aspects of the job? Rewards?
Part B: cases of workplace stress
Talk me through an instance of a specific case in which an employee who you line manage has experienced stress and how you managed this particular case (check if this case was before or after studying the e-learning modules). [Remind respondent of the confidentiality of interviews and how all interview data are anonymised and emphasise that we will fictionalise any cases that we refer to in our writing up of the interviews.]
Prompts
-
What particular competences as a manager did you need in dealing with this case?
-
Having studied (some of) the e-learning modules, is there anything you learned from them that you think would have helped you manage this case or do things differently in any way?
-
[If a recent case] Did you find the e-learning modules informed how you managed this case?
Part C: experiences of the Guided E-learning for Managers study
Talk me through your experience of being involved with the GEM e-learning project.
Prompts
-
What made you decide to participate?
-
Expectations of what you would get out of it. Initial thoughts.
-
Overall thoughts/experiences of it.
-
How did you work your way through the modules? Where, when, how long? Was time allocated/‘protected’ for you to do this?
-
Ease of use.
-
How did it suit your style of learning? In what way?
-
Things you liked about it.
-
Things you disliked about it.
-
Applicability: did the module help you to apply the knowledge to day-to-day practice?
-
What changes (if any) would you recommend if it were being offered to managers in another organisation? (Would they recommend the package?)
-
Acceptability of being in a trial (randomisation, consent, communications from research team, level of information).
-
(For non-completers, explore the reasons for not completing the modules.)
Part D: the Guided E-learning for Managers study and the wider picture
Offering managers an e-learning package is one approach to improving employee well-being in the workplace.
-
Experience of other stress management interventions.
-
What else do you need as a manager to support you in helping to create a healthy workplace?
-
Senior management ‘buy-in’/awareness of the GEM study.
Employee topic guide
-
Tell me about your role. How long have you been in post? Are you responsible for any staff yourself?
-
What skills does your manager need to create a healthy workplace (and to reduce workplace stress)?
-
What needs to be in place at the workplace to reduce stress/promote health?
-
What makes you feel well at work? What makes you unwell at work? What are the positives about the job? What are the stressors?
-
Please give as much detail as possible about a specific instance of feeling stressed. How was it handled?
-
Opinions on the questionnaire: content, layout, etc.
-
Acceptability of the trial: the registration process, information given, technical aspects, being sent login information for an online questionnaire, token codes, views on confidentiality, filling in the questionnaire at work (when found time to complete it), contamination (did you know who else was taking part?).
-
The trial blinding – did you know/suspect your manager was participating?
Appendix 5 Unit costs used for costing health-care services
| Costing item | Unit cost (£) | Cost of consultation (£) | Assumption | Reference |
|---|---|---|---|---|
| GP surgery | 41 | 41 | Average duration of contact 11.7 minutes | Per-patient contact lasting 11.7 minutes, excluding direct care staff costs, with qualification costs (p. 191)60 |
| Nurse surgery | 52 | 22 | Duration of contact 25 minutes | Per hour of face-to-face contact with qualification costs (p. 188)60 |
| Specialist nurse | 49 | 20 | Duration of contact 25 minutes | Per hour with qualification costs (p. 186)60 |
| Out of hours | 41 | 49 | GP surgery contact cost plus 20% for out of hours including night, weekend and bank holiday | Per-patient contact lasting 11.7 minutes, excluding direct care staff costs, with qualification costs (p. 191)60 |
| Health visitor | 71 | 30 | Duration of contact 25 minutes | Per hour of home visit with qualification costs (p. 185)60 |
| Community midwife | 68 | 68 | Visit | National Schedule of Reference Costs 2012–13 – all NHS trusts and NHS foundation trusts – other currencies data. Community midwife, ante natal visits. Currency code N01P61 |
| Community pharmacist | 70 | 12 | Duration of contact 10 minutes | Per hour of patient-related activities with qualification costs (p. 180)60 |
| Dietitian | 35 | 35 | Duration of contact 1 hour | Per hour with qualification costs (p. 226)60 |
| Occupational therapy | 63 | 63 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 65161 |
| Counselling | 58 | 58 | Primary care | Per consultation (p. 54)60 |
| Social worker | 226 | 94 | Duration of contact 25 minutes | Per hour of face-to-face contact with qualification costs (p. 198)60 |
| A&E | 115 | 115 | National average unit cost | All NHS trusts and NHS foundation trusts: national average unit costs61 |
| Non-elective inpatients (long stay) | 2686 | 2686 | National average unit cost | All NHS trusts and NHS foundation trusts: national average unit costs61 |
| Non-elective inpatients (short stay) | 604 | 604 | National average unit cost | All NHS trusts and NHS foundation trusts: national average unit costs61 |
| Hospital day case | 693 | 693 | National average unit cost | All NHS trusts and NHS foundation trusts: national average unit costs61 |
| Consultant breast care | 143 | 143 | outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 10361 |
| Consultant cardiology | 143 | 143 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 32061 |
| Consultant dermatology | 100 | 100 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 33061 |
| Consultant endocrinology | 156 | 156 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 30261 |
| Consultant ear, nose and throat | 96 | 96 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 12061 |
| Consultant general medicine | 161 | 161 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 30061 |
| Consultant general surgery | 133 | 133 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 10061 |
| Consultant gynaecology | 133 | 133 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 50261 |
| Consultant neurology | 178 | 178 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 40061 |
| Consultant obstetrics | 129 | 129 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 50161 |
| Consultant ophthalmologist | 88 | 88 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 13061 |
| Consultant orthopaedic surgeon | 111 | 111 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 11061 |
| Consultant pain management | 146 | 146 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 19161 |
| Consultant plastic surgery | 91 | 91 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 16061 |
| Consultant respiratory medicine | 154 | 154 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 34061 |
| Consultant rheumatology | 147 | 147 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 41061 |
| Cardiology | 131 | 131 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 32061 |
| Chiropractor | 50 | 50 | Physiotherapist | All NHS trusts and NHS foundation trusts: community health services – allied health professionals HRG code A08A161 |
| Dental medicine | 116 | 116 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 45061 |
| Gastroenterology | 137 | 137 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 30161 |
| Lipid clinic | 131 | 131 | Cardiology | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 32061 |
| Medical oncology | 144 | 144 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data, consultant led – service code 37061 |
| Midwife | 65 | 65 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 56061 |
| Ophthalmology | 86 | 86 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 13061 |
| Osteopath | 50 | 50 | Physiotherapist | All NHS trusts and NHS foundation trusts: community health services – allied health professionals – HRG code A08A161 |
| Phototherapy | 91 | 91 | All NHS trusts and NHS foundation trusts: phototherapy, 13 years and over – HRG code JC47A61 | |
| Physiotherapy | 50 | 50 | Community | All NHS trusts and NHS foundation trusts: community health services – allied health professionals HRG code A08A161 |
| Podiatry | 42 | 42 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 65361 |
| Psychology | 134 | 134 | Duration of contact 1 hour | Per hour of client contact (p. 179)60 |
| Trauma and orthopaedics | 110 | 110 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 11061 |
| Audiology | 70 | 70 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 84061 |
| Cardiology tests | 54 | 54 | Direct access | All NHS trusts and NHS foundation trusts: directly accessed diagnostic services, minor cardiac procedures – HRG code EA44B61 |
| Colonoscopy | 270 | 270 | All NHS trusts and NHS foundation trusts: HRG data, diagnostic colonoscopy, 19 years and over – HRG code FZ51Z61 | |
| Colposcopy | 191 | 191 | All NHS trusts and NHS foundation trusts: diagnostic colposcopy – HRG code MA38Z61 | |
| Computerised tomography scan | 90 | 90 | All NHS trusts and NHS foundation trusts: computerised tomography scan, one area, no contrast, 19 years and over – HRG code RA08A61 | |
| Endoscopy | 39 | 39 | Direct access | All NHS trusts and NHS foundation trusts: directly accessed diagnostic services, minor endoscopic or percutaneous, hepatobiliary or pancreatic procedures, 19 years and over – HRG code GB04D61 |
| Optometry | 75 | 75 | Outpatient | All NHS trusts and NHS foundation trusts: outpatient attendances data – service code 66261 |
| Radiography | 28 | 28 | Direct access | All NHS trusts and NHS foundation trusts: directly accessed diagnostic services, direct access plain film – HRG code DAPF61 |
| Ultrasound | 51 | 51 | All NHS trusts and NHS foundation trusts: ultrasound scan, less than 20 minutes – HRG code RA23Z61 |
List of abbreviations
- A&E
- accident and emergency
- APP
- Anderson Peak Performance
- CI
- confidence interval
- CPD
- continuing professional development
- EQ-5D-3L
- European Quality of Life-5 Dimensions three-level version
- FTE
- full-time equivalent
- GEM
- Guided E-learning for Managers
- GHQ-12
- 12-item General Health Questionnaire
- HR
- human resources
- HSE
- Health and Safety Executive
- ICC
- intracluster correlation coefficient
- PHR
- Public Health Research
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SME
- small- and medium-sized enterprise
- VAS
- visual analogue scale
- WEMWBS
- Warwick–Edinburgh Mental Wellbeing Scale