Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 10/3010/21. The contractual start date was in April 2012. The final report began editorial review in November 2014 and was accepted for publication in May 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Kerenza Hood is a member of the National Institute for Health Research Clinical Trials Unit Standing Advisory Committee.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Moore et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Structure of the report
Introduction
This trial aimed to determine the effectiveness of a novel, risk-led intervention delivered by environmental health practitioners (EHPs) to licensed premises across Wales. This was achieved by carrying out a pragmatic randomised controlled trial (RCT). However, trialling the intervention was only one element of the overall project. The project also included an intervention development component, an embedded process evaluation and a cost-effectiveness evaluation. The aim of these developmental and evaluative components was to document how the intervention integrates into the working practice of EHPs and to scrutinise and appraise the iterative design and implementation process.
Intervention development involved focus groups with senior EHPs, information sharing meetings between academic researchers, senior EHPs and stakeholders, and development meetings with design professionals. The purpose of this stage of the trial was to optimise the design of the intervention and to determine the most acceptable method of delivery. The findings from this element of the trial were also used to develop a logic model for the planned intervention.
This trial involved the randomisation of purposively sampled licensed premises into control and intervention arms. The premises in the intervention group were visited by an EHP, who undertook an audit that assessed operational risks associated with alcohol-related violence (ARV). The premises staff in the intervention group were also given access to a website with videos and educational material containing information designed to help the staff proactively identify and reduce the risk. The control group did not receive a visit from EHPs or intervention materials. If risks identified using the intervention audit were substantial or significant enough to warrant a formal notice, the premises were reaudited within 3 months of the initial audit taking place. The objective of this part of the trial was to determine, using police violence data, whether or not the audit, associated materials and follow-up audit (when implemented) could reduce incidences of ARV in and around premises.
The evaluative stage of the trial encompasses the imbedded process evaluation and cost-effectiveness analyses. The process evaluation aimed to understand the implementation of the intervention, to aid interpretation of outcomes and to improve future delivery. The aim of the process evaluation as a whole was to better understand all aspects of the trial and to identify opportunities to improve intervention delivery.
Report chapters
This report is laid out as a series of chapters that provide a description of the rationale, conduct and outcomes resulting from each of the trial components. The chapters are now summarised.
Chapter 2 begins with an introduction to the issue of ARV and provides the motivation for a premises-level risk-led intervention and the rationale for using EHPs to deliver the intervention to the premises.
Chapter 3 summarises the theoretical basis behind the main aspects of the trial, including the reason behind the choice of the primary outcome measure, and describes the processes and methods involved in designing the intervention.
Chapter 4 describes the trial stage methods, cost-effectiveness analysis methods and process evaluation methods.
Chapter 5 presents the main quantitative results, together with a brief summary.
Chapter 6 presents results from the embedded process evaluation along with a short discussion that summarises the main findings and examines their significance in the context of previous research.
Chapter 7 presents the findings from the cost-effectiveness evaluation and a brief discussion.
Chapter 8 synthesises the findings arising from the trial as a whole and assesses the extent to which the aims and objectives set out in the introduction were met. This chapter also identifies implications for future research and practice.
Chapter 2 Introduction
In the UK, the costs of ARV to public services, including the NHS, the economy and society, are substantial, estimated to be between £8B and £11B. 1,2 Between 2011 and 2012 there were over 910,000 violent incidents where the offender was believed to be under the influence of alcohol, accounting for 47% of all violent offences committed in that period. 3 An estimated 2 million emergency department attendances each year are thought to be alcohol related. These figures account for 70% of unscheduled accident and emergency (A&E) attendances during peak hours. 1 Medical treatment following alcohol-related assaults, therefore, places a considerable burden on the NHS. 4
Premises licensed for the on-site sale and consumption of alcohol are implicated in alcohol-related injury and violence. 5,6 ARV is commonly observed in alcohol-focused nightlife, with estimates suggesting that 20% of all violence in England and Wales occurs in or around pubs, bars or nightclubs. 7 Many premises licensed for the sale and consumption of alcohol target young adults, and feature minimal seating, loud music, late licences and other features associated with harm. 8,9 As such, there is a growing literature detailing environment-specific risk factors in the on-licensed trade8,9 and recognition that interventions to address these are required. 10,11
Previous evaluations have examined interventions that focus on single risk factors for alcohol-related harm such as responsible beverage service (RBS) training, licensee accords and staff violence-reduction training. 12 RBS training, the most commonly evaluated intervention type, typically deploys ‘off-the-shelf’ training packages that do not involve any consideration of premises’ underlying risk factors. These unfocused interventions are likely to be less effective than interventions that are responsive to the risks and needs of individual premises. Consequently, there is a need for robust, formally evaluated interventions that can be routinely adopted by partners involved with managing the night-time economy (NTE).
Interventions to reduce alcohol-related violence
The UK Licensing Act 200313 emphasises a harm-minimisation approach. While a number of promising premises-level interventions to promote a more proactive approach to harm reduction have been identified,8,14–16 evidence for their effectiveness is limited. There are very few evaluations employing robust methods such as a RCT design, and none of these interventions has been trialled in the UK. Disparate measures of violence have been used, including data from hospital A&E17 and the local police,18 yet it is unclear if outcomes from these studies can be attributed to interventions at the premises level.
A systematic review undertaken in 2007 examined server training interventions aimed at reducing ARV. This review concluded that interventions focusing on a single risk, such as RBS, fail to account for the complex relationships between staff (i.e. servers, security and management) and the premises environment. It was therefore suggested that research in the context of the NTE should be broadened to develop interventions that address more complex causation and multiple risk factors across the full socioecological environment. 12 Another review8 identified a broader range of approaches to prevention encompassing RBS training (n = 6), enhancing the enforcement of licensing regulations (n = 2), multilevel interventions (n = 6), licensee accords (n = 2) and a risk-focused consultation (n = 1). The review highlighted that, of the available RCT evaluations that have been conducted in this area, only Graham et al. 19 implemented a tailored intervention that was responsive to the idiosyncratic needs of premises, while Toomey et al. 20 evaluated a risk-led intervention using quasi-experimental methods. Both of these studies concluded that premises-level interventions that are designed to offset risk factors in each premises are feasible and potentially effective. However, many studies in this area8,12 were subject to a number of shortcomings, including (1) considerable variation in and poorly defined outcome measures, meaning that studies could not be compared, (2) follow-up periods were decided ad hoc and did not consider intervention sustainability, (3) studies often relied on inappropriate control groups, (4) many failed to achieve random allocation, and (5) participants or evaluators were not blind to trial conditions. The review concluded that, while interventions that address multiple risk factors and interventions that are designed and implemented by multiagency and community partnerships have the potential to be effective, there is little rigorous evidence of effective approaches. The recommendation was to develop and pilot complex interventions that address multiple risk factors as a prerequisite for rigorous evaluation and any subsequent implementation.
In response to these findings, Moore et al. 21 examined the feasibility and efficacy of a risk-led, premises-level intervention in reducing ARV. Using the evidence regarding efficacy in reducing ARV, Moore et al. 21 developed a premises-level risk audit designed to assess environmental risk in discrete areas of a premises with the view to providing bespoke advice designed to target, and reduce, risk where required. In line with reviews which have been critical of the methodology used to explore the efficacy of ARV reduction programmes, the intervention developed by Moore et al. was trialled using a RCT design and incorporated a nested process evaluation. 21 Findings from this feasibility study supported the intervention, strengthening evidence that tackling specific environmental risk factors within at the premises level can reduce the incidence of ARV. However, disappointing levels of intervention adoption within licensed premises led to further reflection, particularly on the need for statutory powers to enforce any intervention.
Identifying risk factors
Risk factors are those characteristics of licensed premises that are associated with an increased likelihood of severe intoxication and disorder. These factors are many and varied and may interact with one another. Furthermore, it is likely that many risk factors have not yet been described or that latent factors may offer a simpler explanation for clusters of the observed risk factors. The theoretical frameworks that motivated our approach were routine activity theory (RAT)22 and ‘broken windows’ theory (BWT). 23,24 Both theories describe factors that are necessary for, or increase, the likelihood of crime taking place. RAT is a situational approach to crime that emphasises three co-occurring phenomena: a motivated offender, a suitable target or victim and the absence of a capable guardian. When considering violence from the perspective of RAT it is understandable how licensed premises can play an important role in managing the convergence of these phenomena. Similarly, the recognition of a victim’s participation and the failure of guardians to prevent the incident also make RAT a suitable theory in which to ground prevention research, as it acknowledges determinants other than the presence and motivation of an offender. BWT suggests that offending is informed by situational cues that indicate an absence of social order such as graffiti, litter, vacant buildings and broken or boarded windows. An absence of social order indicates a lack of capable guardians, making it a convenient environment in which to commit crime. In ‘real-world’ experiments, Keizer et al. 25 have shown that individuals take cues from their environment to inform their behaviour. For example, the sound of fireworks being set off illegally was related to an increase in littering, and the presence of graffiti on a mailbox was related to an increase in opportunistic theft.
Social control is also a central component to our approach in understanding the way violence arises in licensed premises. Social control is defined as ‘. . . those organised responses to crime, delinquency and allied forms of deviant and/or socially problematic behaviour that are actually conceived of as such’ (p. 3). 26 Distinctions are made between ‘formal’ and ‘informal’ social controls, with the former relating to interventions enacted by agencies of the state usually under the auspices of legal authority (e.g. the police, environmental health officers), while the latter is concerned with the regulatory and social ordering functions performed by citizens (including bar staff and private security). Innes27 maintains that social controls are increasingly embedded within the physical environment. Further, Black28 proposed that the quantity of social control tends to stay relatively constant, the changing variable being the proportion of control delivered by formal or informal means. 27,29 Additionally, situational and individual factors contribute,30–34 including the opportunity to offend. 22,35–37
The wide variety of activities available in NTEs brings with them a range of risk factors for disorder and intoxication, and numerous studies have sought to identify those risk factors. These risks are summarised briefly below; for more detailed accounts see comprehensive reviews by Graham and Homel. 9,38
High outlet density
The distribution of licensed premises in urban centres has been identified as a key contributor to levels of alcohol-related harm. 39 Areas with high concentrations of licensed premises have disproportionately higher levels of disorder, suggesting a cumulative, non-linear effect of outlet density. 40–42 Clearly, there can be no causal association between outlet density and harm, as areas with a large number of premises but few patrons would be expected to exhibit low levels of alcohol-related harm. High density most likely encourages behaviours that are associated with harm, such as pub hopping and competition between premises that leads to inappropriate promotions. While outlet density is not in itself in the control of premises staff, it would be possible for premises to mitigate those features that are causally associated with harm and are correlated with heightened outlet density, such as crowding and competition. 15
Customer management
Generalising from BWT, the entrance and façade of a premises inform potential customers of the characteristics within. While it is unclear if customers can accurately predict the risk of disorder in a premises based simply on approach, it is likely that interpretations of social norms are informed by these external characteristics. Therefore, door staff behaviour, queue management and the management of intoxicated or disorderly customers are fundamental in providing cues about descriptive and injunctive norms within. Interactions outside premises also represent potential flashpoints for disorder. The congregation of people outside after closing time represents a considerable risk factor, as this usually occurs at times when staff have finished their shift and are busy emptying the premises of its last few customers. This leaves the external area of the premises without a designated guardian at a time when customers are likely to be most intoxicated.
Security and door management
Generalising the social control theory outlined above, door staff represent both the expression and the actuality of informal social control, or guardianship, in a licensed premises. It is, therefore, important that they are adequately trained and present a professional and welcoming demeanour. In England and Wales it is illegal, under the Licensing Act, to allow disorderly conduct on premises. Furthermore, any member of staff who is authorised to prevent disorder and allows it to happen on the premises is legally culpable. Therefore, the refusal of admission to disorderly customers is regarded as a main role of door staff in England and Wales. The deployment of sufficient numbers is essential and should be informed by the capacity of the premises, the number of expected customers and past history of disorder.
In order to obtain a door licence, applicants are required to complete an examined training course. Moreover, in the event of a violent incident, customer ejection or injury on the premises, all details of the incident should be recorded clearly, accurately and promptly in a log book and subsequently reported to the police and, depending on circumstances, to local authority (LA) environmental health officers. Recording events linked to disorder, extreme intoxication and violence also enables premises managers to explore trends in disorder and to determine how to best allocate door staff.
Vigilant serving staff
Premises serving staff play a key role in the safe service of alcohol and the prevention of disorder, as they are responsible for refusing service to underage customers and intoxicated customers and for identifying signs of disorder within the premises. It is essential that serving staff are aware of their legal responsibilities and that they take these responsibilities seriously. Server training has been shown to have limited, short-term effects in improving serving practices in respect of the refusal of service to intoxicated patrons. 8 As serving staff act as informal guardians, it is important that sufficient numbers of staff are deployed in order to facilitate this role. Insufficient numbers of serving staff are associated with increased levels of disorder in a premises, as this increases competition for service between customers,43 as well as crowding. 15 Furthermore, a premises with a high proportion of male staff is associated with disorder in licensed premises,44 although this phenomenon may be a reaction to past disorder as opposed to a causal factor. Clarke45 further suggests that an overly sexualised dress code for female serving staff can contribute to heightened levels of arousal in a premises and this is further implicated in disorder.
Environmental factors
A number of studies have aimed to identify the environmental aspects of a premises that influence the likelihood of disorder. Graham et al. 46 conducted a detailed multilevel analysis of risk factors for bars in Toronto, ON, while Green and Plant38 collated a detailed description of these risk factors. Evidence suggests that showing sport in premises increases the length of customers’ visits47 and is associated with increased levels of aggression. Music has also been related to levels of disorder and intoxication. For example, poor-quality bands can be an irritant,48 while slower tempo country music is associated with an increase in drinking speed. 49 Loud music may further impair communication between customers, preventing the de-escalation of fractious encounters. A range of other environmental factors can act as irritants such as poor air quality,43 increased temperature50–52 and uncomfortable furniture. 43,53 Moreover, dim lighting reduces the capacity for formal surveillance by premises guardians, impairs communication and increases the likelihood of collisions. Areas that are difficult to view and guard, such as thoroughfares and stairways, can also provide increased opportunities for collisions and injuries. Glassware also presents a significant risk factor for serious injury owing to its portability, accessibility and the level of harm that can be caused with a single blow. 12 Furthermore, the presence of empty glasses and other litter on tables may signal low levels of social order, and there is a relationship between untidy premises and disorder. 19,44,48,53,54
Promotions
Stockwell et al. 55 found that alcohol promotions were associated with intoxication but not associated with the risk of alcohol-related harm. More recently, however, studies suggest that promotions and becoming drunk are associated with police-recorded violence. 14
Customer behaviour and characteristics
Disorderly customer behaviour, according to BWT, contributes to perceptions of a permissive environment, thereby increasing the likelihood of further disorder. However, the relationship between gender ratio and disorder risk is unclear and evidence is scarce. 9 Although men are at far greater risk of violence,4 the presence of women may actually serve as a risk factor for violence owing to competition for sexual resources. Similarly, while a younger age is associated with increased risk of violence, customer age is not a strong predictor of disorder. However, age may interact with several other factors, such as premises type, which ultimately contributes to disorder. Typically, persistent offenders who are frequently violent when intoxicated56 are usually well known, emphasising the need for door staff and premises managers to share data across premises in an area.
The importance of partnerships
While identifying and addressing risk at the premises level may help to reduce violence, a part of any intervention is likely to require input from a range of organisations able to assist premises make the required changes. Accordingly, tackling alcohol-related harm and violence is a focus of partnerships involved with managing night-time environments,10,11 including the police, NHS, and local and national government. The aim of partnership-working is to mobilise a power base whereby politics and policy work smoothly together to enable change. 57 Partnerships that cross traditional organisational boundaries have become the accepted approach when addressing health and social problems that require complex solutions. 58 Indeed, Section 17 of the UK Crime and Disorder Act 199859 places an obligation on statutory bodies to work together in partnership to reduce crime and the UK government’s Alcohol Harm Reduction Strategy for England suggests that tackling alcohol misuse and related harm relies on the creation of partnerships between national and local government and health care, policy services, individuals and communities. 60 For city-centre ARV, the Department of Health’s Alcohol Improvement Programme encourages partnership-working to address alcohol-related hospital admissions. 61 The importance of partnerships are further emphasised in the UK’s Alcohol Strategy,1 which sets out proposals to reduce alcohol-fuelled violence and excessive alcohol consumption.
In 2003 alcohol licensing systems were reorganised in England and Wales through the introduction of the Licensing Act 2003 (implemented in 2005). 13 This shifted responsibility to LAs, which were obliged to manage applications in relation to the sale of alcohol through a licensing committee comprising responsible authorities. These responsible authorities, which include the police, the fire service and Trading Standards, are expected to work towards four licensing objectives: the prevention of crime and disorder, public safety, the prevention of public nuisance and the protection of children from harm. Responsible authorities can comment on all applications and also call for the review of an existing licence if there are legitimate concerns that a premises has breached one or more of the licensing objectives. For the first time, through a 2013 amendment, the responsible authorities include the NHS and environmental health, a government agency that is chartered nationally but managed separately within respective LA boundaries.
The UK government has called on LAs to use existing powers to reduce alcohol-related harm. As statutory partners in reducing crime and disorder, and responsible authorities under the Licensing Act, EHPs are well placed to implement effective strategies to prevent workplace violence. EHPs are chartered environmental health professionals who have a history of enforcement and partnership-working and are trained to deliver risk-reduction interventions and advice to small and medium-sized businesses. The primary objective for EHPs is to promote positive relationships between regulators and those they regulate, to protect the public and to encourage business growth,62 and they are the only responsible authority with this remit. EHPs intervene proportionately to the evidence for risk, with the emphasis on a dialogue that helps those they regulate achieve compliance and reduce risk. 63
Given this, an opportunity exists for EHPs to become more involved in ensuring that the on-licensed trade works to reduce risk and maximise public safety. Assault data implicating a premises could be interpreted as an indicator of risk that the premises may not have done all that is reasonably possible to prevent that assault. These data could then be used to trigger an inspection to identify whether or not known causes of violence are present, the expectation being that EHPs would use their regulatory authority to determine whether or not licensed premises are meeting their obligations to maintain public safety. As the link between episodes of violence and risk of harm falls within the remit of the Health and Safety at Work etc Act 197464 (HSWA) and enforceable legislation, is it feasible for EHPs to identify the risks of harm within their statutory remit and work with premises to lessen those risks? This paper addresses that question.
The role of environmental health practitioners
All businesses with five or more employees are obliged under the HSWA to have a written policy that describes how risks are identified and managed. 64–67 The expectation is that all businesses conduct risk assessments and take reasonable actions to reduce risk. The risk assessment, therefore, provides the point through which formal control (i.e. the HSWA and the Licensing Act) can operate to increase informal governance, whereby premises managers work to identify areas in which harm (including alcohol-related harm and disorder) might arise and what can be done to minimise those risks. Risk assessments should be reviewed regularly and employees are expected to be aware of what measures are in place. Dissemination is through formal induction processes for new employees and regular refresher sessions for existing staff, which in turn are expected to increase informal governance within premises. The HSWA therefore provides an important opportunity to manage risk in licensed premises and to encourage appropriate informal governance across the entire premises environment.
The HSWA aims to ensure that business practices are safe for staff and customers. Evidence suggests, however, that some businesses focus more on profitability and ignore the potentially harmful effects of their operation. 68 The concept of social corporate responsibility acknowledges that staff attitudes and ethics can influence business management and practice. Attempts to implement interventions to combat ARV through a social corporate lens can thus lead to difficulties if costly changes are required without a mandate that obliges intervention adoption.
The process evaluation from an earlier feasibility study21 appears to corroborate the lack of enthusiasm and urgency in tackling health and safety issues. Feedback from those delivering the intervention indicated that due diligence was not overly apparent in many premises, indicating that enforcement was, therefore, both critical and necessary. This led to the logical conclusion that intervention implementation was likely to be improved if delivered by a statutory authority.
Of the groups able to enforce organisational change on premises (e.g. the police, LA licensing officers and EHPs), EHPs are most accustomed to surveillance-led activities, particularly in the case of food-poisoning outbreaks. However, unlike the police, they are accustomed to working with small businesses to proactively reduce harm. In the light of this, and given their knowledge, expertise and experience, EHPs may provide a foundation for the development of licensed premises interventions.
Currently, EHPs have no prescribed role in respect to violence reduction in licensed premises and are primarily responsible for enforcing the HSWA and related legislation. However, in upholding the HSWA, EHPs have, among other powers, a right of entry to a premises at reasonable times, the right to investigate and examine, the right to see documents and take copies, the right to request assistance from colleagues, including the police, and the right to ask questions under caution. Where enforcement is necessary, EHPs have several options available to them. They can give legal notices, which are written documents requiring persons to do/stop doing something of which there are two kinds. First, if an EHP is of the opinion that a person is currently contravening the HSWA, or has contravened it in the past, they can be serve that person with an improvement notice that details what is wrong and how to put it right within a set period of time. Second, if an EHP is of the opinion that activities are being carried on, or are likely to be carried on, that involve the risk of serious personal injury then they may serve a prohibition notice, which prohibits the use of equipment and/or unsafe practices immediately. In extreme circumstances EHPs can also prosecute both employers and employees; this can include unlimited fines and a jail sentence.
Implementing a risk-led intervention
As statutory partners in reducing crime and disorder, and responsible authorities under the Licensing Act, EHPs are well placed to drive local action and implement effective strategies that are designed to prevent workplace violence. We therefore sought to identify how risk reduction might be enforced by EHPs under the HWSA.
In order to enhance the ownership and agency of bar staff, the intervention was framed as a risk audit, findings from which informed a subsequent action plan (if necessary). The expectation is that, should the action plan be adopted, the risks linked to premises-level harm will have been addressed and a reduction in alcohol-related harm would be expected. The action plan would require premises to make changes to operating procedures (e.g. reducing capacity, changing how security staff are deployed, checking patrons’ age at the door) that have been identified as contributing to the risk of alcohol-related harm. Although this intervention is framed as a supportive process, designated premises supervisors (DPSs) are still under a legal obligation to respond to the audit action plans.
Furthermore, in an attempt to enforce change through the threat of punishment, parliament has increased the penalties for serving alcohol to intoxicated and/or disorderly customers. An element of the audit will therefore be to establish how much DPSs and servers understand about the behaviour of an intoxicated and/or disorderly individual, and to determine whether or not staff know how to identify and defuse potentially violent encounters. In line with the collaborative aspect of the intervention, premises staff will be encouraged to use an online educational tool developed to aid staff in acknowledging, understanding and addressing customer behaviour.
Rationale for the All-Wales Licensed Premises Intervention trial to reduce alcohol-related violence
The evidence thus far has indicated that interventions addressing multiple risk factors and designed and implemented by multiagency and community partnerships have the potential to be effective in reducing ARV. An evaluation of a UK pilot RCT made significant headway in the delivery and implementation of a risk-led intervention aimed at reducing ARV, while substantial progress was also made to better understand the theoretical mechanisms of a successful risk-led intervention. The All-Wales Licensed Premises Intervention (AWLPI) trial aimed to build on this earlier research by developing a context-based risk-led intervention and to determine its effectiveness in a RCT. If the intervention, designed to be implemented by EHPs, was to prove successful the potential benefits could be substantial. It was calculated that, if the potentially low-cost implementation of the AWLPI succeeds in reducing violence, there could be substantial tangible (e.g. reducing costs to health services and the police) and intangible (e.g. reducing fear of crime and the psychological impact of victimisation) benefits. Furthermore, the research team reasoned that this project could offer the prospect of implementing routine surveillance and proactive violence reduction in EHPs’ practice through engagement with the Chartered Institute of Environmental Health and the Health and Safety Executive (HSE).
Overview of the All-Wales Licensed Premises Intervention trial
The trial described in this report was conducted in two stages. The first stage of the trial involved developing the intervention. The second stage of the trial encompassed training, site recruitment and randomisation, implementation of the intervention, data collection, and the process and economic evaluations.
Intervention development and refinement
In order to develop a suitable and workable intervention, the AWLPI trial incorporated an intervention refinement stage, which involved collaboration with senior EHPs, researchers and web media experts. The specific aim of this stage was to transfer the theoretical and empirical motivations for the intervention into a practicable and accessible evidence-based intervention programme. The intervention refinement stage of the trial is described fully below.
Trial stage
The effectiveness of the intervention developed in the intervention refinement stage of the trial was assessed using a RCT design described more fully in Chapter 4. The primary outcome in this trial was the difference in police-recorded violence between intervention and control premises over the follow-up period. Secondary outcomes were assessed using an embedded process evaluation (see Chapter 6) and economic evaluation (see Chapter 7).
Summary
The costs to society of violence associated with the on-licensed trade are substantial.
There is a statutory requirement of licence holders to reduce the risk of violence, research evidence suggesting that this is possible and strong theoretical positions indicating that an effective approach is feasible.
An earlier feasibility study indicates that, while a trial of interventions to reduce risk in premises is feasible, significant barriers include access to, and therefore the provision of intervention materials in, licensed premises.
Environmental health practitioners have both the skills required to deliver interventions in licensed premises and the statutory authority to gain access.
Environmental health practitioner-delivered interventions in licensed premises also have implications for the NHS, which is a responsible authority under the Licensing Act but has no formal representation on licensing committees or regulatory relationship with licensed premises.
Aims
-
To refine an intervention that can be mainstreamed into EHP usual practice.
-
To test EHPs’ capacity to reduce ARV in a RCT.
-
To determine the effectiveness, acceptability and cost-effectiveness of a risk-led intervention designed to reduce ARV.
Objectives
-
To develop intervention materials that:
-
translate formative work for use in EHP normal practice
-
encompass a risk audit to cover multiple risks and that are therefore responsive to each premises’ unique circumstances.
-
-
To map premises-specific police-recorded violence data across time to determine whether or not the impact of the intervention reduces violence and whether or not any effect changes over time.
-
To identify the costs associated with Safety Management in Licensed Environments (SMILE) implementation and delivery and to approximate the extent to which it can be regarded as an efficient use of public funds.
-
To use qualitative and quantitative data from the embedded process evaluation to:
-
understand intervention development and integration into normal practice
-
assess intervention reach, fidelity, dose and receipt
-
identify if and how the design and implementation of the risk-led intervention delivered by EHPs in this trial could be further optimised and
-
critically appraise the quantitative and qualitative outcomes alongside one another in order to develop a revised logic model of the intervention.
-
Chapter 3 Developing SMILE
Introduction
Overview
The previous chapter described the theory behind premises-level interventions and areas of premises operation that could be targeted so that improvements would bring about a reduction in alcohol-related harm. This chapter describes how formative work was translated for use by EHPs and into a format that would be acceptable to premises staff.
Key research findings from a feasibility study of a risk-led intervention showed that (1) an enhanced multiple risk-audit approach can successfully identify appropriate targets and approaches to prevention; (2) the engagement of licensed premises and intervention efficacy were maximised when implemented by statutory authorities; and (3) police-recorded data on violent incidents were a valid measure of harm, sensitive to change at the premises level. 69
The theoretical basis to the intervention was that identifying risk of alcohol-related harm and motivating changes in premises to mitigate those risks would be expected to reduce alcohol-related harm. This approach is enabled by current legislation. The Licensing Act 2003 places a requirement on DPSs to adjust premises operation if they become aware that their operation increases the risk of harm. 13 Therefore, practitioners who are able to identify and advise premises staff on such risks should expect their advice to be heeded and that premises will respond to such advice. Furthermore, and specific to EHPs, the HSWA facilitates practitioners’ access to premises and premises staff and also affords EHPs the statutory remit to investigate workplace violence. 64 Thus, EHPs provide formal governance and are able to require change in small businesses to reduce harm.
While EHPs were not susceptible to the intervention barriers identified in the feasibility trial, there still existed a need to translate formative theoretical work into a format that was both consistent with EHPs’ normal working practice and acceptable to premises staff. Intervention materials were coproduced with EHPs to translate formative work into a format that communicated premises, obligations to minimise harm in a way that was acceptable to all premises staff (e.g. via an accessible website and informative films). The expectation was that these materials would engage all staff in the premises hierarchy, from door security staff to servers and management. Second, a risk audit was developed that covered multiple risks. This comprised a written booklet that both outlined the statutory and research evidence for areas in which EHPs should attend and provided a uniform means of identifying and collating evidence for risk in premises (see Appendix 1). The risk audit was intentionally developed from earlier audits used by EHPs.
All-Wales Licensed Premises Intervention aims and objectives
The primary research aim for this component of the trial was to refine a risk-led intervention that aimed to identify environmental risks in premises and that could be subsequently mainstreamed into EHP usual practice.
Intervention development
During the first 6 months of the trial (March to September 2012), senior EHPs, industry representatives and web consultants were involved in a consultation process with the research team to develop intervention and training materials. These consisted of the risk audit tool, a website, short instructional films and additional materials such as incident reporting templates and health and safety guidance. Collectively, these were designed to facilitate the risk audit and to standardise the risk audit. The intervention development meetings with the senior EHPs were conducted separately from the meetings with the media and web consultants.
The intervention was planned and constructed during subgroup meetings using a framework structure to guide development. The framework adopted an iterative process informed by subgroup discussion and the literature.
A stakeholder intervention coproduction group was, therefore, established that consisted of four senior EHPs from across Wales and three academics involved in the initial feasibility trial. The first meeting focused on presentation and discussion of feasibility study results. Early on it was recognised that the intervention would map strongly onto current EHP work practices and that the underlying research aims and objectives met with those of the environmental health agency, an agency concerned with anything that was a risk or hazard to the environment generally or to members of the public specifically (see Chapter 4, Process evaluation). In initial meetings it was clear that the value of SMILE had been understood and the organisation was keen to be involved. The meetings also improved academic understanding of the organisational context and the remits of routine EHP practice, which was to investigate accidents, educate and work in partnership with groups and stakeholders who have an interest in public health or the health of the environment.
Three subsequent meetings focused around delivery systems for and design of SMILE. For delivery, EHPs suggested that health and safety EHPs should implement the intervention, as these specialists were likely to have gained useful experience and knowledge of RIDDOR (Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 2013), regulations that require employers, the self-employed and those in control of premises to report specified workplace incidents. 66 Further deliberation about possible changes needed to adapt the risk-audit intervention to the environmental health context resulted in the agreement of senior EHPs to coproduce SMILE with the aim of ensuring that the audit mapped on to existing work practice as closely as possible. Initial iterations of the risk audit tool were developed by the academics based on feasibility trail results and systematic review evidence. This was adapted by the EHPs to conform to existing audit tools used in normal practice. This was then piloted by the senior EHPs with their teams in three premises in each of their areas. Feedback resulted in a revised third and final iteration of the audit tool. For the video, an initial meeting between the stakeholder group, project advisory group and a design company identified potential aims and objectives and suitable content. A follow-up meeting of the stakeholder group reviewed draft videos and recommended revisions. The final videos were agreed by the stakeholder group in a third meeting but these were not piloted with the wider EHP organisation owing to time limitations.
The overall goal was to design an intervention that included a follow-up audit that was deliverable, effective and could yield the data needed to answer the research question. The framework used to structure the intervention development phase is now described.
Key questions:
-
What are the key elements of the intervention?
-
Which components of the current audit are currently performed by EHPs/other agencies?
-
Which components not currently captured by the audit should be included?
-
What policy documents already exist for licensed premises?
-
What supportive materials would be appropriate (i.e. content of videos)?
-
Should follow-up be included as part of the intervention and, if so, what should it assess?
-
-
When should the intervention take place?
-
Should audits take place during the day or at busiest periods?
-
When should follow-ups take place?
-
-
How should the intervention be implemented?
-
Should all aspects of the audit be conducted by EHPs?
-
How should action plans be delivered (e.g. in person/by e-mail/by post)?
-
What is the best format for the action plan (e.g. CD-ROM/hard copy/booklet/web upload)?
-
Should follow-ups be conducted by EHPs only, or in conjunction with other agencies, or solely by other agencies?
-
How should training videos be disseminated [e.g. YouTube (LLC, San Bruno, CA, USA; www.youtube.com), e-mail, newsletter, dedicated sessions at work, dedicated website]?
-
Secondary questions:
-
What will be the main challenges to implementation?
-
What will be the main barriers to premises implementing the action plans and can these be addressed in the development phase?
-
How will other EHPs react to the intervention – anticipated objections/resolutions?
-
What structures and resources would be needed to make the intervention sustainable if it were rolled out?
-
How will the implementation process be monitored? This includes issues such as type and frequency of contact with premises, acceptance of intervention from DPSs, barriers/facilitators to implementation.
-
Are there existing reporting structures that EHPs follow that could be adapted?
-
What are the best ways to capture issues with implementation (e.g. diary/log/telephone call/online form)?
-
Audit development
Three core members of the research team and five senior EHPs were involved in the AWLPI audit development. Development began initially by identifying the most pertinent indicators on an EHP health and safety audit that had previously been developed by EHPs. Selected indicators were translated into a series of items and mapped onto a spreadsheet to provide a comprehensive matrix whereby each item was associated with a potential response. This matrix was sent to the subgroup EHPs for feedback. This process was repeated during the development phase until all parties were satisfied. The finalised matrix was then formatted in the style of a health and safety audit (see Appendix 1). The AWLPI audit was then piloted by EHPs (naive to the AWLPI trial) to check for completeness, accuracy and ease of use. Final iterations of the audit were made as recommended in the piloting feedback.
Web-based training and instructional materials
Representatives from a web development company, a graphic design company, the British Association of Anger Management, an organisation representing door supervisors and a communications consultancy along with three core members of the research team were involved in the development of the AWLPI website and online training films.
The focus of the short films was explored during the developmental meetings between the research team and EHPs. The overarching topics chosen for the films were influenced by the literature, previous research conducted in licensed premises and industrial experience of both the researchers and the EHPs. The visual concepts of the films were developed using storyboards.
Once built, the system underwent user acceptance testing by the research team and all content on the website was checked by EHPs to ensure legal compliance.
Summary of website specifications
-
Technical specification:
-
four videos, each 5 minutes long
-
website and videos to be accessible to smartphones and tablets
-
bilingual (Welsh and English)
-
linked to HSE website (www.hse.gov.uk/)
-
internal database metrics (e.g. to determine usage).
-
-
Design concepts:
-
Enhancing practitioner engagement by:
-
catering for different levels of employee
-
catering for different types of premises
-
‘buy-ins’ for those using the website (e.g. opportunity to gain transferable skills).
-
-
-
Video content:
-
Need to engage audience in four areas:
-
security and communication
-
particular emphasis to be placed on pro-active de-escalation
-
environment
-
crowding/intoxication.
-
-
-
Website structure:
-
The homepage will direct the user to:
-
information about the issues
-
the short films
-
a ‘diligence’ page where users can demonstrate using a feedback mechanism that they have accessed and assimilated the information
-
contact page using a standard e-mail form.
-
-
-
Website design and function:
-
include references to involved parties – the university and funding body
-
function for premises staff to provide feedback/demonstration of diligence to content
-
include links to AWLPI trial Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) page and Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) account.
-
Content of intervention materials
Risk audit
The risk audit included items that could be used to describe basic features of the premises being audited. This included the number of full- and part-time staff, whether or not food was served and whether or not the premises hosted live music. The date and time of the audit was also recorded as well as the distance travelled by the EHP to the premises.
Eleven operational domains were examined and included:
-
Records management: written risk assessments, related policies, premises opening/closing logs and incident logs must be available and up to date. Incidents logged should be cross-referenced with policies and risk assessments to assess whether or not action had been taken to minimise the risk of further harm.
-
Visibility and lighting: visibility and lighting should be good throughout the premises. Blind areas can impede surveillance by premises staff, as can low levels of lighting.
-
Health and safety observations and checks: heating, ventilation and the overall condition of the premises were assessed.
-
Surveillance: surveillance arrangements should be sufficient to protect health and safety. This includes where security staff are usually located and the use of closed-circuit television (CCTV).
-
Noise and communication: staff should be able to communicate with each other effectively about potential risks during times when the premises is open.
-
Risk planning: there should be evidence of regular engagement with PubWatch (www.nationalpubwatch.org.uk) or similar. There should be no evidence of irresponsible drinks promotions. There should be sufficient numbers of front-of-house staff present during busy periods.
-
Door management: effective door management during busy periods should be in place. This includes maintaining appropriate door-staff registers and policies.
-
Managing people: visibly intoxicated and/or disorderly patrons should be effectively managed. Those who are disorderly must be escorted off the premises and those who are intoxicated must not be served alcohol.
-
Staff training: there should be evidence of staff induction and ongoing training that encompasses disorder, violence and aggression.
-
Incident reporting: it is a legal requirement to record violent incidents that have occurred on the premises, records that should inform future practice.
-
Glassware policy: literature suggests that the use of toughened glass or plastic reduces risk of injury.
Risk score and action required
Each of the 11 sections included a risk control indicator (RCI) score. The RCI is a standard instrument used by EHPs to record the perceived level of risk in the environment. Using the RCI, a score of 1 represents a situation where the EHP believed that no further improvements were possible (based on current legislation and guidance); scores of 2 and 3 represent situations where enforcement action may be appropriate; a score of 4 or higher denotes situations requiring legal enforcement. The guidance indicated that EHPs should give a RCI score of 0 to non-applicable areas of premises operation. Each section required EHPs to record any action they had taken (none, verbal advice, written advice, improvement notice or prohibition notice).
Web-based training and instructional materials
Films
Training and educational films were designed to increase awareness of the physical and social environment, and increase knowledge of policies and practices that prevent and reduce excessive alcohol consumption and violence (Figure 1 and Table 1). Each film included animations, summary text and a spoken script. The messages of the films were positively framed by focusing on the benefits to be enjoyed from implementing the techniques demonstrated in the films rather than dramatising the consequences.
FIGURE 1.
An example of a storyboard used to inform the design of the short films. ID, identification; VO, voiceover.

| Chapter One: the benefits of a safer environment | |
|---|---|
| Voiceover: creating a safe environment not only provides a better atmosphere for your customers; it can also help to improve staff retention by making your venue a more pleasant place to work. And with happy customers and happy staff, your reputation can bring you more business Everyone working at the venue can play a role to help reduce risk within your venue. And it needn’t be time-consuming; this video provides a quick snapshot of the ways staff can get involved and work together to provide a safer environment |
Visual: presenter piece to camera, walking through scene of happy customers, happy staff, and busy bar |
| Duration: 30 seconds | |
The training and educational films provided guidance in the following areas: premises environment, security, crowding and how to de-escalate fractious encounters between customers. The four film topics were:
-
safety and your colleagues
-
keeping them happy
-
tables and chairs
-
staggering crowds.
Angling the films towards depictions of emotions, and anger in particular, was felt to be a good inclusion, as staff may feel empowered to recognise and understand conflict at the bar more easily. The films also aimed to communicate that customers’ pride (or ‘power base’) needs to be kept intact throughout interventions in order to avoid escalating or displacing aggression.
Website
The intervention website contained information about harm-reduction practices in licensed premises and provided guidance documents that could be downloaded and used by premises staff (Figure 2). The website also contained a due-diligence quiz that was designed to provide instruction on how premises staff can reduce excessive alcohol consumption and violence. The website was made available in English and Welsh. 70 A diagram of the site layout is in Appendix 2.
FIGURE 2.
The homepage of the SMILE website.

Due-diligence quiz
The due-diligence quiz comprised 25 questions that assessed understanding and knowledge gained through viewing training films. Members of premises staff answering ≥ 50% of questions correctly received a certificate of achievement that could be displayed in premises. Reference materials were also provided. These were downloadable guidance documents, document templates and posters that collectively aimed to help premises staff reduce ARV in their premises. Business cards were also used to advertise the website address. The quiz used is included in Appendix 3.
Intervention training
In order to enhance intervention fidelity, EHPs who were to deliver the intervention attended one of three training workshops held in North, West and South Wales. The training was mainly delivered by senior EHPs and academic staff with a research interest in reducing violence. However, presentations were also given by medical consultants, who were able to highlight the extent and severity of violence within the NTE.
The training sought to increase awareness of ARV in and around premises and to elucidate the potential impact EHPs could have on reducing ARV. Additionally, EHPs were presented with information about the AWLPI trial and the SMILE intervention tools. This part of the training entailed navigating the risk audit and associated website in detail, and advice on how to implement these tools to the best effect.
The finalised intervention
Prior to outlining the intervention for the AWLPI trial, it is worth highlighting that the professionals delivering the intervention were, to some extent, embedded within the intervention itself. The fact that EHPs have statutory powers in the area of workplace health and safety meant, in theory, that the intervention could be delivered with some authority and as such removed the need to gain consent from participating premises. In Wales, the intervention was adopted as EHPs’ annual project, which meant that all EHPs were committed to delivering the intervention as part of their standard practice for that year.
EHPs were programme advocates for the AWLPI trial and also delivered the intervention as auditors. During the training it was emphasised that those delivering the intervention should do so in a standardised manner, to ensure that the mechanisms through which the intervention worked functioned as intended. Figure 3 depicts a logic model of the intervention.
FIGURE 3.
Logic model of the intervention for the AWLPI trial.

Intervention input
The key ingredients during this phase of the intervention are (1) the auditor, (2) the audit and (3) the training films.
-
The auditor is an EHP who has been trained to conduct the audit in a systematic and standardised way.
-
The audit materials consist of:
-
the 11-point audit of the premises, this is grouped into:
-
– the physical environment
-
– policies and procedures
-
– staff training
-
– risk assessment and planning
-
-
guidance leaflets and notices, to be given at the end of the audit if necessary.
-
-
Training films, which were accessed using the SMILE website.
Activities
The audit was conducted in person with each premises’ DPS. The audit took place at a time suitable to both the auditor and the DPS, when they would not be interrupted. It was expected that the audit would take approximately 1 hour. The DPS from each premises should have been informed approximately 2 weeks prior to interview that the auditor would request to see as many of the following documents as possible:
-
health and safety policy
-
drugs and search policy
-
staff training records
-
incident log book
-
accident book (if appropriate)
-
door staff register
-
written procedures for opening/closing bar
-
health and safety checklists
-
fire alarm checks.
Intervention and control groups
In summary, intervention premises received SMILE as described above. Control and intervention premises both received ‘usual practice’, the normal regulatory attention ascribed by partners involved in managing harm in the night-time environment. While this may vary across LAs, in so far as LA licensing, the police and other agencies are differentially involved according to local requirements, such variance will be at the LA level. Because control and intervention premises were stratified by LA in this RCT, such local variation is expected to be balanced across groups.
Following the audit, auditors were asked to discuss the arising risk factors with DPSs to ensure that each risk factor was justified in relation to relevant legislation or evidence. During the audit visit EHPs were to provide the DPS with information about the SMILE website and how to navigate it effectively. DPSs were urged by the EHPs to cascade information about the SMILE website to all their staff and to encourage engagement with the website and its associated training films.
Expected output arising from the audit
The second component of the intervention is the generation of an action plan arising from the audit itself. The action plan given to the DPS should be tailor made for each premises as a result of the findings from the audit. There is a need for this to be a list of points (‘tell me what to do’) rather than a long document. The way the action plan is written should take HSE reports on how small businesses perceive and implement legislation into consideration.
Conducting a follow-up audit
Depending on the severity of the risks identified during the initial audit the EHP would serve an improvement notice or a prohibition notice, or arrange for a second audit to take place. When a formal notice is served the EHP would specify the provision(s) that had been contravened and give reason(s) why they feel these had been contravened. The requirements necessary to remedy the contravention should then be given followed by a reasonable time period in which to comply with the notice (not fewer than 21 days). A second audit would be arranged to ensure that premises had complied with directions.
As a part of the intervention, second audits were expected to have been completed within 3 months after the intervention to check that actions had been taken. In premises where no risks were found, no further visits would be necessary and usual practice would resume.
Expected outcome
It was expected that, through dialogue with auditors immediately following the audit, DPSs would feel some ownership over the action plan they receive. This was key in facilitating premises to carry out the action points, as any disagreement over risk factors should have been resolved and there should not have been any surprises in the action plan.
Summary
Developing and refining an intervention to be delivered by EHPs was undertaken through a period of preparation involving a multidisciplinary team. The basis of the intervention was developed through meetings between environmental health agency managers and academic research staff where the objectives of the intervention were developed from the rationale behind the trial, the literature and previous experience of working with licensed premises to reduce ARV. The underpinnings of the intervention, guided by the overall research objectives, were further developed by the core research team using key questions to guide and focus progression. Industry representatives and web consultants took the visual aspects of the website and video elements of intervention forward with the guidance and feedback from the research team. The audit was finalised between the research team and senior EHPs. With respect to time scales, development of intervention materials occurred concurrently to meetings concerning intervention delivery, data collection and overall trial design in order to maximise intervention feasibility and collecting the data needed to answer the primary research objective. Preparation to conduct the trial, which included intervention development and refinement, took 6 months. By the end of this period a premises-specific, risk-led intervention had been coproduced through collaboration with senior EHPs. This notionally gave the intervention the best chance of being mainstreamed into EHP usual practice. Additionally, consideration of the materials and their implementation alongside the overall trial design throughout this process increased the likelihood of successfully trialling the finalised intervention in licensed premises in Wales.
Chapter 4 Methods
Trial design
The project included a randomised controlled effectiveness trial, with licensed premises as the unit of randomisation. Figure 4 depicts the trial schema. The trial was preceded by an initial intervention refinement period and included an embedded process evaluation and economic evaluation. The trial received ethical approval from Cardiff University Dental School Research Ethics Committee (reference 12/08).
FIGURE 4.
All-Wales Licensed Premises Intervention trial schema.

Trial population
The population comprised premises licensed for the on-site sale and consumption of alcohol residing within any of the 22 Welsh LAs.
Premises eligibility
Licensed premises were eligible if, between the months May 2011 and April 2012, they had one or more violent incidents associated with them. Incidents inside and in the immediate vicinity of licensed premises were identified from police data. Other inclusion and exclusion criteria are presented in Table 2. In order to determine eligibility, premises were cross-referenced with licensing data and, where feasible, premises’ own online web pages.
| Inclusion criteria | Exclusion criteria |
|---|---|
| On-licence premises that are based within the 22 LAs in Wales | On-licence premises that are cafes, restaurants and entertainment venues such as sports facilities and concert halls |
| On-licence premises that are public houses, nightclubs or hotels with public bars | |
| On-licence premises that have one or more violent incidents recorded by the police (including Section 18/20, Section 47, common assault, affray, assault of a police officer) in the 12 months up to May 2012 |
Baseline violent crime data
In order to access police data, data sharing agreements were prepared and signed between Cardiff University and all four police forces in Wales. The agreements covered the period from May 2011 to the end of the trial follow-up period. These data were used to identify eligible premises (see above) and to provide baseline characteristics required for stratification.
All violence against the person data for Wales were requested from all four police forces in Wales. These data included incident location, coded as both Global Positioning System (GPS) co-ordinates (recorded by the attending police officer) and a free-text description of the incident location (also entered by the attending officer). The data from North and South Wales territories were extracted using the NICHE Records Management System. In the Dyfed and Gwent territories the data were extracted using the CIS Records Management System (Computer Information Systems, Inc., Skokie, IL, USA) and Guardian Records Management System (Victorville, CA, USA), respectively, which introduced minor coding differences between each police force data set. Data were handled according to the data sharing agreements in place; original data were encrypted, stored and accessed by two named individuals. Only anonymised data or data with premises details but not crime information were available to members of the research team for screening.
Baseline premises address data were manually checked by two independent researchers. All addresses that identified a licensed premises were marked as such. Licensed premises were identified using online search tools and LA licensing data. Contact (telephone number) and address information were appended to the data, as well as licensable hours of business. Premises were telephoned to ensure that they were open and this was rechecked through contacting LA licensing teams. Premises that were open at baseline and deemed eligible by the research team were then stratified (the variables used to stratify the premises are outlined below). This produced a total of 837 licensed premises with one or more violent incidents associated with them that were eligible for inclusion in the trial. The 600 premises selected for trial participation were chosen randomly, resulting in 300 premises in the intervention group and 300 in the control group. The remaining 237 premises were reserved as replacement premises in the event that intervention premises were closed by the time audits began. A list of intervention premises was then split by LA, weighted by LA size and sent to the respective EHP responsible for premises in that LA, along with intervention materials.
Closure and replacement premises
It was anticipated that a number of premises screened and allocated to the intervention or control groups might cease business or become ineligible (e.g. changing to a restaurant) before the intervention was to be conducted. If premises in the intervention arm became ineligible before the intervention phase began, it was replaced with a premises randomly selected from a list of any remaining premises in that LA, matched by strata. When a replacement premises meeting the necessary strata criteria was unavailable the premises was not replaced. Following the intervention period, the research team investigated closure of premises (in both experimental arms) by contacting LAs. Duplicate premises, or premises in the intervention arm that did not co-operate with EHPs or could not be accessed by EHPs in the allotted intervention period, were not replaced with any of the remaining premises.
Permission to participate
Permission for environmental health practitioners to deliver the intervention
Environmental health practitioners across Wales have allotted time to engage in projects each year. The All-Wales Technical Panel agreed in 2012 that the AWLPI trial would be that year’s project of choice.
Consent from environmental health practitioners
As the EHPs delivering the intervention have statutory powers in the areas of workplace health and safety, and assess risk in small and medium-sized businesses as part of their usual activities, the trial was essentially a natural experiment (albeit with allocation to group being randomised). Therefore, as a part of EHP routine practice, it was unnecessary for premises to provide consent to participate in the trial and/or to receive the intervention.
Trial procedures
Environmental health practitioner intervention training
At least one EHP from each LA attended one training workshop. The EHPs were provided with a training manual and were supported throughout the trial period by the research team.
Data collection
Audit data
Staff at intervention premises were contacted about their forthcoming audit by a letter which was sent by the EHP responsible for that premises. The letter provided information about the trial and explained that an EHP would contact the DPS to arrange a convenient time to undertake the audit. The same template letter was used across all LAs.
The audit was completed by an EHP at a mutually convenient time. Parts of the audits were completed through interactive discourse with the DPS and beverage servers in order to find out more about a particular procedure or when physical evidence of certain artefacts, for example certificates of training, were required. On completion, EHPs fed back to the premises staff on areas where further action was required, if any. Feedback on changes required was given verbally, by letter or through formal notices (prohibition or improvement notices).
Once the forms were completed the EHPs photocopied the completed parts of the form and returned the original version to the research team and kept a photocopy for their files. Inconsistencies or omissions in the audit were clarified with the EHPs before the audit was scanned electronically and stored within a password-protected domain of the Cardiff University shared drive. The paper versions of the audits were stored in a locked cupboard. Audit completion was tracked using a Microsoft Access® database (Microsoft Corporation, Redmond, WA, USA).
Responses from the audit forms were entered manually (using double data entry) into an Access database; these data were then converted into a Stata data file (StataCorp LP, College Station, TX, USA). The researchers entering the data were provided with a metadata template enabling them to match each question/response field on the audit with its shortened variable name and providing them with information about what type of data should be entered (i.e. single response, integer, text, etc.) and how data should be labelled/transformed. The audits also included a section for EHPs to complete that consisted of a checklist and space for reflective feedback regarding each premises. This part of the audit was scanned/e-mailed/faxed/posted and entered into a separate spreadsheet to be used to inform the process evaluation.
The procedure for collecting, storing and entering follow-up audit responses was the same as that for the initial audit.
Feedback from the SMILE website
The SMILE website was coded such that usage statistics could be derived (unique visitors), providing an indication of use. In addition, the site was further coded so that it would not be included in search engines, to reduce the possibility that traffic had been generated from non-project activity.
Police outcome data
Between April and May 2014, data were received from four police forces, Dyfed-Powys, Gwent, North Wales and South Wales, in response to the original data sharing agreements with each. Data were received as four Microsoft Excel® files in different formats (Microsoft Corporation, Redmond, WA, USA). All files contained information related to offence (classification), time (date) and location (GPS and street address). These files were amended so that the data from the four authorities appeared in the same format.
Premises closure
All premises were checked for closure throughout the follow-up period. Premises closures and reopenings were tracked on an Excel spreadsheet. In addition, intervention premises closures were also determined by EHPs reporting that premises were closed when they were unable to gain access to premises for audit visits.
It was initially planned to use LA licensing data to identify premises that were economically active. These data were not available in most LAs, with data quality being at best below the expected standards.
At the end of the follow-up period a freedom of information request to all LAs requested business rate information on all study premises. All businesses are required to pay business rates unless they temporarily or permanently cease trading. These data were accessed to determine temporary and permanent premises closures in both trial arms.
Premises that were closed at the time of intervention delivery (and did not receive an initial audit) were dropped from the study. Premises that received the audit but were temporarily closed had their outcomes censored.
Follow-up data
Police data from January 2013 for 455 days were accessed from the four Welsh police forces. Two data sets were created, one using similar manual search methods used with the baseline data and one using automated search algorithms trained using baseline data. Primary outcome data were in the data file generated using automated procedures; sensitivity analyses used the manually produced data and a combination of both manual and automated.
Manual data
All violence against the person data were manually screened, comparing each entry with the list of trial premises. For each police force, a random subset of entries was independently rechecked using similar methods by a second researcher. Both data sets were compared and inter-rater reliability was calculated as the proportion of records that were identically identified, where a score of 1 was assigned where both raters agreed and 0 otherwise.
Automatic data
The GPS co-ordinates associated with each trial premises, derived from the baseline data, were used to extract a second data set of follow-up data. Data were received from four police forces: Dyfed-Powys, Gwent, North Wales and South Wales. Data were received as four Excel files in different formats. All files contained information related to offence (classification), time (date) and location (address). In order to classify crimes within the violence against the person category, we used Home Office crime classifications. 71 First, different coding systems used by different police forces were normalised to the latest version of the Home Office crime codes. A document called Crime Tree: Mapping of Crime Codes sets out how individual crime codes map to the branches of the crime tree. Level 3 of the tree was used to extract offences related to the violence against the person category. All crime codes corresponding to the violence against the person category at levels 3, 4 and 5 were extracted from the tree and cross-referenced against the crime data.
In the next step, offences not related to premises were removed from consideration. A list of lexical clues was assembled to automatically remove the bulk of the non-relevant data. Examples of such lexical clues include words and phrases such as car park, school, play area, road, footpath, mini market, etc.
Third, the goal of this step was to uniquely identify premises based on their address, which included the premises names. Three crime data files used postcodes as part of an address provided as the location where an offence occurred. Offence data from these three files were cross-referenced to the master file using the postcode. As there was no one-to-one mapping between addresses and postcodes, the cross-referenced data were manually curated to remove incorrect mappings. Manual curation involved comparing the premises names and addresses. The one remaining file contained geographic co-ordinates instead of postcodes. Geographic co-ordinates were converted to postcodes and manually compared against those in the master file by using premises name and address. Close geographic distance between the two postcodes was used to link non-exact matches on postcode, where the premises name and address were consistent with a premises in the master file. As a result of step 3, all offence data were mapped to premises in the master file. By normalising time information to the same date format, all data were normalised and ready to use as a single data set in a coherent format that enabled further statistical analysis.
Finally, the data set was anonymised by removing the premises names and their addresses, leaving only their locally introduced identification (ID). The finalised data set was structured into an Excel file with four columns: premises ID, offence date, offence code and offence description.
Statistical methods
Sample size calculation
A previous exploratory trial21 suggested that an overall group size of 274 premises provided a power of 90% to detect a 10% reduction in the failure rate (a day in which one or more violent incidents occurred) at a significance level of 0.05. Attrition was not a factor in this trial, as EHPs have a statutory authority to enter premises and therefore adjustments for withdrawals were not applicable. Temporary and permanent suspensions of premises licences are valid outcomes, as they represent a form of intervention and are, therefore, accounted for in the group size. A 12-month follow-up period was chosen (12 months following delivery of the first audit), as the earlier exploratory trial suggested that this offered the most likely opportunity to detect a significant effect in a full trial and could control for annualised cyclical variation within premises.
Randomisation
The unit of randomisation was each licensed premises within the 22 LAs in Wales. There were two groups (intervention and control). The total sample size of eligible premises for the randomisation was 837. A minimum sample size of 274 licensed premises per arm was required but this was rounded up to 600 total for simplicity. Therefore, 600 premises, stratified by LA, were randomly selected from the total eligible population for randomisation. Licensed premises were randomly assigned to intervention and control in a 1 : 1 ratio. Optimal allocation was used to randomise licensed premises to intervention or control, stratified by LA. Opening hours [low (0–4 hours after 11 p.m.), high (≥ 5 hours after 11 p.m.)] and number of incidents [low (1 and 2 incidents), high (≥ 3 incidents)] were used to balance the randomisation. 72 LAs that did not have the capacity to carry out as many audits as required for the randomisation were not supplemented with other LA premises, as EHPs do not generally go beyond their boundary, and also the approaches can differ. Premises that were closed prior to intervention delivery were replaced with premises randomly selected from a matched list of any remaining premises within that LA. However, as these spare premises were not randomised they were included only in sensitivity analyses.
Allocation by local authority
The number of premises in each LA receiving the intervention was determined by LA population. Table 3 shows the available number of eligible premises by LA and the number of required premises for the intervention group according to LA population. For information, the same allocation process was repeated for total violent crime by each LA and the number of audits conducted by EHPs in a similar but unrelated project completed the year before the current project began.
| Total available | Area names (English/Welsh) | Estimated audits | Previous inspections | |
|---|---|---|---|---|
| By LA population | By LA violence | |||
| 12 | Blaenau Gwent/Blaenau Gwent | 7 | 8 | 20 |
| 26 | Bridgend/Pen-y-bont ar Ogwr | 13 | 13 | 12 |
| 42 | Caerphilly/Caerffili | 17 | 16 | 20 |
| 78 | Cardiff/Caerdydd | 37 | 42 | 52 |
| 48 | Carmarthenshire/Sir Gaerfyrddin | 17 | 14 | 20 |
| 14 | Ceredigion/Ceredigion | 8 | 5 | 19 |
| 42 | Conwy/Conwy | 10 | 12 | 20 |
| 48 | Denbighshire/Sir Ddinbych | 9 | 13 | 19 |
| 50 | Flintshire/Sir y Fflint | 15 | 13 | 21 |
| 50 | Gwynedd/Gwynedd | 12 | 14 | 20 |
| 22 | Ynys Môn | 7 | 7 | 20 |
| 10 | Merthyr Tydfil/Merthyr Tudful | 6 | 6 | 20 |
| 22 | Monmouthshire/Sir Fynwy | 8 | 6 | 20 |
| 24 | Neath Port Talbot/Castell-nedd Port Talbot | 14 | 11 | 20 |
| 44 | Newport/Casnewydd | 14 | 19 | 25 |
| 40 | Pembrokeshire/Sir Benfro | 11 | 9 | 19 |
| 40 | Powys/Powys | 12 | 9 | 20 |
| 52 | Rhondda Cynon Taf/Rhondda Cynon Taf | 24 | 23 | 20 |
| 58 | Swansea/Abertawe | 24 | 23 | 20 |
| 16 | The Vale of Glamorgan/Bro Morgannwg | 12 | 10 | 19 |
| 18 | Torfaen/Tor-faen | 9 | 9 | 17 |
| 52 | Wrexham/Wrecsam | 13 | 18 | 20 |
Because the number of available premises was not sufficient to meet what was required for some LAs, these LAs had their number reduced to the maximum available. The number of premises required to meet the target sample size was met through increasing the number of premises in those areas where there were sufficient premises and according to LA population (Table 4).
| Total available | Area names (English/Welsh) | Premises | |
|---|---|---|---|
| By LA population | Adjusted | ||
| 12 | Blaenau Gwent/Blaenau Gwent | 7 | 6 |
| 26 | Bridgend/Pen-y-bont ar Ogwr | 13 | 13 |
| 42 | Caerphilly/Caerffili | 17 | 19 |
| 78 | Cardiff/Caerdydd | 37 | 39 |
| 48 | Carmarthenshire/Sir Gaerfyrddin | 17 | 18 |
| 14 | Ceredigion/Ceredigion | 8 | 7 |
| 42 | Conwy/Conwy | 10 | 10 |
| 48 | Denbighshire/Sir Ddinbych | 9 | 9 |
| 50 | Flintshire/Sir y Fflint | 15 | 16 |
| 50 | Gwynedd/Gwynedd | 12 | 12 |
| 22 | Ynys Môn | 7 | 7 |
| 10 | Merthyr Tydfil/Merthyr Tudful | 6 | 5 |
| 22 | Monmouthshire/Sir Fynwy | 8 | 8 |
| 24 | Neath Port Talbot/Castell-nedd Port Talbot | 14 | 12 |
| 44 | Newport/Casnewydd | 14 | 15 |
| 40 | Pembrokeshire/Sir Benfro | 11 | 11 |
| 40 | Powys/Powys | 12 | 12 |
| 52 | Rhondda Cynon Taf/Rhondda Cynon Taf | 24 | 25 |
| 58 | Swansea/Abertawe | 24 | 26 |
| 16 | The Vale of Glamorgan/Bro Morgannwg | 12 | 8 |
| 18 | Torfaen/Tor-faen | 9 | 9 |
| 52 | Wrexham/Wrecsam | 13 | 13 |
Treatment of trial data
Trial populations
Analysis was on an intention-to-treat (ITT) basis using all randomised premises in the groups they were randomised to, regardless of the intervention received. The per-protocol population was defined as baseline premises that were randomised (excluding those found to be duplicates or closed), those found to be trading during the intervention and those that actually received the intervention. The non-randomised population comprised the per-protocol population in addition to the replacement spare premises in the intervention arm and the remaining spare premises in the control arm. Analyses were conducted on both automatic and manual data sets.
Analytic strategy
The primary analysis was a comparison of police-recorded violence between intervention and control premises over the follow-up period, with time-zero being 1 January 2013, the earliest conceivable date an audit could be delivered to a licensed premises, for the ITT group. No interim analyses were undertaken. The primary data set used those data extracted using automated search procedures; sensitivity analyses were conducted on the manually extracted data.
Using the date and time of violent incidents, incidents were organised into sessions. A session was defined as 12 p.m. to 12 p.m. the following day and took the date of the first 12-hour period. Each session was coded with a binary (0, 1) indicator. If a premises had registered one or more violent incidents in a session that session was coded 1; otherwise, it was coded 0.
The Andersen–Gill model was used to analyse failure in premises in the follow-up period in order to account for potential time-varying covariates, censoring, multiple events and discontinuous risk intervals. 73 All incidents of violence at premises from the police forces records were recurrent events with the intervention effect as one predictor, also adjusted by opening hours and number of previous incidents strata (both coded 0, 1) at baseline. As the randomisation was stratified by LA the primary analysis was further explored by the addition of LA as shared frailty. This allowed for any potential clustering to be examined.
Sensitivity analyses were conducted on the per-protocol and non-randomised groups.
Dose was primarily explored through nature of feedback provided by EHPs (none, formal advice) and by any additional follow-up audits undertaken to enforce changes recommended to premises.
Secondary analysis of primary outcomes was undertaken using the Andersen–Gill model to assess the hypothesised intervention wane over the follow-up period. This was achieved by the use of a time by treatment interaction term.
In addition, secondary analyses were used to explore the effect of the intervention on the volume of violence (total counts of incidents) attributable to trial premises, to inform the economic analyses.
Additional exploratory analyses considered the relationship between health and safety issues, incident reporting and EHP confidence in management. In premises with repeat audits the changes were examined in relation to reports of violent incidents. Audit data were also used as part of the process evaluation detailed in Chapter 6.
Cost-effectiveness analysis
A cost-effectiveness analysis was undertaken from a societal perspective.
Intervention costs
We report the costs that would be incurred if the intervention was to be introduced into routine practice. Costs associated with developing the intervention are thus considered as historic and are excluded. As SMILE was additional to usual practice, all costs are incremental. All costs are reported in 2014 prices. As the study period was 1 year, no discounting has been applied.
There are three main elements to the costing of this intervention: training EHPs, the audit process and costs incurred by the licensees as a direct result of advice received during the intervention.
Training costs were all recorded prospectively. These included trainer and trainee time, travel costs, venue fee and administration costs. The hourly value of trainer and trainee time was based on reported salary plus on-costs assuming a 42-week working year and a 37.5-hour working week (assumption from Curtis). 74 Where these details were not provided, the median salary/on-costs were imputed. Travel costs included both time spent travelling and car mileage cost of 40 pence per mile. 75 Other costs such as materials and travel expenses were recorded in money terms.
The cost of printing training manuals, audit documentation, etc., was based on number of pages charged at 5 pence per page (assuming black-and-white printing). Postage was via the Royal Mail’s price finder for first-class postage of large envelopes at £0.93 and small parcels at £5.45. 76
While training could be considered a one-off investment producing a flow of benefits over time, we attributed the whole of training to the sites which received the intervention during the period of study on the basis that retraining would be required annually owing to changes in legislation, etc. It was likely that costs of retraining would be lower than those of initial training and this was explored via sensitivity analysis.
Audit costs included EHP time and travel for the audit (initial plus follow-up, where these occurred) of each premises.
As EHPs have a statutory right to undertake the audit, participation in the study did not require informed consent from licensees of intervention premises or their DPSs. Accordingly, we felt that attempting to identify the costs of implementing any improvements that arose as a result of the audit by questionnaire would produce a low response rate, which would be potentially biased. However, intervention and control premises that participated in the process evaluation did so via informed consent. This provided an opportunity to gain information on licensee-borne costs through the addition of a number of questions to the interview schedules.
Cost of violent incidents
As our data on violent incidents include only those which have been reported to the police, our cost estimates should be regarded as minimal.
The costs of violent incidents were taken from the Home Office data on crimes against the person77 in line with Dubourg,78 which was the basis of many of the Home Office estimates. However, as the Home Office estimates currently exclude three elements which were in Dubourg,78 ‘lost output’, ‘physical and emotional impact on direct victim’ and ‘NHS costs’, we have included these here using the estimates in Dubourg inflated to 2014 prices. As not all violent incidents will incur criminal justice system costs, we have explored via sensitivity analysis the effect of reducing the percentage of incidents which incur criminal justice system costs. These base-case unit costs of a violent incident are reported in Table 5.
| Costs | Magistrates’ Court | Crown Court | Total |
|---|---|---|---|
| Criminal justice system costsa | |||
| Police cost per arrest | 242 | 242 | 484 |
| Pre-charge decision cost (CPS) | 45 | 45 | 90 |
| CPS costs | 160 | 2796 | 2956 |
| HMCTS costs | 296 | 453 | 749 |
| Legal Aid costs | 529 | 4696 | 5225 |
| Cost per month of immediate custody | 2788 | 2788 | 5576 |
| Cost per month of probation | 252 | 252 | 504 |
| Cost of community sentence | 3019 | 3019 | 6038 |
| Total criminal justice system costs | 21,622 | ||
| Other costsb | |||
| Health service | 1879 | ||
| Lost output | 2322 | ||
| Physical and emotional impact on direct victims | 7834 | ||
| Total other costs | 12,035 | ||
| Total | 33,657 | ||
This cost estimate of a violent incident was then multiplied by the number of total incidents that occurred during the follow-up period in order to calculate costs of crimes at premises level.
Effects
The unit of effectiveness for the cost-effectiveness analysis was number of sessions with one or more violent incidents, based on police records.
Cost-effectiveness
The cost-effectiveness analysis was carried out on premises in the ITT sample. The total cost for intervention premises includes the intervention cost plus costs of violent incidents that occurred during the follow-up period. For control premises this was only the cost of violent incidents. As costs data are likely to be skewed, a non-parametric bootstrapped approach was applied to estimate bias-corrected accelerated (BCa) 95% confidence intervals (CIs) for differences in costs. The mean differences in total costs were further adjusted for baseline incidence group and opening hours, in line with the primary analyses.
If the intervention group was less costly and more effective, the intervention would be shown to be unambiguously cost-effective. If the intervention group was more effective but more costly, then results will be reported in the form of an incremental cost-effectiveness ratio showing the additional cost per unit of effect. This would provide an evidence-based benchmark for comparison in future cost-effectiveness evaluations of interventions aimed at reducing violence in the NTE. As some premises had follow-up audits, a separate exploratory economic analysis was done to investigate the cost-effectiveness of the intervention where it included a follow-up audit.
Dealing with uncertainty
Two one-way sensitivity analyses were undertaken to examine how sensitive cost-effectiveness results are to changes in base-case parameters. In the first, the assumption that training costs are apportioned to premises that received the intervention during the study period was replaced by an assumption that training lasts for 5 years. In the second, it was assumed that only 50% of police-recorded violent incidents incur criminal justice system costs.
To explore whether or not the intervention represents good value for money, a stochastic sensitivity analysis was carried out using a non-parametric bootstrapped approach on the joint distribution of costs and effects. Results are reported in the form of a cost-effectiveness acceptability curve (CEAC) showing the probability that the extra cost per unit of effect lay below a range of societal willingness-to-pay thresholds.
Process evaluation
Although the RCT sought to assess the effectiveness of the SMILE intervention, it was accompanied by an embedded process evaluation to aid understanding of the mechanisms operating during SMILE adoption and implementation and provide insight into what works, for whom and in what context. This is particularly important as the implementation of SMILE introduced new practices into established organisational methods of working, a process often affected by normative beliefs, resources and the actions of people and groups involved. 79 The importance of understanding such processes and their subsequent influence on intervention reach, fidelity and receipt within the evaluation of complex interventions has received increasing attention in recent years. 80 A useful framework for assessing these processes exists in RE-AIM81 that focuses on the constructs of intervention reach, efficacy, adoption, implementation and maintenance. These constructs were used to identify the key research objectives for the process evaluation.
A trans-disciplinary action research (TDAR) approach was used in the development and implementation of SMILE to promote intervention adoption and implementation. TDAR facilitates innovation implementation and sustainability through early and sustained engagements with policy and practice,82 with the aim of coproducing ecologically valid interventions through an ongoing cycle of knowledge exchange. Normalisation process theory (NPT)79 offers a framework to assess the effectiveness of such an approach by focusing on the work that takes place when understanding and assimilating new organisational practices (coherence), how individuals and organisations are enrolled to implement new practices (cognitive participation), the work undertaken by individuals and organisations to enact new practices (collective action) and how new sets of practices affect individuals and others around them (reflexive monitoring).
The NPT therefore provides a theoretical framework to assess the extent to which the TDAR approach facilitated SMILE’s adherence to the RE-AIM framework. In doing so it highlights potential recommendations for intervention reconfiguration and sustainability and provides key process data that can facilitate an understanding of main trial outcomes.
Aims and objectives
The process evaluation aimed to explore the intrinsic processes operating during SMILE adoption and implementation and their influence on what was delivered.
The process evaluation objectives were to:
-
understand the adoption of the intervention by EHPs and the adaptation required to integrate SMILE into normal practice
-
assess intervention implementation – reach, fidelity and dose delivered
-
assess intervention efficacy – receipt and acceptability
-
understand the implementation context for intervention maintenance and any intervention reconfiguration
-
construct a logic model of the intervention as delivered.
Process evaluation design
Table 6 outlines the research design and associated methods that were used to explore each of the research aims in three successive phases. Phase 1 explored the intervention codevelopment and adoption within the environmental health organisation; data were obtained from focus groups with senior EHPs involved in SMILE coproduction and implementation. Phase 2 investigated intervention implementation through interviews with EHPs responsible for delivering the intervention and explored issues of reach, fidelity, dose delivered and longer-term maintenance. Phase 3 examined how the intervention was received by licensed premises. Its perceived efficacy, acceptability and likely sustainability were explored through semistructured interviews with a sample of licensed premises staff. Results from these phases were drawn together to construct a logic model of intervention delivery (research objective 5) and refine the intervention. Ethical approval for the process evaluation was given by the Cardiff University Dental School Research Ethics Committee.
| Phase | Source | Method | Areas to be addressed | Research objective |
|---|---|---|---|---|
| Phase 1: SMILE coproduction and adoption by EHPs | Senior EHPs: involved in intervention development and implementation (n = 4) | Pre- and post-intervention focus groups | To understand EHPs’ role in intervention development To explore any organisational change needed to adopt SMILE To assess implementation processes and integration with usual EHP practice, including any barriers and facilitators |
1, 2, 4 |
| Phase 2: SMILE implementation | EHPs (n = 22): one from each LA engaged in the delivery of the intervention | Post-intervention semistructured interviews | To understand usual practice and intervention integration To assess practitioner participation and responsiveness to the intervention To explore intervention reach and the intensity of what was delivered To explore whether or not the intervention was delivered as intended and is sustainable in normal practice To assess the perceived efficacy of the intervention To assess whether or not any reconfiguration is necessary for long-term maintenance |
1, 2, 3, 4 |
| Phase 3: SMILE reception, acceptability and sustainability in licensed premises | Premises staff in 16 intervention and 14 control premises | Post-intervention semistructured interviews | To assess how the intervention was received and its perceived efficacy To explore whether or not the intervention was acceptable and sustainable in premises’ usual practice To assess whether or not any reconfiguration is necessary for long-term maintenance |
3, 4 |
| Phase | Source | Method | Aims and objectives | Process evaluation component (research aim) |
| Phase 1: SMILE adoption, coproduction and implementation by EHPs | Senior EHPs: involved in trial development and implementation (n = 4) | Pre- and post-intervention focus groups | Understand role in intervention development Gain perceptions of organisational change needed to adopt SMILE Description of implementation processes and integration with usual EHP practice, including barriers and facilitators |
Implementation and context (1) Fidelity and adaptation (2) Comparison of traditional practice with intervention (5) |
| EHPs (maximum 22): one from each LA engaged in the delivery of the intervention | Post-intervention semistructured interviews Routine monitoring data | Description of role of EHPs in licensed premises pre SMILE Description of practitioner participation, reception and responsiveness to the intervention Process of intervention delivery, including fidelity, barriers and facilitators and extent of interagency collaboration Description of location, size suitability of intervention/control premises |
Implementation and context (1) Fidelity and adaptation (2) Comparison of traditional practice with intervention (5) |
|
| Phase 2: SMILE delivery, reach and dose | Routine programme data | Audit assessment and outcomes | Audit delivery, reach and dose | Delivery, reach and dose (3) |
| Phase 3: SMILE reception, implementation and sustainability in licensed premises | Premises staff in 16 intervention and 14 control premises | Post-intervention semistructured interviews Routine monitoring data | Intervention premises:
|
Implementation and context (1) Receipt and acceptability (4 – intervention premises only) Comparison of traditional practice with intervention (5) |
Sampling and recruitment
The process evaluation explored SMILE development and implementation with senior EHPs and a representative sample of EHPs who delivered SMILE. Two focus groups were conducted with senior EHPs (n = 4). The first focus group that was conducted after the main phase of SMILE coproduction had been completed sought to explore SMILE codevelopment and adoption. The second focus group took place following delivery of the intervention and was concerned with intervention implementation. The senior EHPs were invited to take part verbally; information sheets and consent forms were completed at one of the regular research group meetings.
Telephone interviews were conducted with one EHP from each LA in Wales (n = 22) who had been involved in the delivery of SMILE. EHP recruitment took place by e-mail or telephone, with information and consent forms supplied and returned electronically. Purposive sampling ensured that practitioners working in premises with the greatest possible variation of risk in both control and intervention arms and significant experience of delivering SMILE were invited to participate. In order to explore the reach and impact of the AWLPI training, three EHPs who had not attended SMILE training workshops were also purposively sampled.
To explore intervention receipt and its relationship with normal practice within premises, a sample of licensed premises were drawn from control (n = 321) and intervention premises (n = 285). Purposeful sampling ensured that these premises represented those found in a range of geographical areas across Wales (North, West and South East) and location (urban, rural, town/fringe) and previous incidences of violence (high/low). EHPs who had delivered SMILE to each premises were asked to provide the owner/manager with details of the study and request permission for a researcher to contact them to discuss participation. Where the EHP failed to gain a response (n = 4) or the DPS refused participation (n = 2), a researcher contacted the DPS directly or selected new premises and conducted recruitment themselves. Recruitment continued until theoretical saturation was reached. This resulted in data from 30 premises across Wales (Table 7).
| Premises | Area of Wales | Location and violence levels | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| North | West | South East | Urban | Town/fringe | Rural | |||||||
| Total | High | Low | Total | High | Low | Total | High | Low | ||||
| Total (N = 30) | 4 | 2 | 24 | 14 | 8 | 6 | 13 | 3 | 10 | 3 | 1 | 2 |
| Intervention (n = 16) | 2 | 1 | 13 | 8 | 5 | 3 | 7 | 1 | 6 | 1 | 0 | 1 |
| Control (n = 14) | 2 | 1 | 11 | 6 | 3 | 3 | 6 | 2 | 4 | 2 | 1 | 1 |
Data collection
Each focus group with senior EHPs was facilitated by two researchers. The focus group schedules for the two focus groups contained different guides and prompts, designed to focus on the RE-AIM framework (see Appendices 4 and 5). The initial focus group was held to gain better understanding of the routine work of the environmental health agency; organisational views on increasing their role in addressing ARV; and some insight into senior environmental health managers’ role in adopting and developing SMILE. The post-implementation focus group encouraged reflection on the process of SMILE implementation, and on how well the interventions had been embedded in environmental health practice.
Semistructured interview schedules for EHPs again drew on the RE-AIM framework (see Appendix 4) and were conducted by a single researcher. Most EHP interviews were conducted by telephone, although one EHP requested a face-to-face meeting. All interviews took place as soon as possible after the intervention phase had ended, as the aim was to identify and explore the process of intervention delivery in varied premises and different parts of Wales, with particular interest in barriers and facilitators experienced during SMILE delivery and assimilation.
Interviews with premises managers/owners (n = 30) were conducted face to face when possible (n = 18) or by telephone (n = 12). All semistructured interviews were held shortly after the intervention phase had ended and were organised around RE-AIM constructs (see Appendix 5).
Data analysis
All focus groups and interviews were audio recorded. Recordings of interviews and focus groups were transcribed, anonymised and entered into password-protected university files before analysis using NVivo 10 (QSR International, Warrington, UK). All transcripts were scrutinised for errors. The first phase of analysis categorised data into dominant themes determined a priori by the constructs of the RE-AIM:81
-
SMILE adoption and diffusion
-
SMILE implementation – reach, fidelity and dosed delivered
-
SMILE efficacy – acceptability and receipt
-
SMILE maintenance – reconfiguration and sustainability.
Subsequent analysis drew on NPT constructs to explore whether or not and to what extent the use of a TDAR approach facilitated these processes. Using this approach, an analytical framework matrix was generated and used to construct a logic model, which visually describes the entire intervention process.
Public and patient involvement
While violence has serious repercussions in communities and is a significant cause of attendances in unscheduled care, it was not deemed necessary to involve the public and patients in the current project. The main reason for this is that those groups involved with the project were mostly premises staff and EHPs. As such, there was no clear means through which public and patient involvement could shape the development of the project and this group was not therefore developed. There may be opportunities for the public, in particular those who have been assaulted in premises, to advise on aspects of the study, and this could be assessed in future work.
Chapter 5 Intervention effectiveness results
Aims and objectives
Aims
-
To investigate the impact of the SMILE intervention on police-recorded violence.
-
To assess the reach and dose delivered of the intervention.
Objectives
-
To analyse police data from 1 January 2012 for 455 days and determine whether or not the intervention was associated with a change in violent-event frequency.
-
To conduct sensitivity analyses to determine the robustness of any intervention effect.
-
To analyse police data from 1 January 2012 for 455 days and determine whether or not the effect of the intervention, if any, changed over time (e.g. intervention wane).
-
To use data on delivery of the audits to determine the proportion of premises that received the intervention (reach) and what actions resulting from the audits were needed to reduce premises-level risk (dose).
Consolidated Standards of Reporting Trials
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram (Figure 5) documents the flow of premises through the trial including the number of audits carried out and reasons for any missing audits.
FIGURE 5.
The CONSORT flow diagram.

There were 837 premises available for randomisation. At randomisation, 300 premises were allocated to each treatment group. Premises were checked to make sure that they were open and still eligible (see Chapter 4); 453 premises remained from the initial randomisation (see Figure 5).
Closed intervention premises were replaced from the remaining pool premises not originally randomised to control or intervention group, matched by strata, to give the non-randomised group. The remaining ‘spare’ premises were added to the control group.
Three premises that had been allocated to the original intervention group were reported as closed by EHPs and replaced, but were subsequently found to be open by EHPs. EHPs audited these ‘false-negative’ premises, as they reopened within the time available to deliver the audit. Of the replacements offered to EHPs, two were believed closed by EHPs but were subsequently found to be open by EHPs and were audited.
The primary analyses are conducted on the premises originally allocated to control and intervention groups (ITT), excluding premises dropped as a result of closure or duplication.
Sensitivity analyses are conducted on the per-protocol and non-randomised groups.
Premises that were dropped were dropped because they were not open, they had become ineligible (e.g. changed from a pub to a restaurant), they were duplicates (some larger premises, for example, might have had entrances on two streets and, therefore, two addresses were registered in the police data for them) or they refused. Refusals were not strictly possible, as EHPs had statutory authority to visit these premises. However, there were occasions where premises claimed that there had been no occasions of violence on-site (e.g. one premises name was identical to that of the village in which it was situated and, thus, it was not possible to disambiguate the exact location of the incident in police data); another premises had recently been reviewed for licensing violations, and a third refused as the premises manager felt that it put his business in a poor light and EHPs indicated that they did not wish to audit this particular premises. In total, three premises refused; the remaining seven premises were dropped owing to other issues, including one that was ineligible because of its size (EHPs are concerned with small and medium-sized businesses, whereas the HSE are concerned with large organisations).
This provides two data sets (manual and automatic) and three levels of analysis (per-protocol, ITT and non-randomised). The primary analyses are conducted on the ITT group using the automatic data. Other analyses are to test sensitivity.
Outcome data
The outcome of interest was police-recorded violent crime associated with premises involved in the study (see Chapter 4). Baseline data were the data initially used to identify eligible premises (premises were eligible if they had one or more violent crimes associated with them). These data also served as a covariate in subsequent analyses.
Follow-up data, covering 455 days from 1 January 2013 (the earliest that a premises could have been audited), with a 12-month follow-up period from the estimated last date of audit (end of March 2013), were derived using two methods: manual and automatic. The automated data were created using bespoke algorithms informed through exploratory analysis of baseline data and are used for primary analyses. Manual data were created through a manual search of police data and are used for sensitivity analyses.
Manual data
Police-recorded violent crime data were manually checked by researchers who sought to identify all premises included in the study: 20% of the data from each of the four police forces was randomly selected and sent to an independent researcher, who completed the same matching process. Proportion of agreement was calculated for each force (0.97, 0.98, 0.97, 0.98) and yielded an overall proportion, where raters agreed, of 0.973.
Automatic data
Baseline data, together with study premises name and address information, were used as a training data set for a bespoke automated text search algorithm that was created to identify study premises in police violent crime data (see Chapter 4, Automatic data).
Summing the total number of incidents identified using each method by day suggests the manual process identified more incidents [daily mean = 6.69, standard deviation (SD) = 5.27] than the automated approach (mean = 3.74, SD = 3.04; t = 19.38, p < 0.001); although there was a robust association over time (Spearman’s ρ = 0.83, p < 0.0001) indicating that rank was preserved over the two approaches.
The reason for these differences is that free text in police data would occasionally use abbreviations that were not picked up in the automated search, particularly where GPS codes were missing. Similarly, records would occasionally not have address information and just provide GPS co-ordinates.
Strata
The baseline violent crime data were used to stratify premises into high-violence (> 2 incidents across the baseline period) and low-violence (≤ 2 incidents) premises. Cut-points were determined through k-means cluster analysis. Opening hours past 11 p.m. on Friday and Saturday nights was also used to stratify premises. Premises open a total of ≥ 4 hours on Fridays and Saturdays constituted the ‘high’ group; premises open for < 4 hours in total constituted the ‘low’ group. Dummy variables were created for each (low = 0, high = 1 for each) and were entered into analyses as covariates.
Capacity was not used to stratify premises, the reason being that these data are not reliably available. Of the 837 eligible premises, capacity data were available for 144 from LA licensing records. For these 144 premises, baseline total violence was associated with capacity (Spearman’s ρ = 0.38, p < 0.0001), suggesting that stratifying on baseline violence was sufficient.
Censoring
All businesses are expected to pay business rates, a form of local taxation. Businesses, including licensed premises that cease to trade whether temporarily or permanently, do not pay these rates. LA business data were, therefore, accessed for all study premises to determine periods of economic inactivity. Violent offences recorded for a premises during a period of inactivity were dropped (many premises are also private residences and can, therefore, experience violence even if they are not operational). In total, six incidents were dropped from automated data and 17 were dropped from the manual data.
Audit completion rate
All intervention premises were audited by EHPs from January 2013 onwards. All premises had received the initial audit by 29 April 2013. A subset of premises received a follow-up audit. All follow-up audits (n = 18) had been completed by 4 June 2013. Figure 6 presents the temporal distribution of completed audits and follow-up audits and suggests that EHPs delivered the intervention in the expected time frame.
FIGURE 6.
Proportion of intervention premises audited by analysis time (0 = 1 January 2013).
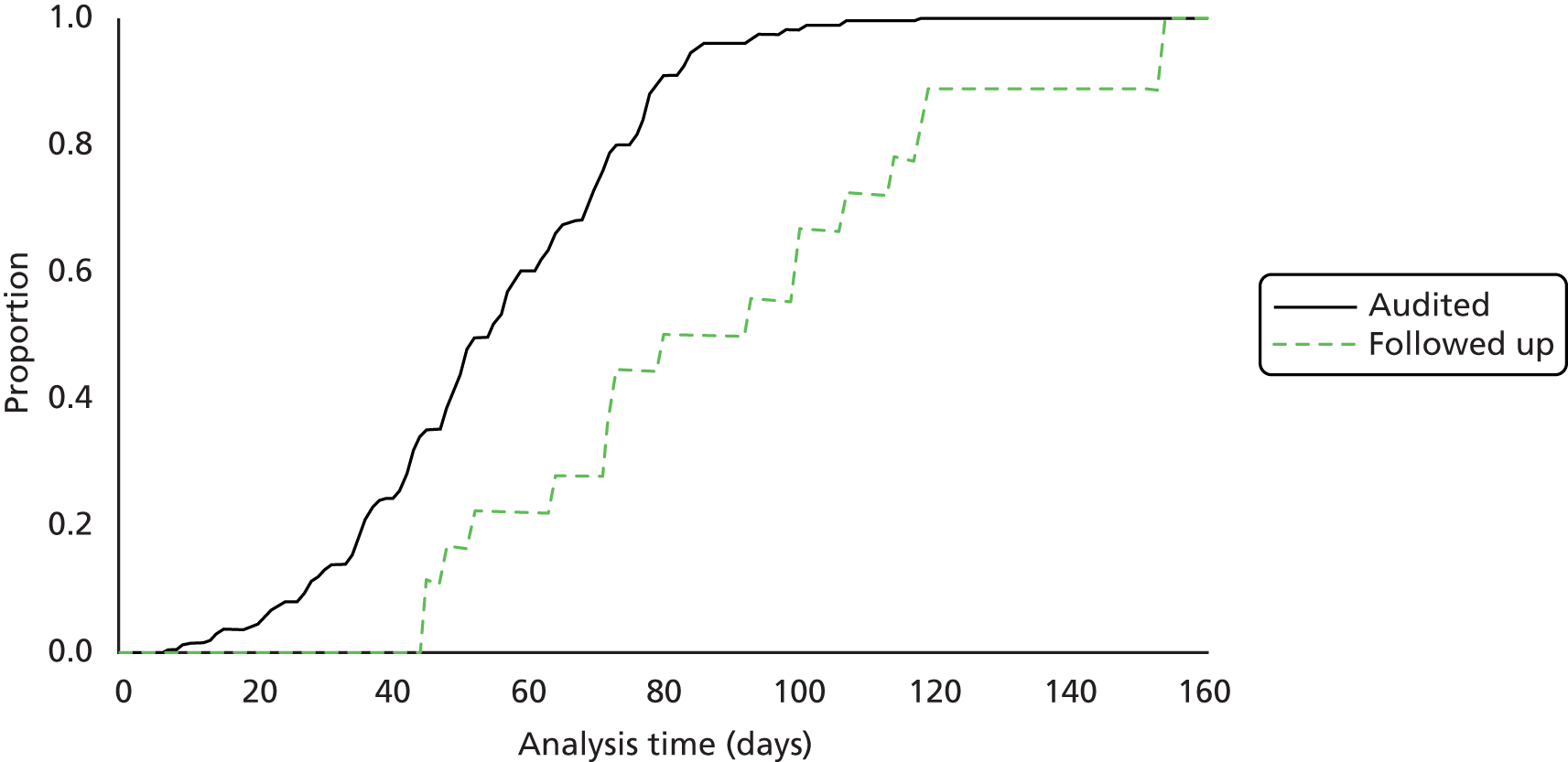
Descriptive statistics
Baseline data
Premises were stratified by opening hours and baseline violence. Table 8 presents descriptive statistics for each group.
| Group | Control | Intervention | ||
|---|---|---|---|---|
| n high | Mean (SD) | n high | Mean (SD) | |
| ITT | ||||
| Violence | 54 | 2.41 (3.03) | 73 | 2.93 (4.75) |
| Opening hours | 97 | 4.35 (2.86) | 109 | 4.49 (2.86) |
| Per-protocol | ||||
| Violence | 54 | 2.41 (3.03) | 72 | 2.92 (4.75) |
| Opening hours | 97 | 4.35 (2.86) | 106 | 4.47 (2.86) |
| Non-randomised | ||||
| Violence | 103 | 2.64 (4.31) | 73 | 2.78 (4.46) |
| Opening hours | 172 | 4.32 (2.75) | 109 | 4.34 (2.80) |
Follow-up data
Incidents and failures
In the automated data a total of 1829 incidents were observed and in the manual data a total of 1762 incidents were observed. These included murders and violence against the person but not sexual offences. Two police forces were willing to share sexual offence data but, on examination, fewer than three such offences were observed in each force. For the ITT group, overall there were 891 failures, with an average of 1.19 (SD = 0.70) violent incidents per failure. Whether or not premises received an audit or follow-up audit was entered into the data as a time-varying covariate (0 up to the date of the audit and 1 thereafter). For premises that had received a follow-up audit, there were 17 failures, representing 19 violent incidents (average violence per failure = 1.12, SD = 0.49); for premises receiving an audit but no follow-up there were 512 failures representing 620 violent incidents (average violence per failure = 1.21, SD = 0.72).
Analyses
Primary analyses are conducted on the ITT group, with sensitivity analyses conducted on per-protocol and non-randomised groups (Table 9). All analyses were conducted on a binary failure indicator, defined as a session (12 p.m. to 12 p.m. the following day) in which premises experienced one or more incidents. The analytic strategy used a derivation of the Cox proportional hazards model for recurrent event analysis. The audit and follow-up audit were entered as time-varying covariates (0 for the control group; for the intervention group 0 until the audit was conducted, 1 thereafter). Opening hours and incident group binary control variables were entered as covariates and premises’ LA membership was entered as shared frailty.
| Group | Data | |||||
|---|---|---|---|---|---|---|
| Automated | Manual | |||||
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| ITT | ||||||
| Audit | 1.34 | 1.20 to 1.51 | < 0.01 | 1.23 | 1.07 to 1.41 | < 0.01 |
| Follow-up audit | 0.43 | 0.26 to 0.71 | < 0.01 | 0.39 | 0.19 to 0.79 | 0.01 |
| Violence group (1 = high) | 2.55 | 2.21 to 2.94 | < 0.01 | 3.45 | 3.00 to 4.01 | < 0.01 |
| Opening hours group (1 = high) | 2.52 | 2.22 to 2.85 | < 0.01 | 2.00 | 1.69 to 2.37 | < 0.01 |
| Per-protocol | ||||||
| Audit | 1.35 | 1.20 to 1.52 | < 0.01 | 1.24 | 1.07 to 1.42 | < 0.01 |
| Follow-up audit | 0.43 | 0.26 to 0.70 | < 0.01 | 0.38 | 0.19 to 0.79 | < 0.01 |
| Violence group (1 = high) | 2.54 | 2.24 to 2.88 | < 0.01 | 3.49 | 3.00 to 4.07 | < 0.01 |
| Opening hours group (1 = high) | 2.51 | 2.17 to 2.89 | < 0.01 | 1.96 | 1.65 to 2.32 | < 0.01 |
| Non-randomised | ||||||
| Audit | 1.33 | 1.20 to 1.48 | < 0.01 | 1.15 | 1.02 to 1.29 | < 0.05 |
| Follow-up audit | 0.71 | 0.49 to 1.03 | 0.68 | 0.81 | 0.50 to 1.30 | 0.38 |
| Violence group (1 = high) | 2.78 | 2.48 to 3.12 | < 0.01 | 3.74 | 3.28 to 2.47 | < 0.01 |
| Opening hours group (1 = high) | 2.44 | 2.15 to 2.77 | < 0.01 | 2.13 | 1.84 to 2.47 | < 0.01 |
For all analyses the likelihood test for LA heterogeneity (θ = 0) yielded a significant result (χ¯2 > 150, p < 0.001 for each test). All models performed significantly better than the null (χ2 > 470 and p < 0.001 for each model).
The net resultant hazard ratio (HR) for the effect of a follow-up audit can be determined through multiplying the audit HR with the follow-up audit HR; these are presented in Table 10 with the number of premises receiving a follow-up audit.
| Group | n | Automated | Manual |
|---|---|---|---|
| ITT | 16 | 0.58 | 0.48 |
| Per-protocol | 16 | 0.58 | 0.47 |
| Non-randomised | 18 | 0.94 | 0.93 |
Figure 7 presents the Nelson–Aalen cumulative hazard estimates (ITT, automatic data) over time for control and intervention (both audited and follow-up audited) premises.
FIGURE 7.
Nelson–Aalen cumulative hazard estimates (using automated data for the ITT group).

As the intervention effect may wane after a certain time period (dose effect), the intervention was treated as a time-varying covariate (interacted with e–0.03t), where t was analysis time, controlling for opening hours and violence groups and with shared frailty for LAs. For all models the likelihood ratio test of LA heterogeneity (θ = 0) yielded a significant effect for each model. However, in each model no significant interaction with time was noted.
Subgroup analysis
To further explore the effect of the intervention on violence, intervention premises were divided into two groups, according to nature of the feedback given: (1) premises where EHPs did not identify any areas of risk and therefore premises received no advice and (2) premises where EHPs did identify areas of risk and provided advice (Figure 8). For the ITT group, using the automated data and controlling for violence and opening hours groups, premises receiving feedback (n = 217) yielded a lower incident rate than those that did not (n = 21; HR = 0.51, 95% CI 0.42 to 0.63).
FIGURE 8.
Subgroup analysis comparing intervention premises receiving EHP feedback with those receiving no feedback.
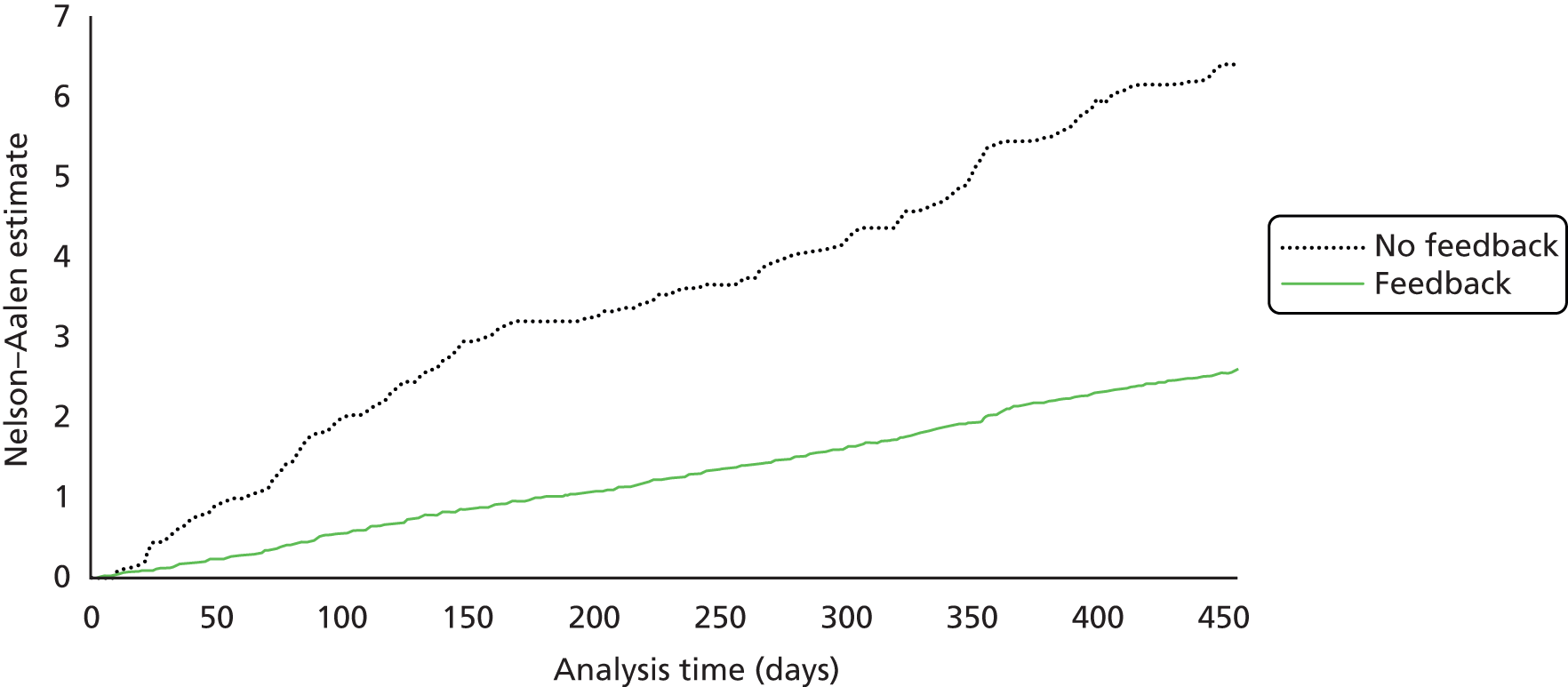
Secondary analyses
One explanation for an increase in police-recorded violence in this context was that premises receive greater attention from the police. As licensing committees involve the police, LA licensing practitioners and other responsible authorities, it is feasible that referral to any of these responsible authorities would mean that premises are placed under greater scrutiny and, therefore, the police are more likely to record violence associated with these premises. In the audit data there are two proxies for greater scrutiny: whether intervention premises received a referral to a responsible authority or were issued a formal notice. In the ITT group, 27 premises were referred to at least one responsible authority, seven premises received a formal notice and two premises received both. To simplify analyses a single referral indicator was created (1 if referred to a responsible authority or received a formal notice, 0 otherwise). Rerunning the main analyses (ITT group, automated data), interacted with the audit indicator yields a significant positive effect (Table 11). No premises receiving a follow-up audit received a referral or notice.
| ITT | HR | 95% CI | p-value |
|---|---|---|---|
| Audit and no referral | 1.26 | 1.12 to 1.42 | < 0.01 |
| Audit and referral | 1.98 | 1.59 to 2.48 | < 0.01 |
| Follow-up audit | 0.46 | 0.28 to 0.76 | < 0.01 |
| Violence group (1 = high) | 1.08 | 1.07 to 1.09 | < 0.01 |
| Opening hours group (1 = high) | 2.77 | 2.40 to 3.18 | < 0.01 |
A Wald test on the equivalence of coefficients on audited with and without referral suggests additional referral activity increases event frequency (χ2 = 16.39, p < 0.001).
Intervention reach, dose and delivery
Duration of audits
Data presented here are for the full non-randomised group.
The first audits took, on average, 82.62 minutes (SD = 34.49 minutes), with an average travel time to the premises of 17.8 minutes (SD = 11.75 minutes). Follow-up audits (n = 18) took, on average, 28.44 minutes (SD = 13.87 minutes), with an average travel time to premises of 13.39 minutes (SD = 7.99 minutes). All follow-up audits were conducted within 3 months of the initial audit (Figure 9).
FIGURE 9.
Number of premises by duration of audit.

Evidence of risk assessments
Of all premises, 73% (n = 204) had ≥ 5 members of staff and were, therefore, eligible to have completed a written risk assessment. Of these, 204 premises (70%) did not have a written risk assessment. In addition, 12 premises with < 5 members of staff did have a written risk assessment.
Risk control indicator outcomes
For each domain, EHPs completed a RCI, a Likert scale that ranged from 0 to 6. A score of 0 denotes not applicable and these scores were dropped from summary statistics. A score of 1 denotes good practice, while a score of 6 denotes heightened levels of risk for that domain. The expectation was that scores of 4–6 would warrant further action in respect of that domain. Figure 10 presents results from the RCI scores and shows that the areas requiring most attention included, first, record keeping (including written risk assessments), second, health and safety and, third, incident reporting.
FIGURE 10.
Mean RCIs (with standard error bars) and percentage of premises scoring ≥ 4 and, therefore, requiring further action.
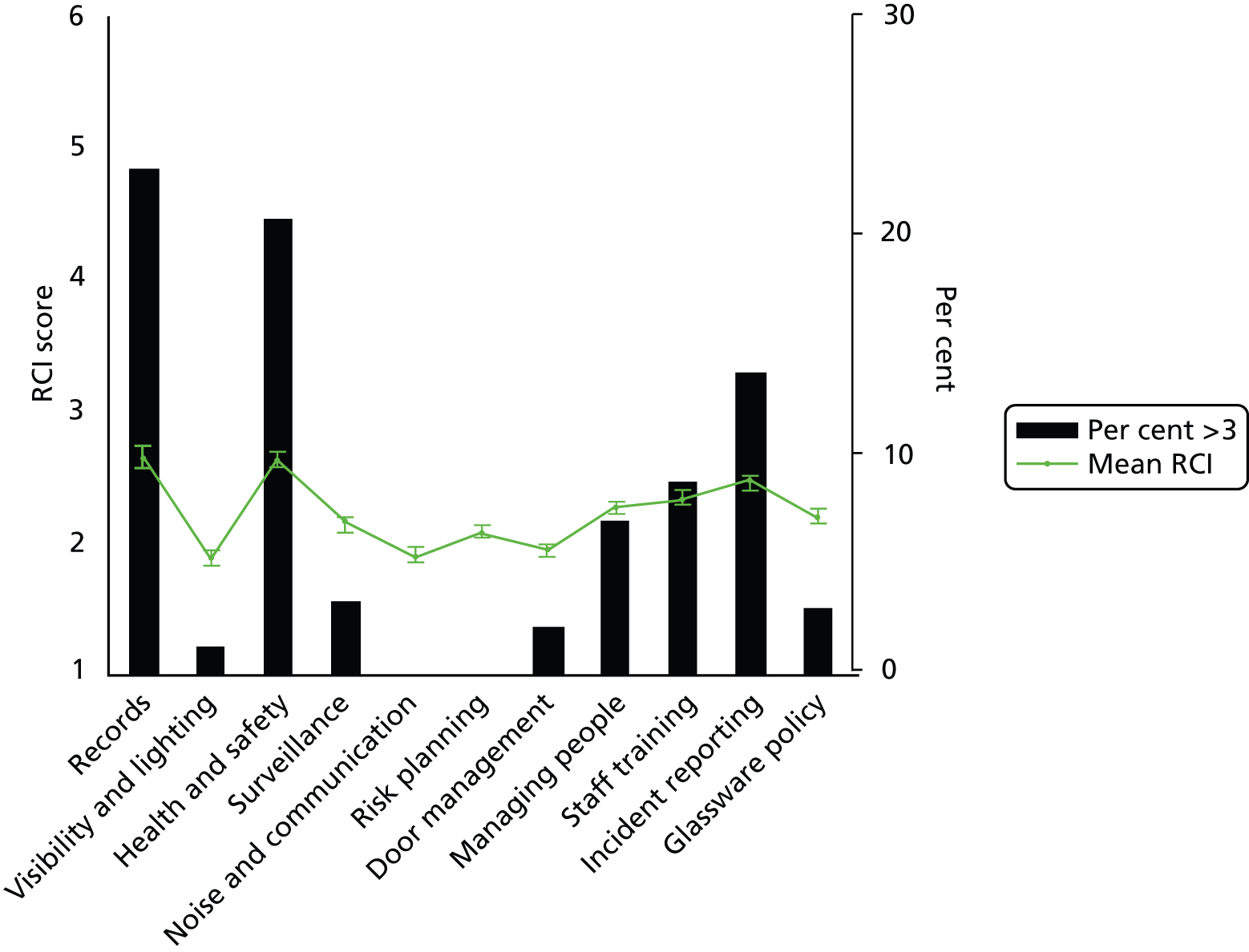
Overall, 34.88% of premises audited scored > 3 on at least one RCI, warranting enforcement, while 6.41% received a follow-up audit.
Actions resulting from the audit
Actions available to EHPs were written and verbal advice, improvement notices (five premises received one, one premises received two) and prohibition notices (three premises received one prohibition notice) and referral to the police (none were referred to the police), referral to fire services (six premises received one referral and one premises received referrals for two issues), and referral to LA licensing (14 premises were referred for one issue, four premises were referred to two reasons and two premises were referred for three reasons). Reasons for referral to LA licensing were for premises not operating according to their licensing conditions. Notices covered lack of safety policies and records (n = 3), inadequate staff training (n = 1), poor condition of the premises (n = 2), poor lighting (n = 1) and significant failing in respect of gas safety (n = 1). In addition, one premises received a prohibition notice for inadequate fire safety but also demonstrated failings with regard to adequate CCTV and staff training.
In total, 24 premises (8.5%) received no verbal or written advice and no prohibition or improvement notices. Written and verbal advice could be given once for each audit domain, yielding a maximum of 11 for both verbal and written advice for each premises (Figure 11). On average, verbal advice was given more frequently (mean = 5.62 per premises, SD = 3.91 per premises) than written advice (mean = 1.97 per premises, SD = 2.22 per premises; t = 16.41, p < 0.001).
FIGURE 11.
The number of premises receiving written and verbal advice. The maximum number of areas on which premises could receive advice was 11.

Follow-up visits
Eighteen premises received follow-up visits from EHPs (16 in the ITT group). In each case all areas of concern had been addressed or were in the process of being addressed (e.g. work was ongoing to make repairs and improvements). Typically, premises received follow-up visits for failings (RCI > 3) in more than one domain (mean = 2.88, minimum = 1, maximum = 4). Table 12 presents the number of premises failing in each audit domain. Some premises failed in more than one area. Of note, there was an expectation that health and safety processes are up to date, fit for purpose and, critically, communicated to staff. Those premises that received follow-up visits for matters relating to health and safety, observation and checks would, owing to their inadequacy, be unable to train staff appropriately. Accordingly, follow-up visits usually required premises to improve how their staff were trained as well.
| Area of concern | Premises | |
|---|---|---|
| Q6a | Records | 7 |
| Q7 | Visibility and lighting | 1 |
| Q8 | Health and safety, observation and checks | 13 |
| Q9 | Surveillance | 4 |
| Q10 | Noise and communication | 0 |
| Q11 | Risk planning | 2 |
| Q12 | Door management | 1 |
| Q13 | Managing people | 1 |
| Q14 | Staff training | 13 |
| Q15 | Incident reporting | 7 |
| Q16 | Glassware policy | 0 |
Perceived efficacy in premises management
Environmental health practitioners rated their confidence in premises management on a Likert 1–6 scale across eight domains (Figure 12). Overall, items varied little both across and within premises and were associated with the numbers of domains receiving verbal advice (Spearman’s ρ > 0.15 and p < 0.01 for each comparison, except organising co-operation and communication, where Spearman’s ρ = 0.12 and p = 0.06) and the number of domains receiving written advice (Spearman’s ρ > 0.32 and p < 0.001 for each comparison) with lower confidence being associated with a greater likelihood of verbal or written advice.
FIGURE 12.
Confidence in management (6 indicates low confidence, 1 indicates high confidence).
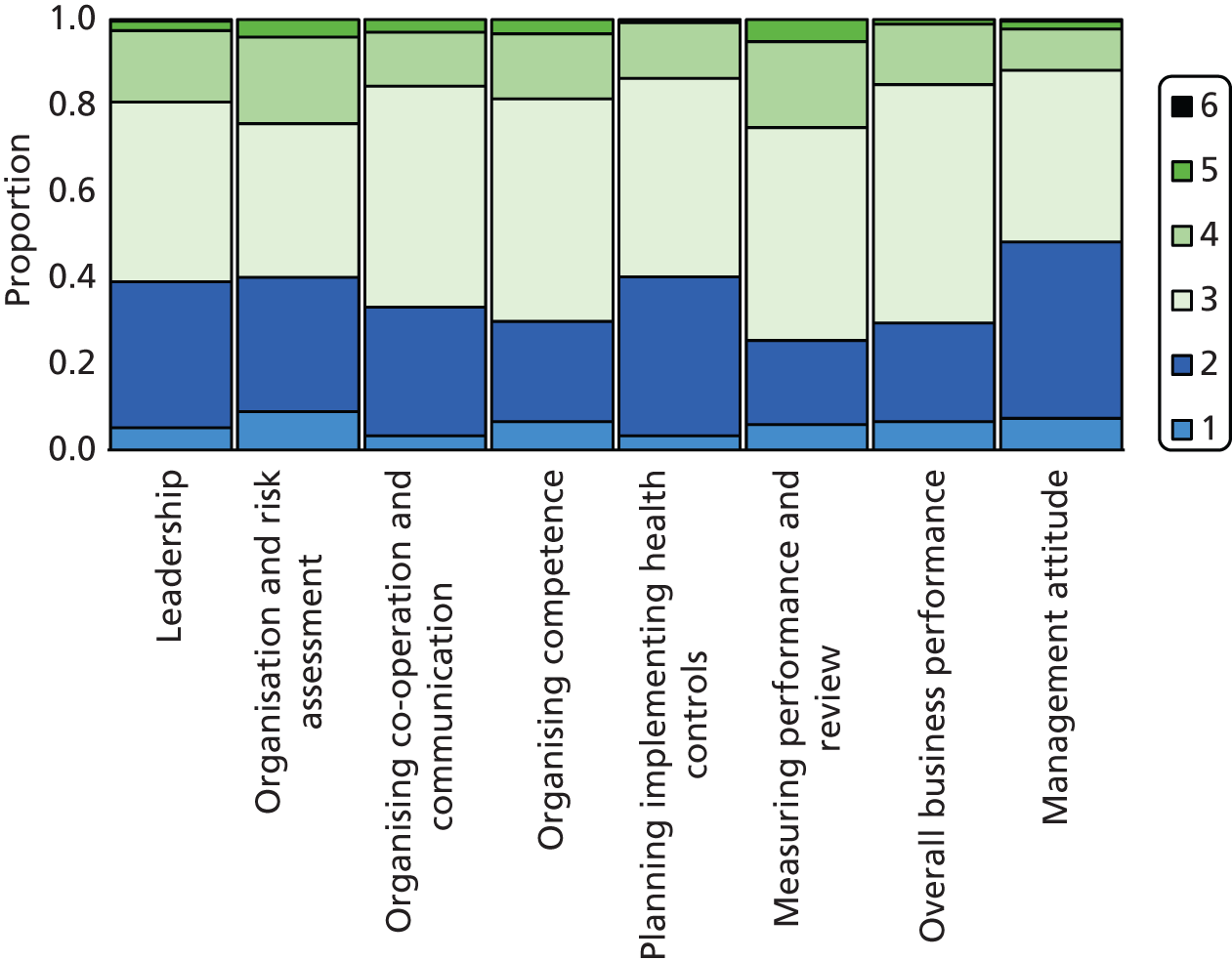
Exploratory analyses
Intervention premises characteristics
Staff-to-customer ratio
Premises ranged from smaller establishments with one owner/occupier to large nightclubs. On average, premises employed 4.4 members of full-time staff (minimum = 0, maximum = 100), lower than the average number of part-time staff, which was 8.4 (minimum = 0, maximum = 80; t = 6.85, p < 0.001). At their busiest time premises would expect to have on average 200.6 customers on-site (minimum = 10, maximum = 3100) and on average 5.78 staff working on-site (minimum = 1, maximum = 60). On average there were 38 customers for every member of staff (minimum = 3.75, maximum = 1033.33) and the staff-to-customer ratio was associated with number of baseline violent incidents in that premises (Spearman’s ρ = 0.19, p < 0.01), such that the more customers per member of staff, the greater the levels of earlier violence.
Opening and closing times
Premises were more likely to stay open later on Friday and Saturday evenings, with 8 p.m. to 11.30 p.m. being those times when premises were busiest (Figures 13 and 14). In total, 99% of premises were open both on a Friday and on a Saturday; with regard to these premises they would be open on average for 3.34 hours in total after 11 p.m. on a Friday and Saturday evening, with those premises open longest also experiencing greater levels of baseline violence (Spearman’s ρ = 0.30, p < 0.001).
FIGURE 13.
Intervention premises self-report busiest periods.
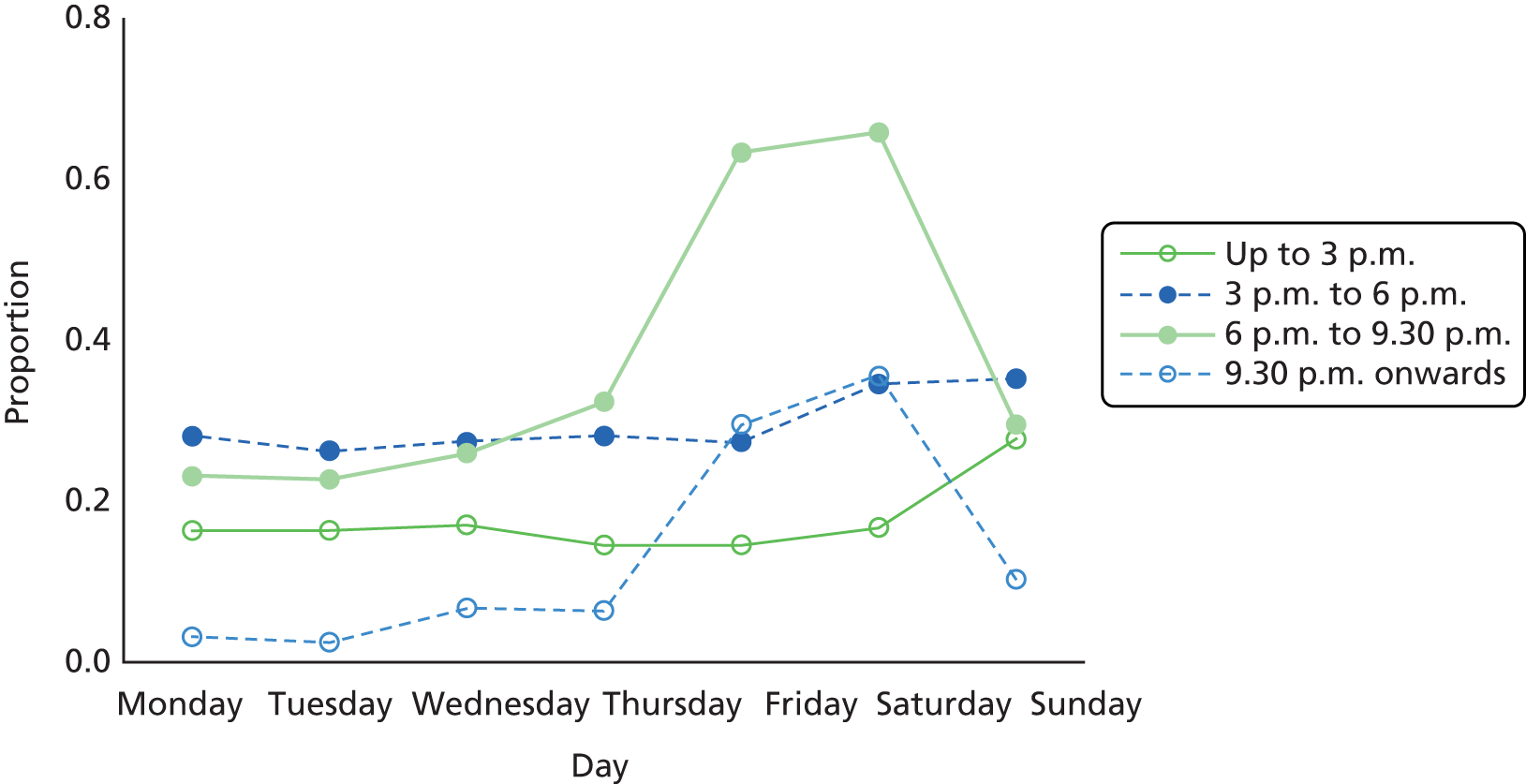
FIGURE 14.
Mean (with standard error bars) premises hours open after 12 p.m. by day of the week.

Door security staff
On average, intervention premises employed 2.04 (minimum = 0, maximum = 18) door security staff when busiest, with more violent premises at baseline being more likely to employ more door security (Spearman’s ρ = 0.44, p < 0.001).
Other characteristics
-
Music, sport and food service.
-
Of the premises audited, 58% had either recorded or live music and 71% showed sport on televisions. Fifty-four per cent of the premises audited served food.
-
-
Organised premises vigilance.
-
Of the 281 premises audited, 62% were involved in PubWatch.
-
-
Area classification.
-
EHPs classified 24% of the audited premises as situated in a non-urban environment.
-
Associations between intervention premises characteristics and baseline violence
A negative binomial regression model (accounting for potential clustering at the LA level) assessed the relationship between past violence and potential predictors of violence, also including whether or not premises had completed a written risk assessment [model χ2(6) = 42.92, p < 0.001]. This model confirms that more customers per member of staff, longer opening hours, and lack of a written risk assessment, a key component of the health and safety advice given by EHPs, were associated with past levels of violence (Table 13). Numbers of door security staff were not included, as these values were collinear with staff numbers (Spearman’s ρ = 0.45).
| Historical violence | Coefficient | z-value | p-value |
|---|---|---|---|
| Customer-to-staff ratio | 0.001 | 2.12 | 0.034 |
| Total hours open | 0.11 | 2.74 | 0.006 |
| Serves food | –0.05 | –0.35 | 0.728 |
| Urban location | 0.29 | 1.86 | 0.062 |
| Written risk assessment | –0.36 | –3.15 | 0.002 |
| Member of PubWatch | 0.25 | 1.56 | 0.118 |
| Constant | 0.13 | 0.57 | 0.567 |
Results summary
The results summarised in this chapter indicate that the reach of an EHP-delivered intervention is high; virtually all premises eligible to receive the audit received one. However, undertaking an initial audit in premises resulted in an increase in violence in intervention premises, compared with control premises. EHPs’ preference was to offer advice and guidance to premises with very few follow-up enforcement visits. However, subgroup analysis showed that conducting a follow-up audit was associated with a reduction in violence. Exploratory analyses further suggest that those premises receiving a follow-up audit did alter processes and respond to feedback. However, while significantly associated with a reduction in violence, numbers in this follow-up group were low, affecting the generalisability of these results. The intervention effect was successfully mapped over time, although the results do not indicate a wane in the intervention effect over time.
The primary result of this audit is, therefore, that EHPs are able to implement an intervention to identify causes of violence in premises and provide advice consistent with the ways they would engage with any business. EHPs, however, were unlikely to use enforcement options that may be associated with intervention effectiveness.
Chapter 6 Process evaluation
Aims and objectives
The process evaluation explored the processes operating during intervention development, adoption and implementation, and the influence of such procedures on delivery.
The process evaluation objectives were to:
-
understand the adoption of the intervention by EHPs and the adaptation required to integrate SMILE into normal practice
-
assess intervention implementation – reach, fidelity and dose delivered
-
assess intervention efficacy – receipt and acceptability
-
understand the implementation context for intervention maintenance and any intervention reconfiguration
-
construct a logic model of the intervention as delivered.
Results
SMILE adoption
Initial intervention adoption
The AWLPI project was adopted after a series of meetings between academics and environmental health managers. Evidence suggests that the meetings facilitated a better understanding of the intervention, its constituent parts and how it was to be evaluated. These meetings also provided the research team with a better understanding of the routine roles and practices of EHPs. However, a more mixed reaction in the wider EHP body suggested that the positive reaction at managerial level did not extend to the broader workforce, highlighting the importance of training and diffusion activities.
The early meetings between academics and senior EHPs included presentations from the feasibility study which gave managers insight into the rationale for AWLPI and increased understanding of the aims and benefits of SMILE. These positive effects were strengthened by recognition that SMILE would map strongly onto current EHP work practice and appreciation that the underlying research aims and objectives of the project met well those of the environmental health agency: ‘I thought “hang on that sounds like some the work that we do, so how come we are not joined up and doing something together?” ’ (senior EHP2). These meetings also improved academic understanding of the remit of routine EHP practice ‘investigating accidents . . . umm, they educate, they work in partnership with groups, other stakeholders who have an interest in public health or the health of the environment’ (senior EHP1).
Subsequent discussion was centred on SMILE design and delivery. Managers suggested that health and safety EHPs should implement the intervention as these specialists were most likely to have gained useful experience in conducting RIDDOR66 investigations in earlier projects: ‘[A]n [earlier] alcohol and violence project, not necessarily for Licensed Premises, but in bookmakers, uhh nightclubs . . . restaurants as well’ (senior EHP1). As changes to adapt SMILE to an environmental health context promised to aid SMILE adoption by the EHP workforce, senior EHPs agreed to work with the academic team to coproduce the intervention.
Wider organisational adoption
Initial news of AWLPI reached much of the wider EHP community more informally through managers. Although all local authorities had chosen to participate in AWLPI, half of the EHPs (n = 11) interviewed felt that inclusion had been imposed. Nonetheless, despite perceptions of a ‘forced adoption’, a recognised barrier to innovation acceptance, most EHPs reacted well to AWLPI, appeared to understand and internalise its demands and believed that they already possessed the necessary skills. This generally positive reception was accompanied by some anticipation that SMILE may help routine work progress into a new legitimate arena:
[W]e are a responsible authority for licensed premises I don’t think that we are finding out enough about what is happening at these premises . . . and if they are not managing violence at their premises then I think that is something that we should be doing.
EHP19
The greatest concern of practitioners came from the realisation that environmental health was to be the sole delivery agent: ‘[L]icensing might have been better placed to deal with this’ (EHP22). Additional disquiet appeared to grow from limited understanding of the rationale of the project – ‘[W]e would deal with violence but not specifically alcohol-related violence and certainly we wouldn’t have had a role with regards alcohol-related violence between customers’ (EHP8) – and lack of understanding of how it differentiated from earlier projects: ‘[W]e had done two violence at work projects in the preceding 2 years and so the general feeling from the team was “oh no not again” ’ (EHP8). These comments raise initial questions about whether or not allowing project information to trickle through organisations in this manner is risky and emphasised the importance of providing diffusion activities throughout organisational hierarchies when introducing innovations into complex institutions.
Contrary to managerial expectation, EHP accounts at this stage suggested that previous experience in addressing work-related violence among EHPs was low. One-quarter reported little or no experience: ‘Not up until the project, no, like I say it wasn’t something that we really, we didn’t look at really’ (EHP1). Of those who had experience, 11 had gained little within licensed premises: ‘I wouldn’t say they was a massive emphasis on it, you know we may look at, if we were going to a licensed premises’ (EHP17). Of the remaining five practitioners, only one had previously worked on a local project similar to AWLPI, ‘for about 4 years . . . through local knowledge and police statistics, I targeted out problem areas and visited all of those’ (EHP5). Others had worked with or as part of LA multiagency teams addressing violence in licensed premises, but involvement ranged from occasional – ‘they meet on a regular basis, now as environmental health officers we don’t sit on that on a regular basis’ (EHP12) – to fuller integration: ‘we apply this scheme in [X] . . . it basically looks at all the issues in terms of NTE, sort of drinking related, alcohol-related problems, underage sales, all these kinds of things’ (EHP10). It was also discovered that EHPs had conducted little work on ARV through RIDDOR: ‘to be honest I don’t recall ever having one’ (EHP13). Despite these findings, there was no evidence suggesting that EHPs felt that lack of experience in these fields would pose a barrier to project adoption and participation.
During the early phase of SMILE adoption the initial discussions were vital as they introduced the concept of involving EHPs in addressing violence in licensed premises to managers and made organisational involvement understandable, relevant and pertinent to them. Subsequent meetings increased mutual understanding and led to agreements to coproduce the intervention and in doing so to draw on the knowledge of senior EHPs with the intent of adapting SMILE to established organisational tools and practices as much as possible. This positive experience at managerial level contrasted with a more negative reaction in less senior EHPs. Although concerns were only expressed by a few EHPs, it may be possible to circumvent such barriers and achieve better levels of early legitimation and enrolment in any roll-out of interventions if more work to give all practitioners a better understanding of the intervention rationale and potential benefits is undertaken earlier. However, the subsequent training offered to LA EHPs did seem to meet initial concerns and generate a more positive response as the intervention was diffused.
Intervention training
Following coproduction of the intervention at least one EHP from each of the 22 Welsh LAs attended a training day. These days aimed to increase wider organisational understanding at both group and individual levels by increasing knowledge and understanding of the intervention format and rationale within the extended EHP body. The training days consisted of expert presentations drawing attention to the extent of violence within the NTE, the potential role of EHPs and the aims and objectives of SMILE. The days also saw senior EHPs presenting the SMILE risk audit in detail and discussing it with the wider EHP body. SMILE audit tools and contact details for allocated intervention premises were distributed to LA environmental health teams once the training days were complete.
In total 74 EHPs attended the training days, a high attendance level which increased the organisational reach of SMILE. Comments from attendees suggested the days increased both individual and communal understanding of the intervention by providing details of project background, rationale and the proposed role of EHPs within it. Most EHPs felt that the research team presentations were useful as they gave ‘[G]ood insight to the background, you know to see where it comes from, the thought behind it and, you know, what you hoped to achieve from doing the project’ (EHP2) while additional medical presentations offered ‘visual sort of displays of injuries that were in A&E from the, from the medical practitioner that was on site, was, was quite . . . Well it was hard hitting’ (EHP5). In addition, the sessions appeared to play an important role in increasing the personal enrolment of EHPs in the project, and providing justification for their involvement in intervention delivery: ‘it did, you know, sort of get me sort of more enthusiastic about trying to tackle it’ (EHP5). The role of senior EHPs in coproducing SMILE was also perceived as important, both in facilitating EHP enrolment – ‘[B]ecause our colleagues had been involved in it from the start that did help because, you know, you weren’t sort of actually preaching to people who had no sort of feedback from peers’ (EHP10) – and in ensuring that the resulting intervention tools met existing skill sets: ‘[T]he actual forms I think are pretty self-explanatory in terms of, you know, filling them in, obviously you know we are used to going on site and taking various different forms with us, you know’ (EHP17). This positive view was later reinforced by the EHPs who did not attend a training day – ‘I had a look through [the risk-audit form] myself and any questions that I had about it I could ask my colleagues and they would sort of clear it’ (EHP6) – which suggests that the SMILE audit fitted into work practices easily even without training being given.
Despite this generally encouraging response, concerns about the exclusion of LA licensing teams remained: ‘the violence and the procedures around that, with regards to CCTV and all that, would have been better suited to licensing’ (EHP18) and ‘it would have been nice to have had the feedback and the input from the licensing officer side of it’ (EHP15). A minority of EHPs were concerned that ‘we don’t want to step on their [licensing’s] toes!’ (EHP18), thus highlighting the importance of agency boundaries within work practices and relationships. 83 A minority of EHPs also felt that the health and safety questions removed the project focus: ‘there were other more general health and safety questions . . . risk assessments and those types of things, maybe they could have been more specific and kind of into more detail perhaps on the violence and aggression’ (EHP9). This response can be attributed to lack of understanding of the role that these factors can play in levels of violence and highlights the importance of providing this knowledge clearly and ensuring that it is disseminated widely during this phase of the project.
Although most EHPs were impressed by the website and films – ‘I felt that I could say to the publicans oh you know it does give you a lot of good information, you know such as challenge 25. And so I thought there was a lot of good information on the DVD’ (EHP2) – two practitioners voiced concerns about one section of one film:
[A]s a team we were slightly horrified by was the contents of the training video which, you know, indicated that premises should put staff into harm’s way in order to protect customers, which is just abhorrent, it is just everything that we would advise against.
EHP8
Consequently, the videos were not extensively promoted by these practitioners.
Overall, the training days appeared to have a beneficial effect. They remedied or limited most EHP concerns by improving levels of understanding, and promoted individual legitimation and enrolment more widely throughout environmental health. The largely positive reaction to SMILE tools and delivery methods was also a testimony to the ability of coproduction to generate interventions that are perceived as valid and relevant to users84 and to the professional attitudes of EHPs, an attribute that was further evidenced during SMILE delivery.
Intervention reach
Although the subsequent delivery of SMILE by EHPs led to significant intervention reach, it is must be noted that a number of premises closed down before the intervention could be delivered, and a small number proved uncontactable or refused to participate. Among the 300 original intervention premises selected, 92 were ineligible owing to premises closure and four refused. Within the four premises refusals, one was as a result of an ongoing prosecution, while one landlord declined because he had recently been part of a similar project and another refused because he felt that SMILE selection reflected poorly on the premises: ‘he got quite upset about it and I think [research team member] got involved as well and you know he had to send you know an apology out’ (EHP21). The final refusal was based on disbelief: ‘they were like well, well, why, why are you here. You know I can’t remember the last time there was even an incident’ (EHP22). This was a feeling shared by managers of many premises in rural or quiet locations. Consequently, EHPs delivered the intervention to 69% of the initial sample.
As per protocol, replacement premises for premises closures and refusals were allocated. In total EHPs delivered SMILE to all but four of the available intervention premises that were open and could be contacted. Such a high implementation rate is consistent with studies in other areas involving statutory partners and strengthens the evidence that agents without legal powers are inferior when compared with those that do have legal power. 69,85 Indeed, nearly all managers consulted reported feeling obligated to co-operate with authorities: ‘it’s going to happen, so may as well go with it’ (DPS 342).
Intervention fidelity and dose delivered
The collaborative approach to intervention development appeared to have produced an intervention that was acceptable and proved to be usable by most EHPs, with high levels of implementation fidelity. However, a similar level of intervention dose was delivered across premises regardless of premises context and level of violence, with EHPs relying on less intensive verbal/written feedback rather than follow-up enforcement visits.
Visits typically consisted of study explanations, an internal and external inspection of premises and necessary documents, a talk ‘that gave information about ‘health and safety at work and that kind of thing’ (DPS 347), and some discussion of the project website and DVD. Although collective EHP accounts provided strong evidence that SMILE delivery was conducted with high levels of fidelity, individual approaches to delivery varied. Some practitioners –
They were always looking at what you were writing and stuff, and it was quite easy for then for me to explain to them with the tick boxes, well you know, you just ‘well look, there is the question, this is the box that I am ticking’.
EHP11
– used more open attitudes than others:
I didn’t score in front of them, I would fill in the pro forma and then come back and do my scores back in the office, so I wouldn’t say to them at the end because obviously that would be quite confrontational.
EHP7
There was evidence that all EHPs found the risk audit easy to use and could provide the necessary advice and guidance: ‘I thought it was all very, the layout and everything was all sort of easy to use and I thought that it was fine’ (EHP1). Some used the audit exclusively – ‘I think that we just utilised your guidance’ (EHP9) – but many drew on previous experience and/or interaction with premises staff:
You work on the response of the person that you are talking to, you know how proactive they are, how responsive they are to what you are talking about. There is no point in serving notices on somebody who is very willing and very happy to put things in place.
EHP7
The EHPs in one LA doubly scored premises: ‘your rating system for this is different to our rating system on our system and so basically we had to rate them twice, we had to rate them for you and then for our own purposes’ (EHP12).
Full description and findings of the audit are reported elsewhere in the report (see Chapter 5). However to summarise, the risk audit involved completion of a RCI (Likert scale 1–6) that indicated levels of risk in 11 separate areas and recorded subsequent requests and actions. Descriptions of visits and the records produced indicated that premises tended to receive a similar dose of the intervention regardless of premises context. Overall, only 24 (8.5%) premises failed to receive some request for action (see also Chapter 5). The vast majority (91.5%) received verbal advice – ‘always verbal on site’ (EHP6) – with over half receiving additional written advice detailing changes that the premises were required to undertake. However, incidence of follow-up visits was low. Only 18 were made in total, most related to health and safety checks (n = 13) and staff training (n = 13). EHPs reported reverting to more formal procedures only when actions were not made or legislation had been compromised:
With issues then which I did pick up on it was written advice, I didn’t need to take any further enforcement action after the written advice and revisiting them, they had done all the, you know they had done all the issues which I had picked up.
EHP6
Few problems in promoting the website and DVD were reported, although the two practitioners who had held concerns about the advice in one film distributed DVDs with warnings to ignore the section in question.
Reports that SMILE delivery was easy together with high prescription fidelity leant further support to claims that use of a coproduction approach produces interventions that fit well into organisational systems. While the high levels of reach and implementation fidelity strengthen arguments that statutory authorities should deliver such interventions, this may need to be considered alongside evidence that EHPs preferred to deliver SMILE using verbal/written advice rather than enforcement and follow-up visits. The effect of this on premises’ response to intervention, therefore, needs to be considered in an examination of intervention receipt and acceptability.
Intervention receipt and acceptability
Findings suggest that the statutory nature of the intervention promoted receipt. However, there was a perception that premises were more responsive to SMILE if they were already engaged with prevention. This was most likely if they were in an urban area, were a large chain and had existing systems and structures in place. Smaller independent premises seemed to find the intervention less acceptable and appeared to require enforcement to promote action.
Half of the EHPs interviewed felt that premises reacted to the SMILE audit positively. Some ascribed this to the statutory nature of visits, others to pre-existing positive relationships with premises:
All of them were accommodating and you know quite a few of them were actually happy then . . . because . . . maybe they hadn’t had an inspection or visit off us for you know a number of years.
EHP6
Some owners supported this view: ‘if you are doing it with the local authority you know that you have covered everything and there is nothing that you have missed out yourself’ (DPS336). In general, EHPs reported that managers of large, often chain, premises tended to react more positively to SMILE – ‘some of the bigger ones . . . where they have got good procedures in place and well trained managers and a well-run place that are receptive to it’ (EHP3) – with poorer responses often coming from long-time owners of smaller pubs:
They said ‘have you ever worked in a pub’ and I said ‘no’, ‘well’ they said ‘well there we are, I have worked in a pub for 30 years, I know exactly what goes on here, I know exactly what to look for’.
EHP3
These EHP descriptions of visits were supported by 16 intervention premises owners/managers (chain, n = 7; independent, n = 9). In reaction to SMILE, managers of large chain premises tended to feel that issues were already being addressed by established in-house policies, practices, training and support: ‘all I have got to do is phone head office, and they are like there with an answer’ (DPS347). However, this opinion was not universal: four managers of chain premises, including two where SMILE identified no concern, felt that the intervention had benefited them by raising personal awareness of ARV and refocusing attention on the issue – ‘it pushes me to the right direction that you have got to be focused on these types of things you know’ (DPS84). In addition, some proprietors noted how having SMILE delivered by EHPs had encouraged maintenance of present standards and updated knowledge:
[F]resh eyes, do you know what I am saying, so I mean and anything new or anything I mean it is like if I have been here 6 years and . . . maybe, she will come and say oh why don’t you try it that way because it is a fresh idea you know. Sometimes so anything new really is always a good idea I think.
DPS124
Within independent premises, despite one reacting very positively –
[T]here are new things coming along . . . and I don’t have the information and there are lots of different things she brought with her, booklets and that as well but especially that DVD, it has just highlighted different zones . . . and say ok I am taking time out here now and I am doing this and showing the staff this as well, and it is all good isn’t it really. It is positive.
DPS131
– a significant number were unhappy at the idea of receiving SMILE. A couple of owners insisted that the intervention had no place in their premises and saw it as an unwelcome burden: ‘I suppose if you hadn’t ticked a lot of the boxes then yes it would be an eye opener and it would be of value. But personally speaking I had a lot of the work already done’ (DPS179). Others participated without complaint, but gave SMILE little thought afterwards, and did not remember it positively: ‘once is bad enough!’ (DPS100).
Participants managing premises near or in towns or city centres appeared more responsive to the aims of the intervention. All agreed that violence was an established ongoing problem, with the majority feeling that the situation had worsened in recent years as escalating use of stimulant drugs had compounded matters: ‘[i]t has got a lot worse over the last few years because there is so much, there is so much drugs in the [location redacted] now it’s sort of an accumulation of the two’ (DPS174). Despite this, a minority of managers working in urban environments perceived violence as something that occurred outside their premises or their area of responsibility –
[P]eople walking down from X Street two of them seen each other . . . history of a feud between them and they started fighting outside. And it has ended up our doormen have got involved because it is literally our doorstep and other people have got, and it just escalated and escalated and it was my doorman that got into trouble for it – for stepping off their door.
DPS33
– or as a consequence of drinking elsewhere either at other premises or through preloading. This inference that premises prefer to distance themselves from customer violence was reinforced by comments such as ‘[t]he biggest issue is once people have become intoxicated is having the foresight, as managers and door staff, to remove those people from the venue’ (DPS28). Such a comment supports evidence that violence and aggression are often displaced onto the street,86 which strengthens a call for some premises to be given stronger support to help them take responsibility for their role in ARV.
Intervention reconfiguration and sustainability
Most EHPs felt that SMILE had been an effective intervention that had had a beneficial impact on the knowledge and practices of EHPs and fitted well with routine work practices. However, initial unease and a lack of confidence in dealing with violence as part of their routine practice remained. Some suggestions to reconfigure SMILE to improve implementation targeting, efficacy and sustainability were also offered. Of particular importance was the involvement of other agencies to promote enforcement and premises receipt.
Using SMILE had raised awareness of ARV and the factors affecting it for many EHPs – ‘it has got to be done, as in like I didn’t realise the scale of the issue’ (EHP21) – and made the potential to address ARV within premises more explicit: ‘I would much prefer to go out there and give them all the information and the guidance that they need you know to help them you know make the premises a safer place rather than going in as an enforcement’ (EHP19). There was wide agreement among EHPs that SMILE fitted the organisational context well: ‘seems to be certainly something that would tie in naturally with the Health and Safety at Work Act and it is sometimes it is a very real, erm, safety issue to employees and to members of the public’ (EHP20). The importance of sustaining and integrating this work into professional practice rather than as a ‘one-off’ intervention was also stressed: ‘I know from like, from personal experience and they have got good intentions for that, the next few months and then it sort of slips off and it goes off their agenda and then something else’ (EHP13).
In contrast, most owners and managers were surprised to find EHPs delivering SMILE. Regardless of this, most felt that EHPs had a role in assessing risk factors given their knowledge and statutory powers: ‘you would make double sure that, you know on that night, you know, it is one of those things that you shouldn’t work like this, you do you just say I will go and double check’ (DPS308). EHPs agreed that statutory powers encouraged actions within premises:
[T]hese interventions highlight the issue to the managing agent and as a result, as is generally the case when we book an assessment, the first thing those in control of the business does is review their own risk assessments on that subject.
EHP8
Further reflection produced some suggestions for SMILE reconfiguration. The major concern stemmed from the data used to identify participant premises. Although virtually all EHPs felt that the premises visited had been representative of their areas, over half felt that the wrong premises had been selected: ‘some of the ones perhaps that I would have classed as being a problem pubs weren’t within that list. . .’ (EHP5). Many respondents agreed, feeling that SMILE effectiveness would have been increased if delivery had been confined to premises whose managers had little experience or knowledge of ARV and how to minimise it – ‘the ones that weren’t part of a chain, independent, no controls, ones with no, no real understanding’ (EHP22) – or which were known to have larger levels of problematic behaviours and violence. Many EHPs suspected that the police violence records were unreliable: ‘you said that a lot of the data came through from the police but when I checked up, certainly on the one pub they had nothing, there was nothing against it whatsoever’ (EHP7). Police violence records were also criticised for associating incidents with nearby premises – ‘three of the pubs in particular, they have called the police for problems outside the premises, you know it is nothing to do with their premises but yet they are, you know they are brought up on the list’ (EHP3) – and for not differentiating between police attendance to prevent trouble and managing ongoing violence: ‘people believed they were serving under age but they were very pro-active in wanting to kind of clean that up . . . and I think that is why they had a higher number of police incidents’ (EHP18).
Post implementation, the feeling that SMILE should have included licensing officers had strengthened – ‘a lot of things that sort of licensees have to do which ties in with this and [licensing] have got a lot of hands on knowledge of individual premises, individual licensees’ (EHP4) – even among some proprietors ‘if a policeman had come in and done that study with me I would have found it more appropriate than the EHP woman coming in to do it’ (DPS22). However, a few managers were concerned that SMILE drew more agencies into a field already negatively affected by decreased funding for police and local authorities in licensing over the last decade: ‘I think that perhaps bringing more bodies into the kind of . . . maybe . . . Yeah I think that, as I say at the moment there is way too much conditions on licences and stuff like that’ (DPS157). SMILE also introduced or reinforced appreciation of the value of multiagency work, especially for EHPs with similar earlier experience: ‘people like the health board, the police, you know fire service, other agencies . . . you know getting everybody interested’ (EHP17). EHPs also maintained that:
it is important to forge these links with everybody . . . so that they can actually, you know raise concerns and perhaps you know change licence conditions and deal with all these things rather than you know do it in isolation.
EHP10
SMILE website
The website containing materials to support the SMILE intervention was organised so that the number of unique visitors visiting the site could be counted. In addition, the bandwidth (the number of data delivered to visitors) was recorded. Figure 15 presents these data and shows that from January 2013 to the end of May 2013 the site received 343 unique visitors and delivered 580 MB of data.
FIGURE 15.
Number of unique visitors to the SMILE website, and bandwidth.

In total, nine intervention premises staff completed the online multiple-choice questionnaire; this was far fewer than expected. In addition, one participant contacted a lead researcher on the project and indicated that they had intentionally answered all questions incorrectly and then put the contact name and address for competing premises.
Conclusions
Study findings suggest that use of a collaborative approach aided the successful adoption, development and implementation of SMILE within environmental health working practices, with high levels of implementation fidelity. The statutory nature of the intervention promoted intervention reach. However, the intervention dose delivered appeared far from optimum, with very few follow-up enforcement visits to premises. This suggests partial intervention failure. This appears particularly problematic, as premises receipt was strongly influenced by the statutory nature of the intervention and the fact that smaller independent premises less engaged in prevention may require such visits in order to overcome intervention resistance.
Initial meetings during the early stages of AWLPI led to better understanding of the rationale for SMILE and its use within environmental health at managerial level, which led to high levels of motivation to integrate the SMILE intervention into EHP work tools and practices among senior staff. Although some LA EHPs reacted less positively when first hearing about SMILE, most concerns appeared to be met by the training days which increased awareness of the need for SMILE, and promoted EHP confidence in their ability and suitability to implement the intervention at both agency and individual levels. Reports of SMILE implementation show that the intervention, generally, was found to be easy to use, was delivered as prescribed and achieved high levels of fidelity.
The statutory nature of the intervention promoted high levels of reach, particularly when compared with results from the previous feasibility trial. However, this needs to be viewed in the light of the relatively high number of premises closures that occurred before the intervention could be delivered and a very small number of premises that refused to participate. For this minority of refusers, a multiagency approach, involving licencing officers, may encourage full premises participation. There were also some concerns about whether or not police data were robust enough to identify at-risk premises and questions regarding whether or not the intervention was targeted at those most in need of it.
In terms of intervention dose delivered, EHPs demonstrated a lack of confidence in dealing with ARV at the start of the project and, although the training appeared to address this, they subsequently relied on advice and guidance rather than enforcement to deliver the intervention, regardless of premises type or level of previous incidence of violence. In this, it appears that the audit acted as a motivational rather than an enforcement tool. At the end of the project EHP concerns in dealing with ARV remained. This may change over time as SMILE becomes more embedded in organisational practice, but, significantly, there was strong support for a multiagency approach, including the police, that promoted enforcement and full intervention implementation.
Addressing such implementation failure appears particularly important, as it was identified as one of the most important mechanisms of action by premises. Acceptability and receipt was largely dependent on the statutory nature of the intervention and the powers of EHPs as delivery agents. For larger chain- or brewery-owned premises in urban areas, SMILE was seen as supporting existing infrastructure and preventative efforts, an extension to routine practice.
In this, there appeared a certain level of complacency, with premises, despite having been being identified as a violence risk, maintaining that they were already dealing with the issue well and busy dealing with competing demands and numerous outside agencies. Follow-up enforcement in such premises may be an effective mechanism to reinforce their classification as a risk premises and prioritise action. Independent premises, on the other hand, seemed to have a stronger need for the intervention. The risk audit identified multiple areas of concern in three-quarters of the independent intervention premises participating in the process evaluation. SMILE acceptability was lower and receipt was poorer in such premises. Managers tended to see the intervention as an added burden, which they lacked the resources to respond to. Such cases demand further consideration of how additional resources/support could be provided for these and similar premises as motivational approaches are unlikely to promote change in the face of such resistance.
Recommendations for intervention reconfiguration and an outline of the intervention as delivered are summarised in the SMILE logic model in Figure 16.
FIGURE 16.
Revised logic model of the AWLPI intervention. EH, environmental health; LP, licensed premises; TD, training day.

In conclusion, process evaluation findings suggest that environmental health is an agency that possesses the required infrastructure, expertise and skills to address the incidence of violence in licensed premises. Analyses indicate that use of the collaborative approach within AWLPI contributed positively to the coproduction and implementation of the SMILE intervention, particularly in the areas of organisational buy-in, intervention development, and EHP participation and action during delivery. The use of regulatory authorities appears an efficient way to promote high levels of premises-level intervention reach to address violence. Findings identify some areas where SMILE could be refined: there were concerns about whether or not the intervention was of sufficient intensity to promote effectiveness and indications that premises may require more follow-up visits and a multiagency approach to counteract assumptions that the issue is already being dealt with adequately or failure to engage in the issue. Concerns regarding the robustness of police data in identifying at-risk premises also suggest the need to consider alternative sources of data for intervention targeting.
Chapter 7 Cost-effectiveness
Aims and objectives
The objectives of this embedded cost-effectiveness analysis were to identify the costs associated with SMILE implementation and delivery and to approximate the extent to which the intervention can be regarded as an efficient use of public funds.
Environmental health practitioner training
Training involved nine trainers and 70 trainees over three training events across Wales (Conwy, Carmarthen and Cardiff) lasting approximately 3.5 hours each. Data on salaries were missing for 17 of 70 trainees and the median (£28,127) was imputed. The total cost of training was £24,314, as shown in Tables 14–18.
| Activity | Hours | Cost |
|---|---|---|
| Obtaining and examining data | 10 | 278 |
| Preparing for and arranging training sessions | 31 | 522 |
| Travelling to and from training venue | 94 | 2712 |
| Delivering (or observing delivery of) training sessions | 90 | 2540 |
| Sending e-mails and making telephone calls | 4 | 120 |
| Providing feedback to licensed premises | 4 | 107 |
| Communicating with licensing officers | 34 | 809 |
| Total cost | 267 | 7088 |
| Item | Cost |
|---|---|
| Stationery: risk audit and follow-up documents, training manuals, envelopes, etc. | 898 |
| DVDs | 549 |
| Business cards | 372 |
| Website | 4569 |
| Postage | 404 |
| Total cost | 6792 |
| Expense | Cost |
|---|---|
| Mileage at £0.40 per mile | 392 |
| Train travel | 355 |
| Parking | 17 |
| Taxis and subsistence | 42 |
| Total cost | 806 |
| Venue | Room hire | Food/drink | Equipment hire | Total cost |
|---|---|---|---|---|
| Conwy | 348 | 374 | 72 | 794 |
| Carmarthen | 210 | 406 | 324 | 940 |
| Cardiff | 0 | 359 | 0 | 359 |
| Total cost | 558 | 1139 | 396 | 2093 |
| Trainee expenses | Total cost |
|---|---|
| Time at training sessions (3.5 hours) (n = 70) | 5197 |
| Travel time | 1142 |
| Mileage expenses | 1012 |
| Other (rail travel, parking, etc.) | 184 |
| Total cost | 7535 |
Audit costs
There were 281 audits held in total, which includes the ITT sample (n = 241) plus the replacements (n = 40) added to the non-randomised sample. Data on EHP salaries were missing for 42 audits and the median salary (£30,311) was imputed. Data were missing on the duration of 2 of 18 follow-up audits and the median follow-up audit time (25 minutes) was imputed. The total cost of auditing (initial plus follow-up) was £10,882, as shown in Tables 19 and 20 (details of audit times are provided in Chapter 5, Intervention reach, dose and delivery).
| Item | Cost |
|---|---|
| EHP time at 281 audits (total hours 383.25) | 8146 |
| Travel time | 1785 |
| Mileage expenses | 717 |
| Total cost | 10,648 |
| Item | Cost |
|---|---|
| EHP audit time at 18 events | 140 |
| Travel time | 66 |
| Mileage expenses | 28 |
| Total cost | 234 |
Licensee premises improvement costs
Of the 281 sites included in the study, 16 intervention and 14 control sites responded to premises’ improvement-related questions during the interviews. Identifying costs to premises that could be attributed to having received an intervention audit proved to be problematic. Licensees were often unsure if some of their improvements were carried out during the audit period and some of these were reported as being requirements of other regulatory bodies (police, LA, etc.) and would have been carried out without the EHP intervention, although the EHP process might have encouraged licensees to comply with these regulations.
In the light of the above, we have not attempted to put a monetary figure on the costs of premises improvements resulting from the audit, but report here some indicative actions taken by licensees in both intervention and control premises. In very few cases these could be identified as a consequence of the audit in intervention premises:
-
maintaining staff training [awareness of violence, abusive behaviour, drug, alcohol, glass and security policies, health and safety training, Challenge 21 training (www.beerandpub.com/industry-briefings/challenge-21), etc.]
-
providing additional bar and door staff at busy times
-
providing female door staff employed to diffuse male–female arguments and check female toilets
-
installing or upgrading CCTV equipment
-
maintaining regular toilet checks
-
using plastic glasses at busy times
-
closing early if high student volume
-
attending PubWatch meetings and joining the After Dark scheme
-
holding regular or increasing risk assessments
-
providing wide spacing between tables
-
maintaining cleanliness of premises, and creating a warm atmosphere, to ‘increase respect from patrons’
-
playing music that appeals to patrons over 25 years of age
-
carrying out random drug searches on every seventh to tenth person
-
keeping a police radio behind bar
-
installing water dispensers near exit
-
selling ‘top-shelf’ products to encourage a ‘better’ demographic of clientele
-
not selling Red Bull (Red Bull GmbH, Salzburg, Austria) and popular shot drinks that are often associated with negative behaviours
-
avoiding ‘2-for-1’ offers on drinks and promoting food offers instead
-
issuing life-bans when absolutely necessary
-
offering coffee to patrons who are heavily under the influence of alcohol
-
limiting opening hours
-
offering club membership that requires a level of good behaviour and respect
-
providing staff uniforms so patrons are aware of them monitoring behaviour
-
immediately stopping bar services upon any disturbance breaking out
-
guarding against going over premises capacity.
Associated costs for most of these preventative measures were rarely reported. Reported costs were mainly for structural changes to premises in order to comply with health and safety requirements and time spent by the manager or other staff. Only some of the following measures could be directly attributable to the EHP audit:
-
collating documents for EHP audit: half an hour of manager’s time (uncosted)
-
CCTV installation and upgrade: costs ranged between £1000 and £3000
-
structural work to premises: costs ranged between £70 and £800
-
more extensive staff training: manager and staff time.
Effectiveness of the intervention
The primary analyses (see Chapter 3, Process evaluation, Conclusions) show that the failure (violent sessions with one or more incidents) was significantly increased by 35% (HR 1.35, 95% CI 1.20 to 1.52) in intervention premises compared with controls during the follow-up period. However, the small number of premises that had follow-up audits (n = 16) showed statistically significant reductions in failure by 57%, compared with all other premises, that is, controls plus intervention premises which were audited only once (HR 0.43, 95% CI 0.26 to 0.71). The net effect of follow-up audits in terms of HRs would be 1.35 × 0.43 = 0.58, suggesting a 42% reduction in failure.
Total costs and cost-effectiveness
Table 21 provides a summary of the total cost of training 70 trainees and auditing 281 licensed premises. The total training cost was £24,314, or £86.53 per premises. The total cost of the intervention, including audit costs, was £35,196, or £125 per premises.
| Type of cost | Cost |
|---|---|
| Training costs (n = 70 trainees) | 24,314 |
| Total audit cost (initial audit n = 281, follow-up audit n = 18) | 10,882 |
| Total intervention cost | 35,196 |
Cost-effectiveness of the intervention
Table 22 shows the mean (SD) costs of training, audit, crimes, total costs and total cost differences, with p-values and 95% CIs. The results show that intervention premises incurred higher costs. The mean difference in total costs between intervention and control premises is £28,831.24, which is not statistically significant (p = 0.17, 95% CI –£12,748.34 to £70,602.91). When adjusted for opening hours and baseline incidents group (binary), the adjusted mean difference is decreased to £24,137.33 and remains not statistically insignificant (p = 0.22, 95% CI –£14,069.34 to £62,151.38).
| Audited (n = 241) | Not-audited (n = 208) | Difference in costs (audited – not audited) | p-value | 95% CIa | |
|---|---|---|---|---|---|
| Training costs | 86.53 | 0.00 | |||
| Audit costs | 38.10 (18.32) | 0.00 | |||
| Costs of crimes against individuals | 124,014.17 (241,612.89) | 95,307.56 (205,182.93) | 28,706.61 | 0.176 | –12,872.78 to 70,477.40 |
| Total costs | 124,138.80 (241,614.42) | 95,307.56 (205,182.93) | 28,831.24 | 0.174 | –12,748.34 to 70,602.91 |
| Difference in total costs (adjusted) | 24,137.33 | 0.222 | –14,069.34 to 62,151.38 |
As the intervention group is more costly and less effective, it is dominated by the control.
Exploratory cost-effectiveness of intervention with follow-up audit
Results in Table 23 show that intervention premises that had follow-up audits incurred significantly lower costs than those not audited (controls) or audited once only. The mean difference in total costs between these two groups is –£64,572, which is statistically significant (p = 0.005, 95% CI –£104,888 to –£18,752). When adjusted as above, the mean difference in total cost is reduced to –£47,795.50, but this difference remains (marginally) statistically significant (p = 0.051, 95% CI –£105,200 to –£1167).
| Follow-up audit (n = 16) (£) | Not audited and audited only once (n = 433) (£) | Difference in costs (£) (follow-up audit – not audited and audited only once) | p-value | 95% CIa (£) | |
|---|---|---|---|---|---|
| Training costs | 86.53 | 44.96 (43.28) | 41.57 | < 0.001 | 37.57 to 45.69 |
| Audit costs | 30.93 (25.65) | 20.06 (23.12) | 10.86 | 0.115 | –1.34 to 26.35 |
| Follow-up audit costs | 12.32 (5.83) | 0.00 | |||
| Costs of crimes against individuals | 48,381.94 (71,628.29) | 113,019.12 (219,107.13) | –64,637.18 | 0.005 | –104,960.40 to –18,800.21 |
| Total costs | 48,511.71 (71,626.45) | 113,084.14 (229,112.62) | –64,572.43 | 0.005 | –104,888.47 to –18,751.64 |
| Difference in total costs (adjusted) | –47,795.50 | 0.051 | –105,199.99 to –1166.72 |
This suggests that an intervention that includes a follow-up audit is more effective and less costly than no intervention or a single audit. This intervention leads to a 42% reduction in violent sessions in the group, which is equivalent to a reduction by seven sessions with violent incident. An intervention that includes a follow-up audit, therefore, could produce savings to society of £47,796, or £6828 per violent session averted.
Stochastic uncertainty in the above results (joint uncertainty in mean failures and costs) are presented via a cost-effectiveness plane that is based on 10,000 bootstrapped replications (Figure 17). The bootstrapped samples consider the mean number of failure sessions and mean total costs. Note that in conventional economic analysis a positive difference in effect means an intervention is more effective than control; here, a negative difference in effects means that the intervention is more effective. Most of the bootstrapped replications are in the south-east quadrant, which means that the intervention (initial audit with follow-up) is more effective and less costly and hence unambiguously more cost-effective.
FIGURE 17.
Cost-effectiveness plane showing the joint uncertainty in mean differences in costs and failures: intervention (including follow-up audit) vs. all other premises.

The CEAC (Figure 18) shows an intervention that includes a follow-up audit that has a 99% probability of being cost-effective over any value the society is willing to pay to avert a violent session.
FIGURE 18.
Cost-effectiveness acceptability curve showing the probability that the intervention (follow-up audits) is cost-effective at different willingness-to-pay values.

One-way sensitivity analysis
As not all violent incidents lead to a criminal justice system cost, we have considered a 50% reduction in this cost in sensitivity analyses. The new estimate of the total cost incurred from a violent incident is £22,846 or (£10,811 + £12,035). A sensitivity analysis is also carried out for training costs amortised over 5 years at a rate of 3.5%. Results are given in Table 24, showing that the intervention (follow-up audits) still remains as a cost saving. However, considering a lower estimate of criminal justice system costs indicates that the adjusted mean difference in total costs is now marginally not statistically significant (p = 0.054, 95% CI –71,687.95 to 2.69).
| Follow-up audit (n = 16) (£) | Not audited and audited only once (n = 433) (£) | Difference in costs (£) (follow-up audit – not audited and audited only once) | p-value | 95% CIa (£) | |
|---|---|---|---|---|---|
| Baseline total costs | 48,511.71 (71,626.45) | 113,084.14 (229,112.62) | –47,795.50 | 0.051 | –105,199.99 to –1166.72 |
| 50% reduction in criminal justice system costs | 32,970.89 (48,618.66) | 76,781.16 (15,520.88) | –32,422.38 | 0.054 | –71,687.95 to 2.69 |
| Training cost amortised over 5 years at 3.5% | 48,444.34 (71,626.45) | 113,049.14 (229,110.11) | –47,827.74 | 0.053 | –106,545.96 to –1572.89 |
Summary
The total cost of the SMILE intervention (training 70 EHPs, auditing 281 premises with further follow-up audit to 18 premises with higher risks of criminal incidents) was £35,196, or £125 per premises.
The intervention was shown to be less effective and more costly and hence not cost-effective (dominated by controls). However, those premises receiving the follow-up audit showed a statistically significant reduction in violent sessions and costs, suggesting that the second audit is cost-effective (dominant). A sensitivity analysis capturing joint uncertainty in costs and effects indicates that the probability of a follow-up audit being cost-effective is almost 100%.
Chapter 8 Discussion and conclusions
Summary of main outcomes and findings
Intervention development
To date, EHPs have not been routinely involved in addressing ARV in premises licensed for the on-site sale and consumption of alcohol, despite having a violence in the workplace remit. LA licensing teams take responsibility in this area and at the expense of EHP involvement, even to the extent that EHPs would rarely visit premises for health and safety reasons. This is of concern. While Licensing are able to enforce the Licensing Act, they have neither health and safety remit nor expertise. Important issues such as fire safety and health and safety training in the workforce and other areas have, therefore, been neglected. This is evidenced in the audit data collected here, where it was found that some premises were operating in ways that placed their customers at risk. Recognising that a number of EHPs felt that licensing should be involved in such intervention work suggests that, at a minimum, joint visits with licensing should be undertaken so that both health and safety and licensing legislation are brought to bear. Alternatively, practitioners skilled in both areas could be trained.
While EHPs have considerable expertise in the area of intervening with small businesses, material and knowledge of what works in respect of reducing the risk of ARV in premises was lacking. An aim of the current study was therefore to develop materials that developed the existing academic knowledge base but also remained within EHPs’ statutory remit. This remit was fairly broad, as under Health and Safety at Work legislation there is an expectation that businesses conduct risk assessments and ensure that their staff are appropriately trained on the processes required to mitigate risk. Staff training is a theme in many interventions in licensed premises and is typically focused on responsible service and similar areas of operation. However, the EHP approach to staff training is that businesses should first understand what risks they are subject to, what the solutions are, who is responsible for mitigating these risks and what can be done. This highlights the need for premises staff to collectively work together to mitigate risk and, thus, generic training programmes are likely to cover only a portion of what is required, and idiosyncrasies will be missed, thereby highlighting opportunities for EHPs to help premises identify and manage risk.
In order to develop materials for EHPs’ use in licensed premises, a series of multidisciplinary development meetings were scheduled. These enabled the development and refinement of a programme model of SMILE, and developed programme models and materials to support EHPs. The final intervention package included a risk audit, a website and a quiz. The risk audit was the primary intervention vehicle. It contained clear instructions on the legislative basis for EHPs to intervene to target specific risk factors in premises, allowed for the quantification of those risks, provided instruction on what changes might reduce those risks and included materials that facilitated a follow-up audit. Instructions for the follow-up audit departed from the original feasibility trial. 21 Originally, all intervention premises in the feasibility study received a follow-up visit, whereas in the current study this requirement was relaxed to fit with EHPs usual working practice in which follow-up visits are scheduled only if a business has more serious issues. For EHPs, dose is commensurate with EHPs’ perceived risk. This reflects recent government guidance62 that aims to reduce the administrative load on small and medium-sized businesses. 88
The website and associated films (available online and on DVD) aimed to provide to premises staff with a positive reason for engaging in harm reduction (e.g. increased footfall), provided template forms consistent with those that EHPs would recommend that small businesses use and further inform premises staff (from senior managers to servers and door security personnel) on how a premises as a whole can work to mitigate harm.
Throughout the development process EHPs engaged with the project fully and played a central role in the coproduction of these materials. The end result was an intervention, SMILE, which proved acceptable to EHPs and was delivered with a high degree of engagement and fidelity.
The intervention
The SMILE intervention was evaluated in a RCT where police-recorded violence was the primary outcome measure. Police violence data were followed for 455 days following randomisation. The reason for following premises for this extended period was to assess any effect of the intervention over time. For example, if a reduction in violence was observed, would this effect be sustained over time or would it wane? Licensed premises are characterised by a high staff turnover and it was hypothesised that this may undermine any initial intervention effect.
Originally, the target sample was 300 premises recruited into each control and intervention group, with sample size estimates suggesting that a minimum of 274 in the intervention group would be required. Historical police data were accessed to identify premises that had experienced one or more violent incidents and these premises constituted the population from which premises were randomly allocated to each experimental group. Twelve months of police data were accessed in order to identify premises, together with a 6-month period in which data were analysed and material prepared. This meant that premises were identified in police data through incidents that occurred up to 18 months previously. Accordingly, a large number of premises were no longer amenable to receive the intervention. Reasons for this included closure and change of purpose (e.g. from a traditional pub to a restaurant). In order to confirm both control and intervention premises were operating further, attempts were made to access LA public licensing registers, although information in these proved to be, at best, sparse and not fit for purpose. Thus, business rate information was also accessed (as small business premises are expected to pay business rates if they are operating). This allowed us to note when premises closed, if they did so, during the follow-up period. In addition, and at the point of implementation, premises were dropped from the study for additional reasons. These included duplicates (e.g. some nightclubs may operate a bar in the same venue that differs in name from the nightclub itself), ongoing prosecution by either environmental health or a related agency, and occasions where premises claimed there had been no occasions of violence on-site (e.g. one premises name was identical to the village in which it was situated and thus it was not possible to disambiguate the exact location of the incident in police data). An advantage of working with EHPs was their capacity to access premises; all small businesses must provide access within 24 hours of receiving notice that they are to be visited. Despite this, three premises refused to participate. In these cases it was the local EHP who asked that they did not pursue the premises in question, mostly because of a preference to avoid conflict in what was effectively a project. These refusals were, therefore, anomalous.
The high level of attrition, mostly a result of closure, from the study meant that ITT analyses were underpowered, according to initial sample size estimates. Accordingly, and to mitigate this feature, sensitivity analyses were planned where the remaining population of premises were added into analyses. Effectively, fewer than expected premises in the analyses means that there is more uncertainty and these sensitivity analyses offer one method to assess the impact of increased uncertainly in analyses. No matter which way we looked at the data the results were consistent. The intervention was associated with an increase in police-recorded violence.
Over 98% of premises eligible to receive the intervention and that were open at the time received a visit from an EHP, suggesting a high level of engagement. Furthermore, analysis of data derived from the initial audit indicates that EHPs did find evidence of risk in premises. These risks varied considerably in form and severity and, therefore, the form of advice given to premises by EHPs also varied. It is usual EHP practice to titrate their response to findings in a manner that is commensurate with the risks they observe. Thus, for fairly mild incursions premises would receive verbal advice on how they might address issues and for much more serious issues EHPs’ response went as far as formal notices that placed a legal duty on premises to enact the required changes. If premises failed to make changes under a formal notice then they became liable to criminal proceedings. A small number of premises exhibited a range of problems to such a serious level that EHPs were obliged to issue formal notices. The review process, under the Licensing Act (2003, Section 53 A), takes 28 days for initial consultation followed by a 20-day period in which a hearing will be held. It is led by a senior police officer and is mostly focused on serious crime; there are opportunities for an expedited review, but these are rare. This process does not cover broader issues concerned with health and safety.
Although instruction was given on the criteria for conducting follow-up visits to premises in the audit materials, and at least one-third of premises met these criteria according to audit data, far fewer than expected premises received a follow-up audit. This may be a result of reluctance on the part of EHPs.
Both primary and secondary sensitivity analyses yielded a consistent intervention effect whereby police-recorded violence increased following the intervention and showed no change in this effect over time (it did not wane). Although the trial was underpowered, secondary exploratory analyses and comparisons with the original feasibility study21 provide insights into the possible reasons for this effect.
In the original feasibility study, all premises received an initial and follow-up audit. Further, audits were conducted by private contractors who, while experts in health and safety in the workplace, were not affiliated with statutory bodies. This meant that engaging premises in the feasibility study proved difficult, with few interested in any voluntary harm-reduction initiative; this was effectively overcome through collaboration with EHPs who delivered the intervention to nearly 100% of eligible premises. However, the process evaluation found that in many instances EHPs sought the advice of partners in LA licensing teams. It is therefore possible that this caused premises in the intervention group to receive greater attention across partners than control premises. As the police are able to record only the violence they are aware89 of, it is feasible that this increased attention meant that more violence was recorded in intervention premises than in control premises, an effect that has been observed in similar studies using police data. 17
A more pertinent issue is whether or not premises in the intervention group made any changes in consequence of the intervention and advice received from EHPs. The only group in which reliable data are available to establish whether or not premises made the recommended changes is those premises that received a follow-up visit from EHPs. In this case, analysis of the audit data strongly suggests that those premises receiving a second follow-up visit had, in fact, made the changes recommended by EHPs. While the process evaluation had covered this matter to some extent, how reliable these data are is open to question. Premises staff, in particular those in premises that are exhibiting greater risk of alcohol-related harm, are unlikely to be reliable, particularly if changes are viewed as being voluntary, which, without a follow-up visit, might have been the case. Further secondary analyses, in particular comparing premises in which written or verbal advice had been given with premises in which no advice had been given, appear to support this. Those that received advice showed lower levels of violence over the follow-up period. We therefore suggest, accepting issues concerned with the fewer than expected premises, that dose would appear to be a key component in the effect of the intervention. As EHPs provided greater motivation for premises to make changes, levels of violence appear to have fallen.
Process evaluation
Study findings suggest that environmental health is an agency that possesses the required infrastructure, expertise and skills to become more involved in addressing the incidence of ARV in licensed premises. Their existing professional practice and audit tools provide a context for the development of appropriate interventions that draw on their professional skills and statutory powers.
The provision of a developmental phase and coproduction approach in intervention development ensured high levels of intervention approval and implementation fidelity as the intervention mapped well on to existing working practices. Utilising a TDAR approach in future intervention development phases appears to be a promising approach. However, adequately addressing professional skills and understanding how to achieve sustainable changes in professional practice is also important. There was some professional reluctance and a lack of confidence in dealing with ARV as a new area of work among some EHPs at the start of the project. This appeared to have been addressed by the training days and diffusion of the intervention within the organisation. However, these concerns remained at the end of the study and might have contributed to the intervention implementation failure of a key mechanism of action for intervention effectiveness, the use of statutory enforcement.
Statutory powers appeared to be key in facilitating the high level of reach of the intervention and were identified as an important influence on promoting intervention acceptability and receipt in premises. However, EHPs rarely drew on these powers. Enforcement follow-up visits were hardly ever used, regardless of premises context or levels of violence associated with premises. Examining the potential mechanisms of action, premises’ responses suggested that these visits could be key in promoting responsibility and addressing resistance at the premises level. Larger premises engaged in prevention may require more follow-up visits and the involvement of licensing officers to counteract assumptions that the issue is already being dealt with adequately and smaller premises appear to need more support and follow-ups to adequately engage in the issue.
Engaging with and supporting a professional group in a new area of work may require a longer period of intervention diffusion and normalisation in order to promote full implementation. Confidence to draw on statutory powers may come as familiarity increases and responsibilities are assumed within routine practice rather than within the context of a research study. Significantly, suggestions that the intervention should utilise a multiagency approach were identified throughout the project. Collaboration with the police in intervention delivery may promote enforcement, or its threat, and promote a crucial mechanism of action for effectiveness. There are also some issues to consider in the targeting of the intervention and its assessment of effectiveness, with a need to examine alternative sources of data to identify at-risk premises and identify change over time.
Cost-effectiveness
The total cost of the SMILE intervention (training 70 EHPs and auditing 281 premises with further follow-up audit to 18 premises with higher risks of criminal incidents) was £35,196, or £125 per premises. The intervention was shown to be less effective and more costly and hence not cost-effective (dominated by controls).
Although there is considerable uncertainty on the observed significant effect of the follow-up visit on police-recorded violence, those premises receiving the follow-up audit also showed a statistically significant reduction in violent sessions and costs, suggesting that the second audit is possibly cost-effective (dominant). A sensitivity analysis capturing joint uncertainty in costs and effects indicates that the probability of a follow-up audit being cost-effective is almost 100%.
Summary
There is a need to join up the NHS, which is a responsible authority under the 2003 Licensing Act as is environmental health, with action in premises so that health service data of violence are appropriately acted on. It is feasible for EHPs to fulfil this role, although traditionally, while they have a violence in the workplace remit, EHPs have not been involved in the on-licensed trade. These responsibilities have typically fallen to LA licensing teams and the police (usual practice in the context of this study). Given that licensed premises are required to meet health and safety legislation and EHPs have the skills required to work with business to reduce risk of violence, and can do so with a degree of immediacy that the 2003 Licensing Act does not afford practitioners, this project has highlighted opportunities for EHPs to become more involved in the management of licensed premises. In particular, their risk-oriented model fits well with the provision of health data, which does not meet evidential requirements required to prosecute but would indicate risks of violence are present. The need to become more generally involved in licensed premises was noted by some EHPs, although a minority were also reluctant to do this. This may be a result of some EHPs seeing their role more in the area of food hygiene and not embracing the increased responsibility under the Licensing Act.
While the intervention was broadly acceptable to EHPs, for premises managers the audit was met with either resignation in smaller premises or a certain level of complacency in larger premises. From website traffic there is evidence that premises staff did engage with the intervention materials to some extent, although very few completed the online questionnaire, and in one case there is evidence that one employee attempted to mislead investigators by purposely entering incorrect answers. Nevertheless, the initial audit was delivered to almost all premises successfully, thereby overcoming one of the main barriers identified in the feasibility trial.
It is feasible that increased police recording of violence following this first audit simply reflects increased police ascertainment of violence rather than any real increase, but this in itself is evidence that previously hidden violence (from the police) was brought to light. This, of course, is a desirable effect. This interpretation is consistent with increased police ascertainment of violence as a result of other violence prevention interventions: greater violence visibility is also the result of public-space CCTV and data from A&E departments. 90,91
Overall, it appears that the intervention was not fully implemented, with very few follow-up enforcement visits. Despite audit data indicating that nearly 40% of intervention premises should have received some form of follow-up visit, fewer than 10% received one. This represents implementation failure for what was seen as a key mechanism of action. In part this may be a result of EHPs’ reluctance to draw on enforcement in what was a new area of practice and substantial changes in EHP approach (originating from the UK government) over the course of this project to small and medium-sized businesses, where there has been a growing emphasis on fewer routine visits and less ‘red-tape’. 88 We conclude that the responsibility for controlling violence in the on-licensed trade cannot be left to the responsibility of the industry itself, but that EHPs require further support for enforcement through the involvement of the police in a multiagency approach to prevention.
Limitations
The trial was underpowered owing to an unexpected number of premises closing between identification of premises in police data and delivery of the intervention. Premises were eligible if they had registered police-recorded violence in the 12 months leading up to the start of the project. It was expected that a number of premises would close and that, therefore, trial arms were oversampled to account for this. However, a larger number of premises were identified in police data that were open for business at the time of audit. One reason for this was the inadequacy of LA licensing data, the initial source from which premises were assessed for their economic activity. It would appear that many LAs do not hold accurate information on the premises in their catchment. Another source of this variation was duplication. Some premises were identified in the police data with more than one address. Large premises in particular would have more than one entrance or exit on more than one street. This is the nature of the data to hand in this trial, where event data were reduced to identify at-risk premises. Nevertheless, future work should consider how police information on violent crime is linked with LA licensing data and how information on premises can be improved. There is a potentially rich source of information that might inform practice if it were adequate. As a minimum, future work needs to consider the availability and use of A&E data.
A similar issue concerns measures of violence. This trial relied on police-recorded violence, a source with known recording biases. These biases are, potentially, one reason for the observed increase in violence for the intervention group, that intervention premises received greater attention. The alternative, health data, in particular A&E data on assaults, do not have the same level of coverage as police data, but are less susceptible to recording biases.
Generalisability
While this trial focused on premises licensed in Wales, it is likely that the approach adopted here is generalisable to the rest of the UK and internationally. Our approach in developing intervention materials was theoretically robust, focusing on risks and adopting theoretical models identified in the international research literature. Fundamentally, however, and as identified above, the sole reliance on police-recorded violence as an outcome measure reduces the external validity of the results presented here.
The expectation was that, should a significant effect be observed, the 12-month follow-up period would allow us to test for sustainability: whether the effect wore off because of staff turnover in premises or for other reasons. Under the circumstances this was not feasible. Nevertheless, the model presented here, one where EHPs respond to violence in licensed premises, would provide one that could be implemented in the long term. Premises that fail to heed advice would be expected to show heightened levels of violence, thereby warranting further visits from EHPs.
Finally, RCTs are generally seen as a suitable and fairly robust method for capturing meaningful evidence to inform service development. However, this approach is underused and, therefore, opportunities exist for further development. Such areas include addressing the needs of practitioners, upskilling the practitioner workforce and more fully involving robust evaluations into policy development.
Implications for practice
Intervention
Environment Health is now a responsible authority under the 2003 Licensing Act and, despite having a violence at work remit, has had little input into licensing decisions. It is, therefore, appropriate that theoretically robust intervention materials are developed for use by EHPs. The intervention materials developed for use in the current project make important inroads into this objective but should be regarded as a working model on which further development can be enacted. While our endeavours did bring what is known about risks in licensed premises into the area of health and safety, there are opportunities for further development. Notably, many EHPs recognised a need to involve other partners, in particular licensing, and so further development could seek to develop materials that make these collaborations explicit.
Further work needs to be undertaken to determine the effect of follow-up visits. Work on both the earlier feasibility trial21 and, to a lesser extent, the current project found a general lack of enthusiasm in premises for harm-reduction initiatives. Indeed, the main reason for working with EHPs was their authority in enforcing change on small businesses. It is plausible that a second visit to ensure premises have responded to advice is a critical active ingredient. Without it, premises may only pay lip service to the idea of change, rather than engage with it fully. Any future work in this area needs to make this requirement explicit.
Stakeholder engagement
One reason why collaboration with EHPs was deemed necessary was a lack of interest in violence-reduction interventions of premises staff during earlier feasibility trials. EHPs have a statutory authority providing them with access to premises. While inconclusive, the results in this study suggest that this reluctance may have continued into the current trial. While EHPs were able to able to access intervention premises, it is feasible that there was very little engagement beyond that initial visit. It is feasible that premises’ engagement with EHPs was limited and that without any further follow-up visit from EHPs requested changes were not made. Further work in this area may consider this further and investigate opportunities for more robust follow-up visits.
Research
Previous work has highlighted the need for objective measures of violence associated with licensed premises,8,16,21,69,89,92,93 in particular the use of data from A&E departments. Health data are not subject to the same biases as police data, as they are driven by patient need rather than police attention. Further work is required to make full use of these data in trials. Secondary analyses suggest that the follow-up visit could be essential to ensure that suggested changes have been made. This warrants further testing.
Conclusions
This project has demonstrated that a RCT methodology can be deployed to assess service innovations in challenging environments. The project successfully translated fundamental research into practice and developed processes that supported EHPs in delivering interventions to licensed premises. While the project did not show that a reduction in police-recorded violence was associated with the intervention, some evidence suggests that this was a result of partial implementation failure and that it may be effective if risk audit advice is more formally enforced.
Acknowledgements
The trial is funded by the National Institute of Health Research (NIHR) Public Health Research (PHR) programme (project number 10/3010/21). This paper is independent research commissioned by NIHR. The views and opinions expressed in this publication are those of the authors and not necessarily those of the NIHR PHR programme or the Department of Health. The work was undertaken with the support of the Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UK Clinical Research Collaboration Public Health Research Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council (RES-590–28–0005), Medical Research Council, the Welsh Government and the Wellcome Trust (WT087640MA), under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. The South East Wales Trials Unit is funded by the National Institute for Social Care and Health Research (NISCHR). Thanks are due to Claire Simpson and Mayu Heikkinen for administrative work on the project and Sophie Rhodes-Martin for her contribution to the report. We would also like to thank the senior EHPs (Richard Henderson, Sarah Jones, Iwan Llewellyn, Simon Morse, Liz Vann and Gweirydd Williams) for their help during the development stage of the trial and their useful comments and suggestions throughout, and all EHPs who delivered the intervention to licensed premises in Wales.
Contributions of authors
Simon C Moore conceived the study and was the overall lead.
Mohammed Fasihul Alam and David Cohen conducted the cost-effectiveness analyses and write-up.
Kerenza Hood contributed to the overall design and analytic strategy.
Chao Huang conducted statistical modelling.
Simon Murphy managed the process evaluation.
Rebecca Playle contributed to the statistical modelling.
Laurence Moore contributed to the study design.
Jonathan Shepherd contributed to the report.
Vaseekaran Sivarajasingam contributed to the report.
Irena Spasic contributed to the methods and analytic strategy.
Helen Stanton contributed to the report.
Anne Williams contributed to the process evaluation.
All authors contributed to the final report.
Contribution of others
Claire Shovelton contributed to the report.
Data sharing statement
Anonymised data from this study can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- The Government’s Alcohol Strategy. London: Home Office; 2012.
- Alcohol-Use Disorders: Preventing Harmful Drinking. Costing Report. London: National Institute for Health and Care Excellence; 2010.
- Focus on: Violent Crime and Sexual Offences, 2011/12. Newport: Office for National Statistics; 2013.
- Sivarajasingam V, Shepherd JP, Matthews K, Jones S. Violence-related injury data in England and Wales an alternative data source on violence. Br J Criminol 2003;43:223-7. http://dx.doi.org/10.1093/bjc/43.1.223.
- Brantingham PL, Brantingham PJ. Mobility, notoriety and crime: a study of crime patterns in urban nodal points. J Environ Syst 1982;11:89-9. http://dx.doi.org/10.2190/DTHJ-ERNN-HVCV-6K5T.
- Global Status Report on Alcohol 2004. Geneva: World Health Organization; 2004.
- Walker A, Flatley J, Kershaw C, Moon D. Crime in England and Wales 2008/09. London: Home Office; 2009.
- Brennan I, Moore SC, Byrne E, Murphy S. Interventions for disorder and severe intoxication in and around licensed premises, 1989–2009. Addiction 2011;106:706-13. http://dx.doi.org/10.1111/j.1360-0443.2010.03297.x.
- Graham K, Homel R. Raising the Bar: Preventing Aggression in and Around Bars, Pubs and Clubs. Cullompton: Willan Publishing; 2008.
- Mulvihill C, Taylor L, Waller S, Naidoo B, Thom B. Prevention and Reduction of Alcohol Misuse: Evidence Briefing Summary. London: NHS Health Development Agency; 2005.
- Bellis MA, Hughes K, Hughes S. WHO Policy Briefing: Interpersonal Violence and Alcohol. Liverpool: Centre for Public Health, Liverpool John Moores University; 2006.
- Ker K, Chinnock P. Interventions in the alcohol server setting for preventing injuries. Cochrane Database Syst Rev 2006;2. http://dx.doi.org/10.1002/14651858.cd005244.pub2.
- Licensing Act 2003. London: The Stationery Office; 2003.
- Moore SC, Brennan I, Murphy S. Predicting and measuring premises-level harm in the night-time economy. Alcohol Alcohol 2011;46:357-63. http://dx.doi.org/10.1093/alcalc/agr011.
- Moore SC, Flajšlik M, Rosin P, Marshall D. A particle model of crowd behavior: exploring the relationship between alcohol, crowd dynamics and violence. Aggress Violent Behav 2008;13:413-22. http://dx.doi.org/10.1016/j.avb.2008.06.004.
- Moore SC, Jones T, Shepherd J. Red alert. Janes Police Rev 2006;114:22-3.
- Burns L, Coumarelos C. Policing Pubs: Evaluation of a Licensing Enforcement Strategy. Sydney, NSW: New South Wales Bureau of Crime Statistics and Research; 1993.
- Felson MR, Berends R, Richardson B, Veno A, Homel R. Policing for Prevention: Reducing Crime, Public Intoxication and Injury. Monsey, NY: Criminal Justice Press; 1997.
- Graham K, Osgood WD, Zibrowski E, Purcell J, Gliksman L, Leonard K, et al. The effect of the Safer Bars programme on physical aggression in bars: results of a randomized controlled trial. Drug Alcohol Rev 2004;23:31-4. http://dx.doi.org/10.1080/09595230410001645538.
- Toomey TL, Wagenaar AC, Gehan JP, Kilian G, Murray DM, Perry CL. Project ARM: alcohol risk management to prevent sales to underage and intoxicated patrons. Health Educ Behav 2001;28:186-99. http://dx.doi.org/10.1177/109019810102800205.
- Moore SC, Murphy S, Moore SN, Brennan I, Byrne E, Shepherd JP, et al. An exploratory randomised controlled trial of a premises-level intervention to reduce alcohol-related harm including violence in the United Kingdom. BMC Public Health 2012;12. http://dx.doi.org/10.1186/1471-2458-12-412.
- Cohen LE, Felson M. Social change and crime rate trends: a routine activity approach. Am Sociol Rev 1979;44:588-60. http://dx.doi.org/10.2307/2094589.
- Skogan WG. Disorder and Decline: Crime and the Spiral of Decay in American Neighbourhoods. New York, NY: Free Press; 1990.
- Wilson JQ, Kelling GL. Broken windows. Atl Mon n.d.;249:29-38.
- Keizer K, Lindenberg S, Steg L. The spreading of disorder. Science 2008;322:1681-5. http://dx.doi.org/10.1126/science.1161405.
- Cohen S. Visions of Social Control. Cambridge: Polity; 1985.
- Innes M. Understanding Social Control: Deviance, Crime and Social Order. Buckingham: Open University Press; 2003.
- Black D. The Behaviour of Law. New York, NY: Academic Press; 1976.
- Jones T, Newburn T. Private Security and Public Policing. Oxford: Clarendon Press; 1998.
- Becker GS. Crime and punishment: an economic approach. J Polit Econ 1968;76:169-217. http://dx.doi.org/10.1086/259394.
- Dahlback O. Analysing Rational Crime Models and Methods. Dordecht: Kluwer Academic; 2004.
- Polinsky AM, Shavell S. The economic theory of public enforcement of law. J Econ Lit 2000;38:45-76. http://dx.doi.org/10.1257/jel.38.1.45.
- Cornish D, Clarke RV. The Reasoning Criminal. New York, NY: Springer-Verlag; 1986.
- Cornish D, Clarke RV, Henry S, Einstadter W. Criminology Theory Reader. New York, NY: New York University Press; 1998.
- Danner TA. Violent times: a case study of the Ybor city historic district. Crim Justice Pol Rev 2003;14:3-29. http://dx.doi.org/10.1177/0887403402250926.
- Felson M, Clarke RV. Opportunity Makes the Thief. London: Research, Development and Statistics Directorate, Home Office; 1998.
- Felson M. Routine activities and involvement in violence as actor, witness, or target. Violence Vict 1997;12:209-21.
- Green J, Plant MA. Bad bars: a review of risk factors. J Subst Use 2007;12:157-89. http://dx.doi.org/10.1080/14659890701374703.
- Campbell CA, Hahn RA, Elder R, Brewer R, Chattopadhyay S, Fielding J, et al. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am J Prev Med 2009;37:556-69. http://dx.doi.org/10.1016/j.amepre.2009.09.028.
- Livingston M. A longitudinal analysis of alcohol outlet density and assault. Alcohol Clin Exp Res 2008;32:1074-9. http://dx.doi.org/10.1111/j.1530-0277.2008.00669.x.
- Livingston M. Alcohol outlet density and assault: a spatial analysis. Addiction 2008;103:619-28. http://dx.doi.org/10.1111/j.1360-0443.2008.02136.x.
- Pridemore WA, Grubesic TH. A spatial analysis of the moderating effects of land use on the association between alcohol outlet density and violence in urban areas. Drug Alcohol Rev 2012;31:385-93. http://dx.doi.org/10.1111/j.1465-3362.2011.00329.x.
- Homel R, Clark J, Clarke RV. Crime Prevention Studies 3. New York, NY: Criminal Justice Press; 1994.
- Quigley B, Leonard K, Collins R. Characteristics of violent bars and bar patrons. J Stud Alcohol 2003;64:765-72. http://dx.doi.org/10.15288/jsa.2003.64.765.
- Clark RV. Situational Crime Prevention: Successful Case Studies. Boulder, CO: Lynne Rienner Publishers; 1997.
- Graham K, Bernards S, Osgood DW, Wells S. Bad nights or bad bars? Multi-level analysis of environmental predictors of aggression in late-night large-capacity bars and clubs. Addiction 2006;101:1569-80. http://dx.doi.org/10.1111/j.1360-0443.2006.01608.x.
- Single E, Pomeroy H, Peele S, Grant M. Alcohol and Pleasure. Philadelphia, PA: Taylor & Francis; 1999.
- Homel R, Thommeny JL. Public drinking and violence: not just an alcohol problem. J Drug Iss 1992;22:679-97.
- Bach PJ, Schafer JM. Tempo of country music and the rate of drinking in bars. J Stud Alcohol 1979;40:1058-9. http://dx.doi.org/10.15288/jsa.1979.40.1058.
- Baron RA, Bell PA. Aggression and heat: mediating effects of prior provocation and exposure to an aggressive model. J Pers Soc Psychol 1975;31:825-32. http://dx.doi.org/10.1037/h0076647.
- Anderson CA. Temperature and aggression: effects on quarterly and yearly city rates of violent and nonviolent crime. J Pers Soc Psychol 1987;52:1161-73. http://dx.doi.org/10.1037/0022-3514.52.6.1161.
- Griffit W, Veitch R. Hot and crowded: influences of population density and temperature on interpersonal behavior. J Pers Soc Psychol 1971;17:92-9. http://dx.doi.org/10.1037/h0030458.
- Homel R, Carvolth R, Hauritz M, McIlwain G, Teague R. Making licensed venues safer for patrons: what environmental factors should be the focus of interventions?. Drug Alcohol Rev 2004;23:19-2. http://dx.doi.org/10.1080/09595230410001645529.
- Homel R, Hauritz M, Wortley R, McIlwain G, Carvolth R. Preventing Alcohol-Related Crime through Community Action: The Surfers Paradise Safety Action Project. Policing for Prevention: Reducing Crime, Public Intoxication, and Injury. Monsey, NY: Criminal Justice Press; 1997.
- Stockwell T, Lang E, Rydon P. High risk drink settings: the association of serving and promotional practices with harmful drinking. Addiction 1993;88:1519-26. http://dx.doi.org/10.1111/j.1360-0443.1993.tb03137.x.
- McMurran M, Gannon TA, Ward T, Beech AR, Fisher D. Aggressive Offenders’ Cognition: Theory, Research and Practice. Forensic Clinical Psychology. London: John Wiley; 2007.
- El Ansari W, Phillips CJ, Zwi AB. Public health nurses’ perspectives on collaborative partnerships in South Africa. Public Health Nurs 2004;21:277-86. http://dx.doi.org/10.1111/j.0737-1209.2004.021310.x.
- Wildridge V, Childs S, Cawthra L, Madge B. How to create successful partnerships – a review of the literature. Health Info Libr J 2004;21:S3-S19. http://dx.doi.org/10.1111/j.1740-3324.2004.00497.x.
- Crime and Disorder Act 1998. London: The Stationery Office; 1998.
- Alcohol Harm Reduction Strategy for England. London: Prime Minister’s Strategy Unit; 2004.
- Thom B, MacGregor S, Godfrey C, Herring R, Lloyd C, Tchilingirian J, et al. The alcohol improvement programme: evaluation of an initiative to address alcohol-related health harm in England. Alcohol Alcohol 2013;48:585-91. http://dx.doi.org/10.1093/alcalc/agt052.
- Environmental Health: A New Relationship for Regulators. London: Chartered Institute of Environmental Health; 2011.
- Regulators’ Code. London: Better Regulation Delivery Office; 2014.
- Health and Safety at Work etc Act. London: The Stationery Office; 1974.
- The Management of Health and Safety at Work Regulations 1999: 3. Risk Assessment. London: The Stationery Office; 1999.
- Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 2013. Bootle: HSE; 2013.
- Graham K, Bernards S, Osgood DW, Homel R, Purcell J. Guardians and handlers: the role of bar staff in preventing and managing aggression. Addiction 2005;100:755-66. http://dx.doi.org/10.1111/j.1360-0443.2005.01075.x.
- Carroll AB. A three-dimensional conceptual model of corporate performance. Acad Manage Rev 1979;4:497-505.
- Moore SC, O’Brien C, Alam MF, Cohen D, Hood K, Huang C, et al. All-Wales licensed premises intervention (AWLPI): a randomised controlled trial to reduce alcohol-related violence. BMC Public Health 2014;14:21-3. http://dx.doi.org/10.1186/1471-2458-14-21.
- Chartered Institute of Environmental Health . SMILE 2012. www.smileproject.co.uk (accessed 6 July 2015).
- Counting Rules for Recorded Crime. London: Home Office; 2015.
- Carter B, Hood K. Balance algorithm for cluster randomized trials. BMC Med Res Methodol 2008;8. http://dx.doi.org/10.1186/1471-2288-8-65.
- Cook RJ, Lawless JF. The Statistical Analysis of Recurrent Events. New York, NY: Springer; 2007.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: PSSRU, University of Kent; 2013.
- Automobile Association . Motoring Costs n.d. www.theaa.com/motoring_advice/running_costs/index.html (accessed 6 July 2015).
- Royal Mail . Price Finder n.d. www.royalmail.com/price-finder (accessed 23 October 2014).
- User Guide to Crime Statistics. London: Home Office; 2011.
- Dubourg R, Hamed J, Thorns J. The Economic and Social Costs of Crime Against Individuals and Households 2003/04. London: Home Office; 2005.
- May C, Finch T. Implementation, embedding, and integration: an outline of Normalization Process Theory. Sociology 2009;43:535-54. http://dx.doi.org/10.1177/0038038509103208.
- Glasgow R, Klesges L, Dzewaltowski D, Estabrooks P, Vogt T. Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res 2006;21:688-94. http://dx.doi.org/10.1093/her/cyl081.
- Bruun D, Bjerre E, Krustrup P, Brasso K, Johanson C, Rorth M, et al. Community based recreational football: a novel approach to promote physical activity and quality of life in prostate cancer survivors. Int J Environ Res Public Health 2014;11:5567-85. http://dx.doi.org/10.3390/ijerph110605567.
- Stokols I. Toward a science of transdisciplinary action research. Am J Community Psychol 2006;38:63-77. http://dx.doi.org/10.1007/s10464-006-9060-5.
- Zietsma C, Lawrence T, Fraser S. University institutional work in the transformation of an organizational field: the interplay of boundary work and practice work. Adm Sci Q 2010;55:189-221. http://dx.doi.org/10.2189/asqu.2010.55.2.189.
- Damanpour F, Schneider M. Characteristics of innovation and innovation adoption in public organizations: assessing the role of managers. JPART 2009;19:495-522. http://dx.doi.org/10.1093/jopart/mun021.
- Rowe SC, Wiggers J, Wolfenden L, Francis JL, Freund M. Evaluation of an educational policing strategy to reduce alcohol-related crime associated with licensed premises. Can J Public Health 2012;103:eS8-14.
- Warbuton AL, Shepherd JP. Tackling alcohol related violence in city centres: effect of emergency medicine and police intervention. Emerg Med J 2006;23:12-7. http://dx.doi.org/10.1136/emj.2004.023028.
- Efron B, Tibshirani RJ. An Introduction to the Bootstrap. London: Chapman and Hall; 1993.
- Temple M. Triennial Review Report: Health and Safety Executive. An Independent Review of the Function, Form and Governance of the Health and Safety Executive (HSE). London: Department for Work and Pensions; 2014.
- Shepherd J, Shapland M, Scully C. Recording by the police of violent offences; an accident and emergency department perspective. Med Sci Law 1989;29:251-7.
- Sivarajasingam V, Shepherd JP, Matthews K. Effect of urban closed circuit television on assault injury and violence detection. Inj Prev 2003;9:312-16. http://dx.doi.org/10.1136/ip.9.4.312.
- Florence C, Shepherd J, Brennan I, Simon T. Effectiveness of anonymised information sharing and use in health service, police, and local government partnership for preventing violence related injury: experimental study and time series analysis. BMJ n.d.;342. http://dx.doi.org/10.1136/bmj.d3313.
- Shepherd J. Victim services in the National Health Service (NHS): combining treatment with violence prevention. Crim Behav Ment Health 2005;15:75-81. http://dx.doi.org/10.1002/cbm.38.
- Sivarajasingam V, Shepherd JP, Newcombe RG. Why public health must contribute to reduce violence. BMJ n.d.;343. http://dx.doi.org/10.1136/bmj.d4453.
Appendix 1 The SMILE audit tool
Appendix 2 The SMILE website map
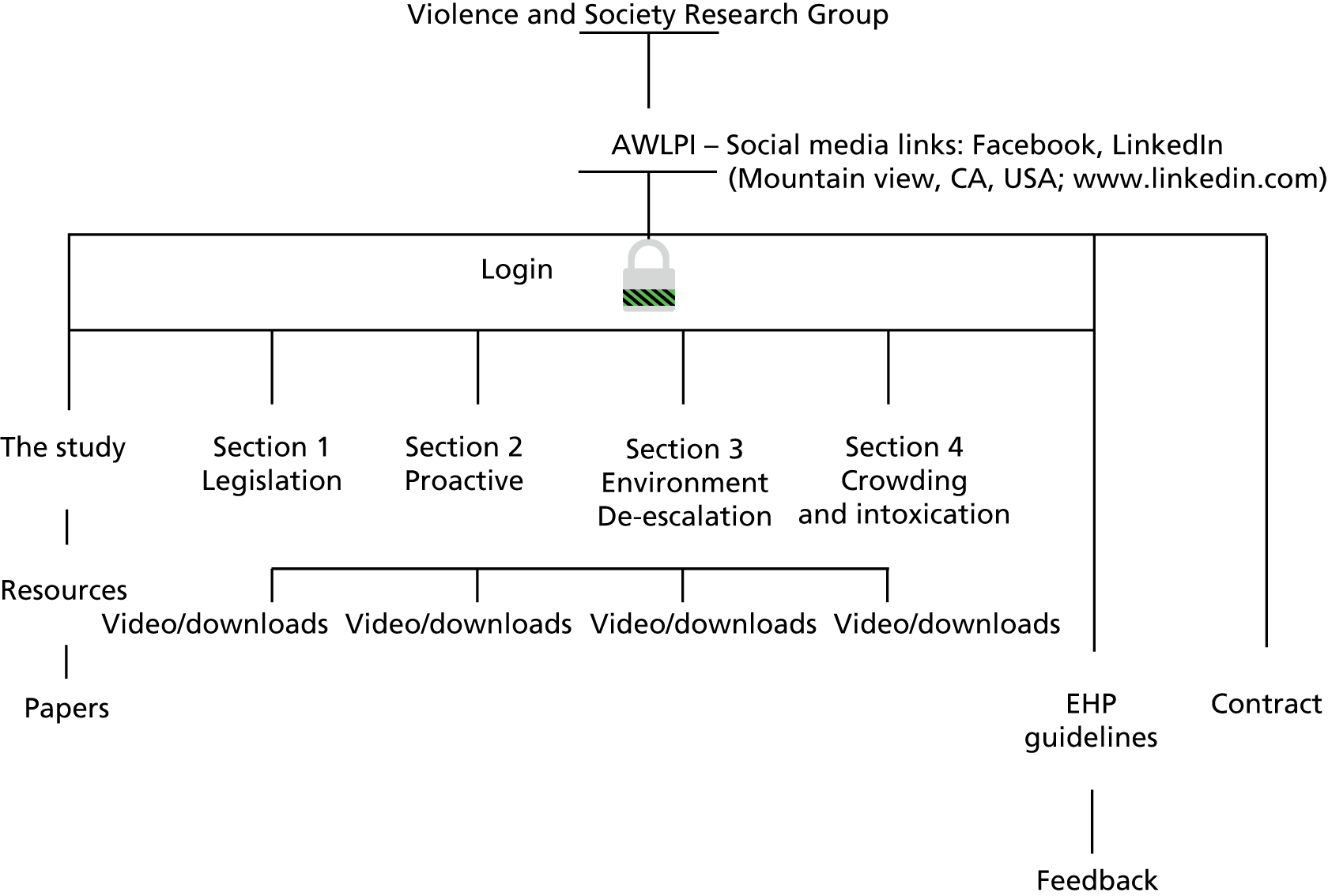
Appendix 3 Web-based materials
The following are the questions included on the SMILE website.
Q1. Which of the following can the use of drugs in a venue lead to?
-
A1. Penalty.
-
A2. Loss of licence.
-
A3. Conviction.
-
A4. All of the above.
Q2. Which are more effective: routine door searches or random door searches?
-
A1. Routine door searches.
-
A2. Random door searches.
Q3. How can disputes be avoided at the door when asking for ID?
-
A1. By maintaining an authoritative manner.
-
A2. By having a policy such as Challenge 25 publicly displayed.
-
A3. By asking everyone for their date of birth.
-
A4. By separating males from females.
Q4. Whose responsibility is it to monitor customers once they are inside premises to ensure they are not too intoxicated or rowdy?
-
A1. Door staff.
-
A2. Everyone.
-
A3. DPS.
-
A4. Bar staff.
Q5. What are the three stages of anger development?
-
A1. Cause, action, effect.
-
A2. Argument, shouting, fighting.
-
A3. Trigger, escalation, crisis.
-
A4. Incident, conflict, reaction.
Q6. Identify three signs that anger is beginning to develop.
-
A1. Physical agitation.
-
A2. Stretching arms.
-
A3. Looking at the floor.
-
A4. Raised voice.
-
A5. Eyeballing someone.
Q7. Which of these should you NOT do when trying to diffuse a situation at the TRIGGER stage?
-
A1. Maintain an open and relaxed body posture.
-
A2. Request that people calm down.
-
A3. Introduce yourself and ask if there is anything you can do to help.
-
A4. Let people express themselves and show you’re listening.
Q8. Which TWO sets of signals would help you recognise that someone is in the ESCALATION stage of anger?
-
A1. Salivating mouth and colour drained from face.
-
A2. Looking tense and taking up more space.
-
A3. Red face, dry mouth and sweaty hands.
-
A4. Looking down with crossed arms.
Q9. Which of these should you NOT do when trying to diffuse a situation at the ESCALATION stage?
-
A1. Touch someone, for example to usher them to a quieter place.
-
A2. Listen and smile.
-
A3. Move to a quieter area to distract their attention.
-
A4. Suggest you both go to get some fresh air.
Q10. How can you spot that someone is in the CRISIS stage?
-
A1. They are pacing the floor, looking down and not talking to anyone.
-
A2. They are vigorously dancing.
-
A3. They are in a trance-like state and completely irrational, possibly being abusive/violent.
-
A4. It’s impossible to tell.
Q11. What should you do if you feel that there is the possibility of physical danger?
-
A1. Ask the person to leave immediately.
-
A2. Call for a member of door staff/manager.
-
A3. Approach the person face-on and ask them to stop their behaviour.
-
A4. Ask other customers for help.
Q12. In relation to antisocial behaviour, why is it important to keep a clean, well-maintained bar environment?
-
A1. It means you can easily identify people who are behaving antisocially.
-
A2. It helps to stop germs from spreading.
-
A3. It gives customers the impression that the venue does not tolerate vandalism, criminal or disrespectful behaviour.
-
A4. It means less time has to be spent tidying up at the end of your shift.
Q13. What could you do to help prevent glasses causing injuries (deliberate or accidental)?
-
A1. Keep a dustpan and brush behind the bar.
-
A2. Ask customers to return their glasses to the bar when they have finished their drinks.
-
A3. Get door staff to clear tables when they have some spare time.
-
A4. Use plastic glasses at busy times and regularly clear tables of glasses.
Q14. Which TWO ways can help you reduce the risks of crowding outside your venue?
-
A1. Have a cordon to separate queues for your venue and other things such as cashpoints.
-
A2. Have separate queues for males and females.
-
A3. Make everybody line up in pairs.
-
A4. Ensure the smoking area does not interfere with the venue’s entrance.
Q15. Why is crowding in internal areas such as the bar and toilets a risk factor?
-
A1. It is a fire risk.
-
A2. Customers may buy more than one drink at the bar increasing their chance of getting drunk quickly.
-
A3. Close physical contact between customers may lead to agitation.
-
A4. All of the above.
Q16. What is a key risk factor to consider when special events (e.g. large sporting events, live music) attract more customers than usual to your venue?
-
A1. People may not be able to see the television screen/band clearly.
-
A2. Crowding at the bar during half-time/breaks.
-
A3. Having extra cash in the tills.
-
A4. Not being able to close on time.
Appendix 4 Environmental health practitioner interview schedule
Q1. What were your feelings about ARV before this project?
-
Prompts:
-
Did you think alcohol use caused problems?
-
What did you think the costs were to society, communities, individuals?
-
Do you know the financial cost of alcohol-related harm to England and Wales? (If no, what would your guess be?) (£21B)
-
Did you think there was a relationship between alcohol and violence?
-
Did you think ARV was a problem?
-
What kind of problem?
-
Any specific times, locations, groups of people?
-
What caused/affected ARV:
-
in society (national legislation, policy, economics, culture)
-
in communities (local policy, economics, culture)
-
in your local area (local policy, economics, culture, work type/patterns, leisure)
-
in the NTE (all above)
-
in the NTE within the local authority you work in?
-
-
Have you noticed any changes over the last 5 years? In the NTE?
-
Do you think the recession has had an impact on the work and actions of licensed premises in relation to ARV this area? In the NTE?
-
Did you think licensed premises (policy, practice) have a role in ARV?
-
Can you describe this?
-
Q2. Can you describe your typical type of work before this project began?
-
Prompts:
-
What area of environmental health do you work in?
-
Can you describe your job generally?
-
Was the identification of risk factors part of your work?
-
To what extent was dealing with violence in the workplace part of your work?
-
Was ARV part of your remit?
-
Have you taken part in project work before?
-
How do you feel about research and the value of evidence-based research?
-
Q3. Can you describe your organisation’s role in addressing ARV and injury in licensed premises or associated risks before this project began?
-
Prompts:
-
Do you think your organisation had a role?
-
Can you describe it?
-
Was there any specific guidance about referral to RIDDOR after accidents/injury due to ARV?
-
How did your managers feel about this role?
-
Did you feel it was adequate?
-
Did your organisation work with other agencies?
-
Can you describe it?
-
Did you feel it was adequate?
-
Q4. Can you describe your work role in licensed premises before this project began?
-
Prompts:
-
Did it include any risk assessment?
-
Were you aware of any risk factors in licensed premises that influenced ARV?
-
Was dealing with violence in licensed premises in a workplace part of your work?
-
How about dealing with any aggression or violence in licensed premises whatever the cause?
-
Certain accidents and injuries have to be reported to RIDDOR. How does this apply to injuries from violence and aggression in licensed premises? In your opinion what percentage of accidents/injuries related to ARV are RIDDOR reported?
-
Did your work in licensed premises include work with other agencies? Can you describe it?
-
Did you feel you it was adequate?
-
To your knowledge what did other EHPs (in your LA/in wider LAs) do?
-
Q5. Can you describe how you became involved in the project (AWLPI)?
-
Prompts:
-
What was your first contact with the project?
-
How was the project presented or described to you?
-
Who was consulted about your team’s involvement?
-
What did you think about it?
-
How did the project map on to work you did already?
-
How widespread was knowledge of the project in your office?
-
What was the general attitude to the project in the office?
-
Do you know why some have performed audits and others haven’t?
-
-
Did you attend a training day?
-
If yes:
-
What did you think of the day (good/poor bits)?
-
Would you change anything about the training day?
-
How did you feel about the project afterwards?
-
Did you feel confident you could deliver the interventions?
-
Did the training day/manual provide enough resources?
-
-
If no:
-
Did you get a training manual?
-
Were you given any related information and/or training?
-
How did you feel about the project?
-
Did you feel confident you could deliver the interventions?
-
Did you use your organisational hub?
-
Did you access the project website? What did you think of it?
-
Did you feel you had been supplied with enough resources?
-
-
All:
-
Could you envisage any barriers to implementing the project?
-
Any ideas on how this could be overcome?
-
-
Q6. (Only for those attending training days) Do you feel your organisation and your office/you were involved in the development of the project interventions (audit, website and films) enough?
-
Prompts:
-
Through the training day?
-
Through feedback after use?
-
Q7. Can you describe your reaction to the Audit and Guidance document?
-
Prompts:
-
How did you feel about it?
-
What did you think about its layout? Content?
-
When did you get the audit? Was there enough time to prepare for visit?
-
What was the document like to read?
-
Would you make any changes to it? Any risks we should have included?
-
Anything we should add to guidance?
-
Do you feel it had a use in preventing violence in licensed premises?
-
Did you feel it was the role of EHPs to undertake such an audit?
-
What do you feel were the most important part(s) of the audit in addressing factors associated with violence in licensed premises?
-
How did colleagues react to the audit?
-
Q8. Can you describe your reaction to the website and films?
-
Prompts:
-
How did you feel about it?
-
What did you think about the website form and content?
-
What did you think about the film content?
-
If you tried it what was it like to use?
-
Did you feel it was the role of EHPs to promote the website and films?
-
What was your colleagues’ reaction to the website and films?
-
Q9. Can you tell me a little about the premises you audited?
-
Prompts:
-
How many audits did you do?
-
Can you tell me a little about the premises you audited?
-
Size.
-
The area it is located in (NTE, recognised area of alcohol problems).
-
The premises history and reputation for ARV.
-
Existing policy and practice in relation to preventing ARV.
-
Existing policy and practice in relation to dealing with ARV.
-
-
Were all owners/duty managers aware of RIDDOR?
-
Are alcohol-related violent incidents included in reports and accidents?
-
Can you describe the owner’s/manager’s/DPS’s feelings about regulating ARV?
-
Do you feel overall that you conducted audits at a wide range of premises?
-
Do you think the right premises were identified and involved?
-
Q10. Can you describe your experiences doing the audit and promoting the website?
-
Prompts:
-
What were the interventions like to use?
-
Can you tell me about arranging the inspections (easy, difficult)?
-
Did you conduct the audit alone, with other EHPs or with staff from other agencies?
-
If with others, can you tell me about that?
-
Who did you deal with while conducting the audit at the premises?
-
Do you feel this was the most appropriate staff (owner, manager, DPS)?
-
Did you get to speak to other staff members?
-
What were bar staff attitudes to the audit (typical, variations)?
-
Did you promote the website and leave access details?
-
What were bar staff attitudes to the website/films (typical, variations)?
-
Can you describe any problems implementing the interventions?
-
Do you think it was a worthwhile process? In what ways?
-
How does it compare with colleagues’ experiences?
-
Q11. Can you tell me about scoring and actions that resulted from the audit?
-
Prompts:
-
How did you decide on scores?
-
Actions within the premises.
-
What did you do?
-
How did actions relate to scores?
-
What was the staff response?
-
What was the outcome?
-
Referrals to other authorities.
-
To whom?
-
Why?
-
What was the reaction of the other agencies?
-
How did your actions compare with your colleagues’?
-
Q12. Can you tell me about any monitoring/reaudits you did?
-
Prompts:
-
Can you describe any changes in the premises?
-
Were there any changes in the attitudes, policies and practices of staff?
-
Q13. Looking back would you make any changes to the way the audit and/or website was developed? Or changes that would help implementation for future use? Will the new enforcement code that identifies hazard rather than risk as the focus have any effect on audit use or scoring in the future?
Q14. In the light of your work on the project what are your current thoughts about the role of EHPs in intervening in licensed premises to address factors affecting ARV?
Q15. Do you think the changes in the licensed premises you audited that you described will have a positive impact on the levels of ARV in those licensed premises? Could this apply to the NTE in other premises and in districts generally?
-
Do you think this will be sustained?
-
Is there anything else you think the environmental health organisation can do?
-
Your work in this project has stemmed from police data: what are your thoughts on this interagency working?
-
What are your thoughts on strengthening this by sharing environmental health data – such as the RIDDOR data on assaults in licensed premises with the police? What impact do you think it may have?
-
What are your thoughts on extending this to more interagency work and data sharing with other agencies such as fire services, licensing panels and the health services?
Appendix 5 Licensed premises staff interview schedule
Intervention premises
Q1. Can you tell me a little about your work in the licensed trade?
-
Prompts:
-
How long and where?
-
Have you worked in a range of different environments?
-
Have they been local, other parts of the UK or abroad?
-
Have you worked in similar premises to these (organisation, size, location, clientele)?
-
Q2. What are your feelings about the alcohol and violence debate?
-
Prompts:
-
Do you think there is a relationship?
-
Do you think ARV causes problems in:
-
society
-
communities
-
licensed premises generally
-
your premises?
-
-
What kind of problems?
-
Are they related to any specific times, locations, groups of people?
-
What do you think caused them?
-
Did you have any policies or practices to deal with these problems within your premises?
-
Did you feel this was your responsibility to do?
-
Were there any other actions you can think of that you could have taken?
-
Who else do you feel is/should be responsible?
-
Q3. Can you describe how your premises became involved in the project (AWLPI)?
-
Were you aware of the incident that led to the police record(s)?
-
What was your first contact with the EHP?
-
What information were you given?
-
What did you think about the contact, your premises being involved?
-
Did this lead to any response or action?
-
Did you know what the EHP visit was about? What were you expecting?
-
How was the appointment date and time agreed?
-
Did you do anything to prepare for the visit?
Q4. Can you describe what happened when the EHP inspection took place?
-
Prompts:
-
What did the EHP ask about?
-
What did the EHP look at?
-
Who did the EHP talk to?
-
What did the EHP do?
-
What information did the EHP give you?
-
Were you shown the website and/or films?
-
What did you think about the visit?
-
What was the visit outcome (informal advice, formal written advice, and referral)?
-
Could you see how the visit was related to alcohol and violence in your premises?
-
Q5. Can you describe any actions taken by the EHP/other authorities after the inspection?
-
Prompts:
-
What did the EHP do?
-
Did you receive any letters or notices?
-
Were any referrals made to other authorities (LA licensing officers, police, fire)?
-
If they were, what did they do?
-
Q6. Can you tell me about any changes made in your premises, or in premises policy or practices, after the audit and how much you think these have cost you?
-
Prompts:
-
changes in equipment (CCTV, mirrors, glassware, communication)
-
structural changes
-
staff changes
-
staff training
-
records, assessments, risk planning and checks
-
membership of PubWatch or similar
-
door management
-
any other changes
-
costs:
-
-
buying items
-
fitting
-
paying for specialist services (gas, electricity, decorators, plumbers, etc.)
-
employing new staff (security, door, extra staff for busy periods)
-
training
-
lost staff time
-
travelling (purchase items, attend courses).
-
-
Q7. Do you have any plans for changes in the near future (by Easter) to reduce the chance of violence; any idea of how much this will cost?
-
Prompts:
-
See Q6.
-
Q8. To return to the EHP visit, can you tell me what use you made of the website after the inspection?
-
Prompts:
-
Did you access it?
-
If so which bits did you view?
-
Did you complete the quiz?
-
Did you use any resource links? If so which ones?
-
What did you think of the site?
-
Can you describe any effects website use had on you and/or your premises?
-
Did you tell any other staff about the site?
-
Do you know if they use it?
-
Q9. Did the EHP make a follow-up visit?
-
Prompts:
-
If yes, do you know why?
-
Can you describe what happened?
-
What was the outcome?
-
Will you have any further contact with the EHP?
-
Q10. In your opinion did this experience have any impact, both negative and positive?
-
Prompts:
-
On your premises?
-
On premises policy and practice?
-
On the levels of violence in your premises?
-
On your/your staff’s awareness of the link between alcohol and violence?
-
On your/your staff’s awareness of what can be done within the premises to reduce the risk of ARV?
-
Do you think EHPs have a role in preventing violence in licensed premises?
-
Q11. Is there anything else you think health and safety can do to help you reduce the risk of ARV in your premises?
Control premises
Q1. Can you tell me a little about your work in the licensed trade?
-
Prompts:
-
How long and where?
-
Have you worked in a range of different environments?
-
Have they been local, in other parts of the UK or abroad?
-
Have you worked in similar premises to these (organisation, size, location, clientele)?
-
Q2. What are your feelings about alcohol and violence?
-
Do you think there is a relationship?
-
Do you think ARV causes problems in society/communities/licensed premises generally?
-
In your premises?
-
What kind of problems?
-
Are they related to any specific times, locations, groups of people?
-
What do you think caused them?
-
Did you have any policies or practices to deal with these problems within your premises?
-
Did you feel this was your responsibility to do?
-
Were there any other actions you can think of that you could have taken?
-
Who else do you feel is/should be responsible?
Q3. Can you describe how your premises became involved in the project (AWLPI)?
-
What was your first contact about the project?
-
What information were you given?
-
Do you know why your premises were included in the project?
-
What did you think about your premises being involved?
-
Did this lead to any response or action?
Q4. Can you think of any factors in or around your premises that may affect ARV?
-
Prompts:
-
hours of opening/serving
-
safety policy and risk assessments
-
visibility, lighting
-
health and safety around the premises
-
noise and communication
-
sharing information with other premises
-
alcohol promotions
-
staff levels at busy times
-
door management
-
people management: staff training re: drunk disorderly clients; barriers to training
-
provision of RBS staff training
-
log book/accident book
-
glassware policy.
-
Q5. Have there been referrals to authorities since the incident(s) that led to the police notification in the last year?
-
Prompts:
-
EHP?
-
LA?
-
Fire and rescue?
-
Police?
-
If there were, what did they do?
-
Q6. Can you tell me about any changes made in your premises, or in premises policy or practices, this year that may influence levels of ARV, and can you estimate just how much these changes or actions have cost you?
-
Prompts:
-
Changes in:
-
equipment (CCTV, mirrors, glassware, communication)
-
structural changes
-
staff changes
-
staff training
-
records, assessments, risk planning and checks
-
membership of PubWatch or similar
-
door management
-
any other changes.
-
-
Costs:
-
in buying items
-
fitting
-
paying for specialist services (gas, electricity, decorators, plumbers, etc.)
-
employing new staff (security, door, extra staff for busy periods)
-
training
-
lost staff time
-
travelling (purchase items, attend courses).
-
-
Q7. Do you have any plans for changes in the near future (by Easter) to reduce the chance of violence . . . any idea of how much this will cost?
-
Prompts:
-
See Q6.
-
Q8. In your opinion have your actions in the last year had any impact, both negative and positive?
-
Prompts:
-
On your premises?
-
On premises policy and practice?
-
On the levels of violence in your premises?
-
On your/your staff’s awareness of the link between alcohol and violence?
-
Of your/your staff’s awareness of what can be done within the premises to reduce the risk of alcohol-related awareness?
-
Do you think environmental health officers have a role in preventing violence in licensed premises?
-
Q9. Is there anything else you think can be done to help you reduce the risk of ARV in your premises?
Appendix 6 Focus group schedule for initial focus group with senior environmental health practitioners
Interview schedule for chief executive officers and senior management.
Q1. We are really interested in the role of health and safety in the licensed trade: can you tell me about your organisation’s relationship with health and safety?
-
Have health and safety been involved with the organisation to date?
-
What was the result of the contact?
-
Did this contact impact on health and safety within licensed premises (staff and clients)?
-
Did you feel it was a positive experience?
-
Could they have been more helpful? How?
-
Do you feel the involvement of EHPs was standardised across the licensed field in England and Wales?
-
Was there/do you feel there would there be a benefit to this?
Q2. On a more general level, how do you think people living in the UK feel about alcohol use?
-
Do you think it is seen as a normal part of our culture?
-
Does this vary with different populations and contexts? Age, gender, geography, culture, ethnicity, venue, daytime, night-time, NTE?
-
Has acceptability changed over time?
-
What do you think has influenced any changes?
Q3. What about drinking and related violence?
-
Do you think people drink too much?
-
Do you think this is related to aggression and violence?
-
Is this also seen as a normal part of our culture?
-
Again does this vary with different populations and contexts? Age, gender, geography, culture, ethnicity, venue, daytime, night-time, NTE?
-
Has attitude to excessive alcohol use and consequences changed over time?
-
What do you think has influenced any changes?
-
How do we get to know about levels in the UK?
-
How do those who work in the industry hear about ARV, both single incidents and general levels?
-
What are your feelings about binge drinking? Do you think it impacts on business in the licensed trade? For good or bad?
Q4. It has been argued that ARV is linked to many different factors. What do you think promotes violence in and around pubs and clubs?
-
External: culture – national/local/area licensed premises set in.
-
Population: young, male/female split.
-
Economics: preloading.
-
Failure of feeder pubs to stop further drinking.
-
Failure of other authorities to address problem.
-
Within industry: risk factors – refer to audit.
Q5. If any risks are identified in your organisation’s licensed premises (licensed premises your organisation supplies) do you have a set procedure for reporting and dealing with them?
-
Are you made aware of all incidents?
-
Only incidents leading to actions such as referrals, involvement of other officials?
-
Only if a RIDDOR notification is needed or made?
-
Whose responsibility is it to plan resultant actions and follow up?
Q6. Again more generally, where do you feel responsibility for regulating ARV in the NTE should lie?
-
National legislation and policy?
-
Policy and action with/by:
-
police
-
fire and rescue
-
Trading Standards
-
licensing officers
-
local councils
-
(health and safety – don’t prompt if they don’t volunteer this)
-
the industry
-
licensed premises staff/managers
-
individuals?
-
-
Does that reflect the national picture or do you think it varies locally?
Q7. What are the benefits and challenges of addressing ARV in licensed premises from your company’s perspective?
-
Disadvantages: cost (staff, security, fewer promotions, decreased number of clients).
-
Advantages: safer environment, better atmosphere, attract more clients.
Q8. Has your organisation ever discussed or formulated policy or practices to address ARV on premises?
-
What were they?
-
Would you say they were proactive or reactive?
-
How often are they implemented?
-
Is this standard across establishments or applied on a site-to-site basis?
Q9. Some feel that action to address ARV from within the industry would be best: do you agree or do you feel actions from other agencies or sources (police, legislation, health and safety, licensed officers) would be better?
-
What would be positive about internally driven change?
-
Would this produce any problems?
-
Problems and benefits of external changes?
Q10. Should there be a standard approach across the UK to address ARV, or do you think local schemes would be better? Explain rationale.
Q11. Do you know how one of your premises became involved in the project (AWLPI)?
-
Were you aware of the incident that led to the police record(s)?
-
What was your first contact with the EHP?
-
What information were you given?
-
What did you think about the contact, your premises being involved?
-
Did your staff do anything to prepare for the visit?
Q12. Do you know anything about the EHP inspection?
-
If yes, prompts:
-
What did the EHP ask about?
-
What did the EHP look at?
-
Who did the EHP talk to?
-
What did the EHP do?
-
What information did the EHP give?
-
Were you or your staff shown the website and/or films?
-
What did you think about the visit?
-
What was the outcome of the visit (nothing, informal advice, formal written advice, referral)?
-
Could you see how the visit was related to alcohol and violence on the premises?
-
(If yes to Q12) Q13. Can you describe any actions taken by the EHP/other authorities after the inspection?
-
Prompts:
-
What did the EHP do?
-
Did your staff receive any letters or notices?
-
Were any referrals made to other authorities (LA licensing officers, police, fire)?
-
If they were, what did they do?
-
(If yes to Q12) Q14. Do you know if any changes were made in the premises, policy or practices after the audit? Did this extend to other premises?
-
Prompts:
-
changes in equipment (CCTV, mirrors, glassware, communication)
-
structural changes
-
staff changes
-
staff training
-
records, assessments, risk planning and checks
-
membership of PubWatch or similar
-
door management
-
any other changes.
-
(If yes to Q12) Q15. Do you know if any use was made of the website after the inspection?
-
Prompts:
-
Did you access it?
-
If so which bits did you view?
-
Did you complete the quiz?
-
Did you use any resource links? If so, which ones?
-
What did you think of the site?
-
Can you describe any effects website use had on you and/or your premises?
-
Did you tell any other staff about the site?
-
Do you know if they use it?
-
(If yes to Q12) Q16. Did the EHP make a follow-up visit?
-
Prompts:
-
If yes – do you know why?
-
Can you describe what happened?
-
What was the outcome?
-
Will you have any further contact with the EHP?
-
(If yes to Q12) Q17. In your opinion did this experience have any impact, negative or positive?
-
Prompts:
-
On your premises/organisation?
-
On premises/organisation policy and practice?
-
On the levels of violence in your premises?
-
On organisational awareness of the link between alcohol and violence?
-
On organisational awareness of what can be done within the premises to reduce the risk of alcohol-related awareness?
-
Q18. Is there anything else you or other authorities could do to help you reduce the risk of ARV in your organisational premises?
Appendix 7 Focus group schedule for second focus group with senior environmental health practitioners
Interview schedule: senior EHPs (involved in development).
In each box the major question is in the top row. The following row contains prompts to ensure that pertinent data is collected.
Q1. Before the project what did you feel about the role of EHPs in licensed premises?
-
Did you feel they had a role?
-
What was the extent of that role?
-
What were the main issues that brought EHP involvement?
-
To what extent were events related to RIDDOR a part of this?
-
Do you feel poor RIDDOR reporting prevented more EHP involvement?
Q2. What were your feelings about alcohol before this project?
-
Prompts:
-
Did you think alcohol use caused problems?
-
Did you think there was a relationship between alcohol and violence?
-
Did you think ARV was a problem?
-
What kind of problem?
-
In society (national legislation, policy, economics, culture)?
-
In communities (local policy, economics, culture)?
-
In your local area (local policy, economics, culture, work type and patterns, leisure)?
-
In the NTE (all above)?
-
-
Any specific times, locations, groups of people?
-
Have you noticed any changes over time?
-
Any additional problem in the NTE?
-
Did you think licensed premises (policy, practice) had a role in ARV?
-
Can you describe this?
-
Q3. To your knowledge, who should be responsible for regulating ARV in the licensed trade?
-
Prompts:
-
police
-
fire and rescue
-
Trading Standards
-
licensing officers
-
local councils
-
(health and safety – don’t prompt if they don’t volunteer this)
-
licensed premises staff/managers
-
individuals?
-
-
Does that reflect the national picture or do you think it varies locally?
Q4. To your knowledge did health and safety play a role in combating alcohol-induced violence and injury in licensed premises before this project began?
-
If yes to above:
-
Can you describe it?
-
Did it involve interagency work with any other responsible bodies (authorities and licensed premises)?
-
Can you describe that?
-
Did you feel it was adequate?
-
How did it impact on your organisation’s workload?
-
Was that a national policy or did it very locally?
-
Q5. Can you describe the usual work of environmental health officers before the project?
-
Prompts:
-
in general
-
in the retail sector
-
in licensed premises.
-
Q6. Can you describe how you became involved in the project (AWLPI)?
-
Prompts:
-
What was your first contact with anyone about the project?
-
Did you know anything about this type of work before?
-
How was the project described to you?
-
Why did you become involved?
-
Were any colleagues involved?
-
Could you envisage any barriers to implementing the project?
-
Q7. Can you describe what you did and who you worked with during development of the project interventions (audit, website, films)?
-
Prompts:
-
Initial development – can you tell me about your work in relation to the intervention development with Cardiff University?
-
Were you involved enough?
-
Can you describe any problems that arose during your involvement?
-
Did you have sufficient impact on the development process?
-
Would you make any changes to the developmental process?
-
Q8. After the audit had been completed can you tell me about its finalisation and production?
-
Prompts:
-
Were you consulted before the final go-ahead?
-
If so, what happened during consultation?
-
If any further changes were made were you informed?
-
Q9. Can you describe your reaction to the completed Audit and Guidance document?
-
What did you think about the audit?
-
What did you think about the form of the document?
-
The timing of receipt?
-
What was the document like to read?
-
Would you make any changes to it?
-
Did you feel it promised to have a use in preventing violence in licensed premises?
-
What did you think was the EHPs’ reaction to the audit?
-
Did you feel it was the role of EHPs to undertake such an audit?
-
What do you feel were the most important part(s) of the audit in addressing factors associated with violence in licensed premises?
Q10. Can you describe EHPs’ reaction to the concept of the project?
-
What did they think about it?
-
Did responses vary?
-
How did it meet perceptions of their roles?
Q11. Can you describe what you thought about the running of the training days?
-
Was it easy to disseminate knowledge about it?
-
How was the process of getting EHPs to attend?
-
What did you think of the:
-
organisation
-
content
-
timing?
-
-
Have you received any feedback from EHPs who attended?
-
How did you feel about your role in it? Enough? Too limited?
Q12. Can you describe general EHP reaction to the Audit and Guidance document?
-
What did they think about the audit?
-
What did they think about the form of the document?
-
The timing of receipt?
-
How did they find the document to read?
-
Do you think they felt it was their role to undertake such an audit?
-
Did responses vary?
Q13. Can you describe EHPs’ reaction to the website and films?
-
What did they think about the website form and content?
-
What did they think about the film content?
-
What was is it like to use?
-
Did they feel it was the role of EHPs to promote the website and films?
-
What did you think was the EHPs’ reaction to the website and films?
-
Did responses vary?
Q14. Looking back would you make any changes to the way the audit and/or website was developed or implemented?
Q15. How would you describe your organisation’s response to the project?
-
Overall.
-
LAs.
-
Managers.
-
EHPs.
Q16. What are your current thoughts about regulating alcohol and violence in licensed premises? Have there been any changes during your involvement in the project?
Q17. Is there anything else you think EHPs/health and safety could do to address factors in licensed premises affecting ARV?
Appendix 8 Descriptive statistics: audit
| Q6. Records | Visible evidence | No evidence | N/A | Missing |
|---|---|---|---|---|
| R1A. Safety policy | 119 | 71 | 88 | 3 |
| R2A. Written risk assessment | 128 | 73 | 75 | 5 |
| Per cent | ||||
| R2C. Includes violence and aggression | 40.65 | |||
| R2D. Includes lone working | 24.10 | |||
| R3A. Opening checks and walkabouts | 145 | 116 | 17 | 3 |
| Q7. Visibility and lighting | Yes | No | N/A | Missing |
| V1. Entrances/exits clearly visible? | 276 | 5 | ||
| V2. Entrances/exits well lit? | 276 | 5 | ||
| V3. Suitable lighting in indoor areas? | 274 | 7 | ||
| V4. Suitable lighting in outdoor area? | 259 | 7 | 9 | 6 |
| Q8. Health and safety, observation and checks | Yes | No | N/A | Missing |
| HS1. Are electricity safety records available and up to date? | 176 | 101 | 4 | |
| HS2. Are gas safety records available and up to date? | 154 | 84 | 39 | 4 |
| HS3. Are fire checks evident? | 241 | 40 | ||
| HS4. Are fire extinguishers maintained and serviced? | 254 | 26 | 1 | |
| HS5. Do the fire exit external routes have any hazards or risks preventing their safe use? | 45 | 236 | ||
| HS6. Are there any visible risks? | 29 | 249 | 1 | 2 |
| Risk | No risk | N/A | Missing | |
| HS7. Condition of floors | 33 | 248 | ||
| HS8. Housekeeping | 19 | 261 | ||
| HS9. Ventilation | 7 | 273 | 1 | |
| HS10. Heating | 13 | 267 | 1 | |
| HS11. Public WC condition | 18 | 261 | 2 | |
| HS12. First aid | 16 | 261 | 4 | |
| Q9. Surveillance | Yes | No | N/A | Missing |
| SR1. CCTV at premises? | 224 | 39 | 18 | |
| SR2. Signage displayed? | 162 | 68 | 47 | 4 |
| SR3. Position of cameras suitable? | 218 | 10 | 50 | 3 |
| SR4. Blind areas from the bar? | 110 | 134 | 33 | 4 |
| SR5. Blind areas from door staff? | 44 | 110 | 121 | 6 |
| SR8. Is CCTV storage adequate? | 212 | 10 | 52 | 7 |
| Q10. Noise and communication | Music | Customers | Other | Missing |
| What sources of noise might affect communication between staff (tick all that apply)? | 208 | 177 | 19 | 28 |
| Verbally | Radio | Other | Missing | |
| How do staff communicate during busy periods? | 266 | 70 | 23 | 5 |
| Q11. Risk planning | Yes | No | N/A | Missing |
| RP1. Is there regular engagement with PubWatch or similar? | 173 | 92 | 16 | |
| RP2. Is there visible evidence of alcohol promotions? | 103 | 176 | 2 | |
| Mean | SD | |||
| RP4. Number of front-of-house staff at busy times? | 5.78 | 6.12 | 3 | |
| Q12. Door management | Yes | No | N/A | Missing |
| DS1. Are all security staff SIA licensed? | 140 | 7 | 132 | 2 |
| DS2. Is there a door staff register? | 117 | 27 | 135 | 2 |
| DS3. Are SIA registration numbers present on the door staff register? | 119 | 15 | 144 | 3 |
| DS4. Do security staff monitor the internal environment as well as the door? | 140 | 5 | 133 | 3 |
| DS6. Is there a policy for ID checks? | 236 | 4 | 39 | 2 |
| DS7. Is there a policy for refusal of entry to intoxicated/disorderly customers? | 234 | 5 | 41 | 1 |
| DS8. Queuing system in place? | 77 | 68 | 132 | 4 |
| Q13. Managing people | Yes | No | N/A | Missing |
| MP1. Are staff trained to manage intoxicated/disorderly customers? | 243 | 31 | 6 | 1 |
| Staggering gait | Slurred speech | Othera | Missing | |
| MP3. What characteristics are used to decide whether or not someone is too drunk by staff? | 263 | 257 | 62 | 2 |
| Refuse service | Asked to leave | Otherb | Missing | |
| MP5. What action is taken in respect of severely intoxicated customers? | 238 | 260 | 46 | 3 |
| MP7. What action is taken in respect of disorderly customers? | 263 | 232 | 38 | 4 |
| Yes | No | N/A | Missing | |
| MP9. Are there barriers that prevent staff/management from following the correct procedures | 12 | 259 | 8 | 2 |
| Q14. Staff training | Yes | No | N/A | Missing |
| ST1. Is there an induction programme for both PT and FT staff that includes information on disorderly and/or intoxicated customers? | 222 | 41 | 17 | 1 |
| ST2. Is there ongoing training and refreshers for both PT and FT staff that includes information on disorderly and/or intoxicated customers? | 195 | 64 | 20 | 2 |
| ST3. Is there health and safety training, including fire training? | 211 | 53 | 14 | 3 |
| Q15. Incident reporting | Yes | No | N/A | Missing |
| IR1. Is there an accident book/accident log sheets? | 232 | 48 | 1 | |
| IR2. Is a written record of reportable incidents kept? | 196 | 67 | 16 | 2 |
| IR3. Evidence of RIDDOR reportable incidents? | 56 | 204 | 20 | 1 |
| IR4. Were these reported to RIDDOR? | 43 | 41 | 194 | 3 |
| IR5. Evidence of any ‘near misses’ (i.e. serious but not reportable)? | 53 | 152 | 74 | 2 |
| IR6. Are incidents used in future planning, risk assessment? | 134 | 62 | 83 | 2 |
| Q16. Glassware policy | Yes | No | N/A | Missing |
| GP1. Glass only | 177 | 97 | 6 | 1 |
| GP2. Some polycarbonate (or similar) | 143 | 98 | 32 | 8 |
| GP3. All polycarbonate (or similar) | 31 | 181 | 60 | 9 |
| GP4. No glass after midnight | 22 | 166 | 87 | 6 |
| GP5. Are customers allowed to take glass outside (e.g. smokers)? | 152 | 112 | 16 | 1 |
| GP6. If yes, are staff assigned the role of collecting empties from outside? | 187 | 6 | 86 | 2 |
Glossary
- Designated premises supervisor
- The designated premises supervisor is a named person whose role is identified in the UK Licensing Act 2003 (Great Britain. Licensing Act 2003. London: The Stationery Office; 2003) as one who is accountable for the day-to-day running of the licensed premises and acts as the primary contact for local government and the police.
- Environmental health practitioner
- Environmental health practitioners are primarily responsible for enforcing the 1974 Health and Safety at Work etc Act (Great Britain. Health and Safety at Work etc Act 1974. London: The Stationery Office; 1974) and related legislation. The Health and Safety at Work etc Act requires businesses, including licensed premises, to work towards high standards of health and safety in the workplace and to protect employees and the public from harm. Such responsibilities include the provision of information and training to staff to ensure a safe working environment, the provision of written safety policies and risk assessments, and looking after the health and safety of others. In upholding the Health and Safety at Work etc Act, environmental health practitioners have a right of entry at reasonable times to investigate and examine a premises, the right to view and copy documents, and the right to ask questions under caution. Where enforcement is necessary, environmental health practitioners can also give written legal notices. If an environmental health practitioner is of the opinion that a premises is contravening the Health and Safety at Work etc Act, that premises can be served with an improvement notice, which details what needs to be addressed within a set period of time. However, if an environmental health practitioner believes that activities are occurring that put employees and the public at immediate risk of harm then they may serve a prohibition notice, which prohibits unsafe practices immediately. In very extreme circumstances environmental health practitioners can also bring about criminal prosecutions of both employers and employees.
- RE-AIM
- The RE-AIM framework is used to explore the implementation of health promotion interventions in community settings. The acronym represents five key evaluative components (‘reach’, ‘efficacy’, ‘adoption’, ‘implementation’ and ‘maintenance’), which are used to structure exploration of the data.
- Safety Management in Licensed Environments
- This intervention, known as SMILE, encompassed several elements: the risk audit adapted for the All-Wales Licensed Premises Intervention trial and used by the environmental health practitioners; the bespoke action plan provided to the designated premises supervisor in response to the risks identified by the All-Wales Licensed Premises Intervention risk audit; and the intervention’s website for premises staff (including educational films).
List of abbreviations
- A&E
- accident and emergency
- ARV
- alcohol-related violence
- AWLPI
- All-Wales Licensed Premises Intervention
- BCa
- bias-corrected accelerated
- BWT
- ‘broken windows’ theory
- CCTV
- closed-circuit television
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- DPS
- designated premises supervisor
- EHP
- environmental health practitioner
- GPS
- Global Positioning System
- HR
- hazard ratio
- HSE
- Health and Safety Executive
- HSWA
- Health and Safety at Work etc Act 1974
- ID
- identification
- ITT
- intention to treat
- LA
- local authority
- NPT
- normalisation process theory
- NTE
- night-time economy
- NWP
- North Wales Police
- RAT
- routine activity theory
- RBS
- responsible beverage service
- RCI
- risk control indicator
- RCT
- randomised controlled trial
- RE-AIM
- reach, efficacy, adoption, implementation and maintenance
- RIDDOR
- Reporting of Injuries, Diseases and Dangerous Occurrences Regulations
- SD
- standard deviation
- SMILE
- Safety Management in Licensed Environments
- SWP
- South Wales Police
- TDAR
- trans-disciplinary action research