Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3000/03. The contractual start date was in January 2011. The final report began editorial review in January 2015 and was accepted for publication in August 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dr Stallard reports support from Pathways, the organisation that markets the FRIENDS programme, during project dissemination. Accommodation was paid for by Pathways whilst presenting the results of this study at the ‘train the trainer’ conference in Brisbane in August 2014.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Stallard et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Nature, extent and course of emotional problems in children
Anxiety and depressive disorders in children are common. The American Great Smoky Mountain Study found that 2.4% of children aged 9–16 years fulfilled diagnostic criteria for an anxiety disorder and 2.2% for a depressive disorder over a 3-month period. 1 Similar rates were found in the British Mental Health Survey, where 3.7% of 5- to 15-year-olds had a current anxiety disorder and 1% had a depressive disorder. 2 Comorbidity between anxiety and depression is common,3,4 with cumulative rates suggesting that by age 16–17 years 15–18% of children will have experienced an impairing emotional disorder of anxiety or depression. 1,4
Emotional problems have a persistent and unremitting course, with longitudinal studies highlighting that child mental health disorders persist into adulthood. In the Dunedin birth cohort study approximately 52–55% of young adults with depression or anxiety met diagnostic criteria for a mental health disorder before the age of 15 years, with 75% having a first diagnosis before the age of 18 years. 5 Childhood anxiety increases the risk of anxiety, depression, substance misuse and educational underachievement in early adulthood. 6,7 Similarly, childhood depression increases the risk of suicide, subsequent depression and substance misuse. The associated health-related burden and economic and societal costs are considerable and the need to improve the mental health of children is being increasingly recognised as a national and global priority. 8–10
Limited reach of treatment services
Improving the emotional health of children is an important public health issue that has become a major tenet of UK governmental policy. 11–13 Effective psychological treatments are available for children with mental health disorders, although few children actually receive them. 14,15 Surveys in the UK and USA found that approximately one-third of children with anxiety disorders and under half with depressive disorders had sought or received specialist help over a 1- to 3-year period. 16,17 Those with emotional disorders were less likely than those with other mental health disorders to have contact with specialist services. The limited reach and availability of specialist treatment services alongside a policy shift towards early intervention has led to a growing interest in preventative approaches and a move from clinical to community settings.
School-based preventative approaches
In the UK, almost eight million children and young people attend primary and secondary schools. 18 As such, schools provide an important environment for public health initiatives, offering the potential for delivering both primary prevention (i.e. promoting well-being and reducing the occurrence of new problems) and secondary prevention (i.e. stopping mild or moderate problems from worsening). Schools provide a familiar and natural environment, reaching a high percentage of children. Their central role in promoting emotional well-being has been emphasised in the national Social and Emotional Aspects of Learning (SEAL) initiative. 13
The effectiveness of school-based emotional health prevention programmes for primary school children has been the subject of two National Institute for Health and Care Excellence (NICE) reviews. 18,19 In the first, 31 studies were identified that adopted a universal approach (i.e. interventions were provided to all children regardless of need), with only one having been undertaken in the UK. 18 The second focused on targeted/indicated approaches in which interventions were provided to children at high risk or already displaying mild or moderate problems. 19 Ten studies that focused on internalising problems (anxiety and mood) were identified, but none was undertaken in the UK.
Both reviews found evidence that universal and targeted/indicated mental health programmes could have an effect on mental health. In terms of content, multicomponent programmes (i.e. teaching different skills such as relaxation, problem-solving and cognitive awareness) based on a clear theoretical framework, particularly cognitive–behavioural therapy (CBT), and which included some parental input (e.g. training/information) had the strongest evidence. This conclusion was also endorsed in a review of 27 randomised controlled anxiety prevention trials. 20 The results indicate that most universal, selective and indicated prevention programmes were effective in reducing anxiety symptoms. Although not formally tested, the authors note that the effects of CBT programmes were marginally larger than those of non-CBT interventions, with the median effect size for CBT programmes of 0.57 indicating a moderate effect. However, there was considerable variation in effect size between studies, suggesting that, although the content is important, mediating variables such as adherence to programme fidelity, leader rapport, levels of participation and audience appeal are also important factors that will influence effectiveness.
The reviews also identified a number of important methodological limitations, including small sample sizes, use of non-standardised mental health outcome measures and an absence of follow-up assessments. In addition, the comparative effectiveness of teacher-delivered and mental health-delivered interventions is unclear and has been directly investigated in only one study. 21 Before school-based emotional health programmes can be endorsed, implementation trials in which efficacious interventions are provided under diverse everyday conditions are required. The replication of treatment effects under everyday conditions cannot be assumed, with a number of recent school-based prevention studies failing to find positive effects on depression,22–25 anxiety26,27 and general emotional well-being. 28
The FRIENDS cognitive–behavioural therapy prevention programme
Cognitive–behavioural therapy is concerned with the way that children think about their world and the meanings and interpretations they make about the events that occur. It provides a framework for helping children to understand the link between what they think, how they feel and what they do. During CBT they are helped to explore and become aware of their cognitions and how these are associated with their feelings and affect their behaviour. This process allows unhelpful cognitions to be identified, tested and re-evaluated in more helpful ways that allow the child to experience more pleasant feelings and to become more motivated and able to face challenges and problems. In addition to understanding and challenging cognitions, CBT helps children to develop better emotional awareness, so that they can become better at identifying their different emotions, and a range of emotional management skills. Finally, CBT includes many behaviour techniques to facilitate behaviour change such as positive reinforcement, contingency management, monitoring and graded exposure.
Expected outcomes of CBT relate to each of the three core domains of the model: first, cognitive changes such as reductions in worries or negative thoughts; second, improved emotional management resulting in reduced symptoms of anxiety and depression; and, third, changes in behaviour resulting in improvements in self-esteem as the child learns to successfully overcome and cope with challenges. Another outcome that has been observed from the small group process that is an integral part of child CBT programmes such as FRIENDS is improvements in relationships and reductions in bullying.
Of the school-based CBT preventative programmes that have been developed, the FRIENDS programme is one of the better evaluated and has more consistent evidence of effectiveness. 20,29 This was noted by the World Health Organization,30 who identified the FRIENDS programme as having strong evidence of being effective as a school-based intervention for anxiety. The programme addresses a number of the issues identified in the previous reviews. It has a clear theoretical model, sufficient sessions, age-appropriate materials, enjoyable and fun activities, a structured leader manual with detailed session plans, standardised leader training, ongoing supervision to ensure fidelity, a parent session and weekly parent contact sheets.
In an initial randomised controlled trial (RCT) involving 489 children aged 10–12 years, significant post-intervention reductions in anxiety were reported following the FRIENDS programme. 21 These results were replicated in a subsequent study involving 594 children aged 10–13 years and were found to be maintained at 12 months. 31,32 The FRIENDS programme also had a positive effect on mood in the high-anxiety group. In terms of those with more significant problems, 85% of those in the FRIENDS group who initially scored above the clinical cut-off for anxiety and low mood were diagnosis free at 12 months compared with 31% in the comparison group. In the most recent study involving 692 children, the FRIENDS group demonstrated significant reductions in anxiety 3 years after the FRIENDS programme. 33 In addition, comparison between children aged 9/10 years and those aged 14/16 years showed that, although both age groups benefited from the FRIENDS programme, the younger group demonstrated the greatest changes in anxiety symptoms. 34 Although these results are promising, recent trials in Canada failed to find additional benefits for the FRIENDS programme, as either a universal or a targeted intervention. 26,27 Finally, no RCTs of the FRIENDS programme have been undertaken in the UK and so it is unclear whether the programme is effective when delivered in UK educational settings.
The current study
The systematic reviews summarised above indicate that school-based programmes can have benefits in terms of both secondary (post-intervention reductions in symptoms) and primary (preventing the development of significant symptoms) prevention. Programmes with a clear theoretical model based on CBT appear the most effective for anxiety and mood disorders. In addition, multicomponent programmes that teach children skills in different areas and which involve parents (e.g. relationship building/skill enhancing) appear particularly promising.
Of the available programmes fulfilling these criteria, the FRIENDS programme has a strong evidence base. Small-scale cohort studies of the FRIENDS programme have been undertaken in the UK and demonstrate the feasibility of delivering the programme within the UK educational system. These studies have found encouraging post-intervention results, with gains being maintained 1 year after the programme. 35,36 Similarly, a recent small-scale evaluation has found preliminary evidence to suggest that the FRIENDS programme may also have a primary preventative effect. 37
In the UK studies, the FRIENDS programme was delivered by trained school nurses from outside the school. This method of delivery is consistent with findings from a systematic review of school-based anxiety prevention programmes which noted that programme leaders were more likely to be mental health professionals. 20 However, the review also noted that, in one-quarter of studies, programmes were led by trained teachers and delivery by school staff also resulted in significant reductions in anxiety. 20 In terms of the FRIENDS programme, only one study has directly compared leader effects and found school leaders to be as effective as health leaders. 21 However, this study was underpowered and recent implementation trials of the FRIENDS programme delivered by trained school staff failed to find a positive effect. 26,27 It is therefore unclear whether school leaders are as effective as health staff in delivering the FRIENDS programme.
This trial compared the relative effectiveness of the FRIENDS programme delivered by trained school and health staff compared with usual school lessons (personal, social and health education, PSHE). The study addressed the methodological concerns identified above, had adequate power to detect predicted differences between groups and included an assessment of treatment fidelity; included follow-up at 12 and 24 months; and included an analysis of primary and secondary preventative effects and an evaluation of cost-effectiveness and acceptability. If found to be effective, the FRIENDS programme could be made widely available in the UK; it could be integrated within the school PSHE curriculum and would complement and build on other school initiatives.
Objectives
-
Primary outcome: to evaluate the effectiveness of the FRIENDS programme in reducing symptoms of anxiety and low mood at 12 months.
-
Primary outcome: to evaluate the effectiveness of the FRIENDS programme for children with low and high anxiety at baseline in terms of symptoms of anxiety and low mood at 12 months.
-
Secondary outcomes: to examine the effectiveness of the FRIENDS programme in terms of self-esteem, worry, bullying and overall well-being at 12 months.
-
Medium term: to examine the medium-term effects of the FRIENDS programme on symptoms of anxiety and low mood at 24 months.
-
Medium term: to evaluate the effects of the FRIENDS programme for children with low and high anxiety at baseline in terms of symptoms of anxiety and low mood at 24 months.
-
Medium term: to examine the effects of the FRIENDS programme on secondary outcomes of self-esteem, worry, bullying and overall well-being at 24 months.
-
Cost-effectiveness: to assess the cost-effectiveness of the FRIENDS programme in terms of health-related quality of life (and cost–utility) at 6 months.
-
Acceptability: to assess the acceptability of the FRIENDS programme including participant perceptions of usefulness, examples of ongoing skill usage and satisfaction (6 months).
Chapter 2 Methods
The study protocols for the 12- and 24-month assessments have been published. 38,39
Design
Preventing Anxiety in Children through Education in Schools (PACES) was a pragmatic, cluster, three-arm RCT; the three arms consisted of the FRIENDS programme delivered by health staff or school staff and the usual school curriculum (Table 1). The key difference in the two FRIENDS conditions was the person leading the sessions. In the health-led FRIENDS programme the leaders were health professionals from outside the school whereas in the school-led FRIENDS programme the leader was the teacher or a member of the school staff with responsibility for delivering PSHE.
| Trial arm | Content | Delivery |
|---|---|---|
| Treatment as usual | Normal school curriculum | One member of the school staff (one person per class) |
| School-led FRIENDS | Structured CBT programme | School staff leader with two facilitators (three people per class) |
| Health-led FRIENDS | Structured CBT programme | Two health staff leaders with teacher (three people per class) |
Ethical approval, consent and trial monitoring
The study was approved by the Department for Health Research Ethics Committee at the University of Bath.
Six- and 12-month follow-ups
Consent/assent involved three stages. First, eligible schools were provided with information about the study and interested head teachers were required to provide written confirmation that their school wished to participate. Second, information was sent to the home address of the parents of all eligible children. Parents were invited to return a form opting out of the study if they did not wish their child to complete the study assessments. Finally, children were provided with information about the study and were required to provide signed assent before completing the baseline assessment. Dual carer/child consent/assent was therefore required for assessment completion.
Twenty-four-month follow-up
The PACES cohort transitioned to secondary school in September 2013. A new opt-in recruitment process was approved for the 24-month assessment, which required signed parent and child consent. Participants received a £30 financial incentive to compensate parents and children for their time in completing the assessments.
Trial monitoring
The ongoing conduct and progress of the trial was monitored by an independently chaired Data Monitoring and Ethics Committee and a Trial Steering Committee. The trial steering committee included a teacher and a parent representative.
Participants, recruitment and randomisation
Sample size
The study was powered to detect a difference between the FRIENDS programme (health and school led) and usual PSHE. Based on an intracluster correlation coefficient of 0.02, 28 pupils per class, 90% consent and 80% retention, effect sizes in the range of 0.28–0.30 standard deviations (SDs) are detectable with 80% power and 2.7% Dunnett-corrected two-sided alpha with 45–54 schools (i.e. 1134–1360 consenting pupils). A standardised treatment effect size of 0.3 is equivalent to an estimated difference on the Revised Child Anxiety and Depression Scale (RCADS) of 3.6 points based on a SD of 12.
Recruitment of schools
A list of primary schools in Bath and North East Somerset and Swindon and Wiltshire within a 50-mile radius of the University of Bath was compiled from local authority information (n = 268). Project information sheets were sent to the head teachers and meetings arranged with the 45 schools who expressed an interest. Four schools did not return signed letters confirming participation before randomisation and were therefore excluded. In total, 41 schools were randomised with one school subsequently withdrawing (usual school provision arm) before baseline assessments were completed. The cohort therefore consisted of 40 schools (1448 eligible children).
Inclusion/exclusion criteria
Interventions were provided during the school day as part of the school PSHE curriculum. All children aged 9–10 years (Years 5 and 6) were eligible unless they were not attending school (e.g. because of long-term sickness or because they were excluded from school) or did not participate in PSHE lessons for religious or other reasons.
Randomisation
Allocation of schools on a 1 : 1 : 1 ratio took place once all schools had been recruited. Balance between trial arms with respect to key characteristics [school size, number of classes, number of children in Year 5 classes, preferred term of delivery, preferred day of delivery, numbers of mixed Year 5 classes (i.e. classes that were Years 4/5 combined and classes that were Years 5/6 combined) and single Year 5 classes and level of educational attainment] was achieved by calculating an imbalance statistic for a large random sample of possible allocation sequences. 40 A statistician with no other involvement in the study randomly selected one sequence from a subset with the most desirable balance properties.
Interventions
FRIENDS: a universal cognitive–behavioural therapy programme
The FRIENDS programme is a manualised CBT programme designed to improve children’s emotional health. 41 Each child has his or her own workbook and group leaders have a comprehensive manual specifying key learning points, objectives and activities for each session. The intervention trialled in this study involved nine 60-minute weekly sessions delivered to whole classes of children (i.e. universal delivery). Written work is kept to a minimum and each session uses a variety of different materials and activities to engage and maintain interest. The feasibility and viability of delivering the FRIENDS programme in UK schools has previously been established. 35–37
The FRIENDS programme is based on the principles of CBT and develops skills to counter the cognitive, emotional and behavioural aspects of anxiety. Children develop emotional awareness and regulation skills to enable them to identify and replace anxiety-increasing cognitions with more balanced and functional ways of thinking and to develop problem-solving skills to confront and cope with anxiety-provoking situations and events. The programme therefore teaches children skills to identify and manage their anxious feelings, develop more helpful (anxiety-reducing) ways of thinking and face and overcome fears and challenges rather than avoid them. A detailed summary of each session is provided in Table 2.
| Session | Primary focus | Core tasks |
|---|---|---|
| 1 | Introduction to FRIENDS |
|
| 2 | Introduction to feelings |
|
| 3 | Identify feelings and learn to relax |
|
| 4 | Helpful and unhelpful thoughts |
|
| 5 | Changing thoughts and facing challenges |
|
| 6 | People who can help and problem-solving |
|
| 7 | Reward yourself for being brave |
|
| 8 | Practise the FRIENDS plan |
|
| 9 | Review and celebrate |
|
An additional session for parents/carers was conducted to provide parents with an overview of the programme, the CBT rationale and the skills that the children learned. In addition, parents received a summary sheet detailing the key learning points of each session and the skills that their child would be practising so that they were able to reinforce and encourage their use at home.
Health-led FRIENDS programme
The FRIENDS programme was delivered by two health facilitators (e.g. school nurses, psychology assistants) external to the school with the class teacher providing support. These were not mental health specialists but health professionals with a lower level of training and/or expertise. All 11 facilitators had at least an undergraduate university degree in a relevant discipline (psychology n = 3; art therapy n = 1) or an appropriate professional background (school nurses n = 6; teaching n = 1) and experience of working with children or young people.
School-led FRIENDS programme
Each participating school identified school staff members (e.g. class teachers, special educational needs co-ordinators, teaching assistants) to deliver the FRIENDS programme. In total, there were 14 school-led leaders (five class teachers; four PSHE co-ordinators; three learning support assistants and two head teachers).
School staff were assisted in delivering the programme by two health facilitators external to the school. This ensured that there were at least three adults present during session delivery. The health facilitators were not responsible for leading the session but for supporting the school leader. The school leader therefore led the session, introduced the session topic, planned the content and led the delivery of the exercises. The facilitators worked as class helpers, being organised and directed by the teacher to work with small groups or individual children to help them engage in the exercises and express their ideas.
FRIENDS programme training and supervision
The FRIENDS leaders from the health- and school-led arms attended a 2-day training event to familiarise them with the nature, extent and presentation of anxiety and depression in children and the CBT model. Participants worked through each of the FRIENDS sessions and practised the exercises to familiarise themselves with the materials and key learning points.
During delivery of the programme, fortnightly group supervision was provided by an accredited FRIENDS trainer. Health and school leaders attended together. During these sessions the aims and content of the FRIENDS sessions were reviewed and any problems with implementation were addressed.
Usual school provision
Children participated in their usual PSHE sessions provided by the school. All schools were following a UK national curriculum programme designed to develop self-awareness, management of feelings, motivation, empathy and social skills. 13 The sessions were planned and provided solely by the teacher and did not involve any external input from the research team.
To more specifically define PSHE within each school the head teacher and the school PSHE co-ordinator and/or the Year 5 class teacher participated in a semistructured interview. The interview was undertaken at the end of the school term and assessed whether the school was following the national curriculum and what additional interventions might be running in the school and their content. The interview clarified the PSHE topics covered by the 9- and 10-year-old children during the study period, the way that they were addressed (dedicated sessions, integration, circle time, etc.), the length of time devoted to the PSHE curriculum and the number of adults (e.g. teachers, assistants, volunteers, trainees) in the classroom.
Treatment fidelity
Treatment fidelity was assessed by randomly assessing audiotape recordings of 10% of the FRIENDS sessions. Sessions were rated by an independent assessor to determine whether core tasks (detailed in Table 2) were delivered.
Delivery of the FRIENDS programme
At the end of each FRIENDS session leaders rated a range of possible mediating variables including child engagement, participation and contributions, school support, personal confidence in delivering the FRIENDS programme, personal enjoyment of the group and their perception of group benefit.
Acceptability of the FRIENDS programme
All children who received the FRIENDS programme were asked at the end to assess the programme on 10 dimensions including enjoyment, acquisition and use of new skills and whether they would recommend the programme to another child.
Demographics and context
Family, demographic and socioeconomic status
At baseline children completed a questionnaire assessing age, sex, who they lived with, number of siblings and ethnicity. In addition, they completed the Family Affluence Scale (FAS), which provides an indicator of socioeconomic status. 42,43 This short questionnaire asks children to rate the following four items relating to family affluence: family ownership of a car, child has own bedroom, number of family holidays in the past year and how many computers the family own.
School context
Data on a number of socioeconomic indices that might be related to outcome were collected for each participating school. These included the number of children receiving free school meals, the number of children in care, the number of children with educational statements, the level of educational attainment on standardised assessment tests, class size and the number of teaching assistants in study classes. In addition, the dominant pedagogical orientation of each school was profiled.
Outcome measures
Assessments were completed at baseline and 6, 12 and 24 months and involved a combination of child-, parent- and teacher-completed questionnaires and semistructured interviews.
Child report questionnaires: psychological functioning
All child outcome data were collected by self-completed questionnaires administered by researchers blind to children’s trial allocation. Questionnaires were completed at school, in groups in classes, at baseline and 6 and 12 months. The researchers and any teaching assistants working in the class helped individual children with literacy problems. At 24 months they were completed individually by each child in the home.
Revised Child Anxiety and Depression Scale
This was the primary outcome measure. The RCADS44 is a recent modification of the Spence Children’s Anxiety Scale,45 which was revised to correspond more closely to Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition criteria for anxiety and depression. 46 The 30-item scale was used (RCADS-30), which assesses anxiety in the areas of social phobia, separation anxiety, obsessive–compulsive disorder, panic disorder and generalised anxiety disorder and also assesses major depressive disorder. The RCADS-30 has good internal consistency, test–retest stability and convergent and divergent validity. 47,48
Rosenberg Self-Esteem Scale
The Rosenberg Self-Esteem Scale49 is a self-completed questionnaire that assesses self-worth and acceptance and requires the child to rate each of 10 questions on a four-point scale, ranging from ‘strongly agree’ to ‘strongly disagree’. The Rosenberg Self-Esteem Scale has demonstrated good reliability and validity across a large number of different sample groups, including young children aged 7–12 years, and is one of the most commonly used and best-known measuring tools for self-esteem.
The Penn State Worry Questionnaire for Children
The tendency for children to engage in excessive, generalised and uncontrolled worry was assessed by the Penn State Worry Questionnaire. 50 Each item is rated on a 4-point Likert scale assessing how strongly it applies to the child (0 = ‘not at all’ through to 3 = ‘always true’). The original scale consists of 14 items although a subsequent evaluation found that with children aged 8–12 years it was preferable to remove the three reverse-scored items. 51 The 11-item version was used here, which has good psychometric properties with this age group.
The Olweus Bully/Victim Questionnaire
The degree to which children have bullied others or have been the victim of bullying was assessed with the two global items from the Olweus Bully/Victim Questionnaire. 52
Well-being
Overall life satisfaction and happiness with six aspects of everyday life were assessed on a 7-point scale. 53 These items were selected from the 12 domains identified within The Good Childhood Report54 and pragmatically seemed more relevant for our (younger) cohort. The items selected assessed satisfaction with school, appearance, family, home, friendships and health and overall life satisfaction.
The School Concerns Questionnaire
The School Concerns Questionnaire (SCQ)55 was completed by children at the 24-month assessment only. The SCQ is a 20-item scale assessing worries about starting secondary school. Items cover organisational (e.g. changing classes, remembering equipment), social (e.g. making new friends, being bullied) and academic (e.g. homework, being able to do the work) concerns. Each item is rated on a 10-point scale assessing the extent of worry.
Health-related quality of life: child health utility
Children completed the Child Health Utility 9 Dimensions (CHU-9D) (licensed by the University of Sheffield)56 at baseline and 6, 12 and 24 months. The CHU-9D, a validated measure of health-related quality of life, is short (nine items) and has been specifically developed for use with children aged 7–11 years. 57 The use of the CHU-9D allowed us to assess how improvements in mental health (anxiety and depression) might translate into changes in overall health-related quality of life.
Parent report questionnaires: child psychological functioning
Questionnaires for parents at baseline and 6 and 12 months were sent home and returned in a prepaid stamped addressed envelope. At 24 months, parents completed the questionnaires either over the telephone or during an interview with a researcher.
Strengths and Difficulties Questionnaire
The Strengths and Difficulties Questionnaire (SDQ)58 is a brief, widely used behavioural screening questionnaire. The SDQ consists of 25 items that assess emotional symptoms, conduct problems, hyperactivity and/or inattention, peer relationship problems and pro-social behaviour. 58,59 Parents also rate overall distress and the social impact of their child’s behaviour on home life, friendships, classroom learning and leisure activities.
Revised Child Anxiety and Depression Scale – Parent Version
The parent-completed Revised Child Anxiety and Depression Scale (RCADS-30-P)60 is a 30-item parent version of the primary outcome measure completed by children. The RCADS-30-P has high internal consistency and test–retest reliability and good convergent and divergent validity.
School Concerns Questionnaire
The SCQ55 is the parent version of the questionnaire completed by children. It was completed at the 24-month assessment only, after children had transitioned to secondary school.
Teacher report questionnaires: psychological functioning
Class teachers were asked to complete the overall distress and impact rating of the SDQ for all children in their class. This assesses the teacher perception of whether a child has a problem with his or her emotions, concentration or behaviour or being able to get on with other people. If so, the teacher completes questions about chronicity, distress, interference with peer relationships or classroom activities and burden.
Child interviews
Semistructured interviews were undertaken with a self-selecting group of approximately 10% of the children who received the FRIENDS programme to discuss their experience in more detail. The interview explored what they had learned, whether they had used any new skills, what aspects of the programme were most helpful and what could be improved. Areas of satisfaction and dissatisfaction were assessed and views about the materials, activities and specific sessions obtained.
Parent interviews
A letter was sent to all of the parents of participating children through their child’s school inviting them to participate in a semistructured interview. Those who agreed to be interviewed at baseline (n = 308) were invited to repeat the interview at 6 (n = 284) and 24 (n = 252) months. The interviews were thus conducted with a self-selected (non-random) subsample of all parents of trial participants. Parents were offered a cash voucher to cover the cost of their time. Interviews were conducted at the parent’s home or at a convenient location of their choice. A copy of the parent interview is provided in Appendix 1.
Client Services Receipt Inventory
The Client Services Receipt Inventory (CSRI)61 is a semistructured interview used for economic analysis that was used to assess children’s use of health, social and educational services over the past 6 months. The CSRI was adapted following experience from a previous study and further piloting, with more optional specification of the types of other professionals who may have been seen for worry, anxiety or unhappiness. There was also a revised question to capture how many days out of paid employment a parent or other adult may have taken off to look after their child and another to capture whether their child had received extra support or input at school to help with learning or because of their behaviour. Similarly structured questions elicited information about help or support from social services or help or support from voluntary organisations for their child.
Screen of parental health and mental health
Parents completed the mental health screening tools routinely used by the Improving Access to Psychological Therapies (IAPT) project. This includes a measure of anxiety (Generalised Anxiety Disorder seven-item scale, GAD-7),62 depression (Patient Health Questionnaire-9 items, PHQ-9)63 and the IAPT phobia scale. 64
Parents also completed the 8-item Short Form Health Survey (SF-8)65 and the adult version of the Penn State Worry Questionnaire. 66 The SF-8 assesses eight aspects of health including pain, energy, everyday impairment and emotional problems.
Additional areas
Finally, parents completed an inventory of recent life events and were surveyed about the recreational and leisure time pursuits of their child.
The 24-month interview covered all of the above and in addition parents were asked to complete the SCQ, which provided their perceptions of how well their child had transitioned to secondary school.
School interviews
At the end of each FRIENDS programme the class and head teachers in the intervention schools were invited to participate in a semistructured interview to obtain their views about the programme. They were asked whether they had noticed any particular benefits, whether they had identified any problems in terms of delivery, materials and integration within the school curriculum and whether they felt that the programme was sustainable.
Assessment summary
A summary of the assessments completed at each assessment point is presented in Table 3.
| Assessment | Who | Baseline | 6 months | 12 months | 24 months |
|---|---|---|---|---|---|
| Child questionnaire | All participating children |
|
|
|
|
| Parent questionnaire | Postal questionnaire responders |
|
|
|
|
| Teacher questionnaire | All participating teachers |
|
|
|
|
| Parent interviews | Parents who opt in for interview |
|
|
|
Statistical analysis
Statistical analysis was conducted using IBM Statistical Product and Service Solutions (SPSS) Statistics version 22 (IBM Corporation, Armonk, NY, USA) and was undertaken blinded to allocation. Analysis and presentation of data are in accordance with Consolidated Standards of Reporting Trials (CONSORT) guidelines and in particular the extension to cluster randomised trials. 67–69
The effects on the primary outcome (RCADS score at 12 months’ follow-up) were assessed by intention-to-treat analysis without imputation. To take account of the hierarchical nature of the data, we used multivariable mixed-effects models to compare the mean RCADS score at 12 months for health-led FRIENDS with that for school-led FRIENDS and usual school provision, with adjustment for baseline RCADS score, sex and school effects. These analyses were repeated for secondary outcomes. Group comparisons were Bonferroni corrected for multiple testing.
For RCADS score we undertook a further planned analysis. We used repeated-measures mixed-effects analysis of variance models to investigate convergence/divergence between trial arms over time. We carried out preplanned subgroup analyses using interaction terms in the regression models between randomised arm and the baseline variable [RCADS score 0–48 (low anxiety), ≥ 49 (high anxiety)].
We conducted sensitivity analyses to assess the potential effect of missing data. Completion rates for all groups at 12 months were high (91.8–92.7%) although non-completers tended to be more symptomatic on our primary outcome measure (RCADS) at baseline (data not shown). Using multiple imputation methods 20 data sets were created and showed that imputation for missing data made no material difference to the overall results (see Table 10).
Qualitative analysis
Qualitative interviews were undertaken with staff from all 28 schools who received the FRIENDS programme. Children from 19 of these schools participating in the first two terms of the programme volunteered to take part in focus groups. A total of 115 children participated, a sample that was sufficient to ensure that all themes had been identified. Interviews followed topic guides informed by previous research on the FRIENDS programme to assess programme acceptability.
Interviews and focus groups were digitally audio recorded and transcribed verbatim. The transcripts were thematically analysed following the guidelines of Braun and Clarke. 70 Recordings were transcribed using NVivo 10 software (QSR International, Warrington, UK). The data were then openly coded, that is, without trying to fit them into the pre-existing coding frame. The coding was conducted at a semantic level, that is, by explicit or surface meaning of the data, without looking beyond what a participant said, and was allowed to form as many codes as appropriate.
Coding reliability and validity were checked by two researchers independently coding three randomly selected transcripts. Inter-rater reliabilities were calculated using NVivo 10. The coding agreement was in the range of 79–100%, indicating satisfactory agreement and consistency.
Transcripts were then independently coded and analysed by four researchers. A final coding framework was generated by discussion and consensus. The final analysis identified six distinctive themes relating to programme overview, programme content and delivery, the FRIENDS workbook, positive aspects of the programme, programme benefits and continued use of skills. The themes were checked for internal consistency. Further analysis involved building detailed data maps and examining data prevalence.
Economic analysis
An analysis comparing the two versions of the FRIENDS programme and treatment as usual was undertaken. The cost-effectiveness analysis was based on the primary outcome measure (i.e. cost per extra point reduction per child on the primary outcome measure RCADS) and quality-adjusted life-years (QALYs) (i.e. cost–utility analysis). The analysis of costs and cost-effectiveness was conducted using prices from the year 2013. It was carried out according to current best practice methods for conducting economic evaluation alongside trials71,72 and alongside cluster RCTs. 73,74
Both the cost analysis and the cost-effectiveness analysis were from the joint perspective of the health sector (NHS) and the education/social services sector (e.g. capturing children’s within-trial contacts with mental health services as well as those opportunity costs incurred by schools in order to participate). They encompassed resources needed to provide the intervention (teacher and health professional time, training time and materials, recruitment of schools) and estimated resource impacts of altered outcomes (e.g. mental health service consultations and treatments). The study identified, measured and valued the resource consequences of each alternative (applying opportunity costs as the main principle for valuation), including the separate identification of those costs/resources associated with the provision and evaluation of the interventions within the context of a research trial (i.e. those costs that would probably not be incurred should the programme be more widely implemented). The opportunity cost of a consumed resource is the value of the benefits foregone by using the resource for the next best alternative; conventionally, in most circumstances, market rates (e.g. pay per hour) or prices paid are assumed to represent opportunity costs.
Service use data
Individual-level resource use data was collected during interviews with parents of a subsample of the trial participants, using an adapted version of the CSRI61 at baseline and 6 months’ follow-up. The range of services assessed is summarised in Table 4.
| Type of service use | Details recorded | Notes or limits |
|---|---|---|
| Overnight hospital stays | Number of days in hospital and reasons for stays | For up to three stays |
| Accident and emergency visits | Number of visits and reasons for visits | Up to three reasons |
| Hospital outpatient appointments | Number of visits and reasons for visits | Up to three reasons |
| Visits to the GP | Number of visits and number of visits for worry, anxiety or unhappiness | |
| ‘Has your child seen anyone else for psychological problems (such as worry, anxiety or unhappiness)’ | Number of times seen (for each of nurse at a GP practice, school nurse, counsellor, child mental health service, child psychologist, social worker or ‘Someone else, please say who’) | |
| Taking medication (for anxiety or depression) | Name of medicine and how long taken | Up to three medicines |
The unit costs applied to different types of health service use and for visits to different types of professionals or services because of anxiety or depression are provided in Table 5. The two main sources for the unit costs were the Department of Health’s NHS reference costs76 (for primary care trusts and NHS trusts combined) and the Personal Social Services Research Unit’s unit costs of health and social care75 (hourly costs of patient or client contact for various types of health or social care professional).
| Resource type and unit | Unit cost (£) | Source |
|---|---|---|
| Visit to GP | 37 | aSection 10.8 (11.7-minute consultation)75 |
| GP practice nurse consultation | 12 | aSection 10.6 (nurse GP practice, per consultation)75 |
| School nurse time (per hour) | 60 | aSection 10.1 (community nurse, per hour with patient)75 |
| Counsellor (per hour)b | 63 | aSection 2.8 (counselling services in primary medical care, per hour with patient or per contact hour)75 |
| Child mental health service (per hour)b | 65 | aSection 10.2 (mental health nurse, per hour with patient)75 |
| Child psychologist (per hour)b | 134 | aSection 9.5 (clinical psychologist, per hour with patient)75 |
| Consultant psychiatrist (per contact)b | 261 | aSection 15.7 (consultant: psychiatric, per face-to-face contact)75 |
| Social worker (per hour)b | 55 | aSection 11.3 [social worker (children), per hour with client]75 |
Costing the intervention
The resource use involved in delivering the FRIENDS programme was costed using project records of staff time and other expenditure, based on as detailed a breakdown as possible of different resources used (i.e. a microcosting approach). This included the paid time of facilitators or teachers delivering the programme, the cost of their training and ongoing supervision and management, travel costs, printing costs for course booklets and an apportionment of the cost of recruiting schools. The calculated intervention costs excluded the costs of developing or adapting the new materials (these were treated as ‘sunk costs’ as it was assumed that they would not be incurred again). We also excluded the proportion of the facilitators’ delivery time that was spent completing additional research measures. The costs did, however, include the initial training costs of the facilitators (time of trainers and facilitators, room hire and subsistence). Usual school provision involved no intervention costs.
All costs were calculated as either the amount of resource used multiplied by a unit cost or the total amount incurred over the trial period divided by the number of pupils in participating classes, the number of sessions delivered or the number of schools, depending on the level at which the cost was incurred. Teacher time costs were based on hourly average pay rates for mid-grade primary school teachers, whereas the cost of the health facilitators was based on hourly actual salary costs of those employed over the relevant period of intervention delivery (see Appendix 2).
Economic analysis
The cleaning and correction of resource use and CHU-9D data and the calculation of service use costs were conducted in PASW Statistics v21 (SPSS Inc., Chicago, IL, USA). Some educational resource use data that were collected were not costed, for example additional help and support for maths and literacy (spelling, reading), because it was considered unlikely to be associated with changes in low mood or anxiety. Similarly, although child absence from school because of worry, anxiety or unhappiness was reported, we did not estimate any cost impact associated with this.
The models for analysing incremental cost-effectiveness were fitted using Stata 12 software (StataCorp LP, College Station, TX, USA). Given the short time frame of the trial and follow-up, neither costs nor outcomes were discounted to present values.
Two cost-effectiveness analyses were conducted, one using the RCADS score and another using QALYs based on responses to the CHU-9D questionnaire. The derivation of the per-person QALYs from baseline to 6 months for each child involved (1) converting complete CHU-9D raw responses into CHU-9D utility values using the established algorithm57 and (2) estimating the mean of the CHU-9D utility at baseline and at 6 months and dividing this by two (i.e. half a year). QALYs were therefore calculated only for children who had complete CHU-9D data at both time points.
Incremental costs, incremental effects and, when relevant, incremental cost-effectiveness ratios (ICERs) were estimated, comparing the classroom-based CBT arm with the usual school provision arm. The incremental cost per unit decrease in RCADS score (as lower scores on the RCADS indicate better outcome) and the incremental cost per unit QALY increase were estimated. Both unadjusted and adjusted analyses were carried out, adjusting for year level for all outcomes and additionally for RCADS score at baseline when analysing the RCADS outcome. The remaining factors used to balance the randomisation were not adjusted for because of the relatively small number of clusters.
Random-effects bivariate linear regression models were fitted to model cost and effectiveness (RCADS or QALY) simultaneously, allowing for correlation within randomised clusters and correlation between cost and effectiveness score within participants. 77 These models produced estimates of the mean difference in cost and its standard error; the mean difference in effect and its standard error; and (indirectly through the variance–covariance matrix of the regression coefficients) the correlation between the mean cost difference and the mean effect difference.
Both the RCADS- and QALY-based cost-effectiveness results are based on those in the economic subsample who had valid cost and outcome data. A sensitivity analysis combining the cost data from the economic subsample with the effectiveness data from the whole sample was also conducted.
The findings reported here are based on analyses of complete cases. Within the economic subsample levels of missing data for the key outcomes were low. Also, the economic subsample was deemed too small to justify imputation of any missing data.
The potential value of extrapolating the trial results using a decision model was originally suggested. This was proposed when our follow-up was going to be 12 months and would have been valuable if there was a convincing between-group difference in effectiveness and/or service use costs at 6 and 12 months. However, at 24 months, after the trial extension, our results showed no between-group differences in effectiveness and, as such, we felt that no model-based extrapolation would be plausible.
Chapter 3 Results
Recruitment and participant flow
In total, 45 primary schools were enrolled in the study, with 41 providing signed consent by the specified deadline. Following randomisation, one school allocated to the usual school provision arm withdrew before the baseline assessment. The remaining 40 schools were retained throughout the study and the flow of participants is summarised in Figure 1.
FIGURE 1.
The PACES CONSORT flow diagram.
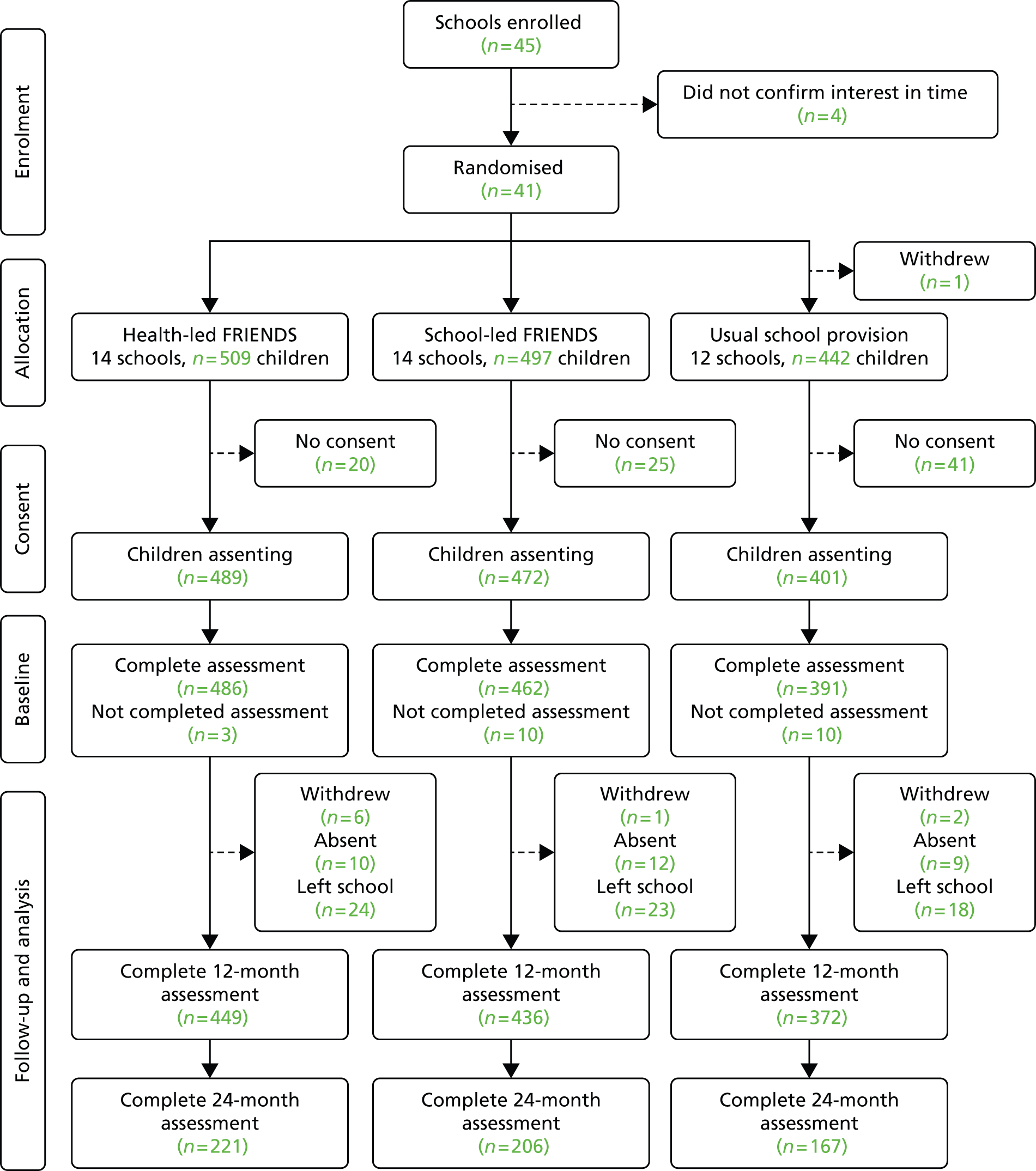
Of the 1448 eligible participants, 1362 (94%) consented to participate in the study with 1339 (98%) completing baseline assessments. Of these, 489 were allocated to health-led FRIENDS, 472 to school-led FRIENDS and 401 to usual school provision. Interventions were delivered to all participating schools in the academic year September 2011–July 2012.
At 12 months, 65 (4.8%) children had left school, nine (0.7%) withdrew consent and 31 (2.3%) were absent on the day(s) of assessment, resulting in 1257 children (92.3%) being assessed.
By the 24-month assessment children had transitioned to secondary school. For this assessment we had to initiate a new recruitment and consent process. We wrote to all of our initial cohort and asked parents to opt in to this assessment by returning a signed consent form and contact details. Data were obtained from 594 children, 43.6% of those who initially consented to participate. The 24-month assessments were completed by 221 (45.2%) in the health-led FRIENDS arm, 206 (43.6%) in the school-led FRIENDS arm and 167 (41.6%) in the usual school provision arm.
School demographics
Table 6 summarises the 40 participating schools by trial arm. On average, the schools were representative of the UK in terms of academic attainment (i.e the percentage of children achieving Key Stage 2 level 4 in maths and English). However, there were more children with special educational needs [23.2% vs. 17.1%; t = 4.180, degrees of freedom (df) = 39; p < 0.001] and lower rates of pupil absence (4.4% vs. 5.1%; t = –4.513, df = 38; p < 0.001) and eligibility for free school meals (12.4% vs. 18.2%; t = –3.540, df = 39; p < 0.001) in the study cohort than the national average.
| School ID | Trial arm | Number of pupils | Last Ofsted ratinga | Eligible for free school meals (%) | Educational needs (%) | Overall absence (%) | % achieving Level 4 English and maths |
|---|---|---|---|---|---|---|---|
| 2 | 1 | 183 | 1 | 2.2 | 15.8 | 2.8 | 96 |
| 8 | 1 | 215 | 3 | 9.5 | 27.4 | 4.9 | 67 |
| 38 | 1 | 149 | 2 | 0 | 34.9 | 3.6 | 95 |
| 13 | 1 | 394 | 3 | 11.3 | 26.1 | 3.8 | 64 |
| 29 | 1 | 50 | 2 | 6.4 | 18.0 | 3.8 | n/a |
| 4 | 1 | 126 | 2 | 9.5 | 11.9 | 6.8 | 79 |
| 15 | 1 | 108 | 4 | 45.4 | 49.1 | 4.5 | 71 |
| 24 | 1 | 288 | 2 | 9.3 | 18.4 | 2.7 | 95 |
| 40 | 1 | 220 | 3 | 30.5 | 33.2 | 5.0 | 71 |
| 19 | 1 | 274 | 1 | 4.4 | 1.5 | 4.3 | 91 |
| 25 | 1 | 258 | 2 | 8.2 | 20.9 | 3.9 | 85 |
| 11 | 1 | 253 | 2 | 10.6 | 34.0 | 5.0 | 64 |
| 34 | 1 | 354 | 2 | 8.9 | 29.1 | 4.8 | 73 |
| 32 | 1 | 238 | 1 | 7.2 | 15.1 | 3.6 | 98 |
| 1 | 2 | 260 | 2 | 22 | 39.2 | 6.0 | 73 |
| 37 | 2 | 381 | 3 | 6.7 | 12.1 | 4.5 | 88 |
| 3 | 2 | 188 | 1 | 2.7 | 18.1 | 3.0 | 87 |
| 14 | 2 | 49 | 1 | 2 | 26.5 | 3.6 | 67 |
| 27 | 2 | 205 | 2 | 17.1 | 16.1 | 3.5 | 87 |
| 30 | 2 | 140 | 2 | 32.2 | 30.0 | 6.2 | 94 |
| 18 | 2 | 346 | 1 | 7.8 | 16.2 | 3.0 | 81 |
| 21 | 2 | 182 | 4 | 27.8 | 36.8 | 6.8 | 58 |
| 6 | 2 | 117 | 2 | 10 | 24.8 | 4.8 | 57 |
| 39 | 2 | 239 | 2 | 19.2 | 18.4 | 3.6 | 79 |
| 9 | 2 | 488 | 1 | 4.5 | 22.5 | 4.2 | 88 |
| 5 | 2 | 107 | 2 | 1.9 | 11.2 | 4.3 | 88 |
| 7 | 2 | 405 | 3 | 11.4 | 15.1 | 4.5 | 85 |
| 36 | 2 | 411 | 1 | 11.9 | 18.7 | 3.4 | 94 |
| 28 | 3 | 356 | 2 | 10.3 | 21.3 | 4.8 | 81 |
| 16 | 3 | 183 | 2 | 7.1 | 16.9 | 3.4 | 100 |
| 26 | 3 | 150 | 2 | 27.5 | 20.0 | 4.9 | 81 |
| 17 | 3 | 396 | 2 | 5.6 | 18.2 | 4.2 | 81 |
| 23 | 3 | 94 | 3 | 6.3 | 22.3 | 4.1 | 91 |
| 33 | 3 | 348 | 2 | 4.8 | 17.8 | 4.1 | 85 |
| 31 | 3 | 180 | 3 | 7.7 | 16.7 | 4.1 | 70 |
| 35 | 3 | 414 | 2 | 16.2 | 32.9 | 4.9 | 76 |
| 41 | 3 | 119 | 2 | 27.7 | 30.3 | 4.6 | 73 |
| 22 | 3 | 93 | 2 | 16.8 | 32.3 | 5.9 | 67 |
| 20 | 3 | 197 | 2 | 1.5 | 25.9 | 3.7 | 78 |
| 12 | 3 | 243 | 3 | 22.6 | 33.3 | 5.1 | 88 |
| Average | 235 | 12.4 | 23.2 | 4.4 | 78.7 | ||
| National average | 18.2 | 17.1 | 5.1 | 79.0 | |||
| Average by trial arm | |||||||
| 1 | 222 | 2.1 | 11.7 | 24.0 | 4.3 | 74.9 | |
| 2 | 251 | 1.9 | 12.7 | 21.8 | 4.4 | 80.4 | |
| 3 | 231 | 2.3 | 12.8 | 24.0 | 4.5 | 80.9 | |
There were no significant differences for any variable between trial arms.
Balance between trial arms
Demographic and baseline symptomatology for the three groups is summarised in Table 7. The proportion of boys in the usual PSHE group (42%) was lower than that in each of the other two trial arms (52% and 50%) but otherwise the arms were well balanced at baseline.
| Characteristic | Trial arm | ||
|---|---|---|---|
| Health-led FRIENDS | School-led FRIENDS | Usual PSHE | |
| No. of children | 489 | 472 | 401 |
| No. of schools | 14 | 14 | 12 |
| No. of schools with two or more classes | 6 | 7 | 5 |
| Class size of schools, mean (SD) | 19.56 (6.56) | 18.15 (7.68) | 20.05 (8.29) |
| Missing baseline assessment, n (%) | 3 (0.6) | 10 (2.1) | 10 (2.5) |
| Sex, n (%) | |||
| Male | 255 (52.1) | 237 (50.2) | 170 (42.4) |
| Female | 234 (47.9) | 235 (49.8) | 231 (57.6) |
| Ethnicity, n (%) | |||
| British white | 455 (94.2) | 439 (95.2) | 359 (92.1) |
| Non-white | 28 (5.8) | 22 (4.8) | 31 (7.9) |
| Living situation, n (%) | |||
| Mum and dad | 347 (71.4) | 315 (68.2) | 268 (68.5) |
| Parent and partner | 43 (8.8) | 55 (11.9) | 37 (9.4) |
| Single parent | 67 (13.8) | 68 (14.8) | 58 (14.8) |
| Other | 29 (6.0) | 24 (5.2) | 28 (7.2) |
| Number of siblings, n (%) | |||
| 0 | 49 (10.1) | 30 (6.5) | 32 (8.2) |
| 1 | 221 (45.5) | 214 (46.5) | 184 (47.1) |
| 2 | 129 (26.5) | 134 (29.1) | 92 (23.5) |
| 3 or more | 87 (17.9) | 82 (17.8) | 83 (21.2) |
| Family affluence, n (%) | |||
| Low (0–2) | 6 (1.5) | 11 (2.4) | 13 (3.3) |
| Medium (3–5) | 142 (29.4) | 139 (30.1) | 128 (32.9) |
| High (6–8) | 331 (69.1) | 311 (67.5) | 249 (63.8) |
| Child-reported assessment | |||
| Child total RCADS score, mean (SD) | 26.24 (15.56) | 24.91 (14.32) | 26.78(16.32) |
| Penn State Worry Questionnaire for Children score, mean (SD) | 10.63 (8.14) | 10.99 (8.24) | 10.46 (8.35) |
| Rosenberg Self-Esteem Scale score, mean (SD) | 18.94 (5.34) | 19.43 (5.39) | 19.57 (5.98) |
| Total life satisfaction, mean (SD) | 14.21 (6.77) | 13.32 (5.71) | 13.76 (6.82) |
| Bullied more than two or three times a month, n (%) | 142 (29.3) | 124 (26.8) | 112 (28.6) |
| Parent-reported assessment | n = 217 | n = 201 | n = 153 |
| Total RCADS score, mean (SD) | 12.55 (8.81) | 10.99 (8.60) | 12.52 (9.34) |
| Total SDQ score, mean (SD) | 9.09 (6.32) | 8.31 (6.28) | 9.00 (6.24) |
| Total SDQ threshold | |||
| Abnormal ≥ 17, n (%) | 22 (10.5) | 25 (13.0) | 21 (14.4) |
| Teacher-reported assessment | n = 487 | n = 466 | n = 396 |
| Teacher-rated SDQ impact | |||
| Difficulty, n (%) | 119 (24.4) | 125 (26.8) | 109 (27.5) |
Usual school provision
Semistructured interviews were completed with each school in the usual PSHE arm to determine the nature, extent and content of the PSHE that was provided. An overall rating of the emphasis that each school placed on academic attainment and social and emotional well-being on a 10-point Likert scale (0 = ‘not important’; 10 = ‘very important’) was obtained. Data are summarised in Table 8.
| School | Main PSHE model | Dedicated PSHE sessions | Time per Week | No. of PSHE leaders | PSHE content covered | Academic attainment importance | Social and emotional well-being importance |
|---|---|---|---|---|---|---|---|
| 16 | SEAL | Yes | 5 hours per term | 1 + TA | New beginnings; getting on and falling out | 8 | 10 |
| 26 | Learning 4 Life | Yes | 45 minutes | 1 + TA | My family and friends; healthy bodies, healthy minds | 9 | 10 |
| 17 | SEAL | Yes | 45 minutes | 1 | New beginnings; getting on and falling out | 7.5 | 7.5 |
| 23 | Learning 4 Life | Yes | 45 minutes | 1 | Going for goals; my family and friends | 7 | 10 |
| 33 | SEAL | Fortnightly assembly | 40 minutes | 1 | Getting on and falling out; good to be me | 8 | 8 |
| 31 | Interpersonal Curriculum model (SEAL based) | Weekly assembly | 30 minutes | 1 | Adaptability; communication | 8 | 8 |
| 35 | Spiritual, Moral, Social and Cultural Development model (not SEAL based) | Yes | 30–60 minutes | 1–2 | Caring and sharing; staying healthy; safety first | 9 | 8 |
| 22 | Learning 4 Life | Yes | 60 minutes | 1 | Our happy school; out and about | 8 | 8 |
| 20 | SEAL | Yes | 60–90 minutes | 1 | New beginnings; getting on and falling out | 9 | 8 |
| 12 | SEAL | Yes | 30 minutes | 1 | Going for goals; new beginnings; good to be me | 9 | 9 |
| 41 | SEAL | Yes | 60 minutes | 1 | Good to be me; going for goals | 9 | 10 |
| 28 | SEAL | Yes | 30–40 minutes | 1 | Could not recall | 10 | 8 |
The PSHE lessons were typically delivered by a single teacher as dedicated weekly sessions of 30–60 minutes. Academic attainment and social and emotional well-being were both rated equally highly by the schools.
In terms of content, all but one school were following the national SEAL curriculum13 or a programme informed by it (Learning 4 Life). 78 The SEAL curriculum aims to develop the underpinning qualities and skills that help promote positive behaviour and effective learning. It focuses on five social and emotional aspects of learning: self-awareness, managing feelings, motivation, empathy and social skills. SEAL is organised into seven main themes: new beginnings, getting on and falling out, say no to bullying, going for goals, good to be me, relationships and changes. Each theme is designed for a whole-school approach and includes a whole-school assembly and suggested follow-up activities in all areas of the curriculum.
The Learning 4 Life programme was developed in Wiltshire. It is based on the SEAL curriculum and includes a range of emotional literacy materials that can be integrated within the wider PSHE curriculum. The programme has six main themes that closely map onto the SEAL curriculum. The SEAL and Learning 4 Life programmes are summarised in Table 9.
| Social and Emotional Aspects of Learning | Learning 4 Life |
|---|---|
| New beginnings: exploring feelings of happiness, excitement, sadness, anxiety and fearfulness. Learning to calm down and problem solve | Our happy school: working in a group, respect others, personal responsibility for own behaviour |
| Getting on and falling out: developing social skills for friendships; learning to work well in a group, manage anger, resolve conflict | Out and about: keeping safe and managing risk, discrimination and stereotyping, protecting oneself online |
| Say No to Bullying: antibullying work | |
| Good to be me: understand effect of feelings on behaviour, feel good about self; manage feelings, relax, cope with anxiety, stand up for yourself and assertiveness | Healthy bodies, healthy minds: healthy lifestyles (diet, alcohol, drugs) and promoting positive physical and mental well-being; managing risk, building resilience, making safe choices around drugs, work/life balance |
| Going for goals: reflecting on self and strengths, taking responsibility, building confidence and self-efficacy | Looking forward: looking at choices with reference to finance, saving, budgeting |
| Relationships: exploring feelings in terms of important relationships (family and friends) and coping with loss | My family and friends: coping with issues such as loss, self-image and media influence; pubertal changes and sex education and relationships |
| Changes: understanding different types of change (positive and negative) and responses to it | Ready, steady, go: exploring difficult changes around loss and bereavement; planning to transition to secondary school |
Within the usual provision schools, PSHE had a wide focus. During the intervention phase PSHE addressed issues including personal safety, healthy eating, coping with loss and social skills, as well as emotional awareness and management. Although the focus on emotional regulation and problem-solving overlapped with the focus of the FRIENDS programme, the specific PSHE focus on anxiety was less systematic and intensive.
Intervention dosage and fidelity
The complete nine-session FRIENDS programme was delivered to all classes in the health-led and school-led groups. Session attendance was not recorded although average school absence rates in participating schools were very low (health-led 4.25% vs. school-led 4.4%).
To assess intervention fidelity, 49 sessions (one from each class in the 28 schools delivering the FRIENDS programme) were audio recorded and independently rated to determine how many core tasks had been delivered. All specified core tasks and home activities were delivered in the 24 health-led sessions assessed. In the 25 school-led sessions, 15 (60%) delivered all of the core tasks and the home activity, eight (32%) delivered all except the home activity and the remaining two (8%) did not deliver one core task and the home activity.
Outcomes
Objective 1: to evaluate the effectiveness of the FRIENDS programme in reducing symptoms of anxiety and low mood (primary outcome) at 12 months
At the 6-month asssessment, data were available from 1317 children, 96.7% of those who completed the baseline assessments. Our analysis revealed no significant between-arm differences in total RCADS score (health-led FRIENDS: baseline 26.24 (SD 15.56) vs. 6 months 22.99 (SD 14.52); school-led FRIENDS: baseline 24.91 (SD 14.32) vs. 6 months 24.32 (SD 15.95); usual school provision: baseline 26.78 (SD 16.32) vs. 6 months 24.70 (SD 15.84).
Our primary outcome was the child-reported RCADS score at 12 months. Data at 12 months were available for 1257 children, 92.3% of those who completed the baseline assessments (health-led FRIENDS 91.8%; school-led FRIENDS 92.4%; usual school provision 92.7%). Tables 10 and 11 summarise the total and subscale scores by trial arm at baseline and 12 months.
| RCADS scale | Health-led FRIENDS, mean (SD) | Adjusted difference (95% CI), health-led FRIENDS vs. usual school provision | Usual school provision, mean (SD) | Adjusted difference (95% CI), health-led FRIENDS vs. school-led FRIENDS | School-led FRIENDS, mean (SD) | p-valuea | |||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 489) | 12 months (n = 449) | Baseline (n = 401) | 12 months (n = 372) | Baseline (n = 472) | 12 months (n = 436) | ||||
| Depression | 4.04 (2.60) | 3.15 (2.53) | –0.36 (–0.76 to 0.04) | 3.85 (2.77) | 3.47 (2.,72) | –0.34 (–0.82 to 0.14) | 3.68 (2.34) | 3.34 (2.51) | 0.120 |
| Social anxiety | 5.28 (3.28) | 4.39 (3.32) | –0.41 (–0.94 to 0.12) | 5.13 (3.26) | 4.68 (3.37) | –0.79 (–1.42 to-0.16) | 5.05 (3.23) | 5.04 (3.43) | 0.013 |
| Separation anxiety | 3.81 (3.34) | 2.48 (2.94) | –0.42 (–0.97 to 0.12) | 4.23 (3.45) | 3.07 (3.14) | –0.42 (–1.07 to-0.23) | 3.68 (3.14) | 2.89 (2.96) | 0.190 |
| Generalised anxiety | 5.79 (3.80) | 4.43 (3.56) | –0.77 (–1.40 to –0.14) | 5.97 (3.94) | 5.15 (3.70) | –0.89 (–1.64 to-0.14) | 5.64 (3.54) | 5.19 (3.64) | 0.011 |
| Panic | 2.85 (2.87) | 2.03 (2.56) | –0.34 (–0.78 to 0.09) | 2.97 (3.11) | 2.42 (3.00) | –0.37 (–0.89 to 0.15) | 2.68 (2.79) | 2.33 (2.74) | 0.157 |
| OCD | 4.56 (3.31) | 3.43 (3.10) | –1.99 (–0.71 to 0.31) | 4.61 (3.22) | 3.79 (3.20) | –0.51 (–1.12 to 0.10) | 4.45 (3.12) | 3.99 (3.20) | 0.124 |
| Total RCADS | 26.24 (15.56) | 19.49 (14.81) | –2.66 (–5.22 to –0.09) | 26.78 (16.32) | 22.48 (15.74) | –3.91 (–6.48 to-1.35) | 24.91 (14.32) | 22.86 (15.24) | 0.009 |
| RCADS scale | School-led FRIENDS, mean (SD) | Adjusted difference (95% CI), school-led FRIENDS vs. usual school provision | Usual school provision, mean (SD) | Adjusted difference (95% CI), school-led FRIENDS vs. health-led FRIENDS | Health-led FRIENDS, mean (SD) | p-valuea | |||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (n = 472) | 12 months (n = 436) | Baseline (n = 401) | 12 months (n = 372) | Baseline (n = 489) | 12 months (n = 449) | ||||
| Depression | 3.68 (2.34) | 3.34 (2.51) | –0.02 (–0.43 to 0.38) | 3.85 (2.77) | 3.47 (2.,72) | –0.34 (–0.82 to 0.14) | 4.04 (2.60) | 3.15 (2.53) | 0.120 |
| Social anxiety | 5.05 (3.23) | 5.04 (3.43) | 0.38 (–0.16 to 0.91) | 5.13 (3.26) | 4.68 (3.37) | –0.79 (–1.42 to-0.16) | 5.28 (3.28) | 4.39 (3.32) | 0.013 |
| Separation anxiety | 3.68 (3.14) | 2.89 (2.96) | 0.00 (–0.54 to 0.55) | 4.23 (3.45) | 3.07 (3.14) | –0.42 (–1.07 to-0.23) | 3.81 (3.34) | 2.48 (2.94) | 0.190 |
| Generalised anxiety | 5.64 (3.54) | 5.19 (3.64) | 0.12 (–0.52 to 0.75) | 5.97 (3.94) | 5.15 (3.70) | –0.89 (–1.64 to-0.14) | 5.79 (3.80) | 4.43 (3.56) | 0.011 |
| Panic | 2.68 (2.79) | 2.33 (2.74) | 0.03 (–0.41 to 0.47) | 2.97 (3.11) | 2.42 (3.00) | –0.37 (–0.89 to 0.15) | 2.85 (2.87) | 2.03 (2.56) | 0.157 |
| OCD | 4.45 (3.12) | 3.99 (3.20) | 0.31 (–0.21 to 0.83) | 4.61 (3.22) | 3.79 (3.20) | –0.51 (–1.12 to 0.10) | 4.56 (3.31) | 3.43 (3.10) | 0.124 |
| Total RCADS score | 24.91 (14.32) | 22.86 (15.24) | 1.28 (–1.30 to 3.87) | 26.78 (16.32) | 22.48 (15.74) | –3.91 (–6.48 to-1.35) | 26.24 (15.56) | 19.49 (14.81) | 0.009 |
Our analysis was adjusted for school, baseline symptomatology (RCADS score) and sex. There was a significant difference in adjusted mean total RCADS score at 12 months between health-led FRIENDS and school-led FRIENDS [–3.91, 95% confidence interval (CI) –6.48 to –1.35; p = 0.0004] and usual school provision (–2.66, 95% CI –5.22 to –0.09; p = 0.043). The 95% CIs include our predefined clinically important difference of 3.6 points on the RCADS. Analysis of the RCADS subscales (see Table 11) showed a difference in generalised (p = 0.011) and social (p = 0.013) anxiety but not depression (p = 0.12).
Missing data analysis
Although data completion at 12 months was very high (93.9%), an analysis of missing data was undertaken to compare baseline RCADS scores of those who did and those who did not complete the 12-month assesments (Table 12). On our primary outcome measures (RCADS), child non-completers at 12 months had higher baseline scores (indicating more symptomatology) on the total RCADS and all subscales.
| Characteristic | Health-led FRIENDS, mean (SD) | School-led FRIENDS, mean (SD) | Usual school provision, mean (SD) | p-value (interaction) |
|---|---|---|---|---|
| Completers, n (%) | 449 (91.8) | 436 (92.4) | 372 (92.8) | 0.867 |
| Non-completers, n | 40 | 36 | 29 | |
| Sex male, n (%) | ||||
| Completers | 234 (52.1) | 220 (50.5) | 159 (42.7) | 0.649 |
| Non-completers | 21 (52.5) | 17 (52.8) | 11 (37.9) | |
| Child-reported RCADS score | ||||
| Depression | ||||
| Completers | 4.01 (2.58) | 3.62 (2.31) | 3.73 (2.68) | 0.001 (0.140) |
| Non-completers | 4.41 (2.89) | 4.46 (3.04) | 5.43 (3.45) | |
| Separation anxiety | ||||
| Completers | 3.84 (3.43) | 3.63 (3.15) | 4.07 (3.36) | 0.015 (0.012) |
| Non-completers | 3.54 (2.18) | 4.24 (3.04) | 6.29 (4.03) | |
| Social anxiety | ||||
| Completers | 5.24 (3.28) | 4.97 (3.14) | 5.00 (3.20) | 0.001 (0.298) |
| Non-completers | 5.72 (3.24) | 5.97 (4.13) | 6.79 (3.65) | |
| General anxiety | ||||
| Completers | 5.71 (3.76) | 5.65 (3.56) | 5.76 (3.79) | 0.001 (0.010) |
| Non-completers | 6.64 (4.13) | 5.54 (3.35) | 8.64 (4.75) | |
| Panic | ||||
| Completers | 2.85 (2.89) | 2.65 (2.72) | 2.84 (3.01) | 0.020 (0.045) |
| Non-completers | 2.84 (2.70) | 3.00 (3.54) | 4.64 (3.88) | |
| OCD | ||||
| Completers | 4.49 (3.26) | 4.42 (3.10) | 4.48 (3.17) | 0.002 (0.361) |
| Non-completers | 5.38 (3.84) | 4.91 (3.38) | 6.18 (3.47) | |
| Total RCADS score | ||||
| Completers | 26.10 (15.66) | 24.63 (14.13) | 25.88 (15.78) | 0.001 (0.025) |
| Non-completers | 27.87 (13.53) | 28.21 (16.32) | 37.96 (18.99) | |
Sensitivity analyses were conducted to assess the potential effect of missing data. Twenty imputed data sets were created using imputations based on RCADS total and subscale scores (Table 13).
| RCADS scale | Health led FRIENDS (n = 489), mean (SD) | School led FRIENDS (n = 472), mean (SD) | Usual school provision (n = 401), mean (SD) | p-valuea |
|---|---|---|---|---|
| Depression | 3.10 (2.85) | 3.39 (2.87) | 3.44 (2.84) | 0.163 |
| Separation anxiety | 2.55 (3.78) | 2.952 (3.82) | 2.900 (3.77) | 0.209 |
| Social anxiety | 4.34 (3.74) | 5.04 (3.69) | 4.62 (3.69) | 0.021 |
| General anxiety | 4.36 (4.27) | 5.20 (4.28) | 4.94 (4.23) | 0.013 |
| Panic | 2.03 (2.99) | 2.38 (3.00) | 2.32 (2.96) | 0.170 |
| OCD | 3.47 (3.43) | 4.03 (3.45) | 3.69 (3.42) | 0.052 |
| Total RCADS score | 19.79 (17.18) | 23.01 (17.23) | 21.89 (17.00) | 0.020 |
Imputation for missing data made no material difference to the overall results. There continued to be a between-group difference in total RCADS score and on the generalised and social anxiety subscales.
Objective 2: to evaluate the effectiveness of the FRIENDS programme for children with low and high anxiety at baseline in terms of symptoms of anxiety and low mood at 12 months
We were interested to explore the effects of the programme on those children with elevated symptoms of anxiety. Within community surveys 3–4% of children will be suffering with an anxiety disorder. In addition, a further group of children will have significant symptoms but may not fulfil all diagnostic criteria. We therefore chose to identify the 10% with the highest RCADS scores to cover both of these groups.
The distribution of child-reported total RCADS scores at baseline was examined. A total RCADS score of ≥ 49 identified 10.1% of children and was used as a cut-off to categorise children as having either high anxiety (n = 130) or low anxiety (RCADS score of ≤ 48, n = 1151). Using this cut-off, 99 high-anxiety and 1029 low-anxiety children completed the RCADS at 12 months. Table 14 summarises the total RCADS score at baseline and 12 months by trial arm for the high- and low-anxiety subgroups.
| Subgroup | Health-led FRIENDS, mean (SD) | School-led FRIENDS, mean (SD) | Usual school provision, mean (SD) | p-value overall group effecta |
|---|---|---|---|---|
| High anxiety (RCADS score of ≥ 49) | n = 36 | n = 31 | n = 32 | |
| Baseline | 57.59 (8.18) | 55.66 (7.16) | 57.57 (7.90) | 0.288 |
| 12 months | 35.31 (19.24) | 40.65 (21.40) | 33.97 (21.15) | 0.368 |
| Low anxiety (RCADS score of ≤ 48) | n = 374 | n = 360 | n = 295 | |
| Baseline | 22.78 (11.86) | 22.01 (11.05) | 22.51 (12.03) | 0.623 |
| 12 months | 17.68 (13.40) | 21.06 (13.42) | 20.74 (14.12) | 0.006 |
There were significant within-group reductions for the high-risk group at 12 months but no between-group effects. For the low-risk group, there were significant within-group reductions and between-group differences in mean RCADS scores at 12 months (p = 0.006). Adjusted mean differences showed an effect for health-led FRIENDS compared with school-led FRIENDS (–3.78, 95% CI –6.16 to –1.40; p = 0.003) and for health-led FRIENDS compared with usual school provision (–3.13, 95% CI –5.61 to –0.65; p = 0.015). Post hoc analysis indicated that this related to a reduction on the social (p = 0.013) and generalised anxiety (p = 0.006) subscales in the health-led FRIENDS group.
Objective 3: to examine the effectiveness of the FRIENDS programme in terms of self-esteem, worry, bullying and overall well-being (secondary outcomes) at 12 months
At the 6-month assessment, data were available from 1317 children and 479 parents. Analysis of our secondary outcomes revealed no significant between-group differences (data not reported here).
Our primary assessment point was 12 months post baseline assessment. Table 15 summarises the secondary outcomes (child-reported outcomes and parent and teacher assessments) at baseline and 12 months by trial arm.
| Outcome | Health-led FRIENDS | School-led FRIENDS | Usual school provision | p-value overall group effecta | |||
|---|---|---|---|---|---|---|---|
| Baseline | 12 months | Baseline | 12 months | Baseline | 12 months | ||
| Child reported | |||||||
| n | 489 | 449 | 472 | 436 | 401 | 372 | |
| Penn State Worry Questionnaire for Children score, mean (SD) | 10.63 (8.14) | 8.19 (7.93) | 10.99 (8.24) | 9.62 (8.30) | 10.46 (8.35) | 9.03 (8.52) | 0.0136 |
| Rosenberg Self-Esteem Scale score, mean (SD) | 18.94 (5.34) | 20.90 (6.22) | 19.43 (5.39) | 20.77 (5.82) | 19.57 (5.98) | 20.87 (5.95) | 0.639 |
| Total life satisfaction, mean (SD) | 14.21 (6.77) | 13.87 (6.00) | 13.32 (5.71) | 13.73 (6.08) | 13.76 (6.82) | 13.95 (5.88) | 0.770 |
| Bullied more than two or three times a month, n (%) | 142 (29.3) | 74 (16.5) | 124 (26.8) | 98 (22.5) | 112 (28.6) | 86 (23.2) | 0.156 |
| Not bullied or bullied once or twice, n (%) | 343 (70.7) | 374 (83.5) | 338 (73.2) | 337 (77.5) | 279 (71.4) | 285 (76.8) | |
| Parent reported | |||||||
| n | 217 | 173 | 198 | 159 | 152 | 119 | |
| Total RCADS score, mean (SD) | 12.55 (8.81) | 10.76 (8.90) | 10.99 (8.60) | 9.82 (7.13) | 12.52 (9.34) | 10.03 (7.31) | 0.816 |
| Total SDQ score, mean (SD) | 9.09 (6.32) | 7.06 (6.00) | 8.31 (6.28) | 6.67 (5.62) | 9.00 (6.24) | 7.32 (9.95) | 0.767 |
| Total SDQ threshold ≥ 17, n (%) | 22 (10.5) | 15 (9.3) | 25 (13.0) | 11 (7.3) | 21 (14.4) | 9 (7.9) | 0.333 |
| Teacher reported | |||||||
| n (%) | 487 (99.6) | 454 (92.8) | 466 (98.7) | 445 (94.3) | 396 (98.8) | 375 (93.5) | |
| Teacher SDQ impact, mean (SD) | 119 (24.4) | 131 (28.9) | 125 (26.8) | 143 (32.1) | 109 (27.5) | 117 (31.2) | 0.538 |
There were no between-group differences on any measure after adjusting for baseline, sex and school-level effects.
Objective 4: to examine the medium-term effects of the FRIENDS programme on symptoms of anxiety and low mood (primary outcome) at 24 months
A total of 594 children completed assessments at 24 months. A comparison of the baseline characteristics of those who did and those who did not complete the 24-month assessment is shown in Table 16.
| Characteristic | Completers (n = 594) | Non-completers (n = 768) | p-value |
|---|---|---|---|
| Study arm, n | |||
| Health-led FRIENDS | 221 | 268 | 0.568 |
| School-led FRIENDS | 206 | 266 | |
| Usual school provision | 167 | 234 | |
| Sex, n | |||
| Male | 279 | 383 | 0.288 |
| Female | 315 | 385 | |
| Family affluence, mean (SD) | 6.18 (1.46) | 5.96 (1.53) | 0.009a |
| Child baseline RCADS score, mean (SD) | |||
| Depression | 3.98 (2.61) | 3.77 (2.54) | 0.139 |
| Separation anxiety | 3.92 (3.32) | 3.86 (3.31) | 0.758 |
| Social anxiety | 5.21 (3.12) | 5.12 (3.37) | 0.61 |
| Generalised anxiety | 5.91 (3.69) | 5.69 (3.80) | 0.286 |
| Panic | 2.98 (3.06) | 2.71 (2.80) | 0.106 |
| OCD | 4.66 (3.26) | 4.45 (3.19) | 0.25 |
| Total anxiety RCADS score | 22.57 (13.58) | 21.76 (13.68) | 0.288 |
| Total RCADS score | 26.50 (15.29) | 25.52 (15.47) | 0.255 |
| Child baseline worries, mean (SD) | 11.20 (8.33) | 10.32 (8.14) | 0.056 |
| Child baseline self esteem, mean (SD) | 19.25 (5.30) | 19.33 (5.74) | 0.794 |
| Child baseline CHU-9D score, mean (SD) | 8.12 (6.12) | 7.76 (6.23) | 0.299 |
| Child baseline total happiness, mean (SD) | 14.12 (6.58) | 13.50 (6.32) | 0.085 |
| n = 383 | n = 183 | ||
| Parent baseline RCADS score, mean (SD) | |||
| Depression | 1.55 (1.47) | 1.40 (1.74) | 0.289 |
| Separation anxiety | 2.08 (2.34) | 2.11 (2.69) | 0.907 |
| Social anxiety | 4.38 (2.77) | 3.84 (2.68) | 0.029a |
| Generalised anxiety | 2.87 (2.36) | 2.70 (2.54) | 0.458 |
| Panic | 0.52 (1.04) | 0.69 (1.42) | 0.111 |
| OCD | 1.06 (1.41) | 0.93 (1.52) | 0.301 |
| Total anxiety RCADS score | 10.68 (7.58) | 10.16 (8.50) | 0.504 |
| Total RCADS score | 12.19 (8.43) | 11.59 (9.86) | 0.499 |
| Parent baseline SDQ score, mean (SD) | |||
| Prosocial | 8.22 (1.83) | 8.34 (1.83) | 0.471 |
| Hyperactivity | 3.51 (2.56) | 3.46 (2.50) | 0.808 |
| Emotional symptoms | 2.21(2.27) | 2.24 (2.50) | 0.885 |
| Conduct problems | 1.56 (1.74) | 1.57 (1.80) | 0.919 |
| Peer problems | 1.48 (1.77) | 1.49 (1.93) | 0.978 |
| Total SDQ score | 8.75 (6.15) | 8.89 (6.59) | 0.81 |
The only differences were in family affluence (higher in completers) and parent-rated social anxiety (higher in completers).
Table 17 summarises the total and subscale mean scores for the primary outcome measure (child-reported RCADS) at baseline and 12 and 24 months. Paired t-tests were undertaken to compare within-group change over time (baseline to 24 months). Anxiety symptomatology in all groups on the RCADS total scale and each subscale, including depression, had reduced by 24 months.
| RCADS scale | Baseline, mean (SD) | 12 months, mean (SD) | 24 months, mean (SD) | Paired t-test baseline to 24 months p-value |
|---|---|---|---|---|
| Health-led FRIENDS | n = 204–19 | |||
| Depression | 4.04 (2.60) | 3.15 (2.53) | 2.63 (2.03) | < 0.001 |
| Separation anxiety | 3.81 (3.34) | 2.48 (2.94) | 1.82 (2.26) | < 0.001 |
| Social anxiety | 5.28 (3.28) | 4.39 (3.32) | 4.01 (2.59) | < 0.001 |
| General anxiety | 5.79 (3.80) | 4.32 (3.56) | 3.68 (2.63) | < 0.001 |
| Panic | 2.85 (2.87) | 2.03 (2.56) | 1.39 (2.18) | < 0.001 |
| OCD | 4.56 (3.31) | 3.43 (3.10) | 2.62 (2.61) | < 0.001 |
| Total RCADS score | 26.24 (15.56) | 19.49 (14.81) | 15.87 (11.26) | < 0.001 |
| School-led FRIENDS | n = 180–201 | |||
| Depression | 3.68 (2.34) | 3.34 (2.51) | 2.12 (1.90) | < 0.001 |
| Separation anxiety | 3.68 (3.14) | 2.89 (2.96) | 1.83 (1.85) | < 0.001 |
| Social anxiety | 5.05 (3.22) | 5.04 (3.43) | 4.23 (3.01) | < 0.001 |
| Generalised anxiety | 5.64 (3.54) | 5.19 (3.64) | 3.81 (2.80) | < 0.001 |
| Panic | 2.68 (2.79) | 2.33 (2.74) | 1.21 (1.68) | < 0.001 |
| OCD | 4.45 (3.12) | 3.99 (3.20) | 2.56 (2.41) | < 0.001 |
| Total RCADS score | 24.91 (14.32) | 22.86 (15.24) | 15.58 (10.40) | < 0.001 |
| Usual school provision | n = 151–64 | |||
| Depression | 3.85 (2.77) | 3.47 (2.72) | 2.56 (1.95) | < 0.001 |
| Separation anxiety | 4.23 (3.45) | 3.07 (3.14) | 2.36 (2.41) | < 0.001 |
| Social anxiety | 5.13 (3.26) | 4.68 (3.37) | 4.48 (2.70) | < 0.001 |
| Generalised anxiety | 5.97 (3.94) | 5.15 (3.70) | 3.89 (2.58) | < 0.001 |
| Panic | 2.97 (3.11) | 2.42 (3.00) | 1.40 (1.90) | < 0.001 |
| OCD | 4.61 (3.22) | 3.78 (3.21) | 2.75 (2.49) | < 0.001 |
| Total RCADS score | 26.78 (16.32) | 22.48 (15.73) | 17.40 (10.89) | < 0.001 |
At 24 months, there were no between-group effects on the primary outcome after adjusting for baseline, sex and school effects. Children in each condition achieved similar reductions in anxiety symptoms and depression at 24 months (Table 18).
| RCADS scale | Health-led FRIENDS (n = 218–20), mean (SD) | School-led FRIENDS (n = 201–6), mean (SD) | Usual School Provision (n = 164–7), mean (SD) | p-valuea |
|---|---|---|---|---|
| Depression | 2.63 (2.03) | 2.12 (1.90) | 2.56 (1.95) | 0.069 |
| Separation anxiety | 1.82 (2.26) | 1.83 (1.85) | 2.36 (2.41) | 0.224 |
| Social anxiety | 4.01 (2.59) | 4.23 (3.01) | 4.48 (2.70) | 0.183 |
| Generalised anxiety | 3.68 (2.63) | 3.81 (2.80) | 3.89 (2.58) | 0.683 |
| Panic | 1.39 (2.18) | 1.21 (1.68) | 1.40 (1.90) | 0.697 |
| OCD | 2.62 (2.61) | 2.56 (2.41) | 2.75 (2.49) | 0.831 |
| Total RCADS score | 15.87 (11.26) | 15.58 (10.40) | 17.40 (10.89) | 0.182 |
Objective 5: to evaluate the medium-term effects of the FRIENDS programme for children with low and high anxiety at baseline on symptoms of anxiety and low mood (primary outcome) at 24 months
A total of 535 children had baseline and 24-month data available, of whom 48 had high anxiety and 487 had low anxiety at baseline. Data on child-reported total RCADS scores are summarised in Table 19.
| Subgroup | Health-led FRIENDS, mean (SD) | School-led FRIENDS, mean (SD) | Usual school provision, mean (SD) | p-value overall group effecta |
|---|---|---|---|---|
| High anxiety | n = 20 | n = 15 | n = 13 | |
| Baseline | 57.59 (8.18) | 55.66 (7.16) | 57.57 (7.90) | |
| 12 months | 35.31 (19.24) | 40.65 (21.40) | 33.97 (21.15) | 0.763 |
| 24 months | 25.20 (14.99) | 23.60 (13.14) | 27.00 (15.93) | 0.773 |
| Low anxiety | n = 184 | n = 165 | n = 138 | |
| Baseline | 22.78 (11.86) | 22.01 (11.05) | 22.51 (12.03) | |
| 12 months | 17.68 (13.40) | 21.06 (13.42) | 20.74 (14.11) | 0.020 |
| 24 months | 14.68 (10.10) | 14.62 (9.82) | 16.36 (9.76) | 0.184 |
The number of high-anxiety children with 24-month follow-up data available was low [health-led FRIENDS 20/36 (55.6%); school-led FRIENDS 15/31 (48.4%); usual school provision 13/32 (40.6%)] and appropriate caution needs to be exercised in interpreting these data. Paired t-tests revealed a significant within-group reduction in total RCADS score from baseline to 24 months for all high-risk children (health-led FRIENDS: t = 8.52, df = 19, p < 0.001; school-led FRIENDS: t = 8.96, df = 14, p < 0.001; usual PSHE: t = 6.99, df = 12, p < 0.001). However, there were no between-group effects.
Approximately half of the children identified with low anxiety at baseline completed the 24-month assessment [health-led FRIENDS 184/374 (49.2%); school-led FRIENDS 165/360 (45.8%); usual school provision 138/295 (46.8%)]. Paired t-tests revealed a significant within-group reduction in total RCADS scores from baseline to 24 months for all children (health-led FRIENDS: t = 9.10, df = 183, p < 0.001; school-led FRIENDS: t = 8.85, df = 164, p < 0.001); usual school provision: t = 7.209, df = 137, p < 0.001). However, there were no between-group effects when baseline to 24-month total RCADS scores were examined.
Objective 6: to examine the effects of the FRIENDS programme on secondary outcomes of self-esteem, worry and overall well-being at 24 months
Table 20 summarises baseline and 24-month scores for the secondary child outcomes of worry, self-esteem and happiness (life satisfaction) and parent-reported anxiety and general behaviour. The results indicate no between-group effects for any outcome.
| Outcome | Health-led FRIENDS, mean (SD) | School-led FRIENDS, mean (SD) | Usual school provision, mean (SD) | p-value overall group effecta | |||
|---|---|---|---|---|---|---|---|
| Baseline | 24 months | Baseline | 24 months | Baseline | 24 months | ||
| Child reported | |||||||
| n | 489 | 212–20 | 472 | 201–6 | 401 | 164–7 | |
| Penn State Worry Questionnaire for Children score | 10.63 (8.14) | 7.08 (6.40) | 10.99 (8.24) | 7.78 (7.01) | 10.46 (8.35) | 7.51 (5.99) | 0.685 |
| Rosenberg Self-Esteem Scale score | 18.94 (5.34) | 21.58 (5.71) | 19.43 (5.39) | 22.75 (5.37) | 19.57 (5.98) | 21.80 (5.35) | 0.218 |
| Total life satisfaction | 14.21 (6.77) | 12.05 (4.50) | 13.32 (5.71) | 11.69 (4.03) | 13.76 (6.82) | 12.26 (4.21) | 0.770 |
| Parent reported | |||||||
| n | 217 | 181–8 | 198 | 184–93 | 152 | 145–7 | |
| Total RCADS score | 12.55 (8.81) | 13.06 (8.60) | 10.99 (8.60) | 11.64 (7.16) | 12.52 (9.34) | 11.28 (7.17) | 0.719 |
| Total SDQ score | 9.09 (6.32) | 8.79 (6.55) | 8.31 (6.28) | 7.42 (5.16) | 9.00 (6.24) | 7.86 (6.20) | 0.161 |
Similarly, there were no between-group differences on the SCQ (health-led FRIENDS 43.67 (SD 25.87); school-led FRIENDS 43.49 (SD 23.94); usual school provision 45.87 (SD 25.12). Although 67 (11.2%) children had not yet transitioned to secondary school, the mean ratings for this group did not differ from those of the group who had transitioned.
Objective 7: to assess the cost-effectiveness of the FRIENDS programme in terms of health-related quality of life (and cost–utility) at 6 months
A total of 308 parents volunteered to be interviewed, with 284 providing data about service usage at both baseline and 6 months. Within this subgroup, 268 had valid child-reported RCADS data at 6 months and 273 had valid CHU-9D-derived QALY data (for 0–6 months). The differences in the baseline characteristics of those supplying service use data (interviewed) and those not interviewed are shown in Table 21.
| Variable | Interviewed (n = 308) | Not interviewed (n = 1054) |
|---|---|---|
| Study arm, n | ||
| 1 | 122 | 367 |
| 2 | 96 | 376 |
| 3 | 90 | 311 |
| Sex, n (%) | ||
| Male | 151 (49.0) | 511 (48.5) |
| Female | 157 (51.0) | 543 (51.5) |
| Family affluence, mean (SD) | 6.12 (1.50) | 6.04 (1.50) |
| Child baseline RCADS score, mean (SD) | ||
| Depression | 4.16 (2.62) | 3.77 (2.55) |
| Separation anxiety | 3.96 (3.34) | 3.87 (3.30) |
| Social anxiety | 5.50 (3.07) | 5.05 (3.31) |
| Generalised anxiety | 6.19 (3.77) | 5.67 (3.74) |
| Panic | 3.29 (3.16) | 2.69 (2.83) |
| OCD | 5.11 (3.37) | 4.37 (3.16) |
| Total anxiety RCADS score | 24.18 (13.73) | 21.49 (13.55) |
| Total RCADS score | 28.35 (15.73) | 25.22 (15.22) |
| Child baseline worries, mean (SD) | 11.90 (8.76) | 10.35 (8.04) |
| Child baseline self-esteem, mean (SD) | 18.96 (5.30) | 19.39 (5.62) |
| Child baseline CHU-9D, mean (SD) | 8.95 (6.60) | 7.61 (6.08) |
| Child baseline total happiness, mean (SD) | 15.02 (7.11) | 13.40 (6.19) |
| n = 306 | n = 254 | |
| Parent baseline RCADS score, mean (SD) | ||
| Depression | 1.85 (1.78) | 1.08 (1.12) |
| Separation anxiety | 2.44 (2.74) | 1.66 (1.97) |
| Social anxiety | 4.70 (2.84) | 3.63 (2.52) |
| Generalised anxiety | 3.20 (2.65) | 2.35 (2.01) |
| Panic | 0.71 (1.35) | 0.41 (0.90) |
| OCD | 1.25 (1.55) | 0.74 (1.26) |
| Total anxiety RCADS score | 12.06 (8.63) | 8.62 (6.33) |
| Total RCADS score | 13.87 (9.82) | 9.71 (6.95) |
| Parent baseline SDQ score, mean (SD) | ||
| Prosocial | 8.06 (1.92) | 8.51 (1.68) |
| Hyperactivity | 3.74 (2.69) | 3.20 (2.31) |
| Emotional symptoms | 2.62 (2.50) | 1.74 (2.06) |
| Conduct problems | 1.77 (1.91) | 1.31 (1.52) |
| Peer problems | 1.75 (1.98) | 1.17 (1.56) |
| Total SDQ score | 9.91 (6.70) | 7.46 (5.47) |
Table 21 highlights that those in the group interviewed for the cost-effectiveness analysis were more symptomatic on child- and parent-reported measures on almost every scale and subscale, including the primary outcome measure (child-reported RCADS: t = 3.07, df = 1279; p = 0.002) and the health-related quality of life measure for deriving utility (child-reported CHU-9D: t = 3.36, df = 1331; p = 0.001).
Intervention costs
The health-led and school-led FRIENDS groups had similar intervention costs of £52.25 and £55.92 per student respectively (Table 22).
| Resource | Health-led FRIENDS (£) | School-led FRIENDS (£) |
|---|---|---|
| Leader training (leaders’ time) | 1197 | 11,572 |
| Leader training (trainers’ time) | 1299 | 1299 |
| Leader manuals (printing) | 159 | 625 |
| Supervision of delivery (receivers’ time) | 2432 | 7232 |
| Supervision of delivery (supervisors’ time) | 1918 | 1918 |
| Supervision travel costs | 0 | 2250 |
| Delivery (teachers’ time) | 0 | 3255 |
| Delivery (facilitators’ time) | 13,468 | 5693 |
| Travel | 9720 | 0 |
| Booklet/printed materials (£4.25 per child) | 2673 | 2784 |
| Total | 32,866 | 36,628 |
| No. of classes in trial arm | 24 | 25 |
| Mean no. of children per participating class (data from 33 schools in the study) | 26.2 | 26.2 |
| Total no. of children | 629 | 655 |
| Mean intervention cost per child | 52.25 | 55.92 |
Although the overall costs are similar, this conceals a different mix of cost components. Having fewer and externally based staff delivering the intervention in the health-led FRIENDS group meant higher travel costs and higher facilitator costs for the actual time delivering the programme (two people per class per session). In contrast, the school-led FRIENDS group needed to train and supervise more people delivering the intervention, at least one per school, but only had to pay for the extra preparation time of teachers, not their classroom intervention delivery time (as this would have already been used as part of PSHE lessons).
Health-care usage
Table 23 shows the very similar health and social care service usage and care costs for the trial arms in the 6 months before and during and after the intervention.
| Resource | Health-led FRIENDS | School-led FRIENDS | Usual school provision | |||
|---|---|---|---|---|---|---|
| No. of children (% of 122) | Mean (SE) cost (£) | No. of children (% of 96) | Mean (SE) cost (£) | No. of children (% of 90) | Mean (SE) cost (£) | |
| Over the 6 months previous to baseline | ||||||
| GP visits | 2 (1.6) | 0.61 (0.43) | 6 (6.2) | 2.70 (1.13) | 4 (4.4) | 2.06 (1.07) |
| Seeing other professionals | 10 (8.2) | 7.02 (4.02) | 15 (15.6) | 6.54 (3.01) | 17 (18.9) | 14.73 (5.22) |
| Total cost of service use | 7.63 (4.04) | 9.24 (3.26) | 16.79 (5.86) | |||
| Resource | No. of children (% of 112) | Mean (SE) cost (£) | No. of children (% of 89) | Mean (SE) cost (£) | No. of children (% of 82) | Mean (SE) cost (£) |
| From baseline to 6 months | ||||||
| GP visits | 2 (1.8) | 1.65 (1.36) | 5 (5.6) | 2.49 (1.15) | 5 (6.1) | 3.61 (1.99) |
| Seeing other professionals | 10 (8.9) | 9.27 (5.36) | 13 (14.6) | 5.88 (3.42) | 14 (17.1) | 12.62 (6.54) |
| Total cost of service use | 10.92 (5.56) | 8.37 (3.65) | 16.23 (7.16) | |||
| Change in cost of service use between the two time periods | +3.29 | –0.87 | –0.56 | |||
Tables 24 and 25 show the incremental costs, RCADS scores and QALYs and incremental cost-effectiveness of the interventions. Incremental analysis compares the gain or loss in effectiveness with the additional costs, or cost savings, for one intervention compared with another.
| Outcome | Health-led FRIENDS, mean (SD)a | Usual school provision, mean (SD)a | Mean difference (95% CI),a adjusted | p-value | ICER (95% CI), adjusted |
|---|---|---|---|---|---|
| Cost (£) | 63.68 (60.2) | 11.19 (44.15) | 52.50 (36.70 to 68.30) | < 0.001 | |
| RCADS score | 25.61 (16.0) | 27.70 (16.7) | –2.56 (–6.20 to 1.08) | 0.49 | 18 (7 to infinity) |
| QALYs | 0.388 (0.057) | 0.390 (0.056) | –0.004 (–0.021 to 0.014) | 0.69 | –14,617 (3407 to –2243) |
| Outcome | Health-led FRIENDS, mean (SD)a | School-led FRIENDS, mean (SD)a | Mean difference (95% CI),a adjusted | p-value | ICER (95% CI), adjusted |
|---|---|---|---|---|---|
| Cost (£) | 63.68 (60.2) | 64.37 (34.82) | 0.041 (–14.01 to 14.09) | 0.995 | |
| RCADS score | 25.61 (16.0) | 23.98 (14.0) | –1.68 (–5.80 to 2.44) | 0.43 | 0 (undefined) |
| QALYs | 0.388 (0.057) | 0.401 (0.051) | –0.015 (–0.031 to 0.002) | 0.08 | –3 (undefined) |
The only statistically significant difference between groups in either costs or effects at 6 months was the cost difference between health-led FRIENDS and usual school provision. Correspondingly, the ICERs have extremely wide uncertainty limits (when they can be calculated). This is clearly depicted by the scatterplots on the cost-effectiveness plane and cost-effectiveness acceptability curves for the two analyses based on QALYs (Figures 2 and 3). Compared with usual school provision, health-led FRIENDS never reaches more than a 35% probability of being cost-effective at any willingness to pay for a QALY.
FIGURE 2.
Cost-effectiveness acceptability curve and scatterplot of health-led FRIENDS vs. usual school provision, QALY outcome, adjusted analysis. (a) Cost-effectiveness plane: health-led FRIENDS vs. usual school provision; and(b) probability that health-led FRIENDS is cost-effective vs. usual school provision. Note that cost differences in GBP and effect differences in QALYs.

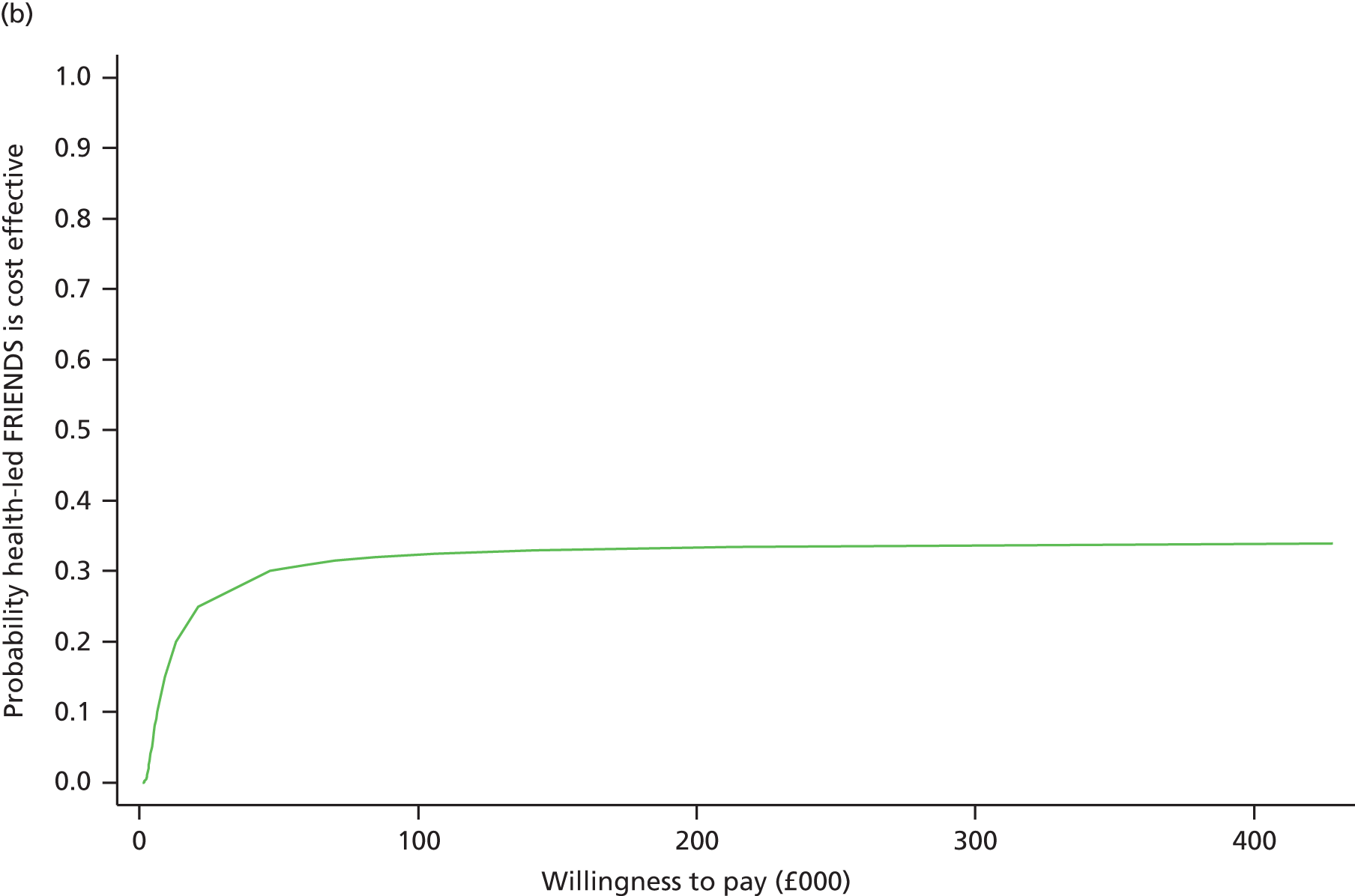
FIGURE 3.
Cost-effectiveness acceptability curve and scatterplot of health-led vs. school-led FRIENDS, QALY outcome, adjusted analysis. (a) Cost-effectiveness plane: health-led FRIENDS vs. school-led FRIENDS; and (b) probability that health-led FRIENDS is cost-effective vs. school-led FRIENDS. Note that cost differences in GBP and effect differences in QALYs.

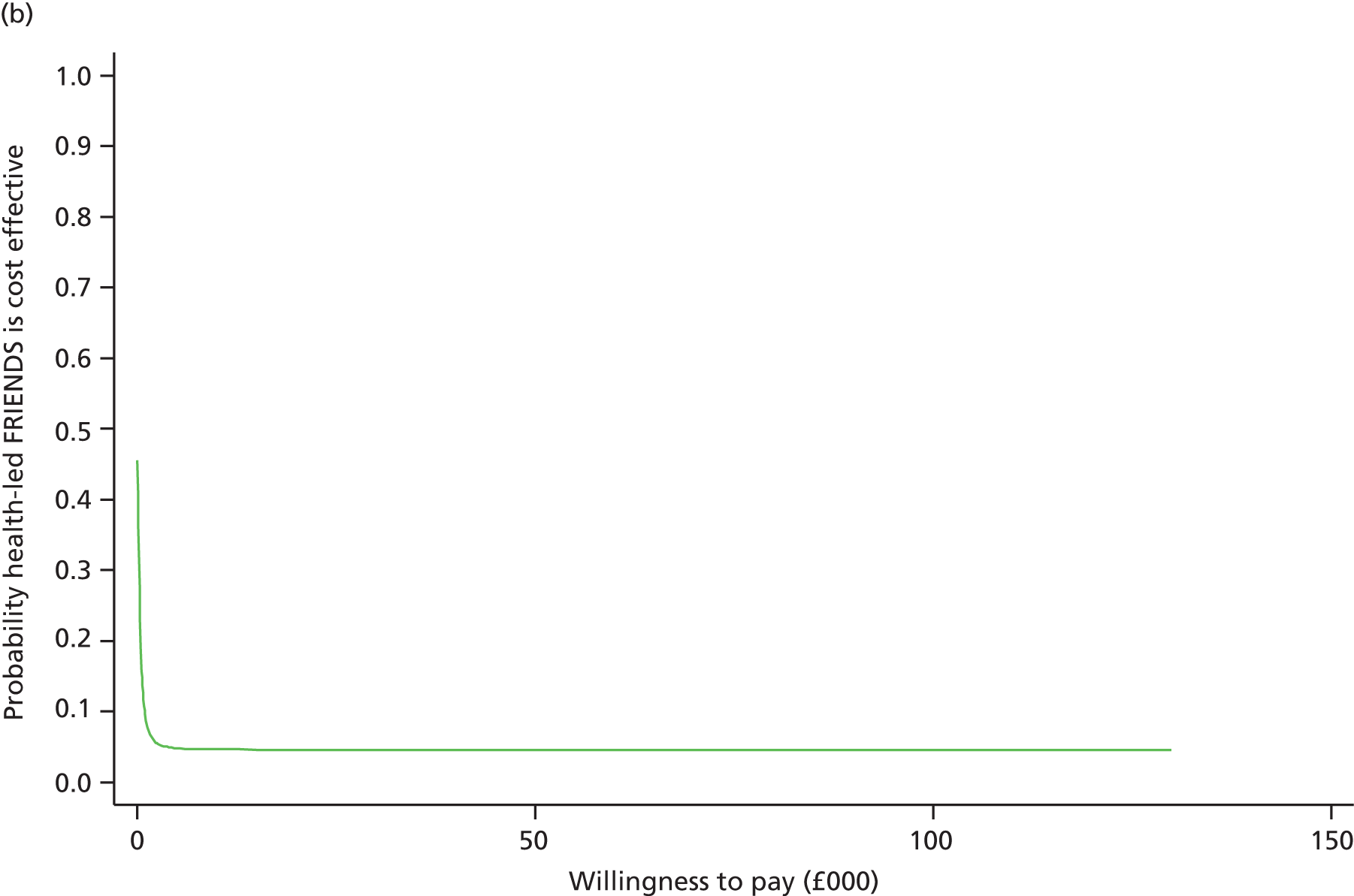
Overall, whether considering the impact on quality of life or on anxiety, the FRIENDS programme is unlikely to be cost-effective, at least over the short term. However, this conclusion needs to be treated with caution as the subgroup used for the economic analysis was different in a number of ways from the total cohort (see Table 21).
We did not conduct an economic evaluation at the 24-month time point. This was because (1) there were no statistically significant between-group effects at 24 months and (2) the interview subsample of parents and their children who supplied resource use data was substantially different from the group of non-interviewed parents/children (see Table 21) and was also smaller again at the 24-month follow-up time point (only 252 parents were interviewed at this follow-up point compared with 308 at baseline).
Sensitivity analysis
In a sensitivity analysis, we combined the cost data from the interview subsample at 6 months with the effectiveness data from the whole trial sample followed up at 6 months. These results are shown in Tables 26 and 27. They show that the uncertainty surrounding the incremental cost-effectiveness estimates is as large as in the base-case analysis using only data from the economic interview subsample. Our conclusion, that the FRIENDS programme is unlikely to be cost-effective, is therefore unaltered.
| Outcome | Health-led FRIENDS, mean (SD)a | Usual school provision, mean (SD)a | Mean difference (95% CI),a adjusted | p-value | ICER (95% CI), adjusted |
|---|---|---|---|---|---|
| Cost (£) | 63.68 (60.2) | 11.19 (44.15) | 52.50 (36.70 to 68.30) | < 0.001 | |
| RCADS score | 22.99 (14.5) | 24.70 (15.8) | –1.71 (–3.59 to 0.17) | 0.07 | –27 (12 to infinity) |
| QALYs | 0.402 (0.054) | 0.401 (0.057) | –0.002 (–0.005 to 0.010) | 0.51 | 20,757 (4635 to –9211) |
| Outcome | Health-led FRIENDS, mean (SD)a | Usual school provision, mean (SD)a | Mean difference (95% CI),a adjusted | p-value | ICER (95% CI), adjusted |
|---|---|---|---|---|---|
| Cost (£) | 63.68 (60.2) | 64.37 (34.82) | 0.041 (–14.01 to 14.09) | 0.995 | |
| RCADS score | 22.99 (14.5) | 24.32 (16.0) | –2.17 (–3.99 to –0.36) | 0.02 | –2 (undefined) |
| QALYs | 0.402 (0.054) | 0.404 (0.05) | < 0.001 (–0.007 to 0.007) | 0.999 | 14,738 (undefined) |
Objective 8: to assess the acceptability of the FRIENDS programme including participant perception of usefulness, examples of ongoing skill usage and satisfaction (6 months)
Evaluation of delivery of the FRIENDS programme
At the end of each FRIENDS session all adults present (i.e. leaders, facilitators, classroom helpers) were asked to rate the session on nine variables. These variables assessed how well the children engaged with the session; how much they participated; whether they were interested; how much they understood; whether they enjoyed the session; whether the session was disrupted by challenging behaviour; whether the session would help the children; how confidently the session was delivered; and whether there was enough support available in the class. Each variable was rated on a 5-point scale (0 = ‘not at all’; 1 = ‘a little’; 2 = ‘somewhat’; 3 = ‘quite a lot’; 4 = ‘a great deal’). For each session, the total number of ratings received ranged from 64 to 89. Average session ratings are summarised in Table 28.
| Session | Children engaged | Children participated | Children interested | Children understood | Children enjoyed | Disruptive behaviour | Helped children | Confident delivery | Support available |
|---|---|---|---|---|---|---|---|---|---|
| Session 1: introduction | 3.34. (0.57) | 3.26 (0.74) | 3.06 (0.68) | 3.16 (0.62) | 3.07 (0.69) | 0.63 (0.88) | 2.26 (0.77) | 3.39 (0.62) | 3.54 (0.51) |
| Session 2: recognition of feeling | 3.29 (0.70) | 3.37 (0.68) | 3.06 (0.67) | 2.84 (0.73) | 2.98 (0.75) | 0.78 (0.99) | 2.59 (0.78) | 3.41 (0.70) | 3.53 (0.53) |
| Session 3: emotional management | 3.21 (0.68) | 3.28 (0.84) | 3.07 (0.81) | 3.09 (0.72) | 3.19 (0.67) | 0.85 (0.95) | 2.74 (0.65) | 3.35 (0.70) | 3.46 (0.66) |
| Session 4: helpful and unhelpful thoughts | 3.23 (0.62) | 3.27 (0.68) | 3.13 (0.69) | 3.15 (0.65) | 2.92 (0,82) | 0.56 (0.89) | 2.94 (0.73) | 3.24 (0.73) | 3.48 (0.59) |
| Session 5: changing thoughts | 2.90 (0.81) | 2.97 (0.78) | 2.78 (0.77) | 2.80 (0.64) | 2.65 (0.80) | 0.65 (0.87) | 2.64 (0.84) | 3.24 (0.77) | 3.37 (0.73) |
| Session 6: problem-solving | 3.41 (0.65) | 3.51 (0.61) | 3.28 (0.67) | 2.93 (0.82) | 3.53 (0.67) | 0.83 (0.99) | 2.82 (0.80) | 3.36 (0.69) | 3.42 (0.72) |
| Session 7: rewards | 2.89 (0.77) | 2.89 (0.87) | 2.76 (0.91) | 2.84 (0.91) | 2.65 (0.99) | 0.89 (1.04) | 2.51 (0.82) | 3.32 (0.73) | 3.47 (0.65) |
| Session 8: practise FRIENDS | 2.91 (0.90) | 2.96 (0.87) | 2.85 (0.91) | 2.98 (0.90) | 2.74 (0.86) | 0.71 (0.90) | 2.71 (0.90) | 3.40 (0.73) | 3.35 (0.79) |
| Session 9: review and celebration | 3.37 (0.77) | 3.46 (0.71) | 3.34 (0.83) | 3.41 (0.67) | 3.48 (0.75) | 0.71 (1.00) | 2.76 (0.87) | 3.57 (0.70) | 3.68 (0.59) |
| Overall average (n = 637–758 ratings) | 3.17 (0.75) | 3.22 (0.76) | 3.03 (0.80) | 3.02 (0.77) | 3.02 (0.84) | 0.74 (0.95) | 2.64 (0.81) | 3.36 (0.71) | 3.34 (0.65) |
Overall, there was little disruptive behaviour and the sessions were rated highly. Children were perceived to be engaged, participated well, were interested, understood and enjoyed the sessions. Sessions were delivered confidently and there was enough support in the class. The lowest rating related to the extent to which the session would be helpful for the children.
End of programme evaluation
At the end of the FRIENDS programme all participating children were asked to evaluate what they thought of the programme and whether it had helped them. A total of 1264 children completed the end of programme survey and the results are summarised in Table 29. The results show high levels of satisfaction: the programme ideas were understood by most participating children, three-quarters rated the programme as fun and 70% felt that they had learned new skills that had helped them. In addition, one-third of children reported that they had used their new skills to help someone else. The area in which children expressed least satisfaction related to time to complete the work, with < 50% feeling that they had sufficient time to complete it.
| Area evaluated | Yes, n (%) | No, n (%) | Not sure, n (%) |
|---|---|---|---|
| Did you understand most of the sessions? | 1045 (83.5) | 49 (3.9) | 158 (12.6) |
| Did you feel safe talking about yourself? | 757 (60.5) | 186 (14.9) | 309 (24.7) |
| Did you feel people listened to you? | 662 (53.1) | 160 (12.8) | 425 (34.1) |
| Was it fun? | 934 (75.0) | 140 (11.2) | 171 (13.7) |
| Do you think it has helped you? | 742 (60.0) | 117 (14.3) | 318 (25.7) |
| Did you learn anything new? | 876 (70.9) | 152 (12.3) | 207 (16.8) |
| Did you have enough time to do the work? | 579 (46.5) | 337 (27.1) | 329 (26.4) |
| Have you helped anyone with your new skills? | 434 (35.0) | 495 (40.0) | 310 (25.0) |
| Have you talked to your family about FRIENDS? | 589 (47.3) | 539 (43.3) | 118 (9.5) |
| Would you recommend it to a friend? | 787 (62.9) | 176 (14.1) | 289 (23.1) |
Qualitative interviews
More detailed qualitative interviews were undertaken with staff (n = 47) from all 28 schools who received the FRIENDS programme. In addition, children (n = 115) from 19 of the 28 FRIENDS schools volunteered to take part in focus groups. These groups were undertaken at school and we recruited children until no new themes were identified. Parents (n = 20) were also randomly selected from a group of 308 who volunteered to take part in detailed interviews and were interviewed individually, mostly at home.
Participants were asked for their overall views about the programme, their most positive and negative experiences, the skills that the children learned, the contribution of the programme to the school PSHE curriculum and how the children had benefited. In addition, parents were asked about any changes in their child’s mood and anxiety, general behaviour, overall confidence, friendships, engagement in out-of-school social and recreational activities and educational progress.
Analysis identified six major themes relating to programme overview; programme content and delivery; the FRIENDS workbook; positive aspects of the programme; programme benefits; and continued use of skills.
Overall, children found the FRIENDS programme to be ‘helpful’ and ‘fun’, with the majority of teachers valuing the conceptual underpinning of the programme and the sequential development of skills:
providing children with the skills and the resilience at this stage, made sense to us and seemed to fit with what we know about teaching year five.
Teacher
I liked the idea of building something step by step each week; there was very obvious progression within it.
Teacher
Children and teachers were particularly positive about the active FRIENDS sessions, with children enjoying the hands-on activities, group work, role plays, creative tasks and games:
I liked the one where you put the book on your head with a piece of paper, you draw with a pencil and you had to draw things without you looking so it was like, you were confident and you could do it.
Child
The amount of time required for the programme was identified as an issue, with children wanting additional or longer sessions and almost half of the teachers wanting fewer or shorter sessions:
the lessons could have been longer so we had more time to do the work book.
Child
The hour was quite a long time to take out of a whole school week, I must admit, um, a 40 minute session would be probably what you’d want to devote to PSHE.
Teacher
Teachers noted an overlap between the skills taught during the FRIENDS sessions and those taught in PSHE classes. However, a number commented that because the FRIENDS programme was more focused and explicit in teaching these skills it usefully complemented PSHE:
there is some overlap but I do not actually mind that. I think these things are good to be done more than once.
Teacher
There were, however, different views from the teachers about how well the FRIENDS programme could be fitted within a busy school timetable:
I think it was enough time to obviously really, kind of, embed their understanding of like the thoughts and things and um, to obviously talk about previous lessons, so I think it was a reasonable amount of time actually.
Teacher
It doesn’t, 9 weeks doesn’t fit into a term at all but . . . I don’t think there is anything you could take out of the programme to make it, make it fit.
Teacher
Overall, children and teachers were positive about the workbook, finding it helpful and attractive:
I really liked the workbooks, how they explained things in not really complicated detail, and pictures were really good in them as well.
Child
However, many teachers felt that there was too much reading and writing in the workbook, which sometimes distracted the children from actively participating in discussions:
I think sometimes the children found that the booklet a little bit difficult . . . they didn’t really express what they were feeling in the booklet. And for some of the children, the actual writing of the booklet was really hard.
Teacher
Children particularly liked the sessions that focused on problem-solving, with teachers and children commenting positively about the relaxation exercises:
I think some of the activities in the groups that we had to get the balloon across the classroom, they were quite good because you got to construct a thing and you get to work as a team and I found that quite helpful, to let us work as a team and share our ideas.
Child
I think that the relaxation part of it . . . the children particularly liked.
Teacher
Overall, teachers felt that the most positive skill that the children learned was the ‘red and green thoughts’, a way of describing negative and unhelpful ways of thinking, which increase anxiety (red thoughts), and positive, helpful ways of thinking, which reduce anxiety (green thoughts):
they’ve really taken that on board, I think it was really visual and I think it was really clear to them what they were and they were identifying them.
Teacher
Children identified improvements in emotional awareness and management and peer relationships:
It’s helped me to control my feelings and my sister annoys me and I’ve learned how to control not getting angry with her.
Child
Because it helped me work with some people who I didn’t normally work with it helped me realise how different people react to different situations.
Child
Teachers also noted improvements in emotional literacy and the children’s ability to deal with challenging and worrying situations. However, almost half of the teachers could not identify any particular changes in the children’s behaviour:
Whether or not that’s had any long lasting impact, I think is doubtful.
Teacher
Parents had limited direct knowledge of the programme. Although participating schools were asked to run a parent session to explain the FRIENDS programme, only 15 of the 28 schools arranged a parent session. These were very poorly attended, with around 10% of parents attending.
Parents had observed an increase in their child’s confidence and a general sense of being calmer. However, they did not attribute this to the FRIENDS programme but to changes in development and increased maturity:
His confidence has improved and now he doesn’t take any more that he has to, he’ll walk away from situations. The other day there was somebody saying something to him and he just went ‘whatever’ and walked away. Whereas before he would have come home and probably burst into tears.
Parent
She’s calmer; she seems more in control of her feelings . . . When she does have a fall out with friends or someone’s nasty to her . . . she copes with it a lot better now.
Parent
I’d sort of put it down to hormones.
Parent
Children and teachers identified a number of examples of ongoing skill usage in which the FRIENDS programme had been applied to everyday problems:
it helped me overcome my fear of getting in the water, ‘cause now I can swim 5 metres.
Child
my cousin was feeling a bit grumpy a couple of weeks ago and I just, I just knew by the way she was just looking, I just knew that OK I’d better give her some space.
Child
There was also evidence of some vicarious effects whereby siblings, peers, parents and teachers benefited from the FRIENDS programme. Children reported sharing skills with family and friends, for example relaxation, problem-solving and thought challenging, and found this useful:
Sometimes my Mum gets angry and I say in my head my mum’s thinking red thoughts and then I say to her, can you think a green thought.
Child
Teachers also commented that they had found the programme beneficial for themselves. They reported having learnt a lot about emotional health (language and skills) for their own personal development, as well as gaining more emotional insight into the children:
it’s given me a strategy to know how to help them, rather than just saying ‘oh, sit down, yeah, you’re fine, you’re fine, it’ll be OK’.
Teacher
Chapter 4 Discussion
Principal findings
This is the first large pragmatic randomised trial undertaken in the UK comparing a universally provided classroom-based CBT anxiety prevention programme (FRIENDS) led by health and school staff with usual school provision. At 12 months we assessed 92.3% of those who completed our baseline assessments. There were no baseline differences in anxiety and only one difference between our groups (sex), which was controlled for in all subsequent analyses. In view of this we feel confident in our findings, which show that, at 12 months, when transported to everyday settings, health-led FRIENDS was effective in reducing child-reported symptoms of anxiety compared with school-led FRIENDS or usual school provision. Children with high anxiety levels in each group showed reductions in anxiety symptoms over time although the effect for health-led FRIENDS was particularly evident in the low-anxiety group.
The overall completion rate for the 24-month assessment was low (43.6%) although there were few differences in baseline characteristics between completers and non-completers. By 24 months, child-reported anxiety in all three groups had reduced. There were no longer any between-group effects on total anxiety for the whole sample or in the low- or high-anxiety subgroups. Similarly, there were no between-group effects on any of the child- or parent-reported secondary outcomes.
The FRIENDS programme was accommodated within primary school timetables with all nine sessions being delivered to all participating schools. Intervention fidelity was good and the qualitative evaluation indicated that the FRIENDS programme was acceptable to teachers and children, who found the programme enjoyable and useful. The qualitative evaluation also found evidence of ongoing skill usage and a ripple effect whereby those who were not the direct target of the intervention benefited from the programme.
The cost of delivering the 9-week FRIENDS programme was £52–56 per child. Determining cost-effectiveness was difficult as the subgroup who volunteered for the economic analysis was not representative of the total cohort on key baseline assessments and health service use over a 12-month period was low. Although our results do not provide evidence of the cost-effectiveness of the FRIENDS programme over the short term, this conclusion should be treated with considerable caution.
Intervention leader
Our results indicate that outcomes depended on who delivered the programme. Despite intervention leaders in the school- and health-led FRIENDS groups receiving the same initial training and following a manualised programme, school leaders achieved smaller reductions than health leaders in child-reported anxiety at 12 months. Only one previous study has directly compared the FRIENDS programme led by trained psychologists with the FRIENDS programme led by school staff;21 although both leaders were effective the study lacked statistical power. Our study was appropriately powered and is consistent with a review in which the intervention leader was found to moderate programme effectiveness. 29 Our findings are also consistent with other implementation trials in which teacher-led FRIENDS was not found to be effective. 26,27 Although training teachers to deliver mental health prevention programmes offers a way of increasing anxiety awareness and embedding anxiety management skills within schools, our results suggest that this approach is not as effective, in the short term, as programme delivery by health professionals. Further exploration identified three potentially important differences between health and school leaders.
First, although programme fidelity was high, the home assignment was not undertaken in 40% of the school-led sessions that were assessed. Ongoing practice of newly acquired skills is an integral part of CBT programmes and the absence of this may have compromised the effectiveness of session leaders who were new to this approach. 79 However, this possibility needs to be balanced against the increased opportunities for class teachers to integrate and consolidate programme skills more intensively through their daily contact with children.
Second, although both groups had the same initial training, comparatively few teachers attended ongoing supervision, a key aspect of effective training in CBT. 80 Although teachers will be competent in some of the areas addressed in supervision, such as classroom management and engaging children of differing abilities, they will be less familiar with the underlying cognitive model. Limited ongoing opportunities to consolidate the theoretical model, share good practice, discuss challenging issues and refine skills may therefore have compromised programme delivery in the school-led group.
A further possible difference, which we did not assess in this study, was the manner in which the programme was delivered. The majority of school leaders delivered the programme only once and so were less familiar with the materials. Health leaders delivered more sessions and may have developed a more thorough understanding of the materials and become more confident and enthusiastic in their delivery. These factors have been noted as potentially important in systematic reviews and need to be assessed in future studies. 20
Although our results suggest that, in the short term, the FRIENDS programme should be led by health providers, it is possible that school staff could become more effective with additional training, practice and supervision. Further training in the cognitive model may help to develop a greater understanding of the theoretical underpinning of the programme and the subtleties of the techniques and skills taught. The importance of and rationale for home-based practice could be highlighted and inducements to attend supervision sessions might improve short-term outcomes for the school-led condition. However, this will increase delivery costs and so the relative effectiveness and costs associated with health- and school-led models of delivery need to be carefully detailed and assessed. This is important as it is often assumed that it will be cheaper and more sustainable to train and support school staff to deliver emotional health prevention programmes. Our findings suggest that this may not be the case and raises a key question about how these programmes would be funded if they are rolled out across the UK.
Universal delivery
The FRIENDS programme was delivered as a universal intervention to all 9- to 10-year-old children in participating classes. Children classified as having high and low anxiety on the basis of baseline assessments showed significant reductions in anxiety symptoms over time. There were no group effects for the high-anxiety children, although numbers were small and our study was not powered to compare between-arm differences within this subgroup. The absence of between-group effects may therefore be a power issue or alternatively may reflect regression to the mean. This issue needs to be clarified in further suitably powered studies with highly anxious children.
Our study was, however, sufficiently powered to detect differences within the low-anxiety group. We found a marked between-group reduction in favour of the health-led FRIENDS group at 12 months. Although this reduction in symptomatology was maintained at 24 months, all groups improved over time and there were no longer any between-group effects. This result is promising and suggests that universally delivered anxiety prevention programmes may result in a faster reduction in anxiety symptoms, which is maintained over time. However, our study was not able to demonstrate a primary preventative effect as we were not able to assess changes in rates of emerging anxiety disorders. This would have been very time-consuming and expensive, requiring diagnostic interviews, which could potentially be stigmatising and unacceptable within a community population. 3 Nonetheless, our study does support the use of universal anxiety prevention programmes and highlights that both high- and low-anxiety children show reductions in anxiety symptomatology at 12 months, which are maintained at 24 months. Given that fears, anxiety and stress are common in children, anxiety prevention programmes may be particularly suited to universal delivery. 29 Furthermore, universal approaches are less stigmatising and can be better accommodated within school timetables.
Programme effects
Our study found a significant effect on our primary outcome of anxiety in the health-led FRIENDS groups at 12 months. There were no between-group differences for any secondary outcome suggesting that the intervention effects were specific to anxiety. The FRIENDS programme is designed as an anxiety prevention programme and specifically develops skills known to reduce anxiety, that is, anxiety awareness and management, replacing anxiety-increasing cognitions and reducing avoidance. The specific effect that we found is therefore consistent with the underlying theoretical model and programme focus. However, given the comorbidity between anxiety and depressive disorders and the shared elements of many CBT programmes, this absence of a positive effect on depressive symptoms, worries, self-esteem and reported bullying is disappointing. 81 Although positive effects had been noted in our previous uncontrolled studies,35–37 these effects do not appear robust compared with treatment as usual. The results of this trial suggest that, although anxiety prevention programmes may have a positive effect on anxiety symptoms, they cannot be assumed to enhance the general emotional well-being of children.
The effect was also specific to child report as although parent and teacher ratings of symptomatology reduced over time there were no between-group differences. These findings may suggest a greater change in internal, anxious distress rather than in observable, anxiety-related behaviours. Changes such as these would be less likely to be identified by the SDQ, which is better at detecting behavioural rather than emotional disorders. Our results therefore highlight the difficulty of assessing changes in internal emotional symptoms and cognitions that are not directly observable by parents or teachers.
Other possible explanations include the low parental reponse rate, the lack of sensitivity of our measures and/or floor effects. The response rate for parent-completed baseline questionnaires was only 42% and as such our findings may not be representative of the total cohort. The teacher assessment involved a global rating and as such may be insensitive to specific changes in anxiety symptoms.
Further evidence that the quantitative measures did not capture changes in symptoms and behaviour is provided by the qualitative analysis. Although our qualitative data were obtained from a small, self-selected sample, all parents interviewed noted improvements in their child’s confidence, a variable that was not directly assessed by our structured questionnaires. However, parents attributed this change to increased maturity and there is some evidence from community surveys to suggest that anxiety does reduce in early adolescence. For example, using our main outcome measure (RCADS), a study of a community cohort in the Netherlands found a natural reduction in anxiety between the ages of 10 and 12 years. 82 The possibility of a naturally occurring decrease in anxiety symptoms in our cohort needs to be acknowledged, although the average total size of our reduction (9–10 points) is double that found in a general population over a similar time frame (4 points). 82
Finally, baseline symptom levels in this predominantly subclinical sample were relatively low. This will result in floor effects, which will make it difficult to detect any small but important changes in symptomatology.
Cognitive–behavioural therapy in the classroom
The FRIENDS programme is based on CBT, a model and psychotherapeutic approach that is typically used to treat mental health disorders. When providing school-based universal emotional health programmes the majority of children will be healthy and will not require treatment. It would be inappropriate to provide individual treatment in a classroom context where personal information would be publicly shared. It is therefore important to emphasise that the aim of the FRIENDS programme in this study was not to provide treatment but to use the CBT framework to help children develop emotional, cognitive and behavioural skills that they can then apply to everyday life. Developing ‘skills for life’ within the school context fits with the recognition that schools are not just concerned with developing academic skills but also have an important role in enhancing the emotional development of children. 13,83
Our qualitative analysis highlighted how teachers valued the underlying CBT model, commenting that the logical and sequential structure of the programme facilitated the gradual introduction and learning of new skills. Skills from all three core elements of the CBT model (e.g. cognitive, emotional and behavioural) were highlighted as valuable. Children particularly commented on the behavioural (coping step plan and problem-solving) and emotional (relaxation techniques) elements whereas teachers were particularly positive about the cognitive (‘red and green thoughts’) and emotional (relaxation techniques) elements. Although many teachers felt that the skills being taught in the FRIENDS programme were similar to those that children would be learning through their usual classes, a number felt that the CBT model provided a more focused approach that complemented the usual classes well.
Fit with schools
The FRIENDS programme was successfully accommodated within the timetables of our primary schools, with all nine sessions being delivered to participating classes. In primary schools there is less competing pressure on academic activities and so the delivery of emotional health prevention programmes is easier than in secondary schools. For example, in a previous study evaluating a universal depression prevention programme in secondary schools, we experienced regular requests to reduce the length of the nine-session intervention and in some schools had to shorten the programme. 84 The amount of time required to deliver the programme was nonetheless identified as an issue, particularly by teachers. Children wanted more or longer sessions whereas teachers were divided in their views. Some felt that nine sessions were not enough whereas others felt that the programme content could be compacted and delivered in fewer sessions.
In addition to securing dedicated time to focus on pupil well-being and emotional health, primary schools are facing significant financial challenges, which will impact on their ability to maintain this focus. Although the health-led FRIENDS programme resulted in quicker reductions in anxiety, the staff resources required were higher than those typically available for usual PSHE in schools. The delivery method that we evaluated involved having three people in the classroom for the FRIENDS programme compared with the single teacher who typically delivers PSHE. The education sector has been subject to significant cuts, with central funding for some well-being initiatives such as the National Healthy Schools Programme and SEAL ceasing and PSHE being removed from the statutory national curriculum. 85,86 Although the costs of delivering the nine-session FRIENDS programme are comparatively reasonable (i.e. £52–56 per child), this nonetheless represents a significant financial commitment for schools with limited funds. Thus, although schools offer a convenient location for delivering mental health programmes, primary schools will continue to have many competing demands for their limited time and resources, which will limit their ability to take up and implement prevention programmes such as this.
The above pressures also highlight a key challenge for school-based emotional health prevention, namely the need to ensure flexibility to adapt the programme to the local situation, balanced against the need to maintain programme fidelity. This is a particular issue if school staff are trained to lead the programme. They will be more directly and readily influenced by competing demands and pressures from within the school, which may result in the programme being more prone to adaptation and fidelity being compromised. With external (health) leaders there is a degree of external scrutiny and accountability. The programme would need to be contracted with the school and the number of sessions agreed so that session cancellation would therefore be harder. The health leaders would inevitably be delivering the programme in a number of schools, potentially increasing programme familiarity and fidelity.
A further consideration, likely to influence uptake and fit within schools, is the effect of emotional health prevention programmes on academic outcomes. Emotional health prevention programmes typically focus on mental and psychological outcomes and little attention has been paid to the effect on educational attainment. The primary goal of schools is to improve learning and as such they will be more interested in adopting emotional health programmes if they benefit educational attainment as well as psychological well-being.
Cost-effectiveness
Our study raises a number of questions about economic evaluations of universal mental health prevention programmes for children. Although anxiety disorders are relatively common, they tend to be poorly identified and comparatively few children receive treatment. 16,17 With poor identification, service usage amongst those with anxiety disorders will be low. Furthermore, in universal trials the majority of children will be healthy and therefore will not need to use health services. Therefore, potential savings from trials of universal interventions, where the target condition is of low frequency and service use limited, will be hard to identify. With indicated anxiety prevention programmes, which are delivered only to those identified with the condition, the benefits are easier to demonstrate, with a recent evaluation demonstrating that a targeted approach is cost-effective. 87
In view of the low service usage and the fact that the intervention was primarily aimed to prevent rather than treat existing low mood and anxiety, a time frame longer than the 6 months that we used to capture pre and post intervention service use may be required to accurately capture potential changes in outcomes and related health service use. Similarly, cost-effectiveness analyses of universal approaches need to include a wider range of potential resources other than the typical focus on health and social care resources. These include education service usage, parental productivity loss and loss of child’s leisure time, factors that we did not assess in our current study.
Although service use data were not collected at 12 months’ follow-up, the main trial had estimated a statistically significant effect on the trial’s primary outcome, RCADS, at this time point. In a speculative analysis it is possible to compare this favourable effect (–2.66, 95% CI –5.22 to –0.09; p = 0.009) with the cost of delivering the health-led FRIENDS programme compared with usual school provision. This implies an ICER of £20 per point reduction in RCADS score. As with all such cost-effectiveness estimates in relation to clinical outcome scores, it is impossible to know whether this represents good value for money.
Although the estimated mean QALY gain at 12 months’ follow-up was very small and imprecise (0.0093, 95% CI –0.007 to 0.026; p = 0.265), this would imply an ICER of £5600 per QALY gained. If the mean additional cost of the intervention is £52, then the lowest mean QALY gain required for the ICER to be < £30,000 per QALY (the current policy-making threshold of affordability for the NHS in England) is 0.0017. If such small mean gains could be demonstrated with greater precision then relatively cheap group-delivered programmes such as the FRIENDS programme are more likely to be judged as cost-effective without assuming downstream savings from any improvements in mental health.
Strengths and limitations
Our study has many strengths. We used a manualised anxiety prevention programme that has proved efficacious and has been piloted in UK schools. 29,35–37 We had a large and appropriately powered cohort, recruitment and retention at 12 months were high, absenteeism was low and programme fidelity was good. However, our study does have a number of limitations.
First, children were not blind to the intervention that they received. We relied on child-completed self-report measures and did not undertake any diagnostic interviews. Although anxiety symptoms were reduced in our health-led FRIENDS group at 12 months, it is unclear whether this reflected changes in diagnostic status or impairment. Similarly, it is unclear whether this statistically significant change in symptom score reflects clincally important changes in everyday functioning.
Second, although our study included a representative sample of UK schools, our cohort was less disadvantaged and had more white British participants than the average UK state school. It is therefore unclear whether similar results would be obtained with a more disadvantaged or ethnically diverse population. Although our schools were well matched on a number of objective dimensions, there could be differences in more subjective factors such as school culture and ethos, which we did not comprehensively assess.
Third, although the health- and school-led FRIENDS facilitators had the same initial training, the health-led group had lower levels of anxiety at 12 months. This suggests that a manualised programme may result in different outcomes depending on who delivers it. Exploring reasons for this are important and, although our study assessed content fidelity, that is, the number of core tasks delivered, we did not assess how they were delivered. Health leaders may therefore have been more familiar with the materials and more enthusiastic in their delivery than school leaders. Additionally, although our qualitative analysis included the views of children, parents and school staff, we did not directly assess the views of the health leaders. It is therefore unclear why health leaders were more effective at 12 months or whether, with additional input, teachers could become more effective at delivering the FRIENDS programme.
Fourth, although recruitment and retention were very high at 12 months, we were able to assess only 43.6% of our cohort at 24 months. This is disappointing but understandable given that this assessment occurred after our cohort transitioned to secondary school and we had to initiate a new recruitment and consent process. All parent contact was made through schools as we did not have direct access to the home details of our study participants. We are therefore unclear whether our poor uptake was because information was not being passed by the schools to parents or because parents were actively refusing to consent. Although there were few differences between 24-month completers and 24-month non-completers on baseline variables, with such a low response rate our 24-month data will lack statistical power and need to be treated with appropriate caution.
Our qualitative evaluation provides additional data to complement our quantitative results and is the first to assess the views of children, teachers and parents. We used a robust qualitative methodology for data collection, analysis and reporting and data were obtained from a large sample, allowing saturation of dominant themes. However, the children who participated in our qualitative interviews were self-selected and, as such, may be more vocal, confident and positively disposed to the FRIENDS programme. Similarly, the parents who we interviewed were selected from a subgroup of more engaged parents who volunteered for additional interviews. These parents may therefore have been more motivated and engaged with our project and their views may be different from those of the wider population.
Finally, our cost-effectiveness analysis was carried out according to current best practice for conducting economic evaluation alongside randomised trials. 71–74 However, data for the economic analysis were obtained from a subgroup of our cohort by retrospective recall rather than using real-time diaries or service/practitioner records. Our subsequent analysis identified that, although we had a large sample, at baseline this group was not representative of our whole cohort on a number of factors, including our primary anxiety (RCADS) and utility (CHU-9D) outcomes. We are therefore not confident that the cost-effectiveness and service use data are representative of our full cohort.
Chapter 5 Conclusions
Main findings
-
Our study suggests that a school-based anxiety prevention programme informed by CBT (FRIENDS) is effective in the short term when transported to everyday schools. The programme had good acceptability and was delivered with fidelity although teachers were unsure about the amount of time (9 hours) needed for the programme.
-
Effectiveness depends on who delivers the programme, with school leaders being less effective than health leaders.
-
At 24 months’ follow-up anxiety had reduced across all trial arms although significant reductions were achieved more quickly in the health-led FRIENDS group. In this group anxiety symptoms had reduced by 12 months and were maintained at 24 months.
-
The effects were specific to anxiety and were observed only for child-completed measures. Although parents and teachers reported a number of more general improvements during the qualitative interviews, these were not reflected in the standardised assessments that we used. Anxiety prevention programmes cannot therefore be assumed to enhance the general emotional well-being of children.
-
Fears, anxiety and stress are common in children and our study suggests that anxiety prevention programmes may be particularly suited to universal delivery. At 12 months there was evidence that the FRIENDS programme particularly benefited children with low levels of anxiety.
-
We were unable to assess the cost-effectiveness of the FRIENDS programme. Although our sample for the economic analysis was large, it was more symptomatic and differed from our full cohort on almost every measure. However, health service usage within this predominantly healthy group was low. It is therefore not possible to conclude whether the level and certainty of the additional effectiveness gains in terms of RCADs score would warrant the additional costs of providing the intervention in schools.
Implications
The FRIENDS anxiety prevention programme is acceptable to children and school staff and can be implemented with good fidelity in primary schools. Short-term effectiveness depended on who delivered the programme, with quicker reductions in anxiety occurring when the FRIENDS programme was delivered by health leaders. Children with low levels of anxiety benefited from the programme, suggesting that a universal delivery approach may be beneficial in terms of primary as well as secondary prevention. Although the cost-effectiveness and longer-term benefits of the programme need to be demonstrated, our results suggest that universal delivery will result in significant costs that may be beyond the finances available to most schools.
Research recommendations
Our study raises a number of questions for future research.
-
Although using the same programme, school leaders were less effective than health leaders. Further research should explore potential programme moderators such as delivery variables (e.g. leader confidence, understanding of CBT and enthusiasm), school factors (e.g. school ethos and commitment to emotional health) and student variables (e.g. sex, motivation and disruption).
-
Given the pressures on school time and the concerns of teachers about the length of the programme, identifying the core ‘active ingredients’ and exploring how these can be delivered to maximise engagement and use time allocated effectively would be helpful.
-
Although children with high levels of anxiety showed reduced symptoms our sample was not sufficiently large to reliably determine whether there were between-group differences in this subgroup. The effectiveness of the FRIENDS programme delivered as a universal intervention for high-anxiety children needs to be investigated.
-
Our cohort consisted of predominantly white British children and was less disadvantaged than the UK population as a whole. The effectiveness of anxiety prevention programmes based on CBT needs to be demonstrated with more ethnically diverse and disadvantaged children and with those who have additional leaning needs.
-
The cost-effectiveness of universal anxiety prevention programmes needs to be determined. Given the low service usage that we found, cost-effectiveness needs to be assessed over a longer time frame and should capture a wide range of resources including health, social care and educational resources and impacts on parental productivity.
-
The effect of emotional health prevention programmes on academic outcomes needs to be investigated.
-
Future studies should define more clearly the content of interventions received by comparison groups. This will determine any differences and overlaps between the content of usual school classes and the content of active interventions.
Acknowledgements
This study was funded by the National Institute for Health Research Public Health Research programme (09/3000/03). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Department of Health.
The authors would like to thank the schools and students who participated in this project and the facilitators who helped with intervention delivery. We would like to thank the research team: Lucy Georgiou, Ellen Cook, Esther Mugweni, Charlotte Mcleod, Sarah Rook, Danielle Byrne, Joanna Morris, Nichola Harkin, Sarah Sedman and Karen Spillard. We are grateful to Professor Paula Barrett who developed the FRIENDS programme. We would also like to acknowledge the support and guidance of the Trial Steering Committee and Data Monitoring and Ethics Committee and in particular their respective chairs, Professor Alan Emond and Professor Tamsin Ford. Finally, we would like to thank the reviewers of this report for their helpful and thoughtful suggestions.
Contribution of authors
All authors had access to all study data and participated in interpretation of the findings, contributed core ideas and were involved in critically revising the paper for important intellectual content. All authors read and agreed the final report.
Paul Stallard (Professor of Child and Family Mental Health) was the chief investigator on the study and took overall responsibility for the study and the writing of the report.
Elena Skryabina (Research Fellow) was the trial manager and contributed to the design of the 24-month follow-up and led the qualitative analysis.
Gordon Taylor (Reader in Medical Statistics) contributed to the design of the study and undertook the statistical analysis.
Rob Anderson (Associate Professor of Health Economics and Evaluation) contributed to the design of the study and led the cost-effectiveness analysis.
Obioha C Ukoumunne (Senior Lecturer in Medical Statistics) undertook the analysis of costs and cost-effectiveness.
Harry Daniels (Professor of Education) contributed to the design of the study and advised on educational issues.
Rhiannon Phillips (Research Fellow) contributed to the design of the study and advised on the qualitative analysis.
Neil Simpson (Consultant Paediatrician) contributed to the design of the study and advised on intervention delivery.
Publications
Stallard P, Taylor G, Anderson R, Daniels H, Simpson N, Phillips R, et al. School based intervention to reduce anxiety in children: study protocol for a randomised controlled trial (PACES). Trials 2012;13:227.
Stallard P, Skryabina E, Taylor G, Phillips R, Daniels H, Anderson R, et al. Classroom-based cognitive behaviour therapy (FRIENDS): a cluster randomised controlled trial to Prevent Anxiety in Children through Education in Schools (PACES). Lancet Psychiatry 2014;1:185–92.
Stallard P, Taylor G, Anderson R, Daniels H, Simpson N, Phillips R, et al. The prevention of anxiety in children through school based interventions: study protocol for a 24 month follow-up of the PACES project. Trials 2014;15:77.
Data sharing statement
The project data archive can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Costello EJ, Mustillo S, ErkanI A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 2003;60:837-44. http://dx.doi.org/10.1001/archpsyc.60.8.837.
- Ford T, Goodman R, Meltzer M. Service use over 18 months among a nationally representative sample of British children with psychiatric disorder. Clin Child Psychol Psychiatry 2003;8:37-51. http://dx.doi.org/10.1177/1359104503008001006.
- Garber J, Weersing VR. Comorbidity of anxiety and depression in youth: implications for treatment and prevention. Clin Psychol Sci Pract 2010;17:293-306. http://dx.doi.org/10.1111/j.1468-2850.2010.01221.x.
- Essau CA, Conradt J, Petermann F. Frequency, comorbidity, and psychological impairment of anxiety disorders in German adolescents. J Anxiety Disord 2000;14:263-79. http://dx.doi.org/10.1016/S0887-6185(99)00039-0.
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry 2003;60:709-17. http://dx.doi.org/10.1001/archpsyc.60.7.709.
- Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry 2001;40:1086-93. http://dx.doi.org/10.1097/00004583-200109000-00018.
- Bittner A, Egger HL, Erkanli A, Costello EJ, Foley DL, Angold A. What do childhood anxiety disorders predict?. J Child Psychol Psychiatry 2007;48:1174-83. http://dx.doi.org/10.1111/j.1469-7610.2007.01812.x.
- Kieling C, Baker-Henningham H, Belfer M, Conti G, Erterm I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet 2011;378:1515-25. http://dx.doi.org/10.1016/S0140-6736(11)60827-1.
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS. Grand challenges in global mental health. Nature 2011;475:27-30. http://dx.doi.org/10.1038/475027a.
- Snell T, Knapp M, Healey A, Guglani S, Evans-Lacko S, Fernandez JL, et al. Economic impact of childhood psychiatric disorder on public sector services in Britain: estimates from national survey data. J Child Psychol Psychiatry 2013;54:977-85. http://dx.doi.org/10.1111/jcpp.12055.
- The National Service Framework for Children, Young People and Maternity Services. London: HMSO; 2004.
- Every Child Matters: Change For Children. London: Department for Education and Skills Publications; 2004.
- Excellence and Enjoyment: Social and Emotional Aspects of Learning. Guidance. London: Department of Education and Skills; 2005.
- James AC, James G, Cowdrey FA, Soler A, Choke A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev 2013;6. http://dx.doi.org/10.1002/14651858.cd004690.pub3.
- Reynolds S, Wilson C, Austin J, Hooper L. Effects of psychotherapy for anxiety in children and adolescents: a meta-analytic review. Clin Psychol Rev 2012;32:251-62. http://dx.doi.org/10.1016/j.cpr.2012.01.005.
- Ford T, Hamilton H, Meltzer H, Goodman R. Predictors of service use for mental health problems among British school children. Child Adolesc Ment Health 2008;13:32-40. http://dx.doi.org/10.1111/j.1475-3588.2007.00449.x.
- Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics 2010;125:75-81. http://dx.doi.org/10.1542/peds.2008-2598.
- Adi Y, Killoran A, Janmohamed K, Stewart-Brown S. Systematic Review of the Effectiveness of Interventions to Promote Mental Wellbeing in Children in Primary Education. Report 1: Universal Approaches (Non-Violence Related Outcomes). London: NICE; 2007.
- Shucksmith J, Summerbel C, Jones S, Whittaker V. Mental Wellbeing of Children in Primary Education (Targeted/Indicated Activities). London: NICE; 2007.
- Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin Psychol Rev 2009;29:208-15. http://dx.doi.org/10.1016/j.cpr.2009.01.002.
- Barrett P, Turner C. Prevention of anxiety symptoms in primary school children: preliminary results from a universal school-based trial. Br J Clin Psychol 2001;40:399-410. http://dx.doi.org/10.1348/014466501163887.
- Araya R, Fritsch R, Spears M, Rojas G, Martinez V, Barroilhet S, et al. School intervention to improve mental health of students in Santiago, Chile: a randomized controlled trial. JAMA Pediatr 2013;167:1004-10. http://dx.doi.org/10.1001/jamapediatrics.2013.2361.
- Challen AR, Machin SJ, Gillham JE. The UK Resilience Programme: a school-based universal nonrandomized pragmatic controlled trial. J Consult Clin Psychol 2014;82:75-89. http://dx.doi.org/10.1037/a0034854.
- Stallard P, Sayal K, Phillips R, Taylor JA, Spears M, Anderson R, et al. Classroom based cognitive behaviour therapy in reducing symptoms of depression in high risk adolescents: pragmatic randomised controlled trial. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e6058.
- Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, et al. School-based prevention of depression: a randomised controlled trial of the beyond blue initiative. J Child Psychol Psychiatry 2006;74:401-15.
- Miller LD, Laye-Gindhu A, Liu Y, March JS, Thordarson DS, Garland EJ. Evaluation of a preventive intervention for child anxiety in two randomized attention-control school trials. Behav Res Ther 2011;49:315-23. http://dx.doi.org/10.1016/j.brat.2011.02.006.
- Miller LD, Laye-Gindhu A, Bennett JL, Liu Y, Gold S, March JS, et al. An effectiveness study of a culturally enriched school-based CBT anxiety prevention program. J Clin Child Adolesc Psychol 2011;40:618-29. http://dx.doi.org/10.1080/15374416.2011.581619.
- Humphrey N, Kalambouka A, Bolton J, Lendrum A, Wigelsworth M, Lennie C, et al. Primary Social and Emotional Aspects of Learning (SEAL) – Evaluation of Small Group Work. Manchester: Department for Children, Schools and Families; 2008.
- Fisak BJ, Richard D, Mann A. The prevention of child and adolescent anxiety: a meta-analytic review. Prev Sci 2011;12:255-68. http://dx.doi.org/10.1007/s11121-011-0210-0.
- Prevention of Mental Disorders: Effective Interventions and Policy Options. Geneva: WHO; 2004.
- Lowry-Webster H, Barrett P, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: preliminary data from an Australian study. Behav Change 2001;18:36-50. http://dx.doi.org/10.1375/bech.18.1.36.
- Lowry-Webster H, Barrett P, Lock S. A universal prevention trial of anxiety symptomatology during childhood: results at one-year follow-up. Behav Change 2003;20:25-43. http://dx.doi.org/10.1375/bech.20.1.25.24843.
- Barrett PM, Farrell LJ, Ollendick TH, Dadds M. Long-term outcomes of an Australian universal prevention trial of anxiety and depression symptoms in children and youth: an evaluation of the FRIENDS programme. J Clin Child Adolesc Psychol 2006;35:403-11. http://dx.doi.org/10.1207/s15374424jccp3503_5.
- Lock S, Barrett PM. A longitudinal study of developmental differences in a universal preventive intervention for child anxiety. Behav Change 2003;20:183-99. http://dx.doi.org/10.1375/bech.20.4.183.29383.
- Stallard P, Simpson N, Anderson S, Carter T, Osborn C, Bush S. An evaluation of the FRIENDS programme – a cognitive behaviour therapy intervention to promote emotional resilience. Arch Dis Child 2005;90:1016-19. http://dx.doi.org/10.1136/adc.2004.068163.
- Stallard P, Simpson N, Anderson S, Hibbert S, Osborn C. The FRIENDS emotional health programme: initial findings from a school based project. Child Adolesc Ment Health 2007;12:32-7. http://dx.doi.org/10.1111/j.1475-3588.2006.00421.x.
- Stallard P, Simpson N, Anderson S, Goddard M. The FRIENDS emotional health prevention programme: 12 month follow-up of a universal UK school based trial. Eur Child Adolesc Psychiatry 2008;17:283-9. http://dx.doi.org/10.1007/s00787-007-0665-5.
- Stallard P, Taylor G, Anderson R, Daniels H, Simpson N, Phillips R, et al. School-based intervention to reduce anxiety in children: study protocol for a randomized controlled trial (PACES). Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-227.
- Stallard P, Taylor G, Anderson R, Daniels H, Simpson N, Phillips R, et al. The prevention of anxiety in children through school-based interventions: study protocol for a 24-month follow-up of the PACES project. Trials 2014;15. http://dx.doi.org/10.1186/1745-6215-15-77.
- Raab GM, Butcher I. Balance in cluster randomized trial. Stat Med 2001;20:351-65. http://dx.doi.org/10.1002/1097-0258(20010215)20:3<351::AID-SIM797>3.0.CO;2-C.
- Barrett P. FRIENDS for Life: Group Leaders Manual for Children. Bowen Hills, QLD: Australian Academic Press; 2004.
- Boyce W, Torsheim T, Currie C, Zambon A. The family affluence scale as a measure of national wealth: validation of an adolescent self-report measure. Soc Indic Res 2006;78:473-87. http://dx.doi.org/10.1007/s11205-005-1607-6.
- Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M. Researching health inequalities: the development of the Health Behaviour on School-Aged Children (HBSC) family affluence scale. Soc Sci Med 2008;66:1429-36. http://dx.doi.org/10.1016/j.socscimed.2007.11.024.
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behav Res Ther 2005;43:309-22. http://dx.doi.org/10.1016/j.brat.2004.02.004.
- Spence SH, Sclare I. Child Psychology Portfolio. Windsor: NFER-Nelson; 1997.
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child and anxiety scale. Behav Res Ther 2000;38:835-55. http://dx.doi.org/10.1016/S0005-7967(99)00130-8.
- Sandin B, Chorot P, Valiente RM, Chorpita BF. Development of a 30 item version of the Revised Child Anxiety and Depression Scale. Rev Psicopatol Psicol Clin 2010;15:165-78. http://dx.doi.org/10.5944/rppc.vol.15.num.3.2010.4095.
- Muris P, Meesters C, Schouten E. A brief questionnaire of DSM-IV-defined anxiety and depression symptoms among children. Clin Psychol Psychother 2002;9:430-42. http://dx.doi.org/10.1002/cpp.347.
- Rosenberg M. Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press; 1965.
- Chorpita BF, Tracey SA, Brown TA, Collica TJ, Barlow DH. Assessment of worry in children and adolescents: an adaptation of the Penn State Worry Questionnaire. Behav Res Ther 1997;35:569-81. http://dx.doi.org/10.1016/S0005-7967(96)00116-7.
- Muris P, Meester C, Gobel M. Reliability, validity, and normative data of the Penn State Worry Questionnaire in 8–12-yr-old children. J Behav Ther Exp Psychiatr 2001;32:63-72. http://dx.doi.org/10.1016/S0005-7916(01)00022-2.
- Solberg ME, Olweus D. Prevalence estimation of school bullying with the Olweus Bully Victim Questionnaire. Aggr Behav 2003;29:239-68. http://dx.doi.org/10.1002/ab.10047.
- Rees G, Goswami H, Bradshaw J. Developing an Index of Children’s Subjective Well-Being in England. London: Children’s Society; 2010.
- Rees G, Goswami H, Pople L. The Good Childhood Report 2012; A Review of our Children’s Well-Being. Leeds: Children’s Society; 2012.
- Rice F, Frederickson N, Seymour J. Assessing pupil concerns about transition to secondary school. Brit J Ed Psychol 2010;81:244-63. http://dx.doi.org/10.1348/000709910X519333.
- Stevens K. Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy 2001;9:157-69. http://dx.doi.org/10.2165/11587350-000000000-00000.
- Stevens K. Valuation of the Child Health 9D Index. Pharmacoeconomics 2012;30:729-47. http://dx.doi.org/10.2165/11599120-000000000-00000.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Goodman R, Scott S. Comparing the Strengths and Difficulties Questionnaire and the Child Behavior Checklist: is small beautiful?. J Abnorm Child Psychol 1999;27:17-24. http://dx.doi.org/10.1023/A:1022658222914.
- Ebesutani C, Chorpita BF, Higa-McMillan CK, Nakamura BJ, Regan J, Lynch RE. A psychometric analysis of the Revised Child Anxiety and Depression Scales – parent version in a school sample. J Abnorm Psychol 2011;39:173-85. http://dx.doi.org/10.1007/s10802-010-9460-8.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. http://dx.doi.org/10.1001/archinte.166.10.1092.
- Spitzer RL, Kroenke K, Williams JB, . Validation and utility of a self-report version of PRIME MD. JAMA 1999;282:1737-44. http://dx.doi.org/10.1001/jama.282.18.1737.
- NHS Improving Access to Psychological Therapies (IAPT) Programme . The IAPT Data Handbook: Guidance on Recording and Monitoring Outcomes to Support Local Evidence-Based Practice. Version 2.0.1 2011. http://iapt.nhs.uk/silo/files/iapt-data-handbook-v2.pdf (accessed 28 September 15).
- Ware JE, Kosinski M, Dewey JE, Gandek B. How to Score and Interpret Single-Item Health Status Measures: a Manual For Users of the SF-8 Health Survey. Lincoln, RI: Quality Metric Incorporated; 2001.
- Meyer TJ, Miller ML, Metzgar RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 1990;28:487-95. http://dx.doi.org/10.1016/0005-7967(90)90135-6.
- Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b2393.
- White IR, Horton N, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d40.
- Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c869.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2007.
- Ramsay S, Willke R, Briggs A, Brown R, Buxton M, Chawla A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force Report. Value Health 2005;8:521-0. http://dx.doi.org/10.1111/j.1524-4733.2005.00045.x.
- Diaz-Ordaz K, Kenward M, Grieve R. Handling missing values in cost-effectiveness analyses that use data from cluster randomised trials. J R Stat Soc Ser A (Stat Soc) 2014;177:457-74. http://dx.doi.org/10.1111/rssa.12016.
- Gomes M, Grieve R, Nixon R, Edmunds WJ. Statistical methods for cost-effectiveness analyses that use data from cluster randomized trials: a systematic review and checklist for critical appraisal. Med Decis Making 2012;32:209-20. http://dx.doi.org/10.1177/0272989X11407341.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: PSSRU, University of Kent; 2013.
- NHS Reference Costs 2012 to 2013. London: Department of Health; 2013.
- Goldstein H. Multilevel Statistical Models. London: Arnold; 2003.
- Wiltshire Council . Learn 4 Life: Integrating PSHE Education and SEAL 2011. www.wiltshirehealthyschools.org/documents/learn-for-life/ (accessed 2 October 2015).
- Glenn D, Golinelli D, Rose RD, Roy-Byrne P, Stein MB, Sullivan G, et al. Who gets the most out of cognitive behavioural therapy for anxiety disorders? The role of treatment dose and patient engagement. J Consult Clin Psychol 2013;81:639-49. http://dx.doi.org/10.1037/a0033403.
- Manassis K, Ickowicz A, Picard E, Antle B, McNeill T, Chahauver A, et al. An innovative child CBT training model for community mental health practitioners in Ontario. Acad Psychiatry 2009;33:394-9. http://dx.doi.org/10.1176/appi.ap.33.5.394.
- Mannassis K. Anxiety prevention in schools. Lancet 2014;3:164-5. http://dx.doi.org/10.1016/s2215-0366(14)70285-8.
- Van Oort FVA, Greaves-Lord K, Verhulst FC, Ormel J, Huizink AC. The developmental course of anxiety symptoms during adolescence: the TRAILS study. J Child Psychol Psychiatry 2009;50:1209-17. http://dx.doi.org/10.1111/j.1469-7610.2009.02092.x.
- Department for Education . The Importance of Teaching – The Schools White Paper 2010 2010. www.education.gov.uk/publications/eOrderingDownload/CM-7980.pdf (accessed 24 September 2015).
- Stallard P, Phillips R, Montgomery A, Spears M, Anderson R, Taylor J, et al. A cluster randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of classroom-based cognitive–behavioural therapy (CBT) in reducing symptoms of depression in high-risk adolescents. Health Technology Assess 2013;17. http://dx.doi.org/10.3310/hta17470.
- National Healthy Schools Programme. n.d.
- Department for Education . Guidance: Personal, Social, Health and Economic (PSHE) Education 2013. http://webarchive.nationalarchives.gov.uk/20130903123545/http:/www.education.gov.uk/schools/pupilsupport/pastoralcare/a0075278/healthy-schools (accessed 28 September 2015).
- Simon E, Dirksen C, Bogels S, Bodden D. Cost-effectivness of child-focused and parent-focused interventions in a child anxiety prevention program. J Anxiety Disord 2012;26:287-96. http://dx.doi.org/10.1016/j.janxdis.2011.12.008.
Appendix 1 Parent interview
Appendix 2 Intervention costs: detailed breakdown
Data sources are trial records unless otherwise footnoted.
| Health-led FRIENDS | School-led FRIENDS |
|---|---|
| 14 schools | 14 schools |
| 24 classes | 25 classes |
| n = 509 children | n = 497 children |
| 21.21 children per class | 19.88 children per class |
| Leader training: leaders | |
| Six health leaders | 25 school staff |
| Six × 2 days (16 hours) | 25 × 2 days (16 hours) |
| Total 96 hours | Total 400 hours |
| Hourly rate £12.47 | Teacher hourly rate £28.93a |
| Total £1197 | Total £11,572 |
| Leader training: trainers | |
| Clinical psychologist + programme manager | Clinical psychologist + programme manager |
| 2 days (16 hours) | 2 days (16 hours) |
| Hourly rate (£59 + £22.16) | Hourly rate (£59 + £22.16) |
| Total £1299 | Total £1299 |
| Leader manual | |
| £159 | £625 |
| Supervision of delivery | |
| Six leaders × 13 sessions × 2.5 hours | 25 school staff × four sessions × 2.5 hours |
| Attended supervision over three terms | Attend four sessions per delivery of FRIENDS |
| Total 195 hours | Total 250 hours |
| Hourly rate £12.47 | Teacher hourly rate £28.93a |
| Total £2432 | Total £7233 |
| One provider × 13 sessions × 2.5 hours | One provider × 13 sessions × 2.5 hours |
| Delivered supervision over three terms | Delivered supervision over three terms |
| Total 32.5 hours | Total 32.5 hours |
| Supervisor hourly rate £59b | Supervisor hourly rate £59b |
| Total £1918 | Total £1918 |
| Supervision travel cost | |
| No additional travel cost | 25 teachers × four sessions × £22.50 round trip |
| Total £0 | Total £2250 |
| Delivery | |
| (1) Teacher costs | |
| No additional cost for supporting teacher | Teacher needs 30 minutes of preparation time per session |
| 25 classes × nine sessions × 0.5 hours = 112.5 hours | |
| Teacher hourly rate £28.93 | |
| Total £0 | Total £3255 |
| (2) Facilitator costs | |
| 24 classes × nine sessions × two leaders | 25 classes × nine sessions × two supporters (probably teaching assistant) |
| 2.5 hours per session | 1 hour per session (no preparation) |
| Total 1080 hours | Total 450 hours |
| Hourly rate (trial records) £12.47 | Hourly rate (teaching assistant) £12.65c |
| Total £13,468 | Total £5693 |
| Travel | |
| 24 classes × nine sessions × two leaders | No cost, staff will be at the school |
| £22.50 per trip | |
| Total £9720 | |
| Children booklets | |
| 24 classes = 629 children | 25 classes = 655 children |
| £2673 | £2784 |
| Total health-led cost = £32,866 | Total school-led cost = £36,629 |
List of abbreviations
- CBT
- cognitive–behavioural therapy
- CHU-9D
- Child Health Utility 9 Dimensions
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CSRI
- Client Services Receipt Inventory
- df
- degrees of freedom
- IAPT
- Improving Access to Psychological Therapies
- ICER
- incremental cost-effectiveness ratio
- PACES
- Preventing Anxiety in Children through Education in Schools
- PSHE
- personal, social and health education
- QALY
- quality-adjusted life-year
- RCADS
- Revised Child Anxiety and Depression Scale
- RCADS-30
- Revised Child Anxiety and Depression Scale 30-item version
- RCADS-30-P
- parent version of the Revised Child Anxiety and Depression Scale 30-item version
- RCT
- randomised controlled trial
- SCQ
- School Concerns Questionnaire
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SEAL
- Social and Emotional Aspects of Learning
- SF-8
- 8-item Short Form Health Survey
- SPSS
- Statistical Product and Service Solutions