Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 12/182/14. The contractual start date was in May 2014. The final report began editorial review in November 2015 and was accepted for publication in March 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Karl Atkin is a member of the National Institute for Health Research Public Health Research Funding Board. Chris Hatton’s salary is part-funded by Public Health England through his role as a codirector of their Learning Disabilities Public Health Observatory.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Berghs et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Note on terminology
In this project, we tried to be inclusive of all theories and models of disability. The language used reflects this. Impairment and disability are used interchangeably. In doing so, we acknowledge that these words assume different meanings depending on the paradigms or social movements with which they become associated. It is equally important to acknowledge that disabled people might wish to choose their own definitions, which may or may not accord with standard classifications. We did not want to impose contested definitions on the experiences of people with disabilities, although, to be helpful, we provide a summary of common approaches, reflected in the literature and with which our report engages.
Medical models tend to define disability in terms of a biological pathology located in an individual body, which requires medical technology, medicine or rehabilitation to make a person well. Human rights approaches use person-first definitions, such as ‘persons with disabilities’, and are keen to establish legal, political, cultural, social and economic rights, consistent with the normative values associated with the society within which a disabled person lives. A social model of disability makes a distinction between disability as the experience of oppression and disadvantage and impairment as a physical, sensory, cognitive or mental health condition. Therefore, when a person refers to himself or herself as a disabled person, they are referring to his or her identification with the experience of disablement. Critical disability studies approaches use terminology such as ‘differently able’ or view disability along a continuum of human diversity. This includes people who might take pride in their specific form of disability or their social experiences of disability, such as ‘psychiatric system survivors’. Finally, there are people who have impairments but who do not define themselves as having disabilities or do not want to be associated with disability. They might prefer to use a medical description, which can be linked to cultural, social and political understandings (as in the case of people with dementia), or they may wish to connect with other identities associated with family, kinship, ethnicity, religion or other social or political movements.
Chapter 1 Background to the study
The research was commissioned by the National Institute for Health Research (NIHR) Public Health Research (PHR) programme in response to a call, ‘Implications for public health research of models and theories of disability’ (see www.nets.nihr.ac.uk/__data/assets/pdf_file/0004/129559/CB-12-182-14.pdf). Consistent with the scope of this commissioned call, the project presents a critical and informed discussion of how best to encourage more inclusive research practices, in a way that enables public health research evidence to better reflect the diverse experiences of people with a range of different disabilities. This introductory chapter explains why the research is important.
Disability and public health
According to the Family Resources Survey,1 estimates of disability in the UK have remained stable, at 19% of the population. Consequently, 10 million people in England experience significant difficulty with day-to-day activities linked to long-term conditions; this population includes those with lifelong and later-life conditions. 1 As ageing is associated with functional decline, nearly half of those living with impairments are aged 60 years or over. 2 Many disabled people also live with other physical conditions, such as coronary heart disease, diabetes and respiratory conditions, alongside mental health problems. 1
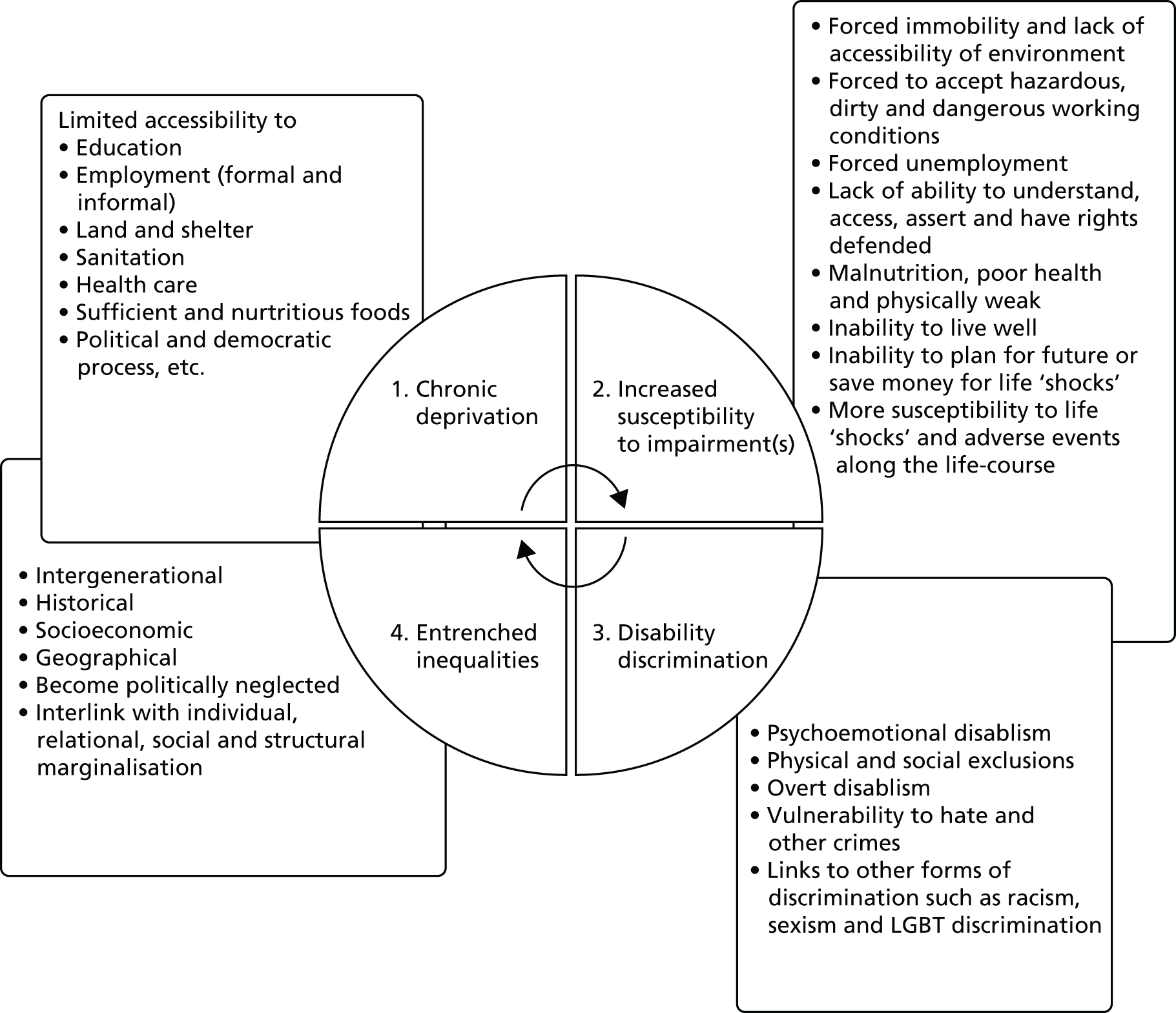
There are marked social gradients in disability across the life-course, with evidence of enduring effects associated with childhood circumstances. 3–10 In addition, and at each stage of the life-course, people with disabilities are disproportionately exposed to the social factors that contribute to health inequalities, including proximal risk factors such as smoking, obesity and lack of physical activity,11,12 alongside broader determinants associated with educational and employment opportunities, poverty and poor housing, and inequitable access to services. 6,13,14 These environmental disadvantages are, in turn, disabling and create further barriers to social inclusion. 12,15,16
There is growing appreciation of the diversity of disabling experiences, with different impairments having their own aetiologies and trajectories, acquired in a wide range of circumstances, and mediated by individual, social and political contexts. The public face of impairment is also challenging previous perceptions by encouraging a more encompassing understanding of ‘being disabled’. 17 Disability, although socially patterned, can affect anyone, including those with pre-existing chronic conditions, mental health problems and intellectual and cognitive impairments. 6,18–20 Furthermore, international understandings have moved away from a strictly medical definition, where ‘disability’ is ‘caused’ by functional deficits (such as physical injury or intellectual disability), to one that is sensitive to environmental determinants and in tune with how people experience disability as they go about their day-to-day lives. 21 This shift is a fundamental aspect of our analysis.
The United Nations (UN) Convention on the Rights of Persons with Disabilities (CRPD) reflects these changes, such that disability is understood to result ‘from the interaction between persons with impairments and attitudinal and environmental barriers that hinders their full and effective participation in society on an equal basis with others’. 22 Human rights and equality frameworks are also increasingly employed to articulate the moral claims and service needs of people with disabilities,12,23,24 in order to reflect impairment complexity. 25,26 The CRPD, for example, sets out an international framework for citizens’ rights and state obligations on health-care provision, rehabilitation, accessibility and research with and for disabled people. 22 The UK is a signatory to this framework, which is further supported at a national level by the Human Rights Act (1998)27 and the Equality Act (2010)28 which make discrimination on the basis of disability illegal, while also requiring an equality duty in health-care provision. 29 The duty to involve and support people in decisions linked to their health and well-being is also defined in the Mental Capacity Act (2005)30 and the Care Act (2014),31 respectively.
Public health research
Public health interventions have a critical part to play in advancing the status and well-being of people with disabilities. Interventions to tackle underlying causes of ill-health and reduce health inequalities have the potential to transform lives. 6 These interventions also support wider policy objectives to promote independent living and care at or close to home. 32 However, there are significant challenges to developing an evidence base,33 and four broad inter-related concerns can be identified: a lack of engagement with more theoretical conceptualisations of disability; a lack of methodological sophistication in including and capturing the experiences of disability; limited public engagement; and failing to ensure that research findings produce evidence that reflects the diverse experiences associated with disabling conditions. These challenges explain why public health research has been criticised for largely overlooking the experiences of disabled people and has been slow to accommodate shifts in understandings of – and the politics around – disability,34–39 despite equity being an increasingly salient feature of public health interventions. 40 Perspectives and assumptions can, for example, be outmoded and inappropriate, with disability represented as a ‘burden’ and a ‘cost’ to society. 41–43
Consequently, there is limited evidence on the types of public health interventions that are likely to be effective and on the kinds of measures that should be used when evaluating effectiveness. 44 There remains a dearth of public health material discussing intervention design, methods, including economic evaluation, and strategies to actively make mainstream disability-sensitive research by adapting universal and inclusive designs. 45–48 There is also little debate about how best to actively engage disabled adults, young people and children, particularly when trying to identify interventions consistent with disabled people’s preferences. 49–54 Further difficulties are associated with accommodating the differences generated by lifelong, acquired or fluctuating conditions, where experience is further mediated by sociodemographic factors such as gender, social class, ethnicity, sexuality and age. 10,55–57 Few studies, for example, assess the impact of public health interventions aimed at specific groups of disabled people, with diverse circumstances across the life-course. 58,59
This report seeks to fill these gaps by facilitating a discussion on the most appropriate ways in which to generate research evidence that is sensitive to a broad range of disabling experiences. 21,60 This is challenging. Nonetheless, disability studies and allied perspectives offer alternative ways of defining and engaging with disability, which can improve future intervention research. 61–66 However, these perspectives typically derive from a different epistemological and ontological starting point to that informing mainstream public health research and policy. 67–70 They might, for example, encourage a suspicion of any public health interventions that seek to ‘rehabilitate’ or ‘normalise’ behaviour, believing them to be a form of oppression and to deny the rights of disabled people. 23,71
Such perspectives – aligned to social and political movements – conceptualise disability as generated by the wider structures of social inequality and as a human rights issue. 72 Research perspectives and methods that have been built from these perspectives are grounded in an appreciation that disability is – and is experienced as – a dynamic interplay between impairment, attitudes and the environment. 73 Consequently, disability seen to be generated by normative values and assumptions, embedded in discursive practices, where failure to accommodate diversity and difference denies the experiences of people with disabilities, generates oppression and produces inequalities.
These approaches have generated a rich literature on disability – including that developed by the World Health Organization (WHO) – which accommodates social, relational, ecological, economic and medical models. 12 Recent international reviews, for example, have examined the application of different theories to public health interventions in terms of measurement, applicability and standardisation. 62,63,74 These reviews challenge mainstream practices and generate alternative ways of doing research. Some reviews, for example, have examined how public health theories could connect to specific disability measurements. 75 There are also studies assessing the relevance of public health outcome measurements to the experiences of people with disabilities. 43,61,76–79 Other work, although oriented to specific forms of impairments or groups, such as intellectual disabilities, mental health or younger populations, explores how disability impacts on and is affected by public health interventions,55,58,80–82 including health information;83 health-promotion interventions;57,84,85 health checks;86 self-management;87 personalisation;88 self-advocacy;89,90 and access to health care. 82,91 Despite providing valuable insights into more inclusive research strategies,36,51,65 this disparate literature has yet to be synthesised in a way that makes it accessible to those commissioning and undertaking public health research. 92 Connecting this more critical literature on the experiences of disability to the models and theories associated with public health is an important starting point, from which more inclusive research may emerge.
Why do the research?
Public health interventions aim to improve population health and reduce inequalities. As we have seen, people with disabilities are at particular risk of poor health and are disproportionately disadvantaged vis-à-vis the social factors that contribute to health inequalities. Although people with disabilities constitute a major recipient group for public health interventions, research has not engaged in any systematic way with the experiences of people with disabilities. 93 This undermines the ability of public health research to promote equity and social inclusion. 40
An appreciation of how different models of disability can inform the development and evaluation of public health interventions, together with the provision of guidelines on the most appropriate ways in which to incorporate the perspectives and experiences of those with disabilities, could be especially beneficial to research and policy. 94,95 It can help connect evidence-based practice to the diverse needs of those with disabilities, while also being sensitive to broader concerns about social disadvantage, accessibility and inclusion.
It is against this background that the NIHR PHR programme commissioned research on the public health implications of models and theories of disability. Public health interventions have been a key feature of successive governments’ policies, with a focus on developing interventions that both improve overall population health and reduce health inequalities. This drive has occurred against the backdrop of an ageing and increasingly diverse disabled population, and a cost-saving agenda that places a premium on people with impairments remaining in the community and accessing – and remaining in – the labour market, supported by effective health- and social-care interventions.
Increasing attention is being given to understanding how public health can deliver appropriate models of support and ensure better outcomes for disabled people, in which their rights are respected. 96 The Department of Health, for example, began a partnership with the Disability Rights Commission (now part of the Equality and Human Rights Commission) to ‘improve information and services, communications and levels of awareness of disability issues’. 97,98 Such strategies promote the inclusion of disabled people, their rights and needs in all public services,99 including public health. 100–102
There are particular advantages of integrating current public health research to emerging ideas that see those with disabilities as active citizens, part of wider social networks (such as partners and parents) and as stakeholders in the services that they use. 56,103 Incorporating such perspectives, while maintaining a commitment to understanding what – and how – interventions work, can lead to a range of public health benefits. 104 These include the promotion of health, social inclusion and equality. For example, the life expectancy of those with mental health problems is 20 years lower than the population norm. 105 One of the reasons for this includes the difficulty of maintaining a healthy lifestyle. 106,107 Smoking cessation raises particular challenges, particularly given that evidence suggests that current interventions are not sensitive to the experiences of those with mental health problems or the ways in which people have to negotiate social disadvantages associated with their disability. 108 A more inclusive approach, committed to ensuring that differences do not become the basis of inequalities, not only would empower people but would also have the potential to achieve significant public health gains. 109
Aims of the study
As we have argued, the complex and nuanced nature of disability is rarely considered in public health debates, especially when evaluating interventions. With a large and growing population of disabled people, the UK needs a strong evidence base on which to build future intervention research, and one that specifically offers advice on how to reconcile established research designs with those informed by more inclusive models. Without this, we shall continue to know little about what will work, for whom and under what circumstances. In line with the commissioning brief, our research questions are:
-
How can different models and theories of disability appropriately inform research into the effectiveness of public health interventions? To what extent can intervention research be sensitised to accommodate different configurations of diversity within and among general and disabled populations?
-
How do different models of disability map on to current research on public health interventions? What are the implications of commissioning research into public health interventions that are inclusive of, or for, disabled people in a way that accommodates appropriate terminology and measurement and takes account of different causes and types of impairment, while being sensitive to the experience and needs of different demographic groups associated with gender, socioeconomic position, ethnicity, sexuality and age?
-
How should participants, the public and stakeholders be involved in research and what does inclusive research practice look like?
-
What study designs and relevant outcomes best capture the experiences of impairment and disability in a way that maximises health benefits and that ensures that mainstream research reflects the experiences of people with disabilities?
To answer these questions, the project was organised in two parts (see Appendix 1). First, we scoped models and theories of disability and explored their relevance for public health paradigms; and, second, we assessed their implications for public health by reviewing a sample of systematic reviews of public health interventions, explored how far current intervention designs incorporated approaches consistent with disability models and theories. Our analysis, along with discussions with politically active disabled people and professionals working in public health, informed the iterative development of a decision aid. The decision aid aimed to critically evaluate current research practices and evidence bases, while looking to the future by enabling commissioners to assess the likelihood that commissioned public health research will produce more inclusive evidence relevant to the experiences of those with disabilities.
Conclusion
This opening chapter established the context for the research and the reasons why it is necessary. To be relevant, public health research needs to reflect a diverse range of disabling experiences. Otherwise, current evidence will struggle to engage with social disadvantage, accessibility and inclusion and thereby will risk generating inappropriate responses and wasting valuable resources. Our research explores how mainstream public health research can be more sensitive and inclusive of disability, in terms of how research is commissioned and how interventions are developed and researched. This includes connecting theoretical debates about how disability is conceptualised with current research practice to assess how current research design captures, engages and explains the experiences of disability. Our final conclusions will enable commissioners to judge the likelihood that research on a particular intervention will apply to a range of different disabilities, as experienced in different social contexts. It will also encourage researchers to adapt more inclusive approaches, including examples of best practice, from which successful public health interventions can be developed. Chapter 2 outlines how we operationalised our research questions by discussing the methodological basis of our work.
Chapter 2 Methods
The previous chapter established the broad aim of the project, which is to explore whether or not, and how, current research on public health interventions captures a diverse range of disabling experiences. Our analysis has to connect the more theoretical and sometimes polemical literature on the experiences of disability, in which various critical voices question the underlying assumptions of the research and policy process, with the mainstream public health literature, concerned with generating an evidence base on effectiveness. This required us to provide an overarching account of the different ways in which disability is conceptualised and to translate this into a language accessible to those engaged with public health. In this chapter, we explain:
-
how we carried out a two-stage scoping review to investigate what implications differing theories and models of disability could have for understanding the effectiveness of public health interventions
-
how we generated and analysed public health interventions of two types:
-
generic public health interventions potentially relevant to the lives of disabled people, in order to gain insights into the ability of mainstream research to capture the experiences of disability
-
specific public health interventions targeted at people with disabilities, which enabled us to explore the potential of more inclusive designs
-
-
how our analysis informed the development of a decision aid/toolkit
-
how we organised a consultation with politically and socially active disabled people and public health professionals to deliberate our findings.
Our first scoping review identified the range of disability theories and models and considered their strengths and possible limitations in generating inclusive approaches and capturing diverse experiences. We assessed the potential contribution of these theories and models to public health research and policy by developing a decision aid to evaluate and inform more inclusive research practice. The second stage of the project examined purposively selected public health reviews from the Cochrane (international) Library of Intervention Reviews and, to further support diversity, relevant databases held by the Campbell Collaboration and Joanna Briggs Institute. A total of 30 Cochrane reviews deal with mainstream, generic interventions. This enables the research to consider the potential for more inclusive designs. Another 30 Cochrane reviews include people with disabilities as a key target group, thereby enabling the research to assess the extent to which a more inclusive research question was able to capture the experiences of disabled people. Two reviews from each arm of the review were then purposively sampled and subjected to more detailed analysis. Finally, deliberation panels with socially and politically active disabled people and public health professions helped to refine our conclusions.
In preparing the chapter – and consistent with our iterative approach – we had an awareness of how the different stages of the project influenced each other. We have, however, adapted a pragmatic approach in describing this. This chapter outlines the different stages of the project, while acknowledging the difficulties of providing a conventional and discrete methodological account. This is why we introduce our initial reflections of the literature, as way of explaining why certain decisions were taken.
Stage 1: scoping different models of disability
We sought to identify, appraise and summarise relevant works on disability according to an explicit and reproducible methodology. Typically, scoping reviews are inclusive, and encompass relevant literature, concept or policy mapping, in addition to stakeholder consultations. 110–112 This can be a strength when assessing the depth and breadth of a research field and particularly one characterised by diverse approaches. 113–115 However, it can also be a potential weakness, which underplays specificity and encourages imprecision,112 while the perceived lack of defined quality assessment can affect empirical robustness and, in turn, policy uptake. 114,116
Aware that we had to provide a broad (theoretical) overview of a research field, while mindful of potential weaknesses in our approach, we relied on Arksey and O’Malley’s110 widely used framework to establish transparency, which helpfully parallels those used for more conventional systematic reviews. This framework informs a structured approach to reviewing, while incorporating an iterative searching process, with search terms subject to refinement in the light of the studies identified. The framework also enables us to contextualise our discussion in broader debates. We further supplemented our approach with reference to Levac et al. ’s115 and Daudt et al. ’s117 recommendations of enhancement, which include (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; (5) collating, summarising and reporting the results; and (6) a consultation exercise.
To this extent, our approach is more akin to a knowledge review. Such reviews, developed by the Social Care Institute for Excellence (see www.scie.org.uk/), provide a thematic, explanatory exploration of the relevant literature. Knowledge reviews are especially useful in informing more reflexive commissioning, policy and practice112,114 and more broadly in assessing theory and models. 118 They also allow an appraisal through ‘mapping’ the literature rather than giving an ‘assessment’ of the ‘quality of the individual studies’, while highlighting gaps in current available reviews. 112 Moreover, knowledge reviews do not take the available evidence at face value but generate important questions about, for example, what research is commissioned and whose priorities it reflects. 112
Aims of first scoping review
The stage 1 scoping review offers a critique of different (largely theoretical) understandings of disability and explores six inter-related themes by:
-
identifying and summarising the range of disability models, definitions and theories and assessing their potential contribution to public health research and policy
-
locating different definitions, models and theories within the field of disability studies and the social and political movements of disabled people
-
appraising how well different definitions capture the diverse range of experiences associated with disability, with a particular focus on how different causes, aetiologies and trajectories mediate this experience, including a consideration of the impact of comorbidities
-
assessing whether or not, and how, the different consequences of impairment and the context in which it is realised inform debates, including a focus on how well different theories of disability take account of broader sociodemographic variables and experience
-
investigating the consequences of adapting particular terminologies, study designs and outcome measures when evaluating public health interventions
-
examining different approaches to public/stakeholder involvement.
We began by developing a protocol, outlining all major methodological decisions taken. Identified references were entered into an EndNote (version 7.4, Thomson Reuters, CA, USA) library. This enabled studies to be retrieved by key word, subject heading or medical subject heading (MeSH) searches. We intended to identify relevant studies through:
-
searches of major electronic databases
-
cross-checking with major publications in the field of disability studies, history and policy
-
scanning reference lists of relevant papers
-
internet searches
-
searches of key books and book chapters (an important source of literature on this subject)
-
examining major policy documents
-
consulting experts in the field by cross-checking key texts with members of the project steering committee.
As can be seen in Initial inclusion criteria, we had to refine our initial approach to one that was more focused and consistent with the aims of the project. We next explain the development of our thinking and how we arrived at our eventual methodological approach.
Initial inclusion criteria
All resources were searched from 1990 onwards, as this is when critiques and new models begin to appear in the UK (as seen in the work of writers such as Nasa Begum and Gerry Zarb,66 Colin Barnes and colleagues,67 Mike Oliver72 and Jenny Morris119). These authors also capture the history of the various disability and civil rights movements, thereby adding further context, enabling us to locate material within broader social movements.
We then set about identifying MeSH terms. In doing so, we included a range of different physical, intellectual and mental impairments, while reflecting the different political, economic and cultural disabling consequences of having a lifelong, acquired or fluctuating condition. These were cross-referenced against those terms used in disability studies, sociological literature and public health policy. Our MeSH terms included: ‘model*’, ‘theor*’, ‘disab*’, ‘handicap*’, ‘persons with disabl*’, ‘mentally disabled*’, and ‘chronic disab*’. We used Boolean operators such as ‘AND’ to widen or narrow the searching in our databases. Our search strategy included the following electronic databases: Scopus, MEDLINE, Cumulative Index to Nursing and Allied Health Literature, PsycINFO and Social Sciences Citation Index. We set an inclusion and exclusion date (1990 and 2014, respectively). We supplemented the electronic database searches with hand-searching of key journals, along with website and grey literature searches (such as the Conference Proceedings Citation Index).
Our inclusion criteria mean that an output was considered relevant only if it was in English; informed by one or more of the key guiding issues highlighted in the review questions; clearly focused on models and theories; and met our operationalisation of the study objectives/review questions. Studies were excluded if they were not in the English language. Studies published before 1990 or after May 2014 were excluded. If the studies did not incorporate our MeSH terms, they were also excluded. Box 1 illustrates preliminary results when using the SCOPUS database.
(1990 to May 2014) AND (‘disabilit*’ AND ‘theor*’) = 4970.
(1990 to May 2014) AND (‘disabilit*’ AND ‘model*’) = 26,415.
(1990 to May 2014) AND (‘model* of disabilit*’) = 26,415.
We had a large number of ‘hits’, but closer scrutiny revealed that many of the included studies were not unequivocally discussing models or theory linked to ‘disability’. We realised that the scoping in the databases was rather unwieldy, as the overview of theories and models of disability was too extensive. We checked if this would be the case in the PubMed database using the same MeSH terms. ‘Hits’ were still in the thousands. On further analysis, the way in which ‘theory’ could be defined was too diffuse for the purposes of our review. There were also different conceptual levels of theories, comparisons and meta-analysis, based in a plethora of paradigms evident across psychology, law, social sciences, medicine, statistics and public health. We discussed this as a team and with our project steering committee.
Following these discussions, the research team decided to refine and refocus our scoping approach to ensure that we adequately captured the theoretical richness and diversity of ‘disability’ in a way that was consistent with our aims. 118,120 Consequently, we oriented our search towards specific journals in which we felt that this diversity would be reflected. This not only offered a more manageable approach, but also ensured the inclusion of different disability theories and models. Following discussions with the project steering committee, we made a list of the 10 most influential peer-reviewed journals considered likely to contain articles about theories or models of disability and, at the same time, to capture the experiences of various impairments, different social and political experiences of disability and perspectives that took account of intersectionality.
Using this more focused approach, we hand-searched 10 journals and followed up key papers, reports and texts. The 10 journals were Disability & Society; Scandinavian Journal for Disability Research; Disability Studies Quarterly; Journal of Intellectual Disability Research; British Journal of Social Work; Human Rights Quarterly; Journal of Disability Policy Studies; Social Science & Medicine; Ethnicity & Health; and Social Theory and Health. We did not include journals such as the Disability and Health Journal or Disability and Rehabilitation, as we wanted to avoid a focus on rehabilitation. We also wanted the selected journals to ensure representation across not only impairments, age, socioeconomic class, geography and ethnicity but also the political and social spectrum.
We searched the archives of each of these journals from January 1990 to May 2014. For each journal, we kept a record of the possible articles of interest. In keeping with both a conceptual and genealogical approach, we decided to make our MeSH terms more flexible and inclusive to accommodate the historically changing language and policy landscape. The abstract or title of a paper thus had to include at least one of the following search terms: ‘model’, ‘paradigm’, ‘perspective’, ‘approach’, ‘formulation’, ‘conceptual frame’, ‘discourse’, ‘definition’, ‘understanding’, ‘theory’ or ‘framework’. We were especially aware that early articles may not use the word ‘model’. There also had to be an explicitly named perspective of viewing disability in the title or abstract. If we were unsure, but the title included possible MeSH terms that could be linked to a specific way of viewing disability, we included it. For example, we included papers that were about ‘human rights’, ‘social understanding’, ‘United Nations Convention on the Rights of Persons with Disabilities’, ‘International Classification of Impairments, Disability and Handicap’ (ICIDH), ‘International Classification of Functioning, Disability and Health’ (ICF), ‘ecological’, and ‘critical disability studies’ (CDS). Finally, we tried to be inclusive of language that was applicable to specific disabilities or language that may now be considered politically incorrect, such as ‘normalisation’ or ‘retardation’.
Ideally, we would have liked to have included a journal with an explicit focus on childhood disability. However, potential journals such as Archives of Disease in Childhood had a biomedical focus, whereas more specialist journals, with a large number of papers on childhood, such as Autism, were too broad in scope. The 10 journals selected, however, did include papers on childhood disability, although we acknowledge a potential gap in our approach, which we attempted to address when interrogating reviews of intervention studies.
Data selection
We located 182 articles from the 10 journals and printed these for further hand-searching. We mapped these papers according to the guidelines of Arksey and O’Malley110 by providing a summary of each paper. 110 Methodologically, Campbell et al. 118 noted that there are no real guidelines linked to theoretical reviews. Particular challenges include charting the relationship of a model vis-à-vis a theory, theoretical explanation and/or development. 121 We also realised that, in order to understand the applications of some models, we had to be methodologically inclusive of how they had been translated. As we have seen, scoping reviews are especially useful in allowing an appraisal through ‘mapping’ of the literature rather than giving an ‘assessment’ of the ‘quality’ of the individual studies. They are also useful in highlighting gaps in current available reviews. 112
Conceptually, we wanted to understand theory development and implications of use. This informed our approach to charting. A data extraction sheet was designed to quickly map details on the five inter-related themes (see Appendix 2). This enabled us to identify and summarise a range of disability models, assess their potential contribution to public health research and policy, and appraise how well different definitions capture the diverse range of experiences associated with disability. Following discussions with our project steering committee, we wanted to ensure balance in how we represented theories and models, by illustrating both their strengths and their weaknesses.
Refinement of inclusion criteria
In charting each article, we further refined the explicit discussion of theoretical models by offering an analysis of a particular model, paradigm or perspective; a comparative analysis or comparison between models, paradigms or perspectives; and a meta-analysis of models, paradigms or perspectives. We included grey literature if relevant, for instance, an extensive book review presenting a critique of a particular model and any subsequent rebuttals. We excluded applications of a model to a specific impairment or group of impairments, research-based papers or testing of a model or paradigm. We also excluded sociocultural understandings of disability, statistical approaches and in-depth theoretical or philosophical analyses unless specific to a model, paradigm or perspective. Although some commentaries and editorials were interesting, we excluded them if they referred to a study that was already included or critiques made more extensively elsewhere.
The refinement of the inclusion criteria through the mapping exercise meant that we were left with 121 articles. After scoping by the primary reviewer (MB), a second reviewer (KA) examined the validity of the findings of the primary reviewer. The second reviewer also checked and charted the 27 articles about which the first reviewer was unsure. As most of these articles were concerned with explicit discussions about disability and were not research-based, the first and second reviewer did not have to engage in an analysis of the methods and methodology or robustness of the research undertaken.
The results of our initial search strategy finally identified 104 articles explicitly about disability models, paradigms and theories (Figure 1). We used these articles to identify relevant secondary sources and grey literature such as major books and theories on disability theory and sociological theory linked to disability (such as that on chronic and long-term illness) as well as public health policy documents from national and global institutions such as the Human Rights Commission, the WHO, the UN, the UN Children’s Emergency Fund, the International Monetary Fund and the World Bank. An initial list was drawn up largely based on the volume of citations. We also discussed and agreed with our project steering committee what the more influential and most important texts (books and chapters) on disability theory, models and definitions were. This literature provided important and nuanced theoretical context to our analysis, while reflecting current debates about disability and how these have changed over time. To this extent, our account is a broad and extensive map of current theories and models of disability.
FIGURE 1.
Scoping flow chart.

Reflections on the literature
When looking across the set of papers, we noted four distinct models: medical models; human rights models; social models; and CDS models. Although the core elements of the models demonstrated a degree of consistency over time, perhaps not surprisingly, the definitions, terminology and theoretical background of the models kept changing and were dynamic, gradually becoming more reified – and perhaps less innovative – over time. Our analysis reflects this.
More theoretically informed articles were found in two journals, namely Disability & Society and Scandinavian Journal of Disability Research. Furthermore, although we assumed that journals such as Human Rights Quarterly would include discussion about disability rights, our review suggested otherwise. Ethnicity & Health had no discussions of models and Social Theory & Health, for example, contained only one article that was relevant (Table 1). The journal Disability & Society was largely UK focused, although it published foundational work on the social model and functioned as a genealogical review through which to find books, articles and grey literature. The Scandinavian Journal for Disability Research focused on Scandinavian or European thought on disability with well-established international academics and was especially strong on linking more relational and psychological accounts of disability.
| Journal | Number of articles |
|---|---|
| Disability & Society | 49 |
| Scandinavian Journal of Disability Studies | 16 |
| Journal of Disability Policy Studies | 12 |
| Social Science & Medicine | 8 |
| Disability Studies Quarterly | 7 |
| Journal of Intellectual Disability Research | 5 |
| British Journal of Social Work | 2 |
| Human Rights Quarterly | 2 |
| Social Theory and Health | 1 |
| Ethnicity & Health | 0 |
The most geographically diverse journal was the Journal of Intellectual Disability Research. By way of contrast, the Journal of Disability Policy Studies was completely US based. Social Science & Medicine was heavily biased towards the international application of more medical models of disability and Disability Studies Quarterly was the most innovative by linking disability with cultural studies. We would have expected there to be a lively debate on models of disability in the British Journal of Social Work or Social Theory and Health; however, this rarely occurred. Furthermore, despite an interest in disability and human rights, especially in an international context, ‘disability’ tended to be undertheorised in Human Rights Quarterly. Although research on disability had been published in Ethnicity & Health, no conceptual discussions were found.
Geographically, most discussion of theoretical models were located in the Global North (the UK, the USA and Europe) rather than the Global South, where, it is argued, more disabled people are located. 12,122 Across our review period, we found only one article discussing a rights-based model from the Global South (Table 2).
| Region | Number of articles |
|---|---|
| UK | 44 |
| USA | 26 |
| Europe | 15 |
| International | 7 |
| Canada | 6 |
| Australia | 5 |
| India | 1 |
Stage 2: reviewing public health interventions
We now turn to the second stage of the scoping review and explore its relationship with stage 1. Our second stage explored three components, namely:
-
broader public health interventions potentially relevant to the lives of disabled people, in order to gain insights into the ability of mainstream research to capture the experiences of disability (n = 30 reviews)
-
public health interventions targeted at people with disabilities, which enabled us to explore the potential of more inclusive designs (n = 30 reviews)
-
an analysis of the applicability and feasibility of a decision aid applied to the two reviews of interventions, to assess the potential for a more inclusive approach, reflecting the diverse experiences of disability.
Key analytical questions, applied to both reviews, included:
-
Was an inclusive approach considered and used to inform the design and conduct of studies?
-
Did the study design privilege the inclusion of some impairment types and disability groups over others and, if so, what types of disabilities are more likely to be accommodated?
-
What possible accommodations could be identified to make for a more inclusive research design?
-
Were accommodations – potential or otherwise – identified by authors as having the potential to jeopardise the scientific integrity of the research evidence?
-
Were communication difficulties used to justify the exclusion of certain people and to what extent could these be regarded as legitimate?
-
How were those with disabilities treated when recruiting to the study?
-
How was disability discussed in the findings?
-
Did the authors consider the extent to which their findings could be generalised to include the experiences of those with disabilities?
-
To what extent could the findings produce relevant and universal evidence?
-
To what extent could study designs be perceived to be disablist (excluding disabled people) or ableist (premised on able bodied norms).
Similarly to in stage 1, we followed Arksey and O’Malley’s110 framework. This provided a structured and iterative searching process, with search terms subject to refinement in light of the studies identified. We did an initial pilot search using The Cochrane Library before beginning our formal full searches. The combined MeSH terms of ‘disability’ and ‘interventions’ generated > 5000 hits. However, the joining of the MeSH term of ‘disability’ AND ‘intervention’ generated a more manageable 643 results. We used this to generate a sample of 30 reviews; each, on average, included 16 studies (with a range of 3 to 51 studies). This potentially gave us material on 480 studies. However, when we reviewed these studies in more detail, we found that many of these interventions were not reviews of randomised controlled trials (RCTs) that were sufficiently specific to the public health policy context or inclusive of ‘disability’. We checked to see how many studies were specifically about ‘public health’ AND ‘disability’ and found only 13 results out of a possible 8664 records. The pilot search, therefore, demonstrated the feasibility of our approach but also the importance of assuming a more iterative approach to the literature, particularly given the broad and flexible use of terms such as ‘public health’, ‘intervention’ and ‘disability’. To further facilitate this approach, we compared an expansive search with a theoretically specific search to assess how best to proceed.
The expansive search was extensive to the extent that it identified how many interventions were linked to public health and how many interventions were linked to disability in The Cochrane Library. The theoretically specific approach was informed by an analysis of disability theory and models linked to both ecological public health and disability rights models, in addition to reflecting differing impairments, intersectionality and life-course (see Chapter 3). This approach also had the advantage of focusing on individual, social–relational, social and macrostructural levels, linked to differing public health issues as well as to disabilities. Contrasting an expansive with a theoretically informed searching process also allowed a check of The Cochrane Library in terms of what would be identified by the Library as relevant.
Our focus on public health interventions and their evaluation using RCTs offered a good reflection of current policy, research and funding priorities in the UK. Furthermore, policymakers, researchers and professionals frequently used The Cochrane Library to inform decision-making. The Cochrane Library, although not covering a broad range of evaluative methodologies, does provides a good account of mainstream public health research and this is what we wanted to capture.
The results of our expansive approach allowed us to gain an overview of and to identify relevant systematic review studies for our topic of interest (see Appendix 3). We found 181 results from 8660 records from a search on ‘public health’ in the title, abstract or keywords, and we found 541 results from 8660 records from a search on ‘disability’ in title, abstract or keywords in The Cochrane Library. We printed out a list of the first 40 studies for public health interventions to check mainstreaming and the first 40 most relevant disability interventions to check inclusion. We had a list of studies for public health and a list for disability, and two reviewers (MB and KA) checked each study for relevance.
Having undertaken the expansive scope, we cross-checked the findings by means of a theoretically specific scope to find out how that would compare. When scoping the disability literature, we found that disability concepts such as ‘theory’ and ‘model’ were rarely linked to evaluation of reviews. 118,120 Bonner123 argues that theory-based evaluations can be of great use in identifying why interventions do or do not work in specific contexts and can be linked to realist pragmatic outcomes. Moore et al. 124 note the greater importance of theory and its contribution to how the Medical Research Council (MRC) guidance of complex interventions was framed. This is why we decided that it was important to understand the role of theory in public health interventions. We used the theoretical paradigms of the different but interconnected levels on which public health and disability interventions should ideally be working.
We combined our search on interventions with insights generated from our theoretical search to guide the scoping and to ensure that it covered issues across individual, social, institutional and policy perspective, both in terms of a ‘public health’ and a ‘disability’ focus. Furthermore, and to ensure consistency with the NIHR PHR brief, we decided that our scoping should be guided by individual public health policy priority issues (such as obesity) as well as by areas in which we thought that future individual public health issues would probably lie (such as gambling, new forms of infectious diseases and disaster preparedness) or more social public health issues (such as the use of green and public spaces, urban renewal and impact of environmental change). We cross-referenced for possible variations on terminology and to ensure consistency with the brief, and included current public health themes as reflected in recently funded interventions by the NIHR PHR, such as health literacy, binge drinking, physical activity and smoking cessation (Table 3).
| Individual | obesity | cardiovascular disease | gambling |
| respiratory health | diabetes | sexual health | |
| mental health | alcohol | maternal health | |
| dental | smoking | cancer | |
| injury | violence | substance abuse | |
| Relational/life-course | pregnancy | infant | teenager |
| adult | older person/elderly | ||
| Social | education | housing | employment |
| recreation | transport | ||
| Macrostructural | socio-economic | environmental | political |
| historical/policy | cultural |
We printed out the first three hits for each of the headings. The first (MB) and second (KA) reviewer went through the results to assess relevance for public health. Although there was a plethora of material on public health priorities such as obesity and smoking cessation, there was, perhaps not surprisingly, not much evidence on effectiveness of interventions on possible future public health policy issues such as gambling, the environment or recreation. This is an important consideration when interpreting our findings.
Our review of public health and disability followed the same approach (Table 4), although we additionally conducted a mapping exercise identifying common forms of impairment by noting the number of hits when we cross-checked with public health (i.e. ‘public health’ AND ‘intellectual disab*’).
| Individual | intellectual disabilities | hearing impairment | chronic conditions |
| dementia | stroke | ADHD | |
| frailty | spinal cord injuries | pain | |
| visual impairment | arthritis | depression | |
| musculoskeletal (back pain) | HIV | autism | |
| Relational/life-course | pregnancy | infant | teenager |
| adult | older person/elderly | ||
| Social | education | housing | transport |
| employment | recreation | ||
| Macrostructural | socio-economic | environmental | political |
| historical/policy | cultural |
To ensure consistency with the brief, we checked our findings against common forms of ‘disability’ in Britain,1 alongside what we thought would be future public health priorities in terms of improving health, well-being and quality of life (QoL) (e.g. dementia, depression and mental health). Terminology often had to be clinical to access the interventions we were looking for. We tried to be exhaustive by cross-checking interventions on disability issues (i.e. work disability and behavioural interventions), while also including terms such as ‘sustainable’, ‘investment’ and ‘social protection’. We had, however, few public health and disability hits, despite disability models and theories indicating that public health research was moving in this direction. This explained our use of supplementary databases.
Many of theories and models of disability identified disability as an affirmative identity and examined disabling barriers that impede independence and health. The idea of ‘independence’ was foundational to the creation of many disability theories and models. To ensure that such paradigms were not excluded, we further verified our approach against the Derbyshire Coalition for Inclusive Living’s ‘seven needs for independent living’. 125 This approach consists of information, peer-support, housing, technical aids, personal assistance, transport and access. 125 Unfortunately, we could not find sufficient public health evidence linked to peer-support, technical aids, communication and personal assistance.
To conclude, neither an expansive nor a theoretical scoping on disability was as relevant as the combined, more focused, results that we gained from MeSH terms such as ‘public health’ AND ‘disability’. We increased hits a little by adding variations of (disab*). Additional piloting indicated that the Campbell Collaboration Library of Systematic Reviews and Joanna Briggs Institute Database of Systematic Reviews and Implementation Studies were important in accessing more specific information on public health and disability, particularly with regard to future priorities. We decided to use these three databases (the Cochrane Library, the Campbell Collaboration Library of Systematic Reviews and the Joanna Briggs Institute Database of Systematic Reviews and Implementation Studies) together to build our review of specific interventions about disability and public health. The results of the theoretical scoping were slightly better for public health, in that this ensured a more general overview in terms of accessing public health issues in accordance with an ecological model on several levels from policy implementation to individual physical interventions. 126 However, the two reviewers found that the same results were obtained within an expansive scoping by rejecting doubles, or reviews of interventions that were on the same theme. To guide the scoping, the two reviewers decided to keep the idea of multilayered framework – combining expansive and theoretical scoping – and use it as an implicit guide (Figure 2). We also note the importance of rejecting interventions on the same theme to ensure an overview of policy issues, while reflecting areas in which research was lacking.
FIGURE 2.
Mapping theoretical approaches on to reviews of interventions.

Scoping public health interventions
In scoping relevant studies, we first assessed how inclusive 30 randomly selected generic public health interventions found in the Cochrane database were of the disability theories or models we identified (see Chapter 3). The piloting demonstrated that the Cochrane database was sufficiently comprehensive to ensure that we accessed a wide variety of reviews of public health interventions. Second, we gathered information about ‘public health’ interventions inclusive of disability for 30 specifically sampled studies. When undertaking the more specific review of disability and public health we checked the Cochrane database first but found insufficient studies (n = 13) and had to supplement this information with studies from the Campbell Collaboration Library of Systematic Reviews and Joanna Briggs Institute Database of Systematic Reviews and Implementation Studies. We manually searched the online archives of the Campbell Collaboration Library of Systematic Reviews from 2004 to 2015 (Volume 11). We manually searched the online archives of the Joanna Briggs Institute Database of Systematic Reviews and Implementation Studies from 1998 to 2014. These searches generated seven reviews. Apart from the use of databases, the methodological principles informing the generic reviews and the reviews more inclusive of disability were similar.
Inclusion criteria
We randomly selected relevant peer-reviewed studies based on our MeSH terms. The review studies had either an explicit public health focus for the generic review or a specific public health and disability focus for our second, more focused, review. The review had to be located in developed or middle- to high-income countries so that they would have relevance to the UK. We were particularly interested in reviews of public health interventions (RCTs). Reviews located in mainly low-income countries were excluded. Reviews that had not been completed and could present only a protocol were also excluded, as were studies still in progress, being updated or withdrawn by the database we were using. If there were reviews in which themes overlapped, we chose the most relevant review and rejected the other review as a ‘double’. When scoping for reviews of disability and public health, we excluded studies about self-care, peer-support, rehabilitation and information unless they had an overt public health focus.
Nonetheless, some of the excluded reviews provide useful analytical insights, which were useful in refining our decision aid. For example, although Godfrey et al. 127 had a relevant and potentially interesting review on intervention strategies across disease and impairment groupings, we had to exclude this because the focus was on ‘self-care’ activities. However, they noted challenges of data synthesis linked to differing ‘types of outcomes measured’; ‘methods of measurement’; and types of ‘priority’ given to outcome measures, preventing comparison of heterogeneous data. 127 This review also raised important issues about scientific rigour and the reporting of systematic review methodologies and appraisal of ‘risk of bias’. 127 The authors point out, for example, that risk of bias is considered internally to a study and does not focus on real-world maintenance or sustainability of an intervention. Similarly, Balogh et al. 82 and Robertson et al. 128 focused on interventions in health and health-care services that fell outside our scoping. Nonetheless, they identified differences not only in outcome measures used by different studies but also the jurisdictions and way that the provision of care would be organised.
Data selection and analysis
The formal content of reviews was appraised by adapting the Effective Public Health Practice Project (EPHPP) Quality Assessment Tool recommended by the Cochrane Public Health Review Group (see Appendix 4). For the purposes of this study, we operationalised the assessment tool to include an examination of how the research question was formulated; sampling strategy; response and follow-up rates; intervention integrity; statistical analyses; and assessment of adjustment for confounders. We used quality appraisal criteria for descriptive rather than exclusion purposes and to highlight variations between reviews (and studies). We also used the Cochrane–Campbell Equity Checklist for Systematic Reviews (or Preferred Reporting Items for Systematic Reviews and Meta-Analyses-Plus) to evaluate the extent to which studies included in the reviews engaged with equity, thereby providing evidence for good research practice, which has successfully engaged with the diverse experiences of disability.
To facilitate this, we used scoping charting methods to help us organise the material selected. 110 We focused on trying to understand if inclusion of disability was linked to the theoretical paradigm being used and if that influenced the methodology and the use of outcome measures. We developed a data extraction table to enable us to scope and review this quickly (see Appendix 5). To aid analysis, we decided to colour code the results similarly to a traffic-light system: red (no inclusion); amber (nominal inclusion); and green (inclusion). 129,130 The term ‘nominal’ indicated that, although disability had been included, there was often no real attempt to define disability theoretically and inclusion appeared to be in name only. 131
In analysing the selected reviews, we became aware of a difference among ‘active exclusion’, in which people with disabilities were excluded from interventions; ‘passive exclusion,’ where the study was designed in such a way to be exclusionary (i.e. owing to exclusions set around ‘literacy’);59 or ‘partial exclusion’ where some – but not all – categories of impairments were seen as problematic (such as mental health). We wanted to keep the scoping open at this stage of the process and focus mainly on categories of inclusion, paradigms used and outcome measures. We initially thought that identifying disability paradigms would be indicative of type of inclusion or exclusion. This was not the case. We discovered that there had been very little theoretical integration of disability paradigms; often, we had to examine the outcome measures or diagnostic definitions of impairment to understand the models being used.
The initial screening of identified reviews was conducted by two reviewers (MB and KA). Discussions resolved any discrepancies. A data extraction sheet collected details on the intervention being evaluated; study designs; target populations; inclusion and exclusion criteria; measures used and their appropriateness to understanding different types of disability; user and public involvement; and relevance of findings to broad and diverse experiences of disability. We noted where reviews included studies with participants from poorer backgrounds, ethnic minority populations and other marginalised groups. We also commented on the extent to which studies – either generic or specific – accommodated the different circumstances in which disability is negotiated and experienced.
The first reviewer (MB) did the initial piloting, scoping and charting of the material. By mapping the reviews, the charting offered a critical commentary on the models and theories of disability (or lack thereof) underpinning (implicit or explicit) evaluations of public health interventions. It also explored whether or not ‘disability’ was included, how it was being defined and what the connection was to the outcome measures and more general concerns of public health. In any review, there is a risk of bias, and, to offer a counter to this, a second reviewer (KA) reviewed the charted data and checked for public health relevance. This was also important in ensuring our iterative process and considering the broader heterogeneity of our approach.
To be consistent with the initial brief, we kept thresholds for inclusion of ‘disability’ as low as possible, but this can be viewed as a limitation to the extent that it might not accord with the lived experiences of disability. We relied mainly on the Cochrane Database of Systematic Reviews but had to interrogate other databases in order to ensure that we had sufficient research evidence. This could be indicative of a lack of ‘disability’ evidence or that we were too narrowly focused on RCTs as providing ‘evidence’. 132 Nonetheless, a more inclusive approach would have generated too much material and greater heterogeneity, thereby making it difficult to draw meaningful conclusions. We were also aware of how our definitions of public health research were influenced by current NIHR practice in terms of research priorities and previously commissioned research. This might have provided a more narrowly defined approach to public health, but was necessary in order to set boundaries consistent with the commissioners’ needs. Furthermore, we were aware that we were assessing reviews of studies on interventions. This is why we decided to select two papers from the different arms of stage 2 scoping and subject them to a more detailed analysis.
Interrogating two selected reviews in more detail
We interrogated the individual studies included in two selected reviews of interventions. We developed a simple charting diagram to collect material (see Appendix 6). Using insights from our earlier scoping, we were especially interested in life-course and fluctuating conditions, the role of intersectionality, and the use and relevance of outcome and effectiveness measures.
In selecting the reviews, we decided to focus on an important cross-cutting public health and disability issue, that is, physical activity. We reasoned that studies would be easy to access and would include a wide variety of outcome measures. Following discussion among the review team, we identified two reviews. The first was a generic physical activity intervention, including 44 studies. 133 The second review focused on physical activity for older people with dementia and included 17 studies and was more purposively specific. 134 The reviewers (MB and KA) read through each article cited in each of the reviews. They were especially sensitive to any reference to disability, including those that might seem more tangential, such as ‘morbidity’. The reviews also explored if any theoretical framework – implicit or explicit – informed the research and, if so, the extent to which this was linked to research design. When formally charting the material, we appraised the extent to which each study was inclusive of the following concepts (see Chapter 4); dignity, inclusion, intersectionality, accessibility and equity in design.
To supplement our material, a member of the project team (MB) e-mailed the corresponding author of each public health study to check whether or not people with disabilities were included and, if so, how. In assessing their responses, the reviewers adapted Feldman et al. ’s92 methods to compare studies; this included asking whether or not the study could have made reasonable accommodations to include disability; the extent to which it could account for intersectionality (such as gender, ethnicity, comorbidities and so on); and if equity was a part of the research design (see Appendix 7). The ‘reasonable accommodation’ question was deliberately ‘open’, as we wanted to get a feel for what authors saw as the key issues. We also asked how easily the intervention could be taken up and whether or not any identified change was sustainable. We gave the corresponding authors 1 month to answer our questions. We received 39 replies out of 44 trials or RCTs which made up the review.
Developing a decision aid and checklist
Our initial analysis suggested the importance of developing a decision aid which could:
-
provide a framework by which to offer a critique of current research practices
-
build capacity and support a more inclusive public health research agenda.
In analytical terms, the decision aid can be seen as an outcome of the first scoping review, which was further developed when evaluating material generated during the second stage of the scoping review and in consultation with our deliberation panels. Our scoping review indicated a need for a greater connection between the disability literature and public health interventions. The lack of explicit engagement with disability that we identified in the public health reviews made this challenging. Nonetheless, we were able to use the material to generate an informed and critical discussion, which connected more theoretical approaches to the more practical, methodological questions raised by the commissioning brief. Chapter 5 provides a more detailed account of our findings, but, as some important themes informed our analysis, we briefly discuss them here.
A study may have been inclusive of ‘disabled people’ but may not have thought about offering a meaningful analysis of disabling experiences by mainstreaming ‘disability’; engaging with disability culture; or considering (dis)ableism in research design. Similarly, most studies had a rudimentary discussion of ethical issues, often confining discussions to confirmation of gaining ethical consent and formal approval. Few, if any, studies engaged with broader ethical issues associated with ensuring ‘inherent dignity’. Only one study, for example, discussed how disability had been ‘dignified’ in terms of inclusive practices. 135 As anticipated, the participation of disabled people in a study’s development and inclusion in samples was rare. Nonetheless, understanding the reasons for inclusions or exclusions was valuable in developing the decision aid. Intersectionality, accessibility and equity assumed similar analytical importance.
Intersectionality was often defined in terms of descriptive categories and reported as such, with little attempt to offer explanatory accounts. It was rare, for example, for sociodemographic categories to be theoretically linked to specific paradigms. Offering an explanation of inequalities was, therefore, the exception rather than the rule. Overall, most studies had examined certain issues of intersectionality but very few put them all into practice, especially comorbidities. For example, papers would note that disability was linked to diabetes and chronic conditions but did not explore this during analysis. More often than not, comorbidities were used as a reasons for exclusion. 136 Accessibility and the broader accommodation of study participants with disabilities were poorly articulated too, with few attempts made to offer a theoretical engagement or to connect to study design. 137,138 Most authors noted that accommodations could have been possible but were not applicable to the study, that study settings, such as schools, would have mainstreamed participants with disabilities and, therefore, did not have to consider it, or ignored the question. Equity was a particularly difficult issue to define. Many of the problems were linked to the empirical design of interventions and, although most studies had theoretically considered equity, they could not provide evidence of long-term sustainability, sensitive to the needs of disabled people or how their intervention could be maintained in the long term. We thus had to focus on methodological design in terms of equity, particularly given that inclusion could occur within an ethical and empirical environment not conducive to equity. 136
Deliberation panels
Consultation with stakeholders is an essential but often neglected part of scoping methodologies. 115,117 We were committed to debating our findings with key stakeholders, particularly given that we believed it would prove useful in identifying gaps in the accommodation of disability in public health. Such consultation would also enable our research (and public health) to reflect the social and political context of disability. 139–141 We first deliberated our findings with politically and socially active disabled people. This ensured that our findings had some grounding in the expectations and experiences of different stakeholders, including those likely to be critical of our approach. We felt this to be especially important, as we wanted our account to reflect the challenges facing public health research when engaging with people with disabilities. We also recruited participants from different regions, to reflect the local dynamics of disability politics. Our agenda was deliberately broad, and the deliberation panels offered expertise, criticisms and advice on the relevance of our work. 142 A fifth deliberation panel comprised researchers, public health professionals and commissioners. The purpose of these deliberation panels was to ensure that our discussion was located in the practicalities and challenges of undertaking public health research. We could also contrast the priorities of professional stakeholders with those of politically active disabled people.
We engaged four partner organisations to help us organise and recruit people to these panels. These voluntary organisations were geographically spread across the country in London (Inclusion London), Manchester (Greater Manchester Coalition of Disabled People), Sheffield (BME Network) and Leeds (Sisters of Frida). The organisations were very small, locally run and located in areas linked to social disadvantage and deprivation, such as Brixton (London) and Moss Side (Manchester). Potential participants were all given information sheets explaining the study and a copy of the ethical decision-aid to discuss before the panel happened (see Appendix 8). The voluntary organisations were given recruitment fees and the participants were paid a fee plus travel expenses for participation.
Although we wanted the deliberation panels to reflect diversity, we did have issues in terms of how inclusive we were of various impairments and identities. Initially, we contacted the Mental Health Foundation/Joseph Rowntree Foundation (Dementia Engagement and Empowerment Project)143 with regard to organising a group with people in the early stages of dementia. We wanted to capture the experiences of people not yet politically organised as ‘disabled’. 96,144 Owing to time constraints, this was not possible. We also wanted to capture the recommendations of people with various types of impairment who may not ascribe to an identity of ‘disabled’ or ‘disability’ but who may be socially and politically organised. We had more success in achieving this.
Five deliberation panels took place during late July and early August of 2015. A total of 34 participants were involved. Formal ethical approval (see Appendix 9) was granted by the Department of Health Sciences’ Governance Committee (University of York). In gaining approval, we were aware that our work occupied a grey area between consultation and research. We decided to gain ethical approval, however, as it would enable us to publish our findings.
Before each deliberation panel began, participants were asked if they had any questions about the information sheet or study. Participants were assured of anonymity and confidentiality. The consent process and form was also explained to participants. A moderator from the partner organisation was always present and ensured oversight of the deliberation process. The deliberation panels were recorded and lasted between 60 and 100 minutes. The deliberation was structured into three parts: the meaning of public health; how to conduct public health research; and the relevance of our decision aid. Our sampling strategy attempted to be as inclusive and diverse as possible. In total, 30 disabled people participated in four panels. They had a wide range of backgrounds and impairments (Table 5). These included social activism within an organisation or community work, in addition to political activism, lobbying and representation. Parents of disabled children were involved, alongside young people with disabilities. Adults participating included those with hidden disabilities, undiagnosed conditions, fluctuating conditions, multiple impairments and mental health issues. We did note a slight predominance of people with visual impairments and wheelchair users. People with hearing impairments were under-represented, whereas people with learning disabilities were not represented. We also noted a slight gender bias, with more women than men in all but one of the panels. The panel with health-care professionals recruited four people. When we explored this low uptake further, we found that many public health professionals thought that disability was a specialised issue or not directly linked to public health. Many, therefore, declined because they thought that they would have nothing to say.
| Panels | Participants | Gender | Focus |
|---|---|---|---|
| London | 4 | 3 women, 1 man | Professionals |
| London | 8 | 4 women, 4 men | Disability |
| Manchester | 8 | 4 women, 4 men | Disability |
| Sheffield | 8 | 6 women, 2 men | Disability |
| Leeds | 6 | 6 women | Disability |
Deliberation panels were digitally recorded, transcribed, anonymised and analysed using NVivo (version 10, QSR International, Doncaster, VIC, Australia). Analyses were conducted using a constructionist grounded theory. We started data analysis using line-by-line coding, then developing categories, which we coded thematically. The object of the thematic stage of coding was not to develop a theory per se, but to assemble the insights of our participants to refine the decision aid. 145
Role of the project steering committee
To ensure the relevance and quality of our scoping review, we established a project steering committee. This met three times during the project. The committee include research commissioners, policymakers, researchers and representatives of disabled people’s organisations. They offered advice on the conduct of research in relation to key milestones, helped the research team to interpret findings, provided critical feedback on project outcomes and advised and supported dissemination activities.
Some of the more politically active disabled people who we approached declined to take part. This was attributable to a perceived emphasis on public health at the expense of disability. Those involved in public health regarded disability as a specialist issue, outside the scope of their expertise. It was also not a particular priority for them.
The first meeting of the steering committee discussed the research project, protocol and the research team’s proposed approach to scoping models and theories of disability. Although supportive of the project, members expressed concern that disabled stakeholders had not been involved in drafting the initial commissioning brief. They also made various methodological comments, which were incorporated into the study design (see Initial inclusion criteria), and emphasised the importance of finding a common ground on which those working in disability-related fields could engage with those doing public health research. The second meeting discussed the scoping of public health interventions and the development of the decision aid. The committee agreed with the emphasis on human rights. The final meeting discussed the findings from the deliberation panels and how best to disseminate the findings of the project.
The committee found this a difficult and challenging project. This made for interesting debate, which demonstrated the difficulties of establishing a more inclusive public health research agenda. Those with a background in disability studies, for example, sometimes felt ill at ease engaging with public health paradigms, particularly if there was a perceived association with rehabilitation. Some also expressed concern that people with disabilities faced more fundamental problems associated with access to basic care and what was seen as a more general assault on their rights resulting from the current reorganisation of welfare provision. (As we shall see, members of our deliberation panels made similar observations; see Chapter 6.) Those working in public health sometimes struggled to reconcile more inclusive approaches with the need to maintain the ‘scientific’ integrity of research.
Conclusion
This chapter presented our methodological approach, although, as we have noted, we used an iterative approach, meaning that this is not a conventional methodological chapter per se. Nonetheless, it provides a transparent account, outlining in some detail what we did and how our methods informed our findings. Our account, which synthesises information from a variety of sources, employed a narrative, thematic and interpretative approach. This synthesis linked different models and theories of disability to an understanding of public health research. The synthesis demonstrated the breadth and depth of the literature on disability, including possible (theoretical) tensions when applied to public health research. This was connected to an assessment of the more practical aspects of research design and inclusive research strategies.
In the chapters that follow, we begin by outlining four inter-related models explaining disabling experiences and then assess potential strategies for connecting these models to public health research, by exploring the value of a ‘decision aid’. This decision aid offers various options for both a critical appraisal of current research practices and a strategy for developing a more inclusive public health. It provides a bridge between the different models of disability and the concerns of public health by outlining a range of options with which commissioners, practitioners and research could engage.
By integrating the findings from the different reviews, we are in a position to provide best practice guidelines on terminology and categorisation; deployment of life-course perspectives; participant, public and stakeholder involvement; and the appropriateness of study designs and outcome measures to explore the diverse range of experiences associated with different disabilities. By evaluating a range of strategies, our findings seek to inform the commissioning of both future research on targeted public health interventions and generic interventions designed to mainstream disabled people/groups. However, it is important not to give definite guidance in what is a rapidly changing field. There is also a limited evidence base on which to inform decision-making. This is why we discuss possible choices and their consequences. We are especially sensitive to the needs of more social and emancipatory models of doing research, while recognising the practical demands of producing evidence-based public health research.
Chapter 3 Scoping models and theories of disability
This chapter presents the findings from our first scoping review, in which we offer a synthesis of the research discussing and critiquing models, definitions and theories of disability. We identify the range of models and theories (including strengths and possible limitations in generating inclusive approaches and capturing diverse experiences); their place within the field of disability studies and within the social and political movements of disabled people; the dialogue between them; and their potential contribution to mainstream public health research and policy. This chapter identifies four broad models in the disability literature:
-
The medical model: this model views impairment as a problem located in an individual.
-
The human rights model: accords fundamental human rights to persons with disabilities.
-
The social model: makes a distinction between impairment (physical/mental/sensory) and disability (as the experience of social oppression).
-
The CDS model: questions the dualism between impairment and disability.
We offer a contextual account of the assumptions underpinning these models before discussing, in Chapter 4, the potential implications for how public health research is undertaken, including reflecting on a potential dissonance between public health and disability discourses. We begin, however, with a reflective and historical note on the difficulties we faced when mapping a shifting debate.
Mapping a shifting debate
We found a wide variety of models (statistical, professional, psychological, rehabilitative, policy, ecological), including models that focused on specific impairments (i.e. autism, arthritis, depression). Most of these models were located in the Global North, although a number of large quantitative studies were based, for example, in China. There was much less meta-analysis of models or in-depth (theoretical) exploration of strengths and weaknesses of a particular model. The earliest models that we found were linked to rehabilitative public health146 and were located mainly in the USA. 21 Many of the models also had an economic basis or were concerned with quantifying disability, especially from the early 1990s onwards (see the activities of the World Bank and the WHO). 12,59 The need for international standards of measures was strongly correlated to global development discourses as well as to debates about the definition of health and the meaning of QoL. One of the most influential QoL measures was Amartya Sen’s147 capabilities or capability approach. The capabilities approach has transcended its original economic origins to become a normative framework associated more with human rights approaches. 148–150 Such an approach argues that, when promoting human development, the focus should be on ‘functioning’ in terms of ‘being and doing’, consistent with what people are able to achieve. 151 This has been hugely influential in social justice152 and human rights151 and has been applied to understanding thresholds of deprivation in economic development (the UN’s Human Development Index). Nussbaum and Sen152 argue that human development should be related to an understanding of QoL in terms of people’s capabilities. The capabilities approach was foundational for feminist approaches to, and in indices measuring, gender development. 153 The capabilities approach has also been influential in public health, in particular in linking financial capability, health and disability. 154 These factors tie in with larger international public health programmes and interventions linked to welfare or social security, which, for example, examine the impact of conditional and unconditional cash transfers on health to increase capacity and capabilities. Nevertheless, the capabilities approach, although seemingly positive, is still largely related to the measurement of the economic impact of ill-health and disability,155 although there are signs that this might change, as the capabilities approach has the potential to develop into a paradigm more accessible to empirical researchers. 148,156 Furthermore, and perhaps reflecting its original association with socioeconomic policies, there remains a tendency for capability debates to conceptualise social justice in relation to the distribution of welfare ‘goods’, rather than as a broader connection to social equality and discrimination. Resolving these tensions is likely to be an important consideration when assessing the usefulness or otherwise of capability approaches in engaging with more critical rethinking of disabling experiences.
The most influential approaches to measurement are found in the International Classification of Diseases157 (ICD) and the Global Burden of Disease (GBD). 158 The GBD uses metrics based on ‘disability’ gaps such as disability-adjusted life-years (DALYs). 41,159 DALYs similarly appear in the literature from the 1990s onwards and are used in the World Bank’s World Development Reports160 and Disease Control Priorities Review. 161 DALYs measure health lost as a result of mortality or non-fatal injuries or disease and are calculated by adding years of life lost and years lived with disability. 162 The GBD study is updated each year and calculates the prevalence of disability using a number of measures such as DALYs;44,163 it also increasingly involves the measurement of acute and chronic diseases and injuries. 122,158
In terms of metrics such as health-adjusted life-years, quality-adjusted life-years (QALYs) or DALYs, there has been little discussion about how and why these measures were developed or the ways in which they could be seen to imply that disability or ill-health are ‘costs’. 160 This is a problem to which we shall return. Methodological issues were discussed in the associated literature but this tended to focus on issues relating to weighting of variables and the definition of life expectancy to calculate cost-effectiveness164 rather than to offer a critique of the concept of disability underpinning the quality-adjustment of people’s health.
By the late 1990s, criticisms of the use of DALYs had emerged. These criticisms questioned the norms and values underpinning such a measure, highlighted the dangers of viewing health in a silo without connection to the broader social environment, and asked whether or not such metrics adequately captured disabling experiences. 164–166 Later criticisms of DALYs focused on attempts to understand the influence of self-report, cost-effectiveness and culture on understanding disability. 167–171 For example, a person with a visual impairment may not be in poor health, and being ‘blind’ might be an issue linked to welfare rather than to health. 167 Several critiques note the insufficiency of current measures to capture both the increasing complexity of impairments and political understandings of disability. 63,172 Measurement tools linked to measuring health expectancies in longitudinal data also came to the fore, particularly in the 2000s, as demonstrated by disability-free life expectancy, disability-adjusted life expectancy or healthy life expectancy. 166,173 Similar criticisms about the ability of such tools to capture complexity have emerged. We return to this in Chapter 4.
The tendency to view disability in terms of health measures has sometimes resulted in the neglect of other relevant health policy priorities directly linked to disabled people’s daily lives in the UK, such as independent living, direct payments or the personalisation agenda. 39 Debates about measurement have also struggled to reflect the conceptual debates over how disability is understood. 122,174
From the 1990s onwards, research on development and poverty began to include disability, but epidemiological research on how inequality links to disability did not come to the fore until the 2000s. Even then, most studies were quantitatively driven and rarely reflected more qualitative experiences of disability. 175 However, critical voices, often aligned with the social model of disability, began to have an influence (see A more social model approach below). Mike Oliver’s reworking of the Office of Population Census and Surveys (OPCS) (now the Office for National Statistics survey) demonstrates some of these tensions (Box 2).
What’s wrong with you? (OPCS survey question)
What’s wrong with society? (Mike Oliver’s alternative)
Do you have problems at work or are you unable to get a job because of your illness?
Do you have problems at work or are you unable to get a job because of the physical environment and/or the discriminatory attitudes of others?
Does your health problem mean you are restricted in your daily activities of living?
Do inadequacies in community services, housing and transport mean that you are restricted in your daily activities of living?
Source: adapted from Oliver. 175
Other problems included difficulties over how measurements captured changing debates about health and social care and in particular incorporated ideas about ‘self’ care, management and advocacy. 88 Measurements informed by the political movements of disabled people or advocacy were equally rare. Nonetheless, over the past 5 years, we note an international and national move towards viewing disability as an essential feature of all future public health initiatives, which in turn are strongly influenced by rights-based models. The influence on public health practice, however, appears to have been slow. Most developments continue to focus on screening for disability or its measurement within population groups.
Definitions of ‘impairment, ‘disability’, ‘illness’, ‘disease’, ‘disorder’ and ‘chronic illness’ are constantly shifting, especially in terms of how they are linked to what is understood as ‘disabling’. Armstrong,176 maintaining a critical stance, saw the emergence of concepts such as ‘chronic illness’ as linked to the medical pathologisation of ageing. During the scoping review, we also noticed a further inconsistency in how ‘disabling’ is defined, with terminology more consistent with ‘disease’ or ‘disorder’ noted when discussing addiction and obesity. This may point to a growing emphasis on biomedical understandings171 rather than on more collective experiences of disability and disablement, linked, for example, to austerity. 177,178
Medical definitions and classifications have also been influenced by the WHO’s international global policy priorities and classifications in terms of their differing models, classifications (i.e. ICD) and/or diagnostic manuals [i.e. Diagnostic and Statistical Manual of Mental Disorders179 (DSM)]. However, the language linked to impairment could still be regarded as paternalistic, by, for example, focusing on ‘vulnerability’, or as patronising, by prioritising models for professionals working with disabled people rather than the perspectives of disabled people themselves. 180,181 This is also evident in public health policies linked to disabled people and their emphasis on dependency. 182 The emphasis on the measurement of impairment could also be regarded as particularly unhelpful, as could the discriminatory language (‘retarded’, ‘retardation’, ‘deficiency model’, ‘subaverage’, ‘slow’ or ‘slow-functioning’)183,184 and implicit concern with ableism (‘failure to adapt’ and ‘challenging behaviours’). 185
Despite critical challenges to such views, which have been influential in public health, there remains a tension between viewing impairment as an ‘outcome of disease or impairment’ or as a disability, informed by social limitations connected to discrimination. 21 It is unclear, for example, if mental health, pain or substance abuse issues were viewed as ‘impairments’ or as ‘disability’ when quantified as such in bureaucratic, administrative or professional models.
Current debates about obesity are likely to generate similar confusion. Administrative, legal and medical understandings exist side by side, with each influencing the other but in ways that are not always recognised, questioned or acknowledged.
The growing influence of more holistic measures, however, has been welcome, particularly as more ecological paradigms have become influential. From the early 2000s onwards, for example, we see more analysis in terms of the intersectionality of disability (such as gender, age, ethnicity and socioeconomic class). There has also been a greater willingness to explore how the biosocial, institutional and cultural processes influence understandings of disability. An issue such as ‘addiction’, for instance, has shifted from being understood in terms of a disabling ‘brain disease model’ to ‘ecologies of addiction’,186 ‘neurosocial’187 or even ‘neuroplastic’188 understandings. These models are correspondingly linked to recent (bio)social science challenges and innovations,189 for instance, in terms of the importance of longitudinal analysis and big data. 190
Problems remain, however. Some epidemiological studies, for example, explicitly focus on modelling a particular type of impairment in a delimited setting, for instance by assessing levels of lower back pain as a form of disability affecting the working population in Europe. 191 This growing kind of research demonstrates the importance of ‘risk’ discourses linked to impairment that focuses on the consequences of prognosis and diagnosis for economic and bureaucratic measurement. 192 This has been termed an ‘actuarial model’193 but is also linked to the growing political importance of quantification of health as providing evidence for policy and practice. This is evident in public health research and the influence, however subtle, of more positivist theories, implicit in medical models and governance, remains. 194
Finally, our review demonstrated how theoretical developments in how we understand disability have been recently influenced by other social movements, such as those associated with feminism, queer theory, intersectionality and critical race theory. However, the links between social justice theories and inequalities literature on poverty, although influential, have remained undertheorised, and the practical impact on the operationalisation of more evaluative methodologies used in public health remains small.
To summarise, our initial review demonstrated a variety of different models explaining disability, many of which are sensitive to time and place. Consequently, a historical or genealogical reading of these theories and models is important in understanding the evolution of these debates. During this evolution, it is rare for one model not to be influenced by, and to interact with, the other models. The medical model, for example, has successfully incorporated aspects of the more critical debates associated with the social model (see International Classification of Functioning, Disability and Health below). To this extent, any attempt to provide operational definitions can do little more than provide an ideal type. Nonetheless, these ideal types are a useful starting point in beginning to understand the (potential) connection of different models with public health interventions and research.
The medical model
A medical model of disability was the most discussed model in our first scoping review. This is perhaps not surprising, as the other three models were developed in response to the ways in which medicine has viewed disability. In essence, medical models see impairment as a consequence of some ‘deviation’ from ‘normal’ body functioning, which has ‘undesirable’ consequences for the affected individual. Impairment is seen as indicative of an underlying physical abnormality (pathology), located within the individual body, and medical treatment, wherever possible, should be directed at the underlying pathology in an attempt to correct (or prevent) the abnormality. Critics argue that this is a form of biological reductionism which views disability in terms of an individual deficit/problem that has to be fixed, rehabilitated or prevented rather than in terms of being generated by the social consequences of impairment. 195,196 This tension has come to inform how the medical model has been debated.
Disability has tended to be theoretically conceptualised as a physical rather than a mental health problem, at least initially. There is also some debate about whether the medical model should be viewed as a transactional model or systems approach. Llewellyn and Hogan197 argue that a systems approach views development as ‘synergistic’ within the environment, whereas the transactional model understands development as a transaction or exchange between person and environment. These early understandings heralded the later influences of ecological models and the growing importance of science and technology studies in the sociology of health and illness. More recently, (bio)medical models have been used to consider obesity, smoking, violence, risky sexual behaviour and even climate change, but, as we shall see, they are rarely linked to theoretical (and more inclusive) discussions of disability.
The medical model could be seen as especially weak in conceptualising comorbidities or multimorbidities, which is at odds with the idea that many people will possibly experience various forms of impairment during their lifetime. Disability has been seen as an extraordinary, unusual, life-changing event and has often been viewed as an individual personal tragedy. 198–200 Oliver198 explicitly states that the medical model encapsulates both biomedical and psychological perspectives but that the ‘individual medical model’ has medicalisation as a key aspect. Barnes199 views rehabilitation and the norm of the able body as central to the ‘individual’ medical model and the way in which disability is understood. Nonetheless, most theoretical analyses of disability models, despite containing critical references to ‘a medical model’, do not always expound what they understand by it or reflect ways in which the model has changed. 200
Early articles on health, which were informed by medical models, were nearly always linked to measurements such as the tacit models underlying health status instruments or the need for normative reference case against which deficits and deviations could be compared and measured. 201 The earliest medical models were also linked to defining scales of measurement such as those associated with ‘quality of life’. 202 When focusing on outcome measures for QoL, it was, however, rare for studies to consider environment, opportunity or disabling process. 203,204 The focus tended to be on individual conditions, with little attempt to explore how disability could be socially generated.
In 2001, there was an attempt by the WHO to engage globally with disabled people and use their ideas to rethink medical care. 35 The influence of the medical model remained, as evidenced by the continued refinement of the ICIDH, which is now known as ICIDH-2. The papers included in the scoping review do not reveal why the model espoused by the WHO became configured as ‘the medical model’, particularly when there was a conscious attempt to move beyond it.
International Classification of Impairments, Disability and Handicap
The WHO hired an external consultant, David Wood (University of Manchester), to develop an extension of the 1976 ICD157 to cover ‘chronic illnesses’ and to focus not only on impairments but also on their social and functional consequences. 23,205 Although David Wood was mainly involved in classification, it was the sociologist Mike Bury and the public health epidemiologist Elizabeth Badley who attempted to understand the conceptual links between disability and handicap. This built on previous work, such as variations of the Nagi model,146,206–208 which made distinctions between pathology (as disease), impairment, functional limitations and disability (as societal functioning), and the Quebec model, in which ‘handicap’ was viewed as an outcome of social creation. 209,210 In many ways, revising the ICIDH-2 was a response to an ageing population and people with impairments living longer and having complex health needs. 211 However, the ICIDH-2 tended to be less successful when trying to understand and incorporate models and outcomes of successful ageing, but was successful in developing a classificatory scheme linked to disability. For example, although medical advances enabled people with chronic illnesses to live for longer, a medical model struggled to adapt to their functional needs, as well as to the idea that QoL was equally social in nature.
The WHO’s ICIDH-2212 implies a causal relation between biological processes and social outcomes, whereby disease leads to impairment, which leads to disability, which leads to handicap. It focuses on disease but uses a threefold classification between impairment, disability and handicap, as follows:
-
Impairment: any loss or abnormality of psychological, physiological or anatomical structure or function.
-
Disability: any restriction or lack (resulting from an impairment) of ability to perform an activity in the manner or within the range considered normal for a human being.
-
Handicap: a disadvantage for a given individual, resulting from an impairment or a disability that limits or prevents the fulfilment of a role that is normal (depending on age, gender, social and cultural factors) for that individual. 212
In the first scoping review, myriad applications of ICIDH-2 were found, especially in Social Science & Medicine. For example, there were several applications of the ICIDH-2 to understanding processes of ‘disablement’. 213 Hartley and Wirz214 modified the ICIDH-2 in the development of a ‘communication disability model’, which could be used to positively influence the professional delivery of services. Bickenbach et al. 215 argue that the UK social model or US civil rights minority model represented ‘models of disablement’, and that the ‘universalism’ of ICIDH-2 counted this. Other thinkers view the ICIDH-2 in a more pluralistic environmental sense, with a strong connection to ‘human ecology models’. 216 Despite this, the use of the ICIDH-2 was largely classificatory, as evidenced by its use in the second OPCS national survey of disability. 23,217 As such, it came under considerable criticism, particularly in how it continued to assume a causal link between impairment and ‘disability’, thereby enabling the conceptualisation of impairment primarily as an individual’s medical ‘problem’, which needed to be fixed or rehabilitated. 218 This led to further refinement, in an attempt to capture the social construction of disability and the process of disablement. 219–221
International Classification of Functioning, Disability and Health
Responding to criticism by disabled people and the growing influence of a more social model of disability and the impact of environmental barriers (see A more social model approach below), the WHO commissioned a revision of the ICIDH-2. 215 This revision attempted to bring together an individual medical understanding of impairment, with an acknowledgement, reflecting more social models of disability, that society disables:
Disability and functioning are viewed as outcomes of interaction between health conditions (diseases, disorders and injuries) and contextual factors . . . Among contextual factors are external environmental factors (for example, social attitudes, architectural characteristics, legal and social structures as well as climate, terrain and so forth), and internal personal factors, which include gender, age, coping styles, social background, education, profession, past and current experience, overall behaviour pattern, character and other factors that influence how disability is experienced by the individual.
World Health Organization222
Furthermore, according to the WHO:12
Disability is the umbrella term for impairments, activity limitations, and participation restrictions, referring to the negative aspects of the interaction between an individual (with a health condition) and that individual’s contextual factors (environmental and personal factors).
World Health Organization12
The resulting ICF223 is typically represented in a visual diagram in which the functioning of the body or body part, personal activities and social participation are a central triad (Figure 3). 222 Disability involves any dysfunction of impairments, activity limitations or participation restrictions. The arrows are bidirectional to indicate that components of health are interlinked and affect each other. This responded to the critiques of those advocating a more social model of disability, who question the linear relationships implied by the ICIDH-2.
FIGURE 3.
The ICF (reprinted with permission from Towards a Common Language for Functioning, Disability and Health ICF, World Health Organization, 2002, www.who.int/classifications/icf/training/icfbeginnersguide.pdf.)222

Interventions can also be mapped on to this triad, as different interventions can be used for the body, personal activity or social participation. This is why the ICF is also known as the relational or ‘bio-psycho-social’ approach. The ICF also can be mapped on to interventions or preventions (Table 6). 222 This is potentially useful to public health research, and this is an idea to which we shall return.
| Perceived difficulty | Intervention | Prevention |
|---|---|---|
| Health condition | Medical treatment/care Medication |
Health promotion Nutrition Immunisation |
| Impairment | Medical treatment/care Medication Surgery |
Prevention of the development of further activity limitations |
| Activity limitation | Assistive devices Personal assistances Rehabilitation therapy |
Preventative rehabilitation Prevention of the development of participation restriction |
| Participation restriction | Accommodations Public education Antidiscrimination law Universal design |
Environmental change Employment strategies Accessible services Universal design Lobbying for change |
The literature in our scoping review indicated that the ICF has been richly conceptualised in terms of comorbidities or secondary conditions. 11 However, this has mainly been in terms of risk and a connection to rehabilitation. This is why Rimmer et al. 11 argue that such models need to be interdisciplinary to work. However, Ravesloot et al. 75 found that some categories of the ICF could be mapped on to behavioural change models used in public health promotion. However, they found that neither the ICF nor behavioural change models addressed the reasons behind how people would find ‘meaning’ when participating in interventions. 75 The ICF also continues to be criticised by disabled people. 23,71
Strengths
The ICF was seen in the literature to have a particular value when discussing policy. 224 Advocates of the ICF have argued that it improves on the ICIDH-2217,225 by providing a scientific standard to inform national and international policies on disability at both an individual and population level. To this extent, the ICF has been successfully applied in a range of surveys such as by the WHO (health and disability) and the statistical office of the European Union (Eurostat) (disability and social integration). 226,227 More generally, the ICF has contributed to studies exploring the prevalence of disability and its measurement,228 while also providing the opportunity for comparable data.
The ICF can also be used with other WHO instruments such as the ICD, Tenth Edition (ICD-10) and ICD, Eleventh Edition (ICD-11)229 and an ICF-CY230 specifically for children and youth. Üstün et al. ,231 for example, argue that, although there are many ‘condition specific assessment tools’ (e.g. the Hamilton Rating Scale for Depression232) as well as ‘generic measures’ [i.e. Short-Form questionnaire-36 items (SF-36)], the ICF was specifically developed to counter these ‘data silos’. This is why the ICF is being used to reflect a global public health agenda [i.e. human immunodeficiency virus (HIV), malaria]. The ICF can also accommodate different outcome measures (technical, clinical or patient-oriented) and has ‘linking rules’ to illustrate how to connect health status measures to technical and clinical data or interventions. 233 Cieza et al. 233 explain that the strengths of the ICF are its standard terminology and definitions, an ability to disregard competing and condition specific instruments and the power to distinguish between outcomes and outcome measures.
Although the ICF seems complex in terms of the different ways in which it can be translated, the ways in which people use the ICF can be creative. For example, one study in the review examined the ‘capacity’ of people with psychiatric disabilities to work and measured the gap in terms of their current social participation. 234 In this way, disability is viewed as an environmental construction. The application of the ICF to rehabilitation, in addition to its use globally to collect statistics (i.e. the UN’s Washington Group)235 and to monitor the CRPD, has been particularly successful. 62,236 Bickenbach237 sees the ICF as a ‘bridge’, insofar as statistics are needed as indicators to monitor progress on global policy issues such the Millennium Development Goals and how nations are conforming to legal conventions such as the CRPD.
The link between the ICF and CRPD is not always welcomed by those who take a more critical approach to understanding disability (see A social model approach and Critical disability studies below). However, our scoping review revealed that those working within a more global perspective on disability rights have creatively connected theories such as Sen’s147,151 ‘capabilities’ approach to the ICF149,150,238 and, more recently, to social capital. 239 Furthermore, the versatility of ICF can be seen as an attempt to link it with debates about inequalities or social determinants of health (SDHs),240 in addition to human rights instruments and social justice in global public health. 241 However, our analysis suggests that among those broadly supportive of the ICF, there is uncertainty about how best to connect the ICF to the CRPD or other international instruments and conventions. Baylies242 argues that ideas about ‘participation’ can be used to locate the ICF within discourses of ‘rights, capabilities and human development’ and ‘environment’:
These new elements are specifically intended to link the ICF with the standard Rules on the Equalisation of Opportunities for Persons with Disabilities so as to provide, ‘an appropriate instrument for the implementation of stated international human rights mandates as well as national legislation’ (WHO 2001: 6). In acknowledging the legitimacy of a broadened discourse on disability in terms of rights, inclusiveness and participation, the ICF has enlarged the understanding of the nature of disablement, emphasising the crucial importance of context of the social and physical environment.
Baylies242
Our scoping review suggests that the potential of such an approach is still to be fully realised. 226 Furthermore, tensions have emerged, particularly in terms of how clinicians, bureaucrats and disabled people expect the ICF to do different things. However, overall, the conceptual strength of the ICF is that it has the potential to move from a rehabilitative domain to one informing a broader approach to social welfare.
Potential weaknesses
Although the ICF is an attempt to transcend the medical model, it struggles to escape fully from its associations with it. A systematic review on the use of the ICF, for example, found that most papers were about clinical and rehabilitative use. 243 Applications to public health research are rare, although when used it tends to emphasise a ‘functional’ approach to disability. 213 The perceived association between the ICF and rehabilitation has become a particular social and political focal point in the disability literature for reasons that are not entirely clear. This is despite the links between ICF and CRPD. 221,244 This might reflect a tension between aspiration and practical application. Although the ICF has a broad application,222 its implementation remains narrow. A particular and persistent criticism, for example, is that the ICF is predicated on norms and values that are still fundamentally disablist.
The ICF, despite having considerable influence on defining outcome measures, has been less successful in encouraging an exploration of what happens during an intervention and, in particular, in how measurement is linked to rehabilitation. 38,245,246 A connected problem is the possible confounding of function (i.e. functional limitations or measures) with what it means to live healthily with impairment. 38 This might have particular importance when discussing public health research. Activities of daily living (ADL) and measures of self-reported health such as SF-36 can, for example, confuse function with health. 204 Moreover, the focus on the content of outcome measures entails comparisons. This can sometimes mean that response categories are taken for granted and not linked to conceptual critique. 247 The relationship between health status, biopsychosocial and environmental functioning can, therefore, be unclear. In attempting to make sense of this, Bickenbach248 notes that the ICF is a classification system and neither an ‘assessment instrument’ nor ‘measurement tool’, despite being used as such. He argues:
Despite this, the descriptive qualifiers for Body Functions, Activities and Participation and Environment Factors were scaled, both qualitatively (No problem; Mild; Moderate; Severe; and Complete Problem) but also quantitatively (No problem = 1–4%; Mild problem = 5–24% and so on). Clinicians in the various rehabilitation professions and measurement theorists have developed assessment tools to measure specific Body Functions. Some of these have acceptable statistical properties, are reliable, and are widely accepted by professional communities worldwide. Other such tools have been developed for very local purposes –specific diseases, specialised clinical settings – often primarily designed to regularise professional remuneration or insurance pay-out in specific jurisdictions.
Bickenbach248
Bickenbach goes on to say that the ICF raises issues with the definitions of activity and participation:
The pattern is same: disability is a matter of the body, the person and the person in society. Hence the triads: impairment, disability, handicap (ICIDH and Quebec); and impairment, functional limitation, disability (Nagi). It stands to reason that in the ICF the pattern should be repeated, and it apparently is: Impairment, Activity Limitation, Participation Restriction. But there is a catch. The Activity and Participation classification ‘merges’ the two; or more correctly, the individual categories in the classification are both Activity and Participation categories. But how can Activity and Participation be conceptually different, but identical in terms of their list of categories?
Bickenbach248
Participation and personal factors are especially criticised for being undertheorised. 23 The more critical literature suggests, for example, that the use of the ICF has neglected overarching structural issues, such as the links between poverty and inequality in the creation of impairment and disablement. 242 The use of the ICF in employment fields is viewed as especially problematic, particularly given that disability is conceptualised as a barrier to valorisation. 243 Criticisms, therefore, have focused on how the ICF has rarely been used to challenge or change policy to create a more enabling society in line with the CRPD or social model. 23,242
There are also concerns that the ICD defines impairment as a variation from the statistical norm and that ‘an individual’s capacities are assessed against that of someone without a similar health condition (disease, disorder or injury)’. 23 This raises broader concerns about what it is to be human221,249,250 and about the ability of the medical profession to define what is normal. 251 Kras,252 for example, raises concerns about how public health interventions aimed at disabled people who have autism can become linked to ideas of ‘prevention’ and rehabilitation. Ginsburg and Rapp253 agree and argue that:
Most researchers who ‘count disability’ – demographers, statisticians, economists – are rarely in dialogue with scholars in disability studies, whose concern has been to show how ‘disability counts’ across a range of qualitative fields.
The plethora of visuals, decision aids and assessments associated with ICF is also seen as constraining creativity and innovation and encouraging a rather mechanistic, uncritical application. 239 This is an especially telling critique given the points raised in the previous paragraph.
The recommendation of the WHO and the UN for the ICF to be a universal standard measure is not without its problems, especially given the criticisms of some disabled activists, who are keen to identify theoretical and conceptual weaknesses,254 while arguing that no consensus exists. 39 Those working within more critical disability models argue that there can be no universally applied measures,39 and to think that there can be fails to acknowledge the way in which the ICF reflects a bureaucratic and medical approach divorced from the local sociocultural realities in which people live. 255 The ‘universal’ approach has also been criticised for a lack of sensitivity to gender and ethnicity, in addition to its relationship to western scientific concepts and formulations. 242,256,257 A more human rights-based approach is presented as possible means by which to overcome these difficulties.
The human rights model
Many of the criticisms highlighted above find specific and defined expression in alternative approaches to conceptualising disability. Despite having a long history,258 the human rights model has only recently assumed analytical importance in the context of disability. Nonetheless, it generated the second highest number of papers in our scoping review, taking various national and international forms. 259 The model was initially linked to the 1948 Declaration of Human Rights. 260 Early rights-based models were linked with the political movements of the time, such as civil rights,261–263 feminism264 and children’s rights. 265
Although international treaties incorporated ‘disability’ (see, for example, the 1976 International Covenant on Economic, Social and Cultural Rights266 and International Covenant on Civil and Political Rights267), most early discussions of rights were usually framed in terms of the need for national legislation that made discrimination a crime. Later policy documents such as those from the Disability Rights Commission97,268 and Human Rights and Equality Commission,101,102 supported a human rights paradigm, which eventually became enshrined in legislation in the USA and the UK. The US-based literature focused on the Americans with Disabilities Act (1990),269 while in the UK the legal rights of disabled people were enshrined in the Disability Discrimination Act (1995) which was later incorporated into the Equality Act (2010). 28 In the Equality Act (2010),28 disability was regarded as a protected characteristic, against which discrimination, harassment and victimisation was illegal. The Act also established equality of opportunity and placed a public service duty on public sector organisations to foster good relationships between groups both with and without protected characteristics.
Historically, the 1980s marked the emergence of disability as a global issue. The International Year of Disabled Persons was marked in 1981, and in 1982 the UN published a World Programme of Action Concerning Disabled Persons. 270 By the 1990s, which marked the start date for our scoping review, disability was firmly on the UN agenda and beginning to be mentioned explicitly by conventions such as the International Committee on Economic, Social and Cultural Rights in 1993. There were also mentions of ‘rights models’, with links being made to movements such as the global ‘right to health’ and the health activism of the 1990s and 2000s. There was a strong association of disability with biosocial identities and health inequalities. 271 Our scoping review suggests that, from 2006 onwards, there was a gradual move from general discussions of civil and political rights to more specific discussions associated with the CRPD. 272,273
Researchers and activists involved in the development of the CRPD advocated it use as an explicit ‘new’ human rights paradigm. 274 This meant that research was moving towards a more encompassing, albeit critical, understanding of rights. Most countries have signed up to this international legislative instrument.
Conceptions of citizenship predicated on tacit rights-based approaches have been increasingly applied to understanding the difficulties facing disabled people. 275 For example, the importance of active agency in decision-making by young disabled adults is discussed in the context of transitional care. 276 Disability activists and academics have also taken up rights-based approaches, but this has not been without tensions, particularly among those who espouse a more ‘international’ disability approach12,200,277 and those who see rights-based approaches as failing to fully embrace emancipatory paradigms. 23,71,278,279 Sayce and O’Brien280 argue that ‘rights’ represent both risks and rewards for disabled people, especially if they become medically defined or disconnected from practical outcomes (see also Sayce281).
Early work in disability studies and activism examined what a move from ‘needs based assessments’ to ‘rights based assessments’ would look when applied to independent living. 282 Drewett283 concluded that, although ‘rights’ are presented as ‘fairer’ than the ‘needs-based character of welfare policies’, it is not clear how such an approach would change the delivery of health and social care. This is why some argue for legislative protection, alongside more inclusion in social life, which is informed by normative values and assumptions. For Rioux and Heath,260 quoting Quinn et al. ,284 a more rights-based approach can be defined as follows.
Importantly, it means locating any problems outside the person and especially in the manner by which various economic and social processes accommodate the difference of disability . . . The debate about disability rights is therefore connected to a larger debate about the place of difference in society.
This quotation suggests a more fundamental tension between ‘recognition versus redistribution’,260 which has been identified by several authors. 285,286 Concerns have also been expressed by the demands of both negative and positive rights. Although civil and political rights are understood negatively in terms of protection from discrimination, they do offer legal redress. Cultural and social rights are understood more positively, but, because they are often enforced through the ‘redistribution’ of resources, they become threatened in times of austerity. 260,285,286
Strengths
Advocates view the CRPD as a rights outcomes approach which argues for the removal of barriers to allow both non-discrimination and participation in social life. 272,273 Such an approach, which it is hoped will be embedded in legislation, brings together previous rights-based instruments, which encompass both social needs and political rights. Adopted in 2006, the CRPD is viewed as one of the most innovative and extensive human rights instruments. 22 It contains over 50 articles and an optional protocol. The UK is a signatory to the convention and its optional protocol, which it ratified in 2009. The CRPD is conceptually linked to the ICF but it also ensures that the definition of disability remains dynamic by:
Recognising that disability is an evolving concept and that disability results from the interaction between persons with impairments and attitudinal and environmental barriers that hinders their full and effective participation in society on an equal basis with others.
From Convention on the Rights of Persons with Disabilities, United Nations, © 2006 United Nations. Reprinted with the permission of the United Nations22
Health, for example, is mentioned explicitly in Article 25 of the UN CRPD,22 which states that:
State Parties recognise that persons with disabilities have the right to the enjoyment of the highest attainable standard of health without discrimination on the basis of disability. States Parties shall take all appropriate measures to ensure access for persons with disabilities to health services that are gender-sensitive, including health-related rehabilitation. In particular parties shall:
a) Provide persons with disabilities with the same range, quality and standard of free or affordable health care and programmes as provided to other persons, including in the area of sexual and reproductive health and population-based public health programmes;
b) Provide those health services needed by persons with disabilities specifically because of their disabilities, including early identification and intervention as appropriate, and services designed to minimise and prevent further disabilities, including among children and older persons;
c) Provide these health services as close as possible to people’s own communities, including in rural areas;
d) Require health professionals to provide care of the same quality to persons with disabilities as to others, including on the basis of free and informed consent by, inter alia, raising awareness of the human rights, dignity, autonomy and needs of persons with disabilities through training and the promulgation of ethical standards for public and private health care;
e) Prohibit discrimination against persons with disabilities in the provision of health insurance, and life insurance where such insurance is permitted by national law, which shall be provided in a fair and reasonable manner;
f) Prevent discriminatory denial of health care or health services or food and fluids on the basis of disability.
From Convention on the Rights of Persons with Disabilities, United Nations, © 2006 United Nations. Reprinted with the permission of the United Nations22
Health is also closely linked to Article 26 (rehabilitation), as well as to other articles in the CRPD, such as Article 1 (respect for dignity); Article 2 (communication, respect for dignity, reasonable accommodation and universal design); Article 9 (accessibility, i.e. of medical facilities); Article 17 (protect physical and mental integrity of person); and Article 31 (statistics and data collection to inform policy). Intervention is linked to a right to health but also to minimising and preventing further disabilities. Article 25 begins with accessibility of care in terms of different gendered needs but is also inclusive of population health and a life-course approach. As such, it straddles both the need for prevention and duty of care and health across the life-course. 287 In addition, the CRPD notes that inequalities exist in terms of accessibility and affordability of health care. Perhaps importantly, given the focus of this review, Stein et al. 100 note that Article 4 means that states have an obligation to ensure accessibility to health care, which also includes research.
Inclusivity is at the heart of a rights-based approach to disability. Perhaps because of this, our scoping review revealed that much work explores the link between a rights-based perspective and those anchored in concepts of ‘human development’ or ‘capability’. 242 Discrimination is specifically seen to prevent inclusivity. Article 2 of the CRPD notes how discrimination can be ‘political, economic, social, cultural, civil or in any other field’. 22 Although there is some work linking the CRPD to the effects of discrimination and disablism,69,288,289 our scoping review suggests that this is rather undertheorised. Nonetheless, there is an opening up of debates about how and why certain bodies and people are included or excluded. 253,290,291 Interestingly, our scoping revealed how some ethical arguments on research design are using human rights-based discourses to justify inclusion and mainstreaming of persons with disabilities and children. However, there has been less of a commitment to strengthening evidence and using this to change policy. 292
Potential weaknesses
Most analyses of the impact of the CRPD identify non-enforcement as a problem. Evidence suggests that the CRPD has very little national ‘bite’ in terms of defined sanctions. 99 Furthermore, the links between the CRPD and other legislative bodies such as the European Court of Human Rights remain unclear to disabled people. 293 Conceptual difficulties have also occurred in the UK, where more medical models have been used to define adverse outcomes in legal judgements. 293 Fraser Butlin293 notes that, semantically, the Equality Act (2010)28 seems to shift from a rights-based language to a welfare model that views disabled people in terms of ‘needs’ and, thus, by implication, as not contributing to society.
A frequent issue linked to the implementation and enforcement of the CRPD is how to understand what ‘reasonable accommodation’ means. This has particular implications for research. The way in which environments should be ‘modified’ to accommodate and ensure that disabled people can exercise their rights is open to interpretation. 294,295 These difficulties equally apply to the Equality Act,28 despite the detailed descriptions of what reasonable adjustments contain; consequently, innovation remains a problem, particularly when the CRPD is seen as a defined and unreflective instrument. 296 Inclusion tends to be defined in relation to access and, ignoring diversity among people with disabilities, assumes a universal research design will solve problems for all. Young and Quibell297 argue that, for some categories of impairment such as intellectual disabilities, a rights-based approach is never sufficient. They note that having entitlements to rights and citizenship may not change social and political exclusion or ensure justice. 297 Furthermore, the legal status of people with fluctuating impairments or conditions or comorbidities is ignored. 298
Underpinning these critiques is a more fundamental questioning of the ontological and epistemological foundations of rights and personhood. Such philosophical debates are outside the scope of the review, but the policy consequences are not. Silvers299 calls for a much stronger link between the legal status of ‘disability’ and ‘real justice’. The legislation of disability can also be viewed as a challenge to the unity of the model. 300 Barral301 notes that both user-led activism and European Union policies have led to the proliferation of rights-based frameworks. Like Meekosha and Soldatic,302 Barral is concerned that if these are imposed on people, they can become a form of colonisation in which the interests of the state take precedence over the rights of the people. 301 Despite these misgivings, there has been a move towards the development of standard indicators linked to rehabilitation, health and the CRPD. 303,304 This could be indicative of the lack of an ethical framework. Likewise, Lawson296 argues that, although the public sector has an equality duty to involve disabled people, they can just as easily slide into tokenism or even abandon such processes without an obligation. Isaac et al. 305 note that disability mainstreaming in terms of rights is viewed as a ‘responsibility’ for others and this can have paternalistic overtones. Although the CRPD can be used to advocate for individuals, its use can also be seen as having to ‘protect’ and ‘safeguard’ individuals rather than to ‘enable’ environments. There is a danger, therefore, that, despite the CRPD, disability will still be framed as a ‘problem’ of the individual. This suggests a continued role for the more established social model of disability.
A social model approach
Papers included in the scoping review, regardless of whether they are for or against a social model of disability, were widely seen as foundational to disability studies and advocacy. 198,306–309 A social model of disability developed from the experiences and activism of disabled people in the UK from the early 1970s onwards. It was also heavily influenced by activists in the USA and the independent living movement. It countered an individual medical model that viewed disability as a problem of/or caused by impairment, which had individual consequences (see The medical model). It also reclaimed the experience of disability from the expertise of health-care professionals and social workers. 199,310–312
Disabled people’s activism was founded on the rejection of professional control over their lives. Barnes313 explains how up until the late 1960s, ‘severely disabled people’ did not have access to disability-related welfare and their only options were residential care or ‘poverty and social isolation in the community’. Welfare entitlements, for example, existed only if a person had gained injuries through employment-related activities. In the UK, therefore, early activism was linked to ensuring economic welfare and attracted key disability activists, including Paul Hunt, Vic Finkelstein, Ken Davis and Maggie Hines. 310,313 All were founders of the Union of the Physically Impaired against Segregation (1976) and were committed to the idea that impairment did not ‘disable’; rather they argued that:
It is society which disables physically impaired people. Disability is something imposed on top of our impairments by the way we are unnecessarily isolated and excluded from full participation in society.
Union of the Physically Impaired Against Segregation314
These insights were primarily taken up and further developed along materialist and Marxist lines by Vic Finkelstein,315 Mike Oliver72,316 and Colin Barnes. 313,317 According to Oliver:
This new paradigm involved nothing more or less fundamental than a switch away from focusing on the physical limitations of particular individuals to the way the physical and social environments impose limitations upon certain groups or categories of people.
Oliver318
Disability is thus understood as a form of social oppression generated by barriers, (dis)ableism and exclusion from social life. 23 This interpretation has changed over time in accordance with disabled people’s activism for social change and inclusion.
Early studies focused on barriers in the physical environment and disablement in social life. This changed by the early 2000s, when key thinkers began questioning the dualism between impairment and disability. 307 Goodley319 argued that intellectual disabilities were socially constructed. Shakespeare and Watson stated that disability was caused by bodies (biological and social), as well as by restrictive social barriers. 307 Interesting debates occurred among key thinkers,279,308,309,320 with a concern to make the social model more ‘relational’, and an emphasis on innovation and dynamism. 72 These discussions moved the social model in interesting directions, such as conceptualising what a sociology of disability would look like; the concept of ‘impairment effects’;309,320 psychoemotional disablism;69,321 and intersectionality with chronic illness and gender. 131 Despite this, the social model maintained its importance in unifying people to ‘fight’ against social oppression. 322,323
Strengths
A perceived strength of the social model is that it is socially and politically located in disabled people’s movements and activism for social change. 310,311,324 It also put disabled people in control of their own lives. Research, for example, was encouraged to follow paradigms of participation, coproduction and/or emancipatory research. 23,198,278,325 Furthermore, the social model is regarded as accessible, as it is based on a simple premise of using people’s experiences of exclusion or disablement, to enable them to make the connection between removal of barriers and fight for equality with greater justice in society as a whole. This is why Beresford326 describes the understanding of the social model as a ‘light bulb’ moment for disabled people.
A historical understanding of capitalism as linked to the ‘working’ body was initially fundamental when making sense of the social model. The materialist basis of the model led to work on understanding capitalist modes of production and their relationship to structural inequalities and social exclusion. 312,316,327–329 Not being able to contribute or sell one’s labour in a capitalist system often meant exclusion from social life, which is why social models advocated ideas such as independent living, the right to work and a shared ‘disability’ culture. 313,316,328 Access to meaningful work remains at the heart of the social model,330,331 as does rethinking disability in positive terms. Swain and French332 and Swain et al. 333 argue that the social model should be moving towards an ‘affirmative model of disability’ that celebrates impairment and disability. Celebration of impairment and disability culture lies in direct opposition to more (bio)medical understandings of impairments which states that they should be intervened in, prevented or cured.
A positive framing of disability has also led some authors to rethink a capabilities approach. 242,334 Burchardt,334 for example, emphasises the commonalities between a capabilities framework and the social model in terms of how they view ‘social barriers and individual limitations, the importance of autonomy and the value of freedom, and dissatisfaction with income as a measure of well-being’. She explicitly connects social justice with a focus on how a capabilities approach can lead to combating poverty and social, economic and political exclusions. 334 These arguments have become increasingly influential and also connected to rights-based approaches, although the use of a capabilities approach, within social justice frameworks, has come under considerable philosophical criticism, particularly in terms of the potential neglect of the ethics of caring relationships and the construction of mutual dependency. 335–338 It remains to be seen how influential the more socially oriented capabilities approach will become. 156
Nonetheless, the emphasis on capabilities is illustrative of how the social model can be flexible and innovative, in particular in the way in which it views intersectionality and how disability might vary across the life-course. Attempts to understand multiple discrimination or simultaneous oppression is evidenced by linking gender, ethnicity and disability to explain the high incidence of schizophrenia among Afro-Caribbean populations in the UK. Some of the more interesting theoretical directions and possible renewal of the social model339 have come from movements generated by social model activism, such as that associated with the ‘psychiatric system survivor’ movements326 and newer forms of activism linked to ‘neurodiversity’340,341 and ‘madness and distress’. 342 The ‘neurodiverse’ movement,343 for example, argue that they provide a bridge between the social model and psychiatric survivors. 341 The movement began in the 1990s with people with autism spectrum conditions, dyslexia, dyspraxia and attention deficit hyperactivity disorder (ADHD), and it argues both for the social acceptance of their conditions and a recognition that such conditions are ‘real’. 344 The movement tends to be antinormalisation and sensitive to medical pathologisation.
The social model is able to adapt to changing circumstances and is particularly adept at being able to absorb criticisms and use them to develop more nuanced and sophisticated applications. However, the scoping review also reveals that later innovative theoretical thinking has struggled to impact on political action. This is how strengths can become weakness, as the constant theorising of a model could be seen as failing to generate social action. For example, the social model, although incredibly influential in developing the ICF and CRPD – at least at the conceptual level – has struggled to ensure that a rights-based approach becomes connected to emancipation.
Potential weaknesses
Various critiques of a social model of disability have risen to prominence since the late 1980s. Many of these have developed from within the social model. More fundamental critiques centre on the ontological and epistemological neglect of ‘the body’. Several authors have questioned the basis of ‘impairment’ as purely biological by arguing that impairments are socially constructed, personal and limiting. For example, the social model is seen to struggle to explain where the social and medical overlap, for example in, the physical and psychological pain of impairments. This is why Shakespeare and Watson307 argued that disability is caused by bodies (biological and social) as well as by restrictive social barriers (see A social model approach).
The political framing of ‘disability’ as an inclusive category, in the sense that it posits a political and affirmative disability identity, has also been queried. Disabled people, for example, have questioned the democratic framing and inclusion of ‘diversity’ within a social model, particularly groups such as d/Deaf, those with intellectual disabilities, those with mental health issues and those from neurodiverse categories. Individuals categorised into such groups may not view themselves as ‘disabled’ or adhere to an idea of biological ‘impairment’. For example, d/Deaf people see themselves as having a unique minority group culture,345 and war veterans may prefer to view themselves as ‘war-wounded’ rather than ‘disabled’. 346 Other aspects of a person’s identity, for example in terms of ethnicity or lesbian, gay, bisexual and transgender identity, may be more ‘positive’ and affirmative in an activist or social movement framework than a disability identity (see Corbett347). Disability, therefore, might not be a primary factor in the construction of a person’s identity. Deaf culture, for example, assumes a primary Deaf identify and struggles to accommodate those who wish to express different aspects of who they are, such as their ethnic and cultural identity. 348 More general critiques emerging from feminism,119,349,350 critical ‘race’ theory,351 and cultural studies352 further reflect this and have partly led to the development of CDS,353,354 although, as Priestley355 notes, these positions and theories do not necessarily negate the social model but can be incorporated within it.
Another strand of criticism has focused on the extent to which ‘disability’ can be ‘fixed’, particularly given that the boundaries between disabled and non-disabled are fluid. This has led Goodley319 to question the epistemological framing of a social model. The conceptual difference between impairment and disability is thus seen as reinforcing the Cartesian dualism of the body and the mind that is implicit in biomedicine and the medical profession. 356 In particular, Shakespeare and Watson307 have argued that the social model has become an outdated ‘ideology’ and the dualistic distinction between ‘impairment’ and ‘disability’ cannot be upheld.
Finally, there is an inbuilt hierarchy within the social model that prioritises activism and emancipation that is controlled by disabled people themselves rather than by their allies. Political activism and emancipation by disabled people can be viewed as a strength69,313 but can simultaneously alienate allies and make it difficult to establish links with other social movements. 200,307 Furthermore, a degree of moral policing can occur, with attempts to establish an agreed orthodoxy which can be difficult to challenge. 121 This is the starting point of CDS, which offers a more fluid approach.
Critical disability studies
Critical disability studies is a more recent development. It is also difficult to define, and the boundaries between CDS and the social model are especially blurred. 357–359 CDS is informed by postmodernist and poststructuralist perspectives, such as those offered by Foucault360 and Derrida,361 which question the foundations of concepts such as ‘impairment’ and ‘disability’. This allows for considerable flexibility. In addition, CDS argues against an overarching ‘biomedical’ understanding of disability, focusing instead on the cultural and linguistic construction of ‘disability’ and disableism. 312 It can, however, take on ideas of emancipation or rights-based approaches, although this does not necessarily mean that everyone working within CDS associates with these ideas.
Advocates of CDS argue for a conceptual ‘paradigm shift’,362 which questions the dualism of impairment and disability. CDS is also strong on intersectionality and has links to, for example, critical ‘race’ theory. 363 Critical realism is central to understanding CDS,364 although there is little agreement on what this might mean in practice. Consistent themes, however, include disregarding naive realist/empiricist approaches355,365 and a focus on viewing an individual as simultaneously being part of biological, psychological and social worlds. 366,367 Meekosha and Shuttleworth368 argue that CDS is about rethinking how disabled people become marginalised by using critical social and cultural theory, although in their case, this is aligned with an ‘emancipatory focus’. For Meekosha et al. ,369 critical engagement consists of:
the irreducibility of the social to empirically derived ‘facts’; (2) the necessity to link theory with praxis; (3) a reflexive awareness of the historical development of our own thinking; and (4) an openness to and dialogical engagement with ideas emerging from diverse cultures.
Critical disability studies aim to reframe the ‘disabled bodies/minds along the lines of capacity, potential, interconnection and possibility’. 370,371 CDS has been especially influential in discussion about the origins and operation of ableism and normative assumptions about a functional body, the connection between sexuality and disability, including queer studies, and ‘mad studies’. 372,373 ‘Mad studies’, for example, is an ‘umbrella term’ bringing together critiques of psychiatric diagnosis and interventions with ‘survivor’ movements374,375 to argue for more equal representation and involvement in health policy and practice, thereby politicising a need for not only user involvement but control and representation. 376,377
Strengths
Critical disability studies covers many critical theoretical developments, which offer alternative ways of viewing disability. Questioning existing assumptions, for example on the site of the body, is probably one of its important strengths. 378 CDS is not incompatible with rights-based approaches, and many thinkers remain committed to emancipatory activities302 and, in particular, disability justice,379 in which impairments function as sites of moral blame and shame linked to health inequalities. There has been a recent stream of critical thinking around the norms and values of neoliberalism, the measures being used to ‘count’ disability and what it means to be able-bodied. 380 For example, Jain,381 Puar382 and Fritsch383 examine differences between affect, debility and capacity. They examine the diffusion of the category ‘disability’ and its construction in terms of ‘variability’ and ‘risk coding’381 or as ‘anticipatory’ in terms of a ‘debility’. 382 There are also some interesting applications of CDS that are relevant to public health approaches. These include understanding power dynamics, reconceptualising embodiment as fluid rather than binary, rethinking ‘intersectionality’ in political terms and ensuring a ‘critical’ perspective in how ‘disability’ is constructed.
Potential weaknesses
Although CDS can contribute to our critical understandings of disability, criticisms have invariably concentrated on its refusal to define ‘disability’, its poor link to policy change and its apparent inability to include disabled people in its more theoretical debates. Furthermore, CDS can be so diffuse that it can mean almost anything. 384 When thinking about explicit links to public health and interventions, for example, the constant emphasis on the ‘critical’ runs the risk that evidence is continually deconstructed and rendered unreliable. CDS, therefore, is in danger of leaving a ‘waste-ground devoid of meaning’,385 although ideas such as ableism373 or ‘sanism’375,386 can provide some counter to this by offering the opportunity to rethink interventions to ensure that they do not impose able-bodied or mental health norms. The CDS relationship to ‘rights’ can also be problematic,302 and this explains Shakespeare’s277 attempts to generate ‘a social relational’ model linked to international and institutional understandings of disability. 387
The increasingly specialised language of CDS does not make it especially accessible to disabled people. There is no ‘light-bulb’ moment (see A social model approach) and, as such, CDS is vulnerable to the criticism that it is controlled by a small number of intellectual elites. CDS has struggled to unify disability or rights-based activists or mobilise research to ensure real policy changes or activism. This gives some credence to those who have argued that a focus on theory and the cultural construction of ‘disability’ takes away from the analysis of economic norms of production and political activism. 313 There are also concerns that a focus on the body will lead back to the biological essentialism of a medical model and negative ascriptions of disability as akin to disadvantage and deviance. 313,388
Conclusion
The scoping review revealed that theories and models are rarely used in a ‘discrete’ way but rather create a broad ranging and often polemical debate with no fixed point of reference. This is the first challenge facing those who wish to connect public health research with more inclusive approaches to disability. The different models are presented in perhaps a more static or idealised fashion than is the case in practice, although this was a conscious choice to make the models accessible and to highlight their main thematic elements. The medical model, for example, has changed considerably over the years and has been refined to take account of ongoing critique. Debates, therefore, are dynamic, interdisciplinary and engage with each other, creating fluidity, which is sensitive to practical applications and theoretical development. Current theory, for example, has become more sensitive to the life-course as different elements of identity, belief systems and definitions of disability struggle for predominance.
This flexibility is reflected in how research on disability has been conducted, although the more social models and CDS seem to have had less influence on public health research than, say, the ICIDH-2 or ICF. The ICIDH-2 and ICF are, of course, more closely aligned to the study designs on which evaluations of public health interventions are based. This perhaps explains the interest of public health research in measurements of disability and a movement towards amalgams of definitions based on models or combinations of models so that they are more inclusive of variations in impairment across the life-course. 64,172 There would, however, seem to be less interest in this in theoretical development and the more critical approaches to disability. This creates potential tensions. The need for standardised, comparable measures of disability could be in conflict with the diverse experiences associated with disability and fail to accommodate intersectionality, the impact of the life-course and fluctuating conditions. Experience and skill are needed to apply the nuances implicit in many models, and the historical struggles of public health to engage with more critical approaches to disability might make this problematic.
Public health research is not alone in finding it difficult to reflect disabling experiences. The scoping review, although demonstrating how most models are developed in opposition to ‘a medical model of disability’, also provides evidence about its residual influence. The ICF, for example, could be seen as a classificatory, administrative model that attempts to ensure that medical norms have a more social meaning. 12,389 The scoping review, however, found little evidence of a connection between this arm of the WHO and the WHO plan of action on the SDHs. 390 Our scoping review in particular indicated that measurements of disability are not especially well aligned with definitions of disability found in various paradigms and theories. Examples include the environmental creation (prognosis) of impairment effects, sociocultural barriers to health-care access or how disability discrimination and disablism increase exposure to social determinants of poorer health. 15,289,391,392
To address the commissioning brief, we need to be able to translate the models and theories to work practically in the evaluation of public health interventions. Only the ICF has been easily explained and applied to differing contexts. This perhaps explains its popularity. To focus on only the ICF, however, would ignore the detailed and sophisticated critique of its use and the value of other models outlined by the scoping review. Consequently, an important next step in our analysis is to think about how different models could be visualised, applied and used to critically evaluate interventions in line with various definitions of disability and their measurements. We also need to connect with the theoretical approaches used in public health. We realised, therefore, that it would be useful to define what a public health of disability should look like and to try to link together definitions of disability and public health. This is unlikely to provide a definite answer, but, in keeping with our iterative intent, contributes to a more reflexive framework that has a range of options with which public health research could engage.
Chapter 4 Developing an ethical–empirical decision aid
The scoping review outlined in Chapter 3 provided insights into various models, paradigms and perspectives on disability. It demonstrated how they have matured in conversation with each other, although the lack of a strong connection to public health remains problematic. In an attempt to bridge this gap, this chapter does the following:
-
uses visual and conceptual mapping to explore the relationship between public health and disability
-
examines potential commonalities including the role of inequalities and social inclusion in bringing together disability theories and public health
-
illustrates how a broad human rights model could provide an overarching framework to operationalise commonalities
-
develops an ethical–empirical decision aid or checklist to explore how disability is being addressed in public health research
-
by way of example, assesses the implications of our decision aid for some of the measures used in public health.
Despite suspicion of public health interventions within disability studies, the scoping review revealed thinkers able to innovate and to move between models and to thus develop more pluralist approaches. The challenge is to capture the potential of these debates to contribute to more inclusive public health research. This requires mapping the complex and shifting debates about disability on to understandings of the commonly used theories underpinning public health. By exploring potential commonalities between the two approaches, we outline a range of possible options, which are used to inform a ‘decision aid’. In doing so, our aim is to offer common ground on which those engaged in public health research and those engaged in disability studies can meet. We end the chapter by exploring the potential of the decision aid by considering it in relation to some of the more frequently used measures in public health. Discussion about the decision aid will also provide an analytical framework with which to interrogate the material identified in the second stage of the scoping review. This will further refine its use.
Mapping of models and theories
The medical model connects with public health’s interest in describing populations, measuring outcomes and developing interventions to improve (and rehabilitate) well-being. There is, however, a strand of public health thinking that connects with the more critical models of disability. Ecological approaches, for example, are evident in both public health and disability debates,393 although there is surprisingly little connection between the two. For example, one of the most widely known models used in public health, Dahlgren and Whitehead’s ecological model of the determinants of health,126 was not mentioned by any of the models or theories of disability included in the scoping review.
The ecological approach is typically visualised as beginning with an individual and views health as shaped by the individual’s interactions with their micro-, meso- and macro-environments, ranging from intimate and community relationships to living and working conditions to wider economic and political processes. Addressing social inequalities in health is, therefore, seen to require action on inequalities operating at these multiple and intersecting levels (Figure 4). Throughout the scoping review, it became clear that some disability models worked to a similar set of ideas, which connected individual, social-relational, social-communitarian and macro levels of analysis. 355,365 This creates potential for developing a more inclusive public health agenda.
FIGURE 4.
The public health ecological model. Reprinted with permission from Dahlgren and Whitehead. 126
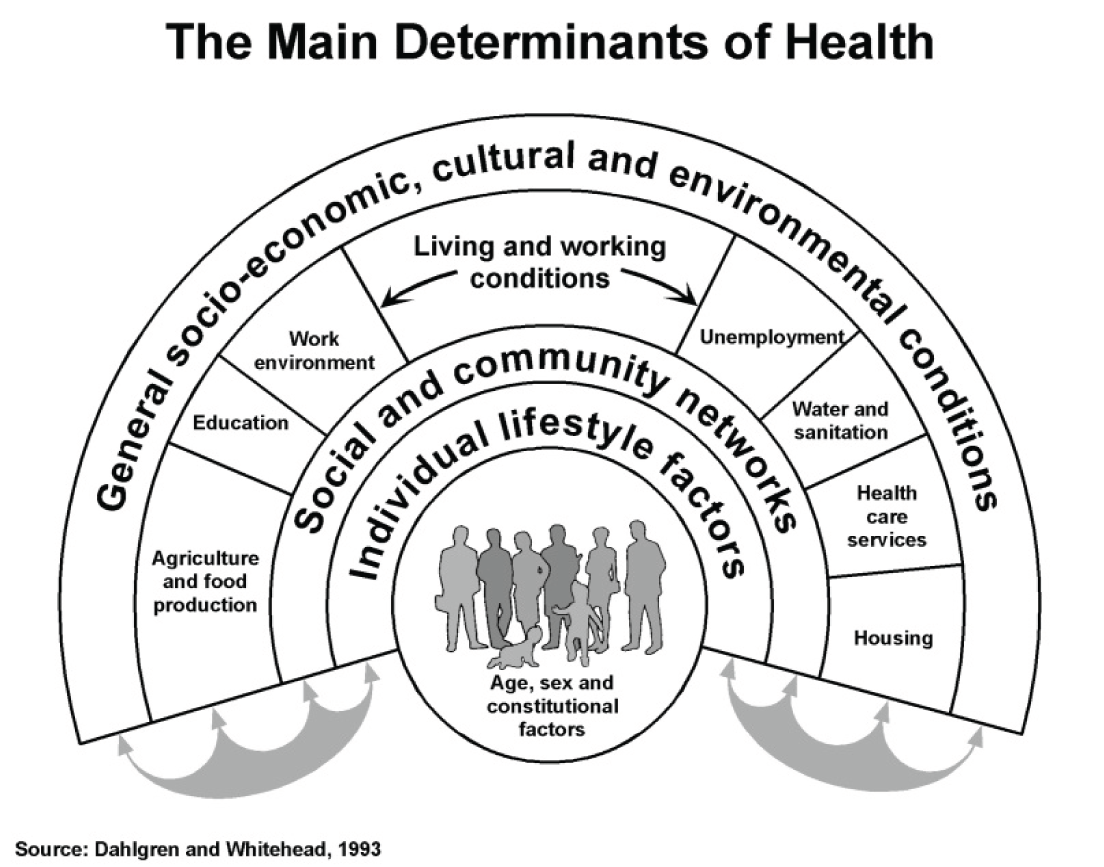
The ecological model can be further refined with reference to the work of Graham and Kelly,394 who argued that interventions are underpinned by one of three approaches to reducing health inequality:
-
Disadvantage: improving the absolute position of the most disadvantaged individuals and groups.
-
Gap: reducing the relative gap between the best- and worst-off groups.
-
Gradient: reducing the entire social gradient. Consequently, when implementing (and evaluating) any public health intervention the aim – theoretically and practically – is to tackle health inequalities and improve equity. The ways in which this can be done include focusing on the most disadvantaged in a society (such as disabled people); reducing inequalities between the most healthy and least healthy; or improving the overall health in a society on all levels so that the entire social gradient changes.
The ecological model has various expressions in public health, and some research has attempted to connect it to an (implicit) understanding of disability. 395,396 Most of these examples align it with more medicalised understandings of disability395,397,398 and use the ecological model to chart ‘risks’ for ill-health, impairment or disability based on epidemiological measurement or SDHs. 399 Nonetheless, ecological approaches prioritise the SDHs,6,400 which can be useful when making sense of disabling experiences and the processes of disablement, particularly when attempting to understand the link between poverty, impairment and disablement across the life-course (Figure 5 provides a visual representation of this).
FIGURE 5.
Social determinants of diversity.
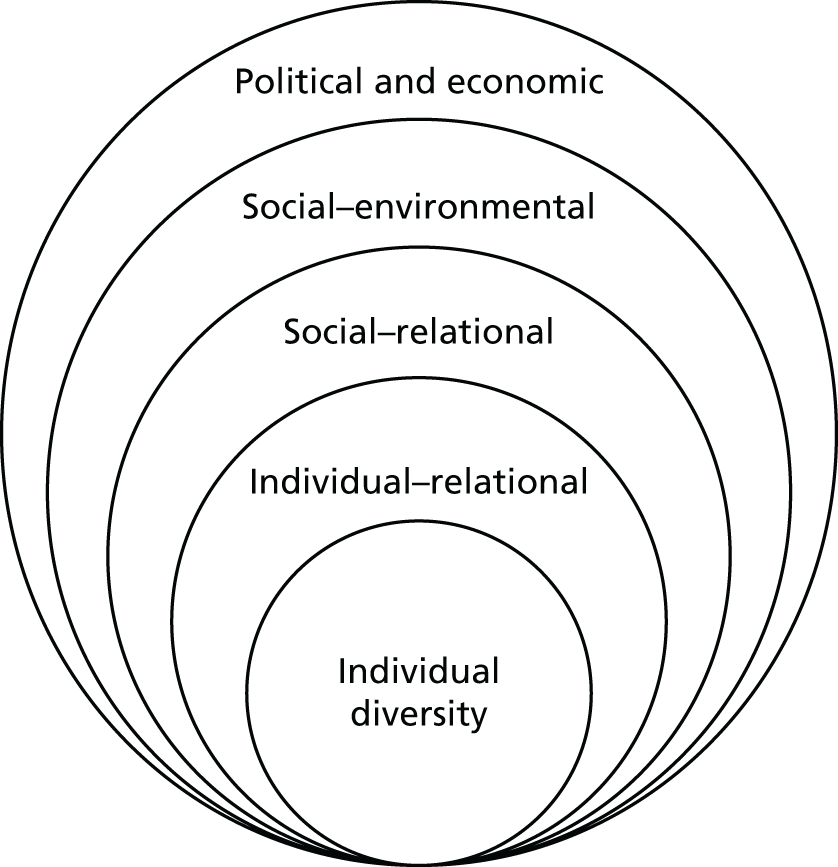
The SDHs have become especially influential following the publication of the WHO Commission for Social Determinants of Health. 401–403
The social determinants of health are the conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels. The social determinants of health are mostly responsible for health inequities – the unfair and avoidable differences in health status seen within and between countries. 404
The WHO is currently working to develop indicators and measurements on the SDHs for the UN’s sustainable development goals (SDGs). 405 Focusing on the determinants and maintenance of inequalities is especially valuable when discussing disability and links with more rights-based and social model approaches. Elements of a more medical model, however, remain in public health perspectives. A recent King’s Fund report, for example, when using a social determinants approach, measures health and health inequalities in terms of disability-free life-years. 406
Disability, poverty and inequality models
In the scoping review, the relationship between poverty (inequality) and disability was identified as foundational to more critical models of disability. 12,327,407–409 Such models emphasise a strong connection between inequalities and disablement and a particularly strong association with ‘entrenched poverty’. These concerns are reflected in the public health literature and this is another important point of potential cross-linkage. For example, children living in poverty who already have an illness or health condition are particularly susceptible to disability. 19,399,410 Income inequalities have also been found to be linked to conditions such as mental health or obesity. 411 Furthermore, disability can affect families in terms of the extra health costs of impairment, time spent caring and loss of income,409 and, more generally, families that have a disabled family member are more likely to live in poverty. 1,412
Consequently, this experiential and statistical association between chronic poverty and disability, as well as its intersections with other dimensions of disadvantage,413 would seem fundamental to understanding the processes of impairment and disablement408 and their wider complexity in differing local and global contexts. 414 Yeo,408 for example, argues that a person with disabilities faces discrimination, which leads to multiple forms of exclusion. Institutional, environmental and attitudinal barriers, for example, result in disabled individuals not having the same opportunities as everyone else, which means that they are more susceptible to poverty, which in turn negatively affects their health. Whitehead et al. 415 and Yeo408 both view this as a cyclical or spiral dynamic of political, sociocultural, economic and environmental processes. Adapting the above in terms of a multidimensional matrix (not necessarily cycle or spiral) means that the situational factors linked to impairment become embodied and potentially (but not necessarily) linked to disability discrimination, which in turn further increases susceptibility to inequalities and the possibility of chronic deprivation. Setting out the factors that can lead to inequality, ill health and disease416 also helps to identify what constitutes enabling environments, explaining why some people who have impairments thrive or are resilient and flourish (Figure 6 provides a visual representation of these arguments).
Poor health, mental health issues and/or impairments have all been identified as factors that increase inequalities. 417–420 MacInnes et al. 420 note that a plethora of issues needs to be tackled but that ‘early interventions’, such as those in workplace settings to prevent physical impairment or mental health issues, in addition to more ‘responsive health care systems’, can contribute to tackling inequalities. Similarly, it was noted that (vocational) rehabilitation can help to ensure that people do not become incapacitated after sickness leave. 409,420,421 This is consistent with a public health agenda and explains why inequality models linked to disability have relevance when evaluating public health interventions, particularly when assessing the potential impact of interventions, and this can be joined with an analytical framework by which to explain disabling experiences.
Difficulties, however, begin to occur over the use of metrics that are used to inform connections between disability and inequalities. As we have seen (see Chapter 3), those who assume a more critical perspective criticise such measures as (dis)ablest and failing to capture the lived experiences of disabled people, while implicitly making assumptions about burden and normality. Measures facing particular criticism include disability-adjusted life expectancy, healthy life expectancy and disability-free life expectancy. 422 As noted, all are seen to reinforce a negative understanding of disability by focusing on the difficulties associated with having a disability rather than on the potential of emancipatory activities to change the social environment. Such measures are also criticised for struggling to accommodate a more dynamic account of disabling experiences, in which disability is likely to be experienced by most people at some time in their lives. 1 Furthermore, the link to inequalities or understanding disadvantage can sometimes be oversimplified, especially if interpreted within the context of a short-term, narrow, cost-focused analysis linked to disability measures, rather than the long-term need for accessible and appropriate care. 423
Recent critical literature from disability studies would prefer to explore inequalities by questioning the able-bodied norms and values which they see as implicit in standard health-related measures. This critical literature also notes a perceived all-embracing concern with ‘ability’ to work,290 adherence to variations of a capabilities approach that still focuses on functioning413 or a misplaced emphasis on producing fine graduations of debility and capacity. 383 This is why, when exploring inequalities and disability, more critical debates emphasise the importance of considering the norms and values implicit in interventions and evaluations designed to measure their effects, alongside the broader value of more inclusive practices associated with a human rights-based approach.
Human rights and public health
A human rights approach considers individual factors, social participation (including family life), and environment and access, within a context of macro-structural factors. 22 Such an approach is probably best reflected in the CRPD (see Chapter 3), which can be mapped on to ecological approaches linked to public health and disability (Figure 7). Not only does a rights-based approach connect well with a public health moral commitment to equality, but it can also support the ethical, practical and methodological decision-making required when undertaking research. 424
FIGURE 7.
Modelling the CRPD.

Public health interventions could be seen to facilitate social justice and equality. 101,425,426 The Joseph Rowntree Foundation’s work to ensure a dementia-friendly city or rights-based interventions to improve welfare rights advice, for example,427 demonstrate the value of a more inclusive paradigm, informed by a respect for rights and a sensitivity to disabling experiences. However, evaluation designs for public health interventions typically remain linked, epistemologically and ontologically, to a (positivist) medical model. 426,428 Interventions, and the research evaluating them, can be disempowering, particularly when individual experience is denied429 or a population is regarded as vulnerable and their rights are framed paternalistically in terms of protection and within able-bodied norms. The scoping review suggested that disabled people often find themselves excluded from research and, in particular, from trial-based research on methodological grounds because they are viewed as ‘hard to reach’; their inclusion is seen as raising difficult ethical issues, especially about consent; or their inclusion would require too much adjustment when generating a sample. 51,59,92,430 Tackling such principles of inclusion are often at the heart of human rights-based approaches:
By inclusion in mainstream research we mean that persons with disabilities are welcome to join most research studies (not just studies about disability); they are treated with dignity and respect; studies are designed and accommodations are provided as needed to allow them to participate (without threatening the integrity of the research); and they are not excluded without a reasonable justification (Iacono, 2006; McDonald, 2012; McVilly and Dalton, 2006). Inclusion also involves being active partners in research, so that the voices of people with disabilities in research can be heard, and research about them is meaningful to them.
Charlton327
A human rights-based approach to health interventions is becoming increasingly applied to ‘persons with disabilities’, as illustrated in the fields of health advocacy,90,431 rehabilitation,303,304 psychiatry or behavioural support. 432 Feldman et al. ,47,90 for example, used the CRPD’s Article 25 on health to develop health self-advocacy training and intervention for persons with intellectual disabilities based on the ‘3Rs’, that is, rights, respect and responsibilities.
Despite the increasing emphasis on public and patient involvement, a rights-based approach has not had a great deal of impact on public health research. 426 The CRPD is, however, highly applicable to Graham and Kelly’s394 account of inequalities, and, by combining the two, it is possible to generate a checklist assessing the inclusivity of public health interventions and research. 433 One can, therefore, use the CRPD to assess the individual factors that are included in an intervention and also what kind of intervention it is, in terms of how it addresses the gap, disadvantage or gradient394 (Table 7).
| Article | General inclusion of the CRPD | Example of intervention | Disadvantage | Gap | Gradient |
|---|---|---|---|---|---|
| Individual factors | |||||
| 1 | Promote, protect and ensure respect and dignity of human rights | CRPD capacity building in public health | |||
| 5 | Equality and non-discrimination | Inclusion in broader public health campaigns (e.g. smoking, alcohol, drug use) | |||
| 6 | Women with disabilities | Screening provisions (e.g. breast and cervical) | |||
| 7 | Children with disabilities | Public health education in schools (e.g. nutrition and fitness) | |||
| 8 | Awareness-raising | Disability and public health training for professionals | |||
| Environmental and access | |||||
| 9 | Accessibility | Universal design as feature of public health provision | |||
| 10 | Right to life | Balanced information on disability (e.g. during antenatal screening) | |||
| 11 | Situations of risk and humanitarian emergencies | Interventions to aid disabled people to flee violence or conflict | |||
| 12 | Equal recognition before the law | Equality inclusions in public health awareness (e.g. stroke symptoms outreach to minority ethnic communities) | |||
| 13 | Access to justice | Right to redress public health exclusions | |||
| 14 | Liberty and security of person | Creation of public health of disability | |||
| 15 | Freedom of torture or cruel, inhuman or degrading treatment or punishment | Ensuring ethics, respect for bodily integrity and dignity in public health | |||
| 16 | Freedom from exploitation, violence and abuse | Preventative policies and actions against disability hate crimes | |||
| 17 | Protecting the integrity of the person | Inclusion in services (e.g. safeguarding, mental health, learning disability, etc.) | |||
| 18 | Liberty of movement and nationality | Disabled children registered and cared for | |||
| Social participation | |||||
| 19 | Living independently and being included in the community | Formal or informal personal assistance (e.g. people with dementia) | |||
| 20 | Personal mobility | Removing barriers to accessible transport (e.g. people with visual impairments) | |||
| 21 | Freedom of expression and opinion, and access to information | Public health choices and participation in interventions and design | |||
| 22 | Respect for privacy | Public health access and confidentiality of health needs (e.g. mental health and HIV) | |||
| 23 | Respect for home and the family | Enabling homes and healthy families (e.g. heating provision) | |||
| 24 | Education | How to live well with secondary conditions (e.g. diabetes, obesity and pain) | |||
| 25 | Health | Access to primary health, mental and dental care | |||
| 26 | Habilitation and rehabilitation | Rehabilitation for offenders (e.g. learning difficulties/disabilities) | |||
| 27 | Work and employment | Evaluating employer resources and policies for reasonable accommodations | |||
| 28 | Adequate standard of living and social protection | Impact of social protection schemes | |||
| 29 | Participation in political and public life | Inclusion in PPI, CCGs, voluntary organisations and public health boards | |||
| 30 | Participation in cultural life, recreation, leisure and sport | Participation in recreational activities (e.g. swimming) | |||
| Macro-structural | |||||
| 31 | Statistics and data collection | Indicators of public health and disability along the life-course | |||
| 32 | International cooperation | Public health and disability policies integrated in the SDGs | |||
| 33 | National implementation and monitoring | Evaluation of public health and disability policies | |||
A rights-based framework and an ethical–empirical decision aid
Table 7 establishes the potential for developing a human rights framework for public health interventions, in a way that could accommodate the complexity and challenges of capturing the disabling experience and reconciling it with the concerns of public health. We are particularly mindful that the human rights approach was respected by proponents of the four models outlined in Chapter 3. In our scoping review, we also noted the move towards thinking of ‘health’ as a right and how, for example, ‘personalisation’ and ‘choice’ were becoming especially prominent in health- and social-care discourses. 24,88,434 This, and the discussion above, informed our decision to explore a rights-based ethical framework based on the CRPD. In particular, we felt that Article 3 was inclusive of ethical principles relevant to public health and public health research and committed to the duty of equality, while also emphasising life-course, intersectionality and gender. Article 3 specifically notes the following:
-
Respect for inherent dignity, individual autonomy including the freedom to make one’s own choices, and independence of persons;
-
Non-discrimination;
-
Full and effective participation and inclusion in society;
-
Respect for difference and acceptance of persons with disabilities as part of human diversity and humanity;
-
Equality of opportunity;
-
Accessibility;
-
Equality between men and women; and
-
Respect for the evolving capacities of children with disabilities and respect for the right of children with disabilities to preserve their identitiesFrom Convention on the Rights of Persons with Disabilities, United Nations, © 2006 United Nations. Reprinted with the permission of the United Nations22
Article 3 connects well with experiences of disability by adapting an inclusive approach and ensuring that experiences are part of mainstream discussions in a meaningful rather than tokenistic way. Dignity, for example, cannot stand alone but is grounded in other facets of mainstreaming disability (Figure 8). A member of our project steering committee, Professor Peter Beresford, asked us to envisage models as three-dimensional structures. If one views accessibility as the base of a stepping-stone structure, it must be considered before equality of opportunity. That in turn provides a stepping stone to ensuring respect for intersectionality. This approach equally respects a social model perspective on social justice and a critical disability reflection on interrogating what inclusion and exclusion of (dis)ablism means.
FIGURE 8.
Modelling Article 3 from the CRPD.
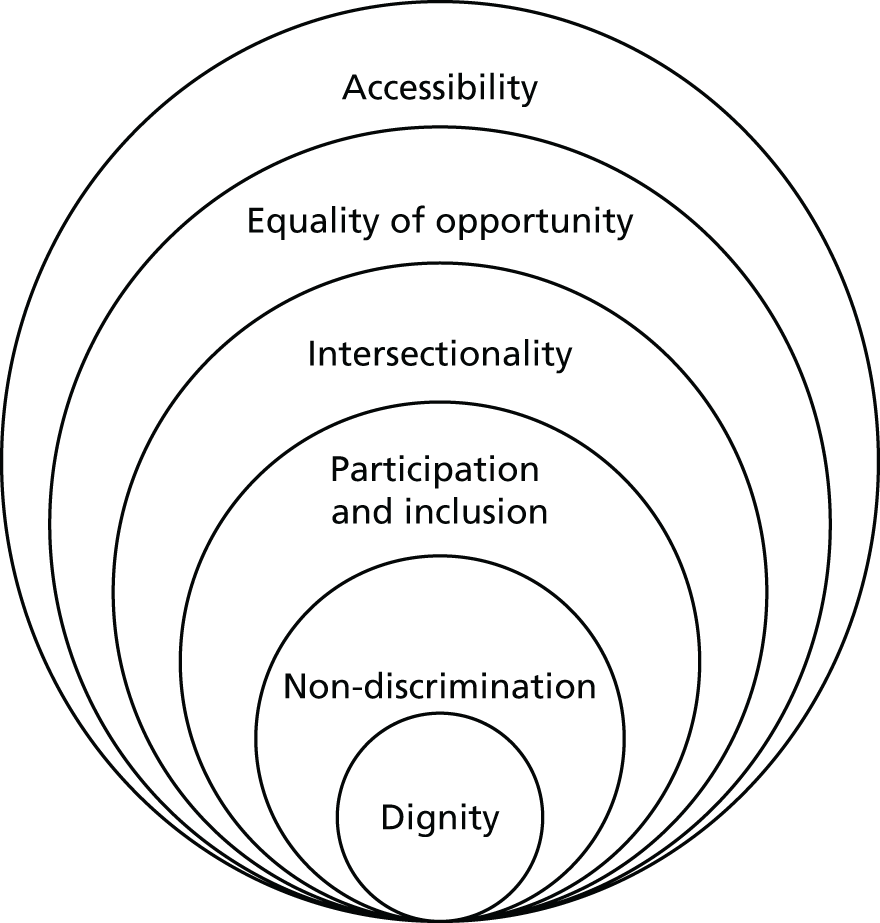
If an intervention, and the research evaluating it, is respectful of disability rights, it can be related to several components of the CRPD and scored accordingly (Table 8). Ethical and empirical design could thereby become mutually reinforcing, whereby ethical design leads to empirically robust public health research that addresses disabling health inequalities.
| CRPD | Dignity (including autonomy and informed choice) | Non-discrimination | Full and effective participation and inclusion | Respect for difference | Equality of opportunity | Accessibility | Gender sensitivity | Sensitivity to age differences, such as those associated with old age, children, young people |
|---|---|---|---|---|---|---|---|---|
| Research design | ||||||||
This forms the basis of our (ethical) decision aid/checklist, which can be further strengthened by being considered in relation to the Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) framework435 and its concern with reach, effectiveness, adoption, implementation and maintenance. One of the strengths of RE-AIM is its orientation to the evaluation of interventions in real-world and complex settings in accordance with robust methodologies. 435 RE-AIM can also be easily mapped on to the CRPD, with five concepts having particular relevance, namely dignity, inclusion, intersectionality, accessibility and equity (Box 3).
The Reach of an intervention or its representativeness is linked to Intersectionality and the kinds of population groups that are typically recruited or neglected in research despite experiencing health inequalities linked to disability; such as women, children, and people from ethnic minority backgrounds or lower-socioeconomic groups. These populations are typically (and stereotypically) framed as ‘vulnerable’ or ‘hard to reach’. Intersectionality should also connect with the diverse nature of the disabling experience and a range of different impairments.
The Effectiveness of an intervention is linked to primary and secondary outcome measures and how they impact on who becomes included (or excluded). It also explains and describes how participation in research is viewed and measured.
Inclusion is important in ensuring the diversity of the disabling experience is captured, which in turn impacts on the use of primary and secondary outcome measures. It also raises questions about how inclusion is defined, negotiated, and measured; and the extent to which participation is an important consideration.
The Adoption of the intervention is linked to the setting of the intervention and how well the setting can be accessed. If a design is universal and accessible, it is more likely to be adopted. In this way, Accessibility is linked to mainstream adoption and uptake.
The Implementation of an intervention or how it is adapted to a particular setting, while generally linked to cost-effectiveness, can also become linked to the dignity of participants. This includes participatory design methods, ensuring ethics and consent and ensuring enabling environment. Implementation, therefore, should not be (dis)ableist and modifications need to take account of the potential consequences of disability.
The Maintenance of an intervention or its uptake and adaption to real-world settings is linked to issues of equity. Equity would address the extent the intervention addresses the social gap, gradient or disadvantage linked to disability.
Graham and Kelly394
A simple scoring system could help one to understand how well rights are being implemented. For example, a rating-scale such as the Pragmatic Explanatory Continuum Indicator Summary436 would give an evaluation or score of an intervention and how well research evaluating that intervention respected ethics and the equity of persons with disabilities (Table 9). A score of 0, 0.5 or 1 (100%) can be given.
| Dignity | Inclusion | Intersectionality | Accessibility | Equity |
|---|---|---|---|---|
| How was informed consent given? How was accountability defined? Was the research a participatory or emancipatory design? Is the research informed by ableist norms? |
How were participants included in the trial? Was this effective? How was inclusion defined? What models of participation were used? Were measurements applicable to disabled people? Do outcome measures adequately reflect the experiences of disability? |
To what extent can the research explore gender; ethnicity; life-course; comorbidities and multimorbidities? What was the reach of the design? To what extent do the findings reflect intersectionality? |
Are this trial and the settings accessible? Were reasonable accommodations or adaptations made? Was there a relationship between accessibility and adoption? |
Is the research connected to an issue linked to equity? Was there or will there be maintenance of the intervention effects? What is the likely uptake in real-world settings? To what extent do the findings reflect the diverse experiences of disability and what are the implications of this for how the research findings should be interpreted? Does the research reflect on the potential universality of its application, while reflecting on potential limitations to engage with equity? Can the effects of the intervention be maintained in real-world settings? |
The use of outcome measures in public health and their relevance to different types of disability
We end this chapter with a practical case study, which explores how our decision aid could relate to measures commonly used in public health research. In Chapter 3, we noted how many of the models and theories of disability were formed in opposition to the medical model. A particular ethical and empirical issue was the use of potentially insensitive measurements, such as DALYs,163 which struggle to accommodate the different social and political contexts of ‘being’ disabled. As we have seen, exclusions create disability, and social inequalities exacerbate disabling effects. This explains why concerns have been raised about the possible relationship between measurement and medical rehabilitation, along with the imposition of able-bodied norms. 290 Critics have also pointed out that commonly used measures struggle to capture temporality or culture,437,438 while also noting that the difficulty of applying some measures to the experiences of disabled people is used to justify exclusion criteria, with little consideration of the extent to which support aides would enable greater inclusion. Consequently, such concerns raise doubts about the validity and reliability of the evidence presented when such measures are used. 172,439 It is, therefore, important to be mindful that a public health landscape that is sensitive to disability does not replicate this. Our discussion illustrates how using models and theories of disability can inform the use of our evaluative tools and begin a critical reflection on the norms and values behind the measures that we use. Our discussion is exploratory, offering an initial introduction. The lack of an informed evidence-based discussion makes this necessary, as do the norms of current practice, which often uncritically apply outcome measures without considering their relevance to the experiences of disabled populations. There are, however, exceptions, and a review of measures and their relevance to childhood neurodisability provides a potential template on which to base future work,440 although care would need to be taken to avoid accusations of ableism. More critical models of disability, for example, would wish to replace ‘neurodisability’ with ‘neurodiversity’.
Consequently, and consistent with our broad approach, our case study specifically considers the applicability of outcome measures to different types of disability and the extent to which such measures are inclusive and accessible, respect dignity and are able to capture intersectionality and equity. To this extent, our concern is thematic, to illustrate the difficulties facing more inclusive research practices. We acknowledge that these practices would need to take account of methodological concerns, such as the meaning of different types of measures and what they aim to assess, while also critically engaging with the often complex relationships between definitions of well-being, QoL, health-related quality of life (HRQoL), functioning (including social, physical, emotional, participation) and health utility. At present, such relationships tend to be confused and the conflation of functioning and well-being concepts within instruments, for example, is common.
Many measures are either generic, focusing on QoL (SF-36 or Health of the Nation Outcome Scale), and/or disease-/condition-specific (Hamilton Rating Scale or Beck Depression Inventory focus on depression), or they focus on comorbidities (Functional Comorbidity Index) and/or multimorbidities (Cumulative Illness Rating Scale and Charlson Index). There are also self-reported outcome measures that focus on pain (the short-form McGill Pain Behaviour scale), pain behaviour (Non-verbal Pain Scale) or the extent to which pain affects function441 or ADL. 439 Furthermore, there are measures that focus on well-being linked to mental health (i.e. the Warwick–Edinburgh Mental Well-being Scale) or how well people with mental health problems function in social situations (i.e. Social Functioning Questionnaire). There are also specific disability measures, which have been developed mainly in rehabilitative contexts, for example, those linked to traumatic brain injuries (Disability Rating Scale or Independent Living Scale). Although many measures focus on functioning, several now focus on capability and what people can do. Common indicators focusing on capabilities are linked to Nussbaum’s or Sen’s models152,153,442 (e.g. Measures of Wellbeing and Capability for Use in Economic Evaluation,443 Novel Multi-dimensional Patient-Reported Capabilities Instrument for Mental Health Research and Policy444), but also increasingly to the work of Robeyns,148 who provide a possible connection to human rights and social justice rather than a focus on functionality. 149,150
To explore the value of such outcome measures in capturing the diverse experiences of disability in public health settings across the life-course, we focus on childhood physical disability, intellectual disability, autism, chronic illness [e.g. multiple sclerosis (MS)], dementia and depression. Our analysis is informed by the need to measure, and the insights provided by, a more critical approach to disability.
Quality-of-life measures attempt to assess well-being from biological, psychosocial, social, emotional, physical, cultural and spiritual aspects of life. Common outcome measures include HRQoL; the Human Development Index; gross national happiness; ADL; variations of the capabilities approach; and the Social Progress Index. EuroQoL is a standardised European HRQoL measurement tool on which the European Quality of Life-5 Dimensions (EQ-5D™) questionnaire is based. The EQ-5D is used in a variety of settings, and since 2009 has been part of NHS quality assurance. The National Institute for Health and Care Excellence (NICE) has also recommended the use of the EQ-5D to (1) carry out population-level surveys; (2) ensure the cost-effectiveness of health technology assessments; and (3) measure conditions or health status across time in services from the perspective of patients. 445,446 Alongside the EQ-5D, the EuroQol visual analogue scale (EQ-VAS) and EQ-Index have also been developed.
European Quality of Life-5 Dimensions
The EQ-5D questionnaire is designed around five themes: (1) mobility; (2) self-care; (3) usual activities; (4) pain and discomfort; and (5) anxiety and depression. The EQ-VAS is a related visual analogue scale that asks people to visually identify the experience on a ruler-like scale of best health to worst health. The EQ-5D can be answered in differing levels of severity. The EQ-5D three-level response requires answers in the form ‘some/moderate/extreme problems’, whereas the EQ-5D five-level response allows five answers on levels of severity: ‘no/slight/moderate/severe/unable to/extreme problems’. 447
From a critical disability perspective, the EQ-5D is predicated on an able-bodied norm. Critical voices also argues that it presupposes a Cartesian division between the body and the mind, which may not be culturally sensitive. More specifically, participation in ‘mobility’, ‘self-care’ and ‘usual activities’ could be seen to be culturally negotiated and might not have a similar meaning for all groups. This creates potential problems in capturing intersectionality and inequalities, in addition to the social context in which disability is experienced. Comorbidity is also difficult to capture, and it is sometimes difficult for people to attribute causes to a particular response. Linking depression to health, for example, might be especially problematic. Other concerns include the following:
-
‘mobility’ is predicated on walking
-
‘self-care’ refers to how independently a person can engage in self-care activities rather than the support they require to be independent
-
‘pain and discomfort’ is viewed as mainly physical in nature
-
routine activities have different meanings depending on disability and context
-
function might be difficult to define for people with a disability
-
physical barriers might have psychological reasons, especially for those with mental health problems or learning disabilities
-
‘anxiety and depression’ are regarded as psychological sensations
-
the discussion of impact on disease might have little meaning when a person does not regard themselves as having a disease.
Quality-of-life measures tend to conceptualise impairment as physiological ‘problems’, with which a person needs help. QoL measures are also criticised for implying that disability is a ‘burden’ for the person and those with whom they live. Some would argue that this is insensitive and contributes to stigma and that more of a focus on ‘flourishing’ with disability would be preferable. QoL measures can, in particular, fail to capture the social experiences of disability and the extent to which the social, political and economic circumstances in which people live are disabling.
Childhood physical disability
The child-friendly version of the EQ-5D, the EQ-5D youth survey,448 allows young people and children under 18 years of age to self-report on their health. Culturally appropriate understandings of self-care and age-specific types of impairment are considered, and there is a focus on ensuring accessibility of language. However, questions about ‘walking about’, ‘problems with walking’ or ‘being confined to a bed’ are not especially relevant to a young person with a physical disability. 448 A young person’s level of independence and participation in social activities might be dependent on his or her carer or parent, his or her access to technology and transport; accessibility of his or her home and his or her facilitated participation in school life. If a young person is a wheelchair user, he or she might not feel any pain or discomfort in his or her lower extremities. Nonetheless, sores located there would be a significant health issue but would be difficult to record. Similarly, the experience of ‘feeling worried, sad or unhappy’ could be linked to experiences associated with being a child or teenager, family life, interactions with professionals, health status and/or being a wheelchair user rather than to the impairment per se. Furthermore, the impairment may not be a ‘problem’ at all, except as a social construction. Consequently, the child or young person might not view their health as being linked with their illness or impairment.
Intellectual disability
The scoping review revealed that patients with intellectual disabilities have some of the greatest health inequalities. Often, a focus on intellectual disability overshadows health issues such as oral health, heart disease, smoking cessation, early-onset Alzheimer’s disease, depression and neglect. Such a heterogeneous population group makes it especially important to ensure that health needs are accessed appropriately and sensitively. If a patient had an intellectual disability, EQ-5D would have to be made accessible and/or be visually translated for them depending on the severity of their disability. This does not always happen, which explains why intellectual disability is sometimes used as an exclusion criterion. Research rarely commits resources to support accessibility and decision-making. There is also the problem of proxy responses, with carers answering questions, such as those relating to self-care, on a person’s behalf. Conceptually, some people might not distinguish pain as either a physical or emotional sensation. Similarly, a person’s physical or emotional expressions of pain or discomfort might be misunderstood or viewed as challenging behaviour, especially if the person in question happens to be male, physically strong and from a black and minority ethnic (BME) group or living in an institutional setting. 449,450 Finally, there are no questions that enable people to give expression to mental suffering, social isolation or neglect.
Autism
Some of the most socially and politically vocal parents’ groups and disability communities are linked with autism. The diagnosis of autism and its ascription on a continuum from low-functioning to high-functioning individuals (i.e. those with Asperger syndrome) can be contentious, reflecting a medical model of classification. People with autism often need support with the verbal and non-verbal communication of information. Depending on the type of autism, the sensory setting of the EQ-5D questionnaire might depend on who is asking the questions as much as on ensuring that it is made accessible. Some people with autism have severe communication difficulties and will need help from a carer or parent in answering the questions. Others might interpret the questions in a literal way. For example, it might make more sense to ask if a person has ever had any trouble walking, rather than if they can walk. The same applies to asking questions about pain. It might make more sense to a person with autism to ask about feeling ill and when that occurred. Asking questions about ‘usual activities’ may also be negatively understood as creating a norm about what should be regarded as usual, and this might be confusing for some. Similarly, questions about function might seem vague and confusing, especially if physical barriers occur for psychological reasons. Many people with autism have difficulties with social interactions and may enjoy activities or have intensive and very specific hobbies that fall outside what is considered ‘usual’. This does not mean that they do not participate socially or do not have a ‘usual’ family life. However, specific types of social participation might generate experiences of anxiety, distress and depression and it is, therefore, important to ask about the context in which that occurs and if it is linked to health status. There are several innovative ways, such as photo voice, to engage with those who have autism. These, however, are rarely connected to the use of outcome measures.
Chronic illness: multiple sclerosis
Chronic illnesses and life-limiting conditions now affect a significant number of people. MS is a neurological chronic illness that can fluctuate in severity over the life-course and/or become progressively worse. Most people are diagnosed between the ages of 20 and 40 years, and the condition affects more women than men. Depending on the day on which the EQ-5D questionnaire is administrated, questions about ‘mobility’, ‘self-care’ and ‘usual activities’ may get a different response. On a particular day, mobility might be impaired but this might be attributable to visual loss. The underlying cause of immobility may not, therefore, be understood. In addition, questions about pain and discomfort do not access experiences that diagnostically fall outside that continuum, such as numbness, changed voice or fatigue, all of which could be significant in attempting to understand illness progression and the experience of health. The concept of ‘usual activities’ is, equally, a shifting one and it may be more relevant to ask about participation in activities in various forms or how that changes depending on experiences of pain. It is also crucial to understand the experiences of chronic and fluctuating pain, use and accessibility of pharmaceutical drugs and how that links to intersectionality. 451
Dementia
Advances in standards of living and medical technologies mean that people in the UK are living longer. There are many intersections between ageing, health and disabling conditions. Dementia, an umbrella term, encapsulates a wide range of conditions linked to cognitive, speech, spatial, temporal and affective impairments such as Alzheimer’s disease or vascular dementia. Dementia affects mainly older people, although it can develop earlier in some young people. Along the life-course it will affect more women than men, making gender a salient feature, although this might reflect differences in life expectancy between genders. Ensuring that the questionnaire is administered in a well-known setting by a familiar person is an important consideration. Although mobility may not be affected, gait or spatial temporal awareness will, and it is important to understand this. Asking about ‘problems’ with self-care activities or ‘usual activities’ could be stigmatising and distressing for people with memory loss; it may be more sensitive to ask if an individual is being supported in ‘self-care’ and any other ‘activities’. Furthermore, people might not be able to express experiences of pain or discomfort, although visual aids might help. Likewise, other experiences that may cause discomfort or anxiety and that are linked to medication use or the progression of dementia, such as nightmares or daytime hallucinations, are not covered, despite the fact that they lead to impaired sleep and thus affect everyday QoL. Anxiety and depression may both be linked to experiences of dementia but in very different ways, although, at present, EQ-5D does not assess this. In addition, asking people to indicate how well they feel on a scale of 1 to 20 may not make any sense to people with severe dementia, and asking about the worst imaginable health state may mean that they confuse health with the experience of having dementia.
Depression
Mental health includes a broad spectrum of conditions, of which depression is one of the most common in the UK. Depression also occurs across the life-course, affecting a heterogeneous population. It can be linked to a wide variety of causes such as work-related stress; being unemployed; bereavement; bullying; loneliness; ill-health; chronic pain; and ageing. Past or present experiences of abuse (physical and emotional) can also be correlated with depression, as can experiences of trauma or stress. Further experiences of stigma, oppression or discrimination are correlated with depression. 2,452,453 Depending on the type of depression and whom it affects, the EQ-5D may have to be translated in different ways, for example, in cases in which depression affects a political refugee from Burundi; a person suffering from severe clinical depression; a d/Deaf person; or a person with intellectual disabilities. This is not straightforward, particularly in terms of ensuring that depression is not further stigmatised. Mobility in people with depression could be affected, but not necessarily in a way that is linked to physical health. Nonetheless, it could affect participation in work and daily life, which perceptions of stigma might further restrict. Mobility can also be affected by underlying conditions. Pain and depression may also be expressed in culturally varied ways and may be linked to psychic, psychosocial, affective and spiritual complaints. Another important factor to also take into consideration is what type of therapy, intervention or medication a depressed person is undergoing when answering the EQ-5D.
Short Form questionnaire-36 items
Many of the more general difficulties faced when using the EQ-5D equally apply to the use of other measures. There might, however, be more specific, contextual factors peculiar to the measure. The SF-36 has been designed by RAND Health (Santa Monica, CA) to gather information about population level health. 454 It is a QoL measure and has been adapted to the ICF. It is also used by health economists to calculate QALYs. It has 36 different questions ordered in eight themes, each of which can be scored. These themes are: (1) physical function; (2) role limitations attributable to physical health; (3) pain; (4) general health; (5) vitality; (6) social function; (7) role limitations attributable to emotional issues; and (8) mental health. It has not been adapted for disease-specific impairments or conditions, and more critical voices argue that it is disableist in both construction and language. Work, for example, is assumed to be an activity in which everyone engages. The SF-36 also creates a clear division between physical and mental health, in a way that might not reflect a person’s experiences. Stevens and Killeen455 argue that, unlike the EQ-5D, which uses a severity approach, the SF-36 seems to take a ‘frequency approach’ in measurement scales. We explore the consequences of this in relation to specific forms of disability.
Childhood physical disability
The SF-36 is not intended for use in children, and more sensitive measures such as the Short Form Health Survey 10 Child Health Questionnaire are recommended. Nonetheless, the SF-36 has been applied to teenagers and young people. The physical function questions are predicated on vigorous or moderate activities such as walking and climbing stairs, which might assume a different context in young people and for those with particular form of disabilities. Similarly, physical health is expressed as a problem related to work.
Intellectual disability
Critics argue that the terminology and language of the SF-36 is inappropriate and difficult to understand. The questionnaire asks if the person feels full of ‘pep’ and also if they feel ‘depressed’. This might not have immediate meaning to someone with an intellectual disability. A question such as ‘As a result of physical or emotional health have you accomplished less in the last four weeks’ presupposes an understanding of differences between various health statuses and how they impact on ‘accomplishments’ as well as an understanding of a sense of time.
Autism
As with the EQ-5D, questions can be interpreted differently (and literally) depending on the kind of autism with which a person is diagnosed. For example, questions such as ‘Have you had any of the following problems with your work or other regular daily activities as a result of your physical health?’ or ‘Have you been a happy person?’ might confuse someone with autism. Others might not have the ability to verbalise emotions such as happiness.
Chronic illness: multiple sclerosis
How much bodily pain a person has had in the past 4 weeks may not be as relevant as asking about when, where and how pain occurs. Questions could also contradict each other, for example, as in the case of asking about feeling ‘calm’ and then asking about feeling ‘worn out’? Furthermore, questions about vitality rather than rest, relaxation or sleep may be more pertinent to understanding physical and emotional health and the broader role limitations that are experienced by someone with chronic illness or MS.
Dementia
The first question asks about perceptions of health in terms of recall and if that has improved or become worse. This is difficult for someone with dementia to answer. More generally, the SF-36 does not ask about the role of the environment, which might be more significant to understanding experiences of dementia than ranking task-based activities.
Depression
Depression can affect all aspects of a person’s life and can lead to deteriorating health function. When answering a questionnaire, therefore, depression may be overshadowed by physical ill health.
Client Service User Receipt Inventory
Cost-effectiveness measures, of which there are many, are an important feature of public health research. One of the most widely used cost-effectiveness measures in public health is QALYs. It considers what health benefits an intervention will add to life-years. As we have noted, cost-effectiveness measures such as QALYs are viewed as problematic by several models and theories of disability because they presuppose ideas of ‘burden’ and ‘problem’ and rarely engage with how the social and political environment creates disability. Furthermore, when researchers rethink outcome measures, for example in terms of ‘capability’, such measures are used mainly to justify the cost-effectiveness of interventions. 148,444 Few measures view disabled people as creating economic ‘wealth’, for example through the employment of others. 23 Likewise, collective indicators or measures of cultural, social, political or innovative contributions to, and participation within, society do not exist. 150
There are different types of economic evaluations associated with cost-effectiveness. NICE now requires both cost–consequences and cost–benefit analyses to be undertaken when assessing interventions. The Client Service User Receipt Inventory (CSRI), for example, measures the costs of services used by people who have long-term, complex, fluctuating or severe conditions. It has been further developed to measure sociodemographics (CSSRI) and pain (CSRI-Pain) in patients. The CSRI asks 30 questions about how frequently and intensively health- and social-care services are being used by a service user. It also contains specific questions about the health-care providers with whom a patient has had contact, inclusive of emergency, primary, mental health, rehabilitative and complementary medicine. The CSRI is, however, predicated on people having access to care, which might not be the case for all disabled people. 181 A ‘right’ and ‘need’ to use services may not be understood by all disabled people. Likewise, the responsibility of health and social care to ensure equity in services might not be understood by professionals or service planners. Evidence indicates that disabled people, such as those with intellectual disabilities, are not accessing health care and dying 20 years earlier than the general population. 14 This suggests that a focus on cost must be ethically balanced by a concern with social justice. Delimiting access to health care because of cost could be viewed as a violation of human rights, particularly if cost value and QoL are considered only when a person is in a ‘healthy’ state.
The CSRI also assumes that people with the most need use services the most intensively. Evidence, however, suggests that this is not always the case,456 particularly given that discrimination and disablism might create barriers to accessing appropriate care. The CSRI does not necessarily engage with this possibility. It also assumes accurate patient recall, which might be difficult for those with cognitive or intellectual impairments or mental health problems.
In addition, the CSRI does not take a life-course approach and thus struggles to accommodate those who use services intensively with high costs but who do not have such high care demands. Finally, differences in how effective services are also occur, and the CSRI, with its focus on the individual, can place the onus of responsibility in the creation of costs on the patient rather than on health- and social-care services or state policies to safeguard population health and well-being. In this respect, it may be useful to have an outcome measure for how well state policies respect equity in public health or an equity index.
Moving forward
When thinking about how measures can be adapted for use in public health research, we note the need for inclusive, generic measures that reflect experiences of living with disabilities and that transcend straightforward notions of embodiment438 and physiological functioning. This would help to understand how ‘problems’ with impairment and health can be linked to social, economic and political barriers as well as to a lack of access to health and social care. Measures, for example, ignore how the environment could be creating disability rather than the individual impairment. They demonstrate a particular lack of connection to stigma and discrimination and how these could correlate with health inequalities. It could be feasible, however, to develop an outcome measure examining how an intervention tackled barriers, enabled participation or encouraged participation. 150 We would also hope that outcome measures would focus on acceptance and diversity, which in turn would help to develop a more critical understanding of capability and perhaps one that is able to critically engage with the use of the WHO/ICF as the sole standard for measuring and screening for disability. We also hope that measures would engage with how people understand their identities and what normatively becomes important for them and their families. Inclusion and accessibility, however, remain an ongoing problem and the adaptability of measures for use by people with a broad range of different disabilities is underdeveloped.
Conclusion
This chapter discussed the potential of an operational decision aid to facilitate more inclusive and methodologically robust research practices. In doing so, we have attempted to make a connection between the theoretical models used to understand and define disability and paradigms associated with public health, in ways that support methodological rigour, ethical engagement and respect for personhood and the rights of the individual. The more critical literature is especially sceptical about the value of public health research in empowering people with disabilities. These criticisms need to be addressed, particularly given that measurement and classification continue to dominate debates. There is not a great deal of enthusiasm among those assuming a more critical voice to engage with public health, which is often treated with suspicion as a form of normalisation and which thereby denies the experiences of disabled people.
The idea that interventions can be simultaneously disabling and enabling is an important consideration, as is an acknowledgement of how interventions and research can (implicitly) embody ableist assumptions. This provides a theoretical basis from which to consider inclusivity, informed by a more rights-based approach to disability. This has many advantages, including a commitment to locating the individual within their broader social context. It is also sensitive to life-course and, more generally, to intersectionality and inequalities, thereby providing a potential bridge between models and theories of disability and more ecological models and theories about the SDHs that inform public health. We are mindful, however, that a more inclusive, rights-based research approach needs to produce methodologically rigorous research. The RE-AIM framework and its commitment to evaluating real-world, complex interventions has a particular value in supporting this. Our exploration of commonly used outcome measures investigated further the importance of methodological rigour and offered potential ways forward when rethinking outcome measures to ensure that they are disability-sensitive.
In the second stage of the project, we used these ideas to try to understand how different models and theories of disability linked up to the current state of research in public health. By referencing our rights-based empirical and ethical decision aid, we explored the extent to which current public health research is inclusive and able to capture the experiences of disabled people. In grounding our account in the current realities of research, our analysis was able to provide a more realistic account of how best to make public health research more sensitive to the experiences of disability. Our intention was to offer a critical discussion about the value of adapting a more socially oriented model of disability and to assess the practicalities of defining appropriate research questions that adapt inclusive sampling strategies, use relevant outcome measures and establish appropriate user involvement and preference.
Chapter 5 Scoping reviews of interventions
In the second part of our scoping review, we evaluated the extent to which the current evidence on public health interventions connects with the different theories and models associated with understanding disability. We were particularly aware of the importance of balancing sensitivity to more social and emancipatory models of doing research while recognising the practical demands of producing robust, evidence-based public health research. To explore this and to make suggestions for improving study designs and outcome measures, we purposively selected the following:
-
a total of 30 generic reviews of public health interventions, which could potentially benefit those with disabilities, to gain insights into the ability of mainstream research to capture the experiences of disability
-
a total of 30 reviews of interventions with a public health focus in which people with disabilities were identified as a key target group to enable us to examine the potential of inclusive designs.
As outlined in Chapter 2, we developed a traffic-light system to assess the extent to which each review was inclusive of disability. This informs the first part of our analysis. We then interrogated each review in detail by providing a summative narrative commentary in relation to our toolkit/checklist outlined in Chapter 4. We payed particular attention to how reviews engage with dignity, inclusion, intersectionality, accessibility and equity. Our account is initially brief, as the lack of engagement with disability gave us little material on which to comment, especially in the more generic public health reviews. It is, however, possible to identify some overarching themes, which help to make sense of the literature. Finally, we selected two reviews – one generic and one focused on disability – and explored the extent to which each included study engaged with disability in accordance with some of the frameworks and decision aids offered in Chapter 4.
Generic reviews of public health interventions
The 30 generic public health reviews of interventions were based on the findings of 668 studies. The lowest number of studies included in a review was two and the highest number was 67 studies. We found no reviews that were wholly and explicitly inclusive of disability, mainstreamed disability or used disability theories or models. None, therefore, was assessed a having green light and, to this extent, our classificatory system was not especially helpful when assessing generic public health interventions. Some of the studies, however, could be regarded as nominally inclusive and we have given these studies an amber ranking. We outline the chosen reviews in Table 10.
| Study | Ranking |
|---|---|
| Dobbins et al.133 | Red |
| Waters et al.457 | Amber |
| Thomson et al.458 | Amber |
| Pega et al.459 | Red |
| Jahanfar et al.460 | Amber |
| Adler et al.461 | Red |
| Dyson et al.462 | Amber |
| Siegfried et al.463 | Red |
| Johnston et al.464 | Amber |
| Ker and Chinnock465 | Amber |
| Cashman et al.466 | Amber |
| Bailey et al.467 | Amber |
| Oringanje et al.468 | Red |
| van den Broek et al.469 | Amber |
| Jefferson et al.470 | Red |
| Langford et al.471 | Amber |
| Joyce et al.472 | Amber |
| Hosking et al.473 | Red |
| Hayes et al.474 | Red |
| Baker et al.475 | Red |
| Spinks et al.476 | Amber |
| Foxcroft et al.477 | Red |
| Grilli et al.478 | Amber |
| Dennis et al.479 | Red |
| Callinan et al.480 | Amber |
| Ehiri et al.481 | Red |
| Coppo et al.482 | Amber |
| Wilson et al.483 | Red |
| Marcano Belisario et al.484 | Amber |
| Yeung et al.485 | Amber |
The reviews reflected a broad range of interventions, relevant to different stages of the life-course, and a mix of preventative strategies and health promotion. Each review had a policy focus of improving health in general, which at least in theory could have included people with disabilities. Three inter-related themes explain why this did not occur:
-
The nominal inclusion of disabled people, while sometimes mistaken for mainstreaming, becomes the basis of analytical exclusion.
-
The theoretical and methodological disconnects with the disability literature make it difficult to produce meaningful findings that are relevant to the experiences of disabled people.
-
There is confusion over what is meant by ethical engagement and social inclusion when discussing mainstreaming.
Nominal inclusions
The nominal mention of models and concepts of disability illustrated some of the difficulties in developing an evidence base that is relevant to the experiences of people with disabilities. We found that half of our reviews could be regarded as nominally inclusive (15/30), although this did not necessarily mean that the reviews provided a meaningful analysis of disability. We included Waters et al. 457 as nominally inclusive because ‘obesity’ can be described as a disability and the authors mention a link to chronic diseases. Thomson et al. 458 was nominally inclusive because the study mentioned ‘vulnerability’ and ‘pre-existing poor health’, in addition to having outcome measures linked to mental health. Two reviews did not define disability but linked the influence of tax credits459 and obesity133 to ‘disability’. Jahanfar et al. 460 examined violence against pregnant women but did not make explicit reference to ‘disability’, despite mentioning physical injuries, mental health ‘problems’, the physical impact on the unborn child, and developmental and behavioural influences on other children in the family. The exclusion of the word ‘disability’ in this context was felt to be significant, in particular given other evidence indicating that ‘disability’, more than any other intersectional factor, is correlated with an increased risk of domestic violence. 486,487
Nominally inclusive reviews could exclude contested definitions and measures of disability. Disablement, for example, was mentioned in some studies in terms of injury or mental health (psychology/psychiatry), for instance, but was not theorised as ‘disability’ (see Generic reviews of public health interventions above). Obesity can be explicitly linked to disablement and disease and to impairments and life-limiting public health conditions across the life-course. 488,489 However, Waters et al. 457 did not explicitly consider this in relation to disability mainstreaming. Similarly, Thomson et al. 458 make reference to poor health and housing but do not conceptualise this within broader debates about disability. Many reviews did use measures that could be associated with disability. Adler et al. 461 and Siegfried et al. 463 viewed the risk of high salt intake and alcohol use, respectively, in terms of DALYs. Neither review, however, explained how international measures of population health were defined or made an attempt to connect them to a disability theory. In most cases, measures of mortality and morbidity dominated and were frequently presented in ways that confused them with measures of living with disability. 165
Theoretical and methodological disconnects
The reviews usually reported international measures of health, using them to provide an overview of general population health and prevalence of specific conditions, without signalling how their use might be methodologically and theoretically contested. 44,122,166 There was no discussion, for example, of how the use of different measures of disability or impairment could have altered findings. 39 Moreover, the empirical or theoretical validity of such measures when understanding disabling experiences was not questioned. 120 Many of the reviews also made implicit and, at times, subtle assumptions, which associated disability with burden, risk or cost. 38,204 Furthermore, most reviews adopted a descriptive empirical approach, usually stating that ‘X’ was an important public health issue and that there was ‘Y’ evidence for this being a problem, hence the need for evaluation of an intervention. Few considered the potential impact of diversity or intersectionality and the relationship for example, between gender, social class, age and ethnicity and the interpretation of a study’s findings. Disability, therefore, was rarely considered, and the reviews linked to smoking cessation interventions illustrate this well. Tobacco use and cessation are rightly presented as population-wide health challenges; however, the evidence base came from studies in which the inclusion criteria were not made clear (i.e. studies may or may not have included people with disabilities). Furthermore, the reviews on the use of tobacco framed smoking as a public health burden, with outcome measures linked to individual behavioural change models. No review linked its findings to discussions about SDHs or inequalities.
The ethics of social inclusion
Many reviews cited studies using exclusion criteria that would have made it difficult to include people who had physical, cognitive or mental impairments. 484 There was often an inbuilt able-bodied bias either in the negotiation of inclusion and consent or in the use of measures. For example, Ehiri et al. 481 note the impact of traffic accidents in terms of lives lost but also in terms of years living with disability, which presupposes that people travelling in cars do not have any prior ill health or disabilities. Concerns about cost-effectiveness tended to exclude a more nuanced discussion about the relevance of an intervention to different types of people, including those with a disability. More generally, although the emphasis on behaviour change oscillated between private (individual) and public (policy) ‘risk’ in many of the reviews, there was little connection with more critical disability measures or the more ecological models associated with public health. There was also little acknowledgement that disability is socially constructed and created throughout the life-course. Furthermore, few reviews reflected on how the evidence base might be skewed to a population that is reflective of diverse experiences, including those relating to disability.
Perhaps not surprisingly, reviews did not discuss the importance of the ethical and effective mainstreaming of disability. Our scoping review indicated that studies struggled with what ‘disability’ was, how to define and measure it and the relevance of outcome measures to the experiences of disability. Wilson et al. 483 argued that traffic accidents were a significant cause of disability and used DALYs in measuring the impact of traffic cameras and calming measures. The outcome measures focused on issues that could be measured and checked easily, such as speeding and mortality and morbidity rates linked to car crashes. The review, however, did not measure how traffic calming influenced the overall public health environment in terms of accessibility or impact on376 pedestrians.
Public health and disability
We explored the 30 reviews of interventions focusing on disability (Table 11). These contained findings from 450 studies. We begin by classifying the reviews according to the traffic-light system outlined in Chapter 2, and we had more success than when classifying the generic interventions. Just under one-third of the reviews were inclusive (9/30) but a large proportion did not engage with disability theory; this was true even when the studies discussed disability issues within a public health context (21/30). Most of the reviews seemed to implicitly display the residual influence of medical models (14/30) and, consequently, disability was viewed as a problem, requiring a fix. Consequently, risk rather than emancipatory discourses dominated the evidence. Furthermore, measures appeared to be used uncritically, with little reflection on how they captured the diverse nature of disability, intersectionality or life-course effects.
| Study | Ranking |
|---|---|
| Fox et al.134 | Amber |
| Ashman and Duggan490 | Green |
| Mayo-Wilson and Montgomery491 | Amber |
| Kaufman et al.492 | Red |
| Curioni et al.493 | Amber |
| Duperrex et al.494 | Amber |
| Austin et al.495 | Amber |
| Jacobson Vann and Szilagyi496 | Red |
| Fong et al.497 | Green |
| Grant et al.498 | Green |
| De La Rue et al.499 | Red |
| Regehr et al.500 | Amber |
| Coren et al.501 | Amber |
| Gensby et al.502 | Green |
| Coren et al.503 | Green |
| Ramsay et al.504 | Amber |
| Mayo-Wilson et al.505 | Green |
| Mayo-Wilson et al.506 | Green |
| Mayo-Wilson et al.507 | Green |
| Mayo-Wilson et al.508 | Green |
| Zwi et al.509 | Amber |
| Heiwe and Jacobson510 | Red |
| Adeniyi and Young511 | Red |
| Martin et al.512 | Amber |
| van Oostrom et al.513 | Amber |
| Kamper et al.514 | Amber |
| De Silva et al.515 | Amber |
| Marteau et al.516 | Red |
| Mastellos et al.517 | Amber |
| Khan et al.518 | Amber |
In interpreting these reviews, we identified four inter-related analytical themes explaining approaches to disability:
-
the continued influence of the medical model
-
the extent to which reviews captured a life-course perspective that was sensitive to disability
-
how reviews engaged with a lack of evidence
-
the role of participation, ethics and equity in public health research.
The continued influence of the medical model
When piloting, it became apparent that studies in the Cochrane Database linked to ‘disability’ were mostly clinical in nature. Our scoping review further supported this. For instance, reviews often framed disability in terms of rehabilitation514,518 or as an individual rather than social experience. 515 The lack of reviews focusing on disability meant that we had also to use the Joanna Briggs Institute Library and Campbell Collaboration Library. These databases were more likely to contain reviews that used theories and models of disability to guide research and interventions (see Chapter 2).
A number of reviews focused on the relationship between various forms of disability and interventions facilitating a return to work. 497,502,513,514,518 The earliest review focused on the return to work after cancer and seemed to take a broad ecological approach in linking behavioural, psychological, educational and vocational frameworks to improve outcomes. 497 However, reviews focusing on specific disabilities such as MS seemed to take a narrow vocational approach, but one that could be said to be inclusive of disability. 518 For example, Gensby et al. 502 recount how disability becomes something to be ‘managed’ within workplaces. This contrasts with another study, which used the ICF rehabilitative framework to politically frame lower back pain in terms of ‘disability’. 514
A public health prevention model seemed evident in weight-management and fitness interventions across the life-course,134,493,510,511,517 although many of these interventions were rehabilitative or clinical. 134,493 Nonetheless, two reviews were linked explicitly to chronic conditions, and focused on exercise training for chronic kidney disease510 and weight loss interventions for chronic asthma, resepectively. 511 Rehabilitation, however, remained implicit. There was little consideration, for example, of more participatory or even emancipatory approaches.
Ageing was often linked to impairment, albeit as a risk to be avoided. For instance, one review on the impact of home visits to older people viewed success in terms of the prevention of ‘impairment’ and deaths. 498 One of the few studies that discussed how prevention and risk might conflict with each other was a study on driving interventions linked to dementia. 519 Driving ensures the mobility and independence of people, but dementia raises important public safety considerations with regard to driving. Discussions of vulnerability, risks and prevention could also be found in studies focusing on sexuality, violence and abuse in relationships. 500,504,509 In these reviews, however, ‘disability’ is largely absent unless negatively framed. Thus, definitions of disability were mostly clinical in nature and used a medical model approach to diagnosis490 (such as the WHO’s DSM) or were linked to biological definitions of impairment. 134,495
It was not always clear how and why the clinical or physiological outcome measures were chosen or how instruments had been validated within the studies. There was a strong predominance of psychological and psychiatric measures, instruments and outcomes. 491,495 Studies also used both self-reported (subjective) measures and functional (objective) measures without demarking clear differences between disability and health.
There was a particular disconnect between the theoretical grounding of disability theories and the use of outcome measures. For instance, Gensby et al. ,502 although inclusive of disability, did not give an explicit definition of ‘disability’ when examining the success of return-to-work disability-management programmes. The primary outcome measures calculated days of sickness leave, whereas secondary outcome measures focused on return to work and job functionality as measured by the ICF and the Work Role Functioning Scheme. There was, however, no reference to the more critical literature, which advocated a rethinking of workplace interventions and associated measures to reflect greater sensitivity with the diverse experiences of physical and mental impairments. 417,420,520
Life-course perspectives and disability
Several of the studies relevant to disability appeared not to see themselves in these terms. 514 Furthermore, many of the studies cited in the reviews used exclusion criteria that would prevent people with mental health or learning disabilities, for example, from participating in the research. 510 Consequently, even when engaging with disability, these public health studies struggle to accommodate the diverse experiences of disability, often preferring to view it in terms of reified measurement rather than as a social, cultural and political experience. We experienced particular difficulties in classifying reviews that were at first glance inclusive of disability. 490,503 Few, however, used theoretical frameworks to offer an analysis of disability, despite making allusions to them. Intersectionality and inequalities were also poorly articulated, as was an elucidation of how they might link to disability. 501
Despite evidence that early interventions improve long-term gains across the life-course, few reviews assessed the long-term implications of interventions. This indicates a possible gap in understanding the association between being poor, living in a deprived neighbourhood, belonging to a marginalised group and experiencing discrimination to higher rates of impairment, on the one hand, and to ill health, on the other, not only in the present but also in future generations. Current research, for example in intellectual disability, is beginning to focus on how neighbourhood and environmental risk factors are related to disability across the life-course, especially in children. 16,399,410 No review engaged with this and, more generally, there was a lack of connection with the more ecological models associated with public health. Interventions beginning early in the life-course are more cost-effective,15,521 and improvements in the social environment can positively impact on the consequences of severe forms of disability. 86,128,522,523 Likewise, the reviews did not reflect these debates.
Engaging with a lack of evidence
Some reviews commented on the lack of evidence for specific interventions linked to disability, such as comorbidities,524 childhood disability,51 ageing,57 mental health, fluctuating conditions or intellectual disability. 92,128 This is consistent with the broader literature and occurred at both a theoretical and methodological level. For example, Curioni et al. 493 examined the prevention of stroke linked to obesity. They did not, however, provide evidence that would enable them to contextualise their findings within debates about other factors that lead to stroke, such as smoking, alcohol use and high blood pressure. This is why many reviews reported outcome measures for which impacts could not be disentangled, by assuming that disability was a static condition with one primary cause. 134 Other neglected issues include the potential impact of secondary and associated conditions such as pain, fatigue, depression and impact of medication.
The few reviews that attempted to be inclusive of disability490,503 and that used paradigms found in disability studies, such as the social model, did not find any robust evidence that reflected the experiences of disability. 505–508 This, however, illustrates how public health interventions can be connected with the needs and aspirations of disabled people,125,129 such as improving social networks and support to live well and independently with disability. 53 There remain, however, few reviews connecting independent living or personal assistance with public health. For example, Lloyd-Evans et al. ’s525 review on peer-support for people with mental illnesses of differing complexity found a lack of evidence and a general lack of scientific rigour. The authors suggest a need for an assessment of ‘theory based interventions’ linked to issues such as ‘peer-support’. Perhaps the strongest evidence of how using disability theory and models can lead to public health research that is sensitive to the needs of disabled people came from the four reviews by Mayo-Wilson et al. 505–508 These reviews focused on the issue of personal assistance and connected intersectionality and inequalities with the life-course, while linking personal assistance with independent living.
Participation, ethics and equity
Evidence-based assessments are important to ensure that interventions improve health. When thinking about the efficacy of public health interventions and their general applicability, inclusion in design would help to strengthen the evidence base. However, the ways in which interventions were designed were often not participatory, despite evidence suggesting that more inclusive approaches could have a positive impact on attrition and sustainability. 59 Inclusive approaches can contribute to strengthening ethical review, as well as help with understanding how concepts such as ‘vulnerability’ or ‘capacity’ relate to particular conceptions of disability. 51,92 Many studies, however, appeared to take a ‘paternalistic’ view of research that was out of touch with the disability movement; intersectionality and more rights-based approaches; developments in cultural competence; and efforts to tackle discrimination. For example, Mastellos et al. ,517 who examined theoretical behavioural change models, observed that studies rarely considered how approaches to inclusion and participation could impact on the validity of the study findings. The review by Coren et al. 501 was one of the few that connected inclusion with a more rights-based framework. The review examined the participation and inclusion of children in the intervention planning as a secondary outcome measure and noted its importance when developing appropriate outcome measure tools that are relevant to the lives of children.
Appraising and assessing public health research studies
Our scoping reviews of interventions demonstrated a lack of disability-inclusive research in both general public health interventions and those more specifically associated with disability. There was little connection with the more critical models of disability and there was a residual tendency to treat disability as a problem or burden, while failing to accommodate variability, intersectionality or comorbidity. Our scoping of models of disability indicate that rights-based discourses are becoming increasingly influential. Some authors advocated the use of CRPD as an ethical foundation for inclusive research,424 although there was no consensus on how to implement this. To explore this further, we illustrate the potential of the decision aid outlined in Chapter 4 by applying it to a selection of individual studies included in the two reviews of interventions. Using insights from our earlier scoping, we were especially interested in life-course and fluctuating conditions, the role of intersectionality, and the use and relevance of outcome and effectiveness measures.
In selecting the reviews, we decided to focus on a cross-cutting public health and disability issue, namely, physical activity. We reasoned that such studies would be easy to access and include a wide variety of outcome measures. Following discussion among the review team, we identified two recent reviews. The first was a generic physical activity intervention, inclusive of 44 studies. 133 The second review focused on physical activity for older people with dementia and included 17 studies. 134 We again used a traffic-light system in which we considered inclusion (green), nominal inclusion (amber) and exclusion (red) across the categories of dignity, inclusion, intersectionality, accessibility and equity. Using a scoring system of green = 1, amber = 0.5 and red = 0, a total score was given for each study. These scores were informed by the research team’s initial assessment of the study and from correspondence with the authors of the generic public health review.
Assessing public health interventions: school-based physical activity programmes
We begin by discussing the studies that make up a generic public health review on physical activity and provide an assessment of the individual papers, in accordance with our decision aid (Table 12, based on studies in Dobbins et al. 133).
The settings for these public health interventions were mostly high- to middle-income countries. Physical activity primarily focused on the prevention of obesity in children and young people. A total of 44 RCTs were included. A total of 24 of these were based in the USA and the rest were located in Australia (6), Belgium (3) and six other European countries (France, Greece, Portugal, Spain, Switzerland and the UK), all of which contributed one study, in addition to Canada, India, Mexico, China and Hong Kong, all of which also contributed one study each. 133 The studies dated back to the 1980s, and the early US studies had particularly large samples. The 44 studies comprised 36,593 participants, including young people, families, teachers, schools and communities. 133 Most of the trials were longitudinal, usually > 6 months in duration, with many of the US studies lasting several years.
| Interventions | Ranking | |||||
|---|---|---|---|---|---|---|
| Dignity | Inclusion | Intersectionality | Accessibility | Equity | Total | |
| Angelopoulos et al.526 | Amber | Red | Amber | Red | Amber | 1.5 |
| Araújo-Soares et al.527 | Amber | Red | Amber | Red | Amber | 1.5 |
| Barbeau et al.528 | Amber | Red | Amber | Red | Amber | 1.5 |
| Bayne-Smith et al.529 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Burke et al.530 | Amber | Red | Amber | Red | Amber | 1.5 |
| Bush et al.531 | ||||||
| Colin-Ramirez et al.532 | Amber | Red | Amber | Amber | Amber | 2 |
| Dishman et al.533 | Amber | Red | Amber | Red | Amber | 1.5 |
| Donnelly et al.136 | Amber | Green | Green | Amber | Amber | 3.5 |
| Dorgo et al.137 | Amber | Green | Green | Green | Red | 3.5 |
| Ewart et al.534 | Amber | Amber | Amber | Amber | Red | 2 |
| Gentile et al.535 | Amber | Red | Amber | Amber | Amber | 2 |
| Haerens et al.536 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Haerens et al.537 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Jones et al.538 | Amber | Red | Amber | Red | Amber | 1.5 |
| Kipping et al.539 | Amber | Amber | Amber | Amber | Red | 2 |
| Kriemler et al.540 | Amber | Red | Amber | Red | Amber | 1.5 |
| Li et al.541 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Lubans et al.542 | Amber | Red | Amber | Amber | Amber | 2.5 |
| Luepker et al.543 | Amber | Green | Amber | Amber | Green | 3.5 |
| Martinez et al.544 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| McManus et al.545 | Amber | Red | Amber | Red | Amber | 1.5 |
| Neumark-Sztainer et al.546 | Amber | Red | Amber | Amber | Amber | 2 |
| Peralta et al.547 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Petchers et al.548 | ||||||
| Reed et al.135 | Green | Amber | Amber | Amber | Amber | 3 |
| Robinson549 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Salmon et al.550 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Simon et al.551 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Singh et al.552 | Amber | Amber | Amber | Amber | Red | 2 |
| Singhal et al.553 | ||||||
| Stephens and Wentz554 | Amber | Red | Amber | Red | Red | 1 |
| Stone et al.555 | Amber | Amber | Amber | Red | Amber | 2 |
| Treviño et al.138 | Amber | Green | Green | Green | Green | 4 |
| Verstraete et al.556 | Amber | Red | Amber | Red | Red | 1 |
| Walter et al.557 | ||||||
| Walther et al.558 | ||||||
| Wang et al.559 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Webber et al.560 | Amber | Red | Amber | Red | Amber | 1.5 |
| Weeks et al.561 | Amber | Red | Amber | Amber | Amber | 2 |
| Williamson et al.562 | Amber | Amber | Amber | Red | Amber | 2 |
| Wilson et al.563 | Amber | Amber | Amber | Amber | Amber | 2.5 |
| Young et al.564 | Amber | Red | Amber | Red | Amber | 1.5 |
When assessing these public health studies we noted three inter-related thematic observations from which to explore the potential of an inclusive disability research agenda, namely, linking theory to empirical design; disability and mainstreaming; understanding intersectionality.
Linking theory to empirical design
Most of the studies could be said to be theoretically informed by public health paradigms, often with an implicit focus on combating inequalities, although some studies did not make this explicit and, more generally, there was little engagement with more theoretical explanations of inequalities or disadvantage. Poverty, for example, was rarely mentioned, despite its importance in exploring obesity and physical activity. 565 Many studies, however, reflected a sustained commitment to health promotion and (theoretical) use of health belief models such as Bandura’s social cognitive theory, theory of planned behaviour or socioecological approaches. The use of behavioural change models were usually focused on the individual (micro) issues rather the broader social (structural) context, in which people made choices. No study engaged with an explicit model of disability.
It was rare for any theoretical connections to be made between inequalities, public health paradigms, diagnosis of conditions or impairments, the outcome measurements being used and how long-term impact was measured for sustainability. When contacted, authors could not provide convincing explanations for this and seemed uncertain what was meant by theory. This explains why many of the studies offered a descriptive rather than explanatory analysis, which made it difficult to assess why an intervention was successful. Most studies gave a narrow quantitative appraisal about what evidence existed to support the intervention and how bias was controlled. 529 For example, Burke et al. 530 discussed a trial of health promotion programmes for 11-year-olds that was geared towards high-risk children and illustrated the statistical robustness of methods as well as the characteristics of the higher risk children who left the intervention. An understanding of why those higher risk children left the study was not, however, part of the analysis.
Disability and mainstreaming
In discussing mainstreaming with authors, we became aware that many studies did not use consistent definitions of disability, with few referencing international conventions or medical definitions. Authors who e-mailed us acknowledged that they were unclear about the definition of ‘disability’ that they should use, or who and what was included in the term ‘disability’. There was confusion over whether or not ‘disability’ was inclusive of illness, learning difficulties (e.g. ADHD), neurodiversity (e.g. Asperger syndrome) or mental health issues. Some authors stated that they had not asked about such issues and felt that they belonged to a private (personal) not public (political or social) realm. In a few cases, authors asked for clarification from the research team, asking what we understood disability to be. Authors also struggled to define what inclusive practices meant. Verstraete et al. 556 had bought a range of robust equipment for their physical activity intervention but admitted that they had not thought about accessibility or accommodation. One author, however, did send us material illustrating how the trial had thought about mainstreaming in physical activity interventions. 135
Some authors thought that disability was ‘probably’ included or ‘could’ have been included or that disabled children had participated, but they could not give specific details. One author stated confidentially via e-mail that they had tried to include disabled children by administering the questionnaire face-to-face. Other authors mentioned how disability became a part of exclusion criteria, such as in the case of walking or running interventions,540 and stated that no disabled children had been included. Some authors qualified this by saying that ‘severe disabilities’ were not included and added that those decisions belonged to the schools. 563 Despite the lack of inclusion, some of the interventions could have been adapted to be accessible to disabled children. 542 The inclusion of families or carers was largely justified on the grounds of ethics rather than analytical or explanatory significance. None of the authors mentioned universal design or what the notion of ‘mainstreaming’ included.
Although cultural sensitivity had been considered in several studies,135,138,528,555 and a link made to ‘well-being’, the majority of studies were not particularly disability sensitive or inclusive of disability culture. Most studies had not adequately defined cultural sensitivity other than in terms of exclusion criteria. Several authors passed the onus of responsibility on to the institution from which the sample was taken, stating that they depended on the institutions to ensure accessibility or to define mainstreaming. One author noted that American schools are required by law to ensure disability mainstreaming but qualified this by stating that this is only if they are ‘able’. These links to legislation are revealing. Although ‘disability’ may have been implicitly included in trials, none of the studies’ analyses discussed disability.
Disability and intersectionality
Some studies successfully related intersectionality to debates about inequalities. These included studies on improving health for girls, which connected ethnicity and lower socioeconomic status to hypertension, obesity and cardiovascular disease. Some studies focused on African American51 and Mexican American children. 138,531 Three studies focused explicitly on African American girls,528,534,564 and others focused on the mixed ethnic and socioeconomic backgrounds of children in inner cities, areas with deprivation or urban–rural divides. 533,538,557,563 Generally, US studies tended to be better at engaging with intersectionality associated with age, gender, ethnic origin and social economic status than some European studies. 535–537,540 However, intersectionality remained poorly conceptualised theoretically. Eight of the US studies that explicitly focused on gender (girls) and health issues linked to obesity528,529,533,534,538,546,560,564 struggled to explain their findings in terms of ethnicity or socioeconomic disadvantage (or disability). Webber et al. 560 focused on ensuring that participating girls came from a range of backgrounds and ethnicities, and they used a combination of qualitative and quantitative techniques linking health promotion in schools and within communities. However, their process evaluation considered gender and ‘race’ as statistical values as part of a broader strategy to understand fidelity. 564 Some smaller studies, however, were more successful, such as the Australian study focusing explicitly on boys, which noted that a ‘one size fits all’ approach might not work and that a more targeted approach might be necessary. 547 However, within the Australian context, indigenous health or ethnicity were seemingly not considered.
Many of the authors said that they had collected data on comorbidities and chronic conditions, usually in a questionnaire. Few of the studies, however, explicitly examined comorbidities or chronic conditions unless they felt obliged to explain them as criteria for exclusion. McManus et al. 545 note that none of the children included had any ‘present illnesses or chronic conditions’ and Treviño et al. 138 excluded children with ‘type 1 and 2 diabetes’. Weeks et al. 561 note that subjects were included if they were in ‘sound general health’ and could participate in a jumping intervention. Wilson et al. 563 noted that:
Adolescents were excluded if they had a medical condition that interfered with PA, (2) were developmentally delayed such that the intervention materials were not cognitively appropriate or, (3) were currently in treatment for a psychiatric disorder.
The inclusion of disability was usually seen to overcomplicate study design and/or be incompatible with outcome measures. Many authors also struggled to reflect on the extent to which the interventions that they were evaluating could function to exclude people with disabilities. Wang et al. 559 positively noted the importance of the cultural sensitivity of their research (as it included a high percentage of African American participants) but did not include disability sensitivity.
Equally, concepts of inclusion, accessibility and theoretical and methodological connections to equity were poorly debated by many of the studies. This is why many studies found it difficult to accommodate the diverse experiences of disability and, more specifically, to offer explanations about the extent to which study findings had any relevance for a broad range of disabled groups.
Assessing public health interventions focusing on disability: physical activity levels with a diagnosis of dementia
Many of the interventions outlined in these studies were set in institutional settings such as nursing homes, community homes or long-term care facilities. Few interventions focused on community settings and this raises an interesting point about the extent to which such a focus was ‘disability sensitive’ and reflected the ‘real-world’ changing demographics and policy implications of impairments. 21,566 The studies focused on physical activity, believing that it ensured a better QoL for those at risk of dementia. 134 Dementia, although measured using a range of subjective and objective criteria, including self-report, generally focused on functional status consistent with a more medical model of disability. Table 13 provides our assessment of the studies, according to the scoring system identified above.
Most of the 17 settings were located in middle- to high-income countries such as the USA (4), Brazil (3) and France (2). European countries such as Germany, Spain, Belgium, the Netherlands and Italy all had one study, as did Canada, Australia and the Republic of Korea. Most studies had small sample sizes and few studies were longitudinal in nature. The total number of participants across the 17 studies was 1163. Fox et al. 134 explain that their review focused on RCTs, non-RCTs and quasi-randomised trials, with 12 studies using two groups (one a control) and the other five using three groups. When assessing the interventions, three themes emerged as important in explaining studies’ approaches to disability, namely, the clinical nature of the interventions, the use of outcome measures and the implication of this for the study’s findings; the ethics of participation; and inclusion, intersectionality and inequalities.
| Intervention | Ranking | |||||
|---|---|---|---|---|---|---|
| Dignity | Inclusion | Intersectionality | Accessibility | Equity | Total | |
| Christofoletti et al.567 | Amber | Green | Green | Green | Amber | 4 |
| Coelho et al.568 | Amber | Green | Green | Green | Amber | 4 |
| Cott et al.569 | Amber | Green | Green | Green | Amber | 4 |
| Eggermont et al.570 | Amber | Green | Green | Green | Amber | 4 |
| Garuffi et al.571 | Amber | Green | Green | Green | Amber | 4 |
| Hauer et al.572 | Amber | Green | Green | Green | Amber | 4 |
| Kemoun et al.573 | Amber | Green | Amber | Green | Amber | 3.5 |
| Kwak et al.574 | Amber | Green | Amber | Amber | Amber | 3 |
| Roach et al.575 | Amber | Green | Green | Green | Amber | 4 |
| Rolland et al.576 | Amber | Green | Green | Green | Amber | 4 |
| Santana-Sosa et al.577 | Amber | Green | Amber | Green | Amber | 3.5 |
| Steinberg et al.578 | Amber | Green | Green | Green | Amber | 4 |
| Stevens and Killeen455 | Amber | Green | Green | Green | Amber | 4 |
| Tappen et al.579 | Amber | Green | Amber | Green | Amber | 3.5 |
| Teri et al.580 | Amber | Green | Green | Green | Amber | 4 |
| Van de Winckel et al.581 | Amber | Green | Green | Green | Amber | 4 |
| Venturelli et al.582 | Amber | Green | Green | Green | Green | 4.5 |
Clinical interventions and outcome measures
Neither public health paradigms nor disability theories or models were mentioned by the studies. Interventions were mostly clinical in nature. Disability, when mentioned, often occurred as an exclusion category or was offered as a reason for dropout. Roach et al. 575 noted that ‘increased illness, disability or death’ explained why participants ‘dropped out’ of the intervention. Rolland et al. 576 defined disability in terms of ADL measures and Cott et al. ,569 who mentioned ‘physical disability’ as a characteristic to be measured in terms of ‘functioning’, noted that they wanted to prevent ‘excess disability’. Correlations were also made between ageing and disability. Stevens et al. 455 linked disability explicitly to the ‘Revised Elderly Persons Disabilities Scale’. Teri et al. 580 called their intervention ‘Reducing Disability in Alzheimer Disease’, but did not define disability. Few studies offered a theoretical reconciliation between their approach and their findings. Teri et al. ,580 like most studies, viewed Alzheimer’s disease as a clinical condition rather than a disability with social consequences. When asked about this, the authors seemed confused by the question. Most studies were concerned with demonstrating the internal validity and effectiveness of the trial design rather than with offering an explanatory account, which reflected, for example, intersectionality, comorbidities or the fluctuating nature of the condition. Perhaps not surprisingly, no study debated emancipation or independence.
Studies seemed to struggle with assessing measurements of (primary and secondary) outcomes and understanding their validity or links to ‘risk’ of health conditions and broader inequalities. Fox et al. 134 noted 10 different measures of cognition and several different measures of ‘functional ability’. There was also a lack of clarity in defining Alzheimer’s disease or dementia more broadly. Most studies used the ICD diagnosis and then the Mini Mental State Examination to measure cognition or other methods of cognitive assessment such as asking respondents to draw a clock (see also Fox et al. 134).
There seemed to be a potential dissociation between the sheer number of outcome measures and their relevance to the success or otherwise of the intervention. 455,576 No study defined disability, and measures were rarely linked to social and political debates about inequalities583 or impairments. 584 Outcome measures tended to conceptualise participants with Alzheimer’s disease as a ‘burden’. 578 The influence of psychiatry and psychology in the use of the DSM and ICD as diagnostic tools was evident, but few studies offered a methodological discussion of their validity or reliability or how they related to intersectionality. 585 More general medical models heavily influenced how impairment was conceptualised and measured and how study findings were explained. Even when dementia was linked to improving QoL, ‘quality’ was presupposed to be medical or was linked to health outcomes that were measurable. 455,572,577,578 Participants were not asked about what QoL meant to them. Moreover, QoL was not linked to other social and political factors that could improve life with dementia.
The ethics of participation
Individual studies often mentioned ethics, and we discussed this further with the authors. One study, for example, noted having to frequently gain consent rather than assume it was a one-off event. 455 One study mentioned gaining the written consent of a primary caregiver, legal guardian or partner in addition to the person with dementia. 569 Another study also ensured that they got medical consent for study participation by contacting a person’s physician. 572 These studies provide interesting examples of how studies can adapt to more inclusive designs, particularly when the issue is regarded as important. Nonetheless, researchers tended to work within established research orthodoxy when obtaining consent, still viewing it in terms of written informed consent. 568 There was little discussion of a more rights-based approach or supported decision-making. Other ethical issues of, for example, having a placebo control arm in an institutional setting in which there might be a lack of physical and cognitive stimulation, or using differing types of activities that could have lesser impact, were not debated. 567,568
Inclusion, intersectionality and inequalities
Few studies included people with severe forms of dementia or mentioned issues of intersectionality such as ethnicity, gender, age or other comorbidities. Comorbidities such as severe heart disease or difficulties with breathing were seen as justifiable exclusion criteria, because of the physical nature of the intervention. 582 Other studies excluded people with Parkinson’s disease, vascular dementia, major depression, schizophrenia and ‘mental retardation’. 579 Most of the studies collected differing forms of cognitive, biological, physiological, psychosocial and genetic data (e.g. apolipoprotein E genotype), which they correlated to questionnaires, surveys and relevant intersectional data such as age, gender, educational level and physical fitness opportunities in the institutional settings. Such data, however, tended to be presented in a descriptive rather than an analytical or theoretical way. One author presented lists of physiological and other data to illustrate whether or not they were correlated. 582 Sometimes relevant data, for example when an intervention involved mostly white men580 or mostly female participants,576 were mentioned almost as an afterthought.
Most studies focused on a walking intervention but did not seem to question norms of ‘mobility’ or ‘balance’. There were exceptions, such as Stevens et al. ,455 whose study included people in wheelchairs and those with Parkinson’s disease, and Van de Winckel et al. ,581 whose dance therapy intervention was accessible to people in wheelchairs and those with limited physical mobility. Roach et al. 575 focused on familiar functional exercises that did not require recall of new information. Teri et al. 580 gave the care-givers autonomy to help decide what activities could increase physical activity and work in home settings, but did not seem to involve those with dementia except in terms of ensuring consent.
Studies rarely used public health or disability theory to explain their findings. Many studies connected physical activity to an individual bodily ‘problem’ of function. Few studies, however, focused on the importance of creating a more enabling environment. The physical surroundings in terms of built environment and sensory settings alongside care-giving support have been found to be important in improving QoL in people with dementia and encouraging them to take part in physical activity. 586 It was rare, however, for studies to take such an ecological approach.
It is debatable if many of the interventions were inclusive of ‘disability’ rather than of a group of people with functional impairments. Many studies did not use the term ‘disability’ or define it other than in terms of clinical terminology. Accessibility was considered but was rarely connected to dignity, environment or to more macro issues associated with equity. Recent debates exploring the experiences of people with dementia have focused on social inclusion;587 the removal of barriers to health care;588 and rights-based approaches more broadly. 96,523 None of the studies engaged with these discussions.
Conclusion
Public health interventions struggle with mainstreaming. Inclusion has tended to be nominal, and disability theories and models have rarely been considered or used to inform the design or conduct of the studies included in scoping. Studies did privilege certain impairment types and disability groups over others. Severe forms of disabilities, rare forms of disabilities and intellectual disabilities were often excluded. The lack of inclusion of the d/Deaf population and those with visual impairments was especially notable. Disability was generally viewed as something that had to be avoided and prevented. Most research, therefore, tended to view disability in terms of burden or economic cost. Intersectionality was also poorly debated, as was the potential for more participatory and emancipatory forms of research. Similarly, much of the research failed to connect with ideas about how the social, political and economic environment could create disability. Disability tended to be seen as an individual problem. Nonetheless, we did not find any evidence of accommodation, which jeopardised the robustness of research evidence. However, more often than not, disability was tacitly used as a reason to exclude people with disabilities. Their inclusion was seen to overcomplicate the research, although the myriad outcome measures used in many studies suggest that the commitment to simplicity might be partial. The studies focusing on dementia were more likely to engage with accommodation, although inclusive strategies did not always consider dignity.
Our decision aid/checklist, outlined in Chapter 4, while offering the basis for a critique of the current literature, also offers potential solutions to the problems identified in our scoping review. Public health research, as reflected in the reviews of interventions, struggles to adapt a more inclusive approach to disability, which is reflected at different stages of the research process. To this extent, it could help to improve the capacity of public health research to engage with disability. Disabled people, for example, often find themselves excluded from research, and, if they are included, analysis struggles to offer a meaningful interpretation of their experience.
Chapter 6 Findings from the deliberation panels
The scoping of the theories of models of disability in Chapter 3 indicated that human rights are an important cross-cutting issue, which are connected to wider public health concerns. This informed our ethical and empirical decision aid, which was used to assess the extent to which public health research engages with different models of disability. We now debate the use of our decision aid with professionals and politically active disabled people to explore its potential application from the perspectives of different stakeholders. In this chapter we present the deliberations of key stakeholders (public health professionals and socially and politically active disabled people) according to three thematic headings, namely, the meaning of public health, the role of public health interventions and the potential of human rights approaches to develop a more inclusive public health landscape.
Our analysis demonstrated that, although stakeholders identified with human rights-based approaches, they were wary of how they could be used to generate research evidence. This wariness – which took many forms – helped us to refine our thinking. This is discussed in Chapter 7.
The meaning of public health
All stakeholders accepted the importance and potential of public health. A disabled female participant viewed it as being ‘of generic importance to all of us as a society’. Public health was seen to have a broad agenda. Often, participants made links to the prevention of specific conditions such diabetes mellitus or interventions associated with smoking cessation. They also spoke of the success of vaccines in eradicating disabling conditions such as polio. Many, however, saw the success of public health as one of its problems, by citing the example of people living longer, as one disabled participant noted.
It has implications for the type of society that we live in . . . it’s not just a medical problem. It’s a social problem as well.
A holistic understanding of public health was expressed as the ideal, both for disabled participants and professionals, as one professional’s comments demonstrate.
I mean public health, for me, is all encompassing, from prevention to awareness of what helps to keep us well. And promoting good health, through to living with whatever condition you have in a healthy well way; and it takes into account all of the broader things in life that impact on physical wellbeing and mental health wellbeing, from the environment that you live in to your upbringing, to your circumstances, to culture, to disability, all of those bits. That’s what it means for me; and it’s the messaging that goes around that and getting people to access things that enable that to happen.
A male disabled participant remarked on ‘Issues around housing and stuff that are once again becoming a real wider threat to health’.
Disabled participants, however, felt that public health struggled with issues of holism and inclusivity. A female disabled participant remarked that ‘Somehow the systems kind of push the narrow view onto you’. Disabled participants felt that the current climate meant that public health was becoming more medicalised, individualistic and privatised. This was seen as unhelpful. Disabled participants across all panels believed that they had become public health ‘burdens’, viewed mainly in terms of a ‘cost’ to society or as ‘drains on the purse strings’ rather than as individuals with rights. This explains why many disabled people expressed cynicism about public health research and a reluctance to engage with it, including one female disabled participant.
We lost an estimated 25 billion in tax avoidance in major corporations and you never hear about that in the kind of mainstream media discourse; and the vilification of disabled people as scroungers and benefit frauds, although it plays very strongly into being able to dial back the social welfare budget, it is hugely damaging and hugely divisive, and until that changes, until that mainstream noise changes, and I’m not sure it will . . . I don’t foresee things getting very much better.
Holism was usually connected to equity. A female disabled participant said that ‘Public health means, to me, access to services and provision as a member of the public’. Most disabled participants felt that this was not always achieved, as the following quotation illustrates: ‘Public health provision that should be available equally to everyone, is not necessarily that way in practice’. All participants acknowledged that health inequalities continued to be strongly linked to how impairment/s became correlated with age, gender, ethnicity, socioeconomic class and geography. Current policy, however, was seen to be widening inequalities, which undermines the public health agenda. In one panel, for example, disabled people debated how people with learning disabilities had difficulty accessing dental health provision and how this could have broader consequences for their health. For many disabled participants, challenging inequalities politically was a greater priority than defining a public health research agenda.
I was the recipient of the Independent Living Fund and I do believe that one of the reasons I am still here in my grand old age is because I’ve always had a decent support package and that is what kept my health as good as it can be.
Several participants felt that current policy change should be the focus of public health research, rather than specific and refined interventions.
I’d be very interested to see any research done about the impact of all the cuts in services and benefits to people’s health, you know, because obviously there’s a massive change in social care provision and there’s a massive change in benefit provision and what actual impact that will have had, because it obviously will have had an impact on people’s physical health, and also on people’s mental health.
Disabled participants believed that professionals were working with outdated stereotypes of disability and, therefore, had limited understanding of their public health needs. Many, for example, felt that the link between health and disablist practice was poorly understood. They also felt that their impairment was used to frame their needs rather than being seen as a consequence of a particular health-care problem. They, in effect, become their disability. Disabled participants felt that people with cross-cutting, fluctuating, undiagnosed or severe forms of impairments, conditions or mental health needs, or with impairments traditionally associated with disability, were particularly sidelined and ignored. They expressed specific unease about how the diagnosis or identification of an impairment or condition with ‘disability’ became not only bureaucratically important but also increasingly linked to deservingness of treatment, public health access and rights to social welfare. This is why many disabled participants felt that their dignity was not always respected, and this further explained their suspicion of public health interventions and research.
Professionals agreed about the challenges of meeting public health needs within current resources, particularly given that these resources were seen as becoming increasingly scarce. Most professionals cited the important influence of the Marmot Review,20 which, as one participant observed, emphasised: ‘a life-course approach . . . on giving a child the best start, a universal offer but proportional to need. I think they call it proportional universalism’. Professionals identified with such sentiments but agreed that this is difficult to achieve in practice. They specifically mentioned how they struggled with ensuring a universal approach while also reducing health inequalities. Professionals identified the lack of evidence, particularly on how intersectionality mediated health outcomes and acknowledged that this created difficulties in providing appropriate support to people with disabilities. One professional, for example, noted that basic statistics on the mental health prevalence in BME communities were not available.
The role of public health interventions
The impact of austerity on welfare tended to dominate discussions in the deliberation panels with disabled people to such an extent that it was sometimes difficult to encourage them to focus specifically on public health. Many disabled people would argue, however, that understanding this broader context was fundamental to making sense of public health. This offered further evidence for their criticisms of public health interventions. A longstanding issue for many, which was articulated by one male disabled participant, was the perception that public health had ‘an emphasis more on curing us than sort of supporting us’. Several participants made allusions to the growing medicalisation of conditions at the preclusion of more inclusive public health approaches, including a female participant, who said that ‘Doctors don’t like us ’cos we’re expensive’, and a male participant.
You’ve got health authorities going bust, being shut down, and where they are losing money they’re then being fined to having their limited resources cut further. So as disabled people we are a smaller percentage of the population, and although people are acquiring age related impairments, they’ll deal with that as a sort of separate funding issue, but the likes of the rest, of the younger disabled people, they, you know, it’s not cost-effective necessarily for them.
A participant in Panel 4 believed that instead of social provision, the response to disabled people was often ‘Go and get a pill from the doctor’. A young BME woman with depression agreed: ‘I’ve just basically just got shoved in a corner; take them tablets and, you know, just keep on them and you’ll be fine.’
Another female participant in Panel 1 noted the following.
I think people, or social workers, they look at it as ‘go get your drugs and come back home and you can’t have a life, you know, like going to go swimming or an activity going to the cinema and funding keep getting cut off and you don’t get that support, and it’s really sad. It’s not about medication. It’s about having, you know, a better life. And like you spoke about obesity and stuff, it’s not about going to the doctors given a drug to lose that weight, that’s what the doctors are doing at the minute, just pump you drugs to lose weight; they could go swimming, go for walks or do something else, you know.
One male disabled participant said that the role of public health interventions was ‘Fixing people we can fix, and everybody else, sorry, we’ve got no money in the coffers’. The perceived instrumental focus and a concern with ensuring productivity/employment and potential economic gain were seen as especially unhelpful. This explains why some disabled participants identified with a human rights approach as a way of encouraging inclusivity and respect for the experiences of disabled people. A commitment to such an approach could also help to overcome many participants’ concerns about the perceived emphasis on individual responsibility and deservingness in current public health interventions, as a disabled participant discussed.
There is a bit of a growing culture, isn’t there, about, you know, apportioning blame to somebody if they get ill and if you get diabetes it’s because, you’ve not looked after yourself, and there’s the association then is obviously the cost.
A female participant explained that ‘you have a general right to services but no individual right to anything’. Pejorative judgements were seen as becoming more common, as the quotation below from a female disabled participant illustrates.
I think that underpins like health care for disabled people, even to the point of when, if you get weighed, if you get with hoisting and things, and you, you get judgements made about your weight because you’ll get told that you’re too heavy or, or you mustn’t be too heavy to be hoisted, or you mustn’t get too heavy to, you know, walk and, and things like that; and our non-disabled people’s choices are their own and we, they seek to make a lot more commentary on our choices than we do on theirs.
This connected to disabled people’s concerns about a lack of respect and loss of dignity mentioned above (see The meaning of public health), as one participant noted.
The woman who had taken her council to Court because they had removed her overnight care and said she should wear incontinence pads instead, and she was fully continent; and that’s an example of, we are not given choices, our choice involves somebody else.
The lack of respect was also associated with paternalism and a denial of choice for disabled people.
Deliberation panels involving disabled people questioned the use of the word ‘intervention’. One participant, for example, pointed out that interventions focus on disabled people rather than on health-care professionals. Such arguments confirmed suspicions that interventions aimed to fix or cure disabled people. Some disabled participants felt that a more inclusive approach could overcome this. Not everyone agreed, however, and several pointed out the ‘tokenism’ of public and patient involvement, which benefited researchers more than disabled people. This led some participants to suggest that research was reluctant to change its current practices. Participants, for example, considered it important to rethink the ethics of mainstreaming, especially within randomisation in RCTs. They advocated purposeful or quota sampling to ensure diversity. Many also gave examples of how their disability excluded them from research, including a female participant.
I had an unofficial experiment two years back, when I was at [name of university], you get regular e-mails around asking for people to take part in psychological research, ‘cos there’s always psychologists trying to do tests. And I’d always emailed back and say, ‘I have a mental health problem’. And most of the time people would e-mail back and say, ‘Oh no, sorry, you know, we’ll exclude you’.
Many disabled participants noted how the need for evidence was often linked to the use of measures. Most regarded these as insensitive, inappropriate and rarely relevant to the experiences of disability. Disabled participants identified research that could generate more relevant measures as a priority. This would help to overcome their concerns about being seen as a burden (see The meaning of public health), while encouraging researchers to focus on long-term health gains for disabled people. Another important consideration for disabled participants was the need for measures to reflect empowerment and independence.
So, you know, people like the New Economics Foundation with the happiness index, you know; and one of the things that might be useful to look at is the decisions that are made for people and the decisions that are made by people and what the difference is in their health, you know, so actually measuring, trying to, the more people are active in the decisions that they make in their lives, what impact does that have on their health as, as opposed to those who have decisions handed down to them, you know, and kind of what that means for us people, but also the individual cases on a wider case, you know, measuring the social impact of decisions right across society.
The residual impact of the medical model was criticised in many of the panels. Disabled participants voiced particular criticisms of the recovery model in mental health, noting that for many disabled people ‘recovery’ was not possible. Cost-effectiveness measures were similarly criticised for being informed by able-bodied norms, although disabled participants believed that researchers were not aware of this. This further undermined their confidence in public health research.
Many disabled participants stressed the importance of getting the ‘basics right’, that is, including disabled people in the design of the research from the outset to ensure ‘disability’ in design, as discussed by a disabled panel member.
I want, in research, an approach of impairments that says, yeah, you’ve got it, yeah, but this is what we could do as a society to empower and enable you, you know, to live a full life; because if you have a socially and economically active disabled person, however you define that, is volunteering, employment, peer support, whatever, you go from being a negative force to a positive force to be able to contribute, whereas a lot of the health research and interventions and stuff are seen in a negative sense.
Comments by the same participant demonstrate that the coproduction of research was a particularly popular idea.
We’re talking about coproduction . . . means involving disabled people right from the beginning . . . you’d avoid half of these pitfalls and problems if that was actually done, but as usual, it’s usually we’re an afterthought to be honest.
Several participants, however, pointed out that coproduction would need to take account of the diversity. A male participant noted the following.
We’re constantly renewing ourselves, there’s always people that become disabled people who weren’t previously; and it’s a complicated area ’cos it goes into personal transitions theory and things like that, but for a large part, a lot of disabled people don’t start off in a very empowered position.
This is why most participants remained critical of ‘a one size fits all’ approach, with several noting that mainstreaming does not ensure appropriate representation.
For professionals, two priorities emerged when discussing public health interventions. First, they focused on what a lack of representation meant for their evidence base.
I think there is a real mismatch between what, in public health, this evidence works for the general public; it doesn’t work for some sections of the disability. So actually by going on commissioning and evidence-based tools such as obesity elements, and some of the proven techniques there, definitely doesn’t work with people with a learning disability.
Public health professionals also noted that intersectional research was lacking, which again undermined the current evidence base.
I don’t think that we have enough like cross-cutting analysis on how different equalities interact with each other. So, I think we have analysis about disability and we have analysis about, for example, race or faith, but I think it would be more, it would be useful to have a more nuanced approach to understand particularly how the two things interrelate because then I think you probably understand how disadvantaged some communities are.
A human rights approach
As we have seen, disabled participants remained suspicious of current public health research (and interventions). They wanted a stronger commitment to health for all and noted how a focus on and understanding of the wider barriers to health and mental health was important in developing more inclusive practices, as noted by one participant.
If you haven’t got accessible housing or you don’t have the right support, you know, if you don’t have support to deal with mental health issues; that, all of those barriers that are out there are going to massively impact on a disabled person’s health anyway.
Disabled participants made a particularly strong connection between human rights and empowerment and how this connection impacted on ideas of citizenship, social inclusion and a more general understanding of who had ‘rights’ in UK society. In effect, a commitment to human rights was seen as fundamental to all forms of human activity, including public health research. This – as we shall see – contrasted subtly with professionals’ views, which saw human rights as a possible means to an end to improve research evidence.
Disabled participants, however, expressed concerns about how ‘rights’ could be manipulated. This is why they felt that any approach had to be informed by an overarching (theoretical) paradigm, which connected to more critical models of disability. One participant noted that the slogan of the social model was especially relevant (‘rights not charity’), before observing that it was legal ‘rights’ that ‘protected’ disabled people. This explains disabled people’s enthusiasm for the CRPD, which they felt could be the basis of more inclusive research practices.
The CRPD, you know, Declaration of Rights for Persons with Disabilities . . . it uses the social model as a tool. See, the thing about the social model, all it is, is a tool for analysis. It’s a tool for understanding . . . It’s used within the rights model. They’re not mutually exclusive.
Many disabled people felt that the social model paradigm was increasingly important, because it challenged the current cultural climate around disability and, in particular, the idea that disabled people are ‘burdens’. Participants in Panel 4, however, took a more nuanced view, believing a human rights model to offer more opportunities than a social model, as explained by one participant.
I think if we can use a human rights framework to our advantage to say, actually you have to listen to us, you have to consult with us, you have to consider us in the policies, because we are real and we are valid and we have human rights, we are equal humans. In that way I think rights is the strongest current political discourse we have for positive change for all minority groups, not just disabled people; and for that reason I think a rights-based discourse in relation to public health is strong, we just have to bear in mind the caveat that the rights, I suppose, can be misused as well.
For many disabled participants, a particular advantage of a more human rights-based approach was its potential use as a legal tool.
So I’d say, are the services implementing things like dignity inclusion and stuff, and also, and the other problem is when funding gets tight they switch straight back to medical model, and that’s a big problem. They try social model, whatever, in the good times, but as soon as the money, everything, their mind set, their systems, switch straight back to medical model which, for a lot of people with disabilities, does not offer dignity, independence, freedom of choice, it’s just back to you need to be looked after.
Despite this, many disabled people were not convinced that their rights would be respected or enforced, as one participant explained.
I know I’ve got human rights on paper, right [other members of the panel laugh] but it’s very difficult to actualise those rights, if that makes any sense? You know, under the Human, the UN Convention, I’ve got the rights to live independently; well the government’s just closed the ILF fund, so, you know; it’s about accountability as well, you know.
A participant in the same group then noted how one of the strengths of the Equality Duty [as outlined in the Equality Act (2010)28] was that responsibility lay with public bodies or society and not with the individual. Others agreed, but expressed concern that human rights did not have this same reach in the UK. Although participants were broadly supportive of a human rights model, they expressed concerns about how seriously it would be taken by researchers and policymakers. Many felt that it would become another ‘tick box’ with no redress if it was not followed. Nonetheless, most disabled participants, however, did find the decision aid attractive.
Professionals noted that, to work, any human rights decision aid would have to be championed at the highest national levels. Professionals questioned the usefulness of the decision aid and wondered whether it would become ‘just another evaluation tool’, which no one took seriously. They did not understand how a decision aid could link to SDHs or other indicators. Some professionals noted that they were already providing public health interventions to disabled people and that they consulted the evidence base provided by the Public Health Observatories. Professionals also questioned if using a human rights framework would necessarily lead to better evidence in RCTs. To this extent, professionals’ commitment to a more human rights approach could be seen as instrumental. There was little discussion among professionals about the more critical models of disability and their relevance to research. One professional saw them as a possible distraction. It was also rare for professionals to see research as a form of empowerment or as the basis for emancipatory activity.
Dignity
Disabled participants, as we have seen, felt that their dignity was often compromised when they become involved in public health RCTs and research. Most believed that rights were their strongest defence against loss of dignity. One panel member said that ‘rights are the strongest argument we have to treat everybody with dignity, to treat everybody as an equal’. Dignity was also associated with returning control to disabled people. Panel 3 specifically noted how sensitivity towards disability culture had to be understood to ensure dignity. Several participants linked definitions of dignity to autonomy and commented that disabled people should have autonomy over their bodies. Others discussed dignity within the context of choice and independence and, more generally, QoL. Overall, participants stated that dignity often encompassed more than simply ‘ethical consent’ and had to be considered at all stages of the research process, which included considering the possibilities raised by coproduction. The professional panel had less to say about dignity, but did see it as a general good.
Inclusion
Most disabled participants currently associated inclusion [including patient and public involvement (PPI)] with tokenism. One participant summarised the views of many.
Inclusion and participation are good buzz words for research and maybe it might be good to have meaningfully included, how are people meaningfully included, rather than just included, because you’re then asking them to go that step further and show how that, that involvement contributed to research findings, how it was used, why it was used, were they included?
Professional participants agreed and argued that inclusion and mainstreaming did not always work for disabled people.
I think also like have an opportunity for disabled people to help shape some of those messaging, and to help shape some of the way the services are being provided; because often there’s like a disjunct between what public health professionals might think is required and what they might think is accessible, but they still might not meet the needs of disabled people so those barriers remain.
This is why several professionals advocated the use of champions.
So we had smoking cessation, we had weight management, we had sexual health, drugs; all of the, the kind of services out there; and they attended; we had the community learning disability team that led on the training and they’re developing action plans now which include sections that are twice the length than they would usually be; that carers are actively welcomed to come along to the events; easy read format. So there are a number of things we are doing; but I would absolutely say without that lead, without that person, that champion, they, the groups are marginalised and overlooked.
Disabled participants were less convinced about champions, questioning how representative they were. All panels mentioned how the individual presence of one disabled, female or BME person, especially as a champion, was not inclusive, democratic or representative of a heterogeneous disability community. Disabled participants were especially concerned that inclusion was imposed rather than discussed. Disabled participants also felt that vulnerability was not appropriately discussed when researchers considered inclusion, although participants were also aware that capacity was used to justify exclusion of disabled people, as one panel member explained.
Well I mean there [are] safeguards within the legislation around the empowerment . . . but I think in terms of mental health and mental capacity that’s another issue. To say it’s perception is that people with mental health, impairments or disabilities lack capacity; or is it that society’s constructed in such a way to exclude those with mental health impairments and learning disabilities?
Other disabled participants expressed concerns about gatekeeping, which they believed further hindered inclusion.
I think the idea of gatekeeping’s quite interesting ’cos I think it works the other way round as well; so, for instance, where people are carrying out research they may not approach disabled people, they may approach their carers, professionals, workers, family members and therefore the research, the information the researchers are getting back has also been edited [laugh from other members in the panel] if that makes sense, because they’re not actually getting the views of disabled people directly, they’re getting them through somebody else.
Disabled participants associated inclusion with political citizenship and active choice rather than with researchers choosing the method of inclusion and the topics under discussion. Some disabled people felt that more should be done to increase the capacity of disabled organisations to engage with research. This, many argued, would help to facilitate a more meaningful inclusion.
I think there’s also the sort of a danger that, you know, research that is expert or professional led and excludes disabled people and then disabled people are almost just the subject
Examples of good practice, however, did emerge. Some participants gave examples of their expertise having been recognised and of feeling that they were making a difference in the design of inclusive spaces, better technology or policy recommendations. This was usually the case in research that used methods of coproduction and included disabled people as partners.
Intersectionality
Both disabled and professional participants emphasised the importance of understanding intersectionality, but felt that this was not reflected in current public health research, which, despite paying lip-service to its value, often did not have anything meaningful to say about it. This was often attributed to the need for public health to offer quick and simple solutions to what are complex issues. The inability of public health research to engage with the complexity of disabling experiences was identified as a particular problem by disabled participants.
I think that lack of awareness of other types of disability, other types of physical disability, other types of sensory or cognitive impairment are really not tackled in public health discourse very much. I think it’s all people stood round smiling from different ethnic minority groups and a person in a wheelchair.
Ethnic minority disabled participants felt especially disadvantaged and believed that research struggled to recognise their ethnic identity alongside their disabled identity.
Because I don’t want to be told by a non-person of colour that the service provision is adequate for me; even though the death toll is rising, the actual service provision is adequate. I don’t want to be told that any more, that’s long gone. We need to get rid of the frontline racist service provision that we have. Racism always comes in a recession, and if you are a person that’s protecting your own purse strings so you have a job, you’re going to be racist too. So, we need to have a fair access, and if they’re not going to give us the positions, because it can’t just be one colour face at that level, there, the services need to be adequately monitored, evaluated and heads must roll. By then, maybe we’ll get a fair access to service provision.
Accessibility
All disabled participants agreed that in order to be empirically robust, interventions, and the research that evaluates them, has to become more socially and politically accessible, as described by one participant.
The way that research ethics committees work is that genuinely if you have any kind of mental health issue or cognitive impairment or psychosocial disability you can’t be involved unless you’re going to jump through a thousand hoops to make sure . . .. The entire structure of how research is conducted excludes disabled people from participation in it and I think there is a fundamental shift that needs to, okay, in universities, at the national research ethics committee levels, to recognise disabled people as being completely able, a lot of the time, much more than the current system gives them credit for, to be involved in research . . . whether they’ve actually been achieved and where the gaps are, and have a reflective process from researchers, and that they have to take into account people’s responses, in where . . . five targets have been met in the research process.
Disabled participants observed that supported decision-making and advocacy were rarely considered by researchers. This frustrated many participants, who pointed out how researchers seemed happier to elicit proxy responses from family carers and health-care professionals than to engage with disabled people. This was seen as a particular problem for those with learning disabilities. Disabled participants also felt that accessibility has become defined in extremely narrow terms, often relying on stereotypical responses rather the experiences of disabled people.
Do they think, is it in large print? Is it easy read? Are there pictorials? Is it audio available? Is it video available? . . . All of that is accessibility. And I don’t think, maybe you need almost like just an example list of things for people to check off, because I think, I think you’re aware of the; I think, I completely see the benefits of simplifying it, I get it, but I think there’s a risk with allowing people to tick yes, we installed a wheelchair ramp, as a blanket for yes, we conducted accessible research.
Disabled participants believed that designing an intervention without having thought about accessibility was unethical. For many, accessibility and assurances of accommodation had a strong connection to equity. Professionals agreed about the importance of accessibility but tended to focus on practical issues such as language or viewed accessibility as an additional cost. There was, however, little debate about how to offer a meaningful analysis if disabled people are included. There was also little connection to equity or human rights.
Equity
Many disabled participants pointed to the need for short- and long-term equity in public health research. They also noted that public bodies had an equality duty but that this did not always inform the commissioning or conduct of research. Professionals tended to associate equity with disadvantage. Disabled participants, however, emphasised discrimination and the need to address human rights issues.
Both professionals and disabled participants debated the current prioritising of certain disabled groups, such as people with dementia or people with learning disabilities. Professionals saw this as valuable as long as it was not at the expense of other disabled groups. Disabled participants took a different view, believing it to be attributable to the fact that people with dementia and learning disabilities are not as politically or socially independent as other disability groups in society and/or may not share the identity of ‘disability’. As such, their inclusion in public health or advocacy may not challenge public health or express criticisms of the way in which public health research is currently being conducted.
Professionals felt that the proposed decision aid was too idealistic and did not understand its legal or human health basis. They were also concerned about the costs of inclusion.
I’m sure many times, because it, I think there might be an issue about equitable access to resources; and adjustments, reasonable adjustments, do cost money; and it’s about having the resourcing, and if you’re having resources focused on that, resources being taken away from other groups and other needs and so I think you would be, so you’d have to have a very clear business case as to why the adjustment or why the change was reasonable, and why this was seen as a free allocation of resources. But I imagine that would be one aspect that might come up.
Many disabled participants questioned the commitment of public health to tackling health inequalities. Several disabled participants also pointed out that even when researchers were inclusive and doing research relevant to the needs of disabled people, the next steps in terms of translating research into practice was not achieved. To this extent, disabled participants were sensitive to the relevance of inclusion and its relationship to equity, at all stages of the research process and not simply at key points, which are usually decided by the researchers. This is why many disabled participants made a strong association between equity and political will to question and change the status quo, as noted by one disabled participant.
It’s called lip service. So, they can do all the research and everything, and you can get your findings, but at the end of the day, if nobody does nothing with that then, you know, it just looks as though things have been put in place when they really haven’t.
Another disabled participant made a similar remark.
There’s entrenched values and principles and there’s a lot of money attached to the way things are, as they are at the minute, so for us to come along and go, you know, to disrupt that, there’s going to be resistance to that, isn’t there, because there’s been hundreds and hundreds of years of this public health professional thing been built up on seeing disabled people as a burden or who need to be cured.
Consequently, for disabled participants any decision aid would need a strong connection to ensuring basic and fundamental rights.
So I would like in a few years that we recharge this decision aid because we can, and we could make it much [laugher from other members of the panel] more, not just about your right but actually your quality of everything, you know? Not just your basic rights.
The value of a human rights checklist
Using the CRPD innovatively and connecting it to RE-AIM (see Chapter 3) as a decision aid/checklist illustrates how models and theories of disability can inform research about the effectiveness of public health interventions. Each of the five deliberation panels gave examples of how intervention research can be sensitised to accommodate different configurations of diversity within disability. They also gave examples of how terminology and measures needed to change, alongside the conduct of research, to ensure that the complexity and diversity of the disabling experience was captured. In many ways, the deliberation panels were reiterating many of the findings of this review and, in particular, the need for better research evidence. However, politically and socially active disabled people argued that this was not an immediate priority for them, as basic access to health care and public health had to be ensured first. They also expressed a suspicion of public health research, which was seen as aligned to a more medical model of disability and, in particular, the idea of rehabilitation. Most of their deliberation was subsumed into theoretical and political debates about tensions between equity and distribution of resources.
Nonetheless, both professionals and participants espoused a holistic vision of public health,589 but neither group felt that this was being adhered to in policy or practice. Professionals, for example, noted tensions between ensuring public health prevention and promotion and taking a life-course approach. Participants in particular felt that there has been a ‘narrowing’ of the meaning of public health and that this has had consequences for how equity and social justice are understood. Furthermore, disabled participants felt that those responsible for public health research may not (yet) have the capabilities or resources to translate social involvement into the necessary political changes (see Beckfield et al. 590) and expressed concerns about how disablism and racism may thwart these efforts. Disabled participants, when speaking about public health research, examined the more general distribution of resources and made implicit links to a second-class citizenship, noting not only the complex relation between deprivation, discrimination and disability but also that any enabling discourses, practices and even research evidence become marginalised by the status quo. They were especially critical of commissioning and of the ability to translate research evidence into policy and practice. Concerns were also expressed about inclusion, which was often seen as instrumental, predetermined by the researchers and tokenistic. Disabled participants would have preferred to see a more political engagement and one that was evident throughout the entire research process.
Professionals struggled to connect the more theoretical debates about disability with the process of doing research, which was largely seen as a technical exercise. This was probably reflected in their concerns about the cost of inclusion rather than its political desirability. Professionals also struggled with issues of intersectionality when discussing disability, which contrasted with how they viewed ethnicity and gender (see Kapilashrami et al. 591). In this respect, professionals did not always see the links between theoretical and empirical innovation and the potential importance of opening up public health research to more critical insights that reflect disabled people’s experiences. Professionals tended to describe a top-down bureaucratic approach to inclusion, often following national leads or prioritising the appointment of designated champions. Professionals did not show a great deal of familiarity about the social and political meaning of disability. Both professionals and disabled participants indicated a sense of powerlessness in changing current public health priorities, which they felt had become defined by economic cost instead of long-term investments in health. For this reason, they questioned the value of the decision aid, although disabled participants expressed some degree of attachment to it and could see its potential value. Professionals expressed particular concerns that it would become another evaluative exercise, to which no one would pay attention.
Conclusion
Our deliberation panels suggested that the use of any decision aid needs to be linked to a human rights-based approach. In this way, the decision aid will be inclusive. Discussions also suggested that the decision aid could be used to build capacity by ensuring greater participation. Disabled participants were especially keen to become coproducers rather than to engage with tokenistic consultation, disconnected from the political and social experiences of disability. Professionals, however, might take more convincing.
Chapter 7 Discussion
This was an ambitious project, that combined theoretical reflection with empirical engagement and evaluated current practice while looking towards the future. We were aware of the considerable ground that it covered and, in particular, the difficulties in reconciling different ways of thinking about disability and public health research. This was not only challenging for us but also perhaps signifies the problems that public health researchers face when engaging with disability. This chapter outlines how we met the aims of the commissioning brief by discussing how we connected the theories and models of disability with the (present and future) conduct of public health research. Our account offers a framework with which to critically evaluate current research practices and evidence bases, and also offers ways in which to enable public health research to engage with the diverse experiences associated with disability. We offer a potential decision aid/checklist to enable commissioners and researchers to assess the likelihood that a research project will produce evidence relevant to the experiences of those with disabilities. The aim is to facilitate informed decision-making while creating the potential to generate a debate among those involved in public health research to question their current and future practices. We structure our discussion around the overall aims of the study (and commissioning brief).
How can different models and theories of disability appropriately inform research on the effectiveness of public health interventions, and to what extent can intervention research be sensitised to accommodate different configurations of diversity within and among general and disabled populations?
The scoping of the various models and theories of disability pointed to a rich, but largely untapped, resource for public health research. We singled out four key contributions that this literature could make to facilitating more inclusive research practices:
-
ensuring that models and theories in public health are informed by a constructive dialogue with the political and social expectations of disabled people
-
enabling the identification of locations at which theories and models of disability intersect with those of public health
-
introducing the potential of a human rights model to strengthen the capacity of public health research to generate robust evidence relevant to the experiences of those with disabilities
-
the creation of disability-sensitive decision aids to aid inclusion in public health interventions.
Our first scoping review identified a range of critical models and theories, in line with the social and political expectations of disabled people. These were developed largely in opposition to a medical model of disability and its view that impairment was a problem located in the individual, which rehabilitation could ‘fix’. Although medicine and rehabilitation are important, these theories and models of disability are committed to generating a more holistic understanding that advocates inclusive practices aimed at tackling discrimination and disadvantage. This led us to explore the potential of more human rights-based approaches, which are concerned with highlighting social exclusion and dismantling barriers to ensure access for disabled people to all aspects of social life.
Human rights-based approaches, along with the more social and critical accounts of disability, align with ecological models of public health, the most widely known of which is Dahlgren and Whitehead’s126 SDH framework. This provides a possible connection between theories of disability and public health paradigms, which we explored through the use of visual representations in Chapter 4. Commonalities include conceptualising the determinants of health as operating on individual, relational, social and structural levels, and a commitment to addressing social and health inequalities.
The use of the CRPD22 can deliver a capacity-building tool by functioning as a link between public health and socially informed understandings of disability. In particular, it provides a framework for dealing with the complex ethical and empirical issues that arise when evaluating public health interventions. The CRPD establishes the importance of inclusion, in addition to the importance of respecting dignity, when engaging with disabled people. There are, for example, important legal considerations which should not be overlooked in study designs, such as the role of the Mental Capacity Act (2005)30 in gaining consent and the importance of supported decision-making in accommodating people with intellectual disabilities. Our review, however, suggests that there has been little debate in public health about what ethical inclusion in research looks like or how it should be respectful of dignity.
Building on these insights, we illustrated one way in which human rights-based models could inform a decision aid that could be used to critically engage with current research evidence, while also supporting public health research to adapt more inclusive practices that are sensitive to the experiences of disability. Our deliberation panels further refined the decision aid by pointing out several tensions, including the risk of it become another tokenistic evaluation tool, which no one takes seriously. They did agree, however, that such an approach had potential, particularly in its commitment to social inclusion.
In presenting our decision aid (summarised in Figure 9), we emphasise that it should be regarded as ‘work in progress’, but it is nonetheless helpful in stimulating debate among commissioners and researchers. The decision aid, for example, could provide a resource, encouraging researchers to think about ways of respecting choice and ensuring the dignity of participants with impairments. It can also be used to evaluate current research evidence. Our review, however, indicated the danger of using rights-based approaches without thinking about how they link to empirical robustness and the needs of research. 588,592,593 This is why we connected our decision aid to the use of RE-AIM (see Developing practical guidance for inclusive research practices). A member of our steering committee, Professor Simon Dyson, suggested that we call it the Inclusion, Dignity, Equality, Accessibility and Intersectionality (IDEAS) decision aid.
FIGURE 9.
The IDEAS decision aid.

How do different models of disability map on to current research on public health interventions?
Our scoping review of public health interventions indicated that theories and models of disability rarely informed evaluative intervention designs, although it could be said such designs were also not particularly sensitive to ecological models of public health. The scoping of interventions in Chapter 5 illustrated that, although the internal validity of research design was frequently mentioned in systematic reviews, theoretical external validity was often ignored. We could not identify a great detail of discussion about inequalities or future public health priorities, such as childhood disability,287,594 ageing10 or multiple impairments and comorbidity. 583
The focus on internal validity, such as in ensuring control groups, randomisation, checking bias and the description of effects of interventions, seemed to encourage methodological disconnects about diagnosis definitions and outcome measures, in addition to dignity and equity. For example, the Cochrane Collaboration Risk of Bias Tool and the EPHPP quality assessment tool examine psychometric properties of outcome measures, and the EPHPP also offers an evaluation of ‘validity’ and ‘reliability’. 595 Neither tool, however, explains or justifies its relevance to the diverse range of disabling experiences or the extent to which it might reflect able-bodied norms. 595 Consequently, the validity of measures is not questioned and is taken for granted, despite more critical theories of disability questioning the sociocultural assumptions implicit in many measures. 596 Ironically, where disability was recognised, it was often used as a criterion of exclusion on the basis that it might undermine the validity of the study.
The theoretical disconnects that we identified between public health paradigms espoused in research and the actual research undertaken requires more critical discussion. 597 This is perhaps why our scoping of public health research suggests that the empirical design of interventions did not always match up with the long-term creation of equity and, in particular, the contribution that public health research makes to policies that contribute to reducing social inequalities. This is despite research indicating that for interventions to support ‘self-efficacy’, they need to be designed in a way that is supportive of an ‘ongoing’ and ‘interactive, multilevel process of mutual inquiry’, sensitive to individual, relational, social and structural levels. 87 Such an approach is in keeping with models and theories of disability as well as with public health models as revealed by our visual mapping. It also links to future directions of public health research. 598
To facilitate this, interventions, and the research that evaluates them, might need to reflect a greater diversity of approaches. Most of the studies that we accessed in the 30 generic and 30 specific public health interventions used behavioural change models that implicitly place the onus of responsibility for change on the individual, rather than on how context and environment may constrain opportunities and outcome. This creates potential tensions with more inclusive, rights-based approaches that may view the onus for change to lie with changing policy or societal norms to ensure that they become more accommodating of disability. 132,599 More critical disability paradigms destabilise the norms of rational choice theory and emphasise the social causes of health inequalities rather than ‘checking’ the health effects of interventions. 597 This is consistent with public health paradigms that advocate complexity and innovation. However, our review suggests that public health research (and the interventions being evaluated) does not always focus on comorbidities or ‘multi-level, multiply determined, complex and interacting’ factors that could affect the outcomes of the interventions. 435 Furthermore, discussions about whether or not the interventions were explanatory or pragmatic in nature were rare. 436 To overcome these problems, some authors advocate using realist approaches when evaluating public health interventions. 600,601 This would connect well with the theoretical and methodological basis of disability models and with holistic and ecological understandings of public health. 602
What are the implications for commissioning research into public health interventions inclusive of or for disabled people in a way that accommodates appropriate terminology and measurement and that takes account of different causes and types of impairment, while being sensitive to the experiences and needs of different demographic groups associated with gender, socioeconomic position, ethnicity, sexuality and age?
Our proposed decision aid enables commissioners to assess the potential of research to reflect the diverse range of disabling experiences, including the role of intersectionality. Commissioners also need to ensure that research is methodologically robust and able to produce findings that can contribute to the existing evidence base. More inclusive research could address these concerns, particularly given that the current evidence base has little to say about the experiences of disabled people. Furthermore, our decision aid could help commissioners to negotiate the political nature of research and to address the concerns of those who advocate a human rights-based approach, which moves beyond the ‘politics of recognition’, where ‘focusing’ on need can be confused with ‘responding’ to need, to establishing a ‘politics of difference’, where acceptance of difference is reconciled with an intent to ensure that such difference does not become a basis for inequalities. 603,604 Our deliberation panels suggest that health-care professionals are well aware of the difficulties that research has in establishing equity, although more politically active disabled people identified the value of using a decision aid to educate and empower disabled people. Locating ethical choice within rights-based structures allows – at least theoretically – participants more control, while ensuring that their legal rights and entitlements are respected. These, however, remain contested debates, which need to be negotiated when undertaking research.
Most of the public health interventions reviewed, even those inclusive of disability, theorised disability in terms of cost to the general public and conceptualised it, albeit subtly, in terms of individual dependency and deservingness. Consequently, interventions were found to be occurring downstream or retrospectively after a health inequality and cost had already been identified (e.g. obesity or dementia) rather than to be concerned with preventing the inequality occurring in the first place (Figure 10).
FIGURE 10.
Retrospective prevention.

This might be appropriate, but we raise it to be mindful of the importance of understanding the norms and values implicit in various paradigms and models, along with the importance of considering the influence of the socioeconomic and political context in which interventions are developed. As we have noted, critical models of disability dispute the emphasis on individual choice and behavioural change. In these models, political, social and economic contexts create disability. Cognitive behavioural therapy, for example, while enabling the individual to cope better with their conditions, can simultaneously encourage them to cope with and adapt to what could be perceived as a repressive social environment. 17 This further justifies a more inclusive rights-based approach, in which the social construction of disability is acknowledged. Critics, therefore, argue for a shift in focus by pointing out how individuals, especially if they are living in poverty, cannot change the disabling environments that cause health inequalities. 178,605 This has led to calls for more prospective interventions, as detailed in Figure 11. 433,602
FIGURE 11.
Prospective promotion.

How should participants, the public and stakeholders be involved in research and what does inclusive research practice look like?
Our decision aid offers various strategies on which more inclusive research practice could be based (although this would also need to connect to more inclusive interventions). If the design of an intervention excludes disabled people, any research evaluating that intervention will replicate this exclusion. Our review discussed how more inclusive practices could be enacted at any stage of the research process, including establishing the types of research questions relevant to the experiences of disabled people; having designs that are inclusive and accessible, able to capture diversity and intersectionality, including the use of sensitive and appropriate measures; and encouraging participatory dissemination and implementation of research findings. We noted, however, the different interests of stakeholders. Our deliberation panels of disabled participants, for example, expressed particular enthusiasm for coproduction. Researchers, however, seem more concerned with using inclusive research to establish methodological robustness, perhaps creating new forms of measurement that capture the experiences of disability or at least ensure that the use of measures does not provide a basis for excluding particular groups of disabled people. This, however, does enable ethical involvement to connect to empirical robustness. Linking our decision aid/checklist to RE-AIM, for example, could help to facilitate this by linking theories of disability to the implementation and outcome of methodologically robust public health research. The links between the human rights-based approaches and robustness of research evidence are especially important, and more inclusive practices need to reconcile their mutual interdependence.
Our scoping review suggests that the inclusion of ‘disabilities’ in public health often follows a top-down approach, with limited or tokenistic public involvement. We also note the particular difficulties faced by public health research in engaging with people with perceived communication difficulties or cognitive problems. Campaigns focused on ensuring involvement in trials (such as It’s Okay to Ask592,606) and the use of disability champions, including partnerships between government and third-sector partners, offer potential solutions to these problems, as do discussions about establishing an ethical framework and available cohort for recruiting people with dementia to trials involving older people. 607 These initiatives, however, are not without their critics, as discussions in our deliberation panels demonstrated. More critical approaches to disability advocate a more bottom-up approach. Involving people, especially if they have typically been under-represented in research, can have a powerful effect on the people themselves, while generating a more inclusive research process. 103
Stakeholder involvement and empowerment are perhaps poorly reflected in intervention studies of effectiveness in public health research, as inclusion is viewed as secondary to the aims of the research. 608 This is perhaps why the role of PPI generated so much discussion in our deliberation panels. Furthermore, we found that interventions were rarely informed by empirical insights generated from the lived experiences of disability. 103 The emancipatory potential of research design was also rarely realised in public health research. Moreover, we did not find evidence of a commitment to accountability among intervention studies. The setting of interventions might exacerbate the problem. Schools or workplace environments may not be typical places in which to find people who experience social isolation, thereby undermining a fundamental aspect of inclusion. For example, people with long-term mental health issues and learning difficulties are particularly at risk of social isolation, as are those in marginalised groups who also have disabilities such as BME women, migrants and family carers. 13,609 These groups might not be particularly visible in the settings from which many samples are drawn.
One possible way of ensuring equity and inclusion is through using the principles of universal design. 610 This involves more than just mainstreaming disability or ensuring nominal compliance with equity (although these issues are undeniably important) but requires careful thought about inclusion and its consequences for research practices. To this extent, universal design is about enabling a sustainable commitment to equity,611 in terms of either facilitating greater inclusivity or reducing inequalities. This might prove difficult, at least in the first instance, as our scoping of public health reviews indicates how empirical practices are not always linked to theory. This creates difficulties when offering meaningful explanations about the implications of disabling experiences for public health’s evidence base. It also creates difficulties when engaging with the implications of inequalities and disadvantage.
The scoping review suggested tensions between improving the general health of a population (universal/utilitarian) and a more focused approach that examines particular inequalities or issues such as dementia which affect a particular subgroup within the general population (targeted/distributional). More universal approaches rarely mainstream disability or connect disability to its more social and political consequences, including the potential for more emancipatory, inclusive practices. This demonstrates how debates about equity and inequality can become sidelined.
If research is to have an impact on a general population, disability needs to be mainstreamed into public health interventions. There is also a need for research that focuses on disability, in addition to research that targets specific inequalities affecting disabled people. Some authors have suggested that a mainstreaming approach to disability should be seen as a category of intersectionality, in that disability would feature alongside age or gender, for example. 487 This is how interventions can be both universal and distributional in nature. For example, an intervention on urban renewal ensuring accessibility for older and disabled people by installing outdoor elevators and escalators also increased walkability, social interactions, safety and socioeconomic regeneration. 608 Such interventions are multilayered and comprehensive in the ways in which they tackle health inequalities. Furthermore, the addition of an observational qualitative arm or process evaluation can help to evaluate the success or failure of an intervention in a way that reflects the complexity and diversity of the disabling experience, as well as provide an insight into participatory approaches.
What study designs and relevant outcomes best capture experiences of impairment and disability in a way that maximises health benefits and ensures that mainstream research reflects the experiences of people with disabilities?
Overcoming the short-term initial difficulties of inclusion by excluding disabled people can have consequences for achieving long-term public health benefits. Our review noted the lack of ‘methodological congruence’ between the theoretical paradigms used and public health research. 612 Quality assessments of systematic reviews, for example, largely concentrate on methodological checks, including discussions of inclusion or exclusion criteria, bias or confounding, rather than on theoretical assessments of the paradigms, definitions or measures being used and how these might relate to the strengths and relevance of the methodological design. 613,614 As we have mentioned, functioning and well-being are often conflated, as is QoL and HRQoL, and the relationship between well-being and health utility is poorly articulated.
This is where more critical models of disability could be useful, along with the use of our proposed decision aid. We have already noted how different models and theories of disability raise questions about the extent to which different measures can capture the different disabling experiences and the implications of this for the validity and reliability of the evidence presented. 172,439 Our scoping review indicates how measures often represent disability, although sometimes subtly, in a negative way, associating it with cost and burden or predicating it on the grounds of able-bodied norms. To this extent, they appeared aligned to professional dominance and paternalism, viewed people as their impairments and relied on a terminology which could be regarded as pejorative. However, an interest in ‘capability’ measures and indicators has begun to challenge such thinking79,155,615 or take it in new directions. 413,566
Public health interventions are increasingly moving into welfare, vulnerability and risk. 616 This is also part of the more holistic approach to public health and the commitment to inequalities, as we have previously noted. In this way discourses on risk and resilience to risks (global and individual) become interlinked. However, measures commonly used in public health research are little informed by these debates. Furthermore, our scoping review noted a difference in some studies on health promotion between a (bio)medical model understanding of the intersections between health and disability and a person’s perceived health and QoL. 64,617 This is known as the ‘disability paradox’ and raises important questions for public health research. 618 Interventions that rely on medical models may not reflect the extent to which those with impairments can continue to have a positive QoL. A disability, for example, might have several secondary causes that can cause pain or mental distress. Nonetheless, an individual might still feel that they have a good QoL because of the social resources available to them. 619
Although ageing is a normal part of the life-course, it has to be distinguished from secondary conditions, such as mental health issues or impairment(s), that have a negative effect on health. Similarly, a person can be born with a congenital disability but can also have serious health and mental health needs which may or may not have a link to impairment. The use of outcome measures can seem disjointed, especially when disability is viewed as a speciality rather than a mainstream issue. If disability is something that potentially affects everyone across the life-course, then outcome measures will have to change to take this into account.
Recognising the broader determinants (social, political and economic) of health would also facilitate a more inclusive research practice, able to locate an individual’s experience within his or her social environment. This is a timely reminder that public health might need to create more enabling measures that can capture the diversity of the disabling experience and are sensitive to individual circumstances, the effects of the life-course and the impact of intersectionality. This could also assume political relevance by empowering people to live well, thrive or ‘flourish’ with impairment(s). 152,153,620,621 The idea of ‘flourishing’ seemed to connect especially well with more affirmative and holistic models of disability. Within this context, to flourish means to thrive. It encompasses ideas of health and well-being that are inclusive of disability. The word flourish also takes a broader and perhaps different ontological and epistemological approach to public health, in which the starting point would be interventions to ensure that people are aided to live well with disability and impairment across the life-course. The understanding of ‘flourish’ also encompasses elements of distinction, which are connected to social and political empowerment. Empirically, this could be translated into measures of societal status/standing, societal accessibility/inclusion or social enablement/emancipation. 622,623 Social sustainability measures indicators are available to facilitate this, but currently they have no connection to disability.
Conclusion
Our proposed decision aid, IDEAS, offers a capacity-building and evaluative aid that can both educate and provide an indicator of equity when analysing reviews. In proposing it, we are nonetheless aware of the importance of combining more inclusive research practices with methodologically robust research design. We are equally aware of the value and importance of practical application and we explore this more in Chapter 8, which also offers a more general overview of our research.
Chapter 8 Conclusion
Our project aimed to draw out the implications of different models and theories of disability for researching the effectiveness of public health interventions. To address this, we undertook a two-part scoping study as well as consultations with public health professionals and socially and politically active disabled people. This provided an overview of current theoretical and empirical debates, including examples of best practice, to help inform a more inclusive evaluative research design in public health research.
Chapter 1 introduced the project and justified its focus. Chapter 2 provided methodological detail by discussing how we conducted the two scoping studies and outlining our approach to analysis and synthesis. Chapter 3 provided an overview of the most common theories and models of disability found in the literature, namely, the medical, rights-based, social and critical disability models. We examined the strengths and weaknesses of each model in terms of their implications for evaluating public health interventions. To help support more inclusive designs, Chapter 4 explored conceptual commonalities (and gaps) among public health and disability models. Although a shared commitment to addressing social inequalities was evident in both public health and disability models, we found that the interest in definitions and measurements of disability employed within public health research would be regarded as problematic from the perspective of most disability models. However, the scoping of disability models indicated that the application of a human rights-based model has the potential to provide a link between disability and public health research approaches. This informed the development of our decision aid, which may be used as the basis of (present) critique and (future) capacity building.
We tested this decision aid in the second part of our scoping study (see Chapter 5), which offered a critical evaluation of the public health literature on interventions. This review indicated that disability mainstreaming was not a part of generic evaluations and that many of the specific evaluations focusing on disability were not disability sensitive. We pointed to a range of ethical and empirical gaps within the evaluation of both generic and specific interventions, including what appeared to be an absence of appropriate outcome measures. Our proposed decision aid also illustrated how different models of disability could inform positively the development and evaluation of public health interventions. Furthermore, our decision aid may help to connect evidence-based practice to the diverse needs of those with disabilities, while also being ethically sensitive to broader concerns about social disadvantage, accessibility and inclusion. In doing so, it can connect the need for methodologically robust research with more inclusive social practices. Chapter 6 described the deliberative consultation with professionals and politically and socially active disabled people and reaffirmed that human rights approaches are considered helpful but that caveats about how the aid would be used exist. Chapter 7 summarised how we met the aims of the research, and the present chapter explores the practical relevance of our work, offers reflections on the research process and makes suggestions for future research.
Reflections on the research
This was a challenging and ambitious review, which attempted to synthesise complex, and at times seemingly incompatible, debates within the defined time frame of an 18-month project. This involved making a range of pragmatic and theoretical decisions, which are outlined in Chapter 2. There are, however, more general considerations that should be taken into account when interpreting our findings.
The research was conducted in response to a commissioned call by the NIHR PHR programme, ‘What are the implications of different models and theories of disability for researching the effectiveness of public health interventions and what factors should be considered for research studies?’. The commissioned brief was broad in scope and required a synthesis of the literature on models of disability as well as advice on terminology, inclusive research practices and the use of appropriate study designs. The brief was particularly interested in life-course approaches and the impact of a broad range of disabilities.
The volume of literature on models of disability was vast and disparate, reflecting a diverse range of priorities, paradigms and languages, and combining specialised methodological and empirical concerns with more nuanced and wide-ranging theoretical debates (see Chapter 3). We had to juxtapose carefully the need for specific detail and recourse to specialist terms and debates with the ability to offer a generic and accessible account of interest to public health research and commissioners. We are aware that commissioners may well have little previous knowledge of the debates associated with different theories and models of disability.
Our review struggled with a general lack of evidence on what a public health of disability should look like. Our analysis, therefore, highlighted the importance of generating a debate among those commissioning and doing public health to question their current and future practices. Our IDEAS decision aid, along with the guidelines, have been produced in response to this challenge and are designed to generate informed decision-making among stakeholders. Without such a starting point, any debate about research design (including outcome measures) that is disconnected from experiences of disability would have been likely to reproduce current difficulties rather than to transcend them. This, for example, explains our emphasis on the importance of understanding the ways in which theories of disability have – and could be – used to make public health interventions (and established research designs) more inclusive and responsive to the needs of disabled people. The failure of public health research to engage with a range of disabling experiences has reinforced this in other ways too (see Chapters 4 and 5). We had, for example, little evidence on which to offer advice for assessing effectiveness and developing appropriate outcome measures for disabled people. This is also why we offered a critical commentary on common outcome measures rather than a redesign of them to establish their validity for capturing the diverse range of disabling experiences.
The commitment to capturing broad themes meant that we had to make compromises over the level of detail that we could provide. Our findings, although relevant to childhood disability, reflect the preference of previous debates to focus on disability in adulthood. We have attempted to counter this ‘bias’, but acknowledge that this is an important area for future investigation. Similarly, emerging, and at times contested, debates on neurodisability (which has important implications for childhood disability) and longstanding debates on sensory impairments suggest the importance of individualised and specialised responses. The need for research exploring what more inclusive practices mean for specific groups of disabled people is an important consideration. This, however, raises an interesting additional tension between universal and more specialist designs, which is also a feature of the literature. The resulting practical and methodological issues are rarely debated. As we have seen, for example, the assumed need for more specialist designs is used uncritically as a reason to exclude those with a disability. A more considered and informed approach, which reconciles practical endeavour with theoretical insight throughout the entire research process, is necessary.
In presenting our models of disability, certain strategic decisions needed to be made to facilitate a coherent narrative. We decided to offer a thematic rather than a strictly chronological account. This was particularly important to ensure that we could capture the ways in which the models and theories informed each other while also changing over time. We did not want to present a schematic or static account. Our advice needed to acknowledge the ongoing influence of the different models on current practice and the process of their continued (and future) evolution, in dialogue with each other.
Our decision to use The Cochrane Library had an impact on the way in which we framed public health. Our use of supplementary databases, associated with the Campbell Collaboration Library and the Joanne Briggs Institute, did not entirely mitigate this. By their nature, Cochrane-style reviews lean towards clinical topics and RCTs and can sometimes seem disconnected from the political, economic and social position of disabled people. Trials, while attracting particular interest among those undertaking public health research, rarely reflect the emerging tensions between ecological approaches and well-established medical models. This explains, for example, why no review linked its findings to theoretical or empirical discussions (or evidence) about SDHs or inequalities. Their purpose was to assess ‘effectiveness’, while following a formula that did not encourage discussion of wider social issues. Furthermore, some of the discussions around the inclusivity of the reviews and their methodology (such as risk of bias assessments and focus on internal validity) may not be fully transferable to other types of reviews (such as mixed methods) or primary studies (such as mixed methods evaluations, qualitative studies and process evaluations). It is, therefore, important to acknowledge that the scope of public health research is much broader than reviews of intervention studies.
Finally, it is important to acknowledge the ‘realities’ of current research priorities (and funding). As our deliberation panels demonstrated, disabled participants expressed serious concerns about the extent to which research was committed to listening to their experiences and to generating evidence that is meaningful to their lives. We accept that the practicalities, and perhaps understandable pragmatism, of public health research can create tensions when attempting to adapt more inclusive research that is able to accommodate diversity. Implementing our decision aid would, for example, enable current key stakeholders to question their current practices, particularly if they wish to avoid accusations of tokenism. This includes a commitment to investing in capacity building to ensure that public health can better engage with disability; allocating additional resources to those researchers who wish to adapt more inclusive designs; challenging those researchers who use disability as an exclusion criterion; and ensuring ethical approvals do not always assume that disabled people are ‘vulnerable’. Admittedly, these changes will create additional financial pressures in an already challenging funding environment, although the long-term gain in facilitating a better informed evidence base undermines the potential for flawed understanding, inappropriate responses and wasted resources. Our advice to researchers and commissioners presented here is a response to these concerns.
Future research
Reflections on the scope of the project have provided some useful insights into possible foci of future research. Evidence on how best to reconcile inclusive research practices with methodologically robust research designs offers an important starting point. Without this, we will continue to know little about what will work, for whom and under what circumstances. We have mentioned the value of exploring the impact of more inclusive practices for a range of different disabilities, which might create specific challenges that need to be accommodated by future research. Life-course is an important consideration, as is the need for research to reflect the specific experiences of disabled children and young people. Underpinning this work is the need for valid and reliable outcome measures that are sensitive to the disabling experience. With one or two expectations,440 we would appear to be a long way from adapting current measures to make them more applicable to populations with a disability; and even development of validated and reliable measures might struggle to convince those who assume a more critical approach to disability. They would prefer a focus on neurodiversity. The tensions raised by the use of measurements, particularly in terms of possible accusations of ableism, reflect the challenges facing public health research. Developments in the application of capability approaches and their potential connection to human rights and social justice offers a possible way forward, although, at present, this remains a theoretical rather than empirical possibility. Furthermore, and in relation to this, a more inclusive research design has to somehow ensure that its findings capture the experiences of disabled people. Current research, for example, struggles to offer a convincing framework, even when disabled people are included within the sampling strategy. This suggests the need for evidence on the use of analytical techniques that would enable researchers to make sense of their findings in ways that are relevant to the experiences of those with disabilities. Finally, there needs to a more robust evidence base on how best to facilitate more meaningful public engagement in public health research. This includes exploring successful strategies of engagement, alongside a discussion about the consequences (and politics) of involvement (Box 4).
-
Understand the theoretical and empirical challenges to methodological rigour when using inclusive research designs.
-
Develop evaluative research methodologies that are able to accommodate a diverse range of disabling experiences, including comorbidities, while also taking into account the influence of life-course.
-
Explore how best to include disabled children and young people in the design of research.
-
Develop valid and reliable research measures that are sensitive to how people and children experience their disability.
-
Develop analytical techniques able to offer explanation, consistent with different understandings and models of disability.
-
Facilitate public engagement in public health research, which is sensitive to the needs of a broad range of different stakeholders.
Developing practical guidance for inclusive research practices
The findings of this report have illustrated the need for more guidance on how to integrate a disability-inclusive approach into robust evaluations of public health interventions. Socially and politically active disabled people as well as professionals agree that having a disability-sensitive paradigm within which research could be designed and implemented would represents a positive step forward. Current evaluation designs, however, do not link into contemporary disability and public health perspectives or develop outcome measures evaluating how people can live well or flourish with disability. Our project has also illustrated how models and theories of disability remain untapped resources for establishing a more sensitive reinvention of public health research practices. Our report gives the specific example of how disability equity could be achieved using a human rights paradigm.
In line with best practice in research, politically and socially active disabled participants and organisations run by disabled people were actively involved as stakeholders in our study. They were an essential resource for the project. Although the project did not follow a coproduction model, we included principles drawn from it, with findings informed through a partnership between the project team and the wider community of politically and socially active disabled people. Their comments and ideas indicated the need for meaningful user involvement in setting public health research priorities and anchoring them in an appreciation of their health needs and the inequalities experienced by disabled people.
In order to support our primary stakeholders, as well as to inform the commissioning of public health research, we have developed tentative guidance and a checklist for the development and evaluation of further inclusive research practices. This guidance may also help to guide intervention design and improve current evidence-based policy. To make it especially accessible to those doing public health research, we have adapted the successful MRC guidance on developing and evaluating complex interventions624 and, ensuring consistency with our approach, have linked it to the internationally recognised human rights convention (CRPD) to help ensure an ethical basis for research (Figure 12). Our use of the MRC guidelines is deliberate, as it provides a potential link between robust design (as reflected in RE-AIM) and more inclusive approaches, which are sensitive to the diverse experiences of disability. As we have mentioned, our intent is to begin a debate about what more inclusive research practices might look like, to enable commissioners and researchers to understand the consequences of the decisions that they make with regard to disability.
FIGURE 12.
Key elements for public health research incorporating disability into the development and evaluation process. Adapted, with the permission of the MRC, from Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. 624

Advice to primary stakeholders: public health and disability checklist
In line with our commitment to a human rights approach, we end our report by using the IDEAS framework outlined in Chapter 7 to offer possible advice to a range of different stakeholders, in the form of a pragmatic public health and disability checklist. We begin by offering a checklist to people with disabilities to encourage them to engage with public health research. This could be adapted to a variety of accessible formats (Figure 13), although our suggested text should be regarded as preliminary and would need to be redrafted following wider consultation with disabled people and their organisations. (This was outside the scope of the current research project.)
FIGURE 13.
Checklist for people with disabilities when engaging with research.
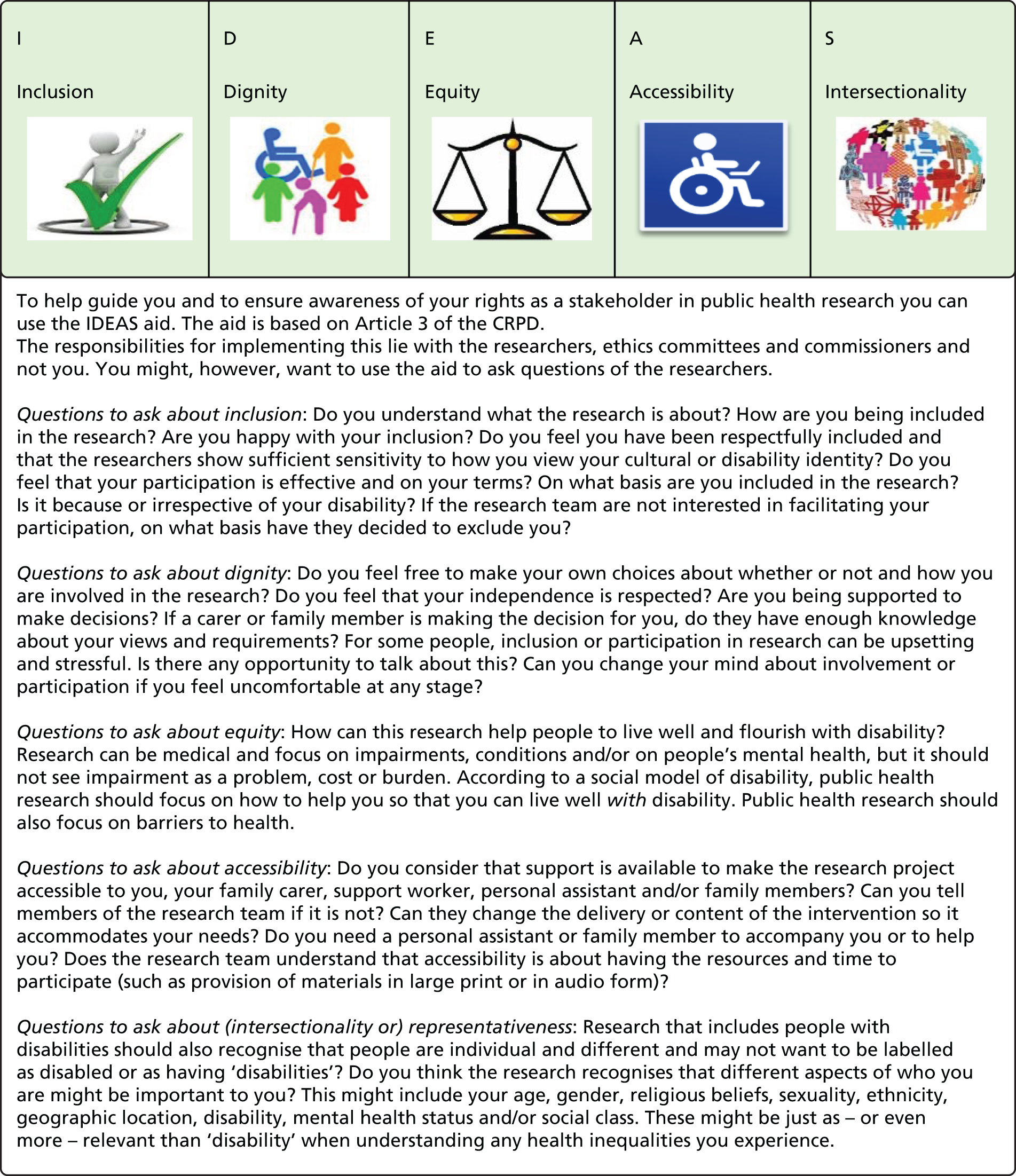
We also present a public health and disability checklist, which researchers might wish to consider when thinking about undertaking public health research in ways that are sensitive to disability (Box 5). This is a little harder to do, as current research practice reflects different degrees of sensitivity. Exclusive practices, for example, occur alongside examples of (inclusive) good practice that are informed by social and political engagement with disability. Consequently, and consistent with our approach, our questions are intended to generate enabling, reflexive engagement rather than to be prescriptive. As we have noted, more inclusive research designs improve the evidence base in public health, enabling a better and more universal understanding of effectiveness and one that is relevant to the experiences of disabled people.
Is it possible for the research to engage in coproduction or to involve disabled stakeholders in the development of the research question or design? What are the implications of participation?
DignityHow well is the research likely to reflect the diverse experiences of disability? Is it important that it does? To what extent does the research either generically or specifically touch on issues related to the experiences of disabled people? How, for example, can disability sensitivity be ensured in design? What ethical issues need to be considered? Are the theoretical and empirical implications of using particular types of measures made explicit?
EquityHow well will the research contribute to improving the conditions for health for people with a range of different impairments, conditions and/or mental health issues? Does it link to social entitlements for well-being and/or enabling social environments? What models of disability/impairment inform the research? Is there a discussion of universality and generalisability and, in particular, the extent to which the research can be said to reflect disability experiences? If not, is this acknowledged and the implications for the evidence base considered?
AccessibilityHas the intervention, and the study through which it will be evaluated, been designed with accessibility in mind? What adjustments are necessary and feasible to ensure accessibility? Are disabled participants needlessly excluded? How well does the research, for example, engage with those who use non-verbal communication strategies or who have cognitive impairments and/or learning disabilities?
IntersectionalityDoes the existing evidence suggest that there is a gap in the literature linked to health inequalities? How well does the research connect to comorbidities and intersectionality? How well will it articulate the link between gender, age, socioeconomic class, sexuality, geography, disability or ethnicity?
Analytical frameworkHow well does the research provide a meaningful analysis of disabling experiences in a way that links to theoretical perspectives/causal framework underpinning the intervention? Are there any disability-oriented recommendations that other researchers could learn from or that are important to the evaluation of the intervention? Does it acknowledge that people with disabilities can ‘flourish’ rather than see disability as a burden? Does it consider how a disabling social and political environment might explain experiences?
Building on this, we now reflect on the potential considerations that commissioners might like to take into account when commissioning public health research (Box 6). These can be connected to the guidance for researchers.
To what extent were disabled people involved in commissioning the research? What participatory models were followed? To what extent does the commissioning brief reflect the diverse experiences of disabled people and the different types of impairments? How was accountability ensured?
DignityHow well will the research enable people to live well with disability? Does it cater for those with complex impairments? Does it address health inequalities in a way that does not treat disability as problem, burden or cost?
EquityHow does the research tackle inequalities? Does the research demonstrate the long-term effectiveness of the intervention? Is change sustainable? Are cost-effectiveness and other measures sensitive to the experiences of disabled people? Is the research producing evidence that is applicable and relevant to the different experiences of disability?
AccessibilityIs the intervention and the research designed to evaluate it accessible to the general population? What extra resources are necessary to ensure accessibility?
IntersectionalityIs the research able to reflect a diverse range of experiences, while being sensitive to the life-course? Has thought been given to physical, cognitive or mental health disability as an intersectional category when presenting the research? Can the research reflect the impact of comorbidities? Have potential differences attributable to age, gender, social class and ethnicity been considered?
Reflecting the potential and positive influence of ethic committees, when ensuring more inclusive research, we next consider the types of questions, such committees might consider asking (Box 7).
Involvement in research evaluating public health interventions should be an open ethical choice which can be rescinded at any time. Ethics committees can help to ensure greater ethical robustness of their research designs by using IDEAS.
InclusionWere stakeholders included in the design of the research? How do the researchers intend to gain ethical consent? Is it sensitive to the experiences of disabled people? Is it respectful of independence or interdependence? Have the researchers considered the possible relevance of the Mental Capacity Act (2005)?30 Is consent gained at different points during the research?
DignityHow is dignity ensured? Are the language/visuals used during the research inclusive and disability-sensitive? Is the research non-discriminatory and culturally sensitive?
EquityHow well does the research connect to debates about equity and health inequalities? Does the research reflect the different and diverse experiences of disability? Does the research consider long-term consequences of the interventions and the extent to which they are sustainable? How well does the research avoid conceptualising disability as a burden, cost or problem?
AccessibilityHow accessible is the research? Are people with physical, cognitive or mental impairment excluded without good reason? Does it include people with complex or severe impairments, health conditions and/or mental health conditions and the variety of settings in which they might live?
IntersectionalityHow well will the research be able to explain health inequalities? Is the analysis able to take account of differences according to age, socioeconomic class, gender, ethnicity or comorbidities?
Conclusion
The research undertaken for this report has produced a review of disability models and theories, a benchmarking report on current practice in intervention research, and an evidence-based and critically informed guide/checklist for research commissioners and researchers that assesses and evaluates the consequences of adapting a more nuanced and socially inclusive approach to disability when undertaking intervention studies. Our report has discussed the extent to which public health research could be made more sensitive to the different models and theories of disability. Our findings outline a range of options available to researchers and commissioners. We pay particular attention to human rights approaches. These can connect more critical models of disability to the ecological models already used in public health research and policy. They, therefore, offer a potential framework by which commissioners and researchers can assess the consequences of choices and decision-making when attempting to develop more inclusive public health research.
Acknowledgements
We wish to thank Tess McManus of Inclusion London, Dr Armineh Soorenian of the Sisters of Frida, Coral Jarrett and Angela Baugh of the BME Network Sheffield, and Caron Blake of the Greater Manchester Coalition for Disabled People for aiding us with the organisation of the deliberation panels.
We acknowledge the participation of public health professionals and the many socially and politically active disabled people who shared their time and critical expertise with us.
We also wish to thank the individual members of our project steering committee who deftly guided this project with their respective expert advice: Professor Simon Dyson, Professor Brett Smith, Professor Peter Beresford, Tess McManus, Dr Armineh Soorenian, Dr Amanda Keeling and Dr Laia Becares.
Sally Stephenson, Jenny Brown and Gavin Macmillan provided excellent administration support to the project.
Contributions of authors
Maria Berghs (Research Fellow and Co-investigator) was responsible for conducting the two stages of the scoping review and oversaw the deliberation panels. She did the primary writing up of the report with the support of Karl Atkin.
Karl Atkin (Principal Investigator) oversaw the day-to-day management of the project, acted as second reviewer and aided the writing up of the project, taking responsibility for the final edits. Alongside Professor Hilary Graham, he ensured theoretical and empirical oversight of the project.
Hilary Graham (Co-investigator) ensured the critical public health focus of the project. She gave her considerable theoretical expertise and technical advice at all stages of the project to ensure its empirical robustness.
Chris Hatton (Co-investigator) gave theoretical and empirical foundation to the project using his expertise in intellectual disability and public health. He reviewed the writing up of the project and gave advice in terms of applicability to a public health audience.
Carol Thomas (Co-investigator) ensured that the theoretical overview of the project linked to disability theory and models. She also gave insights into new directions and developments in disability studies.
Data sharing statement
This is a narrative scoping review and, therefore, the material generated beyond that contained within the report is not suitable for sharing. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Family Resources Survey 2012/2013. London: Department of Work and Pensions; 2015.
- Banks J. Cognitive function, financial literacy and financial outcomes at older ages: introduction. Econ J 2010;120:F357-F62. http://dx.doi.org/10.1111/j.1468-0297.2010.02393.x.
- Graham H. Socioeconomic inequalities in health: evidence on patterns and determinants. Benefits 2006;14:77-90.
- Emerson E, Graham H, Hatton C. The measurement of poverty and socioeconomic position in research involving people with intellectual disability. Int Rev Res Mental Retardation 2006;32:77-108. http://dx.doi.org/10.1016/S0074-7750(06)32003-4.
- Birnie K, Cooper R, Martin RM, Kuh D, Sayer AA, Alvarado BE, et al. Childhood socioeconomic position and objectively measured physical capability levels in adulthood: a systematic review and meta-analysis. PLOS ONE 2011;6. http://dx.doi.org/10.1371/journal.pone.0015564.
- Marmot M, Bell R. Fair society, healthy lives. Public Health 2012;126:4-10. http://dx.doi.org/10.1016/j.puhe.2012.05.014.
- Anderson LL, Humphries K, McDermott S, Marks B, Sisirak J, Larson S. The state of the science of health and wellness for adults with intellectual and developmental disabilities. Intellect Dev Disabil 2013;51:385-98. http://dx.doi.org/10.1352/1934-9556-51.5.385.
- Emerson E, Hatton C. Health Inequalities and People with Intellectual Disabilities. Cambridge: Cambridge University Press; 2013.
- Gore N, Emerson E, Brady S. Rates of breastfeeding and exposure to socio-economic adversity amongst children with intellectual disability. Res Dev Disabil 2015;39:12-9. http://dx.doi.org/10.1016/j.ridd.2014.12.028.
- Morciano M, Hancock RM, Pudney SE. Birth-cohort trends in older-age functional disability and their relationship with socio-economic status: evidence from a pooling of repeated cross-sectional population-based studies for the UK. Soc Sci Med 2015;136–137:1-9. http://dx.doi.org/10.1016/j.socscimed.2015.04.035.
- Rimmer JH, Chen MD, Hsieh K. A conceptual model for identifying, preventing, and managing secondary conditions in people with disabilities. Phys Ther 2011;91:1728-39. http://dx.doi.org/10.2522/ptj.20100410.
- World Report on Disability. Geneva: World Health Organization; 2011.
- Emerson E, Llewellyn G, Madden R, Graham H, Hatton C, Rechel B, et al. Routledge Handbook of Disability Studies. Abingdon: Routledge; 2012.
- Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The confidential inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 2014;383:889-95. http://dx.doi.org/10.1016/S0140-6736(13)62026-7.
- Emerson E. Commentary: Childhood exposure to environmental adversity and the well-being of people with intellectual disabilities. J Intellect Disabil Res 2013;57:589-600. http://dx.doi.org/10.1111/j.1365-2788.2012.01577.x.
- Emerson E, Blacher J, Einfeld S, Hatton C, Robertson J, Stancliffe RJ. Environmental risk factors associated with the persistence of conduct difficulties in children with intellectual disabilities and autistic spectrum disorders. Res Dev Disabil 2014;35:3508-17. http://dx.doi.org/10.1016/j.ridd.2014.08.039.
- Atkin K, Stapley S, Easton A. No one listens to me, nobody believes me: self management and the experience of living with encephalitis. Soc Sci Med 2010;71:386-93. http://dx.doi.org/10.1016/j.socscimed.2010.04.011.
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, et al. Grand challenges in global mental health. Nature 2011;475:27-30. http://dx.doi.org/10.1038/475027a.
- Halfon N, Houtrow A, Larson K, Newacheck PW. The changing landscape of disability in childhood. Future Child 2012;22:13-42. http://dx.doi.org/10.1353/foc.2012.0004.
- Marmot M. Health inequalities and mental life. Advances Psychiatric Treat 2012;18:320-2. http://dx.doi.org/10.1192/apt.bp.112.010132.
- Lollar DJ, Crews JE. Redefining the role of public health in disability. Annu Rev Public Health 2003;24:195-208. http://dx.doi.org/10.1146/annurev.publhealth.24.100901.140844.
- Convention on the Rights of Persons with Disabilities. New York, NY: United Nations; 2007.
- Oliver M, Barnes C. The New Politics of Disablement. Basingstoke: Palgrave Macmillan; 2012.
- Berghs M, Swain J, French S, Barnes C, Thomas C. Disabling Barriers – Enabling Environments. London: Sage Publications Ltd; 2013.
- Gridley K, Brooks J, Glendinning C. Good practice in social care: the views of people with severe and complex needs and those who support them. Health Soc Care Community 2014;22:588-97. http://dx.doi.org/10.1111/hsc.12105.
- Gridley K, Brooks J, Glendinning C. Good practice in social care for disabled adults and older people with severe and complex needs: evidence from a scoping review. Health Soc Care Community 2014;22:234-48. http://dx.doi.org/10.1111/hsc.12063.
- Human Rights Act 1998. London: The Stationery Office; 1998.
- Equality Act 2010. London: The Stationery Office; 2010.
- Department for Education . Equality Act 2010: Guidance 2015. www.gov.uk/equality-act-2010-guidance (accessed February 2016).
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Care Act 2014. London: The Stationery Office; 2014.
- Healthy Lives, Healthy People. London: Department of Health; 2010.
- Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health 2010;64:284-91. http://dx.doi.org/10.1136/jech.2008.082743.
- Oliver M. Theories in health care and research: theories of disability in health practice and research. BMJ 1998;317:1446-9. http://dx.doi.org/10.1136/bmj.317.7170.1446.
- Barnes C. Rethinking Care from the Perspective of Disabled People. Conference Report and Recommendations. Geneva: World Health Organization; 2001.
- Meyers AR, Andresen EM. Enabling our instruments: accommodation, universal design, and access to participation in research. Arch Phys Med Rehabil 2000;81:5-9. http://dx.doi.org/10.1053/apmr.2000.20618.
- Loeb ME, Eide AH, Altman B, Barnartt S. International Views on Disability Measures: Moving Towards Comparative Measurement. Bingley: Emerald Group Publishing Ltd; 2006.
- Krahn GL, Fujiura G, Drum CE, Cardinal BJ, Nosek MA. The dilemma of measuring perceived health status in the context of disability. Disabil Health J 2009;2:49-56. http://dx.doi.org/10.1016/j.dhjo.2008.12.003.
- Molden TH, Tøssebro J. Disability measurements: impact on research results. Scand J Disabil Res 2011;14:340-57. http://dx.doi.org/10.1080/15017419.2011.621654.
- Purdam K, Afkhami R, Olsen W, Thornton P. Disability in the UK: measuring equality. Disabil Soc 2007;23:53-65. http://dx.doi.org/10.1080/09687590701725658.
- Murray CJ, Acharya AK. Understanding DALYs (disability-adjusted life years). J Health Econ 1997;16:703-30. http://dx.doi.org/10.1016/S0167-6296(97)00004-0.
- Andresen EM. Criteria for assessing the tools of disability outcomes research. Arch Phys Med Rehabil 2000;81:15-20. http://dx.doi.org/10.1053/apmr.2000.20619.
- Andresen EM, Lollar DJ, Meyers AR. Disability outcomes research: why this supplement, on this topic, at this time?. Arch Phys Med Rehabil 2000;81:1-4. http://dx.doi.org/10.1053/apmr.2000.20614.
- Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet 2012;380:2129-43. http://dx.doi.org/10.1016/S0140-6736(12)61680-8.
- Universal Design for Learning Guidelines Version 2.0. Wakefield, MA: Center for Applied Special Technology; 2011.
- Williams RW, Harris S, Lomas D, Perkin M, Gallagher G, Nash S, et al. Inclusive research with people with intellectual disability: the Question-Aires way. J Appl Res Intellect Disabil 2014;25.
- Feldman MA, Owen F, Andrews AE, Tahir M, Barber R, Griffiths D. Randomized control trial of the 3Rs health knowledge training program for persons with intellectual disabilities. J Appl Res Intellect Disabil 2016;29:278-88. http://dx.doi.org/10.1111/jar.12186.
- Rowland JL, Malone LA, Fidopiastis CM, Padalabalanarayanan S, Thirumalai M, Rimmer JH. Perspectives on active video gaming as a new frontier in accessible physical activity for youth with physical disabilities. Phys Ther 2016;96:521-32. http://dx.doi.org/10.2522/ptj.20140258.
- Dye L, Hare DJ, Hendy S. Capacity of people with intellectual disabilities to consent to take part in a research study. J Appl Res Intellect Disabil 2007;20:168-74. http://dx.doi.org/10.1111/j.1468-3148.2006.00310.x.
- Nind M. Conducting Qualitative Research with People with Learning, Communication and Other Disabilities: Methodological challenges. Southampton: Economic and Social Research Council National Centre for Research Methods; 2009.
- Feldman MA, Battin SM, Shaw OA, Luckasson R. Inclusion of children with disabilities in mainstream child development research. Disabil Soc 2013;28:997-1011. http://dx.doi.org/10.1080/09687599.2012.748647.
- McDonald KE. We want respect: adults with intellectual and developmental disabilities address respect in research. Am J Intellect Dev Disabil 2012;117:263-74. http://dx.doi.org/10.1352/1944-7558-117.4.263.
- Brooker K, Mutch A, McPherson L, Ware R, Lennox N, van Dooren K. “We can talk while we’re walking”: seeking the views of adults with intellectual disability to inform a walking and social-support program. Adapt Phys Activ Q 2015;32:34-48. http://dx.doi.org/10.1123/apaq.2013-0067.
- Zarb G. Modelling the social model of disability. Critical Public Health 1995;6:21-9. http://dx.doi.org/10.1080/09581599508409049.
- Rimmer JA, Rowland JL. Physical activity for youth with disabilities: a critical need in an underserved population. Dev Neurorehabil 2008;11:141-8. http://dx.doi.org/10.1080/17518420701688649.
- Beresford P. User involvement, research and health inequalities: developing new directions. Health Soc Care Community 2007;15:306-12. http://dx.doi.org/10.1111/j.1365-2524.2007.00688.x.
- Heller T, Fisher D, Marks B, Hsieh K. Interventions to promote health: crossing networks of intellectual and developmental disabilities and aging. Disabil Health J 2014;7:24-32. http://dx.doi.org/10.1016/j.dhjo.2013.06.001.
- Brooker K, van Dooren K, McPherson L, Lennox N, Ware R. A systematic review of interventions aiming to improve involvement in physical activity among adults with intellectual disability. J Phys Act Health 2015;12:434-44. http://dx.doi.org/10.1123/jpah.2013-0014.
- Brooker K, van Dooren K, Tseng CH, McPherson L, Lennox N, Ware R. Out of sight, out of mind? The inclusion and identification of people with intellectual disability in public health research. Perspect Public Health 2015;135:204-11. http://dx.doi.org/10.1177/1757913914552583.
- Lollar DJ. Public health and disability: emerging opportunities. Public Health Rep 2002;117:131-6. http://dx.doi.org/10.1016/S0033-3549(04)50119-X.
- Mont D, Loeb M. Beyond DALYS: Developing Indicators to Assess the Impact of Public Health Interventions on the Lives of Persons with Disabilities. SP Discussion Paper No. 0815. Washington, DC: The World Bank; 2008.
- Madans JH, Loeb ME, Altman BM. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: the work of the Washington Group on Disability Statistics. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-S4-S4.
- Palmer M, Harley D. Models and measurement in disability: an international review. Health Policy Plan 2012;27:357-64. http://dx.doi.org/10.1093/heapol/czr047.
- Drum CE, Krahn GL, Bersani H. Disability and Public Health. Washington, DC: American Public Health Association; 2009.
- McDonald KE, Raymaker DM. Paradigm shifts in disability and health: toward more ethical public health research. Am J Public Health 2013;103:2165-73. http://dx.doi.org/10.2105/AJPH.2013.301286.
- Begum N, Zarb G. Measuring Disablement in Society: Working Paper 5: Measuring Disabled People’s Involvement in Local Planning 1996. http://disability-studies.leeds.ac.uk/files/library/Begum-local-planning.pdf (accessed May 2016).
- Barnes C, Mercer G, Shakespeare T. Exploring Disability: A Sociological Introduction. Cambridge: Cambridge University Press; 1999.
- Priestley M. Disability: A Life Course Approach. Cambridge: Polity Press; 2003.
- Thomas C. Sociologies of Disability and Illness: Contested Ideas in Disability Studies and Medical Sociology. Basingstoke: Palgrave Macmillan; 2007.
- Goodley D. Disability Studies: An Interdisciplinary Introduction. London: Sage Publications Ltd; 2011.
- Oliver M, Barnes C. Back to the future: the World Report on Disability. Disabil Soc 2012;27:575-9. http://dx.doi.org/10.1080/09687599.2012.686781.
- Oliver M. The social model of disability: thirty years on. Disabil Soc 2013;28:1024-6. http://dx.doi.org/10.1080/09687599.2013.818773.
- Barnes C, Mercer G. Exploring Disability. Bristol: Policy Press; 2010.
- Üstün TB, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The International Classification of Functioning, Disability and Health: a new tool for understanding disability and health. Disabil Rehabil 2003;25:565-71. http://dx.doi.org/10.1080/0963828031000137063.
- Ravesloot C, Ruggiero C, Ipsen C, Traci M, Seekins T, Boehm T, et al. Disability and health behavior change. Disabil Health J 2011;4:19-23. http://dx.doi.org/10.1016/j.dhjo.2010.05.006.
- Hays RD, Hahn H, Marshall G. Use of the SF-36 and other health-related quality of life measures to assess persons with disabilities. Arch Phys Med Rehabil 2002;83:4-9. http://dx.doi.org/10.1053/apmr.2002.36837.
- Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ 2004;13:873-84. http://dx.doi.org/10.1002/hec.866.
- Versteegh MM, Leunis A, Uyl-de Groot CA, Stolk EA. Condition-specific preference-based measures: benefit or burden?. Value Health 2012;15:504-13. http://dx.doi.org/10.1016/j.jval.2011.12.003.
- Vergunst F, Jenkinson C, Burns T, Simon J. Application of Sen’s capability approach to outcome measurement in mental health research: psychometric validation of a Novel Multi-Dimensional Instrument (OxCAP-MH). Human Welfare 2014;3:1-4.
- Harrison T. Health promotion for persons with disabilities: what does the literature reveal?. Fam Community Health 2006;29:12-9. http://dx.doi.org/10.1097/00003727-200601001-00004.
- Tennant R, Goens C, Barlow J, Day C, Stewart-Brown S. A systematic review of reviews of interventions to promote mental health and prevent mental health problems in children and young people. J Public Mental Health 2007;6:25-32. http://dx.doi.org/10.1108/17465729200700005.
- Balogh R, Ouellette-Kuntz H, Bourne L, Lunsky Y, Colantonio A. Organising health care services for persons with an intellectual disability. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd007492.
- McConkey R. Accessibility of Healthcare Information for People with a Learning Disability. A Review and Discussion Paper. London: Equality Commission; 2006.
- Holloway S, Lee L, McConkey R. Meeting the training needs of community-based service personnel in Africa through video-based training courses. Leonard Cheshire Foundation International. Disabil Rehabil 1999;21:448-54. http://dx.doi.org/10.1080/096382899297431.
- Seekins T, Kimpton T, Peterson J. Evidence-based Health Promotion Interventions for People with Disabilities: Results of a Systematic Review of Literature. Portland, OR: Research and Training Center on Health and Wellness for People with Disabilities; 2010.
- Robertson J, Roberts H, Emerson E, Turner S, Greig R. The impact of health checks for people with intellectual disabilities: a systematic review of evidence. J Intellect Disabil Res 2011;55:1009-19. http://dx.doi.org/10.1111/j.1365-2788.2011.01436.x.
- Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part II). Health Promot Pract 2005;6:148-56. http://dx.doi.org/10.1177/1524839904266792.
- Sims D, Cabrita Gulyurtlu SS. A scoping review of personalisation in the UK: approaches to social work and people with learning disabilities. Health Soc Care Community 2014;22:13-21. http://dx.doi.org/10.1111/hsc.12048.
- Antao L, Shaw L, Ollson K, Reen K, To F, Bossers A, et al. Chronic pain in episodic illness and its influence on work occupations: a scoping review. Work 2013;44:11-36.
- Feldman MA, Owen F, Andrews A, Hamelin J, Barber R, Griffiths D. Health self-advocacy training for persons with intellectual disabilities. J Intellect Disabil Res 2012;56:1110-21. http://dx.doi.org/10.1111/j.1365-2788.2012.01626.x.
- Alborz A, McNally R, Glendinning C. Access to health care for people with learning disabilities in the UK: mapping the issues and reviewing the evidence. J Health Serv Res Policy 2005;10:173-82. http://dx.doi.org/10.1258/1355819054338997.
- Feldman MA, Bosett J, Collet C, Burnham-Riosa P. Where are persons with intellectual disabilities in medical research? A survey of published clinical trials. J Intellect Disabil Res 2014;58:800-9. http://dx.doi.org/10.1111/jir.12091.
- Dale C, Prieto-Merino D, Kuper H, Adamson J, Bowling A, Ebrahim S, et al. Modelling the association of disability according to the WHO International Classification of Functioning, Disability and Health (ICF) with mortality in the British Women’s Heart and Health Study. J Epidemiol Community Health 2012;66:170-5. http://dx.doi.org/10.1136/jech-2011-200078.
- Rimmer JH. Building a future in disability and public health. Disabil Health J 2011;4:6-11. http://dx.doi.org/10.1016/j.dhjo.2010.04.001.
- Reinhardt JD, Wahrendorf M, Siegrist J. Socioeconomic position, psychosocial work environment and disability in an ageing workforce: a longitudinal analysis of SHARE data from 11 European countries. Occup Environ Med 2013;70:156-63. http://dx.doi.org/10.1136/oemed-2012-100924.
- Dementia, Rights, and the Social Model of Disability. London: Mental Health Foundation; 2015.
- Disability Rights Commission . Equal Treatment: Closing the Gap: Information for Practitioners 2006.
- Improving the Quality of Care in General Practice. Report of an Independent Inquiry Commissioned by the King’s Fund. London: The King’s Fund; 2011.
- Stein MA, Lord JE. Monitoring the Convention on the Rights of Persons with Disabilities: innovations, lost opportunities, and future potential. Human Rights Q 2010;32:689-728. http://dx.doi.org/10.1353/hrq.2010.0003.
- Stein MA, Stein PJ, Weiss D, Lang R. Health care and the UN Disability Rights Convention. Lancet 2009;374:1796-8. http://dx.doi.org/10.1016/S0140-6736(09)62033-X.
- The United Nations Conventions on the Rights of People with Disabilities: A Guide for Disabled People and Disabled People’s Organisations. London: Equality and Human Rights Commission; 2010.
- The Public Sector Equality Duty: A Way Forward for the Health Sector. London: Equality and Human Rights Commission; 2011.
- Beresford P. Beyond the Usual Suspects: Towards Inclusive User Involvement: Research Report. London: Shaping Our Lives; 2013.
- Nilsen ES, Myrhaug HT, Johansen M, Oliver S, Oxman AD. Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database Syst Rev 2006;19. http://dx.doi.org/10.1002/14651858.cd004563.pub2.
- Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry 2014;13:153-60. http://dx.doi.org/10.1002/wps.20128.
- Richardson CR, Faulkner G, McDevitt J, Skrinar GS, Hutchinson DS, Piette JD. Integrating physical activity into mental health services for persons with serious mental illness. Psychiatr Serv 2005;56:324-31. http://dx.doi.org/10.1176/appi.ps.56.3.324.
- Chang CK, Hayes RD, Perera G, Broadbent MT, Fernandes AC, Lee WE, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLOS ONE 2011;6. http://dx.doi.org/10.1371/journal.pone.0019590.
- Gilbody S, Peckham E, Man MS, Mitchell N, Li J, Becque T, et al. Bespoke smoking cessation for people with severe mental ill health (SCIMITAR): a pilot randomised controlled trial. Lancet Psychiatry 2015;2:395-402. http://dx.doi.org/10.1016/S2215-0366(15)00091-7.
- Taylor DH, Hasselblad V, Henley SJ, Thun MJ, Sloan FA. Benefits of smoking cessation for longevity. Am J Public Health 2002;92:990-6. http://dx.doi.org/10.2105/AJPH.92.6.990.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. http://dx.doi.org/10.1080/1364557032000119616.
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005;10:6-20. http://dx.doi.org/10.1258/1355819054308576.
- Anderson S, Allen P, Peckham S, Goodwin N. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res Policy Syst 2008;6. http://dx.doi.org/10.1186/1478-4505-6-7.
- Davis K, Drey N, Gould D. What are scoping studies? A review of the nursing literature. Int J Nurs Stud 2009;46:1386-400. http://dx.doi.org/10.1016/j.ijnurstu.2009.02.010.
- Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J 2009;26:91-108. http://dx.doi.org/10.1111/j.1471-1842.2009.00848.x.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-69.
- Armstrong R, Hall BJ, Doyle J, Waters E. Cochrane Update. ‘Scoping the scope’ of a Cochrane review. J Public Health 2011;33:147-50. http://dx.doi.org/10.1093/pubmed/fdr015.
- Daudt HM, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol 2013;13. http://dx.doi.org/10.1186/1471-2288-13-48.
- Campbell M, Egan M, Lorenc T, Bond L, Popham F, Fenton C, et al. Considering methodological options for reviews of theory: illustrated by a review of theories linking income and health. Syst Rev 2014;3. http://dx.doi.org/10.1186/2046-4053-3-114.
- Morris J. Pride Against Prejudice: Transforming Attitudes to Disability. London: Women’s Press; 1991.
- Threlfall AG, Meah S, Fischer AJ, Cookson R, Rutter H, Kelly MP. The appraisal of public health interventions: the use of theory. J Public Health 2015;37:166-71. http://dx.doi.org/10.1093/pubmed/fdu044.
- Finkelstein V. Modelling Disability n.d.
- Global Burden of Disease Study 2013 Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743-800. http://dx.doi.org/10.1016/S0140-6736(15)60692-4.
- Bonner L. Using theory-based evaluation to build evidence-based health and social care policy and practice. Critical Public Health 2003;13:77-92. http://dx.doi.org/10.1080/0958159031000100224.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h1258.
- Crosby N, Jackson R. The Seven Needs and the Social Model of Disability. Derby: Derbyshire Coalition for Inclusive Living; 2000.
- Dahlgren G, Whitehead M, Dahlgren G, Whitehead M. European Strategies for Tackling Social Inequities in Health: Levelling Up Part 2. Copenhagen: WHO Regional Office for Europe; 2007.
- Godfrey CM, Harrison MB, Lysaght R, Lamb M, Graham ID, Oakley P. Intervention strategies that support self-care activities: an integrative study across disease/impairment groupings. JBI Database Systematic Rev Implement Rep 2010;8:1304-50.
- Robertson J, Hatton C, Baines S, Emerson E. Systematic reviews of the health or health care of people with intellectual disabilities: a systematic review to identify gaps in the evidence base. J Appl Res Intellect Disabil 2015;28:455-523. http://dx.doi.org/10.1111/jar.12149.
- UK’s Disabled People’s Manifesto: Reclaiming our Futures. London: Inclusion London; 2013.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. London: Cochrane; 2011.
- Thomas C. Disability and gender: reflections on theory and research. Scand J Disabil Res 2006;8:177-85. http://dx.doi.org/10.1080/15017410600731368.
- Ogilvie D, Hamilton V, Egan M, Petticrew M. Systematic reviews of health effects of social interventions: 1. Finding the evidence: how far should you go?. J Epidemiol Community Health 2005;59:804-8. http://dx.doi.org/10.1136/jech.2005.034181.
- Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev 2013;2. http://dx.doi.org/10.1002/14651858.cd007651.pub2.
- Fox BB, Hodgkinson B, Parker D. The effects of physical exercise on functional performance, quality of life, cognitive impairment and physical activity levels for older adults aged 65 years and older with a diagnosis of dementia: a systematic review. JBI Database Systematic Rev Implement Rep 2014;12:158-276. http://dx.doi.org/10.11124/jbisrir-2014-1714.
- Reed KE, Warburton DE, Macdonald HM, Naylor P, McKay HA. Action Schools! BC: a school-based physical activity intervention designed to decrease cardiovascular disease risk factors in children. Prev Med 2008;46:525-31. http://dx.doi.org/10.1016/j.ypmed.2008.02.020.
- Donnelly JE, Greene JL, Gibson CA, Smith BK, Washburn RA, Sullivan DK, et al. Physical Activity Across the Curriculum (PAAC): a randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev Med 2009;49:336-41. http://dx.doi.org/10.1016/j.ypmed.2009.07.022.
- Dorgo S, King GA, Candelaria N, Bader JO, Brickey GD, Adams CE. The effects of manual resistance training on fitness in adolescents. J Strength Cond Res 2009;23:2287-94. http://dx.doi.org/10.1519/JSC.0b013e3181b8d42a.
- Treviño RP, Yin Z, Hernandez A, Hale DE, Garcia OA, Mobley C. Impact of the bienestar school-based diabetes mellitus prevention program on fasting capillary glucose levels: a randomized controlled trial. Arch Pediatr Adolesc Med 2004;158:911-17. http://dx.doi.org/10.1001/archpedi.158.9.911.
- Abelson J, Eyles J, McLeod CB, Collins P, McMullan C, Forest PG. Does deliberation make a difference? Results from a citizens panel study of health goals priority setting. Health Policy 2003;66:95-106. http://dx.doi.org/10.1016/S0168-8510(03)00048-4.
- Crosby N, Kelly JM, Schaefer P. Citizens panels – a new approach to citizen participation. Public Administration Rev 1986;46:170-8. http://dx.doi.org/10.2307/976169.
- Raisio H, Valkama K, Peltola E. Disability and deliberative democracy: towards involving the whole human spectrum in public deliberation. Scand J Disabil Res 2013;16:77-9. http://dx.doi.org/10.1080/15017419.2013.781957.
- Abelson J, Forest PG, Eyles J, Smith P, Martin E, Gauvin FP. Deliberations about deliberative methods: issues in the design and evaluation of public participation processes. Soc Sci Med 2003;57:239-51. http://dx.doi.org/10.1016/S0277-9536(02)00343-X.
- Williamson T. A Stronger Collective Voice for People with Dementia. York: Joseph Rowntree Foundation; 2012.
- Thomas C, Milligan C. Dementia and the Social Model of Disability. York: Joseph Rowntree Foundation; 2015.
- Reichertz J. Abduction: the logic of discovery of grounded theory. Forum 2010;11. www.qualitative-research.net/index.php/fqs/article/view/1412/2902 (accessed May 2016).
- Nagi S, Sussman MB. Sociology and Rehabilitation. Washington, DC: American Sociological Association; 1965.
- Sen A, Griffin K, Knight JB. Human Development and the International Development Strategy for the 1990s. Basingstoke: Macmillan Press; 1990.
- Robeyns I. The capability approach: a theoretical survey. J Hum Dev 2005;6:93-117. http://dx.doi.org/10.1080/146498805200034266.
- Morris C. Measuring participation in childhood disability: how does the capability approach improve our understanding?. Dev Med Child Neurol 2009;51:92-4. http://dx.doi.org/10.1111/j.1469-8749.2008.03248.x.
- Trani J-F, Bakhshi P, Bellanca N, Biggeri M, Marchetta F. Disabilities through the Capability Approach lens: implications for public policies. Eur J Disabil Res 2011;5:143-57. http://dx.doi.org/10.1016/j.alter.2011.04.001.
- Sen A. Human rights and capabilities. J Hum Dev 2005;6:151-66. http://dx.doi.org/10.1080/14649880500120491.
- Nussbaum M, Sen A. The Quality of Life. Oxford: Clarendon Press; 1993.
- Nussbaum MC. Women and Human Development: The Capabilities Approach. Cambridge: Cambridge University Press; 2001.
- Allmark P, Machaczek K. Financial capability, health and disability. BMC Public Health 2015;15. http://dx.doi.org/10.1186/s12889-015-1589-5.
- Anand P, Hunter G, Carter I, Dowding K, Guala F, van Hees M. The development of capability indicators. J Hum Dev Capabilities 2009;10:125-52. http://dx.doi.org/10.1080/14649880802675366.
- Nielsen L, Axelsen DV. Capabilitarian sufficiency: capabilities and social justice. J Hum Dev Capabilities 2016. http://dx.doi.org/10.1080/19452829.2016.1145632.
- International Classification of Disease. Geneva: World Health Organization; 1976.
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163-96. http://dx.doi.org/10.1016/S0140-6736(12)61729-2.
- Murray CJ. Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bull World Health Organ 1994;72:429-45.
- Anand S, Hanson K. Disability-adjusted life years: a critical review. J Health Econ 1997;16:685-702. http://dx.doi.org/10.1016/S0167-6296(97)00005-2.
- Jamison DT, Breman JG, Meashman AR, Alleyne G, Claeson M, Evans DB, et al. Disease Control Priorities in Developing Countries. Washington, DC: Oxford University and The World Bank; 2006.
- Haagsma JA, Maertens de Noordhout C, Polinder S, Vos T, Havelaar AH, Cassini A, et al. Assessing disability weights based on the responses of 30,660 people from four European countries. Popul Health Metr 2015;13. http://dx.doi.org/10.1186/s12963-015-0042-4.
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013;380:2197-223. http://dx.doi.org/10.1016/S0140-6736(12)61689-4.
- Fox-Rushby JA, Hanson K. Calculating and presenting disability adjusted life years (DALYs) in cost-effectiveness analysis. Health Policy Plan 2001;16:326-31. http://dx.doi.org/10.1093/heapol/16.3.326.
- Arnesen T, Nord E. The value of DALY life: problems with ethics and validity of disability adjusted life years. BMJ 1999;319:1423-5. http://dx.doi.org/10.1136/bmj.319.7222.1423.
- Gold MR, Stevenson D, Fryback DG. HALYS and QALYS and DALYS, oh my: similarities and differences in summary measures of population Health. Annu Rev Public Health 2002;23:115-34. http://dx.doi.org/10.1146/annurev.publhealth.23.100901.140513.
- Nord E. Disability weights in the Global Burden of Disease 2010: unclear meaning and overstatement of international agreement. Health Policy 2013;111:99-104. http://dx.doi.org/10.1016/j.healthpol.2013.03.019.
- Wiedermann W, Frick U. Using surveys to calculate disability-adjusted life-year. Alcohol Res 2013;35:128-33.
- Haagsma JA, Polinder S, van Beeck EF, Mulder S, Bonsel GJ. Alternative approaches to derive disability weights in injuries: do they make a difference?. Qual Life Res 2009;18:657-65. http://dx.doi.org/10.1007/s11136-009-9484-0.
- Voigt K, King NB. Disability weights in the global burden of disease 2010 study: two steps forward, one step back?. Bull World Health Organ 2014;92:226-8. http://dx.doi.org/10.2471/BLT.13.126227.
- Laurie EW. Who lives, who dies, who cares? Valuing life through the disability-adjusted life year measurement. Trans Institute British Geographers 2015;40:75-87. http://dx.doi.org/10.1111/tran.12055.
- McDermott S, Turk MA. The myth and reality of disability prevalence: measuring disability for research and service. Disabil Health J 2011;4:1-5. http://dx.doi.org/10.1016/j.dhjo.2010.06.002.
- Murray CJ, Lopez AD. Regional patterns of disability-free life expectancy and disability-adjusted life expectancy: global Burden of Disease Study. Lancet 1997;349:1347-52. http://dx.doi.org/10.1016/S0140-6736(96)07494-6.
- Nord E. Uncertainties about disability weights for the Global Burden of Disease study. Lancet Glob Health 2015;3:e661-2. http://dx.doi.org/10.1016/S2214-109X(15)00189-8.
- Oliver M. Changing the social relations of research production?. Disabil Handicap Soc 1992;7:101-14. http://dx.doi.org/10.1080/02674649266780141.
- Armstrong D. Chronic illness: a revisionist account. Sociol Health Illn 2014;36:15-27. http://dx.doi.org/10.1111/1467-9566.12037.
- Lock M, Nguyen V-K. An Anthropology of Biomedicine. Chichester: John Wiley & Sons; 2010.
- Stuckler D, Basu S. The Body Economic: Why Austerity Kills. New York, NY: Basic Books; 2013.
- Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Association; 2013.
- Biley F, Donlan M. A model for mental handicap nursing. Nurs Stand 1990;4:36-9.
- Broyles RW, McAuley WJ, Baird-Holmes D. The medically vulnerable: their health risks, health status, and use of physician care. J Health Care Poor Underserved 1999;10:186-200. http://dx.doi.org/10.1353/hpu.2010.0498.
- Roulstone A. Disability, dependency and the New Deal for disabled people. Disabil Soc 2000;15:427-43. http://dx.doi.org/10.1080/713661962.
- Schmid AH. The deficiency model: an exploration of current approaches to late-life disorders. Psychiatry 1991;54:358-67.
- Mooney RP, Mooney DR, Cohernour KL. Applied humanism: a model for managing inappropriate behavior among mentally retarded elders. J Gerontol Nurs 1995;21:45-50. http://dx.doi.org/10.3928/0098-9134-19950801-11.
- Stevens P, Martin N. Supporting individuals with intellectual disability and challenging behaviour in integrated work settings: an overview and a model for service provision. J Intellect Disabil Res 1999;43:19-2. http://dx.doi.org/10.1046/j.1365-2788.1999.43120169.x.
- Raikhel E, Kirmayer L, Lemelson R, Cummings C. Re-visioning Psychiatry: Cultural Phenomenology, Critical Neuroscience, and Global Mental Health. Cambridge: Cambridge University Press; 2015.
- Rose NS, Abi-Rached JM. Neuro: The New Brain Sciences and the Management of the Mind. Princeton, NJ: Princeton University Press; 2013.
- Simons RL, Klopack ET. Invited address: the times they are a-changin’ gene expression, neuroplasticity, and developmental research. J Youth Adolesc 2015;44:573-80. http://dx.doi.org/10.1007/s10964-014-0245-1.
- Rose N. The human sciences in a biological age. Theory Culture Soc 2013;30:3-34. http://dx.doi.org/10.1177/0263276412456569.
- Butz WP, Torrey BB. Some frontiers in social science. Science 2006;312:1898-900. http://dx.doi.org/10.1126/science.1130121.
- Tousignant M, Rossignol M, Goulet L, Dassa C. Occupational disability related to back pain: application of a theoretical model of work disability using prospective cohorts of manual workers. Am J Ind Med 2000;37:410-22. http://dx.doi.org/10.1002/(SICI)1097-0274(200004)37:4<410::AID-AJIM11>3.0.CO;2-8.
- Moynihan RN, Cooke GP, Doust JA, Bero L, Hill S, Glasziou PP. Expanding disease definitions in guidelines and expert panel ties to industry: a cross-sectional study of common conditions in the United States. PLOS Med 2013;10. http://dx.doi.org/10.1371/journal.pmed.1001500.
- Linton SJ, Gross D, Schultz IZ, Main C, Côté P, Pransky G, et al. Prognosis and the identification of workers risking disability: research issues and directions for future research. J Occup Rehabil 2005;15:459-74. http://dx.doi.org/10.1007/s10926-005-8028-x.
- Hogsbro K, Pruijt H, Pokrovsky N, Tsobanoglou G, Kalekin-Fishman D, Denis AS. The ISA Handbook in Contemporary Sociology. London: Sage Publications Ltd; 2009.
- Solvang P. The emergence of an us and them discourse in disability theory. Scand J Disabil Res 2000;2:3-20. http://dx.doi.org/10.1080/15017410009510749.
- Hogsbro K. SIMREB–towards a systematic inquiry into models for rehabilitation. Scand J Disabil Res 2010;12:1-18. http://dx.doi.org/10.1080/15017410903338812.
- Llewellyn A, Hogan K. The use and abuse of models of disability. Disabil Soc 2000;15:157-65. http://dx.doi.org/10.1080/09687590025829.
- Oliver M. Understanding Disability: From Theory to Practice. London: Palgrave Macmillan; 1995.
- Barnes C. Rehabilitation for disabled people: a ‘sick’ joke?. Scand J Disabil Res 2003;5:7-23. http://dx.doi.org/10.1080/15017410309512609.
- Shakespeare T. Disability Rights and Wrongs Revisited. Abingdon: Routledge; 2013.
- Gross BH, Hahn H. Developing issues in the classification of mental and physical disabilities. J Disabil Policy Studies 2004;15:130-4. http://dx.doi.org/10.1177/10442073040150030101.
- Felce D. Defining and applying the concept of quality of life. J Intellect Disabil Res 1997;41:126-35. http://dx.doi.org/10.1111/j.1365-2788.1997.tb00689.x.
- Patrick DL. Rethinking prevention for people with disabilities. Part I: a conceptual model for promoting health. Am J Health Promot 1997;11:257-60. http://dx.doi.org/10.4278/0890-1171-11.4.257.
- Jette AM, Keysor JJ. Uses of evidence in disability outcomes and effectiveness research. Milbank Q 2002;80:325-45. http://dx.doi.org/10.1111/1468-0009.t01-1-00006.
- Tricot A. Assessments of the Evaluations of the Application of the ICIDH to the Various Spheres of Rehabilitation and Integration of People with Disabilities. Strasbourg: The Council of Europe; 1996.
- Sussman MB. Sociology and Rehabilitation. Washington, DC: American Sociological Association with the Vocational Rehabilitation Administration; 1965.
- Nagi SZ, Pope AM, Alvin R. Disability in America: Toward a National Agenda for Prevention. Washington, DC: National Academy Press; 1991.
- Jette AM. Toward a common language for function, disability, and health. Phys Ther 2006;86:726-34.
- Fougeyrollas P, St-Michel G, Bergeron N, Cloutier R. The handicap creation process: analysis of the consultation. ICIDH International Network 1991;4:8-37.
- Fougeyrollas P. Documenting environmental factors for preventing the handicap creation process: Quebec contributions relating to ICIDH and social participation of people with functional differences. Disabil Rehabil 1995;17:145-53. http://dx.doi.org/10.3109/09638289509166709.
- Haveman M, Heller T, Lee L, Maaskant M, Shooshtari S, Strydom A. Major health risks in aging persons with intellectual disabilities: an overview of recent studies. J Policy Practice Intellect Disabil 2010;7:59-6. http://dx.doi.org/10.1111/j.1741-1130.2010.00248.x.
- International Classification of Functioning, Disability and Health 1980. Geneva: World Health Organization; 1980.
- Verbrugge LM, Jette AM. The disablement process. Soc Sci Med 1994;38:1-14. http://dx.doi.org/10.1016/0277-9536(94)90294-1.
- Hartley SD, Wirz SL. Development of a ‘communication disability model’ and its implication on service delivery in low-income countries. Soc Sci Med 2002;54:1543-57. http://dx.doi.org/10.1016/S0277-9536(01)00136-8.
- Bickenbach JE, Chatterji S, Badley EM, Üstün TB. Models of disablement, universalism and the international classification of impairments, disabilities and handicaps. Soc Sci Med 1999;48:1173-87. http://dx.doi.org/10.1016/S0277-9536(98)00441-9.
- Tøssebro J. Introduction to the special issue: Understanding disability. Scand J Disabil Res 2004;6:3-7. http://dx.doi.org/10.1080/15017410409512635.
- Bury M. A comment on the ICIDH2. Disabil Soc 2000;15:1073-7. http://dx.doi.org/10.1080/713662025.
- Pfeiffer D. The ICIDH and the need for its revision. Disabil Soc 1998;13:503-23. http://dx.doi.org/10.1080/09687599826579.
- Chapireau F, Colvez A. Social disadvantage in the international classification of impairments, disabilities, and handicap. Soc Sci Med 1998;47:59-66. http://dx.doi.org/10.1016/S0277-9536(98)00033-1.
- Üstün T, Bickenback JE, Badley E, Chatterji S. A Reply to David Pfeiffer ‘The ICIDH and the Need for its Revision’. Disabil Soc 1998;13:829-31. http://dx.doi.org/10.1080/09687599826533.
- Pfeiffer D. The devils are in the details: the ICIDH2 and the disability movement. Disabil Soc 2000;15:1079-82. http://dx.doi.org/10.1080/713662020.
- Towards a Common Language for Functioning, Disability and Health (ICF). Geneva: World Health Organization; 2002.
- International Classification of Functioning, Disability and Health 2001. Geneva: World Health Organization; 2001.
- Schalock RL. The emerging disability paradigm and its implications for policy and practice. J Disabil Policy Stud 2004;14:204-15. http://dx.doi.org/10.1177/10442073040140040201.
- Hurst R. To revise or not to revise?. Disabil Soc 2000;15:1083-7. http://dx.doi.org/10.1080/713662026.
- Kostanjsek N. Use of The International Classification of Functioning, Disability and Health (ICF) as a conceptual framework and common language for disability statistics and health information systems. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-S4-S3.
- Sykes W, Groom C. Developing Standard Disability Survey Questions: A Report on Cognitive Testing. London: Office for Disability Issues; 2009.
- Bickenbach JE. Monitoring the United Nation’s Convention on the Rights of Persons with Disabilities: data and the International Classification of Functioning, Disability and Health. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-S4-S8.
- Escorpizo R, Kostanjsek N, Kennedy C, Nicol MM, Stucki G, Üstün TB. Harmonizing WHO’s International Classification of Diseases (ICD) and International Classification of Functioning, Disability and Health (ICF): importance and methods to link disease and functioning. BMC Public Health 2013;13. http://dx.doi.org/10.1186/1471-2458-13-742.
- International Classification of Functioning, Disability and Health: Children and Youth Version. Geneva: World Health Organization; n.d.
- Üstün B, Chatterji S, Kostanjsek N. Comments from WHO for the Journal of Rehabilitation Medicine Special Supplement on ICF Core Sets. J Rehabil Med 2004;44:7-8.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62.
- Cieza A, Geyh S, Chatterji S, Kostanjsek N, Üstün B, Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med 2005;37:212-8. http://dx.doi.org/10.1080/16501970510040263.
- Dalin R, Rosenberg D. An approach to measurement and statistical description of participation in community life for people with psychiatric disabilities. Scand J Disabil Res 2010;12:47-58. http://dx.doi.org/10.1080/15017410903175693.
- United Nations Statistics Division . Washington Group on Disability Statistics n.d. http://unstats.un.org/unsd/methods/citygroup/washington.htm (accessed February 2016).
- Altman B, Altman B, Barnartt S. International Views on Disability Measures: Moving Towards Comparative Measurement. Bingley: Emerald Group Publishing Ltd; 2006.
- Bickenbach J. The World Report on Disability. Disabil Soc 2011;26:655-8. http://dx.doi.org/10.1080/09687599.2011.589198.
- Mitra S. The capability approach and disability. J Disabil Policy Stud 2006;16:236-47. http://dx.doi.org/10.1177/10442073060160040501.
- Koutsogeorgou E, Leonardi M, Bickenbach JE, Cerniauskaite M, Quintas R, Raggi A. Social capital, disability, and usefulness of the International Classification of Functioning, Disability and Health for the development and monitoring of policy interventions. Disabil Soc 2014;29:1104-16. http://dx.doi.org/10.1080/09687599.2014.910106.
- Harley DA, Mpofu E, Scanlan J, Umeasiegbu VI, Mpofu N, Mpofu E. Community-Oriented Health Services: Practices Across Disciplines. New York, NY: Springer Publishing Company; 2015.
- Groce N, Levy BS, Sidel VW. Social Injustice and Public Health. Oxford: Oxford University Press; 2013.
- Baylies C. Disability and the notion of human development: questions of rights and capabilities. Disabil Soc 2002;17:725-39. http://dx.doi.org/10.1080/0968759022000039037.
- Cerniauskaite M, Quintas R, Boldt C, Raggi A, Cieza A, Bickenbach JE, et al. Systematic literature review on ICF from 2001 to 2009: its use, implementation and operationalisation. Disabil Rehabil 2011;33:281-309. http://dx.doi.org/10.3109/09638288.2010.529235.
- Bickenbach J. Ethics, disability and the International Classification of Functioning, Disability and Health. Am J Phys Med Rehabil 2012;91:163-7. http://dx.doi.org/10.1097/PHM.0b013e31823d5487.
- Whiteneck G, Dijkers MP. Difficult to measure constructs: conceptual and methodological issues concerning participation and environmental factors. Arch Phys Med Rehabil 2009;90:22-35. http://dx.doi.org/10.1016/j.apmr.2009.06.009.
- Dijkers MP. Issues in the conceptualization and measurement of participation: an overview. Arch Phys Med Rehabil 2010;91:5-16. http://dx.doi.org/10.1016/j.apmr.2009.10.036.
- Cieza A, Stucki G. Understanding functioning, disability, and health in rheumatoid arthritis: the basis for rehabilitation care. Curr Opin Rheumatol 2005;17:183-9. http://dx.doi.org/10.1097/01.bor.0000151405.56769.e4.
- Bickenbach JE, Watson N, Roulstone A, Thomas C. Routledge Handbook of Disability Studies. Abingdon: Routledge; 2013.
- Pfeiffer D. The philosophical foundations of disability studies. Disabil Stud Q 2002;22:3-23. http://dx.doi.org/10.18061/dsq.v22i2.341.
- Barile M. Globalization and ICF eugenics: historical coincidence or connection? The more things change the more they stay the same. Disabil Stud Q 2003;23:203-23. http://dx.doi.org/10.18061/dsq.v23i2.425.
- Latimer J. The Gene, the Clinic, and the Family: Diagnosing Dysmorphology, Reviving Medical Dominance. Abingdon: Routledge; 2013.
- Kras JF. The ‘Ransom Notes’ affair: when the neurodiversity movement came of age. Disabil Stud Q 2009;30. http://dx.doi.org/10.18061/dsq.v30i1.1065.
- Ginsburg F, Rapp R. Making disability count: demography, futurity, and the making of disability publics. Somatosphere 2015. http://somatosphere.net/2015/05/making-disability-count-demography-futurity-and-the-making-of-disability-publics.html (accessed May 2016).
- Imrie R. Demystifying disability: a review of the International Classification of Functioning, Disability and Health. Sociol Health Illn 2004;26:287-305. http://dx.doi.org/10.1111/j.1467-9566.2004.00391.x.
- Miles MA. ICIDH meets postmodernism, or ‘incredulity toward meta-terminology’. Disability World 2001;7.
- Finkelstein V. Rethinking Care in a Society Providing Equal Opportunities for All. Geneva: World Health Organization; 1998.
- Pfeiffer D. The disability paradigm. J Disabil Policy Stud 2000;11:98-9. http://dx.doi.org/10.1177/104420730001100209.
- Groce N. Disability and the League of Nations: the Crippled Child’s Bill of Rights and a call for an International Bureau of Information, 1931. Disabil Soc 2014;29:503-15. http://dx.doi.org/10.1080/09687599.2013.831752.
- Kanter AS. The Development of Disability Rights under International Law: From Charity to Human Rights. New York, NY: Routledge; 2014.
- Rioux M, Heath B, Swain J, French S, Barnes C, Thomas C. Disabling Barriers, Enabling Environments. London: Sage Publications Ltd; 2012.
- Barton L. The struggle for citizenship: the case of disabled people. Disabil Handicap Soc 1993;8:235-48. http://dx.doi.org/10.1080/02674649366780251.
- Russell M. What disability civil rights cannot do: employment and political economy. Disabil Soc 2002;17:117-35. http://dx.doi.org/10.1080/09687590120122288.
- Fleischer DZ, Zames F. Disability rights: the overlooked civil rights issue. Disability Stud Q 2005;25. http://dx.doi.org/10.18061/dsq.v25i4.629.
- Heumann JE. Gender issues in disability policy. J Disabil Policy Stud 1997;8:231-3. http://dx.doi.org/10.1177/104420739700800211.
- Jones H. Disabled children’s rights and the UN Convention on the Rights of the Child. Disability Stud Q 2000;20. http://dx.doi.org/10.18061/dsq.v20i4.266.
- United Nations (Office of the High Commissioner) . International Covenant on Economic, Social and Cultural Rights 1976. www.ohchr.org/EN/ProfessionalInterest/Pages/CESCR.aspx (accessed May 2016).
- United Nations (Office of the High Commissioner) . International Covenant on Civil and Political Rights 1976. www.ohchr.org/en/professionalinterest/pages/ccpr.aspx (accessed May 2016).
- The Duty to Promote Disability Equality: Statutory Code of Practice: England and Wales. London: The Stationery Office; 2005.
- Americans With Disabilities Act of 1990 n.d.
- United Nations . World Programme of Action Concerning Disabled Persons 1982. www.independentliving.org/files/WPACDP.pdf (accessed May 2016).
- Hunt P, Mesquita J. Mental disabilities and the human right to the highest attainable standard of health. Human Rights Q 2006;28:332-56. http://dx.doi.org/10.1353/hrq.2006.0019.
- Mégret F. The Disabilities Convention: human rights of persons with disabilities or disability rights?. Human Rights Q 2008;30:494-516. http://dx.doi.org/10.1353/hrq.0.0000.
- Harpur P. Embracing the new disability rights paradigm: the importance of the Convention on the Rights of Persons with Disabilities. Disabil Society 2011;27:1-14. http://dx.doi.org/10.1080/09687599.2012.631794.
- Degener T, Blanck P, Flynn E. Routledge Handbook of Disability Law and Human Rights. Oxford: Routledge; 2016.
- Barnes C. Disability rights: rhetoric and reality in the UK. Disabil Soc 1995;10:111-16. http://dx.doi.org/10.1080/09687599550023769.
- Tisdall EKM. Why not consider citizenship?: A critique of post-school transitional models for young disabled people. Disabil Soc 1994;9:3-17. http://dx.doi.org/10.1080/09687599466780011.
- Shakespeare T. Disability Research Today: International Perspectives. Abingdon: Routledge; 2015.
- Oliver M, Barnes C, Mercer G. Doing Disability Research. Leeds: The Disability Press; 1997.
- Sheldon A, Traustadóttir R, Beresford P, Boxall K, Oliver M. Disability rights and wrongs?. Disabil Soc 2007;22:209-34. http://dx.doi.org/10.1080/09687590701195274.
- Sayce L, O’Brien N. The future of equality and human rights in Britain – opportunities and risks for disabled people. Disabil Soc 2004;19:663-7. http://dx.doi.org/10.1080/0968759042000252560.
- Sayce L. From Psychiatric Patient to Citizen Revisited. London: Palgrave Macmillan; 2016.
- Morris J. Community Care or Independent Living?. York: Joseph Rowntree Foundation; 1993.
- Drewett AY. Social rights and disability: the language of ‘rights’ in community care policies. Disabil Soc 1999;14:115-28. http://dx.doi.org/10.1080/09687599926415.
- Quinn G, Degener T, Bruce A, Burke C, Castellino J, Kenna P, et al. Human Rights and Disability: The Current Use and Future Potential of United Nations Human Rights Instruments in the Context of Disability. New York, NY and Geneva: United Nations Publications; 2002.
- Barnes C, Mercer G. Disability. Cambridge: Polity; 2003.
- Fraser N, Gordon L. “Dependency” demystified: inscriptions of power in a keyword of the welfare state. Social Politics 1994;1:4-31. http://dx.doi.org/10.1093/sp/1.1.4.
- Early Childhood Development and Disability: A Discussion Paper. Geneva: World Health Organization; 2012.
- Thomas C. Theorising disability and chronic illness: where next for perspectives in medical sociology?. Social Theory Health 2012;10:209-28. http://dx.doi.org/10.1057/sth.2012.7.
- Emerson E, Roulstone A. Developing an evidence base for violent and disablist hate crime in Britain: findings from the life opportunities survey. J Interpers Violence 2014;29:3086-104. http://dx.doi.org/10.1177/0886260514534524.
- Heath B. Foreword: “From each according to ability”? Capitalism, poverty, and disability. Canadian J Disabil Stud 2015;4:1-11.
- Moore M. Disability: who counts? What counts?. Disabil Soc 2015;30:671-2. http://dx.doi.org/10.1080/09687599.2015.1061772.
- Yousafzai AK, Lynch P, Gladstone M. Moving beyond prevalence studies: screening and interventions for children with disabilities in low-income and middle-income countries. Arch Dis Child 2014;99:840-8. http://dx.doi.org/10.1136/archdischild-2012-302066.
- Butlin SF. The UN Convention on the Rights of Persons with Disabilities: does the Equality Act 2010 measure up to UK international commitments?. Industrial Law J 2011;40:428-38. http://dx.doi.org/10.1093/indlaw/dwr015.
- Lawson A. Disability and Equality Law in Britain: The Role of Reasonable Adjustment. Oxford: Hart Publishing Ltd; 2008.
- Lawson A. People with psychosocial impairments or conditions, reasonable accommodation and the Convention on the Rights of Persons with Disabilities. Law Context 2008;26.
- Lawson A. Disability and employment in the Equality Act 2010: opportunities seized, lost and generated. Industrial Law J 2011;40:359-83. http://dx.doi.org/10.1093/indlaw/dwr021.
- Young DA, Quibell R. Why rights are never enough: rights, intellectual disability and understanding. Disabil Soc 2000;15:747-64. http://dx.doi.org/10.1080/713661998.
- Flynn E. Disabled Justice?: Access to Justice and the UN Convention on the Rights of Persons with Disabilities. Farnham: Ashgate Publishing Ltd; 2015.
- Silvers A. Moral status: what a bad idea!. J Intellect Disabil Res 2012;56:1014-25. http://dx.doi.org/10.1111/j.1365-2788.2012.01616.x.
- Söder M. Tensions, perspectives and themes in disability studies. Scand J Disabil Res 2009;11:67-81. http://dx.doi.org/10.1080/15017410902830496.
- Barral C. Disabled Persons’ Associations in France. Scand J Disabil Res 2007;9:214-36. http://dx.doi.org/10.1080/15017410701680506.
- Meekosha H, Soldatic K. Human rights and the Global South: The case of disability. Third World Q 2011;32:1383-97. http://dx.doi.org/10.1080/01436597.2011.614800.
- Skempes D, Stucki G, Bickenbach J. Health-related rehabilitation and human rights: analyzing states’ obligations under the United Nations Convention on the Rights of Persons with Disabilities. Arch Phys Med Rehabil 2015;96:163-73. http://dx.doi.org/10.1016/j.apmr.2014.07.410.
- Skempes D, Bickenbach J. Developing human rights based indicators to support country monitoring of rehabilitation services and programmes for people with disabilities: a study protocol. BMC Int Health Hum Rights 2015;15. http://dx.doi.org/10.1186/s12914-015-0063-x.
- Isaac R, Dharma Raja BW, Ravanan MP. Integrating people with disabilities: their right – our responsibility. Disabil Soc 2010;25:627-30. http://dx.doi.org/10.1080/09687599.2010.489314.
- Shakespeare T, Watson N. Defending the social model. Disabil Soc 1997;12:293-300. http://dx.doi.org/10.1080/09687599727380.
- Shakespeare T, Watson N, Altman B, Barnartt S. Exploring theories and Expanding Methodologies: Where We Are and Where We Need To Go. Bingley: Emerald Group Publishing Ltd; 2001.
- Shakespeare T. Social models of disability and other life strategies. Scand J Disabil Res 2004;6:8-21. http://dx.doi.org/10.1080/15017410409512636.
- Thomas C. Rescuing a social relational understanding of disability. Scand J Disabil Res 2004;6:22-36. http://dx.doi.org/10.1080/15017410409512637.
- Campbell J, Oliver M. Disability Politics: Understanding Our Past, Changing Our Future. Abingdon: Routledge; 1996.
- Finkelstein V. Phase 3: Conceptualising New Services n.d. http://pf7d7vi404s1dxh27mla5569.wpengine.netdna-cdn.com/files/library/finkelstein-Phase-3-Conceptualising-New-Services.pdf (accessed May 2016).
- Thomas C, Swain J, French S, Barnes C, Thomas C. Disabling Barriers – Enabling Environments. London: Sage Publications Ltd; 2012.
- Barnes C, Watson N, Roulstone A, Thomas C. The Routledge Handbook of Disability Studies. Abingdon: Routledge; 2012.
- Fundamental Principles of Disability. London: UPIAS; 1976.
- Finkelstein V, Brechin A, Liddiard P, Swain J. Handicap in a Social World: A Reader. London: Hodder Arnold; 1981.
- Oliver M. The Politics of Disablement. London: Palgrave Macmillan; 1990.
- Barnes C. Disabled People in Britain and Discrimination: A Case for Anti-Discrimination Legislation. London: C. Hurst & Co. Publishers; 1991.
- Oliver M. Social Work with Disabled People. London and Basingstoke: Macmillan; 1983.
- Goodley D. ‘Learning Difficulties’, the social model of disability and impairment: challenging epistemologies. Disabil Soc 2001;16:207-31. http://dx.doi.org/10.1080/09687590120035816.
- Thomas C. How is disability understood? An examination of sociological approaches. Disabil Soc 2004;19:569-83. http://dx.doi.org/10.1080/0968759042000252506.
- Reeve D. Negotiating psycho-emotional dimensions of disability and their influence on identity constructions. Disabil Soc 2002;17:493-508. http://dx.doi.org/10.1080/09687590220148487.
- Thomas C. Disability: getting it “right”. J Med Ethics 2008;34:15-7. http://dx.doi.org/10.1136/jme.2006.019943.
- Williams-Findlay R. Lifting the lid on Disabled People Against Cuts. Disabil Soc 2011;26:773-8. http://dx.doi.org/10.1080/09687599.2011.602868.
- Hunt P. Stigma: The Experience of Disability. London: Geoffrey Chapman; 1966.
- Barnes C. Reflections on Doing Emancipatory Disability Research. London: Sage Publications Ltd; 2014.
- Beresford P, Barnes CM, Mercer G. Doing Disability Research. Leeds: Disability Press; 2004.
- Charlton JI. Nothing About Us Without Us: Disability Oppression and Empowerment. Berkeley, CA: University of California Press; 1998.
- Gleeson B. Geographies of Disability. London: Routledge; 1999.
- Hahn H, Barnes C, Barton L, Oliver M. Disability Studies Today. Cambridge: Polity Press; 2002.
- Barnes C, Mercer G. Disability, work, and welfare challenging the social exclusion of disabled people. Work Employment Soc 2005;19:527-45. http://dx.doi.org/10.1177/0950017005055669.
- Graby S. Access to work or liberation from work? Disabled people, autonomy, and post-work politics. Can J Disabil Stud 2015;4:132-61.
- Swain J, French S. Towards an affirmation model of disability. Disabil Soc 2000;15:569-82. http://dx.doi.org/10.1080/09687590050058189.
- Swain J, French S, Barnes C, Thomas C. Disabling Barriers – Enabling Environments. London: Sage Publications Ltd; 2013.
- Burchardt T. Capabilities and disability: the capabilities framework and the social model of disability. Disabil Soc 2004;19:735-51. http://dx.doi.org/10.1080/0968759042000284213.
- Bérubé M. Life As We Know It: A Father, A Family, and An Exceptional Child. New York, NY: Pantheon; 1996.
- Young IM. Inclusion and Democracy. Oxford: Oxford University Press; 2002.
- Kittay EF, Jennings B, Wasunna AA. Dependency, difference and the global ethic of longterm care. J Pol Philosophy 2005;13:443-69. http://dx.doi.org/10.1111/j.1467-9760.2005.00232.x.
- Kittay EF. Love’s Labor: Essays on Women, Equality and Dependency. Abingdon: Routledge; 2013.
- Tregaskis C. Social model theory: the story so far …. Disabil Soc 2002;17:457-70. http://dx.doi.org/10.1080/09687590220140377.
- McWade B, Milton D, Beresford P. Mad studies and neurodiversity: a dialogue. Disabil Soc 2015;30:305-9. http://dx.doi.org/10.1080/09687599.2014.1000512.
- Graby S, Spandler H, Anderson J, Sapey B. Madness, Distress and the Politics of Disablement. Bristol: Policy Press; 2015.
- Beresford P, Wallcraft J, Barnes C, Mercer G. Doing Disability Research. Leeds: Disability Press; 1997.
- Silberman S. NeuroTribes: The Legacy of Autism and How to Think Smarter About People Who Think Differently. Crows Nest, NSW: Allen & Unwin; 2015.
- Waltz M. Autism: A Social and Medical History. Basingstoke: Palgrave Macmillan; 2013.
- Ladd P. Understanding Deaf Culture: In Search of Deafhood. Clevedon: Multilingual Matters; 2003.
- Berghs M. War and Embodied Memory: Becoming Disabled in Sierra Leone. Abingdon: Routledge; 2016.
- Corbett J. A proud label - exploring the relationship between disability politics and gay pride. Disabil Soc 1994;9:343-57. http://dx.doi.org/10.1080/09687599466780381.
- Atkin K, Ahmad WI, Jones L. Young South Asian deaf people and their families: negotiating relationships and identities. Sociol Health Illn 2002;24:21-45. http://dx.doi.org/10.1111/1467-9566.00002.
- Morris J. Personal and political: a feminist perspective on researching physical disability. Disabil Handicap Soc 1992;7:157-66. http://dx.doi.org/10.1080/02674649266780181.
- Thomas C. Female Forms: Experiencing and Understanding Disability. Buckingham: Open University Press; 1999.
- Asch A. Critical race theory, feminism, and disability: reflections on social justice and personal identity. Ohio St L J 2001;62.
- Garland-Thomson R. Integrating disability, transforming feminist theory. NWSA J 2002;14:1-32. http://dx.doi.org/10.2979/NWS.2002.14.3.1.
- Corker M, Shakespeare T, Corker M, Shakespeare T. Disability/Postmodernity: Embodying Disability Theory. New York, NY: Continuum; 2002.
- Tremain S, Tremain S. Foucault and the Government of Disability. Ann Arbor, MI: University of Michigan Press; 2005.
- Priestley M. Constructions and creations: idealism, materialism and disability theory. Disabil Soc 1998;13:75-94. http://dx.doi.org/10.1080/09687599826920.
- Hughes B, Paterson K. The social model of disability and the disappearing body: towards a sociology of impairment. Disability Soc 1997;12:325-40. http://dx.doi.org/10.1080/09687599727209.
- Davis LJ. Enforcing Normalcy: Disability, Deafness, and the Body. London: Verso; 1995.
- Mitchell DT, Snyder SL. Narrative Prosthesis: Disability and the Dependencies of Discourse. Ann Arbor, MI: University of Michigan Press; 2000.
- Thomson RG. Extraordinary Bodies: Figuring Physical Disability in American Culture and Literature. New York, NY: Columbia University Press; 1997.
- Foucault M. Madness and Civilisation. London: Vintage Books; 2006.
- Derrida J. Writing and Difference. London: Routledge; 2001.
- Gabel S, Peters S. Presage of a paradigm shift? Beyond the social model of disability toward resistance theories of disability. Disability Soc 2004;19:585-600. http://dx.doi.org/10.1080/0968759042000252515.
- Campbell FAK. Exploring internalized ableism using critical race theory. Disability Soc 2008;23:151-62. http://dx.doi.org/10.1080/09687590701841190.
- Bhaskar R, Danermark B. Metatheory, interdisciplinarity and disability research: a critical realist perspective. Scand J Disabil Res 2006;8:278-97. http://dx.doi.org/10.1080/15017410600914329.
- Gustavsson A. The role of theory in disability research-springboard or strait-jacket?. Scand J Disabil Res 2004;6:55-70. http://dx.doi.org/10.1080/15017410409512639.
- Michailakis D. The systems theory concept of disability: one is not born a disabled person, one is observed to be one. Disabil Soc 2003;18:209-29. http://dx.doi.org/10.1080/0968759032000044184.
- Galis V. Enacting disability: how can science and technology studies inform disability studies?. Disabil Soc 2011;26:825-38. http://dx.doi.org/10.1080/09687599.2011.618737.
- Meekosha H, Shuttleworth R. What is so critical about critical disability studies?. Aust J Hum Rights 2009;15:47-75.
- Meekosha H, Shuttleworth R, Soldatic K. Disability and critical sociology: expanding the boundaries of critical social inquiry. Crit Sociol 2013;39:319-23. http://dx.doi.org/10.1177/0896920512471220.
- Sadjadi R, Conaway M, Cutter G, Sanders DB, Burns TM. Psychometric evaluation of the myasthenia gravis composite using Rasch analysis. Muscle Nerve 2012;45:820-5. http://dx.doi.org/10.1002/mus.23260.
- Goodley D. Dis/entangling critical disability studies. Disabil Soc 2013;28:631-44. http://dx.doi.org/10.1080/09687599.2012.717884.
- Siebers T. Disability Theory. Ann Arbor, MI: University of Michigan Press; 2008.
- Campbell FK. Contours of Ableism: Territories, Objects, Disability and Desire. London: Palgrave Macmillan; 2009.
- Beresford P, Nettle M, Perring R. Towards a Social Model of Madness and Distress. Exploring What Service Users Say. York: Joseph Rowntree Foundation; 2010.
- LeFrançois BA, Menzies R, Reaume G. Mad Matters: A Critical Reader in Canadian Mad Studies. Toronto, ON: Canadian Scholars’ Press; 2013.
- Derbyshire Coalition of Disabled People . ‘Patient’ Empowerment With Specific Reference to Disabled People: A Response to the Department of Health ‘Patients Charter’, 1992 1992. http://disability-studies.leeds.ac.uk/files/library/Derbyshire-CIL-patients.pdf (accessed May 2016).
- Russo J, Beresford P. Between exclusion and colonisation: seeking a place for mad people’s knowledge in academia. Disabil Soc 2014;30:153-7. http://dx.doi.org/10.1080/09687599.2014.957925.
- Shildrick M. Leaky Bodies and Boundaries: Feminism, Postmodernism and (Bio)Ethics. London: Routledge; 1997.
- Soldatic K, Grech S. Transnationalising disability studies: rights, justice and impairment. Disabil Stud Q 2014;34. http://dx.doi.org/10.18061/dsq.v34i2.4249.
- McRuer R. Crip Theory: Cultural Signs of Queerness and Disability. New York, NY: New York University Press; 2006.
- Jain SL. Living in prognosis: toward an elegiac politics. Representations 2007;98:77-92. http://dx.doi.org/10.1525/rep.2007.98.1.77.
- Puar JK, Davis LJ. The Disability Studies Reader. New York, NY: Routledge; 2013.
- Fritsch K. Gradations of debility and capacity: biocapitalism and the neoliberalization of disability relations. Can J Disabil Stud 2015;4:12-48.
- Vehmas S, Watson N. Moral wrongs, disadvantages, and disability: a critique of critical disability studies. Disabil Soc 2013;29:638-50. http://dx.doi.org/10.1080/09687599.2013.831751.
- Bauman Z. Intimations of Postmodernity. Abingdon: Routledge; 2003.
- Perlin ML. Things have changed: looking at non-institutional mental disability law through the sanism filter. NY Law Sch Law Rev 2003;19:165-75.
- Ferrie J, Watson N, Shakespeare T. Disability Research Today: International Perspectives. Abingdon: Routledge; 2015.
- Connell R. Southern bodies and disability: re-thinking concepts. Third World Q 2011;32:1369-81. http://dx.doi.org/10.1080/01436597.2011.614799.
- WHO Action Plan: “Better Health for Persons With Disabilities”. Geneva: World Health Organization; 2015.
- Closing the Gap: Policy Into Practice on Social Determinants of Health: Discussion Paper. Geneva: World Health Organization; 2011.
- Roulstone A, Mason-Bish H. Disability, Hate Crime and Violence. London: Routledge; 2012.
- Sherry M. Disability Hate Crimes: Does Anyone Really Hate Disabled People?. Farnham: Ashgate Publishing; 2012.
- Hollomotz A. Beyond ‘vulnerability’: an ecological model approach to conceptualizing risk of sexual violence against people with learning difficulties. Br J Social Work 2009;39:99-112. http://dx.doi.org/10.1093/bjsw/bcm091.
- Graham H, Kelly MP. Health Inequalities: Concepts, Frameworks and Policy. London: Health Development Agency; 2004.
- Hogg J. Intellectual disability and ageing: ecological perspectives from recent research. J Intellect Disabil Res 1997;41:136-43. http://dx.doi.org/10.1111/j.1365-2788.1997.tb00690.x.
- Barr B, Taylor-Robinson D, Stuckler D, Loopstra R, Reeves A, Whitehead M. ‘First, do no harm’: are disability assessments associated with adverse trends in mental health? A longitudinal ecological study. J Epidemiol Community Health 2015;70:339-45. http://dx.doi.org/10.1136/jech-2015-206209.
- Minkler M, Fadem P. “Successful Aging:”: a disability perspective. J Disabil Policy Stud 2002;12:229-35. http://dx.doi.org/10.1177/104420730201200402.
- Verdugo MA, Navas P, Gómez LE, Schalock RL. The concept of quality of life and its role in enhancing human rights in the field of intellectual disability. J Intellect Disabil Res 2012;56:1036-45. http://dx.doi.org/10.1111/j.1365-2788.2012.01585.x.
- Emerson E, Kariuki M, Honey A, Llewellyn G. Becoming disabled: the association between disability onset in younger adults and subsequent changes in productive engagement, social support, financial hardship and subjective wellbeing. Disabil Health J 2014;7:448-56. http://dx.doi.org/10.1016/j.dhjo.2014.03.004.
- Marmot M, Wilkinson R. Social Determinants of Health. Oxford: Oxford University Press; 2006.
- Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health: Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008.
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 2008;372:1661-9. http://dx.doi.org/10.1016/S0140-6736(08)61690-6.
- Kwok H. A 10-year review of a Hong Kong model for mental health care of people with intellectual disability. Isr J Psychiatry Relat Sci 2006;43:252-7.
- Health in the Post-2015 Development Agenda: NEED for A Social Determinants of Health Approach, Joint Statement of the UN Platform on Social Determinants of Health. Geneva: World Health Organization; 2013.
- Dora C, Haines A, Balbus J, Fletcher E, Adair-Rohani H, Alabaster G, et al. Indicators linking health and sustainability in the post-2015 development agenda. Lancet 2015;385:380-91. http://dx.doi.org/10.1016/S0140-6736(14)60605-X.
- Buck D, Maguire D. Inequalities in Life Expectancy. Changes Over Time and Implications for Policy. London: The King’s Fund; 2015.
- Beresford P. Poverty and disabled people: challenging dominant debates and policies. Disability Soc 1996;11:553-68. http://dx.doi.org/10.1080/09687599627598.
- Yeo R. Chronic Poverty and Disability. Frome: Centre for Action on Disability and Development; 2001.
- Burchardt T. Being and Becoming (Case Report 21 Prepared for the Joseph Rowntree Foundation) 2003.
- Emerson E. Deprivation, ethnicity and the prevalence of intellectual and developmental disabilities. J Epidemiol Community Health 2012;66:218-24. http://dx.doi.org/10.1136/jech.2010.111773.
- Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Soc Sci Med 2015;128:316-26. http://dx.doi.org/10.1016/j.socscimed.2014.12.031.
- Disability-Free Life Expectancy by Upper Tier Local Authority: England 2009-11 and comparison with 2006-08. Newport: Office for National Statistics; 2014.
- Wolff J, De-Shalit A. Disadvantage. Oxford: Oxford University Press; 2013.
- Groce N, Kembhavi G, Wirz S, Lang R, Trani J-F, Kett M. Poverty and Disability. A Critical Review of the Literature in Low and Middle-Income Countries. London: Leonard Cheshire Disability and Inclusive Development Centre; 2011.
- Whitehead M, Dahlgren G, Evans T. Equity and health sector reforms: can low-income countries escape the medical poverty trap?. Lancet 2001;358:833-6. http://dx.doi.org/10.1016/S0140-6736(01)05975-X.
- Nguyen V-K, Peschard K. Anthropology, inequality, and disease: a review. Ann Rev Anthropology 2003;32:447-74.
- Hill D, Lucy D, Tyers C, James L. What Works at Work. Review of Evidence Assessing the Effectiveness of Workplace Interventions to Prevent and Manage Common Health Problems. Norwich: Institute for Employment Studies for Health Work and Wellbeing Executive; 2007.
- Boardman J. Social exclusion and mental health-how people with mental health problems are disadvantaged: an overview. Mental Health Social Inclusion 2011;15:112-21. http://dx.doi.org/10.1108/20428301111165690.
- Ipsos MORI. Disabled People and Financial Wellbeing. London: SCOPE; 2013.
- MacInnes T, Tinson A, Gaffney D, Horgan G, Baumberg B. Disability, Long Term Conditions and Poverty. A Report for the Joseph Rowntree Foundation. London: New Policy Institute; 2014.
- Waddell G, Burton AK, Kendall NAS. Vocational Rehabilitation. What Works, For Whom, and When? Report for the Vocational Rehabilitation Task Group. London: The Stationery Office; 2008.
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 1997;349:1498-504. http://dx.doi.org/10.1016/S0140-6736(96)07492-2.
- Banerjee S. The Use of Antipsychotic Medication for People with Dementia: Time for Action. London: Department of Health; 2009.
- Durham J, Brolan CE, Mukandi B. The Convention on the Rights of Persons with Disabilities: a foundation for ethical disability and health research in developing countries. Am J Public Health 2014;104:2037-43. http://dx.doi.org/10.2105/AJPH.2014.302006.
- Cook D, Moore-Cox A, Xavier D, Lauzier F, Roberts I. Randomized trials in vulnerable populations. Clin Trials 2008;5:61-9. http://dx.doi.org/10.1177/1740774507087552.
- Iacono T, Carling-Jenkins R. The human rights context for ethical requirements for involving people with intellectual disability in medical research. J Intellect Disabil Res 2012;56:1122-32. http://dx.doi.org/10.1111/j.1365-2788.2012.01617.x.
- Mackintosh J, White M, Howel D, Chadwick T, Moffatt S, Deverill M, et al. Randomised controlled trial of welfare rights advice accessed via primary health care: pilot study [ISRCTN61522618]. BMC Public Health 2006;6. http://dx.doi.org/10.1186/1471-2458-6-162.
- Thomson H, Hoskins R, Petticrew M, Ogilvie D, Craig N, Quinn T, et al. Evaluating the health effects of social interventions. BMJ 2004;328:282-5. http://dx.doi.org/10.1136/bmj.328.7434.282.
- Groce NE, Rohleder P, Eide AH, MacLachlan M, Mall S, Swartz L. HIV issues and people with disabilities: a review and agenda for research. Soc Sci Med 2013;77:31-40. http://dx.doi.org/10.1016/j.socscimed.2012.10.024.
- Donovan J, Mills N, Smith M, Brindle L, Jacoby A, Peters T, et al. Quality improvement report: Improving design and conduct of randomised trials by embedding them in qualitative research: ProtecT (prostate testing for cancer and treatment) study. Commentary: presenting unbiased information to patients can be difficult. BMJ 2002;325:766-70. http://dx.doi.org/10.1136/bmj.325.7367.766.
- Brolan CE, Boyle FM, Dean JH, Taylor Gomez M, Ware RS, Lennox NG. Health advocacy: a vital step in attaining human rights for adults with intellectual disability. J Intellect Disabil Res 2012;56:1087-97. http://dx.doi.org/10.1111/j.1365-2788.2012.01637.x.
- Chan J, French P, Webber L. Positive behavioural support and the UNCRPD. Int J Positive Behavioural Support 2011;1:7-13.
- Waters E, Petticrew M, Priest N, Weightman A, Harden A, Doyle J. Evidence synthesis, upstream determinants and health inequalities: the role of a proposed new Cochrane Public Health Review Group. Eur J Public Health 2008;18:221-3. http://dx.doi.org/10.1093/eurpub/ckm127.
- West K. The grip of personalisation in adult social care: between managerial domination and fantasy. Critical Social Policy 2013;33:638-57. http://dx.doi.org/10.1177/0261018313481563.
- Kessler R, Glasgow RE. A proposal to speed translation of healthcare research into practice: dramatic change is needed. Am J Prev Med 2011;40:637-44. http://dx.doi.org/10.1016/j.amepre.2011.02.023.
- Gaglio B, Phillips SM, Heurtin-Roberts S, Sanchez MA, Glasgow RE. How pragmatic is it? Lessons learned using PRECIS and RE-AIM for determining pragmatic characteristics of research. Implement Sci 2014;9. http://dx.doi.org/10.1186/s13012-014-0096-x.
- Babulal GM, Bakhshi P, Kopriva S, Ali SA, Goette SA, Trani JF. Measuring participation for persons with mental illness: a systematic review assessing relevance of existing scales for low and middle income countries. BMC Psychol 2015;3. http://dx.doi.org/10.1186/s40359-015-0093-0.
- Pols J, Limburg S. A matter of taste? Quality of Life in day-to-day living with ALS and a feeding tube [published online ahead of print November 7 2015]. Cult Med Psychiatry 2015. http://dx.doi.org/10.1007/s11013-015-9479-y.
- Macefield RC, Jacobs M, Korfage IJ, Nicklin J, Whistance RN, Brookes ST, et al. Developing core outcomes sets: methods for identifying and including patient-reported outcomes (PROs). Trials 2014;15. http://dx.doi.org/10.1186/1745-6215-15-49.
- Morris C, Janssens A, Allard A, Thompson Coon J, Shilling V, Tomlinson R, et al. Informing the NHS Outcomes Framework: Evaluating Meaningful Health Outcomes for Children With Neurodisability Using Multiple Methods Including Systematic Review, Qualitative Research, Delphi Survey and Consensus Meeting 2014. http://eprints.whiterose.ac.uk/80851/ (accessed May 2016).
- Boonen A, Stucki G, Maksymowych W, Rat AC, Escorpizo R, Boers M. The OMERACT-ICF Reference Group: integrating the ICF into the OMERACT process: opportunities and challenges. J Rheumatol 2009;36:2057-60. http://dx.doi.org/10.3899/jrheum.090357.
- Sen A. Commodities and Capabilities. Oxford: Oxford University Press; 1999.
- Coast J, Flynn TN, Natarajan L, Sproston K, Lewis J, Louviere JJ, et al. Valuing the ICECAP capability index for older people. Soc Sci Med 2008;67:874-82. http://dx.doi.org/10.1016/j.socscimed.2008.05.015.
- Simon J, Anand P, Gray A, Rugkåsa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Soc Sci Med 2013;98:187-96. http://dx.doi.org/10.1016/j.socscimed.2013.09.019.
- Ara R, Wailoo A. NICE DSU Technical Support Document 12: The Use of Health State Utility Values in Decision Models. Sheffield: School of Health and Related Research, University of Sheffield; 2011.
- Longworth L, Rowen D. Mapping to obtain EQ-5D utility values for use in NICE health technology assessments. Value Health 2013;16:202-10. http://dx.doi.org/10.1016/j.jval.2012.10.010.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. http://dx.doi.org/10.1016/j.jval.2012.02.008.
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. http://dx.doi.org/10.1007/s11136-010-9648-y.
- Holland T, Clare IC, Mukhopadhyay T. Prevalence of criminal offending by men and women with intellectual disability and the characteristics of offenders: implications for research and service development. J Intellect Disabil Res 2002;46:6-20. http://dx.doi.org/10.1046/j.1365-2788.2002.00001.x.
- Duxbury J, Aiken F, Dale C. Deaths in custody: the role of restraint. J Learning Disabil Offending Behav 2011;2:178-89. http://dx.doi.org/10.1108/20420921111207873.
- Case A, Deaton A, Wise D. Insights in the Economics of Aging. Chicago, IL: University of Chicago Press; 2016.
- Nosek MA, Hughes RB, Taylor HB, Taylor P. Disability, psychosocial, and demographic characteristics of abused women with physical disabilities. Violence Against Women 2006;12:838-50. http://dx.doi.org/10.1177/1077801206292671.
- McDonald KE, Keys CB, Balcazar FE. Disability, race/ethnicity and gender: themes of cultural oppression, acts of individual resistance. Am J Community Psychol 2007;39:145-61. http://dx.doi.org/10.1007/s10464-007-9094-3.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30:473-83. http://dx.doi.org/10.1097/00005650-199206000-00002.
- Stevens J, Killeen M. A randomised controlled trial testing the impact of exercise on cognitive symptoms and disability of residents with dementia. Contemp Nurse 2006;21:32-40. http://dx.doi.org/10.5172/conu.2006.21.1.32.
- Dixon A, Le Grand J, Henderson J, Murray R, Poteliakhoff E. Is the NHS Equitable? A Review of the Evidence. London: London School of Economics and Political Science; 2011.
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12. http://dx.doi.org/10.1002/14651858.cd001871.pub3.
- Thomson H, Thomas S, Sellstrom E, Petticrew M. Housing improvements for health and associated socio-economic outcomes. Cochrane Database Syst Rev 2013;2. http://dx.doi.org/10.1002/14651858.cd008657.pub2.
- Pega F, Carter K, Blakely T, Lucas PJ. In-work Tax Credits for Families and their Impact on Health Status in Adults. Cochrane Database Syst Rev 2013;8. http://dx.doi.org/10.1002/14651858.cd009963.pub2.
- Jahanfar S, Howard LM, Medley N. Interventions for preventing or reducing domestic violence against pregnant women. Cochrane Database Syst Rev 2014;11. http://dx.doi.org/10.1002/14651858.cd009414.pub3.
- Adler AJ, Taylor F, Martin N, Gottlieb S, Taylor RS, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease. Sao Paulo Med J 2015;133:280-1. http://dx.doi.org/10.1590/1516-3180.20151333T2.
- Dyson L, McCormick FM, Renfrew MJ. Interventions for promoting the initiation of breastfeeding. Cochrane Database Syst Rev 2005;2. http://dx.doi.org/10.1002/14651858.cd001688.pub2.
- Siegfried N, Pienaar DC, Ataguba JE, Volmink J, Kredo T, Jere M, et al. Restricting or banning alcohol advertising to reduce alcohol consumption in adults and adolescents. Cochrane Database Syst Rev 2014;11. http://dx.doi.org/10.1002/14651858.cd010704.pub2.
- Johnston V, Liberato S, Thomas D. Incentives for preventing smoking in children and adolescents. Cochrane Database Syst Rev 2012;10. http://dx.doi.org/10.1002/14651858.cd008645.pub2.
- Ker K, Chinnock P. Interventions in the alcohol server setting for preventing injuries. Cochrane Database Syst Rev 2006;2. http://dx.doi.org/10.1002/14651858.cd005244.pub2.
- Cashman CM, Ruotsalainen JH, Greiner BA, Beirne PV, Verbeek JH. Alcohol and drug screening of occupational drivers for preventing injury. Cochrane Database Syst Rev 2009;2. http://dx.doi.org/10.1002/14651858.cd006566.pub2.
- Bailey JV, Murray E, Rait G, Mercer GH, Morris RW, Peacock R, et al. Interactive computer-based interventions for sexual health promotion. Cochrane Database Syst Rev 2010;9. http://dx.doi.org/10.1002/14651858.cd006483.pub2.
- Oringanje C, Meremikwu MM, Eko H, Esu E, Meremikwu A, Ehiri JE. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database Syst Rev 2009;4. http://dx.doi.org/10.1002/14651858.cd005215.pub2.
- van den Broek N, Dou L, Othman M, Neilson JP, Gates S, Gülmezoglu AM. Vitamin A supplementation during pregnancy for maternal and newborn outcomes. Cochrane Database Syst Rev 2010;11. http://dx.doi.org/10.1002/14651858.cd008666.pub2.
- Jefferson T, Di Pietrantonj C, Al-Ansary LA, Ferroni E, Thorning S, Thomas RE. Vaccines for preventing influenza in the elderly. Cochrane Database Syst Rev 2010;2. http://dx.doi.org/10.1002/14651858.cd004876.pub3.
- Langford R, Bonell CP, Jones HE, Pouliou P, Murphy SM, Waters E, et al. The WHO health promoting school framework for improving the health and wellbeing of students and their academic achievement. Cochrane Database Syst Rev 2014;4.
- Joyce K, Pabayo R, Critchley JA, Bambra C. Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst Rev 2010;2. http://dx.doi.org/10.1002/14651858.cd008009.pub2.
- Hosking J, Macmillan A, Connor J, Bullen C, Ameratunga S. Organisational travel plans for improving health. Cochrane Database Syst Rev 2010;3. http://dx.doi.org/10.1002/14651858.cd005575.pub3.
- Hayes SL, Mann MK, Morgan FM, Kelly MK, Weightman AL. Collaboration between local health and local government agencies for health improvement. Cochrane Database Syst Rev 2012;3. http://dx.doi.org/10.1002/14651858.cd007825.pub6.
- Baker PRA, Francis DP, Soares J, Weightman AL, Foster C. Community wide interventions for increasing physical activity. Cochrane Database Syst Rev 2015;1. http://dx.doi.org/10.1002/14651858.cd008366.pub3.
- Spinks A, Turner C, Nixon J, McClure RJ. The ‘WHO Safe Communities’ model for the prevention of injury in whole populations. Cochrane Database Syst Rev 2008;3. http://dx.doi.org/10.1002/14651858.CD004445.pub3.
- Foxcroft DR, Moreira MT, Almeida Santimano NML, Smith LA. Social norms interventions to reduce alcohol misuse in university or college students. Cochrane Database Syst Rev 2015;1. http://dx.doi.org/10.1002/14651858.CD006748.pub2.
- Grilli R, Ramsay C, Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database Syst Rev 2002;1. http://dx.doi.org/10.1002/14651858.cd000389.
- Dennis JA, Khan O, Ferriter M, Huband N, Powney MJ, Duggan C. Psychological interventions for adults who have sexually offended or are at risk of offending. Cochrane Database Syst Rev 2012;12. http://dx.doi.org/10.1002/14651858.cd007507.pub2.
- Callinan JE, Clarke A, Doherty K, Kelleher C. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev 2010;4. http://dx.doi.org/10.1002/14651858.cd005992.pub2.
- Ehiri JE, Ejere HO, Magnussen L, Emusu D, King W, Osberg JS. Interventions for promoting booster seat use in four to eight year olds traveling in motor vehicles. Cochrane Database Syst Rev 2006;1. http://dx.doi.org/10.1002/ebch.51.
- Coppo A, Galanti MR, Giordano L, Buscemi D, Bremberg S, Faggiano F. School policies for preventing smoking among young people. Cochrane Database Syst Rev 2014;10. http://dx.doi.org/10.1002/14651858.cd009990.pub2.
- Wilson C, Willis C, Hendrikz JK, Le Brocque R, Bellamy N. Speed cameras for the prevention of road traffic injuries and deaths. Cochrane Database Syst Rev 2010;11. http://dx.doi.org/10.1002/14651858.cd004607.pub3.
- Marcano Belisario JS, Bruggeling MN, Gunn LH, Brusamento S, Car J. Interventions for recruiting smokers into cessation programmes. Cochrane Database Syst Rev 2012;12. http://dx.doi.org/10.1002/14651858.cd009187.pub2.
- Yeung A, Hitchings JL, Macfarlane TV, Threlfall A, Tickle M, Glenny A-M. Fluoridated milk for preventing dental caries. Cochrane Database Syst Rev 2005;3. http://dx.doi.org/10.1002/14651858.cd003876.pub2.
- Breckenridge JP, Devaney J, Kroll T, Lazenbatt A, Taylor J, Bradbury-Jones C. Access and utilisation of maternity care for disabled women who experience domestic abuse: a systematic review. BMC Pregnancy Childbirth 2014;14. http://dx.doi.org/10.1186/1471-2393-14-234.
- Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health 2015;105:198-206. http://dx.doi.org/10.2105/AJPH.2014.302182.
- Obesity and Disability. London: Public Health England; 2013.
- Gatineau M. Obesity and Disability: Children and Young People. London: Public Health England; 2014.
- Ashman L, Duggan L. Interventions for learning disabled sex offenders. Cochrane Database Syst Rev 2008;1. http://dx.doi.org/10.1002/14651858.cd003682.pub2.
- Mayo-Wilson E, Montgomery P. Media-delivered cognitive behavioural therapy and behavioural therapy (self-help) for anxiety disorders in adults. Cochrane Database Syst Rev 2013;9. http://dx.doi.org/10.1002/14651858.cd005330.pub4.
- Kaufman J, Synnot A, Ryan R, Hill S, Horey D, Willis N, et al. Face to face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev 2013;5. http://dx.doi.org/10.1002/14651858.cd010038.pub2.
- Curioni C, André C, Veras R. Weight reduction for primary prevention of stroke in adults with overweight or obesity. Cochrane Database Syst Rev 2006;4. http://dx.doi.org/10.1002/14651858.cd006062.pub2.
- Duperrex O, Blackhall K, Burri M, Jeannot E. Education of children and adolescents for the prevention of dog bite injuries. Cochrane Database Syst Rev 2009;2. http://dx.doi.org/10.1002/14651858.cd004726.pub2.
- Austin MP, Priest SR, Sullivan EA. Antenatal psychosocial assessment for reducing perinatal mental health morbidity. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd005124.pub2.
- Jacobson Vann JC, Szilagyi P. Patient reminder and recall systems to improve immunisation rates. Cochrane Database Syst Rev 2005;3. http://dx.doi.org/10.1002/14651858.CD003941.pub2.
- Fong CJ, Murphy K, Westbrook JD, Markle M. Behavioral, psychological, educational and vocational interventions to facilitate employment outcomes for cancer survivors: a systematic review. Campbell Syst Rev 2015;11.
- Grant S, Parsons A, Burton J, Montgomery P, Underhill K, Mayo-Wilson E. Home visits for prevention of impairment and death in older adults: a systematic review. Campbell Syst Rev 2014;3.
- De La Rue L, Polanin J, Espelage D, Pigott T. School based intervention to reduce dating and sexual violence: a systematic review. Campbell Syst Rev 2014;7.
- Regehr C, Alaggia R, Dennis J, Pitts A, Saini M. Interventions to reduce distress in adult victims of sexual violence and rape: a systematic review. Campbell Syst Rev 2013;3. http://dx.doi.org/10.1177/1049731512474103.
- Coren E, Hossain R, Pardo JP, Veras M, Chakraborty K, Harris H, et al. Interventions for promoting reintegration and reducing harmful behaviour and lifestyles in street-connected children and young people: a systematic review. Campbell Syst Rev 2013;6. http://dx.doi.org/10.1002/14651858.cd009823.pub2.
- Gensby U, Lund T, Kowalski K, Saidj M, Klint Jørgensen A-M, Filges T, et al. Workplace disability management programs promoting return to work: a systematic review. Campbell Syst Rev 2012;17.
- Coren E, Hutchfield J, Thomae M, Gustafsson C. Parent-training interventions to support intellectually disabled parents: a systematic review. Campbell Syst Rev 2010;3.
- Ramsay J, Carter Y, Davidson L, Dunne D, Eldridge S, Feder G, et al. Advocacy interventions to reduce or eliminate violence and promote the physical and psychosocial well-being of women who experience intimate partner abuse. Cochrane Database Syst Rev 2009;3. http://dx.doi.org/10.1002/14651858.cd005043.pub2.
- Mayo-Wilson E, Montgomery P, Dennis JA. Personal assistance for adults (19-64) with both physical and intellectual impairments. Cochrane Database Syst Rev 2008;2. http://dx.doi.org/10.1002/14651858.cd006860.pub2.
- Mayo-Wilson E, Montgomery P, Dennis JA. Personal assistance for adults (19-64) with physical impairments. Cochrane Database Syst Rev 2008;3. http://dx.doi.org/10.1002/14651858.cd006856.pub2.
- Mayo-Wilson E, Montgomery P, Dennis JA. Personal assistance for children and adolescents (0-18) with intellectual impairments. Campbell Syst Rev 2008;4.
- Mayo-Wilson E, Montgomery P, Dennis JA. Personal assistance for children and adolescents (0-18) with both physical and intellectual impairments. Cochrane Database Syst Rev 2008;3. http://dx.doi.org/10.1002/14651858.cd006859.pub2.
- Zwi KJ, Woolfenden SR, Wheeler DM, O’Brien TA, Tait P, Williams KW. School-based education programmes for the prevention of child sexual abuse. Cochrane Database Syst Rev 2007;3. http://dx.doi.org/10.1002/14651858.cd004380.pub2.
- Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev 2011;10. http://dx.doi.org/10.1002/14651858.cd003236.pub2.
- Adeniyi FB, Young T. Weight loss interventions for chronic asthma. Cochrane Database Syst Rev 2012;7. http://dx.doi.org/10.1002/14651858.cd009339.pub2.
- Martin AJ, Marottoli R, O’Neill D. Driving assessment for maintaining mobility and safety in drivers with dementia. Cochrane Database Syst Rev 2013;8. http://dx.doi.org/10.1002/14651858.cd006222.pub3.
- van Oostrom SH, Driessen MT, de Vet HC, Franche RL, Schonstein E, Loisel P, et al. Workplace interventions for preventing work disability. Cochrane Database Syst Rev 2009;2. http://dx.doi.org/10.1002/14651858.cd006955.pub2.
- Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev 2014;9. http://dx.doi.org/10.1002/14651858.cd000963.pub3.
- De Silva M, Maclachlan M, Devane D, Desmond D, Gallagher P, Schnyder U, et al. Psychosocial interventions for the prevention of disability following traumatic physical injury. Cochrane Database Syst Rev 2009;4. http://dx.doi.org/10.1002/14651858.cd006422.pub3.
- Marteau TM, French DP, Griffin SJ, Prevost AT, Sutton S, Watkinson C, et al. Effects of communicating DNA-based disease risk estimates on risk-reducing behaviours. Cochrane Database Syst Rev 2010;10. http://dx.doi.org/10.1002/14651858.cd007275.pub2.
- Mastellos N, Gunn LH, Felix LM, Car J, Majeed A. Transtheoretical model stages of change for dietary and physical exercise modification in weight loss management for overweight and obese adults. Cochrane Database Syst Rev 2014;2. http://dx.doi.org/10.1002/14651858.cd008066.pub3.
- Khan F, Ng L, Turner-Stokes L. Effectiveness of vocational rehabilitation intervention on the return to work and employment of persons with multiple sclerosis. Cochrane Database Syst Rev 2009;1. http://dx.doi.org/10.1002/14651858.cd007256.pub2.
- Martin JJ. Benefits and barriers to physical activity for individuals with disabilities: a social-relational model of disability perspective. Disabil Rehabil 2013;35:2030-7. http://dx.doi.org/10.3109/09638288.2013.802377.
- Karanika-Murray M, Weyman AK. Optimising workplace interventions for health and well-being: a commentary on the limitations of the public health perspective within the workplace health arena. Int J Workplace Health Management 2013;6:104-17. http://dx.doi.org/10.1108/IJWHM-11-2011-0024.
- Feldman M. Editorial: cost-benefit of effective interventions. J Developmental Disabil 1998;6:i-vi.
- Emerson E, Hatton C, Robertson J, Baines S. Perceptions of neighbourhood quality, social and civic participation and the self rated health of British adults with intellectual disability: cross sectional study. BMC Public Health 2014;14. http://dx.doi.org/10.1186/1471-2458-14-1252.
- Emerson E, Vick B, Rechel B, Muñoz-Baell I, Sørensen J, Färm I. Social Exclusion, Disadvantage, Vulnerability and Health Inequalities. A Task Group Supporting the Marmot Region Review of Social Determinants of Health and the Health Divide in the EURO Region. Background Paper 5: Health Inequalities and People With Disabilities in Europe n.d. www.researchgate.net/profile/Eric_Emerson/publication/277078091_Health_Inequalities_and_People_with_Disabilities_in_Europe_Background_Paper_5_for_the_Social_Exclusion_Disadvantage_Vulnerability_and_Health_Inequalities_task_group_supporting_the_Marmot_region_review_of_social_determinants_of_health_and_the_health_divide_in_the_EURO_region/links/5561698f08ae9963a119fd50.pdf (accessed May 2016).
- Beavis J, Kerr M, Marson AG, Dojcinov I. Non-pharmacological interventions for epilepsy in people with intellectual disabilities. Cochrane Database Syst Rev 2007;17. http://dx.doi.org/10.1002/14651858.cd005502.pub2.
- Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry 2014;14. http://dx.doi.org/10.1186/1471-244X-14-39.
- Angelopoulos PD, Milionis HJ, Grammatikaki E, Moschonis G, Manios Y. Changes in BMI and blood pressure after a school based intervention: the CHILDREN study. Eur J Public Health 2009;19. http://dx.doi.org/10.1093/eurpub/ckp004.
- Araújo-Soares V, McIntyre T, MacLennan G, Sniehotta FF. Development and exploratory cluster-randomised opportunistic trial of a theory-based intervention to enhance physical activity among adolescents. Psychol Health 2009;24:805-22. http://dx.doi.org/10.1080/08870440802040707.
- Barbeau P, Johnson MH, Howe CA, Allison J, Davis CL, Gutin B, et al. Ten months of exercise improves general and visceral adiposity, bone, and fitness in black girls. Obesity 2007;15:2077-85. http://dx.doi.org/10.1038/oby.2007.247.
- Bayne-Smith M, Fardy PS, Azzollini A, Magel J, Schmitz KH, Agin D. Improvements in heart health behaviors and reduction in coronary artery disease risk factors in urban teenaged girls through a school-based intervention: the PATH program. Am J Public Health 2004;94:1538-43. http://dx.doi.org/10.2105/AJPH.94.9.1538.
- Burke V, Milligan RA, Thompson C, Taggart AC, Dunbar DL, Spencer MJ, et al. A controlled trial of health promotion programs in 11-year-olds using physical activity enrichment for higher risk children. J Pediatr 1998;132:840-8. http://dx.doi.org/10.1016/S0022-3476(98)70315-4.
- Bush PJ, Zuckerman AE, Theiss PK, Taggart VS, Horowitz C, Sheridan MJ, et al. Cardiovascular risk factor prevention in black schoolchildren: two-year results of the Know Your Body program. Am J Epidemiol 1989;129:466-82.
- Colin-Ramirez E, Castillo-Martinez L, Orea-Tejeda A, Vergara-Castaneda A, Keirns-Davis C, Villa-Romero A. Outcomes of a school-based intervention (RESCATE) to improve physical activity patterns in Mexican children aged 8-10 years. Health Educ Res 2010;25:1042-9. http://dx.doi.org/10.1093/her/cyq056.
- Dishman RK, Motl RW, Saunders R, Felton G, Ward DS, Dowda M, et al. Self-efficacy partially mediates the effect of a school-based physical-activity intervention among adolescent girls. Prev Med 2004;38:628-36. http://dx.doi.org/10.1016/j.ypmed.2003.12.007.
- Ewart CK, Loftus K, Hagberg JM. School-based exercise to lower blood pressure in high-risk African American girls: project design and baseline findings. J Health Educ 1995;26:99-105.
- Gentile DA, Welk G, Eisenmann JC, Reimer RA, Walsh DA, Russell DW, et al. Evaluation of a multiple ecological level child obesity prevention program: switch what you do, view, and chew. BMC Med 2009;7. http://dx.doi.org/10.1186/1741-7015-7-49.
- Haerens L, Deforche B, Maes L, Cardon G, Stevens V, De Bourdeaudhuij I. Evaluation of a 2-year physical activity and healthy eating intervention in middle school children. Health Educ Res 2006;21:911-21. http://dx.doi.org/10.1093/her/cyl115.
- Haerens L, Maes L, Vereecken C, De Henauw S, Moreno L, De Bourdeaudhuij I. Effectiveness of a computer tailored physical activity intervention in adolescents compared to a generic advice. Patient Educ Couns 2009;77:38-41. http://dx.doi.org/10.1016/j.pec.2009.03.020.
- Jones D, Hoelscher DM, Kelder SH, Hergenroeder A, Sharma SV. Increasing physical activity and decreasing sedentary activity in adolescent girls – The Incorporating More Physical Activity and Calcium in Teens (IMPACT) study. Int J Behav Nutr Phys Activ 2008;5. http://dx.doi.org/10.1186/1479-5868-5-42.
- Kipping RR, Payne C, Lawlor DA. Randomised controlled trial adapting US school obesity prevention to England. Arch Dis Child 2008;93:469-73. http://dx.doi.org/10.1136/adc.2007.116970.
- Kriemler S, Zahner L, Schindler C, Meyer U, Hartmann T, Hebestreit H, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c785.
- Li YP, Hu XQ, Schouten EG, Liu AL, Du SM, Li LZ, et al. Report on childhood obesity in China (8): effects and sustainability of physical activity intervention on body composition of Chinese youth. Biomed Environ Sci 2010;23:180-7. http://dx.doi.org/10.1016/S0895-3988(10)60050-5.
- Lubans DR, Morgan PJ, Callister R, Collins CE. Effects of integrating pedometers, parental materials, and e-mail support within an extracurricular school sport intervention. J Adolesc Health 2009;44:176-83. http://dx.doi.org/10.1016/j.jadohealth.2008.06.020.
- Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. Outcomes of a field trial to improve children’s dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health (CATCH) collaborative group. JAMA 1996;275:768-76. http://dx.doi.org/10.1001/jama.1996.03530340032026.
- Martinez VM, Aguilar FS, Gutierrez RF, Martinez MS, Lopez MS, Martinez SS, et al. Assessment of an after-school physical activity program to prevent obesity among 9- to 10-year-old children: a cluster randomized trial. Int J Obesity 2008;32:12-2. http://dx.doi.org/10.1038/sj.ijo.0803738.
- McManus AM, Masters RS, Laukkanen RM, Yu CC, Sit CH, Ling FC. Using heart-rate feedback to increase physical activity in children. Prev Med 2008;47:402-8. http://dx.doi.org/10.1016/j.ypmed.2008.06.001.
- Neumark-Sztainer D, Haines J, Robinson-O’Brien R, Hannan PJ, Robins M, Morris B, et al. ‘Ready. Set. ACTION!’ A theater-based obesity prevention program for children: a feasibility study. Health Educ Res 2009;24:407-20. http://dx.doi.org/10.1093/her/cyn036.
- Peralta LR, Jones RA, Okely AD. Promoting healthy lifestyles among adolescent boys: the Fitness Improvement and Lifestyle Awareness Program RCT. Prev Med 2009;48:537-42. http://dx.doi.org/10.1016/j.ypmed.2009.04.007.
- Petchers MK, Hirsch EZ, Bloch BA. A longitudinal study of the impact of a school heart health curriculum. J Community Health 1988;13:85-94. http://dx.doi.org/10.1007/BF01364203.
- Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA 1999;282:1561-7. http://dx.doi.org/10.1001/jama.282.16.1561.
- Salmon J, Ball K, Crawford D, Booth M, Telford A, Hume C, et al. Reducing sedentary behaviour and increasing physical activity among 10-year-old children: overview and process evaluation of the ‘Switch-Play’ intervention. Health Promotion Int 2005;20:7-17. http://dx.doi.org/10.1093/heapro/dah502.
- Simon C, Schweitzer B, Oujaa M, Wagner A, Arveiler D, Triby E, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obesity 2008;32.
- Singh AS, Chin A, Paw MJ, Brug J, van Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med 2009;163:309-17. http://dx.doi.org/10.1001/archpediatrics.2009.2.
- Singhal N, Misra A, Shah P, Gulati S. Effects of controlled school-based multi-component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India. Eur J Clin Nutr 2010;64:364-73. http://dx.doi.org/10.1038/ejcn.2009.150.
- Stephens M, Wentz S. Supplemental fitness activities and fitness in urban elementary school classrooms. Family Med 1998;30:220-3.
- Stone EJ, Norman JE, Davis SM, Stewart D, Clay TE, Caballero B, et al. Design, implementation, and quality control in the Pathways American-Indian multicenter trial. Prev Med 2003;37:13-2. http://dx.doi.org/10.1016/j.ypmed.2003.08.006.
- Verstraete SJ, Cardon GM, De Clercq DL, De Bourdeaudhuij IM. Increasing children’s physical activity levels during recess periods in elementary schools: the effects of providing game equipment. Eur J Public Health 2006;16:415-9. http://dx.doi.org/10.1093/eurpub/ckl008.
- Walter HJ, Hofman A, Vaughan RD, Wynder EL. Modification of risk factors for coronary heart disease. Five-year results of a school-based intervention trial. N Engl J Med 1988;318:1093-100. http://dx.doi.org/10.1056/NEJM198804283181704.
- Walther C, Gaede L, Adams V, Gelbrich G, Leichtle A, Erbs S, et al. Effect of increased exercise in school children on physical fitness and endothelial progenitor cells: a prospective randomized trial. Circulation 2009;120:2251-9. http://dx.doi.org/10.1161/CIRCULATIONAHA.109.865808.
- Wang LY, Gutin B, Barbeau P, Moore JB, Hanes J, Johnson MH, et al. Cost-effectiveness of a school-based obesity prevention program. J Sch Health 2008;78:619-24. http://dx.doi.org/10.1111/j.1746-1561.2008.00357.x.
- Webber LS, Catellier DJ, Lytle LA, Murray DM, Pratt CA, Young DR, et al. Promoting physical activity in middle school girls: Trial of Activity for Adolescent Girls. Am J Prev Med 2008;34:173-84. http://dx.doi.org/10.1016/j.amepre.2007.11.018.
- Weeks BK, Young CM, Beck BR. Eight months of regular in-school jumping improves indices of bone strength in adolescent boys and girls: the POWER PE study. J Bone Miner Res 2008;23:1002-11. http://dx.doi.org/10.1359/jbmr.080226.
- Williamson DA, Copeland AL, Anton SD, Champagne C, Han H, Lewis L, et al. Wise Mind project: a school-based environmental approach for preventing weight gain in children. Obesity 2007;15:906-17. http://dx.doi.org/10.1038/oby.2007.597.
- Wilson DK, Van Horn ML, Kitzman-Ulrich H, Saunders R, Pate R, Lawman HG, et al. Results of the “Active by Choice Today” (ACT) randomized trial for increasing physical activity in low-income and minority adolescents. Health Psychol 2011;30:463-71. http://dx.doi.org/10.1037/a0023390.
- Young DR, Phillips JA, Yu T, Haythornthwaite JA. Effects of a life skills intervention for increasing physical activity in adolescent girls. Arch Pediatr Adolesc Med 2006;160:1255-61. http://dx.doi.org/10.1001/archpedi.160.12.1255.
- Chaufan C, Yeh J, Ross L, Fox P. You can’t walk or bike yourself out of the health effects of poverty: active school transport, child obesity, and blind spots in the public health literature. Critical Public Health 2015;25:32-47. http://dx.doi.org/10.1080/09581596.2014.920078.
- Sherlaw W, Lucas B, Jourdain A, Monaghan N. Disabled people, inclusion and policy: better outcomes through a public health approach?. Disabil Soc 2013;29:444-59. http://dx.doi.org/10.1080/09687599.2013.816628.
- Christofoletti G, Oliani MM, Gobbi S, Stella F, Gobbi LTB, Canineu PR. A controlled clinical trial on the effects of motor intervention on balance and cognition in institutionalized elderly patients with dementia. Clin Rehabil 2008;22:618-26. http://dx.doi.org/10.1177/0269215507086239.
- Coelho FG, Andrade LP, Pedroso RV, Santos-Galduroz RF, Gobbi S, Costa JL, et al. Multimodal exercise intervention improves frontal cognitive functions and gait in Alzheimer’s disease: a controlled trial. Geriatr Gerontol Int 2013;13:198-203. http://dx.doi.org/10.1111/j.1447-0594.2012.00887.x.
- Cott CA, Dawson P, Sidani S, Wells D. The effects of a walking/talking program on communication, ambulation, and functional status in residents with Alzheimer disease. Alzheimer Dis Assoc Disord 2002;16:81-7. http://dx.doi.org/10.1097/00002093-200204000-00005.
- Eggermont LH, Swaab DF, Hol EM, Scherder EJ. Walking the line: a randomised trial on the effects of a short term walking programme on cognition in dementia. J Neurol Neurosurg Psychiatry 2009;80:802-4. http://dx.doi.org/10.1136/jnnp.2008.158444.
- Garuffi M, Costa JLR, Hernández SSS, Vital TM, Stein AM, dos Santos JG, et al. Effects of resistance training on the performance of activities of daily living in patients with Alzheimer’s disease. Geriatr Gerontol Int 2013;13:322-28. http://dx.doi.org/10.1111/j.1447-0594.2012.00899.x.
- Hauer K, Schwenk M, Zieschang T, Essig M, Becker C, Oster P. Physical training improves motor performance in people with dementia: a randomized controlled trial. J Am Geriatr Soc 2012;60:8-15. http://dx.doi.org/10.1111/j.1532-5415.2011.03778.x.
- Kemoun G, Thibaud M, Roumagne N, Carette P, Albinet C, Toussaint L, et al. Effects of a physical training programme on cognitive function and walking efficiency in elderly persons with dementia. Dement Geriatr Cogn Disord 2010;29:109-14. http://dx.doi.org/10.1159/000272435.
- Kwak YS, Um SY, Son TG, Kim DJ. Effect of regular exercise on senile dementia patients. Int J Sports Med 2008;29:471-4. http://dx.doi.org/10.1055/s-2007-964853.
- Roach KE, Tappen RM, Kirk-Sanchez N, Williams CL, Loewenstein D. A randomized controlled trial of an activity specific exercise program for individuals with Alzheimer disease in long-term care settings. J Geriatr Phys Ther 2011;34:50-6. http://dx.doi.org/10.1519/JPT.0b013e31820aab9c.
- Rolland Y, Pillard F, Klapouszczak A, Reynish E, Thomas D, Andrieu S, et al. Exercise program for nursing home residents with Alzheimer’s disease: a 1-year randomized, controlled trial. J Am Geriatr Soc 2007;55:158-65. http://dx.doi.org/10.1111/j.1532-5415.2007.01035.x.
- Santana-Sosa E, Barriopedro MI, López-Mojares LM, Pérez M, Lucia A. Exercise training is beneficial for Alzheimer’s patients. Int J Sports Med 2008;29:845-50. http://dx.doi.org/10.1055/s-2008-1038432.
- Steinberg M, Leoutsakos JM, Podewils LJ, Lyketsos CG. Evaluation of a home-based exercise program in the treatment of Alzheimer’s disease: the Maximizing Independence in Dementia (MIND) study. Int J Geriatr Psychiatry 2009;24:680-5. http://dx.doi.org/10.1002/gps.2175.
- Tappen RM, Roach KE, Applegate EB, Stowell P. Effect of a combined walking and conversation intervention on functional mobility of nursing home residents with Alzheimer disease. Alzheimer Dis Assoc Disord 2000;14:196-201. http://dx.doi.org/10.1097/00002093-200010000-00002.
- Teri L, Gibbons LE, McCurry SM, Logsdon RG, Buchner DM, Barlow WE, et al. Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA 2003;290:2015-22. http://dx.doi.org/10.1001/jama.290.15.2015.
- Van de Winckel A, Feys H, De Weerdt W, Dom R. Cognitive and behavioural effects of music-based exercises in patients with dementia. Clin Rehabil 2004;18:253-60. http://dx.doi.org/10.1191/0269215504cr750oa.
- Venturelli M, Scarsini R, Schena F. Six-month walking program changes cognitive and ADL performance in patients with Alzheimer. Am J Alzheimers Dis Other Demen 2011;26:381-8. http://dx.doi.org/10.1177/1533317511418956.
- Boyd CM, Fortin M. Future of multimorbidity research: how should understanding of multimorbidity inform health system design. Public Health Rev 2010;32:451-74.
- Boyd V. Are some disabilities more equal than others? Conceptualising fluctuating or recurring impairments within contemporary legislation and practice. Disabil Soc 2012;27:459-69. http://dx.doi.org/10.1080/09687599.2012.662828.
- Frances AJ, Nardo JM. ICD-11 should not repeat the mistakes made by DSM-5. Br J Psychiatry 2013;203:1-2. http://dx.doi.org/10.1192/bjp.bp.113.127647.
- Jenkins C, Smythe A. Reflections on a visit to a dementia care village. Nurs Older People 2013;25:14-9. http://dx.doi.org/10.7748/nop2013.07.25.6.14.e478.
- Bartlett R. Citizenship in action: the lived experiences of citizens with dementia who campaign for social change. Disabil Soc 2014;29:1291-304. http://dx.doi.org/10.1080/09687599.2014.924905.
- Tomlinson M, Swartz L, Officer A, Chan KY, Rudan I, Saxena S. Research priorities for health of people with disabilities: an expert opinion exercise. Lancet 2009;374:1857-62. http://dx.doi.org/10.1016/S0140-6736(09)61910-3.
- Whitehead M, Dahlgren G. What can be done about inequalities in health?. Lancet 1991;338:1059-63. http://dx.doi.org/10.1016/0140-6736(91)91911-D.
- Beckfield J, Bambra C, Eikemo TA, Huijts T, McNamara C, Wendt C. An institutional theory of welfare state effects on the distribution of population health. Soc Theory Health 2015;13:227-44. http://dx.doi.org/10.1057/sth.2015.19.
- Kapilashrami A, Hill S, Meer N. What can health inequalities researchers learn from an intersectionality perspective? Understanding social dynamics with an inter-categorical approach?. Soc Theory Health 2015;13:288-307. http://dx.doi.org/10.1057/sth.2015.16.
- Lewis K. Participation of People with a Learning Disability in Medical Research. London: Mencap; 2014.
- Death by Indifference: 74 Deaths and Counting. A Progress Report 5 years on. London: Mencap; 2012.
- Mihalopoulos C, Vos T, Pirkis J, Carter R. The population cost-effectiveness of interventions designed to prevent childhood depression. Pediatrics 2012;129:e723-30. http://dx.doi.org/10.1542/peds.2011-1823.
- Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract 2012;18:12-8. http://dx.doi.org/10.1111/j.1365-2753.2010.01516.x.
- Titchkosky T, Aubrecht K. WHO’s MIND, whose future? Mental health projects as colonial logics. Social Identities 2015;21:69-84. http://dx.doi.org/10.1080/13504630.2014.996994.
- Pawson R, Sridharan S, Killoran A, Kelly MP. Evidence-Based Public Health: Effectiveness and Efficiency. Oxford: Oxford University Press; 2010.
- Hanlon P, Carlisle S, Hannah M, Reilly D, Lyon A. Making the case for a ‘fifth wave’ in public health. Public Health 2011;125:30-6. http://dx.doi.org/10.1016/j.puhe.2010.09.004.
- Ogilvie D, Egan M, Hamilton V, Petticrew M. Systematic reviews of health effects of social interventions: 2. Best available evidence: how low should you go?. J Epidemiol Community Health 2005;59:886-92. http://dx.doi.org/10.1136/jech.2005.034199.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review–a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. http://dx.doi.org/10.1258/1355819054308530.
- Bonell C, Fletcher A, Morton M, Lorenc T, Moore L. Realist randomised controlled trials: a new approach to evaluating complex public health interventions. Soc Sci Med 2012;75:2299-306. http://dx.doi.org/10.1016/j.socscimed.2012.08.032.
- Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health 2013;67:190-3. http://dx.doi.org/10.1136/jech-2012-201257.
- Taylor C, Gutmann A. Multiculturalism: Examining the Politics of Recognition. Chichester: Princeton University Press; 1994.
- Farrer L, Marinetti C, Cavaco YK, Costongs C. Advocacy for health equity: a synthesis review. Milbank Q 2015;93:392-437. http://dx.doi.org/10.1111/1468-0009.12112.
- Schrecker T, Bambra C. How Politics Makes Us Sick: Neoliberal Epidemics. London: Palgrave Macmillan; 2015.
- It’s Okay to Ask. London: NIHR; 2015.
- Join Dementia Research. London: NIHR; 2015.
- Mehdipanah R, Manzano A, Borrell C, Malmusi D, Rodriguez-Sanz M, Greenhalgh J, et al. Exploring complex causal pathways between urban renewal, health and health inequality using a theory-driven realist approach. Soc Sci Med 2015;124:266-74. http://dx.doi.org/10.1016/j.socscimed.2014.11.050.
- Trotter R. Over-Looked Communities, Over-Due Change: How Services can Better Support BME Disabled People. London: Scope; 2012.
- Iwarsson S, Ståhl A. Accessibility, usability and universal design–positioning and definition of concepts describing person-environment relationships. Disabil Rehabil 2003;25:57-66. http://dx.doi.org/10.1080/dre.25.2.57.66.
- Imrie R, Hall P. Inclusive Design: Designing and Developing Accessible Environments. London: Spoon Press; 2001.
- Richards L, Morse JM. README FIRST for a User’s Guide to Qualitative Methods. London: Sage Publications Ltd; 2012.
- Creswell JW. Qualitative Enquiry and Research Design: Choosing Among Five Approaches. London: Sage Publications Ltd; 2007.
- Bradbury-Jones C, Taylor J, Herber O. How theory is used and articulated in qualitative research: development of a new typology. Soc Sci Med 2014;120:135-41. http://dx.doi.org/10.1016/j.socscimed.2014.09.014.
- Lorgelly PK, Lawson KD, Fenwick EA, Briggs AH. Outcome measurement in economic evaluations of public health interventions: a role for the capability approach?. Int J Environ Res Public Health 2010;7:2274-89. http://dx.doi.org/10.3390/ijerph7052274.
- Panter-Brick C. Street children, human rights, and public health: a critique and future directions. Ann Rev Anthropology 2002;31:147-71. http://dx.doi.org/10.1146/annurev.anthro.31.040402.085359.
- Harrison TC, Umberson D, Lin LC, Cheng HR, Cheng HR. Timing of impairment and health-promoting lifestyles in women with disabilities. Qual Health Res 2010;20:816-29. http://dx.doi.org/10.1177/1049732310362987.
- Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med 1999;48:977-88. http://dx.doi.org/10.1016/S0277-9536(98)00411-0.
- Brown I, Hatton C, Emerson E. Quality of life indicators for individuals with intellectual disabilities: extending current practice. Intellect Dev Disabil 2013;51:316-32. http://dx.doi.org/10.1352/1934-9556-51.5.316.
- Sayer A. Class, moral worth and recognition. Sociology 2005;39:947-63. http://dx.doi.org/10.1177/0038038505058376.
- Sayer A. The Moral Significance of Class. Cambridge: Cambridge University Press; 2005.
- Wilkinson RG. Socioeconomic determinants of health: health inequalities: relative or absolute material standards?. BMJ 1997;314. http://dx.doi.org/10.1136/bmj.314.7080.591.
- Marmot MG. The Status Syndrome: How Social Standing Affects our Health and Longevity. Basingstoke: Macmillan; 2004.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
Appendix 1 Implications for public health research of models and theories of disability: a scoping review project flow diagram
Appendix 2 Data extraction table for identifying models and theories of disability
| Article | |
| Summary | |
| Description of model | |
| Visual |
Appendix 3 Flow charts for stage 2 scoping
Appendix 4 Effective public health practice project quality assessment tool
As recommended by the Effective Public Health Practice project website (see www.ephpp.ca/tools.html), there are seven steps in the quality assessment tool, as follows:
-
Question formulation: intended to guide the review process and provide boundaries for the searching of the literature.
-
Literature search and retrieval: electronic databases are searched with a series of terms organised around the topic of interest.
-
Determining relevance criteria: intended to establish unique relevance criteria, including a description of the population of interest, interventions, outcomes and study design.
-
Assessment of literature for relevance and quality: independent assessment by two reviewers using established relevance criteria. Assessment includes an examination of sampling strategy, response and follow-up rates, intervention integrity, statistical analyses and assessment of adjustment for confounders.
-
Data extraction and synthesis: data of relevance to the research question will be extracted from studies that have achieved the highest methodological rating. These findings are presented in a narrative synthesis. Meta-analysis is done when appropriate. The report is peer reviewed, that is the written report is scrutinised by external experts.
-
Peer review of the report: synthesis of information and creation of a written report for peer review by five or more public health experts.
-
Dissemination: this involves active dissemination strategies in order to promote use by public health professionals and uptake of the review results.
Appendix 5 Extraction table for the second stage of the scoping: scoping interventions
| Intervention | Inclusion/exclusion of disability | Paradigm | Outcome measures | Interventions included (if two or more studies are published by the same author in the same year, the first one is taken to interrogate, and if more than one study refers to the same trial, the published one referred to is interrogated) |
|---|---|---|---|---|
Appendix 6 Charting individual evaluations of public health interventions
| Interventions | Dignity | Inclusion | Intersectionality | Accessibility | Equity |
|---|---|---|---|---|---|
| Fox et al.134 | Examples: Informed consent was given? How? Were participants treated in a dignified manner? Was the research disability sensitive? Accountability? Participatory design? Integration in implementation? |
How was disability included in the trial? How was disability defined? Were people excluded if they had disabilities or specific impairments, conditions or mental health issues? Link to outcome measures? Was this effective inclusion to allow participation? |
Attention paid to:
|
Is this trial and the settings accessible? Were reasonable accommodations or adaptations made? Did accessibility reflect adoption? |
Is the review connected to an issue linked to equity? Was theory linked to equity? Was there or will there be maintenance of intervention effects? |
Appendix 7 Contacting the corresponding authors
Dear (name of corresponding author)
My colleagues at the University of York (Professors Graham and Atkin) and Lancaster University (Professors Hatton and Thomas) in the United Kingdom are working on a project funded by the National Institute for Health Research Public Health Research programme called Implications for Public Health: Theories and Models of Disability.
You can read more about the project here: www.york.ac.uk/healthsciences/research/public-health/projects/theories-of-disability/.
This is a review of public health interventions. We are also interrogating some reviews from the Cochrane Database of Systematic Reviews in greater detail. Your study is a part of one review that we are analysing. We would be very grateful if you could give us some further background information about your trial or direct us to where we could find this information.
-
Were any disabled children/adolescents included in the trial? By disability we understand this being inclusive of children/adolescents with physical impairments and/or mental health conditions. (1 = definitely yes; 2 = probably yes; 3 = not sure; 4 = probably no; 5 = definitely no.)
-
If disabled children/adolescents were included did you need to do anything to make your study more accessible or inclusive for them? Please explain. If they were not included do you think your study could have included them with reasonable accommodations? Please explain.
-
You collected data on ethnicity, age and gender but we wondered if you also collected data on socioeconomic status, comorbidities or chronic conditions? (1 = definitely yes; 2 = probably yes; 3 = not sure; 4 = probably no; 5 = definitely no.)
It would be very helpful to us to gain an understanding of these issues. If you have any further questions about our study please do not hesitate to get in touch.
With best wishes
Adapted from Feldman et al. 92
Appendix 8 Briefing
A human rights toolkit for public health research
What is the study about?
Public health interventions that are effective in the general population are often assumed to apply to people with disabilities. However, evidence for this is limited and there is a need for more inclusive and better informed research. Given the public health challenges facing the UK population, it is especially important to ensure that interventions are relevant to people’s lives.
Randomised controlled trials are viewed as the gold standard of research in public health and are becoming increasingly influential in terms of policy. However, these are not always inclusive.
To address this problem, we want to develop a toolkit to help inform ‘disability’-sensitive and ethical research. We want your advice on how to develop this toolkit and, more specifically, on how researchers can do better research. No prior knowledge of research is needed to take part in the discussions.
Why human rights?
Human rights are becoming increasingly influential in informing how research should be conducted. Article 3 of the UN CRPD defines these rights as:
-
respect for inherent dignity, individual autonomy including the freedom to make one’s own choices, and independence of persons;
-
non-discrimination;
-
full and effective participation and inclusion in society;
-
respect for difference and acceptance of persons with disabilities as part of human diversity and humanity;
-
equality of opportunity;
-
accessibility;
-
equality between men and women;
-
respect for the evolving capacities of children with disabilities and respect for the right of children with disabilities to preserve their identities. 22
What does our toolkit look like?
Our proposed toolkit focuses on dignity, inclusion, intersectionality, accessibility and equity.
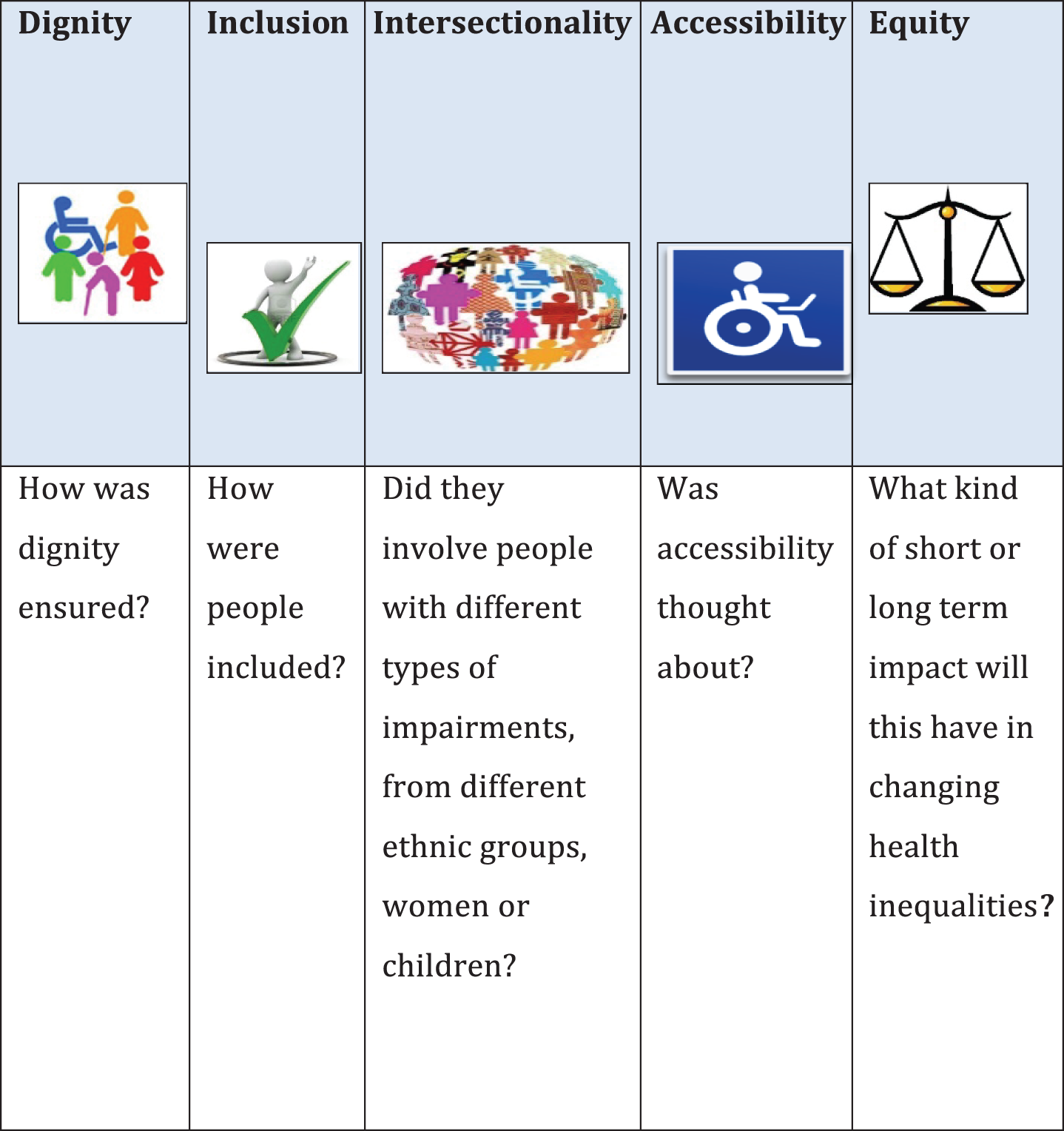
Why a panel?
We are still developing and trying to improve our toolkit. We want to know what you think about it. How well do you think it reflects the needs of people? Will it help researchers to be ethical and respectful and to protect human rights?
Appendix 9 Letter confirming ethical approval
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- ADL
- activities of daily living
- BME
- black and minority ethnic
- CDS
- critical disability studies
- CRPD
- Convention on the Rights of Persons with Disabilities
- CSRI
- Client Service User Receipt Inventory
- DALY
- disability-adjusted life-year
- DSM
- Diagnostic and Statistical Manual of Mental Disorders
- EPHPP
- Effective Public Health Practice Project
- EQ-5D
- European Quality of Life-5 Dimensions
- EQ-VAS
- EuroQol visual analogue scale
- GBD
- Global Burden of Disease
- HIV
- human immunodeficiency virus
- HRQoL
- health-related quality of life
- ICD
- International Classification of Diseases
- ICF
- International Classification of Functioning, Disability and Health
- ICIDH
- International Classification of Impairments, Disability and Handicap
- IDEAS
- Inclusion, Dignity, Equality, Accessibility and Intersectionality
- MeSH
- medical subject heading
- MRC
- Medical Research Council
- MS
- multiple sclerosis
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OPCS
- Office of Population Census and Surveys
- PHR
- Public Health Research
- PPI
- patient and public involvement
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- RE-AIM
- Reach Effectiveness Adoption Implementation Maintenance
- SDG
- sustainable development goal
- SDH
- social determinant of health
- SF-36
- Short-Form questionnaire-36 items
- UN
- United Nations
- WHO
- World Health Organization