Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 11/3002/02. The contractual start date was in February 2013. The final report began editorial review in August 2016 and was accepted for publication in January 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Elizabeth Allen, Joanna Sturgess and Diana Elbourne report grants from the NHS National Institute for Health Research Public Health Programme to the London School of Hygiene and Tropical Medicine during the conduct of the study. Geraldine Macdonald is in the process of completing a Cochrane Review of home-visiting programmes that will include studies of nurse–family partnership. Two predecessor reviews were withdrawn in response to a criticism by David Olds. The criticism did not materially affect the results or conclusions of the reviews, but it was deemed appropriate to correct these and republish. This work is in progress, but the results are not yet available.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Barnes et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2017 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
This report describes the evaluation in a randomised controlled trial (RCT) of the Group Family Nurse Partnership (gFNP) programme, compared with usual care, as a strategy to reduce the likelihood of child abuse and neglect.
Background
Recent estimates show that suboptimal parenting of infants is a major public health issue. As of 31 March 2012, infants (children aged up to 1 year) accounted for 13% of those who were subject to a child protection plan in England. 1 The most common initial category of abuse for infants was neglect (49%), followed by emotional abuse (22%) and physical abuse (16%). Infants also face four times the average risk of homicide, perpetrators being parents in most cases. 2 Non-accidental head injuries are common, resulting in up to 30% mortality and significant neurological impairment for survivors. 3 Furthermore, the abuse of very young children may be up to 25% higher than indicated by official estimates. 4
In addition to preventing childhood injury and abuse, sensitive caregiving during the first year is important for promoting optimal child outcomes because brain development at that time is rapid and vulnerable to negative influences. Brain development is strongly influenced by the environment, the key component being the interactions with primary caregivers. Early research in the field of developmental psychology has, for example, highlighted the significant role that the infant’s primary caregiver plays in regulating the infant. 5 Maternal sensitivity has been shown to be a significant predictor of infant attachment security,6 and recent research has identified the importance of the specific nature or quality of the attunement or contingency between parent and infant,5 and the parent’s capacity for what has been termed ‘maternal mind-mindedness’7 or ‘reflective function’. 8 Research also shows that infant regulatory and attachment problems can best be understood in a relational context, and that disturbances to the parent–child relationship and parental psychosocial adversity are significant risk factors for infant emotional, behavioural, eating and sleeping disorders. 9 Trauma and adverse parent–child interactions in infancy elevate cortisol, a strong indicator of stress, and can lead to attachment difficulties, hyperactivity, anxiety and impulsive behaviour. 10,11
Policy context
A range of cross-party policy documents has now explicitly highlighted the importance of promoting children’s well-being during pregnancy and first 2 years of life,12–14 and recent key documents include Conception to Age 2: The Age of Opportunity15 and The 1001 Critical Days: The Importance of the Conception to Age Two Period. 16
Fair Society, Healthy Lives. Independent Review Into Health Inequalities in England Post 201017 focused on the importance of pregnancy and the first 2 years of life in terms of equalising the life chances of children, and Healthy Lives, Healthy People18 similarly points to the importance of ‘starting well’, focusing in particular on the health of mothers during pregnancy and parenting during the early years. Recent research has identified that this period is key because of the ‘biological embedding of social adversity’ that takes place during sensitive developmental periods. 19,20 This research showed that toxic stress caused by high levels of anxiety and depression during sensitive developmental periods (e.g. pregnancy and the postnatal period) can disrupt the developing brain architecture and other organ systems and regulatory functions, impacting the fetal/infant physiology in terms of hyper-responsive/chronically activated stress response; their resulting behavioural adaption; and the long-term cognitive, linguistic and socioemotional development. The long-term impact occurred in terms of increased stress-related chronic disease, unhealthy lifestyles and widening health disparities.
Evidence context
There is limited evidence available about ‘what works’ to support vulnerable parents during pregnancy and infancy. Although evidence concerning the effectiveness of home-visiting programmes in general in reducing child maltreatment is inconclusive,21 the US-developed Nurse Family Partnership (NFP) was one of nine home-visiting programmes identified as effective by the US Department of Health and Human Services as part of their Home Visiting Evidence of Effectiveness Review. 22 It is commonly named when examples of programmes with high-quality evidence for success are sought. For instance, the US coalition for evidence-based policy, responding to a Congressional directive that funds be directed to programmes with top-tier evidence of effectiveness identified only two programmes for children aged 0–6 years and their families that could be thus categorised, one of which was the NFP. 23 The Blueprints mission of the ‘Center for the Study and Prevention of Violence’ was charged with identifying outstanding violence and drug prevention programmes that meet a high scientific standard of effectiveness and, out of 800 with published research, found 12, one of which was NFP. 24 A similar conclusion was reached by academics seeking evidence-based home-visiting programmes likely to reduce child abuse and neglect. 25 The NFP was found to be effective in both decreasing child maltreatment and improving parenting practices. 22 Long-term follow-up of the NFP in the USA suggests a 48% reduction in cases of child abuse and neglect by the age of 15 years. 26
The NFP curriculum has strong theoretical underpinnings, in terms of both risk and protective factors, and the mechanisms through which change may be produced,27 drawing on ecological,28 self-efficacy29 and attachment30 theories. Ecological theory emphasises the importance of interactions between the characteristics of individuals and their contexts; self-efficacy theory focuses on an individual’s beliefs that they can successfully carry out behaviour required for good outcomes; and attachment theory highlights the importance of the early interactions with the primary caregiver in terms of the child’s later capacity for affect regulation. The cornerstone of the NFP model is the therapeutic nurse–client relationship. Beneficial outcomes found in the US trials included improved prenatal health, fewer childhood injuries, fewer subsequent pregnancies, increased intervals between births, increased maternal employment and improved school readiness;23,26,31–33 it has also been shown to have the potential to be cost-effective. 34 Results from the US trials of NFP found that it was particularly beneficial for women with ‘low psychological resources’, namely a combination of lower intelligence, mental health problems and low self-efficacy. 35
The NFP programme was introduced into England in 2007, renamed the Family Nurse Partnership (FNP),36 and has been offered to first-time teen mothers in more than 70 locations in England, Scotland and Northern Ireland,37 although recent RCT evidence has failed to support it as a way to reduce child abuse and neglect in the UK. 38 An implementation evaluation in the first 10 areas to provide FNP found that the programme was perceived in a positive light by potential clients and the nurses responsible for its delivery and uptake was high, with delivery close to the stated US objectives. 39 Nevertheless, potential sustainability issues were identified and in particular local concerns about its cost set against long-term rather than immediate gains. 40,41 Issues of eligibility were also examined, with the conclusion that, over time, the criteria might have to be changed to include additional risk factors beyond young age, although this could cause difficulties in identifying women early in their pregnancy. 42
In addition to being trained according to the US requirements, UK nurses are trained in ‘motivational interviewing’43 so that they can develop in-depth engagement with families to achieve change. As is the case in the USA, fathers are encouraged to be present for home visits and they have reported positively about the programme, in particular that the nurses invested time in developing relationships with them and identified their strengths in addition to areas that needed support, and that the programme was holistic in its approach. 44
Developing Group Family Nurse Partnership
In response to enquiries for a programme that could be offered to women who are ineligible for FNP, a group-delivered structured-learning programme based on FNP was developed in England by the Family Nurse Partnership National Unit (FNP NU) in collaboration with the NFP National Office at the University of Colorado, Denver. 45,46 gFNP was developed as a way to use the expertise of the FNP nurses, and the learning from the FNP, to reach women whose children were at risk of poor outcomes, but offered in a different context, and to reach those not eligible for FNP. The programme has the same theoretical basis as the home-based programme but is delivered in a local children’s centre (or similar community location). gFNP is, like FNP, aimed at helping young parents develop their health, well-being, confidence and social support in pregnancy and their children’s health and parenting in the first year of life, and at raising aspirations about future education and employment to increase support for the family in the future. 45
The programme was designed on the basis that group care prenatally can improve pregnancy outcomes47,48 and may be less costly than individual support,49 and that postnatal groups are a way of supporting potentially vulnerable mothers. 50,51 Meeting in a group with other mothers can be perceived by non-teenage mothers as more helpful than one-to-one support. 52 However, young mothers can be uncomfortable in groups and are less likely than older mothers to attend, especially if the group includes predominantly older mothers. 53 The main difference from existing group support in the UK for pregnant women or women with new babies, such as that offered by midwives and health visitors delivering the universal Healthy Child Programme (HCP)54 and other support provided in Sure Start Children’s Centres,55 is that gFNP spans both pregnancy and infancy, with ongoing support from the same practitioners over 18 months and ongoing contact with a group of families whose babies are of a similar age. Other group services are more time limited and focus either on pregnancy well-being, preparation for labour and birth or on specific infant issues such as sleep problems or breastfeeding, although the Preparation for Birth and Beyond materials56 are designed to address this by incorporating approaches to supporting families in pregnancy that are holistic and practical.
The gFNP programme uses the materials and approach of the NFP programme,23 aiming to improve maternal and infant health, promote close mother–infant attachment, develop sensitive parenting and effective family relationships, and help women to explore life choices as they become parents. 57 In addition, the programme includes aspects of ‘Centring Pregnancy’, an intervention developed in the USA, which provides groups of between 8 and 12 women with antenatal care during nine 2-hour sessions, with time for discussion about issues such as smoking, healthy eating and breastfeeding, and enables women to understand their own health status by encouraging them to be actively involved in all of the health checks. 47 The group-based Centring Pregnancy is said to be preferred to traditional (individual) antenatal care,47,58,59 and has led to improved prenatal outcomes such as fewer preterm births among high-risk women. 48,60 Experience of Centring Pregnancy in the UK context is limited to a feasibility study carried out in South London. 61 As part of the gFNP programme, during pregnancy clients receive routine antenatal care in accordance with UK National Institute for Health and Care Excellence (NICE) guidelines,62 and in the postnatal phase infants are monitored according to the HCP54 guidelines. To allow for this, one of the practitioners delivering the programme had to have also notified his or her intention to practise as a midwife and the FNP nurses had to have training in the delivery of the HCP.
Although NFP23,26,31 and Centring Pregnancy47,59,60,63 have substantial evidence outside the UK, it was necessary to provide evidence for gFNP, and for the merger and adaption of the two approaches to supporting mothers and their infants. The gFNP programme is a complex intervention made up of many components that have been designed, through education, nurse contact and peer support, to change parent behaviour. 64,65 According to Medical Research Council (MRC) guidelines,64,65 and in line with a framework proposed for developing and evaluating NFP innovations,66 the stages for effectively evaluating and implementing complex interventions are (1) programme development; (2) piloting for feasibility; (3) evaluation of clinical effectiveness and cost-effectiveness, ideally with a RCT; and (4) translation into mainstream practice.
Following programme development and prior to this RCT, the UK Department of Health (DH) and the FNP NU commissioned two feasibility evaluation studies of gFNP. 57,67 The feasibility of delivering gFNP was established68 by asking if there were barriers to reaching the intended population; whether or not any client factors were related to attendance; if programme delivery could be sustained over 18 months; and if gFNP was acceptable to different stakeholders.
Each feasibility study used a mixed-methods design69 involving the parallel collection of quantitative information on attendance, and client characteristics and qualitative data from semistructured interviews or focus groups (depending on resources and participant availability) to provide contextual understanding of the specific study questions. Quantitative data documented the outcome of referrals to gFNP, characteristics of clients and their attendance. Qualitative data covered experiences of the programme and reflections on programme delivery from a range of stakeholders.
Variability in attendance was identified, despite clients reporting strong commitment in interviews. Across the six sites delivering gFNP in the two feasibility studies, the mean number of sessions delivered by sites was 38 out of a potential 44 in the curriculum. 68 Although some clients had attended almost the maximum number of sessions, two never attended any meetings. An examination of whether or not any client factors could be linked to attendance found only that low attendance overall was related to mothers having never been employed (vs. employed full-time), whereas attendance in pregnancy was significantly lower for women living alone than for those living in a household with other adults. 68
Acceptability was high, with clients reporting support from others and enjoying the fact that they could share their baby’s progress with other parents. They also believed that coming together as a group with the babies and mothers helped in their baby’s developmental progress. The majority of clients considered that the inclusion of routine midwifery care in the group was a positive aspect to the programme.
Study aims
Following the results of the two, generally positive, feasibility studies, it was decided, in line with the MRC guidelines for evaluating complex interventions,64,65 to evaluate gFNP’s impact with the highest quality of evidence, in a RCT. The First Steps study’s objective was:
-
to determine whether or not gFNP, compared with usual antenatal and postnatal care, could reduce risk factors for maltreatment in a vulnerable group (namely expectant mothers aged < 20 years who already had a child, and expectant mothers aged 20–24 years with no previous live births and low/no educational qualifications).
In addition, the study aimed to answer the following questions:
-
Would provision of gFNP enhance maternal physical and mental health in pregnancy and the experience of pregnancy and delivery for mothers and fathers?
-
Would provision of gFNP enhance infant birth status and health status in infancy, breastfeeding and immunisation uptake during the first year?
-
How feasible and acceptable would gFNP be as part of routine antenatal and postnatal services?
-
How cost-effective was gFNP as a means of providing antenatal and postnatal services, compared with usual care?
Chapter 2 Methods
Trial design
The study comprised a multisite randomised controlled parallel-group trial in which eligible women were allocated (minimised by site and maternal age group) to one of two arms: (1) gFNP delivered via 44 sessions over 76 weeks or (2) usual care.
Participants
The participants were young (aged < 25 years) pregnant women.
Eligibility criteria
The requirement of the UK FNP NU was that gFNP should be offered to women who were not eligible for FNP, but who would be likely to benefit from the content of programme, based on research in the USA. 23,26 Women eligible for the trial, based on criteria defined by the FNP NU, were expectant mothers with expected delivery dates (EDD) within approximately 10 weeks of each other, for each group in each site. The range of EDDs was specified in relation to the expected date of the first meeting per site so that the majority would be 16–20 weeks pregnant when programme delivery commenced in that site. Specific criteria, beyond similar EDDs and gestation, were that participants should be either:
-
aged < 20 years at their last menstrual period (LMP) with one or more previous live births; or
-
aged 20–24 years at their LMP with no previous live births and low educational qualifications [defined as not having both mathematics and English language General Certificate of Secondary Education (GCSE) at grade C or higher or, if they had both, no more than four GCSEs at grade C or higher].
Exclusions were:
-
expectant mothers aged < 20 years who had previously received home-based FNP
-
mothers in either age group with psychotic mental illness (defined as bipolar disorder or schizophrenia)
-
mothers who were not able to communicate orally in English.
Study setting
Family Nurse Partnership teams are located around England, but with various dates of starting ranging from 2007 to the time that the study was being planned (October 2012). FNP teams were eligible to be part of the trial if:
-
the team had delivered the home-based FNP programme in its entirety (from birth to age 24 months) to a cohort of women
-
the team included at least one family nurse (FN) practitioner who had notified their intention to practise as a midwife.
Invitations were sent by the FNP NU to eligible teams, noting that they could take part if, in addition:
-
they could demonstrate from birth records that sufficient women of the relevant age and parity in the local area had given birth in the previous year for recruitment of two groups of 16–20 women (8–10 intervention, 8–10 control), each recruited within approximately 6 weeks, assuming that at least three times that number would need to be identified to gain sufficient agreement
-
they could confirm good links with community midwifery such that they also signed the expression of interest.
Seventeen teams expressed initial interest and eight sent in formal expressions of interest. Following site visits to discuss the likelihood of sufficient birth data and good midwifery collaboration, seven teams agreed to take part in the trial, located across England in Barnsley, Dewsbury, Lewisham (London), Nottingham, Sandwell (Birmingham), South Tyne and Wear and Waltham Forest (London). The eighth site found that their birth rate would not support the numbers needed for the trial.
The selection of FNs within sites to be involved in the trial was the responsibility of FNP teams. FNs, all of whom had substantial experience of delivering FNP, in general volunteered, and the majority had previous experience of running other types of group. At least one FN at each site had to have an intention to treat (ITT) as a midwife. The FNs received several days of training specific to delivering gFNP, which focused on group dynamics and the different aspects of the curriculum designed to generate interactions between group members. The training, from FNs who had developed the programme materials and been involved in feasibility research, covered topics such as using communication and motivational interviewing skills within a group context. 70 Although in theory FNs could have withdrawn from involvement, any FN withdrawing during the study did so owing to illness. Most sites were not able to send to training more than the two FNs needed for the programme. In cases of short-term absence, the supervisor or another FN from the team usually deputised.
Study intervention
Group Family Nurse Partnership is designed to run from the first trimester of pregnancy until infants are aged 12 months, with 44 group meetings in the curriculum (14 covering pregnancy and 30 covering infancy). 57 It was delivered to a group of women living in relatively close proximity, with similar EDDs (within 8–10 weeks). 46 Meetings lasted around 2 hours and were held in children’s centres, health centres or other suitable community facilities in the local areas served by the FNP teams. Sessions were facilitated by two experienced FNP FNs, one of whom had notified their intention to practise as a midwife. The two FNs exchanged the roles of active leader (facilitating a topic and activity) and active observer, noticing behaviours and body language of members and stepping in to support the leader and maintain a positive and inclusive group environment.
The gFNP programme includes content to improve maternal health and pregnancy outcomes; to improve child health and development by helping parents provide more sensitive and competent care; and to improve parental life course by helping parents develop effective support networks, plan future pregnancies, complete their education and find employment. 23 The curriculum domains were mother’s personal health, the maternal role, maternal life course, family and friends, environmental health and related health and human services, with referrals made when necessary. The gFNP curriculum materials and activities were modified from those used to deliver FNP to reflect group administration. They were designed to avoid a lecture context and to facilitate interaction between group members and between group members and the nurses, providing a range of engaging, often ‘hands-on’ activities. In particular, gFNP had a particular focus on enhancing social support and social networks through dialogue between group members, which is not a specific focus of home-based FNP. 46,57
Specific to the gFNP programme and following NICE guidelines,62 the family nurse midwife (FNMW) provided routine antenatal care during the meeting, taking an approach based on the Centring Pregnancy Programme,47,59,61 which encourages women to monitor their own health (e.g. by testing their own urine or listening to the fetal heartbeat). The Centring Pregnancy approach was perceived to correspond well with the gFNP aims in that both focus on developing self-efficacy and encouraging women to be more self-aware. 46 Once infants were born, both FNs were involved in routine infant checks, conducted in accordance with the UK NHS HCP. 54
An appreciation of the diversity of group members is central to thinking about how the content is delivered, especially for some emotive topics such as ‘safe relationships for our children’. 46 Although there was a curriculum for each meeting, the nurses were sensitive to the need for ‘agenda matching’ related to particular issues raised; this requires the practitioners to listen to the issues that are uppermost for the group members and agree how these can be met, while at the same time ensuring that the session agenda is realised and behaviour adaptation is progressed for everyone. In addition to modelling of infant care, they model respectful relationships and turn-taking,71 which are expected to be of benefit to any group members with poor social skills, especially if they are experiencing difficult interpersonal relationships. 46 Study participants allocated to gFNP could also access any aspect of the HCP usual care that they wished, independently or with the guidance of the gFNP nurses.
Control: usual care
Complete details of the care offered through the NHS to pregnant women and those with infants up to the age of 1 year at the time that the research was conducted can be found in the Healthy Child Programme. Pregnancy and the First Five Years. 54 The HCP, led by health visitors, is delivered through integrated services that bring together Sure Start Children’s Centre staff, general practitioners (GPs), midwives, community nurses and others. In summary, it offers every family a programme of screening tests, immunisations, developmental reviews, and information and guidance to support parenting and healthy choices. There are core universal elements provided for all families with additional progressive, preventative elements for those with medium or high risk. The universal programme includes a neonatal examination, a new-baby review at about 14 days, a 6- to 8-week baby examination, and a review by the time the child is 1 year old and at 2–2.5 years.
It aims to develop strong parent–child attachment and positive parenting, resulting in better social and emotional well-being among children; care that helps to keep children healthy and safe; healthy eating and increased activity, leading to a reduction in obesity; prevention of some serious and communicable diseases; increased rates of initiation and continuation of breastfeeding; readiness for school and improved learning; early recognition of growth disorders and risk factors for obesity; early detection of – and action to address – developmental delay, abnormalities and ill health, and concerns about safety; identification of factors that could influence health and well-being in families; and better short- and long-term outcomes for children who are at risk of social exclusion.
There is a focus on supporting mothers and fathers to provide sensitive and attuned parenting, in particular during the first months and years of life. From the 12th week of pregnancy, women are encouraged to see a midwife or maternity health-care professional for a health and social care assessment of their needs, risks and choices.
Primary outcome measures
Two primary outcome measures of parenting were used because of the difficulties associated with the detection of low frequency events such as child abuse. One is a self-report measure of parenting opinions and the other is an objective measure of maternal behaviour during a parent–infant interaction. Both are known to be able to identify mothers at risk for abusive parenting.
-
The Adult Adolescent Parenting Inventory Version 2 (AAPI-2)72 is a 40-item self-report measure able to discriminate between abusive and non-abusive parents. The total raw score is converted to a standard 10 score, with low scores indicating a higher risk for practising abusive parenting practices. Subscales are also available: ‘inappropriate’ expectations of children (seven items); inability to demonstrate empathy to children’s needs (10 items); strong belief in the use of corporal punishment (11 items); reversing parent–child family roles (seven items); and oppressing children’s power and independence (five items). Responses are on a five-point Likert-type scale ranging from strongly agree to strongly disagree. Internal reliability of the subscales ranges from 0.83 to 0.93, Cronbach’s alphas range from 0.80 to 0.92. The scales were constructed based on factor analysis to demonstrate construct validity and the inventory has discriminant validity comparing abusive and non-abusive parents.
-
The observational CARE-Index73,74 is based on a video recording of 3–5 minutes of mother–child play, and measures three aspects of maternal behaviour (sensitivity; covert and overt hostility; unresponsiveness) and four aspects of infant behaviour (co-operativeness; compulsive compliance; difficultness; and passivity). For this study only maternal sensitivity has been used as the co-primary outcome and has been shown to differentiate between abusing, neglecting, abusing and neglecting, marginally maltreating and adequate dyads. 75 Scores can range from 0 to 14, higher scores indicating better maternal sensitivity and/or infant co-operation. Scoring was conducted blind to allocation. Reliability scoring was completed on a random 10% sample of the recordings.
Secondary outcome measures
Eight secondary outcomes assessed socioemotional aspects of parenting and family life and service use.
-
The observational CARE-Index infant co-operativeness.
-
Maternal depression was assessed (at baseline and at 2, 6 and 12 months post partum) using the Edinburgh Postnatal Depression Scale (EPDS),76 a well-validated 12-item measure of postnatal depression with high reliability (0.88) and internal consistency (0.87), 86% sensitivity and 78% specificity. This questionnaire was scored within 24 hours of its administration so that any woman with a total score above the recommended cut-off indicating a risk of depression, or who responds affirmatively to the question asking about self-harm, could be identified and a health-care professional contacted to give appropriate support.
-
Maternal stress was assessed (at 2 and 12 months post partum) using the Abidin Parenting Stress Index (PSI), Short Form,77 a well-validated 36-item measure of perceived stress in the parenting role with sound test–retest reliability (r = 0.84) and internal consistency (α = 0.91). High scores on the PSI have been associated with abusive parenting,78,79 with some evidence that parenting stress is higher in women with five or more risk factors for child abuse. 80
-
Parenting sense of competence was assessed with the Parenting Sense of Competence (PSOC) scale81 at 2 and 12 months. This 17-item measure has three factors – satisfaction, efficacy and interest – established by factor analysis in a normative non-clinical sample, each with acceptable internal consistency (from 0.62 to 0.72). 82
-
The extent of social support available to the mothers was assessed (baseline and 12 months) using the Medical Outcomes Study (MOS), Social Support Survey. 83 The 20-item scale measures four dimensions of support, established using confirmatory factor analysis (emotional support, tangible support, positive interaction and affection), each with internal consistency of 0.91 or higher, and also provided a total support score (Cronbach’s alpha 0.97); stability over time is also high for each scale (ranging from 0.72 to 0.78). 83
-
Brief questions designed for the study and based on those developed for use when delivering FNP40 asked about maternal smoking and alcohol and drug use.
-
Brief questions designed for the study and based on those developed for use when delivering FNP40 asked about relationship violence.
-
Brief questions designed for the study asked about infant feeding.
Information other than for the primary and secondary outcome at different time points was collected and is shown but was not formally tested (e.g. baby demographics; immunisations; maternal smoking, alcohol and drug use).
Data collection
The trial commenced in February 2013, recruitment and baseline data collection commenced in July 2013, continuing to July 2014, and data collection was completed in March 2016. Data collection was conducted by researchers making four visits to participants’ homes (baseline in early pregnancy, when infants were 2, 6 and 12 months of age), when they administered structured questionnaires, and (at 12 months) made a 3- to 5-minute video recording of the mother and infant together, presented with a standardised set of toys.
At a Project Management Committee meeting (31 October 2014), it was agreed that the target windows for data collection were 2–3.5 months (60–105 days) for the 2-month outcomes, 6–7.5 months (180–225 days) for the 6-month outcomes and 12–14 months (365–425 days) for the 12-month outcomes, although data would still be collected outside those windows if the participant was available. It was also agreed that interviews with mothers whose babies were premature would be timed as much as possible according to their chronological age. The participants were given ‘High Street’ vouchers for £20 at each home visit data collection point to acknowledge their time for participation. All reasonable attempts were made to contact any participants lost to follow-up during the course of the trial to complete the assessments.
Data management
Each participant was allocated a unique identifier (UID) prior to the baseline interview and this UID was recorded on each questionnaire completed for that participant. All questionnaires were anonymous. The researchers sent completed questionnaires by post directly to the London School of Hygiene and Tropical Medicine (LSHTM) Clinical Trials Unit (CTU) and checks were made for receipt. The questionnaires received at the LSHTM CTU were reviewed for errors and omissions and, when possible, these were resolved via communication with the researchers. The questionnaires were stored in a locked cabinet. The data were double entered into a database by trained data personnel. All electronic trial data from questionnaires and electronic management data with personal participant content stored at the LSHTM CTU were password protected and held on secure servers at the LSHTM.
Video-taped play interactions were transferred by the fieldworkers from the camera to encrypted USB flash drives with Advanced Encryption Standard 256-bit military-level security, sent by recorded delivery to the principal investigator (PI), with files deleted from the camera by the fieldworkers. Recordings were decrypted by the PI and saved with full anonymisation of filenames on a dedicated drive separate from any other study information. Copies of recordings were sent on DVDs to the coder by special delivery and codings returned on a password-protected Microsoft Excel (2010; Microsoft Corporation, Redmond, WA, USA) file to the study PI via e-mail. These were converted to a Statistical Product and Service Solutions (SPSS version 22; SPSS Inc., Chicago, IL, USA) data file once all codings had been received and sent by the PI as a password-protected file by e-mail to the trial statistician at the LSHTM CTU.
Sample size calculation
The sample size was calculated for the two primary outcomes: the AAPI-272 and maternal sensitivity from the observational CARE-Index. 73–75 The standard deviation (SD) of the AAPI-2 based on a total sum of the raw scores of 40 items (range 40–200 items) is 10, with differences of 6.7 identified in the normative sample between abusive and non-abusive adult females. 72 The SD for the CARE-Index sensitivity scale (range 0–14) was expected to be around 2.3. 73
For this individually randomised trial, we initially proposed to recruit sufficient mothers and babies (families) to allow the trial to detect a difference between groups of 0.5 SD, with 90% power at a significance level of 0.05 (two-tailed), considered to represent a moderate size of effect. 84 Basing calculation on the AAPI-2, very conservatively assuming a correlation of 0.4 between pre- and post-intervention scores, at least 71 families were needed in each arm of the trial to detect this difference. Allowing for an expected 30% dropout rate (based on the first two applications of the programme in England), we planned to recruit a minimum of 84 families per arm of the trial. We therefore proposed, conservatively, to recruit a minimum of 100 families per arm (n = 200). The proposed sample size would similarly allow us to detect a change of approximately 0.5 SD in the CARE-Index maternal sensitivity score. 73–75 If this was achieved, we expected to be able to detect a difference at follow-up between arms of the trial of approximately 1.2 with 90% power and a 5% level of significance.
However, owing to ongoing slow recruitment, and because two of the Phase I groups with very low numbers were discontinued prematurely, the allocation ratio was changed during the trial from 1 : 1 to 2 : 1 in favour of the intervention arm. As a result of this and the actual recruitment rate, sample sizes were revised to 100 families in the intervention arm and 65 families in the control arm. With the expected dropout rate of 30%, we would still have 82% power to detect the planned differences in the primary outcomes.
Recruitment and consent
Community midwives were initially involved in identifying potentially eligible women based on their age, parity and gestation,85 giving them a study leaflet describing the study (see Report Supplementary Material 1) and asking for written agreement to give their names and contact details to the local researcher as part of a staged consent process, using an ‘agreement to contact’ form (see Report Supplementary Material 2). Owing to a range of factors,86 the identification of potentially eligible participants subsequently involved both Clinical Local Research Network (CLRN) midwives and FNP FNs who generally gained oral agreement for research contact, as approved by the Research Ethics Committee (REC) (amendment #1).
The first research contact was by telephone to confirm eligibility. Women who were not eligible were thanked for their time. Those eligible were given an information sheet about the trial (see Report Supplementary Material 2), and time to think about participation. After at least 24 hours, researchers arranged a home visit, so that written consent could be obtained (see Report Supplementary Material 2) and baseline data could be collected.
Randomisation procedure
The process was overseen by the LSHTM CTU. The UID (which included a site identifier) and age at the LMP of eligible consenting mothers-to-be were passed by the researchers to the central randomisation service at the Health Services Research Unit, Aberdeen, using an automated telephone procedure. Minimisation criteria [site and age group (< 20 years and 20–24 years)] were used to ensure a balance of key prognostic factors. Allocation to one of two arms was securely computer generated and delivered by e-mail to the LSHTM, which conveyed the information to study participants by post and conveyed to each gFNP team the names and contact details of women allocated to the intervention arm by fax or password-protected e-mail, receiving confirmation of receipt by e-mail.
Blinding
The research team collecting the data and the psychologists scoring the videos were blind to treatment allocation.
Statistical analyses
The primary analyses were by ITT and included adjustment for baseline measure of the outcomes when possible (analysis of covariance; ANCOVA). When outcomes were collected at multiple time points to gain power, random-effects models, using a likelihood-based approach, were fitted to the outcomes at all the time points they were measured at simultaneously (Table 1 and see Appendix 1). This has the additional advantage that the data from all participants contribute to the analysis, even if there are missing data at some follow-up time points.
| Measure | Time point | |||
|---|---|---|---|---|
| Baseline, pregnancy | Infant, 2 months | Infant, 6 months | Infant, 12 months | |
| AAPI-2 | ✗ | ✗ | ||
| CARE-Index | ✗ | |||
| Demographics | ✗ | ✗ (update) | ✗ (update) | ✗ (update) |
| EPDS | ✗ | ✗ | ✗ | ✗ |
| Infant feeding | ✗ (plans) | ✗ | ✗ | |
| Infant immunisations | ✗ | ✗ | ||
| Maternal drug use | ✗ | ✗ (update) | ✗ (update) | |
| EQ-5D-5L | ✗ | ✗ | ✗ | ✗ |
| Maternal smoking and alcohol use | ✗ | ✗ (update) | ✗ (update) | |
| PSI, Short Form | ✗ | ✗ | ||
| PSOC | ✗ | ✗ | ||
| Relationship violence | ✗ | ✗ | ||
| Social networks (MOS) | ✗ | ✗ | ||
| Service use | ✗ | ✗ | ✗ | |
Reflecting the discussion at the Project Management Group (31 October 2014), about appropriate time windows for data collected at 2, 6 and 12 months, the statistical analysis plan as agreed with the Data Monitoring Committee in December 2014 was for the primary analysis to exclude all data outside the windows (i.e. after 12 months + 60 days; 6 months + 45 days; and 2 months + 30 days). A sensitivity analysis was then conducted including all data, even those outside the windows.
For the primary outcome of the AAPI-2,72 a linear regression model was used to estimate a mean difference in AAPI-2 score between the two arms of the trial. For the primary outcome maternal sensitivity score, a mixed-effects model was used with a random effect at the mother level (to allow for multiple births), to estimate a mean difference in maternal sensitivity score between the two arms of the trial. However, only one set of twins was available for this analysis and their responses were identical. Therefore, it was not possible to include a random effect and the analysis was carried out at the mother level using a linear regression model.
For the secondary outcomes, appropriate generalised linear models were used to examine the effect of the intervention. Odds ratios (ORs) and mean differences are reported with 95% confidence intervals (CIs). When continuous measures were available at baseline, they were adjusted for in the analysis.
When there was evidence of non-normality in the continuous outcome measures, the non-parametric bootstrapping, with 1000 samples, was used to estimate the effect of the intervention and bias-corrected CIs are reported. 87 When this was done, p-values were estimated using permutation tests.
An adjusted analysis, adjusting for site and maternal age group, was also carried out. A pre-specified subgroup analysis was planned based on ‘looked-after’ history, but, as there was only one participant in the intervention arm (see Chapter 6), this was not carried out.
It was planned that the impact of being a twin would be explored by including a covariate in all models, but owing to the low number of twins this was not carried out. However, exploratory analyses were carried out to examine the impact of premature birth on all outcomes. Further exploratory secondary analyses were also carried out, in which the small group in which the intervention was delivered was fitted as a random effect to allow for any potential clustering by group.
A complier average causal effect (CACE) analysis88 was also carried out. The CACE analysis estimates a measure of the effect of the intervention on those participants who received it as intended by the original allocation.
A reliability analysis was carried out for the CARE-Index. Ten randomly selected videos (stratified by site) were scored by a second scorer and Lin’s concordance correlation coefficient was calculated and Bland–Altman plots were produced to assess reliability.
Health economic study
A prospective economic evaluation, conducted from a NHS and Personal Social Services (PSS) perspective, was integrated into the trial. The economic assessment method adhered as closely as possible to the recommendations of the NICE reference case. 89 Primary research methods estimated the costs of the delivering gFNP, including development and training of accredited providers, the cost of delivering the group sessions, participant monitoring activities and any follow-up/management. Broader resource utilisation was captured through participant questionnaires administered at baseline, 2, 6 and 12 months post partum. Maternal health-related quality of life (HRQoL) was assessed using the EuroQol-5 Dimensions, five-level version (EQ-5D-5L) measure90 at baseline and at 2, 6 and 12 months post partum. This contains a visual analogue scale (VAS) asking patients to rate their current HRQoL on a scale from 0 to 100, and a five-dimension health status classification system, which can then be converted to a multiattribute utility score by applying a UK tariff. 91
In addition, information was collected about service use that could indicate a risk factor for abuse or neglect, namely contact with a social worker and the child’s attendance at hospital accident and emergency (A&E) departments (all based on maternal reports at 2, 6 and 12 months). Confirmation was to be from Hospital Episode Statistics (HES) records, but these could not be obtained. The unit costs for health and social care resources were largely derived from local and national sources and were estimated in line with best practice. For further details, see Chapter 4.
Process study
The uptake rate of women who agreed to the intervention involved an assessment of the ratio of women randomised to receive the intervention who then attended at least one session relative to those who either refused after meeting with the FN or agreed but never attended any sessions based on standardised data forms completed by FNs.
The study attrition rate was estimated in terms of the proportion of women who dropped out relative to those who continued in either arm of the trial and also those who may or may not have taken part in research visits, but ceased to receive the intervention, based on information provided by the nurses delivering the programme. This included both women who stopped attending and women in areas where the programme delivery ended prematurely.
The extent to which the programme was delivered with integrity was assessed through an analysis of data from the programme’s standardised data forms, documenting attendance and the content domains covered in sessions.
A parallel qualitative appraisal was concerned with understanding ‘how’ the gFNP service:
-
was implemented based on data collated by the FNP NU on sessions delivered and attendance of clients, to develop evidence for future roll-out and potential fidelity measures
-
was experienced by families and practitioners, to develop recommendations for improvement
-
impacted on established roles to understand how barriers to and drivers of change manifest in distinct professional knowledge, practice and cultural domains.
The appraisal was informed by both quantitative data and qualitative interviews, which are further detailed with the results in Chapter 5.
Focus on mothers with a ‘looked-after’ history
After the programme concluded, delivery interviews were sought with participants who had identified at 6 months post partum that they had spent time away from their parent(s) during childhood, in the care of social services. Interviews were also conducted with FNs involved in delivering gFNP in sites, which included the self-identified ‘looked-after’ participants, and with other professionals involved in providing support to young parents who had in their childhood or adolescence been ‘looked after’. For further details, see Chapter 6.
Study harms/adverse events
Information was collected on any hospitalisation of mother or infant other than for delivery; congenital anomaly or birth defect; persistent or significant disability; and death identified by information from participants at data collection points or using pre-paid change of circumstances cards. All events were reported to the REC, which gave a favourable opinion within 15 days of the PI becoming aware of the event.
Ethics
Ethics approval for the main study was granted in May 2014 by the National Research Ethics Service (NRES) Committee South West – Frenchay (REC reference 13/SW/0086). Six substantial amendments to the study protocol were also approved, as follows, most of which were changes that were designed to boost the poor recruitment.
October 2013: approval of –
-
FNs with access to midwifery records and Comprehensive Clinical Research Network midwives (when available), having access to midwifery booking lists to identify potentially eligible participants
-
contact with potentially eligible participants to be by telephone to gain ‘agreement to research contact’
-
a study poster to highlight the study in GP clinics and midwifery waiting rooms
-
extending the recruitment period by 2 months
-
adding one additional exclusion criterion – any woman already enrolled in the trial who experiences fetal death and becomes pregnant again within the recruitment period
-
a letter to be sent to any participant experiencing fetal death
-
a change in the original analysis plan, with a CACE analysis to be carried out after the ITT analysis to determine the effect of the intervention on those who received gFNP as intended.
November 2013: approval of –
-
including in the groups a small number of women who are not part of the research study (called in subsequent sections ‘buffer clients’). They were women not eligible for the research because they were aged 20–24 years but had more educational qualifications than were allowed for eligibility. This was to facilitate the groups being of the minimum size (set at eight), which had become a concern with slow recruitment. The presence of buffer clients has been taken into account in the analyses.
December 2013: approval that –
-
owing to ongoing slow recruitment and two of the Phase I groups with very low numbers being discontinued prematurely, the allocation ratio be changed from 1 : 1 to 2 : 1 in favour of the intervention arm (this was predicted to lead to a reduction in the power of the study from 90% to 80%)
-
additional questions added to the process qualitative interviews so that the experience of a group being discontinued could be examined.
April 2014: approval of –
-
a simplification of the eligibility criteria for 20- to 24-year-olds for the final (third) phase of recruitment, removing the requirement for low/no educational qualifications
-
a slightly revised study leaflet removing mention of the educational requirement.
June 2014: approval that –
-
contrary to the original proposal, the 6-month data collection would be by a home visit rather than a telephone call, a change based primarily on feedback from clients when visited at 2 months, that they did not want to talk extensively on the telephone when coping with a baby, and also as a strategy to maximise study retention
-
participants would be provided with a £20 voucher at 6 months rather than the planned £10, as it was a home visit, rather than the original plan of a telephone call and a voucher to be sent in the post
-
one final question be added to the 6-month interview so that participants could identify whether or not they had any history of being ‘looked after’ by the local authority.
November 2014: approval of –
-
all of the study materials (consent form, information sheets, interview guides) to conduct the qualitative interviews with study participants who had been allocated to receive gFNP and with FNs who had delivered gFNP; interviews to begin once gFNP delivery was complete in the area.
Chapter 3 Results: main study
Participant flow and recruitment
Of the 492 women who agreed that the research team could contact them about the study, after their initial eligibility was ascertained on the basis of their age, parity and EDD, 166 were enrolled (99 to the intervention group and 67 to the control group). The full details of the reasons for non-enrolment can be seen in Figure 1. Some (n = 31) declined when they were contacted by researchers before their eligibility could be established and others (n = 27) could not be contacted. Among the 137 found by researchers to be definitely eligible for the study, the main reason for non-enrolment was that they declined (n = 106), whereas other eligible women agreed to consider taking part in the study but then were not available for an interview (n = 17) or were found to live outside the area served by the FNP team (n = 14). Ineligibility was determined for 114 women and was primarily for women in the 20–24 years age range who had more educational qualifications than were specified (n = 60) or were not expecting their first child (n = 16). A small number of the women aged < 20 years were found to be expecting their first child (n = 10), and other women (n = 10) were not within the specified EDD range or could not communicate adequately in spoken English (n = 9).
FIGURE 1.
First Steps Consolidated Standards of Reporting Trials diagram. a, Identified as ineligible after recruitment: one participant outside gFNP service area, one participant previously received one-to-one gFNP; b, includes one 2-month questionnaire (in each arm) completed at the 6-month time point; and c, no 6-month interview data but followed up at 12 months. Figure reproduced from Barnes et al. 92 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
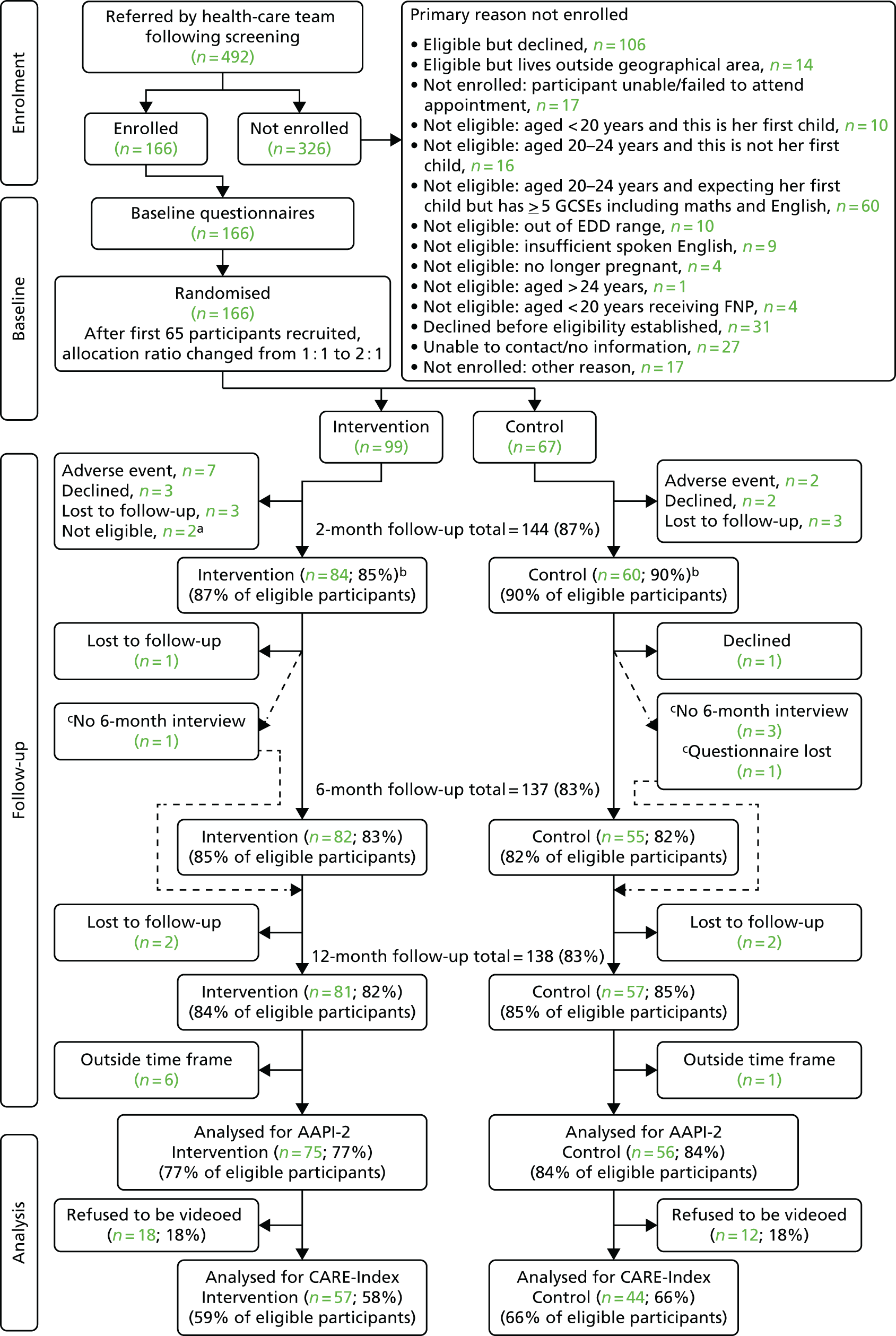
After recruitment, it was found that two women in the intervention arm were ineligible (one was outside the service area and the other had received FNP), and so baseline information is provided for 97 women in the intervention arm and 67 in the control arm. Although information from the follow-up at around 2 months post partum was collected for 144 participants (84 in the intervention arm and 60 in the control arm), 16 participants (nine in the intervention arm and seven in the control arm) were outside the agreed time window, leaving 128 participants (75 in the intervention arm and 53 in the control arm). From the follow-up at around 6 months post partum, information was collected for 137 participants (82 in the intervention arm and 55 in the control arm); however, 16 participants (12 in the intervention arm and four in the control arm) were outside the agreed time window, leaving 121 participants (70 in the intervention arm and 51 in the control arm) (see Figure 1). Although 138 12-month interviews were carried out (81 in the intervention arm and 57 in the control arm), seven (six in the intervention arm and one in the control arm) were outside the agreed time window, leaving 131 interviews (75 in the intervention arm and 56 in the control arm) eligible for the primary analysis. The primary analysis for the CARE-Index (co-primary outcome) was based on 101 videos (57 in the intervention arm and 44 in the control arm) (see Figure 1).
Baseline
The participants in the two randomised arms appear comparable at baseline in terms of their demographic characteristics (Table 2), partner’s demographic characteristics (Table 3), smoking, alcohol consumption and drug use (Table 4) and questionnaires documenting parenting attitudes, depression symptoms, social networks and relationship violence (Table 5). In all tables the denominator is the whole sample, but also given, when relevant, are numbers of missing data and the number of data available when the denominator depends on the answer to a previous question (e.g. if yes, has GCSEs, then how many? If yes, a smoker, then how many cigarettes per day?).
| Category | Trial arm, n (%) | |
|---|---|---|
| Intervention (N = 97) | Control (N = 67) | |
| Age, mean (SD) | 21.7 (1.9) | 21.9 (1.6) |
| Missing, n | 1 | 1 |
| Age at LMP, mean (SD) | 21.0 (1.8) | 21.2 (1.8) |
| Educational qualifications: GCSEs or equivalent? | ||
| Yes | 73 (75.3) | 55 (82.1) |
| No | 24 (24.7) | 12 (17.9) |
| Number of GCSEs, mean (SD) | 6.7 (3.1) | 6.4 (2.7) |
| Data available, n | 70 | 54 |
| Number of GCSEs at grade C or higher, mean (SD) | 3.8 (3.6) | 3 (2.5) |
| Data available, n | 69 | 53 |
| Educational qualifications: other? | ||
| Yes | 79 (82.3) | 56 (83.6) |
| No | 17 (17.7) | 11 (16.4) |
| Ethnicity | ||
| White: British | 61 (63.5) | 48 (71.6) |
| White: Irish | 2 (2.1) | 0 (0.0) |
| Any other white background | 2 (2.1) | 3 (4.5) |
| Asian British: Indian | 0 (0.0) | 0 (0.0) |
| Asian British: Pakistani | 5 (5.2) | 5 (7.5) |
| Asian British: Bangladeshi | 1 (1.0) | 0 (0.0) |
| Black British: Caribbean | 14 (14.6) | 6 (9.0) |
| Black British: African | 3 (3.1) | 2 (3.0) |
| Any other black background | 0 (0.0) | 0 (0.0) |
| Chinese | 0 (0.0) | 0 (0.0) |
| Mixed | 8 (8.3) | 3 (4.5) |
| Prefer not to say | 0 (0.0) | 0 (0.0) |
| Current partner? | ||
| Yes | 83 (85.6) | 59 (88.1) |
| No | 14 (14.4) | 8 (11.9) |
| Current partner: biological father? | ||
| Yes | 83 (100.0) | 59 (100.0) |
| No | 0 (0.0) | 0 (0.0) |
| Marital status | ||
| Married | 10 (10.4) | 8 (11.9) |
| Unmarried/cohabiting | 43 (44.8) | 37 (55.2) |
| Separated | 0 (0.0) | 0 (0.0) |
| Widowed | 0 (0.0) | 0 (0.0) |
| Divorced | 0 (0.0) | 0 (0.0) |
| Single | 43 (44.8) | 22 (32.8) |
| Number of people currently living with, mean (SD) | 2.9 (1.5) | 3.1 (1.6) |
| Missing, n | 1 | |
| Currently living in household | ||
| Own mother/parents | 11 (11.7) | 7 (10.9) |
| Husband/partner | 24 (25.5) | 24 (37.5) |
| Husband/partner and others, not including maternal mother | 10 (10.6) | 6 (9.4) |
| Own mother/parents and others, not including husband/partner | 14 (14.9) | 10 (15.6) |
| Own mother/parents and others, including husband/partner | 6 (6.4) | 5 (7.8) |
| Foster parent | 0 (0.0) | 0 (0.0) |
| Husband/partner and others | 2 (2.1) | 3 (4.7) |
| Other adults (own father, aunt, grandmother, older sibling, friend, etc.) | 12 (12.8) | 6 (9.4) |
| Live alone | 15 (16.0) | 3 (4.7) |
| Where are you living? | ||
| House or bungalow | 68 (70.1) | 49 (73.1) |
| Flat, low rise | 12 (12.4) | 5 (7.5) |
| Flat, high rise, first three floors | 5 (5.2) | 12 (17.9) |
| Flat, high rise, above third floor | 4 (4.1) | 0 (0.0) |
| Room or bedsit | 2 (2.1) | 1 (1.5) |
| Hostel | 2 (2.1) | 0 (0.0) |
| Supported housing | 1 (1.0) | 0 (0.0) |
| In a group home/shelter | 2 (2.1) | 0 (0.0) |
| Confined to an institutional facility | 0 (0.0) | 0 (0.0) |
| Homeless | 0 (0.0) | 0 (0.0) |
| Other | 1 (1.0) | 0 (0.0) |
| Enrolled in any school or educational programme? | ||
| Yes | 12 (12.4) | 9 (13.4) |
| No | 85 (87.6) | 58 (86.6) |
| What course? | ||
| School, up to year 11 | 1 (8.3) | 0 (0.0) |
| School, year 12 or 13/sixth form college | 1 (8.3) | 0 (0.0) |
| Access course | 1 (8.3) | 1 (11.1) |
| Vocational course | 6 (50.0) | 2 (22.2) |
| University | 3 (25.0) | 6 (66.7) |
| Ever worked? | ||
| Yes | 76 (78.4) | 56 (83.6) |
| No | 21 (21.7) | 11 (16.4) |
| Currently working? | ||
| Yes, full-time | 30 (39.5) | 28 (50.0) |
| Yes, part-time | 14 (18.4) | 8 (14.3) |
| No | 32 (42.1) | 20 (35.7) |
| Category | Trial arm, n (%) | |
|---|---|---|
| Intervention (N = 97) | Control (N = 67) | |
| Partner’s educational qualifications: GCSEs or equivalent? | ||
| Yes | 52 (54.7) | 39 (58.2) |
| No | 10 (10.5) | 12 (17.9) |
| Don’t know | 20 (21.1) | 8 (11.9) |
| No partner | 13 (13.7) | 8 (11.9) |
| Number of GCSEs, mean (SD) | 5.9 (2.9) | 7 (2.9) |
| Data available, n | 32 | 28 |
| Number of GCSEs at grade C or higher, mean (SD) | 3.8 (3.0) | 4.3 (3.6) |
| Data available, n | 28 | 24 |
| Educational qualifications: other? | ||
| Yes | 60 (72.3) | 43 (72.9) |
| No | 8 (9.6) | 12 (20.3) |
| Don’t know | 15 (18.1) | 4 (6.8) |
| Ever worked? | ||
| Yes | 73 (88.0) | 56 (94.9) |
| No | 9 (10.8) | 2 (3.4) |
| Don’t know | 1 (1.2) | 1 (1.7) |
| Currently working? | ||
| Yes | 56 (76.7) | 38 (67.9) |
| No | 17 (23.3) | 18 (32.1) |
| Don’t know | 0 (0.0) | 0 (0.0) |
| Current job | ||
| Managers and senior officials | 1 (1.6) | 2 (4.3) |
| Professional occupations | 3 (4.7) | 1 (2.1) |
| Associate professional and technical occupations | 3 (4.7) | 1 (2.1) |
| Administrative and secretarial occupations | 0 (0.0) | 1 (2.1) |
| Skilled trades occupations | 17 (26.6) | 19 (40.4) |
| Personal service occupations | 4 (6.3) | 2 (4.3) |
| Sales and customer service occupations | 11 (17.2) | 6 (12.8) |
| Process, plant and machine operatives | 6 (9.4) | 7 (14.9) |
| Elementary occupations | 12 (18.8) | 1 (2.1) |
| Don’t know | 0 (0.0) | 0 (0.0) |
| N/A | 7 (10.9) | 7 (14.9) |
| Category | Trial arm, n (%) | |
|---|---|---|
| Intervention (N = 97) | Control (N = 67) | |
| Ever smoked? | ||
| Yes | 56 (57.7) | 43 (64.2) |
| No | 41 (42.3) | 24 (35.8) |
| Smoked during pregnancy? | ||
| Yes | 42 (75.0) | 32 (74.4) |
| No | 14 (25.0) | 11 (25.6) |
| Number of cigarettes per day, mean (SD) | 3.7 (4.6) | 3.8 (4.6) |
| Data available, n | 41 | 31 |
| Anyone else in household smoke? | ||
| Yes | 43 (44.8) | 29 (44.6) |
| No | 53 (55.2) | 36 (55.4) |
| Alcohol consumption in the last month? | ||
| One or two times a week | 0 (0.0) | 2 (3.0) |
| One or two times a month | 4 (4.1) | 4 (6.0) |
| Less than once a month | 4 (4.1) | 4 (6.0) |
| Never | 89 (91.8) | 57 (85.1) |
| Last month typical? | ||
| Yes | 60 (61.9) | 37 (55.2) |
| No | 37 (38.1) | 30 (44.8) |
| Typical monthly alcohol consumption (if no)? | ||
| Three or four times a week | 2 (5.6) | 0 (0.0) |
| One or two times a week | 15 (41.7) | 16 (55.2) |
| One or two times a month | 12 (33.3) | 7 (24.1) |
| Less than once a month | 6 (16.7) | 5 (17.2) |
| Never | 1 (2.8) | 1 (3.5) |
| Number of units per day, mean (SD) | 4.6 (6.3) | 4.5 (5.4) |
| Data available, n | 69 | 51 |
| Marijuana use in last month? | ||
| Three or four times a week | 0 (0.0) | 2 (3.0) |
| One or two times a week | 1 (1.0) | 1 (1.5) |
| One or two times a month | 0 (0.0) | 0 (0.0) |
| Less than once a month | 0 (0.0) | 1 (1.5) |
| Never | 95 (97.9) | 63 (94.0) |
| Refused to answer | 1 (1.0) | 0 (0.0) |
| In the past month, on how many days did you use any street drugs? | ||
| Never | 97 (100.0) | 67 (100.0) |
| Plan to breastfeed baby? | ||
| Yes, definitely | 63 (65.0) | 40 (59.7) |
| Possibly, not certain | 22 (22.7) | 15 (22.4) |
| No, definitely not | 12 (12.4) | 12 (17.9) |
| Category | Trial arm, mean (SD) | |
|---|---|---|
| Intervention (N = 97) | Control (N = 67) | |
| AAPI-272 (higher = positive) | ||
| Total (/10) | 7.2 (0.8) | 7.2 (0.9) |
| Missing, n | 9 | 2 |
| Inappropriate expectations (/35) | 21.6 (4.2) | 21.8 (4.0) |
| Empathy (/50) | 36.3 (5.0) | 36.3 (5.4) |
| Corporal punishment (/55) | 43.2 (5.5) | 42.3 (6.1) |
| Role reversal (/35) | 24 (4.1) | 23.9 (4.5) |
| Power independence (/25) | 18.6 (2.1) | 19.3 (2.3) |
| EPDS76 (higher = more depressed) | ||
| Total (/30) | 6.9 (4.7) | 7.7 (5.0) |
| Missing, n | 1 | 1 |
| Possible depression (EPDS ≥ 10) | ||
| Yes | 24 (24.5) | 20 (30.3) |
| No | 74 (75.5) | 46 (69.7) |
| Social networks83 (higher = more support) | ||
| Total (/100) | 85.8 (15.6) | 85.3 (16.4) |
| Missing, n | 2 | |
| Tangible support (/100) | 85.5 (18.1) | 86.4 (17.5) |
| Emotional support (/100) | 85.1 (16.4) | 83.3 (18.9) |
| Affectionate support (/100) | 91.8 (16.4) | 90.8 (17.7) |
| Positive social interaction (/100) | 83.9 (20.6) | 85.1 (19.4) |
| Relationships40 (higher = more abuse) | ||
| Total abuse (/8) | 0.6 (0.9) | 0.5 (0.8) |
| Lifetime abuse (/2) | 0.2 (0.6) | 0.5 (0.8) |
| Physical aggression (/2) | 0.1 (0.3) | 0.1 (0.3) |
| Verbal abuse (/2) | 0.3 (0.4) | 0.3 (0.4) |
| Sexual abuse (/2) | 0 (0.0) | 0 (0.2) |
Attendance at Group Family Nurse Partnership groups
Programme delivery and attendance is covered in detail in Chapter 5 so it is only summarised here. In total, the 97 trial participants were allocated to 16 planned groups; five sites planned to offer two groups (A and B) and two sites planned to offer three groups (A, B and C) (Table 6), although in some cases no sessions were delivered for a planned group. In addition, one participant attended sessions offered in groups A and B as the first group was terminated prematurely.
| Site | Group | Number allocated to group | Mean number of sessions attended (SD) | Median number of sessions attended | Range |
|---|---|---|---|---|---|
| All | 117a | 11.8 (13.8) | 3 | 0–44 | |
| 1 | A | 7 | 12.1 (10.2) | 11 | 0–23 |
| 1 | B | 12 | 6.8 (11.7) | 1 | 0–31 |
| 2 | A | 7 | 30 (12.7) | 33 | 15–44 |
| 2 | B | 7 | 15.1 (13.1) | 13 | 0–32 |
| 3 | A | 5 | 1.4 (1.3) | 2 | 0–3 |
| 3 | B | 10 | 17.1 (13.4) | 23.5 | 0–33 |
| 4 | A | 6 | 3.3 (2.4) | 4 | 0–6 |
| 4 | B | 13 | 17.6 (15.0) | 24 | 0–38 |
| 4 | C | 6 | 0.3 (0.5) | 0 | 0–1 |
| 5 | A | 7 | 12.7 (11.1) | 16 | 0–26 |
| 5 | B | 7 | 0 (0.0) | 0 | 0–0 |
| 6 | A | 7 | 29.3 (13.9) | 35 | 0–39 |
| 6 | B | 10 | 15.1 (14.3) | 14 | 0–34 |
| 7 | A | 5 | 1.2 (2.2) | 0 | 0–5 |
| 7 | B | 5 | 4.2 (4.1) | 5 | 0–9 |
| 7 | C | 3 | 0 (0.0) | 0 | 0–0 |
The mean number of gFNP sessions attended by the 117 clients allocated to groups (see Table 6), comprising 99 trial participants (97 allocated to gFNP and two control group participants mistakenly offered gFNP as buffers by FNP teams) and the 18 buffer clients who were not eligible for the trial owing to educational qualifications but were offered gFNP to boost group sizes to a viable number, was 11.8 (SD 13.8).
Overall, the 97 trial participants in the intervention arm attended a mean of 10.3 sessions (SD 13.4), but a substantial proportion (39, 40%) did not attend any sessions (Table 7). Of the 97 randomised to the intervention, 17 were never allocated a gFNP UID number by the relevant gFNP team and did not attend any sessions. The reasons for this are given in Chapter 5 (see Uptake of the programme). Twenty-two of the remaining 80 participants registered for gFNP did not attend any sessions, 10 of whom were allocated to groups that did not offer any sessions. Five of those were offered one-to-one FNP, but no information was available about how much of that service was received and others were referred back to existing services. Thus, of the 97 study participants allocated to the intervention arm, 58 took part in at least one gFNP session. A summary of attendance overall and by group is given in Table 6 (trial participants and buffer clients), Table 7 (only intervention arm trial participants), Table 8 (only intervention arm trial participants, pregnancy sessions) and Table 9 (only intervention arm trial participants, infancy sessions).
| Site | Group | Number allocated to group | Mean number of sessions attended (SD) | Median number of sessions attended | Range |
|---|---|---|---|---|---|
| All | 97a | 10.3 (13.4) | 2 | 0–44 | |
| 1 | A | 3 | 2.3 (3.2) | 1 | 0–6 |
| 1 | B | 12 | 6.8 (11.7) | 1 | 0–31 |
| 2 | A | 4 | 36.3 (11.7) | 41 | 19–44 |
| 2 | B | 6 | 15.5 (14.3) | 15.5 | 0–32 |
| 3 | A | 5 | 1.4 (1.3) | 2 | 0–3 |
| 3 | B | 8 | 20.6 (12.6) | 25.5 | 0–33 |
| 4 | A | 6 | 3.3 (2.4) | 4 | 0–6 |
| 4 | B | 9 | 19.7 (15.4) | 26 | 0–38 |
| 4 | C | 6 | 0.3 (0.5) | 0 | 0–1 |
| 5 | A | 5 | 12.2 (10.6) | 16 | 0–24 |
| 5 | B | 7 | 0 (0.0) | 0 | 0–0 |
| 6 | A | 4 | 22.8 (15.9) | 28 | 0–35 |
| 6 | B | 9 | 13.1 (13.6) | 13 | 0–34 |
| 7 | A | 5 | 1.2 (2.2) | 0 | 0–5 |
| 7 | B | 5 | 4.2 (4.1) | 5 | 0–9 |
| 7 | C | 3 | 0 (0.0) | 0 | 0–0 |
| Site | Group | Mean number of sessions attended (SD) | Median number of sessions attended | Range |
|---|---|---|---|---|
| All | 4.5 (5.1) | 2 | 0–15 | |
| 1 | A | 2 (2.6) | 1 | 0–5 |
| 1 | B | 2.9 (3.8) | 1 | 0–10 |
| 2 | A | 13 (2.0) | 14 | 10–14 |
| 2 | B | 8.3 (7.1) | 10.5 | 0–15 |
| 3 | A | 1.4 (1.3) | 2 | 0–3 |
| 3 | B | 7 (4.9) | 8 | 0–14 |
| 4 | A | 3.3 (2.4) | 4 | 0–6 |
| 4 | B | 7.9 (6.4) | 11 | 0–14 |
| 4 | C | 0.3 (0.5) | 0 | 0–1 |
| 5 | A | 6.4 (5.3) | 7 | 0–12 |
| 5 | B | 0 (0.0) | 0 | 0–0 |
| 6 | A | 8.5 (6.0) | 10 | 0–14 |
| 6 | B | 4.9 (4.4) | 6 | 0–12 |
| 7 | A | 0.8 (1.3) | 0 | 0–3 |
| 7 | B | 4.2 (4.1) | 5 | 0–9 |
| 7 | C | 0 (0.0) | 0 | 0–0 |
| Site | Group | Mean number of sessions attended (SD) | Median number of sessions attended | Range |
|---|---|---|---|---|
| All | 5.8 (8.2) | 0 | 0–30 | |
| 1 | A | 0.3 (0.6) | 0 | 0–1 |
| 1 | B | 3.8 (8.3) | 0 | 0–22 |
| 2 | A | 23.3 (9.7) | 27 | 9–30 |
| 2 | B | 7.2 (7.7) | 5 | 0–17 |
| 3 | A | 0 (0.0) | 0 | 0–0 |
| 3 | B | 13.6 (8.6) | 16.5 | 0–22 |
| 4 | A | 0 (0.0) | 0 | 0–0 |
| 4 | B | 11.8 (9.5) | 14 | 0–24 |
| 4 | C | 0 (0.0) | 0 | 0–0 |
| 5 | A | 5.8 (5.7) | 7 | 0–13 |
| 5 | B | 0 (0.0) | 0 | 0–0 |
| 6 | A | 14.3 (9.9) | 18 | 0–21 |
| 6 | B | 8.2 (9.4) | 7 | 0–23 |
| 7 | A | 0 (0.0) | 0 | 0–0 |
| 7 | B | 0 (0.0) | 0 | 0–0 |
| 7 | C | 0 (0.0) | 0 | 0–0 |
Baseline demographics for all intervention arm trial participants and for those who attended at least one group session are given in Table 10. There are no apparent differences between the demographic characteristics of women who attended at least one group session and those of the intervention arm trial participants as a whole.
| Category | Intervention (N = 97), n (%) | Attended at least one group session (N = 58), n (%) | Control (N = 67), n (%) |
|---|---|---|---|
| Age, mean (SD) | 21.7 (1.9) | 21.6 (1.8) | 21.9 (1.6) |
| Missing, n | 1 | 1 | 1 |
| Age at LMP, mean (SD) | 21.0 (1.8) | 20.9 (1.7) | 21.2 (1.8) |
| Educational qualifications: GCSEs or equivalent? | |||
| Yes | 73 (75.3) | 46 (79.3) | 55 (82.1) |
| No | 24 (24.7) | 12 (20.7) | 12 (17.9) |
| Number of GCSEs, mean (SD) | 6.7 (3.1) | 6.5 (3.3) | 6.4 (2.7) |
| Data available, n | 70 | 44 | 54 |
| Number of GCSEs at grade C or higher, mean (SD) | 3.8 (3.6) | 3.9 (3.6) | 3 (2.5) |
| Data available, n | 69 | 43 | 53 |
| Educational qualifications: other? | |||
| Yes | 79 (82.3) | 47 (81.0) | 56 (83.6) |
| No | 17 (17.7) | 11 (19.0) | 11 (16.4) |
| Ethnicity? | |||
| White: British | 61 (63.5) | 34 (59.7) | 48 (71.6) |
| White: Irish | 2 (2.1) | 2 (3.5) | 0 (0.0) |
| Any other white background | 2 (2.1) | 1 (1.8) | 3 (4.5) |
| Asian British: Indian | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Asian British: Pakistani | 5 (5.2) | 1 (1.8) | 5 (7.5) |
| Asian British: Bangladeshi | 1 (1.0) | 1 (1.8) | 0 (0.0) |
| Black British: Caribbean | 14 (14.6) | 10 (17.5) | 6 (9.0) |
| Black British: African | 3 (3.1) | 3 (5.3) | 2 (3.0) |
| Any other black background | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Chinese | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mixed | 8 (8.3) | 5 (8.8) | 3 (4.5) |
| Prefer not to say | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Current partner? | |||
| Yes | 83 (85.6) | 51 (87.9) | 59 (88.1) |
| No | 14 (14.4) | 7 (12.1) | 8 (11.9) |
| Current partner: biological father? | |||
| Yes | 83 (100.0) | 51 (100.0) | 59 (100.0) |
| No | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Marital status? | |||
| Married | 10 (10.4) | 6 (10.3) | 8 (11.9) |
| Unmarried/cohabiting | 43 (44.8) | 25 (43.1) | 37 (55.2) |
| Separated | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Widowed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Divorced | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Single | 43 (44.8) | 27 (46.6) | 22 (32.8) |
| Number of people currently living with, mean (SD) | 2.9 (1.5) | 2.8 (1.5) | 3.1 (1.6) |
| Missing, n | 1 | 1 | |
| Currently living in household? | |||
| Own mother/parents | 11 (11.7) | 4 (7.1) | 7 (10.9) |
| Husband/partner | 24 (25.5) | 16 (28.6) | 24 (37.5) |
| Husband/partner and others, not including maternal mother | 10 (10.6) | 5 (8.9) | 6 (9.4) |
| Own mother/parents and others, not including husband/partner | 14 (14.9) | 8 (14.3) | 10 (15.6) |
| Own mother/parents and others, including husband/partner | 6 (6.4) | 3 (5.4) | 5 (7.8) |
| Foster parent | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Husband/partner and others | 2 (2.1) | 2 (3.6) | 3 (4.7) |
| Other adults (own father, aunt, grandmother, older sibling, friend, etc.) | 12 (12.8) | 9 (16.1) | 6 (9.4) |
| Live alone | 15 (16.0) | 9 (16.1) | 3 (4.7) |
| Where are you living? | |||
| House or bungalow | 68 (70.1) | 38 (65.5) | 49 (73.1) |
| Flat, low rise | 12 (12.4) | 9 (15.5) | 5 (7.5) |
| Flat, high rise, first three floors | 5 (5.2) | 2 (3.5) | 12 (17.9) |
| Flat, high rise, above third floor | 4 (4.1) | 2 (3.5) | 0 (0.0) |
| Room or bedsit | 2 (2.1) | 1 (1.7) | 1 (1.5) |
| Hostel | 2 (2.1) | 2 (3.5) | 0 (0.0) |
| Supported housing | 1 (1.0) | 1 (1.7) | 0 (0.0) |
| In a group home/shelter | 2 (2.1) | 2 (3.5) | 0 (0.0) |
| Confined to an institutional facility | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Homeless | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Other | 1 (1.0) | 1 (1.7) | 0 (0.0) |
| Enrolled in any school or educational programme? | |||
| Yes | 12 (12.4) | 9 (15.5) | 9 (13.4) |
| No | 85 (87.6) | 49 (84.5) | 58 (86.6) |
| What course? | |||
| School, up to year 11 | 1 (8.3) | 1 (11.1) | 0 (0.0) |
| School, year 12 or 13/sixth form college | 1 (8.3) | 1 (11.1) | 0 (0.0) |
| Access course | 1 (8.3) | 0 (0.0) | 1 (11.1) |
| Vocational course | 6 (50.0) | 4 (44.4) | 2 (22.2) |
| University | 3 (25.0) | 3 (33.3) | 6 (66.7) |
| Ever worked? | |||
| Yes | 76 (78.4) | 46 (79.3) | 56 (83.6) |
| No | 21 (21.7) | 12 (20.7) | 11 (16.4) |
| Currently working? | |||
| Yes, full-time | 30 (39.5) | 17 (37.0) | 28 (50.0) |
| Yes, part-time | 14 (18.4) | 9 (19.6) | 8 (14.3) |
| No | 32 (42.1) | 20 (43.5) | 20 (35.7) |
Primary outcome
A total of 131 12-month interviews were carried out within the agreed time frame and 101 mothers agreed to be videoed for the CARE-Index. 73,74 The reasons for not agreeing to video recording were as follows: self-conscious about appearing on video (five of these participants were in a later stage of pregnancy) (n = 14); baby not well (n = 4); no time after the interviews and did not want a second appointment (n = 4); family pressure (n = 3); just did not like the idea (n = 3); interview not in the home so not practical (n = 1); and failure of recording and no wish for another appointment (n = 1). The primary outcome data and estimated intervention effects are shown in Table 11.
| Measure | Intervention (n = 75), mean (SE) | Control (n = 56), mean (SE) | Unadjusted effect estimatea | Adjusted effect estimateb | ||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |||
| AAPI-272 (higher = positive) | ||||||
| Total (/10) | 7.5 (0.1) | 7.5 (0.1) | 0.05 (–0.17 to 0.24) | 0.68 | 0.06 (–0.15 to 0.28) | 0.59 |
| Missing, n | 5 | 1 | ||||
| Inappropriate expectations (/35) | 23.5 (0.6) | 22.9 (0.6) | 0.58 (–0.71 to 1.96) | 0.44 (–0.89 to 1.78) | ||
| Empathy (/50) | 38.0 (0.6) | 37.0 (0.7) | 1.2 (–0.11 to 2.49) | 1.21 (–0.03 to 2.57) | ||
| Corporal punishment (/55) | 43.3 (0.7) | 43.3 (0.7) | –0.63 (–2.17 to 0.84) | –0.45 (–1.96 to 1.02) | ||
| Role reversal (/35) | 25.6 (0.5) | 26.1 (0.6) | –0.5 (–1.54 to 0.53) | –0.47 (–1.53 to 0.60) | ||
| Power independence (/25) | 19.5 (0.3) | 19.7 (0.3) | 0.01 (–0.72 to 0.73) | –0.11 (–0.90 to 0.58) | ||
| CARE-Index73,74 (higher = positive) | ||||||
| n = 57 | n = 44 | |||||
| Mother’s sensitivity | 4.0 (0.3) | 4.7 (0.4) | –0.76 (–1.68 to 0.13) | 0.22 | –0.68 (–1.62 to 0.16) | 0.25 |
There was no suggestion of an important effect of gFNP on either of the two primary outcomes in the ITT analysis based on outcomes available within the agreed time frame. The AAPI-272 total was 7.5/10 [standard error (SE) 0.1] in both arms [difference adjusted for baseline, site and maternal age group 0.08 (95% CI –0.15 to 0.28; p = 0.50)]; and mother’s sensitivity in the CARE-Index,73,74 mean 4.0 in intervention arm (SE 0.3) and 4.7 in control arm (SE 0.4) [difference adjusted for site and maternal age group –0.76 (95% CI –1.67 to 0.13, p = 0.21)] (see Table 11).
Three sensitivity analyses were carried out: the first included all participants irrespective of whether or not they were within the pre-specified time window; the second explored the effect of including a random effect for the small group the intervention was delivered in; and the third explored the effect of premature births. All three supported the findings of the primary analysis (see Appendix 2).
Using a CACE analysis88 (see Chapter 2) to take account of compliance made very little difference to the ITT results for the AAPI-2 either when compliance was defined as attending at least one group session (difference 0.14, 95% CI –0.41 to 0.69; p = 0.64), or when it was defined as attending at least 17 group sessions (difference 0.17, 95% CI –0.91 to 1.24; p = 0.76). The corresponding results for mother’s sensitivity in the CARE-Index are difference –1.29 (95% CI –2.78 to 0.19; p = 0.09) when compliance was defined as attending at least one group session and difference –2.61 (95% CI –5.57 to 0.35; p = 0.8) when compliance was defined as attending at least 17 group sessions (Table 12).
| Measure | Intervention (n = 75), mean (SE) | Control (n = 56), mean (SE) | Unadjusted effect estimate, difference (95% CI) | p-value |
|---|---|---|---|---|
| AAPI-272 (higher = positive) | ||||
| Total (/10) attended at least one session | 7.6 (0.2) | 7.4 (0.2) | 0.13 (–0.40 to 0.66) | 0.64 |
| Total (/10) attended at least 17 sessions | 7.9 (0.2) | 7.7 (0.5) | 0.18 (–0.88 to 1.23) | 0.74 |
| CARE-Index73,74 (higher = positive) | ||||
| Total (/10) attended at least one session | 4.1 (0.3) | 5.4 (0.7) | –1.26 (–2.71 to 0.20) | 0.09 |
| Total (/10) attended at least 17 sessions | 4.3 (0.5) | 6.9 (1.4) | –2.55 (–5.44 to 0.35) | 0.09 |
Secondary outcomes
The pre-specified secondary outcomes based on data available within the agreed time frames are shown in Table 13. There was no evidence of any effect of the intervention on any of the secondary outcomes, with the exception that the proportion of women still breastfeeding at 6 months was higher in the intervention arm (adjusted OR 3.2, 95% CI 0.99 to 10.6; p = 0.05). The sensitivity analyses carried out supported the findings of the primary analysis (see Appendix 2).
| Measure | Intervention, mean (SE) | Control, mean (SE) | Unadjusted effect estimatea | Adjusted effect estimateb | ||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |||
| CARE-Index73,74 (higher = more co-operative) | ||||||
| n = 57 | n = 44 | |||||
| Infant co-operativeness | 3.0 (0.3) | 3.5 (0.3) | –0.49 (–1.25 to 0.34) | 0.38 | –0.45 (–1.25 to 0.33) | 0.42 |
| EPDS76 (higher = more depressed) | ||||||
| n = 84 | n = 60 | |||||
| Total (/30): 2 months | 3.4 (0.5) | 3.5 (0.5) | ||||
| Missing, n | 1 | 1 | ||||
| Total (/30): 6 months | 3.1 (0.5) | 3.0 (0.6) | ||||
| Total (/30): 12 months | 3.8 (0.5) | 4.1 (0.6) | –0.07 (–0.76 to 0.62) | 0.85 | 0.05 (–0.68 to 0.77) | 0.90 |
| Missing, n | 1 | 1 | ||||
| PSOC scale82 (higher = more competent) | ||||||
| n = 84 | n = 60 | |||||
| Total (/102): 2 months | 60.6 (0.6) | 60.7 (0.5) | ||||
| Missing, n | 3 | 1 | ||||
| Total (/102): 12 months | 60.9 (0.4) | 60.7 (0.6) | –0.12 (–0.92 to 0.67) | 0.76 | –0.18 (–1.03 to 0.67) | 0.68 |
| Missing, n | 2 | |||||
| PSI77 (higher = more stress) | ||||||
| n = 84 | n = 60 | |||||
| Total (/180): 2 months | 70.5 (1.9) | 68.3 (1.8) | ||||
| Missing, n | 3 | 1 | ||||
| Total (/180): 12 months | 73.4 (1.5) | 74.9 (2.0) | –0.97 (–3.65 to 1.70) | 0.48 | –1.09 (–3.86 to 1.68) | 0.44 |
| Missing, n | 1 | 2 | ||||
| Social networks83 (higher = more support) | ||||||
| n = 75 | n = 56 | |||||
| Total (/100) | 84.6 (2.2) | 84.5 (2.3) | –0.59 (–5.71 to 4.53) | 0.82 | –0.45 (–5.45 to 4.59) | 0.85 |
| Missing, n | 2 | 1 | ||||
| Tangible support (/100) | 81.9 (2.4) | 81.7 (2.8) | 0.12 (–6.35 to 5.98) | –0.31 (–7.21 to 5.56) | ||
| Emotional support (/100) | 84.5 (2.3) | 82.8 (2.7) | 0.07 (–6.00 to 6.36) | 0.05 (–6.09 to 6.12) | ||
| Affectionate support (/100) | 88.6 (2.3) | 92 (1.9) | –3.63 (–9.20 to 1.87) | –4.31 (–10.24 to 1.32) | ||
| Positive social interaction (/100) | 84.5 (2.3) | 85.9 (2.4) | –1.82 (–8.36 to 4.39) | –1.19 (–8.42 to 4.19) | ||
| Relationships (higher = abuse) | ||||||
| n = 75 | n = 56 | |||||
| Total abuse (/6) | 0.4 (0.1) | 0.5 (0.1) | –0.07 (–0.39 to 0.19) | 0.63 | –0.10 (–0.40 to 0.17) | 0.47 |
| Physical aggression (/2) | 0.1 (0.0) | 0.1 (0.1) | –0.08 (–0.24 to 0.05) | –0.09 (–0.24 to 0.04) | ||
| Verbal abuse (/2) | 0.3 (0.1) | 0.3 (0.1) | –0.02 (–0.19 to 0.14) | –0.04 (–0.20 to 0.12) | ||
| Sexual abuse (/2) | 0 (0.0) | 0 (0.0) | ||||
| Smoking, alcohol and drugs | ||||||
| n = 75 | n = 56 | |||||
| Combined substance abuse score (/24) | 17 (0.3) | 16.6 (0.3) | –0.2 (–1.19 to 0.79) | 0.71 | –0.20 (–1.16 to 0.82) | 0.70 |
| Still breastfeeding at 6 months | ||||||
| n = 70 | n = 51 | |||||
| Yes | 15 (21.4) | 4 (7.8) | 3.2 (0.99 to 10.3) | 0.05 | 3.46 (1.02 to 11.75) | 0.05 |
| No | 55 (78.6) | 47 (92.2) | 1 | |||
Reliability of the CARE-Index
Ten videos were analysed for the CARE-Index by two coders. Lin’s concordance coefficient for mother’s sensitivity based on these 10 videos was 0.56 (95% CI 0.27 to 0.85), suggesting poor agreement. Examination of the Bland–Altman plot for this outcome (see Appendix 3) suggests systematic bias for this component of the CARE-Index, with one scorer consistently scoring higher than the other.
Demographics and outcomes at 2, 6 and 12 months
See Appendix 1 for demographic updates. Baby demographics (Table 14), infant feeding (Tables 15 and 16), immunisations (Tables 17 and 18), smoking, alcohol and drug use (Tables 19 and 20), questionnaire scores (Tables 21–23) and all CARE-Index scores (Table 24) follow.
| Category | Intervention (N = 78a) | Control (N = 54b) |
|---|---|---|
| Age of baby | ||
| Age in days, mean (SD) | 73.0 (15.1) | 74.8 (15.4) |
| Sex | ||
| Male, n (%) | 42 (53.8) | 34 (63.0) |
| Female, n (%) | 36 (46.2) | 20 (37.0) |
| Birthweight | ||
| Weight in grams, mean (SD) | 3165.0 (85.8) | 3178.3 (77.0) |
| Missing, n | 1 | |
| Category | Intervention (N = 75), n (%) | Control (N = 53), n (%) |
|---|---|---|
| Ever breastfed? | ||
| Yes | 64 (85.3) | 45 (84.9) |
| No | 11 (14.7) | 8 (15.1) |
| Still breastfeeding? | ||
| Yes | 19 (25.3) | 12 (22.6) |
| No | 56 (74.7) | 41 (77.4) |
| Age last breastfed? | ||
| Age in days, mean (SE) | 18.4 (2.9) | 19.0 (3.7) |
| Data available, n | 41 | 33 |
| Ever had formula? | ||
| Yes | 68 (90.7) | 50 (94.3) |
| No | 7 (9.3) | 3 (5.7) |
| Age first formula? | ||
| Age in days, mean (SE) | 7.1 (1.4) | 10.3 (2.4) |
| Data available, n | 60 | 47 |
| Milk received in last 7 days? | ||
| Only breast milk | 13 (17.8) | 3 (6.0) |
| Only infant formula | 51 (69.9) | 37 (74.0) |
| Breast milk and infant formula | 9 (12.3) | 10 (20.0) |
| Category | Intervention (N = 70), n (%) | Control (N = 51), n (%) |
|---|---|---|
| Ever breastfed? | ||
| Yes | 58 (82.9) | 38 (74.5) |
| No | 12 (17.1) | 13 (25.5) |
| Still breastfeeding? | ||
| Yes | 15 (21.4) | 4 (7.8) |
| No | 55 (78.6) | 47 (92.2) |
| Age last breastfed? | ||
| Age in days, mean (SE) | 43.5 (7.6) | 44.9 (8.3) |
| Data available, n | 43 | 33 |
| Ever had formula? | ||
| Yes | 63 (90.0) | 49 (96.1) |
| No | 7 (10.0) | 2 (3.9) |
| Age first formula? | ||
| Age in days, mean (SE) | 17.3 (7.1) | 18.7 (4.9) |
| Data available, n | 60 | 45 |
| Milk received in last 7 days? | ||
| Only breast milk | 11 (15.9) | 2 (4.1) |
| Only infant formula | 54 (78.3) | 46 (93.9) |
| Breast milk and infant formula | 4 (5.8) | 1 (2.0) |
| Missing, n | 1 | |
| Category | Intervention (N = 75), n (%) | Control (N = 53), n (%) |
|---|---|---|
| Diphtheria vaccination? | ||
| Yes | 51 (68.0) | 36 (67.9) |
| No | 24 (32.0) | 17 (32.1) |
| If no, why | ||
| Decided/advised not to have | 3 (12.5) | 1 (5.9) |
| Appointment booked | 21 (87.5) | 16 (94.1) |
| Tetanus vaccination? | ||
| Yes | 51 (68.0) | 36 (67.9) |
| No | 24 (32.0) | 17 (32.1) |
| If no, why | ||
| Decided/advised not to have | 3 (12.5) | 1 (5.9) |
| Appointment booked | 21 (87.5) | 16 (94.1) |
| Pertussis vaccination? | ||
| Yes | 50 (66.7) | 36 (67.9) |
| No | 25 (33.3) | 17 (32.1) |
| If no, why | ||
| Decided/advised not to have | 3 (12.5) | 1 (5.9) |
| Appointment booked | 21 (87.5) | 16 (94.1) |
| Polio vaccination? | ||
| Yes | 50 (66.7) | 36 (67.9) |
| No | 25 (33.3) | 17 (32.1) |
| If no, why | ||
| Decided/advised not to have | 3 (12.5) | 1 (5.9) |
| Appointment booked | 21 (87.5) | 16 (94.1) |
| Haemophilus influenzae type B vaccination? | ||
| Yes | 51 (68.0) | 36 (67.9) |
| No | 24 (32.0) | 17 (32.1) |
| If no, why | ||
| Decided/advised not to have | 3 (12.5) | 1 (5.9) |
| Appointment booked | 21 (87.5) | 16 (94.1) |
| Pneumococcal infection vaccination? | ||
| Yes | 50 (66.7) | 35 (66.0) |
| No | 25 (33.3) | 18 (34.0) |
| If no, why | ||
| Decided/advised not to have | 3 (13.0) | 1 (6.3) |
| Appointment booked | 20 (87.0) | 15 (93.8) |
| Category | Intervention (N = 75), n (%) | Control (N = 56), n (%) |
|---|---|---|
| Diphtheria vaccination: 8 weeks? | ||
| Yes | 72 (96.0) | 55 (98.2) |
| No | 0 (0.0) | 0 (0.0) |
| Decided/advised not to have | 3 (4.0) | 1 (1.8) |
| Diphtheria vaccination: 3 months? | ||
| Yes | 71 (94.7) | 54 (96.4) |
| No | 1 (1.3) | 0 (0.0) |
| Decided/advised not to have | 3 (4.0) | 2 (3.6) |
| Diphtheria vaccination: 4 months? | ||
| Yes | 70 (94.6) | 54 (96.4) |
| No | 1 (1.4) | 0 (0.0) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 1 | |
| Tetanus vaccination: 8 weeks? | ||
| Yes | 72 (96.0) | 55 (98.2) |
| No | 0 (0.0) | 0 (0.0) |
| Decided/advised not to have | 3 (4.0) | 1 (1.8) |
| Tetanus vaccination: 3 months? | ||
| Yes | 70 (94.6) | 54 (96.4) |
| No | 1 (1.4) | 0 (0.0) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 1 | |
| Tetanus vaccination: 4 months? | ||
| Yes | 69 (94.5) | 54 (96.4) |
| No | 1 (1.4) | 0 (0.0) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 2 | |
| Pertussis vaccination: 8 weeks? | ||
| Yes | 72 (96.0) | 55 (98.2) |
| No | 0 (0.0) | 0 (0.0) |
| Decided/advised not to have | 3 (4.0) | 1 (1.8) |
| Pertussis vaccination: 3 months? | ||
| Yes | 70 (94.6) | 54 (96.4) |
| No | 1 (1.4) | 0 (0.0) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 1 | |
| Pertussis vaccination: 4 months? | ||
| Yes | 70 (94.6) | 54 (96.4) |
| No | 1 (1.4) | 0 (0.0) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 1 | |
| Polio vaccination: 8 weeks? | ||
| Yes | 72 (96.0) | 55 (98.2) |
| No | 0 (0.0) | 0 (0.0) |
| Decided/advised not to have | 3 (4.0) | 1 (1.8) |
| Polio vaccination: 3 months? | ||
| Yes | 70 (94.6) | 54 (96.4) |
| No | 1 (1.4) | 0 (0.0) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 1 | |
| Polio vaccination: 4 months? | ||
| Yes | 69 (94.5) | 54 (96.4) |
| No | 1 (1.4) | 0 (0.0) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 2 | |
| Haemophilus influenzae type B vaccination: 8 weeks? | ||
| Yes | 71 (94.7) | 55 (98.2) |
| No | 1 (1.3) | 0 (0.0) |
| Decided/advised not to have | 3 (4.0) | 1 (1.8) |
| Haemophilus influenzae type B vaccination: 3 months? | ||
| Yes | 69 (93.2) | 54 (96.4) |
| No | 2 (2.7) | 0 (0.0) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 1 | |
| Haemophilus influenzae type B vaccination: 4 months? | ||
| Yes | 68 (93.2) | 53 (94.6) |
| No | 2 (2.7) | 1 (1.8) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 2 | |
| Haemophilus influenzae type B vaccination: 1 year? | ||
| Yes | 19 (43.2) | 18 (50.0) |
| No | 22 (50.0) | 16 (44.4) |
| Decided/advised not to have | 3 (6.8) | 2 (5.6) |
| Missing, n | 32 | 20 |
| Pneumococcal infection vaccination: 8 weeks? | ||
| Yes | 70 (94.6) | 54 (96.4) |
| No | 1 (1.4) | 1 (1.8) |
| Decided/advised not to have | 3 (4.1) | 1 (1.8) |
| Missing, n | 1 | |
| Pneumococcal infection vaccination: 4 months? | ||
| Yes | 68 (93.2) | 53 (94.6) |
| No | 2 (2.7) | 1 (1.8) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 2 | |
| Meningococcal group C vaccination: 3 months? | ||
| Yes | 69 (92.0) | 52 (92.9) |
| No | 3 (4.0) | 2 (3.6) |
| Decided/advised not to have | 3 (4.0) | 2 (3.6) |
| Meningococcal group C vaccination: 4 months? | ||
| Yes | 67 (91.8) | 53 (94.6) |
| No | 3 (4.1) | 1 (1.8) |
| Decided/advised not to have | 3 (4.1) | 2 (3.6) |
| Missing, n | 2 | |
| Meningococcal group C vaccination: 1 year? | ||
| Yes | 19 (42.2) | 18 (50.0) |
| No | 23 (51.1) | 16 (44.4) |
| Decided/advised not to have | 3 (6.7) | 2 (5.6) |
| Missing, n | 30 | 20 |
| Category | Intervention (N = 75), n (%) | Control (N = 53), n (%) |
|---|---|---|
| Baseline smoking status | ||
| Smoker | 23 (31.1) | 21 (39.6) |
| Was smoker but quit | 9 (12.2) | 7 (13.2) |
| Non-smoker | 42 (56.8) | 25 (47.2) |
| Anyone smoking in house since birth? | ||
| Yes | 9 (12.0) | 14 (26.4) |
| No | 66 (88.0) | 39 (73.6) |
| Current smoker? | ||
| Yes | 19 (25.3) | 18 (34.0) |
| No | 56 (74.7) | 35 (66.0) |
| Number of cigarette a day (if yes) | ||
| Mean (SD) | 6.7 (1.2) | 5.4 (1.0) |
| Data available, n | 19 | 17 |
| Are you trying to cut down (if yes)? | ||
| Yes | 2 (66.7) | 5 (55.6) |
| No | 1 (33.3) | 4 (44.4) |
| Have you used nicotine replacement (if yes)? | ||
| Yes | 1 (50.0) | 1 (20.0) |
| No | 1 (50.0) | 4 (80.0) |
| Number of cigarettes a day if cutting down | ||
| Mean (SD) | 5.0 (2.0) | 9 (1.9) |
| Data available, n | 2 | 5 |
| Number of cigarettes yesterday | ||
| Mean (SD) | 5.0 (2.0) | 9.6 (1.6) |
| Data available, n | 2 | 5 |
| Do you drink? | ||
| Yes | 35 (46.7) | 28 (52.8) |
| No | 40 (53.3) | 25 (47.2) |
| How often did you drink in the last month? | ||
| Every day | 0 (0.0) | 0 (0.0) |
| Five or six times a week | 0 (0.0) | 0 (0.0) |
| Three or four times a week | 1 (2.9) | 0 (0.0) |
| Once or twice a week | 4 (11.4) | 4 (14.3) |
| Once or twice a month | 18 (51.4) | 12 (42.9) |
| Less than once a month | 8 (22.9) | 10 (35.7) |
| Never | 4 (11.4) | 2 (7.1) |
| Refused to answer | 0 (0.0) | 0 (0.0) |
| Was last month typical? | ||
| Yes | 26 (74.3) | 22 (78.6) |
| No | 9 (25.7) | 6 (21.4) |
| If no, how often do you drink in a typical month? | ||
| Every day | 0 (0.0) | 0 (0.0) |
| Five or six times a week | 0 (0.0) | 0 (0.0) |
| Three or four times a week | 0 (0.0) | 0 (0.0) |
| Once or twice a week | 2 (22.2) | 1 (20.0) |
| Once or twice a month | 2 (22.2) | 1 (20.0) |
| Less than once a month | 4 (44.4) | 2 (40.0) |
| Never | 1 (11.1) | 1 (20.0) |
| Refused to answer | 0 (0.0) | 0 (0.0) |
| Number of units a day | ||
| Mean (SD) | 4.1 (0.6) | 7.0 (1.7) |
| Data available, n | 34 | 28 |
| How often did you use marijuana in the last month? | ||
| Every day | 0 (0.0) | 0 (0.0) |
| Five or six times a week | 0 (0.0) | 1 (1.9) |
| Three or four times a week | 0 (0.0) | 0 (0.0) |
| Once or twice a week | 0 (0.0) | 1 (1.9) |
| Once or twice a month | 0 (0.0) | 0 (0.0) |
| Less than once a month | 0 (0.0) | 0 (0.0) |
| Never | 75 (100.0) | 51 (96.2) |
| Refused to answer | 0 (0.0) | 0 (0.0) |
| How often did you use street drugs in the last month? | ||
| Every day | 0 (0.0) | 0 (0.0) |
| Five or six times a week | 0 (0.0) | 0 (0.0) |
| Three or four times a week | 0 (0.0) | 0 (0.0) |
| Once or twice a week | 0 (0.0) | 0 (0.0) |
| Once or twice a month | 0 (0.0) | 0 (0.0) |
| Less than once a month | 0 (0.0) | 0 (0.0) |
| Never | 75 (100.0) | 53 (100.0) |
| Refused to answer | 0 (0.0) | 0 (0.0) |
| Category | Intervention (N = 75), n (%) | Control (N = 56), n (%) |
|---|---|---|
| Baseline smoking status | ||
| Smoker | 24 (32.0) | 22 (39.3) |
| Was smoker but quit | 6 (8.0) | 7 (12.5) |
| Non-smoker | 45 (60.0) | 27 (48.2) |
| Anyone smoking in house? | ||
| Yes | 9 (12.3) | 10 (17.9) |
| No | 64 (87.7) | 46 (82.1) |
| Current smoker? | ||
| Yes | 25 (33.3) | 20 (35.7) |
| No | 50 (66.7) | 36 (64.3) |
| Number of cigarettes a day (if yes) | ||
| Mean (SE) | 7.9 (1.1) | 7.4 (1.4) |
| Are you trying to cut down (if yes)? | ||
| Yes | 11 (52.4) | 11 (55.0) |
| No | 10 (47.6) | 9 (45.0) |
| Have you used nicotine replacement (if yes)? | ||
| Yes | 3 (27.3) | 3 (27.3) |
| No | 8 (72.7) | 8 (72.7) |
| Number of cigarettes a day if cutting down | ||
| Mean (SE) | 7.4 (1.7) | 8.7 (1.9) |
| Missing, n | 4 | |
| Number of cigarettes yesterday | ||
| Mean (SE) | 7.7 (1.2) | 6.9 (1.2) |
| Data available, n | 23 | 19 |
| Do you drink? | ||
| Yes | 44 (58.7) | 32 (57.1) |
| No | 31 (41.3) | 24 (42.9) |
| How often did you drink in the last month? | ||
| Every day | 0 (0.0) | 0 (0.0) |
| Five or six times a week | 0 (0.0) | 1 (3.1) |
| Three or four times a week | 1 (2.3) | 0 (0.0) |
| Once or twice a week | 9 (20.5) | 6 (18.8) |
| Once or twice a month | 24 (54.6) | 15 (46.9) |
| Less than once a month | 4 (9.1) | 6 (18.8) |
| Never | 6 (13.6) | 4 (12.5) |
| Refused to answer | 0 (0.0) | 0 (0.0) |
| Was last month typical? | ||
| Yes | 29 (65.9) | 23 (71.9) |
| No | 15 (34.1) | 9 (28.1) |
| If no, how often do you drink in a typical month? | ||
| Every day | 0 (0.0) | 0 (0.0) |
| Five or six times a week | 0 (0.0) | 0 (0.0) |
| Three or four times a week | 0 (0.0) | 0 (0.0) |
| Once or twice a week | 1 (6.7) | 1 (11.1) |
| Once or twice a month | 4 (26.7) | 3 (33.3) |
| Less than once a month | 7 (46.7) | 4 (44.4) |
| Never | 3 (20.0) | 1 (11.1) |
| Refused to answer | 0 (0.0) | 0 (0.0) |
| Number of units a day | ||
| Mean (SE) | 6.2 (0.9) | 4.5 (0.7) |
| Data available, n | 39 | 31 |
| How often did you use marijuana in the last month? | ||
| Every day | 0 (0.0) | 2 (3.6) |
| Five or six times a week | 0 (0.0) | 0 (0.0) |
| Three or four times a week | 0 (0.0) | 1 (1.8) |
| Once or twice a week | 0 (0.0) | 0 (0.0) |
| Once or twice a month | 0 (0.0) | 1 (1.8) |
| Less than once a month | 0 (0.0) | 0 (0.0) |
| Never | 75 (100.0) | 52 (92.9) |
| Refused to answer | 0 (0.0) | 0 (0.0) |
| How often did you use street drugs in the last month? | ||
| Every day | 0 (0.0) | 0 (0.0) |
| Five or six times a week | 0 (0.0) | 0 (0.0) |
| Three or four times a week | 0 (0.0) | 0 (0.0) |
| Once or twice a week | 0 (0.0) | 0 (0.0) |
| Once or twice a month | 0 (0.0) | 0 (0.0) |
| Less than once a month | 0 (0.0) | 0 (0.0) |
| Never | 75 (100.0) | 56 (100.0) |
| Refused to answer | 0 (0.0) | 0 (0.0) |
| Category | Intervention (N = 75) | Control (N = 53) |
|---|---|---|
| EPDS76 (higher = more depressed), mean (SD) | ||
| Total (/30) | 3.4 (0.5) | 3.5 (0.5) |
| Missing, n | 1 | 1 |
| Possible depression (EPDS ≥ 10), n (%) | ||
| Yes | 2 (2.7) | 2 (3.9) |
| No | 72 (97.3) | 50 (96.2) |
| PSOC scale82 (higher = more competent), mean (SD) | ||
| Total (/102) | 60.6 (0.6) | 60.7 (0.5) |
| Missing, n | 3 | 1 |
| PSI77 (higher = more stress), mean (SD) | ||
| Total (/180) | 70.5 (1.9) | 68.3 (1.8) |
| Missing, n | 3 | 1 |
| Category | Intervention (N = 70), mean (SE) | Control (N = 51), mean (SE) |
|---|---|---|
| EPDS76 (higher = more depressed) | ||
| Total (/30) | 3.1 (0.5) | 3.0 (0.6) |
| Possible depression (EPDS ≥ 10), n (%) | ||
| Yes | 4 (5.7) | 5 (9.8) |
| No | 66 (94.3) | 46 (90.2) |
| Category | Intervention (N = 75), mean (SE) | Control (N = 56), mean (SE) |
|---|---|---|
| AAPI-272 (higher = positive) | ||
| Total (/10) | 7.5 (0.1) | 7.5 (0.1) |
| Missing, n | 5 | 1 |
| Inappropriate expectations (/35) | 23.5 (0.6) | 22.9 (0.6) |
| Empathy (/50) | 38 (0.6) | 37 (0.7) |
| Corporal punishment (/55) | 43.3 (0.7) | 43.3 (0.7) |
| Role reversal (/35) | 25.6 (0.5) | 26.1 (0.6) |
| Power independence (/25) | 19.5 (0.3) | 19.7 (0.3) |
| EPDS76 (higher = more depressed) | ||
| Total (/30) | 3.8 (0.5) | 4.1 (0.6) |
| Missing, n | 1 | 1 |
| Possible depression (EPDS ≥ 10), n (%) | ||
| Yes | 4 (5.4) | 6 (10.9) |
| No | 70 (94.6) | 49 (89.1) |
| Social networks83 (higher = more support) | ||
| Total (/100) | 84.6 (2.2) | 84.5 (2.3) |
| Missing, n | 2 | 1 |
| Tangible support (/100) | 81.9 (2.4) | 81.7 (2.8) |
| Emotional support (/100) | 84.5 (2.3) | 82.8 (2.7) |
| Affectionate support (/100) | 88.6 (2.3) | 92 (1.9) |
| Positive social interaction (/100) | 84.5 (2.3) | 85.9 (2.4) |
| Relationships (higher = abuse) | ||
| Total abuse (/8) | 0.4 (0.1) | 0.5 (0.1) |
| Physical aggression (/2) | 0.1 (0.0) | 0.1 (0.1) |
| Verbal abuse (/2) | 0.3 (0.1) | 0.3 (0.1) |
| Sexual abuse (/2) | 0 (0.0) | 0 (0.0) |
| PSOC scale82 (higher = more competent) | ||
| Total (/102) | 60.9 (0.4) | 60.7 (0.6) |
| Missing, n | 2 | |
| PSI77 (higher = more stress) | ||
| Total (/180) | 73.4 (1.5) | 74.9 (2.0) |
| Missing, n | 1 | 2 |
| Category | Intervention (n = 57), mean (SE) | Control (n = 44), mean (SE) |
|---|---|---|
| CARE-Index | ||
| Mother’s sensitivity | 4.0 (0.3) | 4.7 (0.4) |
| Infant co-operativeness | 3.0 (0.3) | 3.5 (0.3) |
| Dyadic synchronicity | 4 (0.2) | 4.7 (0.3) |
| Mother controlling | 3.2 (0.5) | 2.7 (0.5) |
| Mother unresponsive | 6.8 (0.5) | 6.7 (0.6) |
| Infant compulsive | 3.1 (0.4) | 2.2 (0.5) |
| Infant difficult | 3.5 (0.4) | 3.6 (0.5) |
| Infant passive | 4.5 (0.6) | 4.4 (0.7) |
| Mother pattern | ||
| Unresponsive | 37 (64.9) | 28 (65.1) |
| Control | 18 (31.6) | 11 (25.6) |
| Sensitive | 2 (3.5) | 4 (9.3) |
| Infant pattern | ||
| 1 | 26 (45.6) | 17 (39.5) |
| 2 | 13 (22.8) | 11 (25.6) |
| 3 | 16 (28.1) | 11 (25.6) |
| 4 | 2 (3.5) | 4 (9.3) |
Harms/severe adverse events
Information was collected at maternal interview on loss/termination of the pregnancy; hospitalisation of mother or infant other than for delivery (see Chapter 4 for details); congenital anomaly or birth defect; persistent or significant disability; and death of either mother or infant. These were reported to the REC.
Miscarriage or termination before the time that participants could begin attending gFNP sessions occurred in the case of five of the intervention arm participants and one control group member (Table 25). One further potential gFNP client did not respond to researcher contact and communication with her GP indicated that there had not been a live birth, but this was not confirmed by the participant. One additional participant in the intervention group experienced late loss of pregnancy in the eighth month, and the infant of one participant in the control group died at age 3 months. At the time that the information was received regarding loss of pregnancy, the research team did not have information about the participant’s allocation; however, all but one loss occurred early in pregnancy, before the intervention was likely to have been initiated. All participants except the one who experienced unreported miscarriage/termination received letters inviting them to remain in the study, but none wished to do so. No information was requested about any potential reason for the loss of the pregnancy.
| SAE | gFNP | Usual care |
|---|---|---|
| Miscarriage/termination | 5 | 1 |
| Late miscarriage | 1 | |
| Infant death | 1 | |
| Suspected miscarriage/terminationa | 1 |
Chapter 4 Economic evaluation
Overview
A prospective economic evaluation was conducted alongside the RCT with the aim of estimating the cost-effectiveness of the gFNP programme in comparison with standard care. The primary analysis adopted the perspective of the NHS and PSS recommended by NICE and consequently excludes the costs incurred by other sectors of the economy or by families and informal carers. 89
Two main analyses of incremental cost-effectiveness were conducted. The first analysis comprised a cost–utility analysis (CUA) calculating the incremental cost per quality-adjusted life-year (QALY) gained attributable to the gFNP programme, based on maternal HRQoL outcomes. 90,91 The second analysis comprised a cost-effectiveness analysis (CEA) calculating the incremental cost per unit change in each of the primary outcomes [i.e. incremental cost per unit change in the revised AAPI-272 or incremental cost per unit change in the CARE-Index (maternal sensitivity domain)]. 73,74
Measurement of resource use and costs
A comprehensive strategy was adopted to estimate the incremental costs associated with the gFNP programme. This encompassed two broad strands of research: (1) estimation of costs associated with the delivery of the gFNP programme; and (2) estimation of broader health and personal social service resource inputs and broader societal resource inputs.
Costing of the Group Family Nurse Partnership programme
A particular focus of the economic evaluation was the assessment of the cost of delivering the gFNP programme in community settings, including the costs of programme development, training of accredited gFNP practitioners, cost of delivering the group sessions, participant monitoring activities and any follow-up/management. This primarily involved asking each of the gFNP practitioners in each site to prospectively complete detailed weekly activity logs outlining the cost of delivering each gFNP session, including costs associated with preparation time, programme delivery time, indirect administrative activities, home visits and telephone contacts, as well as gFNP-related training and supervision activities. The weekly activity logs also recorded the mode, distance and time spent travelling by each practitioner as a result of gFNP-related activities. They also recorded additional expenditures associated with refreshments, materials, cards or gifts, participant travel, partner travel, child care costs and miscellaneous expenditures associated with weekly gFNP-related activities. The costs of venue hire were estimated separately at each site. A copy of the weekly FN activity log is provided online (see Report Supplementary Material 4). The total costs of delivering the gFNP programme across each group and site were subsequently converted into group- and site-specific estimates of average cost per session per attending woman using separately collected attendance data for each group within each site.
Collection of broader resource use data
Data were also collected about all significant health and personal social service and broader societal resource inputs over the period between randomisation and 12 months post partum. Trial participants were asked to complete detailed resource use questionnaires via researcher-administered face-to-face interviews at baseline and at 2, 6 and 12 months post partum to minimise loss of information due to recall difficulties. The data collected from the trial participants at each time point covered their (and, in the case of the postpartum questionnaires, their babies’) use of hospital care services, community-based health care, community-based social care, and medicines and drugs. Information was also collected regarding the use of legal services and costs borne by the trial participants or their family members or friends as a result of the trial participants’ (and, in the case of the postpartum questionnaires, their babies’) health status, over the relevant time horizons. Medication use was categorised by chemical entity, mode of administration, dosage frequency and duration of use. The service use questionnaires were piloted to assess their acceptability and women’s comprehension levels of the questions. Copies of the service use questionnaires administered at each time point are provided online (see Report Supplementary Material 3).
As part of our strategy to measure broader resource use, an application was also submitted to the Health and Social Care Information Centre (HSCIC) during the course of the study for a new data sharing agreement relating to bespoke data linkage of HES admitted inpatient care, A&E and outpatient data to complement data collected within our battery of research instruments. We wanted to use the HES data for our trial participants to validate the self-reported hospital service utilisation data. Unfortunately, despite following the stipulated guidance from the HSCIC at the time of the study design, our application to the HSCIC was rejected on the following grounds: (1) the original consent material (consent form/patient information sheet) was from Birkbeck University of London and did not mention the University of Warwick CTU (the unit co-ordinating the economic evaluation) on either document; and (2) neither document mentioned the HSCIC or mentioned the flow of identifiable data to the HSCIC. Nevertheless, we proceeded to measure hospital service utilisation on the basis of participant self-reports and are confident that the integrity of the study design, conduct and analysis was not compromised.
Valuation of resource use
Resource inputs were valued using a combination of primary research, based on established accounting methods and data collated from secondary national tariff sets. Direct and indirect staff time associated with the delivery of the gFNP programme was valued using national unit costs per working hour for each Agenda for Change band of staff. 93 These unit cost estimates were inclusive of components for staff salaries, employer salary on-costs, qualifications, and revenue and capital overheads. The travel costs for gFNP practitioners were based on standing and running costs per mile provided by the Automobile Association (AA) for travel by car,94 and values published in the Department for Transport Public Service Vehicle Survey for travel by public transport. 95 Inpatient admissions over the study time horizon were delineated by type and duration and valued using per diem costs extracted from the NHS Reference Costs trusts schedule. 96 The use of other hospital-based care was valued by applying unit costs extracted from national tariffs. 97 Costs for the community-based services were calculated by applying unit costs from national tariffs93,97 to resource volumes. NHS net prices per milligram for the medications were obtained from the British National Formulary98 or the British National Formulary for Children. 99 The costs for individual participants or their children were estimated based on their reported doses and frequencies where these were available, or otherwise on an assumed daily dose based on British National Formulary or British National Formulary for Children recommendations. The costs of time taken off work were estimated by applying sex-specific median earnings data to occupational classifications100 derived from self-reported work status information. Other family-borne costs were valued using data reported by the participants as part of the follow-up resource use questionnaires. Unit costs were inflated where necessary to 2014–15 prices (pounds sterling) using the NHS Hospital and Community Health Services Pay and Prices Index. Costs accrued by each trial participant beyond the first 12 months of follow-up were discounted at 3.5%, as recommended by NICE. 89
Calculation of utilities and quality-adjusted life-years
The economic evaluation estimated maternal QALYs with the view to measuring preference-based health outcomes for the purposes of the CUA. The HRQoL of the mothers was assessed using the EQ-5D-5L90,101 obtained at baseline and at 2, 6 and 12 months post partum as a secondary outcome of the trial. The EuroQol-5 Dimensions (EQ-5D) consists of two principal measurement components. The first is a descriptive system, which defines HRQoL in terms of five dimensions: ‘mobility’, ‘self-care’, ‘usual activities’, ‘pain/discomfort’ and ‘anxiety/depression’. Responses in each dimension are divided into five ordinal levels coded (1) no problems, (2) slight problems, (3) moderate problems, (4) severe problems and (5) extreme problems/unable to perform. For the purposes of this study, the new English tariff set for the EQ-5D-5L developed by researchers at the Office of Health Economics was applied to each set of responses to generate an EQ-5D utility score (preference weight) for each woman. 102 The resulting utility scores range from scores –0.281 to 1.0, with 0 representing death and 1.0 representing full health; values below 0 indicate health states worse than death. The second measurement component of the EQ-5D consists of a 20-cm vertical VAS ranging from 0 (worst imaginable health state) to 100 (best imaginable health state), which provides an indication of the subject’s own assessment of their health status on the day of the survey.
Quality-adjusted life-years were calculated as area under the baseline-adjusted utility curve, and were calculated using linear interpolation between baseline and follow-up utility scores. QALYs accrued by each trial participant beyond the first 12 months of follow-up were discounted at 3.5%, as recommended by NICE. 89
Missing data
Multiple imputation, assuming missing data were missing at random but correlated in an observable way with the mechanism that generated the outcome of interest, was used to impute missing data and avoid biases associated with complete-case analysis. Missing data, particularly in the form of censoring, were a particular issue for the costs and health utility scores collected at 2, 6 and 12 months post partum (with some missing data observed in > 20% of the sample). Multiple imputation using chained equations103 and predicted mean matching were carried out on the EQ-5D-5L, as well as cost estimates, at 2, 6 and 12 months post partum. Predicted mean matching is a semi-parametric imputation approach, and generally performs better than linear regression despite the similarities in method. 104 Maternal age, looked-after status and sex of infant were included as explanatory variables in the imputation models. In addition, the baseline EQ-5D-5L utility score was included as an explanatory variable in the models predicting EQ-5D-5L utility scores at the follow-up points; and the baseline AAPI-2 score was included as an explanatory variable in the models predicting the AAPI-2 score at 12 months post partum. Twins who were trial participants were treated as clusters in the analyses and reflected in the multiple imputations. Five imputed data sets were generated as this has been deemed sufficient to obtain valid responses. 105,106
Analyses of resource use, costs and outcome data
Resource use items were summarised by trial allocation group and follow-up period, and differences between groups were analysed using t-tests for continuous variables and chi-squared tests for categorical variables. Mean (SE) costs by cost category and mean (SE) total costs were estimated by trial allocation group for all time periods. Total costs were estimated from both a NHS and PSS perspective and a broader societal perspective. Cost comparisons were carried out using Student’s t-tests. Differences in mean total costs and their CIs were estimated. Non-parametric bootstrap89 estimates based on 10,000 replications were also calculated for these differences in mean costs and their respective CIs calculated. For each of the five dimensions of the EQ-5D-5L,90 we compared the proportion of women with suboptimal levels of function (defined as some, moderate, severe or extreme problems) at each follow-up point between the trial comparators using the Pearson chi-squared (χ2) test. Differences in the EQ-5D-5L utility scores at each follow-up point between the comparison groups were tested using two-sample t-tests for unequal variance.
In addition, bivariate regression was carried out for both costs and outcomes. These analyses explored the determinants of costs and outcomes using seemingly unrelated regression, and included the pre-specified prognostic factors of trial intervention (referent: standard care), maternal age (continuous variable), sex of infant (referent: boys), looked-after status (referent: none) and the presences of twins within the trial population (referent: none).
Cost-effectiveness analyses
The main CEAs were conducted following multiple imputations of all missing cost and outcomes data. The cost-effectiveness results were primarily expressed in terms of an incremental cost-effectiveness ratio (ICER). This was calculated as the difference in mean costs divided by the difference in mean outcomes (QALYs or maltreatment outcome measure) between the trial comparators. The primary analyses adopted the perspective of the NHS and PSS. The non-parametric bootstrapping approach was used to determine the level of sampling uncertainty surrounding the mean ICER by generating 10,000 estimates of incremental costs and benefits. These were represented graphically on four-quadrant cost-effectiveness planes. Cost-effectiveness acceptability curves (CEACs) showing the probability that the gFNP programme is cost-effective relative to standard care across a range of cost-effectiveness thresholds were also generated based on the proportion of bootstrap replicates with positive incremental net benefits.
Unless otherwise stated, all statements about cost-effectiveness were based on a £20,000 per QALY gained threshold. 89 The probability that the gFNP programme was less costly or more effective than standard care was based on the proportion of bootstrap replicates that have negative incremental costs or positive incremental health benefits, respectively. Published estimates of willingness to pay for unit changes in the maltreatment outcome measures are not available in the public domain. Consequently, statements about cost-effectiveness estimated using either the AAPI-272 or the CARE-Index (maternal sensitivity domain)73,74 are based on a hypothetical range of values for the cost-effectiveness threshold (£0–50,000).
Sensitivity and subgroup analyses
Several sensitivity analyses were undertaken to assess the impact of areas of uncertainty surrounding components of the economic evaluation. These involved re-estimating the main cost-effectiveness outcomes under the following scenarios: (1) adopting a wider societal perspective that includes costs incurred by all sectors of the economy and by families and informal carers; (2) restricting the analyses to complete cases (i.e. those with complete cost and outcome data); (3) recalculating the average cost per gFNP session per attending woman by varying the mean number of gFNP sessions attended to the highest and lowest mean number of sessions observed across all groups across all sites; and (4) recalculating the average cost per gFNP session per attending woman by varying the number of gFNP group participants to the highest and lowest number of participants observed across all groups across all sites.
Subgroup analyses were also conducted for the main cost-effectiveness results to explore heterogeneity in the trial population. These were conducted by (1) programme completers (no, yes), where women who participated in a pre-specified number of group sessions of the gFNP programme (set at ≥ 17 sessions to ensure consistency with the main clinical analyses reported in Chapter 3) were regarded as ‘programme completers’ (i.e. as having complied with the protocol sufficiently); and (2) programme phase (I, II, III) to test whether or not organisational learning may have influenced the cost-effectiveness of the gFNP programme.
Long-term cost-effectiveness model
The trial-based economic evaluation focused on the short- and medium-term costs and consequences of the gFNP programme in expectant mothers aged < 20 years with one or more previous live births or expectant mothers aged 20–24 years with low/no educational qualifications and no previous live births. The study protocol allowed for extrapolation of costs and consequences over a longer time horizon if the trial demonstrated statistically significant differences in medium-term outcomes. This would have required the development of a de novo decision-analytic model. Accepted guidelines for good practice in decision-analytic modelling and the general principles outlined in the NICE ‘reference case’ were to be followed. 89,107 Long-term extrapolation of outcomes were to be expressed in terms of QALYs in the event of differences in medium-term outcomes. Both costs and outcomes accruing beyond the first year post partum were to be discounted using a 3.5% annual discount rate in line with current guidance. 89
Discrete choice experiment
Objective
It was felt that presentation of the results of the economic evaluation in terms of incremental cost per maternal QALY gained had the potential to miss effects of the gFNP programme on the child (or the broader family), whereas presentation of the results of the economic evaluation in terms of incremental cost per unit change (or unit difference) in each of the primary maltreatment outcomes [(1) AAPI-2 or (2) CARE-Index (maternal sensitivity domain)] was likely to miss relevant consequences of the gFNP programme for the mother and be less amenable to overall judgments of cost-effectiveness by decision-makers.
A discrete choice experiment (DCE) was therefore conducted that aimed to quantify people’s preferences for the disparate outcome measures collected in evaluating the gFNP programme. This would allow decision-makers to look explicitly at the trade-offs between different possible outcomes, and help to assess the net benefit of the gFNP programme in a manner that values the plethora of costs and outcomes across several domains. Ethics approval for the DCE was provided by the University of Warwick’s Biomedical and Scientific REC: REGO-2016-1769.
Background to discrete choice experiments
Discrete choice experiments are increasingly being used in health economics to address a wide range of health policy-related concerns. 108,109 The approach draws its microeconomic foundations from the characteristics theory of demand110 and random utility theory (RUT). 111 The characteristics theory of demand assumes that goods, services or types of health-care provision can be valued in terms of their constituent characteristics (otherwise known as attributes). DCEs involve respondents making a number of stated preference choices in response to DCE questions. According to RUT, respondents are assumed to act in a utility maximising manner and make choices contingent on the levels of attributes in DCE scenarios. Therefore, choice data obtained from respondents’ stated preferences can be analysed using econometric methods compatible with RUT. If the specified attributes are significantly related to respondent choices, findings from data analysis should provide information relating to how the average respondent’s utility (or willingness to pay) is affected by changes in the levels of attributes.
There are five identifiable stages in the design and analysis of stated preference DCEs: (1) identifying the attributes to include in the study; (2) assigning levels to these attributes; (3) designing the orthogonal matrix of attributes and levels using design theory; (4) eliciting preferences for these scenarios; and (5) analysing the responses.
Selection of attributes and levels
A number of approaches have been suggested to identify potential attributes for DCEs, including literature reviews, other evidence on the impact of disease or health technology being assessed, expert opinion, qualitative research and other preliminary studies. 112,113 In this DCE, the attributes were framed by the primary and secondary outcomes of the gFNP trial rather than developed de novo. The attributes were chosen to cover a wide range of potential outcomes that could impact on both the mother and the child, with attributes based on questions from the following trial instruments:
-
child abuse potential based on the AAPI-272
-
maternal stress based on the Abidin PSI, Short Form77
-
parenting sense of competence based on the PSOC scale81
-
maternal HRQoL based on the EQ-5D-5L101
-
social support based on the MOS, Social Support Survey. 83
In addition, we aimed to estimate marginal rates of substitution between changes in the EQ-5D-5L attribute and the remaining attributes. The intention was to estimate changes in all the attributes on an overall ‘utility’ scale. To enable accurate quantification on the utility scale, it was decided to include two attributes derived from the EQ-5D-5L.
A key consideration was the levels with which each attribute was delineated for the purposes of the DCE. In selecting the levels for each attribute, a balance had to be struck between keeping the task simple and manageable for the respondents while obtaining the necessary information for assessing the relative importance of these attributes and linking to the gFNP trial outcomes. In the DCE conducted as part of the ‘Building Blocks’ trial,38 each attribute, with the exception of EQ-5D health states, was described in a binary format. The attributes selected for the gFNP DCE are potentially describable in terms of two or more levels. We analysed the outcomes data for the selected attributes within the gFNP data set, blinded to trial allocation, with a view to assessing the distribution of scores for each attribute. We initially selected levels for each attribute based on these distributions. Further refinements of the levels chosen was informed by the opinion of the Trial Management Group (TMG), to ensure that the levels chosen reflected plausible states for individuals eligible for the programme to be in. The final attributes and levels chosen, and the instrument from which they were derived, are shown in Table 26.
| Instrument | Attribute | Levels |
|---|---|---|
| AAPI-2 | Parental empathy | You do not feel you have a high level of understanding of your child’s needs |
| You feel you have a high level of understanding of your child’s needs | ||
| PSI | Maternal stress | You do not feel stressed in your role as a parent |
| You feel stressed in your role as a parent | ||
| PSOC | Parenting sense of competence | You do not feel confident and capable of problem-solving as a parent |
| You do not feel confident and capable of problem-solving as a parent | ||
| EQ-5D-5L | Maternal HRQoL | You do not feel anxious or depressed |
| You feel slightly anxious or depressed | ||
| You have no problems in doing your usual activities | ||
| You have slight problems in doing your usual activities | ||
| MOS | Social support | You do not feel you have enough support from your friends and family |
| You feel you have enough support from your friends and family |
Discrete choice experiment pilot study
Given the preliminary evidence on the likely number of attributes and levels, we anticipated that using a full factorial design for the DCE would prove impractical. Therefore, the range of final choices to be specified in the pilot DCE questionnaire was defined using an orthogonal fractional factorial design within the SAS package (version 9.4; SAS Institute Inc., Cary, NC, USA). Three rounds of piloting of the DCE questionnaire were conducted. First, we conducted eight cognitive debrief interviews among women representative of the gFNP study population who were identified through local health visitors. This initial phase of the piloting aimed to assess respondents’ ability to complete the task. The specific objectives of this part of work were (1) to determine if respondents understood the DCE task in the way that it was intended; (2) to identify any problems with any individual attributes; and (3) to identify any problems with the questions and DCE structure. In the second part of the pilot study, the revised DCE questionnaire was piloted among 10 women representative of the study population who were identified through Sheffield-based health visitors. In the third part of the pilot study, conducted in a sample of 50 representative respondents identified by the online survey company Ipsos MORI Fieldwork International, the DCE was translated into a web-based format and simply catered for ‘main effects’. The issue of which attributes (and their levels) might interact with each other, and how they interact, was explored using data from these 50 pilot DCE questionnaires.
Development of the final discrete choice experiment questionnaire
The design of the final DCE questionnaire was informed by the pilot exercise and followed best practice in DCE design. 114 The final DCE questionnaire adopted an orthogonal fractional factorial design, which was developed using the SAS software package. We also used evidence from the pilot exercise to explore whether or not the adoption of clearly defined labels for models of social care during the antenatal and postnatal periods might be appropriate within the final DCE design. 115 Based on the pilot research, it was decided not to adopt a ‘labelled choice’ DCE design for the final DCE. The final design contained 16 questions, to which a 17th was added, which was a duplicate of a previous question to check for consistency in respondents’ answers. This repeated question was not included in the final analysis of the data set. A copy of the final DCE questionnaire is provided online (see Report Supplementary Material 5).
Participant recruitment and data collection
The final DCE survey was conducted by an online survey company (Ipsos MORI), which was responsible for the design of survey web pages, translation of the paper-based questionnaire to a web-based one, recruitment of study participants, data collection and data cleaning. The participants were invited to complete the online survey by Ipsos MORI and were reimbursed for their participation (£1 per participation). A copy of the DCE participant information leaflet is provided online (see Report Supplementary Material 6). Previous research has indicated that estimation precision in the design of DCEs (which accounts for the potential competing concerns of statistical efficiency and response efficiency) flattens out at around 300 observations. 116 A total of 600 respondents therefore allowed for two samples to be included in the full survey: one composed of women whose characteristics broadly match the trial eligibility criteria, and the other composed of a representative sample of the general population whose values can be considered relevant for social decision-making purposes. For the sample that aimed to match the general population, a stratified probabilistic sampling approach was adopted to ensure that a representative sample was achieved; the strata were defined by age, sex and region. For both populations, questions were presented in a random order to each individual participant to remove potential biases from the order in which they were asked. The quality of retrieved data, both during a ‘soft launch’ and the main study was assessed. Descriptive statistics for responses to each question were estimated. In addition, responders who were classified as ‘speeders’ (i.e. completed the survey much faster than anticipated) were removed by Ipsos MORI from the data set.
Analysis of final discrete choice experiment data
The analysis followed standard practice in the DCE literature, and involved the estimation of a conditional logit model clustered on patient UID (to allow for multiple responses from each respondent). The model also contained a term for whether the option chosen was the first or second one presented in each pairwise choice, to adjust for any potential for individuals to preferentially favour one alternative based on the ordering of options.
Results
Study population
A total of 166 women were randomised into the ‘First Steps’ trial, 99 to the gFNP intervention and 67 to usual care (control). Two women in the intervention arm were ineligible, and baseline information is provided for 97 women in the intervention arm and 67 in the control arm. Consequently, the baseline study population for the bulk of the health economic analyses was 164 women. There were four sets of twins: three in the intervention arm and one in the control arm. A complete profile of resource use was collected for 141 women and their infants at 2 months post partum (representing 86.0% of the baseline study population). A complete profile of resource use was collected for 136 (82.9%) women and their infants and 138 (84.1%) women and their infants for the 2–6 months post-partum period and the 6–12 months post-partum period, respectively. Overall, a complete profile of resource use over the entire follow-up period was available for 129 (78.7%) women and their infants. A complete QALY profile was available for 103 (62.8%) women, whereas QALY calculations based on baseline and 12 months post-partum EQ-5D-5L data were possible for 131 (79.9%) women.
Resource use and costs
Cost of the Group Family Nurse Partnership programme
Estimates of the total costs of delivering the gFNP programme are provided in Table 27 for each group within each study site. The cost components are aggregated into four headings, namely (1) staff costs, inclusive of training activities, planning, direct delivery, administrative activities, home visits, meetings with professionals, telephone calls and supervision activities associated with group delivery; (2) travel costs, based on distances travelled by practitioners by mode of transport; (3) venue costs; and (4) other costs, inclusive of costs of refreshments, materials, cards or gifts, and reimbursed participant travel, partner travel and childcare costs associated with group delivery. Total intervention costs are also presented within each group within each site. These varied between £150 (site 4, group C) and £36,672 (site 2, group B).
| Site | Group | Costs (£) | ||||
|---|---|---|---|---|---|---|
| Staffa | Travelb | Venue | Otherc | Total | ||
| 1 | A | 16,596.30 | 155.50 | 1480.00 | 219.80 | 18,451.60 |
| B | 24,144.30 | 382.40 | 1720.00 | 395.90 | 26,642.60 | |
| 2 | A | 26,421.70 | 906.90 | 1800.00 | 537.70 | 29,666.30 |
| B | 33,001.30 | 768.80 | 2160.00 | 741.40 | 36,671.50 | |
| 3 | A | 1371.00 | 16.70 | 160.00 | 14.00 | 1561.70 |
| B | 21,542.70 | 189.90 | 1640.00 | 299.40 | 23,672.00 | |
| 4 | A | 3144.60 | 15.20 | 760.00 | 54.00 | 3973.80 |
| B | 20,978.80 | 206.50 | 2600.00 | 310.70 | 24,095.90 | |
| C | 110.00 | 0.00 | 40.00 | 0.00 | 150.00 | |
| 5 | A | 5986.30 | 105.40 | 1160.00 | 182.80 | 7434.40 |
| 6 | A | 29,347.00 | 933.00 | 1080.00 | 1334.90 | 32,694.90 |
| B | 22,497.50 | 404.20 | 1040.00 | 438.30 | 24,380.00 | |
| 7 | A | 2447.10 | 38.40 | 320.00 | 33.00 | 2838.50 |
| B | 5704.20 | 168.00 | 480.00 | 42.00 | 6394.20 | |
Group- and site-specific estimates of average cost per gFNP session per attending woman were estimated using the total cost data in Table 27 and data on group size and mean session attendance reported in Chapter 3. These average costs are reported in Table 28, varying from £83.30 in site 4, group C, to £473.10 in site 7, group A. Table 28 also reports group- and site-specific estimates of average cost per gFNP session per attending woman following sensitivity analyses that varied (1) the mean number of gFNP sessions to the highest and lowest mean number of sessions observed across all groups across all sites; and (2) the number of gFNP group participants to the highest and lowest number of participants observed across all groups across all sites. As expected, increases in values for both the session attendance variable and the group size variable had the tendency to decrease the average cost per gFNP session per attending woman.
| Site | Group | Baseline value (£) | Sensitivity analysis 1: mean number of sessionsa | Sensitivity analysis 2: number of participantsb | ||
|---|---|---|---|---|---|---|
| Higher | Lower | Higher | Lower | |||
| 1 | A | 228.80 | 83.4 | 8335.9 | 110.9 | 480.7 |
| B | 326.50 | 74.0 | 7400.7 | 301.4 | 1306.00 | |
| 2 | A | 174.90 | 114.1 | 11,410.1 | 61.4 | 266.2 |
| B | 346.00 | 174.6 | 17,462.6 | 186.3 | 807.4 | |
| 3 | A | 223.00 | 10.4 | 1041.1 | 85.8 | 371.8 |
| B | 138.40 | 78.9 | 7890.7 | 106.5 | 461.4 | |
| 4 | A | 198.70 | 22.1 | 2207.7 | 92.6 | 401.4 |
| B | 105.30 | 61.8 | 6178.4 | 105.3 | 456.4 | |
| C | 83.30 | 0.8 | 83.3 | 38.5 | 166.7 | |
| 5 | A | 98.00 | 30.2 | 3019.6 | 38.4 | 166.4 |
| 6 | A | 118.90 | 116.1 | 11,609.5 | 85.8 | 372.0 |
| B | 216.50 | 109.00 | 10,898.3 | 124.2 | 538.2 | |
| 7 | A | 473.10 | 18.9 | 1892.3 | 182.0 | 788.5 |
| B | 304.50 | 71.0 | 7104.6 | 117.1 | 507.5 | |
Broader resource use
Table 29 presents resource use values for women and their infants, with complete data by trial allocation and by study period. The resource values are presented for subcategories of resource use, including mode of delivery, hospital inpatient and day case admissions by the mother, hospital inpatient admissions by the infant, hospital outpatient service contacts, community health-care contacts, social service contacts, legal service contacts, medication use and other resource items. Notably, of the women for whom delivery data were complete, 20.7% in the intervention arm were delivered by caesarean section, compared with 13.6% in the control arm. The use of hospital inpatient, day case and outpatient services was relatively low in both trial groups. Among women for whom complete resource use data were available over the entire follow-up period, the mean number of contacts with GPs was 9.61 in the intervention arm, compared with 11.97 in the control arm. Among trial participants with complete resource use data over the entire follow-up period, the mean number of visits by mothers and infants to hospital A&E departments was 0.28 and 1.36, respectively, in the intervention arm, compared with 0.13 and 1.25, respectively, in the control arm, with no difference between groups. Among trial participants with complete resource use data over the entire follow-up period, the mean combined number of social worker contacts was 2.03 in the intervention arm and 0.65 in the control arm. The difference was not significant, but a trend (p = 0.066) was evident for more contacts from baseline to 2 months post partum in the intervention arm. Over the entire follow-up period, a higher proportion of women in the control arm incurred travel costs and lost earnings as a result of their health state or their contacts with health and social care professionals. Resource use values were combined with unit costs for each resource item (Table 30) to estimate economic costs for each resource category.
| Service use | Baseline to 2 months | 2–6 months | 6–12 months | Whole follow-up period | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention (N = 82) | Control (N = 59) | Intervention (N = 81) | Control (N = 55) | Intervention (N = 78) | Control (N = 56) | Intervention (N = 77) | Control (N = 52) | |
| Modes of delivery | ||||||||
| Spontaneous vaginal delivery, n (%) | 48 (58.5) | 40 (67.8) | N/A | N/A | N/A | N/A | 45 (58.4) | 34 (65.4) |
| Forceps, n (%) | 7 (8.5) | 5 (8.5) | N/A | N/A | N/A | N/A | 5 (6.5) | 5 (9.6) |
| Ventouse, n (%) | 2 (2.4) | 3 (5.1) | N/A | N/A | N/A | N/A | 2 (2.6) | 3 (5.8) |
| Emergency caesarean section, n (%) | 11 (13.4) | 7 (11.9) | N/A | N/A | N/A | N/A | 11 (14.3) | 6 (11.5) |
| Elective caesarean section, n (%) | 6 (7.3) | 1 (1.7) | N/A | N/A | N/A | N/A | 6 (7.8) | 1 (1.9) |
| Vaginal breech, n (%) | 1 (1.2) | 0 (0) | N/A | N/A | N/A | N/A | 1 (1.3) | 0 (0) |
| Hospital inpatient and day care admissions (mother) | ||||||||
| General ward, mean (SE) | 0.07 (0.03) | 0.07 (0.03) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.07 (0.03) | 0.07 (0.03) |
| Postnatal ward, mean (SE) | 0.07 (0.03) | 0.03 (0.02) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.07 (0.03) | 0.03 (0.02) |
| High-dependency unit, mean (SE) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Intensive care unit, mean (SE) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Medical ward, mean (SE) | 0 (0) | 0 (0) | 0 (0) | 0.02 (0.02) | 0.01 (0.01) | 0.02 (0.02) | 0.01 (0.01) | 0.04 (0.03) |
| Surgical ward, mean (SE) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.04 (0.02) | 0 (0) | 0.04 (0.02) | 0 (0) |
| Day care, mean (SE) | 0.06 (0.03) | 0.07 (0.03) | 0.02 (0.02) | 0 (0) | 0.01 (0.01) | 0 (0) | 0.04 (0.02) | 0 (0) |
| Other, mean (SE) | 0.04 (0.02) | 0.03 (0.02) | 0 (0) | 0.02 (0.02) | 0.09 (0.03) | 0.02 (0.02) | 0.09 (0.03) | 0.04 (0.03) |
| Hospital inpatient admissions (baby) | ||||||||
| Special care baby unit, mean (SE) | 0.04 (0.02) | 0.02 (0.02) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.04 (0.02) | 0.02 (0.02) |
| High-dependency unit, mean (SE) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.14 (0.04) | 0.18 (0.05) | 0.13 (0.04) | 0.17 (0.05) |
| Neonatal intensive care unit, mean (SE) | 0.02 (0.02) | 0.05 (0.03) | 0 (0) | 0 (0) | 0.06 (0.03) | 0.09 (0.04) | 0.09 (0.30) | 0.13 (0.05) |
| Children’s ward, mean (SE) | 0 (0) | 0 (0) | 0.02 (0.02) | 0.18 (0.05) | 0 (0) | 0 (0) | 0.03 (0.02) | 0.17 (0.05) |
| Other, mean (SE) | 0.14 (0.04) | 0.25 (0.06) | 0.02 (0.02) | 0.04 (0.03) | 0 (0) | 0 (0) | 0.16 (0.05) | 0.27 (0.07) |
| Hospital outpatient service contacts | ||||||||
| Hospital A&E, mean (SE) | 0.39 (0.08) | 1.73 (1.35) | 0.41 (0.17) | 0.43 (0.09) | 0.59 (0.12) | 0.46 (0.10) | 1.61 (0.29) | 1.38 (0.26) |
| A&E baby only, mean (SE) | 0.25 (0.06) | 0.22 (0.06) | 0.37 (0.16) | 0.36 (0.16) | 0.47 (0.10) | 0.43 (0.10) | 1.36 (0.26) | 1.25 (0.26) |
| Hospital outpatient clinic, mean (SE) | 0.72 (0.28) | 0.56 (0.18) | 0.35 (0.10) | 0.31 (0.13) | 0.23 (0.08) | 0.77 (0.37) | 0.81 (0.24) | 1.50 (0.77) |
| Community health-care contacts | ||||||||
| GP surgery, mean (SE) | 9.26 (5.40) | 3.92 (0.42) | 2.77 (0.34) | 2.94 (0.47) | 3.17 (0.56) | 4.04 (0.64) | 9.01 (1.27) | 10.84 (1.68) |
| GP home, mean (SE) | 0.01 (0.01) | 0.02 (0.02) | 0 (0) | 0 (0) | 0.01 (0.01) | 0 (0) | 0.03 (0.03) | 0 (0) |
| GP telephone, mean (SE) | 0.70 (0.38) | 0.27 (0.09) | 0.20 (0.10) | 0.31 (0.14) | 0.19 (0.08) | 0.43 (0.15) | 0.57 (0.23) | 1.13 (0.38) |
| Practice nurse, mean (SE) | 1.18 (0.14) | 1.33 (0.20) | 0.91 (0.13) | 1.00 (0.16) | 0.53 (0.09) | 1.16 (0.29) | 1.90 (0.21) | 3.12 (0.69) |
| District nurse, mean (SE) | 0.06 (0.03) | 0.03 (0.03) | 0.01 (0.01) | 0.04 (0.04) | 0.01 (0.01) | 0 (0) | 0.04 (0.03) | 0.04 (0.04) |
| Physiotherapist, mean (SE) | 0.07 (0.03) | 0.32 (0.17) | 0.03 (0.02) | 0.04 (0.03) | 0.01 (0.01) | 0.16 (0.09) | 0.05 (0.03) | 0.23 (0.13) |
| Calls to NHS Direct, mean (SE) | 0.34 (0.09) | 0.52 (0.15) | 0.59 (0.15) | 0.31 (0.09) | 0.73 (0.19) | 0.72 (0.16) | 2.01 (0.44) | 1.76 (0.38) |
| Community psychiatrist, mean (SE) | 0.18 (0.15) | 0.05 (0.05) | 0.03 (0.02) | 0 (0) | 0.04 (0.04) | 0.02 (0.02) | 0.09 (0.09) | 0.04 (0.04) |
| Community psychologist, mean (SE) | 0 (0) | 0 (0) | 0.05 (0.05) | 0 (0) | 0.04 (0.04) | 0.02 (0.02) | 0.08 (0.08) | 0.04 (0.04) |
| Midwife in clinic, mean (SE) | 2.29 (0.54) | 3.07 (0.63) | 0.23 (0.20) | 0 (0) | 0.78 (0.32) | 0.20 (0.11) | 1.83 (0.67) | 0.42 (0.24) |
| Midwife at home, mean (SE) | 2.70 (0.55) | 3.51 (0.50) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Health visitor, mean (SE) | 3.36 (0.39) | 4.25 (0.63) | 7.72 (5.63) | 1.73 (0.54) | 1.46 (0.48) | 2.34 (0.63) | 10.88 (5.97) | 6.38 (1.66) |
| Social service contacts | ||||||||
| Social worker, mean (SE) | 0.63 (0.25) | 0.08 (0.07) | 0.29 (0.14) | 0.06 (0.04) | 1.04 (0.67) | 0.48 (0.28) | 2.03 (0.85) | 0.65 (0.35) |
| Home help/care worker, mean (SE) | 0 (0) | 0 (0) | 0.10 (0.10) | 0 (0) | 0 (0) | 0 (0) | 0.10 (0.10) | 0 (0) |
| Alcohol support, mean (SE) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Drug/substance misuse services, mean (SE) | 0.02 (0.02) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.03 (0.03) | 0 (0) |
| Crèche, mean (SE) | 0.04 (0.03) | 0 (0) | 0.19 (0.19) | 0 (0) | 0 (0) | 0 (0) | 0.23 (0.20) | 0 (0) |
| Family support, mean (SE) | 0.04 (0.03) | 0 (0) | 0.58 (0.37) | 0.02 (0.02) | 0.29 (0.26) | 0.61 (0.40) | 0.92 (0.61) | 0.67 (0.43) |
| Legal service contacts | ||||||||
| Police services, mean (SE) | 0.11 (0.09) | 0.20 (0.13) | 0.17 (0.08) | 0.04 (0.04) | 0.12 (0.05) | 0.36 (0.19) | 0.39 (0.13) | 0.63 (0.29) |
| Probation services, mean (SE) | 0.02 (0.02) | 0 (0) | 0.01 (0.01) | 0 (0) | 0 (0) | 0 (0) | 0.04 (0.02) | 0 (0) |
| Solicitor services, mean (SE) | 0.17 (0.13) | 0.13 (0.07) | 0.03 (0.02) | 0.15 (0.10) | 0.13 (0.09) | 0.11 (0.08) | 0.29 (0.18) | 0.39 (0.21) |
| Legal aid, mean (SE) | 0.01 (0.01) | 0.07 (0.06) | 0.01 (0.01) | 0 (0) | 0.01 (0.01) | 0 (0) | 0.04 (0.04) | 0.08 (0.07) |
| Medication use | ||||||||
| Medication use, n (%) | 63 (76.8) | 46 (77.9) | 61 (75.3) | 40 (72.7) | 63 (80.8) | 40 (71.4) | 67 (87.0) | 43 (82.7) |
| Other resource categories | ||||||||
| Travel costs, n (%) | 28 (34.1) | 18 (30.5) | 11 (13.4) | 8 (14.5) | 14 (17.9) | 13 (23.2) | 28 (36.4) | 23 (44.2) |
| Lost earnings, n (%) | 9 (11.0) | 12 (20.3) | 6 (7.3) | 2 (3.6) | 8 (10.3) | 6 (10.7) | 16 (20.8) | 13 (25.0) |
| Childcare, n (%) | 1 (1.2) | 0 (0) | 0 (0) | 0 (0) | 2 (2.5) | 2 (3.5) | 3 (3.9) | 2 (3.8) |
| Housework help, n (%) | 0 (0) | 0 (0) | 1 (1.2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Resource item | Measurement unit | Unit cost (£) | Source |
|---|---|---|---|
| Mode of delivery | |||
| Spontaneous vaginal delivery | Delivery | 1514.10 | DH96 |
| Forceps | Delivery | 1670.90 | DH96 |
| Ventouse | Delivery | 1670.90 | DH96 |
| Emergency caesarean section | Delivery | 3820.40 | DH96 |
| Elective caesarean section | Delivery | 2922.30 | DH96 |
| Vaginal breech | Delivery | 3153.10 | DH96 |
| Hospital services | |||
| General ward | Day | 295.80 | DH96 |
| Antenatal/postnatal ward | Day | 464.80 | DH96 |
| High-dependency unit | Day | 847.00 | DH96 |
| Intensive care unit | Day | 1176.00 | DH96 |
| Surgical ward | Day | 428.48 | aNICE117 |
| Children’s ward | Inpatient spell | 2837.20 | aCurtis97 |
| Community care services | |||
| GP surgery | Visit | 44.00 | Curtis and Burns93 |
| GP home | Visit | 45.00 | Curtis and Burns93 |
| GP telephone | Contact | 27.00 | Curtis and Burns93 |
| Practice nurse | Visit | 43.00 | Curtis and Burns93 |
| District nurse | Visit | 59.00 | Curtis and Burns93 |
| Physiotherapist | Visit | 34.00 | Curtis and Burns93 |
| Calls to NHS Direct | Contact | 6.10 | Curtis and Burns93 |
| Community psychiatrist | Visit | 62.00 | Curtis and Burns93 |
| Community psychologist | Visit | 61.60 | aCurtis97 |
| Midwife in clinic (other than gFNP midwife) | Visit | 44.00 | Curtis and Burns93 |
| Midwife at home (other than gFNP midwife) | Visit | 55.00 | Curtis and Burns93 |
| Hospital A&E department | Visit | 206.00 | Curtis and Burns93 |
| Hospital outpatient clinic | Visit | 205.00 | Curtis and Burns93 |
| Social and legal services | |||
| Social worker | Visit | 42.00 | Curtis and Burns93 |
| Home help or care worker | Visit | 24.00 | Curtis and Burns93 |
| Alcohol support services | Contact | 122.00 | Curtis and Burns93 |
| Drug/substance misuse services | Contact | 123.00 | Curtis and Burns93 |
| Crèche | Session | 23.10 | Rutter118 |
| Police services | Contact | 18.80 | Curtis and Burns93 |
| Probation services | Contact | 311.20 | aMinistry of Justice119 |
| Solicitors | Contact | 145.00 | aCurits and Netten120 |
| Legal aid | Contact | 93.00 | aCurits and Netten120 |
Economic costs
Economic costs for women with complete data are in Table 31 by trial group, study period and cost category. With the exception of the cost of the gFNP intervention, there were no significant differences between the trial groups in any cost subcategory, for each period of follow-up (baseline to 2 months post partum, 2–6 months post partum, 6–12 months post partum) and for the entire follow-up period. The mean cost of gFNP for women with complete data over the entire period was £2036 (SE £307). Over the entire follow-up period, mean (SE) total NHS and PSS costs, inclusive of the cost of gFNP, were £8877 (SE £1399) in the intervention arm and £6066 (SE £601) in the control arm, generating a mean cost difference of £2810 (bootstrap 95% CI £338 to £6607; p = 0.069). Over the entire follow-up period, mean (SE) total societal costs, inclusive of the cost of gFNP, were £9134 (SE £1435) in the intervention arm and £6362 (SE £631) in the control arm, generating a mean cost difference of £2771 (bootstrap 95% CI £685 to £6865; p = 0.077).
| Cost category by period | Trial arm, mean (SE) cost (£) | Mean difference (£) | p-valuea | Bootstrap 95% CI (£)b | |
|---|---|---|---|---|---|
| Intervention | Control | ||||
| Baseline to 2 months (total, n = 141; intervention, n = 82; control, n = 59) | |||||
| Mother | |||||
| Delivery costs | 1922.60 (114.00) | 1871.70 (118.70) | 50.90 | 0.762 | –292.20 to 369.50 |
| Hospital inpatient (non-delivery) costs | 216.20 (73.80) | 45.80 (29.00) | 170.40 | 0.062 | 18.80 to 344.10 |
| A&E costs | 27.60 (9.30) | 310.70 (278.90) | –283.10 | 0.233 | –1103.60 to 10.60 |
| Outpatient care costs | 50.00 (26.50) | 73.00 (34.90) | –23.00 | 0.595 | –116.00 to 55.10 |
| Community care costs | 337.20 (52.80) | 409.50 (51.60) | –72.30 | 0.344 | –210.00 to 66.80 |
| Medication costs | 121.60 (92.40) | 49.60 (27.70) | 72.00 | 0.520 | –58.20 to 298.70 |
| PSS costs | 1.20 (0.90) | 106.10 (105.60) | –104.90 | 0.243 | –400.80 to 1.90 |
| Legal service costs | 19.80 (10.50) | 17.80 (8.30) | 2.00 | 0.891 | –23.70 to 27.40 |
| Other costs | 82.60 (24.40) | 92.90 (38.80) | –10.40 | 0.813 | –119.00 to 68.30 |
| Total costs | 2778.80 (243.30) | 2977.30 (373.80) | –198.50 | 0.643 | –1178.00 to 563.80 |
| Baby | |||||
| Hospital inpatient care (readmission) costs | 1410.20 (1082.10) | 544.50 (209.40) | 865.70 | 0.503 | –523.00 to 4041.00 |
| A&E costs | 52.80 (12.80) | 45.40 (11.20) | 7.40 | 0.680 | –21.20 to 41.10 |
| Outpatient care costs | 97.50 (50.60) | 41.70 (13.80) | 55.80 | 0.361 | –16.30 to 191.10 |
| Community care costs | 512.00 (237.70) | 268.70 (28.10) | 243.30 | 0.389 | –32.90 to 846.50 |
| Medication costs | 9.00 (3.10) | 4.20 (2.00) | 4.80 | 0.244 | –2.10 to 12.70 |
| Other costs | 43.20 (30.70) | 13.20 (4.20) | 30.10 | 0.41 | –10.30 to 109.80 |
| Total costs | 2124.70 (1130.00) | 917.70 (217.10) | 1207.00 | 0.371 | –354.70 to 4233.80 |
| Total | |||||
| Total mother and baby costs | 4903.50 (1183.80) | 3895.00 (433.10) | 1008.50 | 0.486 | –848.10 to 4045.60 |
| 2–6 months (total, n = 136; intervention, n = 81; control, n = 55) | |||||
| Mother | |||||
| Hospital inpatient readmission costs | 0 (0) | 5.40 (5.30) | –5.40 | 0.226 | –21.90 to 0.00 |
| A&E costs | 10.20 (6.20) | 11.20 (6.30) | –1.10 | 0.908 | –18.70 to 15.80 |
| Outpatient care costs | 7.60 (5.60) | 11.20 (8.20) | –3.60 | 0.711 | –27.10 to 13.70 |
| Community care costs | 223.30 (132.40) | 95.90 (19.40) | 127.40 | 0.432 | –31.70 to 490.80 |
| Medication costs | 7.00 (2.00) | 3.30 (1.10) | 3.70 | 0.160 | –0.30 to 8.40 |
| PSS costs | 0 (0) | 0 (0) | 0 | N/A | N/A |
| Legal service costs | 9.80 (5.00) | 27.30 (18.00) | –17.50 | 0.275 | –68.30 to 7.90 |
| Other costs | 7.90 (3.00) | 3.60 (3.20) | 4.30 | 0.338 | –6.10 to 12.00 |
| Total costs | 265.70 (134.00) | 157.90 (32.70) | 107.80 | 0.515 | –70.30 to 482.40 |
| Baby | |||||
| Hospital inpatient readmission costs | 287.00 (6.30) | 493.50 (95.00) | –206.50 | 0.010 | –424.50 to –54.20 |
| A&E costs | 73.80 (32.40) | 74.90 (18.00) | –1.20 | 0.978 | –55.90 to 90.80 |
| Outpatient care costs | 63.30 (19.60) | 52.20 (23.90) | 11.10 | 0.720 | –55.50 to 72.40 |
| Community health care costs | 138.40 (17.00) | 126.70 (19.50) | 11.60 | 0.658 | –41.50 to 65.90 |
| Medication costs | 51.70 (44.03) | 19.50 (13.60) | 32.20 | 0.559 | –27.50 to 160.00 |
| Other costs | 10.70 (4.20) | 22.30 (12.20) | –11.60 | 0.305 | –41.20 to 9.30 |
| Total costs | 624.70 (69.90) | 789.10 (132.10) | –164.40 | 0.235 | –482.10 to 106.90 |
| Total | |||||
| Total mother and baby costs | 890.40 (151.40) | 947.00 (142.00) | –56.60 | 0.795 | –450.20 to 434.10 |
| 6–12 months (total, n = 138; intervention, n = 81; control, n = 57) | |||||
| Mother | |||||
| Hospital inpatient readmission costs | 25.60 (12.40) | 2.60 (2.60) | 23.00 | 0.127 | 4.30 to 53.40 |
| A&E costs | 22.90 (8.90) | 7.20 (5.00) | 15.70 | 0.172 | –4.50 to 36.40 |
| Outpatient care costs | 38.00 (14.90) | 104.30 (64.50) | –66.30 | 0.246 | –230.90 to 31.30 |
| Community care costs | 121.10 (24.10) | 160.30 (40.80) | –39.20 | 0.381 | –132.70 to 46.70 |
| Medication costs | 69.80 (56.10) | 19.10 (7.60) | 50.70 | 0.452 | –14.80 to 224.20 |
| PSS costs | 0 (0) | 0 (0) | 0 | N/A | N/A |
| Legal service costs | 23.40 (16.10) | 24.20 (14.50) | –0.80 | 0.972 | –39.30 to 50.30 |
| Other costs | 39.60 (15.80) | 58.80 (36.60) | –19.20 | 0.595 | –123.00 to 35.50 |
| Total costs | 340.40 (88.70) | 376.60 (105.50) | –36.20 | 0.793 | –318.60 to 207.20 |
| Baby | |||||
| Hospital inpatient readmission costs | 562.30 (136.20) | 848.80 (200.20) | –286.50 | 0.222 | –764.50 to 154.60 |
| A&E costs | 106.80 (20.80) | 86.70 (19.90) | 20.10 | 0.504 | –33.20 to 75.20 |
| Outpatient care costs | 7.60 (7.60) | 50.40 (17.20) | –42.80 | 0.013 | –79.10 to –6.40 |
| Community care costs | 123.0 (20.80) | 163.40 (21.20) | –40.10 | 0.192 | –95.50 to 21.70 |
| Medication costs | 24.50 (8.50) | 130.00 (99.40) | –105.50 | 0.210 | –377.30 to 19.00 |
| Other costs | 16.10 (7.10) | 54.00 (36.70) | –37.90 | 0.237 | –152.70 to 12.40 |
| Total costs | 840.60 (161.10) | 1333.30 (261.90) | –492.70 | 0.093 | –1120.30 to 90.00 |
| Total | |||||
| Total mother and baby costs | 1181.00 (206.90) | 1709.90 (288.50) | –528.90 | 0.128 | –1203.70 to 130.80 |
| Entire follow-up period (total, n = 129; intervention, n = 77; control, n = 52) | |||||
| Mother | |||||
| Delivery costs | 1945.00 (120.90) | 1846.20 (126.50) | 98.80 | 0.584 | –211.60 to 434.90 |
| Hospital inpatient (non-delivery) costs | 257.20 (78.40) | 60.60 (38.00) | 196.60 | 0.053 | 42.30 to 359.40 |
| A&E costs | 64.20 (14.90) | 364.50 (316.40) | –300.30 | 0.251 | –1029.60 to 40.50 |
| Outpatient care costs | 98.50 (38.00) | 130.10 (73.10) | –31.60 | 0.678 | –237.30 to 99.50 |
| Community care costs | 689.70 (161.50) | 665.90 (87.90) | 23.80 | 0.910 | –288.20 to 441.40 |
| Medication costs | 209.90 (156.80) | 62.10 (30.80) | 147.80 | 0.445 | –52.90 to 555.10 |
| PSS costs | 1.20 (1.00) | 120.40 (119.80) | –119.10 | 0.228 | –488.50 to 2.00 |
| Legal service costs | 46.20 (18.90) | 71.70 (33.40) | –25.60 | 0.477 | –115.40 to 41.70 |
| Other costs | 137.90 (32.80) | 149.60 (60.80) | –11.70 | 0.855 | –163.90 to 108.80 |
| Total costs | 3449.80 (355.10) | 3471.00 (436.70) | –21.10 | 0.970 | –1107.70 to 1016.30 |
| Baby | |||||
| Hospital inpatient readmission costs | 2313.70 (1186.20) | 1747.80 (300.50) | 565.90 | 0.700 | –1070.90 to 3518.00 |
| A&E costs | 232.80 (44.50) | 210.00 (37.70) | 22.80 | 0.716 | –85.90 to 137.60 |
| Outpatient care costs | 175.70 (63.40) | 145.90 (44.80) | 29.80 | 0.728 | –111.50 to 198.30 |
| Community care costs | 765.40 (256.40) | 550.30 (53.60) | 215.10 | 0.497 | –122.10 to 926.30 |
| Medication costs | 87.40 (47.20) | 162.70 (109.50) | –75.30 | 0.481 | –371.00 to 99.60 |
| Other costs | 72.70 (36.90) | 74.60 (41.50) | –2.00 | 0.972 | –113.50 to 95.10 |
| Total costs | 3647.70 (1305.90) | 2891.30 (383.50) | 756.30 | 0.642 | –1074.70 to 4555.70 |
| Total | |||||
| Total mother and baby costs | 7097.50 (1416.80) | 6362.30 (631.00) | 735.20 | 0.684 | –1670.70 to 4762.30 |
| gFNP Intervention costs | 2036.00 (306.90) | 0 (0) | 2036.00 | < 0.0001 | 1501.30 to 2709.60 |
| Total NHS and PSS costs (including intervention) | 8876.60 (1399.00) | 6066.40 (601.00) | 2810.30 | 0.069 | 337.80 to 6607.10 |
| Total societal costs (including intervention) | 9133.50 (1435.40) | 6362.30 (631.00) | 2771.20 | 0.077 | 685.40 to 6865.40 |
Health-related quality-of-life outcomes
There were no statisticaly significant differences between the intervention and control groups in suboptimal levels of function in HRQoL, as measured by five dimensions of the EQ-5D-5L,90 at each of the follow-up time points (Table 32). Similarly, there were no statistically significant differences in the overall EQ-5D-5L utility score or EQ-5D VAS score between the intervention and control groups, at each of the follow-up time points (see Table 32).
| Time/allocation | Mobility | Self-care | Usual activities | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Suboptimal | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Suboptimal | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Suboptimal | |
| Baseline (n = 164) | ||||||||||||||||||
| Intervention (n = 97) | 82 (84.5) | 6 (6.2) | 2 (2.1) | 1 (1.0) | 6 (6.2) | 15 (15.5) | 91 (93.8) | 1 (1.0) | 0 (0) | 0 (0) | 5 (5.2) | 6 (6.2) | 79 (81.4) | 12 (12.4) | 4 (4.1) | 0 (0) | 2 (2.1) | 18 (18.6) |
| Control (n = 67) | 56 (83.6) | 5 (7.5) | 2 (3.0) | 1 (1.5) | 3 (4.5) | 11 (16.5) | 64 (95.5) | 0 (0) | 0 (0) | 0 (0) | 3 (4.5) | 3 (4.5) | 55 (82.1) | 7 (10.4) | 4 (6.0) | 1 (1.5) | 0 (0) | 12 (17.9) |
| p-value | 0.972a | 0.691a | 0.519a | |||||||||||||||
| 2 months (n = 128) | ||||||||||||||||||
| Intervention (n = 75) | 72 (96.0) | 1 (1.3) | 2 (2.7) | 0 (0) | 0 (0) | 3 (4.0) | 74 (98.7) | 1 (1.3) | 0 (0) | 0 (0) | 0 (0) | 1 (1.3) | 71 (94.7) | 2 (2.7) | 1 (1.3) | 0 (0) | 0 (0) | 3 (4) |
| Control (n = 53) | 51 (96.2) | 2 (3.8) | 0 (0) | 0 (0) | 0 (0) | 2 (3.8) | 53 (100.0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 52 (98.1) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) |
| p-value | 0.332a | 0.399a | 0.675a | |||||||||||||||
| 6 months (n = 121) | ||||||||||||||||||
| Intervention (n = 70) | 70 (100.0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 70 (100.0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 69 (98.6) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 1 (1.4) |
| Control (n = 51) | 50 (98.0) | 0 (0) | 1 (2) | 0 (0) | 0 (0) | 1 (2.0) | 51 (100.0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 48 (94.1) | 1 (2.0) | 2 (3.9) | 0 (0) | 0 (0) | 3 (5.9) |
| p-value | 0.239a | N/A | 0.337a | |||||||||||||||
| 12 months (n = 131) | ||||||||||||||||||
| Intervention (n = 75) | 69 (92) | 2 (2.7) | 1 (1.3) | 0 (0) | 3 (4.0) | 6 (8.0) | 74 (98.7) | 0 (0) | 0 (0) | 0 (0) | 1 (1.3) | 1 (1.3) | 68 (90.7) | 4 (5.3) | 1 (1.3) | 0 (0) | 1 (1.3) | 6 (7.9) |
| Control (n = 56) | 54 (96.4) | 1 (1.8) | 0 (0) | 0 (0) | 1 (1.8) | 2 (3.6) | 54 (96.4) | 1 (1.8) | 0 (0) | 0 (0) | 1 (1.8) | 2 (3.6) | 54 (96.4) | 0 (0) | 1 (1.8) | 0 (0) | 1 (1.8) | 2 (3.6) |
| p-value | 0.697a | 0.497a | 0.415a | |||||||||||||||
| Time/allocation | Pain/discomfort | Anxiety/depression | EQ-5D VAS score | EQ-5D-5L utility score | ||||||||||||||
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Suboptimal | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Suboptimal | Mean (SD) | Mean (SD) | |||||
| Baseline (n = 164) | ||||||||||||||||||
| Intervention (n = 97) | 61 (62.9) | 22 (22.7) | 10 (10.3) | 1 (1) | 2 (2.1) | 35 (36.1) | 81 (83.5) | 14 (14.4) | 0 (0) | 0 (0) | 1 (1) | 15 (15.4) | 80.8 (14.2) | 0.845 (0.249) | ||||
| Control (n = 67) | 35 (52.2) | 29 (43.3) | 1 (1.5) | 2 (3) | 0 (0) | 32 (47.8) | 45 (67.2) | 14 (20.9) | 7 (10.4) | 1 (1.5) | 0 (0) | 22 (32.8) | 79.1 (18.4) | 0.820 (0.224) | ||||
| p-value | 0.018a | 0.009a | 0.514b | 0.523b | ||||||||||||||
| 2 months (n = 128) | ||||||||||||||||||
| Intervention (n = 75) | 65 (86.7) | 5 (6.7) | 2 (2.7) | 2 (2.7) | 1 (1.3) | 10 (13.4) | 66 (88) | 4 (5.3) | 5 (6.7) | 0 (0) | 0 (0) | 9 (12) | 80.9 (18.1) | 0.940 (0.145) | ||||
| Control (n = 53) | 44 (83) | 7 (13.2) | 2 (3.8) | 0 (0) | 0 (0) | 9 (17) | 51 (96.2) | 1 (1.9) | 1 (1.9) | 0 (0) | 0 (0) | 2 (3.8) | 86.3 (9.9) | 0.964 (0.079) | ||||
| p-value | 0.447a | 0.261a | 0.051b | 0.292b | ||||||||||||||
| 6 Months (n = 121) | ||||||||||||||||||
| Intervention (n = 70) | 64 (91.4) | 2 (2.9) | 3 (4.3) | 1 (1.4) | 0 (0) | 6 (8.6) | 66 (94.3) | 3 (4.3) | 1 (1.4) | 0 (0) | 0 (0) | 4 (5.7) | 79.8 (19.3) | 0.974 (0.078) | ||||
| Control (n = 51) | 46 (90.2) | 2 (3.9) | 3 (5.9) | 0 (0) | 0 (0) | 5 (9.8) | 48 (94.1) | 2 (3.9) | 1 (2) | 0 (0) | 0 (0) | 3 (5.9) | 83.6 (13.0) | 0.971 (0.076) | ||||
| p-value | 0.805a | 0.970a | 0.224b | 0.825b | ||||||||||||||
| 12 months (n = 131) | ||||||||||||||||||
| Intervention (n = 75) | 53 (70.7) | 11 (14.7) | 7 (9.3) | 3 (4) | 1 (1.3) | 22 (29.3) | 62 (82.7) | 6 (8) | 5 (6.7) | 1 (1.3) | 1 (1.3) | 13 (17.3) | 80.6 (14.8) | 0.875 (0.242) | ||||
| Control (n = 56) | 47 (83.9) | (8.9) | 3 (5.4) | 0 (0) | 1 (1.8) | 9 (16.1) | 47 (83.9) | 6 (10.7) | 2 (3.6) | 0 (0) | 1 (1.8) | 9 (16.1) | 77.7 (18.9) | 0.926 (0.223) | ||||
| p-value | 0.337a | 0.804a | 0.325b | 0.216b | ||||||||||||||
Analyses of incremental costs and incremental health outcomes
A bivariate regression, in the form of a seemingly unrelated regression, was carried out with a view to estimating the incremental costs and incremental health outcomes associated with the gFNP programme (Table 33). The adjusted incremental cost associated with gFNP over the entire follow-up period was £1776 (95% CI –£42 to £3593) when a NHS and PSS perspective was adopted and the analyses were restricted to participants with complete cost and QALY data. The respective values were £1593 (95% CI –£264 to £3451) and £2200 (95% CI £97 to £4304) when the analyses were restricted to participants with complete cost and AAPI-2 data and complete cost and CARE-Index (maternal sensitivity domain) data, respectively. The other pre-specified prognostic factors of maternal age, sex of infant, looked-after status and the presence of twins within the trial population did not have independent significant effects on either costs or health outcomes.
| Participant characteristic | Primary health outcome (95% CI) | ||
|---|---|---|---|
| QALY (n = 101) | CARE-Index (maternal sensitivity) (n = 80) | AAPI-2 (n = 90) | |
| NHS and PSS costs | |||
| Intervention: gFNP | 1775.75 (–41.67 to 3593.17) | 2200.26* (96.75 to 4303.77) | 1593.28 (–264.00 to 3450.56) |
| Twins in trial population: yes | 1681.53 (–7230.27 to 10,593.34) | N/A | 2258.36 (–6143.71 to 10,660.43) |
| Looked-after status: yes | –770.67 (–5352.81 to 3811.48) | –793.34 (–6331.45 to 4744.76) | 424.28 (–4676.30 to 5524.85) |
| Infant sex: female | –896.25 (–2718.46 to 925.95) | –993.85 (–3108.16 to 1120.46) | –655.31 (–2517.19 to 1206.58) |
| Maternal age: continuous | 182.01 (–333.99 to 698.01) | 163.56 (–496.50 to 823.61) | 283.19 (–241.68 to 808.06) |
| Constant | 2088.27 (–8902.18 to 13,078.73) | 2376.74 (–11,672.28 to 16,425.76) | –430.82 (–11,651.02 to 10,789.38) |
| Health outcomes | |||
| Intervention: gFNP | –0.01 (–0.05 to 0.02) | –0.47 (–1.44 to 0.49) | 0.19 (–0.05 to 0.43) |
| Twins in trial population: yes | (–0.10 to 0.26) | 0 (0 to 0) | 0.18 (–0.92 to 1.27) |
| Looked-after status: yes | 0.02 (–0.07 to 0.12) | 0.01 (–2.52 to 2.54) | 0.44 (–0.22 to 1.11) |
| Infant sex: female | 0.01 (–0.03 to 0.05) | 0.38 (–0.59 to 1.35) | –0.01 (–0.25 to 0.23) |
| Maternal age: continuous | 0 (–0.01 to 0.01) | 0.20 (–0.10 to 0.51) | –0.03 (–0.09 to 0.04) |
| Constant | 0.93*** (0.71 to 1.15) | –0.11 (–6.53 to 6.31) | 0.64 (–0.83 to 2.10) |
Cost-effectiveness results
Baseline analysis
The incremental cost-effectiveness of gFNP is shown in Table 34 for the women with costs and health outcomes data subject to multiple imputation, by outcome measure. Adopting a study perspective of the NHS and PSS (i.e. that adopted for the baseline analysis) and measuring health outcomes in terms of QALYs, the average total cost was £8179 in the gFNP intervention group, compared with £6107 in the usual-care group, generating a mean incremental cost of £2072. The mean incremental cost-effectiveness of gFNP was estimated at –£247,485 per QALY gained (i.e. on average the intervention was associated with a net positive cost and a net negative effect). The bootstrapped mean ICERs largely fell in the north-west quadrants of the cost-effectiveness plane (Figure 2). The CEAC shown in Figure 2 indicates that, regardless of the value of the cost-effectiveness threshold, the probability that gFNP was cost-effective does not exceed 3%. If decision-makers are willing to pay £20,000 for an additional QALY, the probability that gFNP was cost-effective is approximately 2.3% (see Table 34). This pattern of results was broadly replicated when outcomes were measured using the AAPI-2 score (Figure 3) or the CARE-Index (maternal sensitivity domain) (Figure 4). It is notable, however, that when outcomes were measured in terms of change in AAPI-2 score between baseline and 12 months post partum, the gFNP intervention was associated with a positive health effect (mean incremental gain in AAPI-2 score 0.02). For this outcome measure, the probability that gFNP was cost-effective reached 25.1% at a notional £20,000 cost-effectiveness threshold.
| Outcome measure | Mean costs (95% CI) | Mean effects (95% CI) | ICER (£) | Probability gFNP intervention is | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (£) | Control (£) | Difference (£) | Intervention | Control | Difference | More effectivea (%) | Less costlya (%) | Cost-effectivea (%)b | Cost-effectivea (%)c | Cost-effectivea (%)d | ||
| QALY | n = 97 | n = 67 | n = 97 | n = 67 | ||||||||
| 8179 (5397 to 10,961) | 6107 (5029 to 7184) | 2072 (–843 to 4988) | 0.92 (0.84 to 1.00) | 0.93 (0.85 to 1.00) | –0.01 (–0.05 to 0.03) | –247,485 (NW) | 19.2 | 2.8 | 2.0 | 2.3 | 3.0 | |
| AAPI-2 | n = 97 | n = 67 | n = 97 | n = 67 | ||||||||
| 8179 (5903 to 10,455) | 6107 (5160 to 7054) | 2072 (–392 to 4537) | 0.27 (0.14 to 0.40) | 0.25 (0.12 to 0.38) | 0.02 (–0.17 to 0.21) | 111,334 (NE) | 58.4 | 1.9 | 19.1 | 25.1 | 32.9 | |
| CARE-Index (maternal sensitivity) | n = 97 | n = 67 | n = 97 | n = 67 | ||||||||
| 8179 (5903 to 10,455) | 6107 (5160 to 7054) | 2072 (–392 to 4537) | 3.97 (3.54 to 4.39) | 4.84 (4.30 to 5.38) | –0.87 (–1.55 to –0.19) | –2382 (NW) | 1.2 | 1.4 | < 1 | < 1 | < 1 | |
FIGURE 2.
(a) Cost-effectiveness plane; and (b) CEAC based on the QALY outcome: imputed data, NHS and PSS perspective (£, 2014–15 prices). Figure reproduced from Barnes et al. 92 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
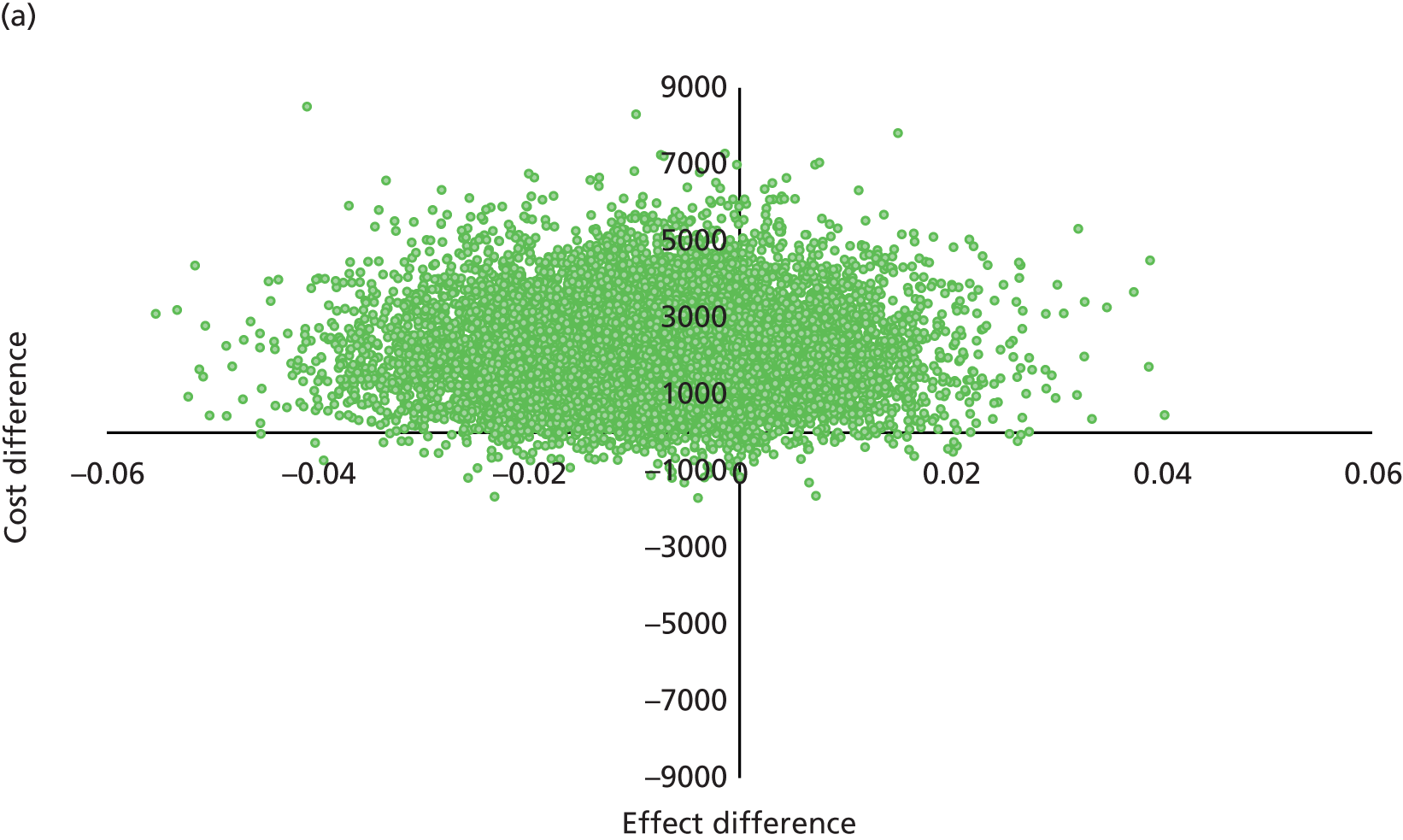

FIGURE 3.
(a) Cost-effectiveness plane; and (b) CEAC based on the AAPI-2 outcome: imputed data, NHS and PSS perspective (£, 2014–15 prices).
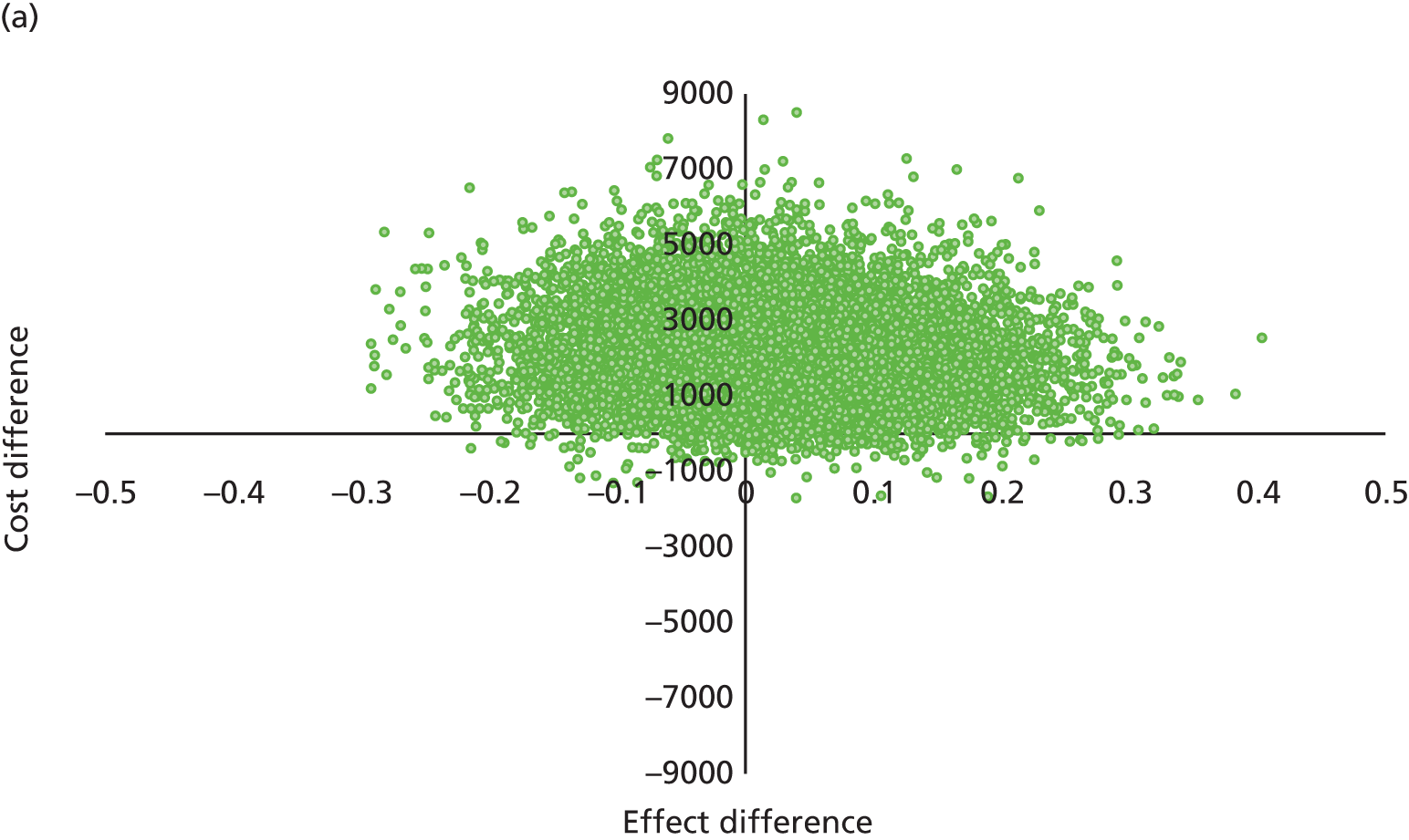
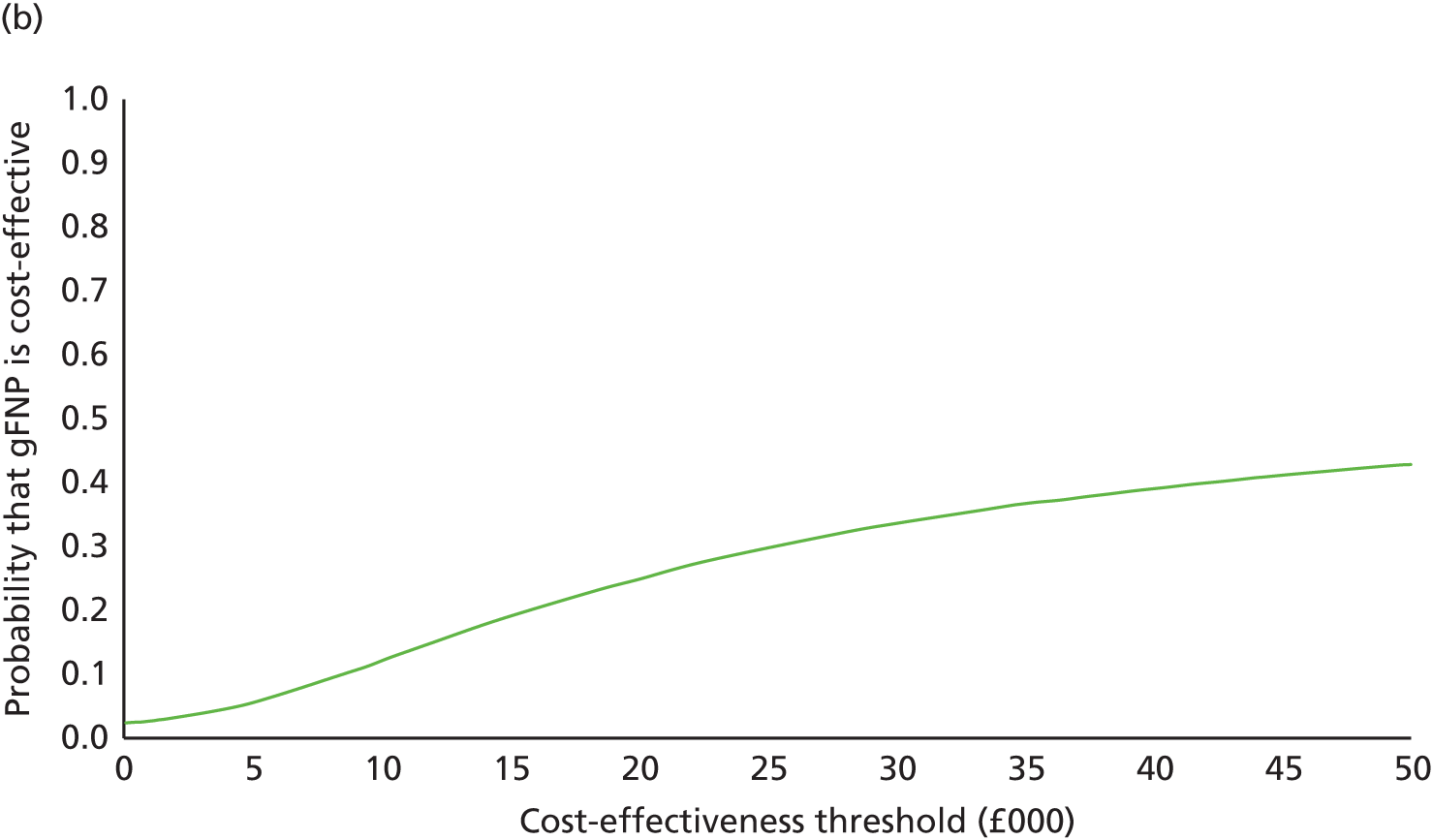
FIGURE 4.
(a) Cost-effectiveness plane; and (b) CEAC based on the CARE-Index outcome: imputed data, NHS and PSS perspective (£, 2014–15 prices).
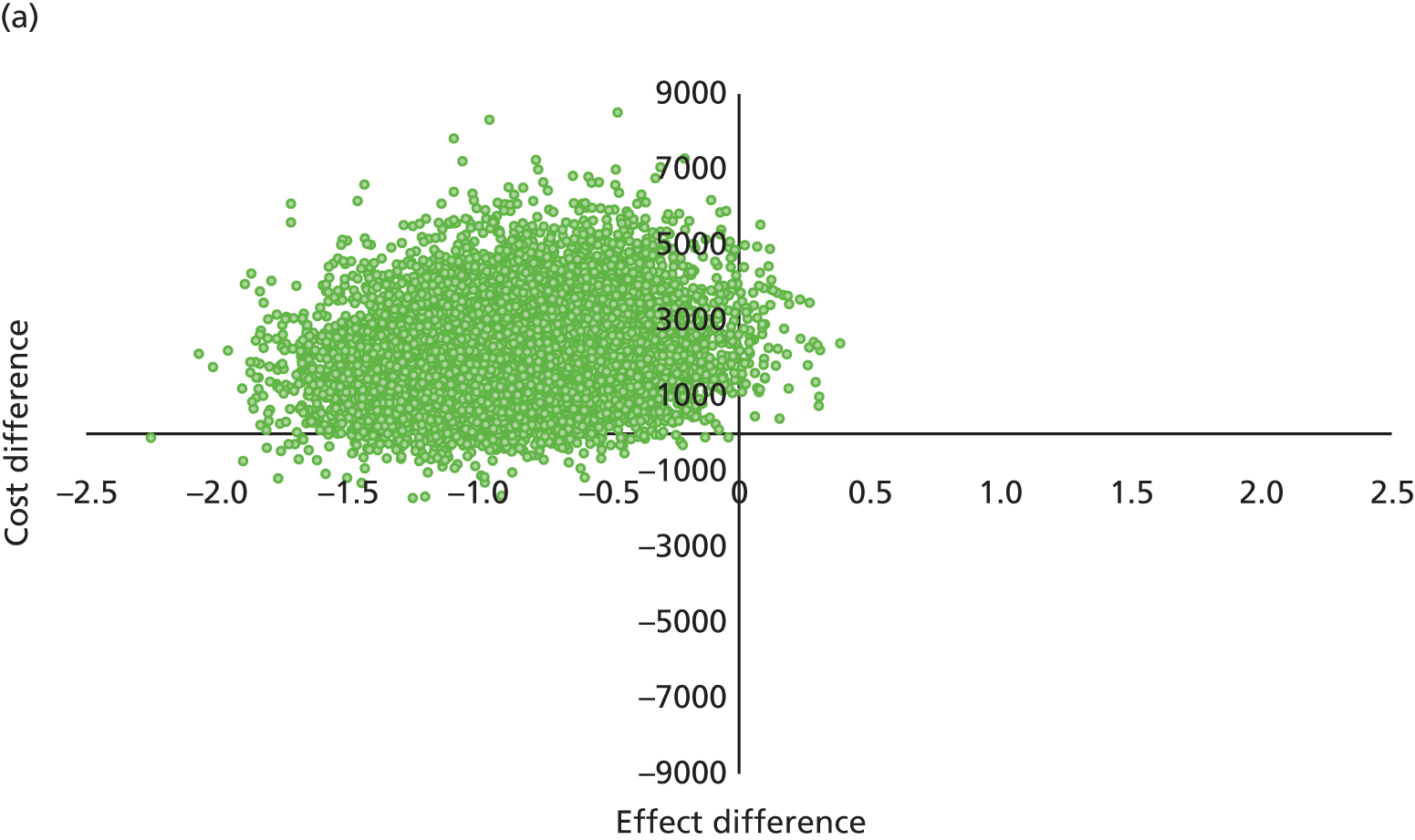
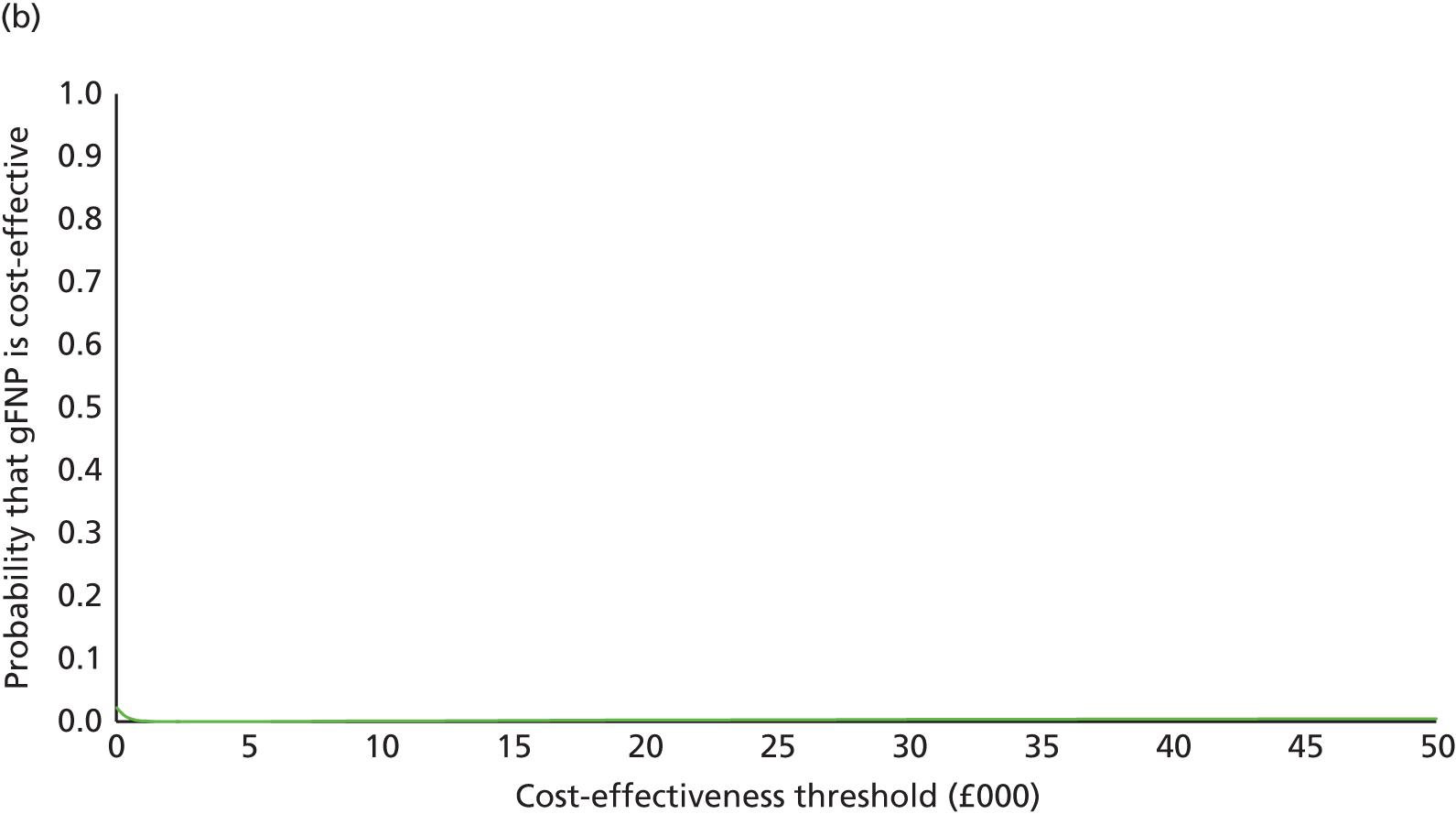
Sensitivity analyses
Several sensitivity analyses were undertaken to assess the impact of uncertainty surrounding key parameters or methodological features on the cost-effectiveness results. Broadening the study perspective to that of society as a whole had little effect on these cost-effectiveness results. In particular, when the QALY metric was adopted as the primary outcome measure, the mean ICER remained in the north-west quadrant of the cost-effectiveness plane and the probability that gFNP was cost-effective at a £20,000 cost-effectiveness threshold remained at 2.5% (Table 35). Similarly, the probability that gFNP was cost-effective remained relatively static following a broadening of study perspective when the CARE-Index (maternal sensitivity) and change in AAPI-2 score were adopted as outcome measures. Table 36 presents recalculations of cost-effectiveness following restriction of the analyses to complete cases (i.e. women and their infants with complete cost and outcome data over the entire follow-up period). These analyses had little notable effect on the overall pattern of results. The results of the final set of sensitivity analyses that varied gFNP session attendance and group size are presented in Table 37. As expected, increasing the mean number of gFNP sessions attended to the highest number of sessions observed across all groups across all sites and increasing the number of gFNP group participants to the highest number of participants observed across all groups across all sites had the effect of decreasing the mean cost difference between the trial groups. Nevertheless, the mean ICER for gFNP remained in the north-west quadrant of the cost-effectiveness plane, and the probability of cost-effectiveness for the intervention did not exceed 20% at a £20,000 cost-effectiveness threshold.
| Outcome measure | Mean costs (95% CI) | Mean effects (95% CI) | ICER (£) | Probability gFNP intervention is | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (£) | Control (£) | Difference (£) | Intervention | Control | Difference | More effectivea (%) | Less costlya (%) | Cost-effectivea (%)b | Cost-effectivea (%)c | Cost-effectivea (%)d | ||
| QALY | n = 97 | n = 67 | n = 97 | n = 67 | ||||||||
| 9074 (6206 to 11,942) | 6279 (5112 to 7445) | 2795 (–277 to 5867) | 0.92 (0.90 to 0.94) | 0.93 (0.91 to 0.94) | –0.01 (–0.03 to 0.02) | –333,775 (NW) | 19.2 | 3.2 | 2.6 | 2.5 | 2.9 | |
| AAPI-2 | n = 97 | n = 67 | n = 97 | n = 67 | ||||||||
| 9074 (6206 to 11,942) | 6279 (5095 to 7463) | 2795 (–302 to 5892) | 0.27 (0.14 to 0.40) | 0.25 (0.12 to 0.38) | 0.02 (–0.17 to 0.21) | 150,152 (NE) | 58.4 | 1.3 | 14.1 | 19.0 | 28.2 | |
| CARE-Index (maternal sensitivity) | n = 97 | n = 67 | n = 97 | n = 67 | ||||||||
| 9074 (6206 to 11,942) | 6279 (5095 to 7463) | 2795 (–302 to 5892) | 3.97 (3.54 to 4.39) | 4.84 (4.30 to 5.38) | –0.87 (–1.55 to –0.19) | –3212 (NW) | 1.2 | 1.0 | < 1 | < 1 | < 1 | |
| Outcome measure | Mean costs (95% CI) | Mean effects (95% CI) | ICER (£) | Probability gFNP intervention is | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (£) | Control (£) | Difference (£) | Intervention | Control | Difference | More effectivea (%) | Less costlya (%) | Cost-effectivea (%)b | Cost-effectivea (%)c | Cost-effectivea (%)d | ||
| QALY | n = 56 | n = 45 | n = 56 | n = 45 | ||||||||
| 9085 (6061 to 12,109) | 6005 (4788 to 7222) | 3080 (–102 to 6262) | 0.84 (0.81 to 0.88) | 0.86 (0.81 to 0.90) | –0.01 (–0.07 to 0.05) | –217,674 (NW) | 32.7 | 1.1 | 1.9 | 2.0 | 2.5 | |
| AAPI-2 | n = 59 | n = 49 | n = 59 | n = 49 | ||||||||
| 9085 (5654 to 12,516) | 6005 (4776 to 7234) | 3080 (–594 to 6754) | 0.25 (0.08 to 0.42) | 0.15 (0.01 to 0.29) | 0.10 (–0.13 to 0.33) | 30,843 (NE) | 77.8 | 2.4 | 28.7 | 37.0 | 47.4 | |
| CARE-Index (maternal sensitivity) | n = 52 | n = 41 | n = 52 | n = 41 | ||||||||
| 9085 (7283 to 10,887) | 6005 (4706 to 7304) | 3080 (885 to 5275) | 4.06 (3.47 to 4.65) | 4.66 (3.90 to 5.42) | –0.60 (–1.55 to 0.35) | –5126 (NW) | 12.2 | 2.8 | 6.6 | 8.0 | 9.0 | |
| Sensitivity analysis | Mean costs (95% CI) | Mean effects (QALYs) (95% CI) | ICER (£) | Probability gFNP intervention is | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (£) | Control (£) | Difference (£) | Intervention | Control | Difference | More effectivea (%) | Less costlya (%) | Cost-effectivea (%)b | Cost-effectivea (%)c | Cost-effectivea (%)d | ||
| Higher mean number of sessions | n = 56 | n = 45 | n = 56 | n = 45 | ||||||||
| 7389 (5137 to 9640) | 6120 (5164 to 7076) | 1269 (–1184 to 3721) | 0.92 (0.90 to 0.94) | 0.93 (0.91 to 0.94) | –0.01 (–0.03 to 0.02) | –151,502 (NW) | 19.2 | 28.8 | 21.5 | 20.1 | 18.4 | |
| Lower mean number of sessions | n = 56 | n = 45 | n = 56 | n = 45 | ||||||||
| 128273 (90,388 to 166,157) | 6264 (5239 to 7290) | 122008 (84,104 to 159,913) | 0.92 (0.90 to 0.94) | 0.93 (0.91 to 0.94) | –0.01 (–0.03 to 0.02) | –4,600,000 (NW) | 19.2 | < 1 | < 1 | < 1 | < 1 | |
| Higher number of women per group | n = 56 | n = 45 | n = 56 | n = 45 | ||||||||
| 7668 (5424 to 9913) | 6117 (5180 to 7053) | 1552 (–882 to 3985) | 0.92 (0.90 to 0.94) | 0.93 (0.91 to 0.94) | –0.01 (–0.03 to 0.02) | –185,300 (NW) | 19.2 | 13.9 | 10.2 | 9.7 | 9.7 | |
| Lower number of women per group | n = 56 | n = 45 | n = 56 | n = 45 | ||||||||
| 12679 (9829 to 15,529) | 6129 (5190 to 7069) | 6550 (3557 to 9543) | 0.92 (0.90 to 0.94) | 0.93 (0.91 to 0.94) | –0.01 (–0.03 to 0.02) | –782,195 (NW) | 19.2 | < 1 | < 1 | < 1 | < 1 | |
Subgroup analyses
Two sets of subgroup analyses were conducted to explore the heterogeneity in our cost-effectiveness results (Table 38). The subgroups considered were (1) whether or not the trial participants completed the gFNP programme, defined by a completion threshold of attendance at ≥ 17 sessions; and (2) programme phase (I, II or III) to test whether or not organisational learning may have influenced the cost-effectiveness of the gFNP programme. Both sets of subgroup analyses were based on cases with complete cost and QALY data at all time points. There was no evidence that either programme completion or the programme phase had a positive effect on the cost-effectiveness of the gFNP programme.
| Sensitivity analysis | Mean costs (95% CI) | Mean effects (QALYs) (95% CI) | ICER (£) | Probability gFNP intervention is | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (£) | Control (£) | Difference (£) | Intervention | Control | Difference | More effectivea (%) | Less costlya (%) | Cost-effectivea (%)b | Cost-effectivea (%)c | Cost-effectivea (%)d | ||
| Programme completers | n = 29 | n = 67 | n = 29 | n = 67 | ||||||||
| 9863 (7552 to 12,174) | 6107 (5170 to 7043) | 3757 (1283 to 6230) | 0.90 (0.87 to 0.93) | 0.93 (0.91 to 0.94) | –0.03 (–0.06 to 0.01) | –140,686 (NW) | 5.3 | < 1 | < 1 | < 1 | < 1 | |
| Programme non-completers | n = 68 | n = 67 | n = 68 | n = 67 | ||||||||
| 7449 (4428 to 10,470) | 6107 (5170 to 7043) | 1342 (–1817 to 4502) | 0.93 (0.91 to 0.95) | 0.93 (0.91 to 0.94) | –0.001 (–0.03 to 0.02) | –1,122,691 (NW) | 45.9 | 20.9 | 20.9 | 20.9 | 20.6 | |
| Programme Phase I | n = 27 | n = 67 | n = 27 | n = 67 | ||||||||
| 7771 (5358 to 10,184) | 6107 (5170 to 7043) | 1665 (–872 to 4201) | 0.91 (0.88 to 0.95) | 0.93 (0.91 to 0.94) | –0.01 (–0.06 to 0.03) | –125,764 (NW) | 22.1 | 8.3 | 5.7 | 5.7 | 5.4 | |
| Programme Phases II and III | n = 44 | n = 67 | n = 44 | n = 67 | ||||||||
| 9783 (7446 to 12,120) | 6107 (5105 to 7108) | 3677 (1146 to 6207) | 0.91 (0.88 to 0.94) | 0.93 (0.90 to 0.95) | –0.02 (–0.06 to 0.02) | –217,390 (NW) | 34.0 | 2.1 | 1.3 | 1.3 | 1.2 | |
Discrete choice experiment
Study population
For the purposes of the DCE, we aimed to recruit a total of 600 respondents, split into two groups, one composed of women whose characteristics broadly match the trial eligibility criteria, and the other composed of a representative sample of the general population whose values can be considered relevant for social decision-making purposes. Ipsos MORI used a wide range of targeting criteria to select the study samples, from simple demographics to more complex behavioural and attitudinal profiling. Once a sample had been selected, e-mail invitations were automatically randomised so as not to induce bias. The sampling was started from a panel of pre-targeted pregnant women for the expectant mothers quota. For the general population quota, randomised e-mail invitations were released in batches corresponding to the size of the quotas required, stratified by age, sex and region. The smaller pool of expectant mothers within the Ipsos MORI panels led to the recruitment of 200 pregnant women and 400 members of the general population in the full DCE.
Results
The results of the repeated question consistency check within the DCE design are presented in Table 39. Across the full sample, approximately 78% of people provided consistent responses, with the consistency among expectant mothers being somewhat lower than in the general population. A sensitivity analysis was conducted excluding those people who did not provide consistent responses, which did not find meaningfully different interpretations to the primary analysis.
| Population | Sample size | Number passing consistency check |
|---|---|---|
| Full sample | 600 | 469 (78.2%) |
| Expectant mothers | 200 | 142 (71.0%) |
| General population | 400 | 327 (81.8%) |
The results of the primary DCE analysis are presented in Tables 40–42 for the three populations of interest: expectant mothers; the general population; and the full study sample combining those two groups.
| Characteristic | Coefficient | SE (coefficient) | Significance |
|---|---|---|---|
| Selecting option B (second choice set) | –0.025 | 0.057 | |
| You do not feel anxious or depressed | –0.116 | 0.056 | * |
| You feel you have a high level of understanding of your child’s needs | 0.930 | 0.054 | *** |
| You have no problems in doing your usual activities | –0.149 | 0.053 | ** |
| You feel you have enough support from your friends and family | 0.318 | 0.054 | *** |
| You do not feel stressed in your role as a parent | 0.398 | 0.054 | *** |
| You feel confident and capable of problem-solving as a parent | 0.936 | 0.053 | *** |
| Characteristic | Coefficient | SE (coefficient) | Significance |
|---|---|---|---|
| Selecting option B (second choice set) | 0.075 | 0.042 | |
| You do not feel anxious or depressed | 0.004 | 0.041 | |
| You feel you have a high level of understanding of your child’s needs | 1.046 | 0.040 | *** |
| You have no problems in doing your usual activities | –0.094 | 0.039 | * |
| You feel you have enough support from your friends and family | 0.449 | 0.039 | *** |
| You do not feel stressed in your role as a parent | 0.576 | 0.040 | *** |
| You feel confident and capable of problem-solving as a parent | 1.359 | 0.040 | *** |
| Characteristic | Coefficient | SE (coefficient) | Significance |
|---|---|---|---|
| Selecting option B (second choice set) | 0.040 | 0.034 | |
| You do not feel anxious or depressed | –0.038 | 0.033 | |
| You feel you have a high level of understanding of your child’s needs | 1.002 | 0.032 | *** |
| You have no problems in doing your usual activities | –0.113 | 0.031 | *** |
| You feel you have enough support from your friends and family | 0.402 | 0.032 | *** |
| You do not feel stressed in your role as a parent | 0.511 | 0.032 | *** |
| You feel confident and capable of problem-solving as a parent | 1.210 | 0.032 | *** |
Across all three populations, the four attributes not based on the EQ-5D-5L,90 namely the AAPI-2,72 Abidin PSI,77 PSOC81 and MOS,83 produced highly significant coefficients, with respondents significantly more likely to select options where the more positive of the two alternatives was present. However, for the two EQ-5D-5L-based attributes (anxiety/depression and usual activities), no such clear pattern was evident, with coefficients often not significant and occasionally with the numerical value of that coefficient in the ‘wrong’ direction (i.e. respondents occasionally favoured options with increased anxiety or a lower ability to perform their usual activities). Although this is unlikely to be an accurate finding in and of itself, the result clearly demonstrates that the two EQ-5D-5L-based maternal HRQoL attributes were viewed as being considerably less important than the other four attributes by both groups of respondents, meaning that an analysis based solely on maternal HRQoL is likely to miss potential benefits in other domains. As a result of the coefficients for the EQ-5D-5L attributes not pointing in the ‘correct’ direction, it was not possible to calculate marginal rates of substitution for the other attributes based on the utility values attached to those attributes.
Interpretation
Although the results of the DCE meant that it was not possible to explicitly incorporate the outputs from the DCE into an augmented CUA to reflect the value in changes in attributes not covered by the EQ-5D-5L, the results clearly demonstrate that, at the levels included in the questionnaire, the EQ-5D-5L attributes are viewed as considerably less important, by both expectant mothers and the general population, than the other factors included. This may imply that CUAs using solely the EQ-5D-5L to measure outcomes may miss important factors when evaluating parenting programmes.
A potential explanation for some of the results not showing the expected pattern is the levels chosen for the EQ-5D-5L attributes in the DCE questionnaire. An earlier questionnaire draft used the moderate levels from the EQ-5D-5L for the anxiety or depression and usual activities attributes, but this was reduced to the ‘slight’ levels after feedback during the piloting process that suggested that higher levels of problems may be too severe for the populations under consideration. It is therefore possible that the EQ-5D-5L levels chosen were insufficiently far apart for people to consider them as part of their trade-offs. These mental health attributes were not statistically significant within the Ipsos MORI pilot of 50 responses and therefore no adjustments could be made prior to the full survey roll-out. Nevertheless, the DCE clearly demonstrates the value placed by both pregnant women and members of the general population on non-health outcomes that are not included in the QALY metric.
Chapter 5 Process evaluation
Introduction
The process evaluation was designed to explore in more detail the delivery and experience of gFNP. It considered the uptake of gFNP for women who agree to the intervention and the attrition from gFNP provision. It also determined the extent to which the programme was delivered with integrity based on anonymised data from standardised data forms documenting sessions delivered, the content domains covered in sessions, attendance and participants’ responses to the content, comparing the information with recommendations for delivery of one-to-one FNP from the US National Office and from the UK FNP NU. It also provided qualitative information to set the results in context by determining the acceptability of the programme for clients and practitioners plus their thoughts on its feasibility in the future, with reference to the findings of the implementation evaluations. 57,67,68,121
Background
Model of the Group Family Nurse Partnership programme delivery used for the First Steps study
Delivery of the programme for the trial participants was by two FNs, one of whom had also notified their intention to practise as a midwife. Groups were scheduled to be held fortnightly from mid-pregnancy to the end of the baby’s first year (44 sessions in all), at an accessible community venue. The programme’s content follows the FNP programme in that six content domains are incorporated: maternal personal health, maternal role, life course development, family and friends, environmental health, and referrals to health and human services. Content is delivered through discussion, specially designed group activities and a range of printed material that clients are encouraged to keep in a folder. FNs record attendance for each registered client, rating their attendance and responses to each session attended and also record for each session the proportion of time spent on each of the content domains.
The two FN facilitators delivering group sessions at each site were also experienced in delivering home-based FNP and continued to deliver this while delivering the group sessions, albeit with a reduced caseload. It was intended that each group would ideally comprise between 8 and 12 women whose partners (if they had them) would be encouraged to attend. The criteria for young women recruited to take part in the study were that they were likely to benefit from the support offered by gFNP but were not eligible for FNP, namely expectant mothers aged < 20 years with one or more previous live births, or expectant mothers aged 20–24 years with low/no educational qualifications and no previous live births. Additionally, their EDDs were to be within 6 to 8 weeks of each other for each group in each site.
Routine antenatal care was provided during the pregnancy group sessions according to NICE guidelines,62 and at the postnatal sessions infancy checks were carried out according to the HCP. 54 The expectant mothers are encouraged to carry out pregnancy checks themselves with guidance from the FNMW, one of the group’s two facilitators. Incorporation of this strategy is based on studies in the USA suggesting that this ‘Centring Pregnancy’ approach61,122 encourages self-efficacy and could promote peer-to-peer learning. 46 In addition, it was anticipated that the group context of gFNP would help young mothers to develop social networks with other young women with babies, reducing social isolation and increasing social capital.
Variants of the gFNP model of programme delivery just described had previously been evaluated and modestly adapted during the 3-year period immediately preceding the trial, with the findings summarised in brief below, indicating that the model described above was appropriate for testing the efficacy of gFNP using a RCT approach.
Findings from the feasibility studies
Following development work in 2009, two feasibility studies were commissioned to evaluate the acceptability of gFNP for both clients and practitioners. The models of delivery differed in the nature of the practitioners providing the programme. In Phases I and II57,123 the programme was provided by two fully trained FNs, one of whom had also notified their intention to practise as a midwife and the second a fully trained health visitor. In Phase III67,121 a modified approach was used, involving only one FN. She was present throughout the programme and the second facilitator for the pregnancy sessions was a local community midwife, who was then replaced by a local children’s centre child and family support worker for the infancy component. All the new non-FNP practitioners in Phase III undertook a short training course developed to support them in group facilitation roles and to provide them with some knowledge of the FNP curriculum and its strength-based mode of delivery. In both studies, recruitment was a balance between conforming to the suggested criteria, especially gestational age and the range of gestational ages to include, and identifying sufficient women. Refinement of the educational qualifications of eligible participants was also made. The initial stage of the formative evaluation in two sites124 concluded that the original eligibility criteria, either being younger than 20 years and expecting a second child or aged 20–25 years and expecting a first child, with gestation ideally 12 weeks at referral, led to two challenges: (1) to identify a sufficient number with due dates close together; and (2) to identify women early enough in their pregnancies, most were recruited after 12 weeks’ gestation. A second phase of feasibility work at the same two sites,57 using additional eligibility criteria of low or no educational qualifications and/or no employment found again that the average gestational age at referral in both groups was beyond the recommendation of 12 weeks and that to identify sufficient women the range of gestational ages needed to be about 2 months rather than 6–8 weeks. This meant that there was some disruption to the programme around the time that infants were born with some women still focusing on antenatal issues, whereas others had newborns. In further feasibility research in four locations,67 criteria for participant recruitment were the same as those described in Phase II and substantial effort was again required to identify sufficient clients, but it was possible to start all groups with between 8 and 12 clients.
The feasibility studies suggested that gFNP was highly acceptable to both service users and to the practitioners delivering the service. Clients liked the idea of meeting other ‘mums’ like themselves and making new friends, and saw the opportunity to discuss parenting issues with other parents in addition to the professionals as an extra advantage. 57,121 In both studies, many clients also commented that they had developed their social networks as a consequence of attending the group. 121,123 A key impact of taking part in gFNP was said to be an increase in personal confidence and in their ability to look after their babies; there was also a reported improvement in mental health from being less isolated and receiving more support from health professionals and other members of the group. 67
When asked about the gFNP approach, and the materials and resources used in delivering the programme agenda, clients generally said that they preferred more practical activities and especially those that they could do with their babies. The majority considered that the inclusion of routine midwifery care in the group was a bonus when deciding to accept the programme, expecting it would allow more contact with a midwife and health visitor than would be the case if receiving routine services. 68 However, there were mixed responses from clients when asked how they felt about carrying out their own health checks. Although the majority of the women interviewed expressed the view that carrying out the checks gave them a sense of independence and control over their own pregnancies, there were some who voiced the opinion that they would prefer a nurse to do the tests for them in case they made mistakes; others were ambivalent about the process. 67,68,121
Attendance at the gFNP sessions was greater during the pregnancy phase than in infancy in both feasibility studies. Attendance was also highly variable; although some clients attended almost all sessions, others attended as few as two. When asked about non-attendance, transport problems were an issue for some and after their babies had been born some clients found it too tiring to organise themselves to get to group sessions or had employment or educational opportunities. 68
The gFNP practitioners found the programme acceptable and they enjoyed working in a group context,67,68 but some reservations were expressed regarding programme delivery by non-FNP professionals. Despite the training provided for non-gFNP health professionals, their lesser knowledge of the FNP approach placed a heavier burden on the FN facilitators. 68 Division of responsibilities was most evident during pregnancy, community midwives being more confident about and concerned with health checks, while taking a more backseat role for other programme content. They reported less confidence in delivering the gFNP content and in the strength-based style of delivery (motivational interviewing),43 which is central to FN training. In contrast, during the infancy sessions the division between FNP and non-FNP professionals was more balanced with both FNs and Sure Start Family Support workers involved with infant health checks and in delivering gFNP content. However, for the First Steps trial the original staffing model was used; all practitioners were FNP professionals.
Quantitative information about service delivery
Method
Data about the acceptance of the offer of gFNP were provided by the relevant gFNP site administrator or FN to the First Steps data manager at the LSHTM. Data about client attendance and response to the content were recorded by FNs after each session for each recruited client on form UK001G and reasons for leaving recorded on form UK004G; the relevant information was collated by the FNP NU and shared with the study PI, anonymised in that only the gFNP UID was available. Matching with study UIDs was completed by the LSHTM data manager to retain blinding for the research team and shared with the PI for analysis after the final research visits had been completed. Data on group size and content covered were recorded on form UK031G by FNs for each session delivered, collated by the FNP NU and shared with the PI for analysis after the end of programme delivery.
Results
Uptake of the programme
Out of the 97 women randomised to receive the intervention (not including two recruited and randomised in error), 80 (82.5%) were allocated a UID number by the relevant gFNP team, indicating that they had been contacted by the FNs and had agreed to receive the intervention. Reasons for not allocating a number for the remaining 17 were as follows: six were contacted and refused the intervention; three were contacted and agreed but did not attend any sessions; one had miscarried by the time the team contacted her; one had moved away; two were not contactable; and for four no information was provided. Thus, the uptake rate based on those contacted was high, at 83 out of 89 (93%), although indicating agreement to attend the groups but then not attending could be perceived as declining without wanting to tell the FN, making the uptake rate 80 out of 89 (90%). However, both of these uptake rates are higher than those found in the process evaluations, which were 74% and 57%. 57,67 Of the 80 who were allocated a UID by the gFNP team, 58 (72.5%) attended at least one session. Reasons for not attending any sessions after agreeing to receive the programme (n = 22) were that their pregnancy ended before groups began (n = 4) or that no sessions were offered in their area due to the number recruited being too low for a group to be viable (n = 13), with no information for the remaining participants (n = 5).
Group size
Although uptake of the offer of participation in the study was good, the slow rate of participant identification meant that group size was adversely affected. The original recruitment plan85 was for community midwives to forward names and telephone numbers of potential participants to the research team, but this had to be amended to involve CLRN research midwives and FNP team members (see Chapter 2, Ethics). Interviews with community midwifery representatives indicated that the reasons for the low number of potential participants identified by their teams to researchers related to a number of issues, including some confusion about their role in identifying potential participants, but not in recruiting to the study; insufficient time during booking appointments; expectations that a group programme would not be acceptable; and concerns about the eligibility criteria. 86 A consequence, even with the amended strategies detailed in Chapter 2, was that recruitment remained slow and the majority of the groups were smaller at the start of programme delivery than the recommended minimum number of eight,46,68 with none reaching the maximum size of 12 mothers-to-be.
The average number recruited to groups at the start of delivery, including ‘buffer’ clients who were not taking part in the trial but who joined at the start of programme delivery, was 6.3 (range 2–11), with all but 3 of the 16 groups starting out smaller than the recommended size (range 8–12), the most typical sizes being seven (n = 5) or six (n = 4). The average number of gFNP clients present at groups was lower, at 3.9 (range 0–8, SD 1.7); 60% of sessions had between three and five clients present, with more than five present for only 15% of groups. Partner attendance was, on average, very low (mean 0.7, range 0–6). For more than half of the group sessions (56%), no partner attended, and generally there were either one (29% of sessions) or two (11% of sessions) partners present.
Sessions delivered
The curriculum has 14 pregnancy sessions and 30 for infancy. The number of pregnancy sessions run in the 16 groups involved in the trial was lower, with an average of 9.2 (range 0–15), with only 9 of the 16 groups running ≥ 13 sessions. The average number of infancy sessions delivered was 13.0 (range 0–31). Only 1 of the 16 groups was able to offer the full number of infancy sessions, with a further eight offering half or more, whereas 7 of the 16 offered no infancy sessions at all, having terminated the programme owing to low attendance.
Attendance
Details of attendance are given in Table 43, first for all those study participants allocated to the intervention (n = 97, not including two recruited and randomised in error), then for all those allocated a UID number by the gFNP teams (n = 80), and finally for those who attended a least one session (n = 58).
| Participant status based on gFNP attendance | Pregnancy sessions (range 0–15) | Infancy sessions (range 0–30) | Total sessions (range 0–44) |
|---|---|---|---|
| Allocated to intervention, n = 97 | 4.5 (SD 5.1) | 5.8 (SD 8.8) | 10.3 (SD 13.4) |
| Given a gFNP UID, n = 80 | 5.4 (SD 5.2) | 7.0 (SD 9.3) | 12.4 (SD 13.8) |
| Attended at least once, n = 58 | 7.5 (SD 4.6) | 9.6 (SD 9.7) | 17.0 (SD 13.5) |
Although uptake was higher than the implementation evaluations,57,67 the extent of attendance for the First Steps trial participants was not as high as had been found in the feasibility work. The average attendances in the feasibility studies were 10.4 and 8.3 sessions, respectively, in pregnancy (14 in the curriculum) and 16.6 and 13.5 in infancy (30 in the curriculum). In comparison the average attendance in the First Steps RCT for the 58 women who attended at least one session was lower, particularly in infancy (pregnancy 7.5 and infancy 9.6; see Table 43). It is likely that the small size of the First Steps trial groups at the outset, not the case for the implementation evaluations, may have contributed to the lower attendance. In addition, the premature termination of programme delivery in many cases clearly reduced the likelihood of optimal attendance for trial participants, a situation much less common in the feasibility studies.
Attrition
The rate of attrition during pregnancy in the home-based FNP was expected to be around 10%. 39 Of the 58 trial participants in the intervention arm who attended at least one gFNP session in pregnancy, only 35 (60.3%) attended the infancy phase of the programme, meaning that, at 39.7% (23/58), attrition in pregnancy was higher than had been found in the two development studies (13% and 19%)67,124 and higher than the target for the home-delivered FNP. However, the majority of the 23 participants who stopped attending (15/58, 26%) were women in areas where programme delivery terminated prematurely in the pregnancy phase owing to low numbers coming to the group, whereas fewer (8/58, 14%) stopped attending groups that were still functioning. Reasons were not available for all leavers. The most frequently cited reason for leaving in pregnancy was that the participant considered that they had sufficient knowledge about child development and parenting (n = 5); FNs reported that two group participants left after an argument with another group member, and two were no longer able to attend as they had moved away. One participant left the infancy programme owing to family pressure and another left as she found it difficult to keep up attendance and also to maintain her baby’s routine. Owing to the low number of groups continuing with the full infancy programme, attrition in infancy has not been calculated.
Participant responses to content
Each time a client or partner attended a session, three ratings (on a scale from one to seven) were made by the FNs of their involvement in the group, their understanding of the content and any conflict or disagreement with the content discussed during that session (Table 44).
| Phase of programme and source of information | Involvement | Understanding of materials | Conflict with materials |
|---|---|---|---|
| Pregnancy | |||
| Study 157 | 4.9 (2–5) | 4.9 (1–5) | 1.0 (1–2) |
| Study 267 | 4.8 (3–5) | 4.8 (2–5) | 1.1 (1–5) |
| First Steps RCT | 6.3 (2–7) | 6.4 (2–7) | 1.3 (1–7) |
| Infancy | |||
| Study 1 | 4.9 (3–5) | 5.0 (2–5) | 1.0 (1–3) |
| Study 2 | 4.9 (3–5) | 4.9 (3–5) | 1.0 (1–3) |
| First Steps RCT | 6.3 (2–7) | 6.4 (2–7) | 1.2 (1–7) |
These ratings cannot be compared directly with those made in the feasibility studies,57,67 as the scale used in feasibility delivery was one to five, but the ratings from the feasibility work are provided in Table 44 for information. The pattern of ratings was comparable to previous work in that clients on average are rated near the top of the scales for involvement and understanding with close to the lowest point on the scale for conflict with the content. However, it should be noted that a range of client ratings was evident, with some situations of low involvement, low understanding or a high level of disagreement with the session’s content.
Delivery of programme content
The extent to which the programme was delivered with integrity was assessed through an analysis of data from the programme’s standardised data forms completed by the FNs to document session attendance and the proportion of time spent on each of the content domains during sessions. The coverage of the six content domains can be seen in Table 45. There are no specific targets for the percentage of time to be spent on each domain when delivering FNP in a group context, but targets developed for the one-to-one home delivered programme36,39,40 correspond closely to those achieved on average in delivering the group programme. However, it needs to be noted when making comparisons that the delivery of home-based FNP does not have a target for the percentage of time spent on referrals to health and human services and FNP FNs apportion the percentage of time spent with clients in visits across only five content domains, whereas gFNP FNs, in their summary of group sessions, apportion the percentage of time spent across six domains.
| Site | Personal health, % | Maternal role, % | Life course, % | Friends and family, % | Environmental health, % | Health/human services, % | Planned content covered, % |
|---|---|---|---|---|---|---|---|
| Pregnancy | |||||||
| One-to-one FNP target | 35–40 | 23–25 | 10–15 | 10–15 | 5–7 | N/A | |
| Total | 32 | 33 | 8 | 12 | 7 | 8 | 94 |
| 1 | 30 | 30 | 10 | 12 | 8 | 11 | 97 |
| 2 | 32 | 33 | 5 | 12 | 8 | 9 | 93 |
| 3 | 28 | 36 | 11 | 13 | 6 | 7 | 88 |
| 4 | 29 | 31 | 10 | 12 | 10 | 9 | 97 |
| 5 | 37 | 31 | 11 | 9 | 6 | 6 | 95 |
| 6 | 34 | 38 | 8 | 12 | 5 | 4 | 91 |
| 7 | 35 | 28 | 7 | 14 | 9 | 9 | 96 |
| Difference | – | – | F 2.28* | – | F 2.95** | F 5.58** | F 1.97a |
| Infancy | |||||||
| One-to-one FNP target | 14–20 | 45–50 | 10–15 | 10–15 | 7–10 | N/A | |
| Total | 19 | 44 | 10 | 11 | 9 | 8 | 92 |
| 1 | 17 | 39 | 13 | 13 | 10 | 9 | 100 |
| 2 | 19 | 41 | 9 | 12 | 8 | 11 | 92 |
| 3 | 16 | 45 | 12 | 11 | 9 | 8 | 88 |
| 4 | 16 | 47 | 10 | 10 | 11 | 7 | 90 |
| 5 | 19 | 43 | 9 | 12 | 9 | 8 | 91 |
| 6 | 21 | 49 | 8 | 9 | 7 | 6 | 90 |
| Difference | – | F 3.20* | F 1.93a | F 2.11a | F 2.63* | F 5.30** | F 1.93a |
The proportion of time recommended for personal health when delivering FNP at home is 35–40% in pregnancy and 14–20% in infancy. The averages for gFNP are comparable, at 32% and 19%. In pregnancy it would be expected that slightly less time would be spent on personal health when delivering gFNP, as women also received routine antenatal checks during the group sessions from the gFNP midwife. The proportion of time spent in pregnancy groups on maternal role (33%) was slightly higher than that suggested for FNP (23–25%), but it was comparable in infancy (44%; FNP target 45–50%).
The average proportion of time spent on planning for the future (life course) in gFNP pregnancy sessions (8%) was low in comparison with the FNP target (10 to 15%), but it was notable that sites showed considerable variability, with mean percentages ranging from 5% to 11%. This may be one area that was influenced by the specific characteristics of the group members. Other site differences can be seen in coverage of environmental health (participants in some groups may have better housing situations) and health and human services, which predominantly concerns referrals to other agencies. Again, some groups may have members with high need for referral and others may not.
It is notable that more variation between sites can be seen during infancy sessions than during pregnancy. This may suggest that ‘agenda matching’ becomes more typical of programme delivery once babies are born and issues are raised in the group about particular parenting topics, or child development concerns.
Qualitative interviews
Following the completion of gFNP programme delivery at each site, qualitative interviews were conducted with:
-
a subsample of trial participants who had been randomised to the intervention arm
-
FNs who had been involved in delivering the programme.
The aim of interviewing trial participants randomised to the intervention arm was to explore acceptability of the programme and any perceived benefits. The aim of interviewing the FNs was to explore their thoughts on delivering the programme and its likely sustainability. The interviews for trial participants took place after completion of the relevant group and for FNs took place after completion of programme delivery in the relevant site so that questions asked during the qualitative interview did not influence their experience of the intervention.
Method
Trial participants
Participants from Phases I and II of the trial and across sites were selected to reflect a range of attendance experiences (not all those randomised to receive the intervention had attended gFNP). However, any participants who had reported that they had been in care (looked-after child; LAC) were excluded from selection, as they were eligible for the interviews described in Chapter 6. Once the 12-month data collection for trial participants had taken place (the final interview in the main study), and on receipt of the relevant questionnaires, the data manager (LSHTM) was able to inform the trial manager (Birkbeck) in blocks (range two to seven), which arm of the trial the participants had been randomised to, as agreed by the Project Management Committee. This procedure was used to preserve blinding for participants who had not yet completed 12 months, while facilitating timely interviewing for those who had completed. Following this staged unblinding procedure, attendance data for the pregnancy phase of the programme was initially used to estimate whether participants were frequent or infrequent attenders to ensure a broad range of participants were approached for inclusion in the qualitative study (infancy attendance data were not available until later).
The original target figure for the qualitative interviews with participants was 20; however, the final number interviewed was 32 in order to ensure a broad range of experiences was captured, including the experiences of women whose group was discontinued prematurely (to explore what this had meant to them and to identify what alternative forms of support were offered). Participants were spread across Phase I (n = 14) and Phase II (n = 18), and included at least one from each of the seven sites. The number of participants interviewed per site was five or six apart from two sites where the programme delivery had been terminated prematurely during Phase I. Total attendance for the interviewed participants across pregnancy and infancy sessions was on average 20 (range 0–39) with a median of 22. Average attendance for them in pregnancy was eight sessions (range 0–14), and average attendance in infancy was 12 sessions (range 0–25), so the desired spread of experiences of gFNP was achieved.
Service providers (family nurses)
The target for interviews was at least one FN and one supervisor in each of the seven sites (n = 14). Although all of the FNs contacted had initially agreed to be interviewed, in some instances due to sickness on the day or prior commitments elsewhere, not all were available. In two sites, FNs who had delivered earlier sessions in the programme had left the team altogether and were unavailable for contact. Some gFNP supervisors declined to be interviewed as they had not been involved in delivering the programme. In all, 16 FNs were interviewed, three of those were also supervisors and five were also FNMWs. At least two were interviewed per site and in one site three were interviewed.
Procedure
Trial participants
After participants had completed the 12-month interviews, the trial manager, was informed by the data manager of the status of participants (intervention or control) and the extent of exposure to gFNP. She then informed fieldworkers which participants had been randomised to receive the intervention (along with any available attendance data). They could then approach these individuals to invite them to take part in a qualitative interview about their experiences.
Fieldworkers, who had previously conducted structured interviews with the participants, contacted prospective interviewees by telephone and invited them to take part in a face-to-face interview about their experiences of gFNP. All fieldworkers were female, and the participants understood that they were university employees and not linked in any way with the delivery of gFNP. The fieldworkers had conducted qualitative interviews previously and also received additional training from the trial manager and the PI. If participants agreed to take part in a qualitative interview the fieldworker arranged a date and time, usually at the participant’s home where their previous trial interviews had been carried out. If a participant felt that she would like to hear more about the interview and why it was being carried out before agreeing to take part, the fieldworker arranged to visit her at home to give her more information and answer any questions she might have. Not everyone who was approached agreed to be interviewed and, in these cases, they were thanked for their time and the telephone call ended.
At the beginning of the visit and prior to the interview the fieldworker gave the participant an information sheet about the qualitative study (see Report Supplementary Material 7) and, after going through it with her, answered any questions that arose. Informed consent was taken once the fieldworker was satisfied that the participant understood what the interview entailed, and this included consent for the interview to be recorded (see Report Supplementary Material 7). The interviews were digitally recorded. At the end of the interview the participant was given a £20 shopping voucher as a thank-you for her time. The interviews lasted between 15 minutes and 1 hour.
Family nurses
The female trial manager, who was known to all gFNP teams to be an independent university employee and who had met with them prior to the trial commencing, with mainly telephone communication throughout the recruitment process, conducted the qualitative interviews with gFNP FNs, all of whom were also female. She was notified when the group sessions were completed at each site and then contacted the gFNP team to arrange a convenient date to visit them at their base to carry out the interviews. On arrival at the gFNP site, on the day arranged for the interviews, the trial manager gave those FNs to be interviewed information sheets about the qualitative study (see Report Supplementary Material 7) and the opportunity to ask any questions that they might have. Informed consent was then taken from the FNs, including permission to record the interview (see Report Supplementary Material 7), and all interviews were carried out individually on a face-to-face basis in a quiet office. The interviews lasted between 40 minutes and 1 hour and were digitally recorded.
Measures
Trial participants
The questionnaire was structured around seven topics, designed to guide the conversation with questions rather than to be a question and answer process (see Report Supplementary Material 7).
-
Attendance at gFNP sessions: the first topic was concerned with attendance and asked how often the participant had been able to go to the group, had their partner attended with them and if they had any transport difficulties getting to the venue. If their attendance had been low or they had stopped attending altogether they were asked about why they thought this had been the case and if they had received any other types of support.
-
Views on group activities: this section asked about any topics or activities that they had found particularly useful or enjoyable as well as whether or not they felt that they could be honest within the group and say what they were really thinking, or raise issues of particular concern.
-
Overall impact of the programme: these questions explored the overall impact of the programme in terms of how they dealt with day-to-day behaviours such as crying, sleeping or weaning and their approach to parenting in the future. They were asked to rate on a scale of 1 to 10 the difference going to the group had made to the way they were looking after their baby, with 1 = not at all and 10 = made all the difference in the world. They were then asked to talk a bit more about why they had made that rating.
-
Relationships in the group: this section looked at relationships in the group, both with other group members and with the FNs who facilitated the sessions.
-
Overall thoughts about gFNP: participants were asked if they would recommend the group to others and if there was anything they would change about the way it was organised.
-
Support as part of a research trial: participants were asked if they thought the group should be routinely available for all young pregnant women rather than just being part of a research study.
-
Final thoughts: the last section gave participants the opportunity to express any final thoughts they had about the support that they had been given through attending the group.
Family nurses
The FN qualitative questionnaire was in four parts, but it was intended that the interview be conducted in a conversational style, letting the discussion be as natural as possible while covering the topics (see Report Supplementary Material 7).
-
Participation: the first part was concerned with participation, focusing on attendance and factors that might affect whether or not people came to the group, such as location, availability of transport, weather, and topics being covered at group or perhaps relationships with other group members.
-
Encouraging self-care: the next section explored their views on participants in the group being active contributors in the sessions so that they could learn from each other, and more specifically being active in their own routine maternity/pregnancy care (while pregnant) and once the babies were born, what they thought about encouraging mothers (and fathers) to be involved in checking their baby’s development.
-
Possible impacts of gFNP: the third part covered whether or not providing midwifery care in the group had any impact for group members on antenatal health or their experience of labour and delivery. There were also questions about improved confidence of the mothers with their infants as a result of attending the group.
-
Delivery and sustainability: the last section was concerned with the delivery and sustainability of gFNP, with a final question asking FNs to sum up what the experience of delivering group sessions had been like for them.
Analysis strategy
All interviews were transcribed with full anonymisation. Simple content analysis125 was used to summarise the interviews conducted by two researchers (JacB and JanS) identifying comments relevant to pre-defined research themes: acceptability and perceived benefits for clients; acceptability and sustainability for practitioners (Table 46). Quotations from participants’ interviews start with P followed by a random number from 01 to 32 (e.g. P24). Quotations from FNs’ interviews start with FN followed by a random number from 01 to 16 (e.g. FN12).
| Interviewee | Main theme | Subthemes |
|---|---|---|
| Clients | ||
| A | Aspects of gFNP that worked well for service users | FN qualities |
| Group structure and size | ||
| Group interactions | ||
| Practical factors | ||
| B | Barriers to engaging with the programme for service users | FN qualities |
| Group structure and size | ||
| Group interactions | ||
| Practical factors | ||
| C | Perceptions of likely impacts of attending gFNP | Fewer mental health problems |
| Learn about child development | ||
| Develop parenting skills | ||
| Extend social networks and support | ||
| FNs | ||
| D | The experience of providing support in a group context | Identify evidence of peer learning and support |
| Able to observe social interactions | ||
| Less knowledge of clients’ home circumstances | ||
| E | Aspects of gFNP that worked well for the practitioners | Creating a ‘safe space’ |
| Providing a varied curriculum | ||
| Agenda matching | ||
| Able to observe progress over time | ||
| F | Particular challenges in delivering gFNP | Providing antenatal care and infant health checks in a group context |
| Encouraging self-care | ||
| G | Training and staffing issues | Initial preparation and training |
| Supervision | ||
| Staff absence for sickness or leave | ||
| H | Suggestions about future sustainability | Improve recruitment pathway and links with community midwives |
| Incorporate within FNP provision | ||
| Amend group size and timing | ||
Results
A: aspects of Family Nurse Partnership that worked well for service users
Family nurse qualities
Once participants had been recruited into the study and had been informed by post which arm of the trial they had been randomised to, those in the intervention arm were contacted by a FN, given a brief outline of the programme and invited to attend their first group session. This first contact was the beginning of an important relationship between the participant and the gFNP team, which has emerged as a key theme in terms of motivation for continued attendance at group sessions. Across the sites, participants reported on the friendliness, approachability and availability of the FNs.
They are really helpful . . . they are not the type of people to make you feel shy but they were so lovely they made you feel confident.
P15
I really liked them, felt very comfortable talking to them and they always made you feel welcomed.
P28
Oh [FN] was so lovely and you could just send a message . . . even when she was on holiday and I was still texting . . .
P24
I just want to thank them [the FNs] and thank them for the opportunity because obviously I got a lot out of it and I think it was brilliant.
P29
They were very nice staff. Very friendly, helpful, fun!
P32
In order to deliver a psychoeducational, theory-based programme to young women who had low or no educational qualifications, information needed to be presented in an informative rather than a didactic manner. Therefore, a mixed-methods approach was taken by the FNs, involving some standard presentation of material but supplemented by interactive techniques (e.g. a ‘hands-on’ activity using a scaling technique to ascertain participants’ knowledge of sugar and salt content in processed baby foods). Appreciation was expressed regarding the FNs checking at the end of a session that everyone had understood the topics that had been presented that day. Participants also liked being given handouts from the session to take home and keep.
. . . if you’re learning something new, if there’s a practical task to go with it as well that’s better, because I know that some people learn better by listening, watching or doing . . . Once we had to stand up from one to five, or whatever the cards said, just to see how much sugar or salt was in certain foods, or what we thought . . . So little like tasks like that open your eyes in a different way.
P07
. . . we do loads of different things . . . writing down on pieces of cardboard that they’ve cut out into love hearts what we love about us baby, we once did like a little chain where she gave us two little strips of paper and entwined them with each other, and everything we thought of that were nice about us baby we would fold a piece over which made like a long chain thing, so it was nice.
P08
There were quite different topics – three or four different topics each group . . . we always got like paper explaining everything, that were good to take home and put them in a folder.
P04
A particular strategy that can improve engagement with the programme is known as ‘agenda matching’, whereby if participants would like to discuss a topic that is programme related but perhaps not due to be delivered at that point, FNs adapt the session to address the issue as well answering other relevant questions. In interviews a number of participants mentioned this flexible approach, appreciating that FNs listened to their immediate concerns rather than sticking rigidly to the schedule for that day.
There were days they didn’t do topics as such, they just asked if anybody wanted to talk about anything in particular . . . we could always ask, or do a topic on it.
P04
They were good [FNs] doing stuff that we wanted to. We didn’t always know what we were going to do; they’d just change if we wanted to talk about something else.
P25
The availability of the FNs for support and advice, both inside and outside the group, was important to participants; they talked about knowing that they could telephone or text for advice if they were at home, or that, if there was a private problem at a gFNP session, it could be discussed away from the group in a side room or later at home.
I know if there’s owt up, I can phone them, I know I can talk to them . . . I trust them . . .
P02
What I really appreciated about them were they give you an option, either you can ask in front of everyone, or you can go in a private room for privacy – that’s really good, I appreciate that.
P10
I knew full well if I did have a problem she’d come and see me which she did once when I was actually feeling quite down . . . if I ever needed her to come and see me she would.
P21
Group structure and size
In addition to appreciating the qualities of the FNs, a second popular theme to emerge from the interviews was related to the way in which the group was structured. Participants liked the fact that they were all at a similar stage of pregnancy and going through a similar experience, as well as being close in age. Being a first-time mother was important in terms of group membership and this was an opinion expressed across sites; there was a feeling of all being in the ‘same boat’, of not knowing what to expect or having any idea of how to look after a baby. Although there were some participants who already had children, this was the exception rather than the rule, and several groups were composed of first-time mothers only.
It were nice to be able to talk to somebody that were going through it at the same time as you, because there’s nowt worse than being pregnant and saying to somebody, ‘I’m having this pain’ or whatever and they’ve already been pregnant like ten year ago or summat, so . . . being in group, people roughly around the same stage, it were nice to be able to compare.
P04
It was nice as well because we was all first time mums so we was all in the same boat as we didn’t know what to expect. So we all really relied on each other for asking for help and stuff like that.
P18
Clients also stated that they preferred a smaller group with approximately six or seven participants rather than larger groups because everyone could get to know each other, which might not happen with higher numbers. Some participants also stated that during the pregnancy stage they would have liked to attend gFNP once per week, but after giving birth, once per fortnight was enough as they were busy taking care of their new baby. Some also felt that 2 hours for a group session was not long enough, as they would only just get through the topics and activities in that time before they had to go home.
I think it would be nice if during the pregnancy stage to have it like once a week, I think more so because it’s more interesting – I think when baby comes along obviously it’s a lot busier time, so once a fortnight’s fine, but I think during the pregnancy stage it’s quite nice to- especially with the first one, I think you’re kind of lonely as it is, so it is kind of nice, to kind of – I think I looked forward to it every fortnight – like I said, I hardly missed a session, so yeah I think . . .
P06
I just wish it lasted longer, 2 hours wasn’t really long enough by the time we have spoken about topics and activities sometimes when people got their taxis they would leave at 2.30/3.00 so too short . . .
P15
Yeah good, there were only six or seven of us. We all clicked and I think the group we had was a good group of girls.
P27
Group interactions
Attending the group sessions on a regular basis afforded participants the opportunity to make friends and establish new social networks. However, group interactions initially involved everyone agreeing to work together to create a ‘safe’ space where the sharing of ideas was possible, respecting each other’s privacy, confidentiality and different approaches to the ideas that were discussed. Once the ‘safe container’ had been established with skilful facilitation by the FNs, participants’ confidence grew and they reported that they were able to exchange ideas and views that might not always coincide but resulted in respectful disagreement.
At first we was all a bit guarded . . . and we knew that we’d all have different views on things . . . but even when a subject would come up, and someone would say something, if someone didn’t agree with it, we’d still like put our point across, but in like a positive way, ‘Like did you look at it from this side?’ and then you know it would open their eyes . . . in the beginning they [FNs] say, ‘If something’s said here in class, we don’t want to hear it outside these walls’ and things like that. So I think from the beginning everybody had that respect there.
P07
I was really worried about everything. I didn’t know how I was going to care for him. The group kind of helped in the sense that everyone kind of inputted different ideas.
P13
Friendships formed and peer learning took place within the group and could extend beyond the sessions, with participants setting up their own virtual groups to enable them to keep in touch with each other and support each other outside sessions.
It was good because we’re all friends. We all talk on Facebook [Facebook, Inc., Menlo Park, CA, USA] and everything.
P26
The ‘hands-on’ activities such as ‘hand painting’ were popular, and the technique of ‘role play’ further encouraged participation and interaction within the group.
. . . since he’s been born we’ve done like hand painting, and pictures and stuff like that – that’s been really good. We’ve done quite a few things – like when I were pregnant, like obviously it were more for me and for other girls, but since we’ve had babies, it’s been more for them . . . it’s been good.
P04
. . . we spoke about the emotional sides a lot . . . we did a lot of role-play and group work so it was quite hands-on. We were comfortable with expressing our own opinions in the group.
P12
Practical factors
At interview participants were asked about a number of practical factors associated with attending gFNP sessions, such as the suitability of the venue, if it was easy to travel to and the time of day the sessions ran. Some sites based their groups in children’s centres that were not always centrally located, and others opted for town centre locations (e.g. the local library), anticipating that these locations might be more convenient for travel. In some instances the venues changed due to unforeseen circumstances, or because they were found to be unsuitable once the sessions were under way. Money for travel was available to encourage attendance, and participants could submit taxi receipts or bus tickets to be reimbursed.
I couldn’t get into town, ‘cause they changed the destination – it was quite far – but they changed it and now I’ve been getting taxis since I had her, so they reimburse you anyway, so I didn’t really find it a problem – I think if I’d had to pay it myself, I probably wouldn’t go.
P02
It was a long way and I don’t know anyone so if X [partner] is working then I couldn’t. I don’t know anyone to take me.
P17
On arrival fresh fruit and healthy snacks were routinely provided by the FNs for group participants, not only to make the group more welcoming, but also to highlight messages given during the sessions about healthy eating, and this was appreciated.
. . . from day one, they were just so welcoming, and every week they’d bring us biscuits and fruit boxes, and make us drinks all the time, so they’ve always been very welcoming, so you just feel as soon as you walk in you just feel straight at home.
P08
B: what are barriers to engaging with the programme for service users?
Effective client engagement is a core concept in gFNP, a key aspect of this is regular attendance at the group sessions. A number of clients attended regularly (although some less frequently than others), whereas several clients appeared to disengage from the programme either stopping suddenly or tailing off their attendance gradually. When clients were asked at interview about any aspects of the group that they found challenging, a variety of reasons were given ranging from their relationship with the FNs and other clients, specific interactions within the group, the perception of it being ‘like school’, the changing structure of the group (when two groups merged), to practical difficulties encountered (such as time of day or transport problems) when attending sessions.
Family nurse qualities
Although the majority of those interviewed for the qualitative study were enthusiastic about their engagement with gFNP, there were some participants who were less positive about their experience of attending the sessions, their relationship with the FNs and the other young women at gFNP. A participant at one site had been expecting a more interactive experience including standard antenatal checks and being supported to carry out self-care checks; when none of these activities took place she stated it was just like attending a lecture.
They need to be more interactive. For example all the checks that they say they’re going to do. You know with the baby’s heartbeat, stuff like that you really want to hear. All of that just didn’t happen. So it felt like you were going to a little lecture. You sit down and they just talk, you take notes and that’s it.
P31
At another site, although midwifery checks were being carried out on a regular basis at group sessions, one participant also continued to receive routine antenatal care from her community midwife, and eventually stopped attending gFNP. She remarked that she regarded the FNs as ‘teachers’ rather than a nurse and a midwife.
I just felt like it were just like a college course . . . the way that they were teaching it and stuff . . . I didn’t feel comfortable in telling them, because I didn’t feel like they were midwives, I felt like they were just teachers – so that’s another reason I stopped going as well . . . I didn’t feel like I had that midwife care or that midwife relationship that you should have had.
P05
Added to this, the participant regarded reminder texts and catch-up telephone calls from the FNs as ‘harassment’, unlike most other participants who perceived this type of contact as supportive and caring; this highlights the delicate approach that may be needed to follow up non-attenders, making sure that they feel able to explain any issues that they have with the programme.
. . . they harassed you with messages constantly, like if you didn’t come to a group or whatever . . .
P05
Group structure and size
Low attendance at early sessions, influenced by the fact that almost all groups started with a smaller than optimal number, was reported as a deterrent to some clients in terms of continuing to attend. One participant explained that she tapered off her attendance because membership was very low; she had anticipated attending a group with young mothers her own age, where bonding would take place and social networks could be built up outside the sessions. However, this did not happen in one of the sites, where groups failed to run beyond the first few sessions.
I would want to go with people my age group and be able to talk and communicate even when you’re not at group . . . the group got cancelled. Before that it’d be just two people turn up so we didn’t do anything. So that’s why as well I didn’t go as much.
P31
. . . there should be more mums in the group [there were] just two! At the beginning it was three but then one of them just stopped.
P32
At another site where programme delivery stopped because of low numbers, one client understood why this had happened and indicated that she would have gone back if the sessions had started up again.
. . . they discontinued the sessions due to the amount of people in the sessions. They didn’t feel that they could move on with the group because it was only basically two of us . . . [however] If they contacted me and they wanted to see us then I’d gladly go.
P12
Group numbers were based on acceptance of the offer of the programme. However, clients might be considered passive accepters, which can be an easier option than explaining to an enthusiastic FN that the programme does not sound acceptable. This can have an impact both for that client, who may well then not be offered other services, and for the eventual group, which will then be smaller than expected. One participant initially agreed and was randomised to receive gFNP, but never attended any sessions because she felt tired and lacked the motivation to go.
Because I just didn’t really have the time . . . because I was tired.
P30
In one site two groups had merged to increase numbers and thus allow for programme delivery to continue, but the merger itself was problematic for one participant. She had built up her confidence attending one group and getting to know other participants, but when her group merged she was reluctant to repeat the exercise with new people.
It were just the merge that did it for me really; if there wasn’t that merge, I’d still be going . . . cause they’re all new faces, and the babies are that bit older, and you just think you don’t know anyone there, so I were a bit hesitant, and you do feel a bit uncomfortable . . . I’m not a confident person as it is.
P10
The habits or views of other clients could be a barrier, even though FNs worked to accommodate diverse opinions and practices. At one site, a client attended only two sessions before stopping because of the smoking habits of other group members.
. . . the mums-to-be basically annoyed me . . . they said, ‘I don’t see why I should stop smoking, just ‘cause I’m pregnant!’ . . . so I just stopped going, and I told them I didn’t want to go any more.
P03
Group interactions
Although some groups worked very well, and group members respected each other’s points of view, took turns in having their say and encouraged those who were quieter, this was not always the case. It could be difficult for other participants if some group members dominated the discussions and made it difficult for others to have their say. One participant explained that this was the reason she stopped attending. However, it was also noted that the FNs were able to manage this type of disruption, and this was appreciated.
I think it worked quite well, there were quite a few girls that kind of spoke out and made it interesting, and had a laugh – that kind of thing. In the beginning I was quite quiet, but then I just said what I thought.
P06
We knew that we’d all have different views on things, and things like that, but even when a subject would come up, and someone would say something, if someone didn’t agree with it, we’d still like put our point across, but in like a positive way.
P07
We all got on though we had disagreements, but we would be nice about it . . . I would be honest if I had something to say I would say it, I would tell them in a good way, I would not be rude.
P15
. . . there were two people that were quite loud, and nobody really got a look-in to any decisions . . . that’s probably why I didn’t go back . . . You just don’t feel comfortable when somebody’s really loud and you’re not even getting any time to say anything- there’s no point being there if you can’t talk.
P01
There was one girl who always had something to say about everything and they were really good at sorting it out . . . saying ‘OK let’s move on now and if you need any more information talk to me after’.
P22
Although most of those interviewed enjoyed learning about new topics related to their pregnancy, appreciated the interactive nature of the group sessions and liked having folders for storing the sheets of information they were given to accompany each session, this was not the case for everyone. Some participants regarded learning within the group negatively, comparing it to being at ‘college’ and expressing a dislike of filling in paperwork to keep in a folder.
. . . the materials and stuff that they were using, it was all like paper; it wasn’t something that I were interested in. I just felt like it were just like a college course, type of thing.
P05
Practical factors
Practical factors such as location, time of day and the venue itself came into the equation when exploring individual participants’ views about their reasons for low attendance or stopping attendance altogether. Distance from the venue was a deterrent, especially if the venue had changed and travelling to the new one involved a longer journey. The timing of the sessions also affected some participants, with afternoon sessions being deemed more acceptable than those in the early mornings in some cases.
I went up until I were about 36 week pregnant and then I couldn’t go any more . . . they changed locations, and it were just a bit harder to get to from that, so that’s why I stopped going.
P01
It was a long way and I don’t know anyone so if X [partner] is working then I couldn’t. I don’t know anyone to take me.
P18
. . . when I got heavily pregnant and I would get tired group would start from 10 or 11 so that meant waking up really early to get there. After I had [baby] it was hard getting there early, very hard, so they had to change the times, and even then getting on the bus, it was just hard.
P23
The provision of taxis was offered at several sites in order to encourage attendance, and although this did prove successful for some it was not the case for everyone at one particular site. One participant stated that she did not feel particularly safe in a taxi on her own, and another mentioned that the drivers would complain about various aspects of providing the service during the journey; however, both views suggest a problem with that particular taxi company and its employees, not officially linked to gFNP, rather than with the mode of transport. In general, providing assistance with transport to group sessions was perceived positively.
It was quite far, but they changed it and now I’ve been getting taxis since I had her.
P02
. . . I’d ring a taxi, or sometimes text class [group] to ring me a taxi, so one way or another I’d get there.
P04
. . . they paid for us to take taxis if we couldn’t get there. So no, it were easy [to get to sessions].
P07
For me getting the taxis by myself felt a bit iffy being in the car with a fella.
P27
. . . it wasn’t that they didn’t turn up but sometimes when we got in the taxis they complained because they used to pick up me and D as well because we got a taxi together. They used to complain that we shouldn’t get a cab because we didn’t have a tab? And one time the group had to be cancelled because we couldn’t get any taxis for some people and not for some.
P28
There was criticism of the venue at a couple of sites; one participant who already had a child commented that the venue was not suitable for young children and that it had probably been booked with the newly pregnant first-time mums in mind. There was also a suggestion that gFNP should have their own centres so that the sessions could carry on longer instead of having to vacate a room when the allocated session time was up.
. . . it was just such a non-child environment where they had it . . . it were just probably for people who were just pregnant at that time . . .
P01
They should probably have their own centre because where we went it was a children’s centre, so we were using different rooms and we were running on their time, and sometimes it’s ‘oh it’s time to go now’. So if they had their own building or something like that then it could be longer, because I did enjoy it, sometimes I was like ‘oh I don’t want to go yet, we’re still talking’.
P23
C: what are the likely impacts of attending Group Family Nurse Partnership?
Fewer mental health problems
A number of participants reported feeling less lonely as a result of attending gFNP and, because of the companionship found there, thought that they were less depressed. Some went further, describing the group members as another family and speculating that they might not have coped had they not attended; there was a feeling that going to gFNP sessions was something to look forward to and that it kept life ‘normal’. One participant stated that she thought she would have had a breakdown without the support from the FNs, especially when she was in hospital just after she had given birth. In contrast, she felt that she had been given no help by hospital staff. Another participant reported that she felt confident that if she was feeling ‘down’ the FNs would support her.
. . . I don’t know how I would have coped without going to group . . . but I feel like it has made a lot of difference, and it’s helped a lot.
P11
Group is like another family for me.
P14
It’s so helpful when I was in the hospital, I didn’t really feel like I had any help whatsoever and I can just remember sitting there thinking if it wasn’t for the FNs I thought I probably would have had a breakdown . . . they came to see me as soon as the baby was born. Definitely reassuring.
P16
I knew full well if I did have a problem she would come and see me which she did once when I was actually feeling quite down . . . there was a point when [the baby] was constantly crying and I just didn’t know what to do . . . if I ever needed her to come and see me she would.
P21
Learn about child development
Learning about infant development struck a chord with several of those who were interviewed, particularly the way a baby’s brain develops and how their own actions might influence that development. Bonding with their babies, emotional states and babies’ well-being were all mentioned as topics that participants remembered and had stood out as activities they not only found useful but also enjoyed.
. . . they told us about the neurons, like brainwaves and stuff like that, and the way they [babies] learn . . . So even from right at the beginning, talking about when you talk to your baby, and you repeat stuff, and the more you repeat it, the more they learn it . . .
P07
. . . one of main ones [topics that influence behaviour] that stuck in my head is how they pick up on your emotions, especially when you’re pregnant . . . so if I am feeling a bit stressed, or a bit moody I try not to do it around him, or if we’re having a bit of a bicker you know, over something stupid, I’m like, ‘No! Shhh!’.
P10
. . . a lot of things really, like the tuning in and tuning out, and the baby states – the different states – that were really useful . . .
P11
I think it’s more about gentle parenting rather than being harsh on baby. We have always tried this as well as trying to think from baby’s perspective.
P14
They showed us how to bond with the babies. We never really did anything outrageous that I can remember, probably just hand and feet paintings, which were good . . . apart from that it was just talking about the baby’s well-being really.
P23
Develop parenting skills
The practical advice about looking after their babies on a day-to-day basis was highly valued, and several participants explained that they had not known how to look after a baby before going to gFNP sessions. Memorable topics mentioned frequently in interviews were bathing, nappy changing and weaning. Some participants had anticipated that the weaning stage was likely to be problematic, but the support given by the FNs gave them confidence to blend different foods and take a healthier approach rather than using only commercially available baby food in jars.
. . . we’d covered everything, from washing us baby, to dressing them, changing their nappy, everything . . . it has helped a lot, because I didn’t know how to bath a baby, a new born baby, and like I didn’t know a lot of things, they gave me the knowledge.
P08
I have learnt a lot of stuff, there are a lot of things that I’ve picked up . . . weaning them, and buying soft foods that have not got sugar in it . . . things that you don’t really think of.
P06
It was very useful . . . stage one and stage two [weaning] . . . when she was so tiny I don’t think she could take food down properly so the weaning tips did help, putting it in jars and blending more so she was eating it fine.
P15
Being given information about the benefits of breastfeeding as well practical advice encouraged some participants to breastfeed their babies, even though they had not considered it as an option before attending the programme.
I was more motivated to breastfeed her after the group.
P14
The one I found most helpful was probably about breastfeeding, showing us how to introduce it and everything . . . I felt more confident putting it into action when she arrived.
P16
Extend social networks and support
Participants made friends with other gFNP clients and particularly enjoyed this aspect of the programme, which allowed them to extend their social networks while learning about their babies and being given practical support by the FNs. In addition to meeting up in gFNP sessions, they reported attending activities such as baby gym sessions together and going to each other’s houses. After the programme had finished many participants reported that they stayed in regular contact with each other either at events or in virtual groups using Facebook and WhatsApp. Participants felt that bonds were strengthened between them because they went through the experience of pregnancy and childbirth together. In one instance, one participant who was not working had offered social support in the form of babysitting to a friend from gFNP who had gone back to work.
I’ve made friends with . . . people that were in my group . . . we went swimming last week with all the kids.
P09
We all get on and we still talk daily on WhatsApp group, so we all talk to each other every day. We message each other see how we are all doing, send videos of the babies.
P16
I found the group extremely useful; it was good so I went to them. It was good because I made friends.
P19
So all of our group we set up a little like Facebook message so that we all talk to each other on that.
P20
We met up with each other for Christmas at one girl’s house and we had a bit of a Christmas party. It was really good fun.
P22
D: the experience of providing support in a group context
Identify evidence of peer learning and support
The programme goals, underpinning theories and themes are the same as those delivered within FNP, but an additional aim of delivering FNP in a group context is to facilitate peer learning and the development of friendships within the group. The idea of peer learning was underlined by one FN who explained that sharing ideas within the group and promoting conversations around specific topics (e.g. weaning) can have a wider impact than perhaps a one-to-one conversation between a FN and a client.
. . . if you are talking about it [weaning/immunisations] in a group and sharing ideas you get a much wider impact, and it’s not just the family nurse saying ‘You shouldn’t wean until . . .’ Peer contact/aspect of learning, the group allows for that to happen, so the group context really promotes these conversations much better than a one to one does.
FN01
Across sites FNs observed examples of peer learning leading to behaviour change. For example, a new mother who slept with her baby, changed so that after group discussion she told her group that the baby was now sleeping in her own cot due to the advice she had received from them. Another instance cited was at a session on weaning where gFNP clients took part in a food testing activity and gave each other advice based on individual experiences.
They have definitely changed behaviour through group discussion . . . one girl who slept with baby, was on medication and drank, but eventually she talked about it and then other girls would say ‘Well I have done this . . .’ then she announced ‘the little one is in her own cot, I don’t bring her into my bed . . . I have only done it through you guys, through listening to group discussion’.
FN11
We did a session on where they tested food, blindfolded, and X [client] came into her own there with the baby led weaning, and they just took advice from each other. One of them would say ‘Well I have tried this, this worked’ . . . or ‘I tried that and it didn’t work’ so they were very open to sharing.
FN08
Noting different needs also encouraged empathy among group members, for example with a client who had learning difficulties or if a client was reluctant to take part in activities designed to help prepare for handling a new baby.
. . . there was one person in group in pregnancy that was very quiet with some learning difficulties, you could see she was quite embarrassed by contributing but what was interesting was how the rest of the group protected her and how they included her.
FN10
One client who we were quite worried about, when we did PIPE [role play activities designed to promote parent–child interaction] in pregnancy she wouldn’t hold the doll . . . and she was one of the last to give birth. It really helped, the other mums encouraging her to hold their babies helped her confidence, before she had her baby she wouldn’t necessarily have any experience and so she found that really useful and she ended up handling her baby really well.
FN07
Able to observe social interactions
There were numerous comments across sites about the emotional support that participants gave each other as the group dynamic strengthened. For example, there was support for a participant who was extremely anxious as she had previously had a miscarriage and was afraid she would not be able to hear the fetal heartbeat during the antenatal self-care checks. Other members of the group gathered round and held her hand to reassure her while this was being done. At another site the group supported an individual experiencing mental health issues who felt that she was not being a ‘good mother’ by pointing out how well her baby was doing and boosting her self-esteem. There were also more general comments about the practical support that group members gave each other such as picking each other up in their cars so that they could attend the group. This could contribute to the development of ‘bridging’ social capital in that group members had varying cultural and educational backgrounds.
There was one girl who was very, very nervous listening to the fetal heart, at the beginning of the midwifery care, but the group members all supported her, all got round and held her hand. She was just scared of not being able to hear the fetal heart having had a miscarriage previously. The group members all got round very quickly that is one of the ways we found that they were gelling really well, the ways they were supporting her.
FN05
We had one client with mental health issues . . . The other girls really well supported her. There were times when she felt like she wasn’t being a good mum and they were able to boost her self-esteem and say ‘Well actually, look how much she [the baby] has come on’.
FN04
We had an extremely mixed group educational achievements and culturally it was powerful for us because there were people in the group who would never ever mix socially and were very supportive of each other to the point of picking them up in their cars and bringing them to group and they are they are still in touch and on Facebook groups together, it’s amazing.
FN010
Facilitating groups gave the FNs the opportunity to observe how the babies interacted and developed socially by playing together. A FN who was not a regular gFNP facilitator, but who had stepped in to cover absence, commented afterwards to the regular group facilitator on her surprise about how well the babies played together and how interactive they were.
It was a joy to watch these babies interact together and we have one little one who always wanted to cuddle the other members . . . all she wanted to do was cuddle them and they just got used to that, they accepted that and that is how they coped. They just played together; shared things had each other’s food, they just got on together really well.
FN05
X was off and I asked another nurse to come along and she said ‘I can’t believe how well these babies are playing together, at the age they are at they should be playing alongside each other but they were more interactive’.
FN11
E: aspects of Group Family Nurse Partnership that worked well for the practitioners
Creating a ‘safe space’
In order for group members to have the confidence to raise any issues or concerns they might have, they need to be able to trust the group and the facilitators. To this end, at the beginning of the programme FNs try to create a ‘safe container’ by setting boundaries and laying down ground rules about confidentiality and information sharing. In this way group members are able to ask about sensitive issues with confidence and share what they understand about a topic, while making sense of new ideas that have been introduced in the session. High levels of client engagement within a group tend to go hand in hand with early development of a ‘safe container’ within that group.
I think it did give them confidence to try out new things within the group, and they knew they were safe.
FN04
I think that is part of getting your group dynamics right at the very beginning. If you have made that safe container and you have group rules, they know they are free to talk and you give them open questions they just go with it.
FN05
Providing a varied curriculum
Programme content, focusing on pregnancy and early parenthood, is based on a number of themes ranging from the development of maternal bonding and attachment-related concepts to consistency of care. Engaging clients in the programme is a skilful process especially where they have had poor school experiences. Thus, FNs adopted a mix of delivery methods to suit different learning styles; although there was some teaching and paperwork involved, there were also ‘hands-on’ activities to maintain interest and enjoyment. Informational leaflets are given out during sessions, to be kept and taken home, but there are also many creative activities which enable group members to actively engage with topics in a different way such as craft type activities, particularly useful to engage clients who have lower literacy levels or poor educational experiences.
The labour time line . . . all the sessions are interactive . . . and also the other one was the home safety, interactive materials are better than just . . . talking through materials.
FN04
We had to look at how we offered the programme not to re-invent but just how to offer it . . . we did a lot more crafty things because we found that worked and they loved it.
FN08
Agenda matching
Within the context of delivering the curriculum, a key aspect of gFNP is that the group facilitators listen and respond to issues raised by individual group members and at the same time deliver the programme content for that session; this is referred to as agenda matching. This is also something that is encouraged when delivering home-based FNP, but is more challenging when there are a number of agendas to be matched.
. . . we’ve always said to them if they have something they want to ask about a particular topic to let us know . . . They raised something about feeding so I said next week’s session is about feeding . . . but if you feel you need an answer today then we can make time for that at the end . . . we always had time for them at the end to ask us anything if they wanted to on their own.
FN02
. . . agenda matching, picking up on your audience essentially, so it is useful having a programme but being able/confident enough to move it slightly if that needs to happen as well.
FN06
It was hard at times and at times probably if a client needed something straight away that did interfere but what we tended to do was if I was managing the programme X [the other FN] would step in and we would manage it that way.
FN08
Able to observe progress over time
A particular advantage of being able to observe the impact of gFNP over time was to see the progress of individuals as they interacted in the group. For example, some women who were initially shy and lacking in confidence at the beginning of the programme were observed to become more confident over time and contribute more to discussions. FNs believed that as their self-esteem increased they became more sociable in successive sessions.
I supported her because she was really quiet, made her come out of her shell, kept asking her ‘what do you think?’ So she felt able to contribute . . . she was able to give them pointers on breastfeeding because her baby was born first and I think that boosted her self-esteem.
FN04
. . . there was one client in particular who was naturally a shy person to begin with, social services were involved with her, she has quite low self-esteem, she didn’t engage at the beginning of group . . . X took a lead, worked with her, hand held her to come and that girl’s journey has been incredible! I think being in the group setting and seeing the positive role models of the other parents had brought her on in her journey and she is a wonderful mummy now. Without her peer group she would still be isolated, she now sees the other girls socially as well as in group . . . social services closed the case a long time ago . . . So I think it has changed her life . . .
FN09
F: particular challenges in delivering Group Family Nurse Partnership
Providing antenatal care and infant health checks in a group context
A significant difference between FNP and gFNP is the provision of midwifery care as part of the offer. The strategy was that in the antenatal period routine antenatal care would take place before the group session, and during the session participants would be encouraged to engage in self-care such as testing their own urine and listening to the fetal heartbeat. These activities were overseen by the group FNMW who had responsibility for providing routine antenatal care, such as blood tests and record-keeping in line with national (NICE) guidance and local policies. After their babies were born the young women in the group were encouraged to participate in infancy checks such as weighing and measuring, overseen by the FN who is a trained health visitor.
However, the FNs who were also midwives needed to ensure that they were up to date with the current requirements for practising midwives, and needed ‘catch up’ training which added to the preparatory training time for providing the gFNP service. Some FNMWs had not practised in the area where they were working as FNs and as a consequence needed to become familiar with the record-keeping systems used for documenting antenatal services, and there was in some areas a delay before all relevant IT access could be arranged. The process of renotifying as practising midwives could also be slow. Several of the FNMWs who were interviewed for the study reported feeling that, although they received additional supervision from a supervisor of midwives, in addition to the gFNP supervisor, they experienced some stress and anxiety about whether or not they were providing excellent antenatal care according to the NICE guidelines62 in the group context.
. . . initially it took a long time for the group midwife to be back on the NMC [Nursing and Midwifery Council] register as a practising midwife, so we did ask the community midwives to take on that role for a short period of time, but I think they thought we were stepping on their toes.
FN04
My only concern is that when you do the midwifery care you are a midwife but you are not actually working in midwifery at this moment in time. Things change very quickly, policies change and if you are not doing that on a day to day basis it is very hard to get up to date . . .
FN05
At the study days with the other midwives throughout the country, we all felt there was so much pressure on us because we are not in practice as midwives, that is not our ‘bread and butter’ day to day work so we were having to really focus what is needed now . . . we are FN’s . . . It took us longer to do an antenatal check than it would if we were a midwife. Going back to midwifery after five years away from it was very hard.
FN09
A number of practical problems were encountered in the delivery of antenatal care. It was reported that there was sometimes insufficient time during the sessions to carry out the antenatal checks according to NICE guidelines,62 as well as trying to cover the topics and activities scheduled for that session. Carrying equipment such as the (examination) couches from where they were stored to the venue and setting them up was described as ‘hard work’. More specifically, and in order to comply with the guidelines, once blood tests had been carried out the samples and all relevant paperwork had to be taken to the local hospital for testing, adding to their administrative burden. The FNMWs also needed to familiarise themselves with hospital systems for updating records regarding the standard antenatal checks and some FNMWs had not practised in the area where they were working as FNs. As a consequence, they were initially unfamiliar with, or sometimes had poor access to, the record-keeping systems for documenting receipt of antenatal services.
When I had to do the NICE care towards the end of one group I had seven more check-ups to do and I said ‘if people can come half an hour early we’ll do it then, then some in the middle’. It was awful so chaotic . . . I had never worked in the town where we were doing it as a midwife. I was unfamiliar with all the paperwork it was an absolute nightmare . . . at the time I was trying to do all the midwifery stuff it felt overwhelming, that side of it. I don’t think I was prepared for that.
FN09
. . . I found it hard work, it’s learning the system at X hospital, it’s the extra stuff that comes with taking the bloods here . . . the fetching and carrying, it’s quite a lot of hard work, all the equipment to the group and back . . .
FN15
We bought couches, all sorts, and they are heavy and we didn’t have a venue where these things could be stored. If we were thinking about it again you would have to think carefully about where you would store things, where you would take bloods.
FN14
Encouraging self-care
An additional aspect of the midwifery care is that gFNP clients are encouraged to engage in self-care activities such as carrying out their own urine testing, monitoring their own blood pressure and listening to the fetal heartbeat. The idea behind these activities is that it encourages self-efficacy through ‘sharing their experiences and learning together as a route to self-awareness and knowledge’. 46 The FNs believed that this was a good approach, but reported that not all clients were enthusiastic about carrying out self-care and responses varied from site to site.
I think it’s really good . . . taking their own blood pressure, testing urine, etc., and for those that want to have the baby listened to while they are there, and those that don’t want to show their bellies can go outside or go into in to the (private) room. I think the ones that were there were all keen to be involved and OK about it.
FN03
. . . we wanted to do it; we were all set up, but I don’t know how well it did really work . . . they were reluctant to do it and they didn’t want to be palpating abdomens in front of other group members. They would go off and listen to their own baby but they didn’t want to do it in the group they would often come back and say ‘You’ll have to do it because I can’t’.
FN11
I think if the women were that way minded it would be fine, I just didn’t know, I tried to sell it but it just didn’t seem to be what this group of women did. I put everything out and they were able to but they weren’t really bothered about participating.
FN15
However, there was more enthusiastic participation during infancy in checking their baby’s development, which involved completing ‘Ages and Stages’ questionnaires, weighing and measuring.
. . . you couldn’t stop them from weighing the babies, and filling out the ASQs [Ages and Stages Questionnaires] . . . No-one would not do it. They all wanted to know about each other, very much a sharing process. They would have their own discussions such as ‘Is anybody teething here or walking yet?’ So they would almost check in with themselves about different developments and have their own discussions.
FN06
Worked brilliantly, weighed them and quite happy to fill out ASQs [Ages and Stages Questionnaires] and we always started with a round of what is new with your baby.
FN11
G: training and staffing issues
Initial preparation and training
When asked about how well prepared they felt by their training, most FNs reported feeling well prepared, although several had worked with group-based programmes previously and felt that this contributed to being confident about delivering gFNP. One noted that, although the training prepared her for working with a group, it did not prepare her for dealing with difficult situations that arose within the group: only experience could do that. Another FN reported that, although the training was very good, she had learnt more by working alongside a FN colleague and seeing how she dealt with certain situations. Nevertheless, those who had had previous training outside FNP on facilitating group work commented that the training for gFNP was much better.
Previously I did parent education and when I think about it the training was really poor, you were just expected to do it . . . the training here is really good and working with another colleague I learnt so much from X, how she handles certain things. I think it was really, really positive.
FN07
I think the training we had was good, though it can only prepare you to a certain extent as you can’t cover every scenario in training . . . there are always going to be situations where something is said and you are floored by it but that’s experience about how you deal with it . . . what this training did prepare us for was how to deal with it in a group.
FN10
I was involved in group work for teenage parents. When I look back now I think I just expected them to sit there and accept the information I was going to give them. I have learnt loads and it has definitely been transferable. When I do one to one and have parents and grandparents I transfer those communication skills.
FN11
Supervision
It was noted that the supervision for FNs delivering gFNP would benefit from taking a different approach to supervision for one-to-one FNP. Specifically, rather than the regular individual supervision (i.e. the supervisor and the FN), which is provided for all FNs, and FNP team supervision, everyone involved in delivering gFNP could attend at the same time so that they would be thinking about the group as a whole, and this would ideally take place fortnightly.
It didn’t feel right to use individual supervision; even the documentation didn’t seem to fit for gFNP. We did do a fair bit of work looking at frequency of supervision . . . how did we document it – stuff like that . . . it looked like once a fortnight, both nurses together . . . so it would be all of us quite often thinking about the group as a whole.
FN14
One particular issue was to ensure that all safeguarding responsibilities were well covered. Unlike in one-to-one FNP, which takes place in a client’s home and affords FNs ample opportunity to assess potentially high-risk situations, the strategy for delivering gFNP does not routinely include home visits. Some FNs remarked that one potential disadvantage of gFNP, compared with FNP, was having less knowledge of clients’ circumstances outside the group. Supervision for the gFNP work was designed to address this difference, discussing the extent to which FNs knew about the individual circumstances of clients, so that home visits could be made as required in addition to the group sessions.
The tricky thing for us in gFNP is that you don’t know the clients in the same depth that you know your individual clients . . . in order to safeguard children . . . whereas in group FNP you didn’t have that depth of knowledge.
FN14
We also dealt with some safeguarding in group. We have got round that, but initially it didn’t feel as safe as we didn’t know the clients quite as well because you were only meeting them in a group, it ended up there were more home visits because the nurses didn’t feel safe.
FN13
Staff absence for sickness or leave
The FNs delivering gFNP had received additional training, but this was not available to all team members, usually only to the two FNS who were to be providing the gFNP programme. Nevertheless, staff sickness and leave cover had to be managed and this was approached in a variety of ways.
It has been problematic, I had one nurse who went off sick . . . then one of the nurses left because she got another job . . . so it was a nightmare, I had stepped in to cover one nurse and now there was 6 months before the programme ends . . .
FN04
There were fewest staffing problems if FN supervisors and FNs who were not part of the team delivering the programme had been able to attend the training. They were able to provide cover when needed although they would not be so familiar to the clients. If this training had not been possible then FNs who were part of the FNP team but had not attended group training came in as replacements. Whether or not they had training, they could be perceived as ‘outsiders’ by the clients and it was noted that clients tended to direct their questions to the regular facilitator rather than the temporary replacement. However, it was emphasised that the temporary cover should be by a nurse with FNP training rather than a non-FNP professional because of the FNP ethos and the ‘safe container’ aspect, considered crucial to developing relationships within the group. In an instance when a children’s centre worker had been invited to contribute to the group on a specific topic the ‘safe container’ aspect had been missing from the session and there was the view that there had been less depth of interaction between group members.
. . . what’s important is the basis of this is the relationship, I felt that they felt very safe and secure with us and we did introduce other FNs to cover holiday and they were absolutely fine with that . . . There was one session where we used a children’s centre worker and she did something around language and the session was fine but there wasn’t that same level, that depth of interaction whereas with the FN I didn’t feel that. It felt like a safe container with the FN.
FN10
I liked the fact that there were two FNs because if one [of those trained to deliver group] is not here you still have the FN training and the FN ethos . . . plus they could prepare together, deliver together and they could look back and reflect together.
FN14
H: suggestions about future sustainability
Improve recruitment pathway and links with community midwives
There were mixed views about improving the client recruitment pathway, and linked to this involving community midwives either in the recruitment process or in delivering midwifery care within the programme. Some held the view that FNs should work more closely with community midwifery as they were up to date with all the local procedures and pathways in the hospital system. On the other hand, even if community midwives were more supportive of the programme (either one-to-one or gFNP), the gFNP teams needed their own access to client records so that they could be recruited directly.
I think you do need a community midwife as they have all the updated pathways to get somewhere.
FN03
. . . we need to get midwives on board but we know that is impossible either for one to one or group. I think it is just getting the clients yourself . . . Better for us to have access to the records so we can approach them so you know what you are telling them and they get a picture straight away of what is going to happen.
FN05
In contrast, some FNs thought that the midwifery component of gFNP should be removed altogether from the programme because clients did not feel that they were getting ‘proper care’ unless it was at the hospital, meaning that the antenatal care was being provided twice, making the cost of delivery high. One suggestion for an alternative way of working was that a community midwife could come to part of the session to work alongside a FNMW. Not only would they instil confidence in the clients, but they would also have good access to all the necessary documentation and databases for recording women’s progress. It would also mean that FNP teams without a FN who had notified their intention to practise as a midwife could offer gFNP.
I don’t think it worked well, I think they felt safe going to the hospital and having their appointments at the hospital. They felt as though they were getting ‘proper care’ rather than a side room, or part of the room where everyone else was. They had someone who had been introduced to them as the midwife . . . so it was a bit hard for them to get their heads around the dual role of family nurse/midwife. We found a lot of our clients continued seeing their midwife at the hospital anyway, in fact nearly all of them did.
FN01
Undertaking competence based learning for the FN/Midwife was extensive and required a significant amount of time and commitment I would therefore suggest that a currently practising/case loading midwife would have the requisite skills available. It may be beneficial to have FN/Midwife alongside the midwife or include the midwife in elements of FNP learning. A midwife based within the maternity unit would also have access to booking information, medical/maternity records which may support delivery of maternity care element.
FN16
On the other hand, FNs also stated that they would rather work with other FNs as they are familiar with the programme, and more specifically with the motivational interviewing technique as a way of communicating with clients. Giving community midwives an element of FNP training may not be enough to satisfy the FNs’ requirement of working with someone who can deliver the same ethos as them.
I think two FNs work really well; we know the programme, the materials and the resources. We’ve got the communication skills, it’s very difficult working with other professionals because they don’t communicate the way we do and you see the client’s resistance and being disengaged. So definitely the two FNs . . .
FN11
Incorporate within Family Nurse Partnership provision
There were suggestions that offering gFNP as an alternative (or in addition) to FNP might reduce the isolation of some of the one-to-one clients and, additionally, if the group sessions were held in children’s centres the isolated client might be encouraged to engage with other activities at the children’s centre. This of course would mean that eligibility for gFNP would expand to include women who were eligible for FNP (i.e. first-time mothers aged < 20 years, who are currently not eligible for the programme). This might be beneficial as it would also increase the pool of potential participants, meaning that acceptable group sizes could be achieved.
They [group members] probably go to all the children’s centres sessions and they are quite happy socialising with other people . . . some of the clients we see on an individual basis who are quite isolated . . . if they were in a group, then at least it might take away social isolation . . . if you see them in the home all of the time some of them are quite reluctant to engage with the children’s centres . . . I am thinking are we doing a dis-service to them because we take everything to them.
FN04
I think that people who are isolated socially . . . a period of one to one would help them to build their confidence . . . then try and ease them into a children’s centre, is the first step, get the outreach workers to come out with them, get them familiar take it step by step, don’t go full on to group, much better to ease them in. to get to grips with being a parent and then introduce them into the group, that would work.
FN01
Amend group size and timing
In development work it was initially expected that groups would be ideally 12 participants, plus theoretically all of their partners – although, in practice, partner attendance is low. Given that not all group members attend every session, and that some clients bring their partners, FNs at every site suggested that an ideal number for a group was between six and eight clients. This reflected closely what clients had reported as an optimally sized group. The FNs suggested that this number enabled all members to contribute and to be able to raise issues or ask questions, and if some of them brought partners the group would still be a manageable size. However, if there were too few participants, for example under five, the group dynamic would fail as there would not be enough variety of input.
I think a group needs to be six to eight to start with plus any partners. Then if you do have any that drop out or miscarry or move areas then you still have a group that can come.
FN05
I think seven is a good number, because not everybody comes every week. If you go with five and people don’t come it’s too small so five is perfect. So if you have a group of seven you usually get five which is perfect.
FN09
I would say six to promote useful discussion anything less particularly if you only have two couples it can be quite tricky if they are of like minds. I think six to eight probably is a good size.
FN14
Discussion
Despite the enthusiasm and many positive comments about the programme, attendance varied across groups and sites (see Table 43). Some clients managed to attend almost all sessions; others could be described as regular but not perhaps frequent attenders, whereas others only stayed in the programme during their pregnancy. Attendance at group can be perceived as an indicator of the programme’s acceptability. Although it is anticipated that clients are unlikely to attend every group session in the programme due to illness or some other unexpected event, it is reasonable to expect a degree of commitment to their group and the programme, demonstrated by regular attendance. Irregular attendance can put the group dynamic at risk as a reasonable number of participants is required for fruitful discussion, which is an integral part of gFNP. This is clear from the extent to which only one of the 16 groups that were initiated was able to maintain delivery of the programme through to its full 44 sessions; others terminated the programme as numbers dwindled to only one or two clients, with this taking place in pregnancy in some cases. Group size appears then to be the main issue that has emerged from an examination of delivering gFNP for the trial, as the qualitative interviews indicate substantial acceptability of the programme content and mode of delivery from clients, and substantial satisfaction in delivering the programme from the professionals. The location of the sessions and ease of travel is also a likely factor influencing attendance.
Consistent with previous findings,57,67 participants expressed enthusiasm for the way the group was structured in that they were close to each other in age, stage of pregnancy, and later the infancy period. This of course presents the first dilemma: the more defined the eligibility criteria are to ensure comparability of the clients, the less likely it is that an appropriate number can be recruited in a short space of time so that their gestation periods are similar.
The second issue is that the programme is delivered to a group. Professionals such as midwives have suggested that many women, and especially young women, are unlikely to find group support acceptable. 86 Some of the participants in this trial expressed reservations about attending the group because it was a different experience and there was mention of being ‘guarded’ about what was said. However, early on in the programme, while the group was forming and as clients started to attend sessions, FNs introduced the notion of a safe space where the group members could feel free to discuss issues within the group. The importance of privacy was emphasised, keeping what was discussed in the group session within the group and respecting the opinions of others, even if they differed from their own. This development of a safe container allowed participants to feel confident in airing their views and exchanging ideas with each other. Respectful interaction led in turn to peer learning taking place and friendships developing, not only with others from similar backgrounds but also with group members from different social cultures and ethnic backgrounds.
Group care allows professionals to encourage peer learning through the facilitated discussion that was part of each session. However, despite being able to observe mothers and their babies within the group context, a downside to delivering gFNP as opposed to FNP was that FNs felt that they had less knowledge of clients’ circumstances outside the group because regular home visits were not part of the programme. The response to this concern differed by site, with a couple of sites routinely scheduling extra home visits outside group sessions and others making extra home visits in response to specific safeguarding issues or, at one site only, carrying out the routine home visits immediately after the baby was born but not making any others.
An examination of the content delivered (see Table 44) showed that, despite the group context and a focus of agenda matching, the FNs were able to deliver all aspects of the six content domains appropriately. Indeed, the possibility of providing the content using craft-based and participatory activities may make the content particularly relevant. Participants were enthusiastic about most aspects of the group sessions, but especially about the variety of topics and the mixed approach taken by the FNs to delivering the programme. Although the practical advice given to participants about looking after their babies on a day-to-day basis, such as nappy changing, washing and dressing the baby, was highly valued, the weaning sessions in particular gave rise to many positive comments. Learning about child development, bonding with their babies and their emotional states was also reported as memorable and interesting.
There was appreciation of the way in which the FNs responded to requests for discussion of topics that may not have been scheduled for a particular session. Known as ‘agenda matching’,46 this flexible approach appears to have made the curriculum more acceptable to the group because it showed that the FNs were listening to their concerns and were prepared to adapt the session where possible to meet their particular needs at the time.
One aspect of gFNP that appears to have been particularly positive for the clients in the present study, reflecting the feasibility studies,57,67 was the development of social networks as a result of attending gFNP sessions. Across the sites new friendships were said to have been formed with participants meeting up and socialising outside the group, as well as forming virtual groups and communicating via social media. Consistent with previous findings,67 one aspect of these new friendships was that clients reported feeling less lonely and that they were less likely to be depressed. Support from both other group members and the FNs increased clients’ confidence in coping with the challenges of being new parents.
Although many comments were positive, it is important to understand why the programme may not have been the best fit for some clients. Several of those interviewed had initially attended their group on a regular basis and appeared to be engaged with the programme, but then either stopped attending or tailed off their attendance. A common theme in these cases was that a particular group member regularly dominated the group discussion, making it difficult for others to have their say. Although the FNs at one site were able to effectively manage the disruption and maintain the group dynamic in which everyone could express their opinion, there were two instances reported in which individuals stopped attending their group because there was a perceived lack of effective group management. This suggests that clients expect to have the opportunity to take part in meaningful group discussion and that this type of interaction is integral to their continued engagement with the programme. This problem of some individuals dominating the conversation in the group was also highlighted in previous findings57 and may need additional attention when training FNs for delivering gFNP.
Although some individuals stopped attending the group because it had become unacceptable for them to continue, others appeared to find the programme acceptable but attended irregularly. Their reasons tended to be organisational and related to the distance they needed to travel to the venue, the choice of venue and its facilities or even the time of day. Attendance across sites tended to be higher during pregnancy, but became less regular at the infancy sessions as clients discovered that organising themselves and their baby was more of a challenge, especially if transport arrangements involved travelling by public transport. These more pragmatic reasons were consistent with previous findings in the feasibility studies. 68
Low attendance was also the result of the gFNP provision never becoming established. In one site where the group failed to develop owing to insufficient numbers, participants were interviewed to gain their perspectives on the situation. They had attended the first few sessions but then attendance tapered off and they explained that starting with a very small group did not meet their expectation of a group. They had anticipated meeting other expectant young mothers and building up a social network, as well as learning about how to look after their babies, and they felt that two people in a group was not enough to start the process. In addition, in a group one does not always have to contribute, but with only one or two participants there is more pressure to do so. The FNs and clients recommended that a good group size is six or seven. Potentially any group starting with a smaller number might soon dwindle but if there is future provision it might be sensible to limit recruitment to a group of eight, whereas according to current guidelines45,46 the ideal size is said to be between 8 and 12.
The provision of midwifery care as part of gFNP raised many issues. Although much of programme facilitation was highly acceptable to FNs, delivering midwifery care stands out as the most challenging aspect. First, most FNMWs had not been practising midwives for some time and needed updating training to renotify their intention to practise. Additionally, most of them had not been practising midwives in the geographical area where they worked as FNs and were unfamiliar with local hospital systems for record keeping, and in some instances encountered difficulties gaining access to the IT systems. At interview most FNMWs reported feeling ‘under pressure’ as some policy and practice had changed since they last worked as a midwife; in particular, there was mention of feeling anxious about knowing all the relevant documentation and data entry that was required. This situation may have been exacerbated by the perception that some local community midwives had expressed reservations about midwifery care as part of gFNP, fearing that pregnant women receiving gFNP might miss antenatal checks or follow-up of clinical problems if their attendance at group sessions was poor. 86 It was uncomfortable for the FNMWs to feel that their professional integrity was being questioned.
Some FNMWs reported practical problems, the most often cited being lack of time during the group sessions to carry out the antenatal checks in addition to trying to deliver the scheduled topics for the session. There was also much ‘fetching and carrying’ in trying to set up the equipment for carrying out the checks at the group venue, and taking any blood samples to be analysed. Strategies such as conducting the care during home visits add to the cost of delivering the programme and also to the time that FNs need to spend delivering gFNP. Although some clients were enthusiastic, resistance was also encountered to the concept of self-care for the antenatal checks, which is consistent with previous findings. 57,67
The gFNP programme is not currently being offered, but, in the future, if it is considered for a mainstream service, questions will need to be addressed concerning the extent to which community midwives might be involved in recruiting potential clients and in delivering antenatal care, if this is retained as an integral aspect of gFNP. Many issues with low attendance can be linked with small group size, which can be linked in this study with slow recruitment and the challenges of engaging community midwives in the process. 86
The FN interviews in this study indicate that FNMWs felt under pressure, but previous development work found that the involvement of community midwives in the delivery of the programme was not optimal in that they were not as familiar with the one-to-one FNP programme or the motivational style used to deliver content. 67 In addition to the role of midwifery care and community midwives, the precise eligibility criteria may need to be changed. Many clients indicated that it was best if all participants were first-time mothers, ‘all being in the same boat’, not knowing what to expect and learning together about impending parenthood and how to look after their babies. One possibility suggested by FNs was that future delivery could include first-time teen mothers who are also eligible for FNP.
Overall, it has been possible to conclude that the programme, although positively received by most clients and delivered according to guidelines for the sessions that did take place, was not provided in as optimal a manner as possible. Groups were too small, leading to low and dwindling attendance in some cases, and most stopped before the whole programme had been delivered. This may have led to the content being delivered in a style that was not optimal, as many gFNP activities were developed to generate discussion and debate between group members. Without much discussion from the group, the delivery may have been more didactic. Thus, any impact that may or may not be identified in the trial needs to be interpreted taking this into account.
Chapter 6 Looked-after children nested study
The results in this chapter are summarised in Datta et al. 126 This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/.
Background
The term ‘looked-after child’ (LAC) was introduced by the Children Act 1989127 and refers to a child subject to a care order granted by a court or a placement order, or who has been accommodated by a local authority for more than 24 hours. Children cease to be ‘looked after’ at age 18 years. The Children (Leaving Care) Act 2000128 makes provision for the continuing needs of young people as they move from public care to adulthood. It requires local authorities to address how a young person’s needs are met regarding education, training and employment and to allocate a personal advisor to support their transition to independence. The Children and Young Persons Act 2008129 places a duty on local authorities to offer further assistance to young people leaving care (care leavers) particularly in supporting their educational attainment. The Children and Families Act 2014130 introduced ‘staying put’ arrangements, which enable young people to continue living with a foster family until they reach 21 years if both the young person and the foster family agree.
A total of 69,540 children were recorded as looked after by local authorities in England on 31 March 2015. 131 This is an increase of 1% compared with the number looked after on 31 March 2014, and an increase of 6% compared with 31 March 2011. This represents an increase in the proportion of children (those aged under 18 years) looked after from 58 per 10,000 in 2011 to 60 per 10,000 in 2015. The majority of children in public care (61% in 2015) are looked after by the state as a result of maltreatment. Most children in care are placed with foster parents, which includes kinship foster care.
In recent years there has been growing recognition that, compared with children not looked after but with similar socioeconomic backgrounds, LACs are at increased risk of a range of adverse outcomes in adulthood, including educational underachievement;132 poor physical health;133 mental ill health, including self-harm;134 poor sexual health;135 early and/or unplanned pregnancy;136,137 risk of homelessness;138 and sexual exploitation. 139 In their follow-up analysis of the 1970 British cohort study and controlling for other causes of disadvantage, Viner and Taylor140 found that a history of being in care as a child could be linked with lower social status as an adult and more problems such as mental and physical health problems and homelessness. There were also sex-specific associations; women who had experienced care were more likely in their teens to have been excluded from school, whereas men with a care history were more likely to be unemployed. The authors point out, however, that the majority of children who experience care do so for < 6 months, and are unlikely to experience significant long-term health effects or social adversity.
In a subsequent analysis of data from the 1970 British Cohort Study, Dregan and Gulliford141 reported that, after adjusting for confounding, children who experienced ‘both foster and residential care, longer placements and multiple placements’ were at increased risk of more extensive adult emotional and behavioural problems than children with no experience of public care. In particular, they concluded that residential care was associated with increased risk of criminality and multiple placements were linked with low self-efficacy in adulthood.
Rees132 reported the findings of a multidimensional, multiple-rater, population-based study of all LACs aged 7–15 years accommodated by one local authority (n = 193). The study aimed to overcome some of the limitations associated with earlier studies, such as small sample sizes and high attrition; restricted access to LACs; a focus on small, purposive samples; and reliance on case file audits. It confirmed previous findings that LACs performed less well on measures of mental health and of emotional literacy, and experienced a higher incidence of learning difficulties; their average performance in reading and spelling fell almost one SD below that of the general population, but not necessarily of comparable peers who were not looked after. 142 The study also identified positive exceptions and so cautioned against an overgeneralisation of the findings.
Few studies have examined the parenting outcomes of LACs. Early observational research indicated that the experience of being in care is a risk factor for parenting problems in adulthood143,144 and between one-quarter and half of care leavers have a child before or within 24 months of leaving care. 145 A review conducted by Hall and Hall146 found that mothers who have been looked after are much less likely to have family support and have many other vulnerabilities: 83% of women who have been looked after and become mothers have no qualifications, compared with 65% of childless women who have been looked after. The children of mothers who have been looked after may themselves be taken into care and, because of this, some young women avoid involvement with services. 147
Botchway and colleagues148 analysed data from the UK Millennium Cohort Study on pregnancy-related outcomes in women who had spent a period of time in care. The study focused specifically on the extent to which these women differed from those with no experience of care, in relation to factors considered important to the health and well-being of infants, namely smoking during pregnancy, symptoms of maternal depression and initiation of breastfeeding. Their definition of being ‘looked after’ was anyone who had spent any time living away from both parents, excluding those who spent time in a boarding school, prison or young offenders’ institution, or with relatives. The study148 also concluded that disadvantages of being looked after as a child could persist to adulthood in ways that may be relevant to parenting:
. . . there are aspects of care itself that may have an effect on the maternal outcomes studied, such as residential instability, disrupted parental attachments and difficulties in resolving history when faced with having children of one’s own.
p. 7148
Compared with women with no care experience, mothers with a care history were more likely to smoke during pregnancy (OR 3.0) and to experience symptoms of depression (after adjusting for confounders). Although not statistically significant after controlling for confounders, women with a looked-after history were more likely to give birth to low-weight babies and less likely to initiate breastfeeding. The authors note that it is not possible to disentangle the impact of the social disadvantages that results in some women becoming looked after from the experience of being looked after, but argue that the point of the care system is to improve a child’s chances of good or better outcomes. This is a difficult argument to make in the absence of research that provides evidence of how similar children would fare if they had not been in care, and it ignores the potential differential impact of short versus long periods of care or of different care placements.
A number of qualitative studies have explored the experiences of small samples of LACs and care leavers when they become mothers. This research outlines the personal vulnerabilities and structural challenges faced by this group,147,149,150 but also notes some more positive aspects of parenthood. Becoming a mother was reported as presenting an opportunity ‘to set “right” the ‘wrong of their past’151 in terms of both young people’s own family history and in motivating them to stabilise their lifestyle and circumstances. 152 Having a child of their own was for many women the first time they could develop a relationship offering a sense of permanency and in a family in which ‘their value and membership could not be questioned’. 153 However, given the young age of many of them, gaining the valued identity and status associated with motherhood was likely to mean the loss of other identities as students or unencumbered young people.
Parenthood was reported to foster a new sense of responsibility and purpose154 and provided a measure of agency and control that was lacking in other aspects of these young women’s lives. 149 In contrast to their childhood experiences, young mothers said they hoped to be an ‘ideal’ good parent, although found the reality to be challenging and sometimes overwhelmingly demanding, expressing self-doubt about their competence. 151 Studies reported women’s mistrust of social services and resulting reluctance to seek professional support. 151,152 However, in general, motherhood was described as rewarding and ‘an opportunity for healing and renewal’,153 despite also putting these women at increased risk.
In summary, these studies describe how motherhood can be positively experienced by this group of women and the authors note their capacity for resilience while also acknowledging the fragility of their circumstances and providing examples of the many challenges they confront. Researchers call for the provision of effective sex and relationships education for LACs,152 tailored antenatal services,149 increased support in developing emotional understanding,153 recognition of the positive achievements of young mothers,148 interventions to promote social inclusion,151,154 and the development of a shared understanding among professionals of why young people may be deterred from seeking help. 147
There is evidence that LACs are undoubtedly a vulnerable group, particularly those who ‘graduate out’ of care into adulthood prematurely (compared with most 18-year-olds), often into early pregnancy155,156 and often without the benefit of a stable relationship or a supportive family. 157
Concerns about the vulnerability of this group of mothers prompted a recognition that more research was needed into interventions that might promote the health of children born to parents who had previously been in care, or to women who became pregnant while in care, or to those in the process of making the transition from care to adulthood, but still entitled to support from children’s services. 158
Having commissioned three studies into the effectiveness of interventions for vulnerable women,38,159,160 the Public Health Research programme, through the Programme Advisory Board, asked each of these three research teams, in addition to the First Steps trial team,85 to include a specific focus on the impact of the programme on parents – particularly, but not exclusively mothers – with a care history. The estimated sample size for the present study nested into the First Steps trial85 was not expected to be large enough for a quantitative subgroup analysis. We therefore undertook to conduct an exploratory, qualitative study of the views on and experiences of gFNP, from the perspective of participants in the trial, and key stakeholders.
Methods
Ethics approval
The First Steps study was approved by the NRES Committee South West – Frenchay (reference 13/SW/00860) on 28 May 2013. Approval for the documentation for the nested LAC study was given as amendment number 6 on 4 November 2014 (information sheets and interview topic guides for the LAC study are available online; see Report Supplementary Material 8).
Aims and objectives
The overall aim of the LAC study was to explore views about, and experience of, gFNP for women with experience of being cared for by the state.
Specific objectives were to conduct interviews with:
-
women participating in the First Steps study who were in care or who had previously spent time in care
-
FNs delivering the gFNP programme who had at least one woman or one partner with a care background allocated to a group they were facilitating in the First Steps study
-
professionals working with LACs and/or care leavers in the seven local authority areas participating in the First Steps study.
Approach to recruitment
-
Mothers: in order to identify women with a care background participating in the First Steps study, 137 participants interviewed face to face at 6 months post partum (and two who were not interviewed at 6 months but were interviewed at 12 months) were asked ‘Have you ever spent any time in care?’. Those who responded positively were asked additional questions about their experience of care, including the kinds of placements they had experienced (e.g. foster home, children’s home), whether or not they were still in care, when they left care and whether or not they received local authority support as a care leaver. Those women with care experience were told about the nested LAC study by the researchers conducting the trial and asked if they would consent for their contact details to be passed to researchers conducting the LAC study. A LAC study researcher then contacted these women by telephone, provided information about the study, explained that participation was voluntary and, if the woman was willing to take part, made arrangements to conduct an interview at a convenient time. At the interview, research participants were provided with written information about the study and given the opportunity to ask questions. All provided written consent to participate. Interviews were confidential and participants’ data were anonymised.
-
FNs: the sample of FNs to be interviewed were those delivering the gFNP programme in sites in which at least one care-experienced woman had been identified at the 6-month interview. In addition, at regular gFNP Trial Steering Committee meetings, the First Steps PI asked if any FNs were aware of any groups in which there was a partner with a care background. It was made clear that this was not in order to interview the fathers for this study, but to identify whether or not there were additional sites relevant to the LAC study because of a partner with a care background. After process study interviews for the First Steps study were completed in each of the identified sites with a LAC client or partner, the trial manager gave the contact details for the FNs delivering gFNP to the LSHTM LAC researchers. These FNs were e-mailed an introductory letter inviting them to take part in an interview with information about the study, given the opportunity to ask questions, and informed that participation was voluntary. If they responded positively, they were sent a consent form to return. FNs were invited to choose between individual interviews and a group interview of the FNs in a particular site, and were offered either a face-to face or a telephone interview. A week before the planned interview, they were e-mailed an interview schedule, together with a covering note that made it clear that the interview would be audio-recorded and that the schedule provided was for general guidance only and would be adapted to their local circumstances.
-
Other professionals: professionals working with LACs and/or care leavers in each of the seven local authority areas were contacted by telephone and/or e-mail and invited to participate in a semistructured interview. Individuals invited for interview were identified by a researcher who approached social services and health departments and asked for the names and contact details of relevant people. Research participants were provided with written information about the study, given the opportunity to ask questions (by e-mail and on the telephone) and informed that participation was voluntary. Interviews were then arranged with those who agreed to participate.
All interviews were confidential and identifying data were anonymised.
Sample achieved
-
Participants: of the 137 women participating in the First Steps study 6-month interview (with an additional two not seen at 6 months but interviewed at 12 months), six (4.3%) reported experience of being looked after by a local authority. Of these, three were allocated to receive gFNP and three to usual care. Of the six, one woman was lost to follow-up by the main trial, one declined to participate in the LAC study and four agreed to be contacted. One of the four had been allocated to receive gFNP and three had been allocated to usual care. One of the four women was not at home at the time the interview had been arranged and, despite numerous telephone calls and attempts to do so, it was not possible to rearrange the interview. Three women participated in interviews. Of these, two were from one local authority and one was from another. One mother had been allocated to receive gFNP and two had been allocated to usual care.
-
FNs: in three of the seven trial sites, a woman with a care background – and in a fourth, a partner with care experience – participated in a group. All the FNs at these four sites consented to take part in an interview. In two sites, there were three interview participants; in the other two sites, there were two. All were women (Table 47).
-
Other professionals: in the seven local authority areas in which the First Steps study was conducted, 14 people were identified and contacted (one from social services and one from health services in each area). Thirteen agreed to take part in an interview and one (in health services) did not feel sufficiently well informed and could not suggest an alternative interview participant. After numerous approaches and attempts to arrange a convenient time and date, it proved impossible to interview 2 of the 13 people (one in social services and one in health services), despite their initial agreement to take part. Eleven interviews were therefore carried out with social services staff in six areas and health staff in five areas. At least one interview was conducted in each local authority area.
The range of practitioners who participated in the study included, among health service staff, two designated nurses and two named nurses for LACs and a clinical nurse specialist for children in care. Among social services staff, two advanced practitioners working with LACs and care leavers, three managers of social work teams working with LACs and/or care leavers, a commissioner of LAC services and six personal advisors to care leavers.
| Site | Professionals interviewed | ||
|---|---|---|---|
| A | FNP supervisor | FN | FNMW |
| B | FNP supervisor | FN | FNMW |
| C | FNP supervisor | FN | |
| D | FN | FNMW | |
None of the social services or health practitioners interviewed was familiar with gFNP, although many were aware of FNP. As some worked with LACs (aged < 18 years), some worked with care leavers (aged ≥ 18 years) and some worked with both groups, responses refer to parents aged from their teens to their early twenties, including those too young to be eligible for gFNP. FNs, whether or not they had worked with LACs or care leavers in gFNP sessions, had experience of working with these groups as FNP practitioners.
Data collection
-
Face-to-face interviews were conducted in the homes of three mothers who had been in care, participants in the First Steps study, between July and September 2015. Interviews lasted between 40 and 60 minutes. Field notes were written up by the researcher shortly after each interview. Each participant was given a £20 high street shopping voucher in recognition of her contribution to the study.
-
The four interviews with FNs were conducted by telephone between October and December 2015. Each one lasted about 1 hour.
-
The interviews with health and social services practitioners took place between September and November 2015. Three interviews were conducted face to face at workplaces. Of these, one was with an individual and one was a paired interview with an advanced practitioner in the looked-after and leaving care service and a commissioner for LAC services. The third was a group interview with a team of five personal advisors to care leavers and the service manager at their team meeting. A further eight interviews were conducted by telephone with individuals. Interviews lasted between approximately 25 and 90 minutes. Interview length depended in part on the extent of participants’ knowledge of FNP and gFNP.
Research tools
-
Two interview schedules were developed by the research team for women who were, or had been, in care: one for those allocated to gFNP and one for those allocated to usual care. Topics included experience of being looked after; feelings about pregnancy; experience of gFNP (if any); experience of health services, including antenatal, midwifery and health visiting; and views on the particular health service needs of mothers with a looked-after background.
-
The interview schedules for FNs asked about the women (and partners) with a care background who attended any of their groups, the possible impacts of gFNP; training and gFNP in a trial context.
-
The interview schedule developed for health and social care practitioners was amended as a result of initial interviews. Topics included perceptions about why young women with experience of care are more likely than peers to have an early pregnancy; the challenges facing these women when they become pregnant/parents; the particular needs of this group and how they might be met; the availability and adequacy of local services; participants’ knowledge of and views about FNP and gFNP; potential challenges for women with a looked-after history taking part in gFNP; the role of gFNP in service provision; and views on whether FNP or gFNP should be offered to all pregnant young women with a looked-after history.
Data analysis
All but one of the interviews was audio-recorded and transcribed verbatim. One of the interviews with a study participant was not recorded because of high levels of background noise. It would have been impossible to hear the details of the recording or transcribe the interview given the background noise from the television and two children present in the small space.
All interview transcripts were read by at least two of the authors. After familiarisation with the transcripts, the data were analysed on a priori themes drawn from the interview schedules using the Framework Approach. 161 These were refined and developed following team discussion. No identifiable details are included in order to protect respondents’ confidentiality and anonymity. Quotations give details of the respondent’s background (study participant, non-FNP health practitioner, social services practitioner, FNP practitioner), but are not numbered to provide anonymity given the small sample size.
Findings
Findings from interview data with mothers and professionals have been incorporated and are reported below.
Early motherhood
As noted in Background, young women with experience of local authority care are more likely than others to become young parents. We asked social care and health professionals for their views on why those with experience of care are more likely to have an early pregnancy.
Responses can be categorised into two broad areas: life events related to young women’s childhood experiences, removal from their birth families and resulting experience of care; and the associated desire to create a family of their own. Lack of strong familial and social networks was reported as being associated with early sexual debut and a potential for involvement in exploitative relationships, as well as with immaturity regarding planning and use of contraceptives. One nurse for LACs commented on their lack of knowledge:
. . . some don’t even understand the actual biology of getting pregnant so they think it’ll never happen to me.
Health practitioner
Disrupted education, which may be caused by changes of placement and, therefore, of school, may mean that young people miss out on sex and relationships education and so are poorly informed about reproductive processes. Disengagement with school may also mean that individuals have limited aspirations for achieving educationally or in employment.
Practitioners associated young women’s naivety and lack of resilience with changes in placements and saw these as hindering their transition to adulthood. These vulnerabilities, along with financial insecurity, unsettled living arrangements and, in some cases, harmful relationships, may cause them to desire a baby to love and be loved by:
It’s something to call their own, isn’t it, it’s their own and they hope that nobody’s going to take that child away from them. For a lot of them it’s the first time they’ve ever had anything that belongs to them; the parents have gone, different foster parents, movements, different social workers and stuff like that. As where having a baby it’s there, it’s yours, you’ve got to look after it and, yeah, definitely your own.
Social services practitioner
Some respondents thought that, although a pregnancy may not be planned, early parenthood may be a norm in young women’s social circles and, given the absence of alternatives, seen as a positive choice:
. . . having a baby forms their own family and, if they see their other peers having babies young and managing to a certain extent, they feel it’s something they can do as well.
Social services practitioner
One of the young mothers interviewed, who had her baby when she was 23 years old, explained that:
. . . all my friends, like, they all had kids so, like, I was the last one out of all of us to have a child.
Participant
Challenges faced by young mothers
The interviewees outlined a number of challenges faced by young women when they become mothers. Moving from foster or residential care to living independently is in itself challenging for an 18-year-old, and having a baby to care for is an enormous additional responsibility. Young women are likely to be short of money and may lack budgeting and housekeeping skills, while aspiring to having expensive, brand-name buggies and other products for their babies. They may have competing priorities on their time, such as having to sign on to claim benefits, meeting with professionals, attending college, working or applying for jobs, and may not have the maturity to make prudent decisions. Those who are care leavers will continue to be supported by a personal advisor, but their level of social support is likely to be reduced and the regular health checks that they are eligible for while in care stop. Unless they are enrolled onto a FNP programme or live in an area where there is a continuity model of maternity care, contact, and therefore opportunities to build relationships with professionals in midwifery and health visiting may be limited.
The professionals noted the isolation experienced by young mothers, which may be especially marked for those with a looked-after background, particularly if they have moved away from the area where they were in care:
A lot of the time, you know, they tend to kind of become a bit of a prisoner in their own home. A lot of the young girls that I work with find it quite hard to make connections with other young girls – they can be quite catty. So to go into like a Sure Start centre and to be vulnerable is quite difficult for them. So they’ll tend to sit in a lot of the time.
Social services practitioner
The three young mothers interviewed had separated from their babies’ fathers and lived alone with their children. Only one had regular contact with birth or foster parents. One mother, who had been prescribed antidepressants, described her isolation:
I felt like after I’d had [baby] I was very isolated, so I felt like it was just me and her in these four walls.
Participant
Despite social isolation, young mothers with a looked-after background may be wary of seeking professional support because of their own experiences. Several respondents talked about how mothers were reluctant to request help, especially from social services, in case this could be seen as admitting failure as a parent. Their ‘ultimate fear’ is that their baby may be removed from their care, and some may not understand or believe that personal advisors can work with them to improve their situation. One of the mothers interviewed who had been removed from her birth family because of her father’s violence, and who had spent time in a women’s refuge as a result of her partner’s ill treatment, acknowledged this fear and her resolve to keep her child:
I just knew, no matter what, nothing was going to take him away from me.
Participant
In other words, those in most need of support may be least likely to engage with services for a range of reasons, and professional respondents talked about having to develop creative strategies to work effectively with them:
It’s young people who are difficult, challenging, oppositional, have mental health problems, have significant emotional problems – they’re the ones who won’t go for whatever reasons.
Social services practitioner
The high thresholds of need for service provision operating in social services may also mean that support for young parents in need is not prioritised and services may be stretched to the extent that those deemed entitled to support may receive a minimum. The three mothers who were interviewed did not have positive opinions of their experiences of social services.
Young people’s own experiences of being parented may have been detrimental to their development, and their lack of positive parental role models means that they may not have insights into and understanding of the physical and developmental needs of a baby. Some of those interviewed explained that young women may inadvertently put their babies at risk:
They may want to keep the baby safe but they can’t stay away from the people that could cause the baby harm [i.e. friends, boyfriends, birth family].
Health practitioner
. . . quite often they don’t see or recognise what they’re doing or not doing is harmful for the child.
Social services practitioner
One of the mothers thought that professionals working with young parents who had been in care should offer support while acknowledging the sensitivities involved:
It’s like if you help them then it feels like you’re judging them but then if you don’t help them and something happens to that child in the future you’re going to get blamed for it anyway . . . But it’s just getting the right balance.
Participant
Despite the numerous challenges faced by these young women, it was reported that many are successful parents and professional research participants cited examples of individuals who have overcome, or who are in the process of dealing with, multiple difficulties.
Not all young people who get pregnant don’t cope or aren’t good parents. We’ve got some really sensible young parents who are very motivated and very successful . . . doing university and having children.
Social services practitioner
Many of those interviewed noted the diversity of young women’s experience of care and in their personalities and the circumstances of their becoming mothers, concluding that it is not possible to make generalisations about their experiences or their needs.
Maternity services
All three of the young women interviewed reported having seen different health-care personnel during their pregnancy, the birth and in their baby’s early weeks, and so had lacked the opportunity to develop rapport with any individual professional. Two said that they had not attended antenatal classes because these took place either during work hours or too late in the evening. Antenatal care was described by a clinical specialist for children in care as ‘very scanty’ and a personal advisor from the same area felt strongly that midwives should visit vulnerable mothers at home before delivery, in order to build trusting relationships and to check that they had what they needed in preparation for the birth. Specialist services such as midwives with expertise in working with young mothers were reported to be facing cuts due to tightening budgets.
Young mothers who lack family involvement are likely to have greater support needs than others. Two of the mothers talked about why they did not breastfeed their babies:
. . . because after I had him they didn’t tell me if, like they just said, oh you need to breastfeed, I was like, well I don’t want to breastfeed, they didn’t show me how to breastfeed, they didn’t show me how to feed him, they didn’t show me how to change him, anything. I had to do it all by myself.
Participant
. . . it was like I was an inconvenience to the hospital for asking for help for [baby] to latch on and in the end I gave up. And I wish I hadn’t given up but I didn’t get the right support from the hospital.
Participant
Some personal advisors working with care leavers develop and maintain links with health professionals, including FNs running FNP programmes, and support young mothers by signposting them to particular services, linking them with professionals and accompanying them to appointments. Some had also acted as birth partners to their clients. In two of the seven research sites, professionals explained that plans were being developed to meet the particular needs of LACs and care leavers when they become parents as it was acknowledged that a gap in services existed. However, local support services for parents with young children were reported to be facing cuts and, in one area, we were told that many local voluntary sector projects (such as mother and toddler groups) had disappeared because the local authority had ceased to fund them and so ‘killed them off’.
Individual women can choose whether or not they want to accept services and they may decide not to if they think that their behaviour is under surveillance from professionals. One social worker explained that, for example, a woman with a violent partner might withhold that information from midwifery services, but if she does disclose it then a package of support can be arranged between her personal advisor and health personnel.
The potential benefits and disadvantages of Group Family Nurse Partnership to mothers who are in care or care leavers
Group Family Nurse Partnership versus one-to-one Family Nurse Partnership
Those social services and health professionals working with children in care and care leavers were universally positive about one-to-one FNP and its role in supporting young mothers with a care background. As noted above, these research participants did not have personal experience of gFNP:
I think with my young person we kind of expected her to go down a negative path when she was pregnant but when we got the FNP on board I think with all the skills and stuff she learned over that period of time of her pregnancy she just took all the skills and ran with it as soon as the baby was born and she’s doing really, really well.
Social services practitioner
We have had some real success stories with our looked after children where they’ve become parents themselves and gone on to successfully parent the children and I think how that’s been successful is because of the input with the FNP because of the support they’ve had and any of the ones who’ve gone through our FNP would sing their praises really.
Health practitioner
These professionals tended to think that the potential benefit to these young people of attending gFNP would depend on individuals’ personalities and preferences. In their view, the more motivated, confident and older mothers would be more likely to be interested in participating in group activities, whereas others might be uncomfortable attending a group in which they did not know anyone, and might feel intimidated and stigmatised because of their looked-after background. It was acknowledged that attending a group made up of strangers in a new environment would be challenging for any young person:
It might either work really well or not at all. And it would just depend on the kind of personality of each of the young women . . . And . . . whether they wanted to engage with peers or, because some really do, some really don’t . . . And so, you know, I couldn’t say categorically but I’d say in some people it would work really well and some probably not.
Health practitioner
The positive, proactive young person would see [gFNP] as a supportive thing. The ones that are more challenging . . . they may have fear of judgement . . . ‘What will other people think of me? I don’t want other people knowing my business’.
Social services practitioner
Compared with the one-to-one FNP model, some thought that those with a care background might have difficulties attending because of the cost of transport or because they may struggle with time keeping and prioritising appointments:
You can’t be rigid with looked after, you need to be flexible.
Health practitioner
It was also mentioned that the lack of a one-to-one relationship with a FN would be detrimental to those with a care background, who might find it difficult to build trust and learn in a group setting where some might struggle ‘to show their vulnerabilities . . . they can tend to get a bit angry or defensive’ (social services). Although personal advisors might accompany young women to the group initially, this might draw attention to their ‘difference’. Another concern was that, in a small town, those in care might know each other and possibly have a history of antagonism, which could lead to social tension in the group.
The views of two of the mothers (not allocated to gFNP) illustrate individuals’ different preferences. One said she would not have wanted to take part in a group activity, as:
I don’t like being around too many people.
Participant
The other thought:
. . . if I could have met other mums similar to my age and made . . . a network of friends with other babies, I think it would have benefited me and [baby].
Participant
Family nurses, however, were more positive and thought that the diversity of backgrounds and circumstances of those attending groups they had run meant that all members faced individual challenges and so those in care or who had left care would not be singled out. The ‘nurturing’ FNP approach encourages peer learning and support from all participants so the involvement of those with a care background may be particularly empowering for them. They suggested that attending and participating in a group builds confidence, and individual women become skilled at particular aspects of caring for a baby, and so can model behaviour and advise others:
. . . we noticed that, specifically with one client who happens to be the client who was cared for by other family members, that she lacked a lot of confidence when she first came and we observed how that confidence grew. So it’s kind of being accepted, you know, that acceptance and, yeah, you’re sharing ideas, you’re all new to it but she had a lot to share and was an expert in weaning at one point, wasn’t she, yeah it was brilliant for her confidence.
FN
The responses of the mothers suggest that, although they might be familiar with young children through their sisters and friends, they lacked confidence and skills in socialising their children. One said that because of isolation from other children, caused in part by her own depression, her child was ‘clingy’ and did not like group activities. Another was concerned about her child’s aggressive behaviour and refusal to eat healthy foods, but did not seem to have strategies to deal with these. The third and youngest was caring for two children under 3 years, was not in touch with her family, had few friends and had limited resources to manage her situation.
Some respondents thought that attending a group can help to address the social isolation often experienced by young mothers. FNs gave examples of the sustained nature of the social networks developed in gFNP. Group members remained in contact and met after the gFNP programme had finished. Some mothers had set up group Facebook pages and continued to support each other’s learning about parenting by posting questions and suggesting solutions while also meeting socially.
Some of the FNs thought that the group model was more effective and powerful than that offered by one-to-one FNP because of this opportunity for group interaction and shared problem-solving. They described how the topics covered in group sessions could be tailored to meet particular individuals’ needs in a way that did not single them out:
I think it supports them to really embrace parenting and really understand it, you know, the relationship between themselves and the baby.
FN
The empathic nature of established groups was described by FNs who explained how members responded to individuals when they shared their concerns within the group. They saw the group setting as an opportunity for those attending to have time away from the other issues they have to deal with to concentrate on becoming or being a parent:
I don’t think looked after mums need anything different in terms of adding anything specific into the group because all they want to do, they want to be part of something that’s taking them away from the everyday things they’re having to go through.
FN
The fact that everyone is treated in the same way was seen by FNs as a positive aspect of gFNP for mothers with a care background:
. . . they wouldn’t necessarily want to be getting preferential treatment because they’re looked after. They just want to get what everyone else is getting within the group . . . the group’s an opportunity to be that sort of normal person like everybody else . . .
FN
This also applied to a father who had been in care and attended gFNP sessions:
He didn’t particularly talk about his childhood but I think he liked the support that he got from attending group . . . just that there were other dads there as well . . .
FN
It was suggested by some social services professionals that a ‘hybrid’ model of FNP could be developed that would encompass both one-to-one and group sessions. The group model does include both elements to an extent. FNs reported that those participating in gFNP have the opportunity to talk to FNs privately at the end of a session and are encouraged to get in touch between sessions if they want to discuss anything, including issues that they do not want shared with the group. However, it was felt that it was not possible to develop such close relationships with mothers as in one-to-one FNP:
. . . you don’t get to know them as well as you do your one–to-ones because you don’t see them in the home environment all the time and we don’t have those one-to-one, intimate conversations about feelings and such like.
FN
For those with a looked-after background, possible disadvantages of gFNP included the potential of feeling stigmatised by one’s family history. Discussions about group members’ own childhood experiences might be uncomfortable for those who were or had been looked after:
Others are expressing an experience that was very positive when they were growing up and they’re reflecting on an experience that wasn’t.
FN
Practical difficulties might include getting childcare for older children because of lack of family support and juggling the demands on individuals’ time by having to attend appointments associated with care plans, making the transition to independence or other meetings:
It’s very hard to fit the programme in . . . They’ve got looked after reviews, they’ve got to follow up their education, you know, there’s all sorts of things going on for them.
FN
Fathers and mothers in their twenties were more likely to be working than younger mothers and might therefore find it difficult to attend group sessions regularly:
Some of the fathers worked so they popped in and out . . .
FN
In the case of one young mother interviewed, the allocation of housing in another area meant that she was unable to continue attending gFNP because of the distance she would have needed to travel and the associated costs.
Dedicated groups for parents with experience of care
Some support was articulated among health and social services professionals for group-based provision tailored to meet the needs of young parents with a care background only, although interview participants were equivocal about the potential benefits, identifying possible disadvantages as well as advantages. Some thought that a special group could provide a ‘safe place’ in which members could find mutual support. This would, however, depend on the individuals involved and might be hampered by relationships already formed via the care system. However, as noted above, others felt that:
. . . it would be incredibly beneficial for them to have the peer support and the social content . . . having other people, not only people from the care system but other young women who are young and pregnant and . . . I think the support they get and learning from role modelling from other young parents who have come from a different background is . . . absolutely hugely beneficial to them, to be honest . . . they do tend to stick with people that they have known from the care system and I think it would be beneficial for them to have that wider experience.
FN
Family nurses felt that the diversity of backgrounds and experiences found in existing groups offered all participants the opportunity to be ‘normal’ and was supportive to all members. As one FN said, a targeted group for those with a care background would lose the ‘wonderful mix’ found in gFNP groups.
Discussion
This nested study was designed as exploratory, not least because the largest number of young people we expected to recruit was 10. In the event, of the 166 study participants, only six identified that they had been looked after as children, one of whom was lost to follow-up. Of the remaining five, four agreed to be interviewed, but – despite strenuous efforts – it was possible to interview only three. This level of success is, however, in keeping with the challenges of engaging vulnerable young people in research.
The limited number of young mothers who had been looked after within the sample also had an impact on the numbers of FNs with direct experience of providing groups whose membership included those with experience of being looked after. Moreover, the other professionals we interviewed, although familiar with the challenges facing LACs, and almost all familiar with FNP, were unware of the existence of gFNP, what this entailed or what gFNP provided. The data collected for the nested study is therefore limited, not only with regard to the experiences of looked-after mothers, but also in terms of the speculative nature of the information provided by FNs and the other professionals who work with LACs and care leavers. We are, therefore, able to offer only observations, rather than conclusions.
The most important observation to make is that this study confirms the vulnerability of young women in care, and the importance of supporting them in their transition to adulthood and parenthood. Recent years of austerity have further undermined the capacity of social services to fulfil their responsibilities to these young people. 162,163 Both the women interviewed and those who routinely work with care leavers, testified to their lack of preparedness for parenthood, and the impact of financial insecurity, unsettled living arrangements and social isolation.
Similarly, current arrangements for maternity services seem poorly equipped to provide the kind of support required by young care leavers. This group of mothers, who lack other forms of support from friends and family, need dedicated care from individuals with whom they can form a relationship. 148 This need not be one person, but it probably does need to be a very small number of people who can establish some degree of trust during pregnancy, and who can provide some follow-up subsequently. Such relationships lie at the heart of FNP but, from the data in the present study, it is not possible to determine whether or not women who receive gFNP benefit to the same extent, or in the same ways, as those who receive individual FNP have been found to benefit in other trials. 26,31,32,164
One of the key issues for this nested study was to explore the relative acceptability and perceived effectiveness of gFNP for women with a looked-after background. As indicated above, although it is not possible to say anything definitive on this issue, a number of views were expressed that would merit further study. Two of the mothers had very different views about the acceptability of group-based antenatal and postnatal provision, and these undoubtedly reflect different personalities and life experiences. Similarly, diverse opinions were expressed by professionals. A potential conclusion is that gFNP is unlikely to be effective as a sole offer in any particular area. Further, for those with the most troubled histories, individual FNP may well be a more effective option. Another empirical question is whether or not gFNP is a cost-effective addition to individual FNP, as some respondents suggest. Unfortunately, this is also a question that data from this study are unable to answer.
Chapter 7 Discussion and conclusions
Principal findings of the randomised controlled trial
The main ITT analyses did not identify any evidence that the gFNP programme, compared with routine antenatal and postnatal services, was efficacious in reducing risk factors for maltreatment, defined as less likelihood that mothers would have attitudes to parenting that are known to be linked with the potential for abusive parenting and more likelihood that they would display sensitive and responsive behaviour when interacting with their 1-year-old infants. Attitudes expressed when infants were 12 months of age and behaviour in mother–infant play did not differentiate mothers who had been offered the gFNP programme from those who had not in absolute levels, although the cost-effectiveness evaluation did identify more change in score for the intervention group. Nor was there any difference according to the CACE analysis in which comparisons focused on mothers who had attended either at least one session or at least 17 and the control group. Only one of the eight secondary outcomes showed evidence on an impact of gFNP. Women in the intervention arm of the trial were more likely to breastfeed their baby up to 6 months. However, this is of note, as exclusive breastfeeding to 6 months is a World Health Organization recommendation for its health benefits, and the length of breastfeeding time has been linked with increased maternal sensitivity. 165–167
There are several potential explanations for the lack of evidence that the intervention could make an impact on parenting attitudes or maternal behaviour. The first explanation is that the programme does not offer effective additional guidance, information or support compared with care as usual and, thus, it is not a viable prospect to offer this approach, which is more costly than care as usual. There is mixed evidence to support this explanation. The gFNP programme is based on the same theoretical background as the home-based one-to-one programme, FNP, which has been shown to reduce the likelihood of abuse and neglect in trials in the USA22,25,26 and Europe,164 but has failed to do so in the UK. 38 However, the group programme has several differences, in particular that it extends only until infants are 12 months of age and not 24 months, the end point for FNP, and that it places a greater emphasis on developing social support networks. Thus far, this is the first trial of gFNP’s potential for impact. Implementation evaluation studies indicated that the programme was feasible and that both clients and the FNs delivering the programme believed that there were positive benefits, but these focused more on social support and on confidence as a parent than on attitudes to discipline and control, or maternal sensitivity. 57,67 Nevertheless, social support and confidence were both examined as secondary outcomes and did not reveal any benefit of gFNP. Thus, a more likely explanation is that the information and attention provided by routine antenatal and postnatal services delivered by midwives and health visitors, in combination with any additional support offered through care as usual, enabled women in the control arm of the study to have parenting attitudes and behaviour that did not differentiate them from the intervention arm participants. This is not to say necessarily that either group received sufficient input. Although attitudes about parenting were generally at the higher end of the AAPI-2 scale, suggesting low risk, this was not the case for observed maternal sensitivity based on the CARE-Index videotapes. Mothers in both arms of the trial had average sensitivity scores placing them only just above the high-risk range (0–4). 73,74 This excluded those mothers who did not want to participate in the assessment through concerns about appearing on videotape. Thus, women of this age group, relatively new or new to parenting, may benefit from interventions that focus specifically on enhancing playful and stimulating mother–infant activities such as the Australian Community Happiness, Understanding, Giving & Sharing (HUGS) programme. 168
Second, the groups were in the majority of cases not of sufficient size at the outset, even when ‘buffer’ clients (clients not taking part in the trial) were included. The feasibility studies showed that attendance was below the actual number enrolled. 57,68 It is possible that the smaller numbers of participants in the groups did not generate sufficient involvement from members to enable the programme to have an impact, particularly on the secondary outcomes of social support. Although in the implementation research the groups created ongoing social networks57 with activities outside the programme, such as outings and contact through electronic media, in a smaller group it may be more likely that only one or two friendships develop. The smaller group size may also mean that there is insufficient input from group members to elicit the kind of debate and discussion that might arise concerning differing views about parenting topics such as discipline or feeding. Finally, some of the smallest groups had such low attendance that the FNs decided to terminate programme delivery prior to delivery of the full 44 sessions, thereby reducing the possibility of having an impact. It is possible, given the larger numbers required to recruit control participants in addition to those assigned to receive gFNP, that it is just not feasible to evaluate gFNP in a RCT with the limitations that are imposed regarding age, EDD and location.
This relates to a third possible explanation for our findings. With some groups being terminated before providing the full complement of sessions, and others not running at all owing to very low initial numbers, the clients in the intervention arm may have been exposed to insufficient ‘dosage’ to make a substantial impact. The study did not reach the initial planned sample size of 200 that would enable differences between groups to be detected, estimated to be at least 71 per arm after attrition. The randomisation was adjusted during the trial to provide more in the intervention arm, but the potential for impact was limited by the proportion not experiencing any intervention sessions. Although additional CACE analyses were conducted after the ITT, to consider those study participants who had experienced at least 17 sessions, the study is underpowered to identify any differences in these much smaller groups.
Fourth, it is possible that this intervention could have an impact, but not with this particular population. The target population was developed by the FNP NU through feasibility work so that it could be offered to mothers likely to benefit from some support, but who would not be eligible to receive the home-based one-to-one FNP programme. 57,67,68 They had some vulnerabilities, principally young age and (for the 20- to 24-year-olds) few or no educational qualifications. However, to make an impact on attitudes and behaviour that could indicate risk for child abuse and neglect, more vulnerability criteria may be required to identify a population in whom change can be identified. It has been demonstrated that responses to parenting intervention can vary depending on vulnerability, with a moderate number of risk factors linked to optimal benefit while those with few risk factors are likely not to change their parenting. 169 Thus, the programme may need to reconsider the eligibility criteria if it is to demonstrate impact on parenting practices. The inclusion of many women with few vulnerabilities apart from young age may lead to groups with women who do not necessarily need this kind of extended and detailed programme. However, the more criteria that are applied, the more difficult it is likely to be to identify a sufficient number of women with EDDs that are similar, living in proximity to a centre providing the gFNP programme, meaning that groups would potentially be too small. Indeed, it may be impossible to implement the programme owing to the reduced number of potential candidates meeting specific criteria. In addition, it has been shown that the identification of vulnerabilities in pregnancy is dependent on information that is not usually available in midwifery or other antenatal records. 42 This trial struggled to gain sufficient numbers of names of potential participants through reliance on community midwives. 86 However, this might be easier if names are sought as referrals to existing services rather than as research participants.
A fifth reason why no impact on the potential for child abuse and neglect was identified may be related to the choice of outcome measures. Questionnaires asking about attitudes have been shown to differentiate between clinical groups and the normal population, but differences may be smaller and, therefore, harder to detect in a group only at potential risk for abuse. In addition, the video measure of maternal sensitivity73,74 was refused by 30 study participants, further reducing statistical power to detect a difference. Although about half gave a reason that they related to their own body image, they may also have had concerns that the video would reveal less than adequate parenting, possibly even more likely in the intervention arm as some had been receiving a programme that aimed to enhance maternal sensitivity. However, the rates of refusal were similar across the two arms of the trial. The range of scores for maternal sensitivity was low, with almost no mothers being rated in the optimal sensitivity range of 11 or higher. Thus, with limited variability in sensitivity scores the possibility of identifying any difference between groups is reduced. There was evidence that the coder completing ratings of all participants made lower ratings on average than a reliability coder, who rated a 10% sample. However, the difference between the two was not great. Nevertheless, a different method of coding the interactions might be able to identify a greater range of aspects of parenting.
A sixth possible reason for the null finding of the main study for the primary outcomes is that the FNs needed more experience in delivering the programme before taking part in a trial. The programme development studies had taken place in five different sites,57,67 but only one of these five sites participated in the trial. Thus, the majority of the FNs had received training, and had substantial experience of FNP, but had not delivered gFNP prior to being involved in the First Steps study. Ideally, a trial would take place after they had experience of delivering the programme, but there were constraints with respect to funding the programme meaning that, as a new development, it was unlikely that commissioners would agree to its widespread delivery unless evidence could be obtained of its potential for impact. Data from the process evaluation interviews indicated that the FNMWs were particularly aware of making sure that they conducted the antenatal care according to guidelines, an aspect of service delivery that differed from their FNP work. They received supervision from a community midwife in addition to their FNP supervision, but for most it was some time since they had been delivering care as midwives. In some cases the venue used for gFNP was not ideally suited to delivering antenatal care; other research has shown that similar infrastructure issues caused difficulties for nurses delivering the related Centring Pregnancy programme. 170 Ensuring that these more medical aspects of gFNP were delivered well may have meant that the gFNP FNs gave them more attention, at the expense of focusing on specific parenting behaviours.
Seventh, the fact that the programme is delivered in a group needs to be considered in terms of its limited impact. The programme was designed on the basis that group care prenatally can improve pregnancy outcomes,47,48 may be less costly than one-to-one home-based support,49 and that groups have been recommended to support potentially vulnerable mothers. 50,51 It is suggested that meeting in a group with other mothers can be perceived by young mothers as more helpful than one-to-one support,52,171 especially if all group members are of a similar (young) age. 53 In particular, group services are perceived as a way to reduce social isolation for young mothers. 50,171 The process evaluation interviews identified some issues in terms of ease of travel to the group meetings. Reimbursement was offered for the cost of travel but some young parents may not always have the personal resources to organise themselves for regular group attendance. To increase viability by maintaining an adequate group size, group sessions might need to be supplemented by some planned home visits from nurses for the more vulnerable group members so that any issues they have about attendance can be addressed in more detail than can be dealt with by a text message or telephone call. Providing care in a group context, therefore, has many potential benefits, but is not without its challenges. In addition, attendance at groups by partners was low and it has been recommended that couples who are vulnerable in terms of parenting should be supported together, ideally in the home environment, in order to make an impact on parenting and also on the couple’s relationship. 172
Economic evaluation
The economic evaluation that was conducted as part of the First Steps RCT was performed in accordance with national methodological standards with a comprehensive analytical strategy adopted to handle missing data and various forms of uncertainty, including sampling uncertainty, decision uncertainty and methodological uncertainty. For participants with complete data and considering the entire follow-up period, mean (SE) total NHS and PSS costs, inclusive of the cost of the intervention, were £8877 (£1399) in the intervention arm compared with £6066 (£601) in the control arm, generating a mean cost difference of £2810 (bootstrap 95% CI £338 to £6607; p = 0.069). The mean incremental cost-effectiveness of the gFNP intervention was estimated at –£247,485 per QALY gained (i.e. on average the intervention was associated with a net positive cost and a net negative effect). The probability that the gFNP intervention is cost-effective did not exceed 3% regardless of the willingness of decision-makers to pay for an additional QALY. This pattern of results was broadly replicated when outcomes were measured using the CARE-Index (maternal sensitivity domain). When outcomes were measured in terms of change in AAPI-2 score (baseline to 12 months), the probability that the gFNP intervention is cost-effective was estimated at 25.1% at a notional £20,000 cost-effectiveness threshold. The results of the economic evaluation remained robust to several sensitivity analyses that assessed the impact of areas of uncertainty surrounding study components. Furthermore, analyses of heterogeneity in the cost-effectiveness results revealed no evidence that either completion of the gFNP programme or the programme phase had a positive effect on the cost-effectiveness of gFNP.
In addition to a within-trial economic evaluation, a DCE was also performed with the view to quantifying the preferences of individuals for the disparate health and non-health outcome measures adopted by the First Steps RCT. The theoretical underpinnings of the gFNP curriculum, which draw on ecological, self-efficacy and attachment theories, suggest that many of the effects of the programme may not manifest in changes in health status. Indeed, the DCE revealed that changes in EQ-5D-5L-based maternal HRQoL attributes were viewed as being considerably less important than changes in AAPI-2, Abidin PSI, PSOC and MOS outcomes by both members of the general population and expectant mothers. The clear implication is that CUAs that solely use the EQ-5D-5L to measure outcomes are likely to exclude important factors to both recipients and non-recipients when evaluating parenting programmes.
A number of caveats to the results of the economic evaluation should be noted. First, a complete profile of resource utilisation, cost and health utility data over the entire study time horizon was available only for 101 of 164 (61.2%) women and their children, despite intensive efforts to follow up the study participants. In response, multiple imputation techniques for handling missing values were applied. A second caveat is that our cost estimates are largely based on reports by trial participants of their and their children’s use of health, social and broader services, and their own incremental expenditures, over extended recall periods. Previous research in the perinatal context has indicated that new mothers may underestimate their and their children’s use of some categories of services (e.g. community service utilisation), over extended recall periods. 173 If this were the case for our study, our absolute costs for some categories of services may be underestimates. Nevertheless, there is no evidence to suggest that our estimates of incremental cost-effectiveness of the gFNP intervention are biased by this concern. 174 A third caveat is that lost productivity in this study was measured on the basis of women’s time off work, and this approach does not value the time losses of the non-working population, which may be relevant. A fourth caveat is that there are currently no published cost-effectiveness thresholds for the child maltreatment outcomes considered by the CEA, namely unit changes in the AAPI-2 or the CARE-Index (maternal sensitivity domain). Our statements about cost-effectiveness based on these outcomes were based on a hypothetical range of values for the cost-effectiveness threshold (£0–£50,000), and we have focused on a notional value of £20,000 for illustrative purposes. It is evident that further research is needed to inform decision-makers’ willingness to pay values for changes in these outcomes.
Finally, and notably, it was not possible to explicitly incorporate the outputs from the DCE into an augmented CUA to reflect the value in changes in attributes not covered by the EQ-5D-5L. Nevertheless, our research highlights the importance of valuing disparate health and non-health outcomes, for mothers, children and broader family members, when evaluating the effects of parenting programmes using preference-based measures. Future research in this area should focus on valuation techniques that are tractable to application within an economic evaluation framework.
Process evaluation
The process evaluation showed that delivery of the gFNP programme was variable in terms of the number of sessions delivered, but was relatively consistent with the balance of content that is recommended for the one-to-one FNP programme and the extent of involvement and understanding of clients, although site comparisons in infancy indicated that the strategy of agenda matching to some or all group members was likely to lead to differences in the focus of sessions. This was particularly evident with respect to time spent on environmental health, and on links with/referrals to other agencies. In a group programme it may be challenging to match all the agendas, but neither of these two domains should have a specific impact in terms of the main outcomes of the study, parental attitudes and maternal sensitivity, unless issues such as depression are not identified and supported with suitable referrals and advice.
There were several reasons why some sites were not able to deliver the recommended number of sessions, the primary one relating to the slow recruitment that led to smaller than ideal numbers in most groups. Some clients reported that they liked the group to be small, but very small groups are not sustainable from a cost-effectiveness or commissioning standpoint and may also lose some of the dynamic interaction that is likely with a larger number of parents holding varying views. In addition, as was the case in one location, a small group with one or two members who are outspoken and dominant may lead to high attrition as others stop attending, whereas in a larger group they do not have such an impact. It is clear that recruitment pathways will need to be very efficient in any future delivery of gFNP,86 to ensure that all potential participants are identified in a timely fashion.
Staffing issues also had an impact on programme delivery. To avoid taking resources away from the home-based FNP programme the residential training for gFNP was offered to the FNs in each site who had been identified to deliver gFNP, and their supervisors. In some instances additional FNs were able to attend, but not for all sites. This meant that, if the trained FN was not available, through sickness or for other reasons, then it was not easy to deliver the programme and in one case led to gFNP not being delivered, although clients had been enrolled. In addition, even if a trained FN was available, the lack of continuity was perceived as somewhat disruptive to the group process. Any future delivery might consider rotating programme delivery between three FNs so that the group members will be comfortable with whichever two deliver a particular session.
Many positive comments were made by gFNP clients about receiving the service and they linked participating in the programme with increased confidence and increased capacity to manage parenting challenges, such as weaning. However, they also noted that transport or timing factors could mean that they were not able to attend. The ideal model in the feasibility work57,67 was that travel would not be an issue, with the groups taking place in a local children’s centre or health clinic. Not only should this enable easy ‘pram pushing’ access, it should also help to join gFNP up with other services for children and families. However, even in the feasibility work it was a challenge to identify and recruit sufficient numbers of pregnant women with similar EDDs living close to a centre. For the trial, double the number needed to be identified so that a control group could be formed. This led many of the trial sites to locate the programme in a more central spot, which was likely to be able to draw in women from around the area with bus routes generally radiating in to town or city centres. This meant that almost all participants had some kind of journey to make rather than being able to ‘walk around the corner’. If that model is used in the future, then funds to reimburse clients’ travel as were provided in the trial would need to be factored in to delivery costs as they have been in the cost estimates in Chapter 4.
Overall, the process evaluation identified many themes that mirrored the implementation evaluations of both FNP36,39,40 and gFNP. 57,67 Those who attended regularly appeared to really like the programme, believing that it had reduced their isolation, improved their mental health and enhanced their capacity to parent. The FNs found it rewarding to work with them and also identified gains. However, the lack of evidence of effectiveness for most outcomes compared with those for women in the control arm would suggest that other families are similarly supported, although both groups would appear to be likely to benefit from more support. Potentially, the group context, and the presence of both peers and medical practitioners able to explain scientifically the benefits, is particularly relevant to supporting breastfeeding where there was evidence of an improvement in the gFNP group, but differing strategies may be needed to make change for parents potentially at risk for abuse or child neglect.
Relevance for parents with ‘looked-after’ experience as children
The practitioners interviewed for this nested study confirmed the vulnerabilities and challenges that were likely to be experienced by young mothers and fathers who had experience of being looked after by social services, and the importance of supporting them in their transition to adulthood and parenthood. It was also noted that current arrangements for maternity services seem poorly equipped to provide the kind of support required by young care leavers.
However, few mothers were identified in the study with a looked-after history and even fewer could be interviewed, reflecting their often unpredictable life experiences, with the result that only tentative conclusions from the nested study are possible. We were surprised that so few participants reported a looked-after history; rates differed substantially from the FNP implementation evaluation. It might be the case that women with a looked-after history, who may have multiple needs, were reluctant to take part in a research trial without knowing if they would receive additional services. In contrast, the FNP implementation participants were identified after they had agreed to receive the FNP service. 36 Of those who were interviewed, differing views were given about the idea of group-based antenatal and postnatal provision, undoubtedly reflecting different personalities and life experiences. More interviews would be needed with other women who had similar childhood experiences to judge whether or not this kind of programme could have particular relevance to this group. Similarly, diverse opinions were expressed by professionals, many of whom were unfamiliar with the gFNP programme, although most had knowledge of FNP. They generally did not consider that gFNP was likely to be effective as a sole offer for ‘looked-after’ young parents, especially those with the most troubled histories who may not cope well in a group setting and may be reluctant to share their experiences or parenting ideas in a group. This view was shared by the FNs, most of whom had experience of delivering FNP to young parents who had been looked after. They too considered that individual circumstances and characteristics would need to be taken into account before offering a group-based programme such as gFNP. Thus no firm conclusions can be made about whether or not gFNP has potential for this population.
Strengths and limitations of the First Steps study
The strengths of the study are as follows.
-
The study was delivered by a multidisciplinary research team, with expertise in trials, statistics, cost-effectiveness, midwifery, social care, child development, parenting and evaluation of interventions.
-
The study protocol pre-specifying all aspects of the study was published in a peer-reviewed journal.
-
The participants were securely randomised.
-
There was a clear separation between the implementation and research teams.
-
Data collection was undertaken blinded.
-
Rigorous statistical methods and reporting have been used.
-
The study has integral process and economics components.
-
Detailed implementation evaluations were undertaken, indicating that the kinds of outcomes to be studied were likely to be identified.
However, the study also has a number of limitations that influence the ability to make generalisations about gFNP based on the findings.
-
The most relevant is the slow rate at which potential participants were identified, documented in several substantial amendments to the protocol. Although an expected strength had been that the PI and the FNP NU spent many months meeting with sites and with midwifery teams to share information about the trial and what would be required, names were not forthcoming on the basis of being approached at routine antenatal contact with midwives, meaning that the FNP teams, in some cases supported by CLRN midwives, had to take on the task of investigating antenatal records and then telephoning potential participants. It should be noted that at the time there had been some changes in maternity sites with changes to senior staff and service reconfigurations. Thus, in any future research service pressures should be acknowledged as key factors in trying to sustain linkages and to follow through on the initial support identified in each site.
-
The slower rate of identification led to groups being smaller and all the associate issues that have already been summarised, in terms of service delivery, dosage and the associated reduced power to detect differences, especially with the video interactions, as some participants did not agree to this procedure.
-
Another limitation is the absence of information from HES data to validate maternal reports of service use, and to provide details of A&E attendance. The consequence of this was that it was not possible to determine the extent to which A&E visits were for injuries or poisoning, both linked to abuse and neglect. This was a result of tightening of procedures for data sharing not in place at the outset of the trial.
-
A further limitation is that almost all the FNs, although they were highly experienced in delivering home-based FNP and the majority had experience of delivering other group programmes, were new to delivering gFNP. In addition, those with a midwifery role had substantial additional aspects to their role with respect to recording antenatal health information.
-
Groups could be offered only to women who could communicate in English, as one aim of the intervention is to generate a high level of debate and discussion between group members and the practitioners, and practitioners were not available who could run a group in any language other than English. Funding was not available to use interpreters, nor would it necessarily be an ideal way to enable a participant to engage in group discussions. However, it is possible that this population, namely women not integrated into services owing to language barriers, might particularly benefit from this approach.
-
The nested study of women who had been looked after as children did not find the expected number, based on what had been identified for clients receiving FNP. Possibly the generally younger age of FNP clients was a factor, with gFNP clients not as vulnerable in terms of age, although the additional requirement of low educational qualifications was included. Thus, most of the evidence is conjectural, from relevant professionals involved in social care or from FNs who have had experience of FNP clients with a looked-after history.
-
Finally, taking part in research may act as an intervention itself with the attention given by interviewers to both the intervention and control groups, although this is more likely to have implications for some of the secondary outcomes such as mental health or social support than for the primary parenting outcomes.
Recommendations for future research
Evidence regarding the effectiveness of other group-based models of supporting vulnerable women in pregnancy (i.e. Centring Pregnancy) in terms of a range of health outcomes, alongside other briefer group-based preparation for parenthood programmes, suggest the value of examining which programme factors appear to be most strongly associated with better outcomes, in order to enhance the existing gFNP model.
Data from the current RCT should be used to identify those women who may be most likely to benefit from future provision of gFNP. This would involve identifying the characteristics of women who showed some change from gFNP pre to post intervention. It would also involve mapping those characteristics against the quality of the gFNP that was provided, as has been done elsewhere with infant massage. 169
It is encouraging that breastfeeding was enhanced in the intervention families and that in the process evaluation important learning about weaning was obtained. This suggests the potential value of postnatal group support that focuses mainly on infant feeding and weaning, possibly to complement one-to-one FNP, where no impact of weaning was identified. However, it should be noted that breastfeeding was only one of eight secondary outcomes. Thus, this finding would need replicating.
It should be noted when making any plans for trials into early interventions, starting in pregnancy, that there are different recording systems and restricted access for primary care and maternity care, which will mean that the identification of potential participants will be challenging.
Conclusions
This trial failed to show any benefit of gFNP compared with receiving care as usual during pregnancy and until infants were 1 year of age, except for an increased likelihood of breastfeeding up to 6 months. Our study results indicate that gFNP is unlikely to represent a cost-effective use of resources targeted at high-risk mothers and their children, but it must be noted that these findings may not be generalisable to gFNP delivered to larger groups, running for the full 44 weeks. The study also indicates that usual care within the NHS in the UK, which is more accessible and potentially more extensive than the medical attention received by participants in the US trials of FNP, is likely to achieve similar outcomes to the offer of a more intensive service.
Given the additional cost involved in delivering gFNP, it does not appear that this programme, in its current form and with the current target population, can be supported as a way of improving parenting or reducing the likelihood of holding views about parenting and children’s development that place the infant at risk of abuse or neglect. However, data from our economic evaluation can be used to inform future health economic studies in this area.
The study was well designed, on the basis of previous knowledge of FNP and on the implementation valuations of gFNP and was rigorously conducted and analysed. However, many months of preparation notwithstanding, it proved challenging to identify potential participants for the study so that they could be approached. The main consequence of this was that almost all the groups delivered were suboptimal in terms of the number of clients, even with the addition of ‘buffer’ clients. Thus, some dynamic exchange between group members in terms of beliefs or parenting practices, and between group members and the FNs facilitating the groups, may have been lost. The groups delivered in feasibility work were larger and many participants perceived substantial benefits, in particular in terms of one of the secondary outcomes in this study, social support, which was not shown to be affected by gFNP.
The smaller sample size, despite amending randomisation part way through so that more would be allocated to the intervention, also reduced the power of the study; this was especially true for the primary outcome (maternal sensitivity), when only just under two-thirds of study participants agreed to being video-recorded.
Not only were overall trial numbers reduced, but of those allocated to receive gFNP a substantial proportion did not receive the intervention, in many cases because insufficient numbers were recruited to make running a group viable. This is challenging for any future research. To establish larger groups, women need not only to live in close proximity, but also to have similar due dates and possibly fewer eligibility requirements. However, this would produce a less vulnerable group who would be less likely to show benefit from the programme. Careful consideration is needed to work out the best focus for this kind of group programme, which could have potential. Peer support has proved successful in helping parents to deal with older children’s challenging behaviour. 175 It remains to be seen how gFNP can be developed so that it can make a difference for potentially vulnerable parents, either in pregnancy or in infancy, or in both.
Acknowledgements
Contributions of authors
Professor Jacqueline Barnes (Professor of Psychology) conceived the original study design; led the grant application, was responsible for all ethical and other approvals for the study, was first author of the published protocol, directed the data collection team for the main study, chaired the TMG, directed the process evaluation conducting all the quantitative analyses and jointly analysing the qualitative data, wrote Chapter 1, co-authored Chapters 2 and 5 and contributed to all other chapters and finalised all aspects of the report.
Dr Jane Stuart (Research Fellow, Psychological Sciences) was trial manager, contributing to the design of the data collection instruments and managing acquisition of the trial data (quantitative and qualitative) from the participants, and gave input as a member of the TMG throughout the project. She jointly analysed the qualitative process evaluation, co-authored Chapter 5 and commented on all other chapters.
Dr Elizabeth Allen (Senior Lecturer, Medical Statistics) was a co-applicant on the grant application, gave input as a member of the TMG throughout the project, conducted the analyses for the main study and prepared the results for publication, also contributing to Chapter 2 (methods) and commenting on all other chapters.
Stavros Petrou (Professor of Health Economics) was a co-applicant on the grant application and was involved in its implementation. He provided oversight of the design, conduct, analysis and reporting of the health economic evaluation and gave input as a member of the TMG throughout the project. He also led on the writing of Chapter 4.
Ms Joanna Sturgess (Research Fellow, Medical Statistics) managed all the quantitative data entry and secure data storage, provided administrative support for the LACs substudy; and gave input as a member of the TMG throughout the project. She contributed to Chapters 2, 3 and 6 and commented on all other chapters.
Jane Barlow (Professor of Public Health in the Early Years) was a co-applicant on the grant application, contributed to the design of the study, gave input as a member of the TMG throughout the project, contributed to Chapters 1–3, 5–7 and commented on all other chapters.
Geraldine Macdonald (Professor of Social Care) was a co-applicant on the grant application, co-led the LACs substudy focusing on the design measures, gave input as a member of the TMG throughout the project and analysis of data, co-authored Chapter 6 and commented on all other chapters.
Helen Spiby (Professor of Midwifery) was involved in developing the protocol, supported recruitment and liaison with midwifery and gave input as a member of the TMG throughout the project. She has contributed to Chapters 1, 2 and 5, and commented on all other chapters.
Ms Dipti Aistrop (FNP Programme Manager) was involved in developing the protocol, gave input as a member of the TMG throughout the project, provided input on study instruments relevant to FNP staff, was involved in the finalisation of the DCE measure and interpretation of the DCE results, and commented on all chapters.
Edward Melhuish (Professor of Human Development) was a co-applicant on the grant application, was involved in developing the protocol, gave input as a member of the TMG throughout the project and commented on all other chapters.
Sungwook Kim (Research Associate in Health Economics) conducted the bulk of the analyses for the health economic evaluation and prepared the economic results for publication.
Dr Joshua Pink (Research Fellow in Health Economics) contributed to the design of the health economic evaluation. He conducted the bulk of the analyses for the DCE and prepared the results for publication.
Ms Jessica Datta (Lecturer, Public Health) conducted fieldwork for the nested LACs substudy, analysed data for the study and co-wrote Chapter 6, reviewing the final version of the report.
Diana Elbourne (Triallist and Professor of Healthcare Evaluation) was a co-applicant on the grant application, was involved in developing the protocol, gave input as a member of the TMG throughout the project, co-led the nested LACs substudy and conducted the related interviews with FNs, co-led the writing of sections of Chapters 2, 3 and 6, and commented on all other chapters.
Other contributors
We thank Claire Snowdon for her contributions to the development of the substudy on LACs, and her more general input into the trial as a member of the TMG from May 2012 to March 2015.
We thank Rachael Sharpe for providing administrative support throughout the trial.
We thank Dr Tracy Rydin-Orwin (Chartered Principal Clinical Psychologist) for conducting the CARE-Index coding for all videos, and Sara Hunnable (Independent Social Worker) for the reliability coding.
Dr Doug Simkiss (Honorary Associate Clinical Professor in Child Health, Warwick Medical School) provided feedback to the LACs substudy.
The delivery of gFNP was supported by local commissioners. The support of Mary Griffiths, Service Development and New Projects Lead at the FNP NU, has been invaluable throughout the project as has been the involvement of all the FNP teams, providing the gFNP programme, documenting their activities for the Economic Evaluation Team and taking part in qualitative interviews.
Publications
Barnes J, Aistrop D, Allen E, Barlow J, Elbourne D, Macdonald G, et al. First Steps: study protocol for a randomized trial of the effectiveness of the Group Family Nurse Partnership (gFNP) program compared to routine care in improving outcomes for high-risk mothers and their children and preventing abuse. Trials 2013;14:285.
Stuart J, Barnes J, Spiby H, Elbourne D. Understanding barriers to involving community midwives in identifying research participants; experience of the First Steps Randomised Controlled Trial. Midwifery 2015;31:779–86.
Barnes J, Stuart J, Allen E, Petrou S, Sturgess J, Barlow J, et al. Randomized controlled trial and economic evaluation of nurse-led group support for young mothers during pregnancy and the first year postpartum versus usual care. Trials 2017;18:508.
Datta J, Macdonald G, Barlow J, Barnes J, Elbourne D. Challenges faced by young mothers with a care history and views of stakeholders about the potential for Group Family Nurse Partnership to support their needs. Child Soc 2017;31:463–74.
Data sharing statement
Data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Statistical First Release SFR27/2010. London: Department for Education; 2012.
- Crime in England and Wales 2001/2002: Supplementary Volume. London: Home Office; 2003.
- Dias MS, Smith K, DeGuehery K, Mazur P, Li V, Shaffer ML. Preventing abusive head trauma among infants and young children: a hospital-based, parent education program. Pediatrics 2005;115:e470-7. https://doi.org/10.1542/peds.2004-1896.
- Sidebotham PD. Patterns of child abuse in early childhood, a cohort study of the ‘children of the nineties’. Child Abuse Rev 2000;9:311-20. https://doi.org/10.1002/1099-0852(200009/10)9:5<311::AID-CAR627>3.0.CO;2-U.
- Beebe B, Jaffe J, Markese S, Buck K, Chen H, Cohen P, et al. The origins of 12-month attachment: a microanalysis of 4-month mother-infant interaction. Attach Hum Dev 2010;12:3-141. http://dx.doi.org/10.1080/14616730903338985.
- De Wolff MS, van Ijzendoorn MH. Sensitivity and attachment: a meta-analysis on parental antecedents of infant attachment. Child Dev 1997;68:571-91. https://doi.org/10.1111/j.1467-8624.1997.tb04218.x.
- Meins E, Fernyhough C, Fradley E, Tuckey M. Rethinking maternal sensitivity: mothers’ comments on infants’ mental processes predict security of attachment at 12 months. J Child Psychol Psych 2001;42:637-48. https://doi.org/10.1111/1469-7610.00759.
- Slade A. Parental reflective functioning: an introduction. Attach Hum Dev 2005;7:269-81. https://doi.org/10.1080/14616730500245906.
- Skovgaard AM. Mental health problems and psychopathology in infancy and early childhood. An epidemiological study. Dan Med Bull 2010;57.
- Gunnar MR, Donzella B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology 2002;27:199-220. https://doi.org/10.1016/S0306-4530(01)00045-2.
- Schore AN. Affect Regulation and the Origin of the Self: The Neurobiology of Emotional Development. Hillsdale, NJ: Lawrence Erlbaum Associates; 1994.
- Field F. The Foundation Years: Preventing Poor Children From Becoming Poor Adults. London: DH; 2010.
- Allen G. Early Intervention: The Next Steps, An Independent Report To Her Majesty’s Government. London: HMSO; 2011.
- Munro E. Change in children’s social care. Br J Soc Work 2011;41:726-43. https://doi.org/10.1093/bjsw/bcr074.
- Conception to Age 2: The Age of Opportunity. London: Wave Trust; 2013.
- Leadsom A, Field F, Burstow P, Lucas C. The 1001 Critical Days: The Importance of the Conception to Age Two Period: A Cross Party Manifesto. London: DH; 2013.
- Marmot M. Fair Society, Healthy Lives. Independent Review Into Health Inequalities in England Post 2010. London: The Marmot Review; 2010.
- Healthy Lives, Healthy People. London: DH; 2010.
- Boyce WT, Ellis BJ. Biological sensitivity to context: I. an evolutionary-developmental theory of the origins and functions of stress reactivity. Dev Psychopathol 2005;17:271-30. https://doi.org/10.1017/S0954579405050145.
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA 2009;301:2252-9. http://dx.doi.org/10.1001/jama.2009.754.
- Mikton C, Butchart A. Child maltreatment prevention: a systematic review of reviews. Bull World Health Organ 2009;87:353-61. https://doi.org/10.2471/BLT.08.057075.
- Avellar S, Paulsell D, Sama-Miller E, Del Grosso P. Home Visiting Evidence of Effectiveness Review: Executing Summary. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2012.
- Olds DL. The nurse–family partnership: an evidence-based preventive intervention. Inf Mental Hlth J 2006;27:5-25. https://doi.org/10.1002/imhj.20077.
- Model Programs. Denver, CO: Centre for the Study and Prevention of Violence, University of Colorado; 2010.
- Macmillan HL, Wathen CN, Barlow J, Fergusson DM, Leventhal JM, Taussig HN. Interventions to prevent child maltreatment and associated impairment. Lancet 2009;373:250-66. http://dx.doi.org/10.1016/S0140-6736(08)61708-0.
- Olds DL, Eckenrode J, Henderson CR, Kitzman H, Powers J, Cole R, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. JAMA 1997;278:637-43. https://doi.org/10.1001/jama.1997.03550080047038.
- Olds D, Kitzman H, Cole R, Robinson J. Theoretical foundations of a program of home visitation for pregnant women and parents of young children. J Community Psychol 1997;25:9-25. https://doi.org/10.1002/(SICI)1520-6629(199701)25:1<9::AID-JCOP2>3.0.CO;2-V.
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. https://doi.org/10.1037/0033-295X.84.2.191.
- Bowlby J. Attachment and Loss. Volume 1. Attachment. New York, NY: Basic Books; 1969.
- Kitzman H, Olds DL, Henderson CR, Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. JAMA 1997;278:644-52. https://doi.org/10.1001/jama.1997.03550080054039.
- Eckenrode J, Campa M, Luckey DW, Henderson CR, Cole R, Kitzman H, et al. Long-term effects of prenatal and infancy nurse home visitation on the life course of youths: 19-year follow-up of a randomized trial. Arch Pediatr Adolesc Med 2010;164:9-15. http://dx.doi.org/10.1001/archpediatrics.2009.240.
- Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, et al. Effects of home visits by paraprofessionals and by nurses: age-four follow-up of a randomized trial. Pediatrics 2004;114:1560-68. https://doi.org/10.1542/peds.2004-0961.
- Aos S, Lieb R, Mayfield J, Miller M, Pennucci A. Benefits and Costs of Prevention and Early Intervention Programs for Youth. Olympia, WA: Washington State Institute for Public Policy; 2004.
- Olds DL, Henderson CR, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics 1986;78:65-78.
- Barnes J, Ball M, Meadows P, McLeish J, Belsky J. Nurse–Family Partnership: First Year Pilot Sites Implementation in England. Pregnancy and the Post-Partum Period. London: Department for Children, Schools and Families; 2008.
- The Family Nurse Partnership Programme. London: DH; 2012.
- Robling M, Bekkers MJ, Bell K, Butler CC, Cannings-John R, Channon S, et al. Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (Building Blocks): a pragmatic randomised controlled trial. Lancet 2016;387:146-55. http://dx.doi.org/10.1016/S0140-6736(15)00392-X.
- Barnes J, Ball M, Meadows P, Belsky J. Nurse–Family Partnership Programme: Second Year Pilot Sites Implementation in England. The Infancy Period. Research Report DCSF-RR166. London: Department for Children, Schools and Families; 2009.
- Barnes J, Ball M, Meadows P, Howden B, Jackson A, Henderson J, et al. The Family–Nurse Partnership Programme in England: Wave 1 Implementation in Toddlerhood and a Comparison Between Waves 1 and 2a of Implementation in Pregnancy and Infancy. London: DH; 2011.
- Ball M, Barnes J, Meadows P. Issues Emerging from the First 10 Pilot Sites Implementing the Nurse–Family Partnership Home-Visiting Programme in England. London: DH; 2012.
- Barnes J, Howden B, Niven L, Ball M. Eligibility for the Family Nurse Partnership Programme. Testing New Criteria. London: DH; 2012.
- Miller WR, Rollnick S. Motivational Interviewing. Helping People Change. New York, NY: Guilford Press; 2012.
- Ferguson H, Gates P. Early intervention and holistic, relationship-based practice with fathers: evidence from the work of the Family Nurse Partnership. Child Fam Work 2015;20:96-105. https://doi.org/10.1111/cfs.12059.
- Family Nurse Partnership National Unit . Research and Development. Group FNP 2015. http://fnp.nhs.uk/evidence/developments (accessed 27 November 2015).
- Griffiths M. Group family nurse partnership: transferable learning from an intensive parenting preparation group. IJBPE 2016;3:29-32.
- Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol 2007;110:330-9. https://doi.org/10.1097/01.AOG.0000275284.24298.23.
- Williams KJ, Zolotor A, Kaufmann L. Clinical inquiries: does group prenatal care improve pregnancy outcomes?. J Fam Pract 2009;58:384a-c.
- Serçekuş P, Mete S. Effects of antenatal education on maternal prenatal and postpartum adaptation. J Adv Nurs 2010;66:999-1010. http://dx.doi.org/10.1111/j.1365-2648.2009.05253.x.
- de Jonge A. Support for teenage mothers: a qualitative study into the views of women about the support they received as teenage mothers. J Adv Nurs 2001;36:49-57. https://doi.org/10.1046/j.1365-2648.2001.01942.x.
- Stevenson MD, Scope A, Sutcliffe PA, Booth A, Slade P, Parry G, et al. Group cognitive behavioural therapy for postnatal depression: a systematic review of clinical effectiveness, cost-effectiveness and value of information analyses. Health Technol Assess 2010;14. https://doi.org/10.3310/hta14440.
- Hoddinott P, Chalmers M, Pill R. One-to-one or group-based peer support for breastfeeding? Women’s perceptions of a breastfeeding peer coaching intervention. Birth 2006;33:139-46. https://doi.org/10.1111/j.0730-7659.2006.00092.x.
- Getting Maternity Services Right for Pregnant Teenagers and Young Fathers. London: Public Health England; 2015.
- Shribman S, Billingham K. Healthy Child Programme. Pregnancy and the First Five Years. London: DH; 2009.
- Anning A, Ball M. Improving Services for Young Children. From Sure Start to Children’s Centres. London: Sage; 2008.
- Preparation for Birth and Beyond. A Resource Pack for Leaders of Community Groups and Activities. London: DH; 2011.
- Barnes J, Henderson J. Summary of the Formative Evaluation of the First Phase of the Group-Based Family Nurse Partnership Programme. London: DH; 2012.
- Ickovics JR, Kershaw TS, Westdahl C, Rising SS, Klima C, Reynolds H, et al. Group prenatal care and preterm birth weight: results from a matched cohort study at public clinics. Obstet Gynecol 2003;102:1051-7. https://doi.org/10.1097/00006250-200311000-00030.
- Robertson B, Aycock DM, Darnell LA. Comparison of centering pregnancy to traditional care in Hispanic mothers. Matern Child Health J 2009;13:407-14. http://dx.doi.org/10.1007/s10995-008-0353-1.
- Grady MA, Bloom KC. Pregnancy outcomes of adolescents enrolled in a CenteringPregnancy program. J Midwifery Womens Health 2004;49:412-20. http://dx.doi.org/10.1016/j.jmwh.2004.05.009.
- Gaudion A, Menka Y, Demilew J, Walton C, Yiannouzis K, Robbins J, et al. Findings from a UK feasibility study of the Centering Pregnancy Model. Br J Midwifery 2011;19:796-802. https://doi.org/10.12968/bjom.2011.19.12.796.
- Antenatal Care. Routine Care for the Healthy Pregnant Woman. London: NICE; 2008.
- Baldwin KA. Comparison of selected outcomes of CenteringPregnancy versus traditional prenatal care. J Midwifery Womens Health 2006;51:266-72. https://doi.org/10.1016/j.jmwh.2005.11.011.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- A Framework for the Development and Evaluation of RCTs for Complex Interventions to Improve Health. London: MRC; 2000.
- Olds D, Donelan-McCall N, O’Brien R, MacMillan H, Jack S, Jenkins T, et al. Improving the nurse–family partnership in community practice. Pediatrics 2013;132:110-17. http://dx.doi.org/10.1542/peds.2013-1021I.
- Barnes J, Stuart J. Evaluation of Group Family Nurse Partnership. Phase. London: Institute for the Study of Children, Families and Social Issues, Birkbeck, University of London; 2014.
- Barnes J, Stuart S. Developing and evaluating a new intervention: the feasibility of Group Family Nurse Partnership (gFNP). J Child Serv 2016;11:170-86. https://doi.org/10.1108/JCS-12-2015-0035.
- Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage; 2011.
- Wagner C, Ingersoll K. Motivational Interviewing in Groups. London: Guilford Press; 2013.
- Hawkins P, Shohet R. Supervision in the Helping Professions. Kent: Open University Press; 2012.
- Bavolek SJ, Keene RG. Adult-Adolescent Parenting Inventory AAPI-2: Administration and Development Handbook. Park City, UT: Family Development Resources; 2001.
- Crittenden PM. Abusing, neglecting, problematic, and adequate dyads: differentiating by patterns of interaction. Merrill Palmer Quart 1981;27:1-18.
- Crittenden PM. CARE-Index Infants and Toddlers: Coding Manual. Miami, FL: Family Relations Institute; 2001.
- Cramer B, Robert-Tissot C, Stern DN, Serpa-Rusconi S, De Muralt M, Besson G, et al. Outcome evaluation in brief mother–infant psychotherapy: a preliminary report. Inf Mental Hlth J 1990;11:278-300. http://dx.doi.org/10.1002/1097-0355(199023)11:3%3C278::AID-IMHJ2280110309%3E3.0.CO;2-H.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. https://doi.org/10.1192/bjp.150.6.782.
- Abidin R. Parenting Stress Index: Professional Manual. Lutz, FL: Psychological Assessment Resources, Inc.; 1995.
- Lacharite C, Ethier LS, Couture G. Sensitivity and specificity of the parenting stress index in situations of child maltreatment. Can J Behav Sci 1999;31:217-20.
- Mash EJ, Johnston C, Kovitz K. A comparison of the mother–child interactions of physically abused and non-abused children during play and task situations. J Clin Child Psychol 1983;12:337-46. https://doi.org/10.1080/15374418309533154.
- Nair P, Schuler ME, Black MM, Kettinger L, Harrington D. Cumulative environmental risk in substance abusing women: early intervention, parenting stress, child abuse potential and child development. Child Abuse Negl 2003;27:997-1017. https://doi.org/10.1016/S0145-2134(03)00169-8.
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. J Clin Child Psychol 1989;18:167-75. https://doi.org/10.1207/s15374424jccp1802_8.
- Gilmore L, Cuskelly M. Factor structure of the Parenting Sense of Competence scale using a normative sample. Child Care Health Dev 2009;35:48-55. http://dx.doi.org/10.1111/j.1365-2214.2008.00867.x.
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705-14. https://doi.org/10.1016/0277-9536(91)90150-B.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Erlbaum; 1988.
- Barnes J, Aistrop D, Allen E, Barlow J, Elbourne D, Macdonald G, et al. First Steps: study protocol for a randomized trial of the effectiveness of the Group Family Nurse Partnership (gFNP) program compared to routine care in improving outcomes for high-risk mothers and their children and preventing abuse. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-285.
- Stuart J, Barnes J, Spiby H, Elbourne D. Understanding barriers to involving community midwives in identifying research participants; experience of the first steps randomised controlled trial. Midwifery 2015;31:779-86. http://dx.doi.org/10.1016/j.midw.2015.04.011.
- Mooney CZ, Duval RD. Bootstrapping: A Nonparametric Approach to Statistical Inference. Newbury Park, CA: Sage; 1993.
- Dunn G, Maracy M, Tomenson B. Estimating treatment effects from randomized clinical trials with noncompliance and loss to follow-up: the role of instrumental variable methods. Stat Methods Med Res 2005;14:369-95. https://doi.org/10.1191/0962280205sm403oa.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- Dolan P. Modelling valuations for EuroQoL health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Barnes J, Stuart J, Allen E, Petrou S, Sturgess J, Barlow J. Randomized controlled trial and economic evaluation of nurse-led group support for young mothers during pregnancy and the first year postpartum versus usual care. Trials 2017;18. https://doi.org/10.1186/s13063-017-2259-y.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- Motoring Costs 2014. Version 2. London: AA; 2014.
- Department for Transport (DfT) Public Service Vehicle Survey: Bus Statistics. London: Department for Transport; 2015.
- NHS Reference Costs 2014–2015. National Schedule of Reference Costs. London: DH; 2014.
- Curtis L. Unit Costs of Health and Social Care 2015. Canterbury: University of Kent, Personal Social Services Research Unit; 2014.
- British National Formulary. London: British Medical Association, Royal Pharmaceutical Society of Great Britain; 2014.
- British National Formulary for Children. London: British Medical Association, Royal Pharmaceutical Society of Great Britain; 2013.
- Annual Survey of Hours and Earnings. London: Office for National Statistics; 2012.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. http://dx.doi.org/10.1016/j.jval.2012.02.008.
- Devlin N, Shah K, Feng Y, Mulhern B, van Hout B. Valuing Health-Related Quality of Life: An EQ-5D-5L Value Set for England. Research Paper 1601. London: Office of Health Economics; 2016.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377-99. http://dx.doi.org/10.1002/sim.4067.
- Horton NJ, Lipsitz SR. Multiple imputation in practice: comparison of software packages for regression models with missing variables. Am Stat 2001;55:244-54. https://doi.org/10.1198/000313001317098266.
- van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 1999;18:681-94. http://dx.doi.org/10.1002/(SICI)1097-0258(19990330)18:6%3C681::AID-SIM71%3E3.0.CO;2-R.
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. Chichester: John Wiley & Sons; 2004.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8. https://doi.org/10.3310/hta8360.
- Mentzakis E, Ryan M, McNamee P. Using discrete choice experiments to value informal care tasks: exploring preference heterogeneity. Health Econ 2011;20:930-44. http://dx.doi.org/10.1002/hec.1656.
- McIntosh E. Using discrete choice experiments within a cost-benefit analysis framework: some considerations. Pharmacoeconomics 2006;24:855-68. https://doi.org/10.2165/00019053-200624090-00004.
- Lancaster K. New approach to consumer theory. J Polit Econ 1966;74:132-57. https://doi.org/10.1086/259131.
- McFadden D, Melvin JR, Moore JC, Riezman R. Essays in Honour of John S. Chipman. Studies in the Modern World Economy. London: Routledge; 1999.
- Bridges JFP, Hauber AB, Marshall D, Lloyd D, Prosser L, Regier D, et al. Conjoint analysis applications in health – a checklist: a report of the ISPOR good research practices for conjoint analysis task force. Value Health 2011;14:403-13. https://doi.org/10.1016/j.jval.2010.11.013.
- Coast J, Al-Janabi H, Sutton EJ, Horrocks SA, Vosper AJ, Swancutt DR, et al. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ 2012;21:730-41. http://dx.doi.org/10.1002/hec.1739.
- Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics 2008;26:661-77. https://doi.org/10.2165/00019053-200826080-00004.
- Kruijshaar ME, Essink-Bot ML, Donkers B, Looman CW, Siersema PD, Steyerberg EW. A labelled discrete choice experiment adds realism to the choices presented: preferences for surveillance tests for Barrett esophagus. BMC Med Res Methodol 2009;9. http://dx.doi.org/10.1186/1471-2288-9-31.
- Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Mühlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health 2013;16:3-13. http://dx.doi.org/10.1016/j.jval.2012.08.2223.
- The E-vita Open Plus for Treating Complex Aneurysms and Dissections of the Thoracic Aorta (MTG16). London: NICE; 2013.
- Rutter J. Childcare Costs Survey 2015. London: Family and Childcare Trust; 2015.
- Probation Trusts Unit Costs Financial Year 2011–12 (Revised). London: Ministry of Justice; 2012.
- Curtis L, Netten A. Unit Costs of Health and Social Care 2005. Canterbury: Personal Social Services Research Unit, University of Kent; 2005.
- Stuart J, Barnes J. Evaluation of Group Family Nurse Partnership Development. Phase 3. Interim Findings. Report to the Family Nurse Partnership National Unit. London: Birkbeck, University of London; 2013.
- Rising SS, Kennedy HP, Klima CS. Redesigning prenatal care through CenteringPregnancy. J Midwifery Womens Health 2004;49:398-404. http://dx.doi.org/10.1016/j.jmwh.2004.04.018.
- Barnes J, Henderson J. Final Report on the Infancy Phase of the Formative Evaluation of the First Phase of the Group-Based Antenatal Care Project. Report Submitted to the Department of Health. London: Birkbeck, University of London; 2011.
- Henderson J, Barnes J. Interim Report on Recruitment and the Pregnancy Phase of the Formative Evaluation of the Group-Based Antenatal Care Project. Report to the Department of Health. London: Institute for the Study of Children, Families and Social Issues, Birkbeck, University of London; 2010.
- Robson C. Real World Research. Chichester: Wiley; 2011.
- Datta J, Macdonald G, Barlow J, Barnes J, Elbourne D. Challenges faced by young mothers with a care history and views of stakeholders about the potential for Group Family Nurse Partnership to support their needs. Child Soc 2017;31:463-74. https://doi.org/10.1111/chso.12233.
- Canova C, Pitter G, Ludvigsson JF, Romor P, Zanier L, Zanotti R, et al. Risks of hospitalization and drug consumption in children and young adults with diagnosed celiac disease and the role of maternal education: a population-based matched birth cohort study. BMC Gastroenterol 2016;16. http://dx.doi.org/10.1186/s12876-015-0415-y.
- Children (Leaving Care) Act 2000. London: The Stationery Office; 2000.
- Children and Young Persons Act 2008. London: The Stationery Office; 2008.
- Children and Families Act 2014. London: The Stationery Office; 2014.
- Zayed Y, Harker R. Children in Care in England: Statistics. House of Commons Library Briefing Paper No. 04470. London: House of Commons Library; 2015.
- Rees P. The mental health, emotional literacy, cognitive ability, literacy attainment and ‘resilience’ of ‘looked after children’: a multidimensional, multiple-rater population based study. Br J Clin Psychol 2013;52:183-98. http://dx.doi.org/10.1111/bjc.12008.
- Zlotnick C, Tam TW, Soman LA. Life course outcomes on mental and physical health: the impact of foster care on adulthood. Am J Public Health 2012;102:534-40. http://dx.doi.org/10.2105/AJPH.2011.300285.
- Simkiss D. Looked-After Children and Young People. Department of Health Chief Medical Officer’s Annual Report 2012: Our Children Deserve Better: Prevention Pays. London: DH; 2013.
- Carpenter SC, Clyman RB, Davidson AJ, Steiner JF. The association of foster care or kinship care with adolescent sexual behavior and first pregnancy. Pediatrics 2001;108. https://doi.org/10.1542/peds.108.3.e46.
- Hobcraft J. Intergenerational and Life-Course Transmission of Social Exclusion: Influences and Childhood Poverty, Family Disruption and Contact with the Police. STICERD Research Paper No. CASE015. London: London School of Economics; 1998.
- Vinnerljung B, Sallnäs M. Into adulthood: a follow-up study of 718 young people who were placed in out-of-home care during their teens. Child Fam Soc Work 2008;13:144-55. https://doi.org/10.1111/j.1365-2206.2007.00527.x.
- Evans A. We Don’t Choose to be Homeless. London: CHAR Housing Campaign for Single People; 1996.
- Jay A. Independent Inquiry into Child Sexual Exploitation in Rotherham 1997–2013. Rotherham: Metropolitan Borough Council; 2014.
- Viner RM, Taylor B. Adult health and social outcomes of children who have been in public care: population-based study. Pediatrics 2005;115:894-99. https://doi.org/10.1542/peds.2004-1311.
- Dregan A, Gulliford MC. Foster care, residential care and public care placement patterns are associated with adult life trajectories: population-based cohort study. Soc Psychiatry Psychiatr Epidemiol 2012;47:1517-26. http://dx.doi.org/10.1007/s00127-011-0458-5.
- Sebba J, Berridge D, Luke N, Fletcher J, Bell K, Strand S, et al. The Educational Progress of Looked After Children in England: Linking Care and Educational Data. Bristol: Rees Centre, University of Bristol; 2015.
- Dowdney L, Skuse D, Rutter M, Quinton D, Mrazek D. The nature and qualities of parenting provided by women raised in institutions. J Child Psychol Psychiatry 1985;26:599-625. https://doi.org/10.1111/j.1469-7610.1985.tb01644.x.
- Quinton D, Rutter M, Liddle C. Institutional rearing, parenting difficulties and marital support. Psychol Med 1984;14:107-24. https://doi.org/10.1017/S0033291700003111.
- Barn R, Andrew L, Mantovani N. Life After Care: The Experiences of Young People From Different Ethnic Groups. London: Joseph Rowntree Foundation; 2005.
- Hall D, Hall S. The ‘Family-Nurse Partnership’: Developing an Instrument for Identification, Assessment and Recruitment of Clients. Research Report DCSF-RW022. London: Department for Children, Schools and Families; 2007.
- Chase E, Maxwell C, Knight A, Aggleton P. Pregnancy and parenthood among young people in and leaving care: what are the influencing factors, and what makes a difference in providing support?. J Adolesc 2006;29:437-51. https://doi.org/10.1016/j.adolescence.2006.01.003.
- Botchway SK, Quigley MA, Gray R. Pregnancy-associated outcomes in women who spent some of their childhood looked after by local authorities: findings from the UK Millennium Cohort Study. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2014-005468.
- Rolfe A. ‘You’ve got to grow up when you’ve got a kid’: marginalized young women’s accounts of motherhood. J Community Appl Soc 2008;18:299-314. https://doi.org/10.1002/casp.925.
- Birtwell B, Hammond L, Puckering C. ‘Me and my bump’: an interpretative phenomenological analysis of the experiences of pregnancy for vulnerable women. Clin Child Psychol Psychiatry 2015;20:218-38. http://dx.doi.org/10.1177/1359104513506427.
- Maxwell A, Proctor J, Hammond L. ‘Me and my child’: parenting experiences of young mothers leaving care. Adopt Foster 2011;35:29-40. https://doi.org/10.1177/030857591103500404.
- Heifetz M, Connolly J, Bohr Y. Pregnancy and motherhood among adolescent girls in child protective services: a meta-synthesis of qualitative research. J Public Child Welf 2012;6:614-35. https://doi.org/10.1080/15548732.2012.723970.
- Pryce JM, Samuels GM. Renewal and risk: the dual experience of young motherhood and aging out of the child welfare system. J Adolescent Res 2010;25:205-30. https://doi.org/10.1177/0743558409350500.
- Barn R, Mantovani N. Young mothers and the care system: contextualising risk and vulnerability. Brit J Soc Work 2007;37:225-43. https://doi.org/10.1093/bjsw/bcl002.
- Dworsky A, Courtney ME. The risk of teenage pregnancy among transitioning foster youth: implications for extending state care beyond age 18. Child Youth Serv Rev 2010;32:1351-6. https://doi.org/10.1016/j.childyouth.2010.06.002.
- Boonstra HD. Teen pregnancy among young women in foster care: a primer. Guttmacher Policy Rev 2011;14:8-19.
- Stein M, Munro ER. The Transition to Adulthood for Young People Leaving Public Care: International Comparisons and Perspectives n.d.
- Looked-After Children and Young People. NICE Guideline PH28. London: NICE; 2010.
- Palmer ML, Henderson M, Sanders MR, Keown LJ, White J. Study protocol: evaluation of a parenting and stress management programme: a randomised controlled trial of Triple P Discussion Groups and Stress Control. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-888.
- White J, Thompson L, Puckering C, Waugh H, Henderson M, MacBeth A, et al. Antenatal parenting support for vulnerable women: an exploratory randomised controlled trial of mellow bumps versus chill-out in pregnancy or care as usual. Br J Midwifery 2015;23:724-32. https://doi.org/10.12968/bjom.2015.23.10.724.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Hastings A, Bailey N, Bramley G, Gannon M, Watkins D. The Cost of the Cuts: The Impact on Local Government and Poorer Communities. York: Joseph Rowntree Foundation; 2015.
- Cann R, Lawson K. Cuts: The View From Foster Carers. London: Fostering Network; 2016.
- Mejdoubi J, van den Heijkant SC, van Leerdam FJ, Crone M, Crijnen A, HiraSing RA. Effects of nurse home visitation on cigarette smoking, pregnancy outcomes and breastfeeding: a randomized controlled trial. Midwifery 2014;30:688-95. http://dx.doi.org/10.1016/j.midw.2013.08.006.
- Health Topics. Breastfeeding. Geneva: World Health Organization; 2016.
- Britton JR, Britton HL, Gronwaldt V. Breastfeeding, sensitivity, and attachment. Pediatrics 2006;118:e1436-43. https://doi.org/10.1542/peds.2005-2916.
- Tharner A, Luijk MP, Raat H, Ijzendoorn MH, Bakermans-Kranenburg MJ, Moll HA, et al. Breastfeeding and its relation to maternal sensitivity and infant attachment. J Dev Behav Pediatr 2012;33:396-404. http://dx.doi.org/10.1097/DBP.0b013e318257fac3.
- Community HUGS. Happiness, Understanding, Giving and Sharing. Heidelberg Heights, Melbourne, VIC; n.d.
- Underdown A, Norwood R, Barlow J. A realist evaluation of the processes and outcomes of infant massage programs. Inf Mental Hlth J 2013;34:483-95. https://doi.org/10.1002/imhj.21408.
- Novick G, Sadler LS, Knafl KA, Groce NE, Kennedy HP. In a hard spot: providing group prenatal care in two urban clinics. Midwifery 2013;29:690-7. http://dx.doi.org/10.1016/j.midw.2012.06.013.
- Keys D. Optimizing Wellbeing: Young Mothers’ Participation in Parents’ Groups. Melbourne, VIC: Key Centre for Women’s Health in Society, School of Population Health, University of Melbourne; 2008.
- Petch J, Halford WK. Psycho-education to enhance couples’ transition to parenthood. Clin Psychol Rev 2008;28:1125-37. http://dx.doi.org/10.1016/j.cpr.2008.03.005.
- Petrou S, Murray L, Cooper P, Davidson LL. The accuracy of self-reported healthcare resource utilization in health economic studies. Int J Technol Assess Health Care 2002;18:705-10. https://doi.org/10.1017/S026646230200051X.
- Clarke PM, Fiebig DG, Gerdtham UG. Optimal recall length in survey design. J Health Econ 2008;27:1275-84. http://dx.doi.org/10.1016/j.jhealeco.2008.05.012.
- Day C, Michelson D, Thomson S, Penney C, Draper L. Evaluation of a peer led parenting intervention for disruptive behaviour problems in children: community based randomised controlled trial. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e1107.
Appendix 1 Demographic updates at each time point
| Category | Intervention (N = 75), n (%) | Control (N = 53), n (%) |
|---|---|---|
| Change in partner since baseline? | ||
| Yes | 11 (14.7) | 8 (15.1) |
| No | 64 (85.3) | 45 (84.9) |
| Change in marital status since baseline? | ||
| Yes | 5 (6.7) | 2 (3.9) |
| No | 70 (93.3) | 50 (96.2) |
| Moved since baseline? | ||
| Yes | 25 (33.3) | 11 (20.8) |
| No | 50 (66.7) | 42 (79.3) |
| Made contact with a refuge? | ||
| Yes | 0 (0.0) | 0 (0.0) |
| No | 74 (100.0) | 53 (100.0) |
| Category | Intervention (N = 70), n (%) | Control (N = 51), n (%) |
|---|---|---|
| Change in partner since baseline? | ||
| Yes | 12 (17.1) | 3 (5.9) |
| No | 58 (82.9) | 48 (94.1) |
| Change in marital status since baseline? | ||
| Yes | 1 (1.6) | 0 (0.0) |
| No | 61 (98.4) | 44 (100.0) |
| Moved since baseline? | ||
| Yes | 14 (21.9) | 12 (25.5) |
| No | 50 (78.1) | 35 (74.5) |
| Change in members of household? | ||
| Yes | 8 (11.6) | 7 (14.0) |
| No | 61 (88.4) | 43 (86.0) |
| Made contact with a refuge? | ||
| Yes | 1 (1.5) | 0 (0.0) |
| No | 68 (98.6) | 51 (100.0) |
| Why was contact made: | ||
| Police | 1 (100) | |
| Length of stay in days | 7 | |
| Category | Intervention (N = 75), n (%) | Control (N = 56), n (%) |
|---|---|---|
| Change in partner since last visit? | ||
| Yes | 9 (12.0) | 7 (12.5) |
| No | 66 (88.0) | 49 (87.5) |
| Change in marital status since last visit? | ||
| Yes | 0 (0.0) | 1 (1.9) |
| No | 74 (100.0) | 53 (98.2) |
| Change in members of household since last visit? | ||
| Yes | 13 (17.8) | 8 (14.3) |
| No | 60 (82.2) | 48 (85.7) |
| Made contact with a refuge since last visit? | ||
| Yes | 1 (1.3) | 2 (3.6) |
| No | 74 (98.7) | 54 (96.4) |
Appendix 2 Sensitivity analyses
First sensitivity analyses: all participants
| Measure | Intervention (N = 81), mean (SE) | Control (N = 57), mean (SE) | Unadjusted effect estimatea | Adjusted effect estimateb | ||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |||
| AAPI-2 (higher = positive) | ||||||
| Total (/10) | 7.5 (0.1) | 7.5 (0.1) | 0.02 (–0.19 to 0.23) | 0.83 | 0.02 (–0.18 to 0.24) | 0.83 |
| Missing, n | 7 | 1 | ||||
| CARE-Index | n = 61 | n = 44 | ||||
| 3.8 (0.3) | 4.7 (0.4) | –0.84 (–1.71 to 0.07) | 0.13 | –0.73 (–1.60 to 0.12) | 0.18 | |
| Measure | Intervention, mean (SE) | Control, mean (SE) | Unadjusted effect estimatea | Adjusted effect estimateb | ||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |||
| CARE-Index | n = 61 | n = 44 | ||||
| Infant co-operativeness | 2.9 (0.3) | 3.5 (0.3) | –0.54 (–1.31 to 0.21) | 0.30 | –0.47 (–1.27 to 0.26) | 0.36 |
| EPDS (higher = more depressed) | n = 84 | n = 60 | ||||
| Total (/30): 2 months | 3.4 (0.5) | 3.5 (0.5) | ||||
| Missing, n | 1 | 1 | ||||
| Total (/30): 6 months | 3.1 (0.5) | 3.0 (0.6) | ||||
| Total (/30): 12 months | 3.8 (0.5) | 4.1 (0.6) | –0.12 (–0.48 to 0.73) | 0.68 | –0.03 (–0.63 to 0.57) | 0.92 |
| Missing, n | 1 | 1 | ||||
| PSOC (higher = more competence) | n = 84 | n = 60 | ||||
| Total (/102): 2 months | 60.6 (0.6) | 60.7 (0.5) | ||||
| Missing, n | 3 | 1 | ||||
| Total (/102): 12 months | 60.9 (0.4) | 60.7 (0.6) | 0.12 (–0.48 to 0.73) | 0.68 | 0.08 (–0.76 to 0.91) | 0.86 |
| Missing, n | 2 | |||||
| PSI (higher = more stress) | n = 84 | n = 60 | ||||
| Total (/180): 2 months | 70.5 (1.9) | 68.3 (1.8) | ||||
| Missing, n | 3 | 1 | ||||
| Total (/180): 12 months | 73.4 (1.5) | 74.9 (2.0) | –0.72 (–3.25 to 1.80) | 0.56 | –0.89 (–3.46 to 1.68) | 0.50 |
| Missing, n | 1 | 2 | ||||
| Social networks (higher = more support) | n = 81 | n = 57 | ||||
| Total (/100) | 85.1 (2.0) | 84.6 (2.3) | –0.03 (–5.09 to 5.08) | 0.99 | 0.07 (–5.18 to 5.00) | 0.98 |
| Missing, n | 2 | 1 | ||||
| Relationships (higher = abuse) | n = 81 | n = 57 | ||||
| Total abuse (/6) | 0.4 (0.1) | 0.5 (0.1) | –0.06 (–0.37 to 0.21) | 0.66 | –0.08 (–0.37 to 0.21) | 0.55 |
| Smoking, alcohol and drugs | n = 81 | n = 57 | ||||
| Combined smoking score (/24) | 3.1 (0.3) | 3.2 (0.4) | –0.12 (–1.07 to 0.90) | 0.83 | –0.09 (–1.02 to 0.95) | 0.86 |
| Still breastfeeding at 6 months | n = 82 | n = 55 | ||||
| Yes | 16 (19.5) | 4 (7.3) | 3.1 (0.97 to 9.81) | 0.06 | 3.51 (1.05 to 11.69) | 0.05 |
| No | 66 (80.5) | 51 (92.7) | 1 | |||
Second sensitivity analyses: with random effect included for groups in which intervention was delivered
| Measure | Intervention (N = 75), mean (SE) | Control (N = 56), mean (SE) | Unadjusted effect estimatea | Adjusted effect estimateb | ||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |||
| APPI-2 (higher = positive) | ||||||
| Total (/10) | 7.5 (0.1) | 7.5 (0.1) | 0.05 (–0.16 to 0.26) | 0.66 | 0.08 (–0.13 to 0.29) | 0.47 |
| Missing, n | 5 | 1 | ||||
| CARE-Index | n = 57 | n = 44 | ||||
| Mother’s sensitivity | 4.0 (0.3) | 4.7 (0.4) | –0.70 (–1.56 to 0.17) | 0.12 | –0.78 (–1.65 to 0.09) | 0.08 |
| Measure | Intervention (N = 75), mean (SE) | Control (N = 56), mean (SE) | Unadjusted effect estimatea | Adjusted effect estimateb | ||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |||
| CARE-Index | n = 57 | n = 44 | ||||
| Infant co-operativeness | 3.0 (0.3) | 3.5 (0.3) | –0.44 (–1.21 to 0.40) | 0.27 | –0.50 (–1.28 to 0.21) | 0.21 |
| EPDS (higher = more depressed) | n = 84 | n = 60 | ||||
| Total (/30): 2 months | 3.4 (0.5) | 3.5 (0.5) | ||||
| Missing, n | 1 | 1 | ||||
| Total (/30): 6 months | 3.1 (0.5) | 3.0 (0.6) | ||||
| Total (/30): 12 months | 3.8 (0.5) | 4.1 (0.6) | 0.23 (–0.86 to 1.32) | 0.68 | 0.25 (–0.84 to 1.34) | 0.58 |
| Missing, n | 1 | 1 | ||||
| PSOC (higher = more competent) | n = 84 | n = 60 | ||||
| Total (/102): 2 months | 60.6 (0.6) | 60.7 (0.5) | ||||
| Missing, n | 3 | 1 | ||||
| Total (/102): 12 months | 60.9 (0.4) | 60.7 (0.6) | –0.12 (–1.30 to 1.05) | 0.84 | –0.14 (–1.32 to 1.04) | 0.82 |
| Missing, n | 2 | |||||
| PSI (higher = more stress) | n = 84 | n = 60 | ||||
| Total (/180): 2 months | 70.5 (1.9) | 68.3 (1.8) | ||||
| Missing, n | 3 | 1 | ||||
| Total (/180): 12 months | 73.4 (1.5) | 74.9 (2.0) | –0.73 (–5.26 to 3.80) | 0.75 | –0.66 (–5.21 to 3.89) | 0.78 |
| Missing, n | 1 | 2 | ||||
| Social networks (higher = more support) | n = 75 | n = 56 | ||||
| Total (/100) | 84.6 (2.2) | 84.5 (2.3) | –0.47 (–6.14 to 5.21) | 0.87 | –0.54 (–6.33 to 5.15) | 0.85 |
| Missing, n | 2 | 1 | ||||
| Relationships (higher = abuse) | n = 75 | n = 56 | ||||
| Total abuse (/6) | 0.4 (0.1) | 0.5 (0.1) | –0.07 (–0.33 to 0.20) | 0.62 | –0.09 (–0.35 to 0.18) | 0.52 |
| Smoking, alcohol and drugs | n = 75 | n = 56 | ||||
| Combined substance abuse score (/24) | 17 (0.3) | 16.6 (0.3) | –0.12 (–1.10 to 0.86) | 0.80 | –0.10 (–1.08 to 0.89) | 0.85 |
| Still breastfeeding at 6 months | n = 70 | n = 51 | ||||
| Yes | 15 (21.4) | 4 (7.8) | 3.12 (0.89 to 10.97) | 0.08 | 3.16 (0.87 to 11.35) | 0.08 |
| No | 55 (78.6) | 47 (92.2) | 1 | |||
Third sensitivity analyses: exploring the impact of premature birth
| Measure | Intervention (N = 75), mean (SE) | Control (N = 56), mean (SE) | Unadjusted effect estimatea | Adjusted effect estimateb | ||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |||
| AAPI-2 (higher = positive) | ||||||
| Total (/10) | 7.5 (0.1) | 7.5 (0.1) | 0.05 (–0.16 to 0.27) | 0.64 | 0.07 (–0.15 to 0.28) | 0.55 |
| Missing, n | 5 | 1 | ||||
| CARE-Index | n = 57 | n = 44 | ||||
| Mother’s sensitivity | 4.0 (0.3) | 4.7 (0.4) | –0.71 (–1.60 to 0.18) | 0.12 | –0.65 (–1.53 to 0.22) | 0.14 |
| Measure | Intervention (N = 75), mean (SE) | Control (N = 56), mean (SE) | Unadjusted effect estimatea | Adjusted effect estimateb | ||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |||
| CARE-Index | n = 57 | n = 44 | ||||
| Infant co-operativeness | 3.0 (0.3) | 3.5 (0.3) | –0.46 (–1.25 to 0.33) | 0.25 | –0.44 (–1.24 to 0.36) | 0.28 |
| EPDS (higher = more depressed) | n = 84 | n = 60 | ||||
| Total (/30): 2 months | 3.4 (0.5) | 3.5 (0.5) | ||||
| Missing, n | 1 | 1 | ||||
| Total (/30): 6 months | 3.1 (0.5) | 3.0 (0.6) | ||||
| Total (/30): 12 months | 3.8 (0.5) | 4.1 (0.6) | 0.26 (–0.82 to 1.34) | 0.64 | 0.35 (–0.63 to 1.33) | 0.49 |
| Missing, n | 1 | 1 | ||||
| PSOC (higher = more competent) | n = 84 | n = 60 | ||||
| Total (/102): 2 months | 60.6 (0.6) | 60.7 (0.5) | ||||
| Missing, n | 3 | 1 | ||||
| Total (/102): 12 months | 60.9 (0.4) | 60.7 (0.6) | –0.16 (–1.34 to 1.02) | 0.79 | –0.21 (–1.38 to 0.96) | 0.72 |
| Missing, n | 2 | |||||
| PSI (higher = more stress) | n = 84 | n = 60 | ||||
| Total (/180): 2 months | 70.5 (1.9) | 68.3 (1.8) | ||||
| Missing, n | 3 | 1 | ||||
| Total (/180): 12 months | 73.4 (1.5) | 74.9 (2.0) | –1.28 (–5.51 to 2.95) | 0.55 | –1.36 (–5.34 to 2.62) | 0.50 |
| Missing, n | 1 | 2 | ||||
| Social networks (higher = more support) | n = 75 | n = 56 | ||||
| Total (/100) | 84.6 (2.2) | 84.5 (2.3) | –0.84 (–6.15 to 4.48) | 0.76 | –0.69 (–5.88 to 4.50) | 0.79 |
| Missing, n | 2 | 1 | ||||
| Relationships (higher = abuse) | n = 75 | n = 56 | ||||
| Total abuse (/6) | 0.4 (0.1) | 0.5 (0.1) | –0.07 (–0.34 to 0.20) | 0.64 | –0.10 (–0.38 to 0.17) | 0.47 |
| Smoking, alcohol and drugs | n = 75 | n = 56 | ||||
| Combined substance abuse score (/24) | 17 (0.3) | 16.6 (0.3) | –0.13 (–1.12 to 0.90) | 0.79 | –0.10 (–1.12 to 0.93) | 0.85 |
| Still breastfeeding at 6 months | n = 70 | n = 51 | ||||
| Yes | 15 (21.4) | 4 (7.8) | 3.12 (0.89 to 10.97) | 0.08 | 3.35 (0.96 to 11.62) | 0.06 |
| No | 55 (78.6) | 47 (92.2) | 1 | |||
Appendix 3 Reliability analysis of CARE-Index maternal sensitivity
A Bland–Altman or difference plot is a graphical method where the differences between the two measurements are plotted against the averages of the two measurements. Bland–Altman plots allow us to investigate the existence of any systematic difference between the measurements (i.e. fixed bias) and to identify possible outliers.
FIGURE 5.
Bland–Altman plot: maternal sensitivity.
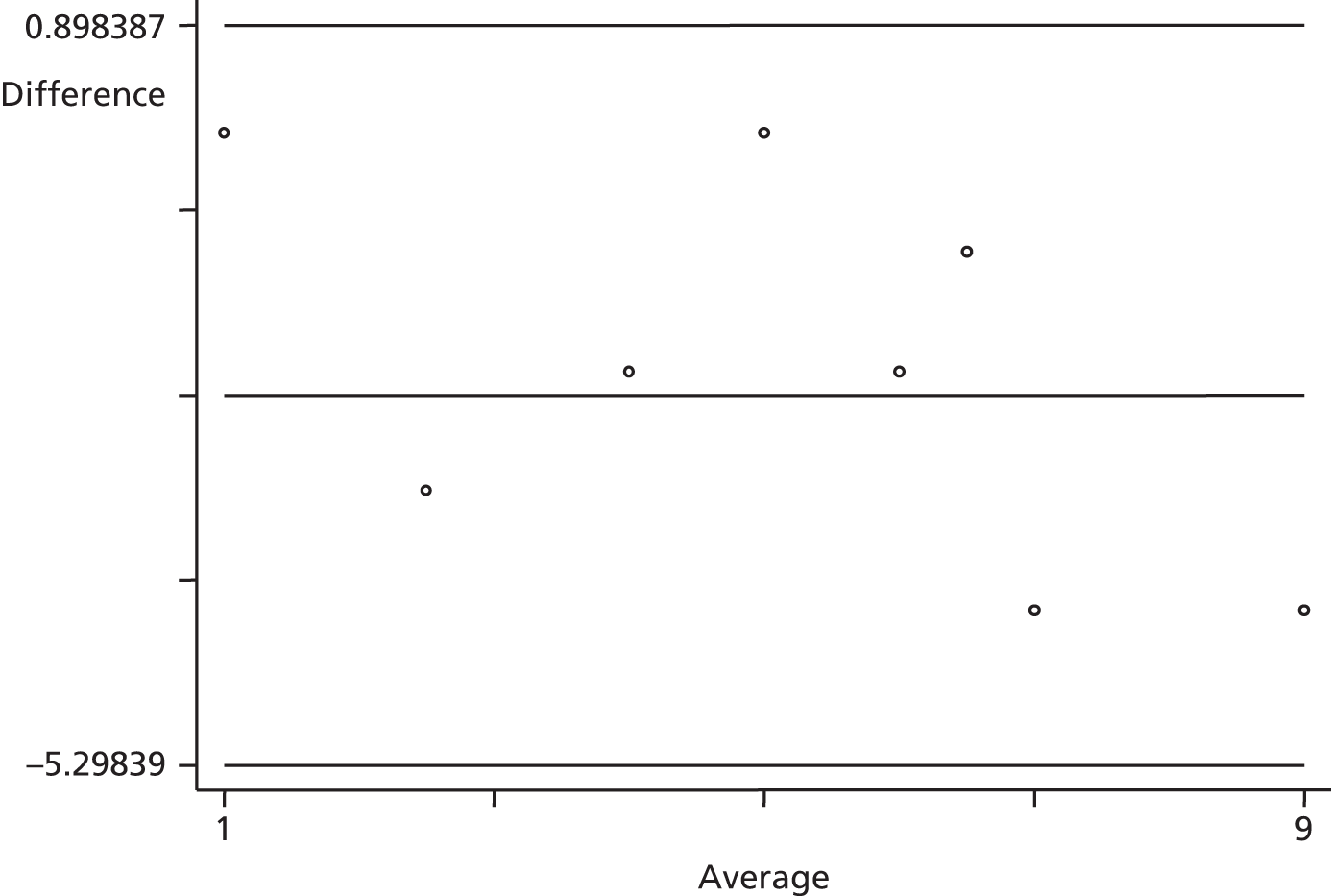
Glossary
- EuroQoL
- The EuroQol Group Association (‘The EuroQol Group’) comprises a network of international, multilingual, multidisciplinary researchers, supporting/instigating/performing scientific research and development of instruments that describe and value health.
- Family nurse
- An individual trained to deliver Family Nurse Partnership according to US Nurse Family Partnership guidelines.
- Family nurse midwife
- A family nurse who has notified his or her intention to practice as a midwife.
- Family Nurse Partnership
- The UK name for Nurse Family Partnership.
- Looked-after child
- A child who is or has been in the care of social services.
- Nurse Family Partnership
- The original US-developed home-visiting programme, renamed Family Nurse Partnership in the UK.
List of abbreviations
- A&E
- accident and emergency
- AAPI-2
- Adult Adolescent Parenting Inventory Version 2
- ANCOVA
- analysis of covariance
- CACE
- complier average causal effect
- CEA
- cost-effectiveness analysis
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CLRN
- Clinical Local Research Network
- CTU
- clinical trials unit
- CUA
- cost–utility analysis
- DCE
- discrete choice experiment
- DH
- Department of Health
- EDD
- expected delivery date
- EPDS
- Edinburgh Postnatal Depression Scale
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FN
- family nurse
- FNMW
- family nurse midwife
- FNP
- Family Nurse Partnership
- FNP NU
- Family Nurse Partnership National Unit
- GCSE
- General Certificate of Secondary Education
- gFNP
- Group Family Nurse Partnership
- GP
- general practitioner
- HCP
- Healthy Child Programme
- HES
- Hospital Episode Statistics
- HRQoL
- health-related quality of life
- HSCIC
- Health and Social Care Information Centre
- ICER
- incremental cost-effectiveness ratio
- ITT
- intention to treat
- LAC
- looked-after child
- LMP
- last menstrual period
- LSHTM
- London School of Hygiene and Tropical Medicine
- MOS
- Medical Outcomes Study
- MRC
- Medical Research Council
- NFP
- Nurse Family Partnership
- NICE
- National Institute for Health and Care Excellence
- NRES
- National Research Ethics Service
- OR
- odds ratio
- PI
- principal investigator
- PSI
- Parenting Stress Index
- PSOC
- Parenting Sense of Competence
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RUT
- random utility theory
- SD
- standard deviation
- SE
- standard error
- TMG
- Trial Management Group
- UID
- unique identifier
- VAS
- visual analogue scale