Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3009/02. The contractual start date was in December 2011. The final report began editorial review in April 2016 and was accepted for publication in October 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
All authors received a grant of £28,000 from the North East Strategic Health Authority in 2012 to cover the costs of delivering the intervention, associated training and other non-research costs of this study. Elaine McColl has been a subpanel member of National Institute for Health Research (NIHR) Programme Grants for Applied Research and Programme Development Grants since June 2008. She was also an editor for the NIHR Journals Library Programme Grants for Applied Research programme from July 2013 to March 2016. Luke Vale has been a panel member of the NIHR Health Technology Assessment Clinical Trials Board since 2014, a panel member for NIHR Programme Grants for Applied Research from March 2008 to June 2016, and Director of the NIHR Research Design Service for the North East of England since April 2012. Martin White is a member of the NIHR Journals Library Editorial Board. He is Programme Director of the NIHR Public Health Research programme and Editor-in-Chief of the NIHR Public Health Research journal (he has held both roles since October 2014).
Dedication
We dedicate this report to Emma Noble, the lead researcher on this project, who died tragically, aged 46, in the second year of the study. Emma was a registered general nurse who worked in the NHS for 14 years prior to her appointment to Newcastle University in September 2004. Emma worked as a researcher in the School of Neurology, Neurobiology and Psychiatry, and the School of Education, Communication and Language Sciences, before she was appointed as a Research Associate in the Institute of Health & Society. Emma worked on the Do-Well study from its inception and was central to establishing the trial. She was a highly valued member of the team. Her sudden and unexpected death was a shock, not only to her family, friends and colleagues, but also to study participants to whom she was a great source of support. She is greatly missed.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Haighton et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Some text in this chapter has been reproduced from our study protocol,1 published under the Creative Commons Attribution License (CC BY 2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited (https://creativecommons.org/licenses/by/2.0/). In addition, some text, boxes, figures and tables have been reproduced from Howel et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution International license (CC BY 4.0), which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Socioeconomic inequalities in health among older people
A vast body of observational evidence on socioeconomic inequalities in health suggests a close relationship between access to resources and health status that is positive, progressive and has no apparent thresholds. 3,4 Health inequalities are universal across time, nations, societies and the human life course. Socioeconomic differences in health persist into old age, and socioeconomic inequalities in self-reported physical and mental health widen in early old age. 5,6 Individuals with mild cognitive impairment exhibit poorer financial and health literacy. 7 Low household wealth is strongly associated with poorer life satisfaction and quality of life. 8 The poorest older people have inadequate access to services essential to health and well-being. 9 Older people, especially those in poor health, therefore often need additional income and support to maintain their independence, including payments for care, domestic help and aids and adaptations to the home. 10–12
Resource-based interventions to promote health
Research into the differential provision of welfare across nations has shown that it can exert an influence on subjective well-being, morbidity and mortality. For example, older people are emotionally better off13 and at lower risk of suicide in welfare states more generous than the UK. 14 Almost half of the reduction in excess winter mortality since 1999/2000 has been attributed to winter fuel payments. 15 Key theories that explain how money influences health include materialist explanations (e.g. money buys health-promoting goods and the ability to engage in a social life in ways that enable people to be healthy, and enables the avoidance of health risks in the environment); psychosocial mechanisms (e.g. the stress of not having enough money may adversely affect health, and having adequate resources may relieve stress); behavioural factors (e.g. people living in disadvantaged circumstances may be more likely to have unhealthy behaviours); and being in poor health may affect education and employment opportunities in ways that affect subsequent health. 16
In theory, increasing individual or group access to material, social or financial resources (so-called ‘assets-based’ approaches)17 should result in improved health,4,18,19 yet little research has directly evaluated the impact of increasing resources on health. 20 Ecological studies following the reunification of Germany have suggested important impacts of increased income on mortality, although a range of other factors may have played a part. 21,22 A systematic review20 of 10 North American randomised controlled trials (RCTs) of income supplementation experiments targeting a range of age groups, carried out in the late 1960s and 1970s, showed that none had reliably assessed the effects of increased income on health. The authors pointed out that, although such experiments are unlikely to be repeated, one way of assessing the health impact of increasing financial resources on health would be to evaluate the impact of assisting claimants to obtain full welfare benefit entitlements. 20
Tackling health inequalities has become a major policy priority for the UK, highlighted, for example, in the White Paper on public health (Saving Lives: Our Healthier Nation). 23 Following publication of the Acheson report24 and the advent of Health Action Zones in the late 1990s,25 there was an increase in welfare rights advice projects linked to primary care in the UK. Welfare rights advice provision in primary health-care settings can reduce, by an estimated 15%, the time general practitioners (GPs) spend on benefits issues, and leads to fewer repeat appointments and fewer prescriptions. 26 In 1999, Reducing Health Inequalities: An Action Report27 highlighted welfare rights advice as a potentially effective intervention for reducing health inequalities. This proposal was endorsed by the UK government’s Marmot review in 2010. 3
Social welfare for older people and the underclaiming of entitlement
In the UK, a range of financial and non-financial welfare benefits is available; these benefits have different purposes and different criteria for entitlement. Some are means-tested (income-related) and others are dependent on an assessment of health or other needs. Means-tested benefits include income-replacement benefits (e.g. income-related pension credit, and income-related financial support with housing costs). Non-means-tested benefits are intended to help meet the additional needs of those with health or social care problems (e.g. meeting the extra costs associated with ill-health or disability, carer’s benefits to supplement/replace earnings for people who provide support or bereavement benefits for people whose legal partner dies). In addition to financial benefits, material support can be offered to those in need (e.g. mobility aids and housing adaptations, such as rails, ramps and bathroom aids). Financial and non-financial benefits are variously administered through the Department for Work and Pensions, local authorities, housing associations and charities. Welfare rights advisors (WRAs) in local authority social services departments and third-sector organisations (e.g. Citizens Advice Bureaux, Age UK and other charities) help by undertaking financial assessments, recommending whether or not a client might be eligible for a benefit and sometimes offering active assistance with completing claims. Active assistance may also involve liaising with health or social care professionals for evidence of diagnosis or care needs.
The non-claiming of welfare entitlements among older people is a long-standing problem, which is currently increasing. 28 A large proportion of eligible welfare benefits remains unclaimed,28 and many of these are health-related benefit entitlements of vulnerable groups, such as older people. 28,29 Failure to claim entitlements is associated with a number of factors including the complexity of the benefits system,30 lack of knowledge about entitlements and difficulty in making claims. 12,31–33 In recent British studies, the bureaucracy associated with applying and uncertainty regarding the outcome of any claim, the amount of the award, autonomy and independence were reasons cited by people who were entitled to but did not claim benefits. 12,31–34 In addition to the state pension, there are a number of means-tested and non-means-tested benefits that can be awarded to older people if entitlement conditions are fulfilled. The level of underclaiming varies depending on the benefit concerned, but it is estimated to be at least 33% for Pension Credit and 40% for Council Tax Benefit. 35 Entitlement to one benefit can often act as a ‘passport’ to others, as many of the benefits aimed at people over the state retirement age are linked together in a complex network of entitlements that is often difficult for people to access without expert assistance.
Welfare rights advice services and their evaluation
Our systematic review of the health, social and economic impacts of welfare rights advice services in health-care settings32 identified numerous studies that demonstrated the financial and material benefits of such services. Welfare rights advice provided by local authorities and third-sector organisations is known to increase the uptake of benefits among those eligible, particularly when this involves ‘active assistance’ with benefit claims. 24,36 Studies have also shown that the receipt of benefit entitlements can be increased by providing information and advice in general practice, particularly in relation to those benefits that are health related. 37–41 However, our systematic review identified only two studies that investigated the health impact of welfare rights advice,42–44 one of which found an improvement in health-related quality of life (HRQoL) in some of the subscales of the Short Form Health Survey-36 (SF-36). 42,43 However, both studies demonstrated the difficulties of identifying and measuring appropriate health outcome measures when assessing the health effects of welfare rights advice in primary care. Neither study used a randomised controlled design, and both suffered from significant methodological weaknesses that rendered them inconclusive. Both studies evaluated a model of welfare rights advice delivery that was based in primary care, required referral from practice staff and did not offer a domiciliary service or active assistance with claims. Qualitative studies exploring the impact of welfare rights advice on clients in primary care have identified a range of health-related outcomes that can potentially result from the receipt of welfare rights advice, including changes in the physical, behavioural and, in particular, psycho-social domains of health. 12,31–33
Since 2006, few studies have added substantively to this literature. Two papers updated analyses included in our systematic review but yielded no new conclusions. 45,46 A study in a hospice setting audited referrals for welfare rights advice and found inconsistency in referral practices and a heavy workload for WRAs, but valuable potential of such referrals in terms of benefit eligibility. 47 A study in a UK musculoskeletal clinic48 examined the use of the Health Assessment Questionnaire49 as a tool to identify patients’ eligibility for welfare benefits. Although the authors found relatively high levels of eligibility for new benefits among those identified, there are inconsistencies in the numbers in the paper that make it difficult to interpret. Nevertheless, it does identify a potential screening tool for use in health care that might be of value in the future. Another study from some of the authors of this report (Moffatt, Noble and White) examined the use of welfare rights advice among 1174 cancer patients, assessing the viability of a service linked to clinical teams using qualitative methods. 50 The service proved feasible, with exceptionally high levels of successful claims (96%) and median benefits returned (£70/patient). Patients and staff valued the service highly, and health outcome evaluation was felt to be warranted. Krska et al. 51 used a cohort study with qualitative interviews among 148 patients in primary care to evaluate a Citizens Advice Bureaux-delivered welfare rights advice service. 51 They reported a decrease in prescription of hypnotic/anxiolytic medications 6 months after referral for advice, compared with 6 months before, but their analysis was uncontrolled. Practitioners felt that the service benefited patients and reduced workloads.
We conducted a pilot RCT to prepare for the definitive RCT described here, evaluating the impact of a domiciliary welfare rights advice service offered to people aged ≥ 60 years identified via primary care in disadvantaged areas. 11,12,52 In this pilot trial, 58% of participants were awarded either financial (median gain £55/week), non-financial (e.g. aids and adaptations to the home) or both types of benefits,11 confirming the feasibility and success of the intervention from the point of view of accessing unclaimed benefits. It also provided vital information on the feasibility of such a trial, which has helped in planning the definitive RCT reported here. In reporting on the pilot trial we identified a number of key design and methodological issues that would need to be addressed in a definitive evaluation. These are discussed below.
Study design, level of randomisation, contamination and dilution
An appropriate trial design was required, preferably with both randomisation and concurrent controls. Individual-level randomisation was considered preferable to cluster randomisation (e.g. at general practice level), as it required a smaller sample size. The potential problem with individual-level allocation was that there could be ‘contamination’ between intervention and control participants in the same general practice. This was more likely to be the case when welfare rights advice was available from an open-access service delivered in the general practice. However, by using a WRA who only saw patients in their own homes, we found in our pilot RCT that contamination did not occur; no control participants reported independently seeking welfare rights advice during a follow-up period, albeit a period of only 6 months. 11
Equipoise and the control condition
A key consideration in designing the proposed trial was whether or not there was genuine equipoise. Welfare rights advice is known to increase access to financial and material resources for eligible clients. However, our systematic review of published and grey literature indicated that there was no conclusive evidence that welfare rights advice leads to positive or negative changes in health. 32 We discussed these findings with WRAs, with directors of adult social services, with a selection of GPs and with members of the public in our target age group. We found each of these groups to be in equipoise with regard to the proposed trial health outcomes. Having established this, we also carefully considered the issue of study design and the ideal and feasible control conditions.
We considered that, ideally, controls should be adults as similar as possible to intervention group participants, but should not receive welfare rights advice, nor claim or receive new benefits, during the period of outcome follow-up. In clinical trials, it is usual to withhold the intervention from the control group because the health benefits of the intervention are not proven (i.e. clinical equipoise exists). Although this is the case with regard to the health impacts of welfare rights advice, as indicated above there is adequate evidence that welfare rights advice leads to significant financial and material gains for a proportion of recipients. Thus, it was considered ethically problematic to identify that control group participants were eligible to receive additional financial benefits, but either to keep this information from them or to tell them of their eligibility but not give them advice or help with claims. To circumvent this dilemma, we proposed that control participants should not receive a welfare rights assessment until the end of the trial period (i.e. following final outcome measurement). The full intervention (i.e. a full benefit assessment and active assistance with claims until resolved) would then be offered.
We had concerns that the WRAs might feel tempted to offer benefits advice to control participants before the 2-year ‘wait period’ had elapsed. We planned to avoid this by not informing the WRAs of the names of control participants until a few weeks before their benefits assessment was due (i.e. 2 years after their baseline assessment). The study team would hold control participants’ names securely during this period.
The design would thus avoid unfairly raising expectations among control participants. It would also help to avoid the potential problem of contamination, which could have arisen if control participants independently sought welfare advice (leading to dilution of the outcome effect), although we did not propose attempting to prevent this as we found little evidence of it in our pilot RCT. The proposed control condition is, therefore, in effect a ‘wait-list’ control, whereby the control group waits to receive the intervention 24 months after the intervention group.
It is, of course, possible that some members of both the intervention and control groups will die during the proposed 24-month follow-up period, which we would expect in the course of any prospective study of this age group. In our pilot study, we recorded seven deaths (four in the intervention group and three in the control group) out of 105 after 24 months’ follow-up. 11
One of the reasons that such interventions to date have not been rigorously evaluated for health impacts is in part because such research has previously been deemed unethical by researchers considering undertaking such evaluations,53 on the grounds that one cannot withhold benefits to which people are entitled. The proposed design of this RCT is fair because, at present, this kind of intervention is not routinely available to primary care patients and is generally only available to those who seek such services or are referred to them by a health or social care professional (e.g. a hospital social worker); these options remain open to patients in this trial. When targeted services are available in primary care, they tend to be short term and ad hoc. If we find any general practices in participating local authority areas with access to such services, they will be excluded from this trial. Genuine uncertainty exists about the proposed health-related outcomes because participants will not be denied any entitlement that they would otherwise receive and, at the time of the study, the health impact of the proposed intervention remains unknown. 32 We have determined that the research team and key stakeholders from health and social services are in equipoise about the proposed health outcomes.
Pragmatic versus explanatory
In the proposed trial, we know that not all participants in the intervention group will be eligible for additional benefits, and that those who are will receive variable amounts of financial and non-financial benefits. Ideally, we wish to examine the health impact of receiving versus not receiving such benefits, as well as examine the potential for a gradient of effect (‘dose–response’ relationship) by the amount of benefit received. However, to do so will require a substantially larger sample size than that proposed. In practice, therefore, the receipt of welfare rights advice is the intervention we will be evaluating (rather than receipt of specific benefits), as ‘welfare rights advice’ is the service being delivered. The proposed trial is, therefore, a pragmatic (intention-to-treat) RCT of this ‘complex’ intervention. 54 Nevertheless, we will also assess the potential for exploratory subgroup analyses looking at differential effects by participant characteristics (such as age and sex), and receipt/non-receipt of and levels of any benefits received. We anticipate that the trial will therefore contribute both to answering the question of whether or not the welfare rights advice intervention is effective in improving health and to providing new evidence on the more fundamental question of whether or not increasing resources leads to better health. 4
Length of follow-up
To enable the accurate assessment of the health and social effects of welfare rights advice, an appropriate length of follow-up is required. Our previous work suggested that considerable time may elapse between the first advice session and the receipt of new financial or material benefits. Often this is between 3 and 6 months, but it can be longer if the case is not straightforward or if there is an appeal. For example, in our pilot RCT, 45% had received their entitlements by 3 months after their welfare assessment, 85% after 6 months, 95% after 9 months and 100% by 12 months. 11 Given such delays in receipt of benefits, as well as the fact that any financial benefits may not be spent immediately, it seemed unlikely that the benefits would have substantial impacts on health within the first 12 months. In our pilot, which was not adequately powered for substantive analyses, we found no suggestion of differences in health-related outcomes between the intervention and control groups after 6, 12 or 24 months (although in the pilot trial control participants did receive the intervention after 6 months). 11 Nevertheless, it seemed likely that the longer the delay between receipt of intervention and measurement of outcomes, the greater the chance of demonstrating a substantive effect on health.
To assess the acceptability of a range of delays in receiving the intervention among control group participants, we undertook an experiment in the context of a focus group discussion with a representative sample of low-income older people. To achieve this, simulations of the RCT randomisation procedures were undertaken. The first simulation concerned a typical drug trial, and participants were given sweets whose colour depended on whether they were randomised to the intervention or the control group. Then, randomisation for the proposed trial was simulated. The concept of equipoise, with regard to the health impacts of welfare rights advice, was explained. Next, each group member was given an envelope from which they found out whether they were in the control group or the intervention group. If in the intervention group, they were allocated various types of benefit (e.g. Attendance Allowance plus Council Tax Benefit plus Housing Benefit), and the monetary value of these was revealed to them. We then talked through the various possible time delays until the control group would also receive their welfare rights assessment and advice. The time delays used were 3, 6, 9, 12, 18, 24, 36 and 60 months. The initial response to the design was that it was unfair to those in the control group. However, when it was explained that (1) although such services exist, they are not routinely targeted at or delivered to all people aged ≥ 60 years but are only available on referral or demand, (2) the findings of this study could influence the development of such services, involving collaboration between health and social services, and (3) that a substantial ‘wait’ between intervention and control groups is needed to establish any differences in health outcome, the consensus of the group was that a delay of 24 months would be acceptable in the context of the proposed trial. We therefore opted for a wait-list design for the proposed RCT, with a 24-month follow-up period for the main outcome assessment, followed immediately by delivery of the full intervention to the control group.
Selection bias
In our pilot RCT, GPs wrote to random samples of people aged ≥ 60 years, inviting them to respond with an indication of their willingness to participate in the trial (i.e. to ‘opt in’). 11 Using this method, 36% initially agreed to participate, 14% declined to participate and 50% failed to respond. Low levels of positive response to an ‘opt-in’ approach carries a risk of participation bias. 55,56 In their work on evaluating the impact of welfare rights advice for the Department for Work and Pensions,57 Corden et al. 58 routinely use an ‘opt-out’ method of recruitment for similar populations. With the approval of the NHS Research Ethics Service (NRES), we proposed using this type of recruitment method in this trial; this should have reduced the potential recruitment bias associated with ‘opt-in’ recruitment methods and increased the efficiency of trial recruitment.
Choice of outcome measures
Previously reported studies of the health effects of welfare rights advice have restricted reported health outcomes to general measures of health or psycho-social functioning (such as the SF-3642,59), together with measurement of financial gains.
In our qualitative research among recipients of welfare rights advice,12,33 we identified a range of potential benefits of advice, including:
-
health (improvements in anxiety, depression, insomnia; reductions in medication or consultation)
-
health-related behaviours (health-promoting changes in smoking, diet, physical activity and alcohol consumption)
-
social (improvements in family or other relationships, reduction of social isolation, increased ability to work, ability to care for relatives, etc.)
-
financial (debt rescheduling and receipt of new benefits, e.g. Attendance Allowance, Disability Living Allowance, Disability Living Allowance mobility component, Invalid Care Allowance, Incapacity Benefit, Housing Benefit, Income Support)
-
material (e.g. access to free prescriptions, Council Tax exemption, entitlement to respite care, Meals on Wheels, rehousing or home modifications).
The qualitative findings of our pilot study12,33 summarised these perceived benefits of the intervention in terms of:
-
increased affordability of necessities
-
increased capacity to manage unexpected future problems
-
decreased stress related to financial worries
-
increased independence, including ability to travel, shop, visit the GP, etc.
-
increased ability to participate in family life and society.
These findings are corroborated by a recent evidence synthesis undertaken to develop a logic model for the health outcomes of welfare rights advice services. 19 The resultant logic model has been used as the basis for a realist evaluation of the health impact of Citizens Advice Bureaux services, for which a protocol has recently been published. 60
In addition to qualitative work with study participants in our pilot RCT, we collected proposed outcome measures and relevant potential confounding factors. 12 The pilot trial was not sufficiently powered for substantive analyses, but the feasibility of measurements was good, and well tolerated by older people. The main outcome measure we assessed was the SF-36 instrument, as used in several previous studies. 42,59,61,62 Although this had demonstrated some potential, albeit in uncontrolled or non-randomised studies (e.g. positive changes in the mental health and emotional role domains),59 we were concerned that its domains did not sufficiently encompass the substantially wider range of reported impacts of welfare rights advice identified in qualitative studies, including our own (see Welfare rights advice services and their evaluation). 12,33 We therefore sought an alternative HRQoL measure that might best encompass key domains, such as independence, social participation and mental health. There is no single, ideal outcome measure that captures all of these domains, but the CASP-19 (Control, Autonomy, Self-realisation and Pleasure) instrument,57,63 developed specifically with a view to measuring quality of life in older people, comes close and has been recommended by Corden et al. 58 as a composite measure of the impact of welfare rights advice. 57 It is a self-reported summative index, comprising 19 Likert scale items in four domains: control, autonomy, self-realisation and pleasure. 63 Its performance has been examined in several prospective studies, including the English Longitudinal Study of Ageing (ELSA). 64,65
Generalisability
Our pilot trial was undertaken in one social services district (Newcastle upon Tyne) and in four general practice populations. 11 However, we know, from other work and discussions locally, that service delivery in welfare rights advice varies from area to area, as do general practice populations. To enhance the potential generalisability of the results, the RCT was, therefore, undertaken across a range of geographical and local authority areas (including urban and rural) and general practices. It seemed possible, indeed likely, that the present welfare regime would change during the course of the trial. The proposed intervention was not dependent on any particular set of benefits and was adaptable to any new regime. This added to its future generalisability.
Target population
Although we recognised that isolated older people who are eligible for benefits may live in all areas, in order to maximise the efficiency (and impact) of welfare rights advice services provided through primary health care, this RCT focused on practice populations in socioeconomically disadvantaged areas. Eligibility for health-related benefits (and failure to claim) increases with age, particularly post retirement; although there are other key target groups, such as single parents, non-claimants most likely to be accessed through primary care are predominantly in older age groups. 33,66–68 This trial therefore focused on a predominantly post-retirement population (those aged ≥ 60 years), residing in areas of economic deprivation.
The North East has some of the poorest health outcomes in England, coupled with high levels of socioeconomic disadvantage. From the 19th century, the regional economy was based on heavy industries such as deep coal mining, shipbuilding and steel making. Since the 1970s and the demise of heavy industry, the area has suffered economic decline due, in particular, to the closure of shipbuilding, coal mines and other heavy manufacturing. The post-retirement population of interest in this trial were born in the pre-and post-Second World War years (from 1920 to 1950), and many would have worked in these industries, which are associated with industrial-related conditions such as musculoskeletal injuries and diseases of the lung.
Nature of the intervention
The intervention delivered in this trial was based on standard advice services of the type found across local authorities in England when this study was designed. Welfare rights advice is not a statutory service, and provision varies across all local authorities in England, Wales, Scotland and Northern Ireland. Conventionally, however, these services are available only on demand or by referral. Thus, for example, an older person admitted to hospital may be referred by a hospital social worker, doctor or nurse for benefits assessment prior to discharge. Only some services have undertaken the targeting of welfare rights advice at a population level. 32 Those that have done so have found that there is a significant level of underclaiming in the general population and, in particular, among older people. 29 The proposed intervention is, therefore, a modification of a standard welfare rights advice service to target proactively a particularly vulnerable population in which we anticipated there would be high levels of underclaiming (i.e. those aged ≥ 60 years in disadvantaged areas). The only reliable population registers in England at a local level are the primary care patient registration lists held by GPs, which were used to sample this target group selectively.
In our pilot RCT, we identified that effectiveness and efficiency (in terms of successful claims) could be maximised by making the service domiciliary, as a substantial proportion of those aged ≥ 60 years have limited mobility, and during assessments clients often need access to information they keep at home. 33 Domiciliary visits also proved more popular with clients. In addition, we found that WRAs need to provide ‘active assistance’ with claims, for example completing claim forms for clients, as being unable to complete the forms is a key barrier to people claiming. 12,31,32 Finally, GPs need to have appropriate awareness of welfare entitlements and, for health-related benefits in particular, an understanding of the medical criteria on which decisions are made, so that they can support reasonable claims effectively in medical assessments requested by the Benefits Agency. Good communication between GPs and WRAs is essential to facilitate this. In our pilot RCT, we delivered education and training on these issues to all GPs in participating practices,11,12 another feature that is included in the proposed definitive RCT.
Process evaluation
Process evaluation is an essential element of designing and testing complex interventions. Process evaluation is used to assess the fidelity and quality of implementation, clarify causal mechanisms and identify contextual factors associated with variation in outcomes. 54 When evaluating the impact of an intervention, the emphasis of process evaluation is on providing greater confidence in conclusions by assessing the quantity and quality of what was delivered, and assessing the generalisability of its findings by understanding the role of context. 69
To draw conclusions about what works, process evaluations aim to assess fidelity (whether or not the intervention was delivered as intended) and dose (the quantity of intervention implemented). Intervention fidelity relates to adherence to the content of the study protocol and the process of ensuring quality and consistency in intervention delivery to all study participants. 70,71 This includes ensuring a clear intervention model, developing an intervention protocol, selecting appropriate staff to deliver the intervention, ensuring adequate training in the implementation of the intervention and providing staff with ongoing supervision. 70 In complex interventions, fidelity is not a straightforward process. In pragmatic trials the standardisation of the intervention to the study protocol will promote internal validity, but limiting variation may affect generalisability. 54
In addition to what is delivered, process evaluation can investigate how the intervention is delivered. This can provide vital information about how the specific intervention might be replicated, as well as generalisable knowledge on how to implement other complex interventions. Issues considered may include training and support, communication and management structures, and how these structures interact with implementers’ attitudes and circumstances to shape the intervention. Process evaluations also investigate the reach of interventions (whether or not the intended audience comes into contact with the intervention, and how). 69
Exploring the mechanisms through which interventions bring about change is crucial to understanding both how the effects of the intervention occurred and how these effects might be replicated by similar future interventions. Process evaluations may test hypothesised causal pathways using quantitative data as well as using qualitative methods to better understand complex pathways or to identify unexpected mechanisms. Context includes anything external to the intervention that may act as a barrier to or facilitator of its implementation, or its effects. Implementation will often vary from one context to another, however; an intervention may have different effects in different contexts even if its implementation does not vary. Complex interventions work by introducing mechanisms that are sufficiently suited to their context to produce change, while causes of problems targeted by interventions may differ from one context to another. Understanding context is, therefore, critical in interpreting the findings of a specific evaluation and generalising beyond it. Even where an intervention itself is relatively simple, unlike welfare rights advice, its interaction with its context may still be highly complex. 69 In the proposed RCT, we collected both quantitative and qualitative data to assess the process of intervention delivery, allowing us to explore the reach, uptake, fidelity and quality of the intervention, as well as provide contextual information that may prove valuable in explaining the observed outcomes.
Chapter 2 Methods
In this chapter we present the objectives of the study and then describe the methods that were used to achieve the objectives. The methods are divided into three main sections: quantitative (trial) methods, embedded qualitative study methods and economic evaluation methods. We conducted a process evaluation, drawing on both quantitative and qualitative data, and the methods for this are presented in relevant sections below, and drawn upon in the corresponding results chapters. The process evaluation aimed to evaluate the trial procedures, assess the fidelity of the intervention and ascertain the reasons for the intervention’s success or failure. It drew on quantitative data collected to assess the fidelity, dose and reach, including socioeconomic patterning, of the intervention, as well as qualitative data to assess the acceptability and perceived impacts of the trial and intervention, and the reasons for success and failure of each component thereof. An initial analysis of process data was conducted before the main outcome analysis to avoid biased interpretation of process data. This allowed process data to provide prospective insights into why we might have expected to see positive or negative overall effects and generate hypotheses about how variability in outcomes may have emerged. 69 They thus informed our secondary, exploratory analyses.
The proposed methods for all analyses were documented in our protocol. 1 Statistical and economic evaluation analysis plans were further pre-specified in greater detail and approved by the Trial Steering Committee (TSC) prior to the analyses being commenced.
Objectives of the randomised controlled trial
The overall aim of the study was to evaluate the effects on health and well-being of a domiciliary welfare rights advice service for independently living, socioeconomically disadvantaged older people (aged ≥ 60 years), recruited from general (primary care) practices.
Primary objective
To establish the effects on HRQoL of a domiciliary welfare rights advice service targeting independently living, socioeconomically disadvantaged older people (aged ≥ 60 years) identified via primary care, compared with usual practice.
Secondary objectives
-
To establish the cost consequences and the cost-effectiveness of a domiciliary welfare rights advice service targeting independently living, socioeconomically disadvantaged older people (aged ≥ 60 years) identified via primary care, compared with usual practice.
-
To establish the acceptability to trial participants and relevant professionals of a domiciliary welfare rights advice service targeting independently living, socioeconomically disadvantaged older people (aged ≥ 60 years) identified via primary care.
-
To identify the unanticipated consequences (positive or negative) of a domiciliary welfare rights advice service targeting independently living, socioeconomically disadvantaged older people (aged ≥ 60 years) identified via primary care.
Trial design
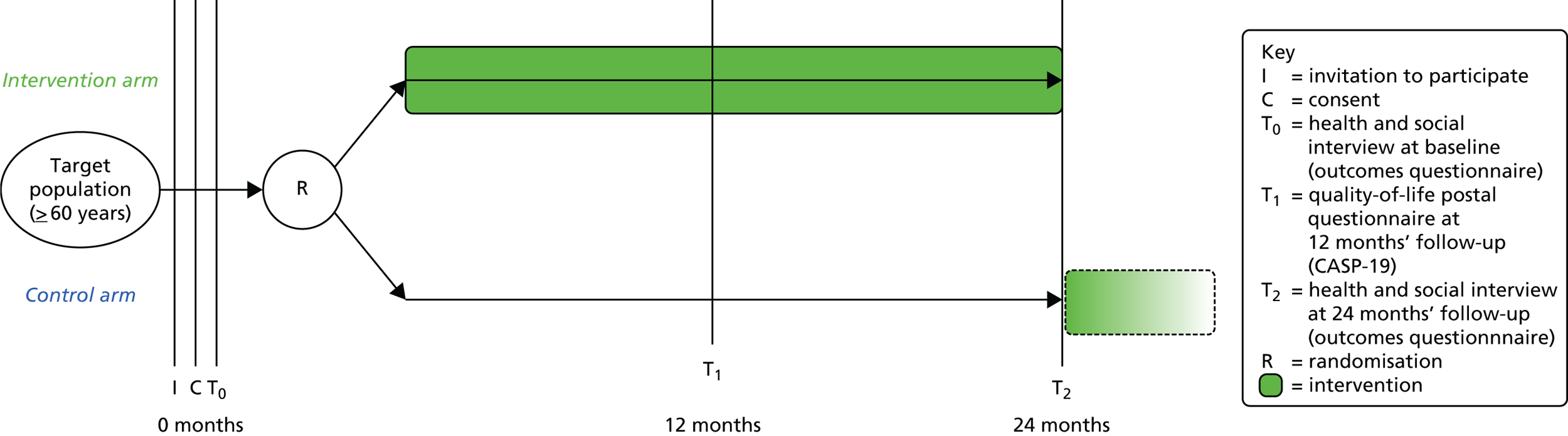
A pragmatic, individually randomised, single-blinded (researchers), parallel-group, wait-list controlled trial of domiciliary welfare rights advice versus usual care, with embedded economic and quantitative and qualitative process evaluations (Figure 1).
FIGURE 1.
Overview of study design.
Setting
The trial took place in socioeconomically disadvantaged areas in the North East of England, which included urban, rural and semirural areas, with no previous access to welfare rights advice services targeted to primary care patients.
The study was planned to take place in 10 of the 12 local authority districts in the North East of England (Stockton, Darlington, Middlesbrough, County Durham, Sunderland, South Tyneside, North Tyneside, Newcastle, Northumberland and Gateshead). Social services departments in these local authorities had agreed in principle to provide domiciliary welfare rights advice services. The intention was to recruit two general practices per local authority district with the help of the Primary Care Research Network – Northern and Yorkshire (PCRN-NY). Lists of all general practices from the local authority districts were obtained from the PCRN-NY and ranked according to deprivation score using the 2010 English Index of Multiple Deprivation (IMD) calculated at middle-layer super output area (MSOA) level for practice premises (main surgery) postcodes, in accordance with the method of Griffin et al. 72 Deprivation covers a broad range of issues and refers to unmet needs caused by a lack of resources of all kinds, not just financial. The English Indices of Deprivation attempt to measure a broad concept of multiple deprivation, made up of several distinct dimensions, or domains, of deprivation. Super output areas are geographical units for the collection and publication of small area statistics. There are currently two layers of super output area: lower-layer super output areas (LSOAs) and MSOAs. LSOAs have an average of 1500 residents and 650 households. MSOAs have a minimum of 5000 residents and 2000 households, with an average population size of 7500, and fit within local authority boundaries. WRAs established whether or not any of the practices in the most socioeconomically deprived two-fifths of the IMD distribution had existing dedicated or targeted welfare rights advice services. Those practices in the lower two-fifths of the deprivation ranking distribution, without existing dedicated or targeted welfare rights advice services, were eligible for inclusion and were sent a letter by the PCRN-NY inviting them to participate (see Appendix 1), along with an information sheet describing the study (see Appendix 2) and an expression of interest form to return directly to the PCRN-NY.
The PCRN-NY provided the study team with a list of all eligible practices that had indicated a willingness to participate in research. If more than two general practices per local authority expressed willingness to participate in the research, the intent was to list the practices randomly and then contact them sequentially until two practices from each local authority district had agreed to participate in the trial. Fourteen eligible practices originally volunteered to participate in the research, representing only eight of the local authority areas for which we had secured the services of domiciliary WRAs. As we did not achieve our target of two general practices per local authority area immediately, we took two further courses of action: (1) we asked those practices that had originally volunteered if they would be willing to recruit additional patients (specifically, twice the number originally requested); and (2) we attempted to recruit further eligible practices through informal research networks across the North East of England. The latter strategy resulted in three further practices volunteering to participate from local authorities already involved in the study. However, it was also necessary to ask three general practices that had expressed willingness to do so, to recruit double the number of participants (Table 1). Owing to the problems with general practice recruitment, the welfare rights advice services in two local authorities that were willing to provide them were ultimately not required and the study took place in eight local authority districts.
| Local authorities (12 approached, 10 offered WRA services, 8 participated) | Domiciliary welfare rights advice services available | First-wave practices volunteered | Second-wave practices volunteered | Number of patients invited to participate by general practice | Number of patients invited to participate by local authority (N = 3912) | ||
|---|---|---|---|---|---|---|---|
| First mailing (N = 1700) | Second mailing (N = 2212) | Both mailings (N = 3912) | |||||
| A | N | a | a | a | a | a | a |
| B | N | a | a | a | a | a | a |
| C | Y | b | b | b | b | b | b |
| D | Y | b | b | b | b | b | b |
| E | Y | 1 | 200 | 187 | 387 | 387 | |
| F | Y | 2 | 100 | 195 | 295 | 695 | |
| 3 | 200 | 0 | 200 | ||||
| 4 | 100 | 100 | 200 | ||||
| G | Y | 5 | 100 | 200 | 300 | 600 | |
| 6 | 100 | 0 | 100 | ||||
| 15 | 0 | 200 | 200 | ||||
| H | Y | 7 | 100 | 0 | 100 | 400 | |
| 8 | 100 | 0 | 100 | ||||
| 16 | 0 | 200 | 200 | ||||
| J | Y | 9 | 100 | 200 | 300 | 600 | |
| 10 | 100 | 200 | 300 | ||||
| K | Y | 11 | 200 | 0 | 200 | 400 | |
| 17 | 0 | 200 | 200 | ||||
| L | Y | 12 | 100 | 230 | 330 | 330 | |
| M | Y | 13 | 100 | 200 | 300 | 500 | |
| 14 | 100 | 100 | 200 | ||||
Participants and recruitment
Participants were volunteer patients aged ≥ 60 years (one individual per household) who were not resident in a nursing home or in hospital, were not terminally ill (as assessed by their GP) and were fluent in written and spoken English.
The PCRN-NY and the Comprehensive Local Research Networks offered personnel and financial resources to participating general practices in the North East of England to identify and approach research study participants. Each participating practice was asked to generate a random sample of up to 300 people aged ≥ 60 years from their practice register. Practice staff scrutinised their list to identify any patients terminally ill or known to be resident in hospital or long-term care, who were excluded. Those who were assessed as not able to participate in the research due to poor mental or physical health, as assessed by their GP, were excluded from the study. Practice staff also checked to ensure that only one person per household had been selected for this list. If two people from the same address were found, one was selected by practice staff at random (by flipping a coin) to be retained and the other was removed from the sample list. Not all practices had sufficient patients registered to be able to generate a list of 300 people aged ≥ 60 years from their practice register; in these circumstances, they listed as many as possible.
This list of up to 300 names (of people believed to meet the eligibility criteria) per practice was randomly ordered and the first 100 patients on the list were sent a letter (see Appendix 3) and patient information sheet (see Appendix 4) signed by the senior GP partner on behalf of the practice, inviting them to participate in the trial. The figure of 100 patients was determined on the basis of the recruitment rate in the pilot study and anticipated to yield the required sample in an optimistic, best-case scenario. The letter on practice-headed paper explained that, unless the participant objected by returning the opt-out form (see Appendix 5) to the practice in the stamped addressed envelope within 2 weeks, their name and contact details would be passed to the research team, who would then contact them directly to discuss the trial further and seek informed consent.
After 2 weeks, the names, addresses and telephone numbers of those who had not opted out were passed to the research team. Research interviewers contacted these individuals by telephone to arrange, if acceptable, a face-to-face meeting at a mutually convenient time in the participant’s own home. At the initial appointment, research interviewers sought written informed consent (see Appendix 6) and then proceeded to collect baseline data.
We monitored recruitment continuously to assess whether or not and when further patients should be invited by each practice. When it became apparent that we would need to approach more than 100 patients to achieve our proposed sample size, practices were asked to write to additional patients from their original list of 300. In two cases, practices contacted all remaining patients aged ≥ 60 years. In these cases, the total number of patients invited was 387 and 330 (practices 1 and 12, respectively). In the three practices that had offered to recruit additional participants, recruitment numbers were doubled at each stage of the process.
Randomisation
Following written consent and baseline assessment, participants were randomised in a 1 : 1 ratio to intervention or control condition, stratified by practice. Research interviewers notified the project administrator after each baseline assessment that a new participant had been successfully recruited. The administrator held sequential allocation tables for each practice, independently generated from random numbers prior to recruitment [generated by a statistician (AB) using Stata version 12 software (StataCorp, College Station, TX, USA]. The administrator allocated all participants to the intervention or control group in the chronological sequence in which they were recruited and immediately sent each participant a standard letter (see Appendix 7) informing them of their group allocation. Only the project administrator had access to the allocation tables, and the allocation was thus concealed from the research team, data collectors and statisticians. The allocation was revealed to the participant and (in the case of intervention group participants) the relevant WRAs. The administrator immediately informed the appropriate local WRA team member of the contact details of each newly allocated intervention group participant and requested that they should be visited for a welfare assessment within 2 weeks. The WRAs were sent lists of control group participants to assess 24 months later, once follow-up had been completed.
Blinding
Research interviewers, who collected data from participants at baseline and 24 months, were not notified of the allocation status of participants to ensure that they remained blinded for the duration of the study.
Intervention
Here the intervention is described as designed and intended, according to Consolidated Standards of Reporting Trials (CONSORT) and Template for Intervention Description and Replication (TIDieR) guidelines. 73,74 In Chapter 3, variations of this intention are documented and the implications are identified. The rationale underpinning the intervention components was rehearsed in Chapter 1.
The domiciliary welfare rights advice service comprised face-to-face welfare rights advice consultations and active assistance with benefit claims, delivered in participants’ own homes and tailored to their individual needs by a qualified WRA employed by local authority departments, or their contracted services, in the North East of England. In one local authority, welfare rights advice services were contracted and delivered by a third-sector organisation. Following randomisation, intervention group participants were given an appointment in their own home with a WRA within 2 weeks, during which participants underwent a full benefit entitlement assessment involving assessment of financial, material and welfare status; assessment of previous benefit entitlement and claims; discussion of current entitlement and options for action, including new claims (financial and non-financial). Active assistance with benefit claims and other welfare issues was given, which included completion of benefit application forms on behalf of the participant. Complex claims or those referred for further assessment or tribunal were managed as per their usual practice by WRAs. It was anticipated that initial assessments would last up to 60 minutes. Participants were followed up at home or by telephone as required by WRAs until they no longer required assistance (cases are usually ‘closed’ once all claims and appeals have been concluded), which could take several months. 11
In area K, one local authority WRA provided the intervention from the start of the project until April 2013, when budget reviews restricted the availability of the WRA for the Do-Well study. A freelance WRA took over and completed the intervention in this area. In area G, the local authority WRA volunteered to provide the intervention for the Do-Well study but withdrew before recruitment began; therefore, a freelance WRA provided the intervention in this area. In area J, a local authority WRA provided the intervention at baseline but was unable to continue at 24 months (i.e. to deliver the intervention to control participants) because welfare rights posts had been lost and a new team had been formed that combined local welfare provision with supported housing. One WRA was retained by the local authority to deal with complex welfare cases but did not have the capacity to continue providing the intervention for the Do-Well study; therefore, a freelance WRA provided the intervention at the 24-month follow-up. In area L, three local authority WRAs provided the intervention throughout the study. In area M, the intervention was provided by paid staff from the Citizens Advice Bureau. In areas H and F, one local authority WRA within each area respectively provided the intervention for the duration of the study. In area E, two local authority WRAs provided the intervention for the duration for the study.
Intervention reach
Intervention reach was assessed as the proportion of those eligible to receive the intervention who actually received it. Causes of participants not receiving the intervention as intended (e.g. participants withdrawing, refusing or being lost to follow-up) and reasons given by participants (in interviews and questionnaires) were recorded when available. We also analysed the socioeconomic patterning of receipt of the intervention, and receipt of welfare benefits using IMD 201072 scores assigned at household level by matching postcode to IMD score at LSOA level.
Eligibility and receipt of welfare benefits was assessed, by type of benefit, as a proportion of those assessed by WRAs in the intervention group at baseline. This was also assessed in the control group at the 24-month follow-up.
At the outset, the intervention was primarily to be funded and provided by welfare rights advice services in the 10 participating local authority areas in the North East. However, a contingency fund of ≈£28,000 was also secured from the North East Strategic Health Authority in 2012, prior to the start of the study, to fund any excess intervention costs and the costs of any training for WRAs and GPs to ensure the effective delivery of this service with a high level of fidelity.
Training and quality control
To ensure consistent approaches to medical assessments related to relevant claims, each participating general practice was visited by a member of the research team and provided with an information pack and guidance on the completion of medical information on benefit application forms (see Appendix 8). This information was developed by the study team, with the help of a senior WRA who was involved in training and quality control in our pilot RCT, and a GP who was a member of the study team for the pilot RCT.
All participating WRAs were invited to attend information sharing events prior to intervention delivery to agree the intervention protocol, which specified the procedures for delivering welfare rights advice and the follow-up actions in a standardised manner. Intervention procedure checklists (see Appendix 9) were then given to all WRAs prior to the commencement of the study to ensure consistent delivery. Study staff closely monitored the progress of intervention delivery and maintained regular contact with all WRAs.
Fidelity assessment
We assessed the fidelity of the intervention in a number of ways. First, we asked WRAs to record the date and time of each initial welfare rights advice assessment, so we could assess whether or not these were delivered on time (within 2 weeks of the baseline study data collection). Second, we assessed whether or not initial welfare rights advice assessments were delivered as intended. This assessment was carried out, as unobtrusively as possible, by analysing audio-recordings of WRAs undertaking this aspect of intervention delivery with a small subsample of study participants. We aimed to analyse one initial welfare advice consultation per WRA (i.e. n = 19). Audio-recorded consultations were assessed by a senior WRA from a local authority not involved in the Do-Well study, selected for her extensive experience as a WRA, supervisor and welfare advice team manager. Each WRA was contacted shortly after the start of the study and asked to audio-record the next consultation undertaken with a consenting participant, and to record a brief commentary explaining the case and the actions recommended. We explained to WRAs that, as part of the research, we needed to understand how they interacted with clients and how outcomes were achieved. We avoided explicit reference to judgements about their practice, as this might have led to practice that was different from usual. Each participant was informed about the nature of the fidelity assessments, and written consent was obtained for audio-recording of the consultation. If a participant refused consent, the WRA was advised to ask the next participant they were due to visit for an initial assessment. The fidelity assessments took place between December 2012 and February 2013. Each consultation was analysed against a checklist of criteria developed by the study team (see Appendix 10). This checklist assessed the overall quality of the consultation, whether or not the correct assessment of needs had been made and that, if warranted, the correct benefits were applied for according to standard procedures. The senior WRA who listened to the recordings completed a confidentiality agreement prior to assessment, as it was felt not possible to fully anonymise the recordings. All data were held in accordance with the Data Protection Act 199875 and all sound files were individually password protected. After analysis of the fidelity assessment, all recorded files were destroyed. The research team was provided with a summary of each consultation based on assessment against the criteria of needs assessment, appropriate benefits applied for and a brief commentary on the justification for the outcomes achieved.
Comparator (wait-list control condition)
Participants randomised to the control group received ‘usual care’ (standard practice) from both health and welfare rights advice services after randomisation until they had completed their 24-month follow-up assessment. They were given no advice regarding welfare rights as a part of the study intervention during this period. However, they were free to seek welfare rights advice independently from their local authority or any third-sector provider at any time. Participants who sought independent advice remained in the trial and were analysed in the control arm on the intention-to-treat principle, and details of any advice and ensuing claims and outcomes were recorded at the 24-month follow-up assessment. Following the 24-month follow-up assessment, participants in the control arm received the intervention, as delivered to the intervention group (described above), including all follow-up visits by WRAs and assistance with claims and appeals over the following months, until all claims had been resolved.
The participants were informed during recruitment, via the patient information sheet (see Appendix 4), that we wanted to recruit 750 people into the study. They were told that one group of 375 people would be given an appointment with the welfare advice service straight away and another group of 375 people would be given an appointment around 24 months later. Potential participants learned that the group they would be put in would be decided by chance, like tossing a coin, but that everyone would receive an appointment within 24 months. Once individuals agreed to participate in the study and completed baseline assessment, they were sent a letter (see Appendix 7) detailing which group they had been assigned to. Wait-list control participants were told that the group they had been assigned to would mean that they would see a WRA approximately 24 months after they entered the study.
Both intervention and control group participants remained clients of the welfare advice service beyond the end of the trial, if necessary, until such time as their help was no longer needed, as per usual welfare rights advice service protocols.
Data collection
Primary outcome measure
The primary outcome measure was HRQoL, measured using the CASP-19 questionnaire. 57,63 CASP-19 comprises 19 questions in the four domains of control, autonomy, self-realisation and pleasure. The range of the scale is 0–57, with higher values indicating better quality of life. 63 CASP-19 was administered by face-to-face interview at baseline (pre randomisation) and at follow-up 24 months post randomisation, and by postal questionnaire (with two reminders at fortnightly intervals including one duplicate questionnaire) at 12 months post randomisation (see Appendix 11).
Secondary outcome measures
The following secondary outcomes were collected by face-to-face interview at baseline (pre randomisation) and at follow-up 24 months post randomisation (see Appendix 11).
Mental health
Mental health was measured by the Patient Health Questionnaire-9 (PHQ-9) depression scale. 76–78 The PHQ-9 examines nine mental health problems. The potential range of the scale is 0–27, with lower values indicating fewer depressive symptoms.
Perceived financial well-being
Perceived financial well-being was measured by the Affordability Index. 79 The 13-item Affordability Index has a potential score range of 4–20, with lower scores indicating fewer financial problems.
Standard of living index
The standard of living index is a 0–24 scale assessing ownership of 24 household items, based on questions used in the British General Household Survey. 80 A higher score indicates a higher standard of living. The items enumerated are listed in question 42 in Appendix 11.
Social support and participation
Social support and participation was measured by social interaction and strength of confiding relationships. 11 The social interaction score has a potential range of 0–27, with higher scores indicating a higher level of social engagement and support. An isolation indicator was created from one item on this scale, categorising whether or not participants reported that they did not see friends and relatives as often as they wished.
General health status
General health status was measured by the EuroQol-5 Dimensions-3 Levels (EQ-5D-3L) instrument. 81,82 The EQ-5D-3L is a five-item scale with three levels of response. The tool has been extensively used in studies and full details are reported on the website of the EuroQoL Group (www.euroqol.org/).
Health-related behaviours
Health-related behaviours were assessed by self-report, to measure change in key indicator behaviours, such as smoking, alcohol consumption,83 diet (consumption of key food groups) and physical activity [Physical Activity Scale for the Elderly (PASE)],84 as in our pilot RCT. 11 The diet score had a potential range of 15–75, with higher scores indicating a healthier diet in terms of salt, fat and sugar consumption. The physical activity score had a potential range of 0–400+, with higher scores indicating higher levels of activity.
Mortality
Mortality was assessed by identifying deaths at 12 months and 24 months from GP records. General practices were sent a list of participants and asked to check their status. This was carried out prior to commencing the 12- and 24-month follow-up assessments, in order to avoid distressing any recently bereaved relatives.
Financial status
Financial status was measured using an assessment tool developed and used in our pilot RCT. 11 This included data on all sources of household income, including benefits, major outgoings (rent/mortgage, fuel bills, etc.), debts and capital assets (i.e. home and savings). As well as these data, at follow-up detailed data were collected (by WRAs) on new benefits received since baseline, including one-off (lump sum) payments and regular, weekly or monthly income.
Independence
Independence was measured by assessing living arrangements and carer status using the following categories: living independently or with carer support, in own home, with relations, in a care home or hospital. We also assessed (by self-report) the number of hours of home care received per week.
Harms
At the outset, we were not aware of any major risks or harms associated with the delivery of the intervention. However, it was possible that older people could spend additional resources in ways that would be potentially harmful. These might include spending additional financial resources on alcohol or tobacco (with known risks of chronic diseases), ‘luxury’ foods, high in fat and sugar (e.g. chocolate), or gambling, which can be addictive and financially ruinous. It was also possible that the increased independence and mobility (which we hypothesised would be associated with access to additional resources) could result in greater environmental exposures outside the home, resulting in infectious diseases or accidental injury. Furthermore, the intervention could lead to greater use of car travel, resulting in lower levels of physical activity. It was also possible that older people would feel obliged to share any additional income with family members, who may be equally socioeconomically disadvantaged, thus negating the beneficial impacts on themselves. Older people may also be more vulnerable to external pressures, such as cold-calling from salespeople. We assessed potential adverse outcomes by (1) identifying negative (unhealthy) changes in all primary and secondary outcome measures; and (2) including additional, semistructured open questions in follow-up questionnaires and interviews on other, potential, unanticipated outcomes in order to document these and develop explanations.
Other quantitative data collected
Demographic variables were collected to characterise the trial participants and adjust for potential confounding in analyses, including age, sex, ethnicity, educational level attained, employment status and living arrangements (number of household members, paying for accommodation, and whether or not emotional support was available). In addition, two scales were used.
Functional ability was measured by the modified Townsend Activities of Daily Living scale,85 which assesses a person’s ability to perform eight activities. The possible range of scores is 0–16, with higher values indicating a greater ability to perform activities of daily living.
Life events score was measured by recording eight potentially serious events, including bereavement and significant illness, that might have occurred in the past 7 months, as well as their impact on the individual. 86
Sample size
A minimum of 318 participants needed to be followed up in each of the intervention and control arms (a total of 636) to provide 90% power at 5% significance level to detect a 1.5-unit difference in mean CASP-19 score57,63 at 24 months between the intervention and control groups, assuming a standard deviation (SD) of 8.7 and a correlation between baseline and 24 months of 0.74. The estimates of SD and correlation coefficients came from the results of ELSA (wave 4) restricting the analyses to those aged ≥ 60 years. 87 Estimating an attrition rate between baseline and 24-month follow-up of 15% (as experienced in our pilot RCT),11 we needed to recruit 750 participants to the study (375 to each group).
There has been no published work to establish a meaningful or clinically important difference on the CASP-19 scale. However, we based the above acceptable difference on data from waves 1 and 2 of the ELSA in those aged ≥ 60 years. We investigated the adjusted mean difference in CASP-19 at wave 2 between groups whose social or health circumstances had changed. 64 Examples of changes in CASP-19 score associated with changes in health or social circumstances that we might have expected to see in the proposed trial included ‘developed limiting illness’, –2.8 units; ‘developed depression’, –2.7 units; ‘lost access to car’, –1.8 units; and ‘increased chance will not meet financial needs’, –1.1 units. These differences on the CASP-19 scale suggest that a difference of 1.5 units would represent a minimally clinically important difference. 65 The chosen sample size also provided power to demonstrate some clinically significant differences in secondary outcomes. For example, 750 participants would provide 90% power to detect a difference between a prevalence of 11% and 4% of clinically significant depressive symptoms (PHQ-9 score of ≥ 10).
Data handling, record keeping and sharing
Baseline and 24-month data were entered directly during interviews, via a tablet computer, into a secure custom-built database for processing and management using a bespoke content management system on Microsoft SQL® Server and ASP.NET (Microsoft Corporation, Redmond, WA, USA). A record was maintained of any changes made to the data post entry. All personal information obtained for the study was held securely at Newcastle University and was treated as strictly confidential. The project administrators undertook entry and verification of data from 12-month posted self-completion questionnaires into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet, with a 10% random sample checked for data entry accuracy. The data collection and transfer in this study complied with NRES88 and Caldicott guidelines89 and the Data Protection Act 1998. 75
All patients were allocated a unique study identifier, which was used on all data collection forms and questionnaires to preserve confidentiality; names or addresses did not appear on completed questionnaires or on other data collection forms. Only a limited number of members of the research team were able to link the unique identifier to patient-identifiable details (name, address and telephone number) that were held on a password-protected Microsoft Access® (Microsoft Corporation, Redmond, WA, USA) database. All study documentation was held in secure offices that were not open to the public, and all members of the research team with access to identifiable or anonymised data operated to a signed code of confidentiality. Transmission of original or hard copy records (e.g. questionnaires, interview recordings) was by secure fax, post or hand delivery by members of the research team or by the WRAs. Participants were informed in the patient information sheet (see Appendix 4) about the transfer of information to the research team and about levels of access to patient identifiable data, and were asked to consent to this.
At the end of the study, original questionnaires, interview transcripts, consent forms and final versions of all data sets will be securely archived in the Institute for Health & Society for 5 years following publication of the last paper or report from the study, in line with sponsor policy and Newcastle Clinical Trials Unit standard operating procedures. This also allows any queries or concerns about the data, conduct or conclusions of the study to be resolved. Anonymised data will subsequently be securely archived and made available for secondary analysis as appropriate. Details of data sharing arrangements are available from the corresponding author.
Trial data analysis
In this section, the methods used to organise and analyse the data are described. This is divided into three sections, covering the quantitative study, economic evaluation and qualitative analysis.
Statistical analysis
Analysis populations
The analysis used the intention-to-treat population, which comprised all participants in the group to which they were randomised, regardless of the intervention that they received. The number of participants who did not receive the intervention to which they were randomised is reported.
Analysis data sets
As interviewers collected most of the data, it was not expected that there would be many missing data on items in particular scales. However, unless specified otherwise by the scale developers, when no more than 20% of items were missing or uninterpretable on specific scales, the scores were calculated by using the mean value of the respondent-specific completed responses on the rest of the scale to replace the missing items. 90
Depending on the extent of missing data on the primary outcome at 24 months, the use of multiple imputation was considered for the primary outcome CASP-19. It was decided that multiple imputation using iterative chained equations was appropriate to obtain a complete data set for the primary outcome at 12 and 24 months, conditional on survival to 12 or 24 months. 91 The variables considered for the multiple imputation model were those thought a priori to be associated with CASP-19 at 12 and 24 months, as well as variables that were predictors of missingness of CASP-19 scores. 92 The final model included baseline characteristics (e.g. age, gender, education, living alone), and CASP-19 at baseline and 12 months. Twenty multiple imputation data sets were produced.
The primary analysis of study end points (listed in the next section) was after the use of the simple imputation method described above to estimate missing items. A sensitivity analysis was carried out to explore the effect of this simple imputation approach. The results of the CASP-19 are also reported after using multiple imputation.
Descriptive analyses (baseline)
Baseline characteristics of the study population were summarised separately within each randomised group. This included primary and secondary outcome variables and covariates. Continuous variables were summarised by numbers of observations and mean and SD, or median and interquartile range (IQR), depending on whether or not the distribution was symmetric. The numbers of observations and percentages are reported for categorical variables. No significance testing for any baseline imbalance was carried out, but any noted differences are reported descriptively.
When covariates were available in both the Do-Well data set and the national ELSA (wave 4),87 their distributions were compared to determine the representativeness of the Do-Well participants.
Analyses of study end points
Descriptive analysis of benefits received
The numbers and percentages of any financial and non-financial benefits (e.g. aids and adaptations) received since baseline were summarised separately within each of the randomised groups.
Primary effectiveness end point
The primary end point, CASP-19, was compared at 24 months between the intervention and control groups using multiple linear regression with adjustment for baseline value and general practice (the stratification variable). The results are reported as a difference in means with a 95% confidence interval (CI). An adjusted analysis included the life events score and functional ability score at 24 months, and baseline covariates age, gender, education and whether or not living alone in the regression model. Bootstrap estimation was used if the distribution was skewed. A similar comparison was also made at 12 months (in this analysis, the life events and functional ability scores at baseline were used instead of those at 24 months).
Secondary effectiveness end points
The following continuous outcomes were assessed at 24 months:
-
mental health PHQ-9
-
Affordability Index
-
Standard of Living Index
-
social interaction score
-
alcohol (timeline follow back)
-
dietary intake score
-
physical activity (PASE)
-
receiving care – hours per week.
Each secondary outcome was compared at 24 months between the intervention and control groups using multiple linear regression with adjustment for baseline and general practice (the stratification variable). The results are reported as a difference in means with a 95% CI. The adjusted analyses also included the baseline covariates of age, gender, education and whether or not living alone in the regression model. Bootstrap estimation was used for CIs when the distribution was skewed.
The following categorical secondary outcomes were assessed at 24 months:
-
living independently (yes or no)
-
mortality
-
change in smoking status since baseline
-
whether or not seeing friends and relations as often as wished.
We used logistic regression with adjustment for general practice (stratification variable) to compare proportions between the intervention and control group. The results are reported as odds ratios with 95% CIs. An adjusted analysis in the regression model also included general practice (stratification variable), age, gender, education and whether or not living alone.
Exploratory analyses
Exploratory analyses were performed in which the linear model for the primary outcome contained terms for intervention, other key variables (sex, age in years and education) and the interaction between them.
In addition, within the intervention group, multiple linear regression explored whether the mean primary outcome (CASP-19) at 24 months differed, first between those receiving and not receiving welfare rights advice, and then between those receiving and not receiving any extra welfare benefits. As a final exploratory analysis, a comparison was made between the CASP-19 scores at 24 months for those in the intervention arm who had previously been awarded a financial welfare benefit and those in the control arm who were later awarded a financial benefit. As they were all eligible for financial welfare benefits, these participants should be similar in their socioeconomic and health profiles. All of these models also included baseline CASP-19 score, general practice, age, gender, level of educational attainment and whether or not living alone.
Analysis of trial process
The analysis for the process evaluation consisted of descriptive statistics for the recruitment and flow of participants through the trial (trial implementation), the time in days between randomisation and visit of WRA, whether or not advice was received, the benefits recorded (receipt of intervention) and the length and number of WRA consultations (dose).
Qualitative study
Sampling
Qualitative interviews were conducted with trial and professional participants. Semistructured interviews with 50 purposively sampled trial participants took place in two phases between January and July 2014 (30 intervention participants) and February and May 2015 (20 control participants). The trial participants were identified from the trial database and recruited to achieve a maximum variation sample with respect to group allocation, gender, age, receipt of benefits and any unanticipated consequences of the intervention identified at follow-up. A sample of 17 professional participants was interviewed between February and June 2015, selected on the basis of their roles in service commissioning, policy, strategy and service delivery. The professional participants were recruited from the Department for Work and Pensions, local authority and Citizens Advice Bureaux welfare rights services, primary care, public health and the third sector. One group of professional participants was directly associated with intervention delivery (i.e. WRAs) and these are identified throughout the report by the code WRA DEL.
Recruitment
All trial participants were asked during the baseline trial assessment and consent procedures if they would be willing to participate in qualitative interviews. Altogether, 657 (327 intervention and 330 control) participants consented to being contacted for a qualitative interview. This excludes one intervention participant who declined a WRA visit and another participant who withdrew consent before their allocation to a trial arm.
Those selected for interview (trial participants and professional participants) were sent a letter of invitation (see Appendix 12) and a participant information sheet (see Appendix 13) by the research team. The researchers’ contact details were provided so that those approached to participate could ask any questions before deciding to participate. Separate written informed consent was obtained for the qualitative interviews (see Appendix 14). Sampling and interviews with trial and professional participants continued until data saturation was achieved. 93 During the initial qualitative fieldwork with trial participants, the partners of trial participants were often present during the interviews and made valuable contributions. After establishing that such partners were also willing to take part, we sought an amendment to the study ethics so that partners who were willing to take part could also be consented and included (see Appendices 15 and 16 for the partner information sheet and consent form). The intervention participants were interviewed between January and July 2014, after their baseline interview was completed and after they had received their welfare rights advice consultation. The control participants were interviewed between February and May 2015, after their 24-month follow-up interview and after receiving the intervention.
Data collection
The interviews with trial participants explored the acceptability of the intervention and research design, and the perceived benefits and unanticipated consequences of the intervention.
The interviews with professional participants explored the acceptability of the intervention, training and research; the fidelity of the intervention; and the probable implications of the intervention for translation into routine policy and practice, both within the North East and more widely.
All interviews were digitally recorded (with permission) and transcribed verbatim. The transcripts were checked by EN, MS and SL for accuracy of transcription. The data were anonymised, and pseudonyms were applied to preserve anonymity.
Analysis
Qualitative data were collected and analysed iteratively so that themes that emerged in early interviews were explored in later ones. A coding framework was developed, applied to an initial 10 interviews, and then revised to accommodate new insights from the initial analysis. Three interviews were double-coded by MS and SL to ensure reliability of the coding framework that was then applied to all the interview data. The data were analysed thematically using the Framework method94 with constant comparison95 and deviant case analysis96 to enhance validity. NVivo 10 software (QSR International, Warrington, UK) was used to code and manage the data.
Economic evaluation
The relative efficiency of the domiciliary welfare rights advice intervention was assessed in within-trial cost–consequences and cost–utility analyses using data collected during the 24 months of the trial follow-up. For the cost–consequences analysis, the costs and consequences of the intervention are reported separately. The cost–utility analysis combined cost data and HRQoL measures to estimate the incremental cost per quality-adjusted life-year (QALY) gained.
Estimates of cost took the perspectives of the public sector services (for the service delivery costs of the Do-Well intervention) and the Treasury (for additional benefits awarded). Sensitivity analyses were performed to assess the impact of different data sources and varying key assumptions and parameters on the cost-effectiveness of the intervention.
Intervention costs
Identification and measurement
Intervention group
The intervention costs were based on resource use and associated costs collected during the trial (supplemented by routine data sources where necessary) for every participant in the intervention group. The intervention costs included the additional time inputs required by WRAs to deliver the intervention. The service costs of delivering the intervention also required data on staff salaries (collected from local authorities) and standard reimbursement rates for the travel distances from participating localities, as well as data on typical caseloads. These data were used to estimate the average total time spent with participants and to calculate the monetary cost of a specific resource use and the average total cost per case of delivering the intervention to participants.
Time spent on visits to clients and additional time inputs were recorded by WRAs in open-format case diaries as part of the casework contact sheet (CCS) for participants in the intervention group (see Appendix 17). The self-completed case diaries enabled WRAs to report categories of their time spent on the intervention [e.g. home visit(s), telephone call(s), writing letter(s)/e-mail(s) and administrative tasks (such as form filling or referring participants to or making follow-up contacts with other agencies)].
Salary costs (including National Insurance and pension) were averaged and a cost per minute was estimated assuming that WRAs worked 46 weeks per year and 37 hours per week. The cost per minute was then applied to the actual time spent for each participant. Table 2 shows the information provided by participating local authorities and the equivalent average cost per minute of staff time and reimbursement rate for travel used in the analyses, together with sensitivity analyses. Only three local authorities were able to supply relevant data, and in two cases this was incomplete. When data were not available from a local authority, this is marked as not available.
| Source (local authority) | Average annual salary (£) (including on-costs for NI, pension and superannuation)a | Salary (£) | Travel reimbursement (£) per mile | ||
|---|---|---|---|---|---|
| Per weekb | Per hourc | Per minute | |||
| F | 35,247 | 766 | 20.71 | 0.35 | n/a |
| G | 31,949 | 695 | 18.77 | 0.31 | n/a |
| K | 37,334 | 812 | 21.94 | 0.37 | 0.396 |
| Analysis scenarios | |||||
| Base case | |||||
| Average salary | 34,843 | 757 | 20.47 | 0.34 | |
| Sensitivity analyses | |||||
| Average salary +20% | 41,812 | 909 | 24.57 | 0.41 | |
| Average salary –20% | 27,875 | 606 | 16.38 | 0.27 | |
| Travel reimbursement +50% | 0.594 | ||||
Given that the intervention was assumed to cause no harm to participants, no additional individual-level resource use (e.g. for adverse events) was collected.
Control group
Ideally, full details of number of tasks and specific durations would have also been collected for participants in the control group to estimate the difference in costs associated with the delivery of the intervention compared with usual practice. Although case-specific activities and durations were collected by means of case diaries in the intervention group, similar information on resource use was not collected from the control group. In the absence of the full details in either arm, the economic analyses considered only the additional activities associated with the delivery of the intervention at home (i.e. travel duration and distance travelled) to calculate the incremental cost between arms.
Aggregation of costs and sensitivity analyses
The data on costs for each participant were summed to produce a total cost per participant. These data were used to estimate the mean total costs for each arm of the trial and incremental costs. All costs are reported in UK pounds sterling (£) for the 2013/14 financial year. As all costs associated with the intervention were assumed to occur during the first year of the 24 months trial period, costs were not discounted.
Given the likely skewed distribution of the cost data, bootstrapping was used to produce 95% CIs. Sensitivity analyses allowed for effects of a variation in the average WRA salary at a range of –20% to +20%. Additionally, a higher rate of reimbursement per mile travelled (£0.594/mile) was considered to account for higher reimbursement rates usually used in health-related and social sciences research.
Outcomes
Our outcome assessments captured the number of new benefits awarded to participants, as well as changes in HRQoL between baseline and 24-month follow-up assessment. New benefit claims could have occurred as a result of the delivery of the domiciliary advice in the intervention group or due to participants in the control group independently seeking welfare rights advice. However, it was expected that the number of new claims in the control arm would be lower than those in the intervention group. As the period of study was 2 years, all outcomes (financial, non-financial, HRQoL) occurring in the second year were discounted at 1.5%, the recommended rate for public health interventions. 97 A sensitivity analysis investigated the impact of discounting at the UK Treasury rate of 3.5%.
Financial and non-financial benefits
Financial benefits included newly awarded monetary payments or tax credits, while non-financial benefits included newly provided aids and adaptations. Whereas financial benefits have an immediate effect on an individual’s income, non-financial benefits do not involve payments to individuals, but capture transfers in some way that may impact on individuals’ income or well-being in the longer term. To avoid a systematic bias when using data from different sources, the initial analysis used questionnaire data for both trial arms when assessing the number of new benefits awarded and weekly amounts per financial benefit. These data were combined with information on durations for financial benefits collected by means of the CCS in the intervention group.
Intervention group
Gains in financial benefits (in terms of weekly amounts for newly awarded benefits) for participants in the intervention arm were self-reported at 24 months and additionally recorded by WRAs in the CCS. The costs of these were presented from the perspective of the UK Treasury.
The total monetary gain in financial benefits per participant was estimated, based on available information on the weekly amount as reported by participants in the 24-month questionnaire and the duration of the award during the follow-up period as recorded by WRAs in the CCS. The duration of financial benefits paid to participants in the intervention group during the trial period was calculated as the number of weeks between the date of the award as documented in the CCS and the end of the study follow-up. Using CCS data allowed for the inclusion of additional information on the payment of arrears (as lump sums) that was not available from questionnaire data.
Control group
For the control group, newly awarded benefits were identified by comparing information collected on welfare benefits received at baseline and at 24-month follow-up.
As data on the duration of each financial benefit were not collected for the control group, we inferred durations for financial benefits received by participants in the control group using information on durations in the intervention group. We used median durations that were less prone to outliers in the data.
Comparison between trial arms
The data described above and multiplying the duration (in weeks) by the amount per week for newly awarded claims provided the total value of each financial benefit per participant during the trial follow-up period. The average values of benefits are reported for those participants who received new benefits in either trial arm. Comparisons between trial arms were possible after mapping questionnaire questions capturing different types of benefits onto all benefits recorded in the CCS (Table 3).
| Financial benefit (from CCS) | Questionnaire equivalent | Question number |
|---|---|---|
| Means-tested | ||
| Council Tax Benefit | Do you receive Council Tax Benefit? | P045 |
| If YES, how much do you receive? Amount (£/week) | P046 | |
| Housing Benefit | Do you receive Housing Benefit? | P049 |
| If YES, how much do you receive? Amount (£/week) | P050 | |
| Pension Credit: Guarantee Credit | Do you receive Pension Credit? | P053 |
| If YES, is it Savings, Guarantee? | P054 | |
| If YES, how much do you receive? Amount (£/week) | P055 | |
| Pension Credit: Savings Credit | Do you receive Pension Credit? | P053 |
| If YES, is it Savings, Guarantee? | P054 | |
| If YES, how much do you receive? Amount (£/week) | P055 | |
| ESA | Do you receive ESA? | P019 |
| If YES, is it contribution based, means-tested? | P020 | |
| If YES, how much do you receive? Amount (£/week) | P021 | |
| Non-means-tested | ||
| DLA: care component | Do you receive DLA (care component)? | P007 |
| If YES, is it paid at lower/middle/higher rate? | P008 | |
| If YES, how much do you receive? Amount (£/week) | P009 | |
| DLA: mobility component | Do you receive DLA (mobility component)? | P013 |
| If YES, is it paid at lower/middle/higher rate? | P014 | |
| If YES, how much do you receive? Amount (£/week) | P015 | |
| Attendance Allowance: low rate | Do you receive Attendance Allowance? | P001 |
| If YES, is it paid at lower rate, higher rate? | P002 | |
| If YES, how much do you receive? Amount (£/week) | P003 | |
| Attendance Allowance: high rate | Do you receive Attendance Allowance? | P001 |
| If YES, is it paid at lower rate, higher rate? | P002 | |
| If YES, how much do you receive? Amount (£/week) | P003 | |
| Carer’s Allowance | Do you receive Carer’s Allowance? | P033 |
| If YES, how much do you receive? Amount (£/week) | P034 | |
| Industrial Injuries Disablement Benefit | Do you receive Industrial Injuries Disablement Benefit? | P029 |
| If YES, how much do you receive? Amount (£/week) | P030 | |
| Severe Disablement Allowance | Do you receive Severe Disablement Allowance? | P037 |
| If YES, how much do you receive? Amount (£/week) | P038 | |
Sensitivity analyses considered IQR values of durations (first and third quartile of the duration distribution observed in the intervention group) to determine if results were robust to a variation in durations when comparing consequences between trial arms. The information on arrears payments was not included in any of the analyses because the relevant data were not available for the control group, and including arrears payments would have increased the apparent effectiveness of the intervention.
Non-financial benefits
Newly awarded non-financial benefits included Blue Badge car parking permits and new household aids and adaptations provided by the Community Equipment Service, which help people to remain independent at home. A list of aids and adaptations items was included in the questionnaire at both baseline and 24-month follow-up (see Appendix 11). Information on relevant non-financial benefits awarded in the intervention group was also recorded by WRAs in the CCS. However, using cross-validation between the CCS and data collected in the 24-month questionnaire revealed discrepancies in the numbers of claims reported by WRAs and those self-reported by participants in the intervention group, while the numbers of new claims for non-financial benefits obtained from questionnaire data for both trial arms were very similar. Therefore, outcomes associated with non-financial benefits were based on questionnaire data only capturing frequencies of newly awarded non-financial benefits for both trial arms.
Unlike the financial benefits, for which weekly amounts per benefit were reported by participants, unit costs were not collected during the trial for the non-financial benefits. Participating local authorities and public sources provided information on unit costs for aids and adaptations that were part of the non-financial benefits and listed separately in the baseline and 24-month questionnaires. The Department of Health and Social Care’s Community Equipment Services National Catalogue and Prescription Scheme (URL: http://psnc.org.uk/services-commissioning/locally-commissioned-services/community-equipment-services/) was used to provide nationally representative unit cost data for Community Equipment Services, which were used to calculate cost implications in absence of unit cost data from the participating local authorities.
Owing to the large number of items listed as aids and adaptations and a lack of variation in the numbers of newly claimed items between trial arms, the costs of installation of those aids and adaptations were not included in the analysis.
Table 4 gives an overview of questions capturing non-financial benefits (including aids and adaptations) claimed at baseline and 24-month follow-up. The associated unit costs for aids and adaptations are shown in Appendix 18.
| Non-financial benefits (including aids and adaptations) (from CCS) | Questionnaire equivalent | Question number |
|---|---|---|
| Blue Badge | Do you or your partner or a relative who drives for you have a disabled person parking badge (Blue Badge)? | C028 |
| Car (Motability Scheme) | Do you or your partner have a car from the Motability Scheme? | C029 |
| Warm Zones referral | CCS only | |
| Amount: Warm Zones referral | CCS only | |
| Help with insulation cost | Have you had any help with insulation costs (e.g. new central heating boiler, loft insulation, cavity wall insulation)? | C018 |
| Grant from HEES | Have you ever received a grant from HEES? | C019 |
| Social tariff (electricity) | Are you on a social tariff for your electricity cost? | C025 |
| Day centre attendance | Do you attend a day centre? | B017 |
| Meals at home | Do you receive a meals at home service? | B019 |
| Financial help with dental treatment charges | Do you receive financial help with dental treatment charges? | R001_2 |
| Amount: dentist | CCS only | |
| Financial help with optical prescription charges | Do you receive financial help with optical prescription charges? | R001_1 |
| Amount: optician | CCS only | |
| Help with health-care costs: travel | CCS only | |
| Amount: NHS travel costs | CCS only | |
| Community Care Alarm | R002 | |
| Aids and adaptations | ||
| Bathing | Do you have any aids, or have any alterations been made in the bathroom that you usually use that make things easier? | D002 |
| Bath/grab rails | D003_1 | |
| Walk-in shower | D003_2 | |
| Bath house | D003_3 | |
| Bath seat/board | D003_4 | |
| Toileting | Do you have any aids to help with toileting? | D004 |
| Grab rails in toilet/bathroom | D005_1 | |
| Commode for day/night use | D005_2 | |
| Bedpan/urinal/bottle | D005_3 | |
| Raised toilet seat | D005_4 | |
| Incontinence pads | D005_5 | |
| Sleeping | Do you have any aids in the bedroom to make things easier for you to get in and out of bed? | D006 |
| Bed hoist | D007_1 | |
| Bed raise/block | D007_2 | |
| Special bed/mattress | D007_3 | |
| Chair/bed | Do you have any of the following aids for your chair or bed? | D008 |
| Sheepskin | D009_1 | |
| Special cushion(s) | D009_2 | |
| Special chair/chair raise | D009_3 | |
| Accessibility | Have any alterations been made to your home to make things easier for you to get around? | D010 |
| Widened doorways | D011_1 | |
| Additional stair rails | D011_2 | |
| Stairlift/vertical lift | D011_3 | |
| Ramp at front/rear entrance(s) | D011_4 | |
| Additional grab rails at front/rear entrance(s) | D011_5 | |
| Door handle(s) | CCS | |
| Mobility | Do you use any aids for getting about? | D012 |
| Manual wheelchair | D013_1 | |
| Electric wheelchair | D013_2 | |
| Walking frame (Zimmer) | D013_3 | |
| Walking stick(s) | D013_4 | |
| Walking trolley | D013_5 | |
| Crutches | D013_6 | |
| Meals | Do you have any aids for helping you with meals? | D014 |
| Kitchen gadgets | D015_1 | |
| Special cutlery/crockery | D015_2 | |
| Meal trolley | D015_3 | |
| Communication | Do you have any services/aids to help you to communicate with people outside your home? | D016 |
| Community Care Alarm scheme | D017_1 | |
| Special telephone | D017_2 | |
| Entrance telecom | D017_3 | |
| Adapted items | Do you have any aids to help you reach or manipulate objects or parts of your body with your hands? | D018 |
| Helping hand for picking up objects while standing | D019_1 | |
| Helping hand for pulling on socks/stockings | D019_2 | |
| Special implements with long handles (e.g. hair brush) | D019_3 | |
Health-related quality of life
Changes in HRQoL over the 24-month trial period were captured by means of the EQ-5D-3L questionnaire. 81 The EQ-5D-3L is a self-completion questionnaire comprising five dimensions of quality of life: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Using the EQ-5D-3L version gave respondents three response options for each of the dimensions: no problems, some problems and severe problems. The responses were recorded as part of the trial questionnaire at baseline and 24-month follow-up and reported separately for each of the five questions in order to observe how responses changed.
Using UK population tariffs, the responses to the EQ-5D-3L questionnaire were converted into scores of participant-specific health state utilities at each time point. The EQ-5D-3L scores were then transformed into QALYs using the ‘area under the curve’ method. 98 From this, the mean QALY score for each group was calculated, along with incremental QALYs gained to capture the change in HRQoL between trial arms over the trial period.
The differences in mean QALYs gained between the two trial arms were estimated both without adjusting for baseline characteristics and with adjusting QALYs for baseline EQ-5D-3L, age, and gender, to account for any imbalance in the characteristics between the two groups at baseline. Imprecision surrounding incremental QALYs was estimated using bootstrapping and the level of imprecision was presented as 95% CIs. 99
Missing data
To assess patterns in missing EQ-5D-3L data, we tested whether or not data were ‘missing at random’100 by creating a binary variable for missing EQ-5D-3L scores at follow-up and analysing the correlation with the primary study outcome, CASP-19 score, at follow-up. If data were missing at random, missing data were addressed by the application of multiple imputation,91 linking the missing EQ-5D-3L data at follow-up to baseline EQ-5D-3L score and a binary variable capturing whether or not participants reported requiring help at home.
Data analysis
The economic analyses estimated differences in costs and outcomes between the intervention and usual care (control group). The measures of variance for all outcomes involved bootstrapping estimates of costs, consequences (financial and non-financial benefits, QALYs gained) and incremental cost per QALY gained. All data were analysed in Stata version 13 software (StataCorp, College Station, TX, USA). In the base-case analysis (complete-case analysis), missing data were assumed to be missing at random.
Cost–consequences analysis
For the cost–consequences analysis, costs and consequences (financial and non-financial benefits as well as HRQoL) of the intervention were assessed separately. Therefore, the implications for participants’ income, based on additional benefits received during the 24-month trial period as well as changes in EQ-5D-3L, were presented in a disaggregated way and presented in the form of a balance sheet. In the balance sheet, outcomes are reported depending on which arm of the trial they favoured. Thus, the cost–consequences analysis can be used to show the trade-offs between different outcomes deemed of importance.
Cost–utility analysis
The cost–utility analysis combined cost data and HRQoL measures to estimate the incremental cost per QALY gained by the intervention group compared with the control group at 24 months. The incremental cost-effectiveness of the intervention compared with usual care was estimated using seemingly unrelated regression (SUR). 101 This allowed for the simultaneous estimation of costs and QALYs gained, which were calculated at individual level, and accounted for unobserved individual characteristics that could affect both costs and QALYs and lead to the potential correlation of these two variables. Using SUR controlled for the potential bias in estimates and ensured efficient estimation. 102 Additionally, the estimation controlled for the baseline covariates of age, gender and EQ-5D-3L.
For the bootstrapping, a common random seed was set and used for regressions of both costs and QALYs, to ensure that each bootstrap iteration for the differences in costs and QALYs was comparable. The results are based on 1000 bootstrap iterations. For each iteration, the SUR analysis was run on the data set, non-parametric bootstrap samples were drawn from the SUR residuals for both trial arms, predicted values of incremental costs and QALYs were calculated using the bootstrapped residuals, and differences in mean costs and QALYs between the intervention and control groups were estimated with 95% CIs to account for uncertainty surrounding the incremental cost-effectiveness ratio (ICER).
The results of the analysis are presented as point estimates for each of the 1000 bootstrap iterations in a cost-effectiveness plane describing the ICERs from each of the 1000 iterations. Finally, the ICERs calculated were compared against willingness-to-pay thresholds of relevance to UK decision-makers [e.g. the National Institute for Health and Care Excellence (NICE)’s current threshold of £20,000–30,000 as society’s willingness to pay (WTP) for one QALY gained]. The probability for the intervention to be cost-effective at different WTP thresholds was then presented in a cost-effectiveness acceptability curve (CEAC).
Ethics arrangements, governance and sponsor
A favourable ethics opinion was received from the UK NRES Committee South West – Exeter (reference number 11/SW/0260). The trial was registered as Current Controlled Trials ISRCTN37380518. The sponsor of the research was NHS North of Tyne.
Changes to protocol
In October 2011 (protocol 1–2), the protocol, participant information sheet and informed consent form were amended to include the possibility of long-term follow-up. In the event of an inconclusive outcome to the study at 24-month follow-up, it would be desirable to follow up participants at a later time point. Therefore, we amended the protocol to seek, at baseline, participants’ consent to contact them again at a later date. It was recognised that long-term follow-up would require further funding and a new protocol.
In May 2013 (protocol 2–3), the protocol was amended to correct some typographical errors. In addition, the covering letters designed to be sent out with the 12-month follow-up questionnaire (cover letter, reminder letter 1 and reminder letter 2) were added.
In August 2013 (protocol 3–3.1) the protocol was amended to increase the number of participants able to take part in the qualitative element of the study from 30 trial participants and 10 professional participants, to up to 70 trial participants and up to 20 professional participants, subject to data saturation.
In February 2014 (protocol 3–4), the protocol was amended to allow us to include other household members in our qualitative interviews. This involved the production of a separate participant information sheet and consent form for other household members (see Appendices 15 and 16).
Protocol version 4, our final approved version, is available at www.nets.nihr.ac.uk/projects/phr/09300902. 103
Independent Trial Steering Committee
An independent TSC provided overall supervision of the trial. The independent TSC comprised Professor Stephen Walters (chairperson), Professor of Medical Statistics and Clinical Trials, School of Health and Related Research (ScHaRR), University of Sheffield; Professor Colin Green (deputy chairperson), Professor in Health Economics and Head of Health Economics Group, Peninsula College of Medicine and Dentistry, University of Exeter; Mr Nick Whitton, Head of Commissioning for Adult Services, Adult and Community Services, Durham County Council; Mrs Sally West, Strategy Adviser – Income and Poverty; Age UK; Dr Anne Corden, Senior Research Fellow, Social Policy Research Unit, University of York; Christine Smith (lay member); John Marshall (lay member); Professor Martin White (Chief Investigator); the study statistician (Ms Denise Howel); and the study project manager (Dr Catherine Haighton). Observers from the National Institute for Health Research Public Health Research programme and our sponsor were invited to all independent TSC meetings. Following the initial pre-study meeting, the independent TSC met annually. Its role was to monitor progress and supervise the trial to ensure that it was conducted to high standards in accordance with the protocol, the principles of good clinical practice, relevant regulations and guidelines, and with regard to participant safety and well-being. A written charter was agreed and used by the independent TSC (see Appendix 19).
Data Monitoring and Ethics Committee
This was a low-risk trial and major safety data were not anticipated; therefore, a Data Monitoring and Ethics Committee was not convened.
Patient and public involvement
We engaged with service users from the outset and throughout the study. The research design was discussed with a representative sample of low-income older people to assess its acceptability. We undertook a simulation experiment in the context of a focus group discussion with a representative sample of low-income older people (discussed in detail earlier, see Length of follow-up). These members of the public provided valuable insight and advice regarding the study design and patient-relevant end points at the outline stage. Throughout the study, direct patient involvement, via a number of focus groups with Age UK members, also supported the development of suitable letters of invitation to participate, participant information sheets and covering letters explaining the study instruments. There were also two lay members of the TSC (Christine Smith and John Marshall), who provided valuable input throughout the course of the study.
Chapter 3 Main trial findings
In this chapter, we present the main findings of the RCT, including quantitative aspects of the process evaluation, a description of the study participants, the main outcome analyses and the exploratory analyses.
Process evaluation
In this section, measures of the implementation of the trial and the intervention will be presented.
Trial implementation
Figure 2 shows the recruitment and flow of participants through the trial, using the CONSORT format. 73 Nearly 4000 primary care patients aged ≥ 60 years were initially approached by 17 general practices. The recruited participants were spread over the 17 general practices, as shown in Table 5. These practices were chosen to be in the lower two-fifths of the deprivation ranking distribution. The average deprivation level of the 17 participating practices (based on the IMD score at the MSOA level for practice postcode) was lower than that among the remaining 363 practices in the North East [IMD score at MSOA level: 27.0 (SD 10.4) vs. 38.5 (SD 11.5)].
FIGURE 2.
The CONSORT flow chart of participants in the Do-Well RCT. WR, welfare rights. Reproduced from Howel et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution International license (CC BY 4.0), which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
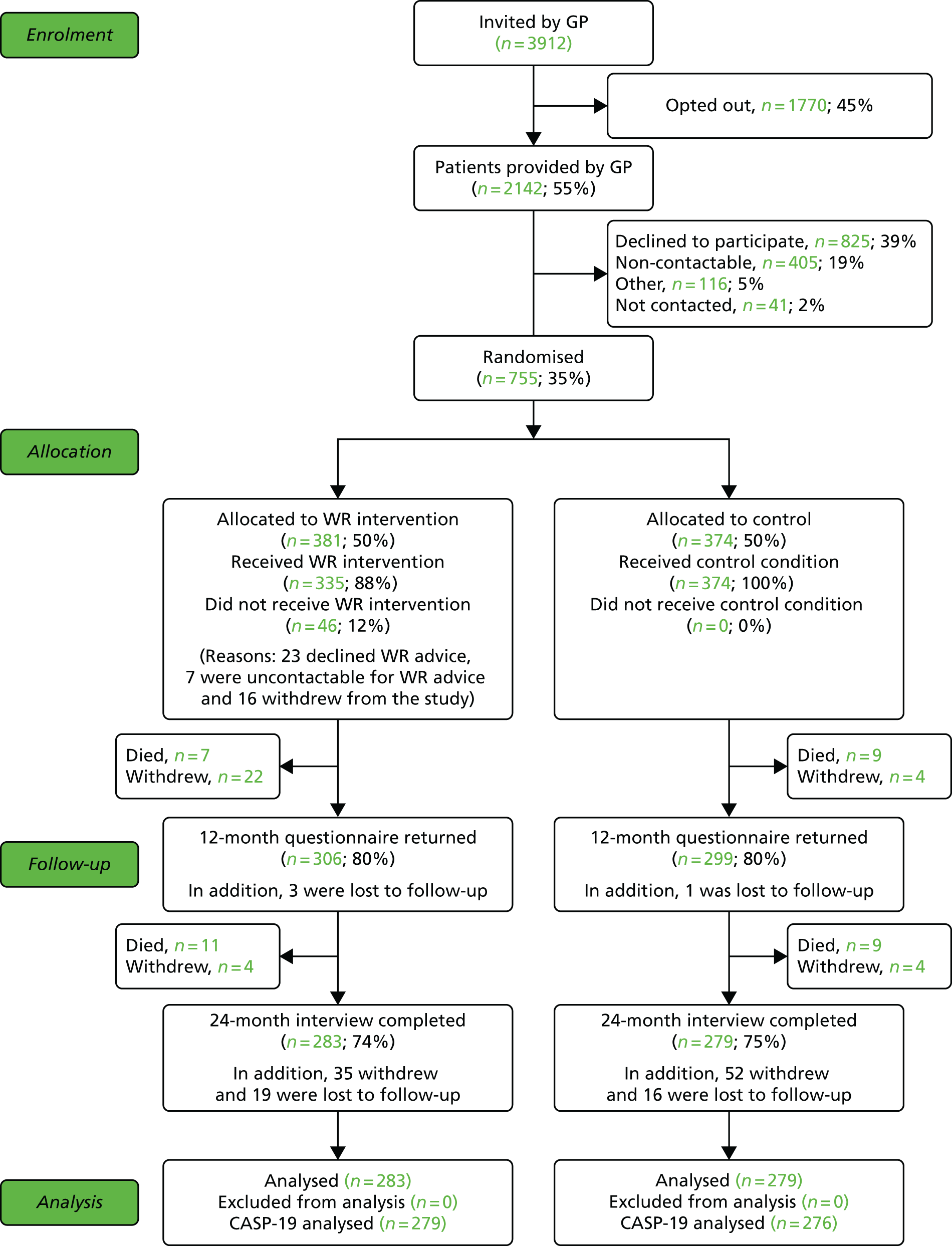
| Practice code | Mailed (n) | Responders (n) | Recruitment rate (%) |
|---|---|---|---|
| 1 | 387 | 52 | 13.4 |
| 2 | 295 | 61 | 20.7 |
| 3 | 200 | 44 | 22.0 |
| 4 | 200 | 51 | 25.5 |
| 5 | 300 | 73 | 24.3 |
| 6 | 100 | 25 | 25.0 |
| 7 | 100 | 17 | 17.0 |
| 8 | 100 | 26 | 26.0 |
| 9 | 300 | 47 | 15.7 |
| 10 | 300 | 70 | 23.3 |
| 11 | 200 | 35 | 17.5 |
| 12 | 330 | 75 | 22.7 |
| 13 | 300 | 54 | 18.0 |
| 14 | 200 | 31 | 15.5 |
| 15 | 200 | 30 | 15.0 |
| 16 | 200 | 47 | 23.5 |
| 17 | 200 | 17 | 8.5 |
| Total | 3912 | 755 | 19.3 |
Of those patients approached, 1770 (45%) opted out of further involvement by returning the invitation slip to their general practice. GPs sent the remaining 2142 names (55% of those approached) and their contact details to the research team. The chief investigator wrote to all of these patients inviting them to participate in the research. Of the 2142 invited, 825 (39%) declined to participate further at that stage, 405 (19%) were not contactable, 116 (5%) initially did not refuse but later declined to participate and 41 (2%) were not contacted as the recruitment target had been reached before they were needed. Those remaining were 755 primary care patients aged ≥ 60 years from participating general practices in socially deprived areas of North East England, all of whom agreed to participate, provided informed consent and were randomised to either the intervention or the control group. The participants were recruited between 11 May 2012 and 28 February 2013.
However, those who agreed to participate (n = 755) were, on average, less socioeconomically disadvantaged [IMD score at LSOA level: 29.0 (SD 16.0)] than non-participants [n = 1387; IMD score: 33.5 (SD 17.9)], and were more likely to be female (53.5% vs. 50.5%).
During the trial, 121 participants withdrew from the study, 36 were lost to follow-up and 36 participants died (see Figure 2 for details). The losses were balanced across allocation groups. In total, 562 participants completed the 24-month follow-up (intervention group, n = 283; control group, n = 279) and were available for analysis.
Receipt of intervention (reach)
As shown in Figure 2, 381 trial participants (50%) were randomly allocated to receive the intervention. The intervention group participants were offered welfare rights advice shortly after recruitment: Figure 3a shows the distribution of the time, in days, between randomisation and the first visit by the WRA, while Figure 3b shows the distribution of time between randomisation and closing the welfare rights advice case, which occasionally took > 12 months. The number seen (as intended) within 2 weeks by their WRA was 5 (1.5%) and within 4 weeks was 37 (11%). The median number of days from study entry to first WRA visit was 58 days (IQR 40–89 days) and the range was 0–403 days. The length of time taken for WRAs to see intervention group participants for their initial assessment increased over time.
FIGURE 3.
Distribution of (a) time (days) between randomisation and first WRA visit; and (b) time (days) from randomisation to welfare rights advice case being closed.
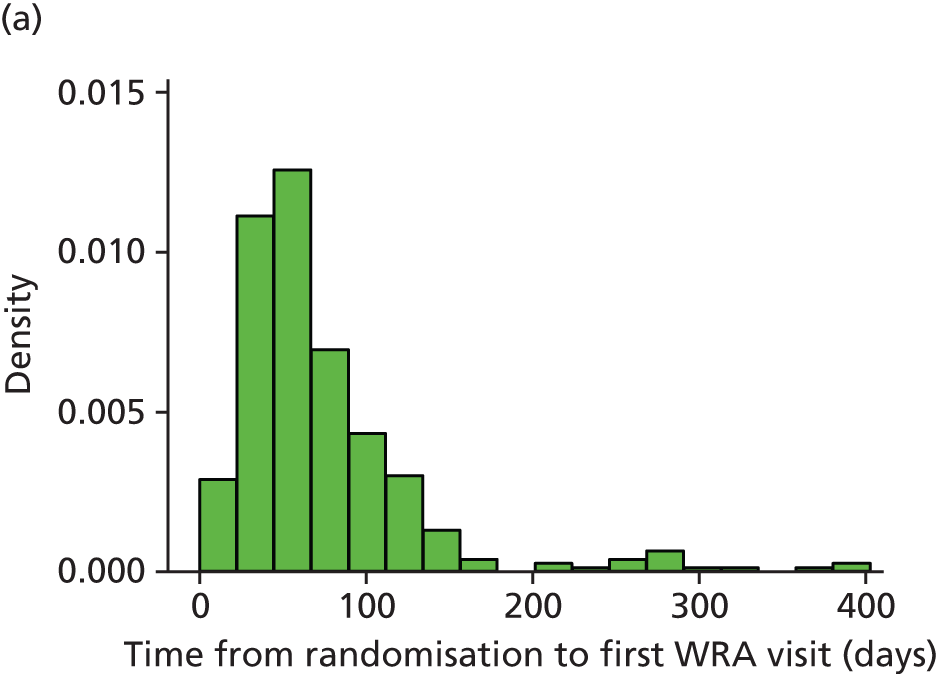
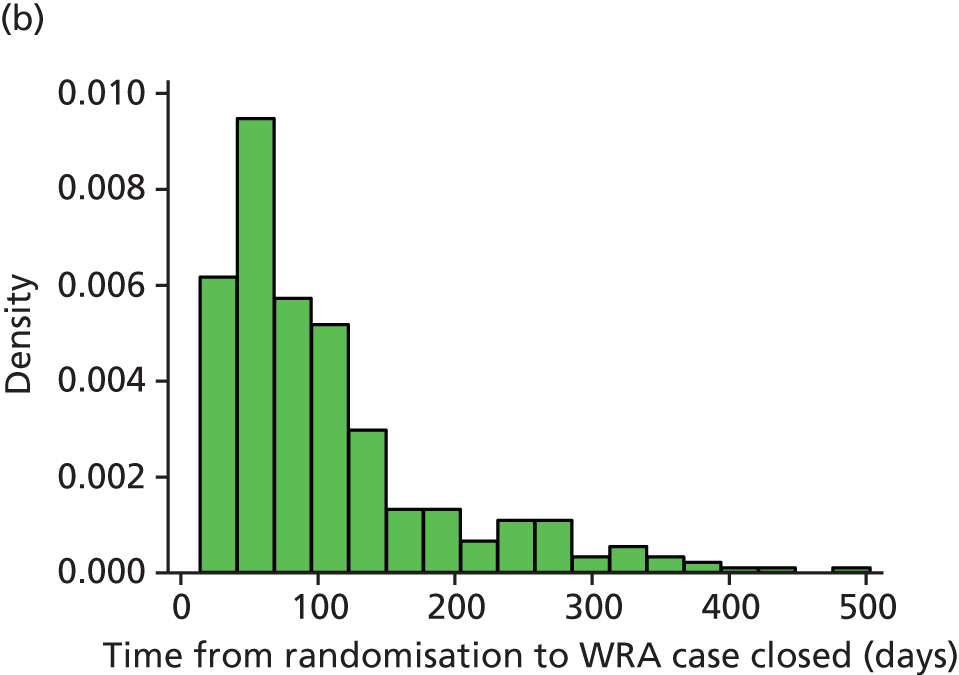
Table 6 shows whether or not the advice was received or if benefits were awarded among the 381 participants in the intervention arm. Of these participants, 335 (88%) actually received the intervention as intended. For those randomised to but not receiving the intervention (n = 46, 12%), the most commonly cited reason for not receiving was that the participant declined the welfare rights advice consultation (n = 23); this represented 6% of all who were eligible and 50% of those not receiving the intervention (in the intervention group). In addition, some participants completely withdrew from the study before intervention delivery (n = 16), while a small number of participants could not be contacted in order to arrange the welfare rights advice appointment (n = 7).
| Number (%) | |
|---|---|
| Welfare rights advice received | |
| Yes | 335 (88) |
| No | 46 (12) |
| Benefits from welfare rights advice | |
| Yes | 84 (22) |
| Eligible but refused | 17 (4.5) |
| Noa | 250 (65.8) |
| Awaiting outcome | 1 (0.3) |
| Withdrawnb | 29 (7.5) |
In total, 84 of the 381 participants (22%) in the intervention arm were awarded an additional benefit, but this rises to 25% when expressed as a percentage of the 335 who received welfare rights advice. Table 7 shows the distribution of the benefits received for those who took up the offer of welfare rights advice. This information came from the records kept by the WRAs (CCS). There were some discrepancies observed between WRA records and those obtained when participants were interviewed at 24 months concerning new benefits that had been awarded. This is explored further in Chapter 5.
| Number (%) | |
|---|---|
| Type of benefit | |
| None | 250 (74.6) |
| Financial | 65 (19.4) |
| Non-financial (aids and adaptations) | 14 (4.2) |
| Both financial and non-financial | 5 (1.5) |
| Not known | 1 (0.3) |
| Of 84 participants who received benefits | |
| Means- or non-means-tested benefits | |
| Means tested | 16 (19.0) |
| Non-means tested | 49 (58.0) |
| Both means and non-means tested | 19 (23.0) |
| Combination of type of benefit and means or non-means tested | |
| Financial (means tested) | 16 (19.0) |
| Financial (non-means tested) | 34 (40.0) |
| Both financial (means and non-means tested) | 15 (18.0) |
| Aids and adaptations (non-means tested) | 14 (16.5) |
| Both financial and aids and adaptations (non-means tested)a | 2 (2.5) |
| Both financial and aids and adaptations (means and non-means tested) | 3 (3.5) |
Table 7 shows that non-means-tested benefits were most commonly received. There were small numbers in each of the categories of different combinations of financial and non-financial benefits received. A detailed description of exactly which financial and non-financial benefits were received is given in Chapter 5.
Dose
The intervention was a standard service and our training and delivery checklist aimed to ensure that the fidelity and ‘dose’ of the intervention was consistent across participants. However, the intervention was also intentionally tailored to individual social welfare needs, and so consultations varied in duration according to the particular circumstances and requirements of each participant. Further details of the duration and number of consultations are given in Chapter 5.
Changes to the intervention
The main alterations to the Do-Well intervention were changes to the personnel delivering the intervention, a consequence of local authority budget cuts resulting from national austerity measures that were out of our control. In May 2012, the WRA from one local authority (G) withdrew from the study without giving a reason (see Table 1 for details of local authorities and general practices). In July 2012, the WRA from another local authority (K) withdrew from the study as a result of staff redundancies. In July 2014, the welfare rights advice team from a further local authority (J) went through a process of restructuring whereby welfare benefits posts were removed and a new team was formed which combined local welfare provision with supported housing. One officer continued dealing with welfare benefits cases but only had a remit for complex issues, and, therefore, was unable to continue with the study. In March 2015, the WRAs in another local authority (H) asked the study team to stop any further referrals, as they had moved into redundancy consultation notice104 and found that they were not be able to provide follow-up appointments. To mitigate the impact of these changes in welfare rights advice provision, we secured the services of two recently retired, qualified WRAs with extensive local authority experience, who were able to work freelance and who stepped in to continue providing the intervention in these local authorities, paid from our contingency budget.
During the course of the study in the eight local authorities, 19 WRAs provided the intervention: three in local authority F; two each in local authorities M and E; two local authority-based and one freelance in local authorities H, J and K; four in local authority L; and one freelance in local authority G.
Fidelity assessment
Seven recordings of WRA initial assessments with participants in the intervention group from five local authorities were made available for fidelity assessment: one local authority refused to allow its WRAs to undergo assessment and two local authorities were unable to complete the assessments within the agreed time frame. In one local authority this was because the welfare advisors were unable to find a client who would consent to the recording within the time frame for the fidelity assessment; in another, local authority budget cuts caused staff shortages that prevented an assessment taking place. In another area, only one WRA was assessed for fidelity owing to staff shortages and time constraints.
All consultations were found to be carried out systematically, and the approach to undertaking each consultation was found to be consistent and in accordance with the protocol for intervention delivery. All consultations were found to have appropriate assessment of financial and health status, and all relevant applications for eligible means- and non-means-tested awards and benefits were carried out.
Contamination
Comparison of the responses to the baseline and 24-month interviews indicated that some control group participants reported receiving new welfare benefits during that period. Despite this, we found no direct evidence that any of the control group participants independently sought welfare rights advice before it was offered following the 24-month interview.
Unanticipated consequences of the intervention
We found no evidence from our quantitative analyses of any unanticipated consequences of the intervention.
Baseline characteristics of trial participants
To illustrate how representative the Do-Well participants were of other residents of England, Table 8 compares the demographic characteristics of the Do-Well participants with those of members of the ELSA cohort in wave 4 who were aged ≥ 60 years. The Do-Well trial participants were recruited from practices in the lower two-fifths of the deprivation ranking distribution in areas of the North East, whereas the ELSA cohort was recruited from the whole population of England. There were clear differences between cohorts on only a couple of variables: higher proportions of Do-Well participants lived alone and ‘were paying rent or mortgage’ (as opposed to owning their own home or, occasionally, living rent free).
| Variable | ELSA cohorta (n = 7321), % | Do-Well trial (n = 755), % |
|---|---|---|
| Sex: male | 43.9 | 46.8 |
| Lives alone | 31.6 | 47.0 |
| In employment | 15.1 | 11.4 |
| Paying rent/mortgage | 26.0 | 42.2 |
| Age (years), mean | 71.7 | 70.6 |
| CASP-19 score, mean | 41.0 | 41.1 |
Tables 9 and 10 show the baseline characteristics of the 755 participants for categorical and numerical outcomes, respectively, by trial arm. The distributions were well balanced between the intervention and control arms. Roughly half of the participants were male, living alone and not paying for accommodation. They were predominantly white, were educated to secondary school level, were retired, were never or ex-smokers and had a satisfactory level of emotional support. The average age was 70 years, while typical Townsend Activities of Daily Living scales were relatively high and stressful life events scores were relatively low.
| Variable | Trial arm, n (%) | |
|---|---|---|
| Intervention (n = 381) | Control (n = 374) | |
| Sex | ||
| Male | 174 (46.0) | 179 (48.0) |
| Ethnicity | ||
| White | 375 (98.5) | 374 (100) |
| Education level | ||
| Primary | 4 (1.0) | 2 (0.5) |
| Secondary | 316 (83.0) | 321 (86.0) |
| Tertiary | 61 (16.0) | 51 (13.5) |
| Living alone | ||
| Yes | 177 (46.5) | 178 (47.5) |
| No | 204 (53.5) | 196 (52.5) |
| Employment status | ||
| Employed | 47 (12.2) | 39 (10.5) |
| Unemployed | 16 (4.2) | 19 (5.0) |
| Retired | 279 (73.2) | 275 (73.5) |
| Other | 38 (10.0) | 39 (10.5) |
| Missing | 1 (0.2) | 10 (0.5) |
| Accommodation | ||
| Not paying | 226 (59.2) | 192 (51.5) |
| Paying | 145 (38.0) | 174 (46.5) |
| Other | 10 (2.5) | 7 (2.0) |
| Missing | 1 (0.3) | 0 (0) |
| Need care at home | ||
| Yes | 97 (25.5) | 115 (31.0) |
| Has emotional support | ||
| Yes | 361 (94.8) | 352 (94.0) |
| No | 11 (2.8) | 17 (4.5) |
| Missing | 9 (2.5) | 5 (1.5) |
| Smoking status | ||
| Never smoked | 124 (33.0) | 118 (31.5) |
| Ex-occasional smoker | 30 (8.0) | 29 (8.0) |
| Ex-daily smoker | 161 (42.0) | 145 (39.0) |
| Occasional smoker | 8 (2.0) | 9 (2.0) |
| Daily smoker | 58 (15.0) | 73 (19.5) |
| Variable | Trial arm | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (n = 381) | Control (n = 374) | |||||||
| n | Mean | SD | Range | n | Mean | SD | Range | |
| Age (years) | 381 | 70.6 | 7.1 | 60–92 | 374 | 70.6 | 7.5 | 60–94 |
| Townsend Activities of Daily Living score (0–16)a | 381 | 10.9 | 4.8 | 0–16 | 373 | 10.7 | 5.0 | 0–16 |
| Life events score (0–32)b | 370 | 4.6 | 4.1 | 0–16 | 371 | 4.4 | 4.2 | 0–24 |
| IMD scorec | 379 | 29.3 | 16.5 | 3.2–74.8 | 373 | 28.7 | 15.5 | 3.2–74.8 |
Table 11 shows the distribution of the primary and secondary outcomes at baseline. The participants had typical values towards the more favourable end of each scale for quality of life, affordability index, standard of living, depression and healthy diet; and towards the less favourable end of the scale for social interaction and physical activity (PASE). The distributions were well balanced between the intervention and control arms.
| Scales (potential ranges) | Trial arm | Observed range | |||
|---|---|---|---|---|---|
| Intervention | Control | ||||
| n | Meana (SD) | n | Meana (SD) | ||
| CASP-19 quality of life score (0 to 57)b | 354 | 41.4 (10.5) | 351 | 40.7 (10.9) | 11.6 to 57 |
| PHQ-9 depression score (0 to 27)c | 372 | 4.4 (5.3) | 366 | 4.6 (5.2) | 0 to 24.8 |
| Affordability index (4 to 20)c | 375 | 13.0 (2.8) | 366 | 13.2 (2.7) | 4 to 20 |
| Standard of living index (0 to 24)b | 381 | 18.7 (2.5) | 374 | 18.6 (2.5) | 7 to 24 |
| Social interaction score (0 to 27)b | 381 | 9.9 (4.6) | 373 | 9.5 (4.3) | 0 to 24 |
| PASE score (0 to 400+)b | 380 | 101.3 (67.5) | 373 | 102.4 (72.3) | 0 to 325.5 |
| Diet score (15 to 75)b | 380 | 46.9 (6.9) | 373 | 46.8 (6.8) | 23 to 66 |
| EQ-5D-3L score (–0.59 to 1)b | 374 | 0.589 (0.332) | 363 | 0.583 (0.356) | –0.594 to 1 |
| Units of alcohol in last week: all | 369 | 6.7 (11.2) | 367 | 6.3 (10.2) | 0 to 84 |
| Units of alcohol in last week: drinkers | 267 | 9.2 (12.3) | 243 | 9.4 (11.3) | 0 to 84 |
| Receiving home care (hours/week)d | 85 | 48.1 (56.1) | 100 | 53.6 (57.5) | 1 to 168 |
Table 12 shows the baseline characteristics of the 755 participants for categorical and numerical outcomes for responders and non-responders at 24 months. Those who dropped out of the trial before the 24-month assessment on average tended to be a little older, slightly more likely to be male and have a lower average CASP-19 score at baseline.
| Characteristic | Responders (n = 555), n (%) | Non-responders (n = 200), n (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| Categorical variables | ||||||||
| Sex | ||||||||
| Male | 251 (45) | 102 (51) | ||||||
| Education level | ||||||||
| Tertiary | 84 (15) | 28 (14) | ||||||
| Continuous variables | n | Mean | SD | Range | n | Mean | SD | Range |
| Age (years) | 555 | 70.0 | 6.9 | 60.2–90.4 | 200 | 72.4 | 8.2 | 60.2–94.2 |
| CASP-19 score at baseline | 522 | 41.6 | 10.4 | 10–57 | 183 | 39.6 | 11.3 | 7–57 |
Outcome analysis
Intention-to-treat analysis of primary and secondary outcomes
Table 13 shows the distribution of the primary outcome, CASP-19 score, at baseline, 12 and 24 months by trial arm: the results are reported on complete cases and, in addition, after the application of multiple imputation. The primary comparison was at 24 months, when the mean CASP-19 scores were 42.9 in the intervention group and 42.4 in the control group: an adjusted mean difference of 0.3 (95% CI –0.8 to 1.5). The unadjusted means showed little difference between trial arms at any time point, and, when the distribution of covariates was taken into account, there was still little or no difference between mean CASP-19 scores. The differences in mean CASP-19 between trial arms remained very similar at all time points when multiple imputation was used to deal with missing primary outcomes for some participants.
| Time point analysed | Observed range | Trial arm | Difference | |||
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| n | Meanb (SD) | n | Meanb (SD) | Adjusted difference in means (I – C) (95% CI)c | ||
| At baseline | 7–57 | 354 | 41.4 (10.5) | 351 | 40.7 (10.9) | n/a |
| At baseline (using MId) | 7–57 | 381 | 41.3 (10.5) | 374 | 40.8 (10.7) | n/a |
| At 12 months | 9–57 | 300 | 38.2 (10.0) | 295 | 37.4 (10.6) | 0.6 (–0.7 to 1.8) |
| At 12 months (using MId) | 9–57 | 371 | 37.9 (10.1) | 365 | 36.9 (10.6) | 0.4 (–0.7 to 1.5) |
| At 24 months | 6–57 | 279 | 42.9 (10.1) | 276 | 42.4 (10.4) | 0.3 (–0.8 to 1.5) |
| At 24 months (using MId) | 6–57 | 320 | 42.7 (10.3) | 317 | 42.6 (10.1) | 0.4 (–0.8 to 1.5) |
The trial was powered to detect a difference of 1.5 units between means on the CASP-19 scale, and there is little evidence of a difference of this size. It should be emphasised that, although all members of the intervention group were offered welfare rights advice, fewer than one-quarter actually received any additional resources, either financial or non-financial, as a result of the advice. The fact that the majority did not receive any welfare benefits means that any potential change in quality of life as a result of receiving welfare rights advice is likely to have been heavily diluted. An exploration of whether or not the difference in means between trial arms varied significantly between subgroups of trial participants was carried out by testing for interactions between trial arm and sex, age group (dichotomised at median age: 68.6 years) and educational group (primary or secondary vs. tertiary): all interaction terms were not statistically significant (p-values of 0.94, 0.15 and 0.22, respectively) and, therefore, dropped from the regression model.
The difference at 24 months in means between the trial arms was small with narrow CIs for all of the secondary outcome scales (Table 14), other than for average hours of care received each week. The average hours per week were higher in the intervention arm (53.7 vs. 42.0; adjusted difference of 26.3 hours/week, 95% CI 0.8 to 56.1 hours/week). However, for this variable, as few reported receiving care and the amount received varied from 1 to 168 hours per week, the estimates of the difference were imprecise and consistent with either a large or virtually no increase in means.
| Outcome measure | Trial arm | Difference | |||
|---|---|---|---|---|---|
| Intervention | Control | ||||
| n | Meana (SD) | n | Meana (SD) | Adjusted difference in means (I – C) (95% CI)b | |
| PHQ-9 depression score (0 to 27)d | 278 | 3.9 (4.8) | 276 | 3.9 (4.7) | 0.2 (–0.4 to 0.9) |
| Affordability index (4 to 20)d | 276 | 11.9 (2.3) | 265 | 12.1 (2.2) | –0.1 (–0.5 to 0.3) |
| Standard of living index (0 to 24)c | 283 | 18.9 (2.3) | 279 | 18.7 (2.3) | 0.1 (–0.2 to 0.3) |
| Social interaction score (0 to 27)c | 282 | 10.5 (4.5) | 277 | 10.3 (4.3) | 0 (–0.5 to 0.5) |
| PASE score (0 to 400+)c | 283 | 95.4 (59.8) | 274 | 95.0 (60.6) | 1.8 (–5.7 to 9.4) |
| Diet score (15 to 75)c | 282 | 47.0 (6.2) | 275 | 47.4 (6.2) | –0.2 (–1.0 to 0.6) |
| EQ-5D-3L score (–0.59 to 1)c | 280 | 0.680 (0.296) | 273 | 0.674 (0.318) | –0.015 (–0.057 to 0.028)d |
| Units of alcohol in last week: all | 281 | 6.3 (11.4) | 278 | 6.1 (10.4) | 0 (–1.3 to 1.2) |
| Units of alcohol in last week: drinkers | 200 | 8.8 (12.6) | 183 | 9.2 (11.6) | –0.1 (–2.0 to 1.7) |
| Receiving home care (hours/week)e | 42 | 53.7 (66.3) | 52 | 42.0 (56.0) | 26.3 (0.8 to 56.1)f |
Table 15 shows the comparison of the four categorical secondary outcomes at 24 months (living independently, mortality, increase in smoking status and social isolation). The proportions were similar across the trial arms, and no associations were statistically significant: the odds ratios were close to 1 and 95% CIs were narrow.
| Categorical outcome | Trial arm, n (%) | Multivariable logistic regression,a OR (95% CI) | |
|---|---|---|---|
| Intervention (n = 283) | Control (n = 279) | ||
| Living independently | |||
| Dependent on others | 52 (18) | 56 (20) | 0.9 (0.6 to 1.4) |
| Mortalityb | |||
| Dead | 18 (5) | 18 (5) | 1.11 (0.5 to 2.3) |
| Smoking status | |||
| Increase since baseline | 19 (7) | 24 (9) | 0.73 (0.4 to 1.4) |
| See friends and relatives | |||
| Not as often as wished | 63 (23) | 65 (24) | 0.9 (0.6 to 1.4) |
Exploratory analyses
A set of exploratory analyses on those in the intervention arm investigated whether the primary outcome (CASP-19) at 24-month follow-up varied between those in subgroups defined by welfare rights advice received or benefits awarded. These subgroups were not likely to be balanced on key covariates, because socioeconomic and health-related variables are key eligibility criteria considered when a welfare award is made. Table 16 shows the distribution of sociodemographic variables for those who did and did not receive any welfare benefits: there were no great differences, but those awarded welfare benefits tended to be slightly older and more likely to live alone and be female, and less likely to be well educated and be able to carry out activities of daily living: there was little difference in mean IMD scores, which might have been expected.
| Characteristic | Benefits, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Benefits awarded and received (n = 84) | No benefits awardeda (n = 267) | |||||||
| Categorical variables | ||||||||
| Sex | ||||||||
| Male | 31 (41) | 121 (47) | ||||||
| Education level | ||||||||
| Primary | 1 (1) | 3 (1) | ||||||
| Secondary | 67 (89) | 209 (81) | ||||||
| Tertiary | 7 (10) | 47 (18) | ||||||
| Marital status | ||||||||
| Living alone | 41 (55) | 111 (43) | ||||||
| Accommodation | ||||||||
| Not paying | 42 (59) | 154 (61) | ||||||
| Continuous variables | n | Mean | SD | Range | n | Mean | SD | Range |
| Age (years) | 84 | 71.4 | 6.8 | 60–88 | 266 | 69.7 | 7.2 | 60–92 |
| Townsend Activities of Daily Living score at 24 months | 60 | 8.5 | 4.1 | 0–16 | 195 | 12.2 | 4.1 | 0–16 |
| Life events score at 24 months | 66 | 4.0 | 3.6 | 0–15 | 209 | 4.7 | 4.1 | 0–18 |
| IMD scoreb | 83 | 29.5 | 16.3 | 6.2–71.7 | 266 | 29.0 | 16.3 | 3.4–74.5 |
Table 17 shows that there was little difference in the crude mean total CASP-19 score at 24-month follow-up between those in the intervention group who did and those who did not receive welfare rights advice, with a small unadjusted difference in means favouring those not receiving welfare rights advice (42.8 for those who received welfare rights advice vs. 44.2 for those who did not). However, after adjustment for key covariates (see Table 17), the direction of difference did not change, but this was not statistically significant (adjusted difference –2.1, 95% CI –5.5 to 1.3).
| Subgroups | n | CASP-19 | |
|---|---|---|---|
| Mean (SD)a | Adjusted difference in means (95% CI)b | ||
| Welfare rights advice received | |||
| Yes | 261 | 42.8 (10.1) | –2.1 (–5.5 to 1.3) (received – not received) |
| No | 18 | 44.2 (9.8) | |
| Welfare benefits awarded | |||
| Yes | 65 | 39.2 (9.4) | –0.7 (–2.8 to 1.4) (awarded – not awarded) |
| No | 208 | 43.8 (10.1) | |
When comparing the subgroups who did and did not receive benefits (as opposed to advice), the lower part of Table 17 shows that there was a lower average CASP-19 score at the 24-month follow-up in those receiving benefits, for both total score and subscales (mean total score 39.2 for those who received benefits vs. 43.8 for those who did not). This might be explained by the fact that those who received benefits tended to be worse off at baseline, in terms of health and socioeconomic variables, than those who did not receive welfare benefits, and this could be reflected in the CASP-19 scores. After adjusting for these covariates, the difference in mean total CASP-19 score was smaller (adjusted difference –0.7, 95% CI –2.8 to 1.4), and there was no indication of a statistically significant or clinically important improvement in average CASP-19 in those receiving welfare benefits.
Secondary outcomes were also compared between those who did and those who did not receive welfare rights advice. Table 18 shows that the adjusted differences in mean between the two subgroups were all small with narrow CIs.
| Questionnaire score at 24 months | Welfare rights advice received | n | Mean (SD)a | Adjusted difference in means (95% CI)b |
|---|---|---|---|---|
| PHQ-9 depression score (0–27)c | Yes | 260 | 4.0 (4.7) | –0.6 (–2.5 to 1.2) (received – not received) |
| No | 18 | 3.0 (5.7) | ||
| Affordability index (4–20)c | Yes | 257 | 11.9 (3.0) | 0.1 (–1.1 to 1.2) |
| No | 19 | 12.0 (3.4) | ||
| Standard of living index (0–24)d | Yes | 264 | 18.8 (2.3) | 0.5 (–0.1 to 1.2) |
| No | 19 | 19.8 (2.5) | ||
| Social interaction score (0–27)d | Yes | 263 | 10.5 (4.5) | 0.9 (–0.6 to 2.4) |
| No | 19 | 10.5 (4.6) | ||
| PASE score (0–400+)d | Yes | 264 | 94.6 (59.3) | 0.2 (–22.1 to 22.6) |
| No | 19 | 106.4 (66.5) | ||
| Diet score (15–75)d | Yes | 264 | 47.0 (6.2) | –0.9 (–3.3 to 1.4) |
| No | 18 | 46.7 (6.9) | ||
| Units of alcohol in last week: all | Yes | 262 | 6.3 (11.4) | 1.0 (–3.1 to 5.0) |
| No | 19 | 5.7 (11.1) | ||
| Units of alcohol in last week: drinkers | Yes | 187 | 8.9 (12.7) | 1.0 (–5.4 to 7.4) |
| No | 13 | 8.3 (12.7) |
A comparison of secondary outcomes between those who did and those who did not receive any benefits was also undertaken. Table 19 shows that the adjusted differences in means between the two subgroups were all small with narrow 95% CIs, except for the physical activity score (PASE). The adjusted mean PASE score was significantly higher in those who were not awarded any benefits (adjusted difference –13.9, 95% CI –27.0 to –0.9); this may reflect the better health of those who did not receive welfare benefits, rather than any effect of non-receipt of welfare benefits on the ability or choice to exercise more.
| Questionnaire score at 24 months | Benefits awarded | n | Mean (SD)a | Adjusted difference in means (95% CI);b awarded – not awarded |
|---|---|---|---|---|
| PHQ-9 depression score (0–27)c | Yes | 65 | 5.2 (4.5) | 0.6 (–0.5 to 1.7) |
| No | 207 | 3.5 (4.9) | ||
| Affordability index (4–20)c | Yes | 65 | 12.2 (2.1) | 0.2 (–0.5 to 0.8) |
| No | 204 | 11.9 (2.3) | ||
| Standard of living index (0–24)d | Yes | 67 | 18.2 (2.1) | 0.1 (–0.3 to 0.5) |
| No | 209 | 19.0 (2.4) | ||
| Social interaction score (0–27)d | Yes | 66 | 9.4 (4.2) | –0.1 (–1.0 to 0.8) |
| No | 209 | 10.8 (4.6) | ||
| PASE score (0–400+)d | Yes | 67 | 69.0 (45.3) | –13.9 (–27.0 to –0.9) |
| No | 209 | 103.0 (61.8) | ||
| Diet score (15–75)d | Yes | 67 | 46.4 (6.0) | –0.6 (–1.9 to 0.8) |
| No | 208 | 47.3 (6.3) | ||
| Units of alcohol in last week: allc | Yes | 67 | 5.9 (9.8) | 0.1 (–2.4 to 2.5) |
| No | 207 | 6.3 (11.5) | ||
| Units of alcohol in last week: drinkersc | Yes | 44 | 9.0 (11.0) | 0.7 (–3.0 to 4.4) |
| No | 149 | 8.7 (12.8) |
A final comparison was between the CASP-19 scores at 24 months for those in the intervention arm who had been awarded a financial welfare benefit and those in the control arm who were later awarded a financial benefit (after 24-month follow-up). As they were all eligible for financial welfare benefits, these participants should be similar in their socioeconomic and health profiles. The 55 in the intervention group who had been awarded financial benefits had a mean CASP-19 score of 39.2 (SD 9.1), whereas the 48 in the control group (who were later found to be eligible) had a mean CASP-19 score of 39.7 (SD 9.4). After adjustment for covariates, the mean CASP-19 score was 1.4 higher in the control group (95% CI –2.0 to 4.7). This comparison shows again that there was little or no evidence that CASP-19 varied between a subgroup who had received benefits and a subgroup who had not.
A further exploration of any association between CASP-19 and receipt of welfare benefits in the intervention group was to look at the weekly amount of financial benefits (in pounds sterling). Figure 4 shows the association between these two variables; it can be seen that there is no indication that CASP-19 at 24 months is higher for those receiving greater financial benefits. However, this does not adjust for the covariates used in previous regression models. When adjustment was made for these, the regression coefficient for CASP-19 on weekly amount was 0.02 (95% CI –0.08 to 0.04) also showing a lack of association.
FIGURE 4.
Association between CASP-19 score at 24 months and weekly amount of financial benefit awarded.

The final exploration looked at the association between the length of time that a person had been receiving additional benefits and the CASP-19 scores at 24 months (Figure 5). It might be expected that among those who had only started receiving welfare benefits shortly before the assessment at 24 months, health may have improved less, and this might be reflected in a smaller change in CASP-19 score. However, the vast majority of people had been receiving benefits for at least a year by the time of final assessment. The correlation between the two variables was 0.39 (95% CI 0.16 to 0.58), a weak positive association.
FIGURE 5.
Association between length of time that participants were in receipt of additional benefits and CASP-19 score at 24-month follow-up.
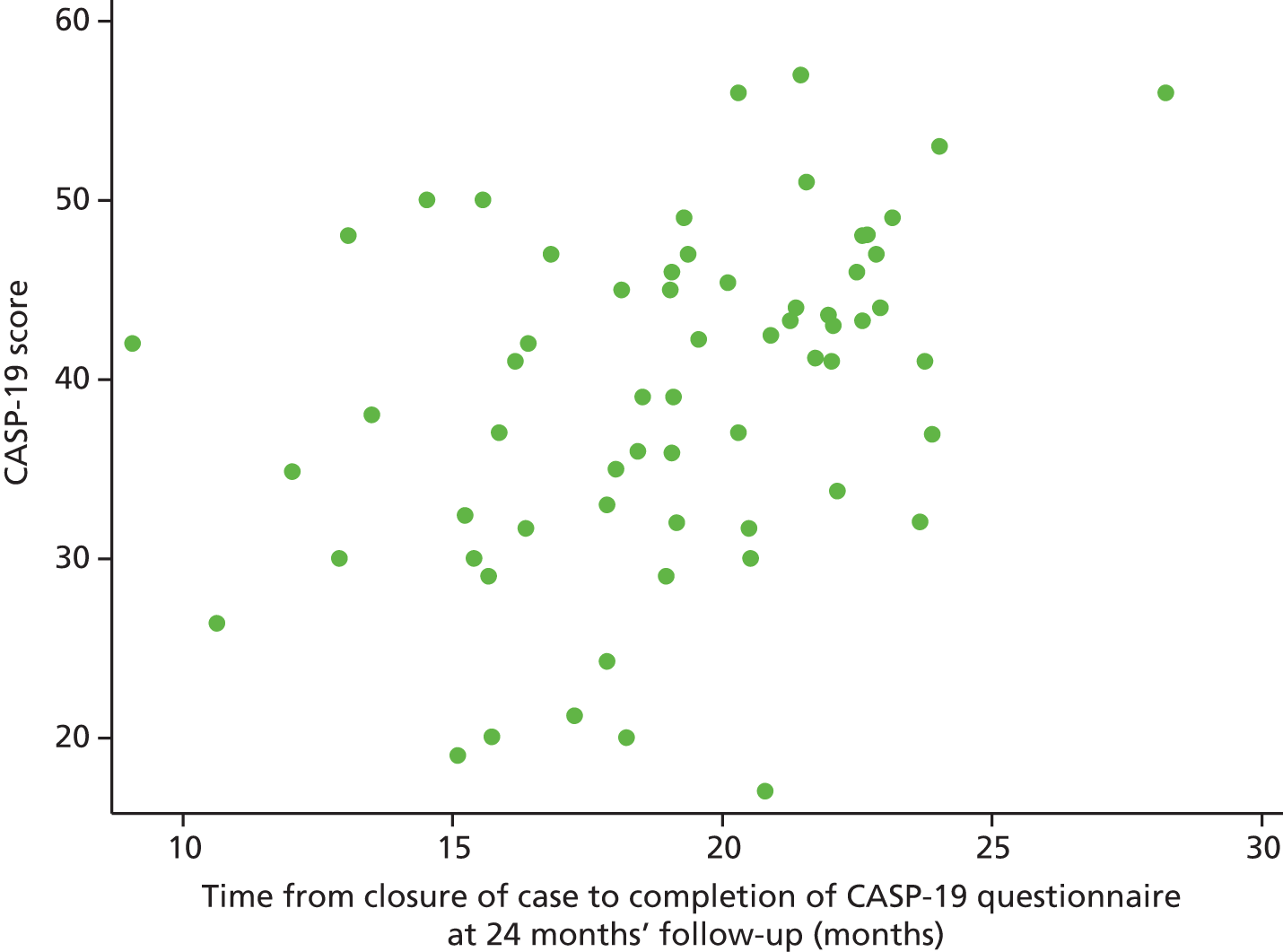
Chapter 4 Qualitative study
Some quotations in this chapter have been reproduced from Howel et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution International license (CC BY 4.0), which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Introduction
This chapter presents the findings of the qualitative study embedded within the RCT. We begin by presenting the sociodemographic characteristics of the qualitative study participants, including household members of trial participants, and professionals (see Tables 20–22). We then present findings on the acceptability of the research design and intervention, followed by those on the impact of the domiciliary welfare rights advice service, as experienced by trial participants and professionals. We then focus on the mechanisms of action and unanticipated consequences of the intervention, before finally examining the impact of external factors, such as cuts to the public sector, on this type of service and its delivery.
The findings are organised around the key themes identified during interviews and are presented for both trial and professional participants. Our presentation of the findings is interspersed with verbatim quotes to illustrate particular points, pseudonyms are used throughout, and any identifying information (e.g. place names) has been removed to preserve anonymity. The participants were made aware that their comments may be used in publications, and informed consent for this was obtained.
Participant characteristics
Tables 20 and 21 present social, demographic and welfare benefit outcome data for the 50 participants in the embedded qualitative study, 30 intervention (see Table 20) and 20 control (see Table 21), all of whom received the intervention as planned. Eight partners were also interviewed alongside trial participants, as indicated in Tables 20 and 21. Thirty-one women and 19 men took part, with six female partners and five male partners also interviewed. The age of the trial participant at the time of the interview is given. The average age was 72 years, ranging from 61 to 86 years. Most of the interviewees were living alone (widowed, n = 19; divorced/separated, n = 8; single, n = 4), with 19 living as part of a couple. Trial participants came from throughout the North East region and from urban, rural and semirural areas; the IMD scores ranged from 7.43 (least deprived) to 71.74 (most deprived). The trial participants were interviewed after receiving a welfare rights intervention and, for those in receipt of a financial or non-financial award, the interview took place after the award was received. The control group trial participants took part in qualitative interviews after their 24-month wait, and following intervention receipt.
| Pseudonym | IMD scorea | Urban/ruralb | Sex | Age in years (baseline) | Marital status | LA | Tenure | Amount (£) gained per week through interventionc | All benefits obtained | Means tested element |
|---|---|---|---|---|---|---|---|---|---|---|
| Nigel | 7.43 | 5 | Male | 61 | Married | Sunderland | O/O | 107 | ESA | |
| Nancy | 7.74 | 6 | Female | 83 | Widowed | Northumberland | Rent free | 77 | AA higher, CTB | Y |
| Gloria | 9.46 | 5 | Female | 72 | Divorced/separated | Sunderland | O/O | 135 | CTB, HB, PC (Guarantee Credit) and AA (lower), Blue Badge | Y |
| William | 12.29 | 5 | Male | 81 | Widowed | Stockton-on-Tees | O/O | 40 | PC (Guarantee Credit and Savings Credit); CTB | Y |
| Barbara (and Derek) | 15.4 | 5 | Female | 75 | Married | Sunderland | O/O | 136 | AA (higher) and Carer’s Allowance (for daughter) | |
| Peter (and Beryl) | 16.23 | 6 | Male | 65 | Married | Durham | SR | 52 | AA (lower) | |
| Finley | 21.21 | 6 | Male | 63 | Widowed | Northumberland | O/O | 41 | DLA (care component) | |
| Brian | 24.6 | 5 | Male | 83 | Married | Newcastle upon Tyne | SR | 0 | None | |
| Diane (and Charles) | 24.94 | 6 | Female | 75 | Married | Northumberland | O/O | 0 | Wheeled Zimmer | |
| Janice | 25.86 | 5 | Female | 70 | Married | Gateshead | O/O | 52 | AA (lower) | |
| Benjamin | 26.57 | 5 | Male | 61 | Divorced/separated | Newcastle upon Tyne | PR | 76 | DLA (care and mobility components); referred to Adult Social Care | |
| Julie | 26.98 | 5 | Female | 72 | Widowed | Sunderland | O/O | 0 | None | |
| Elaine | 27.15 | 5 | Female | 76 | Divorced/separated | Newcastle upon Tyne | SR | 139 | PC and AA (higher) | Y |
| Penny | 28 | 5 | Female | 71 | Married | South Tyneside | O/O | 0 | None | |
| Beatrice | 31.16 | 5 | Female | 74 | Widowed | Sunderland | SR | 139 | AA (higher), Carer’s Allowance | |
| Mabel | 31.91 | 5 | Female | 83 | Widowed | North Tyneside | SR | 0 | None | |
| Jim (and Caron) | 33.46 | 6 | Male | 66 | Married | Northumberland | O/O | 58 | Carer’s Allowance | |
| Emma | 33.6 | 5 | Female | 64 | Married | Sunderland | O/O | 0 | None | |
| Susan | 41.88 | 5 | Female | 74 | Widowed | South Tyneside | O/O | 21 | CTB, PC (Savings Credit); Warm Zone; Health Costs and stair rail | Y |
| Joyce | 42.31 | 5 | Female | 70 | Widowed | South Tyneside | SR | 136 | PC (Guarantee Credit) and AA (higher) | Y |
| Boris (and Shirley) | 43.64 | 5 | Male | 71 | Married | Durham | O/O | 92 | AA (higher), PC (Savings Credit) | Y |
| Natalie | 44.06 | 7 | Female | 64 | Divorced/separated | Northumberland | O/O | 0 | Blue Badge | |
| Myrtle | 46.28 | 5 | Female | 71 | Single | Gateshead | SR | 0 | None | |
| Arthur | 47.06 | 5 | Male | 68 | Divorced/separated | Northumberland | SR | 72 | PC and AA (lower) and SDP and DLA renewal for son | Y |
| Audrey | 57.54 | 5 | Female | 78 | Widowed | Durham | O/O | 139 | AA (higher); PC (Guarantee Credit); CTB | Y |
| Maria | 57.54 | 5 | Female | 77 | Widowed | Durham | SR | 136 | AA (higher); PC (Guarantee Credit) | Y |
| Joan (and Alfred) | 60.28 | 5 | Female | 70 | Married | North Tyneside | O/O | 32 | Industrial Injuries Disablement Benefit | |
| Margaret (and Andrew) | 60.86 | 5 | Female | 63 | Married | Gateshead | O/O | 21 | DLA (care component) | |
| Roger | 61.18 | 5 | Male | 74 | Divorced/separated | Durham | O/O | 0 | Blue Badge | |
| David (and Sandra) | 71.74 | 5 | Male | 72 | Married | Newcastle upon Tyne | O/O | 77 | AA (higher) |
| Pseudonym | IMD scorea | Urban/ruralb | Sex | Age in years (baseline) | Marital status | LA | Tenure | Amount (£) gained per week through interventionc | All benefits obtained | Means tested element |
|---|---|---|---|---|---|---|---|---|---|---|
| Tom | 11.86 | 6 | Male | 69 | With partner | Northumberland | O/O | 7 | CTB | Y |
| Paul | 14.07 | 5 | Male | 76 | Widowed | Newcastle | O/O | 81 | AA (lower) | |
| Lydia | 15.73 | 5 | Female | 68 | With partner | North Tyneside | O/O | 34 | Carer’s Allowance | |
| Stacy | 18.4 | 5 | Female | 65 | Divorced/separated | Newcastle | SR | 50 | PC (Guarantee Credit) | Y |
| Helen (and Ruth) | 22.56 | 5 | Female | 83 | Widowed | Newcastle | SR | 0 | None | |
| Adam | 25.69 | 5 | Male | 70 | Widowed | Sunderland | O/O | 54 | AA (lower); Blue Badge | |
| Jenny | 31.16 | 5 | Female | 69 | With partner | Sunderland | O/O | 27 | AA (higher) | |
| Ian | 31.16 | 5 | Male | 84 | Married | Sunderland | O/O | 0 | None | |
| Harry | 31.91 | 5 | Male | 68 | Divorced/separated | Newcastle | SR | 42 | CTB, HB | Y |
| Laura | 32.45 | 6 | Female | 67 | Widowed | Northumberland | O/O | 10 | CTB and reduced gym membership (amount unknown) | Y |
| Sally | 33.46 | 6 | Female | 79 | Married | Northumberland | O/O | 151 | AA (lower), CTB, PC (Savings Credit) | Y |
| Frida | 35.12 | 6 | Female | 62 | Widowed | Durham | O/O | 0 | None | |
| Sheila (and Carly) | 36.76 | 5 | Female | 77 | Widowed | North Tyneside | O/O | 91 | CTB and AA (lower) | Y |
| Oliver | 39.34 | 5 | Male | 80 | Widowed | South Shields | O/O | 81 | AA (higher) | |
| Debbie | 42.33 | 5 | Female | 61 | Divorced/separated | Gateshead | SR | 78 | DLA renewal (care and mobility components) | |
| Grace | 42.67 | 5 | Female | 62 | Divorced/separated | North Tyneside | SR | 71 | PC (Guarantee Credit and Savings Credit) | Y |
| Rose | 46.87 | 5 | Female | 80 | Widowed | North Shields | SR | 136 | PC (Guarantee Credit and Savings Credit) CTB, HB reassessed and AA (lower) | Y |
| Steven | 51.63 | 5 | Male | 64 | Divorced/separated | South Tyneside | O/O | 0 | None | |
| Gordon | 54.64 | 5 | Male | 86 | Widowed | Newcastle | SR | 0 | None | |
| Mark (and Dawn) | 60.28 | 5 | Male | 68 | With partner | North Shields | SR | 0 | None |
Table 22 presents information about the 17 professional participants in the study. Thirteen women and four men were interviewed from the following sectors: welfare rights, public health, primary care and the civil service. Among the 10 interviewees from the welfare rights sector, four delivered the intervention in the trial, while the remaining six had management or strategic roles within that sector.
| Pseudonym | Sector | Interview | Delivered Do-Well |
|---|---|---|---|
| Alice | Welfare rights | Telephone | No |
| Allan | Welfare rights | Telephone | Yes |
| Anya | Welfare rights | Telephone | Yes |
| Ava | Welfare rights | Telephone | Yes |
| Daniel | Civil service | Telephone | No |
| Fiona | Public health | Face to face | No |
| Holly | Charity | Face to face | No |
| Judith | Public health | Telephone | No |
| Kirsty | Charity | Face to face | No |
| Lucy | Welfare rights | Telephone | No |
| Matthew | Primary care | Telephone | No |
| Melissa | Civil service | Telephone | No |
| Olga | Civil service | Telephone | No |
| Sadie | Welfare rights | Face to face | Yes |
| Samantha | Welfare rights | Face to face | No |
| Stephanie | Primary care | Telephone | No |
| Toby | Charity | Face to face | No |
Acceptability of research design and intervention
Intervention recruitment
Trial participants, alongside professional participants, indicated that being contacted by Newcastle University through their local GP surgeries encouraged them to take part in the study, as both were seen as reputable organisations:
I think the university stamp on the envelope, I think it had some clout on me, you know . . . must be something important . . . made a great deal towards filling it in and taking part.
Elaine, 77 years, intervention, received £139 weekly Attendance Allowance and Pension Credit
The involvement of GP practices appeared to be particularly key to recruitment, as a result of the trust placed in individual GPs by, and the important place of general practice within the lives of, older people, particularly those with health problems:
I trust them [local GP practice] . . . I’ve been with them, well, more or less since I was born . . . I think, well, I’ve been with this practice that lang [long], you got to trust somebody . . . if a letter just comes through the door that says gan [go] on it, that would have went in the bin, I wouldn’t have bothered but because he said, you know, we want you to have a go at this, I thought fair enough, he’s a doctor, he knows what he’s talking about and I just went along with it . . . this way I think was alreet [alright].
Harry, 71 years, control, received £42 weekly Council Tax Benefit and Housing Benefit
One of them [trial participants] told my colleague that they signed up because it was the doctors suggesting it, they were keen to be involved in something the doctor suggested. So they didn’t sign up because they wanted to know if they could get any benefits, they signed up because the doctor has said ‘oh could you participate in this?’, so they did.
Ava, WRA DEL, Welfare Rights Sector
Trust in the institutions involved further assured trial participants that the sensitive information collected for the study, particularly regarding their health and finances, would be kept confidential and secure:
Were you worried about having to provide quite detailed personal information?
I think so. I talk a lot but I’m quite a private person . . . I was a bit anxious but then I thought it’s Newcastle University and they are very trustworthy.
A further factor in recruitment was that the study aims were deemed worthwhile and trial participants appreciated taking part in a project on the potential disadvantages faced by older benefit claimants:
I felt that it may benefit other people like me and other people that don’t know the system and that are struggling making ends meet, it might give them a helping hand.
Emma, 66 years, intervention, received no benefits as a result of the intervention
I think my interest [in the study] was the fact that they were gonna [going to] start putting more information into places like doctors’ surgeries where people who would need the information could get it easier . . . There’s a lot of people out there who need information and that’s just not been targeted to the right people . . . old people only talk to certain people, they might talk to a doctor or a nurse because they are people they see on a regular basis, and if this kind of thing was targeted over doctor surgeries or somewhere where they go like that . . . they might help . . . I thought it was worthy in that respect.
Margaret, 65 years, intervention, received £21 weekly Disability Living Allowance
I think it’s always a good thing to do a study to find out what’s going on . . . it is absolutely fantastic . . . anything that highlights a particular group of people to get advice.
Anya, WRA DEL, Welfare Rights Sector
Only one trial participant expressed that they felt motivated to take part owing to the personal benefit of receiving the welfare rights advice session:
I just thought well it’s only a bit of me time and they’re ganna [going to] tell you what you mightn’t be getting . . . So it was worth it.
Nigel, 63 years, intervention, received £107 weekly Employment Support Allowance
Other trial participants reported being unaware that they might financially benefit from getting involved in the study:
I didn’t realise what was going to happen . . . They didn’t tell us that . . . [they] just asked me questions that was it. I never thought anything about money or anything like that.
Oliver, 82 years, control, received £81 weekly Attendance Allowance
Randomisation
Most trial participants felt that the randomised (wait-list) control trial design of the Do-Well study was an acceptable approach, as the process was clearly explained and they recognised that they would not have received the intervention at all otherwise. Overall, they felt that the study was clearly explained to them so they knew what they were signing up for before becoming involved in the research. They also felt that the randomised controlled method would enable the effects of the intervention to be evaluated:
Would you think that that’s fair that some people do have to wait [to receive the intervention]?
Well yes because you were asked if you wanted to join in, you knew what the terms were so yeah it’s, I mean it was clearly stated that you might be seen and you might not be seen.
Control group trial participants were free to seek independent welfare advice at any time during the study period, and they were specifically asked whether or not being part of the study had encouraged them to think about seeking welfare rights advice elsewhere. Although some interviewees acknowledged that they were aware of welfare rights services, none of our control interviewees reported seeking independent advice prior to receiving the intervention after the 24-month follow-up interview.
Some trial participants highlighted the importance of knowing that they could seek advice independently from the study at any time if they needed to:
If I had been desperate, really desperate . . . somebody would have sorted us out somewhere . . . I could have gone to the council and stuff like that.
Susan, 75 years, intervention, received £21 weekly Council Tax Benefit, Pension Credit and stair rail home adaptation
So you think if you’d been in that situation where things were really bad you might have gone and looked into it yourself?
I would have gone, yes.
Wasn’t bothered [regarding being in the control group], because you can go to Age Concern and the welfare rights to see about your benefits and get them all explained. But I never bothered.
Steven, 67 years, control, received no benefits as a result of the intervention
Although trial participants reported that the study process had been explained and initially agreed to, many went on to admit that they found the process difficult to remember over the period of time that the research was undertaken. Thus, when asked further questions concerning the randomisation element of the study design, many trial participants could not recall whether they had been allocated to the intervention or to the control group, or even that there were two groups at all:
I forgot to tell you the truth, you know. It just went out of my mind till I got a letter to say.
Frida, 65 years, control, received no benefits as a result of the intervention
No, to be honest I would have probably forgotten, my memory is shocking.
Myrtle, 73 years, intervention, received no benefits as a result of the intervention
As time went by I just thought actually that I’d been forgotten about . . . I’ve got all the letters from the past and it does state . . . [random allocation to the wait-list control group] but as time goes by you do forget things.
Tom, 72 years, control, received £7 weekly Council Tax Benefit
This did not deter trial participants from taking part in the trial, as many of those allocated to the wait-list control group did not expect to receive anything from the intervention and so were not worried about having to wait the extra 2 years:
Because I wasn’t expecting anything [from the intervention] like that [receiving benefits] it hasn’t made any difference.
Rose, 83 years, control, received £136 weekly Attendance Allowance, Council Tax Benefit, Housing Benefit and Pension Credit
I never really thought about [receiving benefits] . . . I just thought well didn’t know about it before, so it didn’t matter.
Lydia, 71 years, control, received £34 weekly Carer’s Allowance
I didn’t know there was two groups . . .
And do you think it would have put you off if you had known?
No, no . . . I mean as far as I knew I might have been in the second [wait-list control] group.
On the other hand, a few trial participants were worried that they might be, or be disappointed that they were, allocated to the wait-list control group, delaying their welfare rights assessment by 2 years. Some professional participants also expressed concerns regarding trial participants allocated to the control group, as it was felt that these individuals would unnecessarily miss out on 2 years of benefits:
Well, I worried a little bit, but there again if it’s gonna [going to] happen, it’s gonna happen, if it’s not, it’s just life. It all works out in the end.
Joyce, 72 years, intervention, received £136 weekly Attendance Allowance and Pension Credit
I was a bit disappointed being in the second group . . . as at the time I was going through a hard time with [another welfare rights] caseworker.
Debbie, 64 years, control, renewal of £78 weekly Disability Living Allowance claim
Those individuals [allocated to the control group] have . . . potentially missed out on 2 years [of receiving benefits] . . . it’s their entitlement, why wait 2 years for it when they should be getting it now? . . . that was the main concern.
Daniel, Civil Service
Not surprisingly, some control group trial participants who received a successful benefit claim from the intervention reflected that they would rather have been in the intervention group:
It might have taken a bit more stress off the situation if I had got it 4 or 5 years ago.
Stacy, 67 years, control, received £50 weekly Pension Credit
I think it’s wrong. They shouldn’t wait 2 years. They could have been claiming it for 2 years . . . sooner . . . There are people who are in dire straits, so shouldn’t have to wait 2 years, getting back to that people who deserve it and people don’t deserve it, because I could wait. People who are on the borderline or breadline, they should have priority and be seen straight away, definitely.
Paul, 78 years, control, received £81 weekly Attendance Allowance
However, some intervention group trial participants recognised that they would not have received the welfare rights advice at all if the study had not taken place:
If I hadn’t got the advice, I would be still the way I am now, because I wouldn’t have applied for it myself . . . I wouldn’t know where to have gone for that . . . I would have just put up with it and not had it . . . I don’t think it would have made much difference at all being in that second group.
Elaine, 77 years, intervention, received £139 weekly Attendance Allowance and Pension Credit
In one case, a trial participant stated that the delay was beneficial because an adverse event coincided with being seen in the control group:
So it was just the luck of the draw. As it happened the time I got the advice was the right time for me because if I’d had it previously it wouldn’t have applied to us. It was only after Timothy [husband] died that I became entitled to it.
Laura, 70 years, control, received £10 weekly Council Tax Benefit and reduced gym membership
Overall, intervention group trial participants thought that the randomisation element of the study design was an effective way to answer the research questions and felt that the research was beneficial to future generations of benefit claimants:
It’s the only way you can find out if people [are] happy or unhappy [with the intervention].
Diane, 77 years, intervention, received a wheeled Zimmer frame with seat
The benefits from this [research are] not just for me but for multitudes of people.
Penny, 73 years, intervention, received no benefits as a result of the intervention
Although the randomisation element of the study design was deemed potentially unfair to the control group, it was accepted that (1) this study design was the only way to establish the impact of the intervention on quality of life; (2) welfare rights advice services are not statutory and (3) group allocation was completely random:
I just thought that it was, you know, just the luck of the draw.
Grace, 65 years, control, received £71 weekly Pension Credit
How do you feel knowing that you got welfare advice later on in the study, that you had to wait nearly 2 years?
Makes no difference. It’s a part of life. It happened and that’s it. Nothing you can do about it.
So you don’t mind that you’ve had to wait or anything?
No.
Among those who were interviewed, there was broad agreement that the trial design was an acceptable way to address the research question of the effectiveness of welfare rights advice on health and well-being.
Trial participation
Overall, the trial participants considered the research to be conducted in an appropriate and confidential manner. Most trial participants did not feel that the questions asked were too long or intrusive, with many instead expressing enjoyment of both the researcher’s and the WRA’s company:
You weren’t worried about them asking you questions about your finances?
No, no because it said it was confidential.
I hadn’t felt tensed up you know, waiting for something that’s gonna [going to] be said, that shouldn’t be said or if I put me [my] foot in [it] there or something like that . . . it’s just been nice, comfortable and relaxed. Much better than what I had imagined at first.
Harry, 71 years, control, received £42 weekly Council Tax and Housing Benefit
Do you find it intrusive in any way?
No not at all, no, no, I liked the company . . .
And you didn’t find the initial interview too long . . .?
I was OK with all that . . . in fact, if it’s an elderly person and they are on their own . . . you don’t see anybody from morning till night. Having that person in there talking to you, face to face for a couple of hours is company for you.
None of the trial participants felt that taking part in the study adversely affected or damaged their relationship with their GP, who was associated with the study via the recruitment letter. Trial participants generally felt that their largely positive experiences of taking part in the trial reflected well on their GP:
Well it [participation in the trial] probably made me think more of her [GP] . . . I was surprised when she was amazed that we’d never had any help, ye [you] know.
Finley, 64 years, intervention, received £41 weekly Disability Living Allowance
They [GPs] were quite happy that I was applying actually.
Debbie, 64 years, control, renewal of £78 weekly Disability Living Allowance claim
Did you talk to your doctors at all about your claim for benefits?
No.
OK. Did you think your claim would affect your relationship with the GP?
No, it never entered my head.
One control group trial participant identified a negative experience of taking part in the study, concerning what he perceived as the depressing nature of questions regarding suicide that were asked in the PHQ-9 at baseline and 24-month follow-up:
[The questions on the PHQ-9 questionnaire] . . . were too morbid, so I didn’t fill the second lot in . . . There’s no way am I ever thinking of committing suicide . . . They don’t relate to me in no way whatsoever . . . It was all asking if you felt run down and you felt like topping yourself. Those questions never entered my head . . . I didn’t want to fill it in anymore . . . It was depressing and it could make someone think of committing suicide . . . The people that I met [interviewer and WRA], nothing wrong with them though . . . [and] they said, ‘You don’t need to fill it in’, so I didn’t fill it in.
Paul, 78 years, control, received £81 weekly Attendance Allowance
No other interviewees expressed concerns about the content of the questionnaire.
Acceptability of the intervention
Apart from one, all trial participants interviewed in the qualitative study and the professional participants involved in delivering the intervention reflected positively on the experience of taking part in the Do-Well study. Trial participants expressed gratitude for the advice and monetary benefit received as a result of the intervention:
This has made a big difference to me . . . [the WRA] was just excellent.
Gloria, 74 years, intervention, received £135 weekly Attendance Allowance, Council Tax Benefit, Housing Benefit, Pension Credit and a Blue Badge
Being able to get that money . . . that’s been a great benefit which I wouldn’t have had without taking part.
Tom, 72 years, control, received £7 weekly Council Tax Benefit
Our practice nurse and our assistant practice manager spoke very highly of [the Do-Well project] and patients generally have been really interested in and engaged with it.
Stephanie, Health Sector
Even trial participants who received no benefits as a result of the intervention felt that the intervention was useful for clarifying their benefit entitlement status:
It was useful in the way that we found out that we weren’t entitled to anything else.
Mark, 71 years, control, received no benefits as a result of the intervention
The use of local welfare rights services was highlighted as another positive aspect of the Do-Well study. It gave trial participants the confidence that they could access further welfare advice if their benefit situation were to change, even if the study itself had finished:
And I know how to contact that lady, I have information and I can ring her up . . . I’ve got all her information here.
Right, so if you needed to ring her in the future then you could do?
Oh yes, yeah she said, you know, if things deteriorate get back in touch and I would.
I know where to go should I need help as well and that makes a big difference. Whereas before I thought, ‘Where the heck can I go? Who can help? Who can I talk to?’ Now I know and that makes a difference.
Stacy, 67 years, control, received £50 weekly Pension Credit
Is there anything that you particularly liked about taking part?
Well, the main thing is the fact that you know that you got [a] contact . . . She [WRA] said if there are any problems at all, all I’ve got to do is give her a ring and she’ll come out and see us. Well that’s a good thing.
Impact of the intervention
This section focuses on the impact of the intervention on financial status, health and well-being from the perspectives of trial participants and professional interviewees.
Financial impact
Of the 50 trial participants selected and consented to be interviewed, 34 obtained a successful financial benefit claim as a result of the intervention. Owing to a purposive selection process, and our aim of exploring the perceived effects of additional resources, we sampled a higher proportion (78%) of individuals for the qualitative study who obtained a claim as a result of the intervention than of the proportion in the full trial population (25%). As shown in Tables 20 and 21, a range of previously unclaimed benefits was obtained and most trial participants were entitled to more than one benefit. Eighteen trial participants qualified for means-tested benefits, indicating income thresholds of < 60% of the median income (the most commonly used threshold of low income);105 15 trial participants were eligible for non-means-tested financial benefits only, indicating that they suffered from a range of health and care needs. Two trial participants received non-means-tested non-financial benefits, including disabled parking badges, walking aids and home adaptations. Actual monetary gains ranged from £7 to £151 per week, and the average weekly amount gained was £76, with 25 trial participants also receiving backdated benefits. Many trial participants talked about how the extra money had enabled them to escape a previously precarious financial situation:
[Regarding receiving extra benefit income] It will make us [me] feel better because I’ll not be wondering . . . what do I have to cut out for to pay that bill which I used to do . . . I’m not feeling the pinch as much now whereas before it was a bit of a struggle.
Harry, 71 years, control, received £42 weekly Council Tax Benefit and Housing Benefit
Them years you didn’t get help . . . so I just had to struggle on, I’m used to having no money, you know I had years and years just struggling through, coping, but now I’m getting this, it’s made a big, big difference to my life.
Beatrice, 75 years, intervention, received £139 weekly Attendance Allowance and Carer’s Allowance
Many trial participants mentioned that before the intervention they had been borrowing money from friends and family or relying on continually decreasing savings to afford their basic living costs. The extra income had helped to reduce their debts as well as mitigate the use of their finite savings:
She thought I should [have] had this [benefit] for years like . . . and I think I should have as well . . . ‘cos [because] you couldn’t make ends meet really . . . and you start getting yourself into debt because you borrow money off people and then you try to pay them it back . . . good job you’ve got good parents sometimes . . . you divvint [don’t] want to borrow it, like, but sometime[s] you’ve got to. The money that I had prior to [the intervention], you could sort of live on it but you were just surviving really . . . you just need enough . . . and a little bit extra so you divvint [don’t] sink.
Benjamin, 62 years, intervention, received £76 weekly Disability Living Allowance and referral to Adult Social Care
The savings . . . they just kept going down and down . . .
How well do you think you could manage without the extra income [from the intervention] now?
Well we just wouldn’t be able to manage as long, effectively.
I have more peace of mind about paying for the things that help whereas before I took it all out me [my] savings money which obviously went down . . . so it has given me a lot of peace of mind in that sense.
Audrey, 80 years, intervention, received £139 weekly Attendance Allowance, Council Tax Benefit and Pension Credit
Other trial participants reported the extra income enabled them to start saving to afford future expenses, such as funeral or care costs:
It’s a buffer zone that’s handy you know . . . It’s just left in the bank to accumulate for any eventuality. I put money aside for my funeral and my wife’s funeral.
Tom, 72 years, control, received £7 weekly Council Tax Benefit
Well I know it’s there if I need it, the extra . . . I know it’s there if I needed to fall back on it, you know. I mean they are talking about doing this other knee, there might come a time when I might need somebody coming in a couple a times a day and have to pay them, so I know that that money is there to pay for them.
Elaine, 77 years, intervention, received £139 weekly Attendance Allowance and Pension Credit
The extra benefit income primarily increased trial participants’ ability to meet their basic household bills, transport costs and domiciliary care services. Trial participants reported being better able to heat their homes and afford food without having to worry about the rising cost of fuel and shopping bills. Trial participants also reported being in a better financial position to cope with larger expenses, such as replacing broken household items, without going into debt:
Well I can buy more food than I was able to do before . . . by the time you’ve paid for your heating and one thing and another it was a struggle to get food in. Sometimes I had to go and borrow something off the family . . . from their cupboards and that, you know . . . but it has helped that way.
Beatrice, 75 years, intervention, received £139 weekly Attendance Allowance and Carer’s Allowance
I think the extra money has helped me absorb the changes in the economy . . . everything just costs more.
Sheila, 79 years, control, received £91 weekly Attendance Allowance and Council Tax Benefit
I’ve just had a freezer broke doon [down], a fridge broke doon [down] and the cooker broke . . . I would have probably had to get a loan out if I didn’t have these benefits to replace them.
Arthur, 69 years, intervention, received £72 weekly Attendance Allowance and Pension Credit
Second, the extra income was used to pay for costs associated with travel including taxis, trains, buses and private cars. Access to affordable transport was key to engaging in daily activities and facilitating social interaction. The extra income helped trial participants to retain their independent mobility, to attend hospital appointments and go shopping, as well as socialise with friends and family:
Because I don’t go out on me [my] own at the minute, I could maybe use it to go in the taxi to do things, to be a little more independent . . . go shopping to the supermarket.
Grace, 62 years, control, received £71 weekly Pension Credit
Me [my] sister had a stroke about a year ago and she’s in a home at [place name]. Well, if one of the relatives can’t take me, then I get the taxi and it’s £14 there and back. I couldn’t do that before [the intervention] . . . she’s the only sister I got, she’s stuck in there, she can’t get out . . . and she just lived round the corner there you know so I’ve missed her.
Maria, 80 years, intervention, received £136 weekly Attendance Allowance and Pension Credit
Well I can go out and about in the car . . . and that’s me [my] main escape and I can like put money away so I can go for runs . . . I take Celia and Jane up with us, we have like a girls’ day out . . . daft carry on and a bit of a natter and it’s lovely.
Joyce, 72 years, intervention, received £136 weekly Attendance Allowance and Pension Credit
Third, many trial participants saved up or spent their extra benefit income on domiciliary services, paying formal services or family members to help them with cleaning, shopping and personal care in their homes.
I pay a girl to come and just wait for me in the bathroom while I had me [my] shower while I’m getting in and out just to see I’m all right and I just have to ring another girl, Chloe, she goes and does all me [my] shopping for me, ye [you] know, so I pay her. But that’s how I look at the Attendance Allowance, [it] is [there] to help me with my quality of life, to improve it.
Audrey, 80 years, intervention, received £139 Attendance Allowance, Council Tax Benefit and Pension Credit
A few trial participants reported spending the money on home services to maintain, improve or adapt their properties:
I’ve just had a painter in here. I had a leak in the roof and he had to repair that, so I had to pay for the roof as well, which is a lot of money when you think about it . . . certainly [the extra benefit income] helps. As I say, you don’t realise that you don’t need money [un]til you get a bill in . . . like for the builder and the painters and the joiners.
Paul, 78 years, control, received £81 weekly Attendance Allowance
It helped me a lot. I’ve gotten my fence fixed out the front and I’ve gotten this [mobile thermostat] to help me [my] heating . . . plus I’ve gotten other radiators fitted . . . so it’s a lot warmer now . . . I’m nearly 83, plus me [my] chest, this weather, it kills us. I’ve got that COPD [chronic obstructive pulmonary disease].
Oliver, 82 years, control, received £81 weekly Attendance Allowance
Being able to afford these services and household adaptations, as well as daily living aids such as light, accessible household appliances, was important for those with ill health and disability, as it improved their comfort and well-being by enabling them to carry on living independently in their homes despite being unable to do as much as they could before:
[Owing to receiving extra benefit income] I bought myself a new microwave . . . because I can’t manage pots and pans . . . because I have got a lot of nerve damage in my left arm and hand . . . And, I did go out and buy myself a vacuum cleaner, one of these very lightweight ones because I can’t manage my old vac . . . it is brilliant.
Stacy, 67 years, control, received £50 weekly Pension Credit
I’m going to have to redo my bathroom, because I have difficulty getting out of the bath. In fact, three times I nearly failed . . . I’m back to where I started from, believe it or not, which is basin and flannel . . . the old-fashioned way before bathrooms were invented.
And is that something that you weren’t able to do before [receiving benefit income from the intervention]?
No, I didn’t have the money to do that.
It [benefit income] can make such a difference to older people’s quality of life and being able to live independently . . . bringing in more money that they can use for gardeners, carers, handypersons and cleaners . . . if you’ve got care needs . . . [it] is important . . . We’ve had quite a few people who can’t manage [cleaning] anymore and they’re getting more and more depressed with the state of the place around them. They’re getting embarrassed and becoming more isolated because they don’t want people to come around and see it, so if you get that little bit of extra help to do that . . . Being able to go out, get the occasional taxi, pay off debts or not get into further debt. It’s all those sorts of issues.
Holly, Charity Sector
Additional financial resources also enabled trial participants to access formal services rather than, or as well as, relying on family and friend support networks to provide the help required. The extra benefit income also increased the affordability of council care services:
Instead of relying on them [referring to her daughter and husband] all the time, I can get things done myself.
And that makes you feel better?
It does yes . . . because [they] used to come down, change the bed . . . I can’t make the bed up meself [myself], the state of this arm . . . so somebody’s got to be there. So if some weeks Phillip [daughter’s husband] hasn’t done it, when the cleaner comes, she does it.
Some trial participants reported a sense of pride in being able to reward family and friends for the help they received through offering them money or being able to buy them gifts:
I couldn’t get out at all, and there was a friend of my daughter’s [who] came and helped me with shopping and she wouldn’t, she didn’t want to take any money, but I made her. I says ‘I [have] got money to cover this now, this allowance allows me to pay people for anything they are doing for me’ . . . I didn’t need to pay her, but I did, you know, just for my own satisfaction, so that’s helped.
Elaine, 77 years, intervention, received £139 weekly Attendance Allowance and Pension Credit
Impact on well-being and health
The cumulative impact of being able to afford household, transport and home care costs, as well as receive home adaptations, walking aids and accessible parking badges, had positive effects on trial participants’ ability to engage socially and, consequently, on their overall well-being and health. Trial participants reported improved mental well-being and better access to social support networks, as well as increased ability to cope more independently with existing physical health problems.
Professional and trial participants reported how the improved levels of income had reduced stress, worry and anxiety that had been created by financial uncertainty and/or debt. Many trial participants expressed feeling happier or gaining ‘peace of mind’ after receiving the extra benefit income:
I used to worry at one time but now I don’t, I’ve got no worries at all now. I know I’ve got enough coming in each week to last me that week and put a little bit away for whatever.
William, 83 years, intervention, received £40 weekly, Council Tax Benefit and Pension Credit
I know that loads of older people worry about poverty; it causes stress and anxiety . . . people worry about where they’re going to get meals . . . being able to heat their homes . . . who’s going to look after them. It makes a massive difference . . . for people to be able to get more money in their pockets . . . they end up being wealthier and healthier.
Matthew, Health Sector
Some trial participants identified that decreased financial worries had a positive impact on their physical health:
I think it has done wonders for me, it has taken off a lot of stress problems . . . Generally having that little bit of extra money does . . . improve health slightly because it takes the stress away. If you take the stress away you are not tensing up, you are not damaging any muscles, you are relaxing more and you are sleeping better.
Stacy, 67 years, control, received £50 weekly Pension Credit
The extra income received as a result of the intervention enabled trial participants to afford key transport costs as well as to ‘pay their way’ during social events, both of which facilitated greater social contact despite their increasing age-related health and functional problems. The narratives revealed trial participants’ desire to maximise activities and social opportunities with friendship and family support networks while they were still well enough. Thus, this increased independence to engage in social activities was reported by professional and trial participants as having a positive impact on mental health:
[Regarding receiving a walking aid from the intervention] And does being able to go out and about and have freedom to move, do you think that links to your health?
It is, just getting out, I love getting out, I love talking to people. I go across the square and I see lots of people and he [husband] goes along the river and I think that keeps him, you know. He must have been away about 2 and a half hours this morning . . . I think, just getting out and just chatting to people. I think, because if you don’t, if you cut yourself off, you just turn into a vegetable.
Some of these people may be housebound, or quite socially isolated, so it could have an impact on that particularly if it releases some extra cash into their pocket to enable them to get out and about, and be much more social in their outlook and the way they behave.
Fiona, Public Health
Trial participants had various health issues, including problems with joints, lungs, heart and blood as well as arthritic pain, general fatigue and diabetes. Many did not feel that the monetary increases and non-financial aids received as a result of the intervention could remediate these physical illnesses. However, they did report that the extra benefit income enabled them to cope better with various physical health problems:
Would you say that you think the extra money from benefits has affected your health at all in anyway?
No, not really. It just makes the pain a little bit easier I suppose . . . being able to get a taxi and that.
[On receiving the extra benefit income] It means I was able to get myself a little scooter to go in the back of the car. I can only walk so far without pain . . . I feel in myself better. It doesn’t take away the aches and pains but in myself I feel calmer . . . Everyday life for me, I don’t worry as much anymore, I know I will be able to cope.
Stacy, 67 years, control, received £50 weekly Pension Credit
Some trial participants recounted how being able to afford to keep their heating on for longer had a positive effect on their ability to manage health conditions:
What things do you think affect your health?
The only [thing] I think of is the heating . . . because of me [my] arthritis, when it’s cold everything just seizes up, it’s painful at times. Before I got this lot [extra benefit income], I still wouldn’t put the heating on because . . . if I put it on all day I’m not gonna [going to] be able to afford it . . . I just sat here, I had me [my] gloves on, me [my] hat and me [my] scarf . . . it was freezing in here at times. Then when this [extra benefit income] come along, I put the heating on more.
[On receiving the extra benefit income] It means I can have the heating on all day, without having to worry, because I know I’ve got that extra money to pay . . . I mean Clive [husband] just sits in a wheelchair all day, so he’s on the cold side and I keep thinking well, I can’t have this. I mean, this heating has been on since 8 o’clock this morning and it’s usually on [un]til 11 o’clock at night you know, but I think, well, it doesn’t matter, now, as long as he’s comfortable, we’ve got the money to do it, so that’s fine . . . that is a big weight off my shoulders.
Lydia, 71 years, control, received £34 weekly Carer’s Allowance
Overall, when asked more broadly about the link between income and health, professional participants, and some trial participants, suggested that low income had a negative effect on physical health outcomes:
We all know about social scales, people who are very poor, have poor lifestyles. If you have more income you can have a better lifestyle, can’t you? Have better food, comforts, heating, access to things. So that’s what money brings you, I don’t think it necessarily brings you health but brings you access to things that can give you better health, doesn’t it? That’s what I believe.
Penny, 73 years, intervention, received no benefits as a result of the intervention
Clearly if you’ve more money in your pocket, you can buy different food. You can go to the gym, you can become more active, whether that’s social or physical activity. It’s an enabler for people . . . We know that income is highly correlated to health and well-being.
Fiona, Public Health
Mechanisms of action
Role of the welfare rights advisor in overcoming barriers to older benefit claimants
The main barriers to older people claiming their benefit entitlements can be categorised into (1) knowledge and process and (2) attitudinal. WRAs were pivotal in overcoming barriers to claiming benefits through providing one-to-one advice, support and advocacy. Professional and trial participants reflected that many older people preferred to manage on tight budgets rather than claim welfare entitlements, valuing hard work and independence from state support so highly that they saw accepting benefit income as a personal failure. Additionally, many older benefit claimants did not view welfare as a right but rather as a safety net, designed for others more deserving. Thus, many held further worries about the legitimacy of their claim as well as concerns about inadvertently claiming fraudulently:
I always feel embarrassed at claiming, because I’ve never claimed anything in my life. When you’ve worked all your life it’s strange . . . it never feels as though I’m entitled . . . it’s not in my nature.
Gordon, 88 years, control, received no benefits as a result of the intervention
I didn’t wanna claim it in case I’ve made a mistake, because I couldn’t understand some of the stuff that you had to fill in and I thought if I put my name on the wrong thing here, I could finish off in jail or something, so [I] just never bothered.
Harry, 71 years, control, received £42 weekly Council Tax Benefit and Housing Benefit
I think there is a real attitude [among older people] of having worked all their life and supported themselves . . . they really felt that they’d kind of failed by having to fall back on state support and that they should be able to cope . . . With some of them as well . . . the amounts of money they received were quite substantial . . . They didn’t trust that the system had calculated it correctly and were worried that somebody was going to turn up on their doorstep and tell them that this was all wrong and they had to give it all back. That in itself was a barrier as well.
Melissa, Civil Service
Professional and trial participants reflected how WRAs overcame barriers to claiming by explaining benefit entitlement and addressing concerns about individual claims. The provision of trusted professional support throughout the benefit application process resulted in many successful benefit claims that would not have otherwise occurred:
[The WRA] came and explained all we would be entitled [to], ‘cos [because] you have to do this for him and you have to do that . . . I think it’s understanding the form as well, when you read the form you think, ‘God, you’ve more or less gotta [got to] be completely incapacitated to get this’, but she explained it, you didn’t have to be.
Finley, 64 years, intervention, received £41 weekly care component of Disability Living Allowance
He had his book and he showed me, ‘It is in black and white. It is this law that you will get this’. That really put my mind at rest . . . [my WRA] was spot on, he knew exactly what he was talking about and that made me feel better. I didn’t have to worry . . . It was good, I felt reassured that it was right as well. I would be terrified in case I was claiming something that I shouldn’t get. He explained it all.
Stacy, 67 years, control, received £50 weekly Pension Credit
The staff build up a relationship with the service user and encourage them to claim and not worry about doing it wrong or being accused of fraud because everything will be done with [the WRA] and explained at every step . . . often the people in the most need who are reluctant to claim, they need a friendly face to sit down and talk it through with them.
Alice, Welfare Rights Sector
Trial participants whose benefit applications were initially rejected further highlighted the important advocacy role WRAs held, which gave applicants the confidence to challenge official decisions as well as advice on how to strengthen any reapplication:
Well he [WRA] was like our spokesman, it was like having a solicitor at a trial, you know . . . we were really surprised when we did get it [they received Attendance Allowance on their reapplication], we wouldn’t have got it if it wasn’t for [WRA] . . . when you go in front of that thing [disability capability assessment] and turned out nothing’s wrong with you [when initially turned down for Attendance Allowance], what do you do? How do you fight them? . . . if it wasn’t for [WRA] and you lot [referring to the study], we would never have known.
Boris, 73 years, intervention, received £92 weekly Attendance Allowance and Pension Credit
Overall, domiciliary welfare rights advice was regarded as enabling access to entitlements for vulnerable older populations, particularly when health problems diminished their capabilities and confidence:
You’re in your life of working and ye [you] think ‘ooh I’m alright, I’m independent’, [and] that takes you into a different category, if you know what I mean. But as I got that little bit older . . . there comes a point where you do need it and I came to that stage. I thought now, especially when he’d explained it all to me and after that mini stroke thing, I thought to meself [myself], ‘aye [yes], it’s a good job that I did’ [apply for benefits].
Audrey, 80 years, intervention, received £139 weekly Attendance Allowance, Pension Credit and Council Tax Benefit
Most trial participants expressed surprise and appreciation when their claim was successful, particularly as most had not thought that they would be entitled to anything:
[On receiving benefits] Absolutely shocked to the core, absolutely shocked to the core, I phoned [the WRA] up when the letter came and I just said ‘it’s wonderful, I can’t believe it, can’t thank you enough’ . . . but oh, absolutely gobsmacked when the letter came to say that I was entitled to that money.
Elaine, 77 years, intervention, received £139 weekly Attendance Allowance and Pension Credit
There has been some good results . . . ones with a bit more income and maybe some savings are less likely to [claim] because . . . they didn’t think they’d be entitled to anything and they were and it might just have been a small top-up of the pension credit, but it was something that they didn’t know.
Ava, WRA DEL, Welfare Rights Sector
Primary care as a point of contact for older people
Many professional and trial participants saw the use of GP surgeries as a referral centre for the intervention as an ideal model of service delivery for older populations. Primary care, with its high levels of contact with older people, was regarded as one of the first places where individuals’ changing health circumstances are presented, changes that may lead to new benefit entitlements:
[GP surgeries] are in a good position for vulnerable older people because they have more contact with them than anyone else . . . more so than even maybe the local authority.
Olga, Civil Service
A lot of benefit entitlement is linked to changes that happen to people during their lives, and a lot of those changes will end you up in the GP surgery, so that is the place where you should be trying to identify people and link them into [welfare rights] services.
Melissa, Civil Service
Professional and trial participants felt that older people regarded their local GP surgeries as a respected professional and universal service acting in their best interests. As a result older people were viewed as much more likely to engage with a benefits assessment referral through their local practice, as many trusted the judgement of their GP:
Obviously the health sector is one of the places where people can go and it is universal. That means because it is an open door people don’t feel judged by going to . . . it is a good opportunity for the advice sector but also it very much speaks to things like the Marmot report.
Samantha, Welfare Rights Sector
A lot of older people trust the GPs and the nurses at the GP surgeries. I think there’s certain older people who, if a GP says, ‘I want to refer you on. They’ll help. You can trust them’, they’re more likely to engage initially. I think it is a useful model.
Lucy, Welfare Rights Sector
Domiciliary model
Opinion was divided on the benefits of a domiciliary service delivery model for welfare rights advice. Concerns were primarily about the resources required to deliver the service in this way, but distinct advantages were identified for older populations who have multiple health, income and mobility problems that inhibit their access to services:
I’m housebound . . . Until I get my eyes fixed. Because I’m not safe out in a car, and I’m not very safe on my feet.
Did it help, then, that the welfare rights advisor came to your home?
Yes. That’s helped enormously.
If you asked the clients how they would cope with getting in [to their central offices], half of them wouldn’t get in and half of those that did wouldn’t be able to sit in comfort and go through all the details and the other half would have probably left after the vital paperwork. So I just don’t think it would happen if we didn’t do the [home] visits.
Alice, Welfare Rights Sector
Professional and trial participants further argued that domiciliary visits enabled WRAs to make a wider assessment of clients’ needs, and fostered a safe and confidential environment for trial participants to disclose sensitive information, both of which were felt to strengthen any benefit applications made:
I felt better about it because . . . you are in your own environment so you don’t feel pressured or anything like that, it was more relaxed.
Emma, 66 years, intervention, received no benefits as a result of the intervention
Being in the client’s home gives you an opportunity to make a wider assessment of the client’s needs . . . because you can see how the person lives. Most people will tend to, but not deliberately, play down their care needs because they don’t necessarily see something that is part of their general behaviour, as a care need. It’s how they cope, so they don’t see it, but if you can actually witness some of this stuff, you can make a better application.
Toby, Charity Sector
When I’ve been out to clients’ houses, they seem to be more relaxed, there’s a lot more I can start to ask about, because you’ve already got the trust, if you are at the house you can certainly start to probe a bit more.
Allan, WRA DEL, Welfare Rights Sector
Some professional participants advocated the ‘cost–benefit’ savings domiciliary welfare rights interventions had regarding their potential impact on the use of health and social care services:
I think it’s highly appropriate [model of welfare rights advice] . . . in terms of savings for National Health Service. If you can give people that little bit of extra help at an early stage before they might not be able to manage in their homes anymore, with more depression, more visits to the GP and more spent on them, yes, it’s very important to have home visits available.
Holly, Charity Sector
If you are trying to promote independent living, staying healthy and not being a demand on local authority and health resources which can [be] very expensive you need the preventive work to be effective . . . it’s a good investment.
Alice, Welfare Rights Sector
If they are going out and struggling and you provide an aid and adaptation, it’s gonna [going to] make a big difference to them . . . there’s less risk of falling . . . hav[ing to] go off to hospital . . . that’s the drain on other services.
Anya, WRA DEL, Welfare Rights Sector
However, in addition to resource issues, a minority of professional participants criticised the domiciliary method of service delivery, viewing it as paternalistic and potentially disempowering, limiting understanding of the claimant process and fostering a long-term reliance on welfare rights services. Other professional participants further argued that trial participants might find home visits intrusive and advocated the need for alternative models of service provision for those who prefer to receive advice in a neutral, central location:
It’s a little bit paternalistic in its approach . . . it disempowers clients, and in the longer term, that can be problematic for a client . . . if there is any future problem with the administration of a benefit or the review of a benefit, if you’ve done it all for them, they generally haven’t a clue what that is when it comes in . . . A good I and A [information and advice] service helps someone to assess how much they can do for themselves. It helps tell them how to do it, empowers them to do it, and is there as a safety net if anything goes wrong.
Toby, Charity Sector
Some people might not want to be seen at home anyway . . . It can be very intrusive. They may be embarrassed about the state of their home. There may be someone in the home who they don’t want to know . . . that they’re taking advice . . . [involving] other issues such as domestic abuse.
Holly, Charity Sector
It’s good to have a mix of places to see people . . . some people see [home visiting] as an intrusion . . . one size doesn’t fit all . . . some people might actually prefer to be seen in the GP practice particularly if they are living in poverty and those prouder older people might not want to have strangers coming into their home.
Judith, Public Health
Unanticipated consequences of the intervention
As we have demonstrated, many trial participants were highly satisfied with the intervention, its delivery and its outcomes. Trial participants did not highlight any adverse outcomes, harms or risks associated with the delivery of the intervention. Trial participants did not discuss spending their additional benefit income on potentially anticipated harms such as alcohol, tobacco, ‘luxury’ foods or gambling but rather used it primarily to afford basic household, transport and care costs. Furthermore, trial participants did not associate the independence and mobility received as a result of the intervention with accidental injury or exposure to infectious diseases, but rather with an increased sense of mental well-being as a result of their ability to socialise with family and friends despite their limiting ill health. Although some trial participants used their additional benefit income to afford a new car or taxi fares, trial participants felt that this increased, rather than limited, their levels of physical activity, as they were unable to leave the house without this transport available. No other potential unanticipated harms or risks were discussed throughout the qualitative study. There were, however, a number of unanticipated consequences concerning the intervention delivery identified by the WRAs delivering the intervention.
Intervention delivery
Throughout the study period, progressively larger funding cuts negatively impacted on the capacity of welfare rights organisations to deliver services. Two professional participants reported that their organisation was further stretched by delivering what they regarded as resource-intensive domiciliary visits, which were different from their standard practice:
We’ve had to do them all as home visits . . . it has taken an awful a lot more of our time and we haven’t had the flexibility to deal with it . . . [in our organisation’s service delivery] if it was obvious that [the client] wouldn’t get any benefits than they wouldn’t go through the specialist [WRA], whereas under the Do-Well study the specialists have been doing the whole thing which has been fine and we’d agreed to do it as part of the study, but in the general day-to-day processes without getting the funding for a visit worker to work in that way it does take up more time of the people who are providing advice.
Ava, WRA DEL, Welfare Rights Sector
Two professional participants found they had to take more time explaining the Do-Well intervention, as trial participants had a limited understanding of the study process, especially in the case of control group trial participants who received their intervention 2 years after the study started:
At the beginning it took a little bit of explanation of who we are and why we were coming out . . . at least 2 out of the 13 seemed really resistant to me coming out . . . more the second [control] group. I don’t know whether that was because of the 2-year delay . . . there just seemed to be more of the ‘well, I don’t understand what this is about’ or ‘somebody has already come out to see me’ . . . there was that part of the problem.
Allan, WRA DEL, Welfare Rights Sector
One professional participant described concern about a lack of staggered Do-Well referrals to her organisation:
The only problem I can remember . . . is that the referrals didn’t come through steadily. There were none for a few weeks and then loads, so that put a bit of pressure on . . . [I would have preferred it] more staggered.
Sadie, WRA DEL, Welfare Rights Sector
However, professional participants who raised these concerns also highlighted that the feedback mechanisms were useful in order to raise such concerns and adapt the delivery of the Do-Well intervention to suit their organisation’s needs:
[Regarding limited trial participant understanding of the study process] It was good to have those feedback mechanisms as the project was going along to raise that as an issue.
Allan, WRA DEL, Welfare Rights Sector
I was able to speak to [project administrator] to see if the referrals could be staggered so that we didn’t get a massive batch at once.
Did that happen after that?
Yes, yes. It was just teething problems.
Impact of external factors
Throughout the period of the study, major changes to the UK welfare system were being implemented. Owing to the timing of the intervention delivery (June 2012 to August 2013), none of the changes [e.g. introduction of Universal Credit, Personal Independence Payments and the spare room subsidy (‘bedroom tax’)], affected our intervention trial participants. Overall, in comparison with the adult population below state pension age, those over the state pension age are less affected by the changes, in terms of the key benefits available to older people. However, the cuts in public services disproportionately affected the poorest areas with the worst health outcomes. Welfare rights advice services came under increasing strain from a combination of funding cuts and increasing demands as a result of changes to welfare. 106,107 Thus, the service delivery model that was developed and piloted in 2001–5,11 and that we adopted for the Do-Well study, had to operate under highly constrained budgeting circumstances. We therefore took these external factors into account and examined the suitability of our intervention delivery model in the current economic climate.
Resource-intensive intervention
Despite professional participants advocating a universal, domiciliary intervention as an ideal model of welfare rights service delivery for older people, many recognised that it was a resource-intensive intervention that might not be able to cope with client demand. Owing to rising resource constraints created by the impact of public sector cuts, professional participants felt that this model could not be translated into current routine practice, as it would not be seen as affordable or cost-effective by funders. Many professional participants, and some trial participants, suggested use of a wider range of first- and second-tier service delivery models, prioritising centralised drop-in surgeries and telephone advice lines over face-to-face advice. Some professional participants argued that this would maximise resources, providing welfare rights advice for as many clients as possible despite funding constraints:
There has been a move away from doing home visits . . . money has driven that . . . just not having the capacity . . . [A home visit is] an important part of doing the job and there are some clients where it is the only option, but offering it as a matter of course to everybody, we would probably disagree with . . . in the current climate, where the key driver is cost . . . [and] even telephone advice is often considered too expensive . . . You’re asking for a very expensive approach to the welfare benefit take-up.
Toby, Charity Sector
I think giving a carte blanche home visiting service is probably quite wasteful, in terms of resource, because it costs us time and money to travel to somebody’s home . . . if some of those people were able to travel to a central point then your advisor would have been able to have reached more people . . . if we could offer a premium service to everybody then that is obviously what I would want to do, but I have limited resources and a duty to help as many people as I can with the resources that I do have.
Kirsty, Charity Sector
On the other hand, it was accepted that although a centrally located service provision would make welfare rights advice services available to more people, sole reliance on such a service delivery model would exclude the most ill, disabled and housebound, for whom domiciliary services are still required:
I think that the main driver [in not funding domiciliary services] is that they want locality-based services and want more people to be seen. Now, my argument, my response to that, is that more people will be seen, but those vulnerable people who are relying on home visits will receive no service at all. We will see more people, but we will see more of the less vulnerable, but there doesn’t seem to be a great deal of concern about that.
Kirsty, Charity Sector
Optimally identifying benefit entitlement among older people
Professional participants delivering the Do-Well intervention reflected on the low uptake of benefits among trial participants during the study. It was reported that many of the trial participants seen had comfortable levels of income and no major/limiting health issues, eliminating them from benefit eligibility. Thus, the professional participants highlighted the Do-Well project as having higher levels of ‘redundant’ benefit assessments than their normal welfare rights service provision:
We soon found that a lot of the people who we were coming out to see we ruled out of the entitlement to benefits simply because they had too much capital . . . and they didn’t really have health problems.
Allan, WRA DEL, Welfare Rights Sector
Professional participants advocated an initial triage involving assessment of clients’ care and health needs as part of a first-tier advice service, so that a full benefits assessment, or the use of a domiciliary visit, is undertaken only when appropriate:
I don’t know if there’s a better way of finding the people who are actually missing out . . . Maybe over the phone . . . within a few questions you know they are not going to be entitled because they had no health issues and they were in receipt of some quite decent pension or they had savings for the future, so with those three questions you can virtually rule them out.
Allan, WRA DEL, Welfare Rights Sector
I like the telephone assessments, to start with, because it makes sense . . . [to] identify they are eligible for a benefit first . . . following this up with a mix of home and office visits.
Holly, Charity Sector
I would . . . try and identify how you could segment people, so that the ones who weren’t able to do it for themselves would be the ones prioritised for the domiciliary visits . . . a more tiered approach . . . perhaps get a short questionnaire completed which would allow you to do that segmentation in a more robust way . . . I think the key is targeting in a very personal way, so you are thinking about the person’s needs rather than the groups, so not that you live in a disadvantaged area, therefore you are going to get this, [but] you live in a disadvantaged area and we have evidence that you are not very good at planning . . . I think we just have to think quite carefully how we then target those people.
Judith, Public Health
Many professional participants went on to outline further general points in order to improve welfare rights services that involved timely advice and that recognised that some people used various services at multiple (crisis) points in their lives:
There must be lots of services like us who will see the same people year in, year out with the same problems . . . if the intervention came at an early stage instead of at a crisis point, it’s got to make a difference in the long term . . . in terms of trying to help the poorest and most disadvantaged communities . . . to reduce the need for public services really . . . There’s just so much need out there . . . there’s more than enough work for everybody . . . We have to start working more closely together . . . It’s trying to find ways to maximise your resources as a whole and to trust each other.
Lucy, Welfare Rights Sector
Domiciliary welfare rights advice accessed via primary care was regarded as having a positive impact, by enabling older people to gain their benefit entitlements. Trial and professional participants reflected on how such a model might be translated into policy and practice. User-designed, preventative services were advocated in order to be relevant to local context as well as engaging with vulnerable claimants before they reached a crisis point. Many professional participants stressed the importance of fostering stronger collaboration across the welfare rights sector to maximise sector resources and service delivery. One professional participant suggested that it would be beneficial to train older people as volunteers to aid the delivery of welfare rights advice:
Peers understand their situation because they’re a similar age to them, or in similar circumstances . . . training older people to give benefits advice to other older people would be an interesting model . . . we would always advocate involving older people . . . in the design and the delivery of services . . . to meet their needs . . . which will make them cost-effective as well as efficient in meeting their outcomes.
Melissa, Civil Service
Informally, the sharing of advice and information concerning benefit entitlement occurred between trial participants. Professional and trial participants indicated that welfare rights advice received is passed on to wider networks of family and friends, encouraging wider benefit uptake than for those just involved in the intervention:
I mean, as I says, my friend lost her husband about 8 years ago . . . and I nagged at her, because she, I mean she worked till she was 67 and she was only on like a small pension from Gerry and then her own old age pension and she was struggling. I say ‘Josie, go and ask about housing benefit’, ‘no I’m fighting’. I says, ‘why, what are you fighting for? I think you are entitled to it’. And she eventually went last year and she got her housing benefit [and said] ‘I’m glad I took notice of you’. I says, ‘well if I got it, you’re entitled to it’.
Joyce, 72 years, intervention, received £136 weekly Attendance Allowance and Pension Credit
If you go out to see one person . . . then it’s always a word of mouth that they pass on . . . so they pass it on to the relatives or family.
Anya, WRA DEL, Welfare Rights Sector
Impact of public sector cuts
Professional participants outlined that older people’s demand for welfare rights services was rising. A number of factors were identified: the increase in the older population, particularly the oldest old; an increasingly punitive and complicated welfare benefits system; and the implementation of the Health and Social Care Act 2012108 placing new and additional responsibilities on local authorities to provide advice services to carers as well as those in receipt of care:
There is a definite increase in the number of ‘younger’ older people coming [for welfare rights advice] because . . . the benefit system is now much more punitive . . . with administration problems in the benefits processes [as] there are less people to administer.
Toby, Charity Sector
[The demand for welfare rights advice services] is increasing all the time . . . We can’t possibly deal with everyone who comes to us, there is too high a demand . . . We’ve got this huge ageing population that is going to increasingly need that help to stay in their own homes to keep the costs down, [and stay] independent for as long as possible.
Holly, Charity Sector
However, rather than receiving improved funding allocations, all professional participants reported an intensification of austerity-driven public sector cuts that vastly decreased the resources available for the welfare rights sector. Staff redundancies and organisational restructuring had left many services with fewer advisors coping with an increased workload. Some professional participants described how their organisations had such limited capacity that they had curtailed outreach work to limit client demand:
Legal aid funding has gone which funded a lot of welfare rights . . . the local authority funding is under pressure . . . [and] advice agencies are having more trouble getting funding from charitable trusts. So many people are under pressure and they are on a downward trend.
Alice, Welfare Rights Sector
Because posts have been deleted, we feel like we work on the bare bones of staff, so there are concerns about having enough staff to deal with everything.
Sadie, WRA DEL, Welfare Rights Sector
If you crunch the numbers you know, you need a team three times our size to stick up a flag and say all older people come here for welfare rights advice. We can’t have too high a profile . . . [or else] our waiting list gets too much and that’s bad service for the clients and the staff feel harassed. So we don’t tell everybody all the time that we are here.
Alice, Welfare Rights Sector
Professional participants reported a shift away from guaranteed local and central government funding towards short-term, precarious and competitively tendered contracts from the charity, corporate and health-care sectors. Constant cycles of funding applications were placing a strain on already-stretched resources. At the same time, ‘cost-effective’ interventions were felt to be increasingly prioritised, with an emphasis on providing specialised and targeted interventions using digital, centralised and telephone models of service delivery rather than face-to-face consultations:
I’m under pressure from numerous places to provide more for less . . . the demand for welfare benefits advice far outstrips what we’re able to provide, so we’re having to make decisions all the time as to who receives the service and who doesn’t . . . that’s not a comfortable position to be in.
Kirsty, Charity Sector
Unfortunately that’s how it’s moving now, a lot of the funding rather than being general it’s very targeted . . . it would be good to get funding for a general service available for anybody for specialist benefit advice [rather than just services for people with] leukaemia, young people and mental health.
Ava, Welfare Rights Sector
[Funding] tends to be very much issue-focused and short . . . [but] advice funding should be continual. It shouldn’t be about an innovative new project. There is no innovation in how you provide advice, to be honest. We’ve been doing it to death for years. We generally know what works. It doesn’t need innovation. It just needs to be funded long term, not 2 or 3 years at a time through grants.
Toby, Charity Sector
Some professional participants predicted that this reliance on digital or telephone services would increase barriers to claiming for older people, as many do not have the technical skills to access advice services online:
I think it’s a major shift, the only available services are online and old people don’t necessarily . . . have ready access to the online services, or the confidence to access them.
Stephanie, WRA DEL, Health Sector
Most local authorities are keen to pay for the cheapest option, which means less face to face . . . they would rather people were using self-help tools on the internet . . . it’s as much about cutting costs as it is about saying, ‘This is a sensible approach to giving access to services’, and particularly for older people, it makes no sense. Once you’re over 70, the likelihood of you using the internet is pretty low, and that’s using the internet for anything, not going online and making applications for benefits, which is a quite complex activity.
Toby, Charity Sector
Overall, trial and professional participants depicted a bleak future for the welfare rights sector, predicting further welfare reform and cuts to welfare rights services:
I mean the outlook isn’t great . . . I’m not very confident that we’ll be here in 5 years’ time . . . the only reason that say we might be here in the next couple of years is that welfare reform is massive . . . once those big reforms are gone the general sense seems to be people shouldn’t be on benefits . . . I don’t think there’s really much support for [welfare rights services].
Allan, WRA DEL, Welfare Rights Sector
Impact of widespread negative portrayals of citizens claiming welfare benefits
Trial participants demonstrated a heightened awareness of the stigma attached to claiming welfare benefits. They focused in particular on media and government discourses on benefit entitlement, and how these were negatively influencing the general public’s perceptions of benefit claimants:
They [the government] class every one of them [benefit claimants] as scroungers. They’re not giving any leeway for people who actually need it, you’re all the same. If you’re on benefits you’re an outcast to them . . . They show you the ones they want you to see, yes, but the ones who are entitled to benefits, no, you never see them.
Paul, 78 years, control, received £81 weekly Attendance Allowance
I think the general public has got a bad opinion . . . If they are not on benefits I don’t think they understand what it is like to be on benefits . . . I think they look down on people with benefits. The opinion coming out in the papers . . . I think a lot of people who aren’t on benefits think they [claimants] are all scroungers. Well they are not really.
Debbie, 62 years, control, renewal of £78 weekly Disability Living Allowance
Trial participants did not agree with such negative portrayals of people claiming welfare payments, although there was widespread acknowledgement of dishonest claiming. Trial participants distinguished between ‘deserving’ and ‘undeserving’ claimants. Older citizens were viewed as ‘deserving’ owing to their lifetime contributions into the system, and the fact that, as a group, they were less likely to claim. Trial participants were concerned about the negative stereotyping of people on benefits because they felt that this was exaggerated, lumped a heterogeneous group of individuals together and made it more difficult for ‘genuine’ claimants to access their entitlements:
I think it’s because the papers, they don’t talk about the decent people on benefits. They’ll only talk about the ones that are on benefits, [with] all the children and they’ve got a 52-inch television screen, and they are smoking their head off and having a drink you know. But not all of the benefit people are like that.
Myrtle, 71 years, intervention, no additional resources received
They make you feel as though you are digging you know. Whatever’s out there should be readily available if you need it. You shouldn’t have to get anxious thinking, what if it’s not . . . it’s bad enough to be, struggling . . . dealing with the everyday things that life throws at you when you have got someone who is disabled, without having to fight for something that should be there because you need it.
Laura, 67 years, control, received £10 Council Tax Benefit and reduced gym membership
Summary
The findings of this embedded qualitative study indicate that the research design, in terms of recruitment and randomisation, was acceptable to those interviewed, although there was some concern expressed, primarily by professional informants, about the 24-month wait for the control group to receive the intervention. Without exception among trial participants the intervention was deemed acceptable. The professional informants supported the need for welfare rights advice targeted at older people, but there was some disagreement about the optimal means of service delivery, particularly in the light of recent and continuing cuts to public and voluntary sector services. Trial participants viewed the impact of the intervention as highly positive, in terms of financial, social, health and well-being factors, irrespective of the amount of additional benefit received; professional participants were fully aware of the wide-ranging impact that additional resources could have for older people in need, and reiterated the preventative potential of ‘low-level’ interventions such as welfare rights advice. The mechanisms of intervention delivery – introduced via trusted GPs and domiciliary visits – successfully overcame the well-known barriers to claiming benefit entitlements among older people. However, immediately before and during the execution of the trial the most significant government-led changes to the welfare system since its inception began to be implemented, coupled with austerity-driven public sector and voluntary sector service cutbacks. These external factors were perceived to have considerable implications for the design, commissioning and delivery of welfare rights advice services in the future.
Chapter 5 Economic evaluation findings
Sample characteristics
Table 23 shows the responses to questionnaire data on individual health at baseline and 24-month follow-up for both trial arms. The majority of participants in both trial arms reported having a long-term illness, health problem or disability. At both baseline and 24-month follow-up, and for both trial arms, the largest proportion in each arm described their health status over the previous 6 months as good. The proportion in each arm reporting a long-term illness, health problem or disability, and a health problem limiting their daily activities, decreased over the 24 months of the trial. However, comparing the average baseline EQ-5D-3L score for those participants with missing EQ-5D-3L at 24-month follow-up with the average score for the complete study population showed that those with missing follow-up data had reported a substantially lower EQ-5D-3L at baseline [intervention group 0.589 (complete study population) vs. 0.529 (participants with missing 24-month follow-up EQ-5D-3L score); control group 0.583 vs. 0.457].
| Variable | Trial arm, n (%) | |||
|---|---|---|---|---|
| Intervention | Control | |||
| Baseline (n = 381) | 24-month follow-up (n = 283) | Baseline (n = 374) | 24-month follow-up (n = 279) | |
| Long-term illness/health problem/disability | ||||
| Yes | 327 (86) | 239 (63) | 313 (84) | 236 (63) |
| No | 54 (14) | 43 (11) | 58 (16) | 42 (11) |
| Don’t know | 0 | 0 | 2 (1) | 1 (< 1) |
| Refused to answer | 0 | 1 (< 1) | 0 | 0 |
| Not asked | 0 | 0 | 1 (< 1) | 0 |
| Health problem limiting daily activities | ||||
| Yes | 227 (60) | 166 (44) | 225 (60) | 157 (42) |
| No | 99 (26) | 72 (19) | 87 (23) | 76 (20) |
| Don’t know | 0 | 1 (< 1) | 0 | 3 (1) |
| Not asked | 1 (< 1) | 0 | 1 (0) | 0 |
| Health status (last 6 months) | ||||
| Very good | 38 (10) | 35 (9) | 49 (13) | 45 (12) |
| Good | 119 (31) | 90 (24) | 105 (28) | 83 (22) |
| Neither good/poor | 108 (28) | 71 (19) | 84 (22) | 70 (19) |
| Poor | 94 (25) | 74 (19) | 103 (28) | 64 (17) |
| Very poor | 22 (6) | 13 (3) | 32 (9) | 17 (5) |
| Not asked | 0 | 0 | 1 (< 1) | 0 |
| Missing | 0 | 98 (26) | 0 | 95 (25) |
Cost–consequences analysis
Costs
Table 24 shows the durations of, and associated costs for, the WRAs’ activities required to deliver the intervention to participants in the intervention group. These activities included the home visit itself as well as additional telephone calls, letter or e-mail writing, administrative tasks (such as form filling or referring to other agencies), and other or unspecified activities, as well as travelling to the participants’ homes. Some WRAs recorded durations of 0 minutes for activities or distances of 0 miles for travel. These were considered valid responses as, on occasions, WRAs reported that they combined appointments when these were in close geographical proximity on the same day for efficiency.
| Type of activity | Number of observations | Duration (minutes) or distance (miles) | Costs (£) | ||
|---|---|---|---|---|---|
| Mean | Median (IQR) | Mean | Median (IQR) | ||
| Home visit | 310 | 56.14 | 41.50 (30–72) | 19.04 | 14.16 (10.24–24.57) |
| Telephone call | 210 | 17.19 | 10.00 (5–20) | 5.83 | 3.41 (1.71–6.82) |
| Letter/e-mail writing | 41 | 9.12 | 5.00 (2–10) | 3.09 | 1.71 (0.68–3.41) |
| Administration, form filling, referring to or chasing up other agencies, etc. | 93 | 37.05 | 22.00 (6–55) | 12.57 | 7.51 (2.05–18.77) |
| Other | 9 | 12.22 | 10.00 (10–15) | 4.15 | 3.41 (3.41–5.12) |
| Missing/unspecified | 46 | 32.28 | 22.50 (10–40) | 10.95 | 7.68 (3.41–13.65) |
| Travel time | 328 | 32.21 | 25.00 (15–40) | 10.93 | 8.53 (5.12–13.65) |
| Total time inputs | 347 | 106.61 | 80.00 (54–120) | 36.16 | 27.30 (18.42–40.94) |
| Distance travelled (miles) | 316 | 14.37 | 9.00 (5–19) | 5.69 | 3.56 (1.98–7.52) |
| Total cost | 43.76 | 32.46 (21.78–47.66) | |||
| Total cost (travel duration and distance only) | 16.80 | 12.58 (7.10–21.57) | |||
The average total cost per participant for delivery of welfare rights advice was calculated as £43.76; 38% of these costs (£16.80) were travel costs associated with WRAs travelling to participants’ homes.
Financial benefits
Twelve financial benefits and allowances recorded by WRAs in the CCS were found to have been awarded to participants in the intervention group. Means-tested benefits included Council Tax Benefit, Housing Benefit, Pension Credit (guarantee, savings) and Employment Support Allowance, while non-means tested benefits were Disability Living Allowance (care and mobility components), Attendance Allowance (at high and low rate), Carer’s Allowance, Industrial Injuries Disablement Benefit and Severe Disablement Allowance. For all except two benefits (Employment Support Allowance and Severe Disablement Allowance), information on durations were available from the CCS for participants in the intervention group. The 10 financial benefits for which there was information on the duration of award (i.e. excluding Employment Support Allowance and Severe Disablement Allowance) were therefore considered when comparing the effectiveness of the intervention between trial arms.
Given the limited information collected in the CCS, partner benefits, one-off payments for financial benefits and pending claims were not considered in the initial analyses. In the CCS data, 10 financial benefits received by partners were recorded, but there were no data available to estimate the value of these over the 24-month follow-up period. For instance, for most of the recorded benefits, the only information available was on the recipient of the benefit. No information on the date of award or the weekly amount was recorded. No information on one-off payments was recorded in the CCS. The analysis also excluded pending claims, as the impact of these would not be observed in the 24-month follow-up period.
Table 25 reports the number of financial benefits newly awarded during the 24-month follow-up period and the average total amount (as well as the median and IQR) gained per participant in each trial arm when there were complete data available (a complete-case analysis), as well as the difference in average total amount. The benefits with the highest number of new claims in the intervention group were Council Tax and Attendance Allowance paid at the higher rate, while Council Tax Benefit, Housing Benefit and Disability Living Allowance (care component) were the most frequent new benefits in the control group. There was evidence of statistically significant differences between the trial arms in the weekly amounts for Disability Living Allowance (mobility component) and Carer’s Allowance, for which participants in the control group reported receiving significantly higher weekly amounts.
| Benefit | Trial arm | Difference | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||
| n | n (complete cases) | Mean amount gained (£) | Median (IQR) amount gained (£) | n | n (complete cases) | Mean amount gained (£) | Median (IQR) amount gained (£) | Mean amount (95% CI) gained (£) | |
| Means tested | |||||||||
| Council Tax Benefit | 24 | 8 | 746 | 508 (423–1039) | 29 | 11 | 991 | 889 (423–1585) | –245 (–694 to 204) |
| Housing Benefit | 12 | 5 | 4670 | 6202 (2180–6582) | 12 | 8 | 4920 | 5737 (2855–6543) | –250 (–3387 to 2886) |
| Pension Credit Guarantee | 4 | 4 | 1529 | 1582 (711–2346) | 7 | 4 | 1870 | 1053 (438–3301) | –341 (–2653 to 1971) |
| Pension Credit Savings | 5 | 5 | 872 | 459 (430–845) | 4 | 3 | 955 | 851 (636–1376) | –83 (–977 to 811) |
| Non-means tested | |||||||||
| Disability Living Allowance: Care | 9 | 4 | 5106 | 4023 (2746–7466) | 12 | 8 | 3970 | 4013 (2746–5201) | 1136 (–2742 to 5015) |
| Disability Living Allowance: Mobility | 4 | 1 | 1686 | 1686 (1686–1686) | 7 | 4 | 5030 | 4927 (4380–5680) | –3344 (–4035 to –2654) |
| Attendance Allowance: lower rate | 3 | 2 | 3727 | 3727 (3421–4034) | 5 | 2 | 3941 | 3941 (3867–4016) | –214 (–684 to 256) |
| Attendance Allowance: high rate | 9 | 7 | 7240 | 7387 (7387–7387) | 7 | 3 | 7066 | 6996 (6815–7387) | 174 (–231 to 580) |
| Carer’s Allowance | 2 | 1 | 3895 | 3895 (3895–3895) | 8 | 2 | 5393 | 5393 (4578–6208) | –1499 (–2810 to –187) |
| Industrial Injuries Disablement Benefit | 2 | 2 | 1763 | 1763 (1226–2299) | 5 | 5 | 2257 | 2529 (1229–2545) | –494 (–1673 to 685) |
| Average total amount gained per participant | 36 | 3541 | 2240 (532–6874) | 41 | 3991 | 3756 (1412–6189) | –451 (–1892 to 991) | ||
Contrary to our expectations, the total average value of financial benefits was higher for control group participants awarded new financial benefits than for those in the intervention group. The difference between the intervention and control arms in the total mean amount for newly awarded financial benefits per participant was –£451 (95% CI –£1892 to £991). Although there was no evidence of a statistically significant difference between groups, the CIs were wide enough to include economically important differences favouring either group.
These findings did not change when the discount rate was increased to 3.5% (Table 26). 109 Sensitivity analyses capturing extreme case scenarios assessed the confidence around the imputed missing information on durations in the control group by imputing the missing value with values of either the first (Table 27) or the third quartile (Table 28) from the distribution of duration since receipt of benefit in the intervention group. In both cases, usual care was estimated to be more effective with regard to the average total amount gained per participant across all financial benefits, although this was not statistically significant.
| Benefit | Trial arm | Difference | |||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||
| n (complete cases) | Mean amount gained (£) | Median amount gained (£) (IQR) | n (complete cases) | Mean amount gained (£) | Median amount gained (£) (IQR) | Mean amount gained (£) (95% CI) | |
| Means tested | |||||||
| Council Tax Benefit | 8 | 737 | 502 (418–1026) | 11 | 979 | 878 (418–1566) | –242 (–681 to 197) |
| Housing Benefit | 5 | 4608 | 6119 (2151–6495) | 8 | 4855 | 5661 (2817–6456) | –247 (–3289 to 2795) |
| Pension Credit Guarantee | 4 | 1506 | 1558 (701–2311) | 4 | 1842 | 1038 (432–3252) | –336 (–2626 to 1955) |
| Pension Credit Savings | 5 | 861 | 454 (425–834) | 3 | 943 | 841 (629–1359) | –82 (–962 to 798) |
| Non-means tested | |||||||
| Disability Living Allowance: Care | 4 | 5037 | 3969 (2709–7365) | 8 | 3916 | 3959 (2709–5131) | 1121 (–2715 to 4957) |
| Disability Living Allowance: Mobility | 1 | 1663 | 1663 (1663–1663) | 4 | 4963 | 4862 (4322–5604) | –3300 (–4022 to –2578) |
| Attendance Allowance: low rate | 2 | 3675 | 3675 (3373–3978) | 2 | 3886 | 3886 (3813–3959) | –211 (–677 to 256) |
| Attendance Allowance: high rate | 7 | 7158 | 7303 (7303–7303) | 3 | 6985 | 6916 (6737–7303) | 172 (–226 to 570) |
| Carer’s Allowance | 1 | 3841 | 3841 (3841–3841) | 2 | 5320 | 5320 (4516–6124) | –1478 (–2772 to –184) |
| Industrial Injuries Disablement Benefit | 2 | 1739 | 1739 (1210–2268) | 5 | 2227 | 2495 (1213–2510) | –488 (–1696 to 721) |
| Average total amount gained per participant | 36 | 3496 | 2210 (525–6795) | 41 | 3939 | 3705 (1392–6106) | –443 (–1874 to 988) |
| Benefit | Trial arm | Difference | ||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| n (complete cases) | Mean amount gained (£) | Median amount gained (£) (IQR) | n (complete cases) | Mean amount gained (£) | Median amount gained (£) | IQR | Mean amount gained (£) (95% CI) | |
| Means tested | ||||||||
| Council Tax Benefit | 8 | 746 | 508 (423–1039) | 11 | 917 | 823 | 392–1468 | –171 (–600 to 258) |
| Housing Benefit | 5 | 4670 | 6202 (2180–6582) | 8 | 4166 | 4858 | 2418–5541 | 503 (–2479 to 3485) |
| Pension Credit Guarantee | 4 | 1529 | 1582 (711–2346) | 4 | 1731 | 975 | 406–3057 | –203 (–2382 to 1977) |
| Pension Credit Savings | 5 | 872 | 459 (430–845) | 3 | 879 | 784 | 586–1268 | –8 (–886 to 871) |
| Non-means tested | ||||||||
| Disability Living Allowance: Care | 4 | 5106 | 4023 (2746–7466) | 8 | 3640 | 3679 | 2518–4768 | 1466 (–2392 to 5325) |
| Disability Living Allowance: Mobility | 1 | 1686 | 1686 (1686–1686) | 4 | 4920 | 4819 | 4285–5556 | –3235 (–3951 to –2518) |
| Attendance Allowance: low rate | 2 | 3727 | 3727 (3421–4034) | 2 | 3207 | 3207 | 3147–3268 | 520 (52 to 989) |
| Attendance Allowance: high rate | 7 | 7240 | 7387 (7387–7387) | 3 | 6605 | 6540 | 6370–6905 | 636 (249 to 1023) |
| Carer’s Allowance | 1 | 3895 | 3895 (3895–3895) | 2 | 4656 | 4656 | 3953–5360 | –762 (–1894 to 371) |
| Industrial Injuries Disablement Benefit | 2 | 1763 | 1763 (1226–2299) | 5 | 2257 | 2529 | 1229–2545 | –494 (–1673 to 685) |
| Average total amount gained per participant | 36 | 3541 | 2240 (532–6874) | 41 | 3625 | 3147 | 1307–5431 | –84 (–1473 to 1305) |
| Benefit | Trial arm | Difference | |||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||
| n (complete cases) | Mean amount gained (£) | Median amount gained (£) (IQR) | n (complete cases) | Mean amount gained (£) | Median amount gained (£) (IQR) | Mean amount gained (£) (95% CI) | |
| Means tested | |||||||
| Council Tax Benefit | 8 | 746 | 508 (423–1039) | 11 | 1125 | 1009 (480–1800) | –379 (–853 to 96) |
| Housing Benefit | 5 | 4670 | 6202 (2180–6582) | 8 | 5853 | 6825 (3396–7784) | –1183 (–4409 to 2043) |
| Pension Credit Guarantee | 4 | 1529 | 1582 (711–2346) | 4 | 2423 | 1365 (568–4278) | –894 (–3815 to 2026) |
| Pension Credit Savings | 5 | 872 | 459 (430–845) | 3 | 1060 | 946 (707–1528) | –188 (–1098 to 721) |
| Non-means tested | |||||||
| Disability Living Allowance: Care | 4 | 5106 | 4023 (2746–7466) | 8 | 4212 | 4258 (2914–5518) | 894 (–3017 to 4805) |
| Disability Living Allowance: Mobility | 1 | 1686 | 1686 (1686–1686) | 4 | 5536 | 5422 (4820–6251) | –3850 (–4656 to –3044) |
| Attendance Allowance: low rate | 2 | 3727 | 3727 (3421–4034) | 2 | 4585 | 4585 (4499–4672) | –858 (–1336 to –379) |
| Attendance Allowance: high rate | 7 | 7240 | 7387 (7387–7387) | 3 | 7344 | 7271 (7082–7677) | –103 (–514 to 307) |
| Carer’s Allowance | 1 | 3895 | 3895 (3895–3895) | 2 | 5423 | 5423 (4604–6243) | –1529 (–2848 to –210) |
| Industrial Injuries Disablement Benefit | 2 | 1763 | 1763 (1226–2299) | 5 | 2257 | 2529 (1229–2545) | –494 (–1673 to 685) |
| Average total amount gained per participant | 36 | 3541 | 2240 (532–6874) | 41 | 4420 | 3756 (1678–6727) | –880 (–2406 to 646) |
Missing data were observed for some participants in the intervention group because of missing ‘date awarded’ information. These data were not replaced because no information was available on whether or not the initial claim was successful (i.e. whether or not the benefit was eventually awarded). The average total amount gained per participant and per benefit was estimated by combining information on newly awarded benefits, weekly amounts obtained from questionnaire data for both trial arms and median durations observed in the intervention group.
Non-financial benefits
Non-financial benefits recorded by WRAs in the CCS included the following items in addition to some aids and adaptations: Blue Badge (disabled driver), Warm Zones referral (including amount) and help with health-care costs (optician prescription charges, dental treatment charges, NHS travel costs) (Table 29).
| Benefit | Data source | |||
|---|---|---|---|---|
| CCS | Questionnaire | |||
| Intervention (n = 381) new claims | Intervention (n = 381) new claims | Control (n = 374) new claims | ||
| n (%) | Mean amount (SD) | n (%) | n (%) | |
| Blue Badge | 8 (2) | 21 (6) | 15 (4) | |
| Car (Motability Scheme) | n/aa | 6 (2) | 1 (< 1) | |
| Day centre attendance | n/aa | 2 (1) | 6 (2) | |
| Meals at home | n/aa | 1 (< 1) | 1 (< 1) | |
| Help with insulation cost | n/aa | 24 (6) | 40b (11) | |
| Grant from HEES | n/aa | 10 (3) | 9 (2) | |
| Social tariff (electricity) | n/aa | 16 (4) | 17 (5) | |
| Warm Zones referral | 1 (< 1) | n/aa | n/aa | |
| Amount: Warm Zones referral | 1 (< 1) | 130.00 (n/a) | n/aa | n/aa |
| Financial help with dental treatment charges | 3 (< 1) | 17 (4) | 23 (6) | |
| Amount: dentist | 2 (< 1) | 53.43 (34.20) | n/aa | n/aa |
| Financial help with optical prescription charges | 3 (< 1) | 31 (8) | 36 (10) | |
| Amount: optician | 2 (< 1) | 45.49 (8.84) | n/aa | n/aa |
| Help with health-care costs: travel | 1 (< 1) | n/aa | ||
| Amount: NHS travel costs | 1 (< 1) | 13.08 | n/aa | n/aa |
| Community Care Alarm | 2 (< 1) | 0 (0) | 0 (0) | |
As Table 29 shows, the numbers of new non-financial benefits recorded on the CCS by WRAs for participants in the intervention group were substantially different from the numbers of financial benefits reported by participants in the questionnaire.
To avoid an underestimation of effects in the intervention group, the analysis of non-financial benefits considered the same data source (i.e. questionnaire) for both the intervention and the control group, and so faces the same potential recall bias, thus providing a fair comparison between the two groups.
There was no evidence of statistically significant differences in the number of newly awarded benefits between trial arms, except that significantly more participants in the control group received general help with insulation costs.
One element of non-financial benefits that participants could receive was new aids and adaptations that helped them to remain independent at home. A full list of all items can be found in Table 30. This information was taken from the responses to the questionnaire in order to provide a fair (less biased) comparison. There was no evidence of any statistically significant differences in the number of newly awarded items between trial arms, with the exception of a ‘special telephone’, which was more frequently received in the intervention group.
| Category | Item | Data source, n (%) | ||
|---|---|---|---|---|
| CCS | Questionnaire | |||
| Intervention (n = 381) | Intervention (n = 381) | Control (n = 374) | ||
| Bathing | Bath/grab rail(s) | 17 (4) | 21 (6) | |
| Walk-in shower | 19 (5) | 21 (6) | ||
| Bath house | 2 (< 1) | 0 (0) | ||
| Bath seat/board | 3 (< 1) | 10 (3) | 5 (1) | |
| Toileting | Grab rails in toilet/bathroom | 11 (3) | 13 (3) | |
| Commode for day/night use | 4 (1) | 1 (< 1) | ||
| Bedpan/urinal/bottle | 1 (< 1) | 0 (0) | ||
| Raised toilet seat | 1 (< 1) | 13 (3) | 15 (4) | |
| Incontinence pads | 5 (1) | 1 (< 1) | ||
| Bedroom | Bed hoist | 1 (< 1) | 0 (0) | |
| Bed raise/bed block | 5 (1) | 4 (1) | ||
| Special bed/mattress | 7 (2) | 8 (2) | ||
| Chair/bed | Sheepskin | 0 (0) | 0 (0) | |
| Special cushion(s) | 6 (2) | 5 (1) | ||
| Special chair/chair raise | 3 (< 1) | 9 (2) | 6 (2) | |
| Accessibility | Widened doorways | 2 (< 1) | 2 (< 1) | |
| Additional stair rails | 4 (1) | 10 (3) | 10 (3) | |
| Stairlift/vertical lift | 1 (< 1) | 7 (2) | 4 (1) | |
| Ramp at front/rear entrance(s) | 5 (1) | 5 (1) | ||
| Additional grab rails at front/rear entrance(s) | 17 (4) | 13 (3) | ||
| Door handle(s) | 4 (1) | n/a | n/a | |
| Mobility | Manual wheelchair | 2 (< 1) | 7 (2) | |
| Electric wheelchair | 1 (< 1) | 0 (0) | ||
| Walking frame (Zimmer) | 1 (< 1) | 2 (< 1) | 5 (1) | |
| Walking stick(s) | 22 (6) | 21 (6) | ||
| Walking trolley | 4 (1) | 2 (< 1) | ||
| Crutches | 2 (< 1) | 1 (< 1) | ||
| Meals | Kitchen gadgets | 12 (3) | 12 (3) | |
| Special cutlery/crockery | 4 (1) | 1 (< 1) | ||
| Meal trolley | 2 (< 1) | 0 (0) | ||
| Communication | Community Care Alarm scheme | 14 (4) | 10 (3) | |
| Special telephone | 7 (2) | 1a (< 1) | ||
| Entrance telecom | 3 (< 1) | 1 (< 1) | ||
| Adapted items | Helping hand for picking up objects while standing | 18 (5) | 20 (5) | |
| Helping hand for pulling on socks/stockings | 1 (4) | 1 (< 1) | ||
| Special implements with long handles (e.g. hair brush) | 4 (1) | 3 (< 1) | ||
Table 31 reports the average total value for aids and adaptations per participant. On average, the intervention group received £134 per participant more than the control group in the value of non-financial benefits in the form of aids and adaptations over the 2-year follow-up period (95% CI –£582 to £850).
| Trial arm | Difference | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||||
| n | Mean amount gained (£) | Median amount gained (£) | IQR (£) | n | Mean amount gained (£) | Median amount gained (£) | IQR (£) | Mean difference (£) [intervention-control] | 95% CI (£) | |
| Average total amount gained per participant | 92 | 1514 | 87 | 29–1646 | 92 | 1380 | 130 | 23–4021 | 134 | –582 to 850 |
Health-related quality of life
Changes in HRQoL were captured by a comparison of EQ-5D-3L scores between trial arms. EQ-5D-3L responses are broken down into the responses for each of the five questions so that it is possible to observe how responses to each question may differ between trial arms (see Table 37, Appendix 20). The observed pattern in responses to each of the questions at both baseline and 24 month follow-up was similar between trial arms.
Table 32 reports the mean EQ-5D-3L scores by each group. When converting the responses to the EQ-5D-3L into a score, the 36 participants who died during the trial follow-up period were scored as 0 at the 24 month follow-up, and these data have contributed to the estimation of mean scores. The number of deaths was evenly distributed between the randomised groups.
| Measure | Trial arm | Difference | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||
| n | Mean score | SD | Median score | n | Mean score | SD | Median score | Mean (95% CI) | |
| EQ-5D-3L baseline | 374 | 0.589 | 0.332 | 0.691 | 363 | 0.583 | 0.356 | 0.691 | 0.006 (–0.044 to 0.056) |
| EQ-5D-3L 24 monthsa | 298 | 0.630 | 0.325 | 0.699 | 291 | 0.623 | 0.343 | 0.714 | 0.006 (–0.048 to 0.060) |
| QALYsa | 293 | 1.240 | 0.562 | 1.372 | 282 | 1.242 | 0.613 | 1.415 | –0.002 (–0.098 to 0.094) |
| Adjusted QALYs gainedb | 0.014 (–0.031 to 0.059) | ||||||||
Not all participants who were alive at the end of trial follow-up completed the EQ-5D-3L. To understand if there might be some informative reason why there was not a response to the EQ-5D-3L, the correlation between whether or not EQ-5D-3L was missing and the primary study outcome, CASP-19, was estimated. This analysis showed that there was no evidence that missing EQ-5D-3L values were highly correlated with the CASP-19 (Pearson’s correlation coefficient –0.0886; p = 0.0668). Therefore, it was assumed that missing EQ-5D-3L responses for those who were not known to have died were missing at random.
For both trial arms, EQ-5D-3L scores were slightly higher at 24 months. QALYs calculated from EQ-5D-3L data at both baseline and 24 months were slightly higher on average in the intervention group after adjusting for differences in baseline EQ-5D-3L, age and gender (see Table 32), but there was no evidence of a statistically significant difference between trial arms. The CI is wide enough, however, to include clinically important differences favouring either trial arm.
Balance sheet
The results of the cost–consequence analysis are presented in the balance sheet (Table 33), indicating which arm of the intervention they favour (i.e. in which trial arm a significant positive difference in a particular benefit was observed).
| Outcome favours intervention (I) | Outcome favours control (C) |
|---|---|
|
Qualitative findings For some, the nature of the intervention, involving a domiciliary visit and active assistance with claims, as well as reassurance concerning entitlement, relieved stress and generated positive feelings (e.g. peace of mind) For some, the increased benefits allowed the individual to escape a stressful and precarious financial situation For some, the increased benefits prevented the need for borrowing or reducing savings and helped to reduce or prevent debt, thus increasing their financial security and reducing stress For some, the increased benefits alleviated food and fuel poverty and security against otherwise catastrophic unplanned costs For some, the increased benefits helped to maintain mobility, independence and support formal and informal support with activities of daily living For some, the increased benefits allowed the provision of monetary or non-monetary gifts for informal help receive, increasing their perceptions of self-worth and reinforcing informal support networks |
Financial benefits (mean difference in amount gained) Disability living allowance (mobility component): £3344 (95% CI £2654 to £4035) Carer’s Allowance: £1499 (95% CI £187 to £2810) Non-financial benefits Insulation cost: an additional 16 participants received help with insulation cost [I, 24 (6%); C, 40 (11%); p = 0.030] |
| No evidence that outcome differs between intervention and control group (I – C) | |
| No evidence of a difference in the following financial benefits (mean difference in amount gained), but CIs are wide enough to include economically important differences favouring either group | |
| Financial benefitsa | |
|
Average total amount: –£451 (95% CI –£1892 to £991) Council Tax Benefit: –£245 (95% CI –£694 to £204) Housing Benefit: –£250 (95% CI –£3387 to £2886) Pension Credit (guarantee): –£341 (95% CI –£2653 to £1971) Pension Credit (savings): –£83 (95% CI –£977 to £811) Disability Living Allowance (care component): £1136 (95% CI –£2742 to £5015) Attendance Allowance (low rate): –£241 (95% CI –£684 to £256) Attendance Allowance (high rate): £174 (95% CI –£231 to £580) Industrial Injuries Disablement Benefit: –£494 (95% CI –£1673 to £685) |
|
| No evidence of a difference in the following non-financial benefits (difference in frequency between groups) | |
| Non-financial benefitsa | |
|
Blue Badge: an additional six participants in the intervention group received Blue Badges [I, 21 (6%); C, 15 (4%); p = 0.313] Car: an additional five participants in the intervention group received a car from the Motability Scheme [I, 6 (2%); C, 1 (< 1%); p = 0.057] Day centre attendance: an additional four participants in the control group attended a day centre [I, 2 (1%); C, 6 (2%); p = 0.150] Meals at home: the same number of participants received meals at home in both trial arms [I, 1 (< 1%); C, 1 (< 1%); p = 0.992] Grant from HEES: one additional participant in the intervention group received a grant from HEES [I, 10 (3%); C, 9 (2%); p = 0.828] Social tariff (electricity): one additional participant in the control group reported to be on a social tariff for electricity [I, 16 (4%); C, 17 (5%); p = 0.642] Financial help with optical prescription charges: an additional five participants in the control group received financial help with optical charges [I, 31 (8%); C, 36 (10%); p = 0.356] Financial help with dental treatment charges: an additional six participants in the control group received financial help with dental treatment charges [I, 17 (4%); C, 23 (6%); p = 0.266] |
|
| Aids and adaptations (mean difference in average total amount)a | |
| Average total amount: £134 (95% CI –£582 to £850) | |
| HRQoL (mean difference in QALYs gained) | |
| QALYs gained: 0.009 (95% CI –0.038 to 0.055) | |
Cost–utility analysis
On average, the (adjusted) intervention was found to be more costly and more effective than usual care (Table 34).
| Group allocation | Cost (£) | Incremental cost (£) (95% CI) | QALYs | Incremental QALYs | Incremental cost (£) per QALY gained (ICER) |
|---|---|---|---|---|---|
| Control | 0.00 | 1.242 | |||
| Intervention | 16.80 | 16.80 | 1.240 | –0.002 | Dominated |
| Intervention (adjusteda) | 17.18 (15.37 to 19.05) | 0.009 (–0.038 to 0.055) | 1914 |
However, the differences in QALYs gained were not significant (p = 0.966). The point estimate of incremental cost per QALY gained was £1914. Nevertheless, there is considerable statistical imprecision surrounding these data, and bootstrapping was used to estimate the precision surrounding estimates of cost, QALYs and incremental cost per QALY. The incremental cost-effectiveness plane (Figure 6) visually plots the differences in mean costs and effects from each of the 1000 bootstrap iterations and indicates the level of uncertainty around cost and QALY point estimates (as previously reported by the 95% bootstrapped CIs in Table 34). Every point above the x-axis indicates that the intervention is more costly than usual care. Every point left of the y-axis indicates that the intervention is less effective than usual care, and right of the y-axis is more effective.
FIGURE 6.
Cost-effectiveness plane.
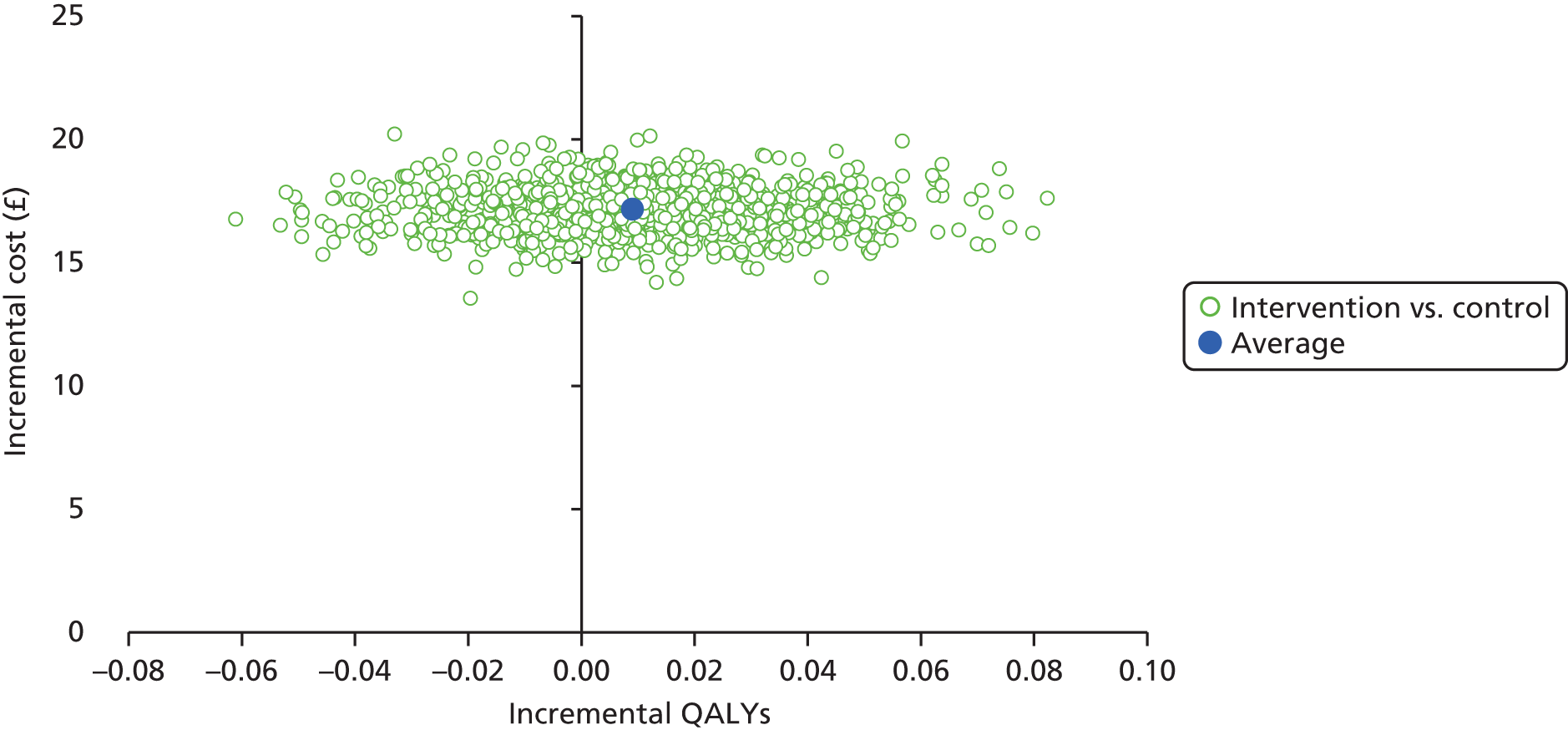
The statistical imprecision surrounding estimates of cost-effectiveness are presented in terms of a CEAC (Figure 7). A CEAC shows the one-sided probability that the intervention is cost-effective at any given value for society’s WTP for a QALY gained. This is analogous to the upper interval in a CI; the lower interval is irrelevant if we believe that the intervention is cost-effective at the upper interval because it must therefore be cost-effective at the lower interval.
FIGURE 7.
Cost-effectiveness acceptability curve.
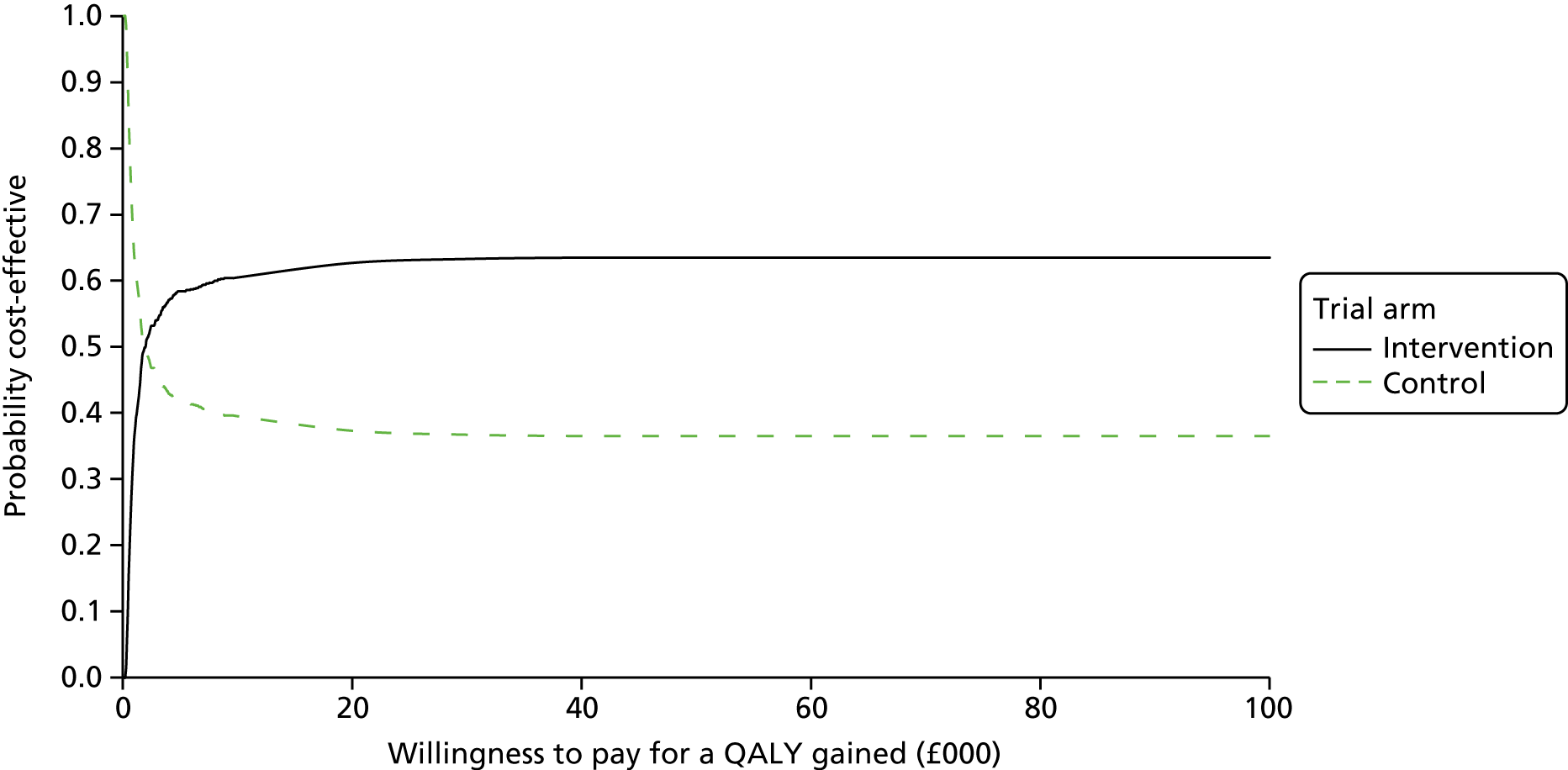
In the CEAC we calculate the number of bootstrap iterations where the intervention arm is likely to be considered cost-effective compared with control over a range of values for society’s WTP for a QALY gain. As we have 1000 bootstrap iterations, we can estimate the probability that the intervention is cost-effective over the range of values. Furthermore, if the intervention is not cost-effective compared with the control then the control is cost-effective.
The probability that the intervention would be cost-effective, should society be willing to pay £20,000 per QALY gained, was around 63%. This suggests, given current evidence, that in economic terms and taking a NHS and local authority perspective we are almost indifferent to whether or not the intervention is implemented.
From an individual perspective, however, the value of the benefits can be considered a gain, albeit one that has not clearly translated into improved health over the 2-year time horizon of the study.
These results were robust to changes in the discount rate and higher costs associated with the delivery of the intervention.
The base-case analysis was based on complete cases. When missing EQ-5D-3L data were imputed using multiple imputation, the QALYs gained in the control group were, on average, 0.019 higher (95% CI –0.068 to 0.029). Therefore, the intervention was, on average, more costly and less effective than the control, and hence the intervention was dominated by usual care (Table 35).
| Scenario | Details | Imputation for missing data | n | Cost differencea | QALY differencea | ICER | Probability cost-effective at WTP £10,000 (%) | Probability cost-effective at WTP £20,000 (%) | Probability cost-effective at WTP £30,000 (%) |
|---|---|---|---|---|---|---|---|---|---|
| Base case | Complete cases only, discount rate 1.5% | n/a (only participants with full data) | 534 | 17.18 | 0.009 | 1914 | 60.5 | 62.7 | 63.3 |
| Higher discount rate | EQ-5D-3L at 24-month follow-up discounted at 3.5% | n/a (only participants with full data) | 534 | 17.18 | 0.009 | 1953 | 60.4 | 62.5 | 63.3 |
| Intervention costs | Mean WRA salary +20%, mileage reimbursement +50% | n/a (only participants with full data) | 534 | 22.39 | 0.009 | 2492 | 59.7 | 61.7 | 62.9 |
| Missing EQ-5D-3L at 24-month follow-up | MI for missing EQ-5D-3L scores at 24-month follow-up | MI using baseline information for EQ-5D-3L and care at home required (binary variable) | 664 | 15.58 | –0.019 | Dominated | 18.6 | 19.3 | 19.8 |
Chapter 6 Discussion
Summary of main findings
Within the intervention group, only 22% of participants were awarded extra financial or non-financial benefits after receiving domiciliary welfare rights advice: the remainder declined the advice, were awarded no benefits or declined the benefits for which they were eligible. Quantitative analyses found little evidence that domiciliary welfare rights advice led to positive impacts on HRQoL over the 24-month follow-up period. There was no significant difference in the primary outcome (CASP-19 score) between intervention and control group participants at 24 months (adjusted mean difference 0.3, 95% CI –0.8 to 1.5), nor was there evidence that the difference varied among subgroups distinguished by age, sex or socioeconomic position. We did find a significant change in the hours of care received per week, which increased more in the intervention group (53.7 vs. 42.0; adjusted difference of 26.3 hours/week, 95% CI 0.8 to 56.1 hours/week), but at the lower end of the CI the difference was of questionable value, while at the upper end of the CI the difference would be of real importance. This range reflected the small numbers receiving care, and the large variation between them in terms of hours of care.
Exploratory analyses indicate that there were no significant differences in primary or secondary outcomes between those in the intervention group who received welfare rights advice versus those who did not, and those in the intervention group who received benefits versus those who did not, excepting that those who did not receive benefits reported significantly higher levels of physical activity at 24 months. We also found no significant differences in CASP-19 score between the 55 participants in the intervention group who were awarded financial benefits compared with the 48 in the control group who were awarded financial benefits after 24 months and were thus comparable on eligibility (adjusted mean difference in CASP-19 score 1.4, 95% CI –2.0 to 4.7). We found no evidence of a dose–response relationship between amount of financial benefit received by those in the intervention group and change in CASP-19 score at 24 months. We did, however, find a weak positive correlation between CASP-19 score at 24 months and the amount of time since receipt of the benefit (0.39, 95% CI 0.16 to 0.58).
The qualitative data suggested that receipt of the intervention was acceptable, and both participants and professionals perceived the receipt of additional financial and non-financial benefits to have had a positive impact on health and HRQoL. For example, for some participants, the increased benefits allowed them to escape a stressful and precarious financial situation; prevented the need to borrow or reduce savings and helped to reduce debt, thereby increasing financial security and reducing stress; alleviated some food and fuel poverty and provided security against otherwise catastrophic unplanned costs; helped to maintain mobility, independence and pay for formal and informal support with activities of daily living; or allowed the provision of monetary or non-monetary gifts for informal help received, increasing perceptions of self-worth and reinforcing informal support networks. Overall, the picture painted by the qualitative findings was one that suggested that the intervention, when leading to additional financial or non-financial benefits, resulted in improvements in HRQoL with the potential to impact on physical or mental health, and could lead to increased independence.
The economic evaluation indicated that, on average, the delivery of domiciliary welfare rights advice was found to be more costly and more effective than standard practice. The average total cost per participant was £44 over 24 months. This included around £17 (95% CI £15 to £19) for additional activities associated with the intervention being delivered in participants’ homes. The mean health gain, although not statistically significant, from the Do-Well intervention after 24 months was 0.009 (95% CI –0.038 to 0.055) QALYs (adjusted for baseline EQ-5D-3L, age and gender), resulting in an ICER of £1914 per QALY gained. However, the probability that the intervention was cost-effective was only 60% when compared with conventional thresholds for society’s WTP for a QALY (£20,000) and any value above. For the majority of financial and non-financial benefits, including aids and adaptations, no difference in the number of new awards was observed between the trial arms over the study period. Using a cost–consequences analysis, from an individual perspective the value of the receipt of benefits was a gain, albeit one that did not clearly translate into improved health over the 2-year time horizon of the study. Imprecision around all estimates was high, and analyses involving multiple imputation to account for missing data yielded differing conclusions, indicating the degree of uncertainty that still exists.
Overall, the economic analyses showed that, despite no significant difference in quality of life being identified, changes in the receipt of benefits might be expected to impact on recipients’ well-being. Nevertheless, there was no evidence of any difference in welfare benefits between the trial arms, although CIs were wide enough to include potentially important differences. Even small increases in relatively small incomes might, therefore, be important.
Strengths and limitations of the study
This is the first RCT to examine the impact of welfare rights advice on health outcomes, and the first to explore specifically the impact of the advice on older people when it is delivered in their own homes. The trial was rigorously, ethically and legally conducted to internationally accepted standards, adhered to accepted reporting protocols and was overseen by an independent TSC. We employed rigorous controls to ensure data quality, and blinding to minimise bias among data collectors. Our primary and secondary outcomes were measured using validated scales, and were chosen on the basis of rigorous pilot work. We demonstrated the potential of the CASP-19 scale to show a clinically important change over time in relevant groups in advance of the trial using analysis of national cohort study data. The study was then powered to be able to demonstrate such a change as a result of the intervention. The intervention and control groups were balanced on all variables, indicating appropriate and effective randomisation.
The trial included a detailed process evaluation with both quantitative and qualitative components providing data that helped to explain the main trial and economic evaluation findings. We optimised the intervention prior to delivery by providing information, training and guidance for WRAs and GPs on their respective roles in ensuring welfare entitlements. We then assessed the fidelity of the intervention by recording and analysing a sample of WRAs’ interactions with clients. We were able to record only seven interactions. Although it is possible that WRAs who were not recorded delivered the service in a different way, resulting in systematically different outcomes, we think that this is unlikely, as a key performance indicator for WRAs is income maximisation, and they are therefore highly motivated to identify eligibility.
The qualitative study was rigorously conducted, with systematic and independent double coding of data to enhance internal validity. The participant data was corroborated using data from professional participants, and triangulated with our pilot study data.
The economic evaluation was conducted from public sector and Treasury perspectives, and comprehensively explored the potential for cost-effectiveness using both cost–utility and cost–consequences analyses. Sensitivity analyses assessed the impact of different data sources and varying key assumptions and parameters on the cost-effectiveness of the intervention.
We intended to conduct the trial in all local authority areas in one region, but found that two out of 12 authorities were unable to provide domiciliary welfare rights advice services, and in a further two local authority areas we were unable to recruit any general practices willing to participate. In the eight local authority areas in which we found willing general practices, there was variation in the ability or willingness of these practices to recruit participants, such that numbers of potential participants who were approached varied from 330 to 695 by local authority area and from 100 to 387 by general practice. Initial recruitment fell short of our target, and a second wave of recruitment, involving the recruitment of additional general practices, was necessary, which required us to seek an extension to the study. We recruited participants from general practices located in areas in the lower two-fifths of the distribution of socioeconomic deprivation, measured using the IMD 2010, using the method described by Griffin et al. 72 However, when we examined the IMD scores assigned to the 17 general practices that agreed to participate in the study, the practices were in fact slightly less deprived on average [mean IMD score at MSOA level 37.0 (SD 10.4)] than the remaining 363 general practices in the North East [mean IMD score at MSOA level 38.5 (SD 11.5)]. Forty-five per cent of older people who were identified by general practices, and who did not opt out after receiving the initial invitation, later declined to participate. We have no information on these 1770 older people, who might have differed significantly (e.g. in terms of benefit eligibility or health status) from those who later participated. Similarly, of the 2142 we invited to participate, only 35% agreed to be randomised. Compared with those who declined, those who participated were, on average, less likely to be socioeconomically disadvantaged [IMD score at LSOA level 33.5 (SD 17.9) vs. IMD score at LSOA level 29.0 (SD 16.0)] and more likely to be women (50.5% vs. 53.5%). Overall, the recruitment rate varied from 8.5% to 26.0% (mean 19.3%; 755/3912) by general practice; it is unclear if this had an impact on outcomes. We compared these data with both the ELSA cohort and equivalent data from our pilot study. In both cases these data suggest that our trial cohort was somewhat more affluent than expected, which is likely to have reduced their eligibility for benefit outcomes and may, to an extent, explain the lower than expected proportion gaining additional benefits.
Participation in the study was limited to those fluent in English, which is likely to have excluded some older people from black and minority ethnic communities. Compared with the rest of the UK, the North East has a lower proportion of people from black and minority ethnic communities. The cost and complexity of providing translation and interpretation services for the very small number of participants (both for the trial and, in particular, for the domiciliary intervention) were considered too great to facilitate the participation of this group. Nevertheless, six people from black and minority ethnic groups participated in the trial (about 0.75% of participants). This does limit the generalisability of the study to black and minority ethnic populations in the UK. The study also excluded individuals deemed unable to participate in the research owing to poor mental or physical health, as assessed by their GP. In studies of this kind, it is usual for GPs to be offered the opportunity to exclude patients from the research who they feel would be unable to participate, or for whom the research might prove too challenging either physically or mentally. Nevertheless, such patients might have benefited from the intervention, and their exclusion may limit generalisability. The exclusion of the above groups may have contributed to the less socioeconomically disadvantaged profile of the trial participants.
One local authority did not deliver its own welfare rights advice services and, instead, contracted such services out to a third-sector organisation. In addition, during the course of the study there was substantial turnover of WRAs and changes in the local authority services available, which may have impacted on intervention delivery. For example, there was an indication that the initial WRA appointments for participants took longer to arrange the more the study progressed. We mitigated this as far as possible by employing independent WRAs as part of the study to provide cover when local authorities could not deliver services in their areas.
We lost 21% of participants through withdrawal or loss to follow-up, which was more than we anticipated from our pilot RCT. 11 However, those lost from the study as a result of death constituted 4.8% of participants, fewer than the 5.6% who died during the 24 months’ follow-up in the pilot study. 11 Those who left the study had poorer health than those who remained at 24 months. We were unable to interview anyone who dropped out of the study, so the reasons for attrition remain unclear.
An important limitation was the lower than anticipated proportion of participants in the intervention group (84/335, 22%) found to be eligible for additional benefits (and, similarly, after 24-month follow-up, in the control group). This had the consequence of significantly reducing the chance that we could detect an overall meaningful effect of the intervention, as any signal from the small number of those eligible was diluted in the intention-to-treat analyses. The relatively small numbers of new benefits recorded and the variation in the observed amounts resulted in substantial imprecision around point estimates for the value of benefits. For most of the financial benefits, owing to a lack of evidence, the economic analysis did not detect any significant differences between trial arms. However, CIs are wide and include economically important differences favouring either the intervention or the control group.
We designed the study to avoid contamination between trial arms. The participants were individually randomised, and those in the control group received no contact from a study WRA until after the 24-month follow-up. However, participants were free to seek welfare rights advice independently or to claim benefits independently during the course of the study. In data collected from the control group by interview at 24 months, a larger than anticipated proportion of participants reported new benefits that were not reported at baseline. When these were financial benefits, they must either have resulted from new claims or be the result of misreporting. When these were non-financial benefits (e.g. aids and adaptations in the home), it is possible that they were acquired by means other than welfare claims. Our qualitative work shed no further light on the source of these benefits (e.g. out of 20 control group participants interviewed, none indicated that participating in the trial had prompted them to seek welfare rights advice independently, yet 14 out of the 20 ultimately reported additional benefits at the 24-month follow-up), and the numbers and amounts of benefits reported, particularly non-financial, differed considerably between the 24-month interview and the CCS forms completed by WRAs at 24 months (see further below). Nevertheless, we are aware that, during the time of the study, a range of third-sector welfare rights advice service providers were operating in the North East, including Citizens Advice Bureaux, Age UK, Advice UK network, Law Centres Network, Shelter and the Money Advice Trust. Family and friends can also be important sources of advice on claiming benefits.
The main outcome (CASP-19) was assessed in interviews at 24 months, and by self-report using a postal questionnaire at 12 months. Such self-reported data may be subject to a variety of biases, in particular due to recall and social desirability. We found that the reports of benefits received at 24-month follow-up differed substantially between interview data and the data collected by WRAs in their CCS forms at 24 months. The reasons for this are unclear and, to ensure comparability with the intervention group, in particular in the economic evaluation, we decided to use the interviewer data. Sensitivity analyses were employed to explore the impact of data source. The discrepancy in self-reported data for additional non-financial benefits was substantial and could have altered the findings. However, comparing the reported numbers between groups suggested no significant effect of the intervention, although we cannot rule out the possibility that a meaningful difference existed. We were unable to obtain all of the CCS forms from the WRAs, resulting in some missing data on benefit outcomes in the control group at 24 months.
In our qualitative study, many participants referred to how benefits alleviated anxiety or worry. In our secondary outcomes measures, although we included the PHQ-9 depression scale, we did not include a specific measure of anxiety, and this is a limitation. We measured activities of daily living using the Townsend Activities of Daily Living scale, which was collected at baseline and at 12 and 24 months. This was included as a potential confounding factor in the outcome analyses. We decided that it would be inappropriate to use this scale as a secondary outcome because, although it reports on the ability to perform activities, it does not take into account whether or not, and from whom, help with activities is needed.
The costs in the control group were probably overestimated compared with those in the intervention group. For example, the durations for all other WRA activities that were not included in the cost analyses may have been higher in the intervention group. This is based on the assumption that, compared with usual practice, more claims for additional benefits may have been picked up by the WRA in participants’ homes, which would have increased the total duration of all activities in the intervention group.
Owing to the number of data collected by means of both participant questionnaires and the CCS that had to be analysed, the aim of the cost-effectiveness analyses was to use as much information as possible to provide an overview of which benefits (out of a potentially large range) were the most frequently awarded. Not all information (e.g. partner benefits and one-off payments from questionnaire data) were included in the final analyses, largely because there were missing duration data. However, as there was no evidence that the number of benefits reported in the questionnaires differed substantially between the trial arms, the results should not have been affected by this decision. Given that the information on durations was essential for the analysis, and was not collected for participants in the control group, estimates of the time a benefit was received in the control group were based on the estimates of the duration of benefits obtained for the intervention group. This may have limited the number of financial benefits considered and, therefore, may have led to an underestimate of the financial benefits in the control group. However, as the intervention was supposed to increase the number of benefits claimed, it was thought that this underestimation would be negligible.
Cross-validation between the CCS and questionnaire data for the intervention group was used to assess the validity of both data sources. This work showed that the number of newly awarded financial benefits recorded for the intervention group in the CCS was slightly higher than in the self-reported questionnaire data. Although a similar pattern of under-reporting may have occurred for those in the control group, the net impact on differences in value of benefits is likely to be small.
Finally, most likely as a result of the age range of the population and the trial period of 2 years, the number of participants lost to follow-up was relatively high, which was reflected, for example, by almost 23% of EQ-5D-3L data missing in each trial arm at the 24-month follow-up. There was also evidence that those remaining in the study at 24 months were healthier than those who dropped out for any reason.
Strengths and limitations in relation to previous studies
The trial was designed carefully to overcome the key methodological weaknesses of previous research. These included a lack of randomisation or controls; a limited range of outcomes without clear theoretical justification; limited statistical power; very short-term follow-up; a lack of economic evaluation; and a lack of process evaluation offering explanatory potential (see Chapter 1 for a detailed discussion of how these limitations were addressed). 42,43
We optimised the intervention to maximise the likelihood of successful claims for those eligible by providing the intervention in people’s own homes, so as to avoid requiring those with health problems to travel;33 ensuring that there was active assistance with claims, so as to avoid the significant challenges that people can face in completing complicated claims forms;12,31,110 and providing training, information and guidance for both WRAs and GPs in assisting claims, so as to ensure that the welfare rights advice was delivered with maximal fidelity. 11,12
We targeted the intervention to ensure that it was delivered most efficiently to those most likely to benefit from the intervention. We did this by identifying general practices in the poorest areas of the North East, using methods similar to those used in previous studies. 72 However, we found that this did not guarantee that either the practices or the individual participants were similarly socioeconomically deprived (i.e. in the lower two-fifths of IMD distribution).
Our qualitative findings were remarkably similar to those identified in our pilot RCT,12 completed more than 10 years earlier. They demonstrated a range of potentially important impacts on HRQoL at an individual level, which we had anticipated might translate into detectable quantitative improvements in CASP-19 and secondary outcomes in this trial. The most notable difference from the pilot study to emerge reflected wider societal discourses on welfare entitlements, particularly the stigma and shame associated with claiming benefits. 111 As has been found elsewhere, being viewed as an undeserving claimant is the key form of benefit stigma,112 and participants went to considerable lengths to justify the legitimacy of their claim by referring to their lifetime contributions into the welfare system. Professionals expressed a range of concerns about the impact of government austerity measures on welfare benefits and services, measures that were not present at the time of our pilot study and that are disproportionately impacting hardest on the poorest areas with the worst health outcomes. 106,107 However, in the context of a rigorously conducted RCT, neither of these issues seems likely to have affected the outcome of the trial, as they would probably have affected both trial arms equally. That said, it is possible that changing views on benefit entitlement adversely affected older people’s willingness to participate in the trial, which may in turn have affected the response rate adversely. It was also evident during the study that the ability of welfare rights advice services to meet the study’s needs became more constrained over time.
Meaning of the study: possible mechanisms and implications for policy and practice
Altogether, the findings of this study do not provide sufficient evidence to support the commissioning of domiciliary welfare rights advice as a means of promoting health among older people. Nevertheless, taking into account the potential limitations of the study, we cannot rule out the possibility that the intervention had a potentially beneficial effect, and that this might be cost-effective. The findings in relation to the trial end points are somewhat surprising, given the qualitative findings, which suggest important impacts on HRQoL at an individual level. There are a number of possible explanations for this. First, the smaller than anticipated proportion of participants in the intervention arm eligible for new benefits will have considerably diluted the effect of the intervention on outcomes, resulting in an undetectable signal from the primary or secondary outcomes. Second, the receipt of additional benefits may take longer to convert into changes in HRQoL than we had time to measure. Third, we may have measured the wrong outcomes. Finally, there may be no measurable effect. Each of these explanations is now discussed further.
Our method of identifying suitable practices yielded ones that, despite being based in relatively poor areas (i.e. in the lower two-fifths of the IMD distribution), did not result in trial participants with equivalent levels of socioeconomic deprivation. This might have been because there were fewer such potential participants in practices than anticipated or because older people at the poorer end of the socioeconomic spectrum were not contactable or were less willing to participate. It is also possible that, when compared with the time our pilot trial was undertaken, there are now fewer older people entitled to unclaimed benefits. However, data collected nationally do not support this proposition. For example, around two-fifths of pensioner households entitled to Council Tax Benefit and one-third of those entitled to Pension Credit are still not claiming these benefits. 35 It seems most likely that our recruitment method failed to identify and engage those most likely to be in need of the intervention. This has important implications for future evaluations and for service delivery models. More targeted approaches to identifying evaluation participants eligible for new benefits are warranted, as suggested by key stakeholders interviewed in our qualitative interviews.
We identified a correlation, albeit one that is relatively weak, between time since receipt of benefit and level of CASP-19 at 24 months in the intervention group. This, coupled with the lack of overall effect at 24 months, and the longer than anticipated time (median 58 days: substantially greater than the intended 14 days) taken by WRAs to conduct initial assessments of participants in the intervention group, suggests that a follow-up of longer than 24 months may have made it possible to detect a stronger effect. The feasibility of such a long-term follow-up (e.g. 36–60 months) in a new randomised trial may be problematic as, in our qualitative work with older people during the design of this trial, participants felt that it would not be acceptable for those in the control group to wait longer than 24 months for the intervention. 1 Nevertheless, further follow-up of this trial cohort would be possible and may yield important new findings.
In developing this trial we focused considerable efforts on identifying the most appropriate outcomes. We based our decisions on existing literature as well as on the findings of our prior qualitative research. 12,52 This work pointed us towards the likelihood that the receipt of additional benefits among those living in socioeconomically disadvantaged circumstances might have its greatest impact on HRQoL. The CASP-19 measure57,63 captured four domains (control, autonomy, self-realisation and pleasure) that most closely mapped onto the theoretical constructs defined in this prior research. Nevertheless, it is possible that this measure failed to capture sufficiently strongly the domain(s) of health or HRQoL that most closely accord with the impacts of increased resources on health. We also failed to detect any effect using a range of secondary outcome measures that we might have expected to demonstrate some change, such as measures of mental health, although our lack of an explicit measure for anxiety is a limitation previously acknowledged. The exact mechanisms of this relationship remain unknown.
It cannot be ruled out that the receipt of additional benefits failed to have any measurable effect on health or HRQoL. Although on first consideration this seems implausible, the context in which this impact is expected to occur needs to be taken into account. The participants in this trial were older people (aged ≥ 60 years), many of whom (particularly those who were more socioeconomically disadvantaged) were in relatively poor health, suffering a range of chronic, non-communicable conditions. These conditions may have resulted from a lifetime of exposure to unhealthy environments or behaviours, consequent on social disadvantage. The potential of these participants’ rate of decline to reduce might therefore be severely constrained by their conditions, such that the amounts of additional income or the advantages of non-financial benefits awarded were too little and too late to result in measurable impact.
Although it has proved all too easy to demonstrate strong socioeconomic patterning of health by measures of socioeconomic position in observational research,3,4 few studies have been able to show, under experimental conditions, that increasing access to resources results in better health. 20 Although this may seem counterintuitive, it is important to remember that we do not yet have a clear understanding of the causal relationship between socioeconomic factors and health outcomes. Some progress has been made in the last 15–20 years, with research identifying some key pathways. 32 This evidence suggests that the relationship is likely to have multiple pathways, some of which may be interdependent, leading to multiple outcomes. Studies such as the trial reported here may have simply not measured the right combination of exposures, outcomes or confounding factors to be able to pick up a measurable signal.
Nevertheless, in this trial we did identify some differences between the intervention and control groups at 24 months that offer tantalising signals that welfare rights advice may have an impact on health. The proportion benefiting from personal care in their home increased in the intervention group compared with controls, indicating that the intervention may have helped participants gain access to much-needed care, which could help them to maintain their independence and access to beneficial social relations. These findings were corroborated by the qualitative data, which provided ample evidence that the intervention led to valued outcomes among those who gained financial or non-financial benefits. Finally, there was weak evidence that the longer participants had benefited from additional financial or non-financial resources, the higher their CASP-19 scores were, an indication that impacts may have been developing over time.
If the intervention is effective, it is probably cost-effective. It proved remarkably cheap to deliver (£44 per case), even in comparison with the usual practice of welfare advice not being delivered in people’s own homes (an average additional cost of £17 per person). The estimated cost per QALY gained was £1914, well below the NICE threshold of £20,000, although with only a 60% chance that the actual cost per QALY was below this value.
Taking into account all of our findings, we remain equivocal about whether or not domiciliary welfare rights advice is effective as a health intervention as assessed in the context of this trial. It is possible that the intervention will yield positive impacts after a longer period of follow-up. It is also possible that important impacts will be identified in further evaluations that overcome the shortcomings of this research. Nevertheless, for those who receive unclaimed benefits as a result, the intervention remains important socially and economically and our research does not suggest that local government or third sector organisations should reduce their efforts in this area. Given that many of the unclaimed benefits for those aged ≥ 60 years are health-related, our research suggests that it will be of value to health care if professionals opportunistically identify and refer people to welfare rights advice services who they believe may be eligible for unclaimed benefits
Unanswered questions and future research
While much fundamental research is still needed to understand the causal pathways between socioeconomic position and health, a significant onus also remains on the research community to provide evidence to demonstrate whether or not improved socioeconomic circumstances result in better health. It would also be prudent to conduct further experimental studies to explore the impact of worsening socioeconomic circumstances on health, particularly in older people, as ecological study evidence suggests that important impacts of austerity measures could be mitigated by interventions such as welfare rights advice. 113
It is unknown if a trial such as this could be replicated using the recruitment of a sample population of those in greater need (as assessed by eligibility) of welfare benefits. The challenges of achieving this are not inconsiderable. It would be important to identify participants on the basis of their own socioeconomic position rather than (or perhaps in addition to) using an ecological measure (e.g. IMD score associated with the general practice), as was used in this study. Recruitment and retention would probably be lower with such a population, and practical and analytical strategies would need to be adopted to minimise and mitigate the effects of the potential bias introduced.
Given the constraints on conducting this trial, it seems unlikely, on ethical grounds, that a similar but necessarily larger trial could be conducted using longer follow-up in order to see whether or not impacts of the intervention emerge over a period of > 2 years. However, it might be possible to conduct an alternative form of evaluation, perhaps taking advantage of a natural experiment in which a cohort of older people, some of whom have and some of whom have not claimed the benefits to which they are entitled, are followed up over an extended period. Such a study would need to make use of routine data to assess outcomes, and could explore the impact of differing lengths of time in receipt of benefits on outcomes. However, without targeted welfare rights advice providing a means to access for those currently not claiming their entitlements, such a study might suffer from similar problems, as sufficient claimants are needed in whom to measure an effect.
Future evaluations of welfare rights advice will need to consider carefully the outcome measures of interest. Taking into account the findings of recent research on psycho-neural pathways that show promise in explaining socioeconomic patterning of health outcomes,114,115 it may be possible to determine more proximal intermediate physiological outcomes, such as cortisol levels, which can be assessed non-invasively and might offer a more sensitive signal.
In the meantime, it may be of value to continue follow-up of this trial cohort to identify whether or not outcomes diverge among the intervention and control groups over a more extended time period (e.g. 2–5 years). The potential costs and burdens of such longer-term follow-up would need to be considered carefully, although follow-up using routine data (from primary care) focusing on independence and morbidity might offer a cost-effective and ethically uncontentious solution.
Acknowledgements
We thank all of the WRAs, general practices and participants who were involved in this research, without whom this study would have not been possible. We particularly thank the participating local authorities for funding and delivering the welfare rights advice services evaluated in this study. The intervention costs were also, in part, supported through a grant from the North East Strategic Health Authority, which ceased to exist in March 2013. This grant also funded the training of the WRAs and primary care staff involved in the study. We thank the Primary Care Research Network and Comprehensive Local Research Network for their support for the study. We are grateful to the Newcastle Clinical Trials Unit and specifically to Christine Harle and Chris Speed for their support with research governance. We would like to thank Erin Graybill, Health Economist, who developed the draft economic analysis plan and contributed to the design and conduct of the economic analysis, before moving on to study for a PhD. We are extremely grateful to our team of interviewers who collected data intermittently over a 3-year period. They are Pat Parr, Jackie Price, Patricia Bell, Victor Ball, Gemma Musson, Ursula Balderson, Susan Clarke, Margaret McDermott, Pauline Winship, Andrea Hird and Nichol Watson. We are grateful to Lavinia Miceli and Astrid Macintyre for their administrative support, Rosemary Bell for her invaluable knowledge and advice of the welfare system, and Sarah Batty, who assessed intervention fidelity. Professor Greg Rubin collaborated on the study and helped with study design. We thank members of the independent TSC for their advice on study management, analysis and interpretation. Thanks must also go to Anne Corden and Peter Allmark for their informal peer review of our final report.
Contributions of authors
Catherine Haighton (Lecturer, Public Health) contributed to the study design and the development of methods, managed the project overall, helped with the data analysis and interpretation, and drafted text in the report.
Suzanne Moffatt (Senior Lecturer, Sociology of Health and Illness) conceived the idea for the study, contributed to the study design and the development of methods, led the embedded qualitative study, helped with the data analysis and interpretation, and drafted text.
Denise Howel (Senior Lecturer, Statistics) conceived the idea for the study, contributed to the study design and the development of methods, led the statistical analysis for the main trial, contributed to the data analysis and interpretation, and drafted text.
Mel Steer (Research Associate) conducted qualitative interviews, contributed to the data analysis and interpretation, and drafted text.
Frauke Becker (Research Associate, Health Economics) contributed to the methods development, collected economic data, conducted the economic analysis, contributed to the data interpretation and drafted text.
Andrew Bryant (Research Associate, Statistics) conducted the statistical analysis for the main trial and contributed to the data interpretation.
Sarah Lawson (Research Associate, Qualitative Research) conducted qualitative interviews, contributed to the data analysis and interpretation, and drafted text.
Elaine McColl (Professor, Health Services Research) contributed to the study design and methods development, oversaw research governance and contributed to the data interpretation.
Luke Vale (Health Foundation Chair, Health Economics) contributed to the methods development, led the economic evaluation, contributed to the data analysis and interpretation, and drafted text.
Eugene Milne (Director, Public Health) contributed to the study design, provided liaison with public health stakeholders and contributed to the data interpretation.
Terry Aspray (Consultant, Geriatric Medicine) contributed to the study design and data interpretation.
Martin White (Professor, Public Health) was chief investigator with overall responsibility for the study, conceived the idea for the study, contributed to the study design and methods development, oversaw the fieldwork, contributed to the data interpretation and drafted text.
All authors commented on drafts of the report and approved the final version.
Emma Noble (deceased) (Research Associate, Public Health) contributed to the development of methods and carried out fieldwork at baseline and at 12-month follow-up.
Publications
Journal articles
Haighton C, Moffatt S, Howel D, McColl E, Milne E, Deverill M, et al. The Do-Well study: protocol for a randomised controlled trial, economic and qualitative process evaluations of domiciliary welfare rights advice for socio-economically disadvantaged older people recruited via primary health care. BMC Public Health 2012;28;12:382. https://doi.org/10.1186/1471-2458-12-382
Moffatt S, Haighton C, Steer M, Lawson S, White M. What impact does welfare rights advice have on health and wellbeing? Qualitative study from the UK. Gerontologist 2015;55:90.
Howel D, Moffatt S, Haighton C, Bryant A, Becker F, Steer M, et al. Does domiciliary welfare rights advice improve health-related quality of life in independent-living, socio-economically disadvantaged people aged ≥ 60 years? Randomised controlled trial, economic and process evaluations in the North East of England. PLoS One 2019;14:e0209560.
Conference presentations
White M, Howel D, Moffatt S, Vale L, McColl E, Haighton C, et al. Does Domiciliary Welfare Rights Advice Improve Health Related Quality of Life in Independent-living, Socio-economically Disadvantaged People aged ≥ 60 years, Recruited via Primary Care? Randomised Controlled Trial with Embedded Economic, Qualitative and Process Evaluations. Presented at The Society for Social Medicine, 60th Annual Scientific Meeting, University of York, York, UK, 14–16 September 2016.
Steer M, Moffatt S, Haighton C, Lawson S, Bryant A, Howel D, et al. A Mixed Methods Approach to Dealing with Discrepant Quantitative and Qualitative Findings: The Case of a Randomised Controlled Trial of a Complex Social Intervention. Presented at the Mixed Methods International Research Association Conference, Durham, UK, 3–5 August 2016.
Moffatt S, Haighton C, Howel D, Steer M, Bryant A, Becker F, et al. Evaluating the Impact of a Welfare Rights Advice Intervention on Older People’s Quality of Life. The Outcomes and Challenges of Undertaking a Randomised Controlled Trial of a Complex Intervention. Presented at the British Society of Gerontology, Stirling, UK, 6–8 July 2016.
Moffatt S, Haighton C, Steer M, Lawson S, Howel D, White M. ‘I Would be Terrified in Case I was Claiming Something I Shouldn’t Get’. Impact of and Barriers to Claiming Welfare Entitlements in Later Life in the UK. Presented at the 23rd Nordic Congress of Gerontology, Tampere, Finland, 19–22 June 2016.
Moffatt S, Haighton C, Steer M, Lawson S, White M. What Impact does Welfare Rights Advice have on Health and Wellbeing? Qualitative Study from the UK. Presented at The Gerontological Society of America Annual Scientific Meeting, Orlando, FL, USA, 18–22 November 2015.
White M, Moffatt S, Lock C, McColl E, Howel D, Deverill M, et al. Is a Randomised Controlled Trial to Evaluate the Health Impacts of Welfare Rights Advice for Older People Safe, Fair and Scientifically Rigorous? Design for a Definitive RCT in North East England, 2011–15. Presented at Population Health – Methods and Challenges Conference, The ICC Birmingham, UK, 24–26 April 2012.
Data-sharing statement
All data requested shoud be submitted to the corresponding author for consideration. Access to available anomymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Haighton C, Moffatt S, Howel D, McColl E, Milne E, Deverill M, et al. The Do-Well study: protocol for a randomised controlled trial, economic and qualitative process evaluations of domiciliary welfare rights advice for socio-economically disadvantaged older people recruited via primary health care. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-382.
- Howel D, Moffatt S, Haighton C, Bryant A, Becker F, Steer M, et al. Does domiciliary welfare rights advice improve health-related quality of life in independent-living, socio-economically disadvantaged people aged ≥ 60 years? Randomised controlled trial, economic and process evaluations in the North East of England. PLoS One 2019;14.
- Marmot M, Atkinson T, Black C, Broadfoot P, Cumberledge J, Diamond I, et al. Fair Society, Healthy Lives (The Marmot Review). London: University College London Institute of Health Equity; 2010.
- Charlton BG, White M. Living on the margin: a salutogenic model for socio-economic differentials in health. Public Health 1995;109:235-43. https://doi.org/10.1016/S0033-3506(95)80200-2.
- Morciano M, Hancock RM, Pudney SE. Birth-cohort trends in older-age functional disability and their relationship with socio-economic status: evidence from a pooling of repeated cross-sectional population-based studies for the UK. Soc Sci Med 2015;136–137:1-9. https://doi.org/10.1016/j.socscimed.2015.04.035.
- Chandola T, Ferrie J, Sacker A, Marmot M. Social inequalities in self reported health in early old age: follow-up of prospective cohort study. BMJ 2007;334. https://doi.org/10.1136/bmj.39167.439792.55.
- Han SD, Boyle PA, James BD, Yu L, Bennett DA. Poorer financial and health literacy among community-dwelling older adults with mild cognitive impairment. J Aging Health 2015;27:1105-17. https://doi.org/10.1177/0898264315577780.
- Jivraj S, Nazroo J. Determinants of socioeconomic inequalities in subjective well-being in later life: a cross-country comparison in England and the USA. Qual Life Res 2014;23:2545-58. https://doi.org/10.1007/s11136-014-0694-8.
- Allin S, Masseria C, Mossialos E. Inequality in Health Care Use among Older People in the United Kingdom: An Analysis of Panel Data. London: London School of Economics and Political Science; 2006.
- Argyle E. Poverty, disability and the role of older carers. Disabil Soc 2001;16:585-95. https://doi.org/10.1080/09687590120059559.
- Mackintosh J, White M, Howel D, Chadwick T, Moffatt S, Deverill M, et al. Randomised controlled trial of welfare rights advice accessed via primary health care: pilot study [ISRCTN61522618.]. BMC Public Health 2006;6. https://doi.org/10.1186/1471-2458-6-162.
- Moffatt S, Mackintosh J, White M, Howel D, Sandell A. The acceptability and impact of a randomised controlled trial of welfare rights advice accessed via primary health care: qualitative study. BMC Public Health 2006;6. https://doi.org/10.1186/1471-2458-6-163.
- Moor N, de Graaf PM, Komter A. Family, welfare state generosity and the vulnerability of older adults: a cross-national study. J Aging Stud 2013;27:347-57. https://doi.org/10.1016/j.jaging.2013.07.002.
- Wu J, Varnik A, Tooding L, Varrnik P, Kasearu K. Suicide among older people in relation to their subjective and objective well-being in different European regions. Eur J Ageing 2014;11:131-40. https://doi.org/10.1007/s10433-013-0297-1.
- Iparraguirre J. Have winter fuel payments reduced excess winter mortality in England and Wales?. J Public Health 2015;37:26-33. https://doi.org/10.1093/pubmed/fdu063.
- Benzeval M, Bond L, Campbell M, Egan M, Lorenc T, Petticrew M, et al. How Does Money Influence Health?. York: Joseph Rowntree Foundation; 2014.
- Asset Based Approaches for Health Improvement: Redressing the Balance. Glasgow: Glasgow Centre for Population Health; 2011.
- McDonough P, Duncan GJ, Williams D, House J. Income dynamics and adult mortality in the United States, 1972 through 1989. Am J Public Health 1997;87:1476-83. https://doi.org/10.2105/AJPH.87.9.1476.
- Allmark P, Baxter S, Goyder E, Guillaume L, Crofton-Martin G. Assessing the health benefits of advice services: using research evidence and logic model methods to explore complex pathways. Health Soc Care Community 2013;21:59-68. https://doi.org/10.1111/j.1365-2524.2012.01087.x.
- Connor J, Rodgers A, Priest P. Randomised studies of income supplementation: a lost opportunity to assess health outcomes. J Epidemiol Community Health 1999;53:725-30. https://doi.org/10.1136/jech.53.11.725.
- Scholz R, Maier H. German Unification and the Plasticity of Mortality at Older Ages. Rostock: Max-Planck-Institute for Demographic Research; 2003.
- Vogt T, Gampe J. Money or Medicine? The Contribution of Rising Income and Improving Health Care to the East-West German Mortality Convergence. Boston, MA: Population Association of America: 2014 Annual Meeting; 2013.
- Saving Lives: Our Healthier Nation. London: The Stationery Office; 1998.
- Acheson D. Independent Inquiry into Inequalities in Health. London: The Stationery Office; 1998.
- Bauld L, Judge K, Barnes M, Benzeval M, Mackenzie M, Sullivan H. Promoting social change: the experience of Health Action Zones in England. J Soc Policy 2005;34:427-45. https://doi.org/10.1017/S0047279405008858.
- The Role of Advice Services in Health Outcomes Evidence Review and Mapping Study. London: Advice Services Alliance; 2015.
- Reducing Health Inequalities: An Action Report. London: Department of Health and Social Care; 1999.
- Income Related Benefits Estimates of Take-Up. London: Department for Work and Pensions; 2010.
- Age Concern . Confusion over Benefits System Keeping Pensioners from Claiming Their Dues – Worrying New Statistics Revealed by Age Concern 2007. www.ageconcern.org.uk/AgeConcern/ACF27D5BD87F43B1B35155C67A628760.asp (accessed 15 June 2009).
- Tackling Pensioner Poverty: Encouraging Take-up of Entitlements. London: National Audit Office; 2002.
- Moffatt S, Scambler G. Can welfare-rights advice targeted at older people reduce social exclusion?. Ageing Soc 2008;28:875-99. https://doi.org/10.1017/S0144686X08007253.
- Adams J, White M, Moffatt S, Howel D, Mackintosh J. A systematic review of the health, social and financial impacts of welfare rights advice delivered in healthcare settings. BMC Public Health 2006;6. https://doi.org/10.1186/1471-2458-6-81.
- Moffatt S, White M, Stacy R, Downey D, Hudson E. The impact of welfare advice in primary care: a qualitative study. Crit Public Health 2004;14:295-309. https://doi.org/10.1080/09581590400007959.
- McConaghy M, Hill C, Kane C, Lader D, Costigan P, Thornby M. Entitled but not Claiming? Pensioners, the MIG and the Pension Credit. Leeds: Department for Work and Pensions; 2003.
- The Poverty Site . Take-up of Benefits n.d. www.poverty.org.uk/66/index.shtml (accessed 17 June 2010).
- Corden A, Ditch J. Introduction to Social Security. London: Routledge; 1999.
- Coppel DH, Packham CJ, Varnam MA. Providing welfare rights advice in primary care. Public Health 1999;113:131-5. https://doi.org/10.1016/S0033-3506(99)00137-7.
- Cornwallis E, O’Neil J. Promoting Health by Tackling Poverty. Scottish RCGP Magazine; 1998.
- Jarman B. Giving advice about welfare benefits in general practice. Br Med J 1985;290:522-4. https://doi.org/10.1136/bmj.290.6467.519-a.
- Paris JA, Player D. Citizens’ advice in general practice. BMJ 1993;306:1518-20. https://doi.org/10.1136/bmj.306.6891.1518.
- Widdowfield H, Rickard P. Health Centre Advice Service Report. Sunderland: Wear Valley Citizens Advice Bureau; 1996.
- Abbott S, Hobby L. An Evaluation of the Health and Advice Project: Its Impact on the Health of Those Using the Service. Liverpool: Health and Community Care Research Unit; 1999.
- Abbott S, Hobby L. Welfare benefits advice in primary care: evidence of improvements in health. Public Health 2000;114:324-7. https://doi.org/10.1016/s0033-3506(00)00356-5.
- Veitch D. Prescribing Citizens Advice. Birmingham: Social Services and Health Authority; 1995.
- Greasley P, Small N. Providing welfare advice in general practice: referrals, issues and outcomes. Health Soc Care Community 2005;13:249-58. https://doi.org/10.1111/j.1365-2524.2005.00557.x.
- Greasley P, Small N. Establishing a welfare advice service in family practices: views of advice workers and primary care staff. Fam Pract 2005;22:513-19. https://doi.org/10.1093/fampra/cmi047.
- Levy J, Payne M. Welfare rights advocacy in a specialist health and social care setting: a service audit. Brit J Soc Work 2006;36:323-31.
- Fruin C, Pitt PI. Welfare benefit promotion within a district general hospital rheumatology centre: a joint project with the local Citizens Advice Bureau. Musculoskeletal Care 2008;6:211-19. https://doi.org/10.1002/msc.133.
- Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum 1980;23:137-45. https://doi.org/10.1002/art.1780230202.
- Moffatt S, Noble E, White M. Addressing the financial consequences of cancer: qualitative evaluation of a welfare rights advice service. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0042979.
- Krska J, Palmer S, Dalzell-Brown A, Nicholl P. Evaluation of welfare advice in primary care: effect on practice workload and prescribing for mental health. Prim Health Care Res Dev 2013;14:307-14. https://doi.org/10.1017/S1463423612000461.
- Moffatt S, White M, Mackintosh J, Howel D. Using quantitative and qualitative data in health services research – what happens when mixed method findings conflict?. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-28.
- Thomson H, Hoskins R, Petticrew M, Ogilvie D, Craig N, Quinn T, et al. Evaluating the health effects of social interventions. BMJ 2004;328:282-5. https://doi.org/10.1136/bmj.328.7434.282.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: New Guidance. Medical Research Council; 2008.
- Angus VC, Entwistle VA, Emslie MJ, Walker KA, Andrew JE. The requirement for prior consent to participate on survey response rates: a population-based survey in Grampian. BMC Health Serv Res 2003;3. https://doi.org/10.1186/1472-6963-3-21.
- Hewison J, Haines A. Overcoming barriers to recruitment in health research. BMJ 2006;333:300-2. https://doi.org/10.1136/bmj.333.7562.300.
- Wiggins RD, Netuveli G, Hyde M, Higgs P, Blane D. The evaluation of a self-enumerated scale of quality of life (CASP-19) in the context of research on ageing: a combination of exploratory and confirmatory approaches. Soc Indic Res 2008;89:61-77. https://doi.org/10.1007/s11205-007-9220-5.
- Corden A, Sainsbury R, Irvine A, Clarke S. The Impact of Disability Living Allowance and Attendance Allowance: Findings from Exploratory Qualitative Research. Research Report No. 649. London: Department for Work and Pensions; 2010.
- Abbott S, Hobby L, Cotter S. What is the impact on individual health of services in general practice settings which offer welfare benefits advice?. Health Soc Care Community 2006;14:1-8. https://doi.org/10.1111/j.1365-2524.2005.00582.x.
- Forster N, Dalkin SM, Lhussier M, Hodgson P, Carr SM. Exposing the impact of Citizens Advice Bureau services on health: a realist evaluation protocol. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009887.
- Abbott S. Prescribing welfare benefits advice in primary care: is it a health intervention, and if so, what sort?. J Public Health Med 2002;24:307-12. https://doi.org/10.1093/pubmed/24.4.307.
- Greasley P, Small N. Welfare Advice in Primary Care. Bradford: University of Leeds; 2002.
- Hyde M, Wiggins P, Higgs P, Blane DB. A measure of quality of life in early old age: the theory, development and properties of a needs satisfaction model (CASP-19). Aging Ment Health 2003;7:186-94. https://doi.org/10.1080/1360786031000101157.
- Netuveli G, Wiggins RD, Hildon Z, Montgomery SM, Blane D. Quality of life at older ages: evidence from the English longitudinal study of aging (wave 1). J Epidemiol Community Health 2006;60:357-63. https://doi.org/10.1136/jech.2005.040071.
- Howel D. Interpreting and evaluating the CASP-19 quality of life measure in older people. Age Ageing 2012;41:612-17. https://doi.org/10.1093/ageing/afs023.
- Craig P. Costs and benefits: a review of research on take-up of income related benefits. J Soc Policy 1991;20:537-65. https://doi.org/10.1017/S0047279400019796.
- Sandell A. Oxford Handbook of Patients’ Welfare: A Doctor’s Guide to Benefits and Services. Oxford: Oxford University Press; 1998.
- Moffatt S, White M, Stacy R, Hudson E, Downey D. ‘If We Had Not Got Referred and Got The Advice, I Don’t Know Where We’d Be, It Doesn’t Bear Thinking About’. The Impact of Welfare Advice Provided in General Practice. A Qualitative Study. Newcastle upon Tyne: Newcastle University; 1999.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Collins A, Colwell N, McClowry S, Melnyk B, Beedy D. Intervention Research: Designing, Conducting, Analyzing, and Funding. New York, NY: Springer; 2012.
- Dumas JE, Lynch AM, Laughlin JE, Phillips Smith E, Prinz RJ. Promoting intervention fidelity. Conceptual issues, methods, and preliminary results from the EARLY ALLIANCE prevention trial. Am J Prev Med 2001;20:38-47. https://doi.org/10.1016/S0749-3797(00)00272-5.
- Griffin T, Peters TJ, Sharp D, Salisbury C, Purdy S. Validation of an improved area-based method of calculating general practice-level deprivation. J Clin Epidemiol 2010;63:746-51. https://doi.org/10.1016/j.jclinepi.2009.07.019.
- Schulz K, Altman D, Moher D. for the Consort Group . CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Trials 2010;11. https://doi.org/10.1186/1745-6215-11-32.
- Hoffmann T, Glasziou P, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: Template for Intervention Description and Replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Data Protection Act 1998. London: The Stationery Office; 2011.
- Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord 2004;81:61-6. https://doi.org/10.1016/S0165-0327(03)00198-8.
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiat Ann 2002;32:1-7. https://doi.org/10.3928/0048-5713-20020901-06.
- Cameron IM, Crawford JR, Lawton K, Reid IC. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br J Gen Pract 2008;58:32-6. https://doi.org/10.3399/bjgp08X263794.
- Ford G, Ecob R, Hunt K, Macintyre S, West P. Patterns of class inequality in health through the lifespan: class gradients at 15, 35 and 55 years in the west of Scotland. Soc Sci Med 1994;39:1037-50. https://doi.org/10.1016/0277-9536(94)90375-1.
- Walker A, Maher J, Coulthard M, Goddard E, Thomas M. Living in Britain. Results from the 2000 General Household Survey. London: The Stationery Office; 2001.
- Szende A, Oppe M, Devlin N. EQ-5D Value Sets: Inventory, Comparative Review and User Guide. Berlin: Springer; 2007.
- The EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Sobell LC, Sobell MB. Alcohol Timeline Followback Users’ Manual. Toronto, ON: Addiction Research Foundation; 1995.
- Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 1993;46:153-62. https://doi.org/10.1016/0895-4356(93)90053-4.
- The Medical Research Council Cognitive Function and Ageing Study Team . The description of activities of daily living in 5 centres in England and Wales. Age Ageing 1998;27:605-13. https://doi.org/10.1093/ageing/27.5.605.
- Marmot MG, Smith GD, Stansfeld S, Patel C, North F, Head J, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet 1991;337:1387-93. https://doi.org/10.1016/0140-6736(91)93068-K.
- Banks J, Lessof C, Nazroo J, Rogers N, Stafford M, Steptoe A. Financial Circumstances, Health and Well-being of the Older Population in England: The 2008 English Longitudinal Study of Ageing (Wave 4). London: Institute for Fiscal Studies; 2010.
- Health Research Authority . Research Ethics 2016. www.hra.nhs.uk/research-ethics-committee-members/guidance-on-ethical-review-for-members/ (accessed 22 March 2016).
- NHS Caldicott Guardians. London: Department of Health and Social Care; 2012.
- Peyre H, Leplège A, Coste J. Missing data methods for dealing with missing items in quality of life questionnaires. A comparison by simulation of personal mean score, full information maximum likelihood, multiple imputation, and hot deck techniques applied to the SF-36 in the French 2003 decennial health survey. Qual Life Res 2011;20:287-300. https://doi.org/10.1007/s11136-010-9740-3.
- Carpenter J, Kenward M. Multiple Imputation and its Application. New York, NY: Wiley; 2013.
- Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338. https://doi.org/10.1136/bmj.b2393.
- Denzin NK, Lincoln YS. Handbook of Qualitative Research. London: Sage; 2000.
- Ritchie J, Lewis J. Qualitative Research Practice. A Guide for Social Scientists. London: Sage; 2003.
- Silverman D. Doing Qualitative Research. London: Sage; 2000.
- Clayman SE, Maynard DW, Have P, Psathas G. Situated Order: Studies in the Social Organisation of Talk and Embodied Activities. Washington, DC: University Press of America; 1994.
- Methods for the Development of NICE Public Health Guidance. London: NICE; 2012.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Drummond M, Sculpher M, Torrance G, O’Brien B, Stoddart G. Methods for The Economic Evaluation of Health Care Programmes. New York, NY: Oxford University Press; 2005.
- Little R, Rubin D. Statistical Analysis with Missing Data. New York, NY: John Wiley & Sons; 2002.
- Fiebig D, Baltagi B. A Companion to Theoretical Econometrics. Oxford: Blackwell Publishing Ltd; 2001.
- Willan AR, Briggs AH, Hoch JS. Regression methods for covariate adjustment and subgroup analysis for non-censored cost-effectiveness data. Health Econ 2004;13:461-75. https://doi.org/10.1002/hec.843.
- White M, Howel D, Deverill M, Moffatt S, Lock K, McColl E, et al. Do-Well Study Protocol Version 3.1 (12th July 2013) 2013. www.nets.nihr.ac.uk/projects/phr/09300902.
- UK Government . Redundancy: Your Rights 2016. www.gov.uk/redundant-your-rights/consultation (accessed 22 March 2016).
- The Poverty Site . Numbers in Low Income 2016. http://poverty.org.uk/01/index.shtml (accessed 16 January 2016).
- Abrahams D, Wood C. Health in Austerity. London: Demos; 2013.
- Whitehead M. Due North: Report of the Inquiry on Health Equity for the North 2014. University of Liverpool and Centre for Local Economic Strategies; 2014.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Moffatt S, Higgs P. Charity of entitlement? Generational habitus and the welfare state among older people in North-east England. Soc Policy Admin 2007;41:449-64. https://doi.org/10.1111/j.1467-9515.2007.00567.x.
- Garthwaite K. ‘The language of shirkers and scroungers?’ Talking about illness, disability and coalition welfare reform. Disabil Soc 2011;26:369-72. https://doi.org/10.1080/09687599.2011.560420.
- Garthwaite K, Bambra C, Warren J. ‘The unwilling and the unwell?’ Exploring stakeholders perceptions of working with long term sickness benefits recipients. Disabil Soc 2013;28:1104-17. https://doi.org/10.1080/09687599.2012.758032.
- Loopstra R, McKee M, Katikireddi SV, Taylor-Robinson D, Barr B, Stuckler D. Austerity and old-age mortality in England: a longitudinal cross-local area analysis, 2007–2013. J R Soc Med 2016;109:109-16. https://doi.org/10.1177/0141076816632215.
- Lazzarino AI, Hamer M, Stamatakis E, Steptoe A. The combined association of psychological distress and socioeconomic status with all-cause mortality: a national cohort study. JAMA Intern Med 2013;173:22-7. https://doi.org/10.1001/2013.jamainternmed.951.
- Serwinski B, Salavecz G, Kirschbaum C, Steptoe A. Associations between hair cortisol concentration, income, income dynamics and status incongruity in healthy middle-aged women. Psychoneuroendocrinology 2016;67:182-8. https://doi.org/10.1016/j.psyneuen.2016.02.008.
Appendix 1 General practitioner recruitment letter
Appendix 2 Information for general practices
Appendix 3 Participant recruitment letter
Appendix 4 Participant information sheet
Appendix 5 Participant opt-out slip
Appendix 6 Participant consent form
Appendix 7 Letter assigning to intervention or control
Appendix 8 Guidance for general practitioners on Attendance Allowance and Disability Living Allowance benefits applications
Appendix 9 Instructions for welfare rights advisors involved in the Do-Well study
Appendix 10 Checklist for internal assessment of welfare rights interviews
Appendix 11 Baseline questionnaire
Appendix 12 Participant recruitment letter (qualitative study)
Appendix 13 Participant information sheet (qualitative study)
Appendix 14 Participant consent form (qualitative study)
Appendix 15 Other household members information sheet (qualitative study)
Appendix 16 Other household members consent form (qualitative study)
Appendix 17 Casework contact sheet
Appendix 18 Non-financial benefits: unit cost of aids and adaptations
| Aid or adaptation | Total average (mean) | Durham (amount) | Northumberland | North Tyneside (mean) | PSSRU 2013/14 | National catalogue and tariff | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amount 1 | Amount 2 | Amount 3 | Mean | Notes | Mean | Notes | Amount | |||||
| Bath or grab rails | 24.64 | 12.66 | 27.40 | 28.00 | 28.40 | 31.00 | 18.00 | Fit handrail to bath | 27.00 | Bath side rail: adjustable height | GR14_v1.2 | 27.00 |
| Walk-in shower | 4021.00 | 3912.00 | 3500.00 | 4651.00 | Level access shower | |||||||
| Bath house | ||||||||||||
| Bath seat/board | 21.86 | 38.33 | 10.21 | 17.05 | Bath seat: 8-inch type | BA08_v1.5 | 16.29 | |||||
| Bath seat: 12-inch type | BA09_v1.5 | 17.80 | ||||||||||
| Grab rails in toilet or bathroom | 28.36 | 27.40 | 28.00 | 28.40 | 31.00 | 27.00 | Bath side rail: adjustable height | GR14_v1.2 | 27.00 | |||
| Commode for day or night use | 117.45 | 344.99 | 15.89 | 57.00 | Commodes | 51.94 | Static commode adjustable height (fixed arms) | TA06_v1.6 | 25.87 | |||
| Mobile commode fixed height (detachable arms) | TA07_v1.5 | 78.00 | ||||||||||
| Bedpan/urinal/bottle | 6.36 | 9.60 | 14.45 | 6.50 | Bed pan | TA10_v1.2 | 6.50 | |||||
| Urinal/bottle | 4.08 | 1.00 | 2.50 | Female urinal bottle | TA08_v1.2 | 2.50 | ||||||
| Male urinal | TA09_v1.2 | 2.50 | ||||||||||
| Raised toilet seat | 16.55 | 31.75 | 5.20 | 12.70 | Raised toilet seat 4 inch | TA02_v1.2 | 10.40 | |||||
| Raised toilet seat 6 inch | TA03_v1.2 | 15.00 | ||||||||||
| Incontinence pads | n/a | |||||||||||
| Bed hoist (bed rails) | 24.95 | 24.95 | ||||||||||
| Bed raise or bed block | 23.44 | 10.79 | 32.00 | Linked bed raisers, pair | 27.53 | Linked double bed raiser | FU15d_v1.2 | 27.53 | ||||
| Linked single bed raiser | FU15s_v1.2 | 27.53 | ||||||||||
| Special bed or mattress | 547.00 | 547.00 | ||||||||||
| Sheepskin | n/a | |||||||||||
| Special cushions | 45.00 | 45.00 | ||||||||||
| Special chair or chair raise | 433.56 | 800.00 | 67.11 | High back chair adjustable height | FU04_v1.3 | 115.60 | ||||||
| Chair raisers for chairs with legs | FU01_v1.2 | 18.62 | ||||||||||
| Widened doorways | 1078.00 | 2412.00 | 292.00 | 530.00 | Widen doorway for wheelchair access | |||||||
| Additional stair rails | 61.52 | 59.55 | 97.00 | 28.00 | Hand rail (internal) | |||||||
| Stairlift or vertical lift | 5729.75 | 3860.00 | 12,412.00 | 4800.00 | 1847.00 | Stairlift (straight) | ||||||
| Ramp at front or rear entrances | 933.82 | 490.45 | 1998.00 | 313.00 | Ramp to front/back door | |||||||
| Additional grab rails at front/rear entrance(s) | 42.00 | 42.00 | Fit handrail (external) | |||||||||
| Manual wheelchair | 263.67 | 243.00 | 173.00 | 375.00 | Self-/attendant-propelled wheelchair | |||||||
| Electric wheelchair | 1850.00 | 1850.00 | Powered wheelchair | |||||||||
| Walking frame (Zimmer) | 18.48 | 13.95 | 23.00 | Standard non-wheeled walking frame: adjustable height | MO29_v1.1 | 22.00 | ||||||
| Standard wheeled walking frame: adjustable height | MO30_v1.1 | 24.00 | ||||||||||
| Walking stick(s) | 17.25 | 4.53 | 38.00 | Walking sticks, choice of six sizes, types £22–54 | 9.21 | Metal walking stick: adjustable height | MO13_v1.3 | 5.64 | ||||
| Metal walking stick anatomical left handed | MO14L_v1.3 | 6.70 | ||||||||||
| Metal walking stick anatomical right handed | MO14R_v1.3 | 6.70 | ||||||||||
| Tripod walking stick: metal | MO15_v1.3 | 13.52 | ||||||||||
| Quadruped walking stick: large | MO16L_v1.0 | 13.52 | ||||||||||
| Quadruped walking stick: small | MO16S_v1.0 | 13.52 | ||||||||||
| Wooden walking stick | MO27_v1.4 | 4.90 | ||||||||||
| Walking trolley | 20.19 | 20.19 | ||||||||||
| Crutches | 12.75 | 9.00 | 16.50 | Metal crutches (double adjustable) | MO17_v1.4 | 16.50 | ||||||
| Kitchen gadgets | 5.91 | 5.91 | Kettle tipper | PL08_v1.3 | 10.00 | |||||||
| Plate guard/surround | PL09_v1.2 | 1.95 | ||||||||||
| Non-spill mug/cup | PL10_v1.2 | 4.00 | ||||||||||
| Long-handled sponge | PL11_v1.2 | 3.50 | ||||||||||
| Bread board | PL12_v1.2 | 4.50 | ||||||||||
| Electrically operated tin opener | PL15_v1.2 | 14.00 | ||||||||||
| Multisize jar and bottle opener | PL16_v2.2 | 9.71 | ||||||||||
| Peeler | PL18_v1.2 | 3.73 | ||||||||||
| Special cutlery/crockery | 9.23 | 4.99 | 13.46 | Cutlery set | PL14_v1.3 | 13.46 | ||||||
| Meal trolley | 26.10 | 20.19 | 32.00 | Trolley adjustable height | FU03_v1.3 | 32.00 | ||||||
| Community Care Alarm scheme | n/a | |||||||||||
| Special telephone | 115.00 | 96.00 | 134.00 | Text phone | SAH10_v1.3 | 233.00 | ||||||
| Corded Amplified Telephone | SAH11_v1.3 | 35.00 | ||||||||||
| Entrance telecom | 286.00 | 286.00 | ||||||||||
| Helping hand for picking up objects while standing | 3.93 | 3.60 | 4.25 | Pick up and reaching aid standard | PL01_v1.2 | 4.25 | ||||||
| Helping hand for pulling on socks or stockings | 3.60 | 3.58 | 3.63 | Sock/stocking aid | PL05_v1.1 | 2.75 | ||||||
| Tights aid | PL06_v1.1 | 4.50 | ||||||||||
| Special implements with long handles (e.g. hair brush) | 7.68 | 7.68 | ||||||||||
Appendix 19 Research governance guidelines for Trial Steering Committee
Appendix 20 EuroQol-5 Dimensions-3 Levels scores at baseline and 24-month follow-up by trial arm
| EQ-5D-3L dimension | Trial arm | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 381) | Control (n = 374) | |||||||||||||||
| Baseline | 24-month follow-up | Baseline | 24-month follow-up | |||||||||||||
| n | Mean score | SD | Median score | n | Mean score | SD | Median score | n | Mean score | SD | Median score | n | Mean score | SD | Median score | |
| EQ-5D-3L | 374 | 0.589 | 0.332 | 0.691 | 298 | 0.639 | 0.330 | 0.710 | 363 | 0.583 | 0.356 | 0.691 | 291 | 0.633 | 0.349 | 0.725 |
| Mobility | 380 | 1.663 | 0.495 | 300 | 1.463 | 0.619 | 374 | 1.615 | 0.487 | 297 | 1.448 | 0.619 | ||||
| No problems | 132 | 127 | 144 | 130 | ||||||||||||
| Some problem | 244 | 153 | 230 | 147 | ||||||||||||
| Confined to bed | 4 | 2 | 0 | 2 | ||||||||||||
| Missing | 1 | 81 | 0 | 77 | ||||||||||||
| Self-care | 381 | 1.289 | 0.498 | 301 | 1.179 | 0.549 | 374 | 1.342 | 0.513 | 297 | 1.165 | 0.536 | ||||
| No problems | 279 | 216 | 253 | 216 | ||||||||||||
| Some problem | 94 | 62 | 114 | 59 | ||||||||||||
| Unable to wash/dress | 8 | 5 | 7 | 4 | ||||||||||||
| Missing | 0 | 80 | 0 | 77 | ||||||||||||
| Usual activities | 381 | 1.593 | 0.585 | 300 | 1.407 | 0.655 | 374 | 1.588 | 0.605 | 297 | 1.404 | 0.656 | ||||
| No problems | 174 | 152 | 177 | 151 | ||||||||||||
| Some problem | 188 | 120 | 174 | 118 | ||||||||||||
| Unable to perform | 19 | 10 | 23 | 10 | ||||||||||||
| Missing | 0 | 81 | 0 | 77 | ||||||||||||
| Pain/discomfort | 380 | 1.963 | 0.624 | 300 | 1.647 | 0.742 | 374 | 1.930 | 0.687 | 297 | 1.653 | 0.791 | ||||
| No pain/discomfort | 81 | 100 | 102 | 108 | ||||||||||||
| Moderate pain/discomfort | 232 | 152 | 196 | 130 | ||||||||||||
| Extreme pain/discomfort | 67 | 30 | 76 | 41 | ||||||||||||
| Missing | 1 | 81 | 0 | 77 | ||||||||||||
| Anxiety/depression | 375 | 1.437 | 0.604 | 301 | 1.229 | 0.609 | 363 | 1.482 | 0.605 | 291 | 1.234 | 0.582 | ||||
| Not anxious/depressed | 233 | 207 | 209 | 192 | ||||||||||||
| Moderately anxious/depressed | 120 | 65 | 133 | 76 | ||||||||||||
| Extremely anxious/depressed | 22 | 11 | 21 | 5 | ||||||||||||
| Missing | 6 | 80 | 11 | 83 | ||||||||||||
Glossary
- Aids and adaptations
- Household equipment and alterations around the home to make life easier for those with disabilities, to help maintain independence.
- Attendance Allowance
- A non-means-tested benefit for people aged ≥ 65 years to help with their personal care costs if they are mentally or physically disabled. The allowance is paid at two different rates, and how much is paid depends on the level of care required.
- Blue Badge
- A non-means-tested parking scheme enabling those with severe mobility issues to park their vehicle in restricted areas.
- Carer’s Allowance
- A non-means-tested benefit payable to someone who earns no more than £110 per week and provides at least 35 hours per week of care for someone who is in receipt of certain benefits.
- Casework contact sheet
- A form completed by welfare rights advisors to record the actions and outcomes of advice and claims assistance provided to study participants.
- CASP-19
- A 19-item, four-domain, health-related quality-of-life questionnaire. The acronym stands for the four domains of Control, Autonomy, Self-realisation and Pleasure.
- Community Care Alarm Scheme
- A pendant and telephone alarm scheme linked to 24-hour warden cover.
- Council Tax Benefit
- A form of support that was replaced in April 2013 by Council Tax Reduction.
- Council Tax Reduction
- A means-tested benefit administered by local authorities to help with payments of council tax for those on a low income. The amount of money received varies depending on where people live, as each council runs its own scheme. The benefit is sometimes referred to as Council Tax Support.
- Department for Work and Pensions
- The government department responsible for administering state pensions and national means-tested and non-means-tested benefits.
- Disability Living Allowance
- A tax-free benefit for disabled people who need help with mobility or care costs. The rate is made up of two components (care and mobility). The amount paid depends on the way in which the disability or health condition affects the claimant. The care component is made up of three levels (lowest, middle and highest) and the mobility component is made up of two levels (lower and higher). Disability Living Allowance ended in April 2013 for people born after 8 April 1948 and existing claimants were invited to claim Personal Independence Payment. New Disability Living Allowance claims can be made only by people < 16 years of age.
- Employment and Support Allowance
- A benefit payable to those aged ≥ 16 years, but under the state pension age, if illness or disability affects their ability to work. The benefit comprises two components (contribution based and income based). Contribution based is a flat-rate amount that is payable for up to 12 months if sufficient National Insurance contributions have been made. Income based is means-tested and is not time limited.
- EuroQol-5 Dimensions-3 Levels
- A descriptive system of health-related quality-of-life states consisting of five dimensions, each of which can take one of three responses referring to three levels of severity.
- Health-care Costs
- The NHS Low Income Scheme, part of the NHS Help with Health Costs scheme, helps people on a low income with prescriptions, dental care, eye care, wigs and fabric support, and health-care and travel costs.
- Home Energy Efficiency Scheme
- Grants to assist people who meet the eligibility criteria to improve the energy efficiency of their home.
- Housing Benefit
- A means-tested benefit for people on low incomes to help pay all or part of their rent. The benefit is administered by local government.
- Income Support
- A means-tested benefit for people aged ≥ 16 years and under the state pension age who are on a low income.
- Industrial Injuries Disablement Benefit
- A non-means-tested benefit for illness or disability caused by accidents or disease at work.
- Pension Credit
- Extra money for people of state retirement age to bring them up to a minimum income. It is a means-tested benefit that consists of two parts (Guarantee Credit and Savings Credit). The Guarantee Credit tops up the weekly income if it falls below a specified amount. The Savings Credit is an extra payment for people who have saved some money towards their retirement.
- Severe Disablement Allowance
- This was phased out and replaced by Employment and Support Allowance in April 2001.
- Short Form Health Survey-36
- A validated, 36-item, health-related quality-of-life questionnaire.
- Spare Room Subsidy
- In April 2013, new rules were introduced for working-age tenants living in local authority or housing association homes. The amount of Housing Benefit paid is based on the number of people in the household and the size of the accommodation. The amount of Housing Benefit is reduced by 14% for one bedroom and by 25% for two or more bedrooms if the bedrooms are considered ‘spare’ under the rules. The subsidy is often referred to as ‘bedroom tax’ in the media.
- Warm Zones
- A not-for-profit agency that helps people on low incomes improve the energy efficiency of their homes. It provides up to 100% grants to improve heating and/or insulation in the home.
List of abbreviations
- CASP-19
- Control, Autonomy, Self-realisation and Pleasure
- CCS
- casework contact sheet
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- ELSA
- English Longitudinal Study of Ageing
- EQ-5D-3L
- EuroQol-5 Dimensions-3 Levels
- GP
- general practitioner
- HRQoL
- health-related quality of life
- ICER
- incremental cost-effectiveness ratio
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- LSOA
- lower-layer super output area
- MSOA
- middle-layer super output area
- NICE
- National Institute for Health and Care Excellence
- NRES
- NHS Research Ethics Service
- PASE
- Physical Activity Scale for the Elderly
- PCRN-NY
- Primary Care Research Network – Northern and Yorkshire
- PHQ-9
- Patient Health Questionnaire-9
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SF-36
- Short Form Health Survey-36
- SUR
- seemingly unrelated regression
- TSC
- Trial Steering Committee
- WRA
- welfare rights advisor
- WRA DEL
- welfare rights advisor delivering the intervention
- WTP
- willingness to pay