Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 12/181/07. The contractual start date was in September 2014. The final report began editorial review in January 2017 and was accepted for publication in July 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dawn Skelton receives personal fees from Later Life Training Ltd outside the submitted work and is a Director of Later Life Training, a company that runs as a not-for-profit organisation delivering Falls Management Exercise (FaME) Postural Stability Instructor (PSI) training to health and fitness professionals across the UK.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Adams et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background and study objectives
The literature search
To contextualise and evidence the Visually Impaired OLder people’s Exercise programme for falls prevenTion (VIOLET) study, a narrative review of the relevant literature was carried out. A literature review was undertaken in January 2016 to support the publication of the study protocol. The search terms ‘falls’, ‘fear of falling’, ‘visual impairment’, ‘sight loss’, ‘elderly’, ‘older people’, ‘older adult’ and their combinations were used to search the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane, MEDLINE (Medical Literature Analysis and Retrieval System Online, or MEDLARS Online) and PubMed databases. The grey literature was also searched to include significant government and other reports, such as work by the Royal National Institute for Blind People (RNIB) and reference lists of key studies provided a further literature source. The results are discussed below.
Falls and visual impairment
In the UK, one in eight people aged > 75 years and one in three aged > 90 years live with significant sight loss. 1 Visual impairment (VI) is associated with a loss of function in activities of daily living,2,3 and visually impaired older people (VIOP) are more likely than sighted peers to move into residential settings, be physically dependent and have poor quality of life (QoL). 4–6 Gleeson et al. 7 state that VI is an independent risk factor for falls. 5,8,9 Poor vision has been related to the recurrence of falls. 10 Waterman et al. 11 cite research identifying a number of falls risk factors associated with VIOP including muscle weakness, impaired balance and – specific to sight – poor visual acuity and contrast sensitivity, decreased depth perception and reduced visual field. 12,13 However, VI is not independently associated with a higher incidence of falls, despite being a risk factor. 14
Among the general population, falls in older people are common and can be life limiting and debilitating, and estimates suggest that, each year, between 30% and 62% of older people fall. 15,16 Falls are seldom due to a single cause6,12 and are associated with considerable morbidity and mortality,17 with approximately 10% of falls resulting in fractures. 18 The economic costs of falls are estimated at 0.07–0.20% of gross domestic product, with falls and their consequences accounting for 0.85–1.5% of Western economies’ total health-care expenditure. 19 In 2015 in the UK alone, falls in the over-65-year-olds were estimated to cost £4.6M per day. 20
Older people with VI have a (1.7-times) higher risk of falling than the general population, more hospital and nursing home admissions and report more contact with their general practitioner (GP) than those who do not have VI. 21,22 Although VI is not independently associated with a higher incidence of falls,14 Boyce22 suggests that in the UK 8% of falls-related hospital admissions are likely to occur in visually impaired people, accounting for 21% of the total cost of treating accidental falls. Such estimates are problematic in that costs to GPs may not be included in treatment costs, reasons for falling may not be known or recorded and aggregate estimates are likely to mask wide geographical variation.
Evidence suggests that multifactorial falls intervention programmes are effective in reducing falls among older people, often tackling underlying health problems, initiating strength and balance training and offering home modifications. 23–25 In 2004, the National Institute for Health and Care Excellence (NICE) guidelines on prevention and assessment of falls in older people25 suggested that by 2005 all NHS boards in the UK should provide a falls service. This echoed the earlier call in 2001 from the National Service Framework for Older People for specialist falls services in both hospital and community settings. 26 A 2008 survey noted that just half of participating falls clinics in the UK assessed for VI and there was little information about how to modify falls prevention programmes for VIOP. 27
Fear of falling and visual impairment
Fear of falling (FoF), with or without a fall, is also common in VIOP and can lead to a cycle of restricting daily activity and mobility, loss of confidence, diminishing physical and mental assets and reduced social participation and overall QoL. 28–30 A UK report by Visibility, a Glasgow-based vision charity, found that older people are highly likely to avoid activity because of VI. 31 Anxiety and depression are also common in those with VI and this may also lead to reduced activity. 1 In a recent randomised controlled trial (RCT) of a cognitive–behavioural therapy-based intervention to reduce FoF in older people, Parry et al. 17 suggest that FoF is likely to affect between 3% and 85% of community-dwelling older people who fall and up to 50% of those who have never fallen. The authors also cite research highlighting that FoF may lead to avoidance of activity, increasing frailty and risk of further falls independent of physical impairment. 32–36
Fear of falling is a significant predictor of a future fall. 37 Clinical and laboratory observations have shown that concerns about falling have a negative impact on older people’s gait patterns. For example, studies of gait and balance in older people’s use of elevated walkways showed both dysfunctional gait adjustments and disproportionately slow walking speeds38 as well as postural balance abnormalities39 when compared with younger subjects. It is also clear that there is a distinction between proper caution around activity and overcaution/a fear–avoidance cycle that perpetuates disability. 40,41 Indeed, a recent review suggests that FoF contributes to falls risk independent of actual gait or balance problems. 42
A recent Cochrane review investigating three-dimensional exercise – yoga, tai chi and strength and resistance training – in community-dwelling older people found that exercise can reduce FoF, but only in the short term, with evidence for long-term efficacy lacking. 43 The authors suggest that future exercise for older people intervention trials should have core outcomes that include FoF. Parry et al. 17 cite a systematic review that identified 12 high-quality RCTs, each with FoF as an outcome,35 but only one of these trials aimed to reduce FoF. 44 The interventions included a range of settings, from community tai chi to home-based multifactorial interventions, and all reported reduced FoF. However, Parry et al. 17 also highlight a more recent multifactorial intervention study, based in a geriatric outpatient setting, that did not find such a benefit. 45
There are also limited health economic data about FoF interventions. 40,42
Measuring the number of falls as a primary outcome does not take into account the more complex impact of an intervention that, by reducing FoF, may increase participants’ confidence in their ability to walk safely and continue to enjoy everyday activities. 46
In relation to VIOP, FoF can also be a barrier to uptake of exercise programmes. Research eliciting the views of VIOP28,31 suggests that perceived risk, stigma, lack of awareness among health professionals, lack of appropriate supporting materials and FoF may be barriers to exercise attendance. Enabling factors could include peer acceptability, appropriate supporting material with demonstration, sensitive explanation, carer involvement and individually tailored interventions.
Fear of falling is thus a vital outcome in falls intervention research, and there are important reasons for its inclusion in studies in VIOP. Any such intervention needs to include targeting of FoF, ameliorating its adverse outcomes and appropriate quantification, FoF being a key outcome measure.
Interventions for falls in visually impaired older people
Gleeson et al. 7 highlight well-designed exercise programmes that reduce falls in the general population44,47 but suggest that such programmes have not been successful in community-dwelling older adults with VI. For example, a recent Cochrane systematic review reports that home safety assessment and multicomponent home-based exercise programmes reduce the rate of falls and risk of falling in community-dwelling older people. 48 However, the New Zealand-based VIP trial49 did not demonstrate such results with VIOP. This study assessed the efficacy and cost-effectiveness of home safety and home exercise interventions for preventing falls and falls-related injuries in community-dwelling people aged ≥ 75 years with severe VI. The VIP trial included 391 participants with visual acuity of 6/24 or worse, of whom 361 (92%) completed 1 year of follow-up. The home safety assessment and modification programme was specifically designed for people with severe VIs and the 1-year home exercise intervention used the Otago exercise programme. 50 This programme includes specific muscle strengthening and balance retraining exercises that increase in difficulty and a walking plan, modified for those with severe visual acuity loss. The home safety modifications, delivered by an occupational therapist (OT), resulted in a significant reduction in the risk of falling while the group receiving home exercise, managed by a physiotherapist, showed a non-significant increase in the risk of falls. However, the authors highlighted that within the exercise programme stricter adherence to the prescription was associated with fewer falls.
Waterman et al. 11 suggest that the VIP study participants who received both home safety and home exercise interventions may have been unwittingly given confusing or conflicting messages from the OT and physiotherapist, this having a negative impact on intervention adherence and study outcome. 28 Adherence to the Otago programme was significantly lower in VIOP than in older people without significant VI in this study (only 18% of VIOP completed all home exercise sessions over a 1-year period)49 and this may have been due to lack of confidence in exercising at home without supervision.
The VIP2UK trial11 was adapted from the VIP Otago home-based programme to increase adherence in VIOP. This community-based feasibility study was carried out in north-west England and recruited 49 community-dwelling VIOP into a three-arm RCT with a control group receiving usual care and social visits, an experimental group receiving a home safety programme and another group receiving a home safety and home exercise programme. The social visits for the group comprised three social visits and two telephone calls and were designed to control for social contact that may reduce falls and influence lifestyle or QoL variables. 11
Falls primary outcome data were collected continuously over 6 months. Secondary outcomes on self-reported and instrumented physical activity and adherence were collected at baseline and at 3 and 6 months for home exercise and at 6 months for the home safety programme. All interventions were delivered by an OT. A total of 43 out of 49 participants (88%) completed the trial and 6-month follow-up. At follow-up, 100% reported partially or completely adhering to home safety recommendations but evidence for adherence to home exercise was equivocal. Whereas self-reported physical activity increased, instrumented monitoring [activPAL™ (PAL Technologies, Glasgow, UK)] showed a decrease in walking activity and there were no statistically significant differences in falls between the groups. However, the authors highlight that the study was not powered to detect a difference.
The VIP2UK authors suggest that further research is needed to explore the differences between the subjective and objective measures of activity and adherence issues. Whereas home safety modifications required a ‘one-off’ input from participants, ongoing adherence to the physical exercise programme (the Otago programme) might have been particularly challenging for the VIOP, some of whom lived alone. Despite the use of mentors, extra telephone calls and audio exercise clips and embedding exercises into daily living, it might have required a lot of effort to follow instructions via large print or audio and continue to be motivated to complete home exercises. The authors conclude that perhaps weekly home visits from an exercise trainer may improve adherence for VIOP or that group exercise with tailored support dependent on VI may lead to better progression in relation to strength and balance and, relatedly, to falls.
Finally, Gleeson et al. 7 highlight three small studies demonstrating that multimodal exercise and tai chi may improve physical functioning in VIOP51–53 in controlled environments when physical and verbal guidance is provided. These were carried out in residential settings and cannot be generalised to community-dwelling adults, who are likely to encounter more environmental hazards and who are more mobile. Gleeson et al. ’s randomised control trial7 with 120 community-dwelling people aged ≥ 50 years investigated the impact of 12 weeks of Alexander Technique lessons on balance and mobility with VIs compared with usual care. There was no impact on the primary outcome: the Short Physical Performance Battery score. However, there were greater intervention effects in the subgroup of multiple fallers, who are at an increased risk of injury compared with non-multiple fallers. Although the study was not powered for falls within the intervention group, trends towards a lower rate of falls and injurious falls were noted. 7 The Alexander Technique uses verbal feedback and manual guidance to teach awareness of previously unnoticed tension and, the authors suggest, may be a suitable intervention for people with VI as it does not require vision or the performance of regular exercises.
Falls Management Exercise and the VIOLET study
With an ageing population, the number of VIOP is predicted to rise. 54 Increasing incidences of key underlying causes such as macular degeneration and diabetes suggest that, without intervention, the number of people with VI in the UK could dramatically increase over the next 25 years. 54 This has implications for the need for falls prevention programmes that are tailored to VIOP. As outlined in The literature search and Falls and visual impairment, falls and FoF in later life are common, falls can be recurring and costs of care for those who fall are a disproportionate drain on local inpatient and adult social care budgets. 55,56 In the UK, falls are a major cause of disability;57 in Scotland, in 2010, three-quarters of people registered as blind or partially sighted (25,609; 74.2%) were aged ≥ 65 years and about one-third (11,158; 32.3%) had additional disabilities. Of the latter, over one-fifth (2476; 22.2%) were also deaf. 58
Our feasibility study draws on the learning from a number of previous studies, including the Falls Management Exercise (FaME)59 programme, the VIP trial49 and the recently completed VIP2UK pilot. 11 A recent Royal College of Physicians report60 demonstrated that 54% of falls exercise services have trained Postural Stability Instructors (PSIs) delivering the FaME programme in groups. A 6-month programme of FaME exercises has also been shown to significantly increase habitual physical activity (i.e. by 15 minutes of moderate to vigorous activity per day) in older people recruited through primary care even at 12 months post intervention, as well as reducing falls. 61 The FaME programme also has significant reach across the UK with a pool of qualified instructors.
A systematic review of falls prevention exercise62 suggested that at least a total of 40 hours of challenging balance and strength work is necessary to reduce falls. In the current study, 12 weeks (with a weekly group session and twice-weekly 1-hour home exercises) equates to 36 hours. We have therefore taken a pragmatic approach to what is achievable when considering roll-outs through NHS- or council-led services using the FaME approach. Indeed, both a scoping report for the Service Development Office27 and the Royal College of Physicians Audit60 suggested that, on average, falls services across the UK should deliver groups or sessions once a week for 8–12 weeks.
There are potential risks and benefits to introducing exercises to this population. As noted in Falls and visual impairment, FoF in VIOP may exacerbate existing gait and balance difficulties, further increasing the risk of falls. Recent research has identified that older people are at increased risk of falling following intensive endurance exercise bouts63 owing to exercise-induced alterations in respiration and muscular fatigue. It was also noted that VI could increase exercise-induced changes to postural control and consequently the risk of falling.
The feasibility study will provide an opportunity for VIOP to contribute to the adaptation and design of an acceptable community-based group exercise programme that could be incorporated into a general health promotion exercise programme. This study will enable VIOP to collaborate with researchers and instructors, and to draw on their expertise and experience to adapt a commonly adopted exercise programme (that is known to reduce falls risk in high-risk frequent fallers59 and low-risk older adults61) to their specific VI needs. This in turn may have a positive impact on gait and balance, increase confidence and lessen FoF. This study will add to an emerging body of work that is using FoF, as assessed by a widely validated cross-cultural tool [Falls Efficacy Scale – International (FES-I)], to address the gap in knowledge of how to successfully manage FoF.
Research aims
The rationale for the study is to provide an opportunity for VIOP to contribute to the adaptation of a group-based falls prevention programme that is prevalent in falls services across the UK. This should facilitate an acceptable, feasible and appealing intervention that will improve uptake and adherence to an intervention known to be effective. The aim of the study is to conduct a mixed-methods feasibility pilot study to inform the design and conduct of a future definitive multicentre RCT and economic evaluation of an adapted group-based exercise programme to prevent falls and reduce FoF among VIOP.
The research questions were:
-
Can an existing exercise programme be adapted for VIOP and successfully delivered in the community?
-
Is it feasible to conduct a RCT of this adapted exercise intervention and what would be the features of a future definitive trial?
Study objectives
The specific objectives were to:
-
explore participants’ ability to act as lay partners in a study to develop a condition-appropriate intervention and what methods enabled them to contribute to research as active partners
-
assess recruitment of VIOP and their willingness to be randomised
-
choose candidate outcome measures for a future RCT from FoF (confidence), activity avoidance, well-being/QoL, anxiety, depression, loneliness and number of falls
-
test the trial methodology and provide outcome data to inform sample size calculations for a definitive RCT
-
explore the capacity to deliver the adapted exercise programme
-
examine delivery of (fidelity) and compliance with the exercise intervention
-
explore participants’ reasons for participating in the exercise programme and acceptability of the exercise programme and trial procedures
-
develop a manualised intervention protocol and training package for a definitive RCT
-
assess the feasibility of collecting service use data for an economic evaluation of the intervention in a future RCT.
Prior to the completion of the feasibility study, the plan was to use the findings of this work to seek funding to conduct a definitive multicentre RCT to evaluate the effectiveness and cost-effectiveness of an adapted group-based exercise programme to prevent falls in VIOP by decreasing their FoF.
Chapter 2 Stakeholder involvement in the adaptation of the Falls Management Exercise programme: conduct and results of focus groups
Introduction
A number of issues have been identified in the literature (see Chapter 1) regarding risk of falling and FoF in those both with and without VI. Despite evidence of the effectiveness of exercise programmes, poor adherence and compliance remain problems and have been found to reduce the effectiveness of any exercise programme. In a RCT carried out in New Zealand with VIOP,49 home safety modifications delivered by an OT resulted in a significant reduction in risk of falling, but the group receiving a home exercise programme (which had already been shown to be highly effective in reducing falls in older people without VI) showed a non-significant increase in risk of falls. On a planned subanalysis, the authors found that adherence to the home exercise component was poor and that those who did adhere to the home exercise programme did see a reduction in falls. 49 A UK study has sought the views of VIOP to help increase adherence to a home exercise programme. 28
In another, smaller, exercise study in people with VI aged ≥ 50 years,7 there was a trend for fewer falls overall, but the rate of falls was not significantly different between those who received 12 lessons on the Alexander Technique and those who did not. Levels of adherence to this programme were high as an instructor visited participants weekly at home. A recent systematic review of exercise in the prevention of falls in VIOP has highlighted the lack of studies in community-dwelling older people, particularly group-based as opposed to home-based exercise. 64
In the UK, two main programmes of exercise are offered as part of falls prevention services: the Otago home exercise programme49,65 and the FaME group exercise programme delivered by PSIs. 59 A Royal College of Physicians report66 showed that 54% of falls exercise services in the UK have trained PSIs delivering the FaME programme. FaME exercise classes are balance-specific, individually tailored and include backward chaining, functional floor exercises and targeted training for dynamic balance, strength, endurance, flexibility, functional skills, gait and ‘righting’ or ‘correcting’ skills to avoid a fall. A full description of the exercise programming and progression has been published. 67
Given the prevalence of both falls and FoF in VIOP, there has been relatively little research into adapting existing falls prevention interventions for this population. This formed the aim of this phase of the VIOLET study.
Aim
The aim of this phase was to recruit and run VIOP stakeholder groups to act as consultants on adapting an existing evidence-based falls prevention programme (FaME) for this population. The findings from this phase were to inform the adaptation of the FaME programme for the subsequent feasibility study.
This chapter reports on the findings of four stakeholder focus groups with VIOP. It explores their main concerns surrounding falls and details their recommendations on adapting a falls prevention programme.
Method
Stakeholder panels were conducted in the two geographical locations of the intervention sites: Newcastle upon Tyne and Glasgow. They took the form of focus groups facilitated by research staff. Two focus groups were completed in each area: the first covered views on falls and falls prevention; the second covered proposed tools to measure the outcomes.
Focus groups were used in this study to explore experiences, views and concerns, to clarify why particular views were held and to facilitate discussion among focus group participants. 68 Ethics approval was gained from both universities’ ethics committees. All participants gave recorded verbal consent.
Participants and recruitment
Participants were accessed through vision-related charitable organisations who were partners in the research project: Visibility in Glasgow and the Newcastle Society for Blind People (NSBP) in Newcastle. The dissemination of the information regarding the project and the focus groups was facilitated locally by the charitable organisations. Inclusion criteria were being aged ≥ 60 years with or without experience of falling and having a VI.
Participants were not excluded from the feasibility study if they had participated in the focus groups.
Focus group structure and prompts
The groups were co-facilitated by two members of the research staff (VD and DS). Also present were representatives of the charitable organisations and observers from within the research team. In a deliberate attempt to make the focus groups accessible, they were held in venues familiar to the VIOP and hosted by the charitable partners. As an aid to participation, the focus groups were held from late morning to early afternoon – that is, during accessible daylight hours. Participant transport costs were covered by the research budget.
Four sessions were held in total, two focus groups at each site, with the same participants in each site being invited to both groups. The groups were scheduled to last for a maximum of 2 hours with a 15- to 30-minute break for refreshments; actual duration was 110–124 minutes. Across the sites, both focus groups opened with a statement of their aims and purposes.
The aim of the first group meeting at each site was to explore how the existing FaME programme should be adapted so that VIOP might best be enabled to participate. The aim of the second set of group meetings was to ascertain the most suitable set of trial outcome measures important to the VIOP and to adapt data collection procedures to maximise participation and minimise participant burden.
The first groups opened with a general discussion in which participants were invited to talk about their experiences of, and opinions around, falls and falling. A member of the research team (DS) then introduced the FaME intervention and verbally described the exercise programme. Large-print excerpts of the home exercise programme booklet that accompanies the group sessions were made available, although most participants were happy with the verbal descriptions. Finally, the participants were invited to try some of the exercises and feedback was sought on acceptability and potential adaptations.
The second groups covered a précis of the information gained in the first focus groups, for member checking, then focused on the outcome measures and trial data collection procedures. Some candidate outcome measures had previously been chosen by the research team. Large-print versions of each tool/questionnaire were available; however, as with the first groups, most participants preferred a verbal description. Each tool was described in detail, including introductions to questionnaires, instructions on how they were completed and questionnaire content. Views were then sought on how participants could best access and complete these measures and preferred modes of interacting with the research team. The second focus groups concluded with a discussion of areas of life that are affected by falls and FoF that were not captured by these candidate measures. Suggestions were sought on how these areas of life could best be captured to allow patient-centred outcome measures to be used in the future feasibility RCT.
The groups were lively and interactive. The facilitators aimed to ensure that every participant had an opportunity to have their opinion heard. Facilitators needed to do little more than present the focus group prompts and discussion followed. A ‘one-at-a-time’ conversational rule was encouraged and on every major topic a group round was conducted to ensure that all opinions were collected.
Analysis
Notes were made during the focus groups and the opinions in the room were précised by the facilitator and checked for accuracy with the group. At the beginning of the second group we member-checked with the participants about the main themes that had come out of the first group. During the second group we discussed, summarised and fact checked throughout, as in the first group. Following this, notes were analysed to both check for accuracy and draw out information on how the intervention should be adapted.
Results
Across both areas, a total of 14 VIOP took part in the four focus groups. The maximum attendance was nine, the minimum five. All but one person at each site attended both focus groups. Participants had a range of VIs including macular degeneration, VIs following stroke and complete blindness. Some had been visually impaired for their whole life and some had started losing their sight more recently. Two people had guide dogs.
Views on falls and falling
As one participant put it, daily life ‘is a pilgrimage into the unknown’ for people with VI. There was a general agreement that falls and FoF were significant issues for this group. FoF was particularly an issue when people were outside their home and in unfamiliar environments. Main areas of concern were street furniture, the state of repair of roads and pavements, steps (on and off, up and down) and unclear or confusing signposting of step edges (leading edges demarcated, last/first step identified). Public transport was a significant issue for all participants, particularly getting on and off, and the wheelchair/pushchair-friendly but VIOP-‘unfriendly’ expanded atriums of newer buses (too large an open space with fewer handholds). People also remarked on the often unhelpful behaviour of drivers (accelerating before VIOP were seated, not informing them of stops). It was also remarked that VI is often ‘invisible’ and not readily apparent to members of the public (i.e. in the absence of a cane or guide dog) and, as a result, other pedestrians/pavement users can cause problems for VIOP. Pain, distraction, overcaution and poor lighting were other issues people mentioned as increasing the likelihood of falls and trips and fear of these.
Most participants reported that they had fallen. On closer questioning, and having agreed on a definition of a fall as ‘an involuntary ending up on the ground or lower level’, it was clear that most participants had not fallen directly to the ground but had experiences that were described as a ‘near miss’. These were slips and trips where the individual had been prevented from falling by either saving themselves or being assisted by another person. However, near misses were thought to affect confidence and curtail activity as much as a fall. So common were trips and slips that the groups talked about them as if they were to be expected, as were minor injuries, bruises and grazes. Most falls, trips and slips had occurred outside the home, though one participant had a significant fall in their own bathroom.
Differing views were expressed regarding the effect the degree of VI would have on FoF and falling. It was felt that this was a complex issue and that it was often influenced by what was referred to as ‘the nature of the person’ – that is, certain people would be more affected by these issues than others depending on their personality. It was also suggested that duration of VI (i.e. from birth or in later life), personal coping strategies, degree of local knowledge of the environment and a desire to be independent would all have an impact on susceptibility to falls and FoF. The views of VIOP in this study resonate with the views of VIOP in the VIP2UK study. 28
Adapting the FaME programme
There was almost universal enthusiasm for the proposed exercises and their perceived potential to increase strength, balance and confidence. Participants were very positive about not just falls prevention but the concept of ‘falling better’ and being enabled to get up off the floor should a fall occur.
Group venue and environment
It was generally thought that somewhere familiar would be less problematic, but if this was not possible then time to become familiar with the venue layout would be appreciated. There was agreement that no music should be played during the exercise sessions in order to hear well and concentrate. There was less consensus around lighting, with some preferring dim and others preferring bright light depending on their particular VI. It was suggested that aids such as ‘anti-glare glasses’ could be utilised by participants who may have a sensitivity to light at certain times.
Group size and personalised support
Specific suggestions regarding modification of FaME were made around group size, for which it was suggested that 6–8 people was the most appropriate number per exercise session. This was mostly to do with feeling confident that the instructor was able to keep an eye on the participants and in order to get to know everyone well, by voice if necessary. During the FaME ‘taster’ exercises, it became apparent that some participants would need one-to-one support depending on their degree of VI and any additional impairment such as deafness. In addition, the participants suggested they should be given the choice to bring another person (friend/relative/carer) with them to give assistance or that another person should be present to assist the VIOP.
Group exercise delivery and instruction
It was also apparent that the pace and content of the class needed to be adjusted to allow for a more detailed verbal instruction, with reinforcement from additional facilitators working with some individuals. There was a consensus on the need for instructors to understand the impact of specific VIs and associated limitations and the need for instructions to be given clearly and at an appropriate pace.
At the Newcastle site, greater anxiety was expressed about learning to get up off the floor, as participants were worried about getting down onto the floor during the exercise classes. They expressed the opinion that once you are down it is hard to get up. Once it was explained that this was precisely why floor exercises were practised and that this was done in a graded manner at their own pace, their anxieties were allayed.
There was a universal preference for the inclusion of a social element, which included the exercise instructor. One of the groups felt that it would be better to have the social element after the exercise class and to ‘get the business out the way first’. Other suggestions centred on multiple classes per week as a catch-up if someone could not attend their usual class and that a peer-support group may develop from the exercise classes in addition to the social aspect that occurred at the end of the classes.
There was no consensus on how instructions were preferred; each individual had their own preference, with some wanting verbal instruction, some hands-on guidance and others retaining enough sight to copy the instructor’s demonstration.
Home exercise programme
It was initially suggested by the research team that each person would complete two 1-hour sessions of exercise at home. Most felt that this was unattainable but that the total of 2 hours per week could be met if it was broken down into 10–20 minutes per session. Some preferred a prompt of some kind, either a booklet or audio disc detailing exercises to follow in ‘chunks’, whereas others preferred incorporating exercises into usual daily activities, such as standing on toes while waiting for the kettle to boil or other exercises while preparing a meal. Again, the consensus was that individual choice and discussion with the instructor about what was best for the individual should determine the home exercise programme.
Measuring meaningful outcomes
Measurement/form of outcome assessment
The key finding that emerged regarding how outcome measures were presented, completed and returned concerned choice. A range of preferences were expressed. Some participants wanted assessment tools to be read to them and to reply (face to face or over the telephone), others wanted large print, some could see large print but not their own writing, and some were happy to receive materials by e-mail as they had screen readers on their computer. Although most participants thought outcome measures would need to be read aloud to them and their responses documented, they also thought that doing this over the telephone would also be acceptable; again, the consensus was that people should be given choice.
In both groups, a considerable amount of time was spent discussing how best to keep a falls diary and how to interpret its contents. This was considered the most ‘heavy’ participant burden, as it needed to be completed every day and submitted weekly. Although there was no overall consensus, most participants, after discussion with the research team, were happy to do this by way of a weekly telephone call.
Content of outcome measures
With a few minor caveats, most participants found all candidate outcome measures acceptable. There was some general discussion about adapting some questionnaires to Likert scales, as this was the group preference for response options. Once it was explained that outcome measures are valid as such only in their existing form, they understood and accepted the difficulty in adapting such questionnaires. However, several participants did express the worry that the questionnaires that focus on limitation and reduced QoL could adversely affect people’s mood, and that this should be highlighted by the interviewer prior to administration.
It was the content of the falls diary that received most discussion. It was felt that falls should be distinguished from ‘near misses’ – trips (tripping on an obstacle) and slips (losing footing) – and that all three should be recorded. The terminology of the falls diary was considered unclear. Most participants were not sure what a soft tissue injury was and they wanted to add ‘graze’ and have a chance to tell someone rather than try to explain it on a form that they could not see well (or at all). Participants also wanted a question on whether or not they were physically or psychologically affected by a fall that, subsequently, reduced their activities or substantially changed their routines, and they wanted to be able to record changing and limiting activity (as opposed to ‘immobilisation’ as currently recorded in the diary). Similarly, the ‘costs’ of a fall were unclear to participants. Again, after discussion with the research team, participants were happy for the falls diary to be a ‘daily yes or no’ document and for all other details to be elicited within a weekly telephone call. Finally, for the Timed Up and Go (TUG) tests, participants wanted to know that they could use the standard aids (or dog) that they normally used to walk.
The groups were asked to reflect on any important outcome measures that they thought were missing and what would be a good outcome for them and important to measure (patient-specific outcome measures). There was a strong feeling among some members that we needed more VI-specific demographics – such as nature of VI; duration of VI (or lifelong); stable, progressive or changeable VI; recent change in VI; personal adaptation and confidence related to VI; and impact of VI on daily activity – in order to fully understand whether or not some people respond better to training than others and what support they would need in the exercise programme. The level of VI (and a person’s ability to cope and function with it) appeared to be an important consideration that they felt was vital for the instructor to understand.
One area that was discussed at some length was the specific impact the intervention could have on QoL, confidence and daily activity as determined by VI. There were various suggestions for capturing this in the form of ‘before and after’ data such as asking specific additional questions, for instance ‘are you impaired in everyday activities as a result of your VI?’. From these discussions, other validated outcome measures were suggested by the research team [e.g. the ConfBal69 scale or the Work and Social Adjustment Scale (WSAS)70], but the groups also felt that it was important to ask about confidence and ability to orientate in new environments and to assess amount of physical activity, degree of general happiness and amount of pain. Finally, several members of the group suggested targets that were meaningful to them and that these could be measured by degree of achievement before and after the groups. From these additional comments, outcome measures were identified to capture these aspects in the feasibility study.
Focus group summary
The opening discussions in both groups highlighted how significant an issue falls and FoF are for this group and the extent to which these concern individuals on a daily basis.
The participants were volunteers recruited from third-sector organisations and thus enthusiastic about the exercise programme. Although some expressed anxieties about practising new skills, they appreciated without exception the usefulness of doing so. Similarly, participants engaged enthusiastically with the process of research and appreciated the necessity of measuring change.
Overall, participants strongly recommended having individual choice and autonomy throughout the proposed intervention, whether this was related to how they participated in the exercise class, completed the outcome measure assessment tools or reported their falls and ‘near misses’. In terms of incidentals, participants gave clear indications of preferring smaller group exercise classes, no music during classes, venue familiarisation, more than one weekly class to choose from, flexibility to bring someone with them, a social element and working with instructors who had an understanding of the impact of living with VI. Thus, many of the recommendations related to the facilitation of the intervention rather than to the actual content of the exercise programme.
Adaptations made to the feasibility randomised controlled trial design
All stakeholder requests were incorporated into the planning and delivery of the classes with the exception of smaller class size and a choice of classes each week. Owing to study resource constraints, class sizes were planned at 10 and offered only once per week. However, this feedback will inform future interventions.
The request for instructor VI training was met. This training was expertly managed by Visibility in Glasgow and incorporated the use of blindfolds and adapted spectacles. All actors from both locations were included. Both exercise instructors and the research team simulated being both a person with VI and a guide and learned invaluable communication and guiding techniques. This training also covered the need for weekly discussions with participants about any changing needs regarding support, aids, position in the class (lighting/hearing) and the importance of social contact and peer support within the group.
An induction session, for introducing the venue and getting to know everyone, formed part of the first session. Participants were encouraged to bring along any carer/family member to the class and extra support personnel were available to help individuals who needed more personalised instruction in the group. The proposed home exercise content was also modified in accordance with the stakeholder panel’s overall feedback. This included adapting the 60-minute FaME home exercise element to graded exercise components of 10 minutes, 15 minutes and 20 minutes. The home exercise booklet used by PSIs71 was adapted to include a series of prompts, particularly focusing on incorporating some of the exercises into everyday activities, and split into smaller ‘chunks’ of exercise that lasted approximately 10 minutes and progressed in duration and intensity/difficulty over time (to a maximum 20-minute session). Audio clips were made available for those who wanted their home exercise programme to be verbal. These could be played on either a compact disc (CD) player or an MP3 player. A digital versatile disc (DVD) was also available to use.
In relation to VIOP’s views on completing the related assessment tools, participants were asked about their preferred mode of assessment tool delivery, such as large print or being read aloud. The preferred solution to the fall diary was implemented in the form of a weekly telephone call between a member of the research team and the participant. This protocol captured falls and ‘near misses’ and allowed a reporting of the financial costs of any such event.
Probably the single biggest impact on the conduct of the feasibility RCT has been a shift in emphasis to interpersonal communication. In trials, the mediating agent between triallists and participants is often the written word. In the case of the VIOLET study we endeavoured to make both the initial and ongoing collection of data based on interpersonal communication. Although this is more burdensome for the research team, we believe it gave the feasibility study a much higher chance of maximising retention and also provided a means of monitoring the impact of the intervention on participants. It also allowed us to address some of the issues that would otherwise be hard to address via written communication. For instance, given the feedback from the stakeholder groups that some of the QoL questions might be upsetting, we were now in a position to highlight and discuss this, both before and after administration of the outcome measures.
Limitations
The participants lived in cities and so would not necessarily represent the experiences of people living in rural areas, who might have different experiences of the accessibility of group classes or external environmental concerns (street furniture, lighting). Participants were recruited from low-vision charities and so were already engaged with external organisations and were less likely to be isolated. Although there was a range of ages, a mix of males and females, people with a history of falls and without, and a range of VIs and histories of sight loss, there was an absence of ethnic minorities and only one person had dual sensory loss. This limits the findings.
One of the focus group facilitators (DS) was the author of the FaME programme, delivers training to specialist exercise instructors and has extensive experience in presenting the exercise programme in a motivating manner. This may have influenced the participants’ enthusiasm for the programme and willingness to try floor-based exercises.
Summary of recommendations from the stakeholder group
These recommendations related to the content of the FaME programme, the way in which it was delivered, the logistics of attending the programme and the design of the subsequent feasibility study. The main recommendation was that personal choice and individual adaptation should be maximised in both the conduct and measurement of the intervention. Specific recommendations centred on venue familiarity, group dynamics and training of facilitators on VI. Additional recommendations were made regarding individual goal setting and choice regarding the methods by which study materials were received and administered.
It was the adaptation of the environment to the needs of a visually impaired person rather than the adaptation of the actual exercises that received most attention from the stakeholder group. Each point was considered in the design and delivery of the subsequent intervention. Recommendations were as follows.
Recommendations for adapting FaME:
-
a fully accessible, familiar venue or the option to get to know an unfamiliar venue before sessions
-
aid getting to and from the venue (e.g. by taxi)
-
a maximum group size of eight persons
-
no music
-
individual adaptation regarding lighting and glare
-
the option to bring another person (or guide dog)
-
a social element (e.g. tea and a chat) after exercise sessions
-
run more than one class (flexibility regarding class time) at the beginning for group bonding
-
home exercises – reduce the length of home exercise sessions to 10–20 minutes; provide a variety of exercises; provide prompts (e.g. in large print, on DVD or audio); integrate exercises with daily living activities
-
train PSIs on (1) the impact of VI, (2) adaptations (aids) that can be used for specific VIs and (3) communication (verbal clarity)
-
more than one instructor or additional person to help VIOP
-
provide the PSI with information regarding individual participants and time to fully understand the nature of the VI, how it may affect the individual and how it may vary across timeframes
-
tailor content to the individual (e.g. floor work).
Recommendations for outcome measures and trial procedures:
-
the possibility to choose how outcome measures are received and administered (e-mail, post, verbal)
-
reduce the content of the falls dairy
-
remove the resources/expenses form so that the researcher administers this
-
incorporate a weekly telephone call to capture data concerning the nature of slips/trips/falls and the impact of these (to ensure capture of ‘near misses’)
-
define ‘slip’, ‘trip’ and ‘fall’
-
patient-centred outcome measures (personal goals)
-
use a tool to capture the impact of VI on an individual and their activities.
Conclusion
Participants expressed very individual preferences and needs regarding the attendance of group exercise to prevent falls. They voiced a strong desire for instructors to be specifically trained in how to tailor instruction and delivery to each individual’s very different functional or visual limitations, which may change week to week. There was an equally strong preference for alternatives and choice in methods of engaging with home exercise and completion of outcome measures. These stakeholders gave clear and useful guidance on ways to adapt an existing falls prevention exercise intervention to maximise both uptake and adherence for VIOP. No matter how good an intervention is, if participants cannot or do not want to engage with it, it is effectively useless. Actively involving stakeholders in the modification of this intervention maximised the possibility that the intervention would be useful for the VIOP population.
Visually impaired older people stakeholder involvement in the adaptation of the FaME programme produced the first health promotion and falls prevention exercise intervention protocol developed collaboratively with older people for community-living VIOP. 46 As detailed in Appendix 1, the intervention protocol manual will enable accurate replication of the feasibility study intervention in a larger multisite study in the future, and can be used to ensure that adaptations of the original FaME intervention for VIOP can be replicated in practice in falls prevention programmes.
Chapter 3 Randomised controlled feasibility trial of the adapted Falls Management Exercise intervention versus usual activities: research process and conduct
Introduction
This chapter describes the methods employed for the research process and conduct of the feasibility study, including identification, screening, consent and recruitment strategy, inclusion/exclusion criteria, flow of participants through the study, design and delivery of the intervention and the outcome measures used for data collection.
The overall aim of this phase was to conduct a feasibility study in order to inform the design and conduct of a future definitive multicentre RCT of an adapted community-based group exercise programme to prevent falls and reduce FoF in VIOP. This was in order to facilitate the development of a feasible and acceptable intervention to improve uptake of, compliance with and adherence to an intervention known to be effective.
The research questions were:
-
Can an existing exercise programme be adapted for VIOP and delivered successfully in the community?
-
Is it feasible to conduct a RCT of this adapted exercise intervention and what are the features of a future definitive trial?
The objectives are presented in Chapter 1.
Study design
This study adapted an existing, effective group-based health promotion intervention for older people (FaME) to reduce falls, with VIOP as experts. Because of the lack of relevant information for a full RCT on this topic, a randomised mixed-methods feasibility study was designed to inform the design and conduct of a future definitive multicentre RCT on an adapted version of FaME. The feasibility study addressed issues relating to the generalisability and transferability of the proposed intervention and investigated the viability of a future definitive RCT.
This was a two-centre randomised pilot trial of an adapted exercise programme for VIOP versus no intervention with embedded qualitative evaluation. An economic evaluation was also carried out (see Chapter 6). Older people with VI were recruited from two study sites (Newcastle and Glasgow) and randomised into one of two groups:
-
group 1 – 12-week exercise programme (1-hour session per week)
-
group 2 – usual activities.
Assessment of the feasibility to progress to a full trial
The criteria to judge the feasibility of progressing to a full trial at 6-month follow-up were as follows:
-
Fifty per cent or more of VIOP eligible for the study were willing to be recruited into the feasibility study.
-
Seventy per cent or more of the participants in the intervention arm have completed 9 to 12 group sessions in the exercise programme (compliance).
-
Data on key outcomes was collected at 6-month follow-up for ≥ 70% of those recruited.
-
Less than 10% of serious adverse events (SAEs) were deemed to be caused by the intervention.
Study population
The study population were drawn from community-living VIOP in Newcastle and Glasgow.
Inclusion criteria
-
Aged ≥ 60 years.
-
Attend a low vision clinic and/or are a member of organisation(s) for the visually impaired such as NSBP in Newcastle or Visibility in Glasgow.
-
Live in own home.
-
Able to walk indoors without the help of another person but may use the assistance of a walking aid.
-
Able to walk outdoors but may need the help of another person and/or walking aid.
-
Have the physical ability to take part in a group exercise class.
-
Have provided informed consent (as appropriate to each older person with VI) to participate in the study prior to any study-specific procedures.
Exclusion criteria
-
Inability to comprehend or follow simple movement instructions in English.
-
Presence of acute or uncontrolled medical problems in addition to VI that the participant’s GP considers would exclude them from undertaking the exercise programme [e.g. uncontrolled heart disease, poorly controlled diabetes, acute systemic illness, neurological problems, severe chronic obstructive pulmonary disease (COPD)].
-
Medical conditions that would necessitate a specialist exercise programme or prevent participants from maintaining an upright seated position or moving around indoors independently (e.g. uncontrolled epilepsy, severe neurological disease or impairment).
-
Current involvement in other falls prevention exercise programmes (with the exception of walking programmes), investigational studies or trials.
Ethics and regulatory issues
The conduct of this study was in accordance with the recommendations for physicians involved in research on human subjects adopted by the 18th World Medical Assembly, Helsinki, 1964, and later revisions.
Ethics approval from the Newcastle and North Tyneside Research Ethics Committee (REC) was sought prior to the commencement of the intervention, as was research and development approval. The REC reference was 15/NE/0057 and the UNN reference was RE-HLS-13-140707-53bb0a7806e37.
Local approvals were sought before recruitment commenced at each site. Newcastle Clinical Trials Unit received a written copy of local approval documentation before initiating each centre and accepting participants into the study. The study was registered as Current Controlled Trials ISRCTN16949845.
Information sheets were provided to all eligible subjects and written informed consent obtained prior to any study procedures. If subjects were unable to sign the consent form, verbal consent was witnessed by a third party, who signed the witness section of the consent form.
Confidentiality
Personal data were regarded as strictly confidential. To preserve anonymity, any data leaving the site identified participants by their initials and a unique study identification code only. The study complied with the Data Protection Act 1998. 72 All study records and investigator site files were kept in offices with restricted access.
Identification, screening, recruitment and consent of participants
The Ophthalmology Department at the Royal Victoria Infirmary (RVI) in Newcastle sees an average of 3138 patients per month aged ≥ 65 years, with approximately 45 patients per month aged ≥ 65 years attending the low-vision clinic. NSBP has approximately 1500 members. NHS Greater Glasgow & Clyde saw approximately 500 patients per month in the general eye clinic, with 20–25 VIOP attending the Glasgow Caledonian University low-vision clinic per month. Visibility ran both a patient support service and an information line and across both they had contact with around 1500 people per year. These organisations identified potential participants and passed on expressions of interest to the research team.
It is known from previous studies that recruitment and adherence in frail older people can be difficult, although data for recruitment and retention rates in VIOP were relatively unknown. In the VIP2UK study,11 only 51% of eligible participants and 10% of those who were originally screened agreed to take part. However, the inclusion/exclusion criteria meant that the study excluded participants who would have been eligible for the VIOLET study.
Visually impaired older people who expressed an interest in participating in the VIOLET study received further information. This information was available in large-print and audio formats. These materials had been designed in consultation with the stakeholder panel and checked to ensure that they met RNIB standards in terms of suitability for those with VI.
The researcher then invited eligible VIOP to participate and answered any questions raised. Signed consent to participate in the feasibility study was sought only when the researcher had ensured that the participant had accessed and understood the information. Once consent had been gained, a letter was sent to the participant’s GP explaining the inclusion and exclusion criteria for the study. This allowed the GP to make a judgement regarding the medical fitness of the participant to take part in the study based on these criteria. Once a participant’s GP confirmation of eligibility had been received, the participant was randomised.
Identification of potential participants
The primary recruiting source at the Newcastle site was NSBP. The organisation raised awareness of the study in its newsletter, which is sent to all members. In addition, members of the research team visited member meetings to discuss the study and how to receive further information. When recruitment began, a dedicated member of NSBP rang the members aged ≥ 60 years to discuss the study and gain permission to forward their contact details to the research team.
Identification of participants from the RVI low-vision clinic proved problematic. The physical space of the clinic area was unsuitable for the research team to approach potential participants. The responsibility for raising awareness of the study was then transferred wholly to the medical and paramedical staff in both the eye clinics and low-vision clinics. Although the managers of these departments and the lead consultant were aware of the study, very few of the staff referred potential participants to the researchers. In an effort to increase recruitment from the NHS site, a minor amendment was made to allow Eye Clinic Liaison Officers (ECLOs) to approach potential participants. They were able to identify potential participants who had recently been seen in their service and, with their permission, forwarded expressions of interest to the research team. These potential participants were then contacted by the research team and assessed for eligibility in the same manner as participants identified through the low-vision clinic and NSBP.
The primary recruiting source at the Glasgow site was Visibility. It raised awareness of the study in its newsletter to members, with expressions of interest being forwarded to the study team. As recruitment via this mode was felt to be slow, Visibility contacted potential participants directly. Expressions of interest were again forwarded to the research staff.
It had been planned to recruit participants from the low-vision clinics held in Glasgow Caledonian University. Unfortunately, recruitment coincided with the summer period when the clinics in the academic setting were not running. Therefore, no recruitment took place from this source.
Screening procedures
Visually impaired older people who expressed a continued interest in participating in the study were screened for eligibility by a researcher over the telephone or at a site mutually convenient to the researcher and the potential participant. Screening was based on the inclusion/exclusion criteria. Eligibility was confirmed by the GP.
To facilitate the first running of the first cohorts in both Newcastle and Glasgow, a staggered start was employed at both sites. This enabled those for whom GP confirmation of eligibility had not been returned promptly to start at any time within the first 3 weeks and continue to complete the 12 sessions. More than 12 weeks of sessions were offered so that each participant was able to attend 12 sessions even with a delayed start.
Consent procedures
Once screening for eligibility had been completed, the researcher invited the VIOP to participate and answered any questions they raised. Following receipt of information about the study, participants were given reasonable time (a minimum of 24 hours) to decide whether or not they wanted to participate. As previously stated, signed or recorded verbal consent to participate in the feasibility study (as appropriate for each VIOP participant) was sought only when the researcher had ensured that the participant had accessed and understood the information provided. If the VIOP was unable to sign the consent form, verbal consent was witnessed by a third party, who signed the witness section of the consent form.
The original signed consent form was retained in the investigator site file, a copy added to the clinical notes (for participants recruited from the NHS) and a copy provided to the participant. The participant specifically consented to their GP being contacted regarding their medical fitness and being informed of their participation in the study.
The right to refuse to participate without giving reasons was respected.
The information sheet and consent form for the study was available in English only. It was decided to exclude participants who were unable to understand simple instructions in English as they would not be able to understand the movement instructions given during the exercise sessions if randomised to the intervention arm of the study.
Randomisation
A computer-based system allocated participants to the intervention and control groups in a 1 : 1 ratio using permuted random blocks of variable length and stratification by centre. This was administered centrally via Newcastle Clinical Trials Unit using a secure web-based system. The principal investigator (PI) at the site, or an individual with delegate authority, accessed the web-based system. Random allocation was determined after a participant screening identification number and initials were entered into the web-based system; participants could then be informed.
Study intervention
The proposed intervention was adapted from the group-based FaME programme, which is widely used as a health-promoting activity in the UK with community-dwelling older people.
For the intervention arm, local qualified FaME PSIs working on each site were trained by a research team member (DS) on adapting the exercises for people with VI following recommendations from the stakeholder panels. The PSIs also received VI training from Visibility.
The exercise programme (the intervention) ran weekly over 12 weeks, with each session lasting up to 1 hour. Two exercise groups were held at each site. In order to maximise recruitment, a further exercise group was held at the Newcastle site. All groups were held in a community venue. In Glasgow, the exercise groups were run at Visibility because this venue was known to the participants. In Newcastle, classes were run at the Trinity Centre. These were city centre venues and required participants to travel into the city centre.
None of the groups had more than 10 participants. The exercises consisted of balance-specific, individually tailored and targeted training for dynamic balance, strength, endurance, flexibility, gait and functional skills and ‘righting’ or ‘correcting’ skills to avoid a fall, as well as backward chaining, that is, retraining of the ability to get down to and up from the floor. The exercises also included functional floor exercises and adapted tai chi exercises. The intervention increased in difficulty over the 12 weeks. Resistance bands and mats were used throughout the study. The details of the methods of delivery, group size, support and timing were decided by the stakeholder panels. A full description of the original exercise programming and progression has been published and an adapted manualised intervention is included as Appendix 1, as this was an important objective of the study.
Prior to commencing the exercise sessions, all participants completed a health screening tool that is normally administered by the exercise instructors prior to delivery of the FaME programme.
The first session was used as an induction to familiarise VIOP with the venue and instructor. Any time remaining after this induction was used for a short exercise session. All following sessions lasted 1 hour and comprised:
-
a 10- to 15-minute warm-up focusing on circulation exercises
-
targeted full-range joint mobilisation and light stretches
-
a standing cardiovascular endurance section lasting 5 minutes in week 2 and increasing to 10 minutes by week 12
-
a balance retraining section of 10 minutes starting with static exercises (such as one-leg stands) and progressing to highly challenging dynamic exercises (such as heel walking and backwards walking)
-
a 10-minute seated resistance component using progressively more challenging resistance bands
-
a 10-minute cool-down including developmental stretches for both the upper and lower limb muscles and one form of adapted tai chi that progressed in difficulty.
The introduction of the backward chaining approach for getting down to and up from the floor was not planned for a specific week of the intervention, given that the VIOP stakeholders had expressed some concern about the ability of the target population to perform this safely. The PSIs were advised to introduce the floor-based exercises at a stage appropriate to the group and no sooner than week 4.
Participants were also advised to exercise at home for up to 2 hours per week using an adapted standardised home exercise programme that has been developed by DS and used in other related studies. Exercises were provided in large-text or audio format and consisted of specific chair and standing exercises to improve balance, bone and muscle strength and flexibility, similar to the exercises carried out in the exercise classes. The home exercises were designed to be completed in 10- to 20-minute blocks, commencing with 10-minute blocks in the first 4 weeks, increasing to 15-minute blocks for a further 4 weeks and increasing again to 20-minute blocks in the last 4 weeks. A greater number of exercises and more challenging balance exercises were included as the duration of the sessions gradually increased. This progressive approach was implemented following VIOP stakeholder advice that 30-minute blocks of home exercise would not be realistic. The exercises were to be performed 6 days per week – that is, every day excluding the day of the exercise class. All home programmes contained ‘prompts’ that linked exercises to daily tasks (e.g. performing heel raises while waiting for the kettle to boil). The prompts were included to increase compliance, following VIOP stakeholder advice. The PSIs supplied participants with the home exercise programmes and were responsible for encouraging participants to adhere to and progress through the programmes. PSIs were asked to ensure that the content of the home exercise programmes had been taught in the group sessions and to help participants with the specific exercise techniques to reduce the risk of any adverse events (AEs) from the home exercises.
Participants were provided with transport by taxi to and from the classes, if required, and invited to bring along someone for support if they wished.
The description of this adapted exercise programme is provided in the manualised intervention, which is available on the National Institute for Health Research (NIHR) website.
Those participants who were randomised to the usual activities group received no intervention. However, they were offered an equivalent exercise programme after the week 24 follow-up data collection at both sites.
Fidelity of the intervention
Postural Stability Instructors were given a flexible framework of lesson plans for the 12-week programme prior to the start of the intervention.
A standardised quality assurance checklist was used to ensure effective and safe delivery of the programme, including progression, adherence to the protocol (i.e. providing home exercise programme, checking on adherence to home exercise and recording any falls mentioned) and completion of all paperwork.
The PSIs compliance with the course content (fidelity) was assessed by videoing two sessions at each site at weeks 3 and/or 4 and weeks 9 and/or 10 respectively.
These videos were examined by a research team member to check that the main components of fitness were covered and progressed sufficiently. Their delivery was signed off by checking against the videos provided.
The quality assurance checklist can be found appended to the manual of the adapted FaME intervention (a copy of this is available from the VIOLET project page on the NIHR website).
Qualitative interviews
As this was a feasibility study, qualitative interviews were conducted to explore acceptability and applicability of the intervention, the research methods and the outcome measures. These interviews are reported in Chapter 5. Structured interviews were also conducted with a purposive sample of the exercise practitioners at two points (before training and at the end of the intervention) to explore their (changing) perspectives on the provision of the intervention over the duration of the intervention (see Chapter 5).
Outcome measures and assessment
A key aim of the feasibility study was to determine whether or not the primary and secondary outcomes for a proposed full trial could be measured for all participants. The feasibility study was not powered to detect significant differences in these measures but was able to describe observed changes between time points and their direction.
The selected candidate outcome measures were standardised assessment instruments that have been used previously in comparable studies. These measures were selected in consultation with the stakeholder panels. The main reasons for this selection were the relevance of the questions to the participants and that the questionnaires were short and, therefore, easier for a person with VI to manage. The proposed measurement tools were reviewed by the stakeholder panels at both sites to ensure that the most appropriate and most acceptable outcome measurement tools were selected and used in the pilot trial. FoF was selected as the primary outcome because, although FoF is common, debilitating and a significant predictor of a future fall particularly among older people, successful management of FoF is limited. Recent reviews show that there is a lack of high-quality research that has FoF as a primary health outcome. There are also limited health economic data about FoF interventions.
Measuring the number of falls as a primary outcome does not take into account the more complex impact of an intervention. Reducing FoF may increase participants’ confidence in their ability to walk safely and continue with everyday activities. Assessing FoF before and after the proposed intervention captures participants’ self-reported change in confidence to continue with physical and social activities. This provides an indication of their perceived QoL and whether or not the negative impacts of FoF, such as social isolation and risk of further falls, have been reduced.
Primary outcome measure
The measures were selected together with VIOP and were modified following the stakeholder panel (see Chapter 2). The final primary outcome of the future RCT would be decided by responsiveness to change, participant burden and participant feedback in this study. A potential candidate outcome was FoF (FES-I). 73
Fear of falling was assessed at baseline and at weeks 12 and 24 by the Short Form FES-I. It captured participants’ self-reported change in confidence to continue with physical and social activities. This in turn gave an indication of their perceived QoL and whether or not the negative impact of FoF, such as social isolation and risk of further falls, had been reduced.
The Short Form FES-I uses seven items – each scored from 1 (not concerned) to 4 (very concerned) – to assess selected activities and provide an indication of how afraid of falling the responder is while doing these activities. The total score for all seven items (range 7–28) is categorised as low (range 7–8), moderate (range 9–13) or high (range 14–28) concern.
Secondary outcome measures
Activity avoidance (two questions)
Activity avoidance can be a consequence of FoF. The degree of activity avoidance was captured using two questions. 34 It was recorded at baseline and at weeks 12 and 24.
There are two stand-alone questions – ‘Are you afraid of falling?’ and ‘Do you avoid certain activities due to fear of falling?’ – scored on a Likert scale with five options: ‘never’, ‘almost never’, ‘sometimes’, ‘often’ or ‘very often’.
Balance/falls risk
Balance/falls risk was assessed by two methods: the TUG test74 and a self-assessment – the Falls Risk Assessment Tool (FRAT),75 which has been used in previous studies in ageing populations. These were assessed at baseline, week 12 and week 24.
The purpose of the TUG test is to assess mobility. Participants can wear their usual footwear and use walking aids if needed. The time taken (in seconds) for them to stand up from the chair, walk to a line 3 metres away at their normal pace, turn around, walk back to the chair and sit down again is recorded using a stop watch.
An older adult who takes ≥ 12 seconds to complete the TUG test can be considered at high risk of falling.
The self-assessment FRAT, developed from the Peninsula FRAT,75 was used. It is a five-item questionnaire (with yes/no responses). Scores of > 3 (yes) indicate that further assessment is required.
Number of falls (falls diary and weekly telephone call)
As well as answering the study questionnaires at the specified time points of baseline, week 12 and week 24, each participant completed a falls diary each week, with assistance from a researcher, during their weekly telephone call. Data were collected for each day, Monday to Sunday, as yes/no responses to the question ‘did you fall’? If a response was ‘yes’, it was coded as follows:
-
0 – no injury
-
1 – bruise and/or cut
-
2 – bruise and/or cut and immobilisation
-
3 – soft tissue injury
-
4 – broken bone
-
5 – other.
Each participant was telephoned 7 ± 2 days from date of previous contact. A suitable time was arranged for each participant and recorded in the trial documentation along with ongoing consent. Details of any AEs and near misses were also recorded at this time and described in the safety analysis.
When a fall did occur, the researcher completed the falls resource/expenses form on behalf of the participant (see Appendix 9).
Physical activity (Phone-Frequency, Intensity, Time and Type)
Physical activity can help to maintain the physical capacity of older adults. The Phone-Frequency, Intensity, Time and Type (Phone-FITT)76 provides an assessment of participants’ perceptions of their own physical activity on various dimensions of physical activity. These are household physical activity, recreational physical activity and total physical activity scores, with two versions of each: frequency and duration (FD) and frequency, duration and intensity (FDI). This was assessed at baseline and at weeks 12 and 24.
For household physical activity, eight items are used to create the summary scores FD and FDI. For recreational physical activity, 13 items are used to create the summary scores. A total score is then calculated.
The methods for calculating summary scores from the questionnaire data are outlined by Gill et al. 76 Individual values of the summary scores have no absolute meaning but rather are interpretable in a relative sense within individuals over time. A zero score indicates no participation in that particular activity. The summary scores are interpretable as absolute measures only in the comparison of those with values of zero (completely sedentary) and those with non-zero values (active to some degree). Other than this contrast, scores are dimensionless.
Loneliness (6-Item Scale for Overall, Emotional, and Social Loneliness)
Social isolation is known to be a potential consequence of FoF and activity avoidance. The degree of perceived loneliness was captured through the 6-Item Scale for Overall, Emotional and Social Loneliness. 77 This was assessed at baseline and at weeks 12 and 24.
The responses to the six items are then split evenly between emotional and social loneliness to give two outcomes as described below.
The three positively formulated items are ‘There are plenty of people I can rely on when I have problems’, ‘There are many people I can trust completely’ and ‘There are enough people I feel close to’; these combine to give the social loneliness score. The three negatively formulated items are:‘I experience a general sense of emptiness’, ‘I miss having people around’ and ‘I often feel rejected’; these combine to give the emotional loneliness scores. The scores are interpreted as follows:
-
Three negatively formulated items – score count (‘more or less’/’yes’) = emotional loneliness score, from 0 (not emotionally lonely) to 3 (intensely emotionally lonely).
-
Three positively formulated items – score count (‘more or less’/’no’) = social loneliness score, from 0 (not socially lonely) to 3 (intensely socially lonely).
Anxiety and depression [Hospital Anxiety and Depression Scale (14 item)]
There is potential for those who become socially isolated to have a degree of anxiety and depression. The Hospital Anxiety and Depression Scale (HADS)78 is a valid and reliable self-rating scale that measures anxiety and depression in both hospital and community settings. HADS gives clinically meaningful results as a psychological screening tool and can assess in both patients with illness and the general population the symptom severity and caseness of anxiety disorders and depression (where caseness is defined as a psychiatric diagnosis made largely on the basis of symptoms – patients’ reports of their subjective experiences – rather than pathognomonic symptoms or signs such as fever). Fully standardised, HADS can detect the presence and severity of mild degrees of mood disorder, anxiety and depression using one brief questionnaire.
The HADS questionnaire has 14 items: seven examining anxiety and seven examining depression. The score is calculated and categorised according to the following scale: 0–7 is considered normal, 8–10 is borderline abnormal and 11–21 is abnormal.
Anxiety and depression were assessed at baseline, week 12 and week 24.
Work and Social Adjustment Scale
The extent to which participants perceived their existing conditions to impact upon areas of their life was assessed using the WSAS. 70 The WSAS is a simple five-item (scored 0–8) questionnaire (total score range 0–40) and a reliable, valid measure of impaired functioning. It is sensitive and useful for comparing between trial arms.
A WSAS score of > 20 suggests moderately severe or worse psychopathology. Scores between 10 and 20 are associated with significant functional impairment but less severe clinical symptomatology. Scores of < 10 are associated with subclinical populations.
Quality of life using the EQ-5D-5L and ICECAP-O
The methods to estimate an incremental cost-effectiveness ratio were rehearsed using the EuroQol-5 Dimensions, five-level version (EQ-5D-5L)79 and ICEpop CAPability measure for Older people (ICECAP-O)80 and administered at baseline, week 12 and week 24. For methods of the cost-effectiveness analysis (see Chapter 6).
Resource use via a health economic self-report service receipt inventory
The cost of each fall to the NHS and social services – along with personal incidental costs and informal caregiver resource use related to falls – was captured by a falls resources/expenses form. This was assessed retrospectively during the weekly telephone call if the participants reported a fall.
Adherence to the group exercise programme (register) and home exercise programme (self-reported)
Participants’ compliance with the exercise programme was assessed by reviewing attendance records (register) at the end of the 12-week course. Participants were classed as compliant if they attended 9 out of 12 of the group sessions.
Current level of activity
Current level of activity had six options to choose from to reflect participants’ level of activity at each time point. This was to capture both exercise, defined as planned and structured exercise, as well as physical activity, which included household and leisure activities. Each participant selected one option from the following six:
-
I do not do any planned physical activity during the week and would find it difficult to start.
-
I am seriously thinking about doing planned physical activity each week.
-
I used to exercise regularly each week but have lapsed.
-
In the last 6 months I have started doing regular activity.
-
I exercise once in a while but not weekly.
-
I exercise regularly each week.
Assessment/data collection
Following consent, a researcher assessed all participants, either on site or in their own home, depending on the participants’ preferences. The participants were also asked a number of questions regarding demographic data, comorbidities, current medication and socioeconomic information and to complete the baseline outcome questionnaires discussed in this chapter.
Because of their VI, assistance was required to fill in the questionnaires, either by the researcher reading out the questions and filling out the forms or by providing the questionnaires in a format accessible to the participant. Sufficient time was allowed for this stage to accommodate each individual’s preference. Once confirmation of eligibility had been received from a participant’s GP, randomisation took place. For both groups of participants, baseline data were collected no more than 4 weeks prior to the intervention start date.
For the intervention group, it was planned that the week 12 visit was conducted ± 2 weeks from the end of the intervention date unless there were prior commitments or extenuating circumstances. For the usual activity group, the week 12 visit was planned to take place 12 ± 2 weeks from the date of their baseline visit. The week 24 visit for all participants was planned to take place 12 ± 2 weeks from the date of their week 12 visit.
The questionnaires were repeated at the week 12 and week 24 visits. All participants were also telephoned each week from their baseline visit up to their week 24 follow-up visit to record any AEs (including falls) that had occurred. A schematic diagram of the intervention is provided in Figure 1. Table 1 outlines the schedule of events.
FIGURE 1.
Schematic diagram of the RCT. Adapted with permission from Adams et al. 81 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
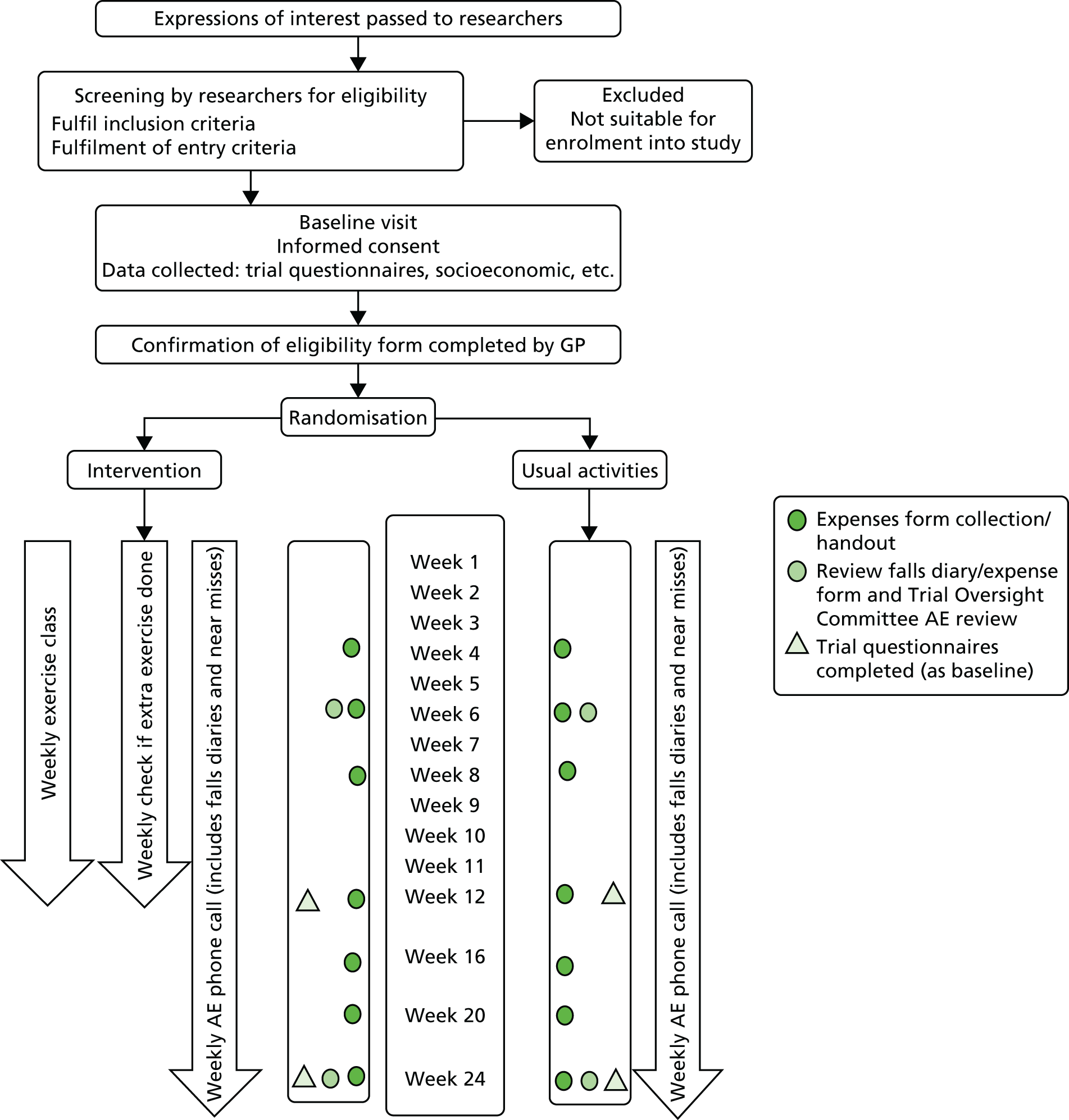
| Processes | Pre-screening | Initial screening | Baseline visit | Intervention or usual care/activities | Final follow-up | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Venue | Post/hand-out | Telephonea/siteb | Siteb/homec | Siteb | Siteb/homec | Siteb/homec | ||||||||||||
| Time (weeks) | 0 | 0a | 0b | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 24 | ||
| Identification: invitation letters participant information sheets sent/handed out | ✗ | |||||||||||||||||
| Screening | ✗ | |||||||||||||||||
| Informed consent | ✗ | |||||||||||||||||
| Letter sent to GP | ✗ | |||||||||||||||||
| Demographic data | ✗ | |||||||||||||||||
| Comorbidities | ✗ | ✗ | ✗ | |||||||||||||||
| Current medication | ✗ | ✗ | ✗ | |||||||||||||||
| Socioeconomic information | ✗ | ✗ | ✗ | |||||||||||||||
| FoF questionnaire | ✗ | ✗ | ✗ | |||||||||||||||
| TUG | ✗ | ✗ | ✗ | |||||||||||||||
| Outcome questionnaires | ✗ | ✗ | ✗ | |||||||||||||||
| QoL questionnaires | ✗ | ✗ | ✗ | |||||||||||||||
| Randomisation | ✗ | |||||||||||||||||
| Falls diaries handed out | ✗ | ✗ | ✗ | ✗ | ||||||||||||||
| Falls diaries collected | ✗ | ✗ | ✗d | ✗ | ||||||||||||||
| Structured interviews with PSIs | ✗ | ✗ | ||||||||||||||||
| Intervention: exercise sessions or usual activities | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Assessment of harms: telephone calls | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗e | ✗ | |||||
| In-depth qualitative interviews with VIOP | ✗ | |||||||||||||||||
| Review of attendance records | ✗ | |||||||||||||||||
Baseline visit procedures (weeks –3 to 0)
The procedures at baseline were:
-
If not already obtained, informed consent was obtained at the beginning of this visit.
-
A research assistant collected information on demographics, comorbidities, current medication and socioeconomic information and carried out the assessments for the outcome measures for participants.
-
Once the confirmation of eligibility had been received from the participant’s GP, randomisation took place, and participants were telephoned by the researcher to inform them of their randomisation outcome.
Intervention group procedures (weeks 1 to 12)
The procedures for the intervention group during this time period were:
-
daily completion of falls diary
-
weekly exercise session lasting up to 1 hour
-
advice to carry out up to 2 hours of additional home exercise per week
-
weekly telephone call to/from researcher to ascertain whether or not the participant had experienced any AEs and completion of the falls resource/expenses form with the researcher (if required)
-
participants asked if they were doing any of the exercises at home.
Usual activity group procedures (weeks 1 to 24)
The procedures for the usual activity group during this time period were:
-
daily completion of falls diary
-
weekly telephone call to/from researcher to ascertain whether or not the participant had experienced any AEs and completion of the falls resource/expenses form with the researcher (if required).
Intervention and usual activity group procedures (week 12 ± 2 weeks)
All participants were seen personally by a researcher at a mutually convenient venue. The researcher collected the following information:
-
comorbidities
-
current medication
-
changes in socioeconomic information
-
incidental costs (intervention group only)
-
completion of the outcome measures.
Intervention group procedures (weeks 12 to 24)
The procedures for the intervention group during this time period were:
-
daily completion of falls diary
-
weekly telephone call to/from researcher to ascertain whether or not the participant had experienced any AEs and completion of the falls resource/expenses form with the researcher (if required).
Intervention and usual activity group procedures (week 24 ± 2 weeks)
All participants were seen personally by a researcher at a mutually convenient venue. The researcher collected the following information:
-
comorbidities
-
current medication
-
changes in socioeconomic information
-
incidental costs (intervention group only)
-
completion of the outcome measures.
Assessment of compliance
Participants’ compliance with the exercise programme was assessed by reviewing attendance records kept by the PSI and the self-reported compliance to the home exercises at the end of the 12-week course. In addition, qualitative interviews, conducted by the researchers after the completion of the exercise classes, provided information on why VIOP attended or did not attend exercise classes and what barriers prevented them from attending. Eligible VIOP who declined the invitation to participate were asked the reason for declining.
Instructors were required to submit basic lesson plans for the 12-week programme prior to the start of the intervention. The PSIs’ compliance with the course content (fidelity) was assessed by a researcher attending a sample of exercise sessions. A standardised checklist was used, similar to that used by researchers in a previously published trial, and these sessions videotaped for quality assurance purposes. Following completion of the intervention, PSIs were also invited to discuss their experiences of delivering the adapted intervention (these discussions are detailed in Chapter 5).
Withdrawal of participants
Participants had the right to withdraw from the study at any time for any reason and without giving a reason. The investigator had the right to withdraw participants from the study in the event of intercurrent illness, AEs, SAEs, protocol violations or if judged to be in the participant’s best interests or for administrative or other reasons. Participants were also withdrawn if the participant’s GP felt they were medically unfit to take part or the participant failed the pre-exercise screening carried out by the exercise instructors.
There were two withdrawal options:
-
withdrawing completely (i.e. withdrawal from both the study treatment and provision of follow-up data)
-
withdrawing partially (i.e. withdrawal from study treatment, including a request to move to another treatment arm, but continuing to provide follow-up data by completing questionnaires).
Consent was sought from participants choosing option 1 to retain data collected up to the point of withdrawal. Participants were asked if they would be happy for the reason for the decision to withdraw to be recorded.
Assessment of harms/adverse event reporting
Participants were telephoned each week from consent to record any AEs that occurred up to their week 24 follow-up. All AEs were assessed for seriousness, severity, duration, causality and expectedness. This included any SAEs reported by the instructors within the exercise sessions or reported in the falls diaries given to participants (if they requested to complete these themselves).
Adverse events were recorded by treatment arm. In addition to splitting up AEs by treatment arm, we made a further distinction for those in the intervention arm by categorising them as occurring (1) from baseline up to the first exercise class of the intervention or (2) after the start of the intervention (following the first exercise class). This was to ensure that the AEs in the two trial arms could be compared over the same period of time. All participants were telephoned weekly from consent because it was not known to which arm they would be assigned until their confirmation of GP eligibility form was completed and returned and the participant could be randomised. However, this led to a potential discrepancy in time periods: for those randomised to the usual activity arm it could be ensured that there were 12 weekly telephone calls between their baseline and week 12 visits; however, for those in the intervention arm there could be a delay between their baseline visit and the start of the intervention, resulting in over 12 weekly telephone calls between their baseline and week 12 visit.
All AEs were treated appropriately. Treatment included one or more of the following: no action taken (i.e. further observation only), concomitant medication given, non-drug therapy given, or patient hospitalised/patient’s hospitalisation prolonged.
The trial oversight committee (TOC) monitored the SAEs to bring the intervention to a close should this have been deemed necessary.
Definitions of seriousness, severity (intensity) of adverse event, causality and expectedness
An untoward occurrence (whether expected or not) was categorised as an SAE if it met the following criteria:
-
resulted in death
-
was life-threatening (i.e. an event in which the subject was at risk of death at the time of the event, not an event that hypothetically might have caused death if it were more severe)
-
required hospitalisation or prolongation of existing hospitalisation
-
resulted in persistent or significant disability or incapacity
-
was otherwise considered medically significant by the investigator.
All AEs were graded on a three-point scale of intensity (mild, moderate or severe):
-
mild – discomfort is noticed but there is no disruption to normal daily activities
-
moderate – discomfort is sufficient to reduce or affect normal daily activities
-
severe – discomfort is incapacitating; inability to work or perform normal daily activities.
Events were also assessed for causality – that is, whether or not they had a reasonable causal relationship to the intervention. Those that did were categorised as ‘related AEs’. Assignment of causality was made as shown in Table 2.
| Relationship | Description |
|---|---|
| Unrelated | There is no evidence of any causal relationship |
| Unlikely | There is little evidence to suggest that there is a causal relationship (e.g. the event did not occur within a reasonable time after administration of the trial intervention). There is another reasonable explanation for the event (e.g. the participant’s clinical condition or other concomitant treatment) |
| Possible | There is some evidence to suggest a causal relationship (e.g. the event occurs within a reasonable time after administration of the trial intervention). However, the influence of other factors may have contributed to the event (e.g. the participant’s clinical condition or other concomitant treatments) |
| Probable | There is evidence to suggest a causal relationship and the influence of other factors is unlikely |
| Definitely | There is clear evidence to suggest a causal relationship and other possible contributing factors can be ruled out |
All AEs judged as having a reasonable suspected causal relationship to a study procedure (i.e. definitely, probably or possibly related) were considered to be related AEs.
Expected AEs included the following:
-
fall/trip/slip and its consequences: cuts and abrasions, soft tissue injury, fracture
-
muscular/joint pain associated with the above or with increased physical activity
-
minor illness not requiring GP intervention (e.g. cold, flu)
-
minor illness requiring GP intervention (e.g. chest infection, urinary tract infection).
Expected SAEs included injurious falls, serious falls and/or hospitalisation due to falls. SAEs excluded:
-
any pre-planned hospitalisations (e.g. elective surgery) not associated with clinical deterioration
-
routine treatment or monitoring of the studied indication not associated with any deterioration in condition
-
elective or scheduled treatment for pre-existing conditions that did not worsen during the study.
Data handling and record keeping
Collected data were entered on a secure validated clinical data management system (MACRO 4.6; Rackspace Inc., Windcrest, TX, USA). Data were handled, computerised and stored in accordance with the Data Protection Act 1998. 72
All study data were retained in accordance with the latest Good Clinical Practice Directive (2005/28/EC)82 and local policy.
Statistical analysis
As this was a feasibility trial, the main analyses were descriptive in order to inform the design of a future definitive study. The main outcomes were feasibility outcomes. The numbers of eligible participants seen over the recruitment period and the resulting rates of recruitment, compliance with randomisation and data completion were presented. Data completeness of the instruments and any potential bias in the completion of follow-up data to inform the choice of instruments in a future trial were ascertained. In Chapter 4, the majority of the outcome data have been presented in simple descriptive tables presenting percentages, means and standard deviations (SDs) or five-number summaries (as appropriate) for each arm of the study. This information was used to inform the design, choice of primary outcome, necessary sample size and approach to the analysis of a future definitive trial. See Chapter 4 for a detailed presentation of findings.
There was potential for clustering effects, particularly class-based clustering in the intervention group. It is part of the function of a pilot trial to investigate and estimate the size of any such effects. As this was a feasibility study, it was hoped that the results would provide estimates of variability in key outcomes both within and between classes and trial arms, which would be used to design a future definitive trial. However, it was understood that there would be very limited information on the size of intraclass correlation coefficient (ICC) in a study with only two centres and two classes per centre and that any estimates of ICC would be very imprecise based on this pilot trial. Estimates of ICC may be obtained from larger relevant trials such as the current ProAct65 study. 61 However, since ProAct65 is a cluster randomised trial as opposed to one in which the clustering effects are due to treatment alone, their estimate of ICC may be larger than those appropriate for use in a future individually randomised trial. 83
Chapter 4 Randomised controlled feasibility study of the adapted Falls Management Exercise intervention versus usual activities: findings
In this chapter, we present the main findings of the feasibility study, including quantitative aspects of the trial processes, a description of study participants and the analyses of the feasibility study data.
Identification of potential participants
Recruiting for the Newcastle site, a dedicated member of NSBP rang members aged > 60 years to gain permission to forward their contact details to the research team. It is not known precisely how many potential participants were approached by NSBP but anecdotal information suggests that > 200 calls were made. From these, 35 expressions of interest were passed to the researchers. Identification of participants from the RVI low-vision clinic in Newcastle proved problematic: very few of the staff referred potential participants to the researchers. After the involvement of ECLOs, 15 potential participants were identified and their expressions of interest forwarded to the research team.
The primary source of potential participants at the Glasgow site was Visibility; no recruitment took place at the low-vision clinic (see Chapter 3 for further details). Anecdotally, > 100 direct contacts were made by Visibility staff. Expressions of interest were again forwarded to the research staff. It is not precisely known how many potential participants were contacted by Visibility; however, the research team received 48 expressions of interest.
All potential participants were contacted by the research team and assessed for eligibility in a consistent manner.
Participant flow
Figure 2 shows the screening, recruitment and follow-up of participants by trial researchers at the two centres. In total, 82 VIOP were screened for eligibility by the researchers. Of these, 16 were eventually found to be ineligible, two declined to participate, 66 consented and 64 were randomised after further loss through failure to meet eligibility criteria. The target for recruitment was 80, with a view to obtaining a minimum of 30 responses in each trial arm at the 6-month follow-up point.
FIGURE 2.
The VIOLET Consolidated Standards of Reporting Trials (CONSORT) flow diagram. Adapted with permission from Adams et al. 81 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
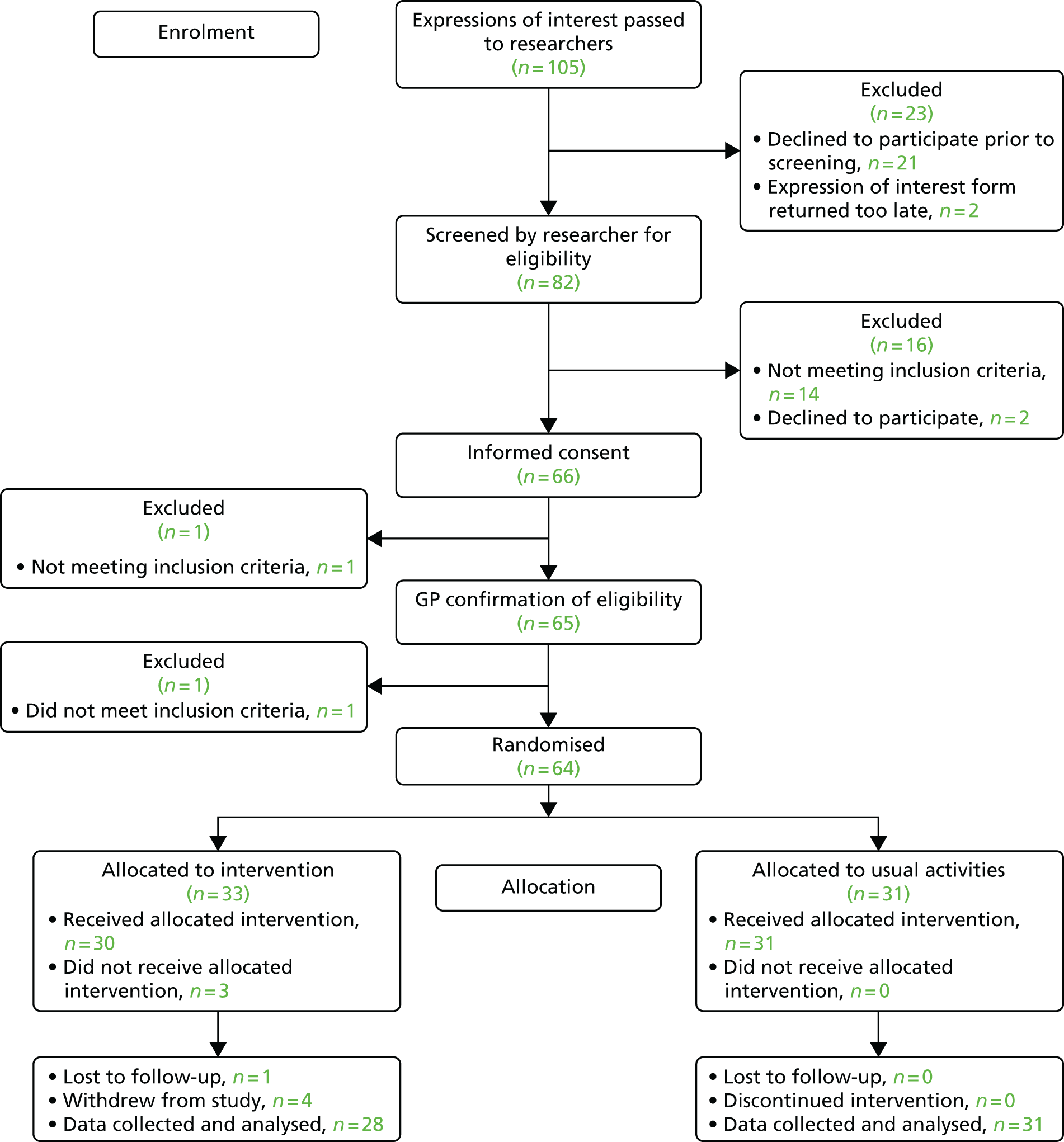
The Newcastle site opened to recruitment in June 2015 whereas the Glasgow site opened in July 2015. The numbers recruited each month (combined across sites) are shown in Table 3.
| Month (2015) | Participants randomised | Cumulative total |
|---|---|---|
| June | 10 | 10 |
| July | 17 | 27 |
| August | 15 | 42 |
| September | 15 | 57 |
| October | 1 | 58 |
| November | 6 | 64 |
The numbers screened, recruited and randomised by site are shown in Table 4.
| Site | Screened, n | Not enrolled for other reasons, n (% of potentially eligible) | Declined, n (% of potentially eligible) | Eligible, n (% of assessed) | Randomised | ||
|---|---|---|---|---|---|---|---|
| Total, n (% of potentially eligible) | To intervention, n | To usual activities, n | |||||
| Newcastle | 45 | 10 (23) | 2 (6) | 33 (73) | 33 (94) | 17 | 16 |
| Glasgow | 37 | 6 (16) | 0 (0) | 31 (84) | 31 (100) | 16 | 15 |
| Total | 82 | 16 (20) | 2 (3) | 64 (78) | 64 (97) | 33 | 31 |
After randomisation, 33 VIOP were allocated to the intervention arm and 31 to the usual activities arm. Of the 33 VIOP allocated to the intervention, three did not attend any classes but two of these nevertheless provided study data. During the study, one person was lost to follow-up and four people in the intervention arm withdrew completely from the study (Table 5). The remaining subjects provided data that was included in the statistical analysis.
| Participant ID | Arm | Date of withdrawal | Reason for not completing trial | Days from randomisation | Exercise classes attended |
|---|---|---|---|---|---|
| VIO/G/001a | Intervention | 19/01/2016 | Deceased | 175 | 6 |
| VIO/G/025b | Intervention | 14/11/2015 | Lost interest in study | 68 | 3 |
| VIO-N-004b | Intervention | 20/10/2015 | SAE: stroke | 124 | 11 |
| VIO-N-014b | Intervention | 29/07/2015 | No longer convenient | 7 | 0 |
| VIO-N-025b | Intervention | 01/09/2015 | Safety concerns | 35 | 2 |
Baseline participant characteristics
Demographic and baseline characteristics at randomisation were compared across treatment groups. Descriptive statistics are tabulated by treatment group and overall in Table 6. The distributions of demographic variables were comparable across the trial arms; the only noticeable difference was that more participants in the usual activities arm lived alone.
| Variable | Intervention arm (N = 33) | Usual activities arm (N = 31) | Total (N = 64) |
|---|---|---|---|
| Gender, n (%) | |||
| Male | 14 (42) | 11 (35) | 25 (39) |
| Female | 19 (58) | 20 (65) | 39 (61) |
| Age (years) | |||
| Median (IQR) | 80 (75–87) | 78 (68–83) | 79 (70.5–84.5) |
| Mean (SD) | 79.3 (8.7) | 76.5 (9.7) | 78.0 (9.2) |
| Range | 61–95 | 62–95 | 61–95 |
| First language, n (%) | |||
| English | 32 (97) | 28 (90) | 60 (94) |
| Other | 1 (3) | 3 (10) | 4 (6) |
| Ethnicity, n (%) | |||
| White | 33 (100) | 29 (94) | 62 (97) |
| Asian or Asian British | 0 (0) | 2 (6) | 2 (3) |
| Marital status, n (%) | |||
| Married/living as married | 16 (48) | 8 (26) | 24 (38) |
| Living with other family members | 0 (0) | 2 (6) | 2 (3) |
| Living alone | 11 (33) | 16 (52) | 27 (42) |
| Widowed | 6 (18) | 5 (16) | 11 (17) |
| Has children aged < 18 years | |||
| Median (IQR) | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| Range | 0–0 | 0–0 | 0–0 |
| Dependant adults, n (%) | |||
| Yes | 2 (6) | 2 (6) | 4 (6) |
| No | 31 (94) | 29 (94) | 60 (94) |
| Employment status, n (%) | |||
| Full-time employment | 0 (0) | 1 (3) | 1 (2) |
| Part-time employment | 0 (0) | 0 (0) | 0 (0) |
| Seeking work | 0 (0) | 0 (0) | 0 (0) |
| Homemaker | 0 (0) | 0 (0) | 0 (0) |
| Student | 0 (0) | 0 (0) | 0 (0) |
| Retired | 29 (88) | 28 (90) | 57 (89) |
| Other | 4 (12) | 2 (6) | 6 (9) |
As would be expected in a group of older people, they reported a number of comorbidities. Summary statistics of the numbers of baseline self-reported comorbidities are shown in Table 7.
| Comorbidities | Intervention arm (N = 33) | Usual activities arm (N = 31) | Total (N = 64) |
|---|---|---|---|
| Any comorbidities reported? n (%) | |||
| Yes | 25 (76) | 20 (65) | 45 (70) |
| No | 8 (24) | 11 (35) | 19 (30) |
| Numbers of comorbidities per participant | |||
| Minimum | 0 | 0 | 0 |
| LQ | 1 | 0 | 0 |
| Median | 2 | 2 | 2 |
| UQ | 5 | 6 | 5 |
| Maximum | 9 | 13 | 13 |
Delivery of intervention and intervention compliance
Two sets of 12-week exercise sessions were intended to be offered at both Newcastle and Glasgow, allowing two potential start dates as recruitment proceeded. However, a staggered start was used to facilitate the running of the first set of classes in both Newcastle and Glasgow. This enabled those for whom the GP confirmation of eligibility had not been returned promptly to start at any time within the first 3 weeks and continue to complete 12 sessions. A total of 14 weeks of sessions was offered so that each participant had the ability to attend 12 sessions even with a delayed start. In Newcastle, a third set of classes was provided for those who had been recruited later or whose eligibility checks took a long time to complete. In Glasgow, the class sizes were six and nine and, in Newcastle, class sizes were six, five and four.
Table 8 summarises the number of sessions attended by participants randomised to the intervention arm on the basis of class registers and how often they exercised at home (self-report) with FD. Four participants withdrew completely from the study and attended 0, 2, 3 and 11 classes prior to withdrawing (see Table 4). One further participant was withdrawn from the trial (deceased) after attending six exercise classes. Two additional participants randomised to the intervention arm did not attend any classes but continued to provide trial questionnaire data. One participant withdrew from the intervention after three classes but continued to provide trial data. In fact, 25 out of 33 participants (76%) attended nine or more classes, which was one of the feasibility criteria for a future trial. The intervention arm participants were encouraged to carry out exercises at home. It can be seen that they spent an average of 50 minutes per week doing home exercises, though there was a large variation in the amount.
| Variable | Minimum | LQ | Median | UQ | Maximum | Mean | SD |
|---|---|---|---|---|---|---|---|
| Number of classes attended | 0 | 9.0 | 10.0 | 12.0 | 12.0 | 8.8 | 3.9 |
| Number of weeks when exercised at home during interventiona | 0 | 5.0 | 9.0 | 11.0 | 14.0 | 7.8 | 4.4 |
| Average weekly exercise frequencyb | 0 | 1.8 | 3.4 | 4.6 | 6.7 | 3.2 | 2.0 |
| Average exercise duration per weekb | 0 | 17.3 | 50.4 | 75.7 | 122.0 | 50.0 | 35.7 |
Data completeness
The trial outcomes were collected at baseline and at weeks 12 and 24, with data collection planned to be within 2 weeks of these time points. Figures 3 and 4 show the time period between baseline and when each of these two assessments actually occurred. A total of 60 out of 64 participants (94%) provided data at the week 12 visit (four had withdrawn completely from the study at this point) and 59 out of 64 participants (92%) completed the week 24 visit (four had withdrawn completely from the study and one was lost to follow-up at this point). In two cases, assessments were completed outside the 2-week limit owing to other commitments or extenuating circumstances.
FIGURE 3.
Time between start of trial and week 12 assessment. Graphs by randomisation arm: (a) intervention arm and (b) usual activities arm. Starting point is baseline visit for usual activities arm and first exercise class for intervention arm (reference lines at ± 2 weeks).
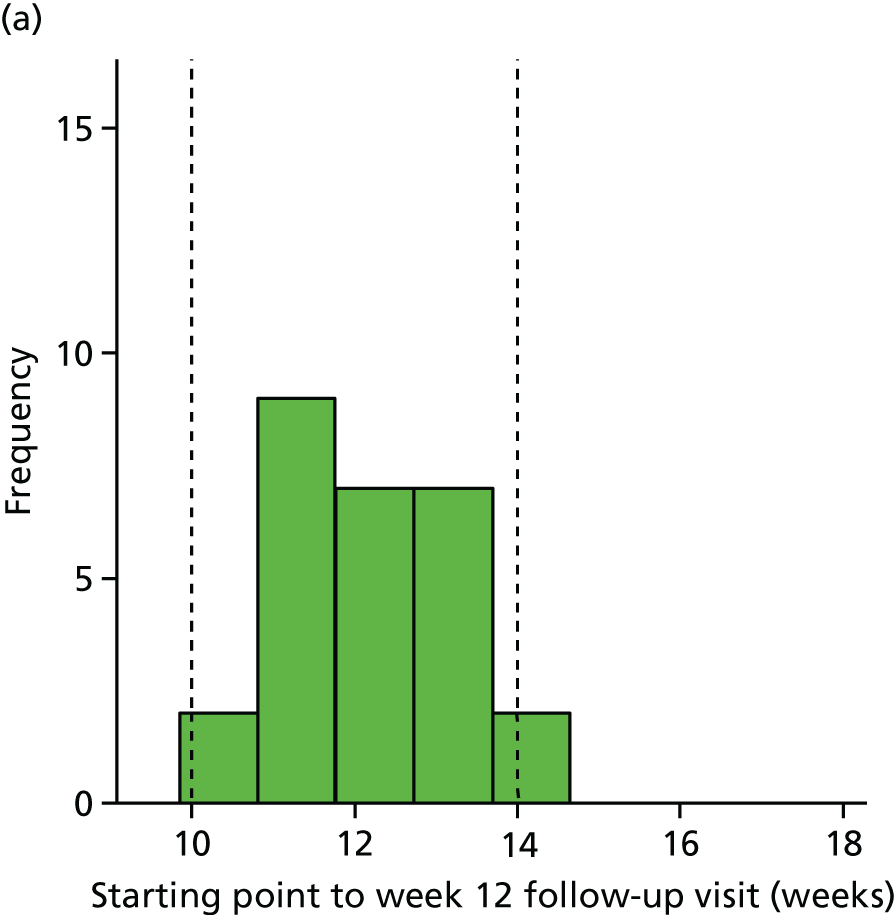

FIGURE 4.
Time between start of trial and week 24 assessment. Graphs by randomisation arm: (a) intervention arm and (b) usual activities arm. Starting point is baseline visit for usual activities arm and first exercise class for intervention arm (reference lines at ± 2 weeks).
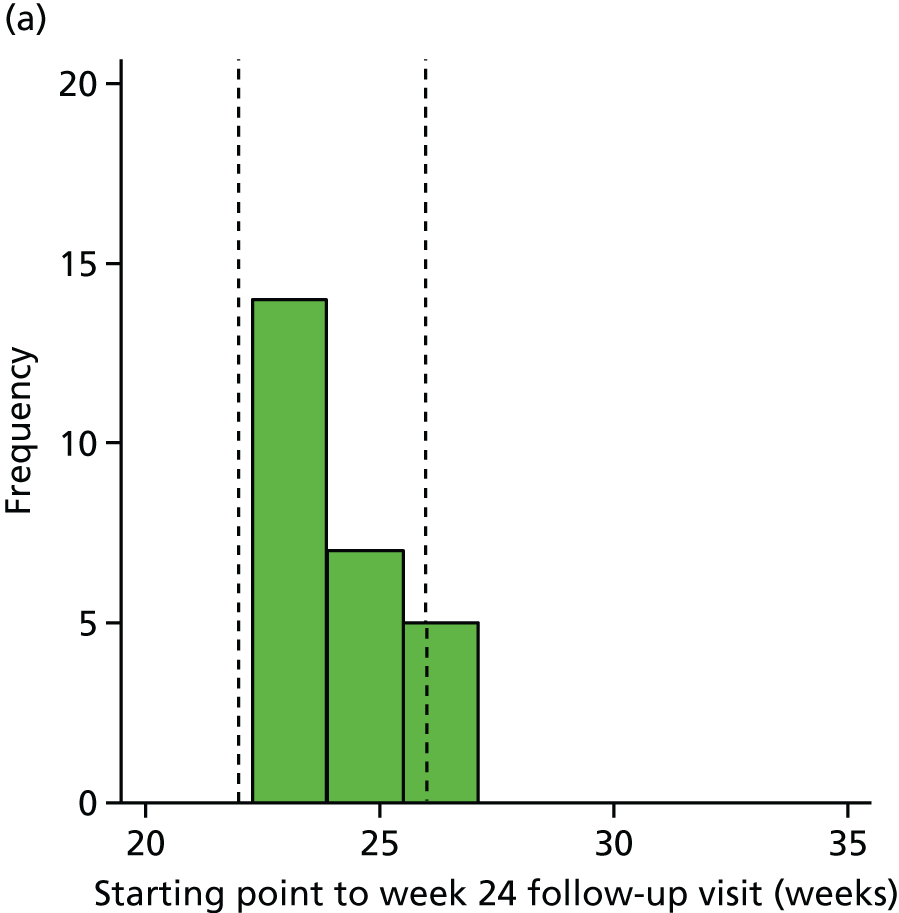
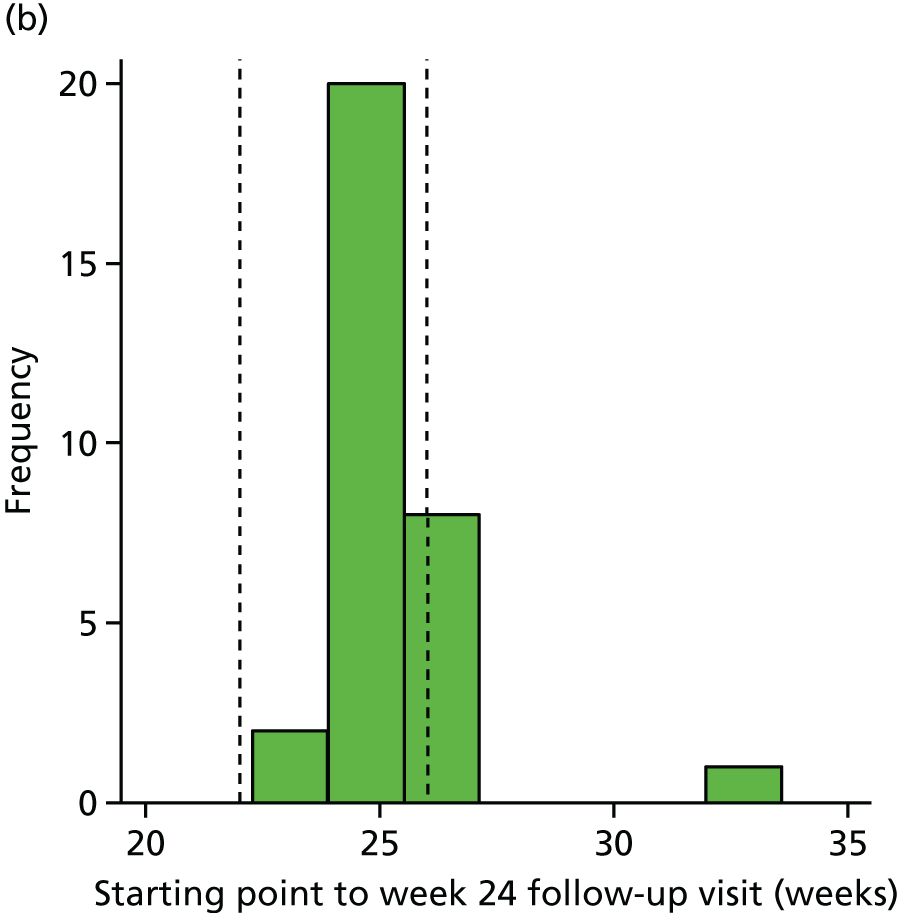
When considering the feasibility of a definitive trial it is important to look at how well alternative outcomes have been completed. Completion rates for each questionnaire at each time point are reported in Table 9 and completion rates for elements of the Phone-FITT questionnaire are reported in Table 10. It can be seen that all those participants in the intervention arm remaining in the trial at each time point completed each of the questionnaires. There were two occasions when participants in the usual activity arms only partially completed a questionnaire (these were nevertheless still usable following missing data rules) and two occasions when whole questionnaires were not completed. All elements of the Phone-FITT questionnaire were completed for all participants remaining in the trial at each time point. This suggests that all chosen scales were suitable for use in a future trial.
| Questionnaire | Time point | Intervention arm (N = 33) | Usual activities arm (N = 31) | ||||
|---|---|---|---|---|---|---|---|
| Complete, n (%) | Partial, n (%)a | Missingb | Complete, n (%) | Partial, n (%)a | Missingb | ||
| Concerns over falling (FES-I) | Week 0 | 32 (97) | 0 (0) | 1 (3) | 29 (94) | 2 (6) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 30 (97) | 0 (0) | 1 (3) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Impact of illness (WSAS) | Week 0 | 32 (97) | 0 (0) | 1 (3) | 30 (97) | 0 (0) | 1 (3) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Anxiety and depression (HADS): anxiety component | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Anxiety and depression (HADS): depression component | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Loneliness: emotional loneliness | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 30 (97) | 0 (0) | 1 (3) | |
| Loneliness: social loneliness | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Functional test (TUG) | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| FRAT | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Questionnaire | Time point | Intervention arm (N = 33) | Usual activities arm (N = 31) | ||||
|---|---|---|---|---|---|---|---|
| Complete, n (%) | Partial, n (%)a | Missingb | Complete, n (%) | Partial, n (%)a | Missingb | ||
| Household FD | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Recreational FD | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Total FD | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Household FDI | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Recreational FDI | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
| Total FDI | Week 0 | 33 (100) | 0 (0) | 0 (0) | 31 (100) | 0 (0) | 0 (0) |
| Week 12 | 29 (88) | 0 (0) | 4 (12) | 31 (100) | 0 (0) | 0 (0) | |
| Week 24 | 28 (85) | 0 (0) | 5 (15) | 31 (100) | 0 (0) | 0 (0) | |
The number of weekly telephone calls is shown in Table 11. Trial participants should have been telephoned each week during the 24-week study period to collect information on falls, near misses and SAEs. If the participant was in the intervention arm, they were also asked about home exercises. However, some participants received more than 24 telephone calls because they were randomised to the intervention arm but had to wait a number of weeks before a programme of exercise classes became available. These participants were still telephoned each week to collect information before the first class and then for the 24 weeks thereafter. Sometimes the classes were offered over 14 weeks (meaning a total of 26 telephone calls up to the week 24 assessment) as extra classes were available to allow participants to catch up if they missed one or two classes.
| Number of weekly telephone calls | |||||||
|---|---|---|---|---|---|---|---|
| Arm | Period of trial | n | Minimum | LQ | Median | UQ | Maximum |
| Intervention arm | Baseline to first class | 15 | 1 | 2 | 3 | 5 | 17 |
| First class to week 24 assessment | 29a | 3 | 22 | 24 | 24 | 26 | |
| No classes attended | 3 | 3 | 13.5 | 24 | 24 | 24 | |
| Usual activities arm | No classes attended | 31 | 20 | 23 | 24 | 24 | 24 |
For participants randomised to the intervention arm, any calls that occurred before the start of the first exercise class are recorded in the ‘Baseline to first class’ row of Table 11. Any calls between the first class and week 24 (with an extra 2 weeks if classes had been offered over 14 weeks) are recorded in the ‘First class to week 24 assessment’ row. The third row of Table 11 shows summary statistics for participants randomised to the intervention arm who did not attend any classes (so there was no ‘start of intervention’). The final row shows summary statistics for the usual activities arm, which start from the baseline visit and should continue for 24 weeks.
Summary statistics on trial outcomes
Numeric outcomes
Table 12 summarises numeric outcome measures (FES-I score, WSAS score, anxiety and depression (HADS), loneliness and FRAT score) by trial arm and data collection point, and the change in these from baseline to the week 12 visit or the week 24 follow-up visit. Based on the FES-I score, the majority of participants had low or moderate concern over falling at baseline. It can be seen that the median change in FES-I score from baseline to week 12 and week 24 was zero in both arms, although there were some large changes in both directions. There was a very wide range of WSAS scores at baseline, but the median changes over time were small, with some large changes in both directions. For anxiety, depression and falls risk assessment scales, the scores were generally low at baseline and median changes over 12 and 24 weeks were zero, with a few larger changes in both directions.
| Outcome measure | Week or change | Intervention arm | Usual activities arm | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Min. | LQ | Median | UQ | Max. | Mean | SD | n | Min. | LQ | Median | UQ | Max. | Mean | SD | ||
|
Concern over falling (FES-I) Score of 7–28 (higher score = more concern) |
0 | 32 | 7.0 | 8.0 | 9.0 | 10.0 | 15.0 | 9.1 | 2.1 | 31 | 7.0 | 7.0 | 9.0 | 11.0 | 23.0 | 9.7 | 3.3 |
| 12 | 29 | 7.0 | 8.0 | 9.0 | 11.0 | 14.0 | 9.3 | 2.2 | 30 | 7.0 | 7.0 | 8.0 | 10.0 | 20.0 | 9.4 | 3.2 | |
| 24 | 28 | 7.0 | 7.0 | 8.0 | 10.0 | 21.0 | 8.9 | 2.9 | 31 | 7.0 | 7.0 | 8.0 | 11.0 | 17.0 | 9.5 | 2.9 | |
| 0 to 12 | 29 | –6.0 | –1.0 | 0.0 | 1.0 | 5.0 | –0.1 | 2.5 | 30 | –12.0 | –1.0 | 0.0 | 1.0 | 10.0 | –0.3 | 3.3 | |
| 0 to 24 | 28 | –7.0 | –2.0 | 0.0 | 0.5 | 8.0 | –0.5 | 2.9 | 31 | –8.0 | –1.0 | 0.0 | 0.0 | 6.0 | –0.3 | 2.6 | |
|
Impact of illness (WSAS) Score of 0–40 (higher score = more illness) |
0 | 32 | 0.0 | 5.6 | 11.9 | 18.1 | 27.5 | 12.7 | 8.5 | 30 | 0.0 | 5.0 | 12.5 | 23.8 | 38.8 | 13.5 | 10.9 |
| 12 | 29 | 0.0 | 10.0 | 15.0 | 20.0 | 35.0 | 15.1 | 7.9 | 31 | 0.0 | 3.8 | 11.3 | 17.5 | 37.5 | 13.3 | 11.6 | |
| 24 | 28 | 0.0 | 12.5 | 20.0 | 25.6 | 40.0 | 19.1 | 10.1 | 31 | 0.0 | 5.0 | 15.0 | 26.3 | 33.8 | 15.4 | 11.8 | |
| 0 to 12 | 28 | –13.8 | –4.4 | 1.3 | 5.6 | 17.5 | 1.1 | 7.8 | 30 | –15.0 | –7.5 | –1.3 | 5.0 | 20.0 | –0.3 | 9.3 | |
| 0 to 24 | 27 | –12.5 | 0.0 | 3.8 | 11.3 | 18.8 | 4.9 | 7.6 | 30 | –12.5 | –5.0 | 1.3 | 6.3 | 17.5 | 1.9 | 7.8 | |
|
Anxiety (HADS component) Score of 0–21 (higher score = more anxiety) |
0 | 33 | 0.0 | 2.0 | 4.0 | 5.0 | 12.0 | 4.1 | 3.1 | 31 | 0.0 | 3.0 | 4.0 | 7.0 | 17.0 | 5.0 | 3.8 |
| 12 | 29 | 0.0 | 1.0 | 4.0 | 7.0 | 11.0 | 4.3 | 3.5 | 31 | 0.0 | 1.0 | 4.0 | 5.0 | 16.0 | 4.4 | 4.2 | |
| 24 | 28 | 0.0 | 1.0 | 4.0 | 7.0 | 14.0 | 4.1 | 3.7 | 31 | 0.0 | 2.0 | 5.0 | 6.0 | 16.0 | 5.0 | 4.2 | |
| 0 to 12 | 29 | –4.0 | –1.0 | 0.0 | 1.0 | 7.0 | 0.4 | 2.3 | 31 | –7.0 | –2.0 | –1.0 | 1.0 | 5.0 | –0.6 | 2.5 | |
| 0 to 24 | 28 | –6.0 | –1.0 | 0.0 | 1.0 | 9.0 | 0.1 | 2.8 | 31 | –10.0 | –1.0 | 0.0 | 1.0 | 5.0 | –0.1 | 2.8 | |
|
Depression (HADS component) Score of 0–21 (higher score = more depression) |
0 | 33 | 0.0 | 1.0 | 3.0 | 5.0 | 14.0 | 3.7 | 3.0 | 31 | 0.0 | 1.0 | 5.0 | 8.0 | 11.0 | 5.0 | 3.5 |
| 12 | 29 | 0.0 | 1.0 | 4.0 | 6.0 | 10.0 | 4.0 | 2.9 | 31 | 0.0 | 2.0 | 4.0 | 7.0 | 12.0 | 4.9 | 3.4 | |
| 24 | 28 | 0.0 | 2.0 | 3.0 | 6.0 | 10.0 | 4.1 | 2.8 | 31 | 0.0 | 2.0 | 4.0 | 8.0 | 12.0 | 5.0 | 3.2 | |
| 0 to 12 | 29 | –4.0 | –2.0 | 0.0 | 1.0 | 6.0 | –0.1 | 2.5 | 31 | –5.0 | –1.0 | 0.0 | 1.0 | 5.0 | –0.1 | 2.2 | |
| 0 to 24 | 28 | –4.0 | –1.5 | 0.0 | 1.0 | 6.0 | 0.0 | 2.3 | 31 | –8.0 | –2.0 | 0.0 | 2.0 | 5.0 | –0.1 | 3.0 | |
|
FRAT Score of 0–5 (higher score = more risk) |
0 | 33 | 0.0 | 0.0 | 1.0 | 3.0 | 5.0 | 1.6 | 1.3 | 31 | 0.0 | 1.0 | 1.0 | 3.0 | 4.0 | 1.8 | 1.3 |
| 12 | 29 | 0.0 | 1.0 | 1.0 | 3.0 | 4.0 | 1.7 | 1.1 | 31 | 0.0 | 1.0 | 2.0 | 3.0 | 4.0 | 2.0 | 1.3 | |
| 24 | 28 | 0.0 | 1.0 | 1.0 | 3.0 | 4.0 | 1.7 | 1.3 | 31 | 0.0 | 1.0 | 2.0 | 3.0 | 4.0 | 1.8 | 1.4 | |
| 0 to 12 | 29 | –2.0 | 0.0 | 0.0 | 1.0 | 2.0 | 0.1 | 1.0 | 31 | –2.0 | 0.0 | 0.0 | 1.0 | 2.0 | 0.2 | 0.8 | |
| 0 to 24 | 28 | –2.0 | 0.0 | 0.0 | 1.0 | 2.0 | 0.0 | 1.0 | 31 | –2.0 | 0.0 | 0.0 | 1.0 | 2.0 | 0.0 | 0.8 | |
Table 13 presents descriptive statistics as above for the various Phone-FITT (physical activity) measures. It can be seen that typical physical activity levels rose slightly over the follow-up period in the intervention arm and less so in the control arm, though no formal comparison was made.
| Outcome measure (Phone-FITT) | Week or change | Intervention arm | Usual activities arm | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Min. | LQ | Med. | UQ | Max. | Mean | SD | n | Min. | LQ | Med. | UQ | Max. | Mean | SD | ||
| Household FD | 0 | 33 | 0 | 12.0 | 28.0 | 38.0 | 76 | 28.3 | 18.5 | 31 | 0 | 12.0 | 22.0 | 40 | 70.0 | 25.8 | 18.3 |
| 12 | 29 | 0 | 13.0 | 25.0 | 46.0 | 92 | 33.3 | 24.7 | 31 | 0 | 11.0 | 27.0 | 47 | 100.0 | 31.3 | 23.9 | |
| 24 | 28 | 0 | 15.5 | 28.5 | 52.5 | 108 | 35.6 | 26.4 | 31 | 0 | 11.0 | 23.0 | 47 | 73.0 | 27.9 | 20.4 | |
| 0 to 12 | 29 | –16 | –2.0 | 6.0 | 13.0 | 29 | 5.8 | 11.1 | 31 | –28 | –3.0 | 2.0 | 18 | 46.0 | 5.5 | 15.9 | |
| 0 to 24 | 28 | –27 | –7.0 | 8.0 | 18.5 | 65 | 7.8 | 19.4 | 31 | –28 | –5.0 | 3.0 | 9 | 30.0 | 2.1 | 13.2 | |
| Recreational FD | 0 | 33 | 0 | 10.0 | 16.0 | 48.0 | 284 | 48.2 | 71.0 | 31 | 0 | 0.0 | 13.5 | 28 | 165.0 | 29.3 | 45.3 |
| 12 | 29 | 0 | 12.0 | 24.0 | 44.0 | 179 | 41.6 | 50.2 | 31 | 0 | 0.0 | 15.0 | 28 | 300.0 | 36.5 | 70.4 | |
| 24 | 28 | 0 | 3.5 | 17.0 | 48.8 | 302 | 49.3 | 79.5 | 31 | 0 | 0.0 | 10.0 | 33 | 1471.3 | 70.5 | 263.1 | |
| 0 to 12 | 29 | –189 | 0.0 | 3.0 | 14.0 | 56 | –6.2 | 46.5 | 31 | –135 | –5.5 | 0.0 | 7 | 272.0 | 7.1 | 62.4 | |
| 0 to 24 | 28 | –153 | –10.3 | 0.0 | 8.0 | 175 | 0.5 | 61.0 | 31 | –161 | –3.0 | 0.0 | 7 | 1306.3 | 41.2 | 239.9 | |
| Total FD | 0 | 33 | 0 | 34.0 | 49.0 | 89.5 | 296 | 76.5 | 75.3 | 31 | 1 | 16.0 | 42.5 | 66 | 222.0 | 55.1 | 53.6 |
| 12 | 29 | 0 | 41.0 | 55.0 | 96.0 | 209 | 74.9 | 57.2 | 31 | 0 | 25.0 | 47.0 | 67 | 377.0 | 67.7 | 84.5 | |
| 24 | 28 | 9 | 30.8 | 52.1 | 100.5 | 410 | 84.9 | 92.0 | 31 | 0 | 18.0 | 43.0 | 66 | 1506.0 | 98.3 | 266.4 | |
| 0 to 12 | 29 | –175 | –4.0 | 8.7 | 27.0 | 69 | –0.4 | 47.6 | 31 | –143 | –19.0 | 4.0 | 27 | 279.0 | 12.7 | 65.3 | |
| 0 to 24 | 28 | –166 | –9.6 | 4.5 | 23.6 | 201 | 8.3 | 70.3 | 31 | –149 | –14.0 | –0.5 | 26 | 1284.0 | 43.3 | 235.8 | |
| Household FDI | 0 | 33 | 0 | 12.0 | 28.0 | 40.0 | 76 | 28.7 | 18.7 | 31 | 0 | 12.0 | 22.0 | 40 | 70.0 | 26.7 | 18.8 |
| 12 | 29 | 0 | 13.0 | 25.0 | 46.0 | 92 | 33.8 | 24.8 | 31 | 0 | 11.0 | 27.0 | 50 | 100.0 | 32.7 | 25.0 | |
| 24 | 28 | 0 | 17.5 | 29.5 | 52.5 | 108 | 36.1 | 26.1 | 31 | 0 | 11.0 | 23.0 | 48 | 73.0 | 29.6 | 21.8 | |
| 0 to 12 | 29 | –16 | –2.0 | 9.0 | 12.7 | 29 | 5.9 | 11.1 | 31 | –28 | –3.0 | 2.0 | 18 | 62.0 | 6.1 | 18.4 | |
| 0 to 24 | 28 | –33 | –7.0 | 9.0 | 19.0 | 65 | 7.8 | 19.8 | 31 | –30 | –5.0 | 2.5 | 9 | 40.0 | 3.0 | 16.4 | |
| Recreational FDI | 0 | 33 | 0 | 10.0 | 16.0 | 48.0 | 284 | 56.9 | 87.8 | 31 | 0 | 0.0 | 13.5 | 28 | 186.0 | 35.1 | 54.3 |
| 12 | 29 | 0 | 12.0 | 24.0 | 47.0 | 217 | 47.5 | 61.4 | 31 | 0 | 0.0 | 15.0 | 42 | 363.0 | 42.5 | 82.7 | |
| 24 | 28 | 0 | 3.5 | 17.0 | 48.8 | 598 | 66.1 | 135.7 | 31 | 0 | 0.0 | 10.0 | 35 | 1622.5 | 77.7 | 289.9 | |
| 0 to 12 | 29 | –178 | –4.0 | 2.0 | 11.0 | 89 | –10.1 | 51.4 | 31 | –126 | –14.0 | 0.0 | 8 | 272.0 | 7.3 | 71.4 | |
| 0 to 24 | 28 | –156 | –11.3 | 0.0 | 7.5 | 325 | 7.1 | 98.7 | 31 | –182 | –6.0 | 0.0 | 8 | 1443.5 | 42.6 | 265.7 | |
| Total FDI | 0 | 33 | 0 | 34.0 | 53.0 | 89.5 | 353 | 85.6 | 93.3 | 31 | 1 | 17.0 | 42.5 | 80 | 236.0 | 61.8 | 62.5 |
| 12 | 29 | 0 | 41.0 | 55.0 | 96.0 | 298 | 81.3 | 70.3 | 31 | 0 | 25.0 | 53.0 | 73 | 421.0 | 75.2 | 95.7 | |
| 24 | 28 | 9 | 32.3 | 54.1 | 100.5 | 706 | 102.2 | 148.5 | 31 | 0 | 18.0 | 49.0 | 75 | 1657.3 | 107.3 | 292.5 | |
| 0 to 12 | 29 | –164 | –8.0 | 5.0 | 27.0 | 102 | –4.2 | 52.2 | 31 | –134 | –25.0 | –1.0 | 32 | 279.0 | 13.4 | 74.7 | |
| 0 to 24 | 28 | –169 | –13.1 | 8.8 | 22.9 | 353 | 15.0 | 106.7 | 31 | –142 | –14.0 | 0.0 | 25 | 1421.3 | 45.6 | 260.9 | |
Table 14 presents the descriptive statistics for the time taken to complete the balance/falls risk (TUG) test. TUG time in seconds is shown in Table 14, but the remaining parts of this questionnaire concerning walking aids and using chair arms to assist in the task are presented separately in Table 15. On average, there was little difference in the TUG test time in either arm between baseline and the week 12 and week 24 assessments.
| Outcome measure (TUG) | Week or change | Intervention arm | Usual activities arm | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Min. | LQ | Median | UQ | Max. | Mean | SD | n | Min. | LQ | Median | UQ | Max. | Mean | SD | ||
| Test completion time (s) | 0 | 33 | 8.8 | 9.8 | 13.3 | 16.8 | 35.6 | 14.6 | 5.9 | 31 | 7.4 | 10.7 | 13.3 | 20 | 120.0 | 20.3 | 21.8 |
| 12 | 28 | 8.9 | 11.0 | 13.5 | 18.4 | 30.2 | 15.9 | 6.5 | 31 | 6.0 | 11.1 | 17.0 | 19.2 | 975.0 | 53.2 | 173.4 | |
| 24 | 28 | 8.2 | 10.3 | 13.8 | 16.3 | 28.5 | 14.4 | 5.3 | 31 | 6.6 | 10.4 | 15.1 | 18.2 | 100.0 | 19.9 | 19.5 | |
| 0 to 12 | 28 | –6.4 | –1.1 | 0.3 | 2.1 | 7.1 | 0.6 | 2.9 | 31 | –6.3 | –2 | 0.3 | 2.2 | 961.2 | 32.8 | 172.5 | |
| 0 to 24 | 28 | –18.4 | –1.9 | –0.4 | 1.3 | 5.9 | –0.7 | 4.2 | 31 | –20.1 | –2.7 | –0.3 | 1.7 | 11.7 | –0.4 | 5.2 | |
| Component | Intervention arm (N = 33) | Usual activities arm (N = 31) | ||||
|---|---|---|---|---|---|---|
| Baseline | Week 12 | Week 24 | Baseline | Week 12 | Week 24 | |
| Unable to do test, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Arms used to get out of chair, n (%) | ||||||
| Yes | 9 (27) | 6 (18) | 7 (21) | 11 (35) | 8 (26) | 10 (32) |
| No | 24 (73) | 22 (67) | 21 (64) | 20 (65) | 23 (74) | 21 (68) |
| Missing | 0 (0) | 5 (15) | 5 (15) | 0 (0) | 0 (0) | 0 (0) |
| Walking aid, n (%) | ||||||
| Yes | 3 (9) | 2 (6) | 2 (6) | 3 (10) | 1 (3) | 2 (6) |
| No | 30 (91) | 26 (79) | 26 (79) | 28 (90) | 30 (97) | 29 (94) |
| Missing | 0 (0) | 5 (15) | 5 (15) | 0 (0) | 0 (0) | 0 (0) |
Change from baseline to week 12 and week 24 in categorical outcomes
A number of the other scales that were used had only a small number of categories, so the distribution at baseline and changes over time have been illustrated in tables showing all possible categories (see Tables 15–18). These tables show the extent of any changes between categories. Colour coding is used to illustrate the direction of changes between time points.
Comparing attitudes in the intervention arm at the week 12 visit to baseline (Table 16), 10 out of 33 participants reported no change in FoF, 12 reported that they were more afraid and seven reported that they were less afraid of falling. Four complete withdrawals were not included.
| Baseline | Week 12 visit (N = 29), n (%) | ||||
|---|---|---|---|---|---|
| Never | Almost never | Sometimes | Often | Very often | |
| Never | 4 (14) | 2 (7) | 1 (3) | 1 (3) | 0 (0) |
| Almost never | 1 (3) | 2 (7) | 6 (21) | 0 (0) | 0 (0) |
| Sometimes | 1 (3) | 3 (10) | 4 (14) | 0 (0) | 1 (3) |
| Often | 1 (3) | 0 (0) | 0 (0) | 0 (0) | 1 (3) |
| Very often | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
Comparing attitudes in the usual activities arm at the week 12 visit to baseline (Table 17), 8 out of 31 participants reported no change in FoF, nine reported that they were more afraid and 14 reported that they were less afraid of falling.
| Baseline | Week 12 visit (N = 31), n (%) | ||||
|---|---|---|---|---|---|
| Never | Almost never | Sometimes | Often | Very often | |
| Never | 3 (10) | 0 (0) | 4 (13) | 0 (0) | 0 (0) |
| Almost never | 3 (10) | 0 (0) | 2 (6) | 0 (0) | 0 (0) |
| Sometimes | 6 (19) | 3 (10) | 5 (16) | 2 (6) | 0 (0) |
| Often | 1 (3) | 0 (0) | 0 (0) | 0 (0) | 1 (3) |
| Very often | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
Comparing attitudes in the intervention arm at week 24 follow-up to baseline (Table 18), 12 participants reported no change in FoF, seven reported that they were more afraid and nine reported that they were less afraid of falling. Four complete withdrawals and one lost to follow-up were not included.
| Baseline | Week 24 visit (N = 28), n (%) | ||||
|---|---|---|---|---|---|
| Never | Almost never | Sometimes | Often | Very often | |
| Never | 5 (18) | 1 (4) | 2 (7) | 0 (0) | 0 (0) |
| Almost never | 2 (7) | 3 (11) | 3 (11) | 0 (0) | 0 (0) |
| Sometimes | 2 (7) | 2 (7) | 4 (14) | 1 (4) | 0 (0) |
| Often | 1 (4) | 0 (0) | 1 (4) | 0 (0) | 0 (0) |
| Very often | 0 (0) | 1 (4) | 0 (0) | 0 (0) | 0 (0) |
Comparing attitudes in the usual activities arm at week 24 follow-up to baseline (Table 19), 12 participants reported no change in FoF, eight reported that they were more afraid and 12 reported that they were less afraid of falling.
| Baseline | Week 24 visit (N = 31), n (%) | ||||
|---|---|---|---|---|---|
| Never | Almost never | Sometimes | Often | Very often | |
| Never | 4 (13) | 1 (3) | 2 (6) | 0 (0) | 0 (0) |
| Almost never | 3 (10) | 1 (3) | 2 (6) | 0 (0) | 0 (0) |
| Sometimes | 4 (13) | 2 (6) | 7 (23) | 2 (6) | 1 (3) |
| Often | 0 (0) | 1 (3) | 1 (3) | 0 (0) | 0 (0) |
| Very often | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
A similar analysis of changes between categories over time (from baseline to week 12 and week 24) is presented for four additional categorical variables in Appendix 13 (avoiding certain activities owing to FoF, emotional loneliness, social loneliness and current level of physical activity). It was common to find no change in any of these variables. Where there was a change, there were few obvious differences between the numbers showing worsening or improving attitudes or between the changes reported in the two trial arms.
Safety analysis
Summary of all adverse events reported
A total of 180 AEs were reported; these were categorised as 16 SAEs and 164 AEs.
There were nine SAEs in the intervention arm and seven SAEs in the usual activities arm. Of the nine SAEs in the intervention arm, four were fractures caused by falls. There were no fractures caused by falls in the usual activities arm. However, of the four participants who sustained fractures caused by falls in the intervention arm, two (VIO-G-016 and VIO-G-019) did not actually begin the intervention. Both of these participants also had a history of falls. Of the other two participants in the intervention arm who sustained fractures, participant VIO-G-001 had taken part in a maximum of seven exercise classes when they tripped and fell in their own home and participant VIO-N-001 had taken part in a maximum of 10 exercise classes when they tripped and fell outside. Participant VIO-N-001 had reported a previous fall when they tripped over the foot of a bed while drawing curtains. Taking into account the fact that two of the participants in the intervention arm who sustained fractures caused by falls did not begin the intervention and had a history of falls, there appears to be no evidence of a link between taking part in the intervention and being at greater risk of a fracture caused by a fall.
With regard to AEs, 81 AEs were reported in the intervention arm and 83 were reported in the usual activities arm.
A total of 17 falls without injury (10 in the intervention arm and seven in the usual activities arm) and 28 near misses (four in the intervention arm and 24 in the usual activities arm) were also reported.
Adverse events
Details of the 164 AEs are shown in Table 20.
| Intervention arm | Usual activities arm | Total | ||
|---|---|---|---|---|
| Baseline to first exercise class | After first exercise class | Randomised to intervention arm but attended no classes | After baseline date | |
| 7 (4) | 70 (43) | 4 (2) | 83 (51) | 164 (100) |
Serious adverse events
Details of the 16 SAEs are shown in Table 21 and their period of occurrence in Table 22.
| Treatment | Participant | Date | Description | Severity | Related to intervention |
|---|---|---|---|---|---|
| Intervention | N-001 | 05/10/2015 | Fracture of ribs caused by trip and fall outdoors | Severe | No |
| Intervention | N-003 | 06/07/2015 | Upper respiratory tract infection | Moderate | No |
| Intervention | N-004 | 11/09/2015 | Stroke | Severe | No |
| Intervention | N-007 | 08/09/2015 | Abdominal cancer | Moderate | No |
| Intervention | G-001 | 26/09/2015- 01/10/2015 | Fracture of two ribs caused by fall | Moderate | No |
| Intervention | G-001 | 10/11/2015 | Suspected light myocardial infarction and pulmonary embolism | Moderate | No |
| Intervention | G-001 | 12/01/2016 | Large bowel obstruction with aspiration pneumonia; participant died | Severe | No |
| Intervention | G-016 | 27/08/2015 | Fractured right humerus caused by fall down some outdoor steps | Severe | No |
| Intervention | G-019 | 15/10/2015 | Fracture of ankle bone caused by fall outdoors | Moderate | No |
| Usual activities | N-015 | 13/07/2015 | Mild heart attack | Severe | No |
| Usual activities | N-015 | 29/09/2015 | Breathlessness | Moderate | No |
| Usual activities | N-022 | 28/07/2015 | Hospitalised as felt unwell; heart was not beating at correct rate | Severe | No |
| Usual activities | N-022 | 21/10/2015 | Bruised left knee in fall | Moderate | No |
| Usual activities | N-022 | 02/12/2015 | Slight heart attack | Moderate | No |
| Usual activities | N-022 | 20/01/2016 | Urinary retention | Moderate | No |
| Usual activities | G-005 | 12/01/2016 | Reaction to medication | Moderate | No |
| Intervention arm | Usual activities arm | Total | ||
|---|---|---|---|---|
| Baseline to first exercise class | After first exercise class | Randomised to intervention arm but attended no classes | After baseline date | |
| 1 (6.25) | 6 (37.5) | 2 (12.5) | 7 (43.75) | 16 (100) |
Falls without injury
Details of the 17 falls without injury are shown in Table 23 and their period of occurrence in Table 24.
| Treatment | Participant | Date | Description |
|---|---|---|---|
| Intervention | VIO-G-030 | 25/09/2015 | Fell over a bowling ball |
| Intervention | VIO-G-030 | 10/01/2016 | Fell off a step |
| Intervention | VIO-N-001 | 30/08/2015 | Fell in bedroom while drawing curtains – tripped over foot of bed |
| Intervention | VIO-N-017 | 19/01/2016 | Fell: lost balance in bedroom and slid from bed to floor |
| Intervention | VIO-N-020 | 22/09/2015 | Overbalanced while catching a jar thrown by a friend and fell onto side |
| Intervention | VIO-N-020 | 17/12/2015 | Stood up on bus; went to sit down again but seat tilted and sat on floor of bus |
| Intervention | VIO-N-020 | 20/12/2015 | Fell over newly carpeted step in church aisle |
| Intervention | VIO-N-020 | 21/12/2015 | Misjudged depths of outdoor steps, lost balance and fell |
| Intervention | VIO-N-025 | 18/08/2015 | Slipped on steps inside house and fell onto bottom |
| Intervention | VIO-N-033 | 21/04/2016 | Stumbled and fell into a snowdrift |
| Usual activities | VIO-G-022 | 27/10/2015 | Fell on bus when bus driver braked suddenly |
| Usual activities | VIO-N-019 | 08/12/2015 | Went to sit on sofa but misjudged distance and fell to floor |
| Usual activities | VIO-N-022 | 12/08/2015 | Fell in bathroom |
| Usual activities | VIO-N-022 | 17/08/2015 | Slipped coming down stairs and fell on bottom |
| Usual activities | VIO-N-022 | 18/08/2015 | Fell into bath; misjudged safety rail |
| Usual activities | VIO-N-024 | 13/12/2015 | Lost balance taking boots off; rocked backwards into kitchen cupboards and onto floor |
| Usual activities | VIO-N-030 | 10/12/2015 | Slipped on steps and fell |
| Type of fall | Intervention arm | Usual activities arm | Total | ||
|---|---|---|---|---|---|
| Baseline to first exercise class | After first exercise class | Randomised to intervention arm but attended no classes | After baseline date | ||
| Falls without injury, n (%) | 2 (12) | 8 (47) | 0 (0) | 7 (41) | 17 (100) |
Near misses
Information on near misses was collected in this study as part of the data collection as members of the stakeholder panel were interested in this as a potential outcome. Near misses are often referred to as ‘slips’ or ‘trips’ where no actual injury is sustained. Table 25 shows occurrences of near misses by trial arm and Table 26 shows period of occurrence. However, data on this could be missing or difficult to interpret (is a ‘near miss’ to be interpreted as a positive event, because they avoided hitting the ground and no injury was sustained, or a negative event, because they had overbalanced?), so no further quantitative analysis was carried out.
| Treatment | Participant | Date | Description |
|---|---|---|---|
| Intervention | VIO-N-006 | 06/07/2015 | Tripped on kerb when exiting taxi |
| Intervention | VIO-N-017 | 15/10/2015 | Went off balance when pottering at home |
| Intervention | VIO-N-020 | 22/01/2016 | Tripped stepping off train |
| Intervention | VIO-N-033 | 09/05/2016 | Got tangled in another person’s wheeled shopping trolley in city centre and tripped |
| Usual activities | VIO-G-003 | 16/09/2015 | Foot caught on the doorstep |
| Usual activities | VIO-G-003 | 21/10/2015 | Foot caught in uneven roadway |
| Usual activities | VIO-G-003 | 21/10/2015 | Foot caught in uneven roadway |
| Usual activities | VIO-G-004 | 11/08/2015 | Almost fell walking on pavement; kept balance using walking stick |
| Usual activities | VIO-G-004 | 08/09/2015 | Wobbled after almost missing a kerb |
| Usual activities | VIO-G-004 | 27/10/2015 | Slight stumble crossing street; corrected using walking stick |
| Usual activities | VIO-G-007 | 18/08/2015 | Tripped when foot caught in pavement crack |
| Usual activities | VIO-G-007 | 15/09/2015 | Stumbled when foot caught in staircase |
| Usual activities | VIO-G-007 | 13/10/2015 | Almost lost balance walking over wooden boards on flat’s veranda during refurbishment |
| Usual activities | VIO-G-007 | 07/01/2016 | Missed the bottom step while going down steps, almost twisting their ankle |
| Usual activities | VIO-G-008 | 26/08/2015 | Almost fell while lifting heavy quilt |
| Usual activities | VIO-G-008 | 15/10/2015 | Almost fell backwards while walking down stairs |
| Usual activities | VIO-G-008 | 26/11/2015 | Feet slipped getting into bath |
| Usual activities | VIO-G-009 | 05/08/2015 | Almost tripped on outside staircase |
| Usual activities | VIO-G-010 | 25/09/2015 | Shins became weak during stroll outside, so gently went down onto pavement in a controlled manner |
| Usual activities | VIO-G-022 | 18/02/2016 | Legs gave way; landed on all fours in a controlled manner |
| Usual activities | VIO-N-009 | 26/10/2015 | Tripped on pavement |
| Usual activities | VIO-N-015 | 06/07/2015 | Lost balance owing to dizziness; hit wardrobe |
| Usual activities | VIO-N-019 | 14/09/2015 | Overbalanced while locking front door; able to regain balance with aid of companion |
| Usual activities | VIO-N-026 | 06/10/2015 | Slipped on water; saved by daughter |
| Usual activities | VIO-N-026 | 06/10/2015 | Tripped on kerb; saved by daughter |
| Usual activities | VIO-N-029 | 08/10/2015 | Stumbled on pavement step |
| Usual activities | VIO-N-029 | 13/08/2015 | Tripped while climbing steps onto bus |
| Usual activities | VIO-N-032 | 15/11/2015 | Tripped on wet ground; saved by daughter |
| Type of fall | Intervention arm | Usual activities arm | Total | ||
|---|---|---|---|---|---|
| Baseline to first exercise class | After first exercise class | Randomised to intervention arm but attended no classes | After baseline date | ||
| Near miss, n (%) | 0 (0) | 4 (14) | 0 (0) | 24 (86) | 28 (100) |
Assessment of the feasibility to progress to a full trial
The agreed progression criteria to judge the feasibility of a definitive trial were:
-
Fifty per cent or more of VIOP eligible for the study are willing to be recruited into the feasibility study.
All but two of those VIOP found to be eligible by the researchers after screening against the inclusion/exclusion criteria were willing to be recruited into the study (66/68 = 97%); although a further two participants were later found to be ineligible, this criterion is judged to have been met. The exact number of potential participants approached by third-sector organisations was not available, but it is known that the number screened by the researchers is much lower than the number of potential participants initially contacted. We therefore feel that meeting this criterion does not reflect the difficulties encountered in recruiting participants to the study.
-
Seventy per cent or more of participants in the intervention arm have completed nine to 12 group sessions in the exercise programme (compliance).
Of the 33 participants randomised to the intervention arm in the trial, 25 (76%) attended between 9 and 12 exercise classes, so this criterion was met. A total of 10 participants (30%) attended all 12 classes, five (15%) attended 11 classes, five (15%) attended 10 classes and five (15%) attended nine classes. Of the eight participants not complying, three (9%) attended no classes. One of these withdrew completely from the trial; the remaining two did not. One participant (3%) attended two classes, two (6%) attended three classes before withdrawing from the intervention, one (3%) attended six classes before dying and one (3%) attended eight classes.
-
Data on key outcomes was collected at 6-month follow-up for ≥ 70% of those recruited.
Overall, 92% of those recruited provided questionnaire data at the week 24 follow-up visit, so this criterion was met. The response rate at week 24 was 85% for all scales in the intervention arm; responses were missing for the five participants who withdrew completely from the study. The response rate at week 24 was 100% for all scales in the usual activities arm; the exception to this was the emotional loneliness questionnaire – one participant did not complete this questionnaire, so the response rate was 97% for this item.
-
Fewer than 10% of SAEs were deemed to be caused by the intervention.
-
There were no SAEs deemed to be caused by the intervention, so this criterion is met.
-
Sample size for definitive trial
We had originally thought that the most appropriate primary outcome measure for a future trial would be FES-I, which measures concerns about falling. We experienced no difficulties in using this scale in the pilot study and so would recommend that it is used in future. Unfortunately, no work has been done to establish the minimum clinically important difference (MCID) for this scale, which is key to a calculation of required sample size. Therefore, indicative calculations have been done using standardised differences of 0.3, 0.4 and 0.5 SDs. A future trial of an exercise class intervention has the potential for the variation between those attending the same class to be smaller than that seen in patients in different classes or in the usual care group, where there is no group interaction. 83 The very small numbers in each class in this pilot study will not provide a reliable estimate of the ICC. Unfortunately, we were not able to obtain appropriate estimates of the ICC from other similar studies. Calculations have been done to show the sensitivity of the sample size estimates by assuming ICC values of 0.01, 0.03 and 0.05. When clustering in the exercise groups needs to be taken into account in the calculations, it is also important to specify the cluster size. After discussions with the stakeholder group, we planned to have exercise classes of no more than eight people, as they felt the visually impaired would need closer attention from the PSIs taking the classes. We found that there was a 15% dropout rate in the intervention group in this study by week 24, which would reduce the class size to seven by follow-up – this is therefore the number in the following calculations. Overall, the dropout rate was 8% across both arms; we have used this figure to work out how many participants need to be recruited to obtain the minimum numbers at follow-up. Note that when there is clustering in only one arm, it is more efficient to have unequal allocation to each arm, marginally increasing the sample size for clustering in the intervention arm. 83
The key parameters necessary to calculate the sample size of a future definitive trial are as follows:
-
type 1 error = 5%
-
power = 80% or 90%
-
MCID = 0.3, 0.4 or 0.5 SD
-
estimate of ICC = 0.01, 0.03 or 0.05
-
cluster size in intervention arm = 7
-
attrition rate = 8%.
Table 27 shows the necessary number of participants to be recruited for each combination of trial parameters.
| Specific trial settings | Sample size required | |||
|---|---|---|---|---|
| Power | Standardised difference in means | ICC | Intervention arm | Usual activities arm |
| 0.8 | 0.3 | 0.01 | 200 | 189 |
| 0.03 | 222 | 189 | ||
| 0.05 | 245 | 189 | ||
| 0.4 | 0.01 | 113 | 106 | |
| 0.03 | 125 | 106 | ||
| 0.05 | 138 | 106 | ||
| 0.5 | 0.01 | 72 | 68 | |
| 0.03 | 80 | 68 | ||
| 0.05 | 89 | 68 | ||
| 0.9 | 0.3 | 0.01 | 267 | 252 |
| 0.03 | 298 | 252 | ||
| 0.05 | 328 | 252 | ||
| 0.4 | 0.01 | 151 | 142 | |
| 0.03 | 168 | 142 | ||
| 0.05 | 185 | 142 | ||
| 0.5 | 0.01 | 97 | 91 | |
| 0.03 | 107 | 91 | ||
| 0.05 | 118 | 91 | ||
Summary of key points
-
The pilot trial was a crucial element of the feasibility study and identified several important issues for the planning of a future definitive trial.
-
The initial screening of potential participants was done by third-sector and NHS partners. Unfortunately, we were unable to collect data on the total numbers contacted at this stage.
-
Most expressions of interest came via the third sector, but staff/volunteers found this to be more time-consuming than anticipated and a future trial would need to consider how this could be supported.
-
The initial method of identifying potential participants by the research team from the Newcastle low-vision clinic was impractical. When the recruitiment source was changed to ECLOs, a small number of VIOP expressed an interest in the trial. The value of recruitment from NHS clinics in a future trial still needs to be considered.
-
The estimate of the proportion of those who met the eligibility criteria was biased upwards: a number of VIOP who had initially expressed an interest told the researchers before the eligibility criteria could be formally addressed that they were unable to take part.
-
Asking GPs to confirm that VIOP were eligible to take part in the study did not lead to a reduction in study numbers: only one participant was excluded by their GP.
-
A total of 64 VIOP were randomised to the intervention or usual care activities trial arms. We had aimed to recruit 80 VIOP. Recruitment was more difficult than anticipated, but this was mitigated by more complete data collection at follow-up.
-
Of the 33 participants in the intervention arm, three did not attend any exercise classes. The median number of classes attended was 10 (out of 12).
-
VIOP were encouraged to practise exercises for 120 minutes per week in addition to the exercise classes; the median achieved was 50 minutes.
-
We aimed to collect outcome data from a total of 60 participants at week 24. We collected outcome data from 59 participants. A total of 95% of trial participants provided data at the week 12 visit and 92% at the week 24 follow-up visit.
-
There were very low levels of missing data at baseline, week 12 and week 24 in both trial arms.
-
There was little or no evidence that exercise and attitudinal outcomes differed between trial arms at follow-up, but this must be interpreted with considerable caution given the small sample size. There were no SAEs deemed to be caused by the intervention.
Chapter 5 An exploration of participants’ views and experiences of the research process and intervention and their acceptability
As part of the evaluation of the VIOLET study, qualitative interviews were completed with two PSIs and nine VIOP who had completed the adapted FaME programme. The interviews were designed to capture the views of both those who delivered and those who took part in the exercise intervention. Findings were triangulated with those of the other data collection streams to explore the acceptability and feasibility of the intervention. This chapter reports on related literature, details the qualitative methodology, reports the findings and concludes with the identification of areas for discussion.
Background
A focused literature review was carried out encompassing falls prevention, VI and evaluation by older people of community-based exercise programmes. Few studies had been carried out with a specific focus on VIOP and falls prevention. There were a number of studies that had focused on older people’s views on falls prevention programmes. 84–91 Specific areas that had been linked to VI were physical activity92 and depression. 93 One review article explored the impact of particular VIs on falls13 and two examined the impact of falls on older people in general. 94,95 No articles were identified that specifically focused on the views of PSIs.
Three seminal papers89–91 set out the motivators for and barriers to older people’s engagement in, and continuation with, community falls prevention programmes. These centred on being interested in and enjoying the exercise process and were linked to being previously active, reduced levels of comorbidities and personal confidence levels. Participants expected to gain both physical and psychological benefits that would help maintain independence. Older people were also more likely to attend sessions if they had received a personal invitation from a health-care professional and gained approval from family and friends.
Barriers to engagement centred on the perception of falls risk. Many older people denied having a falls risk and felt that falls prevention programmes were not beneficial to them. 89 The perceived threat of falling and its potential consequences were not motivating factors. 91 Some older people felt that the advice given was ‘common sense’ and not relevant to them and that programmes were for the more disabled (feelings linked to their denial of a falls risk). 89,90 The studies also suggested that some older people felt that they were too ill or in too much pain or that exercising does more harm than good. 89
Some older people thought the engagement with falls prevention programmes would be a threat to their personal identity, eroding their personal autonomy. 90 These findings were corroborated in a study95 that found that older people were careful to present themselves as not the type to fall, constructing an identity of someone who was physically competent. The study participants perceived falling as negative and discrediting, leading to stigmatisation. This was further explored in a study94 that found that those living with falls spoke of losing confidence, independence and their social identity. These identity and autonomy issues were also highlighted in a qualitative synthesis on falls across the life course,96 in which the majority of the studies focused on older people’s perception of falling in later life.
The projection of a capable and competent person with a denial of their falls risk was also found in a study88 designed to promote uptake of and adherence to exercise-based falls prevention programmes. This study also explored the views of the physiotherapists who were involved in the delivery of the exercise-based falls prevention classes. Uptake was found to be positively influenced by a feeling of maintenance of independence and adherence through an approach that enhanced self-efficacy and self-management. In contrast, the physiotherapists were found to be paternalistic, suggesting that the older people were frail and vulnerable, and this conflicted with the older participants’ projected self-image. The findings suggested that falls prevention programmes and those delivering them should focus on self-management and autonomy and avoid being controlling and overprotective.
A further study84 described what motivated older adults to continue with community group-based exercises to prevent falls. The findings again linked motivation to staying independent and staying healthy. Success was linked to personal confidence, functional capability and the ability to stay in control. Poor balance and pain were highlighted as factors that limited motivation.
A qualitative study92 investigating physical activity and older people with sight loss found that the participants engaged with and enjoyed physical activity when it improved physical, mental and emotional health. Emotional and mental health benefits included meeting others and experiencing a feeling of camaraderie. Health benefits were tangible and described as weight loss and improved cardiovascular function. It was also noted that participants had a competitive edge, comparing their own progress with that of others. The participants felt that their ability to exercise was affected more by other comorbidities than by their VI, and it was suggested this may be a consequence of resilience acquired through developing coping strategies to manage their specific VIs. Other research focusing on the views of VIOP suggests that barriers to the uptake of exercise programmes may be perceived risk, stigma, lack of awareness among health professionals, lack of appropriate supporting materials and FoF. 97,98
Several studies86,87,89,96 have discussed older people’s lack of understanding and knowledge of the falls prevention programmes offered as a barrier to uptake. The conclusions drawn were the necessity to present the positive benefits of exercise programmes, better inform individuals of the benefits of specific exercises for falls prevention and ensure that information in whatever form is non-patronising. 90,95 Lack of engagement was also linked to a fatalistic acceptance that falls and declining health are inevitable in older age. 92,96,97 One paper13 reviewed the literature on visual loss and falls. It discussed the multifactorial nature of falls risk in older people and how visual input was required for coordination, planning movement and maintaining balance. The work focused on the common types of VI and how each may increase falls risk. For example, age-related macular degeneration (AMD) affects the central and reading vision, leaving the peripheral vision mostly unaffected, and this has an impact on the ability to navigate, with two-thirds of those affected having visual motor and balance deficits. Older women with AMD were shown to have more impaired balance, slower visual reaction times and poorer vision than age-matched control subjects.
In conclusion, the body of work reviewed identified facilitators of and barriers to community-based exercise programmes. There is very little research on falls and VI in later life. The majority of work focused on older people in general. The literature also suggests that specific types of VI may impact on physical activity in different ways and that older people do not consider their VI to be a major barrier to exercise.
Methodology
A qualitative methodology and methods enabled the researchers to gain insight into the views and feelings of those delivering the adapted exercise programme (the PSIs) and those who took part in the exercise programme (the VIOP).
Postural Stability Instructors sample
The three PSIs involved in the delivery of the adapted exercise programme were invited to take part in two interviews. Two of the PSIs agreed to be interviewed and were consented. One interview was completed prior to trial-specific training and the second was completed post delivery of the adapted exercise programme. Demographic data collected indicated that both PSIs had worked in the exercise industry for > 20 years and experience included cardiac rehabilitation, aqua-aerobics, athletics and falls prevention. Both had been qualified as PSIs for between 12 and 24 months and were currently delivering the FaME programme in the community setting.
Visually impaired older people’s sample
A pragmatic sampling strategy was utilised for the VIOP participants. Consent for the interviews was included in the original consent for the study. Interviewees were drawn from across all the cohorts of participants, the only additional inclusion criterion being completion of the adapted exercise programme. Wherever possible, the interviews were carried out within 2 weeks of the final exercise session. The final sample consisted of nine participants drawn from across both study sites (Table 28).
| Participant | Age (years) | Gender | Medical history (self-reported) | VI(s) (self-reported) | Degree of VI impact | Age at onset of VI (years) | Physical activity pre intervention | Type of activity |
|---|---|---|---|---|---|---|---|---|
| 1 | 62 | Male | Nil | Glaucoma | Light perception right eye, black blind left eye | Registered blind aged 40, problems started in 20s | Weekly session at local gym | Circuits |
| 2 | 68 | Female | Seasonal acquired depression | Macular degeneration | Central field loss, problems with glare, still reads | 66 | Weekly exercise class | Steps |
| 3 | 62 | Female | Diabetes | Diabetic retinopathy, retinal detachment, cataracts | Depth perception and glare | 27 | Five times per week | Running 5–10 km, spinning, Pilates |
| 4 | 76 | Male | Nil | Macular degeneration | Cannot read, central vision loss | Unknown | Sedentary | N/A |
| 5 | 73 | Male | Diabetes, stroke, osteoarthritis | Refractory problem, diabetic retinopathy, cataracts | Cannot read | 62 | Sedentary | N/A |
| 6 | 82 | Female | Osteoarthritis | Congenital glaucoma | Sees light and dark some shape perception | Birth | Daily joint exercises, weekly walking | Hand and foot exercises, walking around the block |
| 7 | 77 | Female | Hypercholesterolemia | Macular ischaemic retinal vein occlusion, cystoid macular oedema, cataracts | Right eye blind, left eye constantly blurred | 72 | Weekly exercise | Tai chi, swimming, walking |
| 8 | 91 | Female | Atrial fibrillation | Macular degeneration | Central vision loss, reads with magnifier | 85 | Weekly exercise | Yoga, swimming |
| 9 | 81 | Female | Osteoarthritis | Macular degeneration | Central vision loss, reads with magnifier | 75 | Weekly exercise | Line dancing class |
The average age of the participants interviewed was 75 years, ranging from 62 to 91 years, with three males and six females. There was a variety of VIs, with AMD being the most common. Others included glaucoma, diabetic retinopathy and cataracts. Three of the participants reported the onset of their VI between birth and the age of 27 years. The degree of self-reported impact differed across the participants and was dependent on the type of VI reported. Three of the participants classed themselves as blind (1, 6 and 7). Of the nine participants, seven were already exercising on a weekly basis and two described themselves as sedentary. There was wide variation in the type of regular physical activity undertaken, from gym/leisure centre sessions (circuits, steps, Pilates, swimming, yoga) to one person being a regular runner, competing in 5- and 10-km races with a sighted guide. In addition, there were participants who regularly walked in their local area and carried out exercises in the home.
Constituting a pragmatic sample, those interviewed appeared representative of the total sample of the study. Interviewing those who had experienced their sight problems for a long period of time enabled a longitudinal and reflective view to be expressed. The sampling of those more recently affected by their VI provided a view of personal adjustment, resilience and coping strategies.
As part of the evaluation process it had been intended to interview participants who withdrew from the exercise programme. The study had very few withdrawals, and those who did withdraw had clear physical reasons for doing so. Thus, no interviews were carried out with participants who had not completed the exercise programme.
Data collection
Data were collected from both groups (PSI and VIOP) through one-to-one interviews facilitated by the use of topic guides (see Appendix 2). The PSI interviews were structured and focused and the VIOP interviews were semistructured. All interviews were conducted at a mutually convenient time and place and were audio recorded and transcribed.
Postural Stability Instructor interviews
These were conducted by the lead qualitative researcher (DC) employed on the study. The interview, conducted prior to trial training, centred on previous experience, perception of the benefits of the programme and potential issues and views on any specific adaptations. These interviews were analysed prior to the second interview and the findings used to structure the post-delivery interview. The aim of the second interview was to revisit the views expressed prior to delivery, explore what adaptations the PSI may have made and seek recommendations for any future study. The PSIs were encouraged to make notes during the delivery of the adapted exercise sessions and bring these to the second interview as a prompt. This enabled the structured nature of the interview to be maintained.
Visually impaired older people interviews
These one-to-one interviews were conducted by the senior researcher at each study site (L de J and DC). Both researchers have experience of working with older people, including in their own homes. L de J is a physiotherapist and DC is a research nurse. It had been planned to carry out 10 interviews in total, five from each site. It became apparent during data analysis that one of the interviews had been completed using a different method and this was removed from the final analysis. Final analysis is drawn from the transcripts of nine interviews: four from the Glasgow site and five from the Newcastle site.
During the study, it was felt that more detailed information was required regarding the type of VI and the impact it had on the person. This was added to the topic guide and used as the opening area for discussion in all interviews. Additional areas explored were linked to the aims and objectives of the VIOLET study. Specific views were sought regarding reasons for participation and experiences of the research process, including randomisation and data collection. Further detailed views about the exercise sessions and the supporting information were obtained. Open-ended questioning was employed by the interviewers to encourage rich descriptions from the participants. Each interview drew to a close using an approach that enabled the participants to express any other thoughts and views they felt to be important to the research study.
Data analysis
Data analysis involved six steps: (1) organisations of data, (2) reading and memoing, (3) describing, (4) classifying, (5) interpretation and (6) representation. 98 An initial data analysis clinic was held with the interviewers, project manager and one of the PIs (L de J, DC, CB or DS). All transcripts were read and initial categories were identified, discussed and agreed by those present. These initial findings were further refined by the lead qualitative researcher (DC) and themes were produced. Themes were generated in alignment with the research objectives. As part of the data validation process the findings were presented to and discussed by the PAG.
Findings
Postural Stability Instructor pre-trial findings
Three themes were identified in the pre-trial interviews with the PSIs: prior experience, benefits and potential issues.
Prior experience
The PSIs had experience of working with VIOPs in what they referred to as the ‘mainstream’ setting. They were comfortable working with and adapting for people with multiple comorbidities.
Benefits
There was consensus that the adapted FaME programme would be beneficial to those taking part. It was expressed that improved balance, posture and stability would have a positive impact on personal confidence levels: ‘It’s a confidence builder, so people are holding on with two hands, one hand, no hands, so they are going through it nice and steady with build-up’ (PSI2).
Potential issues
Potential issues included six areas. The first area was gauging the ‘level of challenge’. The PSIs were uncertain if, and how, they would be able to progress the participants and linked this to safety issues, participant ability and level of comorbidity. The second area perceived as challenging was the ‘floor work’. This was described as backward chaining,99 in which a person is taught to get down on the floor and rise from the floor in a controlled and safe way. Both PSIs currently avoided the practice of backward chaining in their mainstream classes at the request of their employers (for safety reasons, it was suggested): ‘I’m going to have to read up on floor exercises ’cause as I say we don’t take them down, I haven’t done floor exercises since I qualified’ (PSI1). The third area included concerns around session delivery. The PSIs felt that it would be important to be descriptive, use clear, slow speech and set the room out with VI in mind: ‘I think there will need to be a lot more instruction, more detailed instruction’ (PSI1). The fourth area identified the ‘removal of lifelines’ such as walking aids, sticks/canes and potentially guide dogs as an area of concern: ‘taking walking aids away, lifelines, some might not like you to take their walking aid away (PSI2). There were also expressions of fear of offending and patronising the participants (the fifth area): ‘I’m worried that I offend someone . . . my fear is patronising somebody’ (PSI2). In the final (sixth) area, the PSIs were concerned about what would happen to the participants at the end of the study and if alternative exercise sessions would be offered.
Postural Stability Instructor postdelivery findings
Four main themes were identified: level of challenge, adaptations, home exercise and recommendations. Each theme contained a number of areas.
Level of challenge
A number of areas were suggested by the PSIs to have an impact on the level of challenge that VIOP found appropriate in the exercise sessions. The PSIs discussed that the progression of some participants was hindered by functional ability and comorbidities. This meant that it was challenging to intensify the exercises for more ‘able’ participants as those less physically able were unable to sustain longer periods of intensive exercise. This, they felt, had an impact on the efficacy of the exercise sessions:
There was huge variance in functional capacity, with some really frail, so trying to individualise and really challenge, I personally wasn’t used to that big difference in functional ability. We just need to make sure we challenge them more.
PSI1
Other comorbidities – ‘deafness’, ‘arthritis’ and ‘breathlessness’ – had a greater impact than VI on the delivery of the sessions: ‘I found it very very hard if you had hearing [impairment] and visual [impairment] going on’ (PSI2). Floor work proved problematic as not all participants wished to engage in this activity. The PSIs suggested that during this activity an additional person who had training in and awareness of the moving and handling of persons should be present to assist. ‘Psychological problems’ were also cited – for example, participants compared themselves with others and felt they ‘should be better’ (PSI2). This led to frustration and reduced motivation and appeared to impact on mood. This occurred most frequently when carrying out the dynamic balance exercises:
If the others are marching away no problem and the others have to sit down for some time, they are the ones that would feel like they are holding the class up. It is the ones with more health issues that would feel like they are holding the class up . . . why can’t I be the same as them, I shouldn’t be in this class, I can’t do that, it’s just their way of thinking, I’m holding it up.
PSI2
Adaptations
In relation to the theme ‘adaptations’, PSIs confirmed that a continuous commentary was necessary but that it proved to be more work than they had anticipated. It needed to include what was happening in and around the exercise room, such as who was entering and exiting: ‘every single detail has to be talked through and you have to do it week on week . . . I always said who was in the room’ (PSI1). Using personal forenames enabled the participant to know when comments were directed at them. Strategies were needed to enable voice recognition so that the participants were aware of who was in their vicinity: ‘we did a lot of talking so we’d get to know each other’s voices’ (PSI1). This was also linked to the layout of the room, particularly as different VIs allowed degrees of sight in different ways. For example, participants with AMD retained some peripheral vision so preferred to sit towards the end of rows to ‘see’ the instructor when they were demonstrating. It was also desirable for the PSI to use big gestures and wear clothing that contrasted with the background/room colour.
There were minimal safety issues and the key issue was the need to start the dynamic balance exercises at the same time. Where this did not happen, it led to participants walking into the back of each other and potentially tripping up: ‘When we do the dynamic balance, it is really important that everyone starts at the same time’ (PS1).
The PSIs were clear that no specific exercise had been adapted for the VIOP. Adaptations were in delivery style. They did feel that they were more ‘hands-on’ than in their mainstream classes and described a need to touch the person and place them in the correct positions to enable the pace of the sessions to be maintained: ‘The exercises were as FaME, but there was more hands-on for me, so touching bringing the hands closer together’ (PSI2). The continued need for ‘anchor points’ – that is, solid reference points in the room for participants during the exercise sessions – were noted (PS1). For most this was a chair and for some this helped with their balance; for all it was beneficial to have a reference point to go from and return to.
Home exercise
‘Home exercise’ included the booklet and audio aids given to the participants to facilitate this component of the exercise programme. The study team produced a large-print booklet and audio recording to aid the home exercises. Along with diagrams of the exercises, the team had also added prompts to suggest where and when the exercises could be carried out. The PSIs felt the booklets and audio were useful, although the ordering of the exercises could be changed to better reflect the structure of the sessions. One suggestion was to incorporate the exercises into a story that could be followed by the participants. It was also felt that additional technology could be used, as some participants were unable to operate the audio CD provided. It had been noted that for participants who may have had some memory issues, the home exercise component had not been successful. It was thought that these participants forgot to engage in the home exercise:
We found within the homework book a lot didn’t have readers at home, or they didn’t have CD players to play, or they had dementia and they forgot to do it.
PSI2
Recommendations
Modifications to study processes and the exercise programme were offered. A strong recommendation was that VIOP could and should be integrated into the mainstream falls prevention setting: ‘I couldn’t see any reason why those people couldn’t be in a big group, a mainstream group, I would not segregate them’ (PSI2). The PSIs also suggested that to aid challenge and efficacy, mirroring some mainstream settings, the participants could be stratified by functional ability: ‘you might have something like, level 1 and level 2 and have some sort of functional assessment that you would do at the beginning, then we could really push people’ (PSI1). The addition of another exercise professional would also aid the floor work element, which again would improve challenge and efficacy:
Taking them to the floor, you would certainly need someone strong enough to get them up. I think you need a second person for your frailer people in case there is a fall and if we are taking them to the floor, you need a second person to help someone up if they get stuck, if you are taking them to the floor definitely a second person.
PSI1
The PSIs also felt that the use of stronger TheraBands® (Akron, OH, USA) would have increased challenge and that advice could have been given during the quality assurance processes to increase the overall challenge for the more able participants:
A lot of them progressed very quickly through the bands; we could have done with stronger bands. Going forward more guidance on what exercises to do, what is more beneficial . . . I felt I hadn’t worked them hard enough.
PSI1
Finally, the PSIs discussed the positive impact of the social element of the sessions and suggested that this could be extended and additional information could be given during this time: ‘They liked the social and the bit chat, some of them wouldn’t have come out if it wasn’t for the group’ (PSI2).
From a personal perspective, the PSIs felt that the quality assurance processes used in the study had acted as continued professional development and that this could be replicated in the mainstream exercise setting:
It was good [quality assurance process] and I think it should be done in mainstream, because I think you get a bit lax and you carry on the same old and you are not progressing people and you really need to progress them.
PSI1
Visually impaired older people findings
Four main themes were identified from the interviews with the VIOP who had completed the exercise sessions: reasons for participation, research process, exercise classes and home exercise. These corresponded to the interview topic guide, which was formulated with alignment to the study objectives and any additional findings that emerged from across the data (Table 29). Each of these themes contained areas drawn from within the data. Unless otherwise stated, the findings presented did not differ across the two sites.
| Themes | |||
|---|---|---|---|
| Reasons for participation | Research process | Exercise (class and home) | Self-perception |
| Codes | |||
| Altruism | Fair | Challenge | Independent |
| Progression | |||
| Maintenance | |||
| Usefulness | Understanding/perception | Benefits | Risk free |
| Curiosity | Data collection | Right person? | |
| Relevance | |||
| Subjectivity | |||
| Self-help | Social | ||
| Comparison | Technology | ||
| Falls prevention | Additional person | ||
| Space | |||
Reasons for participation
Altruism was the most common reason for participation, with an expressed desire to be ‘useful’. Additional reasons given were ‘curiosity’, ‘anything to help myself’ and to compare themselves with others who had VIs:
I felt if I could take part in the trials and if that helped somebody else prevent a fall or help the research, then at least I was contributing something back to society. If I can do something to help somebody else, then at least I’ve achieved something.
Participant 1
I’m keen to see how I react within another group of people with a similar disability . . . see how I compare with how other people manage and different degrees of visual impairment.
Participant 3
Two people noted the specific focus on falls prevention and described having had falls in the past. Neither linked their falls to their VI; one suggested it was a balance problem and the other did not know why they had fallen.
Research process
The participants felt the research process and in particular the randomisation was fair. They understood the methodology and knew that should they be randomised to the control/usual activities arm, they would be offered an equivalent exercise programme at the end of the study period. Only one participant suggested they may have withdrawn if they had been allocated to the usual activity arm.
Participants thought that more data were going to be collected on their VI and its impact on their daily activities: ‘questions pertaining more to how my visual impairment affects my life’ (participant 3). There was a perception that the study was more about VI than falls prevention and, therefore, more information should have been collected regarding the VI.
There was discussion regarding the relevance of some of the questionnaires and questions asked, in particular the QoL, anxiety and depression sections. It was felt that some questions were not suited or relevant to an older population. Some of the participants discussed the subjectivity of the questionnaires and how responses could change depending on individual mood on the day of collection:
I don’t think life fits into a tick box thing . . . I don’t see the relevance in that . . . so how accurate is that? . . . it’s just a rough gauge.
Participant 3
What was going through my head was if you’d asked me yesterday I would be down there, if you ask me that today the answer is there . . . so it depends on the day, and it depends on how you are that particular day.
Participant 2
Exercise classes
Four of the participants felt the programme did not physically challenge them and expressed an understanding of ‘exercise’ as something that should be physically demanding and require effort. They would not have continued on the programme should it have been offered after the study period had ended:
I didn’t find the exercises required any effort as such, but it encouraged me to take up the chance of this thing [referring to a more challenging exercise programme] where you’re really working yourself for that hour.
Participant 4
I think they were too easy; I think they could have been developed more. I think I would be speaking for every adult my own age, and beyond, that would like something a bit more . . . a bit more lively.
Participant 2
Linked to this was a perception that the ‘benefits’ gained from attendance, for some, were limited. Benefits were identified as tangible, such as weight loss and increased strength:
I have no ambitions to be Mr Universe again, but surplus fat; I want[ed] to get rid of it.
Participant 4
I decided to go to the study for the muscle part, you know, to build muscle.
Participant 2
Participants did not feel they had an increased risk of falling and, although enjoyable, they did not feel they gained personal benefit from the exercises, although acknowledging that others deemed less frail might do so:
I think the person that thought the whole project up was a real diamond, there were people who had worse sight than me, and it must have helped them a lot more, to get around and keep themselves safe in the house.
Participant 5
Some participants questioned if they were the ‘right’ person to be taking part in the exercise sessions:
I thought I was a bit too young to be there. I think if I have known what it was all about when I applied I don’t think I would have applied.
Participant 4
I just thought, I didn’t fall about much before and I don’t now . . . I feel that I’m not the right sort of person to be doing it.
Participant 8
The positives of the exercise programme were ‘increased balance and confidence’, ‘learning something new’, ‘pitched just right’ and ‘clear and well delivered’. The participants singled out the resistance exercises with the Thera-bands as being the most useful, linked to a feeling of ‘physically’ doing some exercise: ‘I got benefit from them ‘cause I can go upstairs quite quickly now, I measure it by how many stairs I can walk without stopping’ (participant 6).
Three participants had sought out further exercise: one did more strenuous exercise during the intervention period; the other two had begun classes once the study exercise sessions had ceased.
In agreement with the PSI interviews, one participant also suggested that an additional person would be needed for those with multiple comorbidities: ‘The likes of anyone who’s had a stroke that needed a bit more help, that was a bit more infirm’ (participant 3). Participants also agreed that space was important, space to feel comfortable with enough room to feel free: ‘You need to know that you’re free to move about and you’ll not bump into the person next to you’ (participant 2).
Home exercise
Most felt the home exercise component was difficult to maintain, linked to a lack of motivation while ‘on your own’ and the limitations of ‘space’ in the home. Motivation dropped markedly once the exercise sessions had finished:
It’s soulless when you are doing that in the house on your own . . . because there’s a fun element in the class, and there’s a bit of banter, and a cup of tea.
Participant 2
I think in the group situation you are more likely to get on and do them, you are less likely to do them in the home situation.
Participant 6
Participants suggested that, although the booklets provided were useful, they should be available in different modalities [screen reader, voice synthesiser, MP3, Digital Accessible Information System (DAISY) talking book, Braille]. For some the audio CD was too fast, which made it difficult to follow. One participant unable to use the audio CD sent the booklet to a relative, who rang each day to read and describe the exercises over the telephone. In agreement with the PSIs, it was also suggested that the order of the exercises in the booklet should correspond to those performed in the sessions.
There was general agreement that the social interaction gained from both study staff and fellow participants was very enjoyable. The social time at the end of the exercise sessions was viewed by most as very pleasurable. Participants agreed with the PSIs and suggested this aspect could be longer and include elements of information on broad health and well-being subjects:
I think if people are a bit isolated because of the visual impairment or physical disability that affects them a lot, their confidence . . . And I think to bring them out and get them mixing is a huge step for them.
Participant 3
Go a bit broader in chat time, in social time, give them a topic for the week you know, like do you know you might be eligible for a taxi . . . then another week, do you know you can have special treatment on the train.
Participant 7
Two participants expressed an ambivalent view, stating that they would have happily attended the sessions if the social time had not been included.
Self-perception
This was a complex cross-cutting theme. It appeared to influence the views and perception of the participants and was linked to the projection of an independent, risk-free person. The participants felt that their VI was not a hindrance to taking part in the research or the exercise sessions. They suggested they had ‘readjusted already’. These views were linked to a desire to ‘fight age and disease’.
One participant expressed the view that they did not like the use of the word ‘old’ in the title of the research. Another did not like being escorted to and from the taxi when arriving at the venue, feeling this was ‘overprotective’. Fatalistic views were expressed about their health and falls risk. This was linked to the perception that they were too fit for the exercise sessions and were not the ‘right’ type of person to be taking part in the research. There was a reluctance to admit to having a falls risk, and when this was admitted, it was suggested it was an expected part of ageing. The majority of the participants suggested that this project should have been aimed at those more at risk than themselves.
In keeping with the evaluative process, two overarching descriptive themes were drawn from the data. These were facilitators of and barriers to participation (Table 30).
| Evaluative overarching themes | |
|---|---|
| Facilitators of participation | Barriers to participation |
| Being useful | Self-perception and image |
| Relevance | Lack of relevance to person |
| Accessible additional information | Lack of tangible benefits |
| Social interaction | Paternalism |
| Familiar venues | Multiple comorbidities |
| Aid with transport | |
| Building of relationships | |
Facilitators of participation
The main facilitators already identified include usefulness, relevance, additional information (booklet and CD) and social time.
Additional facilitators were venue, transport and relationships (staffs and other participants). Both venues were accessible to visually impaired people and already known to the majority of participants. This was one thing less to ‘worry’ about. Taxis to and from the venues were also appreciated, particularly for those reticent to engage with using public transport: ‘I don’t use public transport at all, when I did go on public transport I had to stop every bus that came along to see where it was going, if it wasn’t the right one I was embarrassed’ (participant 5).
On the whole these participants were already utilising taxi transport for journeys. One participant did not feel the fare reimbursement was necessary: ‘Going there, getting there was no hardship, fiver in a taxi, but you did insist on paying half the time, there was no need for it’ (participant 5).
Those who did not use the taxi transport travelled to the venues by public transport, this being free through the local bus pass schemes.
Participants suggested that although the exercise sessions may not have been challenging, they completed the programme ‘for the study staff’. They did not want to withdraw as they thought this would reflect in a negative way on the research staff. The participants had enjoyed the visits and telephone calls from the research staff and the weekly telephone call became part of their weekly routine:
You and the ladies have a job to do, and I felt that if I skipped it wasn’t myself I was letting down, I was offending other people.
Participant 4
I would know at 10 o’clock there was a phone call coming from [name], it was nice, I would know on Monday I would get a call.
Participant 6
Barriers to participation
It was evident that the participants felt that they had been asked to take part in research focusing on VI. Even those who had previously had a fall did not fully engage with or fully understand the falls prevention aspect of the study. Participants were unsure how the specific exercises were of benefit to them. The overall feeling was that they were not the ‘right’ people to have taken part in the research but continued with it, as the social time was enjoyable and they did not want to ‘let down’ the research team. A limited number of participants also felt that at times the research processes had been paternalistic and detracted from their independence.
Conclusion
The qualitative evaluation of the VIOLET study indicates a number of discussion points.
-
Volunteering for the research project and the exercise programme was primarily driven by an altruistic desire to be useful and contribute to wider society. Although the exercise sessions may not have been as some had expected, the wish to be helpful, fulfil their commitment and have social interaction promoted retention. As noted within other studies96 it is likely that simply volunteering for the study is indicative of these participants having high personal confidence and being resilient problem solvers.
-
The perceived relevance of the exercise intervention acted as both a facilitator of and barrier to participation. It was linked to understanding of the research and the relevance of the information being collected. Where there was a limited understanding or misunderstanding and where relevance was not felt to be strong, the participants suggested this detracted from both the research process and the exercise sessions. Had more information been given on the types of exercise and the benefits of strength and balance exercises, the participants may have been able to see the relevance of this specific exercise programme more readily. However, it may be the case that 12 weeks of sessions was not sufficient for the majority of participants to report tangible benefits.
-
Participants wanted to present themselves as persons who were active, fit and not at risk of falls. There is thus a need to review falls prevention programmes to take into account the use of language and actions that directly challenge self-perception by including an education component to the programmes. Participants’ self-portrayal of not being at increased risk of falling was supported by low falls risk scores.
-
Interviewees would have liked more information to have been collected about their VI and its impact on daily life; this had already been noted by the research team and added to the interview topic guide. In future studies it may be beneficial to address what appears to be an imbalance between the perceived falls risk and the impact of VI on that risk.
-
Like the PSIs, the VIOP also suggested that for less physically able participants it would be beneficial for a second person to assist with the floor work element of the exercise sessions. Further consideration across the mainstream community falls prevention setting is warranted.
-
The participants liked the home exercise information, although access could be improved by both offering a wider range of information technology modalities and enabling participants to progress at their own pace. This could be achieved by providing audio material that can be easily paused, revisited and generally modified to individual preference. Participants suggested formats such as DVD, DAISY, screen reader, voice synthesiser, MP3, talking book and Braille.
-
In agreement with a body of research, home exercising was hard to sustain, particularly once the 12 weekly group classes were completed. Participants missed the peer support, camaraderie and overall social contact. There were also some cognitive (memory) issues and it seems that, in this setting, the home exercise component could not be relied upon to make up the total exercise time required to achieve efficacy.
-
Almost all participants suggested that the social time at the end of the classes was very enjoyable and participant and PSI interviewees suggested that this could be lengthened and may provide a platform for an informal sharing and exchanging of broad health information. This should be considered in further research.
Participants reported that they did not like being referred to as ‘older people’ or considered as ‘old and frail’. It is suggested that such programmes are termed as ‘facilitating independence’ in a community-based sample and may include other aspects such as support and education in addition to an exercise component.
Chapter 6 Health economic analysis of the adapted exercise programme
A prospective economic evaluation was rehearsed to develop and refine methods for a subsequent definitive trial. The main focus was on how to identify, quantify and value accurately the additional costs of delivering the intervention and the potential resource implications versus usual ‘activity’ and also on which measurement tools are appropriate to use with VIOP. The costing approach was initially a broad analytical perspective (NHS, social services and patient/carer costs) to potentially help to detect cost shifting between sectors. The resources used in the exercise group were identified as additional equipment (capital outlay), staff time and consumables. Resource use in terms of out-of-pocket expenses was also explored for all participants in addition to all treatment/care related to the intervention and any falls that may have occurred during the study period. This was assessed retrospectively at the two follow-ups (week 12 and week 24) by piloting the use of a falls resources/expenses form (to include informal caregivers’ time). This was to potentially facilitate the development of a reliable and valid tool to capture resource use. Appropriate unit costs applicable to resource use were identified and sourced from a combination of local costings and national databases. Methods to value informal carer time were also explored and defined.
Methods to estimate an incremental cost-effectiveness ratio for exercise versus usual care in terms of quality-adjusted life-years (QALYs) were rehearsed (using EQ-5D-5L and ICECAP-O administered at baseline and at weeks 12 and 24). In particular, issues relevant to sensitivity analysis were explored to help understand how best to deal with statistical imprecision and other uncertainties in the full trial. The justification for using both EQ-5D-5L and ICECAP-O was that, although it is known that performance on the EQ5D of patients with visual disorders is mixed, it is not known if the EQ-5D-5L instrument is better. This is a rationale for utilising the five-level instrument in this population. Furthermore, there is no current evidence regarding the validity of EQ-5D-5L compared with ICECAP-O in older adults with VI. One study has recently investigated how falls risk, cognitive function and daily function are associated with health-related quality of life (HRQoL) (using the EuroQol-5D) and QoL (using the ICECAP-O) among older adults with mobility impairments. 80 It found that both the EQ-5D-5L and ICECAP-O are reliable and valid markers of falls risk, general balance and mobility, with ICECAP-O capturing more key indicators of impaired mobility and cognitive function. However, to date there has been no comparison of validity of these instruments for use in an older population with VI specifically. The lack of evidence in this population group is therefore a strong rationale for using both instruments with no additional costs to the project.
Methods for health economics and cost-effectiveness
The main focus of the study was on how to identify, quantify and value accurately the additional costs of delivering the exercise programme and the potential resource implications versus usual care.
The study collected data on the use of services within the health-care system, social care costs and patient and carer costs in an attempt to capture relevant components that constitute the overall costs from a health and social services perspective both with and without an exercise programme. Key items included data completeness and the costs of the control and experimental interventions.
Costs
Identification and measurement of resource use
Participants in the usual activities arm did not receive any interventions as part of the trial. It was therefore assumed that the resource use and associated costs would be zero.
The costs associated with the exercise intervention were micro-costed and estimated on a per-patient basis for those in the intervention arm of the trial. The intervention, an adapted exercise programme, was provided at two sites, with a different provider at each site [Later Life Training Ltd (LLT) at Glasgow and HealthWORKS at Newcastle]. The intervention costs comprised three components: staff time associated with their training and delivery of the intervention; the cost of room hire including participant refreshments; and the cost of consumables required for intervention delivery. Each patient received a 12-week exercise programme (one 1-hour session per week). In terms of staff time, each session was supervised by a PSI. Consumables included exercise bands, yoga mats, CDs and DVDs.
Resource use in terms of out-of-pocket expenses and all treatment/care related to the intervention and any falls that occurred during the study period was explored for all participants. This was assessed retrospectively at the two follow-ups (week 12 and week 24) by piloting the use of a falls resources/expenses form (to include informal caregivers’ time) collected by the researcher by telephone. This captured the frequency of use of primary care, community-based health and social care services, secondary care and costs borne by family and carers as a result of having a fall. Primary and community care resources included general practice and home visits from GPs, nurses (visits to a practice nurse at the surgery and district nurse visits in the home), physiotherapists and OTs. Secondary care resources included inpatient stays, accident and emergency (A&E) visits and outpatient visits. Informal caregiving time comprised average time per week spent by family and/or friends helping participants with activities that they would have usually been able to undertake if they had not had a fall. Furthermore, participant out-of-pocket expenses were also captured.
An NHS and personal social services perspective was adopted for the costing component of the feasibility study.
Valuation of NHS and informal caregiving resource use
For each trial participant, all components of treatment costs stratified by category of resource use were computed by multiplying units of resource use by their unit costs. These were then summed over all resource use categories to obtain a total cost for each participant from both an NHS and personal social services perspective. This was then used to generate the average cost per patient in each arm of the trial.
The unit costs for resources used for the costs of the exercise programme were mainly obtained from the VIOLET feasibility study records. This included costs of consumables from the manufacturers and staff time from each of the providers. Unit costs for the health and personal social services used by participants in relation to any falls were obtained from a range of sources including the Personal Social Services Research Unit’s Unit Costs of Health and Social Care 2015100 cost compendium and National Tariff Payment Systems 2014/15. 101 All unit costs were expressed in Great British pounds and valued at 2015–16 prices.
Effectiveness
Health-related quality of life: EuroQol-5 Dimensions, five-level version
In line with NICE recommendations,102 outcomes in the economic analysis were identified and measured using a multiattribute utility measure: EQ-5D-5L. 79 This was used to collect information about participants’ HRQoL at baseline and 5 and 12 weeks post discharge. Both instruments allow HRQoL to be valued on a scale where perfect health and death are 1 and 0 respectively. The values for each health state were obtained from the UK population valuation sets for the two instruments.
The EQ-5D-5L is the generic, multiattribute, preference-based measure preferred by NICE for broader cost-effectiveness comparative purposes. The EQ-5D consists of two principal measurement components. The first is a descriptive system, which defines HRQoL in terms of five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Responses to each of these dimensions are divided into five ordinal levels: no problems, slight problems, moderate problems, severe problems and unable to/extreme problems – generating a total of 3125 possible health states. Index-based values (‘utilities’) are a major feature of the EQ-5D instrument, facilitating the calculation of QALYs that are used to inform economic evaluations of health-care interventions. The responses to the EQ-5D-5L questionnaire were transformed using a standard algorithm to produce a health state utility score at scheduled intervals during the follow-up for each participant in each of the treatment groups. 103
Quality of life: ICECAP-O
We assessed QoL using the ICECAP-O. 104,105 The ICECAP-O is a short five-item multiple-choice questionnaire that measures an individual’s overall QoL according to the following five attributes: attachment (love and friendship), security (thinking about the future without concern), role (doing things that make you feel valued), enjoyment (enjoyment and pleasure) and control (independence). Each domain has four possible options. The ICECAP-O measure covers attributes of capability found to be important determinants of QoL among older adults in the UK; its descriptive system results from an extensive qualitative investigation. The value system for the ICECAP-O provides a single summary score, anchored at zero (‘no capability’) and 1.0 (‘full capability’), for each state described in terms of the five attributes.
Reporting and presenting results
Within the economic analyses, the mean cost of the intervention across the two sites was estimated. Mean differences and 95% confidence intervals (CIs) were not calculated for resource use and associated NHS and personal and social services costs as the number of missing follow-up data rendered it too imprecise and unreliable to do so (see Missing data costs). Utilities were estimated and reported for each trial arm using means, SDs, the median and the range. Furthermore, mean differences in utilities by trial arm and 95% CIs were estimated.
Results
Missing data costs
Five patients withdrew from the study (including one death), leaving a potential sample size of 59 (28 in the intervention arm and 31 in the usual activities arm). Data regarding the intervention and the associated costs were fully recorded. Missing data issues arose following a fall in which all NHS and personal social services were recorded over two follow-up periods (week 12 and week 24) using a participant self-reported falls resources/expenses form (including informal caregivers’ time). There were 20 participants who experienced one or more falls and a total of 31 falls over the duration of the study. Of these, 17 (55%) were in the intervention group and 14 (45%) were in the usual activities group.
However, in terms of NHS and social care resource use, only six participants were recorded as utilising health and social care interventions, and only one of these (a visit to a GP) could be verified. Three patients suggested that they had received an emergency outpatient appointment, but gave no details of the type of clinic attended so it is not clear if this was an A&E attendance, a visit to an ambulatory care service or another service. One patient reported a visit to a GP and a subsequent visit to hospital but no details of the care were provided, for example whom they saw or what interventions, if any, they received. Finally, one participant recorded a secondary care admission to hospital but provided no detail of the type of admission. Personal costs incurred by each trial participant, including informal caregivers’ time, were not included for analysis because of the unreliability of the data. There was uncertainty regarding the units of informal caregivers’ time that participants reported and over what time period; therefore, it was decided that these data were too imprecise to utilise. Two participants had data recorded for utilising informal carers’ time but data on how much time they received were missing. Furthermore, there were no recorded privately incurred costs for any trial participant regarding informal care use. Owing to the quality of the data received regarding use of health and social care resources, informal carers and out-of-pocket expenses, it was decided not to include these costs in the analysis.
Missing data: EuroQol-5 Dimensions, five-level version
There were no missing data for the EQ-5D-5L HRQoL measure with 28 complete responses in the intervention arm and 31 complete responses in the usual activities arm for baseline and both follow-up periods.
Missing data: ICECAP-O
There was one missing data point at baseline for a participant in the intervention arm. This was for the security (thinking about the future without concern) attribute only, with full data recorded for this participant for every other attribute at baseline and both follow-up periods. As part of the complete case analysis this participant was excluded, leaving 27 participants in the intervention arm and 31 in the usual activities arm.
Costs
Costs of exercise intervention
The total cost of providing the exercise intervention was calculated and the average intervention cost per patient across both sites was calculated by dividing the total costs by the number of patients in the intervention arm of the trial by site (n = 14 in both Newcastle and Glasgow sites) and then taking an average of the two mean costs per site. The costs of providing the intervention are detailed in Table 31.
| Resource use | Cost (£) | Unit | Source |
|---|---|---|---|
| Costs of consumables | |||
| Yoga mats and exercise bands | 420.00 | Total cost | VIOLET study files |
| DVDs and CDs | 65.00 | Total cost | VIOLET study files |
| Costs of staff time | |||
| Newcastle PSI (12 sessions × 3 cycles) | 66.66 | Per hour | HealthWORKS |
| Glasgow PSI (12 sessions × 2 cycles) | 61.50 | Per hour | LLT |
| Glasgow PSI set-up time (0.5 hours per session for 24 sessions) | 30.75 | Per 30 mins | LLT |
| Glasgow PSI travel and parking costs (per session) | 7.24 | Per session | LLT |
| Costs of room hire and refreshments | |||
| Newcastle (3 × 12-week cycles) | 1925.00 | Total cost | HealthWORKS |
| Glasgow (2 × 12-week cycles) | 1476.00 | Total cost | Visibility |
The total costs of consumables were split between the two sites equally at £243. The costs of room hire and refreshments differed according to site as this was provided by different organisations with different rates for room hire. The total staffing cost of the exercise intervention at the Newcastle site was based on the delivery of three cycles of the intervention and was £2400. Staff in the Glasgow site were paid £61.50 per hour for the provision of the intervention; in addition, they were paid for half an hour of their time to set up and conduct administrative duties related to the intervention. They were also paid £7.24 for travel and parking expenses for each session delivered. Total staff costs based on two cycles at the Glasgow site amounted to £2388.
The total cost of intervention delivery for three cycles at the Newcastle site was £4568. Based on a sample of 14 study participants in the intervention group across each of the three cycles, the average cost per participant was calculated at £326. The total cost of intervention delivery at the Glasgow site for two cycles of the intervention was £4107. Based on a sample of 14 study participants in the intervention group across two cycles, the average cost per patient was calculated at £293. The average total cost of the intervention per participant across both sites was £310.
Effectiveness
EQ-5D-5L: health-related quality-of-life utility scores
All 59 participants completed the EQ-5D-5L at baseline and the two follow-ups. Therefore, there were no missing data. Table 32 shows the EQ-5D-5L utility scores for both trial arms at baseline and each of the two follow-up periods. Results show that for both treatment groups at baseline, EQ-5D scores indicate a state worse than death, with the health state being worse in the intervention group. However, an independent-sample t-test was performed and found no evidence of a statistically significant difference in mean utility scores between the two study arms.
| EQ-5D-5L utility scores | Intervention arm (N = 28) | Usual activities arm (N = 31) | Mean diff (95% CI) | Significance | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Range | Mean (SD) | Median (IQR) | Range | |||
| Baseline | –0.23 (0.25) | –0.25 (0.39) | 0.83 | –0.15 (0.24) | –0.19 (0.18) | 1.15 | –0.08 (–0.20 to 0.05) | 0.23 |
| Week 12 | –0.2 (0.22) | –0.2 (0.29) | 0.78 | –0.12 (0.27) | –0.15 (0.35) | 0.95 | –0.05 (–0.21 to 0.05) | 0.25 |
| Week 24 | –0.21 (0.27) | –0.26 (0.47) | 0.90 | –0.06 (0.28) | –0.09 (0.43) | 1.14 | –0.15a (–0.30 to –0.01) | 0.04 |
Utility scores at the week 12 follow-up were higher in the control group than in the intervention group, with the difference not statistically significant at the 5% level, but both groups showing an improvement compared with baseline. However, average utility values in both arms still suggest a state worse than death. At the week 24 follow-up, utility was again higher in the control group than in the intervention group with the difference statistically significant at the 5% level. Compared with baseline the utility scores improved for both groups but still showed average HRQoL scores as being in a state worse than death. The range of utility scores and the associated CIs were much larger in the usual activities arm than in the intervention arm with more observations showing positive HRQoL.
ICECAP-O: quality-of-life scores
ICECAP-O QoL capability scores at baseline, and at the week 12 and week 24 follow-ups are presented in Table 33.
| ICECAP-O capability scores | Intervention arm (N = 27) | Usual activities arm (N = 31) | Mean diff (95% CI) | Significance | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Range | Mean (SD) | Median (IQR) | Range | |||
| Baseline | 0.79 (0.14) | 0.84 (0.22) | 0.46 | 0.77 (0.12) | 0.77 (0.2) | 0.43 | 0.02 (–0.05 to 0.08) | 0.59 |
| Week 12 | 0.8 (0.11) | 0.82 (0.13) | 0.46 | 0.80 (0.13) | 0.83 (0.19) | 0.48 | 0 (–0.07 to 0.06) | 0.89 |
| Week 24 | 0.8 (0.14) | 0.83 (0.14) | 0.67 | 0.78 (0.15) | 0.82 (0.24) | 0.54 | 0.01 (–0.07 to 0.09) | 0.83 |
The capability score in the intervention arm was slightly higher in the intervention than in the usual activities arm at baseline but the difference between average scores was not statistically significant at the 5% level. At week 12, capability was slightly higher, with both groups having an average of 80% capability.
At week 24, capability was maintained at an average of 80% in the intervention arm, with a slight reduction in the usual activities arm (78% capability). There were no statistically significant differences in average scores between the trial arms at both follow-up periods.
Summary
The current feasibility study has shown that, although it is possible to collect most of the data necessary for a full cost-effectiveness analysis of the exercise intervention compared with usual care (cost of intervention per se, utility values and capability values), there were some practical issues in accessing information regarding participant self-reporting of resource use post intervention. Participant inputs on use of health and social care services and broader service use were often missing, despite telephone calls by researchers. The data collection instrument for this was the participant self-reported falls resources/expenses form (including informal caregivers’ time). This was based on a series of open-ended questions as it was initially thought by the study team that carers filling out the form would find these types of questions easier to respond to. However, the reality of this form of data capture was that it was not clear in the absence of recorded information whether data were missing or participants had not actually received any formal care. Furthermore, detail of the type of care was also lacking, rendering any estimation of costs of the use of health and personal social care resources impossible. The use of a more structured, previously piloted, data collection tool may have mitigated against some of these issues. Regardless of the design of the data collection tool, it is well documented that reliance on patients/carers as a data collection method is limited by biases in recall, nonresponse and evasiveness. 106 Furthermore, missing data are a common problem for economic evaluations that run alongside clinical trials107 and may be mitigated in a future study by either postal or telephone reminders to participants.
The HRQoL scores showed that participants in both arms of the trial at all time points were in a health state worse than death. However, capability scores were towards the high end of being capable. Perhaps this should not be surprising as the ICECAP measures potentially offer a broader assessment of QoL and well-being than measures routinely used in economic evaluation such as the EQ-5D-3L. 108 This broader assessment may allow measurement of the full effects of an intervention or treatment. Previous research has indicated that the ICECAP-O and EQ-5D-3L measures provide complementary information and are not substitutes for each other. 80 The same may be true for the EQ-5D-5L; however, this is not currently addressed in the literature.
-
Costs of intervention delivery in terms of staff time were cheaper at the Newcastle site than at the Glasgow site. The Newcastle site ran three cycles of the intervention whereas the Glasgow site ran two; however, recruitment to the intervention arm was the same at both sites.
-
There were no missing data for the EQ-5D-5L instrument. Compared with baseline, the utility scores improved in both groups but still showed average HRQoL as being in a state worse than death. Overall, at all three data collection points HRQoL was higher in the usual activities group than in the intervention group.
-
All participants completed the ICECAP-O instrument with the exception of one who failed to complete one domain at one time point. Capability scores differed minimally across trial arms at each of the follow-up times. Furthermore, in both trial arms, there was little difference between average scores from baseline to week 24. Capability scores ranged from 77% to 83% across the two trial groups.
Chapter 7 Discussion, conclusions and recommendations for future research
The following discussion and summary is structured around the study objectives and also considers the underpinning patient and public involvement in the study at all stages. The objectives are presented in accordance with the phases of the study. The feasibility of progressing to a full trial is discussed, along with recommendations for factors that need to be taken into account. Implications for practice are also discussed.
Patient and public involvement
There was patient and public involvement at all stages of the study from inception to completion and dissemination and various methods allowed the participants to contribute to all stages of the study. Of the stakeholder VIOP members (14 participants across the two sites), four expressed an interest in participating in the PAG and attended meetings. We also invited study participants from control and intervention groups to participate in a VIOLET study feedback session in December 2016 to share our findings, elicit their feedback and invite their opinion on next steps. Throughout the duration of the study we also had close contact with our Vision charity partners and, following the launch of the study (hosted by NSBP and with VIOP stakeholders present), we produced a press release announcing the study’s intent to work closely with VIOP to adapt a validated falls prevention programme (FaME) to their needs. This was endorsed by both Visibility – our Glasgow site vision charity partner – and the study PAG representative from the RNIB.
Additionally, the participation and membership of the PAG enabled VIOP to provide valuable input at all stages of the research regarding design, recruitment, adaptation of the intervention and dissemination. Participants also reviewed study materials and made recommendations for both content and presentation of the participant information sheet and Plain English summary.
An exploration of visually impaired older people’s ability to act as lay partners in a study to develop a condition-appropriate intervention (objective 1)
In the first phase of the study, the use of focus groups facilitated VIOP to express individual intervention preferences and needs, such as PSIs being specifically trained to accommodate differing functional and visual needs. There was also a strong preference for a range of choices in the way VIOP engage with home exercise and with the completion of outcome measures, such as the use of weekly telephone calls. The feasibility study enabled VIOP to contribute to the adaptation and design of an acceptable community-based group exercise programme that could be incorporated into a general falls prevention exercise programme.
Visually impaired older people stakeholders also offered guidance on adapting the FaME intervention to maximise uptake and adherence for VIOP. No matter how effective an intervention is, if participants cannot or do not want to engage with it, it is effectively useless. The participant qualitative interviews elicited experiences of undertaking the intervention, which identified many valuable insights into facilitators of and barriers to exercise participation, and highlighted the role of self-perception that underlies exercise participation behaviour.
Assessment of recruitment of visually impaired older people and their willingness to be randomised (objective 2)
Although the study did not recruit the target figure, we feel that the recruitment strategy was largely effective, subject to modifications and suggestions outlined. Variation in the way participants were identified across the two study sites has led to some discrepancies in the recording of eligibility for the study. For participants who had expressed interest in the study, assessment of eligibility was guided by research staff. However, the recruiting organisations did not keep a record of how many initial contacts they made to produce the expressions of interest. Anecdotally, we are aware that > 300 direct contacts (telephone or letter) were made to potential participants, which converted to 105 expressions of interest. For a future study, the recruiting organisations would need to commit to keeping an accurate count of contacts.
Overall, recruiting from third-sector organisations was successful; however, there were lessons learned. Both third-sector recruitment organisations (NSBP and Visibility) identified large numbers of members who they felt would be eligible. These did not convert to actual participants. Organisational feedback suggested that the conversion rate from initial contact to expression of interest was poor. Unfortunately, at this point, we did not collect ‘reason’ for decline, which is needed to fully evaluate the recruitment strategy from this source. In addition, one of the third-sector organisations was able to provide a dedicated member of staff for recruitment whereas the other was not. Identification of potential participants was therefore more burdensome to the third-sector organisations than expected. Furthermore, the available samples from the organisations at Newcastle and Glasgow have now been exhausted and a future study would need to recruit from other sources and sites. In future multisite studies a recruitment strategy should be discussed and agreed across recruiting organisations with additional resource and support for these organisations. It is possible that, in future, a local council register of people who have VI could also be used, as proposed by the recommendations of the VIP2UK study. 11
It proved difficult to recruit from the Newcastle NHS site – the RVI low-vision clinic. Ophthalmologist/optician staff were not always best placed to recruit from within busy and fast-paced outpatient clinics. The RVI is the regional centre of excellence, with many of those attending living outside the Newcastle area and too far away to travel to the classes provided for the intervention group. In a future study, it may be advisable to use the primary care setting with the dual purpose of GP-led assessment of health exclusions and recruitment. Previous research suggests that a ‘personal’ invitation by a health-care professional increases uptake of community exercise classes. 109
On the other hand, the ECLOs based at the RVI were committed to the study, had meetings with the study team from the outset and were able to dedicate a member of staff to identify potential participants and pass on expressions of interest. This recruitment strategy was very successful with a conversion rate of nearly 50%. That said, a lack of accurate data in the pre-screening phase makes it difficult to quantify initial contacts made by the ECLO. In future studies, more information is needed on the pre-screening phase to better articulate commitment/resource requirements. There was no recruitment from the Glasgow Caledonian University eye clinic owing to the summer vacation and we acknowledge that there is a need to take into account the ‘working time’ of all potential recruitment sites.
The impact of GP assessment was negligible as only one participant was screened out on grounds of health according to the inclusion/exclusion criteria.
Only two of those originally found to be eligible for the study declined to take part in the pilot trial. A further two subjects were lost to the study before randomisation as other exclusion criteria came to light. Therefore, we consider this objective to have been successfully achieved.
Delivery of visually impaired older people-appropriate Falls Management Exercise falls prevention intervention and production of manualised intervention (objectives 5, 6 and 8)
A key component of the VIOLET study was the successful delivery of the VIOP-adapted FaME programme by HealthWORKS in Newcastle and Visibility in Glasgow, led by PSIs. The PSIs had established experience of delivering falls prevention intervention programmes in the NHS, including FaME. For each cohort, quality assurance checks were performed, ensuring fidelity of the programmes at both sites. We recommend for future studies that participating PSIs should have an opportunity to attend two workshops, to share and discuss findings regarding successful delivery of the intervention, and that quality assurance is maintained to ensure fidelity.
Guidelines recommend 36 hours of exercise per falls prevention exercise programme; over the 12 weeks of participation, this equates to a total of 3 hours per week. However, VIOLET study participants had a mean time of 110 minutes per week: 50 minutes spent on home exercise and 60 minutes on the weekly group exercise intervention. Both the VIP and VIP2UK studies11,49 reported poor adherence to the home exercise component, although the VIP study suggested that stricter adherence was associated with fewer falls. 49 VIP2UK attempted to increase adherence to home exercise but was not successful. 11 Furthermore, some studies suggest that a 12-week intervention comprising 36 hours of exercise may not provide sufficient balance and strength work to reduce falls. 62 However, as noted earlier, we took a pragmatic approach to what is achievable in order for NHS or local authority-led falls services to be encouraged to adopt the adapted VIOP FaME approach. Research suggests that, on average, falls services across the UK deliver sessions once a week for eight to 12 weeks. 27,60 We strongly support continued development of strategies to increase adherence to home exercise for future studies so that an effective exercise dose is delivered.
Delivery also highlighted the need for an additional exercise professional to support participants with multiple comorbidities such as deafness and assist with the floor work element. In addition, a variable range of participant ability within the exercise classes led to some participants reporting not being physically challenged, which was endorsed by the instructors.
Importantly, VIOP themselves suggest that other comorbidities, such as shortness of breath, may have greater impact on their ability to exercise than their VI. The PSIs did not change the exercise components; rather, they modified their delivery style to the needs of VI in the adapted FaME programme. In their post-intervention interviews, both VIOP and PSIs felt that the majority of VIOP could be integrated into mainstream community classes, which should be stratified by functional ability to address the issues of challenge identified in the interviews by both participants and PSIs. Only those with multiple comorbidities would not be able to be integrated and this would occur in mainstream classes anyway. These individuals should continue to be offered one-to-one exercise interventions as appropriate.
Visually impaired older peoples’ recommendations for the adaptation of FaME delivery and experiences from the perspectives of the PSIs for more effective delivery in future, have been incorporated into the full manualised intervention of the adapted FaME intervention (a copy of this is available from the VIOLET project page on the NIHR website; see www.journalslibrary.nihr.ac.uk/programmes/phr/1218107/#/).
An exploration of visually impaired older people’s reasons for participating in the adapted Falls Management Exercise programme and acceptability of the exercise programme and trial procedures (objective 7)
Volunteering for the study was primarily driven by altruism. Participants expressed a desire to be helpful, fulfil their commitment and enjoy social interaction with other participants, which ultimately promoted retention. Simply volunteering for the study is indicative of these participants having high personal confidence and being resilient problem solvers. 110 Participant interviews also highlighted that interviewees would have liked more information collected regarding their VI and its impact on daily life. In future studies it may be beneficial to address what appeared to be an imbalance between the perceived falls risk and the impact of VI on this risk.
Some participants suggested that they did not understand the relevance of specific exercises. Had more information been given on the types of exercise and the benefits of strength and balance exercises, the participants may have been able to understand the relevance of this specific exercise programme. However, it may be the case that 12 weeks of exercise classes was not sufficient for the majority of participants to notice tangible benefits. Indeed, echoing related studies with VIOP28,31 many of our participants self-presented as active, fit and not at risk of falls or being a ‘faller’. The self-description of ‘not a faller’ was also supported by the falls risk scores, suggesting on the whole that these participants had a low falls risk. A future study should perhaps ensure that those who are at risk of a fall are recruited, as falls services often have the inclusion criterion of a previous fall or distinct FoF.
Self-perception as ‘not a faller’ was common and, as is often highlighted in related literature,40,41 participants also reported a dislike of being described as ‘older people’ or considered as frail. Falls prevention programmes need to emphasise facilitating independence in a community-based sample as well as other positive benefits, such as socialising and receiving useful health education, in addition to the exercise component. In this feasibility study, participants in the intervention group were slightly more afraid and more likely to avoid activity at the end of exercise classes. However, the difference was much smaller at week 24. It is possible that the classes warn people about falling, which initially makes them more likely to avoid activity, and this is well supported in the literature. 111 Conversely, research also highlights how, for some participants, there could be an increase in falls during the initial phase of increasing exercise. 109,111
Home exercising was hard to sustain, particularly once the 12 weekly group classes were completed: this concords with other research. 11,49,111 Although participants were encouraged to exercise for a further 2 hours per week, the median was reported to be 50 minutes per week. Participants missed the peer support, camaraderie and overall social contact. There were also some cognitive (memory) issues and it seems that, in this setting, the home exercise component could not be relied upon to make up the total recommended exercise time. Perhaps one consideration is the ability to attend more group sessions in a week rather than rely on home exercise. Almost all of the participants suggested that the social time at the end of the classes was very enjoyable. Participant and PSI interviewees suggested this could be lengthened and may provide a platform for an informal sharing and exchanging of broad health information. This, as a recommendation, should be considered in further research.
Similar to the PSIs, the VIOP interviewees highlighted that for less physically able participants it would be beneficial for a second person to assist with the floor work element of the exercise sessions. The participants liked the home exercise information, although access could be improved by both offering a wider range of information technology modalities and enabling participants to progress at their own pace. This could be achieved by providing audio material that can be easily paused, revisited and generally modified to individual preference. Participants suggested DVD, DAISY, screen reader, voice synthesiser, MP3, talking book and Braille formats. This area would require further attention should the study progress to a RCT.
Identification of candidate outcome measures for a future randomised controlled trial (objective 3)
The completion rates of the outcome measures were very high. We aimed to collect outcome data from a total of 60 participants at week 24; we collected outcome data from 59 participants. A total of 94% of trial participants provided data at week 12 and 92% provided data at week 24. This was probably due to the completion of the outcome measures with the researchers. Although this resulted in a high completion rate, it is noted that this was very time-consuming for the researchers and that this would need to be considered in future studies. The primary potential (FES-I) provides an assessment of falls risk. In our sample, falls risk was generally low to moderate and thus we did not recruit high-risk fallers for whom the exercise programme may have been more beneficial. This could therefore be used in subsequent studies to stratify participants both in practice and for the purpose of data analysis. The MCID of the FES-I is not known, and thus it was possible to carry out only an estimated sample size calculation based on standardised differences. The measures were acceptable to participants and not perceived to be onerous. The HADS is validated for use in the older population and assesses anxiety, a key predictor of FoF. However, the relevance of some of the QoL questions in the HADS were questionable to the older population. In general, our VIOP took longer to perform the TUG time/functional ability assessment than that reported for healthy community-dwelling subjects aged 65–84 years. 112 Future trials with this population should consider an assessment that is not so reliant on vision. For example, the short physical performance battery is a group of measures that combines the results of gait speed, chair stand and balance tests, although this also requires some vision for safety. 113 It is also suggested that additional outcome measures such as those that assess frailty may be included for this population to provide an indication of whether or not exercise is maintaining levels of resilience even if it does not lead to an improvement. This may be more appropriate and realistic for an older population with many comorbidities. This is a suggestion that may also be useful for assessment in mainstream falls prevention programmes. Further, a longer follow-up period of 12–18 months would also be recommended in future studies, in accordance with related findings. 113
Feasibility of collecting data for health economic analysis (objective 9)
There is evidence to suggest that it is feasible to collect service-use data for an economic evaluation of the intervention in a future RCT, although there were some challenges. It is possible to collect most of the data necessary for a full cost-effectiveness analysis of the exercise intervention compared with usual care (cost of intervention per se, utility values and capability values); however, participant inputs on use of health and social care services and broader service use were often missing owing to the data collection instrument (falls resources/expenses form). It was not clear, in the absence of information recorded, if data were missing or participants had not actually received any formal care. Furthermore, detail of the type of care was also lacking, rendering any estimation of costs of the use of health and personal social care resources impossible. The use of a more structured, previously piloted, data collection tool with either postal or telephone reminders to participants may have mitigated against some of these issues. This could potentially be completed more often to improve recall and accuracy. In addition, processes that allowed access to the required information from the primary medical source may have negated the issue.
The data completion rate was almost 100%. The HRQoL scores identified that some participants in both arms of the trial at all time points were in a health state worse than death. However, capability scores were towards the high end of being capable. The ICECAP-O potentially offers a broader assessment of QoL and well-being than measures routinely used in economic evaluation such as the EQ-5D-3L. This broader assessment may allow measurement of the full effects of an intervention or treatment.
Methodological implications and sample size calculation for future trial (objective 4)
Within the VIOLET feasibility study there was no assessment of VI. This was largely a pragmatic decision; however, we recommend assessment of VI in future studies. Assessment of VI would perhaps have allowed us to stratify VIOP participants, identifying those who might be able to join a mainstream class and those who would require one-to-one intervention or more intensive supervision. The inclusion criteria did not allow screening out for ‘deafness’. People who are profoundly deaf and have a VI are difficult to accommodate in a group setting. The assessment of whether or not potential participants were ‘physically able to take part in a group exercise class’ was, on the whole, carried out when face to face and thus open to individual interpretation. This was also the case when assessing a participant’s ability to walk indoors and outdoors with or without aid. We found that the majority of participants had only low to moderate concern about falling and did not report high levels of anxiety. We would therefore recommend assessment of falls risk in a future study along with assessment of VI.
A number of potential participants ‘self-reported’ an uncontrolled medical condition as a reason for exclusion. There is a need to think about what a potential participant considers to be an uncontrolled medical condition and the degree of concordance with a GP. These issues would be negated to some degree if recruitment was carried out in primary care and assessment was carried out by a GP rather than by a participant or a researcher (who might not be medically trained), although our method replicates current practice in falls services.
The PSIs also suggested stratification by functional ability and some participants discussed not being physically challenged within the exercise classes. Mixing able and less able participants has an impact on the challenge and potential effectiveness of the programme. It is recommended that stratification by functional ability is considered in a definitive trial.
If the same method of recruitment was used in a definitive trial, it would be necessary to allow for a staggered start to the exercise classes to compensate for delays in GP confirmation of eligibility and to maintain timely enrolment into the exercise sessions.
As outlined in Chapter 4, sample size calculations were performed to provide a sample size for varying combinations of trial parameters. For example, at 80% power, a MCID of 0.5 SD, an estimated ICC of 0.01, a cluster size of 7 and an attrition rate of 8%, 72 participants would be required in the intervention group and 68 in the usual activities group. However, this could rise to requiring 328 participants in the intervention group and 252 in the usual activities group if the power was 90%, the MCID was 0.3 SD and the ICC was 0.05.
Does the feasibility study indicate that a full trial should be conducted?
The criteria to determine the feasibility of progressing to a full trial were all met (see Chapter 3); that is, ≥ 50% of VIOP eligible for the study were willing to be recruited into the feasibility study; ≥ 70% of the participants in the intervention arm completed 9 out of 12 group sessions in the exercise programme (compliance); data were collected on key outcomes at the 6-month follow-up for ≥ 70% of those recruited; and, finally, < 10% of SAEs were deemed to have been caused by the intervention itself.
This suggests that this pilot study could be taken to a full study. However, recommendations from the VIOP and the PSIs and discussion within the PAG, trial management group (TMG) and TOC suggest that most VIOP could be integrated into a mainstream class. Training [Continuing Professional Development (CPD)] of PSIs to accommodate a range of VIOP in their mainstream sessions is minimal and easy to facilitate through online training, so would be affordable and have sustainable reach. Only those with multiple comorbidities (such as extreme deafness or extreme frailty) required significantly more supervision. Mainstream classes can be much larger, so, if an elderly person with VI was to join a mainstream class, an extra supervisor may be necessary and should be considered, particularly if the participant’s VI necessitates the adaptations to teaching suggested by the PSIs (e.g. touch, fuller description of the room and the people in it).
However, if a future study were to recruit those more at risk of a fall, those with more defined and limiting VI and those who are not already active in exercise sessions, our recommendations might be different. Should this progress to a future study, these inclusion/exclusion criteria should be refined and recruitment rates may differ.
Limitations
The following limitations were identified:
-
The sample typically exhibited low to moderate falls risk. The programme would have benefited high-risk fallers and these should be targeted for recruitment in future studies.
-
Recruitment proved difficult and we did not recruit the originally planned sample of 80 participants, though retention was better than anticipated.
-
It is possible that there was bias by having the weekly telephone call, which may have acted like an intervention in itself.
-
We recruited only English-speaking participants as one of the exclusion criteria for the trial was being unable to comprehend or follow simple movement instructions in English (in the event that they were randomised to the intervention arm).
-
There was no assessment of VI.
-
The missing data for the health economic evaluation could have been mitigated by the use of previously piloted instruments for data capture.
Conclusions and recommendations for future research
It was possible to recruit and retain participants to the VIOLET study and adapt an existing, widely used exercise intervention for falls prevention (FaME) with VIOP as stakeholders. In future multisite studies, a recruitment strategy should be discussed and agreed across recruiting organisations. It is suggested that recruitment from primary care practices and use of a local register, as proposed by the VIP2UK study,11 should be considered for a community-based intervention.
The intervention was delivered successfully at two sites. Adherence to the study was high with very low attrition rates. This is a strength of the study.
Whereas guidelines recommend 36 hours of exercise per falls prevention exercise programme over the 12 weeks of participation, VIOLET study participants had a mean time of 110 minutes per week: 50 minutes of home exercise and 60 minutes of the weekly group exercise intervention. It is possible that this would be insufficient to bring about any improvement; however, whether exercise had little impact or halted deterioration was not investigated in the VIOLET study. This is an important consideration for future research. Adherence to and duration of exercise is a key consideration in any exercise programme and this should therefore be a critical focus in any future study. Furthermore, PSIs referred to the level of challenge of the exercises for some of the participants, suggesting that there should be stratification based on ability. It is recommended that participating PSIs should have an opportunity to attend two workshops to share and discuss findings regarding successful delivery of the intervention.
Home exercising was hard to sustain, particularly once the 12 weekly group classes were completed. Thus, the home exercise component could not be relied on to make up the total recommended exercise time. The use of technology as prompts may assist in future studies, as may the option, as suggested by the stakeholder panel, for participants to attend multiple groups in a week. Participants enjoyed the social time at the end of the classes, with participant and PSI interviewees suggesting that this could be lengthened and may provide a platform for an informal sharing and exchanging of broad health information. As some participants did not understand the relevance of the exercises and the impact of exercise in maintaining resilience and halting deterioration, it is suggested that the provision of information is also an important part of the exercise intervention. This, as a recommendation, should be considered in further research.
The outcome measures were suitable to assess the study variables and had a high level of completion with very little missing data, with 94% of trial participants providing data at week 12 and 92% providing data at week 24.
Although the progression criteria were met, the following points have been suggested for a future trial.
-
A future definitive trial should consider stratification of participants with low, moderate and high falls risk.
-
There should be an assessment of VI.
-
Recruitment sources could include primary care practices and involve the multidisciplinary team.
-
Non-participants should be interviewed to explore their reasons for not participating.
-
The social element of the exercise programme could be expanded to include an education component addressing the benefit of the exercises to maintain and improve levels of physical and functional ability and thus reduce falls risk.
-
The development of strategies to increase physical activity and structured exercise at home should be explored to reach recommended levels of activity.
-
For the economic evaluation, there should be a resource-use questionnaire that utilises more closed-ended and focused questions, and this should be administered at more time points. This may improve recall and accuracy.
-
Other hard to reach groups could be targeted in future to participate in the FaME programme.
It is concluded that mainstream programmes for falls prevention could be adapted to incorporate VIOP; interviews suggested that it is the delivery style and logistics of attending venues rather than the nature and type of the exercises that is a barrier to participation in exercise programmes. Stratification according to falls risk and functional ability are recommendations of the study. The adapted FaME programme, which has previously published evidence of effectiveness, was found to be both safe and acceptable to participants.
Acknowledgements
We would like to thank Dr Mike Clarke, Consultant Ophthalmologist at the Newcastle Hospitals NHS Foundation Trust, Reader (Ophthalmology) at Newcastle University and Principal Investigator for the study NHS site, for his support with NHS low-vison clinic recruitment and clinical overseeing of the study’s SAEs.
We are especially grateful to Mima Cattan, Emeritus Professor of Public Health, Northumbria University, for her early steer and pioneering development of this study.
The project would not have happened without the tremendous commitment of our participants, to whom we give our sincere thanks. We very much valued the expert advice and feedback we received from the members of the VIOLET study TOC, chaired by Dr Chie Wei Fan. We would like to thank members of the study’s advisory group for their invaluable input and the two organisations, Visibility and the NSBP, for their support in shaping the project and in recruitment. Finally, we thank the study’s PSIs, Vivienne Thompson (HealthWORKS, Newcastle) and Allison Sampson (LLT, Visibility, and Glasgow) for the delivery of our intervention.
This project was funded by the National Institute for Health Research, Public Health Research Programme (project number: 12/181/07).
Contributions of authors
Nicola Adams, Professor of Rehabilitation, was the Chief Investigator, took overall responsibility for the study and the writing of this report.
Dawn Skelton, Professor of Ageing and Health, as Principal Investigator for the Glasgow site of the study, contributed to the design of the study, led on the production of the adaptation of the FaME intervention manual and contributed to the report.
Cathy Bailey, Senior Research Fellow in Ageing, project managed the study and contributed to its design and the writing of the report.
Denise Howel, Senior Lecturer, Statistics, contributed to the design of the study and conduct of the trial, managed the analysis and interpretation of the quantitative and statistical results and co-drafted relevant sections of the report.
Dorothy Coe, Senior Research Assistant, qualitative research, managed the Newcastle site data, co-analysed the qualitative data and produced the qualitative findings chapter.
Rosy Lampitt, Trials Manager, and Jennifer Wilkinson, Senior Trials Manager, both of the Newcastle Clinical Trials Unit, contributed to the design of the study and managed the conduct of the trial, and Rosy Lampitt contributed to the report.
Tony Fouweather performed the statistical analyses and co-drafted the statistical results chapter.
Lex D de Jong, Research Associate and physiotherapist, research managed the Glasgow site, co-analysed the qualitative data and contributed to the report.
Sheena Gawler, Research Assistant at the Newcastle site, managed quality assurance and contributed to the intervention manual and this report.
Vincent Deary, Associate Professor of Psychology, contributed to the design of the study, led on the patient and public involvement and drafted the PPI chapter.
Joanne Gray, Senior Lecturer, Health Economics, contributed to the design of the study, conducted the health-economic analysis and drafted the health-economic analysis chapter.
Heather Waterman, Professor of Nursing and Opthalmology, contributed to the design of the study and the report.
Steve W Parry, Consultant Physician and Clinical Senior Lecturer, contributed to the design of the study and the report.
Publications
Adams N, Skelton DA, Howel D, Bailey C, Lampitt R, Fouweather T, et al. Feasibility of trial procedures for a randomized controlled trial of a community based group exercise intervention for falls prevention for visually impaired older people: the VIOLET study. BMC Geriatrics 2018;18:307.
Skelton DA, Bailey C, Howel D, Cattan M, Deary V, Coe D, et al. Visually Impaired OLder people’s Exercise programme for falls prevenTion (VIOLET): a feasibility study protocol. BMJ Open 2016;6(Suppl. 8):e011996. https://doi.org/10.1136/bmjopen-2016-011996
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. Exclusive use will be retained until the publication of major outputs.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Evans JR, Fletcher AE, Wormald RP, Ng ES, Stirling S, Smeeth L, et al. Prevalence of visual impairment in people aged 75 years and older in Britain: results from the MRC trial of assessment and management of older people in the community. Br J Ophthalmol 2002;86:795-800. https://doi.org/10.1136/bjo.86.7.795.
- Brouwer D, Sadlo G. Limitations in mobility: experiences of visually impaired older people. Br J Occup Ther 2008;71:414-21. https://doi.org/10.1177/030802260807101003.
- Salive ME, Guralnik J, Glynn RJ, Christen W, Wallace RB, Ostfeld AM. Association of visual impairment with mobility and physical function. J Am Geriatr Soc 1994;42:287-92. https://doi.org/10.1111/j.1532-5415.1994.tb01753.x.
- Ivers RQ, Cumming RG, Mitchell P, Attebo K. Visual impairment and falls in older adults: the Blue Mountains Eye Study. J Am Geriatr Soc 1998;46:58-64. https://doi.org/10.1111/j.1532-5415.1998.tb01014.x.
- Klein BE, Moss SE, Klein R, Lee KE, Cruickshanks KJ. Associations of visual function with physical outcomes and limitations 5 years later in an older population: the Beaver Dam eye study. Ophthalmology 2003;110:644-50. https://doi.org/10.1016/S0161-6420(02)01935-8.
- Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci 1998;53:M112-9. https://doi.org/10.1093/gerona/53A.2.M112.
- Gleeson M, Sherrington C, Lo S, Key L. Can the Alexander Technique improve balance and mobility in older adults with visual impairments? A randomised controlled trial. Clin Rehabil 2015;29:244-60. https://doi.org/10.1177/0269215514542636.
- Lamoureux EL, Chong E, Wang JJ, Saw SM, Aung T, . Visual impairment, causes of vision loss, and falls: the Singapore malay eye study. Invest Ophthalmol Vis Sci 2008;49:528-33. https://doi.org/10.1167/iovs.07-1036.
- Lord SR, Smith ST, Menant JC. Vision and falls in older people: risk factors and intervention strategies. Clin Geriatr Med 2010;26:569-81. https://doi.org/10.1016/j.cger.2010.06.002.
- de Boer MR, Pluijm SM, Lips P, Moll AC, Völker-Dieben HJ, Deeg DJ, et al. Different aspects of visual impairment as risk factors for falls and fractures in older men and women. J Bone Miner Res 2004;19:1539-47. https://doi.org/10.1359/JBMR.040504.
- Waterman H, Ballinger C, Brundle C, Chastin S, Gage H, Harper R, et al. A feasibility study to prevent falls in older people who are sight impaired: the VIP2UK randomised controlled trial. Trials 2016;17. https://doi.org/10.1186/s13063-016-1565-0.
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006;35:ii37-ii41. https://doi.org/10.1093/ageing/afl084.
- Dhital A, Pey T, Stanford MR. Visual loss and falls: a review. Eye 2010;24:1437-46. https://doi.org/10.1038/eye.2010.60.
- Lamoureux E, Gadgil S, Pesudovs K, Keeffe J, Fenwick E, Dirani M, et al. The relationship between visual function, duration and main causes of vision loss and falls in older people with low vision. Graefes Arch Clin Exp Opthalmol 2010;248:527-33. https://doi.org/10.1007/s00417-009-1260-x.
- Painter JA, Elliott SJ, Hudson S. Falls in community-dwelling adults aged 50 years and older: prevalence and contributing factors. J Allied Health 2009;38:201-7.
- American Geriatrics Society and British Geriatrics Society . Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148-57. https://doi.org/10.1111/j.1532-5415.2010.03234.x.
- Parry S, Bamford C, Deary V, Finch T, Gray J, MacDonald C, et al. Cognitive-behavioural therapy-based intervention to reduce fear of falling in older people: therapy development and randomised controlled trial – the Strategies for Increasing Independence, Confidence and Energy (STRIDE) study. Health Technol Assess 2016;56:1-206. https://doi.org/10.3310/hta20560.
- American Academy of Orthopaedic Surgeons Panel on Falls Prevention . Guideline for the prevention of falls in older persons. J Am Geriatr Soc 2001;49:664-72. https://doi.org/10.1046/j.1532-5415.2001.49115.x.
- Heinrich S, Rapp K, Rissmann U, Becker C, König HH. Cost of falls in old age: a systematic review. Osteoporos Int 2010;21:891-902. https://doi.org/10.1007/s00198-009-1100-1.
- Age UK . Falls in the Over 65s Cost NHS £4.6 Million a Day 2010. www.ageuk.org.uk/latest-press/archive/falls-over-65s-cost-nhs/.
- Steinman B, Nguyen A, Pynoos J, Leland N. Falls-prevention interventions for persons who are blind or visually impaired. Res Pract Vis Impairment Blindness 2011;4:83-91.
- Boyce T. Falls – Costs, Numbers and Links with Visual Impairment. London: Royal National Institute of Blind People; 2011.
- Gillespie L, Robertson M, Gillespie W, Sherrington C, Gates S, Clemson L, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2009;9. https://doi.org/10.1002/14651858.CD007146.pub2.
- Gates S, Fisher J, Cooke M, Carter Y, Lamb S. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta-analysis. BMJ 2008;336:130-3. https://doi.org/10.1136/bmj.39412.525243.BE.
- Falls: the assessment and prevention of falls in older people. Clinical guideline [CG21]. NICE; 2004.
- National Service Framework for Older People. London: Department of Health and Social Services; 2001.
- Lamb S, Gates S, Fisher J, Cooke M, Carter Y, McCabe C. Scoping Exercise on Fallers’ Clinics. London: NIHR; 2007.
- Brundle C, Waterman HA, Ballinger C, Olleveant N, Skelton DA, Stanford P, et al. The causes of falls: views of older people with visual impairment. Health Expect 2015;18:2021-31. https://doi.org/10.1111/hex.12355.
- Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist 2002;42:17-23. https://doi.org/10.1093/geront/42.1.17.
- Grue E, Finne-Soveri H, Stolee P, Poss J, Wergeland L, Rbye S, et al. Recent visual decline-a health hazard with consequences for social life: a study of home care clients in 12 countries. Curr Gerontol Geriatr Res 2010. https://doi.org/10.1155/2010/503817.
- Campbell S. Deteriorating vision, falls and older people: the links. Glasgow: Visibility; 2005.
- Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008;37:19-24. https://doi.org/10.1093/ageing/afm169.
- Logghe IH, Verhagen AP, Rademaker AC, Bierma-Zeinstra SM, van Rossum E, Faber MJ, et al. The effects of Tai Chi on fall prevention, fear of falling and balance in older people: a meta-analysis. Prev Med 2010;51:222-7. https://doi.org/10.1016/j.ypmed.2010.06.003.
- Zijlstra GA, van Haastregt JC, van Eijk JT, van Rossum E, Stalenhoef PA, Kempen GI. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing 2007;36:304-9. https://doi.org/10.1093/ageing/afm021.
- Zijlstra GA, van Haastregt JC, van Rossum E, van Eijk JT, Yardley L, Kempen GI. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc 2007;55:603-15. https://doi.org/10.1111/j.1532-5415.2007.01148.x.
- Austin N, Devine A, Dick I, Prince R, Bruce D. Fear of falling in older women: a longitudinal study of incidence, persistence, and predictors. J Am Geriatr Soc 2007;55:1598-668. https://doi.org/10.1111/j.1532-5415.2007.01317.x.
- Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 2010;21:658-68. https://doi.org/10.1097/EDE.0b013e3181e89905.
- Delbaere K, Sturnieks D, Crombez G, Lord S. Concern about falls elicits changes in gait parameters in conditions of postural threat in older people. J Gerontol A Biol Sci Med Sci 2009;64:237-42. https://doi.org/10.1093/gerona/gln014.
- Carpenter MG, Adkin AL, Brawley LR, Frank JS. Postural, physiological and psychological reactions to challenging balance: does age make a difference?. Age Ageing 2006;35:298-303. https://doi.org/10.1093/ageing/afl002.
- Parry SW, Finch T, Deary V. How should we manage fear of falling in older adults living in the community?. BMJ 2013;346. https://doi.org/10.1136/bmj.f2933.
- Bailey C, Jones D, Goodall D. What is the evidence of the experience of having a fall across the life course? A qualitative synthesis. Disabil Health J 2014;7:273-84. https://doi.org/10.1016/j.dhjo.2014.02.001.
- Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J Aging Health 2011;23:3-23. https://doi.org/10.1177/0898264310378039.
- Kendrick D, Kumar A, Carpenter H, Zijlstra G, Skelton D, Cook J, et al. Exercise for reducing the fear of falling in older people living in the community. Cochrane Database Syst Rev 2014;28. https://doi.org/10.1002/14651858.CD009848.pub2.
- Cameron I, Gillespie L, Robertson M, Murray G, Hill K, Cumming R, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2012;12. https://doi.org/10.1002/14651858.CD005465.pub3.
- Vind A, Andersen H, Pedersen K, Joergensen T, Schwarz P. Effect of a program of multifactorial fall prevention on health-related quality of life, functional ability, fear of falling and psychological well-being. a randomized controlled trial. Aging Clin Exp Res 2010;22:249-54. https://doi.org/10.1007/BF03324804.
- Skelton D, Bailey C, Howel D, Cattan M, Deary V, Coe D, et al. Visually Impaired OLder people’s Exercise programme for falls prevenTion (VIOLET): a feasibility study protocol. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011996.
- Sherrington C, Tiedemann A, Fairhall N, Close JC, Lord SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull 2011;22:78-83. https://doi.org/10.1071/NB10056.
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9. https://doi.org/10.1002/14651858.CD007146.pub3.
- Campbell A, Robertson MC, La Grow S, Kerse N, Sanderson G, Jacobs R, et al. Randomised controlled trial of prevention of falls in people aged > or =75 with severe visual impairment: the VIP trial. BMJ 2005;331:817-925. https://doi.org/10.1136/bmj.38601.447731.55.
- Campbell AJ, Robertson MC. Otago NZ exercise programme to prevent falls in older adults. A home based individually tailored strength and balance retraining programme. Otago: University of Otago Medical School; 2003.
- Chen EW, Fu AS, Chan KM, Tsang WW. The effects of Tai Chi on the balance control of elderly persons with visual impairment: a randomised clinical trial. Age Ageing 2012;41:254-9. https://doi.org/10.1093/ageing/afr146.
- Cheung K, Au K, Lam W, Jones A. Effects of a structured exercise programme on functional balance in visually impaired elderly living in a residential setting. Hong Kong Physiother J 2008;26:45-50. https://doi.org/10.1016/S1013-7025(09)70007-7.
- Kovács E, Tóth K, Dénes L, Valasek T, Hazafi K, Molnár G, et al. Effects of exercise programs on balance in older women with age-related visual problems: a pilot study. Arch Gerontol Geriatr 2012;55:446-52. https://doi.org/10.1016/j.archger.2012.01.009.
- Royal National Institute of Blind People . Key Information and Statistics on Sight Loss in the UK 2016. www.rnib.org.uk/knowledge-and-research-hub/key-information-and-statistics (accessed 7 June 2017).
- Tian Y, Thompson J, Buck D, Sonola L. Exploring the System-Wide Costs of Falls in Older People in Torbay. London: King’s Fund; 2013.
- Boyce T, Stone MK, Johnson S, Simkiss P. Projecting numbers of falls related to visual impairment. Br J Healthc Manag 2013;19:226-9. https://doi.org/10.12968/bjhc.2013.19.6.284.
- Gribbin J, Hubbard R, Smith C, Gladman J, Lewis S. Incidence and mortality of falls amongst older people in primary care in the United Kingdom. QJM 2009;102:477-83. https://doi.org/10.1093/qjmed/hcp064.
- Mokrovich J. Social Work Area Demographics: Population Estimates, Vulnerability, Disability AND Support, and Analysis of SWS Clients, 2011. Glasgow: Glasgow City Council; 2011.
- Skelton D, Dinan S, Campbell M, Rutherford O. Tailored group exercise (Falls Management Exercise-FaME) reduces falls in community-dwelling older frequent fallers (an RCT). Age Ageing 2005;34:636-9. https://doi.org/10.1093/ageing/afi174.
- Older People’s Experience of Therapeutic Exercises as Part of a Falls Prevention Service. London: Royal College of Physicians; 2012.
- Iliffe S, Kendrick D, Morris R, Masud T, Gage H, Skelton D, et al. Multicentre cluster randomised trial comparing a community group exercise programme and homebased exercise with usual care for people aged 65 years and over in primary care. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18490.
- Power V, Clifford A. Characteristics of optimum falls prevention exercise programmes for community-dwelling older adults using the FITT principle. Eur Rev Aging Phys Act 2013;10:95-106. https://doi.org/10.1007/s11556-012-0108-2.
- Donath L, Zahner L, Roth R, Fricker L, Cordes M, Hanssen H, et al. Balance and gait performance after maximal and submaximal endurance exercise in seniors: is there a higher falls-risk?. Eur J Appl Physiol 2013;113:661-9. https://doi.org/10.1007/s00421-012-2471-0.
- Gleeson M, Sherrington C, Keay L. Exercise and physical training improve physical function in older adults with visual impairments but their effect on falls is unclear: a systematic review. J Physiother 2014;60:130-5. https://doi.org/10.1016/j.jphys.2014.06.010.
- Gardner MM, Buchner DM, Robertson MC, Campbell AJ. Practical implementation of an exercise-based falls prevention programme. Age Ageing 2001;30:77-83. https://doi.org/10.1093/ageing/30.1.77.
- Buttery AK, Husk J, Lowe D, Treml J, Vasilakis N, Riglin J. Older people’s experiences of therapeutic exercise as part of a falls prevention service: survey findings from England, Wales and Northern Ireland. Age Ageing n.d.;43:369-74. https://doi.org/10.1093/ageing/aft182.
- Skelton DA, Dinan SM. Exercise for falls management: rationale for an exercise programme aimed at reducing postural instability. Physiother Theory Pract 1999;15:105-20. https://doi.org/10.1080/095939899307801.
- Morgan DL. Focus Groups as Qualitative Research. London: Sage Publications Ltd; 1997.
- Simpson JM, Worsfold C, Fisher KD, Valentine JD. The CONFbal scale: a measure of balance confidence – a key outcome of rehabilitation. Physiotherapy 2009;95:103-9. https://doi.org/10.1016/j.physio.2008.12.004.
- Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry 2002;180:461-4. https://doi.org/10.1192/bjp.180.5.461.
- Later Life Training . Postural Stability Home Exercise Booklet. Later Life Training 2015 n.d. www.laterlifetraining.co.uk/home-exercise-booklets-free-to-download/ (accessed 7 June 2017).
- Data Protection Act 1998. www.legislation.gov.uk/ukpga/1998/29/section/1 (accessed 5 June 2018).
- Kempen GI, Yardley L, van Haastregt JC, Zijlstra GA, Beyer N, Hauer K, et al. The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 2008;37:45-50. https://doi.org/10.1093/ageing/afm157.
- Podsiadlo D, Richardson S. The timed ‘Up & Go’: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142-8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x.
- Falls Risk Assessment Tool (FRAT). Victoria, Australia: Peninsula Health; 1999.
- Gill DP, Jones GR, Zou GY, Speechley M. The Phone-FITT: a brief physical activity interview for older adults. J Aging Phys Act 2008;16:292-315. https://doi.org/10.1123/japa.16.3.292.
- De Jong Gierveld J, Van Tilburg T. A 6-item scale for Overall, Emotional, and Social Loneliness: confirmatory test on survey data. Research on Ageing 2006;28:582-98. https://doi.org/10.1177/0164027506289723.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Davis JC, Liu-Ambrose T, Richardson CG, Bryan S. A comparison of the ICECAP-O with EQ-5D in a falls prevention clinical setting: are they complements or substitutes?. Qual Life Res 2013;22:969-77. https://doi.org/10.1007/s11136-012-0225-4.
- Adams N, Skelton DA, Howel D, Bailey C, Lampitt R, Fouweather T, et al. Feasibility of trial procedures for a randomised controlled trial of a community based group exercise intervention for falls prevention for visually impaired older people: the VIOLET study. BMC Geriatrics 2018;18. https://doi.org/10.1186/s12877-018-0998-6.
- Official Journal of the European Union L91/13, 9.4.2005. Brussels: European Union; 2005.
- Roberts C, Roberts SA. Design and analysis of clinical trials with clustering effects due to treatment. Clin Trials 2005;2:152-62. https://doi.org/10.1191/1740774505cn076oa.
- de Groot GC, Fagerström L. Older adults’ motivating factors and barriers to exercise to prevent falls. Scand J Occup Ther 2011;18:153-60. https://doi.org/10.3109/11038128.2010.487113.
- Delbaere K, Valenzuela T, Woodbury A, Davies T, Yeong J, Steffens D, et al. Evaluating the effectiveness of a home-based exercise programme delivered through a tablet computer for preventing falls in older community-dwelling people over 2 years: study protocol for the Standing Tall randomised controlled trial. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009173.
- McInnes E, Askie L. Evidence review on older people’s views and experiences of falls prevention strategies. Worldviews Evid Based Nurs 2004;1:20-37. https://doi.org/10.1111/j.1741-6787.2004.04013.x.
- McMahon S, Talley KM, Wyman JF. Older people’s perspectives on fall risk and fall prevention programs: a literature review. Int J Older People Nurs 2011;6:289-98. https://doi.org/10.1111/j.1748–3743.2011.00299.x.
- Robinson L, Newton JL, Jones D, Dawson P. Self-management and adherence with exercise-based falls prevention programmes: a qualitative study to explore the views and experiences of older people and physiotherapists. Disabil Rehabil 2014;36:379-86. https://doi.org/10.3109/09638288.2013.797507.
- Yardley L, Bishop FL, Beyer N, Hauer K, Kempen GI, Piot-Ziegler C, et al. Older people’s views of falls-prevention interventions in six European countries. Gerontologist 2006;46:650-60. https://doi.org/10.1093/geront/46.5.650.
- Yardley L, Donovan-Hall M, Francis K, Todd C. Older people’s views of advice about falls prevention: a qualitative study. Health Educ Res 2006;21:508-17. https://doi.org/10.1093/her/cyh077.
- Yardley L, Donovan-Hall M, Francis K, Todd C. Attitudes and beliefs that predict older people’s intention to undertake strength and balance training. J Gerontol B Psychol Sci Soc Sci 2007;62:P119-25. https://doi.org/10.1093/geronb/62.2.P119.
- Phoenix C, Griffin M, Smith B. Physical activity among older people with sight loss: a qualitative research study to inform policy and practice. Public Health 2015;129:124-30.
- Jones GC, Rovner BW, Crews JE, Danielson ML. Effects of depressive symptoms on health behavior practices among older adults with vision loss. Rehabil Psychol 2009;54:164-72. https://doi.org/10.1037/a0015910.
- Stewart J, McVittie C. Living with falls: house-bound older people’s experiences of health and community care. Eur J Ageing 2011;8:271-9. https://doi.org/10.1007/s10433-011-0202-8.
- Dollard J, Barton C, Newbury J, Turnbull D. Falls in old age: a threat to identity. J Clin Nurs 2012;21:2617-25. https://doi.org/10.1111/j.1365-2702.2011.03990.x.
- Horne M, Speed S, Skelton D, Todd C. What do community-dwelling Caucasian and South Asian 60–70 year olds think about exercise for fall prevention?. Age Ageing 2009;38:68-73. https://doi.org/10.1093/ageing/afn237.
- Child S, Goodwin V, Garside R, Jones-Hughes T, Boddy K, Stein K. Factors influencing he implementation of fall-prevention programmes: a systematic review and synthesis of qualitative studies. Implementat Sci 2012;7:1-14. https://doi.org/10.1186/1748-5908-7-91.
- Creswell JW. Qualitative Inquiry & Research Design Choosing among Five Approaches. London: Sage Publications Ltd; 2007.
- Later Life Training . Getting Down to and Up from the Floor Safely: Home Exercise Programme. 2015. www.laterlifetraining.co.uk/wp-content/uploads/2015/08/Backward-ChainingS_A5.pdf (accessed 7 June 2017).
- Curtis L, Burns A. Unit Costs of Health and Social Care. University of Kent, Canterbury: Personal Social Services Research Unit; 2015.
- National Tariff Payment Systems 2014/15. London: NHS England; 2015.
- Guide to the Methods of Technology Appraisal 2013. Process and Methods [PMG9]. London: NICE; 2013.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Coast J, Flynn TN, Natarajan L, Sproston K, Lewis J, Louviere JJ, et al. Valuing the ICECAP capability index for older people. Soc Sci Med 2008;67:874-82. https://doi.org/10.1016/j.socscimed.2008.05.015.
- Coast J, Peters TJ, Natarajan L, Sproston K, Flynn T. An assessment of the construct validity of the descriptive system for the ICECAP capability measure for older people. Qual Life Res 2008;17:967-76. https://doi.org/10.1007/s11136-008-9372-z.
- Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health 2005;27:281-91. https://doi.org/10.1093/pubmed/fdi031.
- Petrou S, Gray A. Economic evaluation alongside randomised controlled trials: design, conduct, analysis, and reporting. BMJ 2011;342. https://doi.org/10.1136/bmj.d1548.
- Keeley T, Coast J, Nicholls E, Foster NE, Jowett S, Al-Janabi H. An analysis of the complementarity of ICECAP-A and EQ-5D-3 L in an adult population of patients with knee pain. Health Qual Life Outcomes 2016;14. https://doi.org/10.1186/s12955-016-0430-x.
- Bunn F, Barnet-Page E, McInnes E, Dickenson A, Horton K. A systematic review of older people’s perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing Soc 2008;4:449-72. https://doi.org/10.1017/S0144686X07006861.
- McMurdo ME, Roberts H, Parker S, Wyatt N, May H, Goodman C, et al. Improving recruitment of older people to research through good practice. Age Ageing 2011;40:659-65. https://doi.org/10.1093/ageing/afr115.
- WHO Global Report on Falls Prevention in Older Age. Geneva: WHO; 2007.
- Medley A, Thompson M. The effect of assistive devices on the performance of community dwelling elderly on the timed up and go test. Issues Ageing 1997;20.
- Guralmick J, Ferrucci L, Pieper C, Leveille S, Markides K, Ostir G, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. Journal Gerontol A Biol Sci Med Sci 2000;55:M221-31. https://doi.org/10.1093/gerona/55.4.M221.
Appendix 1 Stakeholders report
Appendix 2 Change from baseline to week 12 or week 24 in further categorical outcomes
The distribution at baseline and changes over time for further categorical outcomes have been illustrated in tables (see Tables 34–49) showing all possible categories. These tables show the extent of any changes between categories. For all two-way tables presented for changes from baseline to follow-up (week 12 or week 24), colour coding has been used to illustrate the direction of changes between time points.
Comparing attitudes in the intervention arm to avoidance of certain activities owing to FoF at the week 12 visit to baseline (Table 34), 14 participants reported no change while seven reported that they were more likely and eight that they were less likely to avoid certain activities owing to FoF; four complete withdrawals were not included.
| Baseline | Week 12 visit (N = 29), n (%) | ||||
|---|---|---|---|---|---|
| Never | Almost never | Sometimes | Often | Very often | |
| Never | 9 (31) | 3 (10) | 2 (7) | 0 (0) | 0 (0) |
| Almost never | 2 (7) | 1 (3) | 1 (3) | 0 (0) | 0 (0) |
| Sometimes | 2 (7) | 2 (7) | 3 (10) | 1 (3) | 0 (0) |
| Often | 1 (3) | 1 (3) | 0 (0) | 1 (3) | 0 (0) |
| Very often | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Comparing attitudes in the usual activities arm to avoidance of certain activities owing to FoF at the week 12 visit to baseline (Table 35), 12 participants reported no change and five reported that they were more likely and 14 that they were less likely to avoid activities owing to FoF.
| Baseline | Week 12 visit (N = 31), n (%) | ||||
|---|---|---|---|---|---|
| Never | Almost never | Sometimes | Often | Very often | |
| Never | 6 (19) | 1 (3) | 2 (6) | 0 (0) | 0 (0) |
| Almost never | 2 (6) | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| Sometimes | 8 (26) | 0 (0) | 4 (13) | 1 (3) | 0 (0) |
| Often | 1 (3) | 1 (3) | 1 (3) | 0 (0) | 0 (0) |
| Very often | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 2 (6) |
Comparing attitudes in the intervention arm to avoidance of certain activities owing to FoF at the week 24 visit to baseline (Table 36), 13 participants reported no change and nine reported that they were more likely and six that they were less likely to avoid certain activities owing to FoF; four complete withdrawals and one participant lost to follow-up were not included.
| Baseline | Week 24 visit (N = 28), n (%) | ||||
|---|---|---|---|---|---|
| Never | Almost never | Sometimes | Often | Very often | |
| Never | 9 (32) | 0 (0) | 5 (18) | 0 (0) | 0 (0) |
| Almost never | 0 (0) | 2 (7) | 2 (7) | 0 (0) | 0 (0) |
| Sometimes | 2 (7) | 1 (4) | 2 (7) | 2 (7) | 0 (0) |
| Often | 1 (4) | 1 (4) | 1 (4) | 0 (0) | 0 (0) |
| Very often | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Comparing attitudes in the usual activities arm to avoidance of certain activities owing to FoF at the week 24 visit to baseline (Table 37), 10 participants reported no change and nine reported that they were more likely and 12 that they were less likely to avoid certain activities owing to FoF.
| Baseline | Week 24 visit (N = 31), n (%) | ||||
|---|---|---|---|---|---|
| Never | Almost never | Sometimes | Often | Very often | |
| Never | 5 (16) | 0 (0) | 4 (13) | 0 (0) | 0 (0) |
| Almost never | 2 (6) | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| Sometimes | 5 (16) | 0 (0) | 5 (16) | 2 (6) | 1 (3) |
| Often | 1 (3) | 1 (3) | 0 (0) | 0 (0) | 1 (3) |
| Very often | 0 (0) | 0 (0) | 3 (10) | 0 (0) | 0 (0) |
Comparing responses in the intervention arm to the 3-item emotional loneliness scale at the week 12 visit to baseline (Table 38), 17 participants showed no change and nine reported a worsening of and three an improvement in their emotional loneliness.
| Baseline | Week 12 visit (N = 29), n (%) | |||
|---|---|---|---|---|
| None | Mild | Moderate | Intense | |
| None | 9 (31) | 3 (10) | 1 (3) | 0 (0) |
| Mild | 1 (3) | 4 (14) | 5 (17) | 0 (0) |
| Moderate | 1 (3) | 0 (0) | 1 (3) | 0 (0) |
| Intense | 0 (0) | 0 (0) | 1 (3) | 3 (10) |
In the usual activities arm a similar pattern was observed between week 12 visit and baseline (Table 39): 18 participants reported no change and six reported a worsening of and seven an improvement in their emotional loneliness.
| Baseline | Week 12 visit (n = 31), n (%) | |||
|---|---|---|---|---|
| None | Mild | Moderate | Intense | |
| None | 10 (32) | 1 (3) | 2 (6) | 1 (3) |
| Mild | 0 (0) | 4 (13) | 1 (3) | 0 (0) |
| Moderate | 0 (0) | 1 (3) | 2 (6) | 1 (3) |
| Intense | 0 (0) | 2 (6) | 4 (13) | 2 (6) |
Comparing responses in the intervention arm to the three-item emotional loneliness scale at the week 24 visit to baseline (Table 40), 17 participants showed no change and six reported a worsening of and five an improvement in their emotional loneliness.
| Baseline | Week 24 visit (N = 28), n (%) | |||
|---|---|---|---|---|
| None | Mild | Moderate | Intense | |
| None | 10 (36) | 2 (7) | 1 (4) | 0 (0) |
| Mild | 2 (7) | 4 (14) | 3 (11) | 0 (0) |
| Moderate | 0 (0) | 1 (4) | 1 (4) | 0 (0) |
| Intense | 0 (0) | 0 (0) | 2 (7) | 0 (7) |
In the usual activities arm a similar pattern was observed between week 24 visit and baseline (Table 41): 17 participants reported no change, four reported a worsening of and nine reported an improvement in their emotional loneliness.
| Baseline | Week 24 visit (N = 30), n (%) | |||
|---|---|---|---|---|
| None | Mild | Moderate | Intense | |
| None | 11 (37) | 0 (0) | 3 (10) | 0 (0) |
| Mild | 2 (7) | 2 (7) | 1 (3) | 0 (0) |
| Moderate | 2 (7) | 0 (0) | 2 (7) | 0 (0) |
| Intense | 0 (0) | 3 (10) | 2 (7) | 2 (7) |
Comparing responses in the intervention arm to the social loneliness component at the week 12 visit to baseline (Table 42), 21 participants reported no change and two reported a worsening of and six an improvement in their social loneliness.
| Baseline | Week 12 visit (N = 29), n (%) | |||
|---|---|---|---|---|
| None | Mild | Moderate | Intense | |
| None | 16 (55) | 1 (3) | 0 (0) | 0 (0) |
| Mild | 3 (10) | 1 (3) | 1 (3) | 0 (0) |
| Moderate | 0 (0) | 1 (3) | 3 (10) | 0 (0) |
| Intense | 2 (7) | 0 (0) | 0 (0) | 1 (3) |
In the usual activities arm a similar pattern was observed between week 12 visit and baseline (Table 43): 20 participants reported no change and six reported a worsening of and five an improvement in their social loneliness.
| Baseline | Week 12 visit (N = 31), n (%) | |||
|---|---|---|---|---|
| None | Mild | Moderate | Intense | |
| None | 14 (45) | 2 (6) | 0 (0) | 0 (0) |
| Mild | 1 (3) | 2 (6) | 2 (6) | 1 (3) |
| Moderate | 2 (6) | 0 (0) | 2 (6) | 1 (3) |
| Intense | 1 (3) | 0 (0) | 1 (3) | 2 (6) |
Comparing responses in the intervention arm to the social loneliness component at the week 24 visit to baseline (Table 44), 16 participants in the intervention arm reported no change and four reported a worsening of and eight an improvement in their social loneliness.
| Baseline | Week 24 visit (N = 28), n (%) | |||
|---|---|---|---|---|
| None | Mild | Moderate | Intense | |
| None | 14 (50) | 2 (7) | 0 (0) | 0 (0) |
| Mild | 3 (11) | 0 (0) | 2 (7) | 0 (0) |
| Moderate | 0 (0) | 3 (11) | 1 (4) | 0 (0) |
| Intense | 1 (4) | 0 (0) | 1 (4) | 1 (4) |
For the usual activities arm a similar pattern was observed between the week 24 visit and baseline (Table 45): 19 participants reported no change and four reported a worsening of and eight an improvement in their social loneliness.
| Baseline | Week 24 visit (N = 31), n (%) | |||
|---|---|---|---|---|
| None | Mild | Moderate | Intense | |
| None | 16 (52) | 0 (0) | 0 (0) | 0 (0) |
| Mild | 1 (3) | 2 (6) | 2 (6) | 1 (3) |
| Moderate | 1 (3) | 2 (6) | 1 (3) | 1 (3) |
| Intense | 2 (6) | 1 (3) | 1 (3) | 0 (0) |
Codes for categories of physical activities (see Tables 46–49) were as follows:
-
A: I do not do any planned physical activity during the week and would find it difficult to start.
-
B: I am seriously thinking about doing planned physical activity each week.
-
C: I used to exercise regularly each week but have lapsed.
-
D: In the last 6 months, I have started doing regular activity.
-
E: I exercise once in a while but not weekly.
-
F: I exercise regularly each week.
Comparing levels of activity in the intervention group at the week 12 visit to baseline (Table 46), 16 out of 29 participants reported no change and 12 reported an increase and one a decrease in their level of weekly exercise; four complete withdrawals and one participant lost to follow-up were not included.
| Baseline | Week 12 visit (N = 29), n (%) | |||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |
| A | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (3) | 1 (3) |
| B | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 6 (21) |
| C | 0 (0) | 0 (0) | 2 (7) | 0 (0) | 0 (0) | 2 (7) |
| D | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (3) |
| E | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (3) |
| F | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 14 (48) |
Comparing levels of activity in the usual activities arm at the week 12 visit to baseline (Table 47), 19 out of 31 participants reported no change and seven reported an increase and five a decrease in their level of weekly exercise.
| Baseline | Week 12 visit (N = 31), n (%) | |||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |
| A | 6 (19) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| B | 0 (0) | 1 (3) | 1 (3) | 0 (0) | 0 (0) | 2 (6) |
| C | 2 (6) | 0 (0) | 1 (3) | 0 (0) | 1 (3) | 1 (3) |
| D | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| E | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 1 (3) | 2 (6) |
| F | 1 (3) | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 10 (32) |
Comparing levels of activity in the intervention arm at the week 24 visit to baseline (Table 48), 14 out of 28 participants reported no change and 10 reported an increase and four a decrease in their level of weekly exercise; four complete withdrawals and one participant lost to follow-up were not included.
| Baseline | Week 24 visit (N = 28), n (%) | |||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |
| A | 1 (4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (4) |
| B | 0 (0) | 0 (0) | 2 (7) | 0 (0) | 2 (7) | 2 (7) |
| C | 0 (0) | 0 (0) | 2 (7) | 0 (0) | 0 (0) | 1 (4) |
| D | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (4) |
| E | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (4) |
| F | 0 (0) | 0 (0) | 1 (4) | 1 (4) | 2 (7) | 11 (39) |
Comparing levels of activity in the usual activities arm at the week 24 visit to baseline (Table 49), 15 out of 31 participants reported no change and eight reported an increase and eight a decrease in their level of weekly exercise.
| Baseline | Week 24 visit (N = 31), n (%) | |||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |
| A | 4 (13) | 1 (3) | 0 (0) | 0 (0) | 1 (3) | 0 (0) |
| B | 1 (3) | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 2 (6) |
| C | 2 (6) | 0 (0) | 1 (3) | 1 (3) | 1 (3) | 0 (0) |
| D | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| E | 1 (3) | 0 (0) | 1 (3) | 0 (0) | 1 (3) | 1 (3) |
| F | 1 (3) | 0 (0) | 1 (3) | 0 (0) | 1 (3) | 9 (29) |
Appendix 3 Interview topic guides
Appendix 4 Short form Falls Efficacy Scale – International and Activity Avoidance
Appendix 5 The Phone-Frequency, Intensity, Time and Type
Appendix 6 Loneliness scale
Appendix 7 Hospital Anxiety and Depression Scale
Appendix 8 Work and Social Adjustment Scale
Appendix 9 ICEpop CAPability measure for Older people quality-of-life questionnaire
Appendix 10 Falls resources/expenses form
Appendix 11 Current level of activity
Appendix 12 VIOLET health screening tool
Appendix 13 The VIOLET recruitment graph
Graph of cumulative recruitment against calendar month in 2015
FIGURE 5.
Graph of cumulative recruitment against calendar month in 2015.
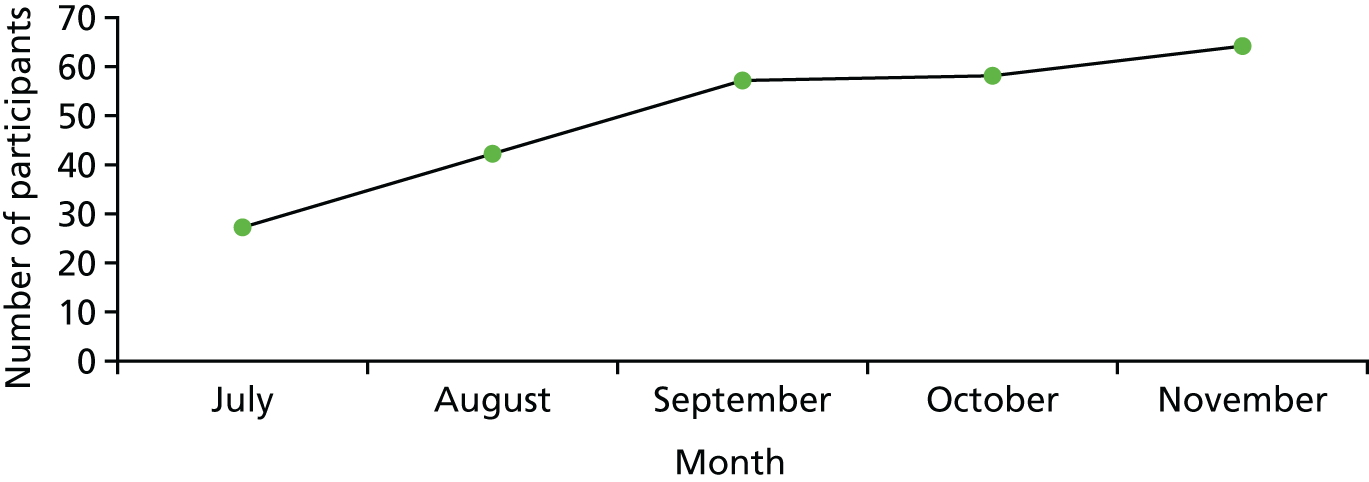
Appendix 14 Ethics approval and protocol amendments
Ethics approval
The study (REC reference: 15/NE/0057) received ethics approval from the National Research Ethics Service Committee North East – Newcastle and North Tyneside 2 on 9 March 2015.
University ethics approval was obtained for the stakeholder focus groups from Northumbria University, Newcastle. Reference: RE-HLS-13-140707-53bb0a7806e37.
Protocol amendments
A minor amendment to the study was submitted to the REC in October 2015 to enable the study team in Newcastle to recruit from additional clinics within the Newcastle Eye Centre at the RVI and not just from the low-vision clinic to aid recruitment.
A substantial amendment was later approved by the REC in January 2016, introducing a usual activities arm participant exercise offer letter and usual activities arm additional GP letter. This was intended to facilitate the offer of a 12-week equivalent exercise programme to the control group at the end of the study – a REC request prior to the original study approval.
A further amendment was submitted in March 2016 regarding a number of minor changes to the protocol. The main change was the removal of reference to the qualitative interviews being transcribed onto NVivo 10 (QSR International, Warrington, UK), a qualitative data management and searching program, as the TMG decided that, as the data set was small and manageable (n = 10, five at each study site), the use of NVivo was unnecessary: interviews at the Glasgow site were transcribed by an experienced transcriber from Northumbria University. Additionally, information regarding thematic analysis was rewritten to give a more accurate picture of the analysis.
List of abbreviations
- A&E
- accident and emergency
- AE
- adverse event
- AMD
- age-related macular degeneration
- CD
- compact disc
- CI
- confidence interval
- COPD
- chronic obstructive pulmonary disease
- DAISY
- Digital Accessible Information System
- DVD
- digital versatile disc
- ECLO
- Eye Clinic Liaison Officer
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FaME
- Falls Management Exercise
- FD
- frequency and duration
- FDI
- frequency, duration and intensity
- FES-I
- Falls Efficacy Scale – International
- FoF
- fear of falling
- FRAT
- Falls Risk Assessment Tool
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- HRQoL
- health-related quality of life
- ICC
- intraclass correlation coefficient
- ICECAP-O
- ICEpop CAPability measure for Older people
- IQR
- interquartile range
- LLT
- Later Life Training Ltd
- MCID
- minimum clinically important difference
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NSBP
- Newcastle Society for Blind People
- OM
- outcome measure
- OT
- occupational therapist
- PAG
- project advisory group
- PI
- principal investigator
- Phone-FITT
- Phone-Frequency, Intensity, Time and Type
- PSI
- Postural Stability Instructor
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RNIB
- Royal National Institute of Blind People
- RVI
- Royal Victoria Infirmary
- SAE
- serious adverse event
- SD
- standard deviation
- TMG
- trial management group
- TOC
- trial oversight committee
- TUG
- Timed Up and Go
- VI
- visual impairment
- VIOLET
- Visually Impaired OLder people’s Exercise programme for falls prevenTion
- VIOP
- visually impaired older people
- WSAS
- Work and Social Adjustment Scale
