Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 13/117/02. The contractual start date was in September 2015. The final report began editorial review in April 2018 and was accepted for publication in August 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Eileen Kaner reports grants from the National Institute for Health Research (NIHR) Public Health Research Funding Board and grants from the NIHR Health Technology Assessment (HTA) programme. Denise Howel is a panel member for the NIHR Programme Grants for Applied Research (PGfAR) programme. Luke Vale is a member of the NIHR NTA Clinical Evaluation and Trials panel, was a panel member for NIHR PGfAR (2008–15), and is co-director of NIHR Research Design Service North East. Colin Drummond is part-funded by the NIHR Biomedical Research Centre at South London and Maudsley NHS Foundation Trust, and the NIHR Collaboration for Leadership in Applied Health Research and Care South London, and is in receipt of a NIHR Senior Investigator Award. Elaine McColl was a member of the NIHR Journals Library Editorial Group (PGfAR) from 2013 to 2016 and a panel member for NIHR PGfAR from 2008 to 2016. Harry Sumnall reports grants from Diageo (Diageo plc, London, UK) outside the submitted work, and he is an unpaid trustee of a drug and alcohol prevention charity, Mentor UK (London, UK), which seeks funding to deliver evidence-based prevention programmes.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Giles et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Structure of the report and background to the research
Key points for Chapter 1
-
The Chief Medical Officer for England recommends that young people and children under the age of 15 years remain alcohol free. If young people aged 15–17 years drink alcohol it is recommended that they do so infrequently and no more than once per week. They should also not exceed adult daily limits.
-
Young people, however, continue to consume alcohol, although the proportion of those who do has been decreasing since 2003.
-
Young people are at increased risk of a range of communicable and non-communicable diseases and longer-term effects from consuming alcohol. Immediate risks include injury, unsafe sex and drug use.
-
Literature shows that alcohol screening and brief interventions (ASBIs) for young people are effective, although there is limited evidence within school settings.
-
There is currently insufficient evidence to be confident about the use of ASBIs to reduce risky drinking and alcohol-related harm in young people in a school setting.
Structure of the report
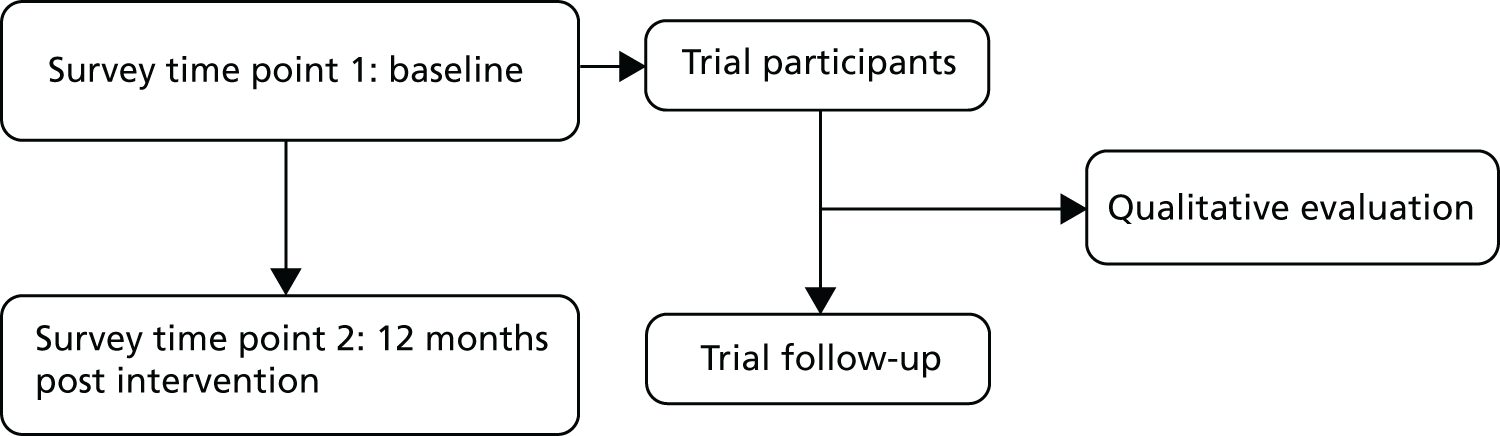
This study assessed the effectiveness and cost-effectiveness of an ASBI (in a school setting) to reduce alcohol consumption in adolescents. This was achieved by way of a two-arm, parallel-group, individually randomised (with randomisation at the level of young person) trial in young people aged 14–15 years in Year 10 at 30 secondary schools across four geographical areas in England: north-east, north-west, Kent and London. The trial involved a baseline and a 12-month follow-up survey. The study included an integrated qualitative process evaluation (Figure 1) with key stakeholders. Young people allocated to the control arm of the trial received a healthy lifestyles information leaflet only; young people allocated to the intervention arm took part in a 30-minute one-to-one structured intervention session based on motivational interviewing (MI) principles with a member of trained school staff (learning mentor) and also received an alcohol information leaflet.
FIGURE 1.
Data time points of the study.
Research questions
This definitive trial builds on a pilot feasibility trial1 that explored the feasibility of offering an ASBI versus ‘standard care’ in this population; the focus of that preparatory study was on rates of eligibility, consent, participation in the intervention and retention for follow-up, as well as the feasibility and acceptability of the intervention for a range of stakeholders (teachers, learning mentors, young people and parents).
The aim of this definitive trial was to evaluate the effectiveness and cost-effectiveness of ASBIs to reduce risky drinking in young people aged 14–15 years in the English school setting, with the primary outcome measure of the trial being total alcohol consumed in standard units in the previous 28 days using the Timeline Follow-Back (TLFB).
Chapters of the report
The report is structured as seven chapters detailing the design, management and outcomes of the main trial study. The report begins by providing the background to the research and outlines the key literature informing the design and conduct of the study. Following this, a chapter is dedicated to each core component of the study. Chapter 2 explores the design of intervention materials as well as the training and support provided to school staff in the delivery of the project. Chapter 3 reports the design, methods and results of the baseline and follow-up survey, as well as the findings in respect of the primary and secondary outcome measures. Chapter 4 provides the design, methods and results of the integrated qualitative evaluation. Chapter 5 details the design, methods and results of the health economic evaluation of the study. Chapter 6 presents a discussion of the key results. Finally, Chapter 7 provides the key conclusions.
Research ethics
The research study was granted ethics approval by Teesside University in September 2015 (reference number 164/15), with Newcastle University acting as the sponsor for the research. The trial is registered as ISRCTN45691494.
Changes to the original study protocol
The study protocol was published in 2016. 2
-
The TLFB was delivered by research co-ordinators, as detailed in the protocol, in all but one school. The remaining school indicated that it would only be willing for young people to complete the TLFB independently, because of staff time and resource constraints. An ethics amendment for this slightly revised procedure was submitted and approved (reference number R164/15, January 2017).
-
The sample size was originally calculated to provide 90% power to detect a standardised difference of 0.3 using a significance level of 5%. Given the difficulty in recruiting sufficient numbers the target for power was reduced from 90% to 80% after discussion with the Trial Steering Committee (TSC) and Data Monitoring and Ethics Committee (DMEC).
-
The EuroQol-5 Dimensions, three-level version (EQ-5D-3L) was used instead of the EQ-5D-Y [EuroQol-5 Dimensions (Youth)]. The study used the EuroQol-5 Dimensions for lack of a better instrument and because it is used extensively in economic evaluations,3 making it a standard for comparing economic outcomes across different interventions.
Research management
The Trial Management Group (TMG) was responsible for ensuring the appropriate, effective and timely implementation of the trial. The TMG met once per month (more or less frequently depending on the needs of the project) and comprised the chief investigator, the project manager, co-applicants, named collaborators and researchers working on the project. A TSC and a DMEC were also appointed to provide an independent assessment of the trial procedures and data analysis. These groups met three times (joint meetings) and their remit was the progress of the trial against projected rates of recruitment and retention, adherence to the protocol, participant safety and the consideration of new information of relevance to the research question. Written terms of reference were agreed and used by the TMG, TSC and DMEC (see Appendix 1).
Research governance
The project complied with the requirements of the Data Protection Act 19984 and the Freedom of Information Act 2000,5 and other UK and European legislation relevant to the conduct of clinical research. The project was managed and conducted in accordance with the Medical Research Council’s Guidelines on Good Clinical Practice in Clinical Trials,6 which includes compliance with national and international regulations on the ethical involvement of patients in clinical research (including the Declaration of Helsinki, 2013). 7 All data were held in a secure environment with participants’ information identified by a unique participant identification number. Master registers containing the link between participant identifiable information and participant identification numbers were stored in a secure area separate from the majority of data. All staff employed on the project were employed by academic organisations and subject to the terms and conditions of service and contracts of employment of the employing organisations. When relevant, research staff were trained in good clinical practice and all staff worked to written codes of confidentiality. The project used standardised research and clinical protocols and adherence to the protocols was monitored by the TMG, TSC and DMEC. We also undertook patient and public involvement (PPI) work (see Appendix 2).
Background
Alcohol use as a public health priority
Consumption of alcohol is a risk factor for mortality and morbidity in adults, and is an important public health issue. Alcohol misuse leads to both societal and economic costs, as well as the burden of disease, yet it is preventable. 8 Although many adults in the UK consume alcohol in line with recommended guidelines, a proportion of adults drink above these recommendations and consume alcohol at harmful and hazardous levels. 9 It has been estimated that 10.8 million adults in the UK drink alcohol at levels that are harmful to their health. 10 Although young adults aged 16–24 years are less likely to drink than individuals in older age groups, when they do choose to drink they consume more alcohol. 11 As a result, this study focused on alcohol consumption in young people.
Prevalence of alcohol consumption in young people
In 2009 the Chief Medical Officer for England recommended that young people and children remain abstinent from alcohol until they are 18 years old. 12 This was accompanied by advice that young people and children should not consume alcohol before the age of 15 years, and, should they choose to consume it thereafter, that they should drink it no more than once per week and only under supervision. If young people aged 15–17 years drink alcohol, it is recommended that they do so on only 1 day per week and do not exceed adult daily limits, and ideally consumption should be below this level. 13
In the UK, the proportion of young people who drink alcohol has steadily decreased between 2003 and 2014. 12 As there was a change in the question around consumption of alcohol in the 2016 version of the ‘Smoking, Drinking, and Drug Use’ survey,14 it is not possible to calculate the change in alcohol consumption in 2016 relative to previous years; however, the direction of effect continues to show decreasing alcohol consumption.
The proportion of young people who have ever had an alcoholic drink in England increases with age, with data from 2016 suggesting that 11% of girls and 9% of boys aged 11–15 years had consumed alcohol in the 7 days preceding the survey. 12 Of these, 1% of 11-year-olds had consumed alcohol in the preceding week, increasing to 24% of 15-year-olds. In total, mean alcohol consumption in ‘the last week’ was lowest in those aged 11–13 years (6.9 units) and highest among 14-year-olds (11.1 units). 12 In terms of the amount of alcohol drunk by 11- to 15-year-olds, in 201712 the mean alcohol consumption in the preceding week was 10.3 units for boys and 8.9 units for girls. 12 For these reasons, this study focused on young people aged 14–15 years, given that the data indicate that more young people start to consume alcohol at this age.
Although alcohol consumption among children and young people is declining, consumption among high-risk children and young people (e.g. those with intellectual disabilities) remains prevalent. 15 In comparison with other European countries, the UK has high levels of drinking among young people. 16 The north-east has one of the highest rates of young people who have ever drunk alcohol, with 49% of 11- to 15-year-olds reporting having ever drunk alcohol. 17 This compares with the lowest prevalence in London of 25% and the highest in the north-west of 50%, with an overall English average of 44%. 12
Consequences of drinking alcohol at a young age
Alcohol consumption at a young age is associated with a number of detrimental outcomes. These include physical and mental health issues, an impact on brain development, and an increased risk of accidents and injury. 12 Longer-term negative outcomes arise in particular from binge drinking, defined as the excessive consumption of alcohol in a limited time and often measured as consuming more than six units in a single session for both men and women. 18 These long-term effects have been observed in a large cohort study (the 1970 British Cohort Study) of > 16,000 babies born between 5 and 11 April 1970, and followed up at ages 5, 10, 16 and 30 years. 19 The findings showed that binge drinking in adolescence was associated with later (adulthood) negative consequences, such as alcohol dependence, homelessness, reduced educational attainment and convictions. In addition, there is evidence that alcohol use tracks over time, from adolescence into adulthood, and also is correlated with other risky behaviours, such as smoking. 20 That study therefore recommended that alcohol interventions target young people, even though the literature suggests that they do not always think that risky or harmful drinking is a concern for them. 21 More immediate consequences of alcohol consumption include school exclusions, with 9.5% of exclusions during 2015–16 in state-funded secondary schools being due to drugs and/or alcohol. 22
Other adverse effects of alcohol consumption in young people include an increased risk of mortality from accidents and suicide as a direct result of drinking alcohol. 23 Additional negative consequences include longer-term impact on brain development, liver damage, and changes in hormones vital for organ development and growth. 23,24 Short-term impacts can also arise from alcohol use in young people, including regretted sexual activity, self-harming, alcohol poisoning, drunk driving and criminal behaviour. 25 It can also lead to weight loss, appetite changes, sleep disturbance, depression and an impact on school performance. 26 In addition, the early consumption of alcohol has been shown to link with the amount of alcohol consumed in older adolescence and adulthood. 27 It is also the case that young people are more likely to binge drink alcohol when they do consume it, which in turn leads to increased risk from accidents. Alcohol use is also linked to non-communicable diseases, such as cancer, cardiovascular disease and gastrointestinal disorders. 28 In terms of short-term benefits, young people report similar reasons for drinking as adults, including for social confidence, for enjoyment26,29 and to celebrate special occasions. 26
Alcohol screening tools
A number of screening tools have been used with young people to identify those who are at risk from their drinking. A systematic review into the clinical effectiveness and cost-effectiveness of alcohol screening tools for adults and young people explored the use of the Alcohol Use Disorders Identification Test (AUDIT),30 Alcohol Use Disorders Identification Test – Consumption (AUDIT-C)31 and AUDIT-QF (first two questions of the AUDIT),32 FAST33 (Fast Alcohol Screening Test), CAGE,34 MAST (Michigan Alcohol Screening Test),35 Paddington Alcohol Test,36 SASSI (Substance Abuse Subtle Screening Inventory) for children and young people,37 ASSIST (Alcohol, Smoking and Substance Involvement Screening Test),38 SASQ (Single Alcohol Screening Question),39 TWEAK (Tolerance, Worried, Rye-opener, Amnesia, K/cut down)40 and T-ACE41 in prenatal screening, as well as laboratory and clinical markers. 42 The review found that alcohol screening tools were more effective at identifying young people drinking at a risky level than laboratory and clinical markers, with the AUDIT a particularly cost-effective measure. 43 The SIPS JR-HIGH pilot trial report discussed the evidence around screening measures in detail,2 although a review of existing reviews25 for ASBIs with young people found that the CRAFFT (Car, Relax, Alone, Forget, Family or Friends, Trouble) was used particularly for older adolescents (15–18 years old), and the AUDIT was found to have greater sensitivity and specificity than other screening tools in young people. In addition, the Adolescent Single Alcohol Question (A-SAQ) was shown to be a reliable single-screening question for drinking frequency44 in the SIPS (Screening and Intervention Programme for Sensible Drinking) research programme in adults. It is a modified version of the Single Alcohol Screening Question (M-SASQ),45 which is adapted for adolescent alcohol consumption. 39
Alcohol primary prevention in the school setting
Primary prevention is a treatment or intervention that seeks to prevent disease occurrence, whereas secondary prevention involves treating/intervening in a disease in its early stages. ASBIs are classified as a form of secondary prevention, in that they typically target individuals who have been identified as drinking alcohol in a pattern that is detrimental to their health. 46
There is limited literature published within the past 5 years that explores primary preventative school-based alcohol brief interventions in the secondary school setting in the UK. The majority of recently published literature focuses on college and university students in other countries, particularly US studies focusing on college students.
Of the previous studies that do exist, they have explored the use of classroom-based curricula and parental interventions as primary prevention with young people. 47 One such is the Steps Towards Alcohol Misuse Prevention Programme trial,47 which explored the effectiveness of a school and parent alcohol intervention. This trial found a significant reduction in heavy episodic drinking in 12- to 13-year-olds; the intervention was delivered at classroom level and not to individuals. 47 The Kids and Adults Together programme trial48 explored the acceptability of primary school classroom-based activities, family events and a digital versatile disc (DVD) to address the effects of alcohol in 9- to 11-year-olds in Wales as a primary preventative measure. The trial found mixed support from the nine primary schools, with two withdrawing from the study. One particular limitation highlighted was the inability to conduct follow-ups within secondary school settings once the young people progressed from primary school. In addition, members of the team conducted a systematic review of peer-led interventions with young people aged 11–21 years; they found 17 studies, of which six were school-based and showed a positive benefit on alcohol use. However, none of the six school-based studies was conducted in the UK and brief interventions were specifically excluded. A meta-analysis of school-based prevention for risky behaviours showed that school settings appear to be effective in reducing alcohol consumption,49 whereas a separate review50 of the prevention of multiple health risk behaviours in schools showed a small positive effect on alcohol consumption. The former review was, however, published in 2001 and the latter was not focused on individually targeted interventions and, therefore, the findings are of limited relevance in the context of the individualised ASBI considered here.
Alcohol screening and brief interventions
Interest in screening and brief interventions for risky drinking has developed since the 1970s. 51 ASBIs have been defined as ‘those practices that aim to identify a real or potential alcohol problem and motivate an individual to do something about it’. 52 Heather, in 1995, offered a more specific definition, stating that brief interventions are ‘a family of interventions varying in length, structure, targets of intervention, personnel responsible for their delivery, media of communication and several other ways, including their underpinning theory and intervention philosophy’. 53 In an early review of brief interventions, Bien54 found that brief interventions were more effective than no intervention or more extensive treatments, with six common elements of brief interventions discussed, based on the FRAMES (Feedback, Responsibility, Advice, Menu, Empathy and Self-efficacy) model. 54 More recent research has reported results of brief interventions in different settings and delivery modes, for example face to face or web based. 55 In terms of implementing a brief intervention, it is often used to provide simple advice for patients with an AUDIT score in the range of 8–15, who may be at risk of injury and chronic health conditions as a result of their alcohol consumption. 52 Given the heterogeneity of brief interventions and settings, it is therefore important to consider the context and components of brief interventions when assessing effectiveness, rather than focusing on general overall effectiveness. Heather53 in particular states the importance of clarifying the length of the intervention when assessing effectiveness, given that the length can range from 5 minutes to at least 3 hours. The same is true of the number of intervention sessions, which can be one or more, and the content of sessions (e.g. MI vs. self-help manual).
The pilot trial focused on the use of simple structured advice based on the FRAMES model, delivered by learning mentors as non-specialists, as opposed to behaviour change counsellors. 1 This approach was found to be acceptable in the school setting and hence was used again in this main trial.
In terms of secondary prevention, a previous review of reviews explored the use of ASBI with young people. 25 The review concluded that MI delivered in school settings is an effective way to reduce alcohol consumption. However, within this review, the definition of young people was wide, ranging from 10 to 21 years, even though the World Health Organization defines ‘young people’ as those aged 10–19 years. 56 An additional systematic review and meta-analysis of ASBIs for young people found that ASBIs led to a decrease in alcohol consumption and alcohol-related problems. However, this work included studies that focused on any level of (alcohol) risk, and also defined eligible participants as those aged 11–25 years. 57
There is some evidence to show school-based group ASBIs can be beneficial,58 but, even then, this has not always been found to be the case for high-risk drinkers. 59 Similarly, there is literature showing that family and school-based interventions can reduce adolescent alcohol use, but this evidence60 is not from a UK setting and does not involve personalised individual ASBIs. A separate systematic review57 of ASBIs with young people showed reductions in alcohol use as a result of ASBIs but included participants up to the age of 30 years, well outside secondary school age.
To focus on young people in particular, and also using recognised definitions for young people, a systematic review [Giles EL, McGeechan GJ, Ferguson J, Byrnes K, Newbury-Birch D. Teeside University. 2018. (In preparation)] was recently conducted to explore the evidence on the efficacy/effectiveness of ASBIs targeting risky drinking in young people (as defined by the World Health Organization) in randomised and non-randomised controlled designs, or quasi-experimental studies. The ASBI had to involve individual one-to-one advice delivered in one to four sessions to constitute a ‘brief’ intervention. Literature searches were conducted in June 2017 of the main databases including PsycInfo, Psycharticles, MEDLINE, Scopus and CINAHL (Cumulative Index to Nursing and Allied Health Literature). Searches combined key alcohol, brief intervention and young people search terms. Papers were eligible for inclusion if they were shown to meet the predefined inclusion criteria, and if their primary focus was around young people aged between 10 and 19 years, engaged in an alcohol brief intervention in any setting, in randomised or non-randomised controlled designs or quasi-experimental studies.
This review identified 16 papers that focused on risky drinking in young people. 61–76 The majority (n = 13) were studies conducted in the USA,61,64–67,69–76 with one in Germany,68 one in Mexico63 and one in Western Australia. 62 The setting was mainly emergency departments (n = 8),62,66,68,70–73,75 with three in universities,61,67,74 one with homeless adolescents,76 one with young people referred from not-for-profit agencies,65 one based in the community64 and two based in schools. 63,69 The ASBIs used largely followed a manual and/or used MI techniques. Findings showed that for the majority of the studies, the ASBI was effective at decreasing alcohol-related outcomes, including a reduction in binge/heavy drinking (n = 4), and/or a reduction in number of typical drinks/alcohol use (n = 10) and/or frequency of drinking (n = 5), and/or a reduction in negative consequences from drinking alcohol (n = 3). One study found no significant differences between the group receiving an ASBI and the control group. 75 Focusing on the two studies conducted in a school setting, one was conducted in Mexico. 63 In this study, the young people were moderate- to high-risk drinkers, mainly male (65%), with an average age of 16 years. The ASBI group received one 90-minute ASBI compared with a waiting list control. At the follow-up points of 3 and 6 months, the ASBI group showed a significant reduction in the amount of alcohol consumed compared with the control. The second study was conducted in the USA with young people who had an alcohol or drug use disorder. 69 The majority of participants were male (52%), with an average age of 16 years. The ASBI were two 60-minute sessions, with one group also receiving a parent session. Significant findings were reported for the number of days alcohol was consumed compared with the assessment-only control group. These two school-based studies therefore suggest that the use of a school setting to deliver ASBI to young people is effective (see Appendix 3).
Results from the SIPS JR-HIGH pilot trial
The pilot trial of SIPS JR-HIGH1 was the first research in England to look at the acceptability and feasibility of a cluster randomised (at the school level) controlled trial of ASBIs in secondary schools with 14- to 15-year-olds. To the best of our knowledge, this current study is the first English research study to examine the effectiveness of ASBIs in young people in the secondary school setting who are identified as risky drinkers.
In the pilot feasibility study, young people who screened positive on a single alcohol screening question and who consented to take part (n = 229) were randomised, at the level of the school, to a control arm of an advice leaflet, to an intervention arm consisting of a 30-minute brief interactive session using structured advice delivered by the school learning mentor and an advice leaflet (intervention 1), or to the same 30-minute brief interactive session and advice leaflet combined with a 60-minute session including family members (intervention 2). Participants were followed up at 12 months (n = 202; 88%) and completed the same survey as at baseline.
Overall, the trial was able to recruit seven schools as originally planned, undertake intervention training with the learning mentors who themselves were able and willing to be trained, and undertake the screening survey with young people. In terms of the acceptability of intervention 1, this arm was found to be the most acceptable. In relation to intervention 2, it was not feasible to engage parents in the third arm of the trial, with qualitative interview findings suggesting that the school staff, the parents and the young people did not think that including parents was acceptable. As a result, intervention 2 was removed from the main trial.
Rationale for the present research
Overall, the pilot feasibility study showed that it was feasible and acceptable to undertake a trial of ASBIs in the school setting with young people, and with learning mentors delivering the intervention. 1 As stated above, given the lack of literature on the use of ASBIs with young people in the secondary school setting in the UK, this trial presented an important step in building the evidence base around the effectiveness of ASBIs with young people for reducing risky drinking.
Aim and objectives
Aim
The aim of this study was to evaluate the effectiveness and cost-effectiveness of ASBIs to reduce risky drinking in young people aged 14–15 years in the English secondary school setting.
Objectives
-
To conduct an individually randomised controlled trial to evaluate the effectiveness and cost-effectiveness of an ASBI for risky drinkers compared with usual practice on alcohol issues conducted by learning mentors with young people aged 14–15 years in the school setting in four areas of England: the north-east, north-west, Kent and London.
-
To measure effectiveness in terms of percentage days abstinence over the last 28 days, risky drinking, smoking behaviour, alcohol-related problems, drunkenness during the last 30 days and emotional well-being.
-
To measure the cost-effectiveness of the intervention in terms of quality of life and health state utility, quality-adjusted life-years (QALYs), service use costs and cost consequences at 12 months post intervention.
-
To monitor the fidelity of an ASBI delivered by learning mentors in the school setting.
-
To explore barriers to, and facilitators of, implementation with staff.
-
To explore young people’s experiences of the intervention and its impact on their alcohol use.
-
If the intervention is shown to be effective and efficient, to develop a manualised screening and brief intervention protocol to facilitate uptake/adoption in routine practice in secondary schools in England.
Outcomes and measurements of the SIPS JR-HIGH effectiveness trial
Validated tools were used in the study to capture the following primary and secondary outcomes measures. 2
Primary outcome
The primary outcome measure was the number of units of alcohol consumed over the previous 28 days, derived using the TLFB completed at 12-month follow-up77 (see documents on project page). The TLFB is designed to be completed retrospectively and employs periodic cues to obtain reliable estimates of daily drinking during a 28-day period.
Secondary outcome measurements
-
The Adolescent Single Alcohol Question (A-SAQ)78 was used to measure risky drinking (scoring ‘4 or more times but not every month’, ‘at least once a month but not every week’, ‘every week but not every day’, or ‘every day’). A score of three or above was considered positive for possible hazardous or harmful drinking. 2
-
Alcohol use frequency, quantity (on a typical occasion) and binge drinking (six or more drinks in one session for men and women)18 was assessed using the 10-question AUDIT. 79,80 Questions 1–8 each have five possible responses relating to how much or how often drinking behaviours occur, and these are scored from 0 to 4. Questions 9 and 10 have three responses and are scored 0, 2 or 4. Scores were summed to give a possible range from 0 to 40. A score of ≥ 4 was indicative of hazardous alcohol consumption in adolescent populations,81 and the adult cut-off point of 8 was also used. 2,30
-
The AUDIT-C was used to assess risky drinking, and comprises the first three questions of the AUDIT. All questions were scored from 0 to 4 and summed to give a range of scores from 0 to 12. An AUDIT-C score of ≥ 3 was indicative of hazardous alcohol consumption and ≥ 5 was indicative of possible dependence in adolescents. 2
-
Alcohol-related problems were assessed using the validated Rutgers Alcohol Problem Inventory (RAPI), which includes measures of aggression. 82 It consists of 23 questions about drinking behaviour, each with four possible responses, all of which are scored from 0 to 3. Responses were summed to give a total score ranging from 0 to 69. A higher RAPI score indicated more problematic drinking behaviour. 2
-
Drunkenness during the previous 30 days was dichotomised as ‘never’ and ‘once or more’. 2,83
-
Drinking motives were assessed using the 20-item Drinking Motives Questionnaire Revised (DMQ-R). 84 There were four sets of five questions designed to assess relative frequency of drinking within each of the subscales of coping, social, enhancement and conformity motives. All questions were on a Likert scale, for which one is ‘almost never/never’, two is ‘some of the time’, three is ‘half of the time’, four is ‘most of the time’ and five is ‘almost always/always’. Higher scores within each domain indicated stronger endorsement of positive reinforcement received through consumption of alcohol. 2,84
-
The percentage days of abstinence during the previous 28 days was calculated from the TLFB questionnaire by dividing the days on which no units were consumed by 28 and multiplying by 100. 2
-
Number of units of alcohol consumed per drinking day was derived by dividing the total number of units of alcohol consumed by the number of days on which > 0 units were consumed. Abstinent pupils were scored as 0. 2
-
Number of days when > 2 units of alcohol were consumed during the previous 28 days was calculated by counting the number of days on which > 2 units were recorded. 2
-
General psychological health was assessed using the 14-item Warwick–Edinburgh Mental Well-being Scale (WEMWBS). 85 This tool used a five-point Likert scale that gives a score of 1–5 per question, giving a minimum score of 14 and maximum score of 70. A higher WEMWBS score indicated better mental well-being. 2,86,87
-
Two questions relating to sexual risk-taking were included. These were the same questions as in the pilot study:1 ‘After drinking alcohol, have you engaged in sexual intercourse that you regretted the next day?’ and ‘After drinking alcohol, have you ever engaged in sexual intercourse without a condom?’ Both questions could be answered with one of the three following options: ‘I have never engaged in sexual intercourse’, ‘yes’ or ‘no’. Information on changes in risky sexual behaviour for the two questions was derived from a cross-tabulation of baseline and follow-up responses to a given question and categorised as ‘never engaged in sexual intercourse’, ‘engaged in sexual intercourse that has been regretted during the last 12 months’ and ‘have engaged in sexual intercourse that has not been regretted’. 2
-
Energy drink consumption was assessed by asking young people how many times per week they consumed energy drinks. Young people could answer ‘never’, ‘less than once a week’, ‘2–4 days a week’, ‘5–6 days a week’, ‘every day once a day’ and ‘every day more than once a day’. Information on changes in the consumption of energy drinks was derived from a cross-tabulation of baseline and follow-up questions and categorised as ‘never consumes energy drinks’, ‘has stopped consuming energy drinks’, ‘has started consuming energy drinks’ and ‘consumes more/less energy drinks’. 2
-
Age of first smoking was asked, as was how many cigarettes had been smoked in the previous 30 days. 88 Information on changes in smoking behaviour was derived from a cross-tabulation of baseline and follow-up responses and categorised as ‘never smoked’, ‘still smoking’, ‘started smoking’ and ‘smoking more/less’. 2,89
-
Demographic information collected included gender, ethnicity and how free time is spent. The first part of the trial participants’ postcode was collected to facilitate calculation of Index of Multiple Deprivation. 2
-
Quality of life was measured using the EQ-5D-3L, which is a valid measure for those aged ≥ 12 years, and was used to measure health-related quality of life. 90 Responses to the five items were converted into utility scores using the UK population algorithm. This was administered at baseline and at 12 months post intervention. 2,90
-
Quality-adjusted life-years were estimated using general population tariffs from responses to the EQ-5D-3L administered and scored at baseline and 12 months; service use was assessed using the modified S-SUQ (Short Service Use Questionnaire) at baseline and 12 months. 2
-
Use of leisure time was assessed using a multiple-choice question that gave suggestions about how free time might be spent and the option to choose multiple answers. 2
-
Incremental cost per QALY gained at 12 months was calculated. 2
-
Modelled estimates of incremental cost per QALY and cost consequences in the longer term were calculated. 2
-
The NHS, educational, social and criminal services data were estimated using a modified S-SUQ91 and via a learning mentor case diary developed in the pilot study,1 measured at 12 months post intervention. 2
-
Cost consequences were presented in the form of a balance sheet for outcomes at 12 months. 2
Chapter 2 Trial process and development of intervention materials and training
Key points for Chapter 2
-
The study incorporated a control condition and a brief alcohol intervention. The brief alcohol intervention was manualised and designed to be delivered on a one-to-one basis to young people who screened positive for risky drinking and left their name on the questionnaire.
-
Young people in the control group were provided with a healthy lifestyle leaflet by the learning mentor.
-
Young people allocated to the intervention received feedback on their positive screen for risky drinking, immediately after which they took part in a 30-minute, six-step interactive intervention led by the learning mentor.
-
Learning mentors were asked to audio-record time spent with participants using a dictaphone. Audio-recorded control and intervention sessions were measured for fidelity using the Behaviour Change Counselling Index (BECCI),92 and control sessions were also assessed for differentiation from the brief alcohol intervention.
Introduction
All young people recruited into the trial, regardless of arm, continued to receive ‘standard alcohol advice’ delivered as part of the school curriculum. The first section of this chapter is concerned with defining what this consisted of in the study schools. In addition, young people allocated to the control condition received a healthy lifestyle information leaflet. No feedback was provided to them on their positive screen for risky drinking. Young people allocated to the brief alcohol intervention met with a trained learning mentor, received feedback on their alcohol screening result and took part in a 30-minute one-to-one structured intervention session. In addition, they received an alcohol advice leaflet. All young people recruited into the trial were followed up 12 months post intervention.
The rest of the chapter describes the design of intervention materials, as well as the training and support provided to learning mentors in the delivery of interventions. The rationale behind, and development of, both the control and the intervention is detailed, and the amendments that were made following the results of the pilot feasibility trial are outlined, with any resultant modifications to intervention materials reported.
Defining ‘standard alcohol advice’
All schools are required to provide Personal, Social, Health and Economic Education (PSHE) to ‘promote children and young people’s personal and economic well-being; offer sex and relationships education; prepare pupils for adult life and provide a broad and balanced curriculum’,93 delivered as part of a wider well-being remit through the National Healthy Schools Programme94 and the Social and Emotional Aspects of Learning strategy. 94 Classroom-based drug and alcohol education is delivered to pupils as part of PSHE classes, and is recognised as an important aspect of the secondary school curriculum (for those aged 11–16 years) in England, Scotland and Wales.
As there are no prescriptive guidelines on what PSHE should actually entail, schools have developed their own versions of PSHE education and different ways to deliver it, rather than following standardised frameworks of study. 93 We asked schools to report their usual practice and found that this varied from school to school, but included advice on drinking responsibly and ‘safe amount of units’, alcohol facts, provision of Addaction95 leaflets, assemblies on alcohol, advice on wider lifestyle choices, an alcohol awareness week, utilisation of Drinkaware96 resources and alcohol-awareness evenings for parents. Schools reported that this advice was delivered by a combination of teachers, pastoral leads, tutors, nurses, learning mentors and external speakers. One school said that it did not currently deliver advice on alcohol. Given the variability in alcohol advice across schools, standard alcohol advice is defined in this study as the regular provision of classroom-based alcohol education to Year 10 pupils as delivered at each particular school site. As a result, many of the young people may have received this standard alcohol advice as usual from their schools, in addition to the ASBI for those randomised to the intervention arm of the trial (see Appendix 4).
Trial process
Study setting and population
Young people aged 14–15 years in Year 10 at secondary schools/academies in four centres, north-east, north-west, Kent and London, were targeted.
In each of the four geographical centres, school performance league tables97 were reviewed and schools from the top, middle and bottom of the league tables were contacted. Efforts were made to recruit a cross-section of schools, including academy schools, schools in deprived areas, faith schools and private schools. Schools were included if they employed learning mentors (or equivalent members of pastoral staff).
In advance of screening, all parents/caregivers (hereafter referred to as ‘parents’) were sent a letter by the school informing them that young people would be screened for risky drinking as part of the study in their child’s school (see documents on project page). Parents had the choice to opt their child out of the study by completing an opt-out form and returning it to the school in a prepaid envelope. Opt-out consent by parents was chosen (instead of opt-in) as this was standard practice in schools (see documents on project page). They were provided with an information sheet to inform consent (see documents on project page). 2
At baseline, all participating schools showed an animation video to pupils who had not opted out of the study. This video detailed the study process. Young people then completed the baseline survey as part of the screening process (see documents on project page). This screening took place in the PSHE or registration class on an individual classroom basis.
Young people had the option to (1) not complete the questionnaire (indicative of lack of assent to screening from the young person), (2) complete the questionnaire anonymously or (3) complete the questionnaire, adding their name and class. 2
Those young people who screened positively on the A-SAQ and left their name were eligible for the trial.
Randomisation
Eligible pupils were individually randomised in a one-to-one ratio to the intervention or control arm of the trial. Randomisation occurred before consent to the trial because of timing constraints: it was not feasible for the learning mentor to access a real-time randomisation system during the session with the young person. Therefore, the randomisation was performed earlier on the list of eligible young people and the allocation was contained in a sealed envelope. Neither the learning mentor nor the young people knew the arm to which they had been allocated until they opened the envelope after consent had been given. Young people aged < 16 years provided assent and those aged 16 years provided consent, as per guidelines issued by the Research Governance and Ethics Committee in the School of Health and Social Care at Teesside University. 1 Hereafter, assent and consent is referred to as consent.
An independent statistician not otherwise involved with the study produced a computer-generated allocation list using random permuted blocks. This statistician was provided with a list of screening identification numbers (identifying the site, school and young person) for eligible participants, in the form of a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet. This statistician also undertook randomisation, and an updated spreadsheet, including allocations to the study arms, was returned to an independent researcher (JF) at Teesside University, where the sealed envelopes containing the allocation were produced. Numbered envelopes containing a slip of paper indicating the arm to which each individual had been allocated were then prepared, sealed and sent to each school, to be opened only when consent had been attained.
School staff identified to deliver interventions
The pilot feasibility trial, which preceded the current trial, identified the learning mentor as the most appropriate role within the school structure to deliver an alcohol intervention. Learning mentors are specifically trained to provide a complementary service to teachers and other school staff, addressing the needs of young people who require assistance in overcoming barriers to learning in order to achieve their full potential. 98 They work with a range of pupils, but they focus on those pupils with multiple disadvantages that have an impact on their education. Within their established role, learning mentors address issues, such as punctuality, absence, bullying, challenging behaviour and abuse, disaffection, danger of exclusion, difficult family circumstances and low self-esteem, as well as underperformance against potential. 99 As part of this role, learning mentors are routinely required to provide advice and support to young people and, as such, are well placed within a school setting to deliver an intervention to young people about alcohol use. In this trial, interventions took place in the learning mentor’s classroom or office space.
Local areas vary in the essential qualifications they look for when appointing learning mentors. However, at a minimum, learning mentors need to have a good standard of general education, especially literacy and numeracy, as well as experience of working with young people. 100 In the present study, learning mentors were defined as the members of school staff trained in the delivery of the control condition/intervention to participating students. However, in practice, within each school, titles, roles and responsibilities varied and this did not constitute a homogenous professional group. Thus, for consistency, the school staff responsible for delivering interventions are referred to only as learning mentors throughout the rest of this report.
Control (healthy lifestyles leaflet)
Young people allocated to the control group met with the learning mentor in school during the week (Monday to Friday). The learning mentor explained the study to them and invited them to participate in the trial. Once a young person had consented to the trial, the learning mentor provided them with the healthy lifestyles leaflet (see documents on project page). This leaflet contained advice on eating less fat, sugar and salt; eating fruit, vegetables and fish; and the importance of breakfast. It also advised readers to ‘move more’. The healthy lifestyle leaflet was chosen as the minimally acceptable intervention that could be provided to young people without giving any alcohol advice. No feedback on the alcohol screening results was provided. The young people in the control group may also have received usual practice advice from the school.
Intervention (brief intervention and alcohol leaflet)
Appendix 5 reports further details on the intervention using the Template for Intervention Description and Replication (TIDieR) checklist. 101 The rest of this section details the intervention.
Young people allocated to the brief alcohol intervention met with the learning mentor face to face in school during the school week (Monday to Friday), in the learning mentor’s office or an alternative suitable space. The learning mentor provided feedback on their positive alcohol screen result and invited them to take part in the trial. Those who consented to the trial received one 30-minute one-to-one interactive session brief alcohol intervention. The session was developed within the pilot feasibility trial. The essential components of brief alcohol interventions were adapted for young people within a school setting after consulting with a PPI group and piloting the intervention. 1 The developed tool was a colourful A3 sheet detailing a six-step intervention, which was intended to lead to an interactive discussion between the young person and the learning mentor (see documents on project page). Based on the principles of MI,102 the intervention sought to increase the young person’s awareness of risks and enable them to consider their motivations for changing their alcohol use. It encompassed the elements of the FRAMES approach for eliciting behaviour change, as outlined in Chapter 1. 54 It was expected that young people would be taken out of class to attend the appointments with learning mentors. The intervention had been found to be feasible and largely acceptable within the pilot feasibility trial and linked qualitative study. The intervention used in the pilot trial, however, had included information about the calorie content of alcoholic drinks. Mixed views were expressed about this content in the pilot feasibility trial and, as such, this was removed from the intervention delivered in the present trial. Table 1 summarises the intervention and control arms.
| Component | Control condition | Brief alcohol intervention condition |
|---|---|---|
| Rationale, theory or goal | Comparison condition | MI to reduce alcohol use |
| Materials | Healthy lifestyle leaflet | Alcohol advice leaflet |
| Procedure | Provision of healthy lifestyle leaflet | Feedback on alcohol screening results, advice on recommended alcohol consumption levels and calculation of participants’ alcohol consumption, raise awareness of risks associated and delivery of behaviour change counselling |
| Intervention provider | Learning mentor | Learning mentor |
| Delivery mode | Information leaflet | Face to face and information leaflet |
| Location | School | School |
| Session duration and frequency | < 1 minute | Up to 30 minutes |
| Tailoring | None | Yes |
| Modifications | None | Adult recommended alcohol consumption reduced from 21 to 14 units per week during study period. The information on the intervention sheet was not changed; however, the learning mentor was advised to communicate this change to participants |
| Fidelity assessment plan | All sessions were to be audio-recorded and a random 20% sample were to be checked by an experienced and qualified alcohol counsellor to ensure differentiation from the brief alcohol intervention. Those in which no advice was given were considered to be at acceptable levels of differentiation | All sessions were to be audio-recorded and a random 20% sample were to be assessed by an experienced and qualified alcohol counsellor using the BECCI |
| Fidelity outcome | 18 sessions were recorded, of which seven were control, and were deemed to be at acceptable levels of differentiation | 11 intervention sessions were audio-recorded. The mean BECCI score was 1.6, indicating that behaviour change counselling was being delivered to ‘some extent’ |
Intervention worksheet
Section 1: how many units are in my drink?
This section sought to raise the young person’s awareness of the units of alcohol in drinks they often consumed. It was comparable with the information commonly provided in simple structured advice. 103 Young people were encouraged to calculate the number of units they drank during a typical drinking day. This calculation was then used as the basis for discussing the recommended levels for adults and the Chief Medical Officer’s recommendation that young people under the age of 15 years should not drink alcohol at all; it was also intended to enable personalised feedback about the risks associated with the young person’s drinking. The Chief Medical Officer’s recommendations on alcohol consumption changed part way through the trial, stating the alcohol guidelines for all adults and not differentiating between men and women, and so learning mentors were advised to verbally update the sheet when speaking with each young person. The young person was also asked how common they perceived alcohol use by young people aged 14–15 years to be. Learning mentors then advised the young people of the actual numbers before asking them to reflect on their thoughts about this. This component was informed by social learning theory. 104 This information was delivered in accordance with the elicit-provide-elicit approach to informing within MI.
Section 2: typical drinking day
In section 2, young people were asked to discuss their typical drinking day in more detail. This background description was intended to provide a useful context for the ensuing discussion about the young person’s drinking, and associated risk and change. The typical drinking day was informed by the SIPS Brief Lifestyle Counselling structure (www.sips.iop.kcl.ac.uk/blc.php). It was developed to provide greater structure and useful prompts about drinking behaviour (with, where, because) for both the young person and the learning mentor. In particular, the additional prompts were intended to provide information relevant to the identification of risk (e.g. the location where a young person consumes alcohol, which may increase or decrease risk) as well as to reinforce positive drinking behaviours (e.g. times when young people drink in ways that are not risky) and to identify the behaviours that may become the focus of change.
Section 3: are there any risks with my drinking?
Section 3 of the intervention built on section 2 and encouraged the young person to consider the risks associated with their alcohol use. The intention was that, by asking the young person to identify personally relevant risks, they would begin to identify motivation for change. It was expected that this would lead naturally on to how important it is for the young person to change their drinking. Young people were then advised of the common risks associated with drinking more than the Chief Medical Officer’s recommended levels before being asked to reflect on this in relation to their own drinking. As well as acting as a further prompt to identifying risks relating to their drinking, the delivery of this information was again in accordance with the elicit-provide-elicit approach to informing within MI.
Section 4: importance/confidence
Section 4 encouraged the young person to rate the importance of changing their drinking, and their confidence at their ability to change, using scaling questions. Importance scales are used in behaviour change counselling to elicit change talk and assess readiness to change. 105 By prompting the young person to consider what would need to happen for this number to increase, ratings may also be positively affected and motivation developed. Confidence scales are useful in identifying barriers to change. Exploration around this can enable the young person to find ways to overcome these barriers and assist in the development of a coping plan in section 6.
Section 5: what do I think about reducing my drinking?
Section 5 asked the young person to consider the ‘bad’ and the ‘good’ things about reducing their drinking. Beginning this section with the bad things before moving on to discussing the good things about reducing consumption enabled pro-change to be reinforced. This is comparable with the ‘Pros and cons of changing your drinking’, which is included in the extended brief intervention tool (www.sips.iop.kcl.ac.uk/blc.php) and discussed by Rollnick et al. 105 The terminology ‘pros and cons’ was changed to ‘good and bad’ to make the language more age-appropriate.
Section 6: what could I do about my drinking?
The final section of the intervention was concerned with developing an action and coping plan for change. It was acknowledged that not all young people would want to agree to such a plan. Those who did were expected to set their own goals, facilitated by the learning mentor, based on the content of the MI. The purpose of this section of the intervention was to elicit commitment talk from the young person,106 as well as to identify existing life skills and develop coping strategies to enable young people to achieve and maintain change. Learning mentors employed a strengths-based approach wherein self-efficacy was promoted. Young people who did not want to agree a plan to change their alcohol use at the present time were encouraged to consider a time when they might want to change their drinking and consider the strategies they would employ.
On completion of the brief alcohol intervention, the young people were provided with an alcohol leaflet, ‘Cheers! Your Health’, designed by the Comic Company (www.comiccompany.co.uk/). This leaflet was identified in the pilot feasibility trial as a suitable, age-appropriate resource that was acceptable to young people (see documents on project page).
Training and support
All learning mentors received training from November 2015 to January 2016 before commencing the study. The training was delivered to learning mentors in group sessions within the school environment by the trial co-ordinator in each study site. The trainers were themselves trained by Ruth McGovern, a senior interventionist. Outreach training has been found to be the most cost-effective implementation strategy for ASBI delivery in other settings. 107 Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) slides were used to guide each training session. This was then followed by an audio-recorded role-play exercise wherein learning mentors practised delivering the intervention with each other to enable the development of skills. Learning mentors were required to record one role-play intervention delivery each. Learning mentors were also trained to issue the participant information leaflet, gather informed consent from the young person and deliver the alcohol information leaflet. Each training session lasted 2–3 hours. An intervention manual was provided to supplement the training (see documents on project page). Following the training session, an experienced alcohol interventionist (RM) listened to the audio-recorded role-plays, rated them using the BECCI and provided feedback on the content. This process was to ensure that learning mentors achieved a minimum standard of fidelity. All learning mentors were required to be rated at a minimum standard (a score of at least 1 on the BECCI) before they delivered the intervention to participating young people within the trial. A total of 80 learning mentors were trained from the four study sites. Four learning mentors were asked to repeat the role-play exercise after detailed feedback was given on their practice. All four learning mentors met the minimum standard following the second exercise. The number of learning mentors per school ranged from one to eight.
The research team provided regular support to the learning mentors, including ongoing guidance on intervention delivery. Co-ordinators made weekly visits/telephone calls and/or sent e-mails to each school throughout the study period to answer questions or concerns, collect materials from completed interventions (such as consent forms and hard copies of intervention tools) and encourage learning mentors to complete outstanding interventions. Finally, learning mentors were provided with a case diary sheet on which they were asked to record any interactions with the individual young people in the trial (see documents on project page). This information was used to calculate the time spent on intervention delivery and inform the cost-effectiveness analysis (see Chapter 5).
Fidelity of the interventions
Fidelity of an intervention within research refers to the extent to which the intervention is true to the therapeutic principles on which it is based. 108 Researchers need to be able to determine whether or not the intervention was delivered as intended; this requires the manualisation of the intervention wherein the philosophy, principles and procedures of the intervention are clearly described. Interventions delivered with high fidelity promote the ability to associate trial results with intervention effectiveness. A manualised intervention with verified fidelity enables the research to be replicated or the intervention to be implemented in practice, if it is shown to be effective.
Learning mentors were asked to audio-record all sessions with consenting participants that they delivered during the trial, from which a 20% sample from various time points would be rated to assess fidelity. However, only 18 recordings (from 11 schools) of the total 443 sessions (control interaction, n = 7, 3%; intervention delivery, n = 11, 5%) were made. Reasons for not recording sessions included the young person’s refusal, unavailable equipment and human error (i.e. forgetting to record the sessions). Because only a limited number of sessions were audio-recorded, all 18 recordings were rated. In this study the control condition was simply assessed as providing no alcohol advice (acceptable levels of differentiation from the alcohol brief intervention) versus providing any alcohol advice (unacceptable levels of differentiation). All seven recordings were free of any alcohol advice and, as such, this small selection of recordings were delivered to an acceptable level of differentiation. The BECCI was used to measure fidelity of the audio-recorded brief alcohol interventions delivered during the trial. BECCI is a tool developed specifically to measure the microskills of behaviour change counselling and MI (e.g. questions, empathic listening statements, summaries). 109 The instrument focuses on the practitioner’s consulting behaviour and attitude rather than the patient’s response. Sessions were rated by an experienced alcohol practitioner within the research team (RM), who is dual qualified in social work and counselling to master’s degree level. Scores were given on a range of 0–4 for 15 different items on a checklist, for which 0 = ’not at all’, 1 = ’minimally’, 2 = ’to some extent’, 3 = ’a good deal’ and 4 = ’a great extent’. A mean score was then calculated. Rating was completed in line with the BECCI Manual for Coding Behaviour Change92 for the purposes of measuring and reporting on the fidelity of intervention delivery within the trial. The mean BECCI scores for the 11 sessions ranged from 0.3 (behaviour change counselling delivered ‘not at all’) to 2.5 (behaviour change counselling skills delivered ‘a good deal’). The mean BECCI score for the 11 recorded interventions was 1.6 and the median BECCI score was 1.5; these scores suggested that overall the learning mentors were found to be delivering behaviour change counselling to ‘some extent’. This is similar to the BECCI scores reported in other studies110 of practitioner-delivered behaviour change counselling. Learning mentors typically performed well when discussing the risks associated with the young person’s alcohol use. Lower scores were observed in respect of microskills relating to discussing and exploring behaviour change.
The small number of interventions recorded is a significant weakness and limits our ability to assess threats to internal validity. 111 It is possible that the learning mentors who did not provide a recording differed in skill from those who did. Learning mentors may have selected recorded sessions in which they felt they performed better.
Chapter 3 Trial methods and results
Key points for Chapter 3
-
A total of 1064 (23.5%) young people screened positive on the A-SAQ.
-
Of those, 443 young people were recruited to the trial from 30 schools in four areas.
-
Follow-up data at 12 months were collected from 84.4% of those recruited.
-
There was evidence of a reduction in drinking across the trial, as reflected in a change in AUDIT score over the 12-month period.
-
Thirty-eight (21%) young people in the intervention arm and 55 (28%) in the control arm reported drinking no alcohol in the previous 28 days on the TLFB.
-
There were few or no differences between the trial arms in the distribution of variables summarising alcohol consumed in the previous 28 days from the TLFB.
-
There were few or no differences between the trial arms in the distribution of survey variables summarising other drinking-related aspects, smoking, psychological well-being and sexual behaviour at 12 months.
Trial summary
Inclusion criteria
-
Young people aged 14–15 years, inclusive.
-
Parents had not opted them out of the study.
-
Scored positive on the A-SAQ and left their names.
-
Were willing and able to provide informed written consent for intervention and follow-up.
Exclusion criteria
-
Were already seeking or receiving help for an alcohol use disorder.
-
Had recognised mental health or challenging behaviour issues, identified by school staff.
Sample size and power
The sample size was calculated to have a 90% power to detect a standardised difference of 0.3 (which equated to a ratio of 1.5 in geometric means) in total alcohol units consumed in 28 days, using a significance level of 5%. Parameter estimates came from the pilot trial1 (mean year group size = 210, 87% completing baseline questionnaire, 80% recruited to trial and 88% providing data at the 12-month follow-up). In the pilot trial we found that 18% of young people had screened positive and left their names. However, given that the numbers screening positive were anticipated to be lower in the south of England, and the extra efforts put in place in the current trial to encourage young people to leave their names on the questionnaires, it was estimated that this figure would be 20% in the full trial. Using these estimates, follow-up data would be required from 235 young people per arm. The number required to have follow-up data if the power was reduced to 80% was 176. Given the difficulty in recruiting sufficient numbers, the target for power was later reduced from 90% to 80%, after discussion with the TSC and DMEC.
Statistical analysis plan
Individual site staff input the trial data into a MACRO™ (Elsevier Limited, London, UK) database held and maintained by the Newcastle Clinical Trials Unit. Data were extracted from MACRO into statistical software package Stata® version 14 (StataCorp LP, College Station, TX, USA). 1 A complete statistical analysis plan providing full details of all statistical analyses, variables and outcomes was finalised and signed before the final database download. Scoring systems for numerical scales are shown in Appendix 6. All analyses were carried out on an intention-to-treat basis, retaining patients in the analysis group to which they had been randomised and including any protocol violator and ineligible participants.
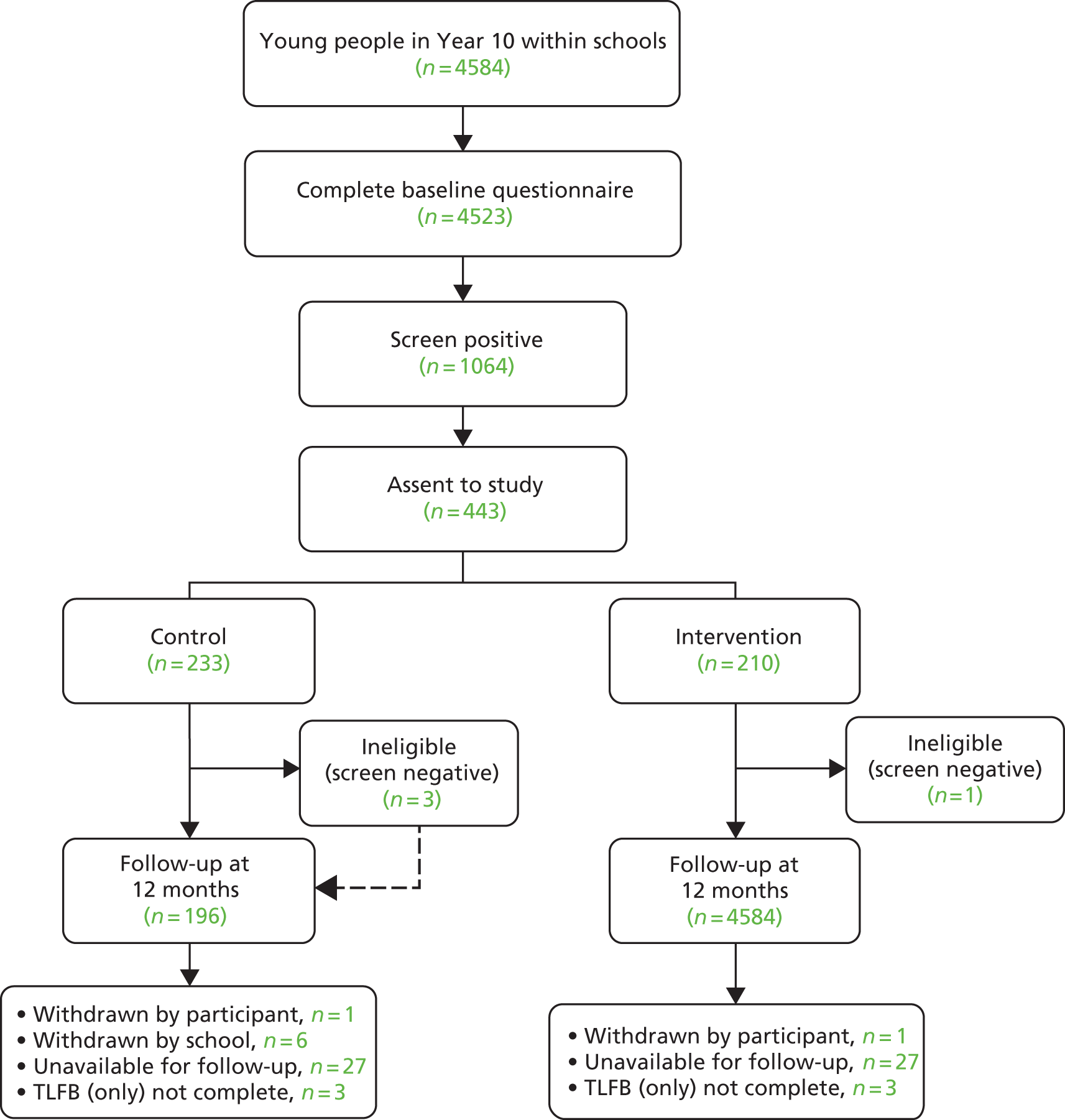
Descriptive analyses
After the recruitment of schools, the flow of young people through the study was presented using a Consolidated Standards of Reporting Trials (CONSORT)2 flow diagram (Figure 2). The number of young people in the age group, how many completed baseline questionnaires, how many screened positive, how many assented and how many completed the 12-month follow-up were reported by region and by school. Any reasons for not completing follow-up were reported when known. Descriptive statistics were used to report the pupil-level baseline data, by arm. These included all measures reported in the baseline questionnaires, reported as comparisons of percentages and means or medians as appropriate.
FIGURE 2.
The CONSORT flow diagram.
Inferential analyses
It was planned to use multiple linear regression to compare the primary outcome (mean number of units consumed in the previous 28 days) between the two trial arms at 12 months, estimating the difference between mean scores and adjusting for any imbalance in key covariates, namely gender, region (north-east, north-west and south), level of deprivation (percentage of free school meals) and baseline AUDIT score. Data from the London and Kent areas were combined as the ‘south’ region as there were very few young people providing responses at baseline and 12 months in London schools. If, as was considered likely, the primary outcome was skewed, the statistical analysis plan stated that there would be a logarithmic transformation and results would be presented as ratios of geometric means. Alternatively, other root transformations could be considered and confidence intervals (CIs) around differences in means would be obtained by bootstrapping. However, at 12 months a substantial minority of participants reported consuming 0 units of alcohol. This made it impossible to use a logarithmic transformation, and root transformations did not deal with the skewness. Hurdle models3 were considered to deal with the zero inflation, but convergence was not achieved for all variables. It was therefore decided to use quantile regression to model the median number of units consumed in the previous 28 days using the same covariates: the results were very similar to those of the Hurdle models when results were available. The majority of secondary outcomes were analysed similarly. The only exception was the comparison of the proportions who had reduced their drinking below hazardous (or dependent) levels between baseline and 12 months; this was done by logistic regression, adjusting for the same covariates as for other outcome variables.
In a post hoc analysis, Bayes factors were calculated to determine the strength of support for the alternative hypothesis (HA: the intervention shows some difference in alcohol consumption between trial arms) versus the null hypothesis (H0: no effect). Bayes factors can determine whether there is simply a lack of evidence for the alternative hypothesis or whether the evidence supports the null hypothesis. A Bayes factor of > 1 indicates support for HA, whereas one of < 1 indicates support for H0. Values of Bayes factors of > 3 or < 1/3 are regarded as substantial evidence for the alternative or null hypothesis, respectively.
Exploratory analyses
Exploratory analysis included investigating differences in the primary outcome by gender, deprivation (percentage of free school meals) and levels of drinking at baseline (A-SAQ). Gender and A-SAQ differences were illustrated by box plots, and associations with deprivation were illustrated by a scatter plot. The levels of drinking according to the A-SAQ at baseline were categorised as those drinking ‘more than 3 units on four or more times in the last 6 months but not every month’, those drinking ‘at least once a month’ and those drinking ‘at least once a week (including those drinking daily)’. It had been planned to look at the extent of the intervention received, but as all of the young people allocated to the brief intervention received it, no such analysis was necessary.
Recruitment and follow-up
The recruitment of schools took place between November 2015 and June 2016. During this period, 154 schools were invited to take part (north-east, n = 44; north-west, n = 35; London, n = 36; and Kent, n = 39). Thirty-three schools were recruited (north-east, n = 13; north-west, n = 7; London, n = 5; and Kent, n = 8); few of the non-participating schools gave reasons for not taking part, but those that did mentioned impending school closure (n = 1), lacking time or staff availability (n = 7), having a policy not to take part in surveys (n = 1) and lacking agreement with elements of the research (n = 2). Two schools that initially agreed to take part subsequently withdrew shortly after recruitment: one in the north-west did not like the sexual health questions, whereas the other, in Kent, withdrew because of school closure. A third school in London later withdrew because of issues with the trial; this was after the young people had been screened but before the meetings to obtain consent had taken place. The number of schools recruited had to be increased from the 20 planned, partly because the average year-group size was much smaller than anticipated from our experiences in the pilot trial.
Recruitment at the young person level is summarised in the CONSORT flow diagram (see Figure 2). Table 2 shows the figures on recruitment, screening, consent and randomisation, by area. Among the schools recruited, 4523 (98.7% of the year groups) pupils completed the baseline questionnaire and 1064 (23.5% of those completing the questionnaire) screened positive. Of those screening positive, 443 (41.6%) consented to take part in the study by providing their names. Using the pilot study data,1 we had expected that 14% of those surveyed would screen positive and consent to take part in the trial, whereas we managed to recruit only 443 out of 4584 (9.7%). The lower than anticipated numbers eligible and willing to take part was largely explained by fewer than expected screening positive on the A-SAQ. Four young people scored negative on the A-SAQ and were incorrectly included, even though they were ineligible, through human error. Three of these were randomised to the control group and completed the 12-month follow-up, but the one randomised to the intervention group withdrew before the intervention. It can be seen that the screen-positive rate varied by area (north-east, 27.4%; north-west, 19.4%; London, 14.6%; and Kent, 24.2%). Table 2 also shows the trial arm to which each young person was randomised. All 210 young people randomised to intervention received the brief intervention. The numbers screening positive and assenting to the study broken down by area and school are shown in Appendix 7. Table 3 summarises the numbers of young people ineligible, withdrawn and lost to follow-up.
| Area | Number of | Consent to study (% of positive) | Randomised to (n) | |||
|---|---|---|---|---|---|---|
| Young people in year | Surveys completed (% of young people in year) | Surveys positive (% of surveys completed) | Intervention | Control | ||
| North-east | 2132 | 2115 (99.2) | 579 (27.4) | 241 (41.6) | 116 | 125 |
| North-west | 734 | 715 (97.4) | 139 (19.4) | 59 (42.4) | 27 | 32 |
| London | 677 | 665 (98.2) | 97 (14.6) | 5 (5.2) | 2 | 3 |
| Kent | 1041 | 1028 (98.8) | 249 (24.2) | 138 (55.4) | 65 | 73 |
| Total | 4584 | 4523 (98.7) | 1064 (23.5) | 443 (41.6) | 210 | 233 |
| Reason | Trial arm (n) | |
|---|---|---|
| Intervention | Control | |
| Ineligible | ||
| Enrolled in trial but had not screened positive on A-SAQ | 1 | 3 |
| Total | 1 | 3 |
| Withdrawal | ||
| Withdrawn: student no longer wished to participate | 2 | 1 |
| Withdrawn by school: poor attendance/disciplinary issues | 0 | 4 |
| Withdrawn by school: health reasons | 0 | 2 |
| Total | 2 | 7 |
| Lost to follow-up/unavailable for follow-up | ||
| Lost to follow-up: participant left school | 10 | 14 |
| Lost to follow-up: reason unknown | 1 | 2 |
| In exam/absent on day of scheduled follow-up | 3 | 6 |
| Lost to follow-up: not contacted within 30 days | 13 | 5 |
| Total | 27 | 27 |
Appendices 8 and 9 show the distribution of the baseline characteristics (categorical and questionnaire responses) of three groups of young people: those screening positive and consenting to the trial, those screening positive and not assenting and those who screened negative. There are similar baseline characteristics between the two subgroups who screened positive, but those who screened negative differed from the screen-positive subgroups in terms of smoking, drinking and sexual behaviour.
Follow-up data at 12 months were collected on 374 young people (84.4% of those recruited to the trial). A few young people did not complete the TLFB, but that information was available for 368 participants (83.0% of those recruited). The numbers providing data on the TLFB and other questionnaires at 12 months in each area are shown in Table 4. Numbers by area and by school can be found in Appendix 10.
| Region | Trial arm | |||||
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| Randomised (n) | TLFB complete, n (%) | 12-month questionnaire complete, n (%) | Randomised (n) | TLFB complete, n (%) | 12-month questionnaire complete, n (%) | |
| North-east | 116 | 98 (84.5) | 98 (84.5) | 125 | 110 (88.0) | 110 (88.0) |
| North-west | 27 | 25 (92.3) | 25 (92.3) | 32 | 27 (84.4) | 26 (81.3) |
| London | 2 | 1 (50.0) | 1 (50.0) | 3 | 3 (100.0) | 3 (100.0) |
| Kent | 65 | 54 (83.1) | 57 (87.7) | 73 | 56 (76.7) | 58 (79.5) |
| Total | 210 | 178 (84.8) | 181 (86.2) | 233 | 196 (84.1) | 197 (84.5) |
Baseline characteristics, by trial arm
Descriptive statistics for all measures reported in the baseline questionnaires are summarised by trial arm in Tables 5 and 6: the distributions were balanced between the intervention and control arms. Overall, 46% of young people randomised admitted ever smoking a whole cigarette, the majority of whom had begun smoking between the ages of 11 and 14 years. However, only 29% stated that they had smoked during the previous 30 days. Fifty-six per cent of young people who responded said that they had never engaged in sexual intercourse. Of those who had, 21% said that they had engaged in intercourse that they had regretted the next day, and 24% said that they had engaged in intercourse without a condom. The median AUDIT score was 6, with a range of 0–40 (the percentages of hazardous and dependent drinking are shown in Table 8). The RAPI score, concerning alcohol-related problems, had a median of 4 and a range of 0–48. The WEMWBS score, measuring psychological health, had a median of 46 and a range of 14–70 (see Tables 5 and 6).
| Variable | Trial arm, n (%) | |
|---|---|---|
| Intervention (N = 210) | Control (N = 233) | |
| Demographics | ||
| Gender | ||
| Female | 106 (50.5) | 115 (49.4) |
| Male | 104 (49.5) | 118 (50.6) |
| Ethnicity | ||
| White | 189 (90) | 213 (91.4) |
| Black | 4 (1.9) | 4 (1.7) |
| Mixed | 14 (6.7) | 12 (5.2) |
| Asian | 1 (0.5) | 2 (0.9) |
| Not known | 1 (0.5) | 0 (0) |
| Other | 1 (0.5) | 1 (0.4) |
| Missing | 0 (0) | 1 (0.4) |
| Use of leisure time | ||
| When you have free time do you mainly | ||
| Go round to a friend’s house (or have them come round to yours) | 59 (28.1) | 75 (32.2) |
| Go out somewhere with friends | 124 (59) | 123 (52.8) |
| Spend time with your family | 25 (11.9) | 32 (13.7) |
| Spend time with brother(s) and/or sister(s) | 9 (4.3) | 19 (8.2) |
| Spend time by yourself | 61 (29) | 58 (24.9) |
| None of these | 13 (6.2) | 14 (6) |
| Did not answer | 3 (1.4) | 2 (0.9) |
| Smoking | ||
| How old were you when you smoked a whole cigarette for the first time? | ||
| I have never smoked a whole cigarette | 115 (54.8) | 122 (52.4) |
| 8 years old or younger | 2 (1) | 6 (2.6) |
| 9 or 10 years old | 5 (2.4) | 8 (3.4) |
| 11 or 12 years old | 32 (15.2) | 40 (17.2) |
| 13 or 14 years old | 47 (22.4) | 44 (18.9) |
| Over 14 years old | 9 (4.3) | 9 (3.9) |
| Did not answer | 0 (0) | 4 (1.7) |
| During the past 30 days, on the days you smoked, how many cigarettes did you smoke per day? | ||
| I did not smoke cigarettes during the last 30 days | 151 (71.9) | 161 (69.1) |
| Fewer than 1 | 13 (6.2) | 12 (5.2) |
| 1 | 8 (3.8) | 9 (3.9) |
| 2–5 | 18 (8.6) | 23 (9.9) |
| 6–10 | 13 (6.2) | 15 (6.4) |
| 11–20 | 7 (3.3) | 5 (2.1) |
| More than 20 | 0 (0) | 6 (2.6) |
| Did not answer | 0 (0) | 2 (0.9) |
| Energy drinks | ||
| How many times per week do you usually drink energy drinks? | ||
| Never | 57 (27.1) | 47 (20.2) |
| Less than once | 57 (27.1) | 69 (29.6) |
| Once | 24 (11.4) | 36 (15.5) |
| 2–4 days | 40 (19) | 44 (18.9) |
| 5–6 days | 11 (5.2) | 11 (4.7) |
| Every day once per day | 9 (4.3) | 8 (3.4) |
| More than once per day | 12 (5.7) | 17 (7.3) |
| Did not answer | 0 (0) | 1 (0.4) |
| Risky sexual behaviour | ||
| After drinking alcohol, have you ever engaged in sexual intercourse that you regretted the next day? | ||
| No | 71 (33.8) | 74 (31.8) |
| Yes | 22 (10.5) | 16 (6.9) |
| I have never engaged in sexual intercourse | 111 (52.9) | 136 (58.4) |
| Did not answer | 6 (2.9) | 7 (3) |
| After drinking alcohol, have you ever engaged in sexual intercourse without a condom? | ||
| No | 71 (33.8) | 68 (29.2) |
| Yes | 22 (10.5) | 23 (9.9) |
| I have never engaged in sexual intercourse | 111 (52.9) | 132 (56.7) |
| Did not answer | 6 (2.9) | 10 (4.3) |
| A-SAQ | ||
| In the last 6 months how often have you drunk more than 3 units of alcohol? | ||
| Never | 0 (0) | 0 (0) |
| Fewer than four times | 1 (0.5) | 3 (1.3) |
| Four or more times but not every month | 79 (37.6) | 98 (42.1) |
| At least once a month but not every week | 92 (43.8) | 92 (39.5) |
| Every week but not every day | 36 (17.1) | 37 (15.9) |
| Every day | 2 (1.0) | 3 (1.3) |
| Measure | n | Minimum | LQ | Median | UQ | Maximum | Mean | SD |
|---|---|---|---|---|---|---|---|---|
| AUDIT | ||||||||
| Intervention | 210 | 0 | 3 | 6 | 11 | 28 | 7.6 | 5.6 |
| Control | 232 | 0 | 3 | 6.5 | 10 | 40 | 7.6 | 6.4 |
| AUDIT-C | ||||||||
| Intervention | 210 | 0 | 2 | 3 | 5 | 10 | 3.8 | 2.1 |
| Control | 232 | 0 | 2 | 4 | 5 | 12 | 4.0 | 2.4 |
| RAPI | ||||||||
| Intervention | 207 | 0 | 1 | 5 | 12 | 45 | 8.1 | 9.9 |
| Control | 225 | 0 | 1 | 3 | 9 | 48.1 | 6.5 | 8.7 |
| WEMWBS | ||||||||
| Intervention | 194 | 14 | 37 | 47 | 53 | 70 | 45.4 | 12.0 |
| Control | 207 | 14 | 40 | 46 | 54.9 | 70 | 46.4 | 11.4 |
| DMQ-R – coping | ||||||||
| Intervention | 206 | 1 | 1 | 1.4 | 2.4 | 5 | 1.8 | 1.0 |
| Control | 228 | 1 | 1 | 1.2 | 2.2 | 5 | 1.7 | 0.9 |
| DMQ-R – social | ||||||||
| Intervention | 207 | 1 | 1.8 | 2.4 | 3.6 | 5 | 2.7 | 1.1 |
| Control | 228 | 1 | 1.6 | 2.4 | 3.3 | 5 | 2.5 | 1.0 |
| DMQ-R – conforming | ||||||||
| Intervention | 206 | 1 | 1 | 1 | 1.2 | 5 | 1.3 | 0.7 |
| Control | 227 | 1 | 1 | 1 | 1.2 | 5 | 1.3 | 0.7 |
| DMQ-R – enhancement | ||||||||
| Intervention | 207 | 1 | 1.2 | 1.8 | 2.6 | 4.4 | 2.1 | 1.0 |
| Control | 228 | 1 | 1.2 | 1.6 | 2.4 | 5 | 2.0 | 1.0 |
Twelve-month outcomes, by trial arm
The four outcome variables derived from the 28-day TLFB are reported in Table 7: this gives the descriptive statistics per trial arm and the unadjusted and adjusted difference in medians with 95% CIs. The distribution of the primary outcome by trial arm and region is shown in Figure 3.
| Measure | n | Minimum | LQ | Median | UQ | Maximum | Mean | SD | Difference (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | |||||||||
| Number of units of alcohol consumed over previous 28 days | ||||||||||
| Intervention | 178 | 0 | 1.8 | 7.3 | 18.5 | 217.4 | 16.2 | 27.9 | –0.5 (–4.2 to 3.1) | 0.8 (–2.5 to 4.0) |
| Control | 196 | 0 | 0 | 7.7 | 18.0 | 88.7 | 13.2 | 17.5 | ||
| Percentage day abstinence over previous 28 days | ||||||||||
| Intervention | 178 | 42.9 | 89.3 | 92.9 | 96.4 | 100 | 92.1 | 9.1 | –3.6 (–4.9 to –2.2) | –0.4 (–2.2 to 1.5) |
| Control | 196 | 57.1 | 89.3 | 96.4 | 100 | 100 | 93.0 | 7.4 | ||
| Number of days > 2 units consumed over previous 28 days | ||||||||||
| Intervention | 178 | 0 | 0 | 1 | 2 | 16 | 1.8 | 2.2 | 0.0 (–0.4 to 0.4) | 0.3 (–0.1 to 0.7) |
| Control | 196 | 0 | 0 | 1 | 2 | 8 | 1.5 | 1.7 | ||
| Drinks per drinking day | ||||||||||
| Intervention | 178 | 0 | 1.5 | 4.2 | 7.8 | 28.8 | 5.3 | 5.2 | 0.0 (–1.3 to 1.3) | –0.5 (–1.6 to 0.6) |
| Control | 196 | 0 | 0 | 3.9 | 7.6 | 29.5 | 4.9 | 5.2 | ||
| AUDIT | ||||||||||
| Intervention | 181 | 0 | 3 | 5 | 8 | 21 | 5.7 | 4.2 | 0.0 (–1.1 to 1.1) | –0.1 (–1.0 to 0.8) |
| Control | 197 | 0 | 2 | 5 | 8 | 23 | 5.5 | 4.3 | ||
| AUDIT-C | ||||||||||
| Intervention | 180 | 0 | 2 | 3 | 5 | 10 | 3.7 | 2.1 | 0.0 (–0.6 to 0.6) | 0.1 (–0.4 to 0.7) |
| Control | 197 | 0 | 2 | 3 | 5 | 9 | 3.4 | 2.2 | ||
| RAPI | ||||||||||
| Intervention | 181 | 0 | 0 | 3 | 7 | 29 | 4.5 | 5.3 | 0.0 (–1.3 to 1.3) | 0.2 (–0.8 to 1.2) |
| Control | 197 | 0 | 0 | 3 | 6 | 35 | 4.0 | 4.8 | ||
| WEMWBS | ||||||||||
| Intervention | 178 | 21 | 43.1 | 50 | 55 | 69 | 48.9 | 9.0 | 1.0 (–1.6 to 3.6) | 1.7 (–0.7 to 4.1) |
| Control | 194 | 24 | 41 | 49 | 55 | 69 | 48.6 | 9.4 | ||
| DMQ-R – coping | ||||||||||
| Intervention | 181 | 1 | 1 | 1.4 | 1.8 | 4 | 1.5 | 0.6 | 0.0 (–0.2 to 0.2) | –0.1 (–0.3 to 0.1) |
| Control | 197 | 1 | 1 | 1.4 | 2 | 4.2 | 1.6 | 0.7 | ||
| DMQ-R – social | ||||||||||
| Intervention | 181 | 1 | 2 | 2.6 | 3.6 | 5 | 2.7 | 1.0 | 0.2 (–0.1 to 0.5) | 0.1 (–0.2 to 0.5) |
| Control | 197 | 1 | 1.8 | 2.4 | 3.2 | 5 | 2.6 | 1.0 | ||
| DMQ-R – conforming | ||||||||||
| Intervention | 181 | 1 | 1 | 1 | 1.2 | 3.6 | 1.1 | 0.4 | 0.0 (–0.2 to 0.2) | 0.0 (–0.04 to 0.04) |
| Control | 197 | 1 | 1 | 1 | 1.2 | 3.4 | 1.1 | 0.3 | ||
| DMQ-R – enhancement | ||||||||||
| Intervention | 181 | 1 | 1.2 | 1.6 | 2.4 | 5 | 1.9 | 0.9 | –0.2 (–0.4 to 0.03) | –0.1 (–0.3 to 0.2) |
| Control | 197 | 1 | 1.2 | 1.8 | 2.4 | 4.4 | 1.9 | 0.8 | ||
FIGURE 3.
Alcohol units consumed in past. (a) Control, London and Kent; (b) control, north-east; (c) control, north-west; (d) intervention, London and Kent; (e) intervention, north-east; and (f) intervention, north-west.

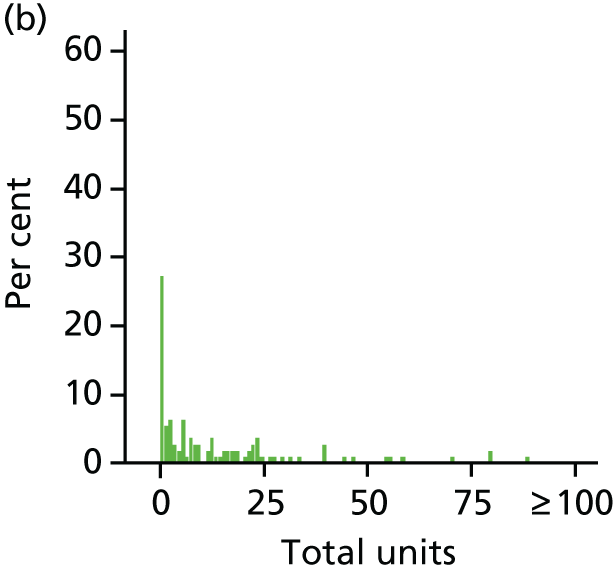
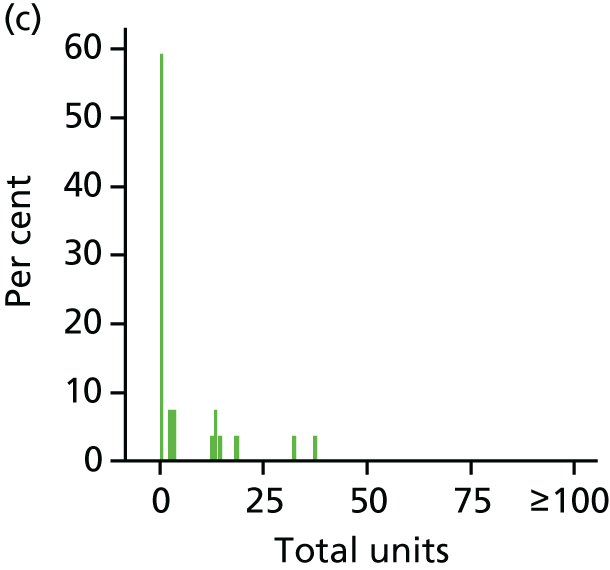


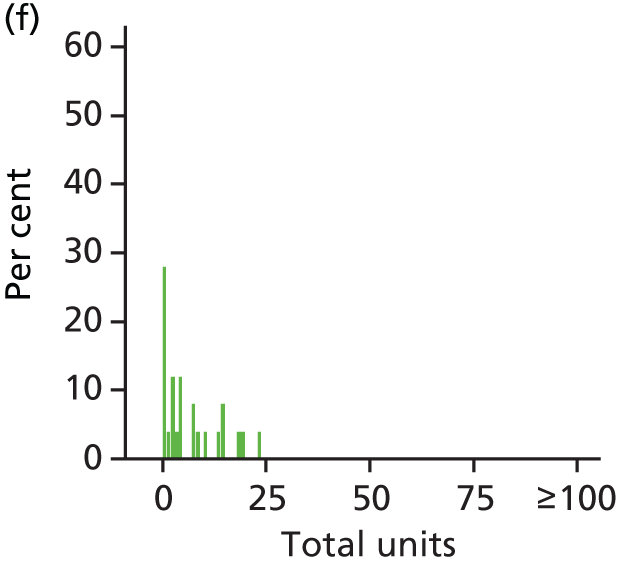
It can be seen that a substantial minority of young people reported consuming no units of alcohol in the previous month (intervention arm, n = 38, 21%; control arm, n = 55, 28%), particularly in the north-west schools. However, a few young people reported consuming a very large number of alcohol units.
The median values of the primary outcome (total units consumed in previous 28 days) were 7.3 in the intervention arm and 7.7 in the control arm. The results of the quantile regression gave an adjusted difference (intervention – control) in median total units of 0.8 (95% CI –2.5 to 4.0), indicating that there was no statistically significant difference in the alcohol consumed by young people, whether or not they received the intervention. It can be seen in Table 7 that the distributions are very similar between trial arms for all four variables derived from the TLFB: the adjusted differences in medians between trial arms were all close to 0. This shows that there were no differences in other aspects of alcohol consumption between young people who received the intervention and those who did not.
The null finding requires further exploration to explore whether it is indicative of being valid, insensitive or invalid. To explore this, we calculated the Bayes factor using the methods outlined by Dienes et al. 112 To estimate the Bayes factor, we estimated the effect size difference between the groups on the primary outcome measure. As the median difference is equivalent to the mean difference for distributions that are similar but not necessarily symmetrical, we tested this assumption by examining the coefficient plots for both quantile and ordinary least squares regression. After confirmation we established the effect size difference and associated CIs using 1000 bootstrap replications stratified by school, 0.0004 (standard error 0.013). We used a recent systematic review of brief interventions for adolescent alcohol users57 and this estimated that the effect size difference on alcohol consumed was of the order of 0.27 (standard error 0.055), similar in magnitude to that proposed in the sample size calculation. The resulting Bayes factor was 0.30, and is strong evidence in support of the null hypothesis, that there is no difference between the groups in alcohol consumed.
Other secondary outcomes were those from questionnaires (AUDIT, AUDIT-C, DMQ-R, RAPI and WEMWBS). Table 7 shows the distribution of questionnaire scores by trial arm at 12 months. It can again be seen that the distributions were very similar by trial arm: the adjusted differences in medians between trial arms were close to 0, with little evidence that the results were consistent with a large difference on any scale.
Those young people who reported risky drinking as defined by AUDIT score are described in Table 8 using cut-off points of 4 (indicating hazardous drinking) and 8 (indicating dependency). Table 8 shows the numbers in each trial arm who reported hazardous and dependent drinking at baseline and 12 months, and the results of the logistic regression compare the odds of reducing levels from hazardous to non-hazardous over 12 months between arms (for those who were hazardous at baseline), and similarly for dependent levels. The adjusted odds ratio comparing those who became non-hazardous between intervention and control arms was 0.91 (95% CI 0.54 to 1.56), indicating little association between trial arm and becoming non-hazardous. That comparing the odds of becoming non-dependent was 0.55 (95% CI 0.29 to 1.04): the odds ratio was further away from 1 in this analysis, but was based on a smaller sample size. For both cut-off points, the number of young people in these categories had reduced at 12 months, although there is little evidence of any difference between control and intervention arms.
| AUDIT score (%) | ||||
|---|---|---|---|---|
| ≥ 4 (hazardous) | ≥ 8 (dependence) | |||
| Intervention (n = 181) | Control (n = 196) | Intervention (n = 181) | Control (n = 196) | |
| Baseline | 71.3 | 66.8 | 40.3 | 42.4 |
| 12 months | 60.8 | 60.7 | 29.8 | 28.6 |
| Odds ratio (95% CI) of baseline hazardous drinkers becoming non-hazardous at 12 monthsa | Odds ratio (95% CI) of baseline dependent drinkers becoming non-dependent at 12 monthsa | |||
| n = 129 | n = 131 | n = 73 | n = 83 | |
| Unadjusted | 0.91 (0.54 to 1.56) | 1.00 | 0.55 (0.29 to 1.04) | 1.00 |
| Adjusted | 1.04 (0.53 to 1.56) | 1.00 | 0.54 (0.28 to 1.02) | 1.00 |
Changes in the A-SAQ score from baseline to 12 months reflected the changes in how much and how regularly young people drank alcohol. At 12 months, 60% of young people in the intervention arm and 59% in the control arm reported that they had reduced their drinking. Only a small proportion of young people said that they were drinking more at 12 months. These changes are shown in Table 9.
| Drinking level | Trial arm, n (%) | |
|---|---|---|
| Intervention (N = 180) | Control (N = 195) | |
| Reduced drinking | 108 (60.0) | 115 (59.0) |
| Drinking at same level | 47 (26.11) | 55 (28.2) |
| Increased drinking | 25 (13.9) | 25 (12.8) |
The changes in smoking status from baseline to 12 months are shown in Table 10. Twenty-three (12.8%) young people had started smoking during this period in the intervention arm, compared with 28 (14.4%) in the control arm. Similar numbers had reported smoking either more or fewer cigarettes over time.
| Smoking status | Trial arm, n (%) | |
|---|---|---|
| Intervention (N = 180) | Control (N = 195) | |
| Never smoked | 76 (42.2) | 83 (42.6) |
| Started smoking | 23 (12.8) | 28 (14.4) |
| Smoking more | 20 (11.1) | 17 (8.7) |
| Smoking less | 25 (13.9) | 28 (14.4) |
| Still smoking (same amount, or amount unknown) | 36 (20.0) | 39 (20.0) |
The changes in risky sexual behaviour are reported in Tables 11 and 12. The number of young people who had engaged in sexual intercourse that they regretted over the 12-month period was 11 in the intervention arm and 12 in the control arm. The number of young people who had engaged in sexual intercourse without a condom over the 12-month period was 12 in the intervention arm and 10 in the control arm. However, data were missing at 12 months for a substantial minority, and there were some inconsistent results (e.g. reporting that they had engaged in risky sexual behaviour at baseline, but that they had never engaged in sexual intercourse at 12 months). The questions were asked as ‘have you ever?’ and so young people reporting risky sexual behaviour at baseline and at 12 months could have been referring to the same event. Any results need to be interpreted with some caution because of these issues.
| Baseline | 12 monthsa (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (N = 210) | Control (N = 233) | |||||||
| No | Yes | Never engaged in sexual intercourse | Missing | No | Yes | Never engaged in sexual intercourse | Missing | |
| No | 45 | 9 | 9 | 8 | 37 | 8 | 15 | 14 |
| Yes | 13 | 3 | 1 | 5 | 8 | 3 | 1 | 4 |
| Never engaged in sexual intercourse | 39 | 2 | 55 | 15 | 61 | 4 | 53 | 18 |
| Did not answer | 3 | 0 | 2 | 1 | 5 | 0 | 2 | 0 |
| Baseline | 12 monthsa (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (N = 210) | Control (N = 233) | |||||||
| No | Yes | Never engaged in sexual intercourse | Missing | No | Yes | Never engaged in sexual intercourse | Missing | |
| No | 45 | 10 | 8 | 8 | 38 | 4 | 14 | 14 |
| Yes | 9 | 7 | 1 | 5 | 6 | 7 | 2 | 8 |
| Never engaged in sexual intercourse | 38 | 2 | 56 | 15 | 56 | 6 | 54 | 16 |
| Did not answer | 3 | 0 | 2 | 1 | 8 | 0 | 2 | 0 |
The changes in consumption of energy drinks from baseline to 12 months are shown in Table 13. Ninety-two (51.1%) young people in the intervention arm either had stopped consuming such drinks or reported consuming fewer during the period; the corresponding number in the control arm was 82 (42.0%).
| Energy drinks intake | Trial arm, n (%) | |
|---|---|---|
| Intervention (N = 180) | Control (N = 195) | |
| Never consumed energy drinks | 37 (20.6) | 29 (14.9) |
| Has stopped consuming energy drinks | 37 (20.6) | 31 (15.9) |
| Has started consuming energy drinks | 13 (7.2) | 13 (6.7) |
| Is consuming more energy drinks | 10 (5.6) | 21 (10.8) |
| Is consuming fewer energy drinks | 55 (30.6) | 51 (26.2) |
| Is consuming the same number of energy drinks | 28 (15.6) | 50 (25.6) |
Exploratory analyses
Exploratory analyses around units consumed by gender and alcohol consumed in relation to free school meals are shown in Figures 4 and 5.
FIGURE 4.
Alcohol units consumed, by gender.

FIGURE 5.
Alcohol units vs. free school meals.
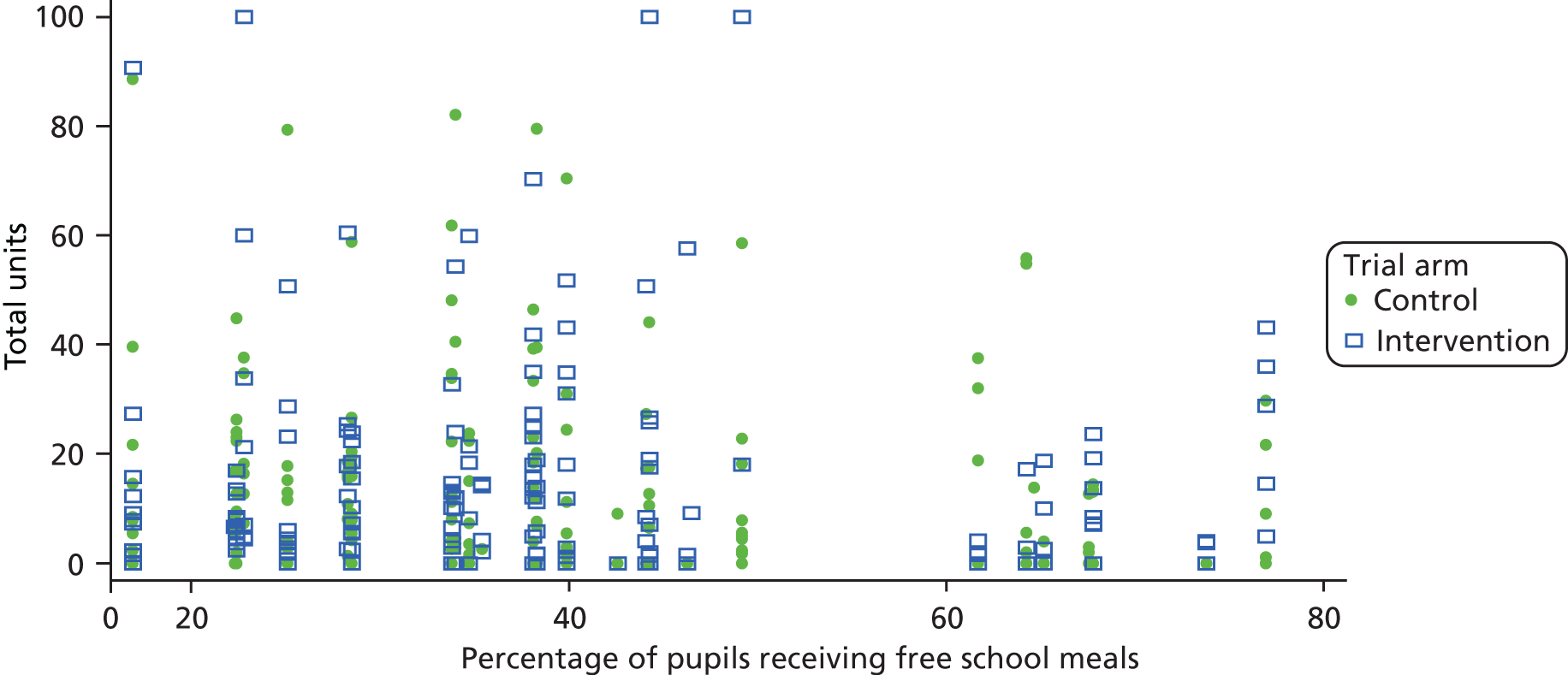
Young people were categorised by level of drinking according to the A-SAQ at baseline. Figure 6 illustrates the total units consumed in the previous 28 days at 12 months for these groups by trial arm. Those who had been drinking more heavily at baseline were also the heaviest drinkers at 12 months, regardless of whether they were in the control or the intervention group. There was no indication that the intervention was more effective in any baseline drinking level subgroups.
FIGURE 6.
Levels of drinking, by trial arm.
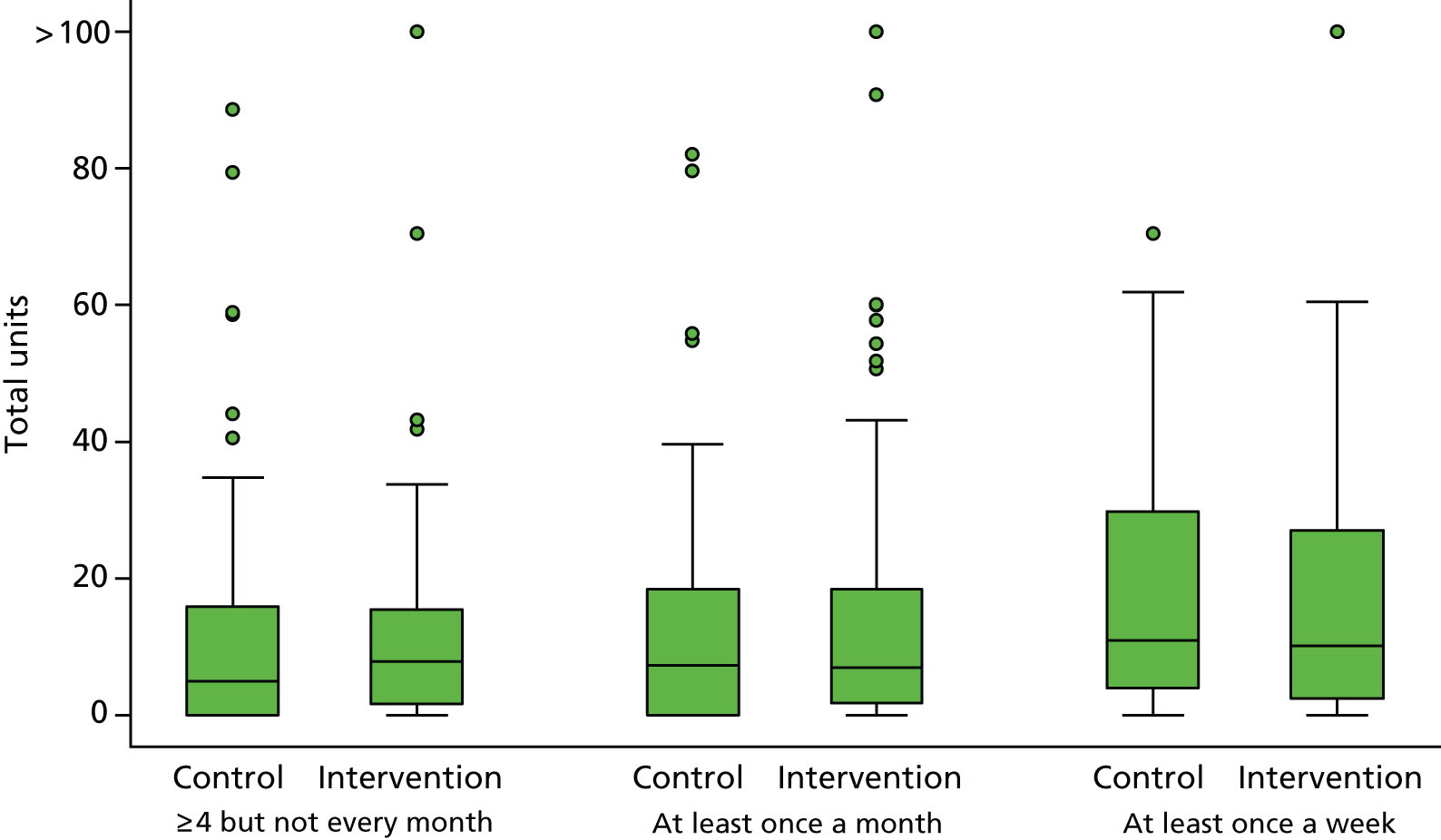
Chapter 4 Qualitative methods and results
Key points for Chapter 4
-
Semistructured interviews were conducted with nine teaching staff, 21 learning mentors, 33 young people and two parents (n = 65).
-
Overall, school-based staff, young people and parents all felt that the intervention was interesting and could have an impact on young people who were drinking alcohol. However, most participants felt that the screening tool was too sensitive and targeted young people who were consuming only small amounts of alcohol, and could be adapted in the future to allow the school to forgo screening and instead target people whom they believed to be drinking excessively and would, in their opinion, warrant an intervention. Given that many young people receiving the intervention were not those whom the school would have known were drinking alcohol, a targeted approach could potentially miss many young people who would benefit from an intervention.
-
The intervention materials were well received by young people and school-based staff. The intervention worksheet was viewed as a useful tool for engaging young people in conversation about risky behaviour. However, school-based staff and young people felt that there was too long an interval between different elements of the study. Whereas the screening was conducted before Christmas in all schools, some intervention and control sessions were not arranged until the following June, although it was up to the school to arrange individual appointments.
-
Overall, the impact on learning mentor workloads within the school was seen as manageable, although this varied greatly. The number of learning mentors within the school, the number of young people randomised and support from other staff within the school all determined the amount of time needed to complete the intervention sessions.
-
The interviews indicated that learning mentors could be well suited to conduct alcohol screening and brief interventions, as these complement the work that they currently do. However, it must be noted that, despite their less formal role within the school, learning mentors may still be viewed as being in a position of authority, which may affect whether or not young people disclose information.
Introduction
To explore the perceptions on delivery of ASBIs in the school setting, a qualitative approach to data collection was adopted, using semistructured interviews with teachers, learning mentors, young people and parents.
Qualitative analysis plan
A complete qualitative analysis plan, providing full details of all qualitative analyses, was finalised and signed before the final analyses were undertaken.
Learning mentor and teacher interviews
Interviews were conducted with learning mentors who delivered the intervention in the school setting, and with teaching staff who approved the study in their school. The aim of the interviews with learning mentors and teachers was to understand the mechanisms and processes of implementing the intervention and also how it could be embedded into the work of staff.
Methods
The interviews with learning mentors and teachers were informed by theory on the likelihood of embedding study interventions in clinical practice, namely normalisation process theory (NPT). 113 The interview guide was linked to intervention implementation, such as role legitimacy (appropriateness of role/parental views, any role conflicts), adequacy (training, how the young people are identified, how the intervention is conducted) and support (time available, support from school and parents). NPT considers factors that affect implementation in four key areas: (1) how people make sense of a new practice (coherence), (2) the willingness of people to sign up and commit to the new practice (cognitive participation), (3) people’s ability to take on the work required of the practice (collective action) and (4) activity undertaken to monitor and review the practice (reflexive monitoring).
Recruitment
All learning mentors who delivered the control or intervention materials to young people in their school (n = 80) and all teaching staff who were involved in facilitating and arranging the ASBIs within schools (n = 30) were invited to take part in a one-to-one interview with their local trial co-ordinator to share their experiences of delivering ASBIs. Invitation letters (see documents on project page) and information sheets (see documents on project page) were e-mailed to all eligible participants, who were asked to complete a pro forma (see documents on project page) indicating their age, ethnicity, role and length of time in current role, if they were interested in taking part in an interview. 2 We aimed to recruit a sample of 24 participants to these interviews: 12 learning mentors and 12 teachers. A sampling framework was used to identify learning mentors and teaching staff for the interviews based on their answers on the pro forma. The populated sampling framework, aiming for sample variation, was based on gender, job role, ethnicity and time in job. It can be seen in Table 14.
| Variable | Region | Total | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| North-east | North-west | London | Kent | ||||||||||||||
| Role | Learning mentor | Teacher | Learning mentor | Teacher | Learning mentor | Teacher | Learning mentor | Teacher | |||||||||
| Target | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 24 | ||||||||
| Recruited | 7 | 2 | 6 | 3 | 1 | 2 | 7 | 2 | 30 | ||||||||
| Role experience (years) | |||||||||||||||||
| < 5 | |||||||||||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | ||||||||
| 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | ||
| Recruited | 3 | 1 | 2 | 1 | 0 | 2 | 5 | 2 | 16 | ||||||||
| 3M | 0F | 1M | 0F | 1M | 1F | 0M | 1F | 0M | 0F | 2M | 0F | 2M | 3F | 0M | 2F | ||
| 5–10 | |||||||||||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | ||||||||
| 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | ||
| Recruited | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 | ||||||||
| 1M | 0F | 0M | 1F | 0M | 1F | 1M | 0F | 0M | 0F | 0M | 0F | 0M | 1F | 0M | 0F | ||
| ≥ 10 | |||||||||||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | ||||||||
| 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | 1M | 1F | ||
| Recruited | 3 | 0 | 3 | 1 | 1 | 0 | 1 | 0 | 9 | ||||||||
| 2M | 1F | 0M | 0F | 0M | 3F | 0M | 1F | 0M | 1F | 0M | 0F | 0M | 1F | 0M | 0F | ||
Data collection
A semistructured interview guide was prepared in advance of the interviews, informed by NPT (see documents on project page). 113 Several other questions were also included to enhance understanding of the school context and priorities in which an ASBI may be implemented. Questions included ‘what are the main issues your school is concerned with at the minute?’ and ‘how does your school normally deal with issues around alcohol use by young people?’ Interviews were conducted on school premises by one of the four trial research co-ordinators in their area (GM, NH, SB and JoF). Informed written consent (see documents on project page) was obtained from each participant immediately before the interview.
Analysis
All interviews were audio-recorded and transcribed verbatim, with any identifying information removed from the transcripts. The interviews were then analysed using a framework analysis technique. Open coding was employed, with the codes grouped into themes and subthemes. Then a coding framework based on the principles of NPT113 was applied (GM, SB and AR). A proportion of transcripts were second coded by an independent researcher (SS and GM), with disagreements resolved through discussion. Following second coding, the framework was further refined before the research team agreed the final themes.
Results
Participants
A total of 30 interviews with learning mentors and school-based staff who took part in the trial were conducted to reach data saturation: 21 learning mentors and nine teachers (one interview involved two learning mentors).
Interviews were conducted in 19 secondary schools across England and, on average, lasted 39 minutes (range 12–102 minutes). Participant characteristics for the learning mentor and teaching staff interviews are given in Table 15.
| Code | Characteristic | |||
|---|---|---|---|---|
| Gender | Ethnicity | Years in job | Region | |
| Learning mentors | ||||
| Learning mentor 1 | Female | White | 5–10 | North-west |
| Learning mentor 2 | Female | Black | > 10 | London |
| Learning mentor 3 | Female | White | < 5 | North-west |
| Learning mentor 4 | Male | White | < 5 | North-east |
| Learning mentor 5 | Male | White | 5–10 | North-east |
| Learning mentor 6 | Female | White | > 10 | North-west |
| Learning mentor 7 | Female | White | > 10 | Kent |
| Learning mentor 8 | Male | White | < 5 | North-east |
| Learning mentor 9 | Female | White | < 5 | Kent |
| Learning mentor 10 | Female | White | < 5 | Kent |
| Learning mentor 11 | Female | White | > 10 | North-east |
| Learning mentor 12 | Female | White | 5–10 | North-west |
| Learning mentor 13 | Male | White | > 10 | North-east |
| Learning mentor 14 | Female | White | > 10 | North-west |
| Learning mentor 15 | Female | White | > 10 | North-west |
| Learning mentor 16 | Male | White | > 10 | North-east |
| Learning mentor 17 | Male | White | < 5 | Kent |
| Learning mentor 18 | Female | White | < 5 | Kent |
| Learning mentor 19 | Male | White | < 5 | North-east |
| Learning mentor 20 | Female | White | < 5 | Kent |
| Learning mentor 21 | Female | White | 5–10 | Kent |
| Teachers | ||||
| Teacher 1 | Male | White | < 5 | London |
| Teacher 2 | Female | White | 5–10 | Kent |
| Teacher 3 | Female | White | < 5 | London |
| Teacher 4 | Male | White | 5–10 | North-west |
| Teacher 5 | Male | White | < 5 | North-east |
| Teacher 6 | Female | White | 5–10 | Kent |
| Teacher 7 | Male | Mixed | < 5 | North-west |
| Teacher 8 | Female | White | 5–10 | North-east |
| Teacher 9 | Female | White | > 10 | North-west |
Interviews
Five themes were identified: (1) learning mentors’ understanding of alcohol use by young people, and of their role in delivering ASBIs; (2) initiating and sustaining ASBIs; (3) factors influencing successful trial delivery; (4) the impact on staff and young people; and (5) embedding the intervention into routine practice. These themes are explained in more detail below. Table 16 illustrates how these themes map on to the core components of NPT. 113
| Theme | ||||
|---|---|---|---|---|
| Learning mentor understanding of alcohol use and their role in delivering alcohol screening and brief interventions | ||||
| Subtheme | Comparison of intervention with existing practice | Understanding of alcohol use by young people | Seeing the benefit for young people | Understanding of the intervention procedures |
| NPT construct | Coherence | Coherence | Coherence | Coherence |
| Initiating and sustaining ASBIs | ||||
| Subtheme | Enrolment in and sustaining ASBIs | Pupil engagement | School support for intervention | Current role complements intervention |
| NPT construct | Cognitive participation | Cognitive participation | Collective action | Cognitive participation |
| Factors influencing successful delivery of intervention | ||||
| Subtheme | External factors impacting on capacity | Confidence that young people are being honest | Confidence in ability to deliver intervention | |
| NPT construct | Collective action | Collective action | Collective action | |
| Reflecting on the impact on staff and young people | ||||
| Subtheme | Appraisal of the intervention on young people’s drinking | Benefits for staff development | ||
| NPT construct | Reflexive monitoring | Reflexive monitoring | ||
| Embedding intervention into routine practice | ||||
| Subtheme | Embedding intervention into routine practice | Changes to intervention to make it more effective | Appraisal of the intervention materials, procedures and training | |
| NPT construct | Cognitive participation | Reflexive monitoring | Collective action | |
Learning mentors’ understanding of alcohol use by young people, and of their role in delivering alcohol screening and brief interventions (coherence)
A common theme that emerged from the interviews centred on the belief that alcohol use among young people has been declining in recent years. Learning mentors’ shared belief that alcohol use is declining is likely to affect their views on the benefits of the intervention. This was indicative of a general feeling that young people’s alcohol use is not something to be concerned about and that only those young people who are putting themselves at immediate risk of harm warrant an alcohol intervention:
That is what we found, is it not, when we did the talking to them, are you putting yourself at risk, and they are like, well, not really. If it is in your house, what risk are you putting yourself into?
Learning mentor 1
I don’t think kids have access anymore . . . I couldn’t see any of our, children going to the corner shop like I used to do.
Learning mentor 2
However, despite feelings that alcohol use among young people is lower than in previous years, and a lack of concern for those who drink in a ‘safe’ environment, there was still a belief that it was important to provide education on the risks associated with drinking alcohol.
There was great variation in the roles of learning mentors within and between schools, with some holding a purely pastoral role and others being involved in some teaching. This meant that there was a difference in the amount of time learning mentors would typically spend discussing issues such as alcohol use with young people and, therefore, a difference in the similarity of the intervention to their usual role and responsibilities. In general, learning mentors did not tend to work on issues relating to alcohol unless these were linked to a specific incident in the school, and even then any action would tend to involve several school staff rather than being one on one:
Initially, if we just pick up on it just by talking to children, we can then pass it on to get further advice or more help for the children if we think it’s needed.
Learning mentor 3
Most learning mentors demonstrated a good understanding of their role in delivering the ASBI. They were aware of their responsibility to work with young people to identify opportunities to change their behaviour, rather than simply telling them not to drink alcohol; however, learning mentors did not demonstrate particularly high fidelity to this component of the intervention. Their understanding of their role in delivering the intervention was demonstrated further by an awareness that, even when they were working with a young person who was resistant to altering their behaviour, there was still an opportunity to effect change:
Realistically, telling a young person don’t ever go out and drink is not only hypocritical, but it’s also naive, and unrealistic, because young people aren’t as daft as we think they are.
Learning mentor 4
Even the ones who were quite adamant that there was nothing wrong with the drinking they did . . . you could still get a little caveat that this is what you could try . . . and I certainly think that was beneficial.
Learning mentor 5
Teaching staff were also aware of the benefits to young people of having a safe space to discuss concerns such as alcohol use. They acknowledged that learning mentors were well placed to provide pastoral support and had a confidential relationship with young people separate from the authority of teaching staff. However, there was also an appreciation that child safeguarding was paramount and, should confidentiality need to be breached, processes were in place to deal with that. This was communicated to young people to help them understand the parameters of confidentiality:
One of the things that when I was delivering the questionnaire . . . the students, were very keen for their teachers not to find out any results.
Teacher 1
We were all told by our child protection officer to make it clear during the intervention that obviously if they say anything where we thought there was a risk of harm, we had to say that.
Teacher 2
Initiating and sustaining alcohol screening and brief interventions (cognitive participation/collective action)
Learning mentors and teachers discussed a variety of methods that were used to implement the ASBI within schools and encourage young people to enrol. The initial screening was seen as quite straightforward to arrange and required nothing more than handing out surveys to all Year 10 pupils and then collecting these:
It was easy to hand them out because we have six tutor groups with 20 students in.
Teacher 2
Support from key stakeholders within the school was identified as an essential component of successfully delivering ASBIs. Although all schools agreed to participate in the trial, not all staff were necessarily made aware of this by senior management. There was a feeling that this contributed to difficulties in releasing young people from classes to participate in the intervention and control sessions. This was further compounded by the time of year at which the intervention and follow-up appointments were due to take place, which for some coincided with exam revision. If the ASBI were to be rolled out in the future, then schools would need to have more control over when to deliver it. Equally, support from teaching staff would be essential to allow young people to leave class to participate:
The time of year, when it comes to it, is not always the best. Possibly after the Easter holidays might be a little bit better.
Learning mentor 6
The number of learning mentors, and the role they had within the school, varied considerably among the participating schools. Whereas some schools had multiple learning mentors, others had only one or two, and this did not necessarily correspond to the number of young people randomised within that particular school. For example, one school had two learning mentors who were responsible for arranging 42 appointments with young people, whereas another school had four learning mentors but only nine appointments. Furthermore, some learning mentors held purely pastoral roles within the school, meaning that they could dedicate time to delivering ASBIs, whereas those who also had teaching commitments could meet with young people only at certain times. This meant that the way in which the learning mentors organised themselves to deliver the interventions was affected by their current role, and the subsequent impact on their workload varied considerably:
I did more than [learning mentor name removed] at that time, I think. I can’t think what [learning mentor name removed] was . . . we didn’t have many anyway. We didn’t have loads.
Learning mentor 3
So in the end I had to pull a few from lessons just to get them done, and I can do that because I’ve got a bit more time on my timetable, cos of my role, to go and pull them out of lessons, but I know some of the other staff who’ve got full teaching hours have struggled with that.
Learning mentor 5
Learning mentors discussed the legitimacy of them undertaking this work, and felt that their relationship with young people could be both a facilitator of and a barrier to effective implementation of the ASBI. Teaching staff, however, were more confident that the pastoral relationship between the learning mentor and young people made the former ideally suited to delivering the intervention:
I think some people, the ones who especially didn’t know us . . . I think they’re still a little bit suspicious of the reasons why they were being asked questions about alcohol, and they were just like ‘no, I just don’t want to do it’.
Learning mentor 4
She’s not a tutor so she never would have had to [have] told a kid off for not wearing their uniform correctly so straight away a student would not associate that member of staff with somebody who’s moany, whingy, don’t want to talk to them.
Teacher 3
Factors influencing successful delivery of the intervention (collective action)
Even when learning mentors organised appointments with young people, the integration of the ASBIs into their existing workload often depended on external factors. For example, if an incident occurred at school that the learning mentor had to deal with, trial-related appointments had to be rearranged. Furthermore, even when young people were allowed out of class, there were occasions when they forgot to turn up. All of this meant that learning mentors had to spend extra time rearranging those missed appointments:
Erm it was just one of those things, I mean my job is very varied, I could turn up in the morning and have a huge . . . disclosure and bang, that’s my day . . . So, it was something that I knew I had to do but it was difficult fitting it in.
Learning mentor 7
So, on paper it didn’t look like it was going to be too bad, because there was, you know, I think I had about eight interventions to do, but when the kids don’t turn up . . .
Learning mentor 5
Many of the learning mentors expressed their concerns around the screening process for the brief intervention, as many young people told them that they did not really drink alcohol. Few participants considered the possibility that young people had been reluctant to disclose the extent of their drinking to them. However, most learning mentors were confident that young people were being honest with them about how much alcohol they drank, and believed that the screening tool was too sensitive. This relates to findings discussed earlier, that some learning mentors accepted that alcohol use by young people is OK if the situations in which they are drinking do not appear to be risky, and so feel that there is no need to intervene in these circumstances. This suggests that the preconceptions of learning mentors are likely to be a barrier to implementing the ASBI, as, if they do not believe that there is a need to intervene, then this could affect any future roll-out of the intervention:
There was a couple that I thought, you must have, you must have lied on your questionnaire, you must have.
Learning mentor 8
Whereas it was quite surprising to see their names on there, in talking to them . . . it wasn’t the concern, it wasn’t justified [the intervention].
Learning mentor 5
For the most part, learning mentors grew in confidence as they delivered a greater number of interventions. Although they found it difficult to remember everything they had to do when they completed their initial appointments, the more they got used to doing them, the easier they became:
Yeah, I mean it was a little bit difficult at first to get myself familiarised with it but I think you know, once I read through it and then it explained it, it was OK after the first [one].
Learning mentor 7
Reflecting on the impact on staff and young people (reflexive monitoring)
Interview participants expressed mixed feelings on the potential impact of the intervention on young people’s drinking, with some participants feeling that the impact could be positive. Learning mentors recognised that the intervention could serve as a teachable moment for young people who perhaps had never considered how much alcohol they were drinking. However, some learning mentors questioned whether or not the intervention would have a lasting impact on young people’s drinking. This was especially the case for those learning mentors who questioned the screening process and the need for an intervention for young people who they felt were not drinking in a risky way:
As I said, I do think it benefited, cos like obviously the units side of things, I do think it made them think ‘Cor, is it, you know, that much?’ so to speak? I do, I think it’s a very good thing, a very good thing.
Learning mentor 9
No, I don’t think it will make them change. But then is that because our cohort wasn’t, they weren’t that bad.
Learning mentor 3
There was also a recognition among teaching staff that participating in the interventions could not only be beneficial for young people, but also that there was also an opportunity for learning mentors to develop and gain new skills that could help them in the future. In particular, they felt that it taught learning mentors to think of the bigger picture, in that alcohol may be playing a part in a range of behaviours that are ongoing in school, and that this could potentially be tackled in a relatively short time:
The staff involved developed a skillset that they could take learning from and apply to other mentoring and support situations in school.
Teacher 4
I think furthermore it’s also meant that our learning mentors to perhaps more quickly, more promptly look at some of the macro-issues around that child.
Teacher 5
Embedding intervention into future practice (cognitive participation/collective action/reflexive monitoring)
There was a general agreement that the intervention was something that could be useful for schools in the future, with the potential to benefit young people. However, it was reported that this would depend on senior school management supporting implementation. In particular, it was seen as important for staff resources to consist of a sufficient number of appropriately trained staff to deal with delivering interventions across all year groups:
No, only just to say really if this is going to be taken further we’d be really interested in being involved because it’s a really good safety net for our students.
Teacher 6
The staffing that we have in place, around the number of students that we have would need to be looked at.
Teacher 5
In general, participants felt that the intervention and related manual were useful. In particular, the A3 worksheet, which was used to facilitate the behaviour change session between learning mentors and young people, was generally well received. Learning mentors also felt that the intervention sessions were long enough. However, despite the positive feedback about the intervention materials, many learning mentors expressed some concern about the length of time between screening and receipt of the intervention. They felt that screening young people before Christmas and then waiting until after the Easter break to conduct the interventions was too long a gap for the students, with many not even remembering that they had completed the baseline survey. However, it should be noted that our protocol allowed for the intervention sessions to take place as soon as the screening had been completed; it was up to schools to arrange individual appointments with young people. Should the ASBI be rolled out in the future, schools themselves would be responsible for scheduling and arranging screening and intervention sessions with young people and could therefore work around their timetables:
I thought the intervention itself was excellent, I thought the piece of work was well thought out, and I think with certain young people it’ll be incredibly effective.
Learning mentor 4
I think the time gap between them actually doing it – especially with it being before Christmas – and us coming to do the interventions . . . I think they actually forgot.
Learning mentor 6
Before they delivered the intervention sessions in schools, learning mentors were trained by a member of the research team on the intervention and trial processes. The consensus was that the training was well thought out and prepared learning mentors for delivering sessions. However, the training took place before the Christmas break and the interventions were not due to begin until January. Some schools did not manage to arrange their intervention and control sessions until between April and June owing to other commitments, and this may have led to a loss in confidence in delivering the intervention. Some learning mentors felt that top-up training could have been provided; however, it may be more beneficial to arrange training for the interventions once it is known when they are likely to take place:
[It] was great, she did a really, sort of brief overview, we had a chance for role play as well, for the longer interventions, which was effective.
Learning mentor 10
When I was doing the interventions I didn’t know whether I was saying the right things. Probably just a bit more training on the best approach, that’s all.
Learning mentor 3
Interviews with young people and parents
Interviews were conducted with young people who took part in any stage of the study within the school setting, and with parents of young people who were involved in the study. The aim of the interviews with young people was to explore their experiences of taking part in the study and their views on any derived benefits, adverse events or improvements resulting from participation, whereas the aim of the parent interviews was to gain their views on school-led interventions for adolescent alcohol use, issues relating to parental consent to take part in such interventions and the appropriateness of school-led health promotion work.
Methods
Recruitment
Young people were eligible for interview if they completed the baseline survey, left their contact details and ticked the appropriate box agreeing to be contacted, so could include those screening positively or negatively on the A-SAQ. We aimed to recruit a purposive sample of 40 participants for the young people interviews. A sampling framework was used to identify participants based on their gender, A-SAQ score, ethnicity and study site. The researchers were blinded to which arm of the trial young people had been randomised and, therefore, we could not sample based on these criteria.
A maximum variation sample was used based on young people’s A-SAQ score (positive and negative), geographical location, trial arm, gender and ethnicity. For example, more young people in the north-east were of a white ethnic background and scored positively on the A-SAQ, whereas more young people in London were of a black ethnic background and scored negatively on the A-SAQ. Recruitment was therefore tailored to take account of these regional variations. From the framework of eligible participants, the first 206 were given an information sheet and invitation letter by their school and asked to inform a learning mentor as soon as possible if they did not want to take part in an interview. The reason for inviting only 206 was that we did not want to over-recruit and thus have to reject a substantial number of potential participants. From these 206, participants were approached sequentially until we reached the desired sample size of 40. However, given time constraints, by the end of the school term only 33 interviews had been conducted.
Parents were eligible for an interview if they had not opted their child out of the study prior to the baseline survey. Schools were asked to text or e-mail to all eligible parents (n = 4245) a link to the participant information sheet and invitation letter, which were hosted on Online Surveys (formerly Bristol Online Surveys; Bristol, UK). Those interested in taking part in an interview were asked to provide their contact details so that the qualitative lead (GM) for the project could contact them to arrange a suitable date and time. The populated sampling frameworks for the young people and parent interviews can be seen in Tables 17 and 18. Although every effort was made to recruit parents to the interviews, by reminding schools to send out texts and e-mails to eligible participants we are not aware of how many parents were contacted by their school. However, we do know that 14 parents opened the link to the invitation letter, five went on to view the information sheet, and only three provided their contact details.
| Variable | Region | Total | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| North-east | North-west | London | Kent | ||||||||||||||
| A-SAQ | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | |||||||||
| Target | 8 | 2 | 4 | 6 | 2 | 8 | 6 | 4 | 40 | ||||||||
| Recruited | 7 | 1 | 3 | 4 | 1 | 7 | 6 | 4 | 33 | ||||||||
| Ethnicity | |||||||||||||||||
| White | |||||||||||||||||
| Target | 6 | 0 | 3 | 1 | 1 | 1 | 4 | 2 | 17 | ||||||||
| 2M | 4F | 0M | 0F | 2M | 1F | 1M | 0F | 1M | 0F | 0M | 1F | 3M | 1F | 1M | 1F | ||
| Recruited | 5 | 0 | 2 | 0 | 0 | 1 | 4 | 2 | 14 | ||||||||
| 2M | 3F | 0M | 0F | 2M | 0F | 0M | 0F | 0M | 0F | 0M | 1F | 3M | 1F | 1M | 1F | ||
| Asian | |||||||||||||||||
| Target | 0 | 1 | 0 | 1 | 0 | 1 | 2 | 1 | 6 | ||||||||
| 0M | 0F | 1M | 0F | 0M | 0F | 0M | 1F | 0M | 0F | 1M | 0F | 0M | 2F | 0M | 1F | ||
| Recruited | 0 | 1 | 0 | 1 | 0 | 0 | 2 | 1 | 5 | ||||||||
| 0M | 0F | 1M | 0F | 0M | 0F | 0M | 1F | 0M | 0F | 0M | 0F | 0M | 2F | 0M | 1F | ||
| Black | |||||||||||||||||
| Target | 0 | 1 | 1 | 2 | 0 | 6 | 0 | 1 | 11 | ||||||||
| 0M | 0F | 0M | 1F | 0M | 1F | 1M | 1F | 0M | 0F | 3M | 3F | 0M | 0F | 0M | 1F | ||
| Recruited | 0 | 0 | 1 | 2 | 0 | 6 | 0 | 1 | 10 | ||||||||
| 0M | 0F | 0M | 0F | 0M | 1F | 1M | 1F | 0M | 0F | 1M | 5F | 0M | 0F | 0M | 1F | ||
| Mixed | |||||||||||||||||
| Target | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 3 | ||||||||
| 1M | 0F | 0M | 0F | 0M | 0F | 0M | 1F | 0M | 1F | 0M | 0F | 0M | 0F | 0M | 0F | ||
| Recruited | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 3 | ||||||||
| 1M | 0F | 0M | 0F | 0M | 0F | 0M | 1F | 0M | 1F | 0M | 0F | 0M | 0F | 0M | 0F | ||
| Chinese | |||||||||||||||||
| Target | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||||||
| 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | ||
| Recruited | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||||||
| 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | ||
| Other | |||||||||||||||||
| Target | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | ||||||||
| 1M | 0F | 0M | 0F | 0M | 0F | 1M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | ||
| Recruited | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | ||||||||
| 1M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | 0M | 0F | ||
| Variable | Region | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| North-east | North-west | London | Kent | ||||||
| Gender | Male | Female | Male | Female | Male | Female | Male | Female | |
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Recruited | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 |
| Ethnicity | |||||||||
| White | |||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1–2 |
| Recruited | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 |
| Asian | |||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1–2 |
| Recruited | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Black | |||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1–2 |
| Recruited | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mixed | |||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1–2 |
| Recruited | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Chinese | |||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1–2 |
| Recruited | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other | |||||||||
| Target | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1–2 |
| Recruited | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Data collection
A semistructured interview guide was prepared in advance of the interviews. A number of questions were included to gain feedback on individual participants’ experiences of the trial. Questions included ‘What are your thoughts on alcohol use by young people?’, ‘Could you tell me about your own drinking?’ and ‘What do you consider to be the most appropriate way for the school to respond to issues relating to alcohol use and young people?’.
Interviews with young people were conducted on school premises, with the local trial research co-ordinators from their region (GM, NH, SB and AA) responsible for arranging and conducting interviews. Participants were asked to sign an informed consent form if they were 16 years old, or an informed assent form if they were 15 years old, immediately before the interview commenced. Interviews with parents were conducted over the telephone (by GM) and participants were asked to provide verbal consent prior to the interview commencing.
Analysis
All interviews were audio-recorded and transcribed verbatim, with any identifying information removed from the transcripts. The interviews were then analysed using thematic analysis, with codes identified inductively. 114 One researcher (GM) conducted the initial coding of the young people and parent interviews. Following this, codes were grouped into themes and subthemes. A proportion of the transcripts were second coded by an independent researcher (EG) to check for validity of the emergent themes. Any disagreements between the first and second coders were resolved by consensus.
Results
Participants
A total of 38 young people (24 girls and 14 boys) initially agreed to be interviewed, with 33 interviews subsequently conducted with young people involved in the trial (20 girls and 13 boys). The remaining five interviews could not be completed as the young person had been withdrawn from the trial (n = 1), had moved school (n = 1) or did not attend school on the day it was arranged (n = 3). Interviews were conducted in 17 out of the 30 study secondary schools and lasted for an average of 20 minutes.
Three parents completed the online pro forma indicating that they were interested in taking part in an interview. Two interviews were conducted (both with women), one in the north-east and one in Kent. The remaining participant could not be contacted to arrange a suitable time for an interview. Interviews lasted an average of 38 minutes. Participant characteristics for the young people and parent interviews are given in Table 19.
| Code | Characteristic | |||||
|---|---|---|---|---|---|---|
| Gender | Age (years) | Ethnicity | A-SAQ | Condition | Region | |
| Young people | ||||||
| Young person 1 | Male | 15 | White | Positive | Intervention | Kent |
| Young person 2 | Female | 16 | White | Positive | Control | North-east |
| Young person 3 | Male | 16 | White | Positive | Control | Kent |
| Young person 4 | Female | 16 | White | Negative | NA | London |
| Young person 5 | Male | 15 | White | Positive | Control | North-east |
| Young person 6 | Female | 16 | Asian | Negative | NA | Kent |
| Young person 7 | Female | 16 | White | Negative | NA | Kent |
| Young person 8 | Female | 16 | White | Positive | Control | Kent |
| Young person 9 | Female | 15 | Black | Negative | NA | London |
| Young person 10 | Female | 16 | Black | Negative | NA | Kent |
| Young person 11 | Male | 16 | White | Positive | Intervention | North-east |
| Young person 12 | Female | 16 | Mixed | Negative | NA | North-west |
| Young person 13 | Female | 15 | Asian | Positive | Intervention | Kent |
| Young person 14 | Male | 16 | White | Negative | NA | Kent |
| Young person 15 | Female | 15 | White | Positive | Intervention | North-east |
| Young person 16 | Male | 15 | Mixed | Positive | Control | North-east |
| Young person 17 | Female | Unknown | Asian | Negative | NA | North-west |
| Young person 18 | Male | 16 | White | Positive | Intervention | Kent |
| Young person 19 | Male | Unknown | Black | Negative | NA | North-west |
| Young person 20 | Female | 15 | Black | Negative | NA | London |
| Young person 21 | Male | 16 | White | Positive | Control | North-east |
| Young person 22 | Male | Unknown | White | Positive | Intervention | North-west |
| Young person 23 | Female | 16 | Black | Negative | NA | London |
| Young person 24 | Female | 16 | Asian | Positive | Control | Kent |
| Young person 25 | Male | 15 | Other | Positive | Intervention | North-east |
| Young person 26 | Male | 16 | White | Positive | Control | North-west |
| Young person 27 | Female | 16 | Black | Negative | NA | London |
| Young person 28 | Male | 15 | Asian | Negative | NA | North-east |
| Young person 29 | Female | Unknown | Black | Negative | NA | North-west |
| Young person 30 | Male | 15 | Black | Negative | NA | London |
| Young person 31 | Female | 16 | Black | Negative | NA | London |
| Young person 32 | Female | 15 | Black | Positive | Control | North-west |
| Young person 33 | Female | 16 | Mixed | Positive | Control | London |
| Parents | ||||||
| Parent 1 | Female | 45 | White | Kent | ||
| Parent 2 | Female | 55 | White | North-east | ||
Interviews with young people
Following analysis of the young people’s interviews, three themes were identified: (1) drinking identities and awareness of risk, (2) access to support and advice in relation to alcohol use and (3) appraisal of the intervention and potential impact on alcohol use. These themes are now outlined with illustrative quotations from participants.
Drinking identities and awareness of risk
A common theme centred on identifying oneself as a drinker. A number of young people distinguished between themselves as someone who only had the occasional drink of alcohol but did not really drink and those ‘other young people’ who were drinkers because they were perceived to drink more often. This very much reflects the results from the learning mentor interviews, in which it was seen as acceptable for young people to consume some alcohol. This shared belief that drinking some alcohol is not risky would probably have an impact on young people’s engagement with an alcohol brief intervention, as if they do not believe their alcohol consumption to be excessive then they do not have much motivation to change their behaviour. As this is also reflected in the beliefs of learning mentors, it could be a significant barrier to future implementation of ASBIs in a secondary school setting. However, although most of the participants felt that others probably drank more than they did, a few participants were quite open about the fact that they drank and seemed to take pride in the fact that they could ‘handle’ drink more than others:
If you are responsible then there is no problem, if you’re drinking in a safe way then it’s OK.
Young person 1
One of my friends is 18 [years] and she can drink a bottle of wine and be drunk whereas I can have like, I could have three of the ones she drinks and I still wouldn’t be that drunk.
Young person 2
There was also variation in young people’s conceptualisation of the risks associated with drinking alcohol at a young age. Much like the learning mentors, those who did not think that there were any risks associated with drinking alcohol at a young age seemed to focus on the short-term risks, such as falling over or being separated from friends. However, those who articulated that there were risks tended to look at the longer-term risks in relation to their health:
Yeah but it’s like, I don’t know, we can stay in the same place or we’re not like harming anybody or anything or we won’t harm ourselves or stuff, we just, I don’t think it’s not safe.
Young person 2
I think it was something to do with like, I can’t remember what it was, but it can lead to cancer and stuff and there’s just loads of illnesses that you can get from it.
Young person 3
Young people put forward a range of reasons for why they did, or did not, drink alcohol. The social aspects of drinking alcohol were discussed by many of the participants, who felt that drinking alcohol made them more confident, made social events more fun and helped them to take their mind off the mental pressures associated with school and exams. Young people also extensively discussed the role of peer pressure in drinking alcohol, with many feeling that it was a big factor in their decision-making around alcohol. However, many more discussed that there was no pressure at all, and often there would be a mix of young people who were and were not drinking:
So it may be, if you don’t do it, you feel like you’re going to be judged by your friends, judged by others, or another reason why you may go drink out, like you go out to parties and, having the like, forced to drink, is, because maybe people, who are this age, think it’s cool to drink and, you know, people are gonna [sic] like you more.
Young person 4
I can just go out and like only two people drink, if they want to drink they can, some people don’t want to, so we’re not bothered.
Young person 5
Another factor that had an impact on whether or not young people consumed alcohol, and how much they consumed, related to their parents’ views on young people drinking. Many of the participants discussed that they only really drank alcohol when their parents allowed it, and usually this was under supervision either as part of a special occasion or when drinking at home with their parents at the weekend. There may be cultural differences in parental consent for alcohol consumption, as outlined in one of the following quotations. However, some young people were aware that, although they could consume some alcohol, if they went too far with it then their parents would not be happy with them. This suggested a level of trust between parents and their children, in that parents were allowing them the freedom to experiment with alcohol but there were still boundaries in place. However, on occasion young people would drink more than they had been allowed, which could lead to repercussions:
She doesn’t like it. Sometimes like if I was at a party she’d go like in the shop for me and get me something to drink so she’d know what I was drinking and stuff but then if I was just saying I was drinking in the street or I drank like 2 days in a row then she’d say [name], don’t drink anymore.
Young person 2
My parents do not allow drinking, but English people, I shouldn’t say this, English people might find it all right to let the children drink at certain age, like 16 is all right.
Young person 6
Access to support and advice on alcohol use
In general, participants felt that there was a lack of formal support and advice for young people around alcohol use in the school setting. There was an acknowledgement that schools did what they could in terms of holding special assemblies or one-off sessions during PSHE lessons. However, there was also a feeling that the information and advice normally provided in school is outdated and does not resonate with young people, thereby limiting its impact. It was felt that if a young person had any concerns about alcohol use, they would need to seek out information by talking to their tutor or head of year, who might be able to refer them to support services. This willingness to engage in dialogue with school staff suggests that school-based alcohol brief interventions may be a feasible delivery model. However, it must be noted that those who seek out advice and support may already be motivated to change their behaviour, and not everyone who is screened by the school will share these motivations. In fact, it was noted in the interviews that not all young people were willing to discuss alcohol use in school:
No, it does pop up in assembly, like, a couple of times, but they don’t go into depth about it. Just like kind of mention it and then go onto something else.
Young person 7
I think you would have to try and find out I think it would be a case of coming to the welfare centre first, there are no posters around but it does fall on the person to find out and this is a problem.
Young person 8
I believe that erm young people should be aware of the drinking and but I don’t feel like what they are giving us is effective enough. I feel like it is just a waste of time, a waste of their money, a waste of our valuable education, etc.
Young person 9
Although there was a sense that advice and support on alcohol use within the school setting was insufficient and often was not relevant to young people, there were a number of avenues for support and advice that young people would use. Young people explained how they would often go to older friends or siblings to ask for advice about drinking and how to stay safe if they did decide to drink. However, there were mixed feelings when it came to discussing alcohol use with their parents; although some were happy talking to a parent, others would never discuss alcohol with them for fear of worrying them, being judged or getting into trouble for underage drinking:
And I’ve also had some advice from my brother as well, he says to make sure you go out with people you’re actually good friends with so they don’t leave you if you’re really drunk.
Young person 10
Probably like my stepdad, my stepdad’s kind of got the whole mentality of like, he kind of realised what it was like because he did it when he was my age and he could probably help me with it.
Young person 11
Well, actually, I dunno [sic], it kind of depends because, like I’m not really, really close to my parents, that I would speak to them, about these things, but, normally, maybe, I would go to, like my older friends.
Young person 4
Appraisal of the intervention and potential impact on drinking behaviour
Young people in general thought that the intervention would have limited impact on their own drinking. However, they felt that the intervention would perhaps be more effective for those young people who drank more alcohol than they did. The perceived effectiveness of the intervention therefore seemed to be very much related to young people’s self-defined identity as being a drinker or not. However, some participants did discuss small changes they had made to their behaviour following the intervention:
I think if I was drinking a lot more, or a little bit more, it would definitely change it, but because I don’t drink that much, it didn’t have too much of an effect.
Young person 1
I was really confused. I was like, ‘Why am I doing this?’ The closest I’ve got to something relating to alcohol is probably sparkling water.
Young person 12
So then like from the session, so I wanted to do it cause like it made me understand why I shouldn’t do it and supported me in thinking why I should probably drink less. She was like you shouldn’t drink that much because these are the reasons why, so basically it supported me into like reducing how much I drink, yeah.
Young person 13
The relationship between the learning mentor and young people was a key factor influencing their experience of the study and intervention. Among those young people randomised to the intervention, most felt comfortable talking to the learning mentors about their drinking behaviour and were reassured that the sessions would be treated as confidential. However, despite having a different relationship with learning mentors from that with teachers, young people were acutely aware that the learning mentors were still school staff. Some were concerned that there may be repercussions from disclosing their alcohol use to learning mentors and, therefore, diluted how much information they gave:
I did like [name], she was funny and engaging, it didn’t feel like it was gonna [sic] be all serious. I did think I could speak to her.
Young person 8
Because I think, I knew that no one would be told about it and it’s like personal and secretive so I knew like my name wouldn’t be like going around and like and that it wouldn’t be broadcast.
Young person 13
I just don’t think it’s one of those things that you’d really want to go and speak to someone about like going and talking to [name], because [name’s] nice but I wouldn’t feel comfortable just sitting there and telling him everything about me, do you know what I mean?
Young person 16
Interviews with parents
Following analysis of the parent interviews, two themes were identified: (1) parents’ thoughts on alcohol use by young people and methods to reduce harm and (2) parents’ thoughts on school-based interventions for alcohol use.
Parents’ thoughts on alcohol use by young people and methods to reduce harm
Mirroring the results presented earlier from the interviews with learning mentors, teachers and young people, there was a belief among parents that it was acceptable for young people to drink some alcohol, with a focus very much on reducing short-term hazards rather than on the long-term risks. Both of the parents who were interviewed discussed that they allowed their children to consume alcohol under age as they believed that this took away curiosity and taught them how to drink responsibly under adult supervision. However, although they allowing their children to drink alcohol, they also discussed the short-term risks associated with drinking too much or putting oneself in a vulnerable situation, demonstrating their belief that allowing their children to consume alcohol in a controlled environment would reduce the associated short-term risks:
I mean my son is 15 and I will allow him to have a drink occasionally erm but just like I said I’ve discussed with him the dangers of drinking and especially of drinking spirits just because obviously that, they can get drunk far quicker drinking spirits.
Parent 2
Yeah, yeah I’m not making it something big and you know clever that they can, you know that they are not proving themselves with adults by drinking because they don’t need to so actually they are more proving themselves as adults by being able to sit with me and have fun you know and enjoy themselves in a sensible way.
Parent 1
Thoughts on school-based interventions for alcohol use
Neither parent demonstrated a great deal of awareness of what approach was taken within their children’s schools for offering advice and support on the risks of alcohol use. However, despite this, both parents felt that the school could do more, especially in discussing the short- and long-term risks. Although one parent was aware that alcohol would fall under the remit of PSHE lessons, they felt it was not discussed in any great detail. The other parent did not know how their child’s school currently approached issues with alcohol because their child had never needed any such support:
I think with like the PSHE thing they um, I think they hardly discuss alcohol at all . . . but I don’t think that they do very much talking to children about the risks of alcohol and trying to be sensible.
Parent 2
Yeah I’ve never had, I’ve never heard of the school’s involvement kind of thing, so I’ve got no experience of it myself.
Parent 1
When discussing the potential impact of delivering the current intervention in the secondary school setting, both parents were particularly enthusiastic and felt that it was a good idea. Both expressed a belief that any intervention that discusses the impact of alcohol and how to minimise risk is worthwhile. However, reflecting what was expressed in the young people and school staff interviews, there was a feeling that the intervention would have limited impact on alcohol consumption. The parents felt that, even though learning mentors have a less formal relationship with young people than teaching staff, young people would still be reluctant to discuss alcohol with them. There was a suggestion that any such intervention would perhaps be better facilitated by an external agency:
Oh well that sounds great but I don’t know if my son actually did that bit, I don’t remember him mentioning it to me.
Parent 2
I think it is giving them a good understanding about what’s healthy as it were and that sort of thing and that’s got to be a lot better. The problem is I think if kids really, really want to drink they are looking for the thing that is highest in alcohol.
Parent 1
Yeah but I think probably it’s, kids will still probably be concerned about what they said . . . Yeah I think someone probably completely like unrelated to the school. Because I’ve worked in a school and I know that people talk to each other.
Parent 2
Chapter 5 Health economics methods and results
Key points for Chapter 5
-
The objective of the economic evaluation of the SIPS JR-HIGH trial was to explore the cost-effectiveness of the brief intervention for alcohol problems in young people compared with usual practice. The evaluation also included a cost–consequences analysis that was used to more broadly compare intervention delivery costs with other gains and costs from the trial.
-
The costs of the intervention included the cost of materials to deliver the intervention, the cost of training learning mentors in schools in the brief intervention techniques and the cost of learning mentors’ time spent preparing and delivering the intervention. The economic outcomes from the trial were the costs of health and other social care resource use, such as general practitioner (GP) visits, hospitalisations and arrests, and the value of QALYs estimated using the EQ-5D-3L scale to capture self-reported quality of life. The use of resources was captured through young persons’ self-reports, and unit costs for the different services were sourced from national databases and a literature search.
-
The average cost of delivering the intervention (learning mentors’ time and the costs of the screening, training and intervention materials) was £31.30 (95% CI 30.9 to 31.7) per intervention participant.
-
The intervention group had lower costs, on average, over 12 months’ follow-up than the control group, but this difference was not statistically significant. The estimated average net cost saving was –£2865 (95% CI –£11,272 to £2707). This value included the effect on costs of missing school days from problems associated with alcohol consumption. When excluding these costs, the average cost saving was –£1324 (95% CI –£5277 to £1727). The CI includes 0, but is wide enough to include economically important differences that could favour intervention or control.
-
The average difference in QALYs between the intervention and control was around –0.004 (95% CI –0.019 to 0.011) QALYs, with lower QALY values for the intervention group. Although the minimum important difference for this population and context is unknown, the mean difference is equivalent to 1.5 days (out of 365 days) in full health over a 12-month period. The CIs surrounding the mean difference in QALYs between intervention and control group above are equivalent to –6.9 to 4.0 days in full health. The lack of difference in QALYs between groups is not unexpected as the trial was not specifically designed to change participants’ reported quality of life (or QALYs). Moreover, the impact on health might be expected to become manifest in the medium or long term if the intervention were to be effective.
-
The intervention has an estimated 74% probability of being cost-effective based on cost per QALY thresholds of between £20,000 and £30,000. This results are based on the service use and costs excluding missing school days from the calculations of differences in costs. These results were similar when the cost of missing school days was included.
-
Given the results reported in Chapter 3 regarding changes in alcohol intake, it is unclear what factors influenced possible differences in cost and the approximately 74% chance of the intervention being cost-effective.
Introduction
This chapter describes the results of the economic evaluation of the SIPS JR-HIGH trial intervention, which included a within-trial cost–utility analysis as well as a cost–consequences analysis. A model-based long-term analysis was originally planned as part of the economic evaluation of the trial, but it was not developed because the within-trial results did not support a need to pursue this approach and because there was a lack of a clear mechanism by which longer-term outcomes could be extrapolated from shorter-term trial data.
Health economics analysis plan
A complete health economics analysis plan, providing full details of all analyses, was finalised and signed before the final analyses were undertaken.
Overview of methods
Within-trial cost-utility
The objective of the within-trial cost–utility analysis was to estimate and compare the costs and effectiveness of the ASBI against usual practice. A cost–utility analysis measures effectiveness in terms of QALYs, and estimates incremental costs with respect to usual practice, incremental QALYs and incremental costs per QALY. The incremental costs per QALY, also called the incremental cost-effectiveness ratio, provide an estimate of the additional cost associated with achieving one more QALY. The perspective for the analyses was the UK public sector (NHS, and educational, social and criminal services).
The estimation of QALYs gained/lost relies on valuations for health states, for which a score of 1 is assigned to full health and 0 to being dead. This in turn relies on measures of the quality of life of study participants. 3 The SIPS JR-HIGH trial used measures of quality of life derived from responses to an EQ-5D-3L scale,115 which is used extensively in economic evaluations. 3 The difference in costs between the intervention and the control participants was based on the cost of delivering the intervention versus current practice plus the difference at follow-up in the young participants’ use of public sector services (e.g. GP appointments, school nurse visits, accident and emergency visits). Given the time horizon of 12 months, no discounting was applied.
Cost–consequences analyses
The cost–consequence analysis presents the cost and effects data of the intervention in the form of a balance sheet. In the balance sheet, a series of comparisons of effects and of costs are presented as pros and cons for the intervention against the control group, that is, information is presented as disaggregated and no attempt is made to formally combine effects with intervention costs as is done in a cost-effectiveness analysis, in which results are summarised in the incremental cost-effectiveness ratio. The approach can potentially capture wider effects than those captured by measures of cost or quality of life. The principle behind a balance sheet is that the analyst should seek to capture all costs and benefits no matter on whom they may fall, the same principles that underpin a cost–benefit analysis. 116
For the cost–consequences analysis, the difference in costs was based on the estimated difference in costs from the within-trial cost–utility analysis. Among the effects under consideration were the levels of service use (primary health care, secondary health care, school, criminal justice system, etc.) listed above. In addition, the effectiveness measures were expanded to include secondary outcome measures of the trial, which included participants’ reported percentage of days of abstinence over the previous 28 days, drinks per drinking day and days drinking more than two units from the 28-day alcohol TLFB, measures of risky drinking (AUDIT) and alcohol-related behavioural problems.
Measures
Quality of life
Quality of life was measured using participants’ responses to an EQ-5D-3L scale,115 which has been validated in young people aged ≥ 14 years. 117 The scale was included alongside other trial outcome measures in the baseline and follow-up questionnaires. The scale contains five dimensions: mobility, self-care, doing usual activities, having pain or discomfort, and feeling anxious/depressed. Each of these dimensions has three possible levels. The permutation of the responses to the different dimensions results in 243 health states. Two further states (unconscious and death) are included, producing a set of 245 possible EQ-5D-3L health states.
The different EQ-5D-3L scores from the young participants’ answers were transformed into the corresponding health states, and these were assigned tariff values or utilities associated with each health state. Tariff values were sourced from UK population tariffs for adults. This resulted in a ‘health state utility’ at each time point for each young person.
Quality-adjusted life-years were estimated using the area under the curve method, calculated for each participant as the arithmetic average of the follow-up and baseline tariff-scaled EQ-5D-3L scores.
Cost of the use of primary care, secondary care and other services
The list of different services used by the young people in the intervention and the control group during the trial was informed by the pilot study. 1 For each participant, their use in the previous 6 months of health, educational, criminal and social care services was recorded using the Short Service Use Questionnaire instrument, administered at baseline and again at follow-up. 91 The answers were captured as the number of appointments, visits, etc., and covered GP visits, social worker visits, school nurse visits, emergency department attendances, hospital admissions and arrests.
In addition to service use, the questionnaire completed by the young people contained a question on missed days (or part of a day) of school or work in the previous 6 months. Responses were collected using a four-point scale with values at 0, 1 or 2 times, 3 to 5 times and > 5 times. To estimate the average number of missed days from school or work, a representative value was used for the second and third categories (1 and 4), with the last category coded as 5.
Each contact with services was matched to a unit cost for that service. Table 20 summarises the unit costs of resource use. The costs of primary health care contacts were the cost per visit reported in the Unit Costs of Health and Social Care 2015118 prepared by the Personal Social Services Research Unit and the Department of Health and Social Care and the Department for Education. Hospital attendances, visits to the emergency department and school nurse visits were costed based on NHS reference costs. These are based on the most recent data available, currently the National Schedule of Reference Costs for 2015–16. 128
| Resource | Unit | Unit cost (average) (£) | Range (£) | Comments | Source | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Health services use | ||||||
| General practice visit | Per visit (patient contact lasting 11.7 minutes) | 44 | NA | NA | Cost including direct care staff costs (nurse FTE 0.51) and cost of qualifications | Unit Costs of Health and Social Care 2015, p. 177118 |
| Emergency department attendance | Attendance | 89 | 67 | 106 | Assumed usual practice to be that a young person who presents as intoxicated is kept in the emergency department until he or she has sobered up (probably assessed by breath test or visual assessment)a | National Schedule of Reference Costs 2014–15 – emergency medicine. Type: 01 non-admitted. Subcategory: ‘no investigation’ with ‘no significant treatment’119 |
| Hospital admission | Admission | 457 | 290 | 587 | Assumed length of stay after admission: 1.8 days |
National Schedule of Reference Costs 2015–16 – non-elective excess bed-days. Currency code WD22Z ‘Mental and behavioural disorders due to use of alcohol: acute intoxication’ and ‘Mental and behavioural disorders due to use of alcohol: Harmful use’121 |
| Social and school services | ||||||
| Social worker visit: London | Per hour of client-related work | 88 | NA | NA | Cost components same as those of social worker visit: non-London times London multiplier to account for higher costs of service provision in London (1.60) | Unit Costs of Health and Social Care 2015, pp. 177, 189. Children’s services118 |
| School nurse visit | Per visit | 54 | 34 | 62 | Assumed cost for specialist community nurse (entry requirements for school nurse position include an approved course in specialist community public health nursing)b | National Schedule of Reference Costs – 2014–15. Service description: nursing. Currency code: N05CO ‘School-based Children’s Health Core Services’, one to one119 |
| Arrest, absenteeism/truancy | ||||||
| Being arrested | Per event | 11 | NA | NA | Assuming young people answered the question based on a broader understanding of the meaning of ‘arrest’ as police involvement (e.g. public cautions) | Expert opinion |
| School/work absenteeism | Per category | 0 | NA | NA | Very low to low (SIPS JR score of ≤ 4). Impacts on the individual assumed to be negligible. The level of absenteeism is not sufficiently high to have an impact on future earnings | Assumptions made based on Hanushek,122 McIntosh and Vignoles,123 Orazem and Gunnarsson,124 Psacharopoulos and Patrinos,125 and Sälzer and Heine126 |
| School/work absenteeism | Per category | 102,612 | NA | NA |
High (SIPS JR score of ≥ 5) Cost from the present value of the lost income over the working life (50 years) (i.e. present value of productivity loss over lifetime earnings) Assuming an effect on annual income from lower numeracy and literacy skills resulting from high absenteeism between 12% and 20% Earnings £/week for full-time employment (30 hours per week) over 52 weeks per year. Weighted average across male and female workers (59% and 41%, respectively) Discount rates for lifetime earnings: 3.5% Duration of working life: 50 years Weighted average using % of population in the UK with higher education or more (40%) as staring working at age of 23 years, and the rest as starting working at age of 16 years |
Assumptions made based on Hanushek,122 McIntosh and Vignoles,123 Orazem and Gunnarsson,124 Psacharopoulos and Patrinos,125 and Sälzer and Heine126 Yearly earnings data estimated from weekly earnings published in Annual Survey of Hours and Earnings: 2016 provisional results (ONS)120 Proportion of the population by education level from ONS ‘KS501UK – qualifications and students’ database120 |
The cost of days of school absenteeism/truancy was taken to be negligible (zero) for school absenteeism of more than four times in the previous 6 months. School absenteeism is expected to influence individuals’ and social returns on education through the impact that school attendance has on gains in cognitive capacity, and the forgone income premiums for higher numeracy and literacy levels. Research suggests, however, that the return to investment penalty from absenteeism is less important in the secondary school years than in the primary school years, and that the most detrimental effects on student performance are from recurrent absenteeism (e.g. missing 2 days per week) rather than from sporadic absenteeism. 125,129 Young people with frequent truancy achieve lower scores on numeracy and literacy tests and lag behind their peers. 126 A large literature has explored the impact of poorer school scores on earnings, and estimates are that children with lower numeracy and literacy could have annual salaries that are between 12% and 20% lower than those of their average-level peers. 122,123 Therefore, for children who reported absenteeism levels of ≥ 5 days in 6 months, the cost of absenteeism was estimated as the present value of the lost working lifetime income using the average yearly earnings during 50 years of working life between the ages of 16 and 66 years and of 23 and 73 years. 130
The cost per young person of service use for each type of service was calculated as the product of the young person’s level of service use multiplied by the appropriate unit cost (see Appendix 11). For each young person, the total service use cost was estimated as the sum across all service categories.
Cost of the intervention
The resources assessed for the delivery of the intervention included only those that would be needed if the intervention were to be provided in practice in the future. 131 Therefore, the resources necessary to develop the intervention materials as well as the resources used in the scientific evaluation of the intervention would not normally be included. Similarly, resources common to both the intervention and the usual practice (control arm) would not normally be included, as these are not relevant for the comparison between the two programmes. 132
As a brief reminder, screening for alcohol problems and the short intervention took place in schools using learning mentors. During the intervention, participants received structured advice/counselling of short duration (anticipated to be, on average, 30 minutes) aimed at reducing alcohol consumption or decreasing problems associated with alcohol, based on theoretical principles of behaviour as a dynamic interaction between the individual, behaviour and environment. 133
The following costs of the intervention were included:
-
Costs of the resources needed for screening the young people for high alcohol drinking levels (printing and postage of information and consent letters to parents informing them of the screening in their children’s school, printing and postage of screening questionnaires).
-
Costs of preparing school learning mentors for interviewing the young people according to the principles of the intervention material (time invested by expert trainers and by the learning mentors).
-
Costs of the interview with the young person (learning mentor time spent preparing the intervention, learning mentor time delivering the intervention and cost of printing of materials for the intervention).
The information on trainer time and cost of printed materials was sourced from the records of the research team. Learning mentors’ time preparing the interview with the young person, and their time with the young person, were captured using the learning mentors’ case diaries. Learning mentors reported the time for preparing the intervention in six categories (0–5 minutes, 6–10 minutes, 11–20 minutes, etc.) with an open-ended question for times exceeding 45 minutes, and time delivering the intervention in intervals of 10 minutes (0–10 minutes, 11–20 minutes, etc.) with an open-ended question for times exceeding 60 minutes. Data on the length of time were transformed from ranges to integer values using the mid-point of the scales (see Table 20).
The cost of learning mentor time was based on published learning mentor gross annual pay statistics for the Local Government Earnings Survey 2013/14 (latest available), adjusted upwards by 1% using the average of public sector salary growth year-on-year from April 2013 to April 2017. 134 The cost of the trainers’ time was based on the pay scale of the 2015/16 (latest available) nationally agreed single pay spine for higher education institutions in the UK, published by the national University and College Union. 135 Costs of time were calculated as average per annum salary plus on-costs (employer contribution to National Insurance and superannuation plans) and training costs, converted to £/minute. Appendix 12 presents details of this calculation. The cost per intervention group participant of the time of the learning mentors in preparing and delivering the intervention was estimated as the product of the salary cost per minute multiplied by the duration in minutes of the preparation time and the interview for each young person.
Total cost
The total costs for each young person in the intervention group for the delivery of the intervention were estimated as the sum of the fixed costs of screening and training plus the individual-level interview costs plus the individual-level costs at follow-up of primary care, secondary care and other services.
Primary and secondary effectiveness measures from the trial
The primary and secondary effectiveness outcomes from the trial were used for the cost–consequences analysis. These measures are described in more detail in Chapter 1, and consisted of the primary outcome measure of the intervention calculated as the number of units of alcohol consumed over the previous 28 days derived from the TLFB questionnaire, as well as to the following secondary outcome measures: percentage of days of abstinence over the previous 28 days, drinks per drinking day and days drinking > 2 units from the 28-day TLFB.
The participant questionnaire also included the AUDIT, AUDIT-C, RAPI, WEMWBS and DMQ-R. Questions on smoking and consumption of energy drinks were used to assess the prevalence of other health risk behaviours.
The measures of interest were the changes at follow-up for these outcomes between the intervention and the control group, which were estimated as part of the statistical analyses of the intervention outcomes (see Chapter 3).
Sociodemographic characteristics
Sociodemographic characteristics of participants included gender, ethnicity and the geographic location of the study site. The four study sites were located in England and were grouped into ‘north’ (north-west, north-east) and ‘south’ (Kent, London).
Data
Data for analyses consisted of responses from participants randomised into intervention and control groups who consented to the trial and completed the follow-up questionnaire. Young people were recruited to the study across schools in the four study sites (London, the north-east, the north-west and Kent) between November 2015 and June 2016, with a 12-month follow-up. More detail about recruitment and randomisation can be found in the study protocol133 and Chapter 2 of this report.
Analyses were carried out on an intention-to-treat basis, that is, participants’ outcomes were analysed according to the group to which they were randomised into rather than according to the treatment they received. By implication, our sample included those participants who did not provide an answer (i.e. missing values) to the final outcome measure of the intervention (the 28-day TLFB). One potential downside, in principle, to using this approach is that estimates of outcomes from the intervention can be very conservative, primarily in trials with high participant non-adherence. On the other hand, the method is used widely in statistical analyses because it can limit biases that would arise from excluding the outcomes of non-compliers, for example, if this group had a worse expected outcome from the start of the study. 131 For the SIPS JR-HIGH trial, the disadvantages of this approach were minimised by the fact that there was little crossover or protocol violation from participants.
Statistical and econometric analyses
Exploratory analyses of the differences between the intervention and control groups in quality-of-life scale (EQ-5D-3L), service use and intervention delivery time and costs were performed to explore trends in the data in terms of missing and extreme values.
Differences in QALYs and costs at follow-up between the intervention and the control group were estimated using a seemingly unrelated regression adjusting for participant characteristics and baseline values. Seemingly unrelated regression estimation was used to allow for the fact that costs and QALYs may be correlated within individuals. 136,137 Adjustment was made to control for the overall variability in costs and QALYs from possible imbalances in baseline characteristics of participants that could have existed even in the presence of randomised assignment to control and intervention groups. Costs were adjusted by baseline service use costs and QALYs were adjusted by baseline EQ-5D-3L scores. Participant characteristics included in both the cost equation and the QALY equation were baseline AUDIT score, baseline score for emotional well-being (WEMWBS), gender, geographical site and an indicator variable identifying if time to follow-up interview was shorter or longer than the target 12-month period (> ± 30 days). The difference in costs was multiplied by two to obtain annual costs given the 6-month recall period of the questionnaires. CIs of the difference between intervention and control groups in costs and QALYs were estimated using non-parametric bootstrap with 1500 replications stratified by gender, intervention group and geographical location. The number of replicates was chosen to achieve a better approximation of the distribution of estimated difference. 137 Histograms of the distribution of the bootstrap estimates were used to decide on the use of bias-corrected or normal-based CIs. The incremental cost-effectiveness ratio was estimated as the ratio between incremental costs and benefits using the results from the between-group difference in costs and difference in QALYs derived from the seemingly unrelated regression.
The cost-effectiveness acceptability curve (CEAC) was estimated using the adjusted (as earlier) incremental costs and incremental QALY values from a seemingly unrelated regression with 1500 bootstrap replicates to calculate the net monetary benefit. The CEAC was produced by estimating the proportion across the bootstrap replicates of positive net monetary benefit values, for different values of the threshold willingness to pay for an additional QALY (see Appendix 13). In addition, the joint distribution of incremental costs and incremental QALYs was explored using a scatterplot of results for each bootstrap iteration of costs and QALYs.
Results
Sample and data characteristics
A total of 443 responses from young participants at baseline were available for analysis. The majority of participants in the sample were from the north-east (55%), followed by Kent (31%), the north-west (13%) and London (1%). There was an almost equal distribution of boys and girls in the sample, and approximately 91% of participants self-reported their ethnicity as ‘white’. Eighty-four per cent of randomised participants who completed a baseline survey also provided a response for the final trial outcome measure at follow-up (the 28-day TLFB).
Tables 21 and 22 present information on the average time spent by learning mentors in preparing and delivering the interviews with the young people. The median time delivering the interview in the intervention group was 16 minutes, with the lowest value for interview delivery at 5 minutes. There were few missing data (< 3%).
| Sessions | Time (minutes) | |
|---|---|---|
| Preparing | Delivering | |
| Total (N) | 210 | 210 |
| % (n) missing | 2.4 (5) | 3.8 (8) |
| Complete (n) | 205 | 202 |
| Minimum | 2.5 | 5 |
| Maximum | 38 | 55.5 |
| Median (IQR) | 8 (9.3) | 15.5 (10) |
| Mean (SD) | 8.7 (7.5) | 20.6 (8.8) |
| Time (minutes) | Responses (%) |
|---|---|
| Preparing interview | |
| 0–5 | 40 |
| 6–10 | 35.1 |
| 11–20 | 17.6 |
| 21–30 | 5.4 |
| 31–45 | 2 |
| Total | 100 |
| Delivering interview | |
| None (withdrewa) | 0.5 |
| 0–10 | 10.3 |
| 11–20 | 39.4 |
| 21–30 | 38.9 |
| 31–40 | 9.9 |
| 41–50 | 0.5 |
| 51–60 | 0.5 |
| Total | 100 |
The distribution of responses to the five dimensions of the EQ-5D-3L are presented in Appendix 14. For each dimension, level 1 represents a better state of health. Most participants in the intervention and control groups reported good levels of mobility, self-care and the ability to perform usual activities. In contrast, scores tended to be lower, indicative of poorer quality of life, for pain/discomfort and anxiety and depression. These trends were observed at both baseline and follow-up. There were slightly more participants reporting better quality of life in each dimension at follow-up across groups. At the same time, there was a larger proportion of missing values in the follow-up questionnaire (13–15%) than at baseline (5–7%), but there was no observable systematic difference between the groups, suggesting a low likelihood of bias arising from the pattern of non-responses.
As would be expected from these types of data, all categories of service use had a distribution of values that was highly skewed to the right (Table 23), reflecting the fact that many participants reported zero service use in the previous 6 months, and a small number of young people reported high levels of GP appointments, nurse visits, etc.
| Level | Service use | ||||||
|---|---|---|---|---|---|---|---|
| GP visit | Social worker visit | School nurse visit | Emergency department attendance | Hospital admission | Being arrested | School or work days | |
| Baseline | |||||||
| Total (N) | |||||||
| Control | 233 | 233 | 233 | 233 | 233 | 233 | 233 |
| Intervention | 210 | 210 | 210 | 210 | 210 | 210 | 210 |
| % (n) missing | |||||||
| Control | 9.4 (22) | 10.7 (25) | 10.7 (25) | 9.0 (21) | 9.9 (23) | 9.0 (21) | 3.0 (7) |
| Intervention | 11 (23) | 8.6 (18) | 7.1 (15) | 7.6 (16) | 7.6 (16) | 7.6 (16) | 1.4 (3) |
| % of maximum | |||||||
| Control | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.9 | 2.2 |
| Intervention | 1.6 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 2.9 |
| Complete (n) | |||||||
| Control | 211 | 208 | 208 | 212 | 210 | 212 | 226 |
| Intervention | 187 | 192 | 195 | 194 | 194 | 194 | 207 |
| Minimum | |||||||
| Control | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Intervention | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Maximum | |||||||
| Control | 100 | 10 | 20 | 21 | 10 | 3 | 5 |
| Intervention | 10 | 7 | 20 | 10 | 10 | 6 | 5 |
| Median (IQR) | |||||||
| Control | 0 (2) | 0 (0) | 0 (0) | 0 (1) | 0 (0) | 0 (0) | 0 (0) |
| Intervention | 1 (2) | 0 (0) | 0 (0) | 0 (1) | 0 (0) | 0 (0) | 0 (0) |
| Mean (SD) | |||||||
| Control | 1.7 (7.1) | 0.2 (0.97) | 0.8 (2.1) | 0.7 (1.9) | 0.3 (0.9) | 0.1 (0.4) | 0.3 (1) |
| Intervention | 1.3 (1.8) | 0.2 (0.9) | 1 (2.7) | 0.7 (1.2) | 0.4 (1.1) | 0.1 (0.5) | 0.4 (1.2) |
| Follow-up | |||||||
| Total (N) | |||||||
| Control | 233 | 233 | 233 | 233 | 233 | 233 | 233 |
| Intervention | 210 | 210 | 210 | 210 | 210 | 210 | 210 |
| % (n) missing | |||||||
| Control | 18.5 (43) | 17.6 (41) | 18 (42) | 17.2 (40) | 17.2 (40) | 16.7 (39) | 15.5 (36) |
| Intervention | 17.6 (37) | 14.8 (31) | 16.7 (35) | 15.2 (32) | 15.2 (32) | 14.8 (31) | 13.8 (29) |
| % of maximum | |||||||
| Control | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 18 |
| Intervention | 0.6 | 0.6 | 0.6 | 0.6 | 2.8 | 0.6 | 0.6 |
| Complete (n) | |||||||
| Control | 190 | 192 | 191 | 193 | 193 | 194 | 197 |
| Intervention | 173 | 179 | 175 | 178 | 178 | 179 | 181 |
| Minimum | |||||||
| Control | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Intervention | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Maximum | |||||||
| Control | 15 | 5 | 10 | 8 | 3 | 2 | 5 |
| Intervention | 20 | 24 | 26 | 8 | 3 | 1 | 5 |
| Median (IQR) | |||||||
| Control | 1 (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Intervention | 0 (2) | 0 (0) | 0 (0) | 0 (1) | 0 (0) | 0 (0) | 0 (0) |
| Mean (SD) | |||||||
| Control | 1.4 (1.9) | 0.1 (0.43) | 0.5 (1.2) | 0.4 (1) | 0.2 (0.5) | 0 (0.2) | 0.2 (0.7) |
| Intervention | 1.1 (2) | 0.2 (1.9) | 0.8 (2.8) | 0.5 (1.1) | 0.2 (0.6) | 0 (0.1) | 0.1 (0.6) |
The highest reported level of service use in the previous 6 months was for GP visits, on average, 1.4 [standard deviation (SD) = 1.9] visits in the control group and 1.1 (SD = 2) visits in the intervention group at follow-up, down from 1.7 (SD = 7.1) and 1.3 (1.8) visits at baseline, respectively. The lowest values were observed for the number of times being arrested. On average, service use decreased across all categories from baseline to follow-up for the intervention and control groups, but the intervention group had higher average values at follow-up of social worker visits, school nurse visits and accident and emergency attendances, whereas the control group had higher average numbers of GP visits and missed school days.
The proportion of the highest reported value (i.e. the proportion of very high values among the responses) tended to be low (< 3%) for the different services; these values were not implausible and, therefore, were included in the main analyses. As with the EQ-5D-3L responses, the proportion of missing values was higher at follow-up than at baseline. The percentage of missing values at follow-up ranged from 18.5% to 13.8%, with no large differences between the intervention and control groups.
Primary and secondary effectiveness outcomes from the trial
The primary and secondary outcomes from the trial are presented in Chapter 3. Very briefly, there were no differences in median values for drinking outcomes measured by the 28-day TLFB between the intervention and control group at follow-up after adjusting for participant characteristics. Similarly, there were no differences in responses to the alcohol problem and well-being scales. Reports of smoking, sexual behaviour and consumption of energy drinks were comparable between the intervention and control groups.
Intervention costs
The total costs per participant for the materials needed for screening and to deliver the intervention, as well as the cost of training the learning mentors, are presented in Appendix 15. The cost of interview materials for the brief intervention per participant in the intervention group was estimated at £1.58, giving a total of £332 for materials for the 210 young people in this group. Screening and training activities in the intervention group were estimated at £14.20 per participant for 210 young people. This included £154 for the screening questionnaires, £1870 for the consent letters and £2875 for the cost of training the 80 learning mentors involved in the study. The cost of the learning mentors was spread over 3 years by dividing this cost by three times the annual number of young people covered by the programme.
The cost of the learning mentor time in preparing for the interview with the young person was, on average, £1.90 and the cost of learning mentors’ time conducting the interview with the young participant in the intervention group was, on average, £4.54 (Table 24).
| Cost | Staff time | ||
|---|---|---|---|
| Preparing for the young person’s interview | Conducting young person’s interview | Total | |
| Mean cost (£) | 1.9 (1.7 to 2.1) | 4.5 (4.3 to 4.8) | 6.5 (6.1 to 6.9) |
Considering the cost of the learning mentors’ time and the costs of the screening, training and intervention materials, the total cost per intervention participant of the intervention was, on average, £22.20 (95% CI £21.83 to £22.57).
Longer-term costs
Health-care and other service use costs at baseline and follow-up are presented in Table 25. The highest costs of health-care use were for hospital admissions, followed by GP visits. The highest social costs that participants faced from risky alcohol drinking levels were for missed school days. These costs represent missed lifetime earnings from underperforming in school as a result of missing classes and were therefore expected to have a higher mean than other social and health-care costs. Costs were lower on average for the intervention group at follow-up for GP visits, arrests and number of missed school days; however, except for arrest costs, the large CIs surrounding these differences indicate the possibility of both decreases and increases in costs of an important economic magnitude, particularly for the cost of missed school days.
| Resource | Cost (£), mean (n) | Difference (95% CI) | |
|---|---|---|---|
| Intervention | Control | ||
| Baseline | |||
| GP visits | 113 (187)a | 154 (211) | –40 (–152 to 20) |
| Social worker visits | 21 (192) | 21 (208) | 0 (–20 to 20) |
| School nurse visits | 104 (195) | 83 (208) | 22 (–22 to 68) |
| Hospital admissions | 358 (194) | 296 (210) | 62 (–110 to 244) |
| A&E attendance | 125 (194) | 131 (212) | –6 (–64 to 38) |
| Being arrested | 1.81 (194) | 1.76 (212) | 0.06 (–1.6 to 2.2) |
| Total resource cost A | 715 (179) | 700 (201) | 14 (–310 to 276) |
| Missed school days | 5949 (207) | 4540 (226) | 1408 (–4356 to 8146) |
| Total resource cost B | 5342 (179) | 4826 (201) | 516 (–5442 to 7028) |
| Follow-up | |||
| GP visits | 98 (173) | 125 (190) | –26 (–62 to 10) |
| Social worker visits | 27 (179) | 9 (192) | 18 (–2 to 60) |
| School nurse visits | 83 (175) | 54 (191) | 28 (–12 to 86) |
| Hospital admissions | 200 (178) | 161 (193) | 40 (–76 to 150) |
| A&E attendance | 91 (178) | 76 (193) | 16 (–24 to 52) |
| Being arrested | 0.1 (179) | 1 (194) | –0.8 (–1.8 to –0.2) |
| Total resource cost A | 501 (169) | 403.2 (184) | 98 (–84 to 252) |
| Missed school days | 1134 (181) | 2083 (197) | –950 (–4320 to 2586) |
| Total resource cost B | 1715 (169) | 2634 (184) | –918 (–4614 to 2802) |
Cost–utility analysis
After adjustment for baseline values and patient characteristics, the mean total costs per participant (the service use costs and the costs of delivering the intervention) in the intervention group at the end of follow-up were £6212 compared with £9077 in the control group, representing a difference of £2865 (95% CI –£11,272 to £2707). The intervention group had, on average, lower QALYs at 12 months than the control group (0.363 and 0.367, respectively), resulting in a difference of –0.004 (95% CI –0.019 to 0.011) between the groups. However, both costs and QALY differences were imprecise, with the 95% CIs including ‘no difference’, but also covering important economic values for costs (the CIs for QALYs might not contain economically important differences, but this is itself unclear). Given these data, an incremental cost per QALY can be calculated only to compare the more costly and more effective control with the less costly and less effective intervention. In this case, the estimated incremental cost per QALY was approximately £723,000 per additional QALY for the control compared with the intervention (Table 26). This is well beyond the £20,000 that the National Institute for Health and Care Excellence typically judges acceptable in its recommendations about the provision of services and treatments. 138 This suggests that the control is, on average, not cost-effective compared with the intervention. Therefore, by implication, the intervention is, on average, cost-effective at a threshold value for society’s willingness to pay for a QALY of £20,000.
| Option | Mean total | Comparison | Incremental | Cost per QALY gained (£) | ||
|---|---|---|---|---|---|---|
| Cost (£) | QALYs | Cost (£) (95% CI) | QALYs (95% CI) | |||
| Control | 9077 | 0.367 | – | – | – | – |
| Intervention | 6212 | 0.363 | Intervention vs. control | –2865 (–11,272 to 2707) | –0.004 (–0.019 to 0.011) | 723,048 |
Figure 7 shows the 1500 bootstrap replicates, stratified by trial group, geographic location and participant sex, of the estimates from a seemingly unrelated regression of the difference between the intervention and control groups, adjusting for baseline resource use costs, baseline EQ-5D-3L score and participant characteristics. Out of 1500 replications, in 54% of observations the intervention was less costly and less effective, in 22% of observations it was less costly and more effective, in 18% of observations it was more costly and less effective, and in 6% the intervention was more costly and more effective. As the figure shows, the majority of the bootstrap replications fall below the diagonal lines, which represent the National Institute for Health and Care Excellence’s cost-per-QALY threshold reference values of £20,000 and £30,000. This indicates that, for the majority of iterations, the intervention would be considered cost-effective.
FIGURE 7.
Incremental cost and QALY plot.
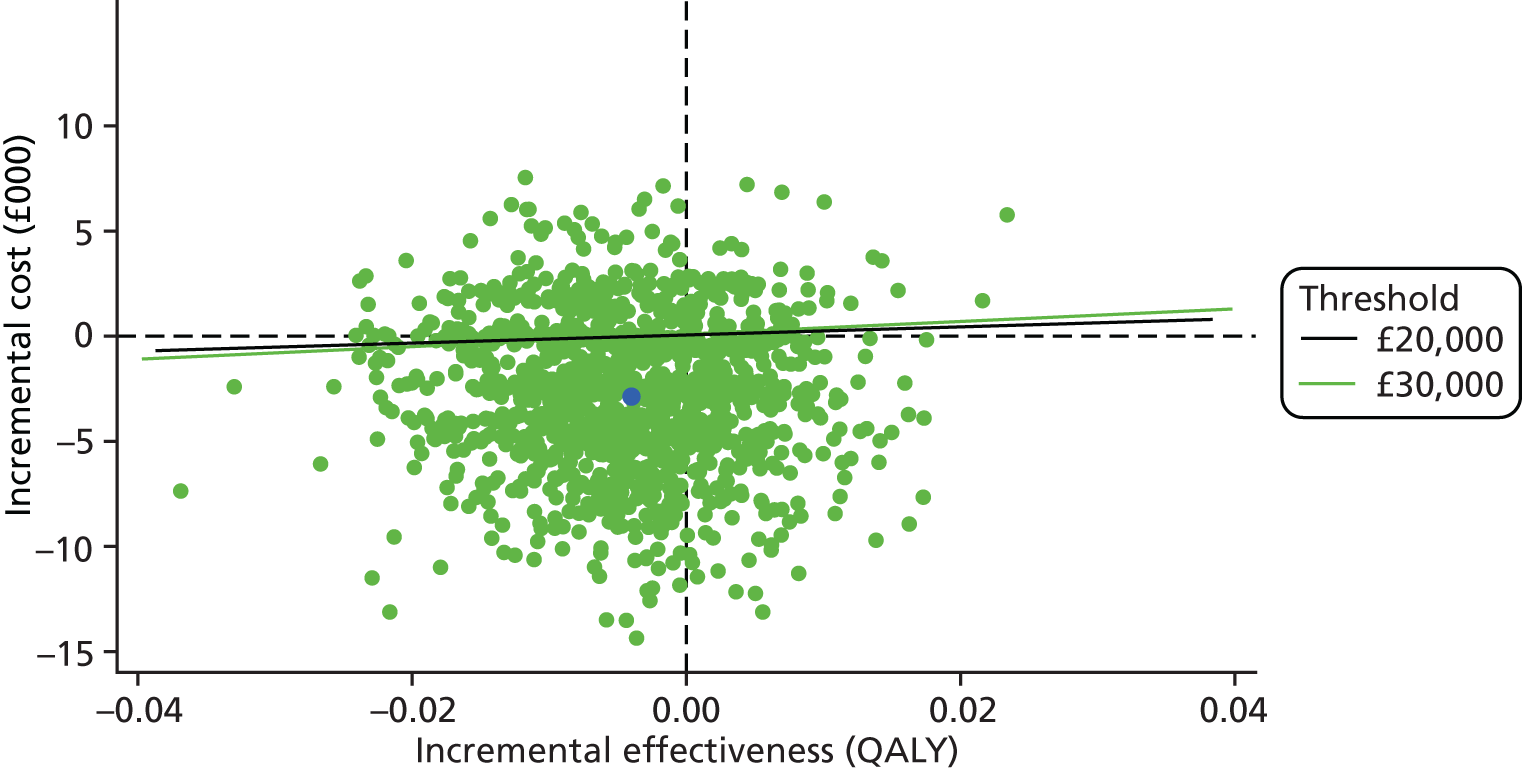
The CEAC (Figure 8) suggests a 76% probability that the brief alcohol intervention is cost saving compared with usual practice. At the same time, at values of £20,000 and £30,000 of willingness-to-pay thresholds for an additional QALY gained, the probability that the intervention could be cost-effective compared with usual practice is 73%. These results were driven by the likelihood that the brief alcohol intervention was cost saving as the mean difference in QALYs was so small.
FIGURE 8.
Cost-effectiveness curve.
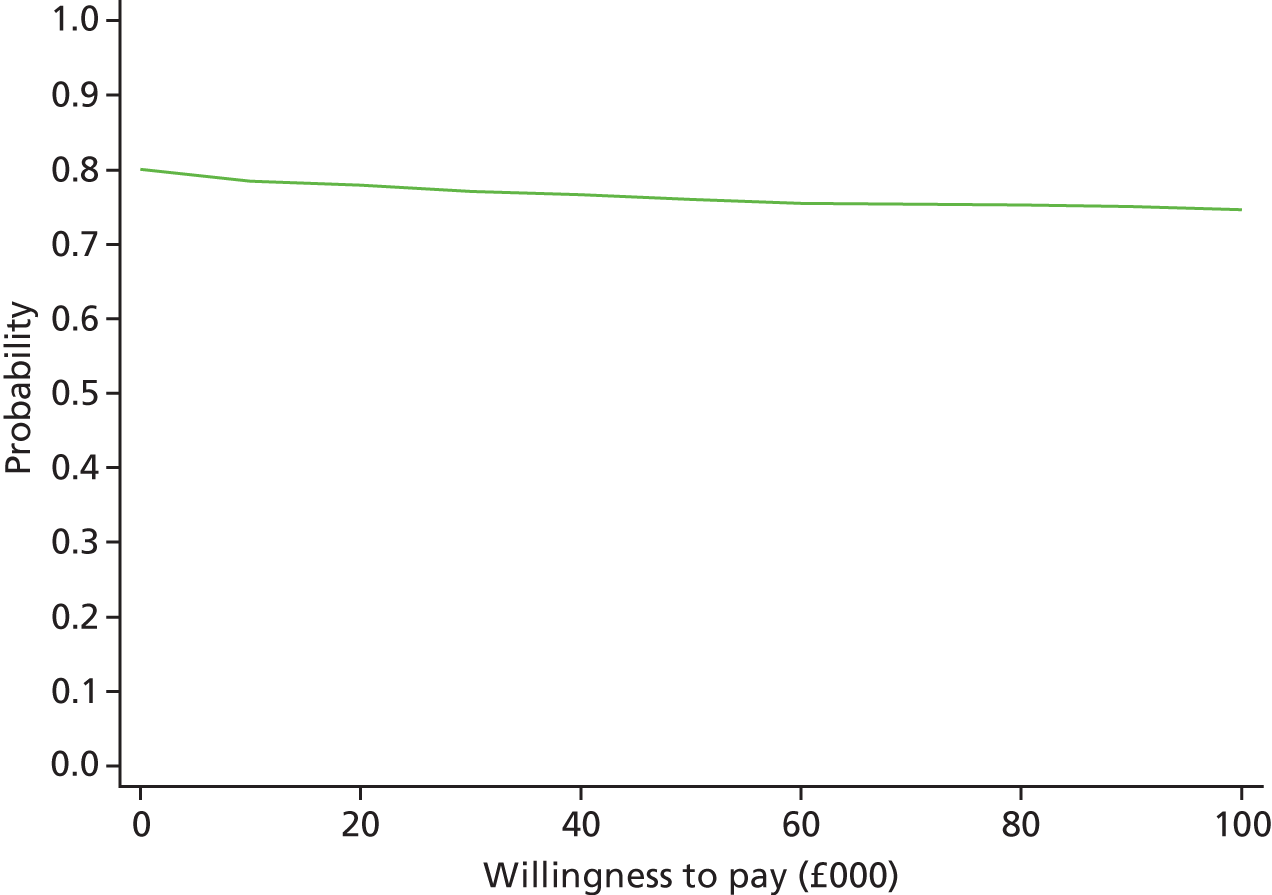
The curve reflects the probability that the intervention will be cost-effective at a given value of society’s willingness to pay for an additional QALY gained. At a willingness to pay equal to zero, the curve shows the probability that the intervention will be cost saving.
Sensitivity analyses of cost–utility results
Sensitivity analysis of cost assumptions
The values obtained for the differences in costs between the intervention and the control groups in a trial are, crucially, determined by the unit costs, the distribution of costs and the assumptions made about the relevant costs to include in the analyses. Two sensitivity analyses were performed to account for these factors. The first explored the potential impact on costs of the very large values of service use, in particular GP visits, social worker visits and nurse visits. The large values were truncated at the 95th percentile of the distribution of each variable. The second analysis excluded the costs associated with missing school days, as these costs are based on future lifetime income lost and can be considered a type of indirect cost, as opposed to the direct realisable costs of service use from, for example, being arrested or going to hospital (Table 27).
| Category | Analysis | ||
|---|---|---|---|
| Original | Sensitivity | ||
| Extreme values | Missed school days | ||
| Incremental costs (£) | –2865 (–11,272 to 2707) | –2911 (–9900 to 4077) | –1324 (–5277 to 1727) |
| Incremental QALYs | –0.004 (–0.019 to 0.011) | –0.004 (–0.019 to 0.011) | –0.004 (–0.019 to 0.011) |
| Cost per QALY gained (£) | 723,048 | 734,804 | 334,537 |
The results were relatively unchanged after truncating the extreme values of GP visits, social worker visits and nurse visits (see Table 26). When excluding the missed school days costs, the mean net savings from the intervention were approximately halved. This resulted in the incremental cost per QALY gained falling to £334,537 compared with £723,048 in the base case analysis (note that this incremental cost-effectiveness ratio is for the more effective but more costly control compared with the intervention). The CEAC obtained when the cost of missed school days was excluded gave a 77% probability of cost saving for the brief intervention, and the probability that the intervention is cost-effective given threshold willingness-to-pay values of £20,000 and £30,000 of 74%. The scatterplot of the joint distribution of incremental costs and QALYs is presented in Appendix 16. Of the 1500 replicates of incremental costs and QALYs, in 54% of observations the intervention was less costly and less effective, in 23% of observations the intervention was less costly and more effective, in 18% of observations the intervention was more costly and less effective, and in 6% the intervention was more costly and more effective.
Multiple imputation
Multiple imputation was used to reduce the proportion of missing values in the total cost at follow-up and in the EQ-5D-3L scores at follow-up. In total, 103 observations, 33% of the number of young people who consented to the study, had missing values of total costs, follow-up EQ-5D-3L or both. Details of the multiple imputation strategy can be found in Appendix 17.
After multiple imputation, the results shown in Table 28 did not differ markedly from those of the main analyses reported in Table 26. The CEAC and the incremental cost/incremental QALY plot (results not shown) were also similar to the plots from the main analyses.
| Option | Mean total | Comparison | Incremental | Cost per QALY gained (£) | ||
|---|---|---|---|---|---|---|
| Cost (£) | QALYs | Cost (£) (95% CI) | QALYs (95% CI) | |||
| Including missed school days costs | ||||||
| Control | 9265 | 0.366 | – | – | – | – |
| Intervention | 6513 | 0.362 | Intervention vs. control | –2752 (–9879 to 4376) | –0.004 (–0.02 to 0.012) | 674,799 |
| Excluding missed school days costs | ||||||
| Control | 4841 | 0.367 | – | – | – | – |
| Intervention | 3630 | 0.363 | Intervention vs. control | –1211 (–4977 to 2566) | –0.004 (–0.02 to 0.012) | 297,105 |
Cost–consequences analysis
The cost–consequences analysis for the SIPS JR-HIGH trial is presented as a balance sheet comparing costs that favour current practice and outcomes that favour the intervention (Table 29). This analysis suggests a very mixed picture, with no clear signal from the other outcomes as to why the intervention has an 80% chance of being cost saving.
| In favour of | |
|---|---|
| Current practice | Brief intervention |
| The additional cost per young person receiving the intervention compared with usual practice was an estimated £22.20 (95% CI £21.83 to £22.57) | 77% probability that the brief intervention is cost saving (results excluding costs from missed school days) |
| Neither in favour of nor against the brief intervention | |
| No negative effect but also no positive effect on the young participants’ QALY values (95% CI –0.019 to 0.011) | |
| No difference between intervention and control groups in the level of alcohol intake: difference in alcohol units consumed in the previous 28 days of 0.8 units (95% CI –2.5 to 4.0 units) | |
| No difference between intervention and control groups in their reported mental well-being (WEMWBS score difference of 1.7, 95% CI –0.7 to 4.1), problem alcohol behaviours (e.g. A-SAQ score percentage reduced drinking: intervention 60%, control 59%; AUDIT score difference of –0.1, 95% CI –1.0 to 0.8) and smoking behaviours (started smoking: intervention 13%, control 14%)a | |
Long-term model analysis
The possibility of developing a long-term model of the cost and effectiveness outcomes of the trial was incorporated into the ex ante economic evaluation analysis plan prepared for this study. This part of the economic evaluation was dependent on the findings from the within-trial evaluation, that is, evidence of effects on costs, economic outcomes (i.e. QALYs) or trial outcomes. The trial did not show any effect on young people’s alcohol intake, with this result unlikely to be different when extrapolating figures to the longer term. 139 Similarly, in terms of the economic outcomes, the results failed to demonstrate statistically significant differences in effects, and data extrapolation from these figures is unlikely to change the main conclusions from the evaluation.
Chapter 6 Discussion
This multicentre, individually randomised controlled trial evaluated the effectiveness and cost-effectiveness of an ASBI in the secondary school setting with young people aged 14–15 years. 2 It follows on from a pilot feasibility study carried out in the north-east of England. 1 That pilot study and a systematic review carried out during this current study highlighted the potential efficacy of ASBIs for young people.
Assumptions from the pilot study indicated that 20 schools were required to participate in the study1 to allow recruitment of the target sample. In fact, an additional 10 schools (making 30 in total) were required to adequately power the study. The prevalence of young people screening positive for risky drinking was considerably lower (23.5%) than that seen in the pilot feasibility study in north-east England (39%). 1 We had expected that the overall risky drinking prevalence rate would be lower, as this trial also included schools in the south of England, where alcohol use is generally lower. 12 However, the prevalence rate in the north-east schools included in this trial (27.4%) was also lower than in the pilot. This is consistent with national surveys that have highlighted a decrease in the prevalence of young people drinking at risky levels. 12 Furthermore, 84.4% of young people were followed up at 12 months, with 83.0% of individuals in the trial completing the primary outcome measure (TLFB), which was slightly lower than the 88% we had expected.
The results would indicate that there is insufficient evidence to recommend adopting an ASBI in the secondary school setting. Overall, the results were consistent across all outcomes: the intervention showed no evidence of benefit for any alcohol-related measure compared with the control arm.
The results we found in relation to the AUDIT are contrary to what we found in the pilot study when we surveyed whole year groups (whether or not in the trial), when the prevalence of dependent drinking increased from 26.0% to 31.8%. 1 We also found a reduction in prevalence (69.0% to 60.7%) using the cut-off point on the AUDIT of 4, which has been shown to be the optimal cut-off point for young people. 81 Furthermore, the prevalence of young people whose alcohol consumption was reported as being reduced using the A-SAQ was 59.6% for the combined trial arms in this study. The field of ASBIs has shown consistent findings in reduced alcohol consumption in both intervention and control groups with adults140–143 and young people. 71 This could, of course be due to regression to the mean; as participants had to score highly on the screening tool at baseline, it is possible that the difference noted is due to a movement towards the population mean at follow-up. 144 We cannot discount this explanation for our findings.
In terms of acceptability, the qualitative findings showed that learning mentors enjoyed the training and found that the intervention was broadly similar to the pastoral work that they already undertake and so could be easily rolled out more widely in schools. They perceived that as the training supported them to discuss and address risky behaviour with pupils, it would help them in their work regarding other health and well-being issues. This could also be a possible explanation for the health economics findings in that the results are capturing spillovers of the intervention on other health and well-being issues. Learning mentors also reported that they grew in confidence as they delivered a greater number of interventions. Research indicates that practitioners can be reluctant to engage in a new service if they fail to see the benefit of that service,145,146 and that such perceptions may act as a barrier to implementing ASBIs in the school setting. 146 In the staff interviews there was a suggestion that, in the future, rather than screening all pupils for alcohol use, the schools could target those individuals believed to be drinking alcohol and who they feel may warrant an intervention. However, this would rely on staff competency in identifying young people at risk from alcohol-related harms; further work would need to be undertaken to assess the validity of staff judgements.
Only 18 learning mentors recorded the sessions with young people, which suggests that staff and/or young people were not happy being recorded or indeed could have forgotten to do so and, therefore, means that we do not know if all sessions were carried out according to protocol. This means that we are unable to make an assessment about the fidelity of implementation of the intervention. It could also be that there was cross-contamination between young people who were randomised to different arms.
The within-trial cost–utility analysis of the brief intervention suggested that there was approximately a 77% chance that the intervention would be cost saving overall when costs of missed school days are excluded. In other words, the cost of the intervention is likely to be offset by lower use of health services and other resources considered. The results were stable regardless of assumptions made about the impact of missed school days, exclusion of high service use and imputation of data. There was no evidence of a difference in QALYs and the CI may be sufficiently narrow to rule out the possibility of an important difference. Using conventional values for willingness to pay for QALY improvements (both £20,000 and £30,000), the intervention had a 74% probability of being cost-effective. The results of the cost–consequences analysis were presented in the form of a balance sheet, which showed that, despite the balance of probabilities being in favour of a cost-saving intervention, there was no evidence of a change in any of the other outcomes. This means that there is no clear evidence about the mechanism that might drive cost savings. This raises questions about whether any cost savings would be real or an artefact of imprecise cost data.
Other studies evaluating the economic outcomes of brief interventions to reduce hazardous and harmful alcohol drinking have been shown to be cost-effective. 147 These, however, have mostly related to interventions delivered in primary care by specialist nurses or GPs. Previous studies have also suggested that intervention costs might be offset by savings in health-care service use148,149 and, potentially, savings elsewhere in society, notably in costs to the criminal justice system from brief interventions to reduce alcohol abuse. 150,151 With this in mind, the finding of potential savings in the SIPS JR-HIGH trial is not wholly unrealistic. Nevertheless, it is unclear, based on the trial data, how the intervention could have caused these.
With respect to QALYs the SIPS JR-HIGH trial found that any differences would be small at best. One recent pilot study with male adults (aged > 18 years) using ASBIs as well as stepped-care sessions found that, on average, intervention participants had lower QALY values than those in the control group, but the difference was very small (0.0027) and the CIs were very wide. 150 The difference in QALYs was also small and non-significant in a large study looking at different counselling-based therapy options to address alcohol problems. 91 The lack of impact on QALYs at least over the short follow-up of a trial is perhaps unsurprising, as interventions target relatively healthy populations. This means that most participants are likely to report no problems on the items of mobility, self-care and usual activities of the EQ-5D-3L scale,117 which was also observed in the SIPS JR-HIGH trial. This means that it may be unlikely that economically relevant changes in QALYs would be observed in the short term. The health impacts of an intervention (either positive or negative) may be felt only in the longer term, which may be difficult to capture within a trial.
Strengths and limitations
The prevalence of risky drinking was found to be lower than anticipated, meaning that we could not recruit sufficient numbers to reach a target power of 90%. This may have been because the screening tool lacked sufficient sensitivity, although A-SAQ is validated for use in this age group. Lower than anticipated prevalence rates meant that the sample size that was originally calculated to provide 90% power to detect a standardised difference of 0.3 using a significance level of 5% had to be revised. As such, the target for power was reduced from 90% to 80% after discussion with the TSC and the DMEC. This reduced power may have had an impact on our ability to determine the effectiveness of an ASBI in this setting, and may indicate a need for a larger, cluster-design trial.
We successfully recruited 30 schools to take part in the study, although recruitment of schools was not evenly split across the sites (north-east, n = 13; north-west, n = 7; London, n = 5; and Kent, n = 8), which may have resulted from the geographical areas chosen. We found that schools in London were less likely to agree to take part in the study. In addition, some parents opted their children out. As we did not collect data on the characteristics of those opted out, we cannot speculate whether or not this biased the result. Once recruited, however, most schools were willing to take part in all aspects of the study. From anecdotal evidence, a range of factors influenced school participation: the project presented direct benefits to participating schools in terms of boosting alcohol education provision through additional staff training and the provision of enhanced support for participating students who needed it. However, some schools that declined to participate did so because they indicated that they did not feel their young people had a problem with alcohol. We also found that there were a small number of young people whom we could not follow up at 12 months. There were a number of reasons but the primary one was related to young people not being at school at the time of follow-up, either because they had left school or were not attending on the days we were there.
Although we used validated tools for the outcome measures, our primary outcome assessments relied on self-reports, the use of which may have led to inaccurate reporting of alcohol use. 152 However, adolescent self-reported alcohol questionnaires are considered to be generally reliable,152,153 although studies of recall in substance use surveys suggest that this may be an understudied recall bias. 154,155 In addition, the use of the self-completed TLFB in one school may have affected the results, with these young people completing the TLFB differently from those who completed it with the research co-ordinator. That said, self-completed TLFB questionnaires have been validated for both interviewer-conducted and self-completed versions. 156 Furthermore, it is possible that other confounders had an impact on the results, given that the intervention and control sessions were in a school setting as opposed to, for example, a tightly controlled laboratory setting.
In addition, not all intervention and control sessions were recorded to assess fidelity. Therefore, the small number of interventions that were recorded is a significant weakness and limits our ability to assess threats to internal validity. Learning mentors may have selected recorded sessions in which they felt that they performed better, and, as such, any potentially poorer sessions may be one reason for the null result. The small number of recordings may also have been because of a lack of confidence, with the qualitative data suggesting that learning mentors felt that there was a long time between training and delivering the sessions. In addition, young people in either arm may have discussed their learning mentor session with their peers, which is a source of contamination, and may have affected the trial result.
One of the fundamental issues in research around ASBIs is that studies include different measurement tools and outcomes (some validated and some not). A piece of work is currently taking place that aims to develop a core outcome set for alcohol brief interventions to improve the measurement of alcohol-related change in adults: Outcome Reporting in Brief Intervention Trials: Alcohol (ORBITAL). 157 We have used validated tools in this trial and it is expected that most of them will be included in the final ORBITAL outcome set.
The interviews showed that young people and school staff did not find the trial procedures excessively onerous and they seemed to welcome the use of a one-to-one alcohol intervention, although some young people did report that the time lag between the various stages of the study was long, which may have had an impact on validity. That said, a 12-month follow-up is a well-used time frame in research. Young people reported that they believed that the intervention could be a helpful way to reduce the risks associated with alcohol use, although they felt that it would have been more appropriate to target those young people who drank more than they did. This relates to social norms, and there is a large body of evidence indicating that young people often underestimate their own, and overestimate their peers’, alcohol consumption. 158,159 However, although most evidence suggests that young people increase their consumption to match perceived social norms,160 the results of these interviews instead show a comparison between young people who drink some alcohol and those other young people who drink more.
We found some issues with the operational work of learning mentors within schools that had an effect on booking appointments and follow-ups with young people. Not all teaching staff were aware that the ASBIs were ongoing and, therefore, some were reluctant to allow young people out of class, especially around exam time. To address this, learning mentors varied the classes that they took young people out of so as not to overly disrupt lessons. This interactional workability of the learning mentors was key to not disrupting existing relationships with teachers in the school and facilitating teachers’ co-operation with the trial. 161
As in our pilot study1 and other studies,162,163 despite the use of different techniques including letters and texts, recruitment of parents to take part in interviews was poor; although all eligible parents (n = 339) were invited to participate, only three expressed an interest and only two interviews were conducted. That said, discussions with these parents reflected many of the perceptions already expressed by school staff and young people as to the acceptability of the trial and embedded procedures.
The economic evaluation used internationally accepted methods of best practice. It was based on an explicit and detailed health economics analysis plan that was finalised before the analysis commenced. In terms of methods the intervention was micro-costed and rigorous attempts were made to capture resource use. The study also sought to use an internationally accepted tool for the measure of quality of life: the EQ-5D-3L. Nevertheless, the trial was not powered to be able to detect economically important differences and hence the results have been presented as the likelihood that the intervention is cost-effective. Furthermore, the cost to attach to some outcomes, such as absenteeism, is debatable. The results appeared stable over a range of sensitivity analyses around costs. Whereas the EQ-5D-3L might be generally accepted for use in economic evaluations, the data from the whole study suggest that short-term health impacts are at best very small but that the intervention might have wider impacts on well-being. An alternative valuation technique, such as contingent valuation, might have been more appropriate. The use of such techniques within a cost–benefit analysis framework has been argued to be valuable for evaluating public health interventions.
Although not strictly a limitation of the study, the results of the trial suggest that the intervention may be cost saving. However, quantitative findings from the trial do not help to provide an explanation for this. One possible explanation suggested from the qualitative findings is that the intervention may have ‘spillover’ effects but how these could influence costs is unclear and would require further investigation.
This research has advanced our understanding of how to carry out research in this setting and provides important information about carrying out public health research in secondary schools. Although this study did not prove the efficacy of ASBIs in this setting, it did show that it is possible to develop a safe and broadly acceptable process to deliver ASBIs to risky drinkers in a secondary school. Further research should include the following.
-
Understanding the prevalence of alcohol consumption within a school at a level that may be detrimental to health is a key component of any educational or psychosocial approach to managing school-aged children’s alcohol use. The findings from this study suggest that a short screening tool, such as AUDIT-C,81 would be feasible and appropriate for screening in the school setting.
-
The process of identification and brief intervention was associated with no adverse events and was found to be feasible and acceptable to deliver in practice. As schools take on a greater role in addressing mental and physical health in adolescence, this study suggests that they should consider the role of brief interventions as first-line strategies in addressing a range of physical health, mental health and educational needs of pupils.
Chapter 7 Conclusions
Implications for public health and education practice
The evidence from this study does not support the implementation of ASBI for young people aged 14–15 years in the secondary school setting.
Recommendations for future research
-
As our results in terms of involvement of schools and prevalence rates of risky drinking were considerably different from what we found in the pilot study, we recommend that, in the future, pilot feasibility studies should include more than one geographical area.
-
In addition, although alcohol consumption among young people is declining, it may be that consumption among high-risk young people remains prevalent. In any future research it may be worth focusing on higher-risk groups, which may include older young people (i.e. 15- to 18-year-olds).
-
Future work is needed around how to involve parents successfully in research on health-related behaviours in the secondary school setting.
-
Research with school staff and pupils is needed to better understand and design school-based research to ensure that it can be carried out in a timely manner and following research design protocols.
-
Despite the economic findings, there is insufficient evidence to recommend adopting ASBIs.
-
More qualitative investigation is needed to explore why the use of services may have fallen, contrary to the trial results.
-
Further exploration of potential reasons why the use of health and other services might have reduced is needed. This would primarily be qualitative to explore reasons for the possible reduction in costs.
-
We found that the animation shown in schools to provide instructions on how to complete the baseline survey, including details on confidentiality and next steps in the study, was well received. Young people indicated that the animation was clear and easy to understand, and school staff indicated that it was easy to inform young people about the study and how to complete the survey (which contained the screening tools). It is therefore recommended that such tools be used in future research.
Acknowledgements
The research team would like to thank all of the school staff, young people and parents who took part in the research. We would like to acknowledge the help of Team Alpha at Teesside University, who were responsible for inputting survey data and preparing the research packs. We would like to thank the following individuals who contributed to this study:
Ms Amanda Atkinson, Public Health Institute, Liverpool John Moores University, UK.
Dr Áine Aventin, School of Nursing and Midwifery, Queen’s University Belfast, UK.
Professor Damon Berridge, Farr Institute CIPHER, Swansea University, UK
Mr Alan Brennan, Health Economics, Sheffield University, UK.
Mr Andy Bryant, Institute of Health and Society, Newcastle University, UK.
Ms Erin Graybill, Institute of Health and Society, Newcastle University, UK.
Mr Sean Harris, Norham High School, Newcastle upon Tyne, UK.
Dr Andrea Hearne, Regional Drug and Alcohol Service, Newcastle upon Tyne, UK.
Professor Matthew Hickman, School of Social and Community Medicine, University of Bristol, UK.
Professor Simon Moore, School of Dentistry, Cardiff University, UK.
Ms Kelly O’Brien, Health Improvement Specialist (Drugs and Alcohol), Central Manchester University Hospitals NHS Foundation Trust, UK.
Mr Les Tate, Strategy and Commissioning Manager, North Tyneside Council, UK.
Ms Alison Steel, Clinical Trials Unit, Newcastle University, UK.
Mr Alan Strachan, North Tyneside Council, Tyne and Wear, UK.
Dr Chris Sutton, Lancashire Clinical Trials Unit, School of Health, University of Central Lancashire, UK.
TeamAlpha, School of Health and Social Care, Teesside University, UK.
All of the schools that have taken part in this research.
Contributions of authors
All authors read, commented on and agreed the final draft report.
Dr Emma L Giles (Senior Research Lecturer in Public Health; Project Manager; specialty – public health) project managed the study and took overall responsibility for the conduct of the study, the writing of the report and conduct of the trial and was a member of the TMG, TSC and DMEC.
Dr Grant J McGeechan (Lecturer in Health Psychology; Qualitative Research Lead and North East Co-ordinator; specialty – psychology) conducted the north-east interviews and both of the parent interviews, coanalysed all aspects of the qualitative work, drafted the qualitative chapter of the final report and was a member of the TMG, TSC and DMEC.
Professor Simon Coulton (Professor of Health Services Research; Kent Chief Investigator and Co-applicant; specialty – health services) contributed to the design of the study and the conduct of the trial, and was a member of the TMG.
Dr Paolo Deluca (Senior Research Fellow; London Co-applicant; specialty – addictions) contributed to the design of the study and the conduct of the trial, and was a member of the TMG.
Professor Colin Drummond (Professor of Addiction Psychiatry; London Site Chief Investigator and Co-applicant; specialty – addictions) contributed to the design of the study and the conduct of the trial, and was a member of the TMG.
Ms Denise Howel (Senior Lecturer; Lead Statistician and Co-applicant; specialty – statistics) contributed to the design of the study and the conduct of the trial, supervised the statistical component of the research, carried out statistical analysis, co-drafted the survey chapter, and was a member of the TMG, TSC and DMEC.
Professor Eileen Kaner (Professor of Public Health Research; Qualitative Lead and Co-applicant; specialty – public health) contributed to the design of the study and the conduct of the trial, was the qualitative lead and was a member of the TMG.
Professor Elaine McColl (Professor of Health Services Research; Trial Manager and Co-applicant; specialty – health services) contributed to the design of the study and the conduct of the trial, and was a member of the TMG, TSC and DMEC.
Dr Ruth McGovern (Senior Research Interventionist; Interventionist and Co-applicant; specialty – health interventions) co-developed the interventions, assessed intervention fidelity, drafted the intervention chapter of the report and was a member of the TMG.
Dr Stephanie Scott (Senior Lecturer in Criminology; Qualitative Study Researcher and Co-applicant; specialty – criminology and medical sociology) contributed to the design of the study and the conduct of the trial, and was a member of the TMG, TSC and DMEC.
Ms Elaine Stamp (Research Associate; Statistician; specialty – statistics) carried out the statistics analysis of the study, co-drafted the survey chapter and was a member of the TMG, TSC and DMEC.
Professor Harry Sumnall (Professor of Substance Use; North West Chief Investigator and Co-applicant; specialty – substance use) contributed to the design of the study and the conduct of the trial, and was a member of the TMG.
Professor Liz Todd (Professor of Educational Inclusion; Co-applicant; specialty – education studies) contributed to the design of the study and the conduct of the trial, and was a member of the TMG.
Professor Luke Vale (Professor of Health Economics; Co-applicant and Lead Health Economist; specialty – health economics) contributed to the design of the study and the conduct of the trial, and was a member of the TMG, TSC and DMEC.
Dr Viviana Albani (Research Associate; Health Economist; specialty – health economics) conducted the health economic analysis, drafted the health economic chapter and was a member of the TMG, TSC and DMEC.
Dr Sadie Boniface (Research Associate; London Research Co-ordinator; specialty – addictions) was the co-ordinator in London, took responsibility for the qualitative work in London and was a member of the TMG.
Mrs Jennifer Ferguson (Graduate Tutor; Independent Researcher; specialty – public health) assisted with the randomisation process, making up research packs and inputting anonymised data.
Professor Eilish Gilvarry (Honorary Professor of Addictions Psychiatry, Consultant Psychiatrist in Addictions; Chairperson of TMG; specialty – addictions) contributed to the study design, co-developed the interventions and chaired the TMG.
Ms Nadine Hendrie (Research Associate; Kent Research Co-ordinator; specialty – substance use) was the second co-ordinator in Kent, assisted with the qualitative work in Kent and was a member of the TMG.
Ms Nicola Howe (Database Manager; specialty – clinical trials) assisted with the database management and was a member of the TMG.
Ms Helen Mossop (Research Assistant; Statistician; specialty – statistics) assisted with the statistical analysis.
Ms Amy Ramsay (Research Associate; London Research Co-ordinator; specialty – health services) assisted with the qualitative work in London and was a member of the TMG.
Dr Grant Stanley (Research Associate; North West Research Co-ordinator; specialty – education studies) was the co-ordinator in the north-west, assisted with the qualitative work in the north-west and was a member of the TMG.
Professor Dorothy Newbury-Birch (Professor of Alcohol and Public Health Research; Overall Chief Investigator; specialty – alcohol and public health) took overall responsibility for the study, co-drafted the report and was a member of the TMG, TSC and DMEC.
Contributions of others
Dr Jo Frankham (Research Associate; North West Research Co-ordinator; speciality – methodology) assisted with the qualitative work in the north-west and school recruitment, and the TMG. Dr Frankham left the study in the early stages.
Dr Jayne Ogilvie (Research Associate; Kent Research Co-ordinator; specialty – public health) was the first co-ordinator in Kent, assisted with the qualitative work in Kent and was a member of the TMG. Dr Ogilvie no longer wanted to be an author on the report.
Mr Les Tate (Strategy and Commissioning Manager; TMG advisory member; specialty – education) contributed to the design of the study and the conduct of the trial, was a member of the TMG and co-ordinated school involvement in the study. Mr Tate left his role halfway through the trial and no longer wanted to be an author on the report.
Publications
Giles EL, Scott S, Coulton S, Deluca P, Drummond C, Graybill E, et al. Development of a multicentre randomised controlled trial of screening and brief alcohol intervention to prevent risky drinking in young people in a high-school setting (SIPS JR-HIGH). Lancet 2015;386:S1–83.
Giles EL, Coulton S, Deluca P, Drummond C, Howel D, Kaner E, et al. Multi-centre individual randomised controlled trial of screening and brief alcohol intervention to prevent risky drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH): study protocol. BMJ Open 2016;6:e012474.
Giles EL, Newbury-Birch D, Coulton S, Deluca P, Drummond C, Howel D, et al. A multi-centre individual-randomised controlled trial of screening and brief alcohol intervention to prevent risky drinking in young people aged 14–15 in a high school setting. Addiction Sci Clin Pract 2017;12(Suppl. 1):A17.
McGeechan GJ, Giles EL, Scott S, McGovern R, Boniface S, Ramsay A, et al. A qualitative exploration of school-based staff’s experiences of delivering an alcohol screening and brief intervention in the high school setting: findings from the SIPS JR-HIGH trial [published online ahead of print October 29 2018]. J Pub Heal 2018.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. Exclusive use will be retained until the publication of major outputs.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Newbury-Birch D, Scott S, O’Donnell A, Coulton S, Howel D, McColl E, et al. A pilot feasibility cluster randomised controlled trial of screening and brief alcohol intervention to prevent hazardous drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH). Public Health Res 2014;2.
- Giles E, Coulton S, Deluca P, Drummond C, Howel D, Kaner E, et al. A multi-centre individual-randomized controlled trial of screening and brief alcohol intervention to prevent risky drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH): study protocol. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012474.
- Szende A, Oppe M, Devlin N. EQ-5D Value Sets. Inventory, Comparative Review and User Guide. Dordrecht: Springer; 2007.
- Data Protection Act 1998. London: The Stationery Office; 1998.
- Freedom of Information Act 2000. London: The Stationery Office; 2000.
- Leading Science for Better Health. London: Medical Reseach Council; 2018.
- WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects. Ferney-Voltaire: World Medical Association; 2018.
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009;373:2223-33. https://doi.org/10.1016/S0140-6736(09)60746-7.
- Alcohol Misuse: Tackling the Epidemic. London: British Medical Association Board of Science; 2008.
- Health Matters: Harmful Drinking and Alcohol Dependence. London: Public Health England; 2016.
- Adult Drinking Habits in Great Britain. Newport: Office for National Statistics; 2018.
- Smoking, Drinking and Drug Use Among Young People. Leeds: NHS Digital; 2016.
- Guidance on the Consumption of Alcohol by Children and Young People. London: DHSC; 2009.
- Smoking, Drinking and Drug Use Among Young People in England in 2016. Leeds: NHS Digital; 2017.
- Emerson E, Robertson J, Baines S, Hatton C. Predictors of self-reported alcohol use and attitudes toward alcohol among 11-year-old British children with and without intellectual disability. J Intellect Disabil Res 2016;60:1212-26. https://doi.org/10.1111/jir.12334.
- Health Survey for England. Leeds: NHS Digital; 2016.
- Fuller E. Smoking, Drinking and Drug Use among Young People in England in 2014. London: NatCen Social Research; 2015.
- NHS Direct . Binge Drinking 2014. www.nhs.uk/Livewell/alcohol/Pages/Bingedrinking.aspx (accessed 11 August 2016).
- Viner RM, Taylor B. Adult outcomes of binge drinking in adolescence: findings from a UK national birth cohort. J Epidemiol Commun Health 2007;61:902-7. https://doi.org/10.1136/jech.2005.038117.
- Paavola M, Vartiainen E, Haukkala A. Smoking, alcohol use, and physical activity: a 13-year longitudinal study ranging from adolescence into adulthood. J Adolesc Health 2004;35:238-44. https://doi.org/10.1016/j.jadohealth.2003.12.004.
- Murgraff V, Parrott A, Bennett P. Risky single-occasion drinking amongst young people – definition, correlates, policy, and intervention: a broad overview of research findings. Alcohol Alcohol 1999;34:3-14. https://doi.org/10.1093/alcalc/34.1.3.
- Permanent and Fixed-period Exclusions in England: 2015 to 2016. London: Department for Education; 2017.
- Matthews S, Brasnett L, Smith J. Underage Drinking: Findings from the 2004 Offending, Crime and Justice Survey. London: Home Office; 2006.
- Clark DB, Lynch KG, Donovan JE, Block GD. Health problems in adolescents with alcohol use disorders: self-report, liver injury, and physical examination findings and correlates. Alcohol Clin Exp Res 2001;25:1350-9. https://doi.org/10.1111/j.1530-0277.2001.tb02358.x.
- Patton R, Deluca P, Kaner E, Newbury-Birch D, Phillips T, Drummond C. Alcohol screening and brief intervention for adolescents: the how, what and where of reducing alcohol consumption and related harm among young people. Alcohol Alcohol 2014;49:207-12. https://doi.org/10.1093/alcalc/agt165.
- Newbury-Birch D, Gilvarry E, McArdle P, Stewart S, Walker J, Lock C, et al. The Impact of Alcohol Consumption on Young People: A Review of Reviews. London: Department for Children, Schools and Families; 2009.
- Bellis MA, Phillips-Howard PA, Hughes K, Hughes S, Cook PA, Morleo M, et al. Teenage drinking, alcohol availability and pricing: a cross-sectional study of risk and protective factors for alcohol-related harms in school children. BMC Public Health 2009;9. https://doi.org/10.1186/1471-2458-9-380.
- Global Status Report on Alcohol and Health, 2014. Geneva: WHO; 2014.
- Reducing Underage Drinking: A Collective Responsibility. Washington, DC: National Academies Press; 2004.
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption – II. Addiction 1993;88:791-804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x.
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 2007;31:1208-17. https://doi.org/10.1111/j.1530-0277.2007.00403.x.
- Kaarne T, Aalto M, Kuokkanen M, Seppä K. AUDIT-C, AUDIT-3 and AUDIT-QF in screening risky drinking among Finnish occupational health-care patients. Drug Alcohol Rev 2010;29:563-7. https://doi.org/10.1111/j.1465-3362.2010.00172.x.
- Hodgson R, Alwyn T, John B, Thom B, Smith A. The Fast Alcohol Screening Test. Alcohol Alcohol 2002;37:61-6. https://doi.org/10.1093/alcalc/37.1.61.
- Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA 1984;252:1905-7. https://doi.org/10.1001/jama.1984.03350140051025.
- Selzer ML. The Michigan alcoholism screening test: the quest for a new diagnostic instrument. Am J Psychiatry 1971;127:1653-8. https://doi.org/10.1176/ajp.127.12.1653.
- Smith SG, Touquet R, Wright S, Das Gupta N. Detection of alcohol misusing patients in accident and emergency departments: the Paddington alcohol test (PAT). J Accid Emerg Med 1996;13:308-12. https://doi.org/10.1136/emj.13.5.308.
- Miller GA. The Substance Abuse Subtle Screening Inventory (SASSI) Adolescent Manual. Bloomington, IN: The SASSI Institute; 1990.
- World Health Organization Alcohol, Smoking and Substance Involvement Screening Test Working Group . The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction 2002;97:1183-94. https://doi.org/10.1046/j.1360-0443.2002.00185.x.
- Williams R, Vinson DC. Validation of a single screening question for problem drinking. J Fam Pract 2001;50:307-12.
- Russell M. New assessment tools for risk drinking during pregnancy: T-ACE, TWEAK, and others. Alcohol Health Res World 1994;18.
- Sokol RJ, Martier SS, Ager JW. The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol 1989;160:863-8. https://doi.org/10.1016/0002-9378(89)90302-5.
- Jackson R, Johnson M, Campbell F, Messina J, Guillaume L, Meier P, et al. Screening and Brief Interventions for Prevention and Early Identification of Alcohol Use Disorders in Adults and Young People. Sheffield: School of Health and Related Research, University of Sheffield; 2010.
- Coulton S, Drummond C, James D, Godfrey C, Bland JM, Parrott S, et al. Stepwice Research Team . Opportunistic screening for alcohol use disorders in primary care: comparative study. BMJ 2006;332:511-17. https://doi.org/10.1136/bmj.38743.421574.7C.
- Screening and Intervention Programme for Sensible drinking (SIPS) . Modified-Single Alcohol Screening Question (M-SASQ) n.d. www.sips.iop.kcl.ac.uk/msasq.php (accessed 23 November 2017).
- O’Neil S, Coulton S, Deluca P, Deverill M, Drummond C, Gilvarry E, et al. Brief intervention to prevent hazardous drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH): study protocol for a randomized controlled trial. Trials 2012;13. https://doi.org/10.1186/1745-6215-13-166.
- Management of Substance Abuse Prevention and Young People. Geneva: WHO; 2018.
- Sumnall H, Agus A, Cole J, Doherty P, Foxcroft D, Harvey S, et al. Steps Towards Alcohol Misuse Prevention Programme (STAMPP): a school- and community-based cluster randomised controlled trial. Public Health Res 2017;5.
- Segrott J, Rothwell H, Hewitt G, Playe R, Huang C, Murphy S, et al. Preventing alcohol misuse in young people: an exploratory cluster randomised controlled trial of the Kids, Adults Together (KAT) programme. Public Health Res 2015;3.
- Wilson DB, Gottfredson DC, Najaka SS. School-based prevention of problem behaviors: a meta-analysis. J Quantitative Criminol 2001;17:247-72. https://doi.org/10.1023/A:1011050217296.
- Bonnell C, Jamal F, Harden A, Wells H, Parry W, Fletcher A, et al. Systematic review of the effects of schools and school environment interventions on health: evidence mapping and synthesis. Public Health Res 2013;1.
- Heather N. Brief Interventions. Chichester: John Wiley & Sons; 2004.
- Babor TF, Higgins-Biddle J. Brief Intervention for Hazardous and Harmful Drinking: A Manual for Use in Primary Care. Geneva: World Health Organization, Department of Mental Health and Substance Dependence; 2001.
- Heather N. Interpreting the evidence on brief interventions for excessive drinkers: the need for caution. Alcohol Alcohol 1995;30:287-96.
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction 1993;88:315-35. https://doi.org/10.1111/j.1360-0443.1993.tb00820.x.
- McCambridge J, Cunningham JA. The early history of ideas on brief interventions for alcohol. Addiction 2014;109:538-46. https://doi.org/10.1111/add.12458.
- Adolescent Health. Geneva: WHO; 2017.
- Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: a systematic review and meta-analysis. J Subst Abuse Treat 2015;51:1-18. https://doi.org/10.1016/j.jsat.2014.09.001.
- Hale DR, Fitzgerald-Yau N, Viner RM. A systematic review of effective interventions for reducing multiple health risk behaviors in adolescence. Am J Public Health 2014;104:e19-41. https://doi.org/10.2105/AJPH.2014.301874.
- Gmel G, Venzin V, Marmet K, Danko G, Labhart F. A quasi-randomized group trial of a brief alcohol intervention on risky single occasion drinking among secondary school students. Int J Public Health 2012;57:935-44. https://doi.org/10.1007/s00038-012-0419-0.
- Toumbourou JW, Gregg ME, Shortt AL, Hutchinson DM, Slaviero TM. Reduction of adolescent alcohol use through family-school intervention: a randomized trial. J Adolesc Health 2013;53:778-84. https://doi.org/10.1016/j.jadohealth.2013.07.005.
- White HR, Morgan TJ, Pugh LA, Celinska K, Labouvie EW, Pandina RJ. Evaluating two brief substance-use interventions for mandated college students. J Stud Alcohol 2006;67:309-17. https://doi.org/10.15288/jsa.2006.67.309.
- Tait RJ, Hulse GK, Robertson SI. Effectiveness of a brief-intervention and continuity of care in enhancing attendance for treatment by adolescent substance users. Drug Alcohol Depend 2004;74:289-96. https://doi.org/10.1016/j.drugalcdep.2004.01.003.
- Martínez Martínez KI, Pedroza Cabrera FJ, de los Ángeles Vacío Muro M, Jiménez Pérez AL, Salazar Garza ML. Consejo breve para adolescentes escolares que abusan del alcohol. Acta Ortop Mex 2008;34:247-64.
- Magill M, Colby SM, Orchowski L, Murphy JG, Hoadley A, Brazil LA, et al. How does brief motivational intervention change heavy drinking and harm among underage young adult drinkers?. J Consult Clin Psychol 2017;85:447-58. https://doi.org/10.1037/ccp0000200.
- Davis JP, Houck JM, Rowell LN, Benson JG, Smith DC. Brief motivational interviewing and normative feedback for adolescents: change language and alcohol use outcomes. J Subst Abuse Treat 2016;65:66-73. https://doi.org/10.1016/j.jsat.2015.10.004.
- Cunningham RM, Chermack ST, Ehrlich PF, Carter PM, Booth BM, Blow FC, et al. Alcohol interventions among underage drinkers in the ed: a randomized controlled trial. Pediatrics 2015;136:e783-93. https://doi.org/10.1542/peds.2015-1260.
- Baer JS, Kivlahan DR, Blume AW, McKnight P, Marlatt GA. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. Am J Public Health 2001;91:1310-16. https://doi.org/10.2105/AJPH.91.8.1310.
- Arnaud N, Diestelkamp S, Wartberg L, Sack PM, Daubmann A, Thomasius R. Short- to midterm effectiveness of a brief motivational intervention to reduce alcohol use and related problems for alcohol intoxicated children and adolescents in pediatric emergency departments: a randomized controlled trial. Acad Emerg Med 2017;24:186-200. https://doi.org/10.1111/acem.13126.
- Winters KC, Leitten W. Brief intervention for drug-abusing adolescents in a school setting. Psychol Addict Behav 2007;21:249-54. https://doi.org/10.1037/0893-164X.21.2.249.
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA 2010;304:527-35. https://doi.org/10.1001/jama.2010.1066.
- Spirito A, Sindelar-Manning H, Colby SM, Barnett NP, Lewander W, Rohsenow DJ, et al. Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: results of a randomized clinical trial. Arch Pediatr Adolesc Med 2011;165:269-74. https://doi.org/10.1001/archpediatrics.2010.296.
- Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, Rohsenow DJ, et al. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. J Pediatr 2004;145:396-402. https://doi.org/10.1016/j.jpeds.2004.04.057.
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol 1999;67:989-94. https://doi.org/10.1037/0022-006X.67.6.989.
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, et al. Screening and brief intervention for high-risk college student drinkers: results from a 2-year follow-up assessment. J Consult Clin Psychol 1998;66:604-15. https://doi.org/10.1037/0022-006X.66.4.604.
- Bernstein J, Heeren T, Edward E, Dorfman D, Bliss C, Winter M, et al. A brief motivational interview in a pediatric emergency department, plus 10-day telephone follow-up, increases attempts to quit drinking among youth and young adults who screen positive for problematic drinking. Acad Emerg Med 2010;17:890-902. https://doi.org/10.1111/j.1553-2712.2010.00818.x.
- Baer JS, Garrett SB, Beadnell B, Wells EA, Peterson PL. Brief motivational intervention with homeless adolescents: evaluating effects on substance use and service utilization. Psychol Addict Behav 2007;21:582-6. https://doi.org/10.1037/0893-164X.21.4.582.
- Sobell L, Sobell M. Alcohol Timeline Followback Users’ Manual. Toronto, ON: Addiction Research Foundation; 1995.
- Engs RC, Hanson DJ. The Student Alcohol Questionnaire: an updated reliability of the drinking patterns, problems, knowledge, and attitude subscales. Psychol Rep 1994;74:12-4. https://doi.org/10.2466/pr0.1994.74.1.12.
- Babor T, De La Fuente J, Saunders J, Grant M. AUDIT, The Alcohol Use Disorders Identification Test, Guidelines for Use in Primary Health Care. Geneva: World Health Organization; 1989.
- Reinert DF, Allen JP. The alcohol use disorders identification test: an update of research findings. Alcohol Clin Exp Res 2007;31:185-99. https://doi.org/10.1111/j.1530-0277.2006.00295.x.
- Coulton S, Alam MF, Boniface S, Deluca P, Donoghue K, Gilvarry E, et al. Opportunistic screening for alcohol use problems in adolescents attending emergency departments: an evaluation of screening tools [published online ahead of print March 26 2018]. J Public Health 2018. https://doi.org/10.1093/pubmed/fdy049.
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol 1989;50:30-7. https://doi.org/10.15288/jsa.1989.50.30.
- Segrott J, Gillespie D, Holliday J, Humphreys I, Murphy S, Phillips C, et al. Preventing substance misuse: study protocol for a randomised controlled trial of the Strengthening Families Programme 10-14 UK (SFP 10-14 UK). BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-49.
- Cooper M. Motivations for alcohol use among adolescents: development and validation of a four-factor model. Psychol Assess 1994;6:117-28. https://doi.org/10.1037/1040-3590.6.2.117.
- Warwick-Edinburgh Mental Well-Being Scale (WEMWBS). Edinburgh: NHS Health Scotland; 2006.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Clarke A, Friede T, Putz R, Ashdown J, Martin S, Blake A, et al. Warwick-Edinburgh Mental Well-being Scale (WEMWBS): validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-487.
- Hibbell B, Guttormsson U, Ahlström S, Balakireva O, Bjarnason T, Kokkevi A, et al. The 2011 ESPAD Report: Substance Use Among Students in 36 European Countries. The European School Survey Project on Alcohol and Other Drugs (ESPAD); 2012.
- The European School Survey Project on Alcohol and Other Drugs (ESPAD) . English Student Master Questionnaires 2015.
- EuroQol . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Team UR . Cost effectiveness of treatment for alcohol problems: findings of the randomised UK alcohol treatment trial (UKATT). BMJ 2005;331. https://doi.org/10.1136/bmj.331.7516.544.
- Lane C. The Behaviour Change Counselling Index (BECCI) Manual for Coding Behaviour Change Counselling. Cardiff: University of Wales College of Medicine; 2002.
- Not Yet Good Enough: Personal, Social Health and Economic Education in English Schools in 2012. Manchester: Ofsted; 2013.
- Emotional, Behavioural and Social Skills: Guidance. London: Department for Education and Skills; 2005.
- Addaction . Addaction 2015. www.addaction.org.uk/ (accessed 23 November 2017).
- Drinkaware . Drinkaware 2016. www.drinkaware.co.uk/ (accessed 23 November 2017).
- Gov.uk . Find and Compare Schools in England 2018. www.gov.uk/school-performance-tables (accessed 8 January 2018).
- Kendall L, O’Donnell L, Golden S, Kae Ridley K, Machin S, Rutt S, et al. Excellence in Cities: The National Evaluation of a Policy to Raise Standards in Urban Schools 2000–2003. Department for Education and Skills; 2005.
- Royal Borough of Kensington Council (RBKC) . Professional Frameworks. Care, Advice and Guidance LM Practice Guide for New Learning Mentors and New Line Managers 2011. www.rbkc.gov.uk/pdf/Professional%20Framework%20(A%20summary%20of%20job%20descriptions,%20pay,%20qualifications%20and%20training)1.pdf.
- Skills for Schools . Learning Mentor 2018. www.skillsforschools.org.uk/roles-in-schools/learning-mentor (accessed 3 November 2016).
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Milner W, Rollnick S. Motivational Interviewing: Helping People Change. New York, NY: Guilford Press; 2013.
- Alcohol-use Disorders – Preventing the Development of Hazardous and Harmful Drinking. London: NICE; 2010.
- Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1997.
- Rollnick S, Miller WR, Butler C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: Guilford Press; 2008.
- Miller W, Rollnick S. Motivational Interviewing: Preparing People for Change. New York, NY: Guilford Press; 2002.
- Kaner EF, Lock CA, McAvoy BR, Heather N, Gilvarry E. A RCT of three training and support strategies to encourage implementation of screening and brief alcohol intervention by general practitioners. Br J Gen Pract 1999;49:699-703.
- Teague GB, Bond GR, Drake RE. Program fidelity in assertive community treatment: development and use of a measure. Am J Orthopsychiatry 1998;68:216-32. https://doi.org/10.1037/h0080331.
- Lane C, Huws-Thomas M, Rollnick S, Hood K, Edwards K, Robling M. Measuring adaptations of motivational interviewing: the development and validation of the Behaviour Change Counselling Index (BECCI). Patient Educ Couns 2005;56:166-73. https://doi.org/10.1016/j.pec.2004.01.003.
- Butler CC, Simpson SA, Hood K, Cohen D, Pickles T, Spanou C, et al. Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: a cluster randomised trial. BMJ 2013;346. https://doi.org/10.1136/bmj.f1191.
- Horner S, Rew L, Torres R. Enhancing intervention fidelity: a means of strengthening study impact. J Spec Pediatr Nurs 2006;11:80-9. https://doi.org/10.1111/j.1744-6155.2006.00050.x.
- Dienes Z, Coulton S, Heather N. Using Bayes factors to evaluate evidence for no effect: examples from the SIPS project. Addiction 2018;113:240-6. https://doi.org/10.1111/add.14002.
- May C, Finch T. Implementation, embedding, and integration: an outline of normalization process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- EQ-5D. Rotterdam: EuroQol Research Foundation; n.d.
- McIntosh E, Thorsen T, Mäkelä M. Changing Professional Practice, Theory and Practice of Clinical Guidelines Implementation. Copenhagen: Danish Institute for Health Services Research and Development; 1999.
- Oluboyede Y, Tubeuf S, McCabe C. Measuring health outcomes of adolescents: report from a pilot study. Eur J Health Econ 2013;14:11-9. https://doi.org/10.1007/s10198-011-0340-0.
- Unit Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- Unit Costs of Health and Social Care 2014. Canterbury: PSSRU, University of Kent; 2014.
- Annual Survey of Hours and Earnings: 2016 Provisional Results. Newport: Office for National Statistics; 2016.
- Meyer S, Steiner M, Mueller H, Nunold H, Gottschling S, Gortner L. [Recent trends in the burden of alcohol intoxication on pediatric in-patient services in Germany. Klin Padiatr 2008;220:6-9. https://doi.org/10.1055/s-2007-972566.
- Hanushek EA, Sykes G, Schneider B, Plank DN. Handbook of Education Policy Research. New York, NY: Routledge; 2009.
- McIntosh S, Vignoles A. Measuring and assessing the impact of basic skills on labour market outcomes. Oxford Econ Papers 2001;53:453-81. https://doi.org/10.1093/oep/53.3.453.
- Orazem PF, Gunnarsson V. Child Labour, School Attendance and Academic Performance: A Review. Geneva: International Labour Organization/International Programme on the Elimination of Child Labour; 2003.
- Psacharopoulos G, Patrinos HA. Returns to investment in education: a further update. Educ Econ 2004;12:111-34. https://doi.org/10.1080/0964529042000239140.
- Sälzer C, Heine J-H. Students’ skipping behavior on truancy items and (school) subjects and its relation to test performance in PISA 2012. Int J Educ Dev 2016;46:103-13. https://doi.org/10.1016/j.ijedudev.2015.10.009.
- Youth Justice Statistics 2013/14. England and Wales. Newport: Office for National Statistics; 2015.
- National Health Service Reference Costs 2015–16. London: DHSC; 2016.
- Wilson V, Malcolm H, Edward S, Davidson J. ‘Bunking off’: the impact of truancy on pupils and teachers. Br Educ Res J 2008;34:1-17. https://doi.org/10.1080/01411920701492191.
- Local Government Association . Local Government Earnings Survey 2013 14 n.d. www.local.gov.uk/sites/default/files/documents/earnings-survey-201314-su-537.pdf (accessed 7 September 2016).
- McAuley KA, Taylor RW, Farmer VL, Hansen P, Williams SM, Booker CS, et al. Economic evaluation of a community-based obesity prevention program in children: the APPLE project. Obesity 2010;18:131-6. https://doi.org/10.1038/oby.2009.148.
- Drummond MF, Sculper MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. New York, NY: Oxford University Press; 2005.
- Giles EL, Coulton S, Deluca P, Drummond C, Howel D, Kaner E, et al. A multi-centre individual-randomized controlled trial of screening and brief alcohol intervention to prevent risky drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH): study protocol. BMJ Open 2016;6.
- Average Weekly Earnings in the Public Sector. Newport; 2018.
- HE Single Pay Spine. London: University and College Union; 2017.
- Cameron A, Triveldi P. Microeconometrics Using Stata. College Station, TX: Stata Press; 2010.
- King G, Tomz M, Wittenberg J. Making the most of statistical analyses: improving interpretation and presentation. Am J Political Sci 2000;44:347-61. https://doi.org/10.2307/2669316.
- National Institute for Health and Care Excellence . The Social Care Guidance Manual 2013. www.nice.org.uk/process/pmg10/chapter/introduction (accessed January 2019).
- Purshouse R, Brennan A, Latimer N, Meng Y, Rafia R, Jackson R, et al. Modelling to Assess the Effectiveness and Cost-effectiveness of Public Health Related Strategies and Interventions to Reduce Alcohol Attributable Harm in England using the Sheffield Alcohol Policy Model version 2.0. Report to the NICE Public Health Programme Development Group. Sheffield: University of Sheffield; 2011.
- Newbury-Birch D, Bland M, Cassidy P, Coulton S, Deluca P, Drummond C, et al. Screening and brief interventions for hazardous and harmful alcohol use in probation services: a cluster randomised controlled trial protocol. BMC Public Health 2009;9. https://doi.org/10.1186/1471-2458-9-418.
- Drummond C, Deluca P, Coulton S, Bland M, Cassidy P, Crawford M, et al. The effectiveness of alcohol screening and brief intervention in emergency departments: a multicentre pragmatic cluster randomized controlled trial. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0099463.
- Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, et al. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.e8501.
- McCambridge J, Kypri K. Can simply answering research questions change behaviour? Systematic review and meta analyses of brief alcohol intervention trials. PLOS ONE 2011;6. https://doi.org/10.1371/journal.pone.0023748.
- Bland JM, Altman DG. Regression towards the mean. BMJ 1994;308. https://doi.org/10.1136/bmj.308.6942.1499.
- Ling T, Brereton L, Conklin A, Newbould J, Roland M. Barriers and facilitators to integrating care: experiences from the English Integrated Care Pilots. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.982.
- Waller G, Finch T, Giles EL, Newbury-Birch D. Exploring the factors affecting the implementation of tobacco and substance use interventions within a secondary school setting: a systematic review. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0659-8.
- Ludbrook A. Effective and Cost-Effective Measures to Reduce Alcohol Misuse in Scotland: An Update to the Literature Review. Edinburgh: Scottish Executive Health Department; 2004.
- Sassi F, Cecchini M, Devarux M, Astolfi R, Sassi F. Tackling Harmful Alcohol Use. Economics and Public Health Policy. Paris: Organization for Economic Co-operation and Development; 2015.
- Westwood G, Meredith P, Atkins S, Greengross P, Schmidt PE, Aspinall RJ. Universal screening for alcohol misuse in acute medical admissions is feasible and identifies patients at high risk of liver disease. J Hepatol 2017;67:559-67. https://doi.org/10.1016/j.jhep.2017.04.017.
- Drummond C, Coulton S, James D, Godfrey C, Parrott S, Baxter J, et al. Effectiveness and cost-effectiveness of a stepped care intervention for alcohol use disorders in primary care: pilot study. Br J Psychiatry 2009;195:448-56. https://doi.org/10.1192/bjp.bp.108.056697.
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res 2002;26:36-43. https://doi.org/10.1111/j.1530-0277.2002.tb02429.x.
- Leigh BC, Gillmore MR, Morrison DM. Comparison of diary and retrospective measures for recording alcohol consumption and sexual activity. J Clin Epidemiol 1998;51:119-27. https://doi.org/10.1016/S0895-4356(97)00262-X.
- Lintonen T, Ahlström S, Metso L. The reliability of self-reported drinking in adolescence. Alcohol Alcohol 2004;39:362-8. https://doi.org/10.1093/alcalc/agh071.
- Shillington AM, Roesch SC, Reed MB, Clapp JD, Woodruff SI. Typologies of recanting of lifetime cigarette, alcohol and marijuana use during a six-year longitudinal panel study. Drug Alcohol Depend 2011;118:134-40. https://doi.org/10.1016/j.drugalcdep.2011.03.009.
- Percy A, McAlister S, Higgins K, McCrystal P, Thornton M. Response consistency in young adolescents’ drug use self-reports: a recanting rate analysis. Addiction 2005;100:189-96. https://doi.org/10.1111/j.1360-0443.2004.00943.x.
- Rueger SY, Trela CJ, Palmeri M, King AC. Self-administered web-based timeline followback procedure for drinking and smoking behaviors in young adults. J Stud Alcohol Drugs 2012;73:829-33. https://doi.org/10.15288/jsad.2012.73.829.
- Shorter GW, Heather N, Bray JW, Giles EL, Holloway A, Barbosa C, et al. The ‘Outcome Reporting in Brief Intervention Trials: Alcohol’ (ORBITAL) framework: protocol to determine a core outcome set for efficacy and effectiveness trials of alcohol screening and brief intervention. Trials 2017;18. https://doi.org/10.1186/s13063-017-2335-3.
- Vallentin-Holbech L, Rasmussen BM, Stock C. Association between personal and perceived peer alcohol drinking among Danish adolescents. Eur J Public Health 2016;26. https://doi.org/10.1093/eurpub/ckw166.045.
- Scalco MD, Meisel SN, Colder CR. Misperception and accurate perception of close friend substance use in early adolescence: developmental and intervention implications. Psychol Addict Behav 2016;30:300-11. https://doi.org/10.1037/adb0000175.
- Erskine-Shaw M, Monk RL, Qureshi AW, Heim D. The influence of groups and alcohol consumption on individual risk-taking. Drug Alcohol Depend 2017;179:341-6. https://doi.org/10.1016/j.drugalcdep.2017.07.032.
- Kennedy A, Rogers A, Bowen R, Lee V, Blakeman T, Gardner C, et al. Implementing, embedding and integrating self-management support tools for people with long-term conditions in primary care nursing: a qualitative study. Int J Nurs Stud 2014;51:1103-13. https://doi.org/10.1016/j.ijnurstu.2013.11.008.
- Heinrichs N, Bertram H, Kuschel A, Hahlweg K. Parent recruitment and retention in a universal prevention program for child behavior and emotional problems: barrier to research and program participation. Prevent Sci 2005;6:275-86. https://doi.org/10.1007/s11121-005-0006-1.
- Axford N, Lehtonen M, Kaoukji D, Tobin K, Berry V. Engaging parents in parenting programs: lessons from research and practice. Children Youth Serv Rev 2012;34:2061-71. https://doi.org/10.1016/j.childyouth.2012.06.011.
- Willan AR, Lin DY. Incremental net benefit in randomized clinical trials. Stat Med 2001;20:1563-74. https://doi.org/10.1002/sim.789.
Appendix 1 Terms of Reference for Trial Management Group, Trial Steering Committee and Data Monitoring and Ethics Committee
Terms of reference for the Trial Management Group
These terms of reference were determined at the beginning of the project and are therefore in future tense. The aim was to guide the scientific, administrative and operational direction of SIPS JR-HIGH.
Chief investigator
Dr Dorothy Newbury-Birch, Health and Social Care Institute, Teesside University.
Aims and objectives
The TMG group has the primary aim of ensuring appropriate, effective and timely implementation of the SIPS JR-HIGH trial.
The TMG will strive to achieve this aim by fulfilling the following objectives to:
-
identify appropriate sites for conducting the SIPS JR-HIGH trial
-
participate in the development and compilation of data collection instruments and other relevant research and intervention manuals
-
determine tasks, schedules and deliverables of the SIPS JR-HIGH trial
-
determine the fidelity of trial interventions
-
produce a working protocol for the trial and ensure adherence to the protocol
-
develop a publication protocol
-
facilitate and support data analysis
-
determine tasks, schedules and deliverables for report writing and publication of findings
-
ensure that adequate supervision/support occurs for research staff.
Membership
Eilish Gilvarry (chairperson), Dorothy Newbury-Birch (chief investigator), Eileen Kaner (Newcastle lead), Emma Giles (project manager), Simon Coulton, Elaine McColl, Denise Howel, Elaine Stamp, Les Tate, Colin Drummond, Paolo Deluca, Ruth McGovern, Stephanie Scott, Harry Sumnall, Liz Todd, Luke Vale, Sadie Boniface, Jo Frankham, Grant McGeechan, Victoria McGowan, Jayne Ogilvie, Grant Stanley, Claire McDonald and Nicola Howe.
Membership of the group will be reviewed as appropriate and as required.
Meeting
The TMG will meet once a month or more often if needed. Members are able to join the meeting by teleconferencing. A meeting will be considered quorate when at least three members are in attendance.
Reporting
The group will report to the TSC.
Duration
The group will function for the entire duration of the SIPS JR-HIGH trial.
Terms of reference for the Trial Steering Committee
These terms of reference were determined at the beginning of the project and are therefore in future tense. The aim was to guide the scientific, administrative and operational direction of SIPS JR-HIGH.
Chief investigator
Professor Dorothy Newbury-Birch, Health and Social Care Institute, Teesside University.
Project manager
Dr Emma Giles, Health and Social Care Institute, Teesside University.
Aims and objectives
The TSC has the primary aims of monitoring implementation of the SIPS JR-HIGH trial and providing an independent assessment of the data analysis and reporting.
The TSC has the following objectives to:
-
provide an oversight role for the trial including providing advice and comments to the trial sponsor and funder and ensure it is conducted to rigorous standards
-
comment on the progress of the trial and adherence to protocol
-
consider new information of relevance to the research question
-
provide advice, through the chairperson, to the chief investigator and trial funder on all appropriate aspects of the trial
-
provide evidence to support any requests for extensions.
Meeting
The TSC will meet biannually. Members are able to join the meeting by teleconferencing. A meeting will be considered quorate when at least three members are in attendance. Dorothy Newbury-Birch and Emma Giles will be responsible for calling, organising and minuting the meeting.
Duration
The group will function for the entire duration of the SIPS JR-HIGH trial.
Membership
Current membership is shown in Table 30.
| Name | Position |
|---|---|
| Chairperson: Professor Mathew Hickman | Professor in Public Health and Epidemiology |
| Professor Damon M Berridge | Professor of Applied Statistics |
| Ms Lisa Lowry | Teacher |
| Ms Louise Jones | Learning Mentor |
| Professor Alan Brennan, Health Economics | Professor of Health Economics and Decision Modelling |
| Mr Alan Strachan | North Tyneside Council, Director of Extended Services |
| Dr Áine Aventin | Research Fellow |
Two young people from the study will be invited to take part in the steering group.
Study team members
Professor Dorothy Newbury-Birch (XXXX).
Dr Emma Giles (XXXX).
Ms Denise Howel (XXXX).
Membership of the group will be reviewed as appropriate and as required.
Terms of reference for the Data Monitoring and Ethics Committee
These terms of reference will guide the scientific, administrative and operational direction of the SIPS JR-HIGH trial.
Chief investigator
Professor Dorothy Newbury-Birch, Health and Social Care Institute, Teesside University.
Project manager
Dr Emma Giles, Health and Social Care Institute, Teesside University.
Aims and objectives
The DMEC has the primary aim of monitoring the study data and make recommendations to the TSC on whether there are any ethical or safety reasons why the trial should not continue.
The DMEC has the following objectives to:
-
consider any ethical or safety reasons as to why the trial should not continue
-
consider the need for any interim analysis advising the TSC regarding the release of data and/or information
-
consider safety, quality and compliance data
-
consider the chain of custody and storage of trial data
-
provide advice, through the chairperson, to the chief investigator and trial funder on all appropriate aspects of the trial
-
provide evidence to support any requests for extensions.
Meeting
The DMEC will meet annually. Members are able to join the meeting by teleconferencing. A meeting will be considered quorate when at least two members are in attendance. Dorothy Newbury-Birch and Emma Giles will be responsible for calling, organising and minuting the meeting.
Duration
The group will function for the entire duration of the SIPS JR-HIGH trial.
Membership
Current membership is shown in Table 31.
| Name | Position |
|---|---|
| Chairperson: Professor Simon Moore | Professor in Public Health Research |
| Dr Chris Sutton, CStat | Associate Director and Principal Lecturer |
| Dr Andrea Hearne | Consultant Psychiatrist |
Membership of the group will be reviewed as appropriate and as required.
Appendix 2 Patient and public involvement work
Patient and public involvement (PPI) was sought at different times and at multiple levels, and is reflected on throughout this report.
Table 32 summarises the PPI activities that were included in the original application, together with the PPI activities undertaken. Not all of the activities were undertaken and this will be discussed.
| Element of the trial | Proposed PPI in application | PPI undertaken |
|---|---|---|
| Design and conduct of study | A strategy and commissioning manager (education) was involved in application and TMG | A strategy and commissioning manager (education) was involved in application and TMG |
| Animation development with two young people (convenience sampling from local schools) | Animation development with two young people (convenience sampling from local schools) | |
| Animation development with focus group at local school who were not involved in the definitive trial | ||
| Management of the research | Management group in each school: co-ordinator, staff/learning mentors and young people. Report to TMG | Focus groups with young people and staff towards the end of the trial to explore trial procedures |
| Two young people, learning mentors and teacher in TMG | ||
| Skype™ (Microsoft Corporation, Redmond, WA, USA) meeting at beginning of study with young people and staff/learning mentors from each site to discuss paperwork/processes | Economic and Social Research Council day to discuss research on 9 November 2016 | |
| Skype/face-to-face meeting at end of study with young people and staff/ learning mentors from each site to discuss paperwork, processes, reporting and dissemination | Mini-research study at a north-east school to teach basic research skills | |
| Reporting of the research | A young person attended the university in June 2017 to discuss how best to report and disseminate the research. A 14-year-old also read the Plain English summary and verified that they were able to understand it, and that it was clear | |
| Dissemination of findings |
Patient and public involvement was imperative to the success of the trial. We consulted with PPI representatives including local authority employees, parents, young people and members of staff at participating school sites. Their contribution to the development, management and delivery of this research included input into the design and conduct of the trial (the local authority lead for education was a co-applicant for this research) and piloting of study documentation and intervention materials (parents and young people) to ensure readability and understanding (see Chapter 2).
We ran a focus group at one school to help design the animation used to introduce the baseline survey (www.youtube.com/watch?v = KM78TwBcOeY; accessed 2 March 2016) and to seek feedback on what should be included and how to ‘pitch’ and design the animation. We also involved two young people in the development of the animation video; they worked at the university over a few days and also spent 2 days with the animation design company to have an input into the animation that was developed to be played to all young people at baseline showing instructions for the survey. The animated video has design work that was drawn by one of the young people while attending the design company. These two young people also commented on the paperwork and process involved with the trial (e.g. information leaflets, consent forms).
For the management of the research, it proved infeasible to hold Skype meetings with schools at the beginning and end of the trial, and to involve young people, staff and learning mentors in the TMG. This was because of school commitments and timetabling issues. To compensate for this, we ran a focus group, after follow-ups, with young people and staff from a Kent school to discuss the trial, a PPI interview with a learning mentor in a London school, a focus group with three staff members from a school in the north-west and, in the same school, a focus group with three young people to discuss how the trial was implemented, and any benefits or difficulties faced.
In addition to this PPI work, a young person attended the university in June 2017 to discuss the dissemination of the trial findings. We also ran an Economic and Social Research Council Festival of Social Science 2016 research day event, when we worked with young people on aspects of research, which included discussing the SIPS JR HIGH project. Members of the Teesside study team worked with one school in the north-east during the academic year 2016–17 to talk about research and teach basic skills, helping them to carry out a piece of research. This provided us with the opportunity to work closely with the young people and to discuss the trial.
Appendix 3 Systematic review results
| Authors (year) | Country (setting) | Design | Participants | Control (n) | Intervention (n) | Alcohol outcome measures | Follow-up points | Included at follow-up (attrition) | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Arnaud et al. (2017)68 | Germany (emergency departments) | RCT. (cluster RCT) | Patients treated for acute alcohol intoxication. Intervention group, 48.9% male; TAU group, 52% male. Age < 18 years; mean age in intervention group 15.7 years, mean age in TAU group 15.8 years | Treatment as usual (n = 175) | Manual guided brief intervention of approximately 45 minutes modelled on HaLT-HART am LimiT counselling session and MI (n = 141) | Screen for alcohol use related risk (CRAFFT); changes in binge drinking frequency (single question): [‘How often do you have 5 or more drinks on one occasion?’ (four drinks for females)], number of alcoholic drinks on a typical drinking occasion and alcohol-related problems (brief RAPI) | 6 weeks post enrolment; 3 and 6 months |
Intervention group: 3 months, n = 124 (86.1%); 6 months, n = 126 (87.5%) TAU group: 3 months, n = 145 (82.4%); 6 months, n = 153 (86.9%) |
Mean changes in binge drinking episodes significant from baseline to 3 and 6 months for both groups, with larger changes in the BI group (3 months –1.35, 95% CI –1.73 to –0.97; p < 0.001; 6 months –1.26, 95% CI –1.63 to –0.88; p < 0.001) Significant mean change in number of alcohol drinks per typical drinking occasion from baseline to 3 and 6 months for both groups, with larger changes in the BI group (3 months –2.24, 95% CI –3.18 to –1.29; p < 0.001; 6 months –1.86, 95% CI –2.85 to –0.86; p < 0.001) |
| Baer et al. (2001)67 | USA (university) | RCT |
508 out of 2041 completed questionnaires. High-risk student drinkers: 45% male Normative comparison sample: 46% male; aged < 19 years |
No intervention (n = not reported) | Self-monitor drinking for 2 weeks pre intervention. A written manual was used to provide individualised feedback and provision of a one-page list of tips for reducing risks related to drinking (n = not reported) | RAPI; Daily Drinking Questionnaire; 6-point scales to report quantity, frequency, and peak occasions of drinking; at baseline alcohol dependence question from the Diagnostic Interview Schedule and consequences from the Brief Drinker Profile. Interview questions were asked to assess family history of alcoholism and personal history of conduct problems. Other questionnaires assessed alcohol expectancies, psychiatric symptomatology, stress, perceived drinking norms and sexual behaviour | Baseline and 12, 24 and 36 months | At the 4-year follow-up, 363 out of the 433 participants (84%) from the two high-risk groups and the normative comparison group completed assessments. Complete data sets at baseline and all four follow-up periods were provided by 328 participants (76%), and 346 participants (80%) provided data at four out of five time points, including year 4 | Findings suggested that much heavy drinking among college students is transitory. Compared with the high-risk control sample, participants receiving brief individual preventative intervention had significantly greater reductions in negative consequences over 4-year period. Over 4 years, the magnitude of change was greatest for measures of negative drinking consequences [F(4321) = 45.65; p < 0.001], compared with those of drinking quantity [F(4321) = 28.22; p < 0.001] and drinking frequency [F(4321) = 7.58; p < 0.001], which demonstrated the smallest effect |
| Baer et al. (2007)76 | USA (homeless young people) | RCT | 117 (out of 254 screened) homeless young people. Mild to moderate substance abusers; 13- to 19-year-olds; mean age 17.9 years; 56% male | Usual care (n = 52) | MI (≤ 4 sessions of average of 32 minutes; first session averaged 17 minutes, subsequent sessions averaged 32 minutes). Feedback was arranged in booklet format (n = 75) | 30-day modified TLFB | Baseline and 1 month and 3 months | Of 117 young people in the sample for analysis, 97 (82.9%) returned for the 1-month interview, and 89 (76.1%) completed all three interviews |
Per-protocol analysis showed there were significant reductions in alcohol use at 3- but not at 1-month follow-up assessments (Cohen’s d = 0.20) Satisfaction was high |
| Bernstein (2010)75 | USA (emergency department) | RCT. (three groups) | 853 patients aged 14–21 years giving positive AUDIT test or positive for binge drinking/high-risk behaviours; 87% aged ≥ 18 years; 45% male | AC (n = 284) and MAC (n = 286) | Peer-conducted MI, referral to community resources and treatment if indicated and 5- to 10-minute booster telephone call (n = 283) | 30-day TLFB | Baseline and 3 and 12 months for BI and AC groups, and baseline and 12 months for MAC group |
Intervention: 3 months, n = 202 (71.4%); 12 months, n = 207 (73.1%) AC group: 3 months, n = 197 (69.4%); 12 months, n = 209 (73.6%) MAC group: 12 months, n = 198 (69.2%) |
No effects were found for between-group consumption or high-risk behaviours. Intervention compared with AC resulted in significant efforts to change behaviour (p < 0.05) |
| Cunningham et al. (2015)66 | USA (emergency department) | RCT | 836 young adults screening positive on the AUDIT-C (aged 14–17 years, score of ≥ 3; aged 18–20 years, score of ≥ 4). Age range 14–20 years; 51.6% male | Enhanced usual care (n = 281) (brochure listing resources) | Computer BI (n = 277), therapist BI (n = 278) and one or two booster conditions administered at the 3-month follow-up interview. Same brochure as control condition was also given | Participants were asked ‘How often did you have a drink containing alcohol?’ (never = 0; monthly or less = 1; 2 to 4 times per month = 2; 2 to 3 times per week = 3; ≥ 4 times per week = 4) and ‘How many drinks containing alcohol did you have on a typical day when you were drinking?’ (1 or 2 drinks = 1; 3 or 4 = 2; 5 or 6 = 3; 7 to 9 = 4; ≥ 10 = 5); multiplied to produce a quantity-frequency index with scores ranging from 0 to 20 | Baseline and 3, 6 and 12 months | 86.8% at 3 months, 87.1% at 6 months and 88.0% at 12 months |
3 months: regression analyses showed that the computer BI and therapist BI significantly decreased the alcohol consumption index score and alcohol consequences compared with control. Cohen’s d effect sizes were as follows: alcohol consumption index, 0.10 (computer BI) and 0.13 (therapist BI); alcohol consequences, 0.11 (computer BI) and 0.14 (therapist BI) 6 months: regression models examining the main effects of the computer BI, therapist BI, and post-emergency department session on alcohol consumption index scores and consequences at 6 months (controlling for 3-month levels of alcohol domain) showed no significant effects for either of the BIs. The main effect of the post-emergency department session was significant for alcohol consequences but not for consumption (Cohen’s d = 0.12) 12 months: at 12 months, the therapist BI and computer BI did not significantly affect alcohol consumption index scores but did reduce alcohol consequences [Cohen’s d effect sizes = 0.12 (therapist BI vs. enhanced usual care) and 0.17 (computer BI vs. enhanced usual care)]. There were no main effects of the post-emergency department session on alcohol-related outcomes at 12 months |
| Davis et al. (2016)65 | USA (referred from not-for-profit treatment agencies) | RCT | 48 adolescents referred for substance-use disorders. Mean age 16.3 years; 77.1% male | n/a |
MI (n = 22) MI plus normative feedback (MI + NF) (n = 26) |
Counts of the number of days of alcohol use in the previous 90 days; binge drinking measured by how many days, in the previous 90 days, that participants got drunk or drank five or more drinks | Baseline and 3 months | Recordings were available for 43 study participants (89.5%) | Adolescents with higher percentage change talk who received the MI + NF had significantly fewer days of alcohol consumption (p = 0.001) and binge drinking (p = 0.047) |
| Magill et al. (2017)64 | USA (community) | RCT | Heavy drinkers. Age range 17–20 years; mean age 18.2 years; 38% male; n = 167 | Mediation and relaxation training (n = 84). 60 minutes | MI session (approximately 60 minutes) (n = 83) | 6-week TLFB | Baseline, 6 weeks and 3 months | Study attrition was 3% | MI compared with relaxation training showed a greater reduction in heavy drinking at 6 weeks (p = 0.000) and 3 months (p = 0.003) |
| Marlatt et al. (1998)74 | USA (university) | RCT | High-risk sample selected from screening pool (n = 348); 45.9% male | Normative sample from screening pool (n = 115) and assessment only control (n = 174) | Individualised MI (n = 174). Delivered winter term of first year college | Frequency of alcohol consumption, daily drinking questionnaire, RAPI. Alcohol dependence scale | Baseline and 6, 12 and 24 months | 24 months n = 403 (88%), of these n = 379 (83%) completed 12 and 24 month assessments | Participants who received the brief intervention showed significantly greater deceleration of drinking rates and problems over time than those in the control group. In comparison with students in the control condition, those in the treatment group reported drinking less frequently over time [F(2, 284) = 3.59; p < 0.029], smaller quantity over time [F(2, 290) = 6.65; p < 0.001] and smaller peak quantity over time [F(2, 294) = 3.63; p < 0.028]. The magnitude of these effects are modest; effect sizes ranged from 0.14 to 0.20 |
| Martínez Martínez et al. (2008)63 | Mexico (schools) | RCT. | Moderate to high risk drinkers. Age range 14–18 years; average age 16 years; 65% male; n = 52 | Waiting list control (n = 26) | 90-minute, single-session BI (n = 26) | Problem Oriented Screening Instrument for Teenagers (POSIT) questionnaire; pattern of alcohol consumption during the last 3 months (quantity and frequency) | Baseline and 6 months | 6-month follow-up: intervention, n = 23 (88.5%); control, n = 17 (65.4%) | Significant differences between the experimental and control groups at 3 (p < 0.01) and 6 months (p < 0.1), showing reduction in alcohol consumption in the BI experimental group |
| Monti (1999)73 | USA (emergency department) | RCT | Treated in emergency department (blood or self-reported consumption). Mean age 18.4 years; n = 94; 64% male | Standard care (n = 42) including a handout | Motivational interview (n = 52). Also given same handout as control arm | Adolescent Drinking Index, young adults drinking and driving questionnaire, Adolescent Injury Checklist, health behaviour questionnaire, adolescent drinking questionnaire | Baseline and 3 and 6 months | 3 months, n = 87 (93%); 6 months, n = 84 (89%) | A time effect [F(l, 79) = 24.55; p < 0.001] showed significant reductions in adolescent drinking questionnaire total scores, with no group difference or interaction |
| Spirito et al. (2004)72 | USA (emergency department) | RCT | Treated in emergency department and had evidence of alcohol use (blood/breath/saliva) or self-report consumption within 6 hours of admittance. Mean age 15.7 years; n = 152; 64% male | Standard care: 5-minute brief advice and handout (n = 74) | Brief MI (one session of 35–45 minutes) (n = 78) | Adolescent drinking questionnaire, Adolescent Drinking Inventory, young adult drinking and driving questionnaire, Adolescent Injury Checklist, health behaviour questionnaire | Baseline and 3, 6 and 12 months | 3 months, n = 142 (93.4%); 6 months, n = 136 (89.5%); 12 months, n = 136 (89.5%) | Both MI and standard care conditions resulted in reduced quantity of drinking during the 12-month follow-up. Adolescents who screened positive for problematic alcohol use at baseline reported significantly more improvement on two out of three alcohol use outcomes (average number of drinking days per month and frequency of high-volume drinking) if they received MI compared with standard care |
| Spirito et al. (2011)71 | USA (emergency department) | RCT | Drug and alcohol users; 46% male; aged 13–17 years, mean age = 15.45 years; n = 125 | n/a |
Individual MI session 45–60 minutes and five monthly parenting booster brochures (n = 63) Individual MI plus family checkup: as above with the addition of family check-up (n = 62) |
Adolescent drinking questionnaire (8-point scale) | Baseline and 3, 6 and 12 months |
Individual MI: 3 months n = 56 (88.9%); 6 months n = 53 9 (84.1%); 12 months n = 47 (74.6%) Family check up: 3 months n = 41 (66.1%); 6 months n = 39 (62.9%); 12 months n = 36 (58.1%) |
Both conditions resulted in a reduction in all drinking outcomes at 3, 6 and 12-month follow-up (p < 0.001). Across groups any drinking in previous month decreased from 100% to 39.3% at 3 months, 55.2% at 6 months and 67.9% at 12 months. High-volume drinking occurrence dropped from 84% at baseline to 24% at 3-month follow-up, 35.3% at 6 months and 53.3% at 12 months; all were significantly less than baseline (p < 0.001). There was one significant between-group difference on high-volume drinking days at 3 months with family check up reporting lower prevalence (14.6%, 95% CI 3.8% and 25.5%) than individual MI (32.1%, 95% CI 19.9% to 44.4%), at 6 months family check up was lower (27%, 95% CI 12.7% to 41.3%) than individual MI (43.6%, 95% CI 30.5% to 56.8%). No difference was shown at 12 months. There were no effects on number of drinking days or quantity per drinking occasion |
| Tait et al. (2004)62 | Western Australia (emergency department) | RCT | Emergency department presentation of alcohol or drug use. Age range 12–19 years; mean age 16.7 years; 55% male; n = 127 | Usual hospital care (n = 67) | Brief intervention (n = 60). (not described) | AUDIT-C with a threshold of five or greater for males and four or more for females | Baseline and 4 months | Intervention, n = 32 (53%); control, n = 51 (76%) | Of those followed up, 64 had hazardous alcohol consumption at baseline: 6 out of 15 (40%) treated adolescents moved to ‘safer’ use, whereas 10 out of 49 (20%) non-treated adolescents moved to ‘safer’ alcohol consumption patterns [χ2 (1) = 2.4, n/s]. It was also noted that there were 17 adolescents in the non-treated group with non-hazardous consumption at baseline, of whom seven (41%) changed to hazardous consumption by 4 months. No such change was seen in the treated group. AUDIT-3 score (change from baseline to 4 months) B 0.13, 95% CI –0.35 to 0.61; p = 0.587 |
| Walton et al. (2010)70 | USA (emergency department) | RCT | Eligible if reported past-year alcohol use and aggression. Mean age 16.8 years, range 14–18 years; n = 726; 44% male | Control group received brochure post screening (n = 235) | SafERteens therapist (n = 254) vs. computer brief intervention (one session of 35 minutes) (n = 237) | AUDIT-C, Problem Oriented Screening Instrument for Teenagers (POSIT), frequency of aggression towards peers | Baseline, 3 and 6 months |
Computerised brief intervention: 3 months n = 205 (86.5%); 6 months n = 209 (87.8%) Therapist brief intervention: 3 months n = 215 (84.6%); 6 months n = 209 (82.3%) Control: 3 months n = 206 (87.7%); 6 months n = 208 (88.5%) |
At 3 months, the therapist intervention showed reductions in the occurrence of peer aggression (therapist, –34.3%; control, –16.4%; relative risk, 0.74; 95% CI 0.61 to 0.90), experience of peer violence (therapist, –10.4%; control, –4.7%; RR 0.70, 95% CI 0.52 to 0.95), and violence consequences (therapist, –30.4%; control, –13.0%; RR 0.76, 95% CI 0.64 to 0.90). At 6 months, both the therapist intervention and computer intervention showed reductions in alcohol consequences compared with controls (therapist, –32.2%; control, –17.7%; odds ratio, 0.56; 95% CI 0.34 to 0.91; computer, –29.1%; control, –17.7%; odds ratio 0.57; 95% CI 0.34 to 0.95) |
| White et al. (2006)61 | USA (university) | RCT | College students violating alcohol policies, n = 222 | Personal written feedback only (n = 104). Two sessions (1 hour) | 30 minute brief intervention (n = 118). Two sessions (1 hour) | Frequency of alcohol use using a 6-point ordinal scale ranging from 0 = not in the last month to 5 = daily; number of occasions of heavy episodic drinking in the past month (five or more drinks for males and four or more for females; questions adopted from the Modified Daily Drinking Questionnaire to assess the number of drinks and the number of hours of drinking each day in a typical week in the last month; RAPI | Baseline and 3 months | Unknown | There were significant decreases in the total number of drinks in a typical week (F = 22.84, 2/219 df, p < 0.001), the number of times of heavy episodic drinking in the past month (F = 4.44, 1/218 df, p = 0.04), the peak BAC in a typical week (F = 45.86, 1/219 df, p < 0.001), the number of alcohol-related problems in the past 3 months (F = 75.16, 1/220 df, p < 0.001) |
| Winters et al. (2007)69 | USA (school) | RCT (three arms) | Adolescents with alcohol/drug use disorder. Mean age 15.6 years, range 13–17 years; n = 79; 62% male | Assessment only (control) (n = 27) |
BI-A: two-session BI-adolescent × 60 minutes (n = 26) BI-AP: two session × 60 minutes BI-adolescent plus BI-parent session (n = 26) |
Adolescent Diagnostic Interview and TLFB. Personal consequences scale (11-item self-report scale) | Baseline, 1 month and 6 months | N = 78 (only one attrition case) | Both intervention groups (BI-adolescent and BI-parent) showed significantly better outcomes than control (p < 0.05) for number of alcohol use days, number of alcohol abuse symptoms and number of alcohol dependency symptoms. Significantly better outcomes for BI-adolescent and BI-parent (compared with control) were found for a number of the drug outcomes but not for alcohol. BI-adolescent was found to be significantly better than BI-parent for number of days abstinent from alcohol in previous 90 days |
Appendix 4 Schools’ usual practice
| School code | Job title | Question | |||||
|---|---|---|---|---|---|---|---|
| Does your school currently teach alcohol advice as part of the curriculum? | Can you provide details? | Where does this advice happen? | Who delivers the advice? | Who would a young person talk to if they had an alcohol issue? | Is there anything else you would like to say about alcohol advice at your school? | ||
| NW06 | Head of PSHE and careers | Yes | PSHE covers various aspects of alcohol education, drinking responsibly, drink spiking, drunk driving, alcohol units and keeping safe | PSHE, one to one when necessary, health days | Form tutors, Young Addaction, pastoral heads | Support manager, who might involve an external agency if considered necessary | |
| NW01 | Lead professional of health and well-being | Yes. They lead health lessons within Year 7 and 8 and this fits into a 6-week block of lessons on drugs and alcohol | They look at the effects of alcohol, peer pressure, units of alcohol, health facts that alcohol affects, side effects of drinking | Classroom lessons. Students can also seek advice from pastoral staff, nurses, teachers | Health teacher (PE), form tutors | Progress leaders, form tutors, nurse, pastoral staff | Should be more free support available to school. For students to use hands-on activities, such as resources, from Manchester Healthy Library |
| NW02 | VP for SMSC and Inclusion | Yes | Formal lessons on healthy lifestyles/choices | In PSHE classes | Teachers of PSHE overseen by the head of year and the VP | The academy health advisor/school counsellor or one of the pastoral team (each year group has a non-teaching pastoral manager) | If they hear that older students have been drinking outside school |
| NW03 | Director of health specialism | Yes | The healthy schools team supports the delivery of alcohol and drugs education. They look at the impact of excessive alcohol intake | PSHE classes, one-to-one targeted pastoral work, school assembly | Healthy schools team, health tutor, head of year, pastoral team | Pastoral year lead, safeguarding lead | |
| NW04 | Manager of social inclusion centre | Yes | It is incorporated into their PSHE lessons along with drugs awareness and uses the Manchester Healthy Schools materials | In PSHE lessons, targeted assemblies, drop-down days as appropriate | PSHE teachers, learning mentors, Wythenshawe Community Housing Youth Workers | Any member of staff they felt comfortable with and then it may be referred on to a more appropriate member of staff | They use a framework for PSHE to ensure that golden threads of learning about values and safe choices are interwoven into the whole curriculum |
| NW05 | Lead co-ordinator for PSHE | Yes | Advice is given to whole school pupils via form during the alcohol awareness week, a lesson is taught to Years 8, 9, 10 and 11, leaflets are available if needed from the school nurse. The nurse is available every Friday | During the alcohol awareness week, a lesson is taught to Years 8, 9, 10 and 11 | Advice is delivered via teachers in PSHE lessons, the school nurse | School nurse, PSHE teacher, head of year, pastoral mentors | Advice is available to all year groups, alcohol awareness relates to drug and social behaviour |
| NE04 | Head teacher | Yes | Advice, leaflets, external speakers | Tutor groups in PSHE, one-to-one support also offered | A mix of people: tutors, heads of year, school nurse | Head of year and student support | |
| NE09 | Special support assistant | In the religious education curriculum and tutor programme | Presentations in school | In school assemblies, tutor groups; in religious education lessons | Class teachers; learning mentors in assemblies | Key stage co-ordinators, learning mentors and safeguarding lead | |
| NE06 | Student support worker | Yes | Alcohol awareness lessons | In religious education classes | Learning mentors/student support | Learning mentors/student support/head of year | |
| NE03 | Not completed | ||||||
| NE01 | Not completed | ||||||
| NE02 | Not completed | ||||||
| NE05 | HoD PE | Yes | Advice information workshops | Tutor groups, PSHE lessons, one-to-one meeting (if necessary) | Tutors/year group teams, PSHE team, external mentors, head of year | Tutor, teacher, head of learning, behaviour and welfare officer | |
| NE07 | Not completed | ||||||
| NE08 | Not completed | ||||||
| NE10 | Not completed | ||||||
| NE11 | Not completed | ||||||
| NE12 | Not completed | ||||||
| NE13 | Year manager | Yes, as part of PSHE | They have delivered as part of focus days over the last 5 years alcohol awareness to three year groups: Years 7, 9 and 11. Y7 has been delivered as part of a day on healthy living. The workshop was delivered by [NAME] (school nurse) or a member of her team. Year 9 have had alcohol awareness delivered as part of the risk and resilience day organised by an outside source in the past | In tutor group but students had the opportunity to speak on a one-to-one basis. Year 11 as part of live and learn day, consequence of alcohol issues delivered by the fire brigade and Cleveland Police. These will continue through the citizenship programme, Year 11 already this year, [NAME] team will deliver in summer term also Year 7 | External providers as named above | Year manager and [NAME], safeguarding officer | |
| L01 | Not completed | ||||||
| L02 | Not completed | ||||||
| L03 | Not completed | ||||||
| L04 | Not completed | ||||||
| K04 | Inclusion lead | Yes | Knowledge development and advice | Discussions within values lessons (PSHE equivalent), tutors may raise issues in response to topical issues and in development of knowledge in science | Various teachers | Pastoral support manager | No |
| K05 | Welfare manager | No, but they introduce some DrinkAware resources into PSHE at times | The Alcohol Education Trust has run an alcohol awareness evening for parents (October 2017) and are running one in February 2018, but attendance has been low | In school, in PSHE and lead lessons | The Alcohol Education Trust and class teachers | A young person would speak to a welfare manager or a member of staff they trust | |
| K03 | Senior pastoral leader | No | Pastoral team | ||||
| K02 | HOD Health and social care | In the health and social care department it looks at health risks so alcohol advice is taught in the syllabus (Year 7, term 5). In lessons around substance misuse, which includes alcohol consumption | Kenwood Trust (local charity) delivers an assembly to Year 9 and 10. This is organised through the assistant head who is in charge of pastoral care. It has also purchased the alcohol goggles to support lessons and health and social care lessons. If a student is caring for a family member because of substance misuse, then it would make a referral to Kent Young Carers and/or Crossroads for them to access support. We have [NAME] to refer to for counselling, CAST mentors for students to talk to in school and then also external agency support via Early Help. There is also Addaction, it takes direct referrals | School assemblies – Year 7 health and social care lessons – Year 11 unit 5 health promotion | Class teachers, external speakers | Student manager, head of year | They can be putting in a lot more support for our students to raise awareness about alcohol consumption in our school. This could be put in place in lessons across all years |
| K07 | Head of PSHE; head of alternative curriculum | Yes | Taught through school nurses intervention on themed education days to Year 9. PSHE lessons on misuse of drugs include alcohol (Years 7–10) | In school in class groups (PSHE) in school in year groups (themed education days) | PSHE teachers, school nurses (visitors) | Director of learning (head of house), form tutor, PSHE teacher, staff with whom they have a good relationship, academic or emotional/social mentor, weekly nurse drop-in clinic, home/school liaison officer, counsellors on staff, counsellors from youth service, referrals can be made by children’s team to appropriate support groups outside school including Open Roads and child and adolescent mental health services | They would welcome any support or contact with agencies that would support students wishing to deal with their own or their carer’s problems with alcohol. They would welcome more advice about agencies available to us to help us offer better support to our students |
| K01 | Assistant principal | Alcohol advice delivered through the tutorial programme/assemblies. Workshops delivered by a senior early help worker | Advice is through tutorial programme Leaflets on offer through addaction, Kenwood Trust and senior early help worker have organised sessions and workshops | Assemblies, tutorial programme, small groups for workshops | Head of house, guidance managers, tutor, external presenters: Addaction, Kenwood Trust, senior worker | Head of house, guidance manager, tutor, safeguarding team | The resources offered through this process have been really effective when discussing alcohol with students |
| K06 | Assistant head teacher | Yes | Within lessons, once a week | Lessons | Teacher | DSL or member of pastoral team. Sometimes ethics teacher when covering topic | n/a |
Appendix 5 The TIDieR checklist
| Item number | Item | Where located | |
|---|---|---|---|
| Primary paper (page numbers) | Other (details) | ||
| Brief name | |||
| 1. | Provide the name or a phrase that describes the intervention | 13 | – |
| Why | |||
| 2. | Describe any rationale, theory, or goal of the elements essential to the intervention | 14 | – |
| What | |||
| 3. | Materials: describe any physical or informational materials used in the intervention, including those provided to participants or used in intervention delivery or in training of intervention providers. Provide information on where the materials can be accessed (e.g. online appendix, URL) | 14–16 | – |
| 4. | Procedures: describe each of the procedures, activities and/or processes used in the intervention, including any enabling or support activities | 14–16 | – |
| Who provided | |||
| 5. | For each category of intervention provider (e.g. psychologist, nursing assistant), describe their expertise, background and any specific training given | 13 | – |
| How | |||
| 6. | Describe the modes of delivery (e.g. face to face or by some other mechanism, such as internet or telephone) of the intervention and whether it was provided individually or in a group | 13 | – |
| Where | |||
| 7. | Describe the type(s) of location(s) where the intervention occurred, including any necessary infrastructure or relevant features | 13 | – |
| When and how much | |||
| 8. | Describe the number of times the intervention was delivered and over what period of time including the number of sessions, their schedule and their duration, intensity or dose | 13 | – |
| Tailoring | |||
| 9. | If the intervention was planned to be personalised, titrated or adapted, then describe what, why, when and how | 14–16 | – |
| Modifications | |||
| 10. | If the intervention was modified during the course of the study, describe the changes (what, why, when and how) | 13–16 | – |
| How well | |||
| 11. | Planned: if intervention adherence or fidelity was assessed, describe how and by whom, and if any strategies were used to maintain or improve fidelity, describe them | 15–17 | – |
| 12. | Actual: if intervention adherence or fidelity was assessed, describe the extent to which the intervention was delivered as planned | 16–17 | – |
Appendix 6 Scoring systems
| Survey | Scale/subscale details | Question scoring | Overall score | Notes |
|---|---|---|---|---|
| A-SAQ | Single question with a choice of six responses to indicate levels of harmful drinking | (1) Never, (2) < 4 times, (3) ≥ 4 times but not every month, (4) ≥ once a month but not every week, (5) every week but not every day, (6) every day | 1–6 | A score of ≥ 3 is considered a positive score for possible hazardous or harmful drinking |
| AUDIT | 10 questions about drinking behaviour with five possible responses for questions 1–8, or three responses for questions 9 and 10 | Score of 0–4 for questions 1–8 and 0, 2 or 4 for questions 9 and 10 | 0–40 when scores from each question are added | An AUDIT score of ≥ 8 is considered to indicate possible hazardous or harmful drinking in adults. There is currently no agreed score to indicate hazardous or harmful drinking in adolescents |
| AUDIT-C | First three questions of the AUDIT | All questions are scored 0–4 | 0–12 when scores from each question are added | An AUDIT-C score of ≥ 4 is considered to indicate possible hazardous or harmful drinking in adults. There is currently no agreed score to indicated hazardous or harmful drinking in adolescents |
| RAPI | 23 questions about drinking behaviour, each with four possible responses | All questions are scored 0–3 | 0–69 when scores from each question are added | Higher RAPI scores indicate more problematic drinking behaviour |
| WEMWBS | 14 questions to assess level of happiness and life satisfaction | Each question is scored 1–5 | 14–70 when scores from each question are added | WEMWBS provides robust results for populations and groups with higher scores indicating higher levels of well-being. It has not yet been validated for monitoring mental well-being in individuals |
| TLFB-28 | Quantitative estimations of daily alcohol consumption | Provides a variety of different estimations of individual consumption levels | The TLFB is a method for assessing recent drinking behaviour. Administered by a learning mentor, it involves asking young people to retrospectively estimate their daily alcohol consumption over a 28-day period prior to the interview. We will specifically derive total alcohol consumed in a 28-day period, percentage of days abstinent, drinks per drinking day and number of days drinking more than 2 units |
Appendix 7 Recruitment numbers
| Region and school | Number of | Consent to study | Randomised to | |||
|---|---|---|---|---|---|---|
| Young people in year | Surveys completed | Surveys positive | Intervention | Control | ||
| North-east | ||||||
| NE12 | 225 | 220 | 56 | 17 | 8 | 9 |
| NE01 | 184 | 183 | 79 | 24 | 13 | 11 |
| NE02 | 89 | 88 | 24 | 8 | 4 | 4 |
| NE11 | 239 | 238 | 58 | 26 | 13 | 13 |
| NE10 | 223 | 221 | 69 | 24 | 9 | 15 |
| NE09 | 81 | 79 | 18 | 9 | 4 | 5 |
| NE03 | 186 | 185 | 34 | 23 | 12 | 11 |
| NE06 | 188 | 188 | 50 | 36 | 15 | 21 |
| NE08 | 213 | 212 | 55 | 23 | 13 | 10 |
| NE04 | 81 | 81 | 11 | 8 | 3 | 5 |
| NE13 | 190 | 189 | 54 | 2 | 2 | 0 |
| NE07 | 105 | 104 | 32 | 15 | 6 | 9 |
| NE05 | 128 | 127 | 39 | 26 | 14 | 12 |
| Subtotal | 2132 | 2115 | 579 | 241 | 116 | 125 |
| North-west | ||||||
| NW06 | 178 | 176 | 46 | 6 | 4 | 2 |
| NW01 | 152 | 149 | 33 | 10 | 0 | 10 |
| NW02 | 82 | 79 | 5 | 5 | 4 | 1 |
| NW03 | 94 | 93 | 19 | 13 | 6 | 7 |
| NW04 | 118 | 114 | 22 | 15 | 9 | 6 |
| NW05 | 110 | 104 | 14 | 10 | 4 | 6 |
| Subtotal | 734 | 715 | 139 | 59 | 27 | 32 |
| London | ||||||
| L04 | 89 | 86 | 2 | 1 | 0 | 1 |
| L02 | 123 | 120 | 4 | 1 | 1 | 0 |
| L03 | 92 | 89 | 7 | 0 | 0 | 0 |
| Withdrawn | 261 | 258 | 72 | 0 | 0 | 0 |
| L01 | 112 | 112 | 12 | 3 | 1 | 2 |
| Subtotal | 677 | 665 | 97 | 5 | 2 | 3 |
| Kent | ||||||
| K01 | 136 | 135 | 32 | 19 | 10 | 9 |
| K06 | 113 | 112 | 37 | 24 | 11 | 13 |
| K02 | 137 | 135 | 26 | 13 | 7 | 6 |
| K03 | 171 | 170 | 35 | 25 | 11 | 14 |
| K07 | 119 | 118 | 44 | 18 | 9 | 9 |
| K05 | 136 | 136 | 20 | 11 | 6 | 5 |
| K04 | 229 | 222 | 55 | 28 | 11 | 17 |
| Subtotal | 1041 | 1028 | 249 | 138 | 65 | 73 |
| Total | 4584 | 4523 | 1064 | 443 | 210 | 233 |
Appendix 8 Baseline characteristics
| Characteristic | Screening | ||
|---|---|---|---|
| Screened positive and gave consent (N = 439),a (n %) | Screened positive and did not give consent (N = 625), n (%) | Screened negative (N = 3459),a n (%) | |
| Demographics | |||
| Gender | |||
| Female | 221 (50.3) | 351 (56.2) | 1636 (47.3) |
| Male | 218 (49.7) | 261 (41.8) | 1779 (51.4) |
| Missing | 0 (0) | 13 (2.1) | 44 (1.3) |
| Ethnicity | |||
| White | 398 (90.7) | 524 (83.8) | 2542 (73.5) |
| Black | 8 (1.8) | 22 (3.5) | 293 (8.5) |
| Chinese | 0 (0) | 2 (0.3) | 31 (0.9) |
| Mixed | 26 (5.9) | 28 (4.5) | 183 (5.3) |
| Asian | 3 (0.7) | 14 (2.2) | 251 (7.3) |
| Other | 2 (0.5) | 13 (2.1) | 90 (2.6) |
| Not known | 1 (0.2) | 12 (1.9) | 29 (0.8) |
| Missing | 1 (0.2) | 10 (1.6) | 40 (1.2) |
| Use of leisure time | |||
| When you have free time do you mainly | |||
| Go round to a friend’s house (or have them come round to yours) | 134 (30.5) | 236 (37.8) | 781 (22.6) |
| Go out somewhere with friends | 245 (55.8) | 370 (59.2) | 1251 (36.2) |
| Spend time with your family | 57 (13) | 81 (13) | 824 (23.8) |
| Spend time with brother(s) and/or sister(s) | 28 (6.4) | 41 (6.6) | 328 (9.5) |
| Spend time by yourself | 117 (26.7) | 134 (21.4) | 1231 (35.6) |
| None of these | 27 (6.2) | 38 (6.1) | 221 (6.4) |
| Did not answer | 5 (1.1) | 8 (1.3) | 22 (0.6) |
| Smoking | |||
| How old were you when you smoked a whole cigarette for the first time? | |||
| I have never smoked a whole cigarette | 233 (53.1) | 266 (42.6) | 2980 (86.2) |
| ≤ 8 years old | 8 (1.8) | 24 (3.8) | 16 (0.5) |
| 9 or 10 years old | 13 (3) | 26 (4.2) | 22 (0.6) |
| 11 or 12 years old | 72 (16.4) | 110 (17.6) | 97 (2.8) |
| 13 or 14 years old | 91 (20.7) | 159 (25.4) | 235 (6.8) |
| > 14 years old | 18 (4.1) | 31 (5) | 44 (1.3) |
| Did not answer | 4 (0.9) | 9 (1.4) | 59 (1.7) |
| Missing | 0 (0) | 0 (0) | 6 (0.2) |
| During the past 30 days, on the days you smoked, how many cigarettes did you smoke per day? | |||
| I did not smoke cigarettes during the last 30 days | 308 (70.2) | 395 (63.2) | 3189 (92.2) |
| < 1 | 25 (5.7) | 36 (5.8) | 62 (1.8) |
| 1 | 17 (3.9) | 24 (3.8) | 28 (0.8) |
| 2–5 | 41 (9.3) | 72 (11.5) | 64 (1.9) |
| 6–10 | 28 (6.4) | 54 (8.6) | 32 (0.9) |
| 11–20 | 12 (2.7) | 16 (2.6) | 11 (0.3) |
| > 20 | 6 (1.4) | 16 (2.6) | 9 (0.3) |
| Did not answer | 2 (0.5) | 12 (1.9) | 55 (1.6) |
| Missing | 0 (0) | 0 (0) | 9 (0.3) |
| Energy drinks | |||
| How many times per week do you usually drink energy drinks? | |||
| Never | 103 (23.5) | 136 (21.8) | 1452 (42) |
| Less than once per week | 123 (28) | 175 (28) | 973 (28.1) |
| Once per week | 60 (13.7) | 83 (13.3) | 397 (11.5) |
| 2–4 days per week | 84 (19.1) | 136 (21.8) | 383 (11.1) |
| 5 or 6 days per week | 22 (5) | 21 (3.4) | 63 (1.8) |
| Every day, once per day | 17 (3.9) | 36 (5.8) | 91 (2.6) |
| More than once per day | 29 (6.6) | 34 (5.4) | 82 (2.4) |
| Did not answer | 1 (0.2) | 4 (0.6) | 18 (0.5) |
| Risky sexual behaviour | |||
| After drinking alcohol, have you ever engaged in sexual intercourse that you regretted the next day? | |||
| No | 142 (32.3) | 230 (36.8) | 741 (21.4) |
| Yes | 38 (8.7) | 92 (14.7) | 73 (2.1) |
| I have never engaged in sexual intercourse | 246 (56) | 274 (43.8) | 2495 (72.1) |
| Did not answer | 13 (3) | 26 (4.2) | 144 (4.2) |
| Missing | 0 (0) | 3 (0.5) | 6 (0.2) |
| After drinking alcohol, have you ever engaged in sexual intercourse without a condom? | |||
| No | 137 (31.2) | 225 (36) | 736 (21.3) |
| Yes | 44 (10) | 92 (14.7) | 54 (1.6) |
| I have never engaged in sexual intercourse | 242 (55.1) | 280 (44.8) | 2518 (72.8) |
| Did not answer | 16 (3.6) | 27 (4.3) | 149 (4.3) |
| Missing | 0 (0) | 1 (0.2) | 2 (0.1) |
Appendix 9 Comparison of baseline survey data, by screening and assent subgroups
| Survey | n | Minimum | LQ | Median | UQ | Maximum | Mean | SD |
|---|---|---|---|---|---|---|---|---|
| AUDIT | ||||||||
| Screened positive and gave consent | 436 | 0 | 3 | 6.7 | 10 | 40 | 7.7 | 6.1 |
| Screened positive and did not give consent | 614 | 0 | 4 | 7 | 12 | 40 | 9.1 | 7.2 |
| Screened negative | 3428 | 0 | 0 | 0 | 1.25 | 34.4 | 1.3 | 2.4 |
| AUDIT-C | ||||||||
| Screened positive and gave consent | 433 | 0 | 2 | 4 | 5 | 12 | 4.0 | 2.3 |
| Screened positive and did not give consent | 620 | 0 | 3 | 4 | 6 | 12 | 4.6 | 2.5 |
| Screened negative | 3412 | 0 | 0 | 0 | 1 | 12 | 0.8 | 1.3 |
| RAPI | ||||||||
| Screened positive and gave consent | 429 | 0 | 1 | 4 | 10.5 | 48.1 | 7.3 | 9.3 |
| Screened positive and did not give consent | 604 | 0 | 2 | 6 | 14 | 69 | 10.4 | 12.7 |
| Screened negative | 3260 | 0 | 0 | 0 | 1 | 63 | 1.6 | 4.8 |
| WEMWBS | ||||||||
| Screened positive and gave consent | 398 | 14 | 39 | 46.2 | 54 | 70 | 45.8 | 11.7 |
| Screened positive and did not give consent | 572 | 14 | 36.5 | 44 | 52 | 70 | 43.7 | 12.3 |
| Screened negative | 3197 | 14 | 41 | 49 | 56 | 70 | 48.0 | 11.8 |
| DMQ-R – coping | ||||||||
| Screened positive and gave consent | 430 | 1 | 1 | 1.4 | 2.2 | 5 | 1.8 | 1.0 |
| Screened positive and did not give consent | 594 | 1 | 1 | 1.6 | 2.4 | 5 | 2.0 | 1.1 |
| Screened negative | 3060 | 1 | 1 | 1 | 1 | 5 | 1.1 | 0.5 |
| DMQ-R – social | ||||||||
| Screened positive and gave consent | 431 | 1 | 1.8 | 2.4 | 3.4 | 5 | 2.6 | 1.1 |
| Screened positive and did not give consent | 595 | 1 | 2 | 2.8 | 3.8 | 5 | 2.9 | 1.1 |
| Screened negative | 3064 | 1 | 1 | 1 | 1.4 | 5 | 1.4 | 0.7 |
| DMQ-R – conforming | ||||||||
| Screened positive and gave consent | 430 | 1 | 1 | 1 | 1.2 | 5 | 1.3 | 0.7 |
| Screened positive and did not give consent | 594 | 1 | 1 | 1 | 1.4 | 5 | 1.4 | 0.7 |
| Screened negative | 3053 | 1 | 1 | 1 | 1 | 5 | 1.1 | 0.4 |
| DMQ-R – enhancement | ||||||||
| Screened positive and gave consent | 431 | 1 | 1.2 | 1.8 | 2.6 | 5 | 2.0 | 1.0 |
| Screened positive and did not give consent | 594 | 1 | 1.4 | 2.2 | 3 | 5 | 2.3 | 1.1 |
| Screened negative | 3060 | 1 | 1 | 1 | 1 | 5 | 1.2 | 0.5 |
Appendix 10 Follow-up data
| Region and school | Trial arm (n) | |||||
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| Randomised | TLFB complete | 12-month questionnaire complete | Randomised | TLFB complete | 12-month questionnaire complete | |
| North-east | ||||||
| NE12 | 8 | 8 | 8 | 9 | 8 | 8 |
| NE01 | 13 | 13 | 13 | 11 | 10 | 10 |
| NE02 | 4 | 4 | 4 | 4 | 4 | 4 |
| NE11 | 13 | 6 | 6 | 13 | 12 | 12 |
| NE10 | 9 | 3 | 3 | 15 | 11 | 11 |
| NE09 | 4 | 4 | 4 | 5 | 5 | 5 |
| NE03 | 12 | 11 | 11 | 11 | 11 | 11 |
| NE06 | 15 | 15 | 15 | 21 | 19 | 19 |
| NE08 | 13 | 13 | 13 | 10 | 10 | 10 |
| NE04 | 3 | 1 | 1 | 5 | 4 | 4 |
| NE13 | 2 | 1 | 1 | 0 | 0 | 0 |
| NE07 | 6 | 5 | 5 | 9 | 5 | 5 |
| NE05 | 14 | 14 | 14 | 12 | 11 | 11 |
| Subtotal | 116 | 98 | 98 | 125 | 110 | 110 |
| North-west | ||||||
| NW06 | 4 | 4 | 4 | 2 | 1 | 1 |
| NW01 | 0 | 0 | 0 | 10 | 8 | 8 |
| NW02 | 4 | 4 | 4 | 1 | 1 | 1 |
| NW03 | 6 | 4 | 4 | 7 | 7 | 7 |
| NW04 | 9 | 9 | 9 | 6 | 5 | 4 |
| NW05 | 4 | 4 | 4 | 6 | 5 | 5 |
| Subtotal | 27 | 25 | 25 | 32 | 27 | 26 |
| London | ||||||
| L04 | 0 | 0 | 0 | 1 | 1 | 1 |
| L02 | 1 | 0 | 0 | 0 | 0 | 0 |
| L03 | 0 | 0 | 0 | 0 | 0 | 0 |
| Withdrawn | 0 | 0 | 0 | 0 | 0 | 0 |
| L01 | 1 | 1 | 1 | 2 | 2 | 2 |
| Subtotal | 2 | 1 | 1 | 3 | 3 | 3 |
| Kent | ||||||
| K01 | 10 | 9 | 9 | 9 | 8 | 8 |
| K06 | 11 | 5 | 8 | 13 | 1 | 4 |
| K02 | 7 | 7 | 7 | 6 | 6 | 6 |
| K03 | 11 | 10 | 10 | 14 | 12 | 12 |
| K07 | 9 | 6 | 6 | 9 | 8 | 8 |
| K05 | 6 | 6 | 6 | 5 | 5 | 5 |
| K04 | 11 | 11 | 11 | 17 | 16 | 15 |
| Subtotal | 65 | 54 | 57 | 73 | 56 | 58 |
| Total | 210 | 178 | 181 | 233 | 196 | 197 |
Appendix 11 Time and salary cost of learning mentors
Mid-point values for the answers to closed questions (time range in minutes) for the preparation and delivery of the control and intervention interview.
| Range (minutes) | Mid-pointa (minutes) | Source |
|---|---|---|
| 0–5 | 2.5 | Case diary: learning mentors (Q1)b |
| 0–10 | 5.0 | Case diary: learning mentors (Q2) |
| 6–10 | 8.0 | Case diary: learning mentors (Q2) |
| 11–20 | 15.5 | Case diary: learning mentors (Q1, Q2) |
| 21–30 | 25.5 | Case diary: learning mentors (Q1, Q2) |
| 31–40 | 35.5 | Case diary: learning mentors (Q2) |
| 31–45 | 38.0 | Case diary: learning mentors (Q1) |
| 41–50 | 45.5 | Case diary: learning mentors (Q2) |
| 51–60 | 55.5 | Case diary: learning mentors (Q2) |
Appendix 12 Salary costs
| Resource | (A) Annual salary | (B) Add on costsa to (A) | (A) + (B) | (C) Week unit cost: divide (A) + (B) by number of working weeks per yearb | (D) Hour unit cost: divide (C) by number of work hours per weekc | (E) Minute cost: divide (D) by 60 minutes per hour |
|---|---|---|---|---|---|---|
| Learning mentor time spent on intervention delivery (£) | 19,905.08 | 3184.81 | 23,089.89 | 501.95 | 13.57 | 0.23 |
| Qualified trainer time on intervention deliveryd (£) | 32,600.00 | 5216.00 | 37,816.00 | 822.09 | 22.22 | 0.37 |
Appendix 13 Net monetary benefit
The value of net monetary benefit (NMB), expressed as costs, was estimated as:
where IE is the incremental effectiveness, in this study the incremental QALYs, IC are the incremental costs of the intervention compared with those of the control group, and λ is the monetary value of an additional unit of effectiveness. 164 λ takes a range of values to evaluate the NMB at different levels of willingness to pay for an additional unit of effectiveness.
Appendix 14 EuroQol-5 Dimensions, three-level version dimensions
| EQ-5D-3L dimension | Proportion | |||||||
|---|---|---|---|---|---|---|---|---|
| Over complete responses | Of missing values in each dimension | |||||||
| Control | Intervention | Control | Intervention | |||||
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Mobility | ||||||||
| Level 1 | 87 | 95 | 87 | 96 | ||||
| Level 2 | 8 | 3 | 10 | 3 | 7 | 15 | 6 | 13 |
| Level 3 | 3 | 0 | 2 | 0 | ||||
| Self-care | ||||||||
| Level 1 | 99 | 100 | 98 | 100 | ||||
| Level 2 | 0 | 0 | 0 | 0 | 7 | 15 | 5 | 13 |
| Level 3 | 0 | 0 | 1 | 0 | ||||
| Usual activities | ||||||||
| Level 1 | 88 | 94 | 90 | 91 | ||||
| Level 2 | 9 | 5 | 9 | 8 | 7 | 15 | 6 | 13 |
| Level 3 | 1 | 0 | 0 | 0 | ||||
| Pain/discomfort | ||||||||
| Level 1 | 78 | 85 | 79 | 83 | ||||
| Level 2 | 19 | 14 | 19 | 16 | 7 | 15 | 5 | 13 |
| Level 3 | 2 | 0 | 0 | 0 | ||||
| Anxiety/depression | ||||||||
| Level 1 | 64 | 69 | 66 | 71 | ||||
| Level 2 | 30 | 28 | 27 | 26 | 7 | 15 | 5 | 14 |
| Level 3 | 4 | 1 | 6 | 2 | ||||
Appendix 15 Details of intervention delivery costs
| Activities | Unit cost (£) | Resource use | Total (£) |
|---|---|---|---|
| Screening and training activities | |||
| Consent letters (opt out)a | 0.30/letter | 6233 letters | 1869.90 |
| Screening questionnaire | 0.03/pack | 4807 | 153.80 |
| Simulated-scenario training material for learning mentorsb | 0.75/pack | 80 packs | 60.00 |
| Trainer time on trainingb | 22.22/hour | 7.5 hours per co-ordinator × four co-ordinators | 666.70 |
| Learning mentor time in training sessionb | 13.43/hour | 2 hours per learning mentor × 80 learning mentors | 2148.80 |
| Interview activities | |||
| Behaviour Change Counselling interview packc | 0.86/pack | 302 packsd | 259.70 |
| Alcohol information leaflet | 0.24/leaflet | 302 leaflets | 72.50 |
| Total over 12 months | 5231.30 | ||
| Number of young people | 210d | ||
| Total over 12 months per young person | 15.80 | ||
Appendix 16 Sensitivity analysis
Incremental cost and incremental QALY scatterplot for the sensitivity analysis excluding the cost of missed school days (Figure 9).
FIGURE 9.
Sensitivity analyses excluding the cost of missed school days.
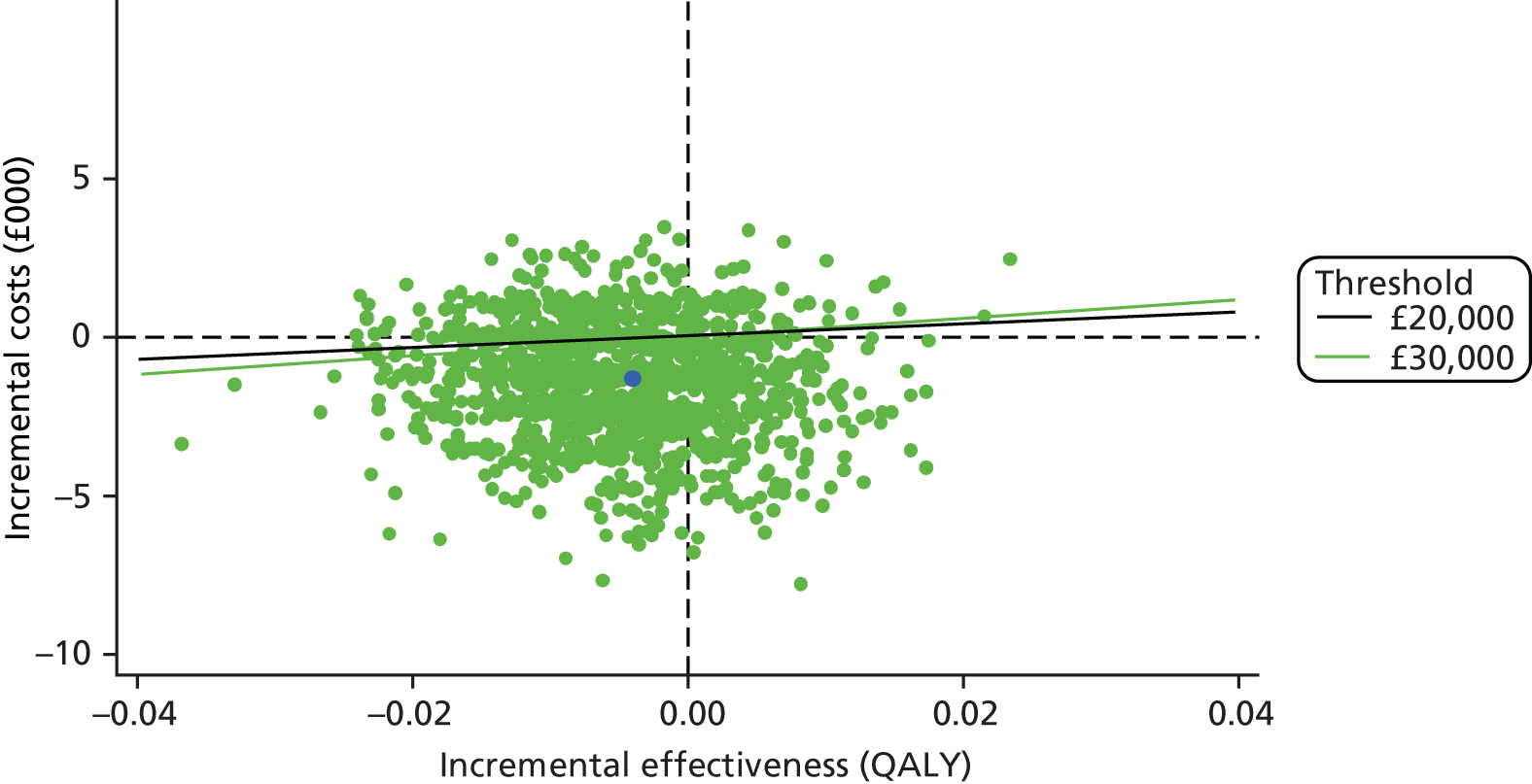
Distribution of incremental costs and incremental QALYs from 1500 bootstrap replicates stratified by trial group, geographical location and participants’ gender of the estimates from a seemingly unrelated regression of the difference between intervention and control group adjusting for baseline resource use costs, EQ-5D-3L score and participant characteristics. Fifty-six per cent (54%) of 1500 bootstrap replicates had lower costs and lower QALYs, 23% had lower costs and higher QALYs, 18% had higher costs and lower QALYs and 5% had higher costs and higher QALYs.
Appendix 17 Multiple imputation of total cost and follow-up EuroQol-5 Dimensions, three-level version scores
The missing values of total cost and follow-up EQ-5D-3L scores were imputed using multiple imputation with chained equations. The method of chained equations is more flexible than the method of using multivariate normal regression, which assumes a normal joint distribution of the variables to be imputed. With chained equations, it is possible to impute each imputed variable with a separate model specification. We used predictive mean matching with the number of closest observations (nearest neighbours) set at 5 to model the imputed values of total cost and EQ-5D-3L. The covariates in both the cost equation and the EQ-5D-3L equation included baseline EQ-5D-3L score, baseline resource costs, gender, geographical area, AUDIT score, WEMWBS score and intervention group. Ten imputations were used with burning of 500 iterations and the procedure was ‘forced’ to continue when the imputed value estimated was a missing value to complete the imputation process. Table 45 shows the initial level and proportion of missing values and the number and proportion of imputed observations after multiple imputation with chained equations.
| Variable | Complete | Missing | Total | Imputed | % over total that was missing | % of missing successfully imputed | % of missing over total after imputation |
|---|---|---|---|---|---|---|---|
| Control | |||||||
| Total cost | 181 | 52 | 233 | 34 | 22 | 65 | 6 |
| EQ-5D-3L | 196 | 37 | 233 | 26 | 16 | 70 | 5 |
| Intervention | |||||||
| Total cost | 161 | 49 | 210 | 35 | 23 | 71 | 7 |
| EQ-5D-3L | 180 | 30 | 210 | 21 | 14 | 70 | 4 |
| Overall | |||||||
| Total cost | 345 | 98 | 443 | 69 | 22 | 70 | 7 |
| EQ-5D-3L | 376 | 67 | 443 | 47 | 15 | 70 | 5 |
Glossary
- Alcohol screening and brief intervention
- A secondary preventative activity aimed at individuals whose consumption level or pattern is likely to be harmful to their health or well-being. It generally consists of screening (to identify relevant recipients) followed by structured advice or counselling of short duration that are aimed at reducing alcohol consumption or decreasing the number or severity of problems associated with drinking.
- Control
- A healthy lifestyle advice leaflet (e.g. fruit and vegetable intake), which was delivered by the school learning mentor.
- Intervention
- A 30-minute brief interactive session that combined structured advice and motivational interviewing techniques delivered by the school learning mentor, and provision of an alcohol advice leaflet.
- Learning mentor
- Specifically trained staff who provide a complementary service to teachers and other school staff, addressing the needs of young people who require assistance in overcoming barriers to learning in order to achieve their full potential. Learning mentors support, motivate and challenge pupils who are underachieving. They help pupils overcome barriers to learning caused by social, emotional and behavioural problems.
- Participants in the trial
- Young people who screened positively on a single alcohol screening question, left their name on the survey and gave consent.
- School teaching staff
- Teachers employed to deliver the curriculum.
List of abbreviations
- A-SAQ
- Adolescent Single Alcohol Question
- ASBI
- alcohol screening and brief intervention
- AUDIT
- Alcohol Use Disorders Identification Test
- AUDIT-C
- Alcohol Use Disorders Identification Test – Consumption
- BECCI
- Behaviour Change Counselling Index
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DMEC
- Data Monitoring and Ethics Committee
- DMQ-R
- Drinking Motives Questionnaire Revised
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- FRAMES
- Feedback, Responsibility, Advice, Menu, Empathy and Self-efficacy
- GP
- general practitioner
- MI
- motivational interviewing
- NMB
- net monetary benefit
- NPT
- normalisation process theory
- PPI
- patient and public involvement
- PSHE
- Personal, Social, Health and Economic Education
- QALY
- quality-adjusted life-year
- RAPI
- Rutgers Alcohol Problem Inventory
- SD
- standard deviation
- SIPS
- Screening and Intervention Programme for Sensible Drinking
- TIDieR
- Template for Intervention Description and Replication
- TLFB
- Timeline Follow-Back
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
- WEMWBS
- Warwick–Edinburgh Mental Well-being Scale
