Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 14/54/19. The contractual start date was in January 2016. The final report began editorial review in October 2018 and was accepted for publication in March 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Siobhan Creanor reports grants from the National Institute for Health Research (NIHR) Public Health Research programme during the conduct of the study, and various other grants from NIHR and UK charities, outside the submitted work. She is also Director of the Peninsula Clinical Trials Unit, which is in receipt of NIHR Clinical Trials Unit Support Funding (current award ends 31 August 2021).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Callaghan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Some text in this chapter has been reproduced from Thompson et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Scientific background
Individuals in the criminal justice system (CJS) have a high prevalence of physical and mental health-care needs, have lower psychological well-being2 and experience significant problems in accessing health and social care services. 3 Services for those with multimorbidities who are under community supervision often appear fragmented. 4 Key barriers to access to health-care services include general practice registration, long waiting times for appointments and a perception of not being supported by services to make contact, such as probation. 5 Furthermore, a lack of trust in health services and health professionals (e.g. in primary care) causes many offenders to avoid medical help despite a high prevalence of emotional problems. 6
Unhealthy behaviours such as problematic alcohol use and smoking are much higher in the offender population than in the general population. 7 For example, 60–80% of the offender population report problematic alcohol use compared with 20–30% of the general population and ≈80% of offenders smoke compared with ≈20% of the general population. 8 In addition, prevalence data from a rapid systematic review showed that 53–69% of adults in the probation setting scored positively for an alcohol use disorder. 9 Both of these behaviours (which are often co-existing) lead to several health problems, and possibly low mental well-being, through a number of plausible processes (e.g. economic, social, psychological). 10 Likewise, substance misuse is particularly prevalent and is also linked to mental health problems. However, services in the substance misuse field are already very well developed for offenders. 11
In 2004, the government’s white paper Choosing Health: Making Healthy Choices Easier12 introduced a new workforce called health trainers, who are often drawn from the communities in which they operate. The introduction of health trainers signalled a shifting focus in the UK towards self-management of health, and on reducing the demands placed on formal care. 13 A health trainer’s main role is to provide one-to-one support to people in disadvantaged areas to facilitate health behaviour change and access health services. A handbook for health trainers was developed in 2008 outlining the approach and evidence-based techniques (e.g. goal-setting, self-monitoring, creating action plans) that health trainers can use to help people change their behaviour. 14 The core work of health trainers includes the support of behaviour changes such as healthy eating, stopping/reducing smoking, increasing physical activity, reducing alcohol consumption and improving mental well-being. Their work has been positively rated but there is still a lack of robust evaluation. 15,16
Our rapid review of published and grey literature, and contact with local probation service leads, revealed that the scope of health trainers has been extended to prison and probation settings, with promising findings,17 especially when the health trainer has experience of the CJS. Although health trainers have typically focused on supporting health behaviour change, there is increasing interest in their role being extended to facilitate improvements in mental well-being. Furthermore, when enhancing well-being has been the main focus, individuals are more likely to attain their planned goals. 17 In parallel work, a screening and brief intervention for reducing alcohol use in individuals in the criminal justice settings18–20 indicated no additional benefit in comparison with feedback on screening and a client information sheet,21 suggesting that a more client-centred intervention with longer engagement may be needed. A 2015 systematic review22 identified 95 studies working with offenders both in and out of prison (42 studies based in the community) on improving health outcomes, of which 59 led to improved mental health, substance use, infectious disease or health service utilisation outcomes, suggesting that interventions can be successful. However, 91 of the studies were judged as having an unclear or high risk of bias and the review highlighted the lack of high-quality rigorous research with a population that is comparatively under-researched. Further rigorous research is therefore needed to evaluate the effectiveness and cost-effectiveness of a health trainer-led intervention aimed at improving mental well-being and health behaviour among people under community supervision, and to understand the change processes involved.
The recent reorganisation of community supervision, as part of the ‘Transforming Rehabilitation’ agenda, saw the split of services into Community Rehabilitation Companies (CRCs) and the National Probation Service (NPS). CRCs manage the majority of offenders, particularly those who are classified as being of low to medium risk, whereas the NPS supervises high-risk offenders. The reforms presented an opportunity to engage those released from prison with sentences of < 1 year (who previously would not have received supervision), as well as those serving community sentences. Providing health trainer support in this context could improve engagement with existing health promotion services23 and stimulate greater ownership and control over health behaviour change and involvement in activities to foster mental well-being. 24
There has been increasing interest in subjective well-being, distinct from lack of mental illness, as an important concept. The following five behaviours to increase mental capacity and well-being were recommended in the Foresight Report:24 (1) Connect with others, (2) keep Learning, (3) be physically Active, (4) take Notice of things around you and (5) Give (CLANG). Subjective well-being is an important outcome in its own right and has the potential to change relatively quickly.
Well-being potentially affects physical health (e.g. hypertension, heart disease) and mental health (e.g. depression, self-harm, substance misuse), health behaviours (e.g. smoking, alcohol use), employment and productivity, crime and society in other ways. 24 Although the role of exercise for improving well-being is clear, changing other specific health-related behaviours, such as smoking, can also improve subjective feelings of well-being for some individuals. 25,26 Individuals’ patterns of current behaviour, motivation to change and potential benefits will be idiosyncratic and require a personal analysis. Assessing the benefit of health promotion interventions is rarely easy and well-being poses particular problems. One method of assessing subjective well-being is through the Warwick–Edinburgh Mental Well-being Scale (WEMWBS). 27 WEMWBS captures the two perspectives of mental well-being: (1) the subjective experience of happiness (affect) and life satisfaction (the hedonic perspective) and (2) positive psychological functioning, good relationships with others and self-realisation (the eudaimonic perspective). The latter, based on self-determination theory,28 includes the capacity for self-development, positive relations with others, autonomy, self-acceptance and competence; therefore, it has the potential to positively enhance further health-promoting behaviours.
The WEMWBS has been widely used at a population level to assess mental well-being, as well as with individuals in specific groups. 29–33 Original data we obtained from the Scottish Prisoner Service in 2014 (personal communication) showed a mean WEMWBS score of 43.2 [standard deviation (SD) 12.3, range 14–70], compared with a general population score of 51.6 (SD 8.71) for England31 and 49.9 (SD 8.5) for Scotland. 34 Lower scores are associated with smoking, lower consumption of fruit and vegetables, high alcohol use and lower socioeconomic status. 33 Although these associations are likely to involve reciprocal causal effects, this does highlight the need for interventions to improve the mental well-being among groups with the lowest scores.
People who receive community supervision from the new NPS and CRC services are particularly suitable for a high-intensity health promotion intervention for four reasons: (1) they are often excluded from ‘usual’ health care and health and well-being-promoting interventions as a result of a combination of access arrangements, lifestyle factors and distrust of authority; (2) they often have low levels of mental well-being and poor health-related behaviours; thus, the gains of the proposed intervention are potentially high; (3) while under supervision, and, therefore, in a period of sustained mandated contact with a service, there is an opportunity to both engage such individuals in an intervention and capture follow-up data in the context of a rigorous evaluation; and (4) being subject to justice supervision can often be a time when individuals wish to improve their life circumstances, particularly towards the start of sentences.
The current research aimed to develop and test the feasibility and acceptability of a client-centred intervention for individuals receiving community supervision, to support them to change one or more health-related behaviours, enhance their well-being and reduce the risk of long-term conditions. The health trainer role has been adapted for specific populations, including offenders17 and smokers,35 with early signs that the support is acceptable and feasible. However, further intervention development and piloting was required to integrate a focus on promoting well-being and multiple health behaviour changes in offenders in the new NPS/CRCs context, and to understand the interactions between well-being and health behaviour changes. These uncertainties were explored, and reduced, in a process evaluation, working with the peer researchers who have lived experience of the CJS. The pilot trial and process evaluation further tested our assumptions, the intervention and cost-effectiveness.
Aims and objectives of the pilot trial
The aim of this pilot randomised controlled trial (RCT) was to develop and implement a health trainer-led intervention to support health and well-being improvements for those under community supervision in the CJS. Furthermore, the pilot study sought to explore uncertainties about the acceptability and feasibility of the trial methods and intervention to inform the design of a full RCT.
The specific objectives were to:
-
assess the acceptability and feasibility of the STRENGTHEN intervention, alongside routine engagement with community supervision services, for the key stakeholders including participants receiving community supervision, CRCs, the NPS and health trainers themselves
-
assess the acceptability of recruitment, randomisation and assessment procedures in a pilot pragmatic RCT
-
determine, from the pilot RCT, completion rates for proposed outcome measurements to assess well-being (i.e. the WEMWBS), behavioural measures (e.g. self-reported alcohol consumption, smoking status, diet, physical activity, substance use) and quality of life [measured using the Short Form questionnaire-36 items (SF-36) and EuroQol-5 Dimensions, five-level version (EQ-5D-5L)] at baseline and at the 3- and 6-month follow-ups
-
provide data to contribute to sample size calculations for a fully powered RCT to primarily assess subjective well-being (measured using the WEMWBS) and to ensure that the effect size (intervention vs. usual care) chosen for powering the definitive trial is plausible
-
use a mixed-methods process evaluation to further refine and understand the acceptability and feasibility of the intervention, its delivery and the trial procedures
-
estimate the resource use and costs associated with delivery of the intervention, and to pilot methods for the cost-effectiveness framework in a full trial.
Chapter 2 Intervention development
Development of the STRENGTHEN intervention
Through original research and literature reviews, we developed an extensive understanding of what are likely to be the effective components of an intervention targeted at health behaviours and improvement of health and mental well-being in this population. A clear starting point logic model of intervention components and aims underpins the intervention, based on the health trainer role in a previous trial of smoking cessation in disadvantaged groups35 and the development of a collaborative care model for prison leavers with multiple health problems. 36
The health trainer role has been adapted for specific populations, including offenders17 and smokers,35 with early signs that the support is acceptable and feasible. However, further intervention development and piloting was required to integrate a focus on promoting mental well-being and multiple health behaviours and to understand the interactions between mental well-being and health behaviour changes. As with our previous research, we used the original health trainer manual with its focus on smoking, alcohol consumption, physical activity and diet as a starting point for possible content and structure, adapting and developing when necessary to meet our specific aims (i.e. a stronger focus on mental well-being).
Through engaging with patient and public involvement (PPI) groups to understand what and how ‘mental well-being’ may be interpreted and understood alongside the target behaviours, we integrated mental well-being and the four target behaviours in the logic model in such a way that they exist independently from, and are interwoven with, each other. It was felt that, for some people, their mental well-being may be so low that it would need to be addressed directly before other changes could be considered. For others, addressing the four behaviours could implicitly lead to improvements in mental well-being. Therefore, the training manual was developed in such a way that health trainers were trained to support people with improving their well-being as a target in and of itself, as well as being able to support change in the four behaviours. In creating the STRENGTHEN training manual [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)], extensive work was given to adapting the way the behaviours can be supported in such a way to implicitly and explicitly maximise the benefit for people’s mental well-being.
Incorporating the Five Ways to Well-being
The framework chosen for promoting mental well-being was the Five Ways to Well-being (5WWB) [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)]. The 5WWB were developed as an accessible public health message based on evidence-based practices people can perform easily every day, which could lead to improvements in mental well-being. 23 PPI work supported the 5WWB as being an acceptable and useful framework that could be applied to the target population.
To incorporate the 5WWB, members of the research team took part in a 1-hour training session during which they were trained to understand and focus on their own well-being to ensure familiarity and understanding of the framework. Following this, the 5WWB were incorporated into the training manual as a stand-alone section for supporting people who want to improve their well-being. A section was also developed that embedded ways to promote the four health behaviours of the original health trainer manual in ways that would maximise their impact on well-being. For example, supporting a reduction in alcohol use could also link to exploring how this might help a client to connect with others (who may be trying to do likewise), learn about the physical and mental health consequences of alcohol use and guidance on safer levels of use, discover how physical activity can help deal with alcohol cravings, notice the effects of alcohol on financial, social, emotional and cognitive functioning, and give support to others to manage their alcohol consumption. A similar set of examples can be developed for each of the health behaviours.
Adapting the health trainer role and intervention
Content from the original health trainer manual that was considered appropriate was adapted for the STRENGTHEN intervention; the central ethos of being client-centred and embedded in the community was carried forward into the STRENGTHEN intervention, as were components such as action-planning, problem-solving, self-monitoring and signposting. The intervention included:
-
a heavy focus on engagement, trust/rapport building
-
a focus on reduction rather than stopping smoking, or pushing guidelines (five a day, 14 units, etc.), as this would be seen as threatening
-
flexibility of timing, frequency and duration.
The core competencies
As with our previous work adapting the health trainer role,35 a set of six core competencies were developed, which were designed to underpin the work of the health trainer (see Appendix 1). They reflected elements that were considered to be crucial to successful delivery of the intervention, and were reinforced throughout the manual, health trainer training and the supervision process. They were (1) active participant involvement, (2) motivation-building for changing a behaviour and improving well-being, (3) set goals and discuss strategies to make changes, (4) review efforts to make changes/problem-solving, (5) integration of concepts: building an association between well-being and behaviour and (6) engage social support and manage social influence. These competencies not only served as a guide for what the health trainers should be mindful of in their delivery, but also for assessing intervention delivery fidelity (as discussed in Chapter 6).
Patient and public involvement and stakeholder input to intervention development
In order to ensure that the intervention was acceptable and tailored to the needs of the target population, intervention development work was undertaken in the form of the establishment of PPI groups and a stakeholder consultation. A summary of the findings that were used to shape the intervention manual and health trainer training is provided in the following sections.
The STRENGTHEN peer researcher input to intervention development
The research team have established a collaborative relationship with a local day service for substance use and alcohol rehabilitation that supports people with multiple and complex needs. The service had recently collaborated in extensive PPI activities for a trial of an intervention to support prison-leavers with common mental health problems to achieve their goals (ENGAGER 2). 36 The research team attended the regular Monday morning group session in order to provide service users with information about the STRENGTHEN pilot trial and invite them to an introductory session to help them decide if they would like to be involved in advising about the development of both the intervention and the trial. It was at this stage that service users advised the research team that, due to the potentially sensitive nature of the topic, there should be separate groups for men and women. It was also seen as beneficial to the development of the intervention, as potential gender-specific aspects of content, implementation and delivery could be teased out in order to maximise acceptability to both women and men.
Group members were keen to adopt the title of ‘peer researcher’ that was used in the ENGAGER 2 PPI groups. 37 This both helped them to define their role in the project and put them on an equal footing in the team, with their expertise being their lived experience and understanding of the context in which the intervention would be delivered. The groups met on a bi-weekly basis for 4 months (with two or three missed sessions to take account of school holidays as a result of parenting responsibilities of some group members). Although there was some fluctuation in the attendance of both the men’s and women’s groups, a ‘core group’ of attendees emerged who attended the majority of peer researcher meetings (approximately five in the men’s group and six in the women’s group). This continuity allowed peer researchers to follow the development of the study and to witness how the outcomes of the previous meeting were implemented. Each meeting was 2 hours long, with a 15-minute mid-point break, and was facilitated by two members of the research team. Each meeting followed a schedule of activities to address issues regarding the design of the intervention and/or the research, with flexibility to discuss other topics that peer researchers raised as relevant to the intervention/research. The start of each group involved a catch-up on progress with the pilot trial and, as the groups progressed, how the advice that the group had provided during the previous meeting had been used and implemented. It was clear that these updates of how the work of the group had been utilised were key to maintaining engagement by showing the changes to and progress with the study to which the peer researchers contributed.
The PPI groups contributed to the intervention in terms of its conceptualisation, content and practicalities of delivery. Each of these will be dealt with in turn, with reference to the contribution and changes made by the groups and illustrative quotes from group meetings, when appropriate.
Conceptualisation
Title and logo
Peer researchers saw it as important that the title of the intervention was one that both attracted potential participants and encapsulated the meaning of the intervention. Both the men’s and women’s groups discussed the aims of the intervention and what these meant to them. Both the men’s and women’s groups were keen to capture the notion of building futures on firm foundations. The men’s group generally used building analogies (‘firm foundations’, ‘scaffolding’) and the women’s group used more analogies from the natural world (‘trees’, ‘strong roots’). Both groups posited that the intervention title should provide the feeling that it would support participants to build their own strength, laying down firm foundations for a healthier future:
It’s about strengthening people so they can take control.
For some reason in my mind I’ve got a picture of a tree. You’ve gotta start with your roots, haven’t you? So you get your group going, your roots. Then a few sessions, the trunk will get stronger and stronger and stronger and then the ideas come and branch out and hopefully, if it works, it will bear fruit.
The outcomes of the peer researcher discussions were delivered to the wider team and an art and photography student from a local school who was on work experience in the Community and Primary Care research team. A range of title options were developed and presented to the peer researchers, who decided that the intervention would be best represented by the word ‘strengthen’, with the tagline, ‘Firm foundations for health and well-being’. The work experience student was provided with anonymised quotations from the peer researcher discussions and provided two draft logos: the first, an outline of a human head with a tree-like structure formed of dendrites within the head, with roots at what would be the brain stem, representing growth and change, and the second, a version of a human figure in the yoga ‘tree’ pose, to represent strength and well-being. Both the peer researcher groups and the research team chose the former logo as that to be used on all trial, intervention and promotional/dissemination materials for the course of the pilot trial.
Practicalities of delivery
Peer researchers discussed a range of practical issues and potential solutions that could encourage both initial participation and intervention engagement that were included in the health trainer training.
Location
It was put to the groups that, when risk assessment outcomes allowed and at the preference of intervention participants, health trainer sessions could be held in locations other than the NPS or CRC offices where participants were initially recruited. Peer researchers provided a range of options for suitable locations in the Plymouth area, which provided a starting point for Plymouth health trainers, and categories of location types (cafes, rooms linked to key services, etc.) for Manchester health trainers to identify during intervention set-up. Both groups considered that the option of attending sessions at a location that was local to participants or somewhere ‘friendlier’ than the probation offices may remove a potential barrier to participation and engagement. It was therefore decided that, following the initial health trainer session in the probation offices and confirmation of risk level with the offender manager, participants would be given the option of meeting at another agreed location. The women’s group also stated the importance of provision for children at session locations. One woman who had experience of prison sentences advised that some women who have recently been released from prison could be subject to orders stating that other people are unable to take care of their children, which would necessitate children being present during sessions.
Mode of delivery
Peer researchers felt that in-person sessions would be more personal than sessions delivered over the telephone, emphasising the more personal aspect of meeting face to face, including developing empathy and picking up on body language. They also saw it as important for participants to have human contact and not, as they put it, ‘talking to another machine’. Peer researchers were clear that all first intervention sessions should be in person, with participants being able to choose if subsequent sessions were delivered in person or by telephone.
Contact
Peer researchers agreed that telephone was generally the best way to contact people. Peer researchers suggested informal, between-session contact via telephone call or text, for example providing information linked to a goal or enquiring after them following an appointment/event, to be important in terms of developing trust. Members of the women’s group said that they would not answer a telephone call if it was from a number that they did not know and so suggested that health trainers and researchers should send a text first saying who they are. Female peer researchers also suggested that some women in abusive relationships would have their text messages read and telephone calls monitored and that health trainers should be mindful of this when sending messages and making telephone calls (i.e. not to leave messages with anyone else answering the telephone/ask if they can talk when making calls).
Building trust
Building trust and rapport with participants was seen by peer researchers as essential in ensuring effective delivery of the intervention. Peer researchers discussed their own and others’ negative interactions with a range of services and also the type and impact of positive interactions with services with which they had worked well. The groups were clear that health trainers should make building trust a priority and not launch straight in to supporting participants to identify target health behaviour(s). It was viewed as important that health trainers be non-judgemental and understand the difficulties and barriers faced by participants in their interactions with other services. The groups described balancing being professional with being a friend. The women’s group in particular talked at length about the importance of health trainers showing that they care and provided a range of ways in which they could do this, for example by taking the time to listen, following participants up in a non-judgemental way if they do not attend an appointment, sending between-session texts during difficult periods/trigger times. They also suggested that, rather than immediately asking how participants had got on with their goals at the start of a session, the health trainer should ensure that they spend some time asking how the participant has been, to ensure that it is clear that the session is focused on them as a person.
The importance of trust and ways in which health trainers could achieve this was included in both the intervention manual and the training. It was made clear that the first two or three sessions should be focused on developing trust and getting to know the participant before moving on to focus on identifying and working towards goals.
Stakeholder input to intervention development
Lynne Callaghan interviewed eight stakeholders from a range of related health trainers and CJSs in order to identify any changes/adaptations that needed to be made to the intervention to meet the needs of the population and deliver the intervention in the current context. Roles included management and delivery of a similar health trainer intervention in probation services; practitioners with a remit of providing well-being and housing services, with a particular focus on women; a court advice and support service; a community-based support worker working alongside custody liaison and diversion workers; and a signposting and support service that worked in collaboration with the CRC and other key services. Most of these services were located in the south-west of England, with two participants located in the south central region. As the second site had not yet been identified and secured at this stage, it was not possible to include services from this area. Interviews had a focus on understanding the facilitators of and barriers to working with men and women in the CJS, in particular those under community supervision; the experiences of supporting clients to change health behaviours and mental well-being; the process of goal-setting used with clients; the mode and frequency of contact and how they worked with clients to support initial and ongoing engagement; and what works well and what does not work so well in supporting clients to change their health behaviours and improve mental well-being.
Interviews were transcribed verbatim and analysed using thematic analysis. A summary of emergent themes is included in the following sections.
Challenges to behaviour change
Some of the challenges to health behaviour change included managing concurrent mental health needs of clients with little support available, low confidence to make changes and difficulties of taking ownership. A large proportion of services to which health trainers can signpost a client in order to support behaviour change are delivered in a group format, which, it was perceived, is often not acceptable to clients. It was also viewed that clients perceive activities to support behaviour change as expensive. Returning to prison was seen as a particular challenge with working with this client group, as well as returning to old patterns of behaviour.
Behaviour change facilitators
-
Trust and rapport with clients was seen as key to effectively supporting behaviour change, achieving something for the client (no matter how small) so ‘they feel quite positive about what you can do’.
-
Focusing on the positive during sessions: ‘I mean, the more that we turn things into a positive the better with this client group . . . because they’re always, you know, talked at in a condescending way’.
-
Helping clients to see the relationship between their goals, ‘allowing them to see how kind of they can build a pathway really for themselves’.
-
Setting simple, achievable goals: ‘and we do a lot around making sure that people achieve and that actually something that seems really, really simple is actually quite a challenge to some people. So they have very simple goals’.
-
Support to access free/inexpensive activities to support behaviour change, for example: ‘I used to try and promote the outdoor gym . . . which is the cheapest gym I know, if you’ve got a dog, go for a walk, if you’ve got a pushbike, go and ride your pushbike . . . you know, it’s cheaper than the gym. ‘Cause a lot of people I worked with were on a very low income’.
-
Clients supported to set their own goals, not goals decided by the health trainer: ‘It’s better to get people to set their own goals . . . because they’re more powerful if it’s your own goal’.
Challenges to conducting the role
-
Location of the service and perceived oppressive environment of CJS premises: ‘But a lot of people say “oh, I’m not going in there, I’m not . . . you know, yeah, you might be lovely and all the rest of it, and give me what I want, but I’m not walking through that door” ’.
-
Limited time in sessions to build trust and rapport: ‘just everything from really getting to know people well. Erm, and that takes time. Erm, and that suffers when we have, you know, a very busy session’.
-
Being seen as part of the probation service: ‘So working for a charity we’ve worked alongside probation very closely and then we get seen as probation by the client, and so we get kind of lumped as “oh yeah, just part of the authorities” . . . I’ve been told, you know, “you’re just one of them”’.
-
Difficulties in keeping in contact via mobile phone: ‘even the ones I work with now, um, don’t have mobile phones cause they’ve probably sold it to buy drugs or more alcohol’.
Facilitators of conducting the role
-
Getting to know the client: ‘so before we did anything about what they actually wanted me to help them with, we’ll have a chat about the footy at the weekend . . . but then you, you get to meet people . . . and people come in just for a chat . . . and then I think you’ve broken most of the barriers then . . .’.
-
Networking with other services for effective signposting/advice: ‘and they’re much more likely to help you, I think, than if it’s sort of, someone random that they don’t know’.
-
In-person contact is important for the client: ‘I just think when you’ve met somebody and you’ve seen their face and you kind of, I meant they’re quite short visits, you know, those initial ones, but you get, probably get a sense, a better sense of what the person can support you with’.
-
Sharing with colleagues and team problem-solving: ‘but it’s also good to throw things around with people. People give you ideas, and people give you sort of advice and, and it’s always good to have those conversations’.
-
Reimbursement of travel expenses.
-
Building and maintaining a directory of organisations and resources.
Findings from the thematic analysis supported writing of the manual and preparation of the training materials and structure. Direct quotations from both stakeholder interviews and PPI sessions were used as reflection points and to exemplify specific points throughout the manual; by doing so, they were ‘bringing the manual to life’ by showing the practical application of key points.
The STRENGTHEN intervention
The STRENGTHEN training manual [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)] provides a detailed insight into the structure, delivery style, components and content of the intervention.
The key components of the piloted intervention were as follows:
-
A health trainer was available for one-to-one sessions over 14 weeks, by either face to face or telephone (the frequency and length of sessions was negotiated with each participant). The face-to-face intervention sessions took place in a variety of settings, including probation services and other local community locations.
-
An initial invitation to engage with the health trainer was described as an ‘open and flexible’ opportunity to receive support for one or more of the target health behaviours and/or improving overall health and mental well-being through other activities, including CLANG (as part of the 5WWB).
-
Health trainers were trained to help participants understand the inter-relationship between health behaviours, such as smoking, alcohol use, diet, physical activity and their relationship to mental well-being, and other positive and negative behaviours, including substance use. Each participant was encouraged to develop a personal plan based on individual behaviour-change goals and motivation to improve mental well-being. Some participants had positive perceived mental well-being but engaged in risky behaviours; others were concerned about emotional distress. The intervention was intended to be flexible enough to support both these extremes.
-
The support was described as ‘open’ to reflect the planned underpinning and overlapping influence of self-determination theory and the client-centred principles of motivational interviewing,38 which were central to the intervention. Health trainers avoided giving ‘advice’ and empowered clients to confirm the desire for change and develop self-regulatory skills such as self-monitoring, setting action plans and reviewing progress. The intervention was tailored to and led by the participants’ needs.
-
The health trainer, informed by the 5WWB, helped clients to build positive behaviours [e.g. initiating and maintaining activities (physical, creative, etc.)] and find opportunities for gaining core human needs (i.e. sense of competence, autonomy and relatedness), as well as to learn and notice, to enhance mental well-being.
-
Any reductions in alcohol consumption (as units per week, alcohol-free days or avoidance of trigger events) or smoking (using different strategies)35,39,40 and increases in physical activity and healthy eating were supported, with the underlying aim (not necessarily explicitly discussed with the participant) to build confidence to meet guidelines for safe alcohol consumption, to quit/reduce smoking, to engage in daily/weekly physical activity and eat healthily.
-
Participants were actively supported to gain help from friends and family, link with other community resources (parks, leisure centres) and services (e.g. Stop Smoking Services, Drug and Alcohol Treatment Service) as a part of achieving their personal plan, and explore options for continued support after the intervention as appropriate.
Training the health trainers
Following the development of the health trainer manual, a training plan was developed, which the training manual supported. The training consisted of various sections covering the key components of the intervention (see Appendix 1). The training was delivered over 3 days at both sites, led by the intervention lead (TPT) with input from key members of staff (LCal, AHT) to support delivery. The training included multiple opportunities for feedback and discussion, as well as skills practice with staff and PPI representatives. Following the training, health trainers were allocated up to three practice participants, who were recruited from the peer researcher groups as a way to develop real-world experience of delivering the intervention.
Supervision of the health trainers
A supervision contract was drawn up [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)] outlining expectations of supervision sessions. Supervision sessions were led by the intervention lead (TPT) and took place bi-weekly with both sites simultaneously via Skype™ (Microsoft Corporation, Redmond, WA, USA). The supervision sessions began following the delivery of the intervention with practice participants. Supervision sessions followed a standing agenda, which allowed for discussion and feedback on specific cases and resolution of any difficulties health trainers may have been facing, and allowed health trainers to feed back any issues that they felt needed to be resolved. Issues included elements that they felt were not working, or elements they felt would be a useful addition; these were fed back by the intervention lead to the project management group who would decide if any changes were necessary as part of the formative process evaluation. Audio-recordings of sessions were also reviewed in some supervision sessions and linked back to the core competencies.
Chapter 3 Trial design and methods
Trial design
The STRENGTHEN pilot trial was a parallel two-group randomised pilot trial with 1 : 1 individual participant randomisation to either the intervention plus standard care (intervention) or standard care alone (control), with a parallel process evaluation. Participants were recruited through CRCs in the south-west and north-west of England, and through the NPS in the south-west only. Participants were recruited through the NPS at only one site to test the feasibility and acceptability of recruitment and engagement of those classified as presenting a high risk of serious harm to researchers or health trainers. Follow-up assessments were carried out at 3 and 6 months post baseline data collection. Ethics approval for the trial was granted by the Health and Care Research Wales Ethics Committee and the former National Offender Management Service, now Her Majesty’s Prison and Probation Service (Research Ethics Committee reference number: 16/WA/0171; National Offender Management Service reference number: 2016-192).
Eligibility criteria
Participants had to satisfy the following criteria to be enrolled in the trial:
-
male or female and aged ≥ 18 years
-
currently receiving community supervision
-
having a minimum of 7 months left of community sentence/supervision
-
having been in the community for at least 2 months following any custodial sentence
-
willing and able to receive support to improve one or more of the four target health behaviours and/or mental well-being
-
willing and able to take part in a pilot randomised controlled trial with follow-up assessments at 3 and 6 months
-
residing in the geographical areas of the study.
Exclusion criteria were as follows:
-
presenting a serious risk of harm to the researchers or health trainers
-
unable to provide informed consent
-
having disrupted/chaotic lifestyles that may have made engagement in the intervention too difficult.
Sample size
A recruitment target of 120 participants was set across the two geographical regions (with the aim of recruiting 60 participants per region). Following consultation with the Trial Steering Committee, the decision was made for a 60 : 40 men-to-women purposive sample to inform understanding of the experience of women in the CJS. Women make up a smaller proportion of those under community supervision, and represent a small number of the total prison population. 41 However, the aim was to over-recruit for women in an attempt to avoid losing that understanding of experience through proportional sampling.
This pilot trial was not powered to detect between-group clinically meaningful differences in the proposed primary outcome. Therefore, the target sample size was primarily set to assess the feasibility objectives of the trial and to inform sample size calculations for a planned definitive trial. When data from a pilot trial are required to estimate the SD of a continuous outcome, to maximise efficiency in terms of the total sample size across pilot and main trials, the recommendation is that a two-group pilot trial should have follow-up data from at least 70 participants (i.e. 35 per group). 42 As most participants would remain engaged with the probation service for the length of the trial, it was anticipated that retention would be reasonably high. A recruitment target of 120 participants, based on an assumed non-differential retention rate of 75% at 6 months, in an aim to obtain follow-up outcome data on a minimum of 45 participants in each of the allocated groups, across both regions. A retention rate of 60% would still provide sufficient data for planning the future trial. 42 Local services suggested that, over a 3-month window, there may be 20–30 ex-offenders entering each of the two local community supervision systems per week. It was estimated that around 10% would decline to participate in a baseline assessment11,17,43 and a further 20% would be found to be ineligible following the baseline assessment. Based on recruitment rates from other probation trials,11 it was estimated that around 50% of eligible subjects would consent to participate.
Recruitment
Recruitment for the trial was over a 14-month period between October 2016 and December 2017; initially, the planned recruitment period was a 3-month period from October to December 2016. This is discussed in more depth in Chapter 4. There were two pathways to participant recruitment: (1) via the CRCs and NPS and (2) via community organisations, including drug and alcohol rehabilitation centres, homeless hostels and day centres (in the Plymouth site only) (Figure 1). Recruitment via community organisations was introduced as an attempt to reach those not engaging regularly with the CRC or NPS services.
FIGURE 1.
Participant pathway to recruitment. CRF, case report form.
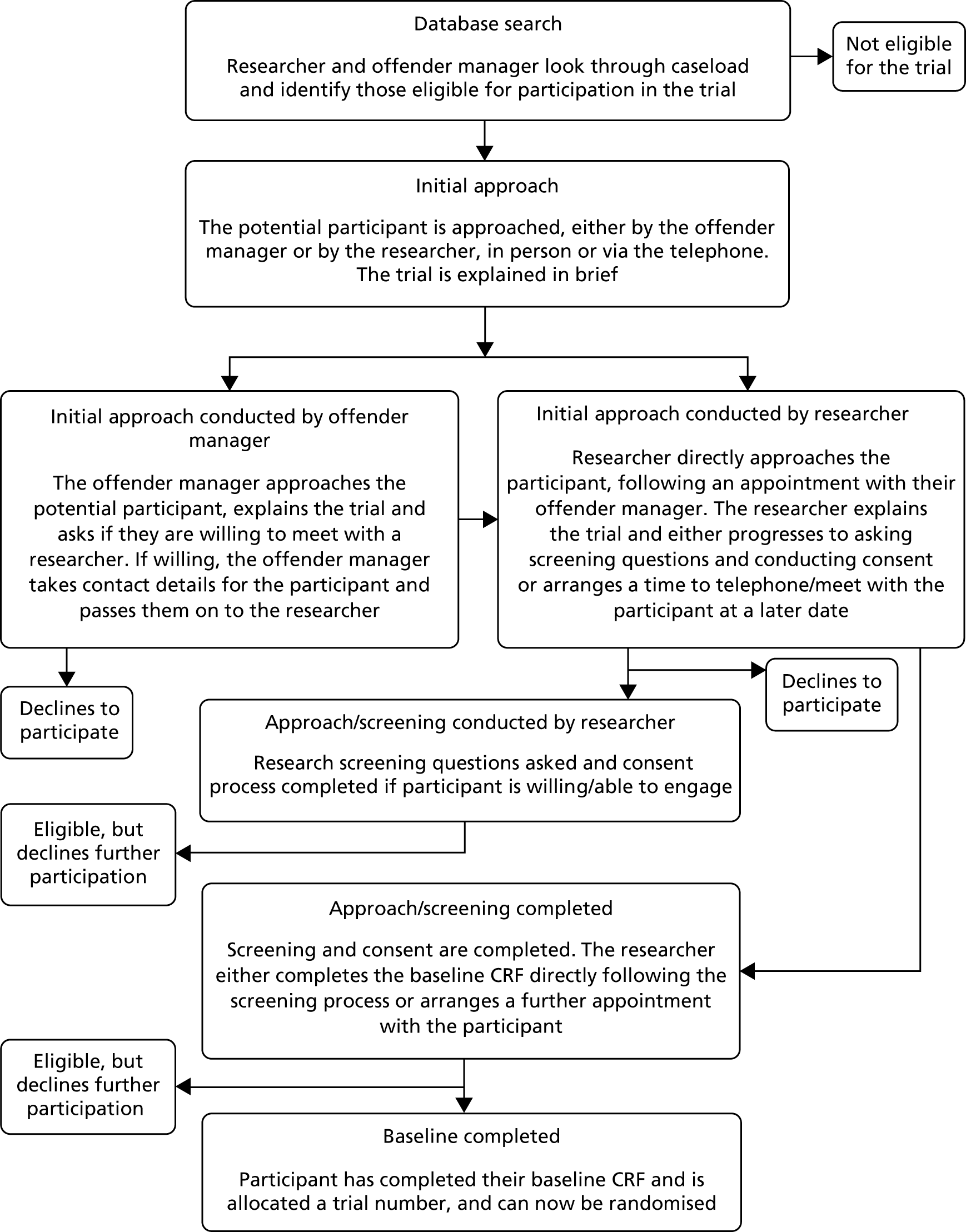
Initially, a single point of access administrator was identified for both the CRC and NPS. The single point of access administrator identified potential participants using the nDelius record system (Beaumont Colson Ltd, Newcastle upon Tyne, UK) for both services. The offender managers of identified individuals were then consulted by the researchers for screening for inclusion/exclusion criteria and assessment of risk. Further into the trial, a decision was made to alter this process, with researchers helping the offender managers to screen caseloads (i.e. sitting alongside them, but without visibility of personal information) to maximise efficiency and reduce overall staff demand [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019) for documents related to the screening process].
Those individuals who were assessed as eligible for participation in the research were initially approached by their offender manager, who explained the trial and asked if clients would be interested in speaking to the researcher directly after their appointment (if researchers were available), at their next scheduled appointment or via the telephone. On receiving verbal agreement to approach the client, the offender manager facilitated this meeting, providing an introduction. All participants were given the opportunity to meet the researchers for the initial appointment at the CRC/NPS offices.
Recruitment via community organisations
Identification of participants through community organisations involved key staff (e.g. day centre managers) initially approaching potential participants and inviting them to talk to a researcher about the trial. On receiving verbal agreement to approach, the researcher made a time and date for a meeting, to explain the project in more detail. The consent form [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)] for potential participants who were identified through the community organisations requested consent for the researcher to make contact with their offender manager, to establish whether or not the individual met the criteria for participation in the trial. Following positive assessment by the offender manager, the researcher made contact with potential participants to arrange a time to conduct baseline data collection. If the offender manager assessed the potential participant as not meeting the inclusion criteria, the researcher made a time to explain to the individual why they were not eligible for participation in the trial.
Participant approach by researcher
During approaches, at both the CRC/NPS and community organisations, the researcher explained the trial, presenting information from the participant information sheet [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)], including the potential time burden for the participant. Emphasis was placed on ensuring that the potential participant understood fully the concept and implications of randomisation, the voluntary nature of the research and their right to withdraw without detriment to their care or legal rights. Confidentiality (including reasons for a breach of confidentiality) and data protection were also presented at this stage. Potential participants were given the opportunity to ask questions and discuss their involvement in the trial. All participants were asked if they were willing and able to:
-
receive support to improve one or more of the target health behaviours and/or improve mental well-being if randomised to the intervention
-
take part in a pilot RCT with follow-up assessments at 3 and 6 months.
If the individual expressed further interest in taking part in the trial, the researcher progressed with the informed consent process, in which both the participant and researcher signed two copies of the consent form [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)] (one retained by the participant and one by the researcher). If the participant expressed a need for time to think about their involvement, the researcher arranged a later date and time to contact the individual to discuss whether or not they wanted to continue with the trial. Individuals who were unwilling or unable to proceed were thanked for their time and reminded that there were no negative consequences of not taking part.
When the consent form was completed, the researcher continued with the baseline data collection during the same appointment if the participant was happy to proceed, or made a further appointment for baseline data collection if not. In addition to the baseline data assessment, the researcher completed a contact form [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)] for each participant, noting contact numbers and addresses, as well as any key services with which they were engaging. The participant signed this form to confirm their permission for the research team to contact them via relevant services.
In regards to the consent process and data collection, individuals who lacked capacity on a particular day (potentially through intoxication) were given additional opportunities to complete assessments before being deemed to be ineligible to proceed. Given the often challenging and chaotic lives that this population can present with, this flexibility was particularly important.
Randomisation and concealment
Allocation to the intervention or control group was 1 : 1 and used a minimisation algorithm with a random element, to ensure balance between allocated groups with respect to age, gender and recruitment region.
On completion of the screening interview and baseline data collection, the researcher entered the participant details into a password-protected web-based randomisation system set up and managed by the Peninsula Clinical Trials Unit (PenCTU), and confirmed that the participant had completed the baseline case report form (CRF). The participant would then be allocated a unique randomisation number, and the participant’s allocated group (STRENGTHEN intervention or control) was then sent to the trial administrator via e-mail. To maintain blinding of the research assistants (RAs), the website would confirm that the allocation process had been successful, but would not display the participant’s allocated group. Health trainers would contact participants (via telephone) who had been allocated to the intervention arm of the trial and arrange an initial date/time to meet. Participants allocated to the control group were contacted by telephone or in person at CRC/NPS offices by either a health trainer or a research administrator, to maintain RA blinding. The conversation included a discussion of the randomisation process, to ensure that the participant had understood which group they had been allocated to.
Blinding of the researchers was tested for feasibility, to see whether it would be possible in a definitive trial. Researchers were asked to record instances when they believed they had been unblinded in the baseline, 3- and 6-month CRFs. We recognised from pilot work in our ENGAGER37 trial that concealment of trial arm may be very difficult because the RA mostly conducted the follow-up assessments in the offender management service, and offender managers or participants themselves may mention their involvement in the intervention in passing.
Data collection
Proposed outcome measures were collected at baseline (at or shortly following recruitment) and 3 and 6 months post baseline. Six months is the proposed primary assessment point for the future definitive trial [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019) for documents related to data collection].
Baseline data collection
The researcher typically continued with the baseline data collection following screening; however, additional sessions were arranged to meet the needs of individual participants. Detail of demographic data, as well as primary and secondary outcome measures collected at baseline, is in Proposed primary and secondary outcomes. Baseline data collection was delivered using a narrative conversational format developed in previous studies. 11 For the proposed primary outcome, the WEMWBS, participants were given the option to complete it themselves or have the researcher read responses aloud (method of completion was recorded). Questions from other measures were incorporated into a constructed, flexible script that avoids duplication to minimise disengagement.
On completion of the baseline assessment, the researchers discussed the 3- and 6-month follow-ups with participants, and agreed the best way to contact the participant for that appointment, depending on a range of scenarios, and changes to modes of follow-up, including any new mobile telephone numbers.
Three- and six-month data collection
Researchers contacted participants to arrange a time and date to complete the 3- and 6-month follow-ups. Contact ranged from initial text messages, to telephone calls and letters (if consent had been given). When researchers struggled to re-contact participants, offender managers were approached for information and to engage participants at appointments by asking if they were willing to meet with the researcher. Researchers arranged to meet with participants either in the CRC/NPS offices or at a suitable location in the community. When possible, assessments were conducted on the premises of services that participants were engaging with, in order to minimise risk to the researcher. When this was not possible, researchers adhered to the project’s lone-working policy [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)] and used buddies as an additional safeguard if required. Data collection could be completed via a telephone call, but the preference was for face-to-face appointments to support continued engagement with the study.
Prior to the follow-up assessment being conducted, the researcher reminded the participant of the contents of the information sheet and consent process, drawing attention to data confidentiality and instances of disclosure for which the researcher would need to breach confidentiality. Identical measures to those collected at baseline were collected for the 3- and 6-month assessments, with the exception of ethnicity, to avoid unnecessary duplication/participant burden.
Feasibility and acceptability questions
A key aim of this trial was to collect data on the following acceptability and feasibility outcomes:
-
proportion of eligible participants
-
recruitment rates
-
rates of attrition and loss to follow-up
-
completion and completeness of data collection
-
estimates of the distribution of outcome measures
-
acceptability of intervention to participants
-
acceptability of trial procedures (e.g. blinding, randomisation) to participants.
Proposed primary and secondary outcomes
The proposed primary outcome for the definitive trial was the WEMWBS, to measure subjective mental well-being, which has good psychometric properties. 27,44 The short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS) was subsequently calculated for the purposes of possible future interest. 44
Secondary outcomes were:
-
self-reported smoking (number of cigarettes smoked per day)
-
Fagerström Test for Nicotine Dependence
-
alcohol use (measured using the Alcohol Use Disorders Identification Test)
-
diet (measured using the Dietary Instrument for Nutrition Education)
-
physical activity (measured using the 7-day Physical Activity Recall questionnaire)
-
substance use (measured using the Treatment Outcomes Profile)
-
confidence, importance (i.e. an individual’s perception of the importance of changing the target behaviour), access to social support, action-planning and self-monitoring measures relating to health behaviours
-
health-related quality-of-life [measured using the EQ-5D-5L and Short Form questionnaire-6 Dimensions (SF-6D) (derived from the SF-36)]
-
intervention costs (related to health trainer time, training, supervision, travel, consumables)
-
health care use, social care use and other resource use data were collected using a participant self-report resource use questionnaire.
The secondary outcome measures were selected as they link on to the four health behaviours and were rated as acceptable to participants during the PPI consultation stage.
Summary of process evaluation methods
The aims of the process evaluation were to:
-
assess whether or not the intervention was delivered as per the manual and training
-
ascertain components of the intervention that are critical to delivery
-
explore reasons for divergence from delivery of the intervention as manualised
-
understand when context is moderating delivery
-
understand the experience and motivation of participants in the control arm of the pilot trial to maximise retention in a full trial
-
explore reasons for declining to participate in the trial
-
explore reasons for disengaging in the intervention before an agreed end
-
understand, from a participant perspective, the benefits and disadvantages of taking part in the intervention.
Data collection
Semistructured one-to-one interviews
One-to-one semistructured interviews were conducted with the following participant groups:
-
participants randomised to the intervention arm of the pilot (n = 11)
-
participants randomised to the control arm of the pilot (n = 5)
-
health trainers across both geographic regions (n = 6)
-
offender managers/probation workers across both geographic regions (n = 6).
Interviews were guided by semistructured interviews schedule [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)]. All interviews were digitally audio-recorded and transcribed verbatim.
Discussions with decliners
Researchers asked up to four potential participants who declined to take part following screening for their reasons for not continuing with participation. The researcher was sensitive to the right to withdraw from the trial without providing a reason and did not question the potential participant further should they decline to divulge their reason for discontinuation. These discussions were not recorded, but notes were taken to inform the process evaluation.
Digital audio-recordings of health trainer sessions (n = 20)
Health trainers were asked to record sessions with participants. The choice of sessions to record was a collaborative decision between the health trainer and the research team based on appropriateness (assessed by the health trainer) and data required (assessed by the research team and guided by their knowledge of each case via the health trainer session report forms). All participants were asked for their consent for sessions to be recorded at the start of the intervention. However, health trainers were requested to seek verbal consent to record each session prior to recording.
Health trainer session report forms
Health trainers kept an electronic record of each session on the bespoke intervention section of the data management system. Each contact and session was recorded, including information on date, location, duration, type (face to face or by telephone), subsidies taken up by participant, primary and secondary goals of participant, goals met (if applicable) and any particular difficulties encountered, for discussion in supervision.
Analysis
Intervention fidelity was assessed through the scoring of audio-recordings of health trainer sessions against a developed list of key intervention processes, or the six core competencies detailed in Chapter 1 [(1) active participant involvement, (2) motivation-building, (3) goal-setting, (4) reviewing efforts to make changes and problem-solving, (5) integration of concepts and (6) engaging social support and managing social influences]. These were scored on two domains: (1) practitioner adherence to the core competencies outlined in the intervention manual and (2) competence of delivery. Recordings were scored independently by two researchers.
Quantitative data were summarised descriptively, with confidence intervals (CIs) as appropriate.
Any factors that were identified as possibly contributing to participants’ intervention engagement, and trial recruitment and retention will be explored in more detail in Chapter 6. All data were organised using NVivo version 11 (QSR International, Warrington, UK). 45 Data related to feasibility and acceptability of trial method and the intervention were analysed using thematic analysis. Interview data and session notes were synthesised into a framework analysis grid to understand the experience of participants in receiving the intervention in order to understand how the intervention works in practice and the components of the intervention that are critical to delivery. This allowed the feasibility and acceptability of the intervention, the intervention delivery and the research data collection to be assessed. Any procedures that needed to be adapted were identified and potential improvements and solutions were suggested.
Statistical analysis
A detailed statistical analysis plan was written by the trial statisticians and approved by the chairperson/independent statistician on the Trial Steering Committee (statistical analysis plan version 1.0, dated 8 June 2018) prior to trial database lock.
Analytical approach
Analyses were undertaken in accordance with the Consolidated Standards of Reporting Trials (CONSORT) extension for randomised pilot and feasibility trials. 46 The primary analysis (in the form of summary statistics, not formal/inferential analysis) was undertaken on an intention-to-treat basis, in which participants are analysed according to their allocated group, regardless of adherence to the protocol or lack of participation/engagement, if allocated to the intervention group.
Statistical significance levels
As this was a feasibility trial, no inferential between-group comparisons were undertaken (i.e. there was no between-group hypothesis testing). Where presented, confidence intervals are at the 95% level, unless otherwise stated.
Interim analysis
There was no planned interim analysis for this trial.
Time points of statistical analysis
The statistical analysis was undertaken once the final group of participants completed the final assessment and the database was locked following final approval and sign-off of the statistical analysis plan by the Trial Steering Committee.
Missing data
One of the objectives of this feasibility trial was to assess the completeness of potential outcome measures for the definitive trial, at the level of both item and outcome measure. Missing outcome data were noted and used to inform the probable pattern of missing data in a full-scale trial.
Imputation methods
No imputation of missing values was undertaken, with the exception of missing values in the proposed primary outcome, WEMWBS. The established method for imputing missing item-level data was implemented when participants were missing between one and three items on the WEMWBS. 44
Statistical software
The statistical analyses were undertaken using Stata® version 14 (StataCorp LP, College Station, TX, USA), supplemented when required by R (The R Foundation for Statistical Computing, Vienna, Austria).
Trial population
Data from the screening process through to the completion of the trial were recorded and presented in a CONSORT-style flow diagram (see Figure 2).
Participants who discontinued, withdrew or were lost to follow-up
It was possible that participants would withdraw consent part-way through the trial. Participants who discontinued were categorised as follows:
-
continued to consent for follow-up and data collection
-
consented to use pre-collected data only.
Reasons for withdrawal or loss to follow-up were summarised, when reported, both prior to and after randomisation.
Participants who withdrew from the trial were not replaced. The extent of discontinuation, withdrawal and loss to follow-up will be used to inform the design of the anticipated fully powered trial, predominantly to ensure a sufficiently powered trial after allowing for losses to follow-up.
Statistical analyses
As this was a pilot trial, it was not powered to be able to support or justify any conclusions regarding intervention effectiveness realised from hypothesis testing;47 indeed, that was not the purpose of the trial. As a result, the analysis of the results did not involve formal/inferential statistical comparisons between groups, but rather was descriptive, with the view to informing the design of a fully powered definitive trial.
Continuous measures were summarised as means, SDs, ranges, medians and interquartile ranges. Categorical data were summarised by frequencies and percentages. When appropriate, parameter estimates (e.g. between-group differences) are presented with 95% confidence intervals.
Baseline characteristics and measures, collected prior to randomisation, were summarised by allocated group to informally check for balance between groups and provide an exploratory overview of the trial sample. An analysis of randomised groups at baseline is not good practice47 and so was not undertaken, but we considered imbalances to assess the efficiency of the randomisation procedures.
Analyses of quantitative data were conducted to summarise feasibility outcomes and to evaluate engagement with the STRENGTHEN intervention and the completion of the planned primary and secondary outcome measures. Summary statistics were calculated for each of the outcome measures at each time point. Between-group differences in WEMWBS scores at the 3- and 6-month follow-ups were calculated, together with 95% confidence intervals (no p-values are presented). The correlation between baseline and follow-up WEMWBS scores was calculated across all participants with available data, with corresponding confidence intervals, together with upper confidence limits for the SD of WEMWBS, to inform sample size calculations for future trials.
Cost-effectiveness and data collection
The pilot trial aimed to estimate the resource use and costs associated with the delivery of the intervention, and develop a framework for estimating the cost-effectiveness of the STRENGTHEN intervention plus usual care, versus usual care alone, in a future economic evaluation alongside a fully powered RCT. We aimed to develop and test economic evaluation methods for the collection of resource use data, for estimating related costs, and also the collection of outcome data appropriate for economic evaluation. Full details of the methods used are presented in Chapter 5.
Patient and public input to trial methods
The peer researcher groups introduced in Chapter 2 reviewed and discussed trial methods, including the following:
-
participant information sheets and consent forms
-
semistructured interview schedules
-
CRFs and associated data collection.
Both peer researcher groups reviewed the information sheets and consent forms for the pilot trial and the process evaluation. The first drafts reviewed were adapted from ENGAGER 2 information sheets and consent forms that themselves had been reviewed by the ENGAGER 2 peer researchers. Peer researchers provided guidance to adapt wording and order of text to aid comprehension and to ensure that the main points of the trial and requirements for participation were clear.
The first draft of the CRF was given to each of the peer researchers (literacy levels had already been assessed by researchers). Over 3 weeks, peer and trial researchers role-played each of the measures in pairs or threes, as appropriate. It was made clear that peer researchers did not need to answer honestly but could play a role in order that they did not have to disclose any confidential or sensitive information. Peer researchers discussed the measures in turn and/or annotated drafts and gave them to the trial researchers. Each of the issues raised by the peer researchers in relation to the CRF are detailed in the following list, with reference to the changes made, when applicable:
-
Removal of the Patient Health Questionnaire-9 items (PHQ-9)
The original STRENGTHEN CRF contained the PHQ-9 (a measure of depression). Peer researchers questioned the use of the PHQ-9 for a trial in which the primary outcome was mental well-being, as opposed to mental illness. They were particularly concerned about the impact that some of the items may have on participants who may be experiencing challenging life circumstances, and potentially have mental health needs, when it was not in a therapeutic context. As one of the peer researchers stated, ‘if someone was just starting a recovery journey, they may not be in a stable headspace and question 6 could be triggering.’ The trial researchers took this issue back to the project team, which supported the PHQ-9’s removal from the CRF as the collection of this outcome was not critical to the aims of the pilot trial.
-
Simplification of response format
There was some concern among peer researchers that some of the formats by which participants could respond to items were complex and in some instances provided too nuanced a set of choices. It was explained to the peer researchers that, in the case of validated measures, the responses could not be amended. However, for the measures included to capture confidence, control and connectedness in relation to changing each of the target health behaviours, where there was originally a 9-point scale, this was amended to a 7-point scale on the advice of the peer researchers. Furthermore, also on the advice of the peer researchers, to assist participants in making the appropriate response to the items contained in the validated measures, the researchers produced laminated A4 ‘answer cards’ that contained the options required for each item.
-
Understanding of item choice
Peer researchers noted that some of the items could be perceived as sensitive by participants and that it was not always clear as to the rationale for including all of the measures. Therefore, it was agreed that the research team would add a short paragraph or script for researchers at the start of each measure to explain why they were asking the items contained in each measure.
-
Wording of items
Similar to response format, peer researchers were aware that the wording of validated measures could not be amended. Concerns were raised about what were considered ‘Americanisms’ in the SF-36, for example ‘blocks’ and ‘pep’. For items such as this, the peer researchers provided alternatives that researchers could use to aid participants’ comprehension.
-
Order of measures
In the first draft of the CRF, the WEMWBS and the items related to offence history were at the start of the booklet. Peer researchers felt that it would be best to start with generic questions before asking those that could be considered more personal. They understood the need to order the WEMWBS near to the start of the CRF to ensure that this was collected if a follow-up appointment was unexpectedly cut short. It was therefore agreed between the peer researchers and the research team that this would be presented after demographic measures and that offence data (considered particularly sensitive) would be collected after measures of target health behaviours.
Chapter 4 Results
This chapter reports on:
-
participant recruitment
-
trial attrition and associated factors
-
baseline participant characteristics for the total sample and by allocated group
-
outcomes (e.g. WEMWBS, health behaviours) over time, by allocated group
-
WEMWBS descriptive data at follow-up, by allocated arm and CRC/NPS
-
intervention engagement
-
the association between intervention engagement and WEMWBS at follow-up
-
factors associated with intervention engagement
-
other methodological considerations
-
the indicative sample size calculation for definitive trial.
Brief overview
A number of barriers to recruitment were overcome, for example by taking on Manchester instead of Southampton as a second site at a late stage (and putting the resources and governance processes in place), and working with offender management services (OMSs) while they were becoming established and overcoming their own challenges. A great deal was learnt about participant flow into the trial and the reasons for excluding those in the service and after having been approached. Having recruited our target of 120 participants, we are now in a strong position to estimate the resources required to recruit participants.
Trial attrition was initially around 50%, but with improved processes throughout the pilot trial this was improved to 60% overall, which partly met our progression criteria. There was no clear influence of trial arm or recruitment service on retention. An acceptable level of retention was achieved without financial incentives.
The characteristics of the sample were described; overall, they had low levels of well-being; unhealthy lifestyles, particularly with respect to diet, alcohol and smoking; and were from low socioeconomic backgrounds.
It was not an aim of the trial to detect statistical significance between group differences, but the reported values for the main outcome variable, WEMWBS, at the 3- and 6-month follow-ups indicated some differences in favour of the intervention arm, from which to provide estimates for a sample size calculation for a definitive trial. There were also some encouraging signs that there was lower tobacco and alcohol consumption at follow-up in the intervention arm than in the control arm. Data for all measures were generally complete because assessments were mainly conducted face to face. Those who had moderate (2–5) intervention sessions appeared to have higher WEMWBS scores at follow-up than those who had lower and higher engagement.
Overall, 28% of participants did not attend any sessions, and 62% attended at least two sessions, which partly met our progression criteria. The overall mean number of sessions attended was 3.7 (SD 3.4), with a median of 3.
Recruitment and retention of participants
The flow of participants through the pilot trial is shown in the CONSORT flow chart (Figure 2) for the whole sample recruited (i.e. n = 120) from identification to recruitment and randomisation, through to completion of follow-ups at 3 and 6 months. Additional data on participant flow through the trial for each OMS are shown in Appendix 2, Figures 5–7.
Table 1 shows reasons for exclusion at steps A (determined by the service), B (from initial screening by the researcher) and C (from further screening or events prior to randomisation by the researcher). Appendix 3 shows the flow of participants through the trial for the services/sites (i.e. Plymouth NPS and CRC, and Manchester CRC).
| Reason | Number excluded |
|---|---|
| Risk | 55 |
| Inability to engage | 43 |
| Less than 7 months to serve after search | 883 |
| Release date < 2 months before search | 665 |
| Other | 481 |
| Back in custody/court | 279 |
| Repeat screen | 113 |
| Unable to engage | 37 |
| Moved out of area | 35 |
| Missing person | 7 |
| Mental health barriers | 5 |
| Passed away | 1 |
| Unknown | 4 |
Chapter 3 provides details on the processes for recruitment from the OMSs, including the inclusion and exclusion criteria.
At step A, offender managers excluded those who clearly did not meet our inclusion criteria. As Figure 2 shows, of the 3237 people considered in the initial search, 2101 were excluded at step A. Table 1 shows the reasons for excluding participants across all sites at step A. In some cases, researchers included multiple exclusion reasons for individual potential participants, hence there being a greater number of exclusions detailed in Table 1 (n = 2127). Most (77%) of the exclusions (n = 1620) were related to ‘risk’, ‘inability to engage’ and timing and duration of the sentence. The remaining 23% (n = 481) were excluded for other reasons, as shown in Table 1. ‘Unable to engage’ includes the following: does not see offender manager (e.g. because they are doing unpaid work), next appointment would be after trial recruitment ends, warrant out for person’s arrest and person in a care home. ‘Mental health barriers’ include those who were considered inappropriate to approach because of their fragile emotional state.
At step B, the offender manager and researcher made contact (or not) with the potential participant, and excluded those who did not meet the inclusion criteria (e.g. level of risk, timing and duration of community sentence, not interested in being in the trial). Across all sites, of the 1095 approached, 841 were excluded for the reasons shown in Table 2. In a full trial, we would make minor changes to the way these reasons were recorded, as it took many hours trawling through records for reasons that had not been recorded on the CRF or that were complex due to delays, which subsequently meant a person was no longer eligible because less than 7 months remained of their community sentence. Among the ‘other reasons’, ‘conflicting commitments’ include those who were working full-time or unsociable shifts, those studying or those with other significant service engagement. ‘Inability to engage’ includes those who did not have face-to-face visits with their offender manager, those who were having their order appealed and those who could not engage on top of the demands of their order. Reasons for ‘mental health barriers’ are described in step A. ‘Unavailability of offender manager’ refers to case managers who were either too busy to engage with the RA or were not physically present as a result of annual leave or sickness. ‘Physical health barriers’ refers to those who were too physically unwell to take part, and those struggling to engage with other services because of physical health needs. ‘Stressful life events’ includes those who had recently suffered a bereavement, or another event, that would make it difficult for them to engage.
| Reason | Number excluded |
|---|---|
| Declined/withdrew | 85 |
| Disruptive lifestyle making intervention engagement too difficult | 92 |
| Less than 7 months left to serve after search | 138 |
| Limited English | 14 |
| Not interested in being supported one to one by a health trainer | 13 |
| Not interested in changing one of four target health behaviours or improving mental well-being | 14 |
| Unable to provide informed consent | 15 |
| Unable to contact | 30 |
| Transferred to another area | 23 |
| Returned to custody | 29 |
| Resides outside target geographical area | 8 |
| Trial already closed | 192 |
| Previously randomised | 3 |
| Risk | 14 |
| Other (total) | 171 |
| Not engaging with CJS services | 74 |
| Conflicting commitments | 25 |
| Not engaging with researcher | 16 |
| Inability to engage | 14 |
| Mental health barriers | 9 |
| Back in court | 7 |
| Repeat screen | 6 |
| Unavailability of offender manager | 6 |
| Physical health barriers | 5 |
| Stressful life events | 4 |
| Missing person | 4 |
| Passed away | 1 |
At step C, some participants were excluded after they had already been approached and were awaiting completion of the baseline assessments. Table 3 shows the reasons why 134 people did not enter the trial. Once again, it was sometimes difficult to ascertain the reason for exclusion, and we will make minor changes to the way recording takes place in a full trial. The large number of people (n = 62) who declined/withdrew at this stage is indicative of the chaotic lives some potential participants had. Any delay between screening and gaining consent and completing the baseline assessment increased the likelihood of a potential participant not being recruited.
| Reason | Number excluded |
|---|---|
| Declined/withdrew | 62 |
| Disruptive lifestyle making intervention engagement too difficult | 1 |
| Less than 7 months left to serve after search | 14 |
| Limited English | 1 |
| Not interested in being supported one to one by a health trainer | 5 |
| Not interested in changing one of the four target health behaviours or improving mental well-being | 20 |
| Unable to contact | 6 |
| Recruitment completed | 1 |
| Returned to custody | 1 |
| Other (total) | 23 |
| Conflicting commitments | 13 |
| Not engaging with the researcher | 6 |
| Inability to engage | 2 |
| Stressful life events | 2 |
In steps B and C, it was not always easy to determine the precise reason for an eligible participant not entering the trial. For example, ‘not being able to contact’, ‘an inability to engage’ and ‘lack of interest’ in being in the trial were not always distinct. Assuming that a total of 199 potentially eligible participants were recorded as ‘declined/withdrew’ or not interested in the intervention (changing lifestyle or well-being) at stage B or C, and 120 eligible participants did enter the trial, we recruited > 30% of eligible participants, suggesting a promising degree of interest and acceptability.
In addition to attempts to quantify why the target population in the OMS did not enter the trial, the process evaluation in Chapter 6 qualitatively describes the challenges in the recruitment pathway.
The conversion rates for participants initially identified in searches, through each step, to ultimately being randomised, are shown in Table 4. The percentages indicate the amount of work completed to achieve randomisation, with the co-operation of the OMSs; the greater the percentage moving from one step to another indicates a more efficient process. Across all sites, 4% of those initially checked by the OMS ended up being randomised, varying from 2% to 7%. Although conversion rates from the initial OMS search to the researcher approaching the potential participant for a face-to-face screening was similar across sites and averaged 34%, there was greater variation across sites from the initial researcher approaching the potential participant to successful randomisation, averaging 7% across all services and varying from 7% to 24% between services. Similarly, the Plymouth NPS converted the greatest proportion (80%) from completing the approach to actual randomisation, with only 30% in the Manchester CRC being randomised after completing the approach.
| Recruitment source | Number of participants recruited | Conversion rate (from initial offender service search to randomisation) (%) | Conversion rate (from initial service search to researcher approach for initial screen) (%) | Conversion rate (from initial approach by RA to randomisation) (%) | Conversion rate (from approach completed by RA to randomisation) (%) |
|---|---|---|---|---|---|
| Plymouth CRC | 47 | 5 | 38 | 12 | 60 |
| Plymouth NPS | 33 | 7 | 31 | 24 | 80 |
| Manchester CRC | 40 | 2 | 32 | 7 | 30 |
| All sites | 120 | 4 | 34 | 11 | 47 |
Retention of participants
Overall, as Figure 2 shows, of the 120 participants recruited and randomised, 60% (n = 72) completed the follow-up assessment at 3 months and 60% completed the 6-month follow-up assessment.
As Table 5 shows, there was no consistent difference in retention at the 3- and 6-month follow-ups between the intervention and control groups across all sites. Retention varied across recruitment site from 48% to 70% at 3 months, and from 48% to 88% at 6 months. Observed differences in retention rates between allocated treatment groups were not consistent at each follow-up assessment, suggesting no systematic bias in retention, but it is something to be wary of in a larger trial. Retention rates were higher among those recruited through the NPS than the CRCs at both the 3- and 6-month follow-ups; again, this is something to be wary of in a full trial. The process evaluation (see Chapter 6) further considers this.
| Recruitment source | Number recruited/randomised | Completion of the 3-month follow-up, by allocated group and overall, n (%) | Completion of the 6-month follow-up, by allocated group and overall, n (%) |
|---|---|---|---|
| Plymouth CRC | 47 |
|
|
| Plymouth NPS | 33 |
|
|
| Manchester CRC | 40 |
|
|
| All sites | 120 |
|
|
Further qualitative information about the factors influencing retention is reported in Chapter 6.
Participant characteristics
Participant demographic characteristics for the total sample and by allocated group are shown in Table 6. The sample, as a whole, was 91% male, had a mean age of 40.5 years, was predominantly white British, had few qualifications above General Certificate of Secondary Education (GCSE) or Ordinary (O) levels and few were in paid employment. The median number of convictions for the sample overall was six.
| Characteristic | Intervention (N = 61) | Control (N = 59) | All participants (N = 120) |
|---|---|---|---|
| Male, n (%) | 55 (90.2) | 54 (91.5) | 109 (90.8) |
| Age (years), mean (SD) [range] | 41.3 (12.9) [20.2–77.9] | 39.6 (10.2) [20.6–63.9] | 40.5 (11.7) [20.2–77.9] |
| Ethnicity, n (%) | |||
| White English, Scottish, Welsh or Irish | 48 (78.7) | 51 (86.4) | 99 (82.5) |
| White other | 2 (3.3) | 0 (0.0) | 2 (1.7) |
| Black British | 2 (3.3) | 1 (1.6) | 3 (2.5) |
| Black Caribbean | 4 (6.6) | 2 (3.3) | 6 (5.0) |
| Other (including Indian, Pakistani, other Asian background, Chinese and mixed background) | 5 (8.0) | 5 (8.0) | 10 (8.0) |
| Living situation, n (%) | |||
| Own your own property | 2 (3.3) | 3 (5.1) | 5 (4.2) |
| Renting through the housing association/local authority | 10 (16.7) | 13 (22.0) | 23 (19.3) |
| Living in a hostel | 4 (6.7) | 7 (11.9) | 11 (9.2) |
| Living in supported accommodation | 5 (8.3) | 4 (6.8) | 9 (7.6) |
| Sleeping rough | 1 (1.7) | 0 (0.0) | 1 (0.8) |
| Renting a property privately | 17 (28.3) | 15 (25.4) | 32 (26.9) |
| Living with parents (or other caregiver) | 15 (25.0) | 7 (11.9) | 22 (18.5) |
| Other (including B&B, sheltered accommodation, sofa surfing) | 6 (10.0) | 10 (17) | 16 (13.3) |
| Have children aged < 18 years, n (%) | 27 (44.3) | 33 (55.9) | 60 (50.0) |
| Have a partner now, n (%) | 19 (31.7) | 22 (39.3) | 41 (35.3) |
| Normally live with, n (%) | |||
| Husband/wife/partner | 12 (19.7) | 16 (27.1) | 28 (23.3) |
| Child or children aged < 18 years | 10 (16.4) | 9 (15.3) | 19 (15.8) |
| Parents/parents-in-law/step-parents | 15 (24.6) | 6 (10.2) | 21 (17.5) |
| Other family or friends | 2 (3.3) | 7 (11.9) | 9 (7.5) |
| On own | 22 (36.1) | 20 (33.9) | 42 (35.0) |
| Other | 7 (11.5) | 11 (18.6) | 18 (15.0) |
| Highest qualification, n (%) | |||
| University degree or equivalent | 5 (8.6) | 1 (1.8) | 6 (5.3) |
| Higher education qualification (below degree level) | 11 (18.7) | 10 (18.2) | 21 (18.6) |
| GCE, A levels or equivalent | 0 (0.0) | 5 (9.1) | 5 (4.4) |
| GCSE, O levels or equivalent | 17 (29.3) | 17 (30.9) | 34 (30.1) |
| Other qualifications at NVQ level 1 or below | 14 (24.1) | 10 (18.2) | 24 (21.2) |
| No formal qualifications | 11 (19.0) | 12 (21.8) | 23 (20.4) |
| Previous prison sentence, n (%) | 36 (59.0) | 38 (64.4) | 74 (61.7) |
| Best description of work situation, n (%) | |||
| Paid employment | 16 (26.2) | 14 (23.7) | 30 (25.0) |
| Voluntary work | 2 (3.3) | 3 (5.1) | 5 (4.2) |
| Unpaid care work (not child care) | 1 (1.6) | 0 (0.0) | 1 (0.8) |
| Child care | 1 (1.6) | 1 (1.7) | 2 (1.7) |
| Student | 0 (0.0) | 1 (1.7) | 1 (0.8) |
| Unemployed | 41 (67.2) | 39 (66.1) | 80 (66.7) |
| Number of hours per week of work, mean (SD) [range] | |||
| Paid employment | n = 15; 35.1 (11.2) [14–60] | n = 13; 37.0 (15.5) [15–60] | n = 28; 36.0 (13.2) [14–60] |
| Voluntary work | n = 2; 18.5 (3.5) [16–21] | n = 3; 28.0 (36.4) [6–70] | n = 5; 24.2 (26.3) [6–70] |
| Unpaid care work (not child care) | n = 1; 40 | n = 0 | n = 1; 40 |
| Child care | n = 1; 84 | n = 1; 37 | n = 2; 60.5 (33.2) [37–84] |
| Student | n = 0 | n = 1; 20 | n = 1; 20 |
Summary of outcome measures at baseline
Table 7 shows baseline summary data, by trial arm and for the whole sample for the WEMWBS scores (long and short version), quality-of-life measures and behavioural measures (alcohol use, dietary intake, smoking status, substance use and physical activity). The WEMWBS scores were low compared with national data, but similar to a Scottish sample of prisoners. Similarly, the EQ-5D-5L and SF-6D data indicated that the sample had a low quality of life. Lifestyle measures indicated a poor diet in terms of diet and fat consumption, a high risk of alcohol dependence (73%) among the 64% who reported drinking alcohol, a high proportion of smokers (72%) (with 75% having at least moderate cigarette dependency), but also a very physically active sample, with the sample averaging 572.5 minutes of moderate–vigorous physical activity over the previous 7 days. Overall, of the 69 participants (58% of the total sample) who reported some substance use, the most frequent substances reportedly used were cannabis (57%), prescription drugs (40%), non-prescription drugs (15%), benzodiazepam (7%), opiates (6%), cocaine (7%) and crack (6%).
| Measure | Intervention | Control | Overall | |||
|---|---|---|---|---|---|---|
| n | Summary statistics | n | Summary statistics | n | Summary statistics | |
| WEMWBS score, mean (SD) [range] | 61 | 43.6 (12.0) [19–63] | 59 | 44.9 (11.6) [15–68] | 120 | 44.2 (11.8) [15–68] |
| SWEMWBS score, mean (SD) [range] | 61 | 20.9 (4.8) [9.5–32.5] | 59 | 21.2 (4.4) [9.5–30.7] | 120 | 21.1 (4.6) [9.5–32.5] |
| SF-6D score, mean (SD) [range] | 59 | 0.681 (0.138) [0.355 to 0.943] | 58 | 0.654 (0.152) [0.362 to 1] | 117 | 0.668 (0.145) [0.355 to 1] |
| EQ-5D-5L score, mean (SD) [range] | 60 | 0.667 (0.288) [–0.158 to 1] | 59 | 0.685 (0.243) [0.007–1] | 119 | 0.677 (0.266) [–0.158 to 1] |
| Self-reported drinker, n (%) | 61 | 42 (68.9) | 59 | 35 (59.3) | 120 | 77 (64.2) |
| Total units of alcohol in previous 4 weeks, median (IQR) [range] | 39 | 36 (16–108) [0–1120] | 31 | 36 (9–120) [0–448] | 70 | 36 (14–108) [0–1120] |
| AUDIT score, mean (SD) [range] | 42 | 13.5 (9.6) [1–36] | 35 | 14.1 (9.3) [2–35] | 77 | 13.8 (9.4) [1–36] |
| AUDIT score indicating high risk of hazardous or harmful drinking or possible dependence (> 7), n (%) | 42 | 30 (71.4) | 35 | 26 (74.3) | 77 | 56 (72.7) |
| Self-reported smoker, n (%) | 61 | 43 (70.5) | 59 | 43 (72.9) | 120 | 86 (71.7) |
| Cigarettes per day, median (IQR) [range] | 42 | 17.2 (11–31.1) [1–126] | 41 | 12 (6.7–15.6) [0–166.7] | 83 | 13.3 (8.9–26.7) [0–166.7] |
| FTND, n (%) | 42 | 40 | 82 | |||
| Low to moderate (score 3–4) | 10 (23.8) | 10 (25.0) | 20 (24.4) | |||
| Moderate (score 5–7) | 21 (50.0) | 24 (60.0) | 45 (54.9) | |||
| High (score ≥ 8) | 11 (26.2) | 6 (15.0) | 17 (20.7) | |||
| Self-reported substance user, n (%) | 61 | 34 (55.7) | 59 | 35 (55.3) | 120 | 69 (57.5) |
| Minutes of moderate activity per week, median (IQR) [range] | 56 | 370 (210–750) [30–4200] | 50 | 580 (360–1080) [30–3780] | 106 | 420 (225–840) [30–4200] |
| Minutes of vigorous activity per week, median (IQR) [range] | 21 | 210 (60–300) [5–3480] | 22 | 375 (190–720) [0–2520] | 43 | 270 (105–630) [0–3480] |
| Total minutes of moderate and vigorous physical activity per week, median (IQR), [range] | 56 | 442.5 (215–1020) [30–4350] | 50 | 795 (420–1440) [30–5880] | 106 | 572.5 (315–1175) [30–5880] |
| Number (%) who reported doing at least 150 minutes of moderate and vigorous physical activity per week | 56 | 49 (87.5) | 50 | 48 (96.0) | 106 | (91.5) |
Data for the demographic variables and proposed primary and secondary outcomes at baseline suggest that the allocated groups were comparable on most measures, that is the minimisation algorithm (with random element) was generally successful. There were some apparent differences observed between allocated groups in the physical activity measures, with greater amounts of moderate and vigorous activity in participants allocated to the control group than in those allocated to the intervention group.
Outcome measures over time, by allocated group
Tables 8 and 9 show the summary data for the WEMWBS (and SWEMWBS) and lifestyle behaviours, respectively, at baseline and at the 3- and 6-month follow-ups, by trial arm, from participants completing assessments. The mean between-group difference (intervention minus control) in the WEMWBS score was 4.6 (–1.7 to 10.8) at 3 months, and 1.9 (95% CI –4.6 to 8.4) at 6 months. We provide similar data for the SWEMWBS in the interests of completeness for other researchers who may be interested in using this version.
| Outcome measure | Time point | Intervention (N = 61) | Control (N = 59) | Mean difference (95% CI) between intervention and control groups | ||||
|---|---|---|---|---|---|---|---|---|
| Completed, n (%) [95% CI] | Mean (SD) [range] | Median (Q1, Q3) | Number (%) completed [95% CI] | Mean (SD) [range] | Median (Q1, Q3) | |||
| WEMWBS | Baseline | 61 (100.0)a | 43.6 (12.0) [19–63] | 45.0 (34, 53) | 59 (100.0)a | 44.9 (11.6) [15–68] | 45.0 (37–55) | NA |
| 3-month follow-up | 34 (55.7) [42.4–68.5] | 50.5 (13.1) [16–68] | 53.5 (47, 59) | 38 (64.4) [50.9–76.4] | 45.9 (13.3) [17–70] | 45.5 (38–56) | 4.6 (–1.7 to 10.8) | |
| 6-month follow-up | 40 (65.6) [52.3–77.3] | 49.6 (13.6) [14–68] | 54.5 (41.5, 60) | 32 (54.2) [40.8–67.3] | 47.7 (13.9) [18–70] | 48.5 (37–61) | 1.9 (–4.6 to 8.4) | |
| SWEMWBS | Baseline | 61 (100.0)a | 20.9 (4.8) [9.5–32.6] | 20.7 (17.4, 24.1) | 59 (100.0)a | 21.2 (4.4) [9.5–30.7] | 20.7 (18.0–23.2) | NA |
| 3-month follow-up | 34 (55.7) [42.4–68.5] | 23.7 (5.4) [9.5–32.6] | 24.1 (21.5, 27.0) | 38 (64.4) [50.9–76.4] | 21.9 (5.0) [12.4–35.0] | 21.1 (18.6–26.0) | 1.7 (–0.7 to 4.2) | |
| 6-month follow-up | 40 (65.6) [52.3–77.3] | 23.1 (6.2) [7.0–35.0] | 25.0 (19.3, 27.0) | 32 (54.2) [40.8–67.3] | 22.9 (6.4) [7.0–35.0] | 23.2 (18.0–28.1) | 0.1 (–2.9 to 3.1) | |
| Outcome variable | Intervention | Control | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3-month follow-up | 6-month follow-up | Baseline | 3-month follow-up | 6-month follow-up | |||||||
| N | Summary statistics | N | Summary statistics | N | Summary statistics | N | Summary statistics | N | Summary statistics | N | Summary statistics | |
| Alcohol | ||||||||||||
| Drinks alcohol, n (%) | 61 | 42 (68.9) | 34 | 19 (55.9) | 40 | 22 (55.0) | 59 | 35 (59.3) | 38 | 23 (60.5) | 32 | 20 (62.5) |
| Number of units in previous 4 weeks for those who drank, median (Q1, Q3) [range] | 39 | 36 (0, 64) [0–1120] | 19 | 21 (4, 36) [3–672] | 21 | 12 (4, 24) [0–120] | 31 | 36 (9, 120) [0–448] | 19 | 42 (15, 200) [3–400] | 20 | 36 (8, 129) [0–240] |
| AUDIT score indicating high risk of hazardous or harmful drinking or possible dependence (> 7), n (%) | 42 | 30 (71.4) | 18 | 10 (55.6) | 22 | 12 (54.5) | 35 | 26 (74.3) | 23 | 15 (65.2) | 20 | 11 (55.0) |
| Overall AUDIT score for those who drink, mean (SD) [range] | 42 | 13.5 (9.6) [1–36] | 18 | 10.4 (8.5) [2–35] | 22 | 8.1 (6.2) [1–30] | 35 | 14.1 (9.3) [2–35] | 23 | 12.1 (8.6) [2–32] | 20 | 11.0 (8.8) [1–33] |
| Diet | ||||||||||||
| DINE fibre total score, mean (SD) [range] | 60 | 31.7 (16.4) [2–84] | 34 | 29.2 (13.1) [6–70] | 39 | 29.8 (14.0) [7–58] | 59 | 30.6 (14.2) [11–83] | 38 | 29.4 (10.8) [12–57] | 31 | 29.7 (12.7) [11–61] |
| DINE fibre category (fibre score), n (%) | ||||||||||||
| Low intake (< 30) | 60 | 31 (51.7) | 34 | 14 (41.2) | 39 | 19 (48.7) | 59 | 32 (54.2) | 38 | 20 (52.6) | 31 | 17 (54.8) |
| Medium intake (30–40) | 12 (20.0) | 15 (44.1) | 12 (30.8) | 14 (23.7) | 12 (31.6) | 8 (25.8) | ||||||
| High intake (> 40) | 17 (28.3) | 5 (14.7) | 8 (20.5) | 13 (22.0) | 6 (15.8) | 6 (19.4) | ||||||
| DINE fat total score, mean (SD) [range] | 60 | 36.9 (14) [14–74] | 29.2 (14.6) [13–69] | 40 | 32.0 (15.4) [13–75] | 58 | 38.2 (15.8) [11–80] | 38 | 38.2 (16.8) [10–75] | 31 | 36.1 (16.8) [10–76] | |
| DINE fat category (fat score), n (%) | ||||||||||||
| Low intake (< 30) | 60 | 23 (38.3) | 32 | 22 (68.8) | 40 | 23 (57.5) | 58 | 19 (32.8) | 38 | 13 (34.2) | 31 | 14 (45.2) |
| Medium intake (30–40) | 13 (21.7) | 5 (15.6) | 8 (20.0) | 13 (22.4) | 13 (34.2) | 6 (19.4) | ||||||
| High intake (> 40) | 24 (40.0) | 5 (15.6) | 9 (22.5) | 26 (44.8) | 12 (31.6) | 11 (35.5) | ||||||
| DINE unsaturated fat total score, mean (SD) [range] | 39 | 8.9 (2.3) [3–12] | 22 | 8.7 (2.0) [6–12] | 35 | 9.0 (2.1) [3–12] | 38 | 9.3 (2.3) [3–12] | 31 | 9.2 (2.4) [3–12] | 28 | 8.8 (2.1) [3–12] |
| DINE unsaturated fat category (unsaturated fat score), n (%) | ||||||||||||
| Low intake (< 30) | 39 | 2 (5.1) | 22 | 15 (68.2) | 35 | 2 (5.7) | 38 | 1 (2.6) | 31 | 3 (9.7) | 28 | 2 (7.1) |
| Medium intake (30–40) | 23 (59.0) | 7 (31.8) | 20 (57.1) | 21 (55.3) | 12 (38.7) | 17 (60.7) | ||||||
| High intake (> 40) | 14 (35.9) | 0 (0.0) | 13 (37.1) | 16 (42.1) | 16 (51.6) | 9 (32.1) | ||||||
| Smoking | ||||||||||||
| Smoker, n (%) | 61 | 43 (70.5) | 34 | 15 (44.1) | 40 | 23 (57.5) | 59 | 43 (72.9) | 38 | 22 (57.9) | 32 | 17 (53.1) |
| Number of cigarettes per day,a median (Q1, Q3) [range] | 42 | 17.2 (11.0, 31.1) [1–126] | 14 | 14.4 (4.4, 20.0) [4–66.7] | 22 | 11.1 (8.0, 20.0) [2–76.7] | 41 | 12 (6.7, 15.6) [0–166.7] | 22 | 12.1 (8.9, 20.0) [4.4–33.3] | 17 | 15.6 (8.9, 22.2) [4.4–66.7] |
| FTND category, n (%) | ||||||||||||
| Low to moderate (score 3–4) | 42 | 10 (23.8) | 14 | 4 (28.6) | 22 | 7 (31.8) | 40 | 10 (25.0) | 22 | 6 (27.3) | 17 | 7 (41.2) |
| Moderate (score 5–7) | 21 (50.0) | 6 (42.9) | 5 (36.4) | 24 (60.0) | 11 (63.6) | 4 (29.4) | ||||||
| High (score ≥ 8) | 11 (26.2) | 4 (28.6) | 7 (31.8) | 6 (15.0) | 2 (9.1) | 5 (29.4) | ||||||
| Physical activity: 7-day Physical Activity Recall questionnaire | ||||||||||||
| Did vigorous activities in previous 7 days, n (%) | 61 | 21 (34.4) | 34 | 14 (41.2) | 40 | 17 (42.5) | 58 | 22 (37.9) | 38 | 17 (44.7) | 31 | 11 (35.5) |
| Total number of minutes of vigorous activity, median (Q1, Q3) [range] | 21 | 210 (60, 300) [5–3480] | 14 | 175 (90, 360) [0–3090] | 17 | 180 (90, 315) [60–3600] | 22 | 375 (190, 720) [0–2520] | 17 | 300 (180, 420) [20–3600] | 11 | 180 (110, 1105) [60–1680] |
| Did moderate activities in previous 7 days, n (%) | 61 | 56 (91.8) | 34 | 30 (88.2) | 40 | 36 (90.0) | 59 | 50 (84.7) | 38 | 35 (92.1) | 32 | 30 (93.8) |
| Total number of minutes of moderate activity, median (Q1, Q3) [range] | 56 | 370 (210, 750) [30–4200] | 30 | 622.5 (300, 1660) [20–3360] | 36 | 332.5 (140, 630) [20–2520] | 50 | 580 (360, 1080) [30–3780] | 35 | 570 (400, 1440) [0–2700] | 30 | 540 (210, 1020) [20–3600] |
| Total minutes of moderate and vigorous activity: median (Q1, Q3) [range] | 56 | 442.5 (215, 1020) [30–4350] | 31 | 685 (330, 1800) [20–4140] | 37 | 600 (220, 1020) [20–3720] | 50 | 795 (420, 1440) [30–5580] | 36 | 795 (470, 1680) [60–3600] | 30 | 640 (260, 1560) [70–3900] |
| Number of hours sleeping each day: mean (SD) [range] | 61 | 6.1 (1.6) [2–10.5] | 34 | 6.0 (1.4) [2–8] | 40 | 6.2 (2.2) [0–12] | 56 | 6.5 (2.3) [1.5–13] | 38 | 6.9 (2.1) [3–12] | 32 | 6.6 (3.1) [0–18] |
| Substance use in the previous 4 weeksb | ||||||||||||
| Opiates, n (%) | 34 | 6 (17.6) | 8 | 1 (12.5) | 10 | 1 (10.0) | 35 | 2 (5.7) | 15 | 1 (6.7) | 10 | 1 (10.0) |
| Crack, n (%) | 3 (8.8) | 0 (0.0) | 0 (0.0) | 1 (2.9) | 1 (6.7) | 1 (10.0) | ||||||
| Cocaine, n (%) | 2 (5.9) | 2 (25.0) | 1 (10.0) | 3 (8.6) | 0 (0.0) | 0 (0.0) | ||||||
| Amphetamines, n (%) | 1 (2.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (6.7) | 2 (20.0) | ||||||
| Cannabis, n (%) | 19 (55.9) | 4 (50.0) | 7 (70.0) | 20 (57.1) | 11 (73.3) | 7 (70.0) | ||||||
| Legal highs, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.9) | 0 (0.0) | 0 (0.0) | ||||||
| Benzodiazepam, n (%) | 5 (14.7) | 2 (25.0) | 2 (20.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||||
| Prescription drugs, n (%) | 15 (44.1) | 4 (50.0) | 2 (20.0) | 13 (37.1) | 7 (46.7) | 4 (40.0) | ||||||
| Non-prescription drugs, n (%) | 5 (14.7) | 1 (12.5) | 1 (10.0) | 6 (17.1) | 4 (26.7) | 2 (20.0) | ||||||
| Other substance(s), n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 (11.4) | 1 (6.7) | 1 (10.0) | ||||||
Table 10 shows the summary data, by allocated group, for the process outcome measures (i.e. perceived importance, confidence, use of support, action-planning and self-monitoring) at baseline and at the 3- and 6-month follow-ups. Only those reporting use of alcohol (64% of total sample) and tobacco (72% of total sample) completed the questionnaire items on beliefs about alcohol and smoking, respectively. We have not undertaken exploratory factor analysis to confirm the merits of creating a composite score by adding the four items for each behaviour concerned with action-planning, and the two items concerned with self-monitoring; the data presented are for reference only.
| Process measure | Intervention arm | Control arm | ||||
|---|---|---|---|---|---|---|
| Baseline (N = 61) | 3-month follow-up (N = 34) | 6-month follow-up (N = 40) | Baseline (N = 59) | 3-month follow-up (N = 38) | 6-month follow-up (N = 32) | |
| Self-reported drinker, n (%) | 42 (68.9) | 19 (55.9) | 22 (55.0) | 35 (59.3) | 23 (60.5) | 20 (62.5) |
| Alcohol, mean (SD) [range] | 42 responses | 19 responses | 22 responses | 35 responses | 23 responses | 20 responses |
| Important to reduce alcohol consumption | 3.05 (1.59) [1–5] | 2.74 (1.28) [1–5] | 2.82 (1.14) [1–5] | 3.00 (1.71) [1–5] | 3.17 (1.67) [1–5] | 3.10 (1.45) [1–5] |
| Confidence in reducing alcohol consumption | 4.40 (0.91) [1–5] | 4.42 (0.69) [3–5] | 4.32 (0.84) [3–5] | 4.51 (0.70) [3–5] | 4.57 (0.73) [3–5] | 4.45 (0.69) [3–5] |
| People close for support | 4.10 (0.98) [2–5] | 3.95 (1.18) [1–5] | 4.05 (0.95) [2–5] | 4.00 (1.21) [1–5] | 4.13 (1.01) [2–5] | 4.00 (1.26) [1–5] |
| Made plans for amount when drinking | a2.56 (1.48) [1–5] | 2.95 (1.39) [1–5] | 2.59 (1.14) [1–4] | 2.74 (1.44) [1–5] | 3.17 (1.56) [1–5] | 2.85 (1.31) [1–5] |
| Made plans for days not drinking | a3.05 (1.40) [1–5] | 3.05 (1.31) [1–5] | 3.00 (1.20) [1–5] | 2.69 (1.32) [1–5] | 2.87 (1.49) [1–5] | 2.70 (1.22) [1–5] |
| Made plans for interferences | a2.46 (1.23) [1–5] | 2.53 (1.22) [1–5] | 2.59 (1.05) [1–4] | 2.26 (1.04) [1–5] | 2.39 (1.16) [1–5] | 2.65 (1.35) [1–5] |
| Made plans for setbacks | a2.34 (1.11) [1–5] | 2.53 (1.31) [1–5] | 2.64 (1.09) [1–4] | 2.49 (1.15) [1–5] | 2.52 (1.20) [1–5] | 2.65 (1.35) [1–5] |
| Self-monitored amount being drunk | a2.51 (1.47) [1–5] | 2.79 (1.47) [1–5] | 2.82 (1.33) [1–5] | 2.66 (1.49) [1–5] | 2.70 (1.66) [1–5] | 3.00 (1.45) [1–5] |
| Thought about amount being drunk | a2.95 (1.52) [1–5] | 2.84 (1.46) [1–5] | 2.73 (1.35) [1–5] | 2.91 (1.52) [1–5] | 2.83 (1.67) [1–5] | 3.05 (1.50) [1–5] |
| Diet, mean (SD) [range] | 61 responses | 34 responses | 40 responses | 59 responses | 38 responses | 32 responses |
| Important to eat a healthy diet | 3.79 (1.11) [1–5] | 4.35 (0.92) [2–5] | 4.18 (0.87) [1–5] | 4.02 (0.99) [1–5] | 4.11 (1.01) [1–5] | 4.00 (1.16) [1–5] |
| Confident in eating a healthy diet | 3.77 (1.07) [1–5] | 4.18 (1.00) [1–5] | 3.88 (1.22) [1–5] | 3.86 (1.15) [1–5] | 4.05 (0.77) [2–5] | 3.75 (0.95) [2–5] |
| People close for support | 3.48 (1.26) [1–5] | 3.94 (1.10) [1–5] | 3.95 (0.93) [1–5] | 3.49 (1.19) [1–5] | 3.55 (1.08) [1–5] | 3.69 (1.00) [2–5] |
| Plans for what/how much food to eat | 2.85 (1.49) [1–5] | 3.47 (1.56) [1–5] | 3.38 (1.23) [1–5] | 2.73 (1.30) [1–5] | 3.05 (1.25) [1–5] | 3.06 (1.16) [1–5] |
| Plans for replacing things with healthier options | 3.10 (1.39) [1–5] | 3.62 (1.44) [1–5] | 3.65 (1.23) [1–5] | 3.00 (1.34) [1–5] | 3.45 (1.27) [1–5] | 3.59 (1.24) [1–5] |
| Made plans for interferences | 2.34 (1.01) [1–5] | 2.59 (1.33) [1–5] | 2.98 (1.17) [1–5] | 2.44 (1.04) [1–5] | 2.55 (0.95) [1–5] | 2.75 (0.98) [1–5] |
| Made plans to cope with setbacks | 2.39 (1.02) [1–4] | 2.68 (1.34) [1–5] | 2.95 (1.15) [1–5] | 2.39 (1.02) [1–4] | 2.55 (0.86) [1–4] | 2.81 (1.03) [1–5] |
| Monitored amount of food eaten | 2.25 (1.21) [1–5] | 3.24 (1.50) [1–5] | 3.25 (1.260) [1–5] | 2.29 (1.29) [1–5] | 2.76 (1.24) [1–5] | 2.75 (1.16) [1–5] |
| Regularly thought about what they were eating | 2.92 (1.38) [1–5] | 3.68 (1.34) [1–5] | 3.50 (1.20) [1–5] | 3.10 (1.34) [1–5] | 3.32 (1.30) [1–5] | 3.22 (1.18) [1–5] |
| Five portions of fruit/vegetables most days | 2.52 (1.35) [1–5] | 3.06 (1.39) [1–5] | 2.98 (1.39) [1–5] | 2.64 (1.39) [1–5] | 2.79 (1.23) [1–5] | 2.53 (1.02) [1–5] |
| Five portions of fruit/vegetables in a single day | 2.57 (1.42) [1–5] | 3.15 (1.64) [1–5] | 3.23 (1.42) [1–5] | 2.86 (1.43) [1–5] | 3.08 (1.32) [1–5] | 3.06 (1.16) [1–5] |
| Self-reported smoker, n (%) | 43 (70.5) | 15 (44.1) | 23 (57.5) | 43 (72.9) | 22 (57.9) | 17 (53.1) |
| Smoking, mean (SD) [range] | 43 responses | 15 responses | 23 responses | 43 responses | 22 responses | 17 responses |
| Important to reduce smoking | 3.74 (1.29) [1–5] | 3.73 (1.62) [1–5] | 3.78 (1.41) [1–5] | 4.37 (0.79) [2–5] | 4.27 (1.16) [1–5] | 4.53 (0.87) [2–5] |
| Important to quit smoking | 3.35 (1.34) [1–5] | 3.53 (1.64) [1–5] | 3.87 (1.39) [1–5] | 4.05 (1.15) [1–5] | 3.82 (1.26) [1–5] | 4.24 (1.15) [2–5] |
| Confident in reducing smoking | 3.47 (1.40) [1–5] | 3.53 (1.06) [2–5] | 3.22 (1.35) [1–5] | 3.49 (1.37) [1–5] | 3.23 (1.41) [1–5] | 3.41 (1.18) [2–5] |
| Confident in quitting smoking | 2.86 (1.44) [1–5] | 3.20 (1.21) [1–5] | a3.27 (1.16) [1–5] | 3.16 (1.29) [1–5] | 2.82 (1.37) [1–5] | 3.00 (1.37) [1–5] |
| People close for support | 3.28 (1.52) [1–5] | 3.40 (1.35) [1–5] | 3.39 (1.31) [1–5] | 3.35 (1.57) [1–5] | 3.50 (1.14) [1–5] | 3.71 (1.05) [2–5] |
| Plans for how much will smoke | 2.40 (1.43) [1–5] | 3.00 (1.77) [1–5] | 2.96 (1.26) [1–5] | 2.77 (1.49) [1–5] | 2.91 (1.31) [1–5] | 3.12 (1.17) [2–5] |
| Plans for strategies to reduce smoking | 2.67 (1.36) [1–5] | 3.20 (1.57) [1–5] | 3.26 (1.25) [1–5] | 2.86 (1.39) [1–5] | 2.86 (1.25) [1–5] | 3.12 (1.22) [2–5] |
| Plans for interferences with plans | 2.09 (0.87) [1–4] | 2.20 (1.32) [1–5] | 2.52 (1.04) [1–5] | 2.63 (1.07) [1–5] | 2.45 (1.18) [1–5] | 2.59 (1.00) [1–5] |
| Plans for coping with setbacks | 2.12 (0.88) [1–4] | 2.40 (1.40) [1–5] | 2.52 (1.12) [1–5] | 2.58 (1.10) [1–5] | 2.50 (1.14) [1–5] | 2.65 (1.06) [1–5] |
| Plans for quitting smoking | 2.37 (1.36) [1–5] | 2.93 (1.62) [1–5] | 2.91 (1.31) [1–5] | 2.28 (1.42) [1–5] | 2.45 (1.18) [1–5] | 3.18 (1.24) [2–5] |
| Monitored amount of smoking | 2.84 (1.51) [1–5] | 2.87 (1.73) [1–5] | 2.91 (1.35) [1–5] | 2.74 (1.43) [1–5] | 2.95 (1.40) [1–5] | 3.18 (1.13) [2–5] |
| Thought about amount of smoking | 3.35 (1.48) [1–5] | 3.53 (1.55) [1–5] | 3.09 (1.24) [1–5] | 3.56 (1.33) [1–5] | 3.64 (1.14) [1–5] | 3.82 (1.01) [2–5] |
| Physical activity, mean (SD) [range] | 61 responses | 34 responses | 40 responses | 59 responses | 38 responses | 32 responses |
| Important to be physically active | a3.97 (1.18) [1–5] | 4.56 (0.66) [2–5] | 4.35 (0.89) [1–5] | 4.29 (0.93) [1–5] | 4.39 (0.86) [2–5] | 4.19 (1.15) [1–5] |
| Confidence in being physically active | a4.17 (0.98) [1–5] | 4.32 (0.77) [2–5] | 4.23 (0.92) [1–5] | 4.05 (1.12) [1–5] | 3.89 (1.25) [1–5] | 4.09 (1.12) [1–5] |
| People close for support | a3.47 (1.24) [1–5] | 3.94 (1.10) [1–5] | 3.88 (1.14) [1–5] | 3.75 (1.11) [1–5] | 3.89 (1.06) [1–5] | 3.78 (1.04) [1–5] |
| Made plans for when to be physically active | 3.23 (1.41) [1–5] | 3.85 (1.21) [1–5] | 3.68 (1.25) [1–5] | 3.19 (1.46) [1–5] | 3.29 (1.33) [1–5] | 3.44 (1.32) [1–5] |
| Made plans for where to be physically active | 3.23 (1.41) [1–5] | 4.06 (1.13) [1–5] | 3.73 (1.22) [1–5] | 3.25 (1.37) [1–5] | 3.24 (1.34) [1–5] | 3.50 (1.30) [1–5] |
Warwick–Edinburgh Mental Well-being Scale descriptive data by time, allocated arm and Community Rehabilitation Company/National Probation Service
Based on fairly small numbers of participants, we explored if there were noticeable differences in WEMWBS scores at each time point by trial arm and overall, for participants recruited via the CRCs and NPS. As shown in Table 11, baseline scores were slightly lower for the CRC participants. Differences in WEMWBS scores between trial arms were most noticeable at follow-up among the NPS participants.
| Service | Time point | Intervention arm (N = 61) | Control arm (N = 59) | Overall (N = 120) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) [range] | Median (IQR) | n | Mean (SD) [range] | Median (IQR) | n | Mean (SD) [range] | Median (IQR) | ||
| CRC | Baseline | 43 | 42.2 (12.5) [19–63] | 43 (33–53) | 44 | 45.6 (11.9) [15–68] | 45 (37.8–55.0) | 87 | 43.9 (12.2) [15–68] | 44 (36–55) |
| 3-month follow-up | 22 | 49.0 (14.7) [16–66] | 52.5 (43–59) | 27 | 46.3 (14.4) [17–70] | 44 (38–59) | 49 | 47.5 (14.4) [16–70] | 51 (39–59) | |
| 6-month follow-up | 24 | 47.7 (14.3) [14–65] | 49 (40.5–59.5) | 19 | 48.3 (16.1) [18–70] | 47 (37–63) | 43 | 48.0 (15.0) [14–70] | 48 (37–61) | |
| NPS | Baseline | 18 | 46.9 (10.3) [31–63] | 48 (37–54) | 15 | 42.8 (10.9) [20–58] | 47 (36–50) | 33 | 45.1 (10.6) [20–63] | 48 (37–51) |
| 3-month follow-up | 12 | 53.3 (9.3) [35–68] | 54.5 (50.5–58.5) | 11 | 45.1 (10.8) [23–61] | 46 (36–56) | 23 | 49.4 (10.7) [23–68] | 53 (44–56) | |
| 6-month follow-up | 16 | 52.3 (12.4) [22–68] | 55 (45–62) | 13 | 46.7 (10.6) [28–61] | 51 (39–53) | 29 | 49.8 (11.8) [22–68] | 53 (41–57) | |
Intervention engagement
This section describes the level of engagement with the intervention. Further exploration of the views of participants and health trainers is described in Chapter 6.
Table 12 shows the number (percentage) of sessions with a health trainer that participants in the intervention group had in Plymouth, Manchester and overall. Overall, only 28% of participants did not attend any sessions, with a slightly higher proportion in Manchester not attending any sessions. The progression criterion for the trial was to achieve a target of at least 70% of participants who attended at least two sessions for automatic progression. Overall, 63% attended at least two sessions, varying from 50% in Manchester (albeit with small numbers) to 68% in Plymouth. Drawing on the process evaluation, we are seeking to understand these small differences and whether or not they may be a result of chance. The overall mean number of sessions attended was 3.7 (SD 3.4), with median of 3. Very few participants had more than nine sessions.
| Number of health trainer-led sessions attended | Participants, n (%) | ||
|---|---|---|---|
| Plymouth (N = 41) | Manchester (N = 20) | Total (N = 61) | |
| 0 | 10 (24.4) | 7 (35.0) | 17 (27.9) |
| 1 | 3 (7.3) | 3 (15.0) | 6 (9.8) |
| 2–5 | 14 (34) | 6 (30) | 20 (33) |
| 6–9 | 12 (29) | 3 (15) | 15 (25) |
| 10–12 | 2 (5) | 1 (5) | 3 (5) |
Association between intervention engagement and change in Warwick–Edinburgh Mental Well-being Scale score
Table 13 shows the WEMWBS score over time for those who had low (up to one session), moderate (two to five sessions) and high (six or more sessions) intervention engagement, among those completing the WEMWBS assessments. It is noticeable that a smaller proportion of those assessed at baseline in the ‘low engagement’ group provided data at 3 and 6 months, compared with in the moderate and high engagement groups. It would appear that those with moderate engagement had higher WEMWBS scores at the 3- and 6-month follow-ups than those with the lowest and highest engagement.
| Level of engagement | Baseline | 3-month follow-up | 6-month follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) [range] | Median (IQR) | n | Mean (SD) [range] | Median (IQR) | n | Mean (SD) [range] | Median (IQR) | |
| High engagement (≥ 6 sessions) | 18 | 44.7 (13.3) [19–63] | 47.5 (33–54) | 16 | 48.9 (13.2) [16–66] | 53.0 (43.5–55.5) | 16 | 46.7 (15.6) [14–68] | 51.5 (37–57.5) |
| Moderate engagement (2–5 sessions) | 20 | 45.2 (10.9) [21–63] | 44.5 (37–54.5) | 12 | 53.9 (14.7) [16–68] | 58.0 (51–63.5) | 15 | 53.9 (10.3) [35–68] | 55.0 (43–63) |
| Low engagement (0–1 sessions) | 23 | 41.3 (11.9) [20–59] | 44.0 (32–52) | 6 | 48 (9.2) [33–59] | 49.5 (43–54) | 9 | 47.4 (14.5) [14–62] | 49.0 (45–59) |
Factors associated with intervention engagement
Table 13 shows the WEMWBS scores at baseline for those with different levels of intervention engagement. The scores were lowest for those who went on to have no more than one session with the health trainer.
Other methodological considerations
Recruitment issues
Table 14 presents the planned and actual recruitment to the trial. We originally anticipated, based on expected numbers of probable eligible participants coming through the OMSs, that we would recruit approximately 10 participants per month (for 4 months) per OMS from September 2016. In the first 7 months after the first participant was recruited, we had recruited only 22 participants. Once recruitment processes were established across the three OMSs, it took 9 months to recruit 90 participants (i.e. 3.3 per OMS per month).
| Project month | Month of recruitment | Planned accumulated recruitment target (n) | Actual recruitment per month (n) | Actual accumulative recruitment (n) |
|---|---|---|---|---|
| 9 | September 2016 | 30 | 0 | 0 |
| 10 | October 2016 | 60 | 3 | 3 |
| 11 | November 2016 | 90 | 9 | 12 |
| 12 | December 2016 | 120 | 2 | 14 |
| 13 | January 2017 | 1 | 15 | |
| 14 | February 2017 | 3 | 18 | |
| 15 | March 2017 | 4 | 22 | |
| 16 | April 2017 | 8 | 30 | |
| 17 | May 2017 | 17 | 47 | |
| 18 | June 2017 | 13 | 60 | |
| 19 | July 2017 | 5 | 65 | |
| 20 | August 2017 | 18 | 83 | |
| 21 | September 2017 | 10 | 93 | |
| 22 | October 2017 | 7 | 100 | |
| 23 | November 2017 | 19 | 119 | |
| 24 | December 2017 | 1 | 120 |
Given that the CRCs were still being established at the time of the original bid, the target was somewhat speculative. Our original bid included plans to recruit from offender services in Plymouth and Southampton. During trial set-up in Southampton, we discovered that health trainers had been commissioned to support offenders in the community, and we decided against comparing the STRENGTHEN health trainer intervention with the local health trainer support. Plymouth and Manchester were already collaborating on another trial involving support for offenders leaving prison, so we set Manchester up as a second site. This caused a delay in recruitment until contracts and excess treatment costs were confirmed, and researchers and health trainers were appointed. The first recruitment took place in April 2017 in Manchester. In Plymouth, the first recruitment in the CRC took place in October 2016, just a few weeks after intended. Recruitment via the Plymouth NPS eventually began in April 2017.
The conversion of potential participants from being approached and then randomised was more efficient in the NPS. One explanation for the NPS service having such efficient recruitment processes is that clients had less chaotic lives and once a step had been completed, there were fewer interruptions. It is not clear why the Plymouth CRC was more efficient at recruiting than the Manchester CRC, but we will seek to better understand this ahead of a full trial to maximise our resource efficiency in all CRCs.
The importance of the co-operation of the OMS for recruitment was very evident in December 2016 and January 2017 when the Plymouth CRC was unable to support us as a result of corporate and staffing difficulties. Several staff were on sick leave and others resigned, which meant searching through service records of potential participants stopped. Later dips in recruitment were due to researcher sick leave.
Retention issues
We originally defined our longest follow-up assessment to coincide with when we expected participants to have a 6-month follow-up with their offender manager, and, in many cases, to coincide with the end of their community sentence. As the study evolved, it became clear that the OMSs had not found it easy to ensure that a formal (face-to-face) 6-month session took place; therefore, we attempted to remain in contact with our sample and complete follow-up assessments around 6 months whenever they could be arranged. In three cases, this extended to 6 weeks after the assessment was scheduled to take place. Given that it was our aim to demonstrate that we could assess participants after at least 6 months, this is not seen as a major issue, but it did delay database cleaning and lockdown. No participant who withdrew from the trial requested that their previously collected data be removed from the trial database.
The slightly higher 6-month follow-up rate for the intervention group for the whole sample was particularly influenced by the large difference between the two trial arms among participants recruited in the south-west CRC, as shown in Appendix 2 (see Figure 5). Among the 47 south-west CRC participants randomised, 65% and 38% were followed up in the intervention and control groups, respectively. It is not clear why there was a between-trial arm difference in the south-west CRC participants, but not in the north-west CRC. As Figures 5–7 in Appendix 2 show, follow-up rates were, overall, considerably lower in participants from the two CRCs (51% in the south-west, and 48% in the north-west) than in the NPS participants (88%).
Data completeness
The completeness of data collection for all variables at baseline and follow-up assessments is shown in Appendix 6. Researchers reported few difficulties with the data collections that were mostly administered by the RA in face-to-face format. For the administration of the WEMWBS, almost all participants completed the measure themselves. As one might expect, our researchers reported that sensitive questions about substance use were probably incomplete. Throughout the rest of this chapter, summary statistics (including percentages) are based on the number of participants responding to the given questions; therefore, the number of respondents is also given.
Blinding of researchers at follow-up assessments
Table 15 shows the extent of possible bias in capturing follow-up data. As is common in studies involving complex interventions such as a health trainer intervention, participants may mention something associated with the intervention they have or have not received to a researcher when collecting follow-up data. Researchers were more likely to become aware of the assigned trial arm if a participant had been allocated to the intervention group than if a participant had been allocated to the control group. The data indicate that it will be very challenging to ensure that outcome measures are assessed by blinded researchers in a full definitive trial.
| Follow-up | Trial arm, n/N (%) | Overall, n/N (%) | |
|---|---|---|---|
| Intervention | Control | ||
| 3 months | 29/34 (85.3%) | 14/38 (36.8%) | 43/72 (59.7%) |
| 6 months | 34/40 (85.0%) | 20/32 (62.5%) | 54/72 (75.0%) |
Data were analysed to determine how well the protocol was followed in terms of the screening and randomisation processes and in completing follow-up assessments in a timely manner, given the challenges in working with a considerable proportion of the sample. Table 16 shows the number of days it took between screening and completing the baseline assessment, and between completing the baseline assessment and randomisation. From the point of satisfactory screening and gaining informed consent to being assigned to the trial group was approximately 9 days.
| Event time (days) | n | Mean (SD) [range] | Median (IQR) |
|---|---|---|---|
| Screening and baseline | 120 | 8.7 (25.4) [0–237] | 0 (0–9.5) |
| Baseline and randomisation | 120 | 0.6 (2.8) [0–28] | 0 (0–0) |
| Randomisation and 3-month follow-up | 72 | 99.5 (16.9) [74–169] | 96 (89–111) |
| Randomisation and 6-month follow-up | 72 | 196.4 (36.6) [152–407] | 188.5 (178–206.5) |
The mean time between completing the baseline and 3- and 6-month follow-ups was 14 and 28 weeks, respectively, suggesting some slippage, but this may not be surprising given the challenges of keeping in contact with the participants in this trial. There was no noteworthy difference between trial groups in terms of the times between key events (data are not shown).
Data to inform future sample size calculations
One of the key objectives of the STRENGTHEN pilot trial was to collect data to contribute to indicative sample size calculations for a definitive trial to assess the effectiveness (and cost-effectiveness) of the STRENGTHEN intervention in terms of the proposed primary outcome, WEMWBS score, at the primary end point of 6 months post baseline.
As the planned primary analyses would include adjustment for baseline WEMWBS score, the pilot data have been used to estimate the correlation between the baseline and 6-month WEMWBS scores, as well as estimating the SD of the 6-month WEMWBS score. Table 17 shows the point estimates for these two parameters, together with the lower one-sided 80% confidence bound for the estimated correlation and the upper one-sided 80% bound for the estimated SD. 48 For reference, estimates are shown for the intervention and control groups separately, as well as for the pooled groups (i.e. pooled across all participants) for both WEMWBS and SWEMWBS scores, with estimates also presented for 3 months, for completeness.
| Measure | Follow-up | Intervention group | Control group | Pooled groups | |||
|---|---|---|---|---|---|---|---|
| SD (80% upper confidence limit) | Correlation with baseline (80% lower confidence limit) | SD (80% upper confidence limit) | Correlation with baseline (80% lower confidence limit) | SD (80% upper confidence limit) | Correlationa with baseline (80% lower confidence limit) | ||
| WEMWBS | 3 months | 13.1 (14.72) | 0.72 (0.64) | 13.3 (14.89) | 0.47 (0.36) | 13.3 (14.38) | 0.58 (0.51) |
| 6 months | 13.6 (15.19) | 0.61 (0.51) | 13.9 (15.76) | 0.77 (0.70) | 13.7 (14.81) | 0.68 (0.63) | |
| SWEMWBS | 3 months | 5.4 (6.08) | 0.70 (0.62) | 5.0 (5.63) | 0.36 (0.23) | 5.2 (5.67) | 0.52 (0.45) |
| 6 months | 6.2 (6.93) | 0.53 (0.43) | 6.4 (7.24) | 0.73 (0.66) | 6.3 (6.76) | 0.61 (0.54) | |
Indicative sample size for a definitive trial of the STRENGTHEN intervention
As specified in the agreed statistical analysis plan, indicative sample size calculations are based on estimates from the STRENGTHEN pilot data of the required parameters. The data in Table 18 have been used to produce potential target sample sizes for a definitive trial of the STRENGTHEN intervention, to detect a between-group difference of three units44,49,50 for the proposed primary outcome of WEMWBS score at the primary end point of 6 months post baseline, under a range of plausible assumptions.
| Between-group difference at 6 months | SD | Unadjusted total sample size required to be followed up (n) | Total sample size required to be recruited – adjusted for LTF only (n) | Total sample size required to be followed up – adjusted for correlation only (n) | Total sample size required to be recruited – adjusted for correlation and LTF (n) | |
|---|---|---|---|---|---|---|
| Base case | 5 | 14.8 | 1028 | 1470 | 620 | 886 |
| Vary standard deviation | 3 | 12 | 676 | 966 | 408 | 582 |
| 3 | 13 | 792 | 1132 | 478 | 682 | |
| 3 | 14 | 918 | 1312 | 554 | 792 | |
| 3 | 15 | 1054 | 1506 | 636 | 908 | |
| 3 | 16 | 1200 | 1714 | 724 | 1034 | |
| Vary correlation | 3 | 0.5 | 1028 | 1470 | 772 | 1102 |
| 3 | 0.6 | 1028 | 1470 | 658 | 940 | |
| 3 | 0.7 | 1028 | 1470 | 524 | 750 | |
| Vary LTF | 3 | 50% | 1028 | 2056 | 620 | 1240 |
| 3 | 60% | 1028 | 1714 | 620 | 1033 | |
| 3 | 70% | 1028 | 1470 | 620 | 886 | |
| 3 | 80% | 1028 | 1286 | 620 | 776 |
The base case for the sample size calculation conservatively assumes a SD of 14.8 units (i.e. the upper one-sided confidence bound from the pilot data), with calculations also shown for SDs ranging from 12 to 16 units.
As the planned analyses would include adjustment for baseline WEMWBS, the effect of allowing for the correlation between the baseline and 6-month WEMWBS scores has also been considered. 51 From the STRENGTHEN pilot trial, the point estimate of the correlation between baseline and 6 months across all participants was 0.68, with the one-sided 80% lower bound being 0.63. The base case for the sample size calculation assumes a correlation of 0.63, with calculations also shown for correlations of 0.5 to 0.7.
Finally, an allowance is made for the estimated follow-up rate at 6 months. In the STRENGTHEN pilot trial, the overall retention rate at 6 months was 60%. However, a recent trial,43 funded by the National Institute for Health Research Programme Grants for Applied Research programme, in the CJS observed an increase in retention rate from 50% to 67% at the 3-month follow-up following the introduction of a small financial incentive for completing the trial. Therefore, the target sample size in the base case assumes a retention rate of 70%.
In summary, the base case assumes detecting a between-group difference of 3 units (SD of 14.8 units), a correlation between the baseline and 6-month WEMWBS scores of 0.63 and a follow-up rate of 70%; with two-sided 5% alpha and 90% power.
Based on Table 18, the number of participants required to be followed up at the 6-month primary end point ranges from ≈970 to ≈2060, before allowing for the correlation between baseline and follow-up. After including adjustment for this correlation, the number of participants required to be recruited reduces to a range of 580–1240.
Chapter 5 Economic analysis
Research question
A full economic evaluation of the STRENGTHEN intervention would address the following research question: is the health trainer-led motivational intervention plus usual care cost-effective, versus usual care alone in a UK setting, for people under community supervision?
The purpose of this pilot study was to estimate the resource use and costs associated with the delivery of the intervention and to develop a framework for estimating the cost-effectiveness of the STRENGTHEN intervention plus usual care, versus usual care alone, in a future economic evaluation alongside a fully powered RCT. This involved developing and testing economic evaluation methods for the collection of resource use data and the estimation of related costs, and piloting the collection of outcome data appropriate for economic evaluation.
Methods
Design
The economic analysis was conducted concurrently with the pilot randomised controlled trial, using within-trial intervention, resource use and outcome data, over a 6-month time horizon.
The incremental cost for the delivery of the STRENGTHEN intervention was considered when provided in addition to usual care, and costs associated with health/social care service use and quality-adjusted life-years (QALYs) were estimated for the intervention and control groups.
Intervention and comparator
The intervention arm (see Chapter 2) received the STRENGTHEN intervention plus usual care and the control arm received usual care alone.
Perspective
We adopted the primary perspectives of the UK NHS and Personal Social Services (PSS), with broader aspects of care also reported from a societal perspective.
Time horizon
The pilot trial time horizon of 6 months’ follow-up was employed in the economic analysis, with outcome assessments at both the 3- and 6-month follow-ups.
Intervention resource use and costs
The additional (incremental) costs associated with delivery of the STRENGTHEN intervention, when added to usual care, were estimated using resource use data collected within-trial.
The health trainers who delivered the intervention kept a record of participant contact on the intervention section of the data management system on which they collated details of face-to-face, telephone, text, e-mail and letter contacts. These were grouped according to whether the contact was a predesignated intervention session, a planned contact or another form of contact. The health trainer also recorded the time spent travelling in relation to these contacts (whether or not the participant attended the appointment) and documented any additional time spent unsuccessfully attempting to contact participants.
Other resources required for the delivery of the intervention were identified via a questionnaire and discussion with the intervention developers after the intervention had been delivered. Such resources included the health trainers’ handbook, worksheets and folders for participants, training and supervision of the health trainers, and additional administrative and management activities undertaken by the health trainers and the health trainer co-ordinator. The health trainer co-ordinator prospectively recorded their time involved in intervention-related activities.
Costs were applied to the intervention resources in Great British pounds at 2017 costs. Unit cost estimates were drawn from nationally recognised, published sources (Unit Costs of Health and Social Care52,53 and NHS reference costs54,55), with the project-specific information about costs provided by those who delivered the intervention. These unit costs are set out in Table 19.
| Resource item | Unit cost (£, 2017) | Source of cost estimate | Basis of cost estimate |
|---|---|---|---|
| Health trainer time | 28 per working hour | PSSRU 2017, page 154.52 AfC band 4, annual salary £21,579a | Health trainers are expected to be employed on AfC band 4 |
| Health trainer co-ordinator time | 33 per working hour | PSSRU 2017 page 154.52 AfC band 5, annual salary £23,439 | Health trainer co-ordinators are expected to be employed on AfC band 5 |
| Health trainer handbook | 18 per handbook | Intervention providers | Production costs |
| Participants’ worksheets and folders | 5.00 per set | Intervention providers | Printing costs |
| Training | 13 per participant |
|
See Table 21 |
| Supervision | 94 per participant |
|
See Chapter 5, Supervision |
Health, social care and broader societal resource use and costs
Self-report resource use was collected via interviewer-administered questionnaires at baseline and at the 3- and 6-month follow-ups (covering the prior 2-, 3- and 3-month periods, respectively). (The first reporting time period was 2 months as, in line with the trial inclusion criteria, participants may have been in the community for only 2 months following a custodial sentence.) The questions enquired about health care, social care and other services that participants may have used, such as criminal justice and education resources, in addition to assistance provided by relatives or friends [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)].
We combined health and social care follow-up resource use data with nationally recognised, published unit costs52–55 to estimate the mean (SD) resource costs per participant. Costs were in Great British pounds at 2017 costs or adjusted for inflation if costs for 2017 were not available (Table 20).
| Resource item | Unit cost (£, 2017) | Source of cost estimate | Basis of cost estimate |
|---|---|---|---|
| Primary care | |||
| GP contacts (surgery) | 31.00 per contact | PSSRU 2017,52 page 162 | Surgery consultation of 9.22 minutes |
| GP contacts (home) | 38.76 per contact |
|
|
| GP telephone calls | 24.14 per contact |
|
|
| Practice nurse contacts (surgery) | 9.30 per contact | £36 per hour: 15.5-minute consultation | |
| Practice nurse contacts (telephone) | 7.90 per contact | PSSRU 2017,52 page 164 | £36 per hour: 6.6-minute consultation |
| Community nurse contacts (home) | 37.00 per contact | NHS Reference Costs 2016/17 54 | Community health services, district nurse, adult face to face54 |
| Community mental health nurse contacts (home) | 36.00 per contact | PSSRU 2017,52 page 159 | £36 per hour: 1-hour visit |
| Community psychiatric nurse contacts (home) | 36.00 per contact | PSSRU 2017,52 page 159 | £36 per hour: 1-hour visit |
| Counsellor contacts | 43.00 per contact | PSSRU 2017,52 page 155 | Band 6 Scientific and Professional staff, £43 per hour: 1-hour consultation |
| Physiotherapist contacts | 53.00 per contact | NHS Reference Costs 2016/17 54 | Community health services, physiotherapist, adult, one to one54 |
| Occupational therapist contacts | 77.00 per contact | NHS Reference Costs 2016/17 54 | Community health services, occupational therapist, adult, one to one54 |
| Dietitian contacts | 33.00 per contact | PSSRU 2017,52 page 155 | Band 5 Scientific and Professional staff, £33 per hour: 1-hour consultation |
| NHS Stop Smoking Services | 129.67 per intervention | PSSRU 2017,52 page 115 | Mean cost of therapies for smoking cessation |
| Alcohol services contacts | 45.00 | PSSRU 2017,52 page 63 | Alcohol health worker: 1-hour consultation |
| Drug services contacts | 134.00 | PSSRU 2017,52 page 59 | Community contact (adult) for drug services |
| Walk-in centre attendances | 42.80 |
|
|
| Secondary care | |||
| A&E visits | |||
| General A&E visits | 147.80 | NHS Reference Costs 2016/17 54 | Outpatient attendances data, A&E |
| Mental health A&E visits | 193.00 | NHS Reference Costs 2016/17 54 | Mental Health Specialist Teams, A&E Mental Health Liaison Services, Adult and Elderly |
| Day cases | 727.00 | PSSRU 2017,52 page 110 | Weighted average of all day-case stays |
| Hospital admissions | |||
| General medical admissions (nights) | 324.99 | NHS Reference Costs 2016/17 54 | Regular day or night admissions |
| Outpatient appointments | |||
| General | 137.00 | PSSRU 2017,52 page 110 | Weighted average of all outpatient attendances |
| Psychologist | 55.00 | PSSRU 2017,52 page 203 | Band 7 Scientific and Professional staff, £55 per hour: 1-hour consultation |
| Psychiatrist | 108.00 | PSSRU 2017,52 page 211 | Psychiatric consultant, £108 per hour: 1-hour consultation |
| Alcohol appointments | 45.00 | PSSRU 2017,52 page 63 | Alcohol health worker: 1-hour consultation |
| Social care | |||
| Home help/care worker contacts | 6.90 | PSSRU 2017,52 page 160 | Mean hourly cost of all home care: £18. 23-minute visit |
| Social worker contacts | 59.00 | PSSRU 2017,52 page 174 | Per hour of client-related work |
Outcomes
Our primary economic end points were costs and QALYs at the 6-month follow-up. QALYs are a commonly used summary measure of health-related quality-of-life, taking account of both quality and quantity of life,57,58 and are the metric used by the National Institute for Health and Care Excellence (NICE) when considering the cost-effectiveness of interventions across a broad range of health and social care contexts. 59 We estimated QALYs over the 6-month trial follow-up using the EQ-5D-5L trial data and applying the internationally recognised ‘cross-walk’ algorithm60 to provide QALY weights from a UK general population survey to value the EQ-5D-3L (EuroQol-5 Dimensions, three-level version) health states. 61 This methodological approach adheres to the current ‘position statement’ of NICE regarding use of the EQ-5D-5L. 62
Given the uncertainty of the appropriateness of the EQ-5D-5L for this population, we also used trial data from the SF-36 to estimate QALYs using the SF-6D. 63
Analysis
Intervention resource use and costs
We calculated quantities (mean and SD) of each component of resource use, applied unit costs to these data (means and SDs), and estimated the mean (SD) cost per participant for the intervention.
Health, social care and broader societal resource use and costs
We calculated the mean (SD) resource use, by item, at baseline and for resource use reported at the 3- and 6-month assessments. Unit costs were applied to the disaggregated health/social care data over the period of the 6-month follow-up, and the mean (SD) cost for each of these items was calculated, by treatment arm. Costs of resource use were then calculated for the following subcategories by treatment group: primary care, secondary care and social care.
Outcome data
We derived QALY estimates, for both the EQ-5D-5L and the SF-6D, using data from the baseline, 3-month and 6-month assessments, applying the area-under-the-curve approach, a recognised method for assessing repeated-measures data, and specifically recommended for cost-effectiveness analyses. 57
Results
Resource requirements and cost of the STRENGTHEN intervention
Sixty-one people were provided with the STRENGTHEN intervention. This included 20 from the centre in Manchester, 23 from the Plymouth CRC and 18 from the Plymouth NPS. The resources used to provide the intervention, and their quantities and costs, are detailed in Tables 21–24.
| Resource item | Unit cost (£, 2017) | Source of cost estimate | Cost (£, 2017) |
|---|---|---|---|
| Trainer’s time: one experienced health trainer for 3 days | 33 per working hour | PSSRU 2017,52 page 154. Agenda for Change band 5, annual salary £23,439 | 693 |
| Service user consultant: half a day | 10 per hour | Intervention providers | 35 |
| Trainer and service user consultant travel expenses | 10 each, per day | Intervention providers | 40 |
| Approximate cost to train a health trainer | 384 | ||
| Approximate cost per participant | £384 to train a health trainer who is retained for approximately 2 years, during which time they work with approximately 30 people: £384 ÷ 30 = £12.80 | 13 |
| Resource item | Basis of resource use estimate |
|---|---|
| Health trainer handbook | One per eight participants (one handbook per health trainer, seven health trainers, 61 participants) |
| Participant worksheets and folder | One set per participant |
| Training | As described in Table 21 |
| Supervision | As described in Chapter 5, Supervision |
| Additional health trainer co-ordinator time |
|
| Additional health trainer time |
|
| Health trainer time | n (%) | Number of contacts | |||
|---|---|---|---|---|---|
| Mean | SD | Minimum | Maximum | ||
| Intervention sessions (N = 61) | |||||
| Face to face | 41 (72.1) | 2.90 | 2.81 | 0 | 11 |
| Telephone | 15 (24.6) | 0.82 | 1.74 | 0 | 8 |
| Contacts (N = 61) | |||||
| Face to face | 7 (11.5) | 0.11 | 0.32 | 0 | 1 |
| Telephone | 60 (98.4) | 7.80 | 6.24 | 0 | 32 |
| Text | 57 (93.4) | 15.39 | 11.58 | 0 | 56 |
| 15 (24.6) | 0.90 | 2.99 | 0 | 21 | |
| Letter | 16 (26.2) | 0.28 | 0.49 | 0 | 2 |
| Unsuccessful contact attempts | 7 (11.5) | 0.21 | 0.76 | 0 | 5 |
| Other (N = 61) | |||||
| Face to face | 5 (8.2) | 0.08 | 0.28 | 0 | 1 |
| Telephone | 21 (34.4) | 0.70 | 1.19 | 0 | 5 |
| Text | 6 (9.8) | 0.11 | 0.37 | 0 | 2 |
| 23 (37.7) | 1.34 | 2.39 | 0 | 9 | |
| Unsuccessful contact attempts | 31 (50.8) | 3.28 | 5.82 | 0 | 23 |
| Total time per participant (minutes) (N = 61) | |||||
| Intervention sessions | |||||
| Face to face | 136.21 | 153.17 | 0 | 855 | |
| Telephone | 26.28 | 71.67 | 0 | 445 | |
| Contacts | |||||
| Face to face | 0.69 | 2.62 | 0 | 15 | |
| Telephone | 14.20 | 17.83 | 0 | 101 | |
| Text | 12.31 | 12.73 | 0 | 51 | |
| 1.92 | 6.56 | 0 | 45 | ||
| Letter | 3.13 | 7.31 | 0 | 30 | |
| Unsuccessful contact attempts | 0.16 | 0.76 | 0 | 5 | |
| Other | |||||
| Face to face | 2.23 | 15.37 | 0 | 120 | |
| Telephone | 2.11 | 4.77 | 0 | 25 | |
| Text | 0.18 | 0.81 | 0 | 6 | |
| 1.97 | 4.02 | 0 | 22 | ||
| Unsuccessful contact attempts | 8.39 | 20.94 | 0 | 120 | |
| Total travel time per participant (minutes) (n = 61) | |||||
| Intervention sessions | |||||
| Face to face | 94.67 | 104.21 | 0 | 420 | |
| Planned face to face, but participant did not attenda | 0.33 | 2.56 | 0 | 20 | |
| Contacts | |||||
| Face-to-face | 1.31 | 5.91 | 0 | 30 | |
| Planned face to face, but participant did not attenda | 24.39 | 47.73 | 0 | 215 | |
| Other | |||||
| Face-to-face | 1.80 | 9.92 | 0 | 60 | |
| Planned face to face, but participant did not attenda | 1.20 | 5.51 | 0 | 30 | |
| Resource item | Cost per participant (£, 2017) | |||
|---|---|---|---|---|
| Mean | SD | Minimum | Maximum | |
| Health trainer handbook | 2.25 | |||
| Worksheets and folders | 5.00 | |||
| Health trainer training | 12.80 | |||
| Health trainer supervision | 93.72 | |||
| Additional health trainer co-ordinator time | 58.58 | |||
| Additional health trainer time | 19.88 | |||
| Health trainer time | ||||
| Intervention sessions | ||||
| Face to face | 63.57 | 71.48 | 0 | 399.00 |
| Telephone | 12.26 | 33.45 | 0 | 207.67 |
| Contacts | ||||
| Face to face | 0.32 | 1.22 | 0 | 7.00 |
| Telephone | 6.63 | 8.32 | 0 | 47.13 |
| Text | 5.75 | 5.94 | 0 | 23.80 |
| 0.90 | 3.06 | 0 | 21.00 | |
| Letter | 1.46 | 3.41 | 0 | 14.00 |
| Unsuccessful contact attempts | 0.08 | 0.35 | 0 | 2.33 |
| Other | ||||
| Face to face | 1.04 | 7.17 | 0 | 56.00 |
| Telephone | 0.99 | 2.23 | 0 | 11.67 |
| Text | 0.08 | 0.38 | 0 | 2.80 |
| 0.92 | 1.87 | 0 | 10.27 | |
| Unsuccessful contact attempts | 3.92 | 9.77 | 0 | 56.00 |
| Total costs of health trainer time | 97.90 | 88.72 | 0.47 | 417.67 |
| Health trainer travel time | ||||
| Intervention sessions | ||||
| Face to face | 44.18 | 48.63 | 0 | 196.00 |
| Planned face to face, but participant did not attenda | 0.15 | 1.20 | 0 | 9.33 |
| Contacts | ||||
| Face to face | 0.61 | 2.76 | 0 | 14.00 |
| Planned face to face, but participant did not attenda | 11.38 | 22.27 | 0 | 100.33 |
| Other | ||||
| Face to face | 0.84 | 4.63 | 0 | 28.00 |
| Planned face to face, but participant did not attenda | 0.56 | 2.57 | 0 | 14.00 |
| Total costs of health trainer travel time | 57.73 | 52.34 | 0 | 196.00 |
| Total mean cost per participant | 347.86 | 128.44 | 192.70 | 805.90 |
Health trainer time
The mean cost for health trainers’ time in contact and non-contact activities in relation to participants was £98 (SD £89). They spent a mean of 136 (SD 153) minutes providing face-to-face intervention sessions per participant, and a mean of 26 (SD 71) minutes providing telephone sessions. They spent an additional mean of 14 (SD 18) minutes and 12 (SD 13) minutes contacting participants by telephone and text, respectively. Health trainers spent an average of 9 minutes per participant making unsuccessful contact attempts.
Health trainers’ travel time cost a mean of £58 (SD £52) per participant. This was mainly accounted for by the mean cost of £44 (SD £49) to travel to meet participants for face-to-face intervention sessions, although it is of note that the estimated average cost of health trainers travelling to meet participants who did not attend the appointment was £12 per participant. Health trainer mileage rates were not included in the estimate of the cost of the intervention as they are included in the overhead costs of the unit cost of health trainer time.
Training
Based on data provided by the intervention developers, and the future potential implementation of the intervention in practice, we assumed the following resource requirements for training health trainers: a health trainer co-ordinator for 3 days, a service user consultant for half a day, travel expenses, venue costs for the provision of the training and consumables (e.g. handouts).
The estimated costs associated with these resources were £693, £35 and £40 for the health trainer co-ordinator, the service user consultant and travel expenses, respectively, with venue and consumable costs being covered in the overhead costs of the health trainer co-ordinator’s hourly rate. In addition, we did not include health trainers’ time in the training costs, as we assumed that this would be included in the overhead costs component of their hourly rate, as described in the Unit Costs of Health and Social Care 2017. 52
These figures equated to approximately £768 for a training ‘block’ (see Table 21). We assumed that at least two people would be trained concurrently, resulting in a cost to train each health trainer of approximately £384. The model used in the pilot suggests that pairs of health trainers would manage a caseload of approximately 30 people per centre, per year. Assuming that health trainers were retained in post for 2 years, this implied a training cost attributable to each participant of approximately £12.80.
Supervision
Supervision was provided by a health trainer co-ordinator and, if implemented in practice, would be expected to take a form similar to approximately 1 hour of contact per health trainer per week, to include check-in, debriefing and any group supervision. This equated to approximately 2 hours of the health trainer co-ordinator’s time per week (assuming two health trainers per centre). Based on an approximate caseload of 30 people per centre, per year, and an estimated working time for the health trainer co-ordinator of 42.6 weeks per year,52 this implied a supervision cost attributable to each participant of approximately £93.72. The costs of health trainers’ time were not included in the supervision costs as these were included in the overhead costs of their hourly rate.
Additional intervention costs
Additional intervention costs were the health trainer co-ordinator’s time spent in other administrative/management activities (approximately £59 per participant), health trainers’ time in other discussions with the co-ordinator (£20 per participant), health trainer handbooks (£2.25 per participant) and participant worksheets/folders (£5).
Health and social care resource use and costs
Table 25 presents quantities of resources used from the primary economic perspective of the NHS/PSS, across the 6-month follow-up, described by treatment arm. These resources are disaggregated by item and grouped as primary care, secondary care and social care services. Table 26 presents the costs associated with this disaggregated resource use. Total NHS/PSS costs were £773 in the control group and £585 in the intervention group. The largest contributors to overall costs were general practitioner (GP) surgery appointments, counselling sessions, community drug or alcohol services, hospital day cases and social worker contacts. Tables 36–38 in Appendix 4 present the health and social care resource use of the intervention and control groups.
| Resource item | Intervention group | Control group | ||
|---|---|---|---|---|
| n (%) | Mean (SD) [range] | n (%) | Mean (SD) [range] | |
| Primary care services | 29 | 29 | ||
| GP at surgery/health centre | 18 (62.07) | 2.44 (3.11) [0–12] | 22 (75.86) | 2.75 (2.32) [0–8] |
| GP via telephone | 8 (27.59) | 1.00 (2.47) [0–10] | 9 (31.03) | 1.17 (2.40) [0–9] |
| GP at home | 0 | 0 | 0 | 0 |
| Practice nurse at surgery/health centre | 9 (31.03) | 0.51 (0.98) [0–4] | 9 (31.03) | 0.89 (1.63) [0–5] |
| Practice nurse via telephone | 1 (3.45) | 0.03 (0.18) [0–1] | 1 (3.45) | 0.03 (0.18) [0–1] |
| Practice nurse at home | 0 | 0 | 1 (3.45) | 0.06 (0.37) [0–2] |
| Community mental health nurse | 3 (10.34) | 0.55 (2.59) [0–14] | 3 (10.34) | 0.34 (1.07) [0–4] |
| Community psychiatric nurse | 3 (10.34) | 0.17 (0.53) [0–2] | 6 (20.69) | 0.37 (0.94) [0–4] |
| Physiotherapist at surgery/health centre | 0 | 0 | 2 (6.9) | 0.20 (0.81) [0–4] |
| Physiotherapist at home | 0 | 0 | 0 | 0 |
| Occupational therapist at surgery/health centre | 0 | 0 | 0 | 0 |
| Occupational therapist at home | 0 | 0 | 0 | 0 |
| Dietitian | 0 | 0 | 1 (3.45%) | 0.03 (0.18) [0–1] |
| Counsellor | 7 (24.14) | 1.65 (4.22) [0–19] | 7 (24.14) | 1.75 (4.01) [0–14] |
| NHS Stop Smoking Servicesa | 1 (3.57) | 0.13 (0.74) [0–4] | 3 (10.34) | 0.31 (1.16) [0–6] |
| Alcohol services – community | 2 (6.9) | 0.51 (1.97) [0–9] | 5 (17.24) | 1.65 (4.32) [0–18] |
| Drug services – community | 4 (13.79) | 0.72 (2.37) [0–12] | 2 (6.9) | 0.34 (1.31) [0–6] |
| Walk-in-centre | 0 | 0 | 1 (3.45) | 0.03 (0.18) [0–1] |
| Secondary care services | 30 | 29 | ||
| A&E visits | ||||
| General A&E visits | 3 (10) | 0.10 (0.31) [0–1] | 3 (10.34) | 0.13 (0.44) [0–2] |
| Mental health A&E visits | 1 (3.33) | 0.03 (0.18) [0–1] | 1 (3.45) | 0.06 (0.37) [0–2] |
| Day cases | 2 (6.67) | 0.1 (0.40) [0–2] | 4 (13.79) | 0.34 (1.04) [0–4] |
| Hospital admissions | ||||
| General medical admissions | 2 (6.67) | 0.16 (0.74) [0–4] | 0 | 0 |
| ICU admissions | 0 | 0 | 0 | 0 |
| Alcohol services admissions | 0 | 0 | 0 | 0 |
| Drug services admissions | 0 | 0 | 0 | 0 |
| Outpatient appointments | ||||
| General appointments | 7 (23.33) | 0.3 (0.59) [0–2] | 5 (17.24) | 0.31 (0.84) [0–4] |
| Psychologist appointments | 0 | 0 | 0 | 0 |
| Psychiatrist appointments | 0 | 0 | 2 (6.9) | 0.13 (0.58) [0–3] |
| Talking therapy appointments | 0 | 0 | 0 | 0 |
| Mental health clinic appointments | 0 | 0 | 0 | 0 |
| Alcohol appointments | 0 | 0 | 0 | 0 |
| Drug services appointments | 0 | 0 | 0 | 0 |
| Criminal justice liaison appointments | 0 | 0 | 0 | 0 |
| Social care services | 29 | 29 | ||
| Social worker | 7 (24.14) | 0.93 (2.56) [0–12] | 4 (13.79) | 0.93 (3.21) [0–13] |
| Home help/care worker | 1 (3.45) | 0.03 (0.18) [0–1] | 1 (3.45) | 0.34 (1.85) [0–10] |
| Resource item | Intervention group | Control group | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Primary care services | ||||
| GP at surgery/health centre | 29 | 75.90 (96.47) [0–372] | 29 | 85.52 (72.06) [0–248] |
| GP via telephone | 29 | 24.14 (59.83) [0–241] | 29 | 28.3 (58.09) [0–217] |
| GP at home | 29 | 0 | 29 | 0 |
| Practice nurse at surgery/health centre | 29 | 4.81 (9.17) [0–37] | 29 | 8.34 (15.19) [0–47] |
| Practice nurse via telephone | 29 | 0.27 (1.47) [0–8] | 29 | 0.27 (1.47) [0–8] |
| Practice nurse at home | 29 | 0 | 29 | 2.55 (13.74) [0–74] |
| Community mental health nurse | 29 | 19.86 (93.57) [0–504] | 29 | 12.41 (38.82) [0–144] |
| Community psychiatric nurse | 29 | 6.21 (19.41) [0–72] | 29 | 13.66 (33.9) [0–144] |
| Physiotherapist at surgery/health centre | 29 | 0 | 29 | 10.97 (43.38) [0–212] |
| Physiotherapist at home | 29 | 0 | 29 | 0 |
| Occupational therapist at surgery/health centre | 29 | 0 | 29 | 0 |
| Occupational therapist at home | 29 | 0 | 29 | 0 |
| Dietitian | 29 | 0 | 29 | 1.14 (6.13) [0–33] |
| Counsellor | 29 | 71.17 (181.81) [0–817] | 29 | 75.62 (172.63) [0–602] |
| NHS Stop Smoking Services | 28 | 4.63 (24.51) [0–130] | 29 | 13.41 (40.19) [0–130] |
| Alcohol services – community | 29 | 23.28 (88.88) [0–405] | 29 | 74.48 (194.4) [0–810] |
| Drug services – community | 29 | 97.03 (318.1) [0–1608] | 29 | 46.21 (176.45) [0–804] |
| Walk-in-centre | 29 | 0 | 29 | 1.48 (7.95) [0–43] |
| Primary care subtotal | 28 | 334.64 (526.06) [0–2124] | 29 | 374.35 (402.95) [0–1353] |
| Secondary care | ||||
| General appointments | 30 | 41.10 (81.65) [0–274] | 29 | 42.52 (116.38) [0–548] |
| Psychologist appointments | 30 | 0 | 29 | 0 |
| Psychiatrist appointments | 30 | 0 | 29 | 14.9 (62.74) [0–324] |
| Alcohol appointments | 30 | 0 | 29 | 0 |
| General medical admissions | 30 | 54.17 (242.65) [0–1300] | 29 | 0 |
| Day cases | 30 | 72.7 (292.67) [0–1454] | 29 | 250.69 (759.4) [0–2908] |
| General A&E visits | 30 | 14.78 (45.1) [0–147.8] | 29 | 20.39 (65.2) [0–296] |
| Mental health A&E visits | 30 | 6.43 (35.24) [0–193] | 29 | 13.31 (71.68) [0–386] |
| Secondary care subtotal | 30 | 189.18 (445.48) [0–1728] | 29 | 341.8 (877.56) [0–3456] |
| Social care services | ||||
| Social worker | 29 | 54.93 (151.19) [0–708] | 29 | 54.93 (189.83) [0–767] |
| Home help/care worker | 29 | 0.24 (1.28) [0–7] | 29 | 2.38 (12.81) [0–69] |
| Social care subtotal | 29 | 55.17 (151.68) [0–708] | 29 | 57.31 (199.27) [0–836] |
| Total cost to NHS and PSS (excluding intervention cost) | 28 | 584.69 (774.66) [0–2832] | 29 | 773.46 (995.74) [0–3707] |
Details of NHS and social care resource use and costs for the 2 months prior to baseline, and separately at the 3- and 6-month follow-up assessments, for the intervention and control groups, are given in Appendix 5 (see Tables 39–41) and Appendix 6 (see Tables 42–44).
Broader societal resource use
Table 27 gives details of broader societal resources that intervention and control group participants reported using over the 6 months of follow-up. These items are disaggregated and grouped by education services, other services and informal care. Appendix 6 provides additional details of use of these resources in the 2 months prior to the baseline assessment, and separately for the 3- and 6-month follow-ups. Similar patterns of resource use were apparent in the intervention and control groups at baseline and at follow-up.
| Resource item | Intervention group | Control group | ||
|---|---|---|---|---|
| n (%) | Mean (SD) [range] | n (%) | Mean (SD) [range] | |
| Other service providers (e.g. criminal justice, employment, education services) | 30 | 29 | ||
| Probation worker | 26 (86.67) | 5.56 (4.44) [0–19] | 25 (86.21) | 6.93 (6.12) [0–27] |
| Community rehabilitation worker | 8 (26.67) | 0.93 (1.68) [0–6] | 6 (20.69) | 1.17 (3.21) [0–16] |
| Employment worker/officer | 2 (6.67) | 0.16 (0.74) [0–4] | 0 (0) | 0 (0) [0–0] |
| Citizen’s Advice Bureau | 0 | 0 | 1 (3.45) | 0.03 (0.18) [0–1] |
| Job centre | 12 (40) | 2.83 (5.33) [0–20] | 11 (37.93) | 2.06 (3.65) [0–12] |
| Enhanced Thinking Skills | 0 | 0 | 0 | 0 |
| Cognitive Skills Booster | 0 | 0 | 0 | 0 |
| Cognitive Self-Change Programme | 0 | 0 | 0 | 0 |
| Police custody | 3 (10) | 0.20 (0.66) [0–3] | 1 (3.45) | 0.03 (0.18) [0–1] |
| Focus on Resettlement | 0 | 0 | 0 | 0 |
| Solicitor/lawyer | 4 (13.33) | 0.33 (0.95) [0–4] | 4 (13.79) | 0.20 (0.61) [0–3] |
| Barrister | 1 (3.33) | 0.06 (0.36) [0–2] | 0 | 0 |
| Legal advocate | 1 (3.33) | 0.03 (0.18) [0–1] | 0 | 0 |
| Informal care from relatives and friends | 30 | 29 | ||
| Hours per week | 10 (33.33) | 1.75 (3.79) [0–16] | 10 (34.48) | 1.82 (4.80) [0–24] |
| Days taken off work | 2 (6.67) | 0.20 (0.80) [0–4] | 2 (6.9) | 0.06 (0.37) [0–2] |
Outcomes
Quality-adjusted life-years
Table 28 reports EQ-5D-5L health state values at baseline and at the 3- and 6-month follow-ups, and QALYs based on the EQ-5D-5L values, for the intervention and control groups. The intervention group had slightly lower mean EQ-5D-5L health state values at baseline, with an increase in values at the 3- and 6-month follow-ups. The EQ-5D-5L data showed a minimal difference in QALYs in favour of the intervention group over the 6 months of follow-up.
| Measure: time point | Intervention group | Control group | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| EQ-5D-5L: baseline | 60 | 0.667 (0.288) [–0.158 to 1] | 59 | 0.685 (0.243) [0.007 to 1] |
| EQ-5D-5L: month 3 | 34 | 0.760 (0.267) [0.083 to 1] | 38 | 0.743 (0.284) [–0.087 to 1] |
| EQ-5D-5L: month 6 | 39 | 0.768 (0.255) [–0.162 to 1] | 32 | 0.765 (0.238) [0.088 to 1] |
| EQ-5D-5L QALYs (6 months) | 29 | 0.358 (0.121) [0.116 to 0.5] | 29 | 0.354 (0.122) [0.015 to 0.5] |
| SF-6D: baseline | 59 | 0.681 (0.138) [0.355 to 0.943] | 58 | 0.654 (0.152) [0.362 to 1] |
| SF-6D: month 3 | 32 | 0.753 (0.156) [0.473 to 1] | 37 | 0.719 (0.155) [0.37 to 1] |
| SF-6D: month 6 | 39 | 0.753 (0.158) [0.491 to 1] | 30 | 0.696 (0.186) [0.301 to 1] |
| SF-6D QALYs (6 months) | 26 | 0.376 (0.065) [0.262 to 0.475] | 26 | 0.345 (0.078) [0.175 to 0.494] |
When the SF-6D was used to estimate QALYs, a greater difference was found in favour of the intervention group, but the groups differed in their SF-6D scores at baseline.
Data completeness
Follow-up rates
Table 29 presents the numbers and proportions of participants who provided follow-up data, grouped by intervention and control groups. The proportion of participants who provided data at baseline and at the 3-and 6-month follow-up points (49%) was the same in the two groups. But, overall, 60% of participants completed baseline and 3 months, and 60% completed baseline and 6 months (see Appendix 3, Table 35, for completion rates for a selection of secondary outcomes, with 95% CIs).
| Group | n | Follow-up behaviour | n | % |
|---|---|---|---|---|
| Intervention group | 61 | Both follow-ups completed | 30 | 49 |
| Month 3 only completed | 4 | 7 | ||
| Month 6 only completed | 10 | 16 | ||
| No follow-up data | 17 | 28 | ||
| Control group | 59 | Both follow-ups completed | 29 | 49 |
| Month 3 only completed | 9 | 15 | ||
| Month 6 only completed | 3 | 5 | ||
| No follow-up data | 18 | 31 | ||
| All participants | 120 | Both follow-ups completed | 59 | 49 |
| Month 3 only completed | 13 | 11 | ||
| Month 6 only completed | 13 | 11 | ||
| No follow-up data | 35 | 29 |
Missing resource use data
Among those who provided data at baseline and at the 3-month follow-up, rates of missing data for individual resource use items were very low. There were no missing data among those who provided data at the 6-month follow-up.
The largest number of missing data was among primary care and social care services. One participant in the intervention group did not complete this section of the CRF for the 3-month follow-up; other than this, primary and social care data for this period were complete. The extent of missing primary care resource use data at baseline is presented in Table 30. This suggests that some participants and/or interviewers were not clear about the definition of ‘walk-in centres’.
| Resource item | Intervention (n) | Control (n) |
|---|---|---|
| Primary care services – baseline | ||
| GP at surgery/health centre | Complete | Complete |
| GP via telephone | Complete | Complete |
| GP at home | 1 | Complete |
| Practice nurse at surgery/health centre | 1 | Complete |
| Practice nurse via telephone | 2 | Complete |
| Practice nurse at home | 1 | Complete |
| Community mental health nurse | 1 | Complete |
| Community psychiatric nurse | 1 | Complete |
| Physiotherapist at surgery/health centre | 1 | Complete |
| Physiotherapist at home | 1 | Complete |
| Occupational therapist at surgery/health centre | 1 | Complete |
| Occupational therapist at home | 1 | Complete |
| Dietitian | 1 | Complete |
| Counsellor | 1 | Complete |
| NHS Stop Smoking Services | 1 | Complete |
| Alcohol services – community | 1 | Complete |
| Drug services – community | 1 | 1 |
| Walk-in-centre | 2 | 3 |
| Other | Complete | Complete |
| Social care services – baseline | ||
| Social worker | 1 | Complete |
| Home help/care worker | 1 | 1 |
| Outcome data | ||
| EQ-5D-5L: baseline | 1 | Complete |
| EQ-5D-5L: month 3 | Complete | Complete |
| EQ-5D-5L: month 6 | 1 | Complete |
| EQ-5D-5L QALYs (6 months) | 1 | Complete |
| SF-6D: baseline | 2 | 1 |
| SF-6D: month 3 | 2 | 1 |
| SF-6D: month 6 | 1 | 2 |
| SF-6D QALYs (6 months) | 4 | 3 |
All secondary care data were complete for baseline and both follow-up periods, with the exception of one missing data point in the intervention and one in the control group at baseline for day cases. All data on education and other services were complete at baseline and follow-up. All data on help from relatives and friends were complete, with the exception of one missing data item in the intervention group at the 3-month follow-up, for days taken off work.
Missing outcome data
Table 30 also shows the extent of missing data for the EQ-5D-5L and SF-6D. We might expect a higher rate of missing data for the EQ-5D-5L and SF-6D than for the resource use items, because these instruments require respondents to answer a number of questions in order to produce a health state value. Missing data for any one of these constituent questions will result in a missing health state value. Completeness of data for the EQ-5D-5, however, was no different from completeness of the resource use data, with only one missing value for the intervention group at baseline and at the 6-month follow-up; data for the control group and for the intervention group at the 3-month follow-up were complete. There were slightly more missing data for the SF-6D, although there were only one or two observations missing from each group at each time point.
Discussion
To the best of our knowledge, this is the first report of a pilot trial of the effectiveness and cost-effectiveness of a health trainer-led motivational intervention for people under community supervision in the UK. As part of this pilot, we have estimated the resource use and costs associated with the delivery of the STRENGTHEN intervention, and considered, developed and tested economic evaluation methods for the collection of resource use and cost and outcome data for a future, policy-relevant, full cost-effectiveness analysis alongside a definitive RCT.
The cost of the STRENGTHEN intervention
We estimated the mean cost of the STRENGTHEN intervention to be approximately £348 (SD £128) per participant. The main cost drivers for the intervention, determined by data prospectively collected using health trainer/participant contact sheets, activity logs of the health trainer co-ordinator and a questionnaire for completion by the intervention providers, were: (1) staff time of the health trainers and the health trainer co-ordinator and (2) supervision of the health trainers.
Supervision of the health trainers cost approximately £94 per participant, and involved approximately 1 hour of contact between the health trainer co-ordinator and each health trainer per week. This degree of supervision and support is considered imperative for the nature of the intervention, working with this population under community supervision, and would probably be replicated in a definitive trial and if, longer-term, the intervention is implemented more widely. In other work involving health trainer support for reducing smoking, we have managed to create a more cost-effective supervision process with shared virtual sessions involving up to eight health trainers across four sites. In a full STRENGTHEN study, we would therefore expect to reduce supervision costs with an economy of scale.
Costs for training the health trainers amounted to approximately £13 per participant, but there were significant uncertainties regarding the resource requirements for training and the allocation of costs across caseload, given the high staff turnover in the pilot. It is anticipated that the cost of training would be reduced in a larger trial, and if the intervention is shown to be effective and cost-effective and is put into practice across the UK. Economies of scale might mean that more health trainers could be trained simultaneously. With implementation, a more formalised training programme might be established, for example in relation to a City and Guilds qualification. A further developed training approach would affect resource requirements and costs of the intervention, and would warrant additional consideration and investigation in the context of a definitive trial.
It is notable that it cost approximately £12 per participant in health trainers’ time travelling to meet participants who did not attend appointments. It may be that this is a realistic component of providing an intervention to this population. The tenacity of health trainers in repeated attempts to contact and support participants may be an important feature in contributing to the potential effectiveness and cost-effectiveness of the intervention.
The estimated cost of the STRENGTHEN intervention is greater than that of the health trainer intervention provided in the Exercise Assisted Reduction then Stop (EARS) pilot study (£192). 35 This difference in cost appears largely attributable to more time spent training, supervising and supporting health trainers in the STRENGTHEN trial. This is a necessary requirement for the health trainers to be appropriately skilled and supported given the focus in the STRENGTHEN trial on a broader range of health behaviours and well-being and the greater need to build trust and rapport in the first session before moving on to behaviour change.
A future full trial and cost-effectiveness analysis could usefully consider other aspects of the structure of the intervention that might alter if it were to be implemented in practice, and how this might affect resource requirements and their costs. Such differences could be planned for in sensitivity analyses in a definitive cost-effectiveness analysis. For example, in examining the association between intervention engagement and WEMWBS scores at follow-up (see Chapter 4), it appeared that the scores were greater for those who attended 2–5 sessions rather than more (or fewer). Limiting the number of sessions to no more than five may help reduce the intervention cost.
Health/social care resource use and costs
The pilot found a lesser cost of health/social care resource use (excluding the intervention) in the intervention group over the 6 months of follow-up. When the cost of the intervention was also considered, the incremental cost in the intervention group was greater than that of the control group (over the 6-month follow-up period). However, differences in health/social care resource use were largely accounted for by a small number of costly drivers (e.g. hospital day cases) and the groups also differed in the cost of their resource use in the 2 months prior to baseline. The groups may, therefore, have been imbalanced at baseline, and the small sample size susceptible to the effect of a limited number of outliers and costly resource events.
Outcomes
At the 6-month follow-up, the intervention group had higher WEMWBS scores, more QALYs based on the SF-6D and marginally more QALYs based on the EQ-5D-5L; however, the pattern of scores at baseline indicated that the intervention group had higher SF-6D health state values, but poorer EQ-5D-5L and WEMWBS scores.
Learning from the pilot for a full cost-effectiveness analysis alongside a definitive trial
There are many learning points from this pilot for a future cost-effectiveness analysis, the most important of which are as follows.
Costing the intervention
The prospectively collected data regarding health trainer contacts with participants required some clarification. Contact information was captured by health trainers on the data management system. This included key information on the time that health trainers spent in contact and non-contact activities with participants. As the trial progressed, the health trainers deviated from this format and collected additional information. This provided further contextual information regarding the intervention, but lacked some specificity. For example, the distinction between ‘contacts’ and ‘other’ was somewhat unclear, and the fact that telephone calls, texts and e-mails could have travel time attributed to them required explanation (health trainers had travelled to meet participants who did not attend the appointment, resulting in the health trainer contacting them by alternative means). A future economic evaluation should use a brief, straightforward contact sheet with unambiguous instructions for its completion.
Resource use
The resource use questionnaire was developed with the involvement of individuals under community supervision. This application of public involvement64 should have served to make the resource use questions as relevant and accessible to the population as possible. However, there was a fairly large number of ‘other’ responses in terms of the health and social care resources that people used, particularly in relation to education, criminal justice and other services, but no consistent groupings for these ‘other’ responses were apparent. Steps might be usefully taken to elucidate any specific other key resources to enquire about in a main trial, particularly if a wider-reaching, broader societal perspective is to be adopted in sensitivity analyses. This said, it may be possible to ‘cost’ such data only if methodologically reliable unit costs for such resources can be identified. Our scoping searches have not identified rigorous, transparently devised unit costs for all the resource items currently included under this broader perspective.
There were issues with the quality of the data collected on participants’ use of medications, which arose in part because of the practice of recording these data as free text (see Appendix 7, Table 45). For the main study, we recommend identifying a manageable number (a maximum of 10) of medications that are frequently used by this population, and collecting data on the use of these drugs in a more structured format. This could also be tied into plans for improving the collection of data on illicit drug use.
Quality-adjusted life-years measures
The profile of health state values differed for the intervention and control groups across the three assessment points dependent on whether the EQ-5D-5L or the SF-6D was used for the estimation of QALYs. This may imply greater relevance and/or responsiveness of one of the measures over the other for use with this population. The EQ-5D-5L is the QALY measure preferred by NICE for use in cost-effectiveness analyses,59 but given the different pattern of responses compared with the SF-6D, we would continue to use the SF-36 in a definitive trial, and analyse SF-6D QALY data in a sensitivity analysis.
The WEMWBS had excellent data quality, with no missing data points. As research plans are under way to produce QALY weights for the WEMWBS (Stavros Petrou, UK Health Economists’ Study Group meeting, Bristol, June 2018, personal communication), this would indicate including the measure in a definitive trial of the effectiveness and cost-effectiveness of the intervention.
Baseline assessments and covariates
The differences between the groups in resource use costs and outcome scores at baseline highlight the importance of following the recommendation for full cost-effectiveness analyses of adjusting for baseline costs/outcome scores with the use of regression analyses. 58 In addition, key baseline covariates would be accounted for, with good practice being to account for covariates consistent with those used for the effectiveness analyses.
Data completeness
The follow-up rates were higher for the economic outcome measures than for the resource use questionnaire, a finding not usual in the collection of economic evaluation data. 65 Of specific note is that the pilot data were characterised by very little ‘missingness’, that is the measures relevant to the economic evaluation that were completed at follow-up were comprehensively completed with very few missing data points. This was particularly significant for the responses to the resource use questionnaire, given that such questionnaires often suffer from poor response rates and patchy completion. 65 The mode of interviewer administration is very likely to be a contributing factor to this provision of ‘complete’ data. 66 We would strongly advise retaining this mode of administration in a future definitive trial, particularly given the difficulties of retaining contact and response with this population.
Development of an economic evaluation framework for a definitive trial
In addition to our learning described above, for a future full economic evaluation and cost-effectiveness analysis we would follow good practice guidelines67 and national policy guidance. 59 Our base-case approach of an NHS/PSS perspective follows the methodological guidance for cost-effectiveness analyses set out by the NICE,59 and a broader societal perspective will be further explored in future sensitivity analyses, as recommended by the second panel on cost-effectiveness. 68
For the full trial, we will assess the cost-effectiveness of the STRENGTHEN intervention in relation to the threshold of £20,000 to £30,000 per QALY used by NICE for recommending treatments or interventions for funding in the NHS. 59 Our primary economic analysis will estimate mean costs and mean QALYs by treatment allocation, and estimate differences between groups over the follow-up period. We will calculate incremental costs and incremental effects, and combine these to present incremental cost-effectiveness ratios (ICERs), to enable decision-makers to assess value for money using cost-per-QALY estimates [ICER = (costSTRENGTHEN – costusual care)/(QALYSTRENGTHEN – QALYusual care)].
To present the level of uncertainty regarding the cost-effectiveness estimates, we will use the cost-effectiveness plane to present combinations of incremental costs and incremental QALYs from bootstrap replicates. We will also use the cost-effectiveness acceptability curve (CEAC),69 with the net benefit statistic [(incremental QALYs × willingness to pay per QALY) – incremental cost],58 to present the probability that the STRENGTHEN intervention is cost-effective (i.e. incremental net benefit statistic is > 0), against a range of potential cost-effectiveness thresholds.
We will analyse the data on an intention-to-treat basis and, as the follow-up period will not be > 12 months, no discounting of future costs or outcomes will be undertaken. We will explore the extent of missing data, with the intention of using regression-based multiple imputation as required in sensitivity analyses.
Conclusion
The successful completion of this pilot implies the feasibility of conducting a larger definitive trial with full cost-effectiveness analysis. Piloting the framework for a future economic evaluation via the collection of intervention resource use and cost data; data on health, social care and broader societal resource use; data on the potential primary outcome measure for the trial; and policy-relevant QALY outcome measures has led to a number of specific indications for how to structure and conduct such a cost-effectiveness analysis of the STRENGTHEN intervention.
Chapter 6 Process evaluation
Introduction
This chapter focuses on the assessment of the acceptability and feasibility of the intervention, the trial methods and any potential adaptations indicated. We have included the perspectives of the participants (control and intervention), STRENGTHEN health trainers and the offender managers who worked with the researchers. The findings are presented for each method of data collection, brought together in a case study and then summarised with regard to our stated aims.
Aims
The aims of the process evaluation were to:
-
assess whether or not the intervention was being delivered as per the manual and training
-
ascertain components of the intervention that are critical to delivery
-
explore reasons for divergence from delivery of the intervention as manualised
-
understand when context is moderating delivery
-
understand the experience and motivation of participants in the control arm of the pilot in order to maximise retention in a full trial
-
explore reasons for declining to participate in the trial
-
explore reasons for disengaging in the intervention before an agreed end
-
understand, from a participant perspective, the benefits and disadvantages of taking part in the intervention.
Assessment of fidelity of delivery of the STRENGTHEN intervention
Delivery (treatment) fidelity70 was assessed in the trial to examine the extent to which the intervention was delivered as intended. This allows greater confidence that any changes in the dependent variables can be reasonably attributed to the intervention70 and allows planning for future improvements to intervention delivery by identifying areas that may have been delivered below an expected standard.
The health trainer training, manual and supervision were designed to equip the health trainers with the skills to effectively deliver and engage the participant in six core competencies across the duration of the intervention. In summary, the six core competencies were:
-
active participant involvement
-
motivation-building for changing a behaviour and improving well-being
-
set goals and discuss strategies to make changes
-
review efforts to make changes/problem-solving
-
integration of concepts – building an association between well-being and behaviours
-
engaging social support and managing social influence.
These core competencies were intended to be transient across sessions, with acknowledgement that not all of them may necessarily be applicable in every session (except for core competency 1, which was considered fundamental to the intervention in terms of being client-centred and building trust and rapport). All competencies were intended to be delivered in a client-centred approach drawing on motivational interviewing techniques and principles (see Appendix 1 for a detailed description).
Methods
Audio-recordings of health trainer-delivered sessions (n = 18) were purposively sampled across participants who had also taken part in a process evaluation interview to allow for the potential to triangulate process evaluation data. Methods employed were those used in previous research conducted by members of the research team for assessing treatment fidelity,71 albeit to assess the competence of three health trainers in supporting change in two health behaviours: physical activity and smoking. The health trainers in the present study had the opportunity to support change in four health behaviours and well-being, but we were interested in the generic competencies, irrespective of the behaviour(s) that the participant wished to work on. In this pilot trial, we also aimed to test the methods for assessing intervention fidelity, given the difference in aims of the STRENGTHEN intervention.
The participants sampled (n = 9) had a minimum of a first session and a subsequent audio-recorded session. The first session and a later session for each participant were listened to and scored as a whole, independently, by two researchers, in order to capture competencies that may not have been present in the first session (e.g. core competency 4). The Dreyfus system for skill acquisition72 was used to assign a score for each of the six core competencies on a 7-point Likert scale (0–6) reflecting six levels of competence (from incompetent to expert). Written guidance was provided to the researchers to inform their scoring (see Appendix 1, Figure 4, for rating criteria for delivery fidelity). A score for each participant was generated based on the health trainer’s performance across two sessions to attempt to reflect their experience of the intervention delivery as designed around the six core competencies. Owing to the comparatively large number of health trainers (n = 6) across the two sites, no comparison between individual health trainers was planned.
As part of an initial standardisation procedure, a recorded session was listened to simultaneously by both researchers who independently scored the health trainers’ levels of competence. The scores were then discussed and agreement reached over interpretation of the scoring scales. A further three sessions were scored independently and subsequently discussed between researchers to ensure that both researchers employed similar interpretations, before independently reviewing and scoring the remaining sessions.
Scores classed as ‘competent delivery’ were considered acceptable delivery, those as ‘advanced beginner’ may need further development in future training and any below ‘novice’ may represent problematic performance and warrant further investigation.
Results
Table 31 shows the mean scores for each of the six core competencies, overall and for each coder.
| Mean score | Core competency, mean (SD) | Overall, mean (SD) | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| Researcher 1, mean (SD) | 3.94 (0.81) | 3.00 (0.66) | 2.72 (0.57) | 2.78 (0.57) | 2.89 (0.49) | 2.39 (1.02) | 2.95 (0.83) |
| Researcher 2, mean (SD) | 3.67 (0.83) | 3.06 (0.77) | 3.00 (0.75) | 2.89 (0.86) | 2.83 (0.75) | 2.67 (1.00) | 3.02 (0.85) |
| Overall mean (SD) | 3.81 (0.81) | 3.03 (0.70) | 2.86 (0.66) | 2.83 (0.71) | 2.86 (0.61) | 2.53 (0.99) | 2.99 (0.84) |
Inter-rater reliability was assessed across all items using a two-way mixed, consistency, average measures intraclass correlation coefficient (ICC). The resulting ICC was in the excellent range (ICC = 0.84), suggesting that coders had a high level of agreement, which indicated that the ratings scales were employed consistently. Overall, the total mean scores for intervention delivery differed by 0.07 between coders, and the mean for overall delivery was scored at 2.99 (SD 0.84), suggesting overall competent delivery.
Active participant involvement (core competency 1) scored highest, approaching the proficient level of delivery, whereas engaging social support and managing social influence (core competency 6) scored the lowest. All other items were rated as approaching the mid-point of the scale for competent delivery (Figure 3).
FIGURE 3.
Overall mean (SD) fidelity scores by core competency.
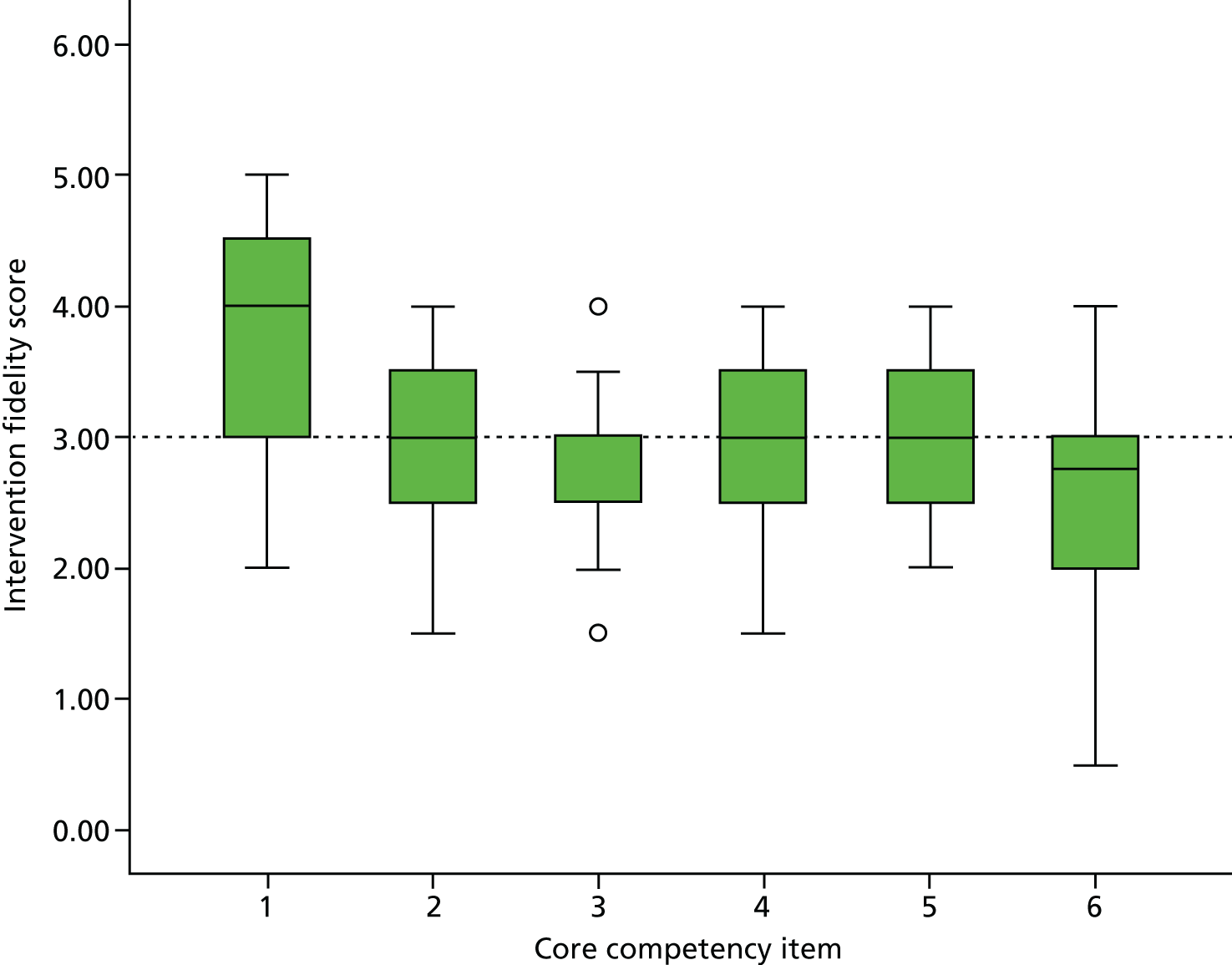
Discussion
Overall intervention delivery fidelity was judged to be acceptable, with some areas for improvement. The overall score for competence of delivery was judged to sit between ‘advanced beginner’ and ‘competent’. Given that this was a novel intervention being delivered with a complex target population, delivery can be deemed to be acceptable within the context of a pilot trial, albeit limited by the small number of sessions analysed.
Active participant involvement scored notably higher than the other competencies; this is probably due to the importance placed on it during intervention development and health trainer training. The population was acknowledged as being potentially very distrustful of services; therefore, rapport- and trust-building (a key component in core competency 1) were key aims emphasised throughout training and supervision. They were particularly evident as aims of the first session, and through a function of the sampling procedure, more opportunity to demonstrate core competency 1 was observed because 50% of the sessions sampled being a first session.
Engaging social support and managing social influence (core competency 6) showed a trend of being the least well-delivered competence. Anecdotally, this may be due to the difficulties this population faces in feeling trapped by their social circles and influences, unable to relocate from a community of offending, and perceived barriers to what are considered new socially acceptable activities owing to their being labelled as an offender with the attached stigma. Conversely, some participants had consciously isolated themselves in attempt to move away from a culture of offending. Future training and intervention development would benefit from increased understanding of how the population perceive their social influences and identify acceptable ways to help participants to positively manage negative social influence and engage positive social support.
Although the other four competencies scored reasonably well, they were all slightly below the threshold for competent delivery. It is possible that this occurred as a result of over-emphasis on actively engaging the participant, which occurred at the expense of the other competencies; it also possibly occurred as a result of the sampling procedure. Additional scoring of sessions other than the first sessions may have uncovered more examples of proficient delivery of the other competencies. These issues should be considered in more detail in future research and health trainer training.
Participant experience of the STRENGTHEN intervention
Methods
Recruitment and sampling
Participants were purposefully sampled to take part in a semistructured one-to-one interview with Lynne Callaghan on completion of the 6-month follow-up assessment. Given the challenges of retention and participant burden, the sampling focused on participants who engaged well with the intervention; identified by the health trainers and Tom P Thompson. We also aimed to recruit up to six participants who disengaged before an agreed end. Recruiting people who have disengaged from services into research studies is particularly challenging. 73 It was possible to interview only one person who had disengaged, owing to challenges in making contact and reluctance to participate. This participant’s data have been used to inform our understanding of why participants might disengage.
Participants
Eleven intervention and five control participants took part in one-to-one semistructured interviews with Lynne Callaghan (broken down by site in Table 32). Characteristics of interview participants are presented in Table 33.
| Service | Control participants (n) | Intervention participants (n) |
|---|---|---|
| CRC south-west | 2 | 2 |
| CRC north-west | 1 | 5 |
| NPS | 2 | 4 |
| Characteristics | Control (n = 5) | Intervention (n = 11) |
|---|---|---|
| Age (years), mean (SD) | 45.8 (12.5) | 41.1 (12.4) |
| Sex (male/female) | 5/0 | 9/2 |
| Baseline data | ||
| WEMWBS score, mean (SD) | 42.8 (12.5) | 49.6 (11.1) |
Interviews
Most interviews were conducted in person in CRC/NPS offices; one participant (from a CRC) chose to meet in a café. Interviews were between 20 and 90 minutes; intervention participant interviews took longer. Interviews were guided by a semistructured interview schedule [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)] developed for control and intervention (engaged and disengaged) participants. Questions focused broadly on the acceptability of trial methods (both groups) and the intervention (intervention group).
All participants were asked about their experience of being approached to take part in the study, their motivation to participate, their understanding of randomisation and the acceptability of data collection methods. Control participants were asked about their experience of being allocated to the control group and any support that they had accessed to support change in any of the target health behaviours and well-being. Intervention participants were asked about their experience of being allocated to the intervention group, acceptability of the intervention, procedures and style of delivery, behaviour/well-being focus, experience of goal-setting, own behaviour change (single and multiple) and perceived benefits.
Findings
Acceptability and feasibility of methods used to recruit, randomise and assess participants
Process used to recruit participants to the trial
Participants were initially approached by their offender manager during routine appointments or, if necessary, by telephone. We asked them about their experiences of recruitment. Given participants’ mandated requirements to attend CRC/NPS appointments, it was important that they understood the voluntary nature of their participation:
Yeah and was it your, erm, probation officer that introduced you to [name] and, and the research? How did that all happen? Can you remember?
Ah, so I had, yeah I had a, er, a normal meeting with [name].
Yep.
And, erm, she put it to me that there was somebody that was doing a course of some kind and if I was interested would I like to listen about it and make a decision. Made it clear that I didn’t have to and it wouldn’t be coming back on me if I said no, so.
OK, that’s good.
I wasn’t forced into it.
The research team worked closely with offender managers to ensure that participation was not counted towards an enforceable component of their order, although one participant thought that it did. Some offender managers allowed their clients to forgo a probation appointment if they attended a STRENGTHEN appointment. Participants in both groups found the initial introduction process acceptable, and found the study information sufficient to make a decision regarding participation.
Motivations for taking part
Participants in both groups talked about making a contribution to research as their initial motivation for participation and clearly understood that this was a research study, not an offer simply to receive an intervention. Participants were keen to contribute to help people in a similar situation and building knowledge:
Erm, after I heard about it I thought ‘yeh, why not?’ It didn’t seem to require a huge amount for me. But I am all for statistical research to back up information, or to discover things.
Participant 10, south-west NPS, control, male
Intervention participants, in particular, spoke about wanting to make a change in their lives, although this was not always obviously linked to the target health behaviours, for example using the intervention to provide occupation to fill their day and support them in developing a routine.
Others were motivated by concerns about health:
I chose to take part because, erm, I realised that perhaps my health isn’t at it’s great and, erm, over the course of the last few years it’s deteriorated quite rapidly really.
Participant 8, south-west NPS, intervention, male
Randomisation: understanding the process and acceptability
Participants were generally accepting of the process and necessity for randomisation:
Er, and then when she did the initial interview, erm, she said she’d phone back and let me know what group I was in. But I could still, er, doing like, erm, interviews, every 3 month, erm, without intervention so, erm, they could work out, erm, the difference between those that have had intervention and those that haven’t.
Participant 16, north-west CRC, control, male
Although there was some disappointment expressed by control participants interviewed that they were not allocated to the intervention group, it did not reduce their motivation to participate in the study and engage in follow-up appointments. Two of the control participants could not remember being told which group they were in, but it was not clear if this was due to difficulty of recollection or failure in communication. There was some confusion about whether the decision was random or based on their responses to outcome measures:
Get a health trainer or not so . . . Erm, yous a, obviously analysed, I don’t, how it, how is it marked? The questionnaires that I did were assessed and then I got allocated a health trainer.
Participant 7, south-west NPS, intervention, male
Acceptability and feasibility of data collection methods
As described in Chapter 3, the researcher read aloud a script to introduce each measure and completed each item to support engagement and literacy difficulties. Participants were given the opportunity to self-complete the WEMWBS if preferred, as this measure is validated for self-completion or telephone administration. Participants were generally happy to complete outcome measures at baseline and follow-up. Interview participants questioned the wording of the CRF, particularly the SF-36. The STRENGTHEN PPI groups had raised the issue of potentially confusing Americanisms in this measure, which was supported by the interview participants. The RAs were therefore trained to offer alternative words to clarify the meaning of any unfamiliar words or expressions if needed. Although most participants found the length of the CRF and the time taken for completion acceptable, some found a proportion of the items repetitive. Most participants found the experience positive in terms of the interaction and the researcher explaining terms, although one questioned how the presence of a researcher would affect a participant’s honesty. Some participants experienced their positive interaction with the researcher as a motivator for completing follow-up interviews:
[Researcher]’s been nice, so, you know, that does, that does help your motivation to come back.
Participant 8, south-west NPS, intervention, male
There were some frustrations expressed that the measures did not cover areas of participants’ lives that they felt were important to understanding their responses to the outcome measures. One participant expressed difficulty responding to items regarding physical health due to their disability, which was not covered by the CRF. Other participants experienced difficulties in providing appropriate responses as the ‘restrictive’ scales did not allow them to respond in a way that represented their situation.
Acceptability and feasibility of the intervention
Intensity of support
The frequency, duration and mode of support provided by the health trainers was flexible and participant led. Participants were informed at the start of the intervention that they could have up to 12 one-to-one sessions over a 14-week period. The health trainers noted, in the early stages, a gap between randomisation and a participant’s initial contact with their health trainer; it was agreed that the 14 weeks would commence from the date of the first session. All first sessions were in person in the building in which participants met with their offender managers. However, after this, the frequency, mode (in person or telephone) and length of sessions were guided by the participant in conjunction with the health trainer. CRC participants were also given the choice to meet with their allocated health trainer in another location.
Participants were able to make changes to the frequency of sessions in accordance with their needs. Therefore, the intensity of health trainer support could be increased or reduced to support behaviour change goals, to allow for changes in circumstances or other commitments, or as participants took increased control over health and/or well-being and relied less on the support of the health trainer:
There was a greater, you know, at the beginning I was seeing [name] once a week, then went to fortnightly and then three-weekly and then monthly.
Participant 7, south-west NPS, intervention, male
The duration of health trainer sessions was acceptable to participants, with most recalling sessions lasting approximately 30–90 minutes. Participants reported enjoying the sessions and that the time seemed to pass quickly. Participants also appreciated the flexibility of being able to increase sessions when required, appreciating the chance to talk beyond the suggested hour:
Mmm, erm, I sup–, I don’t know, I think everything was sort of, for me, you know, [name], I just, you know, she gave up a lot of time, you know, extra time, you know. I know obviously it was an hour and, like I said at the beginning, sometimes an hour and a half.
Participant 7, south-west NPS, intervention, male
No participant felt that the duration of the intervention was too long; some felt that the intervention was the right length for them, and others would have liked to have received the intervention over a longer period owing to changes in circumstances. Examination of dates of sessions showed that 23 participants had gaps of ≥ 3 weeks during their engagement with the intervention. The flexibility of the duration of the intervention meant that participants could fit the intervention around often very challenging situations in their lives in the 14-week time frame.
Mode of delivery
Participants chose in person sessions, telephone sessions or both. Participants found the modes in which the health trainer sessions were delivered to them acceptable:
Definitely. The first trainer, I feel terrible that I don’t remember their name, was very helpful; I got a lot more phone calls. They chose to do this and I chose as a mutual agreement, to do them on the phone.
Participant 14, north-west CRC, intervention, male
Participants described how health trainers also communicated with them via mobile phones to maintain contact between sessions. This extra communication enabled participants to receive information related to supporting their behaviour-change goals and reminders for intervention appointments. Participants found this to be acceptable:
Erm, I had, you know, texts and erm, and erm, phone calls and stuff, you know. Not overbearing but, you know, just, just enough to, you know, remind me and stuff, so yeah.
Participant 8, south-west NPS, intervention, male
Location
Community Rehabilitation Company participants were given the opportunity to meet with their health trainer at an agreed public place following the initial meeting. This option was not available to NPS participants because of their higher category of risk. As both CRC offices were in busy city centres and in areas where parking charges were enforced, being able to meet in an area that was local to residences or work places facilitated attendance:
Yeah, like a café that was close to me commute, ‘cause I’ve, it was, I was pushed for time each time, it was, ‘cause of obviously working and two kids and stuff, so it was closer to home. It was really handy.
Participant 12, north-west CRC, intervention, male
National Probation Service participants were aware of their assessed level of risk and understood that their health trainer sessions would be held in the probation service offices. One NPS participant stated that, although he would have preferred attend sessions in another location, the flexibility of delivery meant that he was able to arrange sessions to take place immediately after a mandated course. This flexibility, and further strategies for managing his anxiety when in the waiting room, meant that he could maintain his engagement.
Suggested adaptations
Participants in both arms of the pilot trial found their participation in the research and, where relevant, the intervention, to be acceptable. Participants suggested potential improvements including:
-
Researchers should explain potentially hard to understand words within the CRF without the participant having to ask or show that they did not understand.
-
Worksheets could be used more systematically to review overall progress.
-
A participant with a diagnosis of attention deficit hyperactivity disorder suggested that the intervention could be offered alongside activities that could facilitate people with a similar diagnosis to make the most of the support being offered.
-
Signposting to other services.
-
Providing literature and information about events linked to target behaviours.
-
Offering more sessions to follow up their progress or extend the intervention.
Health trainer experience of delivering the STRENGTHEN intervention
The six health trainers (three in the north-west and three in the south-west) who delivered the intervention took part in one-to-one semistructured interviews with Lynne Callaghan in person (south-west) or by telephone (north-west). Interviews were guided by a semistructured interview schedule [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)] that covered questions relating to training; supervision; the intervention manual; their experience of delivery, including barriers to and facilitators of delivery; and motivational interviewing (MI) techniques.
Findings
Key themes from health trainer interviews are presented in the following sections, with example quotations to support each theme.
Training
Seven health trainers were trained across both sites (three in the north-west and four in the south-west; see Chapter 2). One was not available for an interview because he/she had left the role.
Practical application
Health trainers spoke about the chance to practise elements of what they had learned during the training sessions. In particular, the opportunity to practise the MI techniques one to one with one of the STRENGTHEN PPI representatives was valued:
Um, so just having that actual practical experience for me, um, was really useful ‘cause, um, you know, we learnt all about the theory and everything, but I think it’s really important to actually then do that.
Health trainer 1
Training structure
During the course of the pilot study, we had to find and train some replacement health trainers quite quickly. We experimented with offering the health trainer training over 2 days instead of 3 for health trainers brought into the study later on, in one-to-one format with subsequent additional remote training and supervision. The health trainers were generally positive about the structure of the training in a group, but one of those completing it over 3 days did find that a great deal of information was covered in that timeframe:
Um, no, it was all relevant really, um, I think, I think the 3 days was difficult, but then it was probably even more difficult for H ‘cause she’s done it in 2.
Health trainer 3
The value of group training was highlighted by a health trainer who joined the north-west site at a later stage. The existing part-time health trainer was able to join the training, which she felt made a positive difference to her experience:
. . . so I think it was quite useful for him to do it again, but it also meant that both of us kind of with [line manager], just y’know, it was just a bit better having, like, a three-way chat for sessions.
Health trainer 4
Motivational interviewing
Health trainers talked about their experiences of receiving MI informed training. They valued the opportunities to watch videos of the techniques being applied by experts and then to practise the techniques live:
And I’d thought about it before in the last project as well; it’s one thing to watch a video, and you watch what’s-his-face do the motivational interviewing, and he’s brilliant at it, and he makes it look really easy, and it’s a totally different thing when you’re the person, and you don’t know what people are going to present with.
Health trainer 6
The coverage of MI in the training sessions also supported health trainer training and direction in the delivery of the intervention to the population. Using examples in the manual and those provided by the trainers, they were able to gain an understanding of both the specific needs and characteristics of the population and how the MI techniques and principles could be applied to successfully deliver the intervention in the probation/CRC context:
Through descriptions with people and you had to write things with the strength lenses in mind, and then as a weakness. It was just really good to see. I think the whole idea was talking about you might come across an offender manager who speaks really negatively about, like, a participant and it’s like ‘oh they’re rubbish and . . .’ but if you just get the basic facts about them, you can spin it any way. You can make them sound as if they are working really hard to improve themselves, or you can make them sound as the, y’know, just stuff about and do nothing.
Health trainer 4
Manual
Health trainers described a range of ways in which they used the manual following training and during intervention delivery. Revision of key information was one of the most common ways in which the health trainers perceived the manual was supporting them to deliver the intervention. Health trainers talked about the manual supporting general revision of the intervention, for example:
. . . it’s quite a tool to just . . . just keep the knowledge kind of ticking over.
Health trainer 4
It was also used by health trainers for specific revision of MI techniques to give confidence and enable them to retain information that they would require during an intervention session:
Just, um, so I did, like, before I saw the first person I read through the MI techniques, . . . and sort of wrote some key points, um, down in my notebook and just like read them through a bit before the appointment, just so they’re sort of in there.
Health trainer 1
Using the manual to prepare for sessions was seen as particularly useful by one health trainer who used the manual to review and revise the more complex techniques or those that she felt less confident in using prior to delivering a session:
There’s one that’s in there that I’m stronger at than others naturally, so, erm, I like to look at y’know like, I think I’m quite good at reflecting . . . but, it . . . it’s the more complex one and I like to think beforehand if . . . if those things are fresh in my mind before I go into a session.
Health trainer 4
Health trainers also used the manual to keep in mind the range of tools available to them to deliver the intervention, including behaviour change and MI techniques and supplementary materials, including worksheets and diaries. This supported them to be both flexible and responsive to participants’ goals and circumstances:
Yeah very much so, I mean I think with, with a lot of work that I’ve done in the past, obviously I want to make sure that I’m using a range of different techniques as well, so I can sort of make sure that I’m doing a good job basically . . . yeah . . . re-reading over . . . over stuff as well, and it is useful because you can just figure it out and you can just look at a section that [you do not know] and yeah, I find it useful, but that’s me.
Health trainer 4
Health trainers reported that the content and format of the manual were acceptable and accessible. In particular, quotations used to demonstrate and illustrate specific points in the manual were viewed as useful in emphasising what is useful in terms of delivery:
I can’t remember specifically what section it was under, but there was a PPI group saying, um, er, ‘it’s just nice to feel that you’re not being judged, it’s nice to have someone be genuinely interested and care’. Um, it’s all little things like that to do with the delivery and with the techniques that are being used so you can actually see whether those, whether those techniques are actually working.
Health trainer 2
Supervision
Overall, health trainers found supervision to be acceptable and useful. Group supervision was attended every fortnight with south-west health trainers attending in person with the supervisor (TPT) and the north-west health trainers attending virtually by Skype. Health trainers discussed the ways in which they made use of supervision. Stated uses varied from sharing key issues from health trainer sessions, consolidating learning of core competencies, confirmation of practice (e.g. appropriateness of signposting) and receiving support to maintain the person-centred approach of the intervention.
At the start of intervention delivery, time was taken during each supervision session to listen to session recordings and to review practice in terms of both delivery of the core competencies and use of MI techniques. As delivery progressed, health trainers listened to pre-selected sessions in order to discuss a broader range of practice. All health trainers found listening to recordings useful, to review interactions with participants and improve their application of the MI techniques by listening to both their own practice and the suggestions of the supervisor and fellow health trainers:
Good to practise that and, again, just checking if there are ways that you can improve the techniques or, you know, seeking advice or suggestions from the others and ways to maybe approach things differently if you get, like, a similar problem with something that comes up or . . . just, yeah, using it as like a discussion point, um, for how to deal with things really that come up and, so that was useful.
Health trainer 1
Health trainers also spoke about the utility of listening to session recordings to reflect on their own practice:
. . . you know quite difficult listening back to your own voice . . . but it is really useful because you . . . you can kind of reflect on what you’ve done and then go back to your [memory] and think ‘actually I probably could’ve done more if I’d done that or used that technique’. So, yeah, so far I think it’s been . . . it’s been a good experience, yeah.
Health trainer 4
Group supervision was supplemented by short (3- to 5-minute) one-to-one telephone calls following every health trainer session. Although these telephone calls were primarily to provide a safety check-in, they were also perceived by health trainers as facilitating a vehicle for brief one-to-one supervision:
Yeah, we had a bit of a chat, and a bit of a debrief and, so that kind of acts as a bit of one-to-one supervision as well.
Health trainer 5
Furthermore, health trainers felt that they were able to download their experience of their most recent sessions while it was fresh in their minds, and additionally, the call enabled them to feel supported and connected to the intervention team when working at a distance:
Does make you feel like you’re supported, you’re part of a team. Your welfare is important and you get to . . . get to have an immediate debrief. It’s quite useful to kind of articulate out loud, that if you go away from your appointment and you just churn it over in your head.
Health trainer 4
Formal supervision was conducted as a group, with short post-session telephone calls perceived by health trainers as providing one-to-one supervision, as described above. Additional one-to-one supervision and support were also available at other times when required by the health trainers. The focus on group supervision was viewed as acceptable to the health trainers in supporting them to share their practice and develop their learning to enhance their delivery of the intervention:
Um, but I think the advantage of having joint is that you’re learning from each other and, you know, one person might have come, um, had an experience and the other person is like ‘oh, I’ve had that too actually and this is what I did’, you know, and it’s just, it’s really useful for sharing ideas and because, particularly when there’s two of you doing, you know, delivering the same intervention, you know, um, you can learn lots from each other.
Health trainer 1
The supervision structure and agenda was also flexible to take account of the needs and priorities of the health trainers. In addition, the supervisor facilitated a supportive and responsive approach to promote discussion of key issues:
No, I don’t think so, [name] always gives us lots of opportunities to bring up, it’s not like he dictates everything, and goes, ‘right that’s it, it’s all over’. He always gives us plenty of opportunities to ask questions, and bring up any issues that we’re having and things.
Health trainer 5
Barriers to delivery
The main barriers to delivery stated by health trainers related to non-attendance of participants and difficulty with contact. Reasons for non-attendance perceived by health trainers ranged from caring responsibilities to difficulties with both organisation and ability to attend appointments owing to perceived chaotic life circumstances:
When they’ve got chaotic lives, things going on, it’s actually quite a high rate of, you know, cancellation and that’s where you’ve got to be so flexible but, you know, they tend to always do want to actually then just rearrange.
Health trainer 1
Health trainers spoke about dealing with non-attendance and encouraging attendance by being flexible and non-judgemental when participants cancel and/or make contact to rearrange (in some instances multiple times). They also talked about strategies, such as working alongside offender managers, so that they were able to assertively contact participants by co-ordinating with routine appointments in order to make contact. Communication with offender managers also enabled health trainers to understand participants’ needs and that their challenges in attending were not specific to their health trainer sessions:
When I got that e-mail from the offender manager, I was almost quite relieved to be honest, that I was like ‘right it’s not me’. I was a bit like ‘oh god no one really’ y’know ‘no one wants to meet me’ it’s just difficult clients.
Health trainer 4
Location at probation/CRC offices was perceived as a barrier by two health trainers. One viewed this as a barrier due to the intervention being delivered in probation per se, owing to the negative experiences and associations with the location, and the second viewed it as a barrier due to the physical health needs of one of the participants:
So, that could be a barrier to them engaging with the intervention, if they just don’t want to go to the probation.
Health trainer 5
The final barrier offered by two of the health trainers was linked to the person-centred nature of the intervention. Although health trainers supported participants to develop and work towards goals that related to health behaviour(s) and/or mental well-being that were of the participant’s choosing, this was not always viewed by health trainers as the optimal decision for the participant in terms of either improving their health or being the most important choice in terms of reducing their risk of ill health:
Yeah, I mean, I think definitely be able to use the supervision and [unclear] remember after the first one, erm . . . I knew that he would . . . but . . . but . . . I am sure you are going to know exactly what I am saying but you could see what he should probably be focusing on, but unless he said he wants to focus on it, he’s can’t focus on it.
Health trainer 4
Suggested adaptations
Health trainers suggested adaptations to enhance their delivery of the intervention, including the following:
-
training –
-
more time to practice MI techniques and receive feedback
-
wider range of modes of delivery throughout the training sessions to break up time with activities
-
-
manual –
-
add inclusion of a clear definition of the role and remit of the health trainer
-
provide guidance regarding the use of the data management system for reference post training
-
provide guidelines and suggested wording for telephone calls and text messages to participants to support effective communication
-
-
supervision –
-
allocation of more time for discussion of core competencies and how they are applied in practice to enhance learning.
-
Two proposed additions to supporting materials were actioned in the early stages of delivery:
-
Development of a working document of local services and schemes to which participants could be signposted. The original health trainers in both sites were able to use their time as their caseloads built up to identify local services to collate a list of signposting options.
-
It was suggested that the participants should be provided with some paperwork to support their engagement with the intervention. This led to the development of a participant pack containing information about the intervention remit, the health trainer and local services. This was presented in a folder in which any further information and worksheets used by participants during the intervention could be stored.
Offender managers’ experiences of working with the research team
Six offender managers who had identified and approached potential participants took part in one-to-one semistructured interviews, two from each OMS. Interviews were conducted in person by Lynne Callaghan during the final phase of intervention delivery and follow-up assessments. Interview participants were purposively sampled with direction and support from site researchers. Interviews were guided by a semistructured interview schedule [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/145419/#/ (accessed 30 August 2019)]. Questions focused on caseload characteristics, experience of working with researchers, understanding of the pilot trial, approaching clients to take part in the trial, perceptions of the intervention and their current and recent experience of the impact of Transforming Rehabilitation. 74
Findings
Key themes from offender manager interviews are presented in the following sections with quotes to support each theme.
Working with women
Offender managers discussed women both in terms of their needs, and how their service had sought ways of meeting those needs. NPS and CRC offender managers who took part in interviews had similar experiences and perceptions of women in terms of the complexity and level of their needs. Accentuated areas of need included safeguarding (often because of being past and/or current victims of abuse), mental health, alcohol and substance use, and child care:
I suppose their level of need can be higher, I think. I think the ones that tend to come our way do need a lot of support.
Site 1, offender manager 2
There was understanding of the need to offer women alternative locations to the main probation offices for them to feel comfortable and safe to access probation support:
I suspect they’re better at turning up at those [community organisations] kind of places than they are here, you know it always can be quite daunting for female offenders to come in here.
Site 1, offender manager 2
Offender managers in both CRC services talked about various ways in which their services worked to enhance women’s access to and to promote engagement with probation support. In both sites, this has involved provision of services in a location separate from the main CRC office. In site 1, this was a drop-in centre with a more relaxed ethos at a community organisation separate from the building and organisation of the CRC:
Well, offering different ways of working, so the drop-in on a Tuesday in [name of service] for women, the women’s space, is run differently, it’s quite a – I’ve never been, being a man! – it’s much more relaxed and less structured.
Site 1, offender manager 1
Similarly, in site 3, very few women use the main city centre probation offices and are able to see their offender managers through more local specialised women’s hubs with a more open and flexible approach, which enable them to attend with children:
Um, we have specialised women’s hubs where it’s a little bit more flexible in terms of, say, half term when they’ve got the children there, you know, that kind of thing and, um, looking at . . . there seems to be, especially in Manchester, a lot more kind of support and interventions for females, um, I don’t know if that is just the Manchester, but that’s how it feels. I do think that they have very different needs and there’s different crisis when it comes to the male and female.
Site 3, offender manager 2
Sources of community support
Offender managers talked about the range of support services in the community and the perceived barriers to accessing these services for their clients. Participants spoke about the need for, and/or provision of, services to meet the varied needs of their clients including the target health behaviours of the STRENGTHEN intervention (including alcohol, physical activity and smoking) and mental well-being/mental health, as well as other health and social needs including GPs, housing, probation services, risk management, employment and access to dentists. All offender managers talked about barriers for their clients in accessing support services to meet these health and social needs in the community. One of the main barriers to access was the lack of service resource to meet the level of need in the community. One offender manager talked about the lengths that he and his colleagues went to in order to manage a client experiencing a mental health crisis, and the inability of mental health services to be able to provide timely support because of low resource availability:
Yeah. I mean we had a guy in reception last week, he’d come in at the beginning of the week and said he was suicidal, he was going to throw himself in front of a car, [name] managed to talk him out of that and got him down to the housing office and got him some B&B [bed and breakfast] accommodation, he then came back 2 days later, he did have a mental health appointment but it wasn’t til the 7th of March. He came back 2 days later and said that he’d taken this whole packet of tablets the night before, so we just had to sit with him, got an ambulance, just sat with him ‘til the ambulance came. So yeah, that’s always–
Site 1, offender manager 2
But there’s just not enough out there, it’s not that easy to do it. I know other, the agency that we work with have got a massive waiting list so if somebody turns up and they’re homeless it’s like, ‘right, OK, you can get seen in 6 to 8 weeks’.
Site 3, offender manager 1
Some clients are also excluded from being able to access services because of their living circumstances, such as homelessness, which means that they are unable to provide an address. For NPS clients, the nature of their offence and subsequent conviction(s) often resulted in loss of family, employment (and in many cases, chances of future employment) and home, and they may have needed to move to another area to live. Furthermore, some services exclude individuals owing to the nature of the offence. For example, a local mental health service in one site would not allow sex offenders to access its services despite the arguable need in terms of isolation and loss. Similarly, the same offender manager identified a need for support services for sexual abuse among her clients that the main local service could not meet because of their exclusion of victims of sexual abuse/violence who had been convicted of sex offences:
Um, and, you know, I went to [name of service] and said ‘will you work with him?’, you know, ‘you don’t need to touch the sexual offending, I am doing that work, but he desperately needs to work on his sense of loss and his identity, his sense of identity’ and they just wouldn’t touch him. You know, and who else is going to do that work?
Site 2, offender manager 2
Working with the STRENGTHEN pilot trial
Offender manager participants shared their perceptions of the parameters and processes of the trial in terms of their experience of working with the research team to identify and recruit participants.
Inclusion and exclusion criteria
Offender managers discussed the inclusion and exclusion criteria in terms of their applicability to their clients and their appropriateness, both in enabling a balance of those who might benefit from the intervention and in ensuring, as far as possible, that participants who were recruited would be able to engage in both the research and the intervention if they were allocated to the intervention group. One of the inclusion criterion considered by the offender managers was that of potential participants having to be released from prison (when applicable) for at least 2 months before the search was conducted. One CRC offender manager commented that this might be more appropriate for NPS participants than for those in the CRC:
I suppose it’s probably different for us [CRC] and the guys upstairs [NPS] as well; they, probably, at the 2-month stage would be fairly settled, because probably for those that aren’t settled by that time they’d be looking probably to send them back to prison.
Site 1, offender manager 2
Although the other offender manager participant at the same site concurred that basic needs had not always been met in his client group within this timeframe, he felt that having the 2-month limitation was a useful starting point and ensured that potential participants could develop a relationship with him, which he believed supported the initial approach to take part in the study:
It also meant that they had a chance to get to know me, ‘cause if they’d just come out of prison and they’ve not worked with me before, they’re perhaps less likely to be interested or willing to consider it.
Site 1, offender manager 1
Other issues stated included the need to exclude potential participants owing to the length of time that they had left to serve on their order, which reduced the proportion of the caseload that could be approached.
Conducting the search
Offender manager participants spoke about their involvement in the identification of potential participants in terms of using the inclusion and exclusion criteria to search for potential participants on their caseload. Generally, offender managers felt that their involvement in this process was valuable in supporting accurate identification of people who might want to take part in the trial:
I mean, someone can look through a whole caseload and say, on the dates we have, yes, this person’s eligible and they’re not, but they can’t say whether they’re motivated, or potentially interested, or there are other thing going on which mean that they’re unlikely to be able to take part.
Site 1, offender manager 1
Offender manager participants found the process of working with the researchers to be acceptable as they were able to fit this in alongside their routine work. It was also noted that this was facilitated by the flexibility of the researcher being based in the organisation (or for site 2, in the same building) and being flexible about when they were able to meet with the offender manager. Furthermore, two offender managers commented on the minimal burden that this process involved:
It was fine, it was really straightforward and really quick.
Site 2, offender manager 2
Recruitment
The co-location and flexibility of researchers was viewed by offender managers as helpful for the recruitment process, by enhancing communication and maximising opportunities to approach potential participants with perceived chaotic lifestyles. Initial approaches, in most cases, were made by offender managers asking their client if they would be willing to talk to a researcher about taking part in the pilot trial. Following a positive response, they were able to immediately invite the researcher into the room to make the approach to participate:
What I normally do is, um, explain that she’s here, are they OK to just have a little chat with her and she can explain more about what the study is . . . um, and then they can either go away and have a think about it or they can let her know if they want to be involved or not. And then introduce [name of researcher] and she’ll explain what it’s about.
Site 3, offender manager 2
It was also important for offender managers to feel that they could introduce the study appropriately, either if the researcher was not able to be there at the time of a routine appointment or for some of their clients who may not have responded well to the initial approach being undertaken by the researcher:
Yeah, because some of them, you know my less motivated people, might be very angry, so I will just test the water first, and if they poke it, I won’t waste [researcher name]’s time. Or it might be that no one can make it on the Tuesday, so I will run it through with them, and they can meet the following Tuesday.
Site 2, offender manager 1
During this initial introduction made by the offender manager, they spoke about both what the intervention would involve, in terms of the health behaviour and well-being focus, and the research, in particular the voluntary nature of the study and randomisation. Offender manager participants not only emphasised to their clients that taking part in the pilot trial was voluntary, but also believed that the voluntary nature of participation in research was important for successful engagement:
If they’re only doing it ‘cause they think their probation officer wants them to do it and they think that it’s part of a, er, a statutory instrument then . . . that could undermine the, the study because the study is all about it being voluntary.
Site 2, offender manager 2
This understanding contributed to the decision not to link involvement in the trial and/or intervention as a contribution to rehabilitation activity requirements (RARs); as well as potentially incentivising participation, the enforceable nature of RAR days (i.e. if they did not attend a researcher or health trainer session, they could be called to see their offender manager or to court) meant that ongoing participation could not be considered voluntary:
Yeah, endorsement of [this is] worth considering about, but making sure that they were aware it was entirely voluntary and that it didn’t affect their work with me, that it could fit in with that, but if they didn’t want to take part that had no bearing on what I was working on with them.
Site 1, offender manager 1
In general, offender managers understood both how randomisation worked and that it was necessary for the pilot trial. However, there was some disappointment and frustration for those who were allocated to the control group and did not receive the intervention who were perceived as needing further support:
It’s frustrating but I suppose, I don’t entirely understand the how and why, ‘cause it’s like if you’ve got somebody who does need it, why not give it to them?
Site 3, offender manager 1
Barriers to and facilitators of engagement and retention
Offender managers described a range of barriers to and facilitators of engagement and retention both in terms of what has worked and not worked in their management of clients and also their views about what would and would not work in terms of engaging and retaining participants in the trial and intervention. Having both busy and chaotic lives was seen as a barrier to engagement. Common challenges included child care and other caring-related commitments (particularly for women), which clients may perceive as making them too busy to take on further appointments, and substance/alcohol abuse and homelessness that contributed to perceived chaotic lives:
‘Cause they’re just all over the place, it’s like herding cats really, with some of those.
Site 1, offender manager 1
So current homeless people. I think relevant, I mean it would be of use to them, ‘cause, you know, really ‘cause a lot of times their health, well-being is terrible . . . but they’re also more likely to not turn up.
Site 3, offender manager 1
Related to the perceived chaotic lifestyle of a proportion of (mainly CRC) clients are the competing priorities of these individuals in terms of accessing interventions when their basic needs have not been met. Offender managers from both CRC sites cited homelessness as one of the main priority areas for people that needs to be addressed prior to accessing health and well-being interventions:
And I suppose, if they’re worrying about where they’re going to sleep at night, or, how they’re gonna pay their bills, what they’re going to eat that day, or anything like that, because quite often that’s what we’re dealing with, and you know, I suppose it’s just prioritising.
Site 1, offender manager 2
The association of STRENGTHEN with probation was also viewed as a potential barrier to engagement because of (potential) participants being suspicious and defensive in that context:
Sometimes they associate it with probation sort of thing, even once they’re through the door, so people think, they’ve got their own barriers just because they’re here. You know, so they’ve got their defences up all the time, sometimes.
Site 3, offender manager 1
Lack of motivation to change was also perceived as being a barrier to engagement. First, through not wanting to take part in anything above what they are already doing and, second, not having an insight into their current situation and therefore not perceiving a need for support from an intervention designed to help them to make changes. Other practical barriers suggested by offender managers included distance required to travel to access the support/intervention and lack of finance to pay for travel:
Their lack of motivation, thinking they haven’t got any issues.
Site 2, offender manager 1
A range of facilitators of engagement and retention were provided by offender manager participants, often in response to the barriers stated above. Accessibility of the researcher and having someone known to the individual who was present in the building was seen as supporting initial engagement, through direct introduction by offender managers:
Because their lives are that chaotic and stuff so it’s a case of, so we almost need like somebody in-house, just here all the time, who can do that. So when they are here it’s like, just gonna go and get them, can just be like, yeah.
Site 3, offender manager 1
Flexibility of location was also perceived as being facilitative of engagement. As presented above, provision of services in a location other than probation offices was seen as being supportive of women’s engagement. This could be extended to individual men, for example meeting in cafes, when they did not want to be seen by others in the building. There were opposing views about the extent to which delivering an intervention in the probation offices, or in partner agencies generally, enhances presentation/engagement, with one offender manager from one CRC site suggesting that meeting in a neutral location would be beneficial, whereas the other offender manager from the same service suggested that location in the CRC would support engagement:
You need to be flexible enough. ‘Cause we do it. I see some of my clients in coffee shops and stuff because they’ve got so much anxiety of coming into the building and being seen by other people, or we’ve got people in gangs and stuff like that and they’re not allowed to cross certain boundaries so you go and see them in local places. As long as it’s safe to do so, obviously.
Site 3, offender manager 1
The nature of sex offenders as ‘compliant’ was viewed by two offender managers (one in a CRC and one in NPS) as making them more likely to engage. However, the NPS offender manager did offer a note of caution that, although they may present, that does not automatically translate into engagement:
Plus the fact that they are kind of naturally very compliant in all aspects of the way they work with us . . . at least, ah, certainly on the surface.
Site 2, offender manager 2
It was proposed that a small incentive may support initial engagement. However, it was recognised not only that doing something that may support changes to health may be sufficient incentive for some, but also that the offer of support needs to come at a point in someone’s life when they are ready to make a change:
I think that would probably be quite successful; I think you’re getting a population of people who are wanting to make a change of some kind, and then if there’s an opportunity offered, then, it’s kind of a happy accident they’ll go, ‘yeah, OK, maybe I’ll have a chat with somebody then’.
Site 1, offender manager 2
Benefits of the intervention
Offender managers did not directly collect information about the trial or intervention; however, their feedback is insightful. Two offender manager (CRC and NPS) participants had received feedback about progress of their clients who received the intervention. The CRC offender manager recalled that one of his clients had completely stopped using cannabis while he was receiving STRENGTHEN health trainer support. The NPS offender manager described the benefits of the intervention for two participants who reported health behaviour changes including healthy eating, reduced alcohol consumption and improved mental well-being. Furthermore, she perceived positive experience of the intervention as potentially contributing to reducing re-offending:
But, you know, as he left, you know, his, um, order he was saying that, you know, it had been really positive, he was still eating better, he was drinking less, he was walking more, I think he’d lost some weight and I think he was just generally feeling more in control and more positive about himself and his health, so I think that, you know, if anything to boost self-esteem with that group of offenders is a positive thing ‘cause, a lot of time they’re, you know, just way down here, um, ‘cause they know that, you know, they’ve thrown away so much of their lives and they know that, you know . . . they, their offending is part of an incredibly dark part of their lives and anything which can raise their self-esteem and make them feel a little bit better about themselves also will be a bit of a protective factor against going back to that sort of very dark time when they were offending so, you know, it is a positive thing for them to feel a little bit good about themselves.
Site 2, offender manager 2
Probation service context and changes
Offender managers were asked about the service changes that had occurred as a result of Transforming Rehabilitation and the impact of the change on the service. Participants spoke about a range of impacts on staff such as changing to new roles and locations, staff changes and losses due to both redundancy and sickness. One of the main impacts on staff stated by offender manager participants was that of increased caseloads and associated burden. These issues were compounded by staff shortages due to a perceived underestimation of the number of individuals who would be eligible for support:
In terms of how many, how much staff they would need. And when the sentencing guidelines changed, um, in 2014 I think it was, so when the people who got short sentences who initially, they didn’t have probation, they went on licence when they came out so that’s created so much more work.
Site 3, offender manager 2
Higher caseloads, and other service changes, were perceived as having changed the role of probation workers because of the restricted time that they are able to spend on one-to-one support, necessitating increased signposting to other services, with a shift towards increasing group work. Furthermore, referral processes are not viewed as facilitating timely engagement.
Another way in which the changes have affected client support in the CRCs is the development of support by telephone. The ‘in-touch’ team has been developed for low-risk offenders to be supervised via telephone rather than in person on CRC premises. Furthermore, the other CRC site had restructured during the recruitment period of the pilot trial to form specialised teams that focus support on specific needs, including those of homeless people and women. There was a sense that the organisations were operating in a state of constant change:
It’s just kind of constantly changing in terms of the interventions that we deliver and how those are supposed to operate.
Site 1, offender manager 1
Another major impact on the structural and continuous changes to the services is the implementation and functionality of systems that are required to support the work of the offender managers and the service as a whole. This has created difficulty for offender managers not only in terms of learning and using new systems following the division of services, but also in having the required operational resources to enable functions that now need to be shared across two services that were previously managed by one:
And that just takes time ‘cause it’s a bit job and sometimes people will come in and they’ll be coming in for an induction and we won’t be able to see them on the system because it’s not been transferred yet.
Site 3, offender manager 1
The STRENGTHEN intervention at work
Health trainer case notes were used to identify the primary and secondary target behaviours of the intervention participants interviewed for the process evaluation. Table 34 presents the number of intervention sessions attended by interview participants and their original target behaviours. The majority of participants aimed to change at least two of the target behaviours and/or well-being. Of the 10 participants who identified a target behaviour early in intervention delivery, seven reported how they had changed that behaviour in their process evaluation interview, examples of which are also included in Table 34. Of the remaining three participants who identified a target behaviour, one reported changing different behaviours (smoking and alcohol consumption) to the original targets (healthy eating and mental well-being) and two did not report change in their behaviour during their interview. One participant who did not identify target behaviours reported change in his diet due to the intervention.
| Participant | Number of sessions attended | Primary target | Secondary target | Participant perspective of benefit of the intervention |
|---|---|---|---|---|
| Participant 1 (south-west CRC, male) | 4 | Reducing smoking | N/A | Smoking:Oh, I was really bad at the time, I was sort of smoking in excess of like 15 fags a day, 20 fags a day . . . So. And within a few weeks of like speaking to [health trainer] and stuff I changed onto the electric fags . . . And that . . . worked really well, I didn’t smoke for about 4 weeks, 5 weeks . . . And broke my electric fag and went straight back to sort of like smoking, but I’ve noticed I have really, really, really cut down |
| Participant 2 (south-west CRC, female) | 8 | Increasing physical activity | Healthy eating | Unable to make changes due to personal circumstances:A few, well I’d say, I’d, because of all the stuff that was going on I didn’t keep up with it, if you know what I mean |
| Participant 5 (south-west NPS, male) | 7 | Healthy eating | Reducing alcohol | Healthy eating:When this came along [STRENGTHEN], one of things I said was ‘well OK, I sometimes have a couple of cakes after my lunch, I could cut that down to one cake, and that’s 50% off that already’ |
| Alcohol:With the alcohol I knew I was drinking on at least three occasions a week and I would drink a whole bottle of wine or a couple of beers or something like that. I tried to get it down, mainly successful, to twice a week . . . and I try to keep it down to the 11 units, but I don’t worry if it goes a little bit above. But I have certainly been keeping it below 20 units | ||||
| Participant 6 (south-west NPS, male) | 7 | Healthy eating | Increasing physical activity | Healthy eating:To me I wasn’t starving, I just wasn’t eating properly. . . I’d only eat biscuits and pasties or whatever but . . .There wasn’t, you know I wasn’t eating but, I do, I did, certainly start. And I bought myself a little thing to cook some stuff in as well. ‘Cause I’ve got a little grill, you know, grill. I didn’t have an oven because I didn’t cook |
| Physical activity:Now I do it on a regular, I mean, whereas I was a bit lazy and went for a walk once, twice a week, I do it everyday | ||||
| Participant 7 (south-west NPS, male) | 11 | Other stated target (return to work) | Reducing alcohol | Alcohol:You know, so that, and then it was just, it sort of weened itself off. And then I used to sort of, you know, when I seen [name] erm, on a Thursday, as I say, usually on a Thursday, I used to sort of say, ‘right, OK, treat of the week this, once you’ve seen [name], you’ve done your two thing, right, go and have a pint’. That’s what I did, it was just my little treat |
| Participant 8 (south-west NPS, male) | 2 | Increasing physical activity | N/A | Physical activity:I was thinking about it for a while before, but erm, I never really put anything into action. Erm, but I, I started looking at erm, the unhealthy snacks I’d been eating, erm . . . binge eating er, and erm, and the reasons as to why I’ve been doing it. Erm, so erm, a lot of it’s food boredom erm, and I’ve, I’ve been addressing the, the boredom by er, taking my dog out on lots of walks |
| Participant 11 (north-west CRC, male) | 11 | No stated target | N/A | Healthy eating:The only thing that was helpful to me about was me diet because even though I thought I was eating quite healthy when I actually did the food plans and I wrote it down . . . I did realise that I was eating too much red meat . . . erm, and so I did cut, cut back on the red meat er . . . content, content |
| Participant 12 (north-west CRC, male) | 5 | Healthy eating | Enhancing mental well-being | Alcohol:Give up, stopped drinking. On holiday, went on holiday without having a drink |
| Smoking:Yeah, that’s what I was doing, cutting down over the sessions and . . . stuff like that, yeah | ||||
| Participant 13 (north-west CRC, female) | 4 | Reducing smoking | Enhancing mental well-being | Smoking:So yeah, from like 20 a day of pre-packed cigarettes to a couple of hand-rolled, um, cigarettes . . . So, yeah, I’m almost there |
| Participant 14 (north-west CRC, male) | 5 | Increasing physical activity | Healthy eating | Physical activity:I wasn’t great before, rubbish to be honest. I was a bit low at times, not really exercising. So I kind of changed everything |
| Participant 15 (north-west CRC, male) | 4 | Other stated target (own accommodation) | Increasing physical activity | No stated change in behaviour:Felt helpful to kind of talk through stuff and try and sort some positive targets out and stuff |
Case study: Jack’s story
This case study presents the experience of an individual who engaged well with the intervention and who focused on and changed multiple behaviours. Jack’s focus was on healthy eating, physical activity and mental well-being. All personal identifiers, including distinguishing features of his presentation, have been carefully modified or removed to ensure anonymity. The case study was selected as an example of multiple health behaviour change alongside change in mental well-being. The case study makes use of transcribed health trainer session recordings, health trainer session notes and participant interview to describe Jack’s journey through the intervention.
Participant description
Jack is a male aged between 50 and 59 years who suffers from social anxiety and finds attending the probation offices very stressful. Jack has a casual job and tends to avoid social contact. During the course of the intervention, he moved from a shared house into a self-contained flat. Jack found the process of arrest, court and sentencing traumatic. He has built up a good working relationship with his offender manager, which he finds supportive.
Early engagement with the intervention
Jack’s health trainer had difficulty in making initial contact to arrange the first session. Through Jack’s offender manager, his health trainer was able to arrange an initial meeting at a routine probation appointment so that his offender manager could introduce his health trainer, which helped him to meet her in a way that he was comfortable with.
Through this interaction with Jack’s offender manager, his health trainer was aware of his social anxiety and mindful of the impact that this may have on building trust. However, she felt that he had relaxed to some extent by the end of the first session:
I think it will take some time for Jack and me to develop trust as he is very anxious and wary of people. However he did seem to relax a little in this middle of the session . . . he has agreed to attend another session, and made a joke on his way out, which suggests he might feel a little more comfortable than at the start of the session.
Health trainer session notes
With knowledge of Jack’s social anxiety, she adapted her approach in the first session to actively involve Jack in the session. This involved the use of one of the worksheets to take the focus away from general conversation. This helped to focus discussion on how he felt about the health behaviours and his mental well-being, using MI techniques to support rapport-building:
This session was more directive than other sessions, in that I felt the best way to engage with Jack was to focus on the project as he didn’t seem like he would find it easy to talk more generally at this stage. Using the pentagon was particularly useful in this session, as it gave us a focus for discussions. I tried to be gentle, e.g. in terms of my tone of voice and taking things at his speed. I was careful about my body language. I used open questions, affirmation and praise and empathy.
Health trainer session notes
Jack’s use of the pentagon worksheet provided a score out of 10 for each health behaviour and mental well-being (0 being the worst it could be and 10 being the best it could be). Jack scored his diet at 5, physical activity as 5 and his mental well-being as 3. Jack’s primary target was healthy eating, with a secondary target of increasing physical activity. Jack lived primarily on takeaway foods and did not cook. With a focus on healthy eating in the first session, Jack used this as an opportunity to review his eating and relationship with food and the processes that he needed to engage in to eat food that he prepared himself, namely shopping, preparing food and cooking. One of his early observations was about cooking:
I haven’t had a cooked meal for about 18 months.
Session 1 recording
Furthermore, as Jack felt more comfortable opening up to his health trainer, he spoke about the impact of his social anxiety on his ability to buy healthy foods:
I don’t go Tesco’s or Sainsbury’s and all of that, there’s too many people now, I couldn’t go there. I’m no good with people at the minute.
Session 1 recording
Exploring motivation
As the health trainer supported Jack to review his recent eating behaviours, he revealed that he had recently bought food in his local corner shop to make himself a sandwich. This was a big step for Jack, as he explains:
I bought a loaf of bread and some cheese and made myself a cheese sandwich . . . I mean, that’s how unusual . . . because I felt it was unusual for me to be doing it.
Session 1 recording
The health trainer actively explored Jack’s motivation for wanting to change his eating habits and, in particular, why this was important to him. She noticed that Jack had talked about being normal or wanting to feel normal and used reflection to test this out with him:
You’ve said ‘normal’ a couple of times, isn’t it? There’s sort of, feeling normal seems something that’s sort of quite important to you, doesn’t it?
Health trainer session 1
Jack agreed with this and went as far as to say that the act of buying food and making a sandwich for him to eat made him feel:
Bit back to normality.
Session 1 recording
Although it was clear that his confidence for shopping in supermarkets was low, he felt confident buying food in his local corner shop:
‘Cause I know the corner shop and they know me . . . so I can just go there, buy my stuff.
Feel safe there?
Yeah, that’s it. Then come away.
Session 1 recording
By understanding why it was important for Jack to focus on and change this behaviour, and by exploring his current level of confidence for performing behaviours to support healthy eating, the health trainer was able to start offering suggestions related to Jack’s review of his current eating and link that to his aim to improve his eating habits:
So maybe think about, maybe it’s just next time you’re in there buying your kind of, your regular stuff, think, have a little look at what else they’ve got in there that you might fancy. I’m just thinking you know, what’s gonna move you. So you’re a 4 at the moment and I’m you know, wondering what’s gonna kind of, what we could do to get, to move it up a little bit.
Health trainer session 1
Early goals
Owing to the way in which the health trainer actively engaged Jack from the outset, progress was made in the first session in terms of both identifying target behaviours, and developing goals, both long term and short term. By the end of the first session, Jack had explored foods that he enjoyed, which formed the basis of a shopping list and made a plan to shop in his local corner shop and prepare simple food:
But that’s an idea, maybe I’ll write erm, and I’ll go and get some stuff. Maybe at the weekend.
Session 1 recording
The health trainer and Jack also discussed using a food diary following their session. Jack was keen to use this both to review what he was currently eating and to make plans for what he would eat in the week ahead:
‘Cause what I might do is, I think I’ll write down what I’m eating but try and put a plan. Not every day but for certain days to have certain meals.
Session 1 recording
Furthermore, although the majority of the first session was focused on healthy eating, Jack and his health trainer discussed physical activity, first talking about his past experience:
Played football every week, you know, did training twice a week. Do running [inaudible] none of that now but . . .
Session 1 recording
Although there was limited time to discuss this area because of the focus on healthy eating, because Jack had already stated physical activity as a target, the health trainer suggested using a pedometer, which was available for Jack to take away with him and use following the session. Jack responded positively to this and made a plan to make use of it with a view to increasing his walking:
No, I will use it, you know, to see how much I walk . . . I might walk just to more, higher, you know.
Session 1 recording
Further progress
Approximately halfway through intervention delivery (session 4 of the seven sessions Jack attended), Jack had progressed further in attaining his goals around healthy eating and physical activity. Regarding healthy eating, Jack had managed his social anxiety and shopped in two large supermarkets to buy some food items from a list that he and his health trainer had written together:
Yes, that’s what I took and I had a look at some of the things on there . . . and yeah and at least I did it . . . not a drastic amount but . . . but the thing was, I did it.
Session 4 recording
Jack was supported to review and reflect on what had motivated this change in behaviour, which he concluded was due to goal-setting:
I have to set myself a goal to do something . . . otherwise I don’t do it . . . and the way my life is at the moment, it’s easier not to do something.
Session 4 recording
Now that Jack was also cooking, he was also supported to reflect on how he felt after he ate a cooked meal:
But it’s my food has got better just slowly but–
Do you feel like you’ve got a bit more energy from eating a bit better?
I do, I feel different after I’ve eaten.
Session 4 recording
Further, Jack had also used his pedometer and had increased his physical activity to 35,000 steps in a week.
Reflection
Jack made changes to both his eating and physical activity, which affected his mental well-being. His WEMWBS scores increased from 31 when recruited to the study to 35 when the 3-month outcome measures were collected and increased again to 41 on the collection of the 6-month outcome measures. In his one-to-one interview with Lynne Callaghan, he reflected on the challenges that he had faced and overcome to enhance his diet, particularly around shopping:
But I know that I did go into and I have since, not all the time but been into the bigger shops, if you understand. Didn’t buy very much but the thing was just going in there with what I knew I wanted to buy and just went in to buy them. Then come out the shop. And to me that was, I hadn’t done that for a long time because of my anxiety and stuff like that, so.
Interview recording
He also reflected on the impact that his cooking had on the food that he was now eating compared with what he was eating prior to the intervention:
Spaghetti bolognese, shepherd’s pie, that sort of thing, you know, mince and that. And I made, I think I did sausage, peas and potatoes . . . You know, just generally easy stuff, nothing you know, nothing too much but to me, compared to what I was eating, before it was a meal.
Interview recording
Jack also increased his physical activity and even found ways to combine healthy eating and physical activity:
Now I do it on a regular, I mean, whereas I was a bit lazy and went for a walk once, twice a week, I do it every day . . .
And then I used to, like I’d go for a walk out on the moors or down, wherever I’d go for a walk . . . and I’d stick a bit of fruit in the pocket for the walk. So I was really doing two things . . . at the same time.
Interview recording
Finally, increasing physical activity also positively affected Jack’s mental well-being by giving him more opportunities to be in the countryside and take notice and connect with his environment:
I feel, sorry, mentally I go to a calm place now and like, you know, it’s erm, it’s erm, yeah it calms me down . . . Even if I’m not stressed I just, I can go in there and I’m calm and I, I just looking at different things that there I’m walking past, you know. It could be animals, it could be the trees, it could be the birds, it could be people just cycling past, you know . . . But all these little things, they just send me into my own little world . . . ‘cause, yeah, ‘cause with my anxiety I just, when I’m in me own space there’s nobody else there . . . so, so it’s quite cool.
Interview recording
Researcher observations on recruitment and follow-up
Research assistants kept logs on issues of recruitment and follow-up during data collection. The points below summarise the main observations of RAs across both geographic areas that affected recruitment and retention:
-
Services were observed as being extremely busy. Researchers were aware that they were working with services during a challenging time of restructuring and change. RAs had difficulty in making time to meet with offender managers. Meeting offender managers one to one supported rapport-building, which aided supporting follow-up.
-
There were some issues with offender managers acting as gatekeepers – suggesting that some potential participants would not be suitable despite meeting the inclusion criteria.
-
Research assistants were aware that they, and therefore the pilot trial, might be seen as part of probation. There was a general feeling that this was more of a problem for CRC participants than for those under NPS. For some participants, offender managers supporting the project was seen as being in partnership with probation. For others (mainly NPS) it seemed to help that the offender manager was supportive of their involvement and that it was, to some extent, endorsed by the organisation. However, being aligned with probation made it difficult to meet with participants for the 6 month follow-up if they had finished the terms of their order early.
-
Delays in conducting searches and screening potential participants occurred because of the reliance of the RAs on OMS staff to conduct this role as the research team did not have access to the record system. This also affected follow-up appointments as RAs were not able to directly access up-to-date information that would support securing appointments with participants.
Summary of findings against aims
-
We have assessed whether the intervention is being delivered as per manual and training:
Assessment of delivery fidelity considered delivery of the intervention by health trainers to be acceptable within the context of a pilot trial, with the overall score for competence of delivery rated between ‘advanced beginner’ and ‘competent.’ Feedback from health trainers showed clear use of the manual to support consolidation of learning from training, which was further supplemented through supervision.
-
We have explored the key components of intervention that are critical to delivery:
The core competencies were seen as critical to delivery, with ‘active participant involvement’ viewed as the foundation on which the remaining core competencies could be delivered. Other components of the intervention critical to delivery include flexibility and person-centeredness in terms of location, time, duration of intervention and behavioural focus of the intervention. A full trial would permit mediation analysis to determine if key components were important for change in the respective outcomes.
-
We have explored reasons for divergence from delivery of the intervention as manualised:
There were few reports of divergence from manualised delivery, owing to the inbuilt flexibility of the intervention and acceptability and feasibility of delivering the intervention core competencies using the vehicle of the MI techniques (with the support of training, manual and supervision). The example of divergence presented in the case study in terms of using the first session for goal-setting rather than solely for rapport-building (as manualised) remained supported by the manual as the delivery was led by the participant.
-
We have attempted to understand when context is moderating delivery:
Participants and health trainers generally found the location of the intervention acceptable. There was some indication from participants that meeting health trainers in a location other than the CRC facilitated rapport-building. Furthermore, some NPS participants suggested that they would have preferred to have met health trainers away from NPS offices. In a definitive trial, we could explore individual risk assessments for NPS participants to enable those assessed as being low risk to the health trainer to be seen in another safe location. The CRC was in flux, which affected recruitment and retention; however, there was no evidence that this affected intervention delivery.
-
We have attempted to understand the experience and motivation of participants in the control arm of the pilot trial to maximise retention in a full trial:
Participants in the control arm found the trial methods to be acceptable and generally understood and accepted the process of randomisation. Initial motivation of control participants was that of wanting to help others in similar circumstances and contribute to the evidence base by taking part in research. Some participants found the engagement with the researcher at recruitment and follow-up to be a motivating factor, affecting retention. Although some control participants expressed some disappointment at their group allocation, this did not demotivate them to continue their participation. It should be noted that those control participants who took part in the process evaluation had completed the 6-month follow-up and, therefore, may have perceived their experience of participation differently from those who were not retained in the study.
-
We have explored reasons for declining to participate in the trial:
Researchers noted the reasons provided for declining to participate on the data management system; these are provided as exclusion reasons (see Tables 1–3). When potential participants provided a reason for declining to take part in the study, these were –
-
conflicting commitments (unsociable shifts, full-time working)
-
stressful life events that meant that they did not want to take part (bereavement, sexual assault)
-
physical health issues that they perceived would be a barrier to engaging with the intervention.
-
-
We have explored reasons for disengaging in intervention before an agreed end:
Recruiting participants to take part in a process evaluation interview who disengaged from the intervention before an agreed end was problematic owing to difficulty in making contact and arranging a time to participate. One participant who took part in an interview and who had disengaged from the intervention indicated that he disengaged because of a change in life circumstance and would have liked to have returned to the intervention but was ready to do so only following the end of the 14-week time frame.
-
We have explored from a participant perspective, the benefits and disadvantages of taking part in the intervention.
This chapter has presented a range of perceived benefits of the intervention in terms of health and well-being behaviour change and associated impacts. Participants have also benefited from understanding the links between (1) health behaviours in relation to behaviour change, (2) health behaviours and mental well-being and (3) emotions, well-being and behaviour. Participants spoke little about disadvantages of the intervention, which would need to be explored further in a full trial.
Chapter 7 Discussion and conclusions
Context
This research was conducted as a result of commissioned National Institute for Health Research (NIHR) (Public Health Research programme) call to fill a gap in the understanding of the effectiveness and cost-effectiveness of interventions to improve the health of offenders in the community. A proposal was initially submitted to conduct a full trial but, given the uncertainties about conducting a randomised trial with the target group, we were funded to conduct a pilot trial. This report considers those uncertainties and what we have learned to take into a full trial.
Just before the research began, offenders were managed by either a NPS or a CRC. The latter was introduced in February 2015 and our proposal, in anticipation of this, aimed to recruit through CRCs and NPSs in two sites: Plymouth and Southampton. In the lead-up to the start of the study, health trainer support became available for offenders in Southampton; as a result, we had to seek an alternative second site. We chose Manchester because the University of Plymouth had an ongoing collaboration in another NIHR trial under way with the University of Manchester, but, to avoid delay, we set up recruitment only in the CRC.
Building on a previous single-site pilot trial to examine the effectiveness and cost-effectiveness of health trainer support to help promote exercise-assisted reduction to stop smoking (the EARS trial),35 we explored how health trainers around the country interacted with offenders. Our PPI work also involved considerable engagement to inform the intervention and trial design. A significant adaptation to the EARS intervention took place to accommodate promoting the 5WWB and supporting changes in smoking, physical activity, alcohol consumption and diet for the STRENGTHEN study.
The STRENGTHEN pilot RCT was developed to assess the feasibility and acceptability of the health trainer intervention and trial methods. Criteria were identified on which to judge recruitment, trial retention and intervention engagement. Data collection involved mixed methods to fully explore how the intervention and trial procedures were viewed by stakeholders and to identify areas for improvement.
This chapter will consider issues associated with the following: trial design and methods; recruitment; study attrition and follow-up data completion; participant characteristics and reach; outcomes at follow-up; intervention content, design, acceptance and feasibility; describing usual care; health economics and plans for a full trial; strengths; limitations; implications for health and social care; and implications for future research.
At the end of the chapter, we will summarise the strengths and weaknesses of the trial and implications for future research, with a particular focus on conducting a full trial.
Trial design and methods
Based on what is reported in Chapters 4–6, this study provides support for the trial design and methods being acceptable and feasible to progress to a full trial, with some minor changes.
Recruitment
We eventually recruited the planned 120 participants, albeit over a longer time scale owing to a number of delays beyond our control. The pilot trial has helped us to better understand the recruitment constraints experienced in three different offender services in two cities as well as the resources needed to recruit participants in a timely manner, from both quantitative and qualitative data. Given that the CRCs in both Plymouth and Manchester were only just finding their feet at the beginning of the study and at times were under extreme operating pressures, it was an extra challenge to build vital relationships with the offender managers and the service leads. We are indebted to those working in the services who ran searches for potentially suitable participants, informed us of when appointments were taking place to allow our researchers to make contact, and for their support in many other ways. We have used all our experience of working in the CJS to make it work; should further changes occur to services, we feel we will be even more equipped to minimise barriers to recruitment, across different services and recruitment sites, to a larger trial.
At the start of the trial, there were uncertainties about the conversion rates within the recruitment processes and we largely addressed these. Early experiences of working with the OMS led to more consistent and informative understanding of the numbers of potentially eligible participants and the probable recruitment rates. The main reasons for not including potential participants in the pool to be screened was that that they did not fit in a predefined window of having lived in the community for at least 2 months (following release from prison, if relevant) or they had < 7 months of community supervision remaining within their court order ‘typical’ lifestyles and levels of well-being. The CRC and NPS data management systems were mostly resource efficient for completing this prescreening, although our researchers still had to remove people from our pool of potential participants because of lapses in time between the initial search by the service and further screening.
Many potential participants were also not included in the pool of potential participants or were subsequently excluded owing to the risk they posed to the trial researchers and health trainers in the community. Making such assessments was understandably resource intensive, involving both objective and subjective criteria for the OMS, and delayed the recruitment process at times of high pressure on staffing in the services. Owing to this screening and subsequent lone-worker policy procedures, there were only a few minor incidents in which researchers and health trainers felt uncomfortable and these were efficiently resolved.
We also wanted to ensure a balance between including participants who had appeared to have a chaotic life (e.g. were hard to establish contact with and perhaps often missed OMS appointments) and low levels of well-being, who may have the most to gain from the health trainer intervention, and excluding those who were likely to be lost to follow-up, given that we had set a challenging progression criterion for the pilot trial. We also wanted to include only those who were likely to remain in the same geographic area to maximise follow-up rates and intervention engagement. The results provisionally indicate a possible association between baseline WEMWBS scores and intervention engagement: those with the lowest WEMWBS scores at baseline tended to have the lowest levels of intervention engagement, and they tended to be more likely to be lost to follow-up. Leading into a full trial, we would continue to review our processes for including and excluding those with a chaotic life, and ways to maintain intervention engagement and completion of follow-up assessments.
The process evaluation also tried to identify why, through interviews, some participants had chosen not to take part in the study. The reasons largely mirrored those recorded by researchers during screening, and it was not always easy to differentiate between whether they simply did not want to take part and did not value what was on offer, or had other conflicts and chaotic lives meaning that even a brief follow-up meeting or intervention session would have been difficult. Interviews with staff in the OMS also identified a tension between the objectives of the pilot trial to assess client-centred health trainer support, and the need for the OMS to provide opportunities for their clients to gain credits for community engagement. The research team agreed to resist this as it would have changed the dynamics of the intervention. We could probably have increased recruitment had the intervention been badged as something to provide ‘credits’ but we resisted this.
The trial and intervention procedures were generally well understood, based on our process evaluation. Participants in the control group were occasionally disappointed at not receiving the intervention but, in general, they were happy to feel that they were contributing to the research evidence. We had developed participant information sheets with our PPI groups and these seemed to generally be well understood. The idea of being in a RCT and having a chance of receiving (or not) a complex intervention was not always easy to convey, but there were few examples of misunderstanding. Describing a complex intervention, such as health trainer support to explore change in four health behaviours and well-being, with a largely open-ended format in terms of intervention aims, frequency and location of sessions and intervention duration, is not easy. The overall levels of engagement suggest that we had considerable success in recruitment and intervention engagement. Ahead of a full trial, we would seek to explore, with our PPI group, further ways to improve understanding of the trial methods and nature of the intervention, but it is anticipated that only minor changes would be necessary.
Study attrition and follow-up data completion
As we indicate above, a full trial could have improved follow-up rates by including only those who have less chaotic lives but we have learnt a lot about getting the right balance between selective recruitment and maximising the potential for the intervention to support those with the greatest need. A full trial will be about producing effectiveness and cost-effectiveness information on the health trainer intervention and also understanding for whom it is beneficial. It will be important to maximise recruitment and retention from the range of people with community sentences.
Over the course of the pilot trial, we did improve follow-up completion rates in a number of ways, such as making contact directly with participants rather than waiting for planned service offender meetings (which did not always take place), using social media to stay in touch and by putting more focused staffing resource into the process across sites. We will further explore the socioeconomic, demographic and other factors influencing study attrition, but propose that, in a full trial, we will include a financial incentive to improve follow-up rates.
We found only limited evidence that the trial assessment procedures were overly burdensome, and thereby contributed to lower follow-up rates. All follow-up assessments were completed in face-to-face format with our researchers and, once a meeting was under way, the level of data completion was very good for most outcomes.
Participant characteristics and reach
We cited information in Chapter 1 from other sources that show that the offender population have typically lower levels of well-being and poorer lifestyles than the general population. The demographic characteristics, lifestyle behaviours and measures of well-being in this pilot study mirror those in the literature, and therefore indicate good reach and generalisability for the findings. For example, original data obtained from the Scottish Prison Service in 2014 (personal communication) showed a mean WEMWBS score of 43.2 (SD 12.3) (range 14–70), compared with a general population score of 51.6 (SD 8.71) for England31 and 49.9 (SD 8.5) for Scotland. 34 Our overall sample had a mean WEMWBS score of 44.2 (SD 11.8). Lower WEMWBS scores are typically associated with smoking, lower consumption of fruit and vegetables, high alcohol intake and lower socioeconomic status. The data in this pilot trial indicate similarly unhealthy lifestyle behaviours, low levels of educational attainment and other sociodemographic indices.
Quality-of-life scores (EQ-5D-5L and SF-6D) for the present sample are also very low compared with the general population. 75–78
The sample, overall, was 91% male, and this reflects the overall low proportion of females in the UK CJS. In the process evaluation, we interviewed offender managers who spoke about the gender balance among the clients they worked with, and the focus of the OMS on risk level, with NPS participants being mainly males who had committed sexual offences or serious assault.
Outcomes at follow-up
As we have noted, this pilot trial did not aim to identify the effectiveness of the intervention at follow-up. The planned sample size of 120 participants was aimed at informing sample size calculations from data collected at follow-up to inform sample sizes for a full trial. The main focus, as the probable primary outcome in a full trial, was on the WEMWBS scores. Higher scores in favour of the intervention were reported at 3 and 6 months. There also appeared to be less alcohol consumed at 3 and 6 months, and fewer cigarettes smoked at 6 months in the intervention group than in the control group. We captured survey data on processes associated with individual behaviour changes and presented the data in Table 10 for information only and confirmed that we could collect this information. These data would be used to explore if changes in such processes, aligned closely to our intervention logic model, would mediate changes in health behaviour.
The SF-6D scores at 6 months were 0.753 (SD 0.158) in the intervention group and 0.696 (SD 0.186) in the control group; a difference of 0.041 has been described as a meaningful difference. 79
Intervention content, design, acceptance and feasibility
One of the primary aims of the STRENGTHEN study was to develop an acceptable and feasible intervention. We built on previous work adapting health trainers to support changes in physical activity and smoking reduction, through engagement with PPI groups and individuals to develop and manualise the STRENGTHEN intervention addressing physical activity, smoking, alcohol use and diet, and incorporating an exclusive focus on mental well-being, with health trainer training materials and supervision processes established in parallel. Six part-time health trainers were trained and involved in delivering the STRENGTHEN intervention in Plymouth and Manchester. Quantitative and qualitative data were captured to help understand the processes and acceptance and feasibility of the intervention for the target population, and to identify further ways to improve the intervention.
Both quantitative and qualitative data indicated that the intervention was acceptable and well received by participants. The flexibility in the number and timing of support sessions received, the way support was offered (by telephone or face to face), the location where sessions took place, the pace of the intervention (from building trust and rapport to working on changing well-being and/or lifestyle) and signposting to additional tailored support (e.g. drug and alcohol services, employment agencies) all contributed to the delivery of a client-centred and empowering intervention.
We also recorded 18 health trainer support sessions with participants and coded these to check intervention delivery fidelity. Provisional analysis (see Chapter 6) of two sessions with the same participant (n = 9) showed acceptable intervention delivery fidelity for all six core competencies (i.e. active participant involvement; motivation-building for changing a behaviour and improving well-being; set goals and discuss strategies to make changes; review efforts to make changes/problem-solving; integration of concepts: building an association between well-being and behaviours; and engaging social support and managing social influence) against a prior agreed level of acceptability. Health trainers’ overall mean competency was 2.99 (SD 0.84) on our 6-point scale. Given the sometimes challenging nature of the sessions, with a good proportion of the sample with somewhat chaotic lives, the scores for delivery were considered acceptable, and although some parts were delivered better than others, no component was delivered to an unacceptable standard, suggesting that it is feasible for the health trainers to deliver the intended intervention.
As in our previous trial,71 the competence ‘engaging social support and managing social influence’ was the least well delivered, and ways to further improve this competence will be considered ahead of training staff for future delivery of the intervention with this population. ‘Active participant involvement’ was the highest-rated competence, which reflects the focus of the intervention on building trust and empowering the participants, and confirms that the health trainers offered a client-centred intervention, as embedded in the intervention manual and training. There was also consistency across health trainers in intervention delivery fidelity in terms of competency ratings. The initial session, always included in the ratings, confirmed that our focus on building trust and respect to empower participants to return for repeat sessions, and then to work on changes in lifestyle or well-being, was an effective approach leading to mostly good intervention engagement.
We also aimed to empower participants by offering choice around the mode of delivery and where the health trainer sessions took place if in face-to-face mode. Interviews with intervention participants and health trainers highlighted that it was valuable to hold meetings away from the offices of the OMS, to separate the health trainer support from sentence requirements and the CJS.
A significantly novel aspect of the intervention was how to raise awareness of the 5WWB and integrate these with initiating plans for lifestyle change using evidence-based behaviour change techniques. We have learned a lot about how the intervention was delivered and received from both quantitative and qualitative data. The health trainers valued the training and opportunity to build new skills. With further refinement to training and delivery, as a result of the learning experiences in the pilot trial, the acceptability and effectiveness could be further enhanced and fidelity improved.
Describing usual care
Interviews with offender managers highlighted how limited the opportunities in the community were for supporting well-being and lifestyle change. The services that are available tend to focus on acute needs. Our resource use survey successfully tested the acceptability of collecting these data, with very high levels of data completeness.
Health economics and plans for a full trial
In this first pilot trial of the cost-effectiveness of a health trainer-led motivational intervention for people under community supervision in the UK, we have estimated the resource use and costs associated with the delivery of the STRENGTHEN intervention, and considered, developed and tested economic evaluation methods for the collection of resource use, cost and outcome data for a full cost-effectiveness analysis alongside a definitive RCT. Overall, because all assessments were completed in face-to-face mode, data completeness was very good. Some minor changes in capturing health and social care resource use will be needed to more efficiently capture costs recorded as ‘other’ for the database in a full trial. The data provide tangible evidence of the resources needed to maintain contact (by a variety of means) between health trainers and the participants in an effort to deliver the intervention.
Sample size estimations for a full trial
Assuming the need to detect a between-group difference of 3 units, a SD of 14.8 units with a correlation between baseline and 6 months of 0.63 for the WEMWBS and a follow-up rate of 70%, and with two-sided 5% alpha and 90% power, the number of participants required for a full trial falls within the range of 580–1240. Without that correlation, the range would be between ≈970 and ≈2060. The pilot trial has enabled us to estimate with greater precision what the required sample size for a full trial would be.
Strengths
-
This is the first study to explore the acceptability and feasibility of conducting a rigorous evaluation of the effectiveness and cost-effectiveness of a health trainer intervention to improve well-being and health behaviours among an offender population under community supervision.
-
The mixed-methods process evaluation provided valuable information to inform some changes to improve the trial methods.
-
The mixed-methods process evaluation provided valuable information to inform some changes to improve the intervention in terms of practitioner training, standard of delivery, and acceptability.
-
A bespoke, centralised, secure information technology system has allowed us to make a detailed assessment of the resources needed to deliver the STRENGTHEN intervention, provide an opportunity to maintain some degree of intervention delivery fidelity and subsequently assess the costs of intervention delivery and what degree of intervention engagement (i.e. dose) would be required to have the desired benefits on well-being and lifestyle change.
-
The health economic analysis provides a solid basis for designing the economic analysis for a full-scale trial.
-
The study provides a rigorous assessment of the resources required to deliver a full trial, with respect to recruitment and follow-up assessments.
Limitations
-
We experienced challenges approaching and recruiting women. This was due to limited offender manager capacity to support initial approach, the location of probation support for women away from main OMS offices and the complexity of the lives of potential female participants that challenged their being able to participate.
-
We worked with only one NPS service; therefore, the differences in resources needed to recruit and retain participants, and engage them in the intervention, are less well understood.
-
Recruitment: although we attempted to recruit a representative sample of the target population, from both CRCs and NPS, our inclusion/exclusion criteria may have biased the sample, and, therefore, the generalisability of the findings. Conducting randomised trials with people under community supervision with long-term follow-up is a challenge and, although we tried to accommodate a broad range of participants, our trial methods inevitably excluded some of the most hard-to-reach people. Conversion of participants from the RA approaching a potential participant to randomisation was lower via the Manchester CRC than via the two OMSs in Plymouth, and especially the NPS. This may suggest that the findings were less generalisable in Manchester, or it may just indicate that the RAs and OMS were more risk averse in interpreting the exclusion criteria.
-
Trial retention: the study was designed to synchronise the capture of follow-up data with scheduled meetings for the participants with offender managers. Owing to the fluidity of the OMS, especially early in the study, the OMS did not consistently hold these meetings and this contributed to a lower trial retention than would be optimal. We explored if OMS was associated with trial retention, albeit with small numbers of participants in subgroups, and again follow-up rates were higher among participants recruited via the NPS (in Plymouth). It is probable that participants in the NPS had less chaotic lives and were easier to keep in touch with owing to the nature of their offences.
-
Intervention engagement: we set in our progression rules, based on another health trainer intervention trial delivered in a disadvantaged community, a goal for 70% of the sample to attend at least two intervention sessions. In Plymouth, and especially in the NPS, this target was all but met (68%), but only 50% met this target in Manchester, albeit among only 20 participants randomised to the intervention.
-
Intervention delivery: we coded only 18 audio-recorded sessions between participants and health trainers from which to assess delivery fidelity (as defined by the core competencies) for this pilot trial report. Further analysis is planned to ensure that we have a robust measure to assess delivery fidelity in the future.
-
To ensure high data completion at follow-up assessments, the trial RAs mostly met participants face to face and were trained to minimise bias. We also used health trainers and a RA to notify participants at baseline of their allocated trial arm, to attempt to keep the RAs blinded. Despite these measures, overall, RAs noted that they had become unblinded in assessing 60% and 75% of participants at 3 and 6 months, respectively, with a higher proportion of intervention participants inadvertently indicating their trial arm to RAs. We cannot therefore be certain that the RA did not introduce bias in the way the survey items in the follow-up assessments were answered, although meetings and supervision with RAs did not suggest that this had happened.
Implications for health and social care
There is currently little or no evidence available to determine what an effective and cost-effective intervention would look like to support offender populations under community supervision, and what the improvements in well-being and health behaviours would be. We have estimated the mean cost of the STRENGTHEN intervention to be approximately £348 (SD £128) per participant from the recorded staff time of the health trainers and the health trainer co-ordinator (for training and supervision). The pilot trial has provided valuable information about the implementation of such an intervention in terms acceptability and feasibility. The WEMWBS has undergone extensive psychometric assessment and plans are under way to produce QALY weights for the WEMWBS (S Petrou, personal communication).
Although there is an association between WEMWBS scores and health behaviours (with lower scores linked to poorer diet, alcohol consumption and cigarette use), it is unknown if there is a causal direction. In a full trial, the process evaluation would seek to further explore, through mediation analysis, whether changes in lifestyle influence well-being, or vice versa, or if there is a bi-directional effect. This pilot study provides provisional support for improvements in well-being, particularly for alcohol use, among those receiving the intervention. Our logic model suggests that by empowering the target population they can make choices to change behaviour and find ways to improve well-being.
The present study did not seek to assess if the intervention had an effect on re-offending. It is possible that changes in alcohol consumption, and feeling more competent, in control and being connected to others, which are components of well-being alongside the feeling and functioning aspects of mental well-being captured by the WEMWBS, could have impact on re-offending. A full trial would seek to determine this with potentially significant implications for the CJS and support options provided alongside the OMS.
Owing to the limited rigorous evidence for the effectiveness and cost-effectiveness of providing health training support among disadvantaged populations, more broadly, on multiple health behaviours and well-being, the present study provides some valuable insights into the possible effects of such an intervention compared with usual care.
During the course of the study, we were asked by staff in one of the OMSs, if the health trainer support could be ‘badged’ as a RAR for which clients could be awarded credits. Because the intervention was underpinned by self-determination theory and MI principles, it was designed to empower participants to make changes to lifestyle and things that might improve a sense of well-being. Our PPI group strongly indicated that the OMS building and personnel were part of the ‘controlling’ CJS and that linking credits to our intervention would change the interpersonal relationship between a health trainer and a participant. We have therefore concluded that the health trainer support as a future possible intervention would be best delivered outside (physically and organisationally) the CJS, in community settings where the client is more comfortable, with safeguarding processes in place as appropriate.
Implications for future research
We have conducted a detailed pilot trial to address uncertainties in conducting a full RCT, and estimated the probable sample size needed for a full trial. We believe that such a full trial involving ≈900 participants (determined from between-group differences at follow-up in this pilot trial), recruited from 16 different OMSs (eight NPSs and eight CRCs) across the UK would optimise the generalisability of the findings, and inform future health care, public health and CJS policy. Research is also urgently needed to examine the effects of health trainer support for disadvantaged groups, more broadly, with poor health and well-being; the proposed study will make a significant contribution to our understanding of if and how change occurs, thereby adding value for money. Our proposed full trial has drawn from findings of the reported pilot trial, but overcoming the identified limitations will improve the efficiency of the trial methods and intervention delivery. We therefore propose that the following actions take place before trial recruitment commences to address limitations relating to recruitment, trial retention, intervention engagement and blinding.
Recruitment
-
We will seek further PPI input into how to disproportionally over-recruit females to our sample to maximise the generalisability of the findings.
-
We have already approached and will work closely with all 16 OMSs to identify trial procedures including recruitment processes. The OMSs that we have already engaged with are very keen to be involved again, and we are aware that they can be powerful advocates for bringing new OMSs into the study. We propose a full trial to recruit from eight cities, paired into four regions, with a NPS and CRC in each city, to maximise researcher efficiency.
-
We envisage more efficient recruitment from our NPS partners, and will therefore consider the balance of research resources needed to recruit similar numbers of participants from each OMS.
-
We have found from initial RA training that maintaining RA engagement is essential for recruitment in the challenging OMS environments. We will establish bi-weekly virtual RA meetings to share learning about recruitment processes and opportunities, as in the pilot trial and in another NIHR health trainer trial. 80
-
The addition of a £10 shopping voucher as a reward for completing the 3-month follow-up assessment and £20 at 6 months may also provide an extra incentive for potential participants, as identified by our PPI group.
-
There is a risk of bias in terms of which participants will be identified as being suitable for the trial by offender managers. RAs at each site will be trained to provide each OMS with a clear brief on our inclusion/exclusion criteria and how health trainers work with those with more chaotic lives, to try to ensure that only the most high-risk clients are excluded. We will build on the procedures used in the pilot trial to monitor and report on risk of bias in the recruitment process. For example, the reasons for exclusion were sometimes reported retrospectively in the pilot trial, which was resource intensive; with revised procedures and RA training, this could be done proactively, and linked to the PenCTU database system.
-
Given the range of recruitment efficiencies (i.e. conversion rates from approach to randomisation) between Manchester and Plymouth and NPS/CRC, we will review processes at all sites and carefully monitor recruitment rates, with the addition of support as needed.
-
We recruited just six participants via the community (i.e. without searching NPS and CRC databases) at a time when we were struggling to recruit to the trial. These few participants were not subjectively different from other participants in the trial but required additional resources. We would not plan to use such an approach in a full trial.
-
Finally, there are proposed changes to the organisation of OMSs; NPS will take over offender management from CRCs in England when their contracts expire in spring 2021. There will be 10 regions, each led by a ‘Regional Probation Director’. Other probation services including unpaid work, accredited programmes and resettlement/rehabilitation interventions will be commissioned from private and voluntary sector providers. CRCs in Wales will be taken over by NPS from 1 December 2019.
Trial retention
-
To improve trial retention (i.e. increase follow-up assessments to at least 70%), we would introduce the following changes to a full trial protocol: (1) the attendance at follow-up assessments would be incentivised, with participants receiving a shopping voucher on completion of 3-month (£10) and 6-month (£20) visits; (2) we would maintain close working relationships with offender managers to facilitate the need for RAs to conduct follow-up assessments in conjunction with the 3- and 6-month supervisory visits to the OMS, or elsewhere if needed; (3) we would reflect on pilot trial processes and those in another trial (ENGAGER)37 to optimise ways to stay in touch with participants outside the OMS; and (4) special attention would be given by RAs to improve retention rates for those participants under supervision in the CRCs, to limit bias in the findings.
-
In a full trial, we would focus process evaluation resources on trying to determine the reasons for loss to follow-up using OMS information and participant interviews.
-
We will conduct further exploratory analysis from the pilot trial data to describe the characteristics of participants who did/did not complete follow-up assessments to inform strategies to further boost trial retention.
Intervention engagement
-
We will conduct further exploratory analyses from the pilot trial data to describe the characteristics of participants who completed more/less/no intervention sessions to inform strategies to further boost intervention engagement, especially among CRC participants.
-
We will further explore the association between the number of intervention sessions attended and WEMWBS scores at follow-up.
-
We will further use the data captured in the process evaluation of the intervention in the pilot trial to identify what the health trainers found difficult to do and what was well received by participants, and how the intervention affected generating trust and rapport, and changes in well-being and lifestyle. This would be used to inform PPI discussion groups and make what we anticipate to be relatively minor changes to the intervention and training materials ahead of a full trial.
-
We would also use ongoing data gathered from the delivery of a health trainer intervention in our four-site RCT (TARS)80 with a focus on changing smoking and physical activity, involving 450 participants who are being offered health trainer support. In this trial, we have developed training materials for a single training event for eight health trainers over 3 days, with subsequent regular virtual training. All health trainers have remained in post over 12 months to date, and ongoing process evaluation is helping us to reflect on training and supervision processes and intervention content. Leading into a full STRENGTHEN trial, this experience will be added to the learning from the pilot trial to produce more efficient and effective training and delivery of the health trainer intervention and assessment of intervention fidelity.
Intervention delivery
The training for the practitioners should be adapted to incorporate more focus on delivering the competencies that were not so well delivered in the pilot trial (e.g. engaging social support and managing social influence). Although an active participant is central to the intervention, such a strong focus on training, including throughout ongoing supervision, possibly came at the expense of the other competencies. This should be accounted for through extra time for training and supervision, particularly early on.
Blinding
In response to the finding that RAs had become unblinded in assessing 60% and 75% of participants at 3 and 6 months, respectively, with a higher proportion of intervention participants inadvertently indicating their trial arm to RAs, we would explore, with PPI input, ways to best minimise unblinding ahead of a full trial. Unblinding in studies of this kind are notoriously difficult to maintain, as in another NIHR trial involving offenders (ENGAGER). 37 It is possible that blinding would have been even more unlikely without the steps that we put into place, namely using an administrator to notify participants as to which arm they had been allocated to, instead of using the RAs. So we would propose to use a similar system to that in the pilot trial, with some minor changes. The process evaluation revealed that unblinding resulted from participants mentioning if they had been involved in the intervention, and sometimes the offender manager (often present at follow-up assessments) mentioned it. We would train RAs to reinforce to participants and offender managers the need to not discuss intervention involvement (or not) until after any assessment is completed. We will also conduct sensitivity analyses in the main analysis to determine the possible effects of unblinding.
Conclusions
The pilot trial has provided a platform from which to develop a multicentred randomised trial to rigorously assess the effectiveness and cost-effectiveness of health trainer support for people under community supervision. In this chapter we have made recommendations for reviewing some methods (e.g. offering financial incentives for returning surveys at follow-up, which appeared to improve trial retention in the ENGAGER study), with further analysis of the pilot trial findings, engagement with our PPI groups and learning from the NIHR-funded ENGAGER trial (completed in spring 2019) and the NIHR-funded TARS trial which moved into the analysis phase in autumn 2019. The retention rates in this study meant that sufficient data were provided for planning a full trial. 42 The research question about improving health and well-being among those under community supervision remains a high priority, irrespective of probable changes to the organisations who deliver community supervision.
Acknowledgements
This pilot trial has been dependent on the time and goodwill of numerous people and organisations. First, we would like to thank the service users and staff of Hamoaze House in Plymouth. Hamoaze House service users were instrumental in the adaptation of the STRENGTHEN intervention, health trainer training and the development of the trial methods. We would also like to thank service users from the Revolving Doors Agency for their contribution to the Trial Steering Committee, as well as independent members, including Professor Richard Morris (Chairperson, University of Bristol), Professor Sarah Stewart-Brown (University of Warwick) and Dr Emma Plugge (Public Health England), whose advice and guidance was invaluable at key points during the study. The STRENGTHEN team would also like to thank staff at the PenCTU for supporting the design, development and delivery of the trial.
For their enthusiasm, hard work and dedication, we would like to thank the STRENGTHEN health trainers, including Alex Gude, Chris Whittingham, Hayley-Jane Sims, Rebecca Harris and Lucy Cartwright. Thank you also to Dr Glenn Roberts who advised on the incorporation and use of the 5WWB. We would also like to express our gratitude to Dr Lyndsey Withers (volunteer, Well Connected, Plymouth University) who guided and supported community recruitment. The team would also like to extend their thanks to Kira Butters (student, University of South Wales) for her innovative and thoughtful work in creating a logo based on the discussions of the STRENGTHEN PPI group. We are also grateful for the support of Dr Lauren Weston (Plymouth University) in recruiting and following up participants.
The team are grateful to the OMSs at the south-west and north-west sites for the support provided to the researchers and health trainers. Finally, we would like to thank the participants who gave so generously of their time and shared their experiences with us.
This research was supported by the NIHR Collaborations for Leadership in Applied Health Research and Care South West Peninsula (PenCLAHRC).
Contributions of authors
Lynne Callaghan (https://orcid.org/0000-0002-0766-645X) (Senior Research Fellow) co-led the overall drafting and development of the final report, particularly Chapters 1, 2, 3 and 6.
Tom P Thompson (https://orcid.org/0000-0002-6366-9743) (Senior Research Fellow) and Jane Horrell (https://orcid.org/0000-0001-7284-7647) (RA) led the assessment and reporting of intervention fidelity in Chapter 6 and contributed to the overall report writing.
Siobhan Creanor (https://orcid.org/0000-0002-7373-8263) (Associate Professor in Medical Statistics), Doyo Gragn Enki (https://orcid.org/0000-0003-1532-8992) (Research Fellow in Medical Statistics) and Ben Jones (https://orcid.org/0000-0001-7374-1107) (RA) led the data analysis and estimation of sample size calculations for a possible full trial and contributed to the overall report writing.
Cath Quinn (https://orcid.org/0000-0003-4644-4603) (Senior Research Fellow) contributed to the overall report writing, particularly Chapter 6.
Jane Senior (https://orcid.org/0000-0002-7133-4898) (Senior Lecturer in Forensic Mental Health) and Jenny Shaw (https://orcid.org/0000-0003-2569-7687) (Professor of Forensic Psychiatry) contributed to the overall report preparation, and led input on trial processes at the Manchester site.
Colin Green (https://orcid.org/0000-0001-6140-1287) (Professor in Health Economics), Annie Hawton (https://orcid.org/0000-0002-1336-5899) (Senior Research Fellow in Health Economics) and Elizabeth Goodwin (https://orcid.org/0000-0003-1351-9170) (Research Fellow) contributed to the writing of the final report, particularly Chapter 5.
Richard Byng (https://orcid.org/0000-0001-7411-9467) (Professor in Primary Care Research) contributed to the writing of final report.
Gary Wallace (https://orcid.org/0000-0003-3753-1270) (Associate Director of Public Health) contributed to the writing of the final report with insight on the future implementation of the intervention.
Julia Sinclair (https://orcid.org/0000-0002-1905-2025) (Associate Professor of Psychiatry) and Jill Annison (https://orcid.org/0000-0002-5441-6525) (Associate Professor of Criminology) contributed to the writing of the final report.
Amy Kane (https://orcid.org/0000-0002-9483-5193), Emma Hazeldine (https://orcid.org/0000-0003-0152-6322), Samantha Walker (https://orcid.org/0000-0002-2684-1081), Rebecca Crook (https://orcid.org/0000-0002-3557-5731) and Verity Wainwright (https://orcid.org/0000-0002-9876-250X) (all RAs) contributed to the writing of the final report and prepared data on trial methods.
Lucy Cartwright (https://orcid.org/0000-0001-8733-1379) (Professional Services) contributed to the preparation of the final report.
Adrian H Taylor (https://orcid.org/0000-0003-2701-9468) (Professor in Health Services Research) was the chief investigator and co-led the overall drafting and development of the final report, particularly Chapters 4 and 7.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following reviews and provided necessary agreements are in place.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Thompson T, Callaghan L, Hazeldine E, Quinn C, Walker S, Byng R, et al. Health trainer-led motivational intervention plus usual care for people under community supervision compared with usual care alone: a study protocol for a parallel-group pilot randomised controlled trial (STRENGTHEN). BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-023123.
- Sirdifield C. The prevalence of mental health disorders amongst offenders on probation: a literature review. J Ment Health 2012;21:485-98. https://doi.org/10.3109/09638237.2012.664305.
- Carswell C, Noble H, Farrow D. Barriers between offenders and primary health care after release from prison: a case study. Practice Nursing 2017;28:386-9. https://doi.org/10.12968/pnur.2017.28.9.386.
- Hertfordshire Probation Trust . A Health Needs Assessment of the Hertfordshire Probation Trust Caseload 2011.
- Binswanger IA, Nowels C, Corsi KF, Long J, Booth RE, Kutner J, et al. ‘From the prison door right to the sidewalk, everything went downhill,’ a qualitative study of the health experiences of recently released inmates. Int J Law Psychiatry 2011;34:249-55. https://doi.org/10.1016/j.ijlp.2011.07.002.
- Howerton A, Byng R, Campbell J, Hess D, Owens C, Aitken P. Understanding help seeking behaviour among male offenders: qualitative interview study. BMJ 2007;334. https://doi.org/10.1136/bmj.39059.594444.AE.
- Light M, Grant E, Hopkins K. Gender Differences in Substance Misuse and Mental Health Amongst Prisoners: Results from the Surveying Prisoner Crime Reduction (SPCR) Longitudinal Cohort Study of Prisoners 2013. www.justiceacademy.org/iShare/Library-UK/gender-substance-misuse-mental-health-prisoners.pdf (accessed 24 January 2019).
- Public Health England . Specification No.29 Section 7A Public Health Services for Children and Adults in Secure and Detained Settings in England. Public Health Services for People in Prison or Other Places of Detention, Including Those Held in the Children &Amp; Young People’s Secure Estate 2012. www.england.nhs.uk/wp-content/uploads/2017/04/Gateway-ref-08483-180913-Service-specification-No.-29-Health-and-Justice.pdf (accessed 24 January 2019).
- Newbury-Birch D, McGovern R, Birch J, O’Neill G, Kaner H, Sondhi A, et al. A rapid systematic review of what we know about alcohol use disorders and brief interventions in the criminal justice system. Int J Prisoner Health 2016;12:57-70. https://doi.org/10.1108/IJPH-08-2015-0024.
- Willey H, Eastwood B, Gee IL, Marsden J. Is treatment for alcohol use disorder associated with reductions in criminal offending? A national data linkage cohort study in England. Drug Alcohol Depend 2016;161:67-76. https://doi.org/10.1016/j.drugalcdep.2016.01.020.
- Byng R, Quinn C, Sheaff R, Samele C, Duggan S, Harrison D, et al. COCOA: Care for Offenders, Continuity of Access: NIHR Service Delivery and Organisation Programme 2012. www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1713-210_V01.pdf (accessed 24 January 2019).
- Department of Health and Social Care . Choosing Health: Making Healthy Choices Easier 2004. https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4094550 (accessed 24 January 2019).
- Visram S. Impact and acceptability of lay health trainer-led lifestyle interventions delivered in primary care: a mixed method study. Prim Health Care Res Dev 2017;18:333-43. https://doi.org/10.1017/S146342361700010X.
- Michie S, Rumsey N, Fussell S, Hardeman W, Johnston M, Newman S, et al. Improving Health – Changing Behaviour: NHS Health Trainer Handbook. London: Department of Health and Social Care and British Psychological Society; 2008.
- Attree P, Clayton S, Karunanithi S, Nayak S, Popay J, Read D. NHS health trainers: a review of emerging evaluation evidence. Crit Public Health 2012;22:25-38. https://doi.org/10.1080/09581596.2010.549207.
- Visram S, Clarke C, White M. Making and maintaining lifestyle changes with the support of a lay health advisor: longitudinal qualitative study of health trainer services in northern England. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0094749.
- Dooris M, McArt D, Hurley MA, Baybutt M. Probation as a setting for building well-being through integrated service provision: evaluating an Offender Health Trainer service. Perspect Public Health 2013;133:199-206. https://doi.org/10.1177/1757913913486036.
- Newbury-Birch D, Bland M, Cassidy P, Coulton S, Deluca P, Drummond C, et al. Screening and brief interventions for hazardous and harmful alcohol use in probation services: a cluster randomised controlled trial protocol. BMC Public Health 2009;9. https://doi.org/10.1186/1471-2458-9-418.
- Coulton S, Newbury-Birch D, Cassidy P, Dale V, Deluca P, Gilvarry E, et al. Screening for alcohol use in criminal justice settings: an exploratory study. Alcohol Alcohol 2012;47:423-7. https://doi.org/10.1093/alcalc/ags048.
- Orr KS, McAuley A, Graham L, McCoard S. Applying an Alcohol Brief Intervention (ABI) model to the community justice setting: learning from a pilot project. Criminol Crim Justice 2015;15:83-101. https://doi.org/10.1177/1748895813509636.
- Newbury-Birch D, Coulton S, Bland M, Cassidy P, Dale V, Deluca P, et al. Alcohol screening and brief interventions for offenders in the probation setting (SIPS Trial): a pragmatic multicentre cluster randomized controlled trial. Alcohol Alcohol 2014;49:540-8. https://doi.org/10.1093/alcalc/agu046.
- Kouyoumdjian FG, McIsaac KE, Liauw J, Green S, Karachiwalla F, Siu W, et al. A systematic review of randomized controlled trials of interventions to improve the health of persons during imprisonment and in the year after release. Am J Public Health 2015;105:e13-33. https://doi.org/10.2105/AJPH.2014.302498.
- Lang N, Hillas A, Mensah M, Ryan S, Glass L. Linking probation clients with mainstream health services: experience in an outer London borough. Probat J 2014;61:278-85. https://doi.org/10.1177/0264550514536757.
- Foresight Projects . Mental Capital and Wellbeing: Final Project Report 2008. www.gov.uk/government/publications/mental-capital-and-wellbeing-making-the-most-of-ourselves-in-the-21st-century (accessed 24 January 2019).
- Malcolm E, Evans-Lacko S, Little K, Henderson C, Thornicroft G. The impact of exercise projects to promote mental wellbeing. J Ment Health 2013;22:519-27. https://doi.org/10.3109/09638237.2013.841874.
- Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ 2014;348. https://doi.org/10.1136/bmj.g1151.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68-7. https://doi.org/10.1037/0003-066X.55.1.68.
- Bartram DJ, Yadegarfar G, Sinclair JM, Baldwin DS. Validation of the Warwick–Edinburgh Mental Well-being Scale (WEMWBS) as an overall indicator of population mental health and well-being in the UK veterinary profession. Vet J 2011;187:397-8. https://doi.org/10.1016/j.tvjl.2010.02.010.
- Bartram DJ, Sinclair JM, Baldwin DS. Further validation of the Warwick–Edinburgh Mental Well-being Scale (WEMWBS) in the UK veterinary profession: Rasch analysis. Qual Life Res 2013;22:379-91. https://doi.org/10.1007/s11136-012-0144-4.
- NHS Digital . Health Survey for England 2013 n.d. https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/health-survey-for-england-2013 (accessed 24 January 2019).
- Elsey H, Farragher T, Tubeuf S, Bragg R, Elings M, Brennan C, et al. Assessing the impact of care farms on quality of life and offending: a pilot study among probation service users in England. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019296.
- Stranges S, Samaraweera PC, Taggart F, Kandala NB, Stewart-Brown S. Major health-related behaviours and mental well-being in the general population: the Health Survey for England. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005878.
- The Scottish Government . Scottish Health Survey 2013 n.d. www.gov.scot/Publications/2014/12/9982/0 (accessed 24 January 2019).
- Taylor AH, Thompson TP, Greaves CJ, Taylor RS, Green C, Warren FC, et al. A pilot randomised trial to assess the methods and procedures for evaluating the clinical effectiveness and cost-effectiveness of Exercise Assisted Reduction then Stop (EARS) among disadvantaged smokers. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18040.
- Kirkpatrick T, Lennox C, Taylor R, Anderson R, Maguire M, Haddad M, et al. Evaluation of a complex intervention (Engager) for prisoners with common mental health problems, near to and after release: study protocol for a randomised controlled trial. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-017931.
- Taylor C, Gill L, Byng R, Quinn C. Engaging ‘seldom heard’ groups in research and intervention development: Offender mental health. Health Expectations 2018;21:1104-10. https://doi.org/10.1111/hex.12807.
- Markland D, Ryan RM, Tobin VJ, Rollnick S. Motivational Interviewing and Self Determination Theory. J Soc Clin Psychol 2005;24:811-3. https://doi.org/10.1521/jscp.2005.24.6.811.
- Nutt DJ, Rehm J. Doing it by numbers: a simple approach to reducing the harms of alcohol. J Psychopharmacol 2014;28:3-7. https://doi.org/10.1177/0269881113512038.
- Lindson N, Aveyard P, Ingram JT, Inglis J, Beach J, West R, et al. Rapid reduction versus abrupt quitting for smokers who want to stop soon: a randomised controlled non-inferiority trial. Trials 2009;10. https://doi.org/10.1186/1745-6215-10-69.
- Ministry of Justice . Women and the Criminal Justice System Statistics 2015 n.d. www.gov.uk/government/statistics/women-and-the-criminal-justice-system-statistics-2015 (accessed 24 January 2019).
- Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-264.
- Byng R. Developing and Evaluating a Collaborative Care Intervention for Prisoners, With Common Mental Health Problems, Near to and After Release (ENGAGER 2) n.d. www.journalslibrary.nihr.ac.uk/programmes/pgfar/RP-PG-1210-12011/#/ (accessed 29 August 2019).
- Taggart F, Stewart-Brown S, Parkinson J. Warwick–Edinburgh Mental Well-being Scale (WEMWBS) user guide – version 2. Edinburgh: NHS Health Scotland; 2016.
- NVivo Qualitative Data Analysis Software; QSR International Pty Ltd 2015.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- Lee EC, Whitehead AL, Jacques RM, Julious SA. The statistical interpretation of pilot trials: should significance thresholds be reconsidered?. BMC Med Res Meth 2014;14.
- Browne RH. On the use of a pilot sample for sample size determination. Stat Med 1995;14:1933-40. https://doi.org/10.1002/sim.4780141709.
- Kidger J, Evans R, Tilling K, Hollingworth W, Campbell R, Ford T, et al. Protocol for a cluster randomised controlled trial of an intervention to improve the mental health support and training available to secondary school teachers – the WISE (Wellbeing in Secondary Education) study. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3756-8.
- Powell J, Hamborg T, Stallard N, Burls A, McSorley J, Bennett K, et al. Effectiveness of a web-based cognitive-behavioral tool to improve mental well-being in the general population: randomized controlled trial. J Med Internet Res 2012;15. https://doi.org/10.2196/jmir.2240.
- Borm GF, Fransen J, Lemmens WA. A simple sample size formula for analysis of covariance in randomized clinical trials. J Clin Epidemiol 2007;60:1234-8. https://doi.org/10.1016/j.jclinepi.2007.02.006.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- NHS Improvement . NHS Reference Costs 2016 17 n.d. https://improvement.nhs.uk/resources/reference-costs/ (accessed 24 January 2019).
- Department of Health and Social Care . Reference Costs 2011 12 n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213060/2011-12-reference-costs-publication.pdf (accessed 24 January 2019).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: Personal Social Services Research Unit, University of Kent; 2016.
- Brazier J, Ratcliffe J, Salomon J, Tsuchiya A. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford: Oxford University Press; 2007.
- Glick H, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2007.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013 n.d. www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781 (accessed 24 January 2019).
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- National Institute for Health and Care Excellence . NICE Position Statement on the EQ-5D-5L n.d. https://euroqol.org/nice-position-statement-on-the-eq-5d-5l/ (accessed 24 January 2019).
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002;21:271-92. https://doi.org/10.1016/S0167-6296(01)00130-8.
- Goodwin E, Boddy K, Tatnell L, Hawton A. Involving members of the public in health economics research: insights from selecting health states for valuation to estimate quality-adjusted life-year (QALY) weights. Appl Health Econ Health Policy 2018;16:187-94. https://doi.org/10.1007/s40258-017-0355-5.
- Hughes D, Charles J, Dawoud D, Edwards RT, Holmes E, Jones C, et al. Conducting economic evaluations alongside randomised trials: current methodological issues and novel approaches. PharmacoEconomics 2016;34:447-61. https://doi.org/10.1007/s40273-015-0371-y.
- Noble SM, Hollingworth W, Tilling K. Missing data in trial-based cost-effectiveness analysis: the current state of play. Health Econ 2012;21:187-200. https://doi.org/10.1002/hec.1693.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) – explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health 2013;16:231-50. https://doi.org/10.1016/j.jval.2013.02.002.
- Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA 2016;316:1093-103. https://doi.org/10.1001/jama.2016.12195.
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8. https://doi.org/10.1192/bjp.187.2.106.
- Lambert JD, Greaves CJ, Farrand P, Cross R, Haase AM, Taylor AH. Assessment of fidelity in individual level behaviour change interventions promoting physical activity among adults: a systematic review. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4778-6.
- Thompson TP, Lambert JD, Greaves, CJ, Taylor AH. Intervention delivery fidelity assessment of a counselling based intervention for multiple behaviours. Health Psychol 2018;37:627-37. https://doi.org/10.1037/hea0000613.
- Dreyfus HL, Burke J. Competency Based Education and Training. London: Falmer Press; 1998.
- Marshall D, Quinn C, Child S, Shenton D, Pooler J, Forber S, et al. What IAPT services can learn from those who do not attend. J Ment Health 2016;25:410-15. https://doi.org/10.3109/09638237.2015.1101057.
- Ministry of Justice . Transforming Rehabilitation: A Strategy for Reform 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/228744/8619.pdf (accessed 29 August 2019).
- Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ 2004;13:873-84. https://doi.org/10.1002/hec.866.
- Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ 1998;316:736-41. https://doi.org/10.1136/bmj.316.7133.736.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: Centre for Health Economics, University of York; 1999.
- van den Berg B. SF-6D population norms. Health Econ 2012;21:1508-12. https://doi.org/10.1002/hec.1823.
- Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 2005;14:1523-32. https://doi.org/10.1007/s11136-004-7713-0.
- Taylor A. A Multicentred Trial of Physical Activity-Assisted Reduction of Smoking (TARS). Health Technol Assess 2019. www.journalslibrary.nihr.ac.uk/programmes/hta/1511101/#/ (accessed 15 October 2019).
- Joint Formulary Comittee . British National Formulary 2017.
Appendix 1 Health trainer core competencies and fidelity scales
Core competency 1: active participant involvement
Key features
The health trainer should encourage the client to be actively involved in the consultation. The idea is to maximise the client’s autonomy as the main agent of change, developing intrinsic rather than extrinsic motivation, and encouraging her/him to be the person coming up with ideas for improving the situation. However, the client should not be allowed to ramble excessively in an unstructured way and the consultation should be guided through skilful use of MI techniques. A collaborative/shared decision-making style is appropriate and the health trainer may share his/her own expertise and ideas, using techniques such as elicit–provide–elicit. Overall, the client should be increasingly empowered to take control of her/his behaviours and decisions. Interactions should be encouraging, respectful and non-judgemental (the opposite of a didactic, telling or persuading style of interaction). The client should ideally talk for at least half of the time. The interaction should also be individually tailored to the participant’s specific information needs, beliefs, motivations and barriers. The health trainer should engender a clear sense of warmth, genuineness and empathy (within professional boundaries) to develop trust.
Intervention techniques
The intervention techniques used were the following: open questions, affirmation, reflective listening and summaries (OARS). Reflective listening may include simple reflections of content but may also be more sophisticated (e.g. amplified reflection, reflection with a twist) and used to direct the conversation or highlight key strengths or barriers. The elicit–provide–elicit technique should be used to exchange information (e.g. to address misconceptions or offer helpful new information, and to provide vicarious experience). Empathy-building techniques and individual tailoring should be used throughout the consultations: from the initial consultation through to action-planning through to review/maintenance sessions.
Core competency 2: motivation-building for changing a behaviour and improving well-being
Key features
The health trainer should work with the client to explore initial beliefs and motivations about why they want to make any changes. The client’s motivation for making change is built up/enhanced through the exchange of information and techniques to assess and enhance motivation, that is to enhance the perceived benefits (importance) of making a change and confidence (self-efficacy) to take the actions needed.
Intervention techniques
Open questions, affirmation, reflective listening and summaries should be used specifically to explore current behaviour and the pros and cons of changing, and to develop discrepancies between current behaviour and desired behaviour (or outcomes). The decisional balance technique or 0–10 questions may be used to explore importance and confidence. Information should be exchanged on the pros and cons of changing and this and other techniques (exploring possible futures, discussing past attempts) should be used to explore barriers and possible solutions to increase confidence about cutting down/quitting. Motivation building should ideally happen around the start of the intervention process, although it can be further explored and reinforced at later (action-planning, review and maintenance) stages. Establishing self-rewards or incentives (e.g. saving money in a jar, planning rewards) may be part of the process for maintaining motivation.
Core competency 3: set goals and discuss strategies to make changes
Key features
The health trainer should work with the client to discuss a range of strategies for making the desired changes. They should agree a verbal plan of action, seeking to make this as specific as possible. They should discuss the use of self-monitoring to keep track of progress. Written goals and self-monitoring can be implemented if appropriate.
Intervention techniques
The intervention techniques used were the following: goal-setting (with gradual/graded progression), action planning, self-monitoring and deconditioning strategies. Any or all of the strategies presented in the manual may be presented and discussed. The action plan should normally be made verbally, but the health trainer should seek to make this as specific as possible in terms of ‘what, where, when and who with’ and making the goal as specific, measurable, achievable, relevant and time-related (SMART) as possible. The health trainer should introduce and discuss with the client the usefulness of self-monitoring of behaviours (level of behaviour, pattern of behaviour, how behaviours link). A specific plan for self-monitoring should be included in the action plan. The health trainer may also encourage self-monitoring of the contexts (social or environmental or emotional circumstances) in which problems/relapses might occur. Pre-empting and thinking of solutions for possible problems (making a coping plan, if/then plans, barriers/facilitators) is also appropriate here and may involve the use of other recognised behaviour change techniques (e.g. engaging social support, stress management).
Core competency 4: review efforts to make changes/problem-solving
Key features
The health trainer should work with the client to reflect on progress with goals. The health trainer should affirm/reinforce any successes. The client and health trainer should discuss any setbacks (reframing to normalise them, identifying barriers and exploring ways to overcome them). The health trainer and client should then set new targets, either progressing from the old one or establishing new ones that help avoid successive failure.
Intervention techniques
Use of OARS specifically to reinforce successes, to discuss setbacks, to identify barriers (including social or environmental contexts that hinder progress) and explore ways to overcome them (problem-solving). Reframing should be used to normalise setbacks. Goals/action plans should then be reviewed. There may also be some reflection on, and reinforcement of, the client’s skills in avoiding or managing relapse to undesired behaviour (building skills and self-efficacy). Problem-solving may involve the use of other recognised behaviour change techniques (e.g. engaging social support, stress management).
Core competency 5: integration of concepts – building an association between well-being and behaviours/understanding the rationale and how behaviour, mood and emotions link
Key features
The health trainer should work with the client specifically to help her/him gain an appreciation of the relationship between behaviours and well-being. A clear rationale should be presented for how behaviours and feelings/mood are linked and can influence one another. However, both explicit processes (encouraging the client to complete activities to specifically enhance their well-being) and implicit processes (encouraging clients to embrace approaches to changing their behaviour that incorporate the 5WWB) should be facilitated by the health trainer.
Intervention techniques
Use of OARS, goal-setting (with gradual/graded progression), action planning, self-monitoring and deconditioning strategies. Health trainers should present the rationale to the client in an appropriate way and time (after the client is well engaged) and invite clients to reflect on if/how it relates to their own behaviour and well-being. Health trainers could encourage clients to use self-monitoring approaches and treat it as an experiment, to see how their well-being is on a day-to-day basis in relation to how their other behaviours are. Using MI principles and guiding clients towards plans that incorporate the 5WWB (e.g. connecting with non-drinkers to help reduce their alcohol intake).
Core competency 6: engaging social support and managing social influences
Key features
The health trainer should encourage the client to engage social support (to assist on making or carrying out plans) or manage social influences on their behaviour. Social support can be informational (helping to make plans, providing ideas), emotional (not putting pressure on the person to perform unwanted behaviour/accepting their decision to change) or practical (e.g. helping to monitor progress). They should also look to support people to engage social support as a way to connect with others wherever possible.
Intervention techniques
Open questions, affirmation, reflective listening and summaries may be used to explore social influences and to identify possible problems and solutions relating to social influences.
Below is some guidance on how these core competencies may be scored as part of the research process when session recordings are being reviewed. If it is helpful, a scoring approach could also be used in supervision sessions.
The rating scale
The present 7-point scale (i.e. a 0–6 Likert scale) extends from 0, meaning the health trainer did not deliver the intervention element appropriately – either they did not do it well or did not do it sufficiently (low fidelity) to 6, meaning the element was delivered appropriately (high fidelity). Thus, the scale assesses a composite of adherence to the intended intervention method and skill of the health trainer. To aid with the rating of items, an outline of the key features of each item is provided at the top of each section above for each of the competencies. A description of the various rating criteria is given in Figure 4. The examples are intended to be used as useful guidelines only, providing illustrative anchor points, rather than prescriptive scoring criteria.
FIGURE 4.
Rating criteria for delivery fidelity. The scale incorporates the Dreyfus system72 for denoting competence. Note that the ‘top’ marks (i.e. near the ‘expert’ end of the continuum) are reserved for those health trainers demonstrating highly effective skills, particularly in the face of difficulties (i.e. clients with high resistance to change, high levels of emotional expression and complex situational barriers). Note that there are six competence levels but seven potential scores.
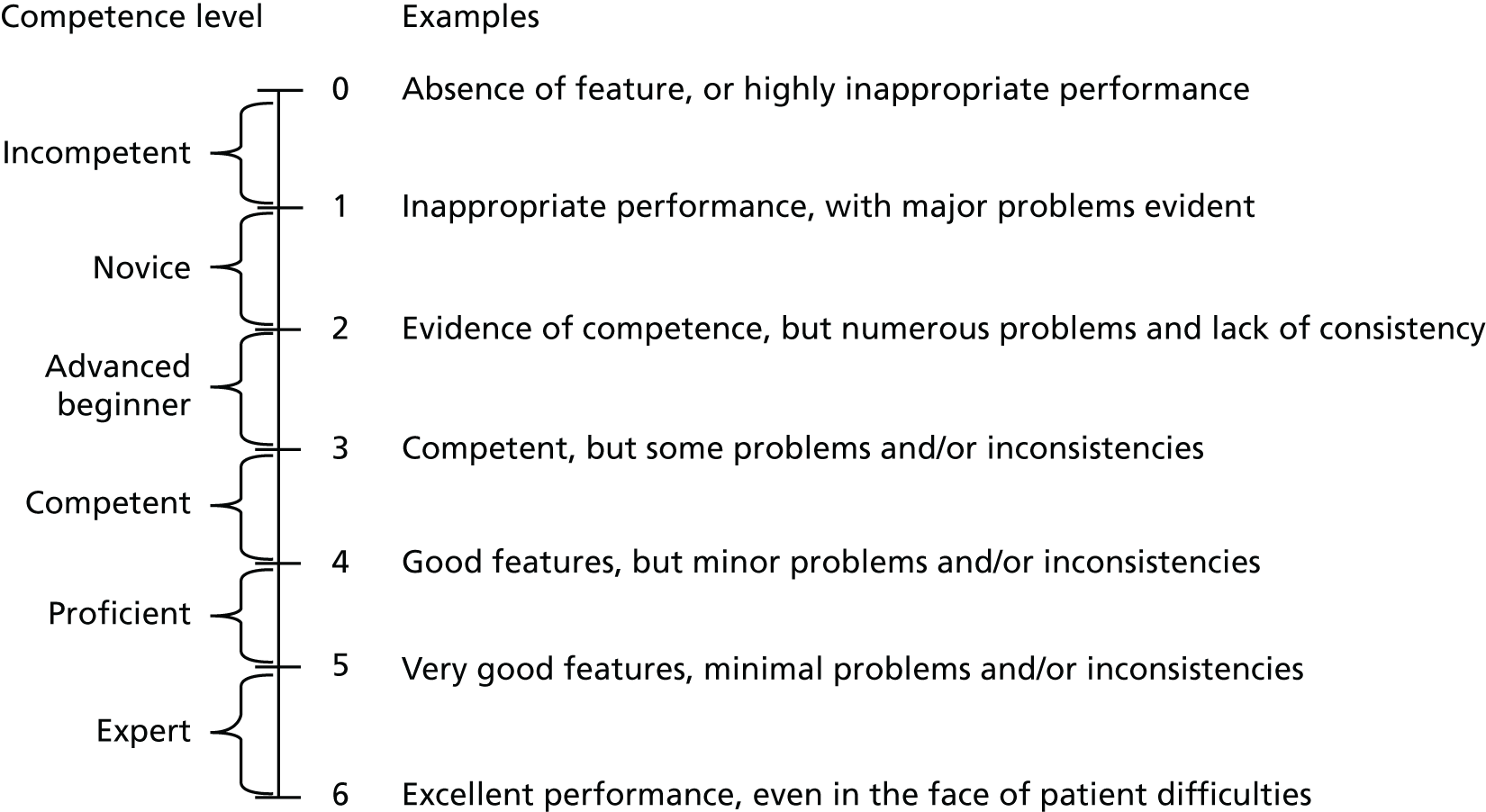
Adjusting for the presence of participant difficulties
Adjustments may be needed when participant difficulties are evident (e.g. excessive avoidance or resistance). In such circumstances, the rater needs to assess the health trainer’s therapeutic skills in the application of the methods. Even though the health trainer may not facilitate change, credit should be given for demonstrating appropriate skillful interaction.
When rating the item, you should first identify whether some of the ‘key features’ are present. If the health trainer includes most of the key features and uses them appropriately (i.e. misses few relevant opportunities to use them and delivers them well), the health trainer should be rated very highly. It is also possible that not every item will be applicable in every consultation. It is important to remember that the scoring profile for this scale should approximate to a normal distribution (i.e. a mid-point of 3), with relatively few scoring at the extremes.
Appendix 2 Flow of participants to recruitment (south-west Community Rehabilitation Company)
FIGURE 5.
Flow of participants to recruitment (south-west CRC).

FIGURE 6.
Flow of participants to recruitment (south-west NPS).

FIGURE 7.
Flow of participants to recruitment (north-west CRC).
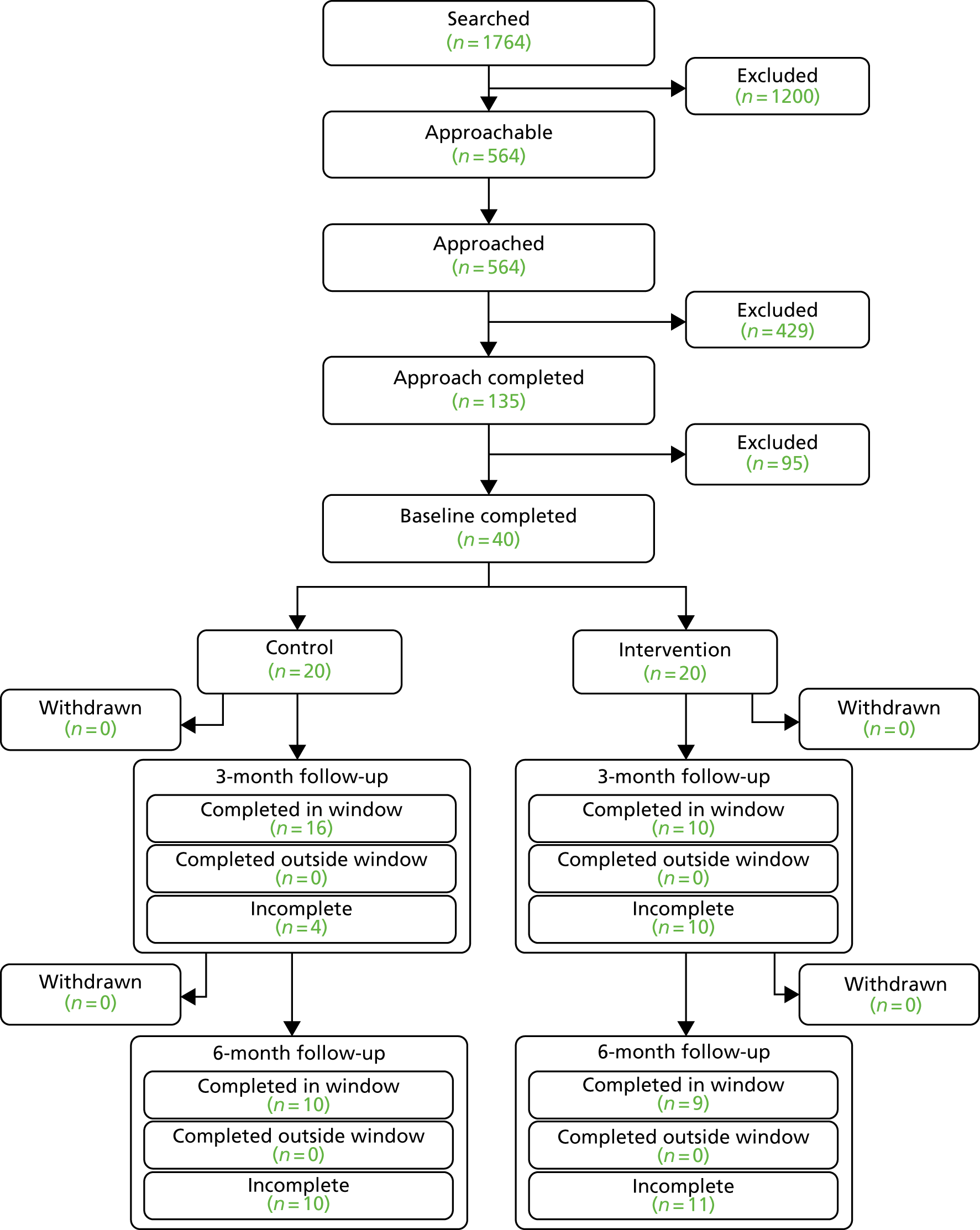
Appendix 3 Completeness of data collection at baseline and follow-up
| Outcome variable | Baseline (N = 61) | 3-month follow-up (N = 34) | 6-month follow-up (N = 40) | Baseline (N = 59) | 3-month follow-up (N = 38) | 6-month follow-up (N = 32) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | |
| Overall AUDIT score among those who drink | 42 | 100.0 (91.6 to 100.0) | 18 | 94.7 (74.0 to 99.9) | 22 | 100.0 (0.85 to 100.0) | 35 | 100.0 (90.0 to 100.0) | 23 | 100.0 (85.2 to 100.0) | 20 | 100.0 (83.2 to 100.0) |
| DINE fibre total score | 60 | 98.4 (91.2 to 100.0) | 34 | 100 (89.7 to 100.0) | 39 | 97.5 (86.8 to 99.9) | 59 | 100.0 (93.9 to 100.0) | 38 | 100.0 (90.7 to 100.0) | 31 | 96.9 (83.8 to 99.9) |
| DINE fat total score | 60 | 98.4 (91.2 to 100.0) | 32 | 94.1 (80.3 to 99.3) | 40 | 100.0 (91.2 to 100.0) | 58 | 98.3 (90.9 to 100.0) | 38 | 100.0 (90.7 to 100.0) | 31 | 96.9 (83.8 to 99.9) |
| DINE unsaturated fat total score | 39 | 63.9 (50.6 to 75.8) | 22 | 64.7 (46.5 to 80.3) | 35 | 87.5 (73.2 to 95.8) | 38 | 64.4 (50.9 to 76.4) | 31 | 81.6 (65.7 to 92.3) | 28 | 87.5 (71.0 to 96.5) |
| Smoker | 61 | 100.0 (94.1 to 100.0) | 34 | 100.0 (89.7 to 100.0) | 40 | 100.0 (91.2 to 100.0) | 59 | 100.0 (93.9 to 100.0) | 38 | 100.0 (90.7 to 100.0) | 32 | 100.0 (89.1 to 100.0) |
| FTND | 42 | 97.7 (87.8 to 99.9) | 14 | 93.3 (68.1 to 99.8) | 22 | 95.7 (78.1 to 99.9) | 40 | 93.0 (80.9 to 98.5) | 22 | 100.0 (84.6 to 100.0) | 17 | 100.0 (80.5 to 100.0) |
| Substance use | 34 | 55.7 (42.4 to 68.5) | 8 | 23.5 (10.7 to 41.2) | 10 | 25.0 (12.7 to 41.2) | 35 | 59.3 (45.7 to 71.9) | 15 | 39.5 (24.0 to 56.6) | 10 | 31.3 (16.1 to 50.0) |
Appendix 4 Health/social care resource use of the intervention and control groups at baseline and at the 3- and 6-month follow-ups
| Resource item | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Primary care services (number of contacts) | ||||
| GP at surgery/health centre | 61 | 1.78 (2.15) [0–10] | 59 | 1.89 (1.90) [0–10] |
| GP via telephone | 61 | 0.42 (1.47) [0–10] | 59 | 0.83 (1.46) [0–6] |
| GP at home | 60 | 0 | 59 | 0.03 (0.18) [0–1] |
| Practice nurse at surgery/health centre | 60 | 0.33 (0.75) [0–4] | 59 | 0.62 (2.15) [0–16] |
| Practice nurse via telephone | 59 | 0.05 (0.22) [0–1] | 59 | 0.05 (0.22) [0–1] |
| Practice nurse at home | 60 | 0 | 59 | 0.33 (2.60) [0–20] |
| Community mental health nurse | 60 | 0.11 (0.37) [0–2] | 59 | 0.13 (0.39) [0–2] |
| Community psychiatric nurse | 60 | 0.05 (0.38) [0–3] | 59 | 0.05 (0.28) [0–2] |
| Physiotherapist at surgery/health centre | 60 | 0 | 59 | 0.37 (1.27) [0–8] |
| Physiotherapist at home | 60 | 0 | 59 | 0 |
| Occupational therapist at surgery/health centre | 60 | 0 | 59 | 0 |
| Occupational therapist at home | 60 | 0 | 59 | 0.01 (0.13) [0–1] |
| Dietitian | 60 | 0.13 (1.03) [0–8] | 59 | 0 |
| Counsellor | 60 | 0.63 (1.72) [0–8] | 59 | 0.66 (3.30) [0–24] |
| NHS Stop Smoking Services | 60 | 0.08 (0.53) [0–4] | 59 | 0.03 (0.26) [0–2] |
| Alcohol services – community | 60 | 0.8 (2.69) [0–16] | 59 | 0.94 (3.37) [0–20] |
| Drug services – community | 60 | 0.96 (2.64) [0–16] | 58 | 0.37 (1.12) [0–6] |
| Walk-in centre | 59 | 0.32 (1.20) [0–8] | 56 | 0.28 (1.38) [0–10] |
| Other | 61 | 0.11 (0.58) [0–4] | 59 | 0.50 (1.68) [0–10] |
| Secondary care (number of events) | ||||
| A&E visits | ||||
| General A&E visits | 61 | 0.14 (0.44) [0–2] | 59 | 0.22 (0.72) [0–4] |
| Mental health A&E visits | 61 | 0 | 59 | 0 |
| Day Cases | 60 | 0.18 (0.70) [0–4] | 58 | 0.25 (0.98) [0–6] |
| Hospital admissions | ||||
| General medical admissions | 61 | 0.03 (0.17) [0–1] | 59 | 0.10 (0.35) [0–0] |
| ICU admissions | 61 | 0 | 59 | 0 |
| Alcohol services admissions | 61 | 0 | 59 | 0 |
| Drug services admissions | 61 | 0 | 59 | 0 |
| Other hospital admissions | 61 | 0 | 59 | 0.01 (0.13) [0–1] |
| Outpatient appointments | ||||
| General appointments | 61 | 0.19 (0.67) [0–4] | 59 | 0.18 (0.47) [0–2] |
| Psychologist appointments | 61 | 0 | 59 | 0.01 (0.13) [0–1] |
| Psychiatrist appointments | 61 | 0 | 59 | 0.01 (0.13) [0–1] |
| Talking therapy appointments | 61 | 0 | 59 | 0 |
| Mental health clinic appointments | 61 | 0 | 59 | 0 |
| Alcohol appointments | 61 | 0 | 59 | 0.03 (0.26) [0–2] |
| Drug services appointments | 61 | 0 | 59 | 0 |
| Criminal justice liaison appointments | 61 | 0 | 59 | 0 |
| Other outpatient appointments | 61 | 0.04 (0.38) [0–3] | 59 | 0.03 (0.26) [0–2] |
| Social care services (number of contacts) | ||||
| Social worker | 60 | 0.63 (1.89) [0–8] | 59 | 0.35 (1.48) [0–8] |
| Home help/care worker | 60 | 0.05 (0.38) [0–3] | 58 | 0.13 (1.05) [0–8] |
| Resource item | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Primary services (number of contacts) | ||||
| GP at surgery/health centre | 33 | 1.45 (1.87) [0–6] | 38 | 1.65 (1.68) [0–6] |
| GP via telephone | 33 | 0.36 (1.14) [0–6] | 38 | 0.55 (1.20) [0–5] |
| GP at home | 33 | 0 | 38 | 0 |
| Practice nurse at surgery/health centre | 33 | 0.27 (0.62) [0–3] | 38 | 0.55 (1.05) [0–4] |
| Practice nurse via telephone | 33 | 0.03 (0.17) [0–1] | 38 | 0.02 (0.16) [0–1] |
| Practice nurse at home | 33 | 0 | 38 | 0 |
| Community mental health nurse | 33 | 0.12 (0.41) [0–2] | 38 | 0.10 (0.64) [0–4] |
| Community psychiatric nurse | 33 | 0.06 (0.34) [0–2] | 38 | 0.23 (0.81) [0–4] |
| Physiotherapist at surgery/health centre | 33 | 0 | 38 | 0.18 (0.72) [0–4] |
| Physiotherapist at home | 33 | 0 | 38 | 0 |
| Occupational therapist at surgery/health centre | 33 | 0 | 38 | 0.10 (0.64) [0–4] |
| Occupational therapist at home | 33 | 0 | 38 | 0 (0) [0–0] |
| Dietitian | 33 | 0 | 38 | 0 |
| Counsellor | 33 | 0.66 (2.32) [0–12] | 38 | 0.52 (1.53) [0–8] |
| NHS Stop Smoking Services | 33 | 0.12 (0.69) [0–4] | 38 | 0.15 (0.71) [0–4] |
| Alcohol services – community | 33 | 0.18 (1.04) [0–6] | 38 | 1.07 (3.07) [0–12] |
| Drug services – community | 33 | 0.30 (0.84) [0–3] | 38 | 0.13 (0.57) [0–3] |
| Walk-in centre | 33 | 0 | 38 | 0.02 (0.16) [0–1] |
| Other | 33 | 0.24 (0.50) [0–2] | 38 | 0.10 (0.38) [0–2] |
| Secondary care (number of events) | ||||
| A&E visits | ||||
| General A&E visits | 34 | 0.06 (0.24) [0–1] | 38 | 0.18 (0.45) [0–2] |
| Mental health A&E visits | 34 | 0 | 38 | 0 |
| Day cases | 34 | 0.02 (0.17) [0–1] | 38 | 0.15 (0.67) [0–4] |
| Hospital admissions | ||||
| General medical admissions | 34 | 0.08 (0.37) [0–2] | 38 | 0.02 (0.16) [0–1] |
| ICU admissions | 34 | 0 | 38 | 0 |
| Alcohol services admissions | 34 | 0 | 38 | 0 |
| Drug services admissions | 34 | 0 | 38 | 0 |
| Other hospital admissions | 34 | 0 | 38 | 0 |
| Outpatient appointments | ||||
| General appointments | 34 | 0.20 (0.47) [0–2] | 38 | 0.15 (0.43) [0–2] |
| Psychologist appointments | 34 | 0 | 38 | 0 |
| Psychiatrist appointments | 34 | 0 | 38 | 0.10 (0.50) [0–3] |
| Talking therapy appointments | 34 | 0 | 38 | 0 |
| Mental health clinic appointments | 34 | 0 | 38 | 0 |
| Alcohol appointments | 34 | 0 | 38 | 0 |
| Drug services appointments | 34 | 0 | 38 | 0 |
| Criminal justice liaison appointments | 34 | 0 | 38 | 0 |
| Other outpatient appointments | 34 | 0.02 (0.17) [0–1] | 38 | 0.05 (0.32) [0–2] |
| Social care services (number of contacts) | ||||
| Social worker | 33 | 0.18 (0.72) [0–4] | 38 | 0.28 (1.62) [0–10] |
| Home help/care worker | 33 | 0 | 38 | 0.26 (1.62) [0–10] |
| Resource item | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Primary services (number of contacts) | ||||
| GP at surgery/health centre | 40 | 1.22 (1.64) [0–6] | 32 | 1.15 (1.27) [0–5] |
| GP via telephone | 40 | 0.8 (1.98) [0–10] | 32 | 0.62 (1.56) [0–6] |
| GP at home | 40 | 0 | 32 | 0 |
| Practice nurse at surgery/health centre | 40 | 0.35 (1.14) [0–6] | 32 | 0.31 (0.69) [0–3] |
| Practice nurse via telephone | 40 | 0.15 (0.94) [0–6] | 32 | 0 |
| Practice nurse at home | 40 | 0 | 32 | 0.06 (0.35) [0–2] |
| Community mental health nurse | 40 | 0.3 (1.89) [0–12] | 32 | 0.18 (0.78) [0–4] |
| Community psychiatric nurse | 40 | 0.15 (0.48) [0–2] | 32 | 0.06 (0.24) [0–1] |
| Physiotherapist at surgery/health centre | 40 | 0.17 (0.78) [0–4] | 32 | 0 |
| Physiotherapist at home | 40 | 0 | 32 | 0 |
| Occupational therapist at surgery/health centre | 40 | 0 | 32 | 0 |
| Occupational therapist at home | 40 | 0 | 32 | 0 |
| Dietitian | 40 | 0 (0) [0–0] | 32 | 0.03 (0.17) [0–1] |
| Counsellor | 40 | 0.65 (2.23) [0–12] | 32 | 1.15 (3.12) [0–12] |
| NHS Stop Smoking Services | 40 | 0 | 32 | 0.18 (0.64) [0–3] |
| Alcohol services – community | 40 | 0.22 (1.04) [0–6] | 32 | 0.46 (1.54) [0–6] |
| Drug services – community | 40 | 1.12 (4.26) [0–24] | 32 | 0.5 (1.60) [0–6] |
| Walk-in centre | 40 | 0.65 (3.79) [0–24] | 32 | 0 |
| Other | 40 | 0.1 (0.49) [0–3] | 32 | 0.28 (1.11) [0–6] |
| Secondary care (number of events) | ||||
| A&E visits | ||||
| General A&E visits | 40 | 0.05 (0.22) [0–1] | 32 | 0.03 (0.17) [0–1] |
| Mental health A&E visits | 40 | 0.02 (0.15) [0–1] | 32 | 0.06 (0.35) [0–2] |
| Day cases | 40 | 0.05 (0.31) [0–2] | 32 | 0.12 (0.55) [0–3] |
| Hospital admissions | ||||
| General medical admissions | 40 | 0.1 (0.44) [0–2] | 32 | 0 |
| ICU admissions | 40 | 0 | 32 | 0 |
| Alcohol services admissions | 40 | 0 | 32 | 0 |
| Drug services admissions | 40 | 0 | 32 | 0 |
| Other hospital admissions | 40 | 0 | 32 | 0 |
| Outpatient appointments | ||||
| General appointments | 40 | 0.07 (0.34) [0–2] | 32 | 0.15 (0.57) [0–3] |
| Psychologist appointments | 40 | 0 | 32 | 0 |
| Psychiatrist appointments | 40 | 0.02 (0.15) [0–1] | 32 | 0 |
| Talking therapy appointments | 40 | 0 | 32 | 0 |
| Mental health clinic appointments | 40 | 0 | 32 | 0 |
| Alcohol appointments | 40 | 0 | 32 | 0 |
| Drug services appointments | 40 | 0 | 32 | 0 |
| Criminal justice liaison appointments | 40 | 0 | 32 | 0 |
| Other outpatient appointments | 40 | 0.07 (0.47) [0–3] | 32 | 0 |
| Social care services (number of contacts) | ||||
| Social worker | 40 | 0.52 (2.09) [0–12] | 32 | 0.5 (2.17) [0–12] |
| Home help/care worker | 40 | 0.02 (0.15) [0–1] | 32 | 0 |
Appendix 5 Costs of health/social care resource use of intervention and control groups at baseline and at the 3- and 6-month follow-ups
| Resource item | Health trainer intervention | Usual care | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Primary care services (number of contacts) | ||||
| GP at surgery/health centre | 61 | 55.39 (66.76) [0–310] | 59 | 58.85 (59.18) [0–310] |
| GP via telephone | 61 | 10.29 (35.66) [0–241.4] | 59 | 20.05 (35.34) [0–144.84] |
| GP at home | 60 | 0 | 59 | 1.31 (7.07) [0–38.76] |
| Practice nurse at surgery/health centre | 60 | 3.1 (6.99) [0–37.2] | 59 | 5.83 (20.06) [0–148.8] |
| Practice nurse via telephone | 59 | 0.4 (1.75) [0–7.9] | 59 | 0.4 (1.75) [0–7.9] |
| Practice nurse at home | 60 | 0 | 59 | 12.54 (96.34) [0–740] |
| Community mental health nurse | 60 | 4.2 (13.41) [0–72] | 59 | 4.88 (14.11) [0–72] |
| Community psychiatric nurse | 60 | 1.8 (13.94) [0–108] | 59 | 1.83 (10.41) [0–72] |
| Physiotherapist at surgery/health centre | 60 | 0 | 59 | 19.76 (67.4) [0–424] |
| Physiotherapist at home | 60 | 0 | 59 | 0 |
| Occupational therapist at surgery/health centre | 60 | 0 | 59 | 0 |
| Occupational therapist at home | 60 | 0 | 59 | 1.31 (10.02) [0–77] |
| Dietitian | 60 | 4.4 (34.08) [0–264] | 59 | 0 |
| Counsellor | 60 | 27.23 (74.25) [0–344] | 59 | 28.42 (142.3) [0–1032] |
| NHS Stop Smoking Services | 60 | 4.32 (23.47) [0–129.67] | 59 | 2.2 (16.88) [0–129.67] |
| Alcohol services – community | 60 | 36 (121.15) [0–720] | 59 | 42.71 (151.67) [0–900] |
| Drug services – community | 60 | 129.53 (354.07) [0–2144] | 58 | 50.83 (150.24) [0–804] |
| Walk-in centre | 59 | 13.78 (51.78) [0–342.4] | 56 | 12.23 (59.26) [0–428] |
| Primary care subtotal | 58 | 233.58 (310.32) [0–1494] | 56 | 271.87 (329.15) [0–1503.6] |
| Secondary care (number of events) | ||||
| General appointments | 61 | 26.95 (92.98) [0–548] | 59 | 25.54 (64.73) [0–274] |
| Psychologist appointments | 61 | 0 | 59 | 0.93 (7.16) [0–55] |
| Psychiatrist appointments | 61 | 0 | 59 | 1.83 (14.06) [0–108] |
| Alcohol appointments | 61 | 0 | 59 | 1.53 (11.72) [0–90] |
| General medical admissions | 61 | 10.66 (58.35) [0–324.99] | 59 | 33.05 (116) [0–649.98] |
| Day cases | 60 | 133.28 (509.55) [0–2908] | 58 | 188.02 (714.91) [0–4362] |
| General A&E visits | 61 | 21.81 (65.19) [0–295.6] | 59 | 32.57 (106.54) [0–591.2] |
| Mental health A&E visits | 61 | 0 | 59 | 0 |
| Secondary care subtotal | 60 | 193.69 (604.94) [0–3603.8] | 58 | 277.46 (848.56) [0–5285.98] |
| Social care services (number of contacts) | ||||
| Social worker | 60 | 37.37 (111.82) [0–472] | 59 | 21 (87.49) [0–472] |
| Home help/care worker | 60 | 0.35 (2.67) [0–20.7] | 58 | 0.95 (7.25) [0–55.2] |
| Social care subtotal | 60 | 37.71 (111.74) [0–472] | 58 | 22.31 (88.27) [0–472] |
| Total cost to NHS and PSS (excluding intervention cost) | 57 | 480.17 (789.5) [0–4675.8] | 54 | 567.4 (1042.79) [0–6484.78] |
| Resource item | Health trainer intervention | Usual care | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Primary care services (number of contacts) | ||||
| GP at surgery/health centre | 33 | 45.09 (58.04) [0–186] | 38 | 51.39 (52.11) [0–186] |
| GP via telephone | 33 | 8.78 (27.54) [0–144.84] | 38 | 13.34 (29) [0–120.7] |
| GP at home | 33 | 0 | 38 | 0 |
| Practice nurse at surgery/health centre | 33 | 2.54 (5.82) [0–27.9] | 38 | 5.14 (9.84) [0–37.2] |
| Practice nurse via telephone | 33 | 0.24 (1.38) [0–7.9] | 38 | 0.21 (1.28) [0–7.9] |
| Practice nurse at home | 33 | 0 | 38 | 0 |
| Community mental health nurse | 33 | 4.36 (14.95) [0–72] | 38 | 3.79 (23.36) [0–144] |
| Community psychiatric nurse | 33 | 2.18 (12.53) [0–72] | 38 | 8.53 (29.51) [0–144] |
| Physiotherapist at surgery/health centre | 33 | 0 | 38 | 9.76 (38.68) [0–212] |
| Physiotherapist at home | 33 | 0 | 38 | 0 |
| Occupational therapist at surgery/health centre | 33 | 0 | 38 | 8.11 (49.96) [0–308] |
| Occupational therapist at home | 33 | 0 | 38 | 0 |
| Dietitian | 33 | 0 | 38 | 0 |
| Counsellor | 33 | 28.67 (100.08) [0–516] | 38 | 22.63 (66.12) [0–344] |
| NHS Stop Smoking Services | 33 | 3.93 (22.57) [0–129.67] | 38 | 6.82 (29.34) [0–129.67] |
| Alcohol services – community | 33 | 8.18 (47) [0–270] | 38 | 48.55 (138.16) [0–540] |
| Drug services – community | 33 | 40.61 (113.53) [0–402] | 38 | 17.63 (77.39) [0–402] |
| Walk-in centre | 33 | 0 | 38 | 1.13 (6.94) [0–42.8] |
| Primary care subtotal | 33 | 144.57 (232.65) [0–1011] | 38 | 197.03 (218.64) [0–799.71] |
| Secondary care (number of events) | ||||
| General appointments | 34 | 28.21 (65.57) [0–274] | 38 | 21.63 (59.81) [0–274] |
| Psychologist appointments | 34 | 0 | 38 | 0 |
| Psychiatrist appointments | 34 | 0 | 38 | 11.37 (54.95) [0–324] |
| Alcohol appointments | 34 | 0 | 38 | 0 |
| General medical admissions | 34 | 28.68 (123.11) [0–649.98] | 38 | 8.55 (52.72) [0–324.99] |
| Day cases | 34 | 21.38 (124.68) [0–727] | 38 | 114.79 (493.55) [0–2908] |
| General A&E visits | 34 | 8.69 (35.30) [0–147.8] | 38 | 27.23 (67.47) [0–295.6] |
| Mental health A&E visits | 34 | 0 | 38 | 0 |
| Secondary care subtotal | 34 | 86.96 (213.78) [0–797.78] | 38 | 183.57 (557.03) [0–3232] |
| Social care services (number of contacts) | ||||
| Social worker | 33 | 10.73 (42.89) [0–236] | 38 | 17.08 (95.93) [0–590] |
| Home help/care worker | 33 | 0 | 38 | 1.82 (11.19) [0–69] |
| Social care subtotal | 33 | 10.73 (42.89) [0–236] | 38 | 18.89 (107.07) [0–659] |
| Total cost to NHS and PSS (excluding intervention cost) | 33 | 244.89 (305.52) [0–1011] | 38 | 399.5 (632.98) [0–3640.88] |
| Resource item | Health trainer intervention | Usual care | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Primary care services (number of contacts) | ||||
| GP at surgery/health centre | 40 | 37.98 (50.86) [0–186] | 32 | 35.84 (39.46) [0–155] |
| GP via telephone | 40 | 19.31 (48.03) [0–241.4] | 32 | 15.09 (37.67) [0–144.84] |
| GP at home | 40 | 0 | 32 | 0 |
| Practice nurse at surgery/health centre | 40 | 3.26 (10.65) [0–55.8] | 32 | 2.91 (6.44) [0–27.9] |
| Practice nurse via telephone | 40 | 1.19 (7.49) [0–47.4] | 32 | 0 |
| Practice nurse at home | 40 | 0 | 32 | 2.31 (13.08) [0–74] |
| Community mental health nurse | 40 | 10.8 (68.31) [0–432] | 32 | 6.75 (28.09) [0–144] |
| Community psychiatric nurse | 40 | 5.4 (17.39) [0–72] | 32 | 2.25 (8.85) [0–36] |
| Physiotherapist at surgery/health centre | 40 | 9.28 (41.38) [0–212] | 32 | 0 |
| Physiotherapist at home | 40 | 0 | 32 | 0 |
| Occupational therapist at surgery/health centre | 40 | 0 | 32 | 0 |
| Occupational therapist at home | 40 | 0 | 32 | 0 |
| Dietitian | 40 | 0 | 32 | 1.03 (5.83) [0–33] |
| Counsellor | 40 | 27.95 (96.18) [0–516] | 32 | 49.72 (134.26) [0–516] |
| NHS Stop Smoking Services | 39 | 0 | 32 | 12.16 (38.4) [0–129.67] |
| Alcohol services – community | 40 | 10.13 (47.24) [0–270] | 32 | 21.09 (69.51) [0–270] |
| Drug services – community | 40 | 150.75 (571.9) [0–3216] | 32 | 67 (215.26) [0–804] |
| Walk-in centre | 40 | 27.82 (162.63) [0–1027.2] | 32 | 0 |
| Primary care subtotal | 39 | 309.43 (844.61) [0–4872.24] | 32 | 216.15 (287.85) [0–933.67] |
| Secondary care (number of events) | ||||
| General appointments | 40 | 10.28 (47.94) [0–274] | 32 | 21.41 (78.66) [0–411] |
| Psychologist appointments | 40 | 0 | 32 | 0 |
| Psychiatrist appointments | 40 | 2.7 (17.08) [0–108] | 32 | 0 |
| Alcohol appointments | 40 | 0 | 32 | 0 |
| General medical admissions | 40 | 32.5 (143.46) [0–649.98] | 32 | 0 |
| Day cases | 40 | 36.35 (229.9) [0–1454] | 32 | 90.88 (402.45) [0–2181] |
| General A&E visits | 40 | 7.39 (32.62) [0–147.8] | 32 | 4.62 (26.13) [0–147.8] |
| Mental health A&E visits | 40 | 4.83 (30.52) [0–193] | 32 | 12.06 (68.24) [0–386] |
| Secondary care subtotal | 40 | 94.04 (321.52) [0–1728] | 32 | 128.96 (492.69) [0–2592] |
| Social care services (number of contacts) | ||||
| Social worker | 40 | 30.98 (123.89) [0–708] | 32 | 29.5 (128.04) [0–708] |
| Home help/care worker | 40 | 0.17 (1.09) [0–6.9] | 32 | 0 |
| Social care subtotal | 40 | 31.15 (124.36) [0–708] | 32 | 29.5 (128.04) [0–708] |
| Total cost to NHS and PSS (excluding intervention cost) | 39 | 437.83 (952.49) [0–4980.24] | 32 | 374.61 (590.62) [0–2675.3] |
Appendix 6 Broader societal resource use of the intervention and control groups at baseline and at the 3- and 6-month follow-ups
| Resource item | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Education services (number of contacts) | ||||
| Education courses | 61 | 0.40 (2.01) [0–14] | 59 | 0.67 (3.47) [0–24] |
| Employment worker/officer | 61 | 0.26 (2.04) [0–16] | 59 | 0 |
| Citizen’s Advice Bureau | 61 | 0 | 59 | 0.01 (0.13) [0–1] |
| Job centre | 61 | 1.81 (6.86) [0–40] | 59 | 0.79 (1.90) [0–8] |
| Enhanced Thinking Skills | 61 | 0.26 (2.04) [0–16] | 59 | 0 |
| Cognitive Skills Booster | 61 | 0 | 59 | 0 |
| Cognitive Self-Change Programme | 61 | 0 | 59 | 0 |
| Other | 61 | 2.13 (7.94) [0–58] | 59 | 1.52 (8.05) [0–60] |
| Other service providers (number of contacts) | ||||
| Probation worker | 61 | 3.29 (2.71) [0–8] | 59 | 3.55 (2.40) [0–9] |
| Social worker | 61 | 0.62 (1.88) [0–8] | 59 | 0.38 (1.52) [0–8] |
| Community rehabilitation worker | 61 | 0.93 (2.64) [0–16] | 59 | 0.23 (1.17) [0–8] |
| Police custody | 61 | 0.04 (0.21) [0–1] | 59 | 0.03 (0.18) [0–1] |
| Focus on Resettlement | 61 | 0 | 59 | 0 |
| Solicitor/lawyer | 61 | 0.09 (0.47) [0–3] | 59 | 0.18 (1.05) [0–8] |
| Barrister | 61 | 0 | 59 | 0.05 (0.28) [0–2] |
| Legal advocate | 61 | 0 | 59 | 0 |
| Other | 61 | 1.09 (5.28) [0–40] | 59 | 0 |
| Help from friends and relatives | ||||
| Hours per week | 61 | 1.70 (4.66) [0–24] | 59 | 1.16 (4.23) [0–28] |
| Days off work in the previous 2 months | 61 | 0 | 59 | 0.05 (0.28) [0–2] |
| Resource item | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Education services (number of contacts) | ||||
| Education courses | 34 | 1.5 (6.55) [0–36] | 38 | 0.52 (2.06) [0–10] |
| Employment worker/officer | 34 | 0.14 (0.70) [0–4] | 38 | 0.13 (0.81) [0–5] |
| Citizen’s Advice Bureau | 34 | 0 | 38 | 0.02 (0.16) [0–1] |
| Job centre | 34 | 1.55 (3.50) [0–12] | 38 | 1.57 (2.77) [0–10] |
| Enhanced Thinking Skills | 34 | 0 | 38 | 0 |
| Cognitive Skills Booster | 34 | 0 | 38 | 0 |
| Cognitive Self-Change Programme | 34 | 0 | 38 | 0 |
| Other | 34 | 2.55 (10.8) [0–62] | 38 | 2.71 (10.3) [0–62] |
| Other service providers (number of contacts) | ||||
| Probation worker | 34 | 2.70 (2.55) [0–8] | 38 | 3.39 (3.14) [0–12] |
| Social worker | 34 | 0.17 (0.71) [0–4] | 38 | 0.28 (1.62) [0–10] |
| Community rehabilitation worker | 34 | 0.55 (1.18) [0–4] | 38 | 0.68 (2.09) [0–12] |
| Police custody | 34 | 0.11 (0.40) [0–2] | 38 | 0.05 (0.22) [0–1] |
| Focus on Resettlement | 34 | 0 | 38 | 0 (0) [0–0] |
| Solicitor/lawyer | 34 | 0.20 (0.68) [0–3] | 38 | 0.15 (0.49) [0–2] |
| Barrister | 34 | 0 | 38 | 0.02 (0.16) [0–1] |
| Legal advocate | 34 | 0.02 (0.17) [0–1] | 38 | 0 |
| Other | 34 | 0.26 (0.86) [0–4] | 38 | 0.92 (5.67) [0–35] |
| Help from friends and relatives | ||||
| Hours per week | 34 | 1.38 (3.44) [0–14] | 38 | 1.23 (2.81) [0–14] |
| Days off work in the previous 2 months | 33 | 0.12 (0.69) [0–4] | 38 | 0.05 (0.32) [0–2] |
| Resource item | Intervention | Control | ||
|---|---|---|---|---|
| n | Mean (SD) [range] | n | Mean (SD) [range] | |
| Education services (number of contacts) | ||||
| Education courses | 40 | 0.22 (0.91) [0–5] | 32 | 0.71 (2.59) [0–14] |
| Employment worker/officer | 40 | 0 | 32 | 0 |
| Citizen’s Advice Bureau | 40 | 0 | 32 | 0 |
| Job centre | 40 | 1.15 (2.15) [0–8] | 32 | 0.71 (1.70) [0–6] |
| Enhanced Thinking Skills | 40 | 0 | 32 | 0 |
| Cognitive Skills Booster | 40 | 0 | 32 | 0 |
| Cognitive Self-Change Programme | 40 | 0 | 32 | 0 |
| Other | 40 | 3.77 (11.7) [0–62] | 32 | 0.21 (0.79) [0–4] |
| Other service providers (number of contacts) | ||||
| Probation worker | 40 | 3.2 (2.61) [0–12] | 32 | 3.71 (4.84) [0–24] |
| Social worker | 40 | 0.57 (2.13) [0–12] | 32 | 0.03 (0.17) [0–1] |
| Community rehabilitation worker | 40 | 0.32 (0.85) [0–3] | 32 | 0.40 (1.10) [0–4] |
| Police custody | 40 | 0.1 (0.44) [0–2] | 32 | 0 |
| Focus on Resettlement | 40 | 0 | 32 | 0 |
| Solicitor/lawyer | 40 | 0.12 (0.46) [0–2] | 32 | 0.06 (0.24) [0–1] |
| Barrister | 40 | 0.07 (0.34) [0–2] | 32 | 0 |
| Legal advocate | 40 | 0 | 32 | 0 |
| Other | 40 | 0.05 (0.22) [0–1] | 32 | 0.06 (0.35) [0–2] |
| Help from friends and relatives | ||||
| Hours per week | 40 | 1.62 (5.13) [0–30] | 32 | 2.15 (8.57) [0–48] |
| Days off work in the previous 2 months | 40 | 0.07 (0.34) [0–2] | 32 | 0 |
Appendix 7 Medications data
Table 45 reports medications used during each reporting period, grouped by the main reported reason for prescription. In total, 60 different drugs were identified by participants as medication that they had used at some point over the baseline and follow-up periods (plus unspecified vitamin supplements). Prescription rates for most individual drugs were very low, with fewer than five users. The medications with more than five users at any assessment point were citalopram, co-codamol, codeine, ibuprofen, mirtazapine, paracetamol, pregabalin, quetiapine, salbutamol and sertraline. Owing to the small numbers, Table 45 reports medication use for the intervention and control groups combined. The drugs listed are grouped according to the main types of health problem for which participants said they were prescribed.
| Medication by reported reason for prescription | Number of participants | ||
|---|---|---|---|
| Baseline | Month 3 | Month 6 | |
| Mental health | |||
| Non-psychosis | |||
| Mirtazapine | 22 | 12 | 9 |
| Pregabalin | 10 | 1 | 6 |
| Sertraline | 9 | 4 | 6 |
| Citalopram | 6 | 3 | 3 |
| Propranolol hydrochloride | 5 | 2 | 2 |
| Fluoxetine | 4 | 2 | 2 |
| Venlafaxine | 2 | 2 | 4 |
| Amitriptyline hydrochloride | 4 | 1 | 2 |
| Diazepam | 3 | 0 | 3 |
| Buprenorphine | 3 | 2 | 0 |
| Methadone hydrochloride | 2 | 2 | 1 |
| Methylphenidate hydrochloride | 2 | 2 | 1 |
| Zopiclone | 2 | 0 | 2 |
| Temazepam | 1 | 1 | 0 |
| Duloxetine | 0 | 1 | 0 |
| Naltrexone hydrochloride | 1 | 0 | 0 |
| Paroxetine | 1 | 0 | 0 |
| Promazine hydrochloride | 1 | 0 | 0 |
| Psychosis | |||
| Quetiapine | 7 | 3 | 5 |
| Trazodone hydrochloride | 1 | 1 | 3 |
| Olanzapine | 0 | 1 | 1 |
| Risperidone | 1 | 1 | 0 |
| Valproic acid | 1 | 1 | 0 |
| Amisulpride | 1 | 0 | 0 |
| Chlorpromazine hydrochloride | 0 | 0 | 1 |
| Pain | |||
| Paracetamol | 9 | 3 | 2 |
| Codeine phosphate | 9 | 3 | 1 |
| Co-codamol | 8 | 2 | 1 |
| Ibuprofen | 6 | 1 | 3 |
| Naproxen | 2 | 3 | 4 |
| Gabapentin | 2 | 2 | 2 |
| Aspirin | 0 | 0 | 2 |
| Diclofenac sodium | 0 | 2 | 0 |
| Tramadol hydrochloride | 1 | 1 | 1 |
| Morphine (Oramorph) | 1 | 0 | 0 |
| Pizotifen | 1 | 0 | 0 |
| Gastric problems | |||
| Omeprazole | 1 | 2 | 4 |
| Lansoprazol | 2 | 0 | 0 |
| Peppermint oil | 0 | 1 | 1 |
| Osmorol | 1 | 0 | 0 |
| Asthma | |||
| Salbutamol | 7 | 3 | 4 |
| Fluticasone with salmeterol inhaler (Seretide) | 1 | 3 | 2 |
| Beclometasone dipropionate | 0 | 0 | 1 |
| Other | |||
| Carvedilol | 1 | 0 | 4 |
| Thiamine | 3 | 2 | 0 |
| Amoxicillin | 0 | 3 | 0 |
| Vitamin supplement (unspecified) | 2 | 2 | 2 |
| Metformin hydrochloride | 2 | 1 | 1 |
| Insulin (not specified) | 2 | 0 | 0 |
| Lactulose | 1 | 1 | 1 |
| Lisinopril | 1 | 1 | 1 |
| Apixaban | 1 | 1 | 0 |
| Cetirizine hydrochloride | 1 | 1 | 0 |
| Folic acid | 0 | 1 | 1 |
| Ascorbic acid | 0 | 0 | 1 |
| Co-amoxiclav | 1 | 0 | 0 |
| Finasteride | 0 | 0 | 1 |
| Loratadine | 0 | 0 | 1 |
| Penicillin | 0 | 1 | 0 |
| Rivaroxaban | 1 | 0 | 0 |
| Sodium valproate | 1 | 0 | 0 |
| Non-identifiable medication use | |||
| Participant did not know the name of the drug | 42 | 17 | 34 |
| Unable to match to the British National Formulary81 | 4 | 2 | 4 |
There were issues with the quality of the data collected on participants’ use of medications, which arose in part because of the practice of recording these data as free text. This led to considerable data quality issues, with many misspellings across a mixture of brand and generic drug names. As a result, for every data entry, the spelling of the drug name and reason for prescription provided on the CRF was checked against the British National Formulary (BNF) (online access provided by NICE) to ensure that the medication was correctly identified, using consistent naming conventions. This process would not be feasible with a full trial data set. In a high proportion of cases, the participant was unable to name the medication that they were prescribed. In addition, there were some drug names that we were unable to match to a drug listed in the BNF. Overall, the percentage of drugs reported by participants that were unidentifiable for one of these two reasons was 22% at baseline (18% at the 3-month follow-up and 28% at the 6-month follow-up). Other issues that would cause problems for costing medication use were that the ‘length of prescription (in days)’ was not always completed, and the dose was seldom recorded. In some cases, it was not clear whether the medication had been prescribed or purchased over the counter. These issues prevented us from including the use of medication in the analysis of resource use and costs. For the main study, we recommend identifying a manageable number of (around 10) medications that are frequently used by this population, and collecting data on the use of these drugs in a more structured format. This could also be tied into plans for improving the collection of data on illicit drug use.
List of abbreviations
- 5WWB
- Five Ways to Well-being
- BNF
- British National Formulary
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CJS
- criminal justice system
- CLANG
- Connect with others, keep Learning, be physically Active, take Notice of things around you and Give
- CONSORT
- Consolidated Standards of Reporting Trials
- CRC
- Community Rehabilitation Company
- CRF
- case report form
- EARS
- Exercise Assisted Reduction then Stop
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GP
- general practitioner
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- MI
- motivational interviewing
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPS
- National Probation Service
- OARS
- open questions, affirmation, reflective listening, summaries
- OMS
- offender management service
- PenCTU
- Peninsula Clinical Trials Unit
- PHQ-9
- Patient Health Questionnaire-9 items
- PPI
- patient and public involvement
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- RA
- research assistant
- RAR
- rehabilitation activity requirement
- RCT
- randomised controlled trial
- SD
- standard deviation
- SF-36
- Short Form questionnaire-36 items
- SF-6D
- Short Form questionnaire-6 Dimensions
- SWEMWBS
- Short Warwick–Edinburgh Mental Well-being Scale
- WEMWBS
- Warwick–Edinburgh Mental Well-being Scale

